Advanced CRISPR Gene Editing Protocols for Precision Correction of Stem Cell Mutations
This article provides a comprehensive guide for researchers and drug development professionals on the latest CRISPR-based strategies for correcting disease-causing mutations in stem cells.
Advanced CRISPR Gene Editing Protocols for Precision Correction of Stem Cell Mutations
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the latest CRISPR-based strategies for correcting disease-causing mutations in stem cells. It covers the foundational principles of stem cell biology and CRISPR technology, details cutting-edge methodological approaches including AI-designed editors and prime editing, addresses critical troubleshooting aspects like delivery and off-target effects, and outlines robust validation frameworks. By synthesizing recent advances and practical protocols, this resource aims to accelerate the translation of edited stem cells into reliable research tools and transformative clinical therapies.
Stem Cell Biology and CRISPR Fundamentals: From Mechanisms to Disease Modeling
The convergence of stem cell biology and precision gene editing represents a transformative frontier in biomedical research and therapeutic development. Pluripotent stem cells, including induced pluripotent stem cells (iPSCs), alongside adult stem cells such as mesenchymal stem/stromal cells (MSCs) and neural stem cells (NSCs), provide versatile platforms for modeling human disease and developing regenerative therapies. The integration of CRISPR-based technologies with these cellular platforms has dramatically accelerated our ability to correct disease-causing mutations, create precise disease models, and develop next-generation cell therapies. This article provides a comprehensive overview of current protocols, applications, and reagent solutions for gene editing across NSC, iPSC, and MSC platforms, with a specific focus on CRISPR-Cas9 methodologies for correcting stem cell mutations.
Stem Cell Platforms for Gene Editing: A Comparative Analysis
The selection of an appropriate stem cell platform is fundamental to experimental design in gene editing research. Each platform offers distinct advantages and limitations based on origin, differentiation potential, and therapeutic applicability.
Table 1: Comparative Analysis of Stem Cell Platforms for Gene Editing
| Platform | Origin | Differentiation Potential | Key Advantages | Primary Applications | Editing Considerations |
|---|---|---|---|---|---|
| iPSC | Reprogrammed somatic cells | Pluripotent (all germ layers) | Autologous source, unlimited self-renewal, patient-specific disease modeling | Disease modeling, drug screening, regenerative medicine | High editing efficiency, but requires careful characterization to maintain pluripotency |
| MSC | Bone marrow, adipose tissue, umbilical cord | Multipotent (osteocytes, chondrocytes, adipocytes) | Immunomodulatory properties, trophic factor secretion, clinically relevant | Immunomodulation, tissue repair, graft-versus-host disease | Primary MSCs have limited expansion; iPSC-derived MSCs offer superior scalability [1] |
| NSC | Fetal brain, iPSC-derived | Multipotent (neurons, astrocytes, oligodendrocytes) | Region-specific subtypes, relevant for neurological disease modeling | Neurodegenerative disease modeling, CNS repair | Editing must preserve neuronal differentiation capacity |
The emergence of iPSC-derived cell types (iPSC-MSCs or iMSCs, iPSC-NSCs) has created exciting new opportunities by overcoming limitations of primary cell sources. Studies demonstrate that iMSCs generated from urinary epithelial cells show homogeneous autologous highly proliferative characteristics and may provide an alternative source to primary MSCs for treating various diseases [1]. These iMSCs maintained MSC characteristics without chromosomal abnormalities even at later passages (P15), during which umbilical cord-derived MSCs (UC-MSCs) started losing their MSC characteristics [1].
CRISPR Gene Editing Approaches and Workflows
CRISPR-Cas9 Systems and Delivery Methods
CRISPR-Cas9 has become the predominant system for gene editing in stem cells due to its precision and programmability. The system consists of two core components: the Cas9 nuclease enzyme that creates double-strand breaks in DNA, and a guide RNA (gRNA) that directs Cas9 to specific genomic sequences [2]. Editing outcomes depend on the repair pathway employed:
- Non-Homologous End Joining (NHEJ): Error-prone repair resulting in insertions or deletions (indels) that disrupt gene function, suitable for gene knockouts.
- Homology-Directed Repair (HDR): Precise editing using a DNA repair template to introduce specific point mutations or insertions, requiring a donor template.
Table 2: Advanced Gene Editing Systems for Stem Cell Research
| Editing System | Editing Mechanism | Key Advantages | Efficiency in Stem Cells | Primary Applications |
|---|---|---|---|---|
| CRISPR-Cas9 (Nuclease) | Creates double-strand breaks | High efficiency for gene knockout | 50-90% in various setups [2] | Gene knockout, large insertions |
| Base Editing | Chemical conversion of single bases (C→T or A→G) | No double-strand breaks; reduced off-target effects | 26-92% base conversions reported [3] | Point mutation correction |
| Prime Editing | Search-and-replace editing using reverse transcriptase | Versatile; all12 possible base-to-base conversions | Varies based on cell type and target | Transition and transversion mutations |
Recent advances in delivery systems have significantly improved CRISPR efficiency in stem cells. Lipid nanoparticle spherical nucleic acids (LNP-SNAs) have demonstrated enhanced delivery, entering cells up to three times more effectively than standard lipid particles and boosting gene-editing efficiency threefold while reducing toxicity [4]. For difficult-to-transfect cells, electroporation of ribonucleoprotein (RNP) complexes (Cas9 protein pre-complexed with gRNA) remains the gold standard, minimizing off-target effects and reducing time spent in culture.
Inducible Gene Editing Systems
Traditional constitutive expression of editing enzymes can lead to unwanted cellular stress, genotoxicity, and selection against edited cells. Inducible systems provide temporal control over editor expression, enabling editing within a specific time window. A recent protocol describes the generation of iPSCs with doxycycline-inducible ABE8e adenine base editor expression at the AAVS1 safe harbor locus [3]. This system enables:
- Temporal control: Editing only during desired time windows
- Reduced cellular stress: Avoids prolonged editor expression
- Tunable expression: Doxycycline concentration modulates editing levels
- Multiplexed editing: Simultaneous editing of multiple genomic loci
The workflow for establishing inducible editing lines involves electroporation of the donor plasmid (containing the inducible editor cassette) alongside AAVS1-specific zinc-finger nuclease plasmids, followed by puromycin selection and junction PCR verification of correct integration [3].
Application Notes and Experimental Protocols
Protocol: CRISPR-Cas9 Mediated Gene Editing in Human iPSCs
This protocol adapts established methods for precise gene editing in human iPSCs [5], optimized for high efficiency while maintaining pluripotency.
Materials and Reagents
Table 3: Essential Research Reagent Solutions for Stem Cell Gene Editing
| Reagent/Category | Specific Examples | Function/Purpose | Notes for Selection |
|---|---|---|---|
| Stem Cell Culture Media | Essential 8, mTeSR Plus, StemFlex | Maintains pluripotency and self-renewal | Feeder-free formulations recommended for editing workflows |
| CRISPR Delivery | Lipofectamine Stem Transfection Reagent, Neon Transfection System | Introduces CRISPR components into cells | RNP electroporation preferred for minimal off-target effects |
| gRNA Design | CRISPR-GPT AI tool [6] | Optimizes guide RNA sequences for specificity and efficiency | AI tools can predict off-target effects and suggest improvements |
| Base Editing Systems | Inducible ABE8e system [3] | Enables precise single-base changes without double-strand breaks | Doxycycline-inducible systems allow temporal control |
| Characterization | Alkaline phosphatase kits, Pluripotency markers (OCT4, NANOG, SOX2) | Validates stem cell quality and pluripotency post-editing | Essential quality control step before and after editing |
Step-by-Step Procedure
iPSC Culture and Preparation:
- Maintain iPSCs in mTeSR Plus medium on Matrigel-coated plates at 37°C with 5% CO₂ [3].
- Passage cells at 70-80% confluency using EDTA or enzyme-free dissociation reagents to maintain viability.
- Ensure cells have >90% expression of pluripotency markers (OCT4, NANOG, SOX2) before editing.
gRNA Design and Complex Formation:
- Design gRNAs using AI-assisted tools like CRISPR-GPT, which leverages 11 years of published data to optimize experimental design and predict off-target effects [6].
- For RNP delivery, complex purified Cas9 protein with synthetic gRNA at 3:1 molar ratio and incubate 10-15 minutes at room temperature.
Electroporation:
- Harvest iPSCs as single cells using Accutase.
- Resuspend 1×10⁶ cells in 100μl R buffer with prepared RNP complexes (10-20μg Cas9 protein).
- Electroporate using Neon Transfection System (1300V, 30ms, 1 pulse) [3].
- Plate transfected cells in pre-warmed Essential 8 medium with 10μM ROCK inhibitor.
Selection and Clonal Isolation:
- For HDR edits, begin antibiotic selection 48 hours post-electroporation.
- For clonal isolation, perform single-cell sorting into 96-well plates 5-7 days post-editing.
- Expand clones for 2-3 weeks with medium changes every other day.
Genotype Validation:
- Screen clones by PCR amplification of target locus and Sanger sequencing.
- Confirm HDR edits by restriction fragment length analysis if silent cutter site was introduced.
- Validate biallelic editing through TA cloning or next-generation sequencing.
Pluripotency Confirmation:
- Verify edited clones maintain pluripotency markers via immunocytochemistry (OCT4, NANOG, SOX2, TRA-1-60, SSEA4) [1].
- Perform in vitro trilineage differentiation potential assay to confirm developmental capacity.
Protocol: Generation of iMSCs from Edited iPSCs
This protocol describes the differentiation of gene-edited iPSCs into mesenchymal stem/stromal cells (iMSCs) for regenerative applications [1].
Materials and Reagents
- Edited iPSC line with validated genotype and pluripotency
- MSC differentiation medium: DMEM supplemented with 10% FBS, 1% GlutaMAX, 1% NEAA
- MSC characterization antibodies: CD73, CD90, CD105 (positive markers); CD34, CD45 (negative markers)
- Trilineage differentiation kits: adipogenic, osteogenic, chondrogenic
Step-by-Step Procedure
Initiate Differentiation:
- Harvest edited iPSCs as small clumps using Gentle Cell Dissociation Reagent.
- Transfer to ultra-low attachment plates in MSC differentiation medium.
- Culture for 7 days as embryoid bodies with medium changes every other day.
Select MSC Progenitors:
- Plate embryoid bodies on 0.1% gelatin-coated plates in MSC differentiation medium.
- Allow outgrowth of mesenchymal-like cells over 7-10 days.
- Passage adherent cells using trypsin-EDTA upon reaching 80% confluency.
Expand and Characterize iMSCs:
- Culture expanded cells through multiple passages to enrich for MSC population.
- Confirm MSC phenotype by flow cytometry for CD73, CD90, CD105 (≥95% positive) and CD34, CD45 (≤5% positive).
- Validate trilineage differentiation potential by culturing in specific induction media:
- Adipogenic: Lipid droplet formation with Oil Red O staining
- Osteogenic: Mineralization with Alizarin Red staining
- Chondrogenic: Glycosaminoglycan production with Alcian Blue staining
Functional Assays:
- Perform migration assays to confirm wound-healing capacity [1].
- Evaluate immunomodulatory function through T-cell suppression assays.
Troubleshooting and Optimization
Even with optimized protocols, researchers may encounter challenges in stem cell gene editing. Common issues and solutions include:
- Low editing efficiency: Optimize gRNA design using AI tools like CRISPR-GPT; increase RNP concentration; test different delivery methods.
- Poor cell viability post-electroporation: Reduce RNP concentration; optimize cell density; ensure prompt plating with ROCK inhibitor.
- Incomplete HDR: Increase repair template concentration; use single-stranded DNA donors; synchronize cells in S-phase.
- Loss of pluripotency: Limit culture time post-editing; minimize single-cell passaging; frequently validate pluripotency markers.
The integration of advanced CRISPR systems with pluripotent and adult stem cell platforms has created unprecedented opportunities for disease modeling, drug discovery, and regenerative medicine. The protocols outlined here provide a foundation for efficient gene editing in iPSCs, NSCs, and MSCs, while highlighting critical reagent solutions and troubleshooting approaches. As the field progresses, emerging technologies including AI-assisted experimental design [6], improved delivery systems [4], and more precise base editors [3] will further enhance our ability to harness pluripotency for therapeutic genome engineering. The ongoing clinical translation of these approaches, evidenced by the growing number of FDA-authorized trials involving edited stem cells [7], underscores the transformative potential of these combined technologies for addressing previously untreatable genetic disorders.
The application of CRISPR-based gene editing technologies has revolutionized stem cell research, enabling precise genetic modifications for disease modeling, drug discovery, and therapeutic development. These technologies offer complementary approaches for manipulating the genome of stem cells, including induced pluripotent stem cells (iPSCs), with varying levels of precision, versatility, and practical implementation requirements. CRISPR-Cas nucleases introduce double-strand breaks (DSBs) that are repaired by non-homologous end joining (NHEJ) or homology-directed repair (HDR). Base editors (BEs) facilitate direct chemical conversion of one base to another without DSBs, while prime editors (PEs) offer precise "search-and-replace" functionality through a reverse transcriptase-mediated process. Each system presents distinct advantages and limitations for stem cell engineering applications, with selection dependent on the specific research goals, desired precision, and available delivery methods.
The selection of appropriate CRISPR technology is particularly critical for stem cell research, where maintaining genomic integrity is paramount. iPSCs derived from somatic cells of patients with genetic disorders like Alzheimer's disease (AD) can be reprogrammed into disease-relevant cell types, creating powerful models for studying pathogenesis and screening therapeutics. The integration of stem cell technology with precise gene editing enables researchers to correct pathogenic mutations in genes such as APP, PSEN1, and PSEN2, which are implicated in familial AD, providing insights into disease mechanisms and potential regenerative medicine approaches.
Technology Comparison and Selection Guide
Comparative Analysis of CRISPR Systems
Table 1: Comparison of Major CRISPR-Based Gene Editing Technologies
| Technology | Editing Mechanism | Editing Outcomes | Key Advantages | Key Limitations | Stem Cell Applications |
|---|---|---|---|---|---|
| CRISPR-Cas Nucleases | Creates DSBs repaired by NHEJ or HDR | Insertions, deletions, gene knock-ins, knock-outs | Broad applicability, efficient gene disruption | Off-target effects, indel byproducts, low HDR efficiency in stem cells | Gene knock-out studies, disease modeling via mutation introduction |
| Base Editors (BEs) | Direct chemical conversion without DSBs | C•G to T•A or A•T to G•C point mutations | High efficiency, no DSBs, low indel formation | Restricted to specific base changes, bystander editing, limited targeting scope | Correcting point mutations in monogenic diseases, introducing specific single nucleotide polymorphisms (SNPs) |
| Prime Editors (PEs) | Reverse transcription of edited sequence from pegRNA | All 12 possible base substitutions, small insertions, deletions | Versatile editing, no DSBs, high precision, reduced off-target effects | Variable efficiency, complex pegRNA design, large construct size | Precise correction of pathogenic mutations without donor DNA templates |
Performance Metrics for Technology Selection
Table 2: Efficiency and Specificity Metrics of CRISPR Systems
| Parameter | CRISPR-Cas Nucleases | Base Editors | Prime Editors |
|---|---|---|---|
| Editing Efficiency Range | 10-80% (highly variable by cell type) | 10-70% (dependent on sequence context) | 10-50% (improving with newer versions) |
| Indel Formation Rate | High (5-60%) | Very low (<1%) | Minimal (<1%) |
| Off-Target Effects | Moderate to high | Moderate (DNA/RNA deaminase activity) | Low |
| Targeting Scope | Limited by PAM availability | Restricted by editing window position | Broadest (flexible PAM requirements) |
| Stem Cell Viability Post-Editing | Variable (DSB-induced toxicity) | Generally high | Generally high |
Application Notes for Stem Cell Engineering
CRISPR-Cas Nuclease Applications
CRISPR-Cas nuclease systems remain widely utilized for stem cell engineering applications where complete gene knockout is desired. The technology is particularly valuable for functional genomics screens in stem cells, enabling researchers to identify genes essential for pluripotency maintenance, differentiation, and disease pathogenesis. In Alzheimer's disease research, CRISPR-Cas9 has been employed to introduce disease-associated mutations in APP, PSEN1, and PSEN2 genes into healthy stem cells, creating isogenic disease models that recapitulate pathological features including Aβ plaque formation and tau hyperphosphorylation.
The implementation of virus-free editing methods using synthetic guide RNAs and electroporation has significantly improved the safety profile of CRISPR-Cas9 in therapeutic applications. This approach avoids random viral integration into the host genome and reduces unwanted DNA edits, making it particularly suitable for clinical translation. Research demonstrates that this method enables efficient knock-in of large DNA sequences, including chimeric antigen receptors (CARs) for cancer immunotherapy, with high specificity and cell viability.
Base Editing Applications
Base editors provide a powerful alternative to nuclease-based approaches for precise single-nucleotide modifications in stem cells without inducing DSBs. These systems are particularly valuable for correcting point mutations associated with genetic disorders or for introducing protective polymorphisms that may modify disease risk. In stem cell models of Alzheimer's disease, base editors can precisely modify risk genes such as TREM2, CD33, and ABCA7, which are primarily expressed in microglia and play important roles in neuroinflammation.
The application of base editing in stem cells is especially advantageous for modifications that require high efficiency with minimal genotoxic stress. Since base editors do not rely on HDR, which is inefficient in many stem cell types, they can achieve higher correction rates while maintaining cell viability and pluripotency. However, the potential for bystander editing, where adjacent nucleotides within the editing window are unintentionally modified, requires careful consideration and design optimization.
Prime Editing Applications
Prime editing represents the most versatile precise editing technology, capable of installing all possible base-to-base substitutions, small insertions, and deletions without DSB formation. This technology is particularly valuable for correcting pathogenic mutations in stem cells with high precision, making it ideal for generating genetically corrected patient-specific iPSCs for regenerative medicine applications. The ability to perform precise edits without donor DNA templates simplifies the editing process and reduces the risk of random integration.
Recent advancements in prime editing systems have significantly improved their efficiency for stem cell applications. The development of engineered pegRNAs (epegRNAs) with structured RNA motifs at the 3' end protects against degradation and improves editing efficiency by 3-4-fold across multiple human cell lines, including primary fibroblasts. Additionally, the split prime editor (sPE) system addresses delivery challenges associated with the large size of traditional prime editors by allowing nCas9 and reverse transcriptase to function independently, enabling delivery via dual AAV vectors.
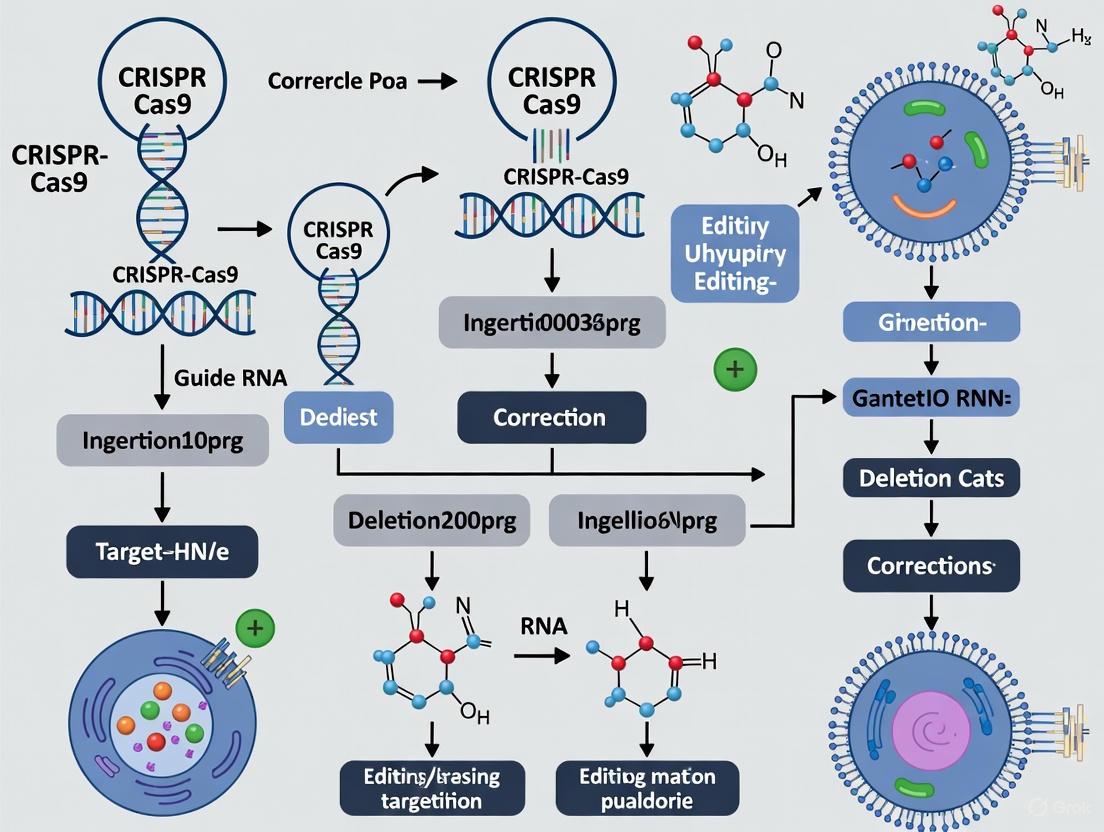
Prime editing workflow showing the stepwise process of precise genome editing.
Experimental Protocols
Protocol 1: Virus-Free CRISPR Editing in Stem Cells Using Synthetic gRNA
This protocol describes a method for editing stem cells using synthetic guide RNAs and electroporation, eliminating the need for viral vectors and reducing the risk of off-target integration.
Materials Required:
- Cultured stem cells (iPSCs, NSCs, or MSCs)
- Synthetic guide RNA (synthesized commercially)
- Cas9 protein (commercially available)
- Electroporation system (e.g., Neon Transfection System)
- Stem cell culture medium with appropriate supplements
- DNA donor template (for HDR-mediated editing)
- Validation reagents (T7 Endonuclease I, sequencing primers)
Procedure:
Guide RNA Design and Preparation:
- Design gRNAs targeting the genomic region of interest using established design tools
- Order synthetic gRNAs with chemical modifications to enhance stability
- Resuspend gRNAs in nuclease-free water to a working concentration of 100 μM
Ribonucleoprotein (RNP) Complex Formation:
- Combine 10 μg of Cas9 protein with 5 μg of synthetic gRNA in electroporation buffer
- Incubate at room temperature for 15-20 minutes to allow RNP complex formation
Stem Cell Preparation:
- Culture stem cells to 70-80% confluency in appropriate conditions
- Dissociate cells using enzyme-free dissociation reagent to maintain viability
- Wash cells twice with PBS and resuspend in electroporation buffer at a concentration of 1×10^7 cells/mL
Electroporation:
- Mix 10 μL of cell suspension with 5 μL of RNP complex
- Transfer to electroporation cuvette and electroporate using optimized parameters (typically 1300-1600V, 10-30ms for stem cells)
- Immediately transfer cells to pre-warmed culture medium
Post-Transfection Culture:
- Plate transfected cells onto matrix-coated plates at appropriate density
- Monitor cell viability daily and change medium after 24 hours
- Allow 48-72 hours for expression and editing before analysis
Validation of Editing:
- Extract genomic DNA 72 hours post-transfection
- Amplify target region by PCR using flanking primers
- Analyze editing efficiency using T7 Endonuclease I assay or sequencing
Virus-free CRISPR editing workflow using synthetic gRNA and electroporation.
Protocol 2: Prime Editing in Stem Cells Using epegRNAs
This protocol outlines the implementation of prime editing in stem cells using engineered pegRNAs (epegRNAs) to enhance editing efficiency through improved RNA stability.
Materials Required:
- Prime editor expression plasmid (PE2, PE3, or newer versions)
- epegRNA expression vector or synthetic epegRNA
- Stem cell line of interest
- Transfection reagent (lipofection or electroporation system)
- Appropriate antibiotics for selection
- Validation primers for targeted sequencing
Procedure:
epegRNA Design and Preparation:
- Design pegRNA with spacer sequence (17-20 nt) and RTT encoding desired edit
- Incorporate evopreQ1 or mpknot RNA motifs at 3' end to enhance stability
- For plasmid-based expression, clone into appropriate backbone with U6 promoter
- For synthetic epegRNA, order with chemical modifications and resuspend to 100 μM
Stem Cell Transfection:
- Culture stem cells to 60-70% confluency in optimal conditions
- For lipofection: Combine 2 μg prime editor plasmid + 1 μg epegRNA plasmid with transfection reagent
- For electroporation: Mix 5 μg prime editor mRNA + 3 μg synthetic epegRNA with cells in buffer
- Transfert using optimized method and parameters for specific stem cell type
Post-Transfection Culture and Selection:
- Culture transfected cells for 48 hours in standard conditions
- If using selection markers, apply appropriate antibiotic 24 hours post-transfection
- Maintain selection for 5-7 days, changing medium every 2-3 days
Editing Efficiency Analysis:
- Harvest cells 7 days post-transfection for genomic DNA extraction
- Perform PCR amplification of target locus
- Use targeted next-generation sequencing to quantify editing efficiency
- Analyze sequencing data for precise edit incorporation and byproduct formation
Clone Isolation and Validation (Optional):
- For single-cell analysis, perform limiting dilution or FACS sorting
- Expand individual clones for 2-3 weeks
- Screen clones by PCR and sequencing to identify correctly edited isolates
- Validate pluripotency markers in edited clones to ensure stemness maintenance
Research Reagent Solutions
Essential Reagents for CRISPR-Stem Cell Research
Table 3: Key Research Reagents for CRISPR-Based Stem Cell Engineering
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| CRISPR Nucleases | Cas9 Nuclease (S. pyogenes), HiFi Cas9 variants | DNA cleavage for gene disruption or HDR | HiFi variants reduce off-target effects in sensitive stem cell applications |
| Base Editors | BE4max, ABE8e | Direct base conversion without DSBs | BE4max for C->T conversions; ABE8e for A->G conversions with improved efficiency |
| Prime Editors | PE2, PE3, PE6 systems | Precise search-and-replace editing | PE6 systems with compact RT show improved efficiency and delivery capability |
| Editing Validation | T7 Endonuclease I, Authenticase, Next-generation sequencing kits | Detection and quantification of editing events | Authenticase outperforms T7 Endo I in detecting diverse mutation types |
| Delivery Systems | Lipid nanoparticles (LNPs), Electroporation systems, AAV vectors | Introduction of editing components into cells | LNPs show promise for in vivo delivery; electroporation preferred for ex vivo stem cell editing |
| Stem Cell Culture | Matrices (Matrigel, Laminin), Defined media, Rho-associated kinase (ROCK) inhibitor | Maintenance of pluripotency and viability | ROCK inhibitor improves survival post-editing procedures |
The integration of advanced CRISPR technologies with stem cell biology has created powerful platforms for disease modeling, drug discovery, and therapeutic development. The evolving CRISPR toolbox, encompassing nucleases, base editors, and prime editors, provides researchers with multiple options for genetic manipulation, each with distinct advantages for specific applications. Selection of the appropriate technology depends on the required precision, efficiency, and practical considerations for stem cell engineering.
Future developments in CRISPR-stem cell applications will likely focus on enhancing editing efficiency, specificity, and delivery methods. The emergence of newer prime editing systems with improved efficiency and reduced size addresses current limitations, potentially enabling broader therapeutic applications. Additionally, advances in delivery systems, particularly lipid nanoparticles and virus-free methods, will facilitate safer clinical translation. As these technologies mature, their integration with stem cell research promises to accelerate the development of personalized regenerative therapies for genetic disorders, including neurodegenerative diseases like Alzheimer's.
The ability to recapitulate human pathology in vitro is a cornerstone of modern biomedical research. Gene-edited stem cells have emerged as a powerful platform for this purpose, enabling the precise investigation of genetic contributions to disease mechanisms and the development of novel therapeutic strategies. The integration of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) technology with stem cell biology has been particularly transformative, allowing for the creation of highly accurate and standardized disease models. These models are instrumental for drug discovery, functional genomics, and personalized medicine, providing a human-relevant context that is often lacking in animal models [8] [9].
This protocol details the application of CRISPR-Cas9 for introducing disease-relevant mutations into mouse embryonic stem cells (mESCs) to model complex neurodevelopmental disorders, as exemplified by recent research into autism spectrum disorder (ASD) [8]. The methodology can be adapted to model a wide range of genetic conditions, providing a robust framework for studying pathology in a controlled, scalable system.
Key Quantitative Data from a Representative Study
A recent large-scale study created a bank of 63 mouse embryonic stem cell lines, each with a distinct autism spectrum disorder (ASD)-associated mutation, providing a standardized platform for pathological investigation [8]. Key quantitative outcomes from the characterization of these models are summarized below.
Table 1: Quantitative Outcomes from a CRISPR-Edited mESC Disease Model Bank
| Parameter | Result / Value | Context and Significance |
|---|---|---|
| Number of Cell Lines | 63 | A bank of mESC lines, each with a different genetic variant strongly associated with Autism Spectrum Disorder (ASD) [8]. |
| Model Fit (R-value) | 0.97 | Demonstrates a high-efficiency, precise editing outcome in a monoclonal cell line derived from a single cell [10]. |
| Protein Reduction (Therapeutic Effect) | ~90% reduction | Observed in clinical trials for hereditary transthyretin amyloidosis (hATTR) using an LNP-delivered CRISPR therapy, showcasing the therapeutic potential of this approach [11]. |
| Key Discovered Pathology | Disrupted protein quality control in neurons | A key pathological mechanism identified through the mESC model bank; neurons were unable to eliminate misshapen proteins [8]. |
Experimental Protocols
Protocol 1: Design and Production of CRISPR Constructs
This protocol covers the initial design and cloning steps for preparing the CRISPR-Cas9 components for stem cell transfection.
Materials:
- gRNA Design Tool: CRISPR-GPT AI tool or similar design software [6].
- Plasmid Backbone: e.g., PX330 (Addgene) for expressing Cas9 and sgRNA [9].
- Oligonucleotides: For synthesizing target-specific guide RNA (gRNA) sequences.
- Cloning Enzymes: Restriction enzymes, ligase, etc.
Method:
- gRNA Design: Identify a 20-nucleotide target sequence adjacent to a 5'-NGG-3' Protospacer Adjacent Motif (PAM) in the gene of interest (e.g., Tex15 for infertility studies) [10]. Tools like CRISPR-GPT can predict optimal gRNA sequences and potential off-target effects [6].
- gRNA Cloning: Synthesize and anneal oligonucleotides corresponding to the target sequence. Ligate them into the gRNA cloning site of the Cas9 plasmid (e.g., PX330) using appropriate restriction enzymes [9].
- Validation: Transform the ligated plasmid into competent bacteria. Select positive clones and validate the plasmid sequence via Sanger sequencing.
Protocol 2: Culturing and Transfection of Mouse Embryonic Stem Cells
This protocol outlines the maintenance and genetic modification of mESCs.
Materials:
- Cell Line: Mouse Embryonic Stem Cells (mESCs) [8].
- Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS) and 1% penicillin-streptomycin [10].
- Transfection Reagent: Lipid-based transfection reagent (e.g., DNAfectin) [10].
- Selection Antibiotic: e.g., Puromycin.
Method:
- Cell Culture: Maintain mESCs in pre-coated T-25 flasks with complete DMEM medium. Incubate at 37°C in a 5% CO₂ environment. Passage cells upon reaching 90% confluence using trypsinization [10].
- Antibiotic Optimization: Perform a cytotoxicity assay to determine the optimal concentration of puromycin (e.g., range of 5.0 μg/mL to 0.01 μg/mL) required to eliminate 95% of non-transfected cells within 48 hours [10].
- Transfection: Plate cells in a multi-well plate. The following day, transfect the cells with the CRISPR-Cas9 plasmid complexed with the lipid-based transfection reagent at an optimized ratio (e.g., a 1:3.5 DNA:DNAfectin ratio) [10].
- Selection: Apply the pre-determined optimal concentration of puromycin 24-48 hours post-transfection to select for successfully transfected cells.
Protocol 3: Validation of Gene Editing
This protocol describes the confirmation of successful genetic modifications in the stem cell population.
Materials:
- Lysis Buffer: For genomic DNA extraction.
- PCR Reagents: Polymerase, primers flanking the target site, dNTPs.
- Restriction Enzyme: For mutation site enzyme cut analysis if the edit disrupts a restriction site.
- Sanger Sequencing Reagents.
Method:
- Genomic DNA Extraction: Harvest transfected and selected cells. Extract genomic DNA using a standard lysis-protocol precipitation method.
- Initial Screening: Amplify the target genomic region by PCR. Perform a restriction fragment length polymorphism (RFLP) assay if the edit alters a restriction site. Cleavage failure indicates potential indel mutations [10].
- Sequence Verification: Purify the PCR product and subject it to Sanger sequencing. Analyze the sequencing chromatograms for the presence of insertions or deletions (indels) around the cut site, which indicate a successful knockout. For heterozygous edits, two distinct indel variants may be present [10].
- In-silico Analysis: Use software to translate the DNA sequence and predict the effect of indels on the reading frame and protein function.
Experimental Workflow and Signaling Pathways
The following diagram illustrates the complete experimental workflow for creating and differentiating a gene-edited stem cell disease model, from design to pathological analysis.
The pathological mechanism discovered through this workflow, specifically for certain autism models, involves a critical disruption of protein quality control in neurons. The diagram below outlines this key signaling and cellular process.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for CRISPR-Stem Cell Disease Modeling
| Item | Function / Application | Example / Note |
|---|---|---|
| CRISPR Plasmid | Expresses both the Cas9 nuclease and the single-guide RNA (sgRNA) for targeted DNA cleavage. | The PX330 vector is a widely used example [9]. |
| Lipid Nanoparticles (LNPs) | A non-viral delivery system for in vivo delivery of CRISPR components; shows promise for future clinical applications. | Effective for liver-targeted therapies; allows for re-dosing [11] [9]. |
| Mouse Embryonic Stem Cells (mESCs) | A self-renewing cell type that can be differentiated into various cell lineages, serving as the foundation for in vitro disease models. | Used to create a standardized bank of 63 ASD models [8]. |
| Lipid-based Transfection Reagent | Facilitates the delivery of CRISPR plasmid DNA into stem cells in vitro. | A 1:3.5 DNA:DNAfectin ratio was identified as optimal for SSCs [10]. |
| AI Design Tool (CRISPR-GPT) | An AI agent that assists in designing CRISPR experiments, predicting off-target effects, and troubleshooting. | Speeds up experimental design and flattens the learning curve [6]. |
| Adeno-Associated Virus (AAV) | A viral delivery vector with high transduction efficiency, but limited packaging capacity. | Commonly used in gene therapy; packaging capacity is a key constraint [9]. |
The convergence of CRISPR-based gene editing with stem cell biology represents a transformative paradigm in therapeutic development, enabling researchers to move beyond symptom management toward curative interventions. This approach allows for the precise correction of pathogenic mutations in patient-derived stem cells, creating powerful disease models and autologous cell therapies. For monogenic disorders, the strategy often involves direct correction of the causal variant, while for complex diseases, it requires targeting key genetic nodes within pathological networks. The protocols outlined in this application note provide a framework for identifying these therapeutic targets and executing their correction using state-of-the-art CRISPR technologies, with particular emphasis on stem cell applications relevant to drug development and clinical translation.
Therapeutic Target Classification and Prioritization
The strategic selection of therapeutic targets is fundamental to successful gene editing outcomes. Targets can be systematically categorized based on disease etiology, with distinct editing strategies employed for each category.
Table 1: Classification of Gene Editing Therapeutic Targets
| Target Category | Disease Examples | CRISPR Strategy | Editing Outcome |
|---|---|---|---|
| Monogenic Loss-of-Function | Spinal Muscular Atrophy, Ornithine Transcarbamylase Deficiency [12] | HDR-mediated correction [12], Base Editing [13] | Restore protein function |
| Monogenic Gain-of-Function | Early-onset Alzheimer's (APP, PSEN1/2 mutations) [14] | NHEJ-mediated knockout [15], Base Editing [13] | Disrupt pathogenic allele |
| Risk Alleles in Complex Diseases | Late-onset Alzheimer's (APOEε4, TREM2) [14] | Gene silencing (CRISPRi), Base Editing [13] | Modulate disease susceptibility |
| Regulatory Elements for Cell Therapy | Universal CAR-T [16], Hypo-immunogenic stem cells [16] | Multiplex gene knockout (HLA disruption) [16] | Evade immune rejection |
The prioritization of targets for stem cell-based protocols requires additional considerations, including gene expression in relevant stem cell derivatives, the feasibility of achieving high editing efficiency without compromising stemness, and the ability to differentiate corrected stem cells into therapeutically relevant cell types.
Experimental Protocols for Target Validation and Correction
Protocol: In Vitro Disease Modeling using Patient-Derived iPSCs
Application Note: This protocol is essential for studying disease mechanisms and screening candidate therapeutic targets, particularly for neurological disorders like Alzheimer's disease where patient neurons are inaccessible [14].
Workflow Diagram:
Methodology:
- iPSC Generation: Reprogram patient dermal fibroblasts or peripheral blood mononuclear cells using non-integrating Sendai virus or episomal vectors expressing OCT4, SOX2, KLF4, and c-MYC. Culture established iPSC lines in mTeSR1 or Essential 8 medium on Matrigel-coated plates [14].
- CRISPR-mediated Gene Correction: Design a sgRNA targeting within 50 bp upstream of the pathogenic mutation. For base editing applications, ensure the target base falls within the activity window (typically positions 4-8 for ABE, 3-9 for CBE) of the editor [13]. Deliver ribonucleoprotein (RNP) complexes comprising 5 µg SpCas9 protein and 2 µg synthetic sgRNA via nucleofection (Lonza 4D-Nucleofector).
- Neural Differentiation: Differentiate corrected and uncorrected iPSCs into cortical neurons using a dual-SMAD inhibition protocol. Treat cells with 100 nM LDN-193189 and 10 µM SB431542 for 10 days to induce neural induction, followed by maturation in neurobasal medium containing BDNF, GDNF, and cAMP for 6-8 weeks [14].
- Phenotypic Analysis:
- Aβ42/Aβ40 Ratio: Quantify using ELISA from conditioned media at day 50 of differentiation. A significant reduction in the Aβ42/Aβ40 ratio in corrected lines indicates phenotypic rescue [14].
- Tau Phosphorylation: Perform western blot analysis using antibodies against phosphorylated tau (AT8, PHF-1) and total tau. Calculate the p-tau/total tau ratio.
- Synaptic Function: Assess using multi-electrode array (MEA) to measure spontaneous neural activity.
Protocol: HDR-Mediated Correction in Hematopoietic Stem Cells (HSCs)
Application Note: This ex vivo editing protocol is foundational for treating monogenic blood disorders and can be adapted for introducing protective mutations. The use of HDR allows for precise nucleotide conversion.
Workflow Diagram:
Methodology:
- HSC Pre-stimulation: Isolate CD34+ hematopoietic stem cells from human mobilized peripheral blood using magnetic-activated cell sorting (MACS). Pre-stimulate cells in StemSpan SFEM II medium supplemented with 100 ng/mL SCF, 100 ng/mL TPO, and 100 ng/mL Fit3-L for 48 hours at 37°C, 5% CO₂ [16].
- RNP Complex Formation: Combine 40 µg HiFi Cas9 protein with 30 µg synthetic sgRNA (resuspended in nuclease-free water) and incubate at room temperature for 10 minutes to form RNP complexes.
- HDR Donor Design: Design a single-stranded oligodeoxynucleotide (ssODN) donor template with ~100 bp homology arms flanking the correction. Incorporate silent mutations (PAM-disruption) within the protospacer to prevent re-cleavage. Add a 5' phosphorothioate modification to enhance stability.
- Electroporation: Mix 2×10⁵ pre-stimulated CD34+ cells with the RNP complex and 2 µL of 100 µM ssODN donor. Electroporate using the Lonza 4D-Nucleofector (pulse code DS-138) in 20 µL P3 Primary Cell Solution.
- Engraftment and Functional Assessment: Transplant 5×10⁵ edited CD34+ cells into sublethally irradiated (250 cGy) NSG mice via tail vein injection. After 16 weeks, analyze bone marrow for human CD45+ cell engraftment by flow cytometry. Assess lineage-specific correction rates via next-generation sequencing of colony-forming unit (CFU) assays [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for CRISPR-Stem Cell Research
| Reagent Category | Specific Product/System | Research Application | Key Considerations |
|---|---|---|---|
| CRISPR Nucleases | HiFi Cas9, SpCas9-NG [15], ABE8e [13] | Target gene knockout, base editing | PAM flexibility (NG/G), reduced off-targets, high efficiency |
| Stem Cell Culture | mTeSR1, Essential 8, Matrigel, Recombinant Vitronectin | iPSC maintenance and expansion | Support pluripotency, xeno-free formulations |
| Delivery Systems | Lipoplex nanoparticles [16], Neon Transfection System, 4D-Nucleofector | RNP/sgRNA delivery to stem cells | Cell viability, editing efficiency, scalability |
| HDR Enhancers | NHEJ inhibitors (e.g., SCR7), RS-1 [16] | Improve precise editing rates | Cytotoxicity optimization required |
| Validation Tools | T7 Endonuclease I, Next-Generation Sequencing, Flow Cytometry | Edit efficiency and off-target analysis | Multiplexed amplicon sequencing for comprehensive profiling |
Advanced Editing Modalities for Complex Disease Targets
For complex diseases influenced by multiple genetic and environmental factors, targeting individual pathogenic mutations is often insufficient. Instead, strategies focus on modulating key pathways or creating protective genetic modifications.
Base Editing for Pathogenic Transition Mutations
Cytosine Base Editors (CBEs) and Adenine Base Editors (ABEs) enable precise conversion of C•G to T•A and A•T to G•C base pairs, respectively, without inducing double-strand breaks. These editors theoretically correct ∼95% of pathogenic transition mutations cataloged in ClinVar [13]. In a recent preclinical study for Alpha-1 Antitrypsin Deficiency (AATD), a single dose of CRISPR base editor CTX460 achieved over 90% mRNA correction and restored circulating protein more than five-fold in rodent models [16].
Application Workflow:
- Target Analysis: Confirm the pathogenic single-nucleotide variant (SNV) is within the activity window of the selected base editor.
- Editor Selection: For A•T to G•C corrections, use ABE8e; for C•G to T•A corrections, use BE4max. For enhanced specificity, employ high-fidelity versions with reduced off-target effects [13].
- Delivery: For in vivo applications, package ABE mRNA into liver-tropic LNP formulations (10 mg/kg dose). For ex vivo stem cell editing, use electroporation of RNP complexes.
- Validation: Perform deep sequencing of the target locus and computationally predicted off-target sites. Assess protein restoration via ELISA or mass spectrometry.
Multiplexed Editing for Cell Therapy Engineering
The creation of universal allogeneic cell therapies requires simultaneous disruption of multiple genes to prevent immune rejection while introducing therapeutic transgenes. This approach has been successfully applied to engineer "universal" regulatory T cells for off-the-shelf transplant therapy by using CRISPR to disrupt HLA class I and II genes while inserting an HLA-E fusion protein [16].
Protocol Overview:
- gRNA Array Design: Clone up to 7 gRNAs targeting HLA-A, HLA-B, HLA-C, and CIITA into a multiplex tRNA-gRNA vector system [15].
- Stem Cell Editing: Electroporate hematopoietic stem cells or T cells with Cas9 RNP complexes and AAV6 donor vectors containing the HLA-E transgene.
- Selection and Expansion: Use FACS to isolate HLA-negative populations. Expand cells in GMP-grade media with cytokines (IL-2, IL-7, IL-15).
- Functional Validation: Perform mixed lymphocyte reaction assays to confirm reduced alloreactivity. Evaluate in vivo persistence in humanized mouse models.
The systematic identification and validation of therapeutic targets across the disease spectrum, combined with optimized CRISPR editing protocols for stem cells, provides a powerful roadmap for developing transformative genetic medicines. The integration of base editing and multiplexed gene disruption technologies enables addressing both monogenic disorders and complex diseases with unprecedented precision. As delivery technologies continue to advance and long-term safety data accumulate, these protocols will form the foundation for a new generation of stem cell-based therapeutics that move beyond palliative care to offer durable, potentially curative outcomes for patients with previously untreatable genetic conditions.
Cutting-Edge Editing Techniques and Workflows for Stem Cell Correction
The development of clustered regularly interspaced short palindromic repeats (CRISPR)-based systems has revolutionized biomedical research, providing scientists with an unprecedented ability to manipulate genetic material with precision. For researchers focused on correcting stem cell mutations, selecting the appropriate gene-editing protocol is paramount to experimental success. This article provides a comprehensive comparison of four fundamental genome-editing approaches: homology-directed repair (HDR), non-homologous end joining (NHEJ), base editing, and prime editing. Each technology offers distinct advantages and limitations, with optimal selection dependent on specific research goals, target cell types, and desired editing outcomes. Understanding the mechanistic basis, efficiency, and applications of these systems is essential for designing effective stem cell gene correction strategies, particularly as these technologies advance toward clinical applications in precision medicine [17].
The evolution from traditional nuclease-based systems to newer precision editing tools reflects the field's ongoing pursuit of greater specificity and reduced unintended consequences. While early programmable nucleases like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) established the feasibility of targeted genome manipulation, their intricate design requirements limited widespread adoption [18]. The discovery of RNA-programmable CRISPR systems dramatically accelerated gene-editing applications due to their remarkable efficiency, ease of programmability, and versatility [17]. This review focuses on the current state of genome-editing technologies, with particular emphasis on their applicability to stem cell research, where precision and safety considerations are of utmost importance.
Mechanism of Action and Key Applications
Double-Strand Break Repair Pathways: HDR and NHEJ
Homology-Directed Repair (HDR) is a high-fidelity DNA repair pathway that utilizes a homologous donor template to enable precise genetic modifications, including targeted insertions, deletions, and substitutions. When a double-strand break (DSB) occurs, the MRN complex (MRE11–RAD50–NBS1) identifies the break and initiates limited end resection with CtIP, creating 3' single-stranded overhangs [18]. Further resection by Exo1 and the Dna2/BLM helicase complex generates extended 3' ssDNA tails, which are protected by replication protein A (RPA). RAD51 then displaces RPA to form nucleoprotein filaments that perform a homology search and initiate strand invasion using a donor template, leading to precise DNA repair through synthesis-dependent strand annealing (SDSA) or double-strand break repair (DSBR) pathways [18]. A significant limitation for stem cell research is that HDR is predominantly active in the S/G2 phases of the cell cycle, making it inefficient in many therapeutically relevant cell types, including quiescent stem cells [17].
Non-Homologous End Joining (NHEJ) represents the cell's primary "first responder" to DSBs and operates throughout all cell cycle phases. In canonical NHEJ, the Ku70–Ku80 heterodimer immediately recognizes and binds to broken DNA ends, preventing extensive resection and recruiting DNA-dependent protein kinase catalytic subunit (DNA-PKcs) [18]. The complex may employ nucleases like Artemis to process ends and polymerases such as Pol μ or Pol λ to fill small gaps before XRCC4 and DNA ligase IV perform final ligation [18]. While NHEJ is highly efficient and effective for gene disruption strategies, it is inherently error-prone, often resulting in small insertions or deletions (indels) that disrupt the target site. In stem cell research, NHEJ is particularly valuable for creating gene knockouts, though its unpredictable outcomes present challenges for precision applications.
Alternative repair pathways such as microhomology-mediated end joining (MMEJ) also contribute to DSB repair outcomes. MMEJ utilizes microhomologies (2-20 nucleotides) to guide annealing of opposing DNA ends, typically mediated by DNA polymerase theta (Pol θ) and PARP1 [18]. This pathway often generates moderate-to-large deletions and is considered highly error-prone, further complicating editing outcomes when using DSB-dependent approaches.
Precision Editing Without Double-Strand Breaks: Base and Prime Editing
Base Editing enables direct chemical conversion of one DNA base to another without requiring DSBs or donor DNA templates. Base editors are modular fusion proteins comprising a catalytically impaired Cas9 nickase (nCas9) fused to a nucleotide deaminase enzyme [17]. Two primary classes have been developed: cytosine base editors (CBEs), which mediate C•G to T•A conversions using a cytidine deaminase domain, and adenine base editors (ABEs), which facilitate A•T to G•C conversions using an engineered tRNA-specific adenosine deaminase (TadA) [17] [19]. When the complex binds to target DNA, the deaminase chemically alters bases within a narrow editing window, achieving highly efficient point mutations with minimal indel formation [17]. This makes base editors particularly suitable for correcting specific pathogenic point mutations in stem cells without activating DNA damage response pathways.
Prime Editing represents a more versatile "search-and-replace" technology capable of introducing all 12 possible base-to-base conversions, small insertions, and deletions without requiring DSBs or donor DNA templates [19]. The system employs a prime editor protein consisting of a Cas9 nickase (H840A) fused to an engineered reverse transcriptase (RT), programmed with a specialized prime editing guide RNA (pegRNA) [19] [20]. The pegRNA both specifies the target site and contains an extended reverse transcriptase template (RTT) encoding the desired edit. After nicking the target DNA, the released 3' flap hybridizes with the primer binding site (PBS) on the pegRNA, priming reverse transcription using the RTT as a template [20]. The resulting edited flap is then incorporated into the genome through cellular repair processes. This multi-step hybridization process enhances editing specificity while providing unprecedented versatility for precise genetic modifications in stem cells [19].
Table 1: Comparison of Key Features of Genome Editing Technologies
| Feature | HDR | NHEJ | Base Editing | Prime Editing |
|---|---|---|---|---|
| DNA Break Type | Double-strand break | Double-strand break | Single-strand nick | Single-strand nick |
| Donor Template Required | Yes | No | No | No (encoded in pegRNA) |
| Editing Precision | High | Low (error-prone) | High | Very High |
| Primary Applications | Precise gene correction, insertions | Gene knockouts, disruptions | Point mutations (C>T, A>G) | All point mutations, small insertions/deletions |
| Theoretical Editing Scope | Unlimited | Disruptions only | Transition mutations only | All 12 possible base substitutions, insertions, deletions |
| Stem Cell Efficiency | Low (cell cycle dependent) | High | Moderate to High | Variable (improving with newer systems) |
| Indel Formation | Low (but competing NHEJ) | High | Very Low | Very Low |
| Key Limitations | Low efficiency, cell cycle dependence | Unpredictable outcomes, indels | Restricted to specific base changes, bystander edits | Efficiency challenges, complex pegRNA design |
Experimental Protocols and Workflows
HDR-Mediated Gene Correction in Stem Cells
Protocol Overview: This protocol describes HDR-based precise gene correction in human pluripotent stem cells (hPSCs) using CRISPR-Cas9 and single-stranded oligodeoxynucleotide (ssODN) donor templates. The procedure spans 7-10 days from nucleofection to genotyping.
Step-by-Step Workflow:
- gRNA Design and Validation: Design gRNAs targeting adjacent to the mutation site using established tools (e.g., CRISPOR, ChopChop). Select targets with high on-target and low off-target scores. Validate editing efficiency using a T7E1 or tracking indel/decomposition by evolution (TIDE) assay before proceeding with HDR experiments.
Donor Template Design: Design ssODN donor templates (90-200 nt) with the desired correction flanked by homologous arms (35-90 nt each). Incorporate silent mutations in the PAM site or protospacer to prevent re-cutting of corrected sequences. Include a restriction site for diagnostic digestion if possible.
Stem Cell Preparation: Culture hPSCs in feeder-free conditions, ensuring >90% viability and optimal growth. Passage cells 2 days before nucleofection to ensure actively dividing cultures, which improves HDR efficiency.
Ribonucleoprotein (RNP) Complex Formation: Combine 10 µg of purified Cas9 protein with 5 µg of synthetic gRNA in nucleofection buffer. Incubate at room temperature for 10-20 minutes to form RNP complexes.
Nucleofection: Harvest 1×10^6 hPSCs using gentle dissociation reagent. Centrifuge and resuspend in stem cell-optimized nucleofection solution. Add RNP complexes and 2-4 µM ssODN donor to cell suspension. Transfer to nucleofection cuvette and electroporate using manufacturer's recommended program (e.g., CA-137 for hPSCs).
Post-Transfection Recovery: Immediately transfer cells to pre-warmed culture medium with 10 µM ROCK inhibitor. Plate at appropriate density on matrix-coated plates. Refresh medium after 24 hours, removing ROCK inhibitor.
HDR Enrichment (Optional): For difficult-to-edit cells, implement chemical enrichment using 1-5 µM NU7026 (DNA-PKcs inhibitor) or 1 µM Scr7 (Ligase IV inhibitor) for 48-72 hours post-nucleofection to suppress NHEJ and favor HDR.
Clonal Isolation and Screening: After 5-7 days, harvest and dissociate cells to single-cell suspension. Seed at low density (1-10 cells/cm²) for clonal expansion. Pick individual colonies after 10-14 days, expand, and genotype using PCR/restriction digest and Sanger sequencing to identify correctly modified clones.
Troubleshooting Notes: Low HDR efficiency may be improved by optimizing donor design, using chemical enhancers, or synchronizing cells in S/G2 phase. High cytotoxicity may require titration of RNP concentrations or alternative delivery methods.
Prime Editing in Stem Cells
Protocol Overview: This protocol describes prime editing in hPSCs using the PEmax editor system with optimized pegRNA designs. The complete workflow requires 10-14 days from transfection to genotyping.
Step-by-Step Workflow:
- pegRNA Design: Design pegRNAs with 10-15 nt primer binding site (PBS) and 10-30 nt reverse transcriptase template (RTT) containing desired edits. Use computational tools (PE-Designer, pegFinder) to optimize designs. Select pegRNAs with predicted strong binding and minimal secondary structure.
Stabilized pegRNA Construction: Incorporate evopreQ1 or mpknot RNA motifs at the 3' end of pegRNAs to enhance stability and resist degradation. Synthesize as chemically modified RNA or clone into expression vectors with appropriate RNA polymerase III promoters.
Prime Editor Delivery: For hPSCs, use ribonucleoprotein (RNP) delivery of PEmax protein complexed with pegRNA. Combine 15 µg PEmax protein with 7.5 µg stabilized pegRNA and 5 µg nicking gRNA (for PE3b system) in nucleofection buffer. Incubate 15 minutes at room temperature.
Stem Cell Nucleofection: Harvest 1×10^6 log-phase hPSCs. Resuspend in P3 Primary Cell Nucleofector Solution with supplement. Add RNP complexes and transfer to nucleofection cuvette. Electroporate using program CA-137.
Post-Nucleofection Recovery: Plate cells in pre-warmed stem cell medium with 10 µM ROCK inhibitor. Refresh medium after 24 hours. Allow recovery for 48-72 hours before assessing editing efficiency.
Efficiency Assessment: Harvest a portion of cells (day 3-4) for initial efficiency assessment using next-generation sequencing or droplet digital PCR. For quantitative analysis, extract genomic DNA and amplify target region with barcoded primers for sequencing.
Clonal Isolation: At day 7, dissociate to single cells and plate at clonal density (0.5-1 cell/well) in 96-well plates. Expand colonies for 14-21 days with regular medium changes.
Screening and Validation: Screen clones by PCR and sequencing of the target locus. Validate top candidates through expanded culture and functional assays where appropriate.
Optimization Notes: Editing efficiency can be improved by using engineered pegRNAs (epegRNAs), optimizing PBS length (12-16 nt typically works best), and including MMR suppression agents such as dominant-negative MLH1 (MLH1dn) for certain edits [21]. The PE3 system, which includes an additional nicking gRNA to the non-edited strand, typically provides 2- to 4-fold higher editing efficiency but may slightly increase indel rates [19].
Table 2: Quantitative Performance Comparison of Editing Technologies
| Parameter | HDR | NHEJ | Base Editing | Prime Editing |
|---|---|---|---|---|
| Typical Efficiency in Stem Cells | 0.5-5% | 20-80% | 10-70% | 1-50% (version-dependent) |
| Indel Formation Rate | 5-30% (at target site) | 20-60% | <1-5% | 0.5-5% |
| Editing Purity | Low (mixed outcomes) | High (disruptions) | High (specific conversions) | High (precise edits) |
| Off-Target Effects | DSB-dependent off-targets | DSB-dependent off-targets | DNA/RNA off-target deamination | Minimal reported |
| Optimal Delivery Format | RNP + ssODN | RNP | RNP or mRNA | RNP with epegRNA |
| Time to Clonal Isolation | 10-14 days | 10-14 days | 10-14 days | 10-14 days |
| Key Efficiency Factors | Cell cycle, donor design, NHEJ inhibition | gRNA efficiency, cell health | Editing window, sequence context | pegRNA design, MMR status |
Pathway Diagrams and Editing Mechanisms
Diagram 1: Genome Editing Pathway Selection. DSB-dependent methods (HDR, NHEJ) rely on double-strand breaks, while newer precision techniques (base editing, prime editing) avoid DSBs to enhance safety and reduce unwanted mutations.
Diagram 2: Prime Editing Mechanism. The prime editing process involves target recognition, DNA nicking, hybridization with the primer binding site (PBS) of pegRNA, reverse transcription using the RT template (RTT), and final incorporation of the edit through flap resolution.
Research Reagent Solutions
Table 3: Essential Reagents for Genome Editing in Stem Cells
| Reagent Category | Specific Examples | Function | Considerations for Stem Cell Research |
|---|---|---|---|
| Editor Proteins | S. pyogenes Cas9-NLS, BE4max, PEmax, PE6 variants | Core editing enzymes | Purified proteins for RNP delivery reduce off-target effects and immune activation |
| Guide RNAs | Synthetic sgRNAs, pegRNAs, epegRNAs with stability motifs | Target specification | Chemically modified RNAs enhance stability; epegRNAs improve prime editing efficiency |
| Delivery Tools | Neon Transfection System, Amaxa Nucleofector | Physical delivery method | Stem cell-optimized programs and solutions maximize viability and editing efficiency |
| Stem Cell Media | mTeSR Plus, StemFlex, Essential 8 | Cell culture maintenance | Chemically defined media supports pluripotency during editing workflow |
| Enhancer Compounds | ROCK inhibitor (Y-27632), NHEJ inhibitors (NU7026, Scr7) | Improve cell survival and editing outcomes | ROCK inhibitor critical for single-cell survival; NHEJ inhibitors favor HDR in dividing cells |
| Validation Tools | T7E1 assay, TIDE analysis, NGS panels, ddPCR | Edit confirmation and quantification | Multiplexed approaches recommended to assess on-target efficiency and potential off-target effects |
The selection of an appropriate genome-editing protocol for correcting stem cell mutations requires careful consideration of research goals, technical constraints, and desired outcomes. HDR remains valuable for large insertions but suffers from low efficiency in many stem cell types. NHEJ is highly efficient for gene disruption but inappropriate for precise correction. Base editing offers exceptional efficiency for specific point mutations but is restricted to transitional changes. Prime editing provides unprecedented versatility for diverse edits but requires optimization and efficiency improvements.
Future developments in genome editing will likely focus on enhancing efficiency and specificity while addressing delivery challenges. For base editing, ongoing efforts aim to expand targeting scope and minimize off-target deamination [17]. Prime editing systems are evolving rapidly, with newer versions (PE4, PE5, PE6) showing marked improvements in efficiency through engineered reverse transcriptases and suppression of DNA mismatch repair pathways [21] [20]. The development of smaller editor proteins, such as those utilizing Cas12f1, may alleviate delivery constraints for therapeutic applications [22].
For stem cell researchers, the optimal editing strategy often involves matching the technology to the specific mutation being corrected. Base editing excels for known transition mutations, while prime editing offers a more versatile approach for diverse corrections without DSBs. As these technologies continue to mature, they promise to unlock new possibilities for modeling and treating genetic diseases through precise manipulation of stem cell genomes.
The advent of artificial intelligence has catalyzed a paradigm shift in the development of genome-editing technologies. AI-designed gene editors, such as OpenCRISPR-1, represent a new class of molecular tools that bypass evolutionary constraints to offer optimized properties for research and therapeutic applications. These proteins are not simple modifications of natural systems but are generated de novo by large language models (LLMs) trained on vast biological datasets [23] [24]. For researchers focused on correcting stem cell mutations, these editors provide a platform with the potential for enhanced specificity, reduced immunogenicity, and tailored functionality that can improve the efficacy and safety of stem cell therapies.
The development of OpenCRISPR-1 demonstrates the power of this approach. Created by Profluent Bio, OpenCRISPR-1 is a functional Cas9-like nuclease that maintains the prototypical Type II Cas9 architecture but contains 403 amino acid differences from the commonly used Streptococcus pyogenes Cas9 (SpCas9) and is nearly 200 mutations away from any known natural CRISPR-associated protein [25] [26]. This significant sequence divergence translates to tangible functional benefits, including reduced off-target effects and lower immunogenicity, while maintaining robust on-target activity comparable to SpCas9 [23] [27].
Key Advantages for Stem Cell Research
For researchers developing protocols to correct stem cell mutations, AI-designed editors offer several distinct advantages that address critical challenges in the field:
Enhanced Specificity: OpenCRISPR-1 demonstrates a 95% reduction in off-target editing across multiple genomic sites compared to SpCas9, with median indel rates of 0.32% versus 6.1% for SpCas9 [24]. This high precision is crucial when editing therapeutically relevant stem cells, where off-target mutations could have profound consequences.
Reduced Immunogenicity: Initial characterizations indicate that OpenCRISPR-1 lacks immunodominant and subdominant T cell epitopes for HLA-A*02:01 that are present in SpCas9 [24]. This suggests potentially lower immune recognition in therapeutic contexts, a valuable property for ex vivo stem cell editing and subsequent transplantation.
Functional Flexibility: OpenCRISPR-1 has been successfully adapted for base editing applications when combined with deaminase enzymes, demonstrating its compatibility with diverse editing modalities [23] [25]. This versatility enables researchers to employ the same editor backbone for different types of genetic corrections required in stem cell research.
Novel PAM Compatibilities: While OpenCRISPR-1 maintains similar PAM preferences to SpCas9 (NGG), the AI-driven design approach can generate editors with tailored PAM specificities [23] [24]. This expands the targetable genomic space for correcting disease-causing mutations in stem cells.
Experimental Characterization and Performance Data
Comparative Performance Analysis
Independent evaluations have provided quantitative data on OpenCRISPR-1's performance relative to other CRISPR systems. A comprehensive 2025 study systematically compared FrCas9, SpCas9, and OpenCRISPR-1 across multiple genomic loci using GUIDE-seq and AID-seq methodologies [27]. The results provide critical insights for researchers selecting appropriate editors for stem cell applications.
Table 1: Comparative Performance of CRISPR-Cas9 Systems
| Editor | On-Target Efficiency (Median Indel %) | Off-Target Activity (Median Indel %) | Specificity (Log2 Ratio On:Off Target) | Key PAM Preferences |
|---|---|---|---|---|
| OpenCRISPR-1 | 55.7% | 0.32% | -2.06 | NGG (69.33%), NGA (17.1%) |
| SpCas9 | 48.3% | 6.1% | -3.95 | NGG (76.89%), NGA (12.23%) |
| FrCas9 | Higher than SpCas9 | Fewer off-targets | 4.12 | NNTA (93.93%) |
Structural Validation
Structural analysis through AlphaFold2 predictions confirmed that over 80% of AI-generated proteins, including OpenCRISPR-1, had high-confidence folds (pLDDT > 80), with structural architectures highly similar to natural Cas9 proteins despite significant sequence divergence [23] [26]. Core functional domains including the HNH and RuvC nuclease domains, PAM-interacting domain, and target recognition lobe were preserved in most generated proteins at rates comparable to natural sequences [24].
Protocol: Implementing OpenCRISPR-1 in Stem Cell Editing
Molecular Cloning and Vector Design
To implement OpenCRISPR-1 in your stem cell research, begin with proper molecular cloning strategies:
Expression Vector Construction: Clone the OpenCRISPR-1 sequence (publicly available through AddGene) into your preferred mammalian expression backbone under the control of a constitutive promoter such as EF1α or CAG [25] [24]. The OpenCRISPR-1 coding sequence is 1,380 amino acids in length and should be human-codon optimized for efficient expression in stem cells.
Guide RNA Design: Utilize the companion AI-generated guide RNA sequences specifically designed for OpenCRISPR-1, which are available alongside the editor sequence [25]. Alternatively, design custom sgRNAs using the standard 20-nucleotide spacer length, as OpenCRISPR-1 maintains compatibility with conventional guide RNA architectures.
Delivery Vector Selection: For hematopoietic stem cells, consider lentiviral delivery systems with appropriate safety profiles. For induced pluripotent stem cells (iPSCs), plasmid or mRNA delivery may be preferable to minimize genomic integration concerns.
Delivery Methods for Stem Cells
Different stem cell types require optimized delivery approaches:
Lipid Nanoparticle (LNP) Delivery: For primary hematopoietic stem cells, consider mRNA-based LNP delivery systems. Formulate OpenCRISPR-1 mRNA and sgRNA into LNPs using commercially available kits, with optimization of the N:P ratio for stem cell transfection.
Electroporation of Ribonucleoprotein (RNP): For precise editing with minimal off-target effects, complex purified OpenCRISPR-1 protein with sgRNA to form RNP complexes. Electroporate using stem cell-optimized settings (e.g., 1600V, 10ms, 3 pulses for human iPSCs).
Viral Delivery: For difficult-to-transfect stem cell populations, package OpenCRISPR-1 and sgRNA into lentiviral or AAV vectors. Note that AAV capacity limitations may require dual-vector systems or the use of smaller editors.
Validation and Quality Control
Comprehensive validation is essential for stem cell editing:
On-Target Efficiency Assessment: Extract genomic DNA 72-96 hours post-editing and amplify target loci via PCR. Quantify editing efficiency using T7E1 assay or TIDE analysis, or through next-generation sequencing for absolute quantification.
Off-Target Profiling: Employ GUIDE-seq or AID-seq for genome-wide off-target detection [27]. Focus particularly on sites with 1-4 nucleotide mismatches to your target sequence, as OpenCRISPR-1 shows variable tolerance to mismatches depending on their position.
Stem Cell Potency Validation: After editing, confirm that stem cells maintain their differentiation potential and colony-forming capacity through appropriate functional assays specific to your stem cell type.
Research Reagent Solutions
Table 2: Essential Reagents for Implementing AI-Designed Editors
| Reagent/Catalog | Supplier | Function in Protocol |
|---|---|---|
| OpenCRISPR-1 Expression Plasmid | AddGene (publicly available) | Source of AI-designed editor for cloning and expression |
| Stem Cell-Specific Lipofectamine | Thermo Fisher | Chemical delivery of plasmids or RNPs to stem cells |
| Human Stem Cell Nucleofector Kit | Lonza | Electroporation reagent optimized for stem cell delivery |
| Cas9 ELISA Kit | Multiple suppliers | Detection and quantification of OpenCRISPR-1 expression |
| GUIDE-seq Kit | Integrated DNA Technologies | Genome-wide identification of off-target editing events |
| StemFlex Medium | Thermo Fisher | Culture medium supporting pluripotency during editing process |
| Recombinant Albumin | Sigma-Aldrich | Serum-free culture supplement for edited stem cells |
Troubleshooting and Optimization
Implementing novel editors like OpenCRISPR-1 may require protocol adjustments:
Low Editing Efficiency: If observing suboptimal editing rates, verify OpenCRISPR-1 expression via Western blot using anti-Cas9 antibodies. Ensure sgRNA is specifically designed for OpenCRISPR-1 rather than SpCas9, as the AI-designed guide RNAs may show optimized performance [25].
Cellular Toxicity: Monitor stem cell viability and proliferation rates post-editing. If toxicity is observed, consider reducing RNP concentrations or switching to mRNA delivery, which typically shows transient expression and reduced cellular stress.
Inconsistent Editing Between Clones: For single-cell derived clones, screen multiple colonies to account for heterogeneity. Consider using early-passage stem cells with robust growth characteristics to minimize variability.
Future Perspectives
The successful implementation of OpenCRISPR-1 marks the beginning of a new era in precision genome editing. The AI-driven design process that created OpenCRISPR-1 can generate millions of diverse CRISPR-Cas proteins, representing a 4.8-fold expansion of diversity compared to natural CRISPR-Cas proteins [23]. This vast sequence space enables researchers to potentially request editors tailored to specific stem cell applications, with custom PAM preferences, size constraints, or enzymatic activities.
Furthermore, the integration of AI tools like CRISPR-GPT can assist researchers in designing optimal editing strategies for their specific stem cell mutation correction projects [28]. These systems can select suitable CRISPR systems, design guide RNAs, and recommend delivery methods based on the target cell type and desired edit.
As the field progresses, we anticipate the development of specialized AI-designed editors optimized for particular stem cell types—such as hematopoietic stem cells with enhanced editing in quiescent populations or neural stem cells with improved nuclear import characteristics. These advances will expand the therapeutic potential of stem cell gene editing for treating genetic disorders.
Prime editing is a versatile "search-and-replace" genome editing technology that enables the precise installation of targeted insertions, deletions, and all 12 possible base-to-base conversions without requiring double-strand DNA breaks (DSBs) or donor DNA templates [29]. This technology combines a Cas9 nickase (H840A) fused to an engineered reverse transcriptase (RT) with a specialized prime editing guide RNA (pegRNA) [30]. The pegRNA both specifies the target site and contains the desired edit, serving as a template for the reverse transcriptase [29]. The editing process initiates when the Cas9 nickase domain creates a single-strand nick at the target DNA site. The exposed 3' end then hybridizes to the primer binding site (PBS) on the pegRNA, allowing the reverse transcriptase to synthesize a DNA flap containing the edited sequence using the reverse transcription template (RTT) of the pegRNA [30] [31]. This newly synthesized edited flap is then incorporated into the genome through cellular DNA repair mechanisms [31].
Compared to traditional CRISPR-Cas9 approaches, prime editing offers significantly greater precision with minimal indel formation and reduced off-target effects [30] [32]. While base editing can efficiently correct certain point mutations, it is restricted to specific transition mutations (C•G to T•A, A•T to G•C, and C•G to G•C) and can cause unwanted bystander editing within its activity window [30] [29]. Prime editing overcomes these limitations, enabling correction of a much broader range of mutations, including transversions, small insertions, and small deletions, without the constraint of a narrow editing window [30] [29]. Its mechanism also makes it less dependent on cellular replication and endogenous DNA repair pathways than homology-directed repair (HDR), allowing for more efficient editing in non-dividing cells [31].
Evolution of Prime Editing Systems
Since the initial development of the PE1 system, successive optimizations have substantially improved prime editing efficiency:
- PE2: Incorporates an engineered M-MLV reverse transcriptase with five mutations that enhance thermostability, processivity, and template binding, resulting in a 1.6- to 5.1-fold increase in editing efficiency compared to PE1 [30] [29].
- PE3/PE3b: Adds a second nicking sgRNA to nick the non-edited strand, biasing DNA repair to use the edited strand as a template and increasing editing efficiency 2-3 fold compared to PE2 [30] [29]. PE3b designs the nicking sgRNA to target the edited strand specifically, reducing indels by 13-fold [29].
- PE4/PE5: Incorporates transient inhibition of mismatch repair (MMR) through a dominant-negative MLH1 variant to prevent repair of the heteroduplex back to the original sequence, improving editing efficiency by 7.7-fold (PE4) and 2.0-fold (PE5) compared to PE2 and PE3, respectively [29] [31].
- PEmax: Features a codon-optimized RT, additional nuclear localization signals, and Cas9 mutations that improve nuclease activity and editor expression [29].
- PE6: Includes specialized prime editors derived from evolved RT domains (PE6a-d) and Cas9 domains (PE6e-g) for improved efficiency with specific edit types and size constraints [29].
- epegRNAs: Incorporate RNA pseudoknots at the 3' end of pegRNAs to protect against degradation and improve stability, thereby enhancing prime editing efficiency [29].
Prime Editing Application: Correcting PRPH2 Splice Site Mutations
PRPH2 and Inherited Retinal Diseases
The human Peripherin 2 (PRPH2) gene encodes a tetraspanin protein essential for the structure and function of photoreceptor outer segments [33]. Mutations in PRPH2 are associated with various inherited retinal diseases (IRDs), including autosomal dominant retinitis pigmentosa, macular dystrophy, and cone-rod dystrophy, contributing to 5-10% of autosomal dominant retinitis pigmentosa cases worldwide [33]. PRPH2-associated IRDs exhibit remarkable phenotypic variability, presenting unique challenges for disease modeling and therapeutic development [33]. Experimental evidence suggests PRPH2 is highly dosage-sensitive, with rods more vulnerable to haploinsufficiency and cones more affected by toxic, dominant-negative mutations [33].
The c.828+1G>A PRPH2 splice site variant is a pathogenic mutation that disrupts normal splicing [33]. This mutation leads to activation of a cryptic splice site and intron retention, forming a mutant transcript that was previously detected in peripheral white blood cells from PRPH2 patients with the prevalent c.828+3A>T variant [33]. The c.828+1G>A variant is rare, making acquisition of patient-derived induced pluripotent stem cells (iPSCs) particularly challenging, necessitating the development of precise gene editing approaches for disease modeling and potential therapeutic correction [33].
Quantitative Outcomes of PRPH2 Correction
Table 1: Prime Editing Efficiency for PRPH2 c.828+1G>A Correction in hiPSCs
| Editing Parameter | Value | Experimental Context |
|---|---|---|
| Overall editing efficiency | ~24% | In pooled GFP-positive hiPSCs [33] |
| Homozygous editing | 7% | Of edited clones [33] |
| Heterozygous editing | 17% | Of edited clones [33] |
| Indel rate | <0.5% | In pooled GFP-positive cells [33] |
| Off-target mutations | Not detected | By dideoxy sequencing at predicted sites [33] |
| Karyotype abnormalities | Not detected | In edited hiPSC clones [33] |
| Functional correction | Canonical transcript restored | In hiPSCs and retinal organoids after correction [33] |
Table 2: Comparison of Genome Editing Technologies
| Editing Technology | Editing Capabilities | Advantages | Limitations |
|---|---|---|---|
| Prime Editing | All base substitutions, small insertions, deletions [30] | High precision, no DSBs, minimal indels, versatile [30] [29] | Variable efficiency requiring optimization [30] |
| Base Editing | C•G to T•A, A•T to G•C, C•G to G•C [30] | High efficiency, no DSBs, few indels [30] | Restricted to specific changes, bystander editing [30] [29] |
| Cas9 Nuclease + HDR | All possible changes [30] | Broad capability in principle [30] | Inefficient, requires DSBs, high indel rate, cell-cycle dependent [30] [29] |
Experimental Workflow for PRPH2 Prime Editing
The following diagram illustrates the complete experimental workflow for implementing prime editing to correct pathogenic mutations in PRPH2 using human induced pluripotent stem cells and retinal organoids:
Detailed Protocol: Prime Editing in hiPSCs
Reagent and Resource Preparation
Table 3: Essential Research Reagents for Prime Editing
| Reagent/Resource | Specification | Purpose |
|---|---|---|
| Prime Editor Protein | PEmax (optimized Cas9 nickase-reverse transcriptase fusion) | Engineered editor with improved expression and nuclear localization [29] |
| pegRNA | Designed with ~13-nt PBS and ~10-30-nt RTT with edit | Specifies target locus and templates desired edit; epegRNAs with pseudoknots enhance stability [29] |
| nicking sgRNA | Targets non-edited strand, avoiding PE3-induced DSBs | Enhances editing efficiency in PE3/PE5 systems [29] |
| Delivery Vector | All-in-one plasmid with GFP reporter | Enables co-expression of all components and identification of transfected cells [33] |
| Cell Line | hiPSCs (e.g., DD50/DD100 precursor cells) | Disease modeling platform capable of retinal organoid differentiation [33] |
| Transfection Reagent | Lipofectamine Stem | Optimized for hiPSC transfection with large plasmids [33] |
| Selection Method | Fluorescence-activated cell sorting (FACS) | Enriches transfected (GFP-positive) population [33] |
Step-by-Step Experimental Procedures
pegRNA and Nicking sgRNA Design
- Identify target sequence: For the PRPH2 c.828+1G>A mutation, design pegRNA with spacer sequence complementary to genomic target site including the splice site mutation [33].
- Design primer binding site (PBS): Create a 13-nucleotide PBS sequence complementary to the 3' end of the nicked DNA strand [31].
- Design reverse transcription template (RTT): Incorporate the desired correction (G to A reversion) along with sufficient homologous sequence on both sides; include silent PAM-disrupting mutations if necessary to prevent re-recognition [31].
- Test multiple pegRNA designs: Empirical testing is critical as editing efficiency can vary up to 50-fold between different pegRNA designs [32].
- Design nicking sgRNA: For PE3/PE5 systems, design nicking sgRNA to target the non-edited strand at a safe distance from the pegRNA-induced nick to avoid creating a double-strand break [29] [31].
Vector Construction and Validation
- Select prime editing system: For PRPH2 correction, researchers used a PE3 approach with an all-in-one construct containing pegRNA, nsgRNA, and GFP reporter [33].
- Clone components: Assemble the prime editor, pegRNA, and nicking sgRNA into your chosen delivery vector. The all-in-one design with GFP reporter facilitates identification of successfully transfected cells [33].
- Verify sequence integrity: Confirm accurate cloning of all components through restriction digest and Sanger sequencing.
- Test editing efficiency: Validate system performance using a reporter cell line (e.g., HEK293T) before proceeding to hiPSCs [33].
hiPSC Transfection and Clone Isolation
- Culture hiPSCs: Maintain hiPSCs in feeder-free conditions using essential supplements like ROCK inhibitor (Y-27632) to enhance viability after dissociation [33].
- Transfect cells: Use Lipofectamine Stem with optimal DNA-to-reagent ratios. For PRPH2 editing, researchers found that varying the amount of DNA and Lipofectamine did not significantly impact editing efficiency, enabling use of lowest amounts to conserve reagents [33].
- Enrich transfected cells: At 48-72 hours post-transfection, use FACS to isolate GFP-positive cells. Both high and low GFP-expressing populations showed similar editing rates (~24%) in the PRPH2 study [33].
- Culture and expand clones: Plate sorted cells at clonal density and culture until colonies form. For PRPH2 editing, both heterozygous and homozygous knock-in hiPSC clones were successfully generated [33].
- Pick and expand clones: Manually pick individual colonies and expand them for genomic analysis.
Molecular Validation of Edited Clones
- Extract genomic DNA: From expanded clonal lines using standard methods.
- Amplify target region: Design PCR primers flanking the edited site in PRPH2.
- Confirm editing: Perform Sanger sequencing to verify precise installation of the c.828+1G>A mutation in heterozygous or homozygous state [33].
- Assess byproducts: Check for unwanted indels at pegRNA and nicking sgRNA target sites; in optimized PRPH2 editing, indel rates were below 0.5% [33].
- Validate pluripotency: Confirm that edited hiPSCs maintain expression of key pluripotency markers and normal karyotype [33].
Functional Validation in Retinal Organoids
- Differentiate retinal organoids: Use established protocols to differentiate corrected and control hiPSCs into 3D retinal organoids [33].
- Analyze transcript correction: Perform RT-PCR and sequencing to assess restoration of canonical PRPH2 splicing in corrected lines compared to uncorrected controls [33].
- Quantify editing outcomes: Use high-throughput sequencing to precisely measure editing efficiency and byproduct formation [32].
Safety and Off-Target Assessment
- Predict potential off-target sites: Use computational tools to identify genomic loci with sequence similarity to pegRNA and nicking sgRNA.
- Perform targeted analysis: Use dideoxy sequencing to screen predicted off-target sites; in the PRPH2 study, no off-target mutations were detected at predicted sites [33].
- Conduct comprehensive genomic analysis: For therapeutic applications, consider whole-genome sequencing of edited clones; studies have shown prime editing does not increase genome-wide mutation rates above background [32].
Technical Considerations and Optimization
Prime Editing Mechanism and Heteroduplex Resolution
The following diagram illustrates the molecular mechanism of prime editing and the critical heteroduplex resolution process that determines editing success:
Critical Optimization Parameters
Successful prime editing requires careful optimization of several parameters:
- pegRNA design: Systematically test multiple PBS and RTT lengths; efficiency can vary dramatically based on pegRNA architecture [32].
- Cellular mismatch repair: Transient inhibition of MMR through PE4/PE5 systems or silent mutations that evade MMR recognition can significantly improve editing outcomes [29] [31].
- Delivery optimization: Balance delivery efficiency with cytotoxicity, particularly when working with sensitive cell types like hiPSCs [33].
- Cell type considerations: Account for variations in transfection efficiency, cell cycle distribution, and DNA repair capacity across different cell types [31].
Prime editing represents a significant advancement in precision genome editing technology, offering researchers the ability to precisely correct pathogenic point mutations like the PRPH2 c.828+1G>A splice site variant with high efficiency and minimal byproducts. The methodology outlined here for correcting PRPH2 mutations in hiPSCs and retinal organoids provides a framework for applying prime editing to other disease-relevant mutations. As the technology continues to evolve with improved editors (PE4/PE5, PEmax), enhanced pegRNA designs (epegRNAs), and optimized delivery strategies, prime editing is poised to become an increasingly powerful tool for disease modeling and therapeutic development for inherited retinal diseases and other genetic disorders.
The emergence of CRISPR-Cas genome engineering has fundamentally transformed the approach to treating monogenic hematologic disorders. Ex vivo gene editing of autologous hematopoietic stem cells (HSCs) presents a promising therapeutic strategy that avoids the risks of graft-versus-host disease and rejection associated with allogeneic transplantation [34]. For disorders such as pyruvate kinase deficiency, a hereditary hemolytic anemia caused by mutations in the PKLR gene, this technology enables the precise correction of genetic defects in a patient's own HSCs. These corrected cells can then be reinfused to establish a permanently corrected hematopoietic system. This Application Note details current protocols and methodologies for the ex vivo correction of HSCs, framing them within the broader research context of CRISPR-based therapies, with specific considerations for pyruvate kinase deficiency.
Current Research Status and Quantitative Data
Recent preclinical and clinical advances highlight the rapid evolution of this field. The table below summarizes key quantitative findings from recent studies relevant to HSC editing for hematologic disorders.
Table 1: Key Quantitative Findings from Recent HSC Editing Research
| Study Focus | Experimental Model | Key Outcome Metric | Result | Source |
|---|---|---|---|---|
| Gene Editing for PK Deficiency | Human HSPCs (PKLR mutation) | Optimization of editing protocol | Implementation of GMP-grade media, NHEJ inhibitors, and shortened transduction times. [16] | |
| Ex Vivo HSC Expansion | Human Cord Blood & Adult HSCs | Expansion of phenotypic LT-HSCs | ~4-fold increase in standard serum-free culture; ~50-fold increase in chemically defined cytokine-free culture. [35] | |
| HSC Ferroptosis Inhibition | Human CB HSPCs in NBSGW mice | In vivo repopulation capacity | Significantly greater long-term engraftment in BM and spleen at 16 weeks post-transplantation. [35] | |
| Allogeneic CAR-T for Autoimmunity | NMO Spectrum Disorder patient | Clinical outcome post universal CAR-T | Patient successfully cleared target cells and was discharged after discontinuing immunosuppressants. [16] | |
| Base Editing for Hemoglobinopathies | Clinical Trial (NCT05456880) | Therapeutic target | Base editors targeting the γ-globin promoter to induce fetal hemoglobin. [34] |
Detailed Experimental Protocol for Ex Vivo HSC Correction
The following section provides a detailed, step-by-step methodology for the ex vivo correction of hematopoietic stem and progenitor cells (HSPCs) for disorders like pyruvate kinase deficiency, integrating the latest technological optimizations.
The following diagram illustrates the complete experimental workflow from cell collection to final validation of the edited hematopoietic stem cells.
Step-by-Step Protocol
Step 1: HSPC Collection and Thawing
- Collect mobilized peripheral blood CD34+ cells from the patient and cryopreserve them.
- Thaw frozen HSPCs rapidly at 37°C using a thawing medium containing DNase I (100 U/mL) to prevent clumping [36].
- Wash cells to remove cryoprotectant and resuspend in a suitable serum-free medium, such as StemSpan or a chemically defined cytokine-free medium [35].
Step 2: Pre-culture and Activation
- Pre-culture HSPCs for 24-48 hours in medium supplemented with a cytokine cocktail (e.g., SCF, TPO, FLT3-L) to promote cell cycle entry, which is crucial for efficient HDR [34] [36].
- To enhance HSC fitness and mitigate culture-induced stress, supplement the medium with a ferroptosis inhibitor (e.g., 10 µM Liproxstatin-1 or Ferrostatin-1) for the entire culture duration [35].
- Integrate a p38 MAPK inhibitor during the ex vivo culture to reduce detrimental stress responses and improve the long-term repopulating capacity of edited HSCs [36].
Step 3: CRISPR-Cas9 RNP Electroporation
- For gene correction (e.g., of the PKLR gene), use a homology-directed repair (HDR) approach.
- Ribonucleoprotein (RNP) Complex Formation: Pre-complex a high-fidelity Cas9 protein with a synthetic sgRNA targeting the genomic locus of interest (e.g., near the disease-causing mutation in PKLR). Use a final concentration of 50-100 µM RNP complex.
- Electroporation: Use a certified electroporator (e.g., Lonza 4D-Nucleofector) and appropriate human HSPC kit. Electroporate the RNP complex into the pre-activated HSPCs. Using RNP delivery, as opposed to mRNA, minimizes the duration of Cas9 exposure and reduces p53-mediated DNA damage response and genotoxicity [34].
Step 4. HDR Template Delivery
- Simultaneously with or immediately after electroporation, transduce the cells with a recombinant adeno-associated virus serotype 6 (rAAV6) donor template.
- The AAV6 template should contain the therapeutic transgene (e.g., a correct PKLR cDNA) or a minigene, flanked by homology arms (~500-800 bp) corresponding to the sequence surrounding the Cas9-induced double-strand break [16] [34].
- Recent protocols suggest using low AAV6 titers to minimize HSC differentiation and exhaustion, though this requires careful optimization [34].
Step 5. Ex Vivo Expansion and Post-Editing Culture
- Following gene editing, transfer the cells into an expansion medium. The choice of medium is critical.
- Chemically defined, cytokine-free media have been shown to support robust HSC expansion over several weeks [35] [37].
- Maintain the supplementation with ferroptosis inhibitors (Lip-1/Fer-1) throughout the culture period, which has been shown to dramatically expand long-term HSCs without compromising their function or causing genotoxicity [35].
- Culture the cells for a defined period (e.g., 2-5 days) to allow for recovery and initial expansion before transplantation.
Step 6. In Vivo Functional Validation
- The gold standard for validating the function of edited human HSCs is xenotransplantation into immunodeficient mouse models (e.g., NBSGW mice) [35].
- Transplant edited HSPCs into sublethally irradiated mice via tail vein or intra-femoral injection.
- Monitor engraftment in the peripheral blood over 16-20 weeks. Subsequently, analyze bone marrow and spleen for the presence of human multilineage hematopoietic cells (CD45+), and specifically for the presence of the genetic correction, to confirm that long-term repopulating HSCs were successfully edited [35] [36].
The Scientist's Toolkit: Essential Research Reagents
The table below catalogues the key reagents and their functions that are essential for successful execution of ex vivo HSC correction protocols.
Table 2: Key Research Reagent Solutions for Ex Vivo HSC Correction
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| CRISPR-Cas9 System | Creates a precise double-strand break in the DNA at the target locus. | High-fidelity SpCas9 protein; Synthetic sgRNA targeting the mutant gene (e.g., PKLR). [34] |
| HDR Donor Template | Serves as a corrective template for the cell's repair machinery. | Recombinant AAV6 (rAAV6) is most common; contains homology arms and corrective sequence. [16] [34] |
| Culture Medium | Supports the survival, activation, and expansion of HSCs ex vivo. | Serum-free media (e.g., StemSpan); Novel chemically defined, cytokine-free media. [35] [37] |
| Small Molecule Inhibitors | Enhances HSC fitness, editing efficiency, and long-term engraftment. | Ferroptosis inhibitors (Lip-1, Fer-1); p38 MAPK inhibitor; NHEJ inhibitors (to boost HDR). [16] [35] [36] |
| Cytokines | Promotes HSC activation and proliferation, necessary for HDR. | Stem Cell Factor (SCF), Thrombopoietin (TPO), FMS-like tyrosine kinase 3 ligand (Flt3-L). [36] |
| Cell Selection Reagents | Enriches for successfully modified cells or specific HSC populations. | Antibodies for phenotypic HSCs (e.g., CD34, CD90, CD45RA, EPCR). [35] |
Critical Pathways and Workflow Optimization Logic
Understanding the biological pathways involved in the cellular response to editing is key to protocol optimization. The following diagram outlines the core challenges and the corresponding strategic solutions integrated into the protocol.
The protocols detailed herein represent the current state-of-the-art in ex vivo correction of HSCs for metabolic disorders like pyruvate kinase deficiency. The integration of precise CRISPR-Cas9 tools with optimized culture conditions—notably the inhibition of ferroptosis—and sophisticated delivery methods creates a powerful therapeutic platform. As demonstrated by the ongoing clinical trials and recent approvals for other hematologic diseases, this field is rapidly moving from research to clinical reality. Future directions will focus on further improving the safety profile by minimizing off-target effects, enhancing the efficiency of HDR in the most primitive HSCs, and streamlining manufacturing processes to make these transformative therapies more accessible. The continuous refinement of these ex vivo correction protocols is paving the way for durable and curative treatments for a wide array of inherited hematological disorders.
The development of "off-the-shelf" or allogeneic cell therapies represents a paradigm shift in regenerative medicine and cancer treatment. Unlike autologous approaches that require custom manufacturing for each patient, allogeneic therapies derived from healthy donors or universal stem cell sources offer the promise of immediate availability, standardized quality, and reduced costs [38] [39]. However, a fundamental biological barrier impedes this vision: the host immune system rapidly recognizes and eliminates donor cells through T cell-mediated rejection directed against mismatched human leukocyte antigen (HLA) molecules and natural killer (NK) cell activation via "missing-self" recognition [38].
Hypo-immunogenic engineering addresses this challenge by genetically modifying donor cells to evade immune detection. This approach employs multiplexed CRISPR genome editing to simultaneously disrupt endogenous HLA expression while introducing protective transgenes, creating universal cell products suitable for any recipient without HLA matching [38]. The strategic ablation of HLA class I and II molecules prevents CD8+ and CD4+ T cell recognition, while the introduction of non-polymorphic HLA-E engages the inhibitory receptor NKG2A on NK cells, circumventing "missing-self" activation [38]. This protocol details the application of this strategy to human pluripotent stem cells, enabling the creation of a renewable source of universal therapeutic cells.
Key Reagents and Research Solutions
Table 1: Essential Research Reagents for Hypo-immunogenic Stem Cell Engineering
| Reagent Category | Specific Examples | Function in Protocol |
|---|---|---|
| CRISPR Nucleases | S. pyogenes Cas9 (SpCas9), Adenine Base Editor (ABE) | Creates double-strand breaks in B2M and CIITA genes; introduces precise point mutations |
| Guide RNAs | sgRNAs targeting B2M exon 2, CIITA | Directs Cas9 to specific genomic loci for knockout |
| Donor Templates | rAAV6 containing HLA-E-B2M fusion construct with homology arms | Provides template for homologous recombination at the B2M locus |
| Stem Cell Culture | Human iPSCs, Essential 8 Medium, Vitronectin | Provides starting cellular material and maintenance conditions |
| Delivery Methods | Electroporation, Lipofection, rAAV6 transduction | Introduces editing components into hard-to-transfect stem cells |
| Validation Antibodies | Anti-HLA-ABC, Anti-HLA-DR, Anti-HLA-E, Anti-FOXP3 | Confirms successful protein-level knockout and knock-in via flow cytometry |
Experimental Workflow and Protocol
The following diagram illustrates the comprehensive workflow for generating hypo-immunogenic universal stem cells, from initial design to functional validation.
Protocol Part 1: Guide RNA Design and Complex Formation
Materials:
- Chemically modified sgRNAs (Synthego or equivalent)
- Alt-R S.p. Cas9 Nuclease V3 (IDT)
- Nuclease-Free Duplex Buffer
Procedure:
- Design sgRNAs targeting exon 2 of the B2M gene (to disrupt HLA class I) and key exons of the CIITA gene (master regulator of HLA class II) [38].
- Design the rAAV6 donor template containing an HLA-E-B2M fusion gene flanked by homology arms (approximately 800bp) specific to the B2M locus.
- Form RNP complexes by pre-complexing 60pmol of Cas9 protein with 60pmol of each sgRNA in nuclease-free duplex buffer. Incubate at room temperature for 10-20 minutes before delivery [40].
Protocol Part 2: Stem Cell Electroporation and Transduction
Materials:
- Cultured human iPSCs (>90% viability)
- Neon Transfection System (Thermo Fisher) or similar
- rAAV6 donor vector (≥1×10¹³ vg/mL titer)
- Stem cell-specific recovery medium
Procedure:
- Prepare iPSCs as single-cell suspension using Accutase. Wash and resuspend in appropriate electroporation buffer at 1×10⁷ cells/mL [40].
- Electroporation: Mix 10μL cell suspension with pre-formed RNP complexes. Electroporate using stem cell-optimized parameters (e.g., Neon System: 1400V, 10ms, 3 pulses) [40].
- Immediately post-electroporation, transduce cells with rAAV6 donor vector at an MOI of 100,000 in recovery medium.
- Plate cells on vitronectin-coated plates in Essential 8 Medium supplemented with 10μM ROCK inhibitor. Culture at 37°C, 5% CO₂.
Protocol Part 3: Clonal Isolation and Genotypic Validation
Materials:
- Flow cytometer with cell sorter
- Lysis buffer for genomic DNA extraction
- PCR reagents and sequencing primers
Procedure:
- Clonal Isolation: At 7-10 days post-editing, dissociate cells and sort single cells into 96-well plates using either:
- FACS for cells with high expression of a knock-in reporter (if included in donor design) [40], or
- Antibiotic selection if the donor construct contains a resistance marker.
- Expand clonal lines for 3-4 weeks until sufficient cells are available for analysis.
- Genotypic Validation:
- Extract genomic DNA from expanded clones.
- Perform 'In-Out' PCR using one primer binding within the integrated transgene and one primer binding in the genomic flanking region outside the homology arm [40].
- Confirm precise integration and sequence the edited loci via Sanger sequencing.
- Screen for potential off-target edits at top-predicted off-target sites for each sgRNA.
Results Analysis and Validation
Table 2: Expected Outcomes and Validation Benchmarks for Hypo-immunogenic Engineering
| Validation Metric | Expected Outcome | Assessment Method |
|---|---|---|
| B2M Knockout Efficiency | >90% INDEL frequency | Tracking of indels by decomposition (TIDE) or next-generation sequencing |
| CIITA Knockout Efficiency | >85% INDEL frequency | TIDE analysis or sequencing |
| HLA-E-B2M Knock-in | 20-40% of alleles (with rAAV6 donor and Cas9 RNP) [40] | Flow cytometry for HLA-E surface expression; 'In-Out' PCR |
| HLA Class I Loss | >99% reduction in HLA-ABC+ cells | Flow cytometry with anti-HLA-ABC antibody |
| HLA Class II Loss | >99% reduction in HLA-DR+ cells | Flow cytometry with anti-HLA-DR antibody |
| Pluripotency Retention | Maintenance of embryonic stem cell markers | Flow cytometry for TRA-1-60, SSEA4; differentiation potential |
| In Vivo Graft Survival | Significant prolongation vs. unmodified allogeneic cells (MST >80 days vs. <30 days) [38] | Humanized mouse skin graft model |
Phenotypic and Functional Validation
The engineered cells must be thoroughly validated to confirm successful immunoevasion while maintaining therapeutic potential. The schematic below illustrates the key genetic modifications and their functional consequences for immune evasion.
Flow Cytometry Analysis:
- Confirm HLA profile by staining with antibodies against HLA-ABC, HLA-DR, and HLA-E. Successful engineering should show:
- Near-complete loss of HLA-ABC and HLA-DR surface expression
- Robust expression of HLA-E in edited clones [38]
- Verify pluripotency maintenance through staining for canonical markers (OCT4, SOX2, NANOG, TRA-1-60, SSEA4).
- Differentiation capacity: Subject edited clones to directed differentiation into target lineages (e.g., cardiomyocytes, neural progenitors, hematopoietic cells) to confirm multilineage potential is retained post-editing.
In Vivo Functional Validation
The ultimate validation of hypo-immunogenic properties requires testing in immunocompetent models that mimic human immune responses.
Humanized Mouse Skin Graft Model [38]:
- Engraft immunodeficient NSG mice with human PBMCs to create a functional human immune system.
- Transplant human skin grafts followed by administration of:
- Unmodified allogeneic T cells (negative control)
- HLA-matched T cells (positive control)
- Engineered hypo-immunogenic T cells (experimental)
- Monitor graft survival over 100 days, with successful engineering demonstrated by significant prolongation of graft survival comparable to autologous cells [38].
- Endpoint analysis: Perform histology and spatial transcriptomics on surviving grafts to assess immune infiltration and tissue repair programs.
Troubleshooting and Technical Considerations
- Low Editing Efficiencies: Optimize RNP concentrations and electroporation parameters. Use chemically modified sgRNAs with 2'-O-methyl 3'phosphorothioate modifications to enhance stability and efficiency.
- Reduced Cell Viability: Include ROCK inhibitor (Y-27632) in recovery medium. Plate cells at high density immediately after electroporation and ensure careful handling.
- Incomplete HLA Knockdown: Validate multiple sgRNAs for each target. Consider using dual sgRNAs to excise larger genomic regions for more reliable knockout.
- Karyotypic Abnormalities: Perform routine karyotyping on expanded clones, as extended culture and editing stress may induce chromosomal abnormalities.
This protocol provides a robust framework for generating universal hypo-immunogenic stem cells through multiplexed HLA engineering. The resulting cell lines evade both T cell and NK cell recognition, addressing the major immunological barriers to allogeneic cell therapy [38]. These engineered cells serve as a renewable source for deriving various therapeutic cell types – including cardiomyocytes, neural cells, pancreatic islets, and immune effector cells – without requiring patient-specific matching [41] [39].
The application of orthogonal CRISPR systems that combine nuclease-dependent targeted integration with base editors, as demonstrated in CAR-T cell engineering [42], provides a promising direction for further enhancing the safety and efficiency of this approach. By minimizing double-strand break-induced genotoxicity, these advanced editing strategies may enable more complex multiplexed engineering while maintaining genomic integrity.
This technology platform establishes a foundation for the next generation of universally compatible cellular therapeutics, potentially transforming treatment paradigms for degenerative diseases, cancer, and traumatic tissue injury.
Solving Key Challenges: Delivery, Specificity, and Functional Integration
Efficient intracellular delivery of CRISPR-Cas9 components remains a fundamental challenge in stem cell research and therapy. The ideal delivery vehicle must protect its genetic cargo, ensure precise targeting of stem cells, achieve high transfection efficiency, and maintain cell viability and pluripotency. For gene editing in hematopoietic stem and progenitor cells (HSPCs), these challenges are particularly pronounced, as prolonged ex vivo culture and manipulation can trigger detrimental cellular responses that compromise long-term functionality [36]. This Application Note examines three leading delivery platforms—viral vectors, lipid nanoparticles (LNPs), and extracellular vesicles (EVs)—within the context of CRISPR-based gene editing protocols for correcting stem cell mutations. We provide a structured comparison of these technologies, detailed experimental methodologies, and essential reagent solutions to facilitate robust and reproducible research outcomes.
Comparative Analysis of Delivery Platforms
The selection of a delivery system is critical for balancing editing efficiency with the preservation of stem cell properties. The table below summarizes the key characteristics of viral, LNP, and EV-based delivery systems for stem cell applications.
Table 1: Quantitative Comparison of Delivery Platforms for Stem Cell Gene Editing
| Platform | Typical Payload Capacity | Editing Efficiency in HSPCs | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Viral Vectors (e.g., AAV) | <4.7 kb [43] | Varies by serotype and target | High transduction efficiency; well-established protocols [43] | Limited packaging capacity; immunogenicity concerns [43] |
| Lipid Nanoparticles (LNPs) | mRNA, ribonucleoprotein (RNP) [44] | High (e.g., >80% reported with optimized Ab-LNPs [44]) | High payload capacity; potential for in vivo use; reduced immune response [45] | Predominant liver tropism without targeting [44] |
| Extracellular Vesicles (EVs) | Proteins, nucleic acids [46] | Data emerging | High biocompatibility; natural homing capabilities; low immunogenicity [46] [47] | Heterogeneity; challenges in scalable production and loading [46] |
Detailed Experimental Protocols
Protocol: Optimizing Culture Conditions for CRISPR Editing in Human HSPCs
This protocol is adapted from della Volpe et al. and focuses on mitigating the detrimental effects of ex vivo culture on HSPCs during gene editing, thereby preserving their long-term repopulating capacity [36].
Summary of Steps:
- HSPC Thawing: Thaw mobilized human CD34+ HSPCs rapidly in a 37°C water bath. Transfer cells to pre-warmed culture medium and centrifuge to remove cryoprotectant. Resuspend in a specialized cytokine-rich medium.
- Ex Vivo Pre-conditioning and Gene Editing: Pre-treat cells with a p38 inhibitor (e.g., 1-5 µM) for 6-24 hours to reduce stress responses. Complex the CRISPR-Cas9 RNP (e.g., 5 µg Cas9 protein with 3 µg sgRNA) and deliver via electroporation. For HDR-mediated correction, include a single-stranded or double-stranded DNA donor template.
- Post-Editing Culture and Analysis: After editing, maintain cells in culture with the p38 inhibitor for 24-48 hours. Analyze editing efficiency via flow cytometry (for fluorescent reporter expression) or next-generation sequencing (NGS) for on-target and off-target modifications.
- In Vivo Functional Validation: Transplant the gene-edited HSPCs into immunodeficient mouse models (e.g., NSG mice). After 12-16 weeks, analyze bone marrow for human cell engraftment and multi-lineage differentiation to confirm the preservation of stem cell functionality [36].
Workflow: Generating Antibody-Targeted LNPs for Precise Stem Cell Delivery
This workflow describes the creation of antibody-targeted LNPs (Ab-LNPs) for the specific delivery of mRNA to HSPCs, based on the strategy pioneered by the Weissman lab [44].
Summary of Steps:
- LNP Formulation: Prepare LNPs using a standard microfluidic mixer. The lipid mixture should include an ionizable lipid (e.g., DLin-MC3-DMA), phospholipid, cholesterol, and a PEG-lipid (e.g., DMG-PEG2000). Encapsulate the mRNA payload (e.g., CRISPR-Cas9 mRNA or base editor mRNA).
- Nanobody Functionalization: Employ a site-specifically conjugated anti-Fc nanobody (e.g., TP1107optimal) to decorate the LNP surface. This nanobody serves as a universal capture agent for antibodies [48].
- Antibody Conjugation: Incubate the nanobody-functionalized LNPs with an antibody specific to a stem cell surface marker, such as anti-CD117 (c-Kit) for targeting hematopoietic stem cells. The nanobody captures the antibody via its Fc region, ensuring optimal orientation for target binding [48] [44].
- Validation and Transfection: Characterize the size and polydispersity of the final Ab-LNPs using dynamic light scattering. Treat CD117+ HSPCs with the Ab-LNPs and quantify mRNA delivery and protein expression efficiency compared to non-targeted LNPs.
Strategy: Engineering Extracellular Vesicles for CRISPR RNP Delivery
This strategy outlines methods for loading CRISPR machinery into EVs and modifying their surface for targeted delivery [46] [47].
Summary of Steps:
- EV Isolation and Purification: Culture parent cells (e.g., mesenchymal stem cells). Collect the conditioned medium and isolate EVs using sequential centrifugation: 2,000 × g to remove cells, 10,000 × g to remove debris, and finally, 100,000 × g to pellet EVs. Purify further using density gradient centrifugation.
- CRISPR Payload Loading:
- Post-isolation Loading: Use electroporation to load pre-assembled Cas9-sgRNA ribonucleoprotein (RNP) complexes into the isolated EVs.
- Pre-isolation Loading (Genetic Engineering): Transduce parent cells to stably express Cas9. When designing sgRNAs, ensure they are specific to the target genomic locus in the recipient stem cells, not the EV-producing cells.
- Surface Functionalization (Post-isolation): Employ chemical conjugation (e.g., click chemistry) to attach stem cell-homing peptides or single-chain variable fragments (scFvs) to proteins on the EV surface, such as Lamp2 [47].
- Functional Assay: Incubate engineered EVs with target HSPCs. Measure the efficiency of gene editing via T7E1 assay or NGS, and assess cell viability and differentiation potential.
Workflow Visualization
The following diagram illustrates the logical decision-making process for selecting and applying the appropriate delivery platform based on research goals.
Diagram 1: Delivery Platform Selection Guide
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of the protocols above requires specific, high-quality reagents. The table below lists essential materials and their functions.
Table 2: Key Research Reagents for Stem Cell Gene Editing Delivery
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| p38 Inhibitor | Enhances HSPC fitness during ex vivo culture by reducing stress-induced responses [36]. | Integrate into culture medium pre- and post-electroporation. |
| Anti-CD117 (c-Kit) Antibody | Targeting moiety for directing Ab-LNPs to hematopoietic stem cells [44]. | Critical for in vivo hematopoietic stem cell targeting. |
| TP1107optimal Nanobody | Enables optimal antibody orientation on LNP surfaces for enhanced targeting efficiency [48]. | Site-specifically conjugated to LNP via azide-DBCO chemistry. |
| DSPE-PEG-Maleimide Lipids | Facilitates conjugation of targeting ligands (e.g., antibodies, peptides) to the LNP surface [44]. | Used in Capstan Therapeutics' CPTX2309. |
| Ionizable Cationic Lipids | Core structural component of LNPs; encapsulates and protects mRNA payloads [44]. | e.g., DLin-MC3-DMA, SM-102. |
| CRISPR-GPT AI Tool | AI-powered assistant for designing CRISPR experiments, predicting off-target effects, and troubleshooting [6]. | Stanford Medicine; useful for novice and expert researchers. |
| Transportan (TP) Peptide | Cell-penetrating peptide that enhances viral vector transfection efficiency via co-incubation [49]. | Particularly useful for difficult-to-transfect primary cells. |
Concluding Remarks
The evolving landscape of delivery systems for CRISPR-based stem cell editing offers powerful and complementary tools for research and therapeutic development. Viral vectors remain a mainstay for ex vivo applications, while advanced LNP technologies, particularly antibody-targeted platforms, are breaking new ground for in vivo precision delivery. Extracellular vesicles represent a promising biocompatible alternative, though their manufacturing requires further standardization. The integration of AI tools like CRISPR-GPT can significantly accelerate experimental design and optimization across all these platforms [6]. By applying the detailed protocols and reagent solutions provided herein, researchers can systematically overcome delivery hurdles and advance the frontier of gene editing in stem cells.
The emergence of CRISPR-Cas systems has revolutionized genome editing, enabling precise modification of target genes with unprecedented efficiency. However, the clinical translation of these technologies, particularly for therapeutic stem cell applications, faces a substantial barrier: off-target effects. These unintended genetic modifications occur when the CRISPR system cleaves or edits DNA at sites other than the intended target, raising concerns about genotoxicity and potential malignant transformations [50]. The absence of standardized guidelines for quantifying and reporting these effects further complicates therapeutic development, leading to inconsistent practices across studies [50].
For stem cell research and therapy, where edited cells may persist long-term in patients, minimizing off-target activity is not merely an optimization goal but a fundamental safety requirement. This Application Note details validated strategies employing high-fidelity Cas variants and engineered guide RNAs to achieve precise genome editing while minimizing off-target risks, with specific protocols tailored for stem cell applications.
High-Fidelity Cas Variants: Enhanced Specificity Without Sacrificing Efficiency
Mechanism and Performance of High-Fidelity Variants
High-fidelity Cas9 variants have been engineered through strategic mutations that alter protein-DNA interactions, particularly in the REC3 domain which is critical for DNA binding and verification [51]. These modifications increase the energy threshold for DNA cleavage, thereby enhancing the system's ability to discriminate between perfectly matched target sequences and those with mismatches.
Recent systematic evaluations of high-fidelity variants reveal important performance characteristics. When comparing Wild-Type (WT) SpCas9 against HiFi and LZ3 variants, research demonstrates that approximately 20% of sgRNAs show significantly reduced efficiency with high-fidelity variants, highlighting the importance of variant-specific sgRNA design [51]. This efficiency loss is strongly dependent on the sequence context in the seed region of sgRNAs and at positions 15–18 in the non-seed region that interacts with the REC3 domain of Cas9 [51].
Table 1: Performance Comparison of High-Fidelity Cas9 Variants
| Variant | On-Target Efficiency | Off-Target Reduction | Key Mutations | Optimal Application Context |
|---|---|---|---|---|
| WT SpCas9 | High | Baseline | None | Initial screening studies |
| HiFi Cas9 | Moderate to High (variant-dependent) | Significant | A262T, R324L, S409I | Therapeutic applications requiring high specificity [51] |
| LZ3 Cas9 | Moderate to High (variant-dependent) | Significant | E1219V, D1135V, N497A, R661A, Q695A, Q926A | Complex genomic regions with high homology [51] |
| eSpCas9 | Moderate | Significant | K848A, K1003A, R1060A | Basic research applications |
| SpCas9-HF1 | Moderate | Significant | N497A, R661A, Q695A, Q926A | Targets with known off-target sites |
Experimental Protocol: Evaluating High-Fidelity Variants in Stem Cells
Objective: To systematically compare the editing efficiency and specificity of high-fidelity Cas9 variants in human induced pluripotent stem cells (iPSCs).
Materials:
- Human iPSCs (maintained in feeder-free culture)
- High-fidelity Cas9 expression plasmids (lentiHiFi-Puro, lentiLZ3-Puro) [51]
- WT SpCas9 control (lentiCas9-Puro) [51]
- sgRNA constructs targeting genes of interest
- Lipofectamine Stem Transfection Reagent
- Puromycin for selection (2 µg/ml)
- T7 Endonuclease I or ICE assay for editing efficiency
- GuideVar software for sgRNA prioritization [51]
Procedure:
- Cell Preparation: Culture iPSCs in essential 8 medium on Geltrex-coated plates until 70-80% confluent.
- Plasmid Transfection: Complex 2 µg of Cas9 plasmid (WT, HiFi, or LZ3) with 3 µl Lipofectamine Stem in Opti-MEM medium. Incubate for 20 minutes at room temperature before adding to cells.
- Selection: Begin puromycin selection 48 hours post-transfection for 72 hours.
- Monoclonal Expansion: Harvest cells and seed at limiting dilution to establish monoclonal lines.
- Efficiency Assessment: Extract genomic DNA from expanded clones. Amplify target regions by PCR and analyze using T7E1 assay or next-generation sequencing.
- Off-Target Screening: Identify potential off-target sites using CIRCLE-seq or GUIDE-seq. Amplify and sequence top 10 predicted off-target loci for each variant.
- Data Analysis: Calculate editing efficiency as percentage of modified alleles. Compare indel frequencies at on-target and off-target sites across variants.
Troubleshooting Note: iPSCs are particularly sensitive to CRISPR-mediated DNA damage. Implement a p38 MAPK inhibitor (1-5 µM) during editing to reduce detrimental cellular responses and maintain stem cell functionality [36] [52].
Advanced Guide RNA Engineering for Enhanced Specificity
Innovative Guide RNA Architectures
Beyond Cas protein engineering, significant advances have been made in guide RNA design to minimize off-target effects while maintaining high on-target activity.
CRISPR Hybrid RNA-DNA (chRDNA) Guides: These guides incorporate 2'-deoxynucleotides (dnt) at strategic positions within the guide sequence. Structural studies reveal that chRDNA guides create distorted guide-target duplex geometry and allosteric modulation of Cas9 conformation, increasing specificity by perturbing DNA hybridization and modulating Cas9 activation kinetics [53]. The positioning of DNA nucleotides affects guide activity and specificity in a target-dependent manner, requiring empirical optimization for each target site.
Circular Guide RNAs (cgRNAs): Engineered cgRNAs utilize a covalently closed loop structure that offers enhanced protection against exonuclease degradation, resulting in greater stability and extended half-life compared to linear guides [54]. Real-time PCR quantification shows that cgRNA expression levels can be 192-392 times higher than normal linear guides, with significantly improved durability in extended culture systems [54].
Table 2: Comparison of Engineered Guide RNA Platforms
| Guide Type | Structure | Key Features | Editing Efficiency | Specificity Enhancement |
|---|---|---|---|---|
| Traditional sgRNA | Linear RNA | Standard scaffold | Baseline | Baseline |
| chRDNA | RNA-DNA hybrid | Strategic DNA substitutions; Alters Cas9 kinetics | Target-dependent; May require optimization | Substantially reduced off-target effects [53] |
| cgRNA | Circular covalently closed | Extreme stability (392.9x higher expression); Extended activity window | 1.9-19.2-fold enhancement in activation [54] | High on-target specificity with minimal off-targets |
| epegRNA | Engineered extension | Modified 3' structure; Prime editing applications | ~70-90% with PE6 system [21] | Reduced indel formation |
Experimental Protocol: Implementing cgRNAs in Stem Cell Editing
Objective: To design, construct, and validate circular guide RNAs for enhanced specificity in stem cell genome editing.
Materials:
- Tornado expression system for cgRNA production [54]
- Poly-AC and poly-U RNA linkers
- dCas12f-VPR or Cas9 expression plasmids
- HEK293T cells for initial validation
- Human iPSCs for therapeutic editing
- Actinomycin D for RNA stability assays
- FACS equipment for efficiency quantification
Procedure: cgRNA Design and Construction:
- Spacer Design: Select 23-nt target-specific spacer sequences with optimal GC content (40-60%).
- Linker Incorporation: Flank the guide sequence with 5-10 nucleotide flexible poly-AC RNA linkers between the 5' ribozyme and gRNA scaffold.
- Vector Construction: Clone the cgRNA sequence into the Tornado expression vector using Gibson assembly.
- Validation: Verify circularization by RT-PCR with outward-facing primers, which only amplify successfully circularized RNAs [54].
Stem Cell Editing with cgRNAs:
- Transfection Preparation: Culture iPSCs to 70% confluency in essential 8 medium.
- RNP Complex Formation: Complex 500 ng of Cas9 protein with 200 ng of in vitro transcribed cgRNA. Incubate for 10 minutes at room temperature.
- Stem Cell Transfection: Deliver RNP complexes using lipofectamine stem transfection reagent.
- Stability Assessment: Treat parallel cultures with actinomycin D (5 µg/mL) at 24 hours post-transfection. Harvest cells at 0, 12, 24, 48, and 72 hours for RNA extraction and cgRNA quantification by qRT-PCR.
- Efficiency Analysis: Harvest cells at 72 hours for genomic DNA extraction. Amplify target regions and quantify editing efficiency by NGS.
Optimization Notes:
- For Cas12f systems, a 23-nt spacer with AC5 linkers demonstrates optimal performance [54].
- Combining cgRNAs with phase-separation systems (e.g., FUSIDR fusion) can further enhance activation efficiency by 2.3-3.9-fold [54].
- For hematopoietic stem and progenitor cells (HSPCs), include a p38 inhibitor in the culture medium to reduce proliferation stress and DNA damage during editing [36].
Integrated Workflow for Stem Cell Genome Editing
The following diagram illustrates the complete optimized workflow for precise stem cell editing, integrating high-fidelity Cas variants and engineered guide RNAs:
Table 3: Essential Research Reagents for Precision Stem Cell Editing
| Reagent/Resource | Function | Example Applications | Key Considerations |
|---|---|---|---|
| HiFi Cas9 | High-fidelity nuclease with reduced off-target activity | Therapeutic editing of stem cells; Disease modeling [51] | 20% of sgRNAs may show reduced efficiency; Requires validation |
| LZ3 Cas9 | Evolved high-fidelity variant with maintained on-target efficiency | Complex genomic targets; Hematopoietic stem cell editing [51] | Sequence-dependent performance; Use GuideVar for prediction |
| chRDNA Guides | Hybrid RNA-DNA guides for enhanced specificity | T cell engineering; Therapeutic applications [53] | DNA positioning is target-dependent; Requires optimization |
| Circular gRNAs | Highly stable guide RNA architecture | Long-term gene activation; In vivo applications [54] | 392.9-fold higher expression than linear guides; Enhanced durability |
| p38 Inhibitors | Small molecules reducing editing-induced stress | HSPC editing; Improving long-term stem cell function [36] [52] | Critical for maintaining repopulation capacity in HSPCs |
| Prime Editors (PE6) | Precise editing without double-strand breaks | Point mutation correction; Insertions/deletions [21] | Editing efficiency 70-90% in HEK293T cells; Reduced indels |
| GuideVar Software | Machine learning framework for sgRNA design | Predicting efficiency of high-fidelity variants [51] | Improves signal-to-noise ratios in screening applications |
The strategic integration of high-fidelity Cas variants and engineered guide RNAs represents a transformative approach for minimizing off-target effects in therapeutic stem cell editing. The experimental protocols detailed herein provide a framework for achieving the precision necessary for clinical applications, with particular relevance for correcting disease-causing mutations in hematopoietic stem cells and iPSCs.
Future directions in this field include the development of cell-type-specific delivery systems for high-fidelity editors, the refinement of machine learning algorithms for predicting variant-specific sgRNA efficiency, and the creation of all-in-one systems that combine multiple specificity-enhancing technologies. As these precision editing tools continue to evolve, they will undoubtedly accelerate the translation of CRISPR-based stem cell therapies from research laboratories to clinical applications, enabling new treatments for genetic disorders with unprecedented safety and efficacy profiles.
Within the broader scope of developing CRISPR gene editing protocols for correcting stem cell mutations, ensuring the clonal purity of edited hematopoietic stem cells (HSCs) is a critical translational challenge. A primary concern is that the transplanted cell population, despite initial diversity, can become dominated by only a few clones, potentially leading to therapeutic failure or unforeseen side effects [16]. To address this, researchers have developed a barcoded AAV6 system that enables high-resolution tracking of individual gene-edited HSC clones throughout the editing and transplantation process [16]. This application note details the protocol for using this system to optimize editing and ensure the engraftment of a diverse, therapeutically relevant stem cell population.
Utilizing the barcoded AAV6 tracking system revealed crucial insights into clonal dynamics and informed specific optimizations for editing HSCs, summarized in the table below.
Table 1: Key Quantitative Findings from Barcoded AAV6 Tracking Studies
| Finding / Parameter | Before Optimization | After Optimization | Key Implication |
|---|---|---|---|
| Post-Transplant Clonal Diversity | Dominated by few clones [16] | Improved diversity (inferred) | Reduces risk of monoclonality and supports sustainable engraftment. |
| Protocol Optimization Focus | N/A | Use of GMP-grade media [16] | Enhances cell viability and fitness during the editing process. |
| Protocol Optimization Focus | N/A | Addition of NHEJ inhibitors [16] | Favors precise homology-directed repair (HDR) over error-prone NHEJ. |
| Protocol Optimization Focus | N/A | Shortened transduction times [16] | Reduces AAV exposure, minimizing cellular stress and off-target effects. |
| Target Disease Model | Pyruvate kinase deficiency [16] | N/A | Protocol validated for correcting PKLR mutations. |
Experimental Protocol
This section provides a detailed methodology for using the barcoded AAV6 system to track edited HSC clones.
The following diagram illustrates the complete experimental workflow, from library preparation to final data analysis.
Detailed Methodology
Step 1: Barcoded AAV6 Library Preparation
- Design and Synthesis: Generate a recombinant AAV6 library where each viral particle carries a unique, heritable DNA barcode within its genome. AAV6 is selected for its high efficiency in transducing HSCs [16] [55].
- Quality Control: Purify and titrate the viral library to ensure a high multiplicity of infection (MOI) and sufficient barcode diversity to tag a vast number of individual HSCs.
Step 2: HSC Isolation and Activation
- Cell Source: Isolate CD34+ HSCs from human donor tissue (e.g., mobilized peripheral blood, bone marrow, or cord blood).
- Pre-stimulation: Activate the quiescent HSCs by culturing in a cytokine-rich, GMP-grade media for 24-48 hours to increase susceptibility to AAV6 transduction and CRISPR editing [16].
Step 3: Co-transduction and Genome Editing
- Editing Strategy: The goal is to correct disease-causing mutations, such as in the PKLR gene. The CRISPR-Cas9 components (e.g., as ribonucleoprotein complexes - RNPs) and the barcoded AAV6 library are delivered to the activated HSCs.
- Delivery Method: Use an optimized transduction protocol. Electroporation or Nucleofection is highly effective for delivering CRISPR RNPs into HSCs, offering high efficiency and limited nuclease exposure time to reduce off-target effects [55]. The barcoded AAV6 library is added simultaneously or shortly after.
- Critical Optimization: The protocol was refined by:
- Using GMP-grade media to maintain cell health.
- Adding NHEJ inhibitors to promote precise, HDR-mediated gene correction.
- Shortening transduction times to minimize cellular stress and improve viability [16].
Step 4: Transplantation and In Vivo Tracking
- Transplantation: The edited and barcoded HSC population is transplanted into conditioned immunodeficient mouse models (e.g., NSG mice).
- Longitudinal Tracking: Monitor engraftment and hematopoietic reconstitution in vivo over time.
Step 5: Analysis of Clonal Output
- Sample Collection: At experimental endpoints, harvest bone marrow from transplanted mice to isolate the engrafted human HSCs and their progeny.
- Barcode Sequencing: Extract genomic DNA and amplify the integrated barcode regions via PCR for high-throughput next-generation sequencing.
- Data Analysis: Bioinformatically count the unique barcodes and their frequencies. This identifies which initial HSC clones contributed to long-term engraftment and reveals the degree of clonal dominance [16].
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Barcoded AAV Tracking
| Item | Function & Role in the Protocol |
|---|---|
| Barcoded AAV6 Library | Delivery vehicle for introducing unique, heritable DNA barcodes into individual HSCs, enabling clonal tracking. |
| CRISPR-Cas9 RNP | The editing machinery; a pre-complexed guide RNA and Cas9 protein complex for efficient and transient cleavage of the target genomic locus (e.g., PKLR). |
| NHEJ Inhibitor | A small molecule (e.g., SCR7) that suppresses the non-homologous end joining DNA repair pathway, thereby enhancing the rate of precise HDR-mediated gene correction. |
| GMP-grade Culture Media | A high-quality, xeno-free medium formulation critical for maintaining the viability, potency, and therapeutic potential of HSCs during the ex vivo editing process. |
| HSC Isolation Kits | Immunomagnetic beads (e.g., anti-CD34) for the positive selection of pure populations of hematopoietic stem cells from donor tissue. |
The use of a barcoded AAV6 system provides an unprecedented and essential view into the clonal dynamics of edited hematopoietic stem cells. The methodology and data presented here, framed within the larger thesis on CRISPR protocols for stem cell mutation correction, highlight that successful therapy depends not only on high editing efficiency but also on preserving a diverse stem cell population post-transplant. The protocol optimizations enabled by this tracking system—such as using GMP-grade media, NHEJ inhibitors, and shortened transduction—are critical steps toward developing safe and effective clinical-grade gene therapies for hematological diseases.
In the field of CRISPR gene editing protocols for correcting stem cell mutations, achieving high editing efficiency is a paramount objective. The therapeutic application of CRISPR, exemplified by the first approved therapy, Casgevy for sickle cell disease and transfusion-dependent beta thalassemia, underscores the critical need for optimized protocols [56] [11]. While CRISPR systems enable targeted genetic modifications, the inherent efficiency of precise editing, particularly via homology-directed repair (HDR), remains a significant challenge in therapeutically relevant primary cells, including hematopoietic stem and progenitor cells (HSPCs) [56] [36]. This application note details systematic approaches to enhance editing efficiency through small molecule interventions and optimized culture conditions, providing validated methodologies for researchers developing stem cell-based gene therapies.
Small Molecule Enhancers of CRISPR Editing
Small molecules that modulate DNA repair pathways and cell cycle progression present powerful tools for shifting the balance toward desired CRISPR editing outcomes. The tables below summarize key small molecules and their effects on different editing pathways.
Table 1: Small Molecule Enhancers for HDR-mediated Precise Editing
| Small Molecule | Target Pathway | Effect on HDR Efficiency | Optimal Concentration | Cell Viability Impact |
|---|---|---|---|---|
| Nedisertib | DNA-PK inhibitor (NHEJ suppression) | 21-24% increase | 0.25 µM | Maintained ~74% viability |
| NU7441 | DNA-PK inhibitor | 11% increase | Not specified | Reduced at higher concentrations |
| Alt-R HDR Enhancer | Commercial HDR enhancer | No significant increase | As manufacturer recommends | Negative impact on viability |
| SCR-7 | DNA ligase IV inhibitor (NHEJ suppression) | No significant increase | Not specified | No significant negative impact |
Table 2: Small Molecule Enhancers for NHEJ-mediated Gene Knockout
| Small Molecule | Target Pathway | Effect on NHEJ Efficiency | Fold Increase | Delivery System |
|---|---|---|---|---|
| Repsox | TGF-β signaling inhibitor | Significant enhancement | 3.16-fold | RNP system |
| Zidovudine (AZT) | Thymidine analog (HDR suppression) | Moderate enhancement | 1.17-fold | RNP system |
| GSK-J4 | Histone demethylase inhibitor | Moderate enhancement | 1.16-fold | RNP system |
| IOX1 | Histone demethylase inhibitor | Mild enhancement | 1.12-fold | RNP system |
| Repsox | TGF-β signaling inhibitor | Moderate enhancement | 1.47-fold | Plasmid system |
The mechanism of Repsox, one of the most effective NHEJ enhancers, involves reducing the expression levels of SMAD2, SMAD3, and SMAD4 in the TGF-β pathway, thereby increasing the efficiency of CRISPR NHEJ-mediated gene editing [57].
Experimental Protocol: Small Molecule Screening for HDR Enhancement
Materials:
- BEL-A erythroid cell line or target HSPCs
- CRISPR ribonucleoprotein (RNP) complex (3 µg Cas9, 1:2.5 gRNA:Cas9 ratio)
- ssODN repair template (100 pmol)
- Small molecule stock solutions (Nedisertib, NU7441, etc.)
- Amaxa 4D-Nucleofector system with 16-well nucleocuvette strips
- Flow cytometry equipment for GFP-based HDR reporter assay
Method:
- Cell Preparation: Culture BEL-A cells following standard protocols. On the day of nucleofection, harvest and count cells, preparing 5×10⁴ cells per nucleofection condition.
- RNP Complex Formation: Incubate Cas9 protein with target-specific gRNA at room temperature for 10 minutes at a 1:2.5 ratio.
- Small Molecule Treatment: Prepare small molecule working concentrations in culture medium (e.g., 0.25 µM Nedisertib, 1 µM NU7441).
- Nucleofection: Use program DZ-100 on the Amaxa 4D-Nucleofector, which provides optimal HDR efficiency (52%) while maintaining high viability (88%).
- Post-nucleofection Recovery: Immediately transfer cells to small molecule-containing media and culture for 48-72 hours.
- Efficiency Assessment: Analyze HDR efficiency using flow cytometry for GFP-positive cells in the BFP-to-GFP reporter system.
- Viability Check: Perform cell viability assessment using trypan blue exclusion or similar method.
This protocol achieved 73% precise editing efficiency for introducing the E6V A>T sickle cell mutation in BEL-A cells, with 48% of clones being homozygous for the mutation [56].
Culture Condition Optimization
Optimized culture conditions are essential for maintaining stem cell fitness during the editing process, particularly for primary cells with limited ex vivo expansion capacity.
Experimental Protocol: Optimized Culture Conditions for HSPC Editing
Materials:
- Human hematopoietic stem and progenitor cells (HSPCs)
- p38 inhibitor (e.g., SB203580)
- Serum-free expansion media optimized for HSPCs
- Cytokines (SCF, TPO, FLT3-L)
- Nucleofection equipment
- In vivo transplantation reagents (NSG mice for functional validation)
Method:
- HSPC Thawing and Recovery: Quickly thaw HSPCs and transfer to pre-warmed culture medium. Centrifuge and resuspend in fresh medium containing DNase I (100 U/mL). Incubate for 4 hours at 37°C before proceeding.
- Pre-stimulation Culture: Culture HSPCs in serum-free medium supplemented with SCF (100 ng/mL), TPO (100 ng/mL), and FLT3-L (100 ng/mL) for 24-48 hours to promote cell cycle entry, which is essential for HDR.
- p38 Inhibitor Treatment: Add p38 inhibitor to culture medium at determined optimal concentration (e.g., 1-5 µM SB203580) to reduce detrimental stress responses during ex vivo culture.
- CRISPR Editing: Perform RNP nucleofection using optimized parameters for HSPCs.
- Post-editing Recovery: Continue culture in p38 inhibitor-containing medium for 24-48 hours post-editing.
- Functional Assessment:
- In vitro analyses: Perform clonogenic assays in methylcellulose to assess progenitor capacity. Use flow cytometry to evaluate differentiation potential.
- In vivo repopulation assay: Transplant edited HSPCs into immunodeficient NSG mice. Analyze bone marrow engraftment and multi-lineage differentiation at 12-16 weeks post-transplantation.
This protocol significantly reduces detrimental cellular responses during extended ex vivo culture, preserving the long-term repopulating capacity of gene-edited HSPCs [36].
Diagram 1: HSPC Culture Optimization Workflow
Integrated Workflow for Enhanced Editing
Combining small molecule treatment with optimized culture conditions creates a synergistic effect on editing efficiency. The diagram below illustrates the integrated workflow for achieving high-efficiency editing in stem cells.
Diagram 2: Integrated Editing Enhancement Strategy
Critical Safety Considerations
While enhancing editing efficiency is crucial, recent findings highlight important safety considerations. The use of DNA-PKcs inhibitors to enhance HDR, such as AZD7648, can lead to exacerbated genomic aberrations including kilobase- and megabase-scale deletions as well as chromosomal arm losses [58]. These structural variations (SVs) raise substantial safety concerns for clinical translation. Traditional short-read amplicon sequencing often fails to detect these large-scale deletions, potentially leading to overestimation of HDR rates and underestimation of indels. For therapeutic applications, it's essential to implement comprehensive genomic integrity assessment using methods like CAST-Seq and LAM-HTGTS to detect SVs [58].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for CRISPR Editing Optimization
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| HDR Enhancers | Nedisertib, NU7441, NU7026 | DNA-PK inhibition to suppress NHEJ and promote HDR |
| NHEJ Enhancers | Repsox, Zidovudine, GSK-J4 | Enhance non-homologous end joining for efficient knockout |
| Cell Culture Additives | p38 inhibitors, Nocodazole | Reduce stress responses and synchronize cell cycle |
| Delivery Systems | Amaxa 4D-Nucleofector, Lipid nanoparticles (LNPs) | Efficient RNP delivery to target cells |
| Editing Assessment | BFP-to-GFP reporter systems, CAST-Seq, LAM-HTGTS | Quantify efficiency and detect structural variations |
| Stem Cell Media | Serum-free expansion media, Cytokine cocktails | Maintain stemness during ex vivo culture |
The strategic integration of small molecule enhancers with optimized culture conditions provides a powerful approach for maximizing CRISPR editing efficiency in stem cell research. DNA-PK inhibitors like Nedisertib and TGF-β pathway inhibitors like Repsox offer substantial improvements in HDR and NHEJ efficiency, respectively. Combined with p38 inhibition and proper cytokine stimulation during ex vivo culture, these approaches maintain stem cell fitness while achieving high editing rates. As CRISPR-based therapies advance, balancing efficiency with comprehensive safety assessments remains paramount for successful clinical translation. The protocols outlined here provide a foundation for researchers developing gene editing approaches for correcting stem cell mutations.
The success of CRISPR-Cas9 gene editing in stem cells represents a transformative frontier in regenerative medicine and the treatment of genetic disorders. However, a critical challenge persists: ensuring the survival, functional integrity, and successful engraftment of these edited cells in vivo. Ex vivo gene editing protocols, particularly for hematopoietic stem and progenitor cells (HSPCs), often require prolonged culture that triggers detrimental cellular responses, compromising long-term repopulating capacity [36]. Furthermore, upon transplantation, the host immune system can mount a rejection response against both allogeneic and edited autologous cells, undermining therapeutic efficacy [59]. This application note provides a detailed framework of optimized culture conditions and engineered strategies designed to overcome these hurdles, enhancing the fitness and engraftment potential of CRISPR-edited stem cells for research and therapeutic development.
The integration of specific small molecules and genetic engineering techniques has shown significant promise in improving the outcomes of stem cell therapies. The following table summarizes the core approaches and their quantified impacts on stem cell fitness and engraftment.
Table 1: Key Strategies for Improving Edited Stem Cell Engraftment
| Strategy | Mechanism of Action | Quantified Outcome | Key Findings |
|---|---|---|---|
| p38 Inhibitor Integration [36] | Reduces detrimental stress responses during ex vivo culture. | Improved long-term functionality and repopulating capacity of GE-HSPCs. | Protocol optimizes culture conditions to maintain stem cell fitness throughout the gene editing workflow. |
| Base Editing (vs. CRISPR-Cas9) [60] | Minimizes genotoxic DNA double-strand breaks; uses chemical conversion of base pairs. | Higher editing efficiency in competitive transplants; reduced red cell sickling in a SCD model. | Considered a more effective and potentially safer therapeutic strategy for certain applications like sickle cell disease. |
| CAR-Treg Cell Co-transplantation [61] | Engineered T-regulatory cells suppress immune attack on transplanted cells. | Achieved immune tolerance; allowed engineered beta cells to engraft in immunodeficient mice with an aggressive immune challenge. | A "lock and key" system using EGFRt-tagged stem cells and matching CAR-Tregs protects grafts from rejection. |
| Lipid Nanoparticle (LNP) Delivery [11] | Enables in vivo gene editing; avoids immune reactions associated with viral vectors; allows re-dosing. | Sustained ~90% reduction in disease-related protein (TTR) over 2 years; safe administration of multiple doses demonstrated. | Overcomes a major delivery challenge and enables re-dosing, which is typically not feasible with viral vectors. |
Detailed Experimental Protocols
Protocol for Optimizing HSPC Culture Conditions with p38 Inhibition
This protocol is adapted from della Volpe et al. and provides a step-by-step guide to enhance HSPC fitness during the CRISPR-Cas9 gene editing workflow [36].
3.1.1 Materials
- Human HSPCs: Cryopreserved CD34+ hematopoietic stem and progenitor cells.
- Culture Medium: Serum-free expansion medium supplemented with cytokines (e.g., SCF, TPO, FLT3-L).
- p38 Inhibitor: Reconstituted in DMSO according to manufacturer's instructions.
- CRISPR Components: Cas9 protein/gRNA ribonucleoprotein (RNP) complexes.
- Transfection Reagent: Such as a neon electroporation system.
3.1.2 Procedure
- Thawing and Seeding: Rapidly thaw cryopreserved CD34+ HSPCs and seed them in pre-warmed culture medium at a density of 1-2x10^6 cells/mL.
- p38 Inhibitor Pre-treatment: Add the optimized concentration of the p38 inhibitor to the culture medium. Incubate the cells for 6-24 hours prior to gene editing.
- CRISPR-Cas9 Electroporation: Harvest the pre-treated cells and resuspend them in an electroporation buffer. Mix the cells with pre-complexed Cas9 RNP and electroporate using the recommended settings for HSPCs.
- Recovery Culture: Immediately transfer the electroporated cells into fresh culture medium containing the p38 inhibitor. Continue the culture for 48-72 hours to allow for gene editing and recovery.
- Downstream Analysis: Harvest cells for in vitro analyses (e.g., flow cytometry for viability and editing efficiency, CFU assays) or transplant into immunodeficient mice (e.g., NSG) for in vivo assessment of engraftment and long-term repopulation capacity.
3.1.3 Critical Steps and Troubleshooting
- Dose Optimization: The concentration of the p38 inhibitor must be titrated for each specific HSPC source and donor to maximize benefits while minimizing toxicity.
- Culture Timing: Prolonged culture, even with inhibitors, can be detrimental. The total ex vivo culture time should be minimized as much as possible.
- Control Groups: Always include untreated and non-electroporated controls to accurately assess the impact of the editing process and the p38 inhibitor.
Protocol for Establishing Immune Tolerance with Engineered CAR-Tregs
This protocol outlines a combinatorial strategy to protect stem cell-derived grafts from immune rejection, based on a study for type 1 diabetes treatment [61].
3.2.1 Materials
- Stem Cell Line: A pluripotent stem cell line (e.g., iPSC).
- T-regulatory Cells (Tregs): Isolated from peripheral blood.
- Engineering Constructs: Lentiviral vectors for expressing:
- Inactive EGFRt (EGFRt) in stem cells.
- Chimeric Antigen Receptor (CAR) specific for EGFRt in Tregs.
- Differentiation Kit: For directing stem cells into the desired cell type (e.g., beta cells, neurons).
3.2.2 Procedure
- Engineer Stem Cells: Differentiate the iPSCs into the target cell type (e.g., beta cells). During the process, transduce the cells with a lentivirus to express the cell surface tag EGFRt.
- Engineer CAR-Tregs: Isolate human Tregs and activate them. Transduce the Tregs with a lentivirus encoding a CAR whose extracellular domain is designed to recognize and bind the EGFRt tag.
- In Vivo Co-transplantation: Transplant the EGFRt-expressing target cells (e.g., under the kidney capsule of an immunodeficient mouse). Systemically administer the anti-EGFRt CAR-Tregs.
- Immune Challenge: To model an aggressive immune response, expose the transplanted mice to effector immune cells.
- Assessment: Monitor graft survival and function (e.g., insulin production for beta cells). Analyze the grafts post-mortem for immune cell infiltration and evidence of rejection.
3.2.3 Critical Steps and Troubleshooting
- Tag Design: The EGFRt tag must be inactive to avoid interfering with native signaling pathways in the target cells.
- Treg Purity: The starting population of Tregs must be highly pure to prevent the expansion of unwanted, pro-inflammatory T cells.
- Dosing Ratio: The ratio of CAR-Tregs to target cells needs to be optimized to ensure sufficient immune suppression without causing pathology.
Signaling Pathways and Workflows
p38 MAPK Stress Signaling in HSPC Culture
The following diagram illustrates the signaling pathway targeted by p38 inhibitors during ex vivo culture to enhance stem cell survival.
CAR-Treg Mediated Immune Protection Workflow
This workflow details the sequential steps for developing a combined cell therapy strategy to achieve immune tolerance for stem cell grafts.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of the protocols above requires a suite of specialized reagents. The following table lists essential materials and their functions.
Table 2: Essential Research Reagents for Stem Cell Engraftment Studies
| Reagent / Material | Function | Application Notes |
|---|---|---|
| p38 MAPK Inhibitor | Small molecule that blocks the p38 stress signaling pathway, reducing apoptosis and preserving stemness during ex vivo manipulation [36]. | Requires dose and timing optimization. Use appropriate vehicle controls (e.g., DMSO). |
| CRISPR-Cas9 RNP Complex | Pre-assembled ribonucleoprotein of Cas9 protein and guide RNA. Enables high-efficiency gene editing with reduced off-target effects and faster kinetics compared to plasmid delivery. | The preferred method for sensitive primary cells like HSPCs. |
| Lipid Nanoparticles (LNPs) | Non-viral delivery vehicles for CRISPR components or mRNA. Favors liver accumulation; enables in vivo editing and allows for re-dosing due to low immunogenicity [11]. | Critical for systemic in vivo delivery. Organ tropism is a key selection criterion. |
| Lentiviral Vectors | Efficient delivery systems for stably integrating genetic constructs into target cells, such as genes for reporter tags (EGFRt) or chimeric antigen receptors (CARs) [61]. | Biosafety Level 2 practices are required. Monitor integration sites for safety assessments. |
| EGFRt Tagging System | A cell surface marker (truncated, inactive EGFR) expressed on engineered stem cells. Serves as a target for companion CAR-Tregs, localizing immune protection to the graft [61]. | The tag is inert and does not initiate downstream EGFR signaling. |
| CAR-Treg Cells | Genetically engineered T-regulatory cells expressing a CAR that recognizes the EGFRt tag. They locally suppress immune responses against the tagged graft, promoting tolerance [61]. | Requires ex vivo expansion and validation of suppressive function prior to infusion. |
Rigorous Assessment and Benchmarking of Edited Stem Cell Products
In the field of CRISPR gene editing protocols for correcting stem cell mutations, comprehensive on-target analysis is paramount for confirming intended genetic modifications while detecting unwanted alterations. Next-generation sequencing (NGS), particularly amplicon sequencing, has emerged as the gold standard for this verification process, enabling researchers to accurately quantify editing efficiency and characterize editing outcomes with high precision [62].
The necessity for rigorous on-target analysis stems from the inherent challenges of CRISPR-based editing in stem cells. While CRISPR-Cas9 can create precise double-strand breaks, the subsequent DNA repair processes can yield a spectrum of outcomes—from perfect on-target edits to imperfect indels and complex rearrangements. In clinically relevant stem cells such as human induced pluripotent stem cells (hiPSCs) and human embryonic stem cells (hESCs), where low knock-in efficiencies (often ≈2–20%) are common, robust verification methods become especially critical for identifying correctly edited clones amidst predominantly unmodified or incorrectly modified cells [63].
Amplicon sequencing addresses these challenges by providing a highly sensitive, quantitative approach for analyzing specific genomic loci of interest. This targeted NGS method facilitates the detection and quantification of diverse editing outcomes, including precise knock-in events, small insertions and deletions (indels), and to some extent, larger structural variations, thereby providing a comprehensive picture of on-target editing efficiency and accuracy [62] [64].
Amplicon Sequencing Workflow for CRISPR Verification
The following diagram illustrates the core amplicon sequencing workflow for CRISPR on-target verification, from initial sample preparation to final data analysis.
Library Preparation Protocol
The amplicon sequencing workflow begins with careful experimental design and sample preparation, followed by a two-step PCR approach to create sequencing-ready libraries.
Primer Design and Experimental Considerations:
- Target Region Selection: Design primers to flank the CRISPR target site, ensuring the modification site is centered within the amplicon [64].
- Amplicon Length Optimization: Keep total amplicon length under 450 bp for paired-end 250 bp sequencing to ensure complete coverage of both ends [64].
- Primer Positioning: Place primer binding sites at least 50 bp away from the cut site to avoid interference with editing outcome assessment [64].
- Specificity Validation: Use tools like Primer-Blast to verify primer specificity and minimize off-target amplification [64].
Two-Step PCR Library Preparation:
Step 1: Target Amplification with Partial Adapters
- Amplify the target region using gene-specific primers with partial Illumina adapter sequences appended to their 5' ends [64].
- Forward primer partial adapter: 5'-CTACACGACGCTCTTCCGATCT-3'
- Reverse primer partial adapter: 5'-CAGACGTGTGCTCTTCCGATCT-3'
- Use high-fidelity DNA polymerase to minimize PCR errors
- Validate amplification success by agarose gel electrophoresis
Step 2: Indexing and Library Completion
- Use the PCR #1 product as template for a second amplification with indexing primers containing unique dual indices (UDIs) [64].
- These primers add complete Illumina adapter sequences and sample-specific barcodes
- Enables multiplexing of hundreds of samples in a single sequencing run
- Purify final libraries using bead-based cleanups to remove primer dimers and nonspecific products
Sequencing and Data Analysis
Sequencing Configuration:
- Utilize Illumina platforms (MiSeq, NextSeq, or NovaSeq) with paired-end 250 bp sequencing chemistry
- Include 5-10% PhiX control to improve base calling accuracy for diverse sequences
- Adjust sequencing depth based on application needs: 1,000-5,000x for bulk edited populations; 10,000x+ for sensitive variant detection
Bioinformatic Analysis Pipeline:
- Demultiplexing: Assign reads to samples based on unique dual indices
- Quality Control: Assess read quality using FastQC and perform adapter trimming
- Alignment: Map reads to reference genome using optimized aligners (BWA, Bowtie2)
- Variant Calling: Identify and quantify editing outcomes using specialized tools:
- CRIS.py: Python-based tool for analyzing genome editing outcomes from NGS data, capable of processing multiple samples simultaneously and detecting user-defined modifications [64].
- CRISPResso2: Popular tool for quantifying CRISPR-induced indels and HDR efficiency
- rhAmpSeq Analysis System: Integrated solution for on- and off-target quantification [62]
Analytical Approaches for Different Editing Outcomes
The optimal analytical approach for CRISPR verification depends on the specific type of edit being evaluated. The decision workflow below guides researchers in selecting the appropriate method based on their experimental goals.
Knock-out and Indel Analysis
For gene knock-out experiments where non-homologous end joining (NHEJ) introduces insertion/deletion mutations (indels), amplicon sequencing provides comprehensive characterization of the resulting mutational spectrum.
Key Analytical Parameters:
- Indel Percentage: The proportion of sequences containing non-wild type indels [65]
- Knock-out Score: The proportion of cells with frameshift mutations or large indels (21+ bp) that likely result in functional gene disruption [65]
- Indel Spectrum: Distribution of different indel types and sizes
- Model Fit (R²): Quality metric indicating confidence in the editing efficiency calculation [65]
Specialized Methods for Challenging Scenarios: In stem cell editing where knock-in efficiencies can be very low (<1%), alternative approaches can enhance clone identification:
- NGS with Low-Density Seeding: Combines low-density cell seeding with NGS screening to identify rare correctly edited clones without antibiotic selection, achieving successful identification even with <1% knock-in efficiency [63]
- CLEAR-time dPCR: A digital PCR method that quantifies DNA repair precision, revealing prevalent scarless repair after DSBs and recurrent nuclease cleavage events [66]
Knock-in and HDR Analysis
For homology-directed repair (HDR) mediated knock-in experiments, verification requires specialized approaches to distinguish precise template integration from spurious editing events.
HDR Efficiency Quantification:
- Knock-in Score: The proportion of sequences containing the desired precise knock-in edit [65]
- HDR-Specific Primers: Design validation primers that span the junction between genomic DNA and inserted sequence
- Donor-Specific Probe Systems: Implement probe-based detection to distinguish integrated donor sequences from episomal templates [66]
Multiplexed Assessment Strategy: The "Edge assay" within the CLEAR-time dPCR framework enables simultaneous quantification of:
- Wildtype sequences
- Small indels
- Total non-indel aberrations This multi-faceted approach provides a more complete picture of editing outcomes beyond simple HDR efficiency calculations [66].
Quantitative Comparison of CRISPR Analysis Methods
Table 1: Performance Characteristics of CRISPR On-Target Analysis Methods
| Method | Detection Capability | Sensitivity | Throughput | Cost Considerations | Best Applications |
|---|---|---|---|---|---|
| Amplicon Sequencing (NGS) | Full indel spectrum, HDR efficiency, some large deletions | 0.1-1% variant frequency [62] | High (multiplexed) | Moderate (decreasing with multiplexing) | Comprehensive characterization, clinical applications [62] |
| Sanger + ICE Analysis | Indel efficiency, KO score, KI score | ~5% variant frequency [65] | Medium | Low | Rapid screening, initial optimization [65] |
| CLEAR-time dPCR | DSBs, large deletions, aneuploidy, targeted integration | Absolute quantification [66] | Medium | Moderate | DNA repair kinetics, therapy safety assessment [66] |
| rhAmpSeq System | On/off-target editing, multiplexed sites | High (detects low-frequency edits) [62] | High | Moderate | Standardized workflows, multi-target assessment [62] |
Table 2: Key Research Reagent Solutions for CRISPR On-Target Analysis
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| rhAmpSeq CRISPR Analysis System | Targeted amplicon sequencing for on- and off-target editing quantification | End-to-end solution with cloud-based analysis; ideal for standardized workflows [62] |
| CRIS.py | Python-based NGS data analysis for genome editing outcomes | Processes multiple samples simultaneously; detects user-defined modifications [64] |
| ICE (Inference of CRISPR Edits) | Sanger sequencing analysis platform | ~100-fold cost reduction vs. NGS; provides KO/KI scores and editing efficiency [65] |
| CLEAR-time dPCR | Digital PCR ensemble for DNA repair quantification | Absolute quantification of DSBs, large deletions; normalizes against reference assays [66] |
| Alt-R CRISPR-Cas9 System | Efficient editing reagents | High-efficiency Cas9 variants; compatible with electroporation and lipofection [62] |
| Edge Assay Components | Primers and probes for integrity assessment | Quantifies wildtype, indels, and total non-indel aberrations simultaneously [66] |
Advanced Applications in Stem Cell Research
Clinical Translation and Safety Assessment
For stem cell therapies advancing toward clinical applications, comprehensive genetic integrity testing becomes essential. Recent advances include:
Multi-Parameter Quality Control:
- SNP Array Analysis: Validates genomic integrity after editing procedures [63]
- Karyotyping and CNV Analysis: Detects large-scale chromosomal abnormalities
- Optical Genome Mapping: Bridges resolution gap between karyotyping and NGS techniques [66]
Stem Cell-Specific Optimization: In hiPSC and hESC editing, the NGS-based footprint-free approach combining low-density seeding with sequencing has achieved remarkable efficiencies up to 64% in hiPSCs and 51% in hESCs, while preserving genomic integrity across subcloning rounds [63].
Troubleshooting and Optimization Guidelines
Common Challenges and Solutions:
- Low Editing Efficiency: Optimize sgRNA design using bioinformatic tools; enhance HDR with timing and TIEs [67]
- PCR Artifacts: Use high-fidelity polymerases; minimize amplification cycles; include appropriate controls
- Variant Detection Sensitivity: Increase sequencing depth; implement duplicate removal; use unique molecular identifiers (UMIs)
- Complex Rearrangements: Combine amplicon sequencing with long-read technologies for comprehensive structural variant detection
Quality Control Metrics:
- Sequencing Depth: Minimum 1000x for bulk populations; 10,000x+ for sensitive variant detection
- Coverage Uniformity: >90% of target bases covered at 0.2x mean depth
- Control Performance: PhiX error rates <1%; positive controls detected at expected frequencies
Amplicon sequencing and NGS-based verification represent cornerstone technologies in the CRISPR gene editing workflow for stem cell research. The methods outlined in this protocol enable researchers to thoroughly characterize on-target editing outcomes, from basic knock-out mutations to precise knock-in corrections. As CRISPR-based stem cell therapies advance toward clinical applications, these comprehensive verification approaches will play an increasingly critical role in ensuring both the efficacy and safety of genetically-corrected cell products. The continuous development of improved analytical methods—including emerging techniques like CLEAR-time dPCR and enhanced bioinformatic tools—promises to further strengthen our ability to validate CRISPR editing outcomes with unprecedented precision and reliability.
The clinical application of CRISPR-based gene editing, particularly in sensitive areas such as correcting stem cell mutations, is heavily dependent on comprehensive off-target profiling. Unintended CRISPR nuclease activity at off-target sites can lead to genotoxic consequences, including the disruption of vital genes, creation of cryptic splice sites, or potential oncogenic mutations [50] [68]. The FDA now recommends using multiple methods, including genome-wide analysis, to measure off-target editing events, a standard highlighted during the approval of the first CRISPR-based therapy, Casgevy (exa-cel) [69]. For stem cell research, where edited cells have the potential for long-term persistence and differentiation, ensuring genomic integrity is paramount. Genome-wide unbiased screening methods like GUIDE-seq and CIRCLE-seq provide the sensitivity and comprehensiveness required for pre-clinical safety assessment, helping to bridge the gap between basic research and clinical translation [50] [69].
Comparative Analysis of GUIDE-seq and CIRCLE-seq
Selecting the appropriate off-target detection assay requires a clear understanding of the strengths, limitations, and applications of each method. The table below provides a detailed comparison of GUIDE-seq and CIRCLE-seq to inform experimental design.
Table 1: Comparative Analysis of GUIDE-seq and CIRCLE-seq Methodologies
| Feature | GUIDE-seq [69] [62] | CIRCLE-seq [69] [68] |
|---|---|---|
| Full Name | Genome-wide, Unbiased Identification of DSBs Enabled by Sequencing | Circularization for In vitro Reporting of Cleavage Effects by Sequencing |
| Core Principle | Captures DSBs in living cells via integration of a double-stranded oligodeoxynucleotide tag. | Uses circularized genomic DNA incubated with Cas9-gRNA in vitro to identify cleavage sites. |
| Detection Context | Living cells (in situ); native chromatin and cellular repair machinery. | Purified genomic DNA (in vitro); no chromatin or cellular repair context. |
| Key Strength | Reflects true cellular activity and identifies biologically relevant edits. | Ultra-sensitive, comprehensive, and standardized; requires minimal sequencing depth. |
| Primary Limitation | Requires efficient delivery of oligonucleotide tag and nuclease; less sensitive for rare off-targets. | May overestimate cleavage due to absence of biological context (e.g., chromatin, repair). |
| Workflow Duration | Approximately 1-2 weeks (including cell culture and sequencing). | Approximately 2 weeks [68]. |
| Sensitivity | High sensitivity for off-target DSB detection in a cellular environment. | Very high sensitivity; can detect rare off-targets with reduced false negatives. |
| Ideal Application | Validation of clinical relevance of off-target effects; studies where cellular context is critical. | Broad discovery and nomination of potential off-target sites; initial gRNA safety screening. |
Application Notes for Stem Cell Mutation Correction Research
In the context of correcting stem cell mutations, the choice between GUIDE-seq and CIRCLE-seq is not mutually exclusive but rather complementary. A robust safety workflow often employs CIRCLE-seq for its high sensitivity in the initial gRNA selection and candidate nomination phases. Its ability to interrogate off-target potential without the constraints of cell culture viability or delivery efficiency is particularly valuable when working with precious or difficult-to-transfect stem cell lines [69] [68]. Subsequently, GUIDE-seq is critical for validating the top candidate gRNAs in the actual stem cell type being developed for therapy. This step confirms which of the potential off-target sites identified by CIRCLE-seq are actually cleaved within the physiological environment of the stem cell, which possesses a unique chromatin landscape and DNA repair profile [69]. This two-tiered approach—combining the comprehensive, context-free power of CIRCLE-seq with the biologically relevant validation of GUIDE-seq—provides a strong foundation for ensuring the safety of gene-corrected stem cells intended for therapeutic use.
Experimental Protocols
Protocol for GUIDE-seq
GUIDE-seq is a cellular method that maps double-strand breaks (DSBs) directly in living cells, capturing the influence of the native cellular environment [69].
Table 2: Key Reagents for GUIDE-seq
| Reagent / Equipment | Function | Example / Comment |
|---|---|---|
| Cells of Interest | Provides the genomic and cellular context for the assay. | Use the target stem cell line (e.g., iPSCs). |
| Cas9-gRNA RNP | The editing complex to be tested. | Alt-R S.p. Cas9 Nuclease V3 or similar. |
| GUIDE-seq Oligo | Double-stranded oligodeoxynucleotide tag that is captured at DSBs. | A proprietary, blunt-ended, phosphorylated double-stranded oligo [69]. |
| Transfection Reagent / Electroporator | For efficient delivery of RNP and oligo into cells. | Neon NxT Electroporator or similar systems for stem cells. |
| Genomic DNA Extraction Kit | To isolate high-quality DNA after editing. | Gentra Puregene Cell Kit or equivalent. |
| PCR and NGS Reagents | For library preparation and sequencing. | Kapa HTP Library Preparation Kit, Illumina sequencing platforms. |
Detailed Step-by-Step Methodology:
- Cell Preparation and Transfection: Culture the target induced pluripotent stem cells (iPSCs) under standard conditions. Co-deliver the Cas9-gRNA ribonucleoprotein (RNP) complex and the GUIDE-seq double-stranded oligodeoxynucleotide tag into the cells using a high-efficiency method such as electroporation. The optimal ratio of RNP to tag must be determined empirically [69] [62].
- Incubation and DNA Extraction: Incubate the transfected cells for 48-72 hours to allow for genome editing and tag integration. Subsequently, harvest the cells and extract high-molecular-weight genomic DNA using a standard kit protocol [69].
- Library Preparation and Sequencing: Shear the purified genomic DNA by ultrasonication. Prepare a sequencing library that enriches for genomic fragments containing the integrated GUIDE-seq tag. This typically involves a tag-specific PCR amplification step followed by Illumina adapter ligation and a second round of PCR to index the samples for multiplexing [69] [62].
- Data Analysis: Process the paired-end sequencing data through the GUIDE-seq bioinformatics pipeline. This aligns reads to the reference genome, identifies genomic locations with tag integration, and nominates off-target sites based on the frequency of tag reads and sequence similarity to the on-target site [62].
GUIDE-seq Workflow: From cell transfection to off-target identification.
Protocol for CIRCLE-seq
CIRCLE-seq is a biochemical, NGS-based off-target assay that offers ultra-sensitive, genome-wide profiling using purified genomic DNA, independent of cellular delivery [68].
Table 3: Key Reagents for CIRCLE-seq
| Reagent / Equipment | Function | Example / Comment |
|---|---|---|
| Purified Genomic DNA | The substrate for in vitro cleavage. | Micrograms of gDNA from the relevant cell type (e.g., iPSCs). |
| Cas9 Nuclease | The active enzyme for cleavage. | Commercially available, e.g., S. pyogenes Cas9 (NEB #M0386M). |
| In vitro transcribed gRNA | Guides Cas9 to target and off-target sites. | Synthesized using kits or commercial synthesis. |
| Focus Ultrasonicator | For controlled shearing of genomic DNA. | Covaris ME220 or similar. |
| Exonucleases (e.g., Lambda, Exo I) | Digests linear DNA, enriching circularized molecules. | New England BioLabs M0262L and M0293L. |
| Plasmid-Safe DNase | Digests remaining linear DNA fragments. | - |
| Ligase | Circularizes sheared genomic DNA fragments. | - |
Detailed Step-by-Step Methodology:
- Genomic DNA Isolation and Shearing: Extract genomic DNA from the desired cell source (e.g., human iPSCs). Using a focused ultrasonicator, shear the DNA to a target fragment size to make it amenable for circularization [68].
- DNA Circularization and Purification: Treat the sheared DNA with exonucleases to digest linear DNA molecules, thereby enriching for successfully ligated, circularized DNA. Purify the circularized DNA using methods such as plasmid-safe DNase treatment to remove any residual linear DNA [68] [62].
- In vitro Cleavage Reaction: Incubate the purified circular DNA library with the pre-complexed Cas9 protein and the gRNA of interest. This allows the nuclease to cleave the DNA at both on-target and off-target sites, linearizing the circular molecules at the points of cleavage [68].
- Library Preparation and Sequencing: Repair the ends of the linearized DNA fragments and ligate Illumina sequencing adapters directly to the break sites. Amplify the library via PCR and sequence using an Illumina platform. The CIRCLE-seq bioinformatics pipeline then maps the paired-end reads, which contain the breakpoint information, to the reference genome to identify all nuclease cleavage sites with high sensitivity [68].
CIRCLE-seq Workflow: From DNA isolation to off-target nomination.
Within the broader scope of a thesis on CRISPR gene editing protocols for correcting stem cell mutations, this document provides detailed application notes and protocols for the critical functional validation phase. Successfully correcting a mutation in a stem cell is only the first step; rigorous demonstration that the edit restores normal protein function and cellular metabolism is essential to confirm therapeutic efficacy [11] [6]. This phase moves beyond genomic sequencing to confirm that the corrected cells can functionally emulate their wild-type counterparts, a prerequisite for their use in disease modeling, drug development, and regenerative cell-based therapies [70].
The protocols herein are framed around the differentiation of pluripotent stem cells (PSCs), whether wild-type or CRISPR-corrected, into hepatocyte-like cells (HLCs) as a model system. Primary human hepatocytes (PHHs) remain the gold standard for studying human liver biology and pathology; thus, the quality of in vitro-generated HLCs must be benchmarked against 24-hour cultured PHHs to ensure they are a phenotypically and functionally accurate model [70]. The following sections provide a consolidated guide for researchers to assess the success of their gene editing and differentiation protocols through a multi-faceted validation of protein expression and metabolic activity.
Key Biological Assays for Functional Validation
A robust evaluation of HLC quality requires a combination of morphological, transcriptomic, proteomic, and functional assays. The table below summarizes the core phenotypic profiling methods used to characterize HLCs against the PHH standard.
Table 1: Biological Assays for Phenotypic Profiling of Hepatocyte-like Cells (HLCs)
| Assessment Category | Specific Assay/Method | Key Targets / Measured Output | Reference Standard |
|---|---|---|---|
| Cell Morphology & Ultrastructure | Phase-contrast & Immunofluorescence Microscopy | Cell polygonal shape, reestablished polarity, cytoskeleton organization | Primary human hepatocyte (PHH) morphology [70] |
| Transmission Electron Microscopy (TEM) | Ultrastructure of organelles (RER, Golgi), bile canaliculi, tight junctions, glycogen granules | PHH ultrastructure [70] | |
| Transcriptomic Profiling | qRT-PCR & RNA-sequencing (Bulk) | Expression dynamics of stemness, hepatic specification, and maturation genes | Gene expression profile of 24-h cultured PHHs [70] |
| Single-Cell RNA-Seq (scRNA-seq) | Cell-to-cell heterogeneity within HLC population, identification of subpopulations | PHH transcriptomic atlas [70] | |
| Protein Expression & Localization | Immunocytochemistry / Immunofluorescence | Presence and correct subcellular localization of hepatic proteins (e.g., ALB, A1AT, HNF4α) | Protein expression and localization in PHHs [70] |
| Western Blot | Semi-quantitative analysis of specific protein expression levels (e.g., CYP enzymes) | Protein levels in PHH lysates [70] | |
| Metabolic Functional Analysis | Cytochrome P450 (CYP) Activity Assay | Metabolism of isoform-specific substrates (e.g., CYP1A2, 2C9, 3A4); measured via luminescence/fluorescence | Metabolic activity of 24-h cultured PHHs [70] |
| Urea Production Assay | Quantification of urea in cell culture supernatant via colorimetric methods | Urea cycle function in PHHs [70] | |
| Albumin Secretion ELISA | Quantification of albumin secreted into the culture medium over a defined period | Albumin secretion rate of PHHs [70] | |
| Low-Density Lipoprotein (LDL) Uptake Assay | Fluorescently-labeled LDL internalization and visualization/quantification | Functional transporter activity in PHHs [70] |
Experimental Workflows and Signaling Pathways
Workflow for HLC Differentiation and Validation
The following diagram illustrates the overarching experimental workflow from stem cell culture to the functional validation of CRISPR-corrected Hepatocyte-Like Cells (HLCs).
Metabolite-Sensing Pathway Regulating Gene Expression
A key aspect of functional validation is ensuring that corrected cells can properly respond to metabolic signals. The diagram below illustrates a pathway where intracellular metabolites directly regulate gene expression by interacting with nuclear proteins, a function that should be restored in metabolically active HLCs.
Detailed Experimental Protocols
Protocol: Immunofluorescence Staining for Hepatic Proteins
Objective: To visualize the presence and subcellular localization of key hepatic proteins in fixed HLCs.
Materials:
- Cells: Fixed HLCs on glass coverslips.
- Primary Antibodies: Mouse anti-Albumin, Rabbit anti-HNF4α.
- Secondary Antibodies: Alexa Fluor 488-conjugated goat anti-mouse, Alexa Fluor 594-conjugated goat anti-rabbit.
- Other Reagents: Phosphate Buffered Saline (PBS), 4% Paraformaldehyde (PFA), 0.1% Triton X-100, Bovine Serum Albumin (BSA), DAPI, mounting medium.
Method:
- Fixation: Aspirate culture medium from cells and wash gently with PBS. Add 4% PFA to cover cells and incubate for 15 minutes at room temperature.
- Permeabilization: Remove PFA and wash cells 3x with PBS. Permeabilize cells with 0.1% Triton X-100 in PBS for 10 minutes.
- Blocking: Wash cells 2x with PBS. Incubate with 1% BSA in PBS for 60 minutes to block non-specific binding.
- Primary Antibody Incubation: Prepare primary antibodies in 1% BSA/PBS at the manufacturer's recommended dilution. Apply to cells and incubate overnight at 4°C in a humidified chamber.
- Washing: The next day, remove primary antibody and wash cells 3x with PBS, 5 minutes per wash.
- Secondary Antibody Incubation: Prepare fluorophore-conjugated secondary antibodies in 1% BSA/PBS, protected from light. Apply to cells and incubate for 1 hour at room temperature in the dark.
- Nuclear Staining: Wash cells 3x with PBS. Incubate with DAPI (1 µg/mL in PBS) for 5 minutes.
- Mounting: Wash cells 2x with PBS. Mount coverslips onto glass slides using an anti-fade mounting medium.
- Imaging: Acquire images using a laser scanning confocal microscope. Compare the fluorescence pattern and intensity to PHH controls.
Protocol: Cytochrome P450 (CYP3A4) Activity Assay
Objective: To quantitatively measure the metabolic activity of the key drug-metabolizing enzyme CYP3A4 in live HLCs.
Materials:
- Cells: HLCs or control PHHs cultured in a 96-well plate.
- Assay Kit: Luminescent CYP3A4 Assay Kit (e.g., Promega P450-Glo).
- Substrate: Luciferin-IPA (provided in kit).
- Inducer: Optional: Rifampicin for CYP3A4 induction.
- Equipment: Multi-mode microplate reader capable of detecting luminescence.
Method:
- Cell Preparation: Culture HLCs in a 96-well plate to near-confluency. Optionally, pre-treat with a CYP3A4 inducer like 10 µM Rifampicin for 48 hours prior to the assay.
- Substrate Addition: Equilibrate the assay buffer and Luciferin-IPA substrate to room temperature. Replace the cell culture medium with the buffer containing the substrate.
- Incubation: Incubate the plate for the recommended time (e.g., 30-60 minutes) at 37°C to allow metabolism of the substrate by intracellular CYP3A4.
- Signal Development: Transfer an aliquot of the supernatant to a white-walled 96-well plate. Add an equal volume of luciferin detection reagent to each well and mix gently.
- Luminescence Measurement: Incubate at room temperature for 20 minutes to stabilize the luminescent signal. Read the plate using a luminometer.
- Data Analysis: Normalize luminescence values to total cellular protein content (determined by a BCA assay) or cell number. Express CYP3A4 activity as Relative Luminescence Units (RLU) per µg protein/hour. Compare the activity of HLCs directly to 24-hour cultured PHHs.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents required for the differentiation and functional validation of HLCs.
Table 2: Essential Research Reagents for HLC Differentiation and Validation
| Reagent/Material | Function/Application | Example Targets/Usage |
|---|---|---|
| CRISPR-GPT AI Tool | AI "copilot" to assist in designing and troubleshooting CRISPR gene-editing experiments; accelerates design and predicts off-target effects [6]. | Generating sgRNA designs for mutation correction in stem cells. |
| Lipid Nanoparticles (LNPs) | A delivery vehicle for in vivo CRISPR therapy; shows high liver tropism and allows for re-dosing due to low immunogenicity [11]. | Systemic delivery of CRISPR-Cas9 components to the liver. |
| Growth Factors & Cytokines | Directs stepwise differentiation of PSCs through definitive endoderm, hepatic specification, and maturation stages [70]. | Activin A (Definitive Endoderm), BMP4/FGF2 (Hepatic Specification), HGF/Oncostatin M (Maturation). |
| Primary Human Hepatocytes (PHHs) | The "gold standard" reference cell for benchmarking the quality, gene expression, and functional maturity of in vitro-generated HLCs [70]. | Used as a 24-hour cultured control in all validation assays. |
| Hepatocyte-Specific Antibodies | Detection and visualization of key hepatic proteins via immunofluorescence and Western blot. | Albumin (ALB), Alpha-1-Antitrypsin (A1AT), Hepatocyte Nuclear Factor 4 Alpha (HNF4α), Asialoglycoprotein Receptor (ASGPR). |
| Functional Assay Kits | Quantitative measurement of specific hepatic metabolic functions in live cells. | CYP450 Activity Assays, Urea Assay Kit, Albumin ELISA Kit. |
| qPCR Primers / RNA-seq Services | Transcriptomic profiling to monitor the expression of genes marking different stages of hepatic differentiation and maturity [70]. | Pluripotency (OCT4), Endoderm (SOX17), Hepatic Progenitor (AFP), Maturity (ALB, CYP enzymes, Urea cycle genes). |
The transition of CRISPR-based gene therapies from research concepts to clinical applications hinges on robust preclinical assessment of their in vivo potency and safety. Humanized mouse models, which are immunodeficient mice engrafted with functional human biological systems, have emerged as indispensable tools for this critical testing phase. They provide a human-relevant in vivo context for evaluating gene editing therapies, particularly for hereditary diseases affecting the hematopoietic system [71] [72]. This document outlines application notes and protocols for utilizing these models within a broader thesis on CRISPR gene editing protocols for correcting stem cell mutations.
Quantitative Efficacy and Safety Data from Humanized Mouse Studies
Data from recent studies demonstrate the performance of CRISPR-based therapeutics in humanized mouse models. The following table summarizes key quantitative findings related to efficacy and safety.
Table 1: Summary of Quantitative Efficacy and Safety Data from Preclinical Studies
| Model / Study Focus | Editing Efficiency / Outcome | Safety Observations | Reference |
|---|---|---|---|
| β-thalassemia patient-derived HSCs in mice (LNP-delivered base editing) | >40% target site editing in the HBG promoter; ~2x increase in fetal hemoglobin (HbF) [71]. | Minimal immune activation; no liver damage; negligible off-target DNA editing; rapid mRNA clearance [71]. | |
| SOD1-ALS transgenic model (CRISPR/Cas9 transgene) | 100% of transgene copies edited; prevention of ALS-like disease [73]. | No tumorigenesis or inflammatory disease observed over 2 years; rare off-target edits; frequent large deletions mediated by Alu elements [73]. | |
| GNAO1 encephalopathy model (CRISPR for humanization) | Successful humanization of the Gnao1 locus [74]. | No abnormal brain histology; no detected off-target modifications in founder mouse [74]. | |
| In vivo HSC editing (Targeted LNP delivery) | Efficient base editing in engrafted human HSCs [71]. | Low immunogenicity; potential for repeat dosing [71]. |
Essential Research Reagent Solutions
The following table catalogizes critical reagents and their applications in developing and testing gene therapies in humanized models.
Table 2: Key Research Reagent Solutions for Humanized Mouse Model Studies
| Research Reagent | Function and Application | Example Use Case |
|---|---|---|
| Next-Generation Humanized Mice (e.g., NSG SGM3xIL15, NSG FLT3xIL15) | Support robust, multilineage human hematopoiesis (T cells, NK cells, myeloid cells) for evaluating immune responses, vector targeting, and long-term therapeutic effects [72]. | Preclinical testing of in vivo CAR cell generation and AAV vector immunogenicity [72]. |
| Cytokine-Expressing Models | Express human cytokines (e.g., IL-3, IL-15, GM-CSF, FLT3L) to enhance development and function of specific human immune cell lineages [72]. | Studies requiring robust human NK cell or myeloid cell populations. |
| Lipid Nanoparticles (LNPs) | In vivo delivery of CRISPR machinery (e.g., mRNA, sgRNA); engineered for targeted delivery to specific tissues like bone marrow [71]. | In vivo base editing of human HSCs engrafted in mouse bone marrow [71]. |
| AAV Vectors | In vivo delivery of CRISPR nucleases, base editors, or donor DNA templates for homology-directed repair. | In vivo gene correction in neural or muscular tissues [71]. |
| Base Editors (e.g., ABE8e) | Mediate precise single-base changes without creating double-strand breaks, reducing indel formation. | Reactivation of fetal hemoglobin by promoter editing in β-thalassemia models [71]. |
Experimental Protocols
Protocol: In Vivo Gene Editing of Engrafted Human HSCs Using Targeted LNPs
This protocol describes a method for editing human hematopoietic stem cells (HSCs) that have previously been engrafted into a humanized mouse model, using systemically administered lipid nanoparticles (LNPs) [71].
Materials:
- Humanized mice engrafted with human CD34+ HSCs (e.g., from β-thalassemia patients).
- LNP formulation containing ionizable lipid (e.g., Lipid-168), base editor mRNA (e.g., ABE8e), and sgRNA (e.g., sgRNA-25).
- Control LNPs (e.g., containing non-targeting sgRNA).
- Equipment for intravenous injection (e.g., syringe, needles, warming chamber).
Procedure:
- Mouse Conditioning: Confirm stable engraftment of human HSCs in NSG or similar immunodeficient mice via flow cytometry analysis of peripheral blood for human CD45+ cells.
- LNP Preparation: Thaw and dilute LNP formulations in an appropriate sterile buffer according to manufacturer specifications. Keep on ice until administration.
- Intravenous Injection: Administer the LNP formulation via tail-vein injection. A typical dose may range from 1-5 mg mRNA per kg of mouse body weight.
- Monitoring: Monitor mice for acute adverse reactions for several hours post-injection.
- Tissue Collection and Analysis: Euthanize mice at predetermined endpoints (e.g., 1-2 weeks post-injection).
- Bone Marrow Harvest: Isolate bone marrow from femurs and tibiae for analysis.
- Potency Assessment:
- Genomic DNA Analysis: Extract genomic DNA from human CD45+CD34+ cells sorted from bone marrow. Use deep sequencing (e.g., Illumina) of the target locus to quantify editing efficiency and profile editing outcomes (indels, base conversions).
- Functional Readout: For hemoglobinopathies, use HPLC to measure fetal hemoglobin (HbF) levels in derived erythroid cells.
- Safety Assessment:
- Off-Target Analysis: Use unbiased methods like CIRCLE-seq on treated human cell genomic DNA to identify potential off-target sites, followed by deep sequencing of these loci from edited mouse tissues.
- Histopathology: Collect and examine tissues (liver, spleen, bone marrow) for signs of toxicity or immune infiltration.
- Plasma Analysis: Measure liver enzymes (e.g., ALT, AST) in plasma to assess hepatotoxicity.
Protocol: Humanized Mouse Model for Allele-Specific RNA Therapeutics Safety
This protocol details the creation and use of a "humanized" mouse model to test the safety of allele-specific RNA therapeutics (e.g., ASOs, RNAi) by ensuring they do not unintentionally silence the wild-type allele [74].
Materials:
- (C57BL/6xCBA/lac) F1 mice for oocyte generation.
- Cas9 protein or mRNA.
- sgRNA targeting the murine locus (e.g.,
GCTTTCCCTGACTCCCTGCfor Gnao1). - Single-stranded oligodeoxynucleotide (ssODN) donor template containing the desired human sequence and a silent restriction site for genotyping.
- Microinjection equipment.
Procedure:
- Design and Preparation: Design an ssODN donor template with homologous arms flanking the human sequence and the desired single-base substitution. The template should also introduce a silent mutation that creates a novel restriction enzyme site for rapid genotyping.
- Microinjection: Co-inject Cas9 protein/mRNA, sgRNA, and the ssODN donor into fertilized mouse oocytes.
- Genotyping Founders: Screen founder pups by PCR and restriction fragment length polymorphism (RFLP) analysis, followed by Sanger sequencing to confirm precise "humanization" of the target locus.
- Establishment of Mouse Line: Breed positive founders to establish a stable mouse line.
- Model Validation:
- Expression Analysis: Use RT-qPCR and Western blot on brain tissues to confirm that the "humanized" allele expresses Gnao1 mRNA and Gαo protein at levels comparable to wild-type mice.
- Histology: Perform histological staining (e.g., H&E) on brain sections to confirm the absence of abnormal changes due to the genetic modification.
- Off-Target Analysis: Use whole-genome sequencing or targeted deep sequencing of in silico-predicted off-target sites to rule out unintended modifications.
- Safety Testing of RNA Therapeutic:
- Administer the candidate allele-specific RNA therapeutic (e.g., via intracerebroventricular injection for CNS targets) to humanized mice.
- Quantify the transcript levels of both the "humanized" and wild-type murine alleles using allele-specific RT-qPCR assays to confirm selective silencing of the intended target without affecting the wild-type allele.
Workflow and Pathway Visualizations
Comparative Editor Analysis: Evaluating SpCas9 vs. Novel AI-Generated Editors
The application of CRISPR-Cas9 technology in correcting stem cell mutations represents a transformative approach for disease modeling and regenerative medicine. The prototypical Streptococcus pyogenes Cas9 (SpCas9) has been the cornerstone of this revolution. However, challenges such as off-target effects and efficiency variability have prompted the exploration of novel protein engineering strategies [75]. Recently, Artificial Intelligence (AI) has emerged as a powerful tool to design next-generation gene editors with enhanced properties [76]. This Application Note provides a comparative analysis of the classic SpCas9 editor versus novel AI-generated editors, specifically OpenCRISPR-1, within the context of stem cell research. We present structured quantitative data, detailed experimental protocols for validation in human pluripotent stem cells (hPSCs), and essential resources to guide researchers in adopting these advanced tools.
Quantitative Comparison of Gene Editors
The performance of a gene editor is primarily evaluated based on its on-target efficiency and specificity. The following tables summarize key quantitative metrics and functional characteristics of SpCas9 and the AI-generated OpenCRISPR-1, based on recent peer-reviewed findings [23] and company reports [77].
Table 1: Performance Metrics of SpCas9 and OpenCRISPR-1 in Human Cells
| Performance Metric | SpCas9 | OpenCRISPR-1 | Measurement Context |
|---|---|---|---|
| Average On-Target Editing Efficiency | 48.3% | 55.7% | Editing at endogenous sites in human cells [77]. |
| Off-Target Editing Rate | 6.1% | 0.32% | Measurement at known promiscuous off-target sites [77]. |
| Reduction in Off-Target Effects | (Baseline) | ~95% reduction | Compared to SpCas9 activity [77]. |
| Sequence Divergence from SpCas9 | (Self) | 403 mutations | Indicates a high degree of novel AI-based design [23] [77]. |
Table 2: Functional and Application Characteristics
| Characteristic | SpCas9 | OpenCRISPR-1 | Implications for Stem Cell Research |
|---|---|---|---|
| PAM Compatibility | NGG | NGG (Interoperable) | Allows targeting of the same genomic loci, enabling direct experimental comparison [77]. |
| sgRNA Scaffold | Native spCas9 scaffold | Native spCas9 scaffold (Compatible) | Utilizes the same well-established sgRNA design tools and protocols [77]. |
| Base Editing Compatibility | Yes | Yes | Successfully paired with deaminase enzymes for precise base editing [23] [77]. |
| Primary Advantage | Well-characterized, widely adopted | High specificity, novel sequence | OpenCRISPR-1 may offer a superior safety profile for therapeutic development. |
Experimental Protocols for Editor Validation in Stem Cells
Before deploying a novel editor like OpenCRISPR-1 in a complex stem cell gene correction project, its performance must be rigorously validated against SpCas9 in your specific experimental system. The protocol below adapts established CRISPR/Cas9 workflows in hPSCs [75] for this comparative purpose.
Protocol: Side-by-Side Validation of Editing Efficiency and Specificity
This protocol outlines the steps to compare SpCas9 and OpenCRISPR-1 activity at selected genomic loci in hPSCs.
1. Design and Cloning of sgRNAs
- Design: Select 3-5 target genomic loci. For each locus, design a sgRNA using reputable online tools (e.g., CHOPCHOP [78]). The target site should be close to the intended future repair site and have a known, quantifiable off-target site [75].
- Cloning: Clone the identical sgRNA sequence into both a SpCas9 expression plasmid and an OpenCRISPR-1 expression plasmid. Using the same sgRNA sequence is critical for a direct comparison.
2. Delivery into hPSCs
- Cell Preparation: Culture and passage hPSCs (e.g., H9 hESCs or patient-derived hiPSCs) as high-quality colonies in feeder-free conditions [75].
- Transfection: For each target locus, transfect hPSCs with the following conditions:
- Condition A: SpCas9 plasmid + sgRNA plasmid
- Condition B: OpenCRISPR-1 plasmid + sgRNA plasmid
- Condition C: Untransfected control
- Methodology: Use an electroporation-based system (e.g., Neon) optimized for hPSCs. Include a fluorescent reporter (e.g., GFP) in the plasmids to enable enrichment of transfected cells 48-72 hours post-transfection via Fluorescence-Activated Cell Sorting (FACS) [75].
3. Analysis of Editing Outcomes
- Genomic DNA Extraction: Harvest sorted cells and extract genomic DNA using a silica-column-based method [75].
- On-Target Efficiency Assessment:
- PCR Amplification: Amplify the on-target region from the genomic DNA using high-fidelity polymerase.
- Next-Generation Sequencing (NGS): Prepare NGS libraries from the PCR products. Sequence to a high depth (>50,000x coverage).
- Data Analysis: Use tools like CRISPResso2 [78] to quantify the percentage of indels at the on-target site for each condition.
- Off-Target Assessment:
- PCR Amplification: Amplify the pre-identified potential off-target sites.
- NGS Analysis: Sequence these amplicons and use CRISPResso2 to detect and quantify any low-frequency indels, comparing the rates between SpCas9 and OpenCRISPR-1.
Workflow Visualization
The following diagram illustrates the logical workflow for the comparative validation protocol:
The AI Design Pipeline for Novel Editors
The creation of OpenCRISPR-1 exemplifies a new paradigm in protein engineering. The process involves training large language models (LLMs) on massive-scale biological data to generate functional proteins de novo [23] [77]. The diagram below outlines this pipeline.
Key Stages:
- Data Curation: Construction of the "CRISPR-Cas Atlas" by mining 26 terabases of genomic and metagenomic data, resulting in over 1.2 million CRISPR operons and expanding known Cas9 diversity by 4.1-fold [23].
- Model Training: Fine-tuning of protein language models (e.g., ProGen2) on this custom atlas to learn the sequence-function relationships of CRISPR systems [23].
- Protein Generation & Filtering: The model generates millions of novel protein sequences, which are bioinformatically filtered. This process achieved a 4.8-fold expansion of diversity across CRISPR-Cas families compared to nature [23].
- Experimental Validation: The most promising generated proteins, such as OpenCRISPR-1, are synthesized and tested in human cell assays for activity and specificity, as detailed in Section 3 [23] [77].
The Scientist's Toolkit: Research Reagent Solutions
Successful gene editing in stem cells requires a suite of reliable reagents and tools. The following table lists essential materials for conducting the comparative analyses described in this note.
Table 3: Essential Research Reagents for Stem Cell Gene Editing
| Reagent / Tool | Function / Description | Example Use Case |
|---|---|---|
| OpenCRISPR-1 Expression System | Plasmid encoding the AI-generated nuclease. | Direct comparison against SpCas9 in validation experiments [77]. |
| SpCas9 Expression System | Benchmark plasmid for comparison. | Baseline control for all experiments [75]. |
| hPSC-Qualified Transfection Kit | Electroporation system optimized for sensitive stem cells. | High-efficiency delivery of CRISPR plasmids into hPSCs with low cytotoxicity [75]. |
| NGS Library Prep Kit | Reagents for preparing sequencing libraries from PCR amplicons. | Assessing on-target and off-target editing frequencies [75]. |
| CRISPResso2 Software | Open-source computational tool for analyzing NGS data from CRISPR experiments. | Quantifying indel percentages and visualizing alignment statistics [78]. |
| Flow Cytometer with Sorter | Instrument for analyzing and isolating cells based on fluorescence. | Enriching transfected cell populations to increase the signal-to-noise ratio in editing analysis [75]. |
The advent of AI-generated gene editors like OpenCRISPR-1 marks a significant leap beyond the capabilities of the foundational SpCas9. Quantitative data demonstrates that these novel editors can achieve comparable or superior on-target efficiency while drastically reducing off-target effects [23] [77]. For researchers focused on correcting stem cell mutations, this enhanced specificity is paramount for generating clean, isogenic cell lines without confounding genomic alterations. The protocols and tools provided here offer a roadmap for integrating these advanced editors into existing stem cell workflows. As AI-driven design pipelines continue to evolve [23] [79], we can anticipate a new generation of bespoke editors with tailored properties, further accelerating the therapeutic application of CRISPR technology in regenerative medicine.
Conclusion
The integration of advanced CRISPR protocols with stem cell biology is fundamentally advancing our capacity to correct pathogenic mutations with high precision. The progression from foundational knowledge to sophisticated methods like AI-designed editors and prime editing, coupled with robust troubleshooting and validation frameworks, creates a powerful pathway for therapeutic development. Success in this field hinges on overcoming persistent challenges in delivery efficiency and long-term safety. Future directions will focus on translating these precise ex vivo editing protocols into scalable, off-the-shelf cell therapies for a broad range of genetic diseases, moving from CRISPR for disease models to CRISPR for cures.
References
- 1. Comparative analysis of human induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8435459/]
- 2. CRISPR Statistics and Facts (2025) [https://media.market.us/crispr-statistics/]
- 3. Efficient gene editing in induced pluripotent stem cells ... [https://www.nature.com/articles/s41598-023-42174-2]
- 4. CRISPR's Efficiency Triples With Spherical Nucleic Acid ... [https://news.feinberg.northwestern.edu/2025/09/05/crisprs-efficiency-triples-with-spherical-nucleic-acid-delivery-system/]
- 5. Comprehensive Protocols for CRISPR/Cas9-based Gene ... [https://pubmed.ncbi.nlm.nih.gov/27532820/]
- 6. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 7. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 8. - CRISPR reveal hidden causes of... | ScienceDaily edited stem cells [https://www.sciencedaily.com/releases/2025/06/250614034240.htm]
- 9. Expanding the CRISPR/Cas toolkit: applications in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1713700/full]
- 10. Frontiers | Genome in mouse spermatogonial editing lines... stem cell [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1599598/full]
- 11. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 12. Progress and challenges in CRISPR-mediated therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8038532/]
- 13. CRISPR-dependent base editing as a therapeutic strategy ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1553590/full]
- 14. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417523/]
- 15. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 16. CMN Weekly (17 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-17-october-2025-your-weekly-crispr-medicine-news/]
- 17. From bench to bedside: cutting-edge applications of base editing and prime editing in precision medicine | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05957-3]
- 18. Fine-Tuning Homology-Directed Repair (HDR) for Precision Genome Editing: Current Strategies and Future Directions | MDPI [https://www.mdpi.com/1422-0067/26/9/4067]
- 19. Emerging trends in prime editing for precision genome ... [https://www.nature.com/articles/s12276-025-01463-8]
- 20. Prime editing: therapeutic advances and mechanistic insights [https://www.nature.com/articles/s41434-024-00499-1]
- 21. Emerging trends in prime editing for precision genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322275/]
- 22. Comparison of CRISPR-Cas9, CRISPR-Cas12f1, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131857/]
- 23. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 24. OpenCRISPR-1: Generative AI Meets CRISPR [https://crisprmedicinenews.com/news/opencrispr-1-generative-ai-meets-crispr/]
- 25. Profluent Modalities | Gene Editing [https://www.profluent.bio/modality/opencrispr]
- 26. Profluent Publishes AI-Designed Genome Editor in Nature ... [https://www.biopharmatrend.com/news/profluent-publishes-ai-designed-genome-editor-in-nature-releases-largest-crispr-dataset-1322/]
- 27. Systematic high-throughput evaluation reveals FrCas9's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939069/]
- 28. AI in Biotech: 2025 Trends, Discoveries, and Game-Changing ... [https://blackthorn.ai/blog/ai-in-biotech-trends-discoveries-and-game-changing-technologies/]
- 29. Prime Editing: Adding Precision and Flexibility to CRISPR ... [https://blog.addgene.org/prime-editing-crisp-cas-reverse-transcriptase]
- 30. Prime editing for precise and highly versatile genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10989687/]
- 31. Designing and executing prime editing experiments in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9799714/]
- 32. Prime editing for functional repair in patient-derived ... [https://www.nature.com/articles/s41467-020-19136-7]
- 33. Prime editing for the investigation of aberrant splicing defect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594906/]
- 34. The future of ex vivo hematopoietic stem cell gene editing [https://pmc.ncbi.nlm.nih.gov/articles/PMC11951688/]
- 35. Inhibiting ferroptosis enhances ex vivo expansion of ... [https://www.nature.com/articles/s41556-025-01814-7]
- 36. Protocol for optimizing culture conditions for ex vivo ... [https://www.sciencedirect.com/science/article/pii/S2666166725001285]
- 37. advances in ex vivo cell culture systems for haematopoietic ... [https://www.sciencedirect.com/science/article/pii/S2352320425001555]
- 38. HLA matching or CRISPR editing of HLA class I/II enables ... [https://www.nature.com/articles/s41467-025-64945-3]
- 39. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 40. Multiplexed genetic engineering of human hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5656432/]
- 41. CRISPR Editing in iPSCs [https://www.synthego.com/ipsc-crispr/]
- 42. Orthogonal CRISPR systems for targeted integration and ... [https://www.sciencedirect.com/science/article/pii/S1525001625006628]
- 43. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 44. Advances in Antibody-Targeted Lipid Nanoparticles (Ab- ... [https://www.biochempeg.com/article/449.html]
- 45. The Hope for Lipid-Based Nanoparticles in Blood Disorders [https://www.sciencedirect.com/science/article/pii/S2452318625000546]
- 46. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 47. Extracellular vesicles for targeted drug delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486671/]
- 48. A versatile antibody capture system drives specific in vivo ... [https://www.nature.com/articles/s41565-025-01954-9]
- 49. Improving viral-based gene delivery to mammalian cells ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925003727]
- 50. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 51. Guide-specific loss of efficiency and off-target reduction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10570041/]
- 52. Protocol for optimizing culture conditions for ex vivo ... [https://pubmed.ncbi.nlm.nih.gov/40173037/]
- 53. Conformational control of Cas 9 by CRISPR hybrid RNA -DNA guides ... [https://pubmed.ncbi.nlm.nih.gov/34478654/]
- 54. Engineered circular guide RNAs enhance miniature ... [https://www.nature.com/articles/s41467-025-58367-4]
- 55. CRISPR Transfection Protocols Guide: How To Select The ... [https://www.synthego.com/guide/how-to-use-crispr/transfection-protocols/]
- 56. Optimizing CRISPR methodology for precise gene editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580712/]
- 57. Improving the Efficiency of CRISPR/Cas9-Mediated Non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384319/]
- 58. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 59. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 60. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 61. A combination strategy for stem cell graft rejection [https://www.regmednet.com/a-combination-strategy-for-stem-cell-graft-rejection/]
- 62. CRISPR off-target detection with NGS | IDT [https://www.idtdna.com/pages/technology/crispr/crispr-genome-editing/crispr-detection/next-generation-sequencing]
- 63. An NGS-based approach for precise and footprint-free ... [https://www.sciencedirect.com/science/article/pii/S1046202325001197]
- 64. High Throughput Analysis of CRISPR-Cas9 Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10427880/]
- 65. How To Use ICE: A Detailed Guide for Analyzing CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/ice-analysis-guide/]
- 66. Unveiling the cut-and-repair cycle of designer nucleases in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583642/]
- 67. Genetic integrity testing of genome-edited pluripotent stem ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3677/genetic-integrity-testing-of-genomeedited-pluripotent-stem-cell-lines-used-for-cell-therapy-applications]
- 68. CIRCLE-seq for interrogation of off-target gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912817/]
- 69. BLOG: Selecting the Right Gene Editing Off-Target Assay [https://seqwell.com/guide-to-selecting-right-gene-editing-off-target-assay/]
- 70. Standard Protocols for Characterising Primary and In Vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11798750/]
- 71. Effectively Edits In Blood Vivo Engrafted... CRISPR Human Stem Cells [https://www.insideprecisionmedicine.com/topics/translational-research/in-vivo-crispr-effectively-edits-human-blood-stem-cells-engrafted-in-mice/]
- 72. Redefining Preclinical Gene Delivery Testing: Humanized ... [https://resources.jax.org/jax-blog/redefining-preclinical-gene-delivery-testing-humanized-mouse-models-as-an-ethical-and-effective-alternative-to-nhps]
- 73. Efficacy and long-term safety of CRISPR/Cas9 genome ... [https://www.nature.com/articles/s42003-021-01942-4]
- 74. CRISPR/Cas9-generated mouse model with humanizing ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2023.1034720/full]
- 75. Comprehensive protocols for CRISPR /Cas9-based gene editing in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 76. a systematic review of AI predictors in CRISPR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11796103/]
- 77. Profluent | Editing the Human Genome with AI [https://www.profluent.bio/media/editing-the-human-genome-with-ai]
- 78. -Powered AI Design Tools CRISPR [https://www.linkedin.com/pulse/ai-powered-crispr-design-tools-mudassir-mohammed-ph-d--7805e]
- 79. AI-guided Cas9 engineering provides an effective strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583830/]