Decoding the Balance: Molecular Mechanisms of Stem Cell Self-Renewal and Differentiation in Development and Disease
This article provides a comprehensive analysis of the sophisticated molecular networks governing the critical balance between stem cell self-renewal and differentiation.
Decoding the Balance: Molecular Mechanisms of Stem Cell Self-Renewal and Differentiation in Development and Disease
Abstract
This article provides a comprehensive analysis of the sophisticated molecular networks governing the critical balance between stem cell self-renewal and differentiation. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational concepts with cutting-edge methodological applications. We explore intrinsic regulators like piRNAs and PIWI proteins, key signaling pathways including TGF-β, mTOR, and Notch, and the crucial role of niche communication. The content extends to troubleshooting in vitro culture challenges, optimizing differentiation protocols for clinical translation, and validating mechanisms through current FDA-approved therapies and clinical trials. By integrating basic science with therapeutic applications, this review serves as a strategic resource for advancing regenerative medicine and targeted drug discovery.
Core Principles and Key Molecular Regulators of Stem Cell Fate
Stem cell fate is governed by two primary division modes: symmetric cell division (SCD) and asymmetric cell division (ACD). These division patterns are fundamental to the processes of self-renewal and differentiation, balancing the maintenance of a stem cell reservoir with the generation of specialized tissues [1]. Self-renewal can be defined as the process by which a stem cell undergoes mitosis to produce at least one daughter cell possessing the same self-renewal and differentiation capacity, thereby creating a complete phenocopy [1]. The decision between symmetric and asymmetric division represents a crucial regulatory point in development, tissue homeostasis, and regeneration, with dysregulation potentially contributing to tumorigenesis [2] [3].
In the context of a broader thesis on stem cell self-renewal and differentiation mechanisms, understanding these division modes provides critical insight into how stem cells navigate fate decisions. ACD generates cellular diversity by producing two differentially fated daughter cells—one retaining stem cell identity and the other committing to differentiation [1] [2]. Conversely, SCD either expands the stem cell pool (symmetric self-renewal) or produces two differentiated progeny (symmetric differentiation) [1] [2]. Recent advances in genetic labeling and single-cell tracking have revealed that many mammalian stem cells exhibit remarkable plasticity, capable of switching between these division modes in response to physiological demands and microenvironmental cues [4] [2].
Core Concepts and Definitions
Characterizing Division Modes and Cell Fate Outcomes
The distinction between symmetric and asymmetric divisions lies in the fate of the daughter cells relative to their parent. The following table summarizes the key characteristics and outcomes of each division mode.
Table 1: Characteristics of Symmetric and Asymmetric Cell Divisions
| Feature | Symmetric Division | Asymmetric Division |
|---|---|---|
| Daughter Cell Fate | Two identical daughters | Two differentially fated daughters |
| Primary Role | Expansion or depletion of stem cell pool | Homeostatic maintenance of stem cell pool while generating differentiated progeny |
| Prevalence in Development | Early embryonic development (transient stem cells) [1] | Later embryonic stages and adult homeostasis (permanent stem cells) [1] |
| Fate Determinants Distribution | Equal distribution of cell fate determinants (e.g., transcription factors, organelles) [4] | Unequal (asymmetric) distribution of cell fate determinants [4] |
| Histone Variant Distribution | Symmetric (e.g., H3.1 and H3.3 in mouse muscle stem cells) [4] | Symmetric (observed in mouse muscle stem cells, unlike some invertebrate models) [4] |
| Spindle Orientation | Can be parallel or perpendicular to basement membrane, yielding symmetric outcomes [3] | Typically perpendicular to basement membrane, yielding asymmetric outcomes [3] |
Quantitative Analysis of Division Modes Across Biological Systems
The propensity for symmetric versus asymmetric division varies significantly across tissue types, developmental stages, and species. Quantitative data from lineage tracing and division tracking reveal this diversity.
Table 2: Quantitative Analysis of Division Modes in Different Biological Systems
| Biological System / Context | Symmetric Division Proportion | Asymmetric Division Proportion | Key Findings and Implications |
|---|---|---|---|
| Mouse Muscle Stem Cells (In Vivo) | Observed [4] | Observed [4] | Cells can switch from ACD to SCD ex vivo, indicating no obligate division mode [4]. |
| Developing Prostate Epithelium (Basal Cells, P15) | ~35% (Horizontal divisions) [3] | ~65% (Vertical divisions) [3] | Horizontal divisions yield two basal cells (symmetric); vertical divisions yield one basal and one luminal cell (asymmetric) [3]. |
| Mathematical Model of Mutagenesis | Variable parameter (θ) [2] | Variable parameter (1-θ) [2] | Symmetric divisions may generate double-hit mutants at a lower rate than asymmetric divisions, potentially delaying cancer onset [2]. |
| Prostate Luminal Cells (Developing) | ~100% [3] | ~0% [3] | Luminal cells divide almost exclusively symmetrically, with spindles horizontal to the basement membrane [3]. |
Experimental Methodologies for Investigating Division Modes
Single-Cell Tracking and Clonogenic Tracing on Artificial Niches
This methodology enables the direct observation of stem cell division patterns and fate outcomes in a controlled environment.
Protocol Workflow:
- Cell Isolation and Labeling: Muscle stem cells (MuSCs) are isolated from reporter mice, for example, expressing fluorescently tagged proteins for key transcription factors (e.g., Pax7) or using a histone H3-SNAP-tag for tracking chromatin inheritance [4].
- Seeding on Artificial Niches: Single cells are plated at low density on engineered substrates that mimic the native stem cell niche, such as specific extracellular matrix (ECM) components like laminin or fibronectin, within micro-patterned wells or soft hydrogels [4].
- Time-Lapse Live-Cell Imaging: Cultures are placed under a live-cell imaging microscope, capturing phase-contrast and fluorescence channels at regular intervals (e.g., every 10-30 minutes) over several days to track cell divisions and movements [4].
- Lineage Tracing and Fate Analysis: The recorded videos are analyzed to construct lineage trees. Division symmetry is assessed by tracking the fate of each daughter cell—whether it remains a stem cell or initiates differentiation (e.g., by expressing Myogenin) over multiple generations [4].
- Quantification of Asymmetry: Asymmetry is quantified by measuring the differential distribution of fate determinants (e.g., fluorescence intensity of Pax7 between daughter cells) or old vs. new DNA strands using pulse-chase labeling [4].
In Vivo Lineage Tracing and Division Axis Analysis
This approach investigates division modes within the intact tissue context, preserving native niche interactions.
Protocol Workflow:
- Genetic Labeling: Use of inducible, cell-type-specific Cre-loxP systems in transgenic mice (e.g., K14CreER for basal cell lineage tracing) [3]. Administration of tamoxifen induces permanent fluorescent labeling (e.g., RFP) in a specific stem or progenitor population.
- Tissue Collection and Sectioning: Harvest tissues of interest (e.g., prostate) at defined time points post-induction. Tissues are fixed, processed, and sectioned for immunohistochemistry [3].
- Immunofluorescence and Spindle Orientation: Tissue sections are stained with antibodies against:
- Cell Lineage Markers: e.g., p63/CK5 for basal cells, CK8/CK18/AR for luminal cells [3].
- Mitotic and Polarity Markers: e.g., γ-tubulin (centrosomes), Survivin (midbody), Phospho-Histone H3 (mitotic cells), Par3/aPKC (cell polarity) [3].
- Junctional Markers: e.g., ZO-1 (tight junctions), E-cadherin (adherens junctions) [3].
- Confocal Microscopy and 3D Reconstruction: High-resolution z-stack images of mitotic cells are acquired using confocal microscopy. The angle of the mitotic spindle relative to the basement membrane is measured in 3D [3].
- Fate Mapping of Daughter Cells: The identity of newly formed daughter cells in anaphase/telophase is determined by colocalization of the midbody marker (Survivin) with lineage-specific markers (e.g., p63 and CK8), confirming whether the division was symmetric (daughters of same lineage) or asymmetric (daughters of different lineages) [3].
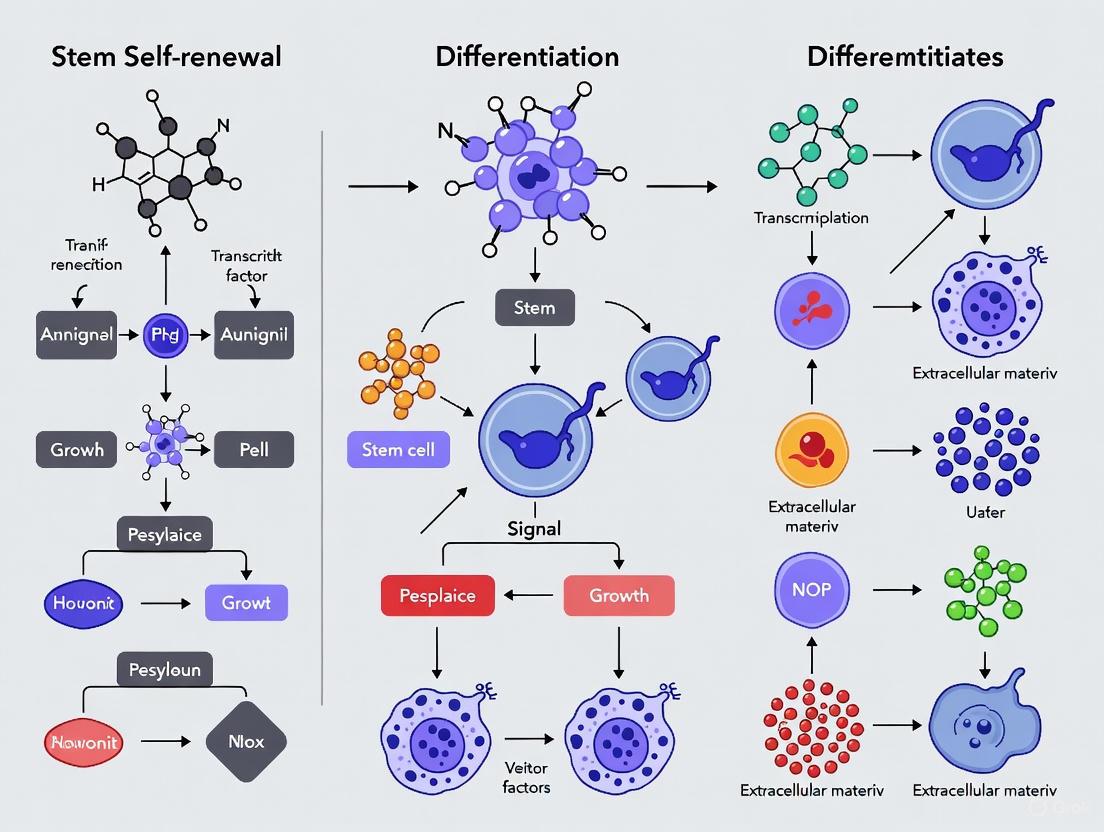
Diagram 1: Experimental workflows for analyzing stem cell division modes.
Molecular Regulators and Signaling Pathways
Key Molecular Players in Division Asymmetry
The execution of asymmetric cell division requires the coordinated action of several conserved molecular systems that establish cell polarity, orient the mitotic spindle, and ensure the asymmetric segregation of cell fate determinants.
Diagram 2: Molecular network regulating asymmetric and symmetric division.
The Scientist's Toolkit: Essential Research Reagents
Investigating stem cell division modes requires a specialized set of reagents and tools. The following table details key resources for designing experiments in this field.
Table 3: Essential Research Reagents for Studying Stem Cell Division Modes
| Reagent / Tool Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Genetically Modified Mouse Models | Pax7-reporter mice; H3-SNAP-tag mice; K14CreER; RosaRFP (or RosaYFP/tdTomato) [4] [3] | Enables lineage tracing, fate mapping, and live imaging of specific stem cell populations and their progeny in vivo and ex vivo. |
| Cell Surface & Lineage Markers | CD73, CD90, CD105 (MSC positive); CD34, CD45 (MSC negative) [5]; p63, CK5 (basal); CK8, CK18, AR (luminal) [3] | Identifies and isolates pure populations of stem cells and their differentiated progeny via FACS or immunohistochemistry. |
| Polarity & Mitosis Protein Antibodies | Anti-Par3, Anti-aPKC, Anti-Gαi, Anti-LGN/Pins [3]; Anti-γ-tubulin, Anti-Survivin, Anti-Phospho-Histone H3 [3] | Visualizes the establishment of cell polarity and the orientation of the mitotic apparatus in fixed tissues. |
| Live-Cell Imaging Tools | SNAP-tag substrates (for histone pulse-chase) [4]; Fluorescent ubiquitination-based cell cycle indicator (FUCCI) | Tracks cell cycle progression, division kinetics, and the inheritance of cellular components in real time. |
| Artificial Niche Components | Laminin, Fibronectin, Collagen; Polyethylene glycol (PEG) hydrogels; Micropatterned surfaces [4] | Provides controlled extracellular environments (e.g., stiffness, ligand density) to study the impact of the niche on division mode. |
Discussion: Implications for Development, Regeneration, and Disease
The strategic balance between symmetric and asymmetric divisions has profound implications beyond basic development. From a therapeutic perspective, the ability of stem cells to switch from asymmetric to symmetric divisions, as observed in mouse muscle stem cells ex vivo, highlights a fundamental plasticity that could be harnessed for regenerative medicine [4]. Expanding stem cell populations through symmetric self-renewal is a critical step in generating sufficient material for cell-based therapies aimed at treating conditions like Parkinson's disease, diabetes, and liver disease [6].
Furthermore, the choice of division mode has significant consequences for tissue-level robustness and cancer risk. Theoretical modeling suggests that tissues relying on symmetric divisions may have a mechanism to delay the accumulation of oncogenic mutations, such as the two-hit process required for tumor suppressor gene inactivation [2]. This is because the stochastic fate decisions in a symmetrically-dividing population can lead to the passive loss of intermediate mutant clones, a phenomenon less likely in a rigidly asymmetric system where every stem cell division retains a stem daughter. This provides a potential evolutionary hypothesis for the prevalence of symmetric divisions in mammalian tissues [2].
Dysregulation of the molecular machinery governing asymmetric division is increasingly linked to tumorigenesis. In the prostate, for example, both basal and luminal cells can serve as cancer cells of origin, and the disruption of polarity proteins like PTEN, which interacts with the Par complex, is a common event [3]. This underscores the critical importance of understanding the molecular regulation of stem cell division modes not only for regenerative medicine but also for uncovering the fundamental origins of cancer and developing novel therapeutic strategies.
Transcriptional and Post-Transcriptional Control Mechanisms
Stem cell fate, encompassing the fundamental processes of self-renewal and differentiation, is governed by a complex interplay of regulatory mechanisms that operate at multiple levels. Transcriptional control establishes the foundational gene expression programs through the action of transcription factors and epigenetic modifications, while post-transcriptional regulation provides a refined layer of control that fine-tunes protein synthesis in response to dynamic cellular cues. Operating as an integrated network, these mechanisms ensure precise temporal and spatial control of gene expression that is essential for maintaining pluripotency, directing lineage specification, and enabling stem cells to contribute to development, tissue homeostasis, and regeneration. A comprehensive understanding of these regulatory hierarchies is paramount for advancing stem cell biology and unlocking their therapeutic potential in regenerative medicine and drug development. This review synthesizes current knowledge of these control mechanisms, framing them within the context of stem cell self-renewal and differentiation, and provides detailed methodologies for their experimental investigation.
Transcriptional Control Mechanisms
Transcriptional regulation constitutes the primary tier of control in stem cell fate determination, establishing the specific gene expression patterns that define cell identity and potential.
Core Transcription Factor Networks
The maintenance of pluripotency in embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) is orchestrated by a core set of transcription factors that form autoregulatory loops to sustain their undifferentiated state. These core pluripotency factors include OCT4, SOX2, and NANOG, which collaboratively bind to and activate their own promoters as well as those of other genes essential for self-renewal, while simultaneously repressing genes involved in differentiation [7]. The forced expression of these and other factors (such as Klf4 and c-Myc) is sufficient to reprogram somatic cells into iPSCs, demonstrating their powerful role in establishing pluripotency [7]. In adult stem cell populations, transcription factor networks become more tissue-specific. For example, in hematopoietic stem cells (HSCs), a distinct set of transcription factors including PU.1, RUNX1, and GATA2 regulates the balance between self-renewal and differentiation into various blood lineages [8]. The directed manipulation of these networks is a primary strategy in controlling stem cell fate for therapeutic applications.
Epigenetic Regulation
Epigenetic modifications provide a heritable, yet reversible, layer of transcriptional control that does not alter the underlying DNA sequence. These mechanisms are critical for locking in cell fate decisions during differentiation.
- DNA Methylation: The addition of methyl groups to cytosine residues in CpG islands is generally associated with transcriptional repression. In stem cells, the promoters of developmental genes often exist in a "bivalent" state, bearing both activating and repressing histone marks, allowing them to be rapidly activated or permanently silenced upon differentiation cues. DNA methyltransferases (DNMTs) and TET proteins, which catalyze demethylation, are essential for these dynamic changes [8].
- Histone Modifications: Post-translational modifications of histone tails, including acetylation, methylation, phosphorylation, and ubiquitination, alter chromatin structure and accessibility. For instance, histone acetylation by co-activators like p300 and CBP is typically linked to open chromatin and active transcription, as seen at pluripotency gene promoters in ESCs. Conversely, repressive complexes such as Polycomb group (PcG) proteins deposit H3K27me3 marks to silence developmental genes, maintaining them in a poised state until differentiation [9] [8].
Table 1: Key Transcriptional Regulators in Stem Cell Fate
| Regulator/Modification | Type | Function in Stem Cells | Experimental Evidence |
|---|---|---|---|
| OCT4/SOX2/NANOG | Transcription Factor Network | Maintain pluripotency; form autoregulatory loops; repress differentiation genes. | iPSC generation; ChIP-seq shows co-occupancy at target promoters [7]. |
| Polycomb Repressive Complex (PRC2) | Chromatin Modifier | Catalyzes H3K27me3 for facultative heterochromatin formation, poising developmental genes for activation. | Loss-of-function leads to premature differentiation; ChIP-seq reveals bivalent domains [9]. |
| p300/CBP | Transcriptional Co-activator | Histone acetyltransferases that open chromatin; interact with β-catenin and other transcription factors. | Genetic ablation impairs self-renewal; regulates Wnt/β-catenin enhanceosome [10]. |
| BMP-SMAD | Signaling Pathway & Transcription Mediator | Promotes self-renewal in ESCs (via ID proteins) and differentiation in adult stem cells. | SMAD4 knockout ESCs show differentiation defects; phospho-SMAD1/5/8 ChIP [9]. |
Signaling Pathways and Transcriptional Integration
Extracellular signals from the stem cell niche are transduced to the nucleus and integrated by transcription factors to dictate cell fate. The Wnt/β-catenin pathway is a quintessential example. In the absence of Wnt signaling ("OFF state"), a destruction complex containing AXIN, APC, CK1α, and GSK3β phosphorylates β-catenin, leading to its ubiquitination by SCF^β-TrCP and proteasomal degradation. Upon Wnt binding ("ON state"), the destruction complex is disassembled, allowing β-catenin to accumulate and translocate to the nucleus. There, it partners with transcription factors from the TCF/LEF family (and others like SOX factors) to form an enhanceosome that activates target genes such as MYC and CCND1, which promote self-renewal and proliferation [10] [11]. Other critical pathways include TGF-β/BMP, Notch, and Hedgehog, each engaging specific SMAD or other transcription factors to regulate distinct aspects of stem cell behavior, from maintaining quiescence to inducing lineage-specific differentiation [9].
Post-Transcriptional Control Mechanisms
After a gene is transcribed, its expression can be extensively modulated through a diverse array of post-transcriptional mechanisms. These controls are particularly critical in stem cells and during early development, where rapid and localized changes in protein synthesis are required in response to environmental signals.
mRNA Stability and Translation: The Role of the Poly(A) Tail
A major hub for post-transcriptional control is the 3' poly(A) tail of mRNAs. This tail interacts with the 5' cap structure to promote mRNA circularization and facilitate translation initiation. It also protects the mRNA from exonucleolytic degradation. The length of the poly(A) tail is dynamically regulated by opposing enzymes: poly(A) polymerases add adenosine residues, while deadenylases remove them [12]. Shortening of the tail (deadenylation) is often the first and rate-limiting step in mRNA decay but can also lead to translational repression without decay. Recent breakthroughs in high-throughput sequencing methods, such as those detailed by Miao et al., have enabled precise measurement of poly(A) tail lengths genome-wide, revealing the central role of this regulation in stem cell fate and early embryonic development [12]. Key deadenylase complexes, like the CCR4-NOT complex, are crucial for controlling mRNA turnover in developing systems, including early lymphocyte development [12].
RNA-Binding Proteins and Their Functions
RNA-binding proteins (RBPs) are effectors of post-transcriptional control, recognizing specific sequences or structures in target mRNAs to influence their fate.
- Pumilio Proteins: These RBPs bind to the 3' untranslated regions (UTRs) of mRNAs and typically repress their translation. In stem cells, different family members have distinct roles; PUM1 promotes differentiation, whereas PUM2 supports self-renewal by regulating the translation of a network of over a thousand mRNAs [13].
- PIWI Proteins and piRNAs: A novel layer of regulation involves PIWI-interacting RNAs (piRNAs), small non-coding RNAs that partner with PIWI proteins. These complexes are capable of silencing transposable elements and post-transcriptionally regulating mRNAs through endonucleolytic cleavage ("slicing"), thereby safeguarding the genomic integrity and functional repertoire of stem cells [13].
Table 2: Key Post-Transcriptional Regulators in Stem Cell Fate
| Regulator | Type | Mechanism of Action | Impact on Stem Cells |
|---|---|---|---|
| CCR4-NOT Complex | Deadenylase Complex | Catalyzes mRNA deadenylation, leading to translational repression and/or decay. | Regulates early lymphocyte development; controls mRNA stability in stem cells [12]. |
| Pumilio (PUM1/PUM2) | RNA-Binding Protein (RBP) | Binds 3' UTRs to repress translation of target mRNAs. | PUM1 promotes differentiation; PUM2 enhances self-renewal [13]. |
| PIWI/piRNA Complex | Small Non-coding RNA & RBP | Binds piRNAs to degrade complementary mRNAs (e.g., transposons). | Maintains genome stability; novel regulatory pathway in stem cells [13]. |
| β-Catenin | Signaling Molecule & RBP Regulator | Can bind RNAs and influence pre-mRNA splicing (e.g., ER-β, PSA). | Non-canonical role beyond transcription; generates splice variants with altered function [10]. |
Alternative Splicing and Localization
Alternative splicing allows a single gene to produce multiple protein isoforms with distinct functions. Evidence suggests that even canonical transcriptional regulators can influence this process. For instance, β-catenin, the central effector of Wnt signaling, has been shown to modulate splice site selection. In HeLa cells, β-catenin transfection induced the expression of a specific estrogen receptor-β (ER-β) variant (ER-β Δ5-6) that acts as a dominant-negative isoform [10]. This indicates that signaling pathways can exert multifaceted control over gene expression by influencing both transcription and RNA processing. Furthermore, the subcellular localization of mRNAs, directed by RBPs, allows for localized protein synthesis, which is crucial in polarized cells such as neurons and during asymmetric stem cell divisions.
Integrated Experimental Analysis of Transcriptional and Post-Transcriptional Control
To fully understand gene regulation during stem cell differentiation, it is essential to employ integrated methodologies that capture both transcriptional and post-transcriptional events. A powerful approach involves combining total RNA-seq (reflecting the transcriptome) with polysome profiling (reflecting the translatome) [14].
Experimental Protocol: Polysome Profiling for Translational State Analysis
The following protocol, adapted from research published in BMC Genomics, allows for the separation and analysis of mRNAs based on their translational efficiency [14].
- Cell Culture and Differentiation: Human embryonic stem cells (e.g., H1 line) are cultured and induced to differentiate into the three germ layers (endoderm, mesoderm, neuroectoderm) using established monolayer protocols with specific factors (e.g., CHIR99021 and Activin A for endoderm) [14].
- Cycloheximide Treatment and Lysis: At desired time points (e.g., day 4 for endoderm), cells are treated with cycloheximide (0.1 mg/mL for 10 min) to arrest ribosomes on mRNA. Cells are then lysed in a buffer containing MgCl₂, NaCl, Triton X-100, and RNase inhibitors [14].
- Sucrose Gradient Centrifugation: The cell lysate is layered onto a 10-50% linear sucrose gradient and centrifuged at high speed (e.g., 270,000 × g for 120 min at 4°C) to separate ribosomal complexes based on density [14].
- Fractionation and RNA Isolation: The gradient is fractionated using a system that monitors UV absorbance at 254 nm. The resulting profile shows peaks for 40S/60S subunits, 80S monosomes, and polysomes (mRNAs bound by multiple ribosomes). Polysome-containing fractions are pooled, and RNA is extracted for subsequent sequencing [14].
- Data Analysis: Sequencing data from total RNA and polysome-bound RNA are analyzed (e.g., using HISAT2 for alignment and DESeq2 for differential expression). Comparing these datasets identifies genes subject to post-transcriptional regulation—e.g., those whose transcript levels remain unchanged but which show significant changes in polysome association [14].
This integrated analysis has revealed substantial post-transcriptional modulation during germ layer commitment, highlighting that the translatome captures regulatory nuances often missed by transcriptomics alone [14].
Visualization of an Integrated Regulatory Pathway
The diagram below synthesizes the canonical Wnt/β-catenin signaling pathway with its non-canonical, post-transcriptional roles, illustrating the multi-level control it exerts on stem cell fate.
Diagram 1: The Wnt/β-catenin pathway integrates transcriptional and post-transcriptional control. In the "OFF" state, β-catenin is degraded, and TCF/LEF factors recruit repressors. In the "ON" state, stabilized β-catenin enters the nucleus to activate transcription. Non-canonically, nuclear β-catenin can also modulate pre-mRNA splicing and interact with RBPs, adding a layer of post-transcriptional regulation to its function in stem cell fate [10].
The Scientist's Toolkit: Key Reagents and Methodologies
Table 3: Essential Research Reagent Solutions for Studying Gene Regulation in Stem Cells
| Reagent / Tool | Function/Application | Example Use Case |
|---|---|---|
| CHIR99021 | Small molecule inhibitor of GSK3β; activates Wnt/β-catenin signaling. | Used in differentiation protocols (e.g., endoderm, mesoderm) to direct stem cell fate [14]. |
| Activin A | Cytokine; activates TGF-β/SMAD2/3 signaling pathway. | Key component in definitive endoderm differentiation from hESCs [14]. |
| Y-27632 (ROCK inhibitor) | Small molecule inhibitor of ROCK kinase; reduces apoptosis in single cells. | Improves survival of hESCs after passaging or thawing during experimental setup [14]. |
| Cycloheximide | Translation inhibitor; arrests ribosomes on mRNA. | Essential for polysome profiling experiments to "freeze" translating ribosomes [14]. |
| CRISPR/Cas9 System | Gene editing technology; enables knockout, knockin, or mutagenesis of specific genes. | Studying the functional role of transcription factors (e.g., OCT4) or RBPs in stem cell self-renewal and differentiation [9] [8]. |
| Single-Cell RNA Sequencing (scRNA-seq) | High-resolution profiling of gene expression in individual cells. | Resolving cellular heterogeneity in stem cell populations and identifying rare subpopulations [15] [7]. |
| Poly(A) Tail Sequencing Kits | High-throughput measurement of poly(A) tail length for transcriptome-wide analysis. | Investigating the role of deadenylation in mRNA stability during stem cell differentiation [12]. |
PIWI-interacting RNAs (piRNAs) are a distinct class of 24-31 nucleotide small non-coding RNAs that form complexes with PIWI proteins to play multifaceted roles in epigenetic regulation and mRNA stability maintenance. Originally characterized in the germline for transposable element suppression, these molecules have emerged as critical regulators in stem cell biology, particularly in balancing self-renewal and differentiation. This technical review synthesizes current mechanistic insights into piRNA biogenesis, their epigenetic functions through DNA methylation and histone modifications, and their post-transcriptional regulatory roles via mRNA cleavage and translational control. Within the context of stem cell self-renewal and differentiation mechanisms, we detail experimental approaches for investigating piRNA pathways and provide key research tools. The growing evidence positions the PIWI/piRNA pathway as an essential epigenetic regulator in stem cell fate determination with significant implications for regenerative medicine and therapeutic development.
PIWI-interacting RNAs (piRNAs) are single-stranded RNA molecules typically 24-31 nucleotides in length, making them the longest class of small non-coding RNAs [16]. They are distinguished from other small RNAs by their strong preference for a 5' uridine residue, 2'-O-methylation at their 3' terminus, and their Dicer-independent biogenesis pathway [17]. These molecules were initially discovered in Drosophila germline cells and have since been identified across diverse species, with approximately 30,000 piRNAs documented in the human genome [17].
piRNAs function through association with PIWI proteins, a conserved subfamily of Argonaute proteins predominantly expressed in germline cells [16] [18]. These PIWI/piRNA complexes form the core of a sophisticated genomic defense system that silences transposable elements (TEs) and regulates gene expression at both transcriptional and post-transcriptional levels [16]. The PIWI protein family includes multiple members across species: humans possess four PIWI proteins (PIWIL1/HIWI, PIWIL2/HILI, PIWIL3/HIWI3, and PIWIL4/HIWI2), while Drosophila has three (Piwi, Aubergine/Aub, and Argonaute 3/Ago3) [19].
Structurally, PIWI proteins contain four conserved domains: N-terminal, PAZ, MID, and PIWI domains, connected by L1 and L2 linkers [16]. The PIWI domain possesses endonucleolytic "slicer" activity mediated by a conserved catalytic triad that enables precise cleavage of RNA targets guided by bound piRNAs [16]. Beyond their canonical role in germline development, PIWI/piRNA pathways have gained significant attention for their functions in somatic stem cells and their dysregulation in various pathological conditions, including cancer [16] [20].
Table 1: Key Characteristics of piRNAs Compared to Other Small Non-Coding RNAs
| Feature | piRNA | miRNA | siRNA |
|---|---|---|---|
| Length (nt) | 24-31 | 19-25 | 20-25 |
| 5' End Bias | Uracil | None | None |
| 3' Modification | 2'-O-methylation | None | None |
| Biogenesis | Dicer-independent | Dicer-dependent | Dicer-dependent |
| Primary Function | TE silencing, gene regulation | mRNA degradation, translation repression | Viral defense, transgene silencing |
| Expression Pattern | Germline, somatic stem cells | Ubiquitous | Ubiquitous |
| Protein Partners | PIWI proteins | AGO proteins | AGO proteins |
piRNA Biogenesis Pathways
piRNA biogenesis occurs through two interconnected yet distinct pathways that ensure a diverse and abundant piRNA population: the primary processing pathway and the secondary "ping-pong" amplification pathway. Both pathways are essential for generating mature, functional piRNAs that maintain genome integrity and regulate gene expression.
Primary Biogenesis Pathway
The primary biogenesis pathway begins with the transcription of piRNA cluster regions in the genome by RNA polymerase II [16]. These piRNA clusters are specific genomic regions rich in transposable element fragments and can be either unistrand (transcribed from one strand) or dual-strand (transcribed from both strands) [19]. In Drosophila, dual-strand cluster transcription in germ cells depends on the Rhino-Deadlock-Cutoff (RDC) complex that recognizes H3K9me3 marks and facilitates non-canonical transcription [20]. In contrast, unistrand clusters in somatic cells are transcribed through canonical Pol II mechanisms dependent on the Cubitus interruptus transcription factor [20].
Following transcription, precursor transcripts are exported to the cytoplasm via specific nuclear export complexes (Nxf3-Nxt1 for germline clusters; Nxf1-Nxt1 for somatic clusters) [20]. These long precursor transcripts are processed at cytoplasmic perinuclear foci known as nuage in germ cells or Yb-bodies in somatic cells [21]. The endonuclease Zucchini (Zuc in Drosophila; PLD6 in mice) cleaves the precursor transcripts, generating pre-piRNAs with 5' monophosphate ends [16] [19]. These intermediates are then loaded onto PIWI proteins, after which their 3' ends are trimmed by the exonuclease Trimmer (PNLDC1) to achieve final length [16]. The mature piRNAs undergo 2'-O-methylation at their 3' terminus catalyzed by the methyltransferase Hen1, which enhances their stability [16] [19]. The resulting PIWI/piRNA complexes are then trafficked to their appropriate cellular compartments—nuclear localization for transcriptional silencing or cytoplasmic retention for post-transcriptional regulation.
Secondary Biogenesis and Ping-Pong Amplification
The secondary biogenesis pathway, known as the ping-pong cycle, amplifies piRNA populations through a reciprocal cleavage mechanism that occurs predominantly in germ cells [16] [21]. This cycle involves two cytoplasmic PIWI proteins: in Drosophila, Aub and Ago3 [21]. The cycle initiates when a primary piRNA bound to Aub (with antisense orientation to TEs) recognizes and cleaves complementary transposon transcripts. This cleavage generates the 5' end of a new piRNA fragment that is loaded onto Ago3 [21] [19]. The Ago3-bound piRNA (with sense orientation) then reciprocally cleaves precursor transcripts from piRNA clusters, generating the 5' end of a new Aub-bound piRNA [21]. This reciprocal relationship creates a self-sustaining amplification loop that efficiently targets active transposable elements.
A distinctive feature of ping-pong-derived piRNAs is their 10-nucleotide complementarity at the 5' ends—Aub-bound piRNAs typically begin with uridine (1U bias), while Ago3-bound piRNAs exhibit adenine at position 10 (10A bias) [21]. This signature results from the precise cleavage mechanism occurring 10 nucleotides upstream of the 5' end of the guiding piRNA [19]. The ping-pong cycle dramatically amplifies piRNA populations, enabling robust suppression of actively transposing elements while maintaining a diverse piRNA repertoire capable of recognizing emerging TE threats.
Epigenetic Regulation by piRNAs
The PIWI/piRNA pathway constitutes a major epigenetic regulatory system that maintains genome stability primarily through silencing transposable elements and regulating gene expression at the transcriptional level. This regulatory capacity is particularly critical in stem cell populations, where maintaining epigenetic integrity is essential for proper self-renewal and differentiation potential.
Transcriptional Gene Silencing Mechanisms
Nuclear-localized PIWI/piRNA complexes mediate transcriptional gene silencing through multiple interconnected epigenetic mechanisms. The best-characterized function involves repression of transposable elements through histone modifications and DNA methylation [19]. In Drosophila, the Piwi/piRNA complex recruits histone methyltransferases that catalyze H3K9 methylation, creating repressive chromatin marks that inhibit transcription initiation [18] [19]. This heterochromatin formation spreads to adjacent genomic regions, effectively silencing embedded transposable elements.
In mammalian systems, PIWI/piRNA complexes play a crucial role in guiding de novo DNA methylation during gametogenesis. The MIWI2/piRNA complex in mice interacts with SPOCD1 to recruit DNA methyltransferases to transposable element loci, establishing DNA methylation patterns that persist through development [19]. This DNA methylation-dependent silencing represents a more stable, long-term repression mechanism that is particularly important for maintaining germline genomic integrity across generations.
Beyond transposable element control, PIWI/piRNA complexes also regulate protein-coding genes through similar epigenetic mechanisms. In germline stem cells, Piwi-mediated silencing of key developmental regulators helps maintain the undifferentiated state by preventing premature expression of differentiation factors [18] [21]. The specificity of this regulation depends on sequence complementarity between piRNAs and target genomic loci, often involving piRNAs derived from specific regions of the genes they regulate.
Chromatin Remodeling and Organization
PIWI/piRNA complexes contribute to higher-order chromatin organization and nuclear architecture. By directing heterochromatin formation to specific genomic loci, these complexes help establish repressive nuclear compartments that limit accessibility of transcriptional machinery [18]. In germline stem cells, this chromatin remodeling function extends to the regulation of genes involved in self-renewal and differentiation decisions.
Recent evidence suggests that piRNAs can guide chromatin modifications beyond H3K9 methylation, including H3K27 methylation and histone deacetylation [19]. The combinatorial effect of these modifications creates a repressive chromatin state that is resistant to activation signals. Additionally, PIWI proteins interact with various chromatin remodeling complexes, facilitating nucleosome repositioning and chromatin compaction at target loci [18].
The epigenetic regulatory functions of PIWI/piRNA complexes exhibit remarkable adaptability, as the piRNA population can rapidly evolve to target newly active transposable elements or regulate different gene sets in response to developmental cues. This dynamic regulation is particularly important in stem cell niches, where epigenetic states must balance stability with plasticity to enable proper differentiation capacity.
Table 2: Epigenetic Modifications Mediated by PIWI/piRNA Complexes
| Epigenetic Modification | Molecular Mechanism | Biological Outcome | Stem Cell Context |
|---|---|---|---|
| H3K9me3 | Recruitment of H3K9 methyltransferases | Heterochromatin formation, transcriptional repression | Maintains undifferentiated state by silencing differentiation genes |
| De novo DNA methylation | Recruitment of DNMTs via SPOCD1 | Stable long-term gene silencing | Imprints transposon silencing during germline development |
| Histone deacetylation | Recruitment of HDAC complexes | Chromatin compaction, reduced accessibility | Prevents premature activation of developmental genes |
| Chromatin remodeling | Interaction with remodeling complexes (SWI/SNF) | Altered nucleosome positioning | Regulates accessibility of self-renewal gene promoters |
piRNA-Mediated mRNA Stability and Translation Control
Beyond their nuclear functions in epigenetic regulation, PIWI/piRNA complexes play crucial roles in the cytoplasm through post-transcriptional regulatory mechanisms that impact mRNA stability and translation. These functions are particularly important for the rapid gene expression changes required during stem cell differentiation and fate determination.
Post-Transcriptional Gene Silencing
Cytoplasmic PIWI/piRNA complexes mediate post-transcriptional gene silencing through mechanisms analogous to RNA interference pathways. The endonucleolytic "slicer" activity of PIWI proteins enables direct cleavage of target mRNAs when guided by perfectly complementary piRNAs [22] [19]. This mechanism is particularly effective for degrading transposable element transcripts, preventing their translation and subsequent transposition [18].
In addition to direct cleavage, PIWI/piRNA complexes can recruit additional RNA degradation machinery to target transcripts. In Drosophila, Aub/piRNA complexes interact with the CCR4-NOT deadenylase complex, leading to removal of the mRNA poly(A) tail and subsequent degradation [22] [18]. This mechanism allows for more regulated control of mRNA stability compared to direct cleavage and is employed for fine-tuning expression of protein-coding genes involved in stem cell maintenance and differentiation.
The ping-pong cycle itself represents a form of post-transcriptional regulation, as it directly consumes transposon transcripts to generate secondary piRNAs while simultaneously degrading these potentially harmful RNAs [21]. This dual functionality creates an efficient defense system that both neutralizes immediate threats and enhances future response capability through piRNA population amplification.
Translational Regulation
Emerging evidence indicates that PIWI/piRNA complexes can directly regulate translation of target mRNAs without necessarily inducing their degradation [21]. In germline stem cells, Aub/piRNA complexes have been shown to associate with specific mRNAs and either promote or repress their translation depending on cellular context and associated protein partners [21].
For instance, in Drosophila germline stem cells, Aub promotes translation of glycolytic enzymes by interacting with translation initiation factors, including PABP and eIF3 [21]. This enhanced glycolytic flux supports the unique metabolic state of stem cells. Conversely, Aub can repress translation of differentiation-promoting factors like Cbl through recruitment of translational repressors [21]. This dual capacity for activation and repression allows for precise control of the proteome in response to developmental signals.
The regulatory specificity of cytoplasmic PIWI/piRNA complexes is determined by both sequence complementarity between piRNAs and target mRNAs, and the particular suite of protein cofactors associated with the complex in different cellular contexts. This contextual regulation enables the same molecular machinery to produce opposing outcomes depending on the stem cell state, contributing to the delicate balance between self-renewal and differentiation.
piRNAs in Stem Cell Self-Renewal and Differentiation
The PIWI/piRNA pathway plays a pivotal role in regulating the balance between stem cell self-renewal and differentiation, particularly in germline stem cells (GSCs) where these molecules were first characterized. Recent evidence indicates similar functions in various somatic stem cell populations, highlighting the conserved importance of this regulatory system in stem cell biology.
Regulation of Germline Stem Cell Maintenance
In Drosophila germline stem cells, Piwi maintains the self-renewal capacity through both cell-autonomous and non-cell-autonomous mechanisms [18] [21]. Within GSCs, Piwi mediates transcriptional silencing of transposable elements and specific differentiation-promoting genes through epigenetic mechanisms, preserving genomic integrity and maintaining the undifferentiated state [18]. The loss of Piwi function leads to TE derepression, DNA damage accumulation, and eventual GSC depletion [18].
In somatic niche cells surrounding GSCs, Piwi regulates key signaling pathways that support stem cell maintenance. In escort cells, Piwi suppresses the expression of Dpp (BMP) signaling components, preventing excessive self-renewal signals that could disrupt the balance between stem cell maintenance and differentiation [18] [21]. Additionally, Piwi directly targets and cleaves c-Fos mRNA in niche cells, reducing AP-1 signaling and maintaining proper niche architecture and function [18].
The Aub protein contributes to GSC maintenance through translational control of metabolic regulators. Aub promotes translation of glycolytic enzymes in GSCs, supporting the glycol metabolic state characteristic of stem cells [21]. During differentiation, mitochondrial maturation facilitates a shift toward oxidative phosphorylation, and Aub-mediated translational control helps coordinate this metabolic transition.
Control of Differentiation Programs
As germline stem cells initiate differentiation, the PIWI/piRNA pathway facilitates this transition through regulated control of differentiation factors. Aub plays a particularly important role in promoting differentiation by modulating the expression of key differentiation regulators at both transcriptional and translational levels [18].
Aub directly regulates the expression of differentiation factors such as Bam (bag of marbles) through post-transcriptional mechanisms [18]. In GSCs, Aub represses Cbl mRNA via recruitment of the CCR4-NOT complex, but this repression is alleviated in cystoblasts, allowing increased Cbl expression that promotes differentiation [21]. This dynamic regulation enables precise control of the timing and progression of differentiation.
Beyond germline stem cells, PIWI/piRNA pathways function in various somatic stem cell populations. In Drosophila intestinal stem cells, Piwi regulates genome integrity and metabolic pathways that impact longevity and gut homeostasis [21]. In highly regenerative species like planarians, PIWI proteins are essential for somatic stem cell function and regenerative capacity [21]. These conserved functions highlight the broad importance of PIWI/piRNA pathways in stem cell biology across tissues and species.
Table 3: PIWI/piRNA Functions in Stem Cell Regulation
| PIWI Protein | Stem Cell Type | Molecular Function | Biological Outcome |
|---|---|---|---|
| Piwi | Germline Stem Cells | Transcriptional silencing of TEs and differentiation genes | Maintains undifferentiated state, prevents premature differentiation |
| Piwi | Escort Cells (niche) | Repression of Dpp signaling, c-Fos mRNA cleavage | Regulates niche signaling, maintains proper stem cell niche architecture |
| Aubergine (Aub) | Germline Stem Cells | Translational activation of glycolytic enzymes | Supports stem cell metabolism, promotes self-renewal |
| Aubergine (Aub) | Cystoblasts | mRNA degradation of self-renewal factors | Promotes differentiation, prevents excessive self-renewal |
| PIWI proteins | Somatic Stem Cells | Genome stability maintenance, gene expression regulation | Supports regenerative capacity, tissue homeostasis |
Experimental Approaches and Methodologies
Investigating PIWI/piRNA functions requires specialized methodological approaches tailored to their unique biogenesis, molecular interactions, and regulatory mechanisms. This section outlines key experimental protocols for studying piRNA biology in the context of stem cell research.
piRNA Identification and Characterization
Small RNA Sequencing: piRNA identification typically begins with small RNA sequencing using protocols that capture the 2'-O-methylated 3' terminus characteristic of mature piRNAs [23]. Standard small RNA-seq libraries should be prepared with 3' adapter ligation methods optimized for 2'-O-methylated RNAs. Bioinformatic analysis involves mapping sequences to piRNA clusters and transposable elements, with particular attention to the 1U/10A bias characteristic of ping-pong cycle products [24].
PIWI Protein Immunoprecipitation: PIWI/piRNA complexes can be isolated through immunoprecipitation using specific antibodies against PIWI proteins, followed by RNA extraction and sequencing to identify associated piRNAs [17]. This approach, often termed piRNA CLIP-seq, provides information about the specific piRNA repertoire associated with each PIWI protein and can reveal context-dependent binding patterns in different stem cell states.
In situ Hybridization and Localization: Cellular localization of piRNAs and PIWI proteins can be visualized using fluorescence in situ hybridization (FISH) for piRNAs combined with immunofluorescence for PIWI proteins [21]. This technique is particularly valuable for identifying subcellular compartments where piRNA biogenesis and function occur, such as nuage in germ cells or mitochondrial membranes where phased biogenesis takes place.
Functional Analysis of PIWI/piRNA Pathways
Genetic Manipulation: Loss-of-function studies using RNA interference or CRISPR-Cas9-mediated knockout of PIWI genes remain the gold standard for determining PIWI/piRNA functions [18] [21]. In stem cell systems, inducible knockout systems allow temporal control of gene disruption to distinguish between developmental and maintenance functions. Transgenic rescue experiments with wild-type or mutant PIWI proteins can dissect functional domains required for specific activities.
Target Validation: Experimental validation of piRNA targets involves luciferase reporter assays with wild-type and mutant target sequences to confirm direct regulation through complementary base pairing [19]. For epigenetic targets, chromatin immunoprecipitation (ChIP) for histone modifications or DNA methylation analysis can confirm transcriptional silencing at specific genomic loci.
Metabolic Labeling and Turnover Studies: Investigating piRNA effects on mRNA stability requires metabolic labeling approaches such as 4-thiouridine incorporation to measure transcript half-lives in the presence and absence of functional PIWI/piRNA pathways [18]. Similarly, ribosomal profiling can reveal translational regulation by providing snapshots of ribosome occupancy on target mRNAs under different conditions.
Research Reagent Solutions
The following table compiles essential research tools and reagents for investigating PIWI/piRNA functions in stem cell systems, with particular emphasis on applications in self-renewal and differentiation research.
Table 4: Essential Research Reagents for PIWI/piRNA Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| PIWI Antibodies | Anti-PIWI, Anti-Aub, Anti-Ago3 (Drosophila); Anti-HIWI, Anti-HILI (Human) | Immunoprecipitation, Western blot, Immunofluorescence | Species specificity critical; validate in knockout controls |
| piRNA Detection | 3' 2'-O-methyl sensitive adapters, PANDH2 antibody | Small RNA library preparation, piRNA detection | Standard small RNA protocols may underrepresent piRNAs |
| Genetic Tools | PIWI mutant flies, Conditional knockout mice, RNAi lines | Loss-of-function studies | Consider functional redundancy between PIWI family members |
| Stem Cell Models | Germline stem cells, Embryonic stem cells, Planarian stem cells | Functional studies in stem cell context | Species-specific piRNA characteristics may limit generalizability |
| Bioinformatic Tools | piRNA cluster annotation, Ping-pong signature analysis, TE expression analysis | piRNA identification, functional annotation | Custom pipelines often needed for specific experimental designs |
| Reporters | Luciferase reporters with target 3'UTRs, Heterochromatin reporters | Target validation, Silencing quantification | Include mismatch controls to confirm specificity |
The PIWI/piRNA pathway represents a sophisticated regulatory system that integrates epigenetic and post-transcriptional control mechanisms to maintain genome stability and regulate gene expression programs. In stem cell biology, this pathway plays particularly important roles in balancing self-renewal and differentiation, with functions identified in both germline and somatic stem cell populations. The dual capacity of PIWI/piRNA complexes to enact stable epigenetic silencing through chromatin modifications and rapidly respond to cytoplasmic transcripts through slicer activity makes them uniquely suited to stem cell regulation.
Future research directions should focus on elucidating the complete repertoire of piRNA functions in somatic stem cells, particularly in mammalian systems where these roles are less characterized. The development of more refined tools for piRNA detection and manipulation, especially in rare stem cell populations, will advance our understanding of their contributions to tissue homeostasis and regeneration. Additionally, the emerging connections between PIWI/piRNA pathways and cellular metabolism in stem cells warrant further investigation, as these links may reveal novel mechanisms coordinating metabolic state with fate decisions.
From a therapeutic perspective, the frequent dysregulation of PIWI/piRNA pathways in cancer and other diseases highlights their potential as therapeutic targets. The restricted expression of PIWI proteins in normal somatic tissues offers promising opportunities for targeted interventions with reduced off-target effects. As our understanding of PIWI/piRNA biology continues to expand, particularly in stem cell contexts, these insights will undoubtedly inform novel approaches to regenerative medicine, cancer therapy, and the manipulation of cell fate for therapeutic purposes.
Cellular quiescence, a reversible state of cell cycle arrest, is a fundamental property of stem cells that enables long-term tissue maintenance and regeneration. The precise control of quiescence is orchestrated by an intricate network of signaling pathways, with Transforming Growth Factor-beta (TGF-β), Bone Morphogenetic Protein (BMP), and the mechanistic Target of Rapamycin (mTOR) representing central regulators. The TGF-β/BMP signaling pathway is involved in the vast majority of cellular processes and is fundamentally important during the entire life of all metazoans, with deregulation of TGF-β/BMP activity almost invariably leading to developmental defects and/or diseases, including cancer [25]. The proper functioning of the TGF-β/BMP pathway depends on its constitutive and extensive communication with other signaling pathways, leading to synergistic or antagonistic effects and eventually desirable biological outcomes [25]. In stem cell biology, these pathways collectively maintain the delicate balance between self-renewal and differentiation, ensuring a protected reservoir of stem cells capable of responding to physiological demands.
The interplay between these pathways creates a sophisticated signaling network that interprets both intracellular and extracellular cues to determine stem cell fate. This network exhibits tremendous complexity and context-dependency, with the nature of signaling cross-talk being overwhelmingly complex and highly context-dependent [25]. In the context of stem cell self-renewal and differentiation mechanisms research, understanding these signaling networks provides critical insights for regenerative medicine applications, including the development of stem cell-based therapies that harness the therapeutic potential of stem cells for treating numerous debilitating illnesses and injuries [15].
Pathway Fundamentals and Molecular Mechanisms
TGF-β Signaling Pathway
The TGF-β pathway operates through a canonical signaling cascade that transmits extracellular signals to the nucleus. Ligand binding to type II TGF-β receptors leads to recruitment and phosphorylation of type I receptors, which subsequently phosphorylate receptor-regulated SMADs (R-SMADs), specifically SMAD2 and SMAD3. These activated R-SMADs form complexes with the common mediator SMAD4 and translocate to the nucleus, where they regulate the transcription of target genes involved in cell cycle arrest, apoptosis, and differentiation [25]. The pathway is tightly regulated by inhibitory SMADs (I-SMADs), including SMAD6 and SMAD7, which compete with R-SMADs for receptor binding or promote receptor degradation.
In stem cell quiescence, TGF-β signaling maintains hematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs) in a reversible dormant state through transcriptional regulation of cyclin-dependent kinase inhibitors p15 and p21. The cytostatic function of TGF-β is mediated through its effects on cell cycle regulators, effectively preventing premature stem cell exhaustion while preserving genomic integrity. Research has shown that TGF-β signaling is crucial for preventing HSC exhaustion and maintaining their long-term repopulating capacity, highlighting its fundamental role in stem cell homeostasis.
BMP Signaling Pathway
As part of the TGF-β superfamily, BMP signaling follows a similar canonical pathway with distinct components and functional outcomes. BMP ligands bind to type II BMP receptors, which phosphorylate type I receptors (ALK1, ALK2, ALK3, ALK6). These activated receptors then phosphorylate R-SMADs 1, 5, and 8, which form complexes with SMAD4 and translocate to the nucleus to regulate transcription of target genes involved in differentiation, proliferation, and survival [25]. The BMP pathway exhibits significant cross-talk with other signaling pathways, creating a sophisticated regulatory network that controls stem cell behavior.
In stem cell biology, BMP signaling plays contrasting roles depending on cellular context. In neural stem cells, BMP promotes differentiation and suppresses self-renewal, while in embryonic stem cells, it supports pluripotency. This contextual functionality demonstrates the complexity of BMP signaling in maintaining quiescence and controlling cell fate decisions. The balance between BMP and TGF-β signaling is particularly important in stem cell niches, where these pathways often exert opposing effects to maintain tissue homeostasis.
mTOR Signaling Pathway
The mTOR pathway functions as a central regulator of cellular metabolism and growth in response to nutrient availability, energy status, and growth factors. mTOR exists in two distinct complexes: mTORC1, which is rapamycin-sensitive and regulates cell growth, autophagy, and protein synthesis through phosphorylation of S6K1 and 4E-BP1; and mTORC2, which is rapamycin-insensitive and controls cell survival and metabolism through phosphorylation of AKT. The mTOR pathway integrates signals from multiple upstream regulators, including PI3K/AKT, AMPK, and growth factor receptors, to coordinate cellular processes with available resources.
In stem cell quiescence, mTOR activity is typically suppressed, reducing anabolic processes and conserving energy. Low mTORC1 activity is a hallmark of quiescent stem cells across multiple tissues, including HSCs, muscle stem cells, and neural stem cells. Activation of mTOR signaling drives stem cells out of quiescence and promotes proliferation and differentiation, making it a crucial switch in stem cell fate decisions. The careful regulation of mTOR activity ensures that stem cells remain protected from metabolic stress while maintaining their capacity for activation upon tissue demand.
Pathway Integration in Quiescence Regulation
The regulation of stem cell quiescence emerges from the sophisticated integration of TGF-β, BMP, and mTOR signaling pathways, which communicate through extensive cross-talk mechanisms. TGF-β/BMP signaling communicates with the Mitogen-activated protein kinase, phosphatidylinositol-3 kinase/Akt, Wnt, Hedgehog, Notch, and cytokine pathways, creating a network that determines stem cell fate decisions [25]. This cross-talk enables stem cells to respond appropriately to diverse environmental cues while maintaining the quiescent state.
A critical integration point occurs between TGF-β and mTOR signaling, where TGF-β can suppress mTORC1 activity through several mechanisms, including upregulation of negative regulators and modulation of AKT signaling. This suppression maintains stem cells in a quiescent, energy-conserving state. Conversely, BMP signaling often exhibits context-dependent interactions with mTOR, in some cases promoting mTOR activation to support stem cell differentiation. The interplay between these pathways creates a dynamic equilibrium that can be perturbed by changes in the microenvironment or systemic factors.
Table 1: Key Molecular Interactions in Quiescence Signaling Networks
| Pathway Interaction | Molecular Mechanism | Functional Outcome in Stem Cells |
|---|---|---|
| TGF-β to mTOR | SMAD-mediated transcription of mTOR inhibitors; regulation of AKT activity | Suppression of mTORC1; maintenance of quiescence |
| BMP to TGF-β | Competition for receptor complexes; modulation of I-SMAD expression | Context-dependent synergy or antagonism in fate decisions |
| mTOR to TGF-β/BMP | Regulation of SMAD phosphorylation and degradation; control of receptor expression | Modulation of pathway sensitivity and output |
| PI3K/AKT to mTOR | Direct activation of mTORC1 via TSC2 Rheb regulation | Exit from quiescence; promotion of proliferation |
The balance between these pathways is particularly important in the stem cell niche, where specialized microenvironmental cells provide precise combinations of ligands and regulators to maintain quiescence. In the bone marrow HSC niche, for example, TGF-β produced by niche cells maintains HSC quiescence, while BMP signaling contributes to the regulation of niche size and function. The integration of these signals with metabolic cues through mTOR allows stem cells to align their fate decisions with available resources and tissue needs.
Experimental Approaches for Signaling Network Analysis
Quantitative Proteomic and Phosphoproteomic Analysis
Advanced mass spectrometry-based techniques enable comprehensive quantification of signaling networks in stem cell populations. As demonstrated in studies of glioblastoma multiforme, quantitative proteomic and phosphoproteomic analysis can identify activated signaling networks from limited biological samples [26]. The experimental workflow involves:
Sample Preparation: Cells are homogenized in ice-cold 8M urea lysis buffer supplemented with protease and phosphatase inhibitors. Protein concentration is quantified using bicinchoninic acid (BCA) assay.
Protein Digestion: Proteins are reduced with 10mM DTT, alkylated with 50mM iodoacetamide, and digested with sequencing-grade trypsin at an enzyme-to-substrate ratio of 1:100.
Peptide Labeling: Peptides are labeled with isobaric tags (iTRAQ or TMT) to enable multiplexed quantification across multiple samples.
Phosphopeptide Enrichment: Phosphotyrosine peptides are enriched using a cocktail of anti-phosphotyrosine antibodies followed by immobilized metal affinity chromatography (IMAC).
Mass Spectrometry Analysis: Fractionated peptides are analyzed by liquid chromatography coupled to tandem mass spectrometry.
Data Processing: Raw data are processed using specialized software to identify proteins and phosphorylation sites, with quantification based on reporter ion intensities.
This approach allows researchers to simultaneously monitor multiple signaling pathways and their activation states, providing a systems-level view of signaling networks in quiescent stem cells.
Organoid-Based Signaling Studies
Three-dimensional organoid cultures provide a physiologically relevant model system for investigating signaling pathways in stem cell biology. Organoids mimic human tissue architecture and function, making them particularly valuable for studying the role of TGF-β signaling in stem cell maintenance and differentiation [27]. The methodology for organoid-based signaling studies includes:
Organoid Generation: Stem cells are embedded in extracellular matrix hydrogels and cultured with specific growth factor combinations to promote self-organization.
Pathway Modulation: Small molecule inhibitors, recombinant proteins, or genetic approaches are used to selectively activate or inhibit specific signaling pathways.
Phenotypic Readouts: Organoids are analyzed using microscopy, immunohistochemistry, and single-cell RNA sequencing to assess morphological changes and differentiation status.
Signaling Analysis: Pathway activity is monitored through phospho-specific antibodies, reporter constructs, or transcriptional targets.
Organoid systems enable the study of TGF-β, BMP, and mTOR signaling in a context that preserves native cell-cell interactions and microenvironmental cues, providing insights that may be missed in traditional 2D culture systems.
Table 2: Experimental Models for Studying Quiescence Signaling Networks
| Experimental System | Key Applications | Technical Advantages | Limitations |
|---|---|---|---|
| Primary Stem Cell Cultures | Direct analysis of quiescent stem cells; functional assays | Physiological relevance; maintenance of native properties | Limited expansion capacity; heterogeneity |
| Organoid Models | Study of niche interactions; tissue-level organization | 3D architecture; cell-cell interactions; long-term culture | Technical complexity; variable reproducibility |
| Genetically Engineered Models | In vivo pathway manipulation; lineage tracing | Physiological context; systemic factors examined | Compensatory mechanisms; developmental effects |
Research Reagent Solutions
Table 3: Essential Research Reagents for Quiescence Signaling Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Pathway Inhibitors | SB431542 (TGF-β RI inhibitor), LDN-193189 (BMP inhibitor), Rapamycin (mTOR inhibitor) | Acute pathway inhibition; functional validation | Specificity; off-target effects; dosage optimization |
| Recombinant Proteins | TGF-β1, BMP4, Noggin | Pathway activation; differentiation assays | Bioactivity verification; concentration optimization |
| Antibodies for Detection | Phospho-SMAD1/5/9, Phospho-SMAD2, Phospho-S6 Ribosomal Protein | Pathway activity assessment; immunohistochemistry | Specificity validation; application-specific optimization |
| Cell Surface Markers | CD34, CD45, CD73, CD90, CD105 [5] | Stem cell isolation and characterization | Context-dependent expression; species specificity |
| Reporters | SMAD-binding element luciferase, BRE-luciferase | Pathway activity quantification; high-throughput screening | Transduction efficiency; background signal |
Signaling Pathway Diagrams
Diagram 1: TGF-β Signaling Pathway. This diagram illustrates the canonical TGF-β signaling cascade from ligand binding to target gene transcription.
Diagram 2: BMP Signaling Pathway. This diagram illustrates the canonical BMP signaling cascade, highlighting similarities and distinctions from TGF-β signaling.
Diagram 3: mTOR Signaling Pathway. This diagram illustrates the mTORC1 activation pathway in response to growth factors and nutrient availability.
Diagram 4: Quiescence Signaling Network Integration. This diagram illustrates the integrative network of TGF-β, BMP, and mTOR signaling in maintaining stem cell quiescence.
The signaling networks centered on TGF-β, BMP, and mTOR pathways represent a sophisticated control system that maintains stem cell quiescence and regulates the balance between self-renewal and differentiation. Understanding these networks at a quantitative level provides critical insights for both basic stem cell biology and therapeutic applications. As research in this field advances, several emerging areas hold particular promise:
First, the application of single-cell technologies will enable researchers to dissect the heterogeneity within stem cell populations and identify distinct quiescent states with different functional properties. Second, the integration of organoid models with CRISPR-based screening approaches will facilitate functional validation of pathway components in physiologically relevant contexts. Finally, the manipulation of these signaling pathways ex vivo could enable the expansion of therapeutic stem cell populations while maintaining their regenerative potential.
The comprehensive understanding of TGF-β, BMP, and mTOR signaling networks in quiescence will ultimately inform the development of novel regenerative medicine approaches [15] and therapeutic strategies for cancer and degenerative diseases where stem cell function is compromised. As these pathways continue to be elucidated in increasing detail, they offer promising targets for manipulating stem cell behavior in clinical applications.
Stem cell biology has evolved from a cell-centric view to a holistic understanding where the microenvironment, or stem cell niche, is recognized as a central determinant of cellular fate. The behavior of stem cells—including their self-renewal, quiescence, and differentiation—is governed not solely by intrinsic genetic programs but by highly specialized microenvironments that integrate structural, biochemical, and mechanical cues [28] [29]. The niche concept, first proposed by R. Schofield in 1978 for hematopoietic stem cells (HSCs), posits that specific microenvironmental 'niches' maintain stem cell self-renewal, guide differentiation and maturation, and can even revert progenitor cells to an undifferentiated state [30]. These niches dynamically respond to injury, oxygen levels, mechanical forces, and signaling molecules, creating a dynamic regulatory system that is fundamental to tissue homeostasis and repair [30] [28].
This review delineates the architecture and function of stem cell niches within the broader context of stem cell self-renewal and differentiation mechanisms. We argue that successful regenerative interventions must treat stem cells and their microenvironment as an inseparable therapeutic unit [28] [29]. Emerging therapeutic strategies are now shifting the regenerative paradigm from a stem-cell-centric to a niche-centric model, which may unlock regenerative outcomes that surpass classical cell therapies [28].
The Architectural Blueprint of Stem Cell Niches
Stem-cell niches are anatomically discrete microenvironments where resident stem cells, their stromal neighbors, and a specialized extracellular matrix (ECM) scaffold cooperate to balance quiescence, self-renewal, and lineage commitment [28].
Core Cellular and Extracellular Constituents
The functional unit of a niche comprises several core components that work in concert:
- Cellular Constituents: Immediate stromal neighbors—such as osteoblasts in bone marrow, fibroblasts in skin, and pancreatic telocytes—govern stem-cell fate through juxtacrine contacts and paracrine factors [28]. Accessory populations including endothelial cells, pericytes, macrophages, adipocytes, mast cells, and sympathetic neurons integrate systemic signals with local demands, modulating circadian mobilization or stress-induced recruitment [28].
- Extracellular Matrix (ECM) Scaffolds: The ECM provides both a structural lattice and a reservoir of biochemical and mechanical cues [28]. Laminin, collagen, fibronectin, and proteoglycans organize spatial relationships between niche residents, create morphogen gradients, and transmit force. Integrins and cadherins on the stem-cell surface translate ECM stiffness, viscoelasticity, and topography into intracellular signaling cascades that steer proliferation or differentiation [28].
Tissue-Specific Niche Architectures
Although built from similar building blocks, niche architecture diverges dramatically across organs to meet distinct regenerative demands. The table below summarizes key characteristics of major adult stem cell niches.
Table 1: Architecture and Characteristics of Major Adult Stem Cell Niches
| Tissue/Organ | Niche Location/Type | Stem Cell Types | Key Supporting Cells | Primary Regulatory Functions |
|---|---|---|---|---|
| Bone Marrow | Endosteal & Perivascular niches | Hematopoietic Stem Cells (HSCs) | Osteoblasts, Endothelial cells, CAR cells | Maintains HSC quiescence (endosteal) and proliferation/differentiation (perivascular) [28]. |
| Skin | Hair follicle bulge, Interfollicular epidermis | Epithelial stem cells | Fibroblasts, Adipocytes | Regenerates epidermis, follicles, and sebaceous glands; maintains barrier function [28] [31]. |
| Intestine | Crypt base | Intestinal stem cells | Paneth cells, Stromal cells | Symmetric division expands pool; asymmetric division yields transit-amplifying cells for continuous renewal [28]. |
| Nervous System | Sub-ventricular zone, Sub-granular zone | Neural stem cells (NSCs) | Endothelial cells, Astrocytes | Maintains neurogenic capacity; interfaces with vasculature and cerebrospinal fluid [28]. |
| Skeletal Muscle | Beneath basal lamina | Satellite cells | Myofibers, Fibroblasts | Repairs muscle fibers after mechanical insult; maintained in quiescent state until activation [28]. |
Molecular Signaling Axes Governing Fate Decisions
Stem-cell self-renewal and lineage specification are regulated by a conserved set of signaling pathways that originate during embryogenesis and remain active throughout adult tissue maintenance [28]. The following diagram illustrates the core signaling pathways and their primary functions in fate decisions.
Figure 1: Core Signaling Pathways in Stem Cell Fate Decisions. These evolutionarily conserved pathways integrate niche-derived cues to determine stem cell behavior.
Key Pathway Functions and Crosstalk
Wnt/β-catenin Pathway: This pathway plays a critical role in tissue homeostasis, supporting both stem cell self-renewal and differentiation, and is considered a key regulator of stem cell function [9] [28]. In the hematopoietic system, Wnt signaling promotes HSC maintenance and interacts with Notch signaling to support long-term self-renewal [28]. Similarly, in the epidermis and intestinal crypts, Wnt activity is critical for tissue homeostasis and cellular differentiation [28].
Bone Morphogenetic Protein (BMP) Pathway: BMP signaling often counterbalances Wnt activity by imposing a quiescent state on stem cells [28]. This is particularly evident in the cycling of hair follicle stem cells where Wnt promotes entry into the growth phase while BMP maintains dormancy [28]. BMPs also play crucial roles in directing differentiation into specific lineages, including bone and cartilage formation [9].
Notch Signaling: The Notch pathway operates primarily through juxtacrine signaling between adjacent cells and plays a fundamental role in directing differentiation and maintaining the stem cell pool through lateral inhibition [9] [28]. In the hematopoietic system, Notch interacts with Wnt signaling to support stem cell maintenance [28].
Transforming Growth Factor-β (TGF-β) Signaling: The TGF-β superfamily consists of diverse proteins including TGF-β (1-3), activins, inhibits, and BMPs [9]. This pathway regulates tissue homeostasis, immune responses, extracellular matrix deposition, and cell differentiation [9]. TGF-β, along with Activin A and Nodal signaling pathways, is crucial for stimulating the self-renewal of primed pluripotent stem cells [9].
These pathways exhibit complex crosstalk, where modulation of one can influence others, providing multiple pharmacological entry points to fine-tune stem cell behavior for therapeutic purposes [9].
Quantitative Methodologies for Niche Analysis
Computational and Single-Cell Approaches
Advances in experimental and computational biology have dramatically improved our ability to resolve stem cell heterogeneity and niche interactions. The following table summarizes key quantitative methodologies and their applications in niche biology.
Table 2: Computational and Analytical Methods for Stem Cell Niche Research
| Methodology | Key Applications in Niche Biology | Resolution | Output Parameters |
|---|---|---|---|
| Single-cell RNA sequencing (scRNA-seq) | Resolves transcriptional states of both stem and niche cells; identifies novel subtypes [32]. | Single-cell | Gene expression profiles, Cell type classification, Differential expression |
| Chromatin Immunoprecipitation Sequencing (ChIP-seq) | Maps epigenetic landscape and transcription factor binding sites [32]. | Single-cell (newer methods) | Histone modifications, Transcription factor occupancy, Enhancer/promoter activity |
| Network Inference Algorithms | Reconstructs gene regulatory networks (GRNs) from expression data [32]. | Network-level | Regulatory interactions, Key transcription factors, Network topology |
| Machine Learning | Predicts stem cell fate outcomes; identifies novel regulatory elements [32]. | Predictive modeling | Fate prediction accuracy, Feature importance, Classification models |
| 3D Vertex Modeling | Simulates mechanical competition for space in epithelial tissues [31]. | Single-cell & tissue | Cell shape metrics, Division patterns, Fate outcomes |
Experimental Protocols for Key Analyses
Protocol: scRNA-seq for Niche Deconstruction
Purpose: To resolve cellular heterogeneity within stem cell niches and characterize transcriptional states of both stem and supporting cells [32].
Workflow:
- Tissue Dissociation: Gentle enzymatic digestion to create single-cell suspension while preserving RNA integrity.
- Cell Sorting: Fluorescence-activated cell sorting (FACS) to enrich for stem cell and niche cell populations using established surface markers.
- Library Preparation: Use droplet-based encapsulation systems (e.g., 10X Genomics) with unique molecular identifiers (UMIs).
- Sequencing: High-depth sequencing on Illumina platforms (recommended: ≥20,000 reads/cell).
- Computational Analysis:
- Quality control with FastQC [32].
- Alignment using STAR or CellRanger.
- Dimensionality reduction (PCA, UMAP).
- Cluster identification and marker gene detection.
- Trajectory inference (pseudotime) using Monocle or PAGA.
Key Reagents: Collagenase/Dispase for dissociation, FACS antibodies against niche-specific surface markers (e.g., CD34 for HSCs), single-cell RNAseq kit, bioinformatic tools (Seurat, Scanpy).
Protocol: Mechanical Fate Mapping in Epidermal Niches
Purpose: To quantify relationships between cell shape, mechanical forces, and fate decisions in skin epidermis [31].
Workflow:
- Tissue Preparation: Generate murine epidermal whole mounts or sectioned tissues.
- Immunofluorescence Staining: Label cell borders (E-cadherin), basement membrane (laminin), and nuclei (DAPI).
- Confocal Imaging: Acquire high-resolution z-stacks of interfollicular epidermis.
- 3D Segmentation: Use image analysis software (e.g., Imaris, MorphoGraphX) to extract cellular morphometrics.
- Shape Parameter Quantification: Measure cell height, cross-sectional area, basal surface area, and apical surface area.
- Lineage Tracing: Combine with inducible genetic labeling to track clonal dynamics.
- Computational Modeling: Input morphological data into 3D vertex models to predict fate outcomes.
Key Reagents: Primary antibodies (anti-E-cadherin, anti-laminin), fluorescent secondary antibodies, mounting medium with DAPI, tamoxifen for Cre induction, vertex modeling software (Chaste, or custom Python/MATLAB code).
The Scientist's Toolkit: Essential Research Reagents
The following table compiles key research reagents and their applications in stem cell niche research, as derived from the experimental methodologies cited.
Table 3: Essential Research Reagents for Stem Cell Niche Investigations
| Reagent Category | Specific Examples | Research Application | Function/Mechanism |
|---|---|---|---|
| Cell Surface Markers | CD34, CD150, CD48 (HSCs); LGR5 (intestinal); α6-integrin (epidermal) [28] [32] | Identification and isolation of specific stem cell populations | Antibody-based recognition of cell surface proteins for FACS sorting |
| Cytokines & Growth Factors | SCF, CXCL12, BMP-4, Wnt3a, FGF2 [9] [28] | Modulation of niche signaling in vitro and in vivo | Activation of specific signaling pathways (e.g., Wnt, BMP, FGF) |
| Small Molecule Inhibitors/Activators | CHIR99021 (Wnt activator), SB431542 (TGF-β inhibitor), LDN193189 (BMP inhibitor) [9] | Pharmacological manipulation of fate decisions | Targeted modulation of key signaling pathways |
| Extracellular Matrix Components | Laminin-511, Collagen IV, Fibronectin, Matrigel [28] | Recreation of niche environments in 3D culture | Structural support and presentation of biochemical cues |
| Viral Vectors | Lentivirus (for reprogramming), Retrovirus (for gene delivery) [33] [9] | Genetic modification of stem cells and niche cells | Introduction of exogenous genes (e.g., reprogramming factors) |
| Lineage Tracing Systems | Tamoxifen-inducible CreER[T2]; Confetti reporter [31] | Tracking cell fate decisions in vivo | Genetic labeling of cells and their progeny to trace lineage relationships |
Mechanical Forces as Determinants of Cell Fate
Beyond biochemical signaling, mechanical forces represent a fundamental layer of regulation within stem cell niches. Recent research has established that physical cues from the microenvironment can directly influence stem cell fate decisions [28] [31].
Biomechanical Regulation of Epidermal Fate
In the skin epidermis, mechanical competition for space naturally gives rise to homeostasis and neutral drift dynamics observed experimentally [31]. A 3D vertex-based model of the interfollicular epidermis demonstrates that:
- Force Balance Determines Fate: When basal cells divide, the fate of daughter cells (whether they remain basal or differentiate suprabasally) emerges spontaneously as a result of force balance and mechanical competition for space, without pre-specified fate assignments [31].
- Tension Heterogeneities Drive Imbalance: Relatively small tension heterogeneities (as low as 10% decrease in basal tension) can heavily tilt cellular dynamics toward exponential growth by making symmetric renewal divisions mechanically favorable [31].
- Cell Shape Predicts Fate: A master relationship exists between cell shape and long-term clonal dynamics, where basal cells with reduced tension exhibit distinct morphological changes that predict biased fate outcomes [31].
This mechanical model was validated during basal cell carcinoma initiation in mouse epidermis, where oncogenic Hedgehog signaling pathway activation drove a well-defined tilt of fate outcomes toward symmetric renewal that correlated with measurable changes in cellular shape [31].
The following diagram illustrates how mechanical forces are integrated with biochemical signaling to determine stem cell fate decisions within the niche.
Figure 2: Integration of Mechanical and Biochemical Cues in Fate Decisions. Mechanical inputs from the niche are transduced into biochemical signals that converge on fate-determining pathways.
Therapeutic Implications and Niche-Targeted Strategies
Understanding niche biology has profound implications for regenerative medicine, disease modeling, and therapeutic development. The shift from cell-centric to niche-centric approaches is opening new therapeutic avenues.
Pharmacological Modulation of Niche Signaling
Pharmacological interventions represent powerful tools to overcome barriers in stem cell therapy by enhancing stem cell survival, directing differentiation, and modulating the stem cell niche [9]. Key strategies include:
- Small Molecule Pathway Modulators: Compounds that activate or inhibit key niche signaling pathways (Wnt, BMP, Notch, Hedgehog) can be used to direct stem cell fate decisions ex vivo or enhance endogenous stem cell activity in vivo [9].
- Immunomodulatory Agents: Drugs that suppress immune rejection of transplanted stem cells or modulate inflammatory environments that disrupt niche function [9].
- Niche Component Targeting: Agents that specifically target dysfunctional niche components, such as fibroblast activation protein (FAP) inhibition in fibrotic niches [28].
Bioengineering Approaches for Niche Recreation
Tissue engineering technologies that combine material science, cell transplantation, and microengineering are being used to develop functional organoids and engineered scaffolds that replicate native niche mechanics [9] [28]. These approaches include:
- Biomimetic Scaffolds: 3D scaffolds that replicate the mechanical properties, topography, and biochemical composition of native niches to support stem cell engraftment and function [28].
- Extracellular Vesicle Therapies: Vesicles derived from niche cells that deliver paracrine cues to support regeneration without cell transplantation [28].
- Composite Constructs: Engineered tissues that preserve endogenous cell-matrix interactions and spatial relationships critical for niche function [28].
Clinical Translation and Challenges
While niche-targeted therapies hold great promise, several challenges remain in their clinical translation. These include optimizing delivery methods for niche-modifying factors, ensuring long-term safety and efficacy, and overcoming regulatory hurdles for complex therapeutic approaches [9]. A multidisciplinary approach integrating personalized medicine, pharmacological modulation, and tissue engineering holds the key to addressing these limitations [9].
In hematopoietic stem cell transplantation, for example, clinical failures often reflect niche misalignment rather than intrinsic stem cell deficits [28]. Improving transplantation outcomes may therefore require complementary therapies that enhance niche function in addition to the stem cell graft itself.
Stem cell niches represent sophisticated microenvironments that integrate structural, biochemical, and mechanical cues to precisely regulate stem cell fate decisions. The emerging paradigm recognizes that successful regenerative interventions must treat stem cells and their microenvironment as an inseparable therapeutic unit [28] [29]. Future advances in the field will depend on high-resolution niche mapping, mechanobiologically informed scaffold design, and niche-targeted clinical trials [28]. As research continues to unravel the complex dialogue between stem cells and their niches, we move closer to a new era of microenvironmentally integrated medicine that may unlock regenerative outcomes surpassing classical cell therapies.
From Bench to Bedside: Techniques and Therapeutic Applications
The advent of human induced pluripotent stem cells (hiPSCs) has marked a revolutionary shift in biomedical research and drug discovery. By reprogramming adult somatic cells into a pluripotent state, hiPSCs provide an unprecedented platform for generating patient-specific cells capable of differentiating into nearly any tissue type [34]. This technology builds directly on foundational knowledge of stem cell self-renewal and differentiation mechanisms, enabling researchers to recreate human disease pathology in culture dishes and accelerate the development of novel therapeutics [35]. The core discovery by Takahashi and Yamanaka that four transcription factors—OCT4, SOX2, KLF4, and c-MYC (OSKM)—could reprogram somatic cells opened new avenues for disease modeling, drug screening, and regenerative medicine [36] [34].
The significance of hiPSC technology extends beyond its ethical advantages over embryonic stem cells. It represents the practical application of stem cell biology principles, particularly the molecular regulation of pluripotency and differentiation decisions [37]. Understanding these mechanisms has been crucial for optimizing directed differentiation protocols that yield functional cardiomyocytes, neurons, and other cell types relevant to human disease [35] [36]. This technical guide examines current hiPSC-based model systems, with a focus on their application in disease modeling and drug discovery, while framing these advances within the broader context of stem cell self-renewal and differentiation research.
Core hiPSC Technology: Reprogramming and Differentiation Methodologies
Reprogramming Approaches and Factors
The fundamental process of generating hiPSCs involves reprogramming somatic cells (typically fibroblasts or blood cells) back to a pluripotent state. While the original OSKM factors remain foundational, significant optimization has occurred to enhance safety and efficiency. Research has demonstrated that c-MYC, an oncogene, can be omitted or replaced with L-MYC to reduce tumorigenic risk [36]. Alternative factor combinations including OCT4, SOX2, NANOG, and LIN28 (OSNL) have also proven effective [36]. Small molecules such as RepSox can replace SOX2, while epigenetic modulators like valproic acid (VPA) and sodium butyrate can enhance reprogramming efficiency by up to 6.5-fold [36].
Table 1: Comparison of hiPSC Reprogramming Methods
| Method | Genetic Material | Genomic Integration | Reprogramming Efficiency | Safety Profile | Primary Applications |
|---|---|---|---|---|---|
| Retrovirus/Lentivirus | DNA (OSKM factors) | Yes | Moderate | Lower (insertional mutagenesis risk) | Basic research, proof-of-concept studies |
| Sendai Virus | RNA | No | High | Higher (cytoplasmic, transient) | Clinical application research |
| Episomal Plasmid | DNA | No (typically) | Low to Moderate | Higher | Clinical grade iPSC generation |
| Synthetic mRNA | mRNA | No | Moderate | High | Clinical applications, gene editing |
| Recombinant Protein | Protein | No | Very Low | Highest | Specialized research applications |
Delivery systems for reprogramming factors have evolved substantially, with non-integrating methods now preferred for clinical translation. Sendai virus, episomal plasmids, synthetic mRNAs, and recombinant proteins each offer distinct advantages, with the common goal of minimizing genomic alteration while maintaining reprogramming efficiency [36] [34]. The field has also seen the emergence of chemical reprogramming using entirely small-molecule combinations, representing the safest approach for potential clinical applications [36].
Directed Differentiation Strategies
The controlled differentiation of hiPSCs into specific lineages leverages knowledge of developmental biology to recapitulate embryonic development in vitro. For cardiomyocyte generation (hiPSC-CMs), protocols typically employ sequential activation and inhibition of key signaling pathways including WNT, BMP, and TGF-β [35] [38]. These approaches yield cardiomyocytes that express characteristic markers and exhibit functional properties, though immaturity remains a significant challenge [35].
Advanced culture techniques have been developed to enhance maturation, including:
- Long-term culture (up to 120-180 days) to promote structural and functional maturation
- Metabolic manipulation by switching from glucose-dependent to fatty acid-dependent media
- Mechanical stimulation through cyclic stretching to promote sarcomere alignment
- Electrical pacing to mimic physiological cardiac contraction patterns
- 3D culture systems including engineered heart tissues (EHTs) and cardiac organoids that better replicate the native microenvironment [35] [39] [38]
Similar progressive differentiation strategies have been optimized for generating specific neuronal subtypes, including motor neurons for modeling amyotrophic lateral sclerosis (ALS) and dopaminergic neurons for Parkinson's disease research [36] [34].
Figure 1: hiPSC Generation and Cardiac Differentiation Workflow. This diagram illustrates the key steps in reprogramming somatic cells to hiPSCs and subsequent directed differentiation into mature cardiomyocytes, highlighting critical signaling pathways and maturation techniques.
hiPSC-Based Disease Modeling: From Mechanisms to Therapeutic Insights
Cardiac Disease Modeling
hiPSC-derived cardiomyocytes have proven particularly valuable for modeling inherited cardiac disorders, where patient-specific cells recapitulate key pathological features in culture. In arrhythmogenic cardiomyopathy (ACM), hiPSC models have revealed disease mechanisms involving impaired desmosomal function, aberrant Wnt/β-catenin signaling, and metabolic alterations that promote fibrofatty infiltration [40]. These models successfully replicate characteristic pathological features including cardiomyocyte apoptosis, electrical instability, and structural remodeling [40].
Similar approaches have advanced understanding of hypertrophic cardiomyopathy, long QT syndrome, and drug-induced arrhythmias. The ability to model these conditions in patient-specific cells has been transformative for investigating genotype-phenotype correlations and identifying novel therapeutic targets [35] [40].
Neurodegenerative Disease Modeling
In the neurological domain, hiPSC-based models have provided unprecedented insights into disease mechanisms. For amyotrophic lateral sclerosis (ALS), motor neurons derived from patient-specific iPSCs recapitulate disease-specific pathology including protein aggregation, mitochondrial dysfunction, and excitotoxicity [36]. These models serve as robust platforms for investigating molecular mechanisms underpinning ALS and accelerating discovery of novel therapeutic strategies [36].
Similar advances have been achieved with hiPSC models of Parkinson's disease, Alzheimer's disease, and other neurodegenerative conditions, where patient-derived neurons exhibit disease-relevant phenotypes including α-synuclein aggregation, tau pathology, and selective vulnerability of specific neuronal populations [34].
Advanced Model Systems: Beyond 2D Monolayers
While 2D monolayer cultures have provided valuable insights, more physiologically relevant 3D model systems have emerged to better capture tissue-level complexity:
- Cardiac Organoids and Engineered Heart Tissues (EHTs): These 3D structures better mimic the native myocardial environment, exhibiting more mature structural organization and functional properties [35] [38]
- Neural Organoids: Complex 3D models that recapitulate aspects of human brain development and connectivity, enabling study of circuit-level dysfunction in neurological disorders
- Microfluidic Systems: Organ-on-a-chip platforms that integrate fluid flow, mechanical forces, and multiple cell types to create more physiologically relevant microenvironments [38]
Table 2: hiPSC-Based Disease Models and Key Applications
| Disease Category | Specific Models | Recapitulated Pathologies | Key Research Applications |
|---|---|---|---|
| Arrhythmogenic Cardiomyopathy | 2D hiPSC-CMs, 3D EHTs | Desmosomal impairment, arrhythmias, metabolic shift | Path mechanism studies, anti-arrhythmic drug testing |
| Hypertrophic Cardiomyopathy | hiPSC-CMs, cardiac organoids | Sarcomeric disarray, hypercontractility, calcium handling defects | Disease modeling, therapeutic screening |
| Amyotrophic Lateral Sclerosis | hiPSC-derived motor neurons | Protein aggregation, axonal transport defects, excitotoxicity | Drug discovery, biomarker identification |
| Parkinson's Disease | hiPSC-derived dopaminergic neurons | α-synuclein pathology, mitochondrial dysfunction, selective vulnerability | Cell replacement therapy, neuroprotection studies |
| Long QT Syndrome | hiPSC-CMs, 2D monolayers | Action potential prolongation, delayed afterdepolarizations | Cardiotoxicity screening, personalized medicine |
Technological Advances in hiPSC-Based Drug Screening
Functional Screening Platforms
hiPSC technology has revolutionized early drug discovery by providing human-relevant models for compound screening. Advanced functional assays now enable medium- to high-throughput screening of potential therapeutics:
- Calcium Imaging: Fluorescent indicators (e.g., Cal-520, Fluo-4) allow monitoring of calcium handling abnormalities in cardiomyocyte models of arrhythmia [39]
- Multi-electrode Arrays (MEAs): These systems record extracellular field potentials in hiPSC-CMs, enabling detection of arrhythmias and assessment of contractile properties [35]
- High-Content Imaging: Automated microscopy combined with machine learning algorithms quantifies structural features like sarcomere organization, mitochondrial function, and morphological changes [39]
- Traction Force Microscopy: Measures contractile force generation in engineered heart tissues, providing functional readouts of cardiotoxicity or therapeutic efficacy [39]
Integration with CRISPR Screening
The combination of hiPSC technology with CRISPR-based functional genomics has created powerful platforms for target identification and validation. "Perturbomics" approaches systematically analyze phenotypic changes resulting from targeted gene modulation, enabling identification of genes with therapeutic potential for diseases including cancer, cardiovascular disorders, and neurodegeneration [41].
CRISPR screens in hiPSC-derived cells can identify genetic modifiers of disease phenotypes, essential genes for specific cell types, and mechanisms of drug action/resistance. Recent technical advances include:
- CRISPRi/a Screens: Using catalytically dead Cas9 (dCas9) fused to repressive (KRAB) or activating (VP64) domains for loss- and gain-of-function studies [41]
- Single-Cell CRISPR Screening: Combining genetic perturbations with single-cell RNA sequencing to resolve transcriptomic consequences of gene modulation [41]
- Base Editing Screens: Using precise base editors to model disease-associated single-nucleotide variants and assess their functional impact [41]
Figure 2: Integrated CRISPR-hiPSC Screening Workflow. This diagram outlines the key steps in combining CRISPR perturbation with hiPSC-based models for functional genomics and drug target discovery, highlighting major phenotypic readouts.
Computational and AI-Enhanced Analysis
The complexity and scale of data generated from hiPSC-based screening platforms has driven development of sophisticated computational tools. Machine learning algorithms now enable:
- Automated Morphological Analysis: Tools like SarcGraph use deep learning to quantify sarcomere organization and structural features in hiPSC-CMs, even in immature or diseased cells with disorganized structures [39]
- Pattern Recognition: Unsupervised learning approaches identify subtle phenotypic patterns that might be missed in conventional analysis [39]
- Predictive Modeling: AI-guided differentiation improves reproducibility and quality control in hiPSC manufacturing [34]
These computational advances have been essential for extracting meaningful biological insights from high-content screening data and establishing standardized, quantitative metrics for assessing hiPSC-derived cells.
The Scientist's Toolkit: Essential Research Reagents and Technologies
Table 3: Essential Research Reagents and Platforms for hiPSC-Based Modeling
| Category | Specific Tools | Function/Application | Key Considerations |
|---|---|---|---|
| Reprogramming Systems | Sendai virus vectors, episomal plasmids, mRNA kits | Non-integrating reprogramming | Efficiency, safety, cost, compatibility with target cell type |
| Differentiation Kits | Commercial cardiomyocyte, neuronal differentiation kits | Directed lineage specification | Protocol reliability, batch consistency, cost-effectiveness |
| Gene Editing Tools | CRISPR-Cas9 systems, base editors, prime editors | Genetic engineering, disease modeling, correction | Efficiency, off-target effects, delivery method, toxicity |
| Characterization Reagents | Antibodies for pluripotency (OCT4, NANOG) and lineage markers (cTnT, MAP2) | Quality control, differentiation validation | Specificity, compatibility with imaging platforms |
| Functional Assays | Calcium dyes (Fluo-4), voltage-sensitive dyes, contractility sensors | Functional assessment of derived cells | Signal-to-noise ratio, phototoxicity, compatibility with live-cell imaging |
| Advanced Culture Systems | 3D scaffolds, microfluidic devices, engineered tissue platforms | Enhanced maturation, physiological relevance | Throughput, reproducibility, analytical compatibility |
| Computational Tools | SarcGraph, custom machine learning pipelines | Quantitative structural and functional analysis | Required expertise, compatibility with existing data systems |
hiPSC-based model systems represent a powerful convergence of stem cell biology, engineering, and genomics. These platforms have dramatically advanced our ability to model human disease and accelerate drug discovery by providing patient-specific, human-relevant systems for mechanistic studies and compound screening. The continued evolution of these technologies—particularly in enhancing cellular maturation, integrating multi-omics approaches, and leveraging artificial intelligence—promises to further bridge the gap between preclinical models and human physiology.
As the field progresses, key challenges remain in standardization, scalability, and clinical validation. However, the rapid advances in hiPSC technology over the past decade suggest these hurdles will be overcome, paving the way for more predictive disease models and effective, personalized therapeutic strategies. By building on fundamental mechanisms of stem cell self-renewal and differentiation, hiPSC-based approaches continue to transform our approach to understanding and treating human disease.
High-Throughput Screening (HTS) in Stem Cell-Based Drug Discovery
High-Throughput Screening (HTS) represents a paradigm shift in stem cell-based drug discovery, enabling the rapid and systematic evaluation of thousands of compounds or genetic modifiers on stem cell behavior. This approach leverages automated technologies to unlock the potential of immune and stem cells to drive more effective cell-based therapies [42]. The integration of HTS with stem cell biology is particularly powerful for investigating the fundamental mechanisms governing stem cell self-renewal and differentiation—processes crucial for regenerative medicine and pharmaceutical development.
Stem cells possess unique properties, including self-renewal and differentiation into specialized cell types, making them indispensable for regenerative medicine applications [15]. When framed within the context of stem cell self-renewal and differentiation mechanisms research, HTS provides an unparalleled toolset for deconstructing the complex signaling networks and environmental cues that dictate cell fate decisions. The application of HTS in this field has been accelerated by several key technological advancements: the widespread adoption of induced pluripotent stem cell (iPSC) technology, which enables the production of patient-specific stem cell lines; innovations in automated cell culture and analysis; and the development of sophisticated bioinformatics tools for processing complex datasets [15] [43].
Core Principles of HTS Workflows
Fundamental HTS Components and Process
The implementation of HTS in stem cell research follows a structured workflow designed to maintain cell integrity while maximizing data quality and throughput. The fundamental process involves screening a diverse library of compounds or genetic factors against stem cell populations under controlled conditions to identify modulators of self-renewal or differentiation. New high-throughput screening methods are unlocking unprecedented potential by combining automated plate handlers, liquid dispensers, and high-sensitivity detectors to generate robust, statistically significant datasets [42].
A typical HTS workflow incorporates several critical stages: assay development and miniaturization, automated reagent dispensing, controlled incubation periods, high-speed detection, and sophisticated data analysis. For stem cell applications, particular attention must be paid to maintaining pluripotency throughout the screening process or precisely controlling differentiation conditions, depending on the screening objectives. The Misvik high throughput screening setup, for example, enables rapid toxicity assessment of multiple materials using a set of well-established toxicity endpoints adapted for stem cell models [44].
HTS Workflow Visualization
The following diagram illustrates a generalized HTS workflow for stem cell-based screening:
Table: Critical Stages in HTS Workflow Implementation
| Stage | Key Activities | Technical Considerations for Stem Cells |
|---|---|---|
| Assay Development | Optimization of cell density, endpoint measurement, controls | Maintain pluripotency or direct differentiation; ensure reproducibility across plates |
| Library Preparation | Compound dilution, plate formatting, positive/negative controls | Include known self-renewal promoters or differentiation inducers as controls |
| Cell Seeding | Automated dispensing of cell suspensions | Ensure uniform cell distribution and viability; minimize edge effects in plates |
| Compound Incubation | Addition of library compounds; controlled environment | Optimize duration to capture early and late effects on cell fate |
| Detection | Measurement of phenotypic endpoints | Validate assays against stem cell-specific markers (e.g., pluripotency factors) |
| Data Analysis | Normalization, hit selection, quality assessment | Implement specialized algorithms for stem cell morphology and colony analysis |
Integration of Stem Cell Models in HTS
Stem Cell Types for HTS Applications
The selection of appropriate stem cell models is crucial for successful HTS campaigns focused on self-renewal and differentiation mechanisms. Different stem cell types offer distinct advantages for specific applications:
Induced Pluripotent Stem Cells (iPSCs) have emerged as particularly valuable tools because they can be routinely produced from patients and healthy individuals and efficiently differentiated into various somatic cell types affected by genetic diseases or that represent specific drug targets [43]. iPSCs offer the key advantage of being patient-specific and ethically non-controversial (non-embryonic), making them ideal for disease modeling and personalized medicine approaches [45]. Biotechnology companies have optimized reagents and differentiation protocols such that they are now widely applicable across many hiPSC lines, enabling more consistent HTS results [43].
Embryonic Stem Cells (ESCs) exhibit characteristics that distinguish them in stem cell biology, most notably their pluripotency, which is defined by distinct features enabling differentiation into any human body cell [15]. This adaptability makes them highly valuable for comprehensive screening of differentiation pathways. However, their use is more ethically complex and regulated than iPSCs.
Adult Stem Cells (ASCs) stand out in the realm of regenerative biology because of their distinctive properties and vital roles in maintaining tissue homeostasis [15]. While they are less potent than pluripotent cells, their multipotency and presence in specific tissue niches make them particularly suitable for screening compounds targeting tissue-specific regeneration and lineage commitment.
Stem Cell Differentiation Mechanisms
Stem cell differentiation is a critical process in developmental biology where a less specialized cell matures into a more distinct form and function [46]. This transformation involves the differential activation of specific genes and the repression of others, which changes the cell's size, shape, function, and metabolic activity. In the context of HTS, understanding these mechanisms is essential for designing appropriate assays that can accurately measure perturbations in differentiation pathways.
The process is driven by intricate signaling pathways that regulate gene expression, ensuring that cells develop the necessary characteristics for their specific functions [46]. These signals can be influenced by both internal genetic factors and external environmental conditions, including:
- Complex signaling pathways: Governed by growth factors, cytokines, and epigenetic modifications like DNA methylation and chromatin remodeling
- Influence of the extracellular microenvironment: Dictates differentiation direction by manipulating culture conditions
- Physical and mechanical forces: Factors such as mechanical forces, extracellular matrix geometry, and cell-to-cell contacts
- Developmental cues: Depending on their stage of development, stem cells exhibit varying differentiation potentials
Experimental Design and Protocol Implementation
Comprehensive HTS Protocol for Stem Cell Applications
A standardized HTS-derived human cell-based testing protocol can combine multiple assays into a broad toxic mode-of-action-based hazard value, an approach that can be adapted for stem cell self-renewal and differentiation studies [44]. The following protocol outlines key considerations for implementing HTS focused on stem cell fate decisions:
Step 1: Assay Development and Optimization
- Select appropriate stem cell type (iPSCs, ESCs, or ASCs) based on research objectives
- Define primary screening endpoints relevant to self-renewal or differentiation:
- Pluripotency markers (OCT4, NANOG, SOX2) for self-renewal studies
- Lineage-specific markers for differentiation studies
- Morphological changes via high-content imaging
- Metabolic activity shifts
- Optimize cell culture conditions for miniaturized format (96, 384, or 1536-well plates)
- Determine optimal cell density, differentiation timeline, and endpoint measurement parameters
- Establish positive and negative controls for both self-renewal and differentiation states
Step 2: Library Management and Compound Handling
- Prepare compound libraries in DMSO at standardized concentrations (typically 10mM stocks)
- Transfer compounds to assay plates using acoustic dispensing or pin tools
- Include control wells containing:
- DMSO only (vehicle control)
- Known self-renewal promoters (e.g., small molecule replacements for LIF/Y-27632)
- Established differentiation inducers (e.g., retinoids, growth factors)
- Implement quality control measures to ensure compound integrity and accurate transfer
Step 3: Cell Seeding and Compound Treatment
- Harvest stem cells as single-cell suspension using appropriate dissociation reagents
- Seed cells into assay plates using automated liquid dispensers
- Maintain consistency in cell number across all wells (critical for reproducible results)
- Add compounds at predetermined timepoints based on differentiation protocol
- Incubate under standard stem cell culture conditions (37°C, 5% CO2) with precise humidity control
Step 4: Endpoint Measurement and Data Acquisition
- For self-renewal screens: Measure pluripotency marker expression via immunofluorescence or reporter assays
- For differentiation screens: Quantify lineage-specific markers at appropriate timepoints
- Implement high-content imaging systems to capture morphological changes
- Utilize multi-parameter readouts to comprehensively assess cell state:
- Cell viability assays (CellTiter-Glo)
- Apoptosis markers (Caspase-Glo 3/7)
- DNA damage indicators (gammaH2AX)
- Oxidative stress markers (8OHG)
- Ensure consistent imaging parameters and focal plane across all plates
HTS Experimental Workflow
The experimental workflow for HTS in stem cell applications follows a logical progression from initial setup to data interpretation, as shown in the following diagram:
Data Analysis and Hit Identification
The complexity of HTS data requires sophisticated analytical approaches, particularly for stem cell applications where multiple parameters define cell state:
Primary Data Analysis:
- Normalize data using plate-based controls to account for positional effects
- Apply statistical methods (Z-score, B-score) to identify significant deviations from controls
- Implement quality metrics (Z-prime factor) to assess assay robustness
- For multi-parameter data, use multivariate analysis to identify correlated responses
Hit Selection Strategies:
- Establish threshold-based criteria for hit identification (typically >3 standard deviations from mean)
- Employ cluster analysis to group compounds with similar effects on stem cell phenotype
- Prioritize hits based on potency, efficacy, and chemical structure
- Apply machine learning algorithms to predict compound mechanisms based on phenotypic profiles
Secondary Validation:
- Confirm primary hits in dose-response format (8-12 point dilution series)
- Assess specificity through counter-screens against unrelated cell types
- Evaluate structure-activity relationships (SAR) through analog testing
- Validate mechanisms through orthogonal assays (qPCR, Western blot, RNA-seq)
Advanced HTS Applications in Stem Cell Research
Toxicity Screening and Safety Assessment
HTS platforms are particularly valuable for toxicity screening using stem cell-derived models. The development of standardized protocols that combine multiple toxicity endpoints into an integrated assessment represents a significant advancement. One approach integrates dose-response parameters from different endpoints and conditions (time points, cell lines, concentrations) into a final toxicity score, with each slice showing the bioactivity and weight of each specific endpoint [44]. This Tox5-score approach integrates key metrics (statistically significant effect, AUC and maximum effect) that are separately scaled and normalized to allow for comparability, then compiled to end- and time-point-specific toxicity scores [44].
This methodology is particularly powerful for stem cell applications because it can transparently visualize the overall assessment, allowing chemicals and materials to be ranked from most to least toxic and compared with known chemical toxicants included in the screens. The system enables clustering based on endpoint, timepoint and cell line specific toxicity scores, enabling grouping and read-across, including transparency on the grouping hypothesis—the underlying bioactivity associated with the detected hazard-based similarity [44].
Disease Modeling and Drug Discovery
iPSC-based platforms have revolutionized disease modeling and drug discovery by enabling the development of patient-specific stem cell lines for a wide range of applications. The use of iPSC-based platforms in disease modeling is increasing, with iPSCs developed from patient biospecimens for specific diseases helping to uncover disease mechanisms more accurately [45]. This approach also facilitates the development of innovative treatment approaches and can help discover targets for drugs.
The applications of iPSCs in drug discovery are particularly significant for diseases where animal models don't achieve perfect success in predicting human pathophysiology, because animals differ from humans in physiology, the immune system and individual genetic backgrounds [43]. iPSC technology enables researchers to routinely produce human iPSC lines and induce their efficient differentiation into different types of body cells that are affected by genetic diseases or are specific drug targets [43].
Table: HTS Applications by Stem Cell-Derived Cell Type
| Cell Type | Primary Applications | Key Readouts | Market Share/Importance |
|---|---|---|---|
| Cardiomyocytes | Cardiotoxicity screening, disease modeling, drug testing | Contractility, electrophysiology, cytotoxicity | 31% share in iPSC-based platforms market [45] |
| Neural Progenitors & Neurons | Neurotoxicity, neurodegenerative disease modeling | Neurite outgrowth, synaptic activity, cell viability | Fastest-growing segment in iPSC market [45] |
| Hepatocytes | Hepatotoxicity, metabolic disease modeling | Albumin production, cytochrome P450 activity, toxicity | Critical for ADME-Tox profiling (80% of drug failures relate to liver/heart) [43] |
| Other Specialized Cells | Tissue-specific toxicity, disease mechanism studies | Lineage-specific markers, functional assays | Expanding portfolio for targeted applications |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of HTS in stem cell-based drug discovery requires a comprehensive set of research tools and reagents specifically optimized for stem cell applications. The following table details key solutions essential for HTS experiments in this field:
Table: Essential Research Reagent Solutions for Stem Cell HTS
| Reagent Category | Specific Examples | Function in HTS Workflow | Technical Considerations |
|---|---|---|---|
| Stem Cell Maintenance Media | mTeSR, StemFlex, PluriSTEM | Maintain pluripotency during expansion and assay setup | Quality control for batch-to-batch consistency; formulation stability in miniaturized formats |
| Differentiation Kits | Cardiomyocyte, neuronal, hepatocyte differentiation kits | Direct stem cells toward specific lineages for screening | Protocol optimization for HTS compatibility; efficiency validation across cell lines |
| Extracellular Matrices | Matrigel, Geltrex, laminin-521, vitronectin | Provide appropriate surface for stem cell attachment and signaling | Coating consistency across microplates; lot-to-lot variability testing |
| Viability/Cytotoxicity Assays | CellTiter-Glo, PrestoBlue, Calcein-AM | Assess compound toxicity and general cell health | Compatibility with stem cell metabolism; optimization for 3D culture systems |
| Apoptosis Detection | Caspase-Glo 3/7, Annexin V assays | Quantify programmed cell death in response to compounds | Timing of measurement relative to treatment; distinction from necrosis |
| DNA Damage Markers | gammaH2AX, COMET assays | Genotoxicity assessment in stem cell populations | Baseline level establishment in control cells; assay sensitivity optimization |
| High-Content Imaging Reagents | Live-cell dyes, immunofluorescence antibodies | Multi-parameter phenotypic characterization | Photostability for automated imaging; validation for stem cell-specific markers |
| Gene Expression Analysis | qPCR assays, RNA-seq kits | Molecular profiling of differentiation state | Compatibility with high-throughput RNA extraction; minimal sample requirements |
Data Analysis and FAIRification in HTS
Data Management and FAIR Principles
The substantial data generated through HTS campaigns requires sophisticated management approaches to ensure findability, accessibility, interoperability, and reusability (FAIR). Data management based on FAIR guiding principles supports consistent machine-driven curation and reuse of the accumulated data by the nanosafety, cheminformatics and bioinformatics communities [44]. Traditional HTS results documentation approaches, such as using spreadsheets for data collecting and preprocessing are time-consuming and error-prone, necessitating more robust solutions.
Tools supporting FAIRification of safety data are available, with platforms providing flexible findability of data gathered and/or generated by a wide variety of European nanosafety projects [44]. The data entry for newly generated data is streamlined through template systems that facilitate efficient processing of widely accepted excel data format by means of user-friendly online forms that allow users to specify essential experimental information.
Advanced Data Analysis Techniques
For stem cell-based HTS, specialized analytical approaches are required to extract meaningful biological insights from complex phenotypic data:
Multi-parameter Integration:
- Combine data from multiple endpoints (viability, differentiation, morphology) into integrated scores
- Apply multivariate statistics to identify correlated responses across assay parameters
- Use machine learning to classify compounds based on multi-dimensional profiles
Temporal Dynamics Analysis:
- Monitor stem cell responses across multiple timepoints to capture kinetic profiles
- Identify early and late responders in differentiation screens
- Model time-dependent transitions between cell states
Pathway and Network Analysis:
- Map screening hits onto known signaling pathways regulating self-renewal and differentiation
- Construct interaction networks to identify key regulatory nodes
- Integrate with omics data (transcriptomics, proteomics) for systems-level understanding
The creation of data-handling workflows has the advantage of facilitated conversion of the FAIR HTS data into formats capable of integrating all data and metadata into a single file and multidimensional matrix amenable to interactive visualizations and selection of data subsets [44]. The resulting FAIR HTS data includes both raw and interpreted data (scores) in machine-readable formats distributable as data archive, enabling broader collaboration and data reuse.
Emerging Trends and Technologies
The field of HTS in stem cell-based drug discovery continues to evolve rapidly, driven by several key technological advancements:
AI and Machine Learning Integration: With the use of AI in an iPSC-based platform, large datasets can be rapidly analyzed, along with the detection of the outcomes [45]. This helps in reducing the time and errors of the process and also identifies cell morphology and abnormalities. In drug development, AI helps in predicting drug efficacy and toxicity, and in personalized medicine, it helps provide the best treatment approaches by analyzing data from iPSC cells and the patient's genetic profile.
Advanced Stem Cell Models: Organoid and 3D culture platforms represent the fastest-growing technology segment in the iPSC-based platforms market [45]. These platforms promote the modeling of various complex diseases and are being used in drug discovery and testing. The development of these more physiologically relevant models enables more predictive screening outcomes, particularly for complex tissues like brain, liver, and kidney.
Automation and Scalability: Companies are developing innovative approaches to scale stem cell production for HTS applications. For example, bit.bio's opti-ox precision cell programming and manufacturing technology enables the conversion of iPSCs into any desired human cell type in a single step within days and at industrial scale, while maintaining exceptional purity and unparalleled consistency [43]. Such advances address critical bottlenecks in stem cell-based screening.
High-Throughput Screening represents a transformative approach in stem cell-based drug discovery, providing powerful tools for investigating the fundamental mechanisms of self-renewal and differentiation. The integration of advanced stem cell models, particularly iPSCs, with sophisticated screening technologies and computational analysis has created unprecedented opportunities for understanding cell fate decisions and identifying novel therapeutic interventions.
As the field advances, key developments in AI integration, 3D culture systems, and automated cell production are poised to further enhance the efficiency and predictive power of HTS platforms. These advancements, coupled with rigorous experimental design and data management practices, will continue to drive innovation in both basic research and drug development, ultimately accelerating the translation of stem cell research into clinical applications.
The future of HTS in stem cell research lies in increasingly sophisticated multi-parameter assays, longer-term dynamic monitoring of cell behavior, and the integration of multi-omics data to create comprehensive models of cell fate regulation. By embracing these approaches, researchers can continue to unravel the complexity of stem cell biology and harness this knowledge for therapeutic development.
Gene editing, particularly CRISPR-Cas9 technology, has emerged as a transformative tool for the precise manipulation of stem cell fate and function. This whitepaper provides an in-depth technical guide to CRISPR-based genome engineering within the context of stem cell self-renewal and differentiation mechanisms research. We detail the core mechanisms of CRISPR-Cas9, its application in controlling stem cell signaling pathways, and provide validated experimental protocols for generating gene-edited human pluripotent stem cell (hPSC) lines. The integration of these technologies enables researchers to construct more accurate disease models, perform sophisticated drug screens, and develop novel cell-based therapies with enhanced precision. This document serves as a comprehensive resource for researchers and drug development professionals seeking to leverage gene editing to decode and direct stem cell fate.
The ability to precisely control stem cell self-renewal and differentiation is a fundamental goal in regenerative medicine and developmental biology. Stem cell fate is governed by complex signaling pathways and gene regulatory networks [9]. Gene editing technologies, especially the CRISPR-Cas9 system, provide researchers with the unprecedented ability to interrogate and manipulate these networks with high specificity and efficiency.
The application of CRISPR in stem cell research has revolutionized our approach to disease modeling, drug screening, and therapeutic development [47]. By enabling the generation of isogenic cell lines that differ only at a single genetic locus, CRISPR facilitates the precise attribution of cellular phenotypes to specific genetic variants, which is crucial for discerning subtle phenotypes in stem cell-derived models [47]. Furthermore, the combination of human pluripotent stem cells (hPSCs), including both embryonic and induced pluripotent stem cells, with CRISPR editing creates a powerful platform for studying human development and disease in vitro [15] [47].
Technical Foundations of CRISPR-Cas9
Core Mechanism and Components
The CRISPR-Cas9 system functions as a programmable DNA-endonuclease. Its operation relies on two core components [48]:
- Guide RNA (gRNA): A short synthetic RNA composed of a scaffold sequence necessary for Cas-binding and a user-defined ~20-nucleotide spacer that defines the genomic target to be modified.
- Cas9 Nuclease: An enzyme that creates double-strand breaks (DSBs) in DNA at locations specified by the gRNA.
The genomic target of the gRNA must be unique and must be located immediately adjacent to a Protospacer Adjacent Motif (PAM). For the most commonly used Cas9 from Streptococcus pyogenes (spCas9), the PAM sequence is NGG [48] [47]. Once the Cas9-gRNA complex binds to a DNA target with sufficient homology, particularly in the seed sequence (8-10 bases at the 3' end of the gRNA targeting sequence), the Cas9 nuclease domains (RuvC and HNH) cleave opposite strands of the target DNA, resulting in a DSB approximately 3-4 nucleotides upstream of the PAM sequence [48].
Figure 1: Core Mechanism of the CRISPR-Cas9 System. The process begins with the formation of a ribonucleoprotein complex between the guide RNA and Cas9 nuclease, which then identifies target DNA sequences adjacent to a PAM sequence, leading to a double-strand break and subsequent repair via cellular pathways.
DNA Repair Pathways and Editing Outcomes
The cellular response to CRISPR-induced DSBs leads to different editing outcomes through two primary DNA repair pathways [48] [47]:
Non-Homologous End Joining (NHEJ): An efficient but error-prone repair pathway that directly ligates break ends without a template. This frequently results in small insertion or deletion mutations (indels). When targeted to open reading frames, these indels can introduce frameshift mutations and premature stop codons, leading to gene knockouts [48]. This is particularly useful for disrupting genes in stem cells to study their function.
Homology-Directed Repair (HDR): A less efficient but high-fidelity pathway that uses a homologous DNA template to repair the break. This enables precise gene editing, including the introduction of specific point mutations, reporter tags, or conditional alleles when a donor template is provided [47]. HDR is essential for creating precise disease-associated mutations in stem cells or correcting pathogenic variants.
Table 1: CRISPR-Cas9 Editing Outcomes Based on DNA Repair Pathways
| Repair Pathway | Template Required | Efficiency | Fidelity | Primary Outcome | Common Applications in Stem Cells |
|---|---|---|---|---|---|
| Non-Homologous End Joining (NHEJ) | No | High | Error-prone | Insertions/Deletions (indels) | Gene knockouts, functional screening |
| Homology-Directed Repair (HDR) | Yes (donor DNA) | Lower | High | Precise edits | Point mutations, reporter knock-ins, gene correction |
Precision Control of Stem Cell Fate
Key Signaling Pathways Regulating Stem Cell Behavior
Stem cell self-renewal, differentiation, and migration are collectively regulated by essential signaling pathways that offer strategic targets for CRISPR-mediated manipulation [9]. Key pathways include:
- TGF-β Signaling: Plays a crucial role in maintaining pluripotency and directing differentiation. TGF-β along with Activin A and Nodal signaling pathways stimulates self-renewal of primed pluripotent stem cells [9].
- Wnt Pathway: Essential for tissue homeostasis and supporting both stem cell self-renewal and differentiation. Considered a key regulator of stem cell function [9].
- Notch Signaling: Regulates cell fate decisions through cell-cell communication. Targeting Notch pathway components can direct differentiation toward specific lineages [9] [15].
- Hedgehog (Hh) Pathway: Critical for embryonic development, particularly in limb and bone formation via regulation of epithelial-mesenchymal interactions [9].
- BMP Signaling: Bone Morphogenetic Proteins regulate various aspects of stem cell fate, including self-renewal and differentiation into multiple lineages [9].
These pathways often exhibit complex crosstalk, where modulation of one can influence others, providing multiple pharmacological entry points to fine-tune stem cell behavior for therapeutic purposes [9].
Advanced CRISPR Systems for Fate Control
Beyond standard gene editing, engineered CRISPR systems enable sophisticated control over stem cell behavior:
CRISPRa (Activation) and CRISPRi (Interference): Using catalytically inactive "dead" Cas9 (dCas9) fused to transcriptional regulatory domains, these systems can selectively activate or repress target genes without altering the DNA sequence [49] [48]. This allows for precise modulation of stem cell signaling pathways and differentiation regulators.
Base Editing: This technology enables direct, irreversible conversion of one DNA base pair to another without requiring DSBs [49]. This is particularly valuable for correcting point mutations associated with genetic disorders in stem cells while minimizing indel formation.
Prime Editing: Functions as a "search-and-replace" system capable of making all 12 possible base-to-base conversions, as well as small insertions and deletions, without DSBs [49]. This expands the range of correctable mutations in stem cells for disease modeling.
Epigenome Editing: Using dCas9 fused to epigenetic modifiers, researchers can write specific chromatin marks to influence stem cell differentiation potential and create stable epigenetic states [48].
Table 2: Advanced CRISPR Systems for Stem Cell Engineering
| Technology | Key Components | Editing Mechanism | Advantages for Stem Cell Research |
|---|---|---|---|
| CRISPRa/i | dCas9 fused to transcriptional activators/repressors | Gene regulation without DNA cutting | Reversible modulation of signaling pathways; no genomic alterations |
| Base Editing | Cas9 nickase fused to deaminase enzymes | Direct chemical conversion of DNA bases | High efficiency correction of point mutations; minimal indel formation |
| Prime Editing | Cas9 nickase fused to reverse transcriptase & PE guide RNA | "Search-and-replace" using RNA template | Broad editing capability without DSBs; versatile for various mutation types |
| Epigenome Editing | dCas9 fused to chromatin modifiers | Targeted epigenetic modification | Studying and controlling epigenetic memory in stem cells |
Experimental Protocols for Stem Cell Genome Editing
Comprehensive Workflow for hPSC Genome Editing
The following protocol outlines the critical steps for successful CRISPR-Cas9-mediated gene editing in human pluripotent stem cells, based on established methodologies [47].
Figure 2: Experimental Workflow for CRISPR-Cas9-Mediated Gene Editing in Human Pluripotent Stem Cells. The process begins with careful sgRNA design and validation, followed by vector construction, delivery to hPSCs, clonal isolation, genotypic screening, and functional validation.
Detailed Methodologies
Critical Parameters:
- Select target sequences with high predicted on-target activity and minimal off-target activity using bioinformatic tools (e.g., CHOPCHOP, CRISPR Design Tool).
- The sgRNA should be located as close as possible to the intended edit site, ideally within 30 bp.
- Ensure the target sequence is unique compared to the rest of the genome and is adjacent to a PAM (NGG for spCas9).
Protocol Steps:
- sgRNA Design: Input genomic coordinates of your target region into a sgRNA design tool. Select 3-5 candidate sgRNAs based on high on-target and low off-target scores.
- Cloning into Expression Vector: Incorporate selected sgRNA sequences into an appropriate expression vector that enables co-expression of the sgRNA, Cas9 nuclease, and a selectable marker (e.g., puromycin resistance or GFP).
- In Vitro Transcription: Alternatively, sgRNAs can be generated by in vitro transcription for delivery with Cas9 protein or mRNA.
hPSC Culture Techniques:
- Maintain hPSCs in defined, feeder-free culture conditions to ensure reproducibility and minimize experimental variability.
- Culture cells to 70-80% confluence before passaging and editing to ensure optimal health and recovery post-transfection.
CRISPR Delivery Methods:
- Electroporation: Most common method for delivering CRISPR components to hPSCs. Optimize voltage and pulse duration for your specific cell line.
- Lipid-based Transfection: Suitable for some hPSC lines with high transfection efficiency.
- Viral Transduction: Lentiviral or adenoviral delivery for difficult-to-transfect cells or for creating stable cell lines.
Genomic DNA Extraction:
- Harvest cells 72-96 hours post-transfection for initial assessment of editing efficiency.
- For clonal isolation, harvest individual clones after 10-14 days of expansion.
Editing Efficiency Assessment:
- Barcoded Deep Sequencing: The gold standard for quantifying editing efficiency and characterizing the spectrum of induced mutations.
- T7 Endonuclease I Assay: Rapid, cost-effective method for initial screening of editing efficiency.
- Restriction Fragment Length Polymorphism (RFLP): Useful when an edit creates or destroys a restriction enzyme site.
Clonal Isolation and Validation:
- Isolate single cells by fluorescence-activated cell sorting (FACS) or limiting dilution.
- Expand individual clones for 3-4 weeks with careful monitoring of pluripotency markers.
- Screen clones by PCR and Sanger sequencing across the target site to identify correctly edited clones.
- Validate pluripotency maintenance post-editing through flow cytometry for characteristic markers (OCT4, NANOG, SOX2).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Based Stem Cell Engineering
| Reagent / Tool | Function | Examples & Specifications |
|---|---|---|
| Cas9 Variants | DNA cleavage with different specificities | spCas9 (standard); Cas12a (multiplexing); High-fidelity variants (eSpCas9, SpCas9-HF1) for reduced off-targets [48] |
| Guide RNA Vectors | gRNA expression | U6-promoter driven vectors; Multiplex gRNA vectors for targeting 2-7 loci [48] |
| Delivery Systems | Introducing CRISPR components into cells | Electroporation systems; Lipid nanoparticles (LNPs); AAV vectors (for in vivo) [50] [47] |
| Stem Cell Culture Media | Maintaining pluripotency during editing | Defined, feeder-free media (e.g., mTeSR, StemFlex) [47] |
| Selection Markers | Enriching transfected cells | Puromycin resistance; GFP/RFP reporters; Antibiotic resistance cassettes for HDR [47] |
| HDR Donor Templates | Precise genome editing | Single-stranded oligodeoxynucleotides (ssODNs; <200 bp); Double-stranded DNA donors (plasmid or AAV) [47] |
| Analysis Tools | Validation of edits | T7E1 assay kits; Next-generation sequencing; Flow cytometry for reporter expression [47] |
Emerging Trends and Future Perspectives
Clinical Translation and Therapeutic Applications
The clinical application of CRISPR-edited stem cells is advancing rapidly, with several notable developments:
- In Vivo vs. Ex Vivo Approaches: Gene editing can be delivered into cells using in vivo or ex vivo methods. In vivo delivery involves direct administration of editing components into the patient, while ex vivo approaches involve removing cells, editing them in a specialized laboratory, and returning them to the patient [49].
- Clinical Trial Progress: As of September 2025, multiple clinical trials are underway using CRISPR-engineered therapies for conditions including non-small cell lung cancer (NSCLC), gastric cancer, colorectal cancer, and acute myeloid leukemia (AML) [50].
- Novel Delivery Systems: Advances in delivery technologies, particularly lipid nanoparticles (LNPs) and engineered AAV vectors with tissue tropism, are enhancing the efficiency and specificity of in vivo gene editing [50].
Technological Innovations
The gene editing landscape continues to evolve with several cutting-edge technologies:
- Single-Cell Multiomics: Emerging single-cell multiomics technologies enable comprehensive characterization of CRISPR-edited cells, detecting off-target edits and correlated gene expression changes at single-cell resolution [51].
- Gene Writing Platforms: New technologies like prime editing and FiCAT gene writing platforms offer enhanced precision and safety profiles for therapeutic applications [49] [50].
- Market Growth: The global gene editing market is projected to grow from USD 11.29 billion in 2025 to USD 42.13 billion by 2034, at a CAGR of 15.76%, reflecting the rapid expansion and investment in this field [49].
Addressing Technical Challenges
Several challenges remain in CRISPR-based stem cell engineering, with ongoing research developing solutions:
- Off-Target Effects: Continued engineering of high-fidelity Cas9 variants (eSpCas9, HypaCas9, evoCas9) with reduced off-target activity [48].
- Mosaicism: A particular challenge in embryonic editing where edited cells contain mixed populations of edited and unedited cells [49].
- Delivery Efficiency: Optimizing delivery methods to improve editing efficiency while maintaining cell viability and pluripotency [47].
- Complex Trait Engineering: Developing approaches for multiplex editing to address polygenic diseases and complex cellular phenotypes [48].
The integration of CRISPR-based gene editing with stem cell biology continues to provide unprecedented opportunities for understanding and controlling cell fate decisions. As technologies advance, the precision, efficiency, and safety of these approaches will continue to improve, accelerating both basic research and clinical applications in regenerative medicine.
Hematopoietic Stem Cell Transplantation (HSCT) remains a cornerstone cellular therapy for a spectrum of hematologic diseases. Its successful clinical translation serves as a paradigm for the broader field of stem cell-based interventions, which is rapidly advancing through pharmacological modulation of key signaling pathways and the adjunct use of supportive cells like Mesenchymal Stem Cells (MSCs). The field is moving beyond traditional HSCT towards sophisticated manipulations and applications of pluripotent and adult stem cells. However, this progress is tightly coupled with the imperative for rigorous scientific rationale, robust preclinical evidence, and comprehensive regulatory oversight to ensure patient safety and therapeutic efficacy. The future of clinical translation lies in a multidisciplinary approach that integrates insights from stem cell biology, immunology, pharmacology, and tissue engineering, all underpinned by a deep understanding of the molecular mechanisms governing stem cell self-renewal and differentiation [52] [9] [53].
Hematopoietic stem cell transplantation (HSCT), first performed over five decades ago, stands as the most established and widely practiced stem cell-based therapy globally. It involves the intravenous infusion of hematopoietic stem cells (HSCs) to re-establish hematopoietic function in patients with damaged or defective bone marrow. The clinical success of HSCT has provided a critical framework for developing other stem cell-based interventions, demonstrating both the immense therapeutic potential and the significant challenges inherent in this modality. The procedure has evolved from a last-resort intervention to a standard of care for many life-threatening hematologic malignancies, such as acute leukemias and lymphomas, as well as non-malignant disorders including aplastic anemia and certain genetic immunodeficiencies [54] [53].
The core principles learned from HSCT—including donor selection, cell sourcing, processing, and infusion, management of immune compatibility (Graft-versus-Host Disease) and rejection, and supportive care during the vulnerable period of engraftment—are directly applicable to the development of novel therapies derived from other stem cell types. Furthermore, the global tracking of HSCT activity and outcomes provides a model for how emerging stem cell therapies should be monitored and evaluated on a population level. Quantitative data reveals that HSCT activity is increasing worldwide, with the highest relative growth in the Asia Pacific region, though significant disparities in access and utilization persist, strongly associated with national economic indicators such as Gross National Income (GNI) per capita [54]. This established clinical foundation makes HSCT an ideal starting point for examining the broader landscape of clinical translation in stem cell medicine.
Core Scientific and Mechanistic Foundations
Molecular Regulation of Stem Cell Fate
The behavior of stem cells, including self-renewal, differentiation, and quiescence, is collectively regulated by a network of evolutionarily conserved signaling pathways. These pathways represent the fundamental mechanistic links between basic research on stem cell fate and their clinical application.
- TGF-β/BMP Signaling: The TGF-β superfamily, including TGF-βs, BMPs, and activins, plays a dual role in maintaining stem cell pluripotency and directing differentiation. TGF-β along with Activin A and Nodal signaling is crucial for stimulating the self-renewal of "primed" pluripotent stem cells. Conversely, BMP-4 promotes the self-renewal of embryonic stem cells (ESCs). This pathway primarily signals through SMAD proteins (SMAD1/5/8 and SMAD2/3) to regulate the expression of genes involved in the cell cycle and differentiation [9].
- Wnt/β-catenin Signaling: The Wnt pathway is a principal regulator of stem cell function, crucial for tissue homeostasis, and supports both self-renewal and differentiation decisions. Its activity is tightly controlled in stem cell niches, and its dysregulation is often associated with tumorigenesis, making its precise modulation a key therapeutic goal [9] [55].
- Notch Signaling: This pathway mediates direct cell-cell communication and is instrumental in cell fate determination. In hematopoietic stem cells (HSCs), Notch signaling helps to maintain the stem cell pool, while in other contexts it can drive lineage-specific differentiation. It is also a key target in strategies to eliminate cancer stem cells [9].
- Hedgehog (Hh) Signaling: Critical for embryonic development, particularly in limb and bone formation, the Hh pathway regulates epithelial-mesenchymal interactions. Like Notch and Wnt, it is a strategic target for inhibiting cancer stem cells to prevent tumor recurrence [9].
- Cell Cycle Coupling: Stem cells, particularly ESCs, exhibit a unique cell cycle structure characterized by a shortened G1 phase and a prolonged S phase. This rapid cycle is closely linked to the maintenance of a pluripotent, undifferentiated state. Core pluripotency factors such as Nanog and Oct4 are intimately connected with the expression of key cell cycle regulators, including cyclins and cyclin-dependent kinases (CDKs). Pathways like Jak1/Stat3 and PI3K/Akt, as well as a metabolic shift towards glycolysis, underpin this unique cell cycle configuration and its role in stemness maintenance [55].
These pathways do not operate in isolation; they exhibit extensive crosstalk, forming a complex regulatory network that can be pharmacologically targeted to fine-tune stem cell behavior for therapeutic purposes [9].
Visualizing Stem Cell Signaling and Fate Regulation
The following diagram illustrates the complex interplay between key signaling pathways and internal processes that govern stem cell self-renewal and differentiation fate, forming the mechanistic basis for therapeutic interventions.
Clinical Translation of Hematopoietic Stem Cell Transplantation
Current Global Landscape and Clinical Applications
HSCT has seen a consistent global increase in application, with data from 2006-2008 showing 146,808 first HSCTs reported from 1,411 teams across 72 countries. The distribution of this activity, however, is highly asymmetric, closely linked to a country's economic status. Europe accounts for the largest share (51%), followed by the Americas (29%), Asia (18%), and the Eastern Mediterranean/Africa region (3%). The transplant rate (number of first HSCTs per 10 million inhabitants) is strongly associated with GNI/capita (R² = 61%), highlighting the significant economic barriers to accessing this advanced therapy. The main indications for HSCT are lymphoproliferative disorders (53%) and leukemias (36%), with solid tumors and non-malignant disorders constituting smaller proportions [54].
Qualitative differences in HSCT practice are also evident. There is a preferential use of allogeneic transplants in lower-income countries compared to autologous ones, a higher reliance on related family donors, and a greater proportion of transplants for non-malignant diseases. These patterns reflect the substantial infrastructure, specialized personnel, and financial resources required, particularly for unrelated donor transplants and the management of complex post-transplant courses associated with malignant diseases [54].
Hematopoietic Stem Cell Products: A Comparative Analysis
The source of hematopoietic stem cells is a critical variable in transplantation, influencing engraftment kinetics, immune reconstitution, and complications such as Graft-versus-Host Disease (GVHD). The table below provides a detailed comparison of the primary HSC products used in clinical practice.
Table 1: Comparison of Hematopoietic Stem Cell Products [56]
| Product Characteristic | Peripheral Blood Stem Cells (PBSCs) | Bone Marrow (BM) | Cord Blood | T-cell–Depleted BM/PBSCs | Haploidentical T-cell–Depleted BM/PBSCs |
|---|---|---|---|---|---|
| T-cell content | High | Moderate | Low | Very low | Very low |
| CD34+ content | Moderate–High | Moderate | Low (but higher potency) | Moderate–High | Moderate–High |
| Time to Neutrophil Recovery | Rapid: median, 16 d | Moderate: median, 21 d | Slower: median, 23 d | Rapid: median, 16 d | Rapid: median, 13 d |
| Risk of Graft Rejection | Low | Low–Moderate | Moderate–High | Moderate–High | Moderate–High |
| Risk of Acute GVHD | Moderate | Moderate | Moderate | Low | Low |
| Risk of Chronic GVHD | High | Moderate | Low | Low | Low |
| Time to Immune Reconstitution | Rapid (6–12 mo) | Moderate (6–18 mo) | Slow (6–24 mo) | Slow (6–24 mo) | Slow (9–24 mo) |
| Early Post-HCT Infection Risk | Low–Moderate | Moderate | High | Very High | Very High |
Experimental Protocol: MSC Co-infusion to Accelerate Engraftment
A key advancement in improving HSCT outcomes is the use of mesenchymal stem cell (MSC) co-infusion. The following is a detailed methodology based on a comprehensive systematic review of clinical studies (2000-2025) [53].
Objective: To evaluate the safety and efficacy of MSC co-infusion in accelerating hematopoietic recovery, particularly platelet and neutrophil engraftment, following HSCT.
Study Design:
- Type: Randomized controlled trials, cohort studies, or single-arm studies.
- Population: Patients (both pediatric and adult) undergoing autologous or allogeneic HSCT for malignant or non-malignant hematologic diseases.
- Intervention vs. Control: Intravenous infusion of MSCs derived from bone marrow or umbilical cord, compared to standard HSCT without MSC infusion.
Methodology:
- MSC Preparation:
- Source: Isolate MSCs from donor bone marrow aspirate or human umbilical cord tissue (Wharton's Jelly).
- Expansion: Culture and expand MSCs in vitro for 3-5 passages under Good Manufacturing Practice (GMP) conditions or phase-appropriate conditions for early-stage trials [52].
- Quality Control: Perform characterization per International Society for Cellular Therapy (ISSCR) guidelines, including flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45, CD11b) markers, and differentiation assays into osteocytes, adipocytes, and chondrocytes.
- Release Testing: Test for viability (>70%), sterility (bacterial/fungal), mycoplasma, and endotoxin prior to cryopreservation and infusion.
MSC Administration:
- Timing: Infuse MSCs intravenously either on the day of HSC infusion (day 0) or shortly thereafter (e.g., day +1 to +5).
- Dosing: A common dose range is 1-5 x 10^6 MSCs per kilogram of recipient body weight. The cells are thawed and administered in a sterile saline solution.
Outcome Measures (Primary Endpoints):
- Neutrophil Engraftment: Defined as the first of three consecutive days with an absolute neutrophil count (ANC) ≥ 0.5 x 10^9/L.
- Platelet Engraftment: Defined as the first of seven consecutive days with a platelet count ≥ 20 x 10^9/L without transfusion support.
- Safety: Monitor for acute infusion-related reactions (e.g., fever, allergic symptoms) and long-term adverse events for at least 100 days post-transplant.
Expected Results: Based on the systematic review of 47 studies and 1777 patients, MSC co-infusion is safe and associated with accelerated engraftment. The average time to neutrophil engraftment in MSC recipients is approximately 14 days, and platelet engraftment is approximately 21.6 days. Approximately 79% of studies report enhanced engraftment, with the most consistent benefit observed for platelet recovery [53].
Visualizing the MSC Co-Infusion Workflow
The following diagram outlines the key stages in the manufacturing and clinical application of MSCs for enhancing hematopoietic recovery post-HSCT.
Regulatory and Manufacturing Framework
The clinical translation of any stem cell-based intervention, including novel applications beyond HSCT, demands rigorous oversight. According to ISSCR guidelines, stem cells and tissues that are "substantially manipulated" or used in a "non-homologous" manner must be regulated as drugs, biologics, or Advanced Therapy Medicinal Products (ATMPs) [52].
- Substantial Manipulation: This involves processing steps that alter the original biological characteristics of the cells (e.g., enzymatic digestion of adipose tissue, prolonged culture and expansion, genetic manipulation). Such products require comprehensive preclinical and clinical testing to establish safety and efficacy for each specific indication [52].
- Non-homologous Use: This occurs when cells are used for a different basic function than they performed in their original tissue location (e.g., injecting adipose-derived stromal cells into the eye to treat macular degeneration). This practice carries documented risks and must be rigorously evaluated by national regulatory agencies like the FDA and EMA [52].
- Manufacturing Oversight: Cellular products are considered manufactured entities. Their production must be subject to quality control systems and standard operating procedures, ideally under Good Manufacturing Practice (GMP) conditions. Critical aspects include donor screening and informed consent for allogeneic products, rigorous testing of cell banks for adventitious agents, and meticulous control over reagents and processes to ensure product consistency, purity, and potency [52].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Stem Cell Research and Therapy Development
| Reagent/Material | Primary Function in Research & Development |
|---|---|
| Cytokines and Growth Factors (e.g., SCF, TPO, FGF, BMPs) | To direct stem cell differentiation, maintain pluripotency in culture, and support ex vivo expansion of specific cell types. Essential for mimicking the native stem cell niche [9] [53]. |
| Small Molecule Pathway Modulators (e.g., Wnt agonists/antagonists, Notch inhibitors) | To pharmacologically fine-tune key signaling pathways (Hedgehog, TGF-β, Wnt, Notch) for precise control over stem cell self-renewal, differentiation, and eradication of cancer stem cells [9]. |
| Cell Culture Media & Supplements (Serum-free formulations, defined media) | To provide a consistent, xeno-free environment for the expansion and differentiation of stem cells, reducing batch-to-batch variability and risk of contamination, crucial for clinical translation [52]. |
| Characterization Antibodies (e.g., for CD34, CD45, CD73, CD90, CD105, OCT4, NANOG) | For flow cytometry and immunocytochemistry to identify, isolate (e.g., FACS), and validate stem cell populations and their differentiated progeny based on surface and intracellular markers [52] [53]. |
| Gene Editing Tools (e.g., CRISPR/Cas9 systems) | For genetic manipulation of stem cells to study gene function, create disease models, or correct genetic defects in autologous cell therapies. Requires stringent quality control to ensure safety [52] [9]. |
| Biomaterial Scaffolds (e.g., hydrogels, decellularized matrices) | To provide a three-dimensional structural and biochemical support system for tissue engineering, enhancing stem cell survival, integration, and functional tissue formation upon transplantation [9]. |
The field of stem cell clinical translation is rapidly evolving beyond traditional HSCT. Key future directions include:
- Pharmacological Enhancement: Using small molecules to improve the survival, integration, and targeted differentiation of transplanted stem cells, while mitigating risks like tumorigenesis and immune rejection [9].
- Endogenous Stem Cell Activation: Developing drugs to stimulate a patient's own resident stem cells to participate in tissue repair, potentially obviating the need for complex transplantation procedures for some conditions [9].
- Advanced Engineering: Combining gene editing technologies, such as CRISPR-Cas9, with stem cell therapies to correct genetic defects ex vivo before autologous transplantation. Furthermore, the integration of stem cells with sophisticated biomaterials and tissue engineering approaches is paving the way for the generation of complex functional tissues and organoids [9].
- Standardization and Personalization: Addressing the current heterogeneity in cell manufacturing and clinical protocols is critical. Future efforts must focus on developing universal standards for cellular identity, purity, and potency, while also moving towards personalized therapies tailored to individual patient needs and disease contexts [52] [53].
In conclusion, hematopoietic stem cell transplantation continues to serve as a vital therapy and a foundational model for the entire field of regenerative medicine. Its ongoing evolution, coupled with breakthroughs in our understanding of stem cell biology and the development of powerful new pharmacological and engineering tools, promises a new era of safer, more effective, and more accessible stem cell-based treatments for a wide range of debilitating diseases.
Tissue Engineering and Regenerative Medicine Applications
Tissue Engineering and Regenerative Medicine (TERM) represents a revolutionary frontier in biomedical science, aiming to repair or replace damaged tissues and organs through the integration of stem cell biology, biomaterial science, and bioengineering principles [57]. This interdisciplinary field has undergone significant advancements, moving from theoretical concept to clinical reality by leveraging the unique properties of stem cells—self-renewal and differentiation capacity—to generate functional tissues [15]. The fundamental paradigm involves harnessing stem cells as building blocks, guiding them through specific differentiation pathways using biochemical and biophysical cues, and supporting their organization into three-dimensional tissues using advanced scaffold systems and bioreactors [57] [58].
The clinical translation of TERM strategies offers promising solutions for millions of patients suffering from debilitating conditions, organ failure, and tissue loss [58]. By directing stem cell differentiation along specific lineages, researchers can now generate patient-specific tissue constructs for transplantation, disease modeling, and drug screening [15]. The field continues to evolve rapidly, with recent breakthroughs in 3D bioprinting, induced pluripotent stem cell (iPSC) technology, and decellularized scaffolds accelerating the development of increasingly complex tissue architectures [59] [58]. This technical guide examines the current state of TERM applications within the broader context of stem cell self-renewal and differentiation mechanisms, providing researchers and drug development professionals with a comprehensive overview of methodologies, clinical applications, and emerging technologies.
Pluripotent Stem Cells and Lineage Specification
Embryonic Stem Cells (ESCs) and induced Pluripotent Stem Cells (iPSCs) represent the most versatile cell sources for TERM applications due to their pluripotency—the ability to differentiate into any cell type derived from the three germ layers [15] [60]. ESCs are isolated from the inner cell mass of blastocysts through microsurgery or immunological targeting of trophoblast cells, while iPSCs are generated by reprogramming somatic cells through the introduction of specific transcription factors [15]. The molecular regulation of self-renewal and differentiation decisions in pluripotent stem cells involves complex interplay between cell cycle regulators, transcription factors, and epigenetic mechanisms. Research has identified CDK2AP1 (CDK2 associating protein 1) as a critical competency factor in embryonic stem cell differentiation, while OCT3/4 maintains pluripotency through epigenetic control mechanisms [37].
Table 1: Pluripotent Stem Cell Applications in Tissue Engineering
| Application Area | Cell Type | Target Conditions | Development Stage |
|---|---|---|---|
| Ophthalmology | iPSC-derived retinal cells | Retinitis pigmentosa, Cone-rod dystrophy | Phase I/IIa trials [60] |
| Neurology | iPSC-derived dopaminergic neural progenitors | Parkinson's disease, ALS, Spinal cord injury | Phase I trials [60] |
| Oncology | iPSC-derived natural killer (NK) cells | Gynecologic cancers | Clinical trials (NCT06342986) [60] |
| Musculoskeletal | iPSC-derived muscle progenitors | Duchenne Muscular Dystrophy (DMD) | Phase I trial (NCT06692426) [60] |
| Reproductive Medicine | iPSC-derived ovarian support cells | In vitro oocyte maturation | Phase III trial (Fertilo) [60] |
The following diagram illustrates the fundamental signaling pathways and transcriptional regulators governing the balance between self-renewal and differentiation in human pluripotent stem cells:
Adult and Perinatal Stem Cells in Regenerative Applications
Adult Stem Cells (ASCs), also known as tissue-specific stem cells, reside in various specialized niches throughout the body and maintain tissue homeostasis through their multipotency—the ability to differentiate into a limited range of cell types within their tissue of origin [15]. Mesenchymal Stem Cells (MSCs) represent the most widely utilized adult stem cell population in TERM, capable of generating bone, cartilage, and fat cells [61]. These cells can be isolated from multiple sources including bone marrow, adipose tissue, and dental pulp [61]. Perinatal Stem Cells derived from umbilical cord, amniotic fluid, and placental tissues offer a unique combination of accessibility, multipotency, and reduced immunogenicity, making them attractive for allogeneic applications [15].
The therapeutic efficacy of MSCs in regenerative medicine stems from both their differentiation capacity and their paracrine signaling capabilities, through which they secrete immunomodulatory factors and extracellular vesicles that modulate the tissue microenvironment [61]. Recent advances have led to the development of iPSC-derived MSCs (iMSCs) that offer enhanced consistency, scalability, and functionality compared to primary MSCs [60]. Clinical trials are currently investigating iMSCs for conditions including High-Risk Acute Graft-Versus-Host Disease (HR-aGvHD), osteoarthritis, and various tissue repair applications [60].
Experimental Methodologies in Tissue Engineering
Stem Cell Differentiation Protocols
Directing stem cell differentiation along specific lineages requires precise control of biochemical and biophysical cues that mimic developmental processes. The following experimental workflow represents a generalized protocol for directed differentiation of pluripotent stem cells:
Specific Differentiation Protocols:
Neural Differentiation: Pluripotent stem cells are first aggregated into embryoid bodies and exposed to dual SMAD inhibition (using Noggin and SB431542) to induce neural induction. Subsequent patterning with morphogens like SHH (Sonic Hedgehog) or FGF8 (Fibroblast Growth Factor 8) generates specific neuronal subtypes, including dopaminergic neurons for Parkinson's disease applications [60].
Cardiac Differentiation: Monolayer cultures of pluripotent stem cells are treated with activated BMP4 (Bone Morphogenetic Protein 4) and FGF2 to induce mesodermal commitment, followed by WNT inhibition to promote cardiac specification. The resulting cardiomyocytes can be further matured using 3D culture systems and electromechanical stimulation [15].
Hepatic Differentiation: Definitive endoderm is induced through ACTIVIN A treatment, followed by hepatic specification using FGF and BMP signaling pathway activation. Final maturation involves exposure to glucocorticoids, oncostatin M, and culture in 3D configurations that enhance metabolic functionality [59].
Scaffold Fabrication and 3D Bioprinting Techniques
Advanced biomaterial scaffolds provide the structural and biochemical framework that supports stem cell differentiation, organization, and functional tissue formation. Recent innovations in scaffold technology include:
Injectable Biomimetic Hydrogels: These water-swollen polymer networks mimic the natural tissue environment and can be delivered through minimally invasive procedures. They incorporate cell-adhesive motifs (e.g., RGD peptides) and matrix metalloproteinase (MMP)-sensitive crosslinkers that permit cell-mediated remodeling [59]. Alginate, hyaluronic acid, and polyethylene glycol (PEG) constitute commonly used hydrogel platforms that can be functionalized with tissue-specific extracellular matrix (ECM) components.
Decellularized Extracellular Matrix (dECM) Scaffolds: Tissues or organs are treated with detergents to remove cellular components while preserving the intrinsic ECM architecture and bioactive factors [58]. These scaffolds provide tissue-specific biological cues that direct stem cell differentiation and organization. Recellularization with patient-specific stem cells or progenitor cells creates functional tissue constructs with potential for clinical transplantation.
3D Bioprinting: Additive manufacturing techniques enable precise spatial patterning of stem cells, biomaterials, and signaling molecules to create complex tissue architectures. 4D and 5D bioprinting approaches incorporate dynamic temporal components, where printed structures evolve over time in response to environmental stimuli [58]. These technologies allow recreation of critical tissue features such as metabolic zones, vascular networks, and multicellular interfaces [59].
Table 2: Advanced Biomaterial Platforms for Stem Cell-Based Tissue Engineering
| Biomaterial Platform | Key Characteristics | TERM Applications | References |
|---|---|---|---|
| Synthetic Hydrogels (PEG, PLA, PLGA) | Tunable mechanical properties, reproducible fabrication, controlled degradation | Cartilage repair, bone regeneration, neural tissue engineering | [59] [58] |
| Natural Polymer Hydrogels (Collagen, Fibrin, Alginate) | Innate bioactivity, cell adhesion motifs, enzymatic degradability | Cardiac patches, adipose tissue engineering, skin regeneration | [59] [58] |
| Decellularized ECM Scaffolds | Tissue-specific biochemical and biomechanical cues, preserved ultrastructure | Whole organ engineering, musculoskeletal tissue regeneration | [58] |
| Nanofibrous Scaffolds (Electrospun) | High surface area-to-volume ratio, biomimetic of native ECM topography | Vascular grafts, ligament/tendon repair, nerve guidance conduits | [59] |
| Bioactive Glass/Ceramic Scaffolds | Osteoconductivity, ion release, high compressive strength | Bone regeneration, dental applications, osteochondral interfaces | [57] |
Clinical Translation and Regulatory Landscape
FDA-Approved Stem Cell-Based Therapies
The clinical translation of TERM technologies has accelerated significantly, with several stem cell-based products receiving FDA approval recently. These pioneering therapies demonstrate the viability of stem cell-derived products for treating various conditions:
Ryoncil (remestemcel-L): Approved in December 2024, this allogeneic bone marrow-derived MSC therapy represents the first FDA-approved MSC product for pediatric patients with steroid-refractory acute graft-versus-host disease (SR-aGVHD) [60]. The MSCs modulate the immune response and mitigate inflammation through paracrine signaling mechanisms.
Omisirge (omidubicel-onlv): Approved in April 2023, this cord blood-derived hematopoietic progenitor cell product accelerates neutrophil recovery in patients with hematologic malignancies undergoing umbilical cord blood transplantation [60]. The nicotinamide-modified stem cell graft reduces infection risk following myeloablative conditioning.
Lyfgenia (lovotibeglogene autotemcel): Approved in December 2023, this autologous cell-based gene therapy treats sickle cell disease in patients aged 12 years and older [60]. The therapy involves genetic modification of the patient's own hematopoietic stem cells to produce hemoglobin that reduces sickling.
Clinical Trial Landscape and Safety Profile
The global clinical trial landscape for pluripotent stem cell-based therapies has expanded substantially, with 115 registered clinical trials involving 83 distinct PSC-derived products as of December 2024 [60]. These trials have collectively dosed over 1,200 patients with more than 10¹¹ cells, demonstrating an encouraging safety profile with no class-wide safety concerns identified [60].
Table 3: Clinical Outcomes of Selected Stem Cell-Based Therapies
| Therapy/Indication | Patient Population | Primary Outcomes | Reported Success Rates |
|---|---|---|---|
| Mesenchymal Stem Cell Therapy (Various inflammatory/autoimmune conditions) | Patients with degenerative conditions, autoimmune diseases | Reduction in inflammation, symptomatic improvement | ~80% success rate based on patient-reported outcomes [61] |
| Hematopoietic Stem Cell Transplantation (Blood cancers) | Patients with hematologic malignancies | Reconstitution of blood and immune cell populations | 60-70% success rate [61] |
| Bone Marrow-Derived Mononuclear Cells (Multiple Sclerosis) | Patients with relapsing-remitting MS | Reduction in relapses, decreased symptom severity | Significant reduction in relapses in clinical studies [46] |
| Autologous Hematopoietic Stem Cell Transplantation (Multiple Sclerosis) | Patients with MS | Improvement in disability scores, decreased relapses | Significant improvement in disability scores [46] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful TERM research requires carefully selected reagents and materials that ensure reproducibility, efficacy, and safety. The following table details essential research solutions for stem cell-based tissue engineering:
Table 4: Essential Research Reagents for Stem Cell-Based Tissue Engineering
| Reagent Category | Specific Examples | Function in TERM Applications |
|---|---|---|
| Stem Cell Culture Media | mTeSR, StemFlex, E8 medium | Maintain pluripotency or support directed differentiation through defined formulations |
| Extracellular Matrix Substrates | Matrigel, Laminin-521, Vitronectin, Recombinant Collagens | Provide adhesion support and biochemical cues for stem cell attachment and differentiation |
| Small Molecule Inhibitors/Activators | CHIR99021 (WNT activator), SB431542 (TGF-β inhibitor), Y-27632 (ROCK inhibitor) | Direct lineage specification through modulation of key signaling pathways |
| Growth Factors & Cytokines | FGF, BMP, EGF, VEGF, Neurotrophins | Promote specific differentiation programs and support tissue maturation |
| Biomaterial Polymers | Alginate, Chitosan, Polycaprolactone, Polyethylene Glycol | Form 2D/3D scaffolds that provide structural support and biochemical cues |
| Gene Editing Tools | CRISPR/Cas9 systems, mRNA for reprogramming, Lentiviral vectors | Genetic modification, cellular reprogramming, lineage tracing |
| Characterization Antibodies | Anti-OCT4, NANOG, SSEA (pluripotency); lineage-specific markers | Assessment of stem cell status and differentiation efficiency |
Emerging Technologies and Future Directions
Converging Technologies Accelerating TERM Advancements
The future of TERM lies at the intersection of multiple disruptive technologies that collectively address current limitations in tissue complexity, vascularization, and functional integration:
Advanced Bioprinting and Biofabrication: 4D and 5D bioprinting technologies incorporate dynamic temporal components and enable the creation of tissues that evolve their structure and function over time or in response to environmental stimuli [58]. These approaches allow engineering of tissues with enhanced physiological relevance, including recapitulation of metabolic zones, cell polarity, and vascular networks [59].
Artificial Intelligence and Machine Learning: AI algorithms optimize biomaterial design, predict stem cell behavior, and refine bioprinting parameters by analyzing complex multivariate datasets [58]. Machine learning models can identify previously unrecognized patterns in stem cell differentiation, potentially revealing novel regulatory mechanisms of self-renewal and lineage commitment.
Gene Editing and Cellular Engineering: CRISPR-based technologies enable precise genetic modifications in stem cells, creating enhanced cell sources with improved differentiation capacity, immune evasion properties, or additional therapeutic functions [15] [59]. These tools also facilitate the development of sophisticated disease models for drug screening and pathological studies.
Addressing Current Challenges and Limitations
Despite significant progress, TERM faces several persistent challenges that require innovative solutions:
Vascularization: Engineering thick, complex tissues requires the integration of functional vascular networks to ensure nutrient delivery and waste removal. Current approaches include sacrificial bioprinting, microfluidic patterning, and the use of pro-angiogenic factors to promote blood vessel formation [58].
Innervation: Restoring sensory and motor function in engineered tissues necessitates the integration of appropriate neural networks. Co-culture systems with neural stem cells and the incorporation of neurotrophic factors represent promising strategies.
Immune Compatibility: While autologous iPSCs address rejection concerns, allogeneic approaches offer advantages in cost and immediacy. Technologies to create universal donor cells through genetic modification of immune recognition molecules are under active development [60].
Standardization and Scalability: Reproducible manufacturing of tissue-engineered products requires standardized protocols, quality control measures, and scalable production systems such as bioreactors [58]. The field is working toward establishing consensus standards for characterizing stem cells and their differentiated progeny.
Tissue Engineering and Regenerative Medicine has evolved from a speculative concept to a rapidly advancing field with tangible clinical impacts. The successful application of TERM strategies hinges on a deep understanding of stem cell self-renewal and differentiation mechanisms, enabling researchers to direct cellular fate decisions toward specific therapeutic endpoints. Recent FDA approvals of stem cell-based products, together with an expanding clinical trial landscape, demonstrate the translational potential of these technologies.
The convergence of stem cell biology with advanced bioengineering approaches—including 3D bioprinting, biomimetic scaffolds, and gene editing—continues to push the boundaries of what is possible in tissue regeneration. As the field addresses remaining challenges in vascularization, innervation, and scalable manufacturing, TERM strategies are poised to transform treatment paradigms for a wide range of debilitating conditions. Continued interdisciplinary collaboration among biologists, engineers, clinicians, and regulatory specialists will be essential to fully realize the potential of stem cell-based therapies to restore form and function to damaged tissues and organs.
Overcoming Technical Hurdles and Enhancing Protocol Efficacy
Preserving Stem Cell Function During In Vitro Culture and Expansion
The foundational principle of stem cell biology revolves around two fundamental cellular processes: self-renewal, the ability to generate identical copies of themselves, and differentiation, the capacity to mature into specialized cell types. For researchers and drug development professionals, maintaining this delicate balance during in vitro culture and expansion presents a significant technical challenge. The molecular mechanisms governing stem cell fate are tightly regulated by an orchestrated interplay of intrinsic genetic programs and extrinsic environmental cues [37]. As the field progresses toward clinical applications, preserving genomic integrity, pluripotency, and differentiation capacity through robust, standardized culture systems has become paramount. This technical guide examines the core principles and latest methodologies for maintaining functional stem cell properties throughout in vitro manipulation, framed within the broader context of stem cell self-renewal and differentiation mechanisms research.
Core Principles of Stem Cell MaintenanceIn Vitro
Defining Culture Condition Standards
Recent comparative analyses of over 100 human pluripotent stem cell lines have demonstrated that defined culture conditions significantly reduce inter-line variability compared to undefined systems [62]. This standardization is crucial for reproducible research and reliable therapeutic outcomes. Defined conditions utilize xeno-free, fully formulated media and recombinant matrices such as laminin 521 and vitronectin, which replace variable components like fetal bovine serum and mouse feeder cells [62]. The primary source of transcriptional variability (17% in principal component analysis) has been directly attributed to differences between defined and undefined culture environments, with defined conditions producing a more homogeneous cell population with uniformly low somatic marker expression [62].
Molecular Regulation of Stem Cell Fate
The decision between self-renewal and differentiation is governed by complex signaling networks and epigenetic regulators. Research has highlighted the significance of cell cycle regulatory molecules like CDK2AP1 as competency factors in differentiation initiation [37]. Furthermore, studies under defined culture conditions have revealed the importance of Ca2+ signaling in maintaining pluripotency, with inhibition of SERCA pumps—which control intracellular calcium storage—disrupting pluripotency gene expression [62]. These findings underscore the intricate connection between metabolic pathways and stem cell identity maintenance.
Quantitative Analysis of Phenotypic Changes During Long-Term Culture
Long-term in vitro expansion inevitably induces phenotypic changes that can compromise therapeutic utility. Understanding these alterations is essential for developing effective countermeasures.
Table 1: Phenotypic Changes in Bone Marrow-Derived Mesenchymal Stem Cells During Long-Term In Vitro Expansion
| Parameter Assessed | Change with Long-Term Culture | Functional Impact |
|---|---|---|
| Self-Renewal Capacity | Decreased colony-forming unit-fibroblast potential [63] | Reduced expansion efficiency and yield |
| Senescence | Increased β-galactosidase staining [63] | Permanent growth arrest and altered secretome |
| Cell Morphology | Increased cell size [63] | Altered physical characteristics and potentially function |
| Osteogenic Potential | Decreased differentiation capacity [63] | Compromised utility for bone regeneration |
| Adipogenic Potential | No consistent change [63] | Preserved utility for fat tissue engineering |
| Surface Marker Expression | Remains similar for positive/negative markers [63] | Maintained phenotypic identity despite functional changes |
| Immunosuppressive Potential | Unchanged CD4+ T lymphocyte suppression [63] | Preserved immunomodulatory function |
| Secretome Profile | Shift in cytokine/chemokine expression [63] | Altered paracrine signaling capabilities |
These quantitative findings highlight that while certain functions remain stable during extended culture, critical properties like self-renewal and specific differentiation pathways become compromised, necessitating careful monitoring and culture duration limits for clinical applications.
Signaling Pathways Governing Stem Cell Behavior
Stem cell fate is collectively regulated by essential signaling pathways that represent potential intervention points for pharmacological modulation. The Hedgehog, Wnt, Hippo, TGF-β, FGF, BMP, and Notch pathways form a complex regulatory network with significant crosstalk [9].
Diagram 1: Key signaling pathways regulating stem cell behavior. Multiple extracellular signals converge to determine stem cell fate decisions through integrated intracellular signaling networks.
The TGF-β superfamily plays a particularly crucial role, with different branches contributing to distinct aspects of stem cell regulation. TGF-β itself, along with Activin A and Nodal, stimulates self-renewal of primed pluripotent stem cells, while BMP signaling contributes to both pluripotency maintenance and lineage specification [9]. These pathways ultimately influence gene expression networks that determine whether stem cells remain in a self-renewing state or commit to differentiation programs.
Advanced Methodologies for Functional Preservation
Defined Culture Protocol for Pluripotent Stem Cells
The transition from undefined to defined culture systems represents one of the most significant advances for preserving stem cell function during in vitro culture. The following protocol outlines key steps for maintaining human pluripotent stem cells under defined conditions:
- Culture Surface Preparation: Coat tissue culture vessels with recombinant laminin-521 (10-20 µg/mL in DPBS) or vitronectin for at least 1 hour at room temperature [62].
- Medium Formulation: Use fully defined medium such as Essential 8 (E8) containing bFGF, TGF-β, insulin, and other essential components without serum or conditioned media [62].
- Passaging Technique: Employ gentle cell dissociation reagents without enzymatic digestion when possible. For enzymatic passage, use minimal concentrations of recombinant enzymes like Accutase or Dispase for the shortest effective duration [62].
- Calcium Homeostasis Monitoring: Regularly assess intracellular calcium signaling, as SERCA pump inhibition has been shown to disrupt pluripotency maintenance under defined conditions [62].
- Quality Control Assessment: Regularly monitor pluripotency marker expression (OCT3/4, NANOG, SOX2), karyotype stability, and differentiation potential through trilineage differentiation assays.
Three-Dimensional Niche Reconstruction Approaches
Recent advances have shifted from conventional two-dimensional culture toward three-dimensional biomimetic models that better replicate the native stem cell microenvironment [64]. These innovative approaches include:
- Bone Marrow Organoids: Utilizing 3D printing, organoid technology, and bone marrow-on-a-chip platforms to recreate architectural and physiological features of the hematopoietic stem cell niche [64].
- Biomaterial Integration: Employing natural and synthetic polymers such as gelatin methacrylamide hydrogel, hyaluronic acid, and polylactic acid to provide appropriate mechanical cues and biochemical signaling [64].
- Niche Component Incorporation: Co-culturing stem cells with supportive cell types like bone marrow stromal cells, endothelial cells, and perivascular stromal cells to replicate cellular crosstalk [64].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Stem Cell Culture and Analysis
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Defined Matrices | Laminin-521, Vitronectin [62] | Replace variable feeder cells; provide consistent adhesion signals |
| Defined Media | Essential 8 (E8) [62] | Supply standardized nutrients and growth factors without serum |
| Signaling Modulators | SB431542 (TGF-β inhibitor), CHIR99021 (Wnt activator) [9] | Precisely control differentiation and self-renewal pathways |
| Gene Editing Tools | CRISPR/Cas9, siRNA [65] | Manipulate gene expression to study function or enhance properties |
| Calcium Indicators | Fluo-4, Fura-2 [62] | Monitor intracellular Ca2+ dynamics in live cells |
| Biomaterial Scaffolds | Gelatin methacrylamide, Hyaluronic acid [64] | Provide 3D structural support mimicking native extracellular matrix |
| Differentiation Inducers | Bone Morphogenetic Proteins (BMPs), Retinoic acid [9] | Direct lineage-specific differentiation through pathway activation |
| Senescence Detectors | β-galactosidase substrates [63] | Identify and quantify senescent cells in culture |
Experimental Workflow for Assessing Culture-Induced Changes
A comprehensive assessment of culture-induced changes requires a multi-faceted approach examining functional, molecular, and phenotypic parameters throughout the expansion process.
Diagram 2: Experimental workflow for assessing culture-induced changes. A multi-parameter approach is essential for comprehensively evaluating how extended in vitro culture affects stem cell properties and function.
This systematic evaluation enables researchers to identify the "critical passage point" beyond which stem cells undergo unacceptable functional decline, providing crucial guidance for establishing safe expansion limits in therapeutic applications.
Preserving stem cell function during in vitro culture requires integrated approaches addressing both intrinsic regulatory mechanisms and extrinsic microenvironmental cues. The implementation of defined culture systems significantly reduces technical variability and enhances reproducibility, while three-dimensional niche reconstruction approaches better mimic physiological conditions. Ongoing research into signaling pathway modulation, particularly those involving Ca2+ dynamics and TGF-β superfamily signaling, continues to reveal new opportunities for optimizing culture conditions. As the field advances, the integration of bioengineering, gene editing technologies, and single-cell omics approaches will further enhance our ability to maintain functional stem cell populations through extended culture, ultimately supporting more effective clinical translation of stem cell-based therapies.
Addressing Tumorigenicity and Uncontrolled Differentiation
The capacity for self-renewal and differentiation positions stem cells as a cornerstone of regenerative medicine. However, these same properties present significant safety challenges, primarily tumorigenicity and uncontrolled differentiation [46]. These risks are intrinsically linked to the very signaling pathways that govern stem cell fate, such as Wnt, TGF-β, and Notch [9]. For researchers and drug development professionals, understanding and mitigating these risks is not merely a translational hurdle but a fundamental aspect of stem cell biology research. Tumorigenic potential arises from the propensity of undifferentiated pluripotent stem cells, including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), to form teratomas, while uncontrolled differentiation can lead to heterogeneous, impure cell populations with unpredictable in vivo behavior [15]. This whitepaper delves into the molecular mechanisms underlying these challenges and outlines rigorous experimental strategies to address them, framing the discussion within the broader thesis of mastering stem cell self-renewal and differentiation mechanisms.
Molecular Mechanisms Governing Fate Decisions
The balance between self-renewal and differentiation is tightly regulated by a complex interplay of intrinsic genetic and epigenetic factors and extrinsic signaling pathways. Disruption of this balance is a primary cause of tumorigenicity and uncontrolled differentiation.
Key Signaling Pathways and Their Crosstalk
The behavior of stem cells is collectively regulated by essential signaling pathways, which offer multiple pharmacological entry points to fine-tune stem cell behavior for therapeutic purposes [9]. The following diagram illustrates the core signaling network and its role in fate decisions:
The Wnt/β-catenin pathway is a primary regulator of stem cell self-renewal, and its dysregulation is strongly associated with tumorigenicity [9]. Conversely, the TGF-β/BMP signaling branch plays a crucial role in directing differentiation into diverse embryonic and extraembryonic lineages [9]. The Notch pathway, vital for cell-fate determination, can inhibit differentiation and maintain a progenitor state, while Hedgehog signaling contributes to embryonic development and tissue patterning. These pathways do not operate in isolation; complex crosstalk, such as that between Wnt and TGF-β, creates a regulatory network that determines the final cellular outcome [9].
Epigenetic Regulation and Cell Cycle Control
Beyond signaling pathways, epigenetic mechanisms exert critical control over stem cell fate. The epigenetic control of core pluripotency factors like OCT3/4 is essential for maintaining pluripotency and functional contribution to the stem cell self-renewal and differentiation decision [37]. Furthermore, cell cycle regulatory molecules play a surprisingly significant role; for instance, CDK2AP1 has been identified as a competency factor in embryonic stem cell differentiation [37]. Disruption of these delicate controls can lead to epigenetic heterogeneity, a phenomenon also observed in cancer stem cells, which contributes to tumor heterogeneity and complicates treatment strategies [66].
Experimental Strategies for Risk Mitigation
A multi-pronged experimental approach is essential to effectively address tumorigenicity and uncontrolled differentiation. The following workflow outlines a comprehensive strategy from cell line establishment to in vivo validation:
Pre-Differentiation Characterization and Banking
Rigorous characterization of starting cell populations is fundamental. This includes:
- Karyotype Analysis: Standard G-banding to identify gross chromosomal abnormalities that could confer growth advantages.
- Pluripotency Verification: Testing through assays like PluriTest [60] or teratoma formation to confirm the capacity to differentiate into all three germ layers.
- Cell Line Authentication: STR profiling to confirm cell line identity and prevent cross-contamination.
Directed Differentiation and Purification Protocols
Precise differentiation protocols are the first defense against uncontrolled differentiation and residual undifferentiated cells.
Neural Differentiation Protocol (Example) This protocol generates dopaminergic neurons for Parkinson's disease research [60]:
- Pluripotent Stem Cell Culture: Maintain human ESCs or iPSCs on recombinant laminin-521 (1 µg/mL) in defined, feeder-free conditions using mTeSR1 medium.
- Dual SMAD Inhibition: Induce neural induction by replacing mTeSR1 with neural induction medium containing:
- DMEM/F-12 with N2 supplement (1X)
- SB431542 (10 µM), a TGF-β receptor inhibitor
- LDN193189 (100 nM), a BMP receptor inhibitor
- Culture for 10-12 days with daily medium changes until neural rosettes form.
- Neural Progenitor Cell (NPC) Expansion: Manually pick rosettes and plate on poly-ornithine/laminin-coated plates in NPC medium (DMEM/F-12 with N2 and B27 supplements, 20 ng/mL FGF-2).
- Dopaminergic Differentiation: Plate NPCs at 100,000 cells/cm² and differentiate for 28 days in:
- Neurobasal medium with B27 supplement
- BDNF (20 ng/mL), GDNF (10 ng/mL), ascorbic acid (200 µM), dBcAMP (500 µM)
- SHH C25II (100 ng/mL) and FGF8 (100 ng/mL) for the first 10 days.
Cardiac Differentiation Protocol (Example) This protocol generates cardiomyocytes for cardiac repair [9]:
- Mesoderm Induction: Culture pluripotent stem cells to 85% confluence in RPMI 1640/B27-insulin medium. Add CHIR99021 (6-8 µM), a GSK-3β inhibitor activating Wnt signaling, for 24 hours.
- Cardiac Specification: At day 3, add IWP4 (5 µM), a Wnt inhibitor, to direct cardiac mesoderm specification. Culture for 48 hours.
- Metabolic Selection: From day 5, replace medium with RPMI 1640/B27-supplemented medium without glucose, supplemented with lactate (4 mM) to selectively eliminate non-cardiomyocytes. Continue for 5-7 days.
- Functional Maturation: Maintain beating cardiomyocytes in RPMI 1640/B27 complete medium with occasional medium changes for up to 90 days for electrophysiological and metabolic maturation.
Pharmacological and Genetic Strategies
Both small molecules and genetic approaches can enhance safety:
Pharmacological Modulation: Small molecules can direct differentiation and suppress tumorigenic tendencies. For example, modulating the Hedgehog, TGF-β, Wnt, Hippo, FGF, BMP and Notch pathways with specific inhibitors or activators can fine-tune stem cell behavior [9]. These compounds can be incorporated into differentiation protocols to enhance efficiency and purity.
Genetic Safety Switches: Introduce suicide genes (e.g., herpes simplex virus thymidine kinase) that can be activated with ganciclovir to eliminate proliferating cells if tumor formation is detected [15]. CRISPR/Cas9 technology can be used to knock in these safety switches at safe-harbor loci like AAVS1.
Purification and Characterization of Differentiated Cells
Efficient purification is critical for removing residual undifferentiated cells:
- Fluorescence-Activated Cell Sorting (FACS): Using cell surface markers specific to the target cell type (e.g., NCAM for neural lineages, CD56 for mesenchymal lineages) while excluding pluripotency markers (TRA-1-60, SSEA-4).
- Magnetic-Activated Cell Sorting (MACS): For larger-scale purification using antibody-conjugated magnetic beads.
- Reporter-Based Sorting: Using genetically engineered stem cell lines with fluorescent reporters under the control of lineage-specific promoters (e.g., NKX2-5 for cardiac cells).
Table 1: Key Characterization Assays for Assessing Tumorigenic Risk
| Assay Type | Specific Method | Measured Parameters | Acceptance Criteria |
|---|---|---|---|
| In Vitro Pluripotency | Flow cytometry for pluripotency markers (OCT4, SOX2, NANOG) | Percentage of TRA-1-60+/SSEA-4+ cells | <0.1% positive cells |
| In Vivo Tumorigenicity | Teratoma assay in immunodeficient mice (e.g., NOD/SCID) | Tumor formation at 12-20 weeks; histology of three germ layers | No tumor formation or only well-differentiated teratomas |
| Oncogenic Transformation | Soft agar colony formation assay | Colony formation in semi-solid medium | No colony formation |
| Karyotypic Stability | G-banding karyotype analysis | Chromosomal number and structure | Normal diploid karyotype (46, XY/XX) |
| Molecular Profiling | RNA-seq for gene expression signatures | Pluripotency and lineage-specific gene expression | Absence of pluripotency network expression |
Table 2: Research Reagent Solutions for Fate Control Experiments
| Reagent/Category | Specific Examples | Function/Mechanism | Application Context |
|---|---|---|---|
| Small Molecule Pathway Modulators | CHIR99021 (Wnt activator), IWP4 (Wnt inhibitor), SB431542 (TGF-β inhibitor), LDN193189 (BMP inhibitor) | Precise control of key signaling pathways (Wnt, TGF-β, BMP) to direct differentiation | Stage-specific use in directed differentiation protocols [9] |
| Extracellular Matrix Proteins | Recombinant laminin-521, Matrigel, poly-ornithine/laminin | Provide structural and biochemical support mimicking native stem cell niche | Coating substrate for cell culture plates to enhance attachment and differentiation |
| Cell Surface Marker Antibodies | Anti-TRA-1-60, Anti-SSEA-4 (pluripotency), Anti-CD44, Anti-CD73 (mesenchymal), Anti-NCAM (neural) | Identification and isolation of specific cell populations by FACS/MACS | Purity assessment and purification of differentiated cells; depletion of undifferentiated cells |
| Gene Editing Tools | CRISPR/Cas9 systems, suicide gene vectors (e.g., HSV-TK) | Genetic modification for lineage tracing, safety switches, or gene correction | Insertion of fluorescent reporters; incorporation of safety mechanisms to eliminate errant cells |
| Cell Culture Media Formulations | mTeSR1 (pluripotent stem cell maintenance), Neural Induction Medium, Cardiomyocyte Differentiation Medium | Defined formulations with specific growth factors and supplements | Maintenance of stemness or directed differentiation into specific lineages |
Analytical Methods for Safety Assessment
Comprehensive safety assessment requires multiple complementary analytical approaches to quantify and mitigate risks.
In Vitro and In Vivo Tumorigenicity Assays
The gold standard for assessing tumorigenic potential remains the teratoma assay in immunocompromised mice [15]. A quantitative approach involves:
- Cell Preparation: Harvest test cells and positive control (undifferentiated stem cells) using standard procedures.
- Inoculation: Inject 1×10^6 to 1×10^7 cells intramuscularly, subcutaneously, or under the testis capsule of NOD/SCID mice (n=10 per group).
- Monitoring: Palpate weekly for tumor formation over 12-20 weeks.
- Endpoint Analysis: Measure tumor size, perform histopathology with H&E staining to identify tissues from all three germ layers, and quantify teratoma incidence and latency.
Alternative In Vivo Models: For higher-throughput screening, the chick embryo chorioallantoic membrane (CAM) assay provides a more rapid, ethically favorable alternative for assessing tumorigenic potential.
Genomic and Epigenomic Stability Assessment
Long-term culture can introduce genetic and epigenetic abnormalities that increase tumorigenic risk:
- Copy Number Variation (CNV) Analysis: Using SNP microarrays or whole-genome sequencing to identify acquired chromosomal abnormalities.
- Whole-Exome Sequencing: To detect point mutations in oncogenes and tumor suppressor genes.
- DNA Methylation Profiling: Bisulfite sequencing to assess epigenetic stability and ensure proper erasure of somatic cell memory in iPSCs.
Table 3: Quantitative Data from Stem Cell Safety Studies
| Study Focus | Experimental Model | Key Quantitative Findings | Implications |
|---|---|---|---|
| PSC-derived cell safety | Global clinical trial data (115 trials, 83 products) [60] | >1,200 patients dosed with >10¹¹ PSC-derived cells; no class-wide safety concerns | Encouraging preliminary safety profile for properly differentiated cells |
| Residual pluripotent cell risk | Teratoma formation assay [15] | As few as 10 undifferentiated mouse ESCs can form teratomas in immunodeficient mice | Extremely sensitive detection methods needed for residual cells |
| Genetic stability in culture | Karyotype analysis of long-term hESC cultures [37] | 30-40% of hESC lines acquire chromosomal abnormalities after extended culture (>30 passages) | Regular monitoring and early passage use recommended for clinical applications |
| Tumorigenicity mitigation | Suicide gene therapy in iPSC-derived cells [15] | >99% elimination of proliferating cells upon ganciclovir administration in HSV-TK models | Safety switches can effectively address post-transplantation concerns |
Clinical Translation and Regulatory Considerations
Translating stem cell therapies from bench to bedside requires navigating a complex regulatory landscape while implementing rigorous safety monitoring.
Current Regulatory Framework and Approved Therapies
The International Society for Stem Cell Research (ISSCR) guidelines emphasize maintaining scientific and ethical integrity through rigor, oversight, and transparency [67]. The FDA's regulatory pathway for stem cell-based products is stringent:
- Investigational New Drug (IND) Application: Required before initiating clinical trials, demonstrating sufficient preclinical safety data [60].
- Biologics License Application (BLA): Required for market approval after successful clinical trials [60].
Recently approved stem cell products demonstrate this regulatory pathway in action:
- Ryoncil (remestemcel-L): First FDA-approved MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (December 2024) [60].
- Omisirge (omidubicel-onlv): Nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cells to accelerate neutrophil recovery (April 2023) [60].
Monitoring and Managing Risks in Clinical Trials
For clinical applications, several strategies help manage risks:
- Cell Dosage Optimization: Balancing therapeutic efficacy with safety, as higher dosages may provide better therapeutic effects but could increase risks [68].
- Long-Term Patient Follow-Up: Essential for detecting delayed adverse events, including tumor formation.
- Imaging Surveillance: Regular MRI or CT scans for patients receiving cell therapies with tumorigenic potential.
- Immunological Safety Nets: Using allogeneic cells from immunoprivileged sources or incorporating inducible suicide genes as safety switches.
Addressing tumorigenicity and uncontrolled differentiation requires a comprehensive approach spanning basic science, translational research, and clinical regulation. The future of safe stem cell therapies lies in several promising directions:
- Advanced Gene Editing: CRISPR-based technologies for more precise genetic modifications and enhanced safety switches.
- Synthetic Biology Approaches: Designing circuits that trigger cell death upon detection of oncogenic transformation.
- Improved Biomaterials: Developing scaffolds that provide spatial and temporal control over differentiation signals.
- Single-Cell Technologies: Enabling better characterization of cellular heterogeneity within therapeutic products.
- Computational Modeling: Predicting tumorigenic potential based on multi-omics data.
As the field progresses, the balance between harnessing stem cells' remarkable potential and ensuring patient safety will continue to rely on rigorous science, thoughtful regulation, and transparent communication between researchers, clinicians, and regulators. By deepening our understanding of the fundamental mechanisms governing self-renewal and differentiation, we can develop increasingly sophisticated strategies to address these critical safety challenges.
Optimizing Differentiation Protocols for Homogeneous Cell Populations
The optimization of differentiation protocols to generate homogeneous cell populations represents a cornerstone in translational stem cell research. This process requires a precise disruption of the inherent self-renewal mechanisms that maintain stem cells in an undifferentiated state. Self-renewal is defined as the process by which stem cells divide to produce more stem cells, thereby perpetuating the stem cell pool throughout life while maintaining an undifferentiated state [69]. This fundamental property balances proto-oncogenes that promote self-renewal, gate-keeping tumor suppressors that limit it, and care-taking tumor suppressors that maintain genomic integrity [69]. Understanding these mechanisms is critical for developing robust differentiation protocols, as the process essentially involves redirecting these inherent programs toward specific lineage commitments.
The drive for homogeneous populations stems from pressing applications in disease modeling, drug screening, and regenerative medicine, where inconsistent cellular compositions can severely compromise experimental validity and therapeutic safety [70] [71]. Recent advances in in silico modeling and quantitative single-cell analysis have begun to unravel the complex dynamics of cell populations during differentiation, providing novel insights for protocol optimization beyond traditional brute-force experimental approaches [70] [72]. This guide synthesizes these advanced methodologies into a comprehensive framework for achieving superior population homogeneity.
Theoretical Foundations: From Self-Renewal to Lineage Commitment
Stem cell fate is governed by a balance between symmetric and asymmetric division. Symmetric division results in two identical daughter cells, both either stem cells (expanding the pool) or differentiated cells, while asymmetric division yields one stem cell and one differentiated progeny, maintaining homeostasis [11]. The shift from self-renewal to differentiation involves complex signaling networks that are both cell-intrinsic and regulated by extrinsic niche signals [69].
The differentiation potential, or potency, varies by stem cell type:
- Pluripotent stem cells (PSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), can differentiate into any of the three germ layers [11].
- Multipotent stem cells differentiate into a limited number of cell types within a closely related family [11].
Directed differentiation protocols for PSCs, particularly toward endoderm derivatives, begin with definitive endoderm (DE) induction as a critical first step [70]. The efficiency of this initial stage fundamentally impacts the homogeneity and quality of resulting populations.
Quantitative Modeling for Protocol Optimization
Mathematical modeling provides a powerful in silico tool for optimizing differentiation protocols without extensive laboratory experimentation. Calibrated differential equation models can predict population dynamics, including proliferation, differentiation, and death, offering quantitative insights for improving yield and homogeneity [70].
Key Findings from Mathematical Modeling of iPSC to DE Differentiation
Recent modeling of iPSC to DE differentiation has yielded critical quantitative insights, summarized in the table below.
Table 1: Key Optimization Parameters from a Mathematical Model of iPSC to DE Differentiation
| Parameter | Optimal Value or Finding | Impact on Differentiation Efficiency |
|---|---|---|
| Optimal Differentiation Period | 1.9 - 2.4 days [70] | Ensures maximum population conversion before efficiency declines. |
| Optimal Plating Population | ~300,000 cells per well [70] | Maximizes yield efficiency in a space-limited growth model. |
| Primary Population Driver | iPSC differentiation outperforms DE proliferation [70] | Highlights the importance of targeting the differentiation rate. |
| Prediction Error of Validated Model | 26.4% [70] | Below the 30% acceptability threshold, indicating model reliability. |
| Superior Growth Model | Logistic and Gompertz growth [70] | Outperforms exponential growth, reflecting spatial constraints. |
Model Structure and Application
The mathematical framework assumes discrete, homogeneous intermediate stages during differentiation. Models incorporate:
- Live Cell Populations: Undifferentiated iPSCs (ns), definitive endoderm (nd), and potential transitional states (nt1, nt2) [70].
- Cellular Processes: Defined by per capita rates for death (dⱼ), proliferation (bⱼ), and differentiation (pⱼⱼ') [70].
- Model Selection: Rigorous testing of 27 candidate models combining different lineage, growth, and error distribution structures identified the most accurate representation of the biological process [70].
This modeling approach enabled in silico investigation of culture modifications, predicting that supplementation with growth modulators could increase DE yield by up to 39% under specific plating conditions [70].
Diagram 1: Multi-State Differentiation Model. iPSCs transition through intermediate states before becoming Definitive Endoderm, with cell death occurring at every stage. Rates 'p' and 'd' are per capita.
Advanced Single-Cell Technologies for Monitoring Heterogeneity
Cutting-edge technologies that quantify cellular behavior at the single-cell level are crucial for assessing and achieving population homogeneity. These approaches move beyond snapshot analyses to capture dynamic temporal kinetics, revealing heterogeneity that bulk or endpoint measurements cannot detect [73] [72].
Quantitative Phase Imaging (QPI) and Kinetic Profiling
A recent groundbreaking study integrated single-HSC ex vivo expansion with time-lapse QPI and machine learning [72]. This label-free, non-invasive imaging technique allows continuous monitoring of individual cells, extracting kinetic features such as dry mass, sphericity, and velocity.
Key findings from this approach include:
- Proliferation Heterogeneity: After 96 hours, 12.5% of single HSCs produced >20 cells, while 21.9% produced <4 cells [72].
- Morphological Diversity: Output cells showed significant variation, with 10.9% of HSCs producing cells with dry masses >200 pg and 17.2% producing cells with <100 pg [72].
- Division Patterns: While 91.3% of divisions were normal, 8.21% showed interrupted cytokinesis, and 0.48% exhibited abnormal patterns (e.g., single cell dividing into three) [72].
Machine learning analysis of these kinetic parameters enabled the classification of HSCs into distinct functional clusters, predicting future stem cell status and functional quality based on past cellular behavior [72].
Diagram 2: QPI Workflow for Predicting Stem Cell Diversity. The process from single-cell seeding to functional prediction.
Experimental Protocol: Single-Cell Kinetic Analysis
Objective: To profile single-cell heterogeneity during differentiation using QPI. Materials:
- Purified stem cell population (e.g., CD201+CD150+CD48-KSL for murine HSCs)
- 96-well U-bottom plate
- Appropriate expansion medium
- Quantitative phase imaging system
Procedure:
- Single-Cell Sorting: Flow-sort one cell per well into a 96-well U-bottom plate [72].
- Time-Lapse Imaging: Culture cells and acquire QPI images at regular intervals (e.g., every 5-20 minutes) for the duration of the experiment (e.g., 96 hours) [72].
- Kinetic Feature Extraction: Analyze images to quantify parameters for each cell, including:
- Dry mass
- Cellular volume and sphericity
- Velocity and motility
- Division timing and symmetry [72]
- Data Integration and Clustering: Perform UMAP analysis or similar dimensionality reduction on kinetic features to identify distinct cellular clusters [72].
- Functional Correlation: Correlate kinetic clusters with functional stemness assays (e.g., transplantation, differentiation potential) to validate predictive power [72].
Systematic Optimization Using Design of Experiments (DOE)
Traditional "one factor at a time" (OFAT) optimization is inefficient for complex differentiation processes involving multiple interacting factors. Statistical Design of Experiments (DOE) provides a framework for multifactorial screening and quantitative modeling, dramatically reducing experimental runs while improving robustness [71].
DOE Methodologies for Differentiation Optimization
Table 2: Design of Experiments (DOE) Approaches for Protocol Optimization
| Method | Key Principle | Best Use Case in Differentiation |
|---|---|---|
| Full Factorial Design | Investigates all possible combinations of factors and levels [71]. | Small-scale optimization with few critical factors (e.g., 2-3 factors). |
| Fractional Factorial Design | Screens a fraction of the full factorial combinations, sacrificing some interaction effects [71]. | Initial screening of a larger number of factors to identify the most influential ones. |
| Orthogonal Array Design | Uses predetermined arrays to efficiently estimate main effects with multiple levels [71]. | Robust parameter design, especially when dealing with noise factors like lot-to-lot variability. |
| Response Surface Methodology (RSM) | Models quadratic responses to locate optimal conditions [71]. | Fine-tuning concentrations of key factors (e.g., growth factors, small molecules) after initial screening. |
| Definitive Screening Design (DSD) | An emerging design that efficiently estimates main effects and quadratic effects with minimal runs [71]. | Screening and optimization when the number of factors is moderate, and curvature is suspected. |
Experimental Protocol: DOE for Media Optimization
Objective: To optimize a differentiation media formulation using a Response Surface Methodology. Materials:
- Pluripotent stem cells
- Basal differentiation medium
- Stock solutions of factors to be optimized (e.g., Growth Factor A, Small Molecule B)
- Cell culture plates and equipment
- Assays for outcome measurement (e.g., flow cytometry, qPCR)
Procedure:
- Factor Selection: Choose 2-3 critical factors identified from prior screening (e.g., growth factor concentration, small molecule concentration, cell seeding density) [71].
- Experimental Design: Create a central composite design (a type of RSM) with 3-5 levels for each factor. This typically requires 15-20 experimental runs for three factors [71].
- Execution: Perform the differentiation protocol according to the designed matrix of conditions.
- Response Measurement: Quantify the key response variable(s), such as the percentage of target cells (e.g., CXCR4+/c-KIT+ for DE) or cell yield [70] [71].
- Model Fitting and Optimization: Fit a quadratic model to the data and use statistical software to identify the factor concentrations that predict the optimal response [71].
- Validation: Confirm the model's prediction by running the recommended optimal condition in triplicate.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Optimizing Definitive Endoderm Differentiation
| Reagent / Tool | Function / Purpose | Example Product / Target |
|---|---|---|
| Surface Markers for DE | Identification and purification of definitive endoderm cells via flow cytometry [70]. | CD117 (c-KIT), CD184 (CXCR4) [70]. |
| Commercial Differentiation Kit | Provides a standardized baseline protocol and reagents for initial differentiation attempts. | STEMdiff Definitive Endoderm Kit [70]. |
| Extracellular Matrix (ECM) | Provides the physical substrate and biochemical signals necessary for cell attachment and differentiation. | Matrigel [70]. |
| ROCK Inhibitor | Increases survival of single cells during passaging, improving plating efficiency and initial yield [70]. | Y-27632 [70]. |
| Chemically Defined System | Promotes differentiation in a controlled, reproducible, and cost-effective manner, free of variable recombinant proteins [74]. | Small-molecule-based induction platforms [74]. |
| Quantitative Phase Microscope | Enables non-invasive, label-free monitoring of single-cell kinetics for heterogeneity analysis [72]. | Ptychographic QPI systems [72]. |
Achieving homogeneous cell populations through optimized differentiation protocols requires a multi-faceted approach that integrates fundamental biological principles, advanced single-cell analytics, and sophisticated experimental design. The convergence of in silico modeling, which predicts optimal timing and plating conditions, with high-resolution kinetic profiling, which reveals hidden functional heterogeneity, provides an unprecedented toolkit for researchers. Furthermore, the application of statistical DOE principles ensures that protocol development is both efficient and robust, meeting the stringent requirements for therapeutic applications. By moving beyond empirical optimization to a model-guided, data-driven paradigm, scientists can systematically enhance the yield, purity, and functional quality of stem cell derivatives, accelerating progress in regenerative medicine and disease modeling.
Managing Immunological Rejection and Engraftment Efficiency
The success of any stem cell-based regenerative medicine application is fundamentally constrained by two interconnected biological challenges: immunological rejection and engraftment efficiency. These barriers stand between the laboratory potential of stem cells and their clinical application. The core therapeutic promise of stem cells lies in their dual capacities for self-renewal and differentiation—the ability to divide indefinitely and mature into specialized cell types [75]. However, after transplantation, the very signals that govern these fundamental processes, including complex molecular pathways that maintain pluripotency or initiate lineage specification, are disrupted by the host's immune response and the failure of donor cells to properly integrate into the niche [37]. This whitepaper examines the current scientific strategies designed to overcome these barriers, focusing on technical approaches that enable donor cell survival, functional integration, and long-term therapeutic efficacy without provoking detrimental immune reactions. The goal is to bridge the foundational knowledge of stem cell biology with the practical requirements for clinical translation.
Mechanisms of Immune Rejection and Engraftment Failure
Transplanted allogeneic stem cells face a multi-faceted immune attack. The primary mechanisms include:
- T-Cell Mediated Rejection: This is the most potent response. Host T cells recognize foreign peptides presented by Major Histocompatibility Complex (MHC) molecules on donor cells. The ensuing activation and clonal expansion of cytotoxic T lymphocytes leads to direct destruction of the graft [76] [77].
- Natural Killer (NK) Cell Cytotoxicity: NK cells identify and lyse "non-self" cells that lack expression of "self" MHC class I molecules. This poses a significant challenge for strategies that involve knocking down MHC to evade T-cell recognition [77].
- Antibody-Mediated Rejection: Pre-existing or de novo generated host antibodies can bind to donor HLA antigens, activating the complement system and causing inflammatory damage to the graft [76].
- Engraftment Failure: Even in the absence of robust immunity, donor cells may fail to engraft due to insufficient niche space, apoptosis triggered by inadequate survival signals, or functional incompatibility with the host tissue, preventing functional integration [78] [53].
The interplay between these immune mechanisms and the stem cell's intrinsic capacity for self-renewal and differentiation defines the success or failure of a transplant. An inflammatory microenvironment can aberrantly alter differentiation fates and disrupt the delicate balance between symmetric and asymmetric cell division that is crucial for populating a graft.
Engineering Immune-Evasive and Engraftable Cells
The generation of "off-the-shelf" allogeneic cell products requires deliberate engineering to circumvent immune surveillance. The following table summarizes the key genetic modifications used to create hypoimmune cells.
Table 1: Key Genetic Modifications for Creating Hypoimmune Stem Cells
| Target Molecule | Engineering Approach | Primary Immune Mechanism Addressed | Intended Outcome |
|---|---|---|---|
| MHC Class I/II | Knockout (e.g., via CRISPR/Cas9) | T-cell recognition | Eliminates direct allorecognition by host T cells [77]. |
| CD47 | Overexpression | Phagocytosis (macrophage) | Delivers a "don't eat me" signal, inhibiting phagocytosis by host macrophages [77]. |
| PD-L1 | Overexpression | T-cell cytotoxicity | Engages PD-1 on activated T cells, inducing local immune tolerance and energy [77]. |
| HLA-G | Overexpression | NK cell & T-cell inhibition | Suppresses NK cell cytotoxicity and inhibits T-cell function, promoting tolerance [77]. |
These modifications can be applied to both pluripotent stem cell (PSC)-derived therapeutic cells, such as pancreatic islets for diabetes, or to primary cadaveric islets, aiming to create universal cell products that do not require extensive HLA matching or long-term immunosuppression [77].
Visualizing the Hypoimmune Engineering Strategy
The following diagram illustrates the coordinated molecular strategy for creating immune-evasive cells.
Quantitative Data on Engraftment Enhancement Strategies
Clinical and preclinical studies have quantified the benefits of various supporting strategies on engraftment metrics. The systematic synthesis of data, particularly from adjunct cell therapies, provides robust evidence for their utility.
Table 2: Impact of Mesenchymal Stem Cell (MSC) Co-Infusion on Engraftment after HSCT (Systematic Review of 47 Studies, n=1777 Patients) [53]
| Parameter | Findings with MSC Co-Infusion | Clinical Significance |
|---|---|---|
| Overall Engraftment | 79% of included studies reported enhanced engraftment. | Consistent positive effect across diverse patient populations and transplant settings. |
| Neutrophil Engraftment | Average time to engraftment: 13.96 days. | Reduces duration of neutropenia, lowering risk of severe infections. |
| Platelet Engraftment | Average time to engraftment: 21.61 days.Most consistently benefited parameter. | Reduces bleeding risk and transfusion dependence; major morbidity reducer. |
| Safety Profile | No serious adverse events related to MSC infusion were reported. | Favorable risk-benefit profile for a supportive therapy. |
The proposed mechanism involves MSC secretion of supportive cytokines—such as SCF, TPO, IL-6, and TGF-β—which help to recreate a supportive bone marrow niche, promote angiogenesis, and modulate post-transplant inflammation, thereby facilitating the survival and proliferation of donor hematopoietic stem cells [53].
Detailed Experimental Protocols for Advanced Models
This protocol demonstrates a targeted approach to overcome the blood-brain barrier and achieve high-level engraftment without full-body toxic preconditioning.
Step 1: Microglia Depletion
- Objective: Create physical "space" in the niche for donor cells.
- Method: Administer a microglia-depleting drug (e.g., a CSF1R inhibitor) to the recipient mouse to eliminate the native microglia population.
Step 2: Focal Irradiation
- Objective: Further condition the brain niche to favor donor cell engraftment.
- Method: Apply targeted irradiation specifically to the brain, sparing the rest of the body from systemic toxicity.
Step 3: Cell Transplantation
- Objective: Deliver healthy donor cells.
- Method: Intracranially inject microglial precursor cells (a specialized subset of hematopoietic stem cells) derived from a non-genetically matched donor. This localized injection ensures high local cell concentration.
Step 4: Systemic Immune Blockade
- Objective: Prevent immune rejection of the non-matched donor cells.
- Method: Administer a short-course of two drugs that transiently block the activation of host immune cells that would otherwise attack the donor cells.
Outcome: This sequence resulted in >85% donor-derived microglia engraftment at 8 months, without graft-versus-host disease, and significantly prolonged survival and improved motor function in a Sandhoff disease mouse model [79].
This Phase 1 clinical trial protocol replaces genotoxic chemotherapy and radiation with a targeted antibody for preconditioning.
Step 1: Targeted Stem Cell Clearance
- Objective: Remove host blood-forming stem cells to create niche space.
- Method: A single intravenous infusion of an antibody (briquilimab) against CD117 (c-Kit), a protein expressed on the surface of hematopoietic stem cells. The antibody selectively depletes these cells without the toxic side effects of chemotherapy or radiation.
Step 2: Graft Engineering
- Objective: Minimize graft-versus-host disease (GvHD) while retaining engraftment potential.
- Method: The donor bone marrow graft is processed to enrich for CD34+ hematopoietic stem cells and deplete alpha/beta T-cells, the primary mediators of GvHD. This allows the use of haploidentical (half-matched) donors, such as a parent.
Step 3: Transplant and Immunosuppression
- Objective: Support initial graft acceptance.
- Method: Patients receive standard immune-suppressing medications around the time of transplant, but omit busulfan chemotherapy and radiation entirely.
Outcome: In three pediatric patients with Fanconi anemia, the protocol led to successful donor chimerism (near 100% at 2 years) with no graft rejection and no procedure-related toxicity [78].
Visualizing the Non-Toxic Conditioning Workflow
The following diagram outlines the key steps of this novel conditioning regimen.
The Scientist's Toolkit: Key Research Reagents and Models
Advancing the field requires a specific set of research tools to develop, test, and validate new strategies for immune evasion and engraftment.
Table 3: Essential Research Tools for Rejection and Engraftment Studies
| Tool / Reagent | Function in Research | Example Application |
|---|---|---|
| CRISPR/Cas9 Systems | Gene knockout (MHC) or knock-in (CD47, PD-L1) in stem cells. | Creating universally compatible "hypoimmune" PSC lines [77]. |
| Anti-CD117 Antibody | Selective ablation of host hematopoietic stem cells in vivo. | Non-genotoxic conditioning in mouse models and clinical trials [78]. |
| Microglia Depleting Agents | Transient removal of resident microglia from the brain niche. | Enabling donor microglia engraftment in CNS therapy models [79]. |
| Immunodeficient Mouse Strains | In vivo assessment of human cell survival, proliferation, and differentiation without acute rejection. | Initial proof-of-concept for tumorigenicity and differentiation potential. |
| Humanized Mouse Models | Evaluation of human cell function and persistence in the context of a functional human immune system. | Testing the efficacy of hypoimmune modifications against a realistic human immune response. |
| Cytokine Arrays / ELISAs | Quantifying secretory factors (e.g., from MSCs) that support niche function. | Mechanistic studies on how MSC co-infusion promotes hematopoietic recovery [53]. |
The convergence of stem cell biology, immunology, and gene editing is producing a new generation of regenerative therapies. Strategies like hypoimmune engineering and targeted, non-toxic conditioning are directly addressing the historical challenges of immunological rejection and poor engraftment. The future of the field lies in refining the safety and precision of these approaches—such as using inducible safety switches in engineered cells to mitigate tumorigenicity risk—and in combining them synergistically. Furthermore, the insights gained from treating rare diseases, like the role of microglia in supporting neuronal health, may illuminate pathways relevant to common neurodegenerative disorders [79]. As these technologies mature, the fundamental principles of stem cell self-renewal and differentiation can be more effectively harnessed to deliver on the promise of safe, effective, and universally accessible regenerative medicine.
Stem cell populations utilize sophisticated fail-safe mechanisms to ensure their maintenance during homeostasis and regeneration. This whitepaper examines how the cell fate determinant Numb functions as a critical fail-safe in intestinal stem cell (ISC) self-renewal, particularly when primary signaling pathways are compromised. We explore the parallel signaling circuitry involving Bone Morphogenetic Protein (BMP) and Numb that provides robustness to stem cell systems, with significant implications for regenerative medicine and cancer biology. Through detailed experimental analysis in Drosophila models and complementary studies in mammalian systems, we delineate the molecular mechanisms whereby redundant pathways secure stem cell fate decisions, offering insights for therapeutic development.
Stem cell self-renewal represents a fundamental process wherein stem cells divide to generate additional stem cells, thereby perpetuating the stem cell pool throughout life while maintaining an undifferentiated state [69]. This process is precisely regulated by both cell-intrinsic mechanisms and cell-extrinsic signals from the niche microenvironment [69] [11]. The concept of fail-safe mechanisms in biological systems refers to backup regulatory circuits that ensure core functions are maintained when primary systems are compromised.
In stem cell populations, such fail-safe systems provide robustness against genetic lesions, environmental perturbations, and signaling fluctuations. The Drosophila midgut has emerged as a powerful model system for elucidating these mechanisms, particularly through studies of intestinal stem cells (ISCs) and their regulatory networks [80]. Here, we examine how Numb and BMP signaling constitute a parallel fail-safe system that ensures ISC maintenance during both homeostasis and tissue regeneration.
The Drosophila Midgut: A Model System for Studying Stem Cell Fail-Safe Mechanisms
The Drosophila midgut epithelium is maintained by intestinal stem cells (ISCs) that undergo asymmetric division to produce both renewed ISCs and enteroblasts (EBs) that differentiate into enterocytes (ECs) or enteroendocrine cells (EEs) [80]. The decision between ISC self-renewal and differentiation is primarily controlled by Notch (N) signaling, where Notch activation drives ISC differentiation into EB [80]. Approximately 80% of ISC divisions are asymmetric, while 20% are symmetric, producing either two ISCs or two EBs [80].
Experimental Model: Genetic Tools for Drosophila ISC Studies
Key genetic tools enabling the dissection of fail-safe mechanisms in Drosophila include:
esg-Gal4 tub-Gal80ts (esgts) system: A temperature-sensitive Gal4/Gal80 system that allows temporal control of gene expression specifically in progenitor cells (ISC/EB) [80]. When combined with UAS-GFP, this system enables visualization and tracking of precursor cells.
MARCM (Mosaic Analysis with a Repressible Cell Marker): This technique permits the generation of genetically mosaic tissues, allowing researchers to analyze mutant clones in an otherwise wild-type background [80].
Su(H)-lacZ reporter: A transcriptional reporter of Notch signaling activity used to monitor Notch pathway activation and identify EBs [80].
Numb and BMP Signaling: A Parallel Circuit for ISC Maintenance
The Role of BMP Signaling in ISC Self-Renewal
The BMP signaling pathway in the Drosophila midgut is activated by epithelium-derived BMP ligands (Dpp and Gbb heterodimers) that are secreted basally and concentrated on the basement membrane [80]. After asymmetric ISC division, basally localized daughter cells transduce higher levels of BMP signaling activity than apically localized daughters [80]. This differential BMP signaling promotes ISC self-renewal by antagonizing Notch pathway activity through mechanisms that remain partially characterized [80].
Genetic studies demonstrate that loss of BMP signaling through depletion of the type II receptor Punt (Put) results in precocious ISC-to-EB differentiation, leading to stem cell loss [80]. In Put-deficient progenitor cells, Notch pathway activation occurs even in the absence of detectable Notch ligand Delta (Dl), suggesting that BMP signaling normally suppresses ligand-independent Notch activity [80].
Numb as a Notch Inhibitor in Asymmetric Cell Division
Numb is a conserved cell fate determinant that functions as a Notch inhibitor [81] [82]. During asymmetric cell division in Drosophila, Numb is preferentially segregated into the basally localized daughter cell that becomes the future ISC [80] [82]. Molecularly, Numb antagonizes Notch signaling through multiple mechanisms:
- Ubiquitination pathway: Numb's phosphotyrosine-binding domain interacts with the E3 ubiquitin ligase Itch to promote ubiquitination of the full-length membrane-tethered Notch receptor and subsequent degradation of the Notch intracellular domain (NICD) after activation [82].
- Sanpodo interaction: Numb converts the membrane protein Sanpodo from a Notch activator to a Notch inhibitor in daughter cells that inherit Numb [82].
- Endocytic regulation: Numb promotes the endocytosis and degradation of Notch receptors, limiting their availability for activation [81] [82].
Surprisingly, despite Numb's asymmetric segregation and well-established role as a Notch inhibitor, loss of Numb does not typically lead to ectopic Notch activation or ISC depletion under normal homeostatic conditions [80]. This observation suggested the existence of complementary mechanisms that compensate for Numb loss.
Genetic Evidence for Parallel Pathway Function
Genetic epistasis experiments reveal the fail-safe relationship between BMP signaling and Numb [80]. Whereas neither depletion of the BMP signal transducer Mad nor numb mutation alone leads to significant ISC loss under homeostasis, combined inactivation results in profound stem cell depletion due to precocious ISC-to-EB differentiation [80].
The following genetic interactions demonstrate this functional redundancy:
Table 1: Genetic Interactions Between BMP Signaling and Numb in Drosophila ISC Maintenance
| Genetic Condition | ISC Maintenance | Notch Activity | Differentiation Outcome |
|---|---|---|---|
| Control | Normal | Asymmetric | Balanced self-renewal/differentiation |
| Mad RNAi/numb⁺ | Normal | Elevated but compensated | Normal ISC pool |
| Mad⁺/numb mutant | Normal | Elevated but compensated | Normal ISC pool |
| Mad RNAi + numb mutant | Severe loss | Constitutively high | Preoccious ISC-to-EB differentiation |
| Put RNAi | Impaired | Ectopic activation | Progressive ISC loss |
| Put RNAi + Dl RNAi | Impaired | Ectopic activation (ligand-independent) | Progressive ISC loss |
These genetic interactions indicate that BMP signaling and Numb function in parallel pathways that both converge on Notch inhibition to ensure proper ISC self-renewal. The system is buffered such that loss of one pathway can be compensated by the other, but simultaneous disruption of both pathways collapses the fail-safe system.
Numb's Crucial Role During Regeneration
The functional importance of Numb becomes particularly evident during midgut regeneration following epithelial damage. When flies are fed bleomycin (which causes EC damage and BMP signaling fluctuation), numb mutations result in significant stem cell loss [80]. This demonstrates that the asymmetrical segregation of Numb into the future ISC provides a critical fail-safe mechanism for ISC self-renewal by offsetting BMP pathway fluctuations during regenerative responses [80].
Visualization of the Numb-BMP Fail-Safe Mechanism
The following diagram illustrates the parallel circuit of BMP signaling and Numb in regulating Drosophila ISC self-renewal:
Experimental Approaches for Investigating Fail-Safe Mechanisms
Protocol: Genetic Epistasis Analysis in Drosophila ISCs
Objective: Determine the functional relationship between BMP signaling and Numb in ISC maintenance.
Methods:
Genetic Crosses: Utilize the esgts system to spatially and temporally control gene expression in progenitor cells:
- Cross esg-Gal4 tub-Gal80ts UAS-GFP; Su(H)-lacZ (esgts) females with males carrying UAS-Put-RNAi, UAS-Dl-RNAi, and/or numb mutant alleles.
- Include appropriate balancer chromosomes to identify progeny with desired genotypes.
Temperature Shift Protocol:
- Maintain 3-5 day-old adult female progeny at 18°C (permissive temperature, Gal80ts active) for 5 days post-eclosion.
- Shift to 29°C (restrictive temperature, Gal80ts inactive) for 10 days to induce RNAi expression or gene inactivation.
Tissue Dissection and Immunostaining:
- Dissect midguts in PBS and fix in 4% formaldehyde for 20 minutes.
- Perform immunostaining using primary antibodies:
- Mouse anti-β-galactosidase (1:500) to detect Su(H)-lacZ (Notch activity)
- Chicken anti-GFP (1:1000) to visualize esg>GFP+ progenitor cells
- Additional cell type markers (e.g., anti-Delta, anti-Prospero)
- Incubate with fluorophore-conjugated secondary antibodies (1:500).
Imaging and Quantification:
- Image posterior region (R4) of midguts using confocal microscopy.
- Quantify the percentage of esg>GFP+ cell pairs showing symmetric vs. asymmetric Notch activity.
- Count total ISC numbers per gut area using established morphological criteria.
Statistical Analysis:
- Perform ANOVA with post-hoc tests to compare ISC numbers and Notch activation patterns across genotypes.
- Analyze at least 15-20 guts per condition to ensure adequate statistical power.
Protocol: Assessing Regeneration-Induced Stem Cell Loss
Objective: Evaluate Numb's essential role during damage-induced regeneration.
Methods:
Bleomycin Feeding:
- Transfer experimental flies to vials containing filter paper soaked in 5% sucrose solution with 25μg/ml bleomycin.
- Maintain for 48 hours before dissection.
Clone Analysis:
- Generate wild-type and numb mutant clones using MARCM system.
- Analyze clone composition and ISC retention at multiple timepoints post-induction.
Proliferation Assessment:
- Incorporate EdU labeling (10μM, 2h pulse) to detect actively cycling cells.
- Co-stain with anti-phospho-histone H3 (pH3) to identify mitotic cells.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Studying Fail-Safe Mechanisms in Stem Cell Biology
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Genetic Tools | esg-Gal4 tub-Gal80ts (esgts) system | Temporal-spatial control of gene expression in progenitors |
| MARCM system | Clonal analysis of mutant cells in wild-type background | |
| Reporters | Su(H)-lacZ (Su(H)GBE-lacZ) | Monitoring Notch signaling activity |
| UAS-GFP | Cell lineage tracing and visualization | |
| Antibodies | Anti-β-galactosidase | Detection of Notch reporter activity |
| Anti-GFP | Identification of genetically targeted cells | |
| Anti-Delta | Marker for ISCs | |
| Anti-Prospero | Marker for enteroendocrine cells | |
| Chemical Agents | Bleomycin | Epithelial damage induction and regeneration studies |
| Ganciclovir | Suicide gene activation in engineered systems | |
| Mutant Alleles | numb mutants (multiple alleles) | Loss-of-function studies of Numb |
| Mad hypomorphic mutants | Compromised BMP signaling studies | |
| Cell Culture Systems | Drosophila primary midgut culture | Ex vivo studies of signaling pathways |
| hPSC-derived neural progenitors | Translation to mammalian systems |
Mammalian Parallels and Clinical Implications
NUMB in Mammalian Systems and Cancer
In mammals, the NUMB gene (located on chromosome 14q24.2-q24.3) encodes an endocytic adaptor protein that exists in multiple isoforms (p72, p71, p66, p65) generated through alternative splicing [81] [83]. These isoforms differ in their PTB and PRR domains, leading to distinct functions in development and disease [81] [83].
NUMB plays crucial roles in various human pathologies:
- Cancer: NUMB functions as a tumor suppressor in many contexts, and its loss or altered isoform expression is associated with breast cancer, non-small cell lung cancer, and colon adenocarcinoma [81] [83]. NUMB helps maintain genomic stability through regulation of the p53-MDM2 axis [81].
- Alzheimer's Disease: NUMB interacts with the amyloid precursor protein (APP) and is involved in APP trafficking and processing, positioning it within Alzheimer's disease pathogenesis [81].
Engineered Fail-Safe Systems in Regenerative Medicine
The concept of parallel fail-safe mechanisms has inspired the development of engineered safety systems for stem cell-based therapies. Two prominent approaches include:
1. Suicide Gene Systems:
- Inducible caspase-9 (iCaspase9): A chemically inducible system that triggers apoptosis upon administration of a small molecule dimerizer [84]. This system has demonstrated efficacy in eliminating undifferentiated iPSCs and iPSC-derived neural stem/progenitor cells, preventing teratoma formation after transplantation [84].
- HSV-Thymidine Kinase (HSV-TK) with cyclinD1 promoter: A FailSafe technology that links suicide gene expression to cell cycle progression [85]. In Parkinsonian rat models, ganciclovir administration following transplantation of FailSafe hPSC-derived neural progenitors significantly reduced graft size by eliminating proliferative cells while preserving functional dopamine neurons [85].
Table 3: Comparison of Engineered Fail-Safe Systems for Cell Therapies
| System | Activation Mechanism | Applications Demonstrated | Efficiency | Advantages |
|---|---|---|---|---|
| iCaspase9 | Chemical inducer (AP20187) | iPSC-NS/PCs in spinal cord injury | ~95% ablation in vitro | Rapid activation, high efficiency |
| HSV-TK/CyclinD1 (FailSafe) | Ganciclovir administration | VM progenitors in Parkinsonian rats | Complete proliferative cell ablation | Cell cycle-dependent, preserves post-mitotic cells |
| HSV-TK (conventional) | Ganciclovir administration | Various cell types | Variable | Clinically validated system |
The parallel circuit of BMP signaling and Numb in Drosophila ISCs exemplifies how evolutionarily conserved fail-safe mechanisms ensure robust stem cell maintenance amid fluctuating environmental conditions and genetic perturbations. This redundant architecture provides biological insurance against system failure, particularly during tissue regeneration when demand for stem cell activity increases.
Future research directions should focus on:
- Identifying additional components of these fail-safe networks across different stem cell systems
- Elucidating how fail-safe mechanisms become compromised during aging and disease
- Developing more sophisticated engineered safety systems for clinical applications
- Exploring the therapeutic potential of modulating fail-safe pathways in cancer and regenerative medicine
Understanding these fundamental mechanisms of stem cell resilience not only advances basic science but also informs the development of safer, more effective stem cell-based therapies with built-in safeguards against potential adverse outcomes like tumorigenicity or stem cell exhaustion.
Clinical Evidence and Comparative Analysis of Stem Cell Platforms
Stem cell therapeutics represent a paradigm shift in regenerative medicine, leveraging the fundamental properties of self-renewal and differentiation to address complex diseases. These core mechanisms enable stem cells to both replenish their own population and generate specialized effector cells, forming the biological basis for novel treatments [46]. The recent FDA approvals of Omisirge, Lyfgenia, and Ryoncil mark significant milestones in translating these mechanistic principles into clinical reality. Each product exemplifies a distinct approach: ex vivo expansion of hematopoietic progenitors, genetic modification of autologous stem cells, and immunomodulation using mesenchymal stromal cells. This whitepaper provides a technical analysis of these therapies for researchers and drug development professionals, focusing on their relationship to stem cell biology, experimental methodologies, and clinical applications.
Technical Profiles of Approved Therapies
Omisirge (omidubicel-onlv)
Mechanism and Indication: Omisirge is a nicotinamide (NAM)-modified allogeneic hematopoietic progenitor cell therapy derived from umbilical cord blood. It is indicated for adults and pediatric patients (12 years and older) with hematologic malignancies who are planned for umbilical cord blood transplantation following myeloablative conditioning [86]. Its primary mechanism involves enhancing the expansion and functionality of cord blood-derived stem and progenitor cells. The NAM modification works by inhibiting differentiation, allowing for the ex vivo expansion of a more primitive cell population while maintaining engraftment potential [87]. This process directly manipulates the self-renewal pathways in hematopoietic stem cells, addressing the historical limitation of low cell numbers in cord blood units.
Clinical Trial Data and Efficacy: The approval was based on a Phase III clinical trial demonstrating significant reduction in neutrophil recovery time and infection incidence.
Table 1: Key Clinical Efficacy Endpoints for Omisirge [86] [60]
| Parameter | Omisirge Arm | Standard UCB Arm | P-value |
|---|---|---|---|
| Median Time to Neutrophil Recovery | 12 days | 22 days | P<0.001 |
| Incidence of Bacterial/Fungal Infections | 37% | 57% | P<0.01 |
| Overall Survival at 100 Days | 95% | 91% | Not Significant |
Experimental Protocol:
- Source Material: Allogeneic hematopoietic stem cells are collected from umbilical cord blood.
- Ex Vivo Culture and Expansion: Cells are processed and cultured with nicotinamide, which modulates the NAD+ pathway to inhibit differentiation and promote the expansion of CD34+ cells.
- Final Product Formulation: The final product consists of two fractions: a Cultured Fraction (CF) and a Non-cultured Fraction (NF), which are cryopreserved.
- Administration: After myeloablative conditioning, patients receive a single intravenous infusion. The CF bag is administered first, followed by the NF bag within 1 hour.
- Premedication: Patients receive antihistamine, hydrocortisone, and acetaminophen 30-60 minutes prior to infusion [86].
Lyfgenia (lovotibeglogene autotemcel)
Mechanism and Indication: Lyfgenia is an autologous hematopoietic stem cell-based gene therapy for patients 12 years of age or older with sickle cell disease (SCD) and a history of vaso-occlusive events [88] [89]. Its mechanism centers on ex vivo genetic modification to address the underlying genetic defect in SCD. A patient's own CD34+ cells are harvested and transduced with a lentiviral vector encoding a modified β-globin gene (βA-T87Q-globin). This gene produces anti-sickling hemoglobin (HbAT87Q), which reduces the proportion of pathological sickle hemoglobin (HbS), thereby decreasing hemolysis and vaso-occlusion [88]. This therapy fundamentally alters the differentiation trajectory of the patient's hematopoietic stem cells to produce erythrocytes with a stabilized, functional hemoglobin.
Clinical Trial Data and Efficacy:
Table 2: Key Clinical Efficacy and Safety Data for Lyfgenia [88] [60]
| Parameter | Result | Follow-up Period |
|---|---|---|
| Complete Resolution of VOEs | 88% of patients | 6 to 18 months post-infusion |
| Most Common Adverse Reactions | Stomatitis, thrombocytopenia, neutropenia, febrile neutropenia | Throughout trial |
| Key Warnings/Precautions | Delayed platelet engraftment, insertional oncogenesis, hypersensitivity | - |
Experimental Protocol:
- HSC Collection: Autologous CD34+ hematopoietic stem cells are collected from the patient via apheresis.
- Ex Vivo Genetic Modification: The cells are transduced with the BB305 lentiviral vector encoding the βA-T87Q-globin gene.
- Myeloablative Conditioning: Patients undergo busulfan myeloablation to create marrow space for the modified cells.
- Product Infusion: The cryopreserved, transduced cell product is thawed and administered via a single intravenous infusion [88].
- Monitoring: Patients require long-term follow-up for the detection of vector integration sites and monitoring for potential insertional oncogenesis.
Ryoncil (remestemcel-L-rknd)
Mechanism and Indication: Ryoncil is an allogeneic bone marrow-derived mesenchymal stromal cell (MSC) therapy. It is the first FDA-approved MSC product, indicated for the treatment of steroid-refractory acute graft-versus-host disease (SR-aGvHD) in pediatric patients 2 months and older [90] [91]. Unlike the previous therapies, Ryoncil's primary mechanism is not engraftment and differentiation, but immunomodulation. The administered MSCs are thought to modulate the immune response by secreting bioactive factors that suppress T-cell proliferation and dendritic cell activity, and reduce inflammation, thereby mitigating the life-threatening immune attack on host tissues [91]. This leverages the paracrine signaling properties of MSCs, a key aspect of their differentiation-independent therapeutic function.
Clinical Trial Data and Efficacy: Approval was based on a single-arm trial (MSB-GVHD001) in 54 pediatric patients with SR-aGvHD.
Table 3: Key Clinical Efficacy and Safety Data for Ryoncil [91]
| Parameter | Result | Notes |
|---|---|---|
| Day 28 Overall Response Rate (ORR) | 70% (95% CI: 56.4, 82.0) | Combined Complete and Partial Response |
| Complete Response (CR) Rate | 30% (95% CI: 18.0, 43.6) | - |
| Median Duration of Response | 54 days (range 7, 159+) | - |
| Common Adverse Reactions | Viral/bacterial infections, pyrexia, hemorrhage, edema, abdominal pain | Incidence ≥20% |
Experimental Protocol:
- Cell Source: Allogeneic MSCs are derived from the bone marrow of healthy adult donors.
- Manufacturing: Cells are expanded ex vivo to create a standardized, off-the-shelf product.
- Dosing Regimen: The recommended dose is 2 x 10^6 cells per kg body weight, administered via intravenous infusion twice weekly for four weeks (total of 8 infusions). Infusions are given at least 3 days apart [91].
- Response Assessment: Treatment may be continued based on clinical response evaluated at 28 days after initiation.
Research Reagent Solutions and Experimental Tools
The development and quality control of these advanced therapies rely on a suite of specialized research reagents and tools.
Table 4: Essential Research Reagents and Tools for Stem Cell Therapy Development
| Reagent/Tool | Function | Application Example |
|---|---|---|
| Nicotinamide (NAM) | Inhibits differentiation, promotes expansion of HSCs in culture. | Critical reagent in the ex vivo manufacturing process of Omisirge [86] [87]. |
| Lentiviral Vectors | Engineered viruses for stable gene delivery into the genome of target cells. | Used in Lyfgenia to introduce the modified β-globin gene into patient HSCs [88]. |
| Cell Culture Media & Supplements | Provides nutrients and specific signals for cell survival, expansion, and maintenance of phenotype. | Essential for all three therapies; e.g., expansion of MSCs for Ryoncil and HSCs for Omisirge and Lyfgenia. |
| CD34 Microbeads | Magnetic-activated cell sorting (MACS) reagent for isolation of CD34+ hematopoietic stem cells. | Used to isolate the target cell population for Lyfgenia manufacturing and in process control for Omisirge. |
| CRISPR/Cas9 Systems | Precision gene-editing tool for knocking in/out or correcting genes. | While not used in these approved products, it is a key reagent in the broader field, e.g., in the related therapy Casgevy [15]. |
| StemRNA Clinical iPSC Seed Clones | GMP-compliant, clinically-suitable induced pluripotent stem cell lines. | Used as a starting material for developing novel, scalable iPSC-derived therapies, as referenced in ongoing trials [60]. |
Visualizing Core Mechanisms and Workflows
The following diagrams illustrate the fundamental biological pathways and manufacturing workflows for these therapies.
Omisirge Mechanism: NAM-Mediated Stem Cell Expansion
Lyfgenia Workflow: Autologous Gene Therapy
Ryoncil Mechanism: MSC Immunomodulation in GvHD
The approvals of Omisirge, Lyfgenia, and Ryoncil demonstrate the successful clinical translation of distinct stem cell biological principles: controlled self-renewal, directed differentiation via genetic engineering, and immunomodulation. These products provide powerful new treatment options for patients with hematologic malignancies, sickle cell disease, and steroid-refractory GvHD, respectively. For the research community, they serve as foundational benchmarks. The future trajectory of the field points toward the increasing use of allogeneic, off-the-shelf iPSC-derived products [60], enhanced precision through advanced gene-editing technologies like CRISPR [15], and the development of more complex tissue-engineered products. Continued research into the fundamental mechanisms controlling stem cell fate, coupled with innovations in manufacturing and quality control, will be essential to fully realize the potential of regenerative medicine.
The clinical application of pluripotent stem cell (PSC)-derived therapies represents a transformative frontier in regenerative medicine. As of 2025, the global landscape includes over 115 clinical trials involving 83 distinct PSC-derived products, primarily targeting ophthalmology, neurology, and oncology indications. More than 1,200 patients have been dosed with over 10¹¹ cells, with no class-wide safety concerns reported to date, indicating a promising safety profile for these innovative therapies. The field is supported by evolving regulatory frameworks and standardized best practices that aim to accelerate the translation of PSC-based therapies from research to clinical application while ensuring patient safety and therapeutic efficacy.
Pluripotent stem cells (PSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), are defined by two fundamental properties: self-renewal (the ability to proliferate indefinitely) and pluripotency (the capacity to differentiate into virtually any cell type in the body) [92]. These cells are derived from the inner cell mass (ICM) of the blastocyst (ESCs) or generated by reprogramming somatic cells through the activation of specific factors including Oct4, Nanog, Klf4, and c-Myc (iPSCs) [92]. The molecular mechanisms governing pluripotency and self-renewal are finely orchestrated by precise networks including epigenetic modifications, transcription factors, signaling pathways, and histone modifications [92]. Understanding these mechanisms is crucial for developing safe and effective PSC-derived therapies, as they directly impact differentiation potential, genomic stability, and ultimate therapeutic efficacy.
The clinical translation of PSC-derived products represents one of the most promising applications of regenerative medicine, offering potential treatments for a wide range of conditions including neurodegenerative diseases, retinal disorders, and cardiovascular conditions. This whitepaper examines the current global clinical trial landscape for PSC-derived products, with specific focus on safety and efficacy data emerging from human trials, technical requirements for product development, and regulatory considerations essential for research and drug development professionals working in this rapidly advancing field.
Global Clinical Trial Landscape: Quantitative Analysis
The global clinical pipeline for PSC-derived therapies has expanded significantly, with current trial activity consolidating around three primary therapeutic areas: ophthalmology, central nervous system (CNS) disorders, and oncology [60]. The cumulative number of PSC clinical trials has shown steady growth from 2010 through 2025, reflecting increasing research investment and clinical translation efforts [60].
Table 1: Global PSC-Derived Clinical Trial Landscape (as of December 2024)
| Parameter | Statistical Data | Timeframe/Notes |
|---|---|---|
| Total Clinical Trials | 115 trials | Global, as of Dec 2024 [60] |
| Distinct PSC-Derived Products | 83 products | In clinical testing [60] |
| Patients Dosed | >1,200 patients | Cumulative across trials [60] |
| Cells Administered | >10¹¹ cells | Total dose volume [60] |
| Leading Therapeutic Areas | Ophthalmology, Neurology, Oncology | Areas with greatest trial concentration [60] |
| Safety Profile | No class-wide safety concerns | Across all trials to date [60] |
Notable PSC-Derived Products in Clinical Development
Several PSC-derived products have reached advanced stages of clinical development, representing key milestones in the field. These products employ diverse technological approaches and target various therapeutic indications.
Table 2: Select PSC-Derived Products in Clinical Development (2024-2025)
| Product Name | Cell Type | Indication | Development Stage | Key Updates |
|---|---|---|---|---|
| Fertilo | iPSC-derived ovarian support cells (OSCs) | In vitro oocyte maturation | Phase III (U.S.) | First iPSC-based therapy to enter U.S. Phase III; FDA IND clearance in Feb 2025 [60] |
| OpCT-001 | iPSC-derived therapy | Retinal degeneration (retinitis pigmentosa, cone-rod dystrophy) | Phase I/IIa | FDA IND clearance Sept 2024; first iPSC-based therapy for primary photoreceptor diseases [60] |
| FT819 | iPSC-derived CAR T-cell | Systemic lupus erythematosus (SLE), lupus nephritis (LN) | Phase I | FDA RMAT designation April 2025 [60] |
| Neural progenitor cell therapies | iPSC-derived neural progenitors | Parkinson's disease, spinal cord injury, ALS | Phase I | FDA IND clearance June 2025 [60] |
| MyoPAXon | iPSC-derived CD54+ allogeneic muscle progenitor cells | Duchenne muscular dystrophy (DMD) | Phase I | ClinicalTrials.gov NCT06692426 [60] |
| Autologous iPSC-derived Dopaminergic Neural Progenitor Cells | Autologous iPSC-derived neural progenitors | Parkinson's Disease | Phase I | ClinicalTrials.gov NCT06687837 [60] |
| FT536 | iPSC-derived natural killer (NK) cells | Gynecologic cancers | Clinical trials | From gene-edited clonal master hiPSC line; ClinicalTrials.gov NCT06342986 [60] |
| Cymerus iMSCs (CYP-001) | iPSC-derived MSCs (iMSCs) | High-Risk Acute Graft-Versus-Host Disease (HR-aGvHD) | Clinical trials | In combination with corticosteroids; ClinicalTrials.gov NCT05643638 [60] |
Safety and Efficacy Profile of PSC-Derived Products
Aggregate Safety Data
The comprehensive safety profile of PSC-derived products has been remarkably favorable across the clinical trial landscape. Cumulative data from over 1,200 dosed patients reveals no class-wide safety concerns associated with PSC-based therapies [60]. This encouraging safety record is particularly noteworthy given the theoretical risks associated with pluripotent cell transplantation, including teratoma formation, immunogenicity, and ectopic tissue formation.
The therapeutic context and administration route appear to influence risk profiles. Ophthalmology applications, which benefit from local administration and the immune-privileged status of the eye, have demonstrated particularly favorable safety outcomes [60]. For CNS applications, managing durability, tumorigenicity controls, and immunosuppression remain critical considerations, though no major safety signals have emerged thus far [60].
The field has benefited from progressive refinement of differentiation protocols, purification methods, and safety switches that mitigate potential risks. Additionally, the establishment of master cell banks and comprehensive characterization assays has contributed to product consistency and safety.
Efficacy Signals Across Indications
While many PSC-derived products remain in early to mid-stage clinical development, promising efficacy signals have emerged across multiple therapeutic areas:
- Ophthalmology: PSC-derived retinal cells have demonstrated positive clinical outcomes in treatments for macular degeneration, with FDA approval anticipated in the near future based on encouraging trial results [93].
- Neurology: Early trials of PSC-derived dopaminergic neurons for Parkinson's disease have shown improved motor functions and reduced symptoms in patients, marking a potential turning point for treating this neurodegenerative condition [93].
- Oncology: iPSC-derived natural killer (NK) cell therapies and CAR T-cell products have demonstrated antitumor activity in early trials, particularly for gynecologic cancers and hematologic malignancies [60].
The efficacy assessment of PSC-derived products requires specialized endpoints tailored to each therapeutic application. For neurological applications, functional improvement measures are essential, while ophthalmology applications benefit from standardized visual acuity and retinal imaging assessments.
Molecular Mechanisms of Pluripotency: Foundation for Therapeutic Applications
Signaling Pathways Governing Pluripotency and Self-Renewal
The therapeutic application of PSC-derived products depends fundamentally on understanding the molecular mechanisms that maintain pluripotency and direct differentiation. These mechanisms differ significantly between murine and human PSCs, reflecting distinct pluripotency states – "naïve" in mESCs and "primed" in hESCs [92].
Murine ESC Pathways:
- LIF (Leukemia inhibitory factor) and BMP4 (bone morphogenetic protein-4) are crucial for maintaining self-renewal in mESCs [92].
- LIF activates transcription factor STAT3, while BMP induces inhibitory differentiation (Id) genes through the Smad pathway [92].
- BMP sustains pluripotency by suppressing the ERK/MAPK pathway and activating MEK5/ERK5 [92].
- Nanog protects self-renewal potential even in absence of LIF, repressing Gata4 and upregulating Rex1 and LIF-responsive genes [92].
Human ESC Pathways:
- The TGF-β/Activin A/Nodal pathway maintains pluripotency by activating Smad2/3 [92].
- Smad2/3 supports self-renewal through activation of Nanog expression [92].
- Low concentrations of Activin A (5 ng/mL) sustain pluripotency, while high concentrations (50-100 ng/mL) induce endodermal differentiation [92].
The following diagram illustrates the key signaling pathways governing pluripotency and self-renewal in human and murine ESCs:
Core Transcription Factor Network
The pluripotent state in ESCs is maintained by a core network of transcription factors that includes Oct4 (POU5F1), Nanog, and Sox2 [92]. These factors work in concert to promote the expression of genes related to pluripotency while suppressing differentiation pathways:
- Oct4: Sustains intrinsic signaling in a LIF-independent manner to promote ES cell pluripotency and self-renewal [92].
- Nanog: Protects self-renewal potential even in absence of LIF, generally considered a master regulator of pluripotency [92].
- Sox2: Works cooperatively with Oct4 to maintain pluripotency and self-renewal.
This core regulatory network interacts with epigenetic modifiers, including chromatin remodeling proteins and histone modifications, to establish a permissive chromatin state that supports pluripotency while allowing for rapid activation of differentiation programs when needed.
Technical Requirements for PSC-Derived Product Development
PSC Line Selection and Culture Optimization
The starting biological material for PSC-derived products fundamentally influences their safety and efficacy profiles. Key considerations include:
- PSC Line Characterization: Comprehensive characterization of PSC lines including karyotype stability, pluripotency marker expression, differentiation potential, and genomic integrity is essential before initiating product development [94].
- Culture Condition Optimization: The differentiation potential of PSCs is significantly influenced by culture conditions. Research demonstrates that PSCs retain higher differentiation potential when cultured in media supporting the glycolytic pathway, with high expression of chromodomain-helicase-DNA-binding protein 7 (CHD7) serving as a positive biomarker for differentiation potential [95].
- Cell Adhesion Substrates: Seeding cells on less potent cell-binding materials can minimize the inclusion of spontaneously differentiated cells, as differentiated cells exhibit reduced adhesive properties compared to undifferentiated PSCs [95].
The following workflow diagram illustrates the key stages in developing PSC-derived cellular therapies:
Essential Research Reagent Solutions
The development of PSC-derived therapies requires specialized reagents and materials to ensure product quality, consistency, and safety. The following table details key research reagent solutions essential for this field:
Table 3: Essential Research Reagent Solutions for PSC-Derived Product Development
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Reprogramming Factors | Oct4, Nanog, Klf4, c-MYC | Generation of iPSCs from somatic cells | Non-integrating delivery methods preferred for clinical applications [92] |
| Culture Media | mTeSR1, Essential 8, Repro FF2 | Maintenance of undifferentiated PSCs | Media supporting glycolytic pathway enhance differentiation potential [95] |
| Extracellular Matrices | Recombinant laminin 521, Vitronectin | Cell culture substrates for feeder-free culture | Defined, xeno-free matrices required for clinical applications [95] |
| Differentiation Inducers | Growth factors, small molecules | Directed differentiation to specific lineages | Concentrations must be optimized (e.g., Activin A: 5 ng/mL for pluripotency vs. 50-100 ng/mL for endoderm) [92] |
| Cell Separation | Magnetic/fluorescence-activated cell sorting | Purification of target cell populations | Marker selection critical for product purity and safety |
| Characterization Tools | Pluripotency markers (Oct4, Nanog, Sox2), Karyotyping, Teratoma formation assays | Quality control and safety assessment | Multiple orthogonal methods required for comprehensive characterization [94] |
Regulatory Landscape and Best Practices
International Regulatory Considerations
The regulatory landscape for PSC-derived products continues to evolve, with several important developments shaping the field:
- Best Practices Framework: The International Society for Stem Cell Research (ISSCR) has released "Best Practices for the Development of Pluripotent Stem Cell-Derived Cellular Therapies," a comprehensive resource designed to accelerate the translation of PSC-derived therapies into clinical trials and commercial use [94].
- Jurisdictional Coverage: Regulatory guidance across nine jurisdictions (Australia, Brazil, Canada, China, European Union, Japan, South Korea, United Kingdom, and United States) is now available, providing the scientific community with consolidated access to vital regulatory requirements [94].
- FDA Designations: Expedited FDA designations including Regenerative Medicine Advanced Therapy (RMAT) and Fast Track are increasingly supporting PSC-based therapy development, facilitating regulatory engagement and trial acceleration [60].
Quality Control and Safety Testing
Robust quality control systems are essential for ensuring the safety and consistency of PSC-derived products. Key considerations include:
- Genomic Stability: Comprehensive testing for genomic alterations, with recommendations for using both sequencing and cytogenetic methods to ensure thorough safety assessments [96].
- Tumorigenicity Assessment: Rigorous evaluation of tumorigenic potential through in vitro and in vivo studies, particularly important for products containing residual undifferentiated PSCs.
- Potency Assays: Development of quantitative assays that measure biological activity specific to the intended therapeutic function.
The global clinical trial landscape for PSC-derived products demonstrates encouraging progress, with expanding trial activity, promising safety profiles, and early efficacy signals across multiple therapeutic areas. The field has reached a significant maturation point, with over 1,200 patients dosed and no class-wide safety concerns identified. Continued advancement will depend on several key factors:
- Standardization: Further development and implementation of standardized protocols for PSC differentiation, purification, and characterization to enhance product consistency and reliability [96].
- Manufacturing Innovation: Advancement of scalable manufacturing platforms, including automated bioreactors and integrated quality control systems, to support commercial viability [96].
- Regulatory Alignment: Continued harmonization of regulatory requirements across jurisdictions to facilitate global development of PSC-derived therapies [94].
- Long-Term Monitoring: Establishment of comprehensive long-term follow-up programs to fully characterize the safety profile of PSC-derived products over extended timeframes.
As the field continues to evolve, the integration of advanced technologies including gene editing, single-cell analytics, and artificial intelligence is expected to further enhance the safety, efficacy, and manufacturability of PSC-derived therapies. With a robust clinical pipeline and ongoing technological innovations, PSC-derived products are poised to make significant contributions to the treatment of numerous conditions with high unmet medical needs.
Stem cell research represents a cornerstone of regenerative medicine, offering unprecedented potential for understanding human development and treating degenerative diseases. The core of this field lies in comparing the three principal stem cell types: Embryonic Stem Cells (ESCs), adult stem cells (ASCs), and induced Pluripotent Stem Cells (iPSCs). Each possesses distinct biological properties, therapeutic applications, and technical considerations that researchers must navigate [97] [98]. ESCs, derived from the inner cell mass of blastocysts, define the gold standard for pluripotency but are entangled with ethical concerns [97] [98]. ASCs, particularly Mesenchymal Stem Cells (MSCs), are multipotent cells readily available from adult tissues, offering a clinically translatable option with immunomodulatory properties [97] [61]. The discovery of iPSCs, somatic cells reprogrammed to an embryonic-like state, presented a revolutionary source free from ethical constraints and capable of enabling patient-specific therapies [99]. This analysis provides a technical comparison of these cell sources, focusing on their molecular signatures, functional characteristics, and experimental protocols, framed within the broader context of stem cell self-renewal and differentiation mechanisms.
Core Characteristics and Comparative Analysis
Defining Properties and Origins
- Embryonic Stem Cells (ESCs): Sourced from the inner cell mass of a blastocyst, ESCs are pluripotent, capable of differentiating into any cell type derived from the three germ layers. Their use is characterized by significant ethical and legal restrictions, which have limited the scope of related research [97] [98].
- Adult Stem Cells (ASCs): Also known as tissue-specific stem cells, ASCs are multipotent and reside in various adult tissues like bone marrow, adipose tissue, and the umbilical cord. They function in tissue maintenance and repair. Mesenchymal Stem Cells (MSCs) are a prominent type of ASC widely used in therapy due to their availability, lack of ethical issues, and immunomodulatory capacities [97] [98] [61].
- Induced Pluripotent Stem Cells (iPSCs): These are generated by reprogramming adult somatic cells through the forced expression of specific transcription factors, such as OCT4, SOX2, KLF4, and MYC (the Yamanaka factors). iPSCs mirror the pluripotency of ESCs but avoid ethical concerns and offer potential for autologous patient-specific treatments [99].
Quantitative Comparison of Molecular and Functional Features
The functional and molecular characteristics of ESCs, ASCs, and iPSCs are defined by their origin and pluripotency state, which directly influence their research and clinical applications. The table below summarizes these key attributes.
Table 1: Comparative Analysis of Stem Cell Source Characteristics
| Feature | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs, e.g., MSCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|---|
| Origin | Inner cell mass of blastocyst [97] | Adult tissues (e.g., bone marrow, adipose tissue) [97] [61] | Reprogrammed somatic cells (e.g., fibroblasts) [99] |
| Pluripotency/Multipotency | Pluripotent [97] | Multipotent [97] [61] | Pluripotent [99] |
| Key Molecular Markers | OCT4, SOX2, NANOG [97] [99] | TGF-β, IL-10, VEGF (secreted factors) [97] | OCT4, SOX2, NANOG, LIN28 [97] [99] |
| Proliferation Capacity | Unlimited self-renewal [97] | Limited self-renewal in culture [61] | Unlimited self-renewal [99] |
| Genetic Stability | Generally stable | Variable, can be affected by donor age | Can harbor epigenetic memory; genetic instability from reprogramming [99] [100] |
| Tumorigenic Risk | Risk of teratoma formation [97] | Low risk [97] [61] | Risk of teratoma formation; potentially lower than ESCs [97] [99] |
| Ethical Considerations | Significant concerns; destruction of embryos [97] [98] | Minimal to no ethical concerns [97] | Minimal to no ethical concerns [97] [99] |
| Therapeutic Strengths | Gold standard for pluripotency studies | Immunomodulation, tissue repair, homing ability [97] [61] | Patient-specific models, disease-in-a-dish, drug screening [99] [101] |
Functional Heterogeneity and Mitochondrial Profiles
A critical consideration in stem cell biology is the inherent functional heterogeneity within a seemingly pure population. Advanced technologies like Quantitative Phase Imaging (QPI) coupled with machine learning have revealed remarkable diversity in the kinetic behaviors of individual hematopoietic stem cells (HSCs), such as variations in proliferation rate, cell division patterns, and morphology, which are not detectable through snapshot genetic analyses [72]. This heterogeneity directly impacts functional quality and must be accounted for in experimental design.
Furthermore, while ESCs and iPSCs are both pluripotent, their functional equivalence upon differentiation is a key area of investigation. A comparative study of mitochondrial function during neural differentiation revealed that while ESCs and iPSCs are similar at the pluripotent stage, significant differences emerge at differentiated stages. Specifically, iPSC-derived neural stem cells showed decreased ATP production compared to their ESC-derived counterparts, and iPSC-derived astrocytes exhibited increased mitochondrial activity and biogenesis [100]. These findings underscore the importance of validating functional outcomes when using iPSCs as substitutes for ESCs in disease modeling and therapeutic development.
Experimental Protocols and Workflows
Protocol for Directed Differentiation of Pluripotent Stem Cells to Astrocytes
Differentiating pluripotent stem cells (PSCs) into specific lineages is fundamental for their application. The following protocol, adapted from a study comparing ESCs and iPSCs, details the process of generating astrocytes [100].
Neural Induction and NSC Generation:
- Culture PSCs (ESCs or iPSCs) under feeder-free conditions on Geltrex-coated plates in Essential 8 medium.
- Perform neural induction to convert PSCs into Neural Stem Cells (NSCs). The specific methodology can vary but often uses dual SMAD inhibition.
- Maintain the resulting NSCs in StemPro NSC Serum-Free Medium as a monolayer on Geltrex-coated surfaces. Use cells between passages 4 and 9 for experiments to ensure consistency [100].
Astrocyte Differentiation:
- Plate NSCs onto poly-D-lysine (PDL)-coated coverslips or culture dishes.
- Culture the cells in Astrocyte Differentiation Medium for four weeks. This medium consists of:
- Basal Medium: DMEM/F-12, GlutaMAX
- Supplements: 1X N2 supplement, 1X B27 supplement
- Growth Factors: 200 ng/ml insulin-like growth factor-I (IGF-I), 10 ng/ml heregulin 1β, 10 ng/ml activin A, 8 ng/ml Fibroblast Growth Factor 2 (FGF2)
- Serum: 1% Fetal Bovine Serum (FBS)
- Change the medium every other day for the first week, every two days for the second week, and every three days for the third and fourth weeks [100].
Astrocyte Maturation:
- Following the differentiation phase, transfer the cells to a specialized Astrocyte Growth Medium (e.g., AGM from Lonza) for maturation.
- Maintain the cells in this maturation medium for up to three months to achieve a mature, stellate-like astrocyte morphology and phenotype [100].
Workflow for Quantitative Phase Imaging (QPI) and Kinetic Analysis of Stem Cells
To assess the functional heterogeneity of stem cells non-invasively, QPI can be employed. The following workflow outlines the key steps [72]:
- Cell Sorting and Culture: Sort a single stem cell (e.g., a murine HSC from the CD201+CD150+CD48-KSL fraction or a human HSC) into a 96-well U-bottom plate containing an appropriate expansion culture medium [72].
- Time-Lapse QPI Acquisition: Place the culture plate in a QPI system (e.g., a ptychographic QPI microscope). Acquire images of the living cell every few minutes over a prolonged period (e.g., 36 to 96 hours) without using labels or high-intensity light [72].
- Feature Extraction: From the time-lapse data, extract multiple kinetic parameters for each individual cell. These can include:
- Dry mass
- Cellular sphericity
- Velocity (for motility)
- Length/Width ratio
- Division Gap (time between first and second divisions) [72]
- Data Integration and Machine Learning: Integrate the extracted kinetic parameters and perform dimensionality reduction using algorithms like Uniform Manifold Approximation and Projection (UMAP). This allows for the identification of distinct cellular clusters based solely on kinetic behavior, which can then be correlated with functional stemness assays [72].
The diagram below visualizes this integrated experimental workflow.
Diagram 1: QPI-ML Workflow for Stem Cell Analysis
Signaling Pathways and Molecular Mechanisms
Core Regulatory Network of Pluripotency and Reprogramming
The pluripotent state of ESCs and iPSCs is maintained by a core transcriptional network and specific signaling pathways. The key genetic regulators include transcription factors OCT4, SOX2, and NANOG, which form an autoregulatory loop to activate genes essential for self-renewal while suppressing those involved in differentiation [97] [99]. The WNT/β-catenin signaling pathway promotes self-renewal, while TGF-β/Activin/Nodal signaling is also critical for maintaining pluripotency in human ESCs. During somatic cell reprogramming to iPSCs, the process involves an initial stochastic phase followed by a deterministic phase, with key events including the silencing of somatic genes, activation of pluripotency genes, and a Mesenchymal-to-Epithelial Transition (MET) [99].
Diagram 2: Key Regulators of Stem Cell Fate
Molecular Mechanisms of iPSC Induction
The groundbreaking discovery of iPSCs by Shinya Yamanaka demonstrated that somatic cell fate is reversible. The reprogramming process, initiated by the Yamanaka factors (OCT4, SOX2, KLF4, MYC), erases the somatic epigenetic memory and reinstates a pluripotent epigenetic landscape [99]. This process involves global changes in chromatin structure, DNA methylation, and histone modifications, effectively reversing the "downhill" progression of Waddington's epigenetic landscape. The molecular dynamics begin with the silencing of somatic genes, followed by the activation of early and then late pluripotency-associated genes, ultimately establishing a stable, self-renewing pluripotent state [99].
The Scientist's Toolkit: Essential Research Reagents
Successful stem cell research requires a suite of specialized reagents and tools. The following table details essential items for working with ESCs, ASCs, and iPSCs.
Table 2: Essential Research Reagents for Stem Cell Research
| Reagent/Material | Function/Application | Example Usage |
|---|---|---|
| Geltrex | A basement membrane matrix used as a substrate to coat culture surfaces, promoting the attachment and growth of pluripotent stem cells. | Coating 6-well plates for the maintenance of human ESCs and iPSCs in feeder-free conditions [100]. |
| Essential 8 Medium | A defined, xeno-free culture medium optimized for the feeder-free maintenance and expansion of human pluripotent stem cells. | Routine culture of human iPSC and ESC lines [100]. |
| StemPro NSC SFM | A serum-free medium (SFM) formulated for the selective expansion and maintenance of human neural stem cells (NSCs). | Maintaining NSCs derived from PSCs as a monolayer after neural induction [100]. |
| Yamanaka Factor Cocktail | A set of transcription factors (OCT4, SOX2, KLF4, MYC) used to reprogram somatic cells into iPSCs. | Delivered via retroviral or Sendai viral vectors to human fibroblasts to generate iPSCs [99] [100]. |
| MitoTracker Green (MTG) | A cell-permeant fluorescent dye that accumulates in mitochondria, used for staining and measuring mitochondrial mass/volume. | Co-staining with TMRE to assess mitochondrial volume and membrane potential in live PSCs and their derivatives [100]. |
| Tetramethylrhodamine Ethyl Ester (TMRE) | A cell-permeant, fluorescent dye that is absorbed by active mitochondria in proportion to their membrane potential (ΔΨm). | Used alongside MTG in flow cytometry to measure the mitochondrial membrane potential [100]. |
| Poly-D-Lysine (PDL) | A synthetic polymer used to coat cultureware, enhancing the attachment of adherent cells, particularly neurons and glia. | Coating coverslips for the differentiation of NSCs into astrocytes [100]. |
| N2 & B27 Supplements | Chemically defined supplements providing hormones, proteins, and lipids essential for the survival and differentiation of neural cells. | Used as key components in astrocyte differentiation medium [100]. |
The comparative analysis of ESCs, ASCs, and iPSCs reveals a landscape of complementary tools for regenerative medicine and biological research. ESCs remain the benchmark for pluripotency, ASCs like MSCs offer a readily applicable and safe option for specific therapeutic strategies, and iPSCs provide a flexible, patient-specific platform for disease modeling and drug discovery. The choice of stem cell source is ultimately dictated by the specific research or clinical objective, balancing factors such as pluripotency, scalability, tumorigenic risk, and ethical considerations. As the field advances, the integration of these cell sources with cutting-edge technologies like 3D bioprinting, gene editing, and high-resolution kinetic imaging, as detailed in this analysis, will continue to unlock their full therapeutic potential and deepen our understanding of stem cell self-renewal and differentiation mechanisms.
The fields of regenerative medicine and cellular immunotherapy are being transformed by two emerging platforms: induced pluripotent stem cell-derived mesenchymal stem cells (iMSCs) and iPSC-derived chimeric antigen receptor T-cells (CAR-T). These technologies represent a convergence of breakthroughs in stem cell biology and genetic engineering, offering solutions to longstanding challenges in therapeutic cell manufacturing. Both platforms are fundamentally rooted in the precise control of stem cell self-renewal and differentiation—the processes by which stem cells divide to make more stem cells or commit to specialized lineages [102] [69].
The property of self-renewal enables stem cells to undergo numerous cycles of cell division while maintaining their undifferentiated state through a balance of symmetric division (producing two identical stem cells) and asymmetric division (producing one stem cell and one differentiated daughter cell) [11]. This balance is regulated by intricate networks of transcription factors, epigenetic modifiers, and signaling pathways that maintain pluripotency in embryonic stem cells (ESCs) and iPSCs [103]. For iPSC-derived therapies, mastering these regulatory networks is essential for generating the large quantities of consistent, functional cells required for clinical applications.
This whitepaper provides an in-depth technical examination of iMSC and iPSC-derived CAR-T cell platforms, focusing on their biological foundations, manufacturing methodologies, current clinical landscape, and the technical challenges that remain for full clinical translation.
Fundamental Biological Mechanisms
Molecular Regulation of Stem Cell Self-Renewal
Stem cell self-renewal is orchestrated by core transcriptional networks and extracellular signaling pathways that maintain the undifferentiated state while permitting expansion. The transcription factors OCT4, SOX2, and NANOG form the core pluripotency network in both ESCs and iPSCs, promoting expression of self-renewal genes while suppressing differentiation programs [103]. These factors work in concert with epigenetic regulators, including Polycomb group proteins and chromatin remodeling complexes, to maintain a transcriptionally permissive state [104].
Multiple signaling pathways precisely regulate the balance between self-renewal and differentiation. In murine ESCs, Leukemia Inhibitory Factor (LIF) activates STAT3 signaling to maintain pluripotency, while Bone Morphogenetic Protein (BMP) signaling suppresses differentiation [103]. Human ESCs and iPSCs rely more heavily on TGF-β/Activin A/Nodal signaling, which activates Smad2/3 to sustain NANOG expression [103]. The Wnt/β-catenin pathway also plays a crucial role across species, with β-catenin degradation maintaining pluripotency in the absence of differentiation signals [11].
Table 1: Key Signaling Pathways Regulating Pluripotency and Self-Renewal
| Pathway | Key Components | Role in Self-Renewal | Species Specificity |
|---|---|---|---|
| LIF/STAT3 | LIF, gp130, STAT3 | Promotes self-renewal via STAT3 phosphorylation | Primarily murine |
| TGF-β/Activin/Nodal | TGF-β, Activin, Nodal, Smad2/3 | Sustains NANOG expression, suppresses BMP | Primarily human |
| BMP/Smad | BMP4, Smad1/5/8 | Induces Id genes, suppresses ERK/MAPK | Both (context-dependent) |
| Wnt/β-catenin | Wnt, β-catenin, GSK3β | Regulates differentiation; inhibition maintains pluripotency | Both |
| PI3K/AKT | PI3K, AKT, mTOR | Promotes proliferation, suppresses differentiation | Both |
From Pluripotency to Lineage Commitment
The transition from pluripotent stem cells to differentiated progeny involves precise lineage commitment through the stepwise activation and repression of developmental pathways. For iMSC generation, this typically involves guiding iPSCs through a mesodermal lineage commitment, followed by specification to a mesenchymal stromal cell fate. For CAR-T cell production, iPSCs are directed through hematopoietic specification followed by T-lineage commitment and maturation.
Critical to these processes is the concept of the stem cell niche—the specialized microenvironment that provides cues for self-renewal and differentiation through cell-cell contacts, soluble factors, and mechanical signals [104]. In vitro recapitulation of these niche signals is essential for efficient differentiation protocols. Key regulators include HOX genes, which establish positional identity during differentiation, and metabolic shifts from glycolysis to oxidative phosphorylation that accompany lineage commitment [104].
iPSC-Derived Mesenchymal Stem Cells (iMSCs)
Manufacturing and Differentiation Protocols
The production of iMSCs from iPSCs requires precise control of differentiation conditions to generate cells that meet the International Society for Cellular Therapy (ISCT) criteria for MSCs: adherence to plastic, specific surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-, CD11b-, CD19-, HLA-DR-), and tri-lineage differentiation potential (osteogenic, chondrogenic, adipogenic) [5].
Detailed iMSC Differentiation Protocol:
- iPSC Maintenance Culture: Maintain iPSCs in Essential 8 medium on vitronectin-coated plates with daily medium changes until 70-80% confluent.
- Mesodermal Induction: Dissociate iPSCs with EDTA and plate as single cells in STEMdiff APEL 2 medium supplemented with 10µM CHIR99021 (GSK-3β inhibitor), 50ng/mL BMP4, and 20ng/mL FGF2 for 3 days.
- MSC Specification: Switch to α-MEM medium supplemented with 10% fetal bovine serum, 1% GlutaMAX, 1% non-essential amino acids, and 0.1mM β-mercaptoethanol for 7-10 days.
- MSC Expansion and Purification: Passage cells using TrypLE Select and purify based on plastic adherence, removing non-adherent cells.
- Characterization: Confirm MSC phenotype via flow cytometry for surface markers and tri-lineage differentiation assays.
This protocol typically yields iMSCs with enhanced proliferation capacity compared to tissue-derived MSCs and reduced donor-to-donor variability. The use of feeder-free systems and defined media is critical for clinical-grade manufacturing.
Advantages Over Tissue-Derived MSCs
iMSCs offer significant advantages over conventional tissue-derived MSCs (from bone marrow, adipose tissue, or umbilical cord). Scalability is dramatically improved, as a single iPSC line can theoretically generate an unlimited supply of iMSCs, overcoming the limited expansion capacity of primary MSCs [105]. This enables the creation of master cell banks with consistent quality and functionality.
iMSCs also demonstrate improved functional properties, including enhanced immunomodulatory capabilities through increased secretion of PGE2, IDO, and TGF-β, and superior tissue repair potential via paracrine factor secretion [5]. Their derivation from iPSCs allows for genetic engineering at the pluripotent stage, enabling the creation of enhanced iMSC lines with improved therapeutic potential.
Clinical Applications and Trial Landscape
iMSCs are being investigated for diverse clinical applications leveraging their immunomodulatory and regenerative properties. Key areas include:
- Graft-versus-Host Disease (GvHD): Cymerus iMSCs (CYP-001) are in an FDA-approved clinical trial for High-Risk Acute GvHD (NCT05643638) in combination with corticosteroids [60].
- Orthopedic Applications: Multiple trials are exploring iMSCs for osteoarthritis, leveraging their chondrogenic differentiation potential and anti-inflammatory effects.
- Cardiovascular Diseases: iMSCs are being tested for critical limb ischemia and other vascular conditions through their angiogenic paracrine activity.
Table 2: Clinical Trials Involving iMSC Therapies
| Product/Company | Indication | Phase | Key Features | Identifier/Status |
|---|---|---|---|---|
| Cymerus iMSCs (Cynata) | High-Risk Acute GvHD | I/II | Allogeneic, manufactured via proprietary technology | NCT05643638 |
| iMSCs (Citius Pharma) | Inflammatory conditions | Preclinical | Allogeneic cGMP master cell bank | Development phase |
| iMSCs (Bone Therapeutics) | Orthopedic diseases | Preclinical | Partnership with Implant Therapeutics | Development phase |
iPSC-Derived CAR-T Cells
Engineering and Manufacturing Platforms
iPSC-derived CAR-T cells represent a paradigm shift from autologous CAR-T manufacturing, offering an "off-the-shelf" approach to cancer immunotherapy. The production process involves genetic engineering at the iPSC stage followed by directed differentiation into functional T-cells.
Detailed iPSC-Derived CAR-T Manufacturing Protocol:
- iPSC Engineering: Electroporate iPSCs with plasmid encoding the CAR construct (typically second-generation with CD3ζ plus CD28 or 4-1BB costimulatory domains) using CRISPR/Cas9 for targeted integration into safe harbor loci (e.g., AAVS1).
- CLP Generation: Differentiate CAR-iPSCs into hematopoietic progenitors using Spin Embryoid Body formation in serum-free differentiation medium with BMP4, VEGF, and SCF for 10-12 days.
- T-Lineage Specification: Coculture CD34+ hematopoietic progenitors with OP9-DL1 or OP9-DL4 stromal cells in the presence of IL-7, FLT3L, and SCF to induce T-cell commitment over 21-28 days.
- T-Cell Maturation: Transfer developing T-cells to plates coated with CD3/CD28 antibodies in the presence of IL-2, IL-7, and IL-15 to promote maturation and expansion over 14-21 days.
- Product Harvest and Formulation: Harvest cells, remove residual non-T-cells via magnetic sorting, and formulate in cryopreservation medium for banking.
This process generates a homogeneous population of CAR-T cells with defined specificity and functionality. The platform allows for multiple genetic modifications, including "off-switches" (e.g., inducible caspase 9), enhanced persistence features (e.g., membrane-bound IL-15), and resistance to the hostile tumor microenvironment (e.g., dominant-negative TGF-β receptor) [106] [105].
Advantages Over Conventional CAR-T Cells
iPSC-derived CAR-T cells offer transformative advantages over conventional autologous CAR-T products. The "off-the-shelf" nature enables immediate treatment availability, eliminating the 3-5 week manufacturing delay associated with autologous products. This is critical for patients with rapidly progressive diseases.
The platform provides unprecedented quality control through extensive characterization and banking at the iPSC stage, ensuring consistent product potency and safety across batches. Cost reductions are substantial, as a single manufacturing run can produce thousands of doses from a master iPSC line, compared to one dose per run with autologous approaches [105].
Additionally, the platform enables rational engineering of enhanced functionalities that are difficult to implement in primary T-cells, including precision gene editing to prevent allorejection (e.g., HLA deletion, HLA-G expression) and incorporation of safety switches.
Clinical Applications and Trial Landscape
iPSC-derived CAR-T platforms are advancing rapidly through preclinical development into clinical testing. Notable programs include:
- FT819 (Fate Therapeutics): The first off-the-shelf, iPSC-derived CAR T-cell therapy targeting CD19 for B-cell malignancies, featuring a novel 1XX CAR signaling domain and HLA engineering to reduce alloreactivity [105].
- FT536 (Fate Therapeutics): An iPSC-derived CAR-NK product targeting multiple tumor antigens (MICA/MICB, CD19) with enhanced functional persistence, currently in trials for gynecologic cancers (NCT06342986) [60].
- BCMA-Targeted CAR-NKT Cells (Cellistic/BrightPath): iPSC-derived CAR-NKT cells targeting BCMA for multiple myeloma, manufactured using a 3D bioreactor platform [105].
Additional companies advancing iPSC-derived CAR programs include Century Therapeutics, Editas Medicine, and Cytovia Therapeutics, with targets spanning hematological and solid tumors.
Research Reagents and Experimental Tools
Table 3: Essential Research Reagents for iMSC and iPSC-Derived CAR-T Development
| Reagent Category | Specific Examples | Function | Application |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Somatic cell reprogramming | iPSC generation |
| Pluripotency Maintenance | Y-27632 (ROCKi), CHIR99021 (GSK3βi), LIF | Enhance iPSC survival and self-renewal | iPSC culture |
| Differentiation Inducers | BMP4, FGF2, VEGF, SCF, IL-7 | Direct lineage specification | Hematopoietic/T-cell differentiation |
| Stromal Cell Lines | OP9-DL1, OP9-DL4, MS-5 | Support T-cell development | T-lineage specification |
| Cytokines/Growth Factors | IL-2, IL-7, IL-15, FLT3L | Promote T-cell maturation and expansion | CAR-T cell culture |
| Gene Editing Tools | CRISPR/Cas9, TALEN, AAVS1 targeting vectors | Precise genetic modification | CAR integration, HLA deletion |
| Characterization Antibodies | CD73, CD90, CD105, CD34, CD45 | Phenotypic validation | iMSC characterization |
| Characterization Antibodies | CD3, CD4, CD8, TCRαβ, CD56 | Lineage confirmation | CAR-T cell validation |
Technical and Regulatory Challenges
Manufacturing and Scalability Hurdles
Despite their promise, both iMSC and iPSC-derived CAR-T platforms face significant manufacturing challenges. For iMSCs, achieving consistent differentiation efficiency at commercial scale remains difficult, with variability in critical quality attributes like immunomodulatory potency and differentiation potential. The development of bioreactor systems capable of large-scale iMSC production while maintaining phenotype is an active area of research.
For iPSC-derived CAR-T cells, the lengthy differentiation protocol (typically 5-7 weeks from iPSC to mature T-cell) presents operational challenges. The use of stromal co-culture systems creates scalability limitations and regulatory concerns about introducing animal-derived components. Development of defined, feeder-free differentiation systems is essential for clinical translation.
Safety and Regulatory Considerations
Tumorigenicity risk represents the primary safety concern for both platforms. Residual undifferentiated iPSCs or early progenitors with proliferative potential could form teratomas or other tumors in vivo. Strategies to address this include:
- Purification methods (e.g., magnetic or flow sorting for specific surface markers)
- Suicide genes (e.g., inducible caspase-9 systems)
- Sensitive detection assays for residual pluripotent cells (<1 in 10^6 sensitivity)
Genomic instability from extended culture and genetic engineering requires comprehensive characterization, including karyotyping, whole genome sequencing, and tumorigenicity studies. Regulatory agencies require extensive proof of product consistency and potency assays correlating with clinical activity.
Visualizing Key Workflows and Signaling Pathways
iPSC Differentiation to iMSCs and CAR-T Cells
Key Signaling Pathways in Pluripotency and Differentiation
The emergence of iMSC and iPSC-derived CAR-T platforms represents a significant advancement in cellular therapeutics, addressing critical limitations of current approaches through standardized, scalable manufacturing. Both technologies build upon our fundamental understanding of stem cell self-renewal mechanisms and lineage differentiation pathways.
Future development will focus on manufacturing innovation, including closed automated systems, 3D bioreactor platforms, and real-time quality monitoring. Product enhancement through genetic engineering will continue, with next-generation iMSCs featuring optimized immunomodulatory profiles and CAR-T products with resistance to tumor microenvironment suppression.
As these platforms advance through clinical trials, establishing robust correlation between potency assays and clinical outcomes will be essential for regulatory approval. The full potential of these technologies will be realized when they can be consistently manufactured at scale while maintaining predefined quality specifications, ultimately making advanced cellular therapies accessible to broader patient populations.
Regulatory Frameworks and the Path from IND Authorization to BLA Approval
The journey from Investigational New Drug (IND) authorization to Biologics License Application (BLA) approval represents a critical pathway for bringing innovative biologic products, including those derived from stem cell research, to market. For researchers developing therapies based on stem cell self-renewal and differentiation mechanisms, understanding this regulatory framework is essential for successful translation from laboratory discovery to clinical application. The process is designed to ensure that biological products—which include gene therapies, cell therapies, and therapeutic vaccines—are safe, pure, and potent before they reach patients [107] [108].
This pathway balances rigorous scientific evaluation with the need to deliver breakthrough treatments to patients. For stem cell researchers, navigating this process requires not only scientific excellence in understanding pluripotency and differentiation pathways but also strategic regulatory planning that begins early in the development process. The molecular mechanisms that govern stem cell fate—including transcription factors like Oct4, Nanog, and Sox2, signaling pathways such as TGF-β/Activin A/Nodal, and metabolic switches from glycolysis to oxidative phosphorylation—directly impact both therapeutic potential and regulatory requirements [109] [103].
The IND Application: Gateway to Clinical Trials
IND Types and Legal Basis
An Investigational New Drug (IND) application is the mandatory first step in the drug development process, serving as a formal request for FDA authorization to administer an investigational drug to humans [110]. From a legal perspective, the IND provides sponsors with an exemption from the Federal Food, Drug, and Cosmetic Act requirement that drugs must have an approved marketing application before being transported across state lines. This exemption is necessary because sponsors typically need to ship the investigational drug to clinical investigators in multiple states [110].
The FDA recognizes several IND types relevant to stem cell research:
- Investigator IND: Submitted by a physician who both initiates and conducts the investigation under whose immediate direction the investigational drug is administered [110].
- Emergency Use IND: Allows FDA to authorize use of an experimental drug in emergency situations without time for conventional IND submission [110].
- Treatment IND: For experimental drugs showing promise in clinical testing for serious or immediately life-threatening conditions while final clinical work and FDA review take place [110].
IND Content Requirements
A complete IND application must contain information in three broad areas [110]:
Animal Pharmacology and Toxicology Studies: Preclinical data to assess whether the product is reasonably safe for initial testing in humans, including any previous experience with the drug in humans.
Manufacturing Information: Details pertaining to composition, manufacturer, stability, and controls used for manufacturing the drug substance and drug product to ensure the sponsor can adequately produce consistent batches.
Clinical Protocols and Investigator Information: Detailed protocols for proposed clinical studies to assess whether initial-phase trials will expose subjects to unnecessary risks, plus qualifications of clinical investigators and commitments to obtain informed consent and IRB review.
For stem cell-based products, the manufacturing information section is particularly crucial due to the complex nature of these products and their sensitivity to manufacturing process changes. The biological characteristics of stem cells—including their reliance on specific metabolic states such as glycolysis in undifferentiated cells and a shift toward oxidative phosphorylation upon differentiation—must be carefully controlled and documented [109].
Table: Key IND Application Components for Stem Cell-Based Products
| Application Section | Key Elements for Stem Cell Products | Relevance to Stem Cell Biology |
|---|---|---|
| Preclinical Data | Proof-of-concept studies, toxicity, biodistribution | Must address pluripotency risks, tumorigenicity (teratoma formation) |
| Chemistry, Manufacturing, and Controls (CMC) | Cell sourcing, characterization, differentiation protocols, quality controls | Links to self-renewal/pluripotency markers (Oct4, Nanog, Sox2) |
| Clinical Protocols | Patient selection, monitoring, differentiation endpoints | Must account for variable differentiation efficiency in vivo |
The FDA Review Process and Clinical Hold
Once an IND is submitted, the sponsor must wait 30 calendar days before initiating any clinical trials. During this period, the FDA reviews the IND for safety to ensure research subjects will not be subjected to unreasonable risk [110]. If the FDA identifies significant safety concerns or deficiencies, it may place the clinical trial on "clinical hold," preventing the study from moving forward until issues are resolved [111].
Successful IND preparation requires reviewing data from the FDA's perspective with particular attention to safety concerns. As noted by regulatory experts at Cardinal Health Regulatory Sciences, "Generally, safety is a big concern for the FDA at the IND stage. They will focus on safety relative to the quality of the product, whether the animal studies support the design of the clinical study, and whether any toxicity was noted in animal studies" [111].
The Transition from IND to BLA: Clinical Development Phases
Phase 1 Trials: Initial Safety Assessment
Phase 1 trials represent the first stage of clinical testing in humans and primarily focus on safety assessment. These studies typically involve a small number of participants (20-80) and aim to determine the drug's safety profile, pharmacokinetics, and often the appropriate dosage range [108]. For stem cell-based therapies, Phase 1 trials must carefully monitor for unique risks such as off-target differentiation, uncontrolled proliferation, and immune reactions to allogeneic cells.
The design of Phase 1 trials for stem cell products should be informed by preclinical studies that have thoroughly characterized the product's differentiation potential and tumorigenic risk. Understanding the molecular switches that control the balance between self-renewal and differentiation—such as the core pluripotency factors Oct4, Nanog, and Sox2—is essential for predicting in vivo behavior and establishing appropriate safety monitoring [103].
Phase 2 Trials: Preliminary Efficacy
Phase 2 trials expand the study to a larger group of people (typically several hundred) to assess the drug's efficacy and further evaluate its safety [108]. These studies provide preliminary evidence of biological activity and help refine the optimal dosing regimen for later-stage trials.
For products based on stem cell differentiation mechanisms, Phase 2 trials should include biomarkers and functional assessments that can objectively measure the intended biological effect. For example, therapies designed to leverage the differentiation potential of human ESCs or iPSCs into specific lineages must demonstrate evidence of successful engraftment and functional integration into target tissues [109].
Phase 3 Trials: Confirmatory Evidence
Phase 3 trials are large-scale studies involving a larger patient population (typically hundreds to thousands) that aim to confirm effectiveness, monitor side effects, and compare the biologic to standard treatments [108]. These trials provide the comprehensive data needed to demonstrate the product's therapeutic value and identify potential risks that may only become apparent in larger populations.
Throughout the clinical trial process, sponsors must ensure compliance with Good Clinical Practice (GCP) guidelines, and the trials are overseen by an Institutional Review Board (IRB) to protect participants' rights and welfare [108]. The data collected during these trials forms the evidentiary foundation for the Biologics License Application.
Table: Clinical Development Pathway for Stem Cell-Based Therapies
| Development Phase | Primary Objectives | Stem Cell-Specific Considerations |
|---|---|---|
| Phase 1 | Safety, tolerability, preliminary dosage | Monitor for teratoma formation, off-target differentiation, immune rejection |
| Phase 2 | Efficacy, optimal dosing | Assess functional differentiation, engraftment, mechanism-specific biomarkers |
| Phase 3 | Confirmatory efficacy, safety in expanded population | Long-term safety monitoring, persistence of therapeutic effect, comparative effectiveness |
The BLA Submission: Comprehensive Evidence for Approval
BLA Content and Requirements
A Biologics License Application (BLA) is the formal submission through which a sponsor requests permission from the FDA to commercially distribute a biologic product in the United States [107]. For gene therapies and other complex biologics, the BLA is reviewed by the FDA's Center for Biologics Evaluation and Research (CBER), specifically its Office of Therapeutic Products (OTP) [107].
A complete BLA must provide comprehensive evidence demonstrating that the biologic product is safe, pure, and potent. Key components include [107] [112]:
- Clinical Data: Safety and efficacy results from Phase I-III trials
- CMC Information: Detailed documentation of chemistry, manufacturing, and controls
- Nonclinical Safety Data: Results from animal and in vitro studies
- Labeling: Draft prescribing information and product labeling
- Pharmacovigilance: Post-marketing surveillance plans and long-term follow-up strategies
For stem cell-based products, the CMC section is particularly critical and must thoroughly describe the manufacturing process, characterization methods, and quality controls that ensure product consistency. The metabolic state of stem cells—with undifferentiated cells exhibiting lower mitochondrial mass, reduced oxidative phosphorylation, and preferential use of glycolysis—can serve as important quality attributes and should be carefully monitored throughout manufacturing [109].
Special Considerations for Stem Cell Products
Stem cell-based therapies face unique regulatory challenges that must be addressed in the BLA:
Product Characterization and Potency Stem cell products require robust characterization methods to demonstrate identity, purity, and potency. This includes monitoring pluripotency markers (Oct4, Nanog, Sox2) for undifferentiated cells or specific differentiation markers for committed progenitors [103]. The biological activity of the product must be linked to its intended mechanism of action, whether through direct tissue regeneration, paracrine effects, or other pathways.
Tumorigenicity Risk Assessment The pluripotency and self-renewal capacity that make stem cells therapeutically promising also represent significant safety concerns. Products must be thoroughly evaluated for potential tumor formation, with particular attention to residual undifferentiated cells that could give rise to teratomas [109]. Understanding the molecular regulation of pluripotency—including transcription factors, signaling pathways, and epigenetic modifiers—is essential for developing appropriate safety tests.
Long-Term Follow-Up Due to the potential for delayed adverse events such as unintended differentiation or late-onset proliferation, stem cell therapies typically require long-term patient monitoring. The FDA may require follow-up periods of up to 15 years to monitor for delayed adverse events [107].
Strategic Regulatory Considerations for Stem Cell Researchers
Expedited Development Pathways
Several FDA programs can accelerate the development and review of promising stem cell therapies:
- Regenerative Medicine Advanced Therapy (RMAT): Offers intensive FDA guidance, eligibility for priority review, and potential accelerated approval for regenerative medicine therapies [107].
- Fast Track: Speeds up the review of drugs for serious conditions with unmet needs [107].
- Breakthrough Therapy: Provides intensive FDA interaction if preliminary clinical evidence indicates substantial improvement over existing therapies [107].
These programs may be available for stem cell products that address serious or life-threatening conditions and demonstrate potential advantages over existing treatments.
Manufacturing and Quality Control
The complex biology of stem cells presents unique manufacturing challenges that must be addressed throughout development:
Process Consistency As products move from early to late-stage development, manufacturers must demonstrate process consistency and product comparability. Changes in culture conditions, differentiation protocols, or scale can significantly impact the product's biological characteristics and therapeutic profile [112].
Metabolic Monitoring Emerging research suggests that mitochondrial function and cellular metabolism play regulatory roles in stem cell fate decisions. Undifferentiated pluripotent stem cells display lower levels of mitochondrial mass and oxidative phosphorylation, instead preferentially using non-oxidative glycolysis as a major energy source [109]. Monitoring these metabolic parameters may provide valuable quality control indicators during manufacturing.
Scalability The transition from research-scale to commercial-scale manufacturing requires careful planning and validation. Automation and standardized analytics can help reduce batch variability and streamline product release [107].
Pre-Submission Meetings and Regulatory Interactions
Strategic engagement with regulatory authorities throughout development is critical for success. Key meetings include:
- Pre-IND Consultation: Early discussion of development plans and data requirements [110].
- INTERACT Meeting: Early-phase meeting for innovative products to discuss development plans [111].
- Pre-BLA Meeting: Critical meeting to align on content and format expectations for the BLA submission [107].
As noted by regulatory experts, "Maintaining communication between the sponsor and the FDA at every stage of drug development may ultimately facilitate early patient access to safe and effective drugs" [111].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagents for Studying Stem Cell Self-Renewal and Differentiation
| Reagent/Material | Function | Regulatory Relevance |
|---|---|---|
| Pluripotency Markers (Oct4, Nanog, Sox2 antibodies) | Identify and quantify undifferentiated stem cells | Critical for product characterization and safety assessment |
| Directed Differentiation Kits | Generate specific cell lineages from pluripotent stem cells | Important for demonstrating manufacturing control and potency |
| Metabolic Assays (Glycolysis, OXPHOS) | Monitor metabolic state of stem cells | Quality attribute given link between metabolism and stem cell state |
| Cell Culture Media Formulations | Maintain stem cells or direct differentiation | Major process parameter that must be controlled and documented |
| Viral Vector Systems | Introduce genes for reprogramming or tracking | Require thorough characterization and safety testing |
Visualization of Regulatory Pathways and Biological Mechanisms
FDA Regulatory Pathway for Stem Cell Products
Diagram 1: FDA Regulatory Pathway for Stem Cell Products. This visualization outlines the key stages from preclinical development through BLA approval, highlighting major decision points and typical timelines.
Molecular Regulation of Stem Cell Fate
Diagram 2: Molecular Regulation of Stem Cell Fate. This diagram illustrates key molecular factors governing stem cell behavior and their connections to critical regulatory considerations for product development.
The pathway from IND authorization to BLA approval represents a rigorous scientific and regulatory journey that ensures stem cell-based therapies meet stringent standards for safety and efficacy before reaching patients. For researchers working at the intersection of stem cell biology and therapeutic development, understanding this framework is not merely a regulatory requirement but an integral component of successful translation.
The molecular mechanisms that control stem cell self-renewal and differentiation—from core transcription factors like Oct4, Nanog, and Sox2 to metabolic switches between glycolysis and oxidative phosphorylation—directly inform both product development and regulatory strategy. By integrating deep biological understanding with proactive regulatory planning, researchers can navigate this complex pathway more effectively, accelerating the delivery of transformative stem cell therapies to patients in need.
As the field advances, continued dialogue between the research community and regulatory agencies will be essential for developing appropriate standards and frameworks that balance innovation with patient safety. Through strategic development and thorough characterization of products based on sound scientific principles, researchers can successfully bridge the gap between laboratory discovery and clinical application.
Conclusion
The precise balance between stem cell self-renewal and differentiation is orchestrated by a complex, interconnected network of intrinsic factors, signaling pathways, and extrinsic niche signals. Understanding these mechanisms, from piRNA-mediated regulation to the integrated signaling of BMP and Notch, is no longer just a biological pursuit but a clinical imperative. The successful translation of this knowledge is already evident in FDA-approved therapies and a robust global clinical trial landscape. Future progress hinges on overcoming persistent challenges in in vitro culture, scaling manufacturing, and enhancing the safety profile of emerging iPSC-based platforms. The synergy between advanced gene editing, single-cell technologies, and precision medicine promises a new era where manipulating stem cell fate becomes a cornerstone treatment for degenerative diseases, cancer, and genetic disorders, fundamentally transforming regenerative medicine.
References
- 1. Mechanisms of Stem Cell Self-renewal [https://www.sciencedirect.com/science/chapter/edited-volume/abs/pii/B9780123747297000081]
- 2. Symmetric vs. Asymmetric Stem Cell Divisions: An Adaptation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3812169/]
- 3. Symmetrical and asymmetrical division analysis provides ... [https://www.nature.com/articles/ncomms5758]
- 4. Report Dynamics of Asymmetric and Symmetric Divisions ... [https://www.sciencedirect.com/science/article/pii/S2211124720301315]
- 5. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 6. | NIH Intramural Research Program Stem Cell Biology [https://irp.nih.gov/our-research/scientific-focus-areas/stem-cell-biology]
- 7. Stem cell revolution: bridging the gap between research ... [https://link.springer.com/article/10.1186/s13287-025-04784-7]
- 8. Frontier progress and translational challenges of ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1583391/full]
- 9. Pharmacological modulation of stem cells signaling pathway ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 10. Post-transcriptional control of gene expression by β-catenin [https://www.nature.com/articles/s41388-025-03470-5]
- 11. Stem Cell Self-Renewal - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/stem-cell-self-renewal]
- 12. Poly(A) tail regulation in stem cells and early development [https://pubmed.ncbi.nlm.nih.gov/41288893/]
- 13. 'A completely new world': Yale Stem Cell Center director ... [https://www.browndailyherald.com/article/2025/09/a-completely-new-world-yale-stem-cell-center-director-discusses-novel-gene-regulation-research]
- 14. Post-transcriptional regulation in early cell fate commitment of ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11400-8]
- 15. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 16. piRNA-Mediated Maintenance of Genome Stability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295023/]
- 17. From biogenesis to biomarkers: the role of piRNAs and PIWI ... [https://jmhg.springeropen.com/articles/10.1186/s43042-025-00735-2]
- 18. Roles and mechanisms of piRNAs in self-renewal ... [https://www.sciencedirect.com/science/article/abs/pii/S0301468125000647]
- 19. The epigenetic regulatory mechanism of PIWI/piRNAs in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01749-3]
- 20. The potential role of PIWI-interacting RNAs in non-small ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1660236/full]
- 21. PIWI proteins and piRNAs: key regulators of stem cell biology [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1540313/full]
- 22. Roles and mechanisms of piRNAs in self-renewal ... [https://pubmed.ncbi.nlm.nih.gov/40753855/]
- 23. miRNA and piRNA differential expression profiles in ... [https://www.sciencedirect.com/science/article/pii/S0531556525000749]
- 24. A model that integrates the different piRNA biogenesis ... [https://www.sciencedirect.com/science/article/pii/S2666515825000034]
- 25. cross-talk between Signaling -beta/ TGF and other BMP pathways [https://pubmed.ncbi.nlm.nih.gov/19002158/]
- 26. Quantitative Analysis of Signaling Networks across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4227552/]
- 27. - TGF in organoids: The mechanisms and applications in 3D β signaling [https://www.sciopen.com/article/10.26599/CO.2025.9410015]
- 28. Stem-Cell Niches in Health and Disease [https://www.mdpi.com/2073-4409/14/13/981]
- 29. Stem-Cell Niches in Health and Disease [https://pubmed.ncbi.nlm.nih.gov/40643502/]
- 30. Stem Cell Niche Concept: Search for Current Expert ... [https://pubmed.ncbi.nlm.nih.gov/40943342/?utm_source=SimplePie&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1pq-4TZ0w1pIimA2HHLJZYTkSjaU335U-aRSFRxJ31Blahz9sN&fc=20220524061305&ff=20250916025017&v=2.18.0.post9+e462414]
- 31. Mechanical control of cell fate decisions in the skin epidermis [https://www.nature.com/articles/s41467-025-62882-9]
- 32. Unlocking hematopoietic stem cell potential [https://pubmed.ncbi.nlm.nih.gov/40970097/]
- 33. Stem cell revolution: bridging the gap between research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12659346/]
- 34. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 35. Human induced pluripotent stem cell-derived ... [https://pubmed.ncbi.nlm.nih.gov/41180839/]
- 36. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 37. Novel Mechanism in Self-Renewal/Differentiation of Human ... [https://www.cirm.ca.gov/our-progress/awards/novel-mechanism-self-renewal-differentiation-human-embryonic-stem-cells/]
- 38. Human iPSC Modeling of Heart Disease for Drug Screening [https://www.frontiersin.org/research-topics/64703/human-ipsc-modeling-of-heart-disease-for-drug-screeningundefined]
- 39. Quantifying HiPSC-CM structural organization at scale with ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013436]
- 40. Advances in arrhythmogenic cardiomyopathy modeling ... [https://www.sciencedirect.com/science/article/pii/S1547527125027535]
- 41. Perturbomics: CRISPR–Cas screening-based functional ... [https://www.nature.com/articles/s12276-025-01487-0]
- 42. How High-Throughput Screening Advances Cell Therapies [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-techniques-to-improve-cellular-drug-discovery-396948]
- 43. How Human iPSCs are Revolutionizing Drug Discovery in ... [https://bioinformant.com/ipsc-drug-discovery/]
- 44. High-throughput screening data generation, scoring and ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01001-8]
- 45. iPSC-based Platforms Market 2025 Report and Trends [https://www.towardshealthcare.com/insights/ipsc-based-platforms-market-sizing]
- 46. Stem Cell Differentiation: Explained (2025) [https://www.dvcstem.com/post/stem-cell-differentiation]
- 47. Comprehensive protocols for CRISPR/Cas9-based gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 48. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 49. Gene Editing Market Size to Surpass USD 42.13 Billion by [https://www.globenewswire.com/news-release/2025/11/04/3179998/0/en/Gene-Editing-Market-Size-to-Surpass-USD-42-13-Billion-by-2034.html]
- 50. CMN Weekly (12 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-12-september-2025-your-weekly-crispr-medicine-news/]
- 51. White Paper: CRISPR/Cas9 Gene Editing [https://www.bioskryb.com/crispr-cas9-gene-editing/]
- 52. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 53. Mesenchymal stem cell infusion to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500263X]
- 54. Quantitative and qualitative differences in use and trends of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3729910/]
- 55. Coupling of stemness maintenance with cell cycle control ... [https://pubmed.ncbi.nlm.nih.gov/41133217/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1NUQW1ZjQGx_nb-pMgaoPrMklqK0auREP7aSv3aS0vtcmHckEh&fc=None&ff=20251031220401&v=2.18.0.post22+67771e2]
- 56. Table 3. Comparison of Hematopoietic Stem Cell Products [https://www.ncbi.nlm.nih.gov/books/NBK84260.2/table/CDR0000700000__64/?report=objectonly]
- 57. Tissue Engineering and Regenerative Medicine 2025 [https://www.frontiersin.org/research-topics/73076/tissue-engineering-and-regenerative-medicine-2025---quo-vadisundefined]
- 58. Editorial: Tissue engineering and regenerative medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949865/]
- 59. Top 5 Latest Advances in Stem Cell Applications for Tissue ... [https://www.mtmlaboratory.com/top-5-latest-advances-in-stem-cell-applications-for-tissue-engineering]
- 60. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 61. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 62. Defined culture conditions robustly maintain human stem ... [https://www.nature.com/articles/s42003-025-07658-z]
- 63. Phenotypic changes associated with continuous long term ... [https://pubmed.ncbi.nlm.nih.gov/40209891/]
- 64. Reconstruction of Hematopoietic Stem Cell Niches In Vitro [https://www.sciencedirect.com/science/article/pii/S259000642501107X]
- 65. Protocols for the application of human embryonic stem cell- ... [https://www.sciencedirect.com/science/article/pii/S2666166725000395]
- 66. Overcoming Barriers in Cancer Biology Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248693/]
- 67. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 68. Stem Cell Clinics in the United States: Explained (2025) [https://www.dvcstem.com/post/stem-cells-usa]
- 69. Mechanisms of stem cell self-renewal [https://pubmed.ncbi.nlm.nih.gov/19575646/]
- 70. In silico modeling of directed differentiation of induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404646/]
- 71. Clever Experimental Designs: Shortcuts for Better iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8700474/]
- 72. Quantitative phase imaging with temporal kinetics predicts ... [https://www.nature.com/articles/s41467-025-61846-3]
- 73. Quantitative Single-Cell Approaches to Stem Cell Research [https://www.sciencedirect.com/science/article/pii/S1934590914004664]
- 74. Protocol for differentiation of human pluripotent stem cells ... [https://www.sciencedirect.com/science/article/pii/S2666166725002953]
- 75. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 76. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 77. Hypoimmune stem cells and islets: hype or a true ... [https://pubmed.ncbi.nlm.nih.gov/41039199/]
- 78. Stem cell transplant without toxic preparation successfully ... [https://med.stanford.edu/news/all-news/2025/07/stem-cell-transplant.html]
- 79. Replacing brain immune cells in mice slows ... [https://med.stanford.edu/news/all-news/2025/08/brain-immune-cells.html]
- 80. Numb provides a fail-safe mechanism for intestinal stem ... [https://elifesciences.org/articles/104723]
- 81. The Multitasker Protein: A Look at the Multiple Capabilities of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856935/]
- 82. NUMB (gene) [https://en.wikipedia.org/wiki/NUMB_(gene)]
- 83. NUMB alternative splicing and isoform-specific functions in ... [https://www.sciencedirect.com/science/article/pii/S0021925825000626]
- 84. Fail-Safe System against Potential Tumorigenicity after ... [https://pubmed.ncbi.nlm.nih.gov/28262544/]
- 85. Human stem cells harboring a suicide gene improve the ... [https://www.nature.com/articles/s41467-021-23125-9]
- 86. Omisirge (omidubicel-onlv) FDA Approval History [https://www.drugs.com/history/omisirge.html]
- 87. NO MORE LIMITATIONS FOR CORD BLOOD USE [https://www.famicord.com/groundbreaking-no-more-limitations-for-cord-blood-use]
- 88. Lyfgenia (lovotibeglogene autotemcel) FDA Approval History [https://www.drugs.com/history/lyfgenia.html]
- 89. LYFGENIA [https://www.fda.gov/vaccines-blood-biologics/lyfgenia]
- 90. Ryoncil [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/ryoncil]
- 91. FDA approves remestemcel-L-rknd for steroid-refractory ... [https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-remestemcel-l-rknd-steroid-refractory-acute-graft-versus-host-disease-pediatric]
- 92. Molecular Mechanisms Underlying Pluripotency and Self ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10179698/]
- 93. Stem Cell Therapy Market Size to Lead USD 54.45 Billion ... [https://www.biospace.com/press-releases/stem-cell-therapy-market-size-to-lead-usd-54-45-billion-by-2034-driven-by-advancements-in-regenerative-medicine-and-personalized-treatments]
- 94. The ISSCR releases new resource to accelerate ... [https://www.news-medical.net/news/20251009/The-ISSCR-releases-new-resource-to-accelerate-the-development-of-PSC-derived-therapies.aspx]
- 95. Improving the differentiation potential of pluripotent stem ... [https://www.nature.com/articles/s41598-022-18400-8]
- 96. Stem Cell Therapy Market Size, Price, Trends [https://www.novaoneadvisor.com/report/stem-cell-therapy-market]
- 97. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 98. A comprehensive review of clinical trials and Progress in ... [https://pubmed.ncbi.nlm.nih.gov/41079454/]
- 99. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 100. Comparing the mitochondrial signatures in ESCs and iPSCs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9518993/]
- 101. Stem cells in regenerative medicine: Unlocking therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2667099225000283]
- 102. Mechanisms that mediate stem cell self-renewal ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/17647265/]
- 103. Molecular Mechanisms Underlying Pluripotency and Self- ... [https://www.mdpi.com/1422-0067/24/9/8386]
- 104. Coordinated regulation of the balance between stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1391626/full]
- 105. The Pipeline for of iPSC-Derived Cell Therapeutics in 2026 [https://bioinformant.com/ipsc-derived-cell-therapeutics/]
- 106. Recent advances in CAR-MSCs: the new engine of cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557984/]
- 107. BLA Filing Process for Gene Therapy Products: 2025 Guide [https://insights.forgebiologics.com/bla-filing-process-for-gene-therapy-products-2025-guide]
- 108. IND to BLA: The FDA Approval Pathway for Biologic Drugs [https://synapse.patsnap.com/article/ind-to-bla-the-fda-approval-pathway-for-biologic-drugs]
- 109. Empowering self-renewal and differentiation: the role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3006229/]
- 110. Investigational New Drug (IND) Application [https://www.fda.gov/drugs/types-applications/investigational-new-drug-ind-application]
- 111. Building a Regulatory Roadmap for IND, NDA, and BLA [https://www.pharmasalmanac.com/articles/building-a-regulatory-roadmap-for-ind-nda-and-bla]
- 112. How to prepare early for regulatory submissions from IND ... [https://www.biolifesolutions.com/resource-center/insights-blog/how-to-prepare-early-for-regulatory-submissions-from-ind-to-bla/]