Bone Marrow vs. Adipose-Derived MSCs: A Comprehensive Characterization Guide for Research and Translation
This article provides a systematic comparison of mesenchymal stromal cells (MSCs) derived from bone marrow (BM-MSCs) and adipose tissue (AD-MSCs) for researchers and drug development professionals.
Bone Marrow vs. Adipose-Derived MSCs: A Comprehensive Characterization Guide for Research and Translation
Abstract
This article provides a systematic comparison of mesenchymal stromal cells (MSCs) derived from bone marrow (BM-MSCs) and adipose tissue (AD-MSCs) for researchers and drug development professionals. It covers foundational biological characteristics, including immunophenotype, proliferation rates, and trilineage differentiation potential. The content details validated isolation methods, culture protocols, and therapeutic applications, supported by recent pre-clinical and clinical data. It also addresses critical troubleshooting aspects, such as donor variability and culture standardization, and offers a rigorous framework for the comparative validation of MSC products, essential for guiding source selection in specific regenerative medicine and immunomodulatory applications.
Defining the Core Biology: Origin, Phenotype, and Basic Properties of BM-MSCs and AD-MSCs
The therapeutic potential of Mesenchymal Stem Cells (MSCs) has garnered significant interest in regenerative medicine and drug development. However, MSCs are not a uniform cellular entity; their biological properties and functional capabilities are profoundly influenced by their tissue of origin and the specific anatomical niche they inhabit. The anatomical niche provides a unique microenvironment comprising distinct biological, chemical, and mechanical cues that shape MSC identity and function [1]. This comparison guide objectively analyzes the implications of tissue origin on MSC identity, focusing on the two most extensively studied sources: bone marrow-derived MSCs (BM-MSCs) and adipose tissue-derived MSCs (AD-MSCs). Understanding these source-dependent differences is crucial for researchers and drug development professionals in selecting the appropriate MSC type for specific therapeutic applications, optimizing isolation protocols, and interpreting experimental outcomes within the broader context of MSC characterization research.
MSCs were first isolated from bone marrow, but have since been identified in nearly all connective tissues, including adipose tissue, umbilical cord, dental pulp, and placenta [1] [2]. The anatomical niche of these cells encompasses the specific in vivo microenvironment, including neighboring cell populations, oxygen tension, mechanical stresses, and soluble signaling factors, which collectively govern their physiological role and inherent properties [1].
Bone Marrow Niche: BM-MSCs reside in a perivascular niche within the bone marrow stroma, closely associated with hematopoietic stem cells (HSCs) and the complex bone matrix. This niche is characterized by relatively low oxygen tension (hypoxia) and mechanical influences from the surrounding bony architecture. Their native functions include supporting hematopoiesis and contributing to bone and cartilage maintenance [2] [3].
Adipose Tissue Niche: AD-MSCs, also termed Adipose-derived Stem Cells (ASCs), predominantly occupy the perivascular space of adipose tissue stromal vascular fraction. Their native niche is rich in lipid-laden adipocytes and vascular networks. The primary physiological role of this niche is tissue homeostasis and repair within adipose depots [4] [5].
The process of in vitro culture expansion, essential for obtaining clinically relevant cell numbers, significantly alters the MSC phenotype away from its native state. Cultured MSCs represent an adaptation to plastic surfaces and standard oxygen conditions, which selectively expands certain subpopulations and masks the original niche-specific characteristics to some degree [3].
Table 1: Key Characteristics of MSC Anatomical Niches
| Feature | Bone Marrow (BM-MSC) | Adipose Tissue (AD-MSC) |
|---|---|---|
| Primary Physiological Role | Support hematopoiesis, bone/cartilage maintenance [2] | Adipose tissue homeostasis and repair [4] |
| Native Microenvironment | Hypoxic, bony matrix, close to HSCs [3] | Vascularized, lipid-rich environment [5] |
| Isolation Yield | Low (0.001-0.01% of nucleated cells) [6] | High (500x more cells per gram than bone marrow) [6] |
| Harvesting Procedure | Invasive, painful bone marrow aspiration [6] | Minimally invasive (e.g., liposuction) [5] [6] |
| Donor Site Morbidity | Significant risk [5] | Low risk [5] |
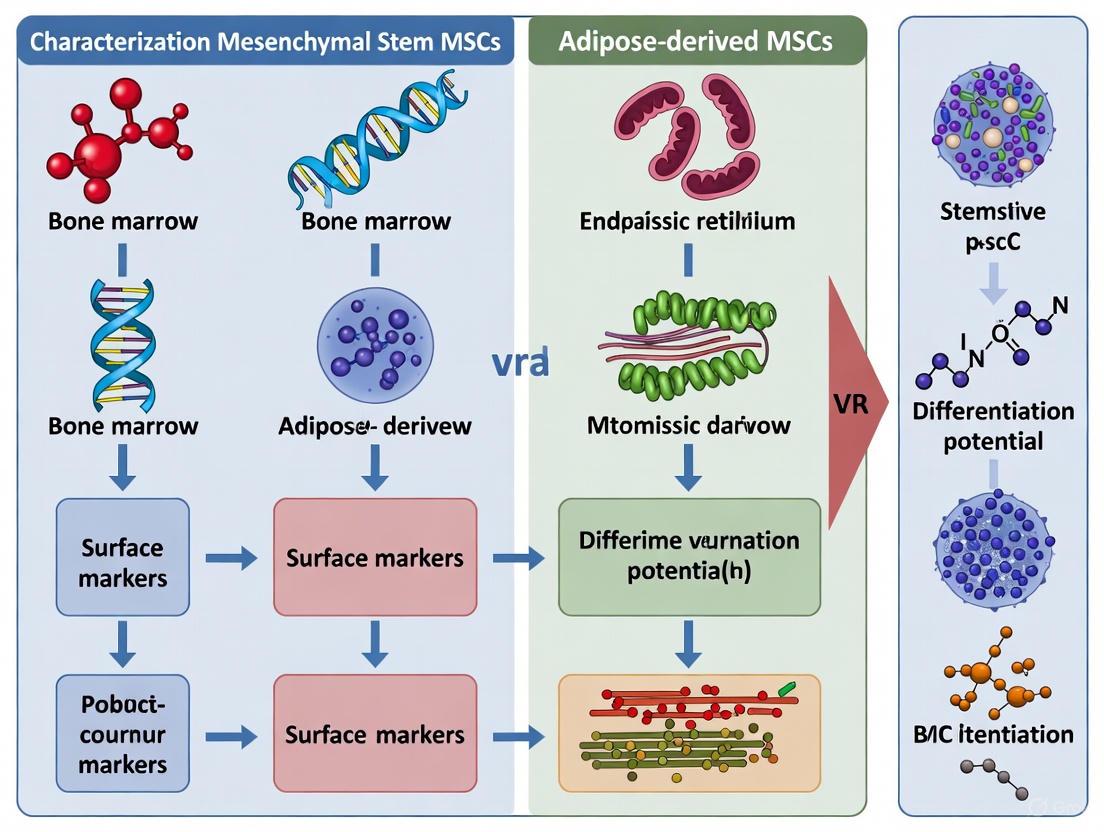
Diagram 1: Anatomical Niche Influences on MSC Identity. The specific microenvironment of each tissue source imprints distinct functional characteristics on resident MSCs.
Comparative Characterization of BM-MSCs and AD-MSCs
Surface Marker Expression
While both BM-MSCs and AD-MSCs adhere to the International Society for Cellular Therapy (ISCT) minimal criteria for MSC definition—being plastic-adherent, expressing CD73, CD90, and CD105, and lacking expression of hematopoietic markers (CD45, CD34, CD14, CD19, HLA-DR)—significant differences exist in their surface marker profiles beyond these core markers [2] [5].
Key Distinguishing Markers:
- CD106 (VCAM-1): BM-MSCs typically show positive expression, while AD-MSCs generally lack this marker [6].
- CD49d (Integrin α4): AD-MSCs express CD49d, whereas BM-MSCs are typically negative for this marker [5] [6].
- Stro-1: BM-MSCs demonstrate positive expression, while AD-MSCs show low or negative expression [5].
These differential marker profiles reflect the distinct adhesive and migratory capacities required for each cell type within their native niches and have implications for their homing potential in therapeutic applications.
Table 2: Surface Marker Profile Comparison
| Surface Marker | BM-MSC Expression | AD-MSC Expression | Functional Significance |
|---|---|---|---|
| CD73, CD90, CD105 | Positive (≥95%) [5] | Positive (≥95%) [5] | Standard MSC-defining markers [2] |
| CD34, CD45, CD14 | Negative (≤2%) [5] | Negative (≤2%) [5] | Hematopoietic lineage exclusion [2] |
| CD106 (VCAM-1) | Positive [6] | Negative/Low [6] | Cell adhesion, hematopoietic stem cell support |
| CD49d (Integrin α4) | Negative [5] [6] | Positive [5] [6] | Cell adhesion and migration |
| Stro-1 | Positive [5] | Negative/Low [5] | Primitive progenitor cell marker |
Proliferation and Clonal Dynamics
AD-MSCs generally exhibit superior proliferative capacity compared to BM-MSCs. Studies demonstrate that AD-MSCs have a faster population doubling time and can undergo more population doublings before reaching senescence [5] [7]. This enhanced expansion capability makes AD-MSCs particularly attractive for applications requiring large cell numbers.
A critical consideration for researchers is the substantial donor-to-donor variability in proliferation rates observed in both cell types, influenced by factors such as donor age, health status, and genetic background [1] [5]. Furthermore, both BM-MSC and AD-MSC populations exhibit significant functional heterogeneity, containing subpopulations with varying differentiation potentials and growth kinetics [1] [3].
Multilineage Differentiation Potential
Despite their shared capacity for trilineage differentiation, BM-MSCs and AD-MSCs display distinct lineage preferences that mirror the functional requirements of their tissue of origin.
Osteogenic Differentiation: BM-MSCs demonstrate superior osteogenic potential compared to AD-MSCs. Donor-matched comparative studies show that BM-MSCs exhibit earlier and higher alkaline phosphatase (ALP) activity, enhanced calcium deposition, and increased expression of osteogenesis-related genes (e.g., osteopontin) [5]. Mechanical stimulation further enhances this innate osteogenic advantage in BM-MSCs [8].
Chondrogenic Differentiation: BM-MSCs generally show greater chondrogenic capacity than AD-MSCs, with more robust expression of chondrogenesis-related genes and extracellular matrix production [5]. This makes BM-MSCs a preferred cell source for cartilage tissue engineering applications.
Adipogenic Differentiation: AD-MSCs possess significantly greater adipogenic capacity, forming lipid vesicles more readily and expressing higher levels of adipogenesis-related genes compared to BM-MSCs [5]. This strong predisposition toward adipogenesis reflects their tissue origin.
Table 3: Functional Differentiation Capacities
| Lineage | BM-MSC Potential | AD-MSC Potential | Supporting Experimental Evidence |
|---|---|---|---|
| Osteogenic | High [5] | Moderate [5] | Higher ALP activity, mineral deposition [8] [5] |
| Chondrogenic | High [5] | Moderate [5] | Superior cartilage matrix gene expression [5] |
| Adipogenic | Moderate [5] | High [5] | Enhanced lipid vesicle formation [5] |
| Immunomodulatory | Strong [2] [3] | Strong, potentially superior [4] [7] | T-cell inhibition, macrophage polarization [7] |
Diagram 2: Lineage Differentiation Preferences. BM-MSCs and AD-MSCs show distinct differentiation biases that reflect their tissue of origin.
Experimental Methodologies for MSC Comparison
Isolation and Culture Protocols
Standardized isolation and culture methods are essential for obtaining reproducible, comparable MSC populations from different tissue sources.
BM-MSC Isolation Protocol:
- Sample Collection: Bone marrow aspirate (typically 10-50 mL) is collected from the iliac crest into heparinized syringes to prevent coagulation [5].
- Processing: The aspirate is filtered through a 70 μm cell strainer, diluted with culture medium (e.g., DMEM with 10% FBS), and centrifuged at 1800 rpm for 10 minutes [5].
- Plating and Expansion: The cell pellet is resuspended in culture medium and plated in tissue culture flasks. After 24 hours, non-adherent cells are removed by washing with PBS. Adherent cells are cultured with medium changes twice weekly [5].
- Passaging: At 80% confluence, cells are detached using trypsin/EDTA and subcultured at appropriate densities [5].
AD-MSC Isolation Protocol:
- Sample Collection: Adipose tissue is obtained through liposuction or surgical resection and washed extensively with PBS containing antibiotics [5].
- Digestion: The tissue is minced and digested with 0.1% collagenase type I for 60 minutes at 37°C with agitation [5].
- Stromal Vascular Fraction (SVF) Separation: The digest is centrifuged (2000 rpm for 5 minutes) to separate the SVF (pellet) from mature adipocytes (supernatant) [5].
- Expansion: The SVF pellet is resuspended in culture medium, plated, and cultured similarly to BM-MSCs [5].
Differentiation Assays
Osteogenic Differentiation:
- Induction Medium: DMEM supplemented with 10% FBS, 10 mM β-glycerophosphate, 50 μM ascorbate-2-phosphate, and 100 nM dexamethasone [5].
- Duration: 21-28 days.
- Assessment Methods: Alkaline phosphatase (ALP) activity staining (early marker), Alizarin Red S staining for calcium deposition (late marker), and osteogenic gene expression analysis (e.g., Runx2, osteocalcin) [8] [5].
Chondrogenic Differentiation:
- Induction Method: Pellet culture system (250,000-500,000 cells per pellet) in serum-free DMEM supplemented with 1% ITS+1, 100 nM dexamethasone, 50 μM ascorbate-2-phosphate, and 10 ng/mL TGF-β3 [5].
- Duration: 21-28 days.
- Assessment Methods: Histological staining (Safranin O for proteoglycans, Toluidine Blue for sulfated glycosaminoglycans), and chondrogenic gene expression analysis (e.g., SOX9, aggrecan, collagen type II) [5].
Adipogenic Differentiation:
- Induction Medium: DMEM with 10% FBS, 0.5 mM isobutylmethylxanthine, 1 μM dexamethasone, 10 μM insulin, and 200 μM indomethacin [5].
- Duration: 14-21 days.
- Assessment Methods: Oil Red O staining of lipid vesicles, and adipogenic gene expression analysis (e.g., PPARγ, FABP4) [5].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for MSC Research
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Isolation Enzymes | Collagenase Type I [5] | AD-MSC isolation from tissue | Concentration (0.1%) and digestion time (60 min) critical for viability |
| Culture Media | DMEM, α-MEM [5] | Basal medium for expansion | Typically supplemented with 10% FBS; serum-free alternatives available |
| Characterization Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR [2] [5] | Flow cytometry immunophenotyping | Essential for ISCT compliance; include appropriate isotype controls |
| Osteogenic Inducers | β-glycerophosphate, Ascorbate-2-phosphate, Dexamethasone [5] | Osteogenic differentiation assay | ALP activity early marker; Alizarin Red for mineralization [8] |
| Chondrogenic Inducers | TGF-β3, ITS+ Supplement, Ascorbate-2-phosphate [5] | Chondrogenic differentiation assay | Pellet culture system mimics 3D environment |
| Adipogenic Inducers | IBMX, Insulin, Indomethacin, Dexamethasone [5] | Adipogenic differentiation assay | Oil Red O stains neutral lipid droplets |
| Analysis Kits | ALP Staining Kit, Alizarin Red S, Oil Red O [8] [5] | Differentiation outcome assessment | Quantitative and qualitative methods available |
The tissue origin and anatomical niche fundamentally shape MSC identity, resulting in functionally distinct cell populations with unique advantages for specific applications. BM-MSCs demonstrate superior osteogenic and chondrogenic potential, making them well-suited for musculoskeletal regeneration. In contrast, AD-MSCs offer practical advantages including higher yield, less invasive harvesting, and robust proliferative and adipogenic capacity, along with potentially enhanced immunomodulatory properties for inflammatory disorders [4] [7].
For researchers and drug development professionals, these differences inform critical experimental and therapeutic decisions. The selection between BM-MSCs and AD-MSCs should be guided by the target application, required cell numbers, and desired mechanism of action. Furthermore, the significant donor-to-donor variability and functional heterogeneity within each population necessitate careful experimental design, including donor-matched comparisons when possible and single-cell approaches to deconstruct subpopulation dynamics [1] [4]. As the field advances, understanding how niche-specific cues determine MSC fate and function will enable more precise manipulation of these cells for enhanced therapeutic outcomes in regenerative medicine and drug development.
In the field of regenerative medicine, Mesenchymal Stromal Cells (MSCs) have emerged as a cornerstone for cell-based therapies. The International Society for Cell & Gene Therapy (ISCT) established minimal criteria to define these cells, creating a essential benchmark for the field [2]. These criteria stipulate that MSCs must be adherent to plastic under standard culture conditions, possess trilineage differentiation potential (osteogenic, adipogenic, and chondrogenic), and express a specific set of surface markers—CD73, CD90, and CD105—while lacking expression of hematopoietic markers [2] [9]. This framework provides foundational standards; however, a critical question persists: do MSCs from different tissue sources uniformly meet these criteria?
The ISCT-proposed markers are not merely identifiers but are proteins with significant biological functions. CD73 functions as a 5'-exonuclease, catalyzing the hydrolysis of adenosine monophosphate to adenosine, which may play a role in cell signaling within the bone marrow and modulate cellular interactions [2]. CD90 (Thy-1), an N-glycosylated glycoprotein, is part of the immunoglobulin superfamily and mediates cell–cell and cell–extracellular matrix interactions [2]. CD105 (Endoglin) is a type I membrane glycoprotein that is part of the TGF-β receptor complex and is essential for angiogenesis and cell migration [2]. Despite the established criteria, significant heterogeneity in reporting and characterizing MSCs exists in both preclinical and clinical literature, with one scoping review finding that only 18% of articles explicitly referred to the ISCT minimal criteria [10]. This analysis delves into the comparative adherence of bone marrow-derived MSCs (BM-MSCs) and adipose tissue-derived MSCs (AD-MSCs) to the ISCT surface marker criteria, examining the quantitative evidence and exploring the functional implications beyond mere phenotypic definition.
Comparative Analysis of Surface Marker Expression in BM-MSCs and AD-MSCs
Quantitative Expression of CD73, CD90, and CD105
Extensive research confirms that both BM-MSCs and AD-MSCs consistently demonstrate high expression of the positive ISCT markers. A comprehensive analysis of the literature reveals that the expression of these markers is a reliable constant, irrespective of the tissue source, when cells are isolated and expanded under standard conditions.
Table 1: Quantitative Expression of ISCT-Defining Surface Markers in BM-MSCs and AD-MSCs
| Surface Marker | Reported Expression in BM-MSCs | Reported Expression in AD-MSCs | Key Function |
|---|---|---|---|
| CD105 (Endoglin) | 82.9% (in vitro studies) [9] | >90% positive [11] | Component of TGF-β receptor complex; angiogenesis [2] |
| CD90 (Thy-1) | 75.0% (in vitro studies) [9] | >90% positive [11] | Cell adhesion, migration, and cell-cell interactions [2] |
| CD73 | 52.0% (in vitro studies) [9] | >90% positive [11] | Ecto-5'-nucleotidase; produces adenosine [2] |
A donor-matched comparative study further reinforced these findings, confirming that isolated ASCs and BMSCs from all donors demonstrated immunophenotypic characteristics of MSCs with strong expression of these standard markers [12]. This high-level expression is maintained across different culture supplements. A direct head-to-head comparison of BM-MSCs and AD-MSCs cultured in human platelet lysate (hPL)-supplemented medium—an alternative to fetal bovine serum for clinical-scale expansion—found that both cell types exhibited similar expression patterns of these surface markers [13]. Furthermore, the expression of these markers, while stable through several passages, has been observed to potentially decrease with extensive passaging, as seen in AD-MSCs where expression was confirmed even at the 13th passage despite a noted decline [14].
Expression of Additional Markers and Donor Variability
While CD73, CD90, and CD105 expression is consistently high, studies often reveal differences in the expression profiles of other, non-ISCT markers. A donor-matched study highlighted that unlike BM-MSCs, AD-MSCs showed high expression of CD49d and low expression of Stro-1 [12]. This suggests that while the core ISCT criteria are met, the tissue of origin imprints a distinct molecular signature on the cells.
It is also critical to acknowledge the role of donor variability. The same donor-matched study concluded that the proliferation and differentiation capacity of both AD-MSCs and BM-MSCs varied significantly among donors, a factor that can influence both marker expression and functional potency [12]. This inherent biological variation underscores the necessity for thorough and lot-specific characterization of MSCs intended for clinical applications.
Experimental Protocols for Isolating and Characterizing MSCs
Standardized Isolation and Culture Workflow
The reliable comparison of MSC surface markers hinges on robust and reproducible isolation and culture methods. The following workflow diagram outlines the standard protocols for deriving and characterizing MSCs from bone marrow and adipose tissue.
Detailed Methodologies for Key Experiments
The characterization of surface markers relies heavily on specific, well-established laboratory techniques. Below are the detailed protocols for the core methodologies cited in comparative studies.
1. Flow Cytometry for Surface Marker Analysis This is the gold-standard technique for quantifying the expression of CD73, CD90, CD105, and other markers [12].
- Cell Preparation: Harvest MSC populations (e.g., at passage 3-5) using a trypsin/EDTA solution. Wash cells twice with phosphate-buffered saline (PBS).
- Antibody Staining: Suspend approximately 4 × 10^5 cells in PBS. Incubate with fluorescently conjugated antibodies against target surface antigens (e.g., CD73, CD90, CD105, CD34, CD45, HLA-DR) and relevant isotype controls for 30 minutes at 4°C in the dark [12].
- Analysis: Wash cells to remove unbound antibody and resuspend in PBS. Acquire data using a flow cytometer (e.g., BD LSRFortessa), collecting a minimum of 50,000 events per sample. Analyze data with specialized software (e.g., FlowJo V10), gating on the live cell population and reporting the percentage of positive cells for each marker [12]. The ISCT defines positivity as ≥95% for CD73, CD90, and CD105, and ≤2% for hematopoietic markers [2].
2. MSC Isolation from Bone Marrow
- Initial Processing: Filter heparinized bone marrow aspirate through a 70 μm cell strainer. Dilute 1:1 with culture medium (e.g., DMEM + 10% FBS + antibiotics) and centrifuge at 1800 rpm for 10 minutes [12].
- Plating and Expansion: Resuspend the cell pellet in culture medium and plate in a culture flask. After 24 hours, wash the flask with PBS to remove non-adherent cells. Refresh the medium twice weekly and passage cells upon reaching 80% confluence [13] [12].
3. MSC Isolation from Adipose Tissue
- Tissue Preparation and Digestion: Minced adipose tissue is washed extensively with PBS containing antibiotics. Digest the tissue with 0.1% collagenase type I (or type IV) for 30-60 minutes at 37°C with agitation [13] [12].
- Stromal Vascular Fraction (SVF) Isolation: Neutralize the collagenase with an equal volume of culture medium. Centrifuge the digest; the resulting pellet is the SVF, which contains the AD-MSCs [12].
- Plating and Expansion: Resuspend the SVF pellet in culture medium and plate in a flask. Culture and passage as described for BM-MSCs [13].
The Scientist's Toolkit: Essential Reagents for MSC Characterization
The consistent isolation and characterization of MSCs depend on a suite of key research reagents. The following table details essential materials and their functions based on the protocols from the cited literature.
Table 2: Key Research Reagent Solutions for MSC Isolation and Characterization
| Reagent / Material | Function in Experimental Protocol | Examples from Literature |
|---|---|---|
| Collagenase Type I / IV | Enzymatic digestion of the extracellular matrix in adipose tissue to release the stromal vascular fraction (SVF). | 0.1% Collagenase Type I [12], 0.2% Collagenase Type IV [13] |
| Density Gradient Medium | Separation of mononuclear cells from whole bone marrow aspirate based on density. | Lymphoprep, Percoll [13] [15] |
| Culture Medium + Supplements | Ex vivo expansion and maintenance of MSCs. Provides necessary nutrients and growth factors. | DMEM/IMDM supplemented with 10% FBS [12] or 5% Human Platelet Lysate (hPL) [13] |
| Fluorescent-Conjugated Antibodies | Detection and quantification of specific cell surface markers (positive and negative) via flow cytometry. | Antibodies against CD73, CD90, CD105, CD34, CD45, etc. [12] |
| Trypsin/EDTA Solution | Detachment of adherent MSCs from the plastic culture flask for passaging or analysis. | Standard reagent for cell harvesting [13] [12] |
Functional Correlations and Implications for Therapeutic Development
While surface marker expression is a necessary defining characteristic, it is insufficient to predict the functional potency of MSCs. The expression levels of CD73, CD90, and CD105 have been shown to have little correlation with cell function [11]. Consequently, a deeper analysis of functional differences is required when selecting a cell source for a specific application.
- Proliferation and Differentiation: Under comparable culture conditions, AD-MSCs often demonstrate greater proliferative potential than BM-MSCs [13] [12]. Regarding differentiation, the tissue source strongly influences lineage preference. BM-MSCs consistently show a higher capacity for osteogenic and chondrogenic differentiation, while AD-MSCs possess a superior adipogenic differentiation potential [13] [12] [11].
- Immunomodulatory Capacity: A critical therapeutic function of MSCs is their immunomodulatory capacity, often assessed by the activity of indoleamine 2,3-dioxygenase (IDO). Notably, AD-MSCs have been reported to display more robust immunomodulatory activity than BM-MSCs, showing significantly higher IDO activity upon stimulation with IFN-γ [11]. This functional advantage is not predicted by the core ISCT marker panel.
- Secretome and Angiogenic Potential: The therapeutic effects of MSCs are largely mediated by their secretome. Comparative studies have identified differences in the secretion of cytokines and growth factors. For instance, AD-MSCs may secrete different levels of factors like FGF-2, HGF, and VEGF under inflammatory priming compared to BM-MSCs [11]. Furthermore, AD-MSCs have been suggested to be more efficient at stimulating angiogenesis [11].
The adherence to ISCT criteria for surface marker expression provides a crucial foundation for the identity of MSCs. Both BM-MSCs and AD-MSCs robustly and consistently meet the minimal criteria for CD73, CD90, and CD105 expression, making this panel a reliable tool for basic identification and quality control [13] [9] [12]. However, this phenotypic similarity belies significant functional heterogeneity. The choice between BM-MSCs and AD-MSCs should not be based solely on ISCT marker expression but must be guided by the intended therapeutic application, considering the documented advantages of BM-MSCs in skeletal regeneration and the potential superior immunomodulatory and proliferative capacity of AD-MSCs [13] [11]. As the field advances, characterisation must extend beyond minimal criteria to include functional potency assays relevant to the mechanism of action, ensuring that the MSC populations used in research and therapy are not only correctly identified but also functionally fit for purpose.
Within the field of regenerative medicine, Mesenchymal Stromal Cells (MSCs) from bone marrow (BM-MSCs) and adipose tissue (AD-MSCs) are the most extensively studied and utilized sources for both research and clinical applications [13] [4]. A fundamental characteristic shared by MSCs from these and other tissues is their typical fibroblast-like, spindle-shaped morphology and their capacity for plastic-adherence in vitro [16] [17]. This common appearance, however, can obscure significant underlying biological differences. For researchers and drug development professionals, a precise understanding of the subtle morphological distinctions and divergent in vitro growth dynamics between BM-MSCs and AD-MSCs is critical. Such knowledge is essential for selecting the optimal cell source for specific therapeutic applications, ranging from treating immunological disorders to facilitating the repair of bone, cartilage, or cardiac tissue [13] [18]. This guide provides a direct, data-driven comparison of these two cell types, framing the analysis within the broader context of MSC characterization research.
Tabular Comparison of Key Characteristics
The following table summarizes the core morphological and growth properties of BM-MSCs and AD-MSCs based on current experimental evidence.
Table 1: Comparative Analysis of BM-MSC and AD-MSC Morphology and In Vitro Growth
| Characteristic | Bone Marrow-MSCs (BM-MSCs) | Adipose Tissue-MSCs (AD-MSCs) | Experimental Context |
|---|---|---|---|
| General Morphology | Fibroblast-like, spindle-shaped [13] | Fibroblast-like, spindle-shaped [13] | Culture in 5% human platelet lysate (hPL)-supplemented medium [13] |
| Proliferation Capacity | Lower proliferative potential [13] | Greater proliferative potential [13] | Serial passaging; calculation of cumulative population doublings [13] |
| Cell Size | Information not specified in search results | Information not specified in search results | |
| Colony Formation | No significant difference in CFU-F efficiency observed [13] | No significant difference in CFU-F efficiency observed [13] | Colony-forming unit-fibroblast (CFU-F) assay at 1x10^3 cells/well [13] |
| Senescence & Stability | May exhibit genetic instability or accelerated senescence after long-term culture [17] | Tends to proliferate at a higher rate than BM-MSCs [7] | Dependent on culture conditions and passaging [17] |
Detailed Experimental Insights and Methodologies
Direct Head-to-Head Comparison Under hPL Conditions
A seminal 2015 study provided a direct comparison of BM-MSCs and AD-MSCs cultured under identical conditions using human platelet lysate (hPL), a clinically relevant alternative to fetal bovine serum (FBS) [13].
Isolation and Culture Protocol:
- BM-MSCs: Bone marrow aspirates were collected from human donors. Mononuclear cells were isolated using a lymphoprep density gradient by centrifugation at 2,000 rpm for 30 minutes. These cells were then plated at a density of 2x10^5/cm² in culture flasks [13].
- AD-MSCs: Lipoaspirate tissues were washed and digested with 0.2% collagenase type IV at 37°C for 30 minutes. The stromal vascular fraction (SVF) was isolated via centrifugation at 300 x g, and viable cells were plated at a density of 1x10^6 cells per flask [13].
- Both cell types were cultured in Iscove’s Modified Dulbecco’s Medium (IMDM) supplemented with 5% hPL and maintained at 37°C with 5% CO₂. At 80-90% confluence, cells were harvested using trypsin-EDTA and replated at 2,000 cells/cm² for expansion [13].
Key Quantitative Findings:
- Morphology: Both BM-MSCs and AD-MSCs exhibited a similar fibroblast-like morphology under hPL conditions [13].
- Proliferation: AD-MSCs demonstrated a significantly greater proliferative potential than BM-MSCs, as measured by cumulative population doubling over serial passages [13].
- Clonogenicity: The CFU-F assay revealed no significant difference in colony-forming efficiency between the two cell types when plated at a low density (1x10^3 cells/well) [13].
Functional Morphology in Tendon Regeneration
A 2023 study investigated the response of BM-MSCs and AD-MSCs to cyclical tensile loading, a model for tendon regeneration, providing insight into how morphology adapts to mechanical cues [19].
Experimental Workflow:
Key Findings:
- Both AD-MSCs and BM-MSCs underwent similar morphological changes and realigned themselves perpendicular to the direction of the stretching force [19].
- No significant differences were observed in tenogenic gene expression or total collagen production between the two cell types under this specific loading regime, suggesting comparable tenogenic potential when mechanically stimulated [19].
Diagram 1: Experimental workflow for comparative MSC analysis.
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their functions for the isolation, culture, and characterization of BM-MSCs and AD-MSCs, as derived from the cited experimental protocols.
Table 2: Essential Reagents for MSC Isolation and Characterization
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Collagenase Type IV | Enzymatic digestion of adipose tissue to isolate the Stromal Vascular Fraction (SVF) for AD-MSC culture. | 0.2% collagenase type IV for 30 min at 37°C [13]. |
| Lymphoprep / Ficoll-Paque | Density gradient medium for isolation of mononuclear cells from bone marrow aspirates for BM-MSC culture. | Lymphoprep gradient centrifuged at 2,000 rpm for 30 min [13]; Ficoll-paque solution [19]. |
| Human Platelet Lysate (hPL) | Xeno-free supplement for clinical-scale expansion of MSCs; promotes growth and maintains differentiation potential. | 5% hPL in IMDM medium [13]. |
| Fetal Bovine Serum (FBS) | Traditional serum supplement for basal MSC culture medium. | 10% FBS in DMEM [18] [19]. |
| Trypsin-EDTA | Proteolytic enzyme solution for detaching adherent cells during subculturing. | Standard protocol for cell detachment at ~80% confluence [13] [16]. |
| Crystal Violet | Stain used to visualize and count cell colonies in the Colony-Forming Unit Fibroblast (CFU-F) assay. | Staining of fixed cell layers on day 14 of culture [13]. |
Signaling Pathways Governing Identity and Function
Distinguishing MSCs from ordinary fibroblasts, which they closely resemble, requires a deep understanding of the molecular pathways that define their identity and regenerative potential. Computational analyses of gene expression and DNA methylation have been instrumental in elucidating these pathways [20].
Diagram 2: Key molecular pathways defining MSC identity versus fibroblasts.
- Identity and Stemness: A strong signature for KRAS signaling is upregulated in MSCs compared to fibroblasts. This pathway is known to play an essential role in the maintenance of stemness [20].
- Immunomodulatory Capacity: MSCs show enriched expression of genes involved in the regulation of coagulation and complement cascades, processes decisive for resolving inflammatory processes. This aligns with their known potent immunosuppressive effects [20] [7].
- Regenerative Potential: Pathways associated with wound healing are particularly important for the regenerative capacity of MSCs. This is mediated through the secretion of a complex cocktail of growth factors, cytokines, and chemokines [13] [20].
- The HOX Code and Epigenetics: The identity of MSCs is further defined by a specific HOX code (a pattern of HOX gene expression). This code is linked to their developmental origin and is associated with differentially methylated regions in HOX genes, providing potential biomarkers for distinguishing MSCs from fibroblasts [20].
Mesenchymal stromal cells (MSCs) represent a cornerstone of regenerative medicine and cell-based therapies, with sources ranging from bone marrow (BM-MSCs) to adipose tissue (AD-MSCs). Proliferation dynamics—encompassing population doubling time (PDT) and growth kinetics—serve as critical indicators of cellular health, expansion potential, and therapeutic suitability. Understanding these parameters is essential for researchers and drug development professionals seeking to optimize cell culture protocols, scale up production, and ensure consistent quality in clinical applications. This guide provides a comprehensive comparison of proliferation dynamics between BM-MSCs and AD-MSCs, synthesizing experimental data and methodologies to inform evidence-based decision-making in MSC selection and application.
Comparative Analysis of Population Doubling Time and Growth Kinetics
Extensive research has demonstrated significant differences in the proliferation capacities of MSCs derived from bone marrow versus adipose tissue. The following synthesis of experimental findings provides a quantitative basis for comparing their growth kinetics.
Table 1: Comparative Population Doubling Time (PDT) of BM-MSCs and AD-MSCs
| Cell Source | Passage Number | Population Doubling Time (Days) | Study Model | Reference |
|---|---|---|---|---|
| BM-MSCs | Passage 3-6 | 1.90 ± 0.45 to 2.25 ± 0.46 | Human | [21] |
| BM-MSCs | Passage 3-6 | 1.85 ± 0.36 to 1.99 ± 0.55 | Human (α-MEM) | [21] |
| BM-MSCs | Multiple passages | Increased with higher passages | Guinea pig | [22] |
| AD-MSCs | Multiple passages | Lower than BM-MSCs | Guinea pig | [22] |
Table 2: Growth Kinetics and Expansion Potential of MSCs from Different Sources
| Parameter | BM-MSCs | AD-MSCs | Experimental Context |
|---|---|---|---|
| Proliferation Rate | Lower than AD-MSCs | Significantly higher | Guinea pig model [22] |
| Response to Passage | PDT increases with passages | PDT increases with passages | In vitro expansion [22] |
| Culture Medium Impact | Higher expansion in α-MEM vs DMEM | Information not specified | Human cells [21] |
| Donor Health Impact | Significantly reduced in CLI patients | Information not specified | Clinical trial [23] |
| Therapeutic Yield | Limited by low initial yield and expansion | Abundant source, minimal morbidity | Comparative review [22] |
The body of evidence consistently indicates that AD-MSCs exhibit superior proliferation capacity compared to BM-MSCs. A fundamental study in guinea pigs demonstrated that the "proliferation rate of AT-MSCs in the analyzed passages was more than BM-MSCs," with both cell types showing increased PDT as passage number increased [22]. This proliferation advantage positions AD-MSCs as a promising source for clinical applications requiring rapid cell expansion.
In human studies, research has further elucidated the impact of culture conditions on MSC proliferation. BM-MSCs cultured in α-MEM medium demonstrated a marginally higher expansion ratio compared to those cultured in DMEM, though the difference was not statistically significant [21]. This highlights the importance of culture medium optimization regardless of cell source.
Donor health status represents another critical factor influencing proliferation dynamics. BM-MSCs isolated from patients with critical limb ischemia (CLI) exhibited significantly longer population doubling times and reduced final cell yields compared to those from young healthy donors [23]. This finding has profound implications for autologous therapy approaches in diseased populations, potentially favoring AD-MSCs sources in such clinical scenarios.
Experimental Protocols for Assessing Proliferation Dynamics
Standardized methodologies are essential for obtaining reliable, reproducible data on MSC proliferation kinetics. This section outlines key experimental approaches referenced in the comparative studies.
Cell Isolation and Culture
BM-MSCs Isolation: Human BM-MSCs are typically isolated from bone marrow aspirates using density gradient centrifugation with Ficoll-paque solution (density 1.077 g/mL). The mononuclear cell layer is collected after centrifugation at 2,200 rpm for 25 minutes, followed by plating in complete growth medium (e.g., DMEM or α-MEM supplemented with 10% FBS or human platelet lysate) [21] [19]. The cultures are maintained at 37°C in a humidified 5% CO2 atmosphere, with medium changes every 3-4 days until 80-90% confluence is reached [22].
AD-MSCs Isolation: Adipose tissue is rinsed with PBS, minced into small pieces, and digested with 0.1% collagenase type I at 37°C for 20-60 minutes. The digested tissue is neutralized with culture medium, centrifuged at 1,200 rpm for 5-7 minutes, and filtered through a 200μm mesh to remove undigested fragments. The resulting stromal vascular fraction (SVF) is plated in culture flasks with appropriate medium [22] [19]. AD-MSCs can also be obtained through mechanical fragmentation methods without enzymatic digestion [16].
Population Doubling Time (PDT) Assessment
For PDT calculation, cells at specific passages are seeded in multi-well plates at a density of approximately 5×10^4 cells per well in triplicate. Cells are counted daily for 7 days post-seeding using automated counters or hemocytometers. The PDT is calculated using the standard formula:
PDT = T × ln(2) / ln(Xe / Xb)
Where T is incubation time in hours, Xb is the cell number at the beginning of the incubation time, and Xe is the cell number at the end of the incubation time [22]. Studies typically compare PDT across multiple passages (e.g., passages 2, 5, and 8) to assess the impact of in vitro expansion on proliferation capacity [22].
Growth Curve Analysis
Cells at specific passages are seeded in 24-well plates at standardized densities (e.g., 5×10^4 cells/well) in triplicate. Cell counts are performed daily for 7-10 days, with medium replenishment every 3-4 days. Growth curves are generated by plotting cell numbers against time, typically displaying the characteristic sigmoidal pattern with lag, log, and plateau phases [22]. The GraphPad Prism software is commonly used for curve plotting and analysis [22].
Diagram 1: Experimental workflow for MSC isolation and proliferation assessment. This flowchart illustrates the parallel processes for isolating MSCs from bone marrow and adipose tissue, followed by standardized proliferation analysis protocols common to both cell types.
Molecular Regulation of MSC Stemness and Proliferation
The proliferation capacity of MSCs is intrinsically linked to their "stemness" - the maintenance of an undifferentiated state with robust self-renewal capabilities. Understanding the molecular basis of MSC stemness provides insights into the observed differences in proliferation dynamics between BM-MSCs and AD-MSCs.
Table 3: Key Molecular Regulators of MSC Stemness and Proliferation
| Regulator Category | Key Factors | Function in MSC Stemness/Proliferation |
|---|---|---|
| Transcription Factors | TWIST1, TWIST2 | Promote proliferation, inhibit senescence via EZH2-mediated silencing of p14 and p16 [24] |
| OCT4 | Enhances cell cycle progression, proliferation, and CFU-F capacity; suppresses senescence markers [24] | |
| SOX2 | Maintains stemness; reduced expression associated with senescence markers p16 and p21 [24] | |
| HOX Genes | HOXA5, HOXB7 | Regulate proliferation and differentiation; deletion induces cell cycle arrest [24] |
| Epigenetic Regulators | EZH2, DNMT1 | Mediate silencing of senescence genes through histone modification and DNA methylation [24] |
| Cell Cycle Regulators | p16, p21, p53 | Accumulate in senescent MSCs; suppression enhances proliferation capacity [24] |
The molecular basis for proliferation differences between MSC sources remains an active research area. Evidence suggests that transcriptional networks vary between MSCs from different tissue sources, potentially explaining their distinct growth kinetics and differentiation capacities [24]. The heterogeneous nature of MSCs—influenced by tissue origin, donor age, and health status—further complicates direct comparisons [25].
Diagram 2: Molecular regulation of MSC stemness and proliferation. This diagram illustrates key genetic and epigenetic factors that maintain MSC stemness, promoting proliferation capacity while suppressing cellular senescence pathways.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents for MSC Proliferation Studies
| Reagent/Category | Specific Examples | Function in Proliferation Assays |
|---|---|---|
| Culture Media | DMEM, α-MEM, Low-glucose DMEM | Base nutrients for cell growth and maintenance [22] [21] |
| Serum Supplements | Fetal Bovine Serum (FBS), Human Platelet Lysate (hPL) | Provides essential growth factors and adhesion proteins [22] [21] |
| Enzymes for Isolation | Collagenase Type I, Trypsin-EDTA | Tissue dissociation and cell harvesting [22] [19] |
| Growth Factors | FGF-2, EGF, PDGF | Enhance proliferation and maintain stemness [24] |
| Cell Detachment | Trypsin-EDTA, Accutase | Gentle cell detachment for subculturing and counting [16] |
| Characterization Antibodies | CD105, CD73, CD90, CD45, CD34, HLA-DR | Flow cytometry verification of MSC identity [25] [19] |
The comprehensive analysis of proliferation dynamics between BM-MSCs and AD-MSCs reveals a consistent pattern: AD-MSCs demonstrate superior proliferation capacity with shorter population doubling times compared to BM-MSCs. This advantage, coupled with their abundant tissue availability and minimally invasive extraction, positions AD-MSCs as a highly promising source for clinical applications requiring rapid cell expansion. However, BM-MSCs remain valuable for specific indications where their differentiation preferences or paracrine signatures may be advantageous.
Future research directions should focus on standardizing culture protocols to minimize heterogeneity, further elucidating the molecular mechanisms underlying proliferation differences, and establishing donor selection criteria based on proliferation competence. As the field advances toward more personalized medical approaches, understanding these fundamental proliferation dynamics will be essential for optimizing MSC-based therapies across diverse clinical applications.
The Colony-Forming Unit Fibroblast (CFU-F) assay stands as a fundamental in vitro technique in regenerative medicine for quantifying the clonogenic potential and self-renewal capacity of Mesenchymal Stem Cells (MSCs). Within the broader context of characterizing MSCs from different tissue sources, particularly bone marrow and adipose tissue, the CFU-F assay provides critical quantitative data on precursor cell frequency and viability. This guide objectively compares the clonogenic performance of Bone Marrow-derived MSCs (BM-MSCs) and Adipose-derived MSCs (AD-MSCs), supporting the comparison with experimental data and detailing the protocols essential for obtaining reliable, reproducible results.
Quantitative Comparison of Clonogenic Potential
Extensive characterization of MSCs from various sources reveals consistent differences in their growth kinetics and clonogenic properties, which are pivotal for selecting the appropriate cell source for specific research or therapeutic applications.
Table 1: Comparative Clonogenic and Functional Properties of MSC Sources
| Property | Bone Marrow-MSCs (BM-MSCs) | Adipose Tissue-MSCs (AD-MSCs) | References |
|---|---|---|---|
| Defining Markers (Positive) | CD73, CD90, CD105 (≥95% positivity) [2] [26] | CD73, CD90, CD105 [27] | |
| Defining Markers (Negative) | CD34, CD45, CD14, CD19, HLA-DR (≤2% expression) [2] | CD34, CD45 [26] | |
| Clonogenic Ability | Demonstrated from small-volume forearm bone marrow aspirates [26] | Not explicitly quantified in search results for AD-MSCs specifically | |
| Osteogenic Potential | Robust [27] | Present, but slightly lower efficacy than BM-MSCs in some models [27] | |
| Adipogenic Potential | Present [26] | Enhanced lipid storage capacity [28] | |
| Therapeutic Efficacy (e.g., in Septic Arthritis) | Significant reduction in inflammation and promotion of cartilage repair [27] | Slightly lower efficacy than BM-MSCs, requires optimization [27] | |
| Key Advantages | Considered the "gold standard"; high differentiation potential [27] | Less invasive harvesting; comparable immunomodulatory properties [27] |
Furthermore, a distinction exists even within the same anatomical cavity. A 2025 study highlighted that Bone Marrow Adipose Tissue-derived MSCs (BMAT-MSCs) exhibit significantly higher osteogenic and adipogenic differentiation potential compared to their concurrent BM-MSC counterparts from the same donor, as indicated by increased calcium accumulation and lipid storage [28]. In pathological conditions like Fanconi Anemia (FA) and Acute Myeloid Leukemia (AML), the osteogenic potential of both BM-MSCs and BMAT-MSCs becomes limited, indicating impaired differentiation under disease conditions [28].
Experimental Protocols for CFU-F Assays
The core protocol for a CFU-F assay involves isolating MSCs, plating them at a low density, and allowing them to form colonies over 1-2 weeks. The following workflow and detailed methodology are adapted from standard characterization procedures [26] [29].
Detailed Methodological Steps
Cell Isolation and Preparation:
- BM-MSCs: Harvest bone marrow aspirates from donor tissue (e.g., femur, tibia, or even forearm bones [26] [27]). Isolate the mononuclear cell fraction using density-gradient centrifugation. For BMAT-MSCs, the adipose layer on top of the centrifuged bone marrow aspirate is collected, washed, and cultured [28].
- AD-MSCs: Minced adipose tissue is digested with collagenase to release the stromal vascular fraction (SVF), which contains the progenitor cells [27].
- The isolated cells are then cultured in complete media (e.g., α-MEM supplemented with fetal bovine serum) to form a homogeneous monolayer of fibroblast-like, plastic-adherent cells [26].
Plating and Culture for CFU-F:
- Passage the cells and plate them at a low density (e.g., 100-1,000 cells per well in a multi-well plate) to allow individual cells to form distinct colonies [30].
- Culture the plated cells for 10-14 days under standard conditions (37°C, 5% CO₂), without disturbing the plates, to allow for colony formation [29].
Staining and Quantification:
- After the incubation period, remove the culture medium, wash the plates, and fix the cells with a fixative such as 4% formaldehyde.
- Stain the fixed cells with 0.5% Crystal Violet or other suitable dyes like Giemsa to visualize the colonies [31].
- Count the colonies manually under a microscope. A colony-forming unit (CFU-F) is typically defined as a cluster of 50 or more cells [30]. The CFU-F frequency is calculated as: (Number of Colonies Counted / Number of Cells Initially Plated) × 100.
Signaling Pathways Governing Differentiation
The superior clonogenic and differentiation potential of MSCs is governed by complex signaling pathways and gene expression networks. The following diagram summarizes the key regulators involved in adipogenic and osteogenic differentiation, pathways that are particularly enhanced in BMAT-MSCs [28].
Key Pathway Notes:
- Adipogenic Commitment: PPARG (Peroxisome Proliferator-Activated Receptor Gamma) acts as the master regulator. Its activation leads to the upregulation of key genes like ADIPOQ (critical for energy metabolism), PLIN1 (involved in lipid droplet formation), and LPL1 (regulates lipid metabolism) [28].
- Osteogenic Marker: COL2A1 (Collagen Type II Alpha 1 Chain) is a significant regenerative marker upregulated in effective MSC therapies [27].
- Secretory Profile: The therapeutic efficacy of MSCs is also mediated by their paracrine secretion of bioactive factors. Key molecules include IGF-1 (Insulin-like Growth Factor 1) and GDF-15 (Growth Differentiation Factor 15), which are often downregulated in pathological states like FA and AML, reflecting adipogenic dysregulation [28]. IL-10 is an immunomodulatory cytokine associated with positive therapeutic outcomes [27].
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Key Research Reagent Solutions for CFU-F Assays
| Item | Function/Description | Example Product/Citation |
|---|---|---|
| MethoCult Medium | Semi-solid methylcellulose-based medium for colony formation; can be supplemented with specific cytokines. | MethoCult (StemCell Technologies) [31] [29] |
| Density-Gradient Medium | Isolates mononuclear cells from bone marrow aspirates or stromal vascular fraction from adipose tissue. | Ficoll-Paque PREMIUM [27] |
| Collagenase | Enzyme for digesting adipose tissue to release the Stromal Vascular Fraction (SVF). | Collagenase Type I/II [27] |
| Characterization Antibodies | Flow cytometry panels for confirming MSC phenotype (positive and negative markers). | Anti-CD73, CD90, CD105, CD34, CD45 [2] [26] |
| Differentiation Media | Induce and assess trilineage potential (osteogenesis, chondrogenesis, adipogenesis). | Osteo-, Chondro-, Adipo-Induction Media [26] |
| Staining Reagents | Fix and visualize colonies for counting (e.g., Crystal Violet) or detect specific lineages (Alizarin Red, Oil Red O). | 0.5% Crystal Violet, Alizarin Red S, Oil Red O [31] |
| Cytokines & Growth Factors | Supplement media to promote specific lineage growth (e.g., for hematopoietic CFU assays). | mSCF, mIL-3, hIL-6 [29] |
The CFU-F assay remains an indispensable tool for evaluating the fundamental quality and self-renewal capacity of MSC populations. Objective comparison through this assay reveals that while BM-MSCs are a robust benchmark with high clonogenic and differentiation potential, AD-MSCs present a viable alternative with easier harvest and comparable immunomodulatory functions. Notably, BMAT-MSCs demonstrate that even sub-populations within a single niche can possess distinct and enhanced clonogenic properties. Understanding these differences is crucial for researchers and drug development professionals in selecting the optimal cell source, developing relevant potency assays [32], and advancing effective MSC-based therapies in regenerative medicine.
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine, offering tremendous potential for treating degenerative and inflammatory diseases due to their multipotent differentiation capacity and immunomodulatory properties. The therapeutic efficacy of MSCs is fundamentally governed by their transcriptional and epigenetic landscapes, which dictate stem cell pluripotency, lineage commitment, and senescence. Bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs) emerge as the most extensively studied and clinically relevant cell sources, each possessing distinct biological characteristics. Within the broader thesis of bone marrow versus adipose derived MSC characterization research, this comparison guide objectively analyzes the molecular machinery controlling their fate decisions. We provide a comprehensive examination of the transcriptional networks, epigenetic modifiers, and signaling pathways that differentially regulate BM-MSC and AD-MSC biology, supported by experimental data and detailed methodologies to inform research and drug development efforts.
Molecular Mechanisms Governing MSC Pluripotency and Senescence
Transcriptional Regulation of Stemness
The stemness of MSCs—their capacity for self-renewal and multilineage differentiation—is finely regulated by a network of transcription factors. Key families include the TWIST, HOX, OCT4, and SOX genes, which demonstrate varying expression patterns and functional significance between BM-MSCs and AD-MSCs [24].
TWIST Family: TWIST1 and TWIST2 are highly expressed in undifferentiated MSCs, with levels decreasing during in vitro expansion. Overexpression of TWIST1 in BM-MSCs increases expression of STRO-1 (a stemness marker), promotes proliferation and adipogenesis, but inhibits osteogenesis and chondrogenesis, suggesting a role in maintaining stemness. Mechanistically, TWIST1 increases EZH2, which silences senescence genes p14 and p16 through H3K27me3 modification [24].
HOX Family: The "HOX code" is stable throughout life and reflects the tissue origin of MSCs, potentially contributing to functional differences between BM-MSCs and AD-MSCs. For instance, HOXA5 promotes osteogenic differentiation and proliferation in dental pulp MSCs, while HOXB7 expression declines with age and its overexpression enhances MSC proliferation, reduces aging markers, and improves bone and cartilage differentiation [24].
OCT4: Expression of OCT4 is highly influenced by serum composition, hypoxia, and passage number. OCT4 overexpression promotes proliferation, colony-forming unit fibroblast (CFU-F) capacity, and chondrogenesis of MSCs. In human hair follicle MSCs, OCT4 enhances cell cycle progression, proliferation, and osteogenesis by upregulating DNMT1 to suppress p21 [24].
SOX Family: SOX2 plays an important role in maintaining MSC stemness and suppressing senescence. Reduced SOX2 expression correlates with increased senescence markers p16 and p21 in MSCs [24].
Epigenetic Control Mechanisms
Epigenetic modifications, including DNA methylation and histone modifications, serve as critical regulators of gene expression and cellular differentiation in MSCs without altering the DNA sequence itself [33].
DNA methylation is established by DNMT3a and DNMT3b and maintained by DNMT1, transferring methyl groups to cytosine in CpG dinucleotide sequences. This process plays crucial roles in genomic imprinting, regulation of tissue-specific gene expression, and X chromosome inactivation [33].
Histone modifications include several key mechanisms:
- Acetylation: Controlled by histone acetyltransferases (HATs) and deacetylases (HDACs), this process neutralizes the positive charge of histones, reducing chromatin condensation and facilitating gene transcription [33].
- Methylation: Histone methyltransferases transfer methyl groups to lysine and arginine residues, which can either repress or activate transcriptional processes depending on the specific region and number of modifications [33].
- Ubiquitination: Attachment of ubiquitin to lysine residues of histones H2A and H2B, with H2A monoubiquitinylation often associated with transcriptional repression and H2B with activation [33].
Table 1: Key Epigenetic Regulators in MSC Biology
| Epigenetic Mechanism | Key Enzymes | Functional Role in MSCs | Effect on Chromatin State |
|---|---|---|---|
| DNA Methylation | DNMT1, DNMT3a, DNMT3b | Genomic imprinting, tissue-specific gene expression | Generally repressive when at promoter regions |
| Histone Acetylation | HATs, HDACs | Controls accessibility to transcription machinery | Open chromatin (euchromatin) when acetylated |
| Histone Methylation | HMTs, HDMs | Can activate or repress transcription based on context | Variable depending on residue modified |
| ATP-dependent Remodeling | SWI/SNF, ISWI, CHD, INO80 | Nucleosome positioning and accessibility | Energy-dependent chromatin restructuring |
Aberrant epigenetic modifications have been identified in aging MSCs, affecting their self-renewal, survival, and differentiation potential. A set of epigenetic enzymes that write or erase these modifications play critical roles in regulating MSC aging [34].
Comparative Functional Analysis of BM-MSCs and AD-MSCs
Proliferation and Differentiation Capacities
Direct head-to-head comparisons of BM-MSCs and AD-MSCs under human platelet lysate (hPL) conditions—a clinical-grade alternative to fetal bovine serum—reveal significant functional differences [13]. AD-MSCs demonstrate superior proliferative potential compared to BM-MSCs, while BM-MSCs possess higher capacity toward osteogenic and chondrogenic differentiation. Both cell types show similar adipogenic differentiation potential [13].
A comprehensive analysis of four mouse MSC sources (including immortalized mouse bone marrow stromal stem cells [imBMSC] and immortalized mouse adipose-derived mesenchymal stem cells [iMAD]) found that iMADs exhibited the strongest osteogenic and adipogenic capabilities upon BMP9 stimulation in vitro. In in vivo studies employing ectopic osteogenesis and critical-sized calvarial defect repair models, iMAD and immortalized mouse calvarial mesenchymal progenitors (iCAL) cells exhibited the highest osteogenic capability [35].
Table 2: Functional Comparison of BM-MSCs and AD-MSCs
| Parameter | BM-MSCs | AD-MSCs | Experimental Context |
|---|---|---|---|
| Proliferation Capacity | Lower | Higher [13] | hPL-supplemented culture |
| Osteogenic Potential | Higher [13] | Lower | hPL-supplemented culture |
| Chondrogenic Potential | Higher [13] | Lower | hPL-supplemented culture |
| Adipogenic Potential | Similar [13] | Similar | hPL-supplemented culture |
| Immunomodulatory Effects | Lower | More potent [13] | T-cell suppression assays |
| Secretion Profile | Higher SDF-1, HGF [13] | Higher bFGF, IFN-γ, IGF-1 [13] | Protein array analysis |
| Bone Regeneration | Moderate | High [35] | BMP9-induced ectopic bone formation |
Secretome and Immunomodulatory Properties
The secretory profiles of BM-MSCs and AD-MSCs show distinct patterns that contribute to their differential therapeutic effects. Significant differences exist between BM-MSCs and AD-MSCs for several secreted proteins, including cytokines (interferon-γ), growth factors (basic fibroblast growth factor, hepatocyte growth factor, and insulin-like growth factor-1), and chemokines (stem cell-derived factor-1) [13].
These differences in secretome likely underlie the observed superior immunomodulatory effects of AD-MSCs compared to BM-MSCs [13]. AD-MSCs have demonstrated better restorative capacity than BM-MSCs in a cerebellar ataxic rat model, with both cell types improving motor performance and restoring the disrupted Purkinje cell layer, but AD-MSCs showing superiority in the improvement of some motor performance parameters and cerebellar VEGF and IGF-1 levels [36].
Experimental Protocols for MSC Characterization
Isolation and Culture Methods
BM-MSC Isolation Protocol [13]:
- Collect bone marrow aspirates (25 mL) from donors with informed consent.
- Layer BM over a lymphoprep gradient and centrifuge at 2,000 rpm for 30 minutes.
- Wash mononuclear cells twice with phosphate-buffered saline (PBS).
- Plate cells at a concentration of 2 × 10^5/cm² in 75 cm² flasks for 2 days in 5% hPL-supplemented medium.
- Remove nonadherent cells and maintain adherent cells at 37°C, 5% CO₂.
- Change medium twice weekly.
AD-MSC Isolation Protocol [13]:
- Harvest lipoaspirate tissues (25 mL) from donors.
- Wash tissues with PBS and digest with an equal volume of 0.2% collagenase type IV at 37°C for 30 minutes.
- Isolate stromal vascular fraction cells by centrifugation at 300 × g at room temperature.
- Culture 1 × 10^6 viable cells in 75 cm² flasks in 5% hPL-supplemented medium.
- After 2 days, replace medium to remove unattached cells.
- Change medium twice weekly.
For both cell types, at 80-90% confluence, harvest with trypsin-ethylenediaminetetraacetic acid and replate at 2,000 cells/cm².
Assessment of Proliferation and Differentiation
Proliferation Assay [13]:
- Serially passage cells and count when 80-90% confluent.
- Calculate population doubling (PD) using the formula: PD = log₁₀(Nh) - log₁₀(Np) / log₁₀(2), where Nh is the collected cell number and Np is the plated cell number.
- Cumulative population doubling (CPD) is the sum of PD for each passage.
Colony-Forming Unit Fibroblast (CFU-F) Assay [13]:
- Plate single-cell suspensions at passage 1 in six-well culture plates at densities of 1 × 10³ per well.
- Culture in IMDM with 5% hPL for 14 days.
- Fix cell layer with methanol and stain with crystal violet.
- Count individual colonies composed of at least 50 cells.
Osteogenic Differentiation Protocol [35]:
- Culture cells in osteogenic medium (0.1 μM Dexamethasone, 50 μM vitamin C, and 10 mM β-sodium glycerophosphate).
- Maintain cultures for varied time periods with medium changes twice weekly.
- Assess mineralization by Alizarin Red staining or alkaline phosphatase activity.
Signaling Pathways in MSC Differentiation
Transcriptomic analysis of multiple MSC lines reveals that despite each line regulating a distinct set of target genes upon stimulation, all undergo osteogenic differentiation by regulating several conserved signaling pathways, including Wnt, TGF-β, PI3K/AKT, MAPK, Hippo, and JAK-STAT pathways [35].
Diagram 1: Signaling pathways regulating MSC osteogenic differentiation. Multiple pathways converge to activate transcription factors that drive bone formation.
The epigenetic control of MSC differentiation involves specific modifications for each lineage [33]:
- Adipogenic differentiation: C/EBPα (encoded by CBPA) and PPARγ (encoded by PPARG) serve as master regulators. The expression of CEBPA depends on HDAC1 activity, while the opening of the PPARG promoter region depends on the SWI/SNF complex and simultaneous acetylation of histone H3 residues.
- Osteogenic differentiation: RUNX2 and OSX are major orchestrators controlled by methylation at histone H3 residues, acetylation at histone H3 and H4 residues, and DNA methylation signatures.
- Chondrogenic differentiation: Depends on MSC condensation to form 3D structures. SOX9 is a major transcription factor in early chondrogenesis, with expression controlled by histone H3/H4 acetylation.
Diagram 2: Epigenetic control of MSC lineage commitment. Specific epigenetic modifications regulate master transcription factors for each differentiation pathway.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for MSC Studies
| Reagent/Category | Specific Examples | Function in MSC Research | Application Notes |
|---|---|---|---|
| Culture Media Supplements | Fetal Bovine Serum (FBS), Human Platelet Lysate (hPL) | Provides essential growth factors and nutrients | hPL preferred for clinical applications to avoid xenograft risks [13] |
| Isolation Enzymes | Collagenase Type IV | Digests extracellular matrix for cell isolation | Critical for AD-MSC isolation from adipose tissue [13] |
| Osteogenic Induction Cocktail | Dexamethasone, Vitamin C, β-sodium glycerophosphate | Indces osteogenic differentiation | Standardized formulation enables comparison across studies [35] |
| Epigenetic Modulators | HDAC inhibitors, DNMT inhibitors | Probes epigenetic mechanisms in MSC differentiation | Enables mechanistic studies of lineage commitment [33] |
| Growth Factors | BMP9, FGF, VEGF, IGF-1 | Directs differentiation and enhances proliferation | BMP9 identified as potent osteoinductive factor [35] |
| Antibodies for Characterization | CD73, CD90, CD105, CD14, CD34, CD45 | Confirms MSC phenotype via flow cytometry | Essential for quality control and standardization [13] |
| Senescence Assay Kits | β-galactosidase staining, p16/p21 detection | Identifies senescent cells in culture | Critical for monitoring MSC quality during expansion [24] |
The transcriptional and epigenetic landscapes of BM-MSCs and AD-MSCs reveal both shared regulatory principles and source-specific characteristics that influence their therapeutic potential. AD-MSCs demonstrate advantages in proliferative capacity, immunomodulatory effects, and secretion of specific growth factors, while BM-MSCs retain superior osteogenic and chondrogenic differentiation potential under standard conditions. These biological distinctions must be considered systematically when selecting the appropriate MSC source for specific clinical applications. The molecular insights and experimental protocols provided in this comparison guide offer researchers a foundation for advancing MSC-based therapies through informed cell source selection and targeted manipulation of transcriptional and epigenetic pathways to maintain stemness and prevent senescence. As single-cell technologies and epigenetic editing tools continue to evolve, our understanding of these landscapes will deepen, enabling more precise control over MSC fate decisions for regenerative medicine applications.
From Bench to Bedside: Isolation, Expansion, and Therapeutic Mechanisms
The field of regenerative medicine increasingly relies on mesenchymal stromal cells (MSCs) for therapeutic applications, with bone marrow (BM) and adipose tissue (AD) serving as two primary somatic sources. The isolation technique employed represents a critical initial step that significantly influences the yield, purity, functional characteristics, and ultimately, the clinical potential of the derived cells [37] [38]. Within research and clinical practice, two methodologies predominate: density gradient centrifugation and enzymatic digestion. This guide provides a detailed, objective comparison of these techniques, framing them within the broader research context of characterizing BM-derived versus AD-derived MSCs. It synthesizes current protocols and performance data to inform researchers, scientists, and drug development professionals in their experimental design and process development.
Density Gradient Centrifugation
This technique separates cells based on their buoyant density. When a heterogeneous cell suspension is layered onto a dense medium and centrifuged, cells migrate to the interface where the medium's density matches their own, effectively partitioning different cell populations [38].
- BM-MSC Isolation: For bone marrow, this method is used to enrich the mononuclear cell (MNC) fraction, which contains the MSCs, from whole bone marrow aspirates. Common media include Ficoll (density ~1.077 g/mL) and Percoll (adjustable density) [38]. The process can be automated using systems like the Sepax device, enhancing reproducibility for clinical-grade production [38].
- AD-MSC Isolation: While enzymatic digestion is standard for adipose tissue, density gradient centrifugation can be applied as a subsequent step to further purify the stromal vascular fraction (SVF) obtained after digestion, helping to remove residual red blood cells and cellular debris [39].
Enzymatic Digestion
This approach uses enzymes to disrupt the extracellular matrix of tissues, thereby liberating the embedded cells into a suspension [40].
- AD-MSC Isolation: This is the most common method for isolating MSCs from adipose tissue. It typically uses type I collagenase to digest the lipid-filled adipocytes and ECM, releasing a heterogeneous cell population called the SVF [40] [41]. The AD-MSCs are then obtained from the SVF based on their plastic adherence [39].
- BM-MSC Isolation: Although less common than for adipose tissue, enzymatic digestion can also be applied to bone marrow fragments, particularly when obtained from surgical procedures like femoral shaft osteotomies, to enhance MSC yield [38].
Workflow Diagrams
The following diagrams illustrate the standard experimental workflows for isolating MSCs from bone marrow and adipose tissue using the discussed techniques.
Comparative Performance Analysis
Quantitative Comparison of Isolation Techniques
The choice of isolation method significantly impacts critical process outcomes such as cell yield, viability, and population composition. The table below summarizes experimental data comparing the performance of these techniques for BM and AD tissues.
Table 1: Performance Comparison of Density Gradient vs. Enzymatic Digestion
| Parameter | Density Gradient (BM) | Enzymatic Digestion (AD) | Experimental Context & Notes |
|---|---|---|---|
| Starting Material | 60 mL bone marrow aspirate [42] | Adipose tissue (lipoaspirate) [41] | Material volumes are typical for clinical processing. |
| Cell Yield | Enriches the MNC fraction; Final BMAC concentrate: ~8 mL [42] | SVF yield increased 3-fold with enzymatic + mechanical method [41] | Mechanical disruption synergizes with enzymatic action for higher AD-MSC yield [41]. |
| Purity/Composition | Isulates MNCs (MSCs & hematopoietic cells); further purified by plastic adherence [38] | Heterogeneous SVF (MSCs, endothelial cells, pericytes, etc.); purified by plastic adherence [39] | Initial product is a mixed population. Final MSC purity is achieved through culture adherence. |
| Key Advantages | • Effective erythrocyte removal• Amenable to automation [38] | • High MSC yield from a rich source• Well-established, standardized protocol [40] [39] | |
| Major Limitations | • Low initial MSC frequency (0.001-0.01%) [43] [44]• Invasiveness of BM harvest [38] | • Requires enzyme neutralization & washing• Collagenase use is a regulatory consideration [39] | Enzymatic methods are considered less suitable for direct clinical application by some [39]. |
| Primary Cell Source | Iliac crest [42] | Subcutaneous abdominal fat [42] | These sites are preferred for their MSC potential and accessibility. |
Protocol Details and Methodological Variations
Detailed Protocol: Enzymatic Digestion of Adipose Tissue A standardized protocol for isolating Adipose-Derived MSCs (AD-MSCs) involves the following steps [40]:
- Wash: The lipoaspirate is washed extensively with phosphate-buffered saline (PBS) to remove blood contaminants.
- Digest: The tissue is minced and digested with Type I collagenase (e.g., 0.075% concentration) under controlled temperature (37°C) and agitation for approximately 30-60 minutes [40] [39].
- Neutralize: Enzyme activity is neutralized by adding a complete growth medium supplemented with serum or human platelet lysate.
- Centrifuge: The cell suspension is centrifuged (e.g., 1200× g for 10 minutes) to pellet the stromal vascular fraction (SVF).
- Filter & Culture: The pellet is resuspended, filtered through a 100-μm mesh to remove undigested tissue, and then plated. AD-MSCs are selected based on their adherence to plastic [40] [39].
- Enhancement: Yield can be significantly increased by combining enzymatic digestion with mechanical distortion (e.g., using the Medi-King tissue dissociator), which increases the surface area for enzyme action without impairing cell viability or differentiation potential [41].
Detailed Protocol: Density Gradient Centrifugation for Bone Marrow For isolation of Bone Marrow-derived MSCs (BM-MSCs):
- Harvest: Bone marrow is aspirated from the iliac crest [42].
- Layer: The aspirate is diluted and carefully layered over a density gradient medium such as Ficoll-Paque (density 1.077 g/mL) or Percoll [38].
- Centrifuge: The preparation is centrifuged (e.g., 400× g for 30 minutes) without braking.
- Collect MNCs: The mononuclear cell layer (a buffy coat) at the sample/medium interface is carefully collected.
- Wash & Culture: The MNCs are washed with PBS to remove residual gradient medium and then plated. The BM-MSC population is enriched through subsequent passaging due to their plastic adherence [38].
Table 2: The Scientist's Toolkit: Key Reagents and Materials
| Item | Function/Application | Specific Examples / Notes |
|---|---|---|
| Collagenase Type I | Enzymatic digestion of adipose tissue ECM. | Critical for releasing SVF; concentration and time must be optimized [40] [39]. |
| Density Gradient Media | Separation of mononuclear cells based on density. | Ficoll (ready-to-use, 1.077 g/mL) or Percoll (adjustable density) [38]. |
| Serum-Free/Xeno-Free Media | Clinical-grade MSC expansion, avoiding FBS. | MSC NutriStem XF, StemMACS MSC XF; ensures compliance with GMP standards [43] [44]. |
| Human Platelet Lysate (hPL) | FBS substitute in culture media; provides growth factors. | Enhances MSC proliferation and is preferred for clinical manufacturing [43] [44]. |
| Automated Bioreactors | Large-scale, closed-system expansion of clinical-grade MSCs. | Quantum Cell Expansion System, CliniMACS Prodigy; ensure reproducibility and reduce manual steps [44]. |
| Chemically Defined Surface Coatings | Enhance cell adhesion and isolation efficiency in xeno-free conditions. | isoMATRIX; improves initial MSC yield and quality during isolation [45]. |
Discussion and Research Context
The comparison between density gradient centrifugation and enzymatic digestion is intrinsically linked to the biological source. Enzymatic digestion is the unequivocal method for adipose tissue due to the need to break down the dense extracellular matrix of adipocytes. In contrast, density gradient centrifugation is more suited for liquid tissues like bone marrow aspirate, where the goal is to fractionate different cell populations based on density.
From a broader research perspective comparing BM-MSCs and AD-MSCs, the isolation technique is a fundamental variable. It directly influences the initial cellular product—MNCs versus SVF—which have different compositions and, consequently, different paracrine and therapeutic potentials. This is critical for applications like treating knee osteoarthritis, where both BMAC (obtained via density gradient) and MFAT (obtained via enzymatic/mechanical processing) are being evaluated in randomized controlled trials [42]. Preclinical studies suggest that AD-MSCs in MFAT may respond better to inflammatory environments, potentially offering a clinical advantage [42].
A significant trend in the field is the move away from animal-derived components like fetal bovine serum (FBS) towards xeno-free or serum-free media and chemically defined biomimetic surfaces for both isolation and expansion [43] [45]. This shift, driven by regulatory requirements for Good Manufacturing Practice (GMP), aims to enhance product consistency and safety [44]. Furthermore, automated, closed-system platforms are becoming essential for scaling up production to meet clinical demand while maintaining quality control [44].
The selection between density gradient centrifugation and enzymatic digestion is primarily dictated by the tissue source—bone marrow or adipose tissue, respectively. While both methods effectively isolate MSCs based on the fundamental property of plastic adherence, they differ significantly in initial yield, procedural complexity, and the heterogeneity of the initial cell product. Enzymatic digestion, particularly when enhanced with mechanical disruption for adipose tissue, provides higher MSC yields. In contrast, density gradient centrifugation offers a cleaner initial separation for bone marrow.
Ongoing research and technological development are focused on standardizing and optimizing these protocols within a GMP-compliant framework. The future of MSC isolation and manufacturing lies in the integration of xeno-free reagents, automated closed systems, and chemically defined tools to ensure the consistent production of high-quality, clinically efficacious mesenchymal stromal cells for regenerative medicine.
The clinical-grade expansion of Mesenchymal Stem Cells (MSCs) is a critical step in regenerative medicine and advanced therapy medicinal product (ATMP) development. The choice of culture medium supplement profoundly influences cell yield, phenotypic stability, functional characteristics, and ultimately, therapeutic efficacy and safety. For decades, fetal bovine serum (FBS) has been the standard supplement, but its use in clinical applications is fraught with significant challenges, including ethical concerns, risk of xenogenic immune reactions, and batch-to-batch variability [46] [47]. Human platelet lysate (hPL) has emerged as a potent, xeno-free alternative, offering a more physiologically relevant human-derived cocktail of growth factors and cytokines [48] [49]. This comparison guide objectively evaluates FBS versus hPL for MSC expansion, with experimental data contextualized within the broader thesis of characterizing bone marrow-derived (BM-MSC) and adipose-derived (AD-MSC) mesenchymal stem cells.
Comprehensive Supplement Comparison: FBS vs. hPL
The selection between FBS and hPL requires a detailed understanding of their fundamental characteristics and how they impact manufacturing processes and final cell products. The table below provides a systematic, point-by-point comparison.
Table 1: Fundamental Characteristics of FBS and hPL
| Parameter | Fetal Bovine Serum (FBS) | Human Platelet Lysate (hPL) |
|---|---|---|
| Source | Blood from bovine fetuses via cardiac puncture [47] | Human platelet concentrates from donated blood; can use expired stocks [48] [46] |
| Key Growth Factors | Bovine-derived factors; generally lower concentrations of key mitogens [50] | High levels of human PDGF, TGF-β1, VEGF, EGF, FGF, IGF-1 [46] [50] |
| Ethical Concerns | Significant; related to animal welfare and collection methods [48] [47] | Minimal; utilizes donated human blood products, aligning with recycling principles [46] |
| Xenogenic Risk | High; potential for immune response against bovine antigens and zoonotic transmission [47] | None; autologous or allogeneic human proteins minimize immunogenicity [47] |
| Batch Consistency | High lot-to-lot variability; requires extensive pre-testing [47] | Variable, but modern pooling and standardization efforts are improving consistency [51] |
| Regulatory Status | Tolerated in Phase I trials but discouraged for later phases and clinical products [47] | Preferred xeno-free alternative for clinical-grade cell manufacturing [46] [51] |
| Cost & Supply | Increasing cost and demand; potential "peak serum" supply limitations [48] [49] | Cost-effective; sustainable supply from blood donation networks [46] [52] |
Experimental Performance Data and Methodologies
Robust experimental data is essential for an objective comparison. The following section details key performance metrics and the methodologies used to generate them, with a focus on proliferation, differentiation, and immunomodulation, particularly between BM-MSCs and AD-MSCs.
Cell Proliferation and Expansion
Experimental Protocol Overview: MSCs from bone marrow and adipose tissue are isolated and cultured in parallel using standard protocols. Basal media (e.g., α-MEM or DMEM) are supplemented with either 10% FBS or 5-10% hPL. Cells are serially passaged upon reaching 80-90% confluence, and population doublings are calculated at each passage. Metabolic activity assays like MTT are often used as a proxy for viability and cell number [12] [53].
Key Findings:
- Superior Proliferation with hPL: Multiple independent studies consistently demonstrate that hPL significantly accelerates the proliferation of both BM-MSCs and AD-MSCs compared to FBS. Cells cultivated in hPL exhibit shorter doubling times and achieve higher cumulative population doublings [46] [47]. One study on Stem Cells from Human Exfoliated Deciduous Teeth (SHED) found comparable viability and growth between FBS and hPL, confirming the safety of transition [53].
- Donor and Tissue Source Variability: While hPL generally enhances growth, the proliferation rate and maximal cell yield can be influenced by the MSC tissue source and inherent donor-to-donor variability [12] [11].
Table 2: Quantitative Proliferation and Functional Data in FBS vs. hPL
| Cell Type / Assay | Performance in FBS | Performance in hPL | Context & Notes |
|---|---|---|---|
| MSC Doubling Time | Longer doubling time [46] | Significantly faster doubling [46] [51] | Consistent across BM-MSC and AD-MSC [11] |
| Adipogenic Differentiation | Lower efficiency, slower [11] | Highly efficient, rapid lipid vacuole formation [11] | AD-MSC inherently more adipogenic than BM-MSC [12] |
| Osteogenic Differentiation | Robust calcium deposition [12] [11] | Supports osteogenesis; may be qualitatively different [46] [11] | BM-MSC often show superior osteogenic capacity [12] |
| Immunomodulatory (IDO Activity) | Lower kynurenine production post-IFN-γ stimulation [11] | ≈3.5-fold higher kynurenine production post-IFN-γ stimulation [11] | AD-MSCs showed more robust activity than BM-MSCs in hPL [11] |
| Cryopreservation Recovery | Effective recovery post-thaw [50] | Comparable or better recovery with PLS (Platelet Lysate Serum) [50] | PLS (coagulated lysate) may be superior to plain PL for freezing [50] |
Differentiation Potential and Functional Characterization
A donor-matched comparison of BM-MSCs and AD-MSCs reveals that, while both meet the ISCT criteria for MSCs, they exhibit tissue-specific differentiation biases that are maintained regardless of the culture supplement [12].
- Adipogenic Differentiation: AD-MSCs demonstrate significantly higher adipogenic capacity than BM-MSCs, forming more lipid vesicles and expressing higher levels of adipogenesis-related genes. This superior performance is evident in both FBS and hPL, though the process is often accelerated in hPL-supplemented media [12] [11].
- Osteogenic Differentiation: BM-MSCs generally show higher osteogenic and chondrogenic potential compared to AD-MSCs. They exhibit earlier and higher alkaline phosphatase activity, greater calcium deposition, and stronger expression of osteogenesis-related genes and proteins like osteopontin [12]. hPL supports successful osteogenic differentiation, though some qualitative differences in matrix deposition may occur compared to FBS [46] [11].
- Immunomodulatory Capacity: A critical therapeutic function of MSCs is their immunomodulation, often assessed in vitro by measuring indoleamine 2,3-dioxygenase (IDO) activity. When stimulated with interferon-gamma (IFN-γ), AD-MSCs cultured in hPL consistently displayed a ≈3.5-fold higher IDO activity (measured by kynurenine production) than parallel cultures of BM-MSCs [11]. This suggests that the choice of both cell source and supplement can significantly impact immunotherapeutic potential.
Standardization and Manufacturing Workflow
A major challenge in clinical translation is achieving lot-to-lot consistency. Recent multinational efforts have demonstrated the feasibility of standardizing hPL production across different blood establishments [51].
Diagram 1: hPL Manufacturing and Quality Control Workflow. The process begins with platelet concentrate preparation and proceeds through pooling, lysis, and clarification to yield final hPL. PLS (Platelet Lysate Serum) is an optional variant involving a coagulation step. Stringent Quality Control (QC) is required before batch release. Adapted from [51] [50].
The workflow for hPL production is more standardized than often perceived. A key finding is that pooling hPL units from multiple donors and across international centers significantly reduces batch-to-batch variability compared to single-donor or single-center batches, enhancing reproducibility for clinical manufacturing [51].
Practical Implementation for Clinical-Grade Expansion
Transitioning from FBS to hPL requires careful consideration of protocols and reagents. The table below outlines a toolkit of essential materials and their functions for setting up an hPL-based MSC expansion system.
Table 3: Research Reagent Solutions for hPL-Based MSC Expansion
| Reagent / Material | Function & Role in Culture | Example & Notes |
|---|---|---|
| hPL (Lysate) | Xeno-free supplement providing growth factors, adhesion factors, and nutrients. | Commercially available or manufactured in-house from expired platelet concentrates [46]. |
| Basal Medium | Provides essential salts, vitamins, and amino acids. | Alpha-MEM or DMEM are commonly used [12] [53]. |
| Heparin | Anticoagulant added to prevent gelation of hPL-medium due to fibrinogen. | Required for most non-defibrinated hPLs; note porcine heparin introduces xeno-components [46]. |
| Pathogen Inactivation | Reduces risk of viral or bacterial transmission from human blood products. | Methods like amotosalen/UV light treatment are used by blood establishments [51]. |
| Trypsin/EDTA | Enzymatic detachment of adherent MSCs for passaging. | Standard cell culture reagent, compatible with hPL-expanded cells [12]. |
| Defined MSC SFM | Serum-free, chemically defined media alternative. | Some require pre-coating and may induce proteostatic stress; cost is high [48] [52]. |
Critical Considerations for Implementation
- hPL Concentration: While 10% is common, studies show that 5% hPL can also effectively support MSC expansion, potentially reducing costs [52]. Optimization is recommended.
- Heparin Management: The necessity and concentration of heparin are critical. Some protocols use fibrinogen-depletion during hPL manufacturing to create a heparin-free, truly xeno-free product [46].
- Cell Seeding Density: MSCs in hPL often proliferate rapidly and may require a lower seeding density than in FBS to avoid premature over-confluence and optimize yield.
- Defined vs. Undefined Supplements: While "serum-free" media (SFM) are marketed as defined alternatives, recent analyses detected significant levels of human serum components (e.g., myeloperoxidase, glycocalicin) in some self-reported SFM, essentially reclassifying them as hPL [52]. This highlights the need for careful supplier evaluation and transparency.
The collective body of evidence strongly supports human platelet lysate (hPL) as the superior supplement for the clinical-grade expansion of MSCs. It mitigates the ethical, safety, and scientific limitations of FBS while enhancing cell proliferation and maintaining critical stem cell functionalities. The choice between BM-MSC and AD-MSC remains application-dependent, driven by their inherent functional biases in differentiation and immunomodulation. Future efforts should focus on the international standardization of hPL production [51] and the development of even more defined, cost-effective formulations to further advance the field of regenerative medicine. For researchers embarking on clinical therapy development, adopting hPL is no longer just an alternative but a necessary step toward safer and more effective cell products.
The characterization of mesenchymal stromal cells (MSCs) from different tissue sources represents a critical area of research in regenerative medicine, with significant implications for developing targeted therapeutic applications. According to standards established by the International Society for Cellular Therapy (ISCT), MSCs must demonstrate plastic-adherence, express specific surface markers (CD73, CD90, and CD105), lack hematopoietic markers (CD34, CD45, CD14, CD19, HLA-DR), and possess trilineage differentiation potential into osteogenic, chondrogenic, and adipogenic lineages [2]. While MSCs can be isolated from various tissues, bone marrow and adipose tissue have emerged as the most prevalent sources for research and clinical applications [5] [54].
Despite sharing fundamental characteristics, inherent biological differences between bone marrow-derived MSCs (BMSCs) and adipose-derived stem cells (ASCs) significantly impact their proliferation capacities and differentiation potentials [5] [54]. Understanding these distinctions is crucial for selecting the appropriate cell source for specific clinical applications. This comparative guide analyzes the quantitative differences in trilineage differentiation capacity between BMSCs and ASCs, provides detailed experimental protocols, and explores the underlying molecular mechanisms governing these differentiation processes.
Quantitative Comparison of Trilineage Differentiation Potential
Osteogenic Differentiation Capacity
BMSCs demonstrate superior osteogenic potential compared to ASCs across multiple quantitative measures. A donor-matched study using cells from patients aged 8-14 years revealed that BMSCs exhibited earlier and higher alkaline phosphatase (ALP) activity, enhanced calcium deposition, and increased expression of osteogenesis-related genes and proteins such as osteopontin [5]. The same study quantified mineralized matrix formation using Alizarin Red staining, with BMSCs showing significantly higher concentrations of calcium deposits compared to ASCs [5].
Research comparing MSCs from different anatomical regions of bone marrow further supports these findings. Cells isolated from the femoral diaphysis/metaphysis (FD) region, which contains more hematopoietic tissue, demonstrated significantly higher osteogenic differentiation compared to cells from the femoral epiphysis (FE), as measured by ALP specific activity and mineralization assays [55]. These regional differences within bone marrow itself highlight the importance of the tissue microenvironment in determining differentiation capacity.
Adipogenic Differentiation Capacity
In direct contrast to osteogenic potential, ASCs exhibit markedly superior adipogenic differentiation compared to BMSCs. When induced with adipogenic differentiation media, ASCs show more extensive lipid vesicle formation and higher expression of adipogenesis-related genes including PPARγ and FABP4 [5]. Quantitative analysis via Oil Red O staining confirms enhanced lipid accumulation in ASCs compared to BMSCs under identical induction conditions [54].
The molecular basis for this differential adipogenic capacity appears linked to the epigenetic memory of the source tissue. Studies of DNA methylation patterns reveal that the PPARγ promoter in ASCs is hypomethylated, favoring adipogenic differentiation, while the same promoter in BMSCs is hypermethylated, suppressing adipogenic commitment [54]. This fundamental epigenetic difference explains the tissue-specific differentiation biases observed in experimental outcomes.
Chondrogenic Differentiation Capacity
BMSCs generally demonstrate enhanced chondrogenic potential compared to ASCs, though the differences may be less pronounced than in osteogenic differentiation. Under chondrogenic induction conditions, BMSCs show increased expression of chondrogenesis-related genes including SOX9, COL2A1, and ACAN (aggrecan) [5]. Immunofluorescence staining reveals stronger SOX9 protein expression in BMSC-derived chondrogenic pellets compared to ASC-derived pellets [5] [55].
Quantitative PCR analyses further support the superior chondrogenic capacity of BMSCs. One study comparing femoral diaphysis-derived cells to epiphysis-derived cells found the former exhibited significantly higher ACAN expression following chondrogenic induction [55]. This correlation between bone marrow regional identity and chondrogenic potential has implications for understanding osteosarcoma development near growth plates where bone marrow conversion occurs [55].
Table 1: Quantitative Comparison of Trilineage Differentiation Potential Between ASCs and BMSCs
| Differentiation Lineage | Cell Source | Key Markers Quantified | Assessment Methods | Relative Performance |
|---|---|---|---|---|
| Osteogenic | BMSCs | ALP activity, Osteopontin, Calcium deposition | ALP assay, Alizarin Red staining, Immunofluorescence | Superior [5] |
| ASCs | ALP activity, Osteopontin, Calcium deposition | ALP assay, Alizarin Red staining, Immunofluorescence | Inferior | |
| Adipogenic | BMSCs | PPARγ, FABP4, Lipid vesicles | Oil Red O staining, qPCR | Inferior |
| ASCs | PPARγ, FABP4, Lipid vesicles | Oil Red O staining, qPCR | Superior [5] | |
| Chondrogenic | BMSCs | SOX9, COL2A1, ACAN | Pellet culture, Immunostaining, qPCR | Superior [5] [55] |
| ASCs | SOX9, COL2A1, ACAN | Pellet culture, Immunostaining, qPCR | Inferior |
Table 2: Optimal Marker Genes for Quantitative Differentiation Assessment
| Differentiation Lineage | Early Stage Markers | Late Stage Markers | Recommended Quantitative Methods |
|---|---|---|---|
| Osteogenic | ALP (ALPL) | Collagen Type I (COL1A1), Mineralization | ALP activity assay, Alizarin Red quantification, qPCR for COL1A1 [55] [56] |
| Adipogenic | PPARγ | FABP4 | Oil Red O quantification, qPCR for FABP4 [56] [54] |
| Chondrogenic | SOX9 | Aggrecan (ACAN), Collagen Type II (COL2A1) | Pellet culture with sulfated GAG quantification, qPCR for ACAN [55] [56] |
Detailed Trilineage Differentiation Protocols
Osteogenic Differentiation Protocol
Standard Induction Medium Formulation:
- Basal medium: Dulbecco's Modified Eagle's Medium (DMEM) or α-MEM
- Supplements: 10% Fetal Bovine Serum (FBS)
- Induction agents:
Experimental Procedure:
- Plate MSCs at density of 4×10³ cells/cm² in multiwell plates
- Culture in basal medium until cells reach 80-100% confluence
- Replace medium with osteogenic induction medium
- Maintain cultures for 21-28 days, changing medium twice weekly
- For quantitative analysis:
- Assess early osteogenic differentiation (days 7-14) via ALP activity assay
- Evaluate mineralization (days 21-28) by Alizarin Red S staining and quantification [54]
Key Considerations: The osteogenic potential of MSCs shows significant donor-dependent variation [5]. BMSCs typically demonstrate earlier and higher ALP activity and more extensive mineralization compared to ASCs under identical induction conditions [5].
Adipogenic Differentiation Protocol
Standard Induction Medium Formulation:
- Basal medium: DMEM with high glucose (4.5 g/L)
- Supplements: 10% FBS
- Induction cocktail:
- 500 nM dexamethasone
- 0.5 mM isobutylmethylxanthine (IBMX)
- 50 μM indomethacin
- 10 μg/mL insulin [54]
Experimental Procedure:
- Plate MSCs at density of 4×10³ cells/cm²
- Culture until complete confluence (contact-inhibition enhances adipogenesis)
- Replace medium with adipogenic induction medium
- Maintain induction for 21 days, changing medium every 3-4 days
- For quantitative analysis:
- Stain lipid droplets with Oil Red O at day 21
- Extract and quantify Oil Red O dye using isopropanol for normalization
- Analyze adipogenic gene expression (PPARγ, FABP4) via qPCR [54]
Key Considerations: ASCs consistently demonstrate superior adipogenic capacity with more extensive lipid vesicle formation and higher expression of adipogenic markers compared to BMSCs [5] [54]. The epigenetic state of ASCs, with hypomethylated PPARγ promoters, predisposes them to adipogenic differentiation [54].
Chondrogenic Differentiation Protocol
Standard Induction Medium Formulation:
- Basal medium: High-glucose DMEM
- Supplements:
- 1:100 diluted ITS+ Premix (insulin, transferrin, selenous acid)
- 50 μg/mL ascorbate-2-phosphate
- 40 μg/mL proline
- 100 μg/mL sodium pyruvate
- Growth factors:
- 10 ng/mL transforming growth factor-β3 (TGF-β3)
- 500 ng/mL bone morphogenetic protein-2 (BMP-2)
- 100 nM dexamethasone [54]
Experimental Procedure:
- Use micromass culture system: pellet 2.5×10⁵ MSCs in conical tube or create micropellets in 24-well plates
- Centrifuge at 500× g for 10 minutes to form pellets
- Maintain pellets in chondrogenic induction medium for 21-28 days
- Change medium every 2-3 days
- For quantitative analysis:
- Assess sulfated glycosaminoglycan (GAG) content using Dimethylmethylene Blue (DMMB) assay
- Analyze chondrogenic gene expression (SOX9, COL2A1, ACAN) via qPCR
- Evaluate cartilage matrix production histologically with Safranin O or Alcian Blue staining [54]
Key Considerations: BMSCs generally show superior chondrogenic differentiation compared to ASCs, with higher expression of SOX9 and ACAN [5]. Pellet or micromass culture is essential for proper chondrogenesis, as monolayer culture suppresses cartilage-specific matrix production [55].
Molecular Mechanisms Governing Differentiation
The differentiation biases observed between ASCs and BMSCs are governed by complex molecular mechanisms involving transcriptional regulation, epigenetic modifications, and signaling pathway activation. Understanding these mechanisms provides insight into the inherent differences between MSC populations from various tissue sources.
Transcriptional Regulation
Each differentiation lineage is controlled by master transcription factors that coordinate the expression of lineage-specific genes:
- Osteogenesis: Runx2 serves as the master regulator, activating osteoblast-specific genes including osteocalcin, osteopontin, and collagen type I [54]. BMSCs demonstrate hypomethylated Runx2 promoters, facilitating osteogenic commitment [54].
- Adipogenesis: PPARγ and C/EBP family members coordinate adipocyte differentiation. ASCs exhibit hypomethylated PPARγ promoters, predisposing them to adipogenic differentiation [54].
- Chondrogenesis: SOX9 regulates chondrocyte differentiation and cartilage matrix gene expression including collagen type II and aggrecan [55].
Epigenetic Control
DNA methylation patterns established during tissue specification create an epigenetic memory that influences differentiation potential [54]. The methylation status of key transcription factor promoters varies significantly between ASCs and BMSCs:
- Runx2 promoters are hypomethylated in BMSCs but hypermethylated in ASCs
- PPARγ promoters are hypomethylated in ASCs but hypermethylated in BMSCs
- Sox9 promoters show only slight methylation differences between ASCs and BMSCs [54]
These epigenetic differences explain the tissue-specific differentiation biases observed between ASCs and BMSCs and persist through multiple population doublings in vitro.
Signaling Pathways
Multiple signaling pathways interact to regulate MSC fate decisions:
- Wnt/β-catenin signaling promotes osteogenesis while inhibiting adipogenesis
- BMP signaling enhances both osteogenic and chondrogenic differentiation
- Notch signaling modulates osteoblast differentiation and function
- Hedgehog signaling promotes osteogenesis and chondrogenesis
The balance between these pathways, influenced by both intrinsic factors and extracellular cues, determines the ultimate differentiation outcome of MSCs.
Diagram 1: Molecular Regulation of MSC Differentiation. This diagram illustrates the key transcriptional regulators, marker genes, and epigenetic factors that govern trilineage differentiation of MSCs, highlighting the tissue-specific preferences between BMSCs and ASCs.
Essential Research Reagent Solutions
Table 3: Essential Reagents for Trilineage Differentiation Studies
| Reagent Category | Specific Products | Application & Function | Considerations |
|---|---|---|---|
| Cell Culture Media | DMEM (high glucose), α-MEM | Basal medium for MSC expansion and differentiation | α-MEM often preferred for BMSCs [5] |
| Differentiation Inducers | Dexamethasone, Ascorbic acid-2-phosphate, β-glycerophosphate | Osteogenic induction | Concentration critical for optimal differentiation [54] |
| IBMX, Indomethacin, Insulin | Adipogenic induction | IBMX concentration affects differentiation efficiency [54] | |
| TGF-β3, BMP-2 | Chondrogenic induction | Growth factor quality significantly impacts outcomes [54] | |
| Analysis Kits | ALP assay kits | Quantitative osteogenic differentiation | Measure early osteoblast differentiation [5] |
| Alizarin Red S | Mineralization assessment | Extract and quantify for objective comparison [54] | |
| Oil Red O solution | Lipid droplet staining | Isopropanol extraction enables quantification [54] | |
| Molecular Biology Tools | qPCR kits with SYBR Green | Gene expression analysis | Validate primer efficiency for differentiation markers [56] |
| Antibodies for CD73, CD90, CD105, CD34, CD45 | MSC characterization by flow cytometry | Essential for verifying MSC phenotype pre-differentiation [5] [57] |
Standardized Quantitative Assessment Methods
Gene Expression Analysis
Quantitative PCR (qPCR) represents the gold standard for assessing differentiation progression at the molecular level. Based on validation studies, the most reliable marker genes for each lineage include:
- Osteogenesis: Col11a1 demonstrates superior performance as an osteogenic indicator compared to other collagen genes [56]
- Adipogenesis: FABP4 serves as an optimal late-stage adipogenic marker with consistent expression patterns across multiple donor samples [56]
- Chondrogenesis: ACAN provides the most consistent indicator of chondrogenic differentiation across different cell passages [56]
Proper normalization using reference genes (e.g., GAPDH, β-actin) and calculation via the 2−ΔΔCT method is essential for accurate cross-comparison between studies [56] [54].
Protein-Level Assessment
Immunofluorescence staining provides protein-level validation of differentiation outcomes:
- Osteogenic cultures: Collagen type I and osteopontin antibodies confirm extracellular matrix production [5]
- Chondrogenic pellets: SOX9 antibodies verify chondrocyte differentiation [55]
- Adipogenic cultures: FABP4 antibodies confirm adipocyte maturation
Functional Assays
Quantitative functional assays provide objective measures of differentiation extent:
- ALP activity assay: Early osteogenic differentiation (days 7-14) [5] [55]
- Alizarin Red S quantification: Mineralization extent (days 21-28) via dye extraction and absorbance measurement [54]
- Oil Red O quantification: Lipid accumulation (day 21) via isopropanol extraction and normalization [54]
- Sulfated GAG quantification: Cartilage matrix production (day 28) via DMMB assay [54]
Diagram 2: Experimental Workflow for Trilineage Differentiation Analysis. This diagram outlines the standardized process from MSC isolation through differentiation and quantitative assessment, culminating in comparative analysis between BMSCs and ASCs.
The comprehensive analysis of trilineage differentiation protocols reveals fundamental biological differences between BMSCs and ASCs with direct implications for both basic research and clinical applications. The quantitative data demonstrate that BMSCs possess superior osteogenic and chondrogenic potential, while ASCs exhibit enhanced adipogenic capacity. These differences are rooted in the epigenetic memory of the source tissue, particularly the methylation status of key transcription factor promoters [54].
For researchers designing differentiation studies, these findings highlight the importance of:
- Selecting the appropriate MSC source based on the target differentiation lineage
- Implementing standardized quantitative methods to enable cross-study comparisons
- Considering donor-matched designs to minimize confounding variables in comparative studies [5]
From a clinical perspective, these results inform cell source selection for specific regenerative applications:
- Bone regeneration: BMSCs represent the preferred cell source due to their enhanced osteogenic capacity
- Cartilage repair: BMSCs show superior chondrogenic potential for cartilage engineering
- Soft tissue reconstruction: ASCs provide optimal adipogenic potential for soft tissue regeneration
Future research directions should focus on manipulating epigenetic programming to enhance desired differentiation pathways, developing standardized potency assays for clinical applications, and exploring the paracrine effects of differentiated MSCs in various therapeutic contexts. As single-cell transcriptomic technologies advance, our understanding of the heterogeneity within MSC populations will continue to refine these differentiation protocols and applications [4].
The therapeutic application of Mesenchymal Stem Cells (MSCs) has undergone a fundamental paradigm shift over the past decade. Initially valued for their differentiation potential, MSCs are now recognized primarily for their paracrine activity [58] [59]. The secretome—the complete set of bioactive factors secreted by these cells—has emerged as the principal mediator of their therapeutic effects, which include immunomodulation, angiogenesis, and tissue repair [59] [60]. This cell-free approach offers significant advantages over whole-cell therapies, including reduced risks of immune rejection, tumorigenicity, and embolization [61] [62]. Within the context of comparative characterization research between bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs), understanding the nuanced differences in their secretome profiles is critical for selecting the optimal cell source for specific therapeutic applications. This guide provides a structured comparison of the secretory profiles of BM-MSCs and AD-MSCs, supported by experimental data and detailed methodologies.
Quantitative Comparison of MSC Secretome Profiles
The composition of the MSC secretome is highly heterogeneous, influenced by factors such as tissue source, donor characteristics, and culture conditions [58] [63] [60]. The tables below summarize key cytokines, growth factors, and microRNAs identified in the secretome of MSCs from different sources, with a focus on bone marrow and adipose tissue.
Table 1: Key Soluble Factors in the MSC Secretome and Their Primary Functions
| Biological Function | Key Growth Factors & Cytokines | Key MicroRNAs (miRNAs) |
|---|---|---|
| Angiogenesis | VEGF, bFGF, MCP-1, PDGF, HGF, IL-6, IL-8 [58] [61] | miR-21, miR-23, miR-27, miR-126, miR-130a, miR-210, miR-378 [58] |
| Immunomodulation | IDO, HGF, PGE2, TGF-β1, TSG-6, IL-7, IL-10 [58] [2] | miR-21, miR-146a, miR-375 [58] |
| Anti-apoptosis | VEGF, bFGF, G-CSF, HGF, IGF-1, STC-1, IL-2, IL-6 [58] | miR-25, miR-214 [58] |
| Anti-fibrosis | HGF, PGE2, IDO, IL-10 [58] | miR-26a, miR-29, miR-125b, miR-185 [58] |
Table 2: Comparative Secretome Profile of MSCs from Different Tissues (Representative Data)
| Secretome Component | Bone Marrow (BM)-MSCs | Adipose (AD)-MSCs | Umbilical Cord (UC)-MSCs |
|---|---|---|---|
| VEGF (Angiogenesis) | High [58] | High [58] | Very High [63] |
| HGF (Immunomodulation) | Present [58] [64] | Present [58] [65] | Present [63] |
| TGF-β1 (Immunomodulation/Chondrogenesis) | Present [58] | Present [58] | Present [63] |
| FGF-2 (bFGF) (Proliferation) | Present [58] [64] | Present (enhanced with bFGF priming) [65] | Present [63] |
| CXCL-1/IL-8 (Angiogenesis/Migration) | Information Missing | Highly upregulated by bFGF priming [65] | Information Missing |
| Immunomodulatory Potency | Strong, induces T-cell cycle arrest [60] | Information Missing | Strongest reported suppression of T-cell proliferation [60] |
| Key Differentiating Factors | Classical, well-characterized profile; supports hematopoiesis [60] | Responsive to inflammatory priming; high yield [63] [2] | Highly proliferative; potent immunomodulation [63] [60] [2] |
Extracellular Vesicles: The Nanoparticulate Mediators of Paracrine Action
A significant portion of the MSC secretome's bioactivity is encapsulated within Extracellular Vesicles (EVs), including exosomes and microvesicles [61] [62]. These lipid-bilayer nanoparticles facilitate intercellular communication by transferring functional proteins, lipids, and nucleic acids to recipient cells [61].
- Biogenesis and Composition: Exosomes (30-200 nm) are formed within multivesicular bodies (MVBs) and released upon MVB fusion with the plasma membrane. They are enriched with tetraspanins (CD63, CD81, CD9), ESCRT complex proteins (Alix, TSG101), and nucleic acids like miRNAs. Microvesicles (100-1000 nm) are generated by the direct outward budding and fission of the plasma membrane [61] [62].
- Therapeutic Advantages: As a cell-free therapy, MSC-EVs mitigate risks associated with whole-cell transplantation, such as pulmonary embolism and tumorigenicity. Their nanoscale size, biocompatibility, and low immunogenicity allow them to cross biological barriers and be stored at -80°C without significant loss of activity [61] [62].
- Functional Evidence: In skin wound healing, MSC-EVs promote angiogenesis, regulate inflammation, and stimulate fibroblast migration and collagen synthesis, effectively accelerating tissue repair and reducing scarring [61].
The following diagram illustrates the biogenesis pathways of different extracellular vesicles and key experimental isolation techniques.
Experimental Protocols for Secretome Analysis
Robust experimental design is essential for the accurate characterization and comparison of MSC secretomes. The following section outlines standard protocols for conditioning, analyzing, and testing the functional capacity of MSC-derived factors.
Conditioned Media (CM) Preparation and Cytokine Profiling
Objective: To collect and analyze the soluble secretory profile of MSCs from different tissue sources.
- Cell Culture & Conditioning:
- Isplicate and culture MSCs (e.g., BM-MSCs, AD-MSCs) from human donors under standardized conditions (e.g., α-MEM + 10% FBS) [63].
- At 80-90% confluence, wash cells and incubate with serum-free medium for 24-72 hours. To study priming effects, add stimuli like bFGF (10-50 ng/mL) [65] or culture under hypoxic conditions (1-5% O₂) [64].
- Collect the supernatant, which is now the Conditioned Media (CM). Centrifuge (e.g., 2000 × g, 10 min) to remove cells and debris. Aliquot and store at -80°C [63] [65].
- Cytokine Analysis:
- Multiplex Immunoassays (Luminex) or ELISA: Use commercially available kits to quantify specific cytokines/growth factors (e.g., VEGF, HGF, IL-8, CXCL-1) [63] [65]. This provides quantitative, targeted data.
- Proteomic Profiling (LC-MS/MS): For an unbiased, global analysis of secreted proteins, subject trypsin-digested CM to Liquid Chromatography with Tandem Mass Spectrometry [58].
Extracellular Vesicle (EV) Isolation and Characterization
Objective: To isolate and characterize EVs from MSC-conditioned media.
- Isolation Methods:
- Differential Ultracentrifugation: The most common method. Sequential centrifugations remove cells (300 × g), apoptotic bodies (2,000 × g), and large debris (10,000 × g). Finally, ultracentrifuge at 100,000 × g for 70-120 min to pellet EVs [61] [62].
- Size-Exclusion Chromatography (SEC): Separates EVs from soluble proteins based on size, often resulting in higher purity and preserved vesicle integrity compared to ultracentrifugation [61].
- Ultrafiltration: Concentrates CM and isolates EVs using membranes with specific molecular weight cut-offs (e.g., 100 kDa) [62].
- Characterization:
- Nanoparticle Tracking Analysis (NTA): Determines EV particle size distribution and concentration.
- Transmission Electron Microscopy (TEM): Visualizes the morphology and ultrastructure of EVs.
- Western Blot: Confirms the presence of EV marker proteins (CD63, CD81, TSG101) and absence of negative markers (e.g., calnexin) [61] [62].
Functional In Vitro Assays
Objective: To validate the biological activity of the MSC secretome and MSC-EVs.
- Immunomodulation Assay:
- Isolate human peripheral blood mononuclear cells (PBMCs) and differentiate macrophages (e.g., using GM-CSF for M1).
- Treat M1 macrophages with MSC-CM or MSC-EVs.
- Analyze polarization by flow cytometry (CD80/86 for M1, CD206/163 for M2) and qPCR (iNOS for M1, Arg-1 for M2) [63].
- Angiogenesis Assay:
- Seed human umbilical vein endothelial cells (HUVECs) on Matrigel.
- Treat with MSC-CM or MSC-EVs.
- Quantify tube formation by measuring number of branches, nodes, and total tube length after 4-18 hours [65].
- Migration Assay (Scratch/Wound Healing):
- Create a scratch in a confluent monolayer of fibroblasts (e.g., NIH/3T3) or other relevant cell types.
- Treat with MSC-CM and monitor wound closure over 24-48 hours using live-cell imaging [65].
The workflow below summarizes the key experimental stages from cell culture to functional validation.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for MSC Secretome Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Serum-Free Media (e.g., DMEM/F12, α-MEM) | Base medium for conditioning; eliminates confounding factors from serum. | Essential for preparing clean, defined Conditioned Media (CM) for downstream profiling and functional assays [63]. |
| Recombinant Human bFGF (FGF-2) | Pre-conditioning agent; enhances proliferation and modulates secretome. | Used to prime AD-MSCs to upregulate secretion of pro-angiogenic factors like CXCL-1 and IL-8 [65]. |
| Hypoxia Chamber/Workstation | Pre-conditioning equipment; creates a low-oxygen environment (1-5% O₂). | Mimics the physiological niche of MSCs and boosts the angiogenic and survival factors in the secretome [64]. |
| Collagenase Type I/II | Enzymatic digestion of tissues for initial MSC isolation. | Used for the extraction of MSCs from adipose tissue (Type I) and gingival tissue (Type II) [63]. |
| Luminex Multiplex Kits / ELISA Kits | Quantification of specific cytokines, chemokines, and growth factors. | For targeted, quantitative analysis of key secretome components (e.g., VEGF, HGF, IL-8) in CM [63] [65]. |
| CD63/CD81/CD9 Antibodies | Markers for characterization of extracellular vesicles (exosomes). | Used in Western Blot analysis to confirm the successful isolation of EVs and assess their purity [62]. |
The transition from cellular to cell-free therapies represents the future of MSC-based regenerative medicine. The comparative analysis of secretomes reveals that while BM-MSCs and AD-MSCs share a core set of therapeutic factors, source-specific specializations exist. The choice between them, or the use of UC-MSCs, should be guided by the desired therapeutic outcome—be it potent immunomodulation, robust angiogenesis, or efficient tissue remodeling. Furthermore, the ability to engineer and precondition MSCs to tailor their secretory output offers a powerful strategy for optimizing patient-specific treatments. As the field progresses, overcoming challenges related to the standardization of secretome production, isolation protocols, and quality control will be paramount for the successful clinical translation of these promising cell-free therapeutics.
Mesenchymal Stem Cells (MSCs) have emerged as a cornerstone of regenerative medicine and immunotherapy, distinguished by their potent capacity to modulate immune responses. Sourced from various tissues including bone marrow (BM-MSCs) and adipose tissue (AD-MSCs), these cells interact with both innate and adaptive immune cells to restore immunological homeostasis [2] [66]. Their therapeutic potential is largely attributed to mechanisms mediated through direct cell-to-cell contact and the secretion of soluble factors [67] [68]. This review provides a detailed, evidence-based comparison of the immunomodulatory mechanisms employed by BM-MSCs and AD-MSCs, with a specific focus on their interactions with T-cells, B-cells, and macrophages. We synthesize findings from direct comparative studies to offer researchers and drug development professionals a clear understanding of their distinct functional profiles, supported by experimental data and standardized methodologies.
Comparative Immunomodulatory Profiles of BM-MSCs and AD-MSCs
BM-MSCs and AD-MSCs, while sharing fundamental characteristics defined by the International Society for Cell & Gene Therapy (ISCT), exhibit source-dependent differences in their immunomodulatory strategies and efficacy [69] [70] [2]. These functional specializations are influenced by their unique tissue microenvironments.
Table 1: Functional Specialization of BM-MSCs and AD-MSCs
| Feature | Bone Marrow-MSCs (BM-MSCs) | Adipose Tissue-MSCs (AD-MSCs) |
|---|---|---|
| Primary Immunomodulatory Strength | Potent suppression of T-cell responses; hematopoietic support [69] [70] | Angiogenic repair; metabolic regulation; potent cytokine secretion (e.g., CXCL9, CXCL10) [69] [7] |
| Key Soluble Factors | Galectin-1, TGF-β1, PGE2, TSG-6, IL-10 [69] [68] [66] | IDO, PGE2, TGF-β, IL-6, CCL2 [7] [66] |
| T-cell Inhibition | Strong inhibition of CD4+ and CD8+ T-cell proliferation; promotes Treg activity via IL-10 and TGF-β1 [69] [68] | Inhibits T-cell proliferation via IDO and PGE2; promotes Tregs [7] |
| Macrophage Polarization | Induces anti-inflammatory M2 phenotype via PGE2 and TSG-6 [68] [66] | Promotes M2 polarization; modulates inflammation via secreted factors [7] |
| B-cell Modulation | Inhibits B-cell development and differentiation [7] | Suppresses B-cell proliferation and antibody production [70] |
| Experimental Evidence | Superior in mixed lymphocyte reactions (MLR) and in vivo transplant models [70] [68] | Effective in preclinical models of inflammatory skin diseases and metabolic disorders [7] |
Direct comparative analyses reveal nuanced differences in their immunomodulatory potency. A head-to-head study showed that while AD-MSCs demonstrated superior capacity to inhibit T and NK cell proliferation, BM-MSCs were equally effective at inhibiting B-cells, a function not observed in umbilical cord MSCs [70]. Another comparison concluded that AD-MSCs possessed a greater immunomodulatory capacity than BM-MSCs or UC-MSCs, as measured by inhibition of mitogen-stimulated T-cell proliferation [70]. These findings underscore the importance of selecting the MSC source based on the specific immune cell population targeted for therapy.
Mechanisms of Interaction with Immune Cells
T-cell Regulation
MSCs modulate T-cell responses through a multifaceted approach that is critical for managing autoimmune diseases and facilitating transplant tolerance.
- Inhibition of Effector T-cells: Both BM-MSCs and AD-MSCs suppress the proliferation and activation of CD4+ and CD8+ T-cells [68]. BM-MSCs achieve this through the secretion of factors like galectin-1, which directly inhibits T-cell proliferation [69]. They also shift the immune balance from a pro-inflammatory Th1 profile (characterized by IFN-γ) to an anti-inflammatory Th2 profile (characterized by IL-4) [69] [68]. AD-MSCs heavily utilize indoleamine 2,3-dioxygenase (IDO), an enzyme that degrades tryptophan essential for T-cell survival, and prostaglandin E2 (PGE2) to suppress T-cell responses [7] [66].
- Promotion of Regulatory T-cells (Tregs): A key mechanism of MSC-mediated immunomodulation is the induction and expansion of CD4+CD25+Foxp3+ Regulatory T-cells (Tregs) [69] [68]. BM-MSCs secrete TGF-β1 and IL-10, which are pivotal for Treg differentiation and function [69]. Cell contact-dependent mechanisms, such as the interaction between PD-L1/PD-L2 on MSCs and PD-1/CTLA-4 on T-cells, are also crucial. This interaction triggers intracellular phosphatases (SHP-1/SHP-2) that dephosphorylate key signaling molecules like ZAP70 and PKCθ, leading to cell cycle arrest in the G0/G1 phase and suppressing T-cell activation [67].
The following diagram illustrates the key signaling pathways MSCs use to communicate with and regulate T-cells.
Macrophage Polarization
MSCs significantly influence the innate immune response by directing macrophage polarization towards an anti-inflammatory, tissue-repairing phenotype.
- Phenotype Switching: MSCs drive the conversion of pro-inflammatory M1 macrophages to the anti-inflammatory M2 phenotype [68] [66]. This is a cornerstone of their therapeutic effect in inflammatory diseases. M2 macrophages are characterized by high IL-10 secretion and decreased production of TNF-α and IL-12p70 [68].
- Key Soluble Mediators: The switch to the M2 phenotype is primarily mediated by soluble factors. PGE2 secreted by MSCs binds to EP2 and EP4 receptors on macrophages, stimulating IL-10 production [66]. TNF-stimulated gene 6 (TSG-6), released by MSCs in response to inflammatory signals, interacts with CD44 on macrophages to inhibit the NF-κβ signaling pathway, thereby exerting a powerful anti-inflammatory effect [68] [66]. MSC-derived extracellular vesicles (EVs) can also modulate this process by delivering regulatory microRNAs [66].
- Cell Contact and Phagocytosis: Interestingly, a cytokine-independent pathway exists where the phagocytosis of MSCs by monocytes/macrophages itself instructs the polarization toward an immunosuppressive M2-like phenotype. These primed monocytes subsequently enhance Treg formation [68].
The diagram below summarizes the mechanism by which MSCs drive macrophage polarization toward the M2 phenotype.
B-cell Modulation
MSCs exert a direct inhibitory effect on B-cells, impacting their proliferation, differentiation, and antibody production.
- Inhibition of Proliferation and Differentiation: MSCs can suppress the proliferation of B-cells and impede their differentiation into antibody-producing plasma cells [7]. This effect varies with the MSC source; for instance, one study indicated that BM-MSCs and AD-MSCs inhibited B-cell proliferation, while umbilical cord MSCs did not [70].
- Soluble Factor-Mediated Suppression: The suppression of B-cells is largely mediated by soluble factors. MSC-secreted CCL2 is a key chemokine involved in this process [7]. Furthermore, the enzyme IDO, which is often upregulated in MSCs by inflammatory cytokines like IFN-γ, also plays a significant role in inhibiting B-cell development and function [7].
Experimental Data and Methodologies
To ensure reproducibility and validate findings, this section outlines standard experimental protocols used to characterize MSC immunomodulation.
Key Experimental Protocols
T-cell Proliferation Assay (Mixed Lymphocyte Reaction - MLR):
- Purpose: To evaluate the capacity of MSCs to suppress T-cell proliferation in response to allogeneic (non-self) immune stimulation [70].
- Methodology: Peripheral blood mononuclear cells (PBMCs) from a donor are labeled with a fluorescent dye (e.g., CFSE) and co-cultured with irradiated PBMCs from an allogeneic donor (stimulator cells). MSCs are added to the culture. After several days, T-cell proliferation is quantified by measuring fluorescence dilution using flow cytometry. Suppression is calculated relative to control wells without MSCs [70] [68].
Macrophage Polarization Assay:
- Purpose: To assess the ability of MSCs to induce a shift from M1 to M2 macrophage phenotype.
- Methodology: Human monocytes are isolated and differentiated into M1 macrophages using IFN-γ and LPS. These M1 macrophages are then co-cultured with MSCs in a transwell system (which allows factor exchange but prevents direct contact) or treated with MSC-conditioned medium. After co-culture, macrophages are harvested. Polarization is assessed by:
Quantitative Data Comparison
The following table consolidates experimental data from direct comparative studies to highlight the differential immunomodulatory effects of BM-MSCs and AD-MSCs.
Table 2: Comparative Experimental Data on MSC Immunomodulation
| Immune Cell Target | Experimental Readout | BM-MSC Effect | AD-MSC Effect | Comparative Findings & References |
|---|---|---|---|---|
| T-cells (CD4+/CD8+) | Proliferation Inhibition (MLR) | Strong inhibition via Galectin-1, TGF-β [69] | Strong inhibition via IDO, PGE2 [7] | AD-MSCs showed superior inhibition of T/NK cell proliferation than BM-MSCs and UC-MSCs in a direct comparison [70]. |
| Regulatory T-cells (Tregs) | Induction/Expansion (Flow Cytometry: CD4+CD25+FOXP3+) | Promotes Treg activity via IL-10, TGF-β1, and cell contact [69] [68] | Promotes Treg proliferation via IL-10 [7] | Both sources are effective; BM-MSC mechanism is well-documented in direct co-culture studies [69] [67]. |
| Macrophages | M2 Polarization (Cytokine: IL-10; Surface Marker: CD206) | Induces M2 via PGE2, TSG-6; Phagocytosis of MSCs instructs M2 phenotype [68] [66] | Promotes M2 polarization [7] | BM-MSCs have been shown to increase anti-inflammatory Ly6Clow monocytes in vivo [68]. |
| B-cells | Proliferation Inhibition | Inhibits B-cell development [7] | Suppresses B-cell proliferation via CCL2, IDO [7] | BM-MSCs and AD-MSCs were both effective at inhibiting B-cells, while UC-MSCs were not in one study [70]. |
| General | Soluble Factor Secretion | High levels of immunosuppressive factors (e.g., Galectin-1) [69] | High levels of CXCL1, CXCL9, CXCL10 [69] | AD-MSCs secrete more chemokines, while BM-MSCs produce more broadly immunosuppressive factors [69]. |
The Scientist's Toolkit: Essential Research Reagents
Successful research into MSC immunomodulation relies on a standardized set of reagents and tools.
Table 3: Essential Research Reagents for MSC Immunomodulation Studies
| Research Reagent / Tool | Function and Application in MSC Research |
|---|---|
| Flow Cytometry Antibodies | Used to identify MSCs (CD73, CD90, CD105) and hematopoietic contaminants (CD34, CD45), and to analyze immune cell populations (e.g., CD4, CD8, CD25, FOXP3 for T-cells; CD14, CD16, CD163, CD206 for monocytes/macrophages) [2]. |
| Pro-inflammatory Cytokines (IFN-γ, TNF-α) | Used to "license" or prime MSCs in vitro. Pre-treatment with these cytokines enhances the expression of key immunomodulatory enzymes like IDO and COX2, thereby boosting the immunosuppressive capacity of MSCs [72] [66]. |
| ELISA / Multiplex Assay Kits | Essential for quantifying the concentration of soluble factors (e.g., TGF-β, PGE2, IL-10, IFN-γ) in MSC-conditioned media or co-culture supernatants, providing a direct measure of paracrine activity [70] [68]. |
| Transwell Co-culture Systems | Permeable supports that allow for the exchange of soluble factors between MSCs and immune cells while preventing direct cell contact. Critical for distinguishing between contact-dependent and soluble factor-mediated mechanisms [67] [68]. |
| Cell Viability/Proliferation Assays (e.g., CCK-8, CFSE) | Used to measure the proliferation and metabolic activity of immune cells (e.g., T-cells) in response to mitogenic stimulation (e.g., CD3/CD28 antibodies) in the presence or absence of MSCs [70] [72]. |
| IDO & COX2 Inhibitors | Small molecule inhibitors used in functional studies to block the activity of specific enzymes. Their use helps confirm the mechanistic role of IDO or PGE2 in observed immunomodulatory effects [66]. |
The immunomodulatory prowess of MSCs is a multifaceted process involving a sophisticated network of interactions with T-cells, B-cells, and macrophages. Direct comparative studies reveal that while BM-MSCs and AD-MSCs share overarching mechanisms, they exhibit distinct functional specializations. BM-MSCs appear to be particularly potent in T-cell suppression and hematopoietic support, making them a strong candidate for treating T-cell-mediated autoimmune disorders and in transplant medicine. In contrast, AD-MSCs excel in angiogenic repair and secretion of specific chemokines, positioning them as a promising tool for conditions involving vascular dysfunction and certain inflammatory pathologies. The choice between MSC sources should be guided by the specific pathological context and target immune pathways. Future research, leveraging standardized experimental protocols and engineered MSCs, will further refine their application, paving the way for more effective and targeted cell-based immunotherapies.
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine due to their multipotent differentiation potential, immunomodulatory properties, and paracrine secretion capabilities. While MSCs can be isolated from virtually all tissues, bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs) have emerged as the most extensively investigated sources for clinical applications [2]. These cells share fundamental biological characteristics but exhibit critical differences in their isolation, expansion capabilities, and functional properties that influence their therapeutic translation [73] [6]. The selection between BM-MSCs and AD-MSCs requires careful consideration of scientific evidence, factoring in disease pathophysiology, patient-specific variables, and practical clinical constraints. This review provides a systematic comparison of BM-MSCs and AD-MSCs, evaluating their characterization, preclinical performance, and clinical trial outcomes across specific disease entities to inform evidence-based therapeutic decisions.
Biological Characterization: A Side-by-Side Comparison
Isolation, Yield, and Surface Marker Profiles
BM-MSCs and AD-MSCs fulfill the International Society for Cellular Therapy (ISCT) minimal defining criteria: adherence to plastic, specific surface marker expression (CD73, CD90, CD105; lacking hematopoietic markers CD45, CD34, CD14, CD19, HLA-DR), and trilineage differentiation potential [2] [6]. However, significant practical differences exist in their procurement and initial characteristics.
Table 1: Comparative Isolation and Basic Characterization of BM-MSCs vs. AD-MSCs
| Parameter | Bone Marrow-Derived MSCs (BM-MSCs) | Adipose-Derived MSCs (AD-MSCs) |
|---|---|---|
| Isolation Procedure | Bone marrow aspirate (iliac crest) [6] | Liposuction, lipoplasty, or lipectomy [6] |
| Invasiveness of Harvest | Invasive, painful, risk of infection [6] | Minimally invasive [74] |
| Typical Cell Yield | 0.001–0.01% of mononuclear cells [6] | ~5,000 stem cells per gram of tissue; 500x higher yield than equivalent BM [6] |
| Proliferation Capacity | Lower proliferation rate and lifespan [7] | Higher proliferation rate and expansion potential [7] [74] |
| Key Positive Markers | CD73, CD90, CD105, CD166 [6] | CD73, CD90, CD105, CD166, CD49d [6] |
| Key Negative Markers | CD34, CD45, CD14 [6] | CD45, CD14 [6] |
| Variable/Discordant Markers | Expresses CD106 [6] | Lacks CD106, may express CD34 in early passages [6] |
Differentiation Potential and Secretome
The functional capacity of MSCs extends beyond their surface identity. Both types demonstrate trilineage differentiation, but with varying efficiencies, and possess distinct secretomes that drive their therapeutic effects.
- Differentiation Potential: BM-MSCs are often considered the "gold standard" for osteogenic and chondrogenic differentiation [75]. AD-MSCs reliably differentiate into adipogenic, osteogenic, and chondrogenic lineages, though some studies suggest BM-MSCs may have superior chondrogenic potential [73] [75].
- Paracrine Secretome: Both MSC types exert a significant portion of their therapeutic effects through paracrine signaling. They secrete growth factors (VEGF, HGF, FGF), cytokines, and chemokines that promote angiogenesis, inhibit apoptosis, and modulate immune responses [2] [7]. The secretome's composition can be dynamically altered by "licensing" the cells with inflammatory cytokines like IFN-γ to enhance their immunomodulatory potency [76].
- Extracellular Vesicles (EVs): A major fraction of the MSC secretome consists of EVs, particularly exosomes. These nanoscale vesicles transfer proteins, lipids, and nucleic acids (mRNAs, microRNAs) to recipient cells, mediating intercellular communication [77]. MSC-derived exosomes are emerging as cell-free therapeutic agents with reduced immunogenicity and risks compared to whole cells [77] [78].
Preclinical and Clinical Performance in Specific Disease Models
Septic Arthritis in Aged Hosts
A 2025 preclinical study directly compared the therapeutic efficacy and safety of BM-MSCs and AD-MSCs in an aged murine model of septic arthritis, providing high-quality, head-to-head comparative data [75].
Table 2: Efficacy Outcomes in Aged Murine Septic Arthritis Model [75]
| Therapeutic Group | Reduction in Inflammation | Cartilage Repair | Key Molecular Regulators |
|---|---|---|---|
| BM-MSC1 (Trabecular) | Significant | Significant | Upregulation: IL-10, COL2A1Downregulation: TNF-α, MMP-13 |
| AD-MSCs | Moderate (lower than BM-MSC1) | Moderate (lower than BM-MSC1) | Favorable modulation, but less pronounced than BM-MSC1 |
| Untreated Controls | Severe inflammation | Severe tissue degradation | Sustained high pro-inflammatory markers |
Experimental Protocol Summary [75]:
- Disease Induction: Septic arthritis was induced in aged (22-24 months) C57BL/6 mice via intra-articular injection of Staphylococcus aureus.
- Treatment Groups: Mice were divided into control, treated (BM-MSC1, BM-MSC2, AD-MSC1, AD-MSC2), and untreated groups.
- Cell Administration: Treated groups received MSC therapy after arthritis induction.
- Outcome Measures: Inflammation, cartilage repair, immune response modulation (via IL-10, TNF-α, COL2A1, MMP-13), and MSC retention/engraftment were analyzed.
The study concluded that BM-MSCs, particularly the trabecular bone-derived subpopulation (BM-MSC1), demonstrated superior performance in reducing inflammation, promoting cartilage repair, and modulating immune responses, suggesting they may be better suited for treating septic arthritis in elderly populations [75].
Neurodegenerative and Autoimmune Diseases
Clinical trials have explored both MSC sources for complex conditions like Amyotrophic Lateral Sclerosis (ALS) and Multiple Sclerosis (MS).
- Amyotrophic Lateral Sclerosis (ALS): A phase I/II clinical trial investigated the safety and efficacy of three intravenous doses of autologous AD-MSCs in 40 ALS patients [74]. The therapy was found to be safe and feasible, with no significant adverse events related to treatment. However, the study did not demonstrate statistically significant efficacy in slowing disease progression across various functional and neurophysiological measures, highlighting the challenge of translating preclinical promise into clinical success [74].
- Multiple Sclerosis (MS): A systematic review of clinical trials up to 2025 indicated that MSC therapy (from various sources, including bone marrow) shows potential for immunomodulation and neuroprotection in MS [79]. Some studies reported decreased lesion activity on MRI and improved disability scores. However, the review emphasized that long-term efficacy and optimal administration protocols remain uncertain, necessitating larger, standardized trials [79].
Inflammatory Skin Diseases
AD-MSCs have shown particular promise in treating immune-mediated inflammatory skin diseases like psoriasis and atopic dermatitis due to their potent immunomodulatory functions [7].
Mechanism of Action: AD-MSCs exert therapeutic effects through cellular interactions and paracrine signaling. They promote M2 macrophage polarization and T regulatory cell (Treg) proliferation via IL-10, while inhibiting the proliferation of CD8+ and CD4+ T lymphocytes and natural killer (NK) cells via indoleamine 2,3-dioxygenase (IDO), prostaglandin E2 (PGE2), and TGF-β [7]. They also secrete factors that promote angiogenesis and inhibit apoptosis, facilitating skin lesion healing.
Figure 1: Mechanism of AD-MSC Action in Inflammatory Skin Diseases. AD-MSCs modulate both innate and adaptive immunity through direct cellular interactions and paracrine secretion of soluble factors, leading to reduced inflammation and promotion of tissue repair [7].
Experimental Workflows and the Scientist's Toolkit
Core Experimental Protocols
Standardized protocols are critical for reproducible MSC research and therapy development.
Generic MSC Isolation and Expansion Workflow [6]:
Figure 2: Standard Workflow for MSC Isolation and Culture. This general flowchart outlines the key steps from tissue harvest to application, with variations at the processing stage depending on the tissue source [6] [76].
Detailed Characterization Assays:
- Flow Cytometry: Confirmation of MSC phenotype using antibodies against CD73, CD90, CD105 (≥95% positive) and CD34, CD45, CD14, CD19, HLA-DR (≤2% positive) [2] [6].
- Trilineage Differentiation: Inducing differentiation using specific media. Osteogenic: Cells cultured with dexamethasone, ascorbate, and β-glycerophosphate, with mineralization detected by Alizarin Red staining. Chondrogenic: Pellet culture with TGF-β, assessed for sulfated glycosaminoglycans with Safranin O or Alcian Blue. Adipogenic: Induction with dexamethasone, insulin, and indomethacin, with lipid vacuoles stained with Oil Red O [2].
- Licensing Protocol: To enhance immunomodulatory potency, MSCs are pre-treated (licensed) with cytokines such as IFN-γ (e.g., 50 ng/mL for 24-48 hours) prior to experimentation or administration [76].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC Research and Their Applications
| Research Reagent / Tool | Primary Function in MSC Research |
|---|---|
| Collagenase Type I/II | Enzymatic digestion of adipose tissue to isolate the stromal vascular fraction containing AD-MSCs [6]. |
| Ficoll-Paque PREMIUM | Density gradient medium for isolation of mononuclear cells from bone marrow aspirates [6]. |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Immunophenotypic characterization of MSCs to confirm identity and purity according to ISCT criteria [2] [6]. |
| Recombinant Human IFN-γ | Licensing agent to pre-condition MSCs, enhancing their immunomodulatory potency by upregulating IDO and PD-L1 [76]. |
| Trilineage Differentiation Kits (Osteo/Chondro/Adipo) | Standardized media formulations to assess the multipotent differentiation capability of MSCs in vitro [2]. |
| Nanoparticle Tracking Analysis (NTA) Instrument | Characterizing size and concentration of MSC-derived extracellular vesicles (e.g., exosomes) [78]. |
Discussion and Clinical Translation Trends
The choice between BM-MSCs and AD-MSCs involves a careful trade-off. AD-MSCs offer clear practical advantages: they are easier to harvest with minimal patient discomfort, provide a much higher initial yield, and generally possess a stronger capacity for in vitro expansion [73] [7]. BM-MSCs, historically the "gold standard," are associated with more invasive harvesting and are thought to be more susceptible to age-related declines in function [75]. However, as the septic arthritis model showed, they can demonstrate superior therapeutic efficacy in specific pathological contexts, potentially due to a more robust immunomodulatory or tissue-regenerative profile [75].
A significant trend in clinical translation is the shift toward cell-free therapies using MSC-derived extracellular vesicles (exosomes) [77] [78]. These vesicles encapsulate the therapeutic cargo of MSCs while offering benefits such as lower immunogenicity, no risk of tumorigenesis from cell proliferation, easier storage, and a potentially better safety profile [77]. As of early 2024, 66 clinical trials were registered investigating MSC-EVs for a range of conditions, with intravenous infusion and aerosolized inhalation being the most common routes of administration [78]. Dose optimization remains a critical challenge for the future of this promising modality.
BM-MSCs and AD-MSCs are both powerful tools in regenerative medicine with distinct strengths. AD-MSCs present clear practical and logistical benefits for widespread clinical application, including easier harvest and high cell yield. BM-MSCs may, in certain disease-specific contexts like joint disorders, offer superior therapeutic efficacy. The emerging field of MSC-derived exosomes and other secretome-based, cell-free products represents the next frontier, potentially obviating the need for source selection altogether. Future research must focus on standardizing isolation and characterization protocols, conducting more direct comparative preclinical studies, and elucidating the precise mechanisms that dictate the functional differences between MSC populations to fully realize their clinical potential.
Navigating Challenges: Donor Variability, Standardization, and Functional Assays
Impact of Donor Age and Health Status on MSC Yield and Potency
Mesenchymal stromal cells (MSCs) represent a cornerstone of regenerative medicine and cell-based therapies, with their therapeutic potential heavily influenced by the characteristics of the cell donor. Donor age and health status significantly impact the yield, expansile capacity, and functional potency of isolated MSCs, creating critical considerations for both autologous and allogene therapeutic applications [80] [81] [82]. As the field advances toward standardized clinical applications, understanding these donor-related variables becomes paramount for optimizing product consistency and therapeutic efficacy. This review synthesizes current evidence on how donor factors influence bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (ASCs), providing a comparative analysis essential for researchers, scientists, and drug development professionals working in cellular characterization and therapeutic development.
Donor Age: A Critical Determinant of MSC Characteristics
Cellular Fitness and Expansion Potential Across Age Groups
The relationship between donor age and MSC fitness reveals a complex picture with clinically relevant nuances. Studies evaluating MSC expansion from a wide donor age range (8 months to 58 years) under hypoxic conditions (5% O₂) demonstrated that while cellular fitness remains largely comparable across age groups, modest reductions in expansion potential occur with advancing age [83] [84]. Specifically, MSCs from older donors (38-58 years) produced slightly fewer cells over a 28-day culture period and exhibited longer population doubling times (54 hours versus 42 hours) compared to those from younger donors (8 months-6 years) [84]. Despite these kinetic differences, a clinically sufficient product (≥10⁶ cells/kg recipient body weight) was consistently obtainable regardless of donor age, with even the poorest expansion yielding approximately 14 doses for a 70kg patient [83].
Markers of cellular aging and oxidative stress showed no significant differences between age cohorts. Telomere length, lipofuscin accumulation, iNOS expression, PGE2 production, p16INK expression, and superoxide dismutase (SOD) activity remained equivalent between younger and older donor-derived MSCs [83] [84]. Similarly, apoptosis rates following oxidative challenge (150μM H₂O₂ exposure) did not differ significantly (1% vs. 1.5%, p=0.14) between groups [84]. These findings suggest that while expansion kinetics may slow modestly with donor age, fundamental cellular fitness parameters remain intact through at least the sixth decade of life when using appropriate culture conditions.
The impact of donor age on MSC properties varies significantly between tissue sources, as demonstrated by comparative studies using matched donors. When BM-MSCs, muscle-derived stem cells (MDSCs), and ASCs were isolated from the same young (4-6 months) and old (4-5 years) rabbit donors, age-related impairment was most pronounced in BM-MSCs, which exhibited diminished proliferation, increased senescence, and reduced chondrogenic potential [82]. In contrast, ASCs and MDSCs showed relative resistance to these age-related declines, maintaining robust expansion and differentiation capabilities in older donors [82].
All MSC populations experienced some age-related changes, including reduced initial cell yield following isolation and diminished adipogenic potential [82]. However, osteogenic capacity and clonogenicity remained preserved across all age groups and tissue sources [82]. This tissue-specific vulnerability to aging has profound implications for cell source selection in clinical applications, particularly for older patients who might benefit more from ASCs than BM-MSCs for autologous therapies.
Table 1: Impact of Donor Age on MSC Properties from Different Tissue Sources
| Parameter | Bone Marrow MSCs | Adipose-Derived MSCs | Muscle-Derived Stem Cells |
|---|---|---|---|
| Proliferation Rate | Significantly reduced with age [82] | Minimally affected by age [82] | Minimally affected by age [82] |
| Senescence | Increased with age [82] | No significant age effect [82] | No significant age effect [82] |
| Osteogenesis | Preserved with age [82] | Preserved with age [82] | Preserved with age [82] |
| Chondrogenesis | Reduced with age [82] | Not reported | Not reported |
| Adipogenesis | Reduced with age [82] | Reduced with age [82] | Reduced with age [82] |
| Clonogenicity | Preserved with age [82] | Preserved with age [82] | Preserved with age [82] |
Donor Health and Biological Status
Donor Sex as a Determinant of MSC Heterogeneity
Beyond chronological age, donor sex represents a significant biological variable affecting MSC potency and functional characteristics. Sex-specific differences manifest across multiple MSC parameters, including proliferation kinetics, differentiation bias, immunomodulatory capacity, and gene expression profiles [80] [81].
Regarding proliferative capacity, female BM-MSCs demonstrate higher clonogenic potential and faster division rates compared to male-derived cells [81]. This enhanced expansion capability is particularly pronounced in BM-MSCs from younger female donors [81]. Conversely, umbilical cord-derived MSCs (UC-MSCs) from male donors exhibit superior proliferation, attributed to higher expression of pluripotency markers including NANOG, TERT, OCT4, and SOX2 [81].
Differentiation capacity also shows sex-dependent variation. Female ASCs demonstrate greater predisposition toward adiopogenic differentiation, while male ASCs show enhanced osteogenic potential [80] [81]. This divergence has practical implications for tissue-specific regenerative applications. Additionally, female BM-MSCs exhibit superior immunosuppressive potency, more effectively suppressing T-cell proliferation compared to male counterparts [81].
Table 2: Donor Sex-Related Differences in MSC Properties
| Characteristic | Male-Donor MSCs | Female-Donor MSCs |
|---|---|---|
| Proliferation | Higher in UC-MSCs [81] | Higher in BM-MSCs [81] |
| Osteogenesis | Enhanced in ASCs [80] [81] | Reduced in ASCs [80] [81] |
| Adipogenesis | Reduced in ASCs [80] | Enhanced in ASCs [80] |
| Immunomodulation | Moderate T-cell suppression [81] | Superior T-cell suppression [81] |
| Gene Expression | Higher OCT4, DNMT1 in UC-MSCs [80] | Distinct transcriptomic profiles [80] |
| Therapeutic Effects | Variable tissue protection [80] | Enhanced protection in lung and myocardial models [80] |
Tissue Source as a Determinant of MSC Potency
The tissue origin of MSCs significantly influences their functional properties and therapeutic potential, with implications for donor selection strategies. While BM-MSCs represent the most extensively characterized population, ASCs offer practical advantages including greater abundance and less invasive harvesting procedures [85] [86].
Comparative studies reveal that ASCs generally demonstrate higher proliferation rates than BM-MSCs, potentially offering expansion advantages in clinical manufacturing [80] [70]. Conversely, BM-MSCs appear superior in supporting hematopoietic function and forming functional hematopoietic niches, reflecting their physiological role in the bone marrow microenvironment [70].
Immunomodulatory properties also vary between tissue sources, though study results show some inconsistency. Some investigations report enhanced immunosuppressive capacity in ASCs compared to BM-MSCs, while others demonstrate equivalent potency [70] [86]. These discrepancies may reflect methodological differences or donor variable influences rather than fundamental biological distinctions.
Experimental Approaches for MSC Characterization
Standardized Methodologies for MSC Isolation and Culture
Robust comparison of MSC properties across donor groups requires standardized isolation and culture methodologies. For BM-MSCs, isolation from bone marrow harvest filters using density gradient centrifugation with Isolymph (density: 1.077-1.080 g/mL) effectively separates mononuclear cells [83] [84]. Subsequent plastic adherence in α-MEM medium supplemented with 10% fetal bovine serum, 1X Glutamax, and 1X penicillin-streptomycin under hypoxic conditions (5% O₂) selects for the MSC population while mimicking physiological niche conditions [83] [84].
ASC isolation typically employs enzymatic digestion of adipose tissue samples using collagenase-based solutions, followed by centrifugation to separate stromal vascular fraction from adipocytes [82]. Culture expansion uses DMEM/F-12 or high-glucose DMEM supplemented with serum [82].
Critical culture parameters include maintaining cells at subconfluent levels (harvesting at 80% confluency) using trypsin/EDTA solutions, and replating at standardized densities (approximately 500 cells/cm²) to ensure consistent population dynamics [83] [84]. Culture duration should typically not exceed 21-28 days (approximately 3 passages) to minimize senescence and genomic instability risks [83] [84].
Diagram 1: Experimental Framework for Evaluating Donor Impact on MSC Properties. This workflow outlines the key factors and methodologies for systematic characterization of donor influences on MSC biology.
Comprehensive Characterization Assays
Evaluation of donor age and health status effects requires multiparameter assessment strategies. Essential characterization assays include:
- Growth Kinetics: Population doubling time calculations and cumulative cell yield quantification over standardized culture periods (e.g., 28 days) [83] [84]
- Senescence Markers: Senescence-associated β-galactosidase staining and lipofuscin quantification using Sudan Black staining [83] [82]
- Oxidative Stress Response: SOD activity assays, apoptosis measurement via Annexin V staining after H₂O₂ challenge (150μM, 1 hour) [83] [84]
- Telomere Length Analysis: Southern blotting or qPCR-based methods to assess replicative history [83]
- Immunophenotyping: Flow cytometry verification of standard MSC markers (CD73, CD90, CD105 ≥95%; CD34, CD45, CD14, CD19, HLA-DR ≤2%) [83] [2] [85]
- Differentiation Potential: Tri-lineage differentiation assays using lineage-specific induction media and quantitative assessment of differentiation extent [2] [85] [82]
- Immunomodulatory Function: Mixed lymphocyte reactions or T-cell proliferation suppression assays to quantify immunosuppressive potency [70] [81]
Table 3: Essential Research Reagents for MSC Donor Characterization Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Culture Media | α-MEM, DMEM/F-12, High-glucose DMEM | Baseline MSC expansion and maintenance [83] [82] |
| Serum Supplements | Fetal Bovine Serum (10-20%), Horse Serum | Essential growth factors and adhesion support [83] [82] |
| Isolation Reagents | Collagenase, Dispase, Trypsin/EDTA, Density Gradient Media (Isolymph) | Tissue dissociation and MSC population enrichment [83] [82] |
| Differentiation Kits | Osteo-, Adipo-, Chondrogenic Induction Media | Tri-lineage differentiation capacity assessment [2] [85] |
| Antibody Panels | CD73, CD90, CD105, CD34, CD45, CD14, CD19, HLA-DR | Immunophenotype verification by flow cytometry [83] [2] |
| Senescence Assays | Senescence-associated β-galactosidase Kit, Sudan Black | Cellular aging marker detection [83] [82] |
| Oxidative Stress Kits | Superoxide Dismutase Assay Kit II, Annexin V Apoptosis Detection | Response to oxidative challenge quantification [83] |
Donor age and health status significantly influence critical characteristics of both bone marrow and adipose-derived MSCs, with implications for therapeutic product development. While BM-MSCs demonstrate greater susceptibility to age-related functional decline, particularly in proliferation and chondrogenic capacity, ASCs maintain more stable properties across donor age groups [82]. Beyond chronological age, donor sex introduces important functional variation in differentiation bias, immunomodulatory potency, and expansion potential [80] [81].
Optimal donor selection and MSC source determination must consider the specific therapeutic application, with BM-MSCs potentially preferred for hematopoietic support and ASCs offering advantages for autologous therapies in older patients. Standardized isolation methodologies and comprehensive characterization pipelines are essential for meaningful comparison across donor groups and tissue sources. As the field progresses toward broader clinical application, understanding and accounting for these donor-related variables will be crucial for developing consistent, potent MSC-based therapies with predictable clinical performance.
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine, with bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs) standing as the most extensively investigated types for clinical applications [13] [2]. These multipotent cells are defined by three key criteria established by the International Society for Cellular Therapy (ISCT): adherence to plastic, specific surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-, CD14-, CD19-, HLA-DR-), and tri-lineage differentiation potential into osteocytes, chondrocytes, and adipocytes [2] [87]. Despite their therapeutic promise, the field faces a significant translational roadblock: substantial batch-to-batch variability that compromises product consistency, therapeutic reliability, and regulatory approval pathways [88] [89].
This variability manifests across multiple dimensions, including donor-dependent differences (age, health status, genetic background), isolation method inconsistencies (enzymatic digestion protocols, tissue processing techniques), and culture condition fluctuations (media composition, supplement sources, passaging techniques) [88] [21]. The emergence of human platelet lysate (hPL) as a xenogeneic-free alternative to fetal bovine serum (FBS) has addressed some safety concerns but introduced new dimensions of variability in expansion and potency characteristics [13]. A comprehensive understanding of these sources of variability, particularly within the context of comparative BM-MSC and AD-MSC biology, is essential for developing robust standardization strategies that can propel MSC therapies from research curiosities to reliable clinical products.
Direct Comparison: BM-MSCs vs. AD-MSCs Under Standardized Conditions
Head-to-head comparisons under standardized culture conditions reveal fundamental biological differences between BM-MSCs and AD-MSCs that impact their therapeutic utility and susceptibility to variability. When cultured under identical hPL-supplemented conditions, both cell types maintain similar fibroblast-like morphology and surface marker expression patterns consistent with ISCT criteria [13]. However, critical functional differences emerge that inform their application-specific advantages and standardization challenges.
Table 1: Functional Comparison of BM-MSCs and AD-MSCs Under Standardized Culture Conditions
| Parameter | Adipose-Derived MSCs (AD-MSCs) | Bone Marrow-Derived MSCs (BM-MSCs) | References |
|---|---|---|---|
| Proliferation Capacity | Higher proliferative potential | Moderate proliferative potential | [13] [90] |
| Cell Yield per mL Tissue | ~500,000–2,000,000 cells | ~5,000–100,000 cells | [90] |
| Osteogenic Differentiation | Moderate capacity | Higher capacity | [13] |
| Chondrogenic Differentiation | Moderate capacity | Strong capacity | [13] [90] |
| Adipogenic Differentiation | Strong capacity | Similar strong capacity | [13] |
| Immunomodulatory Effects | More potent effects | Moderate effects | [13] |
| Secretome Profile | Higher bFGF, IFN-γ, IGF-1 | Higher SDF-1, HGF | [13] |
These functional differences originate from distinct biological characteristics that must be accounted for in standardization protocols. AD-MSCs demonstrate a significant advantage in terms of initial cell yield, with approximately 500,000–2,000,000 cells obtainable per milliliter of adipose tissue compared to only 5,000–100,000 cells per milliliter of bone marrow aspirate [90]. This abundance makes AD-MSCs particularly attractive for applications requiring extensive expansion. Conversely, BM-MSCs retain superior chondrogenic and osteogenic differentiation capacity, positioning them as preferred candidates for musculoskeletal regeneration [13] [90].
The secretory profiles further distinguish these cell types, with AD-MSCs secreting higher levels of basic fibroblast growth factor (bFGF), interferon-γ (IFN-γ), and insulin-like growth factor-1 (IGF-1), while BM-MSCs produce more stem cell-derived factor-1 (SDF-1) and hepatocyte growth factor (HGF) [13]. These differences directly impact their mechanistic actions in therapeutic contexts, with AD-MSCs demonstrating more potent immunomodulatory effects, while BM-MSCs excel in applications requiring homing and tissue remodeling functions [13].
Molecular Insights: Cellular Senescence as a Source of Variability
Recent single-cell transcriptomic analyses have illuminated a fundamental molecular source of batch-to-batch variability: progressive and heterogeneous cellular senescence during in vitro expansion [89]. This aging process directly compromises therapeutic efficacy by downregulating critical immunomodulatory molecules like PD-L1, resulting in impaired immunosuppressive function [89]. The senescent state is characterized by permanent proliferative arrest, altered differentiation capacity, and modified secretome profiles that collectively diminish therapeutic potency and introduce variability.
Table 2: Senescence-Associated Markers and Their Functional Consequences in MSCs
| Senescence Aspect | Key Molecular Markers | Functional Impact on MSCs | References |
|---|---|---|---|
| Cell Cycle Arrest | ↑ p53, p21, p16 | Decreased proliferative capacity | [89] |
| SASP Profile | ↑ IL-6, COL1A1, IGFBP5 | Altered paracrine signaling | [89] |
| Metabolic Shift | ↑ GLB1, HSP proteins | Compromised cellular fitness | [89] |
| DNA Damage | ↓ DNA repair genes | Genomic instability | [89] |
| Immunomodulation | ↓ PD-L1 expression | Reduced T-cell suppression | [89] |
Single-cell RNA sequencing has revealed that clinically expanded MSC products contain multiple subpopulations with distinct senescence states [89]. These subpopulations range from rapidly self-renewing cells with high proliferative capacity (C1-C3 clusters) to fully senescent cells (C5-C7 clusters) with upregulated senescence markers like TP53, CDKN1A, IL6, GLB1, and HSP families [89]. The proportion of these subpopulations varies between donors, tissue sources, and culture passages, creating substantial batch-to-batch functional differences.
Proteomic and transcriptomic integration has identified GATA2 as a key regulator of MSC senescence, with its expression delaying aging processes and enhancing PD-L1 expression [89]. Perinatal MSCs (from umbilical cord and placental chorionic membrane) demonstrate fewer senescence features and more potent immunosuppressive activity compared to adult sources (adipose tissue and bone marrow) [89], suggesting that tissue origin significantly impacts replicative lifespan and consistency.
Experimental Approaches: Standardization Protocols and Assessment Methods
Standardized Isolation and Culture Protocols
Robust standardization protocols have been developed to minimize technical variability in MSC manufacturing. For human umbilical cord-derived MSCs (hUC-MSCs), a method validated across 90 donors demonstrates that processing initiation within 48 hours of collection, removal of blood vessels before explant cultures, and expansion in Minimum Essential Medium α (α-MEM) supplemented with hPL significantly improves reproducibility compared to Dulbecco's Modified Eagle's Medium (DMEM) with FBS [91]. This protocol achieves consistent purity (~98.9%), viability (>97%), and proliferative capacity across donors [91].
For BM-MSCs, comparative media assessments reveal that culture in α-MEM yields higher expansion ratios and slightly lower population doubling times compared to DMEM, though these differences were not statistically significant [21]. Both media were supplemented with 10% hPL, underscoring the importance of consistent supplement quality across manufacturing batches. BM-MSCs cultured in α-MEM also produced higher yields of small extracellular vesicles (sEVs) per cell (4,318.72 ± 2,110.22 particles/cell) compared to those in DMEM (3,751.09 ± 2,058.51 particles/cell) [21], indicating that culture conditions influence both cellular and acellular therapeutic products.
Assessment of Senescence and Functionality
Comprehensive characterization protocols are essential for quantifying batch-to-batch variability. Senescence-associated β-galactosidase staining provides a direct measurement of aging cells, with studies showing increased β-galactosidase activity in long-term expanded MSCs at passage 10 compared to earlier passages [88]. Flow cytometric analysis of surface markers (CD73, CD90, CD105, CD34, CD45, HLA-DR) confirms phenotypic stability across passages [88] [21], while trilineage differentiation assays assess functional potency retention.
Population doubling time calculations offer a quantitative measure of proliferative capacity, with formulas such as:
[ \text{PD} = \frac{\log{10}(Nh) - \log{10}(Np)}{\log_{10}(2)} ]
where (Nh) represents harvested cell number and (Np) represents plated cell number [13]. Cumulative population doubling tracks expansion potential across multiple passages.
For functional assessment, T-cell proliferation inhibition assays quantitatively measure immunomodulatory potency [91], while sEV characterization includes nanoparticle tracking analysis for particle concentration and size distribution, transmission electron microscopy for morphological confirmation (cup-shaped morphology), and Western blotting for marker detection (CD9, CD63, TSG101) [21].
The Scientist's Toolkit: Essential Reagents and Solutions
Standardizing MSC manufacturing requires carefully selected research reagents and quality control tools. The following table details essential solutions for overcoming variability challenges in MSC products.
Table 3: Research Reagent Solutions for MSC Standardization
| Reagent/Solution | Function | Standardization Benefit | References |
|---|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free culture supplement replaces FBS | Eliminates xenogeneic antigens, enhances safety, promotes proliferation | [13] [91] |
| α-MEM Medium | Basal culture medium optimized for MSC expansion | Superior expansion ratios and sEV yields compared to DMEM | [21] [91] |
| Xeno-Free Supplement (XFS) | Defined, animal-free growth supplement | Enhances anti-inflammatory properties, GMP compliance | [88] |
| Senescence β-Galactosidase Staining Kit | Detects senescent cells in culture | Quantifies aging-related variability between batches | [88] [89] |
| MSC Phenotyping Cocktail | Multiparameter flow cytometry panel | Verifies identity and purity (CD73+/CD90+/CD105+/CD34-/CD45-/HLA-DR-) | [88] [21] |
| Tangential Flow Filtration (TFF) | sEV isolation method | Higher particle yields than ultracentrifugation, better scalability | [21] |
Overcoming batch-to-batch variability in MSC products demands a multi-faceted approach that acknowledges the inherent biological differences between tissue sources while implementing robust technical controls. The comparative analysis of BM-MSCs and AD-MSCs reveals distinct functional profiles that should guide source selection for specific clinical applications—BM-MSCs for orthopedics requiring robust chondrogenesis, and AD-MSCs for immunomodulation-focused therapies where higher cell yields are advantageous [13] [90].
Strategic standardization must address both intrinsic (donor-related, tissue source-specific) and extrinsic (isolation, culture expansion) variability factors. Implementation of standardized protocols using defined media like α-MEM with hPL supplementation, rigorous senescence monitoring through β-galactosidase staining and molecular markers, and functional potency assays beyond surface marker characterization are essential components [21] [91]. Emerging technologies such as single-cell RNA sequencing for quality control [89], TFF for consistent sEV production [21], and genetic engineering to enhance PD-L1 expression in senescent cells [89] represent promising avenues for next-generation standardization.
Ultimately, recognizing that some biological variability is inherent to MSC biology should not deter standardization efforts but rather focus them on controlling critical quality attributes that directly impact therapeutic efficacy and safety. Through systematic implementation of these strategies, the field can advance reliable MSC-based products that fulfill their considerable promise in regenerative medicine.
The development of cell-based advanced therapy medicinal products (ATMPs), including mesenchymal stem cells (MSCs), necessitates robust quality control measures to ensure their safety and efficacy in clinical applications. While surface marker expression has traditionally been used for product identification and characterization, a growing body of evidence indicates that these markers alone are insufficient predictors of therapeutic efficacy. Functional potency assays have emerged as critical tools that measure the specific biological activity of a cellular product based on its mechanism of action (MoA), thereby providing a more reliable assessment of its in vivo potential [92] [93].
This paradigm shift is particularly relevant when comparing MSCs from different tissue sources, such as bone marrow (BM) and adipose tissue (AT), for regenerative medicine applications. Although BM-MSCs and AT-MSCs exhibit similar fibroblast-like morphology and expression patterns of standard surface markers (CD73, CD90, CD105), they demonstrate significant functional differences that directly impact their therapeutic performance [13]. The field is now moving toward mechanism-based potency testing that can capture these functional distinctions and better predict clinical outcomes, mirroring advancements in other ATMP sectors like CAR T-cell therapy, where multi-omics approaches are revealing a broader spectrum of characteristics that correlate with function [92].
Comparative Functional Analysis of BM-MSCs vs. AT-MSCs
Proliferation, Differentiation, and Secretory Capacity
Direct head-to-head comparisons of BM-MSCs and AT-MSCs under standardized culture conditions reveal fundamental biological differences that surface marker analysis cannot detect. When evaluated in human platelet lysate (hPL)-supplemented medium as an alternative to fetal bovine serum, AT-MSCs demonstrate significantly greater proliferative capacity compared to BM-MSCs, while both cell types show similar colony-forming unit-fibroblast (CFU-F) efficiency [13]. However, their differentiation potential diverges markedly, with BM-MSCs exhibiting superior osteogenic and chondrogenic differentiation capacity, while both cell types show similar adipogenic potential [13].
Their secretory profiles also differ substantially, influencing their respective mechanisms of action in therapeutic contexts. AT-MSCs secrete higher levels of basic fibroblast growth factor (bFGF), interferon-γ (IFN-γ), and insulin-like growth factor-1 (IGF-1), while BM-MSCs produce more stem cell-derived factor-1 (SDF-1) and hepatocyte growth factor (HGF) [13]. These differences in secretome composition translate to varied immunomodulatory effects, with AT-MSCs demonstrating more potent immunomodulatory capabilities [13].
Table 1: Functional Comparison of BM-MSCs and AT-MSCs Under Standardized Culture Conditions
| Functional Parameter | BM-MSCs | AT-MSCs | Experimental Method |
|---|---|---|---|
| Proliferation Capacity | Lower | Higher | Cumulative population doubling (CPD) [13] |
| CFU-F Efficiency | Similar | Similar | Colony-forming unit-fibroblast assay [13] |
| Osteogenic Potential | Higher | Lower | Alizarin Red S staining, gene expression [13] [94] |
| Chondrogenic Potential | Higher | Lower | Alcian Blue staining, gene expression [13] [94] |
| Adipogenic Potential | Similar | Similar | Oil Red O staining, gene expression [13] |
| Immunomodulatory Effects | Lower | Higher | T-cell suppression assays [13] |
| bFGF Secretion | Lower | Higher | ELISA/proteomic analysis [13] |
| SDF-1 Secretion | Higher | Lower | ELISA/proteomic analysis [13] |
In Vivo Bone Regeneration Capacity
Functional differences between BM-MSCs and AT-MSCs become particularly evident in orthotopic large animal models. When seeded on mineralized collagen sponges and implanted into critical-size defects of sheep tibia, BM-MSCs demonstrated significantly superior bone formation compared to AT-MSCs based on radiographic and histological evaluation [94]. This functional superiority in osteogenesis persisted throughout the 26-week study period, highlighting that surface marker similarity does not guarantee equivalent therapeutic performance [94].
The addition of platelet-rich plasma (PRP) to AT-MSCs partially compensated for their inferior osteogenic capacity, suggesting that functional potency can be modulated through scaffold and microenvironment optimization [94]. These findings underscore the importance of using functionally relevant potency assays that can predict in vivo performance rather than relying solely on surface marker characterization.
Key Functional Potency Assays for MSC Characterization
Differentiation Capacity Assays
Osteogenic Differentiation Protocol:
- Seed MSCs at a density of 3.1 × 10^3 cells/cm² in appropriate culture vessels
- Culture in StemPro Osteogenesis Differentiation Medium for 3 weeks
- Change differentiation media every 3 days
- At endpoint, fix cells and perform Alizarin Red S staining to visualize calcium deposition
- Quantify osteogenic gene expression (e.g., Osteocalcin) via RT-PCR [13]
Chondrogenic Differentiation Protocol:
- Use micromass culture system with 2.5 × 10^5 cells per 15 mL polypropylene tube
- Culture in StemPro Chondrogenesis Differentiation Medium for 4 weeks
- Centrifuge cells at 500 g for 5 minutes to form pellet
- Change differentiation media every 3 days
- At endpoint, perform Alcian Blue staining to visualize cartilage matrix
- Analyze chondrogenic gene expression (e.g., COL2α1) via RT-PCR [13]
Adipogenic Differentiation Protocol:
- Seed MSCs at appropriate density for confluence
- Culture in StemPro Adipogenesis Differentiation Medium for 3 weeks
- Change differentiation media every 3 days
- At endpoint, perform Oil Red O staining to visualize lipid droplets
- Assess adipogenic gene expression (e.g., Adiponectin) via RT-PCR [13]
Secretome and Immunomodulatory Assays
The MSC secretome has emerged as a critical mediator of therapeutic effects, particularly for neonatal applications involving bronchopulmonary dysplasia (BPD) and necrotizing enterocolitis (NEC) [95]. Key functional assays include:
Cytokine Secretion Profiling:
- Collect conditioned media from MSC cultures at standardized cell densities and time points
- Analyze using multiplex ELISA or proteomic approaches
- Focus on key therapeutic factors: VEGF, HGF, IGF-1, bFGF, TGF-β, GM-CSF, IL-10, TSG-6 [95]
Immunomodulation Assays:
- Co-culture MSCs with peripheral blood mononuclear cells (PBMCs) at varying ratios
- Measure T-cell proliferation via CFSE dilution or 3H-thymidine incorporation
- Analyze cytokine production in co-culture supernatants
- Assess effects on macrophage polarization (M1 to M2 transition) [93]
Extracellular Vesicle (EV) Characterization:
- Isolate EVs from conditioned media using differential centrifugation or tangential flow filtration
- Characterize particle size and concentration via nanoparticle tracking analysis
- Identify EV-specific surface markers (CD9, CD63, CD81) via flow cytometry
- Evaluate functional capacity in target cell uptake assays [96] [95]
Figure 1: Mechanism of Action of MSC Secretomes. MSCs release extracellular vesicles (EVs) and soluble factors that interact with target cells through multiple pathways to produce therapeutic effects.
In Vivo Tracking and Biodistribution Assays
Understanding the in vivo distribution and persistence of MSCs is crucial for validating functional potency. Recent approaches include:
Fluorescent Labeling and Imaging:
- Label MSCs with lipophilic dyes (e.g., DiD, DiI) at 10 μM concentration for 50 minutes at 37°C
- Validate that labeling does not affect proliferation or differentiation capacity
- Administer labeled cells via intended route (e.g., intra-articular, intravenous)
- Track using non-invasive biofluorescence imaging systems (e.g., IVIS Spectrum)
- Establish detection thresholds (typically 10^4 cells in vitro, 10^5 cells in vivo) [97]
Molecular Biodistribution Analysis:
- Utilize species-specific genetic markers (e.g., human Alu repeats in animal models)
- Apply quantitative PCR with human-specific primers (e.g., β-globin)
- Analyze tissue distribution patterns at multiple time points
- Correlate persistence with therapeutic outcomes [98] [97]
Table 2: Key Functional Potency Assays and Their Methodological Considerations
| Assay Category | Specific Assay | Key Readout Parameters | Regulatory Considerations |
|---|---|---|---|
| Differentiation Capacity | Trilineage differentiation | Osteogenic: MineralizationChondrogenic: GAG depositionAdipogenic: Lipid droplets | Quantitative image analysis;Gene expression validation [13] |
| Secretome Analysis | Multiplex cytokine array | VEGF, HGF, IGF-1, bFGF, IL-10, TSG-6 | Standardized collection protocols;Reference materials [95] |
| Immunomodulation | T-cell suppression | % Inhibition of proliferation;Cytokine shift (IFN-γ/IL-10 ratio) | Donor-to-donor variability;Positive controls [13] [93] |
| In Vivo Tracking | Biofluorescence imaging | Signal intensity and duration;Biodistribution pattern | Detection sensitivity limits;Labeling effects on function [97] |
| Extracellular Vesicles | Nanoparticle tracking | Particle concentration;Size distribution;Surface markers | Standardized isolation;Minimum characterization [96] |
Advanced Approaches and Correlation with Clinical Outcomes
Multi-Omics Profiling for Comprehensive Characterization
The integration of advanced profiling technologies represents the cutting edge of potency assay development. As demonstrated in CAR T-cell therapy, multi-omics approaches—including genomics, epigenomics, transcriptomics, proteomics, and metabolomics—provide unprecedented resolution of product characteristics that correlate with clinical outcomes [92]. For MSCs, these approaches can identify predictive biomarkers of functionality beyond conventional assays.
Genomic and Epigenomic Profiling:
- Assess DNA methylation patterns associated with differentiation potential
- Analyze chromatin accessibility in key regulatory regions
- Identify epigenetic signatures of cellular senescence [92]
Transcriptomic Analysis:
- Utilize bulk and single-cell RNA sequencing to characterize heterogeneity
- Identify gene expression signatures predictive of in vivo performance
- Monitor stability of transcriptional profiles across passages [92]
Proteomic and Metabolomic Characterization:
- Map surface marker expression beyond standard characterization panels
- Identify metabolic signatures associated with robust functionality
- Correlate protein secretion patterns with therapeutic mechanisms [92]
Figure 2: Integrated Workflow for Comprehensive Potency Assessment. Combining multi-omics profiling with functional assays enables correlation with clinical outcomes and identification of predictive biomarkers.
Strategies for Establishing In Vitro-In Vivo Correlation
Establishing correlation between in vitro potency measurements and in vivo efficacy represents the ultimate goal of potency assay development. The following strategic approaches facilitate this correlation:
Accelerated Degradation Studies:
- Subject MSCs or MSC products to controlled stress conditions (thermal, oxidative)
- Generate samples with a range of biological activities
- Test both in vitro potency and in vivo efficacy in parallel
- Establish correlation curves between assay readouts and functional outcomes [99]
Multi-Assay Matrices:
- Implement complementary potency assays measuring different aspects of functionality
- Weight assay results based on mechanistic relevance
- Develop predictive algorithms combining multiple parameters
- Validate against clinical outcomes when available [100]
Pathway-Specific Reporter Systems:
- Engineer reporter cell lines responsive to key MSC-secreted factors
- Quantitate activation of therapeutic pathways (e.g., anti-inflammatory, angiogenic)
- Correlate pathway activation with in vivo effects in disease models [95]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for MSC Potency Assays
| Reagent/Material | Function | Application Examples | Considerations |
|---|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free culture supplement | MSC expansion for clinical applications; comparative studies | Maintains differentiation potential; reduces immunogenicity [13] |
| Trilineage Differentiation Kits | Standardized induction media | Osteogenic, chondrogenic, adipogenic differentiation assays | Ensure lot-to-lot consistency; include appropriate controls [13] |
| Lipophilic Tracers (DiD, DiI) | Cell labeling and tracking | In vivo biodistribution studies; persistence assessment | Validate no functional impact; establish detection thresholds [97] |
| Extracellular Vesicle Isolation Kits | EV purification from conditioned media | Secretome analysis; cell-free therapeutic development | Standardize isolation method; characterize yield and purity [96] |
| Multiplex Cytokine Arrays | Secretome profiling | Quantitative analysis of paracrine factors | Cover relevant analyte panels; ensure appropriate sensitivity [95] |
| Flow Cytometry Panels | Surface and intracellular marker analysis | Phenotypic characterization; purity assessment | Include ISCT-recommended markers; validate antibody specificity [13] |
The evolution of potency testing for MSCs from surface marker-based characterization to mechanism-based functional assays represents significant progress in the field of regenerative medicine. The comparative analysis between BM-MSCs and AT-MSCs clearly demonstrates that while these cell types share superficial phenotypic similarities, they exhibit distinct functional profiles that direct their therapeutic applications. BM-MSCs show superior performance in osteogenic and chondrogenic applications, while AT-MSCs demonstrate advantages in proliferation capacity and immunomodulation.
Implementing robust functional potency assays that measure differentiation capacity, secretome composition, immunomodulatory activity, and in vivo persistence provides essential data for predicting clinical efficacy. The integration of advanced multi-omics approaches with traditional functional assays offers a path toward comprehensive product characterization and identification of novel biomarkers of potency. As the field advances, continued emphasis on establishing correlation between in vitro potency measurements and in vivo outcomes will be crucial for developing reproducible, efficacious MSC-based therapies tailored to specific clinical indications.
The therapeutic application of Mesenchymal Stem Cells (MSCs) has expanded significantly in regenerative medicine, with bone marrow (BM-MSCs) and adipose tissue (AD-MSCs) emerging as two of the most prevalent cell sources. While both fulfill the International Society for Cellular Therapy's minimal criteria for MSCs—plastic adherence, specific surface marker expression, and trilineage differentiation potential—growing evidence reveals fundamental differences in their metabolic and functional profiles [12] [11]. These tissue-specific variations in cellular energy metabolism and secretome composition directly influence therapeutic efficacy for different indications. This guide provides a structured comparison of BM-MSC and AD-MSC characteristics, focusing on metabolomic and respiratory profiling data to inform cell source selection for research and therapeutic development. Understanding these distinctions enables researchers to systematically match MSC source to application, whether for osteogenic regeneration, immunomodulation, or angiogenesis [13].
Comprehensive Comparison of BM-MSCs and AD-MSCs
The following tables synthesize quantitative and qualitative findings from comparative studies, highlighting key performance differences.
Table 1: Functional Comparison of BM-MSCs and AD-MSCs
| Functional Parameter | Bone Marrow-MSCs (BM-MSCs) | Adipose-Derived MSCs (AD-MSCs) | References |
|---|---|---|---|
| Proliferation Capacity | Robust growth in optimized media | Generally higher proliferative potential | [13] [12] [11] |
| Osteogenic Differentiation | Higher capacity; stronger alkaline phosphatase activity & mineralization | Moderate osteogenic potential | [13] [12] [11] |
| Chondrogenic Differentiation | Higher chondrogenic capacity | Lower chondrogenic capacity | [13] [12] |
| Adipogenic Differentiation | Lower adipogenic efficiency | Highly efficient; rapid lipid vacuole formation | [12] [11] |
| Immunomodulatory Potential | Potent immunomodulation | Often more robust suppression; higher IDO activity post IFN-γ priming | [13] [11] |
Table 2: Secretome and Metabolic Profile Comparison
| Characteristic | Bone Marrow-MSCs (BM-MSCs) | Adipose-Derived MSCs (AD-MSCs) | References |
|---|---|---|---|
| Key Secreted Factors | Advantages in HGF and SDF-1 secretion | Advantages in bFGF, IGF-1, and VEGF secretion post-priming | [13] [11] |
| Angiogenic Potential | Promotes angiogenesis | Often superior angiogenic stimulation | [11] |
| Representative Surface Markers | CD73+, CD90+, CD105+, CD45-, CD34- (Variable Stro-1, CD49d) | CD73+, CD90+, CD105+, CD45-, CD34- (Often CD49d+, Stro-1 low) | [12] [11] |
| Metabolic Pathway Inclination | Balanced oxidative phosphorylation and glycolysis | Inclination toward anaerobic metabolism in some studies | [101] |
Experimental Profiling: Methodologies for Cellular Fitness Assessment
Metabolomic Profiling of Energy Pathways
Metabolomics provides a powerful tool for investigating the metabolic phenotypes of MSCs by quantitatively measuring small-molecule metabolites.
- Sample Preparation: Collect serum or cell culture supernatant from MSC cultures under fasting/resting conditions. Deproteinize samples using methanol, then subject them to derivatization for analysis [101].
- Instrumentation and Analysis: Utilize Ultra-High-Performance Liquid Chromatography coupled with Quadrupole Time-of-Flight Mass Spectrometry (UHPLC-Q-TOF/MS). Employ a C18 column with a gradient mobile phase (water and acetonitrile, both with 0.1% formic acid) [101].
- Data Interpretation: Monitor key metabolites in central carbon metabolism. Focus on Tricarboxylic Acid (TCA) cycle intermediates (e.g., citrate, succinate, fumarate) and glycolytic end-products (e.g., lactate, pyruvate). A elevated lactate-to-pyruvate ratio indicates a shift toward anaerobic glycolysis, suggesting metabolic reprogramming [101] [102].
- Application: This approach can identify metabolic signatures associated with MSC proliferation capacity, differentiation potential, and response to pathological stressors [103] [101].
Cellular Respiration and Bioenergetic Profiling
Direct measurement of oxygen consumption provides a functional readout of mitochondrial health and cellular energy metabolism.
- Experimental Setup: Utilize instruments like the Seahorse Analyzer to perform real-time, label-free measurements of the Oxygen Consumption Rate (OCR) and the Extracellular Acidification Rate (ECAR) from live cells [104].
- Mitochondrial Stress Test: This standard assay involves sequential injection of pharmacological agents:
- Oligomycin: Inhibits ATP synthase, revealing ATP-linked respiration.
- FCCP: Uncouples mitochondria to measure maximal respiratory capacity.
- Rotenone & Antimycin A: Inhibit Electron Transport Chain complexes, revealing non-mitochondrial respiration [104].
- Data Interpretation: Key parameters calculated from the assay include basal respiration, ATP-linked respiration, proton leak, maximal respiratory capacity, and spare respiratory capacity. A high spare capacity is often associated with better cellular fitness and ability to handle stress [104].
- Application: This technique is crucial for evaluating the bioenergetic health of MSCs, identifying dysfunction in oxidative phosphorylation, and assessing the impact of culture conditions or therapeutic manipulations on cellular metabolism [104].
Cellular Fitness Assessment Workflow
Trilineage Differentiation Potency Assays
Functional differentiation assays are essential for confirming MSC multipotency and comparing the lineage-specific propensity of BM-MSCs and AD-MSCs.
- Osteogenic Differentiation: Culture MSCs in commercial osteogenic induction medium supplemented with ascorbic acid, β-glycerophosphate, and dexamethasone. Differentiate for 2-4 weeks, then fix and stain with Alizarin Red S to detect calcium deposits. Quantify staining by elution and spectrophotometry or image analysis [12].
- Adipogenic Differentiation: Induce adipogenesis using medium containing isobutylmethylxanthine, dexamethasone, indomethacin, and insulin. After 2-3 weeks, fix cells and stain with Oil Red O to visualize lipid vacuoles. Quantify by elution and spectrophotometry [12] [11].
- Chondrogenic Differentiation: Pellet cultures are often used. Induce chondrogenesis in a defined serum-free medium with TGF-β. After several weeks, analyze pellets for sulfated glycosaminoglycan content (e.g., Alcian Blue or Safranin O staining) and cartilage-specific gene expression [12].
The Scientist's Toolkit: Essential Research Reagents
Successful metabolomic and functional profiling relies on specific reagents and instrumentation.
Table 3: Essential Reagents and Tools for MSC Metabolic Profiling
| Tool/Reagent | Function/Application | Examples/Specifications |
|---|---|---|
| Seahorse Analyzer | Real-time measurement of OCR and ECAR for bioenergetic profiling | XF Analyzer series; requires specialized cell culture microplates |
| UHPLC-Q-TOF/MS | High-resolution separation and accurate mass identification of metabolites | Agilent, Waters, Thermo Fisher systems; C18 columns common |
| Mitochondrial Stress Test Kit | Standardized reagents for assessing mitochondrial function | Includes Oligomycin, FCCP, Rotenone/Antimycin A |
| Trilineage Differentiation Kits | Standardized media for osteogenic, adipogenic, chondrogenic induction | Commercial kits available from STEMCELL Technologies, MilliporeSigma |
| Cytokine Priming Cocktails | Pre-conditioning MSCs to enhance immunomodulatory function | Typically contain IFN-γ and/or TNF-α |
| Flow Cytometry Antibodies | Confirmation of MSC surface marker profile (CD73, CD90, CD105, etc.) | Conjugated antibodies for positive and negative marker panels |
Metabolic Pathways Underlying MSC Function
Cellular metabolism in MSCs is not merely a housekeeping function but a key regulator of cell fate and therapeutic activity.
- Energy Metabolism Plasticity: MSCs utilize both oxidative phosphorylation (OXPHOS) in mitochondria and aerobic glycolysis (Warburg effect) to generate ATP. The balance between these pathways can influence proliferation and differentiation. Shifts toward anaerobic glycolysis have been observed in some pathogenic states and may reflect a less efficient energy generation mode [104] [101].
- Metabolic Signaling: Metabolites themselves can act as signaling molecules. For instance, succinate and fumarate (TCA cycle intermediates) can regulate epigenetic modifications and stabilize hypoxia-inducible factors, thereby influencing gene expression profiles in MSCs and their target cells [103].
- Therapeutic Implications: The metabolic state of MSCs can impact their secretory profile and immunomodulatory functions. For example, the potent immunosuppressive enzyme Indoleamine 2,3-dioxygenase (IDO), highly expressed in primed AD-MSCs, is part of the tryptophan metabolism pathway [11]. Understanding these connections allows for the metabolic priming of MSCs to enhance their therapeutic efficacy for specific applications.
Key Metabolic Pathways in MSCs
The comparative profiling of BM-MSCs and AD-MSCs reveals a clear paradigm: "one size does not fit all" in regenerative medicine. The choice between cell sources should be driven by the target clinical application. BM-MSCs demonstrate superior performance for skeletal regeneration, while AD-MSCs show distinct advantages in immunomodulation and potentially angiogenic contexts. A deep understanding of their metabolic and functional differences, enabled by the profiling techniques outlined in this guide, allows for a rational, evidence-based selection of the optimal MSC source. This strategic approach is fundamental to enhancing the success of future clinical trials and developing more effective, precision-based cellular therapeutics.
The therapeutic application of Mesenchymal Stem/Stromal Cells (MSCs) in regenerative medicine and treatment of immune-mediated diseases requires manufacturing processes that can transition from laboratory scale to industrial production while maintaining strict Good Manufacturing Practice (GMP) standards [105]. The selection of cell source—primarily bone marrow-derived MSCs (BM-MSCs) or adipose tissue-derived MSCs (AT-MSCs)—carries significant implications for bioprocessing strategy, scalability, and ultimate clinical success. While MSC-based therapies hold immense potential, their translation from research to clinical application faces substantial challenges in large-scale production, with the initial frequency of MSCs in native tissues being remarkably low—approximately one MSC per 10⁴–10⁵ mononuclear cells in bone marrow or per 10²–10³ cells from lipoaspirate [105]. This scarcity necessitates extensive in vitro expansion to achieve clinically relevant yields (millions to hundreds of millions of cells), making efficient, standardized bioprocessing not merely advantageous but essential for clinical translation [105].
The fundamental differences between BM-MSCs and AT-MSCs extend beyond their biological characteristics to encompass critical manufacturing considerations including expansion kinetics, growth factor requirements, and performance in automated bioreactor systems. Understanding these distinctions enables researchers and bioprocess engineers to optimize production platforms for specific MSC sources, ultimately advancing the field toward more effective and accessible cell-based therapies.
Comparative Biology of BM-MSCs and AT-MSCs: Implications for Bioprocessing
Isolation Efficiency and Initial Cell Yield
The isolation process for MSCs from different sources yields substantially different cell numbers, directly impacting upstream process design and initial expansion requirements. AT-MSCs demonstrate a significant advantage in initial yield, providing approximately 500,000–2,000,000 cells per milliliter of lipoaspirate, while BM-MSCs yield only about 5,000–100,000 cells per milliliter of bone marrow aspirate [90]. This approximately 10-50 fold difference in initial cell availability means that AT-MSCs require fewer population doublings to reach therapeutic doses, potentially reducing culture duration and associated risks of cellular senescence or genetic instability.
The isolation methodologies also differ substantially. AT-MSCs are typically isolated from subcutaneous fat via minimally invasive liposuction procedures, requiring enzymatic digestion (commonly with 0.1% collagenase type I) followed by centrifugation to separate the stromal vascular fraction [12]. BM-MSCs are obtained from iliac crest aspiration via bone marrow aspiration, which is considered more invasive, with isolation involving density gradient centrifugation to separate mononuclear cells before plastic adherence selection [12]. These procedural differences necessitate distinct upstream processing equipment and validation approaches in GMP-compliant manufacturing.
Proliferation Capacity and Expansion Kinetics
Under standardized culture conditions with human platelet lysate (hPL) supplementation, AT-MSCs consistently demonstrate superior proliferative capacity compared to BM-MSCs. In donor-matched comparisons, AT-MSCs showed significantly higher proliferation rates over 21-day culture periods [12]. This enhanced expansion potential directly translates to reduced time in culture to achieve target cell numbers, potentially improving manufacturing efficiency.
However, this proliferation advantage must be balanced against functional characteristics. While AT-MSCs proliferate more rapidly, BM-MSCs maintain stronger differentiation capacity toward osteogenic and chondrogenic lineages even under identical culture conditions [13]. This fundamental biological difference may influence the selection of cell source for specific clinical applications, particularly those requiring robust bone or cartilage formation.
Table 1: Comparative Growth Characteristics and Differentiation Potential of BM-MSCs and AT-MSCs
| Parameter | Bone Marrow MSCs (BM-MSCs) | Adipose Tissue MSCs (AT-MSCs) | References |
|---|---|---|---|
| Initial Yield per mL Tissue | ~5,000–100,000 cells | ~500,000–2,000,000 cells | [90] |
| Proliferation Rate | Moderate | Higher | [13] [12] |
| Osteogenic Differentiation | Strong | Moderate | [13] [12] |
| Chondrogenic Differentiation | Strong | Moderate | [13] [90] |
| Adipogenic Differentiation | Moderate | Strong | [13] [12] |
| Immunomodulatory Effects | Moderate | Strong | [13] [90] |
Secretory Profiles and Therapeutic Mechanisms
The secretory profiles of BM-MSCs and AT-MSCs show distinct patterns that may influence their therapeutic mechanisms and consequently, bioprocessing considerations. Under human platelet lysate-supplemented culture conditions, significant differences emerge in the secretion of cytokines, growth factors, and chemokines [13]. AT-MSCs secrete higher levels of basic fibroblast growth factor (bFGF), interferon-γ (IFN-γ), and insulin-like growth factor-1 (IGF-1), contributing to their potent immunomodulatory effects [13]. Conversely, BM-MSCs demonstrate advantages in secretion of stem cell-derived factor-1 (SDF-1) and hepatocyte growth factor (HGF) [13]. These differences in secretome composition may necessitate different quality control measures and potency assays for products derived from each source.
Recent research has also revealed that extracellular vesicle (EV) production, an increasingly important therapeutic mechanism of MSCs, varies by tissue source. In comparative studies using standardized bioreactor platforms, BM-MSCs showed the highest EV output per cell compared to AT-MSCs and umbilical cord MSCs [106]. Additionally, RNA cargo and functional markers differed among EVs from different MSC sources, indicating that the therapeutic profile of MSC-derived products is source-dependent [106].
GMP-Compliant Manufacturing Platforms for MSC Expansion
Automated Bioreactor Systems for Large-Scale Production
Traditional in vitro expansion of MSCs using planar culture vessels is increasingly inadequate for clinical-scale production due to extensive space requirements, labor intensity, and open manipulation risks [105]. Automated closed-system bioreactors have emerged as essential platforms for GMP-compliant manufacturing, offering controlled environments that ensure consistency, reproducibility, and quality. Several integrated systems have been developed specifically for adherent cell culture, each with distinct advantages for MSC expansion:
The Quantum Cell Expansion System (Terumo BCT) utilizes a hollow fiber bioreactor providing 21,000 cm² surface area equivalent to 120 T-175 flasks [105]. This system enables continuous medium exchange and can be directly connected to gas mixtures for environmental control. For BM-MSC expansion, a 7-day process starting with 20 × 10⁶ cells typically yields 100–276 × 10⁶ cells while maintaining immunomodulatory function [105]. The system significantly reduces manual operations compared to flask-based methods and has demonstrated therapeutic efficacy in multiple disease models [105].
The CliniMACS Prodigy (Miltenyi Biotec) represents an integrated automated system that performs MSC isolation, inoculation, cultivation, media change, propagation, and harvesting using a single closed tubing set [105]. This system supports processing of primary tissue-isolated BM-MSCs, AT-MSCs, and umbilical cord MSCs using GMP-compliant media like MSC-Brew [105]. Reported outputs range from 29 to 50 million MSCs at passage zero following a 10-day procedure using 1-layer CellSTACK [105].
Additional platforms including the Cocoon Platform (Lonza), Xuri Cell Expansion System W25 (Cytiva), NANT001/XL (VivaBioCell), and CellQualia (Sinfonia technology) provide diverse technological approaches to automated MSC manufacturing, allowing flexibility in process design based on specific cell source requirements [105].
Table 2: Automated Bioreactor Platforms for GMP-Compliant MSC Manufacturing
| Platform | Technology | Scale Capacity | Reported Performance | Compatible MSC Types |
|---|---|---|---|---|
| Quantum Cell Expansion System | Hollow fiber bioreactor | 21,000 cm² | 100–276 × 10⁶ BM-MSCs from 20 × 10⁶ input in 7 days | BM-MSCs, AT-MSCs, UC-MSCs |
| CliniMACS Prodigy | Integrated automation with adherence culture | Vessel-dependent | 29–50 × 10⁶ MSCs at P0 in 10 days | BM-MSCs, AT-MSCs, UC-MSCs |
| Xuri Cell Expansion System W25 | Stirred-tank or fixed-bed bioreactors | Scalable volumes | Compatible with microcarriers | Multiple MSC types |
| Cocoon Platform | Individualized automated cell processing | Patient-scale | Closed system manufacturing | Multiple MSC types |
| NANT001/XL System | Not specified | Not specified | Not specified | Multiple MSC types |
| CellQualia | Not specified | Not specified | Not specified | Multiple MSC types |
Culture Media Optimization for Clinical-Scale Expansion
The transition from research-scale to clinical-scale MSC manufacturing necessitates replacement of fetal bovine serum (FBS) with human-derived alternatives due to safety concerns regarding potential transmission of animal pathogens and immune reactions to xeno-proteins [13]. Human platelet lysate (hPL) has emerged as an effective substitute, demonstrating considerable growth-promoting properties while maintaining MSC immunophenotype, differentiation potential, and immunomodulatory properties [13].
The formulation of culture media significantly impacts MSC characteristics and performance in bioreactor systems. Studies comparing BM-MSCs and AT-MSCs under hPL-supplemented conditions reveal that both cell types exhibit similar fibroblast-like morphology and surface marker expression patterns, but maintain their distinct differentiation capacities [13]. This suggests that media optimization must be tailored to the specific MSC source, as the same formulation may affect BM-MSCs and AT-MSCs differently.
For example, when using the Quantum bioreactor system, substitution of FBS with hPL significantly enhanced expansion of AT-MSCs while sustaining their quality attributes [105]. Additionally, the use of specific GMP-compliant media such as MSC-Brew in the CliniMACS Prodigy system enables consistent manufacturing of clinical-grade MSCs from multiple tissue sources [105].
Experimental Methodologies for MSC Characterization in Bioprocessing
Standardized Isolation and Culture Protocols
To ensure reproducible manufacturing outcomes, standardized protocols for MSC isolation and expansion are essential. For AT-MSC isolation, enzymatic digestion using 0.1% collagenase type I at 37°C for 30-60 minutes is commonly employed, followed by centrifugation to separate the stromal vascular fraction [12]. The cells are then plated in culture vessels with serum-free medium or hPL-supplemented medium, with non-adherent cells removed after 24-48 hours [13]. For BM-MSC isolation, density gradient centrifugation (e.g., with lymphoprep) separates mononuclear cells from bone marrow aspirates, followed by plating in culture vessels and removal of non-adherent cells after 48 hours [13].
Both cell types are typically cultured in basal media such as DMEM or IMDM supplemented with 5-10% hPL and 1% antibiotics, maintained at 37°C in a humidified atmosphere containing 5% CO₂ [13]. Medium changes are performed twice weekly, and cells are harvested at 80-90% confluence using trypsin-EDTA [12]. For large-scale production, these processes are adapted to automated bioreactor systems with controlled parameters.
Critical Quality Attribute Assessment
Comprehensive characterization of MSCs throughout the manufacturing process is essential for ensuring product quality and consistency. Key assays include:
Immunophenotype Analysis by flow cytometry confirms expression of typical MSC markers (CD105, CD73, CD90 ≥95%) and absence of hematopoietic markers (CD45, CD34, CD14, CD19, HLA-DR ≤2%) according to International Society for Cellular Therapy (ISCT) criteria [12] [2]. Additional markers such as CD49d and Stro-1 may show differential expression between BM-MSCs and AT-MSCs [12].
Proliferation Capacity is assessed through population doubling calculations, with cumulative population doubling (CPD) providing a measure of expansion potential over multiple passages [13]. The formula PD = log₁₀(Nʰ) - log₁₀(Nᵖ) / log₁₀(2) is used, where Nʰ is harvested cell number and Nᵖ is plated cell number [13].
Colony-Forming Unit (CFU-F) Assays evaluate clonogenic potential by plating low-density cell suspensions (e.g., 1×10³ cells per well in 6-well plates) and counting colonies of ≥50 cells after 14 days following crystal violet staining [13].
Multi-lineage Differentiation Potential is assessed using specific induction media. Osteogenic differentiation is typically induced with dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate, with mineralization detected by Alizarin Red staining [12]. Chondrogenic differentiation employs TGF-β3, dexamethasone, ascorbate-2-phosphate, and proline in pellet culture, with sulfated glycosaminoglycans detected by Alcian Blue staining [12]. Adipogenic differentiation uses insulin, dexamethasone, indomethacin, and IBMX, with lipid vacuoles visualized by Oil Red O staining [12].
Functional Potency Assays including immunomodulatory capacity measured by T-cell suppression assays and secretome analysis through ELISA or multiplex arrays for cytokines (IFN-γ), growth factors (bFGF, HGF, IGF-1), and chemokines (SDF-1) provide critical data on therapeutic potential [13].
Essential Research Reagent Solutions for MSC Bioprocessing
The transition from research-scale to GMP-compliant manufacturing requires carefully selected reagents that support cell growth while maintaining quality attributes and regulatory compliance.
Table 3: Essential Research Reagent Solutions for MSC Bioprocessing
| Reagent Category | Specific Products | Function & Importance | GMP Considerations |
|---|---|---|---|
| Culture Media | RoosterNourish, MSC-Brew, IMDM with hPL | Provides nutrients for cell growth and expansion | Defined, xeno-free formulations preferred for clinical use |
| Growth Supplement | Human Platelet Lysate (hPL) | Replaces FBS; reduces xeno-risks while promoting proliferation | Pooled from multiple donors to minimize variability; pathogen testing required |
| Dissociation Agents | Trypsin-EDTA, Collagenase Type I/IV | Detaches adherent cells for passaging and harvesting | Recombinant sources preferred over animal-derived for clinical use |
| Cell Separation Media | Lymphoprep, Ficoll-Paque | Density gradient separation for BM-MSC isolation | Quality-controlled lots with certificate of analysis |
| Cryopreservation Media | Cryostor, DMSO-based formulations | Preserves cell viability and function during frozen storage | Defined composition; DMSO concentration optimized for minimal toxicity |
| EV Collection Medium | RoosterCollect-EV | Optimized for extracellular vesicle production during MSC culture | Low-particulate formulation to facilitate downstream processing |
| Characterization Kits | Flow cytometry antibody panels, Differentiation kits | Quality control assessment of identity, purity, and potency | Validated for consistency and reproducibility |
The selection between BM-MSCs and AT-MSCs for large-scale GMP-compliant manufacturing involves careful consideration of multiple factors including therapeutic application, manufacturing constraints, and regulatory requirements. AT-MSCs offer advantages in initial yield and proliferation capacity, potentially reducing expansion time and manufacturing costs. Conversely, BM-MSCs demonstrate superior osteogenic and chondrogenic differentiation potential, making them preferable for orthopedic applications, while their established research history may facilitate regulatory approval.
Automated bioreactor systems have demonstrated capability for expanding both MSC types while maintaining critical quality attributes, though process parameters may require optimization for each specific cell source. The ongoing transition from FBS to hPL-containing media enhances safety profiles without compromising cell growth, and integrated closed systems reduce contamination risks while improving reproducibility.
As MSC therapies continue to advance through clinical development, the implementation of robust, scalable bioprocessing strategies tailored to specific cell sources will be essential for translating cellular potential into clinically effective and commercially viable therapeutics. Future advancements in bioprocessing technology and media formulation will likely further enhance manufacturing efficiency while maintaining the critical biological attributes that underpin therapeutic efficacy.
Addressing Senescence and Maintaining Genomic Stability During Long-Term Culture
The therapeutic efficacy of mesenchymal stromal cells (MSCs) in regenerative medicine depends on obtaining sufficient cell quantities through in vitro expansion. However, long-term culture introduces significant challenges related to cellular senescence and genomic instability that can compromise patient safety and treatment outcomes [107] [108]. Within the context of bone marrow-derived mesenchymal stromal cells (BM-MSCs) versus adipose-derived mesenchymal stromal cells (AD-MSCs), understanding these processes is crucial for developing safe cellular therapies.
During culture expansion, MSCs undergo extensive morphological and functional changes, including diminished differentiation potential and altered immunomodulatory properties [107]. These changes conflict with the high demands for standardization and safety in regenerative medicine applications. This review systematically compares how BM-MSCs and AD-MSCs respond to long-term culture stress, focusing on the onset of senescence, accumulation of DNA damage, and epigenetic reprogramming, while providing standardized experimental approaches for monitoring these parameters.
Senescence Characteristics in MSCs During Long-Term Culture
Morphological and Functional Hallmarks
Cellular senescence represents a state of permanent cell cycle arrest triggered by various stressors, including serial passaging in culture [109]. Senescent MSCs display characteristic enlarged, flattened morphology with more granular cytoplasm, often described as a "fried egg" appearance [109] [110]. This morphological transformation is accompanied by significantly prolonged population doubling times and decreased colony-forming unit (CFU) capacity, indicating diminished self-renewal capability [109].
Functionally, senescent MSCs exhibit biased differentiation potential, with reduced osteogenic capacity and increased adipogenic propensity [109] [110]. This differentiation shift has particular implications for bone regeneration therapies, where the therapeutic objective is osteogenesis rather than adipogenesis. Additionally, senescent MSCs develop a senescence-associated secretory phenotype (SASP), releasing pro-inflammatory cytokines including IL-1, IL-6, IL-8, MMPs, TNF-α, and VEGF [109]. This secretome alteration potentially affects both the therapeutic efficacy of MSCs and their microenvironment through paracrine signaling.
Epigenetic Regulation of Senescence
Epigenetic modifications serve as critical regulatory mechanisms in MSC senescence. Research has identified highly reproducible senescence-associated DNA methylation (SA-DNAm) changes at specific CpG sites, particularly in developmental genes and homeobox genes [107]. These epigenetic alterations correlate with repressive histone marks such as H3K9me3 and H3K27me3 and are enriched in intergenic regions [107] [109].
The emergence of an "Epigenetic-Senescence-Signature" provides a valuable tool for monitoring cellular senescence for quality control purposes [107]. Unlike somatic cells, pluripotent stem cells evade both telomere attrition and SA-DNAm changes, suggesting they possess mechanisms to bypass the 'Hayflick limit' that restricts MSC proliferation capacity [107].
Table 1: Senescence Markers in Long-Term MSC Culture
| Parameter | Early Passage (P1-P4) | Late Passage (≥P5) | Detection Methods |
|---|---|---|---|
| Morphology | Spindle-shaped, fibroblastic | Enlarged, flattened, granular | Phase-contrast microscopy |
| Proliferation Rate | High (24-48h doubling) | Low (>96h doubling) | Population doubling time, CFU assay |
| SA-β-gal Activity | <5% positive cells | >20% positive cells | Histochemical staining |
| DNA Methylation | Youthful methylation pattern | SA-DNAm changes at developmental genes | Whole-genome bisulfite sequencing |
| Secretome Profile | Normal cytokine secretion | SASP (elevated IL-6, IL-8, MMPs) | ELISA, multiplex immunoassays |
| Differentiation Potential | Balanced trilineage potential | Adipogenic bias, osteogenic reduction | Lineage-specific staining, qPCR |
Genomic Instability in Long-Term Culture
DNA Damage Accumulation
Long-term culture of MSCs under artificial conditions imposes significant replicative stress that can compromise genomic integrity. A comprehensive study analyzing AD-MSCs through eleven passages demonstrated a statistically significant increase in DNA damage from passage five onward using the comet assay [108]. The micronucleus test, which detects chromosome loss or fragmentation, showed a significant increase from passage seven onward, indicating potential mutagenic effects associated with extended culture [108].
While the overall genome of MSCs appears relatively stable throughout culture, transient clonal aneuploidies have been observed in some studies [107]. Notably, these cytogenetically abnormal clones typically do not persist in culture and are lost upon prolonged passaging, with MSC preparations ultimately entering senescence with proliferation arrest [107]. This suggests the existence of protective mechanisms that eliminate genetically compromised cells from the population.
Oncogenic Transformation Risks
The risk of malignant transformation in cultured MSCs remains a concern despite their extensive application in clinical trials. Importantly, spontaneous transformation of human MSCs with tumor formation in immunocompromised mice has not been convincingly demonstrated in studies without methodological issues like cell line contamination [107]. Current evidence suggests that senescence acts as a barrier against oncogenic transformation by limiting the expansion of potentially malignant clones [107].
Array-comparative genomic hybridization (aCGH) can detect dominant clones with significant deletions or duplications, but this method may miss smaller genetic alterations or point mutations that could predispose to transformation [107]. Furthermore, oncogenic transformation does not necessarily confer growth advantage in vitro, making detection through standard karyotypic analysis or genomic profiling insufficient to exclude all transformation risks [107].
Table 2: Genomic Stability Assessment in Long-Term MSC Culture
| Assessment Method | Parameter Measured | Critical Passage Threshold | Application in Quality Control |
|---|---|---|---|
| Comet Assay | DNA strand breaks | Significant increase at P5 [108] | Early detection of genotoxicity |
| Micronucleus Test | Chromosomal loss/breakage | Significant increase at P7 [108] | Mutagenicity screening |
| Karyotype Analysis | Chromosomal abnormalities | Transient aneuploidies observed [107] | Detection of gross chromosomal changes |
| aCGH | Copy number variations | No dominant clones reported [107] | Identification of submicroscopic alterations |
| Telomere Length Analysis | Replicative history | Progressive shortening [109] | Replicative senescence monitoring |
Comparative Analysis: BM-MSCs vs. AD-MSCs
Tissue-Specific Senescence Patterns
When comparing MSC sources, proliferation capacity emerges as a distinguishing characteristic. AD-MSCs typically demonstrate higher initial cell yields and faster population doubling times compared to BM-MSCs [16] [90]. Dental pulp stromal cells (DPSCs), which share some characteristics with BM-MSCs, show consistently smaller cell size, Nestin positivity, and higher proliferation rates than AD-MSCs [16]. This enhanced proliferative capacity of AD-MSCs may impact their senescence progression during extended culture.
The secretome profile also varies significantly between MSC sources. Analysis of conditioned media from AD-MSCs and DPSCs revealed significant variations in anti-inflammatory and pro-inflammatory cytokines, chemokines, and growth factors [16]. While both MSC types release comparable numbers of extracellular vesicles, AD-MSCs produce significantly higher quantities of smaller exosomes [16]. MicroRNA expression profiles differ substantially, with DPSC-derived miRNAs primarily involved in oxidative stress and apoptosis pathways, while AD-MSC miRNAs play regulatory roles in cell cycle and proliferation [16].
Implications for Clinical Applications
The functional preservation of MSCs during expansion has direct implications for their therapeutic efficacy. In clinical applications for osteoarthritis, both BM-MSCs and AD-MSCs have demonstrated safety and encouraging outcomes when injected intra-articularly [111]. However, the optimal MSC source may vary depending on the application—while BM-MSCs show stronger chondrogenic differentiation potential, AD-MSCs offer advantages in accessibility, immunomodulation, and proliferation [90].
For elderly patients, the use of autologous MSCs presents particular challenges due to age-related cellular senescence [109]. Allogeneic MSCs from younger donors may circumvent aging-related aberrant microenvironments and inflamed-aging, making them potentially more suitable for certain clinical applications [109].
Experimental Approaches for Monitoring Senescence and Genomic Stability
Essential Methodologies for Quality Control
Comet Assay Protocol for DNA Damage Assessment
The alkaline comet assay represents a sensitive method for detecting DNA strand breaks in individual cells [108]. The standardized protocol involves:
- Cell Preparation: Harvest MSC samples at each passage (P1, P3, P5, P7, P9, P11) and suspend in PBS at 1×10⁵ cells/mL
- Slide Preparation: Mix 100µL cell suspension with 75µL low melting point agarose (0.5%) at 37°C and place on slides pre-coated with agarose
- Lysis: Immerse slides in freshly prepared cold lysis solution (2.5M NaCl, 100mM EDTA, 10mM Tris-HCl, 1% Triton X-100, 10% DMSO) for at least 1 hour at 4°C
- Electrophoresis: After lysis, place slides in electrophoresis tank filled with fresh alkaline buffer (300mM NaOH, 1mM EDTA, pH>13) for 20-40 minutes, then run electrophoresis at 25V for 20-30 minutes
- Neutralization and Staining: Neutralize slides with 0.4M Tris buffer (pH 7.5) and stain with fluorescent DNA-binding dye (e.g., ethidium bromide or SYBR Gold)
- Analysis: Score 100-150 randomly selected cells per sample using fluorescence microscopy; express results as percentage of DNA in tail or tail moment [108]
Micronucleus Test for Chromosomal Damage
The cytokinesis-block micronucleus cytome assay provides a comprehensive measure of chromosome breakage and loss:
- Cell Culture: Seed MSCs at appropriate density in chamber slides or multiwell plates
- Cytochalasin B Treatment: Add cytochalasin B (3-6µg/mL) to cultures after cell attachment to block cytokinesis while allowing nuclear division
- Harvesting: After 48-72 hours of culture, harvest cells and perform mild hypotonic treatment if needed
- Fixation and Staining: Fix cells with methanol:acetic acid (3:1) and stain with DNA-specific fluorochromes (e.g., DAPI)
- Scoring: Examine binucleated cells for the presence of micronuclei; score at least 1000 binucleated cells per sample following standardized criteria [108]
Diagram 1: Comprehensive Senescence Monitoring Workflow for MSC Quality Control. This integrated approach combines morphological, functional, genetic, and epigenetic analyses to determine suitability for therapeutic applications.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Senescence and Genomic Stability Assessment
| Reagent/Category | Specific Examples | Research Application | Quality Control Function |
|---|---|---|---|
| Senescence Detection | SA-β-gal Staining Kit | Histochemical detection of senescent cells | Quantification of senescence percentage |
| DNA Damage Assessment | Comet Assay Kit, γH2AX Antibody | DNA strand break detection | Genotoxicity screening |
| Epigenetic Analysis | Methylation-Specific PCR Kits, Bisulfite Conversion Kits | SA-DNAm pattern analysis | Epigenetic senescence signature monitoring |
| Cytogenetic Analysis | Giemsa Stain, DAPI, Cytochalasin B | Chromosomal aberration detection | Karyotypic stability assessment |
| Flow Cytometry Panel | CD73, CD90, CD105, CD34, CD45, HLA-DR | Immunophenotype verification | MSC identity and purity confirmation |
| Differentiation Media | Osteogenic, Chondrogenic, Adipogenic Induction Kits | Trilineage differentiation capacity | Functional potency assessment |
| Telomere Length Analysis | Telomere PNA FISH Kit, qPCR Assay | Replicative history determination | Replicative senescence monitoring |
Regulatory Considerations and Clinical Translation
Current Regulatory Framework
Regulatory agencies worldwide have established guidelines for MSC-based therapies, classifying them as advanced therapy medicinal products in the European Union [108]. The U.S. Food and Drug Administration (FDA) requires verification of safety, identity, purity, and potency for all cellular therapies [108]. Similarly, Brazil's ANVISA and other national regulatory bodies have implemented standards for Good Practice of Human Cells for therapeutic use [108].
A significant challenge in the regulatory landscape is the absence of specific definitions regarding the maximum number of passages that ensure the lowest possible risk in MSC-based regenerative medicine [108]. This regulatory gap underscores the importance of establishing scientifically validated criteria for culture limits based on robust genomic stability data.
Recommendations for Standardization
Based on current evidence, the following practices are recommended for maintaining genomic stability during MSC expansion:
Establish Passage Limits: Implement strict passage limits, with heightened genomic monitoring beyond passage 5 for AD-MSCs [108]
Comprehensive Genetic Toxicology Assessment: Incorporate both comet assay and micronucleus testing as standard quality control measures at critical passages [108]
Epigenetic Monitoring: Utilize SA-DNAm signatures as biomarkers for cellular senescence state [107]
Functional Potency Verification: Regularly assess differentiation potential and immunomodulatory function throughout culture expansion [109]
Documentation and Traceability: Maintain detailed records of population doubling times, morphological changes, and any deviations from normal growth characteristics
Diagram 2: Risk-Based Quality Control Pathway for MSC Manufacturing. This decision tree incorporates critical testing at passage thresholds informed by genomic stability data to ensure product safety.
The long-term culture of MSCs presents significant challenges related to cellular senescence and genomic instability that must be addressed to ensure patient safety and therapeutic efficacy. Current evidence indicates that passage-dependent genomic damage becomes statistically significant from passage 5 onward for AD-MSCs, as detected by comet assay, with chromosomal abnormalities increasing from passage 7 [108]. While BM-MSCs and AD-MSCs share fundamental senescence mechanisms, source-specific differences in proliferation capacity, secretome profiles, and differentiation potential necessitate tailored quality control approaches.
The implementation of comprehensive monitoring strategies that integrate morphological assessment, functional assays, genetic toxicology testing, and epigenetic analysis provides the most robust approach for identifying senescent and genetically compromised cells. Standardized experimental protocols, including comet assay and micronucleus testing, offer reproducible methods for detecting DNA damage and chromosomal abnormalities at critical passage thresholds.
As the field advances, the development of passage-specific regulatory guidelines based on robust genomic stability data will be essential for standardizing MSC-based therapies across different tissue sources and clinical applications. Future research should focus on establishing validated biomarkers of senescence and genomic instability that can predict therapeutic efficacy and safety in clinical applications.
Head-to-Head Comparison: A Data-Driven Framework for MSC Source Selection
Within regenerative medicine, the selection of an appropriate mesenchymal stem cell (MSC) source is a critical determinant for the success of cell-based therapies. Among the most widely used sources are bone marrow-derived MSCs (BMSCs) and adipose-derived MSCs (ADSCs). A core aspect of their characterization revolves around their proliferation capacity, which directly impacts the ability to obtain sufficient cell numbers for therapeutic applications. This guide provides a direct, data-driven comparison of the growth rates and longevity of BMSCs versus ADSCs, synthesizing key experimental findings to inform researchers and drug development professionals. The evidence indicates that while both cell types meet the criteria for MSCs, ADSCs generally demonstrate superior proliferative potential and delayed senescence, a crucial advantage for large-scale ex vivo expansion [85] [12].
Quantitative Comparison of Proliferation and Growth
The following table summarizes key quantitative findings from direct comparative studies on the proliferation capacity and related characteristics of BMSCs and ADSCs.
Table 1: Direct Comparison of BMSC and ADSC Proliferation Capacity
| Parameter | Bone Marrow-MSCs (BMSCs) | Adipose-Derived MSCs (ADSCs) | Experimental Context |
|---|---|---|---|
| Proliferation Rate | Lower proliferative potential [13] [12] | Significantly higher proliferative potential [13] [12] | Donor-matched comparison under human platelet lysate (hPL) conditions [13]. |
| Cumulative Population Doublings | Lower | Higher; up to 1 billion cells potentially generated from 300g of adipose tissue [85]. | Serial passaging in culture [85] [12]. |
| Senescence Markers | Higher expression of senescence markers (p53, p21, p16) observed in adult-derived MSCs [85]. | Lower expression of senescence markers (p53, p21, p16) compared to adult BMSCs [85]. | In vitro expansion and molecular analysis [85]. |
| Clonogenic Capacity (CFU-F) | Similar colony-forming unit-fibroblast efficiency to ADSCs [13]. | Similar colony-forming unit-fibroblast efficiency to BMSCs [13]. | Colony-forming unit assays [13]. |
| Donor Age Effect | Quality is influenced by donor's age and health [85]. | Proliferation capacity maintained better in younger donors (fetal, calf) [112]. | Studies across different donor age categories [85] [112]. |
Key Experimental Protocols and Methodologies
The comparative data presented rely on standardized experimental approaches. Below are the core methodologies commonly employed in these head-to-head studies.
Cell Isolation and Culture
- BMSC Isolation: Bone marrow aspirates are typically diluted and separated using a density gradient (e.g., Ficoll-Paque) to isolate mononuclear cells. These cells are plated in culture flasks, and after 24-48 hours, non-adherent cells are removed. The adherent cells are cultured and expanded in media often supplemented with fetal bovine serum (FBS) or, for clinical relevance, human platelet lysate (hPL) [13] [12].
- ADSC Isolation: Adipose tissue is washed, minced, and digested with collagenase (e.g., Collagenase Type I or Liberase) to break down the extracellular matrix. The digested tissue is centrifuged to obtain a stromal vascular fraction (SVF) pellet, which is then resuspended and plated. ADSCs are isolated based on their adherence to plastic [12] [112].
Assessment of Proliferation and Longevity
- Population Doubling (PD) and Cumulative Population Doubling (CPD): This is a fundamental metric. At each passage, cells are harvested and counted. The PD is calculated using the formula:
PD = log₂(Nh / Np), whereNhis the number of cells harvested andNpis the number of cells plated. The CPD is the sum of PDs across all passages, providing a measure of long-term expansion capability [13]. - Metabolic Activity Assays: Assays like MTT are used to indirectly assess cell proliferation and viability over time. Cells are seeded at a low density and measured at multiple time points (e.g., days 3, 7, 14, 21). The metabolic activity correlates with the number of viable cells [12].
- Senescence-Associated Beta-Galactosidase (SA-β-gal) Staining: This histochemical stain identifies senescent cells in culture, which express higher levels of β-galactosidase activity at pH 6.0. A higher percentage of SA-β-gal-positive cells indicates reduced longevity and earlier onset of senescence [112].
- Gene Expression Analysis: The expression levels of senescence-associated genes such as
p16,p21, andp53are quantified using techniques like RT-qPCR to molecularly validate observations of cellular aging [85] [24].
Diagram 1: Experimental workflow for comparing BMSC and ADSC proliferation.
Molecular Basis of Proliferation Differences
The differential proliferation rates and longevity between BMSCs and ADSCs are underpinned by distinct molecular regulatory networks.
Table 2: Key Molecular Regulators of MSC Stemness and Proliferation
| Regulator | Function in MSC Stemness/Proliferation | Impact on BMSCs vs. ADSCs |
|---|---|---|
| Twist1 | Maintains stemness, promotes proliferation, and inhibits senescence by suppressing p14 and p16 expression via EZH2 [24]. | Crucial for both types; its downregulation leads to senescence. |
| OCT4 | Enhances cell cycle progression, proliferation, and CFU-F capacity. Suppresses senescence markers p16 and p21 [24]. | Expression levels and stability during culture may vary between sources. |
| SOX2 | Maintains stemness and suppresses senescence. Reduced expression is linked to increased p16 and p21 in senescent MSCs [24]. | Its reduction during in vitro expansion can affect long-term growth. |
| HOX Genes | Stable "HOX code" reflects tissue origin. Some members like HOXB7 enhance proliferation and reduce aging markers [24]. | The unique HOX code of ADSCs may contribute to their robust growth. |
| Senescence Markers (p16, p21, p53) | Induction of these markers leads to cell cycle arrest and entry into senescence, limiting expansion potential [85] [24]. | ADSCs generally show lower expression, contributing to longer lifespan. |
Diagram 2: Molecular network regulating MSC proliferation and senescence.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials critical for conducting rigorous comparisons of MSC proliferation.
Table 3: Essential Research Reagent Solutions for MSC Proliferation Studies
| Reagent/Material | Function in Proliferation Assays | Considerations for Comparison Studies |
|---|---|---|
| Human Platelet Lysate (hPL) | Serum supplement for cell culture; promotes MSC expansion while reducing xeno-contamination risks vs. FBS [13]. | Preferred for clinical-scale expansion. Using hPL standardizes conditions for a more direct comparison [13]. |
| Collagenase Type I/IV / Liberase | Enzymatic digestion of adipose tissue to isolate the stromal vascular fraction (SVF) for ADSC culture [12] [112]. | Enzyme concentration, activity, and digestion time must be optimized and consistent to avoid impacting initial cell viability. |
| Trypsin/EDTA | Proteolytic enzyme used for detaching adherent cells during passaging. | Over-exposure can damage surface markers and affect cell health, confounding proliferation data. |
| Defined MSC Growth Media | Basal media (e.g., DMEM) formulated with specific supplements to support MSC growth and maintain differentiation potential. | Using the same media formulation and supplement batch for both cell types is essential for a fair comparison. |
| Antibodies for Flow Cytometry (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Immunophenotyping to confirm MSC identity and purity before and during proliferation experiments [12] [113]. | Essential quality control to ensure observed differences are not due to cell population heterogeneity. |
| MTT Reagent | A tetrazolium salt reduced by metabolically active cells to a purple formazan, used to assay proliferation and viability [12]. | Provides an indirect measure of cell number. Results should be corroborated with direct counting methods. |
The direct comparison of growth rates and longevity firmly establishes that ADSCs possess a superior capacity for in vitro expansion compared to BMSCs, characterized by higher proliferative potential and a delayed onset of senescence. This makes ADSCs a highly attractive source for applications requiring large cell quantities. However, the choice of source must be balanced against other factors, such as the specific differentiation lineage required, as BMSCs often demonstrate superior osteogenic and chondrogenic potential [13] [12]. Furthermore, donor characteristics—most notably age—significantly impact the proliferation of both cell types and must be carefully considered in experimental design and therapeutic development [112]. Future research focused on standardizing culture protocols and further elucidating the underlying molecular mechanisms will be crucial for fully leveraging these cellular tools in regenerative medicine.
Within the field of regenerative medicine, Mesenchymal Stem/Stromal Cells (MSCs) represent a cornerstone for developing advanced therapies for bone, cartilage, and metabolic disorders. A critical step in their clinical application is the rigorous, quantitative assessment of their differentiation potency, which can reveal significant donor- and tissue source-dependent heterogeneity. This guide objectively compares the differentiation bias of MSCs from two principal sources—bone marrow (BM-MSCs) and adipose tissue (AT-MSCs)—framed within the broader thesis of understanding how tissue origin influences cellular function. We synthesize experimental data and detailed methodologies to provide researchers, scientists, and drug development professionals with a standardized framework for evaluating lineage-specific bias.
Quantitative Comparison of MSC Differentiation Potential
The inherent capacity of MSCs to differentiate into osteogenic, chondrogenic, and adipogenic lineages is not uniform. The following tables summarize quantitative data on the differentiation potential and functional characteristics of BM-MSCs and AT-MSCs, providing a direct, evidence-based comparison.
Table 1: Quantitative Assessment of Trilineage Differentiation Potential
| Lineage | Key Quantitative Markers | BM-MSC Performance | AT-MSC Performance | Notable Assays & Observations |
|---|---|---|---|---|
| Osteogenic | Alkaline Phosphatase (ALP) Activity, Calcium Deposition (Alizarin Red) | Robust ALP activity and matrix mineralization [114] [115]. | Effective osteogenesis; enhanced with specific scaffold concentrations (e.g., 100 mg/ml G-bone) [114]. | ALP assay with p-NPP substrate; quantification at 405 nm [114]. Potency assays using biomarkers (ALPL, DCN, TGFB2) [115]. |
| Chondrogenic | Sulfated Glycosaminoglycans (sGAG, Alcian Blue), Collagen Type II | Forms cartilage matrix rich in proteoglycans and Collagen II [116]. | Comparable chondrogenic capacity to BM-MSCs; produces sulfated proteoglycans and Collagen II [116]. | Pellet or Hyaff-11 scaffold culture with TGF-β3; histological scoring (Bern Score) [116]. |
| Adipogenic | Lipid Droplet Accumulation (Oil Red O), Fabp4, Pparg2 | Capable of adipogenic differentiation [117] [118]. | Strong and reliable adipogenic potential, with clear lipid droplet formation [117] [119] [120]. | Culture with dexamethasone, insulin, indomethacin, IBMX; staining and gene expression analysis (e.g., FABP4, PPARγ2) [121] [120]. |
Table 2: Functional and Immunomodulatory Characteristics
| Characteristic | BM-MSCs | AT-MSCs | Experimental Evidence |
|---|---|---|---|
| Immunophenotype (ISCT Criteria) | Positive for CD73, CD90, CD105 (>95%); Negative for CD34, CD45, HLA-DR (<2%) [2] [117] [119]. | Positive for CD73, CD90, CD105 (>95%); Negative for CD34, CD45, HLA-DR (<2%) [2] [117] [119]. | Flow cytometry analysis confirms similar surface marker profiles between sources [119] [120]. |
| Immunomodulatory Potency | Suppress PBMC proliferation and inhibit dendritic cell differentiation [120]. | More potent suppression at equal cell numbers; higher secretion of IL-6 and TGF-β1 [120]. In vitro co-culture assays with PBMCs and monocytes [120]. | |
| Tissue Source Considerations | Lower frequency in marrow (~0.001-0.01%); invasive aspiration procedure [120]. | High frequency in tissue (~500x BM); easily accessible from liposuction waste [120]. | Cell isolation and expansion from donor tissues [119] [120]. |
Experimental Protocols for Differentiation and Quantification
Quantitative Osteogenic Differentiation and ALP Assay
The following workflow visualizes a standardized protocol for quantifying osteogenic differentiation, particularly in the presence of scaffold materials, using Alkaline Phosphatase (ALP) activity as a key early marker [114].
Detailed Protocol [114]:
- Cell Seeding and Culture: Scaffold particles (e.g., G-bone) are ground and coated onto a 96-well plate at varying concentrations (5, 20, 60, and 100 mg/ml). A consistent number of MSCs (e.g., 3x10³ cells) are seeded onto the scaffold layers in maintenance or osteogenic media. Osteogenic media is typically composed of α-MEM, 10% FBS, dexamethasone (100 nM), ascorbic acid (50 μM), and β-glycerophosphate (10 mM).
- Cell Lysis: After culture (e.g., up to 11 days), cells are washed with PBS and lysed at 4°C for 2 hours using a lysis buffer (e.g., 25 mM Tris-HCl, 0.5% Triton X-100).
- ALP Activity Measurement: 50 µl of the cell lysate is transferred to a new plate and mixed with 50 mmol/l p-nitrophenylphosphate (p-NPP) in a sodium carbonate buffer (pH 10.4). The mixture is incubated at 37°C for 30 minutes.
- Quantification: The enzymatic reaction is stopped, and the amount of released p-nitrophenol (pNP) is determined by measuring the absorbance at 405 nm using a spectrophotometer. The quantity of pNP is calculated using a standard curve.
Chondrogenic Differentiation in Pellet Culture
For chondrogenesis, the standard method involves creating a high-density 3D microenvironment that promotes cartilage matrix formation [116].
Detailed Protocol [116]:
- Pellet Formation: 2x10⁵ MSCs (at passage 2) are placed in a conical polypropylene tube. The tube is centrifuged at 500 g for 5 minutes to form a pellet.
- Induction Culture: The supernatant is carefully removed, and the pellet is cultured in a defined chondrogenic medium. This medium consists of DMEM high glucose, supplemented with ITS-G, 1.0 mg/ml human serum albumin, TGF-β1 (10 ng/ml), dexamethasone (10⁻⁷ M), ascorbic acid (14 µg/ml), and penicillin-streptomycin.
- Culture Maintenance: Pellets are cultured for 14-21 days, with medium changes twice a week.
- Analysis: The resulting pellets are fixed, embedded in paraffin, and sectioned for histological staining (e.g., Safranin-O or Alcian Blue for proteoglycans) and immunohistochemistry (e.g., for Collagen types I and II). A standardized scoring system like the Bern Score can be used for quantitative histological assessment.
Adipogenic Differentiation Protocol
Adipogenic differentiation is induced using a cocktail that promotes the accumulation of intracellular lipid droplets [120].
Detailed Protocol [120]:
- Induction: MSCs are plated at a high density (e.g., 100,000 cells per well in a 24-well plate). Upon confluence, the standard medium is replaced with adipogenic induction medium. A typical formulation includes α-MEM with 10% FBS, dexamethasone (10⁻⁷ M), insulin (10 µg/ml), indomethacin (5 µM), and 3-isobutyl-1-methylxanthine (5 µM).
- Maintenance: Cultures are maintained for 2-3 weeks, with the medium refreshed every 3-4 days.
- Staining and Quantification: After 3 weeks, cells are fixed and stained with Oil Red O to visualize lipid droplets. Staining can be eluted and quantified spectrophotometrically or the number of differentiated cells can be counted manually. Gene expression analysis of markers like FABP4 and PPARG provides additional quantitative data [121].
Signaling Pathways Governing Lineage Commitment
The fate of MSCs is determined by complex and often reciprocal signaling pathways. The following diagram synthesizes key regulators that bias differentiation toward osteogenic, chondrogenic, or adipogenic lineages [117] [115] [118].
Key Pathway Insights:
- Osteogenesis: Driven by master transcription factors RUNX2 and MSX2 [118]. The coactivator TAZ enhances RUNX2 activity while simultaneously suppressing the adipogenic master regulator PPARγ, establishing a reciprocal regulatory switch [118]. TGF-β2 has also been identified as an important inducible biomarker for osteogenic commitment [115].
- Chondrogenesis: Governed by SOX9, which upregulates essential cartilage matrix genes like ACAN (aggrecan) and COL2A1 (collagen type II) [117]. This process is typically induced in 3D cultures with exogenous TGF-β3 [116] [122].
- Adipogenesis: Orchestrated by the sequential activation of C/EBPα and PPARγ, which promote the expression of lipid-handling proteins like FABP4 [121] [117]. PPARγ can directly inhibit RUNX2, thereby repressing osteogenesis [118].
The Scientist's Toolkit: Essential Research Reagents
Successful differentiation experiments rely on a standardized set of reagents and tools. The following table catalogs essential solutions for MSC differentiation research.
Table 3: Key Research Reagent Solutions for MSC Differentiation Studies
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Basal Media | α-MEM, DMEM-high glucose, DMEM/Ham's F12 | Serves as the nutrient base for maintenance and differentiation media [114] [116] [120]. |
| Serum/Supplements | Fetal Bovine Serum (FBS), Human Platelet Lysate (PLTMax) | Provides essential growth factors and attachment factors for cell proliferation [114] [115] [119]. |
| Osteogenic Inducers | Dexamethasone, Ascorbic Acid, β-Glycerophosphate | Core components to induce osteoblast differentiation and matrix mineralization [114] [115] [118]. |
| Chondrogenic Inducers | TGF-β1 or TGF-β3, Dexamethasone, Ascorbic Acid, ITS-G Supplement | Crucial for inducing chondrogenesis in pellet or scaffold cultures [116] [122]. |
| Adipogenic Inducers | Dexamethasone, Insulin, IBMX, Indomethacin | Cocktail to trigger intracellular lipid accumulation and adipocyte maturation [121] [120]. |
| Key Assay Kits | Alkaline Phosphatase Assay (p-NPP), Alizarin Red S, Oil Red O, Alcian Blue | Used for quantitative and qualitative assessment of differentiation endpoints [114] [119] [120]. |
| Critical Biomarkers | mRNA: ALPL, RUNX2, DCN, TGFB2 (Osteo); SOX9, ACAN, COL2A1 (Chondro); PPARG, FABP4, CEBPA (Adipo)Protein: Collagen II, Decorin, TGF-β2 | Measured via qPCR, RNA-seq, or immunohistochemistry to quantitatively gauge differentiation potency and progression [114] [116] [121]. |
A systematic approach to quantifying the trilineage differentiation bias of MSCs is indispensable for predicting their in vivo efficacy and ensuring reproducibility in regenerative medicine. The data and methodologies compiled in this guide demonstrate that while both BM-MSCs and AT-MSCs are multipotent, their quantitative performance and functional biases differ. Key findings indicate that AT-MSCs demonstrate a pronounced propensity for adipogenesis and can exhibit more potent immunomodulatory effects, whereas the osteogenic potential of BM-MSCs remains a benchmark. The choice between them, therefore, should be strategically aligned with the target clinical application. Employing the standardized experimental protocols, reagent frameworks, and biomarker analyses outlined here will enable researchers to make informed, data-driven decisions in both basic research and clinical therapy development.
In regenerative medicine, multipotent mesenchymal stromal cells (MSCs) have emerged as a powerful therapeutic tool, not merely for their differentiation capacity but predominantly for their potent paracrine activity [123]. The secretome—the totality of cytokines, growth factors, bioactive molecules, and extracellular vesicles released by these cells—is now recognized as the primary mediator of their therapeutic effects, including immunomodulation, tissue repair, and angiogenesis [123] [124]. This secretome's composition is not universal; it is deeply influenced by the MSC's tissue of origin, creating a critical variable for clinical translation.
Framed within the broader context of bone marrow versus adipose-derived MSC characterization research, this guide provides a systematic, data-driven comparison of their secretome profiles. For researchers and drug development professionals, understanding these source-dependent differences is essential for selecting the optimal cell type for specific clinical applications, whether for treating neurological, hepatic, or inflammatory diseases.
Comparative Secretome Profiles: Quantitative Analysis
Direct comparative studies under standardized culture conditions reveal significant differences in the secretory output of BM-MSCs and AD-MSCs. The tables below summarize key quantitative data on critical cytokines and growth factors.
Table 1: Comparison of Key Growth Factor Secretion Profiles
| Growth Factor | BM-MSC Secretion | AD-MSC Secretion | Reported Functional Significance |
|---|---|---|---|
| HGF (Hepatocyte Growth Factor) | Higher [13] [125] | Lower | Liver regeneration, anti-apoptotic, mitogenic for hepatocytes, angiogenesis [126] [125] |
| FGF (Fibroblast Growth Factor) | Conflicting Data (Lower [125]) | Conflicting Data (Higher [13]) | Angiogenesis, wound healing, tissue repair [123] |
| IGF-1 (Insulin-like Growth Factor 1) | Lower [13] | Higher [13] | Metabolic regulation, chondrogenesis, osteogenesis |
| SCF-1 (Stem Cell-Derived Factor-1) | Higher [13] | Lower | Chemotaxis, hematopoietic stem cell homing |
| VEGF (Vascular Endothelial Growth Factor) | No significant difference reported [125] | No significant difference reported [125] | Angiogenesis, vascular permeability |
Table 2: Comparison of Key Cytokine and Immunomodulatory Factor Secretion
| Cytokine/Factor | BM-MSC Secretion | AD-MSC Secretion | Reported Functional Significance |
|---|---|---|---|
| IFN-γ (Interferon-gamma) | Lower [13] | Higher [13] | immunomodulation, MHC regulation |
| IL-10 (Interleukin-10) | Not consistently different | Not consistently different | Potent anti-inflammatory cytokine [127] |
| IL-6 (Interleukin-6) | Lower [125] | Higher [125] | Complex role in inflammation & tissue repair |
| IL-1RA (Interleukin-1 Receptor Antagonist) | Not consistently different | Not consistently different | Anti-inflammatory, blocks IL-1 signaling [123] |
| PGE2 (Prostaglandin E2) | Not consistently different | Not consistently different | Immunomodulation, macrophage polarization to M2 phenotype [123] |
Experimental Protocols for Secretome Analysis
To generate the comparative data presented above, robust and standardized experimental protocols are essential. The following methodology outlines a typical workflow for secretome profiling and functional validation.
Cell Culture and Standardization
- Cell Sourcing and Isolation: BM-MSCs are typically isolated from bone marrow aspirates via density gradient centrifugation (e.g., using Lymphoprep) to obtain mononuclear cells [5] [13]. AD-MSCs are isolated from adipose tissue (e.g., lipoaspirate) through enzymatic digestion (commonly with 0.1% collagenase) followed by centrifugation to obtain the stromal vascular fraction (SVF) [5] [128] [124].
- Culture Conditions: To enable a valid comparison, cells from both sources should be cultured in parallel using identical media. The use of xeno-free supplements like human platelet lysate (hPL) is now encouraged for clinical-grade expansion [13] [43] [125]. Cells are typically maintained until passage 3-5 to ensure a consistent, homogeneous population before analysis [5] [13].
- Conditioned Media (CM) Collection: Upon reaching 70-80% confluence, cells are washed and the culture medium is replaced with a serum-free or hPL-free base medium. After a conditioning period (e.g., 48-72 hours), the conditioned media is collected, centrifuged to remove cellular debris, and stored at -80°C for subsequent analysis [124] [125].
Secretome Profiling and Functional Assays
- Multiplex Immunoassays: The concentration of specific cytokines and growth factors (e.g., HGF, FGF, IFN-γ, IL-6) in the CM is quantified using high-sensitivity multiplex platforms like Luminex xMAP technology or ELISA. This provides the quantitative secretome profile [127] [13] [125].
- Macrophage Polarization Assay: To functionally validate immunomodulatory potency, CD14+ monocytes are isolated from human peripheral blood and differentiated into M0 macrophages. These macrophages are then treated with MSC-conditioned media and stimulated with LPS/IFN-γ. Polarization is assessed by flow cytometry analysis of M1 (e.g., CD80, CD86) and M2 (e.g., CD206, CD209) surface markers, and by quantifying secreted inflammatory cytokines [124].
- Neurite Outgrowth Assay: To assess neurotrophic potential, dorsal root ganglion (DRG) neurons are isolated and cultured in the presence of MSC-conditioned media. Neurite outgrowth is quantified microscopically, measuring total neurite length per neuron, demonstrating the functional impact of the secretome on neural tissue [125].
The following workflow diagram illustrates the complete experimental process from cell isolation to data analysis:
Signaling Pathways of Key Secreted Factors
The therapeutic effects of the MSC secretome are mediated through specific signaling pathways activated by its key components in target cells. Understanding these pathways is crucial for rational therapeutic design.
- HGF/c-Met Pathway: HGF is a multifunctional factor secreted by MSCs that binds to its high-affinity receptor, c-Met, on target cells (e.g., hepatocytes, epithelial cells) [126]. This binding induces receptor dimerization and autophosphorylation, activating intracellular tyrosine kinase domains. The downstream signaling cascades—including MAPK/ERK, PI3K/Akt, and STAT—orchestrate diverse biological responses such as cell proliferation, motility, morphogenesis, and survival, which are essential for tissue regeneration and protection [126].
- IFN-γ Immunomodulatory Pathways: IFN-γ, found at higher levels in AD-MSC secretome, plays a complex role in immunomodulation [13]. It can prime MSCs to enhance their immunosuppressive functions. MSC-derived IFN-γ, in concert with other factors, can inhibit T-cell proliferation and drive the polarization of macrophages toward an anti-inflammatory M2 phenotype, thereby resolving inflammation and promoting a regenerative tissue environment [123].
The diagram below illustrates the HGF/c-Met signaling pathway, a key mechanism for MSC-mediated tissue repair:
The Scientist's Toolkit: Essential Reagents for Secretome Research
The following table details key reagents and their functions essential for conducting robust secretome profiling studies, based on the methodologies cited in this guide.
Table 3: Essential Research Reagents for MSC Secretome Analysis
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Human Platelet Lysate (hPL) | Xeno-free supplement for clinical-grade MSC expansion; replaces fetal bovine serum (FBS). | Used as a culture medium supplement for standardized expansion of BM-MSCs and AD-MSCs [13] [125]. |
| Collagenase Type I / IV | Enzymatic digestion of adipose tissue to isolate the Stromal Vascular Fraction (SVF) for AD-MSC culture. | Used for dissociation of lipoaspirate tissues [5] [124]. |
| Lymphoprep / Ficoll-Paque | Density gradient medium for isolation of bone marrow mononuclear cells (BM-MNCs) from aspirates. | Used for separation of BM-MSCs from bone marrow aspirates [5] [13]. |
| Multiplex Bead-Based Immunoassay Kits (e.g., Luminex) | Simultaneous quantification of multiple cytokines/growth factors from a small volume of conditioned media. | Used for secretome profiling and analysis of cytokines (IFN-γ, ILs) and growth factors (HGF, FGF) [127] [124]. |
| CD14+ MicroBeads | Immunomagnetic separation of human monocytes from PBMCs for macrophage polarization assays. | Implied in the isolation of monocytes for subsequent macrophage culture and polarization studies [124]. |
The comparative secretome profiling of BM-MSCs and AD-MSCs reveals a clear dichotomy: AD-MSCs demonstrate a higher proliferative capacity and secrete greater levels of certain immunomodulatory factors like IFN-γ, while BM-MSCs consistently show a stronger propensity for secreting potent regenerative factors like HGF and exhibit superior direct immunomodulatory capacity in co-culture systems [5] [13] [125].
These distinctions have profound implications for therapeutic development. The choice between BM-MSCs and AD-MSCs should be guided by the specific pathophysiology of the target disease. For instance, applications demanding robust tissue regeneration, such as liver repair or possibly bone healing, may benefit more from the BM-MSC secretome rich in HGF and other morphogenic factors [126] [13]. Conversely, for modulating chronic inflammatory conditions, the AD-MSC secretome, with its distinct cytokine cocktail and potent vesicular microRNAs, might be the more effective choice [13] [128]. Future research must focus on standardizing isolation and culture protocols and engineering optimized secretome products tailored to specific clinical indications.
Within the rapidly advancing field of cell-based therapies, mesenchymal stromal cells (MSCs) have emerged as a cornerstone for their potent immunomodulatory capabilities. While MSCs can be isolated from various tissues, bone marrow (BM) and adipose tissue (AT) are the most widely used sources, especially for autologous applications due to their relative abundance and ease of harvest [13]. The central question of which source provides a more effective therapeutic profile for immunomodulation remains a critical area of investigation. This guide provides a systematic, data-driven comparison of the immunosuppressive effects of bone marrow-derived MSCs (BM-MSCs) and adipose tissue-derived MSCs (AD-MSCs), framing the analysis within the broader context of MSC characterization research. It synthesizes evidence from in vitro and in vivo studies to offer researchers and drug development professionals a clear, objective evaluation to inform their therapeutic choices.
Head-to-Head Comparison of Immunomodulatory Properties
Direct, donor-matched comparisons and studies conducted under standardized culture conditions are invaluable for a unbiased comparison of BM-MSCs and AD-MSCs. The table below summarizes key quantitative differences in their proliferation, differentiation, and immunomodulatory capacities.
Table 1: Comparative Biological Characteristics of BM-MSCs and AD-MSCs
| Biological Characteristic | Bone Marrow-MSCs (BM-MSCs) | Adipose-Derived MSCs (AD-MSCs) | Research Context |
|---|---|---|---|
| Proliferation Capacity | Lower proliferative potential [13] | Significantly greater proliferative potential [13] [12] | Culture with human platelet lysate (hPL) [13] |
| Osteogenic Potential | Higher osteogenic capacity; superior bone formation in critical-size defects [13] [94] [12] | Inferior osteogenic capacity [13] [94] [12] | In vitro differentiation & in vivo sheep tibia model [94] [12] |
| Chondrogenic Potential | Higher chondrogenic capacity [13] [12] | Lower chondrogenic capacity [13] [12] | In vitro differentiation [13] [12] |
| Adipogenic Potential | Similar adipogenic potential [13] | Similar, though some studies show higher, adipogenic potential [13] [12] | In vitro differentiation [13] [12] |
| Immunomodulatory Soluble Factors | Higher secretion of HGF and SDF-1 [13] | Higher secretion of bFGF, IFN-γ, and IGF-1 [13] | Analysis of secreted proteins in hPL culture [13] |
| Potency in T-cell Proliferation Inhibition | Potent immunomodulatory effects [13] | More potent immunomodulatory effects in some studies [13] | In vitro co-culture with activated T-cells [13] [129] |
A critical study performing a head-to-head comparison under human platelet lysate (hPL)-supplemented conditions—a clinically relevant alternative to fetal bovine serum—confirmed that while both cell types exhibit standard MSC morphology and surface markers, their functional strengths differ [13]. The study concluded that AD-MSCs possess biological advantages in proliferative capacity and immunomodulatory effects, whereas BM-MSCs have superior osteogenic and chondrogenic differentiation potential [13]. These inherent differences were corroborated by a donor-matched comparison, which also highlighted significant variation in proliferation and differentiation capacity among different donors, a factor that must be considered for clinical translation [12].
Detailed Experimental Protocols for Assessing Immunosuppression
To ensure the reproducibility of immunomodulatory potency assays, this section outlines standardized protocols used in key studies.
In Vitro T-cell Proliferation Inhibition Assay
A common and reliable method to quantify MSC-mediated immunosuppression involves co-culturing MSCs with activated T-cells and measuring the suppression of proliferation [129].
- Step 1 (Day 0 - Mitotic Inactivation of MSCs): MSCs are detached, resuspended, and irradiated (e.g., 30 Gy X-ray) to prevent their proliferation. Varying numbers of irradiated MSCs (e.g., 625 to 10,000 cells/well) are seeded in a 96-well plate in triplicate and incubated overnight [129].
- Step 2 (Day 1 - T-cell Isolation and Labeling): Splenic T-cells or peripheral blood mononuclear cells (PBMCs) are isolated from mice or human donors, respectively. T-cells are then fluorescently labeled with Cell Trace dyes such as Carboxyfluorescein succinimidyl ester (CFSE). The labeled T-cells are added to the MSC cultures along with T-cell activation stimuli, such as CD3/CD28 beads or mitogens like phytohemagglutinin (PHA) [129].
- Step 3 (Day 3 or 4 - Proliferation Analysis): After 72 hours in culture, T-cells are harvested. The proliferation index is determined by flow cytometry, analyzing the dilution of the CFSE signal in daughter cells. The percentage of inhibition is calculated relative to the proliferation of T-cells activated in the absence of MSCs [129]. This assay reliably demonstrates a dose-dependent inhibitory effect of both BM-MSCs and AD-MSCs on T-cell proliferation.
Secretome and Soluble Factor Analysis
The immunomodulatory effects of MSCs are largely mediated by their secretome, which includes soluble factors and extracellular vesicles (EVs). To dissect the mechanism:
- Harvesting: MSC-conditioned medium is collected after a defined production period [130].
- Fractionation: The secretome can be fractionated using techniques like tangential flow filtration (TFF) with membranes of different molecular weight cutoffs (e.g., 5, 10, 30, or 100 kDa) or ultracentrifugation to separate soluble factors from EVs [130].
- Bioassay: The immunomodulatory activity of each fraction is tested. For instance, fractions can be applied to stimulated human PBMCs. The anti-inflammatory effect can be measured by the inhibition of key signaling pathways (e.g., NF-κB and IRF) in reporter cell lines, or by quantifying the release of cytokines like IL-10 and IL-12 from PBMCs [130] [131]. Research has shown that soluble factors below 5 kDa, including Prostaglandin E2 (PGE2), are key mediators of the anti-inflammatory effect on innate immune pathways, while components larger than 100 kDa are also potent inhibitors of T-cell proliferation [130].
Table 2: Key Research Reagents for Immunomodulatory Potency Assessment
| Research Reagent / Solution | Function in Experimental Protocol |
|---|---|
| Human Platelet Lysate (hPL) | A xeno-free, clinically relevant supplement for MSC culture medium that promotes growth while maintaining immunophenotype and function [13]. |
| Carboxyfluorescein succinimidyl ester (CFSE) | A fluorescent cell dye used to track and quantify lymphocyte proliferation via flow cytometry-based dye dilution assays [129]. |
| CD3/CD28 Activation Beads | Synthetic beads that mimic antigen-presenting cells to provide the necessary signals for robust polyclonal T-cell activation in vitro [129]. |
| Tangential Flow Filtration (TFF) | A filtration method used to concentrate and fractionate the MSC secretome based on molecular weight, enabling the study of specific components like soluble factors and EVs [130]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | A plate-based technique used to precisely quantify the concentration of specific immunomodulatory factors (e.g., PGE2, HGF, IFN-γ) in cell culture supernatants [13] [130] [131]. |
Signaling Pathways of MSC-Mediated Immunomodulation
The immunosuppressive actions of MSCs are not mediated by a single pathway but are the result of a complex, integrated network of mechanisms. The following diagram synthesizes the key interactions of BM-MSCs and AD-MSCs with immune cells, highlighting the roles of their distinct secretomes.
This diagram illustrates that both BM-MSCs and AD-MSCs exert immunomodulation primarily through their secretome. The soluble factors (e.g., PGE2), particularly those below 5 kDa, are crucial for inhibiting pro-inflammatory innate immune responses in PBMCs, leading to reduced inflammation [130]. Concurrently, larger components of the secretome (e.g., extracellular vesicles and proteins) directly modulate T-cell activity, effectively inhibiting their proliferation [130] [132]. The distinct efficacy profiles of BM-MSCs and AD-MSCs can be attributed to their differential expression of key factors; AD-MSCs secrete more bFGF, IFN-γ, and IGF-1, potentially contributing to their observed potent T-cell suppression, while BM-MSCs secrete more HGF and SDF-1 [13].
Correlation of In Vitro Findings with In Vivo Efficacy
The ultimate validation of a therapeutic candidate's potential lies in its performance in live animal models. A strong correlation has been demonstrated between in vitro immunomodulatory profiles and in vivo efficacy, not only for MSCs but also for other biologic agents like probiotics [131]. A study using a murine model of trinitrobenzene sulfonate (TNBS)-induced colitis found that bacterial strains which induced a high IL-10/IL-12 cytokine ratio (anti-inflammatory to pro-inflammatory) in human PBMC assays in vitro also provided the best protection against colitis in vivo [131]. This principle is highly relevant for MSC therapy development, suggesting that robust in vitro screening can effectively predict in vivo performance.
For MSCs, their therapeutic effect in vivo is also closely linked to their secretome. MSC-derived extracellular vesicles (EVs) are being increasingly explored as a cell-free alternative, offering comparable immunomodulatory and anti-inflammatory properties [132]. These EVs can be engineered for targeted drug delivery, further enhancing their clinical potential for treating complex conditions like neurodegenerative disorders where neuroinflammation plays a key role [132].
The choice between BM-MSCs and AD-MSCs for immunomodulatory therapy is not a matter of one being universally superior, but rather of selecting the right tool for the specific clinical application. The accumulated evidence indicates that AD-MSCs hold an advantage for strategies prioritizing rapid expansion and potent, direct immunosuppression, as evidenced by their stronger proliferation and T-cell inhibition in some studies. In contrast, BM-MSCs are likely more suitable for applications requiring robust osteogenic or chondrogenic differentiation alongside immunomodulation, such as in orthopedic regenerative medicine. The observed donor-to-donor variability in the potency of both cell types [12] underscores the necessity of implementing rigorous, standardized in vitro potency assays—such as T-cell proliferation inhibition and secretome analysis—as a critical step in the manufacturing process. This data-driven approach ensures the development of safe, effective, and reproducible cell-based immunomodulatory therapies.
The selection of optimal cell sources is a critical foundational step in developing mesenchymal stem cell (MSC)-based therapies. Among the various tissue sources available, bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs) have emerged as the most extensively characterized and clinically utilized populations [2] [85]. While both cell types share fundamental MSC properties defined by the International Society for Cellular Therapy (ISCT) criteria—including plastic adherence, specific surface marker expression, and trilineage differentiation potential—they exhibit significant biological and functional differences that influence their therapeutic performance across various indications [2] [87]. This comparative analysis synthesizes current scientific evidence to create a decision matrix for researchers and therapy developers, enabling strategic selection of MSC sources based on target disease pathophysiology, required mechanism of action, and patient-specific factors.
The burgeoning field of MSC therapeutics has yielded promising clinical applications across diverse medical specialties, including orthopedics, neurology, immunology, and gynecology [85] [87]. As of 2025, sixteen MSC-based therapies have received regulatory approval worldwide, with ten derived from bone marrow, three from umbilical cord, two from adipose tissue, and one from umbilical cord blood [85]. This distribution reflects both historical development patterns and functional distinctions between tissue sources. Understanding the comparative advantages and limitations of BM-MSCs versus AD-MSCs is thus essential for advancing the field and optimizing therapeutic outcomes.
Characterization and Fundamental Properties
Defining Characteristics and Marker Profiles
Both BM-MSCs and AD-MSCs adhere to the minimal criteria established by ISCT for defining MSCs, including plastic adherence in standard culture conditions, expression of characteristic surface markers (CD73, CD90, CD105 ≥95%), absence of hematopoietic markers (CD34, CD45, CD14/CD11b, CD79α/CD19, HLA-DR ≤2%), and trilineage differentiation potential into osteocytes, adipocytes, and chondrocytes in vitro [2] [85]. Despite these shared characteristics, subpopulation heterogeneity exists within both source types, influenced by donor factors, isolation methods, and culture conditions [4] [87].
Recent single-cell RNA sequencing studies have revealed previously unappreciated heterogeneity within AD-MSC populations, identifying distinct subpopulations with varying propensities for differentiation, immunomodulation, and proliferation [4]. Similarly, BM-MSCs demonstrate functional heterogeneity based on their specific niche within the bone marrow microenvironment (e.g., perivascular versus endosteal locations). These subpopulations may be characterized by differential expression of markers beyond the standard ISCT panel, including CD146, CD271, MSCA-1, and SSEA-4 [27] [4].
Tissue-Specific Identification and Isolation
Table 1: Key Markers for MSC Subpopulation Identification
| Marker | BM-MSC Expression | AD-MSC Expression | Functional Significance |
|---|---|---|---|
| CD105 | High | High | Angiogenesis, cell migration [2] |
| CD73 | High | High | Immunomodulation via adenosine production [2] |
| CD90 | High | High | Cell-cell and cell-ECM interactions [2] |
| CD44 | Variable | High (AD-MSC2) | Hyaluronic acid receptor, migration [27] |
| CD146 | Variable | High (AD-MSC2) | Pericyte marker, vascular association [27] |
| CD34 | Negative (≤2%) | Variable/Positive* | Hematopoietic stem cell marker; *may be expressed on fresh AD-MSCs but decreases with culture [2] [85] |
| HLA-DR | Negative (≤2%) | Negative (≤2%) | Prevents immune activation [2] |
The isolation protocols for these cell populations differ significantly due to their tissue origins. BM-MSCs are typically isolated from bone marrow aspirates using density-gradient centrifugation to separate mononuclear cells, followed by plastic adherence to select for the MSC population [27]. The initial yield of BM-MSCs from bone marrow is relatively low (approximately 0.001-0.01% of nucleated cells), necessitating substantial in vitro expansion to obtain clinically relevant cell numbers [85].
In contrast, AD-MSCs are isolated from adipose tissue specimens through a more streamlined process involving collagenase digestion to liberate the stromal vascular fraction (SVF), followed by centrifugation and plating of the cellular pellet [74] [4]. Adipose tissue provides a significantly higher yield of MSCs, with approximately 1 billion cells potentially generated from 300g of adipose tissue [85]. This quantitative advantage makes AD-MSCs particularly attractive for applications requiring large cell numbers without extensive expansion.
Comparative Functional Analysis
Proliferation and Senescence Profiles
AD-MSCs generally demonstrate superior proliferative capacity compared to BM-MSCs, with shorter population doubling times and extended replicative lifespans in culture [85] [7]. This enhanced proliferative potential is particularly evident in MSCs derived from subcutaneous adipose deposits compared to those from omental regions [7]. Several studies have attributed this difference to reduced expression of senescence markers (p53, p21, p16) in AD-MSCs and umbilical cord blood MSCs compared to adult BM-MSCs [85].
The proliferation rates of both MSC types are influenced by donor age, with cells from younger donors generally exhibiting more robust expansion capacity [27]. However, this age-dependent decline appears more pronounced in BM-MSCs, potentially due to the proximity of BM-MSCs to the hematopoietic system and their role in supporting age-associated hematopoiesis [27]. AD-MSCs appear to maintain relatively stable proliferative capacity across donor ages, making them potentially more suitable for autologous therapies in elderly populations [27].
Differentiation Potential and Lineage Propensity
While both MSC sources demonstrate trilineage differentiation capacity, they exhibit distinct lineage propensities that inform their application selection. BM-MSCs traditionally show superior osteogenic and chondrogenic potential, establishing them as the "gold standard" for orthopedic applications [27] [85]. This enhanced bone-forming capacity has been consistently demonstrated in both in vitro differentiation assays and in vivo implantation models [8] [27].
AD-MSCs demonstrate robust adiopgenic differentiation potential, consistent with their tissue origin [87]. While capable of osteogenic and chondrogenic differentiation, this may require more specific induction protocols or scaffolding environments to achieve outcomes comparable to BM-MSCs [27]. Recent studies have identified specific AD-MSC subpopulations with enhanced chondrogenic potential, particularly those isolated from the infrapatellar fat pad (AD-MSC1), suggesting that anatomical harvesting site may significantly influence functional properties [27].
Table 2: Quantitative Comparison of Differentiation Potential
| Differentiation Lineage | BM-MSC Performance | AD-MSC Performance | Key Supporting Evidence |
|---|---|---|---|
| Osteogenesis | High | Moderate | BM-MSC1 showed significant upregulation of osteogenic markers (COL2A1) and superior calcium deposition [8] [27] |
| Chondrogenesis | High | Variable (site-dependent) | BM-MSCs demonstrated enhanced chondrogenic markers; AD-MSC1 (infrapatellar) showed good potential [27] |
| Adipogenesis | Moderate | High | AD-MSCs consistently show efficient lipid accumulation and adipogenic marker expression [87] |
| Neurogenic Potential | Moderate | Moderate-High | Both show transdifferentiation capacity; AD-MSCs studied in ALS clinical trials [74] |
Immunomodulatory Mechanisms and Potency
Both MSC types exert potent immunomodulatory effects through direct cell-cell contact and paracrine signaling, but emerging evidence suggests nuanced differences in their mechanisms and potency. AD-MSCs have demonstrated particularly robust effects on macrophage polarization toward the anti-inflammatory M2 phenotype and inhibition of neutrophil extracellular trap (NET) formation, which may be advantageous for treating inflammatory skin conditions and autoimmune disorders [7].
BM-MSCs have shown superior performance in certain inflammatory disease models. In a recent aged murine model of septic arthritis, BM-MSC1 (trabecular bone-derived) significantly outperformed AD-MSCs in reducing inflammation, promoting cartilage repair, and modulating immune responses [27]. The BM-MSC1 population demonstrated significant upregulation of anti-inflammatory interleukin-10 (IL-10) and downregulation of pro-inflammatory tumor necrosis factor-alpha (TNF-α) [27].
The immunomodulatory effects of both MSC types are not constitutive but are rather licensed by the inflammatory microenvironment. Exposure to interferon-gamma (IFN-γ) and other pro-inflammatory cytokines enhances the immunosuppressive capacity of both cell types through induction of indoleamine 2,3-dioxygenase (IDO) and other mediators [7] [87]. The kinetics and magnitude of this licensing effect may vary between sources, potentially influencing their therapeutic timing and efficacy.
Preclinical and Clinical Evidence
Orthopedic and Musculoskeletal Applications
In orthopedic applications, both MSC sources have demonstrated efficacy in promoting tissue repair and modulating inflammation. A 2025 meta-analysis of randomized and comparative studies on knee osteoarthritis treatment found that both adipose- and bone marrow-derived stromal cells significantly reduced pain scores at 3, 6, and 12 months compared to other orthobiological injections [133]. However, these differences were not reflected in functional outcomes, suggesting that the observed pain reduction did not correspond to substantial improvements in knee functionality [133].
In a direct comparative study using an aged murine model of septic arthritis, BM-MSCs (particularly the BM-MSC1 subpopulation) demonstrated superior therapeutic performance compared to AD-MSCs across multiple parameters [27]. BM-MSC1 treatment resulted in significantly greater reduction in inflammation, enhanced cartilage repair, and more effective modulation of immune responses, with upregulation of regenerative markers (IL-10, COL2A1) and downregulation of destructive mediators (TNF-α, MMP-13) [27]. Imaging studies confirmed superior retention, engraftment, and host tissue interaction for BM-MSCs in this inflammatory joint environment [27].
Neurological Applications
In neurological disorders, both MSC types have been investigated for their neuroprotective and immunomodulatory potential. A phase I/II clinical trial investigating AD-MSCs for amyotrophic lateral sclerosis (ALS) demonstrated safety and feasibility of intravenous administration at doses of 1×10⁶, 2×10⁶, and 4×10⁶ cells/kg, but did not show significant differences in the rate of disease progression compared to placebo [74]. The proposed mechanism of action involves transient paracrine signaling rather than long-term engraftment, with IV-administered MSCs releasing extracellular vesicles, cytokines, and mitochondria that reprogram peripheral immune cells after a brief pulmonary first-pass effect [74].
Preclinical studies in SOD1-G93A murine models of ALS have shown more promising results, with AD-MSC administration delaying motor decline and prolonging survival, potentially through upregulation of glial-derived neurotrophic factor (GDNF) and basic fibroblast growth factor (bFGF) [74]. The differential outcomes between rodent models and human trials highlight the challenges in translating MSC therapies for neurodegenerative conditions and may reflect species-specific differences in disease pathophysiology or MSC responsiveness.
Inflammatory and Autoimmune Conditions
AD-MSCs have shown particular promise in inflammatory skin diseases, where their immunomodulatory properties can target multiple aspects of disease pathophysiology. In psoriasis models, AD-MSCs significantly reduced disease severity, including scaling, thickness, and erythema, through modulation of T cell responses and promotion of M2 macrophage polarization [7]. Similarly, in atopic dermatitis, AD-MSC-derived exosomes alleviated pathological symptoms, including clinical scores, serum IgE levels, eosinophil infiltration, and immune cell recruitment to skin lesions [7].
Notably, cell-free therapies using MSC-derived extracellular vesicles are emerging as a promising alternative to whole-cell therapies, potentially offering similar efficacy with reduced safety concerns [134] [7]. These vesicles contain a complex cargo of proteins, mRNAs, miRNAs, and lipids that can modulate recipient cell behavior while avoiding potential risks associated with cell transplantation, such as ectopic tissue formation or immunogenic reactions to allogeneic cells [134].
Experimental Design and Methodologies
Standardized Isolation and Characterization Protocols
BM-MSC Isolation Protocol:
- Obtain bone marrow aspirate (typically 20-60mL) from iliac crest under local anesthesia
- Dilute with phosphate-buffered saline (PBS) containing anticoagulants (heparin or EDTA)
- Perform density-gradient centrifugation using Ficoll-Paque (1.077 g/mL) at 400-800×g for 20-30 minutes
- Collect mononuclear cell layer from interface
- Wash cells with PBS and plate at density of 50,000-100,000 cells/cm² in MSC culture medium
- Culture in α-MEM or DMEM/F12 supplemented with 10-15% fetal bovine serum and 1% penicillin/streptomycin
- Replace medium after 48-72 hours to remove non-adherent cells, then every 3-4 days thereafter
- Passage at 70-80% confluence using trypsin/EDTA [27] [87]
AD-MSC Isolation Protocol:
- Obtain adipose tissue through lipoaspiration or surgical resection (subcutaneous abdominal region preferred)
- Wash extensively with PBS containing antibiotics to remove blood contaminants
- Digest with 0.075% collagenase Type I or II at 37°C with agitation for 30-60 minutes
- Neutralize enzyme activity with serum-containing medium
- Centrifuge at 300-600×g for 5-10 minutes to separate stromal vascular fraction (pellet) from adipocytes (supernatant)
- Resuspend pellet in erythrocyte lysis buffer (if necessary), then filter through 70-100μm mesh
- Plate cells at density of 10,000-50,000 cells/cm² in MSC culture medium
- Culture conditions similar to BM-MSCs [74] [4]
Key Experimental Workflow
Signaling Pathways in MSC Mechanisms
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC Research
| Reagent Category | Specific Examples | Research Application | Considerations |
|---|---|---|---|
| Surface Markers | CD73, CD90, CD105 (positive) | Phenotypic characterization | Expression levels may vary between sources [2] [27] |
| Negative Markers | CD34, CD45, CD11b, CD19, HLA-DR | Purity assessment | CD34 may be transiently expressed on fresh AD-MSCs [2] [85] |
| Osteogenic Induction | Dexamethasone, β-glycerophosphate, ascorbic acid | Differentiation assessment | BM-MSCs typically show stronger mineralization [27] |
| Chondrogenic Induction | TGF-β3, BMP-6, dexamethasone, ascorbate-2-phosphate | Chondrogenic potential | Pellet or micromass culture systems [27] |
| Adipogenic Induction | IBMX, dexamethasone, indomethacin, insulin | Adipogenic differentiation | AD-MSCs show more efficient lipid accumulation [87] |
| Culture Media | α-MEM, DMEM/F12, MSC-qualified FBS | Cell expansion | Serum-free alternatives available but may affect functionality [87] |
| Characterization Kits | Flow cytometry panels, differentiation kits | Standardized assessment | Essential for comparability between studies [2] |
Decision Matrix for Therapeutic Selection
Indication-Specific Recommendations
Table 4: MSC Source Selection Matrix for Target Indications
| Therapeutic Area | Preferred MSC Source | Rationale | Supporting Evidence |
|---|---|---|---|
| Orthopedic (Bone) | BM-MSC | Superior osteogenic differentiation and bone regeneration | Enhanced osteogenic markers and mineralization [27] [133] |
| Cartilage Repair | BM-MSC or AD-MSC1 (infrapatellar) | Strong chondrogenic potential; site-specific AD-MSC variants | BM-MSCs show enhanced chondrogenesis; specific AD-MSC subpopulations effective [27] |
| Inflammatory Skin | AD-MSC | Robust immunomodulation, particularly for T cells and macrophages | Effective in psoriasis, atopic dermatitis models [7] |
| Autoimmune | AD-MSC or UC-MSC | Potent immunomodulatory capacity; reduced donor variation | Favorable safety profile in Crohn's fistula trial [4] |
| Neurological | Context-dependent | BM-MSC: established safety; AD-MSC: higher cell yield for repeated dosing | ALS trials show AD-MSC safety but limited efficacy [74] |
| Aged Population | AD-MSC | More stable phenotype with aging; less invasive harvesting | Reduced age-related functional decline [27] |
Strategic Considerations for Therapy Development
When designing MSC-based therapies, several strategic considerations should guide source selection:
Autologous vs. Allogeneic Approaches: For autologous therapies, AD-MSCs offer practical advantages due to less invasive harvesting and higher initial cell yields, particularly important for elderly patients or those with compromised bone marrow function [85] [87]. For allogeneic approaches, UC-MSCs may offer advantages in proliferation capacity and immunomodulatory potency, though BM-MSCs have more extensive clinical safety data [85].
Dosing and Administration Requirements: Applications requiring high cell numbers or repeated dosing may favor AD-MSCs due to their expandability [74] [7]. Routes of administration also influence selection; for intravenous delivery, the pulmonary first-pass effect significantly reduces engraftment, making paracrine-potent cells potentially more effective [74].
Manufacturing and Regulatory Considerations: BM-MSCs benefit from established international standards (ISO/TS 24651:2022) and longer clinical track records [85]. AD-MSC therapies face challenges regarding standardization due to heterogeneity and variable tissue harvesting processing methods [4]. Regulatory approvals currently favor BM-MSCs, with ten approved therapies versus two for AD-MSCs globally [85].
The comparative analysis of BM-MSCs and AD-MSCs reveals a complex landscape where tissue source significantly influences therapeutic performance across different disease contexts. Rather than declaring a universally superior source, the evidence supports context-dependent selection based on target indication, mechanism of action, and patient-specific factors. BM-MSCs maintain advantages in orthopedic applications requiring robust osteogenic and chondrogenic differentiation, while AD-MSCs show promise in inflammatory conditions and scenarios requiring large cell numbers.
Future research directions should focus on subpopulation refinement to identify specific MSC subsets with enhanced therapeutic properties, preconditioning strategies to boost functionality, and standardized potency assays to better predict clinical performance [4] [87]. The growing interest in cell-free approaches using MSC-derived extracellular vesicles offers promising alternatives that may circumvent challenges associated with whole-cell therapies while maintaining therapeutic benefits [134] [7].
As the field advances, the development of more sophisticated decision matrices incorporating patient-specific factors, disease staging, and manufacturing considerations will enable more precise matching of MSC sources to clinical applications. This tailored approach will ultimately enhance therapeutic outcomes and accelerate the clinical translation of MSC-based therapies across diverse medical specialties.
The field of regenerative medicine has long been dominated by mesenchymal stem cells (MSCs) derived from classical sources, primarily bone marrow (BM-MSCs) and adipose tissue (AD-MSCs). These cells are defined by the International Society for Cellular Therapy (ISCT) through three key criteria: adherence to plastic, expression of specific surface markers (CD73, CD90, CD105) with lack of hematopoietic markers, and trilineage differentiation potential [2]. While BM-MSCs represent the most extensively studied type with high differentiation potential and strong immunomodulatory effects, and AD-MSCs offer easier harvesting with comparable therapeutic properties, the therapeutic landscape is rapidly evolving [2]. Emerging MSC sources, particularly dental pulp stem cells (DPSCs) and umbilical cord-derived MSCs (UC-MSCs), are demonstrating unique biological properties that may offer distinct advantages for specific clinical applications. UC-MSCs are recognized for their enhanced proliferation, lower immunogenicity, and suitability for allogeneic transplantation, while DPSCs, with their neural crest origin, exhibit powerful neurogenic and angiogenic potential [2] [135]. This review systematically compares these MSC sources within the context of the established BM versus AD characterization framework, providing experimental data and methodologies to guide researchers in selecting appropriate cell sources for specific regenerative applications.
Source-Specific Characteristics and Experimental Profiling
Isolation Methodologies and Cellular Characterization
Dental Pulp Stem Cells (DPSCs) are typically isolated from dental pulp tissue of third molars or orthodontically extracted teeth. The standard protocol involves extracting teeth under sterile conditions, splitting them to access pulp tissue, and then using either enzymatic digestion or explant culture methods. In the mechanical fragmentation approach, pulp tissue is cut into 1-2 mm³ fragments, washed, and seeded in culture plates with αMEM medium supplemented with 10-20% fetal bovine serum (FBS) [16] [136]. Cells migrating from tissue fragments form monolayers within 2-4 weeks and are subcultured at 80-90% confluence [16]. DPSCs demonstrate characteristic MSC surface markers with >90% expression of CD73, CD90, and CD105, and <4% expression of hematopoietic markers CD34 and CD45 [136]. Notably, DPSCs are consistently smaller than ADSCs, Nestin-positive, and exhibit higher proliferation rates [16].
Umbilical Cord-derived MSCs (UC-MSCs) are obtained from Wharton's jelly, the mucoid connective tissue of the umbilical cord. The isolation process involves collecting umbilical cords after birth with informed consent, disinfecting the tissue, and carefully removing blood vessels. The Wharton's jelly is then extracted, minced into small fragments, and cultured using explant methods or enzymatic digestion with collagenase. Cells are expanded in DMEM or αMEM supplemented with 10-15% FBS [2] [137]. UC-MSCs adhere to plastic surfaces and exhibit typical fibroblast-like morphology. They demonstrate the standard MSC immunophenotype (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-) and possess trilineage differentiation capacity [2].
Table 1: Comparative Characterization of MSC Sources
| Parameter | BM-MSCs | AD-MSCs | DPSCs | UC-MSCs |
|---|---|---|---|---|
| Tissue Source | Bone marrow aspirate | Adipose tissue (abdominal, subcutaneous) | Dental pulp (coronal/radicular) | Umbilical cord Wharton's jelly |
| Isolation Yield | ~0.001-0.01% of nucleated cells | ~500,000 cells/gram tissue | Varies by pulp size and donor age | ~1-5 × 10⁵ cells/cm of cord |
| Key Surface Markers | CD73+, CD90+, CD105+ | CD73+, CD90+, CD105+ | CD73+, CD90+, CD105+, Nestin+ | CD73+, CD90+, CD105+ |
| Population Doubling Time | ~30-40 hours | ~30-50 hours | ~32-48 hours | ~20-30 hours |
| Unique Properties | Gold standard, high osteogenic potential | Ease of access, abundant tissue | Neural crest origin, high neurogenic potential | Neonatal source, low immunogenicity |
| Primary Applications | Orthopedic, hematopoietic support | Soft tissue reconstruction, cosmetic | Pulp regeneration, neurological disorders | Allogeneic therapy, immunomodulation |
Differentiation Capacity and Functional Potency
The trilineage differentiation potential represents a fundamental criterion for MSC characterization. Standard protocols for evaluating this capacity involve culturing cells in specific induction media:
Osteogenic Differentiation: Cells are seeded at 3×10³ cells/well in 48-well plates and cultured in DMEM supplemented with 10% FBS, 50µM ascorbic acid-2 phosphate, 10mM β-glycerophosphate, and 0.1µM dexamethasone for 2-3 weeks. Differentiation is confirmed by Alizarin Red S staining detecting calcium deposits [16].
Adipogenic Differentiation: Cells are induced with DMEM containing 10% FBS, 0.5mM isobutylmethylxanthine, 1µM dexamethasone, 10µM insulin, and 200µM indomethacin. Lipid vacuole formation is visualized with Oil Red O staining after 2-3 weeks [16].
Chondrogenic Differentiation: Pellet cultures are established using 2.5×10⁵ cells centrifuged in conical tubes and cultured in DMEM with 1% ITS+ premix, 50µM ascorbic acid-2 phosphate, 0.1µM dexamethasone, and 10ng/mL TGF-β3 for 3-4 weeks. Chondrogenesis is assessed by Alcian blue or Safranin O staining for proteoglycans [16].
Comparative studies reveal significant differences in differentiation capacity across MSC sources. While BM-MSCs demonstrate strong osteogenic potential, DPSCs show limited adipogenic differentiation capacity but enhanced neurogenic potential due to their neural crest origin [16]. AD-MSCs reliably undergo adipogenesis, making them ideal for soft tissue regeneration, while UC-MSCs exhibit balanced multilineage capacity with particularly strong immunomodulatory properties [2] [137].
Secretome Analysis and Cell-Free Therapeutic Approaches
The therapeutic effects of MSCs are increasingly attributed to their paracrine activity rather than direct differentiation and engraftment. The secretome—comprising soluble factors, extracellular vesicles (EVs), exosomes, and microRNAs—mediates tissue repair through immunomodulation, angiogenesis, and anti-apoptotic effects [2] [16].
Comparative Secretome Profiling
Comprehensive analysis of conditioned media from different MSC sources reveals distinct molecular profiles:
DPSC Secretome: DPSCs release factors particularly enriched for neural regeneration and angiogenesis. Their extracellular vesicles contain microRNAs predominantly involved in oxidative stress and apoptosis pathways (e.g., miR-125a-3p, miR-147a, miR-21-3p) [16] [7]. DPSC-conditioned medium demonstrates potent effects on odontogenic differentiation and vascularization, facilitating pulp-dentin complex regeneration [138].
AD-MSC Secretome: AD-MSCs secrete a broad spectrum of anti-inflammatory cytokines (IL-10, TGF-β), chemokines (CCL2, CCL5), and growth factors (VEGF, FGF, IGF-1) that promote angiogenesis and tissue repair [7]. Their EVs contain microRNAs that regulate cell cycle and proliferation pathways, making them particularly effective for inflammatory skin disorders like psoriasis and atopic dermatitis [7].
UC-MSC Secretome: UC-MSCs produce a potent combination of immunomodulatory factors (PGE2, IDO, HLA-G) and tissue-repair molecules that demonstrate efficacy in graft-versus-host disease, COVID-19 ARDS, and neurological disorders [137].
Table 2: Secretome Composition Across MSC Sources
| Secretome Component | BM-MSCs | AD-MSCs | DPSCs | UC-MSCs |
|---|---|---|---|---|
| Anti-inflammatory Factors | IL-10, TGF-β, PGE2 | IL-10, TGF-β, PGE2, IDO | IL-10, TGF-β | IL-10, TGF-β, PGE2, IDO, HLA-G |
| Growth Factors | VEGF, HGF, FGF | VEGF, HGF, FGF, IGF-1 | VEGF, NGF, BDNF | VEGF, HGF, FGF, ANG-1 |
| Extracellular Vesicle Production | ~1-3×10¹⁰ particles/10⁶ cells | ~2-4×10¹⁰ particles/10⁶ cells | ~1-3×10¹⁰ particles/10⁶ cells | ~3-5×10¹⁰ particles/10⁶ cells |
| Characteristic miRNAs | let-7 family, miR-21 | miR-21-3p, miR-31 | miR-125a-3p, miR-147a | miR-146a, miR-21, let-7 |
| Primary Pathways Regulated | Hematopoiesis, osteogenesis | Angiogenesis, adipogenesis | Neurogenesis, apoptosis | Immunomodulation, tissue repair |
Experimental Workflow for Secretome Analysis
Diagram 1: Experimental workflow for comprehensive secretome analysis from MSC cultures.
The standard protocol for secretome analysis begins with MSC culture expansion until 70-80% confluence in complete medium. For conditioning, cells are thoroughly washed and switched to serum-free medium to eliminate FBS-derived protein contamination [16] [138]. Conditioned media is collected after 48-72 hours and centrifuged (2,000×g, 10 minutes) to remove cells and debris. For extracellular vesicle isolation, the supernatant undergoes ultracentrifugation (100,000×g, 70 minutes) or size-exclusion chromatography [16]. Protein components are analyzed via ELISA for specific factors or LC-MS/MS for global proteomic profiling. miRNA content from EVs is assessed using RNA extraction followed by qPCR arrays or sequencing. Functional validation includes in vitro assays (migration, proliferation, tube formation) and in vivo disease models to confirm bioactivity [138].
Signaling Pathways and Molecular Mechanisms
Neural-Like Properties of DPSCs: Cholinergic Signaling
DPSCs exhibit unique basal neural-like properties due to their neural crest origin. Recent investigations have revealed they possess a functional cholinergic system, including type 2 muscarinic receptors (m2AChR) that regulate quiescence [139].
Experimental Protocol for Cholinergic Signaling Analysis:
- Gene Expression Profiling: DPSCs are seeded at 1×10⁵ cells/well in 24-well plates. RNA extraction uses RNAqueous Total RNA Isolation Kit or RNeasy Mini Kit with DNase treatment. cDNA synthesis employs High-Capacity cDNA Reverse Transcription Kit. Gene expression analysis utilizes TaqMan Array human neurotransmitter plates or targeted qPCR with GAPDH normalization [139].
- Immunocytochemistry: Cells plated on coverslips are fixed with 4% paraformaldehyde, permeabilized with 0.1% Triton X-100, and blocked with 1% BSA. Primary antibodies (m2AChR, m3AChR, m5AChR; 1:1000 dilution) are applied overnight at 4°C, followed by Alexa Fluor 488-conjugated secondary antibodies (1:1000) [139].
- Functional Assays: Receptor-specific agonists/antagonists assess functionality. LDH release and CCK-8 assays evaluate viability and proliferation. Cell cycle analysis uses flow cytometry with PI staining. Osteogenic differentiation and wound healing assays determine effects on differentiation and migration [139].
Diagram 2: m2AChR signaling pathway in DPSCs regulating quiescence and differentiation.
Research findings demonstrate that m2AChR activation in DPSCs engages the MAPK/ERK pathway, upregulates CDKN1A (P21), and induces reversible cell cycle arrest at G2/M phase without affecting viability or pluripotency. This quiescent state correlates with impaired migration and reduced osteogenic differentiation capacity, suggesting m2AChR as a potential target for manipulating DPSC behavior in regenerative applications [139].
All MSC sources share common immunomodulatory mechanisms but exhibit source-specific variations in potency and factor production. The general immunomodulatory pathway involves:
Experimental Protocol for Immunomodulation Assessment:
- Immune Cell Coculture: MSCs are cocultured with peripheral blood mononuclear cells (PBMCs) or specific immune cell populations (T cells, macrophages, dendritic cells) in transwell systems or direct contact setups.
- T Cell Suppression Assay: CFSE-labeled T cells are activated with anti-CD3/CD28 antibodies in the presence of MSCs. Proliferation is measured by CFSE dilution via flow cytometry after 3-5 days.
- Macrophage Polarization: MSCs are cocultured with monocyte-derived macrophages. M1/M2 polarization is assessed by surface markers (CD80/CD86 for M1; CD206/CD163 for M2) and cytokine secretion (TNF-α, IL-12 for M1; IL-10, TGF-β for M2).
- IDO/Tryptophan Metabolism: IDO activity is measured by kynurenine production in supernatant via spectrophotometry after incubation with L-tryptophan.
UC-MSCs typically demonstrate superior immunomodulatory potency, producing higher levels of PGE2, IDO, and TGF-β that more effectively suppress T-cell proliferation and promote regulatory T-cell formation compared to BM-MSCs and AD-MSCs [137]. DPSCs show particularly strong effects on neutrophil function and macrophage polarization, while AD-MSCs excel in modulating Th2 responses relevant to allergic inflammation [16] [7].
Clinical Translation and Regulatory Landscape
Clinical Applications and Trial Outcomes
Emerging MSC sources are demonstrating promising results across diverse clinical indications:
UC-MSC Clinical Applications: Clinical studies (2014-2024) show UC-MSCs have a consistent safety profile and therapeutic benefits across multiple indications. In musculoskeletal applications, they improve osteoarthritis pain and function; in hepatology, they sustain gains in decompensated cirrhosis and mitigate acute allograft rejection; in neurology, they improve motor, sensory, and visual function in cerebral palsy, chronic spinal cord injury, and traumatic optic neuropathy; in COVID-19-related ARDS, they enhance oxygenation, radiological recovery, and quality of life [137].
DPSC Clinical Progress: DPSC research has evolved from proof-of-concept studies to clinical trials, successfully achieving functional pulp tissue regeneration containing vasculature and innervation in patients, with some cases promoting further root development [135]. Applications have expanded beyond dentistry to preclinical models of ischemic brain injury, spinal cord injury, kidney injury, and diabetes [135].
AD-MSC Dermatological Applications: AD-MSCs and their exosomes show significant efficacy in immune-mediated skin diseases. They reduce psoriasis symptoms including scaling, thickness, and erythema through immunomodulation, and AD-MSC-derived exosomes effectively alleviate atopic dermatitis symptoms including clinical scores, serum IgE levels, eosinophil counts, and immune cell infiltration [7].
Regulatory Status and FDA Approvals
The regulatory landscape for MSC therapies is evolving with significant recent milestones:
FDA-Approved MSC Product: In December 2024, Ryoncil (remestemcel-L) became the first FDA-approved MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD) in patients aged ≥2 months. This allogeneic bone marrow-derived MSC product modulates immune response and mitigates inflammation associated with SR-aGVHD [140].
iPSC-Derived MSCs (iMSCs): iPSC-derived MSCs are gaining momentum in regenerative medicine trials, offering enhanced consistency and scalability compared to primary MSCs. An ongoing FDA-approved clinical trial is evaluating Cymerus iMSCs (CYP-001) for High-Risk Acute Graft-Versus-Host Disease (HR-aGvHD) in combination with corticosteroids [140].
Table 3: Clinical and Regulatory Status of MSC Sources
| Parameter | BM-MSCs | AD-MSCs | DPSCs | UC-MSCs |
|---|---|---|---|---|
| FDA-Approved Products | Ryoncil (remestemcel-L) for SR-aGVHD | None currently | None currently | Omisirge (cord blood-derived hematopoietic progenitors) |
| Phase III Trials | Multiple completed/ongoing | Several in cosmetic/reconstructive applications | Progressing toward Phase III | Multiple in GvHD, COVID-19 ARDS |
| Primary Clinical Targets | GvHD, orthopedic repair | Soft tissue reconstruction, inflammatory disorders | Pulp regeneration, neurological disorders | GvHD, autoimmune diseases, organ transplantation |
| Cell Banking Potential | Established but limited starting material | Excellent for autologous banking | Long-term viability (13+ years cryopreservation) [136] | Established cord blood banking infrastructure |
| Manufacturing Challenges | Donor morbidity, limited expansion | Donor variability, enzymatic processing | Limited tissue amount, donor age sensitivity | Collection timing, neonatal screening |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for MSC Characterization
| Reagent/Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Culture Media | αMEM, DMEM-KO, DMEM/F12 | Basal nutrient support | αMEM preferred for DPSCs; DMEM-KO for neural differentiation |
| Serum Supplements | Fetal Bovine Serum (FBS) | Growth factors and adhesion factors | Batch testing critical; 10-20% concentration |
| Differentiation Kits | Osteo-, Chondro-, Adipogenic Induction Media | Trilineage differentiation assessment | Serum-free formulations available for standardized assays |
| Surface Marker Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR | Immunophenotyping by flow cytometry | ISCT-defined panel essential for characterization |
| Extracellular Vesicle Isolation Kits | Ultracentrifugation, Size-exclusion chromatography, Precipitation kits | Secretome analysis | Method affects vesicle purity and functionality |
| qPCR Assays | TaqMan Array Human Neurotransmitter Panel | Neural lineage gene expression | Critical for DPSC neural propensity assessment |
| Cell Viability Assays | CCK-8, LDH release, Annexin V/PI staining | Toxicity and proliferation assessment | Multiple assays recommended for comprehensive profiling |
The comparative analysis of MSC sources reveals a complex landscape where tissue-specific properties significantly influence therapeutic applicability. While BM-MSCs remain the gold standard reference with extensive characterization history, and AD-MSCs offer practical advantages of accessibility, emerging sources present compelling opportunities. DPSCs, with their neural crest origin, demonstrate unique neural-like properties and exceptional odontogenic capability, making them ideally suited for dental pulp regeneration and neurological applications. UC-MSCs stand out for their potent immunomodulatory capacity, low immunogenicity, and suitability for allogeneic banking, positioning them as promising candidates for immune-mediated disorders.
Future research directions should address several critical challenges: standardization of isolation and expansion protocols to minimize donor- and method-dependent variability; development of potency assays that predict in vivo efficacy; and optimization of cell banking practices that maintain functional properties during long-term storage. The emerging paradigm shift from cell-based to cell-free therapies utilizing MSC-derived secretomes and extracellular vesicles offers promising alternatives that may circumvent challenges associated with cell transplantation while maintaining therapeutic efficacy. As the field advances, rational selection of MSC sources based on comprehensive molecular and functional profiling matched to specific clinical indications will maximize therapeutic outcomes in regenerative medicine.
Conclusion
The choice between BM-MSCs and AD-MSCs is not a matter of superiority but of strategic application. Key takeaways indicate that AD-MSCs often exhibit superior proliferative capacity and potent immunomodulatory effects, making them strong candidates for therapies targeting inflammatory and immune-mediated diseases. In contrast, BM-MSCs consistently demonstrate a higher potential for osteogenic and chondrogenic differentiation, positioning them as the preferred source for bone and cartilage regeneration. Future directions must focus on developing standardized, potency-based release criteria that move beyond minimal defining characteristics. Furthermore, leveraging advanced omics technologies (proteomics, metabolomics) to create detailed secretome and functional profiles will be crucial for predicting clinical efficacy and advancing the field toward personalized, indication-driven MSC therapies.
References
- 1. ON THE ORIGIN AND IMPACT OF MESENCHYMAL STEM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7735381/]
- 2. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 3. Mesenchymal stem cell perspective: cell biology to clinical ... [https://www.nature.com/articles/s41536-019-0083-6]
- 4. Adipose-derived mesenchymal stromal cells in clinical trials [https://www.sciencedirect.com/science/article/pii/S0024320524003515]
- 5. Adipose-derived and bone marrow mesenchymal stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6008936/]
- 6. A comparison of adult and neonatal tissue-derived MSC | Cell ... [https://biosignaling.biomedcentral.com/articles/10.1186/1478-811X-9-12]
- 7. Adipose-derived mesenchymal stem cells and their ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1617157/full]
- 8. and Adipose Tissue-Derived Mesenchymal Stem Cells under ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0334482]
- 9. Cell surface markers for mesenchymal stem cells related to the... [https://pubmed.ncbi.nlm.nih.gov/36865479/]
- 10. Definition and Characteristics of Mesenchymal Stromal Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8895491/]
- 11. Adipose & Bone Marrow-Derived hMSCs: What's the ... [https://www.roosterbio.com/blog/adipose-and-bone-marrow-derived-hmscs-whats-the-difference/]
- 12. Adipose-derived and bone marrow mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0914-1]
- 13. Comparative analysis of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4453294/]
- 14. Verification of changes in cells and extracellular vesicles ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925001653]
- 15. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 16. Comparative analysis of human Mesenchymal Stromal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616983/]
- 17. Growth Factor-Primed WJ-MSC Secretome Enhances ... [https://www.mdpi.com/2227-9059/13/12/2863]
- 18. The therapeutic efficacy comparison of MSCs derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077008/]
- 19. Adipose and Bone Marrow Derived-Mesenchymal Stromal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9902123/]
- 20. Comparative computational analysis to distinguish ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1270493/full]
- 21. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 22. Isolation, Characterization and Growth Kinetic Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4961111/]
- 23. Marrow changes and reduced proliferative capacity of ... [https://www.sciencedirect.com/science/article/pii/S1465324922007319]
- 24. Understanding the molecular basis of mesenchymal stem ... [https://www.nature.com/articles/s41419-025-08094-x]
- 25. The heterogeneity of mesenchymal stem cells: an important ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03587-y]
- 26. Feasibility of bone marrow mesenchymal stem cells ... [https://www.sciencedirect.com/science/article/pii/S2405844021017424]
- 27. The effect of therapeutic potential and safety of bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12654889/]
- 28. Detailed characterization of bone marrow adipose tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S8756328225000250]
- 29. Mouse Granulocyte-Macrophage Colony-Forming Unit Assay [https://www.ncbi.nlm.nih.gov/books/NBK604939/]
- 30. A high-throughput and low-waste viability assay for microbes [https://www.nature.com/articles/s41564-023-01513-9]
- 31. How to Set Up Hematopoietic Colony-Forming Unit (CFU) ... [https://www.stemcell.com/procedure-for-setting-up-the-cfu-assay.html]
- 32. Analysis of the measurements used as potency tests ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11877884/]
- 33. Mesenchymal stem cells under epigenetic control – the role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10628230/]
- 34. Epigenetic regulation of mesenchymal stem cell aging ... [https://www.sciencedirect.com/science/article/pii/S2352304222003038]
- 35. Adipose-derived mesenchymal stem cells (MSCs) are a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10770370/]
- 36. Adipose tissue-derived mesenchymal stem cells have ... [https://www.archivesofmedicalscience.com/Adipose-tissue-derived-mesenchymal-stem-cells-have-better-restorative-capacity-than,117735,0,2.html]
- 37. Validated methods for isolation and qualification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403454/]
- 38. Towards the standardization of methods of tissue ... [https://link.springer.com/article/10.1007/s10616-021-00474-3]
- 39. Methods of Isolation, Characterization and Expansion ... [https://www.mdpi.com/1422-0067/19/7/1897]
- 40. Isolation of Adipose-Derived Mesenchymal Stromal/Stem ... [https://pubmed.ncbi.nlm.nih.gov/40445288/]
- 41. Isolation of Adipose Tissue-Derived Stem Cells [https://pubmed.ncbi.nlm.nih.gov/30365239/]
- 42. Adipose tissue-derived versus bone marrow-derived cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049959/]
- 43. Expansion and characterization of bone marrow derived ... [https://www.nature.com/articles/s41598-021-83088-1]
- 44. Automated Manufacturing Processes and Platforms for ... [https://link.springer.com/article/10.1007/s12015-024-10812-5]
- 45. A chemically defined biomimetic surface for enhanced ... [https://www.sciencedirect.com/science/article/pii/S1465324922007046]
- 46. Comparative Analysis of Mesenchymal Stem Cell Cultivation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7844400/]
- 47. Evaluation of human platelet lysate versus fetal bovine ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324913007779]
- 48. Frontiers | Towards the standardization of human platelet lysate... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1496231/full]
- 49. Towards the standardization of human platelet lysate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245862/]
- 50. Comparison between Platelet Lysate ... [https://www.mdpi.com/2227-9059/12/1/140]
- 51. Human platelet lysate standardization across three ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04445-9]
- 52. of culture media supplements identifies Comparison ... serum [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04561-6]
- 53. Growth and size of stem cells from human exfoliated deciduous teeth... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12093836/]
- 54. Tissue source determines the differentiation potentials of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-017-0716-x]
- 55. Tri-Lineage Differentiation Potential of Osteosarcoma Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9960605/]
- 56. A new protocol for validation of Chondro, Adipo and Osteo ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816622001951]
- 57. Adipose-Derived Mesenchymal Stromal Cells in Basic ... [https://www.mdpi.com/1422-0067/24/4/3888]
- 58. Effects of Mesenchymal Stem Cell‐Derived Paracrine Signals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7995150/]
- 59. Mesenchymal stem cell secretome for regenerative medicine [https://www.sciencedirect.com/science/article/pii/S2090123224001814]
- 60. The secretion profile of mesenchymal stem cells and ... [https://www.nature.com/articles/s41392-022-00932-0]
- 61. Roles of extracellular vesicles from mesenchymal stem cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11683238/]
- 62. Mesenchymal stem cell-derived extracellular vesicles for ... [https://www.nature.com/articles/s41419-022-05034-x]
- 63. MSCs' conditioned media cytokine and growth factor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10214600/]
- 64. Mesenchymal Stromal Cell Secretome: Influencing ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.02837/full]
- 65. Cytokines released from human adipose tissue-derived ... [https://www.sciencedirect.com/science/article/pii/S2352320424001160]
- 66. Immunomodulatory Mechanisms of Mesenchymal Stem ... [https://www.mdpi.com/1422-0067/23/17/10023]
- 67. The Immunomodulatory mechanism and research ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04333-2]
- 68. Immunomodulation by Mesenchymal Stem Cells (MSCs) [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.01191/full]
- 69. The role and mechanism of mesenchymal stem cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12175325/]
- 70. Comparing the Immunomodulatory Properties of Bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4630659/]
- 71. Comparison of in-vitro immunomodulatory capacity ... [https://www.sciencedirect.com/science/article/pii/S1567576925004709]
- 72. Immunomodulatory properties of mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628475/]
- 73. Same or not the same? Comparison of adipose tissue- derived versus... [https://pubmed.ncbi.nlm.nih.gov/22468918/]
- 74. Adipose-derived mesenchymal stem cells for the treatment ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1655124/full]
- 75. The effect of therapeutic potential and safety of bone marrow ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0335011]
- 76. Immunomodulatory function of licensed human bone ... [https://www.sciencedirect.com/science/article/pii/S1567576923014224]
- 77. Immunomodulatory and Regenerative Functions of MSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383523/]
- 78. Trends in mesenchymal stem cell-derived extracellular ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1625787/full]
- 79. Mesenchymal stem cells in clinical trials for multiple sclerosis [https://pubmed.ncbi.nlm.nih.gov/40902228/]
- 80. The potency of mesenchymal stem/stromal cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC11034072/]
- 81. The potency of mesenchymal stem/stromal cells: does donor ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03722-3]
- 82. Impact of Aging on the Regenerative Properties of Bone ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0115963]
- 83. Mesenchymal Stromal Cells from Donors Varying Widely in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3657201/]
- 84. Mesenchymal stromal cells from donors varying widely in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324910704667]
- 85. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 86. Bone marrow vs. adipose MSCs - Research Article [https://www.foreverlabs.com/articles/blog/bone-marrow-vs-adipose-mscs]
- 87. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 88. Batch variability and anti-inflammatory effects of iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11999995/]
- 89. Multi-omics analysis of human mesenchymal stem cells ... [https://www.nature.com/articles/s41467-023-39958-5]
- 90. Comparative Study of Adipose-Derived and Bone Marrow ... [https://www.genesispub.org/comparative-study-of-adipose-derived-and-bone-marrow-derived-mesenchyme-stem-cells-for-intervertebral-disc-regeneration-in-patients-with-degenerative-disc-disease]
- 91. A robust and standardized method to isolate and expand ... [https://www.sciencedirect.com/science/article/pii/S1465324923010071]
- 92. New insights on potency assays from recent advances and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597888/full]
- 93. Potency assays and biomarkers for cell-based advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288881/]
- 94. Comparison of mesenchymal stem cells from bone marrow ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961210001171]
- 95. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 96. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 97. In vivo human adipose-derived mesenchymal stem cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-016-0420-2]
- 98. In Vivo Distribution of Human Adipose-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4382309/]
- 99. Establishing correlation between in vitro potency and in ... [https://www.nature.com/articles/s41541-025-01181-2]
- 100. How Potency Assay Strategy Can Accelerate Cell Therapy ... [https://slingshotbio.com/how-potency-assay-strategy-can-accelerate-cell-therapy-development/]
- 101. Metabolomic profiling of anaerobic and aerobic energy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8326443/]
- 102. Small molecule metabolites: discovery of biomarkers and ... [https://www.nature.com/articles/s41392-023-01399-3]
- 103. Emerging Biomarkers in Metabolomics - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11642057/]
- 104. Profiling Cellular Energy Metabolism [https://www.sciencedirect.com/science/article/pii/S0022202X2102220X]
- 105. Automated Manufacturing Processes and Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11872983/]
- 106. When Data Blooms: Insights into MSC-EV Bioprocessing [https://www.roosterbio.com/blog/when-data-blooms-insights-into-msc-ev-bioprocessing/]
- 107. Implications of long-term culture for mesenchymal stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3580484/]
- 108. Genomic instability in long-term culture of human adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10361644/]
- 109. Mesenchymal Stem Cell Senescence and Rejuvenation [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00364/full]
- 110. Mesenchymal Stem Cell Senescence and Osteogenesis [https://www.mdpi.com/1648-9144/58/1/61]
- 111. Clinical Trials with Mesenchymal Stem Cell Therapies for ... [https://www.mdpi.com/1422-0067/24/12/9939]
- 112. Donor age and breed determine mesenchymal stromal cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04236-2]
- 113. Expansion of human bone marrow-derived mesenchymal ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03481-7]
- 114. A quantitative method to determine osteogenic differentiation aptness of scaffold - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7254472/]
- 115. Qualifying Osteogenic Potency Assay Metrics for Human Multipotent Stromal Cells: TGF-β2 a Telling Eligible Biomarker - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7760953/]
- 116. Chondrogenic differentiation potential of osteoarthritic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2787268/]
- 117. Adipogenesis, Osteogenesis, and Chondrogenesis of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7362937/]
- 118. The balance of osteogenic and adipogenic differentiation ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961211014153]
- 119. Proliferation, Characterization and Differentiation Potency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7305462/]
- 120. Adipose Tissue-Derived Multipotent Stromal Cells Have a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3673757/]
- 121. Longitudinal expression profiles of key markers during ... [https://www.sciencedirect.com/science/article/pii/S0006291X25005649]
- 122. Chondrogenic potential of mesenchymal progenitors from ... [https://www.sciencedirect.com/science/article/pii/S2352304225002193]
- 123. Mesenchymal stem cell secretome for regenerative medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11976416/]
- 124. MSCs' conditioned media cytokine and growth factor ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03381-w]
- 125. A Comparative Analysis of Multipotent Mesenchymal ... [https://www.nature.com/articles/s41598-020-61167-z]
- 126. The discovery of Hepatocyte Growth Factor (HGF) and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3081175/]
- 127. Gene Expression Profiling and Secretome Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3906387/]
- 128. Comparative analysis of human Mesenchymal Stromal Cells ... [https://biologydirect.biomedcentral.com/articles/10.1186/s13062-025-00697-w]
- 129. A procedure for in vitro evaluation of the immunosuppressive ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02344-3]
- 130. Size-dependent immunomodulation by MSC secretome [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512777/]
- 131. Correlation between in vitro and in vivo immunomodulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4065951/]
- 132. Mesenchymal stromal cell extracellular vesicles as immune ... [https://www.sciencedirect.com/science/article/pii/S0166223625001948]
- 133. Adipose- and bone marrow-derived stromal cells reduce ... [https://link.springer.com/article/10.1007/s00590-025-04322-4]
- 134. MSC beneficial effects and limitations, and MSC-derived ... [https://www.sciencedirect.com/science/article/pii/S2666765723000662]
- 135. The research landscape and trends of dental pulp stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636884/]
- 136. Viability of dental pulp derived stem cells after long-term ... [https://www.sciencedirect.com/science/article/pii/S0099239925005977]
- 137. Advancing regenerative therapies with umbilical cord- ... [https://pubmed.ncbi.nlm.nih.gov/41036706/]
- 138. Dental pulp stem cells conditioned medium-functionalized ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627220/full]
- 139. Investigations into the basal neural-like properties of dental ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04730-7]
- 140. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]