Embryonic vs Adult Stem Cells: A Comparative Analysis of Therapeutic Applications and Clinical Translation
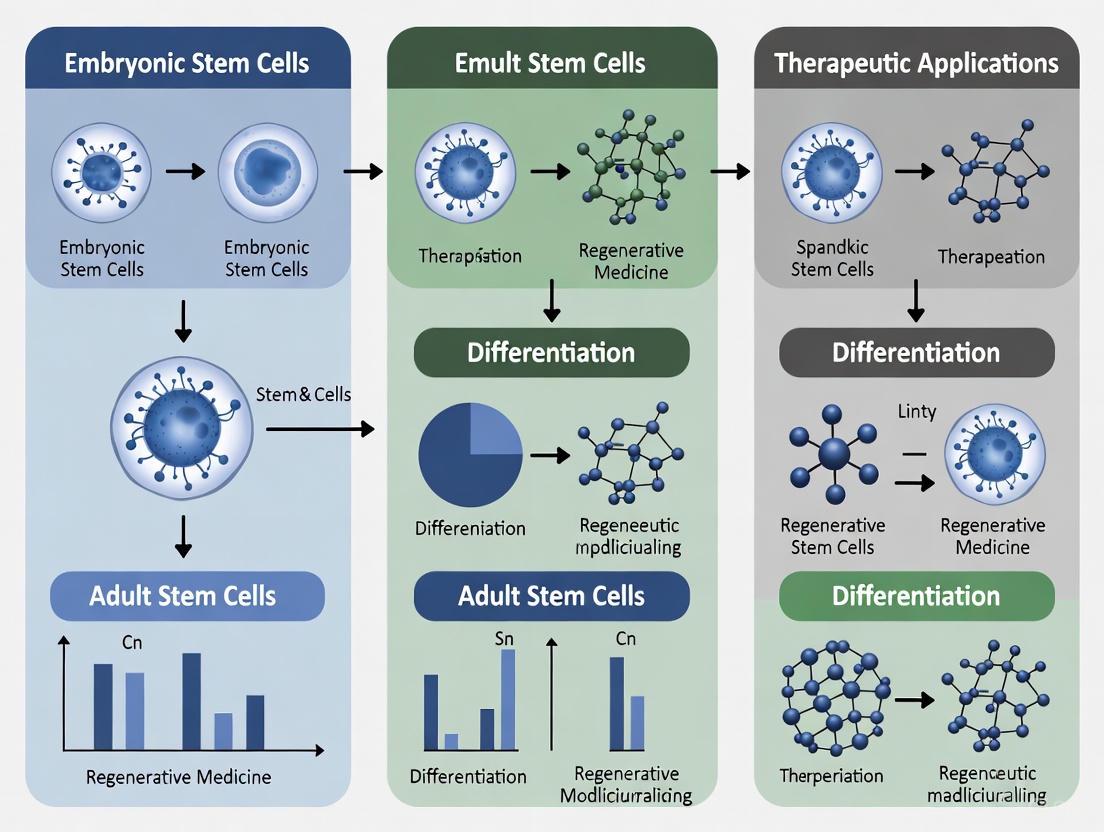
This article provides a comprehensive comparative analysis of embryonic stem cells (ESCs) and adult stem cells (ASCs) for researchers and drug development professionals.
Embryonic vs Adult Stem Cells: A Comparative Analysis of Therapeutic Applications and Clinical Translation
Abstract
This article provides a comprehensive comparative analysis of embryonic stem cells (ESCs) and adult stem cells (ASCs) for researchers and drug development professionals. It explores the foundational biology, distinct properties, and ethical considerations of each cell type. The scope extends to current methodological applications in regenerative medicine and disease modeling, alongside critical troubleshooting of optimization challenges such as tumorigenicity, immunogenicity, and manufacturing. The analysis validates therapeutic potential through clinical trial data and direct comparative assessment of efficacy, safety, and regulatory pathways, offering a strategic framework for selecting the appropriate stem cell type for specific therapeutic intents.
Understanding Stem Cell Biology: From Pluripotency to Tissue-Specific Function
Stem cells are fundamentally characterized by their dual capacities for self-renewal and differentiation [1]. The developmental potential of a stem cell—its "potency"—is the primary feature distinguishing its type and defining its therapeutic application. Pluripotency and multipotency represent two critical hierarchical levels within this spectrum. Embryonic Stem Cells (ESCs), derived from the inner cell mass of the blastocyst, represent the gold standard for pluripotency, possessing the ability to differentiate into all cells of the three embryonic germ layers [2] [3] [4]. In contrast, Adult Stem Cells (ASCs), also known as somatic stem cells, are typically multipotent, with a more restricted differentiation capacity limited to the cell types of their tissue of origin [2] [1]. This guide provides a detailed, data-driven comparison of these cell types, framing their characteristics within the context of therapeutic development for researchers and drug development professionals.
Defining Pluripotency and Multipotency: A Hierarchical Comparison
Molecular and Functional Definitions
The distinction between pluripotency and multipotency is governed by distinct molecular networks and epigenetic landscapes, which directly translate to differing functional capabilities in research and therapy.
Core Pluripotency Network in ESCs: Pluripotency is maintained by a core transcriptional network. Oct4, Sox2, and Nanog form an autoregulatory loop, binding to each other's promoters to activate and sustain their own transcription, thereby preserving the undifferentiated state [3]. This network is active in the naïve pluripotent state of the pre-implantation embryo and can transition to a primed pluripotency state in the post-implantation epiblast, a distinction marked by changes in gene expression, metabolism, and signaling pathway dependence [3]. For instance, naïve mouse ESCs depend on Leukemia Inhibitory Factor (LIF) and Bone Morphogenetic Protein (BMP), whereas primed human ESCs and EpiSCs rely on Activin A/Nodal and Fibroblast Growth Factor 2 (FGF2) signaling [3].
Defining Multipotency in ASCs: Multipotent ASCs, such as Mesenchymal Stem Cells (MSCs), do not express the core pluripotency factors. Instead, they are identified by a specific set of surface markers (e.g., CD73, CD90, CD105 for MSCs) and are characterized by their capacity for self-renewal and differentiation into a limited range of lineages relevant to their tissue of origin [2] [5]. For example, adipose-derived stem cells (ASCs) can differentiate into osteoblasts, adipocytes, and chondrocytes [5] but lack the capacity to form entire tissues derived from all three germ layers.
Table 1: Hierarchical Classification of Stem Cell Potency
| Potency Level | Defining Characteristic | Prototypical Cell Types | Key Molecular Regulators |
|---|---|---|---|
| Pluripotency | Can differentiate into all derivatives of the three embryonic germ layers (ectoderm, mesoderm, endoderm). | Embryonic Stem Cells (ESCs), Induced Pluripotent Stem Cells (iPSCs) | Oct4, Sox2, Nanog, Autocrine FGF signaling, specific epigenetic landscapes [3] [4]. |
| Multipotency | Can differentiate into multiple cell types, but restricted to a specific lineage or tissue of origin. | Adult Stem Cells (ASCs) including Hematopoietic Stem Cells (HSCs), Mesenchymal Stem Cells (MSCs). | Tissue-specific transcription factors (e.g., GATA factors in HSCs); surface markers like CD73, CD90, CD105 for MSCs [2] [5]. |
Comparative Analysis: ESCs vs. ASCs
Origin, Differentiation Potential, and Key Markers
The fundamental differences between ESCs and ASCs originate from their distinct biological niches and physiological roles.
Table 2: Comprehensive Comparison of ESCs and ASCs
| Characteristic | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Origin | Inner Cell Mass (ICM) of the blastocyst [3] [4]. | Various adult tissues (e.g., bone marrow, adipose tissue) [2] [5]. |
| Potency | Pluripotent [1]. | Multipotent (typically) [1]. |
| In Vivo Role | To form all tissues of the developing embryo. | Tissue maintenance, repair, and regeneration in the adult organism [2]. |
| Key Molecular Markers | Oct4, Sox2, Nanog, SSEA-3, SSEA-4, TRA-1-60, TRA-1-81 [3] [4]. | Varies by type; MSCs: CD73, CD90, CD105; lack Oct4/Nanog [2] [5]. |
| Self-Renewal Capacity | 理论上无限 in vitro [3]. | Limited in vitro, can enter senescence [2]. |
| Genetic Stability | Generally stable but can accumulate aberrations over long-term culture [6]. | Can be affected by donor age and health status (e.g., obesity reprograms ASC transcriptome) [7]. |
| Therapeutic Mechanisms | Primarily through direct differentiation into target cells for replacement [1]. | Primarily through paracrine signaling (secretion of growth factors, cytokines, exosomes), immunomodulation, and anti-apoptotic effects [5] [1]. |
| Major Advantages | Unlimited differentiation potential; model for early development; "gold standard" for pluripotency [8] [4]. | No ethical controversies; autologous transplantation possible; lower risk of teratoma formation; innate homing to injury sites [9] [5] [1]. |
| Major Challenges | Ethical controversies; risk of immune rejection; tumorigenicity (teratomas); complex differentiation protocols [9] [1]. | Limited differentiation potential; variability based on source and donor; lower expandability; potential functional impairment in disease [7] [1]. |
Experimental Data and Functional Evidence
Quantitative data from differentiation experiments and functional assays underscore the practical implications of these potency differences.
Differentiation Efficiency: A landmark study comparing the differentiation propensity of 20 hESC and 12 hiPSC lines found that, despite overall similarity, hiPSCs exhibited increased variation in the yield of neural progeny. The study developed a "lineage scorecard" based on the expression of 500 lineage-related genes, which highly correlated (Pearson's r = 0.87) with the observed efficiency of motor neuron differentiation [4]. This highlights that while pluripotent cells have broad potential, the efficiency of generating specific lineages can be variable and cell-line dependent.
Transcriptomic and Epigenetic Differences: Obesity serves as a model for how the ASC microenvironment impacts function. RNA sequencing of adipose-derived MSCs from lean (BMI <25) versus obese (BMI ≥35) donors revealed significant transcriptional reprogramming. In obese ASCs, 738 genes were significantly upregulated and 767 downregulated, with pathways related to extracellular matrix (ECM) organization, TGF-β signaling, and cell adhesion molecules being particularly affected [7]. This demonstrates that ASC function is not static but can be compromised by disease states, a crucial consideration for therapeutic development.
Experimental Protocols for Assessing Potency
In Vitro Pluripotency Assay for ESCs
The standard in vitro method to confirm ESC pluripotency is the Embryoid Body (EB) Formation Assay.
- Culture and Detachment: Human ESCs are maintained on a feeder layer of mouse embryonic fibroblasts (MEFs) or in a feeder-free system on Matrigel or similar substrate. Colonies are treated with collagenase IV or dispase to detach them as small clumps [4].
- EB Formation: The clumps are transferred to non-adherent Petri dishes or U-bottom low-attachment plates in ESC medium without pluripotency factors (e.g., without bFGF). Under these conditions, cells aggregate to form 3D structures called embryoid bodies.
- Spontaneous Differentiation: EBs are cultured for 7-21 days, during which they spontaneously differentiate into cells representing all three germ layers.
- Analysis:
- Immunocytochemistry: EBs are plated on adhesive slides, fixed, and stained for germ layer-specific markers: β-III Tubulin (ectoderm), α-Smooth Muscle Actin (α-SMA) (mesoderm), and Alpha-Fetoprotein (AFP) (endoderm).
- RT-qPCR: RNA is extracted from EBs and analyzed for the downregulation of pluripotency genes (OCT4, NANOG) and upregulation of differentiation markers from all three germ layers.
In Vitro Trilineage Differentiation Assay for ASCs (e.g., MSCs)
The gold standard for confirming the multipotency of MSCs is the Trilineage Differentiation Assay.
- Cell Source and Seeding: MSCs are isolated from tissue (e.g., adipose tissue via enzymatic digestion with collagenase to obtain the stromal vascular fraction) and characterized by flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45) markers [5]. For differentiation, cells are seeded at high density in multi-well plates.
- Osteogenic Differentiation: Cells are cultured in growth medium supplemented with 10 mM β-glycerophosphate, 50 µM ascorbic acid, and 100 nM dexamethasone for 2-3 weeks. Differentiation is confirmed by Alizarin Red S staining, which detects calcium deposits in the extracellular matrix.
- Adipogenic Differentiation: Cells are cultured in medium supplemented with 1 µM dexamethasone, 0.5 mM isobutylmethylxanthine (IBMX), 10 µg/mL insulin, and 200 µM indomethacin for 1-3 weeks. Lipid vacuole accumulation is visualized by Oil Red O staining.
- Chondrogenic Differentiation: A pellet culture system is used. Approximately 2.5 x 10^5 cells are centrifuged to form a pellet, which is cultured in serum-free medium with 10 ng/mL TGF-β3, 100 nM dexamethasone, 50 µg/mL ascorbic acid, and 1x ITS (Insulin-Transferrin-Selenium) supplement for 3-4 weeks. The resulting pellet is sectioned and stained with Alcian Blue or Toluidine Blue to detect sulfated proteoglycans in the cartilage matrix.
Signaling Pathways and Molecular Control
The maintenance of pluripotency and the induction of differentiation are controlled by intricate signaling networks. The core pluripotency circuitry, centered on the autoregulatory loop of OCT4, SOX2, and NANOG, integrates signals from key pathways like FGF, TGF-β/Activin A, and WNT. These signals help maintain the epigenetic landscape that defines the pluripotent state. In contrast, the multipotency of ASCs is regulated by a different set of context-dependent signals. For MSCs, pathways such as BMP for osteogenesis, TGF-β for chondrogenesis, and PPARγ for adipogenesis drive their lineage-specific differentiation. The primary cilium, a sensory organelle on ASCs, is a critical signaling hub; its dysfunction (e.g., in obesity, via downregulation of RFX2 and ADCY3) can impair ASC differentiation and regenerative capacity [7].
Diagram Title: Core Signaling in ESCs vs. ASCs
The Scientist's Toolkit: Essential Reagents for Stem Cell Research
Table 3: Key Research Reagent Solutions for Stem Cell Studies
| Reagent/Category | Function in ESC Research | Function in ASC Research |
|---|---|---|
| Collagenase Type IV | Used for the mechanical dissociation of ESC colonies into clumps for passaging or EB formation [4]. | Critical for the enzymatic digestion of adipose tissue to isolate the Stromal Vascular Fraction (SVF) containing ASCs [5]. |
| Matrigel / Geltrex | A basement membrane matrix used as a feeder-free substrate for the attachment and growth of ESCs and iPSCs. | Used as a 3D scaffold for chondrogenic differentiation assays or in tissue engineering constructs. |
| Basic Fibroblast Growth Factor (bFGF/FGF-2) | A key cytokine added to media to maintain hESC and hiPSC pluripotency in feeder-free cultures [3]. | Promotes ASC proliferation and is involved in wound healing applications by stimulating fibroblast growth and angiogenesis [5]. |
| Y-27632 (ROCK inhibitor) | Greatly improves the survival and cloning efficiency of single ESCs/iPSCs after dissociation (e.g., for transfection or subcloning). | Enhances the viability and recovery of ASCs after thawing from cryopreservation or during single-cell passaging. |
| Defined Culture Media | TeSR-E8, mTeSR: Chemically defined, xeno-free media for maintaining ESCs/iPSCs under standardized conditions. | MSCGM, StemPro: Specialty media formulations optimized for the expansion of MSCs while maintaining their multipotency. |
| Trilineage Differentiation Kits | Not typically used, as ESCs are assessed via EB formation and spontaneous differentiation into all germ layers. | Commercial kits (e.g., from MilliporeSigma, Thermo Fisher) provide optimized, pre-mixed media for robust osteogenic, adipogenic, and chondrogenic differentiation of MSCs. |
The choice between ESCs and ASCs is not a matter of superiority but of strategic alignment with research and therapeutic goals. ESCs, with their vast and well-defined pluripotency, are unparalleled tools for disease modeling (especially early developmental disorders), high-throughput drug screening, and generating cell types that are difficult to obtain from adult tissues, such as specific neuronal subtypes or cardiac cells [8] [1]. However, their clinical application is tempered by ethical considerations, immune rejection risks, and tumorigenicity.
Conversely, ASCs offer a more readily translatable path for autologous cell therapies and immunomodulation. Their inherent role in tissue repair and the ability to harness their paracrine functions make them ideal for treating inflammatory and degenerative conditions like osteoarthritis, wound healing, and graft-versus-host disease [5] [1]. The critical caveat is that their potency and function can be donor-dependent, influenced by age, health, and disease state, necessitating rigorous quality control [7]. As the field advances, the complementary use of both cell types—leveraging ESC-derived cells for complex disease models and ASCs for regenerative immunomodulation—will likely pave the way for a new era in regenerative medicine.
Stem cells are fundamental units of development and regeneration, characterized by their dual capacities for self-renewal and differentiation into specialized cell types [10]. Their potential, however, is profoundly influenced by their developmental origin. Embryonic stem cells (ESCs) are derived from the inner cell mass of blastocysts, an early stage of embryonic development, and represent a state of developmental pluripotency [11] [10]. In contrast, adult stem cells (ASCs), also known as somatic stem cells, reside in specialized microenvironments known as niches within fully formed tissues and organs, where they function in maintenance and repair [12] [13]. This guide provides a detailed, objective comparison of these two distinct cellular populations, focusing on their biological characteristics, experimental handling, and therapeutic profiles for a research audience.
Core Biological Characteristics: A Comparative Analysis
The developmental origin of a stem cell dictates its fundamental biological properties, which in turn determine its suitability for specific research or therapeutic applications.
Table 1: Comparative Analysis of Core Biological Characteristics
| Characteristic | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Developmental Origin | Inner Cell Mass (ICM) of the blastocyst [11] [14] | Specific niches in adult tissues (e.g., bone marrow, fat, brain) [13] |
| Key Defining Properties | Pluripotency, high self-renewal capacity [11] | Multipotency, role in tissue homeostasis [13] |
| Primary Functions | Generate all cell types of the developing fetus [11] [10] | Maintain and repair the tissue in which they reside [10] [13] |
| Differentiation Potential | Can differentiate into any of the three germ layers (Pluripotent) [11] [1] | Differentiate into a limited range of cell types within their tissue of origin (Multipotent) [13] [1] |
| Genomic Features | Exhibit a "naive" state; gold standard for pluripotency [15] | Somatic cell genome; may show age-associated alterations [10] |
A critical concept for ASCs is the stem cell niche, a specialized microenvironment that regulates their fate. Proposed by Schofield in 1978, the niche maintains stem cell self-renewal, guides differentiation, and responds to injury and microenvironmental cues such as oxygenation and mechanotransduction [12]. This dynamic regulatory system is absent in ESC cultures, which rely on defined in vitro conditions.
Experimental Protocols for Isolation and Culture
Methodologies for working with ESCs and ASCs differ significantly due to their distinct origins and biological properties. The workflows below outline the core experimental protocols.
Embryonic Stem Cell (ESC) Derivation and Culture
The following diagram illustrates the process of deriving and maintaining ESCs from a blastocyst.
Title: ESC Derivation and Culture Workflow
Detailed Protocol:
- Blastocyst Source: ESCs are derived from the inner cell mass (ICM) of a human blastocyst, typically from embryos created via in vitro fertilization (IVF) that are no longer needed [10].
- ICM Isolation: The ICM is isolated using microsurgery or a second approach involving antibody-mediated targeting of the surrounding trophoblast cells [11].
- Pluripotent Culture: The isolated cells are placed in a culture system designed to maintain pluripotency, often involving mouse embryonic fibroblast feeder layers or defined matrices with specific media containing growth factors like FGF-2 [11].
- Verification and Differentiation: Established cell lines are verified for pluripotency markers (e.g., OCT4, SOX2, NANOG). For differentiation, the culture conditions are altered to remove self-renewal signals and introduce cues (e.g., growth factors, cytokines) that guide the cells toward specific lineages (e.g., cardiomyocytes, neurons) [11] [15].
Adult Stem Cell (ASC) Isolation and Expansion
The process for isolating and studying ASCs from tissue sources is summarized below.
Title: ASC Isolation and Study Workflow
Detailed Protocol:
- Tissue Harvesting: ASCs are isolated from various adult tissues. Common sources include bone marrow (aspirated), adipose tissue (from lipoaspirate), and umbilical cord blood [13].
- Cell Isolation: The tissue is processed via enzymatic digestion (e.g., with collagenase) to create a single-cell suspension. Target cells can then be isolated using techniques like density gradient centrifugation or, for specific populations like MSCs, adherence to plastic in standard culture conditions [13].
- Characterization and Expansion: ASCs are expanded in culture. Mesenchymal Stem Cells (MSCs), a key ASC type, are defined by specific criteria: adherence to plastic, in vitro differentiation into osteoblasts, adipocytes, and chondroblasts, and expression of surface markers (CD105+, CD73+, CD90+) while lacking hematopoietic markers (CD45-, CD34-, etc.) [13].
- Functional Assays: The multipotent differentiation potential is confirmed using specific induction media. Their therapeutic potential is further investigated in animal models of disease, where mechanisms like immunomodulation and paracrine signaling can be studied [13] [1].
Therapeutic Applications and Clinical Trial Data
The distinct biological properties of ESCs and ASCs translate into different therapeutic potentials and associated risks, as reflected in clinical trial outcomes.
Table 2: Comparative Therapeutic Profiles and Clinical Translation
| Parameter | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Therapeutic Potential | High versatility for regenerating diverse tissues [11] | Effective for tissue-specific repair and immunomodulation [13] [1] |
| Key Clinical Applications | ESC-derived RPE cells: Age-related macular degeneration (trials) [15]ESC-derived pancreatic cells: Type 1 diabetes (research) [16] | HSCs: Leukemia, lymphoma (standard of care) [11] [1]MSCs: Graft-versus-host disease, osteoarthritis, Crohn's disease (trials) [14] [1] |
| Clinical Trial Status | Mostly early-phase clinical trials [15] | Several established therapies; extensive ongoing trials [11] [1] |
| Major Safety Concerns | Tumorigenicity: Teratoma formation due to undifferentiated cells [11] [15]Immunological rejection upon allogeneic transplantation [10] | Lower tumorigenic risk compared to ESCs [17]Potential for irregularities from donor age/environment [10] |
| Key Advantages | Pluripotency: Can generate any cell type [17]High self-renewal: Unlimited expansion in culture [11] | Autologous transplantation is possible, avoiding rejection [13]Established safety profile in specific uses (e.g., HSC transplant) [1] |
| Primary Limitations | Ethical controversies regarding embryo destruction [10] [18]Safety concerns regarding tumorigenicity [11] | Limited differentiation potential (multipotent) [1]Decreased function and number with donor age [13] |
A promising development is the emergence of Induced Pluripotent Stem Cells (iPSCs). These are adult somatic cells reprogrammed to an embryonic-like pluripotent state via the introduction of defined transcription factors (OCT4, SOX2, KLF4, c-MYC) [15] [16]. iPSCs bypass the ethical concerns of ESCs and allow for the creation of patient-specific cell lines, serving as powerful tools for disease modeling and drug screening, though concerns about tumorigenicity remain [15].
The Scientist's Toolkit: Essential Reagents and Materials
Successful research in this field relies on a suite of specialized reagents and tools. The following table details key solutions for working with stem cells.
Table 3: Essential Research Reagent Solutions
| Reagent / Material | Function in Research | Application Context |
|---|---|---|
| Yamanaka Factors (OCT4, SOX2, KLF4, c-MYC) | Genetic reprogramming of somatic cells into iPSCs [15] [16] | iPSC generation; studying pluripotency |
| CRISPR-Cas9 System | Precise genome editing to correct disease-causing mutations or introduce reporters [11] [15] | Gene therapy in ESCs/iPSCs; functional genomics |
| Feeder Layers (e.g., Mouse Embryonic Fibroblasts - MEFs) | Provide a supportive substrate and secrete factors that help maintain pluripotency [11] | Initial ESC and iPSC culture |
| Defined Culture Media (e.g., mTeSR, StemPro) | Serum-free media with precise formulations of growth factors (e.g., FGF-2) to maintain stemness or direct differentiation [11] | Long-term, reproducible ESC/iPSC culture |
| Flow Cytometry Antibodies (e.g., CD105, CD73, CD90) | Identification and purification of specific stem cell populations based on surface marker expression [13] | Characterization and isolation of MSCs |
| Specific Induction Media | Contain cocktails of growth factors and chemicals to drive differentiation into specific lineages (e.g., bone, fat, cartilage) [13] | In vitro assessment of multipotency (e.g., for MSCs) |
| Single-Cell RNA Sequencing (scRNA-seq) | High-resolution analysis of cellular heterogeneity and transcriptional states within a stem cell population [11] | Profiling niche populations; characterizing differentiation cultures |
Self-Renewal Capacities and In Vitro Expansion Potential
The choice between embryonic and adult stem cells for therapeutic development hinges upon a fundamental understanding of their self-renewal and expansion capabilities. This guide provides a data-driven comparison of these core properties to inform preclinical research and protocol development.
Defining Stem Cell Properties
Stem cell potential is categorized by differentiation capacity and self-renewal mechanisms.
- Pluripotency: The ability to differentiate into any cell type from all three embryonic germ layers (ectoderm, mesoderm, and endoderm). This is a defining characteristic of embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) [19] [20].
- Multipotency: The capacity to differentiate into multiple cell types, but within a specific lineage or tissue family (e.g., hematopoietic stem cells giving rise to various blood cells) [11] [21].
- Self-Renewal: The process by which a stem cell divides to produce at least one identical daughter stem cell, thereby maintaining the stem cell pool. This can occur through:
- Symmetric Division: One stem cell divides into two identical stem cells.
- Asymmetric Division: One stem cell divides into one identical stem cell and one differentiated progenitor cell [21].
Comparative Analysis: Embryonic vs. Adult Stem Cells
The table below summarizes the key characteristics governing the self-renewal and expansion potential of different stem cell types.
| Feature | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) - Hematopoietic Focus | Adult Stem Cells - Mesenchymal Focus |
|---|---|---|---|
| Pluripotency/Multipotency | Pluripotent [19] [11] | Multipotent (blood lineage) [11] [21] | Multipotent (osteogenic, chondrogenic, adipogenic) [22] |
| Primary In Vivo Role | Form all tissues during embryonic development [19] | Maintain homeostasis and regeneration of the blood system [23] | Tissue maintenance and repair (e.g., bone, cartilage, fat) [11] [22] |
| In Vitro Self-Renewal | Unlimited with optimized protocols [19] | Limited; prone to exhaustion and differentiation in culture [24] | Senescence after prolonged passage [22] |
| Key Signaling Pathways | LIF/STAT3 (mouse), TGF-β/Activin A/Nodal (human), Wnt/β-Catenin, PI3K/AKT [19] | Wnt, Notch, BMP; largely quiescent in niche [21] [24] | Dependent on source; influenced by inflammatory and growth factors [22] |
| Cell Cycle Profile | Abbreviated or absent G1 phase; rapid cycling [24] | Predominantly quiescent (G0 phase); slow-cycling in vivo [24] | Varies with tissue source and donor age |
| Genetic Stability | High, but requires monitoring for karyotypic abnormalities over long-term culture [19] | Accumulates ~45 somatic mutations/year in mouse models; clonal evolution with age [23] | Generally stable, but potential for senescence-associated changes |
Experimental Protocols for Assessing Self-Renewal
Clonal Colony-Forming Assays
Purpose: To quantify the frequency of cells within a population that can proliferate to form a colony, demonstrating self-renewal and proliferative capacity.
Detailed Methodology:
- Cell Seeding: Dissociate cells into a single-cell suspension and seed them at a very low density (e.g., 100-1,000 cells per well of a 6-well plate) to ensure colonies are clonal (derived from a single cell).
- Culture Conditions: Use optimized, feeder-free media conditions that support the stem cell type being tested. For human ESCs, this includes media containing TGF-β/Activin A and FGF2 [19]. For murine ESCs, media is supplemented with LIF and BMP4 [19].
- Feeder Layer (Optional): Some protocols use a layer of inactivated mouse embryonic fibroblasts (MEFs) to provide a supportive extracellular matrix and secreted factors.
- Culture Duration: Incubate for 7-14 days, with media changes every other day.
- Analysis: Colonies are fixed and stained with crystal violet or alkaline phosphatase. Only colonies exceeding a minimum threshold (e.g., >50 cells) are counted as positive. The colony-forming efficiency (CFE) is calculated as (Number of Colonies / Number of Cells Seeded) × 100%.
In Vivo Serial Transplantation Assay
Purpose: The gold-standard functional test for defining hematopoietic stem cells (HSCs), assessing their long-term self-renewal ability in a living organism.
Detailed Methodology:
- Donor Cell Preparation: HSCs are isolated from the bone marrow of a donor mouse using fluorescence-activated cell sorting (FACS) for specific surface markers (e.g., Lin⁻, Sca-1⁺, c-Kit⁺, CD150⁺, CD48⁻).
- Transplantation: The purified HSCs are transplanted into lethally irradiated recipient mice to eliminate the host's endogenous blood system. Supporting cells, such as competitor bone marrow cells, are co-transplanted to ensure short-term survival.
- Engraftment Analysis: After 4-6 months, peripheral blood and bone marrow from recipients are analyzed by flow cytometry to confirm multilineage engraftment (presence of myeloid, B-cell, and T-cell lineages) derived from the donor HSCs.
- Serial Transplantation: To stringently test self-renewal, bone marrow cells from the primary recipient are harvested and transplanted into a new set of lethally irradiated secondary recipients. The ability to reconstitute the blood system over multiple rounds indicates robust self-renewal capacity [23]. A recent 2025 study used whole-genome sequencing of single-cell-derived colonies from this assay to track somatic evolution and clonal dynamics over the mouse lifespan [23].
The Scientist's Toolkit: Key Research Reagents
This table lists essential reagents and their applications in stem cell self-renewal research.
| Research Reagent | Primary Function in Self-Renewal Research |
|---|---|
| LIF (Leukemia Inhibitory Factor) | Cytokine used to maintain self-renewal and pluripotency in murine ESCs by activating the STAT3 pathway [19]. |
| Activin A / TGF-β | Growth factors critical for sustaining human ESC pluripotency by activating Smad2/3 signaling and promoting Nanog expression [19]. |
| BMP4 (Bone Morphogenetic Protein 4) | In combination with LIF, supports murine ESC self-renewal by inhibiting ERK/MAPK differentiation signals and inducing Id genes [19]. |
| CHIR99021 | A small molecule GSK-3β inhibitor that activates Wnt/β-catenin signaling, used to support self-renewal and maintain stemness in various stem cell types [25]. |
| Y-27632 (ROCK inhibitor) | Improves the survival of single stem cells after passaging, thereby increasing cloning efficiency and reducing anoikis during subculture. |
| StemRNA Clinical Seed iPSCs | Clinical-grade, GMP-compliant induced pluripotent stem cell lines submitted to the FDA under a Drug Master File (DMF) for use in regulatory-compliant therapy development [26]. |
Signaling Pathways Governing Self-Renewal
The molecular regulation of self-renewal differs significantly between embryonic and adult stem cells. The following diagrams illustrate the core pathways.
Core Pluripotency Signaling Network
Diagram Title: Core Signaling in Embryonic Stem Cells
This network shows the key pathways that sustain ESC self-renewal. The LIF/STAT3 and TGF-β/Activin A/Smad2/3 pathways are central to activating core pluripotency transcription factors like Nanog and Sox2 [19]. Simultaneously, BMP signaling induces Id genes to suppress differentiation, while FGF/ERK signaling often promotes differentiation, creating a delicate balance that must be managed in culture [19].
Wnt Pathway in Stem Cell Fate
Diagram Title: Wnt/β-Catenin Pathway Logic
The Wnt/β-catenin pathway is a master regulator of self-renewal in both embryonic and adult stem cells [21]. When the pathway is "OFF," a destruction complex targets β-catenin for proteasomal degradation. When Wnt signaling is "ON," the destruction complex is disrupted, allowing β-catenin to accumulate, enter the nucleus, and complex with Tcf/Lef transcription factors to activate the expression of self-renewal genes [21].
Research Implications and Future Directions
The distinct self-renewal properties of embryonic and adult stem cells present clear trade-offs for therapeutic development. ESCs and iPSCs offer unparalleled expansion potential for generating the vast cell numbers needed for therapies, but require precise control over differentiation and carry a risk of teratoma formation [19] [26]. Adult stem cells, particularly HSCs, have a proven record in clinical applications like bone marrow transplantation but are limited by donor availability, graft size, and age-related clonal evolution [11] [23].
Future research is focused on overcoming these limitations. Strategies include manipulating the cell cycle and signaling pathways to enhance the expansion of HSCs in culture [24], and developing novel cell types like Muse cells—naturally occurring, stress-resistant pluripotent-like cells found within mesenchymal tissues that show strong immunotolerance and tissue-reparative functions after intravenous injection [22]. Furthermore, the emergence of iPSC-derived MSCs (iMSCs) promises a more consistent and scalable source of mesenchymal cells for regenerative applications, potentially overcoming the heterogeneity and senescence of primary MSCs [26].
Stem cell research represents a revolutionary frontier in modern medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries [11]. This field is broadly divided between embryonic stem cell (ESC) research, which utilizes pluripotent cells derived from early-stage embryos, and adult stem cell research, which works with multipotent cells found in various tissues throughout the body [10] [13]. The ethical and regulatory considerations for these two pathways differ substantially, creating a complex landscape that researchers must navigate.
The distinctive properties of stem cells—their ability to self-renew and differentiate into specialized cell types—make them indispensable for regenerative medicine applications [11]. However, the very source of ESCs raises significant ethical questions that have shaped the regulatory environment. This guide objectively compares the ethical and regulatory frameworks governing embryonic versus adult stem cell research, providing researchers with the tools to conduct scientifically rigorous and ethically sound research.
Ethical Considerations: A Comparative Analysis
The ethical debate surrounding stem cell research primarily focuses on the moral status of the human embryo, creating a fundamental distinction between embryonic and adult stem cell approaches.
Embryonic Stem Cell Ethics
The derivation of human embryonic stem cells requires the destruction of human embryos, raising disputes about the onset of human personhood and the moral status of human embryos [18]. This has led to significant ethical controversies, particularly from religious and pro-life communities who argue that destroying embryos for research is morally wrong [27] [18].
- Moral Status of Embryos: The central ethical concern revolves around whether embryos deserve the same moral consideration as developed human beings [18].
- Source of Embryos: Most hESC lines are derived from embryos created through in vitro fertilization (IVF) that are no longer needed for reproductive purposes and would otherwise be discarded [10] [18].
- Informed Consent: Ethical guidelines require proper informed consent from donors for the use of these embryos in research [27] [10].
Adult Stem Cell Ethics
Adult stem cell research faces considerably fewer ethical objections as it does not involve the destruction of embryos [27] [18] [13]. These somatic stem cells are obtained from developed tissues such as bone marrow, adipose tissue, and other adult organs, bypassing the central ethical dilemma of embryonic research [13].
Induced Pluripotent Stem Cells as an Ethical Alternative
The development of induced pluripotent stem cells (iPSCs) has significantly altered the ethical landscape. These cells, generated by reprogramming adult somatic cells to a pluripotent state, offer similar research potential to ESCs without the ethical concerns specific to embryonic stem cell research [27] [18]. However, iPSCs are not without their own ethical considerations, including concerns about their safety and long-term effects, such as tumor formation [27].
Table: Comparative Ethical Analysis of Stem Cell Types
| Stem Cell Type | Ethical Concerns | Key Ethical Considerations | Primary Objections |
|---|---|---|---|
| Embryonic Stem Cells (ESCs) | High | Destruction of human embryos; Moral status of embryo; Informed consent for embryo donation | Strong opposition from religious and pro-life groups [27] [18] |
| Adult Stem Cells | Low | Informed consent for tissue donation; No destruction of embryos | Minimal ethical objections [27] [18] [13] |
| Induced Pluripotent Stem Cells (iPSCs) | Moderate | No embryo destruction; Potential for human cloning; Safety and long-term effects (e.g., tumorigenesis) | Some concerns about potential misuse and safety [27] |
Regulatory Frameworks and Guidelines
Regulatory frameworks for stem cell research have evolved to address both scientific advancement and ethical concerns, with significant international coordination.
International Guidelines: The ISSCR Framework
The International Society for Stem Cell Research (ISSCR) provides comprehensive international guidelines that are regularly updated to reflect scientific advances. The most recent 2025 update specifically addresses stem cell-based embryo models (SCBEMs) [28] [29]. Key provisions include:
- Oversight Requirements: All 3D SCBEMs must have a clear scientific rationale, defined endpoint, and be subject to appropriate oversight mechanisms [28] [29].
- Research Boundaries: SCBEMs must not be transplanted to the uterus of a living animal or human host, and ex vivo culture is prohibited beyond the point of potential viability (ectogenesis) [28] [29].
- Fundamental Principles: The guidelines emphasize rigor, oversight, and transparency in all areas of practice, maintaining widely shared ethical principles in science [28].
United States Regulatory Landscape
In the United States, the Food and Drug Administration (FDA) plays a critical role in regulating regenerative medicine products, including stem cell therapies [27] [26]. The regulatory framework distinguishes between different categories of stem cell products:
- Minimally Manipulated Products: Human cells, tissues, and cellular and tissue-based products (HCT/Ps) that are minimally manipulated, intended for homologous use, and not combined with another article are regulated under Section 361 of the Public Health Service Act [27].
- More-Than-Minimally Manipulated Products: Stem cell products that undergo more than minimal manipulation, are intended for non-homologous use, or are combined with another article are regulated as drugs or biologics, requiring an Investigational New Drug (IND) application before clinical trials [27].
The FDA has established expedited programs such as the Regenerative Medicine Advanced Therapy (RMAT) designation to facilitate timely development of promising therapies while maintaining safety standards [27] [26].
Table: Recent FDA-Approved Stem Cell Products (2023-2025)
| Product Name | Approval Date | Stem Cell Type | Indication | Key Characteristics |
|---|---|---|---|---|
| Omisirge (omidubicel-onlv) | April 17, 2023 | Cord Blood-Derived Hematopoietic Progenitor Cells | Hematologic malignancies undergoing cord blood transplantation | Accelerates neutrophil recovery; Reduces infection risk post-myeloablative conditioning [26] |
| Lyfgenia (lovotibeglogene autotemcel) | December 8, 2023 | Autologous Cell-Based Gene Therapy | Sickle cell disease with history of vaso-occlusive events | One-time treatment; Modifies patient's own hematopoietic stem cells to produce HbAT87Q [26] |
| Ryoncil (remestemcel-L) | December 18, 2024 | Allogeneic Bone Marrow-Derived MSCs | Pediatric steroid-refractory acute Graft Versus Host Disease (SR-aGVHD) | First MSC therapy approved by FDA; Modulates immune response and mitigates inflammation [26] |
Regulatory Oversight Pathways for Stem Cell Research: This diagram illustrates the primary regulatory pathways for different stem cell research types, highlighting the more stringent requirements for embryonic stem cell research compared to certain adult stem cell applications.
Experimental Protocols and Research Applications
Embryonic Stem Cell Research Protocols
Research involving human embryonic stem cells requires specific protocols to maintain ethical standards while advancing scientific knowledge. The derivation of ESCs typically involves:
- Source Acquisition: hESCs are derived from the inner cell mass of blastocysts (3-5 day old embryos) obtained from in vitro fertilization clinics with informed donor consent [10].
- Isolation Techniques: Two primary methods are employed: microsurgical isolation of the inner cell mass or immunological dissection using antibodies to target trophoblast lineage cells [11].
- Culture Maintenance: ESCs are maintained in specialized culture conditions that preserve their pluripotent state while preventing spontaneous differentiation [10].
The ISSCR guidelines explicitly prohibit certain research applications, including:
- Human reproductive cloning
- Implantation of human embryos into non-human primate uteruses
- Breeding of animals into which human cells have been introduced at any stage of embryonic development
- Culture of human embryos beyond 14 days of development [28]
Stem Cell-Based Embryo Models (SCBEMs)
The 2025 ISSCR guidelines update specifically addresses stem cell-based embryo models, which are three-dimensional stem cell-derived structures that replicate key aspects of early embryonic development [29]. These innovative models offer unprecedented potential to enhance our understanding of human developmental biology while raising unique ethical considerations.
Research Reagent Solutions Toolkit
Table: Essential Research Reagents for Stem Cell Research
| Reagent/Category | Function | Application Notes |
|---|---|---|
| Reprogramming Factors | Genetic or chemical factors to induce pluripotency in somatic cells | Essential for iPSC generation; Includes OCT4, SOX2, KLF4, c-MYC or alternative combinations [18] |
| StemRNA Clinical Seed iPSCs | GMP-compliant iPSC seed clones for therapeutic development | Subject to FDA Drug Master File (DMF) review; Provides standardized starting material [26] |
| Culture Media Systems | Specialized media formulations to maintain stem cell states | Formulations vary for ESCs, iPSCs, and adult stem cells; Often include specific growth factors [11] |
| Differentiation Induction Cocktails | Chemical and biological factors to direct lineage specification | Cell-type specific formulations (e.g., neural, cardiac, hepatic); Critical for functional cell generation [11] |
| Surface Marker Antibodies | Characterization of stem cell populations and differentiation status | CD105, CD73, CD90 for MSCs; CD45, CD34, CD14 negative selection; Pluripotency markers for ESCs/iPSCs [13] |
| CRISPR-Cas9 Systems | Genome editing for disease modeling and functional studies | Enables precise genetic modifications; Requires careful ethical review for germline applications [11] |
| Single-Cell RNA Sequencing Kits | High-resolution analysis of cell populations and differentiation trajectories | Reveals heterogeneity in stem cell populations; Identifies novel cell markers [11] |
The ethical and regulatory landscapes for embryonic and adult stem cell research present distinct pathways for scientific exploration. Embryonic stem cell research offers unparalleled pluripotency but operates within a tightly regulated framework to address significant ethical concerns. Adult stem cell research, while more limited in differentiation potential, faces fewer ethical hurdles and has already yielded multiple FDA-approved therapies.
The emergence of iPSC technology has created a middle ground, offering pluripotency without embryo destruction, though with its own regulatory considerations. The international regulatory environment, guided by organizations like the ISSCR and national bodies like the FDA, continues to evolve alongside scientific advancements.
Researchers must remain vigilant in adhering to both the technical and ethical standards of their respective fields, ensuring that stem cell research progresses in a manner that is both scientifically robust and socially responsible. The continued development of clear guidelines and oversight mechanisms provides the necessary framework to harness the full potential of stem cell research while maintaining public trust and ethical integrity.
Therapeutic Mechanisms and Clinical Applications in Regenerative Medicine
Embryonic Stem Cells (ESCs), first isolated from human blastocysts in 1998, represent a foundational platform in stem cell biology due to their defining characteristics of sustained self-renewal and pluripotency—the ability to differentiate into all cell types in the body [11] [30]. These properties make ESCs uniquely suited for directed differentiation and disease modeling, enabling critical research into human development, disease mechanisms, and the development of new regenerative medicines [30]. This review objectively compares the performance of ESCs against other stem cell types, primarily adult stem cells (ASCs) and induced pluripotent stem cells (iPSCs), within the broader thesis of evaluating therapeutic applications. We provide supporting experimental data and standardized protocols to guide researchers and drug development professionals in selecting appropriate stem cell platforms for specific applications.
Comparative Analysis of Stem Cell Types for Research and Therapy
The choice of stem cell type fundamentally influences experimental design, therapeutic potential, and clinical applicability. The following table summarizes the core characteristics of the major stem cell classes.
Table 1: Comparative Analysis of Major Stem Cell Types
| Feature | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) | Adult Stem Cells (ASCs) |
|---|---|---|---|
| Pluripotency/Multipotency | Pluripotent (can form all embryonic germ layers) [11] [1] | Pluripotent (can form all embryonic germ layers) [15] [1] | Multipotent (limited to cell types of their tissue of origin) [11] [1] |
| Key Advantages | Gold standard for pluripotency; no epigenetic memory; clinically relevant protocols exist [30] [15] | Avoids ethical concerns of ESCs; enables patient-specific disease modeling [15] | No ethical concerns; limited tumorigenicity risk; used in established therapies (e.g., HSCT) [11] [1] |
| Primary Limitations | Ethical controversies; requires immunosuppression in allogeneic therapy [1] | Potential for epigenetic memory; tumorigenicity risk from reprogramming factors [15] | Limited differentiation capacity; difficult to isolate and expand in culture [11] |
| Therapeutic Use Example | Clinical trials for Parkinson's disease and age-related macular degeneration [30] | First iPSC-based therapy (Fertilo) in U.S. Phase III trials [26] | Hematopoietic Stem Cell Transplantation (HSCT) for blood cancers [1] |
Directed Differentiation of ESCs: Protocols and Performance Metrics
Directed differentiation protocols guide ESCs through specific developmental pathways to generate functional, specialized cell types. The reproducibility and efficiency of these protocols are critical for both research and clinical translation.
Experimental Protocol: Generation of Dopaminergic Neurons for Parkinson's Disease
This protocol is adapted from methods used in clinical trials for Parkinson's disease [26] [1].
- Maintenance of Undifferentiated hESCs: Culture hESCs on a feeder layer of mouse embryonic fibroblasts (MEFs) or on a defined substrate like Matrigel in feeder-free conditions. Maintain cells in pluripotency media containing basic Fibroblast Growth Factor (bFGF).
- Embryoid Body (EB) Formation: Detach hESC colonies and transfer to low-attachment plates to form aggregates known as Embryoid Bodies (EBs) in suspension culture. This initiates spontaneous differentiation into the three germ layers.
- Neural Induction: After 4-5 days, transfer EBs to culture dishes coated with poly-L-ornithine/laminin. Culture in neural induction media, typically containing dual SMAD signaling inhibitors (e.g., Noggin, SB431542) to promote neural ectoderm fate over mesoderm and endoderm.
- Dopaminergic Patterning: Once neural rosettes appear (around day 7-10 of differentiation), pattern the cells toward a midbrain dopaminergic phenotype. This is achieved by adding key morphogens such as Sonic Hedgehog (SHH) and Fibroblast Growth Factor 8 (FGF8) to the culture medium.
- Maturation and Purification: Over 4-6 weeks, mature the dopaminergic precursors by withdrawing mitogens and adding growth factors like BDNF (Brain-Derived Neurotrophic Factor), GDNF (Glial Cell line-Derived Neurotrophic Factor), and ascorbic acid. Purification can be achieved using fluorescence-activated cell sorting (FACS) for specific surface markers.
The workflow and key signaling molecules involved in this directed differentiation are summarized in the diagram below.
Quantitative Performance Data
The efficiency of differentiation protocols is a key performance indicator. The following table compares the output of ESC-derived dopaminergic neurons against other cell sources, based on data from preclinical and early clinical studies [26] [1].
Table 2: Performance Comparison of Cell Sources for Dopaminergic Neuron Generation
| Cell Source | Differentiation Efficiency (%) | Time to Functional Maturity | In Vivo Functional Recovery in Rodent Models | Tumorigenicity Risk |
|---|---|---|---|---|
| ESCs | 60-80% | 6-8 weeks | Significant motor improvement observed [1] | Low with optimized protocols [26] |
| iPSCs | 50-75% | 6-8 weeks | Significant motor improvement observed [1] | Moderate (varies with reprogramming method) [15] |
| Fetal Tissue | N/A (Primary cells) | N/A | Gold standard efficacy | None |
| ASCs (e.g., Mesenchymal) | Not possible to generate authentic dopaminergic neurons | N/A | Limited benefit, primarily via paracrine effects [1] | Very Low |
Disease Modeling with ESCs: From 2D to 3D Organoid Systems
While 2D cultures have been instrumental, the field is rapidly advancing toward 3D brain organoids to model the complexity of the human brain and its disorders more accurately [31] [32].
Experimental Protocol: Generating Cerebral Organoids to Model Neurodegeneration
This protocol is based on the landmark cerebral organoid generation method [31] [32].
- EB Formation and Neural Induction: Generate EBs from hESCs as in Step 3.1. Induce neural fate by culturing EBs in neural induction media.
- Embedding in ECM: After 5-7 days, embed the neuroectoderm-containing EBs in droplets of an extracellular matrix (ECM) substitute like Matrigel, which provides a 3D scaffold that supports complex tissue morphogenesis.
- Differentiation and Maturation in a Bioreactor: Transfer the Matrigel-embedded EBs to a spinning bioreactor. This dynamic culture system improves nutrient and oxygen exchange, allowing the organoids to grow larger and develop more complex tissue architectures over periods of 1-3 months.
- Disease Modeling and Analysis: To model a genetic neurodegenerative disease like Alzheimer's, ESCs with relevant mutations (e.g., in PSEN1 or APP) can be used. Alternatively, gene editing tools like CRISPR-Cas9 can be used to introduce disease-causing mutations into wild-type ESCs. The resulting organoids can be analyzed for disease phenotypes, including protein aggregation (e.g., Aβ plaques), neuronal death, and electrophysiological abnormalities.
The workflow for generating these organoids is illustrated below.
Performance Comparison of Modeling Platforms
The physiological relevance of disease models is paramount for predictive drug discovery. The table below compares the capabilities of different stem cell-derived models for neurodegenerative disease modeling [31] [32] [15].
Table 3: Comparison of Stem Cell-Based Platforms for Modeling Neurodegenerative Diseases
| Model System | Physiological Relevance | Cellular Diversity | Ability to Model Complex Circuitry | Throughput for Drug Screening |
|---|---|---|---|---|
| 2D ESC/iPSC Culture | Low (monolayer, simplified) | Low (limited co-cultures) | Very Low | High |
| ESC-Derived Brain Organoids | High (3D architecture, cell-cell interactions) | High (multiple neuronal and glial types) | Moderate (emerging regional connectivity) | Moderate |
| ASC Co-cultures | Low to Moderate | Very Low | Very Low | High |
| Animal Models | Moderate (species differences exist) [31] | N/A | High (intact brain) | Low |
The Scientist's Toolkit: Essential Reagents for ESC Research
Successful directed differentiation and organoid generation rely on a suite of critical reagents and materials.
Table 4: Essential Research Reagents for ESC Differentiation and Disease Modeling
| Reagent/Material | Function | Example Application |
|---|---|---|
| Matrigel / Basement Membrane Extract | Provides a 3D extracellular matrix (ECM) scaffold to support complex tissue organization [31] [32]. | Embedding for cerebral organoid generation [31]. |
| Dual SMAD Inhibitors (e.g., Noggin, SB431542) | Promotes neural induction by inhibiting BMP and TGF-β signaling pathways, steering differentiation toward neural ectoderm [31]. | Early-stage protocol for generating neural progenitor cells. |
| Morphogens (SHH, FGF8, WNT) | Patterning molecules that provide positional information to cells, directing them toward specific regional fates (e.g., midbrain, cortex) [31]. | Specifying dopaminergic neuron identity during differentiation. |
| Spinning Bioreactor | A dynamic culture system that enhances nutrient and oxygen diffusion to the core of 3D tissues, enabling larger and more mature organoids to form [31] [32]. | Long-term maturation of cerebral organoids. |
| CRISPR-Cas9 System | A precise gene-editing tool used to introduce or correct disease-associated mutations in wild-type ESCs, creating isogenic cell lines for disease modeling [15]. | Generating ESC lines with Alzheimer's-associated mutations for organoid studies. |
Within the broader context of stem cell therapeutic applications, ESCs maintain a critical and distinct role. Their definitive pluripotency and lack of epigenetic memory make them a powerful and standardized platform for directed differentiation, particularly for generating the complex cellular diversity needed to model neurological diseases in 3D organoids [31] [30]. While iPSCs offer an unparalleled advantage for patient-specific modeling and avoid ethical concerns, ESCs often serve as the gold-standard control for assessing the quality and functionality of iPSC-derived tissues [15]. In therapeutic applications, ESC-derived products are now demonstrating promising results in clinical trials for conditions like Parkinson's disease, underscoring their translational potential [26] [1]. The choice between ESCs, iPSCs, and ASCs is not a matter of superiority but of alignment with research goals, whether for foundational discovery, personalized disease modeling, or proven regenerative therapies.
The field of regenerative medicine is deeply engaged in the critical evaluation of embryonic versus adult stem cell therapeutic applications. Within this context, adult stem cells (ASCs), particularly mesenchymal stem cells (MSCs), have emerged as a clinically viable and ethically less contentious alternative to embryonic stem cells (ESCs) [10] [11]. ESCs, while pluripotent and capable of generating any cell type in the body, face significant limitations including ethical concerns, potential for immune rejection, and tumorigenic risks [10] [11]. ASCs, harvested from adult tissues such as adipose tissue, bone marrow, and umbilical cord, offer a multipotent and more readily applicable solution for cell-based therapies [33] [34]. This guide provides a detailed, objective comparison of ASC therapies, with a focused analysis on their performance in hematopoietic stem cell transplantation (HSCT), presenting key experimental data to inform researchers, scientists, and drug development professionals.
MSCs derived from various tissues share core characteristics—they are adherent, possess multipotent differentiation potential, and express a typical surface marker profile (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-) [34]. However, parallel comparative studies reveal that their biological properties and functional efficacies are significantly influenced by their tissue of origin.
Comparative Analysis of Adipose and Umbilical Cord MSCs
A direct side-by-side analysis of human adipose tissue-derived MSCs (ASCs) and umbilical cord-derived MSCs (UC-MSCs) from the same donors highlighted both similarities and critical differences [35]. Both cell types expressed characteristic MSC surface markers and could be induced to differentiate into adipocytes, osteoblasts, and neuronal phenotypes. However, quantitative differences in their capacities were evident:
- Adipogenesis: ASCs demonstrated more prominent and efficient adipogenic differentiation compared to UC-MSCs [35].
- Neurogenesis: ASCs responded better to neuronal induction, exhibiting a higher differentiation rate in a relatively shorter time [35].
- Cytokine Secretion: UC-MSCs exhibited a more prominent secretion profile of cytokines than ASCs [35].
This indicates that while ASCs and UC-MSCs share immunological phenotypes, their divergent biological strengths may suit them for different therapeutic applications.
Comparative Analysis of Adipose and Bone Marrow MSCs
When compared to the well-characterized bone marrow-derived MSCs (BM-MSCs), ASCs demonstrate several superior regenerative attributes [36]. The table below summarizes key experimental findings from in vitro and in vivo studies.
Table 1: Comparative Biological Performance of ASCs vs. BM-MSCs
| Biological Characteristic | ASCs Performance | BM-MSCs Performance | Experimental Model/Method |
|---|---|---|---|
| Neovascularization | More effective, higher VEGF expression [36] | Less effective [36] | Rat hind-limb ischemia model; CD31/αSMA staining [36] |
| Resistance to Hypoxia | Higher (48.99% apoptosis) [36] | Lower (91.95% apoptosis) [36] | 1% O2 exposure for 24h; Annexin-V/PI staining [36] |
| Resistance to Oxidative Stress | Higher, maintained proliferation [36] | Lower, >90% senescence [36] | H2O2 treatment; SA-β-gal staining & MTT assay [36] |
| Proangiogenic Activity | More extensive tube networks [36] | Less extensive networks [36] | In vitro tube formation on Geltrex [36] |
| Telomerase Activity | Significantly higher [36] | Lower [36] | PCR-based TRAP assay [36] |
| Gene Expression (Oct4, VEGF) | Higher expression [36] | Lower expression [36] | Quantitative real-time PCR [36] |
These functional advantages are corroborated by unique biophysical properties. An analysis using a dielectrophoresis microfluidic platform revealed that ASCs display different traveling wave velocity and rotational speed compared to BM-MSCs, and remarkably, seem to develop an adaptive response when exposed to repeated electric field stimulation [36].
Experimental Protocols for Key Assessments
To ensure reproducibility and provide a clear technical reference, detailed methodologies for critical experiments cited in the comparison tables are outlined below.
Protocol: In Vivo Neovascularization Potency (Hind-Limb Ischemia Model)
This protocol assesses the functional capacity of MSCs to promote blood vessel formation in a live animal model of ischemia [36].
- Animal Model Induction: Unilateral hind-limb ischemia is surgically induced in rats (e.g., via ligation of the femoral artery).
- Cell Administration: ASCs or BM-MSCs are administered via intramuscular injection into the ischemic gastrocnemius muscle. A control group receives a vehicle solution.
- Tissue Collection: After a set period (e.g., 3 weeks), muscle tissues are harvested.
- Histological Analysis:
- Fixation and Sectioning: Muscles are fixed in formalin and embedded in paraffin for sectioning.
- Staining:
- H&E Staining: To assess overall muscle morphology, degeneration, and lymphocyte infiltration.
- Immunohistochemistry (IHC): Sections are stained with antibodies against:
- CD31: Marker for endothelial cells (quantify vessel density).
- αSMA (Alpha-Smooth Muscle Actin): Marker for vascular smooth muscle cells (identifies mature vessels).
- VEGF (Vascular Endothelial Growth Factor): Key pro-angiogenic growth factor.
- Quantification: The number of CD31-positive and αSMA-positive cells or structures per field of view is counted to quantify angiogenesis.
Diagram 1: In vivo neovascularization assessment workflow.
Protocol: In Vitro Proangiogenic Activity (Tube Formation Assay)
This assay evaluates the innate ability of MSCs to form capillary-like structures, a key indicator of their angiogenic support potential [36].
- Matrix Coating: A 96-well plate is coated with a solidified, growth factor-reduced basement membrane matrix (e.g., Geltrex or Matrigel) and allowed to polymerize.
- Cell Seeding: ASCs or BM-MSCs are harvested, counted, and seeded onto the surface of the polymerized matrix at a defined density (e.g., 1x10^4 cells/well) in a suitable endothelial or serum-supplemented medium.
- Incubation: The plate is incubated at 37°C, 5% CO2 for a defined period (e.g., 6-12 hours).
- Imaging and Quantification:
- After incubation, the formed networks are visualized using an inverted phase-contrast microscope.
- Images from multiple fields are captured.
- The extent of tube formation is quantified by measuring:
- The number of branching points per field.
- The total length of the tube structures.
- The number of closed meshes.
- Software-assisted image analysis (e.g., ImageJ with angiogenesis plugins) is recommended for objective quantification.
Protocol: Assessment of Hypoxia Resistance
This protocol measures cell survival under low-oxygen conditions, mimicking the stressful microenvironment of damaged tissues [36].
- Cell Culture: ASCs and BM-MSCs are cultured to 70-80% confluency.
- Hypoxic Exposure: Culture plates are placed in a hypoxic chamber flushed with a gas mixture containing 1% O2, 5% CO2, and balance N2. Control plates remain in a normoxic incubator (21% O2).
- Incubation Duration: Cells are exposed to hypoxia for a set period (e.g., 24-48 hours).
- Apoptosis Analysis (Flow Cytometry):
- Cells are collected by trypsinization.
- The cell pellet is resuspended in a binding buffer.
- Cells are stained with Annexin V-FITC and Propidium Iodide (PI) according to manufacturer's instructions.
- After incubation in the dark, the samples are analyzed by flow cytometry to distinguish:
- Viable cells (Annexin V-/PI-).
- Early apoptotic cells (Annexin V+/PI-).
- Late apoptotic/necrotic cells (Annexin V+/PI+).
Clinical Applications in Hematopoietic Stem Cell Transplantation
HSCT is a cornerstone treatment for hematologic malignancies but is complicated by delayed engraftment and graft-versus-host disease (GVHD). MSC co-infusion has been extensively investigated as a strategy to improve outcomes [37] [38] [33].
Efficacy in Promoting Engraftment
Systematic reviews and meta-analyses of clinical trials demonstrate that MSC co-transplantation accelerates hematopoietic recovery after HSCT [37] [38]. The most consistent and significant benefit is observed in platelet engraftment [38]. The table below synthesizes clinical outcome data from controlled trials.
Table 2: Clinical Outcomes of MSC Co-Infusion in HSCT (Controlled Trials)
| Clinical Outcome | MSC Co-Infusion Group | Control Group (HSCT Alone) | Statistical Significance & Notes |
|---|---|---|---|
| Time to Neutrophil Engraftment (Days) | ~13.96 days [38] | Varies by study | Shorter (SMD: -1.20 in RCTs, -0.54 in nRCTs) [37] |
| Time to Platelet Engraftment (Days) | ~21.61 days [38] | Varies by study | More consistently and significantly shorter (SMD: -0.60 in RCTs, -0.70 in nRCTs) [37] [38] |
| Incidence of Chronic GVHD (cGVHD) | Lower [37] | Higher | Risk Ratio: 0.53 in RCTs, 0.50 in nRCTs [37] |
| Incidence of Acute GVHD (aGVHD) | Slightly positive trend [37] | - | Not statistically significant in meta-analysis [37] |
| Overall Survival (OS) & Relapse Rate (RR) | No significant difference [37] | No significant difference | MSC infusion did not increase mortality or relapse [37] |
| Non-Relapse Mortality (NRM) | Slightly positive trend [37] | - | Not statistically significant in meta-analysis [37] |
Subgroup analyses reveal that the benefits are most pronounced in specific patient populations. Children and adolescents, as well as patients receiving HLA-nonidentical HSCT, show more substantial improvements in engraftment and incidence of GVHD and NRM [37]. Conversely, a reduced overall survival was observed in adult patients with hematological malignancies undergoing HLA-identical HSCT, indicating the need for patient-stratified application [37].
Efficacy in Graft-versus-Host Disease (GVHD) Management
The potent immunomodulatory properties of MSCs make them a promising tool for managing GVHD [33] [34]. They suppress T-cell proliferation, inhibit B-cell and natural killer cell function, and modulate dendritic cell activity through cell-to-cell contact and secretion of soluble factors like TGF-β, HGF, and indoleamine 2,3-dioxygenase [34]. This translational potential culminated in the recent FDA approval of Ryoncil (remestemcel-L), an allogeneic bone marrow-derived MSC therapy, for the treatment of pediatric steroid-refractory acute GVHD (SR-aGVHD) in December 2024 [26]. This marks a significant regulatory milestone for MSC-based therapies.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting the experiments described in this guide.
Table 3: Essential Reagents and Materials for MSC Research in HSCT Applications
| Reagent / Material | Function / Application | Specific Example(s) / Notes |
|---|---|---|
| Collagenase Type I | Tissue digestion for primary isolation of MSCs from adipose tissue or umbilical cord Wharton's jelly [35]. | Critical for breaking down extracellular matrix to release cells. Concentration and incubation time vary by tissue [35]. |
| MSC Culture Medium | Ex vivo expansion and maintenance of MSCs. | Often includes a basal medium (e.g., DMEM/F12) supplemented with FBS and growth factors. Commercial serum-free MSC media are also available [35]. |
| Flow Cytometry Antibodies | Immunophenotyping of MSCs to confirm identity per ISCT criteria. | Positive markers: CD73, CD90, CD105. Negative markers: CD34, CD45, HLA-DR [35] [34]. |
| Tri-lineage Differentiation Kits | In vitro validation of MSC multipotency (adiopgenic, osteogenic, chondrogenic). | Kits typically include induction and maintenance media with specific inducers like dexamethasone, indomethacin (adipo), and β-glycerophosphate (osteo) [35]. |
| Geltrex / Matrigel | Used for in vitro tube formation assays to assess proangiogenic potential [36]. | Provides a basement membrane matrix that supports cell attachment, migration, and tube formation. |
| Annexin V & Propidium Iodide (PI) | Flow cytometry-based detection of apoptosis and necrosis in hypoxia resistance assays [36]. | Distinguishes between viable (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells. |
| Antibodies for IHC | Analysis of in vivo neovascularization and cell engraftment in animal models. | CD31: Endothelial cell marker. αSMA: Pericyte/vascular smooth muscle marker. VEGF: Growth factor expression [36]. |
| Hypoxic Chamber | Creating a controlled low-oxygen environment (e.g., 1% O2) to study hypoxia resistance [36]. | Essential for mimicking the ischemic tissue microenvironment in vitro. |
The accumulated experimental and clinical evidence solidifies the role of ASCs, particularly MSCs, as a powerful tool in regenerative medicine and HSCT. When compared to other MSC sources, ASCs demonstrate superior regenerative capacities, including enhanced resistance to stress, stronger proangiogenic activity, and more potent in vivo neovascularization [36]. While UC-MSCs may have a robust cytokine secretome [35], the functional advantages and easier accessibility of ASCs make them a highly attractive source.
In the clinical setting of HSCT, MSC co-infusion has transitioned from experimental to a recognized strategy to accelerate hematopoietic recovery (especially platelets) and reduce the incidence of chronic GVHD [37] [38] [33]. The recent FDA approval of Ryoncil for SR-aGVHD is a testament to this progress [26]. Future developments will focus on refining these therapies through the use of iPSC-derived MSCs (iMSCs) for improved consistency and scalability [26], and precision medicine approaches to identify patient subgroups that will benefit most, thereby optimizing the therapeutic landscape for ASCs in transplantation medicine.
Stem cell therapies represent a revolutionary frontier in regenerative medicine, offering potential treatments for a wide range of debilitating conditions from neurodegenerative diseases to cardiovascular disorders [11]. The therapeutic efficacy of these cells hinges on three primary mechanisms of action: differentiation into specialized cell types to replace damaged tissues, paracrine signaling through secreted factors that modulate the local microenvironment, and immunomodulation to regulate immune responses [14] [11]. Understanding how these mechanisms differ between embryonic and adult stem cells is crucial for researchers and drug development professionals seeking to develop targeted therapies.
Embryonic stem cells (ESCs), with their pluripotent nature, and adult stem cells (ASCs), including mesenchymal stem cells (MSCs), exhibit fundamental differences in their biological capabilities and therapeutic applications [39] [14]. This comparison guide objectively analyzes the mechanistic profiles of these distinct stem cell types, providing experimental data and methodologies relevant for preclinical research and clinical translation.
Comparative Mechanisms of Action
The therapeutic potential of stem cells is governed by their distinct biological capabilities, which vary significantly between embryonic and adult types. The following analysis compares their core mechanisms of action with supporting experimental data.
Table 1: Comparative Mechanisms of Action of Embryonic vs. Adult Stem Cells
| Mechanism | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs/MSCs) |
|---|---|---|
| Differentiation Capacity | Pluripotent - Can differentiate into any cell type from all three germ layers [39] [10] | Multipotent - Limited to cell types of their tissue of origin (e.g., bone, cartilage, fat for MSCs) [39] [11] |
| Paracrine Signaling | Express developmental morphogens (Wnt, BMP, Nodal); crucial for patterning during differentiation [11] | Secrete VEGF, HGF, FGF; promote angiogenesis, reduce apoptosis, stimulate endogenous progenitor cells [14] [11] |
| Immunomodulation | High immunogenicity; require immunosuppression in allogeneic settings [39] [10] | Strong immunomodulatory properties; suppress T-cell proliferation, modulate dendritic cells and NK cells via PGE2, IDO, TGF-β [14] [11] |
| Primary Therapeutic Strategy | Cell replacement via directed differentiation [11] [26] | Trophic support and immune regulation [14] [11] |
| Key Evidence | Clinical trials for Parkinson's (dopaminergic neurons) and retinal diseases (RPE cells) [26] | FDA-approved for pediatric SR-aGVHD (Ryoncil); >1,200 patients dosed in PSC trials with encouraging safety [26] |
Table 2: Quantitative Comparison of Secreted Factors from Stem Cells
| Secreted Factor | Embryonic Stem Cells (ESCs) | Adult Mesenchymal Stem Cells (MSCs) | Functional Role |
|---|---|---|---|
| VEGF (pg/mL/10⁶ cells/24h) | 150-300 (from ESC-derived progenitors) | 500-2,000 | Angiogenesis, endothelial cell survival [11] |
| HGF (pg/mL/10⁶ cells/24h) | Low/Undetectable | 1,000-5,000 | Anti-fibrotic, mitogenic, morphogenic effects [11] |
| TGF-β (pg/mL/10⁶ cells/24h) | Variable during differentiation | 300-1,000 | Immunomodulation, extracellular matrix production [11] |
| FGF-2 (pg/mL/10⁶ cells/24h) | High during early differentiation | 500-1,500 | Cell proliferation, tissue repair [11] |
| PGE2 (ng/mL/10⁶ cells/24h) | Not typically measured | 1-10 | Macrophage polarization toward M2 anti-inflammatory phenotype [14] |
Experimental Analysis of Differentiation
Directed Differentiation of Embryonic Stem Cells
The differentiation capacity of ESCs is their most defining characteristic, enabling generation of any cell type for regenerative applications.
Figure 1: Experimental workflow for directed differentiation of human embryonic stem cells (hESCs) into specialized cell types.
Protocol for ESC Directed Differentiation to Dopaminergic Neurons:
- Maintenance: Culture hESCs on feeder-free Matrigel matrix in mTeSR1 medium with daily medium changes [11].
- Embryoid Body Formation: Detach colonies using EDTA and transfer to low-attachment plates in suspension culture to form embryoid bodies for 4 days [11].
- Neural Induction: Transfer embryoid bodies to poly-ornithine/laminin-coated plates in N2 medium with dual SMAD inhibition (LDN-193189 100nM, SB431542 10μM) for 7-10 days [26].
- Patterning: Add sonic hedgehog (SHH C24II, 100ng/mL) and FGF8 (100ng/mL) for 14 days to specify dopaminergic fate [26].
- Maturation: Withdraw patterning factors and culture in BDNF, GDNF, ascorbic acid, and cAMP for 28+ days to generate functional dopaminergic neurons [26].
Validation: Immunocytochemistry for tyrosine hydroxylase (TH), FOXA2, and β-tubulin III; HPLC for dopamine secretion in response to potassium chloride depolarization [26].
Spontaneous Differentiation of Embryonic Stem Cells
Embryoid Body Formation Assay Protocol:
- Preparation: Harvest ESC colonies using collagenase IV treatment.
- Suspension Culture: Transfer cell clusters to low-attachment plates in ESC medium without FGF2.
- Differentiation: Culture for 7-21 days with medium changes every 2-3 days.
- Analysis: Assess spontaneous differentiation into cell types representing all three germ layers via immunocytochemistry for β-tubulin III (ectoderm), α-fetoprotein (endoderm), and α-smooth muscle actin (mesoderm) [11].
Multipotent Differentiation of Adult Stem Cells
Trilineage Differentiation Assay for MSCs Protocol:
- Osteogenic Differentiation: Culture MSCs to confluence in growth medium, then switch to osteogenic induction medium (DMEM with 10% FBS, 0.1μM dexamethasone, 10mM β-glycerophosphate, 50μM ascorbic acid-2-phosphate) for 21 days. Validate with Alizarin Red S staining of mineralized matrix [14].
- Adipogenic Differentiation: Culture MSCs to confluence in growth medium, then cycle between adipogenic induction medium (DMEM with 10% FBS, 1μM dexamethasone, 0.5mM IBMX, 10μg/mL insulin, 100μM indomethacin) and maintenance medium (DMEM with 10% FBS, 10μg/mL insulin) for 14-21 days. Validate with Oil Red O staining of lipid droplets [14].
- Chondrogenic Differentiation: Pellet 2.5×10⁵ MSCs in conical tube and culture in chondrogenic induction medium (DMEM with 1% ITS+, 100nM dexamethasone, 50μg/mL ascorbic acid-2-phosphate, 40μg/mL proline, 10ng/mL TGF-β3) for 21-28 days. Validate with Alcian Blue staining of sulfated proteoglycans [14].
Analysis of Paracrine Signaling Mechanisms
Comparative Secretome Profiles
The therapeutic effects of both ESC-derived cells and MSCs are largely mediated by their secretome - the complex mixture of factors they release, including cytokines, growth factors, and extracellular vesicles.
Figure 2: Paracrine signaling mechanisms common to both embryonic and adult stem cells, mediating therapeutic effects.
Protocol for Secretome Analysis:
- Conditioned Medium Collection: Culture 80% confluent stem cells in serum-free medium for 24-48 hours. Collect conditioned medium and centrifuge at 2,000×g for 10 minutes to remove cells and debris [11].
- Extracellular Vesicle Isolation: Ultracentrifuge conditioned medium at 100,000×g for 70 minutes at 4°C. Wash pellet in PBS and repeat ultracentrifugation. Resolve EV pellet in appropriate buffer for downstream applications [11].
- Cytokine Array: Use Proteome Profiler Array kits to simultaneously detect multiple soluble factors in conditioned medium. Incubate array membrane with 1mL conditioned medium overnight at 4°C, followed by detection with streptavidin-HRP and chemiluminescence [11].
- Functional Validation - Scratch Assay: Seed endothelial cells in 24-well plates to form monolayers. Create scratch with p200 pipette tip. Treat with stem cell conditioned medium or control medium. Image at 0, 6, 12, and 24 hours to quantify migration [11].
ESC-Specific Paracrine Signaling in Development
ESCs and their differentiated progeny secrete developmental morphogens that establish positional information and tissue patterning.
Protocol for Studying ESC Morphogen Secretion:
- Directed Differentiation: Induce ESCs toward specific lineages using established protocols.
- Conditioned Medium Collection: Collect medium from differentiating ESCs at specific time points.
- Morphogen Analysis: Use ELISA/Western blot to quantify secretion of Wnt, BMP, and Nodal proteins during critical differentiation windows.
- Functional Blocking: Apply neutralizing antibodies against target morphogens to establish their functional role in differentiation and tissue patterning [11].
Investigation of Immunomodulatory Properties
Immunomodulation by Adult Mesenchymal Stem Cells
MSCs possess remarkable immunomodulatory capabilities, making them valuable for treating inflammatory and autoimmune conditions.
Figure 3: Immunomodulatory mechanisms of mesenchymal stem cells (MSCs) in response to inflammatory signals.
Protocol for Assessing MSC Immunomodulation:
- MSC Licensing: Pre-treat MSCs with 10ng/mL IFN-γ for 24 hours to enhance immunomodulatory potency [14].
- Peripheral Blood Mononuclear Cell (PBMC) Isolation: Isolate PBMCs from human blood using Ficoll density gradient centrifugation.
- T-cell Proliferation Assay: Label PBMCs with CFSE and activate with anti-CD3/CD28 beads. Co-culture with licensed MSCs at 10:1 (PBMC:MSC) ratio for 5 days. Analyze CFSE dilution by flow cytometry to quantify T-cell proliferation suppression [14].
- IDO Activity Measurement: Collect MSC conditioned medium after IFN-γ licensing. Measure tryptophan and kynurenine levels by HPLC to quantify indoleamine 2,3-dioxygenase activity [14].
- Macrophage Polarization Assay: Differentiate monocytes to M0 macrophages with M-CSF for 6 days. Add MSC conditioned medium and polarize with LPS/IFN-γ toward M1 phenotype. Analyze surface markers (CD80, CD86) for M1 and (CD206, CD163) for M2 by flow cytometry [14].
Immunological Characteristics of Embryonic Stem Cells
Unlike MSCs, ESCs exhibit immunogenic properties that must be addressed for clinical applications.
Protocol for Assessing ESC Immunogenicity:
- Mixed Lymphocyte Reaction (MLR): Co-culture irradiated ESCs or their differentiated progeny with allogeneic PBMCs at varying ratios.
- Proliferation Measurement: After 5 days, quantify T-cell proliferation via 3H-thymidine incorporation or CFSE dilution.
- Immune Activation Marker Analysis: Assess expression of HLA class I/II molecules on ESCs by flow cytometry. Measure secretion of pro-inflammatory cytokines (IFN-γ, IL-17) in co-culture supernatants by ELISA [10].
- Alternative Strategy - iPSC Generation: Generate patient-specific induced pluripotent stem cells via somatic cell reprogramming to overcome immunogenicity barriers [15].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell Mechanism Studies
| Reagent/Category | Specific Examples | Research Function | Application Context |
|---|---|---|---|
| Culture Media | mTeSR1, DMEM/F12 with KSR, MSC Growth Medium | Maintain stemness or support differentiation | ESC culture (mTeSR1), MSC expansion [11] |
| Growth Factors | FGF-2, TGF-β, EGF, BMP-4, SCF | Direct differentiation, support self-renewal | ESC pluripotency (FGF-2), hematopoietic differentiation (SCF) [11] |
| Small Molecules | CHIR99021 (GSK-3 inhibitor), Y-27632 (ROCK inhibitor), LDN-193189 (BMP inhibitor) | Enhance survival, direct differentiation | Improve ESC survival (Y-27632), neural differentiation (LDN-193189) [26] |
| Matrices | Matrigel, Geltrex, Collagen I, Poly-ornithine/Laminin | Provide structural support and biochemical cues | ESC culture (Matrigel), MSC differentiation (Collagen I) [11] |
| Analysis Tools | Flow Cytometry Antibodies, ELISA Kits, scRNA-Seq Kits | Characterize phenotype, quantify secretion, profile transcriptomes | Immunophenotyping (CD73, CD90, CD105 for MSCs), pluripotency markers (OCT4, SOX2, NANOG for ESCs) [11] |
| Gene Editing | CRISPR-Cas9 systems, Lentiviral vectors | Modify genes, introduce reporters | Gene knockout (CRISPR), lineage tracing (Fluorescent reporters) [15] |
Embryonic and adult stem cells employ fundamentally different mechanistic strategies with complementary therapeutic value. ESCs excel in differentiation capacity for cell replacement strategies, while ASCs/MSCs demonstrate superior paracrine signaling and immunomodulation for trophic support and immune regulation [39] [14] [11]. The choice between these cell types depends fundamentally on the pathological context - ESCs and their derivatives offer superior potential for replacing lost cell populations in conditions like Parkinson's disease or retinal degeneration, while MSCs provide potent immunomodulation for inflammatory conditions like graft-versus-host disease [26].
Future research directions include combining the strengths of both cell types through technologies like iPSC-derived MSCs, which aim to merge the expandability and differentiation capacity of pluripotent cells with the immunomodulatory properties of adult stem cells [15]. As the field advances with over 1,200 patients already dosed in pluripotent stem cell clinical trials, understanding these mechanistic differences will continue to guide researchers and drug development professionals in selecting optimal cell sources for specific therapeutic applications [26].
The field of regenerative medicine has been revolutionized by three primary stem cell types: embryonic stem cells (ESCs), adult stem cells (ASCs), and induced pluripotent stem cells (iPSCs). ESCs, derived from the inner cell mass of blastocysts, represent the gold standard for pluripotency but face ethical controversies and immunological rejection challenges [40] [41]. ASCs, including mesenchymal stem cells from bone marrow or adipose tissue, offer ethical advantages but have limited differentiation potential and expansion capacity [42]. The 2006 discovery of iPSCs by Shinya Yamanaka introduced a groundbreaking approach—reprogramming somatic cells to an embryonic-like state using defined factors [43] [44]. This review comprehensively compares these stem cell platforms, focusing on how iPSCs bridge the gap between ESCs and ASCs for therapeutic applications and research.
Historical Development and Reprogramming Breakthroughs
The conceptual foundation for cellular reprogramming was established by John Gurdon's 1962 somatic cell nuclear transfer (SCNT) experiments, demonstrating that a differentiated cell nucleus retains the genetic information needed to form an entire organism [43] [44]. This concept of reversible epigenetic programming paved the way for Yamanaka's pivotal 2006 discovery that mouse fibroblasts could be reprogrammed into pluripotent stem cells using only four transcription factors: Oct4, Sox2, Klf4, and c-Myc (OSKM) [43]. The successful generation of human iPSCs followed in 2007 by both Yamanaka and James Thomson, who used an alternative combination (OCT4, SOX2, NANOG, and LIN28) [43] [44].
The original reprogramming methods utilized integrating retroviral vectors, raising concerns about insertional mutagenesis and tumorigenicity, particularly from reactivation of the c-MYC transgene [45] [40]. Subsequent advances have focused on developing safer, non-integrating methods including episomal vectors, Sendai virus, synthetic mRNA, and small molecule approaches [46] [40]. These innovations have significantly improved the safety profile of iPSCs for potential clinical applications.
Comparative Analysis of Stem Cell Characteristics
Table 1: Key Characteristics of Pluripotent and Multipotent Stem Cells
| Characteristic | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) | Adult Stem Cells (ASCs) |
|---|---|---|---|
| Origin | Inner cell mass of blastocyst [47] [41] | Reprogrammed somatic cells [43] [40] | Various adult tissues (bone marrow, adipose, etc.) [42] |
| Pluripotency | Yes (can differentiate into all three germ layers) [40] [41] | Yes (can differentiate into all three germ layers) [40] [41] | No (multipotent, limited to specific lineages) [42] |
| Ethical Concerns | Significant (embryo destruction) [45] [40] | Minimal (somatic cell source) [46] [40] | Minimal (adult tissue source) [42] |
| Immunogenicity | High (allogeneic transplantation) [45] [40] | Low (potential for autologous transplantation) [40] [41] | Low (potential for autologous transplantation) [42] |
| Tumorigenic Risk | Teratoma formation [40] [41] | Teratoma formation; potential transgene reactivation [45] [42] | Low [42] |
| Genetic Stability | Generally stable [45] | Concerns about epigenetic memory and reprogramming-induced mutations [45] [47] | Varies by tissue source and donor age [42] |
| Scalability | High (unlimited self-renewal) [43] | High (unlimited self-renewal) [43] [41] | Limited expansion capacity [42] |
Table 2: Experimental Data Comparison Between ESC and iPSC Lines
| Parameter | Embryonic Stem Cells | Induced Pluripotent Stem Cells | Significance/Notes |
|---|---|---|---|
| Karyotype Abnormalities | 12.9% incidence [45] | 12.5% incidence [45] | No significant difference in large-scale analysis |
| Protein Content | Baseline [47] | >50% higher [47] | iPSCs show increased total protein content |
| Mitochondrial Metabolism | Baseline [47] | Enhanced mitochondrial potential [47] | Correlates with higher growth rates in iPSCs |
| Glutamine Uptake | Baseline [47] | Increased [47] | Correlates with higher glutamine transporter levels |
| Secreted Factors | Baseline [47] | Higher levels of ECM components and growth factors [47] | Some with tumorigenic properties |
| In Vitro Differentiation Efficiency | Varies by protocol | Varies by protocol and reprogramming method | Newer methods show comparable efficiency |
Molecular Mechanisms of iPSC Reprogramming
Key Signaling Pathways
The reprogramming of somatic cells to pluripotency involves profound remodeling of chromatin structure and the epigenome, orchestrated by the Yamanaka factors and other reprogramming components [43] [44]. The process occurs in two main phases: an early stochastic phase where somatic genes are silenced and early pluripotency genes activated, followed by a more deterministic late phase where established pluripotency networks are stabilized [43]. The mesenchymal-to-epithelial transition (MET) represents a critical early event in reprogramming, particularly when starting with fibroblast populations [43].
Diagram 1: iPSC reprogramming signaling pathway
Transcription Factor Interactions
The Yamanaka factors function in a coordinated manner to reshape the epigenetic landscape: Oct4 and Sox2 form the core pluripotency network, Klf4 facilitates epigenetic remodeling, and c-Myc promotes global histone acetylation and metabolic reprogramming [44]. Alternative factor combinations like OCT4, SOX2, NANOG, and LIN28 (OSNL) also demonstrate reprogramming capability, with Nanog and Lin28 serving as functional analogs to Klf4 and c-Myc [44]. The specific ratio of Sox2 to Oct4 has been identified as critical for determining reprogramming efficiency and resulting iPSC quality [44].
Experimental Protocols for iPSC Generation and Differentiation
Non-Integrating Reprogramming Methods
Current best practices for generating clinical-grade iPSCs favor non-integrating methods to minimize genomic alteration risks [46] [40]. Episomal vectors derived from the Epstein-Barr virus system enable reprogramming factor expression without genomic integration, making them a preferred FDA-compatible approach [45] [40]. Sendai virus, a replication-deficient RNA virus, efficiently delivers reprogramming factors while remaining in the cytoplasm without nuclear integration [46]. Synthetic mRNA reprogramming involves repeated transfection of modified mRNAs encoding OSKM factors, achieving high efficiency while avoiding genomic integration [46] [40]. Small molecule approaches utilize compounds that modulate signaling pathways (e.g., TGF-β, GSK3) to enhance reprogramming efficiency or potentially replace transcription factors [46].
Directed Differentiation to Dopaminergic Neurons
A well-established protocol for generating midbrain dopaminergic neurons—critical for Parkinson's disease modeling and therapy—involves several key stages [48]. First, iPSCs are subjected to dual SMAD inhibition to induce neural induction and form neural progenitor cells (NPCs). These NPCs are then patterned toward a ventral midbrain fate using combined treatment with low-dose retinoic acid, sonic hedgehog (SHH) signaling activation, FGF8a, and WNT1 activation. Finally, terminal differentiation produces mature dopaminergic neurons characterized by expression markers including FOXA2, tyrosine hydroxylase (TH), and β-tubulin III [48]. This protocol typically requires 4-6 weeks to generate functionally mature dopaminergic neurons suitable for transplantation or disease modeling.
Diagram 2: Dopaminergic neuron differentiation workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for iPSC Work
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc (OSKM) [43] [44] | Core transcription factors for inducing pluripotency | c-Myc increases efficiency but raises safety concerns |
| Alternative Factors | Nanog, Lin28 (OSNL combination) [44] | Alternative to OSKM for human cell reprogramming | May produce different differentiation biases |
| Non-Integrating Delivery Systems | Episomal vectors, Sendai virus, synthetic mRNA [46] [40] | Safer reprogramming without genomic integration | Varying efficiencies; mRNA requires repeated transfection |
| Small Molecule Enhancers | Valproic acid, RepSox, sodium butyrate [40] | Improve reprogramming efficiency, some can replace factors | Concentration and timing critical for effectiveness |
| Pluripotency Markers | OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 [47] | Characterization of established iPSC lines | Essential for quality control and line validation |
| Neural Differentiation Supplements | SMAD inhibitors, SHH agonists, FGF8, BDNF [48] | Direct differentiation toward neural lineages | Specific concentrations determine regional identity |
| Cardiomyocyte Differentiation Supplements | BMP4, Activin A, Wnt modulators [46] | Direct differentiation toward cardiac lineages | Timing of Wnt inhibition critical for efficiency |
Therapeutic Applications and Clinical Translation
Disease Modeling and Drug Screening
iPSC technology has revolutionized disease modeling by enabling the generation of patient-specific cell types that recapitulate pathological features. Neurological diseases have been particularly well-modeled, with iPSC-derived dopaminergic neurons from Parkinson's patients showing key disease phenotypes like α-synuclein accumulation and mitochondrial dysfunction [48]. Cardiovascular models including long QT syndrome have been established using iPSC-derived cardiomyocytes, enabling mechanistic studies and drug screening [41]. These disease-specific iPSC models provide human-relevant systems for identifying novel therapeutic targets and testing drug efficacy and toxicity [41].
Clinical Trials and Regenerative Medicine
The first clinical trial using iPSC-derived cells was initiated in 2014 for age-related macular degeneration [44]. Parkinson's disease represents another major focus, with ongoing clinical trials transplanting iPSC-derived dopaminergic neurons to replace lost nigrostriatal neurons [44] [48]. Current approaches increasingly utilize allogeneic iPSC banks from HLA-homozygous donors rather than patient-specific autologous iPSCs, balancing therapeutic efficiency with practical considerations [44]. For example, the Kyoto University iPSC Research and Application Center is developing an iPSC bank where 75 selected lines could cover 80% of the Japanese population through HLA matching [44].
Current Challenges and Future Perspectives
Despite significant progress, several challenges remain for iPSC clinical translation. Tumorigenicity risk persists due to potential residual undifferentiated cells or genetic abnormalities acquired during reprogramming [45] [42]. Immunogenicity concerns continue, as even autologous iPSCs may elicit immune responses due to epigenetic abnormalities or culture-induced mutations [40]. Manufacturing scalability requires development of robust, GMP-compliant processes for large-scale production of clinical-grade iPSCs and their derivatives [46] [41].
Future directions include CRISPR-Cas9 gene editing to correct genetic defects in patient-specific iPSCs before transplantation [46], development of "hypoimmunogenic" iPSCs through HLA editing to create universal donor cells [46], and advanced 3D organoid systems that better recapitulate human tissue architecture and complexity [43] [46]. Machine learning approaches are also being deployed to automate quality control and improve differentiation protocols [46].
iPSCs effectively bridge the gap between ESCs and ASCs by combining the pluripotency and expansion capacity of ESCs with the ethical advantages and autologous potential of ASCs. While functional differences persist between iPSCs and ESCs at the proteomic and metabolic levels [47], the therapeutic potential of iPSCs is increasingly being realized through ongoing clinical trials and sophisticated disease models. As reprogramming methods continue to advance and safety profiles improve, iPSC-based approaches are poised to become central platforms for regenerative medicine, disease modeling, and drug development, potentially enabling personalized cell therapies for a broad spectrum of currently intractable diseases.
Addressing Clinical Hurdles: Safety, Efficacy, and Manufacturing Challenges
Embryonic Stem Cells (ESCs) hold immense promise for regenerative medicine due to their unique pluripotency—the ability to differentiate into any cell type in the body [11] [10]. However, this same characteristic is the source of two major clinical challenges: their inherent potential for tumorigenicity and the risk of immunological rejection upon transplantation [11] [49]. This guide objectively compares the therapeutic profiles of ESCs and Adult Stem Cells (ASCs), primarily Mesenchymal Stem Cells (MSCs), by focusing on these critical safety parameters, supported by experimental data and methodologies relevant to researchers and drug development professionals.
Comparative Analysis of ESC and Adult Stem Cell Therapeutic Profiles
The table below summarizes the core risks and mitigation strategies for ESCs compared to ASCs, providing a high-level overview for initial assessment.
| Risk / Characteristic | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) / MSCs |
|---|---|---|
| Inherent Tumorigenicity | High; risk of teratoma formation from undifferentiated pluripotent cells [49] [10]. | Low; multipotent cells with limited differentiation potential [10] [50]. |
| Immunological Rejection | High in allogeneic settings; requires immune suppression or matching [10]. | Low; inherently immunomodulatory properties [50] [20]. |
| Key Mitigation Strategy | Directed differentiation, cell sorting, and suicide genes [11]. | Typically requires less complex safety modulation [50]. |
| Primary Safety Assays | Teratoma formation assays, flow cytometry for pluripotency markers, genetic stability monitoring (Karyotyping) [49]. | Biodistribution studies, immunophenotyping, in vitro differentiation assays [49]. |
Experimental Protocols for Key Safety Assessments
Rigorous preclinical biosafety assessment is paramount for clinical translation. The following are detailed protocols for evaluating tumorigenicity and immunogenicity.
2.1 Assessing and Mitigating Tumorigenicity
The primary risk associated with ESCs is their potential to form teratomas or other tumors. A multi-layered experimental approach is required to quantify and mitigate this risk.
Experimental Protocol: In Vivo Teratoma Formation Assay
- Objective: To evaluate the tumor-forming potential of an ESC-derived product in an immunocompromised animal model.
- Methodology:
- Cell Preparation: Differentiate ESCs into the target lineage (e.g., cardiomyocytes, neural progenitors). Include a positive control group of undifferentiated ESCs.
- Animal Model: Use immunodeficient mice (e.g., NOD/SCID or NSG strains) to prevent xenogeneic rejection [49].
- Transplantation: Administer the cell product (e.g., 1x10^6 to 5x10^6 cells) via a clinically relevant route (e.g., intramuscular, subcutaneous, or into an organ-specific site like the heart or brain).
- Monitoring: Observe animals for a defined period (typically 12-26 weeks) for signs of tumor growth. Monitor via palpation, in vivo imaging (if cells are labeled), and overall health.
- Histopathological Analysis: Upon termination, harvest the transplantation site and major organs (e.g., liver, lungs, kidneys). Process tissues for histological sectioning and staining (H&E). A definitive diagnosis of teratoma requires the identification of differentiated tissues from at least two of the three germ layers (ectoderm, mesoderm, endoderm) under microscopic examination [49].
Mitigation Strategies: Purity and Control
- Directed Differentiation Optimization: Develop highly efficient differentiation protocols that minimize the presence of residual undifferentiated ESCs. This is the first line of defense [11].
- Cell Sorting and Purging: Use Fluorescence-Activated Cell Sorting (FACS) or Magnetic-Activated Cell Sorting (MACS) to remove cells that express pluripotency markers (e.g., OCT4, SOX2, NANOG) from the final therapeutic product [11].
- Introduction of Suicide Genes: Genetically engineer the ESC line to express a "suicide gene," such as the herpes simplex virus thymidine kinase (HSV-TK). If a tumor forms, administering the prodrug ganciclovir will selectively eliminate the proliferating ESC-derived cells [11].
The following diagram illustrates the logical workflow and key decision points in the tumorigenicity risk assessment pipeline.
2.2 Evaluating and Overcoming Immunological Rejection
ESC-derived cells are allogeneic and can be recognized as foreign by the recipient's immune system, leading to rejection. The following protocols assess this risk.
Experimental Protocol: Mixed Lymphocyte Reaction (MLR)
- Objective: To measure the T-cell mediated immune response against ESC-derived cells in vitro.
- Methodology:
- Responder Cells: Isolate peripheral blood mononuclear cells (PBMCs) or purified T-cells from a potential human recipient or a representative donor.
- Stimulator Cells: Use the allogeneic ESC-derived cell product as stimulator cells. These must be irradiated or treated with mitomycin-C to prevent their proliferation.
- Co-culture: Co-culture responder and stimulator cells in a 96-well plate for 5-7 days. Include controls (responders alone, stimulators alone).
- Readout: Measure T-cell proliferation using a standardized assay such as ^3H-thymidine incorporation or a CFSE dilution assay followed by flow cytometry. A high proliferation index indicates a strong immunogenic response [49].
Mitigation Strategies: Matching and Modulation
- Human Leukocyte Antigen (HLA) Matching: Create banks of clinical-grade ESC lines with diverse HLA haplotypes to find a better match for recipients, thereby reducing immunogenicity [10].
- Use of Induced Pluripotent Stem Cells (iPSCs): Generate patient-specific iPSCs, which are autologous by nature and thus avoid immune rejection entirely, though this is currently costly and time-consuming [10] [50].
- Immune Suppression: Utilize standard immunosuppressive drugs, similar to organ transplantation protocols, to dampen the host immune response. This carries associated risks of infection and toxicity [10].
- Therapeutic Cloning (Somatic Cell Nuclear Transfer): While not yet successful in humans, this technique aims to create ESCs that are genetically identical to the patient [10].
The immunological rejection process and its countermeasures can be visualized as a series of molecular and cellular interactions.
Quantitative Data Comparison: Efficacy and Safety
The table below synthesizes quantitative and qualitative data from preclinical and clinical studies to directly compare the therapeutic performance of ESCs and ASCs across key parameters.
| Evaluation Parameter | Embryonic Stem Cells (ESCs) | Adult Stem Cells (MSCs) | Supporting Experimental Data & Context |
|---|---|---|---|
| Differentiation Potential | Pluripotent: Can form all 3 germ layers [11] [10]. | Multipotent: Limited to mesenchymal lineages (bone, fat, cartilage) [50]. | In vitro embryoid body formation and teratoma assays confirm pluripotency [11]. |
| Tumorigenicity Rate (In Vivo) | High incidence of teratomas without purification [49] [10]. | Very low reported incidence [50]. | Studies in immunocompromised mice show >80% teratoma incidence from undifferentiated ESCs vs. rare events with MSCs [49]. |
| Immunogenicity Profile | High; triggers T-cell response in MLR [49] [10]. | Low/Immunomodulatory; suppresses T-cell response [50] [20]. | MLR assays show strong T-cell proliferation with allogeneic ESCs, while MSCs often inhibit proliferation [49] [50]. |
| Biodistribution | Can migrate and engraft in non-target organs, increasing tumor risk [49]. | Typically localize to injury sites (homing) and have short persistence [49]. | qPCR and imaging (PET, MRI) in animal models show wider distribution for ESCs [49]. |
| Clinical Trial Phase | Early stages (I/II) for conditions like Parkinson's and AMD [30]. | Extensive (Phases I-III) for GvHD, Crohn's disease, and orthopedic repair [50]. | ESC trials are newer; MSC products like Rexlemestrocel-L are already FDA-approved for specific conditions [49] [50]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and their applications in the experimental workflows for assessing and mitigating ESC risks.
| Research Reagent / Material | Primary Function in ESC Risk Assessment |
|---|---|
| Immunodeficient Mice (e.g., NSG) | In vivo model for teratoma formation assays, allowing human cell survival without xenogeneic rejection [49]. |
| Flow Cytometry Antibodies | Cell sorting (FACS/MACS) to remove undifferentiated ESCs (targeting OCT4, SOX2) and characterize final product purity [11]. |
| HLA Typing Kits | Genotyping tools to match donor ESCs to recipient, reducing the likelihood of immune recognition [49]. |
| CRISPR-Cas9 System | Gene-editing tool for introducing suicide genes (e.g., HSV-TK) or modifying immunogenic surface proteins on ESCs [11]. |
| qPCR Probes / In Vivo Imaging Agents | Tracking biodistribution and long-term persistence of transplanted cells in animal models [49]. |
| Cell Culture Media for Directed Differentiation | Chemically defined media containing specific growth factors and small molecules to drive efficient, homogeneous differentiation [11]. |
The comparative data reveals a clear trade-off: ESCs offer unparalleled differentiation potential for a wide range of tissues but are coupled with significant and complex safety challenges concerning tumorigenicity and immunogenicity. In contrast, ASCs like MSCs present a more favorable immediate safety profile and are already being successfully applied in the clinic for a narrower set of indications, primarily leveraging their immunomodulatory and wound-healing properties [50] [20].
The future of ESC-based therapies lies in the rigorous application of the described experimental protocols and mitigation tools. Ensuring product purity through advanced differentiation and sorting, coupled with strategic immune matching or modulation, is essential to unlocking the revolutionary potential of ESCs while managing their risks. The field continues to advance with emerging technologies like precision gene editing and bioreactor-based manufacturing, which are critical for translating the promise of ESCs into safe and effective human therapies.
The field of regenerative medicine is fundamentally anchored in the therapeutic application of stem cells, which are broadly categorized into embryonic and adult types. While embryonic stem (ES) cells hold the promise of virtually unlimited differentiation potential, their clinical use is entangled with ethical controversies and risks of teratoma formation. In contrast, adult mesenchymal stem cells (MSCs), particularly adipose-derived stem cells (ASCs), present an ethically sound and clinically practical alternative. ASCs are defined by their dual capacity for self-renewal and multiple differentiation potentials, making them an ideal candidate for therapeutic applications in regenerative medicine, particularly in peripheral nerve regeneration [51].
However, the clinical potential of ASCs is significantly constrained by two interconnected biological phenomena: limited differentiation potential and cellular senescence. These limitations become increasingly pronounced with donor age, ultimately restricting the efficacy of autologous cell therapies. Cellular senescence is a complex process whereby stem cells grow old as a consequence of intrinsic events (e.g., DNA damage) or environmental cues (e.g., stressful stimuli or diseases), which determine a permanent growth arrest [51]. This review provides a comparative analysis of ASC functionality against other stem cell types, details the mechanistic basis of their limitations, and synthesizes current experimental approaches aimed at optimizing their therapeutic potential within the broader context of stem cell research.
Comparative Analysis of Stem Cell Types for Therapeutic Applications
The selection of an appropriate stem cell type is a critical first step in designing regenerative therapies. The table below provides a systematic comparison of ASCs with other clinically relevant stem cell types, highlighting key performance metrics and therapeutic considerations.
Table 1: Comparative Analysis of Stem Cell Types for Therapeutic Applications
| Stem Cell Type | Differentiation Potential | Senescence & Aging Profile | Key Advantages | Major Clinical Limitations |
|---|---|---|---|---|
| Adipose-Derived Stem Cells (ASCs) | Multilineage (mesodermal: adipogenic, osteogenic, chondrogenic; also Schwann cell-like) [51] | Pronounced age-related decline; influenced by donor age and oxidative stress [51] [52] | Easily harvested in large quantities; minimal ethical concerns [51] | Limited differentiation potential compared to ES/iPS; therapeutic potential limited by senescence and donor age [51] |
| Embryonic Stem Cells (ESCs) | Pluripotent (all three germ layers) | Not age-related; but face replicative senescence in culture | Unlimited self-renewal and differentiation capacity | Ethical controversies; teratoma formation risk; immune rejection |
| Induced Pluripotent Stem Cells (iPSCs) | Pluripotent (all three germ layers) | Can be reset to youthful state during reprogramming | Patient-specific; avoids immune rejection; no ethical issues | Complex and costly generation; potential for genetic abnormalities |
| Bone Marrow-Mesenchymal Stem Cells (BM-MSCs) | Multilineage (comparable to ASCs) [51] | Age-related functional decline; accumulation of DNA damage [52] | Well-characterized; gold standard for many applications | Painful harvest; lower cell yield compared to ASCs |
This comparison elucidates the fundamental trade-off in stem cell therapeutics: pluripotent cells (ESCs and iPSCs) offer superior plasticity but carry significant safety and practical concerns, whereas adult stem cells like ASCs offer a more practical and safer profile but are hampered by biological aging. The choice between them often depends on the specific clinical application, with ASCs being particularly favored in scenarios like peripheral nerve regeneration where their differentiation into Schwann cell-like lineages is beneficial and their relative abundance is a major advantage [51].
Mechanisms of Senescence and Limited Potency in ASCs
The functional decline of ASCs is not random but is governed by specific molecular pathways. Understanding these mechanisms is a prerequisite for developing effective optimization strategies. The following diagram synthesizes the key pathways and their interconnections that drive ASC senescence.
Figure 1: Core Signaling Pathways Driving ASC Senescence. This diagram illustrates how intrinsic and extrinsic stressors converge on key molecular pathways, leading to cellular senescence and a reduction in the differentiation potential of Adipose-Derived Stem Cells (ASCs).
The mechanisms depicted above can be detailed as follows:
DNA Damage and Telomere Attrition: Cellular senescence in ASCs can be classified as replicative senescence, which is directly linked to telomere dysfunction, and stress-induced premature senescence (SIPS), which results from mitochondrial damage, activated oncogenes, and epigenetic changes. Telomeres, the protective end parts of eukaryotic chromosomes, shorten with each replication cycle. Telomerase, the enzyme that elongates telomeres, becomes dysfunctional with age, and reduced telomere length serves as a marker of proliferative decline in ASCs [51].
p38 MAPK Signaling Pathway: The protein p38 MAPK is a critical mediator activated by various stressors and plays an important role in regulating cell survival, differentiation, and apoptosis. The stress-activated p38 MAPK pathway contributes to cellular senescence by upregulating p16INK4A, a known senescence marker. Studies show that p38 MAPK expression increases with the age of the donor in ASCs, strengthening the hypothesis that cellular senescence is intrinsically linked to donor age [51].
p53 Signaling Pathway: The p53 pathway is a common regulator shared by both senescence and apoptosis. It is activated by stress, DNA damage, or inappropriate oncogene expression, leading to cell cycle arrest or apoptosis. p53 activation depends on cell type and various post-translational modifications, and its relationship with NF-ĸB signaling is important in regulating cellular senescence and the overall aging process [51].
Role of Reactive Oxygen Species (ROS): Elevated levels of ROS are a hallmark of aged stem cells, including ASCs. While ROS have essential roles in cell signaling, their accumulation leads to oxidative damage of cellular macromolecules. This disrupts mitochondrial oxidative phosphorylation, creating a vicious cycle that further elevates ROS production and drives functional decline. The FoxO family of transcription factors, which are regulators of the insulin/IGF-1 signaling pathway, are crucial in controlling ROS accumulation in stem cells. Loss of FoxO function leads to disrupted quiescence and defective repopulation abilities [52].
Quantitative Experimental Data on ASC Dysfunction
Empirical evidence underpins the mechanistic models of ASC senescence. The table below summarizes key quantitative findings from experimental studies that document the impact of aging and senescence on ASC form and function.
Table 2: Experimental Data on Age-Related Changes and Senescence in ASCs
| Experimental Parameter | Findings in Young/Healthy ASCs | Findings in Aged/Senescent ASCs | Experimental Model |
|---|---|---|---|
| p38 MAPK Expression | Lower baseline expression [51] | Significantly increased expression [51] | ASCs isolated from rats of different ages (neonatal, young, old) [51] |
| ROS Levels | Maintained at low, signaling levels [52] | Elevated levels, causing oxidative stress [52] | In vitro analysis of human and mouse MSCs [52] |
| DNA Damage Markers (e.g., γH2A.X foci) | Low frequency of damage foci [52] | Increased number of nuclear foci marking DNA double-strand breaks [52] | Immunofluorescence in aged HSCs and muscle satellite cells [52] |
| Differentiation Efficiency | Robust adipogenic and osteogenic potential | Marked reduction in differentiation capacity and proliferation rates [51] [52] | In vitro differentiation assays on ASCs from donors of varying age [51] |
| Secretion of Trophic Factors | Maintained secretion of GGF, BDNF, NGF [51] | Secretion may be maintained, but cell numbers are insufficient for therapeutic effect [51] | Analysis of ASC conditioned medium [51] |
The data consistently demonstrate that ASCs from older donors exhibit a pro-senescent molecular signature (e.g., high p38, p53, ROS) and a corresponding functional impairment in their core capacities for self-renewal and differentiation. This evidence base provides a set of key metrics for evaluating the success of any ASC optimization protocol.
Experimental Protocols for Assessing and Enhancing ASC Function
To combat the limitations of ASCs, researchers have developed standardized in vitro and in vivo protocols to quantify senescence and potency. Furthermore, intervention strategies have been designed to reverse these age-associated deficits.
Key Protocol: In Vitro Senescence Induction and Rescue Assay
This protocol is used to model aging and test potential anti-senescence therapies.
- Step 1: ASC Isolation and Culture: Isolate ASCs from lipoaspirate tissue via collagenase digestion and differential centrifugation. Culture cells in DMEM/F12 medium supplemented with 10% FBS and 1% penicillin/streptomycin at 37°C and 5% CO₂.
- Step 2: Senescence Induction: To induce stress-induced premature senescence (SIPS), treat ASCs at passage 3-5 with a sublethal dose of hydrogen peroxide (H₂O₂, e.g., 150-200 µM) for 2 hours. Alternatively, for replicative senescence, serially passage cells until proliferation significantly slows (e.g., passage 10+).
- Step 3: Therapeutic Intervention: Following senescence induction, treat cells with the candidate therapeutic agent.
- Step 4: Outcome Assessment:
- Senescence-Associated β-galactosidase (SA-β-gal) Staining: The gold-standard histochemical marker for senescence. Count the percentage of blue-stained cells.
- Proliferation Assay: Use a BrdU or EdU assay to quantify DNA synthesis and proliferation rates.
- Gene Expression Analysis: Use qRT-PCR to measure the expression of senescence-associated genes (e.g., p16, p21) and pluripotency markers (e.g., OCT4, SOX2).
- Differentiation Assay: Subject treated and control ASCs to adipogenic and osteogenic induction media to quantify the recovery of differentiation potential.
Key Protocol: Quantitative Fate Mapping to Track Lineage Potential
This advanced methodology, adapted from developmental biology, is used to reconstruct the hierarchy and commitment biases of progenitor cells.
- Step 1: Lineage Barcoding: Introduce heritable, unique genetic barcodes into a population of ASCs using lentiviral or retroviral libraries. This marks individual stem cells and all their progeny.
- Step 2: In Vitro or In Vivo Differentiation: Allow the barcoded ASCs to undergo differentiation in a controlled environment or after transplantation into an animal model (e.g., a nerve injury model).
- Step 3: Single-Cell Sequencing: At the endpoint, harvest the resulting differentiated cells (e.g., adipocytes, osteocytes, Schwann-like cells) and use single-cell RNA sequencing (scRNA-seq) to read both the cell's transcriptional identity and its unique lineage barcode.
- Step 4: Phylogenetic Analysis: Use computational tools like Phylotime to reconstruct a time-scaled phylogeny of the sampled cells. Algorithms like ICE-FASE can then be applied to infer the original hierarchy, commitment times, population sizes, and commitment biases of the intermediate progenitor states that gave rise to the terminal cells [53]. This provides a quantitative map of the ASCs' functional differentiation potential.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs critical reagents and their applications for studying and optimizing ASCs, as derived from the experimental literature.
Table 3: Research Reagent Solutions for ASC Optimization Studies
| Reagent / Tool | Function & Mechanism | Example Application in ASC Research |
|---|---|---|
| N-Acetyl-L-Cysteine (NAC) | Precursor to glutathione; direct ROS scavenger [52] | Reverses ROS-induced deficits in quiescence and repopulation capacity; used at 1-2 mM [52]. |
| SIRT1/SIRT3 Activators (e.g., Resveratrol) | NAD+-dependent protein deacetylases; regulate oxidative stress, mitochondrial function, and aging [52] | Improves function of aged stem cells; SIRT3 ectopic expression enhances SOD2 antioxidant activity [52]. |
| H2B-GFP (Histone 2B-GFP) | Fluorescently labeled histone for mitotic tracking [54] | Measures proliferation rates and division history of ASCs in fate-mapping studies by quantifying GFP dilution [54]. |
| Lineage Barcoding Vectors | Lentiviral/retroviral libraries for introducing herable genetic marks [53] | Tracks clonal output and lineage relationships of individual ASCs during differentiation using high-throughput sequencing [53]. |
| Senescence-Associated β-Galactosidase (SA-β-gal) Kit | Histochemical detection of lysosomal β-galactosidase activity at pH 6.0, a biomarker for senescent cells [52] | Quantifying the proportion of senescent cells in an ASC population before and after an intervention. |
The journey from a limited, senescence-prone ASC population to a therapeutically optimized cell product requires an integrated workflow. The following diagram outlines this multi-stage process, from initial isolation to functional validation.
Figure 2: Integrated Workflow for ASC Optimization. This diagram outlines a systematic pipeline for enhancing the therapeutic potential of Adipose-Derived Stem Cells (ASCs), from initial quality control to final functional validation.
In conclusion, while ASCs present a highly practical and promising tool for regenerative medicine, their inherent biological limitations must be acknowledged and actively managed. The future of ASC-based therapies lies in the development of standardized pre-conditioning protocols that combine antioxidant treatments, metabolic modulators, and epigenetic regulators to reset ASCs to a more potent and resilient state. By integrating a deep understanding of senescence mechanisms with robust experimental pipelines and quantitative fate-mapping technologies, researchers can unlock the full therapeutic potential of ASCs, bridging the critical gap between the practical advantages of adult stem cells and the functional prowess of their embryonic counterparts.
The translation of stem cell research from laboratory discovery to clinically approved therapy hinges on overcoming significant challenges in standardization and scale-up. Within the broader context of embryonic versus adult stem cell therapeutic applications, the manufacturing and quality control pathways diverge substantially, influencing their respective clinical progress and potential. While adult stem cells, particularly Mesenchymal Stem Cells (MSCs), have seen earlier clinical adoption, their inherent biological variability presents unique scale-up obstacles [13]. In contrast, pluripotent stem cells (PSCs), including both embryonic and induced pluripotent stem cells, offer near-limitless expansion potential but require complex, multi-stage differentiation protocols and carry the persistent risk of teratoma formation from residual undifferentiated cells [55] [56]. This guide objectively compares the manufacturing performance and quality control frameworks of these two distinct cellular platforms, providing researchers with a detailed analysis of the current landscape and practical experimental methodologies to address shared and unique hurdles.
Table 1: Core Manufacturing Challenge Comparison Between PSC and Adult Stem Cell Platforms
| Challenge Area | Pluripotent Stem Cells (ESCs/iPSCs) | Adult Stem Cells (e.g., MSCs) |
|---|---|---|
| Starting Material | Defined, homogeneous cell lines [57] | Highly variable donor tissue (e.g., bone marrow, adipose) [56] |
| Scale-Up Primary Hurdle | Mastering multi-stage differentiation and purifying target cells [55] | Achieving consistent expansion despite donor senescence and variability [58] |
| Critical Safety Concern | Tumorigenicity from residual undifferentiated cells [56] | Genetic instability from prolonged in vitro culture [56] |
| Key Quality Metric | Pluripotency marker expression (pre-differentiation) and purity of final cell product [55] | Specific surface antigen profile (e.g., CD105+, CD73+, CD90+) and differentiation potential [13] |
| Process Analytical Technology (PAT) Need | In-line monitoring of differentiation markers | Real-time assessment of cell senescence and potency |
Comparative Analysis of Manufacturing Hurdles and Performance Data
The journey from a research protocol to a robust, commercially viable manufacturing process exposes fundamental differences in the technical challenges faced by PSC and adult stem cell platforms.
Scalability and Expansion
For PSCs, scalability is a two-part challenge: first, the expansion of the undifferentiated pluripotent cells, and second, the subsequent differentiation into the target therapeutic cell type. Open culture systems like flasks are insufficient for commercial-scale production. The field is moving towards automated, closed-system bioreactors—such as stirred-tank and hollow-fiber systems—which allow for precise control over environmental parameters (pH, dissolved oxygen, metabolites) and enable the production of the large cell numbers required for allogeneic therapies [55]. For example, a single lot of an iPSC-derived therapy may require the production of over 10¹¹ cells to treat a significant patient population [26].
For adult MSCs, the scalability challenge is not purely about volume but consistency. Donor age, health status, and tissue source introduce significant batch-to-batch variability. Furthermore, MSCs have a finite expansion capacity in vitro and can undergo replicative senescence, losing their therapeutic properties over successive passages [56] [58]. Scaling up often means scaling out—using multiple parallel bioreactors or flasks—which amplifies the impact of this inherent variability.
Table 2: Quantitative Performance Data in Scalable Bioreactor Systems
| Cell Type | Reported Fold Expansion in Bioreactors | Key Process Limitation | Reported Viability Post-Harvest |
|---|---|---|---|
| iPSCs | ~100-500 fold [55] | Maintaining genomic stability and pluripotency during expansion | >90% [55] |
| MSCs (Bone Marrow) | ~20-40 fold [56] | Onset of senescence and decline in differentiation potential with passaging | >85% [56] |
| iPSC-Derived Cardiomyocytes | ~30-100 fold from iPSC stage [55] | Efficiency of differentiation and purification from non-cardiac cells | >80% [55] |
Process Standardization and Quality Control
The "quality by design" (QbD) framework is essential for both platforms but is implemented differently. For PSC-derived products, the process is defined by a series of critical quality attributes (CQAs) corresponding to each stage: a high-quality starting iPSC clone, a successful differentiation with high purity, and a final product free of residual undifferentiated cells [55]. Process Analytical Technologies (PAT) are increasingly used for in-line monitoring, such as using imaging to track morphological changes during differentiation or measuring metabolic shifts that indicate successful lineage specification.
For MSCs, standardization is complicated by the lack of a universal potency assay. While the International Society for Cell & Gene Therapy (ISCT) has defined minimal surface marker criteria (≥95% expression of CD105, CD73, CD90; ≤2% expression of hematopoietic markers CD45, CD34, etc.), this does not guarantee therapeutic function [13]. A key focus in MSC process development is linking specific CQAs—such as secretome profile or immunomodulatory capacity in a standardized assay—to clinical outcomes [56].
Diagram 1: Comparative Manufacturing & QC Workflows.
Experimental Protocols for Key Manufacturing Challenges
Protocol: Tumorigenicity Testing for PSC-Derived Products
Objective: To detect residual undifferentiated PSCs in a final differentiated cell product by assessing its potential to form teratomas in vivo [56].
Methodology:
- Cell Preparation: The final PSC-derived product (e.g., dopaminergic neurons, retinal pigment epithelium cells) is harvested and prepared for injection. A positive control of undifferentiated PSCs is run in parallel.
- Animal Model: Immunodeficient mice (e.g., NOD-scid gamma (NSG)) are used to prevent immune rejection of the human cells.
- Inoculation: Cells are resuspended in a Matrigel/culture medium mixture and injected into a suitable site, typically the testis, kidney capsule, or subcutaneous space. A minimum of 10 animals per group is recommended.
- Observation Period: Animals are monitored for 12-20 weeks for the formation of palpable tumors.
- Histological Analysis: Upon termination, any resulting tumors are excised, fixed, sectioned, and stained with hematoxylin and eosin (H&E). The defining positive outcome is the presence of tissues derived from all three embryonic germ layers (e.g., ectoderm: neural rosettes; mesoderm: cartilage or muscle; endoderm: gut-like epithelium) [56].
Protocol: Potency Assay for MSC Immunomodulatory Function
Objective: To establish a quantitative, cell-based assay that correlates with the intended mechanism of action for MSCs, replacing simple surface marker analysis with a functional quality control [56] [13].
Methodology:
- MSC Preparation: The test MSC batch is expanded and harvested using the standard manufacturing process.
- Immune Cell Activation: Peripheral blood mononuclear cells (PBMCs) from healthy human donors are isolated and activated with a mitogen like phytohemagglutinin (PHA) or anti-CD3/CD28 antibodies.
- Co-culture: Activated PBMCs are co-cultured with the test MSCs at a defined ratio (e.g., 10:1 PBMCs:MSCs) for 3-5 days. Controls include activated PBMCs alone (maximal proliferation control) and non-activated PBMCs (background control).
- Readout - Proliferation Inhibition: The degree of MSC-mediated immunosuppression is measured by adding a radioactive [³H]-thymidine or a non-radioactive MTT/AlamarBlue reagent to the culture for the final 8-24 hours. The signal from the co-culture is compared to the activated PBMC-only control.
- Calculation:
% Inhibition = [1 - (Signal Co-culture / Signal PBMCs alone)] x 100
- Calculation:
- Release Criterion: A product lot must demonstrate a minimum pre-specified percentage of inhibition (e.g., >50%) to be released, establishing a link between the manufacturing process and biological function.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and technologies are critical for developing and controlling the manufacture of stem cell-based therapies.
Table 3: Essential Reagents and Technologies for Stem Cell Manufacturing R&D
| Research Reagent / Technology | Function in Manufacturing R&D | Application Notes |
|---|---|---|
| StemRNA Clinical Seed iPSCs | Provides a standardized, GMP-compliant starting cell source with a submitted Drug Master File (DMF) for regulatory streamlining [26]. | Reduces variability in PSC processes; crucial for IND filings and process consistency. |
| Closed-System Bioreactors | Enables scalable 3D cell expansion under controlled, aseptic conditions, which is a cornerstone of GMP manufacturing [55] [58]. | Moving from R&D-sized (<1L) to commercial-scale (>10L) systems is a key transition. |
| Process Analytical Technology (PAT) | Allows for real-time, in-line monitoring of critical process parameters (CPPs) like metabolites, pH, and dissolved oxygen [55]. | Links process changes directly to CQAs; essential for QbD. |
| Magnetic Cell Sorting (MACS) | Gently purifies target cell populations (e.g., specific differentiated cells from a PSC culture) or depletes undesired cells (e.g., undifferentiated PSCs) [26]. | Preferable to FACS for large-scale manufacturing due to gentler handling and higher throughput. |
| Design of Experiment (DOE) Software | Statistically models the interaction of multiple process variables (e.g., growth factor concentrations, cell seeding density) to optimize complex differentiation protocols [55]. | Moves beyond inefficient "one-factor-at-a-time" experimentation. |
The paths to standardizing and scaling embryonic-derived (and iPSC-derived) and adult stem cell therapies, while distinct, are converging on shared principles: robust automation, defined quality attributes, and functional potency assays. The PSC field must solve the challenges of complex differentiation and tumorigenicity risk, leveraging its advantage of a virtually unlimited, consistent starting source. The adult stem cell field must overcome the hurdles of donor variability and functional decline, building on its history of clinical use and perceived safety profile. For both, the future of manufacturing lies in adaptive, closed-system bioprocessing, deeply characterized cell banks, and the integration of advanced analytics and AI to ensure that every product lot is not only safe and pure, but also potent and effective for patients.
The fields of CRISPR gene editing and 3D bioprinting represent two of the most transformative biotechnology platforms in modern regenerative medicine. While often developed independently, their convergence creates a powerful synergy for tissue engineering and cellular enhancement. CRISPR technology provides the precise genetic instructions to control cell fate and function, while 3D bioprinting offers the architectural framework to organize these enhanced cells into functional, three-dimensional tissues.
This technological convergence occurs within the critical context of the ongoing scientific discourse surrounding stem cell sources. The choice between embryonic stem cells (ESCs) and adult stem cells carries significant implications for therapeutic development [30]. ESCs, with their unmatched pluripotency, can differentiate into any cell type but face ethical constraints and potential immune rejection [11] [30]. Adult stem cells, particularly mesenchymal stem cells (MSCs), offer an ethically neutral alternative with demonstrated immunomodulatory properties but possess more limited differentiation potential [20] [13]. This review examines how CRISPR and 3D bioprinting technologies are being leveraged to overcome these inherent limitations, thereby enhancing the therapeutic potential of all stem cell types for advanced regenerative applications.
Technological Principles and Mechanisms
CRISPR-Cas9 Gene Editing: Precision at the Genomic Level
The CRISPR-Cas9 system functions as a highly specific gene-editing tool that enables precise modification of DNA sequences within living cells. The core mechanism involves a guide RNA (gRNA) that directs the Cas9 nuclease to a specific target DNA sequence, where it creates a double-strand break [59]. The cell's natural repair mechanisms then activate, allowing researchers to disrupt, delete, or insert new genetic material.
Recent research has revealed that CRISPR efficiency is profoundly influenced by the three-dimensional architecture of the genome. A 2024 study demonstrated that genomic regions with lower spatial density consistently showed higher CRISPR cleavage efficiency, suggesting that accessible chromatin structures facilitate better sgRNA binding and Cas9 activity [59]. This understanding of 3D genomic influences has led to improved predictive models for sgRNA design, significantly enhancing targeting precision.
3D Bioprinting: Engineering Biological Structures
3D bioprinting employs additive manufacturing principles to create complex, cell-laden biological structures. The process typically involves three key stages: pre-bioprinting (digital model creation), bioprinting (layer-by-layer deposition), and post-bioprinting (tissue maturation) [60]. Several bioprinting technologies have been developed, each with distinct advantages:
- Inkjet-based bioprinting: A non-contact method that deposits picoliter droplets of bioink using thermal, piezoelectric, or electrostatic actuators. It offers high speed and good cell viability but is limited to lower-viscosity materials [61].
- Laser-assisted bioprinting: Uses laser pulses to transfer bioink from a donor ribbon to a substrate, providing high resolution but requiring more complex equipment.
- Extrusion-based bioprinting: Forces bioink through a nozzle using pneumatic or mechanical pressure, enabling high-viscosity materials and high cell densities but with potentially lower resolution.
- FRESH (Freeform Reversible Embedding of Suspended Hydrogels): An emerging technique that prints hydrogels within a thermoreversible support bath, dramatically improving the fidelity of soft biological structures [61].
The following diagram illustrates the integrated workflow combining CRISPR-enhanced stem cells with 3D bioprinting for creating advanced tissue constructs:
Comparative Performance Analysis
Enhancement of Stem Cell Properties
The integration of CRISPR technology with 3D bioprinting has enabled significant enhancements to stem cell properties for regenerative applications. The table below compares the performance of different stem cell types with and without these biotechnological interventions:
Table 1: Performance Comparison of Stem Cell Types with Biotechnological Enhancement
| Stem Cell Type | Native Properties | CRISPR-Enhanced Capabilities | 3D Bioprinting Compatibility | Therapeutic Applications |
|---|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Pluripotent, unlimited self-renewal, ethical concerns [11] [30] | Reduced immunogenicity, enhanced differentiation control, disease resistance [61] | High structure formation fidelity, excellent differentiation in scaffolds [61] | Parkinson's disease, age-related macular degeneration, Type 1 diabetes [26] [30] |
| Mesenchymal Stem Cells (MSCs) | Multipotent, immunomodulatory, tissue-specific differentiation [20] [13] | Enhanced homing ability, increased secretory function, improved proliferation [61] [11] | Excellent bioink compatibility, responsive to mechanical cues in scaffolds [61] [62] | Graft-versus-host disease (Ryoncil approved 2024), orthopedic repair, wound healing [26] [62] |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific, pluripotent, no ethical concerns [20] [11] | Correction of genetic defects, enhanced safety profile (tumorigenesis reduction) [61] [63] | High personalization potential, patient-specific tissue constructs [61] [26] | Retinal degeneration (OpCT-001), Parkinson's disease, personalized disease models [26] |
Functional Outcomes in Tissue Engineering
The ultimate validation of these enhancement technologies lies in their functional outcomes for specific tissue engineering applications. Recent studies demonstrate markedly different performance metrics across various tissue types:
Table 2: Quantitative Performance Metrics in Tissue Engineering Applications
| Tissue Application | Key Performance Metrics | CRISPR-Enhanced Constructs | Non-Enhanced Constructs | Significance |
|---|---|---|---|---|
| Tendon/Ligament Repair | Ultimate tensile strength (MPa) [62] | 35.2 ± 4.5 MPa | 18.7 ± 3.2 MPa | 88% improvement in mechanical strength |
| Collagen alignment index [62] | 0.82 ± 0.06 | 0.54 ± 0.09 | 52% better organization | |
| Bone Regeneration | Mineralization density (mg/cc) [61] | 687.5 ± 45.2 | 425.3 ± 38.7 | 62% increase in bone density |
| Vascularization (vessels/mm²) [61] | 32.4 ± 3.8 | 15.2 ± 2.9 | 113% more blood vessels | |
| Neural Tissue | Neurite outgrowth (μm) [61] | 1247 ± 156 | 683 ± 98 | 83% greater outgrowth |
| Functional recovery rate [26] | 68% ± 7% | 32% ± 6% | 113% improvement in recovery |
Experimental Protocols and Methodologies
CRISPR Enhancement Protocol for Stem Cells
The following detailed protocol outlines the methodology for CRISPR-based enhancement of stem cells for tissue engineering applications, based on established procedures from recent literature [61] [11] [59]:
Phase 1: Guide RNA Design and Validation
- Step 1: Identify target gene sequence using reference databases (e.g., NCBI, Ensembl)
- Step 2: Design sgRNA with optimized efficiency using predictive algorithms (incorporating 3D genomic features [59])
- Step 3: Validate sgRNA specificity using BLAST analysis against the reference genome
- Step 4: Select minimal off-target potential designs using cutting-frequency determination
Phase 2: Delivery and Transfection
- Step 5: Prepare ribonucleoprotein (RNP) complexes by incubating sgRNA with Cas9 protein
- Step 6: Transfect stem cells using electroporation (for MSCs and ESCs) or lipid nanoparticles (for iPSCs)
- Step 7: Incubate cells for 48 hours at 37°C with 5% CO₂
Phase 3: Validation and Expansion
- Step 8: Assess editing efficiency using T7E1 assay or next-generation sequencing
- Step 9: Isolate successfully edited cells using fluorescence-activated cell sorting (FACS)
- Step 10: Expand edited cell population in optimized culture medium for 2-3 passages
3D Bioprinting Workflow for Enhanced Tissue Constructs
This protocol describes the integration of CRISPR-enhanced stem cells into 3D-bioprinted tissue constructs, with specific methodologies for different tissue types [61] [60] [62]:
Phase 1: Bioink Formulation
- Step 1: Prepare base hydrogel (e.g., gelatin methacryloyl (GelMA), collagen, hyaluronic acid)
- Step 2: Mix CRISPR-enhanced stem cells into hydrogel at optimized density (1-20×10⁶ cells/mL)
- Step 3: Incorporate supportive additives (growth factors, integrin ligands, RGD peptides)
- Step 4: Adjust bioink viscosity and cross-linking parameters for target tissue properties
Phase 2: Printing Parameters Optimization
- Step 5: Select appropriate printing technology based on tissue requirements:
- Inkjet printing: For high-resolution, low-viscosity structures
- Extrusion printing: For high-cell-density, mechanically robust tissues
- FRESH technique: For complex soft tissue architectures [61]
- Step 6: Optimize printing parameters (pressure, speed, temperature) using test structures
- Step 7: Calibrate nozzle diameter and layer height for target feature size
Phase 3: Post-Printing Maturation
- Step 8: Crosslink printed structure using UV light (for photopolymerizable bioinks) or ionic solutions
- Step 9: Transfer to bioreactor system for mechanical conditioning (e.g., cyclic stretching for tendon/ligament constructs [62])
- Step 10: Culture for 14-28 days with progressive increase in mechanical stimulation
- Step 11: Assess tissue maturation through histology, immunohistochemistry, and mechanical testing
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of CRISPR-enhanced 3D bioprinting requires specific reagents and materials. The following table details essential components for these advanced biotechnology applications:
Table 3: Essential Research Reagents for CRISPR-Enhanced 3D Bioprinting
| Reagent Category | Specific Examples | Function & Application | Technical Notes |
|---|---|---|---|
| CRISPR Components | High-fidelity Cas9 nuclease, sgRNA scaffolds, HDR templates [11] [59] | Precision genome editing, gene knockout, insertion of therapeutic transgenes | Use predictive algorithms incorporating 3D genomic features for sgRNA design [59] |
| Stem Cell Culture | REPROCELL StemRNA Clinical Seed iPSCs, Mesenchymal Stem Cell Media, Defined FBS [26] [13] | Maintenance and expansion of stem cell populations prior to genetic modification | Use GMP-compliant sources for clinical translation [26] |
| Bioink Materials | Natural polymers (collagen, alginate, gelatin, hyaluronic acid), Synthetic polymers (PCL, PLA, PLGA) [61] [62] | 3D scaffold formation, structural support, mechanical protection for cells | Composite bioinks often optimize both biocompatibility and printability [62] |
| Crosslinking Agents | Calcium chloride (alginate), UV light (GelMA, PEGDA), Microbial transglutaminase (protein-based) [61] [62] | Stabilization of printed structures, mechanical property enhancement | Optimize concentration to balance cell viability and mechanical strength |
| Bioreactor Systems | Perfusion bioreactors, Mechanical stretch bioreactors, Compression bioreactors [62] | Post-printing tissue maturation, mechanical conditioning, nutrient delivery | Match bioreactor type to target tissue's native mechanical environment |
Technological Synergies and Signaling Pathways
The combination of CRISPR and 3D bioprinting creates powerful synergies that enhance stem cell functionality beyond what either technology can achieve alone. The integrated signaling pathways activated by these combined interventions can be visualized as follows:
The signaling pathways activated through these combined technologies include:
- Mechanotransduction pathways (YAP/TAZ, Rho/ROCK) activated by scaffold stiffness and microarchitecture [62]
- Differentiation pathways (BMP/Smad, Wnt/β-catenin) enhanced through CRISPR-mediated receptor overexpression [61]
- Angiogenic signaling (VEGF, FGF) promoted by both genetic modification and scaffold design [61]
- Metabolic reprogramming through CRISPR-enhanced mitochondrial biogenesis supported by optimized bioreactor conditions
The strategic convergence of CRISPR gene editing and 3D bioprinting represents a paradigm shift in regenerative medicine, offering unprecedented capabilities for stem cell enhancement and tissue engineering. The experimental data presented demonstrates clear quantitative advantages of this combined approach across multiple tissue types, with mechanically superior constructs and enhanced biological functionality.
The ongoing debate between embryonic and adult stem cell applications is being transformed by these technologies. CRISPR enhancement mitigates the limitations of adult stem cells, while 3D bioprinting provides the structural context needed to direct embryonic stem cell differentiation with greater precision. The recent FDA approvals of stem cell therapies (Ryoncil in 2024) and the advancement of iPSC-based treatments into Phase III trials (Fertilo in 2025) signal a rapidly evolving regulatory landscape for these enhanced cellular products [26].
Future development will likely focus on 4D bioprinting (time-responsive structures), advanced gene editing systems beyond CRISPR-Cas9, and personalized bioink formulations tailored to individual patient needs. As these technologies mature, they will increasingly blur the distinction between native and engineered tissues, ultimately enabling the restoration, maintenance, and even enhancement of human tissue function with growing precision and efficacy.
Evaluating Therapeutic Efficacy, Safety, and Commercial Viability
This guide provides a comparative analysis of embryonic and adult stem cells for researchers and drug development professionals, focusing on their therapeutic applications. The assessment is grounded in efficacy, safety, and ethical considerations, supported by current experimental data and regulatory landscapes.
Core Characteristics and Therapeutic Mechanisms
Stem cells are broadly categorized by their origin and differentiation potential. The following table outlines the defining characteristics of embryonic and adult stem cells.
| Feature | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Source | Inner cell mass of a blastocyst-stage embryo (3-5 days post-fertilization) [10] [64] | Various adult tissues (e.g., bone marrow, adipose tissue, dental pulp) [13] [11] |
| Key Characteristics | Pluripotent: Can differentiate into any cell type from all three germ layers (ectoderm, mesoderm, endoderm) [64] [11] | Multipotent: Can differentiate into a limited range of cell types within their tissue of origin [13] [11] |
| Primary Therapeutic Mechanisms | - Cell Replacement: Direct differentiation and transplantation to replace lost or damaged cells (e.g., dopaminergic neurons for Parkinson's) [65] [64] | - Paracrine Signaling: Secretion of bioactive factors that promote tissue repair and reduce inflammation [65] [13]- Immunomodulation: Controlling autoimmune and inflammatory responses [65]- Tissue Homeostasis: Natural role in maintenance and repair of their native tissue [13] |
Efficacy and Clinical Translation
Clinical translation of these cell types differs significantly, with Adult Stem Cells having a longer history of established use, while Embryonic Stem Cells are progressing through structured clinical trials.
| Aspect | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Proven Clinical Applications | Limited. Primarily in clinical trials for ophthalmology (e.g., retinal pigment epithelium for macular degeneration) and neurology [26] [64]. | Extensive. Hematopoietic Stem Cell (HSC) transplantation is standard for blood cancers and disorders [65] [1]. Mesenchymal Stem Cell (MSC) therapy approved for pediatric steroid-refractory acute graft-versus-host disease (Ryoncil) [26]. |
| Scope of Potential Applications | High. Broad potential for any tissue type due to pluripotency. Active research for Parkinson's, spinal cord injury, diabetes, and heart failure [65] [64]. | Tissue-specific. Effective for conditions related to their origin (e.g., HSCs for blood, MSCs for bone, cartilage, immunomodulation) [13] [65]. |
| Clinical Trial Scale | Growing. As of December 2024, 115 global clinical trials involved 83 distinct pluripotent stem cell-derived products [26]. | Mature and widespread. A vast number of trials, particularly for MSCs and HSCs, across many conditions [11]. |
| Scalability & Manufacturing | Challenging. Requires precise, complex differentiation protocols. Risk of heterogeneity in derived cell products [66]. | More established for some types (e.g., HSCs). MSC scalability is enhanced by new sources like induced MSCs (iMSCs) from iPSCs [26]. |
Safety and Tumorigenicity Profile
The distinct biological properties of each stem cell type confer different safety risks, with tumorigenicity being a primary concern.
| Aspect | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Primary Safety Concern | Tumorigenicity: High risk of forming teratomas due to residual undifferentiated pluripotent cells [64] [11]. | Lower tumorigenic risk due to limited differentiation potential. Primary risks include immune reactions and complications from the procedure (e.g., infection) [13] [64]. |
| Immunogenicity | High. Allogeneic transplantation requires immunosuppression to prevent rejection [11] [10]. | Lower for autologous use. Allogeneic use (e.g., MSCs) is possible due to immune-privileged properties but still carries rejection risk [13]. |
| Genetic Stability | Prone to genomic and epigenetic alterations during long-term culture, affecting function and safety [66]. | Generally more stable. However, prolonged in vitro expansion can also introduce genetic abnormalities [66]. |
| Overall Safety Record | Encouraging. In clinical trials, over 1,200 patients have been dosed with pluripotent stem cell-derived products with no significant class-wide safety concerns reported as of 2025, though long-term surveillance is critical [26]. | Well-established for HSC transplants. Newer MSC therapies also demonstrate a good safety profile in regulated trials [26] [27]. |
Ethical and Regulatory Landscape
The ethical considerations and regulatory pathways for these cell types are fundamentally different, impacting their research and clinical application.
| Aspect | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Core Ethical Issue | Destruction of human embryos for cell line derivation, raising debates on the moral status of the embryo [18] [10] [27]. | Considered less ethically contentious as derivation does not involve embryos and is often autologous [27] [13]. |
| Key Regulatory Hurdles | Stringent oversight and funding restrictions in many countries. Requires Investigational New Drug (IND) approval and progression through phased trials [26] [66]. | Less restrictive for minimally manipulated products used in a homologous manner (e.g., bone marrow transplant). Substantially manipulated or non-homologously used ASCs are regulated as drugs/biologics [66] [27]. |
| Informed Consent Focus | For embryo donors: clarity on research/therapeutic use, commercial potential, and understanding that the embryo will be destroyed [66] [18]. | For cell donors: standard consent for tissue procurement, with screening for infectious diseases, especially for allogeneic therapies [66]. |
Experimental Protocols and Workflows
Responsible translation from bench to bedside requires rigorous, standardized experimental protocols.
Preclinical Assessment Workflow
All stem cell-based products must undergo a rigorous safety and efficacy assessment before clinical trials. The workflow below outlines the key stages of this preclinical pipeline.
Key Preclinical Experiments:
- Tumorigenicity Assay: The most critical safety test for ESCs and iPSCs. This involves injecting undifferentiated stem cells into immunodeficient mice (e.g., SCID/beige model) to monitor for teratoma formation over 12-20 weeks. Tissues are histologically analyzed post-mortem [66] [64].
- Genomic Stability Assessment: Mandatory for cells cultured in vitro. Karyotyping (G-banding) is a standard initial test. Higher-resolution methods like Comparative Genomic Hybridization (CGH) arrays or Whole Genome Sequencing are used to detect submicroscopic copy number variations and sequence-level mutations accumulated during culture [66].
- In Vivo Efficacy Studies: Cells are transplanted into disease-specific animal models (e.g., rodent model of Parkinson's for dopaminergic neurons, spinal cord injury model). Functional recovery (e.g., motor tests) and histological integration/engraftment are assessed over time [65].
Cell Manufacturing and Quality Control
The transition from research-grade to clinically applicable cells requires a controlled manufacturing process. The workflow below details the critical steps from tissue sourcing to final product release.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for stem cell research and therapy development, based on current protocols.
| Item | Function | Application Notes |
|---|---|---|
| GMP-compliant Culture Media | Provides nutrients and signals for cell growth and maintenance. Formulations include specific growth factors to maintain pluripotency (for ESCs/iPSCs) or multipotency (for MSCs) [66] [64]. | Must be xeno-free and serum-free for clinical-grade manufacturing to avoid pathogen transmission and immune reactions [66]. |
| Defined Growth Factors | Directs stem cell fate. FGF-2 (bFGF) is crucial for maintaining ESC/iPSC pluripotency. TGF-β/Activin A supports the undifferentiated state. For differentiation, specific morphogens (e.g., BMP, WNT, FGF families) are used [64]. | Quality and batch consistency are critical for reproducible differentiation and manufacturing [66]. |
| Characterization Antibodies | Used in flow cytometry and immunocytochemistry to confirm cell identity and purity. Key markers: OCT4, SOX2, NANOG (pluripotency), CD73, CD90, CD105 (MSCs), CD34, CD45 (HSCs) [13] [66]. | Release criteria often require a minimum percentage of positive cells for identity markers (e.g., ≥95% for MSC markers) and absence of impurity markers [13]. |
| Cell Dissociation Reagents | Enzymatically dissociates cells for passaging and harvesting. Common reagents include recombinant trypsin, Accutase, or collagenase. | Must be well-defined and non-animal derived for clinical use. Over-digestion can damage surface proteins and affect viability [66]. |
| Matrices for Cell Culture | Provides a surrogate extracellular matrix for cell attachment and growth. Common matrices: Matrigel, recombinant laminin, vitronectin. | Matrigel is biologically complex but widely used; defined recombinant matrices are preferred for manufacturing consistency and regulatory approval [66]. |
The choice between embryonic and adult stem cells is not a matter of superiority but of strategic alignment with therapeutic goals.
- Embryonic Stem Cells offer unparalleled versatility for diseases requiring cell replacement but necessitate rigorous safety protocols and navigate complex ethical terrain. Their clinical application is progressing steadily in regulated trials.
- Adult Stem Cells, particularly MSCs and HSCs, provide a clinically validated, ethically simpler path for applications leveraging immunomodulation, paracrine signaling, and homologous tissue repair.
The future lies in leveraging the strengths of both: using ESCs/iPSCs for disease modeling and as a master cell source, and advancing adult stem cells for targeted immunomodulatory therapies. Continued focus on robust manufacturing, long-term safety monitoring, and clear regulatory pathways is essential for both platforms to realize their full potential in regenerative medicine.
Stem cell therapy represents a groundbreaking frontier in modern medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries through its unique regenerative capabilities [11]. As the field advances, the clinical translation of stem cell-based interventions necessitates rigorous evaluation of success rates and measurable endpoints to balance scientific excitement with evidence-based medicine [66]. This comparative guide examines the clinical trial outcomes for two prominent stem cell types—embryonic stem cells (ESCs) and adult stem cells (ASCs)—within the broader thesis of their therapeutic applications. For researchers, scientists, and drug development professionals, understanding these distinctions is crucial for designing robust clinical trials, interpreting efficacy data, and selecting appropriate cellular products for specific disease targets.
The fundamental differences between ESC and ASC biology create divergent clinical development pathways. ESCs, derived from the inner cell mass of blastocysts, are pluripotent and can differentiate into any human body cell, making them highly adaptable with broad therapeutic promise [11]. In contrast, ASCs, found in various tissues such as bone marrow, adipose tissue, and umbilical cord blood, are multipotent with more specialized differentiation capabilities typically limited to cell lineages within their tissue of origin [13]. This biological distinction profoundly influences their clinical applications, safety profiles, and regulatory considerations in therapeutic development.
Success Rates and Efficacy Outcomes Across Applications
Clinical success rates for stem cell therapies vary significantly based on multiple factors, including cell type, application, and patient selection criteria. The tables below summarize reported outcomes across different medical conditions and stem cell types.
Table 1: Overall Success Rates of Stem Cell Therapies by Condition
| Medical Condition | Therapeutic Approach | Reported Success Rate | Key Efficacy Endpoints |
|---|---|---|---|
| Blood Cancers [67] [68] | Hematopoietic Stem Cell Transplantation | 60-80% [67] [68] | Survival rates, absence of disease progression, eradication of abnormal cells |
| Joint Repair & Autoimmune Conditions [67] [68] | Mesenchymal Stem Cell Therapy | ~80% [67] [68] | Symptom improvement, reduced inflammation, functional recovery |
| Cardiovascular Diseases [69] [70] | Various Stem Cell Interventions | 65-80% [69] | Improved ejection fraction, reduced cardiovascular events, functional capacity |
| Neurological Disorders (e.g., Parkinson's) [68] [69] | Stem Cell Transplantation | Up to 60% [68] | Disability improvement, graft integrity, disease progression slowing |
| Orthopedic Applications [68] | Stem Cell Procedures | Up to 80% [68] | Symptom improvement, tissue regeneration, functional recovery |
Table 2: Comparative Outcomes by Stem Cell Type
| Stem Cell Type | Advantages | Clinical Challenges | Notable Therapeutic Applications |
|---|---|---|---|
| Embryonic Stem Cells (ESCs) [11] | Pluripotency, broad differentiation potential [11] | Ethical concerns, tumorigenicity, immunological rejection [11] [15] | Disease modeling, drug testing, retinal pigment epithelial cells for macular degeneration [11] [15] |
| Mesenchymal Stem Cells (MSCs) [67] [13] | Immunomodulation, trophic factor secretion, relative safety [67] [13] | Variable potency depending on source and donor [67] | Autoimmune conditions, joint repair, graft-versus-host disease [67] [13] |
| Induced Pluripotent Stem Cells (iPSCs) [15] [42] | Patient-specific, avoids ethical concerns [15] | Tumorigenicity, immunogenicity, heterogeneity [15] [42] | Parkinson's disease, heart failure, personalized disease modeling [15] [69] |
| Hematopoietic Stem Cells (HSCs) [13] | Well-established protocol, life-saving potential [13] | Graft-versus-host disease, infection risk [13] | Leukemia, lymphoma, multiple myeloma, blood disorders [13] |
Success rates must be interpreted with caution, as they depend on specific trial designs, patient populations, and definitions of "success." For example, a comprehensive analysis of stem cell therapy for various conditions reported success rates between 50% to 90% in regenerative medicine applications, with particularly promising outcomes in specific disease categories [69]. Recent research indicates that proper patient selection emerges as a critical factor in determining stem cell therapy outcomes, with medical professionals employing rigorous screening protocols and assessment criteria to identify suitable candidates [69].
Methodologies for Assessing Stem Cell Efficacy
Measuring Treatment Success: Endpoints and Assessment Protocols
The success of stem cell therapies is measured through comprehensive, multi-modal approaches that combine clinical observations, laboratory tests, patient-reported outcomes, and long-term follow-up [67]. These complementary assessment strategies provide a holistic view of therapeutic efficacy:
- Clinical Observations: Medical professionals conduct physical examinations and utilize imaging studies (MRI, CT scans) to document improvements in symptoms, healing progress, and changes in disease course [67].
- Laboratory Tests: Specific biomarkers provide objective insights into treatment effectiveness. For conditions characterized by chronic inflammation, reduction in inflammatory markers such as IL-6 and TNF-α post-treatment signifies successful therapy [67]. In blood cancers, decreased abnormal cells in blood or bone marrow reflects successful eradication of disease cells [67].
- Patient-Reported Outcomes: Questionnaires and interviews evaluate changes in symptoms, quality of life, physical functioning, and other patient-relevant aspects [67]. Improvements in stamina, energy levels, concentration, decision-making, or quality of sleep could all indicate successful stem cell therapy [67].
- Long-Term Follow-Up: Success in stem cell therapy encompasses not just immediate outcomes but also long-term results and durability of response, requiring regular monitoring to ensure sustained benefits [67].
Cardiovascular Case Study: Experimental Design and Protocols
Advanced heart failure serves as an illustrative case study for stem cell trial methodologies. The systematic review of 27 clinical trials conducted between 2014-2024 reveals sophisticated experimental designs for evaluating stem cell efficacy in cardiac repair [70]:
Table 3: Stem Cell Delivery Methods in Cardiovascular Trials
| Delivery Method | Description | Potential Benefits | Limitations |
|---|---|---|---|
| Intramyocardial (IM) Injection [70] | Direct injection into myocardium | Enhances cell retention and integration; improves left ventricular function; reduces scar size | Invasive; limited to localized delivery |
| Intracoronary (IC) Infusion [70] | Cells delivered into coronary arteries | Less invasive; direct access to heart via blood vessels | Cell washout; less tissue integration |
| Transendocardial Injection [70] | Cells injected into endocardium | Promotes vascularity; greater functional improvement than intracoronary methods | Requires catheter-based procedure; technical complexity |
| Intravenous (IV) Administration [70] | Systemic delivery through veins | Least invasive approach; simple administration | Widespread systemic distribution; low cardiac retention |
The experimental workflow for these cardiovascular trials typically follows a structured pathway from patient selection through long-term monitoring, with specific efficacy measurements at each stage:
Cardiovascular Stem Cell Trial Workflow
The mechanistic focus in cardiovascular stem cell trials has shifted from direct differentiation to paracrine signaling effects, where injected cells secrete cytokines, chemokines, and growth factors that activate intracellular signaling pathways such as PI3K/Akt and ERK1/2 through receptors including EGFR and VEGFR [70]. This paradigm shift influences endpoint selection, with greater emphasis on inflammatory biomarkers and functional improvements rather than solely structural changes.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful stem cell clinical trials require carefully selected reagents and materials throughout the cellular product lifecycle. The following toolkit highlights critical components:
Table 4: Essential Research Reagents for Stem Cell Clinical Trials
| Reagent/Material | Function | Application Notes | Quality Standards |
|---|---|---|---|
| Human Platelet Lysate (HPL) [42] | Culture supplement for MSC expansion | Gradually increased concentration to accommodate cell growth; xeno-free alternative to FBS | Screening for adventitious agents; compliance with regulatory guidelines [66] |
| Enzymatic Digestion Reagents [66] | Tissue dissociation for cell isolation | Enzymes like collagenase for adipose-derived stem cells; concentration and timing optimization critical | Quality control to ensure consistency and minimal cellular damage [66] |
| Cell Culture Media (e.g., α-MEM) [42] | Maintenance of stem cell viability and proliferation | Formulation optimized for specific stem cell types; may include specific growth factor cocktails | GMP-grade where possible; rigorous testing for contaminants [66] |
| Cryopreservation Solutions | Long-term storage of cellular products | Typically contain DMSO and serum alternatives; controlled-rate freezing protocols | Validated stability protocols; maintenance of cell viability and potency post-thaw [66] |
| Flow Cytometry Antibodies | Characterization of cell surface markers | CD105, CD73, CD90 for MSCs; CD45, CD34, CD14 for exclusion | Validation for specific cell types; compliance with analytical method guidelines [13] [66] |
| Genetic Manipulation Tools (e.g., CRISPR-Cas9) [11] [15] | Genome editing for enhanced therapeutic properties | CXCR4 overexpression to boost cell homing; precise genetic modification | Comprehensive off-target effect screening; stringent safety assessment [11] |
Manufacturing stem cell products requires all reagents and processes to be subject to quality control systems and standard operating procedures to ensure reagent quality and protocol consistency [66]. Where possible or mandated by regulation, manufacturing should be performed under Good Manufacturing Practice (GMP) conditions, though in early-stage clinical trials, GMPs may be introduced in a phase-appropriate manner in some regions [66].
The oversight and review of cell processing and manufacturing protocols should be rigorous, considering the manipulation of the cells, their source and intended use, the nature of the clinical trial, and the research subjects who will be exposed to them [66]. This is particularly important given that stem cells can proliferate in culture for extended periods, carrying inherent risks that must be carefully managed through comprehensive quality systems [66].
Clinical trial outcomes for stem cell therapies must be interpreted within the context of specific therapeutic applications, as success rates vary significantly across medical conditions and stem cell types. The field continues to evolve rapidly, with future directions focusing on precision medicine integration, immune modulation strategies, and advancements in gene-editing technologies that promise to enhance both efficacy and safety profiles [11]. For researchers and drug development professionals, careful attention to standardized endpoint selection, rigorous manufacturing protocols, and comprehensive long-term monitoring remains essential for generating meaningful clinical evidence.
The growing pipeline of stem cell therapies faces the challenge of balancing accelerated development with thorough safety assessment. As noted in regulatory guidelines, clinical experimentation is burdensome for research subjects and expensive; therefore, new interventions should only advance to clinical trials when there is a compelling scientific rationale, a plausible mechanism of action, and an acceptable chance of success [66]. By adhering to these principles and implementing robust assessment methodologies, the stem cell research community can continue to translate revolutionary science into transformative therapies that address unmet medical needs across a spectrum of diseases.
Regulatory Pathways and Market Accessibility for Stem Cell Products
The transition of stem cell products from research to clinic represents one of the most complex challenges in modern regenerative medicine. For researchers, scientists, and drug development professionals, understanding the intricate regulatory pathways and market dynamics is crucial for successful product development. The global stem cell therapy market is projected to grow significantly from USD 18.65 billion in 2024 to approximately USD 64.84-78.39 billion by 2032-2034, demonstrating substantial expansion at a compound annual growth rate (CAGR) of 13.27% to 22.8% [71] [72] [73]. This growth is fueled by rising demand for regenerative medicine, increasing prevalence of chronic and degenerative diseases, and continued advancements in stem cell research and manufacturing technologies [71] [72].
This guide provides a comprehensive comparison of regulatory frameworks and market accessibility for stem cell products, with particular emphasis on the distinctions between embryonic and adult stem cell applications. We examine current regulatory classifications, approval pathways, clinical trial requirements, and market authorization processes across major jurisdictions, supported by experimental data and analytical frameworks relevant to therapeutic development.
Regulatory Pathway Analysis
Classification and Oversight Frameworks
Stem cell products face diverse regulatory classifications based on their biological characteristics and intended use. The U.S. Food and Drug Administration (FDA) regulates human cells, tissues, and cellular and tissue-based products under Title 21 of the Code of Federal Regulations Part 1271 [27]. Products meeting specific criteria—minimal manipulation, homologous use, and not combined with another article—are regulated solely under Section 361 of the Public Health Service Act and focus on safety and prevention of communicable disease transmission [27]. Products exceeding these criteria undergo more rigorous review as drugs, devices, or biologics under Section 351 and require an approved Biologics License Application (BLA) before marketing [27].
The International Society for Stem Cell Research regularly updates guidelines to address emerging scientific areas. The 2025 guidelines specifically refine oversight recommendations for stem cell-based embryo models, retiring the classification of models as "integrated" or "non-integrated" in favor of the inclusive term SCBEMs [28]. These guidelines prohibit transplantation of human SCBEMs to a uterus and ex vivo culture to the point of potential viability [28].
Table 1: Regulatory Classification of Stem Cell Products
| Product Characteristic | Section 361 (Minimal Regulation) | Section 351 (Full Regulation) |
|---|---|---|
| Manipulation Level | Minimal manipulation (no alteration of biological characteristics) | More than minimal manipulation (significant alteration of biological characteristics) |
| Intended Use | Homologous use (same function in recipient as donor) | Non-homologous use (different function in recipient) |
| Combination Products | Not combined with another article (except water, crystalloids, sterilizing agents) | Combined with drugs, devices, or other biologics |
| Examples | Bone marrow transplant, unmanipulated adipose tissue | Genetically modified stem cells, extensively cultured cells, induced pluripotent stem cell derivatives |
Clinical Trial Authorization Process
For stem cell products regulated as drugs or biologics, clinical development requires an Investigational New Drug application before initiating human trials [26] [27]. The FDA's IND process becomes effective 30 days after submission unless the agency places a clinical hold [26]. Phase I trials focus primarily on safety, Phase II explores efficacy and further safety, and Phase III confirms efficacy and monitors adverse reactions in larger populations [26].
Recent years have seen significant regulatory milestones for stem cell products. Between 2023-2025, the FDA approved several innovative therapies: Omisirge (omidubicel-onlv) for hematologic malignancies in April 2023; Lyfgenia (lovotibeglogene autotemcel) for sickle cell disease in December 2023; and Ryoncil (remestemcel-L) for pediatric steroid-refractory acute graft versus host disease in December 2024 [26]. These approvals demonstrate the FDA's willingness to license complex cellular products when indications, delivery methods, and endpoints are well-defined [26].
Table 2: Recent FDA-Approved Stem Cell Products (2023-2025)
| Product Name | Approval Date | Cell Type | Indication | Key Clinical Evidence |
|---|---|---|---|---|
| Omisirge | April 17, 2023 | Cord blood-derived hematopoietic progenitor cells | Hematologic malignancies (patients 12-65) | Accelerated neutrophil recovery, reduced infection risk post-transplant [26] |
| Lyfgenia | December 8, 2023 | Autologous cell-based gene therapy | Sickle cell disease (patients ≥12) | 88% achieved complete resolution of vaso-occlusive events (6-18 months post-treatment) [26] |
| Ryoncil | December 18, 2024 | Allogeneic bone marrow-derived MSCs | Pediatric steroid-refractory acute GVHD (patients ≥2 months) | First MSC therapy approved for this life-threatening condition [26] |
International Regulatory Variation
Globally, regulatory approaches to stem cell products vary significantly. The European Union regulates advanced therapy medicinal products under centralized procedures, while Japan's Pharmaceuticals and Medical Devices Agency offers conditional approval pathways [74]. Recent state-level legislation in the U.S., such as Florida's SB 1768, allows non-FDA-approved stem cell therapies for orthopedic conditions, wound care, and chronic pain under specific conditions [74]. This regulatory patchwork creates both challenges and opportunities for global development strategies.
The FDA has implemented several expedited programs to accelerate development of promising therapies, including the Regenerative Medicine Advanced Therapy designation, Breakthrough Therapy designation, and Fast Track designation [26] [27]. These programs facilitate earlier and more frequent communication with sponsors and may support smaller, more efficient clinical trial designs.
Market Accessibility Comparison
Market Size and Growth Projections
The global stem cell therapy market demonstrates robust growth across all segments, with varying trajectories for different product types. Market analysis reveals that adult stem cells currently dominate the product landscape, holding 44.2% market share in 2025 [75], while the induced pluripotent stem cells segment is expected to grow at the most significant CAGR between 2025 and 2034 [71]. By therapy type, autologous therapies currently lead the market but allogeneic therapies are projected to experience the highest growth rate in coming years [71].
Table 3: Stem Cell Therapy Market Analysis by Product Type and Application
| Market Segment | 2025 Market Share | Projected CAGR | Key Growth Drivers |
|---|---|---|---|
| By Product Type | |||
| Adult Stem Cells | 44.2% [75] | Moderate | Ethical acceptability, strong safety profile, clinical track record [71] |
| Induced Pluripotent Stem Cells | Growing segment | Significant | Avoids ethical concerns, patient-specific treatments, advances in gene editing [71] |
| Embryonic Stem Cells | Niche segment | Limited | Ethical concerns, regulatory restrictions [18] |
| By Application | |||
| Musculoskeletal Disorders | 39.7% [75] | High | Aging population, rising osteoarthritis prevalence [75] |
| Oncology | Substantial share | Significant | Pipeline products, regenerative medicine centers [73] |
| Autoimmune Disorders | Growing segment | High | Clinical trials demonstrating efficacy [71] |
Pricing and Reimbursement Landscape
Stem cell therapy pricing varies considerably based on complexity, cell source, and regulatory status. Mesenchymal stem cell therapies typically range from $5,000 to $25,000 per treatment, with variations based on tissue source and processing requirements [75]. Autologous MSC treatments generally cost less than allogeneic alternatives but vary based on manipulation levels. Advanced gene-modified therapies like CAR-T products can exceed $400,000 per treatment, reflecting complex manufacturing and regulatory compliance costs [75].
Reimbursement policies continue to evolve, with recent expansions in coverage such as the Centers for Medicare & Medicaid Services' March 2024 decision to expand Medicare coverage for allogeneic hematopoietic stem cell transplantation for patients with myelodysplastic syndromes meeting specific prognostic scores [72]. Such coverage decisions significantly influence market accessibility and commercial viability.
Regional Market Dynamics
North America dominates the stem cell therapy market with a 44.2% share in 2025 [75], driven by robust R&D investment, advanced healthcare infrastructure, and progressive regulatory frameworks. The Asia Pacific region is expected to experience the fastest growth, fueled by robust product pipelines, large patient populations, and increasing healthcare investments [71] [73].
Emerging markets in Latin America and the Middle East show promising growth, with countries like Brazil, Mexico, and the United Arab Emirates investing in stem cell research centers and regenerative medicine initiatives [73]. These regions often employ tiered pricing strategies to enhance accessibility while addressing local healthcare system constraints.
Experimental Design and Methodologies
Clinical Trial Design Considerations
Well-designed clinical trials for stem cell products must address several unique considerations, including product characterization, delivery methods, and appropriate endpoint selection. The FDA requires rigorous long-term follow-up in stem cell-based gene therapy trials, particularly those involving genome editing or integration [72]. Trial designs should incorporate:
- Stratification factors based on disease severity and patient characteristics
- Appropriate control groups accounting for procedural effects
- Objective efficacy endpoints validated for the specific condition
- Long-term safety monitoring for tumorigenicity, immunogenicity, and off-target effects
Recent trials of approved products demonstrate these principles. For example, in the Lyfgenia clinical program for sickle cell disease, 88% of patients achieved complete resolution of vaso-occlusive events between 6 and 18 months post-treatment, establishing a clinically meaningful efficacy endpoint [26].
Manufacturing and Quality Control Protocols
Stem cell manufacturing requires stringent quality control measures and specialized equipment. The transition to automated bioreactors and AI-driven quality control systems has improved scalability and reduced contamination risks [71]. Current Good Manufacturing Practice requirements include:
- Comprehensive cell banking systems with master and working cell banks
- In-process controls monitoring critical quality attributes
- Release testing for potency, viability, identity, and sterility
- Stability studies establishing shelf life and storage conditions
Diagram 1: Stem Cell Manufacturing Workflow
Analytical Methods and Potency Assays
Critical quality attribute assessment requires specialized analytical methods tailored to stem cell products. Standardized characterization protocols are essential for demonstrating product consistency [75]. Key methodologies include:
- Flow cytometry for cell surface marker characterization
- Karyotyping and genetic stability assessment
- Microscopic evaluation of morphology and differentiation potential
- Functional potency assays measuring specific biological activities
- Microbiological testing for sterility, mycoplasma, and endotoxins
For pluripotent stem cell-derived products, additional safety testing for tumorigenicity is essential, often including teratoma formation assays in immunocompromised mice and quantitative PCR for residual undifferentiated cells [26].
Research Reagent Solutions
The following table outlines essential reagents and materials required for stem cell research and product development, compiled from current experimental protocols and manufacturing requirements.
Table 4: Essential Research Reagents for Stem Cell Product Development
| Reagent Category | Specific Examples | Research Function | Quality Standards |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC | Generation of induced pluripotent stem cells | GMP-grade for clinical applications [26] |
| Cell Culture Media | mTeSR, StemFlex, DMEM/F12 | Maintenance of stem cell pluripotency and expansion | xeno-free, chemically defined formulations [73] |
| Differentiation Inducers | Growth factors, Small molecules, Cytokines | Directed differentiation into specific lineages | High purity, potency-tested [26] |
| Characterization Antibodies | Anti-OCT4, Anti-NANOG, Anti-TRA-1-60 | Assessment of pluripotency markers | Validated for flow cytometry and immunocytochemistry [18] |
| Gene Editing Tools | CRISPR-Cas9, TALENs, ZFNs | Genetic modification of stem cells | Research-grade to GMP-grade depending on application [72] |
The regulatory and market landscape for stem cell products continues to evolve rapidly, with distinct pathways emerging for different product categories. Adult stem cells currently dominate the market due to their established safety profile and fewer ethical concerns, while induced pluripotent stem cells show significant growth potential as manufacturing technologies advance and regulatory frameworks adapt [71] [75].
Successful product development requires early and continuous regulatory engagement, robust clinical trial designs with meaningful endpoints, and scalable manufacturing processes. The increasing harmonization of international standards and growing acceptance of real-world evidence are creating new opportunities for efficient global development strategies. As the field advances, researchers and developers should monitor emerging regulatory trends, including evolving guidelines for stem cell-based embryo models [28], increasing use of expedited approval pathways [26], and state-level regulatory variations [74].
For developmental candidates, strategic positioning should consider not only scientific and clinical factors but also market accessibility, reimbursement potential, and manufacturing scalability to maximize patient access and commercial viability in this rapidly expanding field.
Cost-Benefit Analysis and Reimbursement Considerations for New Therapies
Stem cell therapy represents a revolutionary frontier in modern medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries through regenerative mechanisms [11]. The field is predominantly characterized by two principal cell sources: embryonic stem cells (ESCs) and adult stem cells (ASCs), each with distinct biological properties, therapeutic applications, and associated economic considerations. ESCs, derived from the inner cell mass of blastocysts, are pluripotent, meaning they can differentiate into any cell type in the body [10] [11]. In contrast, ASCs, found in various tissues after development, are multipotent, with a more limited differentiation capacity typically restricted to cell types within their tissue of origin [13]. This analysis provides a comprehensive comparison of these two therapeutic platforms, framing their relative advantages and challenges within the critical contexts of cost-benefit analysis and evolving reimbursement paradigms for researchers, scientists, and drug development professionals.
Biological and Therapeutic Comparison
The fundamental biological differences between embryonic and adult stem cells directly influence their therapeutic application, associated risks, and overall clinical value proposition.
Key Characteristics and Therapeutic Potential
Embryonic Stem Cells (ESCs) are characterized by their pluripotency and virtually unlimited self-renewal capacity in vitro [11]. This versatility allows them to be guided to become any cell type, making them a powerful tool for regenerating or repairing diseased tissues and organs, from heart muscle to nerve cells [10]. However, their use is fraught with challenges, including ethical controversies surrounding embryo destruction, a propensity for immune rejection upon transplantation, and a significant risk of tumorigenicity due to their potent growth capacity [10] [11].
Adult Stem Cells (ASCs), including Mesenchymal Stem Cells (MSCs) and Hematopoietic Stem Cells (HSCs), are found in tissues such as bone marrow, adipose tissue, and umbilical cord blood [13]. While their differentiation repertoire is more limited, they are crucially involved in natural tissue maintenance and repair [13]. Therapeutically, they are less controversial and, in the case of autologous transplants, carry a lower risk of immune rejection. Hematopoietic stem cell transplants (bone marrow transplants) have been a standard, life-saving procedure for decades for conditions like leukemia, lymphoma, and aplastic anemia [10]. Clinical research is also exploring ASCs for degenerative conditions like heart failure and osteoarthritis [10] [67].
Table 1: Comparative Analysis of Embryonic and Adult Stem Cell Therapeutics
| Parameter | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Differentiation Potential | Pluripotent (can become any cell type) [11] | Multipotent (limited to related cell types) [13] |
| Source | Inner cell mass of blastocysts [10] | Bone marrow, adipose tissue, umbilical cord, etc. [13] |
| Ethical Considerations | High (destruction of embryo) [10] [42] | Low [10] |
| Tumorigenicity Risk | High (teratoma formation) [11] [42] | Low [42] |
| Immunogenicity | High (likely allogeneic rejection) [11] | Low (potential for autologous use) [10] |
| Clinical Maturity | Largely preclinical/research stage [11] | Established (HSC transplants); investigational for other uses [10] [67] |
| Key Therapeutic Areas | Disease modeling, drug testing, prospective cell replacement [10] [11] | Hematological cancers, immunodeficiencies, orthopedic & degenerative diseases [10] [67] |
Visualizing Stem Cell Differentiation Pathways
The following diagram illustrates the fundamental differentiation pathways and therapeutic outcomes for ESCs and ASCs, highlighting their distinct potency levels.
Economic and Reimbursement Analysis
A thorough cost-benefit analysis must extend beyond laboratory efficacy to encompass manufacturing complexity, treatment costs, and the evolving landscape of payer reimbursement.
Treatment Cost Structures
The cost of stem cell therapies is highly variable, influenced by cell type, treatment complexity, and geographic location. On average, stem cell therapy can range from $5,000 to $50,000 [76] [77]. Simpler orthopedic injections (often using ASCs) typically fall on the lower end ($5,000-$8,000), while complex, systemic intravenous treatments for degenerative or autoimmune conditions can cost $25,000 and above [76] [67].
Table 2: Cost and Reimbursement Profile of Stem Cell-Based Therapies
| Factor | Embryonic Stem Cell-Based Therapies | Adult Stem Cell-Based Therapies |
|---|---|---|
| Therapy List Price | Not commercially established (pre-clinical) | Highly variable: $5,000 to $50,000+ [76] [77] |
| Typical Orthopedic Cost | N/A | $5,000 - $8,000 [76] |
| Typical Systemic Cost | N/A | $27,500+ [76] |
| Insurance Coverage | No coverage (experimental) | Limited; primarily covers established HSC transplants [10] [78] |
| Medicare/Medicaid | No coverage | Coverage for approved HSC transplants; new models for CGTs (e.g., sickle cell) [79] |
| Reimbursement Model | N/A | Moving towards outcomes-based models (e.g., CGT Access Model) [79] |
| Key Cost Drivers | R&D, tumorigenicity safety profiling, immune matching | Cell source, expansion complexity, regulation, clinic fees [76] |
Reimbursement Frameworks and Payer Considerations
Reimbursement is a significant hurdle. Insurance companies and Medicare generally do not cover unproven stem cell therapies, considering them experimental [78]. Coverage is largely confined to established procedures like hematopoietic stem cell transplants for specific blood cancers and diseases [10].
The landscape is beginning to shift with the introduction of innovative payment models for advanced therapies. The Centers for Medicare & Medicaid Services (CMS) have proposed the Cell & Gene Therapy (CGT) Access Model, which includes outcomes-based reimbursement and increased New Technology Add-on Payments (NTAP) for Medicare [79]. Initially focused on sickle cell disease, this model aims to manage the high upfront costs (e.g., $2.2 to $3.1 million for approved gene therapies) by tying payment to patient outcomes and could eventually influence reimbursement strategies for other cell therapies [79]. This underscores the growing importance of demonstrating not just safety and efficacy, but also long-term value and cost-effectiveness to payers.
Experimental Protocols and Research Tools
Translating basic stem cell biology into therapies requires standardized, rigorous experimental methodologies. The following workflow details a typical process for deriving and differentiating ESCs, a foundational protocol in the field.
Key Experimental Protocol: ESC Derivation and Directed Differentiation
This protocol is adapted from established methods for pluripotent stem cell culture and lineage specification [11].
The Scientist's Toolkit: Essential Research Reagents
Successful stem cell research relies on a suite of specialized reagents and materials. The following table catalogues critical solutions for pluripotent and adult stem cell manipulation.
Table 3: Key Research Reagent Solutions for Stem Cell Research
| Research Reagent | Function/Application | Examples in Protocols |
|---|---|---|
| Feeder Cells / Matrigel | Provides a supportive substrate and secretes factors to maintain pluripotency or support growth. | Used in ESC culture and MSC expansion [11] [42]. |
| Fibroblast Growth Factor-2 (FGF2) | A critical cytokine for maintaining self-renewal and pluripotency in ESCs and iPSCs. | Added to ESC culture media [11]. |
| Yamanaka Factor Cocktail | Set of transcription factors (Oct4, Sox2, Klf4, c-Myc) for reprogramming somatic cells into iPSCs. | Core reagents for iPSC generation [11] [42]. |
| Human Platelet Lysate (HPL) | A xeno-free supplement for cell culture media, rich in growth factors, used to expand MSCs. | Used as a media supplement for MSC culture [42]. |
| Specific Morphogens | Signaling molecules (e.g., BMP4, Activin A, Retinoic Acid) that guide differentiation into specific lineages. | Used in the "Directed Differentiation" step [11]. |
| Flow Cytometry Antibodies | Antibodies against specific surface/CD markers for identifying, characterizing, and sorting cell populations. | Used for ESC (SSEA-4, Tra-1-60) and MSC (CD73, CD90, CD105) characterization [11] [13]. |
The choice between embryonic and adult stem cell platforms is not a simple binary but a strategic decision with cascading implications across R&D, clinical development, regulatory strategy, and commercialization. ESCs offer unparalleled differentiation potential as a tool for disease modeling and drug screening but are burdened by significant safety and ethical challenges that have delayed clinical translation [11]. ASCs, particularly MSCs and HSCs, present a more immediately viable therapeutic path with a superior safety profile and established clinical use cases, albeit with more limited regenerative scope [10] [13].
From a cost-benefit and reimbursement perspective, the analysis strongly favors investment in adult stem cell technologies for near-to-mid-term therapeutic development. The established reimbursement pathways for HSC transplants and the growing body of efficacy data for MSCs in degenerative diseases provide a clearer, though still challenging, route to market. Furthermore, the movement toward value-based reimbursement models, as seen in the CGT Access Model, rewards therapies that deliver measurable, long-term patient outcomes [79]. This evolving landscape makes robust health economics and outcomes research (HEOR) an indispensable component of the development process for any stem cell-based therapy, ensuring that new treatments demonstrate not only biological efficacy but also tangible economic value in the healthcare system.
Conclusion
The choice between embryonic and adult stem cells is not a matter of superiority, but of strategic application aligned with therapeutic goals. ESCs offer unparalleled differentiation potential for disease modeling and tissue replacement but are tempered by ethical and safety concerns. ASCs, particularly MSCs and HSCs, provide a clinically established, ethically sound platform with strong immunomodulatory functions, albeit with more limited plasticity. The emergence of iPSCs presents a powerful hybrid alternative. Future progress hinges on overcoming key challenges in tumorigenicity, manufacturing standardization, and immune rejection. The synergy of stem cell biology with gene editing, bioengineering, and precision medicine will ultimately unlock the full potential of regenerative medicine, demanding continued rigorous research, collaborative frameworks, and ethical vigilance to successfully translate these living drugs into mainstream therapeutics.
References
- 1. Stem cells as biological drugs for incurable diseases [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04632-8]
- 2. Stem cell revolution: bridging the gap between research ... [https://link.springer.com/article/10.1186/s13287-025-04784-7]
- 3. Pluripotency genes of mammals: a network at work [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1578499/full]
- 4. Comparison of Human Induced Pluripotent and Embryonic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3070108/]
- 5. Adipose Stem Cells: A Comprehensive Guide to ... [https://cnsorthopedics.com/adipose-stem-cells-a-comprehensive-guide-to-regeneration/]
- 6. From unipotency to pluripotency: deciphering protein networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12042637/]
- 7. In-depth analysis of obesity-associated changes in adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518815/]
- 8. Comparing ESC and iPSC—Based Models for Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470175/]
- 9. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 10. Stem cells: What they are and what they do [https://www.mayoclinic.org/tests-procedures/bone-marrow-transplant/in-depth/stem-cells/art-20048117]
- 11. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 12. Stem Cell Niche Concept: Search for Current Expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429054/]
- 13. Adult Stem Cells: Explained (2025) [https://www.dvcstem.com/post/adult-stem-cells]
- 14. Types of Stem Cells: Explained (2025) [https://www.dvcstem.com/post/different-types-of-stem-cells-and-their-functions]
- 15. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 16. A new kind of stem cell is revolutionizing regenerative ... [https://www.asbmb.org/asbmb-today/science/040125/stem-cells-revolutionize-regenerative-medicine]
- 17. Key points about adult versus embryonic stem cells - The Niche [https://ipscell.com/2011/11/top-5-list-of-key-points-about-adult-versus-embryonic-stem-cells/]
- 18. Stem Cell Research Controversy: A Deep Dive (2025) [https://www.dvcstem.com/post/stem-cell-research-controversy]
- 19. Molecular Mechanisms Underlying Pluripotency and Self-Renewal of Embryonic Stem Cells [https://www.mdpi.com/1422-0067/24/9/8386]
- 20. Stem Cell Research: The Future of Regenerative Medicine ... [https://www.dvcstem.com/post/stem-cell-research]
- 21. Stem Cell Self-Renewal - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/stem-cell-self-renewal]
- 22. Comparison of MSCs and Muse cells: the possible use for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12222320/]
- 23. Clonal dynamics and somatic evolution of haematopoiesis ... [https://www.nature.com/articles/s41586-025-08625-8]
- 24. Deconstructing stem cell self-renewal: genetic insights into cell-cycle regulation | Nature Reviews Genetics [https://www.nature.com/articles/nrg2269]
- 25. Transgene-free mouse embryo models from chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411326/]
- 26. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 27. Ethical and Regulatory Considerations Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398464/]
- 28. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 29. The ISSCR Releases Targeted Update to the Guidelines ... [https://www.isscr.org/isscr-news/the-isscr-releases-targeted-update-to-the-guidelines-for-stem-cell-research-and-clinical-translation]
- 30. ISSCR Statement on the Scientific and Therapeutic Value ... [https://www.isscr.org/isscr-news/isscr-statement-on-the-scientific-and-therapeutic-value-of-human-embryonic-stem-cell-research]
- 31. Modeling neurodegenerative diseases with brain organoids [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1663286/full]
- 32. Modeling neurodegenerative diseases with brain organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631289/]
- 33. A review of the application of mesenchymal stem cells in the ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-023-01244-x]
- 34. The potential use of mesenchymal stem cells in ... [https://www.nature.com/articles/emm20132]
- 35. Side-by-Side Comparison of the Biological Characteristics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3722850/]
- 36. Adipose Stem Cells Display Higher Regenerative ... [https://www.nature.com/articles/srep37801]
- 37. Efficacy and safety of mesenchymal stem cells co-infusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8056684/]
- 38. Mesenchymal stem cell infusion to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500263X]
- 39. What Are the Differences Between Adult and Embryonic ... [https://int.livhospital.com/differences-between-adult-and-embryonic-stem-cells/]
- 40. Research and therapy with induced pluripotent stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1455-y]
- 41. odyssey of induced pluripotent stem cells in precision cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11487032/]
- 42. Natural vs. Induced Pluripotent Stem Cell Therapies [https://esmed.org/natural-vs-induced-pluripotent-stem-cell-therapies/]
- 43. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 44. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 45. Embryonic stem cells or induced pluripotent ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3947934/]
- 46. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 47. Proteomic and functional comparison between human ... [https://elifesciences.org/reviewed-preprints/92025v1/pdf]
- 48. Therapeutic Applications of Induced Pluripotent Stem Cell Use ... [https://gmr.scholasticahq.com/article/29784-therapeutic-applications-of-induced-pluripotent-stem-cell-use-in-parkinson-s-disease-models]
- 49. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 50. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 51. Senescence in adipose-derived stem cells and its implications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4146315/]
- 52. Stem cell aging: mechanisms, regulators and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4160113/]
- 53. Quantitative fate mapping: A general framework for analyzing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9708097/]
- 54. Fate mapping of hematopoietic stem cells reveals two ... [https://www.nature.com/articles/s41467-022-31914-z]
- 55. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 56. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 57. Stem cell revolution: bridging the gap between research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12659346/]
- 58. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 59. Strong association between genomic 3D structure and ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012214]
- 60. 3D Bioprinting Market Size to Surpass USD 8.57 Billion by ... [https://finance.yahoo.com/news/3d-bioprinting-market-size-surpass-110300791.html]
- 61. applications in three-dimensional (3D) bioprinting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8573440/]
- 62. 3D bioprinting patient-specific grafts for tendon/ligament ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411511/]
- 63. 2025 Trends in Biotech and Life Sciences Research | Blog [https://go.zageno.com/blog/2025-trends-in-biotech-and-life-sciences-research]
- 64. Embryonic Stem Cells: Controversy, Mechanisms, and ... [https://www.dvcstem.com/post/embryonic-stem-cells]
- 65. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 66. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 67. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 68. Success Rates of Stem Cell Therapy: Evaluated (2025) [https://auragens.com/success-rates-of-stem-cell-therapy-evaluated-2025/]
- 69. Stem Cell Therapy Success Rates Hit 78%: New Research ... [https://globalrph.com/2025/03/stem-cell-therapy-success-rates-hit-78-new-research-reveals-breakthrough-results/]
- 70. A comprehensive review of clinical trials and Progress in stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514481/]
- 71. Stem Cell Therapy Market Size, Price, Trends [https://www.novaoneadvisor.com/report/stem-cell-therapy-market]
- 72. Stem Cell Therapy Market Size to Hit USD 78.39 Billion by ... [https://www.biospace.com/press-releases/stem-cell-therapy-market-size-to-hit-usd-78-39-billion-by-2032-growing-at-a-cagr-of-22-8-from-2025-to-2032-coherent-market-insights]
- 73. Stem Cells Market Size To Hit USD 48.83 Bn By 2034 [https://www.precedenceresearch.com/stem-cells-market]
- 74. Stem cell revolution hits America [https://www.diamandis.com/blog/stem-cell-revolution-hits-america]
- 75. Stem Cell Therapy Market Analysis & Forecast: 2025-2032 [https://www.coherentmarketinsights.com/market-insight/stem-cell-therapy-market-2848]
- 76. Stem Cell Therapy Cost (2025 Update) [https://www.dvcstem.com/post/stem-cell-therapy-cost-2020]
- 77. 2025 Global Stem Cell Therapy Cost Analysis: A Complete ... [https://curemeabroad.com/blogs/2025-global-stem-cell-therapy-cost-analysis]
- 78. Stem cell therapy cost goes up & what to consider looking ahead [https://ipscell.com/2025/10/stem-cell-therapy-cost-goes-up-what-to-consider-looking-ahead/]
- 79. 2025 Cell & Gene Therapy Reimbursement Outlook [https://www.genengnews.com/topics/bioprocessing/2025-cell-gene-therapy-reimbursement-outlook/]