Enhancing Stem Cell Integration with Host Tissue: Strategies for Improved Survival, Engraftment, and Therapeutic Efficacy
This article provides a comprehensive analysis of strategies to enhance the integration of transplanted stem cells with host tissues, a critical challenge in regenerative medicine.
Enhancing Stem Cell Integration with Host Tissue: Strategies for Improved Survival, Engraftment, and Therapeutic Efficacy
Abstract
This article provides a comprehensive analysis of strategies to enhance the integration of transplanted stem cells with host tissues, a critical challenge in regenerative medicine. Aimed at researchers, scientists, and drug development professionals, it explores the foundational biological mechanisms of stem cell homing and engraftment, reviews advanced methodological approaches including biomaterial scaffolds and preconditioning strategies, addresses key troubleshooting and optimization hurdles such as poor cell survival and immune rejection, and evaluates validation techniques and comparative efficacy of different cell sources. The goal is to synthesize current scientific knowledge to guide the development of more effective and reliable stem cell-based therapies.
The Biological Blueprint: Understanding the Native Mechanisms of Stem Cell Homing and Engraftment
Stem Cell Integration Technical Support Center
This technical support center provides targeted troubleshooting guides and FAQs to assist researchers in navigating the complex process of stem cell integration, from initial engraftment to full functional reconstitution of host tissue.
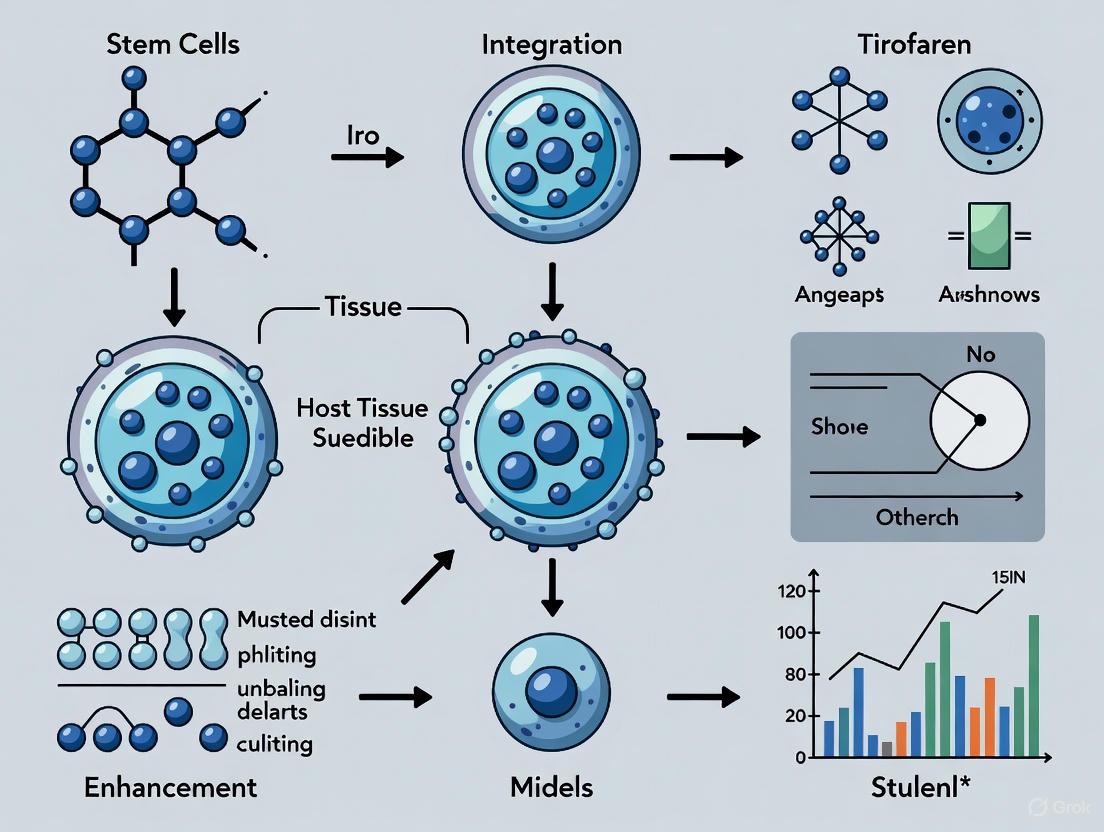
Core Concepts: The Stem Cell Integration Process
Stem cell integration is a multi-stage regenerative cascade where stem cells engraft, self-renew, and reconstitute damaged tissues to restore physiological function [1]. This process is crucial for developing stem cells as "living drugs" that can sense environmental cues, adapt to their microenvironment, and exert sustained therapeutic effects through differentiation, paracrine signaling, and immunomodulation [1].
Stem Cell Integration Pathway
The process begins when tissue injury triggers the release of Damage-Associated Molecular Patterns (DAMPs) from damaged cells [2]. These endogenous molecules activate pattern recognition receptors, initiating inflammatory cascades and stem cell mobilization [2].
Troubleshooting Guide: Common Experimental Challenges
Problem 1: Poor Stem Cell Engraftment Efficiency
Observed Issue: Less than 10% of administered stem cells successfully engraft in target tissues, with remaining cells trapped in reticuloendothelial organs or undergoing apoptosis [3].
Potential Solutions:
- Optimize delivery timing: Administer stem cells during the peak inflammatory phase when SDF-1 chemotactic gradients are strongest [2].
- Enhance vascular support: Implement VEGFR2 activation strategies to promote regeneration of sinusoidal endothelial cells (SECs) essential for engraftment [4].
- Pre-condition stem cells: Expose cells to hypoxic conditions or inflammatory cytokines before transplantation to improve survival and homing capability.
- Utilize scaffold matrices: Provide structural support using biomaterial scaffolds that mimic native extracellular matrix.
Problem 2: Inadequate Functional Tissue Reconstitution
Observed Issue: Stem cells engraft but fail to restore physiological function due to poor differentiation, limited integration, or insufficient cell numbers.
Potential Solutions:
- Modulate microenvironment: Incorporate factors that replicate stem cell niche signaling (Wnt, Notch, BMP pathways) to guide proper differentiation [2].
- Ensure appropriate cell density: Plate at optimal densities to prevent spontaneous differentiation while maintaining proliferative potential [5].
- Monitor differentiation status: Remove areas of unwanted differentiation prior to passaging or transplantation [5].
- Employ combinatorial therapies: Combine stem cell delivery with growth factors or small molecules that enhance functional integration.
Problem 3: Limited Long-Term Cell Survival and Integration
Observed Issue: Transplanted cells show initial engraftment but rapidly decline or fail to integrate with host tissue architecture.
Potential Solutions:
- Address hostile microenvironment: Utilize ROCK inhibitors (Y27632) or RevitaCell Supplement during passaging to prevent extensive cell death [6] [5].
- Promote vascular integration: Enhance angiogenesis through co-delivery of endothelial progenitor cells or pro-angiogenic factors.
- Monitor cell health indicators: Passage cells upon reaching ~85% confluency and avoid overly confluent cultures which can result in poor cell survival [6].
- Implement real-time tracking: Use optoacoustic imaging with exogenous contrast agents to monitor cell distribution, migration, and long-term fate [3].
Experimental Protocols for Assessing Integration
Protocol 1: Evaluating VEGFR2-Mediated Vascular Regeneration for Hematopoietic Reconstitution
Background: VEGFR2 activation is critical for regeneration of VEGFR3+Sca1- sinusoidal endothelial cells (SECs) that are essential for engraftment and restoration of hematopoietic stem and progenitor cells (HSPCs) [4].
Methodology:
- Myelosuppression Model: Induce bone marrow suppression using:
- Chemotherapy: 5-Fluorouracil (5FU)
- Radiation: Sublethal (650 rad) or lethal (950 rad) irradiation
Bone Marrow Analysis:
- Process decalcified bone marrow sections for immunohistochemistry
- Perform polyvariate flow cytometry on crushed, enzymatically processed femurs
- Identify SECs using immunophenotypic signature: VE-cadherin+MECA32+CD31+VEGFR2+VEGFR3+Sca1-
- Identify arterioles as: VE-cadherin+MECA32+CD31+VEGFR2+VEGFR3−Sca1+
VEGFR2 Inhibition Studies:
- Use conditional VEGFR2 knockout mice
- Administer VEGFR2 signaling inhibitors in wild-type mice post-BMT
- Assess SEC reconstruction and HSPC engraftment at 7, 14, and 21 days
Quantitative Assessment Parameters:
- Percentage of SEC regression/regeneration
- HSPC counts (cKit+Lineage−Sca1+ cells)
- Hematopoietic recovery timelines
Protocol 2: Monitoring Stem Cell Migration and Engraftment via Optoacoustic Imaging
Background: Optoacoustic imaging (OAI) enables real-time tracking of stem cell distribution, migration, and engraftment at clinically relevant depths [3].
Methodology:
- Stem Cell Labeling:
- Incubate mesenchymal stem cells with exogenous contrast agents
- Optimize labeling efficiency by testing varying concentrations and incubation times
- Assess cytotoxicity impact on viability, differentiation, and function
In Vivo Tracking:
- Administer labeled cells via appropriate route (IV, local injection)
- Use multispectral optoacoustic tomography (MSOT) with multiple excitation wavelengths
- Acquire signals simultaneously from endogenous chromophores and exogenous contrast agents
- Perform imaging sessions at 24h, 72h, 1-week, and 2-week intervals
Spectral Unmixing Analysis:
- Separate contrast agent signals from background using characteristic spectral profiles
- Quantify inter- and intra-organ distribution of administered cells
- Correlate signal intensity with cell numbers using established calibration curves
Critical Parameters for Contrast Agent Selection:
- Biocompatibility and low toxicity
- Absorption coefficient at available laser wavelengths
- Narrow, characteristic spectral profile distinct from endogenous chromophores
- Efficient cellular uptake without affecting stem cell functionality
Quantitative Data: Integration Efficiency Parameters
Table 1: Stem Cell Integration Efficiency Benchmarks
| Parameter | Optimal Range | Suboptimal Indicators | Experimental Assessment Methods |
|---|---|---|---|
| Engraftment Rate | >10% of administered cells | <1% successful engraftment | Optoacoustic imaging, bioluminescent tracking, histology [3] |
| Initial Cell Survival | >70% viability post-transplantation | <30% viability at 24 hours | Live/dead staining, metabolic activity assays [5] |
| Functional Duration | Sustained >4 weeks | Rapid decline within 7 days | Longitudinal imaging, functional recovery metrics [3] |
| VEGFR2-mediated SEC Regeneration | Complete by 14 days post-injury | Severe regression persisting >21 days | Immunohistochemistry, flow cytometry [4] |
| HSPC Reconstitution | Lineage-specific cells detectable by 7-10 days | Delayed beyond 21 days | Colony-forming unit assays, blood count monitoring [4] |
Table 2: VEGFR2-Dependent Hematopoietic Reconstitution Data
| Experimental Condition | SEC Regeneration | HSPC Engraftment | Hematopoietic Recovery |
|---|---|---|---|
| Steady State (No injury) | Maintained VEGFR3+ SEC network | Normal HSPC maintenance | Homeostatic blood cell production |
| Sublethal Irradiation (650 rad) | Minor SEC regression with spontaneous regeneration | Transient decrease with full recovery | Complete recovery within 14 days |
| Lethal Irradiation (950 rad) + BMT | Severe SEC regression requiring VEGFR2 for regeneration | VEGFR2-dependent HSPC reconstitution | Complete recovery only with VEGFR2 signaling |
| Lethal Irradiation + VEGFR2 inhibition | Severely impaired SEC reconstruction | Blocked engraftment and HSPC reconstitution | Failure of hematopoietic recovery |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Stem Cell Integration Research
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Stem Cell Culture Media | mTeSR Plus, Essential 8 Medium, StemPro hESC SFM | Maintain pluripotency and viability | Use within 2 weeks when stored at 2-8°C; full media change daily [6] [5] |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent, EDTA | Detach and subculture cells | Optimize incubation time (1-2 min adjustments) based on cell line sensitivity [5] |
| Viability Enhancers | ROCK inhibitor Y27632, RevitaCell Supplement | Improve survival after passaging/thawing | Include during passaging of confluent cultures; feed within 18-24h post-passaging [6] |
| Extracellular Matrices | Geltrex, VTN-N, Matrigel, Poly-L-ornithine/Laminin | Provide structural support and signaling cues | Ensure proper coating; use non-tissue culture-treated plates for some matrices [6] |
| VEGFR Signaling Modulators | VEGFR2 agonists/antagonists | Study vascular regeneration for engraftment | Critical for SEC reconstruction post-myeloablation [4] |
| Optoacoustic Contrast Agents | Engineered nanoparticles, dyes | Enable stem cell tracking via OAI | Must have high absorption coefficients and biocompatibility [3] |
VEGFR2 Signaling in Vascular Regeneration
Frequently Asked Questions (FAQs)
Q: What is the critical relationship between vascular regeneration and stem cell engraftment? A: Research demonstrates that VEGFR2-mediated regeneration of sinusoidal endothelial cells (SECs) is essential for hematopoietic stem cell engraftment. Without proper SEC reconstruction, even with bone marrow transplantation, engraftment and reconstitution of hematopoietic stem and progenitor cells is severely impaired [4].
Q: Why do stem cells fail to integrate properly despite successful initial engraftment? A: Failed integration can result from multiple factors: hostile microenvironment at injury site, insufficient vascular support, inflammatory rejection, or lack of appropriate differentiation signals. Studies show less than 10% of administered cells typically achieve successful, lasting integration [3].
Q: What methods are available for real-time monitoring of stem cell integration in preclinical models? A: Optoacoustic imaging (OAI) with exogenous contrast agents enables real-time tracking of stem cell distribution, migration, and engraftment at clinically relevant depths. This provides advantages over MRI (better temporal resolution) and optical imaging (greater penetration depth) [3].
Q: How can I improve survival of stem cells after transplantation? A: Strategies include: using ROCK inhibitors during passaging, ensuring optimal cell density (passage at ~85% confluency), avoiding over-confluent cultures, proper matrix coating, and pre-conditioning cells to hostile microenvironments [6] [5].
Q: What are the key differences between stem cells as "living drugs" versus conventional pharmaceuticals? A: Unlike conventional drugs that are metabolized and excreted, living drugs become part of the damaged tissues, exerting longer-lasting effects. A single dose may have sustained impact, with cells actively homing to injury sites and integrating into tissues [1].
FAQs: Core Cellular Mechanisms
Q1: What are the key mechanisms by which Mesenchymal Stem/Stromal Cells (MSCs) mediate their therapeutic effects? MSCs primarily mediate their therapeutic effects through three core mechanisms: multipotent differentiation, paracrine signaling, and immunomodulation.
- Differentiation: MSCs can differentiate into multiple cell lineages, including osteoblasts, chondrocytes, and adipocytes, to directly replace damaged cells [7].
- Paracrine Signaling: MSCs secrete a broad array of bioactive factors—such as growth factors, cytokines, chemokines, and extracellular vesicles (exosomes)—that modulate the local microenvironment, promote tissue repair, and reduce inflammation. This is now considered a predominant mechanism of action [8] [9] [10].
- Immunomodulation: MSCs interact with both innate and adaptive immune cells (e.g., T cells, B cells, macrophages, dendritic cells) to suppress pro-inflammatory responses and promote anti-inflammatory, regenerative states. This occurs via soluble factors and direct cell-cell contact [11] [7].
Q2: How does the local microenvironment or "niche" influence stem cell behavior? The stem cell niche provides critical cues that determine cell fate [2]. Upon tissue injury, the niche is disrupted, leading to the release of Damage-Associated Molecular Patterns (DAMPs) and pro-inflammatory cytokines [2]. This inflammatory microenvironment not only mobilizes stem cells but also licenses them, enhancing their paracrine and immunomodulatory activities. Key signals include IFN-γ and TNF-α, which induce MSCs to upregulate the production of immunosuppressive factors like PGE2 and IDO [11].
Q3: What is the clinical significance of the MSC secretome? The secretome—comprising all secreted factors and extracellular vesicles—is a major mediator of MSC therapy. Its clinical significance includes:
- Cell-Free Therapy: Using the secretome or isolated exosomes presents a cell-free therapeutic option, avoiding risks associated with whole-cell transplantation, such as pulmonary entrapment or cellular emboli [8] [10].
- Targeted Action: Secreted factors can be engineered or pre-conditioned to enhance specific therapeutic effects, such as amplifying anti-inflammatory responses in osteoarthritis or promoting angiogenesis in ischemic tissues [12] [10].
Q4: What are the primary soluble factors involved in MSC-mediated immunomodulation, and how do they work? MSCs employ a suite of soluble factors to suppress immune responses, particularly in inflammatory environments. The key factors and their mechanisms are summarized below.
Table: Key Soluble Immunomodulatory Factors from MSCs
| Factor | Primary Mechanism of Action | Therapeutic Context |
|---|---|---|
| Indoleamine 2,3-dioxygenase (IDO) | Catalyzes tryptophan degradation into kynurenine, inhibiting T-cell proliferation and function [11]. | Graft-versus-host disease (GvHD), autoimmune disorders [11]. |
| Prostaglandin E2 (PGE2) | Inhibits NF-κB nuclear translocation, reducing pro-inflammatory cytokine (e.g., IL-1β, TNF-α) release. Promotes macrophage shift to anti-inflammatory M2 phenotype [11] [10]. | Osteoarthritis, inflammatory tissue damage [10]. |
| Transforming Growth Factor-β (TGF-β) | Suppresses T-cell and B-cell activity, promotes regulatory T-cell (Treg) generation [11]. | Tissue repair, fibrosis, immune tolerance [12]. |
| Hepatocyte Growth Factor (HGF) | Modulates T-cell and dendritic cell function, supporting anti-inflammatory responses [11]. | Liver regeneration, inflammatory diseases [11]. |
| TNF-α-Stimulated Gene 6 (TSG-6) | Potent anti-inflammatory protein that inhibits NF-κB signaling and neutrophil migration [10]. | Osteoarthritis, degenerative disc disease [10]. |
Troubleshooting Common Experimental Challenges
Q1: Issue - Poor survival or engraftment of transplanted stem cells.
- Potential Causes: Hostile inflammatory microenvironment, anoikis (detachment-induced cell death), inadequate vascularization, or improper delivery method leading to pulmonary entrapment (for intravenous administration) [8] [13].
- Solutions:
- Preconditioning: Treat MSCs with pro-inflammatory cytokines (e.g., IFN-γ) or hypoxia before transplantation to enhance their survival and potency [8] [12].
- Biomaterial Scaffolds: Use 3D biomaterial scaffolds to provide structural support, enhance retention, and protect cells from the hostile environment. These scaffolds can be engineered to deliver bioactive cues [8] [13].
- Optimized Delivery: For systemic administration, consider alternative routes to avoid lung entrapment. Local, direct injection into the target tissue is often more effective for engraftment [8].
Q2: Issue - Inconsistent or uncontrolled differentiation outcomes.
- Potential Causes: Uncontrolled microenvironment, heterogeneity in the starting stem cell population, or undefined culture components [5] [12].
- Solutions:
- Define Culture Conditions: Use fully defined, xeno-free culture media and matrices to reduce variability [5].
- Pharmacological Modulation: Apply small molecules to precisely modulate key signaling pathways (Wnt, TGF-β, BMP) that direct lineage specification [12].
- Biophysical Cues: Utilize engineered substrates with specific stiffness and topography to guide mechanotransduction and fate decisions [13].
Q3: Issue - Low homing efficiency of systemically administered MSCs to the target site.
- Potential Causes: The complex homing process involves mobilization, vascular adhesion, and transmigration, which can be inefficient [8].
- Solutions:
Q4: Issue - Variable immunomodulatory effects of MSCs between experiments.
- Potential Causes: MSC potency is highly dependent on the tissue source, donor variability, culture conditions, and the specific inflammatory signals present in the disease microenvironment [8] [11].
- Solutions:
- Standardize Characterization: Rigorously characterize MSCs using ISCT criteria (plastic adherence, trilineage differentiation, specific surface marker profile: CD73+, CD90+, CD105+, CD34-, CD45-, etc.) and assess their immunomodulatory potency in functional assays [8] [7].
- Inflammatory Priming: License MSCs by exposing them to a defined inflammatory cocktail (IFN-γ + TNF-α) to ensure a consistent, potent immunosuppressive phenotype before application [11].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Investigating Key MSC Mechanisms
| Reagent / Tool | Primary Function | Key Application Notes |
|---|---|---|
| Defined Culture Media (e.g., mTeSR) | Maintains pluripotency and supports consistent growth of human PSCs [5]. | Critical for eliminating variability from serum; less than 2 weeks old for optimal performance [5]. |
| Recombinant Cytokines (IFN-γ, TNF-α) | Used to "license" or precondition MSCs, enhancing their immunomodulatory capacity [11]. | A combination of IFN-γ and TNF-α is often used to maximally induce IDO and PGE2 expression [11]. |
| Small Molecule Pathway Modulators | Pharmacologically manipulate key stem cell signaling pathways (e.g., Wnt, TGF-β/SMAD, BMP) [12]. | Enables precise control over self-renewal and differentiation without genetic manipulation [12]. |
| Non-Enzymatic Passaging Reagents (e.g., ReLeSR) | Gentle dissociation of hPSC colonies into aggregates for subculturing [5]. | Incubation time must be optimized for each cell line to achieve ideal aggregate size (50-200 μm) [5]. |
| Biomaterial Scaffolds (2D & 3D) | Mimics the native extracellular matrix, providing mechanical support and biochemical cues [8] [13]. | 3D scaffolds better maintain cell-cell interaction and support differentiation compared to 2D [8]. |
| Surface Marker Antibodies (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Standardized identification and isolation of MSCs via flow cytometry [8] [7]. | Essential for quality control to ensure population purity according to ISCT criteria [7]. |
| Exosome Isolation Kits | Isolate extracellular vesicles from MSC-conditioned medium for paracrine studies [8] [10]. | Enables investigation of cell-free therapies and the specific cargo (miRNA, lncRNA) responsible for therapeutic effects [10]. |
Essential Signaling Pathway Diagrams
NF-κB Pathway in Inflammation
MSC Immunomodulation Mechanisms
Stem Cell Homing and Recruitment
Within the field of stem cell integration and host tissue enhancement, a profound understanding of the initial injury response cascade is paramount. This cascade, initiated by tissue damage, sets the stage for all subsequent repair and regenerative processes. Central to this event is the release of Damage-Associated Molecular Patterns (DAMPs), which activate innate immunity and establish chemotactic gradients, most notably of the cytokine Stromal Cell-Derived Factor-1 (SDF-1/CXCL12). These gradients are critical for directing the homing and recruitment of various cell types, including mesenchymal stem cells (MSCs), neutrophils, and other progenitors, to the site of injury. This technical support document addresses key experimental challenges and provides foundational knowledge to optimize research in this domain, facilitating the development of advanced regenerative therapies.
Core Concepts FAQ
Q1: What initiates the cellular recruitment cascade following tissue injury? The cascade is initiated by the release of intracellular molecules known as Damage-Associated Molecular Patterns (DAMPs) from necrotic or stressed cells. These molecules, which include ATP, HMGB1, extracellular DNA/RNA, and heat shock proteins, function as danger signals [2] [14]. They are recognized by Pattern Recognition Receptors (PRRs), such as Toll-like receptors (TLRs) and the receptor for advanced glycation end-products (RAGE), on resident immune cells and tissue stromal cells [2]. This recognition triggers intracellular signaling pathways, primarily NF-κB, leading to the production and secretion of pro-inflammatory cytokines and chemokines, including SDF-1, IL-8, and others, which establish the chemotactic gradients necessary for cell recruitment [2] [14].
Q2: What is the role of the SDF-1/CXCR4 axis in stem cell recruitment? The SDF-1 (CXCL12)/CXCR4 axis is one of the most well-characterized pathways governing stem cell homing. Under homeostatic conditions, SDF-1 secreted by bone marrow stromal cells helps retain stem cells within their niche via interaction with its receptor, CXCR4, expressed on stem cells [2]. Upon tissue injury, the damaged site exhibits a marked increase in SDF-1 production, creating a concentration gradient. Stem cells, including hematopoietic stem cells (HSCs), mesenchymal stem cells (MSCs), and endothelial progenitor cells (EPCs), sense this gradient through the CXCR4 receptor and undergo a multistep recruitment process: mobilization from the bone marrow into circulation, vascular rolling and adhesion, transendothelial migration, and finally, migration through the extracellular matrix toward the injury site [2].
Q3: How do neutrophils and stem cells interact during the early injury response? Neutrophils are the first immune responders, arriving at the injury site within hours [15] [14]. Their early recruitment is also guided by DAMPs and chemokines like IL-8 [15]. Beyond their antimicrobial role, neutrophils are now recognized as active contributors to tissue repair. They help clear necrotic debris and, crucially, produce cytokines and factors that modify the microenvironment to support subsequent stem cell recruitment and activity [15]. For instance, our team recently discovered that neutrophils mediate the recruitment of stem cells in the early stages of bone regeneration, thereby triggering important repair processes [15]. The transition from neutrophil-dominated inflammation to a repair phase involving stem cells is a critical step for successful regeneration [14].
Troubleshooting Guides
Challenge: Weak or Unreliable Stem Cell Migration in Chemotaxis Assays
Potential Causes and Solutions:
Cause: Degraded Chemotactic Gradient.
- Solution: The chemotactic gradient formed by SDF-1 bound to vascular and extracellular matrix glycosaminoglycans can extend up to 650 µm [15]. To maintain a stable gradient in vitro, use freshly prepared SDF-1α and ensure the assay chamber is properly sealed to prevent evaporation and convective flow. Consider using microfluidic-based systems that can generate and maintain more stable and complex gradients over longer periods.
Cause: Inappropriate Stem Cell Condition.
- Solution: The homing capacity of stem cells is dependent on their surface receptor expression. Ensure that your MSCs or other progenitor cells express functional CXCR4 receptors. Confirm this via flow cytometry. Passage number can affect receptor expression; use lower-passage cells and consider pre-activation with low-dose cytokines (e.g., IL-6 or SCF) to enhance CXCR4 expression if necessary.
Cause: Incorrect Gradient Concentration.
- Solution: The efficacy of a chemotactic cue is concentration-dependent. An appropriate concentration of IL-8 is required to induce polarization and recruitment of neutrophils; insufficient or excessive levels fail to guide regeneration or cause damage [15]. Systematically titrate the concentration of SDF-1 (e.g., from 10 ng/mL to 200 ng/mL) in your assay to establish the optimal dose for your specific cell type. A bell-shaped response curve is common in chemotaxis.
Challenge: Failure to Detect DAMP-Mediated Signaling in Vitro
Potential Causes and Solutions:
Cause: Non-Physiological DAMP Release.
- Solution: Simply adding recombinant DAMPs to culture media may not recapitulate the sterile injury context. Instead, induce sterile cellular damage in a feeder layer of primary cells (e.g., fibroblasts or keratinocytes) using methods like freeze-thaw cycles, mechanical scratch, or targeted irradiation to release a more physiological mixture of endogenous DAMPs [14].
Cause: Insufficient PRR Expression.
- Solution: The cellular response to DAMPs requires expression of relevant PRRs like TLRs and RAGE. Verify that your sensor cell line (e.g., reporter cells or resident macrophages) expresses the necessary receptors (e.g., TLR4 for HMGB1). If using a standard cell line, consider engineering a reporter system or using primary cells isolated from the target tissue.
Cause: Inadequate Readout of Pathway Activation.
- Solution: DAMP signaling often converges on the NF-κB pathway [2] [14]. Implement robust assays to detect NF-κB activation, such as phospho-specific antibodies for IκBα or p65 NF-κB via western blot, immunofluorescence to visualize p65 nuclear translocation, or using NF-κB luciferase reporter constructs.
Key Experimental Protocols
Protocol: Establishing a DAMP-Mediated Inflammatory Model In Vitro
Objective: To create a reliable in vitro system that mimics the sterile inflammatory response following tissue injury for studying downstream chemokine production and cell recruitment.
Materials:
- Primary fibroblasts or other relevant tissue-resident cells.
- Cell culture plates.
- Phosphate-Buffered Saline (PBS).
- Liquid nitrogen or a mechanical scratcher.
- ELISA kits for SDF-1, IL-8, and other chemokines.
Methodology:
- Cell Preparation: Seed a confluent monolayer of primary fibroblasts in a multi-well plate and allow them to adhere overnight.
- Induction of Injury:
- Option A (Freeze-Thaw): Wash the monolayer with PBS. Place the plate in a -80°C freezer for 30 minutes, then thaw at 37°C. Repeat for 2-3 cycles [14].
- Option B (Mechanical Scratch): Create a uniform scratch wound in the monolayer using a sterile pipette tip or cell scratcher.
- Conditioned Media Collection: After injury, add fresh serum-free medium and incubate the cells for 6-24 hours. Collect the supernatant (conditioned media) and centrifuge to remove cell debris. Aliquot and store at -80°C.
- Validation: Use the conditioned media to treat naïve reporter cells or to perform ELISA to quantify the release of SDF-1 and other DAMPs-induced chemokines.
Protocol: Quantifying Stem Cell Chemotaxis Using a Transwell System
Objective: To accurately measure the directed migration of stem cells toward an SDF-1 gradient.
Materials:
- Transwell plates with porous membranes (5-8 µm pore size).
- Serum-free basal medium.
- Recombinant SDF-1α.
- Cell staining solution (e.g., Crystal Violet or Calcein-AM).
- 4% Paraformaldehyde (PFA).
Methodology:
- Gradient Establishment: Dilute recombinant SDF-1α in serum-free medium to the desired concentration (e.g., 50-100 ng/mL). Add this chemoattractant solution to the lower chamber of the Transwell plate. For a negative control, use serum-free medium only.
- Cell Seeding: Harvest and resuspend stem cells (e.g., MSCs) in serum-free medium. Seed a defined number of cells (e.g., 1x10^5) into the upper chamber of the Transwell insert.
- Incubation and Migration: Incubate the plate for 4-24 hours at 37°C in a 5% CO2 incubator to allow cell migration.
- Quantification:
- After incubation, carefully remove the non-migrated cells from the top of the membrane with a cotton swab.
- Fix the migrated cells on the bottom side of the membrane with 4% PFA for 10 minutes.
- Stain the cells with Crystal Violet or Calcein-AM.
- Count the stained cells manually under a microscope or dissolve the stain and measure the absorbance for quantification.
Signaling Pathway Visualizations
DAMP Sensing and SDF-1 Production
Stem Cell Recruitment via SDF-1/CXCR4 Axis
Data Presentation: Key Chemoattractants in the Injury Cascade
Table 1: Major Chemoattractants and Their Roles in Cell Recruitment Following Injury.
| Chemoattractant | Primary Target Cell(s) | Key Receptor(s) | Core Function in Recruitment | Notes & Experimental Considerations |
|---|---|---|---|---|
| SDF-1 (CXCL12) | MSCs, HSCs, EPCs | CXCR4 | Guides stem/progenitor cell homing from bone marrow to injury site [2]. | The axis is a primary regulator of stem cell retention and mobilization. |
| IL-8 (CXCL8) | Neutrophils | CXCR1, CXCR2 | Primary neutrophil chemotactic factor; establishes a local chemotactic gradient [15]. | Concentration is critical; inappropriate levels can inhibit repair or cause damage [15]. |
| N-formyl peptides (e.g., fMLP) | Neutrophils | FPR1 | Potent bacterial-derived chemoattractant; also acts on mitochondria released from damaged cells [15] [16]. | Useful for inducing strong neutrophil chemotaxis in control experiments. |
| DAMPs (HMGB1, ATP) | Macrophages, Neutrophils, Dendritic Cells | TLRs (e.g., TLR4), RAGE, P2X/P2Y Receptors | Initiate the response by inducing production of other chemokines (SDF-1, IL-8) [2] [14]. | Represent the initial "danger" signal; use a mix for a physiologically relevant model. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Studying DAMPs and Chemotactic Gradients.
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Recombinant SDF-1α / IL-8 | To establish defined chemotactic gradients in Transwell or microfluidic assays. | Verify species specificity and bioactivity. Aliquot to avoid freeze-thaw cycles. |
| CXCR4 Antagonists (e.g., AMD3100) | To chemically inhibit the SDF-1/CXCR4 axis and confirm its specific role in migration. | Can be used to mobilize stem cells from bone marrow in vivo. |
| Anti-CXCR4 Antibody | For flow cytometric analysis of receptor expression on stem cells. | Critical for correlating migration efficiency with receptor presence. |
| TLR4 Agonists (LPS) & Antagonists (TAK-242) | To specifically activate or inhibit a major DAMP (HMGB1) sensing pathway. | Use ultrapure LPS to avoid confounding TLR2 responses. TAK-242 is a specific small-molecule inhibitor. |
| Phospho-specific NF-κB Antibodies | To detect activation of the key downstream signaling pathway of DAMP recognition. | Measures IκBα degradation or p65 phosphorylation/translocation. |
| Transwell Assay Plates | The standard workhorse for quantifying chemotaxis in a semi-in-vivo setting. | Choose membrane pore size (5-8 μm) appropriate for your cell type. |
Fundamental Concepts: The Stem Cell Niche
What is a stem cell niche?
A stem cell niche is a distinct, dynamic, and specialized microenvironment that provides a physical anchor for stem cells and regulates their fate through a complex set of biochemical, biophysical, and cellular cues [17] [18]. First proposed by R. Schofield in 1978 for hematopoietic stem cells (HSCs), the niche concept explains how the local microenvironment maintains stem cell self-renewal, controls the balance between quiescence and proliferation, and guides differentiation and maturation [17]. Think of it as a dedicated "support system" that instructs stem cells on when to rest, divide, or specialize.
What are the core components of a niche?
The niche is an ensemble of multiple components that work in concert. The key elements include:
- Supporting Cells: Other cell types, such as mesenchymal stromal cells, osteoblasts, or endothelial cells, provide direct contact and secrete short-range signaling factors [17] [18].
- Extracellular Matrix (ECM): A sugar-rich, crosslinked gel network of structural proteins (e.g., collagens, laminin, fibronectin) and proteoglycans that provides structural support and biochemical signaling [18].
- Soluble Factors: Signaling molecules like growth factors, cytokines, and morphogens (e.g., WNTs, BMPs, FGFs) that can be freely diffusible or immobilized on the ECM [18].
- Physicochemical Cues: Parameters such as oxygen levels (hypoxia), metabolic signals (e.g., calcium ions, reactive oxygen species), and biomechanical forces [17] [18].
Why is understanding the niche critical for tissue regeneration and integration?
For a transplanted stem cell to successfully integrate into host tissue and restore function, it must receive the correct instructions from its new microenvironment [2] [1]. The niche provides the essential cues that direct stem cell homing, survival, fate decisions, and functional incorporation into the existing tissue architecture [2]. By recreating or manipulating these niche signals in vitro, we can pre-condition stem cells for enhanced in vivo integration potential and therapeutic efficacy [18].
Troubleshooting Guides for Niche-Based Experiments
Problem: Poor Survival or Integration of Transplanted Stem Cells
This is a common failure point in pre-clinical studies, often indicating a mismatch between the delivered cells and the host microenvironment.
- Potential Causes and Solutions:
| Potential Cause | Recommended Action | Rationale |
|---|---|---|
| Hostile host environment at the injury site (inflammation, fibrosis). | Pre-treat cells in vitro with pro-survival cytokines or use biomaterial scaffolds to shield cells. | Enhances cell resilience to inflammatory cytokines and oxidative stress present in damaged tissue [1]. |
| Insufficient homing to the target tissue. | Pre-activate cells by priming with specific chemokines (e.g., SDF-1). | Upregulates homing receptors (e.g., CXCR4), improving navigation along chemotactic gradients to the injury site [2]. |
| Lack of essential niche signals for engraftment. | Co-transplant supportive niche cells (e.g., MSCs) or use ECM-based hydrogels. | Provides immediate, localized paracrine support and cell-matrix interactions that mimic a pro-regenerative niche [1] [18]. |
Problem: Uncontrolled Differentiation In Vitro
When stem cells differentiate unpredictably in culture, the niche-mimicking conditions are likely suboptimal.
- Potential Causes and Solutions:
| Potential Cause | Recommended Action | Rationale |
|---|---|---|
| Inconsistent or low-quality stem cell starting population. | Rigorously remove differentiated areas before passaging and use controlled, high-quality cell lines as controls. | A homogeneous, pluripotent starting population is essential for reproducible response to differentiation cues [6] [5]. |
| Incorrect or uneven presentation of differentiation factors. | Use defined, immobilized growth factors instead of only soluble factors to better control concentration and localization. | Immobilizing morphogens (e.g., BMPs) on the ECM or culture surface more closely mimics the natural niche and prevents diffuse signaling [18]. |
| Suboptimal cell seeding density. | Standardize and optimize initial cell density for differentiation assays; both overly confluent and sparse cultures skew fate decisions. | Cell-cell contact is a critical niche signal; incorrect density disrupts endogenous signaling gradients and paracrine communication [6] [5]. |
Problem: Failure of 3D Niche Model Assembly (e.g., Organoids, Bone Marrow-on-a-Chip)
Advanced 3D models are prone to failure due to their complexity.
- Potential Causes and Solutions:
| Potential Cause | Recommended Action | Rationale |
|---|---|---|
| Incorrect ECM composition or stiffness. | Systematically test different ECM hydrogels (e.g., Matrigel, Geltrex, synthetic peptides) and mechanical properties. | Stem cell fate is profoundly influenced by ECM composition and matrix stiffness through integrin-mediated signaling [19] [18]. |
| Lack of essential cellular co-culture partners. | Introduce relevant supporting cells, such as endothelial cells for vascularization or MSCs for stromal support. | Niches are multi-cellular; the absence of key supporting cells fails to recapitulate essential paracrine and cell-contact signals [19] [17]. |
| Inadequate nutrient or oxygen diffusion. | Optimize the size of 3D constructs and consider using perfused microfluidic systems (organs-on-chips). | Central necrosis in large organoids indicates hypoxia and nutrient deprivation, which disrupts normal morphogenesis and niche function [19] [18]. |
Frequently Asked Questions (FAQs)
How do niches influence stem cell fate decisions?
Niches regulate fate through an integrated signaling network. The diagram below summarizes the key regulatory pathways and their logical relationships within a stem cell niche.
What are the key differences betweenin vivoniches and currentin vitromodels?
While in vitro models have advanced significantly, key disparities remain.
| Feature | In Vivo Niche | Current In Vitro Models | Implication for Research |
|---|---|---|---|
| Complexity | Highly complex, multi-cellular, and vascularized. | Simplified, often lacking full cellular repertoire and vasculature. | Models may miss critical signals from missing cell types or systemic inputs [19] [18]. |
| Dynamic Regulation | Signals change spatiotemporally in response to physiology and injury. | Often static; controlled delivery of multiple factors is challenging. | Fails to fully recapitulate the dynamic sequence of events during repair [2] [17]. |
| Biomechanics | Precise and tissue-specific mechanical properties. | Stiff plastic (2D) or variable hydrogel mechanics (3D). | Altered mechanotransduction can direct cells toward aberrant fates [18]. |
Can we target niches for therapeutic purposes?
Yes, this is a promising frontier. Instead of replacing cells, therapies can be designed to reactivate endogenous niches to enhance the body's own repair mechanisms [17]. For example, after a heart attack, delivering specific niche factors could potentially stimulate resident cardiac stem cells to proliferate and repair the damage, reducing the need for complex cell transplantation procedures [1].
How does the niche concept relate to cancer?
The concept of a "cancer stem cell niche" is critically important. Cancer stem cells are believed to reside in specialized microenvironments that protect them and sustain their self-renewal [18]. These niches can hijack normal signaling pathways to promote tumor growth and confer resistance to chemotherapy and radiation. Therefore, understanding and therapeutically disrupting the cancer stem cell niche is a major focus of oncology research [18].
Experimental Protocols: Key Workflows
Workflow: Establishing a Simplified 2D Niche Model to Study HSC-MSC Interactions
This protocol outlines the creation of a reductionist system to investigate how mesenchymal stromal cells (MSCs) influence hematopoietic stem cell (HSC) fate.
Detailed Methodology:
- Surface Preparation: Coat a tissue culture-treated plate with human fibronectin (5 µg/mL in PBS) for at least 1 hour at 37°C.
- Stromal Layer: Seed human bone marrow-derived MSCs at a density of 5,000-10,000 cells/cm² on the coated surface. Culture them in MSC growth medium until a confluent monolayer is formed.
- HSC Isolation: Isolate CD34+ HSCs from human umbilical cord blood using a clinical-grade immunomagnetic separation kit, following the manufacturer's instructions.
- Co-culture: Plate the isolated HSCs (at 1,000-5,000 cells/cm²) directly onto the pre-established MSC monolayer.
- Culture Conditions: Maintain the co-culture in a defined serum-free hematopoietic support medium, supplemented with key cytokines like Stem Cell Factor (SCF; 50 ng/mL) and FLT3-Ligand (FLT3-L; 50 ng/mL) [19].
- Analysis:
- Phenotype: After 7 days, harvest non-adherent and gently dissociated adherent cells. Analyze for HSC markers (e.g., CD34, CD90, CD45RA) via flow cytometry.
- Functionality: Perform colony-forming unit (CFU) assays in methylcellulose to assess multilineage differentiation potential.
Workflow: Testing the Role of immobilized vs. Soluble Cues on Neural Stem Cell (NSC) Fate
This protocol compares the effect of different growth factor presentations on NSC differentiation.
Detailed Methodology:
- Surface Functionalization:
- Arm 1 (Immobilized): Coat plates with a mixture of laminin (10 µg/mL) and FGF-2 (1 µg/mL) that has been chemically cross-linked to the surface using a sulfo-SANPAH crosslinker protocol [18].
- Arm 2 (Soluble) & Arm 3 (Control): Coat plates with laminin (10 µg/mL) only.
- NSC Culture: Seed human neural stem cells at a density of 2.5 x 10⁴ cells/cm² onto the prepared surfaces. Use fresh, pre-warmed neural induction medium.
- Factor Presentation:
- Arm 1: Use basal neural induction medium without added soluble FGF-2.
- Arm 2: Supplement the medium with soluble FGF-2 (20 ng/mL).
- Arm 3: Use basal medium without any FGF-2.
- Culture and Differentiation: Culture the cells for 7-10 days, changing the medium every other day.
- Analysis:
- Immunocytochemistry: Fix cells and stain for neural lineage markers: β-III-Tubulin (neurons), GFAP (astrocytes), and O4 (oligodendrocytes). Quantify the percentage of cells positive for each marker.
- qPCR: Analyze gene expression markers for the same lineages.
The Scientist's Toolkit: Key Reagent Solutions
Essential materials and reagents for studying and reconstructing stem cell niches in vitro.
| Reagent / Material | Function in Niche Research | Example & Notes |
|---|---|---|
| Defined Culture Media (e.g., mTeSR Plus, Essential 8) | Maintain pluripotency of hPSCs in feeder-free conditions, providing a consistent basal medium for niche studies [6] [5]. | Ensure medium is fresh (<2 weeks old at 2-8°C) to prevent spontaneous differentiation. |
| ECM Hydrogels (e.g., Geltrex, Matrigel, Laminin, synthetic peptides) | Provide a biologically active 3D scaffold that mimics the in vivo ECM, presenting adhesion sites and immobilizing growth factors [6] [18]. | Different stem cell types may require specific ECMs (e.g., VTN-N for hPSCs, Laminin for NSCs). |
| ROCK Inhibitor (Y-27632) | Improves survival of dissociated stem cells (especially hPSCs) after passaging or thawing by inhibiting apoptosis [6] [5]. | Use as a supplement for 18-24 hours post-passaging. Critical for single-cell seeding. |
| Cytokines & Growth Factors (e.g., SCF, BMPs, FGFs, WNTs) | Recreate key signaling pathways of the niche to direct self-renewal, differentiation, and maturation [2] [19]. | Consider immobilization strategies to mimic the natural, spatially restricted presentation in the niche [18]. |
| Small Molecule Agonists/Antagonists | Precisely control key signaling pathways (WNT, BMP, TGF-β) in a time-dependent manner to direct stem cell fate [18]. | Offer advantages over recombinant proteins, including stability, cost, and reversibility. |
| Chemokines (e.g., SDF-1/CXCL12) | Study and enhance the homing potential of stem cells by activating receptors like CXCR4, guiding cells to injury sites [2]. | Used for in vitro migration assays and pre-conditioning cells before transplantation. |
Quantitative Comparison of Stem Cell Types
The table below summarizes the core characteristics, integration mechanisms, and key challenges associated with Mesenchymal Stem Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs), and Tissue-Specific Stem Cells, providing a foundational comparison for researchers [20] [1] [21].
Table 1: Comparative Analysis of Stem Cell Types for Integrative Potential
| Feature | Mesenchymal Stem Cells (MSCs) | Induced Pluripotent Stem Cells (iPSCs) | Tissue-Specific Stem Cells (e.g., HSCs) |
|---|---|---|---|
| Potency & Differentiation | Multipotent (primarily mesodermal lineages: osteo-, chondro-, adipo-genic; reported transdifferentiation) [7] [21] | Pluripotent (can differentiate into all three germ layers) [20] [1] | Multipotent (typically limited to lineages of their tissue of origin) [1] |
| Primary Integration Mechanism | Predominantly paracrine signaling (trophic factors, extracellular vesicles); low-rate, transient engraftment [21] | Direct differentiation and replacement of damaged host cells; potential for functional engraftment [20] [1] | Direct engraftment, self-renewal, and reconstitution of host tissue lineages (e.g., blood, immune cells) [1] |
| Key Markers (Positive) | CD73, CD90, CD105 [7] | OCT4, SOX2, NANOG [20] [22] | Varies by tissue (e.g., CD34 for HSCs) [7] |
| Key Markers (Negative) | CD34, CD45, CD11b, CD19, HLA-DR [7] | - | - |
| Tumorigenic Risk | Low [20] [21] | High (due to reprogramming factors, genomic instability) [20] | Low (in their native context) |
| Immunogenicity | Low; immunomodulatory [7] [21] | Low for autologous use; potential immunogenicity from epigenetic aberrations [20] | High for allogeneic transplantation (requires matching) |
| Major Challenges | Functional heterogeneity, low engraftment efficiency, donor-dependent variations [21] | Tumorigenicity, immunogenicity, genetic and epigenetic heterogeneity [20] | Limited availability, expansion difficulties in vitro |
Experimental Protocols for Assessing Integrative Potential
Protocol 1: Evaluating MSC Migration and Paracrine Activity
Objective: To assess the homing capability and secretome-mediated effects of MSCs, which are central to their integrative potential and therapeutic efficacy [2] [21].
Materials:
- Isolated MSCs (e.g., from bone marrow, umbilical cord, or adipose tissue) [7].
- Complete MSC growth medium (e.g., α-MEM supplemented with human platelet lysate) [20].
- Transwell migration chamber.
- Conditioned medium from MSC cultures.
- Target cells relevant to the disease model (e.g., cardiomyocytes for cardiac repair).
Methodology:
- Homing/Migration Assay: [2] [21]
- Place MSCs in the upper chamber of a Transwell insert.
- Add a chemotactic gradient of a known chemoattractant (e.g., SDF-1) to the lower chamber to simulate injury signals [2].
- Incubate for 6-24 hours under standard culture conditions.
- Fix and stain the cells that have migrated to the lower membrane surface.
- Count the cells under a microscope to quantify migratory capacity.
- Paracrine Effect Assay: [21]
- Culture MSCs until 70-80% confluency.
- Replace the medium with a serum-free option and incubate for 24-48 hours to collect conditioned medium (CM).
- Filter the CM to remove any cells or debris.
- Apply the CM to target cells (e.g., those subjected to oxidative stress or injury).
- Assess target cell viability (e.g., via MTT assay), apoptosis (e.g., caspase activity), and proliferation (e.g., Ki-67 staining) to measure the paracrine-mediated therapeutic effect.
Protocol 2: Assessing iPSC Differentiation and Functional Integration
Objective: To guide iPSCs to differentiate into specific lineages and verify their functional integration into host tissues, a key step for regenerative therapies [20] [1].
Materials:
- Validated iPSC line.
- Essential 8 Medium or similar feeder-free maintenance medium [6] [5].
- Differentiation kits or specific cytokine cocktails for target lineage (e.g., activin A for definitive endoderm).
- ROCK inhibitor (Y-27632) for enhancing cell survival after passaging [6].
- Immunocytochemistry reagents for lineage-specific markers.
Methodology:
- iPSC Culture and Quality Control: [20] [5]
- Maintain iPSCs in a pluripotent state using defined media like Essential 8 on vitronectin (VTN-N)-coated plates.
- Monitor cultures daily for spontaneous differentiation. Remove differentiated areas manually or through selective passaging before starting differentiation protocols [5].
- Passage cells at ~85% confluency using EDTA or gentle dissociation reagents to maintain healthy, undifferentiated cultures [5].
Directed Differentiation: [20]
- Initiate differentiation by switching to specific induction media when iPSCs reach an optimal density.
- For robust results, include control cell lines (e.g., H9 or H7 ESC lines) to account for protocol variability and line-specific differentiation efficiency [6].
- Adjust cell seeding density and induction time based on the target lineage and the specific iPSC line used [6].
Verification of Integration and Function: [1]
- After differentiation, analyze the cells for expression of lineage-specific markers via immunostaining or flow cytometry.
- For in vivo integration studies, transplant the differentiated cells into appropriate animal models.
- Perform long-term follow-up to assess both functional improvement (e.g., motor function, electrical activity) and safety, specifically monitoring for tumor formation [20].
Troubleshooting Guides and FAQs
FAQ 1: How Can We Overcome the Low Engraftment Efficiency of MSCs in Host Tissue?
Challenge: A significant hurdle in MSC therapy is the low rate of cell retention and engraftment at the target site post-transplantation, which limits their direct regenerative contribution [21].
Solutions:
- Cell Priming/Preconditioning: Pre-treat MSCs with inflammatory cytokines (e.g., IFN-γ, TNF-α) or culture under hypoxic conditions before transplantation. This mimics the injury microenvironment, enhancing the cells' survival, homing, and paracrine activity [21].
- Genetic Modification: Engineer MSCs to overexpress homing-related receptors (e.g., CXCR4, the receptor for SDF-1) to improve their recruitment to injury sites [2] [21].
- Biomaterial-Assisted Delivery: Use hydrogel-based scaffolds or other biomaterials to encapsulate MSCs. These materials provide a protective niche, improve localization, and support cell survival and function at the transplantation site [21].
FAQ 2: What Are the Critical Steps to Minimize Tumorigenic Risk in iPSC-Derived Therapies?
Challenge: The use of iPSCs is associated with potential tumor formation, primarily due to residual undifferentiated cells or genetic abnormalities acquired during reprogramming and culture [20].
Solutions:
- Rigorous Purification: Implement stringent purification protocols post-differentiation to remove any residual pluripotent cells. This can be achieved using fluorescence-activated cell sorting (FACS) with antibodies against pluripotency markers (e.g., TRA-1-60) or by using cell surface markers specific to the desired differentiated cell type.
- Vector-Free Reprogramming: Utilize non-integrating Sendai virus vectors or episomal plasmids for reprogramming to prevent insertional mutagenesis. For existing lines, ensure clearance of reprogramming vectors; for example, with the CytoTune-iPS Sendai 2.0 Kit, a temperature shift can be used to clear specific vectors after sufficient passages [6].
- Comprehensive Safety Monitoring: Employ genomic integrity assays (e.g., karyotyping, CNV analysis) throughout the culture and differentiation process. Always include long-term in vivo studies in animal models to monitor for teratoma or tumor formation before clinical application [20].
FAQ 3: How Can Heterogeneity in MSC Batches Be Controlled for Reproducible Experimental Outcomes?
Challenge: MSCs exhibit significant donor-to-donor and source-to-source variability, leading to inconsistent experimental and therapeutic results [21].
Solutions:
- Standardized Characterization: Adhere strictly to the updated International Society for Cell & Gene Therapy (ISCT) criteria, which define markers and functional attributes for MSCs. Perform rigorous batch-level quality control, including trilineage differentiation assays and surface marker profiling [21].
- Use of Defined Culture Systems: Avoid using fetal bovine serum (FBS). Instead, use defined supplements like human platelet lysate (HPL) to reduce batch variability and the risk of xenogenic immune reactions [20] [21].
- Functional Potency Assays: Instead of relying solely on surface markers, implement quantitative functional assays tailored to the intended therapeutic mechanism (e.g., T-cell suppression assay for immunomodulation, angiogenesis tube formation assay for vascular repair) to ensure batch potency [21].
Signaling Pathways and Workflows for Stem Cell Integration
The following diagrams, generated using DOT language, illustrate the key signaling pathways and experimental workflows central to stem cell integration.
Diagram 1: SDF-1/CXCR4 Pathway in Stem Cell Homing
This diagram visualizes the SDF-1/CXCR4 signaling axis, a primary pathway responsible for mobilizing and recruiting stem cells to sites of injury [2]. Following tissue damage, the release of Damage-Associated Molecular Patterns (DAMPs) triggers the production of the chemokine SDF-1, which creates a concentration gradient. Stem cells expressing the CXCR4 receptor sense this gradient, leading to their directed migration (homing) toward the injury site, a prerequisite for subsequent integration [2].
Diagram 2: Stem Cell Integration Workflow
This workflow outlines the general path from stem cell preparation to functional recovery in host tissue. It highlights the critical divergence in the mechanism of action post-homing: MSCs primarily exert effects via paracrine signaling, while iPSCs and Tissue-Specific Stem Cells like HSCs aim for direct integration and replacement of damaged cells [1] [21].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Stem Cell Integration Research
| Reagent | Function | Example & Notes |
|---|---|---|
| Human Platelet Lysate (HPL) | A defined, xeno-free supplement for MSC culture; enhances cell growth and reduces variability compared to FBS [20]. | Can be gradually increased in concentration (e.g., in α-MEM) to accommodate and optimize cell growth [20]. |
| Essential 8 Medium | A defined, feeder-free culture medium designed for the maintenance of human pluripotent stem cells (hESCs and iPSCs) [6] [5]. | Allows for seamless transition of PSCs grown in other systems (e.g., mTeSR on Matrigel) when passaged with EDTA [6]. |
| ROCK Inhibitor (Y-27632) | A small molecule that significantly improves the survival of human pluripotent stem cells after single-cell dissociation, cryopreservation, and passaging [6]. | Sold as RevitaCell Supplement. Critical for use during passaging, especially if cells are overly confluent [6] [5]. |
| Vitronectin (VTN-N) | A defined, recombinant substrate for feeder-free adhesion and culture of human pluripotent stem cells [6] [5]. | Used with Essential 8 Medium. Requires non-tissue culture-treated plates for effective coating [5]. |
| Gentle Cell Dissociation Reagent | A non-enzymatic, gentle solution for passaging adherent pluripotent stem cells as small aggregates, minimizing differentiation [5]. | Preferable to enzymatic digestion for maintaining colony integrity; incubation time may require optimization per cell line [5]. |
Engineering Integration: Advanced Biomaterial and Delivery Strategies for Clinical Translation
Frequently Asked Questions (FAQs)
Hydrogel-Based Scaffolds
Q1: What are the key advantages of using hydrogels as synthetic stem cell niches? Hydrogels are highly hydrated, microporous 3D scaffolds that provide an ideal microenvironment for stem cells. Their key advantages include the ability to stably encapsulate stem cells along with signaling molecules or growth factors, and to act as an immunological barrier that protects implanted cells from host immune attack while remaining permeable to therapeutic molecules [23]. They can be engineered with specific mechanical properties and degradation rates to match the target tissue.
Q2: How can I improve the survival and retention of stem cells delivered via hydrogel? Using specially designed, injectable hydrogels can significantly enhance cell retention. For instance, studies have shown that endothelial progenitor cells seeded into a hyaluronic acid (HA) shear-thinning hydrogel exhibited enhanced engraftment efficiency in rat hearts. Similarly, peptide amphiphile-based hydrogels have been shown to ensure growth factor retention, which increases the proliferation of encapsulated muscle stem cells [23].
Electrospun Fiber Scaffolds
Q3: Why are 3D electrospun scaffolds preferable to traditional 2D membranes for tissue engineering? Traditional 2D electrospun membranes are limited by their thinness and high packing density, which result in poor cellular infiltration and restricted nutrient diffusion [24]. Three-dimensional electrospun nanofiber-based scaffolds (3D ENF-S) overcome these limitations by providing a biomimetic 3D environment with significantly increased thickness and porosity. This architecture facilitates deep cell penetration, supports neo tissue development, and promotes higher genetic material expression related to ECM secretion and cell metabolism [24].
Q4: What are the primary methods for fabricating 3D electrospun nanofiber scaffolds? Fabrication methods can be classified into three main categories [24]:
- Electrospun Nanofiber 3D Scaffolds: Created via post-processing techniques (e.g., stacking, rolling, gas foaming) or by tuning collection techniques (e.g., using patterned collectors, cryogenic electrospinning).
- Electrospun Nanofiber/Hydrogel Composite 3D Scaffolds: Combine the fibrous structure of electrospinning with the high hydrability of hydrogels.
- Electrospun Nanofiber/Porous Matrix Composite 3D Scaffolds: Integrate fibers within other porous matrices to create composite structures.
3D Constructs and Host Integration
Q5: What is the concept of "in situ tissue regeneration" and how do scaffolds facilitate it? In situ tissue regeneration is an approach that bypasses extensive ex vivo cell manipulation by using a target-specific biomaterial scaffold to recruit the host's own endogenous stem or progenitor cells to the site of injury [25]. The implanted scaffold, often incorporating bioactive molecules, provides a template and appropriate microenvironment that guides these recruited cells to proliferate and differentiate into the desired tissue type, effectively regenerating damaged tissue without cell transplantation [25].
Q6: How do the physical properties of a biomaterial scaffold influence stem cell fate? The structural and mechanical properties of a scaffold are critical for regulating stem cell behavior and must be matched to the target tissue. For example, hard tissues like bone require scaffolds with relatively strong mechanical properties for load-bearing, whereas soft tissues like skin need porous, soft, and highly viscous biomaterials [23]. Properties such as surface charges, chemical compositions, and topography all play key roles in directing stem cell adhesion, survival, proliferation, and differentiation [23].
Troubleshooting Guides
Low Cell Viability and Retention after Transplantation
Problem: Poor survival and rapid loss of transplanted stem cells at the injury site, with studies showing less than 5% cell retention on the first day after transplantation [23].
| Possible Cause | Solution | Experimental Example |
|---|---|---|
| Harsh microenvironment at injury site | Use a protective, biocompatible scaffold to shield cells. | Utilize a hyaluronic acid (HA) hydrogel to encapsulate cells, which acts as a physical barrier and improves the local microenvironment [23]. |
| Lack of proper cell-matrix interaction | Provide a 3D scaffold that mimics the native ECM. | Culture stem cells on a 3D electrospun nanofiber scaffold that recapitulates the fibrous structure of native ECM, promoting adhesion and survival [24]. |
| Inadequate pro-survival signaling | Co-deliver growth factors or incorporate bioactive peptides. | Incorporate the RGD peptide (a common cell-adhesion motif) into your hydrogel or fiber scaffold to enhance integrin-mediated cell survival signaling [23]. |
Poor Cellular Infiltration into Scaffolds
Problem: Cells remain on the surface of the scaffold and fail to migrate into its core, leading to limited tissue formation and potentially poor integration with the host.
| Possible Cause | Solution | Experimental Example |
|---|---|---|
| Small pore size and high packing density (common in 2D electrospinning) | Optimize fabrication to create larger, interconnected pores. | Employ cryogenic electrospinning, where ice crystals act as templates to create scaffolds with large pores (10-500 μm) [24]. |
| Insufficient bioactivity to guide cell migration | Functionalize the scaffold with chemoattractants. | Incorporate the neuropeptide Substance P (SP) into your scaffold. SP has been shown to effectively mobilize CD29+ MSC-like cells from bone marrow and drive their migration to injury sites [25]. |
| Scaffold's chemical composition is not conducive to cell attachment | Modify surface chemistry or use natural polymers. | Use natural polymers like collagen or chitosan, which inherently contain cell-binding domains, or coat synthetic scaffolds with these materials [26]. |
Inadequate Differentiation into Target Lineage
Problem: Stem cells within the scaffold do not efficiently differentiate into the desired functional cell type.
| Possible Cause | Solution | Experimental Example |
|---|---|---|
| Lack of specific differentiation cues | Sustained delivery of differentiation-inducing growth factors. | For neural differentiation, incorporate Nerve Growth Factor (NGF) or Brain-Derived Neurotrophic Factor (BDNF) via microspheres for controlled release within the scaffold [26]. |
| Mismatch between scaffold stiffness and target tissue | Tune the mechanical properties of your biomaterial. | For neural tissue engineering (a soft tissue), use soft hydrogels (~0.1-1 kPa) to promote neurogenesis, while for bone tissue, use stiffer scaffolds (>10 kPa) to promote osteogenesis [23]. |
| Uncontrolled differentiation (e.g., excessive spontaneous differentiation) | Ensure pre-differentiation culture conditions maintain cell potency and start with high-quality, undifferentiated cells. | Prior to seeding, ensure your stem cell cultures are healthy and undifferentiated. Refer to standard troubleshooting guides for hPSC culture to manage excessive differentiation [5]. |
Mechanical and Physical Properties of Common Biomaterial Polymers
Table 1: Key characteristics of natural and synthetic polymers used in scaffold fabrication.
| Polymer | Type | Key Properties | Example Applications |
|---|---|---|---|
| Collagen | Natural | Biocompatible, low immunogenicity, FDA-approved for some applications, can be processed into films, fibers, and sponges [25]. | Skin, bone, neural tissue regeneration [26] [25]. |
| Chitosan | Natural (Polysaccharide) | Biocompatible, biodegradable, antimicrobial properties [25]. | Nerve conduits, wound dressings [26]. |
| Poly(lactic-co-glycolic acid) (PLGA) | Synthetic | Biodegradable, thermoplastic, tunable degradation rate, FDA-approved for sutures and devices [25]. | General tissue engineering, drug delivery [26] [25]. |
| Poly(ε-caprolactone) (PCL) | Synthetic | Biodegradable, slow degradation, good mechanical strength [24]. | Long-term implantable scaffolds, bone, nerve guides [26] [24]. |
| Hyaluronic Acid | Natural (Glycosaminoglycan) | Highly hydrated, inherent cell signaling properties, can be modified to form hydrogels [23]. | Injectable hydrogels for cardiac, cartilage repair [23]. |
| Polyaniline (PANI) | Conductive Polymer | Conducts electricity, can help neurite outgrowth and cell activation by carrying electrical impulses [26]. | Neural tissue engineering, biosensors [26]. |
Performance Metrics of Advanced Scaffold Designs
Table 2: Documented outcomes of various scaffold-based strategies in experimental models.
| Scaffold Type | Cell Type | Key Outcome | Reference Model |
|---|---|---|---|
| HA Shear-Thinning Hydrogel | Endothelial Progenitor Cells | Enhanced engraftment efficiency and reduced myocardial fibrosis compared to saline-treated cells [23]. | Ischemic rat heart [23] |
| Peptide Amphiphile Hydrogel | Muscle Stem Cells | Ensured growth factor retention and increased proliferation of encapsulated cells [23]. | Injured mouse muscle [23] |
| 3D PCL with nHA Scaffold | (Not Specified) | Scaffold fabricated via mesh collector and layer-by-layer assembly for bone regeneration [24]. | Bone tissue engineering [24] |
| Cryogenic Electrospun PLLA | (Not Specified) | Produced scaffold with large pores (10-500 μm) facilitating cell infiltration [24]. | General tissue engineering [24] |
Experimental Protocols
Protocol: Fabrication of a 3D Electrospun Nanofiber Scaffold via Gas Foaming
Objective: To transform a standard 2D electrospun nanofiber mat into a thick, porous 3D scaffold to enhance cell infiltration.
Materials:
- Electrospun nanofiber mat (e.g., Poly(ε-caprolactone) - PCL)
- Sodium borohydride (NaBH4) aqueous solutions [24] OR a chemical blowing agent like azodicarbonamide [24]
- Deionized water
- Laboratory oven
Method:
- Prepare Electrospun Mat: Fabricate a 2D electrospun PCL membrane using standard electrospinning techniques.
- Gas Foaming Treatment:
- Option A (NaBH4): Immerse the electrospun mat in an aqueous solution of NaBH4. The processing time in the solution directly controls the distribution of gap widths and layer thicknesses in the final scaffold [24].
- Option B (Azodicarbonamide): Incorporate azodicarbonamide into the polymer solution prior to electrospinning. After fiber deposition, expose the mat to a high temperature (e.g., 100°C for 2-3 seconds) to decompose the blowing agent and generate micro-sized pores [24].
- Rinsing and Drying: Thoroughly rinse the expanded scaffold with deionized water to remove any residual chemicals.
- Drying: Lyophilize or air-dry the scaffold to maintain its 3D porous structure.
- Sterilization: Sterilize the final 3D scaffold using ethylene oxide gas or ethanol immersion followed by UV exposure before cell culture.
Protocol: Functionalization of a Hydrogel with a Bioactive Peptide for Enhanced Cell Recruitment
Objective: To create a hydrogel scaffold that actively recruits host stem cells to a site of implantation for in situ tissue regeneration.
Materials:
- Hyaluronic acid (HA) hydrogel (or other injectable hydrogel)
- Substance P (SP) peptide [25]
- Phosphate Buffered Saline (PBS)
- Sterile mixing vials
Method:
- Hydrogel Preparation: Prepare the precursor solution of your HA hydrogel according to the manufacturer's or standard protocol.
- Peptide Incorporation: Dissolve a determined concentration of Substance P (SP) in sterile PBS and mix it thoroughly into the HA precursor solution. The concentration should be optimized based on preliminary studies.
- Cross-linking and Implantation: Allow the hydrogel to cross-link, encapsulating the SP peptide. If using an injectable system, the solution can be gelled in situ.
- Implantation: Implant the functionalized hydrogel at the target injury site.
- Analysis: The sustained release of SP from the hydrogel will mobilize host MSC-like cells (e.g., CD29+ cells) from the bone marrow and recruit them to the implant site, where they can participate in the repair process [25].
Signaling Pathways and Workflows
Diagram Title: In Situ Tissue Regeneration via Host Cell Recruitment
Diagram Title: Scaffold Mechanotransduction Signaling Pathway
The Scientist's Toolkit
Table 3: Essential research reagents and materials for biomaterial scaffold research.
| Reagent/Material | Function/Application |
|---|---|
| Mesenchymal Stem Cells (MSCs) | A widely used adult stem cell source with multipotent differentiation capability and immunomodulatory properties, derived from bone marrow, adipose tissue, or umbilical cord [23] [27]. |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific pluripotent cells that can be differentiated into any cell type, offering a personalized and ethically non-contentious cell source [23]. |
| Collagen Type I | A natural polymer serving as a primary component of the ECM; used to create biocompatible scaffolds that promote cell attachment and growth [26] [25]. |
| Poly(lactide-co-glycolide) (PLGA) | A versatile, biodegradable synthetic polymer with tunable degradation rates, used for creating both scaffolds and controlled drug delivery systems [25]. |
| Hyaluronic Acid (HA) | A natural glycosaminoglycan used to form highly hydrated hydrogels; particularly useful for creating injectable cell delivery systems and mimicking soft tissue environments [23]. |
| Nerve Growth Factor (NGF) | A neurotrophic factor used to direct stem cell differentiation towards neuronal lineages when incorporated into scaffolds for neural tissue engineering [26]. |
| Substance P (SP) | A neuropeptide used as a bioactive cue to functionalize scaffolds, enhancing the recruitment of host stem cells to the site of implantation for in situ regeneration [25]. |
| Electrospinning Apparatus | Standard equipment for generating nanofibrous scaffolds that morphologically mimic the native extracellular matrix [24]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary causes of mechanical stress on stem cells during delivery, and how do they impact cell survival?
Mechanical stress during delivery primarily arises from shear forces and fluid stretching experienced as cells pass through narrow-gauge needles. These forces can disrupt plasma membrane integrity, trigger apoptotic pathways, and significantly reduce viability. Studies show that delivering stem cells via needle injection of cell suspensions results in a survival rate of only ~30%. High cell mortality not only weakens therapeutic outcomes but can also trigger local immune responses and exacerbate damage to the injured tissue environment [28].
Q2: How do injectable and implantable systems differ in their approach to managing mechanical stress?
- Injectable Systems are typically low-viscosity solutions or shear-thinning hydrogels designed for minimally invasive delivery, often via syringe and needle. The main challenge is protecting cells from shear stress during the injection process. Strategies include optimizing delivery parameters and using bio-inks that lubricate cells [28].
- Implantable Systems often involve pre-formed, solid or semi-solid scaffolds (e.g., hydrogels, sponges) that are surgically placed. These systems avoid the high shear stress of injection but face different challenges related to surgical implantation and ensuring integration with host tissue. The mechanical stress is more related to compression and tension post-implantation [29].
Q3: What are the key signaling pathways activated by mechanical stress that affect stem cell viability?
A key pathway involves calcium (Ca²⁺) signaling. Mechanical stress can be converted into electrical signals via piezoelectric materials, which activate Piezo1 channels on the cell membrane. This leads to an influx of calcium ions, rapidly increasing intracellular free Ca²⁺ concentration. This Ca²⁺ surge triggers two critical mechanisms:
- Endogenous Membrane Repair: Ca²⁺ interacts with sensors like synaptotagmin VII and dysferlin to promote rapid resealing of damaged plasma membranes.
- Ca²⁺-triggered Actin Remodeling (CaAR): The increased Ca²⁺ stimulates actin polymerization and the formation of perinuclear actin rings, enhancing cellular stiffness and resistance to subsequent deformation [28].
Q4: What material strategies can be employed to shield cells from mechanical stress during injection?
Incorporating cells into protective hydrogels is a primary strategy. Ideal hydrogels for injectable delivery are:
- Shear-thinning: Their viscosity decreases under the shear stress of injection, reducing force on cells, and rapidly recovers once injected.
- Self-healing: Able to reform their structure after passing through a needle.
- Bioactive: Modified with peptides (e.g., RGD) to promote cell adhesion and survival.
- Piezoelectric: Can be engineered with nanoparticles like Barium Titanate (BTO) to convert harmful mechanical stress into beneficial electrical signals that actively protect cells [28].
Q5: How can I quantitatively assess cell viability and membrane damage after the delivery process?
Standard laboratory assays can be combined to evaluate delivery success:
- Cell Viability: Use live/dead staining (e.g., Calcein-AM for live cells, propidium iodide for dead cells) followed by fluorescence microscopy or flow cytometry. A viability of >80% post-spraying has been achieved with optimized systems [29].
- Membrane Integrity: Perform an Lactate Dehydrogenase (LDH) release assay. LDH is a cytosolic enzyme that leaks out upon membrane damage, providing a quantitative measure of cytotoxicity.
- Functional Assays: Follow up with tests for metabolic activity (e.g., MTT assay) and differentiation potential to ensure functionality is retained [29].
Troubleshooting Guides
Problem: Low Cell Viability Post-Injection
| Symptom | Possible Cause | Solution |
|---|---|---|
| >50% cell death after passing through needle. | Excessive shear stress from high injection speed or small needle diameter. | Optimize delivery parameters: Reduce injection speed, use a larger needle diameter (e.g., 0.45mm vs. 0.33mm), and ensure medium viscosity is appropriate [28]. |
| High LDH release indicating membrane damage. | Lack of physical protection for cells during injection. | Use a protective hydrogel carrier: Employ a shear-thinning hydrogel (e.g., RGD-OSA/HA-ADH) to lubricate and shield cells from direct fluid forces [28]. |
| Cells fail to engraft or proliferate after delivery. | Activation of apoptosis or loss of stemness due to stress. | Precondition or genetically modify cells: Prime MSCs before delivery to enhance stress resistance. Consider using a hydrogel with "electrical protection" that activates endogenous repair via Piezo1 channels [28] [21]. |
Problem: Inconsistent Cell Distribution and Retention
| Symptom | Possible Cause | Solution |
|---|---|---|
| Clumping of cells during delivery. | High cell density or aggregation in suspension. | Filter cells through a sterile cell strainer before loading into the delivery system. Optimize cell concentration for the chosen carrier [29]. |
| Cells leak from the implantation site. | Lack of a retaining matrix at the target tissue. | Switch to an in-situ gelling system: Use a hydrogel that is liquid during injection but solidifies in the body (e.g., via temperature, ionic crosslinking with Ca²⁺). Low-methyl pectin is one such material that gels upon contact with physiological Ca²⁺ [29]. |
| Poor integration with host tissue. | The delivery vehicle does not support cell-matrix interactions. | Use bioadhesive materials: Incorporate mucoadhesive polymers like pectin or functionalize hydrogels with RGD peptides to improve cell and host tissue adhesion [29]. |
The table below summarizes key performance metrics for different cell delivery methods and enhancement strategies as reported in recent studies.
Table 1: Performance Metrics of Cell Delivery Systems and Strategies
| Delivery Method / Strategy | Reported Cell Viability | Key Measured Outcomes | Reference |
|---|---|---|---|
| Needle Injection (Cell Suspension) | ~30% | Baseline for high shear stress-induced mortality. | [28] |
| Spray Delivery (with syringe-driven device) | 80% - 90% | High viability with uniform cell distribution; suitable for covering surface wounds. | [29] |
| Piezoelectric Hydrogel (BTO/RGD-OSA/HA-ADH) | Significantly higher than control | Enhanced endogenous repair; improved actin remodeling; reduced membrane damage; promoted differentiation in IVD model. | [28] |
| Pectin Hydrogel (Spray Delivery) | >80% (No negative effect from pectin) | Good biocompatibility; effective cell retention due to mucoadhesion. | [29] |
Key Experimental Protocols
Protocol 1: Assessing Cell Viability and Membrane Damage Post-Delivery
This protocol is adapted from methods used to evaluate spray-based delivery systems [29].
Objective: To quantitatively determine the survival rate and membrane integrity of human Mesenchymal Stem Cells (hMSCs) after being subjected to a delivery process.
Materials:
- Confluent culture of hMSCs (Passage 3-5)
- Delivery device (e.g., syringe-driven spray device, injection pump)
- Control (non-processed) hMSCs
- Sheath fluid or hydrogel carrier (e.g., PBS, 1% low-methyl pectin solution)
- Cell culture well plates
- Lactate Dehydrogenase (LDH) Cytotoxicity Assay Kit
- Flow cytometer or fluorescence microscope
- Trypan Blue solution or Calcein-AM/Propidium Iodide (PI) staining solution
Method:
- Cell Preparation: Harvest hMSCs and prepare two samples:
- Test Sample: Re-suspend cells in the chosen sheath fluid or hydrogel at the desired concentration (e.g., 1x10^6 cells/mL). Load into the delivery device.
- Control Sample: Re-suspend cells in the same fluid/carrier but do not process through the device.
- Delivery Simulation: Deliver the test sample into a sterile well plate using the standardized parameters (e.g., needle gauge, pressure, distance).
- Viability Assay (Flow Cytometry):
- Collect delivered and control cells.
- Stain with Calcein-AM (2µM, labels live cells) and Propidium Iodide (4µM, labels dead cells) for 30 minutes at 37°C.
- Analyze using flow cytometry. Calculate viability as: (Calcein-AM+ cells / Total cells) x 100%.
- Membrane Damage Assay (LDH Release):
- Collect the medium from both test and control samples after a set incubation period (e.g., 1 hour).
- Perform the LDH assay according to the manufacturer's instructions.
- Measure absorbance. Higher LDH in the medium indicates greater membrane damage.
Protocol 2: Implementing a Piezoelectric "Electrical Protection" Strategy
This protocol is based on the innovative approach using BTO nanoparticles to mitigate mechanical stress [28].
Objective: To incorporate piezoelectric Barium Titanate (BTO) nanoparticles into a hydrogel to protect hMSCs from injection-induced stress by activating endogenous Ca²⁺-mediated repair pathways.
Materials:
- RGD-oxidized sodium alginate (RGD-OSA)
- Hyaluronate Amine (HA-ADH)
- Piezoelectric Barium Titanate (BTO) nanoparticles
- Calcium Chloride (CaCl₂) solution
- hMSCs
- Syringe and needle setup
Method:
- Hydrogel Preparation: Prepare the RGD-OSA/HA-ADH hydrogel precursor solution according to established synthesis protocols. Encapsulate sterile BTO nanoparticles uniformly within the hydrogel matrix.
- Cell Encapsulation: Gently mix hMSCs with the BTO-hydrogel composite to achieve a uniform cell distribution.
- Crosslinking: Load the cell-hydrogel-BTO mixture into a syringe. Upon injection into the target site (e.g., a disc degeneration model), the hydrogel crosslinks via Schiff base reaction, and endogenous Ca²⁺ ions further stabilize the gel.
- Mechanism of Action: During injection, mechanical stress compresses the BTO nanoparticles, generating a piezoelectric potential. This electrical signal:
- Activates voltage-gated calcium channels and Piezo1 channels on the hMSC membrane.
- Triggers a rapid influx of Ca²⁺ into the cytoplasm.
- The Ca²⁺ surge initiates the "lipid-patch" and "endocytic removal" models of membrane repair.
- Simultaneously, it activates the Ca²⁺-triggered actin reset (CaAR) mechanism, increasing cellular stiffness and resistance to deformation.
Signaling Pathway Visualization
The following diagram illustrates the protective signaling pathway activated by piezoelectric materials during mechanical stress.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Optimizing Cell Delivery
| Reagent / Material | Function in Delivery Optimization | Example Use Case |
|---|---|---|
| Low-Methyl Pectin | A biocompatible, sprayable, and mucoadhesive polysaccharide that forms a hydrogel in the presence of Ca²⁺ ions. Provides a protective matrix for cells and aids in retention at the target site. | Used as a carrier for spraying MSCs onto brain or wound surfaces, improving cell retention post-delivery [29]. |
| RGD-Peptide Modified Hydrogels (e.g., RGD-OSA) | The RGD peptide sequence (Arg-Gly-Asp) promotes cell adhesion to the hydrogel via integrin binding, enhancing cell survival, retention, and integration post-delivery. | Modified into alginate-based hydrogels to improve hMSC adhesion and activity within the injectable matrix [28]. |
| Piezoelectric Nanoparticles (e.g., Barium Titanate - BTO) | Core component of the "electrical protection" strategy. Converts mechanical energy from stress into protective electrical signals that activate cellular repair pathways. | Encapsulated within RGD-OSA/HA-ADH hydrogels to protect hMSCs from shear stress during needle injection [28]. |
| Calcium Chloride (CaCl₂) | A crosslinking agent for ionic hydrogels (e.g., low-methyl pectin, alginate). Also serves as a key signaling molecule; its influx is crucial for triggering membrane repair mechanisms. | Used to gel pectin solutions for cell delivery. Also, its endogenous presence triggers gelation and the Piezo1-Ca²⁺ repair pathway [28] [29]. |
| Shear-Thinning Hydrogels (e.g., HA-ADH based) | Hydrogels whose viscosity decreases under shear stress (e.g., in a needle) and recovers afterward. This property drastically reduces mechanical forces on cells during injection. | Serves as the base injectable material for delivering cells, minimizing shear-induced damage while ensuring the formulation is injectable [28]. |
Within stem cell research aimed at enhancing integration with host tissue, the development of functional vascular networks represents a fundamental bottleneck. Engineered tissues thicker than 100–250 µm face central necrosis without an efficient vascular bed to deliver oxygen and nutrients [30]. Co-culture systems, which combine multiple cell types to mimic natural cellular environments, have emerged as powerful tools to overcome this limitation. These strategies are inspired by developmental processes like vasculogenesis (the de novo formation of blood vessels) and leverage the inherent ability of different cells to communicate and support one another's function [30] [31]. The core principle involves combining endothelial lineage cells, which form the vessel lining, with supporting cells such as mesenchymal stem cells (MSCs), fibroblasts, or perivascular cells, which stabilize the newly formed structures [30] [32]. This technical support center provides a practical guide to implementing these systems, addressing common challenges, and detailing protocols to harness cellular crosstalk for enhanced vascularization and tissue maturation.
Core Concepts and Key Reagents
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary objectives of using a co-culture system in vascularization studies? Co-culture systems serve two primary objectives. First, they aim to prevascularize tissue-engineered constructs in vitro before implantation, creating a pre-formed microvasculature that can more rapidly connect to the host's blood supply upon transplantation, thereby reducing the avascular period and enhancing cell survival [30] [32]. Second, they recapitulate the natural cellular crosstalk that occurs in vivo, such as the interaction between endothelial cells and pericytes, which is crucial for the stabilization, maturation, and long-term function of newly formed vascular networks [30] [33].
FAQ 2: Which supporting cell type is most effective for stabilizing endothelial networks? The choice of supporting cell depends on the target tissue and specific application. The most common supporting cells are Mesenchymal Stem Cells (MSCs), which can be derived from bone marrow (BM-MSCs), adipose tissue (AD-MSCs), or umbilical cord. MSCs support vascular networks by differentiating into perivascular cells or through paracrine signaling [30] [21]. Other effective supporting cells include pericytes, which are natural stabilizers of capillaries, and fibroblasts [30] [34]. Adipose-derived stromal cells (ASCs) and capillary-resident stem cells (CapSCs) have also shown strong pro-angiogenic effects in microvessel-on-a-chip models [33].
FAQ 3: Why do my endothelial networks regress or fail to mature in long-term culture? Network regression often indicates a lack of proper stabilization signals. This can be due to an incorrect cell ratio; a common optimal ratio for HUVECs/MSCs is 5:1, though 1:1 has also been used successfully in spheroid models [30]. Furthermore, the culture medium may be a factor. Osteogenic supplements can abrogate vessel formation, while purely vasculogenic media may inhibit osteogenic differentiation [35]. Implementing a sequential differentiation protocol (vasculogenesis first, then osteogenesis) or using a "hybrid" medium can help balance these processes [35].
FAQ 4: How can I effectively analyze cellular crosstalk and interactions in my 3D co-culture? Advanced imaging and molecular techniques are key. Confocal laser microscopy of 3D models (e.g., microvessel-on-a-chip) allows for the reconstruction of vascular morphologies and the quantification of indices like sprout length, vessel diameter, and surface curvature [33]. Isolating specific cell populations from the co-culture via fluorescence-activated cell sorting (FACS) followed by qPCR or RNA-seq can reveal changes in gene expression related to specific pathways, such as the upregulation of steroidogenic enzymes or adhesion molecules [36] [33].
Troubleshooting Common Co-culture Challenges
Table 1: Troubleshooting Guide for Co-culture Experiments
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Poor Network Formation | Suboptimal cell seeding density or ratio [30].Insufficient pro-angiogenic factors in medium [30].Inappropriate biomaterial (e.g., stiffness, biochemistry) [32]. | - Optimize EC/supporting cell ratio (test 1:1, 5:1).Ensure media contains VEGF and other essential vasculogenic supplements [35].Use soft, natural hydrogels like fibrin or collagen that support morphogenesis [35]. |
| Unstable Vessels | Lack of supporting cell integration [30].Regression after initial formation. | - Ensure supporting cells (MSCs, pericytes) are present and can integrate.Consider co-culture with adipose-derived capillary-resident stem cells (CapSCs), which show strong stabilization properties [33]. |
| Inconsistent Results | Donor-to-donor variability of primary cells [21].Uncontrolled switch from 2D to 3D culture [32]. | - Use standardized, commercially sourced cells where possible.Characterize MSC subpopulations and potency [21].Thoroughly document 3D culture protocol (scaffold, cell density, medium) [32]. |
| Balancing Vascularization & Tissue-Specific Differentiation | Osteogenic medium components inhibiting EC function and vessel stability [35]. | - Use a sequential protocol: prevascularize first (7 days), then switch to osteogenic or hybrid medium [35].Test "hybrid" medium containing both vasculogenic and osteogenic supplements [35]. |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Co-culture Experiments
| Reagent/Material | Function | Example Application |
|---|---|---|
| Human Umbilical Vein Endothelial Cells (HUVECs) | Forms the lumenized structure of blood vessels; expresses markers like CD31 and vWf [30]. | A widely used EC source for prevascularization in bone and adipose tissue engineering models [30]. |
| Mesenchymal Stem Cells (MSCs) | Acts as a supporting cell; differentiates into perivascular cells/osteoblasts and provides trophic support [30] [21]. | Co-cultured with HUVECs in fibrin hydrogels to form stabilized vascular networks for bone tissue engineering [35]. |
| Fibrin Hydrogel | A natural, biodegradable 3D scaffold that supports cell invasion and network formation [35]. | Used as a 3D matrix for encapsulating HUVEC-MSC co-cultures to study coupled vasculogenesis and osteogenesis [35]. |
| VascuLife Medium | A defined medium optimized for the culture and maintenance of endothelial cells [35]. | Used as a base vasculogenic medium to induce and maintain EC network formation in 3D cultures [35]. |
| Type IV Collagen & Laminin | Key extracellular matrix (ECM) proteins that provide biochemical cues for cell adhesion and differentiation [36]. | Coating culture surfaces with these proteins was shown to enhance corticosterone production in steroidogenic cells, mimicking endothelial cell contact [36]. |
| Microvessel-on-a-Chip | A microphysiological system (MPS) that provides a controlled 3D environment to study cell-cell interactions and sprouting angiogenesis [33]. | Used to image and quantify the crosstalk between HUVECs and MSCs/ASCs/CapSCs during sprouting angiogenesis [33]. |
Experimental Protocols for Robust Vascularization
Protocol 1: Prevascularization in 3D Fibrin Hydrogels
This protocol details the creation of a stabilized, prevascularized network within a 3D fibrin matrix, a common scaffold in tissue engineering [35].
- Step 1: Cell Expansion and Preparation. Expand Human Umbilical Vein Endothelial Cells (HUVECs) in VascuLife Endothelial Cell Growth Medium and Mesenchymal Stem Cells (MSCs) in a high-performance basal medium. Use cells between passages 4-6 to ensure vitality and prevent senescence.
- Step 2: Hydrogel Encapsulation. Detach cells and resuspend them in VascuLife medium. Create a fibrinogen solution (4.0 mg/mL in PBS) and keep it on ice. For a 1 mL hydrogel, mix 625 µL of fibrinogen, 100 µL FBS, 20 µL thrombin, and 255 µL of cell suspension to reach a final fibrin concentration of 2.5 mg/mL and a total cell density of 500,000 cells/mL. For a 1:1 HUVEC:MSC co-culture, this would be 250,000 of each cell type per mL. Quickly dispense the solution into a multi-well plate (e.g., 0.25 mL/well of a 48-well plate).
- Step 3: Gelation and Initial Culture. Incubate the plate at 37°C for 30 minutes to allow complete gelation. After gelation, carefully add complete VascuLife medium to cover the hydrogel.
- Step 4: Prevascularization Phase. Culture the constructs for 7 days in VascuLife medium (vasculogenic conditions), changing the medium every 48 hours. During this period, HUVECs will form interconnected capillary-like networks, and MSCs will colocalize with these networks, acting as stabilizing pericytes.
- Step 5: Inducing Tissue Maturation. After 7 days, you can transition the constructs to a differentiation medium. For bone tissue engineering, transfer constructs to a hybrid medium (VascuLife base with both vasculogenic and osteogenic supplements) or a pure osteogenic medium (DMEM base with osteogenic supplements like β-glycerophosphate, ascorbic acid, and dexamethasone) for an additional 14 days. Note that pure osteogenic medium may lead to vessel regression, while hybrid medium can maintain vessel networks but may reduce mineralization [35].
Protocol 2: Image-Based Analysis of Sprouting Angiogenesis
This protocol leverages a microvessel-on-a-chip system to quantitatively analyze the crosstalk between endothelial cells and supporting cells [33].
- Step 1: Microvessel Fabrication. Seed HUVECs into the channels of a microfluidic device designed for 3D cell culture. Allow the cells to adhere and form a confluent monolayer, creating a parent microvessel.
- Step 2: 3D Co-culture Setup. After the microvessel is formed, embed MSCs (e.g., CapSCs or ASCs) at a desired density within a collagen I matrix that is poured into the adjacent tissue chamber of the device, surrounding the parent vessel.
- Step 3: Culture and Stimulation. Culture the device under standard conditions (37°C, 5% CO2) for up to 10 days. The MSCs within the matrix will interact with the parent vessel, promoting sprouting angiogenesis.
- Step 4: Immunofluorescence and Imaging. At designated time points, fix the constructs and perform immunofluorescence staining for markers of interest (e.g., CD31 for HUVECs). Image the entire 3D structure using a confocal laser microscope, capturing z-stacks to obtain full volumetric data.
- Step 5: 3D Reconstruction and Quantitative Morphometry. Use image analysis software (e.g., Imaris, ImageJ) to reconstruct 3D models of the vascular network. Quantify key morphological parameters such as:
- Sprout Length: The length of new vessels growing from the parent vessel.
- Surface Curvature: The smoothness of the vessel surface, which indicates maturation (MSCs smooth irregular surfaces).
- MSC Localization: The spatial distribution of MSCs relative to the vessel (e.g., preferential localization at sprout roots or protrusions) [33].
Visualizing Signaling Pathways and Experimental Workflows
Key Signaling Pathways in Endothelial-Support Cell Crosstalk
The following diagram illustrates the core molecular crosstalk that stabilizes nascent vascular networks, a fundamental process in co-culture systems.
Figure 1: Molecular Crosstalk in Vascular Stabilization. This diagram depicts the bidirectional signaling between endothelial cells (ECs) and support cells like MSCs or pericytes. Key interactions include PDGF-BB secretion by ECs recruiting support cells, and Angiopoietin-1 secretion by support cells promoting EC stability and quiescence. Both cell types also adhere to and remodel the extracellular matrix (ECM), which provides critical biochemical and mechanical cues.
Sequential Prevascularization Workflow
This workflow outlines a sequential strategy for creating a vascularized tissue construct, which is often necessary when target tissue differentiation cues (e.g., for bone) can inhibit vessel formation.
Figure 2: Sequential Prevascularization Workflow. This chart outlines a strategic protocol for engineering vascularized tissues. After encapsulating cells in a 3D hydrogel, a dedicated prevascularization phase is followed by a strategic choice of differentiation medium based on the primary research goal, balancing vessel stability against tissue-specific function.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental purpose of preconditioning stem cells before transplantation? Preconditioning is a strategy designed to enhance the therapeutic efficacy of stem cells. It involves exposing cells in vitro to specific environmental stresses—such as hypoxia, cytokines, or growth factors—that they will encounter after transplantation into the diseased host tissue. This exposure "primes" the cells, activating protective cellular responses and enhancing their resilience, survival, engraftment, and immunomodulatory functions in the hostile in vivo microenvironment [37] [38] [21].
Q2: How does hypoxia preconditioning improve the function of Mesenchymal Stem Cells (MSCs)? Hypoxia preconditioning, typically at low oxygen levels (e.g., 1% O₂), mimics the ischemic and stressed conditions of damaged tissue. This exposure stabilizes Hypoxia-Inducible Factors (HIFs), which act as master regulators, triggering adaptive responses. These responses include:
- Enhanced Angiogenesis: Upregulation of pro-angiogenic factors like VEGF to improve blood vessel formation.
- Metabolic Adaptation: A shift in cell metabolism to promote survival under low-oxygen conditions.
- Increased Paracrine Activity: Boosting the secretion of growth factors, cytokines, and extracellular vesicles that mediate tissue repair and immune modulation [39] [40] [37].
Q3: Can preconditioning reduce the challenges associated with donor-to-donor variability in MSCs? Yes, emerging evidence suggests that preconditioning, particularly with proinflammatory cytokines, can reduce functional heterogeneity between MSCs from different donors. Cytokine priming promotes a more consistent and potent immunomodulatory phenotype across cell populations, thereby standardizing therapeutic performance and making clinical outcomes more predictable [38].
Q4: What is the difference between priming with a single factor versus a combination of factors? Combination preconditioning often yields superior, synergistic results. While a single factor might trigger a specific pathway, a combination (e.g., EGF, TNF-α, and hypoxia) can simultaneously activate multiple, complementary signaling networks. This can lead to a greater enhancement of MSC proliferation, extracellular vesicle (EV) biogenesis, and secretion of therapeutic factors compared to single-factor approaches [40].
Q5: Are the effects of preconditioning sustained over time and after a second inflammatory challenge? Research indicates that the effects of cytokine priming can be durable. Studies show that preconditioned MSCs maintain their enhanced immunomodulatory profile over time and can even mount a robust response to a subsequent inflammatory stimulus. This is crucial for clinical translation, as it suggests the primed phenotype will persist after transplantation into an inflamed disease site [38].
Troubleshooting Guides
Issue: Low Cell Survival Post-Transplantation
| Potential Cause | Diagnostic Steps | Recommended Solutions |
|---|---|---|
| Insufficient Preconditioning | Check expression of HIF-1α or other stress-response markers (e.g., HO-1) post-preconditioning. | Optimize preconditioning intensity (e.g., lower O₂ level, increase cytokine concentration) and duration. Consider combination strategies like ETH preconditioning [40] [37]. |
| Host Microenvironment Inflammatory Stress | Analyze inflammatory cytokine levels (e.g., IFN-γ, IL-1β, TNF-α) in the target host tissue. | Prime MSCs with a proinflammatory cytokine cocktail (e.g., IFN-γ, TNF-α, IL-1β) to "license" them for enhanced survival and anti-inflammatory function [37] [38]. |
| Oxidative Stress | Measure intracellular ROS levels in preconditioned vs. naïve MSCs. | Precondition with mild oxidative stress or use molecules that boost antioxidant defenses. "Disease Microenvironment Preconditioning" (DMP) using patient serum can also build cross-tolerance [37]. |
Issue: Inconsistent Therapeutic Outcomes Between Batches
| Potential Cause | Diagnostic Steps | Recommended Solutions |
|---|---|---|
| Donor-derived Heterogeneity | Compare the transcriptomic profile and immunomodulatory potency (e.g., IDO activity) of MSCs from different donors. | Implement proinflammatory cytokine priming, which has been shown to reduce donor-dependent variability and create a more uniform therapeutic cell population [38]. |
| Unstandardized Preconditioning Protocol | Audit and document critical parameters: O₂ level accuracy, cytokine batch and concentration, and exposure time. | Establish a strict, standardized operating procedure (SOP) for preconditioning. Use an orthogonal design approach to optimize multiple factors simultaneously [40]. |
| Functional Decline with Serial Passaging | Monitor population doubling time and senescence markers (e.g., β-galactosidase) at different passages. | Use low-passage MSCs (e.g., P3-P6) for preconditioning and therapy. Select MSC sources with high inherent proliferative capacity, like umbilical cord-derived MSCs [38] [41]. |
Issue: Suboptimal Production of Therapeutic Extracellular Vesicles (EVs)
| Potential Cause | Diagnostic Steps | Recommended Solutions |
|---|---|---|
| Inefficient EV Biogenesis | Quantify EV yield per cell using nanoparticle tracking analysis (NTA). | Precondition with ETH (EGF, TNF-α, Hypoxia), which has been shown to boost EV production 4- to 5-fold by activating ESCRT and Rab GTPase pathways [40]. |
| Impaired EV Cargo Loading | Perform proteomic analysis on isolated EVs to confirm the presence of key therapeutic factors. | The same ETH preconditioning alters the MSC proteome, leading to EVs with enriched angiogenic and immunomodulatory cargo [40]. |
Key Experimental Protocols & Data
Protocol 1: ETH Preconditioning for Enhanced EV Production
This protocol, adapted from [40], details a combination strategy to significantly increase the yield and potency of MSC-derived Extracellular Vesicles.
Methodology:
- Cell Culture: Culture human MSCs (e.g., from bone marrow) in standard complete medium (e.g., α-MEM with 10% FBS) until 80% confluent.
- Preconditioning Stimuli: Apply the following three stimuli simultaneously for 24-48 hours:
- Epidermal Growth Factor (EGF): 10 ng/mL
- Tumor Necrosis Factor-alpha (TNF-α): 50 ng/mL
- Hypoxia: 1% O₂, 5% CO₂, balanced N₂ in a tri-gas incubator.
- EV Production: Replace the medium with fresh medium containing EV-depleted FBS. Collect the conditioned medium after 48 hours.
- EV Isolation: Iserve EVs via sequential centrifugation:
- Centrifuge at 3,000 × g for 20 min (twice) to remove cell debris.
- Ultracentrifuge the supernatant at 120,000 × g for 70 min at 4°C to pellet EVs.
- Wash the pellet with PBS and repeat ultracentrifugation.
- Resuspend the final EV pellet in PBS and store at -80°C.
Key Quantitative Data:
Table 1: ETH Preconditioning Significantly Enhances MSC-EV Yield and Therapeutic Potential
| Metric | Naïve MSCs | ETH-Preconditioned MSCs | Measurement Method |
|---|---|---|---|
| EV Yield | Baseline | 4- to 5-fold increase | Nanoflow cytometry [40] |
| Angiogenic Potential | Baseline | Significantly enhanced | In vitro endothelial tube formation assay [40] |
| Anti-inflammatory Activity | Baseline | Superior regulation of inflammation | Macrophage polarization assay; T-cell proliferation assay [40] [38] |
Protocol 2: Proinflammatory Cytokine Priming for Immunomodulation
This protocol, based on [38], enhances the immunomodulatory capacity of MSCs for treating inflammatory diseases.
Methodology:
- Cell Seeding: Seed MSCs (e.g., 5 × 10⁵ cells) in a culture flask and allow to adhere for 24 hours.
- Cytokine Cocktail: Prepare a priming cocktail in fresh culture medium containing:
- IFN-γ: 20 ng/mL
- TNF-α: 10 ng/mL
- IL-1β: 20 ng/mL
- Priming: Replace the medium with the cytokine-containing medium and incubate for 24 hours.
- Post-Priming: The cells (now termed CK-MSCs) can be harvested for transplantation. Their enhanced function is maintained over time and is resilient to a secondary inflammatory challenge [38].
Key Quantitative Data:
Table 2: Functional Enhancements in Cytokine-Primed MSCs (CK-MSCs)
| Cell Type/Function | Effect of Priming | Observed Outcome |
|---|---|---|
| T-lymphocytes & NK Cells | Inhibited proliferation | Enhanced immunosuppression [38] |
| Dendritic Cells (DCs) | Inhibited differentiation & allostimulatory capacity | Reduced immune activation [38] |
| Monocytes | Promoted differentiation into immunosuppressive profile | Shift towards anti-inflammatory state [38] |
| Donor Variability | Reduced heterogeneity | More consistent therapeutic performance across donors [38] |
Signaling Pathways & Experimental Workflows
Hypoxia and Cytokine Preconditioning Signaling Network
This diagram illustrates the core signaling pathways activated by hypoxia and proinflammatory cytokine preconditioning, which converge to enhance MSC resilience and function.
Experimental Workflow for Preconditioning MSCs
This workflow outlines the key stages in designing and implementing a preconditioning protocol for stem cells.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Preconditioning and Priming Experiments
| Reagent Category | Specific Examples | Function in Preconditioning |
|---|---|---|
| Growth Factors | EGF, bFGF, VEGF, PDGF | Promote MSC proliferation, survival, and EV biogenesis. EGF is a key component of ETH preconditioning [40]. |
| Proinflammatory Cytokines | IFN-γ, TNF-α, IL-1β | "License" MSCs to enhance their immunomodulatory capacity via induction of IDO, PGE2, and other factors [37] [38]. |
| Hypoxia Mimetics | Cobalt Chloride (CoCl₂), Dimethyloxalylglycine (DMOG) | Chemically stabilize HIF-1α to mimic hypoxia in standard incubators; useful when hypoxic chambers are unavailable. |
| Culture Media & Supplements | EV-depleted FBS, Platelet Lysate | Provide essential nutrients while ensuring that observed effects are due to MSC-derived products, not serum contaminants (e.g., for EV production) [40] [38]. |
| Analysis Kits | CCK-8 for viability, ELISA for cytokine detection, Antibody panels for flow cytometry (CD73, CD90, CD105, etc.) | Critical for characterizing the phenotype, viability, and functional output of preconditioned cells [40] [38]. |
Troubleshooting Guide: Common Issues in Stem Cell Engineering
FAQ: What are the primary causes of excessive differentiation in hPSC cultures and how can this be mitigated? Excessive differentiation (>20%) in human pluripotent stem cell (hPSC) cultures often results from suboptimal culture conditions or handling. Key solutions include using fresh cell culture medium (less than 2 weeks old when stored at 2-8°C), meticulously removing differentiated areas before passaging, and minimizing the time culture plates are outside the incubator to under 15 minutes [5]. Furthermore, ensure cell aggregates after passaging are evenly sized, passage cultures when colonies are large and compact but not overgrown, and decrease colony density by plating fewer aggregates. If the issue persists, reduce incubation time with passaging reagents like ReLeSR, as specific cell lines may have higher sensitivity [5].
FAQ: How can low cell attachment after plating be resolved? Low cell attachment can be addressed by initially plating a higher number of cell aggregates (e.g., 2-3 times higher) to maintain a denser culture. Work rapidly after treating cells with passaging reagents to minimize the duration aggregates spend in suspension [5]. Reducing incubation time with passaging reagents is also critical, especially if passaging occurs before cells form multiple layers within a colony. Avoid excessive pipetting that breaks up aggregates; instead, slightly increase incubation time (by 1-2 minutes) with the passaging reagent to allow natural dissociation, particularly for very dense colonies [5].
FAQ: What methods can improve the survival of genetically engineered stem cells in vivo? Improving the survival of engineered stem cells involves precise genome editing and understanding the delivery system. The CRISPR-Cas9 system allows researchers to permanently modify genes in living cells and organisms, which is foundational for correcting mutations that impair cell survival [42]. Catalytically deactivated Cas9 (dCas9) can be fused to effector domains to create CRISPR interference (CRISPRi) or CRISPR activation (CRISPRa) systems, enabling targeted inhibition or activation of specific genes to enhance survival pathways without cutting DNA [43]. Delivery vectors are crucial; the choice of vector (e.g., viral, non-viral) must maximize efficiency while minimizing toxicity [43].
FAQ: How can CRISPR technology be used to modulate the secretome of engineered stem cells? CRISPR technology can directly target and edit genes encoding for secretory factors to modulate the secretome profile of stem cells. The CRISPR-Cas9 system uses a guide RNA (gRNA) sequence to programmatically target specific stretches of genetic code for editing [42]. By combining customizable gRNA with dCas9, researchers can activate the expression of beneficial trophic factors (CRISPRa) or inhibit harmful ones (CRISPRi) [43]. This precise manipulation allows for the enhancement of the therapeutic secretome to support processes like neural regeneration, bone regeneration, and the treatment of various diseases [43].
Experimental Protocols for Key Procedures
Protocol 1: CRISPR-Cas9 Mediated Gene Editing for Enhanced Cell Homing This protocol describes how to use CRISPR-Cas9 to edit genes in stem cells to improve their homing capabilities—the ability to migrate to and engraft in target tissues [42] [43].
- Guide RNA (gRNA) Design: Design a single guide RNA (sgRNA) sequence of approximately 20 nucleotides that is complementary to the target gene locus involved in homing (e.g., chemokine receptors). Use established databases to ensure specificity and minimize off-target effects.
- Plasmid Construction: Clone the sgRNA sequence into a CRISPR plasmid vector that also expresses the Cas9 nuclease (or dCas9 for activation/repression). For knock-in experiments, include a donor DNA template with the desired homologous sequence.
- Stem Cell Transfection: Culture hPSCs (maintained as per troubleshooting guidelines above) to 60-70% confluency. Transfect the CRISPR vector into the cells using an appropriate method (e.g., electroporation or lipofection).
- Selection and Expansion: After 48 hours, apply appropriate antibiotics (e.g., Puromycin) to select successfully transfected cells. Expand the selected cell population.
- Validation: Extract genomic DNA from the edited cells and perform PCR amplification of the target region. Confirm precise gene editing via Sanger sequencing or next-generation sequencing. Validate functional changes in homing capacity using a trans-well migration assay.
Protocol 2: Assessing Stem Cell Survival and Integration In Vivo This protocol outlines a method to evaluate the survival and integration of engineered stem cells after transplantation into host tissue [43].
- Cell Labeling: Label your genetically engineered stem cells (e.g., from Protocol 1) with a fluorescent cell tracker (e.g., CM-Dil) or express a reporter gene like GFP for in vivo tracking.
- Animal Model Preparation: Utilize an immunodeficient mouse model to avoid graft rejection. For disease-specific studies (e.g., muscular degeneration, blood diseases), use established animal models of the pathology.
- Cell Transplantation: Administer the labeled stem cells via an appropriate route (e.g., intravitreal injection for retinal degeneration, intramuscular injection for muscular degeneration, or systemic infusion for blood diseases).
- In Vivo Imaging: At predetermined time points (e.g., 1, 2, and 4 weeks post-transplantation), use in vivo imaging systems (IVIS) or MRI to track the location and bioluminescence/fluorescence of the transplanted cells as a proxy for survival.
- Histological Analysis: Euthanize the animals at the endpoint and harvest the target tissues. Process the tissues for cryosectioning. Perform immunohistochemistry staining using antibodies against the reporter gene and specific host tissue markers to visualize the precise location and integration of the transplanted cells. Counterstain with DAPI to identify nuclei.
Research Reagent Solutions
Table: Essential Research Reagents for Stem Cell Engineering and Analysis
| Reagent/Material | Function/Application | Example/Citation |
|---|---|---|
| mTeSR Plus Medium | A defined, feeder-free culture medium for the maintenance and expansion of human pluripotent stem cells (hPSCs). | [5] |
| CRISPR-Cas9 System | A genome editing tool comprising Cas9 nuclease and guide RNA (gRNA) for targeted gene knockout, knock-in, or modulation. | [42] [43] |
| dCas9 Effector Systems | Catalytically deactivated Cas9 used for CRISPRi (interference) to repress or CRISPRa (activation) to enhance gene expression without DNA cleavage. | [43] |
| ReLeSR | A non-enzymatic passaging reagent used for the gentle dissociation of hPSC colonies into small aggregates for subculturing. | [5] |
| Vitronectin XF | A defined, human-derived substrate used for coating culture vessels to support the attachment and growth of hPSCs in feeder-free conditions. | [5] |
| Guide RNA (gRNA) | A short RNA sequence that directs the Cas9 protein to a specific DNA locus for cleavage or modulation. | [42] |
Table: Summary of Key Quantitative Parameters in Stem Cell Culture Troubleshooting
| Parameter | Optimal Range or Value | Effect of Deviation | Citation |
|---|---|---|---|
| Medium Age (at 2-8°C) | < 2 weeks | Increased risk of spontaneous differentiation | [5] |
| Time Plate Out of Incubator | < 15 minutes | Stress-induced differentiation | [5] |
| Cell Aggregate Size (Target) | 50 - 200 µm | Smaller (<50µm): poor survival; Larger (>200µm): core necrosis | [5] |
| Incubation Time Adjustment (ReLeSR) | ± 1 - 2 minutes | Fine-tunes aggregate size; reduces differentiation | [5] |
Signaling Pathway and Experimental Workflow Diagrams
Overcoming Translational Hurdles: Strategies to Enhance Survival, Retention, and Safety
Troubleshooting Guide: FAQs on Post-Transplantation Cell Death
Transplanted stem cells, particularly Mesenchymal Stem Cells (MSCs), face a harsh microenvironment that can lead to massive cell death within the first few days after administration [44]. This significantly limits the therapeutic efficacy of regenerative treatments. The table below addresses the core challenges and their underlying causes.
| Challenge | Primary Cause | Key Mechanism |
|---|---|---|
| Anoikis | Loss of cell adhesion to the Extracellular Matrix (ECM) | Detachment from the ECM triggers integrin-mediated intrinsic apoptosis pathways [45] [44]. |
| Hypoxia | Nutrient and oxygen deprivation at the injury site | Inadequate blood supply creates a harsh environment that leads to energy depletion and necrotic cell death [44]. |
| Oxidative Stress | Inflammatory response and reactive oxygen species (ROS) generation | Inflammatory cells (neutrophils, macrophages) recruited to the injury site generate high levels of ROS, inducing apoptosis and inactivating protective nitric oxide [44]. |
Experimental Protocols for Enhancing Cell Survival
Genetic Modification to Inhibit Anoikis
Objective: To enhance MSC resistance to detachment-induced apoptosis (anoikis) through genetic engineering.
Detailed Methodology:
- Target Selection: Select genes involved in anoikis regulation. For instance, knockout of Toll-Like Receptor 4 (TLR4) has been shown to improve MSC survival [44].
- Gene Delivery: Use lentiviral or adenoviral vectors to deliver CRISPR/Cas9 components for knockout or to overexpress anti-apoptotic genes (e.g., Bcl-2, AKT) in MSCs during in vitro culture.
- Validation:
- In Vitro Anoikis Assay: Confirm enhanced anoikis resistance by placing genetically modified MSCs in ultra-low attachment plates to prevent adhesion. After 24-48 hours, measure cell viability using an ATP-based assay and compare to untransfected controls.
- Signaling Analysis: Use western blotting to verify the downregulation of pro-apoptotic proteins (e.g., Bax, active caspase-3) and upregulation of survival pathways (e.g., phosphorylated AKT) in the modified cells when in suspension [46].
Hypoxic Preconditioning
Objective: To prime MSCs for the low-oxygen environment of the transplantation site, improving their tolerance and survival.
Detailed Methodology:
- Preconditioning Culture: Expand MSCs in vitro and then subject them to low oxygen tension (1-3% O₂) in a specialized hypoxia workstation or multi-gas incubator for 24-72 hours prior to detachment and transplantation.
- Mechanistic Insight: This preconditioning activates cellular adaptive responses, primarily through the stabilization of Hypoxia-Inducible Factors (HIFs), which upregulate genes involved in glycolysis, angiogenesis (e.g., VEGF), and cell survival [44].
- Functional Validation: Assess the efficacy of preconditioning by measuring the secretion of pro-survival factors (VEGF, HGF) in cell culture supernatant via ELISA and by demonstrating improved in vivo survival in an animal injury model using cell tracking methods.
Pretreatment with Bioactive Molecules
Objective: To bolster the cells' intrinsic defense mechanisms against oxidative stress and apoptosis.
Detailed Methodology:
- Reagent Selection: Pretreat MSCs with cytokines, growth factors, or antiapoptotic molecules before transplantation. Examples include:
- Growth Factors: Insulin-like Growth Factor-1 (IGF-1) or Fibroblast Growth Factor-2 (FGF-2) [44].
- Antioxidants: Compounds that scavenge ROS, such as N-acetylcysteine (NAC).
- Treatment Protocol: Incubate MSCs with the selected reagent at a determined optimal concentration for a defined period (e.g., 4-24 hours) in standard culture conditions.
- Outcome Measurement: Post-treatment, challenge the cells with oxidative stress (e.g., hydrogen peroxide) and quantify survival rates. Alternatively, analyze the activation of pro-survival signaling pathways like PI3K/AKT via western blot [46].
Research Reagent Solutions
The following table lists key reagents used in the aforementioned experimental strategies.
| Research Reagent | Primary Function in This Context |
|---|---|
| CRISPR/Cas9 System | Gene editing tool for knocking out pro-apoptotic genes or introducing survival genes [44]. |
| Lentiviral Vectors | Efficient delivery system for stable genetic modification of MSCs [44]. |
| Hypoxia Chamber | Sealed chamber that maintains a controlled, low-oxygen environment for cell preconditioning. |
| Recombinant IGF-1 / FGF-2 | Growth factors used in pretreatment to activate PI3K/AKT and other pro-survival pathways [44]. |
| Vitronectin XF / Matrigel | Defined or complex ECM substrates used to enhance cell adhesion and mitigate anoikis in culture [5]. |
| Anoikis Assay Kit | Commercial kit containing ultra-low attachment plates and reagents to quantify detachment-induced cell death. |
Signaling Pathways in Cell Survival and Death
Understanding the molecular pathways is crucial for developing targeted interventions. The following diagrams illustrate the key signaling cascades involved.
Anoikis Activation Pathway
This diagram depicts the integrin-mediated signaling cascade that leads to anoikis, a major challenge in cell transplantation.
Pro-Survival AKT Signaling Pathway
This diagram shows the PI3K/AKT pathway, a key cell survival mechanism that can be targeted to improve post-transplantation outcomes.
The successful integration of transplanted cells into host tissue is a cornerstone of regenerative medicine. A critical determinant of this success is managing immune compatibility, a challenge that requires distinct strategies based on whether the cell source is autologous (derived from the patient) or allogeneic (derived from a donor). This technical support center provides a foundational overview of key concepts, troubleshooting guides, and frequently asked questions to assist researchers in navigating the complex immunological landscape of stem cell therapy, thereby enhancing engraftment and therapeutic efficacy.
Foundational Concepts: Autologous vs. Allogeneic Cell Therapies
What are the core differences between autologous and allogeneic cell sources?
The choice between autologous and allogeneic cell sources dictates the entire research and development pathway, from manufacturing to clinical application. The table below summarizes the fundamental distinctions.
Table 1: Core Differences Between Autologous and Allogeneic Cell Therapies
| Feature | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [47] | Healthy donor's cells [47] |
| Key Advantage | Minimal risk of immune rejection and GvHD; inherent compatibility [47] [48] | "Off-the-shelf" availability; scalable production; potential for cost savings [47] [48] [49] |
| Primary Challenge | Complex, patient-specific logistics; high cost; variable cell quality due to patient health [47] [48] | Risk of immune rejection (GvHD) and host-mediated elimination; requires immunosuppression or matching [47] [48] [49] |
| Manufacturing Model | Customized, small-scale for individual patients [47] | Standardized, large-scale batches for multiple patients [47] |
| Ideal Use Case | Non-urgent treatments where immune compatibility is paramount [47] | Treatments requiring immediate availability and broad patient access [47] [49] |
Troubleshooting Guide for Immune Compatibility
Autologous Cell Therapy Challenges
Problem: Low viability or functionality of patient-derived cells.
- Potential Cause: Patient factors such as age, disease status, or prior treatments (e.g., chemotherapy) can negatively impact the quality and potency of the harvested cells [50] [48].
- Solution Strategy: Implement rigorous donor cell screening and selection criteria. For MSCs, consider using sources from younger donors (e.g., umbilical cord) if autologous therapy is not feasible [51]. Functional assays to check proliferation and differentiation capacity prior to expansion are recommended.
Problem: High rates of cell death upon reinfusion.
- Potential Cause: Transplanted cells undergo mechanical stress during injection and face a harsh microenvironment (e.g., hypoxia, inflammation) at the implantation site, leading to anoikis (detachment-induced apoptosis) and poor engraftment [50].
- Solution Strategy: Utilize a tissue engineering approach. Co-delivering cells with extracellular matrix (ECM) molecules or biomaterial scaffolds can protect cells from anoikis and inflammatory attacks, improve retention, and direct cell fate [50].
Allogeneic Cell Therapy Challenges
Problem: Graft-versus-Host Disease (GvHD) in allogeneic transplantation.
- Potential Cause: Donor T cells present in the graft recognize the recipient's tissues as foreign and mount an immune attack [47] [52].
- Solution Strategy: Employ T-cell depletion from the donor graft [53]. Furthermore, select cell types with inherent low immunogenicity, such as Mesenchymal Stem Cells (MSCs), which are considered immune-privileged and can suppress immune responses [48] [7].
Problem: Host versus Graft rejection leading to poor engraftment.
- Potential Cause: The recipient's immune system recognizes the donor cells as foreign and eliminates them. This is often due to Human Leukocyte Antigen (HLA) mismatches [48] [52].
- Solution Strategy:
- Improve HLA Matching: Utilize high-resolution matching techniques, such as eplet analysis, which assesses mismatch at the epitope level for better risk stratification [52].
- Use "Megadose" Transplants: Administering a very large dose of stem cells can help overwhelm the host's immune rejection mechanisms [53].
- Genetic Engineering: Modify donor cells to evade the host immune system (e.g., knock down HLA molecules) [49].
- Leverage Immunomodulatory Cells: Use regulatory cell populations, such as Veto cells, to promote immune tolerance and engraftment, particularly in haploidentical transplants [53].
Frequently Asked Questions (FAQs)
Q1: What are the key immune actors in graft rejection?
- A: The primary actors are:
- Human Leukocyte Antigens (HLAs): Highly polymorphic cell surface proteins. Mismatches between donor and recipient are the main trigger for rejection [52].
- T Cells: Both CD8+ (cytotoxic) and CD4+ (helper) T cells directly attack donor cells or orchestrate the immune response [52].
- B Cells & Donor-Specific Antibodies (DSAs): B cells produce DSAs that target donor HLA and other antigens, leading to antibody-mediated rejection [52].
- Natural Killer (NK) Cells: Can lyse allogeneic cells that lack "self" HLA molecules [50].
Q2: Beyond cell source selection, what are general strategies to enhance immunocompatibility?
- A: Two primary strategies are preconditioning and co-administration with supportive materials.
- Preconditioning: Treating cells with cytokines (e.g., IFN-γ, TNF-α), growth factors, or hypoxia before transplantation can enhance their immunomodulatory functions, survival, and resistance to the hostile transplant environment [51].
- Supportive Materials: As mentioned in the troubleshooting guide, using biomaterial scaffolds or hydrogels can shield cells from immune attack and provide a supportive ECM, drastically improving engraftment success [50].
Q3: Why are Mesenchymal Stem Cells (MSCs) so prominent in allogeneic therapy research?
- A: MSCs possess unique immunomodulatory properties that make them attractive for allogeneic use. They can suppress T-cell proliferation, modulate macrophage polarization, and promote regulatory T-cell differentiation [54] [7]. Furthermore, they have low immunogenicity and can be derived from multiple sources, including bone marrow, adipose tissue, and umbilical cord, offering flexibility in sourcing [54] [7].
Experimental Protocols for Enhancing Immunomodulation
Protocol: Cytokine Preconditioning of MSCs
This protocol is designed to enhance the immunomodulatory potency of MSCs prior to transplantation [51].
- Cell Preparation: Culture MSCs to 70-80% confluence under standard conditions.
- Priming Reagent Preparation: Prepare a fresh culture medium containing the priming cytokine. For IFN-γ preconditioning, a common effective concentration is 25-50 ng/mL [51].
- Preconditioning Incubation: Replace the standard culture medium with the cytokine-containing medium. Incubate the cells for 24-48 hours. The optimal duration may vary based on the MSC source and target disease.
- Harvesting Preconditioned Cells: After incubation, wash the cells with PBS to remove the cytokine medium. Proceed with standard trypsinization and cell harvesting techniques.
- Validation (Recommended): Validate the preconditioning efficacy by measuring the upregulation of key immunomodulatory factors, such as IDO (Indoleamine 2,3-dioxygenase) activity or PGE2 (Prostaglandin E2) secretion, via ELISA or PCR.
Protocol: T-Cell Depletion for Allogeneic Grafts
This outlines a key step in reducing the risk of GvHD in allogeneic hematopoietic stem cell transplantation (HSCT) [53].
- Graft Collection: Collect the donor graft via apheresis.
- Cell Separation: Isolate mononuclear cells from the apheresis product using density gradient centrifugation.
- T-Cell Depletion: Use immunomagnetic bead selection technology. Incubate the cell product with magnetic beads conjugated to antibodies against T-cell surface markers (e.g., CD3).
- Magnetic Separation: Pass the cell-bead mixture through a magnetic column. The labeled T cells are retained in the column, while the depleted graft (enriched for stem cells) is collected.
- Quality Control: Perform flow cytometry analysis on the final product to confirm the reduction in CD3+ T cells to the desired level.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Immune Compatibility Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Immunomagnetic Beads | Negative or positive selection of specific cell populations [53] | Depletion of CD3+ T cells from an allogeneic donor graft to prevent GvHD [53]. |
| Preconditioning Cytokines (e.g., IFN-γ, TNF-α) | Enhancing the immunomodulatory and survival properties of cells prior to transplant [51] | Priming MSCs to increase secretion of PGE2 and IDO, boosting their ability to suppress T-cell responses [51]. |
| Biomaterial Scaffolds / Hydrogels | Mimicking the extracellular matrix to support cell adhesion and protect from anoikis [50] | Co-delivering MSCs in a hydrogel to a myocardial infarction site to improve cell retention and engraftment [50]. |
| HLA Typing Kits | Determining the HLA profile of donor and recipient cells for match assessment [52] | Screening donors to find the best possible match for a recipient to minimize rejection risk. |
| Cell Viability & Cytotoxicity Assays | Quantifying cell survival and immune-mediated killing in vitro. | Assessing the susceptibility of allogeneic cells to host NK cell or T cell attack in a co-culture model. |
Visualization of Key Workflows and Relationships
Allogeneic vs. Autologous Pathways
Immune Rejection Mechanisms
MSC Preconditioning Workflow
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary challenges in achieving functional synaptic integration of stem cell-derived neurons into a host neural circuit? The main challenges involve the hostile microenvironment of the injured tissue, which leads to low survival and inefficient neuronal differentiation of grafted cells. Furthermore, there is often a lack of robust, functional synapse formation and electromechanical coupling between the transplanted neurons and the host neural network, preventing the restoration of signal transmission [55] [56].
FAQ 2: What is electromechanical coupling in the context of neural circuits, and why is it important? In voltage-gated ion channels, electromechanical coupling refers to the long-range allosteric interactions where the conformational state of the voltage-sensing domain regulates the activity of the pore domain. This process is fundamental for converting electrical signals into mechanical action (ion flow), which is essential for neuronal firing and signal propagation [57]. Successful functional integration requires grafted neurons to properly participate in this electromechanical process.
FAQ 3: Which signaling pathways can be targeted to enhance synapse formation and cell survival? The NT-3/TRKC/AKT signaling pathway is a critical target. Research shows that activating this pathway significantly promotes neuronal differentiation, synapse formation, and the survival of grafted neural stem cells. Electroacupuncture has been identified as a non-invasive strategy that can upregulate this pathway in an injured spinal cord [55].
FAQ 4: Are there non-invasive techniques that can improve the microenvironment for neural integration? Yes, Electroacupuncture (EA) applied at Governor Vessel (GV) acupoints is a safe and effective non-invasive strategy. It has been demonstrated to enhance the level of endogenous neurotrophic factors like NT-3, reduce inflammation, and promote axonal regeneration, thereby creating a more favorable microenvironment for grafted cells [55].
FAQ 5: What are the key markers used to confirm successful synapse formation? Key pre-synaptic markers include Synapsin I (SYN), while a key post-synaptic marker is Post-Synaptic Density 95 (PSD95). The presence and co-localization of these proteins, along with functional evidence from techniques like whole-cell patch clamp recording of miniature Excitatory Post-Synaptic Currents (mEPSCs), are used to confirm functional synaptogenesis [55].
Troubleshooting Guides
Table 1: Troubleshooting Low Grafted Cell Survival and Poor Integration
| Problem Description | Possible Cause | Recommended Solution |
|---|---|---|
| Low survival rate of grafted neural stem cells (NSCs) in the host tissue. | Hostile microenvironment at the injury site; lack of neurotrophic support [55]. | Pre-engineer NSCs to overexpress neurotrophic factors like NT-3 prior to transplantation. Combine with adjunct therapies like electroacupuncture (EA) to boost endogenous NT-3 levels [55]. |
| Grafted cells predominantly differentiate into astrocytes instead of neurons. | Inflammatory cues and a non-permissive microenvironment pushing glial fate [55]. | Genetically modify NSCs to concurrently overexpress NT-3 and its receptor TRKC to drive neuronal lineage commitment. Use 3D scaffold systems to provide a supportive niche [55]. |
| Failure of grafted neurons to form functional synapses with the host circuit. | Absence of necessary pre- and post-synaptic specializations; lack of synaptic proteins and electrical activity. | Co-culture NT-3 and TRKC NSCs in a 3D gelatin sponge (GS) scaffold in vitro to pre-form a neural network with synaptic structures before transplantation [55]. |
| Inability to demonstrate functional electromechanical coupling and signal transmission. | Immature or inefficient voltage-gated ion channel function in derived neurons; poor synaptic transmission. | Validate synaptic function in vitro using whole-cell patch clamp to record action potentials and mEPSCs. Post-transplantation, use trans-synaptic viral tracers (e.g., Pseudorabies virus) to map functional connectivity [55]. |
Table 2: Quantitative Data on Combination Therapy (NN Scaffold + EA)
| Experimental Metric | NN Transplant Only | NN Transplant + Electroacupuncture | Measurement Technique |
|---|---|---|---|
| Grafted Cell Survival | Low number of GFP+ cells at graft site [55]. | Significant increase in GFP+ cell number and volume; cells migrated caudally [55]. | Immunofluorescence, Cell Counting |
| Neuronal Differentiation | Majority of cells differentiated into astrocytes [55]. | >60% of NSCs differentiated into MAP2+ neurons; lowest percentage of GFAP+ astrocytes (~14%) [55]. | Immunofluorescence (IF) Staining |
| Synapse Formation (SYN/PSD95) | Low expression of synaptic markers [55]. | Highest expression of Synapsin I and PSD95 proteins [55]. | Western Blot, IF Staining |
| Synaptic Transmission (mEPSC Frequency) | 0.52 ± 0.18 Hz (in vitro NN construct) [55]. | 0.83 ± 0.20 Hz (in vitro NT-3+NSC+TRKC NSC group) [55]. | Whole-cell Patch Clamp |
| Host-Graft Circuit Integration | Limited synaptic connections with host [55]. | Strengthened synaptic integration, as shown by trans-synaptic viral tracing [55]. | Pseudorabies Virus Tracing |
Detailed Experimental Protocols
Protocol 1: Establishing a 3D Neural Network Scaffold with Synaptic Transmission In Vitro
This protocol details the creation of a tissue-engineered neural network (NN) from neural stem cells (NSCs) designed for subsequent transplantation [55].
Key Reagents:
- NSCs (e.g., from GFP transgenic rat hippocampus).
- Recombinant adenovirus for NT-3 (Ad-NT-3) and TRKC (Ad-TRKC).
- 3D Gelatin Sponge (GS) Scaffold.
- Neuronal differentiation media.
Methodology:
- NSC Culture and Transfection: Harvest and culture NSCs as free-floating neurospheres. Transfect NSCs using Ad-NT-3 or Ad-TRKC.
- 3D Seeding and Co-culture: Seed the transfected NSCs (a co-culture of NT-3 NSCs and TRKC NSCs) into the 3D GS scaffold.
- Differentiation and Maturation: Culture the construct for 14 days in neuronal differentiation media to allow for network formation.
- Functional Validation:
- Immunostaining: Confirm expression of NT-3, TRKC, and synaptic markers (MAP2, SYN, PSD95).
- Electron Microscopy (EM): Visualize ultrastructural synaptic contacts (pre-synaptic vesicles, synaptic cleft, post-synaptic density).
- Electrophysiology: Use whole-cell patch clamp to record mEPSCs and action potentials from derived neurons to confirm functional synaptic transmission.
Protocol 2: In Vivo Transplantation and Electroacupuncture (EA) Enhancement
This protocol describes the transplantation of the pre-formed NN into a spinal cord injury model and the application of EA to promote integration [55].
Key Reagents:
- Anesthetics and surgical equipment.
- Stereotaxic injection system.
- Electroacupuncture apparatus.
Methodology:
- Transplantation: Transplant the mature 3D NN scaffold into the lesion site of a transected spinal cord model.
- Electroacupuncture Application:
- Acupoints: Apply EA to Governor Vessel (GV) acupoints, located in the sunken points between adjacent spinous processes along the spine.
- Parameters: A typical regimen involves treatment administered every other day for 8 weeks post-transplantation.
- Functional and Histological Analysis:
- Locomotor Recovery: Assess functional recovery using standardized behavioral scales (e.g., BBB scale for hindlimb movement).
- Tract Tracing: Inject Pseudorabies virus into a region caudal to the graft to retrogradedly trace synaptic connections from host to graft.
- Histology: Analyze tissue sections for graft cell survival (GFP), neuronal differentiation (MAP2), and synapse formation (SYN/PSD95).
Signaling Pathway and Workflow Visualizations
Diagram 1: NT-3/TRKC/AKT Signaling Pathway
Diagram 2: Experimental Workflow for Neural Relay Construction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Promoting Neural Integration
| Research Reagent | Primary Function in Experiment |
|---|---|
| Neural Stem Cells (NSCs) | The foundational cell source with multi-lineage differentiation potential, used to generate new neurons for circuit repair [55] [58]. |
| Adenovirus (Ad-NT-3 / Ad-TRKC) | Viral vectors for the efficient overexpression of neurotrophin-3 (NT-3) and its high-affinity receptor TRKC, crucial for driving neurogenesis and synaptogenesis [55]. |
| 3D Gelatin Sponge (GS) Scaffold | A biocompatible, porous 3D structure that provides a permissive physical and trophic microenvironment for NSC growth, network formation, and transplantation [55]. |
| Electroacupuncture Apparatus | A device for applying controlled electrical stimulation to specific acupoints (e.g., GV points), used to non-invasively modulate the host microenvironment and boost endogenous NT-3 [55]. |
| Pseudorabies Virus (PRV) | A trans-synaptic, retrograde neuronal tracer used to map and validate the functional synaptic connectivity between the host neural circuit and the grafted neurons [55]. |
| Antibodies (MAP2, SYN, PSD95, GFP) | Essential tools for immunohistochemistry and Western Blot to identify neurons (MAP2), visualize synapses (SYN/PSD95), and track grafted cells (GFP) [55]. |
Technical Support Center
Troubleshooting Guides
Guide 1: Addressing Cell Passage-Induced Variability
Problem: Cell morphology, growth rates, and protein expression change unpredictably at high passage numbers, compromising experimental reproducibility [59].
Investigation & Solution:
- Step 1: Establish a Baseline - Determine the specific passage number range for your cell line where performance remains consistent. This range is cell line-specific and must be empirically defined [59].
- Step 2: Implement Routine Monitoring - Perform frequent checks for changes in cellular morphology and routinely generate growth curve data to monitor proliferation rates [59].
- Step 3: Use Low-Passage Cell Banks - Source cell lines from reputable biological resource centers that provide well-characterized, low-passage stocks to minimize starting variability [59].
- Step 4: Automate Characterization - Utilize automated platforms like the Cell X system for quantitative, image-based analysis of cell and colony attributes to guide standardized passage protocols [60].
Guide 2: Mitigating Scalability and Regulatory Risks in Manufacturing
Problem: Manual, labor-intensive processes do not translate well to larger scales, leading to batch failures and regulatory clinical holds due to Chemistry, Manufacturing, and Controls (CMC) issues [61] [62].
Investigation & Solution:
- Step 1: Adopt Scalable Technologies Early - Implement single-use bioreactors and scalable transfection reagents early in process development. Bioreactor systems scalable from 250 mL to 2000 L can ensure a seamless transition from development to commercial manufacturing [61].
- Step 2: Implement Process Control - Apply Quality by Design (QbD) principles and Design of Experiment (DoE) software to optimize process parameters and define your control strategy [61] [63].
- Step 3: Ensure CMC Compliance - Develop a robust CMC strategy from the outset. Recent FDA data shows that 74% of Complete Response Letters are due to manufacturing deficiencies, including insufficient process control and unvalidated analytical methods [62].
- Step 4: Close and Automate Processes - Utilize closed, automated systems like the Lonza Cocoon to reduce contamination risks, lower cleanroom requirements, and improve batch-to-batch reproducibility [63] [64].
Frequently Asked Questions (FAQs)
FAQ 1: What are the critical passage-related changes we should monitor in our cell lines? Passage number can significantly alter a cell line's characteristics. You should routinely monitor for changes in [59]:
- Morphology: Observable changes in cell shape and structure.
- Growth Rates: Sudden increases or decreases in population doubling times.
- Protein Expression & Transfection Efficiency: Changes in the expression of key proteins or the cell's ability to take up foreign DNA.
- Genotypic and Phenotypic Drift: Evolutionary changes and genomic instability that occur over time in culture.
FAQ 2: Our allogeneic therapy requires massive cell expansion. How can we ensure consistency? Ensuring consistency for large-scale allogeneic therapies requires a multi-faceted approach:
- Scalable Bioreactor Systems: Use single-use bioreactors that allow for controlled, large-volume cell expansion [61].
- Process Automation: Implement automated systems for liquid handling and cell culture to minimize human error and variability [64].
- Advanced Cell Sources: Consider induced pluripotent stem cell-derived mesenchymal stem cells (iMSCs), which offer enhanced consistency and scalability compared to primary MSCs from donors [65].
FAQ 3: What are the most common regulatory pitfalls for cell therapies, and how can we avoid them? The most common regulatory pitfalls are related to Chemistry, Manufacturing, and Controls (CMC). To avoid them [61] [62]:
- Start Early: Integrate CMC strategy into early development, not after clinical proof-of-concept.
- Build a Robust Control Strategy: This includes validated analytical methods, comprehensive product characterization, and thorough process performance data.
- Choose the Right Partners: If using a CDMO, select based on technical capability and cultural alignment, not just cost.
- Generate Comparability Data: Be prepared to demonstrate that changes in your manufacturing process do not impact product safety or efficacy.
FAQ 4: How can automation address the high costs and variability of autologous cell therapies? For autologous therapies, where batches are for a single patient, automation is key to "scaling out" rather than "scaling up." This involves [64]:
- Parallel Processing: Using automated, closed systems (e.g., the Lonza Cocoon) to run multiple patient batches simultaneously.
- Reduced Manual Labor: Automating steps like pipetting and media changes cuts the cost of highly skilled labor and reduces contamination risk.
- Standardized Decision-Making: Replacing subjective technician judgments with automated, quantitative metrics for cell selection and culture management improves batch-to-batch reproducibility [60].
Table 1: Quantitative Effects of Passage Number on Specific Cell Lines [59]
| Cell Line | Low Passage # | High Passage # | Observed Effects |
|---|---|---|---|
| MIN-6 (Mouse insulinoma) | Passage 18 | Passage 40 | Differential expression of nearly 1,000 genes involved in secretion, adhesion, and proliferation. |
| LNCaP (Human prostate) | Passage 25 | Passage 60 | Altered regulation of androgen receptor activity via the PI3K/Akt pathway. |
| Caco-2 (Human colon) | Unpublished Data | Unpublished Data | Increase in GFP reporter gene expression after transfection. |
| MCF7 (Human breast) | Unpublished Data | Unpublished Data | Decrease in GFP reporter gene expression after transfection. |
Table 2: Key Solutions for Manufacturing Challenges in Advanced Therapies [61] [66] [63]
| Challenge Category | Specific Hurdle | Proposed Solution & Technology |
|---|---|---|
| Scalability | Transition from 2D to 3D culture; Large-volume expansion. | Single-use bioreactor systems (e.g., from 250 mL to 2000 L); Micro/mini bioreactors (Ambr) for process optimization [61] [63]. |
| Standardization | High donor-to-donor and batch-to-batch variability. | Automated, closed-system processing (e.g., Lonza Cocoon); QbD and DoE software; Allogeneic iPSC-derived cell sources (e.g., iMSCs) [61] [60] [65]. |
| Regulatory (CMC) | Insufficient process control and product characterization. | Early development of potency assays and validated analytical methods; Strategic CDMO partnerships with proven platforms [62]. |
| Safety | Risk of contamination and tumorigenicity. | Closed-system bioreactors; In vivo tumorigenicity assays in immunocompromised models; Karyotype testing for genetic stability [66]. |
Experimental Protocols
Protocol 1: Automated, Image-Based Selection and Characterization of Stem Cell Colonies
This protocol utilizes the Cell X robotic platform and Colonyze image analysis software for standardized, quantitative management of iPSC or MSC cultures [60].
Methodology:
- Image Acquisition: Culture cells in a dish compatible with the automated inverted fluorescent microscope. Capture large field-of-view (LFOV) brightfield or phase-contrast images. For more detailed analysis, 2D or 3D fluorescence images can be acquired.
- Quantitative Analysis: Use the Colonyze software, which complies with ASTM Standard Method F-2944-12, to analyze the LFOV images. The software quantifies metrics for every cell and colony, including:
- Cell number and confluence.
- Colony number and individual colony attributes (cell number, density, morphology).
- Multimodal attributes (e.g., area and intensity of fluorescence markers).
- Precision Manipulation: Based on the quantitative metrics defined as Critical Quality Attributes (CQAs), program the Cell X robot to perform targeted actions:
- Picking: Select and isolate desired cells or colonies.
- Weeding: Remove undesired cells showing spontaneous differentiation.
- Biopsy: Extract cells or media for further in-process testing.
- Documentation: The platform automatically documents the location, physical/biological attributes of manipulated cells, and all process parameters for full quality control traceability.
Protocol 2: Scalable Expansion of Human iPSCs in Bioreactors
This workflow, developed in collaboration with Stanford University, outlines a process for the scalable production of high-quality human induced pluripotent stem cells (iPSCs) [61].
Methodology:
- Process Development in Micro-Bioreactors: Use a high-throughput automated micro-bioreactor system (e.g., Ambr 250 modular system) for initial process optimization. This includes media screening, and determining critical process parameters (CPPs) like pH, dissolved oxygen, and agitation.
- Small-Scale Model Validation: Scale the optimized process from the micro-bioreactors to small-scale glass bioreactors (e.g., Univessel Glass Bioreactors at 2L) to confirm process performance and product quality (e.g., cell yield, viability, pluripotency marker expression).
- Scale-Up to Production Volume: Once reproducibility is confirmed at the small scale, transfer the process to larger single-use bioreactors (e.g., 10L and beyond) for the production of billions of iPSCs required for clinical or commercial applications.
- Establish Differentiation Protocols: Following expansion, establish efficient differentiation protocols to generate the required specialized cell types (e.g., cardiomyocytes) in the necessary quantities.
Process Visualization Diagrams
Diagram 1: Automated Cell Culture Management Workflow
Diagram 2: Tech Transfer & Scale-Up Pathway for GMP Compliance
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Standardized and Scalable Cell Therapy Manufacturing
| Item | Function & Application | Key Consideration |
|---|---|---|
| Micro/Mini Bioreactor Systems (e.g., Ambr) | High-throughput process development and optimization for suspension or adherent cells in a scaled-down model [61]. | Allows for DoE studies to define CPPs before moving to large, expensive GMP batches. |
| Single-Use Bioreactors | Scalable cell expansion from pre-clinical to commercial scale (e.g., 250 mL to 2000 L) in a closed, sterile system [61]. | Reduces cleaning validation burden and cross-contamination risk, accelerating campaign changeover. |
| GMP-Grade Cell Culture Media & Reagents | Xeno-free, serum-free media, supplements, and transfection reagents for use with clinical-grade cell types [61]. | Essential for regulatory compliance; ensures raw materials are traceable and meet quality standards for human use. |
| Automated Cell Characterization Platform (e.g., Cell X) | Non-invasive, quantitative image analysis to guide automated cell/colony picking, weeding, and biopsy based on CQAs [60]. | Replaces subjective manual selection, standardizes protocols between labs and operators, and provides full documentation. |
| Closed and Automated Therapy Systems (e.g., Cocoon) | Automated, functionally closed system for manufacturing autologous cell therapies at the point-of-care or centrally [63]. | Reduces manual labor and cleanroom grade requirements, enabling scalable and cost-effective personalized manufacturing. |
The Core Scientific Challenge: Understanding Tumorigenicity in Stem Cells
What is the fundamental link between stem cell pluripotency and tumorigenicity?
The capacity for uncontrolled growth is an intrinsic challenge in stem cell research, deeply connected to the very properties that make these cells promising for therapy. Pluripotent stem cells (PSCs), including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), share significant molecular machinery with tumor cells [67]. Core transcription factors used for cellular reprogramming, such as c-MYC and KLF4, are established oncogenes, while others like SOX2 and NANOG are frequently overexpressed in various cancers [68] [67]. The teratoma assay, a standard test for demonstrating a cell's pluripotency, is itself a tumorigenicity test, underscoring this deep biological link [67]. The central, unresolved scientific question is whether the properties of pluripotency and tumorigenicity are inextricably coupled, or if they can be separated [67].
Through what mechanisms can stem cell therapies pose tumorigenic risks?
- *Residual Undifferentiated Cells:* The final cellular product intended for transplantation may contain small populations of PSCs that failed to differentiate. These residual cells retain high proliferative capacity and can lead to teratoma formation in vivo [69].
- *Somatic Mutation Accumulation:* During ex vivo culture and expansion, cells can acquire genetic and epigenetic mutations. Key mutations, such as in the p53 tumor suppressor pathway, not only enhance reprogramming efficiency but also significantly increase tumorigenicity risk [68].
- *Incomplete Reprogramming:* The reprogramming of somatic cells to iPSCs can be inefficient and incomplete, potentially resulting in cells with an unstable epigenetic state prone to malignant transformation [68].
- *Oncogenic Transgene Reactivation:* When using integrating viral vectors for reprogramming, a key risk is the potential lack of silencing of the integrated transgenes. These transgenes may be re-expressed after transplantation, driving uncontrolled growth [68].
Assessment and Evaluation: Preclinical Tumorigenicity Testing
A rigorous, multi-tiered preclinical assessment is critical for evaluating the tumorigenic potential of any cell-based product. The following table summarizes the core methodologies. Note that regulatory requirements vary globally, and no single, universally standardized technical guide exists; the strategy must be tailored to the specific product and its intended use [69].
Table 1: Preclinical Methods for Tumorigenicity Evaluation
| Method Type | Method Name | Key Function | Considerations & Limitations |
|---|---|---|---|
| In Vivo Assay | Teratoma Assay | The gold-standard for assessing pluripotency and tumorigenic potential simultaneously. Tests the ability of cells to form differentiated tissues from all three germ layers (ectoderm, mesoderm, endoderm) upon transplantation into immunocompromised mice [67]. | A positive result confirms tumorigenicity; a negative result can be a false negative due to host immune rejection of the cells [67]. |
| In Vivo Assay | Long-Term Tumorigenicity Study | Evaluates the capacity of the final, differentiated cell product to form tumors over an extended period (e.g., up to 1 year) in immunocompromised animal models [70] [69]. | Requires careful design, including appropriate cell dose, route of administration, and use of highly immunodeficient models to ensure engraftment [69]. |
| In Vitro Assay | Karyotype Analysis / G-Banding | Assesses the genomic stability and identity of major chromosomal abnormalities (e.g., aneuploidy, translocations) in master cell banks and final products [70]. | Has limited resolution; cannot detect small genetic mutations. |
| In Vitro Assay | Soft Agar Colony Formation Assay | Tests anchorage-independent growth, a hallmark of oncogenic transformation, by seeding cells in soft agar and monitoring colony formation [69]. | A common in vitro surrogate for tumorigenic potential. |
| Molecular Assay | PCR-Based Vector Copy Number | For genetically modified cells, this quantifies the number of integrated transgenes (e.g., reprogramming factors) in the host genome [68]. | Critical for products derived from integrating vector systems. |
The workflow below outlines the decision-making process for tumorigenicity evaluation, integrating these methods based on the characteristics of the cell-based product [70] [69].
Troubleshooting Guide: Common Issues in the Lab
This section addresses specific, frequently encountered problems related to controlling stem cell growth and differentiation.
Problem 1: Excessive spontaneous differentiation in pluripotent stem cell cultures (>20%).
- Potential Cause & Solution: The culture medium may be outdated or compromised. Ensure complete culture medium is kept at 2-8°C and is less than two weeks old [5].
- Potential Cause & Solution: Colonies were allowed to overgrow. Passage cultures when colonies are large and compact, with dense centers, and avoid plating cell aggregates at too high a density [5].
- Potential Cause & Solution: Excessive time outside the incubator. Minimize handling time and do not have culture plates out of the incubator for more than 15 minutes at a time [5].
- Potential Cause & Solution: Areas of differentiation were not removed. Manually remove differentiated areas from cultures prior to passaging [5].
Problem 2: Low cell survival or attachment after passaging, leading to poor experimental reproducibility.
- Potential Cause & Solution: Incorrect handling of cell aggregates. After passaging, work quickly to minimize the time cell aggregates are in suspension. Do not excessively pipette to break up aggregates; instead, optimize incubation time with the passaging reagent [5].
- Potential Cause & Solution: Inappropriate seeding density. Plate a higher number of cell aggregates initially (e.g., 2-3 times higher) to maintain a more densely confluent culture, which can improve health and attachment [5].
- Potential Cause & Solution: Incorrect plate coating. Verify that non-tissue culture-treated plates are used with certain substrates (e.g., Vitronectin XF), and tissue culture-treated plates are used with others (e.g., Corning Matrigel) [5].
Problem 3: Failure of neural induction from human PSCs.
- Potential Cause & Solution: Poor starting quality of hPSCs. Remove any differentiated or partially differentiated hPSCs before beginning the induction process [6].
- Potential Cause & Solution: Incorrect cell confluency at induction. Cell counting is recommended. Plating density that is too low or too high will reduce efficiency. The recommended plating density for induction is typically 2–2.5 x 10^4 cells/cm² [6].
- Potential Cause & Solution: Using a single-cell suspension. For many protocols, cell clumps (not single cells) should be plated for induction to improve efficiency [6].
Problem 4: Persistent expression of reprogramming vectors in iPSCs.
- Potential Cause & Solution: Inefficient clearance of non-integrating vectors. For Sendai virus-based systems (e.g., CytoTune-iPS Sendai 2.0 Kit), a temperature-sensitive mutant allows vector clearance. Incubate iPSCs at 38–39°C for 5 days to facilitate the removal of c-Myc and KOS vectors, but only after confirming the absence of other vectors (e.g., Klf4) via RT-PCR [6].
Safety Monitoring and Risk Mitigation Frameworks
What are the key biosafety principles for clinical translation?
A comprehensive biosafety framework for cell-based therapies must be built on several operational principles beyond tumorigenicity. These include assessing toxicity, immunogenicity, biodistribution, and final cell product quality [70]. Biodistribution studies, which track the movement and persistence of cells within the recipient, are crucial and typically use quantitative PCR (qPCR) and imaging techniques like PET or MRI [70]. Furthermore, the immunological safety of the product must be evaluated, including the potential to activate complement, T-cell, and NK-cell responses [70].
How can the risk of tumorigenicity be reduced through technological advances?
- *Use of Non-Integrating Reprogramming Methods:* Shift from integrating viral vectors (retrovirus, lentivirus) to non-integrating systems. Promising methods include Sendai virus (an RNA virus that replicates in the cytoplasm), episomal vectors, and direct delivery of reprogramming proteins or messenger RNA (mRNA) [68] [6].
- *Chemical Reprogramming:* The generation of iPSCs using only small molecules is recognized as a promising and potentially safer strategy for clinical-grade manufacturing, as it avoids genetic manipulation entirely [68].
- *Cell Sorting and Purging:* Implementing rigorous purification processes to remove residual undifferentiated pluripotent cells from the final differentiated cell product before transplantation. This can be achieved by using cell surface markers specific for undifferentiated cells and fluorescence-activated cell sorting (FACS) [69].
- *Introduction of "Suicide Genes":* As a fail-safe mechanism, genetic constructs can be introduced into the stem cells that make them susceptible to a specific pro-drug. If uncontrolled growth is detected post-transplantation, administering the drug can selectively eliminate the transplanted cells [67].
The Scientist's Toolkit: Essential Reagents and Methods
Table 2: Key Research Reagent Solutions for Tumorigenicity Mitigation
| Reagent / Tool | Primary Function | Application in Risk Mitigation |
|---|---|---|
| Sendai Virus Vectors | Non-integrating viral vector for reprogramming somatic cells to iPSCs. | Eliminates risk of insertional mutagenesis; temperature-sensitive variants allow for controlled vector clearance post-reprogramming [68] [6]. |
| ROCK Inhibitor (Y-27632) | Small molecule inhibitor of Rho-associated coiled-coil forming kinase (ROCK). | Significantly improves survival of human PSCs after single-cell passaging and cryopreservation, reducing selective pressure for hardier, potentially mutated cells [6]. |
| Geltrex / Matrigel / Vitronectin | Defined extracellular matrix proteins used as substrate for feeder-free PSC culture. | Provides a consistent, defined, and animal-component-free environment, improving culture reproducibility and reducing undefined variables that could impact genomic stability [5] [6]. |
| RevitaCell Supplement | A cocktail containing a ROCK inhibitor and other components. | Used to enhance cell recovery after thawing or passaging, similar to ROCK inhibitor, supporting the maintenance of normal cell growth characteristics [6]. |
| Flow Cytometry Antibodies | Antibodies targeting surface markers (e.g., TRA-1-60, SSEA-4) for pluripotent cells. | Critical for quality control to quantify and remove residual undifferentiated cells from a differentiated cell product before transplantation [69]. |
The following diagram illustrates the multi-layered strategy required to effectively manage tumorigenicity risk, from initial cell manufacturing through to final clinical application.
Bench to Bedside: Analytical Frameworks for Assessing and Comparing Integrative Efficacy
In stem cell research, the ultimate proof of therapeutic success is the successful integration of transplanted cells into host tissue, where they contribute to restoring structure and function. This process involves a complex cascade: activated stem cells are recruited to the injury site, proliferate, differentiate into specific lineages, and ultimately integrate into the existing tissue architecture [2]. A critical challenge for researchers and drug development professionals is not just achieving this integration, but verifying it. This requires sophisticated in vivo models that can track the fate, persistence, and location of administered cells over time within a living organism.
Longitudinal tracking technologies, particularly bioluminescence imaging (BLI), have become indispensable for this task. They allow for the non-invasive, real-time monitoring of cell viability, migration, and engraftment in preclinical models, providing invaluable data on therapeutic efficacy while adhering to the 3Rs (Replacement, Reduction, and Refinement) by enabling repeated measurements in the same animal [71] [72]. This technical support center outlines the core methodologies, troubleshooting guides, and experimental protocols for utilizing these powerful tools in the context of stem cell integration research.
The primary optical imaging modalities for in vivo tracking are bioluminescence and fluorescence. Understanding their fundamental differences is the first step in selecting the appropriate technology for your experiment.
Technology Comparison Table
| Feature | Bioluminescence Imaging (BLI) | Fluorescence Imaging |
|---|---|---|
| Light Source | Internal (enzyme-substrate reaction) [73] | External (laser or lamp) [73] |
| Background Signal | Very low (minimal auto-bioluminescence) [72] | Higher (due to tissue autofluorescence) [72] |
| Excitation Required | No [74] | Yes [73] |
| Sensitivity | High (due to low background) [71] | Moderate (limited by background) |
| Quantification | More straightforward [73] | Challenging (requires background subtraction) [73] |
| Primary Application | Tracking cell location, number, and viability [71] | Visualizing anatomical structures and protein localization |
Bioluminescence Reporter Systems
BLI relies on engineering cells to express a luciferase enzyme, which catalyzes a light-producing reaction upon administration of its specific substrate [71]. The choice of reporter system is critical and depends on the experimental needs. The table below summarizes the key characteristics of the most commonly used luciferases.
Bioluminescence Reporter Comparison
| Luciferase | Origin | Molecular Weight | Emission Maximum | Substrate | Cofactors | Key Features & Considerations |
|---|---|---|---|---|---|---|
| Firefly Luciferase (FLuc) | Firefly (Photinus pyralis) | 62 kDa | 562 nm (Yellow-green) [71] | D-Luciferin [71] | ATP, Mg²⁺, O₂ [71] | - Glow-type kinetics (signal lasts minutes) [71]- Most commonly used reporter [72]- Signal is pH and temperature sensitive [71] |
| NanoLuc (NLuc) | Deep-sea shrimp | 19 kDa | 460 nm (Blue) [72] | Furimazine [72] | None (ATP-independent) [72] | - Extremely bright, small size [72]- Short exposure times- Blue light has poor tissue penetration; best used with BRET systems [72] |
| Renilla Luciferase (RLuc) | Sea pansy (Renilla reniformis) | 36 kDa | 482 nm (Blue) [71] | Coelenterazine [71] | O₂ [71] | - Flash-type kinetics (signal decays rapidly) [71]- Substrate can be unstable with high background [71]- Red-shifted variant (RLuc8) available for better penetration [71] |
| Gaussia Luciferase (GLuc) | Copepod (Gaussia princeps) | ~20 kDa | 480-600 nm [71] | Coelenterazine [71] | None [71] | - Naturally secreted reporter, useful for blood-based assays [71]- Flash-type kinetics [71]- For cell tracking, membrane-tethered versions are recommended [71] |
Experimental Protocols & Workflows
Core Workflow for Bioluminescence Cell Tracking
The following diagram outlines the fundamental steps for a standard bioluminescence imaging experiment to track stem cells, from model creation to data analysis.
Protocol: Cell-Type-Specific Inflammation Tracking
This protocol, adapted from a study on uveitis, details how to track specific immune cell populations, a method that can be applied to monitor inflammatory responses to stem cell implants [74].
- Objective: To longitudinally track the dynamics of specific immune cell lineages (e.g., myeloid cells, T cells) in a living animal model of inflammation or tissue integration.
- Materials:
- Transgenic mouse with a floxed-stop luciferase gene (e.g., ROSA26-LSL-Luc).
- Cell-type-specific Cre-driver mouse lines (e.g., LyzM-Cre for myeloid cells, Lck-Cre for T cells).
- Appropriate substrate (e.g., D-Luciferin for Firefly luciferase).
- In vivo imaging system (IVIS) with a cooled CCD camera.
- Isoflurane anesthesia system.
- Method:
- Generate Experimental Animals: Cross the ROSA26-LSL-Luc mouse with the cell-type-specific Cre-driver line. In the resulting offspring, luciferase will be expressed only in the target cell lineage.
- Induce Disease/Integration Model: Subject the mice to your specific model (e.g., tissue injury, implant surgery, autoimmune induction).
- Image Acquisition:
- Administer the substrate (e.g., 150 mg/kg D-Luciferin intraperitoneally).
- Anesthetize the mouse and place it in the imaging chamber.
- Acquire images at a standardized time post-injection (e.g., 10-15 minutes for IP D-Luciferin). Use auto-exposure settings for initial experiments.
- Data Analysis:
- Define regions of interest (ROIs) over the area of interest (e.g., the injury site or implant).
- Define a background ROI.
- Quantify the signal in units of Radiance (photons/second/cm²/steradian).
- Validation: Correlate bioluminescence signal with post-mortem analysis (e.g., flow cytometry, histology) at endpoint to confirm the cell populations being tracked.
Protocol: Assessing Tissue-Engineered Cartilage Integration
This in vitro protocol provides a model for assessing the integration of engineered tissues, a key principle in regenerative medicine [75].
- Objective: To develop a reproducible model to study the integration between tissue-engineered cartilage and host native cartilage.
- Materials:
- Host osteochondral explant (e.g., from bovine or porcine joint).
- Tissue-engineered biphasic construct (cartilage layer integrated onto a bone substitute scaffold).
- Control autologous osteochondral plug.
- Culture media (e.g., Ham's F12 with ascorbic acid).
- Method:
- Create Explant and Defect: Create a osteochondral explant with a defined, doughnut-shaped host cartilage ring. Create a matching defect in the center.
- Implant Construct: Press-fit the tissue-engineered construct or the autologous control plug into the central defect.
- Culture: Culture the composite construct for several weeks (e.g., 4-8 weeks).
- Assess Integration:
- Histology: Process and stain sections (e.g., H&E, Toluidine Blue). Measure the percentage of the interface where no gap exists between implant and host tissue.
- Biochemistry: Assay for collagen and proteoglycan content at the integration site.
- Biomechanics: Perform a push-out test to measure the adhesive strength at the interface.
- Cell Migration: Pre-label chondrocytes with a fluorescent dye (e.g., carboxyfluorescein diacetate) prior to implantation to track their migration into the host cartilage.
The Scientist's Toolkit: Key Research Reagents
This table lists essential materials and their functions for setting up in vivo tracking experiments.
| Item | Function / Application | Example & Notes |
|---|---|---|
| D-Luciferin | Substrate for Firefly Luciferase (FLuc) [71] | Potassium salt, in vivo grade. Administered IP at 150 mg/kg. |
| Furimazine | Substrate for NanoLuc (NLuc) [72] | Used with Nano-Glo FFz In Vivo Substrate. Enables bright, ATP-independent imaging. |
| Coelenterazine | Substrate for Renilla (RLuc) and Gaussia (GLuc) [71] | Can be less stable; ViviRen is an engineered variant for reduced background [72]. |
| FLuc-Expressing Stem Cells | Engineered cell product for tracking. | Many pre-engineered cancer cell lines exist; stem cells often require in-house viral transduction. |
| ROSA26-LSL-Luc Mouse | Cre-dependent reporter model for cell-type-specific tracking [74] | Crossing with a cell-specific Cre driver (e.g., LyzM-Cre) restricts luciferase expression. |
| IVIS Imaging System | In vivo optical imaging instrument. | Contains a sensitive CCD camera cooled to -90°C to detect low-light signals [73]. |
| Isoflurane Anesthesia System | To anesthetize animals during imaging. | Essential for immobilizing the animal to prevent motion artifacts during (long) exposures. |
| Depilatory Cream | Hair removal. | Critical step: Fur strongly attenuates light. Use on white or hairless mice for best results [73]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q: How much D-luciferin should I inject, and how long should I wait before imaging? A: A standard dose for intraperitoneal (IP) injection in mice is 150 mg/kg [72]. After IP injection, peak signal for Firefly luciferase is typically reached between 10-15 minutes and can remain stable for up to 25-30 minutes. The optimal time window should be empirically determined for your specific model [72].
Q: My image has saturated pixels. What should I do? A: Saturated pixels mean the signal exceeds the camera's linear detection range. To fix this: 1) Reduce the exposure time, 2) use a smaller binning value, or 3) use a larger f-stop (e.g., f/8 instead of f/1) to reduce the amount of light reaching the camera [73].
Q: Should I use IP or IV injection for the substrate? A: IP injection is most common due to its ease and provides a good balance of signal stability and intensity. IV injection (via tail vein) produces a brighter, sharper peak signal almost immediately but decays very rapidly, requiring precise timing. IP is recommended for most longitudinal tracking studies [72].
Q: Can I image two different cell populations in the same animal? A: Yes, through multiplexing. The most robust way is to use two different luciferase systems with distinct, non-cross-reactive substrates, such as FLuc (D-luciferin) and NLuc (furimazine) [72]. Inject substrates sequentially, allowing the signal from the first to decay before injecting the second and imaging again.
Q: Why is my bioluminescence signal low, even though my cells are viable? A: Low signal can result from several factors:
- Fur/Hair: Ensure the imaging area is completely shaved or depilated, especially with dark-furred mice [73].
- Substrate: Verify substrate preparation, concentration, and injection technique.
- Cell Location: Deep-seated or internally located cells will produce a more attenuated signal due to light absorption and scattering by overlying tissue [71].
- Reporter Expression: Confirm luciferase expression in your cells via an in vitro assay before in vivo use.
Q: What is the correct unit to use for quantitative analysis? A: For bioluminescence, use Radiance (photons/second/cm²/steradian). This is a calibrated unit that accounts for the geometry and sensitivity of the instrument. Avoid using raw "Counts," which are uncalibrated and depend heavily on acquisition settings [73].
Troubleshooting Common Problems
| Problem | Possible Cause | Solution |
|---|---|---|
| Low or No Signal | - Substrate degradation/failure- Poor cell survival/engraftment- Heavy fur or pigmentation- Luciferase expression lost | - Prepare fresh substrate; confirm injection.- Check cell viability pre-injection; optimize delivery.- Shave depilate area; use hairless mice if possible.- Verify reporter gene expression in vitro. |
| High Background Signal | (More common in fluorescence) | - For bioluminescence, background is typically low. Ensure no substrate contamination on the animal's fur. |
| Blurry Image | - Animal movement- Incorrect focus- Too coarse binning | - Ensure proper anesthesia depth.- Check and adjust the focus settings.- Use a smaller binning value (e.g., 2x2 instead of 8x8). |
| Strange Ring Artifact in Fluorescence | - Excitation/emission filters too close in wavelength | - Choose an excitation/emission filter pair with a wavelength difference greater than 30 nm [73]. |
| Signal Inconsistency Between Animals | - Variable substrate injection- Differing animal positioning | - Standardize injection technique (same person, same method).- Position animals consistently, minimizing tissue over the region of interest. |
Visualization of Key Concepts
The Stem Cell Integration Cascade
The process of stem cell integration into host tissue is a multi-stage journey, initiated by damage signals and culminating in functional tissue restoration. The following diagram illustrates this cascade, which forms the biological foundation for the tracking methodologies described in this guide.
In stem cell research, demonstrating that transplanted cells have successfully integrated into host tissue is a fundamental milestone. However, the ultimate therapeutic goal is the restoration of physiological function, not merely cellular presence. A growing body of evidence indicates that cell survival and engraftment do not automatically translate to functional recovery [1]. Consequently, the field requires robust, standardized methods to quantify this functional restoration.
This technical support center provides targeted guidance for researchers navigating the complex process of assessing functional outcomes. The following troubleshooting guides and FAQs address common experimental challenges in verifying that stem cell integration leads to meaningful physiological recovery, focusing on practical methodologies and quantitative measures essential for rigorous scientific validation.
Troubleshooting Guide: Functional Outcome Assessment
Problem 1: Poor Correlation Between Cell Engraftment and Functional Recovery You have confirmed stem cell presence and integration at the injury site via histology or imaging, but pre-clinical models show no significant improvement in functional assays.
- Potential Cause 1: The cells may not have differentiated into the correct, functional phenotype or may not have formed appropriate functional connections with host tissue.
Solution:
- Perform immunohistochemical analysis for mature, cell-type-specific markers beyond initial progenitor markers. For neuronal cells, assess synaptophysin for synapse formation [76].
- Conduct electrophysiological studies to confirm functional activity, such as action potentials in neurons or contractions in cardiomyocytes.
- Utilize calcium imaging to visualize network activity in real-time, confirming integration into functional circuits.
Potential Cause 2: The local microenvironment (e.g., persistent inflammation, fibrosis, or inhibitory factors) may be suppressing functional activity of integrated cells [2].
- Solution:
- Modulate the microenvironment using adjunct therapies. Consider administering:
- Immunomodulatory agents (e.g., low-dose tacrolimus) to control rejection.
- Anti-fibrotic agents (e.g., pirfenidone) to reduce scar tissue.
- Re-evaluate functional outcomes after a suitable treatment period.
- Modulate the microenvironment using adjunct therapies. Consider administering:
Problem 2: High Variability in Functional Outcome Measures Functional data from in vivo models is inconsistent, making it difficult to determine statistical significance for your stem cell treatment.
- Potential Cause: Inconsistent animal models of disease/injury lead to high baseline variability in functional capacity.
- Solution:
- Standardize the injury model meticulously. For spinal cord injury, use an calibrated impactor device. For ischemic models, standardize occlusion time.
- Increase sample size to power your study appropriately for the expected effect size and inherent variability.
- Implement baseline functional testing for all subjects pre-operatively and use stratified randomization to ensure equivalent groups.
- Use multiple, complementary functional assays to triangulate your findings (see Table 1).
Problem 3: Difficulty in Tracking Functional Outcomes in Chronic Models In long-term studies, initial functional gains appear to plateau or diminish over time.
- Potential Cause 1: The survival or phenotype of the transplanted cells is not sustained.
Solution:
- Use long-term cell tracking methods such as luciferase-based bioluminescence imaging (BLI) or magnetic particle imaging (MPI) in live animals.
- Perform terminal immunohistochemistry at the study endpoint to confirm the continued presence and phenotype of the cells.
Potential Cause 2: The underlying disease pathology is progressive, overwhelming the therapeutic benefit.
- Solution:
- Consider repeat dosing of cells or supporting trophic factors.
- Combine stem cell therapy with rehabilitative training [77]. In musculoskeletal and neurological models, targeted physical therapy is proven to enhance and consolidate functional gains from cellular therapy by promoting circuit reorganization and tissue remodeling.
Frequently Asked Questions (FAQs)
Q1: What are the key advantages of functional outcome measures over tracking cell presence alone? Tracking cell presence (e.g., via bioluminescent imaging or histology) only confirms that cells survived and engrafted. Functional outcome measures are the ultimate indicator of therapeutic success, demonstrating that the integrated cells are actively contributing to repair and restoration of physiology. They provide clinically relevant data that is more meaningful for translating therapies to patients [1]. A combined approach, confirming both integration and functional improvement, provides the most compelling evidence for efficacy.
Q2: In a spinal cord injury model, what are the standard functional tests used alongside the ASIA score? In a recent clinical study on complete spinal cord injury, researchers used a multi-modal assessment strategy to thoroughly evaluate recovery [76]. The key standardized measures included:
- ASIA (American Spinal Injury Association) Scores: Quantifies motor and sensory function (light touch, pinprick).
- SCIM-III (Spinal Cord Independence Measure): Evaluates practical functional abilities in self-care, respiration, mobility, and sphincter management.
- WHOQOL-BREF (World Health Organization Quality of Life Brief Version): Assesses the patient's perceived quality of life, a crucial patient-reported outcome.
Q3: How can I determine if the functional recovery is due to my transplanted cells and not endogenous repair? Disentangling the specific therapeutic mechanism requires careful experimental design:
- Use of Control Groups: Include appropriate controls (e.g., vehicle-only injections).
- Cell Tracking: Utilize genetically tagged cells (e.g., GFP+, Luciferase+) to correlate the location and number of integrated cells with functional improvements in individual subjects.
- Mechanistic Blocking Studies: Employ specific inhibitors to block proposed mechanisms of action (e.g., antibodies to neutralize paracrine factors). If function declines, it implicates that mechanism.
- Source of Newly Formed Cells: In animals, you can use lineage-tracing models to definitively determine if new functional cells originated from your transplant or the host.
Q4: What are the common pitfalls in interpreting functional data, and how can I avoid them? Common pitfalls include:
- Observer Bias: Use blinded assessments where the experimenter performing the functional tests is unaware of the treatment group (blinded).
- Over-reliance on a Single Test: No single functional assay is perfect. Use a battery of tests to get a comprehensive picture.
- Insufficient Acclimatization: Animals not properly acclimated to testing equipment may exhibit stress-related behaviors that confound results.
- Ignoring Compensatory Mechanisms: An animal may achieve a functional task using an alternative, compensatory strategy rather than true recovery of the damaged pathway. Use high-resolution motion capture and analysis to differentiate true recovery from compensation.
Quantitative Data on Functional Outcomes
Table 1: Standardized Functional Outcome Measures in Pre-Clinical and Clinical Studies
| Tissue System | Functional Test | Measured Parameters | Significance in Assessing Recovery |
|---|---|---|---|
| Neurological (Spinal Cord) | ASIA Impairment Scale [76] | Motor score, sensory score (light touch, pinprick) | Quantifies neurological status; standard in clinical trials. |
| Basso, Beattie, Bresnahan (BBB) Locomotor Rating Scale | Hindlimb movement, coordination, weight support. | Gold standard for rodent SCI models. | |
| Musculoskeletal | Gait Analysis (Footprint, CatWalk) | Stride length, base of support, swing/stance phase. | Objectively quantifies walking function and coordination. |
| Grip Strength Test | Peak force (grams) | Measures limb-specific muscular strength. | |
| Cardiac | Echocardiography | Ejection Fraction, Fractional Shortening | Assesses global heart pump function. |
| Pressure-Volume Loop Analysis | Stroke Volume, Cardiac Output | Gold-standard for hemodynamic assessment. | |
| General/Clinical | SCIM-III (Spinal Cord Independence Measure) [76] | Self-care, mobility, respiration/sphincter management | Evaluates independence in daily activities. |
| WHOQOL-BREF (Quality of Life) [76] | Physical, psychological, social, environmental domains | Patient-reported outcome on life quality improvement. |
Table 2: Key Research Reagent Solutions for Functional Integration Studies
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Enhances survival of dissociated human pluripotent stem cells (hPSCs) after passaging or thawing. [6] | Improving viability of differentiated neurons prior to transplantation to ensure adequate cell numbers for functional effect. |
| Vitronectin (VTN-N) | Defined, xenofree substrate for feeder-free culture of hPSCs. [5] | Maintaining high-quality, undifferentiated stem cells as a starting material for robust differentiation into functional progenitors. |
| Geltrex/Matrigel | Basement membrane extract providing a complex extracellular matrix for cell culture. | Supporting the differentiation and 3D organization of cells into organoids or tissue-like structures for in vitro functional testing. |
| B-27 Supplement | Serum-free supplement optimized for the survival and functional maturation of neurons. [6] | Promoting synaptic activity and long-term functional maintenance of neuronal cultures derived from stem cells. |
| DAMPs (e.g., HMGB1) | Damage-Associated Molecular Patterns; endogenous molecules released upon injury that activate stem cells. [2] | Used in vitro to mimic the injury niche and study how stem cells are recruited and activated for repair. |
| SDF-1/CXCR4 Chemokine Pair | Critical signaling axis for homing and recruitment of stem cells to injury sites. [2] | Pre-conditioning stem cells to enhance their migration and integration into target tissues in vivo. |
Experimental Protocols for Key Functional Assessments
Protocol: Assessing Locomotor Recovery after Spinal Cord Injury in Rodents
Objective: To quantitatively evaluate the recovery of hindlimb motor function following stem cell transplantation for spinal cord injury using the Basso, Beattie, Bresnahan (BBB) Locomotor Rating Scale.
Materials:
- Rodent spinal cord injury model (e.g., contusion model)
- Open-field testing arena (circular, with smooth, non-slip surface)
- Video recording system
- Trained, blinded observers
Methodology:
- Pre-operative Baseline: All animals should be acclimated to the testing arena for at least 10 minutes per day for 3 days prior to surgery.
- Injury and Transplantation: Perform the standardized spinal cord injury. Administer stem cells or vehicle control at the designated time point post-injury.
- Testing Schedule: Test animals weekly for the duration of the study (e.g., 8-12 weeks post-injury).
- Testing Procedure:
- Place the animal in the center of the open field.
- Record its movement for 4 minutes.
- Two trained observers, blinded to the experimental groups, should independently score the animal's hindlimb movement, trunk stability, and tail position based on the 21-point BBB scale (0=no movement, 21=normal gait).
- Data Analysis: Average the scores from the two observers. Perform statistical analysis (e.g., two-way repeated measures ANOVA) to compare treatment and control groups over time.
Protocol: In Vitro Electrophysiology to Validate Neuronal Differentiation
Objective: To confirm that stem cell-derived neurons have matured into functionally active cells capable of firing action potentials.
Materials:
- Putative stem cell-derived neurons (e.g., iPSC-derived motor neurons)
- Patch-clamp rig (amplifier, micromanipulators, computer with acquisition software)
- Recording chamber and perfusion system
- Solutions: Artificial Cerebrospinal Fluid (ACSF), internal pipette solution.
Methodology:
- Cell Preparation: Plate neurons on coated coverslips at a low density suitable for patch-clamping.
- Whole-Cell Configuration: Bring a glass microelectrode (resistance 3-6 MΩ) close to a neuron. Apply gentle suction to achieve a gigaseal (>1 GΩ), then rupture the membrane patch to achieve whole-cell configuration.
- Current-Clamp Recording: In current-clamp mode, maintain the cell at its resting membrane potential. Inject a series of small, depolarizing current steps (e.g., 10-50 pA increments).
- Data Collection: Record the membrane potential response. Functionally mature neurons will respond to sufficient depolarizing current by firing all-or-nothing action potentials.
- Analysis: Key parameters include resting membrane potential (should be around -60 to -70 mV), action potential threshold, amplitude, and frequency. The ability to generate repetitive action potentials indicates advanced functional maturity.
Signaling Pathways and Experimental Workflows
Stem Cell Integration to Functional Recovery Pathway
Functional Outcome Assessment Workflow
This technical support document underscores that while confirming stem cell integration is a critical first step, the field must demand rigorous evidence of functional efficacy. By employing the standardized measures, troubleshooting common pitfalls, and implementing the detailed protocols outlined herein, researchers can robustly demonstrate that their therapies not only populate a damaged tissue but truly restore its lost function.
Technical Support & Troubleshooting Hub
This support center provides targeted guidance for researchers working with Bone Marrow-Mesenchymal Stem Cells (BM-MSCs), Umbilical Cord-MSCs (UC-MSCs), and induced Pluripotent Stem Cell-Derived Endothelial Cells (iPSC-ECs) in the context of tissue integration and enhancement research.
Frequently Asked Questions (FAQs)
Q1: Our BM-MSCs show reduced proliferation and differentiation capacity after several passages. What could be the cause and solution? A: This is a common issue related to replicative senescence.
- Cause: BM-MSCs are adult stem cells with a finite replicative lifespan. Prolonged in vitro expansion leads to cellular aging, manifested as reduced proliferation, altered morphology, and decreased differentiation potential [78].
- Solutions:
- Consider switching to a alternative cell source like UC-MSCs or induced MSCs (iMSCs), which exhibit enhanced proliferative capacities and reduced age-related variability [78].
- For BM-MSCs, use low-oxygen (physioxic) culture conditions to help maintain stemness.
- Ensure you are not passaging cells from an overly confluent culture, as this can negatively impact cell health and recovery [6].
Q2: When differentiating iPSCs into endothelial cells (iPSC-ECs), we observe high heterogeneity and inconsistent purity. How can we improve the protocol? A: Inconsistent differentiation outcomes often stem from the starting population and differentiation cues.
- Cause: The quality of the parent human pluripotent stem cell (hPSC) line is critical. Pre-existing differentiation or partially differentiated hPSCs can significantly reduce induction efficiency [6].
- Solutions:
- Remove differentiated cells: Before starting differentiation, meticulously remove any differentiated areas from your hPSC culture [5].
- Optimize seeding density: Plate hPSCs for induction as small, uniform clumps at a recommended density (e.g., 2–2.5 x 10^4 cells/cm²). Both overly low and high confluency will reduce efficiency [6].
- Include a control: Always use a well-characterized control hPSC line (e.g., H9 or H7 ESC line) in your differentiation experiments to isolate protocol-specific issues from cell-line-specific variability [6].
Q3: Our UC-MSC cultures are contaminated with hematopoietic cells. What is the best isolation method to prevent this? A: The choice of isolation technique significantly impacts initial purity.
- Cause: Enzymatic digestion of umbilical cord tissue can yield a highly heterogeneous cell population with high hematopoietic contamination [79].
- Solution: Employ the explant culture method. While it increases the initial culture time, this inexpensive process requires little manipulation and produces a more homogeneous cell population, as only cells that can migrate from the tissue explant to the plastic surface will grow [79].
Q4: After transplantation in our in vivo model, we observe poor engraftment of our stem cell population. How can we enhance homing to the target tissue? A: Poor engraftment is often related to inefficient homing.
- Cause: Successful homing is a multi-step process governed by chemotactic signals. The SDF-1 (CXCL12)/CXCR4 axis is one of the most critical pathways for stem cell recruitment to injury sites [2].
- Solution:
- Pre-conditioning: Pre-treat MSCs with inflammatory cytokines (e.g., TNF-α or IFN-γ) to upregulate the expression of homing receptors like CXCR4.
- Bio-engineering: Consider modifying your cells to overexpress CXCR4 to enhance their response to SDF-1 gradients released from injured tissue [2].
Q5: We need a consistent, scalable source of MSCs for drug screening. Which cell source is most suitable? A: Induced MSCs (iMSCs) derived from iPSCs are an excellent candidate for this application.
- Rationale: Unlike donor-limited tissue-derived MSCs, iPSCs can be expanded indefinitely, providing a virtually unlimited starting material. iMSCs generated from them demonstrate higher homogeneity, consistent gene expression, and can be expanded over many more generations while maintaining a normal karyotype compared to BM-MSCs or UC-MSCs [78]. This allows for the creation of standardized, off-the-shelf products for large-scale screening.
Troubleshooting Guides
Guide 1: Low Cell Viability After Thawing
| Observation | Possible Cause | Solution |
|---|---|---|
| Low post-thaw viability for all cell types. | Incorrect thawing procedure causing osmotic shock. | Thaw cells quickly (<2 minutes at 37°C). Transfer to a pre-rinsed tube and add pre-warmed medium drop-wise while swirling. Do not add full medium volume at once [6]. |
| Specific to Neural Stem Cells (NSCs). | Storage or medium error. | Ensure cells were stored in liquid nitrogen. Use the correct, freshly prepared complete medium specified for the specific NSC line [6]. |
Guide 2: Excessive Spontaneous Differentiation in Pluripotent Stem Cell Cultures
| Observation | Possible Cause | Solution |
|---|---|---|
| High differentiation rate (>20%) in hiPSC/hESC cultures. | Old or expired culture medium. | Ensure complete medium (e.g., mTeSR Plus) kept at 2-8°C is used within 2 weeks [5]. |
| Overgrowth or uneven colony size. | Passage cells when colonies are large and compact, before they overgrow. Ensure cell aggregates after passaging are evenly sized [5]. | |
| Over-exposure outside incubator. | Avoid having culture plates out of the incubator for more than 15 minutes at a time [5]. |
The choice of cell source is critical and involves trade-offs between potency, scalability, and safety. The following table provides a quantitative and qualitative comparison to guide selection.
Table 1: Core Characteristics of BM-MSCs, UC-MSCs, and iPSC-ECs
| Feature | BM-MSCs [7] | UC-MSCs [7] [78] | iPSC-ECs (from hiPSCs) [80] [78] |
|---|---|---|---|
| Origin | Bone Marrow (Mesoderm) | Umbilical Cord (Mesoderm) | Reprogrammed Somatic Cells (Ecto/Endo/Mesoderm) |
| Differentiation Potential | Multipotent (Osteo, Chondro, Adipo) | Multipotent (Osteo, Chondro, Adipo) | Pluripotent (All three germ layers) |
| Proliferative Capacity | Limited, senescence with passages | High, >40 population doublings | Very high, >60 population doublings |
| Key Surface Markers | CD105+, CD73+, CD90+, CD45-, CD34- [7] | CD105+, CD73+, CD90+, CD45-, CD34- [78] | CD31+, CD144 (VE-Cadherin)+, vWF+ |
| Immunogenicity | Low, immunoprivileged | Very Low, ideal for allogeneic use | Low, potential for autologous use |
| Tumorigenic Risk | Very Low | Very Low | Low, but requires careful differentiation and purification |
| Key Advantages | • "Gold standard" with extensive data• Strong osteogenic potential | • High proliferation• Low immunogenicity• Youthful genetic characteristics | • Unlimited source material• Enables patient-specific therapy• Consistent, scalable production |
| Key Limitations | • Invasive harvest• Donor-dependent variability• Senescence | • Tissue source availability• Heterogeneity between donors | • Requires complex differentiation• Potential for residual undifferentiated cells |
Table 2: Functional Properties for Tissue Integration
| Property | BM-MSCs | UC-MSCs | iPSC-ECs |
|---|---|---|---|
| Pro-Angiogenic Factor Secretion (e.g., VEGF) | High [80] | High | Very High (Native function) |
| Immunomodulatory Strength | High (potent inhibition of T-cell proliferation) [7] | High, but may be less than BM-MSCs in some studies [78] | Variable; iMSCs can show strong immunosuppression [78] |
| Homing to Injury (SDF-1/CXCR4) | Moderate | Moderate | Can be enhanced via engineering |
| Extracellular Vesicle (EV) Production | High, well-characterized | High, with therapeutic cargo | High, cargo can be tailored via iPSC programming |
| Transcriptomic Profile | Enriched in genes for osteogenesis and immune regulation [78] | Varies; may have higher pro-inflammatory factor expression (e.g., IL6) [78] | Can be directed to resemble specific tissue-specific ECs |
Experimental Protocols for Key Analyses
Protocol 1: Directed Differentiation of hiPSCs to iMSCs
Application: Generating a consistent and scalable source of MSCs for tissue regeneration and immunomodulation studies [78].
Methodology:
- Culture hiPSCs: Maintain hiPSCs on a vitronectin (VTN-N) coated plate in Essential 8 medium until 85% confluent [6].
- Induce Differentiation: Replace Essential 8 medium with a specialized induction medium. A common and effective formulation is:
- Base Medium: DMEM supplemented with 10% Fetal Bovine Serum (FBS).
- Key Additives:
- 10 ng/mL basic Fibroblast Growth Factor (bFGF): Critical for mesodermal transformation and angiogenesis.
- 10 ng/mL Platelet-Derived Growth Factor-AB (PDGF-AB): Promotes proliferation and enrichment of MSCs.
- 10 ng/mL Epidermal Growth Factor (EGF): Supports MSC proliferation.
- Maintain and Passage: Culture the cells in this induction medium for 10-14 days, passaging as needed using standard MSC methods (e.g., trypsin/EDTA) when cells reach 85% confluency.
- Validate iMSCs: The resulting cells should be validated for standard MSC surface markers (CD73, CD90, CD105 positive; CD45, CD34 negative) and tri-lineage differentiation potential (osteogenic, chondrogenic, adipogenic) [78].
Protocol 2: In Vitro Tube Formation Assay for iPSC-ECs
Application: Quantifying the angiogenic potential of derived endothelial cells.
Methodology:
- Prepare Assay Plate: Thaw Geltrex or Matrigel on ice overnight at 4°C. Pipette 50-100 µL of the matrix into each well of a 96-well plate and polymerize at 37°C for 30 minutes.
- Harvest Cells: Detach the iPSC-ECs using a gentle dissociation reagent like EDTA or Accutase. Do not use trypsin as it can damage critical surface receptors.
- Seed Cells: Resuspend the iPSC-ECs at a density of 1.0 x 10^5 cells/mL in endothelial cell medium (e.g., EGM-2). Seed 100 µL of the cell suspension onto the polymerized matrix.
- Incubate and Image: Incubate the plate at 37°C, 5% CO2 for 4-18 hours. Periodically observe the cells under a microscope. The iPSC-ECs should form capillary-like tube structures.
- Quantify: Capture images and use image analysis software to quantify parameters like total tube length, number of branches, and number of meshes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Stem Cell Research
| Reagent / Kit | Function & Application |
|---|---|
| Essential 8 Medium | A defined, xeno-free medium for the feeder-free culture of human pluripotent stem cells (hPSCs), including hiPSCs used as a starting point for differentiation [6]. |
| mTeSR Plus Medium | A robust, serum-free medium for maintaining hPSCs in an undifferentiated state. Critical for ensuring high-quality starting material for differentiation protocols [5]. |
| Geltrex / Matrigel | Basement membrane extracts used as substrate coatings for the adherent culture of hPSCs and for assays like the tube formation assay due to their complex ECM protein composition [6]. |
| ROCK Inhibitor (Y-27632) | A small molecule that significantly increases the survival of hPSCs and iMSCs after single-cell passaging and cryopreservation by inhibiting apoptosis [6] [5]. |
| CytoTune -iPS Sendai Reprogramming Kit | A non-integrating, viral vector-based kit for reprogramming somatic cells into hiPSCs, which can serve as the source for iMSCs or iPSC-ECs [6]. |
| bFGF (basic FGF) | A critical growth factor added to MSC induction and culture media to promote proliferation and maintain multipotency [78]. |
| SB431542 (TGF-β Inhibitor) | A small molecule inhibitor used in some protocols to enhance reprogramming or, as shown in research, to rapidly differentiate hPSCs into MSC-like cells by inhibiting the TGF-β pathway [79]. |
Signaling Pathways and Experimental Workflows
Stem Cell Recruitment to Injury
iPSC to iMSC Differentiation Workflow
Frequently Asked Questions (FAQs)
FAQ 1: What are the key biomaterial properties to consider for stem cell therapy applications? For stem cell therapies, biomaterials are not just passive delivery vehicles; they are active components that can enhance therapeutic outcomes. The key properties are degradation, mechanical properties, and the host immune response. Biomaterials can protect transplanted stem cells from harsh pathological environments, facilitate in vivo tracking, and be engineered to deliver additional functional properties, such as therapeutic genes. The ideal biomaterial should degrade at a rate that matches tissue regeneration, have mechanical properties compatible with the target tissue, and elicit a favorable (or minimally disruptive) immune response to support stem cell integration and survival [81].
FAQ 2: My biomaterial scaffold is degrading too quickly in vitro, compromising its mechanical integrity. What factors should I investigate? Rapid degradation and loss of mechanical integrity can be attributed to several factors. First, review the chemical structure of your polymer; esters, anhydrides, and amides have characteristic hydrolysis rates. Second, consider the porosity and surface area of your scaffold, as higher surface area can accelerate degradation. Third, if your in vitro test uses enzymatic solutions, the enzyme concentration and activity might be too high compared to the in vivo environment. It is crucial to use standardized degradation assessment techniques, such as those outlined in ASTM F1635-11, which include monitoring mass loss, changes in molar mass, and mechanical properties over time [82].
FAQ 3: How can I reliably measure biomaterial degradation and distinguish it from simple dissolution? Distinguishing degradation (the breaking of chemical bonds) from dissolution is critical. A multi-technique approach is recommended:
- Gravimetric analysis (mass loss) infers degradation but can be misleading for soluble materials. Always combine it with chemical methods [82].
- Chemical analysis is the only way to confirm degradation. Techniques like Size Exclusion Chromatography (SEC) can track the reduction in polymer molecular weight, while NMR or FTIR can identify chemical bond cleavage and the formation of degradation by-products [82] [83].
- Fluorescent tagging of the biomaterial polymer allows for non-destructive, real-time monitoring of degradation in situ, providing a more dynamic dataset [83].
FAQ 4: The host's immune response is encapsulating my implant in fibrous tissue, leading to failure. How can biomaterial design mitigate this? Fibrous encapsulation is a classic sign of a chronic foreign body response. Several biomaterial design strategies can modulate this immune reaction:
- Surface Modification: Altering surface topography, chemistry, and charge can significantly improve biocompatibility. For example, creating specific nanopatterns can reduce the activation of pro-inflammatory macrophages [84] [85].
- Mechanical Properties: Matching the stiffness of the implant to the target tissue is crucial. Softer materials, for instance, have been shown to reduce inflammatory reactions in brain-like environments [84].
- Bioactive Coatings: Incorporating anti-inflammatory cytokines or specific agents that shift macrophages from a pro-inflammatory (M1) to an anti-inflammatory (M2) phenotype can promote integration and reduce fibrosis [84].
FAQ 5: How does biomaterial stiffness influence mesenchymal stem cell (MSC) behavior? Substrate stiffness is a potent regulator of MSC fate. Seminal work has shown that MSCs cultured on soft substrates (0.1–1 kPa, mimicking brain tissue) tend to express neuronal markers. On stiffer substrates mimicking muscle (8–17 kPa), they exhibit myogenic differentiation, and on rigid substrates (25–40 kPa, mimicking bone), they undergo osteogenic differentiation. This process is mediated by integrin-based mechanotransduction pathways, such as α2-integrin-mediated ROCK-FAK-ERK1/2 signaling for osteogenesis [86].
Troubleshooting Guides
Problem 1: Inconsistent or Uncontrolled Biomaterial Degradation
Potential Causes and Solutions:
| Problem Area | Specific Issue | Recommended Action |
|---|---|---|
| Material Synthesis | Inconsistent polymer crosslinking density. | Standardize synthesis protocols and use techniques like NMR or rheology to quantify crosslinking degree before degradation experiments. |
| Degradation Media | pH or enzyme concentration not representative of target tissue. | Characterize the pH and enzyme profile (e.g., collagenase, esterase) of the target in vivo environment and mimic it in vitro. |
| Assessment Method | Relying solely on mass loss, mistaking dissolution for degradation. | Implement a combined assessment protocol: use gravimetric analysis alongside SEC for molecular weight analysis and HPLC/MS to identify by-products [82]. |
Detailed Experimental Protocol: Monitoring Degradation In Vitro
- Pre-degradation Characterization: Record the initial mass, dimensions, and molecular weight of your biomaterial samples. Visually examine the surface morphology using Scanning Electron Microscopy (SEM).
- Immersion in Media: Immerse samples in a degradation medium such as phosphate-buffered saline (PBS) at pH 7.4, simulated body fluid, or a buffered enzymatic solution. Maintain the media at 37°C under gentle agitation [82].
- Sampling and Analysis: At predetermined time points, remove samples from the media (n=3-5 is recommended for statistical power).
- Gravimetric Analysis: Rinse samples, dry to a constant weight, and measure mass loss.
- Molecular Weight Analysis: Use SEC to determine the change in the average molecular weight (Mn and Mw) of the polymer.
- By-product Analysis: Analyze the degradation media using techniques like HPLC or mass spectrometry to identify and quantify released fragments [82].
- Mechanical Testing: If applicable, perform tensile or compression tests to track the loss of mechanical strength.
The workflow below outlines the key decision points in a standard degradation assessment protocol.
Problem 2: Mismatch Between Biomaterial and Host Tissue Mechanics
Potential Causes and Solutions:
| Problem Area | Specific Issue | Recommended Action |
|---|---|---|
| Material Selection | Stiffness (Young's Modulus) is orders of magnitude higher or lower than native tissue. | Consult literature or perform tests to determine the native tissue's modulus. Select a polymer (e.g., soft hydrogel for brain, stiff PCL for bone) that can be tuned to match this range [87] [86]. |
| Scaffold Architecture | Porosity and pore size negatively impacting mechanical performance. | Re-evaluate fabrication parameters. Higher porosity often reduces stiffness. Use techniques like gas foaming or 3D printing to create more controlled, mechanically robust architectures [87]. |
| Degradation Mismatch | Material loses mechanical strength too quickly before new tissue forms. | Design a material with a slower degradation profile or a composite material that retains a mechanical scaffold for longer [83]. |
Detailed Experimental Protocol: Correlating Degradation with Stem Cell Behavior
To understand how degradation influences stem cell function, you can calculate a Turnover Index (TI). This metric compares the rate of biomaterial degradation to the rate of cellular activity, such as extracellular matrix (ECM) synthesis [83].
- Fluorescent Tagging: Covalently tag your biomaterial with a fluorescent dye (e.g., FITC) to allow non-destructive tracking.
- Monitor Degradation: Culture MSCs on the fluorescent biomaterial. At set intervals, measure the fluorescence intensity of the material itself (scaffold remaining) and the release of fluorescent peptides into the culture media (degradation by-products). Confirm with SEC.
- Quantify Cellular Activity: Simultaneously, measure specific cellular outputs. For osteogenesis, this could be calcium deposition (via Alizarin Red staining) or osteocalcin secretion (via ELISA). For proliferation, use a DNA quantification assay.
- Calculate Turnover Index (TI): Use the formula below. A higher TI for a specific marker (e.g., mineralisation) indicates that the degradation profile supports that cellular activity [83].
TI = (Rate of Cellular Activity) / (Rate of Biomaterial Remaining)
The following diagram illustrates the inverse relationship observed between scaffold degradation and different MSC activities, which is quantified by the Turnover Index.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Experimental Context |
|---|---|
| Polyethylene Glycol (PEG)-based Hydrogels | A versatile synthetic polymer used to create hydrogels with tunable stiffness and controlled degradation for studying MSC mechanotransduction [86]. |
| Gold Nanorods (AuNRs) | Inorganic nanoparticles used as contrast agents for non-invasive, long-term tracking of stem cells post-transplantation via photoacoustic imaging [81]. |
| Fluorescent Tags (e.g., FITC, RITC) | Molecules covalently bound to biomaterials to enable real-time, non-destructive monitoring of degradation in situ via fluorescence intensity measurement [83]. |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Magnetic nanoparticles used to label stem cells for in vivo tracking with Magnetic Resonance Imaging (MRI) and for magnetic targeting to specific sites [81]. |
| Poly(lactic-co-glycolic acid) (PLGA) | A widely used biodegradable synthetic polymer for scaffolds and particles; its degradation rate can be modified by altering the lactic to glycolic acid ratio [81]. |
| Bioactive Glass (BaG) | A class of ceramics that bond strongly with bone tissue (bioactive), releasing ions that promote osteogenesis and modulate the immune response [84]. |
| Size Exclusion Chromatography (SEC) Standards | Certified polymer standards with known molecular weights essential for calibrating SEC systems to accurately measure biomaterial molecular weight changes during degradation [82]. |
FAQs on Preclinical to Clinical Translation
What are the most common regulatory objections for cell therapy applications, and how can we address them in study design?
Regulatory objections for cell therapies frequently relate to preclinical evidence. Key areas for focus include:
- Mechanism of Action (MoA): Your preclinical studies must provide evidence connecting the therapeutic activity to a disease-relevant pathophysiological process [88].
- Clinically Relevant Models: Use animal models of disease that accurately reflect the human clinical condition and disease progression [88].
- Intervention Parameters: Justify critical parameters like cell dose, route of administration, and timing based on robust preclinical data [88].
- Study Design Rigor: Implement robust design elements often lacking in preclinical studies, including randomization and blinding, to reduce bias and overestimation of treatment effects [88].
How do you define "efficacy" in the context of preclinical stem cell research?
Preclinical efficacy is multi-faceted. The ISSCR guidelines define several key elements [88]:
| Efficacy Component | Definition |
|---|---|
| Mechanism of Action | Evidence that the intervention interacts with a disease-relevant biological process. |
| Disease Modification | Ability to modify disease or injury in biological systems similar to expected clinical trials. |
| Intervention Characteristics | Evidence for optimal conditions (e.g., effective dose, route of administration). |
| Effect Characteristics | Sufficient magnitude or durability of effect to be clinically meaningful. |
Our stem cell therapy shows efficacy in rodent models. What key steps ensure this translates to early-phase clinical trials?
Transitioning from rodent models to human trials requires careful planning:
- Lead Optimization: Chemically modify the compound based on animal studies to improve performance and establish safe, effective dosing [89].
- IND-Enabling Studies: Conduct final safety testing in larger animals that more closely mimic human biology. This is required by regulators like the FDA before human trials [89].
- Submit an Investigational New Drug (IND) Application: This package to the FDA includes all preclinical data, manufacturing information, and clinical trial plans. Approval is required to proceed to human trials [90] [89].
What are the major biological hurdles for stem cell integration into host tissue, and what functional data demonstrates successful integration?
Successful integration is a multi-stage process, and functional data must capture each step [2]:
- Recruitment & Homing: Demonstrate that stem cells migrate to the injury site in response to chemotactic signals (e.g., SDF-1/CXCR4 axis).
- Activation & Differentiation: Show that local microenvironmental cues (e.g., BMP, Wnt signaling) drive stem cell differentiation into functional lineages [41].
- Functional Integration: Provide evidence that newly formed cells establish connections and contribute to restored tissue function, supported by angiogenesis and extracellular matrix remodeling [2].
Troubleshooting Common Experimental Challenges
Problem: Poor stem cell survival and engraftment after transplantation in preclinical models.
- Potential Cause: The ischemic or inflammatory microenvironment of the injury site leads to high cell death and poor integration [41].
- Solutions:
- Preconditioning: Genetically or chemically modify cells to enhance their resilience and secretory profile. Example: Overexpress anti-apoptotic or pro-angiogenic genes [41].
- Bioactive Delivery Platforms: Use injectable hydrogels or 3D-printed scaffolds to provide mechanical protection and a supportive microenvironment, improving cell viability and retention [41].
- Optimize Intervention Parameters: Re-visit your timing of delivery, cell dose, and route of administration based on pilot studies [88].
Problem: Inconsistent differentiation outcomes in stem cell cultures, leading to variable preclinical data.
- Potential Causes: Suboptimal culture conditions, high differentiation pressure, or donor-to-donor variability [41].
- Solutions:
- Quality Control: Rigorously assess and maintain genomic integrity, pluripotency, and morphology of hPSC cultures [5].
- Standardize Protocols: Ensure culture medium is fresh and cell aggregates are evenly sized during passaging. Remove differentiated areas prior to passaging [5].
- Use Controls: Always include a control cell line (e.g., H9 or H7 ESC) in differentiation experiments [6].
- Adjust Parameters: For difficult-to-differentiate lines, adjust cell density or extend the induction time [6].
Problem: The therapeutic effect is significant in small animal models but fails to translate in larger, more clinically relevant models.
- Potential Cause: The small animal model does not adequately recapitulate human disease pathophysiology or the intervention's mechanism of action [88] [91].
- Solutions:
- Model Selection: Prioritize disease models with strong clinical relevance and known predictive utility for your specific condition [88].
- Mechanistic Bridging: Ensure your mechanism of action is consistent and measurable across all model systems, from small animal to large animal [88].
- Rigorous Design: Apply the same level of experimental rigor (randomization, blinding, pre-defined endpoints) in all preclinical studies, regardless of model scale [88].
The Scientist's Toolkit: Research Reagent Solutions
Essential materials for stem cell research and their functions:
| Research Reagent | Function |
|---|---|
| ROCK Inhibitor (Y-27632) | Improves survival of dissociated human pluripotent stem cells (hPSCs) during passaging and freezing [6]. |
| Geltrex / Matrigel | Basement membrane matrix extracts used as substrates for feeder-free culture of hPSCs, providing essential adhesion and signaling cues [6]. |
| mTeSR Plus / Essential 8 Medium | Defined, feeder-free culture media formulated to maintain hPSCs in a pluripotent state [5] [6]. |
| B-27 Supplement | Serum-free supplement optimized for the survival and growth of central and peripheral nervous system neurons [6]. |
| ReLeSR | A non-enzymatic passaging reagent for the gentle dissociation of hPSC colonies into cell aggregates [5]. |
| CytoTune-iPS Sendai Reprogramming Kit | A non-integrating viral vector system for reprogramming somatic cells into induced pluripotent stem cells (iPSCs) [6]. |
Visualizing Key Processes and Workflows
Stem Cell Recruitment Cascade
Preclinical to Clinical Workflow
Experimental Protocols for Key Assessments
Protocol 1: Assessing Stem Cell Homing and Recruitment In Vivo
Objective: To quantitatively evaluate the migration and recruitment of systemically delivered stem cells to a site of injury in an animal model.
Methodology:
- Cell Labeling: Label mesenchymal stem cells (MSCs) with a fluorescent dye (e.g., DiR or GFP-lentivirus) or a radioactive tracer (e.g., 99mTc) for detection.
- Model Establishment: Generate a standardized bone fracture or myocardial infarction model in rodents.
- Cell Administration: Systemically administer labeled MSCs via intravenous or intra-arterial injection at a predetermined post-injury time point.
- In Vivo Imaging: At 24, 48, and 72 hours post-injection, use In Vivo Imaging System (IVIS) for fluorescence or Single-Photon Emission Computed Tomography (SPECT) for radioactivity to track and quantify cell signals at the injury site versus control organs.
- Ex Vivo Validation: Euthanize animals at the endpoint. Excise the target tissue and control organs for quantitative analysis (e.g., fluorescence intensity, gamma counting, or qPCR for human-specific Alu sequences in xenograft models).
Protocol 2: Evaluating Osteogenic Differentiation and Bone Regeneration
Objective: To functionally assess the bone-forming potential of modified MSCs in a critical-sized bone defect model.
Methodology:
- Cell Preparation: Use functionalized MSCs (e.g., BMP-2 overexpressing) and control (naïve) MSCs.
- Delivery Vehicle: Seed cells onto a 3D-printed biodegradable scaffold (e.g., PCL/HA) or within an injectable hydrogel (e.g., methacrylated hyaluronic acid).
- Surgical Implantation: Create a critical-sized calvarial defect in rats. Implant the cell-scaffold constructs into the defect site (test group) versus scaffold-only (control group).
- Longitudinal Analysis:
- Micro-Computed Tomography (μCT): Perform scans at 4, 8, and 12 weeks post-implantation to quantitatively analyze new bone volume (BV), bone mineral density (BMD), and trabecular morphology.
- Histology and Immunohistochemistry: Process explanted bone tissue at 12 weeks. Section and stain with:
- H&E: General morphology.
- Masson's Trichrome: Collagen deposition.
- Immunostaining for Osteocalcin and RUNX2: Specific markers of osteogenic differentiation [41].
- Biomechanical Testing: Perform a push-out test or nanoindentation on regenerated bone to assess restoration of mechanical function.
Conclusion
Enhancing stem cell integration with host tissue is a multifaceted challenge that requires a confluence of biological understanding and engineering innovation. The key takeaways are that successful integration depends on recapitulating a supportive microenvironment through biomaterial design, proactively managing the host immune response, and selecting and priming the optimal cell source for the target tissue. Moving forward, the field must prioritize the development of smart, responsive biomaterials that provide dynamic cues, the standardization of cell products and preconditioning protocols, and the implementation of more sensitive, functional outcome measures in clinical trials. By systematically addressing the hurdles of cell survival, retention, and functional integration, the immense transformative potential of stem cell therapies for repairing incurable diseases can be fully realized, ultimately shifting the paradigm from symptomatic management to true tissue restoration.
References
- 1. Stem cells as biological drugs for incurable diseases [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04632-8]
- 2. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 3. Contrast agents for photoacoustic imaging: a review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8467005/]
- 4. Engraftment and reconstitution of hematopoiesis is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3228275/]
- 5. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 6. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 7. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 8. Mesenchymal Stem/Stromal Cells and Their Paracrine Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875256/]
- 9. Mesenchymal stem cells: Paracrine signaling and ... [https://www.sciencedirect.com/science/article/abs/pii/S0014482710002570]
- 10. Immunoregulatory paracrine effect of mesenchymal stem ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1411507/full]
- 11. Mesenchymal stem cells and immunomodulation [https://www.nature.com/articles/cddis2015327]
- 12. Pharmacological modulation of stem cells signaling pathway ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 13. Biomaterials to enhance stem cell transplantation [https://www.sciencedirect.com/science/article/pii/S1934590922001552]
- 14. Transition from inflammation to proliferation: a critical step ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5021733/]
- 15. Neutrophils in Tissue Injury and Repair - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010766/]
- 16. Video: Chemotaxis and Direction of Cell Migration [https://www.jove.com/science-education/v/12259/chemotaxis-and-direction-of-cell-migration]
- 17. Stem Cell Niche Concept: Search for Current Expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429054/]
- 18. Unlocking the Potential of Stem Cell Microenvironments In ... [https://www.mdpi.com/2306-5354/11/3/289]
- 19. Reconstruction of Hematopoietic Stem Cell Niches In Vitro [https://www.sciencedirect.com/science/article/pii/S259000642501107X]
- 20. Natural vs. Induced Pluripotent Stem Cell Therapies [https://esmed.org/natural-vs-induced-pluripotent-stem-cell-therapies/]
- 21. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 22. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 23. Enhancing Stem Cell-Based Therapeutic Potential by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294278/]
- 24. 3D Electrospun Nanofiber-Based Scaffolds: From Preparations and Properties to Tissue Regeneration Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8225450/]
- 25. In situ tissue regeneration through host stem cell recruitment [https://www.nature.com/articles/emm2013118]
- 26. Exploration of biomaterial and stem cell-based strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574274/]
- 27. Advancements and challenges in stem cell transplantation ... [https://www.sciencedirect.com/science/article/pii/S2405844024118671]
- 28. Endogenous stem cell repair strategy via ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725013968]
- 29. An evaluation of spraying as a delivery method for human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085057/]
- 30. Recent Advances on Cell-Based Co-Culture Strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8655789/]
- 31. Cell-based mechanisms and strategies of co-culture ... [https://www.sciencedirect.com/science/article/pii/S0753332223017055]
- 32. Physical and biological advances in endothelial cell-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1084952123000204]
- 33. Image-based crosstalk analysis of cell–cell interactions during ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03223-1]
- 34. A Co-Culture System for Studying Cellular Interactions in ... [https://www.mdpi.com/2306-5354/11/11/1090]
- 35. Coculture of Endothelial and Stromal Cells to Promote ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8827126/]
- 36. Co-culture of vascular endothelial cells enhances ... [https://www.nature.com/articles/s41598-024-69878-3]
- 37. Disease microenvironment preconditioning: An evolving ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925006915]
- 38. Improving the therapeutic profile of MSCs: Cytokine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1473788/full]
- 39. Interplay of hypoxia, immune dysregulation, and metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174378/]
- 40. EGF, TNF-α, and Hypoxia Preconditioning Enhances the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421495/]
- 41. Functionalized mesenchymal stem cells for enhanced bone ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04699-3]
- 42. Questions and Answers about CRISPR [https://www.broadinstitute.org/what-broad/areas-focus/project-spotlight/questions-and-answers-about-crispr]
- 43. CRISPR innovations in tissue engineering and gene editing [https://www.sciencedirect.com/science/article/pii/S0024320524007100]
- 44. Cell Adhesion and Long-Term Survival of Transplanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4333334/]
- 45. Anoikis in cell fate, physiopathology, and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11401975/]
- 46. Cell Survival and Apoptosis Signaling as Therapeutic Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3587990/]
- 47. Differences Between Autologous and Allogeneic Cell Therapies - Patheon pharma services [https://www.patheon.com/us/en/insights-resources/blog/differences-between-autologous-and-allogeneic-cell-therapies.html]
- 48. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 49. Allogeneic Cell Therapy: Advantages, Challenges and Applications | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/allogeneic-cell-therapy.html]
- 50. Challenges and Strategies for Improving the Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5666769/]
- 51. Functional enhancement strategies for immunomodulation of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01920-3]
- 52. Immunocompatibility in transplantation: adapting to a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454034/]
- 53. Cell Source Protocol [https://cell-source.com/cell-source-protocol/]
- 54. Immunomodulatory Functions of Mesenchymal Stem Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572674/]
- 55. Electroacupuncture Facilitates the Integration of Neural Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6373172/]
- 56. Stem cell-derived neuronal relay strategies and functional ... [https://www.sciencedirect.com/science/article/pii/S0142961221005688]
- 57. Mapping Electromechanical Coupling Pathways in Voltage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8579740/]
- 58. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 59. Passage Number Effects in Cell Lines [https://www.atcc.org/resources/technical-documents/passage-number-effects-in-cell-lines]
- 60. Automated in-process characterization and selection of cell-clones for quality and efficient cell manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7547927/]
- 61. Addressing Performance, Scalability, and Regulatory Challenges to Accelerate Cell Therapy Manufacturing [https://www.biopharminternational.com/view/addressing-performance-scalability-and-regulatory-challenges-to-accelerate-cell-therapy-manufacturing]
- 62. Why gene and cell therapies are stalling at the FDA [https://www.drugdiscoverynews.com/why-gene-and-cell-therapies-are-stalling-at-the-fda-16527]
- 63. Steps to Process Development Optimization [https://www.biopharminternational.com/view/steps-to-process-development-optimization]
- 64. Frontiers | Automation, Monitoring, and Standardization of Cell Product Manufacturing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.00811/full]
- 65. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 66. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 67. Deconstructing Stem Cell Tumorigenicity: A Roadmap to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2733374/]
- 68. Possible Strategies to Reduce the Tumorigenic Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11120835/]
- 69. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 70. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 71. In Vivo Cell Tracking with Bioluminescence Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354780/]
- 72. Navigating In Vivo Bioluminescence Imaging [https://www.promega.ee/resources/pubhub/2024/navigating-in-vivo-bioluminescence-imaging/]
- 73. Guidance - Preclinical Imaging & Testing - MIT [https://preclinical-imaging.mit.edu/preclinical-imaging/guidance/]
- 74. Bioluminescence for in vivo detection of cell-type-specific ... [https://www.nature.com/articles/s41598-020-68227-4]
- 75. Integration of Tissue-engineered Cartilage With Host Cartilage [https://pmc.ncbi.nlm.nih.gov/articles/PMC3171526/]
- 76. Neurological, functional, and quality of life outcomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054327/]
- 77. Regenerative rehabilitation: Mechanisms, clinical ... [https://www.sciencedirect.com/science/article/pii/S2950575525000395]
- 78. Induced pluripotent stem cell-derived mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03968-x]
- 79. MSCs vs. iPSCs: Potential in therapeutic applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9666898/]
- 80. Stem cell derived exosome trilogy: an epic comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186388/]
- 81. Recent advances of biomaterials in stem cell therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10068913/]
- 82. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 83. Defining a turnover index for the correlation of biomaterial ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706116304652]
- 84. Engineering the Immune Response to Biomaterials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12097135/]
- 85. Interplay between biomaterials and the immune system [https://www.sciencedirect.com/science/article/pii/S1742706122007255]
- 86. Biophysical and Biochemical Cues of Biomaterials Guide ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.640388/full]
- 87. Recent Methods for Modifying Mechanical Properties of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10204517/]
- 88. Synthesizing regulatory guidance for demonstrating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11515533/]
- 89. What is Preclinical Research and Why is it so Important? [https://www.als.net/news/what-is-preclinical-research/]
- 90. Preparation for Clinical Trials - Toolkit - NIH [https://toolkit.ncats.nih.gov/module/getting-started/understand-the-rd-process/preparation-for-clinical-trials/]
- 91. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]