CRISPR-Engineered Stem Cells: Revolutionizing Therapeutic Development and Disease Modeling
This article provides a comprehensive analysis of the integration of CRISPR gene editing with stem cell technology, a frontier that is reshaping biomedical research and therapeutic development.
CRISPR-Engineered Stem Cells: Revolutionizing Therapeutic Development and Disease Modeling
Abstract
This article provides a comprehensive analysis of the integration of CRISPR gene editing with stem cell technology, a frontier that is reshaping biomedical research and therapeutic development. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of CRISPR-Cas systems and stem cell biology, detailing advanced methodologies for creating precise cellular models. The content delves into critical challenges such as off-target effects, delivery efficiency, and immune responses, offering troubleshooting and optimization strategies grounded in recent studies. Furthermore, it presents a rigorous validation and comparative framework, evaluating CRISPR against traditional editing platforms and highlighting successful clinical applications. By synthesizing insights from current literature and clinical trials, this article serves as a strategic resource for advancing the translation of CRISPR-engineered stem cells from the laboratory to the clinic.
The Confluence of CRISPR and Stem Cells: Building the Bedrock of Modern Therapies
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated (Cas) proteins constitute an adaptive immune system in prokaryotes that has been repurposed as a revolutionary genome-editing technology. This system provides bacteria and archaea with sequence-specific defense against invading mobile genetic elements such as viruses and plasmids. The transition from a bacterial immune mechanism to a programmable genome-editing tool represents one of the most significant breakthroughs in modern biotechnology, enabling precise modifications to genetic information across diverse organisms and cell types.
The fundamental CRISPR-Cas system consists of CRISPR arrays—short repetitive DNA sequences interspersed with unique "spacer" sequences derived from previous invaders—and adjacent Cas genes encoding the protein machinery for immune function [1]. These systems are categorized into two classes: Class 1 (types I, III, and IV) utilize multi-protein effector complexes, while Class 2 (types II, V, and VI) employ a single large Cas protein such as Cas9, Cas12, or Cas13 [1]. The Type II CRISPR-Cas9 system, in particular, has been engineered into a versatile platform for genome editing, comprising the Cas9 endonuclease and a synthetic single-guide RNA (sgRNA) that directs Cas9 to specific DNA sequences [1].
Fundamental Mechanisms of CRISPR-Cas Systems
Native Biological Function in Prokaryotes
In its native context, CRISPR-Cas functions as an adaptive immune system through three distinct stages: adaptation, expression, and interference. During adaptation, specialized Cas1-Cas2 integrase complexes capture short fragments of foreign DNA (protospacers) and integrate them as new spacers into the CRISPR array, creating a genetic record of infection [1]. In the expression phase, the CRISPR array is transcribed and processed into small CRISPR RNAs (crRNAs). Finally, during interference, these crRNAs assemble with Cas proteins to form effector complexes that recognize and cleave complementary nucleic acids of invading pathogens, thereby neutralizing the threat [1].
CRISPR arrays provide remarkable insights into the dynamics of host-pathogen interactions. Spacer acquisition typically occurs at the leader end of arrays, with trailer-end repeats generally representing older sequences [2]. Analysis of CRISPR arrays in Bacteroides fragilis populations from human gut microbiomes has revealed three distinct system types (I-B, II-C, and III-B) with varying prevalence and activity levels between individuals, highlighting the dynamic nature of these systems in natural environments [3].
Molecular Mechanisms of Genome Editing
The repurposing of CRISPR-Cas systems for genome editing leverages the interference stage of the native immune response. When deployed in non-native contexts, the CRISPR-Cas9 system creates targeted double-strand breaks (DSBs) in DNA approximately 3 base pairs upstream of a Protospacer Adjacent Motif (PAM) sequence [4]. These breaks are subsequently repaired by the cell's endogenous DNA repair mechanisms, primarily either Non-Homologous End Joining (NHEJ) or Homology-Directed Repair (HDR).
NHEJ is an error-prone repair pathway that often results in insertions or deletions (indels) that can disrupt gene function, making it suitable for gene knockout applications. In contrast, HDR uses a donor DNA template to enable precise genetic modifications, including nucleotide substitutions, gene insertions, or conditional alleles [4]. The efficiency of HDR remains a significant challenge in CRISPR applications, as NHEJ typically dominates the repair process in most cell types.
Table 1: CRISPR-Cas System Classification and Key Characteristics
| Class | Type | Signature Protein | Target | Key Features |
|---|---|---|---|---|
| Class 1 | I | Cas3 | DNA | Multi-protein effector complex |
| Class 1 | III | Cas10 | DNA/RNA | Targets both DNA and RNA |
| Class 1 | IV | Unknown | Unknown | Function not fully characterized |
| Class 2 | II | Cas9 | DNA | Single effector protein; most widely used |
| Class 2 | V | Cas12 | DNA | Single effector protein; different PAM requirements |
| Class 2 | VI | Cas13 | RNA | RNA-targeting capability |
Applications in Stem Cell Genetic Engineering
Disease Modeling and Therapeutic Development
CRISPR-Cas9 technology has revolutionized stem cell research by enabling precise genetic modifications in pluripotent stem cells. In Alzheimer's disease (AD) research, human induced Pluripotent Stem Cells (hiPSCs) derived from patients can be reprogrammed into neurons and glial cells that recapitulate core pathological features of AD, including amyloid-beta (Aβ) plaques and neurofibrillary tangles [5]. CRISPR-Cas9 facilitates the introduction of pathogenic mutations in genes such as APP, PSEN1, and PSEN2 into hiPSCs, creating isogenic cell lines that allow researchers to study disease mechanisms in a controlled genetic background [5].
These engineered stem cell models provide platforms for high-throughput drug screening, enabling identification of compounds that modulate β- and γ-secretase activity to reduce Aβ formation [5]. Additionally, CRISPR-edited stem cells offer potential for cell replacement therapies, where gene-corrected autologous cells could be transplanted to restore function in neurodegenerative conditions.
Protocol: Generating Conditional Knockout Models in Stem Cells
The generation of conditional knockout (cKO) models using stem cells requires precise integration of recombinase recognition sites (e.g., loxP sites) flanking critical exons of target genes. The following protocol outlines key steps for efficient homology-directed repair in stem cells:
Guide RNA Design: Design two crRNAs targeting sequences flanking the exon of interest. In vivo studies demonstrate that targeting the antisense strand with two crRNAs improves HDR precision compared to other strategies [4].
Donor DNA Template Design: Create a donor template with homologous arms (60-80 bp) flanking the loxP sites. Incorporation of 5'-end modifications (biotin or C3 spacer) significantly enhances HDR efficiency. 5'-biotin modification increases single-copy integration up to 8-fold, while 5'-C3 spacer modification produces up to a 20-fold rise in correctly edited cells [4].
Ribonucleoprotein (RNP) Complex Formation: Combine Cas9 protein with sgRNAs to form RNP complexes. Delivery as RNP complexes rather than plasmid DNA reduces off-target effects and improves editing efficiency.
Stem Cell Transfection: Transfect stem cells using optimized electroporation parameters. For challenging cell types, perform extensive optimization—testing up to 200 conditions in parallel can identify parameters that increase editing efficiency from 7% to over 80% [6].
Validation and Screening: Isolate single-cell clones and validate correct integration via PCR, Southern blotting, and sequencing. Functional validation through differentiation and gene expression analysis confirms the conditional nature of the knockout.
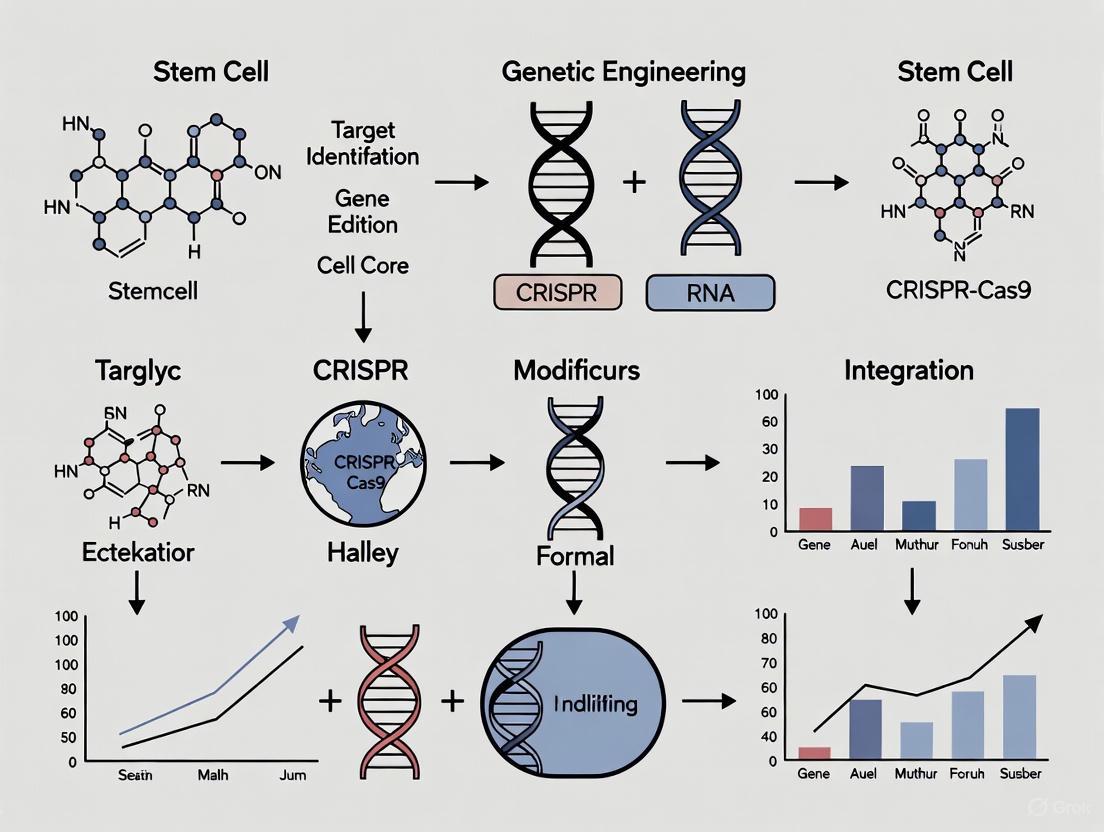
Diagram 1: Workflow for Generating Conditional Knockout Stem Cell Models
Advanced Genome Engineering Technologies
CRISPR-Assisted Transposase Systems
Recent advances have integrated CRISPR systems with transposase enzymes to enable precise, large-scale DNA integration without relying on endogenous DNA repair mechanisms. CRISPR-associated transposase (CAST) systems combine RNA-guided DNA targeting with transposase-mediated DNA insertion, enabling integration of large genetic elements (up to 30 kb) into specific genomic loci [7].
Type I-F CAST systems utilize Cas6, Cas7, and Cas8 proteins forming the Cascade complex, which directs target DNA recognition, while TnsA, TnsB, and TnsC form a heteromeric transposase complex that catalyzes DNA cleavage and transposition [7]. Type V-K CAST systems employ the single-effector protein Cas12k, with DNA integration occurring 60-66 base pairs downstream of the PAM site [7]. These systems have demonstrated nearly complete insertion efficiency in prokaryotic hosts and are being adapted for eukaryotic and mammalian cell applications.
Prime Editing and Precision Modifications
Prime editing represents a versatile "search-and-replace" genome editing technology that enables precise base conversions, small insertions, and deletions without requiring double-strand breaks or donor DNA templates. This system uses a catalytically impaired Cas9 endonuclease fused to an engineered reverse transcriptase enzyme, programmed with a prime editing guide RNA (pegRNA) that specifies the target site and encodes the desired edit [7].
The development of prime editing addresses significant limitations of conventional CRISPR-Cas9 systems, particularly off-target effects and the low efficiency of HDR in post-mitotic cells, including neurons derived from stem cells. This technology shows particular promise for correcting point mutations associated with neurodegenerative diseases in stem cell models.
Table 2: Advanced CRISPR Technologies for Stem Cell Engineering
| Technology | Mechanism | Editing Capacity | Key Advantages | Current Limitations |
|---|---|---|---|---|
| CRISPR-Cas9 HDR | Double-strand break with donor template | < 2 kb | High efficiency knockouts | Low HDR efficiency; off-target effects |
| Base Editing | Chemical modification without DSB | Single nucleotide | High precision; no DSBs | Limited to specific base changes |
| Prime Editing | Reverse transcription without DSB | < 100 bp | Versatile; minimal off-targets | Complex system design |
| CAST Systems | Transposase-mediated integration | Up to 30 kb | Large payload capacity | Early development for eukaryotic cells |
| HITI | NHEJ-mediated integration | 1-5 kb | Works in non-dividing cells | High indel frequency |
Optimization Strategies for Enhanced Efficiency
Improving Homology-Directed Repair
Enhancing HDR efficiency remains a critical focus for precise genome editing applications in stem cells. Recent research has identified several key factors that significantly improve HDR outcomes:
Donor DNA Modifications: Denaturation of long 5'-monophosphorylated double-stranded DNA templates enhances precise editing and reduces unwanted template multiplications. 5'-biotin modification increases single-copy integration up to 8-fold, while 5'-C3 spacer modification produces up to a 20-fold rise in correctly edited cells [4].
Protein Cofactors: Supplementation with RAD52 protein increases single-stranded DNA integration nearly 4-fold, though accompanied by higher template multiplication. This approach demonstrates a 13-fold increase in correct modification compared to dsDNA alone when combined with denatured DNA templates [4].
Strand Targeting: Targeting the antisense strand with two CRISPR RNAs improves HDR precision compared to sense strand targeting, particularly in transcriptionally active genes [4].
Protocol: High-Efficiency Transfection Optimization
Achieving high editing efficiency in stem cells requires careful optimization of transfection parameters. The following protocol outlines a systematic approach:
Cell Line Preparation: Culture stem cells in optimal conditions to ensure >90% viability before transfection. Use early passage cells whenever possible.
Positive Controls: Include species-specific positive controls to distinguish between guide RNA failures and optimization parameter issues [6].
Multi-Parameter Testing: Test an average of seven different transfection conditions, systematically varying parameters such as voltage, pulse length, and reagent concentrations. Advanced platforms can test up to 200 conditions in parallel to identify optimal parameters [6].
Editing Assessment: Measure editing efficiency through genotyping rather than relying solely on transfection efficiency metrics, as successful transfection does not guarantee efficient editing [6].
Balance Optimization: Balance high editing efficiency with cell viability, as there is no benefit to achieving 99% editing efficiency if all edited cells undergo cell death [6].
Diagram 2: Strategies for Enhancing HDR Efficiency in Stem Cells
Clinical Applications and Therapeutic Translation
Current Clinical Landscape
CRISPR-based therapies have begun demonstrating remarkable success in clinical trials, with the first CRISPR-based medicine, Casgevy, receiving approval for treating sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) [8]. This ex vivo therapy involves harvesting a patient's hematopoietic stem cells, editing them to reactivate fetal hemoglobin production, and reinfusing them after myeloablative conditioning.
Recent advances include the development of personalized in vivo CRISPR treatments. In a landmark 2025 case, an infant with CPS1 deficiency received a bespoke in vivo CRISPR therapy developed and delivered in just six months [8]. The treatment utilized lipid nanoparticles (LNPs) for delivery and was administered via IV infusion, with the patient safely receiving multiple doses that progressively reduced symptoms. This case establishes a regulatory pathway for rapid approval of platform therapies and demonstrates the potential for treating rare genetic diseases.
Protocol: Rapid Screening of Gene Editing Outcomes
Monitoring editing outcomes is essential for both research and clinical applications. The following protocol enables rapid screening of CRISPR-Cas9 gene editing outcomes using fluorescent protein conversion:
Generate Reporter Cell Line: Create enhanced Green Fluorescent Protein (eGFP)-positive cells via lentiviral transduction [9].
Design Editing Strategy: Design gRNAs to convert eGFP to Blue Fluorescent Protein (BFP) through specific nucleotide changes. The HDR-mediated conversion to BFP indicates precise editing, while NHEJ-mediated disruption leads to loss of fluorescence [9].
Transfection and Culture: Transfect editing reagents into eGFP-positive cells and culture for sufficient time for protein turnover.
Flow Cytometry Analysis: Analyze cells using fluorescence-activated cell sorting (FACS) to quantify the percentages of BFP-positive (HDR), eGFP-positive (unedited), and non-fluorescent (NHEJ) populations [9].
Data Interpretation: Calculate HDR and NHEJ efficiencies based on fluorescence patterns. This system enables high-throughput, scalable assessment of gene editing techniques and optimization of editing conditions [9].
Table 3: Quantitative Analysis of HDR Enhancement Strategies
| Strategy | Condition | HDR Efficiency | Template Multiplication | Key Findings |
|---|---|---|---|---|
| Donor Type | dsDNA | 2% | 34% | Baseline efficiency |
| Donor Type | Denatured DNA | 8% | 17% | 4-fold HDR increase |
| Protein Addition | RAD52 + ssDNA | 26% | 30% | 13-fold HDR increase |
| 5' Modification | 5'-C3 spacer | 40% | 9% | 20-fold HDR increase |
| 5' Modification | 5'-biotin | 14% | 5% | 8-fold HDR increase |
| Strand Targeting | Antisense + ssDNA | 8% | 5% | Improved precision |
Computational Tools and Future Directions
AI-Powered CRISPR Design
Artificial intelligence tools are revolutionizing experimental design in CRISPR applications. CRISPR-GPT, a large language model developed at Stanford Medicine, functions as a gene-editing "copilot" that assists researchers in generating designs, analyzing data, and troubleshooting flaws [10]. This AI tool leverages 11 years of published experimental data and expert discussions to hone experimental designs, predict off-target effects, and recommend optimization strategies.
The system offers multiple interaction modes: beginner mode provides explanations for recommendations, expert mode collaborates on complex problems without additional context, and Q&A mode addresses specific technical questions [10]. In practice, researchers have used CRISPR-GPT to successfully design experiments on their first attempt, significantly reducing the trial-and-error period typically required for CRISPR experiment optimization.
CRISPR Array Analysis Tools
Bioinformatic tools enable detailed analysis of CRISPR system dynamics in natural environments. The CRISPR Comparison Toolkit (CCTK) provides resources for identifying relationships between CRISPR arrays through several steps [2]:
Array Identification: CCTK Minced identifies CRISPR arrays using a sliding window search to identify regularly spaced repeats without requiring prior knowledge of CRISPR subtypes.
Relationship Analysis: CRISPRdiff visualizes arrays and highlights similarities between them, assigning unique color combinations to spacers present in multiple arrays.
Evolutionary Analysis: CRISPRtree infers phylogenetic relationships between arrays using a maximum parsimony approach, presenting hypotheses about evolutionary history based on spacer patterns.
These tools facilitate exploration of how CRISPR systems evolve in response to environmental pressures, providing insights that can inform engineering of improved CRISPR systems for biotechnological applications.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for CRISPR Stem Cell Research
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| CRISPR Nucleases | Cas9, Cas12a, Cas12k, Nickase variants | DNA cleavage at target sites | Cas9 most widely validated; Cas12k for CAST systems |
| Guide RNA Formats | Synthetic sgRNA, crRNA:tracrRNA duplex | Target specification | Synthetic sgRNA most common for stem cells |
| Donor DNA Templates | dsDNA, ssDNA, 5'-modified donors | HDR template | 5'-biotin or C3 spacer enhances efficiency 8-20x |
| Enhanced HDR Reagents | RAD52, small molecule inhibitors | Increase HDR efficiency | RAD52 increases ssDNA integration 4-fold |
| Delivery Systems | Lipid nanoparticles, Electroporation | Introduce editing components | LNPs enable in vivo delivery and redosing |
| Stem Cell Media | Essential 8, mTeSR, StemFlex | Maintain pluripotency | Varies by stem cell type and application |
| Editing Assessment | T7E1, TIDE, NGS, Flow cytometry | Measure editing outcomes | Fluorescent conversion enables rapid screening |
The journey of CRISPR-Cas systems from bacterial immunity mechanisms to programmable genome editing tools represents one of the most transformative developments in modern biotechnology. As research continues to refine these systems, improve delivery methods, and enhance precision, the applications in stem cell genetic engineering continue to expand. The integration of CRISPR technology with stem cell biology has created unprecedented opportunities for disease modeling, drug discovery, and therapeutic development.
Current challenges, including editing efficiency, off-target effects, and safe delivery in vivo, are being addressed through continued innovation in protein engineering, delivery technologies, and computational design tools. The recent success of clinical trials and the emergence of personalized CRISPR treatments highlight the tremendous potential of these technologies to revolutionize medicine and provide new hope for patients with genetic disorders.
As the field progresses, the combination of stem cell technology and CRISPR genome editing promises to enable increasingly sophisticated approaches to understanding and treating human disease, ultimately fulfilling the promise of personalized regenerative medicine.
Stem cell research has profoundly transformed the landscape of regenerative medicine and therapeutic development. Induced pluripotent stem cells (iPSCs), mesenchymal stem/stromal cells (MSCs), and neural stem cells (NSCs) represent three distinct yet complementary therapeutic vessels with immense potential for treating a wide spectrum of diseases. The convergence of these cell-based approaches with precision gene-editing technologies, particularly CRISPR/Cas9, has opened unprecedented opportunities for modeling human diseases, screening therapeutic compounds, and developing innovative cell therapies. This article provides a comprehensive overview of these stem cell types, their therapeutic applications, and detailed experimental protocols within the context of advanced genetic engineering research.
Stem Cell Characteristics and Therapeutic Potential
Induced Pluripotent Stem Cells (iPSCs)
iPSCs are reprogrammed somatic cells that have regained pluripotency through the ectopic expression of specific transcription factors. The groundbreaking discovery by Takahashi and Yamanaka in 2006 demonstrated that mouse fibroblasts could be reprogrammed into pluripotent stem cells using four factors: Oct4, Sox2, Klf4, and Myc (OSKM) [11]. This was subsequently extended to human cells in 2007, with Thomson's group using a different combination: OCT4, SOX2, NANOG, and LIN28 [11] [12]. The molecular reprogramming process occurs in two phases: an early stochastic phase where somatic genes are silenced and early pluripotency genes are activated, followed by a deterministic phase where late pluripotency-associated genes are activated [11].
Table 1: iPSC Reprogramming Methods and Efficiencies
| Reprogramming Method | Key Features | Reprogramming Efficiency | Advantages | Disadvantages |
|---|---|---|---|---|
| Retroviral/Lentiviral | Original method using OSKM factors | 0.01-0.1% [12] | Well-established, efficient | Integration into genome, tumorigenicity concerns |
| Sendai Virus | RNA virus that does not enter nucleus | 0.1-1% [12] | Non-integrating, high protein production | Requires ~10 passages to dilute out virus |
| mRNA Transfection | Daily transfection of reprogramming mRNAs | 1.4-4.4% [12] | Footprint-free, defined method | Labor-intensive, requires multiple transfections |
| PiggyBac Transposition | Mobile genetic element with excision capability | 0.02% in human MSCs [12] | Footprint-free after excision | Lower efficiency in human cells |
| Protein Transduction | Direct delivery of reprogramming proteins | 0.001-0.006% [12] | Completely DNA-free | Very low efficiency, technically challenging |
| miRNA Transfection | Uses microRNAs to enhance or induce reprogramming | Up to 10% reported [12] | Can enhance efficiency | Not consistently replicated |
Mesenchymal Stem Cells (MSCs)
MSCs are multipotent adult stromal cells capable of self-renewal and differentiation into multiple lineages, including osteoblasts, adipocytes, and chondrocytes [13] [14]. According to International Society for Cellular Therapy (ISCT) guidelines, MSCs must express specific surface markers (CD105, CD73, CD90) while lacking hematopoietic markers (CD45, CD34, CD14, CD11b, CD79α, CD19, and HLA-DR) [13] [14]. MSCs can be isolated from various tissues, including bone marrow, adipose tissue, umbilical cord, and placenta [13] [15]. The therapeutic effects of MSCs are primarily attributed to their immunomodulatory properties and paracrine actions rather than their differentiation potential [14].
Table 2: MSC Sources and Their Characteristics
| Tissue Source | Isolation Method | Key Markers | Differentiation Potential | Therapeutic Strengths |
|---|---|---|---|---|
| Bone Marrow | Enzymatic digestion or explant culture | CD105+, CD73+, CD90+, CD271+ [15] [14] | High osteogenic potential [15] | Standard source, well-characterized |
| Adipose Tissue | Enzymatic digestion | CD105+, CD73+, CD90+, CD36+ [15] | High adipogenic potential [15] | Easily accessible, abundant supply |
| Umbilical Cord | Explant culture or enzymatic digestion | CD105+, CD73+, CD90+, CD45- [15] | High osteogenic, low adipogenic potential [15] | High proliferation, potent immunomodulation |
| Placenta | Enzymatic digestion | CD105+, CD73+, CD90+, CD146+ [14] | Multilineage differentiation | Available as medical waste, primitive properties |
Neural Stem Cells (NSCs)
NSCs are multipotent cells capable of self-renewal and differentiation into the three major central nervous system (CNS) lineages: neurons, astrocytes, and oligodendrocytes [16]. In the mature mammalian CNS, NSCs are primarily localized to two key regions: the subventricular zone (SVZ) lining the lateral ventricles of the forebrain, and the subgranular layer of the dentate gyrus in the hippocampal formation [16]. NSCs can be isolated from embryonic, postnatal, or adult CNS tissue, or generated from PSCs through neural induction protocols [16]. The therapeutic potential of NSCs lies in their ability to replace damaged neurons and glial cells, provide neurotrophic support, and modulate the inflammatory environment in neurological disorders.
CRISPR/Cas9 Applications in Stem Cell Engineering
The CRISPR/Cas9 system has revolutionized stem cell research by enabling precise genetic modifications in stem cells for disease modeling and therapy development. This RNA-guided gene-editing tool consists of two main components: a Cas9 nuclease that cleaves target DNA and a single-guide RNA (sgRNA) that directs Cas9 to specific genomic sequences [17].
CRISPR/Cas9 in iPSC Research
CRISPR/Cas9 technology allows for precise genetic modifications in iPSCs, making it invaluable for disease modeling and therapeutic applications. In Alzheimer's disease research, CRISPR/Cas9 has been used to introduce or correct mutations in genes such as APP, PSEN1, and PSEN2 in iPSCs, enabling the study of disease mechanisms and screening of potential therapeutics [17]. For monogenic disorders like thalassemia, CRISPR/Cas9 can correct disease-causing mutations in patient-derived iPSCs, which can then be differentiated into hematopoietic stem cells for autologous transplantation [18]. This approach offers a potential cure by addressing the genetic root cause of the disease.
CRISPR/Cas9 in MSC Research
While MSCs are already used therapeutically for their immunomodulatory properties, CRISPR/Cas9 can enhance their therapeutic potential through genetic engineering. This includes modifying MSCs to enhance their homing capabilities, increase their secretion of therapeutic factors, or improve their resistance to inflammatory environments [18]. Additionally, CRISPR/Cas9 can be used to study the mechanisms underlying MSC biology, such as the genes involved in their differentiation potential or immunomodulatory functions.
Experimental Protocols
iPSC Generation and Characterization Protocol
Reprogramming Human Fibroblasts to iPSCs Using the PiggyBac Transposition System
Materials:
- Human dermal fibroblasts (commercially available or patient-derived)
- PB-Tre-h4F, PB-Tre-hRL, PB-Tre-P2F, EF1α, and Pbase plasmids [19]
- STO feeder cells
- M15 medium supplemented with doxycycline (1.0 μg/mL)
- mTeSR medium (STEMCELL Technologies, #85850)
- Vitronectin (VTN)-coated plates (Gibco A14700)
Methodology:
- Transfection: Prepare a DNA mixture containing 3.0 μg PB-Tre-h4F, 1.0 μg PB-Tre-hRL, 1.0 μg PB-Tre-P2F, 1.0 μg EF1α, and 1.0 μg Pbase. Transfect into 1.0 × 10^6 fibroblasts using preferred method [19].
- Seeding and Initial Culture: Seed transfected cells on STO feeder cells in a 10-cm dish with M15 medium supplemented with doxycycline (1.0 μg/mL) [19].
- Doxycycline Removal: At day 14 post-transfection, remove doxycycline and switch culture medium to mTeSR [19].
- iPSC Expansion: Monitor cultures for emergence of iPSC colonies. Manually pick and expand colonies to establish stable iPSC lines on VTN-coated plates in mTeSR medium [19].
Characterization Assays:
- Alkaline Phosphatase Staining: Fix cells in 4% paraformaldehyde for 30 minutes, then incubate with AP staining solution. Pluripotent cells show strong AP activity [19].
- Immunofluorescence Analysis: Stain for pluripotency markers (OCT4, SOX2, NANOG) using specific antibodies. Analyze using confocal microscopy [19].
- Karyotyping: Treat cells with 0.2 μg/mL colchicine for 2.5 hours. Process cells through hypotonic treatment, fixation, and Giemsa staining. Analyze chromosomes for numerical and structural abnormalities [19].
- Teratoma Formation: Inject iPSCs into immunodeficient mice. After 8-12 weeks, analyze formed teratomas histologically for presence of tissues from all three germ layers [13].
MSC Isolation and Differentiation Protocol
Isolation and Osteogenic/Adipogenic Differentiation of MSCs
Materials:
- Tissue source (bone marrow aspirate, adipose tissue, umbilical cord)
- Collagenase type I for enzymatic digestion
- Growth medium (EGM-2 kit or DMEM with 10% FBS)
- Adipogenic differentiation medium (Cyagen Biosciences, #GUXMX-90031)
- Osteogenic differentiation medium (Cyagen Biosciences, #GUXMX-90021)
- Oil Red O stain (Sigma-Aldrich)
- Alizarin Red S stain (Sigma-Aldrich)
Methodology:
Isolation from Umbilical Cord Tissue:
- Cut umbilical cord tissue into 1-2 mm³ pieces.
- Enzymatically digest with 3 mg/mL type I collagenase for 3-4 hours at 37°C.
- Culture digested tissue in growth medium, changing medium every 2-3 days [15].
Flow Cytometry Characterization:
Adipogenic Differentiation:
- Culture MSCs in adipogenic differentiation medium for 3 weeks, changing medium twice weekly.
- Fix cells and stain with Oil Red O to visualize lipid vacuoles [15].
Osteogenic Differentiation:
- Culture MSCs in osteogenic differentiation medium for 3 weeks, changing medium twice weekly.
- Fix cells and stain with Alizarin Red S to detect calcium deposition, or use von Kossa staining for mineralization [15].
NSC Differentiation and Deep Learning-Based Identification Protocol
Generation of NSCs from iPSCs and Early Fate Identification
Materials:
- Established iPSC lines
- Neural induction medium
- Imageable flow cytometer
- Specific markers: NeuN (neurons), GFAP (astrocytes), Olig2 (oligodendrocytes) [20]
- Deep learning computational setup
Methodology:
Neural Induction from iPSCs:
- Induce neural differentiation using established protocols (embryoid body or monolayer system).
- Identify and isolate neural rosettes containing NPCs [16].
Lineage-Specific Differentiation:
- For neuronal differentiation: Culture NSCs in neuron differentiation medium with retinoic acid (RA) and sonic hedgehog (SHH) for 1-5 days [20].
- For astrocyte differentiation: Culture NSCs in astrocyte differentiation medium for 0.5-2 days [20].
- For oligodendrocyte differentiation: Culture NSCs in oligodendrocyte differentiation medium for 1-3 days [20].
Deep Learning-Based Identification:
- Collect brightfield images of differentiating NSCs using imageable flow cytometry.
- Train a convolutional neural network (CNN) with annotated single-cell images.
- Use the trained model to identify differentiated cell types from brightfield images alone, enabling early prediction of NSC fate [20].
Signaling Pathways and Molecular Mechanisms
iPSC Reprogramming Mechanisms
The reprogramming of somatic cells to iPSCs involves profound remodeling of the epigenome and global changes in chromatin structure. The process begins with the silencing of somatic genes and activation of early pluripotency-associated genes, followed by activation of late pluripotency genes [11]. Mesenchymal-to-epithelial transition (MET) is a critical early event in reprogramming when starting from fibroblast populations [11]. Signaling pathways such as Wnt play crucial roles in establishing and maintaining pluripotency [19].
MSC Therapeutic Action Mechanisms
MSCs exert their therapeutic effects primarily through paracrine actions rather than differentiation and engraftment. The secretion profile of MSCs includes growth factors, cytokines, chemokines, extracellular matrix components, and metabolic products that contribute to immune modulation, tissue remodeling, and cellular homeostasis during regeneration [14]. MSCs can modulate immune responses by inhibiting T lymphocyte proliferation, inducing cell-cycle arrest and apoptosis [14]. They also express a wide array of chemokines and receptors that form a chemotactic network for guiding circulating cells to injury sites [14].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell Research
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC, NANOG, LIN28 | Induction of pluripotency | Multiple combinations effective; viral and non-viral delivery methods [11] [12] |
| CRISPR/Cas9 Components | Cas9 nuclease, sgRNA, HDR donors | Precision gene editing | Enable specific genetic modifications in stem cells [18] [17] |
| Cell Culture Media | mTeSR, E8, MSC growth media | Maintenance and expansion | Defined media preferred for reproducibility [19] |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG, CD105, CD73, CD90, NeuN, GFAP, Olig2 | Cell type identification | Essential for validating stem cell identity and differentiation [15] [20] [14] |
| Differentiation Inducers | Retinoic acid, SHH, BMPs, specific cytokine cocktails | Lineage-specific differentiation | Direct stem cells toward specific fates [20] [16] |
| Small Molecule Inhibitors/Activators | IWR1 (Wnt inhibitor), SB431542 (TGF-β inhibitor) | Pathway modulation | Enhance reprogramming or direct differentiation [13] [19] |
iPSCs, MSCs, and NSCs represent powerful therapeutic vessels with complementary strengths and applications. iPSCs offer unlimited expansion potential and the ability to model human diseases, MSCs provide potent immunomodulatory and trophic support, while NSCs hold promise for treating neurological disorders. The integration of CRISPR/Cas9 technology with these stem cell platforms has accelerated disease modeling, drug screening, and the development of novel cell therapies. As research continues to address challenges such as tumorigenicity, genomic stability, and functional maturation, stem cell-based therapies are poised to transform treatment paradigms for a wide range of diseases.
The convergence of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 technology with stem cell biology represents a paradigm shift in biomedical research and therapeutic development. This powerful synergy leverages the precision of programmable genome editing with the pluripotency and self-renewal capabilities of stem cells. The CRISPR-Cas system functions as a bacterial adaptive immune system that has been repurposed as a highly specific gene-editing tool, utilizing a guide RNA (gRNA) to direct the Cas9 nuclease to create targeted double-strand breaks in DNA [21]. When applied to stem cells—including induced pluripotent stem cells (iPSCs), embryonic stem cells (ESCs), and adult stem cells—this combination enables unprecedented opportunities for disease modeling, drug discovery, and regenerative medicine.
The molecular architecture of the CRISPR-Cas9 system consists of two key components: the Cas9 enzyme, which acts as molecular scissors to cut DNA, and a customizable gRNA that directs Cas9 to a specific genomic locus. This creates a double-strand break that activates the cell's native DNA repair mechanisms: non-homologous end joining (NHEJ) for gene disruption or homology-directed repair (HDR) for precise gene correction [21]. When deployed in stem cells, these precise genetic modifications can be perpetuated through cell divisions and differentiation processes, creating durable cellular platforms for both research and clinical applications.
Application Notes: Research and Clinical Applications
Disease Modeling and Drug Screening
The combination of CRISPR and stem cell technologies has revolutionized disease modeling by enabling the creation of genetically accurate cellular models that recapitulate human disease pathophysiology. Researchers can introduce patient-specific mutations into healthy iPSCs or correct disease-causing mutations in patient-derived iPSCs to establish isogenic control lines. These paired cell lines provide genetically matched systems for identifying phenotype-specific differences, dramatically improving the signal-to-noise ratio in disease mechanism studies [21].
Table 1: CRISPR-Generated Stem Cell Models for Disease Research
| Disease Category | Stem Cell Type | Genetic Modification | Research Application |
|---|---|---|---|
| Neurodegenerative Disorders | iPSCs | Introduction of PARK2 mutations | Parkinson's disease pathogenesis studies [22] |
| Hematologic Disorders | Hematopoietic Stem Cells (HSCs) | BCL11A enhancer editing | Sickle cell disease and beta-thalassemia modeling [8] |
| Cardiac Diseases | iPSC-derived cardiomyocytes | Editing of sarcomere protein genes | Hypertrophic cardiomyopathy drug screening [22] |
| Metabolic Disorders | iPSC-derived hepatocytes | CPS1 deficiency correction | Urea cycle disorder modeling and therapeutic testing [8] |
| Retinal Disorders | iPSC-derived retinal cells | Correction of photoreceptor genes | Inherited blindness studies and gene therapy development [22] |
For drug screening applications, CRISPR-edited stem cells enable high-throughput compound testing in disease-relevant human cell types. This approach is particularly valuable for identifying candidate therapeutics for monogenic disorders, as demonstrated by screens using iPSC-derived motor neurons for amyotrophic lateral sclerosis (ALS) and iPSC-derived microglia for Alzheimer's disease research. The precision of CRISPR editing allows for the incorporation of reporter constructs and biosensors into safe-harbor loci, facilitating real-time monitoring of disease-associated cellular phenotypes in response to compound libraries.
Cell Therapy Manufacturing and Engineering
CRISPR-Cas9 has transformed cell therapy manufacturing by enabling precise engineering of therapeutic stem cell products with enhanced functionality and safety profiles. In allogeneic cell therapies, CRISPR is utilized to create immune-evasive stem cells through knockout of major histocompatibility complex (MHC) genes, reducing host rejection without the need for toxic immunosuppression. This approach is being applied to develop hypoimmune stem cell lines for regenerative medicine applications, including type 1 diabetes (T1D) treatment [23].
Table 2: CRISPR-Engineered Stem Cell Therapies in Clinical Development
| Therapeutic Product | Stem Cell Type | Genetic Modification | Clinical Indication | Development Stage |
|---|---|---|---|---|
| CASGEVY (exa-cel) | Autologous HSCs | BCL11A enhancer disruption | Sickle cell disease, Transfusion-dependent beta thalassemia | FDA Approved [8] [23] |
| CTX112 | Allogeneic CAR-T cells | CD19 targeting + immune evasion edits | B-cell malignancies, Autoimmune diseases | Phase 1/2 [23] |
| CTX211 | Allogeneic stem cell-derived pancreatic islets | Hypoimmune edits + enhanced fitness | Type 1 diabetes | Phase 1 [23] |
| Hypoimmune hiPSC Lines | Induced pluripotent stem cells | MHC class I/II knockout | Multiple regenerative applications | Preclinical [24] |
The manufacturing process for these therapies involves multiplexed genome editing, where multiple genetic modifications are introduced simultaneously to enhance therapeutic properties. For example, CAR-T cell products incorporate edits to improve potency, reduce exhaustion, and prevent fratricide (killing of fellow therapeutic cells) [23]. For stem cell-derived therapies, additional edits can promote differentiation efficiency, engraftment capability, and long-term persistence of the therapeutic cells in the recipient.
In Vivo and In Vivo Regenerative Applications
CRISPR-edited stem cells are advancing regenerative medicine through both ex vivo and in vivo approaches. In ex vivo applications, stem cells are genetically modified outside the body before transplantation, as exemplified by CASGEVY, where a patient's own hematopoietic stem cells are edited to reactivate fetal hemoglobin production [8]. This approach avoids immune rejection concerns but requires complex manufacturing logistics.
Emerging in vivo strategies directly deliver CRISPR components to stem cells within the body using advanced delivery systems such as lipid nanoparticles (LNPs). The recent landmark case of an infant with CPS1 deficiency who received a personalized in vivo CRISPR therapy demonstrates the potential of this approach [8]. The therapy was developed in just six months and delivered systemically via LNPs, with the patient safely receiving multiple doses that each provided additional therapeutic benefit. This case establishes a precedent for on-demand gene editing therapies for rare genetic diseases and highlights the advantage of LNP delivery, which doesn't trigger the same immune responses as viral vectors and allows for potential redosing [8].
Diagram 1: CRISPR-Stem Cell Synergy Workflow. This diagram illustrates the integration of diverse stem cell sources with CRISPR engineering strategies to generate various therapeutic applications.
Experimental Protocols
Protocol: Generation of CRISPR-Edited iPSCs for Disease Modeling
This protocol describes the complete workflow for creating genetically engineered induced pluripotent stem cells (iPSCs) using CRISPR-Cas9, from guide RNA design to validation of edited clones.
Materials and Reagents
- Human iPSCs (commercially available or patient-derived)
- CRISPR-Cas9 plasmid or ribonucleoprotein (RNP) complex
- Lipofectamine CRISPRMAX or Neon Transfection System
- mTeSR Plus maintenance medium
- Recombinant laminin-521 or Matrigel
- CloneR supplement for enhanced clonal survival
- Puromycin or other appropriate selection antibiotic
- QuickExtract DNA solution for genotyping
- PCR reagents and Sanger sequencing primers
- T7 Endonuclease I or Surveyor mutation detection assay
Procedure
Guide RNA Design and Synthesis
- Identify target genomic sequence using reference databases (e.g., UCSC Genome Browser)
- Design 3-5 gRNAs targeting your locus of interest using CRISPR design tools (e.g., CRISPick, CHOPCHOP)
- Synthesize gRNAs as chemically modified synthetic RNAs or clone into appropriate expression vectors
- Validate gRNA efficiency using predictive scoring algorithms and in vitro cleavage assays
CRISPR Delivery to iPSCs
- Culture iPSCs in essential 8 medium on recombinant laminin-521-coated plates until 60-70% confluent
- Prepare CRISPR-Cas9 ribonucleoprotein (RNP) complex by combining 10μg Cas9 protein with 5μg synthetic gRNA, incubate at room temperature for 10 minutes
- Dissociate iPSCs to single cells using Accutase and resuspend at 1×10^7 cells/mL in electroporation buffer
- Add RNP complex to cell suspension and electroporate using Neon Transfection System (1200V, 20ms, 2 pulses)
- Alternatively, use lipid-based transfection with CRISPRMAX according to manufacturer's protocol
Isolation and Expansion of Clones
- 48 hours post-transfection, dissociate cells to single cells and plate at clonal density (500-1000 cells/10cm plate) in mTeSR Plus supplemented with CloneR
- After 10-14 days, manually pick individual colonies using a pipette tip under microscope guidance
- Transfer each colony to a separate well of a 96-well plate pre-coated with laminin-521
- Expand clones through 24-well and 12-well plates before transferring to 6-well format
Genotypic Validation
- At 70-80% confluence in 6-well plates, harvest portion of cells for genomic DNA extraction using QuickExtract solution
- Perform PCR amplification of the target genomic region using flanking primers
- Analyze editing efficiency using T7 Endonuclease I assay or Surveyor mutation detection kit
- For precise edits, clone PCR products and sequence 10-20 colonies or use next-generation sequencing
- Screen for potential off-target effects at predicted off-target sites
Characterization of Edited Clones
- Confirm pluripotency maintenance through flow cytometry for pluripotency markers (OCT4, SOX2, NANOG)
- Perform karyotype analysis to ensure genomic integrity
- Bank validated clones in liquid nitrogen with appropriate documentation
Timeline: This complete protocol requires approximately 8-10 weeks from CRISPR delivery to validated banked clones.
Protocol: In Vivo Delivery of CRISPR-Edited Stem Cells
This protocol describes the administration of CRISPR-edited stem cells for in vivo therapeutic applications, using hematopoietic stem cells (HSCs) for hematologic disorders as a model system.
Materials and Reagents
- CRISPR-edited CD34+ hematopoietic stem cells
- Cryopreservation media (e.g., CryoStor CS10)
- Pre-transplantation conditioning regimen reagents (e.g., busulfan)
- Sterile saline for infusion
- Patient monitoring equipment
- Flow cytometry reagents for engraftment analysis
Procedure
Pre-transplantation Processing
- Thaw CRISPR-edited CD34+ HSCs rapidly at 37°C and transfer to pre-warmed transplant media
- Wash cells to remove cryopreservatives and resuspend in sterile saline at appropriate concentration
- Perform quality control assessments: viability (trypan blue exclusion), cell count, and sterility testing
- Confirm editing efficiency in the final product via PCR and sequencing of a representative sample
Patient Conditioning
- Administer myeloablative conditioning regimen (e.g., busulfan) according to established protocols
- Monitor patient for conditioning-related toxicities and provide supportive care as needed
- Confirm adequate myeloablation before stem cell infusion
Stem Cell Infusion
- Transport cell product to bedside in approved transport container maintaining appropriate temperature
- Pre-medicate patient with antipyretics and antihistamines per institutional standards
- Administer cell product via central venous catheter using a syringe pump over appropriate duration
- Monitor patient closely during infusion for adverse reactions (fever, hypersensitivity, etc.)
Post-Transplantation Monitoring
- Monitor hematologic recovery through daily complete blood counts
- Assess engraftment starting around day +14 via chimerism analysis (STR-PCR or FISH)
- Evaluate editing persistence in peripheral blood cells at regular intervals (1, 3, 6, and 12 months)
- Monitor for potential off-target effects through comprehensive metabolic panels and organ function tests
- Document therapeutic efficacy through disease-specific parameters (e.g., hemoglobin electrophoresis for hemoglobinopathies)
Safety Considerations
- Monitor for insertional oncogenesis through periodic blood tests and clinical evaluation
- Screen for immune responses to CRISPR components or edited cells
- Implement long-term follow-up according to FDA guidance for gene therapy products [22]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for CRISPR-Stem Cell Research
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| CRISPR Nucleases | SpCas9, HiFi Cas9, Cas12a | Create targeted DNA double-strand breaks | High-fidelity variants reduce off-target effects in sensitive stem cell applications |
| Delivery Systems | Lipid nanoparticles (LNPs), Electroporation, AAV vectors | Deliver CRISPR components to cells | LNPs show promise for in vivo delivery; electroporation works well for ex vivo editing [8] |
| Stem Cell Culture Reagents | mTeSR, Essential 8, Laminin-521 | Maintain pluripotency during editing | Xen-free systems recommended for clinical applications |
| Editing Enhancers | HDR enhancers (e.g., RS-1, L755507), NHEJ inhibitors | Bias DNA repair toward desired pathway | Improve efficiency of precise gene correction in slow-dividing stem cells |
| Selection Markers | Puromycin, GFP, antibiotic resistance genes | Enrich for successfully edited cells | Fluorescent reporters enable sorting without antibiotics |
| Analytical Tools | T7E1 assay, Next-generation sequencing, Digital PCR | Validate editing efficiency and specificity | NGS provides comprehensive assessment of on-target and potential off-target edits |
Diagram 2: CRISPR-Stem Cell Experimental Decision Pathway. This diagram outlines the key decision points when designing CRISPR-stem cell experiments, from strategic approach selection through validation tiers.
Current Challenges and Future Perspectives
Despite the remarkable progress in CRISPR-stem cell applications, several significant challenges remain. Delivery efficiency continues to be a primary obstacle, particularly for in vivo applications where reaching the target stem cell population with sufficient editing components remains difficult [8] [21]. The field is actively addressing this through advances in lipid nanoparticle (LNP) technology and novel viral vectors with improved tissue tropism.
Off-target effects present another critical challenge, as unintended edits could potentially lead to oncogenesis or other pathological consequences [21]. The development of high-fidelity Cas variants and improved computational prediction tools has substantially mitigated this risk, but comprehensive off-target assessment remains essential, particularly for clinical applications. Immunogenicity of bacterial-derived Cas proteins represents an additional concern, especially for in vivo applications where pre-existing immunity could limit efficacy or cause adverse reactions [21].
The regulatory landscape for CRISPR-edited stem cell therapies is rapidly evolving. The FDA has established specific guidance documents including "Human Gene Therapy Products Incorporating Human Genome Editing" and "Studying Multiple Versions of a Cellular or Gene Therapy Product in an Early-Phase Clinical Trial" that provide frameworks for development [25] [22]. The recent establishment of the Office of Therapeutic Products (OTP) within the FDA has created a specialized pathway for reviewing these complex biologics, with increased staffing and expertise in cell and gene therapy products [25].
Future directions for the field include the development of next-generation editing platforms such as base editing and prime editing that offer more precise genetic modifications without creating double-strand breaks. The combination of hypoimmune stem cells with precision editing could enable true off-the-shelf regenerative therapies that avoid immune rejection [24] [23]. Additionally, the success of personalized CRISPR therapies, such as the recent case of an infant with CPS1 deficiency, points toward a future of bespoke genetic medicines for rare disorders [8].
As the field advances, balancing innovation with safety remains paramount. The extraordinary synergistic potential of CRISPR and stem cells continues to drive transformative advances across biomedical research and clinical medicine, offering new hope for addressing previously untreatable genetic diseases.
Key Historical Milestones and Ethical Touchstones in the Field
The convergence of stem cell biology and CRISPR-based genome editing represents a paradigm shift in biomedical research and therapeutic development [26]. This synergy creates a powerful platform for disease modeling, drug discovery, and the development of novel cell-based therapies for a range of intractable conditions, from genetic disorders to neurodegenerative diseases [26] [27]. For researchers and drug development professionals, understanding the integrated historical trajectory and the evolving ethical landscape is crucial for navigating this rapidly advancing field. This application note provides a detailed overview of key milestones, ethical frameworks, and standardized experimental protocols that form the foundation of responsible and effective research in stem cell genetic engineering.
Historical Milestones in Stem Cell Research and CRISPR Technology
The following table summarizes the pivotal discoveries that have shaped the fields of stem cell research and genome editing, leading to their powerful integration.
Table 1: Key Historical Milestones in Stem Cell Research and CRISPR Technology
| Year | Milestone | Key Researchers/Entity | Significance |
|---|---|---|---|
| 1961 | Identification of blood-forming (hematopoietic) stem cells [28] [27] | McCulloch and Till | Provided the first definitive evidence for the existence of stem cells, laying the groundwork for bone marrow transplantation. |
| 1981 | Isolation of embryonic stem cells (ESCs) from mouse embryos [28] | N/A | Established the first in vitro models for studying early mammalian development. |
| 1998 | Derivation of the first human embryonic stem cell (hESC) lines [28] [29] [27] | James Thomson | Opened new avenues for studying human development and regenerative medicine, though raising significant ethical questions [30]. |
| 2006 | Discovery of Induced Pluripotent Stem Cells (iPSCs) [28] [27] | Shinya Yamanaka | Developed a method to reprogram adult somatic cells into a pluripotent state, offering an ethical alternative to hESCs and enabling patient-specific disease modeling [26] [27]. |
| 2012 | Characterization of CRISPR-Cas9 for programmable genome editing [31] | Emmanuelle Charpentier and Jennifer Doudna | Demonstrated a highly specific and easily programmable system for editing genes in their natural chromosomal context, revolutionizing genetic engineering. |
| 2023 | First regulatory approval of a CRISPR-based therapy (Casgevy for sickle cell disease and TBT) [31] [8] | FDA/EMA | Marked the transition of CRISPR from a research tool to an approved clinical modality, validating its therapeutic potential. |
| 2025 | First personalized in vivo CRISPR therapy for a rare genetic disease (CPS1 deficiency) [8] | Innovative Genomics Institute (IGI) and collaborators | Demonstrated the feasibility of rapidly developing and deploying bespoke CRISPR therapies for individuals with ultrarare diseases, setting a new regulatory precedent. |
Ethical Touchstones and Regulatory Framework
The powerful capabilities of stem cell genetic engineering necessitate a robust ethical and regulatory framework. The core ethical principles for research, as outlined by organizations like the International Society for Stem Cell Research (ISSCR), include integrity, transparency, and a primary duty of care to patient welfare [29]. The following diagram illustrates the key ethical considerations and their interrelationships that researchers must navigate.
Diagram 1: Key Ethical Considerations. This map outlines the primary ethical domains (yellow) and their associated specific concerns (red) that arise from the use of genome editing and stem cell technologies.
Key Ethical Considerations
- Safety and Unintended Outcomes: A primary concern is the risk of off-target effects, where CRISPR edits occur at unintended sites in the genome, potentially leading to harmful mutations [31] [32]. Similarly, on-target effects can include unwanted edits at the intended target, and the long-term safety of edited cells, including tumorigenicity, must be rigorously assessed [32] [27].
- Access and Justice: The high cost of emerging therapies (e.g., over $2 million per patient) raises significant concerns about equitable access [32]. There is a tangible risk that these treatments could exacerbate existing health disparities both within and between countries, making justice a central ethical touchstone [28] [32] [29].
- Germline Editing: Modifying the human germline (sperm, eggs, or embryos) to create heritable genetic changes is widely considered an ethical red line [32]. Such interventions would permanently alter the human gene pool and raise profound questions about consent of future generations. The ISSCR guidelines explicitly prohibit the clinical use of germline editing [29].
- Informed Consent and Therapeutic Misconception: Obtaining valid informed consent is particularly challenging in this field. Patients with serious illnesses may be vulnerable to "therapeutic misconception," where they conflate experimental research with proven treatment [28]. Researchers must clearly communicate the experimental nature, potential risks, and uncertain benefits of these interventions [28] [29].
Experimental Protocols for Stem Cell Genetic Engineering
This section details a standard workflow for incorporating CRISPR/Cas9 gene editing into stem cell research, using the generation of a gene-corrected neuronal model from patient-specific iPSCs as an example.
Protocol: Gene Correction in iPSCs for Disease Modeling
Application: Modeling and rescuing pathogenic mutations in neurological disorders such as Familial Alzheimer's Disease (caused by mutations in APP, PSEN1, PSEN2) [26].
Diagram 2: Experimental Workflow. This flowchart outlines the key stages for generating gene-corrected disease models using patient-derived iPSCs.
Step 1: iPSC Generation and Culture
- Methodology: Maintain patient-derived iPSCs in feeder-free culture using essential media such as mTeSR or StemFlex on a suitable substrate (e.g., Geltrex or Matrigel). Culture cells in a humidified incubator at 37°C with 5% CO₂. Passage cells using EDTA or enzyme-free dissociation reagents to maintain pluripotency, confirmed by regular checks for marker expression (e.g., OCT4, NANOG, SOX2) and karyotype stability [26] [27].
Step 2: gRNA Design and Vector Construction
- Methodology: Design a target-specific guide RNA (gRNA) using online in silico tools (e.g., from IDT or Broad Institute) to minimize potential off-target effects [31]. For non-viral delivery, clone the gRNA sequence and the Streptococcus pyogenes Cas9 coding sequence into a single plasmid vector under a U6 and Cbh promoter, respectively. Include a donor DNA template containing the desired corrective sequence with homologous arms (~800 bp) if performing HDR [26].
Step 3: Delivery of CRISPR Components
- Methodology: Deliver the CRISPR plasmid or, for higher efficiency and reduced off-target effects, a pre-assembled Cas9-gRNA ribonucleoprotein (RNP) complex [31]. Use an electroporation-based system (e.g., Neon Transfection System) with optimized parameters for iPSCs. A typical reaction uses 1-2 million cells, 10-20 µg of RNP complex, and a pulse voltage of 1100-1300 V for 20-30 ms. Alternatively, use a non-viral delivery method to mitigate immune response risks associated with viral vectors [31] [8].
Step 4: Isolation and Expansion of Edited Clones
- Methodology: Post-transfection, allow cells to recover for 48-72 hours before applying appropriate antibiotic selection (e.g., Puromycin) for 5-7 days if a selection marker was co-delivered. Then, manually pick and expand single-cell-derived clonal colonies in 96-well plates. This step is critical for ensuring a homogeneously edited population [26].
Step 5: Genotypic Validation of Edited Clones
- Methodology: Extract genomic DNA from expanded clonal lines. Screen for successful editing using a mismatch detection assay (e.g., T7 Endonuclease I or TIDE analysis). Confirm the precise genetic correction in positive clones by Sanger sequencing of the target locus. Perform whole-genome sequencing on at least one correctly edited clone to assess potential off-target effects [31] [26].
Step 6: Functional Differentiation and Analysis
- Methodology: Differentiate the validated, gene-corrected iPSC clones and the original (un-corrected) patient iPSCs into the relevant cell type (e.g., neurons) using a standardized protocol. Compare the isogenic cell lines to assess functional rescue of the disease phenotype. For an AD model, this would involve quantifying the reduction of Aβ plaques and phosphorylated tau protein, as well as evaluating the rescue of electrophysiological function and synaptic activity [26].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Stem Cell Genetic Engineering
| Item | Function/Application | Key Considerations |
|---|---|---|
| Human iPSCs | Patient-specific disease modeling; source for gene-edited therapeutic cells [26] [27]. | Check for stable karyotype and pluripotency markers; use low-passage stocks. |
| CRISPR-Cas9 System | Introduction of targeted double-strand breaks in the DNA for gene knockout or correction. | RNP delivery is preferred for reduced off-target effects and shorter cellular exposure [31]. |
| gRNA | Guides the Cas9 nuclease to the specific genomic target sequence. | Must be designed using in silico tools to predict and minimize off-target activity [31]. |
| Electroporation System | Efficient delivery of CRISPR components (RNP or plasmid) into hard-to-transfect iPSCs. | Optimization of voltage and pulse duration is critical for high efficiency and low cytotoxicity. |
| Cytokines & Small Molecules | Direct differentiation of iPSCs into specific somatic cell lineages (e.g., neurons, cardiomyocytes). | Quality and batch consistency are paramount for reproducible differentiation protocols. |
| Lipid Nanoparticles (LNPs) | In vivo delivery vehicle for CRISPR components; shows promise for liver-targeted therapies [8]. | Enables in vivo editing and allows for potential re-dosing due to low immunogenicity [8]. |
Current Clinical Applications and Future Outlook
The clinical translation of integrated stem cell and CRISPR technologies is advancing rapidly. The first approved CRISPR therapy, Casgevy, is an ex vivo application where a patient's hematopoietic stem cells are edited outside the body to treat sickle cell disease and beta-thalassemia [8]. The field is now moving towards more complex in vivo applications and allogeneic (off-the-shelf) cell therapies.
Promising clinical targets include:
- Hereditary Transthyretin Amyloidosis (hATTR): NTLA-2001 (Intellia Therapeutics) is an in vivo CRISPR therapy that knocks out the TTR gene in the liver, showing sustained protein reduction in clinical trials [8] [33].
- Neurodegenerative Disease: Research is focused on using gene-edited stem cells to deliver neurotrophic factors or correct mutations in models of Alzheimer's and Parkinson's disease [26].
- Cardiovascular Disease: Base editing therapies like VERVE-101 and VERVE-102 aim to permanently inactivate the PCSK9 gene in the liver to lower cholesterol [33].
Future developments will depend on overcoming key challenges in delivery, particularly improving the targeting of LNPs and other vectors to organs beyond the liver [8] [34]. Furthermore, the high cost of therapies necessitates the development of scalable manufacturing processes and innovative financing models to ensure equitable access, aligning with the core ethical principle of distributive justice [32] [29].
From Bench to Bedside: Methodologies and Translational Applications in Disease Modeling and Therapy
The field of stem cell genetic engineering has been revolutionized by CRISPR-based genome editing technologies, which provide unprecedented precision for modeling human diseases and developing regenerative therapies. For researchers and drug development professionals, mastering the transition from traditional knockout techniques to advanced base editing is crucial for tackling complex genetic diseases. These workflows enable precise genetic modifications in human pluripotent stem cells (hPSCs), allowing for the creation of more accurate disease models and the development of potentially curative therapies. The integration of these technologies into stem cell research has accelerated our understanding of developmental biology and opened new avenues for personalized medicine, particularly through the creation of patient-specific stem cell lines with targeted genetic corrections.
Core Genome Editing Technologies
CRISPR-Cas9 Knockout Workflows
CRISPR-Cas9-mediated gene knockout remains the foundational workflow in genome engineering, primarily utilized for loss-of-function studies. This technology creates double-strand breaks (DSBs) in DNA at sequence-specific locations, which are then repaired by the cell's error-prone non-homologous end joining (NHEJ) pathway, resulting in insertion/deletion mutations (indels) that disrupt gene function [7]. The simplicity and efficiency of this approach have made it the most widely used CRISPR method, with approximately 45-54% of researchers in both commercial and non-commercial institutions reporting knockouts as their primary type of CRISPR edit [35].
The standard knockout workflow begins with careful single guide RNA (sgRNA) design targeting the early exons of the gene of interest to maximize the likelihood of generating frameshift mutations. The editing components are then delivered to cells, typically via electroporation or viral vectors, with subsequent steps involving clonal isolation, expansion, and genotypic validation. A critical consideration for stem cell researchers is that CRISPR editing in human induced pluripotent stem (iPS) cells predominantly produces homozygous rather than heterozygous modifications, with frequent identical indels occurring in both alleles of target genes [36]. This property has important implications for therapeutic genome editing applications and requires careful experimental design.
Recent advancements have enhanced traditional knockout approaches. For instance, the development of CRISPRgenee, a dual-action gene-editing system that combines CRISPR-Cas9 knockout with epigenetic silencing using truncated guide RNAs, demonstrates improved gene depletion efficiency while reducing sgRNA performance variance compared to conventional CRISPR approaches [36]. This is particularly valuable in stem cell research where complete gene ablation is often necessary to study developmental pathways.
Table: Comparison of Primary CRISPR Modification Methods Among Researchers
| Editing Method | Commercial Institutions | Non-Commercial Institutions |
|---|---|---|
| CRISPR Knockout | 54% | 45% |
| RNAi | 32.2% | 34.6% |
| Base Editing | Comparable to knock-ins | Comparable to knock-ins |
| CRISPRa/i | Comparable to knock-ins | Comparable to knock-ins |
Base Editing Technologies and Workflows
Base editing represents a significant advancement beyond traditional CRISPR-Cas9 systems by enabling precise, irreversible single-nucleotide changes without creating double-stranded DNA breaks [37]. This technology utilizes engineered fusion proteins consisting of a catalytically impaired Cas nuclease (nickase) linked to a deaminase enzyme, which directly converts one DNA base to another within a small editing window [38]. The two primary classes of base editors are cytosine base editors (CBEs), which convert C•G to T•A base pairs, and adenine base editors (ABEs), which convert A•T to G•C base pairs [39].
The base editing workflow shares initial steps with traditional CRISPR approaches, beginning with careful gRNA design to position the target nucleotide within the effective editing window of the base editor. However, unlike knockout approaches, base editing requires consideration of additional parameters including protospacer adjacent motif (PAM) compatibility, editing window position, and potential bystander edits. After delivery of the base editing components to cells, the process achieves precise nucleotide conversion through a series of enzymatic steps: the Cas nickase moiety binds to the target DNA without creating a DSB, the deaminase enzyme catalyzes the base conversion, and cellular mismatch repair mechanisms complete the permanent genetic change.
Recent research demonstrates the remarkable therapeutic potential of base editing in stem cell applications. A landmark study published in November 2025 reported using adenine base editors to precisely repair two of the most common severe β-thalassaemia mutations (CD39 and IVS2-1), restoring adult haemoglobin production in patient blood stem cells with high correction rates (98% for CD39 and 90% for IVS2-1) and an encouraging safety profile [39]. This approach demonstrated restored HBB transcripts and β-globin protein accompanied by a more balanced α/non-α globin ratio, reduced erythroid apoptosis, and improved maturation. The study confirmed the safety of highly processive ABE8e usage in patients' hematopoietic stem cells in terms of genotoxicity and specificity, with no detectable increase in mutation burden and preserved stem-cell diversity based on whole-exome sequencing and clonal analyses [39].
Table: Base Editing Efficiency in Preclinical Disease Models
| Disease Model | Editor Type | Editing Efficiency | Functional Outcome |
|---|---|---|---|
| β-Thalassaemia (CD39 mutation) | ABE8e | ~98% correction | Restored β-globin production, improved erythroid maturation |
| β-Thalassaemia (IVS2-1 mutation) | ABE8e | ~90% correction | Balanced α/non-α globin ratio, reduced apoptosis |
| Sickle cell-β-thalassaemia | ABE8e | Substantial phenotype correction | Reduced sickling, levels lower than asymptomatic carriers |
Advanced Editing Technologies
Beyond base editing, several advanced CRISPR technologies are expanding the capabilities of stem cell genetic engineering. Prime editing represents a more versatile precise editing technology that can install all possible transition and transversion mutations, as well as small insertions and deletions, without requiring double-strand breaks or donor DNA templates [7]. This "search-and-replace" editing approach uses a catalytically impaired Cas9 nickase fused to a reverse transcriptase enzyme and a prime editing guide RNA (pegRNA) that specifies both the target site and the desired edit.
Epigenome editing technologies, particularly CRISPR activation (CRISPRa), have proven valuable for stem cell research applications. A protocol published in October 2025 detailed using CRISPRa to rapidly verify silent gene reporters in human pluripotent stem cells, providing a method to validate reporter knockins at unexpressed loci without requiring time-consuming cell state transitions [40]. This approach enables efficient transcriptional activation of silent genes in hPSCs through designed single-guide RNA (sgRNA) and delivery of CRISPRa components, allowing for rapid functional assessment of genetic modifications.
For large-scale DNA engineering, CRISPR-associated transposase (CAST) systems enable targeted integration of large genetic elements without creating double-strand breaks [7]. These systems are particularly valuable for introducing complex genetic circuits or synthetic genes into stem cells for therapeutic applications. While currently more efficient in prokaryotic systems, where they enable stable integration of donor sequences up to approximately 15.4 kb with type I-F CAST and up to 30 kb using type V-K variants, ongoing development is improving their efficiency in mammalian cells [7].
Application Notes for Stem Cell Research
Workflow Design and Optimization
Implementing robust genome editing workflows in stem cell systems requires careful consideration of several technical parameters. Research indicates that the entire CRISPR workflow, from guide design to clonal isolation, typically requires repetition 3 times (median value) before researchers achieve their desired edit, with the total process taking approximately 3 months for generating knockouts and 6 months for generating knock-ins [35]. This timeline highlights the importance of systematic optimization and validation in stem cell editing projects.
The choice of cell model significantly impacts editing efficiency and experimental difficulty. Primary cells, including stem cells, present greater challenges compared to immortalized cell lines, with survey data showing that among researchers who found CRISPR "easy," only 16.2% worked in primary T cells, while among those who answered "difficult," 50% worked on primary T cells [35]. This differential difficulty underscores the need for protocol optimization when working with sensitive stem cell populations.
Delivery method selection represents another critical parameter. Lipid nanoparticles (LNPs) have emerged as a promising delivery vehicle for CRISPR components, particularly for in vivo applications, due to their favorable safety profile and potential for redosing [8]. Unlike viral vectors, which typically trigger immune responses that prevent repeated administration, LNPs don't trigger the immune system similarly, enabling multiple doses as demonstrated in both Intellia Therapeutics' hATTR trial and the personalized CRISPR treatment for infant KJ with CPS1 deficiency [8].
Recent advances in automated editing and analysis are addressing workflow challenges. Japanese researchers have developed a high-throughput robotic method for isolating and analyzing genome-edited human iPS cell clones, overcoming the challenge of single-cell survival in these fragile cells [36]. This approach enables more efficient processing of the over 1,000 clones often necessary to identify correctly edited stem cell lines, significantly accelerating the research timeline.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Reagents for Advanced Genome Engineering
| Reagent / Material | Function | Application Notes |
|---|---|---|
| Lipid Nanoparticles (LNPs) | In vivo delivery of CRISPR components | Favorable safety profile, enables redosing; natural affinity for liver; researchers developing versions with affinity for other organs [8] |
| Adenine Base Editor (ABE8e) | A•T to G•C base conversions | High-processivity editor used in β-thalassaemia correction; demonstrated high correction rates with preserved stem-cell diversity [39] |
| Hypo-immunogenic Tregs | Universal allogeneic cell therapy | Created by disrupting HLA class I/II genes while inserting HLA-E fusion protein using CRISPR; evades both T and NK cell rejection [34] |
| Cas12a (Cpf1) enzyme | Alternative to Cas9 for gene editing | Used in Edge's AsCas12a-based system for HBG1/2 editing; different PAM requirements than Cas9 [36] |
| dCas9-epigenetic modifiers | Targeted epigenetic manipulation | Enables precise DNA methylation or histone modification; used in breast cancer epigenetic therapy research [36] |
| Programmable phages | Antimicrobial therapy | CRISPR-armed bacteriophages target dangerous bacterial infections; SNIPR001 in Phase 1b trials for hematological cancer patients [8] |
Experimental Protocols
Detailed Protocol: Base Editing in Hematopoietic Stem Cells for β-Thalassaemia
This protocol outlines the adenine base editing approach for correcting prevalent β-thalassaemia mutations (CD39 and IVS2-1) in patient-derived hematopoietic stem and progenitor cells (HSPCs), based on recently published research [39].
Materials:
- Patient-derived CD34+ HSPCs carrying β-thalassaemia mutations
- ABE8e base editor components (plasmid or mRNA)
- Guide RNA targeting the CD39 or IVS2-1 mutation site
- Cell culture media for HSPC maintenance and differentiation
- Electroporation system
- Genotyping primers for HBB locus
- Antibodies for flow cytometry analysis of erythroid differentiation
- RNA extraction kit and RT-PCR reagents for HBB transcript analysis
Procedure:
- Guide RNA Design: Design guide RNAs matched to the CD39 or IVS2-1 target sites, ensuring the pathogenic nucleotide falls within the editing window of the ABE8e base editor (typically positions 4-8 in the protospacer).
- Stem Cell Preparation: Isolate and expand CD34+ HSPCs from patient samples using cytokine-supported serum-free media. Maintain cells at appropriate densities to preserve stemness.
- Electroporation: Deliver the ABE8e base editor (as mRNA or plasmid) and guide RNA to HSPCs via electroporation. Optimize voltage and pulse parameters for minimal cell toxicity.
- Erythroid Differentiation: Culture edited HSPCs in erythroid differentiation medium containing SCF, IL-3, and erythropoietin for 14-21 days to generate erythroblasts.
- Editing Efficiency Assessment: After 72 hours, harvest a subset of cells for genotypic analysis. Use PCR amplification of the HBB locus followed by Sanger sequencing and tracking of indels by decomposition (TIDE) analysis to quantify base conversion efficiency.
- Functional Validation: Differentiate another portion of edited HSPCs along the erythroid lineage. Analyze for restoration of β-globin production via RT-PCR and Western blot at days 7, 14, and 21 of differentiation.
- Phenotypic Rescue Assessment: Evaluate improved erythroid maturation by flow cytometry analysis of CD71/GPA expression, assess reduction in apoptosis via Annexin V staining, and measure α/non-α globin ratio by HPLC.
- Safety Profiling: Perform GUIDE-seq or whole-exome sequencing to assess off-target effects. Evaluate structural integrity of the HBB locus and perform clonal analysis to confirm preserved stem-cell diversity.
Troubleshooting Notes:
- If editing efficiency is low, optimize guide RNA design or electroporation parameters.
- If cell viability is compromised post-electroporation, adjust nucleofection program or implement additional cytokine support.
- For incomplete phenotypic correction, consider increasing editor dosage or implementing a second editing cycle.
Detailed Protocol: CRISPR Activation for Silent Gene Reporter Validation in hPSCs
This protocol describes using CRISPR activation (CRISPRa) to rapidly verify reporter knockins at unexpressed loci in human pluripotent stem cells, based on a recently published method [40].
Materials:
- Reporter knockin hPSC line (e.g., KLF17-GFP reporter hPSCs)
- CRISPRa system (dCas9-VPR fusion protein)
- Target-specific sgRNAs for silent gene of interest
- Appropriate cloning vectors
- Stem cell culture reagents and extracellular matrix for attachment
- Flow cytometry equipment for reporter detection
- RNA extraction and qPCR reagents
Procedure:
- sgRNA Design and Cloning: Design sgRNAs targeting the promoter region of the silent gene. Clone sgRNA sequences into appropriate CRISPRa backbone vectors using Golden Gate assembly or similar methods.
- hPSC Culture: Maintain reporter hPSCs in defined culture conditions appropriate for the specific cell line, ensuring optimal viability and pluripotency.
- CRISPRa Delivery: Transfect hPSCs with CRISPRa components (dCas9-VPR and sgRNA expression vectors) using lipid-based transfection or electroporation optimized for sensitive stem cells.
- Activation and Detection: Culture transfected cells for 72-96 hours to allow for transcriptional activation. Harvest cells for analysis of reporter gene expression (e.g., GFP fluorescence) via flow cytometry or fluorescence microscopy.
- Validation: Confirm successful activation of the endogenous silent gene using qRT-PCR to measure transcript levels of the target gene.
- Clonal Isolation: If necessary, isolate single-cell clones to establish purified reporter lines exhibiting consistent expression upon activation.
Comparative Analysis and Future Directions
The landscape of CRISPR-based genome engineering in stem cell research continues to evolve rapidly, with each technology offering distinct advantages and limitations. Traditional CRISPR-Cas9 knockout remains the most accessible approach for gene disruption studies but carries risks associated with double-strand breaks and limited precision. Base editing provides superior precision for single-nucleotide corrections while avoiding double-strand breaks, making it ideal for correcting point mutations in stem cells without inducing significant genotoxic stress. Prime editing further expands the scope of precise editing beyond the limitations of base editing but currently faces challenges with efficiency in many stem cell systems.
The therapeutic application of these technologies in stem cell engineering is progressing rapidly. Recent clinical successes include the first personalized in vivo CRISPR treatment for an infant with CPS1 deficiency, developed and delivered in just six months [8]. This landmark case demonstrates the potential for rapid development of bespoke CRISPR therapies for rare genetic diseases using stem cell technologies. Similarly, extended follow-up data for CASGEVY, a CRISPR-Cas9 gene therapy for sickle cell disease and beta-thalassemia, shows sustained clinical benefits in patients after more than 5.5 and 6 years, respectively, with 95.6% of sickle cell patients remaining free from vaso-occlusive crises for at least 12 months [36].
Future directions in stem cell genome engineering include the development of more sophisticated delivery strategies, enhanced specificity systems, and automation technologies. The emergence of AI-assisted tools like CRISPR-GPT, an LLM agent system to automate and enhance CRISPR-based gene-editing design and data analysis, demonstrates the potential for artificial intelligence to accelerate experimental design and optimization [41]. As these technologies mature, they will further democratize access to advanced genome engineering capabilities, enabling more researchers to leverage stem cell models for both basic research and therapeutic development.
Genome Engineering Workflow: This diagram illustrates the comprehensive process from experimental planning through application, highlighting key decision points and considerations at each stage of stem cell genetic engineering.
{#role}
Engineering Stem Cells for Neurodegenerative Disease Modeling (e.g., Alzheimer's, Parkinson's)
The integration of stem cell technology and CRISPR-Cas9 gene editing represents a transformative approach for modeling neurodegenerative diseases. Induced pluripotent stem cells (iPSCs) enable the generation of patient-specific neural cells, while CRISPR-Cas9 allows precise introduction or correction of disease-associated mutations. This combination facilitates the creation of physiologically relevant human in vitro models that recapitulate key pathological features of conditions like Alzheimer's disease (AD) and Parkinson's disease (PD), overcoming limitations of traditional animal models [5] [42] [43]. These advanced models serve as powerful platforms for dissecting disease mechanisms, screening therapeutic compounds, and developing personalized treatment strategies. This application note provides detailed protocols and resources for engineering stem cells to model neurodegenerative diseases, focusing on practical implementation for research and drug development.
Key Experimental Workflows
iPSC Generation and Neural Differentiation
The foundation of disease modeling begins with robust reprogramming and differentiation protocols. Somatic cells from patients or genetically modified donors are reprogrammed into iPSCs using optimized methods, which are then differentiated into disease-relevant neural cell types.
Table 1: Comparison of iPSC Reprogramming Methods
| Method | Key Features | Reprogramming Efficiency | Genomic Integration Risk | Best Use Cases |
|---|---|---|---|---|
| Sendai Virus | RNA virus, can be eliminated from cells | High | Low | Clinical applications, basic research |
| Episomal Plasmids | EBNA-1/OriP elements, daily transfection needed | Moderate | None | Clinical applications, basic research |
| mRNA Transfection | Non-viral, lower mutagenic risk | High | None | Fibroblasts, peripheral blood cells |
| PiggyBac Transposon | Precise excision possible | Low | Low (with excision) | Research requiring footprint-free integration |
| Adenoviral Vectors | Non-integrating viral vector | Low | Low | Basic research |
Current protocols commonly employ Sendai virus or episomal plasmids for reprogramming, balancing efficiency with safety profiles [43]. The CHALP chemical cocktail—containing CHIR99021 (GSK3β inhibitor), PD0325901 (MEK inhibitor), LIF, A-83-01 (TGF-β receptor inhibitor), bFGF, and HA-100 (ROCK inhibitor)—can enhance reprogramming efficiency when used as a supplement [43]. For neural differentiation, iPSCs are sequentially patterned using small molecules and growth factors to generate specific neural populations, including dopaminergic neurons for PD modeling or cortical neurons for AD studies.
CRISPR-Cas9 Mediated Genetic Engineering
CRISPR-Cas9 enables precise genetic modifications in stem cells to introduce disease-associated mutations or correct existing ones. The workflow involves guide RNA design, delivery of editing components, and validation of modified clones.
Table 2: CRISPR-Cas9 Genome Editing in Stem Cells for Neurodegenerative Disease Modeling
| Target Gene | Disease Association | Editing Approach | Key Phenotypic Outcomes | Reference Model |
|---|---|---|---|---|
| APP | Alzheimer's disease | Correct Swedish mutation (APPswe) | Reduced Aβ production, normalized electrophysiological function | iPSC-derived neurons [44] |
| PSEN1/PSEN2 | Familial Alzheimer's disease | Correct point mutations | Normalized Aβ42/40 ratio, improved neuronal function | iPSC-derived basal forebrain cholinergic neurons [44] |
| APOE | Late-onset Alzheimer's risk | Convert APOE4 to APOE2 isoform | Reduced amyloid pathology, neuroprotective effects | Cerebral organoids [44] |
| PINK1 | Parkinson's disease | Knockout via dual sgRNAs | Impaired mitophagy, neuronal loss in substantia nigra | Non-human primate model [45] |
| LRRK2 | Parkinson's disease | Knockout in iPSCs | Reduced oxidative stress, decreased α-synuclein accumulation | iPSC-derived dopaminergic neurons [45] |
For enhanced editing efficiency, dual-targeting sgRNA strategies can be employed where two guides target the same gene, though this may increase DNA damage response [46]. Newly developed AI-designed editors like OpenCRISPR-1 show comparable or improved activity and specificity relative to SpCas9 while being highly divergent in sequence [47].
Figure 1: Integrated workflow for engineering stem cells to model neurodegenerative diseases, showing key steps from somatic cell reprogramming to final applications.
Advanced Modeling Systems
Cerebral Organoids and Assembloids
Three-dimensional cerebral organoids offer more physiologically relevant models by recapitulating aspects of tissue architecture and cellular heterogeneity. For AD research, organoids carrying APP or PSEN mutations exhibit Aβ plaque-like structures and tau pathology [42] [43]. Assembloids—complex systems combining multiple organoid types—enable modeling of circuit-level dysfunction, such as cortical-striatal interactions relevant to PD.
High-Content Screening Platforms
iPSC-derived neural models are increasingly deployed for high-throughput compound screening. Platforms utilizing iPSCs have identified small molecules that modulate β- and γ-secretase activity to reduce Aβ formation [5]. CRISPRi screens in iPSC-derived neurons enable systematic functional genetic analysis with fewer off-target effects compared to RNAi [45].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Stem Cell-Based Neurodegenerative Disease Modeling
| Reagent Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| Reprogramming Factors | OCT3/4, SOX2, KLF4, c-MYC (Yamanaka factors) | Somatic cell reprogramming to pluripotency | OCT3/4, SOX2, KLF4 maintain pluripotency; c-MYC enhances efficiency [43] |
| CRISPR Systems | SpCas9, OpenCRISPR-1, Cas12a | Genome editing, gene knockout, mutation correction | OpenCRISPR-1 shows improved specificity; dual targeting enhances knockout efficiency [46] [47] |
| Neural Induction Media | N2/B27 supplements, SMAD inhibitors | Direct differentiation toward neural lineages | Dorsomorphin, SB431542 for neural induction |
| Small Molecule Modulators | CHIR99021 (GSK3β inhibitor), A-83-01 (TGF-β inhibitor) | Enhance reprogramming, direct differentiation | Part of CHALP cocktail for improved reprogramming [43] |
| Lineage-Specific Markers | PAX6 (neural precursor), TUJ1 (neurons), GFAP (astrocytes) | Characterization of differentiated cells | Immunocytochemistry, flow cytometry validation |
Protocol: Generating an Isogenic iPSC Line with AD-Associated Mutation
Guide RNA Design and Vector Construction (Days 1-3)
- Design sgRNAs: Select two high-efficiency sgRNAs targeting your gene of interest (e.g., APP, PSEN1). Use VBC scores or Rule Set 3 algorithms for optimal guide selection [46].
- Clone sgRNAs: Insert sgRNA sequences into CRISPR plasmid vectors (e.g., px459) with appropriate resistance markers.
- Prepare donor template: For point mutations, design single-stranded oligodeoxynucleotide (ssODN) donors with ~60 nt homology arms flanking the desired mutation and a silent restriction site for screening.
iPSC Transfection and Selection (Days 4-10)
- Culture iPSCs: Maintain iPSCs in feeder-free conditions with essential supplements.
- Transfect cells: Deliver CRISPR plasmids and donor template using electroporation or lipofection.
- Antibiotic selection: Begin puromycin selection (1-2 μg/mL) 48 hours post-transfection for 5-7 days.
Clone Isolation and Validation (Days 11-30)
- Pick colonies: Manually pick 96 individual colonies and expand in 96-well plates.
- Genomic DNA extraction: Use quick alkaline lysis method for initial screening.
- PCR screening: Amplify target region and use restriction digest for initial identification of edited clones.
- Sanger sequencing: Confirm precise editing in potential hits.
- Off-target assessment: PCR-amplify and sequence top 5-10 potential off-target sites predicted by Cas-OFFinder.
Functional Characterization (Days 31-60)
- Differentiate to neurons: Use dual-SMAD inhibition protocol to generate cortical neurons.
- Assess pathology: Measure Aβ42/40 ratio by ELISA, analyze tau phosphorylation by Western blot.
- Electrophysiology: Perform patch-clamp recording to evaluate neuronal function.
Figure 2: Detailed protocol workflow for generating and validating isogenic iPSC lines with disease-associated mutations.
Emerging Technologies and Future Directions
The integration of artificial intelligence (AI) and systems biology (SysBio) is transforming stem cell-based disease modeling. AI-designed CRISPR editors like OpenCRISPR-1 represent a significant advancement beyond naturally derived systems [47]. SysBioAI approaches enable holistic analysis of multi-omics datasets from iPSC-derived models, identifying patient-specific responses and contributing to enhanced treatment safety and efficacy [48]. These technologies facilitate an "Iterative Circle of Refined Clinical Translation" through continuous adaptation cycles based on computational analysis of clinical trial outcomes [48].
As these technologies mature, they are expected to drive clinical applications in the next 5-10 years, potentially revolutionizing treatment landscapes for neurodegenerative diseases [5]. The convergence of stem cell engineering, gene editing, and computational biology represents a powerful framework for developing personalized therapeutic approaches for Alzheimer's disease, Parkinson's disease, and other neurodegenerative conditions.
The advent of CRISPR-based gene editing has marked a transformative era for treating genetic hematological disorders, notably sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT). Approved therapies like Casgevy represent a paradigm shift, moving from symptomatic management to potential curative interventions [8]. These therapies fundamentally operate by disrupting the three-dimensional genome structure of the BCL11A gene enhancer, a key transcriptional repressor of fetal hemoglobin (HbF) [49]. This disruption silences BCL11A, leading to the reactivation of fetal hemoglobin, which compensates for the defective or absent adult hemoglobin in SCD and TBT patients [49]. The ex vivo approach, where a patient's own hematopoietic stem cells (HSCs) are genetically modified outside the body before reinfusion, underpins the first generation of these approved treatments.
Beyond the initial breakthroughs, the field is rapidly advancing. The first half of 2025 alone witnessed the landmark administration of a personalized in vivo CRISPR treatment for an infant with a rare genetic disease, CPS1 deficiency, developed and delivered in just six months [8]. This case serves as a powerful proof-of-concept for the agile development of bespoke gene therapies. Furthermore, the integration of artificial intelligence, through tools like CRISPR-GPT, is now accelerating experimental design, helping to flatten the steep learning curve associated with CRISPR and potentially shortening drug development timelines from years to months [10]. However, the field concurrently faces significant challenges, including market forces that have narrowed therapeutic pipelines and proposed deep cuts to U.S. government funding for basic biomedical research, which threaten to slow the pace of future discovery and clinical translation [8].
Quantitative Data and Clinical Outcomes
The efficacy of ex vivo CRISPR therapies for hemoglobinopathies is demonstrated by robust clinical trial data. The sustained therapeutic effect is driven by the permanent genetic modification of long-lived hematopoietic stem cells, enabling a continuous production of red blood cells that express fetal hemoglobin.
Table 1: Clinical Outcomes from Key CRISPR-based Ex Vivo Therapies for Hemoglobinopathies
| Therapeutic Target / Drug | Trial Phase | Key Efficacy Metric | Result | Duration of Follow-up | Reference |
|---|---|---|---|---|---|
| SCD & TBT (Casgevy) | Approved Therapy | Freedom from severe vaso-occlusive crises (SCD) or transfusion independence (TBT) | High efficacy leading to approval | Sustained response at 2+ years | [8] |
| hATTR (Intellia) | Phase I | Reduction in disease-related TTR protein | ~90% average reduction | Sustained for 2+ years in all participants | [8] |
| Hereditary Angioedema (HAE) (Intellia) | Phase I/II | Reduction in kallikrein protein & number of attacks | 86% avg. reduction in kallikrein; Majority attack-free | 16-week post-treatment period reported | [8] |
The mechanistic data further elucidates the source of this durability. Research from St. Jude Children’s Research Hospital has shown that the CRISPR-mediated break in the BCL11A enhancer disrupts a critical chromatin "rosette" structure, which is essential for high-level BCL11A expression [49]. This structural disruption prevents the gene's reactivation, leading to long-lasting silencing and sustained HbF production. This foundational understanding opens doors for alternative, potentially more scalable therapeutic strategies, such as using antisense oligonucleotides to target the enhancer RNA required for this 3D structure, achieving similar BCL11A silencing without permanent genome modification [49].
Detailed Experimental Protocols
Ex Vivo Manufacturing of Genetically Modified Cell Products
The following protocol for the ex vivo production of genetically engineered cells from human peripheral blood is adapted from scalable manufacturing processes, such as those used for CAR-based therapies, and reflects the core principles of HSC manipulation for disorders like SCD [50].
1. Isolation of Peripheral Blood Mononuclear Cells (PBMCs)
- Procedure: Dilute fresh whole blood or buffy coat (preferably within 24 hours of collection) with sterile PBS at a 1:1 ratio. Gently layer the diluted blood over a Ficoll-Paque gradient in a 50 mL conical tube.
- Critical Step: Centrifuge at 800× g for 20 minutes at room temperature with medium acceleration and no brakes to avoid disturbing the gradient layers.
- Post-Centrifugation: Carefully aspirate the cloudy PBMC layer at the plasma-Ficoll interface. Wash the PBMCs with PBS and centrifuge at 300× g for 10 minutes. Repeat washes until the pellet appears white. If red blood cell (RBC) contamination is observed, lyse with an RBC lysis buffer.
- Resuspension: Resuspend the final PBMC pellet in complete RPMI media [50].
2. Purification of Target Cells (e.g., HSCs or NK cells)
- Procedure: For isolation of specific cell populations, use immunomagnetic bead-based selection. For a pure NK cell product, a purity of over 90% is recommended as a benchmark to minimize contamination in the final product.
- Process: Incubate the PBMCs with relevant antibody-conjugated microbeads (e.g., CD34+ for HSCs). Pass the cell suspension through a magnetic column placed in a MACS separator. The magnetically labeled target cells are retained, while unlabeled cells flow through. Elute the target cells after removing the column from the magnetic field [50].
3. Genetic Manipulation via Lentiviral Transduction
- Pre-coating: Coat non-tissue culture treated plates with Retronectin to enhance viral transduction efficiency.
- Transduction: Seed the purified target cells and add the lentiviral vector carrying the therapeutic transgene (e.g., a CRISPR-Cas9 construct targeting the BCL11A enhancer). Centrifuge the plate to facilitate viral contact (spinoculation).
- Critical Step: Incubate the cells for a defined period (e.g., 24 hours) at 37°C, 5% CO₂ [50].
4. Ex Vivo Expansion using the G-Rex System
- System Advantage: The G-Rex (Gas-permeable Rapid Expansion) system enables high-density, large-volume cultures with enhanced gas exchange, addressing limitations of traditional culture systems.
- Process: Transfer the transduced cells into a G-Rex vessel containing specialized expansion media. For NK cells, this media is typically supplemented with a cytokine cocktail including IL-2 (200–500 IU/mL), IL-15 (5 ng/mL), and IL-21 (25 ng/mL) to promote robust expansion while maintaining cell functionality [50].
5. Final Formulation and Cryopreservation
- Harvesting: Collect the expanded, genetically modified cells and wash them.
- Cryopreservation: Resuspend the cell product in a cryoprotectant solution, such as 90% FBS with 10% DMSO or a specialized commercial medium like CryoStor CS10. Freeze the cells in a controlled-rate freezer (e.g., using a "Mr. Frosty" container) before transfer to liquid nitrogen for long-term storage [50].
Workflow Visualization
The following diagram illustrates the complete experimental workflow for ex vivo cell therapy development.
The Scientist's Toolkit: Research Reagent Solutions
Successful ex vivo cell therapy development relies on a suite of critical reagents and equipment. The table below details essential materials, their functions, and specific examples used in the featured protocols.
Table 2: Essential Reagents and Equipment for Ex Vivo Cell Therapy Protocols
| Category / Item | Function / Purpose | Specific Examples & Notes |
|---|---|---|
| Cell Separation | ||
| Ficoll-Paque | Density gradient medium for isolating PBMCs from whole blood. | Density: 1.077 g/mL [50]. |
| Immunomagnetic Beads | High-purity isolation of specific cell types (e.g., CD34+ HSCs). | CD3/CD56 microbeads for NK cell isolation; critical for >90% purity [50]. |
| Cell Culture & Expansion | ||
| G-Rex System | Gas-permeable bioreactor for scalable, high-density cell culture. | Enables large-volume expansion with enhanced gas exchange [50]. |
| Cytokine Cocktail | Promotes cell survival, proliferation, and maintains functionality during expansion. | IL-2, IL-15, IL-21 for NK cell expansion [50]. |
| Genetic Manipulation | ||
| Lentiviral Vector | Engineered virus for stable delivery and integration of therapeutic genes. | Carries CRISPR machinery or CAR constructs [50]. |
| Retronectin | Recombinant fibronectin fragment used to co-localize target cells and viral vectors, enhancing transduction efficiency. | Used to pre-coat transduction plates [50]. |
| Analysis & Storage | ||
| Cryopreservation Medium | Protects cells from ice crystal damage during freeze-thaw cycles. | CryoStor CS10 or 90% FBS + 10% DMSO [50]. |
Mechanism of Action: From Genomic Disruption to Therapeutic Effect
The therapeutic success of ex vivo CRISPR therapies for hemoglobinopathies hinges on a precisely targeted genomic disruption. The following diagram details the molecular mechanism by which editing the BCL11A enhancer leads to therapeutic fetal hemoglobin reactivation.
This mechanism, elucidated by researchers at St. Jude Children's Research Hospital, reveals that the formation of a specific three-dimensional chromatin structure is critical for BCL11A expression [49]. The CRISPR-induced break in the enhancer does not merely cause a small local mutation; it catastrophically disrupts this higher-order architecture, allowing repressive complexes to silence the BCL11A gene permanently [49]. This deep understanding of the mechanism provides a foundation for exploring next-generation therapies, including the use of antisense oligonucleotides to target and degrade the enhancer RNA essential for the rosette formation, offering a potentially non-integrating and more scalable alternative to CRISPR [49].
High-Throughput CRISPR Screens for Target Identification and Drug Discovery
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 screening technology is redefining the landscape of drug discovery and therapeutic target identification by providing a precise and scalable platform for functional genomics [51]. The development of extensive single-guide RNA (sgRNA) libraries enables high-throughput screening (HTS) that systematically investigates gene-drug interactions across the entire genome [51]. This powerful approach has found broad applications in identifying drug targets for various diseases, including cancer, infectious diseases, metabolic disorders, and neurodegenerative conditions, playing a crucial role in elucidating drug mechanisms and facilitating drug screening [51].
The adaptability of human pluripotent stem cells (hPSCs), which can theoretically be differentiated into any cell type in the body, makes them a particularly powerful tool for CRISPR screening [52]. When combined with CRISPR technology, hPSCs enable sophisticated disease modeling, drug screening, and the identification of novel therapeutic targets in biologically relevant cell types [52]. The utility of hPSCs can be further extended by gene editing, allowing researchers to create precise genetic modifications including gene knock-outs to interrogate gene function, or to introduce specific genetic variants of interest [52].
CRISPR Screening Approaches and Applications
CRISPR Screening Modalities
CRISPR screens can be categorized into three primary types based on their mechanisms of action, each with distinct applications in target identification and drug discovery:
CRISPR Knockout (CRISPRko): Utilizes the Cas9 nuclease to create double-strand breaks in DNA, leading to insertions or deletions (indels) when cells repair the DNA via the non-homologous end-joining (NHEJ) pathway [53]. These mutations typically result in a coding frameshift or premature stop codon, effectively silencing gene expression [53]. CRISPRko is generally preferred for gene depletion studies due to its clearer signals [53].
CRISPR Interference (CRISPRi): Employs a deactivated Cas9 (dCas9) that lacks cleavage activity, fused to transcriptional repressors such as KRAB (Kruppel-associated box) [53]. This system inhibits gene expression at the transcriptional level without permanently altering the DNA sequence. CRISPRi can also be used for functional characterization of regulatory elements and long noncoding RNAs (lncRNAs) [53].
CRISPR Activation (CRISPRa): Uses dCas9 fused to transcriptional activators such as the synergistic activation mediator (SAM) system, which consists of multiple activation domains [53]. This approach allows for targeted upregulation of gene expression, enabling gain-of-function studies that can identify genes whose overexpression drives specific phenotypes.
Applications in Drug Discovery
The application of CRISPR screening in drug discovery has expanded considerably, with several key use cases:
Essential Gene Identification: Pooled CRISPR screens were initially used to identify genes essential for cell viability [53]. This approach helps pinpoint critical pathways that cancer cells or pathogens depend on for survival, revealing potential therapeutic targets.
Drug Mechanism Elucidation: CRISPR screening increases insight into drug mechanisms of action by systematically testing how genetic perturbations affect drug sensitivity or resistance [51]. This can reveal both primary drug targets and resistance mechanisms.
Therapeutic Target Validation: By creating isogenic pairs of cell lines through precise genetic editing, researchers can compare cellular phenotypes attributable to specific genetic variants, enabling more sensitive detection of subtle phenotypic differences than when comparing cells from different individuals [52].
Complex Disease Modeling: The integration of CRISPR screening with organoid models enables more physiologically relevant drug target identification in systems that better recapitulate human biology compared to traditional 2D cell culture [51].
Experimental Design and Workflow
The following diagram illustrates the core workflow for a typical high-throughput CRISPR screen:
sgRNA Design and Library Construction
Successful CRISPR screening depends heavily on proper sgRNA design and library construction:
sgRNA Design Principles: The sgRNA should lead to high levels of on-target Cas9 activity with minimal off-target activity [52]. It should be located as close as possible to the site of gene targeting, generally within 30 base pairs [52]. Most genomic loci will have suitable sgRNAs nearby, though alternatives to Streptococcus pyogenes Cas9 with different PAM requirements may be necessary for some targets.
Library Design Considerations: sgRNAs of interest are typically cloned into expression vectors that enable co-expression of the sgRNA, Cas9 variants, and marker genes such as GFP or selectable markers like puromycin to enable selection of successfully transfected cells [52]. For genome-wide screens, libraries containing thousands of sgRNAs are constructed to systematically target genes across the genome.
Online Design Tools: Multiple online bioinformatic tools are available to identify guide sequences with high predicted activity and minimal predicted off-target activity, including CHOPCHOP and the CRISPR Design Tool [52].
Delivery Methods for CRISPR Components
The delivery of CRISPR components into target cells is a critical step that varies depending on cell type and experimental goals:
Table 1: CRISPR Delivery Methods and Applications
| Method | Principle | Advantages | Limitations | Ideal Cell Types |
|---|---|---|---|---|
| Lipofection | Lipid complexes fuse with cell membrane | Cost-effective, high throughput | Lower efficiency | Immortalized cell lines [54] |
| Electroporation | Electric pulse forms membrane pores | Easy, fast, high efficiency | Requires optimization | Numerous cell types [54] |
| Nucleofection | Electroporation optimized for nuclear delivery | High efficiency, direct nuclear delivery | Requires specialized reagents & equipment | Primary cells, stem cells [54] |
| Microinjection | Microneedle injects components directly | Highest precision | Technically demanding, low throughput | Zygotes, embryos [54] |
| Viral Transduction | DNA/RNA packaged into viral particles | High efficiency, stable expression | Safety concerns, expensive | Difficult-to-transfect cells [54] |
The format of CRISPR components also affects delivery strategy. Guide RNA and Cas9 can be delivered as DNA, RNA, or pre-formed ribonucleoprotein complexes (RNPs) [54]. The DNA and RNA formats require transcription and/or translation after introduction into the cell, while pre-formed RNPs are immediately active and can reduce off-target effects [54].
Specialized Screening Technologies
Recent advances have addressed specific challenges in CRISPR screening:
CRISPR-StAR (Stochastic Activation by Recombination): A novel screening method that uses internal controls generated by activating sgRNAs in only half the progeny of each cell after re-expansion of the cell clone [55]. This approach overcomes both intrinsic and extrinsic heterogeneity as well as genetic drift in bottlenecks by generating clonal, single-cell-derived intrinsic controls, significantly improving screening accuracy in complex models such as organoids or in vivo systems [55].
Single-Cell CRISPR Screening: Technologies such as Perturb-seq, CRISP-seq, and CROP-seq combine CRISPR screening with single-cell RNA sequencing, enabling researchers to assess the effects of genetic perturbations on the entire transcriptome at single-cell resolution [53]. This dramatically expands the phenotypic information that can be captured from a single screen.
The following diagram illustrates the innovative CRISPR-StAR technology for high-resolution screening in complex models:
Protocol: CRISPR Screening in Human Pluripotent Stem Cells
Pre-Screen Preparation
sgRNA Design and Validation (2-3 weeks)
Target Selection: Identify genomic targets based on your research question. For whole-genome screens, use established libraries such as the Brunello library [56].
sgRNA Design: Utilize bioinformatic tools (e.g., CHOPCHOP, CRISPR Design Tool) to design sgRNAs with high on-target and low off-target activity [52]. Design multiple sgRNAs per gene to account for variable efficiency.
In Vitro Validation: Test sgRNA efficiency using in vitro transcription and cutting assays with purified Cas9 protein before proceeding to cellular experiments [52].
Cell Culture Preparation (1 week)
Maintain hPSCs in feeder-free conditions using defined matrices and media [52]. Regularly passage cells to maintain 60-80% confluence.
Check Pluripotency Status through regular monitoring of marker expression (e.g., OCT4, NANOG, SOX2).
Ensure High Viability (>90%) before transfection by optimizing culture conditions.
Library Delivery and Selection
Nucleofection of hPSCs (3 days)
Harvest Cells: Accutase-dissociated hPSCs should be collected at 70-80% confluence.
Prepare RNP Complexes: For RNP delivery, complex purified Cas9 protein with synthetic sgRNAs at a 1:2 molar ratio in nucleofection buffer. Incubate for 10-20 minutes at room temperature to allow RNP formation [54].
Nucleofection: Use cell type-specific nucleofection programs and solutions. For hPSCs, typically use 1-5 million cells per nucleofection with 2-5 µg of RNP complex [52] [54].
Recovery: Plate transfected cells in recovery medium supplemented with ROCK inhibitor (Y-27632) for 24 hours to enhance survival.
Selection and Expansion (1-2 weeks)
Antibiotic Selection: If using vectors with antibiotic resistance, begin selection 48 hours post-transfection with appropriate antibiotics (e.g., puromycin at 0.5-2 µg/mL for hPSCs) [52].
Monitor Selection Efficiency: Assess cell death in non-transfected controls to confirm effective selection.
Expand Pool: Once selection is complete, expand the transfected pool to achieve sufficient cell numbers for screening. Maintain a minimum of 500-1000 cells per sgRNA in the library to ensure adequate representation [55].
Phenotypic Screening and Analysis
Phenotype Application (Timing varies by assay)
Apply Selective Pressure: Depending on the screen design, this may involve drug treatment for sensitivity/resistance screens, growth factor withdrawal, or other phenotypic selections.
Maintain Coverage: Throughout the selection process, maintain minimum coverage of 500 cells per sgRNA to prevent stochastic effects [55].
Harvest Timepoints: Collect cells at baseline (T0) and after selection (Tfinal) for comparison. Include appropriate controls (e.g., non-targeting sgRNAs).
Genomic DNA Extraction and Sequencing (1 week)
Extract gDNA: Use high-salt precipitation or column-based methods to isolate high-quality genomic DNA from at least 1×10^7 cells per sample to ensure adequate representation of the library [52].
Amplify Integrated sgRNAs: Perform PCR amplification of integrated sgRNA sequences using barcoded primers to enable multiplex sequencing.
Sequence: Use high-throughput sequencing (Illumina platforms) to achieve sufficient depth (typically 100-500 reads per sgRNA).
Bioinformatics Analysis
Primary Analysis (1-2 weeks)
Quality Control: Assess raw read quality with FastQC and trim adapters if necessary [56]. For the Brunello library, adapter sequences are located 5' and 3' to the guide sequence.
Read Alignment: Map sequences to the reference sgRNA library to generate count tables for each sample.
Normalization: Normalize read counts to account for differences in sequencing depth between samples.
Hit Identification
Differential Abundance Analysis: Use specialized algorithms (e.g., MAGeCK, BAGEL) to identify sgRNAs significantly enriched or depleted in experimental conditions compared to controls [53].
Gene-Level Scoring: Aggregate sgRNA-level effects to generate gene-level scores. MAGeCK uses a robust rank aggregation (RRA) method to identify positively and negatively selected genes [53].
Pathway Analysis: Identify enriched biological pathways among hit genes using gene set enrichment analysis.
Table 2: Bioinformatics Tools for CRISPR Screen Analysis
| Tool | Year | Statistical Method | Key Features | Applications |
|---|---|---|---|---|
| MAGeCK | 2014 | Negative binomial distribution + Robust Rank Aggregation | Comprehensive workflow, widely used | CRISPRko screens [53] |
| BAGEL | 2016 | Reference gene set distribution + Bayes factor | Benchmarking against essential genes | Essential gene identification [53] |
| CRISPhieRmix | 2018 | Hierarchical mixture model | Improved performance with fewer replicates | Screens with limited replicates [53] |
| JACKS | 2019 | Bayesian hierarchical modeling | Deconvolutes sgRNA efficacy | Improved gene effect estimation [53] |
| scMAGeCK | 2020 | RRA/Linear Regression | Single-cell CRISPR screen analysis | CROP-seq, Perturb-seq [53] |
Data Analysis and Interpretation
Quality Control Metrics
Proper quality control is essential for generating reliable screening data:
Library Representation: Ensure even representation of sgRNAs in the baseline sample. Most sgRNAs should be within 100-fold of the median count [56].
Screen Quality: Assess the separation between positive and negative controls. In essential gene screens, sgRNAs targeting core essential genes should deplete robustly compared to non-targeting controls.
Replicate Concordance: High correlation between biological replicates (typically R > 0.8) indicates reproducible results.
Gini Index: Evaluate the evenness of sgRNA distribution; lower values indicate more uniform representation.
Hit Validation Approaches
Initial screening hits require rigorous validation:
Secondary Screening: Validate hits using orthogonal sgRNAs in smaller-scale screens or arrayed formats.
Mechanistic Studies: Employ complementary approaches (e.g., rescue experiments, orthogonal assays) to confirm target engagement and mechanism.
Physiological Relevance: Assess validated hits in more complex models, such as organoids or in vivo systems, to establish physiological relevance [51] [55].
Advanced Applications and Integration with Emerging Technologies
Integration with Organoid Models
The combination of CRISPR screening with organoid technology represents a powerful approach for target identification in more physiologically relevant systems [51]. Organoids—three-dimensional cell cultures that recapitulate aspects of organ structure and function—provide a more realistic biological context for screening compared to traditional 2D cultures. CRISPR screening in organoids enables the identification of context-specific genetic dependencies that may not be apparent in conventional cell culture models [51].
Artificial Intelligence and CRISPR
Artificial intelligence is increasingly being integrated with CRISPR technology to accelerate therapeutic discovery:
CRISPR-GPT: An AI tool developed at Stanford Medicine that helps researchers design CRISPR experiments, analyze data, and troubleshoot design flaws [10]. This system uses years of published data to hone experimental designs and predict off-target edits, potentially reducing the timeline for developing new therapies from years to months [10].
AtomNet: A convolutional neural network that has demonstrated success in identifying novel bioactive compounds across multiple therapeutic areas and protein classes, providing a computational alternative to physical high-throughput screening [57].
In Vivo CRISPR Screening
Recent advances have enabled more effective CRISPR screening in complex in vivo models:
CRISPR-StAR Implementation: This technology has been used to identify in-vivo-specific genetic dependencies in genome-wide screens in mouse melanoma, demonstrating the ability to uncover potential novel drug targets that would not be identified through in vitro screening alone [55].
Overcoming Bottlenecks: Conventional in vivo screening faces challenges related to engraftment bottlenecks and heterogeneous growth, which introduce significant noise [55]. CRISPR-StAR overcomes these limitations by generating internal controls at the single-cell level, enabling high-resolution genetic screening even in heterogeneous in vivo models [55].
Research Reagent Solutions
Table 3: Essential Reagents for CRISPR Screening
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| CRISPR Nucleases | SpCas9, dCas9, Cpf1 | DNA cleavage or binding | PAM requirements, size constraints [52] |
| sgRNA Libraries | Brunello, GeCKO, CRISPRa/i libraries | Gene targeting | Coverage, specificity, validation [56] |
| Delivery Tools | Nucleofection kits, Lipofectamine, Lentiviral systems | Component delivery | Efficiency, cytotoxicity, scalability [54] |
| Selection Markers | Puromycin, Blasticidin, GFP | Transfected cell enrichment | Concentration, timing, cell sensitivity [52] |
| Detection Reagents | Antibodies, Molecular beacons, Sequencing kits | Outcome assessment | Sensitivity, specificity, multiplexing capability |
Troubleshooting and Technical Considerations
Common Challenges and Solutions
Low Transfection Efficiency: Optimize delivery method and conditions. For difficult cell types, consider viral delivery or pre-established Cas9-expressing lines [54].
Poor Library Representation: Maintain high cell numbers throughout the screen (minimum 500-1000 cells per sgRNA) and avoid bottlenecks during passaging [55].
High False Positive/Negative Rates: Include appropriate controls (non-targeting sgRNAs, essential gene targets) and use robust statistical methods for hit calling [53].
Off-Target Effects: Utilize carefully designed sgRNAs with minimal predicted off-target activity, and consider using high-fidelity Cas9 variants [51].
Ethical and Safety Considerations
The application of CRISPR technology, particularly in stem cells and for therapeutic purposes, requires careful attention to ethical and safety considerations:
Off-Target Effects: CRISPR technology faces challenges with off-target effects that must be carefully evaluated, particularly for therapeutic applications [51].
Ethical Review: All experiments involving genetic modification of human cells, particularly stem cells, should undergo appropriate ethical review.
Regulatory Compliance: As CRISPR-based therapies move toward clinical application, regulatory considerations become increasingly important [8].
High-throughput CRISPR screening has revolutionized target identification and drug discovery by enabling systematic, genome-wide interrogation of gene function in physiologically relevant systems, including stem cells. The integration of CRISPR screening with emerging technologies such as organoid models, single-cell analysis, and artificial intelligence is further enhancing its power and applicability. As these technologies continue to evolve, they promise to accelerate the discovery and validation of novel therapeutic targets across a broad range of diseases.
The advent of CRISPR-based genome editing has heralded a new era in therapeutic development for genetic disorders. While ex vivo approaches, where cells are edited outside the body, have seen clinical success with approved products like Casgevy for sickle cell disease and beta-thalassemia, the broader potential of gene therapy hinges on effective in vivo delivery [8] [58]. In vivo strategies aim to deliver editing machinery directly into a patient's body, overcoming the logistical and economic challenges of ex vivo cell manipulation, such as the need for specialized facilities and toxic pre-transplant conditioning regimens [59]. However, the efficient and safe delivery of CRISPR components to target tissues remains the principal barrier to its widespread clinical application [60] [58]. This application note examines the current landscape of in vivo delivery vectors, details associated challenges, and provides structured experimental protocols to guide researchers in this rapidly evolving field.
Delivery Vector Landscape
The choice of delivery vector is paramount for successful in vivo gene editing. The ideal vector must protect its cargo, evade the immune system, and efficiently reach the target cell nucleus. The table below summarizes the key vectors, their characteristics, and applications for in vivo CRISPR delivery.
Table 1: Comparison of Major Vectors for In Vivo CRISPR Delivery
| Vector | Packaging Capacity | Key Advantages | Primary Limitations | Therapeutic Examples/Applications |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | ~10 kb (mRNA) |
|
|
|
| Recombinant Adeno-Associated Virus (rAAV) | <4.7 kb |
|
|
|
| Lentiviral Vectors (LVs) | ~8 kb |
|
|
|
| Virus-Like Particles (eVLPs) | Varies (for RNP) |
|
|
|
Protocols for In Vivo Delivery
Protocol: LNP-mediated In Vivo CRISPR Delivery to the Liver
This protocol outlines the systemic delivery of CRISPR-Cas9 mRNA and sgRNA encapsulated in LNPs for editing genes in hepatocytes, based on successful clinical and preclinical programs for diseases like hATTR amyloidosis and hereditary angioedema [8].
Key Reagents:
- CRISPR Payload: Cas9 mRNA and target-specific sgRNA.
- LNP Formulation: Ionizable lipid, phospholipid, cholesterol, and PEG-lipid.
- Animal Model: Mice (e.g., C57BL/6) or other relevant disease models.
- Vehicle: Sterile, endotoxin-free phosphate-buffered saline (PBS).
Procedure:
- LNP Preparation: Formulate LNPs using microfluidics or T-tube mixing. Combine the aqueous phase (Cas9 mRNA and sgRNA in citrate buffer, pH ~4.0) with the organic phase (lipids in ethanol) at a specific flow rate ratio. This induces spontaneous nanoparticle formation.
- LNP Purification and Characterization: Dialyze or use tangential flow filtration against PBS to remove ethanol and adjust pH. Characterize the final LNP product for particle size (e.g., 70-100 nm), polydispersity index, encapsulation efficiency, and endotoxin levels.
- In Vivo Administration: Administer the LNP formulation via intravenous (IV) injection into the tail vein of mice. A common dose is 1-5 mg mRNA per kg body weight, diluted in an appropriate volume of PBS.
- Efficacy and Safety Assessment:
- Efficacy: After 48-72 hours, analyze liver tissue for:
- Editing Efficiency: Isolate genomic DNA and use next-generation sequencing (NGS) of the target locus to quantify indel percentages.
- Protein Knockdown: For knock-out strategies, measure reduction in target protein levels in plasma (e.g., TTR for hATTR) via ELISA [8].
- Safety: Monitor animals for signs of toxicity, including cytokine release and liver enzyme levels (ALT/AST).
- Efficacy: After 48-72 hours, analyze liver tissue for:
Protocol: rAAV-mediated In Vivo Genome Editing for Retinal Disorders
This protocol describes a subretinal injection method for delivering compact CRISPR systems to the retina, as pioneered in the EDIT-101 clinical trial for Leber Congenital Amaurosis [58].
Key Reagents:
- CRISPR Construct: A single rAAV vector encoding a compact nuclease (e.g., SaCas9, Nme2Cas9) or a dual AAV system for larger effectors, combined with the required sgRNA(s).
- rAAV Serotype: AAV5 or AAV8, which demonstrate good tropism for retinal pigment epithelium and photoreceptors.
- Animal Model: Wild-type or genetically engineered mouse models of retinal disease.
Procedure:
- Vector Production and Quality Control: Produce rAAV vectors using a triple-transfection system in HEK293 cells and purify via iodixanol gradient ultracentrifugation or affinity chromatography. Titer the vector using digital droplet PCR.
- Subretinal Injection:
- Anesthetize the mouse and dilate the pupil.
- Under a surgical microscope, carefully puncture the sclera with a glass micropipette near the ora serrata.
- Inject 1-2 µL of the rAAV preparation (e.g., 1x10^11 - 1x10^12 vector genomes/mL) into the subretinal space, creating a transient retinal detachment, which confirms successful delivery.
- Analysis:
- In vivo Functional Assessment: Perform electroretinography (ERG) at 4-8 weeks post-injection to measure recovery of photoreceptor function.
- Ex vivo Molecular Analysis: Harvest retinal tissue and assess editing efficiency by NGS. For EDIT-101, this involved quantifying the deletion of the pathogenic IVS26 mutation in the CEP290 gene [58].
- Histology: Process retinal sections for immunohistochemistry to evaluate tissue morphology and protein expression restoration.
Protocol: In Vivo Gene Editing of Hematopoietic Stem Cells (HSCs) in Neonates
This advanced protocol leverages the natural trafficking of HSCs in newborns to achieve in vivo gene editing, as demonstrated in mouse models of ADA-SCID and Fanconi anemia [59].
Key Reagents:
- Delivery Vector: Phagocytosis-shielded Lentiviral Vector (e.g., CD47-high LV) or an engineered rAAV.
- Animal Model: Newborn mice (postnatal day 0-1).
Procedure:
- Vector Administration: Systemically administer the vector (e.g., 1x10^9 TU via temporal vein or facial vein injection) into newborn mouse pups within the first 48 hours of life.
- Mobilization (Optional): To enhance efficiency, administer a mobilization regimen (e.g., G-CSF and plerixafor) at 1-2 weeks of age to increase the number of circulating HSCs available for transduction [59].
- Long-term Monitoring:
- Track vector marking and transgene expression in peripheral blood over months by flow cytometry and qPCR.
- Assess multilineage engraftment and clonality in bone marrow, spleen, and thymus.
- For disease models, monitor for phenotypic rescue (e.g., prevention of bone marrow failure in Fanconi anemia mice).
- Functional Validation via Transplantation: Transplant bone marrow from treated mice into conditioned recipient mice to confirm that long-term, self-renewing HSCs were successfully edited.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for In Vivo CRISPR Research
| Reagent / Tool | Function / Description | Example Application |
|---|---|---|
| Compact Cas Orthologs (SaCas9, CjCas9, Cas12f) | Engineered Cas proteins small enough to be packaged into a single rAAV vector alongside sgRNAs and promoters. | Enables all-in-one rAAV therapy for retinal and liver diseases [58]. |
| High-Fidelity Cas9 Variants (eSpCas9, SpCas9-HF1, HypaCas9) | Engineered versions of SpCas9 with reduced off-target activity by weakening non-specific DNA interactions. | Improves safety profile of CRISPR therapies by minimizing unintended genomic edits [62]. |
| Prime Editing (PE) Systems | A versatile "search-and-replace" technology that can make all 12 possible base-to-base conversions without double-strand breaks. | Correction of pathogenic PRPH2 mutation in human iPSC-derived cardiomyocytes and retinal organoids [34] [61]. |
| ABE8e & CBE Base Editors | Fusions of Cas9 nickase with deaminase enzymes that mediate precise A>G or C>T base conversions without causing DSBs. | Correction of the SERPINA1 Z mutation in models of alpha-1 antitrypsin deficiency (AATD) [34] [58]. |
| Alt-R HDR Enhancer Protein | A recombinant protein that increases the efficiency of homology-directed repair (HDR) in challenging primary cells. | Improves precise gene editing rates in hematopoietic stem cells and induced pluripotent stem cells (iPSCs) [61]. |
Visualizing Workflows and Decisions
The following diagrams illustrate the experimental workflow for a standard in vivo CRISPR study and the logical decision-making process for selecting an appropriate delivery vector.
Diagram 1: In Vivo CRISPR Therapy Development Workflow. This flowchart outlines the key steps from target identification to final efficacy assessment in a preclinical study.
Diagram 2: Decision Pathway for Selecting an In Vivo Delivery Vector. This chart guides the initial selection of a delivery vector based on key experimental requirements such as durability of expression, target tissue, and cargo size.
Navigating the Hurdles: Tackling Off-Target Effects, Delivery, and Manufacturing Challenges
In the realm of stem cell genetic engineering, CRISPR-Cas technology has revolutionized our ability to model diseases and develop therapeutic interventions. However, the persistent challenge of off-target effects—unintended genetic modifications at sites other than the intended target—remains a significant barrier to clinical translation [63]. These effects occur due to the inherent tolerance of CRISPR systems for mismatches between the guide RNA (gRNA) and target DNA sequence, potentially leading to catastrophic consequences such as activation of oncogenes or disruption of tumor suppressor genes [64] [65]. In the context of stem cell research, where edited cells may proliferate and differentiate into multiple tissue types, ensuring genomic integrity is paramount for both experimental validity and clinical safety.
The risk profile varies significantly between different application contexts. Ex vivo editing of stem cells allows for selection and validation of properly edited clones, whereas in vivo therapeutic editing poses greater risks as off-target effects cannot be easily removed or selected against [65]. Understanding and mitigating these risks through sophisticated experimental design, advanced nuclease engineering, and comprehensive validation is essential for advancing stem cell-based therapies into clinical applications.
Comprehensive Strategies for Off-Target Minimization
Guide RNA Design and Optimization
The foundation of specific genome editing begins with meticulous gRNA design and optimization. Careful selection of gRNA sequences significantly reduces the potential for off-target activity while maintaining high on-target efficiency [65].
Critical Considerations for gRNA Design:
- Sequence Specificity: Utilize computational tools to select gRNAs with minimal sequence similarity to off-target sites across the genome, prioritizing those with unique sequences even allowing for 3-5 base pair mismatches [65].
- GC Content: Optimal GC content (typically 40-60%) stabilizes the DNA:RNA duplex, enhancing on-target binding while reducing off-target interactions. Both excessively high and low GC content can compromise specificity [65].
- Chemical Modifications: Incorporation of 2'-O-methyl analogs (2'-O-Me) and 3' phosphorothioate bonds (PS) into synthetic gRNAs reduces off-target editing while potentially increasing on-target efficiency [65].
- Guide Length: Truncated gRNAs (17-19 nucleotides instead of 20) can reduce off-target effects by decreasing the binding energy and increasing specificity requirements, though this may sometimes come at the cost of reduced on-target activity [65].
Table 1: Guide RNA Design Parameters and Their Impact on Specificity
| Design Parameter | Recommendation | Impact on Specificity | Considerations |
|---|---|---|---|
| Sequence Length | 17-20 nucleotides | Shorter guides increase specificity | Balance with on-target efficiency |
| GC Content | 40-60% | Optimal stability reduces off-target binding | Avoid extremes (<20% or >80%) |
| Chemical Modifications | 2'-O-Me, PS bonds | Reduces off-target activity | Requires synthetic guide RNA |
| Specificity Scoring | Use multiple algorithms | Identifies guides with low off-target potential | Cross-validate between tools |
Advanced Nuclease Engineering
The evolution of CRISPR nucleases has produced numerous variants with enhanced specificity profiles, moving beyond the wild-type SpCas9 to address off-target concerns.
High-Fidelity Cas Variants: Engineered Cas9 variants such as HiFi Cas9 demonstrate significantly reduced off-target activity while maintaining robust on-target editing [64] [65]. These proteins contain mutations that destabilize non-specific interactions with DNA, increasing the stringency of complementarity required for cleavage.
Cas12 Family Nucleases: The discovery and engineering of compact Cas12 nucleases, including the recently identified Cas12l family (~850 amino acids), offer alternative editing platforms with distinct specificity profiles [66]. These nucleases recognize cytosine-rich PAM sequences and generate staggered double-strand breaks, potentially contributing to higher editing efficiency and specificity in certain contexts [66].
Nickase-Based Approaches: Paired nickase strategies utilizing Cas9 nickases (nCas9) that create single-strand breaks instead of double-strand breaks can dramatically reduce off-target effects [64]. This approach requires two adjacent gRNAs to generate a double-strand break, significantly increasing the specificity requirement. However, it's important to note that nickase systems can still induce structural variations, albeit at lower frequencies [64].
Next-Generation Editing Modalities
Beyond traditional nuclease-based editing, newer technologies fundamentally alter the editing mechanism to avoid double-strand breaks entirely, offering promising avenues for stem cell engineering where genomic integrity is critical.
Base Editing: CRISPR base editors combine a catalytically impaired Cas nuclease (nickase) with a nucleobase deaminase enzyme, enabling direct chemical conversion of one base pair to another without double-strand break formation [67]. These systems are particularly valuable for correcting point mutations associated with genetic disorders. Cytosine Base Editors (CBEs) facilitate C•G to T•A conversions, while Adenine Base Editors (ABEs) enable A•T to G•C transitions [67]. The recent development of Guanine Base Editors (GBEs) further expands the possible transversions [67].
Prime Editing: Prime editors represent a more versatile precise editing technology that uses a catalytically impaired Cas9 reverse transcriptase fusion and a prime editing guide RNA (pegRNA) to directly copy edited genetic information from the RNA template into the target DNA [67]. This system can mediate all 12 possible base-to-base conversions, as well as small insertions and deletions, without double-strand breaks or donor DNA templates.
Table 2: Comparison of CRISPR Editing Platforms and Their Off-Target Profiles
| Editing Platform | Editing Mechanism | Primary Off-Target Concerns | Ideal Applications in Stem Cell Research |
|---|---|---|---|
| Traditional CRISPR-Cas9 | DSB induction followed by NHEJ/HDR | Off-target indels, structural variations | Gene knockouts in validated safe harbor loci |
| High-Fidelity Cas Variants | DSB with enhanced specificity | Reduced off-target indels | Disease modeling requiring high specificity |
| Base Editors | Direct chemical conversion without DSB | Off-target deamination, gRNA-independent editing | Correcting point mutations in monogenic diseases |
| Prime Editors | Reverse transcription from pegRNA | Off-target nicking, RNA-dependent | Multiple mutation types with minimal genotoxicity |
| Cas12 Nucleases | Staggered DSB with distinct PAM | Alternative off-target profile | Expanding editable genomic regions |
Delivery System Optimization
The method and format of CRISPR component delivery significantly influence off-target effects by controlling the duration and concentration of editing machinery within cells.
Cargo Format Selection: The choice between DNA, mRNA, and ribonucleoprotein (RNP) delivery critically impacts off-target profiles. RNP delivery, consisting of pre-complexed Cas protein and gRNA, offers transient activity that minimizes off-target effects compared to plasmid DNA, which persists longer and leads to sustained nuclease expression [65].
Delivery Vehicle Considerations: Viral vectors, particularly AAV, have limited packaging capacity that may necessitate split systems for larger nucleases or base editors [67]. Lipid nanoparticles (LNPs) have emerged as promising vehicles for in vivo delivery, with natural tropism for liver tissue and reduced immunogenicity compared to viral vectors [8]. The transient nature of LNP-mediated delivery aligns well with minimizing off-target effects.
Detection and Analysis of Off-Target Effects
Methodologies for Comprehensive Off-Target Assessment
Rigorous detection of off-target effects is essential for validating editing specificity, particularly in stem cell applications where long-term expansion and differentiation amplify the consequences of unintended edits.
Computational Prediction Tools: In silico prediction represents the first line of defense against off-target effects. Tools like CRISPOR analyze gRNA sequences against reference genomes to identify potential off-target sites based on sequence similarity, mismatch tolerance, and genomic context [65]. These predictions inform subsequent experimental validation strategies.
Cell-Based Detection Methods:
- GUIDE-seq (Genome-wide Unbiased Identification of DSBs Enabled by sequencing) uses oligonucleotide tag integration at double-strand break sites to comprehensively map CRISPR-induced cleavage events across the genome [65].
- CIRCLE-seq provides an in vitro method for profiling nuclease activity on purified genomic DNA, offering sensitive detection without cellular context constraints [65].
- CAST-seq (CRISPR Affinity for Systematic Translocation Sequencing) specifically detects chromosomal rearrangements and translocations resulting from simultaneous cleavage at on-target and off-target sites [64].
Comprehensive Genomic Analysis: Whole genome sequencing (WGS) remains the gold standard for unbiased detection of off-target effects and structural variations, though cost and analytical complexity limit its routine application [64] [65]. Targeted sequencing of predicted off-target sites offers a more practical alternative for validation studies.
Protocol: Comprehensive Off-Target Assessment in Stem Cells
Objective: Systematically identify and quantify off-target effects in gene-edited stem cells using a tiered approach combining computational prediction and experimental validation.
Materials and Reagents:
- Pluripotent stem cells (iPSCs or ESCs)
- CRISPR editing components (RNP complex preferred)
- Cell culture reagents and differentiation media
- DNA extraction kit
- PCR reagents and primers
- Next-generation sequencing library preparation kit
Procedure:
Week 1: Guide Selection and Computational Prediction
- Input target sequence into multiple prediction tools (CRISPOR, Cas-OFFinder).
- Select 3-5 candidate gRNAs based on high on-target efficiency scores and minimal predicted off-target sites.
- Cross-reference predictions with stem cell-specific epigenomic data (e.g., ATAC-seq, ChIP-seq) to identify open chromatin regions with increased vulnerability.
Week 2-3: Stem Cell Editing and Expansion
- Deliver CRISPR components to stem cells using electroporation (for RNP) or viral transduction.
- Culture and expand edited cells for 10-14 days to allow fixation of edits and sufficient material for analysis.
- Confirm on-target editing efficiency using T7E1 assay or Sanger sequencing with ICE analysis.
Week 4: Experimental Off-Target Detection
- Extract genomic DNA from approximately 1×10^6 edited cells and control unedited cells.
- Perform GUIDE-seq:
- Transfect cells with dsODN tag alongside CRISPR components
- Extract genomic DNA after 72 hours
- Prepare sequencing libraries with GUIDE-seq adapters
- Sequence on appropriate NGS platform
- Alternatively, conduct CIRCLE-seq:
- Fragment genomic DNA (100-500 bp)
- Circularize fragments and digest linear DNA
- Incubate with CRISPR RNP complex
- Purify and sequence cleaved fragments
Week 5-6: Data Analysis and Validation
- Process sequencing data using appropriate bioinformatic pipelines (GUIDE-seq processing, CIRCLE-seq analysis).
- Compile list of potential off-target sites from both computational and experimental methods.
- Validate top candidate off-target sites (10-20 sites) by amplicon sequencing in biological replicates.
- Calculate off-target rates and compare to positive and negative controls.
Expected Outcomes and Interpretation:
- A comprehensive off-target profile specific to your stem cell line and editing conditions
- Quantitative assessment of off-target frequency at validated sites
- Informed decision on whether to proceed with the edited line or redesign the approach
Troubleshooting Notes:
- Low signal in GUIDE-seq may indicate inefficient tag integration; optimize transfection efficiency
- High background in CIRCLE-seq may require additional purification steps
- Discrepancies between prediction and experimental results may reflect cell-type-specific chromatin accessibility
Table 3: Research Reagent Solutions for Off-Target Mitigation
| Reagent Category | Specific Examples | Function in Off-Target Mitigation | Application Notes |
|---|---|---|---|
| High-Fidelity Nucleases | HiFi Cas9, eSpCas9, SpCas9-HF1 | Reduced tolerance for gRNA-DNA mismatches | Balance with on-target efficiency; test multiple variants |
| Alternative Cas Nucleases | Cas12a, Cas12l, CasMINI | Distinct PAM requirements and fidelity profiles | Cas12l offers high efficiency with compact size [66] |
| Base Editing Systems | ABE8e, BE4max, AncBE4max | Avoid DSB generation; higher precision | Monitor gRNA-independent off-target deamination |
| Prime Editing Systems | PE2, PEmax, PE3 | Versatile editing without DSBs; high specificity | Optimize pegRNA design for efficiency |
| Chemical Modifications | 2'-O-Me, 3' PS bonds on gRNA | Enhanced stability and specificity | Commercially available from synthetic RNA providers [65] |
| Detection Kits | GUIDE-seq, CIRCLE-seq kits | Comprehensive off-target identification | Validate sensitivity with positive controls |
| Analysis Software | CRISPOR, Cas-OFFinder, ICE | Prediction and quantification of editing outcomes | ICE tool analyzes Sanger sequencing data for on- and off-target edits [65] |
The landscape of off-target mitigation in CRISPR applications continues to evolve rapidly, with several promising directions emerging for stem cell research. The integration of artificial intelligence tools, such as CRISPR-GPT, is streamlining experimental design and predicting potential pitfalls before laboratory work begins [10]. These AI systems can analyze years of published data to recommend optimal gRNAs, predict off-target sites with greater accuracy, and troubleshoot design flaws, potentially reducing the trial-and-error nature of CRISPR experimentation [10].
As CRISPR therapies advance clinically, regulatory scrutiny of off-target effects intensifies. The FDA now requires comprehensive off-target assessment for clinical trials, emphasizing the need for standardized detection methods and risk assessment frameworks [64] [65]. For stem cell researchers, this underscores the importance of rigorous off-target profiling early in therapeutic development pipelines.
Looking forward, the convergence of improved computational prediction, advanced nuclease engineering, and novel editing modalities that avoid double-strand breaks altogether promises to further enhance the specificity and safety of stem cell genetic engineering. By implementing the comprehensive strategies outlined in this application note, researchers can navigate the challenges of off-target effects while advancing the tremendous potential of CRISPR technologies in regenerative medicine and therapeutic development.
{article content start}
Overcoming Immune Rejection and Ensuring Transplanted Cell Survival
The success of regenerative medicine hinges on the ability of transplanted cells to survive, integrate, and function long-term within the host. A primary barrier to achieving this goal is immune-mediated rejection, a complex process involving both innate and adaptive host immunity that can rapidly destroy allogeneic cell grafts. The advent of CRISPR-based genome editing has provided scientists with a powerful toolkit to directly engineer stem cells and their derivatives, enabling the creation of cell therapies with enhanced compatibility and resilience. This application note, framed within the broader context of stem cell genetic engineering research, details the latest CRISPR strategies and provides actionable protocols for researchers and drug development professionals aiming to overcome the critical challenge of immune rejection.
Understanding the Immune Response to Allogeneic Cell Grafts
Transplanted allogeneic stem cell-derived therapies face a multifaceted immune attack. The response is orchestrated by both the innate and adaptive immune systems, and understanding these pathways is essential for developing effective countermeasures.
- Innate Immunity: The innate immune system provides the first line of defense. Natural Killer (NK) cells are a key component, which target and kill cells that lack or express mismatched self-human leukocyte antigen class I (HLA-I) molecules, a concept known as the "missing-self" hypothesis [68]. Furthermore, the complement system, a cascade of soluble proteins, can opsonize transplanted cells or directly induce cell lysis, as observed in islet and hepatocyte transplantation studies [68].
- Adaptive Immunity: The adaptive immune response is highly specific and confers long-lasting immunity. Host T cells recognize foreign donor antigens primarily through three pathways of allorecognition [68]:
- Direct Pathway: Recipient T cells directly recognize intact donor HLA molecules on the surface of the transplanted cells.
- Indirect Pathway: Recipient antigen-presenting cells (APCs) engulf donor cells, process donor proteins, and present them as peptides on host HLA molecules to T cells.
- Semi-direct Pathway: Recipient APCs acquire intact donor HLA-peptide complexes and present them to T cells. While the direct pathway is potent, its effects may be transient. The indirect pathway is considered the dominant mechanism for chronic rejection of cellular therapies, which typically do not contain professional donor APCs [68]. Activated CD4+ T cells provide help to cytotoxic CD8+ T cells, which directly lyse grafted cells, and to B cells, which produce allospecific antibodies.
The following diagram illustrates these key pathways that lead to the immune rejection of transplanted cells.
CRISPR-Based Strategies for Engineering Immune-Evasive Cells
CRISPR technology enables precise genetic modifications to shield cell therapies from the host immune system. The table below summarizes the primary strategic approaches.
Table 1: CRISPR-Based Strategies for Mitigating Immune Rejection
| Strategy | Molecular Target | Mechanism of Action | Key Evidence |
|---|---|---|---|
| HLA Ablation | Beta-2-microglobulin (B2M) / HLA Class I | Eliminates surface expression of HLA-I, preventing CD8+ T cell recognition via the direct pathway. | A foundational step for creating "universal" donor cells [68]. |
| Expression of Immunomodulatory Molecules | PD-L1, HLA-G, CD47 | Engages inhibitory receptors on immune cells (T, NK cells) to transmit direct "don't eat me" signals or suppress activation. | PD-L1 overexpression restricted T cell activation and prolonged graft survival in diabetic mice [68]. |
| Targeting Pro-Inflammatory Signaling | CXCL10, other IFN-γ-induced mediators | Disrupts chemokine signaling that recruits alloreactive T cells to the graft site, reducing local inflammation. | A whole-genome CRISPR screen identified CXCL10 depletion as beneficial for SC-islet survival against allo-rejection [69]. |
| Utilizing Novel CRISPR Systems | Base Editors / Prime Editors | Enables precise single-nucleotide changes without creating double-strand breaks, improving safety and enabling more sophisticated edits like single amino acid swaps in HLA. | Base editing is being used in clinical trials and allows for precise nucleotide conversion without DSBs [70]. |
The workflow for developing such engineered cells involves multiple stages, from target identification to in vivo validation, as outlined below.
Detailed Experimental Protocols
Protocol: Whole-Genome CRISPR Screening to Identify Immune Evasion Targets
This protocol is adapted from a study that identified key drivers of immunogenicity in stem cell-derived islets (SC-islets) [69].
Objective: To perform an unbiased, genome-wide identification of genes that, when knocked out, enhance the survival of stem cell-derived therapies under allogeneic immune attack.
Materials:
- A genome-scale CRISPR knock-out (GeCKO) library or similar.
- Target stem cell population (e.g., human embryonic stem cells - hESCs).
- Allogeneic Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors.
- Culture media for stem cells and PBMCs.
- FACS sorter and analyzer.
- Next-generation sequencing (NGS) platform.
Methodology:
- Library Transduction: Transduce the target hESC population with the GeCKO library at a low Multiplicity of Infection (MOI) to ensure single guide RNA (sgRNA) integration. Use a coverage of at least 500x to maintain library representation.
- Selection and Differentiation: Apply selection (e.g., puromycin) to eliminate non-transduced cells. Differentiate the pooled, edited hESCs into the desired cell type (e.g., SC-islets).
- Immune Co-culture Challenge: Co-culture the differentiated, edited cells with allogeneic PBMCs at a predetermined effector-to-target ratio. Include control groups (edited cells without PBMCs) to account for fitness effects unrelated to immunity.
- Cell Sorting and Recovery: After a sufficient co-culture period (e.g., 5-7 days), separate and collect surviving target cells using fluorescence-activated cell sorting (FACS) based on cell-specific surface markers.
- Genomic DNA Extraction and NGS: Extract genomic DNA from the pre-challenge pool and the post-challenge surviving cell population. Amplify the integrated sgRNA sequences by PCR and subject them to NGS.
- Data Analysis: Bioinformatically quantify the abundance of each sgRNA in the pre- and post-challenge samples. sgRNAs that are significantly enriched in the surviving population indicate gene knockouts that conferred a survival advantage against immune attack.
Protocol: Knock-out of CXCL10 in Stem Cell-Derived Islets via CRISPR-Cas9
This protocol provides a targeted approach based on the findings of the aforementioned screen [69].
Objective: To genetically ablate the CXCL10 gene in hESCs to reduce T cell recruitment and improve SC-islet graft survival.
Materials:
- hPSC line (e.g., H1, H9).
- sgRNA targeting the CXCL10 promoter or early exons (e.g., 5'-GACATCATCCAGGTGGTCAC-3').
- CRISPR-Cas9 plasmid (e.g., SpCas9) or ribonucleoprotein (RNP) complex.
- Lipofectamine CRISPRMAX or electroporator (e.g., Neon).
- Flow cytometry antibodies for CXCL10 intracellular staining or ELISA kit.
- Chemotaxis assay kit (e.g., to test T cell migration).
Methodology:
- sgRNA Design and Complex Formation: Design and synthesize sgRNAs with high on-target and low off-target activity. Complex the sgRNA with SpCas9 protein to form an RNP complex.
- Stem Cell Transfection: Electroporate the RNP complex into hESCs using manufacturer-optimized protocols for high viability and editing efficiency.
- Clonal Selection and Screening: After recovery, single-cell sort the transfected hESC population into 96-well plates to establish clonal lines. Expand clones and screen for CXCL10 knock-out via:
- Genotypic Validation: Genomic DNA PCR of the target locus followed by Sanger sequencing and TIDE decomposition analysis to confirm indel mutations.
- Functional/Phenotypic Validation: Differentiate validated clones into SC-islets. Stimulate the SC-islets with IFN-γ (e.g., 100 ng/mL for 24h) and measure CXCL10 secretion in the supernatant by ELISA. Successful knock-out clones should show a significant reduction or absence of CXCL10 protein.
- In Vitro Functional Assay: Use a transwell migration assay to confirm functionality. Seed SC-islet cells (wild-type vs. CXCL10-KO) in the lower chamber and allogeneic T cells in the upper chamber. After IFN-γ stimulation, quantify T cell migration. CXCL10-KO SC-islets should demonstrate reduced T cell chemotaxis.
The Scientist's Toolkit: Essential Reagents and Models
Successful research in this field relies on a suite of specialized reagents and experimental models.
Table 2: Key Research Reagent Solutions for Immune Evasion Studies
| Category | Item | Function/Application |
|---|---|---|
| CRISPR Editors | SpCas9, SaCas9, Cas12a (Cpf1), Base Editors | The core effector proteins for inducing DSBs or precise base changes. SaCas9/Cas12a are smaller, facilitating AAV delivery [71] [70]. |
| Delivery Tools | Electroporation systems (e.g., Neon), Lipid Nanoparticles (LNPs), AAV vectors | Methods for introducing CRISPR components into stem cells. LNPs show promise for in vivo delivery and allow for re-dosing [8]. |
| In Vitro Models | Allogeneic PBMCs, NK cell isolation kits, Co-culture media | Used to simulate immune attack in a controlled plate-based setting [69] [68]. |
| In Vivo Models | Humanized mice (e.g., NSG, NOG), Immunocompetent diabetic mice | Mouse models with a humanized immune system or autoimmune diabetes are critical for pre-clinical validation of graft survival and function [69] [68]. |
| Analysis Tools | Flow cytometer, ELISA kits, scRNA-Seq, NGS platform | Essential for characterizing editing efficiency, immune cell profiling, cytokine measurement, and transcriptomic analysis [69]. |
Discussion and Future Perspectives
The integration of CRISPR screening with advanced editing tools like base editors provides a powerful, systematic pipeline for identifying and validating genetic modifications that foster immune tolerance. The recent success of in vivo CRISPR therapies delivered via lipid nanoparticles (LNPs), which allow for re-dosing and show a favorable safety profile, further underscores the translational potential of these approaches [8]. However, significant challenges remain. A primary concern is the immunogenicity of the CRISPR system itself, as pre-existing adaptive immunity to common Cas proteins like SpCas9 and SaCas9 has been detected in a substantial portion of the general population [72]. Mitigation strategies under investigation include the use of engineered "immuno-silenced" Cas9 variants and ex vivo editing with minimal residual Cas9 protein [72]. Looking forward, the combination of multiple strategies—such as HLA ablation with concurrent expression of local immunosuppressants like PD-L1—will likely be necessary to achieve robust, long-term graft survival without systemic immunosuppression. As CRISPR tools continue to evolve in precision and safety, the vision of creating universally compatible "off-the-shelf" stem cell therapies moves closer to reality.
{article content end}
The efficacy of CRISPR-based stem cell genetic engineering is fundamentally constrained by the delivery vector. Selecting between viral and non-viral systems requires careful consideration of cargo requirements, target cell sensitivity, and the intended clinical application. Adeno-associated viral (AAV) vectors offer efficient transduction and sustained expression, making them suitable for long-term transgene expression in hard-to-transfect cells. In contrast, lipid nanoparticles (LNPs) provide a highly versatile platform for delivering large or complex CRISPR payloads with a favorable safety profile and suitability for re-dosing. This application note provides a structured comparison and detailed protocols to guide researchers in selecting and optimizing these delivery systems for stem cell engineering projects.
Vector System Comparison and Selection Framework
The choice between AAV and LNP vectors is multifaceted, impacting experimental design, manufacturing complexity, and therapeutic potential. The following tables summarize key quantitative and qualitative differentiators.
Table 1: Quantitative Performance Metrics of AAV vs. LNP Vectors
| Performance Metric | AAV (Viral Vector) | LNP (Non-Viral Vector) |
|---|---|---|
| Cargo Capacity | Strictly limited to <4.7 kb [73] [58] | Flexible/High; virtually unlimited for mRNA, siRNA, DNA [73] [74] |
| Transduction/Efficiency | High in permissive cells; serotype-dependent [58] | Variable; highly formulation-dependent; endosomal escape is rate-limiting (~2-3%) [73] |
| Genetic Persistence | Long-term, episomal (in non-dividing cells) [73] [58] | Transient (ideal for editing) [73] [74] |
| Typical Manufacturing COGS | High [73] [74] | Low to Medium [73] [74] |
| Empty/Full Particle Ratio | A key CMC bottleneck; requires sophisticated purification [73] | Not Applicable |
Table 2: Qualitative Operational and Safety Considerations
| Consideration | AAV (Viral Vector) | LNP (Non-Viral Vector) |
|---|---|---|
| Primary Use Case | In vivo gene delivery; ex vivo for sensitive primary cells (e.g., stem cells) [75] [58] | In vivo gene editing (e.g., CRISPR); ex vivo for robust cells [73] [76] |
| Immunogenicity | High; pre-existing neutralizing antibodies (NAbs) can exclude patients; re-dosing is not feasible [73] [74] | Low; re-dosable therapy is possible [73] [74] |
| Key Safety Concerns | Off-target integration risk (low), cellular immune response [76] | Reactogenicity, potential lipid-related cytotoxicity [73] |
| Manufacturing Bottleneck | Empty/Full capsid separation; complex cell culture & purification [73] | Lipid purity & consistency; microfluidic fouling [73] |
| Regulatory Path | Well-established but requires long-term follow-up for integrating vectors [73] | Evolving; precedent set by mRNA vaccines; regulatory clarity on lipid classification is needed [74] [77] |
Experimental Protocols for Vector Delivery
Protocol: AAV Transduction of Human Induced Pluripotent Stem Cells (hiPSCs)
Principle: Leverage AAV's high transduction efficiency for introducing CRISPR machinery into hiPSCs for long-term gene expression or correction, a common approach in disease modeling [75].
Materials:
- Research Reagent Solutions:
- hiPSCs: Patient-derived or wild-type control lines [75].
- rAAV Vector: All-in-one encoding compact Cas9 ortholog (e.g., SaCas9) and gRNA, or a dual-vector system for larger payloads [58]. Serotype should be selected for stem cell tropism (e.g., AAV6, AAV-DJ).
- Enhanced Infection Solution: Polybrene or other transduction enhancers.
- Cell Culture Media: Essential 8 or mTeSR1 for hiPSC maintenance.
- Rock Inhibitor (Y-27632): To enhance cell survival post-handling.
Methodology:
- hiPSC Preparation: Culture hiPSCs to 70-80% confluence in a vitronectin-coated plate. Gently dissociate into single cells using Accutase. Quench with DMEM/F-12 + 10µM Rock Inhibitor. Count cells and seed at optimal density for your differentiation protocol.
- AAV Inoculation: Thaw rAAV vector on ice. Prepare infection medium by diluting the rAAV stock to the desired MOI (e.g., 10^4 - 10^5 vg/cell) in culture medium supplemented with 4-8 µg/mL polybrene.
- Transduction: Aspirate culture medium from hiPSCs and gently add the AAV-containing medium. Incubate cells at 37°C, 5% CO2 for 24 hours.
- Medium Replacement: After 24 hours, carefully replace the infection medium with fresh, pre-warmed culture medium.
- Analysis and Differentiation: Allow 48-72 hours for transgene expression. Analyze transduction efficiency via fluorescence microscopy (if reporter is present) or PCR. Proceed with directed differentiation into target lineage (e.g., neurons, cardiomyocytes) for phenotypic analysis [75].
Protocol: LNP-Mediated CRISPR RNP Delivery to Hematopoietic Stem Cells (HSCs)
Principle: Utilize LNPs to deliver pre-assembled Cas9-gRNA Ribonucleoprotein (RNP) complexes for rapid, transient editing with minimal off-target effects, ideal for clinical ex vivo editing of HSCs [76].
Materials:
- Research Reagent Solutions:
- HSCs: Mobilized peripheral blood or bone marrow-derived CD34+ cells.
- CRISPR RNP: Complex of purified Cas9 protein and synthetic sgRNA targeting the gene of interest (e.g., BCL11A for sickle cell disease).
- Custom LNP Formulation: Ionizable lipid (e.g., DLin-MC3-DMA), phospholipid, cholesterol, and PEG-lipid. Formulate to encapsulate RNP.
- Electroporation Buffer: Optional, for comparison to electroporation-based RNP delivery.
Methodology:
- HSC Isolation and Activation: Isolate CD34+ cells from source material using immunomagnetic beads. Activate cells in serum-free medium supplemented with cytokines (SCF, TPO, FLT3-L) for 24-48 hours.
- LNP Incubation: Resuspend activated HSCs in pre-warmed base medium. Add the LNP-RNP formulation at a predetermined optimal concentration (e.g., 0.5-1.0 µg/µL RNP). Mix gently.
- Delivery: Incubate the cell-LNP mixture for 4-6 hours at 37°C, 5% CO2.
- Wash and Recovery: Pellet cells and wash twice with PBS to remove excess LNPs. Resuspend in fresh cytokine-supplemented medium and culture for recovery.
- Editing Analysis: After 72 hours, harvest a subset of cells for genomic DNA extraction. Assess editing efficiency by T7 Endonuclease I assay or next-generation sequencing (NGS). The edited HSCs are now ready for transplantation or further functional assays.
Visual Workflows for Vector Selection and Application
The following diagrams outline the logical decision-making process for vector selection and a standard workflow for stem cell engineering.
Vector Selection Logic
Stem Cell Engineering Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Delivery Vector Optimization
| Research Reagent | Function in Experiment | Key Considerations |
|---|---|---|
| AAV Serotype Library (e.g., AAV2, AAV6, AAV9, AAV-DJ) | Determines cell and tissue tropism; enables targeting of specific stem cell types [78] [58]. | Tropism can vary between species and cell states. Must be screened for optimal performance. |
| Ionizable Lipids (e.g., DLin-MC3-DMA, SM-102) | Critical component of LNPs; enables encapsulation and endosomal escape of cargo [73] [74]. | Chemical structure dictates efficacy, stability, and potential toxicity. IP landscape is complex. |
| Compact Cas Orthologs (e.g., SaCas9, CjCas9) | Enables packaging of Cas nuclease, gRNA, and repair template within a single AAV vector [58]. | Often have different PAM requirements and may have varying editing efficiencies compared to SpCas9. |
| Polybrene | A cationic polymer that reduces electrostatic repulsion between AAV and cell membrane, enhancing transduction [75]. | Can be cytotoxic; concentration must be optimized for each cell type. |
| Rock Inhibitor (Y-27632) | Improves survival of dissociated hiPSCs and other sensitive primary cells post-transduction/transfection [75]. | Essential for maintaining high cell viability during stem cell manipulations. |
| pegRNA for Prime Editing | Guide RNA for prime editing systems that directs the nCas9-reverse transcriptase to the target site and provides the edit template [58]. | Design is more complex than standard sgRNA; efficiency can be suboptimal and requires optimization. |
Addressing Scalability and GMP Manufacturing for Clinical Translation
The transition of CRISPR-based stem cell therapies from research to clinic hinges on overcoming significant scalability and manufacturing challenges. The foundational requirement for clinical application is the production of CRISPR components under Good Manufacturing Practice (GMP), a set of quality guidelines ensuring pharmaceutical products are produced according to recognized quality standards [79]. For stem cell researchers, this means evolving from research-grade reagents to clinical-grade materials that guarantee purity, consistency, and safety. The field is advancing toward a phase-appropriate manufacturing model that aligns manufacturing rigor with clinical intent, bridging the gap between research and full-scale production [80]. This application note provides a structured framework for navigating the critical path from proof-of-concept experiments to clinically translatable CRISPR-engineered stem cell products, with a specific focus on protocol standardization, GMP-compliant manufacturing, and scalability considerations essential for drug development professionals.
GMP Manufacturing Standards for CRISPR Components
GMP Facility Specifications and Quality Systems
Clinical translation of CRISPR-engineered stem cell therapies requires GMP-grade guide RNA and Cas components manufactured in facilities with specific controlled environments. Synthego's GMP facility exemplifies the necessary infrastructure, featuring ISO 7 and 8 clean rooms, packout in ISO 5 Class II Biological Safety Cabinets, and compliance with ICH Q7, Section 19, ICH Q9, and ICH Q10 quality guidelines [79]. These facilities maintain single-pass, HEPA-filtered air systems with continuous monitoring for temperature, relative humidity, and differential pressure, operated by fully gowned staff to ensure product integrity [79]. A phase-appropriate approach to manufacturing allows researchers to utilize "GMP-like" intermediate-grade materials during early development before transitioning to full GMP-grade sgRNA for clinical trials [79] [80]. This strategy balances innovation with operational efficiency while maintaining a path to regulatory compliance.
sgRNA and Cas9 Production Standards
The production of CRISPR components for clinical applications must address critical quality attributes including purity, potency, identity, and stability. Current manufacturing capabilities support custom solutions for small to large-scale research-grade sgRNA, intermediate "GMP-like" sgRNA, and full GMP-grade sgRNA [79]. The streamlined process is strictly controlled by manufacturing and quality experts to ensure seamless order execution from project initiation through product delivery [79]. For stem cell applications, the format of CRISPR components (DNA, RNA, or ribonucleoprotein complex) significantly influences manufacturing strategy and regulatory planning, with pre-complexed ribonucleoproteins (RNPs) gaining prominence for their reduced off-target effects and immediate functionality in stem cell systems [54].
Table: GMP Manufacturing Options for CRISPR Components Across Development Phases
| Development Phase | sgRNA Grade | Key Quality Attributes | Typical Applications |
|---|---|---|---|
| Early Research | Research-grade | Sequence verification, functional activity | Proof-of-concept, target validation |
| Preclinical Development | GMP-like | Higher purity, reduced endotoxins, preliminary QC testing | IND-enabling studies, toxicology assessments |
| Clinical Trials | GMP-grade | Full GMP compliance, extensive QC release testing, documentation | Phase 1-3 clinical trials, commercial manufacturing |
Delivery Methods for Stem Cell Systems
Delivery Method Selection Criteria
Selecting appropriate delivery methods for CRISPR components into stem cells requires careful consideration of multiple factors. The choice between transient versus stable transfection is fundamental; transient transfection limits CRISPR component presence to a limited time window, reducing off-target effects, while stable transfection integrates DNA encoding CRISPR components permanently into the cell's genome for long-term expression [54]. For stem cells, which often have limited expansion capacity, delivery efficiency and cell viability are paramount concerns. The format of CRISPR components significantly influences method selection – DNA must enter the nucleus for transcription, mRNA requires cytoplasmic translation, while pre-formed RNPs can function with direct nuclear delivery [54]. Different stem cell types exhibit varying transfection efficiencies, with induced pluripotent stem cells (iPSCs) generally more amenable to manipulation than embryonic stem cells (ES cells) or hematopoietic stem cells (HSC) [54].
Comparative Analysis of Delivery Modalities
Physical delivery methods, including electroporation and nucleofection, use electrical pulses to create temporary pores in the plasma membrane through which CRISPR components can enter cells [54] [60]. Nucleofection, specifically optimized for nuclear delivery, often demonstrates superior performance with hard-to-transfect stem cells. Chemical methods like lipofection utilize lipid complexes that fuse with the cell membrane, while viral methods employ engineered viruses (AAVs, lentiviruses) for highly efficient delivery [60]. Microinjection provides direct physical injection of components using microneedles, offering high efficiency but with technical demands that limit throughput [54]. Recent advances in lipid nanoparticles (LNPs) have enabled efficient in vivo delivery, as demonstrated in clinical trials for liver-targeted therapies [8], though stem cell-specific LNP formulations remain an area of active development.
Table: Delivery Methods for CRISPR Components in Stem Cell Systems
| Delivery Method | Mechanism | Advantages | Limitations | Stem Cell Compatibility |
|---|---|---|---|---|
| Electroporation | Electrical pulses create membrane pores | Easy, fast, high efficiency | Requires optimization, cell sensitivity | Moderate (varies by cell type) |
| Nucleofection | Electroporation optimized for nuclear delivery | High efficiency, direct nuclear access | Specialized reagents & equipment required | High for many stem cell types |
| Lipofection | Lipid complexes fuse with cell membrane | Cost-effective, high throughput | Lower efficiency in sensitive cells | Low to moderate |
| Viral Vectors | Infectious particles introduce DNA | High efficiency, stable expression | Safety concerns, immunogenicity, size constraints | High (with specific pseudotypes) |
| Microinjection | Mechanical injection via microneedle | High precision, direct delivery | Technically demanding, low throughput | Suitable for zygotes and embryos |
Clinical Translation and Regulatory Framework
Clinical Trial Landscape and Evidence Generation
The clinical translation landscape for CRISPR therapies has evolved significantly, with the first FDA approval of CASGEVY (exagamglogene autotemcel) for sickle cell disease and transfusion-dependent beta thalassemia marking a historic milestone [8] [81]. Clinical trials have demonstrated promising results across multiple disease areas, with sustained effects observed – all 27 participants in a two-year follow-up study of an hATTR treatment maintained approximately 90% reduction in disease-related protein levels [8]. For stem cell researchers, these clinical successes provide valuable insights into regulatory expectations, including the need for comprehensive characterization programs verifying that CRISPR-modified cells maintain stability across multiple passages and produce consistent product quality [82]. Whole genome sequencing of CRISPR-engineered cells has become standard practice, providing regulators with detailed documentation that editing occurred precisely at intended genomic locations [82].
Phase-Appropriate Manufacturing Strategy
Implementing a phase-appropriate manufacturing strategy is critical for navigating the transition from research to clinical application. This approach aligns manufacturing rigor with clinical development stage, avoiding the mismatch between manufacturing requirements and available solutions that often plagues early-stage programs [80]. For preclinical development, GMP-Source materials provide an intermediate quality level that supports regulatory filings without the full cost and complexity of complete cGMP production [80]. As programs advance to Phase 1 trials, Small-Scale cGMP offerings create a seamless transition pathway through unified quality systems and technical infrastructure that minimizes process redevelopment needs [80]. This strategic approach to manufacturing enables smarter decision-making at every development stage, ensuring that quality, compliance, and scalability remain synchronized with clinical progression.
Experimental Protocols and Workflows
GMP-Compliant Workflow for Stem Cell Engineering
The following diagram illustrates the integrated workflow for GMP-compliant CRISPR-based stem cell engineering, encompassing both manufacturing and translational research components:
Protocol: CRISPR Delivery via Nucleofection in Stem Cells
This standardized protocol outlines an efficient method for delivering CRISPR ribonucleoprotein (RNP) complexes into stem cells using nucleofection, optimized for minimal off-target effects and high viability.
Materials Required:
- Stem cell culture (e.g., iPSCs, HSCs)
- Clinical-grade sgRNA (GMP-grade recommended)
- High-purity Cas9 protein
- Nucleofector device and appropriate kit
- Pre-warmed culture medium with supplements
- Matrigel-coated or feeder cell plates
- Rho-associated protein kinase (ROCK) inhibitor
Procedure:
- RNP Complex Formation: Combine 10μg of Cas9 protein with 6μg of sgRNA in a sterile microcentrifuge tube. Incubate at room temperature for 15-20 minutes to allow RNP complex formation.
- Cell Preparation: Harvest stem cells using gentle dissociation reagent. Count cells and prepare 1×10^6 cells per nucleofection reaction. Centrifuge at 300×g for 5 minutes and carefully remove supernatant.
- Nucleofection: Resuspend cell pellet in 100μL of nucleofection solution. Add prepared RNP complexes and transfer to nucleofection cuvette. Select the appropriate stem cell-specific program on the nucleofector device.
- Recovery: Immediately transfer nucleofected cells to pre-warmed culture medium containing ROCK inhibitor. Plate cells at appropriate density on prepared culture vessels.
- Analysis: Assess editing efficiency 48-72 hours post-nucleofection using appropriate methods (T7E1 assay, next-generation sequencing, or flow cytometry for reporter systems).
Troubleshooting Notes:
- Low viability: Optimize cell number, reduce RNP concentration, or test alternative nucleofection programs.
- Low editing efficiency: Verify sgRNA activity, increase RNP concentration, or confirm Cas9 protein integrity.
- Poor cell recovery: Ensure ROCK inhibitor is fresh and culture conditions are optimized for specific stem cell type.
Protocol: Clonal Isolation and Screening
Isolation and characterization of clonal stem cell populations is essential for establishing genetically homogeneous lines for therapeutic applications.
Materials Required:
- Antibiotic selection markers (if applicable)
- Limiting dilution plates or automated cell depositor
- DNA extraction reagents
- PCR amplification reagents
- Sequencing primers
- Karyotyping analysis kit
Procedure:
- Clonal Derivation: 48 hours post-editing, dissociate cells to single-cell suspension. Perform limiting dilution in 96-well plates or use automated cell deposition system to isolate single cells.
- Expansion: Culture clones with appropriate conditioning medium and ROCK inhibitor for initial survival. Monitor daily for colony formation.
- Screening: At approximately 70% confluence, split each clone for parallel expansion and genomic DNA extraction.
- Analysis: Perform PCR amplification of target locus followed by sequencing confirmation of edits. For homozygous edits, screen 24-36 clones; for heterozygous edits, screen 48-60 clones.
- Validation: Select correctly edited clones for expanded characterization including off-target analysis, pluripotency marker confirmation (for iPSCs), and karyotyping to ensure genomic integrity.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for CRISPR Stem Cell Engineering
| Reagent/Category | Function | Clinical-Grade Considerations |
|---|---|---|
| GMP sgRNA | Guides Cas9 to specific genomic loci | ICH Q7 compliance, certificate of analysis, endotoxin testing |
| Cas9 Nuclease | Creates double-strand breaks at target sites | High purity, nuclear localization signal, endotoxin-free |
| Nucleofection Kits | Enables efficient RNP delivery | cGMP manufactured, performance qualification for specific stem cell types |
| Cell Culture Media | Supports stem cell growth and maintenance | Xenogeneic component-free formulation, defined composition |
| ROCK Inhibitor | Enhances single-cell survival | Pharmaceutical-grade, stability data provided |
| Characterization Assays | Validates editing and stemness | Validated methods, standard operating procedures |
Decision Framework for Delivery Method Selection
The following diagram provides a systematic approach for selecting the optimal CRISPR delivery method based on stem cell type and research objectives:
Emerging Technologies and Future Perspectives
AI-Enhanced CRISPR Development
Artificial intelligence is rapidly transforming CRISPR-based stem cell engineering by accelerating experimental design and optimizing editing efficiency. CRISPR-GPT, an AI tool developed at Stanford Medicine, functions as a gene-editing "copilot" that helps researchers generate designs, analyze data, and troubleshoot flaws [10]. This AI model, trained on 11 years of expert discussions and published scientific papers, can predict off-target edits and their potential damage, allowing researchers to select optimal experimental paths [10]. The technology significantly reduces the trial-and-error approach that typically dominates CRISPR experimental design, potentially compressing development timelines from years to months [10]. For stem cell researchers, AI integration promises enhanced precision in guide RNA design and more accurate prediction of editing outcomes in diverse stem cell types.
Advanced Editing Platforms and Delivery Innovations
Novel editing platforms like CRISPR Therapeutics' SyNTase technology demonstrate the rapid advancement of editing capabilities. This system utilizes AI-guided structural modeling and large-scale screening to optimize polymerase activity for gene correction based on synthetic nucleotide templates [81]. When integrated with Cas9, SyNTase editors utilize engineered templates with improved serum stability, enabling higher target correction efficiency – up to 95% editing in human hepatocyte models with undetectable off-target effects (<0.5%) [81]. For stem cell applications, these advances translate to more precise genetic corrections with reduced safety concerns. Concurrently, delivery innovations continue to evolve, with lipid nanoparticles (LNPs) enabling in vivo delivery of CRISPR components and demonstrating potential for redosing strategies previously impossible with viral vectors due to immune concerns [8].
The clinical translation of CRISPR-based stem cell therapies requires meticulous attention to manufacturing quality, delivery efficiency, and regulatory strategy. Implementing a phase-appropriate approach to GMP manufacturing ensures alignment between product quality and clinical development stage, while selecting optimal delivery methods based on stem cell type and research objectives maximizes editing efficiency and cell viability. The rapidly advancing landscape of AI-enhanced design tools and novel editing platforms promises to accelerate this transition, potentially reducing development timelines from years to months. By adopting the structured frameworks, standardized protocols, and decision tools presented in this application note, researchers and drug development professionals can navigate the complex path from bench to bedside with greater confidence and efficiency, ultimately accelerating the delivery of transformative stem cell therapies to patients in need.
The Role of AI and CRISPR-GPT in Accelerating Experimental Design and Troubleshooting
The convergence of artificial intelligence (AI) and CRISPR-based genome editing is revolutionizing stem cell genetic engineering. This synergy is particularly impactful in a field characterized by complex experimental designs and technical challenges. AI technologies are accelerating the entire research pipeline, from initial design to data analysis, making sophisticated genetic manipulations more accessible and efficient. The AI-based clinical trials market, valued at $9.17 billion in 2025 and projected to reach $21.79 billion by 2030, reflects the significant investment and growth in this domain [83].
CRISPR-GPT, developed by researchers at Stanford Medicine, represents a transformative tool in this landscape. It functions as an AI co-pilot for gene-editing experiments, leveraging large language models (LLMs) trained on over a decade of published CRISPR data and expert discussions [10]. This system enables researchers—even those with limited gene-editing experience—to generate precise experimental designs, troubleshoot potential issues, and analyze data with unprecedented speed and accuracy. For stem cell research, where precision and efficiency are paramount for developing therapeutic applications, CRISPR-GPT significantly flattens the steep learning curve traditionally associated with complex genome engineering.
CRISPR-GPT: An AI Co-Pilot for Genome Engineering
System Architecture and Capabilities
CRISPR-GPT is a multi-agent, compositional system that harnesses the reasoning capabilities of large language models for complex task decomposition and decision-making [41]. The system integrates domain expertise through retrieval-augmented generation (RAG) from published protocols and peer-reviewed literature, and incorporates external tools for specialized functions like guide RNA design and off-target evaluation [41].
The architecture comprises several specialized AI agents working in concert:
- LLM Planner Agent: Analyzes user requests, generates reasoning paths, and decomposes complex goals into sequential tasks.
- Task Executor Agents: Handle specific experimental steps (e.g., gRNA design, delivery method selection) through state machines that progress toward defined objectives.
- User-Proxy Agent: Facilitates interaction between the user and the system, providing instructions and integrating feedback.
- Tool Provider Agents: Enable access to external databases and computational tools for specialized analyses [41].
Operational Modes for Different Expertise Levels
CRISPR-GPT offers three distinct modes to accommodate users with varying levels of expertise [41] [10]:
Table: CRISPR-GPT Operational Modes
| Mode | Target User | Key Features | Stem Cell Research Application |
|---|---|---|---|
| Meta Mode | Beginners, new to gene editing | Guided workflow with step-by-step instructions; interactive decision-making | Ideal for stem cell researchers new to CRISPR applications |
| Auto Mode | Advanced domain experts | Freestyle requests; automated task decomposition and workflow creation | Suitable for complex, multi-gene editing projects in stem cells |
| Q&A Mode | All users | On-demand scientific inquiries about gene editing | Quick troubleshooting and protocol optimization |
This flexible approach ensures that both novice and experienced stem cell researchers can leverage the system effectively. As noted by researchers at Stanford, the tool "felt less like a tool and more like an ever-available lab partner" [10].
Application Notes for Stem Cell Genetic Engineering
AI-Optimized Experimental Design Workflow
The integration of CRISPR-GPT into stem cell research follows a structured workflow that enhances traditional experimental planning:
Target Identification and Validation: Researchers input their experimental goals (e.g., "Knock out OCT4 in human induced pluripotent stem cells") into CRISPR-GPT. The system retrieves relevant literature on target gene function and potential pleiotropic effects in stem cells.
CRISPR System Selection: Based on the desired outcome (knockout, knockdown, epigenetic modulation, base editing), CRISPR-GPT recommends the most suitable CRISPR system (e.g., CRISPR-Cas9 for simple knockouts, CRISPR-dCas9 for epigenetic activation) [41].
Guide RNA Design and Optimization: The AI designs highly specific guide RNA sequences with minimal off-target effects, considering stem cell-specific chromatin accessibility and epigenetic landscapes [41] [10].
Delivery Method Selection: CRISPR-GPT recommends optimal delivery methods (viral vs. non-viral) based on stem cell type and editing requirements, noting that lipid nanoparticles (LNPs) show promise for efficient delivery while minimizing toxicity [8].
Experimental Protocol Generation: The system generates step-by-step protocols tailored to stem cell culture requirements, including timing, media formulations, and quality control checkpoints.
The entire process is visualized in the following experimental workflow:
Quantitative Performance Metrics
CRISPR-GPT has demonstrated significant improvements in experimental efficiency and success rates. In validation studies, researchers using CRISPR-GPT achieved successful gene knockout and epigenetic activation on their first attempt—a rarity in conventional CRISPR workflows that often require extensive trial and error [41] [10].
Table: Performance Metrics of CRISPR-Guided vs. Traditional Experiments
| Parameter | Traditional Approach | CRISPR-GPT Guided | Improvement |
|---|---|---|---|
| Experimental Planning Time | Days to weeks | Hours to days | ~70% reduction |
| First-Attempt Success Rate | ~30-40% | ~85-95% | ~2.5x increase |
| Off-Target Prediction Accuracy | Moderate | High | Significant enhancement |
| Multiplexing Capability | Limited | Extensive | Streamlined design |
| Troubleshooting Resolution | Manual, iterative | AI-assisted, predictive | Dramatically faster |
The system's ability to predict off-target effects and suggest optimized experimental conditions is particularly valuable in stem cell research, where maintaining genomic integrity is crucial for downstream therapeutic applications [10].
Detailed Experimental Protocols
Protocol: CRISPR-GPT Guided Gene Knockout in Pluripotent Stem Cells
Objective: Efficient knockout of a target gene in human induced pluripotent stem cells (hiPSCs) with minimal off-target effects.
Materials:
- Table: Essential Research Reagents and Materials
| Reagent/Material | Function | Example/Notes |
|---|---|---|
| Human iPSCs | Target cells for genetic modification | Maintain pluripotency; use low passage numbers |
| CRISPR-GPT Platform | Experimental design and optimization | Access via Agent4Genomics website |
| GMP-grade sgRNA | Targets specific genomic sequence | Synthego; ensures purity and efficacy [84] |
| Cas9 Protein | CRISPR nuclease | True GMP-grade recommended for clinical applications [84] |
| Lipid Nanoparticles (LNPs) | Delivery vehicle | Alternative to viral vectors; enables redosing [8] |
| Stem Cell Culture Media | Maintain pluripotent state | Essential for viability during editing process |
| Genomic DNA Extraction Kit | Post-editing analysis | Validate edits via sequencing |
| Flow Cytometry Antibodies | Assess pluripotency retention | Confirm maintenance of stem cell markers |
Methodology:
Experimental Design Phase:
- Access CRISPR-GPT and select "Meta Mode" for guided workflow.
- Input experimental parameters: "Design knockout of [target gene] in human iPSCs using CRISPR-Cas9."
- CRISPR-GPT will return a complete experimental plan including:
- Recommended gRNA sequences with predicted efficiency and off-target scores
- Optimal delivery method (e.g., LNPs for hiPSCs)
- Suggested controls and validation assays
Guide RNA Preparation:
- Synthesize recommended sgRNA sequences using GMP-grade sources to ensure purity and efficacy [84].
- Resuspend sgRNA in nuclease-free water at working concentration.
Stem Cell Preparation:
- Culture hiPSCs in essential medium under standard conditions.
- Passage cells 24 hours before editing to ensure 70-80% confluency at time of transfection.
Ribonucleoprotein (RNP) Complex Formation:
- Combine sgRNA and Cas9 protein at molar ratio recommended by CRISPR-GPT.
- Incubate 10-15 minutes at room temperature to form RNP complexes.
Delivery via Lipid Nanoparticles:
- Encapsulate RNP complexes in LNPs per manufacturer's protocol.
- Transfert hiPSCs with LNP-RNP complexes using optimized density and volume.
Post-Transfection Culture:
- Replace transfection medium with fresh stem cell medium after 24 hours.
- Monitor cell viability and morphology daily.
Validation and Analysis:
- Harvest cells 72-96 hours post-transfection for genomic DNA extraction.
- Perform T7E1 assay or sequencing to assess editing efficiency.
- Verify retention of pluripotency markers via flow cytometry.
- Expand successfully edited clones for downstream applications.
Troubleshooting:
- Poor Editing Efficiency: Use CRISPR-GPT's troubleshooting mode to analyze potential issues and receive optimization suggestions (e.g., alternative gRNAs, adjusted RNP ratios).
- Cell Toxicity: CRISPR-GPT can recommend alternative delivery methods or buffer modifications to improve viability.
- Pluripotency Loss: The system can suggest culture condition adjustments or early passage timing to maintain stem cell state.
Protocol: Epigenetic Activation via CRISPR-dCas9 in Stem Cells
Objective: Targeted transcriptional activation of endogenous genes in stem cells using CRISPR-dCas9 systems.
Materials:
- Additional materials beyond knockout protocol:
- dCas9 activator (e.g., dCas9-VPR)
- Activator-specific sgRNAs (designed by CRISPR-GPT)
- Differentiation media (if assessing functional outcomes)
Methodology:
System Selection:
- Consult CRISPR-GPT for optimal epigenetic modulation system selection based on target gene and desired expression level.
- The system will recommend appropriate dCas9 architectures (e.g., VPR, SAM) based on published efficacy data.
Multipart Guide RNA Design:
- CRISPR-GPT designs extended gRNAs with appropriate scaffold modifications for activator recruitment.
- The system predicts optimal binding positions relative to transcription start site.
Delivery Optimization:
- For stem cells, CRISPR-GPT often recommends lentiviral delivery of dCas9 components with transient sgRNA expression.
- Follow biosafety guidelines for lentiviral work in stem cell facilities.
Activation Timeline:
- Assess transcriptional activation 48-96 hours post-delivery via qRT-PCR.
- Monitor protein expression 5-7 days post-activation via immunofluorescence or Western blot.
Functional Validation:
- If activating developmental genes, differentiate edited stem cells and assess lineage specification.
- Compare to unedited controls for phenotypic differences.
The following diagram illustrates the key molecular components and their interactions in the CRISPR activation system:
Data Analysis and Validation Framework
AI-Enhanced Quantitative Analysis
Following CRISPR editing in stem cells, rigorous validation is essential. AI-powered quantitative analysis tools like Powerdrill and Excelmatic can streamline this process through:
- Automated Data Cleaning: Handling missing values, outliers, and formatting inconsistencies in sequencing and expression data [85].
- Statistical Analysis: Performing appropriate statistical tests (t-tests, ANOVA, regression) to assess editing efficiency and functional outcomes [86].
- Visualization: Generating publication-ready figures that clearly demonstrate editing outcomes and phenotypic effects [85].
For stem cell researchers, these tools can:
- Compare editing efficiencies across multiple gRNAs or delivery methods
- Analyze correlations between editing efficiency and phenotypic strength
- Assess statistical significance in differentiation outcomes between edited and control cells
Validation Metrics and Quality Control
Table: Essential Validation Parameters for CRISPR-Edited Stem Cells
| Validation Parameter | Method | Acceptance Criteria | AI-Assisted Analysis |
|---|---|---|---|
| Editing Efficiency | NGS sequencing | >70% indels for knockouts | Automated sequence alignment and quantification |
| Off-Target Effects | GUIDE-seq or similar | No significant off-targets (<0.1%) | CRISPR-GPT prediction coupled with experimental validation |
| Pluripotency Retention | Flow cytometry | >90% expression of markers | Automated gating and statistical comparison to controls |
| Genomic Stability | Karyotyping | Normal karyotype | Image analysis algorithms for chromosomal abnormality detection |
| Functional Validation | Differentiation assays | Appropriate lineage specification | Quantitative analysis of marker expression during differentiation |
CRISPR-GPT assists in designing appropriate validation experiments and can recommend optimal sample sizes and controls based on the specific experimental parameters [41] [10].
Troubleshooting and Optimization Guidelines
Even with AI guidance, stem cell genome editing can present challenges. CRISPR-GPT provides systematic troubleshooting for common issues:
Low Editing Efficiency
- Potential Causes: Poor gRNA design, suboptimal delivery, or inaccessible chromatin state in stem cells.
- CRISPR-GPT Solutions:
- Redesign gRNAs with improved on-target scores
- Recommend alternative delivery methods (e.g., electroporation instead of LNPs)
- Suggest chromatin-modifying agents to open target regions
Stem Cell Differentiation or Death
- Potential Causes: Transfection toxicity, off-target effects on essential genes, or excessive handling.
- CRISPR-GPT Solutions:
- Optimize delivery conditions (e.g., lower RNP concentrations, different transfection reagents)
- Predict essential genes to avoid with similar sequences to target
- Recommend culture modifications to maintain pluripotency during editing
Inconsistent Results Across Experiments
- Potential Causes: Stem cell heterogeneity, passage effects, or protocol variations.
- CRISPR-GPT Solutions:
- Standardize protocols using AI-generated detailed workflows
- Recommend appropriate controls for each experiment
- Suggest single-cell cloning to reduce heterogeneity
The AI's ability to draw from vast databases of published troubleshooting cases enables it to provide solutions that might not be immediately apparent to individual researchers [10]. This collective intelligence dramatically shortens the problem-solving timeline.
Future Perspectives and Development
The integration of AI like CRISPR-GPT with stem cell genetic engineering is rapidly evolving. Future developments expected in the near term include:
Enhanced Predictive Capabilities: As more stem cell-specific data is incorporated, AI will better predict lineage-specific editing outcomes and differentiation effects.
Automated Workflow Integration: Full integration with laboratory automation systems for hands-off experimental execution [83].
Expanded Modality Support: Support for newer editing technologies like base editing and prime editing in stem cells [41].
Clinical Translation Tools: AI systems that specifically assist with navigating regulatory pathways for stem cell therapies [83] [84].
The remarkable case of the fully personalized in vivo CRISPR therapy developed for an infant with CPS1 deficiency in just six months demonstrates the accelerated timeline possible with AI-guided approaches [8]. As these technologies mature, stem cell researchers will increasingly rely on AI co-pilots like CRISPR-GPT to design, execute, and analyze complex genetic engineering experiments, ultimately accelerating the development of novel stem cell-based therapies.
Establishing Efficacy and Safety: A Framework for Validation and Comparative Analysis
Gene editing technologies have revolutionized stem cell genetic engineering, enabling precise genomic modifications for therapeutic applications. The primary platforms—CRISPR-Cas9, ZFNs, and TALENs—differ in design, efficiency, and practicality [87] [88]. This analysis compares these tools within the context of stem cell research, providing structured data and protocols to guide researchers and drug development professionals.
Table 1: Key Characteristics of Gene Editing Platforms
| Feature | CRISPR-Cas9 | TALEN | ZFN |
|---|---|---|---|
| Recognition System | RNA-guided (gRNA) | Protein-based (TALE) | Protein-based (Zinc Finger) |
| Nuclease | Cas9 | FokI dimer | FokI dimer |
| Design Complexity | Low (1 week) | Moderate (~1 month) | High (~1 month) |
| Cost | Low | Medium | High |
| Scalability | High (multiplexing) | Limited | Limited |
| Off-Target Risk | Moderate to high | Low | Low |
| Stem Cell Delivery | Viral vectors, LNPs | Plasmid vectors | Plasmid vectors |
CRISPR’s simplicity stems from its guide RNA (gRNA), which can be redesigned rapidly to target new sequences, while ZFNs and TALENs require complex protein engineering for each target [87] [88] [89]. TALENs demonstrate higher specificity due to their protein-DNA binding mechanism, reducing off-target effects in sensitive stem cell applications [88] [89].
Quantitative Efficiency and Precision in Stem Cells
Table 2: Performance Metrics in Stem Cell Editing
| Metric | CRISPR-Cas9 | TALEN | ZFN |
|---|---|---|---|
| Editing Efficiency | High (≥80% KO in HSPCs) | Moderate (~40–60% KI) | Moderate (~50% KI) |
| HDR Efficiency | Moderate (≤20%) | Low (~10%) | Low (~10%) |
| Off-Target Frequency | ≥50% [90] | Low [88] | Low [88] |
| Delivery Efficiency in HSPCs | High (LNPs) [8] | Moderate (electroporation) [91] | Moderate (electroporation) |
- Efficiency: CRISPR achieves high knockout rates in hematopoietic stem and progenitor cells (HSPCs), but homology-directed repair (HDR) efficiency remains limited [90].
- Precision: TALENs show superior specificity in genomic regions with high GC content or repetitive sequences, as demonstrated in HSPC studies using circular ssDNA templates [91].
- Stem Cell Viability: CRISPR with lipid nanoparticles (LNPs) maintains >80% viability in HSPCs, while TALEN-mediated editing preserves pluripotency in mesenchymal stromal cells (MSCs) [8] [92].
Experimental Protocols for Stem Cell Engineering
CRISPR-Cas9 Protocol for HSPC Knockout
Workflow:
- gRNA Design: Select target sequence (e.g., B2M exon 1) with minimal off-target sites using tools like CRISPR-GPT [10].
- Delivery: Electroporate HSPCs with Cas9 ribonucleoprotein (RNP) complex and gRNA.
- Culture: Maintain cells in serum-free media with cytokines (SCF, TPO, FLT3-L) for 72 hours.
- Validation: Assess knockout efficiency via flow cytometry (e.g., B2M surface loss) and NGS for off-target screening.
Key Reagents:
- Cas9 Protein: High-fidelity variants (e.g., HiFi Cas9) to reduce off-target effects.
- Cytokines: Support stem cell survival during editing.
- LNPs: For in vivo delivery to liver-targeting stem cells [8].
TALEN-Mediated Gene Insertion in HSPCs
Workflow [91]:
- TALEN Design: Clone TALE repeats targeting loci (e.g., AAVS1 safe harbor) using modular assembly.
- Template Delivery: Co-electroporate TALEN mRNA and circular ssDNA donor (0.6–2.2 kb) into HSPCs.
- HDR Enhancement: Add HDR-Enh01 mRNA to boost insertion rates.
- Engraftment Testing: Transplant edited HSPCs into NCG mice to assess long-term engraftment.
Key Reagents:
- Circular ssDNA: Resists exonuclease degradation, improving knock-in efficiency by 3–5× compared to linear templates [91].
- HDR Enhancers: Small molecules (e.g., RS-1) to promote homologous recombination.
Figure 1: Stem Cell Editing Workflow. Generic workflow for genetic engineering of stem cells using CRISPR or TALENs.
Signaling Pathways in Stem Cell Immunoengineering
CRISPR-edited MSCs target immune pathways to enhance therapeutic efficacy:
- MHC-I Knockout: Disrupts β2-microglobulin (B2M) to evade CD8+ T-cell recognition [92].
- Anti-Inflammatory Activation: CRISPRa systems (dCas9) overexpress IL-10 and TSG-6 to suppress inflammation [92].
- TLR4/NF-κB Disruption: Knocking out TLR4 reduces pro-inflammatory signaling in autoimmune environments [92].
Figure 2: Immune Engineering Pathways. Key genetic modifications in MSCs for enhanced therapeutic function.
Research Reagent Solutions
Table 3: Essential Reagents for Stem Cell Gene Editing
| Reagent | Function | Example Application |
|---|---|---|
| gRNA Libraries | Targets specific genomic loci | CRISPR knockout screens in HSPCs |
| High-Fidelity Cas9 | Reduces off-target effects | Editing primary MSCs [92] |
| Circular ssDNA | Template for HDR | TALEN-mediated gene insertion [91] |
| Lipid Nanoparticles (LNPs) | In vivo delivery vehicle | Liver-directed stem cell therapy [8] |
| HDR Enhancers | Improves knock-in efficiency | B2M tagging in HSPCs [91] |
| Cytokine Cocktails | Maintains stemness during editing | Expansion of edited HSPCs [91] |
Discussion and Future Directions
CRISPR excels in scalability and ease of use, while TALENs offer higher precision for therapeutic stem cell engineering. Emerging technologies like base editing and prime editing further refine precision by minimizing double-strand breaks [88]. AI tools (e.g., CRISPR-GPT) accelerate gRNA design and reduce off-target predictions, enhancing CRISPR’s reliability [10]. For clinical applications, combining CRISPR with non-viral delivery methods (e.g., LNPs) addresses immunogenicity concerns observed with viral vectors [8] [90].
Functional validation is a critical phase in stem cell genetic engineering, confirming that CRISPR-Cas9-edited stem cells not only carry the intended genetic modification but also possess the expected biological capabilities. This process rigorously assesses the genomic integration of edits, the multilineage differentiation potential of edited cells, and the ultimate functional rescue of disease phenotypes in relevant models. In the context of a broader thesis on stem cell CRISPR applications, this document provides detailed application notes and protocols to standardize these assessments, ensuring that research data is robust, reproducible, and translatable to therapeutic development. The following sections synthesize current clinical evidence and established laboratory methods to create a comprehensive framework for functional validation.
Quantitative Data from Clinical and Preclinical Studies
The success of CRISPR-based therapies hinges on demonstrating functional correction at the molecular, cellular, and organismal levels. The table below summarizes key quantitative outcomes from recent clinical trials and pioneering preclinical studies, providing benchmark data for validation experiments.
Table 1: Key Functional Outcomes from CRISPR-Edited Stem Cell Trials and Studies
| Disease Target | Cell Type | Key Functional Metric | Quantitative Result | Reference / Trial |
|---|---|---|---|---|
| Sickle Cell Disease (SCD) / Transfusion-Dependent Beta Thalassemia (TDT) | CD34+ Hematopoietic Stem and Progenitor Cells | Reduction/elimination of vaso-occlusive crises (SCD) or transfusion requirements (TDT) | Demonstrated in a majority of patients in clinical trials [8] | CASGEVY (exa-cel) |
| Hereditary Transthyretin Amyloidosis (hATTR) | Hepatocytes (via in vivo LNP delivery) | Reduction in serum TTR protein levels | ~90% average reduction sustained over 2 years [8] | Intellia Therapeutics Phase I |
| Hereditary Angioedema (HAE) | Hepatocytes (via in vivo LNP delivery) | Reduction in kallikrein protein and inflammation attacks | 86% avg. reduction in kallikrein; majority of patients attack-free [8] | Intellia Therapeutics Phase I/II |
| Beta-Thalassemia | Patient-derived iPSCs | In vitro differentiation into functional hematopoietic cells and red blood cells | Proof-of-concept established; research ongoing [18] | Preclinical Research |
| Thalassemia Complications | Mesenchymal Stem Cells (MSCs) | Improvement in complications (e.g., osteoporosis, cirrhosis) | Demonstrated potential in animal studies [18] | Preclinical Research |
Detailed Experimental Protocols for Functional Validation
Protocol: Ex Vivo Editing and Functional Analysis of Hematopoietic Stem Cells (HSCs)
This protocol outlines the process for editing CD34+ HSCs for diseases like SCD and TDT, based on the approach used for the approved therapy CASGEVY [23].
I. Materials and Reagents
- CD34+ Hematopoietic Stem Cells: Isolated from patient mobilized apheresis product.
- CRISPR-Cas9 Components: Ribonucleoprotein (RNP) complex of Cas9 nuclease and synthetic sgRNA targeting the BCL11A gene enhancer.
- Electroporation System: For RNP delivery (e.g., Neon Transfection System).
- Culture Media: Serum-free expansion media supplemented with cytokines (SCF, TPO, FLT3-Ligand).
- Analytical Reagents: Flow cytometry antibodies (CD34, CD45, Glycophorin A), Hemoglobin F (HbF) staining kit, qPCR reagents.
II. Step-by-Step Methodology
- Cell Isolation and Preparation: Isolate CD34+ cells using clinical-grade magnetic bead separation. Pre-stimulate cells in cytokine-supplemented media for 24-48 hours.
- CRISPR-Cas9 Electroporation:
- Prepare the RNP complex by pre-incubating Cas9 protein with sgRNA.
- Wash and resuspend pre-stimulated CD34+ cells in electroporation buffer.
- Electroporate cells with the RNP complex using optimized voltage and pulse parameters.
- Post-Editing Culture: Immediately transfer electroporated cells to recovery media. After 24 hours, transfer to expansion media and culture for several days to assess viability and expansion.
- Functional Validation Assays:
- Engraftment and Differentiation Potential: Transplant edited CD34+ cells into immunodeficient mouse models (e.g., NSG mice). Analyze human cell chimerism in bone marrow after 12-16 weeks using flow cytometry for human CD45/CD34 and other lineage markers.
- Fetal Hemoglobin Reactivation: Differentiate edited cells in vitro into erythroid lineages. Use FACS to quantify the percentage of cells expressing HbF.
- Phenotypic Rescue: For SCD models, assess resistance to hypoxia-induced sickling. For TDT models, measure heme production and red blood cell enucleation.
Protocol: In Vivo Functional Validation via LNP Delivery
This protocol describes the assessment of functional rescue after in vivo CRISPR editing, as demonstrated in trials for hATTR and HAE [8].
I. Materials and Reagents
- CRISPR-LNP Formulation: Lipid nanoparticles encapsulating mRNA for Cas9 and the appropriate sgRNA.
- Animal Model: Validated murine or non-human primate model of the target disease.
- Administration Equipment: Syringes, intravenous catheters.
- Sample Collection: Blood collection tubes (serum, plasma), tissue biopsy tools.
- Assay Kits: ELISA kits for target protein quantification (e.g., TTR, kallikrein).
II. Step-by-Step Methodology
- Dosing and Administration:
- Calculate the LNP dose based on animal weight (e.g., mg/kg).
- Administer the CRISPR-LNP formulation via a single intravenous injection.
- Longitudinal Biomarker Monitoring:
- Collect blood samples at baseline and at regular intervals post-injection (e.g., weeks 2, 4, 8, 12, and 24).
- Isolate serum/plasma and quantify the concentration of the target disease-driving protein (e.g., TTR) using ELISA.
- Functional Endpoint Analysis:
- hATTR Model: Perform histological staining of heart and nerve tissues to assess amyloid deposit clearance.
- HAE Model: Monitor and quantify the frequency and severity of vascular leakage or inflammatory attacks post-administration.
- Cardiovascular Models (e.g., CTX310/320): Measure biomarkers like ANGPTL3 for lipid metabolism and Lp(a) for cardiovascular risk [23].
Protocol: Multilineage Differentiation of Edited Pluripotent Stem Cells
This protocol is used to validate the developmental potential of CRISPR-edited iPSCs, crucial for therapies relying on differentiated cell products [18] [93].
I. Materials and Reagents
- CRISPR-Edited iPSCs: Fully characterized clone with sequencing-confirmed edit.
- Directed Differentiation Kits: Commercial kits for mesoderm, endoderm, and ectoderm lineages.
- Cell Culture Vessels: Low-attachment plates for embryoid body formation, Matrigel-coated plates for adherent differentiation.
- Lineage Tracers: Rainbow reporter genes (e.g., fluorescent proteins from jellyfish, sea anemone) for clonal tracking [93].
- Characterization Reagents: Antibodies for lineage-specific markers (e.g., SOX17 for endoderm, TBXT for mesoderm, TUJ1 for ectoderm).
II. Step-by-Step Methodology
- Trilineage Differentiation via Embryoid Body (EB) Formation:
- Detach edited iPSCs and culture in suspension to form EBs for 7-10 days in basal medium.
- Harvest EBs, dissociate, and plate on adhesion-friendly surfaces to allow spontaneous differentiation.
- Directed Differentiation:
- Mesoderm (Cardiomyocytes): Use established protocols with sequential activation/inhibition of BMP, Activin A, and Wnt pathways [93].
- Endoderm (Hepatocytes): Differentiate using protocols involving FGF and BMP signaling.
- Ectoderm (Neurons): Use dual SMAD inhibition (e.g., Noggin, SB431542) to induce neural induction.
- Functional Validation of Differentiated Cells:
- Flow Cytometry: Quantify the percentage of cells expressing definitive lineage-specific markers.
- Cell-Specific Functional Assays:
- Cardiomyocytes: Measure spontaneous contraction and analyze calcium flux.
- Hepatocytes: Assess albumin secretion, LDL uptake, and cytochrome P450 activity.
- Neurons: Perform patch-clamp electrophysiology to confirm action potential generation.
- Clonal Analysis: For cells with integrated rainbow reporters, track the progeny of single iPSCs to assess clonal dominance and differentiation efficiency [93].
Visualization of Experimental Workflows
The following diagrams illustrate the core experimental pathways and workflows described in the protocols.
Diagram 1: HSC Editing & Validation Workflow
Diagram 2: In Vivo LNP Delivery & Analysis
The Scientist's Toolkit: Research Reagent Solutions
A successful functional validation pipeline relies on a suite of specialized reagents and tools. The following table details essential solutions for the experiments described herein.
Table 2: Essential Research Reagents for Functional Validation of CRISPR-Edited Stem Cells
| Reagent/Tool | Specific Example | Function in Validation |
|---|---|---|
| CRISPR-Cas9 Delivery System | Cas9-gRNA Ribonucleoprotein (RNP) Complex | Enables high-efficiency, transient editing with reduced off-target effects in ex vivo HSC and iPSC editing [23]. |
| In Vivo Delivery Vector | Lipid Nanoparticles (LNPs) with Cas9 mRNA/sgRNA | Safely and efficiently delivers CRISPR components to target organs (e.g., liver) for in vivo gene editing [8] [23]. |
| Lineage Tracing System | Rainbow Reporter Genes (e.g., GFP, RFP, iRFP) | Allows tracking of individual stem cells and their progeny (clones) throughout differentiation, revealing clonal dynamics [93]. |
| Stem Cell Differentiation Kits | Defined Media for Mesoderm/Endoderm/Ectoderm | Provides standardized, efficient protocols for differentiating iPSCs into target cell types for functional testing [18] [93]. |
| In Vivo Model System | Immunodeficient NSG Mice | Serves as a gold-standard model for validating the engraftment and long-term repopulation potential of edited human HSCs [8]. |
| Target Protein Quantification | ELISA Kits (e.g., for TTR, Kallikrein) | Precisely measures the reduction of disease-related proteins in plasma/serum, a key biomarker for in vivo therapy efficacy [8]. |
Clinical Trial Success: CRISPR-Engineered MSCs for Immunological Applications
The application of CRISPR in mesenchymal stromal/stem cell (MSC) engineering has shown significant progress in overcoming immunological barriers for regenerative medicine and cancer therapy. Recent preclinical studies demonstrate how precise genetic modifications can enhance MSC survival, function, and therapeutic potential.
Key Preclinical Case Study: Engineering "Immune Stealth" MSCs
A primary challenge in allogeneic MSC therapy is host immune recognition and rejection, primarily mediated by Major Histocompatibility Complex Class I (MHC-I) molecules [94]. CRISPR/Cas9 technology has enabled the creation of hypoimmunogenic MSCs through targeted genetic modifications.
Experimental Protocol: β2-Microglobulin Knockout in Umbilical Cord MSCs [94]
- Objective: Generate universal, "off-the-shelf" MSCs by ablating surface expression of MHC-I to evade CD8+ T-cell recognition.
- Cell Source: Human umbilical cord-derived MSCs (UMSCs) or induced pluripotent stem cell (iPSC)-derived MSCs.
- CRISPR Components: A single guide RNA (sgRNA) targeting the exon of the B2M gene, which codes for the essential light chain of the MHC-I complex, and Cas9 nuclease.
- Delivery Method: Nucleofection of ribonucleoprotein (RNP) complexes.
- Validation: Flow cytometry to confirm loss of MHC-I surface expression; mixed lymphocyte reaction (MLR) assays to demonstrate reduced T-cell proliferation and activation.
- In Vivo Assessment: Transplantation into animal models of cardiac repair showed enhanced cell survival, reduced CD8+ T-cell infiltration, and modulation of the immune microenvironment towards an anti-inflammatory state.
Quantitative Outcomes of Immunological Engineering [94]
| Genetic Target | MSC Type | Experimental Model | Key Functional Outcome |
|---|---|---|---|
| β2-Microglobulin (B2M) | Umbilical Cord MSCs | Cardiac Repair Model | Suppressed CD8+ T-cell activation and infiltration; enhanced cell survival and engraftment. |
| HLA-A, B, C | iPSC-derived MSCs | In Vitro Immunogenicity Assays | Evaded NK cell-mediated cytotoxicity; retained multipotency and chondrogenic differentiation capacity. |
| CIITA (Class II Transactivator) | Bone Marrow MSCs | In Vitro T-cell Assays | Abrogated MHC Class II expression; reduced CD4+ T-cell activation. |
Research Reagent Solutions
Essential materials for CRISPR-mediated MSC engineering include [54] [94] [95]:
- Alt-R S.p. HiFi Cas9 Nuclease V3: A high-fidelity Cas9 enzyme to minimize off-target effects.
- Chemically Modified sgRNA: Enhances stability and reduces immunogenicity.
- Nucleofector System & Kit: Optimized reagents for high-efficiency RNP delivery into primary MSCs.
- CloneR Supplement: Improves survival of single-cell cloned stem cells post-transfection.
- pCXLE-hOCT3/4-shp53-F Plasmid: Allows transient p53 inhibition to enhance Homology-Directed Repair (HDR) efficiency in iPSCs.
High-Efficiency Genome Editing in iPSCs: A Protocol Case Study
A 2024 study established a highly efficient protocol for introducing point mutations in human induced pluripotent stem cells (iPSCs), achieving homologous recombination rates exceeding 90% [95]. This method is critical for creating isogenic cell lines for disease modeling.
Goal: Introduce the APOE R136S (Christchurch) mutation or correct the PSEN1 E280A mutation in human iPSCs [95].
Core Workflow:
- sgRNA Design: Design sgRNA with a cleavage site <10 nucleotides from the target SNP. Incorporate a silent mutation in the repair template's PAM sequence to prevent re-cutting.
- RNP Complex Formation: Complex 0.6 µM sgRNA with 0.85 µg/µL Alt-R HiFi Cas9 V3 nuclease. Incubate 20-30 minutes at room temperature.
- Cell Preparation: Culture iPSCs to 80-90% confluency in feeder-free conditions. Pre-treat with cloning media (StemFlex + 1% RevitaCell + 10% CloneR) 1 hour before nucleofection.
- Nucleofection: Co-deliver RNP complex, 5 µM single-stranded oligodeoxynucleotide (ssODN) repair template, and 50 ng/µL pCXLE-hOCT3/4-shp53-F plasmid (for p53 knockdown) via nucleofection.
- Cloning and Validation: Single-cell clone recovery and expansion. Genotypic validation by sequencing and karyotyping.
Quantitative Data on Editing Efficiency [95]
| Target Mutation | iPSC Line | HDR Efficiency (Bulk ICE) | HDR Efficiency (After Subcloning) | Karyotype Post-Editing |
|---|---|---|---|---|
| APOE R136S | PS 1.9.1 | 49% | 100% (46% Homozygous, 54% Heterozygous) | Normal |
| APOE R136S | ADRC 5.3 Line 1 | 82-99% | 100% | Normal |
| APOE R136S | ADRC 5.3 Line 2 | 87% | 94.4% | Normal |
| PSEN1 E280A Correction | PS 1.9.1 | 97-98% | 100% | Normal |
Clinical Trial Update: In Vivo CRISPR Therapies
The clinical landscape for CRISPR therapies has expanded beyond ex vivo editing, with significant advancements in in vivo delivery and re-dosing capabilities.
Case Study: Lipid Nanoparticle (LNP) Delivery for hATTR
Intellia Therapeutics' phase I trial for hereditary transthyretin amyloidosis (hATTR) represents a landmark case as the first systemic in vivo CRISPR-Cas9 therapy delivered via lipid nanoparticles (LNPs) [8].
Experimental Protocol & Outcomes [8]:
- Therapy: Intravenous infusion of LNPs containing CRISPR-Cas9 components targeting the TTR gene in liver cells.
- Dosing: Single-dose treatment, with an option for re-dosing explored in a subset of patients.
- Efficacy: Rapid, deep (~90% reduction), and sustained reduction of TTR protein levels in blood over two years.
- Safety & Flexibility: No serious side effects reported. The LNP delivery system enabled re-dosing without the severe immune reactions associated with viral vectors, a finding corroborated by the personalized treatment of infant KJ for CPS1 deficiency, who safely received three LNP doses [8].
Signaling Pathway: CRISPR-Cas9 Mediated Gene Disruption for hATTR
The Scientist's Toolkit: Key Reagents for CRISPR Workflows
| Research Reagent | Function & Application | Key Consideration |
|---|---|---|
| Ribonucleoprotein (RNP) Complex | Pre-complexed Cas9 protein and sgRNA; minimizes off-target effects and enables rapid editing. | Gold standard for ex vivo editing (e.g., MSCs, iPSCs) [54] [95]. |
| Lipid Nanoparticles (LNPs) | In vivo delivery vehicle; targets organs like the liver and allows for re-dosing [8]. | Superior safety profile compared to viral vectors. |
| Single-Stranded Oligodeoxynucleotide (ssODN) | Repair template for introducing precise point mutations via HDR [95]. | Requires homology arms; PAM disruption can prevent re-cleavage. |
| HDR Enhancers (e.g., CloneR) | Small molecule cocktails that improve cell survival and HDR efficiency post-transfection [95]. | Critical for challenging edits in sensitive cells like iPSCs. |
| p53 Inhibitors (shRNA) | Transiently inhibits p53 pathway to reduce apoptosis and increase HDR efficiency in stem cells [95]. | Use requires careful validation to avoid selective pressure for karyotypic abnormalities. |
Regulatory Pathways and Standardization for Clinical-Grade Therapies
The regulatory landscape for CRISPR-based therapies is undergoing a significant transformation, shifting from a traditional one-drug-one-disease model toward innovative platform-based approaches that enable faster development of personalized treatments. This evolution is critical for addressing the unique challenges of gene editing therapies, particularly for rare genetic diseases where commercial viability has historically been limited. The field has reached a pivotal moment with the emergence of regulatory frameworks that acknowledge the "plausible mechanism" of CRISPR therapies that directly repair genetic defects, allowing for more efficient approval pathways based on consistent patient outcomes across similar clinical syndromes rather than requiring large patient cohorts for each specific mutation [96].
Recent developments have established actionable pathways for "CRISPR platformization" – a regulatory approach where therapies for different mutations within the same clinical syndrome can be developed under a single master protocol. This framework significantly reduces redundant requirements for each new mutation-specific therapy, with the FDA now considering approval for on-demand gene editing medicines when they (1) treat patients with the same clinical syndrome regardless of the underlying mutation, and (2) demonstrate consistent efficacy that cannot be expected under standard care [96]. This paradigm shift is accelerating the translation of CRISPR therapies from research to clinical application, particularly for diseases affecting accessible tissues like liver and hematopoietic cells.
Current Regulatory Pathways and Framework Developments
Established and Emerging Regulatory Pathways
The regulatory environment for CRISPR therapies has evolved substantially since the first approvals, with distinct pathways now emerging for different therapeutic approaches. The table below summarizes the key regulatory pathways and their current status.
Table 1: Regulatory Pathways for CRISPR-Based Therapies
| Pathway Type | Description | Therapeutic Examples | Current Status |
|---|---|---|---|
| Traditional Disease-Specific Approval | Focuses on a single mutation-disease combination | Casgevy for sickle cell disease and β-thalassemia [8] | Approved therapies available |
| Platform/Umbrella Trial Pathway | Master protocol for multiple mutations causing similar clinical syndromes | Planned urea cycle disorders trial (CHOP, 2026); Severe T cell dysfunction trial (IGI-UCSF) [96] | Phase I trials initiating 2026 |
| "Plausible Mechanism" Pathway | FDA proposal for approval based on mechanistic plausibility and consistent efficacy across small patient cohorts | Proposed for liver and blood stem cell diseases [96] | Regulatory proposal stage |
| Expedited Manufacturing Pathway | Benefit-risk commensurate accelerated small-scale manufacture | IGI-Danaher collaboration for guide RNA production [96] | Development phase |
Standardization Challenges and Solutions for Platform Therapies
The transition to platform regulatory approaches requires addressing significant standardization challenges across multiple domains:
Manufacturing Standardization: Current Good Manufacturing Practice (cGMP) requirements designed for large-scale production present obstacles for personalized therapies. The IGI and Danaher Corporation have collaborated to develop "benefit-risk commensurate" accelerated small-scale manufacturing frameworks that maintain quality while reducing production timelines and costs [96]. This approach is particularly crucial for pediatric patients who require smaller quantities of therapeutic components.
Preclinical Testing Harmonization: Platform approaches enable reduced animal testing requirements for subsequent therapies within the same platform. Once initial safety is established for a delivery system and editing approach, redundant studies can be eliminated, focusing only on elements that address specific risks associated with modifications [96].
Clinical Trial Design Innovation: Master protocol trials allow multiple sub-studies to be conducted under a single overarching framework, significantly improving efficiency. The CHOP-Penn team has publicly shared regulatory filings and FDA correspondence to establish precedents for this approach, creating a roadmap for other institutions [96].
Experimental Protocols for Regulatory-Grade CRISPR Therapy Development
Protocol: Development of Personalized CRISPR Therapy for Rare Metabolic Disease
This protocol outlines the methodology used in the landmark case of an infant with CPS1 deficiency, representing the first personalized in vivo CRISPR therapy developed under an accelerated timeline [8].
Materials and Reagents
Table 2: Essential Research Reagents for Personalized CRISPR Therapy Development
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| CRISPR Nucleases | Cas9, Cas12, engineered variants (hfCas12Max) [33] | DNA cleavage or modification at target sites |
| Delivery Systems | Lipid nanoparticles (LNPs), GalNAc-LNP, AAV vectors, eVLPs [8] [61] [33] | In vivo delivery of editing components |
| Guide RNA Design | sgRNA, crRNA with modified direct repeats [61] | Target specificity and complex stability |
| In Vitro Testing Models | iPSC-derived cells, Patient-derived primary cells [5] | Efficacy and safety assessment pre-clinically |
| Analytical Tools | Next-generation sequencing, INDEL analysis, RNA sequencing [97] | Assessment of editing efficiency and off-target effects |
Step-by-Step Methodology
Target Identification and Validation
- Sequence the patient's genome to identify the specific pathogenic mutation
- Design guide RNAs with high on-target efficiency using computational tools (e.g., CRISPR-GPT) [10]
- Validate guide RNA specificity using in silico off-target prediction algorithms
Therapeutic Construct Design
- Select appropriate CRISPR system based on mutation type (nuclease, base editor, prime editor)
- For the CPS1 case, researchers used Cas9 protein complexed with sgRNA [8]
- Formulate therapeutic using lipid nanoparticles (LNPs) optimized for hepatic delivery
Potency and Specificity Assessment
- Test editing efficiency in patient-derived iPSCs or primary cells
- Evaluate off-target editing using GUIDE-seq or CIRCLE-seq methods
- Assess functional correction through biochemical assays relevant to the metabolic pathway
Safety and Toxicology Studies
- Conduct in vitro immunogenicity assessments
- Perform limited animal studies focusing on biodistribution and acute toxicity
- For platform approaches, leverage previous safety data from similar constructs
Regulatory Documentation
- Prepare Investigational New Drug (IND) application referencing master protocol
- Include comparative analysis to previously approved therapies within the platform
- Propose patient-specific monitoring plan based on established safety profile
Figure 1: Personalized CRISPR Therapy Development Workflow
Protocol: Implementation of Umbrella Trial Design for Multiple Mutations
This protocol describes the methodology for designing and implementing platform trials that can accommodate multiple patient-specific therapies under a single regulatory framework.
Materials and Specialized Reagents
- Platform Core Components: Standardized LNP formulations, quality-controlled Cas protein, sgRNA synthesis system
- Analytical Suite: NGS platform for on-target and off-target assessment, biodistribution assays, immunogenicity testing
- Manufacturing Infrastructure: Small-scale GMP facility capable of rapid therapeutic production
Step-by-Step Methodology
Master Protocol Development
- Define inclusion criteria based on clinical syndrome rather than specific genetic mutations
- Establish standardized endpoints relevant to the disease category
- Create safety monitoring guidelines applicable across all sub-studies
Therapeutic Platform Qualification
- Demonstrate consistent manufacturing quality across multiple lots
- Establish potency assays relevant to the platform mechanism
- Complete comprehensive safety assessment of the core platform components
Mutation-Specific Module Development
- For each new mutation, design and validate guide RNAs using standardized protocols
- Conduct limited in vitro testing to confirm target engagement and efficiency
- Perform comparative analysis to previously approved modules within the platform
Regulatory Integration
- Submit master protocol for FDA review
- Establish precedents for abbreviated requirements for additional mutations
- Implement real-time safety reporting across all modules
Analytical Methods and Quality Control Standards
Quantifying Editing Efficiency and Specificity
Robust analytical methods are essential for regulatory compliance and therapeutic standardization. The following table outlines key quality control parameters and their measurement approaches.
Table 3: Quality Control Metrics for CRISPR Therapy Standardization
| Quality Attribute | Analytical Method | Acceptance Criteria | Regulatory Significance |
|---|---|---|---|
| On-Target Editing Efficiency | NGS of target locus | >70% insertion/deletion or >90% protein reduction for knockout approaches [8] | Primary efficacy indicator |
| Off-Target Editing | GUIDE-seq, CIRCLE-seq | No significant off-target events in predicted sites | Safety profile determination |
| Delivery Efficiency | Biodistribution studies (qPCR) | Tissue-specific accumulation consistent with mechanism | Dosing justification |
| Immunogenicity | Cytokine assays, antibody detection | Minimal immune activation | Repeat dosing potential |
| Product Potency | Functional assays (e.g., protein reduction) | IC50 within established range | Batch-to-batch consistency |
Standardization of Delivery Systems
Delivery method standardization is critical for platform approaches, with lipid nanoparticles (LNPs) emerging as a preferred vehicle for in vivo delivery due to their favorable manufacturing and safety profiles:
- LNP Advantages: Scalable manufacturing, lower immunogenicity than viral vectors, and potential for repeat dosing [8] [61]
- Tropism Optimization: Current LNPs naturally accumulate in the liver, making them ideal for hepatic targets [8]; research continues on engineering LNPs with affinity for other tissues
- Dosing Flexibility: LNP delivery enables dose adjustment and redosing, as demonstrated in the CPS1 case where the patient safely received three doses with incremental improvement [8]
Figure 2: CRISPR Therapy Quality Control Cascade
The standardization of regulatory pathways for CRISPR therapies represents a transformative advancement in genetic medicine. The emergence of platform approaches and umbrella trial designs enables efficient development of treatments for rare diseases that were previously commercially non-viable. Implementation of these pathways requires close collaboration between academic institutions, regulatory agencies, and industry partners to establish standardized frameworks that maintain safety while accelerating access.
The near-term future will see these pathways initially applied to diseases of the liver and hematopoietic system, where delivery technologies are most advanced. For tissues requiring viral delivery, significant challenges remain due to manufacturing constraints and costs. Continued innovation in delivery technologies and manufacturing processes will be essential to expand these regulatory pathways to neurological and other disorders. The successful implementation of these standardized approaches will ultimately determine how quickly the promise of personalized CRISPR medicines becomes a reality for patients across the genetic disease spectrum.
Long-Term Safety and Efficacy Monitoring in Animal Models and Patients
The integration of CRISPR/Cas9 technology with stem cell genetic engineering heralds a transformative era in regenerative medicine, offering potential cures for a range of genetic disorders. However, the long-term biological activity and permanent genomic alterations inherent to these therapies necessitate rigorous, lifelong safety and efficacy monitoring in both preclinical and clinical settings. Ensuring patient safety requires a proactive, risk-adaptive pharmacovigilance model that extends far beyond initial treatment, addressing unique challenges such as genotoxicity, immune complications, and organ-specific effects [98]. This Application Note provides a detailed framework for monitoring the long-term safety and efficacy of CRISPR-engineered stem cell therapies, consolidating current clinical data, standardized protocols, and practical research tools to support researchers and drug development professionals.
Current Landscape and Quantitative Safety/Efficacy Data
Recent clinical trials and preclinical studies have begun to generate crucial long-term data on CRISPR-based interventions. The tables below summarize key quantitative findings on both efficacy and safety from recent investigations.
Table 1: Quantitative Efficacy Data from Preclinical and Clinical Studies
| Therapy / Model | Indication | Key Efficacy Metric | Result | Follow-up Period | Citation |
|---|---|---|---|---|---|
| hSOD1-G93A Transgene Editing | Amyotrophic Lateral Sclerosis (ALS) in mice | Prevention of ALS-like disease | 100% of edited mice (n=15) remained phenotypically normal | >30 months | [99] |
| NTLA-2001 (hATTR) | Hereditary Transthyretin Amyloidosis in humans | Reduction in disease-related TTR protein | ~90% average reduction | Sustained at 2 years (n=27) | [8] |
| NTLA-2002 (HAE) | Hereditary Angioedema in humans | Reduction in plasma kallikrein & inflammation attacks | 86% kallikrein reduction; 8/11 patients attack-free | 16 weeks post-treatment | [8] |
| Personalized in vivo CRISPR | CPS1 Deficiency in an infant | Symptom improvement | Improvement after each of three LNP doses | 6-month development & monitoring | [8] |
Table 2: Long-Term Safety Monitoring Data and Observations
| Therapy / Model | Safety Observation | Incidence / Key Finding | Follow-up Duration | Citation |
|---|---|---|---|---|
| hSOD1-G93A Transgene Editing | Tumorigenesis / Other Diseases | No evidence of tumors or inflammatory disease in 36 mice | Minimum 2 years | [99] |
| CRISPR/Cas9 Transgenic Mice | General Health & Survival | Founder mouse lived 34 months without notable disease | 34 months | [99] |
| hSOD1-G93A Transgene Editing | Large DNA Deletions | Frequent deletions (100s-1000s of bp) mediated by Alu elements | Post-analysis | [99] |
| In vivo LNP Delivery (Intellia) | Re-dosing Capability | Multiple doses safely administered due to non-viral delivery | Multiple weeks | [8] |
Experimental Protocols for Long-Term Monitoring
Preclinical Protocol: Lifetime Assessment in Genetically Engineered Mouse Models
This protocol is designed to maximize the detection of long-term adverse effects from highly efficient, lifelong CRISPR/Cas9 expression [99].
3.1.1 Animal Model Generation:
- Strategy: Utilize a transgenic approach to constitutively express Cas9 and the target-specific gRNA from the zygote stage onward, ensuring maximal editing efficiency in every somatic cell.
- Procedure:
- Clone a 20-nt target-specific sequence (e.g., from human SOD1 exon 2) into the pSpCas9(BB)-2A-GFP (PX458) plasmid.
- Linearize the transgene DNA (SacII/NotI digestion) and microinject it into fertilized eggs from an inbred strain (e.g., C57BL/6J).
- Identify founder lines with high transgene copy numbers and crossbreed them with disease-model transgenic mice (e.g., hSOD1-G93A for ALS).
- Maintain and monitor the resulting double-transgenic (G1H/Cas9) and Cas9-only control mice for their natural lifespan.
3.1.2 Long-Term Phenotypic and Pathological Monitoring:
- Clinical Scoring: Perform twice-weekly assessments for disease-specific signs (e.g., ALS-like phenotype) and general health indicators, including body weight, mobility, and behavior.
- Histopathological Analysis: At endpoint or predefined intervals (e.g., 12, 24 months), conduct full necropsies. Collect and preserve tissues (e.g., CNS, liver, spleen) in formalin. Analyze sections via H&E staining and immunohistochemistry for disease-specific markers (e.g., SOD1, p-62, ubiquitin for ALS), glial activation (e.g., IBA1 for microglia, GFAP for astrocytes), and tumor markers.
- Survival Analysis: Record and compare survival curves between edited and control groups.
3.1.3 Molecular Analysis of Editing and Genomic Integrity:
- Editing Efficiency: Use deep sequencing (e.g., amplicon sequencing of a 512 bp region flanking the Cas9 cut site) on genomic DNA from multiple tissues to characterize the spectrum of insertions/deletions (indels) and confirm editing efficiency.
- Off-Target Analysis: Employ genome-wide methods like CIRCLE-seq or GUIDE-seq on the original gRNA to identify potential off-target sites. Sequencer these loci from long-term animal DNA.
- On-Target Genotoxicity: Design PCR primers flanking the cut site to detect large deletions. Clone and sequence PCR products to characterize the molecular mechanism of any large rearrangements [99].
Clinical Protocol: Risk-Adaptive Pharmacovigilance for CRISPR-Engineered Stem Cell Therapies
This protocol outlines a proactive, long-term monitoring strategy for patients in clinical trials or post-approval, based on a digitally enabled pharmacovigilance model [98].
3.2.1 Pre-Treatment Baseline Assessment:
- Clinical Workup: Comprehensive physical exam, documentation of disease-specific symptoms, and quality-of-life assessments.
- Biomarker Profiling: Establish baseline levels of disease-relevant proteins in blood (e.g., TTR for hATTR, kallikrein for HAE) [8]. Collect biospecimens (blood, PBMCs) for multi-omics analysis (e.g., genomics, transcriptomics).
- Immune Profiling: Test for pre-existing antibodies against the CRISPR nuclease (e.g., Cas9) and the delivery vehicle (e.g., AAV capsid, LNP components).
3.2.2 Multi-Modal Long-Term Patient Monitoring:
- Clinical and Laboratory Monitoring:
- Schedule: Frequent visits (e.g., monthly) in the first year, quarterly in the second year, and bi-annually thereafter.
- Assessments: Track disease-specific clinical endpoints (e.g., vaso-occlusive crises for SCD, angioedema attacks for HAE). Perform standard blood tests, liver/kidney function panels, and inflammatory markers (e.g., CRP, cytokines).
- Pharmacodynamic Biomarker Monitoring: Regularly quantify the level of the target protein in the blood (e.g., TTR, kallikrein) as a surrogate for sustained editing efficacy [8].
- Digital and Patient-Reported Monitoring: Integrate wearable biosensors to track physiological data. Use electronic patient-reported outcome (ePRO) platforms for real-time symptom logging [98].
- Long-Term Genotoxicity Surveillance: Employ droplet digital PCR (ddPCR) or next-generation sequencing (NGS)-based methods to periodically monitor the original edited cell population in blood or tissue biopsies for clonal expansion. This is critical for assessing the risk of malignancies related to oncogene activation or tumor suppressor disruption [98] [99].
3.2.3 Data Integration and Safety Review:
- Integrated Safety Dashboard: Aggregate all clinical, laboratory, biomarker, and digital data into a centralized dashboard for continuous signal detection.
- Review Committee: Establish an independent data and safety monitoring board (DSMB) to review cumulative data at regular intervals and make recommendations on trial continuation, modification, or termination.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRISPR Stem Cell Therapy Monitoring
| Reagent / Material | Function in Monitoring | Specific Example / Application |
|---|---|---|
| GMP-grade gRNAs | Ensures purity and consistency for clinical-grade therapy manufacturing and reduces risk of immune reactions. | Used in INDs for CRISPR therapies; Synthego's INDe gRNAs are for IND-enabling studies [100]. |
| Lipid Nanoparticles (LNPs) | Enables efficient in vivo delivery of CRISPR components to target organs (e.g., liver) and allows for potential re-dosing. | Used in Intellia's NTLA-2001 and NTLA-2002; also in YolTech's YOLT-203 for PH1 [8] [101]. |
| dCas9 Systems (CRISPRi/a) | Allows for transient, reversible modulation of gene expression without double-strand breaks, potentially improving safety profile. | Used in MSC engineering for transcriptional activation of anti-inflammatory genes (e.g., IL-10, TSG-6) [92]. |
| Hypoimmune Gene Edits | Creates "immune stealth" universal donor cells to evade host rejection in allogeneic stem cell therapies. | Knockout of β2-microglobulin (B2M) in MSCs to abrogate HLA class I surface expression [92]. |
| Prime Editors | Enables precise gene correction without double-strand breaks or donor templates, minimizing genotoxicity risks. | Prime Medicine's PM359 for correcting NCF1 mutations in chronic granulomatous disease ex vivo [33]. |
| Bionic Scaffolds | Provides a supportive 3D microenvironment to enhance the survival, engraftment, and directed differentiation of transplanted stem cells. | Directional differentiation of iPSCs into specific cell lineages for tissue repair [5]. |
Visualizing Long-Term Monitoring Workflows
The following diagrams illustrate the integrated workflows for long-term monitoring in both animal models and patients.
Diagram 1: Preclinical Safety Workflow in Mice
Diagram 2: Clinical Pharmacovigilance Workflow
Conclusion
The integration of CRISPR technology with stem cell engineering represents a paradigm shift in biomedical science, offering unprecedented potential for curative therapies and sophisticated disease models. The key takeaways from this analysis underscore the importance of robust foundational knowledge, innovative methodological applications, proactive troubleshooting of delivery and safety issues, and rigorous comparative validation. As the field progresses, future directions will be dominated by the refinement of delivery systems like lipid nanoparticles, the clinical expansion of base and prime editing, the integration of AI tools to de-risk development, and the establishment of clear regulatory frameworks. For researchers and drug developers, mastering this convergence is no longer optional but essential for leading the next wave of breakthroughs in personalized and regenerative medicine.
References
- 1. CRISPR-Cas Systems: Bridging Bacterial Immunity and ... [https://www.mdpi.com/2673-8007/5/4/118]
- 2. Rapid Identification, Visualization, and Analysis of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10457644/]
- 3. Diversity and dynamics of the CRISPR-Cas systems ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-022-08770-8]
- 4. CRISPR-Cas9 HDR optimization: RAD52, denatured, and 5 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616026/]
- 5. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417523/]
- 6. Optimize Your CRISPR Experiments Like a Pro [https://www.synthego.com/blog/crispr-optimization/]
- 7. Advances in large-scale DNA engineering with the ... [https://www.nature.com/articles/s12276-025-01530-0]
- 8. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 9. Protocol to rapidly screen CRISPR-Cas9 gene editing ... [https://www.sciencedirect.com/science/article/pii/S2666166725003569]
- 10. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 11. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 12. A Review of the Methods for Human iPSC Derivation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4176696/]
- 13. MSCs vs. iPSCs: Potential in therapeutic applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9666898/]
- 14. The secretion profile of mesenchymal stem cells and ... [https://www.nature.com/articles/s41392-022-00932-0]
- 15. Differentiation Potential of Mesenchymal Stem Cells Is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5426435/]
- 16. Neural Stem Cells [https://www.stemcell.com/neural-stem-cells-lp.html]
- 17. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches ... [https://www.mdpi.com/2076-3921/14/7/781]
- 18. CRISPR/Cas-edited iPSCs and mesenchymal stem cells [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1595897/full]
- 19. Derivation and characteristics of induced pluripotent stem ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1172385/full]
- 20. Deep learning-based predictive identification of neural stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8110743/]
- 21. Recent applications, future perspectives, and limitations of ... [https://www.sciencedirect.com/science/article/pii/S216225312500188X]
- 22. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 23. CRISPR Therapeutics Highlights Strategic Priorities and ... [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-highlights-strategic-priorities-and]
- 24. A Visual Guide to CRISPR-SNIPER Gene Editing ... [https://www.reprocell.com/blog/a-visual-guide-to-crispr-sniper-gene-editing]
- 25. Understanding FDA Cell and Gene Therapy Guidance [https://www.synthego.com/blog/fda-cell-and-gene-therapy-guidance/]
- 26. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1612868/abstract]
- 27. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 28. Ethical and Regulatory Considerations Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398464/]
- 29. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 30. Stem Cell Research Controversy: A Deep Dive (2025) [https://www.dvcstem.com/post/stem-cell-research-controversy]
- 31. Ethical and Scientific Concerns Relating to CRISPR/Cas Gene ... [https://criticaldebateshsgj.scholasticahq.com/article/144179-ethical-and-scientific-concerns-relating-to-crispr-cas-gene-therapy]
- 32. CRISPR & Ethics [https://innovativegenomics.org/crisprpedia/crispr-ethics/]
- 33. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 34. CMN Weekly (17 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-17-october-2025-your-weekly-crispr-medicine-news/]
- 35. State of CRISPR Gene Editing in the Drug Discovery Sector [https://www.synthego.com/blog/survey-report-crispr-therapeutics/]
- 36. CMN Weekly (13 June 2025) - Your ... [https://crisprmedicinenews.com/news/cmn-weekly-13-june-2025-your-weekly-crispr-medicine-news/]
- 37. CRISPR base editing from gRNA design to analysis [https://www.synthego.com/blog/crispr-base-editing-from-grna-design-to-analysis/]
- 38. In vivo precision base editing to rescue mouse models of ... [https://www.sciencedirect.com/science/article/pii/S2162253125001763]
- 39. Breaking: Base Editing Rescues Severe β-Thalassaemia ... [https://crisprmedicinenews.com/news/breaking-base-editing-rescues-severe-b-thalassaemia-mutations/]
- 40. Protocol to rapidly verify silent gene reporter in human ... [https://pubmed.ncbi.nlm.nih.gov/41201092/]
- 41. CRISPR-GPT for agentic automation of gene-editing ... [https://www.nature.com/articles/s41551-025-01463-z]
- 42. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 43. Current Development of iPSC-Based Modeling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027653/]
- 44. Alzheimer's & CRISPR: How Gene Editing is ... [https://www.synthego.com/blog/alzheimers-crispr/]
- 45. CRISPR in Parkinson's Disease: Research, Gene Therapy, ... [https://www.synthego.com/blog/crispr-parkinson-research/]
- 46. A benchmark comparison of CRISPRn guide-RNA design ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11386-3]
- 47. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 48. Artificial intelligence and systems biology analysis in stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476622/]
- 49. Gene therapy for sickle cell and β-thalassemia works by disrupting three-dimensional genome structure - St. Jude Children’s Research Hospital [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/gene-therapy-for-sickle-cell-and-beta-thalassemia-works-by-disrupting-three-dimensional-genome-structure.html]
- 50. A Scalable Protocol for Ex Vivo Production of CAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452403/]
- 51. CRISPR screening redefines therapeutic target ... [https://www.sciencedirect.com/science/article/pii/S2095177925001741]
- 52. Comprehensive protocols for CRISPR/Cas9-based gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 53. Bioinformatics approaches to analyzing CRISPR screen data [https://pmc.ncbi.nlm.nih.gov/articles/PMC10019185/]
- 54. CRISPR Transfection Protocols Guide: How To Select The ... [https://www.synthego.com/guide/how-to-use-crispr/transfection-protocols/]
- 55. CRISPR-StAR enables high-resolution genetic screening ... [https://www.nature.com/articles/s41587-024-02512-9]
- 56. Genome Annotation / CRISPR screen analysis / Hands-on [https://training.galaxyproject.org/training-material/topics/genome-annotation/tutorials/crispr-screen/tutorial.html]
- 57. AI is a viable alternative to high throughput screening [https://www.nature.com/articles/s41598-024-54655-z]
- 58. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 59. In vivo haemopoietic stem cell gene therapy enabled by ... [https://www.nature.com/articles/s41586-025-09070-3]
- 60. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 61. CMN Weekly (10 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-10-october-2025-your-weekly-crispr-medicine-news/]
- 62. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 63. Guarding the genome: strategies for off-target detection ... [https://pubmed.ncbi.nlm.nih.gov/41241768/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0GaYCevddEDAfC5HA0wlElkFqaKqOUgRmbLrsDcYiaD&fc=None&ff=20251116125141&v=2.18.0.post22+67771e2]
- 64. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 65. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 66. Next-Generation CRISPR Nucleases Expand Therapeutic ... [https://www.the-scientist.com/next-generation-crispr-nucleases-expand-therapeutic-options-73678]
- 67. Next-Generation CRISPR Technologies and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8166939/]
- 68. Immunological considerations and challenges for ... [https://www.nature.com/articles/s42003-021-02237-4]
- 69. Whole-genome CRISPR screening identifies genetic manipulations to reduce immune rejection of stem cell-derived islets - PubMed [https://pubmed.ncbi.nlm.nih.gov/36055241/]
- 70. Advancing CRISPR genome editing into gene therapy clinical trials: progress and future prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 71. Leveraging CRISPR gene editing technology to optimize ... [https://www.nature.com/articles/s41375-024-02444-y]
- 72. Immunogenicity of CRISPR therapeutics—Critical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9978118/]
- 73. Viral vs. Non-Viral Gene Delivery: A Critical Choice for ... [https://www.drugdiscoverynews.com/viral-vs-non-viral-gene-delivery-a-critical-choice-for-gene-therapy-developers-16819]
- 74. The next frontier of in vivo gene therapy: are LNPs the new ... [https://www.darkhorseconsultinggroup.com/post/the-next-frontier-of-in-vivo-gene-therapies]
- 75. Application of CRISPR/Cas9 to human-induced pluripotent ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-020-00276-2]
- 76. Viral and Non-Viral Systems to Deliver Gene Therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11242246/]
- 77. Are LNPs the new AAV? [https://www.cellgenetherapyreview.com/3975-Featured-Articles/621087-Are-LNPs-the-new-AAV/]
- 78. From Discovery to Clinical Impact: The Evolution of AAV ... [https://www.packgene.com/learning-center/evolution-of-aav-vectors/]
- 79. Synthetic sgRNA GMP Manufacturing for CRISPR-based ... [https://www.synthego.com/blog/gmp-sgrna-manufacturing/]
- 80. Making a (Phase-Appropriate) Match [https://www.aldevron.com/blog/align-quality-levels-with-clinical-phase]
- 81. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-present-preclinical-data-alpha-1-antitrypsin]
- 82. CRISPR and Gene Editing: Next-Gen Manufacturing Impacts [https://www.worldpharmatoday.com/biopharma/crispr-and-gene-editing-next-gen-manufacturing-impacts/]
- 83. AI In clinical trials in 2025: the edge of tech [https://clinicaltrialrisk.org/clinical-trial-design/ai-in-clinical-trials-the-edge-of-tech/]
- 84. CRISPR Cell and Gene Therapies: Key Challenges in ... [https://www.synthego.com/blog/crispr-cell-gene-therapy-obstacles/]
- 85. AI-driven Quantitative Data Analysis for ... [https://powerdrill.ai/blog/ai-driven-quantitative-data-analysis-for-research]
- 86. The Key to Streamlining Your Quantitative Analysis [https://excelmatic.ai/blog/the-key-to-streamlining-your-quantitative-analysis/]
- 87. Comparing Gene Editing Platforms: CRISPR vs. Traditional ... [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 88. Precision gene editing: The power of CRISPR-Cas in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590234/]
- 89. CRISPR-Cas9 vs TALEN vs ZFN: Precision Gene Editing ... [https://synapse.patsnap.com/article/crispr-cas9-vs-talen-vs-zfn-precision-gene-editing-compared]
- 90. CRISPR Gene Therapy: Applications, Limitations, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7427626/]
- 91. Circular single stranded DNA potentiates non-viral gene ... [https://www.nature.com/articles/s41467-025-66318-2]
- 92. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574024/]
- 93. Using Color-Coding Genes to Study Stem Cell Biology | ISCRM [https://iscrm.uw.edu/color-coding-technology-reveals-new-insights-about-stem-cell-biology/]
- 94. -mediated CRISPR of mesenchymal stromal/ engineering ... stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04723-6]
- 95. A high efficiency precision genome editing method with ... [https://www.nature.com/articles/s41598-024-60766-4]
- 96. How to get gene-editing medicines to families that need it | STAT [https://www.statnews.com/2025/11/14/fda-gene-editing-medicines-on-demand-pathway/]
- 97. Frontiers | Unraveling the future of genomics: CRISPR , single-cell... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1565387/full]
- 98. Pharmacovigilance in Cell and Gene Therapy [https://pubmed.ncbi.nlm.nih.gov/40783602/]
- 99. Efficacy and long-term safety of CRISPR/Cas9 genome ... [https://www.nature.com/articles/s42003-021-01942-4]
- 100. Understanding CRISPR Clinical Trials [https://www.synthego.com/blog/understanding-crispr-clinical-trials/]
- 101. The Latest Updates From the Gene-Editing Clinical Trials ... [https://crisprmedicinenews.com/news/the-latest-updates-from-the-gene-editing-clinical-trials-february-2025/]