Designing Stem Cell Clinical Trials: A Phase-by-Phase Guide from IND to BLA
This article provides a comprehensive guide to the design and execution of Phase I, II, and III clinical trials for stem cell-based therapies.
Designing Stem Cell Clinical Trials: A Phase-by-Phase Guide from IND to BLA
Abstract
This article provides a comprehensive guide to the design and execution of Phase I, II, and III clinical trials for stem cell-based therapies. Tailored for researchers and drug development professionals, it covers the foundational principles of trial design, from navigating regulatory pathways like the IND and RMAT designation to methodological considerations for different stem cell types (MSCs, iPSCs, HSCs). It further addresses critical challenges in manufacturing, safety monitoring, and efficacy assessment, offering optimization strategies and insights into the validation requirements for successful regulatory approval and market entry.
Laying the Groundwork: From Preclinical Evidence to First-in-Human Trials
For researchers developing stem cell-based therapies, the Investigational New Drug (IND) application represents the critical regulatory gateway from preclinical discovery to clinical investigation. As a formal request to the Food and Drug Administration (FDA) for authorization to administer an investigational drug or biological product to humans [1], the IND process requires meticulous planning and strategic execution. The evolving landscape of stem cell therapeutics, marked by significant regulatory milestones such as the first FDA-approved mesenchymal stem cell (MSC) therapy (Ryoncil) in December 2024 and the first induced pluripotent stem cell (iPSC)-based therapy (Fertilo) to enter U.S. Phase III trials in February 2025 [2], underscores the importance of mastering this process. This document provides application notes and protocols framed within stem cell clinical trial design, offering researchers a structured approach to navigating IND requirements for Phase I-III investigations.
Table: Recent FDA-Approved Stem Cell Therapies (2023-2025)
| Product Name | Approval Date | Cell Type | Indication |
|---|---|---|---|
| Ryoncil (remestemcel-L) | December 2024 | Allogeneic MSC | Pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD) [2] |
| Lyfgenia (lovo-cel) | December 2023 | Autologous cell-based gene therapy | Sickle cell disease [2] |
| Omisirge (omidubicel-onlv) | April 2023 | Cord blood-derived hematopoietic progenitor cells | Accelerate neutrophil recovery in hematologic malignancies [2] |
IND Types and Regulatory Framework
Understanding the appropriate IND pathway is essential for efficient regulatory strategy. The FDA recognizes several IND types, each with distinct purposes and eligibility criteria.
IND Classification
- Investigator IND: Submitted by a physician who both initiates and conducts an investigation, often to study an unapproved drug or an approved product for a new indication or patient population [3].
- Emergency Use IND: Allows FDA to authorize use of an experimental drug in an emergency situation where standard submission timelines are impractical, or for patients not meeting existing study protocol criteria [3] [1].
- Treatment IND: Submitted for experimental drugs showing promise in clinical testing for serious or immediately life-threatening conditions while final clinical work and FDA review are conducted [3].
- Commercial vs. Research IND: All INDs fall into one of two administrative categories: Commercial (for products intended for marketing) and Research (non-commercial, often for investigator-initiated studies) [3].
For complex stem cell-based products, early regulatory engagement is strongly recommended. The Pre-IND Consultation Program fosters early communications between sponsors and FDA review divisions to provide guidance on data necessary to warrant IND submission [3]. For CBER-regulated products, these meetings offer valuable feedback on preclinical study design, initial clinical trial plans, and manufacturing controls needed to initiate human studies [1].
IND Application Components: A Strategic Framework for Stem Cell Products
A complete IND application must contain information across three broad domains: preclinical data, manufacturing information, and clinical protocols [3]. For stem cell therapies, each domain presents unique considerations.
Preclinical Data Package
Preclinical studies for stem cell therapies must establish a rationale for initial human testing and demonstrate reasonable safety. The focus is on determining if the product is reasonably safe for initial use in humans and exhibits pharmacological activity that justifies commercial development [3].
Table: Essential Preclinical Studies for Stem Cell INDs
| Study Type | Key Objectives | Stem Cell-Specific Considerations |
|---|---|---|
| Proof-of-Concept (in vitro) | Demonstrate mechanism of action, target engagement | Differentiation efficiency, potency assays, transcriptomic profiling |
| Biodistribution & Engraftment | Track cell fate, persistence, migration | In vivo imaging, PCR-based tracking, immunohistochemistry |
| Tumorigenicity | Assess unregulated growth potential | Teratoma formation assays (for pluripotent derivatives), karyotyping |
| Toxicology | Identify target organ toxicity, maximum feasible dose | Ectopic tissue formation, infusion-related reactions, alloreactivity |
Experimental Protocol: Tumorigenicity Assessment for iPSC-Derived Products
Purpose: To evaluate the potential for unregulated proliferation and teratoma formation of iPSC-derived cellular products.
Materials:
- Test Article: Fully differentiated iPSC-derived cell product (e.g., dopaminergic neurons, retinal pigment epithelium)
- Control Articles: Undifferentiated iPSCs (positive control), vehicle/matrix alone (negative control)
- Animal Model: Immunodeficient mouse strain (e.g., NOD-scid gamma)
- Reagents: Matrigel Basement Membrane Matrix, PBS, fixatives, histological stains
Methodology:
- Cell Preparation: Prepare the final clinical-formulation test article and controls in the appropriate injection vehicle.
- Administration: Using a sterile technique, administer cells via the intended clinical route (e.g., intracranial, subretinal, intramuscular). Include a positive control group receiving undifferentiated iPSCs.
- Observation Period: Monitor animals for 16-26 weeks, assessing for palpable mass formation, neurological deficits, or other signs of pathology.
- Necropsy and Histopathology: Euthanize animals at study endpoint or upon meeting humane endpoints. Perform gross necropsy and collect injection site, distant organs (brain, liver, lungs, gonads), and any abnormal tissues for histopathological analysis.
- Analysis: Process tissues for H&E staining and immunohistochemistry for pluripotency markers (OCT4, NANOG) to identify residual undifferentiated cells.
Data Interpretation: The test article is considered to have a low tumorigenic risk if no teratomas or tumors are formed, with histology showing only the expected, differentiated cell phenotype at the injection site, in stark contrast to the positive control group.
Chemistry, Manufacturing, and Controls (CMC)
The CMC section must demonstrate the ability to consistently produce and supply the stem cell product. Key elements include comprehensive information on composition, manufacturer, stability, and controls [3]. For stem cell therapies, this is particularly challenging due to product complexity and living nature.
Research Reagent Solutions for Stem Cell Manufacturing
Table: Essential Materials for G-Compliant Stem Cell Manufacturing
| Reagent/Material | Function | Critical Quality Attributes |
|---|---|---|
| StemRNA Clinical Seed iPSCs | Master cell bank for iPSC-derived products [2] | GMP-compliant, documented donor screening, karyotypically normal, pluripotency validated |
| Xeno-Free Culture Medium | Supports cell expansion and differentiation | Defined composition, absence of animal-derived components, performance qualified |
| Cell Dissociation Reagents | Enzymatic or non-enzymatic passaging | High purity, minimal lot-to-lot variability, validated for use with stem cells |
| Characterization Antibodies | Flow cytometry and ICC for identity/purity | Specificity validated, appropriate isotype controls, conjugated for multiparametric analysis |
| Cryopreservation Medium | Long-term storage of cell banks and final product | Formulated with DMSO and serum alternatives, supports high post-thaw viability |
Stem Cell Manufacturing Workflow: This diagram outlines the critical stages in the production of a stem cell-based therapeutic product, from the master cell bank to the final product release.
Clinical Protocol and Investigator Information
The clinical protocol must provide detailed plans for proposed clinical studies to assess whether initial-phase trials will expose subjects to unnecessary risks [3]. For stem cell therapies in Phase I/II, protocols often combine safety and efficacy endpoints to accelerate development for serious conditions with unmet needs [4].
Experimental Protocol: Phase I/II Trial for an iPSC-Derived Neural Progenitor Cell in Parkinson's Disease
Purpose: To assess the safety, tolerability, and preliminary efficacy of allogeneic iPSC-derived dopaminergic neural progenitor cells (DA01) in patients with moderate Parkinson's disease.
Study Design: Open-label, dose-escalation trial with 24-month follow-up.
Key Eligibility Criteria:
- Inclusion: Idiopathic Parkinson's disease diagnosed ≥5 years, Hoehn & Yahr Stage 3-4 in "off" state, responsive to levodopa but with motor complications.
- Exclusion: Atypical parkinsonism, significant neurological comorbidity, contraindication to immunosuppression or MRI.
Intervention:
- Neurosurgical Procedure: Stereotactic implantation of DA01 cells into the postcommissural putamen.
- Immunosuppression: Initiated 1 week pre-operatively (Tacrolimus, Mycophenolate Mofetil) and maintained for 12 months, followed by a 3-month taper.
Primary Endpoints:
- Safety: Incidence and severity of adverse events, including serious adverse events (SAEs) related to the product or procedure, over 12 months.
- Tolerability: Ability to complete the cell implantation procedure and immunosuppressive regimen.
Secondary Endpoints:
- Efficacy: Change from baseline in MDS-UPDRS Part III (motor score) in "off" state at 12 and 24 months.
- Functional Imaging: Change in striatal 18F-DOPA uptake on PET at 12 months.
Exploratory Endpoints: Patient-reported outcomes, reduction in levodopa-equivalent daily dose.
The Submission Process and FDA Review Timeline
Navigating the submission mechanics and post-submission timeline is critical for study activation.
Submission Mechanics
- Commercial INDs: Must be submitted electronically through the FDA's Electronic Submissions Gateway (ESG) in eCTD format [1] [5].
- Research (Non-commercial) INDs: May be submitted electronically via ESG or email, or as paper copies to the appropriate FDA center [1].
- Required Forms: The submission must include completed FDA Form 1571 (IND Application Form) and FDA Form 1572 (Statement of Investigator) for each participating clinical investigator [6].
IND Submission and Review Timeline: This diagram visualizes the pathway of an IND application through the FDA's 30-day review process, culminating in either study activation or a clinical hold.
Post-Submission Expectations and Clinical Hold Scenarios
After submission, the sponsor must wait 30 calendar days before initiating any clinical trials [3] [5]. During this period, the FDA reviews the IND for safety to ensure research subjects will not be subjected to unreasonable risk [3]. If the FDA raises no concerns within this 30-day window, the IND becomes effective, and the study may proceed [6]. Approximately 9% of IND submissions face clinical holds, which can significantly delay development [5]. A clinical hold may be issued if the FDA identifies significant safety concerns or deficiencies in the study protocol [6]. Sponsors must then address these concerns comprehensively and resubmit the application, restarting the 30-day review clock.
Special Considerations for Stem Cell INDs
Expedited Programs and Regulatory Designations
For stem cell therapies targeting serious or life-threatening conditions, several expedited FDA programs can facilitate development:
- Regenerative Medicine Advanced Therapy (RMAT): A designation for regenerative medicine therapies (including stem cell products) that preliminary clinical evidence indicates has the potential to address unmet medical needs [2].
- Fast Track: Designed to facilitate development and expedite review of drugs to treat serious conditions and fill unmet medical needs [2] [4].
Clinical Trial Design and Endpoints
Stem cell trials require unique considerations in trial design. Phase I trials for gene and cell therapies typically enroll a small number of individuals with the disease rather than healthy volunteers [4]. Phases are often combined (e.g., Phase I/II) to make the evaluation process more efficient for serious and rare diseases with clear unmet medical needs [4]. In these combined trials, both safety and efficacy tests are performed on a small group of participants with the disease [4]. For stem cell products, phase 4 post-marketing studies with long-term follow-up are mandatory to continue monitoring safety and outcomes [4].
Recent Regulatory Guidance and Future Directions
The FDA's Center for Biologics Evaluation and Research (CBER) has outlined its 2025 Guidance Agenda, which includes several topics relevant to stem cell therapy developers [7]. Notable planned guidances include "Potency Assurance for Cellular and Gene Therapy Products" and "Post Approval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products" [7]. These documents, when finalized, will represent the FDA's current thinking on these critical topics and should be closely monitored by sponsors [8].
Phase I clinical trials represent the critical first step in translating preclinical stem cell research into human therapies. The primary mission of these studies is to establish the safety and tolerability of investigational cellular products in a small cohort of participants [9]. In the context of stem cell therapeutics, this initial phase focuses on identifying potential risks, determining appropriate dosing, and gathering preliminary data on biological activity before advancing to larger efficacy-focused trials. The fundamental ethical principle governing this stage is the primacy of patient welfare, requiring that researchers never excessively place vulnerable patients at risk and that the welfare of current research subjects is never overridden by promise for future patients [10]. For stem cell-based interventions, which carry irreversible risks including tumorigenicity and immune reactions, rigorous Phase I trial design is particularly crucial for ensuring patient safety while generating meaningful data to guide future development.
Core Objectives and Quantitative Safety Endpoints
Primary Objectives
The design of Phase I stem cell trials is fundamentally guided by clearly defined primary and secondary objectives. The primary objectives universally focus on safety parameters, while secondary objectives explore preliminary signals of biological activity and therapeutic effect.
- Safety and Tolerability Assessment: Comprehensive evaluation of treatment-emergent adverse events (TEAEs) using standardized grading systems such as the Common Terminology Criteria for Adverse Events (CTCAE) [11]. This includes monitoring for both acute reactions and potential delayed effects unique to cellular therapies.
- Maximum Tolerated Dose (MTD) Determination: Identification of the highest dose level with acceptable safety profile, typically using dose-escalation designs such as the 3 + 3 design where cohorts of 3-6 participants receive ascending dose levels [11] [12].
- Dose-Limiting Toxicity (DLT) Characterization: Detailed documentation of toxicities that prevent further dose escalation, defined as specific grade 2 toxicities or any grade 3 toxicity attributable to the investigational product that does not resolve within a predetermined observation period [12].
Secondary Objectives
- Preliminary Efficacy Signals: Initial assessment of potential therapeutic benefits through disease-specific clinical outcome measures, though these trials are not powered for statistical significance [11].
- Pharmacokinetic/Pharmacodynamic Profiles: Evaluation of cell persistence, migration, engraftment, and biological activity through imaging, biomarker analyses, and functional assessments [9].
- Immunogenicity Assessment: For allogeneic stem cell products, evaluation of host immune responses against the transplanted cells that might impact safety or efficacy [12].
Quantitative Safety Endpoints in Recent Stem Cell Trials
Table 1: Safety Endpoints from Recent Phase I Stem Cell Clinical Trials
| Trial Reference | Cell Type | Indication | Cohort Size | Dose Levels | Primary Safety Findings |
|---|---|---|---|---|---|
| MR-MC-01 Trial [11] | hESC-derived MSCs | Interstitial Cystitis | 6 (Phase I) | 2.0×10⁷ & 5.0×10⁷ cells | No DLTs observed; only mild AEs (transient hemorrhage, bladder pain) |
| P-MSC Trial [12] | Placental MSCs | Critical Limb Ischemia | 9 | 20×10⁶ & 60×10⁶ cells | All doses well-tolerated; no treatment-related serious AEs during 6-month follow-up |
| PSC Review [2] | Various PSC-derived | Multiple indications | >1,200 (aggregate) | Variable | No class-wide safety concerns across 115 global clinical trials |
Table 2: Common Safety Monitoring Parameters in Phase I Stem Cell Trials
| Safety Domain | Specific Assessments | Timing/Frequency |
|---|---|---|
| Adverse Event Monitoring | Type, frequency, severity, and relationship to product | Baseline, throughout study, and at all follow-up visits (e.g., 1, 3, 6 months) |
| Laboratory Parameters | Hematology, clinical chemistry, urinalysis | Baseline, post-treatment, and at scheduled intervals |
| Immunological Safety | Host antibody formation, T-cell proliferation assays, cytokine levels | Baseline and multiple post-treatment timepoints |
| Product-Specific Safety | Tumorigenicity, ectopic tissue formation, improper differentiation | Long-term follow-up with appropriate imaging modalities |
| Disease-Specific Safety | Condition-specific exacerbations or complications | Throughout study period using standardized assessment tools |
Experimental Protocols and Methodologies
Phase I Trial Design Considerations
The design of Phase I stem cell trials requires careful consideration of patient population, dosing strategy, and endpoint selection. For stem cell products, traditional dose-escalation designs may be adapted to address product-specific characteristics, including the non-linear relationship between cell dose and biological effect, potential for cell persistence and long-term effects, and unique safety concerns such as tumorigenicity or immunogenicity [13].
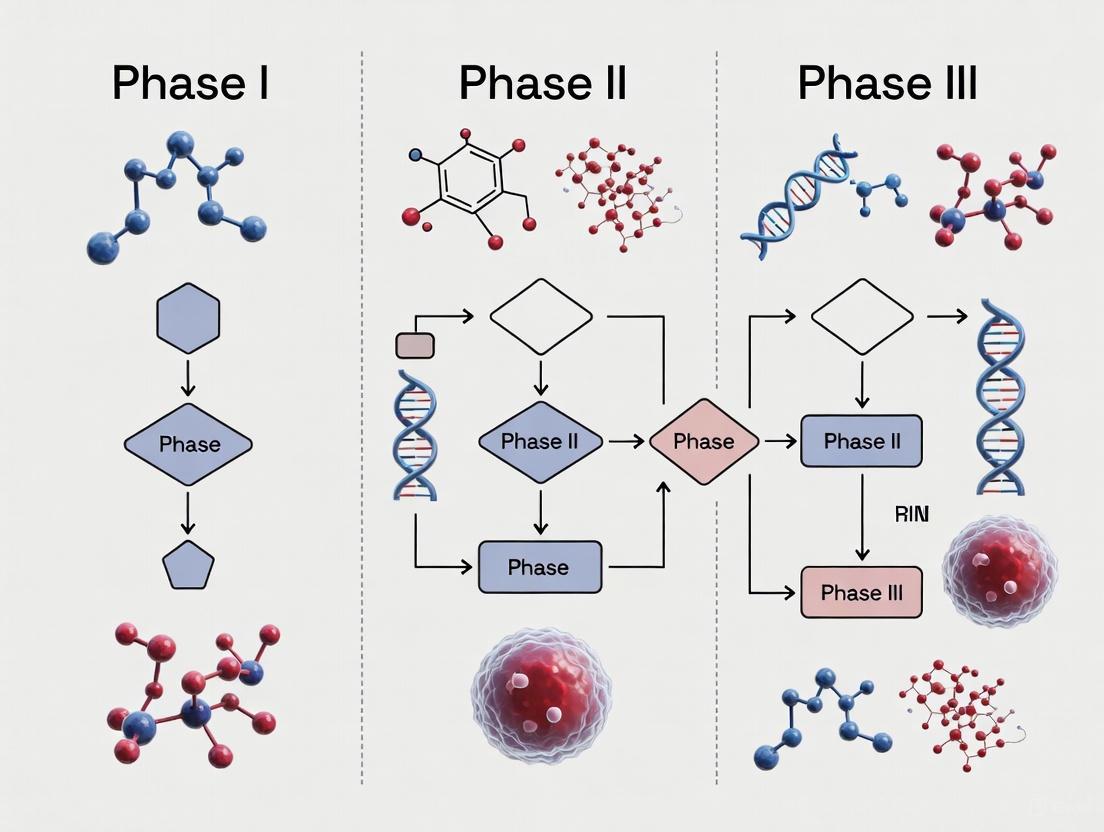
Phase I Stem Cell Trial Workflow diagram illustrates the sequential stages of early-phase clinical development, from regulatory submission through final safety analysis.
Dose Escalation Methodology
The 3 + 3 dose escalation design remains a standard approach for Phase I stem cell trials, though adaptive designs are increasingly employed:
Dose Escalation Decision Methodology visualizes the standard 3 + 3 design used to determine the maximum tolerated dose while prioritizing participant safety.
- Starting Dose Selection: Based on comprehensive preclinical toxicology studies in relevant animal models, typically representing a fraction of the no-observed-adverse-effect-level (NOAEL) with appropriate safety factors applied [13].
- Dose Escalation Scheme: Predefined increments (e.g., 100%, 67%, 50%) based on product characteristics, preclinical data, and anticipated therapeutic window.
- DLT Observation Period: Sufficient duration to capture acute and subacute toxicities, typically 28 days for stem cell products to monitor for early immune reactions or acute safety concerns [11].
- Stopping Rules: Predefined criteria for pausing or terminating dose escalation based on specific safety events, including unexpected severe adverse events or multiple DLTs at a given dose level.
Comprehensive Safety Monitoring Protocol
A robust safety monitoring protocol for stem cell Phase I trials includes multiple assessment modalities conducted at predetermined intervals:
Baseline Assessment Protocol
- Comprehensive medical history and physical examination
- Disease-specific symptom scoring using validated instruments
- Laboratory evaluations (hematology, chemistry, coagulation, urinalysis)
- Immunological profiling ( lymphocyte subsets, HLA typing, pre-existing antibodies)
- Baseline imaging appropriate for target indication and potential safety concerns
Post-Treatment Monitoring Protocol
- Daily safety assessments during initial observation period
- Structured AE documentation using CTCAE criteria [11]
- Protocol-specific laboratory monitoring at days 1, 3, 7, 14, and 28 post-administration
- Disease-specific functional assessments at predefined intervals
- Immunological monitoring for host response to allogeneic cells [12]
Long-Term Follow-Up Protocol
- Regular assessments for at least 1-2 years post-administration
- Tumorigenicity monitoring through appropriate imaging modalities
- Assessment for delayed immune responses or late-onset effects
- Evaluation for potential cell migration to non-target tissues
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent Category | Specific Examples | Function in Therapy Development |
|---|---|---|
| Stem Cell Source | REPROCELL StemRNA Clinical Seed iPSCs [2] | Provides GMP-compliant, quality-controlled starting material for consistent therapy production |
| Cell Culture Media | Defined MSC media, iPSC maintenance media | Supports expansion and maintenance of cellular phenotypes while ensuring reproducibility |
| Differentiation Kits | Neural differentiation kits, cardiomyocyte differentiation kits | Directs stem cell differentiation toward specific therapeutic cell types with high efficiency |
| Characterization Antibodies | Flow cytometry antibodies (CD73, CD90, CD105, SSEA-4, Tra-1-60) | Confirms cell identity, purity, and absence of undifferentiated pluripotent cells |
| Quality Control Assays | Karyotyping kits, mycoplasma detection kits, sterility testing media | Ensures product safety and genetic stability throughout manufacturing process |
| Cryopreservation Solutions | Defined cryomedium with DMSO alternatives | Maintains cell viability and functionality during frozen storage and transport |
Regulatory Framework and Ethical Considerations
The regulatory landscape for stem cell-based therapies continues to evolve, with specific guidance documents addressing unique aspects of cellular product development. The FDA has established expedited programs for regenerative medicine therapies, including the Regenerative Medicine Advanced Therapy (RMAT) designation, which can be applied for based on preliminary clinical evidence [2]. Phase I trials must comply with Investigational New Drug (IND) requirements, focusing particularly on chemistry, manufacturing, and controls (CMC) information, preclinical safety assessment, and clinical protocol design [13].
Ethical conduct of Phase I stem cell trials requires strict adherence to established guidelines, including those from the International Society for Stem Cell Research (ISSCR), which emphasizes rigor, oversight, and transparency in all research activities [10]. Key ethical considerations include:
- Informed Consent Process: Comprehensive disclosure of experimental nature, potential risks, and uncertain benefits, with particular attention to the irreversible nature of some stem cell-based interventions.
- Vulnerable Population Protections: Additional safeguards when enrolling patients with serious conditions lacking effective treatments who may be particularly vulnerable to unrealistic expectations.
- Transparency in Reporting: Timely sharing of both positive and negative results to advance the field and inform future trial participants [10].
Successful completion of a Phase I stem cell trial establishes the fundamental safety profile necessary for advancement to Phase II studies. The data collected informs key decisions for subsequent development, including recommended Phase II dose, patient population refinement, and optimization of administration procedures. Evidence from oncology trials suggests that safety profiles observed in Phase I studies generally predict toxicities in later-phase trials, supporting the validity of this developmental approach [14]. For stem cell therapies, Phase I success enables progression to larger trials that can more rigorously assess therapeutic efficacy while continuing to monitor long-term safety in expanded patient populations.
The transition from preclinical stem cell research to first-in-human (FIH) trials represents a critical juncture in translational medicine, fraught with unique ethical challenges and scientific uncertainties. For stem cell-based interventions, which are often complex, speculative, and involve irreversible procedures, the selection of appropriate research participants and the process of obtaining genuinely informed consent demand exceptional rigor [15] [16]. These considerations are paramount not only for protecting participant welfare but also for ensuring the scientific validity and social value of the research. The International Society for Stem Cell Research (ISSCR) guidelines emphasize that clinical experimentation is burdensome for research subjects and should only proceed when there is a compelling scientific rationale, a plausible mechanism of action, and an acceptable chance of success [15]. This document provides detailed application notes and protocols to guide researchers, scientists, and drug development professionals in navigating the complex ethical landscape of early-phase stem cell clinical trials, framed within the broader context of a comprehensive stem cell clinical trial design thesis.
Ethical Framework for Participant Selection
The principle of primacy of patient welfare requires that the vulnerability and pressing medical needs of patients with serious conditions lacking effective treatments must never be exploited [15] [10]. Participant selection must balance scientific needs with thorough protection of individual rights.
Candidate Populations: Justifications and Considerations
A systematic review of reasons for including different participant groups in FIH trials identified 181 reasons relating to six ethical themes: non-maleficence, beneficence, scientific value, efficiency, respect for persons, and justice [17]. The major candidate populations and their ethical considerations are summarized below:
Table 1: Ethical Considerations for Participant Groups in Early-Phase Stem Cell Trials
| Participant Group | Ethical Justifications | Ethical Concerns & Mitigation Strategies |
|---|---|---|
| Healthy Volunteers | - Simpler data interpretation due to absence of confounding disease pathology- Lower burden of illness promotes altruistic motivation [17] | - Exposure to risk with no direct therapeutic benefit- Robust screening and comprehensive risk disclosure are essential [17] |
| Patients with Less Advanced-Stage Disease (LASD) | - Physiological resilience may better tolerate unknown risks- Potential for early intervention to alter disease trajectory [17] | - Risk of forfeiting proven standard-of-care treatments- Justify why earlier intervention is scientifically necessary [17] |
| Patients with More Advanced-Stage Disease (MASD) | - Often exhausted available treatments, creating potential for direct benefit- May place higher subjective value on risk-benefit ratio [17] | - Compromised health status may increase vulnerability to coercion or TM- Ensure organ function sufficient for valid safety monitoring [17] |
| Vulnerable Populations(e.g., cognitively impaired, economically disadvantaged) | - Justice requires fair access to research participation and potential benefits [10] | - Heightened susceptibility to coercion or unduly influence- Implement additional safeguards: independent advocates, enhanced oversight [17] |
Quantitative Comparison of Trial Populations
Understanding baseline characteristics of patients in different trial phases is crucial for evaluating the generalizability of results. A 2025 analysis compared patient demographics between registrational phase 2/3 and phase 1 trials in oncology, providing a model for similar assessments in stem cell trials.
Table 2: Comparison of Baseline Patient Characteristics in Phase 1 vs. Phase 2/3 Clinical Trials (Adapted from PMC12083001) [18]
| Characteristic | Phase 2/3 TrialsWeighted Mean (SD) | Phase 1 TrialsWeighted Mean (SD) | Mean Difference | P-value |
|---|---|---|---|---|
| Median Age (years) | 60.7 (5.1) | 59.7 (5.6) | 1.0 | 0.051 |
| Female Rate (%) | Not statistically significantly lower | Not statistically significantly lower | -4.9% | 0.999 |
| Performance Status >1 Rate (%) | 2.3% (4.7) | 1.8% (3.5) | 0.5% | 0.374 |
This data demonstrates that significant disparities in age, sex, and performance status are not inevitable across trial phases. Proactive, ethically-justified selection criteria in phase 1 can create a participant cohort that is both protective and scientifically appropriate for later development [18].
Incorporating Patient-Centered Outcomes in Trial Design
Modern trial design increasingly emphasizes patient-focused drug development (PFDD). For complex disorders affecting multiple symptom domains, patient-selected or patient-ranked outcomes can be incorporated to better align endpoints with what matters most to patients [19].
- Patient-Selected Outcomes: Each patient identifies their single most bothersome symptom. Analysis focuses on this patient-selected outcome, often as a co-primary endpoint [19].
- Patient-Ranked Outcomes (Desirability of Outcome Ranking - DOOR): Patients provide a full ranking of all relevant outcomes by personal importance. A composite endpoint then compares patients across treatment arms based on this prioritized ranking, estimating the probability that a randomly selected participant from the experimental arm has a more favorable outcome profile than one from the control arm [19].
In early-phase dose-finding oncology trials (DFOTs), however, a 2023 review found that statistical methods and reporting for Patient-Reported Outcomes (PROs) are often poorly described and inconsistent, highlighting a crucial need for international guidance in this area [20].
Protocol: Comprehensive Informed Consent Process for Stem Cell Trials
Obtaining valid informed consent in early-phase stem cell trials is an ongoing process, not a single event. The following protocol outlines the essential components, with particular attention to challenges specific to stem cell-based interventions.
Pre-Consent Preparation and Assessment
- Protocol Review by IRB/EC: Ensure the trial protocol and consent documents have received approval from an fully constituted, independent ethics committee with specific expertise in stem cell biology and cell-based therapies [15] [16].
- Consent Document Development: Create consent forms using clear, accessible language (typically 6th-8th grade reading level). Avoid overly technical jargon and explicitly use terms like "research" and "experiment." The ISSCR provides patient-friendly resources (
closerlookatstemcells.org) that can be recommended [16]. - Therapeutic Misconception (TM) Mitigation Planning: Develop specific scripts and materials to address the TM—the common confusion between research participation and therapeutic medical care. Explicitly state the primary goal of the trial (e.g., safety/dosing) and the uncertain nature of any potential benefit [16].
Capacity Assessment and Surrogate Decision-Making
- Systematic Capacity Evaluation: For trials involving neurodegenerative diseases (e.g., Parkinson's, ALS) where cognitive impairment is common, implement a formal capacity assessment conducted by a qualified professional (e.g., psychiatrist). Standard clinical rating scales are insufficient; expert judgment is essential [16].
- Early Involvement of Proxy: For populations where progressive cognitive decline is expected, involve a legally authorized representative (proxy) in the initial consent process. This establishes a shared understanding and allows the proxy to make future decisions consistent with the participant's values if capacity is lost [16].
Core Information Disclosure and Discussion
The consent discussion must cover standard elements and issues unique to stem cell trials. The diagram below outlines the workflow for managing capacity assessment and the consent process.
The core information disclosure must cover these key areas:
- Nature and Purpose of Research: Clearly state this is an early-phase trial (Phase I) whose primary objectives are safety, tolerability, and dosing, not therapeutic efficacy. Use phrases like "This is the first time this intervention will be used in humans" [16].
- Risks and Uncertainties: Disclose all known and theoretical risks. For stem cell interventions, this includes:
- Tumorigenicity or unwanted cell proliferation due to the proliferative nature of stem cells [15].
- Immunogenic reactions, even with autologous cells [16].
- Ectopic tissue formation, migration of cells to unintended sites [15] [16].
- Procedural risks specific to the administration route (e.g., intracranial or intraspinal injection) [16].
- Alternative Options: Discuss all available standard-of-care treatments and the alternative of supportive care only, ensuring participants understand they are not forfeiting proven therapies for a guaranteed benefit [16].
- Cell-Specific Disclosures: Disclose the provenance of the cells (e.g., derived from human embryos, iPSCs), as this may raise religious or moral concerns for some participants [15] [16]. Explain the manufacturing process, level of manipulation, and that the product is rigorously tested for quality and safety as per regulatory standards [15].
Assessment of Understanding and Voluntariness
- Interactive Quiz/Feedback: Employ a short, non-coercive quiz or a "teach-back" method where participants explain key concepts in their own words (e.g., the primary purpose of the trial, major risks, and the voluntary nature of participation) to verify comprehension [16].
- Cooling-Off Period: Mandate a 24-48 hour period between the initial consent discussion and the signing of the consent form to allow for reflection and consultation with family, friends, or personal physicians.
- Cultural and Linguistic Competence: When recruiting from diverse populations, provide translated materials and use qualified interpreters. Partner with community representatives to ensure cultural competence, respecting differences in dietary rules, religious practices, and health beliefs [21].
Consent as an Ongoing Process
- Long-Term Follow-Up and Re-Consent: Plan for long-term monitoring (potentially 10-15 years). Establish procedures for ongoing consent or re-assent for participants who may lose decision-making capacity, leveraging the previously involved proxy [15] [16].
- Adverse Event Communication: Develop a transparent plan for communicating new information, including unexpected adverse events, to participants and their proxies throughout the trial.
Advanced Tools and Reagent Solutions
Implementing these protocols requires a combination of sophisticated reagents, validated instruments, and computational tools.
Research Reagent Solutions for Cell Characterization and Safety
Table 3: Essential Research Reagents for Stem Cell Trial Product Characterization
| Reagent/Material | Function in Patient Selection & Safety | Application Notes |
|---|---|---|
| Pathogen Screening Assays | Donor and cell bank screening for infectious diseases (e.g., HIV, HBV, HCV) to prevent pathogen transmission [15]. | Use FDA/EMA-guided test panels. High-specificity tests can sometimes mitigate the need for direct donor screening [15]. |
| Genomic Stability Assays (e.g., Karyotyping, FISH, NGS) | Detecting genetic and epigenetic changes accumulated during prolonged cell culture that could lead to altered function or malignancy [15]. | Conduct at multiple stages: master cell bank, working cell bank, and end-of-production. |
| Pluripotency & Differentiation Markers | Characterizing stem cell lines and confirming the identity of differentiated progeny before transplantation. | Use standardized antibody panels and flow cytometry. Critical for demonstrating cell product consistency. |
| Tumorigenicity Assays (e.g., In Vivo assays in immunocompromised mice, Soft Agar Assay) | Assessing the potential for residual undifferentiated cells to form tumors post-transplantation [15]. | A required safety study in preclinical development. |
| PD-L1 Quantitative Continuous Scoring (QCS) | A computer vision system for objective, granular quantification of biomarker expression from histology slides, enhancing patient stratification [22]. | Identifies patient subpopulations most likely to respond to therapy (e.g., in immuno-oncology). More objective than visual scoring [22]. |
Visualizing the Patient Selection and Stratification Workflow
Advanced biomarker analysis, such as the PD-L1 QCS system, enables more precise patient selection. The following diagram illustrates the integrated workflow from biomarker discovery to final patient stratification.
This workflow, as demonstrated in the MYSTIC trial for non-small-cell lung cancer, can lead to a more precise identification of patients likely to benefit from therapy. For instance, the PD-L1 QCS-PMSTC biomarker maintained a similar hazard ratio (HR = 0.62) as visual scoring but identified a significantly larger biomarker-positive population (54.3% vs. 29.7%), thereby potentially allowing more patients to benefit from effective treatment [22].
Responsible translation of stem cell research into clinical applications hinges on the ethical integrity of trial conduct, with participant selection and informed consent forming its cornerstone. The frameworks and protocols outlined herein provide a roadmap for navigating the complex interplay between scientific necessity and unwavering respect for participant autonomy and welfare. Adherence to these guidelines, coupled with continuous critical reflection and engagement with bioethicists, patient communities, and regulatory bodies, will ensure that the promising field of stem cell-based regenerative medicine advances on a foundation of trust, rigor, and ethical commitment. This approach is not an impediment to progress but a prerequisite for sustainable and socially valuable scientific innovation.
For researchers and drug development professionals working in the dynamic field of stem cell therapies, navigating the regulatory landscape is as crucial as the scientific research itself. The U.S. Food and Drug Administration (FDA) has established several expedited programs specifically designed to accelerate the development and review of promising therapeutics for serious conditions where unmet medical needs exist. These pathways are particularly relevant for stem cell-based interventions, which often target serious or life-threatening diseases with limited treatment options. Understanding the nuances of the Regenerative Medicine Advanced Therapy (RMAT), Fast Track, and Accelerated Approval designations is essential for efficiently translating promising preclinical discoveries into approved therapies for patients. These programs offer strategic advantages that can significantly reduce development timelines while maintaining rigorous standards for safety and effectiveness, though each employs distinct mechanisms and targets different aspects of the development and review process [23].
The traditional drug development pathway can take eight years or more from initial clinical trials to approval [4]. For stem cell therapies targeting rapidly progressive fatal diseases, this timeline is often untenable. Expedited pathways address this challenge by providing more intensive FDA guidance, opportunities for rolling review of marketing applications, and in some cases, altered evidence standards based on earlier-stage clinical data. The 21st Century Cures Act formally established the RMAT designation in 2016, creating a specialized pathway recognizing the unique challenges and opportunities presented by regenerative medicine products [24]. As of September 2025, the FDA has received almost 370 RMAT designation requests and approved 184, with 13 RMAT-designated products ultimately achieving marketing approval [24].
Comparative Analysis of Expedited Pathways
The strategic selection of an appropriate expedited pathway requires understanding their distinct features, eligibility criteria, and benefits. The following table provides a structured comparison of these key designations to inform developmental planning.
Table 1: Comparison of Key FDA Expedited Pathways
| Feature | RMAT | Fast Track | Accelerated Approval |
|---|---|---|---|
| Governing Statute | 21st Century Cures Act [24] | FD&C Act [23] | FD&C Act [23] |
| Primary Scope | Cell therapies, gene therapies, therapeutic tissue engineering products, combination products [24] | Drugs and biologics for serious conditions [23] | Drugs and biologics for serious conditions [23] |
| Unmet Medical Need Requirement | Yes | Yes | Yes |
| Evidence Standard | Preliminary clinical evidence on safety & potential effectiveness [24] | Nonclinical or clinical data demonstrating potential to address unmet need [23] | Effect on a surrogate endpoint reasonably likely to predict clinical benefit, or on an intermediate clinical endpoint [25] [23] |
| Key Benefits | Early interactions, potential for streamlined approval, flexibility in evidence development [24] | Rolling BLA/NDA review, more frequent FDA interactions [23] | Approval based on effect on surrogate or intermediate endpoint [25] |
| Post-Market Requirement | Possible post-approval studies [24] | Not specific to designation | Required confirmatory trials [25] [26] |
Beyond these pathways, the FDA has also proposed a novel Plausible Mechanism (PM) Pathway for highly individualized therapies targeting ultra-rare genetic diseases where traditional trials are nearly impossible. This pathway, introduced in 2025, could be relevant for bespoke stem cell therapies. It centers on mechanistic plausibility and direct clinical responses in a very small number of patients, requiring strong post-market evidence collection [25].
Strategic Application and Protocol Design
RMAT Designation: A Strategic Framework for Stem Cell Therapies
The RMAT designation is the most specialized pathway for regenerative medicine products, including stem cell therapies. To qualify, a therapy must first be classified as a regenerative medicine product, which includes cell therapies, therapeutic tissue engineering products, and combination products. The targeted condition must be serious, and the sponsor must provide preliminary clinical evidence indicating the therapy has the potential to address unmet medical needs for that condition [24]. Unlike other pathways, RMAT designation offers the distinctive potential for flexibility in evidence development, which may include using surrogate or intermediate endpoints, and leveraging real-world evidence (RWE) to support effectiveness claims or satisfy post-approval study requirements [24].
The FDA's September 2025 draft guidance on expedited programs for regenerative medicine therapies provides critical insights for sponsors. It emphasizes that while RMAT designation accelerates clinical development, it does not change the required level of chemistry, manufacturing, and controls (CMC) information needed to assure product quality. Sponsors are therefore advised to pursue a more rapid CMC development program to align with faster clinical timelines. The guidance also encourages sponsors to engage with the Office of Therapeutic Products (OTP) early in development and to seek input from patient communities regarding clinically relevant endpoints [24].
Table 2: Key Considerations for RMAT Designation Requests
| Consideration Area | Key Action Points for Sponsors |
|---|---|
| Manufacturing & CMC | - Develop rapid CMC program to match clinical pace.- Conduct risk assessment for planned manufacturing changes, as post-change product may not qualify for RMAT if comparability is not established [24]. |
| Clinical Trial Design | - Engage FDA early for trial design input.- Consider innovative designs (e.g., basket, umbrella trials) and use of historical controls where populations are adequately matched.- Develop monitoring plans with both short-term and long-term safety assessments [24]. |
| Leveraging Data | - Explore use of real-world evidence (RWE) to support approval applications.- Consider using digital health technologies to collect safety and effectiveness information [24]. |
Integrating Expedited Pathways with Clinical Trial Phases
Strategic use of expedited pathways must be integrated within the traditional framework of clinical development phases. For stem cell therapies, these phases often have unique characteristics.
- Phase I Trials: The primary objective is safety evaluation. For stem cell therapies, these trials are typically conducted not in healthy volunteers but in individuals with the target disease due to the therapy's specificity and potential risks [4] [27]. Key endpoints include identifying dose-limiting toxicities, determining a safe dosage range, and characterizing pharmacokinetics/pharmacodynamics. Early safety and tolerability data from this phase are often critical for supporting a Fast Track or RMAT designation request.
- Phase II Trials: This phase expands the focus to include preliminary efficacy assessment and further safety evaluation in a larger, targeted patient population. Researchers aim to identify the optimal dosing regimen and gather evidence that the therapy provides a meaningful therapeutic effect. The preliminary clinical evidence required for an RMAT designation often originates from well-controlled Phase II studies [28] [24].
- Phase III Trials: These large-scale studies confirm efficacy, monitor adverse effects, and compare the new therapy to standard treatments. For therapies with Accelerated Approval, a positive Phase III trial using a validated surrogate endpoint can form the basis for marketing approval, with confirmatory trials required post-approval [25] [23].
The following diagram illustrates the strategic integration of expedited pathways with the clinical development lifecycle for a stem cell therapy.
Experimental Protocols and Methodologies
Protocol: Designing a Phase I/II Stem Cell Trial for RMAT
Combining Phase I and II trials is a common strategy in stem cell therapy development for serious diseases with high unmet need, allowing for more efficient evaluation of both safety and signals of effectiveness [4]. The following protocol outlines a standardized workflow for such a trial.
Detailed Methodology:
- Protocol Finalization and Regulatory Submission: Develop a comprehensive protocol detailing objectives, patient population, treatment plan, and endpoints. Submit Investigational New Drug (IND) application to FDA, including preclinical data, CMC information, and clinical protocol [4]. Early engagement with FDA is critical to discuss potential for RMAT designation and trial design [24].
- Patient Population and Eligibility: Define clear inclusion/exclusion criteria focusing on the target serious condition. Utilize natural history data to establish baseline expectations. Consider master protocols (basket/umbrella trials) for efficient patient enrollment across multiple sites, as encouraged by recent FDA guidance [24].
- Stem Cell Product Manufacturing: Manufacture the cell product under current Good Manufacturing Practices (cGMP). Use a common manufacturing protocol and quality testing specifications across all clinical sites if it's a multi-center trial [24]. Document the process thoroughly, as any major manufacturing change later may impact RMAT eligibility if comparability cannot be established [24].
- Dosing and Administration: For Phase I, implement a dose-escalation design (e.g., 3+3) to identify the maximum tolerated dose. Administer the product via the intended route (e.g., intravenous, intrathecal, or direct injection). Multiple clinical sites may participate using a shared protocol [24].
- Endpoint Assessment and Monitoring:
- Safety Endpoints: Monitor for adverse events (AEs), serious AEs (SAEs), and adverse events of special interest (AESIs) throughout the study. Given the novel nature of stem cell therapies, include both short-term and long-term safety plans, potentially using digital health technologies for data collection [24].
- Efficacy Endpoints: Select endpoints that are clinically meaningful. For preliminary effectiveness evidence, these may include surrogate endpoints, functional improvement scales, or biomarker data. Engage patient communities for input on relevant endpoints [24].
- Data Analysis and Reporting: Analyze data for safety, tolerability, and preliminary efficacy. This analysis forms the basis for deciding whether to progress to a larger Phase III trial and is crucial for supporting an RMAT designation request or an application for Accelerated Approval.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Stem Cell Therapy Development
| Reagent/Material | Function in Development & Manufacturing |
|---|---|
| Cell Culture Media & Supplements | Supports the expansion and maintenance of stem cells under defined conditions, ensuring consistency and viability of the final product. |
| Cell Separation/Selection Kits | Enriches for specific stem cell populations (e.g., CD34+ hematopoietic stem cells, mesenchymal stem cells) from heterogeneous mixtures like bone marrow or adipose tissue. |
| Characterization Antibodies | Used in flow cytometry and immunocytochemistry to confirm cell identity, purity, and potency by detecting specific surface markers (e.g., CD34, CD73, CD90, CD105). |
| Vector Systems for Genetic Modification | Facilitates the stable introduction or correction of genes in stem cells for therapeutic purposes (e.g., lentiviral vectors for gene delivery). |
| Biomatrices and Scaffolds | Provides a three-dimensional structure for stem cell delivery and tissue formation, enhancing engraftment and functional integration at the target site. |
| cGMP-Grade Cytokines/Growth Factors | Directs stem cell differentiation toward specific lineages (e.g., cardiomyocytes, neurons) in a controlled, manufacturing-compliant environment. |
The strategic utilization of expedited pathways—RMAT, Fast Track, and Accelerated Approval—is transforming the development landscape for stem cell therapies. These designations are not mutually exclusive; a product can potentially qualify for more than one, creating a powerful synergistic effect to accelerate its journey to patients. Success in this evolving environment demands an integrated strategy that combines robust science, meticulous trial design, and proactive regulatory planning. By understanding the distinct advantages and requirements of each pathway, stem cell researchers and drug development professionals can optimize their development plans, increase the efficiency of their clinical trials, and ultimately accelerate the delivery of groundbreaking treatments to patients facing serious diseases with limited options.
Strategic Trial Design for MSCs, iPSCs, and HSCs Across Therapeutic Areas
The transition of stem cell therapies from preclinical research to clinical application hinges on the rigorous development of cell-specific protocols. Unlike traditional pharmaceuticals, living cell therapies present unique challenges due to their complex mechanisms of action, heterogeneity, and dynamic interactions with the host environment. A successful clinical trial protocol must be built on three interdependent pillars: dosing (determining the quantity and quality of cells), administration routes (selecting the method for delivering cells to the target site), and scheduling (optimizing the timing and frequency of administration). This document provides a structured framework for developing these critical components within Phase I-III clinical trials, supported by contemporary data and standardized methodologies.
Quantitative Dosing Benchmarks in Current Clinical Trials
Dosing for cell therapies is not a one-size-fits-all parameter; it is influenced by cell type, source, indication, and route of administration. The following tables summarize key dosing data from recent clinical trials and approved therapies, providing a benchmark for protocol development.
Table 1: Dosing Strategies for FDA-Approved Stem Cell Therapies (2023-2025)
| Product Name | Cell Type | Indication | Dosing Strategy | Key Dosing Consideration |
|---|---|---|---|---|
| Omisirge (Apr 2023) [2] | Cord Blood-Hematopoietic Progenitor Cells | Hematologic malignancies | Allogeneic nicotinamide-modified stem cell graft | Accelerates neutrophil recovery; dose is a prepared graft for transplantation [2] |
| Lyfgenia (Dec 2023) [2] | Autologous CD34+ cells | Sickle Cell Disease | One-time treatment involving genetically modified autologous hematopoietic stem cells | Dose is based on the collection and modification of the patient's own cells [2] |
| Ryoncil (Dec 2024) [2] | Allogeneic Bone Marrow-MSCs | Pediatric Steroid-Refractory aGVHD | First FDA-approved MSC therapy; utilizes cells from a healthy donor [2] | Dose leverages immunomodulatory properties for a life-threatening inflammatory condition [2] |
Table 2: Dosing Ranges in Recent Clinical Trials for Stem Cell-Derived Products
| Therapy / Platform | Indication | Reported Dosing Range | Administration Route |
|---|---|---|---|
| MSC-EVs/Exosomes (General) [29] | Various (e.g., Lung Diseases) | ~10^8 particles (Nebulization); Varies significantly for IV | Intravenous, Nebulization |
| CALEC (Phase I/II) [30] | Limbal Stem Cell Deficiency | Cultivated autologous limbal epithelial cell graft | Surgical transplantation to cornea |
| iPSC-Derived Therapies (General) [2] | Ophthalmology, Neurology, Oncology | Over 10^11 cells administered to >1,200 patients globally (across trials) | Varies by target (e.g., intraocular, intrathecal) |
The data reveals critical dosing challenges. For MSC-derived extracellular vesicles (MSC-EVs), a significant lack of standardized dosing persists, with studies reporting doses in total particles, protein content (µg), or volume, complicating cross-trial comparisons [29]. Furthermore, dose-effect relationships are route-dependent; for instance, nebulized MSC-EV therapy for lung diseases achieved therapeutic effects at doses around 10^8 particles, notably lower than typically required for intravenous routes [29]. This underscores the necessity for route-specific dose optimization.
Administration Routes: Methodologies and Experimental Protocols
The administration route is a critical determinant of cell engraftment, survival, and therapeutic efficacy. It dictates the required cell preparation formulation, viability, and volume.
The selection of an administration route is guided by the pathophysiology of the target disease and the mechanism of action of the cell therapy.
Table 3: Administration Routes for Stem Cell Therapies: Methodologies and Applications
| Route | Methodology & Cell Preparation | Primary Indications | Key Considerations |
|---|---|---|---|
| Intravenous (IV) Infusion [31] | - Cell Prep: Suspension in saline or plasma.- Volume: Typically 1-100 mL.- Procedure: Slow infusion via peripheral vein. | Systemic conditions, autoimmune diseases, GvHD [32] [31] | - Enables systemic distribution via homing.- Risk of pulmonary first-pass effect (cell trapping in lungs).- Requires strict control of infusion rate and cell clumping. |
| Local Injection (e.g., Intraarticular, Intramyocardial) [31] | - Cell Prep: High-concentration suspension.- Volume: Low (e.g., 0.5-5 mL).- Guidance: Often requires ultrasound or fluoroscopy. | Orthopedic conditions (OA), myocardial infarction, localized tissue damage [32] [31] | - Maximizes local cell concentration.- Minimizes systemic exposure.- Technically demanding; risk of leakage from injection site. |
| Intrathecal Injection [31] | - Cell Prep: Suspension in sterile, preservative-free solution.- Volume: 5-15 mL.- Procedure: Lumbar puncture performed by anesthesiologist or neurologist. | Neurological disorders (MS, ALS, spinal cord injury) [32] [31] | - Directly delivers cells to cerebrospinal fluid, bypassing BBB.- Invasive procedure requiring specialized expertise and post-procedure monitoring. |
| Nebulized Inhalation [29] [31] | - Cell Prep: Suspension of cells or extracellular vesicles in a compatible nebulizer fluid.- Procedure: Administration via a mucosal atomization device or nebulizer. | Respiratory diseases (COPD, ARDS, pulmonary fibrosis) [29] [31] | - Directly targets the respiratory epithelium.- For cells, viability post-aerosolization must be rigorously validated. Particularly effective for MSC-EVs [29]. |
| Surgical Transplantation (e.g., CALEC) [30] | - Cell Prep: Cells are expanded into a tissue-engineered graft over 2-3 weeks under GMP.- Procedure: Surgical implantation under anesthesia. | Limbal stem cell deficiency, complex tissue defects [30] | - Provides structural and functional tissue restoration.- Highly invasive, resource-intensive, and requires sophisticated manufacturing. |
Visualizing Administration Route Selection
The following diagram illustrates the logical decision-making process for selecting an administration route based on the disease pathology and target tissue.
Detailed Experimental Protocol: Intrathecal Administration of MSCs
This protocol is adapted from methods described in clinical trials for neurological conditions and reflects current safety data [31].
Objective: To safely administer mesenchymal stem cells (MSCs) into the cerebrospinal fluid (CSF) via lumbar puncture for the treatment of neurological disorders. Key Safety Note: A review of 39 studies concluded that properly performed intrathecal injection of MSCs is "exceedingly safe, with no serious adverse events reported" [31].
Materials:
- Cell Product: Cryopreserved, washed, and formulated allogeneic or autologous MSCs. Final release criteria must include viability >80%, sterility (bacterial/fungal), endotoxin level <5 EU/kg, and identity (e.g., flow cytometry for CD73+, CD90+, CD105+, CD45-).
- Equipment: Standard lumbar puncture kit, sterile drapes, personal protective equipment.
- Imaging: Fluoroscopy or ultrasound for guidance (recommended).
Pre-Procedure:
- Patient Consent: Obtain full informed consent, detailing risks (headache, infection, back pain).
- Cell Preparation: Thaw and wash cells in a closed system. Resuspend in sterile, preservative-free normal saline or lactated Ringer's solution at a final concentration of 10-20 million cells/mL. The total injection volume should not exceed 15 mL. Maintain cells at room temperature and administer within 4 hours of preparation.
- Patient Positioning: Position the patient in the lateral decubitus or sitting position to maximize intervertebral space.
Procedure:
- Aseptic Technique: Cleanse the L3-L4 or L4-L5 interspace with antiseptic and drape sterilely.
- Local Anesthesia: Administer local anesthetic (e.g., 1-2% lidocaine).
- Lumbar Puncture: Perform the puncture with a standard spinal needle (e.g., 22-gauge Quincke). Confirm correct placement by observing CSF flow.
- Cell Administration: Slowly inject the cell suspension over 1-2 minutes. Do not aspirate CSF during injection to avoid turbulence and cell shear stress.
- Needle Removal: Withdraw the needle and apply a sterile dressing.
Post-Procedure:
- Monitoring: Monitor the patient for a minimum of 6 hours for any adverse events (headache, nausea, neurological changes) [31].
- Patient Instructions: Advise the patient to remain flat for 1-2 hours post-procedure to reduce the risk of post-dural puncture headache.
Scheduling and Treatment Regimens
Treatment scheduling—encompassing the timing of the first dose relative to disease stage, the number of doses, and the interval between doses—is a pivotal yet often empirically determined aspect of protocol design.
Scheduling Frameworks Based on Clinical Evidence
- Single vs. Multiple Dosing: A single administration is often evaluated first for safety. The decision to use multiple doses should be hypothesis-driven. For example, in the CALEC trial for corneal damage, 3 out of 14 patients received a second transplant after the initial procedure, which was crucial for achieving complete success in one of these patients [30]. This demonstrates that a rescue or booster dose can be a predefined strategy within a trial protocol.
- Dosing Intervals: The interval between multiple doses should allow for assessment of the initial response and mitigation of potential immunogenicity. In chronic conditions, intervals of 3-6 months are common in early-phase trials to evaluate persistence of effect. For MSC-EVs, the optimal interval is unknown and should be informed by pharmacokinetic and pharmacodynamic (PK/PD) modeling.
- Timing in Acute vs. Chronic Disease: In acute settings, such as myocardial infarction, the timing of cell delivery post-event is critical. Early-phase trials have administered cells days to weeks after the insult (e.g., 3-6 days post-AMI) [28]. In chronic diseases like osteoarthritis, the focus is on long-term symptom modification, and scheduling is more flexible.
Visualizing Protocol Development Workflow
The development of a cell-specific protocol is an iterative process that integrates dosing, route, and scheduling with regulatory and manufacturing considerations. The following workflow outlines this process from foundational research to clinical trial initiation.
The Scientist's Toolkit: Essential Reagents and Materials
The successful execution of a stem cell clinical trial relies on a suite of critical reagents and materials, each serving a specific function in the development and validation chain.
Table 4: Essential Research Reagent Solutions for Stem Cell Clinical Trials
| Reagent / Material | Function in Protocol Development | Key Considerations |
|---|---|---|
| Clinical-Grade iPSC Seed Clones [2] | A standardized, master cell bank serving as the starting material for producing iPSC-derived products (e.g., neurons, cardiomyocytes). | Ensures consistency and scalability. Submission of a Drug Master File (DMF) to regulators provides comprehensive manufacturing data, streamlining IND applications [2]. |
| Defined Culture Media & Supplements | Supports the expansion and maintenance of stem cells without animal-derived components (xeno-free). | Critical for GMP compliance and reducing the risk of immunogenic reactions or pathogen transmission. Serum-free, antibiotic-free protocols are now achievable, as demonstrated in the CALEC trial [30]. |
| Cell Separation & Characterization Kits | Isolates and purifies specific cell types (e.g., CD54+ muscle progenitors) and confirms cell identity and purity pre-administration. | Essential for meeting ISCT criteria for MSCs or other cell types. Kits must be GMP-grade and validated for clinical use. |
| Potency Assay Reagents | Measures the biological activity of the cell product that is linked to its therapeutic mechanism (e.g., immunomodulation, secretion of trophic factors). | A major regulatory requirement. The assay must be quantitative and validated. Lack of standardized potency assays is a key bottleneck in the field, particularly for MSC-EVs [29]. |
| Cryopreservation Media | Allows for long-term storage and transport of the final cell product while maintaining viability and functionality. | Formulation must be optimized for the specific cell type to minimize post-thaw apoptosis and preserve potency. |
The meticulous development of cell-specific protocols for dosing, administration, and scheduling is a non-negotiable prerequisite for generating conclusive safety and efficacy data in stem cell clinical trials. The field is moving toward greater precision, driven by the approval of pioneering products and the maturation of platforms like iPSCs and MSC-EVs. Key to future success will be the adoption of standardized dosing units, the development of clinically relevant potency assays, and the strategic use of combination administration routes. By adhering to a structured, data-driven, and iterative framework for protocol development, researchers can robustly navigate the complexities of clinical trial design and accelerate the delivery of transformative cell therapies to patients.
The design of stem cell-based clinical trials requires a sophisticated understanding of endpoint selection tailored to specific disease pathologies and clinical phases. As regenerative medicine advances, with over 115 global clinical trials involving pluripotent stem cell-derived products reported as of December 2024, the strategic alignment of endpoints with disease mechanisms and patient populations becomes increasingly critical [2]. This application note provides a structured framework for endpoint selection across oncology, autoimmune, and neurodegenerative disorders, contextualized within stem cell clinical trial design. We synthesize current evidence, quantitative outcomes, and methodological protocols to guide researchers in developing rigorous, regulatory-compliant trial designs that effectively capture therapeutic benefits while addressing disease-specific challenges.
Disease-Specific Endpoint Considerations
Oncology Applications
Oncology trials for stem cell therapies require endpoints that capture both direct antitumor effects and supportive care benefits, particularly for therapies involving hematopoietic stem cell transplantation (HSCT).
Table 1: Endpoint Selection in Oncology Stem Cell Trials
| Trial Phase | Primary Endpoints | Secondary Endpoints | Imaging & Biomarkers | Example Therapies |
|---|---|---|---|---|
| Phase I/II | Safety, Dose-Limiting Toxicities (DLTs), Maximum Tolerated Dose (MTD) | Engraftment kinetics, Immune reconstitution | Tumor volume (RECIST criteria), Chimerism analysis | Omisirge (omidubicel-onlv), FT536 (iPSC-NK cells) [2] [33] |
| Phase III | Overall Survival (OS), Progression-Free Survival (PFS) | Graft-versus-Host Disease (GvHD) incidence, Relapse Rate | Minimal Residual Disease (MRD), Positron Emission Tomography (PET) response | Hematopoietic stem cell products for hematologic malignancies [2] [34] |
For engineered stem cell approaches targeting cancer stem cells (CSCs), researchers should incorporate flow cytometry for CSC markers (CD44, CD133) and functional assays measuring sphere formation capacity. Oncolytic virotherapy delivered via mesenchymal stem cells (MSCs) requires assessment of viral replication kinetics and immune cell infiltration in tumor biopsies [33].
Autoimmune Disease Applications
Autoimmune disease trials prioritize endpoints capturing immunomodulation and disease remission, with 83.6% of global stem cell trials for autoimmune diseases in Phase I-II as of 2025 [35].
Table 2: Endpoint Selection in Autoimmune Disease Stem Cell Trials
| Disease Category | Primary Endpoints | Secondary Endpoints | Biomarkers | Cell Types |
|---|---|---|---|---|
| Crohn's Disease (CD) | Clinical Remission (CDAI <150), Endoscopic Response (SES-CD) | Corticosteroid-free remission, Fistula closure | CRP, fecal calprotectin, Treg/Th17 ratio | MSCs (83.6% of trials) [35] |
| Systemic Lupus Erythematosus (SLE) | SRI-4 Response, Renal Response (for LN) | Steroid reduction, BILAG improvement | Anti-dsDNA, complement C3/C4, proteinuria | MSCs, iPSC-derived CAR-T (FT819) [2] [35] |
| Scleroderma | Modified Rodnan Skin Score (mRSS) | ACR-CRISS score, Lung function (FVC) | Autoantibody profiles, inflammatory cytokines | HSCs, MSCs [35] |
Recent trials highlight disease-specific variations in stem cell sourcing and administration. For Crohn's disease, local perianal fistula injection of MSCs demonstrated 50-75% remission rates in Phase II trials, while systemic lupus erythematosus trials employing intravenous MSC administration showed high remission rates (>75%) in 36 registered trials [35]. The FDA's RMAT designation for FT819, an iPSC-derived CAR T-cell therapy for SLE, underscores the regulatory recognition of these approaches [2].
Neurodegenerative Disease Applications
Neurodegenerative disorder trials require endpoints capturing nuanced functional improvements and objective evidence of neuronal integration, with particular challenges in measurement sensitivity and disease progression heterogeneity.
Table 3: Endpoint Selection in Neurodegenerative Disease Stem Cell Trials
| Disease | Primary Endpoints | Secondary Endpoints | Functional Imaging | Novel Technologies |
|---|---|---|---|---|
| Parkinson's Disease | MDS-UPDRS Part III OFF score, Adverse events | ON score, Hoehn & Yahr stage, Quality of Life (PDQ-39) | 18F-DOPA PET (Ki values), fMRI | iPSC-derived dopaminergic progenitors [36] |
| Epilepsy | Seizure frequency reduction (≥50%), Safety/tolerability | Seizure freedom rates, Cognitive function (Neuropsychological battery) | Long-term EEG monitoring, MRI for graft viability | NRTX-1001 (GABAergic interneurons) [37] |
| Alzheimer's Disease | ADAS-Cog, CDR-SB | Brain volume (hippocampal/whole brain), Activities of Daily Living | Amyloid PET, FDG-PET | MSC-derived exosomes, neural progenitors [38] |
Recent advances include the Phase I/II trial of iPSC-derived dopaminergic progenitors for Parkinson's disease, which demonstrated a 44.7% increase in 18F-DOPA uptake in the putamen alongside 20.4% improvement in MDS-UPDRS Part III OFF scores at 24 months [36]. For epilepsy, NRTX-1001 human GABAergic interneuron therapy demonstrated a 92% median reduction in disabling seizures with 80% of subjects showing >80% seizure reduction during the 7-12 month efficacy evaluation period [37].
Experimental Protocols
Protocol: Immunomodulatory Assessment of MSCs in Autoimmune Diseases
This protocol outlines the methodology for evaluating the immunomodulatory capacity of mesenchymal stem cells in autoimmune conditions, particularly for Crohn's disease and SLE.
Materials and Reagents:
- Ficoll-Paque PLUS for PBMC isolation
- Anti-CD3/CD28 activation beads for T-cell stimulation
- Flow cytometry antibodies: CD4, CD25, FOXP3, IL-17, IFN-γ
- MSC culture medium: α-MEM + 10% FBS + 1% Pen/Strep
- ELISA kits: TGF-β1, PGE2, IDO
- Transwell inserts (0.4μm pore) for coculture studies
Procedure:
- Isolate PBMCs from autoimmune disease patients (n≥5 donors) via density gradient centrifugation
- Culture MSCs to 80% confluence in 6-well plates and irradiate (20Gy) to prevent proliferation
- Seed activated CD4+ T cells (1×10^5 cells/well) in Transwell inserts above MSC monolayers at T cell:MSC ratios of 10:1, 5:1, and 1:1
- Collect supernatants at 24, 48, and 72 hours for cytokine analysis via ELISA
- After 96 hours, harvest T cells for flow cytometry analysis of Treg (CD4+CD25+FOXP3+) and Th17 (CD4+IL-17+) populations
- Perform statistical analysis using two-way ANOVA with Tukey's post-hoc test
Quality Controls:
- Verify MSC phenotype (CD73+, CD90+, CD105+, CD45-) before experimentation
- Assess MSC viability >95% post-irradiation
- Include control wells with T cells alone (positive control) and non-activated T cells (negative control)
This methodology underpinned recent trials showing MSC-mediated Treg induction correlating with clinical remission in Crohn's disease, with studies reporting 50-75% remission rates in Phase II trials [35].
Protocol: Functional Assessment of Dopaminergic Progenitors in Parkinson's Disease
This protocol details the assessment of iPSC-derived dopaminergic progenitors for Parkinson's disease, based on the recent Phase I/II trial published in Nature [36].
Materials and Reagents:
- Clinical-grade iPSC line (e.g., QHJI01s04 with specific HLA haplotyping)
- CORIN antibody for FACS sorting of floor plate progenitors
- Neural differentiation medium: DMEM/F12 + N2 supplement + B27 supplement + BDNF + GDNF + ascorbic acid
- Tacrolimus for immunosuppression (target trough: 5-10 ng/mL)
- 6-hydroxydopamine (6-OHDA) for rodent PD models
Procedure:
- Differentiate iPSCs to dopaminergic progenitors using dual SMAD inhibition (LDN193189, SB431542)
- On day 12, sort CORIN+ cells via FACS to enrich for floor plate progenitors (purity >95%)
- Form 3D aggregate spheres in suspension culture for 7 days
- Perform quality control: Flow cytometry for FOXA2+ (midbrain floor plate), LMX1A+ (dopaminergic), and OCT4- (pluripotency exit) populations
- Transplant 2.1-5.5×10^6 cells/putamen using stereotactic neurosurgical navigation
- Maintain tacrolimus immunosuppression (0.06 mg/kg twice daily) for 15 months with gradual taper
- Assess primary safety endpoints: Serial MRI for graft overgrowth, 18F-FLT PET for tumorigenicity, UDysRS for graft-induced dyskinesias
- Evaluate efficacy: MDS-UPDRS Part III OFF/ON scores, Hoehn & Yahr staging, 18F-DOPA PET for dopaminergic activity
Validation Metrics:
- Final product should contain ~60% DA progenitors and ~40% DA neurons
- Exclude TPH2-expressing serotonergic neurons (<1% contamination)
- In rat PD models, grafts should show <1% Ki-67+ proliferating cells at 24 weeks
This protocol enabled the recent demonstration that allogeneic iPS-cell-derived dopaminergic progenitors can survive, produce dopamine (44.7% increase in 18F-DOPA uptake), and improve motor function without tumor formation in PD patients [36].
Visualizing Endpoint Selection Strategy
The following diagram illustrates the strategic framework for endpoint selection across disease domains and clinical phases:
Diagram 1: Endpoint Selection Framework Across Phases and Indications. This framework illustrates the evolution of endpoint priorities from safety-focused early phases to comparative efficacy in late-phase trials, with disease-specific metric selection.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Stem Cell Trial Endpoint Assessment
| Reagent/Category | Specific Examples | Application Function | Disease Relevance |
|---|---|---|---|
| Flow Cytometry Antibodies | CD73/CD90/CD105 (MSC), CD34/CD45 (HSC), CD4/CD25/FOXP3 (Treg) | Cell phenotype validation, immune monitoring | Autoimmune (mechanistic), Oncology (engraftment) |
| Pluripotency Markers | OCT4, SOX2, NANOG, SSEA-4 | Quality control for iPSC/ESC-derived products | All indications (safety) |
| Differentiation Markers | CORIN (dopaminergic), TUBB3 (neuronal), TH (dopamine neurons) | Lineage-specific differentiation assessment | Neurodegenerative (potency) |
| Cytokine Detection | TGF-β, PGE2, IDO ELISA kits, Multiplex cytokine arrays | Immunomodulatory activity quantification | Autoimmune (mechanistic) |
| Functional Assays | Transwell migration, Colony-forming unit (CFU), Phagocytosis | Functional potency assessment | All indications (potency) |
| Imaging Agents | 18F-DOPA (dopaminergic function), 18F-FLT (proliferation), Contrast agents | Graft survival, integration, and safety monitoring | Neurodegenerative, Oncology |
For clinical trial applications, all reagents should be research-grade with documentation supporting potential clinical translation. CORIN sorting for dopaminergic progenitors enabled the recent successful Phase I/II trial of iPSC-derived cells for Parkinson's disease, demonstrating the critical importance of specific differentiation markers [36]. Similarly, flow cytometry panels assessing Treg/Th17 ratios provide crucial mechanistic insights for MSC therapies in Crohn's disease [35].
Strategic endpoint selection in stem cell clinical trials requires integration of disease pathology, therapeutic mechanism, and regulatory considerations. The recent expansion of stem cell therapies—from Ryoncil as the first FDA-approved MSC product for pediatric SR-aGvHD to iPSC-derived dopaminergic progenitors for Parkinson's disease—demonstrates the successful application of these principles [2] [36]. As the field advances with over 1,200 patients dosed in pluripotent stem cell trials without class-wide safety concerns, endpoint strategies must continue evolving to capture meaningful clinical benefits while addressing disease-specific challenges [2]. Future directions include incorporating patient-reported outcomes, standardized potency assays, and novel functional imaging modalities to better assess the therapeutic impact of regenerative medicine approaches across diverse disease indications.
Leveraging Combined Phase I/II Trials for Rare Diseases with Unmet Needs
Combined Phase I/II trials represent a pivotal strategy in accelerating the development of stem cell and other advanced therapies for rare diseases. These seamless trials merge the traditional objectives of Phase I (safety and dosing) and Phase II (preliminary efficacy) into a single, cohesive study, thereby compressing development timelines—a critical advantage for patient populations with serious, life-threatening conditions and no available treatment options [39]. The U.S. Food and Drug Administration (FDA) has recognized the urgency of this approach, explicitly endorsing innovative and efficient trial designs for cell and gene therapies (CGTs) targeting small populations [40] [41]. This regulatory encouragement is embedded within expedited programs such as the Regenerative Medicine Advanced Therapy (RMAT) designation, which promotes earlier and more flexible interactions between sponsors and the agency [40].
The fundamental rationale for using combined trials in rare diseases rests on ethical and practical necessities. In many rare, progressive conditions, assigning patients to a placebo arm is ethically challenging [42] [43]. Furthermore, the very small patient populations make it statistically and logistically difficult to run large, traditional, sequential trials [44]. The FDA has demonstrated a growing willingness to rely on data from single-arm and other innovative trial designs for approval, as evidenced by recent therapies for conditions like recurrent respiratory papillomatosis and steroid-refractory acute graft-versus-host disease [43]. A combined Phase I/II trial, often using patients as their own controls, is therefore not just an efficiency measure but a necessary adaptation to the realities of rare disease research.
Key Design Considerations for Combined Trials
Objectives and Endpoints
The successful design of a combined Phase I/II trial requires the clear and prospective definition of primary objectives for both the Phase I and Phase II portions of the study. These objectives must be supported by appropriate endpoints and a statistical analysis plan that accounts for the seamless nature of the trial.
Table 1: Primary Objectives and Endpoints in Combined Phase I/II Trials
| Trial Phase | Primary Objectives | Recommended Endpoint Types | Data Sources |
|---|---|---|---|
| Phase I Portion | - Assess safety and tolerability- Identify maximum tolerated dose (MTD) or optimal biological dose- Evaluate pharmacokinetics/pharmacodynamics (PK/PD) | - Incidence and grade of adverse events- Dose-limiting toxicities (DLTs)- Laboratory parameters | - Clinical safety labs- Patient diaries- Investigator assessments |
| Phase II Portion | - Determine preliminary efficacy- Further characterize safety profile- Identify a recommended Phase III dose | - Objective clinical outcome measures- Biomarker response- Surrogate endpoints likely to predict clinical benefit | - Clinical outcome assessments (COAs)- Biomarker assays- Digital health technologies (DHTs) |
For the Phase II component, the FDA's draft guidance on innovative designs for CGTs highlights the value of surrogate endpoints and biomarkers, especially in diseases where symptom onset may be delayed or variable [41]. The use of digital health technologies (DHTs) is also encouraged to capture nuanced, real-world data on disease progression and functional changes [40].
Innovative Statistical and Trial Designs
The combined Phase I/II framework is inherently adaptive, allowing for preplanned modifications based on accumulating data. The FDA's recent guidance outlines several innovative designs particularly suited to small populations, which can be integrated into a combined trial structure [40] [41].
- Adaptive Dose-Finding Designs: These designs, such as the continual reassessment method (CRM) or Bayesian logistic regression model (BLRM), are used in the Phase I portion to efficiently identify the optimal dose. They model the relationship between dose and the probability of dose-limiting toxicity (DLT), steering patient assignment to the most informative dose levels.
- Bayesian Trial Designs: These designs are highly useful for leveraging external data, such as natural history data from patient registries, to strengthen the analysis. This is especially powerful in rare diseases, as it allows for a reduction in the required sample size by formally incorporating prior knowledge into the probability models for efficacy and safety [40].
- Single-Arm Trials Using Participants as Their Own Control: In this design, a participant's response to the investigational therapy is compared to their own baseline status. This approach is persuasive when the target condition is universally degenerative and a clear, rapid improvement is expected with an effective therapy [40]. The FDA has approved multiple recent therapies based on this design, including Ryoncil for pediatric SR-aGVHD and Papzimeos for recurrent respiratory papillomatosis [43].
- Externally Controlled Studies: This design uses historical or real-world data (RWD) from patients who did not receive the study therapy as a comparator group. This can serve as the sole control or supplement a small concurrent control arm. Its suitability depends on having a highly predictable and well-documented disease natural history [40].
The diagram below illustrates a representative workflow for a Bayesian adaptive combined Phase I/II trial.
Experimental Protocol and Workflow
This section provides a detailed methodological protocol for a combined Phase I/II trial of an investigational stem cell therapy for a rare neurological disease, incorporating adaptive and Bayesian elements.
- Study Title: A Phase I/II, Open-Label, Adaptive Design Study to Assess the Safety, Tolerability, and Preliminary Efficacy of [Investigational Product] in Patients with [Rare Disease].
- Study Product: Allogeneic iPSC-derived Neural Progenitor Cells.
- Patient Population: N=45 patients (aged 18-65) with genetically confirmed [Rare Disease] and moderate disease severity. Key Inclusion: Progressive symptomatic disease, adequate organ function. Key Exclusion: Contraindications to immunosuppression or MRI; active malignancy.
- Control: Internally controlled via baseline period; supplemented with external natural history cohort data.
Detailed Methodology
1. Preclinical and Regulatory Preparation
- Secure Institutional Review Board (IRBE) and regulatory agency (e.g., FDA) approval under an Investigational New Drug (IND) application [2].
- Establish a Data and Safety Monitoring Board (DSMB) to review interim safety data.
- Finalize a statistical analysis plan detailing all adaptive algorithms and stopping rules.
2. iPSC Product Manufacturing and Quality Control
- Manufacture the investigational product under Good Manufacturing Practice (GMP) conditions [15].
- Implement rigorous quality control testing, including:
- Identity: Flow cytometry for cell-specific surface markers.
- Viability: Trypan blue exclusion or similar assay.
- Purity: Percentage of target cell type vs. undifferentiated cells.
- Potency: In vitro functional assay (e.g., neurotrophic factor secretion).
- Safety: Sterility, mycoplasma, and endotoxin testing.
3. Study Conduct and Dosing
- Screening Period (8 weeks): Confirm eligibility, collect baseline clinical and biomarker data, and establish a pre-treatment progression slope using historical clinical records.
- Phase I Dose Escalation (using Bayesian CRM):
- Dose Levels: 3 pre-specified dose levels (Low, Medium, High).
- Cohorts: Sequential cohorts of 3 patients. Dosing of each new cohort is determined by the updated CRM model based on all accumulated DLT data.
- DLT Observation Period: 4 weeks post-administration.
- Primary Phase I Goal: Identify the Recommended Phase II Dose (RP2D), defined as the dose with a DLT probability closest to the target (e.g., 25%).
4. Phase II Efficacy Expansion
- Once the RP2D is identified, an additional 30 patients are enrolled at this dose level.
- Primary Efficacy Endpoint: Change from baseline to Month 12 on a validated disease-specific functional rating scale.
- Key Secondary Endpoints:
- Proportion of patients with disease stabilization (defined as <20% decline from baseline on the primary scale).
- Change in quantitative biomarker (e.g., neurofilament light chain levels in cerebrospinal fluid).
- Quality of life measures.
5. Data Analysis
- Safety: Summarized descriptively for all dosed patients.
- Efficacy: The primary efficacy analysis will use a Bayesian model. The posterior probability that the change from baseline on the primary endpoint is superior to a pre-specified performance goal (derived from the external natural history data) will be calculated. A probability >90% will be considered a positive result.
The following workflow maps the journey of a patient through this combined trial protocol.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of a complex combined trial relies on a suite of critical reagents and technologies.
Table 2: Essential Research Reagents and Materials for Stem Cell Trial Protocols
| Item/Category | Function/Application | Specific Examples & Notes |
|---|---|---|
| GMP-Grade iPSC Line | Master cell bank serving as the starting material for the therapeutic product. | Requires comprehensive characterization (karyotyping, pluripotency markers, viral screening). REPROCELL StemRNA Clinical Seed iPSCs are an example of a platform with an FDA Drug Master File (DMF) [2]. |
| Directed Differentiation Kits | To differentiate pluripotent stem cells into the desired therapeutic cell type (e.g., dopaminergic neurons). | Xeno-free, GMP-grade media and differentiation factors are critical for regulatory compliance and batch consistency [15]. |
| Cell Characterization Antibodies | To confirm cell identity, purity, and potency through flow cytometry and immunocytochemistry. | Target-specific (e.g., FOXA2, LMX1A for midbrain dopaminergic neurons) and pluripotency (e.g., OCT4, NANOG) markers. |
| Critical Process Parameter Assays | To monitor and control the manufacturing process. | Metabolite analysis (e.g., glucose consumption), cell density, and viability measurements. |
| Biomarker Assay Kits | To measure pharmacodynamic and efficacy biomarkers in patient samples. | ELISA or SIMOA kits for biomarkers like neurofilament light chain (NfL) in CSF/serum; PK/PD assays for gene therapies. |
| Digital Health Technologies (DHTs) | To capture objective, real-world data on disease progression and motor function. | Wearable sensors to quantify gait, tremor, or physical activity in patients' daily lives [40] [41]. |
Combined Phase I/II trials are a powerful, regulatory-endorsed strategy for efficiently advancing promising stem cell therapies to patients with rare diseases. By integrating adaptive designs, Bayesian statistics, and robust biomarker strategies, sponsors can generate the substantial evidence needed for regulatory decisions while respecting the ethical and practical constraints of small populations. As the field progresses, the continued collaboration between researchers, regulators, and patient communities will be essential to refine these designs and accelerate the delivery of transformative treatments.
Incorporating Biomarkers for Patient Stratification and Early Efficacy Readouts
The integration of biomarkers into clinical trial design is transforming the development of stem cell therapies. Biomarkers provide objective, measurable indicators of biological processes, pathogenic processes, or pharmacological responses to therapeutic interventions [45]. In the context of stem cell clinical trials spanning phases I to III, they serve two critical functions: enabling precise patient stratification and providing early efficacy readouts. Well-conducted clinical trials provide data to support decision-making for healthcare policy, guidelines, and clinical practice, and biomarkers are increasingly central to these trials [46]. For stem cell therapies, this is particularly crucial given their complex mechanisms of action, significant costs, and potential variability in patient response.
The paradigm is shifting from traditional clinical endpoints to biomarker-informed approaches. A critical aspect worth emphasizing is that the purpose of most biomarker-guided clinical trials is to assess whether a biomarker demonstrates clinical utility or not—it is not primarily to demonstrate whether a treatment intervention is effective or not [46]. This distinction is fundamental for designing appropriate trials and interpreting their results accurately. For stem cell researchers, this means biomarkers can help determine which patient subgroups are most likely to benefit from specific stem cell products, potentially accelerating development and increasing the probability of technical and regulatory success.
Biomarker-Guided Patient Stratification
Rationale and Strategic Importance
Patient stratification using biomarkers addresses the fundamental challenge of heterogeneity in patient populations. This heterogeneity often obscures treatment effects in unselected populations, leading to failed trials even for potentially effective therapies. Biomarker-guided stratification enables precision medicine approaches by identifying patient subgroups based on molecular profiles, disease mechanisms, or predicted treatment responses.
The power of this approach was demonstrated in a re-analysis of the AMARANTH Alzheimer's trial, where an AI-guided predictive prognostic model (PPM) stratified patients into slow and rapid progressors using baseline biomarkers (β-amyloid, APOE4, and medial temporal lobe gray matter density) [47]. This stratification revealed a 46% slowing of cognitive decline in the slow-progressor subgroup treated with lanabecestat 50 mg compared to placebo—an effect completely masked in the unstratified population [47]. This has direct parallels to stem cell trials, where identifying the right patient subgroups is equally critical.
Biomarker Types and Methodologies for Stratification
Multiple biomarker classes can be employed for patient stratification in stem cell trials, each with distinct applications and methodological considerations:
- Molecular Biomarkers: Genetic, proteomic, and metabolomic profiles can identify patients with specific disease endotypes likely to respond to stem cell mechanisms of action. For autoimmune diseases, biomarkers of specific immune activation pathways (e.g., Th1, Th17) can stratify patients for mesenchymal stem cell (MSC) therapy focused on immunomodulation [48].
- Quantitative Imaging Biomarkers: These provide sensitive, specific, accurate, and reproducible imaging measures of anatomical structures, functional processes, and molecular interactions [45]. In osteoarthritis trials, cartilage volume and composition measurements from MRI can stratify patients for MSC therapies targeting cartilage regeneration [49].
- Multi-Omics Integration: Combining genomics, transcriptomics, and proteomics provides a comprehensive view of biological systems. Multi-omics approaches have transformed cancer research by providing a comprehensive view of tumor biology, enabling stratification based on gene mutations, pathway activity, and immune landscape [50]. Similar approaches can identify distinct patient subgroups in stem cell therapy for degenerative diseases.
- Spatial Biology Technologies: These preserve tissue architecture context, revealing how cells interact within their microenvironment. Key technologies include spatial transcriptomics, spatial proteomics, and multiplex immunohistochemistry [50].
Table 1: Biomarker Types for Patient Stratification in Stem Cell Trials
| Biomarker Category | Specific Modalities | Application in Stem Cell Trials | Technical Considerations |
|---|---|---|---|
| Molecular | Genetic markers, Protein signatures, Metabolic profiles | Identify patients with specific molecular pathways amenable to stem cell mechanisms | Requires validated assays; sample collection standardization |
| Quantitative Imaging | MRI, CT, PET, ultrasound | Assess structural disease severity and progression potential | Standardized acquisition protocols; central reading |
| Multi-Omics | Genomics, Transcriptomics, Proteomics | Comprehensive patient subtyping based on integrated biological data | Data integration challenges; computational resources |
| Spatial Biology | Spatial transcriptomics, Multiplex IHC/IF | Understand cellular interactions in tissue microenvironment | Tissue preservation; complex data analysis |
Protocol: Implementing Biomarker-Guided Stratification
Objective: To stratify patients for stem cell clinical trials using validated biomarkers predictive of treatment response.
Materials:
- Patient biological samples (blood, tissue, biofluids)
- Biomarker analysis platforms (sequencing, immunoassays, imaging)
- Clinical data collection forms
- Statistical analysis software with biomarker analysis capabilities
Procedure:
Biomarker Discovery and Validation:
Clinical Assay Development:
- Develop standardized operating procedures for sample collection, processing, and analysis.
- Establish quality control measures for biomarker measurements.
- Validate assay performance in the target patient population.
Trial Implementation:
- Incorporate biomarker testing into screening procedures.
- Pre-specify stratification algorithms in the statistical analysis plan.
- Randomize patients within biomarker-defined subgroups.
Data Analysis:
- Test for biomarker-treatment interaction effects [46].
- Compare outcomes between biomarker-stratified and non-stratified approaches.
The following diagram illustrates the workflow for biomarker-guided patient stratification:
Figure 1: Workflow for biomarker-guided patient stratification in clinical trials
Early Efficacy Readouts in Stem Cell Trials
The Need for Early Efficacy Assessment
Traditional clinical endpoints in stem cell trials often require extended follow-up periods to detect meaningful changes in disease progression. For chronic conditions such as osteoarthritis, neurodegenerative diseases, and autoimmune disorders, this conventional approach results in prolonged and costly clinical development programs. Early efficacy readouts address this challenge by providing quantitative indicators of biological activity before changes in clinical manifestations become apparent.
In the context of stem cell therapies, early efficacy biomarkers can demonstrate proof-of-concept that the administered cells are engrafting, surviving, and exerting their intended biological effects. For example, in trials of intra-articular MSC injections for knee osteoarthritis, imaging biomarkers can detect structural changes in cartilage months or years before differences in pain or function become statistically significant [49]. Similarly, in neurological applications, quantitative imaging biomarkers and molecular markers can detect therapeutic effects early in the treatment course [45] [47].
Biomarker Classes for Early Efficacy Assessment
Different biomarker classes provide complementary information for early efficacy assessment:
- Quantitative Imaging Biomarkers: In MSC therapy for osteoarthritis, MRI-based cartilage thickness, volume, and composition measurements can serve as early efficacy readouts. The Osteoarthritis Initiative (OAI) has developed public resources to facilitate the scientific evaluation of biomarkers for osteoarthritis as potential surrogate endpoints [45].
- Molecular Biomarkers: For MSC therapies targeting immunomodulation, changes in inflammatory cytokines (e.g., IL-6, TNF-α) and immune cell populations following treatment can provide early evidence of biological activity [52] [48].
- Functional Biomarkers: Electrophysiological measures, metabolic imaging, and physiological testing can detect functional improvements before structural or clinical changes manifest.
Table 2: Early Efficacy Biomarkers in Stem Cell Trials
| Therapeutic Area | Stem Cell Type | Early Efficacy Biomarkers | Endpoint Correlation |
|---|---|---|---|
| Osteoarthritis | Mesenchymal Stem Cells | Cartilage volume/thickness (MRI), biomarker levels (e.g., collagen fragments) [49] | Long-term joint preservation, WOMAC scores |
| Autoimmune Diseases | MSCs, HSCs | Inflammatory cytokines (IL-6, TNF-α), regulatory T-cell populations [52] [48] | Clinical remission rates, disease activity scores |
| Neurodegenerative | MSCs, Neural Stem Cells | Quantitative MRI (volumetry, diffusion), amyloid/tau PET, neurofilament levels [47] | Cognitive decline rates, functional scales |
| Cardiovascular | MSCs, Cardiac Stem Cells | Myocardial perfusion (MRI), ejection fraction, infarct size | Exercise capacity, major adverse cardiac events |
Protocol: Implementing Early Efficacy Assessment
Objective: To establish and validate early efficacy biomarkers for stem cell clinical trials.
Materials:
- Biomarker measurement platforms (imaging, laboratory, functional)
- Standardized operating procedures for biomarker assessment
- Data management systems for longitudinal biomarker data
Procedure:
Biomarker Selection:
- Identify candidate early efficacy biomarkers through preclinical models and prior clinical studies.
- Prioritize biomarkers with strong biological rationale and technical feasibility.
- Establish standardized measurement protocols.
Trial Integration:
- Schedule biomarker assessments at baseline and early post-treatment timepoints (e.g., 1, 3, and 6 months).
- Implement blinding procedures for biomarker assessment.
- Collect concurrent clinical data for correlation analyses.
Statistical Analysis:
- Analyze rate of change in early efficacy biomarkers between treatment groups.
- Establish relationship between early biomarker changes and final clinical outcomes.
- Use longitudinal statistical models to account for repeated measures.
The relationship between early biomarker changes and clinical outcomes follows a predictable temporal sequence:
Figure 2: Temporal sequence of biomarker and clinical outcome assessment
Integrated Protocol: Biomarker Implementation Across Trial Phases
Phase-Specific Biomarker Strategies
Successful incorporation of biomarkers requires phase-appropriate strategies across the clinical development pathway:
Phase I Trials:
- Focus on safety biomarkers and proof-of-concept biomarkers
- Establish biomarker assay feasibility and variability
- Identify potential stratification biomarkers for later-phase trials
- Assess dose-response relationships using pharmacodynamic biomarkers
Phase II Trials:
- Refine patient stratification biomarkers
- Validate early efficacy biomarkers
- Establish correlation between biomarker changes and clinical outcomes
- Use biomarker data to inform phase III trial design and go/no-go decisions
Phase III Trials:
- Implement definitive biomarker-stratified designs
- Validate early efficacy biomarkers as potential surrogate endpoints
- Collect biomarker data for subgroup analyses and personalized medicine applications
Comprehensive Biomarker Validation Protocol
Objective: To establish analytical and clinical validity of biomarkers for stem cell trials.
Materials:
- Sample collection and processing materials
- Biomarker analysis platforms
- Statistical analysis software
- Clinical data collection systems
Procedure:
Analytical Validation:
- Establish precision (intra- and inter-assay variability)
- Determine accuracy and linearity
- Define reference ranges and cut-points using ROC analysis [51]
- Verify sample stability and pre-analytical variables
Clinical Validation:
- Assess biomarker distribution in target population
- Establish association with disease characteristics or clinical outcomes
- Determine biomarker performance characteristics (sensitivity, specificity)
- Validate in independent cohorts when possible
Qualification for Context of Use:
- Demonstrate suitability for intended application (stratification, early efficacy)
- Obtain regulatory feedback on biomarker strategy
- Establish clinical utility for decision-making
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for Biomarker Studies in Stem Cell Research
| Reagent/Solution Category | Specific Examples | Application in Biomarker Research | Key Considerations |
|---|---|---|---|
| Cell Characterization | Flow cytometry antibodies (CD73, CD90, CD105), differentiation kits | Verify stem cell identity and purity prior to administration | Standardized panels for MSC characterization; functional potency assays |
| Molecular Analysis | RNA/DNA extraction kits, PCR/qPCR reagents, sequencing kits | Genetic and transcriptomic biomarker analysis | Sample stability; normalization controls; quality metrics |
| Protein Detection | ELISA kits, multiplex immunoassays, mass spectrometry reagents | Protein biomarker quantification and discovery | Dynamic range; specificity; matrix effects |
| Imaging Contrast Agents | MRI contrast agents, PET tracers, fluorescent labels | Quantitative imaging biomarker acquisition | Dose optimization; kinetic modeling; safety monitoring |
| Cell Tracking Reagents | Magnetic nanoparticles, radiolabels, genetic reporters | Stem cell localization and persistence post-transplantation | Sensitivity; quantification; correlation with efficacy |
| Data Integration Tools | Multi-omics integration platforms, bioinformatics pipelines | Integrative biomarker analysis and patient stratification | Data standardization; computational infrastructure |
The strategic incorporation of biomarkers for patient stratification and early efficacy assessment represents a paradigm shift in stem cell clinical trial design. These approaches address fundamental challenges in drug development by reducing patient heterogeneity, providing earlier indicators of biological activity, and enabling more efficient trial designs. The promising results from biomarker-guided trials in other therapeutic areas, including the demonstrated ability to rescue apparently "failed" trials through post-hoc stratification [47], provide a compelling rationale for their application in stem cell development.
Successful implementation requires careful attention to biomarker validation, appropriate statistical designs, and integration across preclinical and clinical development. As the field advances, biomarkers are poised to play an increasingly central role in realizing the full potential of stem cell therapies through precision medicine approaches. Future directions include the development of novel biomarkers reflecting stem cell-specific mechanisms of action, advanced analytical methods for multi-omics integration, and standardized biomarker frameworks across the stem cell field.
Addressing Critical Challenges in Manufacturing, Safety, and Efficacy
For stem cell therapies transitioning from laboratory research to clinical application, ensuring product quality is a foundational requirement for patient safety and regulatory success. Within the context of Phase I-III clinical trials, this involves establishing a robust framework that integrates Good Manufacturing Practice (GMP) with rigorous donor screening and comprehensive strategies to control genomic instability. Adherence to these principles protects research participants from immediate risks such as contamination and transmission of infectious diseases, while also mitigating long-term oncological risks associated with culture-acquired genetic variants. This document outlines practical protocols and application notes to guide researchers and drug development professionals in building quality-centric development pipelines for stem cell-based Investigational Medicinal Products (ATMPs).
GMP-Compliant Manufacturing in Clinical Trials
Core Principles and Phase-Appropriate Implementation
GMP provides the quality management system for ensuring that stem cell products are consistently produced and controlled according to quality standards appropriate for their intended clinical use [53]. The core objective is to prevent contamination, ensure traceability, and guarantee that the product's critical quality attributes (CQAs)—such as identity, purity, viability, and potency—are consistently met [53]. For early-phase trials, a phased implementation of GMP is often acceptable, where the stringency of controls increases as the product advances through clinical development stages [15].
Key GMP Requirements for Stem Cell-Based ATMPs:
- Aseptic Processing: Traditional sterilization by filtration or heat is not feasible for live cell products. Instead, manufacturing must occur under validated aseptic conditions, supported by media fill simulations to prove process efficacy [53].
- Process Validation: The manufacturing process must be designed and controlled to consistently achieve the CQAs identified during non-clinical, GLP-compliant studies [53].
- Quality Control (QC) Systems: All reagents and processes must be governed by standard operating procedures (SOPs) and a comprehensive quality management system [15].
- Facility and Equipment: GMP-compliant facilities must be designed to minimize contamination risk, often utilizing closed, automated systems like bioreactors for scalable cell expansion [53].
Application Note: A GMP Protocol for Hematopoietic Stem Cell Gene Therapy
The following protocol, adapted from a first-in-man study for Mucopolysaccharidosis type II (MPSII), illustrates a GMP workflow for ex vivo gene therapy [54].
Table: Critical Reagents and Materials for GMP HSC Gene Therapy
| Research Reagent / Material | Function in Protocol | GMP Consideration |
|---|---|---|
| Lentiviral Vector | Gene delivery vehicle for inserting functional gene (e.g., IDS.ApoEII). | Must be produced under GMP; requires full characterization and safety testing (e.g., replication-competent lentivirus assays). |
| Transduction Enhancers (LentiBOOST, Protamine Sulfate) | Improve gene transfer efficiency into HSCs. | Quality must be certified; inclusion can reduce required vector quantity, improving feasibility and safety. |
| CD34+ Cell Selection Kit | Isolation of target Hematopoietic Stem/Progenitor Cells from patient apheresis. | For clinical use, must be a closed-system, validated, and approved for human application. |
| Cell Culture Media & Cytokines | Supports cell survival, maintenance, and expansion during ex vivo culture. | Must be xeno-free or chemically defined where possible; sourced from GMP-compliant suppliers. |
Detailed GMP Protocol:
- Patient Apheresis and Cell Selection: Perform leukapheresis on the conditioned patient. Isulate CD34+ hematopoietic stem cells using a clinical-grade, closed-system magnetic selection kit.
- Pre-Transduction Culture: Culture the selected CD34+ cells in GMP-grade media supplemented with cytokines (e.g., SCF, TPO, FLT3-L) to promote cell viability and priming for transduction.
- Lentiviral Transduction:
- Pre-load the culture bag with the GMP-grade transduction enhancers (e.g., LentiBOOST and protamine sulfate).
- Add the GMP-produced lentiviral vector to the bag at the predetermined Multiplicity of Infection (MOI).
- Introduce the CD34+ cell suspension and incubate for 18-24 hours under controlled conditions (37°C, 5% CO2).
- Post-Transduction Wash and Formulation: Wash the transduced cells to remove residual vector and enhancers. Formulate the final cell product in infusion medium compatible with human administration.
- Quality Control and Release Testing: Perform in-process and lot-release testing. This includes:
- Viability and Cell Count: Using trypan blue exclusion or an automated cell counter.
- Potency Assay: Measure transduction efficiency via flow cytometry for the transgene.
- Sterility Tests: Conduct BacT/ALERT for bacterial and fungal contamination.
- Endotoxin Testing: Limulus Amebocyte Lysate (LAL) assay to ensure levels are below the threshold.
- Vector Copy Number (VCN) Assessment: To confirm appropriate genetic modification and rule out excessive integration.
- Cryopreservation and Storage: Cryopreserve the final product in a controlled-rate freezer and store in the vapor phase of liquid nitrogen until patient infusion.
Donor Screening and Cell Bank Qualification
Regulatory Framework and Screening Requirements
Donor eligibility determination is a critical first step in the supply chain for allogeneic stem cell products. Regulatory agencies like the FDA and EMA require rigorous screening and testing of donors and the resulting cell banks to mitigate the risk of transmitting infectious diseases [55] [15]. This is especially crucial for pluripotent stem cell lines, which can be expanded indefinitely and potentially administered to numerous recipients.
Key Recommendations for Donor Screening [55] [15]:
- Donor Medical History: A comprehensive review including travel history, infectious disease risk factors, and sexual history.
- Physical Assessment: To identify signs of relevant communicable diseases.
- Blood Testing: For specific communicable disease agents, including HIV-1/2, HBV, HCV, HTLV, Syphilis (Treponema pallidum), and Chlamydia trachomatis & Neisseria gonorrhoeae.
- Additional Considerations: For hESC lines derived from donated embryos, direct screening of the gamete donors at the time of derivation may not be feasible. In such cases, the master cell bank must be thoroughly tested for adventitious agents [15].
Application Note: Protocol for Establishing a Qualified Master Cell Bank (MCB) from Donor Tissue
This protocol outlines the steps from tissue procurement to the creation of a clinically usable MCB, with a focus on iPSCs.
Detailed Protocol:
- Informed Consent: Obtain written, legally valid informed consent from the donor. The consent must explicitly cover research and therapeutic use, potential for commercial application, and disclosure of incidental findings [15].
- Tissue Procurement: Collect donor tissue (e.g., skin biopsy, peripheral blood) under universal precautions. The procurement process should follow regulatory guidelines for human tissue, though full GMP may not be mandatory at this initial stage depending on the jurisdiction [15].
- Donor Screening and Testing: Collect a blood sample from the donor for required infectious disease testing, following 21 CFR Part 1271, Subpart C and relevant EMA guidelines [55] [15]. Quarantine the donor tissue until test results are confirmed negative.
- Reprogramming and Clone Selection: Reprogram somatic cells using a non-integrating, clinically compliant method (e.g., Sendai virus, episomal plasmids, or mRNA) [56]. Pick and expand multiple iPSC clones to allow for subsequent selection of the most suitable line.
- Master Cell Bank Generation: Expand a selected iPSC clone under controlled, GMP-guided conditions. Cryopreserve a large number of vials at an early passage to establish the MCB.
- MCB Qualification and Release Testing:
- Identity: Short tandem repeat (STR) profiling to match the MCB to the donor.
- Sterility: Tests for bacteria, fungi, and mycoplasma.
- Viral Safety: In vitro and in vivo adventitious virus assays; specific PCR testing for relevant viruses.
- Potency: Demonstrate pluripotency (e.g., by in vitro trilineage differentiation or PluriTest).
- Genetic Integrity: Perform G-band karyotyping and higher-resolution analysis (see Section 3.2).
- Viability and Cell Count: Post-thaw viability must meet pre-defined release criteria (e.g., >80%).
Table: Donor Screening and MCB Testing Overview
| Stage | Test/Assessment | Method/Standard | Purpose |
|---|---|---|---|
| Donor Screening | Medical & Behavioral History | Donor History Questionnaire (FDA Guidance) | Identify risk factors for communicable diseases [55]. |
| Infectious Disease Serology | FDA-licensed/approved tests for HIV, HBV, HCV, etc. | Detect active or prior infection [55] [15]. | |
| MCB Qualification | Identity | STR DNA Profiling | Confirm donor origin and unique identity of the cell line. |
| Sterility | BacT/ALERT, Mycoplasma PCR | Ensure freedom from microbial contamination [54]. | |
| Viral Safety | In vitro & in vivo virus tests, specific PCR | Confirm absence of adventitious viruses [15]. | |
| Potency | PluriTest / Trilineage Differentiation | Verify functional pluripotency of the iPSC line. | |
| Genetic Integrity | G-band Karyotyping & NGS-based profiling | Detect chromosomal abnormalities and oncogenic variants [57]. |
Controlling Genomic Instability in Stem Cell Products
The Challenge of Culture-Acquired Genetic Variants
Prolonged in vitro culture exerts selective pressure on stem cells, leading to the emergence of clones with genetic mutations that confer a growth advantage [57]. These culture-acquired genetic variants pose a significant safety risk, as they can alter differentiation potential, lead to functional deficiencies, and, most critically, increase the risk of tumor formation (tumorigenicity) upon transplantation [53] [57]. Common recurrent abnormalities in human iPSCs include gains of chromosomes 1, 12, 17, and 20 [57].
Regulatory guidance from the FDA, EMA, and PMDA emphasizes a risk-based, stage-appropriate testing strategy for genetic stability [57]. The extent of testing is informed by factors such as the degree of cell manipulation, route of administration, and the expected persistence of the product in the body.
Application Note: A Risk-Stratified Protocol for Genomic Stability Testing
This protocol provides a methodology for monitoring and controlling genomic instability from the initial clone selection through to the final product.
Detailed Protocol:
- Risk Stratification of iPSC Clones: Early in development, profile multiple clones to select the one with the lowest inherent risk. The risk profile is based on:
- Reprogramming Method: Non-integrating methods (e.g., mRNA) pose lower risk than integrating viruses.
- Donor Age: Older donors may have somatic mutations present in the starting tissue.
- Passage Number: Lower-passage clones are generally preferred to minimize culture-acquired variants.
- Initial Genetic Test Results: Clones with normal karyotypes and no oncogenic mutations are lower risk [57].
- Genetic Stability Monitoring Plan: Implement a testing plan aligned with the clinical development stage.
- Early Research/Clone Selection: Use high-sensitivity Next-Generation Sequencing (NGS) to profile a panel of well-established driver genes (e.g., TP53, KRAS, BCOR) in addition to G-band karyotyping [57].
- MCB & Working Cell Bank (WCB) Testing: Perform G-band karyotyping and high-resolution NGS-based oncogenetic profiling. Low-pass Whole Genome Sequencing (lpWGS) can be a cost-effective alternative for detecting chromosomal abnormalities.
- End-of-Production Cells: Test the final differentiated cell product or cells that have undergone the complete manufacturing process to confirm the absence of genomic alterations induced during differentiation and expansion.
- Tumorigenicity Testing: For pluripotent stem cell-derived products, validate the removal of undifferentiated cells. The gold standard assay is the in vivo teratoma assay in immunocompromised mice to confirm the absence of residual pluripotent cells [53]. For somatic cell-based therapies, tumorigenicity is assessed using in vivo studies in immunocompromised models rather than teratoma tests [53].
Table: Genomic Stability Testing Methods and Applications
| Testing Method | Resolution / Capability | Typical Application | Regulatory Context |
|---|---|---|---|
| G-band Karyotyping | Low (~5-10 Mb). Detects gross chromosomal abnormalities. | MCB release testing; in-process monitoring at key passages. | Standard requirement for identifying aneuploidy and large structural variants [57]. |
| NGS-Based Oncogenetic Profiling | High (single nucleotide). Detects mutations in specific cancer-associated genes. | Risk stratification of clones; lot-release testing for high-risk products. | Recommended by FDA/EMA for detecting oncogenic variants; part of a risk-based strategy [57]. |
| In Vivo Teratoma Assay | Functional assay for pluripotency and tumorigenic potential. | Validation of PSC-derived products to ensure removal of undifferentiated cells. | Required for pluripotent stem cell-based products to assess the risk of teratoma formation [53]. |
| Digital Soft Agar Assay | Sensitive in vitro assay for detecting rare transformed cells. | Alternative or supplement to in vivo tumorigenicity studies for somatic cell products. | Emerging sensitive method recommended over conventional soft agar assays [53]. |
Integrating robust GMP manufacturing, exhaustive donor screening, and vigilant genomic stability control is non-negotiable for the successful and ethical translation of stem cell therapies through clinical trials. The protocols and application notes outlined here provide a actionable framework for researchers. As the field advances with over 115 global clinical trials involving pluripotent stem cells [2], the commitment to product quality will be the ultimate determinant in fulfilling the therapeutic promise of regenerative medicine for patients.
Responsible clinical translation of stem cell-based therapies demands rigorous safety assessment protocols to address unique biological risks. Key challenges include the potential for tumorigenicity from residual undifferentiated cells, immunogenic reactions to allogeneic products, and unknown long-term outcomes [58] [59]. This application note provides a structured framework for preclinical safety assessment and long-term surveillance, aligning with regulatory expectations from the FDA, EMA, and International Society for Stem Cell Research (ISSCR) guidelines [10] [15]. Implementing these standardized protocols ensures patient safety while generating robust data to support phase I-III clinical trial progression.
Tumorigenicity Risk Assessment and Mitigation
Risk Profiling and Elimination Strategies
The tumorigenic potential of stem cell products primarily arises from residual undifferentiated pluripotent stem cells (PSCs) that may form teratomas or acquire oncogenic mutations during culture expansion [58] [59]. Risk correlates with the proportion of residual PSCs, their proliferative capacity, and the tumorigenic potential of the final product.
Table 1: Strategies for Elimination of Tumorigenic Pluripotent Stem Cells
| Method Category | Specific Approach | Mechanism of Action | Reported Efficiency | Key Limitations |
|---|---|---|---|---|
| Physical Separation | Density gradient centrifugation; Membrane filtration | Separates cells based on size/density differences | >80% reduction | Potential for PSC retention in differentiated fraction |
| Antibody-Based | Magnetic-activated cell sorting (MACS); Fluorescence-activated cell sorting (FACS) | Targets PSC-specific surface markers (e.g., TRA-1-60, SSEA-4) | 2-4 log reduction | Cell surface marker disruption; viability loss |
| Pharmacological | Small molecule inhibitors | Targets PSC-specific pathways (e.g., HDAC, ROCK) | >99% elimination | Potential off-target effects on differentiated cells |
| Genetic Modification | Suicide gene insertion | Enables selective ablation of proliferating PSCs | >99.9% elimination | Genetic modification regulatory concerns |
Current elimination strategies predominantly target PSC-specific markers, with no single method achieving perfect clearance. A combination approach is recommended for clinical applications [59].
Experimental Protocols for Tumorigenicity Assessment
Protocol 1: In Vivo Teratoma Formation Assay
- Objective: Assess the potential of residual PSCs to form teratomas in immunocompromised animals.
- Materials: NOD-scid IL2Rgamma[null] (NSG) mice, Matrigel, cell preparation, imaging equipment.
- Procedure:
- Prepare serial dilutions of the final cell product (e.g., 10³, 10⁴, 10⁵, 10⁶ cells per injection).
- Mix cells with Matrigel (1:1 ratio) to enhance engraftment.
- Inject subcutaneously or under the kidney capsule of NSG mice (n=10 per group).
- Monitor weekly for tumor formation over 6-9 months.
- Perform histopathological analysis of suspected tumors for three germ layer differentiation.
- Validation: The assay should detect teratoma formation from as few as 10,000 undifferentiated PSCs [58] [59].
Protocol 2: Soft Agar Colony Formation Assay
- Objective: Evaluate anchorage-independent growth as an indicator of transformation potential.
- Materials: Base agar, top agar, cell culture medium, crystal violet stain.
- Procedure:
- Prepare 1.2% base agar in culture medium and solidify in 6-well plates.
- Mix 5×10³ cells with 0.7% top agar and layer over base agar.
- Culture for 3-4 weeks with regular medium changes.
- Stain colonies with crystal violet and count using automated colony counter.
- Acceptance Criteria: <0.1% colony formation efficiency compared to positive controls [58].
The experimental workflow for tumorigenicity assessment integrates both in vitro and in vivo methods to comprehensively evaluate risk.
Immunogenicity Risk Management
Immunological Safety Criteria
Immunogenicity risks vary significantly between autologous and allogeneic products. Allogeneic cells may trigger host immune responses through allorecognition, while autologous cells may still elicit immune reactions if genetically modified or differentiated into novel cell types [58] [15]. Key immunological safety parameters include:
- Innate immunity activation: Complement activation, neutrophil and macrophage responses
- Adaptive immunity: T-cell and B-cell responses, antibody production
- Human Leukocyte Antigen (HLA) matching: Degree of disparity between donor and recipient
- Immunomodulatory properties: Secretion of cytokines and growth factors that may alter host immune function
Experimental Protocols for Immunogenicity Assessment
Protocol 3: Mixed Lymphocyte Reaction (MLR) Assay
- Objective: Measure T-cell activation in response to allogeneic stem cell products.
- Materials: Peripheral blood mononuclear cells (PBMCs) from healthy donors, irradiated test cells, flow cytometry with activation markers.
- Procedure:
- Isolate PBMCs from multiple donors representing common HLA types.
- Irradiate test stem cell products (3000 rad) to prevent proliferation.
- Co-culture PBMCs with test cells at 10:1 ratio for 5-7 days.
- Measure T-cell proliferation via ³H-thymidine incorporation or CFSE dilution.
- Analyze activation markers (CD69, CD25) and cytokine secretion (IFN-γ, IL-2).
- Interpretation: >2-fold increase in proliferation compared to syngeneic control indicates significant immunogenicity [58].
Protocol 4: Complement-Dependent Cytotoxicity Assay
- Objective: Assess susceptibility of cell products to complement-mediated lysis.
- Materials: Human serum complement, antibody-mediated cross-linking reagents, viability stains.
- Procedure:
- Incubate stem cell products with human serum (10-50%) as complement source.
- Add anti-HLA antibodies for cross-linking where applicable.
- Measure cell lysis after 60-90 minutes using LDH release or flow cytometry with viability dyes.
- Calculate percentage specific lysis compared to no-complement controls.
- Application: Critical for assessing allogeneic products with HLA mismatches [58].
Table 2: Immunogenicity Testing Matrix for Stem Cell Products
| Test Method | Immune Parameter Measured | Cell Product Types | Phase Applicability | Acceptance Criteria |
|---|---|---|---|---|
| Mixed Lymphocyte Reaction | T-cell activation and proliferation | Allogeneic products | Preclinical - Phase I | <2-fold increase vs control |
| Cytokine Release Assay | Pro-inflammatory cytokine secretion | Allogeneic, Genetically modified | Preclinical - Phase I | Absence of cytokine storm profile |
| HLA Typing | Donor-recipient mismatch level | Allogeneic products | Preclinical - Phase III | Match level per trial design |
| Complement Cytotoxicity | Serum-mediated cell lysis | Allogeneic products | Preclinical - Phase I | <20% specific lysis |
| Immunophenotyping | Cell surface marker expression | All products | Preclinical - Phase III | Consistent with product specifications |
Long-Term Safety Surveillance and Biodistribution
Comprehensive Safety Monitoring Framework
Long-term safety surveillance extends beyond initial administration to detect delayed adverse events, including ectopic tissue formation, late-onset immunogenicity, and malignant transformation [58] [60]. The ISSCR guidelines emphasize that "clinical testing should never allow promise for future patients to override the welfare of current research subjects" [10].
Table 3: Long-Term Safety Surveillance Parameters
| Monitoring Category | Specific Parameters | Frequency | Detection Methods |
|---|---|---|---|
| Biodistribution | Engraftment efficiency, ectopic tissue formation | 1, 3, 6, 12 months | qPCR, PET, MRI, bioluminescence |
| Tumorigenicity | Teratoma formation, malignant transformation | 6, 12, 24 months | Physical exam, imaging, histopathology |
| Systemic Toxicity | Multi-organ function, hematological parameters | 1, 3, 6, 12, 24 months | Clinical chemistry, hematology, urinalysis |
| Immunological | Autoimmunity, sensitization, chronic inflammation | 3, 6, 12, 24 months | Antibody detection, T-cell assays, cytokine profiling |
| Functional Outcomes | Product functionality, integration | 6, 12, 24 months | Organ-specific function tests, imaging |
Experimental Protocols for Long-Term Monitoring
Protocol 5: Biodistribution Assessment Using Quantitative PCR
- Objective: Track and quantify stem cell persistence and distribution in target and non-target tissues.
- Materials: Tissue samples (heart, liver, lungs, kidneys, brain, gonads), DNA extraction kit, species-specific primers.
- Procedure:
- Extract genomic DNA from tissues at multiple time points post-administration.
- Design human-specific Alu sequence primers for human cells in animal models.
- Perform quantitative PCR with standard curve of known human cell numbers.
- Normalize results to total DNA content and calculate cells per gram tissue.
- Compare distribution patterns between target and non-target organs.
- Sensitivity: Detection limit of 10-50 human cells per million animal cells [58].
Protocol 6: In Vivo Imaging for Cell Fate Tracking
- Objective: Non-invasive monitoring of cell localization, survival, and proliferation.
- Materials: Firefly luciferase-transduced cells, IVIS imaging system, D-luciferin substrate.
- Procedure:
- Engineer cells to express luciferase reporter gene during manufacturing.
- Administer cells to animal models via intended clinical route.
- Inject D-luciferin substrate (150 mg/kg) intraperitoneally.
- Acquire bioluminescence images at regular intervals (e.g., weekly for 3 months).
- Quantify signal intensity and correlate with cell numbers using standard curves.
- Applications: Real-time monitoring of cell migration, persistence, and clearance [58].
The long-term safety surveillance strategy integrates multiple complementary methods to track cell fate and detect potential adverse effects throughout the product lifecycle.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Safety Assessment
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Cell Culture Media | mTeSR1, StemFlex, Xeno-free media | Maintain stem cell pluripotency and viability | Use defined, GMP-grade for clinical lot production |
| Cell Separation Reagents | MACS PSC Removal Cocktail, FACS antibodies | Deplete undifferentiated PSCs | Combine multiple surface markers (SSEA-4, TRA-1-60) |
| Molecular Analysis Kits | qPCR Alu detection kits, Karyostat+ assay | Biodistribution and genomic stability | Validate species-specific primers for sensitivity |
| In Vivo Imaging Agents | D-luciferin, ¹⁸F-FDG PET tracers | Non-invasive cell tracking | Correlate signal intensity with cell numbers |
| Immunogenicity Assays | IFN-γ ELISpot, multiplex cytokine panels | Detect immune activation | Use human AB serum to avoid xenogeneic responses |
| Toxicity Testing Kits | LDH cytotoxicity, metabolic activity assays | Assess general toxicity | Include positive and negative controls |
| Genomic Stability Tools | Karyotyping, CNV analysis arrays | Detect genetic abnormalities | Monitor throughout culture expansion |
Implementing a comprehensive safety assessment framework is essential for responsible clinical translation of stem cell therapies. The protocols outlined provide a systematic approach to address tumorigenicity, immunogenicity, and long-term safety across all trial phases. As the field advances with emerging technologies like genome editing and complex tissue-engineered products, these risk mitigation strategies must evolve through continued collaboration between researchers, clinicians, and regulators. Adherence to these evidence-based standards ensures patient protection while enabling the legitimate development of transformative stem cell therapies.
The transition of induced pluripotent stem cell (iPSC)-based therapies from research to clinical and commercial reality represents a paradigm shift in regenerative medicine. After more than two decades of development, the approval of iPSCs for manufacturing cell therapies to support clinical trials is now becoming realized [61]. However, manufacturing these therapies at the scale required for patient treatment and clinical trial enabling activities remains a significant challenge that the field must overcome [61]. The unique characteristic of iPSCs—their ability to differentiate into virtually any cell type—offers unprecedented therapeutic potential but introduces substantial complexity in manufacturing processes that must be rigorously controlled from pluripotent state to final differentiated product.
The International Society for Cell and Gene Therapy (ISCT) has recognized these challenges by establishing a Working Group on Emerging Regenerative Medicine Technologies, with iPSC-derived technologies expected to play a key role [61]. This article examines the current state of iPSC manufacturing optimization within the context of clinical trial design, providing researchers and drug development professionals with actionable strategies, detailed protocols, and quantitative frameworks for addressing the critical challenges of scalability and consistency in therapeutic development.
The Clinical Trial Landscape for iPSC-Based Therapies
Current Status and Therapeutic Areas
The clinical application of pluripotent stem cells (PSCs), including both iPSCs and embryonic stem cells (ESCs), has consolidated around several key therapeutic areas. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct PSC-derived products targeting indications primarily in three domains [2]:
- Ophthalmology: The eye offers advantages for initial therapy development, including local administration, relative immune privilege, and straightforward functional assessment.
- Neurology: Central nervous system (CNS) applications are advancing as delivery and differentiation protocols improve.
- Oncology: Investigational approaches include iPSC-derived immune cells for cancer therapy.
To date, more than 1,200 patients have been dosed with over 10¹¹ cells in PSC-based clinical trials, with no class-wide safety concerns identified [2]. This encouraging safety profile has supported continued regulatory approvals for investigational new drug (IND) applications and progression through structured Phase I-III trials, sometimes accelerated through FDA expedited programs such as the Regenerative Medicine Advanced Therapy (RMAT) designation [2].
Regulatory Considerations and Recent Approvals
The regulatory pathway for iPSC-based therapies requires careful navigation. It is crucial to distinguish between FDA authorization to begin clinical trials (IND) and full product approval under a Biologics License Application (BLA) [2]. Recent milestones demonstrate progress on both fronts:
Table 1: Recent FDA-Approved Stem Cell Therapies (2023-2025)
| Product Name | Approval Date | Cell Type | Indication |
|---|---|---|---|
| Omisirge | April 17, 2023 | Cord Blood-Derived Hematopoietic Progenitor Cells | Hematologic malignancies undergoing cord blood transplantation |
| Lyfgenia | December 8, 2023 | Autologous cell-based gene therapy | Sickle cell disease |
| Ryoncil | December 18, 2024 | Mesenchymal Stem Cells (MSCs) | Pediatric steroid refractory acute GVHD |
For iPSC-specific therapies, the landscape is rapidly evolving. In February 2025, the FDA granted IND clearance for Fertilo, the first iPSC-based therapy to enter U.S. Phase III trials, which uses ovarian support cells derived from clinical-grade iPSCs to support ex vivo oocyte maturation [2]. Additional iPSC-derived therapies have recently received FDA clearance for clinical trials, including OpCT-001 for retinal degeneration, neural progenitor cells for Parkinson's disease, spinal cord injury, and ALS, and FT819, an off-the-shelf, iPSC-derived CAR T-cell therapy for systemic lupus erythematosus [2].
Manufacturing Challenges and Scale-Up Considerations
Key Barriers in iPSC Therapy Commercialization
Manufacturing iPSC-based therapies at clinical and commercial scale presents multiple interconnected challenges that must be addressed systematically:
- Process Scalability: Transitioning from 2D adherent culture to 3D suspension systems capable of producing clinically relevant cell quantities
- Cost Management: Balancing expensive manufacturing processes with commercial viability
- Safety Assessment: Implementing robust tumorigenicity profiling and risk assessment protocols
- Regulatory Compliance: Adhering to GMP requirements while maintaining innovation
- Product Characterization: Developing meaningful critical quality attributes (CQAs) for complex living products
The ISCT Working Group has highlighted several specific considerations facing stem cell therapy developers, including development-stage specific manufacturing processes, decisions on when to implement automation, technology selection for expansion and differentiation, and integration of end-to-end manufacturing processes [61].
Quality by Design and Process Analytical Technologies
Implementing Quality by Design (QbD) approaches is increasingly essential for iPSC-based product development [61]. This systematic approach to development emphasizes:
- Quality Target Product Profile (QTPP): Defining the fundamental quality characteristics of the final product
- Critical Quality Attributes (CQAs): Identifying physical, chemical, biological, or microbiological properties that must be controlled
- Critical Process Parameters (CPPs): Determining process variables that directly impact CQAs
Design of Experiment (DOE) approaches are particularly valuable for increased product characterization, allowing researchers to understand complex interactions between multiple process variables efficiently [61]. When combined with Process Analytical Technologies (PAT), these approaches enable real-time monitoring and control of manufacturing processes to ensure consistent product quality.
Protocols for Scalable Manufacturing of iPSC-Derived β-Cells
Background and Rationale
Type 1 diabetes represents an attractive target for iPSC-based therapies due to the well-defined pathophysiology involving loss of pancreatic β-cells. While islet transplantation has demonstrated proof-of-concept, it faces limitations of donor availability and need for immunosuppression [62]. iPSC-derived β-cells offer a potential solution but require manufacturing processes capable of producing clinically relevant quantities of functional cells.
Recent advances have established differentiation protocols capable of generating insulin-producing cells from iPSCs, but most have been optimized in 2D systems that lack scalability [62]. Adherent culture methods become impractical at clinical scales due to surface area limitations, necessitating transition to 3D suspension culture systems.
Three-Stage Suspension Manufacturing Process
Yehya et al. (2024) developed a scalable manufacturing process for iPSC-derived insulin-producing β-cells implemented in 0.5L vertical wheel bioreactors [62] [63]. The process consists of three main stages:
- Transition from adherent to suspension culture using TB2 media to support iPSC growth during scaling
- Stage-wise differentiation with optimized timing and cytokine combinations
- Extended differentiation to enhance marker expression and maturation of islet-like clusters
Table 2: Key Process Parameters for iPSC-Derived β-Cell Differentiation
| Parameter Category | Specific Parameters | Impact on Product Quality |
|---|---|---|
| Bioreactor Operations | Media replenishment rate, Lactate accumulation, Aggregate size control | Influences metabolic profile and differentiation efficiency |
| Temporal Factors | Stage duration, Timing of cytokine exposure | Affects maturation and functional maturation |
| Environmental Conditions | Oxygenation, pH regulation, Shear stress | Impacts viability and differentiation specificity |
| Cell-Specific Factors | Seeding density, Cell line characteristics, Passage number | Affects reproducibility and batch-to-batch consistency |
The methodology employed two iPSC lines (RCP5005N and NCRM-1) maintained under standard conditions before bioreactor transfer [63]. For differentiation initiation, 90 million cells were seeded in 500 mL PBS vertical wheel bioreactors with TB10 media, followed by media replenishment after 24 hours before commencing differentiation protocols.
Process Optimization Using High Dimensional Design of Experiments
The research team employed an optimized High Dimensional Design of Experiments (HD-DoE) protocol specifically designed for scalability [62]. This approach enabled systematic investigation of multiple process parameters simultaneously, revealing that:
- Stage time increase and limited media replenishing with lactate accumulation enhanced differentiation capacity
- Continuous bioreactor runs revealed metabolic shifts toward a more β-cell-like differentiation profile compared to control media change approaches
- Cryopreserved aggregates maintained viability and insulin secretion capacity post-recovery, supporting their potential for storage and transplantation
The differentiation process was monitored through multiple analytical methods, including daily cell counting and aggregate size analysis, quantitative PCR for gene expression profiling, and flow cytometry for characterization of surface and intracellular markers at each differentiation stage [63].
Diagram 1: iPSC to β-cell Differentiation Workflow. This schematic outlines the multi-stage process for generating insulin-producing cells from iPSCs in a bioreactor-based system.
Quality Assessment and Product Characterization
Analytical Methods for Process and Product Monitoring
Robust analytical methods are essential for monitoring both the differentiation process and final product quality. Yehya et al. implemented a comprehensive analytical strategy including [63]:
- Daily monitoring of cell count, viability, and aggregate size distribution
- Quantitative PCR for stage-specific gene expression analysis
- Flow cytometry for intracellular and surface marker characterization
- Functional assessment through glucose-stimulated insulin secretion (GSIS) assays
For aggregate characterization, researchers used ImageJ analysis to determine size distribution and calculated islet equivalency (IEQ) estimates by normalizing aggregates to a theoretical islet size of 150μm using conversion factors [63].
Quantitative Assessment of Organoid Similarity
A significant challenge in the field has been the quantitative assessment of how closely iPSC-derived cells or organoids resemble their target human tissues. To address this limitation, recent research has developed computational approaches for quantitative similarity assessment.
Kim et al. (2021) created a web-based Similarity Analytics System (W-SAS) that calculates organ-specific similarity scores based on organ-specific gene expression panels (Organ-GEPs) derived from the GTEx database [64]. This system uses RNA-seq data from differentiated cells or organoids to compute a quantitative similarity percentage to target organs, including:
- Heart-specific Gene Expression Panel (HtGEP): 144 genes
- Lung-specific Gene Expression Panel (LuGEP): 149 genes
- Stomach-specific Gene Expression Panel (StGEP): 73 genes
This approach moves beyond traditional qualitative assessments based on limited marker analysis to provide a comprehensive, quantitative evaluation of differentiation fidelity, enabling more standardized quality control across different cell lines and differentiation protocols [64].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents for iPSC Differentiation and Manufacturing
| Reagent Category | Specific Examples | Function |
|---|---|---|
| Cell Culture Media | E8 medium, TB2 media, Differentiation media formulations | Support cell growth, maintenance, and stage-specific differentiation |
| Extracellular Matrix | Vitronectin, Laminin-521 | Provide adhesion substrates for cell attachment and signaling cues |
| Dissociation Agents | TrypLE, Accutase | Gentle cell dissociation while maintaining viability |
| Small Molecule Inhibitors | Y-27632 (ROCK inhibitor), CHIR99021 (GSK-3 inhibitor), ALK5 inhibitors | Modulate signaling pathways to direct differentiation |
| Growth Factors/Cytokines | Activin A, BMP4, FGF7, EGF, Retinoic acid | Pattern cells toward specific lineages through developmental cues |
| Analysis Reagents | Live/dead stains, Antibody panels for flow cytometry, RNA isolation kits | Enable comprehensive characterization of cells at multiple stages |
Integration with Clinical Trial Design
Phase-Appropriate Manufacturing Strategies
The manufacturing approach for iPSC-based therapies must align with clinical development phase requirements [61]. Early-phase trials (Phase I/II) may utilize more flexible processes focused on safety evaluation, while late-phase (Phase III) and commercial manufacturing require rigorously controlled, validated processes.
Recent trends show increasing use of combined Phase I/II studies for serious diseases with unmet medical needs, particularly in gene and cell therapy [4]. These combined studies evaluate both safety and preliminary efficacy in a smaller group of patients with the disease, potentially accelerating therapeutic development.
Risk-Based Quality Assessment Framework
The complex nature of living cell products necessitates specialized quality assessment frameworks for clinical trials. A 2020 study developed and validated a quality assessment tool specifically for stem cell clinical trials containing four critical quality attributes [65]:
- Participant Protection: Ethical considerations, informed consent, safety monitoring
- Scientific Value: Study design, endpoint selection, statistical power
- Quality Control: Manufacturing consistency, product characterization
- Stem Cell Products: Potency, purity, identity, and viability assessments
This framework has demonstrated validity in evaluating stem cell trials, with confirmatory trials showing stronger performance in product-related attributes compared to exploratory trials [65].
Diagram 2: Quality Assessment Framework for Stem Cell Trials. This diagram illustrates the four critical quality attributes and their components for evaluating stem cell clinical trials.
The field of iPSC-derived therapies is at an inflection point, with manufacturing scalability and consistency representing the final barriers to widespread clinical application. The protocols, quality assessment frameworks, and manufacturing strategies outlined here provide a roadmap for researchers and drug development professionals to navigate the complex transition from research to clinically viable therapies.
Key to future success will be the continued implementation of QbD principles, DOE approaches for process optimization, and development of quantitative product characterization methods. As the clinical trial landscape evolves, phase-appropriate manufacturing strategies that balance innovation with regulatory requirements will be essential for bringing these promising therapies to patients in need.
The encouraging safety profile established in early trials, combined with manufacturing advances that enhance scalability and consistency, position iPSC-derived therapies to realize their potential as transformative treatments for a range of debilitating diseases. With multiple products advancing through late-stage clinical development, the coming years will likely see an increasing number of iPSC-based therapies achieving regulatory approval and reaching patients.
Adaptive Trial Designs and the Role of AI/SysBio in Refining Clinical Translation
The development of stem cell therapies represents a frontier in modern medicine, offering potential for treating a wide range of degenerative diseases, injuries, and genetic disorders. However, the translation of these advanced therapeutic products from laboratory research to approved clinical applications has been markedly slow and inefficient [66]. Traditional clinical trial designs, developed primarily for small molecule drugs, often prove suboptimal for the unique challenges presented by stem cell-based therapies, which include complex biological mechanisms, heterogeneous patient responses, and intricate manufacturing and delivery requirements.
The convergence of adaptive clinical trial designs, artificial intelligence (AI), and systems biology (SysBio) offers a transformative framework for overcoming these barriers. This integrated approach enables a more nuanced understanding of both product and patient performance, creating what has been termed the "Iterative Circle of Refined Clinical Translation" [66]. By incorporating data-driven adaptations and deep biological insights throughout the clinical development process, researchers can optimize trial efficiency, enhance patient safety, and increase the likelihood of successful regulatory approval for stem cell therapies.
Adaptive Trial Designs: A Paradigm Shift for Stem Cell Development
Fundamental Concepts and Definitions
Adaptive clinical trial designs are defined as studies that include a prospectively planned opportunity for modification of one or more specified aspects of the study design and hypotheses based on analysis of interim data [67]. This flexibility allows trial investigators to respond to emerging information without undermining the trial's statistical validity or integrity. Key characteristics distinguishing adaptive from traditional fixed trials are summarized in Table 1.
Table 1: Comparison of Traditional Fixed Trials vs. Adaptive Trial Designs
| Feature | Traditional Fixed Trial | Adaptive Trial |
|---|---|---|
| Trial Course | Fixed sample size and design; no changes after start | Prespecified interim analyses allow changes to design (e.g., add/drop arms, adjust sample size) |
| Sample Size | Set in advance based on assumptions | Can be re-estimated or reallocated during trial if initial assumptions prove incorrect |
| Flexibility | Rigid, inflexible by design | Built-in flexibility to respond to accumulating data |
| Efficiency | Potentially more patients and time spent even if strong effects emerge early | Often more efficient; may require fewer patients and shorter duration when early trends are clear |
| Ethical Considerations | May continue giving inferior treatments to many patients | Can reduce patient exposure to ineffective treatments by stopping or re-allocating |
| Statistical Complexity | Relatively straightforward | Requires advanced methods and careful control of type I error |
| Operational Complexity | Standard trial operations | More complicated logistics (real-time data capture, DMC oversight, supply chain adjustments) |
Specific Adaptive Designs Relevant to Stem Cell Trials
For stem cell therapies, several adaptive designs have shown particular promise:
Phase I-II Seamless Designs: Conventional phase I trials focusing solely on toxicity are particularly problematic for stem cell therapies where the maximum tolerated dose may not represent the optimal biological dose. Phase I-II designs, such as the EffTox design, overcome this limitation by simultaneously evaluating both efficacy and toxicity to determine the optimal risk-benefit dose [68]. These designs use efficacy-toxicity trade-off contours to quantify each dose's desirability and direct patient assignments toward doses with the most favorable profiles.
Bayesian Adaptive Designs: The BOIN12 design represents an innovative Bayesian approach that combines phase 1 and 2 together [69]. This design assigns utility scores to dose levels based on both safety events (dose-limiting toxicities) and efficacy events (response rates), then calculates composite scores to direct new patients toward safe and effective doses. For example, a dose with responses observed and no DLTs would receive a score of 100, while a dose with DLTs and no efficacy would score 0.
Platform Trials: These master protocol designs allow multiple stem cell therapy candidates to be evaluated simultaneously under a single overarching infrastructure. Arms can be added or removed as new products become available or as interim data indicate promise or failure [67]. This approach is particularly valuable for conditions where multiple stem cell approaches may target different mechanisms.
Quantitative Evidence of Adaptive Trial Performance
Recent analyses demonstrate the tangible benefits of adaptive designs in therapeutic development. Drugs developed using adaptive trials showed a Phase II/III likelihood of launch of 81%, which is 13 percentage points higher than the likelihood of launch for non-innovative trials [70]. Additionally, adaptive trials demonstrated significantly faster recruitment times, requiring approximately 3 months to recruit 100 participants compared to 7 months for non-adaptive controls [70].
Table 2: Performance Metrics of Adaptive Trial Designs Across Therapeutic Areas
| Therapeutic Area | Likelihood of Launch (Adaptive) | Likelihood of Launch (Control) | Time to Recruit 100 Participants (Adaptive) | Time to Recruit 100 Participants (Control) |
|---|---|---|---|---|
| Oncology | 81% | 68% | 8.3 months | 18.7 months |
| Neurology | Similar adaptive advantage | Standard performance | 6.8 months | 10.6 months |
| Rare Diseases | 67% | 85% | 18.2 months | 29.7 months |
Note: The apparently lower performance in rare diseases reflects limited data (only eight cases) and may indicate that different adaptive strategies are needed for these populations [70].
Artificial Intelligence and Systems Biology in Clinical Translation
AI-Driven Clinical Trial Optimization
Artificial intelligence is transforming nearly every aspect of clinical trials, addressing long-standing challenges around cost, speed, and patient selection. The AI in clinical trials market is projected to expand at a compound annual growth rate of nearly 19%, reaching USD 21.79 billion by 2030, reflecting its rapidly increasing adoption [71].
Key applications of AI in stem cell trials include:
Trial Design and Optimization: AI plays a pivotal role in optimizing trial protocols by simulating various scenarios and predicting potential outcomes. This capability allows researchers to refine study designs in advance, minimizing risks and enhancing the likelihood of success [71]. AI-based systems help create protocols that are both patient-friendly and scientifically robust.
Patient Recruitment and Retention: Patient recruitment accounts for approximately 37% of trial postponements [71]. AI addresses this challenge by efficiently identifying potential participants who meet specific trial criteria through analysis of electronic health records, genetic profiles, and demographic information. AI-powered engagement platforms further enhance retention by delivering personalized experiences and timely reminders.
Safety Monitoring and Adverse Event Management: AI enhances safety monitoring by providing real-time alerts for adverse events and monitoring patient adherence to treatment regimens [71]. This proactive oversight helps ensure participants receive intended therapies as planned, reducing the risk of adverse events caused by missed doses or incorrect usage.
Systems Biology Approaches
Systems biology provides a crucial framework for understanding the complex, interconnected biological networks through which stem cell therapies exert their effects. Rather than examining individual components in isolation, systems biology focuses on the dynamic interactions between biological components, offering profound insights into complex biological processes and treatment optimization [66] [72].
For stem cell therapeutics, systems biology approaches enable:
Multi-omics Integration: Combining genomic, proteomic, metabolomic, and transcriptomic data to build comprehensive models of stem cell behavior and therapeutic mechanisms.
Mechanistic Modeling: Moving beyond "black box" correlations to establish causal relationships between therapeutic interventions and clinical outcomes [73]. Biology-first Bayesian causal AI starts with mechanistic priors grounded in biology and integrates real-time trial data as it accrues, inferring causality rather than just correlation.
Patient Stratification: Identifying biologically distinct patient subgroups based on molecular signatures rather than broad clinical categories, enabling more targeted and effective therapy application [73].
The Integrated AI/SysBio Framework: The Iterative Circle of Refined Clinical Translation
The synergy between AI and systems biology creates a powerful framework for stem cell therapy development termed the "Iterative Circle of Refined Clinical Translation" [66]. This continuous learning cycle involves:
- Data Generation: Comprehensive profiling of cell products and clinical outcomes
- SysBio/AI Analysis: Integrated analysis of large-scale multi-omics datasets
- Knowledge Generation: Identification of biomarkers and mechanisms of action
- Protocol Refinement: Adaptation of trial designs and therapeutic applications
- Improved Outcomes: Enhanced safety, efficacy, and potency evaluation
This iterative process allows for continuous refinement of both the stem cell product and its clinical application based on accumulating biological evidence.
Diagram 1: Iterative Circle of Refined Clinical Translation. This continuous learning framework integrates AI and systems biology throughout the clinical development process [66].
Application Notes and Protocols for Stem Cell Trials
Protocol: Implementing a Bayesian Phase I-II Adaptive Design for Stem Cell Dose Optimization
Background: Traditional phase I dose-finding based solely on toxicity is inadequate for stem cell therapies where the therapeutic effect may not correlate directly with maximum tolerated dose.
Objective: To identify the optimal biological dose (OBD) that balances efficacy and toxicity using the EffTox Bayesian adaptive design.
Materials and Methods:
- Stem Cell Product: Characterized according to ISCT criteria with additional potency assays
- Dose Levels: 3-5 dose levels based on preclinical efficacy and safety data
- Patient Population: 40-60 patients with the target condition
- Interim Analyses: Conducted after every 10-15 patients complete the primary endpoint evaluation
Procedural Steps:
Define Efficacy and Toxicity Endpoints:
- Efficacy: A composite endpoint appropriate to the mechanism (e.g., engraftment, biomarker response, functional improvement)
- Toxicity: Dose-limiting toxicities (DLTs) defined according to standard criteria (e.g., CTCAE)
Establish Target Profiles:
- Set minimum acceptable efficacy (AE) and maximum acceptable toxicity (AT) probabilities
- Example: AE = 0.2, AT = 0.3
Define Efficacy-Toxicity Trade-off Contours:
- Construct trade-off contours representing equally desirable combinations of efficacy and toxicity probabilities
- Calculate desirability scores for each contour
Trial Execution:
- Treat initial cohort at a predetermined starting dose
- After each interim analysis:
- Compute posterior probabilities of efficacy and toxicity for each dose
- Identify "acceptable" doses (Pr(efficacy > AE) > threshold AND Pr(toxicity < AT) > threshold)
- Among acceptable doses, select the one with highest desirability score for next cohort
- Continue until maximum sample size reached or stopping rules triggered
Final Analysis:
- Select the dose with the highest desirability score as the recommended phase II dose (RP2D)
- If no doses are acceptable, conclude that no suitable RP2D exists
Statistical Considerations:
- Use Bayesian logistic regression models for efficacy and toxicity
- Conduct extensive simulation studies to evaluate operating characteristics
- Pre-specify decision rules and stopping criteria in the protocol
Protocol: AI-Enhanced Patient Stratification for Stem Cell Trials
Background: Patient heterogeneity significantly impacts stem cell therapy response. AI-driven analysis of multi-omics data can identify biologically distinct subgroups most likely to benefit.
Objective: To develop and validate a predictive biomarker signature for patient stratification in stem cell trials.
Materials and Methods:
Table 3: Research Reagent Solutions for AI-Enhanced Patient Stratification
| Reagent/Technology | Function | Application in Stem Cell Trials |
|---|---|---|
| Single-cell RNA Sequencing | Characterizes transcriptomic profiles at single-cell resolution | Identifies cell subpopulations and molecular response signatures |
| Multiplexed Immunoassay | Simultaneously measures multiple protein biomarkers | Profiles inflammatory and regenerative pathways |
| Mass Cytometry (CyTOF) | High-dimensional analysis of cell surface and intracellular markers | Characterizes immune cell populations and activation states |
| Metabolomics Platform | Comprehensive measurement of small molecule metabolites | Assesses metabolic responses to stem cell therapy |
| AI/ML Integration Software | Integrates and analyzes multi-omics datasets | Identifies complex biomarker patterns predictive of response |
Procedural Steps:
Biospecimen Collection:
- Collect appropriate biospecimens (blood, tissue, etc.) at baseline, during treatment, and at endpoint
- Process and store samples using standardized protocols
Multi-omics Profiling:
- Conduct genomic, transcriptomic, proteomic, and/or metabolomic analyses
- Generate high-dimensional data for each patient
Data Integration and Preprocessing:
- Normalize and quality control all omics data
- Integrate diverse data types into a unified dataset
Predictive Model Development:
- Apply machine learning algorithms (e.g., random forests, neural networks) to identify biomarker patterns associated with clinical response
- Use cross-validation to avoid overfitting
- Generate a response prediction score for each patient
Model Validation:
- Validate the predictive signature in an independent patient cohort
- Assess sensitivity, specificity, and clinical utility
Implementation in Adaptive Trial:
- Use the validated signature for adaptive enrichment
- Adjust patient eligibility criteria based on predictive biomarkers at interim analyses
Protocol: Systems Biology Analysis for Mechanism of Action Elucidation
Background: Understanding the mechanisms through which stem cell therapies exert their effects is crucial for optimizing their clinical application.
Objective: To apply systems biology approaches to elucidate the mechanisms of action of stem cell therapies.
Procedural Steps:
Network Modeling:
- Construct biological networks relevant to the disease pathology and proposed mechanism
- Incorporate protein-protein interactions, signaling pathways, and gene regulatory networks
Multi-omics Data Integration:
- Map transcriptomic, proteomic, and metabolomic data onto biological networks
- Identify significantly perturbed network modules
Dynamic Modeling:
- Develop quantitative models of key signaling pathways
- Incorporate time-series data to model dynamic responses
Causal Inference:
- Apply Bayesian causal network inference to identify driver pathways
- Distinguish causal mediators from correlated biomarkers
Experimental Validation:
- Design targeted experiments to validate key predictions from models
- Use perturbation studies to test causal relationships
Diagram 2: Systems Biology Workflow for Mechanism of Action Studies. This iterative process integrates multi-omics data with network modeling to elucidate therapeutic mechanisms.
Implementation Considerations and Best Practices
Regulatory Landscape and Compliance
Regulatory agencies have demonstrated increasing openness to adaptive designs and AI approaches in clinical development. The FDA has announced plans to issue guidance on the use of Bayesian methods in the design and analysis of clinical trials by September 2025 [73]. This builds on earlier initiatives such as the Complex Innovative Trial Design (CID) Pilot Program and aligns with the European Medicines Agency's Qualification of Novel Methodologies framework.
Key considerations for regulatory compliance include:
- Prospective Planning: All adaptations must be pre-specified in the protocol or statistical analysis plan
- Type I Error Control: Statistical methods must adequately control false positive rates
- Operational Bias Prevention: Processes must prevent unblinding or introduction of bias during interim analyses
- Transparent Reporting: Complete documentation of all design adaptations and their rationale
Practical Guidance for Interim Analyses
The ROBust INterims for adaptive designs (ROBIN) project provides evidence-based recommendations for conducting high-quality and rapid interim analyses [74]. Key recommendations include:
- Early Planning: Consider interim analysis requirements during trial design phase
- Simulation Exercises: Conduct realistic simulations of interim analyses with the study team and data monitoring committee
- Data Quality Focus: Implement rigorous data management processes to ensure clean, timely data for interim analyses
- Efficient Processes: Develop streamlined workflows for data extraction, analysis, and decision-making
- Adequate Resourcing: Ensure sufficient statistical, data management, and operational resources for interim analyses
Stakeholder Engagement and Training
Successful implementation of adaptive AI-enhanced trials requires engagement and training of all stakeholders:
- Investigators and Site Staff: Education on adaptive design concepts and procedures
- Patients and Public: Clear communication about adaptive elements and their ethical benefits
- Regulators: Early consultation on novel design elements
- Statistical and Data Management Teams: Training in advanced statistical methods and data management requirements
The integration of adaptive trial designs with artificial intelligence and systems biology represents a transformative approach to stem cell therapy development. This integrated framework addresses the unique challenges of stem cell translational research by incorporating biological complexity into clinical trial design, enabling continuous learning and optimization throughout the development process.
The protocols and application notes presented here provide practical guidance for implementing these advanced approaches in stem cell clinical trials. As regulatory acceptance grows and methodological advances continue, these strategies offer the promise of accelerating the development of effective stem cell therapies while maximizing patient benefit and ensuring scientific rigor.
The future of stem cell clinical development lies in embracing this integrated, data-driven approach—moving beyond traditional paradigms to create a more efficient, ethical, and biologically-informed pathway from laboratory discovery to clinical application.
Demonstrating Efficacy and Securing Market Approval with Phase III Data
Phase III randomized controlled trials (RCTs) represent the confirmatory stage of clinical development, providing the critical evidence base for regulatory approval and clinical adoption of new therapies. In the context of stem cell therapies for conditions such as advanced heart failure, autoimmune diseases, and advanced cancers, these trials must be meticulously designed to definitively demonstrate both efficacy and safety. The fundamental design principle involves comparing an investigational therapy against a control arm—either placebo or standard of care—through random allocation, which minimizes selection bias and ensures that outcome differences are attributable to the treatment effect rather than confounding factors.
The selection of primary efficacy endpoints is arguably the most crucial design decision, as it forms the basis for sample size calculation, statistical powering, and the ultimate determination of therapeutic success. An analysis of Phase III RCTs in related fields reveals that ordinal scales (e.g., a 7-point clinical status scale) were the most common primary endpoint, utilized in 42.9% of trials, while overall or all-cause mortality—considered the most direct measure of clinical benefit in lethal conditions—was used as the primary endpoint in only 6% of trials [75]. Furthermore, the use of multiple primary endpoints (MPEs) is increasingly common, particularly in oncology; a systematic review found that 12% of Phase III trials in advanced solid tumours adopted MPEs, with this proportion rising from 6% in 2017 to 20% in 2020 [76]. This design complexity necessitates rigorous statistical planning to control Type I error and ensure interpretable results.
Primary Efficacy Endpoint Selection
Endpoint Categories and Applications
The choice of primary endpoint is guided by the therapeutic mechanism, disease context, and regulatory expectations. Endpoints can be broadly categorized into clinician-reported outcomes (ClinROs), patient-reported outcomes (PROs), performance outcomes (PerfOs), and survival outcomes. For stem cell therapies, which often aim for tissue repair and functional improvement, composite endpoints and functional scales are particularly relevant.
Table 1: Common Primary Endpoint Categories in Phase III Trials
| Endpoint Category | Description | Common Examples | Therapeutic Context |
|---|---|---|---|
| Overall Survival (OS) | Time from randomization to death from any cause [76] | Hazard Ratio for death | Oncology trials; considered gold standard for direct clinical benefit [75] |
| Ordinal Scales | Multi-level scale measuring clinical status [75] | 7-point ordinal scale (1=Death, 7=Not hospitalized) | COVID-19 trials; measures spectrum of disease severity [75] |
| Progression-Free Survival (PFS) | Time from randomization to disease progression or death [76] | Hazard Ratio for progression or death | Oncology trials (often paired with OS in MPE designs) [76] |
| Functional/Composite Endpoints | Measures of organ function or composite outcomes | Time to recovery; change in left ventricular ejection fraction | Heart failure trials; stem cell therapy for tissue repair |
| Patient-Reported Outcomes (PROs) | Outcomes reported directly by patients | Quality of life scales, symptom diaries | Chronic disease trials where symptom control is key |
Trends in Multiple Primary Endpoints (MPEs)
The adoption of MPEs is increasing, particularly in complex therapeutic areas like immuno-oncology. A systematic review of Phase III trials in advanced solid tumours found that MPEs were used in 53% of trials testing immunotherapy, compared to 16% of for-profit trials overall and only 4% of non-profit trials [76]. The most common MPE combination was overall survival (OS) and progression-free survival (PFS). When implementing MPEs, two distinct regulatory cases must be considered:
- Multiple "Chances" for Success: The experimental treatment is declared successful if a statistically significant benefit is found on any one of the primary endpoints. This approach requires adjustment for multiplicity to control the overall false-positive rate [76].
- Co-Primary Endpoints: A positive result depends on demonstrating a statistically significant benefit on all specified primary endpoints. In this case, no multiplicity adjustment is needed, as the failure of one endpoint constitutes failure of the entire trial [76].
Despite regulatory guidance, a review found that only 10 out of 27 trials (37%) with MPEs adopted an explicit definition of "co-primary" endpoints, and only one of these declared that positivity on both endpoints was critical for interpretation [76]. Furthermore, among 21 publications with positive conclusions, only 12 (57%) had statistically significant results for both primary endpoints, indicating a frequent disconnect between stated endpoints and conclusions [76].
Statistical Design and Power Considerations
Bridging Phase II and Phase III Evidence
Integrating evidence from earlier phases is critical for efficient Phase III design, especially in orphan diseases or novel fields like stem cell therapy where patient populations may be limited. A Bayesian meta-analytic approach can formally incorporate Phase II data into Phase III planning, treating the Phase II treatment effect estimate as a prior distribution for the Phase III parameter [77]. This approach is particularly valuable when dealing with small numbers of trials, as it accounts for uncertainty in between-trial heterogeneity probabilistically [77]. The meta-analytic-predictive (MAP) prior provides a predictive distribution for the effect in a new trial based on historical data, allowing for more informed sample size calculations and potentially accelerating drug development [77].
A significant challenge in transitioning from Phase II to Phase III is the overestimation of treatment effects in Phase II, which occurs because only promising results (random highs) lead to Phase III initiation [78]. This bias can lead to underpowered Phase III trials. To address this, adjustment methods such as multiplicative (e.g., using a retention factor of 0.9) or additive adjustment of the Phase II treatment effect estimate can be applied when planning the Phase III sample size [78]. Research shows that program set-ups using adjusted treatment effect estimates for Phase III planning are superior to naïve approaches with respect to maximal expected utility [78].
Sample Size and Power Calculation
Sample size calculation for a Phase III trial must account for the chosen primary endpoint, desired power (typically 80-90%), Type I error rate (α, typically 0.05 for a single primary endpoint), and the anticipated treatment effect size. For time-to-event endpoints like OS or PFS, the required number of events is calculated first, followed by the number of patients and study duration needed to accrue these events.
The formula for calculating the number of events required for a time-to-event endpoint is:
Where Z(1-α/2) and Z(1-β) are quantiles of the standard normal distribution, and HR is the anticipated hazard ratio.
For continuous endpoints (e.g., functional scales), the sample size per group is calculated as:
Where σ is the standard deviation of the endpoint, and Δ is the anticipated treatment difference.
When using MPEs with a "multiple chances" design, the α-level must be allocated between endpoints (e.g., using a Bonferroni correction) to maintain the overall Type I error rate. For co-primary endpoints, power is calculated as the probability of achieving statistical significance on all endpoints simultaneously, which requires a larger sample size than for a single endpoint.
Diagram 1: Integrated Phase II/III drug development program workflow
Experimental Protocols and Methodologies
Protocol 1: Randomized Controlled Trial for Stem Cell Therapy in Advanced Heart Failure
Objective: To evaluate the efficacy and safety of allogeneic mesenchymal stem cells (MSCs) versus placebo in patients with advanced heart failure.
Primary Endpoint: Composite endpoint of all-cause mortality or unplanned heart failure hospitalization at 12 months.
Key Inclusion Criteria:
- Adults aged 18-80 years with advanced heart failure (NYHA Class III-IV)
- Left ventricular ejection fraction (LVEF) ≤35%
- Optimized medical therapy for ≥3 months
Randomization and Blinding:
- Stratification Factors: LVEF (≤25% vs. >25%), etiology (ischemic vs. non-ischemic)
- Allocation: 1:1 randomization to MSC therapy or matching placebo
- Blinding: Double-blind design (participants, investigators, outcomes assessors)
Intervention:
- Preparation: Allogeneic MSCs from qualified donor banks, thawed and prepared per protocol
- Administration: Single intracoronary infusion of 1.5 × 10^7 MSCs or placebo
- Concomitant Therapy: Continued guideline-directed medical therapy
Assessment Schedule:
- Baseline, 1, 3, 6, and 12 months: Clinical assessment, biomarkers (NT-proBNP), quality of life questionnaires
- Baseline and 12 months: Cardiac MRI for LVEF and ventricular volumes
- Continuous monitoring: Adverse events, hospitalizations, mortality
Statistical Analysis:
- Sample Size: 300 participants (150 per group) providing 85% power to detect a 35% relative risk reduction in the primary composite endpoint (α=0.05, two-sided)
- Primary Analysis: Cox proportional hazards model for time to first event, with stratification factors as covariates
- Interim Analysis: One interim analysis for efficacy and futility at 50% information fraction
Protocol 2: Multiple Primary Endpoints in Oncology Stem Cell Trial
Objective: To evaluate the efficacy of stem cell-based immunotherapy combined with standard therapy versus standard therapy alone in refractory metastatic cancer.
Primary Endpoints:
- Overall Survival (OS)
- Progression-Free Survival (PFS) per RECIST 1.1
Design: Multiple primary endpoints with "multiple chances" design, with hierarchical testing (PFS tested first, then OS only if PFS is significant) to control overall Type I error.
Key Inclusion Criteria:
- Histologically confirmed metastatic disease
- Progression on at least one prior line of systemic therapy
- Measurable disease per RECIST 1.1
Intervention:
- Experimental Arm: Autologous genetically modified stem cell-derived T-cells + standard chemotherapy
- Control Arm: Standard chemotherapy alone
Assessment Schedule:
- Tumor imaging (CT/MRI) every 8 weeks for first year, then every 12 weeks
- Survival follow-up every 3 months
- Safety monitoring throughout study period
Statistical Analysis:
- Sample Size: 400 participants (200 per group) providing 85% power for PFS (HR=0.65) and 80% power for OS (HR=0.70) with overall one-sided α=0.025
- Alpha Allocation: One-sided α=0.02 for PFS, with α=0.005 carried over to OS testing if PFS is significant
- Analysis: Stratified log-rank tests for both OS and PFS, with Cox proportional hazards models for estimation of treatment effect
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Stem Cell Clinical Trial Monitoring
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| Flow Cytometry Antibodies | Characterization of stem cell surface markers and purity assessment [35] | CD34, CD45, CD73, CD90, CD105, HLA-DR |
| Cell Culture Media | Expansion and maintenance of stem cell populations [35] | Serum-free media with growth factors (FGF, EGF) |
| Differentiation Kits | Assessment of multilineage differentiation potential [60] | Osteogenic, adipogenic, chondrogenic differentiation kits |
| Cytokine Assays | Measurement of paracrine factors secreted by stem cells [60] | ELISA kits for VEGF, HGF, TGF-β, IL-10 |
| qPCR Reagents | Analysis of gene expression in stem cells and recipient tissues | TaqMan assays for pluripotency markers (OCT4, SOX2, NANOG) |
| Immunohistochemistry Kits | Tracking and engraftment assessment of administered cells | Antibodies for specific cell tracking labels |
| Microscopy Reagents | Visualization of cell morphology and integration | Live-cell imaging dyes, cell tracking labels |
Regulatory and Practical Considerations
Endpoint Validation and Regulatory Alignment
Regulatory agencies emphasize that primary endpoints should be "essential to establish effectiveness for approval" [76]. For stem cell therapies, this presents unique challenges, as these treatments may work through multiple mechanisms including immune modulation, tissue repair via growth factors, and anti-inflammatory effects [35]. Consequently, endpoints must capture these diverse potential benefits. The U.S. FDA and European Medicines Agency (EMA) provide specific guidance on MPEs, distinguishing between situations requiring multiplicity adjustment and co-primary endpoints where success on all endpoints is required [76].
A concerning finding from recent literature is that many trials adopting MPEs do not fully respect regulatory recommendations. In a review of oncology trials, only 37% of trials with MPEs provided an explicit definition of "co-primary" endpoints, and only 15% required positivity on both endpoints for study success [76]. Furthermore, 15% of publications with MPEs presented positive conclusions based on only one of the primary endpoints being statistically significant [76]. This highlights the importance of pre-specifying the MPE strategy and maintaining consistency between the statistical plan, results, and conclusions.
Addressing Implementation Challenges
Several practical challenges require consideration in Phase III stem cell trial design:
- Blinding Complexity: Creating convincing placebo controls for invasive administrations (e.g., intracoronary infusion) requires innovative sham procedures.
- Cell Product Consistency: Ensuring batch-to-batch consistency in stem cell products through rigorous quality control measures.
- Long-term Follow-up: Planning extended safety monitoring for potential long-term risks such as tumorigenicity or immune reactions.
- Endpoint Relevance: Selecting endpoints that reflect meaningful clinical benefit while being sensitive to the specific therapeutic effects of stem cells.
Diagram 2: Decision pathway for multiple primary endpoint strategies
Designing pivotal Phase III trials requires meticulous attention to endpoint selection, statistical powering, and regulatory alignment. The increasing adoption of multiple primary endpoints reflects the complexity of demonstrating comprehensive clinical benefit for novel therapies like stem cells. While this approach offers advantages in capturing multidimensional treatment effects, it demands rigorous statistical methods to control Type I error and maintain interpretability.
For stem cell therapies specifically, endpoint selection must align with the proposed mechanisms of action, which may include immunomodulation, tissue repair, and paracrine signaling [35] [60]. Integrating Phase II data through Bayesian methods can enhance Phase III efficiency, while appropriate adjustment for overestimation bias protects against underpowered confirmatory trials. As the field advances, continued attention to regulatory guidance and methodological rigor will be essential for generating compelling evidence that translates promising stem cell therapies into clinical practice.
A Biologics License Application (BLA) is a comprehensive submission to the U.S. Food and Drug Administration (FDA) requesting permission to introduce, or deliver for introduction, a biologic product into interstate commerce [79]. For stem cell-based therapies, the BLA represents the culmination of an extensive research and development journey, demonstrating that the product meets stringent standards for safety, purity, and potency [80]. Unlike small-molecule drugs approved via New Drug Applications (NDAs), biologics including stem cell therapies are regulated under 21 CFR 600-680 and are reviewed by the FDA's Center for Biologics Evaluation and Research (CBER) [79] [80].
The compilation of robust safety and efficacy evidence throughout the clinical development phases is paramount for stem cell products, given their complex biological nature, potential for patient-specific effects, and often novel mechanisms of action. This document outlines the critical evidence requirements and methodological approaches for compiling the necessary data to support a successful BLA submission for stem cell therapies, framed within the context of stem cell clinical trial design across phases I-III.
Clinical Trial Phases: Design and Evidence Generation
Stem cell therapies must progress through phased clinical trials to establish a comprehensive profile of their safety and efficacy. The table below summarizes the key objectives and design elements for each phase.
Table 1: Clinical Trial Phases for Stem Cell Therapy Development
| Phase | Primary Objectives | Typical Design & Population | Key Efficacy Endpoints | Key Safety Monitoring |
|---|---|---|---|---|
| Phase I | Assess safety, determine a safe dosage range, and identify side effects [4] [27]. | Small group (20-100) of patients with the target disease [4] [27]. Open-label, dose-escalation design common [28]. | Preliminary data on biological activity; often not powered for efficacy [28]. | Incidence and severity of adverse events (AEs), dose-limiting toxicities, laboratory parameters, and vital signs [4]. |
| Phase II | Further evaluate safety and assess preliminary efficacy for the condition [4] [27]. | Larger group (up to several hundred) of patients with the target disease [4]. Often randomized and may include a control arm [28]. | Optimal dosing, functional clinical endpoints relevant to the disease (e.g., LVEF for cardiac disease) [28]. | Continued AE monitoring, assessment of common short-term side effects, immunogenicity [4] [27]. |
| Phase III | Confirm effectiveness, monitor side effects, and compare to standard treatments [4] [27]. | Large groups (300-3,000) of patients with the disease [4]. Randomized, controlled, double-blind design is the gold standard [28]. | Definitive clinical outcomes, quality of life measures, comparison to standard of care [81] [28]. | Comprehensive AE profile, identification of rare adverse events, long-term safety within the trial period [27]. |
For stem cell therapies, trial designs often require adaptations. Unlike traditional drug trials, Phase I trials for stem cells typically enroll patients with the target disease rather than healthy volunteers due to the therapy's specificity and potential risks [4] [27]. Furthermore, phases may be combined (e.g., Phase I/II) to make the evaluation process more efficient for serious and rare diseases [4]. Trial design must also account for the cancer stem cell model, where a treatment may eliminate tumorigenic potential without initially reducing overall tumor bulk, necessitating alternative biomarkers and efficacy assessments [81].
Experimental Protocols for Efficacy Assessment
Protocol 1: Assessment of Cardiac Function in Stem Cell Therapy for Ischemic Heart Disease
- Objective: To evaluate the efficacy of stem cell therapy in improving cardiac function post-myocardial infarction.
- Methodology:
- Patient Population: Adults with left ventricular ejection fraction (LVEF) ≤45% after successful percutaneous coronary intervention for acute myocardial infarction (3-7 days post-event) [28].
- Intervention: Intracoronary infusion of autologous bone marrow-derived mononuclear cells (BMMNC) vs. placebo (randomized, double-blind).
- Efficacy Endpoint Measurement:
- Primary Endpoint: Change in global LVEF from baseline to 4-month follow-up [28].
- Imaging Technique: Quantitative left ventricular angiography or Cardiac Magnetic Resonance Imaging (MRI) performed at baseline and 4 months [28].
- Secondary Endpoints: Changes in infarct size, regional wall motion, and perfusion assessed via SPECT or MRI.
Protocol 2: Evaluation of Complex Perianal Fistula Healing in Crohn's Disease
- Objective: To assess the efficacy of allogeneic adipose-derived stem cells (e.g., darvadstrocel) in closing complex perianal fistulas.
- Methodology:
- Patient Population: Patients with Crohn's disease and treatment-refractory complex perianal fistulas [82].
- Intervention: A single local injection of allogeneic expanded adipose-derived stem cells (eASC) vs. control (randomized).
- Efficacy Endpoint Measurement:
- Primary Endpoint: Combined remission at 24 weeks, defined as clinical assessment of closure of all treated fistulas and absence of collections >2 cm on MRI [82].
- Assessment: Clinical evaluation and pelvic MRI at baseline and 24 weeks.
- Long-term Follow-up: Safety and efficacy monitoring continues up to 52 weeks and beyond [82].
The Biologics License Application (BLA): Compiling the Evidence
The BLA is submitted after the final phase of clinical trials demonstrates that the stem cell therapy is safe and effective [4]. It is a consolidated dossier presenting all evidence gathered during development.
Key Components of a BLA for Stem Cell Products
The BLA is organized following the Common Technical Document (CTD) structure. Key modules and their evidence requirements are detailed below.
Table 2: Critical Evidence Components of a BLA for Stem Cell Therapies
| BLA Section / Module | Required Evidence & Documentation | Stem Cell-Specific Considerations |
|---|---|---|
| Form FDA 356h | Official application form with applicant and product information, and summaries of submitted data [79] [80]. | Must specify the product as a somatic cellular therapy. |
| Module 1: Administrative | Prescribing information, patent information, field copy certification [80]. | Draft labeling for the stem cell product, including indications, handling, and administration. |
| Module 2: Summaries | Quality Overall Summary, Nonclinical Overview, Clinical Overview [80]. | Integrated summaries of safety and efficacy across all clinical trials, highlighting the risk-benefit profile. |
| Module 3: Quality (CMC) | Detailed manufacturing process, characterization, controls, stability data, and facility information [80] [83]. | Extensive Chemistry, Manufacturing, and Controls (CMC) data is critical. Must demonstrate process validation, potency assays, cell viability, identity, purity, and freedom from adventitious agents. |
| Module 4: Nonclinical Study Reports | Reports from all pharmacology and toxicology studies [80]. | Biodistribution, tumorigenicity, and immunogenicity studies in relevant animal models. |
| Module 5: Clinical Study Reports | Full study reports from all clinical trials (Phases I-III) [80]. | Case report forms and tabulations for pivotal studies. Must include long-term follow-up data as required. |
For stem cell products, the Chemistry, Manufacturing, and Controls (CMC) section is particularly vital. The principle that "the product is the process" is fundamental for biologics, as small changes in the manufacturing process can significantly impact the final product's quality and performance [80]. This section must provide exhaustive details on the stem cell source (autologous/allogeneic), expansion, differentiation, purification, formulation, and final release specifications [83].
Post-Approval Evidence and Phase IV Studies
After BLA approval, post-market safety monitoring (Phase IV) is essential for stem cell therapies [4] [27]. The FDA emphasizes the importance of continued data collection for cell and gene therapy products due to their potential for long-lasting effects and the limited number of participants treated in pre-approval trials [84]. This often involves:
- Long-Term Follow-up Studies: Required for many gene and cell therapies to monitor for delayed adverse events, sometimes for up to 15 years [4] [83].
- Registries and Post-Approval Studies: Methods to capture real-world safety and efficacy data to better understand the product's long-term profile in a broader patient population [84].
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and materials are essential for conducting the preclinical and clinical assessments critical for BLA compilation.
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent / Material | Function and Application |
|---|---|
| Flow Cytometry Antibodies | Characterization of cell surface markers (e.g., CD34, CD45, CD90, CD105) to confirm stem cell identity and purity during manufacturing and product release [28]. |
| Cell Culture Media & Supplements | For the expansion and maintenance of stem cells under controlled, often GMP-compliant, conditions. Formulations may be designed to direct differentiation. |
| Potency Assay Kits | To measure the biological activity of the stem cell product. For example, an assay that measures the secretion of angiogenic factors for a product intended to promote blood vessel growth [83]. |
| Vector-Specific Assays | For genetically modified stem cells, assays to determine viral vector titer, transgene expression, and copy number are critical Critical Quality Attributes (CQAs) [83]. |
| Animal Disease Models | Preclinical in vivo models (e.g., murine myocardial infarction model) to test hypotheses on mechanism of action, dosing, and initial proof-of-concept for efficacy [28]. |
Visualizing the Path to BLA
The following diagrams illustrate the clinical development pathway and the evidence compilation process for a stem cell therapy BLA.
Diagram 1: Clinical Development Path to BLA. This workflow outlines the sequential phases of clinical development, regulatory submissions, and review that lead from preclinical research to product approval and post-market monitoring. IND = Investigational New Drug Application; BLA = Biologics License Application.
Diagram 2: BLA Evidence Compilation. This diagram illustrates how evidence from Chemistry, Manufacturing, and Controls (CMC), nonclinical studies, and clinical trials across all phases is consolidated into the comprehensive BLA submission.
The transition of stem cell therapies from experimental research to FDA-approved medicinal products marks a significant milestone in regenerative medicine. This analysis examines three pioneering therapies—Ryoncil, Omisirge, and Lyfgenia—that have successfully navigated the rigorous clinical development pathway. Each product addresses distinct clinical needs through unique biological mechanisms: Ryoncil represents the first mesenchymal stromal cell therapy approved for steroid-refractory acute graft-versus-host disease (SR-aGvHD) in pediatric patients [85] [86]. Omisirge, a nicotinamide-modified cord blood-derived product, addresses critical limitations in hematopoietic stem cell transplantation by accelerating neutrophil recovery [87] [88]. Lyfgenia, an autologous cell-based gene therapy, offers a novel treatment for sickle cell disease by genetically modifying patients' hematopoietic stem cells to produce anti-sickling hemoglobin [2] [89]. These case studies provide invaluable insights into effective clinical trial design, regulatory strategy, and manufacturing scale-up for complex biological products.
Case Study 1: Ryoncil (remestemcel-L-rknd)
Clinical Context and Mechanism of Action
Ryoncil was developed to address steroid-refractory acute Graft-versus-Host Disease (SR-aGvHD), a life-threatening complication of allogeneic hematopoietic stem cell transplantation with historically limited treatment options and high mortality. The therapy utilizes allogeneic bone marrow-derived mesenchymal stromal cells (MSCs) from healthy donors, which exert immunomodulatory effects through multiple mechanisms [85] [86]. These cells modulate the inflammatory response in GvHD by inhibiting T-cell proliferation and dendritic cell maturation, while simultaneously promoting the expansion of regulatory T-cells and reducing pro-inflammatory cytokine production. This multifaceted immunomodulatory approach targets the underlying pathophysiology of SR-aGvHD, where conventional steroid therapy has failed to control the dysimmune response.
Clinical Trial Design and Outcomes
The clinical development program for Ryoncil employed a single-arm, multicenter design (Study MSB-GVHD001) in 54 pediatric patients aged 2 months and older with Grade B-D SR-aGvHD (excluding Grade B skin alone) [86]. This patient population represented those with the most urgent unmet medical need. The trial design incorporated key eligibility criteria requiring demonstrated steroid-refractory disease, defined as GvHD progressing within 3 days or not improving within 7 consecutive days of methylprednisolone treatment, ensuring a homogeneous population with true treatment resistance.
Table 1: Key Efficacy Outcomes from Ryoncil Clinical Trial
| Efficacy Parameter | Result | Assessment Timeline |
|---|---|---|
| Overall Response Rate (ORR) | 70% | Day 28 |
| Complete Response (CR) Rate | 30% | Day 28 |
| Partial Response (PR) Rate | 41% | Day 28 |
| Median Duration of Response | 54 days | From Day 28 to progression, new therapy, or death |
The primary efficacy outcome measures were Overall Response Rate at Day 28 and duration of response, with the 70% response rate demonstrating substantial clinical benefit in this critically ill population [86]. The safety profile was characterized by monitoring adverse events expected in this patient population, with the most common non-laboratory adverse reactions (>20% of patients) including viral and bacterial infectious disorders, pyrexia, hemorrhage, edema, abdominal pain, and hypertension. The single-arm design was ethically and practically justified by the life-threatening nature of SR-aGvHD, the lack of effective standard therapies, and the establishment of a clinically meaningful historical control data set for comparison.
Experimental Protocol: MSC Characterization and Potency Assays
Objective: To establish identity, purity, potency, and safety of allogeneic bone marrow-derived mesenchymal stromal cells for treatment of SR-aGvHD.
Materials:
- Bone Marrow Aspirate: Sourced from healthy adult donors under informed consent
- Culture Media: DMEM/F12 supplemented with Fetal Bovine Serum (FBS) or human platelet lysate
- Flow Cytometry Panel: Antibodies against CD73, CD90, CD105, CD45, CD34, HLA-DR
- Cell Differentiation Media: Adipogenic, osteogenic, chondrogenic induction cocktails
- T-cell Suppression Assay Components: Peripheral blood mononuclear cells (PBMCs), phytohemagglutinin (PHA)
- Cryopreservation Solution: Dimethyl sulfoxide (DMSO) in cell culture medium
Methodology:
- Cell Isolation and Expansion: Isolate mononuclear cells from bone marrow aspirate via density gradient centrifugation. Culture selected cells at clonal density (1.5-5.0 cells/cm²) in complete medium with 5% CO₂ at 37°C. Passage cells at 70-80% confluence using trypsin/EDTA.
- Immunophenotypic Characterization (Identity): Harvest cells at passage 3-4. Incubate with fluorochrome-conjugated antibodies against positive markers (CD73, CD90, CD105) and negative markers (CD45, CD34, HLA-DR). Analyze by flow cytometry with ≥95% expression of positive markers and ≤2% expression of negative markers required for product release.
- Trilineage Differentiation (Functionality):
- Adipogenic Differentiation: Culture cells in adipogenic induction medium for 14 days. Fix and stain with Oil Red O to visualize lipid vacuoles.
- Osteogenic Differentiation: Culture cells in osteogenic induction medium for 21 days. Fix and stain with Alizarin Red S to detect calcium deposits.
- Chondrogenic Differentiation: Pellet cells and culture in chondrogenic induction medium for 28 days. Section and stain with Alcian Blue to visualize proteoglycans.
- Potency Assay (T-cell Suppression): Co-culture irradiated MSCs with PHA-stimulated PBMCs at varying ratios (1:2 to 1:20 MSC:PBMC) for 3-5 days. Measure T-cell proliferation via ³H-thymidine incorporation or CFSE dilution by flow cytometry. Include reference standard and acceptance criteria of ≥30% suppression at 1:10 ratio.
- Cryopreservation and Formulation: Harvest cells at target population doubling level. Resuspend in cryopreservation medium with 10% DMSO. Control-rate freeze to -80°C before transfer to vapor phase liquid nitrogen storage.
Diagram 1: MSC Manufacturing and Characterization Workflow
Case Study 2: Omisirge (omidubicel-onlv)
Clinical Context and Mechanism of Action
Omisirge addresses the critical limitation of donor availability in allogeneic hematopoietic cell transplantation (allo-HCT) for patients with hematologic malignancies. Traditional allo-HCT relies on HLA-matched donors, but matched related donors are only available for approximately 30% of patients, with significant disparities across ethnic groups [87]. Only 29% of Black or African American patients find matched unrelated donors compared to 79% of White patients of European descent. Omisirge is a nicotinamide-modified ex vivo expanded cord blood-derived hematopoietic progenitor cell therapy that overcomes the cell dose limitation of conventional cord blood transplants [87] [88]. By expanding the stem and progenitor cell population through nicotinamide modulation of the NAM-NAD+ signaling pathway, the technology inhibits differentiation and promotes self-renewal, resulting in a product with enhanced engraftment potential.
Clinical Trial Design and Outcomes
The clinical development of Omisirge progressed through randomized Phase III trial (NCT02730299) comparing omidubicel to standard umbilical cord blood transplantation in patients with high-risk hematologic malignancies [87]. The trial enrolled patients aged 12-65 years requiring transplantation who lacked a matched related or matched unrelated donor. This randomized controlled design provided robust evidence of superiority over standard cord blood transplantation.
Table 2: Key Efficacy Outcomes from Omisirge Phase III Clinical Trial
| Efficacy Endpoint | Omidubicel Group | Standard UCBT Group | P-value |
|---|---|---|---|
| Median Time to Neutrophil Recovery | 12 days | 22 days | <0.001 |
| Median Time to Platelet Recovery | 34 days | 46 days | 0.03 |
| Incidence of Bacterial Infections | 37% | 57% | 0.03 |
| Incidence of Invasive Fungal Infections | 8% | 21% | 0.02 |
| Grade II-III Acute GvHD | 60% | 45% | 0.04 |
The primary endpoint of time to neutrophil recovery (defined as absolute neutrophil count ≥500/μL for three consecutive days) demonstrated a clinically significant 10-day advantage for Omisirge compared to standard cord blood (12 days vs. 22 days, p<0.001) [87]. This accelerated hematologic recovery translated into meaningful clinical benefits including significantly reduced infection rates and shorter initial hospital stays. The trade-off observed was a higher incidence of Grade II-III acute GvHD in the Omisirge group (60% vs. 45%, p=0.04), consistent with the enhanced immune reconstitution but requiring careful management. The trial successfully established the risk-benefit profile of Omisirge, leading to its approval for patients 12 years and older with hematologic malignancies.
Experimental Protocol: Cord Blood Expansion and Quality Control
Objective: To manufacture nicotinamide-expanded cord blood-derived hematopoietic progenitor cells that accelerate neutrophil recovery after myeloablative conditioning.
Materials:
- Umbilical Cord Blood Unit: Collected under informed consent, cryopreserved
- Expansion Media: Serum-free medium supplemented with nicotinamide, stem cell factor, thrombopoietin, FLT-3 ligand
- Cell Culture Equipment: Gas-permeable cell culture bags, bioreactor system
- Flow Cytometry Panel: Antibodies against CD34, CD45, CD133, CD3, CD19, CD14, CD56
- Colony-Forming Unit (CFU) Assay Components: Methocult medium, cytokines
- Mycoplasma Detection Kit: PCR-based or culture-based method
Methodology:
- Cord Blood Processing: Thaw cryopreserved cord blood unit rapidly at 37°C. Wash to remove cryoprotectant. Isolate mononuclear cells via density gradient centrifugation. Perform CD34+ cell enumeration to establish baseline.
- Ex Vivo Expansion: Seed cells at 1-5×10⁴ cells/mL in serum-free expansion medium containing 10mM nicotinamide, 100ng/mL SCF, 100ng/mL TPO, and 100ng/mL FLT-3 ligand. Culture in gas-permeable bags at 37°C, 5% CO₂ for 21 days. Feed cultures weekly with fresh cytokines.
- Process Monitoring: Sample cultures periodically for cell count, viability, and immunophenotype. Maintain glucose levels >100 mg/dL and pH between 7.0-7.4.
- Final Product Harvest: On day 21, harvest cells by centrifugation. Wash and resuspend in final formulation medium containing 10% DMSO and 1% human serum albumin.
- Quality Control Testing:
- Identity and Purity: Analyze by flow cytometry for CD34+ (target >30% of viable cells) and CD45+ cells. Exclude lymphoid (CD3+, CD19+) and myeloid (CD14+) contaminants.
- Potency Assays: Perform CFU assay by plating 500 cells in methylcellulose medium with cytokines. Count colonies (CFU-GEMM, BFU-E, CFU-GM) after 14 days. Establish correlation with engraftment potential.
- Sterility Testing: Perform BacT/ALERT for bacterial and fungal contamination. Test for mycoplasma by PCR. Endotoxin testing with LAL assay (<5.0 EU/kg).
- Viability Assessment: Determine via trypan blue exclusion or flow cytometry with 7-AAD (requirement >70%).
- Cryopreservation and Storage: Control-rate freeze at -1°C/minute to -80°C, then transfer to vapor phase liquid nitrogen. Maintain chain of custody and temperature monitoring during storage and transport.
Case Study 3: Lyfgenia (lovotibeglogene autotemcel or Lovo-cel)
Clinical Context and Mechanism of Action
Lyfgenia represents a breakthrough in genetic medicine for sickle cell disease (SCD), a debilitating inherited hemoglobinopathy caused by a point mutation in the β-globin gene. This mutation leads to production of abnormal hemoglobin S (HbS), which polymerizes under deoxygenated conditions, causing red blood cell sickling, vaso-occlusive crises, and progressive multi-organ damage. Lyfgenia is an autologous cell-based gene therapy that utilizes a lentiviral vector to genetically modify patients' own hematopoietic stem cells to produce HbAT87Q, a gene-therapy derived hemoglobin that functions similarly to normal adult hemoglobin A but contains a single amino acid substitution (threonine to glutamine at position 87) that inhibits HbS polymerization [89]. This approach addresses the fundamental pathophysiology of SCD at the molecular level.
Clinical Trial Design and Outcomes
The clinical development of Lyfgenia employed a single-arm, 24-month multicenter study in patients aged 12-50 years with sickle cell disease and history of vaso-occlusive events (VOEs) [2] [89]. The trial design focused on demonstrating complete resolution of VOEs, the most clinically meaningful endpoint for patients. All patients underwent myeloablative conditioning with busulfan before infusion with the genetically modified autologous cells.
Table 3: Key Efficacy Outcomes from Lyfgenia Clinical Trial
| Efficacy Parameter | Result | Assessment Period |
|---|---|---|
| Patients Achieving Complete Resolution of VOEs (VOE-CR) | 88% (28/32 patients) | 6-18 months post-infusion |
| Median Hemoglobin AT87Q Levels | ~40% of total hemoglobin | 6-18 months post-infusion |
| Successful Engraftment Rate | 100% | By Day 42 post-infusion |
| Neutrophil Engraftment (ANC ≥500/μL) | Median 21 days | Post-infusion |
| Platelet Engraftment (≥50,000/μL) | Median 39 days | Post-infusion |
The primary efficacy endpoint was complete resolution of VOEs (VOE-CR) between 6 and 18 months after infusion with Lyfgenia, with 88% (28/32) of patients achieving this endpoint [89]. This profound clinical effect correlated with sustained production of the therapeutic HbAT87Q at approximately 40% of total hemoglobin. The safety profile included expected effects of myeloablative conditioning (stomatitis, cytopenias, febrile neutropenia) and a Black Box Warning for hematologic malignancy, which occurred in patients treated with Lyfgenia, necessitating lifelong monitoring [89]. The trial successfully demonstrated a favorable risk-benefit profile for patients with severe SCD, leading to approval with Risk Evaluation and Mitigation Strategy (REMS) requirements.
Experimental Protocol: Lentiviral Vector Transduction and HSC Processing
Objective: To manufacture autologous CD34+ hematopoietic stem cells transduced with lentiviral vector encoding HbAT87Q for treatment of sickle cell disease.
Materials:
- Patient Apheresis Product: CD34+ cells collected via apheresis after mobilizations
- Lentiviral Vector: BB305 LVV encoding HbAT87Q, produced under GMP
- Transduction Media: X-VIVO 15 or StemSpan with cytokines (SCF, TPO, FLT-3 ligand)
- Retronectin: Recombinant fibronectin fragment for transduction enhancement
- Cell Processing Equipment: Closed-system cell processing set, COBE 2991 or similar
- Myeloablative Conditioning Agent: Busulfan
- Cryopreservation Equipment: Controlled-rate freezer, cryobags
Methodology:
- CD34+ Cell Selection: Thaw apheresis product if cryopreserved. Isolate CD34+ cells using immunomagnetic selection (CliniMACS or similar). Determine CD34+ cell count, viability, and purity (target >70%).
- Pre-transduction Culture: Culture CD34+ cells overnight in transduction medium containing 100ng/mL SCF, TPO, and FLT-3 ligand at 1×10⁶ cells/mL. Maintain at 37°C, 5% CO₂.
- Lentiviral Vector Transduction: Coat culture vessels with retronectin (10-20μg/cm²). Seed cells at 1×10⁶ cells/mL with lentiviral vector at target multiplicity of infection (MOI 5-10). Add protamine sulfate (4μg/mL) to enhance transduction. Incubate for 16-24 hours at 37°C.
- Repeat Transduction and Expansion: Harvest cells, centrifuge, and resuspend in fresh transduction medium with vector for second transduction if required. Continue culture for total of 3-5 days.
- Final Product Formulation: Harvest transduced cells, wash to remove vector and cytokines. Resuspend in infusion medium containing Plasma-Lyte A and 1% HSA. Perform final cell count, viability, and vector copy number (VCN) analysis.
- Quality Control Release Testing:
- Vector Copy Number (VCN): Perform qPCR with specific probes for vector sequence and reference gene. Determine mean VCN (target 0.5-5.0 copies/diploid genome).
- Sterility Testing: BacT/ALERT for bacterial and fungal sterility. Mycoplasma PCR. Endotoxin testing (<5.0 EU/kg).
- Potency Assay: Colony-forming unit (CFU) assay with PCR analysis of individual colonies for vector presence. Determine transduction efficiency.
- Identity: Confirm CD34+ cell content and vector-specific sequences.
- Viability: Trypan blue exclusion (requirement >70%).
- Product Administration: Patient undergoes myeloablative conditioning with busulfan. Thaw product at bedside if cryopreserved. Infuse via central venous catheter over 20-30 minutes. Monitor for infusion reactions.
Diagram 2: Autologous Gene Therapy Manufacturing and Treatment Workflow
Cross-Cutting Analysis: Clinical Trial Design Strategies
Endpoint Selection and Patient Population Optimization
The success of these stem cell therapies demonstrates the critical importance of endpoint selection aligned with mechanism of action and careful patient stratification. Ryoncil utilized Day 28 Overall Response Rate as a primary endpoint, appropriate for a rapidly progressing condition like SR-aGvHD where early intervention is critical [86]. This endpoint balanced clinical meaningfulness with practical trial duration. Omisirge selected time to neutrophil recovery as its primary endpoint, directly measuring the proposed biological advantage of the expanded cell product and its potential to reduce early transplant complications [87]. Lyfgenia employed complete resolution of vaso-occlusive events between 6-18 months, capturing the fundamental clinical benefit desired by patients while allowing sufficient time for engraftment and hemoglobin stabilization [89].
Patient population selection reflected strategic clinical development decisions. All three therapies initially targeted populations with high unmet medical need: Ryoncil in pediatric SR-aGvHD where mortality exceeds 80% with conventional treatments; Omisirge in patients lacking matched donors who face significantly worse transplant outcomes; Lyfgenia in sickle cell patients with history of vaso-occlusive events despite standard care [85] [87] [89]. This approach not only addressed urgent medical needs but also created feasible development pathways where dramatic clinical effects could be demonstrated in manageable patient cohorts.
Clinical Trial Phases and Regulatory Strategy
The clinical development pathways for these therapies illustrate how adaptive trial designs and regulatory expedited programs can accelerate availability of promising treatments while maintaining rigorous safety standards.
Table 4: Clinical Trial Phases and Regulatory Pathways for Approved Stem Cell Therapies
| Therapy | Phase I/II Focus | Phase III Design | Expedited Programs | Approval Date |
|---|---|---|---|---|
| Ryoncil | Safety in SR-aGvHD patients | Single-arm, multicenter in 54 patients | Fast Track, RMAT* | December 18, 2024 |
| Omisirge | Dose-finding, engraftment | Randomized vs standard UCBT | Breakthrough Therapy | April 17, 2023 |
| Lyfgenia | Safety, hemoglobin expression | Single-arm, 24-month study in 32 patients | Fast Track, RMAT, Priority Review | December 8, 2023 |
*Regenerative Medicine Advanced Therapy [2] [86] [89]
Ryoncil's development leveraged the Regenerative Medicine Advanced Therapy (RMAT) designation, allowing for rolling submission and increased FDA interactions throughout development [2] [86]. The single-arm trial design was ethically justified by the life-threatening nature of SR-aGvHD and absence of effective alternatives. Omisirge employed a randomized controlled trial, providing robust evidence of superiority over standard cord blood transplantation [87]. This design was feasible because standard cord blood transplantation represented an established, though suboptimal, therapeutic option. Lyfgenia utilized multiple expedited programs including Fast Track and Priority Review, recognizing the transformative potential of this gene therapy for sickle cell disease [89]. The single-arm design with historical controls was appropriate given the predictable natural history of severe sickle cell disease and the magnitude of treatment effect observed.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Key Research Reagent Solutions for Stem Cell Therapy Development
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Serum-Free Cell Culture Media | Provides defined nutrients and growth factors without animal components | X-VIVO 15, StemSpan for hematopoietic cell culture [87] |
| Recombinant Human Cytokines | Stimulates proliferation, maintains stemness, supports differentiation | SCF, TPO, FLT-3 ligand for HSC expansion [87] |
| Immunomagnetic Cell Separation Kits | Isletes specific cell populations with high purity | CD34+ selection for HSC transplantation [89] |
| Flow Cytometry Antibody Panels | Characterizes cell surface markers, purity, and identity | CD73/CD90/CD105 for MSCs; CD34/CD45 for HSCs [85] [86] |
| Lentiviral Vector Systems | Delivers genetic material to target cells for gene therapy | BB305 LVV for HbAT87Q expression in Lyfgenia [89] |
| Colony-Forming Unit (CFU) Assays | Measures functional potency of stem cell products | Methocult for hematopoietic progenitor potency [87] |
| Cryopreservation Solutions | Maintains cell viability during frozen storage | DMSO with human serum albumin for cell banking [86] |
| Mycoplasma Detection Kits | Ensures cell cultures free from mycoplasma contamination | PCR-based methods for rapid screening [86] |
The successful regulatory approval of Ryoncil, Omisirge, and Lyfgenia provides a roadmap for future stem cell therapy development across diverse therapeutic areas. These case studies demonstrate that successful clinical programs share several key attributes: (1) strong biological rationale with robust preclinical data packages; (2) efficient manufacturing processes capable of producing consistent, well-characterized cell products; (3) clinical trial designs that incorporate meaningful endpoints aligned with mechanism of action; and (4) strategic regulatory engagement utilizing expedited programs when appropriate. Furthermore, these successes highlight the importance of patient-centric development—focusing on conditions with severe unmet needs where stem cell therapies can offer transformative benefits. As the field advances, these pioneering products establish benchmarks for quality, efficacy, and safety that will inform the next generation of stem cell-based medicines currently in development.
The development of stem cell therapies represents a frontier in modern medicine, offering potential treatments for a range of serious and life-threatening conditions. However, the pathway from laboratory research to clinically approved therapies is complex and navigates a multifaceted global regulatory landscape. For researchers, scientists, and drug development professionals, understanding the convergent and divergent elements of key regulatory frameworks is crucial for designing efficient and compliant clinical trials. This document provides a detailed comparison of the clinical trial regulations in the United States (U.S.), European Union (EU), and Japan, with a specific focus on implications for stem cell therapy development. It aims to serve as a practical guide for planning and executing phase I-III stem cell clinical trials within these jurisdictions, incorporating the latest regulatory updates for 2025.
Global Regulatory Framework Comparison
Substantial efforts have been made by regulators to accelerate the assessment and approval of transformative therapies, yet variations persist in marketing authorization pathways and expedited approval programs for advanced therapies across the U.S., EU, and Japan [90]. The table below provides a high-level comparison of the core regulatory frameworks, which is essential for strategic trial planning.
Table 1: Comparative Overview of Regulatory Frameworks for Advanced Therapies
| Feature | United States (U.S.) | European Union (EU) | Japan |
|---|---|---|---|
| Governing Legislation | Food and Drug Administration Amendments Act (FDAAA), 21st Century Cures Act [90] [91] | Clinical Trials Regulation (EU) No 536/2014 (CTR) [92] [93] | Pharmaceuticals and Medical Devices Act (PMD Act), Clinical Trials Act [90] [94] |
| Lead Regulatory Agency | Food and Drug Administration (FDA), specifically the Center for Biologics Evaluation and Research (CBER) [90] [2] | European Medicines Agency (EMA) and National Competent Authorities of Member States [90] | Ministry of Health, Labour and Welfare (MHLW) and Pharmaceuticals and Medical Devices Agency (PMDA) [90] [94] |
| Classification of Stem Cell Therapies | Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/P’s); regulated as drugs/biological products [90] | Advanced Therapy Medicinal Products (ATMPs) [90] | Regenerative Medicine Products [90] [95] |
| Key Expedited Pathway(s) | Regenerative Medicine Advanced Therapy (RMAT), Fast Track, Breakthrough Therapy [90] [96] | Conditional Marketing Authorization, Priority Medicines (PRIME) [90] | SAKIGAKE Designation, Conditional Time-Limited Approval [90] |
| Primary Clinical Trial Application System | Investigational New Drug (IND) application via FDA Portal [94] | Clinical Trial Application (CTA) via Clinical Trials Information System (CTIS) [92] [93] | Clinical Trial Notification/Consultation via PMDA [94] |
A significant trend across all regions is the push for greater transparency and harmonization. For instance, in the U.S., the 2025 updates to the FDAAA 801 Final Rule have shortened deadlines for submitting clinical trial results to 9 months and introduced public flags for non-compliance [91]. Similarly, the EU's CTR, fully implemented in 2025, mandates that all clinical trial information be submitted through the CTIS portal, with much of this data becoming publicly accessible [93] [97]. Japan participates in the International Council for Harmonisation (ICH), actively working to harmonize technical requirements and reduce drug lag [94].
Regulatory Pathways and Expedited Programs
For stem cell therapies, which often target serious conditions with unmet medical needs, expedited development pathways are particularly relevant. These programs are designed to accelerate patient access to promising therapies, though they often come with specific obligations for post-market data collection.
United States Expedited Pathways
The FDA offers several expedited programs, with the Regenerative Medicine Advanced Therapy (RMAT) designation being particularly significant for stem cell products. Established under the 21st Century Cures Act, RMAT is available for regenerative medicine therapies intended to treat, modify, reverse, or cure a serious condition [90] [96]. Key benefits include intensive FDA guidance and potential use of surrogate or intermediate endpoints to support accelerated approval. In 2025, the FDA (CBER) released a new draft guidance detailing how sponsors can utilize these expedited development and review pathways for regenerative medicine therapies [96].
European Union Expedited Pathways
In the EU, the Conditional Marketing Authorization (CMA) pathway is available for ATMPs that have a positive benefit-risk balance and are likely to address unmet medical needs. Under CMA, approval can be granted based on less comprehensive clinical data than normally required, provided the sponsor commits to providing full data post-authorization [90]. The Priority Medicines (PRIME) scheme also provides enhanced support and early dialogue for medicines that target an unmet medical need.
Japan Expedited Pathways
Japan's regulatory system features the SAKIGAKE designation, which aims to encourage the development of innovative products and promote marketing authorization ahead of other countries. Designated drugs benefit from prioritized consultation and accelerated review [90]. Furthermore, under the PMD Act, a unique, conditional time-limited marketing authorization can be issued based on preliminary clinical data, with a requirement to submit confirmatory post-marketing evidence within a pre-defined period (up to 7 years) to convert to standard approval [90].
Clinical Trial Application and Submission Processes
The processes for initiating clinical trials differ significantly across regions, impacting trial start-up timelines and operational planning.
United States: IND Process
In the U.S., clinical trials for stem cell therapies require the submission of an Investigational New Drug (IND) application to the FDA. The IND must contain information in three broad areas: animal pharmacology and toxicology studies, manufacturing information, and clinical protocols and investigator information [94] [2]. The FDA has 30 days to review the IND after which the study may proceed if the agency raises no objections [2]. It is critical to note that an IND authorization allows a clinical trial to proceed but is distinct from full product approval, which requires a successful Biologics License Application (BLA) [2].
European Union: CTR and CTIS
The EU's Clinical Trials Regulation (CTR) has centralized the application process through the Clinical Trials Information System (CTIS). This system serves as the single entry point for submitting clinical trial applications in the EU [92] [93]. For multinational trials, the sponsor submits a single application for approval in all concerned Member States, streamlining what was previously a fragmented process. The transition from the previous Clinical Trials Directive to the CTR was completed on January 30, 2025, meaning all clinical trials in the EU/EEA must now be conducted under the CTR using CTIS [92] [97].
Japan: PMDA Consultation and Notification
Japan's process involves consultation with the Pharmaceuticals and Medical Devices Agency (PMDA). For clinical trials aimed at marketing approval, sponsors must comply with the PMD Act and Good Clinical Practice (GCP) standards [94] [95]. The Clinical Trials Act of 2018 created a streamlined process where, after obtaining Institutional Review Board (IRB) approval, sponsors submit an application to the PMDA, which typically responds within 30 days [94].
Figure 1: Generalized Clinical Trial and Approval Pathway for Stem Cell Therapies. While the phase progression is similar, the specific application (IND, CTA, Consultation) and approval (BLA, MAA, MA) mechanisms are region-specific.
Experimental Protocols for Stem Cell Trial Design
Designing robust clinical trials for stem cell therapies requires careful consideration of regulatory expectations, patient safety, and the unique challenges posed by these complex products.
Protocol 1: Phase I Safety and Tolerability Study
Objective: To assess the safety, tolerability, and preliminary characterization of dose-limiting toxicities of an allogeneic iPSC-derived neural progenitor cell therapy in patients with Parkinson's disease.
Methodology:
- Study Design: Open-label, single-arm, dose-escalation study.
- Patient Population: A small cohort (e.g., n=12-15) of patients with confirmed diagnosis, stratified based on disease severity. Inclusion of adolescent patients in adult oncology trials requires special considerations as outlined in FDA guidance [98].
- Dosing: Sequential cohorts receiving progressively higher cell doses. The starting dose is based on rigorous preclinical toxicology data.
- Endpoint Measurements:
- Primary Endpoints: Incidence and severity of adverse events (AEs) and serious adverse events (SAEs), including immunogenic responses.
- Secondary Endpoints: Changes in unified Parkinson's disease rating scale (UPDRS) scores, quality of life measures, and biomarker assessment via neuroimaging.
- Data Collection: Safety monitoring continues for a defined long-term follow-up period (e.g., 5-15 years) to monitor for delayed effects, such as tumorigenicity, as emphasized in the 2025 FDA draft guidance on post-approval data collection for cell/gene therapies [96].
Protocol 2: Phase II/III Pivotal Trial Design
Objective: To evaluate the efficacy and safety of an iPSC-derived retinal pigment epithelium (RPE) cell therapy for geographic atrophy (GA) secondary to age-related macular degeneration.
Methodology:
- Study Design: Randomized, controlled, double-masked, multi-regional trial.
- Patient Population: Larger cohort (e.g., n=100+) with well-defined GA. The FDA encourages enrichment strategies and broader eligibility criteria to enhance the diversity of clinical trial populations where scientifically appropriate [98].
- Intervention: Experimental group receives the cell therapy; control group receives a sham intervention.
- Endpoint Measurements:
- Primary Endpoint: Change in GA area from baseline as measured by fundus autofluorescence (FAF) at 12 months. The use of such digital health technologies for remote data acquisition is supported by recent FDA draft guidance [98].
- Secondary Endpoints: Best-corrected visual acuity (BCVA), low-luminance visual acuity, patient-reported outcomes.
- Statistical Analysis: A detailed statistical analysis plan (SAP) must be pre-specified, incorporating the estimand framework (ICH E9(R1)), which has been adopted by agencies like Australia's TGA and provides clarity on handling intercurrent events [96].
- Data Management: Use of electronic data capture (EDC) systems compliant with 21 CFR Part 11 and aligned with Clinical Data Interchange Standards Consortium (CDISC) standards for electronic submissions, which are required by the FDA and PMDA [94].
The Scientist's Toolkit: Research Reagent Solutions
The successful development and manufacturing of stem cell therapies rely on a suite of critical reagents and materials that ensure product quality, consistency, and safety.
Table 2: Essential Research Reagents and Materials for Stem Cell Therapy Development
| Reagent/Material | Function | Application in Stem Cell R&D |
|---|---|---|
| GMP-Grade iPSC Master Cell Bank | Serves as the standardized, quality-controlled starting material for deriving therapeutic cell types. Ensures batch-to-batch consistency and reduces variability. | Used to generate differentiated cells (e.g., dopaminergic neurons, RPE cells) for transplantation. A filed Drug Master File (DMF) for the master cell bank can streamline regulatory submissions [2]. |
| Xeno-Free Culture Media & Supplements | Provides nutrients and growth factors for cell expansion and differentiation without animal-derived components. Mitigates risk of zoonotic pathogen transmission and immunogenic reactions. | Essential for the in vitro culture of iPSCs and their progeny during the manufacturing process to meet safety standards for clinical applications. |
| Cell Differentiation Kits & Reagents | Directs pluripotent stem cells toward specific somatic lineages (e.g., neural, cardiac, pancreatic) through defined molecular cues. | Critical for producing the target therapeutic cell population with high purity and functional maturity for the intended indication. |
| Characterization Antibodies & Assay Kits | Used for quality control testing, including flow cytometry, immunocytochemistry, and ELISA. Confirms cell identity, purity, potency, and absence of residual undifferentiated cells. | Mandatory for pre-clinical characterization and lot-release testing of the final cell product. Data is included in IND/CTA applications. |
| Cryopreservation Media | Enables long-term storage of the final cell product in a viable state using cryoprotectants like DMSO. Maintains cell viability and functionality during storage and transport. | Used for the final formulation of the cell therapy product, which is often administered as a frozen suspension. |
The global regulatory landscape for stem cell clinical trials is dynamic, with a clear trend towards convergence in key areas such as transparency, ethical standards, and the adoption of expedited pathways for innovative therapies. However, critical differences remain in the specific regulatory architectures of the U.S., EU, and Japan regarding application processes, classification, and approval mechanisms. For drug development professionals, a deep understanding of these frameworks is not merely a regulatory requirement but a strategic component that can significantly influence trial design, operational planning, and ultimately, the successful translation of stem cell research into approved therapies. By leveraging the comparative insights, experimental protocols, and toolkit provided in this document, researchers can navigate this complex environment more effectively, accelerating the delivery of groundbreaking treatments to patients in need.
Conclusion
The successful design of stem cell clinical trials hinges on a meticulous, phase-appropriate strategy that balances scientific rigor with evolving regulatory expectations. Foundational safety in Phase I must be built upon with robust efficacy data in Phase II, culminating in conclusive validation through well-powered Phase III trials. The integration of advanced tools like AI and systems biology, alongside adaptive manufacturing and trial designs, is poised to accelerate development. Future progress depends on continued international regulatory collaboration, the refinement of potency assays, and a steadfast commitment to addressing the unique challenges of stem cell therapeutics to fully realize their potential in regenerative medicine.
References
- 1. Investigational New Drug Applications (INDs) for CBER- ... [https://www.fda.gov/vaccines-blood-biologics/development-approval-process-cber/investigational-new-drug-applications-inds-cber-regulated-products]
- 2. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 3. Investigational New Drug (IND) Application [https://www.fda.gov/drugs/types-applications/investigational-new-drug-ind-application]
- 4. Clinical Trial Phases Explained | ASGCT [https://patienteducation.asgct.org/research-clinical-trials/clinical-trial-phases-explained]
- 5. Master the Investigational New Drug Application Process [https://www.bioaccessla.com/blog/master-the-investigational-new-drug-application-process]
- 6. Submitting an IND Application - One UNC Clinical Research [https://clinicalresearch.unc.edu/playbooks/my-study-lifecycle/study-start-up/fda-regulatory-approvals/investigational-new-drug-ind/submitting-an-ind-application/]
- 7. REGULATORY UPDATE: FDA Releases 2025 Guidance ... [https://www.aabb.org/news-resources/news/article/2025/01/03/regulatory-update--fda-releases-2025-guidance-agenda]
- 8. Guidances [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidances]
- 9. The Different Phases of Clinical Trials [https://www.quanticate.com/blog/bid/63143/the-different-phases-of-clinical-trials]
- 10. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 11. A single-center, phase 1/2a trial of hESC-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087345/]
- 12. Report of a phase 1 clinical trial for safety assessment of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03390-9]
- 13. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 14. Analyses of selected safety endpoints in phase 1 and late- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5620211/]
- 15. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 16. Future needs for informed consent in stem cell clinical trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4774238/]
- 17. Who should be included in first-in-human trials? A systematic ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06550-y]
- 18. Comparison of baseline patient characteristics in phase 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083001/]
- 19. A comparison of approaches to incorporate patient ... [https://arxiv.org/html/2510.11578v1]
- 20. Statistical methods and data visualisation of patient ... [https://www.sciencedirect.com/science/article/pii/S2589537023004054]
- 21. Ethical Considerations in Clinical Research [https://studypages.com/blog/ethical-considerations-in-clinical-research/]
- 22. Enhanced patient selection with quantitative continuous ... [https://www.nature.com/articles/s41698-025-01107-0]
- 23. Expedited Programs [https://friendsofcancerresearch.org/glossary-term/expedited-programs/]
- 24. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 25. FDA's New Plausible Mechanism Pathway [https://www.avancebio.com/fdas-new-plausible-mechanism-pathway-how-it-compares-to-existing-approval-routes/]
- 26. Biopharma RD Faces Productivity And Attrition Challenges ... [https://www.clinicalleader.com/doc/biopharma-r-d-faces-productivity-and-attrition-challenges-in-2025-0001]
- 27. Clinical Trials | UCLA BSCRC [https://stemcell.ucla.edu/clinical-trials]
- 28. Phases I–III Clinical Trials Using Adult Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2975079/]
- 29. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 30. Novel Stem Cell Therapy Repairs Irreversible Corneal Damage in Clinical Trial [https://masseyeandear.org/news/press-releases/2025/03/novel-calec-stem-cell-therapy-clinical-trial-repairs-corneal-damage]
- 31. How Are Stem Cells Administered to the Body? [https://celltexbank.com/blog-delivery-routes/]
- 32. What Conditions Can Stem Cell Therapy Treat in 2025? [https://cellebrationwellness.com/what-conditions-can-stem-cell-therapy-actually-treat-in-2025/]
- 33. The role of stem cells in precision medicine: next-generation ... [https://jenci.springeropen.com/articles/10.1186/s43046-025-00328-5]
- 34. Phases of Clinical Trials [https://www.cancer.org/cancer/managing-cancer/making-treatment-decisions/clinical-trials/phases-of-clinical-trials.html]
- 35. Global clinical trials on stem cell therapy for autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328461/]
- 36. Phase I/II trial of iPS-cell-derived dopaminergic cells for ... [https://www.nature.com/articles/s41586-025-08700-0]
- 37. Neurona Unveils Phase 3 EPIC Study for NRTX-1001 Cell ... [https://www.neuronatherapeutics.com/news/press-releases/022025/]
- 38. Stem cells therapy in neurodegenerative and ... [https://www.sciencedirect.com/science/article/pii/S1043661825003858]
- 39. Clinical Trial Phases: A Guide to Phase I, II, III & IV [https://intuitionlabs.ai/articles/four-phases-clinical-trials]
- 40. Rare Disease Focus: FDA's Trio of Cell and Gene Therapy ... [https://www.ropesgray.com/en/insights/alerts/2025/11/rare-disease-focus-fdas-trio-of-cell-and-gene-therapy-draft-guidances-highlight-expedited-programs]
- 41. FDA targets innovative CGT trial designs in draft guidance [https://www.clinicaltrialsarena.com/news/fda-targets-innovative-cgt-trial-designs-in-draft-guidance/]
- 42. How Precision Medicine is Transforming Rare Disease ... [https://tfscro.com/resources/rare-disease-day-2025-how-precision-medicine-is-transforming-treatment-for-rare-diseases/]
- 43. FDA Lends a Single Arm: Papzimeos Approval Highlights ... [https://www.thefdalawblog.com/2025/09/fda-lends-a-single-arm-papzimeos-approval-highlights-fdas-willingness-to-rely-on-single-arm-trials-for-rare-diseases/]
- 44. Top Clinical Research Organizations for Rare Diseases in ... [https://www.precisionformedicine.com/blog/top-clinical-research-organizations-for-rare-diseases-in-2025]
- 45. Quantitative Imaging Biomarkers: The Application of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3553365/]
- 46. Interpreting results from biomarker-guided clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121256/]
- 47. AI-guided patient stratification improves outcomes and ... [https://www.nature.com/articles/s41467-025-61355-3]
- 48. Global clinical trials on stem cell therapy for autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 49. Efficacy of a single intra-articular injection of mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398016/]
- 50. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 51. Methods of determining optimal cut-point of diagnostic ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02198-2]
- 52. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 53. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 54. Design and validation of a GMP stem cell manufacturing ... [https://www.sciencedirect.com/science/article/pii/S2329050124000871]
- 55. Recommendations for Determining Eligibility of Donors ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/recommendations-determining-eligibility-donors-human-cells-tissues-and-cellular-and-tissue-based]
- 56. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 57. Why Early Genetic Variant Detection in iPSC Cultures Is ... [https://www.reprocell.com/blog/why-early-genetic-variant-detection-in-ipsc-cultures-is-critical-for-safe-and-regulatory-compliant-cell-therapies]
- 58. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 59. Elimination of tumorigenic pluripotent stem cells from their ... [https://www.sciencedirect.com/science/article/pii/S221367112500147X]
- 60. A comprehensive review of clinical trials and progress in ... [https://www.sciencedirect.com/science/article/pii/S2352320425001944]
- 61. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 62. Identifying and optimizing critical process parameters for ... [https://pubmed.ncbi.nlm.nih.gov/39522051/]
- 63. Identifying and optimizing critical process parameters for large ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03973-0]
- 64. Development of a quantitative prediction algorithm for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8302568/]
- 65. Improving Stem Cell Clinical Trial Design and Conduct [https://pmc.ncbi.nlm.nih.gov/articles/PMC7671799/]
- 66. Artificial intelligence and systems biology analysis in stem ... [https://pubmed.ncbi.nlm.nih.gov/41015943/]
- 67. Adaptive Trial Design: A Guide to Flexible Clinical Trials [https://intuitionlabs.ai/articles/adaptive-clinical-trial-design]
- 68. Phase I–II clinical trial design: a state-of-the-art paradigm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5888967/]
- 69. Implementing Adaptive Clinical Trial Designs to Shorten ... [https://theconferenceforum.org/editorial/implementing-adaptive-clinical-trial-designs-to-shorten-timelines-at-bluesphere-bio]
- 70. Adaptive Trial Design - The Innovation Imperative [https://druginnovation.eiu.com/adaptive-trials/]
- 71. AI In clinical trials in 2025: the edge of tech [https://clinicaltrialrisk.org/clinical-trial-design/ai-in-clinical-trials-the-edge-of-tech/]
- 72. iGEM 2025/2026: Systems Biology in Biomedical ... [https://www.frontiersin.org/research-topics/73776/igem-20252026-systems-biology-in-biomedical-innovations-and-healthcare]
- 73. The next generation of clinical trials with AI [https://www.ddw-online.com/the-next-generation-of-clinical-trials-with-ai-36171-202508/]
- 74. Practical guidance for conducting high-quality and rapid ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04362-x]
- 75. Endpoints used in phase III randomized controlled trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7265861/]
- 76. Adoption of multiple primary endpoints in phase III trials ... [https://www.sciencedirect.com/science/article/pii/S0959804921001556]
- 77. Using phase II data for the analysis of phase III studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC5833035/]
- 78. Optimal designs for phase II/III drug development programs ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01093-w]
- 79. Biologics License Applications (BLA) Process (CBER) [https://www.fda.gov/vaccines-blood-biologics/development-approval-process-cber/biologics-license-applications-bla-process-cber]
- 80. The Biologics License Application (BLA) Process Explained [https://www.thefdagroup.com/blog/2014/07/test-the-biologics-license-application-bla-process/]
- 81. Clinical trial design for testing the stem cell model ... [https://pubmed.ncbi.nlm.nih.gov/24212828/]
- 82. Stem Cell Therapy Clinical Trials [https://www.mayo.edu/research/clinical-trials/tests-procedures/stem-cell-therapy]
- 83. BLA Filing Process for Gene Therapy Products: 2025 Guide [https://insights.forgebiologics.com/bla-filing-process-for-gene-therapy-products-2025-guide]
- 84. Postapproval Methods To Capture Safety and Efficacy Data ... [https://www.federalregister.gov/documents/2025/09/25/2025-18650/postapproval-methods-to-capture-safety-and-efficacy-data-for-cell-and-gene-therapy-products-draft]
- 85. Ryoncil [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/ryoncil]
- 86. FDA approval of Ryoncil (remestemcel-L-rknd) for steroid- ... [https://www.fda.gov/drugs/resources-information-approved-drugs/fda-disco-burst-edition-fda-approval-ryoncil-remestemcel-l-rknd-steroid-refractory-acute-graft]
- 87. OMISIRGE® (omidubicel-onlv) | Allogeneic Hematopoietic ... [https://omisirge.com/]
- 88. NO MORE LIMITATIONS FOR CORD BLOOD USE [https://www.famicord.com/groundbreaking-no-more-limitations-for-cord-blood-use]
- 89. FDA Approves First Gene Therapies to Treat Patients with ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease]
- 90. Regulatory Pathways in Europe, the United States, and ... [https://www.ispor.org/publications/journals/value-outcomes-spotlight/vos-archives/issue/view/challenges-in-precision-medicine-aiming-to-align-data-value-and-costs/regulatory-pathways-in-europe-the-united-states-and-japan-and-health-technology-assessments-for-gene-therapies]
- 91. 2025 FDAAA 801 Final Rule Changes Impacting Clinical ... [https://prorelixresearch.com/2025-fdaaa-801-clinical-trial-rule-impact/]
- 92. Clinical trials - Public Health - European Commission [https://health.ec.europa.eu/medicinal-products/clinical-trials_en]
- 93. Clinical trials - Regulation EU No 536/2014 - Public Health [https://health.ec.europa.eu/medicinal-products/clinical-trials/clinical-trials-regulation-eu-no-5362014_en]
- 94. Comparing Clinical Trial Regulations: USA vs. APAC [https://tfscro.com/resources/comparing-clinical-trial-regulations-usa-vs-apac/]
- 95. Healthcare: Medical Devices 2025 - Japan [https://practiceguides.chambers.com/practice-guides/healthcare-medical-devices-2025/japan/trends-and-developments]
- 96. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 97. Prepare for the Implementation of the EU Clinical Trial ... [https://www.ppd.com/blog/prepare-for-eu-clinical-trial-regulation-implementation/]
- 98. Clinical Trials Guidance Documents [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/clinical-trials-guidance-documents]