Combating Stem Cell Senescence: Molecular Mechanisms, Preventive Strategies, and Clinical Applications in Replicative Aging
This article provides a comprehensive analysis of stem cell senescence as a key driver of replicative aging and age-related dysfunction.
Combating Stem Cell Senescence: Molecular Mechanisms, Preventive Strategies, and Clinical Applications in Replicative Aging
Abstract
This article provides a comprehensive analysis of stem cell senescence as a key driver of replicative aging and age-related dysfunction. Tailored for researchers and drug development professionals, it explores the fundamental molecular pathways including lysosomal dysfunction, epigenetic remodeling, and the senescence-associated secretory phenotype (SASP). The scope extends to cutting-edge interventional strategies such as senolytics, senomorphics, and niche modulation, while critically evaluating methodological challenges, optimization techniques, and comparative efficacy of therapeutic approaches. The synthesis of foundational science with translational applications offers a roadmap for developing effective anti-aging interventions and enhancing the efficacy of cell-based therapies.
Decoding the Hallmarks: Molecular Drivers and Biomarkers of Stem Cell Senescence
Technical Troubleshooting Guide
Q1: Our data shows that inhibiting lysosomal hyperacidicity in aged hematopoietic stem cells (HSCs) does not consistently reduce interferon-inflammatory signatures. What could explain this?
- Potential Cause 1: Incomplete lysosomal suppression. The v-ATPase inhibitor concentration or exposure time may be insufficient. Lysosomal hyperacidity in aged HSCs is a robust phenotype, and partial inhibition may not adequately restore lysosomal integrity and downstream metabolic homeostasis [1] [2].
- Potential Cause 2: Persistent mitochondrial DNA (mtDNA) leakage. The cGAS-STING pathway is triggered by misprocessed mtDNA. If lysosomal inhibition does not fully restore the processing of this DNA, inflammatory signaling may persist [1] [3].
- Troubleshooting Steps:
- Confirm the efficacy of your v-ATPase inhibitor using a lysosomal pH indicator (e.g., LysoSensor) to ensure a consistent shift towards a more neutral pH in treated aged HSCs [4].
- Quantify the levels of cytosolic mtDNA via qPCR or immunofluorescence for double-stranded DNA in your treated samples to verify clearance.
- Use a specific STING inhibitor as a positive control to confirm that the inflammatory pathway is indeed cGAS-STING dependent.
Q2: When attempting to replicate the rejuvenation of aged HSCs via lysosomal inhibition, we observe high cell death ex vivo. How can the protocol be optimized?
- Potential Cause: Excessive lysosomal suppression. While slowing lysosomal degradation is beneficial, complete inhibition of this essential organelle is toxic. The "slow degradation" mode is crucial, not a full blockade [1] [2].
- Troubleshooting Steps:
- Perform a dose-response curve for the v-ATPase inhibitor. The goal is to find a concentration that reduces hyperacidity and inflammation without inducing widespread cell death.
- Shorten the treatment duration. The cited study achieved an over eightfold boost in repopulation capacity with ex vivo treatment before transplantation, suggesting a finite, pre-transplantation incubation period is sufficient [1] [2].
- Supplement the culture medium with growth factors and cytokines to support cell survival during the stress of lysosomal modulation.
Q3: How can we reliably distinguish lysosomal hyperactivation in aged stem cells from general autophagy upregulation?
- Solution: A multi-parametric assay is required, as hyperactivation is characterized by more than just increased degradative flux.
- Troubleshooting Steps:
- Measure Lysosomal Activity and pH: Use LysoTracker (stains active lysosomes) in conjunction with a pH-sensitive probe like LysoSensor. Aged HSCs show increased LysoTracker signal coupled with hyperacidity (lower pH) [1] [4].
- Assess Lysosomal Integrity: Evaluate lysosomal membrane permeabilization (e.g., via Galectin-3 puncta assay). Dysfunctional, hyperactive lysosomes in aged HSCs are more prone to damage and leakage [1].
- Analyze Autophagy Flux: Use an LC3 turnover assay (with and without bafilomycin A1). This helps determine if the observed lysosomal activity is coupled to complete autophagic degradation, which may be impaired despite lysosomal hyperactivation [5].
Q4: Are lysosomal dysfunctions consistent across different types of aged stem cells?
- Evidence from Other Systems: While the core principles may be shared, specific manifestations can vary. Research on Mesenchymal Stem Cells (MSCs) has also identified lysosomal acidification dysfunction as a key driver of senescence. In MSCs, this often presents as a loss of acidity and a decline in function, contrasting with the hyperacidity reported in HSCs [4]. This suggests stem cell type-specific contexts are critical.
- Recommendation: Always establish a baseline lysosomal phenotype (pH, activity, mass) for your specific stem cell population and age model before designing interventions.
Experimental Protocols for Key Analyses
Protocol: Assessing Lysosomal pH and Activity in Aged Stem Cells
Objective: To quantitatively evaluate lysosomal hyperacidity and hyperactivity in aged HSCs versus young controls.
Materials:
- Young and aged HSCs (e.g., from 2-3 month and 22-24 month old mice, respectively).
- LysoSensor Green DND-189 (or similar pH-sensitive dye).
- LysoTracker Red DND-99 (or similar acidotropic dye).
- Flow cytometry buffer.
- Flow cytometer.
Method:
- Isolate and purify HSCs (Lin− Sca1+ cKit+ CD48− CD150+ phenotype) from young and aged mice via fluorescence-activated cell sorting (FACS) [1].
- Resuspend the HSCs in pre-warmed buffer.
- Load cells with LysoSensor Green (50 nM) and LysoTracker Red (50 nM) for 20-30 minutes at 37°C.
- Wash cells twice to remove excess dye.
- Analyze immediately via flow cytometry. Use the geometric mean fluorescence intensity (MFI) for quantification.
- Expected Result: Aged HSCs will show a significantly higher LysoSensor signal (indicating lower pH) and an elevated LysoTracker signal (indicating increased lysosomal mass/activity) compared to young HSCs [1] [4].
Protocol: Evaluating Functional Rejuvenation via Transplantation Assay
Objective: To test the functional capacity of aged HSCs following lysosomal inhibition.
Materials:
- Aged HSCs (vehicle-treated control group).
- Aged HSCs treated with v-ATPase inhibitor (e.g., Bafilomycin A1 at optimized concentration).
- Young HSCs (positive control).
- Congenic recipient mice (e.g., CD45.1+).
Method:
- Treat aged HSCs with a v-ATPase inhibitor ex vivo for a defined period (e.g., 16-24 hours) [2].
- Mix treated aged HSCs, control aged HSCs, and young HSCs with competitor bone marrow cells.
- Transplant the mixture into lethally irradiated congenic recipient mice via intravenous injection.
- Monitor peripheral blood chimerism at 4, 8, 16, and 24 weeks post-transplantation using flow cytometry to detect donor-derived (e.g., CD45.2+) myeloid and lymphoid cells.
- Expected Result: The v-ATPase inhibitor-treated aged HSCs will show a significantly higher long-term repopulation capacity and a more balanced lineage output (improved lymphopoiesis) compared to the untreated aged HSCs, approaching the performance of young HSCs [1] [2].
The following table consolidates key quantitative findings from recent research on lysosomal dysfunction in aged hematopoietic stem cells.
Table 1: Key Quantitative Findings in Aged HSCs with Lysosomal Dysfunction
| Parameter | Change in Aged HSCs (vs. Young) | Functional Impact | Citation |
|---|---|---|---|
| Lysosomal Acidity | Increased (Hyperacidic) | Disrupts metabolic/epigenetic homeostasis; triggers inflammation. | [1] [2] |
| Lysosomal Integrity | Decreased (Damaged/Leaky) | Impaired degradation capacity and organelle function. | [1] |
| cGAS-STING Signaling | Activated | Drives interferon-driven inflammatory programs. | [1] [3] |
| Repopulation Capacity | Decreased | Poor transplantation and self-renewal ability. | [1] |
| Repopulation Post v-ATPase inhibition | >8-fold increase | Restores regenerative potential and self-renewal. | [1] [2] |
Table 2: Research Reagent Solutions for Lysosomal Dysfunction Studies
| Reagent / Tool | Function / Target | Application in Research |
|---|---|---|
| V-ATPase Inhibitor (e.g., Bafilomycin A1) | Inhibits vacuolar (H+) ATPase proton pump. | Suppresses lysosomal hyperacidity to restore lysosomal integrity and metabolic homeostasis in aged HSCs [1] [2]. |
| LysoSensor Probes | pH-sensitive fluorescent dyes. | Quantitative measurement of lysosomal pH to identify hyperacidity in aged HSCs [4]. |
| LysoTracker Probes | Fluorescent dyes that accumulate in acidic organelles. | Staining and tracking of active lysosomes; indicates lysosomal mass and activity [1]. |
| cGAS/STING Inhibitors | Pharmacologically inhibits cGAS or STING proteins. | Validates the role of the mtDNA-cGAS-STING axis in driving age-related inflammation in HSCs [1] [3]. |
| Anti-CD150 Antibody | Recognizes SLAM family receptor CD150. | Identifies and isolates phenotypic long-term HSCs (LT-HSCs), which are enriched in aged mice [1]. |
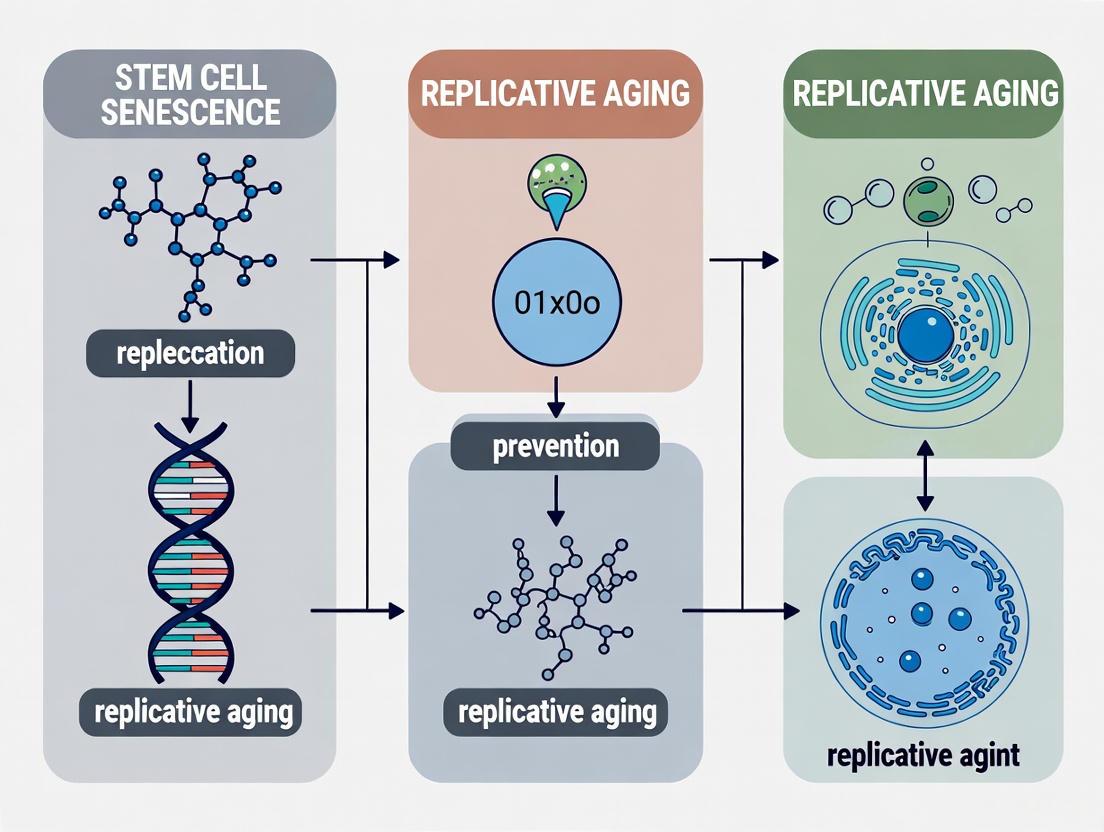
Signaling Pathways and Experimental Workflows
Diagram 1: Lysosomal Dysfunction Drives HSC Aging via cGAS-STING
Diagram 2: Workflow for Reversing HSC Aging
Troubleshooting Guide: Common Experimental Challenges in Senescence Research
This guide addresses frequent issues researchers encounter when studying senescence-associated heterochromatin foci (SAHF) and the senescence-associated secretory phenotype (SASP).
Table 1: Troubleshooting SAHF and SASP Analysis
| Problem | Possible Cause | Solution | Key References |
|---|---|---|---|
| Weak or absent SAHF formation | Incorrect senescence model (e.g., using RS in mouse fibroblasts); Insufficient senescence induction time. | Validate senescence with multiple markers (SA-β-Gal, p16, p21). Use OIS models (e.g., oncogenic RAS in IMR90) for robust SAHF. Ensure adequate induction time (days for OIS, weeks for RS). | [6] [7] [8] |
| Inconsistent SASP expression | Heterogeneous senescent cell populations; Variability between senescence inducers (OIS vs. RS). | Use FACS to sort for SA-β-Gal+ cells. Characterize the specific SASP profile for your model via cytokine array. Confirm NF-κB and C/EBPβ activation. | [6] [9] [10] |
| Difficulty visualizing cytoplasmic chromatin fragments (CCFs) | Low sensitivity of DNA staining; CCFs degraded during protocol. | Use high-sensitivity immunofluorescence (IF) for cytoplasmic DNA. Combine with cGAS/STING pathway markers for functional validation. | [6] [10] |
| SAHF formation but no SASP upregulation | SASP gene loci incorporated into repressive SAHF. | Verify exclusion of key SASP loci (e.g., IL6, IL8) from SAHF via immuno-FISH. Check HMGB2 levels, as its depletion can silence SASP genes. | [6] [9] |
Frequently Asked Questions (FAQs)
Q1: Are SAHF required for the stable cell cycle arrest in senescence? No, SAHF are not strictly necessary for growth arrest. While they help silence proliferation-promoting genes like CCNA2 and CDK1, the arrest is primarily enforced by the p53/p21 and p16/Rb pathways. Disrupting SAHF via HIRA depletion can impair the SASP without fully reversing arrest [6] [10].
Q2: Why do my primary mouse fibroblasts not form punctate SAHF upon senescence induction? Robust, punctate SAHF are primarily a feature of oncogene-induced senescence (OIS) in human fibroblast lines like IMR90 and WI-38. Mouse embryo fibroblasts (MEFs) and replicative senescence (RS) models often fail to form them, instead showing other heterochromatin rearrangements like senescence-associated distension of satellites (SADS) [6] [8].
Q3: What is the functional connection between cytoplasmic chromatin fragments (CCFs) and the SASP? CCFs are released from the nucleus of senescent cells into the cytoplasm. There, they are recognized by the innate immune DNA sensor cGAS. This activates the STING pathway, leading to the induction of the transcription factor NF-κB, a master regulator of the inflammatory SASP [6] [9] [10].
Q4: How can I specifically inhibit the SASP without affecting the senescence growth arrest? This is the goal of senomorphic therapies. Potential strategies include:
- Using small-molecule inhibitors of key SASP regulators like the NF-κB or p38 MAPK pathways.
- Targeting upstream regulators like the cGAS-STING axis [9].
- Inhibiting chromatin regulators that specifically control SASP genes, such as the H3K4 methyltransferase MLL1 [9].
Detailed Experimental Protocols
Protocol 1: Quantifying SAHF via Immunofluorescence and Image Analysis
This protocol is optimized for OIS in IMR90 human lung fibroblasts.
- Key Reagents: Antibodies against H3K9me3 (constitutive heterochromatin core) and H3K27me3 (facultative heterochromatin ring) [7].
- Procedure:
- Induce Senescence: Transduce cells with a vector expressing oncogenic HRAS (e.g., HRASG12V).
- Fix and Permeabilize: At day 6-8 post-induction, fix cells with 4% PFA and permeabilize with 0.5% Triton X-100.
- Stain Chromatin: Incubate with primary antibodies (anti-H3K9me3 and anti-H3K27me3), followed by fluorescent secondary antibodies. Counterstain DNA with DAPI.
- Image and Analyze: Acquire high-resolution confocal images. Quantify the percentage of cells with >5 distinct, DAPI-dense nuclear foci that show the characteristic concentric structure (H3K9me3 core, H3K27me3 ring) [7] [8].
Protocol 2: Inhibiting SASP via MLL1 Inhibition
This protocol tests the role of H3K4me3 in SASP regulation.
- Key Reagents: MLL1 complex inhibitor (e.g., MI-2-2) [9].
- Procedure:
- Induce Senescence: Establish OIS or TIS (e.g., 10 µM Etoposide for 72 hours) in IMR90 cells.
- Apply Inhibitor: Treat senescent cells with the MLL1 inhibitor (e.g., 1-10 µM MI-2-2) for 48 hours. Include a DMSO vehicle control.
- Assay SASP Output:
- Molecular: Perform ChIP-qPCR for H3K4me3 at SASP gene promoters (e.g., IL6, IL8). Expect a significant reduction with inhibitor treatment.
- Secreted: Collect conditioned media and analyze IL-6 and IL-8 levels by ELISA.
- Functional: Test the conditioned media on a cancer cell line (e.g., BJeH) invasion assay; media from inhibitor-treated senescent cells should have reduced pro-invasive capacity [9].
Visualizing Key Mechanisms and Workflows
Diagram 1: Chromatin Reorganization and SASP Regulation in Senescence
Diagram 2: Experimental Workflow for SASP Analysis
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Studying Senescence Epigenetics
| Reagent / Tool | Function / Target | Application in Senescence Research | Example |
|---|---|---|---|
| HIRA sh/siRNA | Depletes HIRA histone chaperone | Disrupts SAHF formation; used to study SAHF's role in SASP and arrest [6]. | siRNA pools |
| HMGB2 Antibody | Detects/Depletes HMGB2 protein | Used in IF, WB; depletion studies show its role in protecting SASP genes from heterochromatin silencing [6] [7]. | Commercial mAb |
| cGAS/STING Inhibitors | Inhibits cytoplasmic DNA sensing | Tests the contribution of the cGAS-STING pathway to SASP initiation (e.g., H-151 for STING) [6] [9]. | H-151, RU.521 |
| MLL1 Inhibitor | Inhibits H3K4 methylation | Specifically reduces H3K4me3 at SASP gene promoters, suppressing their expression (senomorphic effect) [9]. | MI-2-2 |
| HDAC Inhibitors | Inhibits histone deacetylases | Induces a SASP independent of DNA breaks; used to study chromatin-based SASP regulation [10] [11]. | Trichostatin A |
| Antibody: H3K9me3 | Marks constitutive heterochromatin | Key marker for IF analysis of SAHF core structure [6] [7]. | Commercial mAb |
| Antibody: H3K27me3 | Marks facultative heterochromatin | Key marker for IF analysis of SAHF outer ring [6] [7]. | Commercial mAb |
FAQs on Core Concepts & Mechanisms
Q1: How does telomere attrition lead to genomic instability in aging stem cells?
Telomere attrition acts as a persistent form of DNA damage that triggers genomic instability. Telomeres are protective caps at chromosome ends, and their shortening occurs with each cell division in the absence of telomerase. Critically short telomeres are recognized by the cell as double-strand breaks, initiating a DNA damage response (DDR). This can lead to cell cycle arrest, apoptosis, or cellular senescence. In stem cells, this process depletes the functional reservoir, impairing tissue maintenance and regeneration [12]. The dysfunctional telomeres also lose the protection of the shelterin complex, leading to end-to-end chromosome fusions and genomic rearrangements that further drive instability [13].
Q2: What is the role of the cGAS-STING pathway in sensing genomic instability?
The cGAS-STING pathway is a major cytosolic DNA sensor that connects genomic instability to inflammatory signaling. When genomic or mitochondrial DNA leaks into the cytoplasm—a common consequence of DNA damage and nuclear envelope rupture in micronuclei—it is bound by cyclic GMP-AMP Synthase (cGAS). cGAS produces the second messenger 2'3'-cGAMP, which activates STING (Stimulator of Interferon Genes). Activated STING triggers TBK1 and IRF3 phosphorylation, leading to the production of type I interferons and other pro-inflammatory cytokines. This establishes a link between DNA damage, innate immunity, and the senescence-associated secretory phenotype (SASP) [14] [15] [16].
Q3: What are the primary sources of cytosolic DNA that activate cGAS in senescent cells?
The two major sources are:
- Micronuclei: These are small, DNA-containing organelles that form due to chromosome missegregation or fragmentation after genotoxic stress. The nuclear envelope of micronuclei is fragile and often ruptures, exposing self-DNA to the cytosol where it is sensed by cGAS [14].
- Mitochondrial DNA (mtDNA): Mitochondrial dysfunction, a hallmark of aging, can lead to permeability of the mitochondrial membrane and release of mtDNA into the cytoplasm. This has been identified as a key driver of cGAS-STING activation, particularly in aged microglia and other cell types [15] [16].
Q4: How does replication stress contribute to the aging process?
Replication stress refers to the slowing or stalling of DNA replication forks. It is a potent source of genomic instability because stalled forks can collapse into double-strand breaks. This stress is a key driver of cellular senescence, and hereditary premature aging disorders (e.g., Werner syndrome, Bloom syndrome) often involve mutations in genes that help resolve replication stress (e.g., RECQ helicases). Replication stress contributes to multiple hallmarks of aging, including telomere attrition, stem cell exhaustion, and mitochondrial dysfunction [13].
Troubleshooting Guides for Common Research Challenges
Challenge: Detecting cGAS-STING Activation in Aged Stem Cell Cultures
Problem: A researcher is unable to consistently detect markers of cGAS-STING pathway activation in a culture of aged mesenchymal stem cells (MSCs), despite signs of senescence.
| Possible Cause | Diagnostic Experiment | Potential Solution |
|---|---|---|
| Low basal pathway activity | Measure cytosolic cGAMP levels via ELISA or LC-MS [15]. | Pre-treat cells with a low dose of DNA-damaging agent (e.g., 50 µM Etoposide, 24h) to induce cytoplasmic DNA. |
| Compensatory degradation of cGAMP | Quantify expression of enzymes like ENPP1 that hydrolyze cGAMP. | Use a STING agonist (e.g., 2'3'-cGAMP, 2-5 µg/mL) as a positive control to bypass cGAS. |
| Insensitive readout | Perform a time-course analysis of p-STING and p-TBK1 by Western blot in addition to IFN-β mRNA. | Include multiple readouts: qPCR for ISGs (e.g., ISG15, MX1) and ELISA for secreted CXCL10. |
Recommended Workflow:
- Induction: Treat aged MSCs with a STING agonist (e.g., 2'3'-cGAMP) for 6 hours as a positive control.
- Lysis: Harvest cells for RNA extraction (qPCR) and protein extraction (Western blot).
- Analysis:
- qPCR: Analyze expression of IFN-β, ISG15, and CXCL10.
- Western Blot: Probe for total STING, phosphorylated STING (Ser365), and phosphorylated TBK1 (Ser172).
- ELISA: Measure cGAMP from cell lysates or CXCL10 from culture supernatants.
Challenge: Differentiating Senescence-Associated cGAS Signaling from Infection-Related Signaling
Problem: An experiment involves a stem cell model exposed to both genotoxic stress and low levels of environmental microbes, making it difficult to attribute cGAS-STING activation specifically to genomic instability.
| Feature | Senescence-Associated Signaling | Infection-Associated Signaling |
|---|---|---|
| DNA Source | Self-DNA (micronuclei, mtDNA) [14] [15] | Foreign microbial DNA |
| Onset & Duration | Chronic, low-grade, persistent [16] | Acute, strong, typically resolved |
| Key Cytokines | SASP factors (IL-6, IL-8), Type I IFNs [14] [16] | High levels of Type I IFNs, pro-inflammatory cytokines |
| Experimental Inhibition | VDAC inhibitors (e.g., VBIT-4) block mtDNA release [15]. | Antimicrobial agents will prevent signaling. |
Diagnostic Strategy:
- Visualize the Source: Perform immunofluorescence staining for cGAS and γH2AX (DNA damage marker) along with a DNA stain. The co-localization of cGAS with micronuclei is indicative of senescence-associated activation [14].
- Inhibit Specific Sources: Treat cells with VBIT-4 (1-2 µM, 48h), an inhibitor of mitochondrial VDAC oligomerization that blocks mtDNA release. A reduction in signaling implicates mtDNA as a key driver [15].
- Profile the Secretome: Use a multiplex cytokine array. A SASP-rich profile (IL-6, IL-8, MMPs) alongside moderate IFN-β suggests senescence, while a very high IFN-β/IFN-α ratio is more typical of viral infection.
Challenge: High Variability in Telomere Length Measurements
Problem: A team observes unacceptably high variability in telomere length data from qPCR-based assays across replicates of the same primary stem cell population.
| Possible Cause | Diagnostic Experiment | Potential Solution |
|---|---|---|
| Variable DNA quality/quantity | Run all samples on a bioanalyzer to assess DNA integrity and precise concentration. | Use a fluorometric method for DNA quantification and standardize input DNA mass. |
| Primer/dye inefficiency | Check primer dimer formation with no-template controls and analyze amplification efficiency curves. | Optimize primer annealing temperatures and use intercalating dyes specific for dsDNA. |
| Heterogeneous cell population | Analyze cell surface markers via FACS to confirm population purity before extraction. | Use single-cell telomere length measurement techniques, such as quantitative FISH (qFISH). |
Optimal Protocol Checklist:
- DNA Quality: Ensure all DNA samples have an A260/A280 ratio between 1.8-2.0 and are run on a gel or bioanalyzer to confirm high molecular weight and lack of degradation.
- qPCR Validation: Validate primer sets for a single-copy reference gene (e.g., 36B4) and telomere repeats. Ensure amplification efficiencies for both are between 90-110% and within 5% of each other.
- Controls: Include a reference DNA sample in every assay plate to allow for inter-plate normalization and correct for run-to-run variation.
Table 1: Key Markers of Genomic Instability and Associated Pathways
| Marker/Parameter | Young/Healthy Cells | Aged/Senescent Cells | Detection Method | Biological Significance |
|---|---|---|---|---|
| Telomere Length | >10 kbp | <6 kbp [12] | qPCR, TRF, STELA | Indicator of replicative history and onset of senescence. |
| γH2AX Foci | Low (<5 foci/nucleus) | High (>10 foci/nucleus) [17] | Immunofluorescence | Marker of DNA double-strand breaks. |
| Cytosolic cGAMP | Low/Undetectable | Robustly increased [15] | ELISA, LC-MS | Direct indicator of cGAS enzyme activity. |
| p-STING (Ser365) | Low/Undetectable | Elevated [15] | Western Blot | Marker of STING pathway activation. |
| Micronuclei Frequency | Low (<2%) | High (>10%) [14] | Microscopy (DAPI) | Indicator of chromosomal instability and cGAS activator. |
Table 2: Reagents for Modulating the cGAS-STING Pathway in Aging Research
| Reagent | Function | Example Use in Senescence Research | Key Reference |
|---|---|---|---|
| H-151 | Potent and selective STING inhibitor | Suppresses SASP and age-related inflammation in vivo; 1-5 µM in vitro. | [15] |
| 2'3'-cGAMP | STING agonist | Positive control for pathway activation; 2-5 µg/mL in vitro. | [14] [16] |
| VBIT-4 | Inhibitor of VDAC oligomerization | Blocks mtDNA release and subsequent cGAS activation; 1-2 µM. | [15] |
| TREX1 | Cytosolic DNA exonuclease | Ectopic expression degrades cytosolic DNA, suppressing cGAS activation. | [16] |
Essential Signaling Pathways & Workflows
Diagram 1: cGAS-STING Pathway in Aging. This diagram illustrates how triggers of genomic instability (telomere attrition, DNA damage, mitochondrial dysfunction) lead to the accumulation of cytosolic DNA, which activates the cGAS-STING innate immune pathway. This drives the production of pro-inflammatory SASP factors and type I interferons, promoting cellular senescence and tissue aging [14] [15] [16].
Diagram 2: Experimental Workflow for cGAS-STING in Senescence. A generalized workflow for investigating the role of the cGAS-STING pathway in cellular senescence models. The process involves priming cells into senescence, modulating the pathway with specific tools, and analyzing a multi-faceted set of readouts to confirm the relationship [14] [15] [13].
Within the context of stem cell senescence and replicative aging prevention research, mitochondrial dysfunction has emerged as a critical pathophysiological hub. Mitochondria are not only the powerhouses of the cell but also central signaling organelles whose functional decline directly triggers and amplifies the senescent phenotype [18] [19]. In replicative aging, particularly in stem cell populations like mesenchymal stem cells (MSCs), this dysfunction manifests as a self-reinforcing cycle of bioenergetic compromise, metabolic imbalance, and eventual proliferative arrest [20]. The ensuing metabolic shift from oxidative phosphorylation to inefficient glycolysis further depletes the regenerative capacity of stem cell pools, creating a significant barrier to therapeutic application [20]. Understanding the precise mechanistic links between mitochondrial energetics and senescence-associated biomarkers is therefore paramount for developing effective interventions to maintain stemness and combat age-related functional decline.
FAQ: Mitochondrial Dysfunction in Stem Cell Senescence
Q1: How does mitochondrial dysfunction directly trigger a senescent phenotype in human stem cells? Mitochondrial dysfunction induces senescence through several interconnected mechanisms in stem cells. Primarily, it causes a definitive decrease in respiratory capacity per mitochondrion and a lowered mitochondrial membrane potential (ΔΨm) at steady state [19]. This energy crisis is compounded by increased production of reactive oxygen species (ROS), which accelerates damage to proteins, lipids, and DNA, thereby activating persistent DNA damage response pathways that initiate growth arrest [19] [21]. Furthermore, dysfunctional mitochondria in stem cells exhibit specific metabolic alterations, such as a lowered NAD+/NADH ratio. This shift activates AMPK and subsequently p53, establishing a distinct form of growth arrest known as Mitochondrial Dysfunction-Associated Senescence (MiDAS) [22]. The accumulation of damaged mitochondria due to impaired mitophagy further stabil the senescent state [19] [23].
Q2: What are the key mitochondrial biomarkers I should monitor in replicative aging studies? Key mitochondrial proteins serving as reliable biomarkers for cellular senescence include proteins involved in dynamics, quality control, and apoptosis. Analysis of these biomarkers provides valuable information on cellular state at various aging stages [23] [24].
Table: Key Mitochondrial Biomarkers in Cellular Senescence
| Biomarker | Primary Function | Senescence-Associated Change |
|---|---|---|
| DRP1 (Dynamin-related protein 1) | Triggers mitochondrial fission [18] [21]. | Altered expression/activity disrupts mitochondrial network balance [23] [24]. |
| PINK1-Parkin | Initiates mitophagy (clearance of damaged mitochondria) [18]. | Impaired pathway leads to accumulation of dysfunctional organelles [23] [24]. |
| Prohibitin | Regulates mitochondrial respiratory activity and mtDNA stability [24]. | Loss contributes to oxidative stress and functional decline [24]. |
| MFF (Mitochondrial Fission Factor) | Recruits DRP1 to mitochondria to promote fission [21]. | Involved in fission induced by membrane potential loss [24]. |
| VDAC (Voltage-Dependent Anion Channel) | Forms channels in the outer membrane; triggers apoptosis [24]. | Participates in release of pro-apoptotic factors and mtDNA [25] [24]. |
Q3: Why do my late-passage MSCs show a shift from osteogenic to adipogenic differentiation potential? This "osteogenic to adipogenic shift" is a classic hallmark of MSC senescence and is intrinsically linked to mitochondrial metabolic status [20]. As MSCs approach replicative senescence, their mitochondrial function declines, leading to a compensatory increase in mitochondrial mass, but with lower overall efficiency of oxidative phosphorylation (OXPHOS) [19] [20]. This bioenergetic crisis favors a metabolic shift towards glycolysis, which is less efficient at generating ATP but is the preferred metabolic pathway for adipogenesis. In contrast, robust OXPHOS is required to meet the high energy demands of osteogenic differentiation. Therefore, the senescence-associated metabolic reprogramming directly biases stem cell fate towards the less energy-intensive adipogenic lineage, limiting their utility in bone regeneration therapies [20].
Q4: Can mitochondrial transfer or transplantation techniques prevent stem cell senescence? Yes, mitochondrial transplantation represents an advanced and promising therapeutic strategy in regenerative medicine. Preclinical studies have shown that transferring functionally intact mitochondria from healthy donor cells into metabolically compromised recipient cells can reconstitute mitochondrial bioenergetics and rescue cellular function [18]. This approach has demonstrated promise in various disease models and has even been used in pediatric patients receiving ECMO support [18]. For senescent stem cells, this horizontal transfer of healthy organelles could potentially reverse the energetic deficits that underlie the senescent phenotype, thereby restoring proliferative capacity and differentiation potential. However, clinical translation faces challenges, including maintaining mitochondrial vitality post-isolation, ensuring efficient cellular internalization, and achieving sustained therapeutic effects [18].
Troubleshooting Guide: Common Experimental Issues
Problem 1: Inconsistent Senescence Induction via Mitochondrial Disruption
- Potential Cause: Heterogeneous cellular response to the stressor (e.g., oligomycin, rotenone) due to variations in baseline metabolic states.
- Solution: Pre-condition cells in a low-nutrient or uniform metabolic state before induction. Use a combination of biochemical (e.g., mtDNA depletion) and pharmacological stressors for a more synchronized arrest. Always validate induction by measuring multiple senescence markers (SA-β-Gal, p21, Lamin B1) in conjunction with mitochondrial parameters (MMP, ROS) [19] [22].
Problem 2: Failure to Detect mtDNA Release into Cytosol
- Potential Cause: Inefficient cell fractionation methodology or insufficiently sensitive detection assays.
- Solution: Optimize the digitonin-based permeabilization protocol for selective plasma membrane disruption while keeping mitochondrial membranes intact. Use a combination of immunofluorescence for cytosolic mtDNA and highly sensitive qPCR with primers specific for mitochondrial genes (e.g., CYTB, ND1) rather than nuclear DNA to confirm cytosolic presence [25].
Problem 3: Unclear or Weak Mitophagy Flux Data
- Potential Cause: Inadequate inhibition of lysosomal degradation or poor temporal resolution of the assay.
- Solution: Employ a tandem-fluorescent reporter (e.g., mt-Keima, mCherry-GFP-FIS1) that can distinguish neutral (GFP+/mCherry+) from acidic (GFP-/mCherry+) organelles. For pharmacological approaches, use a combination of lysosomal inhibitors (e.g., Bafilomycin A1) and monitor the accumulation of PINK1 and Parkin on mitochondria over a detailed time course [23].
Problem 4: MSC Differentiation Potential is Lost Before Replicative Senescence is Evident
- Potential Cause: Early and subtle mitochondrial dysfunction that precedes overt growth arrest and SA-β-Gal expression.
- Solution: Routinely monitor functional mitochondrial parameters from early passages, including the Respiratory Control Ratio (RCR) in permeabilized cells and NAD+/NADH ratio. Implement interventions like Nrf2 activators or SIRT1 modulators early in the expansion phase to maintain mitochondrial health and stemness [20].
Experimental Protocols for Key Assays
Protocol 1: Assessing Mitochondrial Function in Live Stem Cells via Seahorse XF Analyzer This protocol measures key parameters of mitochondrial function in intact, living MSCs, providing a real-time bioenergetic profile.
- Cell Seeding: Seed 20,000-80,000 early or late-passage MSCs per well in a Seahorse XF cell culture microplate 24 hours before the assay. Use appropriate growth medium.
- Assay Medium Preparation: On the day of the assay, replace growth medium with Seahorse XF Base Medium (supplemented with 1 mM pyruvate, 2 mM glutamine, and 10 mM glucose, pH 7.4) and incubate cells for 1 hour at 37°C in a non-CO2 incubator.
- Sensor Cartridge Loading: Load the Seahorse XFp Sensor Cartridge with modulators:
- Port A: 1.5 µM Oligomycin (ATP synthase inhibitor) to measure ATP-linked respiration.
- Port B: 1.0 µM FCCP (uncoupler) to measure maximal respiratory capacity.
- Port C: 0.5 µM Rotenone & Antimycin A (Complex I & III inhibitors) to measure non-mitochondrial respiration.
- Run the Assay: Place the cell culture plate and sensor cartridge in the XF Analyzer. The instrument will perform a series of mix, wait, and measure cycles to calculate the Oxygen Consumption Rate (OCR) and Extracellular Acidification Rate (ECAR) under basal conditions and after each injection.
- Data Analysis: Calculate key parameters from the OCR profile: Basal Respiration, ATP Production, Maximal Respiration, Proton Leak, and Spare Respiratory Capacity. Normalize all data to total protein content per well [19].
Protocol 2: Quantifying Cytosolic mtDNA Release as a DAMP Signal This protocol details a method to detect the release of mitochondrial DNA into the cytosol, a potent trigger of the innate immune response and SASP.
- Cell Fractionation:
- Harvest 1-5 x 10^6 senescent and control MSCs by trypsinization and wash with PBS.
- Resuspend the cell pellet in 1 mL of ice-cold Digitonin Lysis Buffer (50 µg/mL digitonin in PBS with protease inhibitors).
- Incubate on ice for 10 minutes with gentle tapping. Digitonin selectively perforates the cholesterol-rich plasma membrane while leaving organelle membranes intact.
- Centrifuge at 2,000 x g for 5 minutes at 4°C to pellet the nuclei and intact cells.
- Transfer the supernatant (cytosolic fraction) to a new tube and centrifuge at 16,000 x g for 20 minutes at 4°C to pellet any remaining organelles, including mitochondria.
- Carefully transfer the final supernatant (clean cytosolic fraction) to a new tube.
- DNA Isolation and DNase Treatment: Isolve DNA from the cytosolic fraction using a commercial kit. To ensure the DNA is from within mitochondria and not bound to the outer membrane, treat an aliquot of the fraction with 20 U of DNase I for 1 hour at 37°C before DNA isolation. The DNase will degrade any externally exposed DNA.
- Quantitative PCR (qPCR): Perform qPCR on the isolated DNA using primers specific for a mitochondrial gene (e.g., ND1) and a nuclear gene (e.g., 18S rRNA or B2M). The absence of the nuclear gene signal confirms the purity of the cytosolic fraction. A significant increase in the mtDNA/nuclear DNA ratio in the cytosolic fraction of senescent cells compared to controls indicates mtDNA release [25].
Key Signaling Pathways in Mitochondria-Driven Senescence
The transition of stem cells to a senescent state is orchestrated by specific mitochondrial-driven signaling cascades. The diagram below illustrates the core pathway linking mitochondrial dysfunction to the MiDAS phenotype and the release of mitochondrial DAMPs that promote a pro-inflammatory environment.
Diagram 1: Signaling from mitochondrial dysfunction to senescence. Mitochondrial dysfunction triggers senescence via AMPK-p53 activation from NAD+ decline and ROS-induced DNA damage. Concurrently, released mtDNA activates cGAS-STING, driving a pro-inflammatory SASP [19] [25] [22].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Studying Mitochondria in Senescence
| Reagent / Tool | Function / Target | Example Use in Senescence Research |
|---|---|---|
| MitoTEMPO | Mitochondria-targeted antioxidant (scavenges mtROS) | Testing the causal role of mtROS in initiating senescence; reduces DNA damage and p53 activation [21]. |
| Oligomycin | ATP synthase (Complex V) inhibitor | Inducing metabolic stress and MiDAS; used in Seahorse assays to measure ATP-linked respiration [19] [22]. |
| Nicotinamide Riboside (NR) | NAD+ precursor | Boosting NAD+ levels to counteract the NAD+ decline in senescence, potentially delaying the onset of MiDAS [18]. |
| PINK1 siRNA/shRNA | Gene knockdown of PINK1 kinase | Investigating the role of impaired mitophagy in senescence; knockdown leads to accumulation of damaged mitochondria [23] [24]. |
| Bafilomycin A1 | V-ATPase inhibitor (blocks lysosomal degradation) | Measuring mitophagy flux in conjunction with LC3-II or PINK1/Parkin markers; distinguishes between increased initiation vs. blocked degradation [23]. |
| MitoTracker Red CMXRos | Fluorescent dye that stains active mitochondria (ΔΨm-dependent) | Visualizing mitochondrial mass and membrane potential in live cells; often shows a hyperfused but depolarized network in senescence [19]. |
| JC-1 Dye | Potentiometric fluorescent dye for ΔΨm | Quantifying mitochondrial membrane potential; shift from red (J-aggregates) to green (monomers) indicates depolarization, a hallmark of dysfunction [19]. |
| Coenzyme Q10 | Electron carrier in ETC; antioxidant | Testing therapeutic intervention to improve ETC efficiency and reduce oxidative stress in aging stem cells [18] [26]. |
Cellular senescence is a state of irreversible growth arrest that occurs in response to various stressors, including DNA damage, oxidative stress, and oncogenic activation [27]. A defining feature of senescent cells is the Senescence-Associated Secretory Phenotype (SASP), a complex secretome comprising pro-inflammatory cytokines, chemokines, growth factors, and proteases [28]. In the context of stem cell research and replicative aging prevention, the SASP is a critical therapeutic target. While transient SASP activity can aid tissue remodeling and wound healing, its chronic activation drives inflammation, fibrosis, and tissue dysfunction [27]. In mesenchymal stem cells (MSCs), the accumulation of senescent cells and the persistent SASP secretion can severely impair regenerative potential, immunomodulatory functions, and overall therapeutic efficacy [29]. This technical support guide provides a detailed resource for researchers investigating the profibrotic and pro-inflammatory components of the SASP, with a specific focus on mitigating its effects in stem cell-based therapies and aging research.
Frequently Asked Questions (FAQs)
FAQ 1: What are the core profibrotic and pro-inflammatory components of the SASP most relevant to stem cell aging? The SASP is highly heterogeneous, but several core factors are consistently implicated in driving profibrotic and pro-inflammatory pathways in aging stem cells. Key components include:
- Pro-inflammatory Cytokines: IL-6, IL-8 (CXCL8), IL-1β, and TNF-α. These factors establish a chronic low-grade inflammatory state, often termed "inflammaging," which disrupts the stem cell niche [27] [30].
- Profibrotic Factors: Transforming Growth Factor-beta (TGF-β), IL-11, and SERPINE1 (PAI-1). These molecules directly activate fibroblasts and promote the excessive deposition of extracellular matrix (ECM), leading to tissue fibrosis [27] [31].
- Matrix Remodeling Enzymes: Matrix Metalloproteinases (MMPs) like MMP-1, MMP-3, and MMP-9, along with their inhibitors (TIMPs). They alter the tissue architecture and stem cell microenvironment [28] [27].
- Growth Factors: Vascular Endothelial Growth Factor (VEGF) and Insulin-like Growth Factor-Binding Proteins (IGFBPs). These can paradoxically impair tissue repair and promote senescence in neighboring cells [27].
FAQ 2: How does the SASP contribute to the decline in MSC functionality during in vitro expansion? During serial passaging, MSCs undergo replicative senescence, characterized by an irreversible growth arrest [32]. Senescent MSCs develop a robust SASP, which creates an unfavorable microenvironment through several mechanisms:
- Autocrine and Paracrine Senescence: The SASP factors can reinforce the senescent state in the producing cell and spread senescence to nearby young MSCs and other progenitor cells through the "bystander effect" [29].
- Impaired Immunomodulation: The SASP alters the critical immunomodulatory functions of MSCs. For instance, senescent MSCs may fail to properly suppress T lymphocyte proliferation or promote the differentiation of regulatory T cells (Tregs), undermining their therapeutic utility [29].
- Mitochondrial Dysfunction: Replicative senescence in MSCs is closely linked to mitochondrial defects, including increased reactive oxygen species (ROS) production. This oxidative stress is both a cause and a consequence of the SASP, creating a vicious cycle that accelerates functional decline [32].
FAQ 3: What techniques are recommended for a comprehensive quantification of the SASP in my stem cell models? Accurately measuring the SASP requires a multiparametric approach across different biological levels. The table below summarizes the principal methodologies.
Table 1: Techniques for SASP Quantification
Molecular Level Technique Sample Type Key Applications RNA qRT-PCR Cell culture, tissue Targeted quantification of IL-6, IL-8 transcripts [28] RNA-seq Cell culture, tissue Unbiased discovery of SASP "Atlas"; diversity across cell types [28] Protein ELISA Cell culture, plasma, serum Quantifying specific proteins like IL-6, IL-8 in conditioned media [28] Western Blotting Cell culture, tissue lysate Detecting protein expression and activation states (e.g., mTOR phosphorylation) [28] [32] Multiplex Immunoassays (Luminex, MSD) Cell culture, tissue, plasma Simultaneously measuring dozens of SASP factors in precious samples; used in human studies [28] [33] Mass Spectrometry Cell culture, plasma, serum Comprehensive, unbiased profiling of the SASP secretome [28] Localization Immunofluorescence (IF) Cells, tissues Spatial detection of SASP factors (e.g., IL-6) and co-localization with senescence markers [28] RNA In Situ Hybridization Tissue (fixed sections) Spatial localization of specific SASP factor mRNAs [28]
Troubleshooting Common Experimental Issues
Problem 1: Inconsistent SASP Measurement in Conditioned Media from Senescent MSC Cultures.
- Potential Cause: The heterogeneity of senescent cell populations and variability in the timing of SASP peak expression.
- Solution:
- Standardize Senescence Induction and Validation: Use a combination of biomarkers to confirm a senescent state prior to SASP measurement. This includes Senescence-Associated β-Galactosidase (SA-β-gal) staining [32], and detection of cell cycle inhibitors like p21 and p16 via Western Blot [32].
- Normalize Data: Always normalize SASP protein concentrations (e.g., from ELISA or multiplex assays) to the total cell number or total protein content of the culture.
- Use Multiplex Assays: Employ multiplex platforms (Luminex, MSD) to profile a panel of SASP factors from a single sample to capture the complexity and reduce inter-assay variability [28].
- Collect Time-Course Data: The SASP is dynamic. Collect conditioned media at multiple time points after the induction of senescence to capture its temporal evolution.
Problem 2: Difficulty in Distinguishing SASP-Driven Inflammation from General Inflammatory Responses.
- Potential Cause: Overlap between SASP factors and classic inflammatory cytokines produced during infections or other immune responses.
- Solution:
- Profile Multi-Marker Signatures: Do not rely on a single cytokine like IL-6. Instead, look for a co-expression pattern that is characteristic of senescence, such as the persistent simultaneous upregulation of pro-inflammatory cytokines (IL-6, IL-8), extracellular matrix modulators (MMPs, TIMPs), and growth regulators (IGFBPs) [28].
- Correlate with Senescence Markers: Directly correlate the levels of suspected SASP factors with established cellular senescence markers in your samples (e.g., via combined IF for p21 and IL-6) [28].
- Utilize Published Gene Signatures: Leverage established senescence gene panels, such as the SenMayo gene list, to analyze your transcriptomic data and confirm a senescence-specific signature [34].
Problem 3: Poor Efficacy of Senomorphic Compounds in Suppressing the SASP in Aged MSCs.
- Potential Cause: Inadequate targeting of upstream regulators of the SASP or compound toxicity.
- Solution:
- Target Multiple Pathways: The SASP is regulated by multiple interconnected pathways (NF-κB, C/EBPβ, p38MAPK, cGAS-STING). Consider using a combination of low-dose inhibitors or target a master regulator upstream [27].
- Assess Lysosomal Function: Recent research highlights lysosomal dysfunction as a key driver of stem cell aging. Targeting lysosomal hyperacidity has been shown to reverse age-related defects in hematopoietic stem cells, including reducing inflammatory signaling [2]. Evaluate lysosomal activity (e.g., LysoTracker staining) and consider interventions to restore lysosomal function.
- Check for Iron Accumulation: Iron accumulation has been identified as a key driver of senescence and the SASP in fibrotic diseases [31]. Measure intracellular iron levels (e.g., Perl's Prussian blue staining) and consider iron chelation as an experimental intervention to modulate the SASP.
Key Experimental Protocols
Protocol: Inducing and Validating Replicative Senescence in Human MSCs
This protocol outlines the serial passaging of MSCs to induce replicative senescence in vitro, a key model for studying aging [32].
Materials:
- Human bone marrow-derived MSCs (bMSCs)
- Complete culture medium (e.g., DMEM with 20% FBS, glutamine, penicillin/streptomycin)
- Trypsin-EDTA solution
- Phosphate-buffered saline (PBS)
- SA-β-gal staining kit
- RIPA lysis buffer with protease and phosphatase inhibitors
- Antibodies for p21, p16, and GAPDH
Method:
- Cell Culture and Passaging: Culture bMSCs under standard conditions (37°C, 5% CO2). Serially passage cells at a defined split ratio (e.g., 1:3) upon reaching 80-90% confluence. Record the population doubling level (PDL) at each passage.
- Senescence Validation (at desired PDLs, e.g., P4, P11, P16):
- SA-β-gal Staining: Seed cells on a 24-well plate. Once attached, wash with PBS, fix, and incubate overnight with the X-Gal staining solution at 37°C (without CO2). Count the percentage of blue-stained cells under a bright-field microscope [32].
- Western Blot for Cell Cycle Inhibitors: Lyse cells and extract protein. Perform Western blotting for p21 and p16, using GAPDH as a loading control. A significant increase in these proteins indicates senescence [32].
- Morphological Analysis: Observe cells under a microscope. Senescent MSCs often appear enlarged, flattened, and granular.
Protocol: Quantifying SASP Factors via Multiplex Immunoassay
This protocol describes a method for simultaneously measuring multiple SASP proteins from conditioned media.
Materials:
- Conditioned media from senescent and control MSCs (centrifuged to remove debris)
- Human SASP multiplex assay kit (e.g., from Luminex or MSD)
- Wash buffer
- Microplate reader compatible with the kit
Method:
- Sample Preparation: Collect conditioned media after 24-48 hours of culture in serum-free medium to avoid interference. Clarify by centrifugation and store at -80°C.
- Assay Procedure: Follow the manufacturer's instructions precisely. Typically, this involves:
- Incubating samples with antibody-coated beads or spots.
- Washing to remove unbound proteins.
- Adding a biotinylated detection antibody mixture.
- Adding a streptavidin-conjugated reporter.
- Reading the plate with the appropriate instrument.
- Data Analysis: Use the instrument's software to calculate protein concentrations from standard curves. Normalize values to the total cell count or protein concentration from the corresponding culture well.
Signaling Pathways and Molecular Regulation
The core SASP is primarily regulated by the synergistic activation of the NF-κB and C/EBPβ pathways [27]. DNA damage, oxidative stress, and other senescence triggers activate the cGAS-STING pathway in response to cytosolic DNA, which further potentiates NF-κB activity. The p38 MAPK pathway also plays a key role in SASP regulation. Furthermore, mTOR signaling promotes SASP translation, and its inhibition (e.g., with rapamycin) can suppress the SASP. A critical connection has been established between iron accumulation and the SASP, where iron fuels ROS production, exacerbating the inflammatory secretome [31]. The diagram below illustrates these key regulatory interactions.
SASP Regulatory Network
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SASP and Senescence Research
| Reagent / Assay | Primary Function | Specific Examples & Notes |
|---|---|---|
| Senescence Inducers | To trigger cellular senescence in vitro for experimental models. | Bleomycin: Induces DNA damage. Hydrogen Peroxide: Induces oxidative stress. Etoposide: DNA topoisomerase inhibitor [27] [31]. |
| SASP Modulators (Senomorphics) | To inhibit the production or secretion of SASP factors. | Rapamycin: mTOR inhibitor. Dasatinib + Quercetin: A senolytic cocktail with senomorphic properties. Vacuolar ATPase Inhibitors: Target lysosomal acidity to reduce SASP [27] [2]. |
| Cytokine Multiplex Assays | To simultaneously quantify multiple SASP proteins from a single sample. | Luminex xMAP & Meso Scale Discovery (MSD): Ideal for profiling conditioned media or plasma. Validate panels for key targets like IL-6, IL-8, IL-1β, TNF-α, TGF-β [28] [33]. |
| SA-β-gal Staining Kit | A histochemical marker for detecting senescent cells. | Available from various suppliers (e.g., Sigma, Cell Signaling). Optimal for cells and frozen sections; requires careful pH control [32]. |
| Antibodies for Senescence Markers | For protein-level detection of key senescence effectors via Western Blot or IF. | p21 (CDKN1A), p16 (CDKN2A): Core cell cycle inhibitors. Lamin B1: Often downregulated in senescence. γH2AX: Marker for DNA damage [32]. |
| Lysosomal Probes | To assess lysosomal function and mass, which is often dysregulated in senescence. | LysoTracker: Stains acidic compartments. LysoSensor: Probes lysosomal pH. Useful for investigating the link between lysosomal dysfunction and SASP [2]. |
| Iron Chelators & Sensors | To manipulate and detect intracellular iron, a key SASP driver. | Deferoxamine (DFO): An iron chelator. FerroOrange, FeRhoNox-1: Fluorescent probes for labile iron [31]. |
Therapeutic Arsenal: From Senolytics to Rejuvenation Strategies in Preclinical and Clinical Development
Cellular senescence, a state of irreversible cell cycle arrest, is a fundamental mechanism in aging and a significant contributor to age-related dysfunction. In the context of stem cell research, the accumulation of senescent cells compromises tissue regeneration, impairs stem cell function, and promotes chronic inflammation through the senescence-associated secretory phenotype (SASP) [35] [36]. Senolytic therapies have emerged as promising interventions to eliminate these senescent cells, thereby potentially extending healthspan and mitigating age-related degenerative pathologies [37] [38].
Senotherapeutic agents are broadly classified into two categories: senolytics, which selectively induce apoptosis in senescent cells, and senomorphics, which suppress the deleterious effects of the SASP without eliminating the cells [39] [36]. For research focused on preserving stem cell pools and function, senolytics offer a direct strategy to reduce the senescent burden and create a more hospitable microenvironment for regeneration. This technical support center provides detailed methodologies, troubleshooting guides, and essential resource information for researchers investigating these compounds in models of stem cell senescence and replicative aging.
Detailed Agent Profiles & Quantitative Data
Core Senolytic Classes and Mechanisms
The following table summarizes the primary senolytic agents, their molecular targets, and key functional characteristics relevant to experimental design.
Table 1: Core Senolytic Agent Profiles
| Senolytic Class / Agent | Primary Molecular Targets | Key Mechanisms of Action | Reported Efficacy in Senescent Cells | Key Limitations & Toxicities |
|---|---|---|---|---|
| BCL-2 Family Inhibitors (e.g., Navitoclax/ABT-263) | BCL-2, BCL-xL, BCL-w [36] [38] | Blocks anti-apoptotic proteins, sensitizing senescent cells to intrinsic apoptosis [36] [38]. | Broad-acting across multiple senescent cell types [36]. | Dose-limiting thrombocytopenia due to BCL-xL inhibition in platelets [36] [38]. |
| Dasatinib + Quercetin (D+Q) | Dasatinib: Src family kinases, Eph receptors. Quercetin: PI3K/AKT, BCL-2 family [40] [36]. | Inhibits overlapping pro-survival pathways (SCAPs); broader efficacy in combination [40] [36] [41]. | Effective in senescent preadipocytes, endothelial cells, and VSMCs; reduces p16INK4a, SASP in vivo [40] [41]. | Cell-type specificity; potential for transient chromatin alterations in young cells [40]. |
| Natural Polyphenols (e.g., Fisetin) | PI3K/AKT, NF-κB, ROS pathways; p16–CDK6 interaction [36] [42] [38]. | Induces apoptosis via oxidative stress and suppression of anti-apoptotic signaling; acts as senomorphic [36] [42]. | Reduces senescence markers in multiple tissues; extended lifespan in old mice [38] [43]. | Variable potency; poor bioavailability; extensive first-pass metabolism [42]. |
Quantitative Data for Experimental Planning
Table 2: Experimentally-Validated Dosing and Treatment Schedules
| Experimental Model | Agent | Concentration / Dosage | Treatment Schedule & Duration | Key Outcomes | Source |
|---|---|---|---|---|---|
| Human VSMCs (in vitro) | D+Q | Dasatinib: 100 nM; Quercetin: 5 µM [40] | 48-hour treatment, with or without 24-hour recovery [40]. | Altered chromatin structure; some "rejuvenation" in senescent cells [40]. | [40] |
| Aged Mice (in vivo) | D+Q | Dasatinib: 5 mg/kg; Quercetin: 50 mg/kg [41] | Weekly intraperitoneal injection; treatment initiated at 6, 14, or 18 months; analysis at 23 months [41]. | Ameliorated disc degeneration; decreased p16INK4a, p19ARF, SASP; preserved cell viability [41]. | [41] |
| Progeroid Mice (in vivo) | Fisetin | Not specified in results | Not specified in results | Reduced senescent cell burden across tissues; extended median and maximum lifespan [38]. | [38] |
| Human Clinical Pilot | D+Q | Dasatinib: 50 mg; Quercetin: 500 mg [43] | Oral administration over 6 months [43]. | Increased epigenetic age acceleration at 3 months (mitigated by Fisetin co-administration) [43]. | [43] |
Key Signaling Pathways in Senescence and Senolysis
The efficacy of senolytic agents hinges on targeting specific pro-survival pathways that are upregulated in senescent cells. The diagram below illustrates the key molecular pathways involved in cellular senescence and the points of intervention for major senolytic classes.
Diagram 1: Senescence Signaling and Senolytic Intervention. Key pathways (p53/p21 and p16/RB) establish growth arrest. Senescent cells activate Senescent Cell Anti-apoptotic Pathways (SCAPs) for survival. Senolytics target SCAPs or related nodes to induce apoptosis.
Experimental Protocols for Stem Cell Senescence Research
Protocol: Inducing and Quantifying Replicative Senescence in Stem Cells
This protocol outlines the process of inducing replicative senescence in human mesenchymal stem cells (hMSCs), a common model in aging research, and the subsequent validation of the senescent state.
1. Induction of Replicative Senescence:
- Cell Culture: Culture hMSCs (e.g., from bone marrow or adipose tissue) in standard growth medium. Use cells from low passages (e.g., passage 3-5) as "young" controls.
- Serial Passaging: Continuously passage cells at a standardized seeding density (e.g., 4,000 cells/cm²) until they approach replicative exhaustion [40]. Passage cells when they reach 70-80% confluency.
- Senescence Trigger (Optional): To accelerate senescence, sub-lethal stress can be applied at intermediate passages. Common triggers include:
- Hydrogen Peroxide (H₂O₂): Treat with 50-200 µM H₂O₂ for 1-2 hours, then replace with fresh medium [39].
- Ionizing Radiation: A single dose of 5-10 Gy.
2. Validation of Senescent Phenotype: A senescent population should be confirmed using at least two of the following assays before senolytic testing:
- Senescence-Associated β-Galactosidase (SA-β-Gal) Staining: Fix cells and incubate with X-Gal staining solution at pH 6.0 overnight at 37°C (non-CO₂ conditions) [40] [35]. A population is considered senescent when >70% of cells stain positive (blue-green cytoplasm) [40].
- Proliferation Assay:
- BrdU Incorporation: Measure 5-bromo-2'-deoxyuridine incorporation via immunodetection. A senescent population should have <30% BrdU-positive cells [40].
- Ki67 Staining: Immunofluorescence for the proliferation marker Ki67 should show a significant decrease in senescent cells compared to young controls [41].
- Western Blot or qPCR for Senescence Markers: Confirm upregulated expression of key markers like p16INK4a, p21CIP1, and p53 in senescent cells compared to young controls [41] [44].
- SASP Analysis: Use ELISA or multiplex immunoassays (e.g., Luminex) to detect increased secretion of SASP factors (e.g., IL-6, IL-1β, MMP-13) in the conditioned medium of senescent cultures [41].
Protocol: Testing Senolytic Efficacy In Vitro
1. Treatment of Senescent Stem Cells:
- Agent Preparation:
- Dasatinib: Prepare a stock solution in DMSO. Use working concentrations in the range of 50-200 nM [40].
- Quercetin/Fisetin: Prepare stock solutions in DMSO or ethanol. Use working concentrations of 5-20 µM [40] [38].
- Navitoclax (ABT-263): Prepare stock in DMSO. Use working concentrations of 1-10 µM [36].
- Include vehicle control (e.g., DMSO at the same dilution) for all experiments.
- Treatment Schedule:
2. Assessment of Senolytic Action:
- Viability/Cytotoxicity Assays:
- MTT/XTT Assay: Measure metabolic activity as a proxy for cell viability post-treatment. A successful senolytic will show a significant reduction in viability in senescent cultures but minimal effect in young cultures.
- ATP-based Assays (e.g., CellTiter-Glo): Provide a sensitive measure of viable cell number.
- Apoptosis Assays:
- Caspase-3/7 Activity: Use a luminescent or fluorescent caspase assay to confirm apoptosis is the mechanism of cell death.
- Annexin V/Propidium Iodide (PI) Staining: Perform flow cytometry to quantify early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptotic cells.
- Clearance Confirmation:
- Re-stain for SA-β-Gal after treatment and recovery. A successful treatment should significantly reduce the percentage of SA-β-Gal-positive cells.
- Measure SASP factors in the conditioned medium after treatment. Effective senolysis should lead to a reduction in SASP.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Senescence and Senolytic Research
| Reagent / Assay | Specific Example(s) | Primary Function in Research | Technical Notes |
|---|---|---|---|
| SA-β-Gal Staining Kit | Commercial kits (e.g., Cell Signaling Technology #9860) | Histochemical detection of senescent cells via lysosomal β-galactosidase activity at pH 6.0 [35]. | Standard benchmark; can be combined with immunofluorescence. Not entirely specific [44]. |
| Anti-p16INK4a Antibody | Recombinant monoclonal antibodies for WB, IF, IHC | Protein-level detection of a key cyclin-dependent kinase inhibitor driving senescence [41] [44]. | Critical marker for validation; confirm specificity with knockout controls. |
| Anti-p21CIP1 Antibody | Recombinant monoclonal antibodies for WB, IF, IHC | Protein-level detection of a p53-target gene enforcing cell cycle arrest [44]. | Upstream regulation differs from p16; provides complementary data. |
| SASP Panel | Luminex or ELISA Panels (e.g., IL-6, IL-1α/β, MMP-3, MMP-13) | Multiplexed quantification of soluble SASP factors in cell culture supernatant or serum [41]. | Essential for assessing paracrine effects and senomorphic activity. |
| BCL-2 Family Inhibitors | Navitoclax (ABT-263), ABT-737 | Tool compounds for inducing apoptosis in senescent cells dependent on BCL-2/BCL-xL for survival [36] [38]. | Monitor platelet toxicity in vivo; use as a positive control in vitro. |
| Natural Polyphenols | Fisetin (≥98% purity), Quercetin (≥95% purity) | Tool compounds for studying natural product-mediated senolysis/senomorphics [42] [38]. | Address poor solubility and bioavailability with vehicle optimization (e.g., cyclodextrins) [42]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My senolytic treatment (D+Q) is also killing a significant portion of my young, proliferating stem cells. What could be the cause?
- A: This is a recognized challenge. Evidence shows D+Q can cause transient, reversible chromatin changes in young cells that resemble senescence [40]. To troubleshoot:
- Confirm Senescence Status: Ensure your "young" cell population has a low baseline senescence (<5% SA-β-Gal+, high proliferation). Use early passage cells.
- Titrate Concentration: Perform a dose-response curve. The effective senolytic concentration may be lower than cytotoxic concentrations for young cells. Start with lower doses (e.g., 50 nM Dasatinib + 5 µM Quercetin) [40].
- Shorten Exposure: Reduce treatment time from 48 to 24 hours and include a recovery period to assess if effects on young cells are transient [40].
- Agent Specificity: Consider that your stem cell type might be inherently sensitive to one agent. Test Dasatinib and Quercetin separately to identify the primary driver of toxicity.
Q2: I am not observing a significant reduction in SA-β-Gal positive cells after Navitoclax treatment, despite seeing cell death. Why?
- A: This can occur due to the kinetics of the assay. SA-β-Gal staining is a marker of the senescent state, but its disappearance lags behind actual cell death. The dead cells (which may have been SA-β-Gal+) detach and are washed away during staining, leaving behind the viable, untreated senescent cells. To confirm efficacy:
- Quantify Absolute Cell Death: Use a viability assay (e.g., CellTiter-Glo) and normalize to the total DNA content or protein pre-treatment.
- Measure Apoptosis Directly: Use Annexin V/PI flow cytometry to confirm the induction of apoptosis specifically in the senescent population.
- Use Complementary Markers: Assess clearance by measuring a reduction in other markers, such as p16INK4a protein levels via Western blot or a reduction in SASP factors in the conditioned media, which may provide a more quantitative readout [41].
Q3: The in vitro senolytic efficacy of Fisetin is promising, but I see no effect in my mouse model of stem cell aging. What are potential reasons?
- A: This is a common translational hurdle, primarily attributed to pharmacokinetics and bioavailability.
- Bioavailability: Natural polyphenols like Fisetin have poor oral bioavailability and undergo extensive first-pass metabolism into inactive conjugates [42].
- Solution: Investigate different administration routes (e.g., intraperitoneal injection) or formulated versions of Fisetin designed to enhance bioavailability (e.g., nanoparticles, liposomal carriers, or cyclodextrin complexes) [42].
- Dosing Schedule: The intermittent senolytic dosing used for D+Q (e.g., once weekly) may not be optimal for Fisetin. Explore more frequent dosing or a loading-dose strategy based on published in vivo studies [38].
- Confirm Target Engagement: Analyze the senescent cell burden in the specific tissue of interest (e.g., bone marrow, muscle stem cell niche) after treatment to ensure the compound is reaching its target.
Q4: What are the best practices for defining a cell population as "senescent" for a senolytic experiment?
- A: Relying on a single marker is insufficient due to senescence heterogeneity [37] [44]. A rigorous definition requires a multi-parameter approach:
- Mandatory: Growth Arrest + at least one other marker.
- Gold Standard Panel:
- Proliferation Halt: Demonstrated by <30% BrdU+ or Ki67+ cells [40].
- SA-β-Gal Activity: >70% positive cells is a common benchmark [40].
- Key Marker Upregulation: Elevated protein or mRNA levels of p16INK4a and/or p21CIP1 [41] [44].
- Functional Secretory Phenotype: Increased secretion of SASP factors (e.g., IL-6) [41].
- Emerging Tools: For RNA-seq data, consider using established senescence gene signatures like SenMayo to quantitatively assess senescent burden before and after treatment [44].
FAQ: Core Concepts and Definitions
What is the primary goal of a senomorphic intervention compared to a senolytic? Senomorphic interventions aim to suppress the deleterious effects of the senescence-associated secretory phenotype (SASP) without killing the senescent cell. In contrast, senolytics selectively induce apoptosis in senescent cells to remove them entirely. Senomorphics are particularly valuable in contexts where complete cell clearance is undesirable or when targeting the inflammatory SASP is the primary therapeutic objective. [36] [45]
Why is the SASP considered a "double-edged sword" in stem cell biology and cancer? The SASP has a dual role. Initially, it can facilitate tissue repair and act as a tumor-suppressive barrier by attracting immune cells. However, the chronic presence of SASP factors (cytokines, chemokines, growth factors) creates a pro-inflammatory and pro-tumorigenic microenvironment. In stem cell niches, this can disrupt tissue regeneration, while in cancer, it promotes therapy resistance, metastasis, and immunosenescence. [36] [46] [47]
How do the mTOR, JAK/STAT, and NF-κB pathways interact in regulating the SASP? These pathways form a core signaling network controlling SASP. The DNA damage response often initiates SASP, leading to NF-κB activation. NF-κB and JAK/STAT are primary transcription regulators for many SASP components. mTOR signaling integrates environmental cues to amplify SASP production. There is significant crosstalk; for instance, mTOR can regulate translation of SASP factors, and JAK/STAT can be activated by SASP cytokines in a feed-forward loop. [36] [46] [47]
Troubleshooting Guide: Common Experimental Issues
Issue 1: Failure to Observe Significant SASP Suppression
- Potential Cause: Inadequate pathway inhibition or off-target effects.
- Solution:
- Verify Target Engagement: Use phospho-specific antibodies (e.g., p-S6K for mTOR, p-STAT3 for JAK/STAT, p-p65 for NF-κB) in western blotting to confirm pathway inhibition. [48] [49]
- Titrate Inhibitor Concentration: Start with established IC50 values and perform a dose-response curve. Consider that some senomorphic effects require sub-apoptotic or non-cytotoxic doses. [45]
- Check Senescence Induction: Confirm the senescence model is robust using multiple markers (SA-β-Gal, p16INK4a, p21CIP1). [36] [46]
Issue 2: High Cytotoxicity or Unintended Senolysis
- Potential Cause: Inhibitor concentration is too high, or the compound has off-target senolytic activity.
- Solution:
- Reduce Dosage: Screen lower concentrations and shorten treatment duration. Senomorphics are often effective at non-toxic doses. [45]
- Monitor Viability: Use real-time cell viability assays alongside SASP readouts.
- Select Specific Inhibitors: For mTOR inhibition, consider rapalogs (e.g., Everolimus) which may have a better therapeutic window than pan-inhibitors. [36]
Issue 3: Inconsistent SASP Profiling Results
- Potential Cause: The dynamic and heterogeneous nature of SASP; inappropriate time-points for analysis.
- Solution:
- Multi-timepoint Analysis: SASP composition evolves. Conduct time-course experiments post-senescence induction and after treatment. [46]
- Use a Multi-analyte Approach: Do not rely on a single SASP factor. Use ELISA panels or multiplex assays to profile a suite of key cytokines (e.g., IL-6, IL-8, IL-1α/β, GM-CSF). [46] [47]
- Standardize Conditions: Use consistent serum concentrations in media, as serum can contain variable levels of cytokines and growth factors. [46]
Experimental Protocols for Key Senomorphic Assays
Protocol: Assessing SASP Suppression via Cytokine Array
Objective: To quantitatively measure the effect of senomorphic compounds on the secretion of key SASP factors.
Materials:
- Conditioned media from senescent cells (48-72 hour collection).
- Human Cytokine/Chemokine Magnetic Bead Panel or equivalent ELISA kits.
- Senomorphic compounds (e.g., Rapamycin, Ruxolitinib, BAY 11-7082).
- Multiplex analyzer or plate reader.
Methodology:
- Induce Senescence: Establish a senescence model (e.g., etoposide treatment, irradiation, replicative exhaustion) in your stem cell line. Validate with SA-β-Gal staining and p16/p21 western blot. [36]
- Treat with Senomorphics: After senescence establishment, treat cells with optimized concentrations of senomorphic inhibitors for 48-72 hours.
- Collect Conditioned Media: Aspirate media, wash cells with PBS, and add fresh serum-free media. Collect conditioned media after 24-48 hours. Centrifuge to remove cell debris.
- Perform Multiplex Immunoassay: Follow manufacturer's instructions for the cytokine array. Key analytes should include IL-6, IL-8 (CXCL8), IL-1β, CCL2 (MCP-1), and VEGF. [46] [47]
- Data Analysis: Normalize cytokine concentrations to total cellular protein or cell count. Compare treated senescent cells to untreated senescent and non-senescent controls.
Protocol: Validating Pathway Inhibition via Western Blot
Objective: To confirm the on-target activity of senomorphic compounds by analyzing key phosphorylation sites.
Materials:
- RIPA Lysis Buffer with protease and phosphatase inhibitors.
- Antibodies: p-STAT3 (Tyr705), total STAT3, p-S6 Ribosomal Protein (Ser235/236), total S6, p-NF-κB p65 (Ser536), total p65, β-Actin.
- SDS-PAGE and Western Blotting equipment.
Methodology:
- Cell Lysis: Lyse treated and control cells directly in RIPA buffer. Determine protein concentration.
- Western Blotting: Separate 20-30 µg of protein by SDS-PAGE and transfer to a PVDF membrane.
- Immunoblotting: Probe membranes with phospho-specific antibodies first. After imaging, strip and re-probe with total protein antibodies to assess total protein levels and loading control (β-Actin).
- Expected Outcomes:
Table 1: Key SASP Components and Their Regulation by Target Pathways. This table summarizes core SASP factors that can be used as readouts for senomorphic efficacy.
| SASP Factor | Function | Regulating Pathways | Common Detection Methods |
|---|---|---|---|
| IL-6 | Pro-inflammatory cytokine; promotes chronic inflammation and tumor growth. | NF-κB, JAK/STAT | ELISA, Multiplex Assay |
| IL-8 (CXCL8) | Chemokine; recruits neutrophils, promotes angiogenesis. | NF-κB, JAK/STAT | ELISA, Multiplex Assay |
| IL-1α/β | Pro-inflammatory cytokines; key initiators of inflammaging. | NF-κB | ELISA, Multiplex Assay |
| VEGF | Growth factor; stimulates angiogenesis. | mTOR, NF-κB | ELISA, Multiplex Assay |
| MMP2/MMP9 | Proteases; degrade extracellular matrix, facilitate invasion. | NF-κB, MAPK | Zymography, Western Blot |
| CCL2 (MCP-1) | Chemokine; recruits monocytes/macrophages. | NF-κB | ELISA, Multiplex Assay |
Table 2: Representative Senomorphic Compounds and Their Experimental Use.
| Compound | Primary Target | Common In Vitro Concentration | Key Considerations & Off-Targets |
|---|---|---|---|
| Rapamycin | mTORC1 (via FKBP12) | 10 - 100 nM | Long pre-treatment may be needed; can affect autophagy. [36] [45] |
| Ruxolitinib | JAK1/JAK2 | 1 - 5 µM | Can affect immune cell function; check viability. [48] [49] |
| BAY 11-7082 | IKK/NF-κB | 5 - 10 µM | Can induce apoptosis at higher doses; use short treatments. [46] |
| Tocilizumab (mAb) | IL-6 Receptor | 10 - 100 µg/mL | Neutralizes extracellular IL-6; does not affect production. [46] |
Pathway and Workflow Visualizations
Diagram 1: Core SASP Signaling Network and Senomorphic Inhibition. This diagram illustrates the interplay between the NF-κB, JAK/STAT, and mTOR pathways in SASP production and the points of inhibition for key senomorphic compounds.
Diagram 2: Senomorphic Assay Validation Workflow. A step-by-step guide for evaluating the efficacy of senomorphic compounds in vitro.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Senomorphic Studies
| Reagent / Material | Function / Application | Example Product Types |
|---|---|---|
| Senescence Inducers | To establish in vitro senescence models. | Etoposide, Doxorubicin, Hydrogen Peroxide, Irradiation. |
| Pathway Inhibitors | To selectively target senomorphic pathways. | Rapamycin (mTOR), Ruxolitinib (JAK), BAY 11-7082 (NF-κB). |
| Phospho-Specific Antibodies | To validate on-target inhibition via Western Blot. | Anti-p-S6 (S235/236), Anti-p-STAT3 (Y705), Anti-p-NF-κB p65 (S536). |
| Cytokine Detection Kits | To quantify SASP factor secretion. | Luminex Multiplex Panels, ELLA Automated Immunoassay, ELISA Kits (IL-6, IL-8). |
| SA-β-Gal Staining Kit | A foundational marker for identifying senescent cells. | Commercial kits (e.g., Cell Signaling #9860) or prepared solutions. |
| Flow Cytometry Antibodies | To analyze senescence and SASP markers at single-cell level. | Anti-p16INK4a, Anti-p21CIP1, surface-bound SASP factors (e.g., ICAM-1). |
Frequently Asked Questions (FAQs)
Q1: What is lysosomal hyperactivity in the context of stem cell aging? Lysosomal hyperactivity is a recently identified aging hallmark where lysosomes in aged stem cells become hyperacidic (excessively acidic), depleted, damaged, and abnormally activated. This disrupts the cell's metabolic and epigenetic stability, leading to a loss of regenerative capacity. It is more than just a passive decline; it is an active driver of the aging process in hematopoietic stem cells (HSCs) [2] [3].
Q2: How does lysosomal dysfunction contribute to stem cell aging and inflammation? Dysfunctional lysosomes in aged HSCs fail to properly process damaged mitochondria. This leads to the leakage of mitochondrial DNA (mtDNA) into the cell's cytosol. The cell mistakes this mtDNA for a foreign invader, activating the cGAS-STING immune signaling pathway. This, in turn, triggers harmful inflammatory and interferon-driven responses, which are key drivers of inflammation and aging in stem cells [2] [50] [3].
Q3: Can lysosomal-targeted intervention actually reverse aging in stem cells? Yes, recent evidence demonstrates that aging in blood stem cells is not irreversible. By suppressing lysosomal hyperactivation with a specific v-ATPase inhibitor (ConA), researchers were able to restore lysosomal integrity, renew metabolic and mitochondrial function, and improve the epigenome in aged HSCs. This intervention successfully reset aged stem cells to a younger, healthier state, significantly improving their ability to regenerate blood and immune cells [2] [50].
Q4: What is the key signaling pathway involved in this lysosome-driven aging? The primary pathway is the cGAS-STING pathway. It is activated by cytosolic mtDNA that accumulates due to impaired lysosomal processing in old HSCs. Targeting lysosomal hyperactivity dampens this pathway, reducing inflammation and restoring stem cell function [2] [3].
Q5: Are there endogenous systems for lysosome repair that can be harnessed? Yes, cells have innate mechanisms to repair damaged lysosomes. A key pathway is the Phosphoinositide-Initiated Membrane Tethering and lipid transport (PITT) pathway. Upon lysosomal membrane damage, this pathway is rapidly activated to orchestrate membrane contact sites with the endoplasmic reticulum (ER), facilitating the transfer of lipids like phosphatidylserine and cholesterol to seal and repair the compromised lysosome [51]. The ESCRT (Endosomal Sorting Complexes Required for Transport) machinery is also recruited to directly repair holes in the lysosomal membrane [52].
Troubleshooting Experimental Guides
Issue 1: Low Repopulation Efficiency of Aged HSCs After Intervention
Problem: After attempting a rejuvenation treatment on aged Hematopoietic Stem Cells (HSCs), their in vivo repopulation capacity remains low in transplantation assays.
| Potential Cause | Suggested Solution | Key Parameters to Monitor |
|---|---|---|
| Insufficient lysosomal pH modulation | Titrate the concentration of v-ATPase inhibitors (e.g., Concanamycin A/ConA). Use LysoSensor or similar fluorescent probes to confirm a measurable shift in lysosomal pH towards a more neutral level [2] [50]. | Lysosomal pH, lysosomal membrane integrity (e.g., via Galectin-3 puncta formation). |
| Incomplete suppression of cGAS-STING pathway | Validate the reduction of cytosolic mtDNA and phospho-STING levels via immunofluorescence or Western blot after treatment [2] [3]. | Cytosolic mtDNA levels, p-STING, interferon-stimulated gene (ISG) expression. |
| Prolonged ex vivo culture leading to stem cell exhaustion | Optimize the duration of ex vivo culture with the intervention. The cited protocol used a 4-day treatment [2] [50]. | Cell viability, expression of quiescence markers (e.g., CD34, p57). |
Issue 2: Failure to Reduce Inflammatory Signaling
Problem: The treatment does not lead to a measurable decrease in inflammatory markers.
| Potential Cause | Suggested Solution | Key Parameters to Monitor |
|---|---|---|
| Persistent mitochondrial dysfunction | Assess mitochondrial quality and membrane potential. Combine lysosomal intervention with strategies to improve mitophagy [2]. | Mitochondrial membrane potential (ΔΨm), ROS levels, LC3-II/p62 colocalization with mitochondria. |
| Off-target effects of inhibitors | Include control experiments with selective cGAS-STING pathway inhibitors (e.g., H-151) to isolate the effect [3]. | ISG expression, p-STING levels in inhibitor-only groups. |
| Heterogeneous cell population | Use stringent HSC sorting methods (e.g., SLAM code: CD150+CD48−CD41−Lin−Sca-1+c-Kit+) to ensure a pure population for analysis [2]. | Purity of sorted HSCs pre- and post-treatment. |
Experimental Protocols for Key Assays
Protocol 1: Ex Vivo Rejuvenation of Aged HSCs via Lysosomal Inhibition
This protocol is adapted from the seminal study demonstrating reversal of HSC aging [2] [50] [3].
Objective: To restore youthful function in aged HSCs through short-term ex vivo modulation of lysosomal activity.
Materials:
- Source of HSCs: Bone marrow from aged mice (e.g., 22-24 months old).
- Key Reagent: v-ATPase inhibitor (e.g., Concanamycin A / ConA).
- Culture Media: Serum-free medium supplemented with stem cell cytokines (SCF, TPO, Flt-3L).
- Transplantation Reagents: Recipient mice (e.g., congenically marked, lethally irradiated), supportive bone marrow cells.
Methodology:
- HSC Isolation: Isolate and stringently sort HSCs from aged mouse bone marrow using FACS.
- Ex Vivo Treatment: Culture the sorted HSCs in the presence of a low concentration of ConA (e.g., 100 nM) for 4 days.
- Control Group: Culture a separate aliquot of HSCs in parallel with a DMSO vehicle.
- Transplantation: Transplant a small number (e.g., 100-200) of treated or control HSCs, along with a large number of competitor/supportive bone marrow cells, into lethally irradiated recipient mice.
- Analysis: Monitor peripheral blood chimerism over 16-21 weeks to assess long-term multi-lineage repopulation capacity.
Expected Outcome: HSCs treated with the lysosomal inhibitor should show a significantly enhanced (e.g., >8-fold) ability to reconstitute the blood system compared to vehicle-treated controls, with a more balanced production of myeloid and lymphoid cells [2] [3].
Protocol 2: Assessing Lysosomal Function and Integrity
Objective: To quantitatively evaluate lysosomal pH, activity, and membrane damage.
Materials:
- Lysosensor Yellow/Blue DND-160 or similar ratiometric pH dye.
- DQ-BSA, a self-quenching substrate that fluoresces upon lysosomal proteolysis.
- Antibody for Galectin-3 (for immunostaining of damaged lysosomes).
- LLOMe (L-Leucyl-L-Leucine methyl ester) as a positive control for lysosomal damage.
Methodology:
- Lysosomal pH Measurement:
- Load cells with Lysosensor Yellow/Blue.
- Measure fluorescence emission ratios (e.g., 445 nm / 510 nm) using a microplate reader or confocal microscopy.
- Generate a standard curve using buffers of known pH with ionophores to calculate absolute lysosomal pH [53].
- Proteolytic Activity Assay:
- Incubate cells with DQ-BSA.
- Measure the fluorescence intensity generated by its hydrolysis, which is directly proportional to lysosomal hydrolase activity.
- Membrane Damage Assessment:
Table 1. Key Quantitative Findings from Lysosomal Rejuvenation Studies.
| Parameter | Young HSCs | Aged HSCs (Untreated) | Aged HSCs (Post-Treatment) | Source |
|---|---|---|---|---|
| In Vivo Repopulation Capacity | Baseline (Reference) | Severely Impaired | >8-fold increase | [2] [3] |
| Lysosomal pH | Normal (~4.5-5.0) | Hyperacidic (Lower pH) | Normalized | [2] [50] |
| cGAS-STING Activation | Low | High | Significantly Reduced | [2] [3] |
| Myeloid/Lymphoid Output | Balanced | Myeloid-Biased | Restored Balance | [2] [50] |
Signaling Pathway and Experimental Workflow
Figure 1: Mechanism of Lysosomal Dysfunction in HSC Aging and the Path to Rejuvenation. The diagram illustrates how lysosomal hyperactivity in aged HSCs triggers a cascade of metabolic and inflammatory dysfunction, and how targeted inhibition of v-ATPase can reverse this process.
Figure 2: Experimental Workflow for Ex Vivo HSC Rejuvenation. This workflow outlines the key steps for isolating, treating, and functionally validating the rejuvenation of aged hematopoietic stem cells.
The Scientist's Toolkit: Research Reagent Solutions
Table 2. Essential Reagents for Lysosomal-Targeted Rejuvenation Research.
| Reagent / Tool | Function / Application | Example |
|---|---|---|
| v-ATPase Inhibitors | Pharmacologically suppresses lysosomal hyperacidification to restore normal pH and function. | Concanamycin A (ConA), Bafilomycin A1 [2] [50]. |
| Lysosomal pH Probes | Live-cell imaging and quantification of lysosomal pH. | LysoSensor Yellow/Blue DND-160, pH-sensitive dextrans [53]. |
| Membrane Damage Markers | Detect and quantify lysosomal membrane permeabilization (LMP). | Anti-Galectin-3 antibody (for immunostaining) [52] [51]. |
| cGAS-STING Pathway Assays | Measure activation of the key inflammatory pathway driven by lysosomal dysfunction. | Antibodies for phospho-STING; ELISA for interferon-beta [2] [3]. |
| Inducers of Lysosomal Damage | Positive control agents to study lysosomal repair mechanisms. | L-Leucyl-L-leucine methyl ester (LLOMe), GPN [52] [51]. |
| Metabolic Assays | Evaluate the restoration of mitochondrial function and metabolic homeostasis. | Seahorse Analyzer (for glycolytic and oxidative stress parameters), MitoTracker dyes [2]. |
FAQs: HDAC Inhibitors and SASP in Stem Cell Senescence Research
Q1: How do HDAC inhibitors paradoxically induce a senescence-associated secretory phenotype (SASP) while being investigated as anti-cancer therapeutics?
HDAC inhibitors can induce a SASP in normal fibroblasts, including those in the stromal compartment, by causing chromatin remodeling without necessarily causing physical DNA breaks. This remodeling is sensed by the cell as a stress signal, activating key pathways like the ATM/NF-κB axis, which in turn drives the expression of classic SASP factors like IL-6 and IL-8 [54]. This is a crucial consideration for stem cell research, as a pro-inflammatory SASP in the niche can negatively impact stem cell function and promote a tissue environment conducive to aging [55] [56].
Q2: What is the relationship between the decline of specific HDACs and the onset of cellular senescence?
A general downregulation of canonical HDAC expression is a feature of replicatively senescent cells. Research in human dermal fibroblasts shows that protein levels of HDACs 1-7 decrease significantly during replicative senescence [57]. Functional studies confirm that specifically knocking down HDAC2 or HDAC7 is sufficient to induce senescence biomarkers. Conversely, forcing the expression of HDAC7 in pre-senescent cells can extend their proliferative lifespan, highlighting it as a potential target for modulating cellular aging [57].
Q3: Why do HDAC inhibitors have limited efficacy against solid tumors as a monotherapy, and what does this imply for their use in an aging context?
The molecular mechanisms of HDAC inhibitor action are complex and can induce diverse outcomes like growth arrest, apoptosis, and autophagy in cancer cells [58] [59]. Their limited single-agent activity in solid tumors suggests that the senescent state induced by these drugs might be stable and accompanied by a SASP that could ultimately support tumor growth in a paracrine manner [54] [60]. This dual nature underscores the importance of understanding the specific context—such as cell type and HDAC inhibitor class—when designing therapies aimed at preventing age-related pathologies.
Q4: Can the SASP induced by HDAC inhibitors influence tumor growth in vivo?
Yes, experimental evidence indicates that fibroblasts treated with HDAC inhibitors can promote tumor growth in vivo [54]. This tumor-promoting effect is a direct consequence of the SASP, which creates a pro-inflammatory and pro-tumorigenic microenvironment. For research focused on preventing stem cell senescence, this highlights a critical risk: therapeutic epigenetic modulation must be carefully controlled to avoid generating a deleterious secretome that could disrupt tissue homeostasis and accelerate aging-related decline.
Troubleshooting Experimental Guides
Issue: Inconsistent SASP Induction Following HDAC Inhibitor Treatment
Potential Cause 1: Cell Type-Specific SASP Heterogeneity The SASP composition is highly dependent on the cell type and the specific senescence inducer [55] [60]. A protocol that works in one fibroblast line may not work in another, or in mesenchymal stem cells (MSCs).
- Solution: Always include a positive control for SASP induction, such as etoposide (a DNA-damaging agent) or hydrogen peroxide (oxidative stress). Characterize the baseline SASP profile of your specific stem cell or fibroblast line before testing HDAC inhibitors.
Potential Cause 2: Incorrect HDAC Inhibitor Dosage or Timing Using overly cytotoxic concentrations can push cells into apoptosis rather than senescence, while sub-optimal concentrations may not induce a robust SASP.
- Solution: Perform a dose-response curve to identify a concentration that causes stable growth arrest without significant cell death. Monitor SASP markers over time (e.g., 3-7 days post-treatment) as the phenotype can evolve.
Issue: Different HDAC Inhibitors Producing Variable Senescence Outcomes
Potential Cause: Inhibition of Different HDAC Classes and Non-Histone Targets Pan-HDAC inhibitors (like SAHA/Vorinostat) and class-specific inhibitors (like MS-275 which targets Class I) have distinct targets, leading to different downstream effects [58] [59] [61]. Furthermore, HDACs deacetylate non-histone proteins like HSP90, p53, and RUNX3, affecting their stability and activity [58].
- Solution:
- Select the appropriate inhibitor: Use pan-inhibitors for broad effects or class-selective inhibitors to probe the role of specific HDACs (e.g., HDAC1/2 for cell cycle regulation, HDAC6 for HSP90 modulation).
- Validate target engagement: Measure global histone hyperacetylation (e.g., H3K9ac, H4K16ac) via western blot as a pharmacodynamic marker to confirm inhibitor activity.
- Monitor non-histone targets: Assess acetylation and protein levels of key non-histone substrates like p53 and HSP90 client proteins to get a fuller picture of the inhibitor's mechanism in your system.
Quantitative Data on HDACs and Senescence
Table 1: Changes in HDAC Protein Levels During Replicative Senescence of Human Dermal Fibroblasts [57]
| HDAC | Class | Change in Senescence (vs. Young) | Notes |
|---|---|---|---|
| HDAC1 | I | Decreased | Confirmed in multiple studies |
| HDAC2 | I | Decreased (up to 98%) | Most significant decrease |
| HDAC3 | I | Decreased | |
| HDAC4 | IIa | Decreased | Also reported in 2BS fibroblasts |
| HDAC5 | IIa | Decreased (∼29%) | Least significant decrease |
| HDAC6 | IIb | Decreased | |
| HDAC7 | IIa | Decreased | Ectopic expression extends lifespan |
Table 2: Common HDAC Inhibitors and Their Experimental Use in Senescence Studies
| HDAC Inhibitor | Primary Target | Example Concentration & Duration | Key Experimental Readouts |
|---|---|---|---|
| SAHA (Vorinostat) | Pan-HDAC (I, II, IV) | 3 µM for 6 days [54] | SA-β-Gal, p21, SASP (IL-6, IL-8) |
| Trichostatin A (TSA) | Pan-HDAC (I, II, IV) | 1 mM for 3 days [54] | Histone Acetylation, Cell Cycle Arrest |
| Sodium Butyrate (NaB) | Pan-HDAC (I, IIa) | 4 mM for 72-144 hrs [54] | SASP, DDR markers |
| MS-275 (Entinostat) | Class I (HDAC1, 2, 3) | 6 µM for 6 days [54] | p16INK4A, SASP factors |
Key Experimental Protocols
Protocol 1: Inducing and Validating Senescence with HDAC Inhibitors in Fibroblasts
This protocol is adapted from methods used to establish HDAC inhibitor-induced senescence [54] [57].
- Cell Seeding: Seed early-passage human dermal fibroblasts (e.g., BJ fibroblasts) or your target stem cell/stromal cell line in complete growth medium at a density of 5,000-10,000 cells/cm². Allow cells to adhere for 24 hours.
- HDAC Inhibitor Treatment: Replace the medium with fresh medium containing the desired HDAC inhibitor (e.g., 3 µM SAHA). A vehicle control (e.g., DMSO) is essential.
- Maintenance and Monitoring: Treat cells for 3-7 days, refreshing the inhibitor-containing medium every 48-72 hours. Monitor morphology daily for enlargement and flattening.
- Validation (3-7 days post-treatment):
- Viability/Growth Arrest: Perform a trypan blue exclusion assay or MTT assay to confirm reduced proliferation and viability loss < 30%.
- Senescence-Associated β-Galactosidase (SA-β-Gal) Staining: Fix and stain cells using a commercial SA-β-Gal staining kit. Quantify the percentage of blue-stained cells from multiple fields.
- SASP Analysis: Collect conditioned medium. Measure key SASP factors like IL-6 and IL-8 using ELISA.
- Western Blotting: Analyze lysates for senescence markers (p16INK4A, p21) and HDAC target engagement (increased acetyl-histone H3).
Protocol 2: siRNA-Mediated Knockdown of Specific HDACs to Probe Function
This protocol is used to study the role of individual HDACs, such as HDAC2 or HDAC7, in senescence [57].
- Design and Preparation: Obtain validated siRNA pools targeting your HDAC of interest (e.g., HDAC7) and a non-targeting control (NTC) siRNA.
- Reverse Transfection: Plate cells in antibiotic-free medium simultaneously with the siRNA-lipid complex, prepared according to the manufacturer's instructions (e.g., using Lipofectamine RNAiMAX). A common final siRNA concentration is 10-50 nM.
- Incubation and Analysis:
- 48-72 hours post-transfection, harvest cells to check knockdown efficiency via qPCR and western blot.
- For senescence phenotyping, continue culturing the transfected cells for 5-7 days, passaging as needed, and then assess SA-β-Gal activity, morphology, and SASP secretion as in Protocol 1.
Signaling Pathways and Molecular Mechanisms
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying HDACs and SASP in Senescence
| Reagent / Tool | Function / Application | Key Considerations for Experimental Design |
|---|---|---|
| Pan-HDAC Inhibitors (e.g., SAHA/Vorinostat, TSA) | Induce global histone hyperacetylation; used for initial proof-of-concept studies on SASP induction. | Can induce broad, complex phenotypes. Use class-selective inhibitors for more targeted mechanistic follow-up [58] [54]. |
| Class I-Selective Inhibitors (e.g., MS-275/Entinostat) | Probe the specific role of Class I HDACs (HDAC1, 2, 3, 8) in cell cycle arrest and SASP regulation. | Useful for dissecting the contribution of key nuclear HDACs to the senescent phenotype [54] [61]. |
| siRNA/shRNA for HDACs | Knockdown specific HDAC isoforms (e.g., HDAC2, HDAC7) to validate their individual role in senescence. | Essential for establishing causality. Always include multiple siRNAs and rescue experiments to confirm phenotype is due to specific knockdown [57]. |
| ELISA Kits (for IL-6, IL-8, OPN) | Quantify specific SASP factors in conditioned medium. | Provides quantitative, reproducible data. Crucial for comparing SASP strength across different experimental conditions [54] [57]. |
| SA-β-Gal Staining Kit | Histochemical detection of senescent cells in vitro. | A standard, first-pass biomarker. Can have high false positives/negatives; must be combined with other markers (e.g., p16) for confirmation [57]. |
| Antibodies for Western Blot (e.g., Acetyl-Histone H3, p16INK4A, p21, HDACs) | Assess HDACi activity (histone acetylation) and confirm senescent state. | Monitoring acetyl-histone levels is critical for verifying effective HDAC inhibition in your specific cell model [58] [57]. |
FAQs and Troubleshooting Guides
FAQ 1: Yield and Production Optimization
Q1: Why is my 3D culture system not yielding more EVs than my 2D cultures? A: Suboptimal yield in 3D cultures is often due to inadequate scaling or incorrect bioreactor parameters. Unlike 2D, 3D systems require careful optimization of dynamic conditions. Ensure you are using a system that promotes high cell density and health. Studies show that vertical wheel bioreactors (VWBRs) can significantly enhance EV production and cell productivity compared to both 2D and other 3D systems like spinner flasks [62]. Check that your system provides sufficient nutrient transfer and avoids necrotic cores in large spheroids [63].
Q2: How can I enhance the therapeutic potency of EVs from my 3D cultures? A: The functionality of EVs is tightly linked to the physiological state of the parent cells. To enhance anti-inflammatory or pro-regenerative effects, consider using human Mesenchymal Stem Cells (hMSCs) in a dynamic 3D bioreactor. Research confirms that EVs from hMSCs grown in a VWBR show superior ability to attenuate oxidative stress and suppress pro-inflammatory cytokines (e.g., TNF-α) and NF-κB activation [62]. Priming parent cells with specific stimuli or using scaffold-based 3D cultures to better mimic the native ECM can also enhance EV cargo and function [64] [65].
FAQ 2: Characterization and Functional Analysis
Q3: How do I confirm that the vesicles I'm collecting from 3D cultures are indeed EVs? A: Proper characterization is a multi-step process. You should analyze the isolated vesicles for size, concentration, and specific protein markers.
- Size and Concentration: Use Nanoparticle Tracking Analysis (NTA) to confirm a size profile typically between 30-200 nm for exosomes/small EVs and quantify the yield [62].
- Morphology: Use Transmission Electron Microscopy (TEM) to visualize the lipid bilayer structure [63].
- Surface Markers: Identify positive protein markers (e.g., Tetraspanins like CD63, CD81, TSG101) and negative markers (e.g., Apoptotic body markers) via Western Blot or ELISA [64]. For instance, ELISA can quantify specific markers like Glypican-1 (GPC-1), which was found to be 4-fold higher in exosomes from 3D PANC-1 spheroids [63].
Q4: My EVs have a different miRNA cargo profile in 3D vs. 2D. Is this expected? A: Yes, this is a key finding and an advantage of 3D culture. The 3D microenvironment alters cell signaling and leads to the enrichment of specific EV cargo. In a study on PANC-1 cells, exosomes from 3D spheroids showed significant enrichment of specific miRNAs (like miR-1246, miR-21, miR-17-5p, and miR-196a) compared to 2D cultures [63]. This cargo difference is biologically significant and likely contributes to the enhanced physiological relevance of 3D-derived EVs.
FAQ 3: Technical and Scaling Challenges
Q5: What are the main challenges in scaling up 3D EV production for clinical translation? A: The primary challenges are:
- Bioprocessing: Moving from static cultures to scalable, controlled, and reproducible bioreactor systems that can produce the tens to hundreds of millions of EVs required for a clinical dose [66] [62].
- Standardization: A lack of standardized protocols for EV isolation and purification from 3D cultures leads to batch-to-batch variability [64] [66].
- Characterization and Regulation: Ensuring consistent EV quality, potency, and purity at a large scale is complex. Furthermore, no global drug regulatory agency has yet issued specific technical guidelines for EV-based drugs, creating uncertainty [66].
Q6: How can I prevent the formation of a necrotic core in my 3D spheroids? A: Necrotic cores form due to limited diffusion of oxygen and nutrients in large, dense spheroids.
- Control Spheroid Size: Optimize initial seeding density and culture time to prevent spheroids from becoming too large [63].
- Use Dynamic Culture: Bioreactors like VWBRs or spinner flasks improve nutrient and gas exchange through gentle mixing, reducing the risk of necrosis compared to static 3D cultures [62].
- Incorporate Perfusion: If possible, use systems with continuous medium perfusion to enhance mass transfer.
Table 1: Comparative Analysis of EV Production in 2D vs. 3D Culture Systems
| Culture System | Cell Type | Key EV Output Metric | Observed Outcome (3D vs. 2D) | Key Functional Findings | Reference |
|---|---|---|---|---|---|
| Ultra-low attachment (ULA) plates | PANC-1 pancreatic cancer cells | miRNA content (miR-1246, miR-21, etc.) | Significantly enriched in 3D-derived exosomes [63] | Exosomes from 3D spheroids exhibited a 4-fold increase in GPC-1 levels [63] | [63] |
| ULA plates | PANC-1 pancreatic cancer cells | Protein marker (GPC-1) | 4-fold increase in 3D-derived exosomes [63] | Exosomes from 3D spheroids exhibited a 4-fold increase in GPC-1 levels [63] | [63] |
| Vertical Wheel Bioreactor (VWBR) | Adipose-derived hMSCs | Total EV production & cell productivity | Significantly higher in VWBR vs. 2D and other 3D systems [62] | Attenuated oxidative stress, suppressed TNF-α & NF-κB activation [62] | [62] |
| Spinner Flask Bioreactor (SFB) | Adipose-derived hMSCs | Total EV production & cell productivity | Significantly higher in SFB vs. 2D [62] | Suppressed pro-inflammatory cytokine secretion [62] | [62] |
Table 2: Troubleshooting Common Problems in 3D EV Production
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low EV Yield | - Static culture with poor nutrient/waste exchange- Low cell density or viability- Necrotic core in spheroids | - Transition to a dynamic bioreactor (e.g., VWBR)- Optimize seeding density and culture duration- Implement perfusion or optimize agitation speed [62] |
| Poor EV Purity | - Contamination with cell debris and protein aggregates- Inefficient isolation method | - Use sequential centrifugation steps post-collection- Combine isolation methods (e.g., ExtraPEG-based UC, size-exclusion chromatography) [64] [62] |
| Inconsistent EV Cargo/Function | - Batch-to-batch variation in 3D culture- Uncontrolled culture parameters (pH, O₂)- Parent cell senescence | - Strictly standardize cell culture and EV isolation protocols- Use bioreactors with integrated sensors for monitoring- Use low-passage, healthy cells and monitor senescence markers [66] |
Experimental Protocols
Protocol 1: Enhanced EV Production using a Vertical Wheel Bioreactor (VWBR)
Objective: To produce a high yield of functional EVs from human Mesenchymal Stem Cells (hMSCs) using a scalable 3D bioreactor system.
Materials:
- Cells: Human adipose-derived MSCs (e.g., from Tulane Center for Stem Cell Research) [62].
- Bioreactor: Vertical Wheel Bioreactor (VWBR) system.
- Base Medium: Alpha-Minimal Essential Medium (α-MEM).
- Supplements: 10% exosome-depleted Fetal Bovine Serum (FBS), 1% penicillin-streptomycin.
- Isolation Reagents: ExtraPEG-based ultracentrifugation solution [62].
Method:
- Cell Expansion: Expand hMSCs in 2D culture (e.g., 150 mm dishes) until passage 6, using standard culture conditions (37°C, 5% CO₂).
- Bioreactor Seeding: Seed cells into the VWBR to form 3D aggregates. The specific hydrodynamic properties of the VWBR promote aggregate formation without the need for microcarriers.
- Culture Maintenance: Culture cells in the VWBR with controlled parameters (e.g., agitation speed, temperature, CO₂). Maintain cultures for several days, monitoring cell growth and viability.
- Conditioned Media Collection: After reaching the desired culture density, collect the conditioned media.
- EV Isolation:
- Centrifuge the conditioned media at low speed (e.g., 500 × g) to remove cells and large debris.
- Further clarify the supernatant by centrifugation at a higher speed (e.g., 10,000 × g) to remove apoptotic bodies and other large particles.
- Isolve EVs from the clarified supernatant using the ExtraPEG-based ultracentrifugation method [62].
- EV Characterization: Resuspend the EV pellet and characterize using NTA for concentration/size, TEM for morphology, and Western Blot/ELISA for specific markers.
Protocol 2: Functional Assessment of Anti-inflammatory Effects of EVs
Objective: To evaluate the anti-inflammatory capacity of 3D-derived EVs on target neural cells.
Materials:
- Test EVs: EVs isolated from 3D hMSC cultures (from Protocol 1).
- Cell Model: An in vitro model of neural inflammation, such as brain organoids derived from iPSCs of a sporadic Alzheimer's disease patient [62].
- Assay Kits: Commercial kits for measuring oxidative stress (e.g., ROS detection), TNF-α secretion (ELISA), and gene expression (qRT-PCR for NF-κB pathway genes and neurodegenerative markers).
Method:
- Treatment: Apply the isolated hMSC-EVs to the culture medium of the inflamed neural model. Include a control group treated with a vehicle (PBS).
- Oxidative Stress Measurement: After an appropriate incubation period, lyse the cells and measure levels of reactive oxygen species (ROS) using a fluorescent probe according to the kit's protocol.
- Cytokine Profiling: Collect the conditioned media from the treated cells. Use an ELISA kit to quantify the secretion of the pro-inflammatory cytokine TNF-α.
- Gene Expression Analysis: Extract total RNA from the treated cells. Perform qRT-PCR to analyze the expression of genes involved in the NF-κB signaling pathway and specific neurodegenerative markers.
- Data Analysis: Compare the ROS levels, TNF-α concentration, and gene expression profiles between EV-treated and control groups. A significant suppression in the EV-treated group indicates potent anti-inflammatory functionality [62].
Signaling Pathways and Workflows
EV Biogenesis and Functional Pathway in 3D Culture
3D EV Production and Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D EV Research
| Item | Function/Application in 3D EV Research | Example/Specification |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Promotes scaffold-free 3D spheroid formation by minimizing cell adhesion to the surface. | Plates coated with hydrophilic polymer (e.g., poly-HEMA) [63]. |
| Vertical Wheel Bioreactor (VWBR) | A scalable dynamic 3D culture system that enhances EV yield and quality through optimized hydrodynamics. | Provides efficient mixing with low shear stress, suitable for growing cell aggregates [62]. |
| Exosome-Depleted FBS | Essential supplement for cell culture media to avoid contamination with bovine EVs during EV production. | FBS processed by ultracentrifugation or commercial kits to remove endogenous vesicles [63] [62]. |
| ExtraPEG-based UC Kit | A precipitation-based method for isolating EVs from large volumes of conditioned media. | Offers a potentially scalable alternative to traditional ultracentrifugation [62]. |
| Nanoparticle Tracking Analysis (NTA) | Instrumentation for determining the size distribution and concentration of EV preparations. | Critical for quantifying yield and confirming EV size profile (e.g., 30-200 nm) [62]. |
| miRNA & Protein Assay Kits | For analyzing specific cargo (e.g., miRNAs, surface markers) to confirm EV identity and functionality. | qRT-PCR for miRNAs; ELISA for proteins like GPC-1 [63]. |
Overcoming Translational Hurdles: Specificity, Delivery, and Functional Assessment Challenges
Frequently Asked Questions (FAQs)
FAQ 1: Why is targeting senescent cells so challenging, and what role does heterogeneity play? Senescent cells are challenging to target because they are not a uniform population. Cellular senescence is highly heterogeneous; the specific markers expressed and the strength of the senescence-associated secretory phenotype (SASP) can vary dramatically depending on the cell type of origin, the stimulus that induced senescence, and the tissue microenvironment [67] [68] [69]. For example, a senescent fibroblast will differ significantly from a senescent endothelial cell, and a cell that became senescent due to radiation will have a different SASP profile than one that senesced from an activated oncogene [68]. This means there is no single, universal "senescence marker," making it difficult to design a one-size-fits-all therapy.
FAQ 2: What are the primary strategic approaches for targeting senescent cells? There are two main strategic approaches for targeting senescent cells:
- Senolytics: These are small molecules or other therapeutics that selectively induce apoptosis (programmed cell death) in senescent cells [67] [70]. They aim to clear these cells from tissues.
- Senomorphics (or Senostatics): These compounds do not kill senescent cells but instead suppress the detrimental effects of the SASP—the inflammatory cocktail they secrete [67] [71] [70]. This approach aims to neutralize the harmful influence of senescent cells on their surroundings without removing them.
FAQ 3: Are there functional differences between senescent cell subpopulations that impact therapy? Yes, recent research using high-content imaging has revealed that functionally distinct senescent subpopulations exist even within a uniformly treated culture. A key finding is that the cell cycle phase at the time of senescence induction can determine the cell's functional properties. For instance, senescent cells arrested in the G2 phase have been shown to express higher levels of senescence markers, secrete more IL-6 (a key SASP factor), and demonstrate greater sensitivity to senolytic drugs like ABT263 compared to G1-arrested senescent cells [68]. This indicates that the efficacy of senolytics can depend on the specific subpopulation being targeted.
FAQ 4: What are some emerging technologies for studying senescent cell heterogeneity? Advanced single-cell technologies are crucial for dissecting senescence heterogeneity. Single-cell RNA sequencing (scRNA-seq) allows for the analysis of the unique transcriptomic profiles of individual senescent cells, helping to identify new subtypes and markers [69]. Furthermore, high-content imaging flow cytometry combines the high-throughput capability of flow cytometry with single-cell image acquisition, enabling researchers to analyze multiple senescence markers at the protein level while also assessing cell morphology and excluding artifacts [72].
Troubleshooting Guides
Issue 1: Low Specificity and Efficiency of Senolytic Treatment
Potential Cause: The senolytic compound being used may not be effective against the specific senescent cell subpopulation present in your model system. Heterogeneity in senescence drivers (e.g., p16INK4a vs. p21) and cell cycle status can lead to varied senolytic responses [68].
Recommended Actions:
- Characterize Your Model: Use a panel of senescence biomarkers (see Table 1) to define the primary drivers and features of senescence in your cells. Do not rely on a single marker.
- Combine Senolytics: Consider using a combination of senolytic agents that target different anti-apoptotic pathways (e.g., dasatinib + quercetin) to broaden the spectrum of targetable senescent cells [67].
- Investigate New Modalities: Explore next-generation strategies such as senolytic CAR-T cells or antibody-drug conjugates (ADCs) that target specific senescent cell surface antigens for highly precise elimination [67].
Issue 2: Inconsistent Identification and Sorting of Senescent Cells
Potential Cause: The inherent heterogeneity in size, granularity, and marker expression makes it difficult to reliably identify and isolate a pure population of senescent cells using standard flow cytometry [72].
Recommended Actions:
- Employ Multiplexed Detection: Always use a combination of markers. A common and effective strategy is to use C12FDG (a fluorogenic substrate for SA-β-gal) to detect lysosomal content, combined with analysis of cell size (FSC) and granularity (SSC) [72].
- Utilize Imaging Flow Cytometry: This technology can help distinguish true, large senescent cells from doublets of proliferating cells, which is a common pitfall of traditional flow cytometry [72].
- Validate with Multiple Assays: Correlate your flow cytometry data with other senescence assays, such as the presence of nuclear γH2AX foci (indicating DNA damage) or the loss of Lamin B1 [68].
Quantitative Data on Senescence and Senolysis
Table 1: Common Senescence Biomarkers and Their Detection Methods
| Biomarker | Detection Method | Function/Interpretation | Notes on Heterogeneity |
|---|---|---|---|
| SA-β-Gal Activity | Histochemistry (X-Gal), Flow Cytometry (C12FDG) | Increased lysosomal activity at pH 6.0 [71] [72] | Not exclusive to senescence; levels can vary by cell type and inducer [68]. |
| p16INK4A | Immunocytochemistry (ICC), Western Blot | CDK inhibitor, enforces cell cycle arrest [71] | A robust marker but not universally expressed in all senescent cells [69]. |
| p21 | ICC, Western Blot | CDK inhibitor, responds to p53 and DNA damage [71] | Often associated with initial senescence arrest; expression can be transient [71]. |
| SASP Factors | ELISA, Multiplex Immunoassays | Pro-inflammatory cytokines (e.g., IL-6, IL-8), chemokines, growth factors [67] [71] | SASP composition is highly variable and context-dependent [67] [68]. |
| Nuclear Lamin B1 | ICC | Component of the nuclear lamina [68] | Loss is a common feature of senescence, but the extent of loss can vary [68]. |
| γH2AX Foci | ICC | Marker of DNA double-strand breaks and persistent DNA damage response [68] | Indicates the DNA damage pathway is active; number of foci can be heterogeneous [68]. |
Table 2: Examples of Senotherapeutics and Their Reported Targets
| Therapeutic | Class | Primary Target/Mechanism | Stage / Context |
|---|---|---|---|
| Dasatinib + Quercetin | Senolytic (combination) | Targets BCL-2 family and other pro-survival pathways in SnCs [67] | Clinical trials for age-related diseases [67]. |
| Fisetin | Senolytic (natural product) | Flavonoid that targets SnC pro-survival pathways [67] [70] | Shown to extend healthspan in animal models [67]. |
| Navitoclax (ABT263) | Senolytic | BCL-2/BCL-xL inhibitor [67] | Preclinical studies; sensitivity varies by SnC subpopulation (e.g., G2-arrested more sensitive) [68]. |
| Rapamycin | Senomorphic | mTOR inhibitor; suppresses SASP production [67] [71] | Preclinical and clinical research for aging [67]. |
| Metformin | Senomorphic | AMPK activator; can reduce SASP and inflammatory signaling [67] [70] | Repurposed drug in clinical trials for aging (e.g., TAME) [67]. |
| UBX1325 | Senolytic | BCL-xL inhibitor [68] | Phase 2 clinical trial for diabetic macular degeneration [68]. |
Experimental Protocols for Key Assays
Protocol 1: Evaluating Senolytic Sensitivity in Heterogeneous Populations
This protocol is adapted from research investigating the differential sensitivity of senescent subpopulations to senolytics [68].
Objective: To determine the efficacy of a senolytic compound (e.g., ABT263) on distinct senescent cell subpopulations defined by cell cycle status or marker expression.
Materials:
- Senescent cell model (e.g., primary human fibroblasts or endothelial cells induced by ionizing radiation).
- Senolytic compound (e.g., ABT263 dissolved in DMSO).
- Cell culture plates and standard medium.
- Reagents for immunofluorescence: antibodies against p21, γH2AX, Lamin B1, and a viability dye (e.g., Zombie Yellow [73]).
- High-content imaging system or automated microscope.
Method:
- Induce Senescence: Treat cells with your chosen stressor (e.g., 10 Gy ionizing radiation). Maintain for 10-14 days to establish stable senescence, confirming with markers like SA-β-Gal positivity and lack of EdU incorporation [68].
- Treat with Senolytic: Seed senescent cells and appropriate non-senescent controls. Treat with a range of senolytic concentrations or vehicle control for 24-48 hours.
- Stain and Image: Fix and permeabilize cells. Perform immunocytochemistry for markers of interest (e.g., p21, γH2AX) and a viability dye. Acquire high-resolution images of thousands of cells per condition using an automated microscope.
- Analyze Data: Use image analysis software to segment individual cells. Quantify the intensity of senescence markers and viability status for each cell. Correlate cell death (viability dye positive) with pre-treatment levels of specific markers or use DNA content to gate on G1 and G2 subpopulations [68].
- Interpretation: A successful experiment will show that the senolytic preferentially kills cells with high senescence marker expression and that the killing efficiency is significantly higher in one subpopulation (e.g., G2-arrested) over another.
Protocol 2: Assessing DC Activation by Senescent Tumor Cells
This protocol outlines a method to study the immunogenicity of senescent cells, a key aspect of their heterogeneous biological impact [73].
Objective: To investigate the ability of therapy-induced senescent (TIS) tumor cells to stimulate the maturation and activation of CD103+ dendritic cells (DCs), a critical step in anti-tumor immunity.
Materials:
- Murine tumor cell line (e.g., CT26 colon carcinoma).
- Senescence-inducing drugs (e.g., Etoposide).
- Bone marrow from matched mouse strain.
- Recombinant murine GM-CSF and Flt3-ligand.
- Flow cytometry antibodies: CD11c, CD103, MHC II, CD80, CD86.
Method:
- Generate Senescent Tumor Cells: Treat CT26 cells with a senescence-inducing agent like etoposide for several days. Validate senescence by SA-β-Gal staining and increased p16/p21 expression [73].
- Differentiate CD103+ DCs: Isolate bone marrow from mice and culture with GM-CSF and Flt3-ligand for 8-9 days to generate CD11c+/CD103+ DCs [73].
- Co-culture: Co-culture the differentiated DCs with either senescent or non-senescent (control) CT26 cells for 24-48 hours.
- Flow Cytometric Analysis: Harvest the DCs and stain for surface markers. Analyze by flow cytometry for maturation markers (e.g., MHC II, CD80, CD86). Increased expression of these markers on DCs co-cultured with senescent cells indicates enhanced activation [73].
- Interpretation: This protocol allows you to test whether a specific population of senescent cells can promote an immunogenic response, which is highly relevant for understanding the dual roles of senescence in cancer.
Key Signaling Pathways in Senescence Heterogeneity
The following diagram illustrates the core molecular pathways that drive cellular senescence, highlighting sources of heterogeneity. Variations in the activation level of these pathways contribute to the distinct phenotypes of senescent subpopulations.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Senescence Studies
| Reagent / Tool | Function / Application | Example Product / Citation |
|---|---|---|
| C12FDG | A fluorogenic substrate for SA-β-gal used to detect senescent cells via flow cytometry or microscopy [72]. | Commercially available (e.g., Gold Biotechnology, X4281C [73]). |
| Antibody Panel for ICC/Flow | Multiplexed detection of key senescence proteins (p16, p21, γH2AX, Lamin B1) for phenotypic characterization [72] [68]. | Antibodies from various suppliers (e.g., Cell Signaling Technology). |
| Senolytic Compounds | To selectively eliminate senescent cells in experimental models for functional validation. | ABT263 (Navitoclax), Dasatinib, Quercetin, Fisetin [67] [68]. |
| Recombinant Cytokines | For in vitro differentiation of specific immune cells used in co-culture assays with SnCs. | Recombinant murine GM-CSF and Flt3-ligand for DC differentiation [73]. |
| Flow Cytometry Antibodies for Immune Profiling | To analyze the activation state of immune cells (e.g., DCs, T cells) in response to SnCs. | Antibodies against CD11c, CD103, MHC II, CD80, CD86 [73]. |
| High-Content Imaging Systems | Automated microscopy for single-cell analysis of multiple senescence markers and morphology. | Cytek Amnis ImageStreamX, Nikon Eclipse Ti-PFS [72] [68]. |
Troubleshooting Guide: Common Experimental Challenges in Senescence-Targeting Nanotherapies
FAQ 1: How can I improve the stability and shelf-life of my senolytic-loaded lipid nanoparticles?
Problem: Lipid nanoparticles (LNPs) encapsulating senolytic agents like Dasatinib and Quercetin show aggregation or drug degradation during storage, leading to inconsistent experimental results.
Solution:
- Pre-conditioning: Implement a freeze-drying (lyophilization) process with cryoprotectants such as trehalose (100-200 mM) to enhance storage stability [74].
- Formulation Optimization: Ensure a neutral to slightly negative surface charge (zeta potential between -10 mV to -20 mV) to minimize aggregation. Characterize size and polydispersity index (PDI) using dynamic light scattering (DLS) pre- and post-storage; a PDI below 0.2 indicates a monodisperse, stable formulation [74] [75].
- Quality Control: Establish a stability testing protocol storing batches at 4°C, -20°C, and -80°C. Monitor size, PDI, and drug encapsulation efficiency weekly for one month using HPLC to track drug content [76].
FAQ 2: My nanoparticle system shows poor uptake by senescent mesenchymal stem cells (MSCs). What targeting strategies can I implement?
Problem: Nanoparticles fail to efficiently localize to and internalize within target senescent stem cells, reducing therapeutic efficacy.
Solution:
- Active Targeting: Functionalize nanoparticle surfaces with ligands that bind receptors overexpressed on senescent MSCs. Common ligands include:
- Characterization Workflow:
- Confirm ligand conjugation success using X-ray Photoelectron Spectroscopy (XPS) or Fourier-Transform Infrared Spectroscopy (FTIR).
- Validate targeting efficiency in vitro using flow cytometry and confocal microscopy. Compare cellular uptake in senescent vs. non-senescent MSCs induced by hydrogen peroxide (100-200 µM for 2 hours) or serial passaging (passages 12-15) [29] [78].
FAQ 3: How do I confirm that my nanocarrier is selectively releasing its payload in senescent cells?
Problem: Uncontrolled drug release in the extracellular environment or in non-target cells leads to off-target effects.
Solution: Engineer nanoparticles with stimuli-responsive release mechanisms triggered by the unique microenvironment of senescent cells.
- pH-Responsive Systems: Use polymers or lipids that degrade in the slightly acidic lysosomal environment (pH ~5.0). Incorporate a pH-sensitive dye (e.g., CypHer-5E) to track intracellular release via fluorescence microscopy [77] [78].
- Enzyme-Responsive Systems: Design nanocarriers sensitive to enzymes upregulated in senescence, such as SA-β-Gal. Use substrates like a DDAOG/β-galactosidase probe to visualize enzyme-triggered release [77].
FAQ 4: What are the best practices for quantifying the removal of senescent cells and the resulting rejuvenation of stem cell populations?
Problem: Difficulty in measuring the direct senolytic effect and subsequent functional improvement in stem cell cultures.
Solution: Employ a multi-parametric validation approach.
- Viability Assays: Use a combination of PrestoBlue for overall metabolic activity and a Caspase-3/7 glow assay to specifically quantify apoptosis in treated vs. untreated senescent MSC cultures.
- Senescence Biomarkers: Quantify the reduction of key senescence markers post-treatment using:
- Functional Rejuvenation: Assess the restoration of "youthful" MSC function by conducting:
Experimental Protocols for Key Applications
Protocol: Evaluating Senolytic Nano-Formulations in Aged Mesenchymal Stem Cells
Objective: To test the efficacy and specificity of a senolytic-loaded nanoparticle formulation in clearing senescent MSCs and restoring regenerative functions.
Materials:
- Cell Model: Human bone marrow-derived MSCs (passage 4-5 for "young" control; passage 12-15 for "aged/senescent").
- Induction of Senescence: Treat early-passage MSCs with 150 µM hydrogen peroxide (H2O2) for 2 hours, then recover in complete media for 7 days to establish a stable senescent phenotype [29].
- Nanoparticles: Senolytic-loaded nanoparticles (e.g., Dasatinib + Quercetin in PLGA nanoparticles) and corresponding empty nanoparticles as a control.
Methodology:
- Characterization of Senescence: Confirm the senescent phenotype prior to treatment by staining for SA-β-Gal and analyzing p16 and p21 expression via Western Blot.
- Treatment:
- Seed senescent and young MSCs in 96-well plates (5,000 cells/well).
- Treat with: i) Senolytic nanoparticles, ii) Free senolytic drugs, iii) Empty nanoparticles, iv) Fresh media (untreated control).
- Incubate for 72 hours.
- Efficacy Assessment:
- Cell Viability: Perform PrestoBlue assay at 24, 48, and 72 hours.
- Apoptosis: Measure Caspase-3/7 activity at 48 hours.
- SASP Reduction: Collect conditioned media at 72 hours and analyze IL-6 levels using ELISA.
- Functional Recovery:
- After a 7-day post-treatment recovery, perform a CFU assay by re-seeding 1000 cells in a 10 cm dish and staining with crystal violet after 14 days.
- Induce osteogenic differentiation and quantify mineralization by Alizarin Red S staining after 21 days.
Protocol: Assessing Biodistribution and Off-Target Effects in a 3D Spheroid Model
Objective: To model nanoparticle targeting and penetration in a more physiologically relevant 3D environment containing a mix of senescent and proliferating cells.
Materials:
- 3D Spheroid Model: Co-culture spheroids of GFP-labeled senescent MSCs and mCherry-labeled young MSCs.
- Nanoparticles: Fluorescently labeled (e.g., Cy5) targeted and non-targeted nanoparticles.
Methodology:
- Spheroid Generation: Use a low-adhesion U-bottom 96-well plate to generate co-culture spheroids (500 cells/spheroid) via the hanging-drop method or forced aggregation.
- Treatment and Imaging:
- Incubate spheroids with Cy5-labeled nanoparticles for 24-48 hours.
- Image using a confocal microscope with z-stacking at 24 and 48 hours.
- Analyze fluorescence intensity in the core (senescent cell-rich) versus the periphery (proliferating cell-rich) of the spheroid to quantify targeting precision.
- Viability Analysis: Use a live/dead stain (e.g., Calcein-AM/Propidium Iodide) on the whole spheroid to assess selective cytotoxicity towards senescent cells and minimal damage to healthy cells.
Data Presentation
Table 1: Key Characterization Parameters for Senescence-Targeting Nanoparticles
| Parameter | Target Range | Analytical Technique | Significance for Senescence Targeting |
|---|---|---|---|
| Size (Hydrodynamic Diameter) | 50 - 150 nm | Dynamic Light Scattering (DLS) | Optimal for passive accumulation via EPR effect; facilitates cellular uptake [74]. |
| Polydispersity Index (PDI) | < 0.2 | Dynamic Light Scattering (DLS) | Indicates a uniform particle population, ensuring consistent batch-to-batch behavior [74]. |
| Zeta Potential | ±5 to -25 mV | Electrophoretic Light Scattering | Moderate negative charge often reduces non-specific binding, improving circulation time [75]. |
| Drug Loading Capacity | > 5% w/w | HPLC/UV-Vis Spectrophotometry | Ensures a sufficient therapeutic payload is delivered per particle to elicit a biological effect. |
| Encapsulation Efficiency | > 80% | HPLC/UV-Vis Spectrophotometry | Maximizes cost-effectiveness and minimizes waste of often expensive senotherapeutic agents. |
Table 2: Analysis of Senescence Clearance and Functional Recovery Post-Nanotherapy
| Assay | Expected Outcome (Treated vs. Untreated Senescent MSCs) | Measurement Technique | Interpretation |
|---|---|---|---|
| SA-β-Gal Activity | > 50% reduction | Flow Cytometry / Fluorescence Microscopy | Direct evidence of senescent cell clearance. |
| SASP Factor (e.g., IL-6) | > 60% reduction in secretion | ELISA | Confirms abatement of the pro-inflammatory secretome. |
| Apoptosis Activation | > 3-fold increase in Caspase 3/7 activity | Luminescence-based Caspase-Glo Assay | Validates activation of the intended senolytic (pro-apoptotic) pathway. |
| Clonogenic Capacity (CFU) | 2 to 3-fold increase | Colony-Forming Unit Assay | Demonstrates restoration of critical stem cell self-renewal potential. |
| Osteogenic Potential | Significant increase in mineralization | Alizarin Red S Quantification | Indicates recovery of multi-lineage differentiation capacity. |
Signaling Pathways and Workflows
Diagram: Senescence Signaling and Nanotherapeutic Targeting
Title: Nano-Therapy Targeting of Senescence Pathways.
Diagram: Experimental Workflow for Nano-Senotherapy Validation
Title: Workflow for Validating Nano-Senotherapies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Nanotechnology-Enabled Senescence Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable polymer for nanoparticle fabrication; enables controlled drug release of senolytics [76]. | Vary the lactide:glycolide ratio to tune degradation kinetics from weeks to months. |
| Cremophor-Free Formulations (e.g., nab-paclitaxel) | Clinically approved nanocarrier platform; provides a benchmark for biocompatibility and efficient drug solubilization without toxic solvents [74]. | Useful as a reference when developing novel nano-formulations for hydrophobic drugs. |
| Senescence-Inducing Agents (H2O2, Etoposide) | Tools for generating in vitro models of senescence in stem cell populations for screening nanotherapies [29]. | Optimize concentration and duration (e.g., 100-200 µM H2O2 for 2 hrs) to achieve stable arrest without overwhelming cell death. |
| SA-β-Gal Staining Kit (with C12FDG) | Gold-standard for detecting senescent cells; C12FDG is a fluorescent substrate for flow cytometry, superior to traditional X-Gal for quantification [77] [78]. | |
| FOXO3 Gene Constructs | Genetic tool for creating enhanced "senescence-resistant" stem cells (SRCs) via genetic engineering; a key intervention in anti-aging stem cell studies [80]. | Can be used to pre-condition MSCs before nanoparticle testing to study combination effects. |
| Stimuli-Responsive Linkers (pH-, Enzyme-) | Critical components for constructing "smart" nanoparticles that release payloads specifically in the senescent microenvironment [77] [78]. | Ensure linker activation threshold (e.g., pH 6.0 vs 5.0) matches the target organelle (early vs late endosome). |
| Exosome Isolation Kits | For harvesting natural nanovesicles from engineered young or SRC MSCs; used as therapeutic agents or drug delivery vehicles themselves [80] [78]. | Isolated exosomes can be loaded with anti-senescence miRNAs or drugs for targeted delivery. |
For researchers and scientists in stem cell research and drug development, the accumulation of senescent cells during in vitro expansion poses a major barrier to producing high-quality, therapeutically viable cell products. Cellular senescence, a state of stable cell cycle arrest, is triggered by various stresses encountered during culture, including replicative exhaustion, oxidative stress, and DNA damage [81] [77]. These senescent cells are not merely inert; they actively secrete a plethora of pro-inflammatory cytokines, chemokines, and growth factors—the Senescence-Associated Secretory Phenotype (SASP)—which can compromise the function of neighboring cells, skew differentiation protocols, and potentially impair the safety and efficacy of cell-based therapies [81] [82]. This technical support center provides targeted troubleshooting guides and FAQs to help you identify, prevent, and mitigate cellular senescence in your manufacturing pipeline.
FAQ: Understanding and Identifying Senescence
Q1: What are the primary drivers of senescence in stem cell cultures? Senescence in culture is driven by multiple interconnected factors. Replicative senescence occurs due to progressive telomere shortening with each cell division, ultimately triggering a DNA damage response (DDR) [81] [82]. Oxidative stress from culture conditions can accelerate this process by causing damage to lipids, proteins, and DNA [81]. Furthermore, oncogene-induced senescence can be triggered by excessive proliferative signaling during culture expansion, and even paracrine senescence can occur where SASP factors from a few senescent cells induce senescence in surrounding healthy cells [81].
Q2: Why can't I rely solely on SA-β-Galactosidase staining to identify senescent cells? While SA-β-Galactosidase activity at pH 6.0 is a widely used marker, it is not entirely specific. Its activity can be influenced by factors like high cell confluency and serum starvation, potentially leading to false positives [83]. Given the heterogeneity of senescent cells, a multi-parameter approach is essential for confident identification [83] [84]. SA-β-Gal should be used in conjunction with other markers such as p16INK4a and p21CIP1 (key cell cycle regulators) and γH2AX (a marker of DNA damage) for a more robust assessment [81] [83].
Q3: What are the key differences between senolytic and senomorphic strategies? Senolytics are compounds designed to selectively induce apoptosis in senescent cells, thereby clearing them from the culture. Examples include dasatinib and quercetin [85]. In contrast, senomorphics do not kill senescent cells but instead suppress the detrimental SASP. Urolithin A, for instance, has been shown to potently reduce senescence-related markers and SASP [86]. The choice between strategies depends on your application—whether complete removal of senescent cells is required or if dampening their inflammatory secretome is sufficient.
Q4: How can I modulate the culture environment to slow the onset of senescence? Targeting metabolic and inflammatory pathways is a promising approach. Research shows that suppressing lysosomal hyperactivation can revitalize aged hematopoietic stem cells and improve their regenerative capacity [2]. NAD+ boosters, such as Nicotinamide Riboside, can improve mitochondrial function and have shown potential in extending healthspan in models [77] [85]. Additionally, modulating the cGAS-STING pathway, a key driver of inflammation in aging stem cells, can reduce harmful interferon-driven pathways [2].
Troubleshooting Guide: Common Senescence-Related Issues
Table 1: Troubleshooting Senescence in Cell Culture
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Premature Growth Arrest | Replicative exhaustion, oxidative stress, high seeding density | Check population doubling level; use low-oxygen (physioxic) conditions; ensure sub-confluent passaging [82]. |
| Increased SA-β-Gal Activity | High cell confluency, serum starvation, genuine senescence | Confirm with other markers (e.g., p16, γH2AX); optimize culture conditions to avoid artifacts [83]. |
| Loss of Differentiation Potential | Accumulation of senescent cells, inflammatory SASP | Implement a senolytic treatment (e.g., dasatinib + quercetin) pre-differentiation; test differentiation capacity at lower passages [85] [87]. |
| High SASP-Related Inflammation | Persistent senescent cell population, paracrine signaling | Consider senomorphic agents (e.g., Urolithin A); use culture supplements that inhibit NF-κB signaling [81] [86]. |
| Heterogeneous Senescence in Batch | Stochastic onset, uneven nutrient/waste distribution | Use a multiparameter flow cytometry assay to characterize heterogeneity; improve bioreactor mixing parameters [83]. |
Key Experimental Protocols
Protocol: Multiparameter Flow Cytometry for Senescence Detection
This protocol allows for the simultaneous quantification of multiple senescence markers at single-cell resolution, providing a sensitive and high-throughput alternative to standalone SA-β-Gal staining [83].
- Cell Staining:
- Seed cells and culture for 24 hours.
- Treat with 0.1 µM Bafilomycin A1 to induce lysosomal alkalinization.
- Add 0.02 mM DDAOG, a substrate for β-Galactosidase that generates a far-red fluorescent signal upon hydrolysis. Incubate for 2 hours at 37°C [83].
- Cell Harvesting and Viability Staining:
- Detach cells using a gentle enzyme like TrypLE.
- Stain with a fixable viability dye (e.g., FV450; 1:1000) in PBS for 15 minutes at room temperature [83].
- Fixation and Permeabilization:
- Wash cells and resuspend in BD Cytofix/Cytoperm solution for 30 minutes at room temperature.
- Wash twice with 1x BD Perm/Wash buffer [83].
- Intracellular Antibody Staining:
- Flow Cytometry Analysis:
- Analyze the cells using a flow cytometer capable of detecting multiple fluorophores.
- Gate on live, single cells and quantify the co-expression of SA-β-Gal (via DDAO), p16, and γH2AX.
The workflow for this multi-marker detection protocol is summarized in the following diagram:
Protocol: Testing Senomorphic Compounds for SASP Suppression
This protocol outlines how to evaluate the efficacy of potential senomorphic compounds like Urolithin A in suppressing the SASP [86].
- Induce Senescence:
- Treat your cell type (e.g., human mesenchymal stem cells) with a stressor such as 200 nM Doxorubicin or 5 µM 5’-Aza-2-deoxycytidine for 48 hours.
- Wash the cells with PBS and culture in fresh, drug-free media for an additional 5-7 days to establish senescence [83].
- Apply Senomorphic:
- After senescence is established, add the senomorphic candidate (e.g., Urolithin A) to the culture medium. Include a vehicle control (DMSO) group.
- Incubate for 24-72 hours.
- Analyze SASP Output:
- Conditioned Media Analysis: Collect conditioned media. Analyze levels of key SASP factors (e.g., IL-6, IL-8, MMPs) using ELISA or a multiplex immunoassay.
- Transcriptional Analysis: Harvest cells for RNA extraction. Perform qRT-PCR to measure the expression of SASP-related genes (e.g., IL6, IL8, CXCL2).
Key Signaling Pathways in Senescence
The transition of a cell to a senescent state is governed by a few core signaling pathways. The following diagram illustrates the two primary tumor suppressor pathways, p53-p21 and p16-Rb, which act as central regulators of the senescence growth arrest, and the key drivers that activate them.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Senescence Research
| Reagent / Tool | Function / Target | Example Application in Senescence Research |
|---|---|---|
| DDAOG [83] | Fluorogenic substrate for SA-β-Galactosidase. | Enables live-cell, flow cytometric detection of SA-β-Gal activity when combined with Bafilomycin A1 [83]. |
| Bafilomycin A1 [83] | V-ATPase inhibitor that induces lysosomal alkalinization. | Used alongside DDAOG to optimize the pH for specific detection of SA-β-Gal in flow cytometry protocols [83]. |
| Anti-p16INK4a Antibody [83] | Binds to p16 protein, a central regulator of senescence. | Intracellular staining for flow cytometry or immunohistochemistry to confirm senescent state [81] [83]. |
| Anti-γH2AX Antibody [83] | Detects phosphorylated histone H2AX, a marker of DNA double-strand breaks. | Used to identify DNA damage-associated senescence, often seen as foci within the nucleus [81] [83]. |
| Dasatinib + Quercetin [85] | Senolytic cocktail. | Selectively eliminates senescent cells from a mixed culture population during a pre-treatment step [85]. |
| Urolithin A [86] | Senomorphic compound. | Suppresses the pro-inflammatory SASP in senescent cells, mitigating paracrine damage [86]. |
| ABT263 (Navitoclax) [81] | BCL-2 inhibitor senolytic. | Reverses immunosuppression in the microenvironment and clears senescent cells in vivo and in vitro [81]. |
| Vacuolar ATPase Inhibitor [2] | Targets lysosomal hyperacidity. | Corrects lysosomal dysfunction in aged stem cells, shown to rejuvenate blood-forming stem cells [2]. |
Troubleshooting SA-β-Gal Assays
Q: My SA-β-Gal staining shows high background or non-specific staining. How can I improve the specificity?
A: High background noise is a common limitation of the SA-β-Gal assay, as the enzyme's activity is not entirely specific to senescence. To enhance specificity:
- pH Optimization: Confirm the staining solution is precisely at pH 6.0. Lysosomal β-galactosidase shows maximal activity at pH 4, while the senescence-associated form is detected at this suboptimal pH 6. Even a slight deviation can increase background.
- Include Controls: Always run parallel controls with a known senescent cell population (e.g., cells treated with a DNA-damaging agent like etoposide) and a non-senescent, proliferating cell population. This validates your assay conditions.
- Fixation Time: Do not over-fix cells. Typically, 10-15 minutes with a fixative like 2% formaldehyde/0.2% glutaraldehyde is sufficient. Prolonged fixation can reduce enzyme activity or increase non-specific signal.
- Staining Incubation: Perform the staining incubation at 37°C without CO₂. The presence of CO₂ can acidify the medium and lower the pH, leading to increased lysosomal β-galactosidase activity and higher background. A sealed, CO₂-free environment is crucial.
Q: How can I quantitatively measure SA-β-Gal activity beyond simple cytochemical staining?
A: While cytochemical staining with X-gal is standard, quantitative methods offer more objective data.
- Flow Cytometry: Use a fluorogenic substrate like C₁₂FDG (5-dodecanoylaminofluorescein di-β-D-galactopyranoside). Cells are loaded with the substrate, and the fluorescence intensity, proportional to SA-β-gal activity, is measured by flow cytometry. This allows for quantifying the percentage of senescent cells in a large population.
- Bioluminescence and Fluorescence Imaging: Ratiometric probes for fluorescence imaging or bioluminescence techniques can be applied for more sensitive, quantitative detection in cell cultures or even in vivo samples. These methods are particularly useful for high-throughput screening of senolytic or senomorphic compounds [88].
Troubleshooting Transplantation Efficacy
Q: Our in vitro data on MSCs is promising, but the cells show poor survival and engraftment after transplantation in animal models. What are the potential causes and solutions?
A: This is a major hurdle in translational research. The causes often relate to the harsh in vivo environment and cellular senescence.
- Cause - Replicative Senescence: MSCs undergoing prolonged ex vivo culture enter a senescent state. These aged MSCs exhibit altered morphology, reduced proliferation, poor differentiation ability, and altered paracrine functions, making them therapeutically inefficient [29] [89].
- Solution - Senescence Prevention:
- Molecular Pretreatment: Pre-treat MSCs with molecules that inhibit the aging process. This can include inhibitors of key senescence pathways or compounds that enhance telomere maintenance.
- 3D Culture Systems: Culturing MSCs in three-dimensional (3D) spheroids instead of traditional 2D monolayers can better mimic their natural niche and help maintain their stemness, reducing culture-induced senescence [29].
- Hypoxia Preconditioning: Culturing MSCs under low oxygen conditions (e.g., 1-5% O₂) that mimic their physiological niche can enhance their survival, paracrine activity, and engraftment post-transplantation.
Q: How can we reliably track the fate of transplanted cells in vivo to validate engraftment and function?
A: In vivo tracking is critical for understanding and optimizing cellular therapy.
- Direct Labeling for Short-Term Tracking: Cells can be labeled with superparamagnetic iron oxide (SPIO) particles for MRI tracking or with radionuclides like ¹¹¹In for SPECT/CT imaging. This is excellent for answering questions about initial cell homing and short-term localization. A key limitation is that the label dilutes with cell division and can be retained by phagocytes after cell death, so it primarily indicates the location of the label, not necessarily viable cells [90].
- Reporter Gene Imaging for Long-Term Fate: For long-term monitoring of cell viability, location, and proliferation, genetic engineering is used. Transplanted cells are engineered to express a reporter gene (e.g., luciferase for bioluminescence imaging, GFP for fluorescence, or a receptor for PET imaging). Since the signal depends on the expression of the gene by viable cells, it provides a more accurate picture of long-term cell fate and is the preferred method for assessing functional engraftment [90].
Troubleshooting In Vivo Regeneration Models
Q: We are testing a regenerative therapy in a mouse wound healing model, but the results are difficult to translate to human physiology. What key differences should we consider?
A: Mouse and human skin have critical anatomical and physiological differences that impact healing.
- Skin Structure: Human skin is thicker and more tightly attached to the underlying tissue. Mouse skin is looser and has a thin epidermis with only 2-3 cell layers, compared to 5-10 in humans [91].
- Healing Mechanism: The primary mechanism of wound closure in mice is contraction, mediated by the
panniculus carnosusmuscle. In humans, wound healing relies more on re-epithelialization and the formation of granulation tissue. A therapy that works by inhibiting contraction in mice may not be as effective in humans [91]. - Experimental Design Recommendations:
- Use splinted wound models that prevent contraction, forcing the wound to heal primarily through re-epithelialization, which better mimics human healing.
- Consider incorporating aged or diabetic mouse models to more accurately represent the clinical patient population, where healing is often impaired.
Q: In our stem cell therapy study for ischemic stroke, what advanced techniques can we use to objectively measure functional neurological recovery?
A: Beyond behavioral tests, advanced magnetic resonance imaging (MRI) techniques can provide objective, quantitative biomarkers of recovery.
- Diffusion Tensor Imaging (DTI): DTI measures the microstructural integrity of white matter tracts. An increase in fractional anisotropy (FA) in tracts like the corticospinal tract can indicate axonal reorganization and remyelination, correlating with motor function improvement [92].
- Functional MRI (fMRI): Resting-state fMRI can assess functional connectivity between different brain regions. The restoration of connectivity networks disrupted by stroke can be a powerful indicator of neural circuit repair facilitated by stem cell therapy [92].
- Magnetic Resonance Spectroscopy (MRS): MRS measures metabolic changes in the brain. Changes in metabolites like N-acetylaspartate (NAA, a marker of neuronal health), choline (membrane turnover), and myo-inositol (glial activity) can provide evidence of cellular-level recovery [92].
Research Reagent Solutions
The table below lists key reagents and their functions for studying senescence and transplantation efficacy.
| Reagent/Material | Primary Function | Application Notes |
|---|---|---|
| X-gal (5-bromo-4-chloro-3-indolyl-β-D-galactopyranoside) | Chromogenic substrate for cytochemical detection of SA-β-Gal activity. Turns blue upon cleavage. | Essential for classic senescence staining; requires precise pH 6.0 buffer [88]. |
| C₁₂FDG | Fluorogenic substrate for flow cytometric quantification of SA-β-Gal activity. | Enables quantitative, high-throughput analysis of senescent cell populations [88]. |
| Superparamagnetic Iron Oxide (SPIO) Nanoparticles | MRI contrast agent for direct labeling and in vivo tracking of transplanted cells. | Ideal for short-term cell localization studies; does not indicate cell viability [90]. |
| Lentiviral Reporter Vectors (e.g., Luciferase/GFP) | Genetically engineers cells to express detectable markers for long-term in vivo tracking. | Reporter signal correlates with viable, functioning cells; crucial for engraftment studies [90]. |
| Senolytic Drugs (e.g., SSK1) | Selectively induce apoptosis in senescent cells by targeting lysosomal SA-β-Gal activity. | Used to clear senescent cells from cultures pre-transplantation or to test therapy-induced senescence (TIS) [88]. |
| 3D Culture Scaffolds (e.g., Hydrogels) | Provides a three-dimensional environment for cell culture, mimicking the native stem cell niche. | Helps prevent replicative senescence during in vitro expansion of MSCs [29]. |
Quantitative Data on Senescence and Transplantation
Table 1: SA-β-Gal as a Diagnostic Marker in Human Tumors
This table summarizes clinical findings on SA-β-Gal activity in various cancers, supporting its role as a biomarker.
| Condition / Tissue Type | Number of Patients | Key Finding on SA-β-Gal | Clinical Implication |
|---|---|---|---|
| Primary Ovarian Cancer | 11 | SA-β-gal activity was detected in 100% of cases not subjected to chemotherapy [88]. | Suggests universal presence of senescent cells in this cancer type, potentially related to tumor suppression or SASP. |
| Epithelial Ovarian Adenocarcinoma | Information in source | SA-β-gal activity was detected in primary tumors [88]. | Corroborates the presence of senescence in ovarian cancer pathogenesis. |
Table 2: Stem Cell Clinical Trials in Ischemic Stroke
This table summarizes design and outcomes from key clinical trials, highlighting variables critical for efficacy.
| Study / Phase | Cell Type / Dose | Transplantation Route & Timing | Primary Functional Outcome | Efficacy Result |
|---|---|---|---|---|
| MASTER (Phase II) [92] | MAPCs (Allogeneic); 400 or 1200 million cells | Intravenous (IV); 24-48 hours post-stroke | NIHSS, mRS, BI | Safe but no significant improvement at primary endpoint; earlier timing (24-36h) may be beneficial. |
| TREASURE (Phase II/III) [92] | MAPCs (Allogeneic); 120 million cells | IV; 18-36 hours post-stroke | NIHSS, mRS, BI | Safe but did not improve short-term outcomes; potential benefit in patients with large infarct volumes. |
Signaling Pathways in MSC Senescence
Experimental Workflow for Validating Transplantation Efficacy
Frequently Asked Questions (FAQs)
Q1: What is the fundamental rationale for using intermittent dosing of senolytics in aging research? The primary rationale is to balance efficacy with toxicity. Senolytics are designed to selectively trigger apoptosis in senescent cells, a process that does not require continuous drug exposure. A short-term, intermittent regimen is sufficient to clear a portion of the senescent cell burden. This approach allows time for the tissue to recover and reduces the risk of off-target side effects, which is particularly important as the aging population is more susceptible to adverse drug effects. Chronic, continuous dosing could lead to unnecessary toxicity without providing significant additional benefits in senescent cell clearance [36] [93].
Q2: In a stem cell culture model, how long does it take for senescent cells to re-accumulate after a senolytic treatment, informing the dosing interval? The re-accumulation of senescent cells is not immediate. The rate depends on the initial level of senescence induction and the replication rate of the specific stem cell population. For example, in a model of stress-induced premature senescence, a significant population of senescent cells may re-establish over several days to weeks. Therefore, the dosing interval for in vitro experiments is often empirically determined. A common strategy is to re-treat cultures upon the re-emergence of senescence biomarkers (e.g., SA-β-Gal activity or p16INK4a expression) above a pre-defined threshold, which could range from one to several weeks [94].
Q3: What are the key molecular pathways targeted by intermittent senolytics to preserve stem cell function? Intermittent senolytics preserve stem cell function primarily by eliminating neighboring senescent cells that exert paracrine suppression. This is achieved by targeting the Senescent Cell Anti-apoptotic Pathways (SCAPs) that these cells depend on for survival. Key pathways include:
- BCL-2 Family Pathway: Inhibited by senolytics like Navitoclax (ABT-263) [36] [94].
- Receptor Tyrosine Kinase (RTK) Signaling: Targeted by Dasatinib, often in combination with Quercetin (D+Q) [36] [94].
- p53/FOXO4 Interaction: Disrupted by peptides like FOXO4-DRI, which restores p53-mediated apoptosis in senescent cells [36]. By periodically clearing these inhibitory senescent cells, the microenvironment is improved, allowing for enhanced stem cell self-renewal, reduced SASP-mediated inflammation, and improved regenerative capacity [95].
Q4: How do I choose between a senolytic (killing) and a senomorphic (suppressing) agent for my replicative aging stem cell model? The choice hinges on your research goal.
- Use a senolytic (e.g., Fisetin, D+Q, Navitoclax) if your objective is to permanently remove senescent cells from your culture and study the resulting long-term improvement in stem cell function and replicative potential. This is a "reset" approach [36] [96].
- Use a senomorphic (e.g., Rapamycin, JAK inhibitors) if you wish to temporarily suppress the deleterious effects of the SASP (e.g., chronic inflammation, paracrine senescence) without killing the senescent cells. This is useful for studying the specific role of the SASP or when continuous pathway modulation is needed. Senomorphics may require more continuous dosing to maintain effect [36] [97].
Q5: What are the critical quality control checks for a senolytic agent before use in a sensitive stem cell system?
- Purity and Solubility: Verify the compound's purity and optimize its solubility in a suitable vehicle (e.g., DMSO) to prevent solvent toxicity [94].
- Dose-Response Validation: Perform a pilot dose-response curve specifically on your stem cell type to determine the minimum effective senolytic dose and the maximum tolerated dose that does not induce toxicity in non-senescent cells.
- Senescence Biomarker Panel: Confirm efficacy using a panel of senescence markers (e.g., SA-β-Gal staining, and mRNA/protein levels of p16INK4a, p21CIP1) pre- and post-treatment [94].
- Functional Stem Cell Assays: Assess key stem cell functionalities after treatment, including colony-forming unit assays, differentiation potential, and proliferation kinetics, to ensure the regimen does not impair stemness [95].
Troubleshooting Guides
Issue 1: Lack of Efficacy in Clearing Senescent Stem Cells
Problem: Treatment with a senolytic cocktail does not reduce senescence biomarkers (e.g., SA-β-Gal, p16) in your stem cell culture.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Incorrect Senolytic for Cell Type | Review literature for effective senolytics on your specific stem cell type (e.g., MSCs vs. NSCs). | Switch to a different senolytic class (see Table 1). Test a combination like Dasatinib + Quercetin. |
| Insufficient Dose or Exposure Time | Perform a dose-response assay with a positive control (e.g., a known senescent cell line). | Increase concentration or duration of treatment within cytotoxicity limits. |
| Poor Drug Bioavailability | Check solubility and stability of the compound in your culture medium. | Optimize solvent (e.g., use fresh DMSO), consider using prodrugs or nano-formulations. |
| Senescence Induction Not Robust | Quantify baseline senescence; weak induction may not engage SCAPs strongly. | Re-optimize senescence induction protocol (e.g., increase dose of irradiation or oxidative stress). |
Issue 2: Excessive Toxicity in Non-Senescent Stem Cells
Problem: The senolytic treatment is causing significant death or impaired function in the non-senescent, proliferating stem cell population.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Dose Too High | Perform a viability assay (e.g., MTT, Calcein-AM) on a pure population of young, healthy stem cells. | Titrate down the dose to find the therapeutic window. Adopt an intermittent dosing schedule. |
| Vehicle Toxicity | Include a vehicle-only control group in all experiments. | Reduce the final concentration of the vehicle (e.g., DMSO <0.1%), or switch vehicles. |
| Off-Target Effects | Check for known off-targets of the senolytic (e.g., BCL-xL inhibition in platelets by Navitoclax). | Consider a more targeted senolytic (e.g., a BCL-2 specific inhibitor) or a SenoTAC approach [93]. |
| Prolonged/Continuous Dosing | Compare intermittent vs. continuous dosing schedules for toxicity. | Switch to an intermittent regimen. Treat, then wash out and allow cells to recover. |
Issue 3: Inconsistent Results Between Experimental Replicates
Problem: The reduction in senescence markers or improvement in stem cell function is variable across repeats of the same experiment.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Heterogeneous Senescence | The population of senescent cells may not be uniform. | Use FACS to sort cells based on a senescence marker (e.g., SA-β-Gal) to create a more uniform population for testing. |
| Inconsistent Senescence Induction | Carefully monitor and standardize the senescence induction parameters (e.g., cell density, reagent concentration, time). | Strictly standardize the protocol. Use a validated positive control in every experiment. |
| Drug Degradation | The senolytic compound may degrade in solution over time. | Prepare fresh stock solutions for each treatment, and ensure proper storage conditions. |
Key Experimental Protocols
Protocol 1: In Vitro Assessment of Intermittent vs. Continuous Senolytic Dosing
Objective: To compare the efficacy and toxicity of intermittent versus continuous senolytic dosing in a replicative senescence model of Mesenchymal Stem Cells (MSCs).
Materials:
- Primary human MSCs (early passage)
- Senolytic agent (e.g., Fisetin)
- Growth medium
- Phosphate Buffered Saline (PBS)
- SA-β-Gal Staining Kit
- Antibodies for p16INK4a and p21CIP1
- Cell viability assay kit (e.g., MTT)
Method:
- Induce Replicative Senescence: Culture MSCs until they reach replicative exhaustion (e.g., passage 10+), confirmed by >50% SA-β-Gal positivity.
- Experimental Groups:
- Group 1 (Intermittent): Treat senescent MSCs with a predetermined optimal dose of senolytic (e.g., 10 µM Fisetin) for 24 hours. Wash cells with PBS and return to fresh growth medium for 7 days.
- Group 2 (Continuous): Treat senescent MSCs with the same dose of senolytic, refreshing the drug-containing medium every 48 hours for 7 days.
- Group 3 (Vehicle Control): Treat with vehicle only (e.g., 0.1% DMSO) for the duration of the experiment.
- Assessment:
- Day 1 & Day 7: Quantify senescence markers (SA-β-Gal+ cells, p16/p21 protein levels).
- Day 7: Perform functional assays: colony-forming unit (CFU) assay, and trilineage differentiation potential (osteogenic, adipogenic, chondrogenic).
- Monitor Toxicity: Measure cell viability and apoptosis (e.g., by Caspase-3/7 activity) in all groups at multiple time points.
This protocol directly tests whether short, pulsed treatments can achieve similar or superior clearance of senescent cells with less functional impairment to the remaining stem cell pool compared to continuous exposure [94] [96].
Protocol 2: Validating Senescence Clearance in a 3D Stem Cell Niche Model
Objective: To evaluate senolytic efficacy in a more physiologically relevant 3D co-culture system containing both senescent cells and young stem cells.
Materials:
- Young, healthy MSCs (fluorescently labeled)
- Irradiation-induced senescent fibroblasts (differentially labeled)
- 3D hydrogel matrix (e.g., Matrigel or collagen)
- Live-cell imaging system
Method:
- Establish 3D Co-culture: Embed young MSCs and senescent fibroblasts at a defined ratio (e.g., 1:1) within a 3D hydrogel.
- Senolytic Treatment: After 48 hours, treat the 3D constructs with either an intermittent or continuous senolytic regimen as described in Protocol 1.
- Analysis:
- Imaging: Use live-cell imaging to track the viability and loss of the senescent cell population (via their specific label) over time.
- Functional Readout: After treatment, dissociate the 3D cultures and assay the young MSCs for clonogenicity and migration capacity.
- SASP Analysis: Collect conditioned medium from the 3D cultures pre- and post-treatment and measure key SASP factors (e.g., IL-6, IL-8) via ELISA.
This protocol helps determine if senolytics can effectively penetrate a 3D microenvironment and eliminate senescent cells that are negatively impacting neighboring stem cell function [95].
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Key Senotherapeutic Agents and Their Applications
| Reagent / Tool | Primary Function / Mechanism | Example Application in Stem Cell Aging | Key Considerations |
|---|---|---|---|
| Dasatinib + Quercetin (D+Q) | Tyrosine kinase inhibitor (Dasatinib) & flavonoid (Quercetin) target multiple SCAPs. | Clearance of senescent MSCs and progenitors; improves stem cell function in aged niches [36] [94]. | Effective for intermittent dosing. Cell-type specific; may require optimization of ratio. |
| Fisetin | Natural flavonoid; inhibits pro-survival pathways and induces apoptosis in senescent cells. | Reduction of senescence burden in various human cell types; shown to be effective in aged mouse models [96]. | Good oral bioavailability in vivo; suitable for both in vitro and in vivo intermittent regimens. |
| Navitoclax (ABT-263) | Small-molecule inhibitor of BCL-2/BCL-xL. | Potent senolytic for hematopoietic stem cells (HSCs) and other cell types dependent on BCL-2 family proteins [36] [94]. | Known on-target toxicity of BCL-xL inhibition (thrombocytopenia) limits continuous use. |
| FOXO4-DRI Peptide | Disrupts FOXO4-p53 interaction, reactivating p53-mediated apoptosis in senescent cells. | Rejuvenation of tissue stem cells and restoration of regenerative capacity in aged mouse models [36]. | Peptide delivery can be challenging; more suitable for acute, intermittent treatment. |
| SenoTACs (PROTACs) | Bifunctional molecules that degrade target proteins (e.g., BCL-2 family) via the ubiquitin-proteasome system. | Emerging strategy for highly selective degradation of SCAP proteins with potential for improved safety profiles [93]. | Next-generation technology; offers potential for substoichiometric activity and reduced dosing frequency. |
| SA-β-Gal Staining Kit | Histochemical detection of lysosomal β-galactosidase activity at pH 6.0, a common senescence biomarker. | Standard method to quantify the percentage of senescent cells in a culture pre- and post-senolytic treatment [94]. | A cornerstone assay, but should be used in conjunction with other markers for confirmation. |
Signaling Pathways and Experimental Workflows
Senolytic Induction of Apoptosis in Senescent Cells
Diagram: Senolytic Induction of Apoptosis in Senescent Cells. Senescent cells upregulate pro-survival SCAPs to resist programmed cell death. Senolytic agents specifically target and disrupt these pathways, thereby releasing the brake on apoptosis and leading to the selective clearance of senescent cells [36] [94] [93].
Intermittent vs. Continuous Dosing Workflow
Diagram: Experimental Workflow for Dosing Comparison. This flowchart outlines a parallel experimental setup to directly compare the effects of intermittent (pulsed treatment with recovery) and continuous (constant exposure) senotherapeutic regimens on a senescent stem cell model, with a common endpoint for comprehensive analysis [94] [96].
Bench-to-Bedside Translation: Evaluating Efficacy Across Models and Clinical Trial Outcomes
Frequently Asked Questions (FAQs)
FAQ 1: What are the key biomarkers for reliably identifying and quantifying senescent cells in my preclinical models?
Accurate characterization of senescent cells is fundamental, yet challenging due to their heterogeneity. A combination of biomarkers is recommended, as no single universal marker exists [44].
- Classical Biomarkers:
- Advanced Molecular Characterization: Leverage novel genesets and databases developed through sequencing technologies.
- SenMayo: A geneset of 125 genes enriched in senescent cells, validated to show reduced expression in human adipose tissue after senolytic treatment [44].
- SASP Atlas: A resource defining core and context-specific Senescence-Associated Secretory Phenotype (SASP) factors, including soluble proteins and extracellular vesicles (EVs). Key SASP factors include pro-inflammatory cytokines like IL-6, IL-8, IL-1β, and TNF-α [44] [80] [82].
- Other Markers: DNA damage markers (e.g., γH2AX), elevated lipofuscin, and heterochromatin marks like H3K9me3 [80] [81].
FAQ 2: Why might my senolytic therapy show high efficacy in murine models but fail to translate in primate studies?
This is a common translational challenge often stemming from model organism limitations and senescent cell heterogeneity [44].
- Species-Specific Differences: Rodents have different lifespans, metabolic rates, and immune systems compared to primates. The heterogeneity of senescent cells varies significantly by cell type, tissue, and inducing trigger, meaning vulnerabilities in mouse cells may not be present in human or primate cells [44].
- The Microenvironment: Primate and human systems have more complex tissue microenvironments and systemic factors (e.g., chronic inflammation) that can protect senescent cells or alter drug pharmacokinetics [82].
- Trial Design: The long-term impacts of eliminating senescent cells are understudied, and responses can vary across sexes, which may not be fully accounted for in rodent studies [44].
FAQ 3: How do I choose between a "senolytic" and a "senomorphic" strategy for my research?
The choice depends on your therapeutic goal and the specific research context.
- Senolytics: These are agents that selectively induce apoptosis in senescent cells. They are ideal for scenarios where the physical clearance of senescent cells is the objective, such as testing the causal role of senescent cells in a pathology. Examples include Dasatinib + Quercetin (D+Q) and Navitoclax (ABT-263) [44] [81].
- Senomorphics: These agents suppress the deleterious SASP without killing the senescent cell. This approach may be preferable if senescent cells have beneficial roles (e.g., in wound healing) in your specific model, and you only wish to suppress their inflammatory secretome [81].
FAQ 4: My stem cell cultures are showing high rates of spontaneous differentiation, which confounds senescence analysis. How can I prevent this?
Maintaining high-quality stem cell cultures is critical. Common issues and solutions include [98] [99]:
- Culture Medium: Ensure complete culture medium is fresh (e.g., less than 2 weeks old when stored at 2-8°C) [98].
- Passaging Technique: Passage cells when colonies are large and dense, but before they overgrow. Remove differentiated areas prior to passaging. Ensure cell aggregates after passaging are evenly sized [98].
- Colony Density: Plate an appropriate number of cell aggregates to avoid overly dense or sparse cultures [98].
- Handling Time: Minimize the time culture plates are outside the incubator [98].
The following tables summarize key quantitative findings from seminal studies in rodent, primate, and human organoid models.
Table 1: Efficacy of Senescence-Targeting InterventionsIn Vivo
| Model | Intervention | Key Efficacy Readouts | Reported Results | Reference/Model |
|---|---|---|---|---|
| Aged Cynomolgus Macaque (Primate) | Senescence-Resistant human MPCs (SRCs) with FOXO3 | Cognitive Function, Bone Density, Reproductive Vitality, Inflammation | Systemic rejuvenation; enhanced neural connectivity, fortified skeletal strength, restored reproductive vigor, reduced senescence & inflammation | [80] |
| Aged Mice (Rodent) | Senolytic Cocktail: Dasatinib + Quercetin (D+Q) | Senescent Cell Burden (e.g., SenMayo geneset), Physical Function | Significant reduction in senescent cell burden in adipose tissue; improved healthspan and physical function | [44] |
| Various Preclinical Models | Navitoclax (ABT-263) | Clearance of Senescent Cells, Immunosuppression Reversal | Reversal of myeloid cell immunosuppression in TME; restored CD8+ T cell proliferation | [81] |
Table 2: Efficacy inIn Vitro& Human-Derived Models
| Model | Intervention | Key Efficacy Readouts | Reported Results | Reference/Model |
|---|---|---|---|---|
| Human iPSC-Derived Models | Partial Epigenetic Reprogramming | Epigenetic Clock, Functional Capacity | Rewinding of epigenetic age and restoration of youthful function while maintaining cellular identity | [82] |
| Primary Human Cells (e.g., Fibroblasts) | Metabolic Reprogramming (e.g., Dichloroacetate) | Metabolic Flexibility, Oxidative Phosphorylation | Partial reversal of age-related metabolic changes | [82] |
| Cancer Cell Lines | Navitoclax (ABT-263) | Apoptosis of Senescent Cells | Varied susceptibility to senolysis depending on cell type and context | [44] |
Detailed Experimental Protocols
Protocol 1: Assessing Senescence Reversal in Primate Models Using Engineered Stem Cells
This protocol is based on the landmark study using senescence-resistant mesenchymal progenitor cells (SRCs) in aged macaques [80].
- Cell Engineering:
- Isolate human Mesenchymal Progenitor Cells (MPCs).
- Genetically engineer MPCs to overexpress the geroprotective gene FOXO3 using a lentiviral or other non-integrating vector system to create SRCs.
- Culture and expand SRCs under standard conditions, validating FOXO3 expression and enhanced stress resistance in vitro.
- Animal Dosing:
- Use aged non-human primates (e.g., Cynomolgus macaques).
- Administer SRCs via intravenous infusion. A 44-week trial duration has been demonstrated.
- Include control groups receiving wild-type MPCs or vehicle.
- Tissue Collection and Analysis:
- Collect blood and tissue samples (e.g., brain, bone, reproductive organs) at baseline and endpoint.
- Peripheral Blood Mononuclear Cells (PBMCs) Analysis:
- Flow cytometry for p21 positivity.
- Measure lipid peroxidation (e.g., 4-hydroxynonenal), DNA damage (γH2AX), and inflammatory cytokines (IL-1β, TNF-α, IL-6).
- Assess epigenetic markers like H3K9me3 via immunoblotting or ChIP-seq.
- Tissue Analysis:
- Histology for tissue architecture and senescence markers (SA-β-Gal, p16).
- RNA-seq on tissues to analyze gene expression clusters related to inflammation and innate immunity.
- Assess epigenetic aging clocks (e.g., DNA methylation age).
Protocol 2: Quantifying Senolytic Efficacy in Human Cell Cultures Using the SenMayo Geneset
This protocol utilizes a novel transcriptional signature to measure senescent cell burden [44].
- Induction of Senescence:
- Culture primary human cells (e.g., fibroblasts) or iPSC-derived cells.
- Induce senescence using a relevant stressor (e.g., ionizing radiation, etoposide, replicative exhaustion). Include a non-senescent control.
- Senolytic Treatment:
- Treat senescent cultures with your senolytic compound of interest (e.g., ABT-263, D+Q) at optimized concentrations.
- RNA Extraction and Sequencing:
- Harvest cells and extract total RNA.
- Prepare mRNA-seq libraries and perform high-throughput sequencing.
- Bioinformatic Analysis:
- Map sequencing reads to the reference genome and generate a counts matrix.
- Calculate a score for the SenMayo geneset (125 genes) in your samples. This can be done using gene set variation analysis (GSVA) or single-sample GSEA (ssGSEA).
- Statistical Comparison: Compare the SenMayo score between senescent cultures treated with a senolytic versus those treated with a vehicle control. A significant reduction indicates effective clearance of senescent cells.
Signaling Pathways and Experimental Workflows
Senescence Induction Pathways
Primate Rejuvenation via Engineered Stem Cells
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Senescence Research
| Research Reagent | Function & Application | Example & Notes |
|---|---|---|
| Senescence-Inducing Agents | To establish in vitro models of senescence by causing DNA damage or oxidative stress. | Etoposide: Topoisomerase II inhibitor. Hydrogen Peroxide (H₂O₂): Induces oxidative stress. Alisertib: Aurora kinase A inhibitor [44]. |
| Senolytic Compounds | To selectively eliminate senescent cells in vitro and in vivo. | Dasatinib + Quercetin (D+Q): Common senolytic cocktail. Navitoclax (ABT-263): BCL-2 family inhibitor [44] [81]. |
| FOXO3 Expression Vector | To genetically engineer stem cells for enhanced resistance to senescence. | Used to create Senescence-Resistant Cells (SRCs) for therapeutic application [80]. |
| ROCK Inhibitor (Y-27632) | To improve survival and attachment of human pluripotent stem cells (hPSCs) after passaging or thawing. | Critical for maintaining cell viability in iPSC and organoid culture workflows [99]. |
| TeSR / mTeSR Plus Medium | A defined, feeder-free culture medium for the maintenance of undifferentiated hPSCs. | Essential for culturing human iPSCs and ESCs to ensure consistent, high-quality cell banks [98] [100]. |
| Anti-p16 / p21 Antibodies | For immunohistochemistry and Western blotting to detect and quantify key senescence markers. | Validate senescence induction and assess efficacy of senolytics. |
| Cytokine Profiling Array | To characterize the Senescence-Associated Secretory Phenotype (SASP) from conditioned media. | Measure levels of IL-6, IL-8, IL-1β, TNF-α, and other SASP factors [44] [81]. |
The field of Mesenchymal Stem Cell (MSC) research is transitioning from foundational science to clinical application for age-related conditions. The period from 2023 to 2025 has marked significant regulatory milestones, including the first FDA-approved MSC therapy (Ryoncil) in December 2024 for pediatric steroid-refractory acute graft-versus-host disease [101]. This approval signals a growing regulatory acceptance of cell-based therapies. Concurrently, the research focus is expanding from simply replacing damaged cells to leveraging the complex paracrine signaling and immunomodulatory capacities of MSCs, which are now considered central to their therapeutic effects [102] [103]. These mechanisms are particularly relevant for combating the hallmarks of aging, such as chronic inflammation and stem cell exhaustion.
The clinical pipeline is diversifying, with over 115 global clinical trials involving pluripotent stem cell-derived products, and a significant number utilizing MSCs or their derivatives [101]. Key therapeutic areas include neurology, orthopedics, and immunomediated diseases [102]. A promising development is the advancement of induced Pluripotent Stem Cell-derived MSCs (iMSCs), which offer enhanced consistency and scalability compared to primary MSCs, addressing critical challenges in manufacturing and standardization [101]. Furthermore, research is increasingly focusing on cell-free therapies using MSC-derived extracellular vesicles (EVs), which mimic the rejuvenating effects of MSCs with a potentially superior safety profile [104] [103]. The integration of biological aging clocks is also emerging as a critical tool for objectively measuring the efficacy of interventions in clinical trials [104].
Quantitative Clinical Trial Analysis
The following tables summarize the current state of MSC-based clinical development, highlighting both approved therapies and the expanding pipeline targeting age-related diseases.
Table 1: Recently FDA-Approved Cell Therapies (2023-2025) This table details the key approved products, providing insight into regulatory trends.
| Product Name (Generic) | Brand Name | Cell Type | Indication | Date of FDA Approval |
|---|---|---|---|---|
| Omidubicel-onlv [101] | Omisirge [101] | Cord Blood-Derived Hematopoietic Progenitor Cells [101] | Accelerate neutrophil recovery in patients with hematologic malignancies [101] | April 17, 2023 [101] |
| Lovotibeglogene autotemcel [101] | Lyfgenia [101] | Autologous cell-based gene therapy [101] | Sickle cell disease in patients 12 and older [101] | December 8, 2023 [101] |
| Remestemcel-L [101] | Ryoncil [101] | Allogeneic Bone Marrow-Derived MSCs [101] | Pediatric steroid-refractory acute Graft versus Host Disease (SR-aGVHD) [101] | December 18, 2024 [101] |
Table 2: Select FDA-Authorized Clinical Trials for MSC/iPSC-Derived Therapies (2024-2025) This table showcases the diversity of conditions being targeted in ongoing clinical research.
| Therapy/Product Name | Cell Type | Indication | Trial Status / FDA Designation |
|---|---|---|---|
| OpCT-001 [101] | iPSC-derived therapy [101] | Retinal degeneration (e.g., retinitis pigmentosa) [101] | IND clearance for Phase I/IIa (Sep 2024) [101] |
| FT819 [101] | iPSC-derived CAR T-cell therapy [101] | Systemic lupus erythematosus (SLE) [101] | RMAT designation for Phase I (Apr 2025) [101] |
| Neural progenitor cell therapies [101] | iPSC-based therapies [101] | Parkinson's disease, Spinal cord injury, ALS [101] | FDA IND clearance (Jun 2025) [101] |
| CYP-001 (Cymerus iMSCs) [101] | iPSC-derived MSCs (iMSCs) [101] | High-Risk Acute Graft-Versus-Host Disease (HR-aGvHD) [101] | Ongoing FDA-approved clinical trial [101] |
| Fertilo [101] | iPSC-derived ovarian support cells [101] | In-vitro oocyte maturation [101] | First iPSC-based therapy to enter U.S. Phase III (Feb 2025) [101] |
Core Experimental Protocols in MSC Aging Research
Protocol: Replicative Senescence Induction and Analysis
This foundational protocol is used to model cellular aging in vitro.
- Objective: To induce and quantify replicative senescence in primary MSCs, mimicking age-related functional decline [82].
- Materials: Primary human MSCs (e.g., bone marrow or adipose-derived), standard MSC culture medium (e.g., DMEM with fetal bovine serum), phosphate-buffered saline (PBS), senescence-associated beta-galactosidase (SA-β-gal) staining kit, equipment for flow cytometry.
- Method Steps:
- Cell Culture and Serial Passaging: Culture MSCs under standard conditions (37°C, 5% CO2). Continuously passage cells at a defined seeding density (e.g., 5,000 cells/cm²) until they approach the Hayflick limit [82]. Monitor population doublings at each passage.
- Senescence Induction: Alternatively, induce premature senescence by exposing low-passage MSCs to sublethal doses of oxidative stress (e.g., 200-500 µM H₂O₂ for 2 hours) [104].
- Phenotypic Confirmation (SA-β-gal Staining): Fix cells and incubate with the SA-β-gal staining solution at pH 6.0. Senescent cells will display blue cytoplasmic staining under light microscopy. Quantify the percentage of SA-β-gal positive cells [95].
- Flow Cytometric Analysis: Harvest cells and stain for senescence and DNA damage markers, such as p16INK4a and γH2AX. Analyze using flow cytometry to objectively quantify the senescent population [105].
Protocol: In Vivo Assessment of MSC Efficacy in Aged Rodents
This protocol evaluates the systemic anti-aging effects of MSC administration in animal models.
- Objective: To determine the lifespan-extending and healthspan-improving potential of MSC systemic administration in naturally aging or progeroid rodents [104].
- Materials: Aged or progeroid mice/rats (e.g., 18-24 month old C57BL/6 mice or Ercc1−/− mice), young donor MSCs (1-2 months old), sterile PBS for vehicle control, injection supplies (syringes, needles), equipment for behavioral and cognitive tests.
- Method Steps:
- Cell Preparation: Isolate and expand MSCs from young donor rodents (e.g., bone marrow). Confirm cell viability and phenotype before injection [104].
- Systemic Administration: Randomize aged animals into treatment and control groups. Administer MSCs (e.g., 1x10^6 cells per mouse) via intravenous (i.v.) or intraperitoneal (i.p.) injection. Control groups receive an equivalent volume of vehicle solution [104].
- Regimen: Treatments can be single injections or multiple injections (e.g., monthly until natural death), depending on the study design [104].
- Endpoint Monitoring:
- Lifespan: Record survival daily to calculate median and maximum lifespan extension [104].
- Healthspan: Perform regular assessments of physical activity (e.g., rotarod test), cognitive function (e.g., Morris water maze), and metabolic parameters (e.g., insulin tolerance test) [104].
- Post-Mortem Analysis: Analyze tissues for molecular hallmarks of aging, such as SASP factor levels (IL-6, IL-1β), protein aggregation, and epigenetic age using clocks [82] [104].
Signaling Pathways in MSC-Mediated Rejuvenation
MSCs exert their anti-aging effects through complex interactions with multiple signaling pathways. The diagrams below illustrate two key mechanistic frameworks.
Anti-Aging Signaling Network
Senescence-Associated Secretory Phenotype (SASP)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for MSC Aging Research This table lists critical reagents and their functions for investigating MSC senescence and rejuvenation.
| Research Reagent | Primary Function in MSC Aging Research |
|---|---|
| SA-β-gal Staining Kit [95] | Histochemical detection of senescent MSCs at pH 6.0; a gold-standard biomarker for cellular senescence. |
| FOXO3 Expression Vectors [105] | Genetic engineering tool to create senescence-resistant MSCs (SRCs) by overexpressing this pro-longevity gene. |
| Senolytic Cocktails (e.g., Dasatinib + Quercetin) [85] | Selective elimination of senescent MSCs from culture to study their role or purify cell populations. |
| mTOR Inhibitors (e.g., Rapamycin) [95] | To modulate nutrient-sensing pathways in MSCs, study autophagy induction, and potentially rejuvenate stem cell function. |
| MSC-Derived Exosomes/EVs [104] [103] | Cell-free therapeutic agents; used to isolate and apply the paracrine factors of MSCs in aging models. |
| Cytokine Antibody Array | To profile the Senescence-Associated Secretory Phenotype (SASP) of MSCs, quantifying factors like IL-6, IL-8, and MMPs. |
| StemRNA Clinical iPSC Seed Clones [101] | GMP-compliant, standardized starting material for generating consistent iMSCs, addressing donor heterogeneity. |
Technical Support Center: FAQs & Troubleshooting
FAQ 1: Our primary MSCs show rapid loss of proliferation and high SA-β-gal activity at low passages. What could be the cause?
- Potential Causes: This is often indicative of premature senescence, triggered by suboptimal culture conditions or cellular stress [82] [102].
- Troubleshooting Steps:
- Check Culture Conditions: Ensure physiological oxygen levels (physoxia, ~2-5% O2) instead of standard atmospheric oxygen (21%), which induces oxidative stress. Verify the quality and batch of fetal bovine serum (FBS); consider using validated, low-passage, pooled lots [102].
- Avoid Over-confluence: Do not allow cells to reach 100% confluence. Passage MSCs at 70-80% density to prevent contact inhibition and stress [82].
- Assess Donor Age: Acknowledge that MSCs from older donors have a significantly shorter replicative lifespan in vitro. If possible, use low-passage MSCs from younger donors for experiments requiring extensive expansion [82] [104].
- Test for Mycoplasma: Conduct routine mycoplasma testing, as contamination is a common cause of rapid culture decline.
FAQ 2: We observe high variability in the immunomodulatory potency of our MSC batches. How can we standardize this?
- Potential Causes: Functional heterogeneity is a major challenge in MSC therapy, stemming from donor-to-donor variation, tissue source differences, and culture methods [102].
- Troubleshooting & Enhancement Strategies:
- Implement Potency Assays: Develop and use standardized in vitro potency assays before in vivo use. Examples include measuring T-cell suppression in coculture assays or quantifying IDO (indoleamine 2,3-dioxygenase) activity after IFN-γ stimulation [102].
- Consider iMSCs: Transition to induced Pluripotent Stem Cell-derived MSCs (iMSCs). iMSCs offer a more consistent and scalable cell source, reducing batch-to-batch variability [101].
- Preconditioning (Priming): Prime MSCs prior to application. Expose them to a pro-inflammatory cytokine like IFN-γ or to mild hypoxia. This "licenses" the MSCs, enhancing their immunomodulatory secretome and homing capabilities [102].
- Characterize Thoroughly: Adhere to the updated ISCT Delphi consensus criteria, which go beyond surface markers to include functional attributes like potency and viability, ensuring a more comprehensive product characterization [102].
FAQ 3: What are the primary safety concerns for allogeneic MSC therapy in aged, immunocompromised models?
- Potential Concerns: While MSCs are generally considered low immunogenicity, the aged and inflamed microenvironment may alter their behavior [102].
- Risk Mitigation Steps:
- Tumorigenicity: Although risk is low, perform rigorous checks for genomic stability, especially with long-term cultures or genetically modified MSCs. Karyotype analysis and tumorigenicity assays in immunodeficient mice are recommended for clinical-grade cells [101] [102].
- Immunogenicity: Be aware that repeated administration of allogeneic MSCs can elicit host immune responses in some contexts. Monitor for adverse clinical responses and consider using MSC-derived exosomes, which have even lower immunogenicity [104] [102].
- Cell Fate and Engraftment: Understand that most systemic MSCs are transiently engrafted and are cleared within days to weeks. The therapeutic effects are largely paracrine. Use cell tracking methods (e.g., luciferase imaging) to monitor biodistribution and persistence [102].
FAQ 4: How can we objectively measure the "rejuvenation" effect of our MSC treatment in an animal model?
- Solution: Move beyond chronological age and employ quantitative biomarkers of biological age [104].
- Recommended Approaches:
- Epigenetic Clocks: This is the gold standard. Use DNA methylation-based aging clocks (e.g., based on Horvath's or Hannum's methods) on target tissues (blood, liver, etc.) pre- and post-treatment to quantify reversal of biological age [106] [104].
- SASP Plasma Biomarkers: Measure circulating levels of SASP factors (e.g., IL-6, TNF-α, MMPs) as a proxy for systemic aging and inflammation. A successful intervention should reduce these markers [105].
- Functional Biomarkers: Integrate measures of healthspan, such as improved cognitive performance in memory tests, enhanced physical endurance (grip strength, rotarod), and improved metabolic parameters (glucose tolerance) [104].
Cellular senescence is a fundamental mechanism in aging, marked by irreversible growth arrest and diverse functional changes, including the development of a senescence-associated secretory phenotype (SASP) [36]. In the context of stem cell research, the accumulation of senescent cells impairs tissue regeneration, promotes chronic inflammation, and drives age-related functional decline [36] [107]. Senescent stem cells lose their regenerative capacity, creating a pro-inflammatory microenvironment that further disrupts tissue homeostasis [80].
Senotherapeutics represent a promising class of interventions to counteract stem cell aging, comprising two principal strategies: senolytics, which selectively induce apoptosis in senescent cells, and senomorphics, which modulate deleterious aspects of the senescence phenotype without removing the cells [36] [108]. This technical support center provides troubleshooting guidance for researchers investigating these compounds in stem cell senescence and replicative aging prevention.
Senotherapeutic Mechanisms: Signaling Pathways and Molecular Targets
Key Signaling Pathways in Cellular Senescence
The following diagram illustrates the core molecular pathways involved in cellular senescence and the points of intervention for senotherapeutic agents:
Research Reagent Solutions for Senescence Research
Table 1: Essential Research Reagents for Senotherapeutic Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Senolytic Compounds | Dasatinib, Quercetin, Fisetin, Navitoclax (ABT-263), Piperlongumine | Selective elimination of senescent cells; testing combination therapies | Cell-type specificity varies; intermittent dosing often required to reduce toxicity [36] [109] |
| Senomorphic Compounds | Rapamycin, Metformin, JAK inhibitors (e.g., Ruxolitinib), Curcumin | Suppression of SASP without cell killing; modulating inflammatory microenvironment | Effects are transient; continuous exposure typically needed [108] [107] |
| Senescence Inducers | Doxorubicin, Etoposide, Hydrogen peroxide, High glucose media, Ionizing radiation | Induction of senescence in stem cell models for experimental studies | Dose optimization critical to avoid overt cytotoxicity [108] [110] |
| Detection Reagents SA-β-Gal assay kits, γ-H2AX antibodies, p16/p21 antibodies, SASP cytokine ELISA arrays | Quantification of senescent cell burden and characterization of phenotype | Multiple biomarkers recommended for confident identification [36] [108] |
Troubleshooting Guide: Frequently Asked Questions
Senescence Induction and Model Validation
Q1: Our stem cell cultures show inconsistent senescence induction despite using standardized protocols. What are the key factors to optimize?
A: Inconsistent senescence induction typically stems from several controllable factors:
- Stress dose titration: For chemical inducers like doxorubicin, perform dose-response curves (typically 100-500 nM for 24-48 hours) followed by 3-7 days recovery [108]. Check viability 24h post-treatment - aim for 70-80% survival.
- Cell density effects: Plate cells at consistent densities (30-50% confluence) to prevent contact inhibition from confounding results.
- Validation timing: Assess markers at appropriate timepoints: SA-β-Gal at 3-5 days, p16/p21 protein at 2-4 days, SASP factors at 5-7 days post-induction.
- Passage number control: Use consistent early passages of stem cells, as replicative history affects senescence susceptibility.
Q2: Which senescence biomarkers provide the most reliable validation in stem cell models?
A: Implement a multi-parameter validation approach:
- Essential primary markers: SA-β-Gal activity combined with p16INK4a or p21CIP1 protein detection [108] [110].
- Secondary confirmation: DNA damage markers (γ-H2AX foci) and loss of proliferation markers (Ki-67 or EdU incorporation) [36].
- Functional validation: SASP analysis via cytokine array or RNA-seq of IL-6, IL-8, MMPs [107].
- Stem cell-specific considerations: Assess differentiation capacity alterations and stemness marker changes alongside general senescence markers.
Senotherapeutic Efficacy and Specificity
Q3: Our senolytic treatments show variable efficacy across different stem cell types. How can we optimize for cell-type specificity?
A: Variable efficacy is expected due to heterogeneous anti-apoptotic pathway dependence:
- Mechanism-based selection: Test senolytics targeting different SCAPs: BCL-2 family inhibitors (navitoclax) for mesenchymal stem cells, dasatinib for progenitor cells, fisetin for endothelial differentiation models [36] [37].
- Combination approaches: Implement D+Q (dasatinib + quercetin) for broader targeting [108] [109].
- Dose optimization: Use intermittent dosing (e.g., 24-48 hours followed by washout) to reduce off-target effects while maintaining efficacy [36].
- Cell-type specific markers: Correlate efficacy with expression of targets like BCL-xL, pi3KCD, or tyrosine kinase profiles.
Q4: How do we distinguish true senolytic effects from general cytotoxicity?
A: Implement these specific controls:
- Dose-response in non-senescent cells: Compare IC50 in senescent vs. non-senescent counterparts; true senolytics should show ≥10-fold selectivity [37].
- Apoptosis confirmation: Measure caspase-3/7 activation specifically in SA-β-Gal+ cells using flow cytometry or live-cell imaging.
- Long-term culture recovery: After treatment and washout, monitor regrowth - true senolytic effects permit proliferation renewal from non-senescent populations.
- SASP suppression verification: Even with partial clearance, monitor SASP reduction as secondary efficacy indicator.
Technical Challenges in Assessment Methods
Q5: SA-β-Gal staining shows high background in our stem cell cultures. How can we improve specificity?
A: High background typically results from suboptimal conditions:
- pH precision: Prepare fresh staining solution at precisely pH 6.0 using citric acid/phosphate buffer; deviation even by 0.2 pH units increases lysosomal background [108].
- Hypoxia control: Maintain consistent oxygen tension (5% O2 for many stem cells) as atmospheric oxygen can induce stress-related β-galactosidase.
- Fixation optimization: Fix with 2% formaldehyde/0.2% glutaraldehyde for 5 minutes at room temperature rather than higher concentrations or longer times.
- Appropriate controls: Include known senescent (doxorubicin-treated) and non-senescent (low passage) controls in every experiment.
Q6: Our SASP analysis shows inconsistent results across experimental replicates. What are key technical considerations?
A: SASP heterogeneity requires careful experimental design:
- Conditioned media collection: Use serum-free conditions during collection period (12-24 hours), normalize to cell number, and process immediately or at -80°C.
- Temporal dynamics: Recognize that SASP composition evolves over time - early (72 hours) vs. established (7+ days) senescence shows different profiles [36].
- Multi-analyte approach: Use multiplex cytokine arrays rather than single-analyte ELISAs to capture SASP complexity.
- RNA-seq complement: Combine secretome analysis with transcriptomic SASP factor quantification for comprehensive profiling.
Comparative Efficacy Profiles of Major Senotherapeutic Agents
Table 2: Efficacy, Safety, and Technical Considerations of Key Senotherapeutics
| Senotherapeutic Agent | Mechanism of Action | Efficacy in Stem Cell Models | Key Advantages | Technical Limitations & Safety Concerns |
|---|---|---|---|---|
| Dasatinib + Quercetin (D+Q) | Dasatinib: Tyrosine kinase inhibitor; Quercetin: PI3K/AKT, BCL-2 family inhibitor [36] [108] | Effective in senescent mesenchymal stem cells, pre-adipocytes; reduces p16INK4a, p21CIP1, SASP factors [36] | Broad-spectrum activity; extensive preclinical validation; human trial data available [108] | Dasatinib has potential systemic toxicity; cell-type specific efficacy; intermittent dosing required [109] |
| Fisetin | Flavonoid that suppresses PI3K/AKT, BCL-2 family; induces apoptosis in senescent cells [96] | Reduces senescent cell burden in aged stem cell niches; improves tissue regeneration capacity [96] | Favorable safety profile; natural compound; oral bioavailability | Low bioavailability; rapid metabolism; variable potency across cell types [96] |
| Navitoclax (ABT-263) | BCL-2/BCL-xL inhibitor; disables senescent cell anti-apoptotic pathways (SCAPs) [36] [108] | Potent across multiple senescent phenotypes; effective in hematopoietic stem cell models | Broad-acting across senescent cell types; well-characterized mechanism | Thrombocytopenia due to BCL-xL inhibition in platelets; hematological toxicity [36] |
| SGLT2 Inhibitors (e.g., Dapagliflozin) | Multiple pathways: AMPK activation, mTOR inhibition, reduced inflammation and oxidative stress [110] | Reduces high glucose-induced senescence in endothelial progenitor cells; improves stem cell function | Cardiovascular and renal benefits documented in humans; repurposing potential | Cell-type specific effects; mechanism in stem cells not fully elucidated [110] |
Advanced Methodologies and Emerging Approaches
Experimental Workflow for Comprehensive Senotherapeutic Assessment
The following diagram outlines an integrated experimental approach for evaluating senotherapeutics in stem cell models:
Emerging Technologies and Future Directions
Next-Generation Senotherapeutic Approaches:
- CAR-T Cell Therapy: Engineered chimeric antigen receptor T cells targeting senescent cell surface markers like NKG2DLs show promise in animal models [108].
- Antibody-Drug Conjugates: Targeted delivery of cytotoxic payloads to senescent cells via surface markers like β2-microglobulin [36].
- AI-Driven Discovery: Machine learning approaches screening chemical libraries for novel senotherapeutic compounds with favorable pharmacokinetics [108] [109].
- Lysosomal Targeting: Recent evidence indicates lysosomal hyperactivation drives stem cell aging; targeting vacuolar ATPase reverses aged blood stem cell function [2].
- Gene-Enhanced Stem Cells: FOXO3-engineered senescence-resistant mesenchymal progenitor cells demonstrate rejuvenation potential in primate models [80].
The field of senotherapeutics continues to evolve rapidly, with promising implications for stem cell research and regenerative medicine. While current senolytic and senomorphic strategies show significant potential for counteracting stem cell aging, researchers must carefully consider cell-type specificity, optimal dosing protocols, and appropriate validation methodologies. The continued development of more selective senotherapeutic agents and combination approaches will likely enhance our ability to preserve stem cell function and combat age-related tissue degeneration.
Frequently Asked Questions (FAQs)
Q1: What are the core biomarkers for monitoring stem cell senescence, and what are their primary functions? The core biomarkers encompass three key categories: the cGAS-STING pathway, a cytosolic DNA-sensing mechanism that activates innate immune responses; p16INK4a, a cyclin-dependent kinase inhibitor and cell cycle regulator; and the Senescence-Associated Secretory Phenotype (SASP), a collection of secreted factors like cytokines, chemokines, and proteases. In stem cell senescence, these biomarkers coordinate a stable cell cycle arrest and alter the local tissue microenvironment [111] [112] [28].
Q2: I've observed that p16INK4a-positive cells do not always display a strong inflammatory SASP. Is this expected? Yes, this is a recognized phenomenon. Research indicates that ectopic expression of p16INK4a can induce a durable growth arrest without necessarily triggering a robust SASP. The SASP is often a response to significant macromolecular damage, such as from ionizing radiation or oncogene activation, and is considered separable from the p16INK4a-mediated growth arrest itself. Therefore, the presence of p16INK4a is a strong marker for cell cycle exit but not an exclusive indicator of a full, inflammatory senescent state [113].
Q3: My data shows a dissociation between cGAS-STING pathway expression and senescence signatures in tissue samples. How should I interpret this? This finding is supported by clinical data. A 2025 study on colorectal cancer samples found that significant expression of senescence markers did not correlate with cGAS-STING expression levels. This suggests that the relationship between cGAS-STING and senescence may be highly context-dependent, varying by tissue type, senescence inducer, or disease stage. It is crucial to measure multiple, orthogonal senescence biomarkers (e.g., p16INK4a, SASP factors, and SA-β-Gal) in your specific model to accurately characterize the senescent state [114].
Q4: What are the best practices for quantitatively measuring the SASP? Measuring the SASP is challenging due to its complexity and heterogeneity. A multiparametric approach is recommended:
- RNA Level: Use qRT-PCR for a few key SASP factors (e.g., IL6, IL8) or RNA-seq for an unbiased, transcriptome-wide profile [28].
- Protein Level: Employ ELISA for absolute quantification of specific proteins in cell culture supernatant or plasma. Luminex or Meso Scale Discovery (MSD) multiplex assays are ideal for simultaneously measuring dozens of SASP factors from a small sample volume [28] [115].
- Spatial Context: Immunofluorescence or in situ hybridization on tissue sections can identify which cells are producing SASP factors, providing crucial spatial information [28].
Q5: Can targeting lysosomes impact senescence biomarkers in stem cells? Yes, recent groundbreaking research has shown that lysosomal dysfunction is a key driver of hematopoietic stem cell (HSC) aging. Restoring lysosomal function by suppressing hyperactivation reversed aged HSCs to a more youthful state. This reversal was associated with reduced activation of the cGAS-STING immune signaling pathway, improved mitochondrial function, and dampened harmful inflammatory and interferon-driven pathways [2].
Troubleshooting Guides
Table 1: Common Issues in Biomarker Detection and Resolution
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Weak or no p16INK4a signal in senescent cells | - Insensitive antibody- Epigenetic silencing (promoter hypermethylation) | - Validate antibody with a positive control (e.g., stressed cells).- Treat cells with a DNA methyltransferase inhibitor (e.g., 5-Aza-2'-deoxycytidine) and re-assess [112]. |
| High background in SASP ELISA | - Non-specific antibody binding- Sample components interfering | - Optimize antibody dilution and include a blocking step with 5% BSA.- Dilute sample or use a sample dilution buffer provided in the kit. |
| Inconsistent cGAS-STING pathway activation | - Variable DNA transfection efficiency (if using dsDNA transfection)- Cell-type specific differences | - Use a standardized method for cytosolic DNA delivery (e.g., transfection of a non-metabolizable dsDNA).- Include a positive control cell line known to have a robust STING response (e.g., THP-1) [116]. |
| Dissociation between p16INK4a and SA-β-Gal | - p16INK4a expression may precede SA-β-Gal activity- Different senescence inducers | - Perform a time-course experiment to track the emergence of both biomarkers.- Characterize the type of senescence (e.g., replicative vs. stress-induced) in your model [112] [113]. |
Table 2: Key Research Reagent Solutions
| Reagent / Assay | Function / Application | Key Considerations |
|---|---|---|
| cGAS/STING Knockout Models (e.g., CRISPR/Cas9) | To establish the necessity of the pathway in sustaining stemness and senescence. | cGAS- or STING-knockout impaired tumorsphere formation and tumorigenesis in vivo [111]. |
| Recombinant cGAMP (STING Agonist) | To directly activate the STING pathway and study downstream effects on stem cell function and SASP. | Can be used to polarize Tumor-Associated Macrophages (TAMs) towards an anti-tumor M1 phenotype, influencing the microenvironment [117]. |
| Phospho-STAT3 (Tyr705) Antibody | To detect activation of the STAT3 pathway, a potential downstream effector of cGAS-STING in maintaining cancer stemness [111]. | Use in Western Blot or ICC to correlate cGAS-STING activity with STAT3 phosphorylation. |
| Lysosomal Vacuolar ATPase Inhibitor | To investigate and reverse lysosome-mediated stem cell aging. | Treatment reversed aged HSC lysosomal hyperacidity, restored regenerative capacity, and reduced cGAS-STING-driven inflammation [2]. |
| SASP Proteomic Atlas (www.saspatlas.com) | A comprehensive database for identifying senescence-specific secreted proteins across cell types and inducers [115]. | Use to identify and validate candidate SASP factors (e.g., GDF15, STC1) in stem cell models. |
Experimental Protocols & Data Summarization
Protocol 1: Validating Senescence via Tumorsphere Formation Assay
Application: Assessing the self-renewal and stemness potential of stem/cancer stem cells in vitro, which is potentiated by the cGAS-STING pathway [111].
Detailed Methodology:
- Prepare Single Cell Suspension: Dissociate your stem cell population into a single-cell suspension using enzymatic (e.g., trypsin) or mechanical means.
- Seed Cells: Dilute cells in a serum-free medium supplemented with growth factors (e.g., 20 ng/ml EGF, 10 ng/ml bFGF) and 0.4% BSA. Plate the cells in an ultra-low attachment 96-well plate at a density of < 1000 cells/well to prevent aggregation.
- Culture: Incubate cells for 10-14 days in a 5% CO₂ humidified incubator at 37°C. Change the medium every two days by carefully removing half of the medium and replacing it with fresh pre-warmed medium.
- Image and Quantify: After 10-14 days, acquire multiple images from different fields of view using an inverted microscope. Quantify the number and size of tumorspheres (typically spherical structures with a diameter >50 µm) using image analysis software. Compare the tumorsphere-forming efficiency between control and experimental groups (e.g., cGAS/STING knockout) [111].
Protocol 2: Measuring SASP Factors via Multiplex Immunoassay
Application: Simultaneously quantifying the concentration of multiple SASP proteins from cell culture supernatant, tissue lysate, or plasma/serum.
Detailed Methodology:
- Sample Collection and Preparation: Centrifuge cell culture media to remove cellular debris. Collect plasma or serum using standard protocols. Aliquot and store samples at -80°C until analysis.
- Assay Setup: Following the manufacturer's protocol for your chosen multiplex platform (e.g., Luminex, MSD). Briefly, this involves:
- Adding samples and standards to the pre-coated microplate.
- Incubating to allow analyte binding.
- Washing away unbound material.
- Adding a detection antibody mixture.
- Adding a streptavidin-phycoerythrin (for Luminex) or read buffer (for MSD) for signal development.
- Data Acquisition and Analysis: Run the plate on the appropriate analyzer. Use the standard curve to calculate the concentration of each SASP factor in your samples. Normalize cell culture data to cell number or total protein content [28] [115].
| Biomarker | Primary Mechanism | Impact on Stem Cells | Contextual Notes |
|---|---|---|---|
| cGAS-STING | Detects cytosolic DNA, induces type I IFN and SASP. | Potentiates tumor progression by sustaining cancer stemness; linked to STAT3 activation [111]. | A double-edged sword: can have anti-tumor (immunostimulatory) or pro-tumor (stemness-sustaining) effects [111] [117]. |
| p16INK4a | Inhibits CDK4/6, enforcing G1 cell cycle arrest. | Induces irreversible proliferative arrest, a hallmark of senescence [112]. | Not always associated with an inflammatory SASP; considered a specific but not exhaustive marker of senescence [113]. |
| SASP Factors (e.g., IL-6, IL-8, GDF15) | Paracrine signaling to alter tissue microenvironment. | Can reinforce senescence, promote chronic inflammation, and alter stem cell niche function [28] [115]. | Highly heterogeneous; composition depends on cell type and senescence trigger. A core "SASP Atlas" exists for biomarker discovery [115]. |
Signaling Pathways and Workflows
Diagram 1: cGAS-STING Pathway in Senescence
Title: cGAS-STING-SASP Signaling Axis
Diagram 2: p16INK4a Cell Cycle Arrest
Title: p16INK4a-pRB Cell Cycle Arrest Pathway
Diagram 3: Senescence Biomarker Validation Workflow
Title: Multiparameter Senescence Validation Workflow
Defining Core Longevity Metrics for Experimental Design
FAQ: What is the critical distinction between healthspan and lifespan, and why is it essential for our research on stem cell senescence?
In aging research, precisely defining endpoints is crucial for evaluating the efficacy of interventions. The following table clarifies the core concepts your experiments should measure.
Table: Key Longevity Metrics for Intervention Studies
| Term | Definition | Experimental/Clinical Correlates |
|---|---|---|
| Lifespan | The total time an individual lives, from birth to death [118] [119]. | Primary endpoint: Time until death (or median/mean survival time) in model organisms [118]. |
| Healthspan | The period of life spent in good health, free from serious chronic diseases and significant disability, with preserved physical and cognitive function [118] [119]. | Composite endpoint: Onset of first chronic disease, age-related functional decline (e.g., grip strength, cognitive tests), or independent living capacity [119]. |
| Longevity | The ability to live significantly beyond the average life expectancy under optimal conditions [118]. | Contextual metric: Often used to describe the outcome of interventions that extend lifespan or the trait of long-lived populations. |
Thesis Context: For research focused on stem cell senescence, the primary goal of an intervention is not merely to extend chronological life (lifespan) but to delay the onset of age-related pathology and functional decline (healthspan). A therapy that extends lifespan without improving healthspan could prolong the period of frailty and disability, increasing the healthcare burden. Therefore, your experimental design must track functional healthspan metrics alongside survival data [119]. A global analysis revealed an average 9-10 year gap between total lifespan and healthspan, underscoring the importance of this distinction [119].
Quantitative Data: The Healthspan-Lifespan Gap
FAQ: What quantitative data exists on the global healthspan-lifespan gap, and how can it inform our study targets?
Understanding the current landscape of aging outcomes provides a benchmark for evaluating the success of novel interventions. A 2025 study mapping 183 World Health Organization member states provides critical baseline data.
Table: Global Healthspan-Lifespan Gap Analysis (Garmany & Terzic, 2025) [119]
| Metric | Finding | Implication for Researchers |
|---|---|---|
| Average Global Gap | 9-10 years | This quantifies the scale of the problem; effective interventions should aim to narrow this gap. |
| Variation by Sex | The gap is larger for women. | Study designs must account for sex as a biological variable in aging interventions. |
| Variation by Region | Significant regional differences exist. | The gap is modifiable by environmental, healthcare, and lifestyle factors, proving it is a valid target for therapeutic intervention. |
This data confirms that focusing solely on lifespan can mask declines in population well-being. Healthspan metrics are more effective for capturing the true effectiveness of anti-aging therapies, including those targeting stem cell senescence [119].
Experimental Protocols for Assessing Healthspan and Rejuvenation
Protocol 1: Assessing Stem Cell Rejuvenation via Lysosomal Modulation
This protocol is based on a 2025 study that successfully reversed aging in hematopoietic stem cells (HSCs) by targeting lysosomal dysfunction [2] [120].
Detailed Methodology:
- Cell Isolation: Extract HSCs from the bone marrow of aged donor mice (e.g., 22-24 months old).
- Ex Vivo Treatment: Culture the isolated HSCs in a medium supplemented with a vacuolar ATPase inhibitor, such as Concanamycin A (e.g., 100 nM for 16 hours). This agent suppresses lysosomal hyperacidity.
- Transplantation: Transplant the treated HSCs into lethally irradiated recipient mice (a standard assay for stem cell function).
- Functional Assessment:
- Blood Reconstitution Capacity: Monitor the frequency and diversity of blood cell lineages (myeloid, lymphoid) in peripheral blood weekly for 16 weeks. The cited study showed an eightfold increase in blood-forming capacity post-treatment [2].
- Metabolic & Epigenetic Analysis: Analyze treated cells for restoration of mitochondrial function, reduced inflammatory signaling (e.g., cGAS-STING pathway), and improved epigenomic markers [2] [120].
The following workflow diagram visualizes this experimental protocol:
Protocol 2: Predicting Biological Age with Machine Learning
Machine learning models using blood-based biomarkers can quantify biological age, a key healthspan metric. This protocol is based on a 2025 study that used the China Health and Retirement Longitudinal Study (CHARLS) database [121].
Detailed Methodology:
- Data Collection: Compile a dataset of blood-based biomarkers. The referenced study used 16 markers, including cystatin C, glycated hemoglobin (HbA1c), creatinine, and C-reactive protein [121].
- Model Training:
- Target Variable: Use chronological age for the initial model.
- Algorithms: Train tree-based models (e.g., CatBoost, XGBoost, LightGBM) using the biomarker data.
- Biological Age Calculation: The predicted age from the model is the individual's Biological Age (BA). The difference between BA and chronological age (AgeAccel) indicates accelerated or decelerated aging [122] [121].
- Validation:
- Frailty Correlation: Validate the BA model by testing its ability to predict a separate, functional outcome like frailty status (constructed from deficits in activities of daily living, chronic diseases, etc.) [121].
- Explainability: Apply SHapley Additive exPlanations (SHAP) analysis to identify which biomarkers (e.g., cystatin C) are the most significant contributors to the model's predictions, linking them directly to the aging process [121].
The logical relationship between data, model, and validation is shown below:
Troubleshooting Common Experimental Challenges
FAQ: Our stem cell intervention shows promising lifespan extension in mice, but healthspan metrics are unclear. What went wrong?
- Problem: Lifespan extension without proportional healthspan improvement.
- Solution:
- Implement Composite Healthspan Endpoints: Move beyond simple survival. Incorporate standardized tests for frailty (e.g., mouse clinical assessment battery), cognitive function (e.g., Morris water maze), and physical performance (e.g., grip strength, rotarod) [119].
- Track Onset of Specific Pathologies: Use histopathology and non-invasive imaging to document the delayed onset or reduced severity of age-related diseases (e.g., cancer, kidney disease) in treated cohorts [56].
- Measure Biomarkers of Aging: Utilize epigenetic clocks or panels of blood-based biomarkers (see Protocol 2) to objectively quantify biological aging rates in your treatment groups [121].
FAQ: Our senolytic agent, effective in vitro, fails to reduce senescent cell burden or improve function in aged mice.
- Problem: Failure to translate in vitro senolytic activity to in vivo models.
- Solution:
- Verify Target Engagement: Confirm the agent reaches the target tissues at a sufficient concentration and duration. Use pharmacokinetic analysis and measure downstream effects of senolytic action (e.g., reduced SASP factors in blood) [123].
- Optimize Dosing Regimen: Continuous dosing may cause side effects. Consider intermittent dosing ("hit-and-run" approach), which has shown better efficacy and tolerability in some senolytic studies [123].
- Use a More Translational Model: Standard lab mice are kept in pristine conditions. Consider testing your intervention in mice challenged with a more "real-world" environment (e.g., variable temperatures, pathogen exposure) to better predict human efficacy [123].
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Reagents for Stem Cell Senescence and Longevity Research
| Reagent / Solution | Function / Application | Key Examples / Notes |
|---|---|---|
| Lysosomal Inhibitors | To study and modulate lysosomal function in aged stem cells. Critical for investigating metabolic rejuvenation [2]. | Concanamycin A (V-ATPase inhibitor); Chloroquine. |
| Senolytics | To selectively clear senescent cells and assess their role in aging and healthspan [85] [123]. | Dasatinib and Quercetin (D+Q); Fisetin. Note: Clinical translation has been challenging [123]. |
| mTOR Inhibitors | To mimic caloric restriction and modulate nutrient-sensing pathways, a key longevity mechanism [56] [123]. | Rapamycin (Sirolimus); Everolimus. |
| NAD+ Boosters | To elevate cellular NAD+ levels, activating sirtuins and improving mitochondrial function [85] [123]. | Nicotinamide Riboside (NR); Nicotinamide Mononucleotide (NMN). |
| Yamanaka Factors | For epigenetic reprogramming studies to reverse cellular age [56]. | Inducible expression of Oct4, Sox2, Klf4, c-Myc (OSKM). Requires strict control to avoid tumorigenesis. |
| Key Biomarkers | For constructing biological age clocks and assessing healthspan. | Cystatin C (kidney function, strong predictor), Glycated Hemoglobin (HbA1c, metabolism), CRP (inflammation) [121]. |
| IL-11 Inhibitors | To target the pro-inflammatory cytokine IL-11, a newly identified key driver of "inflammaging" [123]. | Anti-IL-11 antibodies. Shown to extend lifespan in mice by up to 25% [123]. |
Conclusion
The integration of foundational research on stem cell senescence with advanced therapeutic strategies marks a paradigm shift in tackling replicative aging. Key takeaways establish lysosomal and epigenetic dysfunction as central, druggable targets, with senolytics and senomorphics offering complementary approaches for eliminating or modulating senescent cells. Overcoming translational challenges requires improved biomarker development and targeted delivery systems. Future directions must prioritize human clinical validation, combination therapies, and understanding the long-term consequences of senescent cell clearance. The convergence of geroscience with regenerative medicine promises not only enhanced efficacy in cell-based therapies but also novel interventions for extending human healthspan and treating age-related pathologies.
References
- 1. Reversing lysosomal dysfunction restores youthful state in ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925004059?via%3Dihub]
- 2. Mount Sinai Scientists Reverse Aging in Blood Stem Cells ... [https://www.mountsinai.org/about/newsroom/2025/mount-sinai-scientists-reverse-aging-in-blood-stem-cells-by-targeting-lysosomal-dysfunction]
- 3. Reversing lysosomal dysfunction restores youthful state in ... [https://pubmed.ncbi.nlm.nih.gov/41289991/]
- 4. Role of Lysosomal Acidification Dysfunction in ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.817877/full]
- 5. Molecular Mechanisms in Lysosomal Storage Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC9031509/]
- 6. The role of the dynamic epigenetic landscape in senescence [https://www.nature.com/articles/s41514-024-00172-2]
- 7. Dynamic 3D genome reorganization during senescence [https://www.nature.com/articles/s41418-023-01197-y]
- 8. Beyond SAHF: An integrative view of chromatin ... [https://www.sciencedirect.com/science/article/pii/S0955067423000558]
- 9. Chromatin basis of the senescence-associated secretory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9106822/]
- 10. Epigenetic Regulation of Cellular Senescence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8870565/]
- 11. Chromatin remodeling underlies the senescence ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/22422937/]
- 12. Molecular mechanisms of aging and anti-aging strategies [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01663-1]
- 13. Replication stress as a driver of cellular senescence and ... [https://www.nature.com/articles/s42003-024-06263-w]
- 14. The cGAS–cGAMP–STING pathway connects DNA damage to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5940270/]
- 15. cGAS–STING drives ageing-related inflammation and ... [https://www.nature.com/articles/s41586-023-06373-1]
- 16. Activation of cGAS-STING signaling in senescent cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620326/]
- 17. Stem cell aging: mechanisms, regulators and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4160113/]
- 18. Mitochondrial dysfunction: mechanisms and advances in therapy | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-024-01839-8]
- 19. Mitochondrial dysfunction in cell senescence and aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC9246372/]
- 20. Senescence suppressors: their practical importance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11113678/]
- 21. Mitochondria in oxidative stress, inflammation and aging [https://www.nature.com/articles/s41392-025-02253-4]
- 22. Article Mitochondrial Dysfunction Induces Senescence with ... [https://www.sciencedirect.com/science/article/pii/S1550413115005781]
- 23. Mitochondrial proteins as biomarkers of cellular ... [https://pubmed.ncbi.nlm.nih.gov/40856658/]
- 24. Mitochondrial proteins as biomarkers of cellular ... [https://www.aging-us.com/article/206305/text]
- 25. Mitochondrial dysfunction acts as a modulator of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628636/]
- 26. Mitochondrial Diseases: Causes, Symptoms & Treatment [https://my.clevelandclinic.org/health/diseases/15612-mitochondrial-diseases]
- 27. SASP Modulation for Cellular Rejuvenation and Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025513/]
- 28. Measuring the Senescence-Associated Secretory Phenotype [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467123/]
- 29. Preventing MSC aging and enhancing immunomodulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124620/]
- 30. Targeting the senescence-associated secretory phenotype ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725001783]
- 31. Iron accumulation drives fibrosis, senescence and the ... [https://www.nature.com/articles/s42255-023-00928-2]
- 32. Replicative Senescence in Mesenchymal Stem Cells [https://www.mdpi.com/2076-3921/14/4/446]
- 33. The Senescence Associated Secretory Phenotype, a key ... [https://pubmed.ncbi.nlm.nih.gov/40653403/]
- 34. Identification of markers for neurescence through ... [https://www.nature.com/articles/s41514-025-00235-y]
- 35. Senescence and aging: Causes, consequences, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5748990/]
- 36. Targeting Senescence: A Review of Senolytics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190739/]
- 37. Current senolytics: Mode of action, efficacy and limitations ... [https://www.sciencedirect.com/science/article/pii/S0047637423001148]
- 38. Senolytics: from pharmacological inhibitors to ... [https://www.nature.com/articles/s41514-024-00138-4]
- 39. The Antiaging Potential of Dietary Plant-Based Polyphenols [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114605/]
- 40. The senolytic cocktail, dasatinib and quercetin, impacts the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181558/]
- 41. Long-term treatment with senolytic drugs Dasatinib and ... [https://www.nature.com/articles/s41467-021-25453-2]
- 42. Polyphenols show potential for healthy aging and cellular ... [https://www.nutraingredients.com/Article/2025/05/30/polyphenols-show-potential-for-healthy-aging-and-cellular-senescence/]
- 43. Exploring the effects of Dasatinib, Quercetin, and Fisetin on ... [https://www.aging-us.com/article/205581/text]
- 44. Emerging insights in senescence: pathways from ... [https://www.nature.com/articles/s41514-024-00181-1]
- 45. Pharmacological frontiers in senescence [https://www.sciencedirect.com/science/article/abs/pii/S1054358925000511]
- 46. The controversial role of senescence-associated secretory ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02475-8]
- 47. Targeting immunosenescence and inflammaging [https://www.nature.com/articles/s12276-025-01527-9]
- 48. The JAK/STAT signaling pathway: from bench to clinic [https://www.nature.com/articles/s41392-021-00791-1]
- 49. JAK/STAT pathway: Extracellular signals, diseases, immunity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9995824/]
- 50. Fixing Lysosomes Improves Blood Stem Cell Function [https://www.lifespan.io/news/fixing-lysosomes-improves-blood-stem-cell-function/]
- 51. A phosphoinositide signalling pathway mediates rapid ... [https://www.nature.com/articles/s41586-022-05164-4]
- 52. Built to last: Lysosome remodeling and repair in health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9189017/]
- 53. Failure of lysosomal acidification and endomembrane ... [https://www.nature.com/articles/s12276-025-01579-x]
- 54. Chromatin remodeling underlies the senescence-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3605047/]
- 55. Senescence-associated secretory phenotype [https://en.wikipedia.org/wiki/Senescence-associated_secretory_phenotype]
- 56. Recent progress in stem cell and immune cell-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321787/]
- 57. HDAC2 and 7 down-regulation induces senescence in ... [https://www.aging-us.com/article/203304/text]
- 58. Histone deacetylase inhibitors: molecular mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3056563/]
- 59. Histone deacetylase inhibitors: molecular mechanisms of ... [https://www.nature.com/articles/1210620]
- 60. The Senescence-Associated Secretory Phenotype [https://pmc.ncbi.nlm.nih.gov/articles/PMC4166495/]
- 61. Exploring the role of histone deacetylase and histone ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-024-00507-5]
- 62. Extracellular Vesicle Secretion from 3D Culture of Human ... [https://www.mdpi.com/2306-5354/12/9/933]
- 63. improving physiological relevance and yield with 3D cell culture [https://pubs.rsc.org/en-ca/content/articlehtml/2025/nr/d5nr00707k]
- 64. Production and Utility of Extracellular Vesicles with 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9961751/]
- 65. Unlocking the potential of extracellular vesicles: one stimulus ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d5bm01091h]
- 66. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 67. Heterogeneity of Cellular Senescence, Senotyping, and ... [https://pubmed.ncbi.nlm.nih.gov/41096951/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=18y2KI_P1NiQ7OoM-E61YbMjWnlFev64RcvDpSMag7lLnQnUoc&fc=None&ff=20251027171953&v=2.18.0.post22+67771e2]
- 68. Senescent cell heterogeneity and responses to senolytic ... [https://www.aging-us.com/article/206299/text]
- 69. An updated landscape of cellular senescence heterogeneity [https://www.sciencedirect.com/science/article/pii/S2468501123000056]
- 70. Cellular Senescence and Aging: Problems and Solutions [https://www.jinfiniti.com/cellular-senescence-and-aging/?srsltid=AfmBOor9JyIzoQ_Et_LWm7-BYJQm5_Q2X9vNF9XNIycwj6QLfCynOYHw]
- 71. Heterogeneity of Cellular Senescence, Senotyping, and ... [https://www.mdpi.com/1422-0067/26/19/9687]
- 72. Cellular Senescence: Advantages, Disadvantages, and ... [https://fluorofinder.com/cellular-senescence/]
- 73. Protocol for examining the capability of senescent tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10751553/]
- 74. Challenges in Development of Nanoparticle-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326161/]
- 75. Achieving Targeted Delivery with Nanoscale Systems [https://www.pharmtech.com/view/achieving-targeted-delivery-with-nanoscale-systems]
- 76. Nano based drug delivery systems: recent developments and ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-018-0392-8]
- 77. The drug discovery and therapeutic nano-strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605296/]
- 78. Advances in Nanotherapy for Targeting Senescent Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC11365502/]
- 79. Nanotechnology shaping stem cell therapy [https://www.sciencedirect.com/science/article/pii/S0753332221000214]
- 80. Rewriting destiny—gene-hacked stem cells ignite a ... [https://www.nature.com/articles/s41419-025-07958-6]
- 81. Reprogramming cellular senescence and aging clocks for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492661/]
- 82. Cellular Models of Aging and Senescence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384970/]
- 83. Multiparameter flow cytometric detection and quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7541365/]
- 84. Guidelines for minimal information on cellular senescence ... [https://www.sciencedirect.com/science/article/pii/S0092867424006408]
- 85. Life Extension Treatments: A New Era in Anti-Aging (2025) [https://www.dvcstem.com/post/life-extension-treatments]
- 86. Rejuvenation Roundup September 2025 [https://www.lifespan.io/news/rejuvenation-roundup-september-2025/]
- 87. Stem Cells: Anti-Aging Treatment Breakthrough in 2025? [https://www.dvcstem.com/post/anti-aging-stem-cells]
- 88. Senescence-Associated β-Galactosidase Detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9599972/]
- 89. Aging of mesenchymal stem cell: machinery, markers, and ... [https://cmbl.biomedcentral.com/articles/10.1186/s11658-022-00366-0]
- 90. In Vivo Tracking Techniques for Cellular Regeneration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3579215/]
- 91. Key points for translating wound regenerative agents from ... [https://www.sciencedirect.com/science/article/pii/S1465324922007368]
- 92. Clinical trials and advanced MRI techniques with stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505762/]
- 93. SenoTAC: An Emerging Senotherapy for Combating Aging [https://www.sciencedirect.com/science/article/abs/pii/S0022356525402651]
- 94. The potential for senotherapy as a novel approach ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2024.1369153/full]
- 95. Recent progress in stem cell and immune cell-based ... [https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2025.1638168/full]
- 96. Fisetin as a senotherapeutic agent: Evidence and ... [https://www.sciencedirect.com/science/article/pii/S0047637424000952]
- 97. Rejuvenation Roundup July 2025 [https://www.lifespan.io/news/rejuvenation-roundup-july-2025/]
- 98. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 99. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 100. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 101. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 102. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 103. Mesenchymal stem cells and exosomes: A novel ... [https://www.sciencedirect.com/science/article/pii/S053155652500110X]
- 104. Mesenchymal stem cells and their derivatives as potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011939/]
- 105. Rewriting destiny—gene-hacked stem cells ignite a revolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371100/]
- 106. 2025 Biomarkers of Aging Conference [https://www.agingconsortium.org/conference-home]
- 107. Senotherapeutics to Counteract Senescent Cells Are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10855240/]
- 108. Senotherapeutics: Different approaches of discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880081/]
- 109. Computational identification of natural senotherapeutic ... [https://www.nature.com/articles/s41598-024-55870-4]
- 110. SGLT2 inhibitors as a novel senotherapeutic approach [https://www.nature.com/articles/s41514-025-00227-y]
- 111. cGAS-STING signalings potentiate tumor progression via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8968062/]
- 112. P16INK4A—More Than a Senescence Marker - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9501954/]
- 113. Tumor Suppressor and Aging Biomarker p16INK4a ... [https://www.sciencedirect.com/science/article/pii/S0021925820508417]
- 114. Dissociation between the expression of cGAS/STING and a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898089/]
- 115. A proteomic atlas of senescence-associated secretomes for ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000599]
- 116. Activation of a cGAS-STING-mediated immune response ... [https://www.nature.com/articles/s41416-021-01599-0]
- 117. Targeting cGAS-STING pathway for reprogramming tumor ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00750-w]
- 118. Bridging expectations and science: a roadmap for the future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213962/]
- 119. Living Longer vs. Living Better: The Critical Distinction ... [https://foodmedcenter.org/lifespan-vs-healthspan-the-critical-gap-in-modern-aging/]
- 120. Scientists Restore Aging Blood Stem Cells to a More ... [https://www.sciencealert.com/scientists-restore-aging-blood-stem-cells-to-a-more-youthful-state-in-mice]
- 121. Explainable machine learning framework for biomarker ... [https://www.nature.com/articles/s41598-025-98948-3]
- 122. Prediction of biological age using machine learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459789/]
- 123. Could humans live to 150? Why some researchers think ... [https://www.nature.com/articles/d41586-025-03524-4]