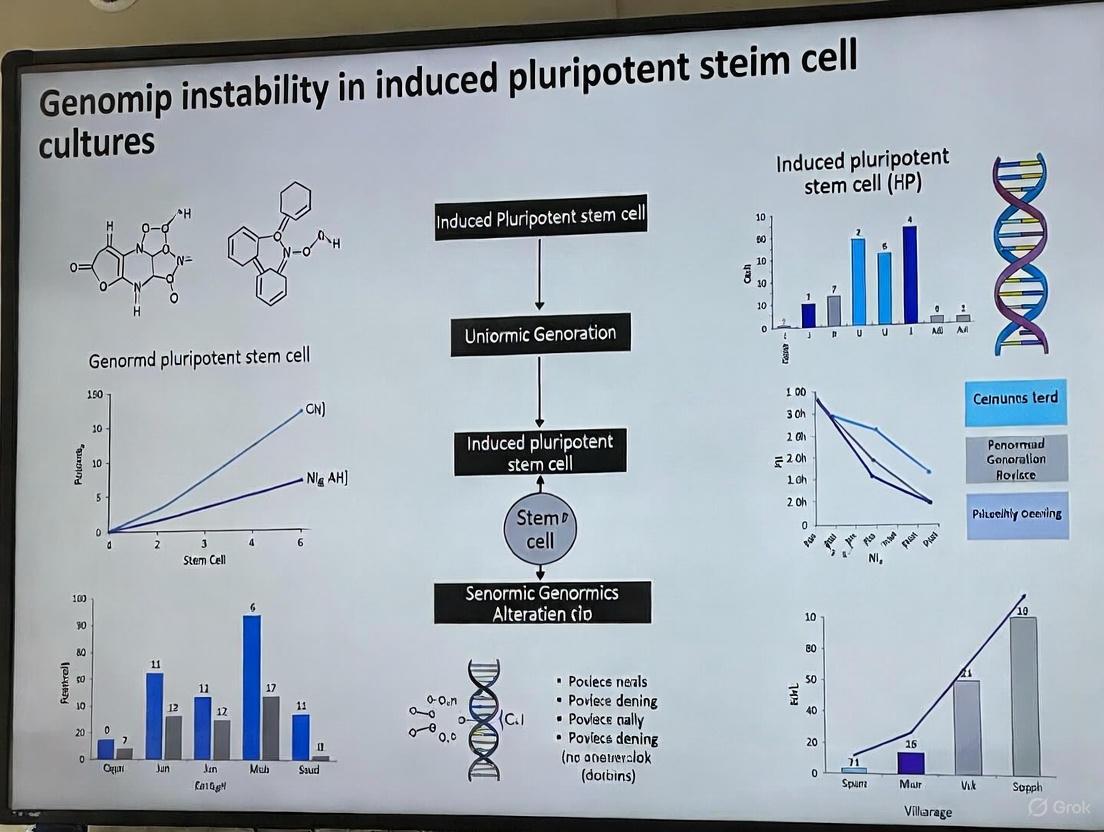
Addressing Genomic Instability in iPSC Cultures: Mechanisms, Monitoring, and Mitigation Strategies for Research and Therapy
The profound therapeutic potential of induced pluripotent stem cells (iPSCs) is tempered by the significant challenge of genomic instability, which can compromise experimental results and pose serious risks in clinical...
Addressing Genomic Instability in iPSC Cultures: Mechanisms, Monitoring, and Mitigation Strategies for Research and Therapy
Abstract
The profound therapeutic potential of induced pluripotent stem cells (iPSCs) is tempered by the significant challenge of genomic instability, which can compromise experimental results and pose serious risks in clinical applications. This article provides a comprehensive resource for researchers and drug development professionals, exploring the molecular origins of instability—from reprogramming-induced replication stress to culture-adapted aneuploidies. It details state-of-the-art methodologies for robust genomic monitoring and compares the fidelity of different reprogramming techniques. Furthermore, the article outlines practical strategies for optimizing culture conditions to minimize instability and establishes a framework for the rigorous validation and safety profiling of iPSC lines destined for preclinical and clinical use.
The Origins and Mechanisms of Genomic Instability in iPSCs
The process of reprogramming somatic cells into induced pluripotent stem cells (iPSCs) places tremendous stress on the cellular machinery, particularly on the fundamental process of DNA replication. This replication stress represents a significant source of genomic instability in iPSCs, potentially compromising their research and therapeutic applications. Central to this phenomenon are the reprogramming factors themselves, especially the oncogene c-Myc, which plays a paradoxical role as both a powerful facilitator of reprogramming and a potent inducer of genomic instability. When activated, c-Myc triggers a cascade of molecular events that can lead to slowing and stalling of replication forks, ultimately resulting in DNA damage and genomic alterations [1]. Understanding these mechanisms is crucial for developing strategies to minimize genomic instability in iPSC cultures, thereby enhancing their safety profile for biomedical applications.
Frequently Asked Questions (FAQs)
Q1: What exactly is replication stress in the context of iPSC reprogramming?
Replication stress refers to the inefficient progression of DNA replication due to slowing, stalling, or collapse of replication forks. During reprogramming, the forced expression of oncogenes like c-Myc creates an environment where the DNA replication machinery encounters obstacles, leading to incomplete genome duplication and potential DNA damage. This is mechanistically distinct from the normal replication process and can compromise genomic integrity [1].
Q2: Why is c-Myc still used in reprogramming if it causes replication stress?
c-Myc remains a component of many reprogramming protocols because it significantly enhances reprogramming efficiency. It functions as a "double-edged sword" by promoting the transition to pluripotency while simultaneously increasing the risk of genomic instability. Research indicates that c-Myc can be dispensable for reprogramming, though its exclusion typically results in substantially lower efficiency [2] [3].
Q3: Are there safer alternatives to using c-Myc in reprogramming?
Yes, several alternatives exist. L-Myc has been identified as a promising substitute that promotes reprogramming with significantly lower transformation activity compared to c-Myc. Additionally, specific c-Myc mutants (such as W136E) that retain reprogramming enhancement while lacking strong transformation capacity have been developed. These alternatives provide researchers with options to balance efficiency and safety concerns [3].
Q4: How does replication stress lead to genomic instability in iPSCs?
Replication stress can directly cause DNA breaks and mutations. When replication forks stall, the DNA becomes vulnerable to breakage, which may result in copy number variations (CNVs), chromosomal rearrangements, and other genetic abnormalities. These alterations can persist in the iPSC population and potentially confer selective growth advantages, leading to their expansion during culture [4] [5].
Q5: What are the practical consequences of replication stress for iPSC-based research?
From a practical standpoint, replication stress-induced genomic instability can compromise experimental reproducibility and disease modeling accuracy. In clinical applications, this instability raises significant safety concerns due to the potential for tumor formation. Research has identified recurrent genomic alterations in iPSCs that overlap with cancer-associated genes, highlighting the importance of careful genomic monitoring [4] [6].
Troubleshooting Guide: Addressing Replication Stress
Problem: High Rates of Genomic Instability in Reprogrammed iPSCs
| Troubleshooting Step | Implementation Details | Expected Outcome |
|---|---|---|
| Alternative Myc Factors | Use L-Myc instead of c-Myc, or utilize c-Myc mutants (W136E) with reduced transformation potential [3]. | Reduced replication stress and tumorigenicity while maintaining reprogramming efficiency. |
| p53 Pathway Modulation | Utilize temporary p53 suppression (e.g., mp53DD dominant-negative mutant) rather than complete knockout [7]. | Enhanced reprogramming efficiency without completely removing critical DNA damage checkpoint. |
| Non-Integrating Methods | Employ Sendai virus or episomal vectors instead of integrating viral systems [7]. | Reduced risk of insertional mutagenesis compounding replication stress-induced damage. |
| Optimized Culture | Avoid prolonged culture; use early passage cells; maintain optimal colony density [8]. | Minimized accumulation of culture-acquired genetic variations. |
| Monitoring Protocols | Implement regular karyotyping and CNV analysis at different passages [4] [6]. | Early detection of genomic abnormalities enabling selective expansion of stable clones. |
Problem: Poor Reprogramming Efficiency When Reducing Replication Stress
| Troubleshooting Step | Implementation Details | Expected Outcome |
|---|---|---|
| Myc Optimization | When using CytoTune Sendai system, optimize Klf4 MOI (try KOS:c-Myc:Klf4 ratios of 5:5:3, 5:5:6, or 10:10:6) [7]. | Balanced reprogramming efficiency with acceptable stress levels. |
| Small Molecule Enhancement | Incorporate small molecules that enhance reprogramming (e.g., ROCK inhibitor Y-27632 for cell survival) [9]. | Improved survival of reprogramming cells without genetic manipulation. |
| Parental Cell Selection | Use early passage ( | More efficient reprogramming with reduced baseline genomic abnormalities. |
| Feeder Condition Optimization | Consider feeder-dependent systems for initial reprogramming (higher efficiency), then adapt to feeder-free [9]. | Maximized reprogramming efficiency before transitioning to defined conditions. |
Experimental Protocols & Methodologies
Assessing Replication Stress in Reprogramming Cells
DNA Fiber Assay Protocol (Adapted from [1])
This protocol measures replication fork progression, a direct indicator of replication stress.
Step 1: Pulse-labeling with Nucleotide Analogs
- Expose reprogramming cells to sequential pulses of CldU (25 μM for 20 minutes) and IdU (250 μM for 20 minutes)
- Ensure precise timing to accurately measure replication speed
Step 2: DNA Fiber Preparation
- Harvest cells and resuspend at low concentration (1,000 cells/μL)
- Spot cells on glass slides and lyse with spreading buffer (0.5% SDS, 200 mM Tris-HCl pH 7.4, 50 mM EDTA)
- Tilt slides to spread DNA fibers, air dry, and fix in methanol:acetic acid (3:1)
Step 3: Immunodetection and Analysis
- Denature DNA with 2.5M HCl, block with 5% BSA
- Incubate with anti-CldU and anti-IdU antibodies sequentially
- Visualize with fluorescence microscopy and measure fiber lengths
- Interpretation: Shorter fiber lengths in c-Myc-expressing cells indicate replication fork slowing, characteristic of replication stress [1]
Safer Reprogramming Using L-Myc Protocol
This protocol leverages L-Myc for efficient reprogramming with reduced genomic instability [3].
Step 1: Preparation of Parental Cells
- Plate human dermal fibroblasts at 50-80% confluence in 6-well plates
- Use early passage cells (
Step 2: Transduction with Reprogramming Factors
- Prepare retroviral vectors encoding Oct3/4, Sox2, Klf4, and L-Myc
- Perform transduction using standard viral delivery methods
- Critical Note: L-Myc generates significantly fewer non-iPSC colonies compared to c-Myc, indicating more specific reprogramming
Step 3: iPSC Selection and Culture
- Transfer transduced cells to feeder layers or feeder-free matrices 3-5 days post-transduction
- Change to human ESC culture medium supplemented with bFGF
- Begin monitoring for iPSC colony appearance at 2-3 weeks
Step 4: Validation
- Pick colonies with ESC-like morphology
- Verify pluripotency markers (Tra-1-60, Tra-1-81, SSEA-3, Oct3/4)
- Perform teratoma assay to confirm differentiation potential
- Key Advantage: iPSCs generated with L-Myc produce high-percentage chimeras competent for germline transmission without increased tumorigenicity [3]
The Scientist's Toolkit: Essential Research Reagents
| Research Need | Recommended Reagents | Specific Function |
|---|---|---|
| Reprogramming with Reduced Risk | CytoTune-iPS 2.1 Sendai Kit (with L-Myc) [7], Epi5 Episomal Kit (with L-Myc/Lin28) [7] | Non-integrating delivery of reprogramming factors with safer Myc alternatives. |
| c-Myc-Specific Reagents | c-Myc antibodies (for monitoring), c-Myc inhibitors (e.g., 10058-F4) | Detection and functional manipulation of c-Myc in experimental systems. |
| Replication Stress Detection | Antibodies against pCHK1, pRPA, γH2AX [1], nucleotide analogs (CldU/IdU) [1] | Markers for monitoring replication stress and DNA damage response activation. |
| Cell Culture Matrices | Geltrex, Matrigel, Laminin-521 [9] | Defined substrates for feeder-free culture supporting pluripotent stem cells. |
| Culture Media | StemFlex Medium, mTeSR Plus, Essential 8 Medium [8] [9] | Optimized formulations for maintaining iPSCs in defined conditions. |
| Cell Survival Enhancement | ROCK inhibitor Y-27632 [9] | Improves survival of dissociated iPSCs and reprogramming cells. |
Signaling Pathways and Experimental Workflows
c-Myc-Induced Replication Stress Mechanism
Safer Reprogramming Experimental Workflow
Data Tables
Comparison of Myc Family Members in Reprogramming
| Property | c-Myc | L-Myc | N-Myc |
|---|---|---|---|
| Reprogramming Efficiency | High | High (superior to c-Myc in human cells) [3] | Moderate |
| Transformation Potential | High | Low | High |
| Specificity (iPSC vs. non-iPSC colonies) | Low | High (significantly higher proportion of true iPSCs) [3] | Low |
| Tumorigenicity in Chimeras | High (increased mortality) [3] | Low (no marked increase) [3] | Not reported |
| Germline Transmission | Promotes | Promotes (comparable quality to ESCs) [3] | Not reported |
| Key Advantages | High efficiency | Specific reprogramming, low tumorigenicity | - |
| Key Limitations | High tumorigenic risk, genomic instability | Less studied | Similar risks to c-Myc |
Common Genomic Alterations in iPSCs and Cancer Associations
| Genomic Region | Type of Alteration | iPSC Context | Cancer Associations |
|---|---|---|---|
| chr20q11.21 | Amplification/CNV | Most recurrent CNV hotspot in iPSCs and ESCs [4] [6] | Frequently amplified in various cancers [4] |
| chr12p | Gain/Trisomy | Frequent in both iPSCs and ESCs [4] | Hallmark of testicular germ cell tumors [4] |
| chr8 | Amplification | Common aneuploidy in pluripotent stem cells [4] | Associated with multiple cancer types |
| chr1, 2, 3, 16 | CNVs | Recurrent regions in hiPSCs across studies [6] | Overlap with cancer-associated genes [6] |
| Key Genes Affected | ID1, BCL2L1, DNMT3B (chr20); NANOG (chr12) | Enriched in pluripotency and anti-apoptosis [4] [6] | Cancer development and progression |
Epigenetic Remodeling and Chromatin Dynamics During Somatic Cell Reprogramming
Frequently Asked Questions (FAQs)
Q1: What are the main epigenetic barriers that resist somatic cell reprogramming? Reprogramming factors must overcome several potent epigenetic barriers to induce pluripotency. Key barriers include:
- Repressive Histone Modifications: Broad heterochromatic regions enriched with H3K9me3 are refractory to initial transcription factor binding and require extensive remodeling for activation [10]. The histone methyltransferase G9a (EHMT2) recruits DNA methyltransferases to pluripotency loci to block their expression [11].
- DNA Methylation: Promoters of key pluripotency genes like OCT4 and NANOG are often hypermethylated in somatic cells. The de novo DNA methyltransferases DNMT3A and DNMT3B act as barriers, and their knockdown improves reprogramming efficiency [11].
- Large Organized Chromatin Modifications (LOCKs): These are large chromosomal regions enriched in H3K9me2 that are prevalent in differentiated cells and cover many lineage-specific genes. They are markedly decreased in pluripotent stem cells, and their persistence impedes reprogramming [10] [12].
Q2: How does the chromatin accessibility of target genes influence the reprogramming timeline? The initial chromatin state of OKSM target genes determines the kinetics of their activation during reprogramming. These targets can be categorized into three classes [10]:
- Class I (Open Chromatin): Genes with an "open" chromatin state (e.g., somatic genes and early MET genes) are characterized by active H3K4me2/3 marks and are bound by OKSM immediately.
- Class II (Permissive Enhancers): Distal regulatory elements with features like H3K4me1 that require additional chromatin remodeling for activation.
- Class III (Refractory Domains): Core pluripotency genes (e.g., NANOG, SOX2) located within broad heterochromatic regions enriched for H3K9me3. These regions are resistant to initial OKSM binding and are the last to be activated, requiring the most extensive chromatin remodeling [10].
Q3: What are the primary sources of genomic instability in iPSC cultures? Genomic instability in iPSCs arises from three main origins [4]:
- Pre-existing Variations: Low-frequency genetic variants present in the parental somatic cell population that are fixed and expanded during the clonal selection of iPSCs.
- Reprogramming-Induced Mutations: Mutations that occur during the reprogramming process itself, which is associated with replication stress and other cellular stresses.
- Passage-Induced Mutations: Mutations that accumulate during prolonged in vitro culture, often due to selective pressures that favor faster-growing variants.
Q4: What methods can improve the safety profile of iPSCs for clinical applications? To enhance safety, focus on using non-integrating reprogramming methods and omitting oncogenes [13]:
- Reprogramming Methods: Use non-integrating methods such as episomal vectors, Sendai virus, or mRNA transfection to avoid insertional mutagenesis [13].
- Factor Selection: Reprogramming with factors that exclude known oncogenes like c-MYC and LIN28 can reduce tumorigenic risk. Some protocols successfully use Oct4, Sox2, Klf4 alone or in combination with small molecules [13].
- Rigorous Screening: Implement comprehensive genetic and genomic screening (e.g., G-banding, CGH/SNP array, whole-genome sequencing) to fully characterize master cell banks before clinical use [4].
Troubleshooting Guides
Problem 1: Low Reprogramming Efficiency
Potential Causes and Solutions:
- Cause: Inefficient epigenetic resetting. Repressive marks at pluripotency loci are not being adequately removed.
- Cause: Suboptimal transcription factor delivery/expression.
- Solution: Utilize a non-integrating, high-efficiency method like Sendai virus or mRNA transfection for robust initial factor expression. For episomal methods, ensure the vectors contain factors like l-Myc or p53 shRNA to boost efficiency without significantly increasing oncogenic risk [13].
- Cause: Inadequate culture conditions.
Problem 2: High Rates of Genomic Instability in Established iPSC Lines
Potential Causes and Solutions:
- Cause: Selective pressure during prolonged culture.
- Solution: Minimize the number of cell passages. Regularly karyotype cells and use genetic screening to monitor for common aberrations. Be aware that certain mutations, such as gains on chromosome 12 (which contains the NANOG gene) or 20q11.21 (containing BCL2L1 and DNMT3B), confer a growth advantage and can rapidly take over a culture [4].
- Cause: Mutations carried over from parental somatic cells.
- Solution: Perform deep sequencing of the parental somatic cell population to identify pre-existing variants. When possible, generate multiple iPSC clones and screen them to select clones with the cleanest genetic background [4].
- Cause: Oxidative and replication stress during reprogramming.
- Solution: Use antioxidants and culture conditions that mitigate cellular stress. The p53 pathway is a key mediator of stress response during reprogramming; transiently modulating this pathway can reduce mutation rates, but requires careful control [4].
Problem 3: Incomplete Reprogramming and Residual Differentiation
Potential Causes and Solutions:
- Cause: Failure to fully activate the core pluripotency network.
- Solution: Extend the reprogramming timeline and ensure exogenous factor expression is maintained long enough for stable endogenous network activation. Analyze the expression of late-pluripotency genes like UTF1 and SOX2 as markers of fully established pluripotency [10] [15].
- Solution: Use advanced assays like ATAC-seq to monitor the chromatin state of key pluripotency loci (e.g., NANOG, SALL4). This reveals whether these genes have transitioned from a "closed" (H3K9me3-rich) to an "open" (accessible) chromatin configuration [10] [16].
- Cause: Persistent expression of somatic genes.
- Solution: Ensure that the silencing of somatic genes, which is an early event in reprogramming, has occurred. This can be facilitated by the recruitment of repressive complexes like PRC2 (which deposits H3K27me3) to somatic loci [10].
The tables below summarize key quantitative findings on genetic instability and chromatin dynamics from the research.
Table 1: Common Genetic Variations in Human iPSCs
| Variation Type | Recurrent Aberrations | Frequency in iPSCs | Potential Functional Impact |
|---|---|---|---|
| Chromosomal Aberration | Trisomy 12, Trisomy 8, Gain of X [4] | Not remarkably different from human ESCs [4] | Selective growth advantage; linked to pluripotency genes (NANOG on Chr12) and cancer [4]. |
| Copy Number Variation (CNV) | Amplification of 20q11.21 [4] | Common hotspot in both iPSCs and ESCs [4] | Contains anti-apoptosis (BCL2L1) and epigenetic (DNMT3B) genes, promoting survival [4]. |
| Single Nucleotide Variant (SNV) | Varies, low recurrence reported [4] | ~10 protein-coding mutations per line [4] | Origins include pre-existing somatic mutations and errors during reprogramming [4]. |
Table 2: Dynamics of Chromatin States During Reprogramming
| Chromatin Category | Description | Example Genes/Regions | Change in Gene Expression During Naïve Reprogramming |
|---|---|---|---|
| Closed-to-Open (CO) | Regions that transition from closed in fibroblasts to open in iPSCs [16]. | DPPA3, KLF4, POU5F1 (OCT4) [16] | Significant and consistent upregulation [16]. |
| Open-to-Closed (OC) | Regions that transition from open in fibroblasts to closed in iPSCs [16]. | AMOTL1, RUNX2 [16] | Marked decrease from day 8 onwards [16]. |
| Permanently Open (PO) | Regions that remain accessible throughout reprogramming [16]. | Genes in TGF-β signaling, apoptosis [16] | Negligible changes [16]. |
Essential Experimental Protocols
Protocol 1: Assessing Chromatin Accessibility with ATAC-seq
This protocol is used to map genome-wide chromatin accessibility and identify open, closed, and dynamically changing regions during reprogramming [16].
- Cell Harvesting: Harvest intermediate cell populations at defined time points (e.g., days 6, 8, 14, 20, 24) during reprogramming, along with the starting somatic cells and final iPSCs.
- Nuclei Isolation: Lyse cells using a mild detergent to isolate intact nuclei. Keep samples on ice to prevent degradation.
- Tagmentation: Incubate the nuclei with the Tn5 transposase. This enzyme simultaneously fragments DNA and inserts adapter sequences exclusively into accessible genomic regions.
- DNA Purification: Clean up the tagmented DNA using a commercial purification kit.
- Library Amplification: Amplify the purified DNA by PCR using primers compatible with the adapters added by Tn5.
- Sequencing and Analysis: Sequence the libraries on a high-throughput platform. Align sequences to the reference genome and call peaks to identify regions of significant accessibility. Compare peaks across time points to define CO, OC, and PO regions [16].
Protocol 2: Tracking Reprogramming Trajectories via Integrated ATAC-seq and RNA-seq
This integrated approach reveals the relationship between chromatin remodeling and transcriptional changes [16].
- Parallel Sampling: From the same sample of reprogramming cells, split the population for simultaneous ATAC-seq and RNA-seq analysis.
- RNA-seq Library Prep: For the RNA-seq arm, extract total RNA. Convert RNA to cDNA and prepare sequencing libraries using a standard kit (e.g., poly-A selection for mRNA).
- Multi-Omics Data Integration: Perform Principal Component Analysis (PCA) on the combined ATAC-seq and RNA-seq datasets to visualize the trajectories of naïve and primed reprogramming.
- Correlation Analysis: Correlate ATAC-seq signals from promoter or enhancer regions with expression levels of associated genes. A positive correlation confirms the functional relevance of the observed chromatin changes [16].
Key Signaling and Regulatory Pathways
The following diagram illustrates the core molecular mechanism of transcription factor-driven somatic cell reprogramming to pluripotency, highlighting the key stages and epigenetic barriers.
Research Reagent Solutions
Table 3: Essential Reagents for Reprogramming and Epigenetic Analysis
| Reagent / Tool | Function / Application | Key Examples / Notes |
|---|---|---|
| Reprogramming Factors | Ectopic expression to initiate reprogramming. | OSKM (Oct4, Sox2, Klf4, c-Myc) or OSNL (Oct4, Sox2, Nanog, Lin28); Use non-integrating delivery systems (Sendai virus, episomal vectors, mRNA) for clinical relevance [15] [13]. |
| Chromatin Remodelers | Enzymes that restructure nucleosomes to open chromatin. | Chd1 (necessary for open chromatin in PSCs); esBAF (ESC-specific SWI/SNF complex) colocalizes with Oct4, Sox2, Nanog [12]. |
| Histone Modifying Enzymes | "Writers" and "Erasers" of histone marks. | Inhibitors of G9a/Dot1L (reduce H3K9me/H3K79me) can enhance reprogramming. PRC2 deposits H3K27me3 to silence somatic genes [10] [11]. |
| DNA Methylation Modulators | Regulate DNA methylation levels at key loci. | DNMT Inhibitors (e.g., 5-azacytidine) promote demethylation of pluripotency gene promoters. DNMT3A/B knockdown improves efficiency [11]. |
| Small Molecule Enhancers | Chemical compounds that improve efficiency/safety. | Used to replace transcription factors (e.g., c-Myc), enhance MET, or inhibit epigenetic barriers (e.g., HDAC inhibitors) [13]. |
| ATAC-seq Kit | To map genome-wide chromatin accessibility dynamics. | Critical for identifying CO, OC, and PO regions during reprogramming [16]. |
Troubleshooting Guides
Guide 1: Managing Culture Dominance by Karyotypically Abnormal Cells
Problem: A rapidly proliferating subpopulation of cells is overtaking your culture, suspected to be a common variant (e.g., trisomy 12, 17, or 20q11.21 gain).
| Observation | Possible Affected Chromosome | Underlying Cause & Functional Consequence |
|---|---|---|
| Rapid culture overgrowth | Trisomy 12 | Increased dosage of pluripotency (e.g., NANOG) and cell cycle genes confers a proliferative advantage [4]. |
| Increased clonal survival post-dissociation | Trisomy 17 (17q25) | Overexpression of ARHGDIA reduces apoptosis and increases clonality after single-cell passaging [17]. |
| Resistance to apoptosis under standard conditions | 20q11.21 Amplification | Overexpression of the anti-apoptotic gene BCL2L1 (Bcl-xL) enhances cell survival [18] [19]. |
| Impaired neuroectodermal differentiation | 20q11.21 Amplification | BCL2L1 overexpression dysregulates TGF-β and SMAD signaling, blocking ectoderm commitment [19]. |
Step-by-Step Diagnostic & Mitigation Protocol:
Detection and Confirmation:
- Karyotyping (G-banding): Perform regular checks (e.g., every 10 passages) to detect gross chromosomal abnormalities. This is a standard first-line test [4].
- High-Resolution Analysis: Use technologies like SNP arrays or array Comparative Genomic Hybridization (aCGH) to identify smaller copy number variations (CNVs), such as the 0.56 Mb amplification at 20q11.21, which may be missed by karyotyping [18] [20] [4].
- PCR or FISH Validation: Confirm specific aberrations, such as the gain of ARHGDIA on 17q25 or BCL2L1 on 20q11.21, using targeted methods [17].
Mitigation Strategies:
- Modify Passaging Technique: Avoid routine single-cell enzymatic passaging, which imposes strong selective pressure. Switch to bulk/clump passaging methods where possible [17].
- Optimize Culture Conditions: Supplement culture medium with a ROCK inhibitor (ROCKi) during single-cell passaging. This can reduce the selective advantage conferred by aberrations like trisomy 17 by promoting general cell survival, thereby allowing normal cells to compete [17].
- Limit Culture Time: Establish a strict schedule for regenerating new cultures from low-passage frozen stocks to prevent the outgrowth of spontaneous mutants [4].
Guide 2: Addressing Poor Differentiation Efficiency
Problem: Your iPSC line differentiates poorly into a specific lineage (e.g., neuronal cells), while other lineages form normally.
| Symptom | Potential Genetic Cause | Mechanistic Insight |
|---|---|---|
| Failure to form neuroectodermal progenitors | 20q11.21 Amplification | BCL2L1 overexpression drives transcriptomic changes that impair TGF-β-dependent signaling, a pathway critical for neuroectoderm commitment [19]. |
| General inefficiency across multiple lineages | Trisomy 12 | Altered balance of pluripotency factors and differentiation regulators can disrupt the coordinated exit from pluripotency [4]. |
Step-by-Step Diagnostic Protocol:
- Genetic Screening: Prioritize genetic screening for 20q11.21 amplification if neuroectodermal defects are observed [19].
- Control Experiment: Differentiate a genetically normal iPSC line in parallel. If the normal line differentiates correctly, the defect is likely intrinsic to the problematic line.
- Lineage Commitment Analysis: Use flow cytometry or qPCR for early lineage-specific markers (e.g., SOX1 for neuroectoderm, SOX17 for endoderm) to pinpoint the differentiation block [19].
- Final Action: If a recurrent aberration is identified and confirmed to impair your target differentiation, bank a new, genetically normal cell line for your experiments.
Frequently Asked Questions (FAQs)
FAQ 1: Why do the same aberrations (trisomy 12, 17, 20q) appear so frequently in different labs?
These aberrations are recurrent because they are not random. They confer a selective advantage under standard culture conditions. The genes within these amplified regions enhance survival (e.g., BCL2L1, ARHGDIA) and proliferation (e.g., genes on chromosome 12), allowing cells carrying them to outcompete normal cells and dominate the culture over time [17] [18] [4].
FAQ 2: My karyotype is normal. Are my cells genetically pristine?
Not necessarily. Conventional karyotyping has limited resolution (typically detecting aberrations >5-10 Mb). Higher-resolution methods like SNP arrays or NGS can detect cryptic lesions (e.g., small CNVs) and low-grade mosaicism, where a subset of cells carries an abnormality [20] [4]. A culture can test normal by karyotype but still contain a small, growing population of aberrant cells.
FAQ 3: Where do these genetic mutations in iPSCs come from?
They can arise from several sources [4]:
- Pre-existing in Somatic Cells: Rare variants present in the parental somatic cell population can be captured and expanded during reprogramming.
- Reprogramming-Induced: The reprogramming process itself can be mutagenic, inducing point mutations and CNVs.
- Culture-Acquired: Mutations can occur during prolonged in vitro expansion, with selective pressure allowing advantageous variants to take over.
FAQ 4: Are these genetically abnormal iPSCs tumorigenic?
They are not necessarily cancerous, but they carry a "first hit" toward oncogenesis. The same genes that provide a culture advantage (e.g., anti-apoptotic BCL2L1) are also frequently amplified in cancers [18]. Transplanting differentiated cells derived from these abnormal iPSCs could pose a long-term risk if these cells acquire additional mutations in vivo.
Experimental Protocols for Cited Key Experiments
Protocol 1: Competition Assay to Model Culture Dominance
This protocol is adapted from experiments investigating the selective advantage of ARHGDIA-overexpressing cells [17].
Purpose: To quantitatively measure the fitness advantage of a test cell population (e.g., mutant or gene-edited) against a reference wild-type population in co-culture.
Materials:
- Wild-type (WT) iPSC line
- Test iPSC line (e.g., with a specific aberration or genetic modification)
- Standard iPSC culture medium
- ROCK inhibitor (e.g., Y-27632)
- Enzyme for single-cell dissociation (e.g., Accutase)
- Flow cytometer
Method:
- Cell Preparation: Maintain WT and test iPSC lines separately. If the test line expresses a fluorescent marker (e.g., GFP), this simplifies tracking.
- Initial Seeding: Mix WT and test cells at a defined ratio (e.g., 1:1). Enzymatically dissociate the mixture into single cells and seed onto culture plates. Culture with and without ROCKi supplementation.
- Serial Passaging: Passage the co-culture every 3-5 days. At each passage, dissociate the culture into single cells.
- Quantification: Analyze an aliquot of cells by flow cytometry to determine the percentage of test cells (e.g., GFP-positive) in the population.
- Data Analysis: Plot the percentage of test cells over multiple passages. A consistent increase indicates a selective advantage.
Protocol 2: Clonal Survival Assay at Low Density
This protocol measures the ability of individual cells to survive and form colonies, a key characteristic of cells with aberrations like trisomy 17 [17].
Purpose: To assess the clonogenicity and survival of iPSCs after low-density seeding, a condition that induces stress.
Materials:
- iPSC lines to be tested
- iPSC culture medium with ROCKi
- Enzyme for single-cell dissociation
- Hemocytometer or automated cell counter
Method:
- Cell Dissociation: Harvest and dissociate iPSCs into a single-cell suspension.
- Low-Density Seeding: Count cells and seed at a very low density (e.g., 500-1,000 cells per well of a 6-well plate) in medium containing ROCKi.
- Culture: Allow cells to grow for 7-10 days, changing the medium every other day. Do not disturb the plates to allow colony formation.
- Analysis: Fix and stain colonies with crystal violet or directly count under a microscope. Compare the number and size of colonies formed by different lines. Lines with a selective advantage will show significantly higher colony-forming efficiency.
Signaling Pathways and Experimental Workflows
Diagram: BCL2L1-Mediated Impairment of Neuroectoderm Differentiation
Diagram: Experimental Workflow for Genetic Instability Monitoring
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| ROCK Inhibitor (ROCKi) | Critical for increasing survival of dissociated iPSCs. Used during passaging to reduce the selective pressure that favors aneuploid cells. Mitigates the advantage of mutations in ARHGDIA [17]. |
| SNP/Array CGH Kits | High-resolution tools for detecting copy number variations (CNVs), including the cryptic 0.56 Mb amplification at 20q11.21, which may be missed by standard karyotyping [18] [20] [4]. |
| Next-Generation Sequencing (NGS) | Provides the most comprehensive genetic analysis. Whole-genome sequencing (WGS) can detect single nucleotide variants (SNVs), CNVs, and structural variants, revealing the full spectrum of genomic instability [4] [21]. |
| Lentiviral ORF Constructs | Used for functional validation. For example, to overexpress candidate genes like ARHGDIA or BCL2L1 in normal iPSCs to test if this recapitulates the selective or differentiation-defective phenotype [17] [19]. |
| qPCR Assays | Rapid, quantitative method to validate gene expression changes associated with aberrations (e.g., elevated BCL2L1 or ARHGDIA mRNA levels) without the need for full genomic screening [17] [19]. |
Within the context of induced pluripotent stem cell (iPSC) research, genomic instability presents a significant challenge for clinical applications. A critical aspect of maintaining genomic integrity is the faithful repair of DNA double-strand breaks (DSBs), with the two major pathways being non-homologous end joining (NHEJ) and homologous recombination (HR). Understanding the balance between these pathways is crucial, as their efficiency and fidelity can be altered during cellular reprogramming and prolonged culture of iPSCs. This technical support article provides troubleshooting guides and FAQs to help researchers identify and address issues related to DNA repair pathway shifts in their iPSC cultures.
FAQs & Troubleshooting Guides
FAQ: What is the relative efficiency and kinetics of NHEJ versus HR in normal human cells?
Answer: In actively cycling normal human fibroblasts, NHEJ is a faster and more efficient DSB repair pathway than HR.
- Kinetics: NHEJ of compatible ends (NHEJ-C) and NHEJ of incompatible ends (NHEJ-I) are fast processes, completing in approximately 30 minutes. In contrast, HR is much slower, taking 7 hours or longer to complete [22].
- Relative Contribution: The ratio of repair events in cycling cells is approximately NHEJ-C : NHEJ-I : HR = 6 : 3 : 1. This makes NHEJ-C twice as efficient as NHEJ-I and three times more efficient than HR [22].
Table 1: Comparison of NHEJ and HR Efficiency and Kinetics [22]
| Repair Pathway | Description | Approximate Completion Time | Relative Efficiency in Cycling Cells |
|---|---|---|---|
| NHEJ-C | NHEJ of compatible DNA ends | ~30 minutes | 6 |
| NHEJ-I | NHEJ of incompatible DNA ends | ~30 minutes | 3 |
| HR | Homologous Recombination | ≥7 hours | 1 |
FAQ: What types of genomic instability are commonly observed in iPSCs?
Answer: iPSCs are prone to acquiring several types of genetic variations, which pose a safety concern for therapeutic use. The main categories are [4] [6]:
- Chromosomal Aberrations: Numerical changes (aneuploidy) and large structural changes. Common recurrent anomalies include trisomy of chromosome 12, and amplifications of chromosomes 8, 20, and X [4].
- Copy Number Variations (CNVs): Deletions or duplications of DNA segments. A recurrent CNV hotspot is an amplification on 20q11.21, a region enriched with genes associated with pluripotency and anti-apoptosis (e.g.,
DNMT3B,ID1,BCL2L1) [4] [6]. - Single Nucleotide Variants (SNVs): Point mutations in the protein-coding regions. Studies have identified an average of ~10 protein-coding mutations per human iPSC line [4].
FAQ: What are the origins of genetic variations in iPSCs?
Answer: The genetic variations found in iPSCs can originate from three main sources [4]:
- Pre-existing Variations: Somatic mutations present at low frequency in the parental cell population can be captured and clonally expanded during the reprogramming process.
- Reprogramming-Induced Mutations: The reprogramming process itself can induce DNA damage and mutations, partly due to replication stress caused by the expression of reprogramming factors [23].
- Passage-Induced Mutations: Genetic changes can accumulate during prolonged in vitro culture of established iPSC lines.
Troubleshooting: How can I reduce replication stress and genomic instability during iPSC reprogramming?
Problem: High levels of replication stress during reprogramming lead to increased DNA damage and de novo CNVs in resulting iPSC lines. Solution:
- Genetic Strategy: Increasing the levels of the checkpoint kinase 1 (CHK1), which helps manage replication stress, has been shown to reduce DNA damage and increase reprogramming efficiency [23].
- Chemical Strategy: Supplementing the culture medium with nucleosides during reprogramming provides the raw materials for DNA synthesis, which reduces the replication stress load. This approach has been demonstrated to lower the levels of DNA damage (γH2AX) and reduce the number of de novo CNVs in the resulting human iPSC lines [23].
Table 2: Strategies to Limit Reprogramming-Induced Genomic Instability [23]
| Strategy | Method | Effect on Reprogramming | Effect on Genomic Instability |
|---|---|---|---|
| Increase CHK1 | Genetic overexpression | Increases reprogramming efficiency | Reduces replication stress and spontaneous chromosomal fragility |
| Nucleoside Supplementation | Chemical supplement | Does not increase efficiency | Reduces DNA damage load and de novo CNVs |
FAQ: How does the disruption of NHEJ impact the repair of fragmented chromosomes?
Problem: In an experimental model of chromothripsis (catastrophic chromosomal shattering), cells lacking core NHEJ components (e.g., LIG4 or XLF) show dramatically reduced survival and decreased frequencies of genomic rearrangements [24].
Solution & Interpretation:
- Canonical NHEJ is the primary DSB repair pathway responsible for reassembling shattered chromosomes and generating complex genomic rearrangements.
- In the absence of NHEJ, alternative end-joining or recombination-based pathways are rarely engaged, leading to persistent DNA damage in the form of 53BP1-labeled "MN bodies" and subsequent cell cycle arrest [24].
- This highlights the critical, and sometimes exclusive, role of NHEJ in repairing severe, clustered DNA breaks.
Experimental Protocols
Protocol 1: Comparing NHEJ and HR Efficiency Using Fluorescent Reporters
This protocol is adapted from a study comparing the kinetics and efficiency of NHEJ and HR in human cells [22].
1. Principle: Chromosomally integrated GFP-based reporter constructs are used. Upon induction of a site-specific DSB by the I-SceI endonuclease, successful repair via NHEJ or HR leads to the reconstitution of a functional GFP gene, which can be quantified by flow cytometry.
2. Reagents and Equipment:
- Reporter cell lines (HCA2-hTERT with single integrated copies of NHEJ-I, NHEJ-C, or HR constructs)
- Plasmid encoding I-SceI endonuclease
- Plasmid encoding DsRed (transfection control)
- Transfection reagent (e.g., Amaxa Nucleofector)
- Flow cytometer
3. Step-by-Step Procedure:
- Step 1: Culture reporter cell lines under standard conditions.
- Step 2: Co-transfect cycling cells with 5 µg of I-SceI plasmid and 0.1 µg of DsRed plasmid to control for transfection efficiency.
- Step 3: Incubate cells for 4 days post-transfection.
- Step 4: Harvest cells and resuspend in cold PBS.
- Step 5: Analyze the samples using a flow cytometer to quantify the percentages of GFP-positive (repaired) and DsRed-positive (transfected) cells.
- Step 6: Calculate repair efficiency as the ratio of GFP+ cells to DsRed+ cells for each independent cell line.
4. Data Analysis:
- The kinetics of repair can be analyzed by performing FACS at multiple time points after transfection (e.g., from 0.5 hours to 24 hours).
- Compare the ratios between different repair pathways to determine their relative contributions.
Protocol 2: Assessing Genomic Integrity in iPSCs Using Copy Number Variation (CNV) Analysis
This protocol outlines methods for detecting structural variations in iPSC lines [4] [6].
1. Principle: Array-based technologies (aCGH or SNP arrays) or next-generation sequencing (Whole Genome Sequencing) are used to identify copy number variations across the genome, revealing regions of amplification or deletion that may have been acquired during reprogramming or culture.
2. Reagents and Equipment:
- iPSC genomic DNA
- aCGH/SNP array platform or NGS platform
- Associated DNA labeling and hybridization kits or NGS library prep kits
3. Step-by-Step Procedure (for array-based methods):
- Step 1: Extract high-quality genomic DNA from iPSC lines and reference control DNA.
- Step 2: Label test and reference DNA with different fluorescent dyes (e.g., Cy5 and Cy3).
- Step 3: Hybridize the labeled DNA mixture to a microarray slide containing probes spanning the genome.
- Step 4: Wash the slide to remove non-specifically bound DNA.
- Step 5: Scan the slide with a microarray scanner to measure fluorescence intensities.
- Step 6: Use dedicated software to calculate log2 ratios of fluorescence intensities and identify genomic regions with significant deviations from the control, indicating CNVs.
4. Data Analysis:
- Focus on recurrent regions of CNVs reported in iPSCs, such as 20q11.21.
- Cross-reference identified CNVs with databases of known cancer genes, fragile sites, and genes involved in pluripotency.
Pathway Diagrams
Origins and Mitigation of Genomic Instability in iPSCs
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents for Studying DNA Repair in iPSCs
| Reagent / Tool | Function / Application | Example Use |
|---|---|---|
| Fluorescent Reporter Constructs (NHEJ/HR) | In vivo, real-time monitoring of specific DSB repair pathway activity. | Comparing the relative efficiency and kinetics of NHEJ vs. HR in different cell types [22]. |
| I-SceI Endonuclease Plasmid | Induction of a specific, reproducible DNA double-strand break at a defined genomic locus. | Activating the repair process in reporter cell lines to measure NHEJ/HR efficiency [22]. |
| Array CGH or SNP Arrays | Genome-wide detection of copy number variations (CNVs) at kilobase resolution. | Identifying acquired structural variations in iPSC lines after reprogramming or extended passaging [4] [6]. |
| Next-Generation Sequencing (WGS/WES) | Comprehensive detection of genetic variations (SNVs, CNVs, indels) at single-nucleotide resolution. | Profiling the full spectrum of mutations in iPSCs and tracing their origin (parental vs. acquired) [4]. |
| CHK1 Expression Vector | Genetic manipulation to increase levels of the checkpoint kinase 1. | Reducing replication stress during reprogramming to lower genomic instability in resulting iPSCs [23]. |
| Nucleoside Supplement | Chemical provision of substrates for DNA synthesis. | Limiting replication stress during reprogramming to reduce DNA damage and de novo CNVs [23]. |
| sgRNAs Targeting DSB Repair Genes | CRISPR/Cas9-mediated knockout of specific DNA repair factors (e.g., LIG4, XLF, POLQ). | Functionally characterizing the role of specific pathways in processing DNA damage in iPSCs [24]. |
The Impact of Culture Conditions and Selective Pressure on the Emergence of Aneuploid Clones
FAQs on Aneuploidy in Stem Cell Cultures
What are the signs that my iPSC culture is developing aneuploidy? While karyotype analysis is needed for confirmation, certain culture observations can signal potential genomic instability. Aneuploid clones often acquire a growth advantage, manifesting as changes in colony morphology, accelerated proliferation rates, and an increased propensity to dominate the culture over passages [4]. Specific recurrent aneuploidies, such as trisomy of chromosome 12 or gains of chromosome 20q11.21, are frequently observed and are associated with genes that promote pluripotency and cell survival [4].
Why does aneuploidy persist in my cultures even though it often reduces cellular fitness? Although aneuploidy can cause proteotoxic stress and reduced fitness under standard conditions, it can provide a crucial selective advantage under specific culture stresses [25]. The extra chromosomes may harbor genes that help cells cope with the culture environment. Consequently, even if aneuploid cells grow slower initially, they can rapidly outcompete normal cells if the culture conditions impose stresses that their specific aneuploidy helps to overcome [4] [25].
Which chromosomes are most commonly gained in iPSC cultures and why? The most recurrent aneuploidies in iPSCs are not random [4]. The table below summarizes the frequently observed chromosomal gains and the key genes within those regions that are thought to drive their selection.
| Chromosomal Abnormality | Key Genes in the Region | Proposed Selective Advantage |
|---|---|---|
| Trisomy 12 | NANOG | Enhances reprogramming efficiency and pluripotency [4]. |
| Gain of 20q11.21 | DNMT3B, ID1, BCL2L1 | Promotes anti-apoptosis and supports pluripotent state [4]. |
| Amplifications of Chromosome 8 and X | - | Frequently recurrent; specific advantages area of active investigation [4]. |
How do my culture practices influence the emergence of aneuploid clones? Two key culture factors are passaging techniques and passage number.
- Passaging: Practices that encourage clonal expansion from single cells or that create uneven colony sizes can increase the risk of an aneuploid clone taking over the culture [8].
- Prolonged Culture: The number of cell passages is a major risk factor. The longer iPSCs are maintained in culture, the more time there is for mutations to occur and for fitter, potentially aneuploid, clones to expand. One study noted that the number of copy number variations (CNVs) was high in early passages but decreased during cell passaging as a result of selective pressure, with deletions of tumor-suppressor genes common early on and duplications of oncogenic genes increasing during later passages [4].
Troubleshooting Guides
Problem: Suspected Aneuploidy Due to Rapidly Overgrowing Clones
Potential Causes and Solutions
| Observation | Potential Cause | Recommended Action |
|---|---|---|
| A subset of colonies appears morphologically distinct and grows significantly faster, outcompeting others. | Emergence of an aneuploid clone with a proliferative advantage. | Verify Genomic Integrity: Perform karyotyping or SNP array analysis on the culture. Isolate Individual Clones: Manually pick and expand colonies with normal morphology away from the overgrowing areas. Bank Early: Use low-passage stocks to minimize culture-induced instability. |
| Culture becomes dominated by a single clone type after several passages. | Selective pressure from suboptimal culture conditions favoring an adapted (possibly aneuploid) clone. | Review Culture Conditions: Ensure media is fresh and not expired. Avoid over- or under-confluency during passaging [8]. Reduce Stressors: Minimize the time culture plates are out of the incubator [8]. |
| Spontaneous differentiation increases concurrently with changes in growth rates. | Genomic instability may be compromising lineage commitment. | Remove Differentiated Areas: Physically scrape or chemically remove differentiated regions before passaging [8]. Check Key Signaling Pathways: Ensure growth factors in media are active and at correct concentrations. |
Problem: Genomic Instability During Reprogramming and Differentiation
Background: Genomic alterations can be introduced during the reprogramming of somatic cells into iPSCs and during subsequent differentiation into target cells. One study found that the reprogramming method itself influences stability, with Sendai virus (SV)-derived iPSCs showing a higher frequency of copy number alterations (CNAs) and single-nucleotide variations (SNVs) compared to those generated with episomal vectors (Epi) [26].
Prevention and Monitoring Strategies
| Phase | Risk | Quality Control Strategy |
|---|---|---|
| Reprogramming | Introduction of CNAs and SNVs [26]. | Choose a Non-Integrating Method: Use episomal vectors over integrating viruses where possible [26]. Characterize Multiple Clones: Genomically screen several independent iPSC clones to select the most stable line. |
| Differentiation | Acquisition of mutations during the process to target cells (e.g., mesenchymal stem cells) [26]. | Monitor Genomic Integrity: Perform spot-checks for CNAs and SNVs in the final differentiated cell product [26]. |
| Long-Term Culture | Passage-induced mutations [4]. | Bank at Low Passages: Create a master cell bank of your iPSC line at an early passage. Limit Passages: Use the lowest possible passage number for final experiments or differentiation. |
Experimental Protocols for Monitoring Genomic Integrity
Protocol 1: Karyotype Analysis by G-Banding
Purpose: To detect numerical chromosomal abnormalities (e.g., trisomy) and large structural changes (e.g., translocations) at a resolution of ~5-10 Mb [4].
- Procedure:
- Cell Harvesting: Treat logarithmically growing iPSCs with a mitotic inhibitor (e.g., colcemid) to arrest cells in metaphase.
- Hypotonic Treatment: Expose cells to a hypotonic solution to swell them and disperse the chromosomes.
- Fixation: Fix the cells repeatedly with a methanol:acetic acid solution.
- Slide Preparation: Drop the fixed cell suspension onto glass slides to achieve well-spread metaphase chromosomes.
- Staining: Stain slides with Giemsa stain to produce a characteristic banding pattern (G-banding) for each chromosome.
- Analysis: Analyze at least 20 metaphase spreads under a microscope to identify chromosomal abnormalities [4].
Protocol 2: Detection of Copy Number Variations (CNVs) using SNP Array
Purpose: To identify submicroscopic copy number gains and losses across the genome at a higher resolution (kilobase level) than karyotyping [4].
- Procedure:
- DNA Extraction: Isolate high-quality genomic DNA from iPSCs and a reference control.
- Digestion and Amplification: Digest the DNA, amplify fragments, and label with fluorescent dyes.
- Hybridization: Co-hybridize the labeled test and reference DNA to a microarray slide containing hundreds of thousands of oligonucleotide probes representing SNPs across the genome.
- Scanning and Analysis: Scan the array to measure fluorescence intensities. Use specialized software to analyze the log intensity ratios and make copy number calls, identifying regions of deviation from the diploid state [4].
Key Signaling Pathways and Workflows
Clonal Expansion of Aneuploid Cells
The following diagram illustrates the conceptual process of how a spontaneous genetic variation can lead to the dominance of an aneuploid clone under selective culture conditions.
Experimental Workflow for Tracking Genomic Instability
This workflow outlines a comprehensive strategy for monitoring the emergence of genomic alterations from reprogramming through to the final differentiated cell product, based on published studies [26].
The Scientist's Toolkit: Essential Reagents for Genomic Stability Research
| Item | Function in Research |
|---|---|
| KaryoStat+ Assay | A commercial SNP-based array solution for comprehensive CNV detection in stem cells. |
| mTeSR Plus Medium | A feeder-free, defined culture medium optimized for the maintenance of hPSCs, helping to reduce undefined culture stressors [8]. |
| ReLeSR Passaging Reagent | A non-enzymatic dissociation reagent for gentle passaging of hPSCs as clusters, minimizing single-cell stress and supporting genomic stability [27]. |
| Vitronectin XF | A defined, human-derived substrate for cell culture, replacing mouse feeder cells or Matrigel to create a more consistent and controlled environment [8]. |
| STEMdiff Mesenchymal Progenitor Kit | A standardized, serum-free kit for the directed differentiation of iPSCs into mesenchymal progenitor cells, enabling controlled studies of instability during differentiation [26]. |
| Dendra2 Protein/Plasmid | A photo-convertible fluorescent protein used in live-cell imaging to track the fate of specific cells, such as those with micronuclei, over multiple divisions [28]. |
Advanced Methods for Detecting and Monitoring Genomic Aberrations
In the field of genomic research, particularly in the study of genomic instability in induced pluripotent stem cell (iPSC) cultures, high-resolution genotyping platforms are indispensable tools. Array-based comparative genomic hybridization (aCGH) and Single Nucleotide Polymorphism (SNP) microarrays enable genome-wide detection of chromosomal abnormalities at a significantly higher resolution than conventional cytogenetic methods [29]. These technologies have become fundamental for identifying genomic variations that arise during iPSC reprogramming and long-term culture, where genomic instability is a major concern for therapeutic applications [30].
The fundamental difference between these platforms lies in their detection capabilities. While aCGH is primarily designed to detect copy number variations (CNVs), SNP arrays can simultaneously identify CNVs, loss of heterozygosity (LOH), and uniparental disomy (UPD), and determine ploidy status [29] [31]. This technical distinction makes each platform uniquely suited for specific research applications, particularly in monitoring the genomic integrity of iPSC cultures intended for regenerative medicine.
Array-Based Comparative Genomic Hybridization (aCGH)
The principle of aCGH is based on the quantitative comparison between a reference DNA and test DNA, typically labeled with Cyanine 3 (green) and Cyanine 5 (red) fluorescent dyes, respectively [32]. The labeled DNA samples are mixed and competitively hybridized to a microarray chip containing thousands of known target DNA sequences. After hybridization, the fluorescence ratio at each probe is measured to detect CNVs throughout the genome [32]. Chromosomal regions with increased copy number in the test sample will show higher green fluorescence, while regions with decreased copy number will show higher red fluorescence [33].
SNP Microarray
SNP microarray technology represents a high-throughput, large-scale genetic testing platform designed for the detection of single nucleotide polymorphisms [33]. The working principle involves the hybridization of fragmented single-stranded DNA to an array containing hundreds of thousands of unique nucleotide probe sequences. SNP arrays take advantage of the differences in SNP loci between individuals. Unlike aCGH, SNP arrays utilize probes featuring different SNP variations that specifically match with SNP sites, allowing determination of the genotype at each locus by measuring hybridization signal intensity [33]. A key advantage of SNP arrays is their ability to detect copy number neutral events such as long contiguous stretches of heterozygosity (LCSH) and uniparental isodisomies, which are undetectable by aCGH alone [29].
Table 1: Key Technological Differences Between aCGH and SNP Microarrays
| Feature | aCGH | SNP Microarray |
|---|---|---|
| Primary Detection | Copy number variations (CNVs) | SNPs and CNVs |
| Genotyping Capability | No | Yes |
| Copy-Neutral LOH Detection | No | Yes |
| Ploidy Determination | Limited | Yes |
| Chimerism Detection | Limited | Yes [29] |
| Resolution | Can detect single-exon CNVs with custom designs [31] | Limited by known SNP distribution [31] |
| Reproducibility | >99.9% for validated SNPs [34] | >99.9% for validated SNPs [34] |
Workflow and Experimental Protocols
Standard Workflow for SNP Microarray
The general workflow of SNP microarray consists of several critical processes that must be carefully optimized for reliable results [33]:
Probe Design: This initial step involves collecting genomic sequence information from target SNP loci. Known SNP information is aligned with the reference genome sequence to determine the position and variable bases of SNP sites. Using sequence information around the SNP sites, specific probes are designed to selectively pair with the variable bases. Probes are typically 20-70 bases in length to ensure stable hybridization and reliable signal detection [33].
SNP Chip Fabrication: Predesigned oligonucleotide probes are arranged orderly and in high density on a solid carrier (usually glass) to create microarrays. Fabrication methods include light-guided in-situ synthesis, chemical spray method, contact dot coating method, and non-contact micromechanical printing. Modern high-density arrays can contain over 400,000 different DNA molecules on a 1 cm² chip [33].
Sample Genomic DNA Preparation: High quality and high molecular weight genomic DNA should always be used, as it directly affects labeling efficiency [32]. The concentration and purity of DNA samples are paramount, typically assessed using spectrophotometric techniques. The A260/280 ratio should be >1.8, and the A260/230 ratio should be in the range of 2.0-2.2 [32]. For short-term storage, DNA should be kept at 4°C to avoid freeze/thaw cycles that can break chromosomes [32].
Labeling, Hybridization, and Scanning: DNA is labeled with fluorescent dyes, with the efficiency of the labeling reaction being critical for success. The labeled genomic DNA hybridizes with the SNP microarray under optimized reaction conditions (temperature, salt concentration, hybridization time). Post-washing, fluorescence is scanned with a specialized scanner, and data is processed through computer image analysis for bioinformatics interpretation [33].
Diagram 1: SNP microarray workflow
Standard Workflow for aCGH
The aCGH workflow shares similarities with SNP arrays but has distinct critical steps:
DNA Quality Assessment: The quality of results is strictly dependent on the quality of probes hybridized on the microarray. Beyond spectrophotometric measurements, DNA integrity should be verified using gel electrophoresis or automated electrophoresis systems [32].
Labeling Reaction Optimization: The labeling reaction typically involves incorporation of cyanine dyes into newly synthesized DNA by random priming. Both denaturation and primer extension steps are crucial. Changing, particularly shortening, the reaction time causes inefficient and incomplete incorporation of Cyanine-labeled deoxynucleotides [32].
Purification and Quality Control: After labeling, DNA must be purified to remove unincorporated nucleotides. This can be achieved through silica membrane-based purification columns, columns with cellulose membranes, or classical DNA precipitation. Ethanol precipitation with NaOAC is preferred for better removal of free nucleotides [32].
Probe Quality Verification: Before hybridization, labeling efficiency should be checked using a NanoDrop in Microarray Measurement Mode. Key parameters include DNA yield (>5.0 µg), dye incorporation (>300 pmoles Cyanine 3 or >200 pmoles Cyanine 5), and specific activity (>60 pmol/µg for Cy3, >40 pmol/µg for Cy5) [32].
Hybridization and Stringency Control: The hybridization mix must be prepared following array manufacturer instructions. The amount of Cot-1 DNA (which blocks non-specific interactions), buffer stringency, and incubation temperature critically affect final results. Incorrect conditions lead to low signal, elevated background, and poor signal-to-noise ratio [32].
Diagram 2: aCGH workflow
Troubleshooting Common Experimental Issues
DNA Quality and Preparation Issues
Problem: Poor DNA quality affecting labeling efficiency
- Potential Cause: Protein or organic compound contamination, or DNA degradation.
- Solution: Re-purify DNA samples if A260/280 ratio is <1.8 or A260/230 ratio deviates from 2.0-2.2. Verify DNA integrity using gel electrophoresis. For freeze/thaw cycles that break chromosomes, store aliquots at -20°C and keep aliquots in use at 4°C for short-term storage [32].
Problem: Suspected DNA contamination with inhibitors
- Solution: Clean up gDNA using the following procedure:
- Add 0.5 volumes of 7.5 M NH4OAc and 2.5 volumes of absolute ethanol (stored at -20°C) to gDNA
- Vortex and incubate at -20°C for 1 hour
- Centrifuge at 12,000 × g for 20 minutes at room temperature
- Remove supernatant and wash pellet with 80% ethanol
- Centrifuge at 12,000 × g for 5 minutes
- Repeat 80% ethanol wash once more
- Resuspend pellet in reduced EDTA TE Buffer [34]
Labeling and Hybridization Issues
Problem: Low signal intensity after hybridization
- Potential Causes: Inefficient labeling reaction, insufficient DNA input, or suboptimal hybridization conditions.
- Solution: Ensure labeling reaction follows manufacturer guidelines for volumes, concentrations, timing, and incubation temperatures. Check dye incorporation and specific activity before hybridization. For limited DNA samples, use specialized labeling kits designed for low input (e.g., 50 ng of DNA) [32].
Problem: Wave effect pattern in hybridization intensities
- Potential Cause: GC content bias of probes or potential bias during DNA isolation.
- Solution: Optimize the amount of Cot-1 DNA and ensure proper denaturing step prior to labeling [32].
Problem: Dye-specific signal reduction
- Solution: Protect Cyanine 5 from ozone effects, which are more pronounced at elevated environmental temperatures. Cyanine 3 is generally not affected by this phenomenon [32].
Data Quality Issues
Problem: High derivative log ratio (DLR)
- Potential Cause: Poor DNA quality and/or labeling efficiency.
- Solution: DLR should be <0.2 for optimal data quality. High DLR values correlate with poor data quality and reduce accurate identification of chromosomal abnormalities [32].
Problem: Suspected sample contamination
- Solution: Check for possible cross-sample contamination using genome analysis software. SNP arrays can detect DNA contamination through genotyping patterns [29] [35].
Table 2: Quality Control Metrics and Thresholds for Array Experiments
| Parameter | Optimal Value | Importance |
|---|---|---|
| DNA A260/280 Ratio | >1.8 | Indicates protein contamination |
| DNA A260/230 Ratio | 2.0-2.2 | Indicates organic compound contamination |
| Signal Intensity | >200 | Measurement of overall fluorescence |
| Background Noise | <25 | Standard deviation of negative controls |
| Signal-to-Noise Ratio | >30 | Ratio between probe signal and background |
| Derivative Log Ratio | <0.2 | Measure of array quality and variation |
| Dye Incorporation (Cy3) | >300 pmoles | Critical for labeling efficiency |
| Dye Incorporation (Cy5) | >200 pmoles | Critical for labeling efficiency |
Application in Genomic Instability Research in iPSCs
The study of genomic instability in induced pluripotent stem cells represents one of the most critical applications of high-resolution genotyping platforms. Human pluripotent stem cells (hPSCs) are known to acquire genomic changes as they proliferate and differentiate, raising concerns about the safety of hPSC-derived cell therapies [30]. Research has shown that hPSCs accumulate specific genomic abnormalities during culture adaptation, with late passage hPSCs being twice as likely to have genomic changes than early passage cells [30].
SNP genotyping has been particularly valuable in identifying common genomic changes in iPSCs, including:
- Recurrent chromosomal abnormalities: Trisomies of chromosomes 1, 12, 17, and X
- Subchromosomal amplifications: Such as the common amplification of 20q11.21, which contains the BCL2L1 (Bcl-xL) gene that enhances hESCs survival
- Copy number variations (CNVs): Both in hESCs and hiPSCs [30]
A recent study systematically investigating genomic alterations from iPSC generation through induced mesenchymal stromal/stem cell (iMS) differentiation observed a total of ten copy number alterations (CNAs) and five single-nucleotide variations (SNVs) during reprogramming, differentiation and passaging [26]. Notably, iPSCs generated using the Sendai virus (SV) method exhibited a higher frequency of CNAs and SNVs compared with those generated with episomal vectors (Epi) [26]. All SV-iPS cell lines exhibited CNAs during reprogramming, while only 40% of Epi-iPS cells showed such alterations [26].
For clinical applications, regulatory agencies require extensive preclinical safety trials in animals to determine whether hPSCs become cancerous or induce cancers [30]. To minimize effects of acquired mutations on cell therapy, it is strongly recommended that cells destined for transplant be monitored throughout their preparation using high-resolution methods such as SNP genotyping [30].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for High-Resolution Genotyping
| Reagent/Material | Function | Application Notes |
|---|---|---|
| CYTAG TotalCGH Labeling Kit | Allows SNP arrays in addition to standard CGH arrays | General purpose labeling for CGH and SNP detection |
| CYTAG SuperCGH Labeling Kit | Designed for limited starting material (e.g., 50 ng DNA) | Ideal for iPSC clones where material may be limited [32] |
| Puregene DNA Blood Kit | DNA extraction from peripheral blood | Standardized DNA extraction for consistent results [31] |
| NH4OAc and Absolute Ethanol | DNA cleanup procedure | Removes inhibitors from gDNA preparations [34] |
| Reduced EDTA TE Buffer | DNA resuspension after cleanup | Maintains DNA integrity for labeling reactions [34] |
| Cot-1 DNA | Blocks non-specific hybridization | Critical for reducing background in hybridization [32] |
| AluI and RsaI Restriction Enzymes | DNA digestion for SNP detection | Enables detection of SNPs located at enzyme recognition sites [31] |
| 8x60K and 4x180K CGH Arrays | Microarray formats for hybridization | 8x60K allows 8 samples/chip; 4x180K provides higher resolution [32] |
Frequently Asked Questions (FAQs)
Q1: Which platform is more suitable for detecting genomic instability in iPSC cultures - aCGH or SNP array? SNP arrays are generally preferred for comprehensive monitoring of genomic instability in iPSCs because they can detect both copy number variations and copy-neutral events such as loss of heterozygosity (LOH) [29] [30]. aCGH may be preferred when targeting specific genes at exon-level resolution is required [31]. For clinical applications, some laboratories use combined arrays that incorporate both CGH and SNP probes to maximize detection capabilities [31].
Q2: What are the critical quality control metrics for array experiments, and what are their acceptable thresholds? Key QC metrics include: DNA purity (A260/280 >1.8, A260/230 2.0-2.2), DNA yield (>5.0 µg for labeling), dye incorporation (>300 pmoles Cy3, >200 pmoles Cy5), specific activity (>60 pmol/µg Cy3, >40 pmol/µg Cy5), signal intensity (>200), background noise (<25), signal-to-noise ratio (>30), and derivative log ratio (<0.2) [32].
Q3: How can we detect low-level mosaicism in iPSC cultures using these platforms? Genomic aberrations smaller than 10Mb can be successfully detected in samples with as low as 10% mosaicism using optimized aCGH protocols [32]. SNP arrays generally show higher sensitivity for detecting low-level mosaic aneuploidies and chimerism compared to aCGH [31].
Q4: What is the typical reproducibility and concordance rate of these technologies? For validated SNPs on quality-controlled arrays, reproducibility rates typically exceed 99.9% among different experiments, and Mendelian consistency rates are approximately 99.96% [34].
Q5: How does the choice of reprogramming method affect genomic instability in iPSCs? Research indicates that Sendai virus (SV)-derived iPSCs show higher frequencies of copy number alterations and single nucleotide variations compared with episomal vector (Epi)-derived iPSCs [26]. All SV-iPS cell lines exhibited CNAs during reprogramming, while only 40% of Epi-iPS cells showed such alterations [26].
Multiplex Fluorescence In Situ Hybridization (M-FISH) for Karyotypic Analysis
Multiplex Fluorescence In Situ Hybridization (M-FISH) is a powerful 24-color karyotyping technique that has become indispensable for the comprehensive detection of complex chromosomal rearrangements. In the context of induced pluripotent stem cell (iPSC) research, where genomic instability is a primary concern, M-FISH provides a critical tool for identifying numerical and structural abnormalities that may arise during reprogramming or prolonged cell culture [4] [36]. This technical support guide addresses common experimental challenges and provides detailed methodologies to ensure accurate detection of chromosomal aberrations, enabling researchers to maintain genomic integrity in their stem cell cultures.
Troubleshooting Common M-FISH Experimental Issues
The following table outlines frequently encountered problems during M-FISH experiments, their potential causes, and recommended solutions.
| Issue | Potential Causes | Troubleshooting Strategies |
|---|---|---|
| Poor or No Signal [37] | Inefficient probe labeling, suboptimal denaturation/hybridization, inadequate permeabilization, low probe concentration | Check probe design and labeling efficiency. Optimize denaturation and hybridization conditions. Ensure complete sample permeabilization. Increase probe concentration or hybridization time [37] [38]. |
| High Background Noise [37] [38] | Incomplete stringent washes, non-specific probe binding, cross-reactivity, sample drying during hybridization | Increase stringency of post-hybridization washes (adjust temperature, salt concentration, and duration). Verify probe specificity and use Cot-1 DNA to block repetitive sequences. Ensure a humidified chamber to prevent drying [37] [38]. |
| Weak or Faded Signal [37] | Fluorophore sensitivity, signal quenching, over-fixed or over-permeabilized samples, improper mounting | Use sensitive fluorophores and anti-fade mounting medium. Minimize light exposure during staining and imaging. Optimize fixation and permeabilization times [37]. |
| Uneven or Patchy Hybridization [37] | Non-uniform probe distribution, air bubbles during mounting, uneven denaturation or permeabilization | Ensure even application of the probe and avoid hard pressure on coverslips. Remove all air bubbles when mounting. Verify consistent sample preparation across the slide [37]. |
| Morphological Distortion [37] | Over-fixation, over-permeabilization, harsh cell dissociation methods | Optimize fixation and permeabilization conditions. Use gentler methods for cell dissociation and spreading [37]. |
| Chromosomal Misclassification [39] | "Flaring" or overlapping fluorescence at translocation junctions, poor chromosome preparations, algorithmic interpretation errors | Corroborate complex rearrangements with whole-chromosome painting (WCP). Ensure high-quality metaphase spreads and optimal hybridization conditions to minimize flaring [39]. |
Frequently Asked Questions (FAQs)
1. How does M-FISH differ from traditional FISH and why is it particularly useful for iPSC research?
Unlike traditional FISH, which typically identifies one or a few targets simultaneously, M-FISH allows for the simultaneous visualization of all 24 human chromosomes in a single experiment using combinatorially labeled whole-chromosome painting probes [40] [36]. This is crucial for iPSC research because it enables the detection of complex chromosomal rearrangements and subtle structural changes that are often missed by other techniques [4] [36]. Identifying these aberrations is essential for ensuring the safety of iPSCs in downstream applications like regenerative medicine.
2. What are the inherent limitations of M-FISH in karyotype analysis?
A key limitation is that M-FISH cannot detect intrachromosomal rearrangements, such as deletions, duplications, or inversions, unless they involve a change in chromosomal paint [39]. Additionally, the technique can produce erroneous interpretations due to "flaring"—the overlapping of fluorescence signals at the junctions of translocated segments, which can lead to false identification of small inserted segments [39]. The resolution for detecting insertions/translocations on metaphase spreads is approximately 1 Mb [39].
3. What steps can be taken to improve the reproducibility of M-FISH results?
To ensure consistent and reproducible results, it is critical to standardize the sample preparation and FISH protocol steps [37]. This includes using healthy, actively growing cells for optimal chromosome morphology, carefully controlling fixation and denaturation times, and using appropriate positive and negative controls with each experiment [37] [38]. Consistent reagent quality and storage conditions are also vital [37].
4. Our M-FISH analysis suggests a complex, multi-chromosomal rearrangement. How can we confirm this finding?
When M-FISH indicates a complex rearrangement, it is highly recommended to validate the result using single-color whole-chromosome painting (WCP) for the specific chromosomes involved [39] [41]. This orthogonal technique helps confirm the origin of chromosomal material and can clarify ambiguities caused by fluorescence flaring, ensuring an accurate karyotype interpretation [39].
Essential M-FISH Protocol for Karyotypic Analysis
This protocol provides a robust methodology for conducting M-FISH, with particular attention to steps critical for analyzing iPSCs.
Sample Preparation and Metaphase Spread Creation
- Cell Culture and Mitotic Arrest: Use healthy, actively growing cells (e.g., iPSCs) at ~75-80% confluency. Treat with Colcemid (e.g., 100 ng/mL for 3 hours) to arrest cells in metaphase [42].
- Hypotonic Treatment: Collect mitotic cells and resuspend the pellet in a pre-warmed hypotonic solution (e.g., 75 mM KCl) and incubate for 15 minutes at 37°C. This swells the cells and helps spread the chromosomes [42].
- Fixation: Centrifuge the cells and fix them in freshly prepared Carnoy's fixative (a 3:1 mixture of methanol to acetic acid). Perform at least two changes of fixative, resuspending the pellet each time. Drop the fixed cell suspension onto clean glass slides and air dry [42].
Slide Pretreatment and Denaturation
- Pretreatment: Treat slides with RNase A and pepsin to remove RNA and digest proteins, respectively, then post-fix in formaldehyde. Dehydrate slides through an ethanol series (70%, 85%, 100%) [38] [41].
- Denaturation: Denature chromosomal DNA by incubating slides in 70% formamide in 2x SSC at 72°C for approximately 2 minutes. Immediately dehydrate through another cold ethanol series and air dry [38] [41].
Probe Hybridization and Washing
- Probe Application: Denature the commercially available 24-color M-FISH probe mix (e.g., SpectraVision Assay) at 72°C for 10 minutes. Apply the denatured probe to the denatured slide, cover with a coverslip, and seal with rubber cement [41].
- Hybridization: Incubate slides in a humidified chamber at 37°C for 48 hours to allow for specific hybridization of the probes to their target chromosomes [41].
Post-Hybridization Washes and Counterstaining
- Stringent Washes: Remove coverslips and wash slides in a solution of 0.4x SSC with detergent (e.g., IGEPAL) at 72°C for 2 minutes, followed by a rinse in 2x SSC with detergent at room temperature [41]. This critical step removes unbound or weakly bound probes, reducing background.
- Counterstaining and Mounting: Apply a counterstain such as DAPI (0.14 μg/mL in an anti-fade mounting medium) to stain all chromosomal DNA. Cover with a coverslip and store in the dark prior to imaging [41].
The Scientist's Toolkit: Key Reagents and Materials
| Reagent/Material | Function | Specific Example/Note |
|---|---|---|
| M-FISH Probe Cocktail [40] [36] | A mixture of whole-chromosome painting probes, each labeled with a unique combination of fluorophores, allowing for 24-color discrimination. | Commercial kits like the SpectraVision Assay (Vysis) are commonly used [41]. |
| Colcemid [42] | Inhibits microtubule polymerization, arresting cells in metaphase to enrich for chromosomes in their most condensed form. | Typically used at ~100 ng/mL for 2-4 hours [42]. |
| Carnoy's Fixative [42] | A 3:1 mixture of methanol and acetic acid that preserves chromosome morphology and prepares cells for spreading. | Must be prepared fresh for optimal results [42]. |
| Formamide [41] | Used in the denaturation buffer to unwind double-stranded chromosomal DNA, making it accessible for probe hybridization. | Used in 70% concentration at 72°C [41]. |
| DAPI (Counterstain) [37] [41] | A DNA-binding fluorescent dye that stains the entire nucleus, providing a reference for overall chromosome and nuclear morphology. | Visualized in the blue channel, distinct from the M-FISH probe colors [37]. |
| Stringent Wash Buffer [38] [41] | A low-salt buffer (e.g., 0.4x SSC) used at a specific elevated temperature to remove probe molecules that are bound non-specifically. | Critical for achieving a high signal-to-noise ratio; temperature is precisely controlled (e.g., 72°C) [41]. |
Whole-Genome Sequencing for Comprehensive SNV and Indel Identification
Frequently Asked Questions (FAQs)
FAQ 1: Why is WGS preferred over whole-exome sequencing (WES) for monitoring genomic instability in iPSCs?
While Whole-Exome Sequencing (WES) is cost-effective for targeting coding regions, Whole-Genome Sequencing (WGS) provides a more comprehensive solution for iPSC research. WGS allows for the analysis of variations across the entire genome, including non-coding regions that may harbor regulatory elements important for pluripotency and oncogenesis [43]. Furthermore, WGS surpasses targeted panels in identifying large-scale copy number variations (CNVs) [44], which are critical genomic aberrations frequently observed in iPSC cultures, such as amplifications on chromosome 20q11.21 [4] [6].
FAQ 2: What are the most common sources of false positives in SNV and Indel calling from iPSC lines?
False positive variant calls can arise from several sources:
- Sequencing Errors: Intrinsic errors from the sequencing platform itself, particularly in challenging genomic contexts like homopolymer runs [45].
- Mapping Errors: Incorrect alignment of reads to repetitive regions or segmental duplications in the reference genome [45] [46].
- Pre-existing Variations in Parental Somatic Cells: Low-frequency somatic variants in the parental cell population (e.g., skin fibroblasts) can be clonally expanded during iPSC generation and mistaken for reprogramming-induced mutations [4].
- PCR Duplicates: Artifacts introduced during library preparation can lead to over-representation of certain sequences [47].
FAQ 3: Our lab is new to NGS bioinformatics. What are the essential steps for variant calling?
A standard bioinformatics pipeline for variant calling from WGS data includes the following key steps [47] [43]:
- Quality Control (QC): Assessing raw read quality using tools like FastQC.
- Preprocessing: Trimming adapter sequences and low-quality bases with tools like Trimmomatic [47].
- Alignment: Mapping quality-controlled reads to a reference genome (e.g., GRCh38) using aligners such as BWA [47] [44].
- Variant Calling: Identifying SNPs and Indels using specialized software like GATK, Strelka2, or VarScan2 [46] [44] [43].
FAQ 4: Which genomic regions should we closely monitor for instability in iPSC cultures?
iPSC cultures show a strong propensity for acquired structural variations in specific genomic regions. Recurrent aberrations include:
- Copy Number Variations (CNVs): Amplification of 20q11.21 is a well-documented hotspot, encompassing cancer-associated genes like BCL2L1 and ID1 [4] [6]. Other recurrent CNVs occur on chromosomes 1, 2, 3, 12, and 16 [4] [6].
- Chromosomal Aneuploidies: Trisomy of chromosome 12 and gains of chromosomes 8 and X are frequently observed and may confer a selective growth advantage in culture [4].
Troubleshooting Guides
Issue 1: High False Positive Variant Calls
Problem: The variant calling pipeline yields an unexpectedly high number of putative SNVs/Indels, many of which are likely artifacts.
Solution:
- Apply Advanced Filtering: Use machine learning-based filtering tools, such as the Variant Quality Score Recalibration (VQSR) in GATK, to distinguish true variants from sequencing and mapping errors [45] [43].
- Implement Context-Aware Error Prediction: Leverage tools like StratoMod, which uses an interpretable machine-learning model to predict variant calling errors based on genomic context (e.g., homopolymer length, difficult-to-map regions) [45].
- Validate with Orthogonal Methods: Confirm critical variants, especially those in clinically relevant genes, using Sanger sequencing [46].
Issue 2: Low Concordance with Genotyping Arrays or Orthogonal Data
Problem: Variant calls from your WGS data show a low concordance rate with known genotypes from SNP arrays or other validated methods.
Solution:
- Re-calibrate Base Quality Scores: Use Base Quality Score Recalibration (BQSR) in GATK to correct for systematic errors in the assigned base quality scores [43].
- Verify Read Mapping: Inspect aligned reads in discrepant regions using a visualizer like the Integrative Genomics Viewer (IGV). Look for mapping quality issues, strand bias, or misalignments around indels [47].
- Check Coverage Depth: Ensure that the coverage depth at discrepant positions is sufficient for reliable variant calling (typically >10-20x) [46].
Issue 3: Detecting Somatic Mutations in iPSCs Versus Pre-existing Variations
Problem: It is challenging to determine if a mutation identified in an iPSC line was acquired during reprogramming or culture, or if it was a pre-existing, low-frequency variant in the parental somatic cell population.
Solution:
- Sequence the Parental Cell Line: The most reliable method is to perform deep sequencing (e.g., >100x coverage) of the parental somatic cells to identify pre-existing variations [4].
- Analyze Multiple Clones: If the parental line is unavailable, sequencing multiple, independently derived iPSC clones from the same donor can help. Mutations shared across all clones are likely pre-existing, while those unique to a single clone are likely acquired during reprogramming or culture [4].
Experimental Protocols
Protocol: A Basic Bioinformatics Workflow for SNV and Indel Calling from iPSC WGS Data
This protocol outlines a standard workflow for identifying genetic variations from iPSC-derived WGS data, based on established pipelines [47] [44] [43].
1. Raw Read Quality Control
- Objective: Assess the quality of the raw sequencing data.
- Procedure:
- Use
FastQCto generate a quality report on the raw FASTQ files. - Check key metrics: per-base sequence quality, sequence duplication levels, adapter contamination, and GC content.
- Use
- Tools: FastQC.
2. Data Preprocessing
- Objective: Remove adapter sequences, trim low-quality bases, and filter poor-quality reads.
- Procedure:
- Run
Trimmomaticto trim Illumina adapter sequences and remove leading/trailing low-quality bases (e.g., quality below Q20). - Drop reads below a minimum length (e.g., 36 bp).
- Run
- Tools: Trimmomatic [47], cutadapt.
3. Alignment to Reference Genome
- Objective: Map the preprocessed reads to the human reference genome.
- Procedure:
- Index the reference genome (e.g., GRCh38) using
BWA index. - Align the cleaned FASTQ files to the reference using
BWA-MEM. - Convert the output SAM file to a sorted BAM file and mark PCR duplicates using
SAMtoolsorPicard.
- Index the reference genome (e.g., GRCh38) using
- Tools: BWA (Burrows-Wheeler Aligner) [47] [44], SAMtools [46].
4. Variant Calling
- Objective: Identify SNVs and short Indels relative to the reference genome.
- Procedure:
- For germline variant calling, use
Strelka2orGATK HaplotypeCallerin single-sample mode. - For best practices, follow the GATK workflow, which may include base quality score recalibration (BQSR) and variant quality score recalibration (VQSR) [43].
- For germline variant calling, use
- Tools: Strelka2 [44], GATK [43], VarScan2 [47].
Workflow Diagram
Data Presentation
Table 1: Recurrent Genomic Aberrations in iPSC Cultures
This table summarizes the most common genomic instability events reported in iPSC studies, which should be prioritized during data analysis [4] [6].
| Type of Variation | Recurrent Genomic Location | Key Genes Involved | Potential Functional Impact |
|---|---|---|---|
| Copy Number Variation (CNV) | 20q11.21 amplification | BCL2L1, ID1, DNMT3B, HCK | Anti-apoptosis, enhanced pluripotency, proliferation advantage [4] [6]. |
| Chromosomal Aneuploidy | Trisomy 12 | NANOG, cell cycle genes | Improved reprogramming efficiency and proliferation [4]. |
| Chromosomal Aneuploidy | Trisomy 8 and X | Various | Selective growth advantage in culture [4]. |
| Copy Number Variation (CNV) | Chromosomes 1, 2, 3, 16 | Cancer-associated loci | Overlap with cancer genes; enrichment for JNK and NFκB signaling [6]. |
Table 2: Performance Comparison of Variant Calling in WGS and WES
This table provides example accuracy metrics from a study evaluating a specific variant calling method (VCMM), highlighting the high accuracy achievable with WGS and WES [46].
| Sequencing Method | False Positive Rate (%) | False Negative Rate (%) | Indel Calling Accuracy (%) | Notes |
|---|---|---|---|---|
| Whole Genome Sequencing (WGS) | 0.0068% | 0.17% | 94.7% | Evaluation based on concordance with genotyping arrays and Sanger validation [46]. |
| Whole Exome Sequencing (WES) | 0.0036% | 0.0084% | 97.3% | Higher accuracy in targeted exonic regions due to greater depth of coverage [46]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for WGS-based iPSC Genotyping
This table lists key reagents, tools, and software essential for preparing and analyzing iPSC samples for WGS.
| Item | Function/Description | Example/Note |
|---|---|---|
| Qubit Fluorometer | Accurate quantification of DNA concentration using fluorescence, unaffected by contaminants. Critical for ensuring sufficient input DNA for library prep [48] [44]. | Preferred over Nanodrop for precise DNA quantification pre-library prep [48]. |
| AllPrep DNA/RNA Kit | Simultaneous isolation of genomic DNA and total RNA from a single sample. Useful for integrated omics studies on the same iPSC line [44]. | |
| SureSelect Human All Exon V7 | Exome capture kit for WES. While this article focuses on WGS, WES remains a cost-effective alternative for targeted sequencing [44]. | |
| BWA (Burrows-Wheeler Aligner) | Short-read alignment software for mapping sequencing reads to a reference genome. A standard tool in NGS pipelines [47] [44] [43]. | |
| GATK (Genome Analysis Toolkit) | A comprehensive software package for variant discovery and genotyping. Provides tools for base quality recalibration and variant filtering [43]. | |
| Strelka2 | A fast and accurate small variant caller for germline and somatic SNVs and Indels. Used in validated clinical and research pipelines [44]. | |
| Integrative Genomics Viewer (IGV) | A high-performance visualization tool for interactive exploration of large genomic datasets. Essential for visually inspecting variant calls and read alignments [47]. |
Relationship Between iPSC Genomic Instability and Analysis Workflow
In the field of induced pluripotent stem cell (iPSC) research, maintaining genomic integrity is paramount. The phosphorylation of the histone variant H2AX on serine 139, forming γH2AX, is one of the earliest cellular responses to DNA double-strand breaks (DSBs) and serves as a critical marker for genomic instability [49] [50]. When DSBs occur, H2AX is rapidly phosphorylated by kinases from the PI3K family, primarily ATM and ATR, leading to the formation of γH2AX foci that can be visualized through immunofluorescence [51] [52]. Each focus represents a single DSB, making this assay exceptionally quantitative for assessing DNA damage levels and replication stress in cells [49] [53].
For iPSC cultures, which are prone to accumulated DNA damage during rapid propagation, the γH2AX assay provides an essential quality control metric [54]. Beyond direct DSBs, γH2AX formation also occurs in response to replication stress—a common challenge in stem cell cultures characterized by stalled replication forks that can lead to genomic instability if unresolved [51] [53]. This technical support document outlines comprehensive protocols, troubleshooting guides, and FAQs to help researchers implement robust γH2AX foci staining in their investigations of genomic instability.
Technical Foundations: Gamma-H2AX Signaling and Detection
Molecular Signaling Pathway
The following diagram illustrates the key molecular events leading to γH2AX formation and detection in response to DNA damage and replication stress:
Experimental Workflow
The standard workflow for γH2AX foci detection and quantification involves multiple critical steps as shown below:
Detailed Experimental Protocols
Standard Immunofluorescence Protocol for Gamma-H2AX Detection
This protocol has been adapted from established methodologies for detecting DNA damage in stem cells and other mammalian systems [54] [55].
Materials Required:
- Cultured cells (iPSCs or differentiated progenitors) grown on chamber slides or coverslips
- phosphate-buffered saline (PBS)
- 4% paraformaldehyde (PFA) in PBS
- Permeabilization solution (0.5% Triton X-100 in PBS)
- Blocking solution (5% BSA in PBS, optionally with 5% normal serum from secondary antibody host species)
- Primary antibody: Anti-phospho-histone H2AX (Ser139) (Clone: Multiple commercial options available)
- Fluorophore-conjugated secondary antibody (e.g., Alexa Fluor 488, 594)
- Nuclear counterstain (DAPI or Hoechst)
- Antifade mounting medium
- Humidified chamber
Step-by-Step Procedure:
Cell Preparation and Fixation
- Culture iPSCs on appropriate substrate (e.g., Matrigel-coated chamber slides) until 60-70% confluent.
- Apply DNA damage-inducing treatments as experimentally required (e.g., etoposide, radiation, replication stress inducers).
- Aspirate culture medium and gently wash cells twice with pre-warmed PBS.
- Fix cells with 4% PFA for 15 minutes at room temperature.
- Wash three times with PBS, 5 minutes each wash.
Permeabilization and Blocking
- Permeabilize cells with 0.5% Triton X-100 in PBS for 10 minutes at room temperature.
- Wash twice with PBS, 5 minutes each.
- Incubate with blocking solution for 1 hour at room temperature to reduce non-specific binding.
Antibody Incubations
- Prepare primary antibody dilution in blocking solution (typically 1:500-1:1000, but titrate for optimal results).
- Apply primary antibody solution to cells and incubate overnight at 4°C in a humidified chamber.
- The next day, wash three times with PBS containing 0.1% Tween-20 (PBST), 5 minutes each.
- Prepare species-appropriate secondary antibody conjugated to preferred fluorophore in blocking solution (typically 1:500-1:1000).
- Apply secondary antibody and incubate for 1 hour at room temperature in the dark.
- Wash three times with PBST, 5 minutes each.
Counterstaining and Mounting
- Prepare DAPI solution (1 µg/mL in PBS) and apply to cells for 5-10 minutes.
- Wash twice with PBS, 5 minutes each.
- For chamber slides, add a drop of antifade mounting medium and carefully apply coverslip. For coverslips, mount on glass slides.
- Seal edges with clear nail polish if necessary.
- Store at 4°C in the dark until imaging.
Quantitative Analysis and Data Interpretation
Image Acquisition Parameters:
- Acquire images using a 60x or 100x oil immersion objective on a fluorescence or confocal microscope.
- Capture Z-stacks (0.2-0.5 µm intervals) for improved foci counting, particularly in thicker cells.
- Maintain consistent exposure settings across all experimental groups.
- Image at least 50-100 cells per condition across multiple fields of view.
Foci Quantification Methods:
- Manual Counting: Visually count discrete foci within each nucleus, excluding diffuse nuclear staining.
- Automated Analysis: Use image analysis software (ImageJ, CellProfiler, or commercial platforms) with appropriate algorithms:
- Identify nuclei using DAPI channel
- Apply intensity thresholding to distinguish foci from background
- Size exclusion to filter out non-specific speckles
- Normalize data as foci per cell or percentage of cells with >10 foci (indicative of significant DNA damage).
Troubleshooting Guide: Common Issues and Solutions
Table 1: Troubleshooting Common Problems in Gamma-H2AX Staining
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| High background fluorescence | Inadequate blocking, antibody concentration too high, insufficient washing | Increase blocking time to 2 hours; titrate antibody to optimal concentration; increase wash times and number of washes; include detergent in wash buffers [56]. |
| Weak or no specific signal | Inefficient fixation, antibody degradation, insufficient permeabilization | Verify antibody activity with positive control; optimize permeabilization time/concentration; try alternative fixatives (e.g., methanol:acetone 1:1); check antibody species reactivity [55]. |
| Diffuse nuclear staining without discrete foci | Over-fixation, incorrect antibody dilution, excessive light exposure during procedures | Reduce fixation time; optimize primary antibody concentration; perform all procedures with minimal light exposure; include positive control (e.g., etoposide-treated cells) [49]. |
| High cell-to-cell variability | Uneven cell culture, inconsistent treatment application, cell cycle effects | Ensure uniform cell seeding density; apply treatments carefully with proper mixing; consider cell cycle synchronization; increase sample size for analysis [49] [54]. |
| Non-specific cytoplasmic staining | Secondary antibody cross-reactivity, incomplete blocking, cell health issues | Include secondary-only control; use cross-adsorbed secondary antibodies; increase serum concentration in blocking buffer; assess cell viability before fixation [56]. |
Frequently Asked Questions (FAQs)
Q1: What constitutes a statistically significant number of γH2AX foci in untreated iPSCs? A: Untreated, healthy iPSCs typically show 1-5 foci per cell, representing endogenous DNA damage from routine cellular metabolism. Values consistently exceeding 5-10 foci per cell may indicate significant replication stress or culture-induced DNA damage requiring investigation [54].
Q2: How quickly do γH2AX foci form after DNA damage induction? A: γH2AX foci formation is rapid, detectable within 1-3 minutes after DSB induction, with peak foci numbers typically observed within 30 minutes to 1 hour post-damage. The timing varies based on damage type and intensity [52] [50].
Q3: Can γH2AX detection distinguish between direct DSBs and replication stress-induced damage? A: While both processes generate γH2AX foci, replication stress often produces more heterogeneous foci patterns and may involve different kinase dependencies (ATR versus ATM). Complementary assays like replication fork labeling or cell cycle analysis can help distinguish these sources [51] [53].
Q4: What are the key considerations for quantifying γH2AX in iPSCs versus differentiated cells? A: iPSCs have more open chromatin architecture, which can affect foci appearance and quantification. They also cycle more rapidly, potentially increasing baseline foci counts. Always include appropriate iPSC-specific controls and consider higher baseline thresholds [54].
Q5: How should γH2AX data be normalized for comparative experiments? A: Common normalization approaches include: (1) foci per nucleus, (2) percentage of cells with >10 foci, or (3) fluorescence intensity quantification when using plate-based assays. The choice depends on experimental design and damage extent [49] [55].
Quantitative Data Interpretation and Standards
Table 2: Gamma-H2AX Foci Quantification Standards and Interpretation
| Experimental Condition | Expected Foci Range per Cell | Biological Interpretation | Recommended Controls |
|---|---|---|---|
| Healthy, untreated iPSCs | 1-5 | Baseline level of endogenous DNA damage | Essential for establishing experimental baseline |
| Moderate replication stress (e.g., mild nucleotide depletion) | 10-25 | Significant replication stress requiring cellular response | Include cell cycle analysis to confirm S-phase arrest |
| Acute DSB induction (e.g., 1-2 Gy ionizing radiation) | 20-40 | Substantial DNA damage activating repair pathways | Dose-response curve with known DSB inducers |
| Severe genotoxic stress (e.g., 10-100 µM etoposide) | 40-100+ | Overwhelming damage often leading to cell death | Include viability assessment and apoptosis markers |
| Delayed timepoint (e.g., 24h post-treatment) | 5-15 | Evidence of ongoing repair or persistent damage | Compare with early timepoints to assess repair kinetics |
Research Reagent Solutions
Table 3: Essential Reagents for Gamma-H2AX Foci Assays
| Reagent | Function | Recommended Specifications |
|---|---|---|
| Anti-γH2AX (Ser139) Antibody | Primary detection antibody for phosphorylated H2AX | Monoclonal recommended for consistency; validate for immunofluorescence; species compatibility with secondary antibodies [54] [55] |
| Fluorophore-conjugated Secondary Antibody | Signal amplification and detection | Cross-adsorbed against serum proteins; choose fluorophores compatible with microscope filters (e.g., Alexa Fluor 488, 594) [56] |
| Nuclear Counterstain | Nuclear identification and segmentation | DAPI or Hoechst 33342; validate concentration to avoid oversaturation [54] |
| Blocking Solution | Reduce non-specific antibody binding | 5% BSA in PBS; consider adding 5% normal serum from secondary antibody host species [56] |
| Permeabilization Agent | Enable antibody access to nuclear antigens | 0.1-0.5% Triton X-100; concentration and time optimization critical [54] [55] |
| Mounting Medium | Preserve fluorescence and reduce photobleaching | Antifade mounting medium with DAPI available for convenience |
Gamma-H2AX foci staining remains an indispensable tool for quantifying DNA damage and replication stress in iPSC cultures. When properly optimized and controlled, this assay provides sensitive detection of genomic instability that might compromise research validity or therapeutic applications. The protocols and troubleshooting guidance provided here address the most common challenges in implementing this technique, enabling researchers to generate reliable, reproducible data for assessing genomic integrity in stem cell systems.
Monitoring Genomic Stability in Differentiated Derivatives and Organoid Models
In the fields of regenerative medicine and drug development, induced pluripotent stem cell (iPSC)-derived differentiated cells and organoid models have become indispensable tools for disease modeling, drug screening, and developmental biology research [57]. These complex three-dimensional structures mimic human tissues more accurately than traditional two-dimensional cultures [58]. However, maintaining genomic stability throughout the culture period presents a significant challenge that directly impacts the validity and reproducibility of experimental results [59]. Genomic instability—ranging from point mutations to chromosomal abnormalities—can arise from various sources including cellular stress during differentiation, extended passaging, and suboptimal culture conditions [60]. This technical support center provides comprehensive troubleshooting guidance and methodological frameworks to help researchers monitor, identify, and address genomic instability in their stem cell models, ensuring data reliability and experimental success.
Troubleshooting Guide: Common Challenges and Solutions
Problem 1: Excessive Differentiation or Spontaneous Differentiation in Cultures
- Potential Causes and Solutions:
- Aging Culture Medium: Ensure complete cell culture medium has been stored correctly at 2-8°C and is less than two weeks old [8].
- Inadequate Differentiation Removal: Manually remove areas of differentiation prior to passaging to prevent spread [8].
- Prolonged Environmental Exposure: Avoid having culture plates outside the incubator for more than 15 minutes at a time to maintain consistent temperature and pH [8].
- Suboptimal Colony Density: Plate fewer cell aggregates during passaging if differentiation exceeds 20% of the culture [8].
- Overgrown Cultures: Passage cultures when colonies are large and compact with dense centers, before they begin to overgrow and spontaneously differentiate [8].
Problem 2: Poor Cell Survival or Low Attachment After Plating
- Potential Causes and Solutions:
- Insufficient Seeding Density: Plate 2-3 times more cell aggregates initially and maintain a more densely confluent culture [8].
- Delayed Processing: Work quickly after cells are treated with passaging reagents to minimize the duration that cell aggregates remain in suspension [8].
- Excessive Manipulation: Reduce pipetting intensity and duration when breaking up cell aggregates to prevent mechanical damage [8].
- Incorrect Plate Selection: Ensure non-tissue culture-treated plates are used when coating with Vitronectin XF; use tissue culture-treated plates when coating with Corning Matrigel [8].
Problem 3: Detection of Karyotypic Abnormalities in Long-Term Cultures
- Potential Causes and Solutions:
- Extended Passaging: Implement a strict passaging schedule and freeze down early-passage stocks to minimize genetic drift [59].
- Oxidative Stress: Include antioxidants in culture media and maintain optimal oxygen tension (typically 5% O₂) to reduce reactive oxygen species-induced DNA damage [59].
- Replication Stress: Optimize feeding schedules to prevent nutrient depletion, which can lead to replication fork stalling and DNA breakage [59].
- Inadequate Checkpoint Function: Regularly monitor p53 pathway integrity, as dysfunction can allow cells with DNA damage to proliferate [60].
Experimental Protocols for Genomic Stability Assessment
Protocol 1: Comprehensive Karyotyping and Chromosomal Analysis
Purpose: Detect gross chromosomal abnormalities and aneuploidy in stem cell cultures and organoids [60].
Materials:
- Colcemid solution (10 µg/mL)
- Hypotonic solution (0.075M KCl)
- Fixative (3:1 methanol:acetic acid)
- Giemsa stain
- Phase-contrast microscope with imaging system
Methodology:
- Culture cells to 60-70% confluency in T25 flasks.
- Add Colcemid to final concentration 0.1 µg/mL and incubate for 4 hours at 37°C.
- Dissociate cells to single-cell suspension using gentle enzymatic treatment.
- Centrifuge at 200 × g for 5 minutes and resusplement pellet in pre-warmed hypotonic solution (0.075M KCl).
- Incubate for 20 minutes at 37°C.
- Add fixative dropwise while gently vortexing.
- Centrifuge and repeat fixation twice more.
- Drop cell suspension onto clean microscope slides and air dry.
- Stain with Giemsa for 8-10 minutes, rinse with distilled water, and air dry.
- Analyze at least 20 metaphase spreads per sample for chromosomal number and structural abnormalities.
Quality Control:
- Include a control cell line with known normal karyotype
- Ensure metaphase spreads show 400-550 band resolution
- Document all abnormalities according to International System for Human Cytogenetic Nomenclature (ISCN) guidelines
Protocol 2: DNA Damage Response (DDR) Assessment via Immunofluorescence
Purpose: Quantify DNA damage markers and DDR activation in differentiated derivatives and organoids [59].
Materials:
- Phospho-histone H2A.X (Ser139) antibody (γH2AX)
- 53BP1 antibody
- Anti-rabbit secondary antibody with fluorescent conjugate
- DNA counterstain (DAPI or Hoechst)
- Paraformaldehyde (4% in PBS)
- Triton X-100 (0.5% in PBS)
- Blocking solution (5% BSA in PBS)
Methodology:
- Culture cells on chambered slides or matrix-coated coverslips.
- Fix with 4% paraformaldehyde for 15 minutes at room temperature.
- Permeabilize with 0.5% Triton X-100 for 10 minutes.
- Block with 5% BSA for 1 hour at room temperature.
- Incubate with primary antibodies (γH2AX and 53BP1) diluted in blocking solution overnight at 4°C.
- Wash 3× with PBS and incubate with fluorescent secondary antibodies for 1 hour at room temperature in the dark.
- Counterstain with DAPI for 5 minutes and mount with antifade medium.
- Image using high-resolution fluorescence or confocal microscopy.
- Quantify foci per nucleus in at least 100 cells per condition.
Interpretation:
- >10 γH2AX foci/nucleus indicates significant DNA damage
- Colocalization of γH2AX and 53BP1 confirms bona fide DNA double-strand breaks
- Compare to positive control (e.g., irradiated cells) and negative control (untreated cells)
Protocol 3: CRISPR-Cas9 Functional Genomic Screening in Organoids
Purpose: Identify genetic dependencies and synthetic lethal interactions in patient-derived organoid models [61].
Table 1: Key Reagents for CRISPR Screening in Organoids
| Reagent | Function | Example/Concentration |
|---|---|---|
| Brunello CRISPR Library | Genome-wide gRNA collection | 78,000 gRNAs targeting ~19,000 genes [61] |
| LentiCRISPR v2.0 | Cas9 and gRNA expression vector | N/A [61] |
| Polybrene | Enhances viral transduction | 8 μg/mL |
| Puromycin | Selection of transduced cells | 1-5 μg/mL (dose determined by kill curve) |
| Organoid culture media | Maintains organoid growth and viability | Dependent on organoid type |
Methodology:
- Library Preparation: Amplify Brunello CRISPR library and produce lentiviral particles in HEK293T cells [61].
- Organoid Transduction: Dissociate organoids to single cells and transduce with CRISPR library at MOI of 0.3-0.5 to ensure single integration.
- Selection: Treat with puromycin for 5-7 days to select successfully transduced cells.
- Screen Execution: Passage organoids regularly, maintaining at least 500x coverage for each gRNA.
- Timepoint Sampling: Collect samples at Day 7 (baseline), Day 21, and Day 36 for genomic DNA extraction.
- gRNA Amplification and Sequencing: PCR amplify integrated gRNAs from genomic DNA and sequence using Illumina platforms.
- Data Analysis: Calculate gRNA depletion/enrichment using MAGeCK or similar algorithms.
Quality Control:
- Ensure >50x coverage for each gRNA in each replicate
- Include control gRNAs targeting essential and non-essential genes
- Validate TP53 status as functional TP53 affects screening outcomes [61]
Signaling Pathways in Genomic Stability
DNA Damage Response Pathway Network
Genomic Stability Monitoring Workflow
Comprehensive Genomic Stability Assessment Workflow
Frequently Asked Questions (FAQs)
Q1: How frequently should I monitor genomic stability in my stem cell cultures? Regular monitoring is essential for maintaining experimental integrity. For ongoing cultures, perform basic assessments (e.g., DNA damage foci staining) every 2-3 passages. Conduct comprehensive karyotyping every 10-15 passages or before initiating critical experiments. Increase frequency if cells show signs of stress, such as slowed growth or morphological changes [59].
Q2: What are the most common genomic abnormalities observed in iPSC-derived models? The most frequent abnormalities include trisomy of chromosomes 12, 17, and 20, segmental amplifications of 20q11.21, and point mutations in TP53. These alterations often confer growth advantages in culture but compromise the biological relevance of the models [60].
Q3: Can I use organoid models for long-term studies given genomic stability concerns? Yes, but with appropriate safeguards. Implement rigorous monitoring protocols, freeze early-passage stocks, and limit the number of passages for individual experiments. For particularly long-term studies, consider periodically regenerating organoids from cryopreserved stocks to minimize genetic drift [57] [61].
Q4: How does the 3D culture environment of organoids affect genomic stability compared to 2D cultures? Three-dimensional cultures may better maintain genomic stability than 2D systems due to more physiological cell-cell interactions, reduced oxidative stress in interior layers, and more natural polarization. However, nutrient and oxygen gradients in larger organoids can create microenvironments where genomic instability may selectively arise [58].
Q5: What emerging technologies show promise for better monitoring of genomic stability? Artificial intelligence (AI) approaches are revolutionizing genomic stability monitoring. Machine learning algorithms can now predict genetic instability from brightfield images alone, while deep learning models can integrate multi-omics data to identify subtle patterns predictive of genomic deterioration long before conventional methods detect abnormalities [62] [63].
Research Reagent Solutions
Table 2: Essential Reagents for Genomic Stability Research
| Reagent Category | Specific Examples | Primary Function | Considerations |
|---|---|---|---|
| DNA Damage Detectors | Anti-γH2AX antibody, Anti-53BP1 antibody, Anti-RAD51 antibody | Detect DNA double-strand breaks and repair machinery | Validate antibody specificity for your model system; optimize fixation methods |
| Chromosomal Analysis | Giemsa stain, FISH probes, Colcemid | Visualize chromosomal number and structure | Ensure metaphase quality; use appropriate banding resolution |
| CRISPR Screening | Brunello library, LentiCRISPR v2.0, Lentiviral packaging plasmids | Identify genetic dependencies and synthetic lethal interactions | Maintain adequate gRNA coverage; confirm Cas9 activity |
| Cell Senescence | β-galactosidase kit, Senescence-associated secretory phenotype (SASP) antibodies | Detect cellular senescence as consequence of genomic instability | Use proper positive controls; distinguish from quiescence |
| Oxidative Stress | CM-H2DCFDA, MitoSOX, Nrf2 pathway inhibitors | Measure reactive oxygen species contributing to DNA damage | Consider compartment-specific ROS probes; account for autofluorescence |
| Apoptosis Detection | Annexin V, Caspase 3/7 assays, TUNEL kits | Quantify programmed cell death resulting from irreparable DNA damage | Distinguish early vs. late apoptosis; use appropriate controls |
Maintaining genomic stability in differentiated derivatives and organoid models requires vigilant monitoring and proactive culture management. By implementing the troubleshooting strategies, experimental protocols, and quality control measures outlined in this technical support center, researchers can significantly enhance the reliability and reproducibility of their stem cell-based models. The integration of traditional assessment methods with emerging AI-driven approaches promises to further advance our capability to preserve genomic integrity throughout long-term culture, ultimately strengthening the validity of research findings in basic science and drug development applications [63].
Strategies to Minimize and Mitigate Genomic Instability
Frequently Asked Questions (FAQs)
Q1: Why should I consider using Myc-independent reprogramming protocols?
The original Yamanaka factors (OSKM) include the proto-oncogene c-Myc, which poses significant risks to the stability and safety of induced pluripotent stem cells (iPSCs). Its overexpression contributes to tumorigenesis, increasing the potential for teratoma formation in downstream applications [64] [65]. Myc-independent protocols address these safety concerns by eliminating or substituting c-Myc while maintaining effective reprogramming. Furthermore, studies have shown that iPSC lines generated without c-Myc may exhibit improved genomic stability, a critical consideration for your thesis research on genomic instability [64] [66].
Q2: What are the primary alternatives to using c-Myc?
Researchers have developed several successful strategies to avoid using c-Myc:
- Direct Omission: Some protocols simply omit c-Myc, using only OCT4, SOX2, and KLF4 (OSK). However, this often comes at the cost of reduced reprogramming efficiency [64].
- Myc Family Substitution: The family member L-Myc can be used as a safer alternative. Research indicates that L-Myc reduces the tumorigenic risk of resulting iPSCs while maintaining reprogramming efficiency [64] [26].
- Alternative Factor Cocktails: The Thomson lab's combination of OCT4, SOX2, NANOG, and LIN28 (OSNL) is a well-established, Myc-free set of factors [64] [66].
- Small Molecule Replacements: Small molecules like RepSox can functionally replace Sox2, and factors like Esrrb or Glis1 can serve as alternatives to c-Myc in somatic cell reprogramming [64].
Q3: How does chemical reprogramming enhance the safety profile of iPSCs?
Chemical reprogramming, which uses defined cocktails of small molecules instead of genetic factors, represents a fundamentally innovative and safer approach [67]. Key advantages include:
- Non-Genomic Integration: It avoids the risk of genomic integration and insertional mutagenesis associated with viral vectors, a significant source of genomic instability [64] [67].
- Standardization and Control: Small molecules are easily synthesized, standardized, and their application can be precisely controlled and reversed, offering a more flexible regulatory path [67].
- Reduced Tumorigenicity: By eliminating the need for potent oncogenes like c-Myc, the risk of tumor formation in derived cells is theoretically lowered [65].
Q4: What are common genomic instability issues observed with different delivery systems?
The method used to introduce reprogramming factors can significantly impact genomic integrity. A 2025 study systematically compared two common methods [26]:
- Sendai Virus (SV) Vectors: These are non-integrating but were associated with a higher frequency of copy number alterations (CNAs) during the reprogramming phase. All SV-iPS cell lines in the study exhibited CNAs. Furthermore, single-nucleotide variations (SNVs) were observed exclusively in SV-derived cells during passaging and differentiation. Late-passage SV-iPSCs also showed upregulation of chromosomal instability-related genes [26].
- Episomal Vectors: These non-integrating plasmids showed a better stability profile. Only 40% of episomal vector-derived iPS cells showed CNAs during reprogramming, and no SNVs were detected during passaging or differentiation [26].
This evidence suggests that episomal vectors may be a preferable choice for research focused on minimizing genomic instability.
Troubleshooting Guides
Problem: Low Reprogramming Efficiency in Myc-Independent Protocols
Potential Causes and Solutions:
- Cause 1: Suboptimal Factor Expression.
- Solution: Ensure the correct stoichiometry of the reprogramming factors. For instance, the ratio of SOX2 to OCT4 is critical for efficiency. If using a three-factor (OSK) protocol, consider fine-tuning the concentrations of each factor [66]. Validate factor expression via qPCR or immunostaining.
- Cause 2: Inefficient Delivery Method.
- Solution: Choose a delivery system that balances efficiency with safety. The table below compares common methods. If using non-integrating methods like episomal vectors, optimize the electroporation conditions or transfection reagent-to-DNA ratio for your specific cell type [26].
- Cause 3: Poor Starting Cell Quality or Type.
- Solution: Use early-passage, healthy somatic cells. Some cell types (e.g., fibroblasts) reprogram more efficiently than others. Consider using chemically defined media conditions to support cell health during the initial transduction phase.
Problem: High Incidence of Genomic Aberrations in Established iPSC Lines
Potential Causes and Solutions:
- Cause 1: Genotoxic Stress from the Reprogramming Process.
- Solution: A key mediator of genotoxic stress is p53. Modulating its pathway can increase efficiency but also raises safety concerns.
- Cause 2: Selective Overgrowth of Aberrant Clones.
- Solution: Implement rigorous genomic screening early and often.
- Action: Perform karyotype analysis and more sensitive techniques like chromosomal microarray on multiple intermediate-stage colonies and the final master cell bank. Do not rely solely on pluripotency marker expression for quality control [26].
- Solution: Implement rigorous genomic screening early and often.
- Cause 3: Use of a High-Risk Delivery System.
- Solution: As highlighted in the FAQ, select a delivery system with a lower inherent risk of inducing mutations.
- Action: Based on current evidence, prefer episomal vectors over Sendai virus systems to minimize CNAs and SNVs [26].
- Solution: As highlighted in the FAQ, select a delivery system with a lower inherent risk of inducing mutations.
The following tables summarize key quantitative data from recent studies to aid in protocol selection and optimization.
Table 1: Comparison of Myc-Independent Reprogramming Factor Cocktails
| Factor Cocktail | Key Components | Reported Efficiency | Genomic Stability Notes | Key Reference |
|---|---|---|---|---|
| OSK | OCT4, SOX2, KLF4 | Lower than OSKM | Avoids c-Myc oncogenic risk; baseline stability. | [64] |
| OSNL | OCT4, SOX2, NANOG, LIN28 | Comparable to OSKM | Avoids c-Myc; Lin28 may accelerate proliferation. | [64] [66] |
| OSK + L-Myc | OCT4, SOX2, KLF4, L-Myc | Maintains efficiency | Reduced tumorigenic risk compared to c-Myc. | [64] [26] |
Table 2: Genomic Instability Associated with Non-Integrating Delivery Systems
| Delivery System | Genomic Integration? | Copy Number Alterations (CNAs) during Reprogramming | Single-Nucleotide Variations (SNVs) | Key Reference |
|---|---|---|---|---|
| Sendai Virus (SV) | No | 100% of cell lines exhibited CNAs | Observed during passaging/differentiation | [26] |
| Episomal Vectors | No | 40% of cell lines exhibited CNAs | No SNVs detected | [26] |
Table 3: Small Molecules to Enhance Reprogramming Efficiency and Safety
| Small Molecule | Function | Effect on Reprogramming | Key Reference |
|---|---|---|---|
| RepSox | TGF-β pathway inhibitor; replaces SOX2 | Increases efficiency; allows factor reduction. | [64] |
| Valproic Acid (VPA) | Histone deacetylase inhibitor | Increases efficiency up to 6.5-fold when combined with 8-Br-cAMP. | [64] |
| 8-Br-cAMP | Cell-permeable cAMP analog | Improves human fibroblast reprogramming by 2-fold. | [64] |
| Sodium Butyrate | Histone deacetylase inhibitor | Enhances robustness of reprogramming. | [64] |
Experimental Workflows and Signaling Pathways
Diagram 1: Myc-Independent Reprogramming Workflow
This diagram outlines the key decision points and steps for establishing iPSC lines using Myc-independent methods, emphasizing quality control for genomic instability.
Diagram 2: p53 Signaling Pathway in Genomic Stability
This diagram simplifies the central role of the p53 pathway in maintaining genomic integrity during the stressful reprogramming process, and common intervention points.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Myc-Independent and Chemical Reprogramming
| Reagent | Function in Reprogramming | Example Use Case |
|---|---|---|
| L-Myc Expression Vector | Safer alternative to c-Myc; maintains efficiency. | Used in the OSK + L-Myc factor cocktail to reduce tumorigenic risk [64] [26]. |
| Episomal Plasmid Vectors | Non-integrating DNA delivery system. | Preferred method for delivering OSK/OSNL factors to minimize CNAs and SNVs [26]. |
| RepSox | Small molecule TGF-β inhibitor; replaces SOX2. | Used in combination with other factors/small molecules to reduce the number of required genetic factors [64]. |
| Valproic Acid (VPA) | Histone deacetylase inhibitor; opens chromatin. | Added to culture medium to enhance reprogramming efficiency, particularly with blood cells [64] [67]. |
| 8-Br-cAMP | Cell-permeable cAMP analog; modulates signaling. | Used in synergy with VPA to significantly boost reprogramming efficiency [64]. |
| CHIR99021 | GSK-3β inhibitor; activates Wnt signaling. | A common component in chemical reprogramming cocktails to promote pluripotency [67]. |
| ALK5 Inhibitor II | TGF-β receptor inhibitor; supports mesenchymal-to-epithelial transition. | Used in chemical reprogramming protocols to create a permissive environment for fate change [67]. |
Optimizing Culture Conditions to Reduce Replicative Stress and Selective Pressure
FAQs on Genomic Instability in iPSC Cultures
What is genomic instability and why is it a concern in iPSC cultures? Genomic instability refers to an increased tendency for mutations and alterations to occur and persist in DNA as cells divide [68]. In iPSC cultures, this is a major concern because disruptions in normal cell division and DNA repair processes can allow cells with errors to proliferate, compromising the safety and validity of research or therapeutic applications [68].
How does replicative stress contribute to genomic instability in iPSCs? Replicative stress occurs when the DNA replication machinery is disrupted or delayed. In the context of iPSCs, the reprogramming process itself and rapid cell proliferation can induce such stress. This stress can lead to DNA replication errors, DNA double-strand breaks, and ultimately, genomic instability, if the cell's damage repair mechanisms are overwhelmed [69].
What selective pressures exist in iPSC cultures? A key selective pressure in iPSC cultures is the continuous proliferation and expansion of cell populations. Cells that acquire mutations conferring a growth advantage, such as those in tumor suppressor genes like TP53, can outcompete normal cells [69]. This can lead to an overrepresentation of genetically abnormal cells in the culture over time.
What are the common genetic changes seen in unstable iPSC cultures? Common changes include mutations in tumor suppressor genes like TP53 and copy number variations (CNVs), which are duplications or deletions of large segments of DNA. These alterations can provide a selective growth advantage to subpopulations of cells [69].
Troubleshooting Guides
Problem 1: Excessive Spontaneous Differentiation in Cultures
Potential Causes and Solutions:
- Cause: Overgrown colonies or uneven colony density creating microenvironments that promote differentiation.
- Solution: Passage cultures when colonies are large and compact but before they become overly confluent. Ensure cell aggregates are evenly sized during passaging to promote uniform growth [8].
- Cause: Old or degraded culture medium.
- Solution: Ensure complete cell culture medium is kept at 2-8°C and is less than two weeks old [8].
- Cause: Prolonged exposure of cultures to non-incubator conditions.
- Solution: Minimize the time culture plates are outside the incubator to less than 15 minutes at a time [8].
Problem 2: Low Cell Survival Post-Passaging (Indicating Replicative Stress)
Potential Causes and Solutions:
- Cause: Passaging cells at an overly high confluency.
- Solution: Passage cells between 40-85% confluency. If cells are overly confluent, use a ROCK inhibitor to improve cell survival [70].
- Cause: Excessive single-cell dissociation and mechanical stress.
- Solution: When using passaging reagents, avoid over-pipetting to generate a single-cell suspension. If aggregates are too large, slightly increase incubation time with the dissociation reagent instead of vigorous pipetting [8] [70].
- Cause: Incorrect seeding density.
- Solution: If low attachment is observed, initially plate 2-3 times the number of cell aggregates to achieve a denser, more supportive culture [8].
Problem 3: Suspected Genetic Aberration and Karyotype Instability
Potential Causes and Solutions:
- Cause: Selective overgrowth of a subpopulation with a growth advantage.
- Solution: Regularly monitor the karyotype and genetic integrity of your cell lines. Avoid culturing cells for an excessively high number of passages. Use controlled freezing to maintain low-passage stock vials [69].
- Cause: Oxidative stress during culture.
- Solution: Consider using antioxidant supplements, though their use should be validated as they can sometimes interfere with differentiation cues.
The following table summarizes key parameters to monitor for maintaining genomic stability.
Table 1: Key Culture Parameters for Genomic Stability Maintenance
| Parameter | Optimal Range | Consequence of Deviation | Reference / Rationale |
|---|---|---|---|
| Passage Confluency | 40-85% | >85%: Increased differentiation, replicative stress, poor survival.<40%: Low seeding efficiency. | [70] |
| Medium Age (at 2-8°C) | < 2 weeks | Degraded components, nutrient depletion, increased pH fluctuation, stress. | [8] |
| Colony Size at Passage | Large, compact, dense centers | Overgrown colonies: Induce spontaneous differentiation and create selective pressures. | [8] |
| Post-Thaw Viability | >80% (aim) | Low viability: High oxidative and replicative stress on the recovering population, favoring selection. | [70] |
Experimental Protocol: Quality Control Assessment for Genomic Integrity
This protocol outlines a routine check for genomic stability in iPSC cultures.
Objective: To periodically assess the genomic integrity of cultured iPSCs through karyotype analysis and pluripotency marker validation.
Materials:
- Log-phase growing iPSC culture (70-80% confluent)
- Appropriate dissociation reagent (e.g., Gentle Cell Dissociation Reagent or ReLeSR)
- ROCK inhibitor (e.g., Y-27632)
- Pre-coated culture plates
- Essential 8 Medium or equivalent
- Fixative solution (e.g., Methanol:Acetic Acid 3:1)
- Giemsa stain
- PCR reagents
- Flow cytometer
Methodology:
- Cell Preparation: Harvest a portion of the iPSC culture using standard passaging procedures. For karyotyping, cells should be in log-phase growth.
- Karyotype Analysis (G-banding):
- Treat cells with a mitotic inhibitor (e.g., colcemid) to arrest them in metaphase.
- Harvest the cells, expose them to a hypotonic solution, and fix them with the fixative solution.
- Drop the cell suspension onto microscope slides, age the slides, and stain with Giemsa stain.
- Analyze at least 20 metaphase spreads under a microscope for chromosomal number and structural abnormalities.
- Pluripotency Marker Confirmation:
- PCR: Extract RNA and perform RT-PCR for core pluripotency factors (OCT4, SOX2, NANOG).
- Flow Cytometry: Dissociate cells into a single-cell suspension, fix, and stain with fluorescently-labeled antibodies against pluripotency surface markers (e.g., TRA-1-60, SSEA-4). Analyze on a flow cytometer. A homogeneous population with >95% positive for these markers suggests a stable, undifferentiated state.
- Documentation and Decision: Compare the karyotype results with the original cell line's profile. If new aberrations are detected or pluripotency marker expression drops below 90%, consider discarding the culture and thawing a new, low-passage vial.
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Maintaining Genomic Stability in iPSC Culture
| Reagent | Function in Context of Genomic Stability | Example |
|---|---|---|
| ROCK Inhibitor | Improves single-cell survival post-passaging and thawing, reducing the selective pressure imposed by massive cell death. | Y-27632 [70] |
| Feeder-Free Culture Medium | Defined formulations (e.g., Essential 8, mTeSR) reduce variability and undefined signals that could induce stress or selective pressures. | Essential 8 Medium [70] |
| Defined Substrate | Provides a consistent, controllable surface for cell attachment and growth, unlike variable basement membrane extracts. | Vitronectin (VTN-N), Recombinant Laminin [70] |
| Gentle Dissociation Reagents | Non-enzymatic or mild enzymatic reagents (e.g., EDTA-based) help maintain cell surface proteins and reduce stress during passaging. | ReLeSR, Gentle Cell Dissociation Reagent [8] [70] |
| Cryopreservation Medium | High-quality, serum-free freezing media ensure high post-thaw viability, minimizing the stressful recovery period and population bottleneck. | Synth-a-Freeze or equivalent |
The Role of the p53 Pathway and Other Checkpoints in Safeguarding Genomic Integrity
Technical Support Center
Troubleshooting Guides
FAQ: My iPSC cultures are showing increased rates of genomic instability. What are the primary cellular mechanisms I should investigate?
Answer: Increased genomic instability in induced pluripotent stem cell (iPSC) cultures frequently results from failures in the DNA damage response (DDR) network, with the p53 pathway being paramount. You should investigate these core mechanisms:
- p53 Pathway Integrity: The p53 protein acts as the "guardian of the genome" [71] [72]. In response to DNA damage, it orchestrates cell cycle arrest, DNA repair, or apoptosis. iPSC reprogramming protocols, especially those involving the c-Myc oncogene, can induce replication stress and genomic aberrations, and p53 inactivation often facilitates this reprogramming by allowing damaged cells to proliferate [5]. Assay for p53 expression, localization, and phosphorylation status.
- DNA Damage Checkpoints: The DDR employs specific checkpoints at the G1/S and G2/M boundaries, as well as intra-S phase, to halt the cell cycle for repair [73] [74]. These checkpoints rely on sensor kinases like ATM and ATR, and effector kinases like Chk1 and Chk2. A failure in these checkpoints, leading to radioresistant DNA synthesis (RDS), is a hallmark of a defective DDR [74].
- Oncogene-Induced Replication Stress: The use of reprogramming factors like c-Myc can cause DNA replication stress, leading to DNA breaks and genomic deletions/amplifications, particularly at common fragile sites [5]. This is a major source of instability during reprogramming and long-term culture.
Recommended Experimental Protocol: Immunofluorescence Analysis of DNA Damage Foci
- Culture and Stress: Grow iPSCs on chambered slides. Treat a sample group with a DNA-damaging agent (e.g., 5 Gy ionizing radiation) and maintain an untreated control.
- Fixation and Permeabilization: Fix cells with 4% paraformaldehyde for 15 minutes, then permeabilize with 0.5% Triton X-100 for 10 minutes.
- Staining: Incubate with primary antibodies against γH2AX (a marker for DNA double-strand breaks) and p53 overnight at 4°C [74].
- Visualization: Incubate with fluorescently-labeled secondary antibodies for 1 hour at room temperature. Mount slides with DAPI-containing medium to stain nuclei.
- Analysis: Image using a fluorescence microscope. Co-localization of bright γH2AX and p53 foci in the nucleus indicates active DNA damage response sites. A failure to form these foci after damage suggests a defective DDR.
FAQ: How can I determine if observed genomic variations in my iPSC lines are common, culture-adapted changes or unique aberrations?
Answer: Human pluripotent stem cells (hPSCs) acquire recurrent genomic changes under selective pressure in culture. Distinguishing these common adaptations from random aberrations is crucial for assessing the safety of your lines for downstream applications [30].
The table below summarizes the most frequent genomic alterations observed in hPSCs:
Table 1: Common Genomic Variations in Human Pluripotent Stem Cells (hPSCs)
| Genomic Alteration | Chromosomal Location | Potential Functional Impact | Frequency & Notes |
|---|---|---|---|
| Trisomy 12 | Chromosome 12 | Confers a growth advantage in culture. | One of the earliest identified and most common aneuploidies [30]. |
| Amplification of 20q11.21 | Chromosome 20 | Contains the BCL2L1 (Bcl-xL) gene, which enhances cell survival [30]. | Found in up to 34% of hPSC lines examined; a classic sign of culture adaptation [30]. |
| Trisomy 1 | Chromosome 1 | Unknown. | Detected in multiple cell lines [30]. |
| Trisomy 17 | Chromosome 17 | Unknown. | Detected in multiple cell lines [30]. |
| Trisomy X | X Chromosome | Unknown. | Observed in female hPSC lines [30]. |
Recommended Experimental Protocol: High-Resolution Genotyping
- Sample Collection: Extract genomic DNA from your iPSC lines at different passages (e.g., early, mid, and late).
- SNP Genotyping: Use a high-resolution method like Single Nucleotide Polymorphism (SNP) genotyping arrays. This technique can detect not only full chromosome aneuploidies but also subchromosomal copy number variations (CNVs) [30].
- Data Analysis: Compare the genotyping profiles of your late-passage cells to the early-passage or parental cells. Use bioinformatics tools to identify regions of duplication or deletion.
- Interpretation: Cross-reference any identified aberrations with databases of common hPSC variations (as listed in the table above). Recurrent changes in regions like 20q11.21 strongly suggest culture-induced selection.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents essential for studying genomic integrity and the p53 pathway in iPSC research.
Table 2: Essential Research Reagents for Genomic Integrity Assays
| Research Reagent | Primary Function | Example Application in Genomic Stability Research |
|---|---|---|
| Anti-p53 Antibody | Detects p53 protein levels and localization via immunofluorescence (IF) or Western blot (WB). | Monitor p53 stabilization and nuclear accumulation in response to DNA damage induced by reprogramming or culture stress [71] [72]. |
| Anti-γH2AX Antibody | Marker for DNA double-strand breaks (DSBs). Forms discrete nuclear foci at damage sites (IF) [74]. | Quantify the number of DSBs in iPSCs after exposure to genotoxic stress or as a result of oncogene-induced replication stress [5] [74]. |
| Anti-phospho Chk1 (Ser345) / Chk2 (Thr68) Antibodies | Detect activated forms of the effector kinases in the DDR pathway (WB, IF) [74]. | Assess the functionality of the DNA damage checkpoint signaling upstream of p53. |
| MDM2 Inhibitor (e.g., Nutlin-3) | Disrupts p53-MDM2 interaction, leading to p53 stabilization and activation [71]. | Used as a tool compound to activate the p53 pathway and test its functional integrity in your cell system. |
| KU-0060648 (DNA-PK Inhibitor) | Inhibits DNA-PKcs, a key enzyme in the Non-Homologous End Joining (NHEJ) repair pathway [75] [74]. | Investigate the contribution of specific DNA repair pathways to maintaining genomic stability in iPSCs. |
Key Signaling Pathways Visualized
p53 Activation and Downstream Signaling
DNA Damage Response and Checkpoint Signaling
Routine Karyotyping and Genomic Screening as Part of Quality Control Pipelines
Frequently Asked Questions (FAQs)
1. Why is routine karyotyping essential for iPSC quality control? Karyotyping provides a global view of the genome, allowing researchers to identify gross chromosomal abnormalities that can arise during the reprogramming of somatic cells into induced pluripotent stem cells (iPSCs) or during subsequent culture. These abnormalities, such as aneuploidy (an abnormal number of chromosomes) or large translocations, can compromise the genomic integrity of the cell line, potentially altering its function and differentiation capacity, and even predisposing it to malignant transformation [76] [77]. Regular karyotyping is a fundamental step to ensure that only karyotypically normal iPSC lines are used for downstream experiments or clinical applications.
2. What specific chromosomal errors are most commonly observed in iPSC cultures? iPSC cultures are particularly susceptible to errors in chromosome number, a condition known as aneuploidy. This includes trisomy (gaining an extra chromosome) or monosomy (losing a chromosome). These errors occur due to nondisjunction, where chromosomes fail to separate correctly during cell division [76]. Specific chromosomes, such as 12, 17, and 20, have been frequently reported to be trisomic in human pluripotent stem cells. Changes in chromosome structure, such as deletions or duplications, can also occur [77].
3. My karyotype results are normal, but my iPSCs show unexpected differentiation patterns. What could be wrong? A normal karyotype only rules out large-scale chromosomal abnormalities. The issue you describe may be caused by more subtle genomic changes that are not detectable by conventional karyotyping. These can include:
- Small Copy Number Variations (CNVs): Deletions or duplications of DNA segments that are too small to be seen under a microscope.
- Point Mutations: Single nucleotide changes in critical genes.
- Epigenetic Instability: Changes in DNA methylation or histone modification that affect gene expression without altering the DNA sequence itself [77]. In such cases, moving to a higher-resolution genomic screening method, such as SNP-based microarrays or whole-genome sequencing, is recommended to identify these subtler anomalies [78].
4. How often should I perform karyotyping on my iPSC lines? It is considered a best practice to perform karyotyping at a minimum when a new iPSC line is established and again before initiating a major set of experiments or differentiation protocols. For long-term cultures, regular screening is advised, for example, every 10-20 passages, as genomic instability can accumulate over time [77]. The frequency should be determined by the specific needs of your research and the known stability of your cell lines.
Troubleshooting Guides
Issue 1: Detection of Chromosomal Abnormalities in iPSC Cultures
Problem: A routine karyotype analysis reveals an abnormal chromosome number, such as trisomy 12 or monosomy X.
Explanation: The forced reprogramming of somatic cells into iPSCs and the subsequent pressure to rapidly proliferate in culture can induce replication stress, leading to errors in chromosome segregation. This is a known challenge in iPSC biology and indicates genomic instability [76] [77].
Solution:
- Confirm the Result: Repeat the karyotyping test on a new sample of cells from the same passage to rule out a technical error [78].
- Isolate a Normal Clone: If the culture is a mixed population (mosaic), use single-cell cloning to isolate sub-clones that have a normal karyotype.
- Characterize the Line: If the abnormal line is to be used for research purposes (e.g., modeling a specific syndrome), fully document the abnormality using a higher-resolution method like microarrays to define the exact breakpoints or regions of gain/loss [78].
- Bank Early: Always cryopreserve low-passage, karyotypically normal stocks of your iPSC lines to minimize the need for extensive passaging.
Issue 2: Inconsistent Results Between Karyotyping and Genomic Screening
Problem: A cell line shows a normal karyotype but a subsequent genomic screen (e.g., microarray) identifies a sub-chromosomal deletion or duplication.
Explanation: This is expected due to the differing resolutions of the techniques. Standard G-banding karyotyping has a resolution limit of approximately 5-10 Megabases (Mb). Genomic microarrays can detect copy number variations down to a scale of kilobases (kb), far below the visibility threshold of a light microscope [78].
Solution:
- Adopt a Tiered QC Strategy: Implement a quality control pipeline where karyotyping is used as a first-line, high-level screen. For lines intended for critical experiments, follow up with a higher-resolution method like SNP microarrays to identify smaller structural variations [79] [78].
- Integrate Methods: Understand that these tests are complementary, not redundant. A combined approach provides the most comprehensive assessment of genomic integrity.
Issue 3: Poor Quality Chromosome Spreads for Karyotyping
Problem: Metaphase chromosome preparations from iPSCs are of poor quality, with overly long, tangled, or broken chromosomes, making analysis impossible.
Explanation: This is typically a technical issue related to the cell culture and harvesting process. Over-confluent cultures, incorrect concentration of colchicine (which arrests cells in metaphase), or overly harsh fixation can all lead to poor chromosome spreading [76] [80].
Solution:
- Ensure Optimal Cell Growth: Harvest cells when they are in a logarithmic growth phase and not over-confluent.
- Troubleshoot the Protocol:
- Colchicine Exposure: Titrate the concentration and duration of colchicine treatment. Too little results in few metaphase spreads; too much causes over-contracted chromosomes.
- Hypotonic Treatment: The hypotonic solution (e.g., potassium chloride) is critical for swelling the cells. Optimize the incubation time and temperature.
- Fixation: Perform the fixative (methanol:acetic acid) changes gently and ensure the fixative is fresh. Dropping the cell suspension onto cold, wet slides can improve spreading.
Experimental Protocols
Protocol 1: G-Banding Karyotype Analysis of Human iPSCs
Purpose: To assess the chromosomal number and gross structure of an iPSC line.
Materials:
- Log-phase growing iPSCs
- Colchicine or Colcemid solution
- Hypotonic solution (e.g., 0.075 M KCl)
- Fresh fixative (3:1 methanol:glacial acetic acid)
- Giemsa stain, phosphate buffer, Gurr buffer
- Microscope slides
Methodology:
- Metaphase Arrest: Add colchicine to the culture medium to a final working concentration (e.g., 0.1 µg/mL) and incubate for 1-4 hours. This inhibits spindle formation, arresting cells in metaphase.
- Harvesting: Dissociate the cells into a single-cell suspension using an enzyme like Accutase. Transfer the cell suspension to a centrifuge tube and pellet the cells.
- Hypotonic Treatment: Resuspend the cell pellet gently in a pre-warmed hypotonic KCl solution. Incubate at 37°C for 15-20 minutes. This causes the cells to swell, separating the chromosomes.
- Fixation: Add fresh, cold fixative drop-wise to the cell suspension while gently vortexing. Pellet the cells and resuspend in fresh fixative. Repeat this fixation process 2-3 times.
- Slide Preparation: Drop the fixed cell suspension onto clean, wet microscope slides and allow them to air dry.
- G-Banding (Trypsin-Giemsa):
- Age the slides (e.g., overnight at 60°C or for a few days at room temperature).
- Treat the slides briefly with a trypsin solution.
- Rinse and stain with a diluted Giemsa stain solution for a few minutes.
- Rinse, air dry, and mount for microscopy.
- Analysis: Under a light microscope, capture digital images of at least 20 well-spread metaphase cells. Arrange the chromosomes into a karyogram using specialized software to analyze their number and banding pattern [78] [80].
Protocol 2: Genomic DNA Extraction for Microarray or PCR-Based QC
Purpose: To obtain high-quality, high-molecular-weight genomic DNA for downstream genomic screening assays.
Materials:
- iPSC pellet or directly from a culture well
- Lysis buffer (e.g., with Proteinase K)
- RNase A
- Phenol-chloroform-isoamyl alcohol or commercial DNA purification kit (e.g., silica column-based)
- Ethanol (100% and 70/75%)
- TE buffer or nuclease-free water
Methodology:
- Lysis: Resuspend the cell pellet in lysis buffer containing Proteinase K and incubate at 56°C until the solution is clear (1-3 hours).
- RNA Removal: Add RNase A to the cooled lysate and incubate at room temperature for a few minutes.
- Extraction: If using phenol-chloroform, add an equal volume, mix thoroughly, and centrifuge to separate phases. Carefully transfer the upper aqueous phase containing the DNA to a new tube.
- Precipitation: Add 2 volumes of 100% ethanol to the aqueous phase to precipitate the DNA. Spool the DNA strand with a pipette tip or glass rod.
- Wash: Wash the DNA pellet with 70% ethanol to remove salts.
- Resuspension: Air-dry the pellet briefly and resuspend in TE buffer or nuclease-free water.
- Quality Control: Quantify the DNA using a fluorometric method (e.g., Qubit) and assess purity and integrity by spectrophotometry (A260/A280 ratio ~1.8) and agarose gel electrophoresis [79].
Data Presentation
Table 1: Common Chromosomal Abnormalities in iPSC Cultures and Their Detection
| Abnormality Type | Description | Detection Method | Potential Impact on iPSCs |
|---|---|---|---|
| Aneuploidy | Gain or loss of entire chromosomes (e.g., Trisomy) | Karyotyping, Microarray | Altered growth, skewed differentiation, genomic instability |
| Polyploidy | Gain of entire chromosome sets (e.g., Tetraploidy) | Karyotyping | Altered cell function, failure to differentiate correctly |
| Deletions | Loss of a chromosomal segment | Microarray, NGS | Loss of tumor suppressor genes, haploinsufficiency |
| Duplications | Gain of a chromosomal segment | Microarray, NGS | Gene dosage effects, oncogene activation |
| Translocations | Exchange of genetic material between chromosomes | Karyotyping (large), NGS (small) | Gene disruption, creation of fusion genes |
Table 2: Comparison of Genomic Integrity Assessment Methods
| Method | Resolution | What It Detects | Throughput | Key Advantage | Key Limitation |
|---|---|---|---|---|---|
| Karyotyping | ~5-10 Mb | Overall chromosome number, large structural changes | Low | Low cost, provides a global view | Low resolution, requires dividing cells |
| FISH | ~50 kb - 1 Mb | Specific chromosomal regions, translocations, aneuploidy | Low | Can be used on interphase/non-dividing cells | Targeted; only looks at pre-selected regions |
| Microarray | ~10 kb - 100 kb | Genome-wide copy number variations (CNVs) | High | High resolution, automated analysis | Cannot detect balanced rearrangements |
| NGS | Single base | SNVs, Indels, CNVs, Translocations | High | The most comprehensive single solution | Higher cost, complex data analysis |
Visualization of Workflows
Quality Control Pipeline for iPSC Genomic Integrity
Karyotype Analysis and Interpretation Logic
The Scientist's Toolkit
Table 3: Essential Research Reagents for Karyotyping and Genomic Screening
| Reagent / Kit | Function |
|---|---|
| Colchicine/Colcemid | Arrests cells in metaphase by inhibiting spindle fiber formation. |
| Hypotonic Solution (e.g., 0.075 M KCl) | Swells cells, dispersing chromosomes for clearer analysis. |
| Giemsa Stain | Creates a characteristic banding pattern (G-bands) on chromosomes for identification [76] [80]. |
| Microarray Kit (e.g., SNP-array) | Provides a high-resolution, genome-wide platform for detecting copy number variations and loss of heterozygosity. |
| NGS Library Prep Kit | Prepares genomic DNA for next-generation sequencing to detect a full range of variants. |
| DNA Quantification Kit (Fluorometric) | Accurately quantifies double-stranded DNA for downstream genomic applications [81]. |
Banking and Utilizing Low-Passage, Karyotypically Normal iPSC Clones for Critical Applications
Troubleshooting Guides
Troubleshooting iPSC Genomic Instability
Problem: Spontaneous differentiation in culture
- Potential Causes: Suboptimal culture conditions, over-confluent cultures, outdated or improperly prepared culture media.
- Solutions: Visualize cells daily and manually remove differentiated areas [82]. Passage cells during log-phase growth, typically at 70-80% confluency [82]. Use advanced, chemically defined media like HiDef B8 Growth Medium, which is specifically formulated to support robust iPSC expansion and minimize spontaneous differentiation [82].
- Prevention: Maintain a consistent passaging schedule using quality-tested reagents. Implement strict quality control for media preparation and use supplements like Ready-CEPT to enhance cell viability during passaging and thawing [82].
Problem: Low editing efficiency in CRISPR experiments
- Potential Causes: Low efficiency of Homology-Directed Repair (HDR) in iPSCs, unsynchronized cell cultures, suboptimal transfection protocols.
- Solutions: Synchronize the cell cycle in your iPSC population to increase the proportion of cells in the HDR-prone S/G2 phases [83]. Use high-quality, validated CRISPR reagents and optimize delivery methods (e.g., electroporation parameters) specifically for your iPSC line.
- Prevention: Begin gene editing projects with low-passage, karyotypically normal clones, as they generally demonstrate better performance and stability in culture [83].
Problem: Detection of chromosomal abnormalities
- Potential Causes: Abnormalities can be pre-existing in parental somatic cells at low frequencies, induced by the stress of reprogramming, or acquired during extended culture [4] [82]. Common recurrent abnormalities include gains of chromosomes 12, 8, X, and copy number variations (CNVs) at 20q11.21 [4].
- Solutions: If abnormalities are detected, the clone should be banked and characterized immediately. For critical applications, it is safest to discard the abnormal clone and select a normal one from your bank. Investigate culture conditions and passaging frequency.
- Prevention: Bank multiple low-passage clones and perform rigorous quality control at the Master Cell Bank stage. Regular monitoring, recommended every 10-15 passages, is crucial for detecting changes during culture [84].
Quantitative Data on Genomic Instability in iPSCs
Table 1: Types and Frequencies of Genetic Variations in iPSCs
| Variation Type | Detection Method | Common Aberrations | Reported Frequency |
|---|---|---|---|
| Chromosomal Aberration | G-banding Karyotyping [4] [84] | Trisomy 12, Trisomy 8, Trisomy X [4] | Recurrently observed; frequency not significantly different from ESCs [4] |
| Copy Number Variation (CNV) | Array CGH, SNP Array [4] | Amplification of 20q11.21 [4] | Numerous CNVs in early passages, decreasing with passaging [4] [84] |
| Single Nucleotide Variant (SNV) | Whole Genome/Exome Sequencing [4] | No strongly recurrent mutations reported to date [4] | ~10 protein-coding mutations per human iPSC line [4] |
Table 2: Recommended Monitoring Schedule for iPSC Banks
| Test | Frequency | Key Purpose | Acceptance Criteria |
|---|---|---|---|
| Karyotype Analysis (G-banding) | At banking (Master Cell Bank); every 10-15 passages during culture [84] | Detect numerical and large structural chromosomal changes [4] [84] | Normal, karyotypically female or male, with no major aberrations [84] |
| Viability Assay | Post-thaw | Determine recovery rate after cryopreservation | >70% viability |
| Pluripotency Marker Assay | At banking | Confirm undifferentiated state | High expression of OCT4, SOX2, NANOG |
| Mycoplasma Testing | Quarterly | Ensure culture is free of contamination | Negative |
Experimental Protocols
Protocol 1: Routine Karyotype Analysis of iPSCs using G-Banding
Purpose: To regularly monitor the chromosomal integrity of iPSC cultures and ensure their suitability for critical applications.
Materials:
- Actively dividing, sub-confluent iPSC culture.
- Karyotype analysis service provider or in-house materials (hypotonic solution, fixative, Giemsa stain, microscope) [84].
Method:
- Sample Preparation: Harvest 2-3 million healthy, actively dividing iPSCs [84].
- Cell Harvesting: Treat cells with a mitotic inhibitor to arrest them in metaphase. Subject cells to hypotonic treatment to swell them and spread the chromosomes, then fix them in a methanol-acetic acid solution [84].
- Slide Preparation and Staining: Drop the fixed cell suspension onto slides. Partially digest the chromosomes with trypsin and stain with Giemsa stain to produce a characteristic banding pattern (G-banding) [84].
- Microscopy and Analysis: Analyze at least 20 metaphase spreads under a high-resolution microscope. Count chromosomes and identify their banding patterns. Arrange the chromosomes into a karyogram [84].
- Interpretation and Reporting: A detailed report should be generated, including the total number of chromosomes, sex chromosome complement, and description of any abnormalities using standard ISCN notation [85] [86]. For example, a normal female karyotype is noted as
46,XXand a male karyotype with a deletion on the short arm of chromosome 5 would be46,XY,del(5p)[85].
Protocol 2: Establishing a Low-Passage Master Cell Bank
Purpose: To create a characterized and secure repository of low-passage iPSC clones, preserving their genomic integrity for future use.
Materials:
- A newly established, karyotypically normal iPSC clone (e.g., passage 5-10).
- Chemically defined culture medium (e.g., mTeSR Plus, TeSR media) [27].
- High-quality cryopreservation medium (e.g., CryoStor CS10) [27].
Method:
- Clone Expansion: Expand the selected clone under optimal conditions, ensuring log-phase growth and daily inspection to remove any spontaneously differentiated cells [82].
- Quality Control Check: When the cells are sufficiently expanded, perform a full suite of quality control tests. This must include karyotype analysis and should also assess pluripotency (e.g., by immunostaining for markers like OCT4, SOX2, NANOG) and confirm the absence of mycoplasma contamination [27].
- Cryopreservation: Only proceed with banking if the clone passes all QC checks. Harvest healthy cells, resuspend them in cryopreservation medium at a defined concentration, and aliquot into cryovials. Freeze the vials using a controlled-rate freezer and store long-term in the vapor phase of liquid nitrogen (-196°C) [27].
- Post-Thaw Viability Check: After banking, thaw a representative vial to confirm cell viability and recovery post-cryopreservation. This validates the banking process.
Frequently Asked Questions (FAQs)
Q1: How often should I perform karyotype analysis on my iPSC cultures? It is recommended to perform karyotype analysis at the time of creating a master cell bank and then at regular intervals during culture, typically every 10 to 15 passages [84]. This frequency should be increased if the cells are subjected to significant stress, such as genetic manipulation or suboptimal culture conditions.
Q2: What kind of chromosomal abnormalities can karyotype analysis detect? Karyotype analysis is excellent for detecting large-scale chromosomal abnormalities, including:
- Aneuploidy: Gain or loss of entire chromosomes (e.g., Trisomy 12 or 8) [4].
- Structural Aberrations: Translocations, large deletions, duplications, inversions, and ring chromosomes [84]. It cannot detect very small deletions/duplications or single nucleotide variants, which require higher-resolution techniques like SNP arrays or next-generation sequencing [4].
Q3: What is the difference between a pre-existing mutation and a reprogramming-induced mutation?
- Pre-existing Variations: These are mutations that already existed in a small subset of the parental somatic cells (e.g., skin fibroblasts) and were captured and clonally expanded during the reprogramming process to create the iPSC line [4].
- Reprogramming-Induced Mutations: These are new mutations that occur during the reprogramming process itself, likely due to the immense cellular stress and rapid proliferation involved in reverting a somatic cell to a pluripotent state [4]. Whole-genome sequencing of iPSCs and their parental cells is required to distinguish between these two origins [4].
Q4: Can karyotype analysis detect mosaicism in my iPSC culture? Yes. By examining multiple metaphase spreads (e.g., 20-40 cells) from the same culture, karyotype analysis can identify mosaicism—the presence of two or more cell populations with different karyotypes within the same culture [84]. This provides critical information about the genetic heterogeneity and stability of your iPSC line.
Q5: Why is it crucial to use low-passage iPSCs for CRISPR gene editing? Low-passage iPSCs are karyotypically normal and have accumulated fewer genetic mutations compared to high-passage cells [4] [82]. Their genetic stability provides a cleaner, more reliable background for interpreting the results of your gene editing experiments. Furthermore, low-passage cells are generally more robust and respond better to the stress of transfection and single-cell cloning, which are essential steps in most CRISPR workflows [83].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Banking and Quality Control of iPSCs
| Reagent/Material | Function | Example Products |
|---|---|---|
| Chemically Defined Culture Medium | Supports robust expansion and maintenance of pluripotency while minimizing spontaneous differentiation. | TeSR media [27], mTeSR Plus [27], HiDef B8 Growth Medium [82] |
| Cryopreservation Medium | Protects cell viability during freezing and long-term storage in liquid nitrogen. | CryoStor CS10 [27] |
| Cell Dissociation Reagent | Enables gentle passaging of iPSC colonies as single cells or clumps. | ReLeSR [27] |
| Karyotyping Kit/Services | Provides materials or access to services for chromosomal analysis via G-banding. | Commercial services [84] |
| Cell Viability Assay Kit | Quantifies the percentage of live cells post-thaw to validate banking success. | - |
| Mycoplasma Detection Kit | Ensures iPSC cultures and banks are free from mycoplasma contamination. | - |
Assessing iPSC Genomic Fidelity for Preclinical and Clinical Translation
Genomic instability is a critical parameter in stem cell research, impacting the safety and reliability of these cells for disease modeling and clinical applications. For scientists and drug development professionals, understanding the fundamental differences in genomic stability between induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs) is essential for experimental design and risk assessment. This guide provides a technical overview of the causes, consequences, and troubleshooting methods for managing genomic instability in these cell lines.
FAQs: Genomic Stability in Pluripotent Stem Cells
1. Why are iPSCs generally considered less genomically stable than ESCs?
The lower genomic stability of iPSCs is attributed to their origin and reprogramming process. Research indicates that a key factor is an imbalance in DNA damage repair pathways. One study found that, compared to ESCs, iPSCs have a greater reliance on the error-prone non-homologous end joining (NHEJ) pathway for repairing DNA double-strand breaks, rather than the high-fidelity homologous recombination (HR) pathway. This lower fidelity in DNA damage repair leads to a higher accumulation of somatic mutations and short insertions/deletions (indels) [87].
2. What are the most common types of genetic abnormalities found in iPSCs and ESCs?
Both iPSCs and ESCs can acquire genetic variations, with some common and some distinct recurrent abnormalities:
- Chromosomal Aberrations: Recurrent aneuploidies include trisomy of chromosomes 12, 17, 8, and X in both cell types [4] [88].
- Copy Number Variations (CNVs): The most recurrent CNV hotspot is an amplification of 20q11.21, which contains genes associated with pluripotency and anti-apoptosis (e.g., BCL2L1, ID1). This is observed in both iPSCs and ESCs [4] [6].
- Single Nucleotide Variants (SNVs): iPSCs have been found to carry an average of approximately 6-12 protein-coding point mutations per line. The origin of these can be pre-existing in the parental somatic cell, acquired during reprogramming, or accumulated during prolonged culture [4] [89].
3. How does the reprogramming method impact the genomic integrity of iPSCs?
The method used to generate iPSCs is a major factor in their genomic stability. Integrating methods, such as those using retroviral or lentiviral vectors, pose a risk of insertional mutagenesis, which can disrupt tumor suppressor genes or activate oncogenes [13]. Non-integrating methods (e.g., Sendai virus, episomal vectors, mRNA reprogramming) were developed to improve safety. However, some non-integrating methods may still require careful screening for residual vector components, and reprogramming efficiency can vary between methods [13]. The use of certain reprogramming factors, particularly the oncogene c-Myc, is also associated with increased tumorigenic risk [13].
4. What are the functional consequences of genomic instability in pluripotent stem cells?
Genomic instability can have several critical consequences:
- Tumorigenicity: The acquisition of mutations in genes like TP53 or amplifications of regions containing oncogenes (e.g., 20q11.21) raises significant safety concerns for cell therapies, as it may lead to malignant outgrowth [88] [6].
- Impact on Differentiation and Phenotype: Genetic changes can alter the growth, differentiation potential, and functionality of the stem cells and their derivatives, potentially compromising their use in disease modeling [89] [88].
- Cell Culture Adaptation: Genetically variant cells often have a selective growth advantage in culture, allowing them to outcompete karyotypically normal cells over passages, a phenomenon observed in both ESCs and iPSCs [88].
Technical Guide: Assessing Genomic Stability
Key Methodologies for Detection
A tiered approach is recommended for comprehensive genomic assessment. The following table summarizes the common techniques and their applications [4] [88]:
| Method | Detection Capability | Key Applications | Typical Resolution/Limit |
|---|---|---|---|
| G-banding Karyotyping | Numerical changes (aneuploidy), large structural changes (translocations, inversions) | Initial, standard cytogenetic screening. | ~5-10 Mb; mosaicism detection limit ~5-20% [4] [88] |
| SNP/Array CGH | Copy Number Variations (CNVs: deletions, duplications) | Genome-wide CNV screening at higher resolution than karyotyping. | Kilobase resolution; cannot detect balanced translocations [4] |
| Whole Genome/Exome Sequencing | Single Nucleotide Variants (SNVs), small indels, CNVs | Most comprehensive profiling; identifies mutations at single-base resolution. | Single nucleotide resolution; can detect low-frequency variants with sufficient depth [4] [87] |
Experimental Protocol: Assessing DNA Repair Fidelity
The following protocol is adapted from a study that directly compared the DNA repair capacity of mouse iPSCs and ESCs [87].
Objective: To evaluate the fidelity of DNA double-strand break (DSB) repair in iPSCs versus ESCs by assessing the number of induced mutations after gamma-irradiation.
Materials:
- Cell Lines: iPSCs (e.g., lentivirus-derived and chemically induced) and ESCs.
- Equipment: Cobalt-60 irradiator (or other calibrated ionizing radiation source).
- Reagents: Cell culture media, trypsin, DNA extraction kit (e.g., QIAamp DNA Mini Kit).
- Analysis Platform: Illumina sequencing platform and associated bioinformatics tools (e.g., BWA for alignment, GATK/SAMTools for variant calling).
Procedure:
- Cell Culture: Maintain all pluripotent stem cell lines in optimal, undifferentiated conditions. Passage cells one day prior to irradiation.
- Irradiation: Expose cells to a 4 Gy dose of gamma-irradiation. Immediately return cells to the incubator.
- Recovery: Culture the irradiated cells for 4 hours to allow for DNA repair mechanisms to act.
- DNA Extraction: Harvest cells and extract high-quality genomic DNA using a commercial kit.
- Whole-Genome Sequencing: Prepare DNA libraries and perform whole-genome re-sequencing (e.g., 2x101bp paired-end reads on an Illumina HiSeq platform).
- Bioinformatic Analysis:
- Map sequencing reads to the reference genome (e.g., mm9 for mouse).
- Call somatic mutations (SNVs and indels) by comparing irradiated samples to non-irradiated control samples from the same cell line.
- Apply stringent filters (e.g., minimum coverage >20, base quality >15, mutant frequency >0.2 in irradiated samples).
Expected Outcome: iPSCs, particularly those generated with integrating methods, are expected to show a higher number of somatic mutations post-irradiation compared to ESCs, indicating lower fidelity of DNA damage repair [87].
DNA Repair Pathway Disparity
The diagram below illustrates the finding that iPSCs have a greater tendency to use the error-prone NHEJ pathway over the high-fidelity HR pathway for DNA repair, a key reason for their relative genomic instability [90] [87].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their functions for studying genomic stability, as cited in the experimental protocols [87].
| Research Reagent | Function/Biological Role |
|---|---|
| Anti-γH2AX Antibody | Immunofluorescence detection of nuclear foci marking sites of DNA double-strand breaks; used to quantify DNA damage. |
| Anti-Phospho-ATM Antibody | Western blot detection of activated ATM kinase, a primary sensor and initiator of the DNA damage response. |
| Anti-H3K9me3 Antibody | Western blot analysis of a repressive histone mark; changes in histone modification can be linked to reprogramming and epigenetic stability. |
| QIAamp DNA Mini Kit | Silica-membrane-based spin column technology for the purification of high-quality, polymerase-ready genomic DNA from cells. |
| Mouse Leukemia Inhibitory Factor (LIF) | Cytokine added to culture media to maintain the pluripotent state of mouse ESCs and iPSCs by signaling through the STAT3 pathway. |
The table below consolidates key comparative data on genomic instability from the research [4] [87] [6].
| Stability Metric | Induced Pluripotent Stem Cells (iPSCs) | Embryonic Stem Cells (ESCs) |
|---|---|---|
| DNA Repair Fidelity | Lower fidelity; biased towards error-prone NHEJ [87] | Higher fidelity; biased towards accurate HR [90] [87] |
| Mutation Load (Post-Irradiation) | Higher number of somatic mutations and indels [87] | Fewer somatic mutations and indels [87] |
| Common CNV Hotspots | 20q11.21 amplification (most recurrent) [4] [6] | 20q11.21 amplification (most recurrent) [4] [88] |
| Common Aneuploidies | Trisomy 12, 8, X, 17 [4] | Trisomy 12, 8, X, 17 [4] [88] |
| Origin of Mutations | Pre-existing, reprogramming-induced, culture-acquired [4] [89] | Primarily culture-acquired [88] |
Impact of the Somatic Cell Source and Genetic Background on Resulting iPSC Lines
Frequently Asked Questions
FAQ 1: How does the genetic background of the donor affect the generation of iPSCs? The genetic background of the somatic cell donor significantly impacts the efficiency of iPSC generation and the stability of the resulting cell lines. Studies using mouse embryonic fibroblasts (MEFs) from genetically diverse strains found that strains like NON/LtJ and CAST/EiJ were more efficient at generating iPSCs and produced more proliferative parent MEFs compared to other strains like C57BL/6J or BALB/cJ [91]. Furthermore, some genetic backgrounds, such as BALB/cJ, required modified culture conditions (e.g., a 5x higher concentration of Leukemia Inhibitory Factor) to establish stable, doxycycline-independent iPSC lines [91]. These findings confirm that genetic background is a key variable in reprogramming experiments.
FAQ 2: Does the tissue origin of the somatic cell influence the properties of the resulting iPSCs? While the tissue of origin can leave a subtle "epigenetic memory" in iPSCs, which may slightly bias their differentiation potential, the genetic variability between different human donors has a far greater impact on the molecular and functional characteristics of iPSC lines [92]. Research shows that transcriptomic, epigenetic, and differentiation profiles are more similar between isogenic iPSCs (those derived from the same donor but different tissues like fibroblasts and blood) than between iPSCs from different donors [92]. Therefore, for biobanking, integrating integration-free iPSC lines from various practical tissues like fibroblasts and blood is a valid strategy, provided a large number of donors are included to capture human genetic diversity [92].
FAQ 3: What are the primary sources of genetic instability in iPSC cultures? Genetic instability in iPSCs arises from three main origins [4] [93]:
- Pre-existing variations in parental somatic cells: Low-frequency genetic variants present in the source somatic cell population can be captured and clonally expanded during the reprogramming process.
- Reprogramming-induced mutations: The reprogramming process itself can be mutagenic. The expression of reprogramming factors induces replication stress, a form of DNA damage that can lead to copy number variations (CNVs) and single nucleotide variants (SNVs) [23].
- Passage-induced mutations: Genetic errors can accumulate during prolonged in vitro culture of established iPSC lines, often conferring a selective growth advantage [4].
FAQ 4: What are the functional consequences of genetic instability in my iPSC line? Genetic instability can severely compromise your research and clinical applications:
- Inconsistent or Impaired Differentiation: Altered expression of genes critical for pluripotency and differentiation can render iPSC lines unable to reliably differentiate into specific cell types, skewing disease modeling and drug screening data [93].
- Increased Risk of Tumorigenicity: The accumulation of mutations, particularly in genes associated with cancer (e.g., recurrent CNVs on chromosome 20q11.21), raises serious safety concerns for cell therapies, as it increases the risk of malignant transformation upon transplantation [4] [6].
- Culture Heterogeneity: Genetic alterations can cause variable functional characteristics, growth rates, and differentiation potential within an iPSC culture, complicating experimental reproducibility and interpretation [93].
Troubleshooting Guides
Problem: Low Reprogramming Efficiency or Failure in iPSC Generation
| Potential Cause | Investigation | Solution |
|---|---|---|
| Non-permissive Genetic Background | Check literature for your specific mouse strain or cell donor background. | Optimize culture conditions; for example, increase the concentration of LIF in the culture medium [91]. |
| Low Proliferative Capacity of Somatic Cell Source | Assess the growth rate of the parent somatic cells before reprogramming. | Select a more proliferative somatic cell type or source from a more permissive genetic background [91]. |
| High Replication Stress | Monitor for markers of DNA damage like γH2AX during reprogramming. | Supplement the culture medium with nucleosides (e.g., 200 µM) during the reprogramming process to reduce replication stress and DNA damage [23]. |
Problem: Inconsistent Differentiation Outcomes Between iPSC Lines
| Potential Cause | Investigation | Solution |
|---|---|---|
| Underlying Genetic Variability | Confirm that the iPSC lines are isogenic. For human lines, genotype to confirm different donors. | When comparing disease-specific phenotypes, use multiple iPSC lines from different donors to account for natural genetic variation [92]. |
| Residual Epigenetic Memory | Perform epigenomic analysis (e.g., methylation arrays) to check for source-tissue signatures. | Perform more rounds of passaging before differentiation, as epigenetic memory tends to diminish over time. |
| Acquired Genetic Aberrations | Conduct routine genetic screening (e.g., karyotyping, aCGH) on your master cell bank. | Regularly screen iPSC lines and discontinue use of lines with known detrimental mutations (e.g., gains of chromosome 12 or 20q11.21) [4] [94]. |
Problem: Excessive Differentiation in iPSC Culture
| Potential Cause | Investigation | Solution |
|---|---|---|
| Overgrown Colonies | Inspect colony size and density. Centers should be dense, not over-confluent. | Passage cultures when colonies are large and compact but before they overgrow. Remove differentiated areas prior to passaging [8]. |
| Old or Unstable Culture Medium | Check the age and pH of the complete medium. | Ensure complete cell culture medium is less than 2 weeks old. Avoid having culture plates out of the incubator for extended periods (>15 minutes) [8]. |
| Suboptimal Passaging | Assess the size and uniformity of cell aggregates after dissociation. | Ensure cell aggregates after passaging are evenly sized. Decrease colony density by plating fewer aggregates. Optimize incubation time with dissociation reagents [8]. |
Detailed Experimental Protocols
Protocol 1: Assessing the Impact of Genetic Background on Reprogramming Efficiency
This protocol is adapted from a study that systematically compared iPSC generation across six mouse strains [91].
Key Materials:
- Mouse Strains: Genetically diverse strains (e.g., NON/LtJ, C57BL/6J, DBA/2J, BALB/cJ, 129S1/SvlmJ, CAST/EiJ).
- Reprogramming Vectors: Doxycycline-inducible lentiviral vectors for murine Oct4, Klf4, Sox2, and c-Myc.
- Critical Reagents: Doxycycline, Leukemia Inhibitory Factor (LIF), Alkaline Phosphatase staining kit, SSEA1 antibody for flow cytometry.
Methodology:
- MEF Isolation: Isolate Mouse Embryonic Fibroblasts (MEFs) from E13.5 embryos of the strains to be tested.
- Lentiviral Transduction: Transduce passage 2 (P2) MEFs with the viral supernatant in the presence of doxycycline (2 µg/mL) to induce factor expression.
- iPSC Culture & Colony Quantification: Plate transduced cells on feeder layers and culture in ESC media with doxycycline. Refresh media daily.
- Quantitative Endpoints:
- Count the total number of emerging colonies.
- Perform Alkaline Phosphatase (AP) staining and report the percentage of AP-positive colonies.
- Use flow cytometry to determine the percentage of cells positive for the pluripotency surface marker SSEA1.
- Quantitative Endpoints:
- Data Analysis: Compare the total colony counts, AP-positive percentage, and SSEA1-positive percentage across the different strains. Strains like NON/LtJ and CAST/EiJ are expected to show higher efficiency across all parameters [91].
Protocol 2: Reducing Genomic Instability During Reprogramming
This protocol describes methods to limit replication stress, a key source of de novo genetic mutations during iPSC generation [23].
Key Materials:
- Nucleoside Supplement: Commercially available nucleoside solution (e.g., 1000X stock).
- Somatic Cells: The fibroblasts or other somatic cells to be reprogrammed.
- Monitoring Reagents: Antibodies for γH2AX for immunofluorescence or Western blot.
Methodology:
- Reprogramming Initiation: Begin standard reprogramming of somatic cells using your method of choice (e.g., lentiviral OSKM).
- Nucleoside Supplementation: Add nucleosides to the culture medium at a final concentration of 200 µM for the duration of the reprogramming process.
- Monitor Replication Stress (Validation):
- Immunofluorescence: Fix cells at various time points (e.g., day 5-7 of reprogramming) and stain for γH2AX, a marker of DNA double-strand breaks.
- DNA Combing: Use DNA combing to directly measure replication fork speed in control and nucleoside-treated, reprogramming-factor-expressing cells.
- Outcome Assessment: Upon establishment of iPSC lines, analyze genomic stability.
- Copy Number Variation (CNV) Analysis: Perform array Comparative Genomic Hybridization (aCGH) on genomic DNA from treated and untreated iPSC clones. The expected outcome is a lower number of de novo CNVs in nucleoside-supplemented lines [23].
- Telomere Instability Analysis: Score multi-telomeric signals (MTS) on metaphase spreads as a readout for chromosomal fragility.
Table 1: Impact of Genetic Background on iPSC Generation in Mouse Models
| Mouse Strain | Reprogramming Efficiency | Pluripotent Stability | Notes |
|---|---|---|---|
| NON/LtJ | High [91] | Stable [91] | Parent MEFs were highly proliferative. |
| CAST/EiJ | High [91] | Stable [91] | Parent MEFs were highly proliferative. |
| 129S1/SvlmJ | Moderate [91] | Stable [91] | A strain considered permissive for ESC derivation. |
| C57BL/6J | Low [91] | Stable [91] | Requires standard LIF concentration. |
| DBA/2J | Low [91] | Stable [91] | Requires standard LIF concentration. |
| BALB/cJ | Low [91] | Conditionally Stable [91] | Required 5x higher LIF concentration to establish stable lines. |
Table 2: Comparison of Common Somatic Cell Sources for Human iPSC Generation
| Somatic Cell Type | Accessibility | Reprogramming Efficiency | Key Considerations |
|---|---|---|---|
| Skin Fibroblasts | High (invasive biopsy) | High, well-established [94] | Gold standard; may carry mutations from sun exposure. |
| Peripheral Blood Cells | High (minimally invasive) | High for CD34+ cells [94] | Preferred for clinical applications; no transgene integration in T-cells requires specific methods. |
| Urine-derived Cells | High (non-invasive) | Moderate [94] | Contain renal epithelial cells; convenient for biobanking. |
| Hair Keratinocytes | High (non-invasive) | High [94] | Easily accessible; show a slight epigenetic memory. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Investigating and Mitigating Genetic Instability in iPSCs
| Reagent / Material | Function | Application Example |
|---|---|---|
| Nucleoside Supplement | Reduces replication stress by providing substrates for DNA synthesis. | Added during reprogramming to decrease DNA damage and lower the load of de novo CNVs [23]. |
| CHK1 (Expression Vector) | Key kinase in the DNA damage response pathway that stabilizes replication forks. | Overexpression during reprogramming reduces replication stress and can increase reprogramming efficiency [23]. |
| Sendai Virus (SeV) Vectors | Non-integrating, cytoplasmic RNA viral vector for factor delivery. | Generates footprint-free iPSCs, avoiding insertional mutagenesis and allowing clinical use [94]. |
| Episomal Vectors | Non-integrating DNA vectors that are gradually diluted from cells. | A common non-viral method for generating clinical-grade iPSCs, though persistence must be monitored [94]. |
| Doxycycline-Inducible System | Allows precise temporal control of reprogramming factor expression. | Enables the study of reprogramming dynamics and can improve the quality of resulting iPSCs [91]. |
Visual Experimental Guide
Diagram: Replication Stress in iPSC Reprogramming and Mitigation Strategy
Diagram: Experimental Workflow for iPSC Line Characterization
Frequently Asked Questions (FAQs)
1. How quickly do mutations accumulate in cultured stem cells? Mutation rates vary significantly between cell types and are influenced by culture conditions. Quantitative studies have determined that human pluripotent stem cells (PSCs) accumulate approximately 3.5 ± 0.5 base substitutions per genome per population doubling. In contrast, adult stem cells (ASCs), such as those from intestine and liver, show higher rates of 7.2 ± 1.1 and 8.3 ± 3.6 base substitutions per doubling, respectively [95]. When expressed as an annual rate, the accumulation in cultured adult stem cells can be nearly 40-fold higher than the natural, in vivo mutation rate [95].
2. What are the most common types of genetic alterations found? The spectrum of genomic instability includes:
- Single Base Substitutions (SBS): The predominant mutation type acquired in culture, often driven by oxidative stress [95].
- Copy Number Variations (CNVs): Recurrent CNVs are frequently observed, with amplifications being more common than deletions. Hotspots often occur on chromosomes 12, 20 (specifically 20q11.21), and X [4] [96] [6].
- Chromosomal Aberrations: Aneuploidy, such as trisomy of chromosomes 8, 12, or X, can arise and may confer a selective growth advantage in culture [4].
- Structural Variants: These include larger-scale rearrangements, which can be a hallmark of replication stress [23].
3. Does culturing under low oxygen reduce mutation rates? Yes. Research demonstrates that a primary driver of in vitro mutations is oxidative stress. Culturing human PSCs under reduced oxygen tension (3% O₂) instead of atmospheric oxygen (20% O₂) significantly reduced the mutation load from 3.5 to 2.1 ± 0.3 base substitutions per genome per doubling [95]. This is a recommended strategy to mitigate genomic instability.
4. Can I use my cell line indefinitely if it looks healthy and grows well? No. Genomic instability can be subclinical. Studies on human umbilical cord mesenchymal stem cells (hUC-MSCs) have shown that a majority of long-term cultured clones (7 out of 9 in one study) developed CNVs, even while maintaining normal morphology, growth, and multipotency [96]. Relying solely on phenotypic appearance is insufficient; periodic genomic monitoring is essential.
5. Are there ways to reduce genomic instability during the reprogramming of iPSCs? Yes. The reprogramming process itself induces replication stress, a key source of DNA damage. Strategies to limit this stress have proven effective:
- Genetic: Increasing the levels of the checkpoint kinase 1 (CHK1) reduces replication stress and DNA damage in the resulting iPSCs [23].
- Chemical: Supplementing the culture medium with nucleosides during reprogramming provides the substrates for DNA synthesis, which lowers the load of DNA damage and reduces the number of de novo CNVs in the resulting iPSC lines [23].
Troubleshooting Guides
Problem: Observed High Mutation Rate in Pluripotent Stem Cell Culture
Potential Causes and Solutions:
| Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Oxidative Stress | • Measure intracellular ROS levels.• Analyze mutation spectrum for a high percentage of C>A transversions, a signature of oxidative damage [95]. | • Switch to culture under reduced oxygen tension (3-5% O₂) [95].• Consider adding antioxidants to the media (use with caution and validate). |
| Replication Stress | • Perform immunofluorescence for γH2AX and 53BP1 foci to detect DNA damage [97] [23].• Analyze fork speed via DNA combing [23]. | • Supplement culture media with nucleosides to support DNA replication [23]. |
| Selective Pressure | • Perform regular karyotyping and high-resolution CNV analysis (e.g., aCGH or sequencing) to detect recurrent aberrations [4] [96]. | • Limit passaging. Use low passage banks for key experiments.• Avoid over-confluency and standardize passaging protocols. |
Problem: Detected Copy Number Variations (CNVs) in an Established Cell Line
Action Plan:
- Confirm the Result: Verify the CNV using an orthogonal method (e.g., confirm aCGH results with SNP array or digital PCR).
- Assess the Impact:
- Make a Go/No-Go Decision:
- For research use, a line with a low number of CNVs in non-critical regions may be acceptable, but this must be documented.
- For clinical applications, any cell line with known oncogenic CNVs should be discarded. Regulatory guidelines typically require detailed genomic characterization prior to therapeutic use.
- Implement Preventative Measures: The presence of CNVs underscores the need for rigorous genomic monitoring and culture condition optimization to prevent their emergence.
Experimental Protocols & Data
Standard Workflow for Mutation Accumulation Analysis
The following diagram outlines a robust method for tracking de novo mutations in individual stem cells over time [95]:
Signaling Pathway: Replication Stress Response During Reprogramming
The ectopic expression of reprogramming factors induces replication stress. The following diagram shows the key players in this DNA damage response pathway and two intervention points [23]:
Quantitative Data on Mutation Accumulation
Table 1: Measured Mutation Rates in Human Stem Cells During In Vitro Culture [95]
| Stem Cell Type | Base Substitutions per Genome per Population Doubling (Mean ± SD) | Annual Mutation Accumulation (vs. In Vivo) |
|---|---|---|
| Pluripotent Stem Cells (PSCs) | 3.5 ± 0.5 | Not Specified |
| Intestinal Adult Stem Cells | 7.2 ± 1.1 | ~40x higher than in vivo |
| Liver Adult Stem Cells | 8.3 ± 3.6 | ~40x higher than in vivo |
| PSCs (at 3% O₂) | 2.1 ± 0.3 | Not Specified |
Table 2: Common Genomic Alterations and Their Functional Consequences
| Alteration Type | Recurrent Genomic Locations | Potential Functional Impact |
|---|---|---|
| Copy Number Variation (CNV) | 20q11.21 (genes: BCL2L1, ID1, DNMT3B) [4] [6] | Enhanced anti-apoptosis, pluripotency, and proliferation [4]. |
| Aneuploidy | Trisomy 12, 8, X [4] | Possible selective advantage for growth in culture; contains pluripotency genes (e.g., NANOG on chr12) [4]. |
| Single Nucleotide Variants (SNVs) | Genome-wide, but depleted in genic and promoter regions [95] | Can lead to nonsynonymous mutations; risk of oncogenic transformation if affecting cancer genes [95]. |
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Genomic Stability Studies
| Item | Function/Benefit | Key Consideration |
|---|---|---|
| Low-Oxygen Incubator | Maintains physiological oxygen levels (3-5% O₂) to significantly reduce oxidative stress and mutation accumulation [95]. | Critical for long-term maintenance of stem cell genomic integrity. |
| Nucleoside Supplement | Provides building blocks for DNA synthesis, reducing replication stress during reprogramming and cell proliferation [23]. | A simple chemical strategy to lower DNA damage and CNVs. |
| γH2AX / 53BP1 Antibodies | Used in immunofluorescence to detect DNA double-strand break foci, a direct measure of DNA damage and replication stress [97] [23]. | Standard assay for quantifying genomic instability in cell populations. |
| aCGH or SNP Array Kits | High-resolution methods for detecting CNVs and loss of heterozygosity (LOH) across the genome [4] [96]. | Higher resolution than traditional karyotyping for submicroscopic changes. |
| Whole Genome Sequencing (WGS) | Provides base-pair resolution for detecting single nucleotide variants, indels, and structural variants in a single, comprehensive assay [95] [4]. | The gold standard for comprehensive genomic characterization. |
Induced pluripotent stem cells (iPSCs) hold transformative potential for regenerative medicine, disease modeling, and drug discovery due to their capacity for unlimited self-renewal and differentiation into any cell type in the human body [14]. However, the same properties that make them clinically valuable also present significant safety risks, particularly their potential to form tumors upon transplantation [98]. The intrinsic tumorigenicity of pluripotent stem cells poses a formidable obstacle to their clinical implementation, as even a small number of residual undifferentiated cells within a differentiated therapeutic product can lead to teratoma formation [99] [98]. Teratomas are benign tumors containing randomly distributed differentiated structures arising from all three germ layers, but their growth can impair organ function and lead to serious clinical complications [98].
A recent clinical case underscores the gravity of this risk, where a patient receiving autologous iPSC-derived pancreatic beta cells for diabetes treatment developed an immature teratoma at the injection site that had already metastasized to regional lymph nodes within two months post-transplantation [98]. This case highlights the critical need for robust tumorigenicity assessment as part of the functional validation pipeline for iPSC-based therapies. Within the broader context of genomic instability research in iPSC cultures, tumorigenicity assays serve as an essential final checkpoint to ensure that genetic and epigenetic alterations acquired during reprogramming or prolonged culture do not enhance the tumor-forming potential of these cells [4] [100]. This technical support center provides comprehensive guidance for implementing and troubleshooting these crucial safety assays within your research framework.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental purpose of performing tumorigenicity assays for iPSC-derived products?
These assays are designed to detect the presence of residual undifferentiated pluripotent stem cells in differentiated cell populations intended for therapeutic use [98]. Even highly efficient differentiation protocols may leave a small population of undifferentiated cells that retain the capacity for uncontrolled proliferation and teratoma formation in vivo [98]. The assays provide a critical safety assessment by quantifying this tumorigenic potential before clinical application. Furthermore, within genomic instability research, these assays help determine whether specific genetic variations acquired during culture (such as trisomy 12 or 20q11.21 amplification) confer selective growth advantages or enhanced tumor-forming capacity [4].
Q2: What are the key differences between in vivo and in vitro tumorigenicity assays?
The table below summarizes the core distinctions between these complementary approaches:
| Parameter | In Vivo Assays | In Vitro Assays |
|---|---|---|
| Biological Context | Provides a complex physiological environment with host-tissue interactions [98] | Simplified, controlled system lacking full physiological complexity [99] |
| Detection Sensitivity | Varies with model; can detect teratomas from 20-100 murine ESCs [98] | Superior sensitivity; digital PCR can detect rare hPSC-specific RNA [99] |
| Time to Results | Several weeks to months for tumor development [98] | Typically days to a few weeks [99] |
| Regulatory Relevance | Historically considered the "gold standard" [99] | Gaining acceptance as technologies improve [99] |
| Key Advantage | Models the complete biological process of tumor formation [98] | Higher throughput, more quantitative, and avoids animal use [99] |
Q3: Which immunodeficient mouse models are most appropriate for these assays?
The selection of an appropriate immunodeficient model is crucial for successful engraftment and tumor development. The following table compares commonly used models:
| Mouse Model | Genetic Characteristics | Key Features for Tumorigenicity Studies |
|---|---|---|
| NOD/SCID | Non-obese diabetic with severe combined immunodeficiency [98] | Reproducible teratoma formation; lacks T and B cells but retains innate immunity [98] |
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl) | Lacks T, B, and NK cells; defective dendritic cells and macrophages [99] [98] | Enhanced engraftment efficiency; requires fewer cells for tumor formation (e.g., 2×10^5 iPSCs) [98] |
| NOG (NOD.Cg-PrkdcscidIL2rgtm1Sug) | Similar to NSG with different IL2rg mutation [99] | Comparable high engraftment potential to NSG models [99] |
Q4: What is the minimum number of undifferentiated cells required to initiate teratoma formation?
Studies using murine embryonic stem cells (ESCs) have demonstrated that as few as 20-100 undifferentiated ESCs within a population of differentiated cells can eventually lead to teratoma formation [98]. For human iPSCs specifically, systemic administration of 2×10^5 iPSCs into immunodeficient NSG mice was sufficient to induce teratoma growth in multiple organs [98]. It is important to note that these thresholds can vary based on the differentiation status of the cells, the specific mouse model used, the transplantation site, and the genetic stability of the cell line.
Q5: How does genomic instability in iPSC cultures impact tumorigenicity risk?
Genomic instability in iPSCs significantly elevates tumorigenicity risk through several mechanisms. Certain chromosomal aberrations commonly acquired during prolonged culture—particularly trisomy of chromosome 12, trisomy of 12q, and gains of chromosome 20q11.21—are associated with enhanced proliferation and survival advantages [4]. These abnormalities activate pluripotency-associated genes and anti-apoptotic pathways, potentially allowing cells to resist differentiation and maintain tumor-forming capacity [4] [100]. Furthermore, replication stress and chromosome condensation defects in aneuploid iPSCs can drive ongoing chromosomal instability, increasing the likelihood of additional oncogenic transformations [100].
Troubleshooting Guides
Problem 1: Failure to Form Teratomas Despite Known Undifferentiated Cell Contamination
| Possible Cause | Potential Solution |
|---|---|
| Insufficient cell numbers | Conduct a cell dose titration experiment. Increase cell numbers incrementally (e.g., 10^5 to 10^7) to establish the minimum tumorigenic dose [98]. |
| Suboptimal injection site | Compare alternative transplantation sites. Intramuscular, subcutaneous, and kidney capsule injections often show higher tumor formation efficiency compared to other sites. |
| Innate immunity in mouse model | Switch to a more severely immunocompromised model. NSG and NOG mice, which lack NK cell activity, often provide superior engraftment rates [99] [98]. |
| Poor cell viability post-injection | Optimize the cell preparation and injection technique. Use Matrigel or similar matrices to enhance cell retention and survival at the injection site. |
Problem 2: High Variability in Teratoma Formation Between Experimental Replicates
| Possible Cause | Potential Solution |
|---|---|
| Inconsistent cell preparation | Standardize the cell dissociation protocol and ensure uniform cell viability assessment before transplantation. |
| Genetic drift in iPSC culture | Regularly karyotype and authenticate iPSC lines. Use low-passage cells and minimize extended culture periods to reduce genomic instability [4] [100]. |
| Technical injection variability | Designate a single trained operator for all injections or implement comprehensive training to ensure consistent technique across multiple operators. |
| Uncontrolled environmental factors | Monitor and standardize mouse housing conditions, including stress minimization and consistent diet, as these can subtly influence engraftment success. |
Problem 3: Excessive Non-Teratoma Tumor Formation or Abnormal Teratoma Pathology
| Possible Cause | Potential Solution |
|---|---|
| Oncogenic genetic alterations | Perform comprehensive genomic analysis of the injected cell population. Screen for common oncogenic mutations (e.g., in TP53, MYC) and chromosomal abnormalities [4] [100]. |
| Contamination with progenitor cells | Improve differentiation protocol efficiency. Implement additional purification steps such as fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) to remove unwanted progenitor populations [98]. |
| Transgene reactivation | Use integration-free iPSCs or ensure complete silencing of reprogramming factors. Consider using footprint-free reprogramming methods to eliminate this risk [98]. |
Experimental Protocols
Standardized Teratoma Formation Assay
This protocol provides a detailed methodology for assessing the tumorigenic potential of iPSC-derived products in immunodeficient mice, based on established procedures from current literature [99] [98].
Materials Required
Cell Preparation:
- iPSC-derived cell product or undifferentiated iPSCs (positive control)
- Appropriate differentiation media or culture media
- Enzyme-free cell dissociation buffer
- Phosphate-buffered saline (PBS) without calcium and magnesium
- Viability stain (e.g., Trypan Blue)
Animal Model:
- 6-8 week old immunodeficient mice (NSG recommended) [98]
- Anesthesia equipment and reagents (e.g., isoflurane system)
- Sterile surgical instruments
Injection Materials:
- Matrigel or similar extracellular matrix
- Insulin syringes (0.5 mL with 28G-30G needles)
- Ice bucket for maintaining Matrigel at low temperature
Histology:
- Neutral buffered formalin (10%)
- Ethanol series for dehydration
- Paraffin embedding system
- Microtome
- Hematoxylin and Eosin (H&E) stain
- Immunohistochemistry supplies for pluripotency markers (OCT4, SOX2, NANOG)
Step-by-Step Procedure
Cell Preparation and Validation (Day -3 to -1)
- Culture undifferentiated iPSCs or differentiated products using standard protocols.
- For differentiated products, confirm differentiation efficiency using flow cytometry for cell type-specific markers and qPCR for pluripotency gene downregulation.
- Harvest cells using enzyme-free dissociation to maintain surface marker integrity.
- Resuspend cells in PBS:Matrigel (1:1 ratio) at a concentration of 1-5×10^6 cells/100 μL, maintaining the mixture on ice to prevent Matrigel polymerization.
Cell Transplantation (Day 0)
- Anesthetize mice according to your institutional animal care protocol.
- For subcutaneous injection: Lift the loose skin on the dorsal flank, insert the needle horizontally, and inject 100-200 μL of cell suspension.
- For intramuscular injection: Target the tibialis anterior or quadriceps muscle, injecting 50-100 μL of cell suspension.
- Include appropriate controls: Matrigel-only negative control and undifferentiated iPSCs positive control.
- Monitor animals for immediate adverse reactions and allow recovery.
Post-Transplantation Monitoring (Weeks 1-12)
- Palpate injection sites weekly to detect tumor formation.
- Measure any developing masses with calipers in two dimensions, calculating approximate volume using the formula: Volume = (Length × Width^2)/2.
- Monitor animal health status, including weight, activity, and signs of distress.
- If using luciferase-expressing cells, perform weekly bioluminescence imaging to track cell survival and proliferation.
Endpoint Analysis (Week 12 or when tumor reaches 1.5 cm diameter)
- Euthanize mice according to approved protocols.
- Excise tumors and photograph for documentation.
- Weigh each tumor and record dimensions.
- Divide each tumor: one portion fixed in 10% neutral buffered formalin for histology, another portion snap-frozen for molecular analysis, and a third portion preserved for possible cell re-isolation.
Histological Processing and Analysis
- Fix tissue samples in formalin for 24-48 hours at 4°C.
- Process through ethanol dehydration series, clear with xylene, and embed in paraffin.
- Section at 5-7 μm thickness using a microtome.
- Perform H&E staining following standard protocols.
- For immunohistochemistry, antigen retrieval may be required before incubation with primary antibodies against pluripotency markers (OCT3/4, SOX2, NANOG).
- Image slides using brightfield microscopy.
Teratoma Scoring and Validation
- Examine H&E stained sections for the presence of tissues representing all three germ layers:
- Ectoderm: Neural tissue, pigmented cells (retinal epithelium), stratified squamous epithelium
- Mesoderm: Cartilage, bone, muscle, adipose tissue
- Endoderm: Respiratory epithelium, intestinal epithelium, glandular structures
- Confirm the absence of undifferentiated stem cell regions, which appear as compact, rapidly dividing cells with high nuclear-to-cytoplasmic ratio.
- Score tumors as "teratomas" only if organized tissues from multiple germ layers are present.
- Examine H&E stained sections for the presence of tissues representing all three germ layers:
Highly Efficient Culture (HEC) Assay for Residual Pluripotent Cells
This sensitive in vitro method serves as a complementary approach to animal studies for detecting rare undifferentiated cells within differentiated populations [99].
Materials Required
Cell Culture:
- Test cell population (differentiated iPSC product)
- Undifferentiated iPSCs (for standard curve)
- Rho kinase inhibitor (Y-27632)
- Pluripotent stem cell culture media with appropriate supplements
Analysis:
- Alkaline phosphatase (ALP) staining kit
- Flow cytometry antibodies for pluripotency markers (TRA-1-60, SSEA-4, OCT4)
- Digital PCR system with primers for pluripotency-associated genes
Procedure
Sample Preparation
- Prepare a single-cell suspension from the test population and determine viable cell count.
- Prepare a standard curve by spiking known numbers of undifferentiated iPSCs (0, 10, 100, 1000) into a fixed number of differentiated cells (e.g., 10^6 cells).
Culture Conditions
- Plate cells at high density (10^4 - 10^5 cells/cm^2) in pluripotency-supporting media supplemented with Rho kinase inhibitor to enhance survival of single pluripotent cells.
- Culture for 7-14 days with media changes every other day.
- Include control wells with known numbers of undifferentiated iPSCs for standard curve generation.
Analysis of Results
- Alkaline Phosphatase Staining: Fix cells and stain for ALP activity following kit instructions. Count ALP-positive colonies.
- Flow Cytometry: Dissociate colonies and stain for pluripotency surface markers (TRA-1-60, SSEA-4). Analyze using a flow cytometer.
- Digital PCR: Isolve RNA from a portion of the cells and perform digital PCR for pluripotency-associated genes (POUSF1, NANOG) to achieve absolute quantification.
Calculation of Sensitivity
- Plot the standard curve of known spiked-in cells versus detected colonies or positive signals.
- Determine the limit of detection (LOD) and limit of quantification (LOQ) for the assay.
- Calculate the frequency of residual pluripotent cells in the test sample based on the standard curve.
Signaling Pathways and Experimental Workflows
Molecular Pathways in Teratoma Formation
The following diagram illustrates the key molecular events leading from genomic instability to teratoma formation, highlighting critical pathways and checkpoints.
Tumorigenicity Assay Workflow
This workflow diagram outlines the complete experimental pipeline for conducting tumorigenicity and teratoma formation assays.
Research Reagent Solutions
The following table outlines essential reagents and materials for conducting tumorigenicity and teratoma formation assays, with specific applications in genomic instability research.
| Reagent/Material | Primary Function | Application Notes |
|---|---|---|
| NSG Mice (NOD.Cg-Prkdcscid Il2rgtm1Wjl) | In vivo tumorigenicity assessment | Preferred model due to complete lack of adaptive immunity and reduced innate immunity; enhances engraftment efficiency [98]. |
| Rho Kinase Inhibitor (Y-27632) | Enhances survival of pluripotent stem cells | Critical for Highly Efficient Culture (HEC) assay; improves cloning efficiency of single pluripotent cells [99]. |
| Matrigel Matrix | Extracellular matrix for cell transplantation | Provides structural support and survival signals for injected cells; improves consistency of tumor formation [98]. |
| Anti-TRA-1-60 Antibody | Detection of undifferentiated pluripotent cells | Cell surface marker with high specificity for pluripotent stem cells; used in flow cytometry and immunocytochemistry [99]. |
| Digital PCR System | Absolute quantification of residual PSCs | Superior sensitivity for detecting rare undifferentiated cells in differentiated populations; does not require standard curves [99]. |
| Pluripotency Marker Panel (OCT4, SOX2, NANOG) | Immunohistochemistry of teratomas | Confirms pluripotent origin of tumors; identifies residual undifferentiated regions within teratomas [98]. |
| Karyotyping/SNP Array Reagents | Genomic instability monitoring | Detects chromosomal abnormalities and copy number variations acquired during culture that may affect tumorigenicity [4]. |
| Luciferase-Expressing iPSCs | In vivo cell tracking | Enables longitudinal monitoring of cell survival and proliferation without sacrificing animals; useful for kinetics studies [98]. |
Establishing Safety and Potency Criteria for iPSC Lines in Regulatory Submissions
FAQs: Genomic Instability in iPSC Cultures
What are the most common genomic instability issues in iPSC cultures? Human PSCs (hPSCs) are prone to genetic changes during reprogramming, in vitro cultivation, and gene editing. Recurrent karyotypic abnormalities often involve trisomy of chromosome 12, 17, or X, or amplification of chromosome 1, 12p, 17q, or the 20q11.21 region. A genetically abnormal clone can completely overtake a culture in less than five passages, compromising research and therapeutic utility [101].
How does genomic instability affect the safety and efficacy of iPSC-based therapies? Genomic instability can lead to chromosomal aberrations that impact differentiation efficiency, functionality of differentiated cells, and the safety of cell replacement therapies. Aberrant cells may exhibit altered growth properties or potential tumorigenicity, posing significant risks for clinical applications [101].
What environmental stressors can induce genomic instability in neural stem cells? Recent research demonstrates that hyperthermia (heat stress) at clinically relevant temperatures (41°C) can induce DNA double-strand breaks in neural stem cells, triggering a p53-mediated DNA damage response. This stress leads to lasting genomic damage including single-nucleotide polymorphisms (SNPs) and gene fusions in key neurodevelopmental genes, potentially contributing to neuronal developmental deficits [102].
How can I monitor my iPSC cultures for genomic instability? Regular quality control is essential. Traditional G-banding karyotyping provides a genome-wide overview and detects structural abnormalities, but has limited resolution (5-10 Mb). SNP array analysis offers higher resolution (detecting abnormalities >350 kb) and can identify copy number variations and copy-neutral loss of heterozygosity, which G-banding cannot detect. A combination of both methods is recommended for comprehensive monitoring [101].
Troubleshooting Guides
Problem: Excessive Differentiation (>20%) in iPSC Cultures
Potential Causes and Solutions:
- Old Culture Medium: Ensure complete cell culture medium (e.g., mTeSR Plus or mTeSR1) kept at 2-8°C is less than 2 weeks old [8].
- Inadequate Passaging: Remove differentiated areas prior to passaging. Ensure cell aggregates are evenly sized and passage cultures when colonies are large, compact, and dense in the centers [8].
- Environmental Stress: Avoid having culture plates out of the incubator for more than 15 minutes at a time [8].
- Culture Density Issues: Decrease colony density by plating fewer cell aggregates during passaging. For sensitive cell lines, reduce incubation time with passaging reagents like ReLeSR [8].
Problem: Poor Cell Attachment After Passaging
Potential Causes and Solutions:
- Initial Plating Density: Plate 2-3 times more cell aggregates initially and maintain a more densely confluent culture [8].
- Procedure Timing: Work quickly after treatment with passaging reagents to minimize time cell aggregates spend in suspension [8].
- Passaging Conditions: Reduce incubation time with passaging reagents, especially if cells are passaged prior to multi-layering within colonies [8].
- Physical Manipulation: Avoid excessive pipetting to break up cell aggregates; instead increase incubation time with passaging reagent by 1-2 minutes [8].
- Culture Vessels: Ensure non-tissue culture-treated plates are used when coating with Vitronectin XF; use tissue culture-treated plates when coating with Corning Matrigel [8].
Experimental Protocols for Genomic Stability Assessment
Protocol 1: SNP Array Analysis for Chromosomal Aberration Detection
Purpose: To detect chromosomal abnormalities and copy number variations in hPSCs with high resolution [101].
Materials:
- QIAamp DNA Blood Mini Kit (Qiagen)
- Global Screening Array v3.0 (Illumina)
- GenomeStudio V2.0.5 software with cnvPartition plug-in
Method:
- Extract genomic DNA using QIAamp DNA Blood Mini Kit
- Process DNA on Global Screening Array v3.0
- Perform SNP calling using GenomeStudio with GenCall threshold of 0.2
- Conduct CNV analysis using cnvPartition 3.2.0
- Evaluate call rates (recommended threshold: 95-98%)
- Analyze B-allele frequency and log R ratio for CNV detection
Quality Control Metrics:
| Parameter | Threshold | Purpose |
|---|---|---|
| Call Rate | >95% | Ensure sufficient SNP detection |
| B-allele Frequency | - | Detect loss of heterozygosity |
| Log R Ratio | - | Identify copy number variations |
Protocol 2: Karyotyping by G-Banding
Purpose: To detect large-scale structural and numerical chromosomal abnormalities [101].
Materials:
- KaryoMax Colcemid (ThermoFisher)
- Hypotonic solution (0.075M KCl)
- Carnoy's fixative (methanol:acetic acid, 3:1)
- Giemsa stain
Method:
- Treat cells with 0.04 μg/mL colcemid for 2 hours
- Create single-cell suspension using Accutase
- Incubate in hypotonic solution for 60 minutes at 37°C
- Fix cells with Carnoy's fixative
- Perform G-banding analysis
- Evaluate at least 20 metaphases structurally with 300-500 band resolution
Signaling Pathways and Experimental Workflows
Genomic Instability Monitoring Pathway
Genomic Stress Response Pathway
Research Reagent Solutions
Essential Materials for Genomic Stability Research:
| Reagent | Function | Application |
|---|---|---|
| mTeSR Plus/M1 | Defined culture medium | Maintain hPSC pluripotency |
| ReLeSR | Passaging reagent | Gentle cell dissociation |
| Vitronectin XF | Culture substrate | Feeder-free culture |
| QIAamp DNA Blood Mini Kit | DNA extraction | Prepare samples for SNP array |
| Global Screening Array | SNP genotyping | Detect chromosomal aberrations |
| KaryoMax Colcemid | Metaphase arrest | Prepare cells for karyotyping |
| Senescence Cell Staining Kit | Detect SA-β-gal | Identify senescent cells |
| Protein Carbonyl ELISA Kit | Measure oxidative stress | Quantify protein carbonylation |
| γH2AX Antibody | DNA damage marker | Detect double-strand breaks |
Conclusion
Genomic instability in iPSC cultures is not an insurmountable barrier but a defined and manageable challenge. A multi-pronged approach—combining a deep understanding of the molecular mechanisms, implementing rigorous and continuous genomic monitoring, and adopting optimized culture and reprogramming protocols—is essential for success. For the field to advance toward safe and effective clinical applications, the standard must be the generation of genomically stable, well-characterized iPSC master cell banks. Future research must focus on refining non-integrating reprogramming methods, developing advanced gene-editing tools to correct acquired mutations, and establishing universally accepted, high-resolution benchmarking standards for genomic integrity. By systematically addressing instability, the immense potential of iPSCs for disease modeling, drug screening, and regenerative medicine can be fully realized.
References
- 1. Oncogenic c - Myc by increasing cohesins... induces replication stress [https://www.nature.com/articles/s41467-024-45955-z?error=cookies_not_supported&code=a3cc1785-4121-4f91-9d62-72789c2b545e]
- 2. Emerging roles of Myc in stem cell biology and novel tumor therapies [https://pubmed.ncbi.nlm.nih.gov/30053872/]
- 3. Promotion of direct reprogramming by transformation- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2922531/]
- 4. Genomic Instability of iPSCs: Challenges Towards Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5346115/]
- 5. Genomic instability in induced stem cells [https://www.nature.com/articles/cdd20119]
- 6. Genomic integrity of human induced pluripotent stem cells ... [https://www.sciencedirect.com/science/article/pii/S1873506120301057]
- 7. Cell Reprogramming - PSC Resource Handbook [https://www.thermofisher.com/us/en/home/life-science/stem-cell-research/stem-cell-research-learning-center/stem-cell-research-resource-library/pluripotent-stem-cell-handbook/psc-handbook-stem-cell-reprogramming.html]
- 8. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 9. Tips and tricks for successfully culturing and adapting human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8640166/]
- 10. Chromatin Dynamics during Cellular Reprogramming - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4216318/]
- 11. The dynamics of chromatin states mediated by epigenetic ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1097780/full]
- 12. Epigenetic regulation of open chromatin in pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4163141/]
- 13. The Challenges to Advancing Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 14. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 15. Induced Pluripotent Stem Cells: Reprogramming Platforms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7194323/]
- 16. Chromatin landscape dynamics during reprogramming ... [https://www.nature.com/articles/s41420-024-02230-w]
- 17. ARHGDIA Confers Selective Advantage to Dissociated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8309423/]
- 18. Gains of 20q11.21 in human pluripotent stem cells - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10828824/]
- 19. Gain of 20q11.21 in Human Pluripotent Stem Cells Impairs ... [https://www.sciencedirect.com/science/article/pii/S2213671119301729]
- 20. High-Resolution Genomic Arrays Facilitate Detection of ... [https://www.sciencedirect.com/science/article/pii/S0301472X06006370]
- 21. Optimizing genomic instability assessment in cancer [https://www.sophiagenetics.com/resource/optimizing-genomic-instability-assessment-in-cancer/]
- 22. Comparison of nonhomologous end joining and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2695993/]
- 23. Limiting replication stress during somatic cell ... [https://www.nature.com/articles/ncomms9036]
- 24. Non-homologous end joining shapes the genomic ... [https://www.nature.com/articles/s41467-024-49985-5]
- 25. Aneuploidy is a Prevalent Strategy in Fungal Adaptation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6826469/]
- 26. Tracing genomic instability in induced mesenchymal ... [https://www.nature.com/articles/s12276-025-01439-8]
- 27. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 28. Origins of chromosome instability unveiled by coupled ... [https://www.nature.com/articles/s41586-025-09632-5]
- 29. The advantages of SNP arrays over CGH arrays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4044733/]
- 30. Genomic Instability in Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3931019/]
- 31. Combined array CGH plus SNP genome analyses in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3865406/]
- 32. Tips for Successful aCGH [https://www.enzo.com/note/tips-for-successful-acgh/]
- 33. The Principles and Workflow of SNP Microarray [https://www.cd-genomics.com/the-principles-and-workflow-of-snp-microarray.html]
- 34. Genotyping Support - Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/microarray-analysis-support-center/genotyping-support/genotyping-support-troubleshooting.html]
- 35. Troubleshooting [https://knowledge.illumina.com/microarray/general/microarray-general-troubleshooting-list]
- 36. Multicolor FISH (M-FISH) Analysis [https://www.creative-bioarray.com/services/multicolor-fish-m-fish-analysis.htm]
- 37. FISH Tips and Troubleshooting [https://www.creative-bioarray.com/support/fish-tips-and-troubleshooting.htm]
- 38. In Situ Hybridization Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/gene-expression-analysis-genotyping-support-center/in-situ-hybridization-support/ish-support-troubleshooting.html]
- 39. Limitations of Chromosome Classification by Multicolor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1275623/]
- 40. Multiplex fluorescence in situ hybridization (M-FISH) [https://pubmed.ncbi.nlm.nih.gov/20809305/]
- 41. Three-Color Chromosome Painting as Seen through the ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2016.00052/full]
- 42. mFISH karyotyping [https://bio-protocol.org/exchange/minidetail?id=8768293&type=30]
- 43. Bioinformatics Workflow for Whole Genome Sequencing [https://www.cd-genomics.com/bioinformatics-workflow-for-whole-genome-sequencing.html]
- 44. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 45. StratoMod: predicting sequencing and variant calling errors ... [https://www.nature.com/articles/s42003-024-06981-1]
- 46. A practical method to detect SNVs and indels from whole ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3703611/]
- 47. Bioinformatic Analyses of Whole-Genome Sequence Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5572866/]
- 48. WES Sample Preparation Guide: Steps for Accurate ... [https://3billion.io/blog/sample-preparation-guide-for-wes]
- 49. Detection and quantification of γ-H2AX using a dissociation ... [https://www.nature.com/articles/s41598-021-88296-3]
- 50. Review H2AX: A key player in DNA damage response and ... [https://www.sciencedirect.com/science/article/pii/S075333222400547X]
- 51. The Role of γH2AX in Replication Stress-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10619570/]
- 52. Strategies for the evaluation of DNA damage and repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5452911/]
- 53. Hallmarks of DNA Replication Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9219557/]
- 54. Assessing Stem Cell DNA Integrity for Cardiac Cell Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC8881784/]
- 55. Quantitative γ-H2AX immunofluorescence method for DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7080928/]
- 56. Protocol for FACS Staining and Considerations for Gating [https://www.stemcell.com/protocol-for-facs-staining.html]
- 57. The Emergence of Organoids in Cellular Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10047824/]
- 58. Navigating stem cell culture: insights, techniques, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586186/]
- 59. Maintenance of Genome Stability - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4936602/]
- 60. The Consequences of Chromosome Segregation Errors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5372005/]
- 61. Comprehensive genomic dependency landscape of a ... [https://www.nature.com/articles/s42003-025-07822-5]
- 62. The use of artificial intelligence in induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11108174/]
- 63. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 64. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 65. Current advances and future prospects of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1546423/full]
- 66. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 67. Chemical reprogramming of human blood cells to ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925002607]
- 68. Genomic Instability [https://www.carislifesciences.com/genomic-instability/]
- 69. Genomic instability in human cancer: Molecular insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4600419/]
- 70. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 71. Targeting p53 pathways: mechanisms, structures ... - Nature [https://www.nature.com/articles/s41392-023-01347-1]
- 72. Unraveling the Guardian: p53's Multifaceted Role in the DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11641486/]
- 73. Molecular mechanisms of mammalian DNA repair ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/15189136/]
- 74. DNA Damage Response - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/dna-damage-response]
- 75. DNA Damage Response - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3003462/]
- 76. Errors in Chromosome Number | Biology for Majors I [https://courses.lumenlearning.com/suny-wmopen-biology1/chapter/outcome-errors-in-chromosome-number/]
- 77. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 78. Karyotyping Information | Mount Sinai - New York [https://www.mountsinai.org/health-library/tests/karyotyping]
- 79. Quality Control Procedures for Genome Wide Association ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3066182/]
- 80. Karyotype [https://en.wikipedia.org/wiki/Karyotype]
- 81. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 82. iPSC Maintenance Challenges and How to Overcome Them [https://definedbioscience.com/blogs/news/ipsc-maintenance-challenges-and-how-to-overcome-them?srsltid=AfmBOopH5gMM3px8n4DEfpvyGxYj3EQDTivnS8s-PU5mTu5bfJhFUhW5]
- 83. Overcoming Barriers of CRISPR Gene Editing in iPS Cells [https://www.synthego.com/blog/ipsc-crispr-editing/]
- 84. Karyotype Analysis for iPSC [https://www.creative-biolabs.com/stem-cell-therapy/karyotype-analysis-for-ipsc.htm]
- 85. Cytogenetic notation [https://en.wikipedia.org/wiki/Cytogenetic_notation]
- 86. Help File - ISCN Symbols and Abbreviated Terms [https://www.coriell.org/0/Sections/Support/Global/iscn_help.aspx?PgId=263]
- 87. Lower genomic stability of induced pluripotent stem cells ... [https://cancercommun.biomedcentral.com/articles/10.1186/s40880-018-0313-0]
- 88. PSC Genomic Integrity and Stability | Cell Quality [https://www.stemcell.com/psc-cell-quality/genomic-integrity]
- 89. Genomic integrity of human induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6828592/]
- 90. Maintenance of genome integrity and active homologous ... [https://www.nature.com/articles/s12276-020-0481-2]
- 91. Genetic background affects induced pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3580468/]
- 92. Genetic Variability Overrides the Impact of Parental Cell ... [https://www.sciencedirect.com/science/article/pii/S2213671115003744]
- 93. Genetic instability of iPSCs: Why does it matter? [https://www.cellgs.com/blog/genetic-instability-of-ipscs-why-does-it-matter.html]
- 94. Human Induced Pluripotent Stem Cells: From Cell Origin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9216482/]
- 95. The mutational impact of culturing human pluripotent and ... [https://www.nature.com/articles/s41467-020-16323-4]
- 96. Long-term cultured mesenchymal stem cells frequently ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3877551/]
- 97. Tools used to assay genomic instability in cancers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8891418/]
- 98. Elimination of tumorigenic pluripotent stem cells from their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277835/]
- 99. Evaluating teratoma formation risk of pluripotent stem cell- ... [https://www.sciencedirect.com/science/article/pii/S146532492500684X]
- 100. Genomic Instability in Human Pluripotent Stem Cells Arises ... [https://www.sciencedirect.com/science/article/pii/S1934590915005019]
- 101. Chromosomal quality control in hPSCs: A practical guide to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259632/]
- 102. Heat Stress-Induced Genomic Instability in Neural Stem ... [https://pubmed.ncbi.nlm.nih.gov/40834973/]