From Bench to Bedside: The Historical Evolution of Stem Cells in Precision Medicine
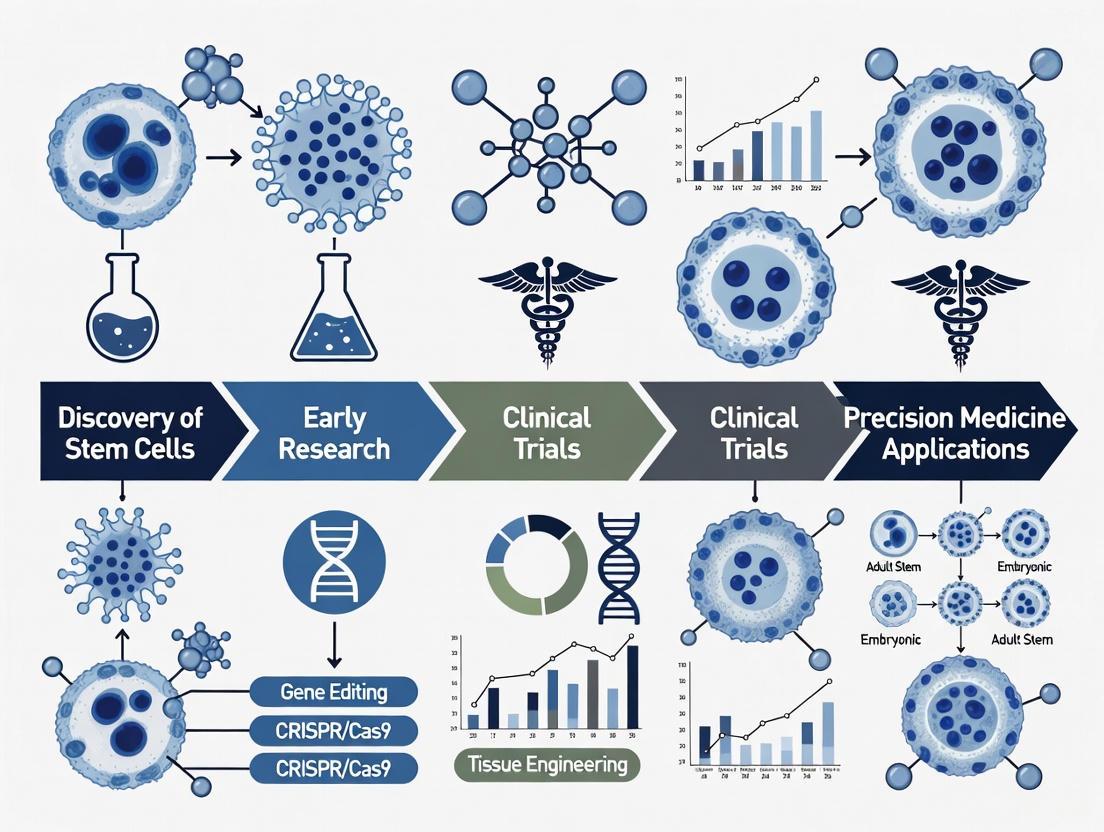
This article traces the transformative journey of stem cell technology and its integration into the paradigm of precision medicine.
From Bench to Bedside: The Historical Evolution of Stem Cells in Precision Medicine
Abstract
This article traces the transformative journey of stem cell technology and its integration into the paradigm of precision medicine. It explores the foundational discoveries, from early embryonic stem cell isolation to the revolutionary development of induced pluripotent stem cells (iPSCs), which enabled patient-specific disease modeling. The review details methodological advances in stem cell engineering, including their application in targeted drug delivery, immune modulation, and the creation of sophisticated disease models for drug screening. It further addresses the critical challenges of tumorigenicity, immune rejection, and manufacturing scalability, while outlining the rigorous regulatory and clinical validation pathways. Finally, the article synthesizes how the convergence of stem cell biology with next-generation sequencing and gene-editing technologies is reshaping personalized therapeutic development for researchers, scientists, and drug development professionals.
Pioneering Discoveries: From Pluripotency to Patient-Specific Models
The isolation of the first human embryonic stem cell (hESC) line in 1998 marked a paradigm shift in regenerative medicine and biomedical research, establishing the conceptual and technical foundation for modern precision medicine approaches [1]. This breakthrough represented the culmination of decades of foundational work in cell biology and embryology, providing researchers with unprecedented access to the primitive cells that give rise to all human tissues. Pluripotency—the capacity of a single cell to differentiate into any of the approximately 200 specialized cell types that comprise the human body—emerged as the defining biological property that would captivate the scientific imagination and fuel two decades of intensive research [2]. For the first time, scientists could explore the intricate signaling pathways and molecular mechanisms that govern human development, disease progression, and tissue regeneration using an unlimited, genetically stable cell source [1].
The historical significance of this achievement extends beyond the laboratory, encompassing ethical considerations, political dimensions, and technological innovations that collectively shaped the trajectory of stem cell research. As Dr. James Thomson, who led the pioneering work, reflected: "For the first time, we had unlimited access to all of the basic cellular building blocks of the human body. And if you make an embryonic stem cell line, that's infinite. You can make as many cells as you want" [2]. This newfound capacity to maintain pluripotent cells in culture indefinitely while retaining their developmental potential created unprecedented opportunities for drug screening, disease modeling, and the development of cell-based therapies targeting conditions that had previously been considered untreatable [3] [1]. The following sections examine the historical context, methodological framework, and conceptual advances that defined this transformative period in stem cell biology.
Historical Context and Prelude to the 1998 Breakthrough
The conceptual foundation for stem cell biology emerged gradually over more than a century, with critical discoveries paving the way for the isolation of human embryonic stem cells. The term "stem cell" was first introduced in 1868 by German biologist Ernst Haeckel, who used "Stammzelle" (stem cell) to describe the unicellular ancestor from which all multicellular organisms evolved [3] [4]. This terminology was further refined in 1888 by zoologists Theodor Heinrich Boveri and Valentin Haecker, who identified a distinct cell population in embryos capable of differentiating into specialized cells [3]. The modern conceptualization of stem cells began to take shape in the early 20th century with Russian histologist Alexander Maksimov's proposal of hematopoietic stem cells in 1908 [4], followed by the first successful bone marrow transplant between identical twins by Dr. E. Donnall Thomas in 1956 to treat leukemia [5] [4].
The subsequent decades witnessed critical advances in understanding stem cell biology, including the seminal 1961 demonstration by Ernest McCulloch and James Till of self-renewing cells in bone marrow, which established the functional definition of stem cells [4]. Research progressed with the identification of mesenchymal stem cells by Alexander Friedenstein in 1970 [4], the discovery of hematopoietic stem cells in umbilical cord blood in 1974 [4], and the first isolation of embryonic stem cells from mouse embryos by Dr. Martin Evans and Matthew Kaufman in 1981 [4] [1]. This progression from conceptual framework to experimental validation in model systems set the stage for the landmark achievement in 1998, with each discovery building upon the previous to establish the methodological and theoretical principles necessary for working with human embryonic material.
Table: Major Historical Developments Preceding Human Embryonic Stem Cell Isolation
| Year | Discovery | Key Researchers | Significance |
|---|---|---|---|
| 1868 | First use of term "stem cell" | Ernst Haeckel | Introduced conceptual framework for ancestral cells |
| 1908 | Concept of hematopoietic stem cells | Alexander Maksimov | Proposed existence of blood-forming stem cells |
| 1956 | First successful bone marrow transplant | E. Donnall Thomas | Demonstrated therapeutic potential of stem cells |
| 1961 | Confirmation of self-renewing bone marrow cells | McCulloch and Till | Provided experimental evidence for stem cell theory |
| 1981 | Isolation of mouse embryonic stem cells | Evans and Kaufman | Established methodology for pluripotent cell culture |
The Landmark 1998 Isolation: Technical Methodology and Experimental Framework
Source Materials and Ethical Considerations
The derivation of the first human embryonic stem cell lines required meticulous attention to both technical and ethical considerations. Thomson's team utilized 36 surplus embryos from patients undergoing in vitro fertilization (IVF) treatment, who provided explicit consent for research use of embryos that would otherwise have been discarded [1]. All embryos were donated voluntarily with informed consent, establishing an ethical framework that would become standard for subsequent hESC derivation [2]. The researchers worked with blastocyst-stage embryos (5-6 days post-fertilization), which contain approximately 100-200 cells organized into an outer trophectoderm layer and an inner cell mass (ICM)—the population of cells that would give rise to the embryonic stem cell lines [1]. This approach built upon previous experience with non-human primate models, as the same research team had successfully derived embryonic stem cells from rhesus macaque embryos in 1994, providing crucial technical expertise in primate stem cell culture [1].
Core Experimental Protocol: Immunosurgery and Pluripotent Cell Culture
The isolation and culture of hESCs followed a multi-stage protocol that required precise execution under sterile conditions. The complete methodology is summarized below.
Table: Detailed Protocol for Isolation and Culture of Human Embryonic Stem Cells
| Step | Procedure | Purpose | Key Reagents/Solutions |
|---|---|---|---|
| 1. Blastocyst Selection | Morphological assessment of embryo development | Identify viable blastocysts with distinct inner cell mass | Sterile phosphate-buffered saline (PBS) |
| 2. Immunosurgery | Removal of trophectoderm using antibody-mediated complement lysis | Isolate intact inner cell mass | Anti-human whole antiserum, Guinea pig complement |
| 3. Plating | Transfer of ICM to culture dish | Initiate stem cell proliferation | Mitotically-inactivated mouse embryonic fibroblast (MEF) feeder layer |
| 4. Initial Culture | Maintenance in specific media conditions | Support stem cell growth while preventing differentiation | KO-DMEM, FBS, L-glutamine, β-mercaptoethanol, Non-essential amino acids |
| 5. Passage | Mechanical dissociation of stem cell colonies | Expand cell lines while maintaining pluripotency | Collagenase IV, Mechanical scraping tools |
The critical innovation in the isolation process was immunosurgery, a technique that selectively removed the trophectoderm layer while preserving the intact inner cell mass [1]. This procedure involved incubating blastocysts with anti-human whole antiserum, followed by exposure to guinea pig complement, which selectively lysed the trophectoderm cells while leaving the ICM undamaged [1]. The intact ICM was then plated onto a feeder layer of mitotically-inactivated mouse embryonic fibroblasts (MEFs) in a specific culture medium formulation that supported stem cell proliferation while inhibiting differentiation [2] [1].
The culture system represented a crucial advancement in maintaining pluripotency in vitro. The MEF feeder layer provided essential extracellular matrix components and signaling molecules that mimicked the natural stem cell niche, while the culture medium contained specific growth factors and nutrients optimized for undifferentiated cell growth [1]. Of the 14 inner cell masses successfully isolated through immunosurgery, five stable hESC lines were established that demonstrated long-term proliferative capacity while maintaining their developmental potential [1]. These lines, including the renowned H9 line that would later be used in clinical trials, could be continuously passaged while retaining normal karyotypes and pluripotent characteristics [1].
Characterization and Validation of Pluripotency
The researchers employed multiple validation strategies to confirm the pluripotent status of the derived cell lines. In vitro differentiation assays demonstrated the capacity of the cells to spontaneously generate derivatives of all three embryonic germ layers—ectoderm, mesoderm, and endoderm—when removed from supportive culture conditions [1]. Teratoma formation assays, conducted by injecting the cells into immunodeficient mice, confirmed their ability to generate complex tissues representative of multiple lineages, a gold standard test for pluripotency [1]. Additionally, the cells expressed characteristic molecular markers of pluripotency, including specific surface antigens and transcription factors that distinguished them from differentiated cell types [2].
Diagram Title: hESC Isolation and Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful derivation and maintenance of human embryonic stem cells depended on a carefully optimized system of reagents and culture conditions. The following table details the essential components required for hESC work during this pioneering period.
Table: Essential Research Reagents for Human Embryonic Stem Cell Culture
| Reagent Category | Specific Examples | Function | Technical Considerations |
|---|---|---|---|
| Feeder Cells | Mitotically-inactivated mouse embryonic fibroblasts (MEFs) | Provide extracellular matrix and secreted factors that support pluripotency | Required inactivation by irradiation or mitomycin C; Batch variability concerns |
| Basal Media | KO-DMEM (Knockout Dulbecco's Modified Eagle Medium) | Nutrient foundation specifically formulated for pluripotent cells | Contains optimized glucose and nutrient concentrations |
| Serum Alternatives | Knockout Serum Replacement | Defined replacement for fetal bovine serum | Red variability and supports undifferentiated growth |
| Growth Factors | Basic fibroblast growth factor (bFGF) | Key signaling molecule that maintains pluripotent state | Concentration critical (typically 4-20 ng/mL); Must be replenished frequently |
| Enzymatic Dissociation Agents | Collagenase IV, Trypsin/EDTA | Enable passage and expansion of cell colonies | Concentration and exposure time must be carefully controlled |
| Supplemental Factors | β-mercaptoethanol, Non-essential amino acids, L-glutamine | Reduce oxidative stress and support proliferation | Essential for cell viability during routine passage |
The feeder layer system represented a particularly critical component, with mouse embryonic fibroblasts providing not only physical support but also essential signaling molecules that maintained the stem cells in their undifferentiated state [1]. The culture medium formulation represented a significant advancement beyond previous systems used for animal stem cells, with KO-DMEM and serum replacement products specifically developed to support human pluripotent cells while reducing batch-to-batch variability [2]. Basic fibroblast growth factor (bFGF) emerged as a crucial cytokine for maintaining self-renewal, with specific concentrations required to prevent spontaneous differentiation [1]. The mechanical and enzymatic methods for cell passage also required careful optimization, as stem cell colonies demonstrated particular sensitivity to dissociation methods, with approaches varying from precise mechanical dissection to controlled enzymatic treatment [2].
Classification Framework: Understanding Stem Cell Potency and Lineage
The isolation of human embryonic stem cells highlighted the importance of precise classification systems for understanding stem cell biology. Researchers established a hierarchical framework based on differentiation potential that remains fundamental to the field.
Table: Classification of Stem Cells by Differentiation Potential
| Potency Category | Differentiation Capacity | Representative Examples | Key Characteristics |
|---|---|---|---|
| Totipotent/Omnipotent | Can form all embryonic and extra-embryonic tissues | Fertilized oocyte (zygote), early blastomeres | Can generate a complete organism; Most undifferentiated cell type |
| Pluripotent | Can differentiate into all three embryonic germ layers | Embryonic stem cells, induced pluripotent stem cells | Forms all body tissues but not extra-embryonic structures |
| Multipotent | Can differentiate into multiple cell types within a specific lineage | Hematopoietic stem cells, mesenchymal stem cells | Tissue-specific; Differentiation limited to related cell types |
| Oligopotent | Can differentiate into a few closely related cell types | Vascular stem cells, lymphoid stem cells | Further restricted differentiation capacity |
| Unipotent | Can produce only one cell type | Muscle stem cells, epidermal stem cells | Most restricted adult stem cell type |
This classification system provided critical context for understanding the unique position of embryonic stem cells in the developmental hierarchy [6] [5]. The pluripotent status of hESCs distinguished them from adult stem cells that had been previously characterized, explaining their broad developmental potential and unlimited self-renewal capacity [6]. This fundamental understanding of potency hierarchies would later prove essential for directing differentiation along specific pathways and for comparing the properties of various stem cell populations isolated from different sources [5] [7].
Diagram Title: Stem Cell Potency Hierarchy
Challenges and Limitations in Early Stem Cell Research
Despite the groundbreaking nature of the 1998 breakthrough, several significant challenges emerged that would require years of additional research to address. The dependence on mouse feeder layers raised concerns about potential xenogeneic contamination and the transfer of animal pathogens, limiting the clinical applicability of the cell lines [2] [1]. The initial culture systems also showed limited ability to precisely control differentiation, with spontaneous, heterogeneous differentiation occurring frequently and complicating efforts to generate pure populations of specific cell types [1]. Additionally, the ethical controversies surrounding the use of human embryos created significant political and funding challenges that would shape the regulatory landscape for years to come [6] [2].
The technical hurdles were equally substantial. The phenomenon of spontaneous differentiation presented a constant challenge for maintaining pure stem cell cultures, requiring meticulous daily attention to culture conditions and colony morphology [2]. As noted by Palmer Yu, a postdoctoral fellow in the Thomson lab: "It can be difficult to keep embryonic stem cells happy. They have the potential to differentiate to all the other cell types, and if you aren't careful, they'll start to spontaneously do so without direction from the scientist. It's actually a constant challenge for us to keep all cells in our culture, in a petri dish, in that undifferentiated state" [2]. Additionally, the field lacked standardized protocols for characterizing and quantifying pluripotency, making comparisons between different cell lines and research groups challenging [1].
The isolation of human embryonic stem cells in 1998 established a fundamentally new platform for understanding human development and disease, creating the technical and conceptual infrastructure that would enable the development of precision medicine approaches. This breakthrough provided researchers with their first unlimited access to the foundational cellular building blocks of the human body, opening unprecedented opportunities for disease modeling, drug screening, and the development of cell-based therapies [2] [1]. The rigorous experimental methodologies established during this period—from immunosurgery techniques to defined culture systems—created standards that would guide subsequent innovations in the field.
The impact of this work extends far beyond the initial achievement, having spawned entirely new research domains including induced pluripotency, organoid technology, and cell-based therapeutic screening platforms. As Dr. Janet Rossant, Senior Scientist at SickKids, noted: "The transition from mouse embryonic stem cells to human embryonic stem cells was a big breakthrough and a fundamental shift. Now we have stem cells with this capacity to make every cell type in the body. Can we harness that capacity?" [2]. This fundamental shift continues to resonate through biomedical research, with the foundational principles established during the early years of stem cell isolation continuing to inform emerging technologies and clinical applications in regenerative medicine and precision therapeutics.
The development of induced pluripotent stem cell (iPSC) technology represents a fundamental paradigm shift in regenerative medicine and biomedical research. This breakthrough, which demonstrated that terminally differentiated somatic cells could be reprogrammed to an embryonic-like pluripotent state, has fundamentally altered our approach to studying human development, disease modeling, and therapeutic development. The discovery by Shinya Yamanaka in 2006 that a small set of transcription factors could reverse the developmental clock provided researchers with a powerful new tool that bypassed the ethical concerns associated with embryonic stem cells while offering unprecedented opportunities for personalized medicine [8]. This technology has since become a cornerstone of precision medicine research, enabling the creation of patient-specific disease models and opening new avenues for drug discovery and regenerative therapies.
Historical Context: The Path to Reprogramming
The conceptual foundation for iPSC technology was built upon decades of pioneering research in cellular biology and development. The historical trajectory reveals how successive discoveries progressively challenged the dogma of irreversible cell differentiation:
Key Milestones in Stem Cell Research
Table 1: Historical Foundations of iPSC Technology
| Year | Discovery | Key Researchers | Significance |
|---|---|---|---|
| 1962 | Somatic Cell Nuclear Transfer (SCNT) | John Gurdon [8] | Demonstrated nuclear totipotency; showed that differentiated cell nuclei could support embryonic development in Xenopus frogs |
| 1981 | Isolation of mouse Embryonic Stem Cells (ESCs) | Martin Evans, Matthew Kaufman, Gail Martin [8] | Established in vitro pluripotent cell culture systems |
| 1998 | Derivation of human ESCs | James Thomson [4] [8] | Provided human pluripotent cells for research and therapy |
| 2006 | Creation of mouse iPSCs | Shinya Yamanaka [9] [8] | First reprogramming of somatic cells to pluripotency using defined factors |
| 2007 | Generation of human iPSCs | Yamanaka and Thomson groups [9] [8] | Extended reprogramming technology to human cells |
The critical theoretical breakthrough came from John Gurdon's seminal SCNT experiments in 1962, which demonstrated that the nucleus of a differentiated somatic cell retained all the genetic information needed to generate an entire organism [8]. This discovery directly contradicted the prevailing Weissman barrier theory and Waddington's concept of irreversible epigenetic landscapes, suggesting instead that cell differentiation was reversible under appropriate conditions [8]. The subsequent isolation of embryonic stem cells from mice (1981) and humans (1998) provided the crucial reference point for what constituted a pluripotent state, while simultaneously highlighting the ethical and immunological challenges that would motivate the search for alternative approaches [4] [8].
The iPSC Breakthrough: Molecular Mechanisms
The Yamanaka Factors
Shinya Yamanaka's pioneering work began with a systematic screening of 24 candidate genes that were known to be important for maintaining pluripotency in embryonic stem cells [8]. Through iterative testing, his team made the remarkable discovery that only four transcription factors—Oct4, Sox2, Klf4, and c-Myc (collectively known as OSKM or the Yamanaka factors)—were sufficient to reprogram mouse embryonic fibroblasts into pluripotent stem cells [8]. The same factors (with Thomson's group demonstrating that Oct4, Sox2, NANOG, and LIN28 could also work) successfully generated human iPSCs in 2007 [10] [9] [8].
The reprogramming process initiates a profound transcriptional and epigenetic remodeling of somatic cells. The mechanism operates through distinct phases:
Evolving Reprogramming Methods
Since the initial viral vector approach, numerous reprogramming methods have been developed to enhance efficiency and safety:
Table 2: Evolution of iPSC Reprogramming Methodologies
| Method | Key Features | Efficiency | Safety Considerations | Applications |
|---|---|---|---|---|
| Retroviral Vectors (Original) | Stable integration, high efficiency | Moderate | Insertional mutagenesis, oncogene activation | Basic research |
| Lentiviral Vectors | Can infect non-dividing cells | Moderate | Insertional mutagenesis | Basic research |
| Excisable Vectors | Allows removal after reprogramming | Moderate | Reduced long-term integration risk | Therapeutic applications |
| Non-integrating Episomes | No genomic integration | Low | Higher safety profile | Therapeutic applications |
| Sendai Virus | RNA-based, non-integrating | High | Cleared after reprogramming | Clinical applications |
| mRNA Transfection | No genetic material integration | Moderate | High safety, requires repeated transfection | Clinical applications |
| Protein Transduction | No genetic material | Low | Highest safety profile | Clinical applications |
| Small Molecule | Chemical induction only | Improving | High safety, easy delivery | Future clinical use |
The field has progressively moved toward integration-free methods such as Sendai virus, mRNA transfection, and small molecule approaches to enhance the safety profile of iPSCs for therapeutic applications [10]. Particularly noteworthy are advances in fully chemical reprogramming, first reported in 2013, which may eventually enable completely defined, xeno-free generation of clinical-grade iPSCs [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for iPSC Generation and Characterization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc (OSKM) or Oct4, Sox2, NANOG, LIN28 | Initiate and drive reprogramming process | Delivery via integrating/non-integrating vectors; chemical alternatives emerging |
| Culture Media | Pluripotent stem cell-specific media (e.g., mTeSR, StemFlex) | Maintain pluripotency and self-renewal | Defined, feeder-free systems preferred for reproducibility |
| Quality Control Assays | Pluripotency markers (Nanog, SSEA-4, TRA-1-60), Karyotyping, Short Tandem Repeat analysis | Verify pluripotent state and genetic integrity | Essential for confirming successful reprogramming |
| Differentiation Inducers | Specific growth factors, small molecules | Direct differentiation toward specific lineages | Protocol-dependent; often sequential activation/inhibition of key pathways |
| Gene Editing Tools | CRISPR-Cas9, TALENs | Introduce or correct disease-relevant mutations | Enables creation of isogenic controls and disease models |
Applications in Precision Medicine and Drug Discovery
The integration of iPSC technology into precision medicine frameworks has created unprecedented opportunities for understanding disease mechanisms and developing targeted therapies.
Disease Modeling and Drug Screening
iPSCs have revolutionized disease modeling by enabling the creation of patient-specific cellular models that recapitulate pathological features in vitro. This "clinical trial in a dish" approach allows for studying disease mechanisms and screening therapeutic compounds in human genetic backgrounds [10]. Notable applications include:
- Neurological Disorders: Modeling of amyotrophic lateral sclerosis (ALS), Alzheimer's disease, Parkinson's disease, and spinal muscular atrophy using patient-specific neurons [11]
- Cardiovascular Diseases: Creation of disease-specific cardiomyocytes for conditions like long QT syndrome, catecholaminergic polymorphic ventricular tachycardia, and hypertrophic cardiomyopathy [10]
- Drug Screening and Toxicity Testing: iPSC-derived cells provide human-relevant systems for evaluating drug efficacy and safety, with particular value in cardiotoxicity testing and hepatotoxicity assessment [12] [9]
The application of iPSC technology in drug discovery is exemplified by several clinical trials that have emerged from iPSC-based screening platforms, including trials of bosutinib, ropinirole, and ezogabine for ALS, and WVE-004 and BII078 for ALS/FTD [11].
Market Growth and Clinical Translation
Table 4: iPSC Market Outlook and Clinical Progress
| Parameter | Current Status | Projected Growth | Key Drivers |
|---|---|---|---|
| Global Market Value | $2.01 Billion (2024) | $4.69 Billion by 2033 [12] | Expanding applications in drug discovery and regenerative medicine |
| Compound Annual Growth Rate | — | 9.86% (2025-2033) [12] | Rising investments and technological advancements |
| Clinical Trial Stage | Phase 3 for osteoarthritis (CYP-004) [9] | Multiple Phase 2 and 3 trials anticipated | Demonstrated safety and efficacy in early trials |
| Key Companies | Fujifilm CDI, Evotec, Ncardia, Cynata Therapeutics [12] [9] | Increased strategic collaborations | Expanding product pipelines and therapeutic applications |
| Major Applications | Disease modeling, drug discovery, toxicology testing [12] [9] | Cell therapies, personalized medicine | Regulatory support (FDA Modernization Act 2.0) |
The clinical translation of iPSC technology reached a significant milestone in 2013 when the first iPSC-derived cell product was transplanted into a human patient for treating macular degeneration [9]. This was followed by Cynata Therapeutics receiving approval in 2016 for the first formal clinical trial of an allogeneic iPSC-derived cell product (CYP-001) for graft-versus-host disease [9]. The ongoing Phase 3 trial of Cynata's CYP-004 product for osteoarthritis represents the largest and most advanced clinical trial of an iPSC-derived therapeutic to date [9].
The discovery of induced pluripotent stem cells has fundamentally transformed biomedical research and regenerative medicine. By providing an unlimited source of patient-specific cells, iPSC technology has enabled unprecedented opportunities for modeling human diseases, screening drug candidates, and developing personalized cell therapies. The continued refinement of reprogramming methods, differentiation protocols, and genome editing technologies promises to further enhance the safety, efficiency, and applicability of iPSCs.
As the field progresses, key challenges remain, including the need for standardized quality control measures, improved differentiation efficiency, and addressing potential genomic instability during reprogramming [12] [8]. However, with the integration of emerging technologies such as artificial intelligence, organoid systems, and 3D bioprinting, iPSCs are poised to remain at the forefront of precision medicine initiatives, potentially enabling truly personalized treatments tailored to an individual's genetic makeup and disease characteristics [9] [11]. The paradigm shift initiated by Yamanaka's discovery continues to unfold, promising to reshape our approach to understanding and treating human diseases in the decades to come.
The historical evolution of precision medicine is deeply intertwined with advances in stem cell biology. The identification and characterization of distinct stem cell lineages—embryonic, adult, and perinatal—have provided researchers with a sophisticated toolkit for modeling human disease, screening therapeutic compounds, and developing regenerative therapies. These cellular tools exhibit fundamental differences in their developmental origins, differentiation potentials, and therapeutic applications, making them uniquely suited for specific research and clinical contexts. Embryonic stem cells (ESCs), derived from the inner cell mass of blastocysts, represent the foundational pluripotent platform capable of generating any cell type in the body [13]. Adult stem cells (ASCs), also known as somatic stem cells, are multipotent tissue-specific residents responsible for maintenance and repair [14]. Perinatal stem cells, harvested from birth-associated tissues such as umbilical cord and amniotic fluid, occupy a unique developmental intermediate position, often exhibiting enhanced plasticity and immunomodulatory properties compared to their adult counterparts [15] [16]. This technical guide examines the defining biological properties, experimental methodologies, and precision medicine applications of these three core stem cell lineages, providing researchers with a framework for their appropriate selection and utilization.
Defining the Core Stem Cell Lineages
Embryonic Stem Cells (ESCs)
Key Characteristics: ESCs are defined by their pluripotent nature, enabling differentiation into any of the three germ layers: ectoderm, mesoderm, and endoderm [13]. They are isolated from the inner cell mass of pre-implantation blastocysts through microsurgery or immunological targeting of trophoblast cells [13]. ESCs possess a virtually unlimited self-renewal capacity in culture, maintaining their undifferentiated state through specific signaling pathways and transcription factor networks [13]. Their primary research applications include disease modeling, drug discovery, and developmental biology studies, leveraging their broad differentiation potential [13].
Historical Context and Ethical Framework: The first human ESCs were isolated in 1998, marking a pivotal moment for regenerative medicine [17]. However, their use involves the destruction of human embryos, creating ongoing ethical considerations that have shaped research policies and funding landscapes worldwide [17]. These concerns directly motivated the development of induced pluripotent stem cells (iPSCs) as an alternative approach [17].
Adult Stem Cells (ASCs)
Key Characteristics: ASCs are multipotent stem cells found in various tissues of the adult organism, where they function in tissue maintenance, repair, and regeneration [14]. Unlike pluripotent ESCs, their differentiation potential is generally restricted to cell types within their tissue of origin [13] [14]. They reside in specific tniche microenvironments that regulate their quiescence, activation, and fate decisions [14]. ASCs can be harvested from multiple sources, including bone marrow, adipose tissue, dental pulp, and even salivary glands, making them accessible for autologous transplantation [14].
Major Subtypes and Functions:
- Hematopoietic Stem Cells (HSCs): Located in bone marrow, HSCs give rise to all blood cell lineages and form the biological basis for bone marrow transplantation [13] [14].
- Mesenchymal Stem Cells (MSCs): Initially isolated from bone marrow but present in all vascularized adult tissues, MSCs can differentiate into osteoblasts, adipocytes, and chondroblasts [18] [14]. Defined standards require them to express specific surface antigens (CD105, CD73, CD90) while lacking hematopoietic markers [14].
- Neural Stem Cells (NSCs): Found in specific brain regions, NSCs generate neurons, astrocytes, and oligodendrocytes [14].
- Epithelial Stem Cells: Reside in the lining of the digestive tract and skin, enabling continuous renewal of these tissues [14].
Perinatal Stem Cells
Key Characteristics: Perinatal stem cells are derived from tissues associated with the prenatal and perinatal period, including umbilical cord blood, Wharton's jelly, amniotic membrane, amniotic fluid, and placenta [15] [16]. These cells exhibit multipotent capabilities but often demonstrate greater plasticity and proliferative capacity compared to adult stem cells [13]. Their collection is non-invasive and poses no ethical controversies, as the tissues are typically discarded after birth [15]. These cells also show reduced immunogenicity, making them promising candidates for allogeneic transplantation [19].
Research Trends and Therapeutic Promise: Bibliometric analysis reveals remarkable expansion in perinatal stem cell research, with over 33,273 publications appearing between 2000 and 2025 [15] [16]. The dominant research categories include hematology, immunology, cell biology, experimental medicine, and tissue engineering [15]. Recent studies highlight their potential in treating diabetic cardiomyopathy, generating hepatocyte-like cells, and repairing neurological damage [15] [16].
Table 1: Comparative Analysis of Stem Cell Lineages
| Characteristic | Embryonic Stem Cells (ESCs) | Adult Stem Cells (ASCs) | Perinatal Stem Cells |
|---|---|---|---|
| Developmental Origin | Inner cell mass of blastocyst | Various adult tissues (bone marrow, adipose, etc.) | Umbilical cord, placenta, amniotic fluid |
| Differentiation Potential | Pluripotent | Multipotent | Multipotent with enhanced plasticity |
| Self-Renewal Capacity | Virtually unlimited | Limited in vitro | Higher than ASCs |
| Ethical Considerations | Significant (embryo destruction) | Minimal | Minimal |
| Immunogenicity | High (allogeneic) | Low (autologous possible) | Reduced immunogenicity |
| Key Research Applications | Disease modeling, developmental biology, drug screening | Tissue repair, hematopoietic reconstitution, immunomodulation | Regenerative medicine, tissue engineering, immunomodulation |
| Primary In Vivo Role | Embryonic development | Tissue maintenance and repair | Fetal development |
Experimental Protocols for Lineage-Specific Analysis
iPSC Generation and Characterization
Reprogramming Methodology: The generation of induced pluripotent stem cells (iPSCs) represents a cornerstone technique for modern precision medicine, enabling the creation of patient-specific pluripotent cells without ethical concerns [17]. The standard protocol involves introducing the Yamanaka factors (OCT4, SOX2, KLF4, and c-MYC) into adult somatic cells, typically dermal fibroblasts or blood cells [17]. This can be achieved using viral vectors (retroviruses or lentiviruses) or non-integrating methods (episomal vectors, Sendai virus, or mRNA transfection) [17]. Following transduction, cells are transferred to ESC culture conditions and monitored for colony formation. Putative iPSC colonies are typically isolated 3-4 weeks post-transduction [17].
Characterization and Validation: Validated iPSC lines must demonstrate:
- Pluripotency Marker Expression: Immunocytochemistry for OCT4, SOX2, NANOG, and SSEA-4 [17].
- Trilineage Differentiation Capacity: In vitro differentiation via embryoid body formation followed by analysis of germ layer markers [17].
- Genetic Stability: Karyotype analysis to confirm chromosomal integrity [17].
Precision Medicine Applications: iPSC technology enables the generation of patient-specific disease models, particularly for neurological disorders, cardiac conditions, and genetic diseases [17]. For example, researchers have successfully generated insulin-producing pancreatic β-cells from iPSCs for diabetes treatment [17].
MSC Isolation and Differentiation
Isolation Protocol: Mesenchymal stem cells can be isolated from multiple tissue sources using standardized protocols. For bone marrow-derived MSCs, aspirates are diluted with phosphate-buffered saline (PBS) and separated via density gradient centrifugation [14]. The mononuclear cell fraction is plated in culture flasks with MSC-specific media, and non-adherent cells are removed after 48-72 hours [14]. Adipose-derived MSCs are isolated through enzymatic digestion (collagenase) of lipoaspirate samples, followed by centrifugation and plating [14]. Umbilical cord-derived MSCs are obtained through explant culture or enzymatic digestion of Wharton's jelly [14].
In Vitro Differentiation Assays:
- Osteogenic Differentiation: Culture in media containing β-glycerophosphate, ascorbic acid, and dexamethasone for 2-3 weeks; validate with Alizarin Red S staining for calcium deposits [14].
- Adipogenic Differentiation: Culture in media containing insulin, dexamethasone, indomethacin, and IBMX for 2-3 weeks; validate with Oil Red O staining for lipid vacuoles [14].
- Chondrogenic Differentiation: Pellet culture in media containing TGF-β3 for 3-4 weeks; validate with Alcian Blue staining for glycosaminoglycans [14].
Characterization Standards: According to International Society for Cellular Therapy guidelines, human MSCs must express CD105, CD73, and CD90 (≥95% positive), while lacking expression of CD45, CD34, CD14/CD11b, CD79a/CD19, and HLA-DR (≤2% positive) [14].
Organoid Generation from Pluripotent Stem Cells
Intestinal Organoid Protocol: Organoid technology represents a revolutionary approach for disease modeling and drug screening [20]. To generate intestinal organoids from iPSCs or ESCs, a stepwise differentiation protocol is employed:
- Definitive Endoderm Induction: Culture pluripotent stem cells in media containing Activin A for 3-5 days [20].
- Mid/Hindgut Specification: Transfer to media containing FGF4 and WNT3A to promote intestinal lineage commitment [20].
- 3D Matrigel Culture: Embed developing intestinal spheroids in Matrigel and culture in media containing EGF, Noggin, and R-spondin to promote crypt-villus structure formation [20].
- Maturation: Maintain organoids for 2-4 weeks with periodic passaging to allow structural maturation [20].
Advanced Co-culture Systems: To enhance physiological relevance, researchers have developed sophisticated co-culture systems:
- "Apical-out" Organoids: Reverse polarity to enable direct host-microbe interaction studies [20].
- Immune Cell Co-cultures: Incorporate macrophages or T cells to study epithelial-immune interactions [20].
- Neural Co-cultures: Combine intestinal organoids with enteric nervous system components to model gut-brain axis signaling [20].
Table 2: Key Research Reagent Solutions for Stem Cell Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Factors | Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) | Conversion of somatic cells to iPSCs |
| Culture Matrices | Matrigel, Laminin-521, Recombinant Vitronectin | Provide structural support for pluripotent stem cell growth |
| Lineage Tracing Systems | Cre-loxP, Dre-rox, Brainbow, R26R-Confetti | Fate mapping and clonal analysis |
| Differentiation Factors | Activin A, BMP4, FGFs, WNT agonists, Retinoic Acid | Direct differentiation toward specific lineages |
| Characterization Antibodies | CD105, CD73, CD90, OCT4, NANOG, SSEA-4 | Identification and validation of stem cell populations |
| Gene Editing Tools | CRISPR-Cas9, TALENs, ZFNs | Genetic modification for disease modeling |
Signaling Pathways and Molecular Regulation
The distinct behaviors of different stem cell lineages are governed by specific signaling pathways and molecular networks. Understanding these regulatory mechanisms is essential for manipulating stem cell fate for precision medicine applications.
The following diagram illustrates the core signaling pathways that regulate self-renewal and differentiation in pluripotent stem cells:
Diagram 1: Core signaling pathways regulating pluripotent stem cell fate. The diagram illustrates how external signals (LIF, BMP, WNT, FGF) activate intracellular pathways that ultimately influence the balance between self-renewal and differentiation.
In adult stem cells, niche-specific signals create localized microenvironments that maintain stem cell quiescence or activate proliferation and differentiation as needed. The following diagram depicts key niche signaling components:
Diagram 2: Niche signaling in adult stem cell regulation. The diagram shows how localized signals from the stem cell niche (Notch, TGFβ, WNT, FGF) influence the balance between quiescence and activation in adult stem cell populations.
For perinatal stem cells, particularly those with therapeutic applications in inflammatory conditions, immunomodulatory pathways play crucial roles. The following diagram outlines key molecular mechanisms involved in their therapeutic actions:
Diagram 3: Therapeutic signaling mechanisms of perinatal stem cells. The diagram illustrates molecular pathways (TLR4/NF-κB/NLRP3 and TGF-β/Smad) through which perinatal stem cells exert immunomodulatory and tissue repair effects, as demonstrated in models of diabetic cardiomyopathy [15].
Applications in Precision Medicine and Therapeutic Development
Disease Modeling and Drug Screening
Stem cell-based models have revolutionized preclinical drug development by providing human-relevant systems for efficacy and toxicity testing. iPSC-derived neurons, cardiomyocytes, and hepatocytes enable patient-specific drug response profiling and identification of subpopulation-specific toxicities [17] [20]. Organoid technology has been particularly transformative for studying complex diseases like inflammatory bowel disease (IBD), where patient-derived intestinal organoids retain disease-specific epigenetic and transcriptional signatures [20]. These models have enabled the identification of novel drug targets, such as components of the ATF6 pathway as a branch of the unfolded protein response [20]. Cerebral brain organoids co-cultured with microglia have provided unprecedented insights into neuroinflammatory processes in Parkinson's disease, demonstrating how mitochondrial stress-associated STING/IFN-I responses drive pathology [20].
Regenerative Medicine and Clinical Applications
The therapeutic application of stem cells represents a paradigm shift in treating degenerative conditions. The FDA-approved stem cell product landscape has expanded significantly between 2023-2025, with notable approvals including [18]:
- Omisirge (omidubicel): Approved in April 2023 for hematologic malignancies, this cord blood-derived hematopoietic progenitor cell product accelerates neutrophil recovery after transplantation [18].
- Lyfgenia (lovotibeglogene autotemcel): Approved in December 2023 as an autologous cell-based gene therapy for sickle cell disease, with 88% of patients achieving complete resolution of vaso-occlusive events in clinical trials [18].
- Ryoncil (remestemcel-L): Approved in December 2024 as the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease [18].
Beyond these approved products, the clinical pipeline includes promising investigational therapies. Fertilo received FDA IND authorization in February 2025 as the first iPSC-based therapy to enter U.S. Phase III trials, using ovarian support cells derived from clinical-grade iPSCs to support ex vivo oocyte maturation [18]. Multiple iPSC-derived therapies targeting retinal degeneration (OpCT-001), systemic lupus erythematosus (FT819), and neurodegenerative conditions have received FDA clearance for clinical trials [18].
Emerging Technologies and Future Directions
The convergence of stem cell biology with bioengineering and gene editing technologies is creating unprecedented opportunities for precision medicine. Lineage tracing technologies have evolved from simple dye labeling to sophisticated genetic systems like Cre-loxP, Brainbow, and dual recombinase approaches (Cre-loxP/Dre-rox) that enable high-resolution fate mapping in developing tissues [21]. The integration of single-cell RNA sequencing with lineage tracing provides multidimensional data on cell fate decisions [21]. CRISPR-Cas9 genome editing enables precise genetic correction in patient-specific iPSCs, creating autologous cell sources for transplantation without immune rejection concerns [13]. The development of direct reprogramming approaches that convert somatic cells between lineages without passing through a pluripotent state offers potentially safer and more efficient routes to therapeutic cell types [17]. As these technologies mature, they promise to accelerate the development of personalized regenerative therapies tailored to an individual's genetic makeup and disease characteristics.
The strategic integration of embryonic, adult, and perinatal stem cell lineages into the precision medicine toolkit has fundamentally transformed biomedical research and therapeutic development. Each lineage offers complementary strengths: ESCs provide the gold standard for pluripotency; ASCs enable tissue-specific regeneration with minimized ethical concerns; and perinatal stem cells offer an accessible, potent intermediate with unique immunomodulatory properties. The ongoing refinement of differentiation protocols, lineage tracing technologies, and genome editing tools continues to enhance the resolution at which we can manipulate cell fate for therapeutic benefit. As the field advances, the convergence of stem cell biology with bioengineering, genomics, and computational modeling promises to unlock increasingly sophisticated approaches for understanding human disease and developing personalized regenerative therapies. The historical evolution of stem cell applications in precision medicine reflects a journey from fundamental biological discovery to transformative clinical applications, with each stem cell lineage contributing unique capabilities to this rapidly advancing field.
Regenerative medicine represents a revolutionary frontier in medical science, aiming to repair, replace, and regenerate damaged tissues and organs [13]. This whitepaper examines the foundational role of stem cell biology in this field, framing it within the historical evolution toward precision medicine. We detail the core cell types driving these advances, provide actionable experimental protocols, and analyze the current clinical and regulatory landscape. Supported by quantitative data and technical workflows, this document serves as a guide for researchers and drug development professionals navigating the transition from foundational biology to therapeutic application.
Regenerative medicine is an emerging branch of medicine that leverages the body's innate repair mechanisms to address conditions previously considered incurable, such as organ failure, myocardial infarction, and neurodegenerative diseases [22]. Its potential to transform the treatment landscape for millions of patients worldwide is unprecedented [13]. Stem cells, with their dual capabilities of self-renewal and differentiation into specialized cell types, are the cornerstone of this field [13] [23]. The historical journey—from the early foundational work in the 19th and 20th centuries to the isolation of human embryonic stem cells (ESCs) in 1998 and the landmark discovery of induced pluripotent stem cells (iPSCs) in 2006—has set the stage for the current therapeutic revolution [13] [24] [25]. This document explores how these biological tools are being systematically bridged to clinical therapy, focusing on the technical methodologies, safety considerations, and regulatory frameworks that underpin this translation.
Stem Cell Types: Characteristics and Therapeutic Potential
Stem cells are broadly categorized based on their origin and differentiation potential. The following table summarizes the key types central to regenerative medicine.
Table 1: Key Stem Cell Types in Regenerative Medicine Research
| Stem Cell Type | Origin | Key Characteristics | Primary Research & Therapeutic Applications |
|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocysts [13] | Pluripotent; can differentiate into any cell type in the body [13] [23] | Disease modeling, drug testing and development, fundamental studies of development [13] |
| Induced Pluripotent Stem Cells (iPSCs) | Genetically reprogrammed somatic cells (e.g., skin, blood) [24] [23] | Pluripotent; avoid ethical concerns of ESCs; enable patient-specific modeling [24] [25] | Personalized disease modeling, drug screening, cell replacement therapies (e.g., Parkinson's, retinal diseases) [24] [18] |
| Adult Stem Cells (ASCs) | Various tissues (e.g., bone marrow, adipose, blood) [13] [23] | Multipotent; limited to differentiating into cell types of their tissue of origin [13] [23] | Tissue-specific regeneration; hematopoietic stem cell transplantation (HSCT) for blood cancers [13] [24] |
| Mesenchymal Stem Cells (MSCs) | Tissues including bone marrow, umbilical cord, adipose [24] [23] | Multipotent; strong immunomodulatory and anti-inflammatory properties [24] [23] | Treatment of graft-versus-host disease (GVHD), inflammatory disorders, musculoskeletal repair [18] [23] |
Core Experimental Protocols and Workflows
Protocol for Generating and Differentiating iPSCs
The creation of patient-specific iPSCs is a fundamental protocol enabling personalized regenerative medicine.
- Somatic Cell Isolation and Culture: Obtain somatic cells, typically dermal fibroblasts or peripheral blood mononuclear cells, from the patient via biopsy or blood draw [24]. Culture and expand these cells under standard conditions.
- Reprogramming Factor Delivery: Introduce the four core transcription factors (Oct3/4, Sox2, Klf4, and c-Myc) into the somatic cells using a non-integrating method, such as Sendai virus or episomal vectors, to minimize the risk of tumorigenicity [24] [26].
- iPSC Colony Culture and Expansion: Transfer the transfected cells onto a feeder layer of mouse embryonic fibroblasts (MEFs) or a synthetic substrate. Culture in a defined medium that supports pluripotency. Colonies with embryonic stem cell-like morphology will appear in 2-4 weeks [24].
- Characterization of Pluripotency: Validate successful reprogramming through:
- Immunocytochemistry: Detection of pluripotency markers (e.g., Oct4, Sox2, Nanog).
- In vitro Differentiation: Formation of embryoid bodies and subsequent differentiation into cells of the three germ layers.
- Directed Differentiation: Differentiate the validated iPSCs into target cells (e.g., dopaminergic neurons, cardiomyocytes) using specific cytokine cocktails and small molecules to mimic developmental signaling pathways [24]. For example, to generate dopaminergic progenitors for Parkinson's disease, activation of the Sonic Hedgehog (SHH) and Wnt pathways is critical [18].
The following diagram illustrates the logical workflow of this protocol:
Diagram 1: iPSC Generation and Differentiation Workflow
Preclinical Assessment of Stem Cell-Based Therapies
Before clinical application, stem cell-derived products must undergo rigorous preclinical testing.
- In Vitro Functional Assays: Assess the functionality of differentiated cells. For iPSC-derived cardiomyocytes, this includes measuring electrophysiological activity via patch clamping or microelectrode arrays. For dopaminergic neurons, measure dopamine release via HPLC [24] [23].
- In Vivo Transplantation and Tracking:
- Animal Models: Utilize immunodeficient rodent models (e.g., NSG mice) of human disease, such as a Parkinson's model induced by 6-hydroxydopamine (6-OHDA) [18].
- Cell Delivery: Transplant the stem cell-derived product (e.g., dopaminergic neural progenitors) into the target site (e.g., striatum) using stereotactic surgery.
- Outcome Measures: Monitor for functional recovery using behavioral tests (e.g., apomorphine-induced rotation). Post-mortem histological analysis confirms cell survival, maturation, and integration into host circuitry [18].
- Tumorigenicity Safety Assessment: A critical step is to monitor for aberrant growth. This involves long-term observation of transplanted animals and sensitive assays like PCR to detect any residual undifferentiated pluripotent cells in the final product [24] [18].
The Scientist's Toolkit: Essential Research Reagents
Successful research in regenerative medicine relies on a suite of high-quality reagents and platforms.
Table 2: Key Research Reagent Solutions
| Reagent / Platform | Function in Research | Specific Example |
|---|---|---|
| Reprogramming Vectors | Deliver transcription factors to somatic cells to induce pluripotency. | Non-integrating Sendai virus or episomal plasmids [24]. |
| Defined Culture Media | Support the growth and maintenance of stem cells or direct differentiation. | mTeSR1 for iPSC maintenance; media with activin A/BMP4 for mesoderm differentiation [24]. |
| GMP-Compliant iPSC Lines | Provide a standardized, clinically relevant starting material for therapy development. | StemRNA Clinical Seed iPSCs with an established Drug Master File (DMF) [18]. |
| CRISPR-Cas9 Systems | Enable precise genome editing for gene correction (e.g., in monogenic diseases) or insertion of therapeutic transgenes. | Used to correct mutations in iPSCs in diseases like sickle cell anemia [13] [24]. |
| Single-Cell RNA Sequencing | Characterize cellular heterogeneity, validate differentiation purity, and identify novel cell populations. | Critical for quality control of differentiated products and analyzing tumor microenvironment interactions [13] [27]. |
Clinical Translation and Regulatory Landscape
The transition from lab to clinic is a carefully regulated process. As of December 2024, 115 global clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products were identified, with over 1,200 patients dosed and no class-wide safety concerns reported [18]. The therapeutic areas of highest focus are ophthalmology, the central nervous system (CNS), and oncology [18].
Table 3: Select FDA-Approved and Late-Stage Stem Cell Therapies (2023-2025)
| Therapy / Product | Indication | Cell Type | Status & Key Details |
|---|---|---|---|
| Ryoncil | Pediatric steroid-refractory acute Graft-versus-Host Disease (SR-aGVHD) | Allogeneic bone marrow-derived MSCs | FDA Approved (Dec 2024). First MSC therapy approved in the U.S. [18]. |
| Lyfgenia | Sickle cell disease with history of vaso-occlusive events | Autologous hematopoietic stem cells (gene-modified) | FDA Approved (Dec 2023). One-time gene therapy that reduces red blood cell sickling [18]. |
| Omisirge | Hematologic malignancies (post-umbilical cord blood transplant) | Nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cells | FDA Approved (Apr 2023). Accelerates neutrophil recovery [18]. |
| Fertilo | Support for ex vivo oocyte maturation | iPSC-derived ovarian support cells (OSCs) | FDA IND Cleared (Feb 2025). First iPSC-based therapy to enter U.S. Phase III trials [18]. |
| OpCT-001 | Retinal degeneration (e.g., retinitis pigmentosa) | iPSC-derived therapy | FDA IND Cleared (Sep 2024) for Phase I/IIa trial targeting photoreceptor diseases [18]. |
It is critical to distinguish between FDA authorization for a clinical trial and full product approval. An Investigational New Drug (IND) application allows a company to begin human trials, whereas formal marketing approval requires a Biologics License Application (BLA) after successful trials demonstrate safety and efficacy [18]. Initiatives like the NIH's Regenerative Medicine Innovation Project (RMIP) are pivotal in accelerating progress by supporting clinical research on adult stem cells and promoting scientific rigor [28].
The future of regenerative medicine is being shaped by several converging technological trends. The integration of stem cells with gene-editing tools like CRISPR-Cas9 allows for the precise correction of genetic defects in patient-specific iPSCs before therapy [13] [24]. The field is also advancing through the development of 3D bioprinting and organoid systems, which create more physiologically relevant models for drug screening and disease modeling, and may eventually serve as engineered tissue grafts [22] [26]. Furthermore, the combination of next-generation sequencing (NGS) with stem cell platforms enables deep molecular profiling of tumors and differentiated cells, refining patient selection and personalizing therapeutic interventions [27].
The initial foray into regenerative medicine has successfully bridged fundamental stem cell biology with tangible therapeutic strategies. The establishment of robust protocols for cell manipulation, coupled with a growing body of clinical evidence and a mature regulatory framework, has moved the field from theoretical promise to clinical reality. While challenges related to tumorigenicity, immunogenicity, and manufacturing scalability remain, the continuous refinement of gene-editing, delivery systems, and differentiation protocols is steadily addressing these hurdles. For researchers and drug developers, this era represents an unprecedented opportunity to contribute to a new therapeutic paradigm that moves beyond managing symptoms to achieving true tissue regeneration and cure.
Engineering Therapies: Stem Cells as Tools for Precision Targeting and Modeling
The historical journey of stem cell applications in precision medicine has witnessed a significant evolution, shifting from a primary focus on cell replacement to harnessing the sophisticated paracrine and immunomodulatory functions of specific stem cell types. Within this paradigm, Mesenchymal Stem Cells (MSCs) have emerged as a cornerstone for advanced therapeutic strategies. Initially identified in the bone marrow by Friedenstein and colleagues in the 1960s for their osteogenic potential, MSCs were primarily conceived as progenitor cells for skeletal tissues [29]. The contemporary understanding, however, recognizes MSCs as non-hematopoietic, multipotent stromal cells with potent capacities for immunomodulation and tissue repair, positioning them as powerful tools for treating a broad spectrum of human diseases [29] [30].
The therapeutic profile of MSCs is defined by their unique characteristics: the ability to self-renew, differentiate into multiple mesodermal lineages (osteoblasts, chondrocytes, adipocytes), and, most importantly, modulate the immune system [29]. According to the International Society for Cellular Therapy (ISCT), MSCs are defined by their adherence to plastic, specific surface marker expression (CD73, CD90, CD105), and lack of hematopoietic marker expression (CD34, CD45, HLA-DR) [29]. Their effects are primarily mediated through the release of a diverse array of bioactive molecules—including growth factors, cytokines, and extracellular vesicles (EVs)—that orchestrate local tissue environments, promote repair, stimulate angiogenesis, and exert profound anti-inflammatory effects [29] [31]. This review delves into the molecular mechanisms and clinical applications of MSCs, framing their role within the next chapter of precision medicine aimed at harnessing innate biological systems for immunomodulation and tissue repair.
Molecular Mechanisms of Action
The therapeutic efficacy of MSCs is not attributed to a single action but to a multifaceted mechanism involving complex interactions with the host immune system and injured tissue. The primary pathways include direct cellular interactions, paracrine signaling, and the release of extracellular vesicles.
Immunomodulatory Properties and Immune Cell Interactions
MSCs possess a remarkable capacity to modulate both innate and adaptive immune responses. They interact with a wide range of immune cells, including T cells, B cells, dendritic cells, macrophages, and natural killer cells, through direct cell-to-cell contact and the release of soluble factors [29]. This immunomodulation is not constitutive but is licensed by inflammatory cytokines, such as interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α), present in the injury microenvironment [32].
Upon activation, MSCs release a cocktail of immunoregulatory molecules. Key among these are:
- Prostaglandin E2 (PGE2): Promotes the polarization of macrophages toward an anti-inflammatory M2 phenotype and inhibits the activity of natural killer (NK) cells [32].
- Indoleamine 2,3-dioxygenase (IDO): Catalyzes the degradation of tryptophan, which suppresses T-cell proliferation and effector functions [32].
- Tumor necrosis factor–stimulated gene 6 (TSG-6): Reduces the recruitment of monocytes and macrophages to sites of inflammation, thereby dampening the inflammatory response [32].
- Growth Factors (e.g., VEGF): Promote angiogenesis and endothelial cell function, which is crucial for supporting tissue repair [32].
The following diagram illustrates the key immunomodulatory pathways activated in MSCs within an inflammatory microenvironment:
Paracrine Signaling and Extracellular Vesicles
A pivotal shift in understanding MSC therapy has been the recognition that their benefits are largely mediated through paracrine effects rather than direct differentiation and engraftment [29] [31]. MSCs release a vast portfolio of bioactive factors, often referred to as the "secretome," which includes lipids, proteins, RNA, and entire organelles packaged into Extracellular Vesicles (EVs) [31].
MSC-derived EVs are emerging as a promising cell-free therapeutic alternative. These nanoscale vesicles can traverse biological barriers and deliver their cargo—including microRNAs, mRNAs, and proteins—to recipient cells, thereby modulating recipient cell behavior [31]. They exhibit strong anti-inflammatory and immunomodulatory properties, which are particularly relevant for treating neurodegenerative diseases and other inflammatory disorders [31]. Furthermore, EVs can be bioengineered to enhance brain targeting or drug loading, increasing their therapeutic potential and moving the field closer to clinical application [31].
Tissue Repair and Regenerative Capabilities
The role of MSCs in tissue repair is a coordinated process that integrates with the body's natural response to injury. The regenerative cascade begins with the release of Damage-Associated Molecular Patterns (DAMPs) from injured cells, which act as distress signals [33]. These signals elicit an acute inflammatory response and mobilize stem cells from their niches.
A critical mechanism for MSC recruitment is the SDF-1/CXCR4 axis. Upon tissue injury, stromal cell-derived factor-1 (SDF-1) is upregulated and creates a chemotactic gradient. MSCs, which express the CXCR4 receptor, follow this gradient, homing to the site of damage [33]. Once localized, MSCs contribute to tissue regeneration by:
- Reducing excessive inflammation via the immunomodulatory mechanisms described above.
- Secreting trophic factors that promote the survival and proliferation of resident progenitor cells.
- Stimulating the formation of new blood vessels (angiogenesis) to restore blood supply.
- Remodeling the extracellular matrix (ECM) to support the formation of new, functional tissue [33].
Advanced Experimental Models and Protocols
Translating the therapeutic potential of MSCs into clinical reality requires robust and reproducible experimental models that closely mimic the in vivo environment. Traditional 2D culture systems often fail to capture the complexity of native tissues, leading to the development of more advanced 3D culture platforms.
3D Collagen Matrix Model for Assessing MSC Immunomodulation
A key protocol for investigating MSC function in a biomimetic environment involves embedding the cells within three-dimensional (3D) collagen hydrogels. This model allows researchers to study how physical parameters, such as matrix stiffness and cell density, influence MSC viability and immunomodulatory activity under inflammatory conditions [32].
Detailed Methodology:
- Hydrogel Preparation: A neutralized collagen solution is prepared from bovine dermis-derived atelocollagen. The solution is mixed with 10x DMEM, 7.5% NaHCO₃, 1M NaOH, and ultrapure water to achieve a physiologically neutral pH [32].
- Cell Encapsulation: Human MSCs are mixed with the neutralized collagen solution to achieve final cell densities typically ranging from 1x10⁶ to 7x10⁶ cells/mL. The mixture is dispensed into culture plates [32].
- Gelation: The plates are incubated at 37°C for 1 hour to allow the collagen-MSC mixture to form a solid hydrogel [32].
- Inflammatory Stimulation: The MSC-laden hydrogels are cultured in a medium supplemented with proinflammatory cytokines, specifically 10 ng/mL TNF-α and 25 ng/mL IFN-γ, to simulate an inflammatory microenvironment. The medium is replaced every two days [32].
- Analysis: Constructs are harvested for analysis at various time points (e.g., 24 hours and 5 days). Key readouts include:
- Gene Expression: Analysis of immunomodulatory genes (e.g., IDO, TSG-6) via qRT-PCR or RNA sequencing.
- Hydrogel Contraction: The surface area of the hydrogels is measured over time to quantify contraction, which is influenced by cell density and matrix stiffness.
- Cell Viability: Assessed using assays like CCK-8 or live/dead staining (e.g., calcein-AM/propidium iodide) [32].
The workflow for this essential experiment is outlined below:
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials used in the aforementioned 3D collagen matrix model, along with their critical functions in the experimental protocol.
Table 1: Key Research Reagent Solutions for 3D MSC Immunomodulation Studies
| Research Reagent | Function and Application in the Protocol |
|---|---|
| Bone Marrow-derived MSCs | Primary cellular component; sourced from human bone marrow and expanded in vitro to study their immunomodulatory behavior [32]. |
| Atelocollagen (Bovine Dermis) | Main structural polymer for forming the 3D hydrogel; provides a biomimetic extracellular matrix that supports cell adhesion and viability [32]. |
| Pro-inflammatory Cytokines (TNF-α, IFN-γ) | Used to simulate an inflammatory microenvironment in vitro; "license" the MSCs to activate their immunomodulatory gene expression and secretory profile [32]. |
| Cell Viability Assay (CCK-8) | Colorimetric assay used to quantify metabolic activity and estimate the number of viable cells within the hydrogel constructs at different time points [32]. |
| Live/Dead Staining (Calcein-AM/PI) | Fluorescent staining method that distinguishes live (green, calcein-AM) from dead (red, propidium iodide) cells, providing a visual assessment of cell viability and distribution in 3D [32]. |
MSC Biomarkers and Functional Characterization
Precise characterization is fundamental for ensuring the identity, purity, and functional competence of MSCs in both research and clinical settings. This is defined by specific surface markers and validated differentiation assays.
Table 2: Key Markers for the Identification and Characterization of MSCs
| Marker Category | Specific Markers | Significance and Function |
|---|---|---|
| Positive Surface Markers (≥95% Expression) | CD105, CD73, CD90 | CD105 is essential for angiogenesis; CD73 an enzyme producing anti-inflammatory adenosine; CD90 mediates cell-cell and cell-ECM adhesion [29]. |
| Negative Surface Markers (≤2% Expression) | CD34, CD45, CD14/CD11b, CD19/CD79α, HLA-DR | These are hematopoietic lineage markers (CD34, CD45, CD14, CD19) and an immunogenic MHC-II molecule (HLA-DR). Their absence confirms the non-hematopoietic nature of the MSC population [29]. |
| Functional Differentiation Potential | Osteogenic, Chondrogenic, Adipogenic | In vitro differentiation into these three mesodermal lineages is a mandatory functional criterion for defining MSCs, as per ISCT guidelines [29]. |
Clinical Translation and Delivery Strategies
A significant challenge in MSC therapy has been the poor retention and survival of transplanted cells at the target site, with studies indicating that less than 5% of administered cells remain viable hours after delivery [32]. To overcome this, biomaterial-based delivery systems, particularly hydrogels, have been developed to enhance therapeutic efficacy.
Hydrogel-Based Delivery Systems
Hydrogels are water-swollen, crosslinked polymer networks that closely mimic the physical and biochemical properties of the native ECM [34]. When used as MSC carriers, they provide a protective 3D microenvironment that supports cell viability, retention, and function upon transplantation [34] [32]. The properties of hydrogels can be finely tuned to modulate MSC behavior:
- Mechanical Properties: Substrate stiffness (elastic modulus) directs stem cell fate. Softer hydrogels (1–10 kPa) promote adipogenic/neurogenic differentiation, while stiffer matrices (25–40 kPa) favor osteogenic commitment [34].
- Biochemical Functionalization: Incorporation of bioactive molecules like RGD peptides (for adhesion), VEGF (for angiogenesis), or BMP-2 (for osteogenesis) can enhance MSC integration and direct therapeutic outcomes [34].
- Injectable Formulations: Hydrogels based on natural polymers (alginate, collagen, hyaluronic acid) can be designed to be injectable, allowing for minimally invasive administration and conformation to irregular defect geometries [34].
Recent advances include the development of "smart" hydrogels that respond to physiological stimuli (e.g., pH, enzymes) for controlled release, and bio-hybrid systems that combine decellularized ECM with synthetic polymers to couple biochemical functionality with structural stability [34]. Early-phase clinical trials have begun to support the feasibility, safety, and therapeutic potential of MSC-laden hydrogels, paving the way for broader clinical application [34].
The journey of MSCs from stromal progenitors to key mediators of immunomodulation and tissue repair mirrors the broader evolution of precision medicine towards biologically integrated therapies. The future of MSC-based therapeutics lies in moving beyond generic cell administration towards precision-engineered, patient-specific solutions. Key future directions include:
- Engineering and Delivery: Enhancing efficacy through advanced biomaterial scaffolds like tunable hydrogels and by developing engineered MSC-derived products, such as extracellular vesicles, which can be loaded with specific therapeutic cargo [34] [31].
- Combination with Advanced Technologies: Integrating MSC platforms with next-generation sequencing (NGS) and single-cell RNA sequencing (scRNA-Seq) to decipher patient-specific disease heterogeneity and identify novel targets, thereby enabling truly personalized treatment regimens [13] [27].
- Overcoming Translational Hurdles: Addressing challenges related to donor variability, scalable manufacturing, and standardized production to ensure consistent, safe, and potent therapeutic products [29] [31].
In conclusion, MSCs represent a paradigm-shifting tool with immense potential to treat a wide range of debilitating diseases. By continuing to unravel their molecular mechanisms and refining our ability to deliver and control their functions, MSC-based therapies are poised to become a cornerstone of next-generation precision regenerative medicine.
{#context}
Weapons Against Cancer: Engineered Stem Cells for Targeted Oncolytic Virotherapy and Drug Delivery
The historical evolution of stem cell applications in precision medicine has reached a pivotal convergence with oncolytic virotherapy, creating a novel therapeutic paradigm for cancer treatment. This synergy addresses one of the most significant challenges in oncology: the precise delivery of potent anticancer agents to tumor sites while sparing healthy tissues. Stem cells, with their innate tumor-homing properties and regenerative capacities, have emerged as sophisticated biological vehicles for oncolytic viruses (OVs), engineered pathogens designed to selectively replicate in and destroy cancer cells [13] [35]. This combination represents a monumental leap from early virotherapy concepts in the 20th century, when sporadic observations of tumor regression followed viral infections, to today's era of rationally designed, genetically engineered "soldiers" equipped with sophisticated "weapons" to combat cancer [36] [37].
The foundational principle of this approach leverages the unique biology of different stem cell types. Mesenchymal stem cells (MSCs), for instance, are attracted to inflammatory and tumor microenvironments, making them ideal delivery vehicles [23]. When loaded with oncolytic viruses, these stem cells serve as protective trojan horses, shielding the therapeutic viruses from premature immune clearance while navigating them to metastatic and primary tumor sites [35]. Upon reaching the tumor, the stem cells release the oncolytic viruses, which then initiate a multi-mechanistic attack: direct lysis of cancer cells, induction of immunogenic cell death, and activation of systemic antitumor immunity [36] [37]. This whitepaper provides an in-depth technical examination of this innovative platform, detailing the core stem cell and virus technologies, their mechanisms of action, essential research methodologies, and the translational pathway from laboratory research to clinical application.
Core Components: Stem Cell Vehicles and Oncolytic Payloads
Stem Cell Platforms: From MSCs to iPSCs
The selection of an appropriate stem cell vehicle is critical for the success of this therapeutic strategy. The most advanced platforms are derived from adult stem cells, which circumvent the ethical concerns and tumorigenicity risks associated with embryonic stem cells [23].
Mesenchymal Stem Cells (MSCs): Sourced from bone marrow, adipose tissue, or umbilical cord, MSCs are the most extensively utilized cellular vehicle in clinical development [23] [18]. Their clinical appeal stems from three key properties: immunomodulatory capabilities that allow allogeneic use without severe rejection, inherent tumor-tropism driven by chemokine signaling in the tumor microenvironment, and a favorable safety profile [23]. The recent FDA approval of Ryoncil (remestemcel-L) for pediatric steroid-refractory acute graft-versus-host disease in December 2024 validates the therapeutic potential of MSCs and paves the way for their use in advanced delivery systems [18].
Induced Pluripotent Stem Cells (iPSCs): iPSCs represent a more recent, technologically advanced platform. These are adult somatic cells genetically reprogrammed to a pluripotent state, offering an unlimited, scalable source for deriving consistent, therapeutic-grade cells [13] [23]. iPSC-derived MSCs (iMSCs) are gaining momentum in regenerative medicine trials due to their enhanced consistency and scalability compared to primary MSCs [18]. For research and development, clinical-grade iPSC seed clones, such as the REPROCELL StemRNA Clinical iPSC Seed Clones, are now available with submitted Drug Master Files (DMF) to streamline regulatory submissions for clinical trials [18].
Table 1: Comparison of Key Stem Cell Platforms for OV Delivery
| Stem Cell Type | Sources | Key Advantages | Current Clinical Status | Primary Applications in OV Therapy |
|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone Marrow, Adipose Tissue, Umbilical Cord | Tumor-homing, immunomodulatory, allogeneic use, well-established safety profile [23] [18] | FDA-approved product (Ryoncil); Multiple clinical trials for OV delivery (e.g., CLD-201) [35] [18] | Protective vehicle for intravenous delivery; Modulates tumor immune microenvironment |
| Induced Pluripotent Stem Cell-derived MSCs (iMSCs) | Genetically reprogrammed somatic cells | Unlimited scalability, batch-to-batch consistency, avoids donor variation [18] | Early-phase clinical trials (e.g., CYP-001 for GvHD) [18] | Next-generation, standardized, off-the-shelf cellular vehicle production |
Oncolytic Virus Platforms and Engineering Strategies
Oncolytic viruses are the therapeutic payload carried by stem cells. They can be broadly classified into DNA and RNA viruses, each with distinct replication cycles, engineering capacities, and oncolytic mechanisms [36] [37].
Herpes Simplex Virus (HSV): A double-stranded DNA virus with a large genome (~150 kb), allowing for the insertion of large or multiple transgenes [36]. Its natural neurotropism can be harnessed for targeting brain tumors. Engineering typically involves deleting the ICP34.5 gene to reduce neurovirulence and enhance tumor-specific replication [36]. T-VEC (talimogene laherparepvec), an HSV-1 engineered to express GM-CSF, was the first OV approved by the FDA in 2015 for advanced melanoma [35] [36].
Adenovirus (AdV): A non-enveloped double-stranded DNA virus known for high transduction efficiency and ease of genetic manipulation [36]. A common strategy to confer tumor-selectivity is the deletion of the E1B-55kDa gene, which is necessary for viral replication in normal cells but dispensable in p53-deficient cancer cells [36]. The adenovirus H101 was approved in China for nasopharyngeal carcinoma in 2005 [36].
Vaccinia Virus (VacV): A large, enveloped double-stranded DNA virus with a strong history as a vaccine and a high capacity for foreign genes [36] [35]. Its rapid replication cycle and cytoplasmic replication (avoiding genomic integration) make it a potent oncolytic agent. Clinical candidates like JX-594 and OLVI-VEC are based on this platform [38] [35].
Modern OV engineering focuses on creating "armed" viruses that not only lyse cells but also manipulate the tumor microenvironment. Key strategies include:
- Enhancing Safety and Selectivity: Using tumor-specific promoters (e.g., hTERT) or deleting viral genes essential for replication in healthy cells (e.g., E1A in AdV) [36].
- Arming with Immunomodulatory Transgenes: Insertion of genes for cytokines (e.g., GM-CSF, IL-12), immune checkpoint inhibitors (e.g., anti-PD-1), or T-cell engagers to stimulate potent anti-tumor immunity [36] [37].
- Improving Delivery and Spread: Incorporation of genes that degrade extracellular matrix (e.g., hyaluronidase) or modify viral surface proteins to enhance infectivity of specific cancer types [37].
Table 2: Key Engineered Oncolytic Virus Platforms for Stem Cell Loading
| Virus Platform (Genetic Material) | Exemplary Engineering Modifications | Key Armed Transgenes | Clinical Candidate Examples |
|---|---|---|---|
| Herpes Simplex Virus (dsDNA) | Deletion of ICP34.5 and ICP47; Insertion of GM-CSF [36] | GM-CSF, IL-12, immune checkpoint inhibitors [36] | T-VEC (Imlygic), RP2/3, SEPREHVIR [38] [35] |
| Adenovirus (dsDNA) | Deletion of E1B-55kD gene; Fiber knob modifications for targeting [36] | p53, TRAIL, bispecific T-cell engagers [36] | H101, Onyx-015, VCN-01 [38] [35] |
| Vaccinia Virus (dsDNA) | Deletion of thymidine kinase (TK) gene; use of synthetic promoters [35] | GM-CSF, CD40 ligand, anti-CTLA-4 [35] | JX594 (Pexa-vec), Olvi-Vec, BT-001 [38] [35] |
| Newcastle Disease Virus (ssRNA-) | Naturally oncolytic; can be engineered for stability [38] | Cytokines, tumor-associated antigens | NDV commonly used in clinical trials [38] |
Mechanism of Action: From Targeted Delivery to Systemic Immunity
The therapeutic efficacy of stem-cell-delivered OVs is a multi-stage process that begins with systemic delivery and culminates in the establishment of lasting anti-tumor immunity. The diagram below illustrates this complex, multi-component pathway.
Stage 1: Protected Delivery and Tumor Homing
Upon intravenous administration, the stem cell vehicle serves a critical protective function. It shields the oncolytic virus from neutralizing antibodies present in the bloodstream, which would otherwise inactivate the virus before it reaches its target [35] [37]. The stem cells, particularly MSCs, then actively migrate toward the tumor site guided by chemotactic signals released by the tumor and its surrounding stroma, such as CXCL12, VEGF, and PDGF [23]. This tumor-homing property enables the delivery of the therapeutic payload not only to the primary tumor mass but also to invasive margins and micrometastases that are often inaccessible via direct injection [35].
Stage 2: Viral Replication and Direct Oncolysis
Once the stem cells localize to the tumor microenvironment, they begin to produce and release the oncolytic viral progeny. These viruses then infect neighboring tumor cells. The selectivity for cancer cells is engineered through multiple mechanisms: many cancer cells have impaired antiviral interferon responses, making them susceptible to viral replication [36] [37]. Furthermore, genetic modifications to the virus, such as placing critical viral genes under the control of tumor-specific promoters (e.g., a promoter active in telomerase-positive cells), ensure that viral replication is largely restricted to malignant cells [36]. The infected cancer cells are subsequently destroyed through viral lytic replication, a process known as direct oncolysis.
Stage 3: Immune Activation and Systemic Anti-Tumor Response
The most significant long-term benefit of this therapy lies in its ability to generate systemic immunity. The virally lysed tumor cells undergo immunogenic cell death (ICD), a process that releases a suite of immunostimulatory signals [36] [37]. These include:
- Tumor-Associated Antigens (TAAs)
- Damage-Associated Molecular Patterns (DAMPs) such as ATP and HMGB1
- Pathogen-Associated Molecular Patterns (PAMPs) from the virus itself [37]
This "antigen tsunami" is captured by resident dendritic cells (DCs), which mature and migrate to draining lymph nodes to prime naive T-cells. The result is the expansion of tumor-specific cytotoxic T lymphocytes (CTLs) that can recirculate, infiltrate both primary and distant tumor sites, and clear malignant cells—an effect known as the abscopal effect [37]. Simultaneously, the pro-inflammatory environment can help to "heat up" immunologically "cold" tumors, making them more susceptible to checkpoint inhibitors and other immunotherapies [35] [39]. The stem cells themselves can contribute to this process by secreting immunomodulatory factors that further shape the anti-tumor immune response [23].
The Scientist's Toolkit: Essential Reagents and Research Protocols
Translating the stem cell-OV concept from theory to practice requires a specific toolkit of reagents, cell models, and analytical methods. The table below outlines core components for establishing a research program in this field.
Table 3: Essential Research Reagents and Experimental Tools
| Reagent / Tool Category | Specific Examples & Models | Critical Function in R&D |
|---|---|---|
| Stem Cell Sources | Primary human MSCs (bone marrow, adipose), Umbilical cord tissue-derived MSCs, Clinical-grade iPSC lines (e.g., REPROCELL StemRNA) [23] [18] | Provide the cellular delivery vehicle; require rigorous characterization of homing ability, immunophenotype, and differentiation potential. |
| Viral Vectors | Engineered HSV (e.g., with ICP34.5 deletion), Oncolytic Adenovirus (e.g., with E1B deletion), Vaccinia virus (e.g., JX-594 backbone) [36] [38] | Constitute the oncolytic payload; must be engineered for tumor selectivity and often "armed" with transgenes. |
| In Vitro Tumor Models | 2D cancer cell line panels, 3D tumor spheroids, Co-culture systems with cancer-associated fibroblasts [40] | Used for initial validation of OV tropism, replication kinetics, and stem cell-mediated delivery efficiency in a controlled system. |
| In Vivo Models | Immunodeficient mice (e.g., NSG) for human tumor xenografts, Immunocompetent syngeneic mouse models, Humanized mouse models [36] | Essential for evaluating homing, biodistribution, therapeutic efficacy, and safety in a physiologically complex environment. |
| Key Assays | Viral Titer Assay (Plaque Forming Units), Flow Cytometry for immune profiling, scRNA-Seq for tumor heterogeneity, Immunohistochemistry for tumor infiltration [13] [40] | Quantify viral replication, characterize immune cell populations in the TME, and assess overall treatment impact. |
Core Experimental Workflow
A standardized research protocol for evaluating stem-cell-delivered OVs involves a sequence of key steps, from initial virus loading into cells to final analysis of therapeutic outcomes. The following diagram maps this workflow.
Detailed Protocol Description:
Virus Loading and Stem Cell Characterization: Stem cells (e.g., MSCs) are transduced with the oncolytic virus at a pre-optimized multiplicity of infection (MOI). The loading efficiency is quantified via flow cytometry (for fluorescent reporter viruses) or qPCR for viral genomes. Critical quality controls include confirming that the stem cells remain viable and retain their migration capacity post-loading [35].
In Vitro Functional Assays:
- Migration Assay: Use a transwell system with a chamber containing tumor cell-conditioned medium as a chemoattractant. Quantify the number of stem cells that migrate through the membrane over 12-24 hours to confirm retained tumor-homing capability [23].
- Cytotoxicity and Viral Replication: Co-culture loaded stem cells with target cancer cells. Monitor cancer cell death over time (e.g., via live-cell imaging or MTT assay) and quantify viral progeny released into the supernatant using a plaque assay on permissive cell lines [36].
In Vivo Therapeutic Evaluation:
- Model Establishment: Implant tumor cells subcutaneously or orthotopically in mice. When tumors reach a predefined volume (e.g., 100-150 mm³), randomize animals into treatment groups: untreated control, OV alone, stem cells alone, and MSC-OV combination [35].
- Delivery and Monitoring: Administer therapies via intravenous or intratumoral injection. Monitor tumor volume regularly with calipers and overall animal health. Use bioluminescent imaging if the OV expresses a reporter gene (e.g., luciferase) to track stem cell localization and viral replication in real time [35] [36].
- Endpoint Analysis: At the end of the study, analyze tumors, blood, and organs. Key analyses include immunohistochemistry for immune cell markers (CD8, CD4, NK cells), cytokine profiling in serum, and qPCR on tissue homogenates to measure viral biodistribution [39] [37]. A full histopathological examination is crucial for assessing off-target toxicity.
Clinical Translation and Future Directions
The path from preclinical validation to clinical application is actively being navigated, with several therapies reaching advanced stages of development. Calidi Biotherapeutics' CLD-201, which consists of adipose-derived stem cells loaded with an oncolytic vaccinia virus, received FDA Fast Track designation for treating soft tissue sarcoma [35]. Preliminary data suggest that the stem cell delivery system protects the virus from immune clearance and amplifies its potency, leading to enhanced immune activation and efficacy in preclinical models [35].
The clinical trial landscape for oncolytic viruses is extensive, with numerous ongoing Phase I-III studies investigating viruses such as HSV, Adenovirus, and Poxvirus for cancers including liver carcinoma, melanoma, and glioblastoma [38]. The recent approvals of stem cell products like Ryoncil and the advancement of iPSC-based therapies into Phase III trials (e.g., Fertilo) demonstrate a maturing regulatory framework for complex cell-based products, which will facilitate the clinical development of stem-cell-delivered OVs [18].
Future directions in this field are focused on enhancing the precision and power of this platform through several key strategies:
- Next-Generation Engineering: Combining OVs with chimeric antigen receptor (CAR) technologies to create off-the-shelf, iPSC-derived CAR-T or CAR-NK cells (e.g., FT819, FT536) that can be delivered alongside OV therapy for a coordinated attack [39] [18].
- Rational Combination Therapies: Systematically pairing MSC-OV therapy with other modalities, particularly immune checkpoint inhibitors (e.g., anti-PD-1) [39] [37]. The OV-induced inflammation can make "cold" tumors "hot," thereby sensitizing them to checkpoint blockade, while the stem cell vehicle ensures sufficient virus reaches the tumor to initiate this process.
- Advanced Delivery and Targeting: Further engineering stem cells to enhance their tumor-specific homing or to express additional therapeutic proteins themselves, effectively creating a synergistic, dual-therapeutic cell factory [13] [37].
- Overcoming Immunosuppression: Using OVs armed with transgenes that directly counter the immunosuppressive tumor microenvironment, such as cytokines that inhibit Tregs or MDSCs, or enzymes that deplete metabolic inhibitors like adenosine [37].
The strategic fusion of stem cell biology with oncolytic virotherapy represents a watershed moment in the historical evolution of precision medicine. This platform elegantly addresses the long-standing challenges of targeted delivery and immune activation in oncology. By leveraging stem cells as guided missiles for engineered oncolytic viruses, researchers have developed a powerful, multi-mechanistic weapon that orchestrates direct tumor lysis, remodels the tumor microenvironment, and ignites a systemic and durable immune response against cancer. As the field advances, propelled by more sophisticated stem cell sources like iPSCs and smarter, multi-armed viral vectors, this approach is poised to become a cornerstone of next-generation cancer immunotherapy, offering new hope for patients with treatment-resistant and metastatic disease.
The field of stem cell research has undergone a revolutionary transformation, fundamentally altering the landscape of precision medicine. This evolution began with embryonic stem cells (ESCs), first isolated in 1981, which provided the initial foundation for studying human development and disease in vitro [13]. However, ethical concerns and immune rejection limitations constrained their clinical utility. The field experienced a paradigm shift in 2006 when Shinya Yamanaka's team discovered that somatic cells could be reprogrammed into induced pluripotent stem cells (iPSCs) through the introduction of just four transcription factors: Oct4, Sox2, Klf4, and c-Myc [41] [42]. This groundbreaking achievement, recognized with a Nobel Prize within six years, enabled the generation of patient-specific pluripotent stem cells without the ethical concerns of ESCs [41].
The concept of "disease-in-a-dish" modeling emerged as a powerful application of iPSC technology, capitalizing on the idea of personalized medicine by using a patient's own cells to model diseases, discover new drugs, and increase the likelihood of favorable therapeutic outcomes [41] [43]. This approach represents a conceptual departure from traditional drug screens, proposing a closed-loop system from sample collection from the diseased patient, to in vitro disease modeling, to drug discovery and FDA approval, and finally to delivering the therapy back to the same patient [41]. Over the past decade, iPSCs have become an indispensable tool for basic biomedical research, disease modeling, pharmacological testing, and personalized cell-based therapies, radically expanding what is possible in regenerative medicine and drug development [42] [44].
Fundamental Principles of iPSC Technology
Somatic Cell Reprogramming
The generation of iPSCs begins with the isolation of somatic cells from a donor. The choice of cell source is critical as it directly influences reprogramming efficiency, quality of resulting iPSC lines, and their subsequent applications [42]. Historically, dermal fibroblasts obtained from skin biopsies were the first cell type used for iPSC generation and remain widely used due to their high genomic stability and ease of expansion [42]. However, less invasive strategies are now preferred, including:
- Peripheral blood mononuclear cells (PBMCs): Offer comparable reprogramming efficiency to fibroblasts with minimally invasive collection [42].
- Urinary epithelial cells: Provide a completely non-invasive, reproducible sampling method with robust reprogramming capacity [42].
- Keratinocytes from hair follicles: Deliver higher reprogramming efficiency compared to fibroblasts, though cell yields are lower [42].
The core reprogramming process involves the introduction of four transcription factors (Oct4, Sox2, Klf4, and c-Myc) that restore pluripotency and self-renewal capacity [42]. These factors work through two principal mechanisms: chromatin remodeling and DNA methylation resetting. Initially, the transcriptional program of the somatic cell is silenced, followed by activation of pluripotency-associated genes, with endogenous reactivation of the Oct4 promoter serving as the central stabilizing mechanism of the pluripotent state [42].
Pluripotency Induction Methods
Various delivery methods have been developed for introducing reprogramming factors, each with distinct advantages and limitations:
Table 1: Comparison of iPSC Reprogramming Methods
| Method | Mechanism | Efficiency | Genomic Integration | Safety Concerns | Primary Applications |
|---|---|---|---|---|---|
| Retroviral/Lentiviral | Integrates into host genome | High | Yes | Insertional mutagenesis, tumorigenesis | Basic research |
| Sendai Virus | Non-integrating RNA virus | Moderate | No | None known | Clinical applications |
| Episomal Vectors | DNA plasmids maintained episomally | Low | No | Low transformation risk | Clinical applications |
| Synthetic mRNA | Transient expression of reprogramming factors | Low | No | Immune response | Clinical applications |
| Recombinant Proteins | Direct protein transduction | Very Low | No | None known | Basic research |
Early approaches relied on retroviral and lentiviral vectors, which were highly efficient but carried risks of insertional mutagenesis and tumorigenesis due to genomic integration [42]. To mitigate these risks, integration-free methods have been developed, including episomal DNA vectors, synthetic mRNA, recombinant protein delivery, and Sendai virus-based systems [42]. While these strategies significantly enhance biosafety, they generally offer lower reprogramming efficiency (typically <0.1-several percent), which varies based on technical factors (vector type, transfection method) and biological factors (donor age, cell type, epigenetic profile) [42].
Technical Methodologies for Disease Modeling
iPSC Culture and Maintenance
Following successful reprogramming, maintaining iPSCs under in vitro culture conditions is essential to preserve their proliferative capacity and pluripotency. Suboptimal environments may trigger spontaneous differentiation or loss of stem cell properties, significantly limiting downstream applications [42].
Early iPSC culture protocols employed feeder layers of mitotically inactivated mouse embryonic fibroblasts, which secreted supportive factors. However, to enhance reproducibility and minimize xenogeneic contamination, feeder-free systems are increasingly used [42]. These rely on extracellular matrix coatings such as Matrigel or recombinant human proteins like laminin [42]. The culture medium typically consists of chemically defined formulations, such as mTeSR1 or E8, supplemented with essential growth factors (e.g., FGF2) and inhibitors of differentiation pathways (e.g., TGF-β/activin A) [42]. These media enable greater standardization and are considered more suitable for translational and clinical applications.
To sustain long-term viability, iPSCs require routine passaging, either mechanically or enzymatically (e.g., using dispase or EDTA). Long-term cryopreservation is achieved using cryoprotectants such as 10% DMSO, allowing stable reconstitution of iPSC lines after thawing [42]. Despite advances in culture technology, challenges persist, including genomic instability during extended passaging and spontaneous differentiation due to fluctuations in culture conditions [42].
Quality Control and Characterization
Rigorous quality control is essential to verify the pluripotent state of iPSCs and ensure genomic integrity. The following characterization methods are routinely employed:
- Pluripotency marker expression: Assessment of canonical markers including Oct4, Nanog, and Sox9 via PCR, immunocytochemistry, or flow cytometry [42].
- Functional pluripotency assays: Directed differentiation into all three germ layers (ectoderm, mesoderm, endoderm), generating representative cell types such as neurons (ectoderm), cardiomyocytes (mesoderm), and hepatocytes (endoderm) [42].
- Genomic integrity evaluation: Karyotyping and whole-genome sequencing to identify chromosomal abnormalities or epigenetic alterations that may compromise differentiation efficiency or predispose cells to malignant transformation [42].
Reprogramming can introduce mutations and DNA damage due to the forced expression of transcription factors, making continuous genomic monitoring essential throughout the reprogramming and culture process [42].
Directed Differentiation Protocols
A critical aspect of disease modeling is the efficient differentiation of iPSCs into relevant somatic cell types. The following table summarizes key differentiation protocols for commonly studied lineages:
Table 2: iPSC Differentiation Protocols for Disease Modeling
| Cell Type | Key Induction Factors | Differentiation Time | Characterization Markers | Primary Disease Applications |
|---|---|---|---|---|
| Cardiomyocytes | Activin A, BMP4, FGF2 | 10-15 days | cTnT, α-actinin, MLC2v | Cardiomyopathy, channelopathies [45] |
| Dopaminergic Neurons | SHH, FGF8, BDNF, GDNF | 30-45 days | Tyrosine hydroxylase, FoxA2, Nurr1 | Parkinson's disease [42] |
| Hepatocytes | Activin A, HGF, FGF4, Oncostatin M | 20-25 days | Albumin, CYP450 enzymes, AAT | Wilson's disease, metabolic disorders [42] |
| Motor Neurons | Retinoic acid, SHH, BDNF, GDNF | 30-40 days | Hb9, ChAT, Islet1 | Amyotrophic lateral sclerosis [42] |
| Corneal Epithelial Cells | BMP4, EGF, PNS | 25-35 days | K12, PAX6, CX43 | Corneal diseases [46] |
A significant challenge in iPSC differentiation is the tendency of derived cells to exhibit an immature, fetal-like phenotype upon differentiation [44]. Achieving functional maturity remains a critical barrier to the use of iPSCs in disease modeling and drug discovery. Recent approaches to enhance maturation include:
- Biomimetic 3D environments: Using hydrogels to mimic not only composition but also architecture of native tissues [44].
- Co-culture systems: Combining multiple cell types to better recapitulate tissue microenvironments [44].
- Mechanical and electrical stimulation: Applying physiological cues to promote functional maturation [43].
For example, researchers have demonstrated that hiPSC-derived cardiomyocytes (hiPSC-CMs) produce higher expression of cardiac maturation markers when co-cultured with human coronary artery endothelial cells in a 3D gelatin methacryloyl hydrogel compared to classic 2D monocultures [44].
Applications in Disease Modeling and Drug Discovery
Neurodegenerative Diseases
iPSC-derived neuronal models have provided new insights into Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS). Patient-specific neurons allow the analysis of pathogenic mechanisms and evaluation of pharmacological interventions [42].
For Alzheimer's disease, iPSC-derived neurons and glia reproduce hallmarks such as tau hyperphosphorylation and β-amyloid deposition, offering a platform for targeted therapeutic development [42]. Parkinson's disease models have recapitulated dopaminergic neuron degeneration in the substantia nigra and revealed the pathogenic role of α-synuclein aggregation, advancing understanding of both sporadic and familial PD [42]. ALS models using iPSC-derived motor neurons have enabled the identification of disease biomarkers and therapeutic compounds [43].
These models support phenotypic screens that have identified compounds capable of rescuing neuronal function in vitro. For example, researchers have developed CRISPR-Cas9 high-throughput machine-learning platforms for modulation of genes involved in Parkinson's disease-associated PINK1-mitophagy in iPSC-derived dopaminergic neurons [43].
Cardiovascular Diseases
iPSCs differentiated into cardiomyocytes enable the study of arrhythmogenic disorders, heart failure, and myocardial injury [42] [45]. Patient-specific iPSC-derived cardiovascular cells allow unprecedented opportunities to discover new drug targets and screen compounds for cardiovascular disease [45].
Specific applications include:
- Disease modeling: Models of congenital arrhythmias linked to KCNQ1 mutations provide a basis for precision cardiology [42].
- Drug screening: iPSC-derived cardiomyocytes are now used routinely to screen for drug-induced arrhythmia risk and have been integrated into regulatory safety initiatives like CiPA [43].
- Regenerative applications: In myocardial damage, iPSC-derived cardiomyocytes, fibroblasts, vascular smooth muscle cells, and endothelial cells have been explored for regenerative transplantation strategies, with promising improvements in cardiac function [42].
iPSC-derived cardiomyocytes have become a standard in cardiac safety screening and are gaining traction in drug discovery for cardiovascular diseases [43].
Metabolic and Genetic Disorders
iPSCs represent a powerful platform for studying genetic and metabolic diseases, as they preserve the patient's genotype in vitro [42]. Key applications include:
- Cystic fibrosis: iPSC-derived airway epithelial cells reproduce defective chloride transport and excessive mucus secretion caused by CFTR mutations, facilitating evaluation of targeted drugs such as ivacaftor and lumacaftor [42].
- Duchenne muscular dystrophy (DMD): iPSC-derived myocytes allow mechanistic studies of muscle degeneration, and gene editing has restored dystrophin expression in vitro, highlighting therapeutic potential [42].
- Wilson's disease: iPSC-derived hepatocytes reproduce copper accumulation and oxidative stress, providing a platform for preclinical drug testing [42].
- Familial hypercholesterolemia: Hepatocyte-like cells derived from iPSCs have been used to model this condition and test potential lipid-lowering therapies [43].
The "disease-in-a-dish" approach is particularly valuable for monogenic disorders like DMD, which is caused by mutations in the dystrophin gene and has a frequency of 1:3500 male births [41]. Modeling such diseases using iPSCs overcome limitations of animal models that may not accurately represent human pathology [41].
Figure 1: Workflow for iPSC-Based Disease Modeling and Drug Screening. This diagram illustrates the closed-loop system from patient sample collection to personalized therapy development.
High-Throughput Screening Applications
Technological Platforms
iPSC-derived cells are not just biologically relevant—they are also compatible with high-throughput screening (HTS) platforms. They can be plated in 384- or 1536-well formats, imaged automatically, and generate rich phenotypic data at scale [43]. Industrial phenotypic screens use these models to identify new drugs, predict toxicity, and uncover mechanisms of action.
Key technological advances enabling HTS with iPSCs include:
- Automated differentiation systems: Bioreactors and automation equipment that allow reproducible, large-scale production of differentiated cells [43] [47].
- High-content imaging: Automated microscopy systems that quantify changes in cell morphology, protein localization, or organelle health across thousands of wells [43].
- Machine learning algorithms: Advanced computational tools that analyze complex phenotypic data to identify compounds that reverse disease features, even when the molecular target isn't known [43].
These systems are particularly valuable for target-agnostic phenotypic screening, which can identify therapeutic compounds without predefined molecular targets, potentially leading to novel therapeutic mechanisms [43].
Cardiac Safety Screening
A prominent success story in iPSC-based screening is their application in cardiotoxicity testing. iPSC-derived cardiomyocytes are now used routinely to screen for drug-induced arrhythmia risk and have been integrated into regulatory safety initiatives like the Comprehensive in Vitro Proarrhythmia Assay (CiPA) [43]. Companies like Roche and Takeda use these cells for preclinical cardiac profiling [43].
This application demonstrates how iPSC-based models can bridge the gap between high-throughput assays and meaningful clinical predictions, potentially reducing late-stage drug attrition due to cardiac safety concerns.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for iPSC-Based Disease Modeling
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc | Dedifferentiation of somatic cells to pluripotent state | Delivery via integration-free methods preferred for clinical applications [42] |
| Culture Matrices | Matrigel, recombinant laminin-521 | Support iPSC attachment and growth | Feeder-free systems enhance reproducibility [42] |
| Defined Culture Media | mTeSR1, Essential 8 (E8) | Maintain pluripotency and self-renewal | Chemically defined formulations reduce batch variability [42] |
| Differentiation Factors | Activin A, BMP4, FGF2, Retinoic Acid | Direct lineage-specific differentiation | Concentration and timing critical for efficiency [42] [45] |
| Cryopreservation Reagents | DMSO, trehalose | Long-term storage of iPSCs and differentiated cells | Controlled-rate freezing improves viability [42] |
| Quality Control Assays | Pluripotency markers, Karyotyping, PCR | Verify pluripotent state and genomic integrity | Essential for clinical-grade lines [42] |
Current Clinical Trial Landscape and Regulatory Framework
Clinical Trial Progress
The clinical translation of iPSC-based therapies has gained significant momentum in recent years. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products targeting indications in ophthalmology, neurology, and oncology [18]. Over 1,200 patients have been dosed with more than 10¹¹ cells, with no significant safety concerns reported to date [18].
Recent systematic reviews have identified 10 published clinical studies and 22 ongoing registered trials utilizing iPSCs to treat a wide range of diseases, including cardiac conditions, ocular disorders, cancer, graft-versus-host disease, and as a source of platelets for transfusion [46]. However, published studies have been mostly small (only 2 studies reported on more than 4 patients) and uncontrolled, with a total of 115 patients treated across all published studies [46].
Recent Regulatory Milestones
Several recent FDA approvals and designations highlight the growing clinical acceptance of stem cell-based therapies:
- Ryoncil (remestemcel-L): Received FDA approval in December 2024 as the first MSC therapy for pediatric steroid-refractory acute graft versus host disease [18].
- Fertilo: In February 2025, received FDA IND clearance as the first iPSC-based therapy to enter U.S. Phase III trials for supporting ex vivo oocyte maturation [18].
- OpCT-001: An iPSC-derived therapy targeting retinal degeneration that received FDA IND clearance in September 2024 for Phase I/IIa trials [18].
- FT819: An off-the-shelf, iPSC-derived CAR T-cell therapy for systemic lupus erythematosus that received FDA RMAT designation in April 2025 [18].
The overall safety profile of iPSC-based clinical trials to date is encouraging, with no class-wide safety concerns observed [18]. However, specific considerations remain regarding the disease being treated and administration methods, highlighting the need for continued long-term surveillance [18].
Challenges and Future Perspectives
Current Limitations
Despite the considerable promise of iPSC technology, several challenges remain that limit its full clinical implementation:
- Functional maturation: Frequently, iPSC-derived cells exhibit an immature, fetal-like phenotype upon differentiation, which may limit their physiological relevance [44].
- Genomic instability: Reprogramming and long-term culture can introduce genetic abnormalities that must be carefully monitored [42].
- Tumorigenicity risk: Residual undifferentiated iPSCs could lead to teratoma formation, requiring rigorous purification of differentiated cell products [46].
- Protocol standardization: Considerable variability exists in differentiation protocols across laboratories, complicating result comparison [43].
- Cost and scalability: Media, reagents, and culture time can be prohibitively expensive for large-scale applications [43].
Considerable variability among studies and ongoing trials in terms of study design, medical conditions examined, and cell source used for iPSC generation may complicate and delay our understanding of the safety and efficacy of iPSC-based therapies [46].
Emerging Solutions and Future Directions
Several innovative approaches are being developed to address these limitations:
- Advanced maturation protocols: Combining 3D culture, mechanical stimulation, and co-culture systems to enhance functional maturity of iPSC-derived cells [44].
- Gene editing technologies: CRISPR/Cas9 systems allow precise genetic correction of disease mutations in patient-derived iPSCs [13] [42].
- Automation and bioprocessing: Advanced bioreactors and automated systems for large-scale, reproducible production of iPSCs and differentiated cells [47].
- Extracellular vesicle therapies: Investigating vesicles derived from iPSC-MSCs as cell-free alternatives that may be safer and less immunogenic [44].
- Standardized characterization: International efforts to establish consistent criteria for iPSC quality control and differentiation validation [46].
As these technologies mature, iPSC-based disease modeling is poised to have a significant impact on clinical care for patients with conditions such as cardiac disease, cancer, and ocular disorders [46]. However, researchers anticipate a period of several more years before the safety and efficacy of iPSC-based therapies can be definitively determined [46].
Figure 2: Challenges and Future Directions in iPSC Technology. This diagram maps current limitations to emerging solutions and anticipated outcomes in the field.
The "disease-in-a-dish" paradigm using iPSCs represents a transformative approach in precision medicine, enabling patient-specific disease modeling and drug discovery that was unimaginable just two decades ago. By providing a virtually unlimited supply of any cell type from individual patients, iPSC technology has created unprecedented opportunities to model human diseases in vitro, screen potential therapeutics, and develop personalized treatment strategies.
While challenges remain in achieving full functional maturation of differentiated cells and standardizing protocols for clinical applications, the rapid progress in this field is evident in the growing number of clinical trials and recent regulatory approvals. The ongoing integration of iPSC technology with advances in gene editing, bioengineering, and artificial intelligence promises to further enhance the predictive power of these models.
As the field continues to evolve, standardized study protocols and adherence to consistent iPSC-derived product characterization criteria will be essential to accelerate the development and approval of safe and effective iPSC-based therapies [46]. With these advances, iPSC-based disease modeling is positioned to dramatically improve our ability to understand disease mechanisms, develop targeted therapeutics, and ultimately deliver on the promise of personalized medicine.
The field of regenerative medicine has undergone a profound evolution, transitioning from foundational stem cell discoveries to the sophisticated bioengineering paradigms of today. This journey finds a pivotal convergence in the integration of 3D bioprinting with organoid development, a synergy that is redefining the boundaries of tissue engineering. Organoids, which are three-dimensional, self-organizing microtissues derived from pluripotent or adult stem cells, meticulously replicate the complex structures and functions of native organs [48]. They have emerged as indispensable tools for disease modeling, drug screening, and personalized medicine. However, traditional methods for cultivating organoids often result in structures with significant limitations, including inadequate reproducibility, insufficient vascularization, and a lack of precise spatial control [48] [49].
The emergence of 3D bioprinting addresses these challenges directly. As an additive manufacturing technology, bioprinting enables the precise, layer-by-layer deposition of living cells, bioactive molecules, and biomaterials—collectively known as bioinks—to construct complex, living architectures [48] [50]. This capability is transformative for organoid science, offering unparalleled control over cell distribution and the regulation of cell behavior and interactions. The fusion of these disciplines creates a powerful pipeline: bioprinting provides the initial, guided spatial framework, while the innate self-organization potential of stem cells fosters the development of sophisticated, functional tissue units [48]. This review explores how 3D bioprinting is advancing organoid development, its critical role within the broader context of stem cell-driven precision medicine, and the detailed methodologies propelling this innovative field forward.
Technical Foundations of 3D Bioprinting for Organoids
A comprehensive understanding of the available bioprinting technologies is essential for selecting the appropriate method for specific organoid applications. Each technique offers distinct advantages and limitations in terms of cost, resolution, cell viability, and compatibility with different bioinks. The table below provides a comparative overview of the four primary bioprinting modalities.
Table 1: Comparison of Primary 3D Bioprinting Technologies
| Feature | Inkjet-Based Bioprinting | Laser-Assisted Bioprinting | Extrusion-Based Bioprinting | Photo-curing Bioprinting |
|---|---|---|---|---|
| Cost | Low | High | Medium | Low |
| Speed | Fast | Medium | Slow | Fast |
| Resolution | ~75 µm | 10-100 µm | 200-500 µm | ~50 µm |
| Cell Density | 10⁶-10⁷ cells/mL | >10⁸ cells/mL | 10⁸-10⁹ cells/mL | >10⁷ cells/mL |
| Cell Viability | High | High (>95%) | Relatively Low | High |
| Key Features | Piezoelectric/thermal drive; multiple nozzles; low-viscosity bioinks. | No nozzle clogging; high-viscosity bioinks; no mechanical cell damage. | Printable high-viscosity materials; wide biomaterial range; most common. | Selective cross-linking with light; high efficiency; simple device. |
| Limitations | Cannot print high-viscosity materials; potential nozzle clogging; mechanical/thermal cell damage. | Complex control; limited hydrogel materials; low printing efficiency; laser side effects. | High mechanical shear stress; relatively low cell viability. | UV light and initiators can damage cells. |
The workflow for bioprinting organoids is a multi-stage process. It begins with imaging and design, often using patient-derived data (e.g., from CT or MRI scans) to create a digital 3D model [51]. This is followed by the selection and preparation of bioinks, a critical step that involves combining the appropriate stem cells with a supportive hydrogel matrix. The printing process itself uses one of the technologies outlined in Table 1 to fabricate the structure. Finally, the printed construct undergoes a maturation phase in a specialized bioreactor that provides the necessary biochemical and mechanical cues to guide the stem cells' self-organization and differentiation into a functional organoid [48] [49].
Diagram 1: A generalized workflow for creating iPSC-derived, 3D-bioprinted organoids, illustrating the key stages from somatic cell reprogramming to final mature tissue.
The Biological Engine: Stem Cells in Organoid Development
The successful development of organoids is fundamentally powered by stem cells, which serve as the foundational "seed cells" due to their unique capacities for self-renewal and differentiation into specialized cell types [13] [27]. The integration of specific stem cell types within bioprinted constructs has been a critical driver in the historical evolution of precision medicine, enabling the creation of patient-specific disease models.
Table 2: Key Stem Cell Types for Bioprinted Organoids
| Stem Cell Type | Origin | Key Characteristics | Role in Organoid Bioprinting |
|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocysts [13] | Pluripotent; can differentiate into any cell type; unlimited self-renewal [13]. | Provides a potent source for various tissue lineages; used in chondrogenic differentiation for cartilage organoids [49]. |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells (e.g., skin, blood) [13] [9] | Patient-specific; pluripotent; avoids ethical concerns of ESCs [13] [27]. | Cornerstone for personalized disease modeling and autologous transplants; used for bone/cartilage, cardiac, and neural organoids [49] [9]. |
| Mesenchymal Stem Cells (MSCs) | Adult tissues (bone marrow, adipose, umbilical cord) [23] [49] | Multipotent; immunomodulatory properties; supports tissue regeneration [23] [27]. | Frequently used for bone and cartilage organoids; UC-MSCs show high proliferative capacity and low immunogenicity [49]. |
The selection of stem cells is a critical determinant of the organoid's phenotype. For instance, the creation of bone and cartilage organoids often relies on Mesenchymal Stem Cells (MSCs) derived from bone marrow (BMSCs) or umbilical cord (UC-MSCs) due to their well-characterized osteogenic and chondrogenic potential [49]. In contrast, the development of neural or cardiac organoids typically utilizes iPSCs because they can be patient-derived and directed to differentiate into cell types like cardiomyocytes or neurons [9]. The combination of CRISPR-Cas9 gene editing with iPSC technology is particularly powerful, allowing researchers to introduce or correct disease-specific mutations, thereby creating highly accurate in vitro models for drug screening and pathological study [13] [49].
Experimental Workflow: A Protocol for Bioprinting Bone/Cartilage Organoids
The following detailed protocol outlines the key steps for fabricating a bone or cartilage organoid using extrusion-based bioprinting, a common method for processing high-viscosity bioinks containing MSCs or iPSCs.
Seed Cell Expansion and Differentiation
- Cell Source: Isolate human Bone Marrow-derived MSCs (BMSCs) or generate iPSCs from patient dermal fibroblasts using non-integrating Sendai virus vectors expressing OCT4, SOX2, KLF4, and c-MYC (Yamanaka factors) [49] [9].
- Culture: Maintain iPSCs in feeder-free conditions using mTeSR1 medium. For MSCs, use α-MEM supplemented with 10% FBS, 1% L-glutamine, and 1% penicillin/streptomycin.
- Pre-differentiation (Optional): To enhance osteogenic or chondrogenic commitment, pre-differentiate cells for 7-10 days in induction media. Osteogenic media contains dexamethasone, ascorbic acid, and β-glycerophosphate. Chondrogenic media contains TGF-β3, dexamethasone, ascorbic acid, and insulin-transferrin-selenium [49].
Bioink Preparation and Formulation
- Base Biomaterial: Prepare a sterile, cell-compatible hydrogel. A blend of GelMA (Gelatin Methacryloyl) and Hyaluronic Acid is highly suitable, providing excellent printability, biocompatibility, and tunable mechanical properties [49].
- Supplementation: Incorporate bioactive cues into the hydrogel precursor solution. This includes RGD peptide (to enhance cell adhesion) and, for chondrogenic induction, the growth factor TGF-β3 (at 10 ng/mL).
- Cell Encapsulation: Harvest the expanded/pre-differentiated MSCs or iPSC-derived progenitors and resuspend them in the hydrogel precursor solution at a high density of 5-20 x 10⁶ cells/mL [48] [49]. Keep the bioink on ice to prevent premature crosslinking.
Bioprinting Process and Post-Printing Maturation
- Printing Setup: Load the cell-laden bioink into a sterile extrusion bioprinter cartridge. Use a nozzle diameter between 200-400 µm.
- Printing Parameters: Set the pneumatic pressure or mechanical piston speed to achieve a consistent filament flow. Maintain the print bed temperature at 15-18°C to improve structural fidelity. Print the structure layer-by-layer based on a pre-designed CAD model, which could be a simple grid or a more complex anatomical shape.
- Crosslinking: Immediately after printing, expose the construct to blue light (405 nm) for 60-120 seconds to photopolymerize the GelMA and stabilize the 3D structure.
- Maturation Culture: Transfer the crosslinked construct to a bioreactor for dynamic culture. Maintain it in chondrogenic or osteogenic medium for 4-6 weeks, changing the medium every 2-3 days. The bioreactor's perfusion system enhances nutrient/waste exchange and provides mechanical stimulation, promoting tissue maturation and the deposition of a functional extracellular matrix, such as collagen type II for cartilage or mineralization for bone [49].
Table 3: Essential Research Reagents for Bioprinting Bone/Cartilage Organoids
| Reagent Category | Specific Examples | Function |
|---|---|---|
| Stem Cells | Bone Marrow MSCs (BMSCs), iPSCs | The foundational "seed" cells with multi/pluripotent differentiation capacity. |
| Hydrogels | GelMA, Hyaluronic Acid, Alginate, Collagen | Serves as the printable 3D scaffold that mimics the native extracellular matrix (ECM). |
| Bioactive Factors | TGF-β3, BMP-2, Dexamethasone, Ascorbic Acid | Directs stem cell differentiation toward specific lineages (osteogenic, chondrogenic). |
| Cell Adhesion Molecules | RGD Peptide | Promotes integrin-mediated cell attachment to the hydrogel, enhancing survival and function. |
| Culture Media | Osteogenic & Chondrogenic Differentiation Media | Provides the biochemical environment necessary for tissue-specific maturation. |
Applications and Impact on Precision Medicine and Drug Development
The integration of 3D bioprinting with organoid technology is producing advanced models that are directly impacting pharmaceutical research and regenerative medicine. These models bridge the gap between traditional 2D cell cultures and complex in vivo physiology.
Advanced Disease Modeling: Bioprinted organoids allow for the creation of highly personalized disease models. For example, patient-derived iPSCs can be used to generate organoids that mimic specific cancer subtypes. Researchers have developed patient-derived lymphoma organoids (PDLOs) for disease-specific modeling and high-throughput pharmacological screening [49]. Similarly, bioprinted bone organoids from patient-specific iPSCs are being used to model genetic disorders like osteogenesis imperfecta and to study the pathogenesis of osteoporosis [49].
High-Throughput Drug Screening and Toxicology: The reproducibility and scalability of bioprinting make it ideal for creating uniform organoid arrays for high-content screening. iPSC-derived organoids, such as cardiomyocytes for cardiotoxicity or hepatocytes for hepatotoxicity, provide a more physiologically relevant human platform for evaluating drug efficacy and safety, aligning with the FDA Modernisation Act 2.0 which now permits the use of human-cell-based assays in lieu of animal testing for certain applications [52] [9]. This leads to more predictive data and can reduce late-stage drug attrition.
Regenerative Medicine and Implants: A primary long-term goal is the creation of functional, implantable tissues. 3D-bioprinted bone and cartilage organoids are at the forefront of this endeavor. By using a patient's own cells (e.g., MSCs or iPSCs), the resulting constructs can theoretically be used for autologous grafts to repair bone defects or cartilage damage, thereby avoiding immune rejection and the challenges associated with donor shortages [51] [49]. Clinical trials are already underway, such as a Phase 3 trial utilizing an iPSC-derived MSC product for the treatment of osteoarthritis [9].
Current Challenges and Future Directions
Despite the remarkable progress, several technical and biological hurdles must be overcome to fully realize the potential of bioprinted organoids.
A significant challenge is vascularization. Current organoids often lack a perfusable vascular network, which limits their size and maturity due to inadequate nutrient and oxygen diffusion deep into the tissue [48] [49]. Future research is focused on co-printing endothelial cells alongside stem cells to create intricate, self-assembling capillary networks within the organoids. Another major hurdle is standardization and reproducibility. Variability in stem cell differentiation, bioink properties, and printing parameters can lead to inconsistencies between batches [49]. The integration of Artificial Intelligence (AI) and machine learning for process control is a promising solution. For instance, a recently developed modular monitoring technique uses a digital microscope and AI-based image analysis to compare printed layers with the intended design in real-time, identifying defects and enabling adaptive correction [53]. This enhances reproducibility and reduces material waste.
Looking ahead, the field will see increased multi-material and multi-cellular bioprinting to create complex, multi-tissue interfaces, such as the bone-cartilage unit or liver-islet axis [50]. The synergy between NGS (Next-Generation Sequencing) and bioprinting will also deepen, allowing for the creation of organoids that not only mimic tissue structure but also reflect the intricate tumor heterogeneity found in patients, further refining personalized cancer treatment strategies [27]. As these technologies mature, the vision of generating fully functional, implantable organs using 3D bioprinting and organoid principles moves closer to reality, promising to bridge the critical gap between organ demand and availability [51].
Navigating Translational Hurdles: Safety, Scalability, and Standardization
The historical evolution of stem cell applications in precision medicine is marked by a pivotal challenge: reconciling their immense therapeutic potential with the persistent risk of tumorigenicity. Stem cell therapy represents a revolutionary frontier in modern medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries through unique properties of self-renewal and differentiation into specialized cell types [13]. However, this transformative potential is intrinsically linked to oncogenic risk, as the same biological mechanisms that enable regenerative applications—proliferation, differentiation plasticity, and persistent engraftment—can also initiate malignant transformation.
The progression of precision medicine now demands sophisticated strategies to control these risks, focusing specifically on ensuring genomic stability throughout stem cell processing and transplantation. Genome instability, characterized by the accumulation of mutations and chromosomal alterations, is a well-recognized hallmark of carcinogenesis [54]. Each cell in the human body suffers an estimated 70,000 DNA lesions per day that arise spontaneously or from genotoxic insult, and these adducts, if not repaired, can cause mutations which influence the faithful passage of genetic material from mother to daughter cells [54]. This technical guide examines current methodologies for mitigating oncogenic risk, framing them within the critical context of genomic stability to advance safer therapeutic applications.
Mechanisms of Oncogenic Risk in Stem Cell Systems
Endogenous and Exogenous Risk Pathways
The tumorigenic potential of stem cell products originates from multiple interconnected pathways that can be categorized as endogenous cell-autonomous risks and exogenous procedure-related risks. Endogenous risks include the inherent potential of residual undifferentiated cells to form teratomas or the acquisition of somatic mutations during in vitro expansion that confer selective growth advantages. Exogenous risks emerge from the technical procedures used in cell manipulation, including genotoxic stress from culture conditions, enzymatic passaging, and cryopreservation.
A primary mechanism of oncogenesis lies in insertional mutagenesis, which occurs when viral vectors used to deliver therapeutic genes integrate into the host genome in a semi-random manner [55]. Such integrations can disrupt critical regulatory regions, such as promoters or enhancers, or directly inactivate tumor suppressor genes or activate proto-oncogenes [55]. Lentiviral and gamma-retroviral vectors, common delivery systems in cell engineering, exhibit distinct genomic integration patterns that influence their oncogenic potential, with gamma-retroviral vectors preferentially integrating near transcriptionally active regions including promoters of proto-oncogenes [55].
Genomic Instability Triggers
Multiple factors trigger genomic instability in stem cell populations:
- Replicative stress during in vitro expansion leads to telomere erosion, DNA polymerase errors, and replication fork collapse
- Oxidative damage from mitochondrial dysfunction or pro-inflammatory pathways creates DNA adducts that promote mutagenesis [54]
- Environmental genotoxic stress from factors such as sunlight, radon, and air pollution introduces DNA lesions that require sophisticated repair mechanisms [54]
Advanced stem cell applications further compound these risks through genome editing technologies. CRISPR/Cas9-mediated editing introduces additional risks: off-target double-strand breaks (DSBs) may lead to chromosomal translocations or inactivation of tumor suppressors, particularly in hematopoietic progenitors [55]. The cumulative impact of these challenges necessitates comprehensive risk mitigation strategies spanning the entire therapeutic development pipeline.
Strategic Framework for Tumorigenicity Risk Mitigation
Genomic Safe Harbor (GSH) Integration
The development of secondary malignancies following cell therapy has spurred interest in site-directed transgene integration into genomic safe harbors (GSHs)—loci validated for stable, high-level transgene expression without oncogenic consequences [55]. GSHs such as AAVS1 (19q13.42), CCR5, and TRAC (T-cell receptor alpha constant) meet stringent criteria: they reside distal to oncogenes, avoid fragile sites, and resist epigenetic silencing [55].
Site-directed integration leverages CRISPR/Cas9, transcription activator-like effector nucleases (TALENs), or zinc finger nucleases (ZFNs) to precisely insert therapeutic constructs into GSHs via homology-directed repair (HDR) [55]. Compared to viral vectors, this approach eliminates positional variability in transgene expression, reducing clonal dominance and exhaustion. For instance, targeting the TRAC locus enables dual benefits; CAR integration disrupts endogenous TCR expression, reducing graft-versus-host disease risk in allogeneic products, while maintaining uniform CAR activity [55].
Table 1: Validated Genomic Safe Harbors for Therapeutic Transgene Integration
| GSH Locus | Genomic Location | Validation Status | Key Advantages | Therapeutic Context |
|---|---|---|---|---|
| AAVS1 | 19q13.42 | Preclinical & Clinical | High transcriptional activity; resistant to silencing | Pluripotent and adult stem cells |
| TRAC | 14q11.2 | Clinical trials | Endogenous TCR disruption; uniform expression | T-cell therapies, CAR constructs |
| CCR5 | 3p21.31 | Preclinical & Clinical | Well-characterized safe location; disease resistance | Hematopoietic stem cells, HIV therapies |
| ROSA26 | 6q22.1 | Preclinical | Ubiquitous expression; open chromatin structure | Multiple cell types, reporter genes |
| CLYBL | 13q32.1 | Preclinical | Transcriptionally permissive; safe integration profile | Metabolic engineering, enzyme expression |
Advanced Genome Editing with Safety Engineering
Next-generation genome editing approaches incorporate multiple safety layers to minimize oncogenic risk:
- High-fidelity CRISPR systems with reduced off-target activity
- Base and prime editing technologies that minimize DNA double-strand breaks
- Anti-CRISPR proteins that limit editing duration and reduce off-target effects
- Co-delivery of DNA repair templates that favor precise homology-directed repair
Researchers have engineered stem cells using AAV-based (closed-ended linear duplex DNA) CELiD vectors for precise, safe integration into the AAVS1 locus. Co-electroporating CD19-CAR CELiD vectors with pCMV-Rep achieved 22.8% site-specific integration, with engineered cells producing elevated cytokines and demonstrating target-cell killing in vitro [55]. This non-viral method minimizes genomic risks by avoiding random viral integration [55].
Cell Sorting and Purification Strategies
Effective removal of undifferentiated stem cells from final therapeutic products is critical for minimizing teratoma risk. Advanced purification approaches include:
- Fluorescence-activated cell sorting (FACS) with pluripotency marker-specific antibodies
- Magnetic-activated cell sorting (MACS) for scalable processing
- Density gradient centrifugation for residual cell removal
- Affinity chromatography with surface marker-specific ligands
- Microfluidic separation technologies for high-precision isolation
Table 2: Critical Quality Attributes for Tumorigenicity Risk Assessment
| Risk Category | Analytical Method | Target Specification | Frequency | Acceptance Criteria |
|---|---|---|---|---|
| Genetic Stability | Karyotyping (G-banding) | Normal diploid karyotype | Master Cell Bank & End of Production | No abnormal clones >5% |
| SNP microarray | Copy number variations | Master Cell Bank & End of Production | <3 megabase aberrations | |
| Whole genome sequencing | Single nucleotide variants | Master Cell Bank | No mutations in oncogenes/tumor suppressors | |
| Oncogenic Potential | Soft agar colony formation | No colony formation | Final Product | 0 colonies in >10^6 cells |
| In vivo tumorigenicity | No tumor formation | Final Product (as needed) | No tumors at 16 weeks | |
| Residual Undifferentiated Cells | Flow cytometry (Pluripotency markers) | <0.1% | Final Product | <1 in 10,000 cells |
| PCR (Pluripotency genes) | Threshold cycle values | Final Product | Below detection limit |
Experimental Protocols for Tumorigenicity Assessment
1In VitroTransformation Assay Protocol
Purpose: To detect anchorage-independent growth as a indicator of transformation potential in stem cell populations.
Materials:
- Low-melting point agarose
- Base agar layer (0.6% agar in complete medium)
- Top agar layer (0.3% agar with 1×10^4 cells/mL in complete medium)
- Positive control cells (known transformed line)
- Negative control cells (primary fibroblasts)
- Colony staining solution (0.005% Crystal Violet)
Methodology:
- Prepare base layer in 6-well plates by adding 2 mL of 0.6% agar-medium mixture and allow to solidify at 4°C for 15 minutes.
- Trypsinize test cells, count viability (must be >90%), and resuspend in complete medium at 2×10^4 cells/mL.
- Mix cell suspension 1:1 with 0.6% agar solution (pre-equilibrated to 42°C) to create final 0.3% agar concentration with 1×10^4 cells/mL.
- Layer 2 mL of cell-agar mixture over base layer and allow to solidify.
- Add 1 mL of complete medium on top of solidified agar to prevent drying.
- Culture plates at 37°C, 5% CO2 for 3-4 weeks, replenishing top medium weekly.
- After incubation, stain colonies with 0.5 mL Crystal Violet for 1 hour and count colonies >50μm diameter using automated colony counter.
Interpretation: Compare colony formation efficiency between test articles and controls. Significant increase in colony formation (>5% of plated cells) or colony size distribution shift indicates transformation potential.
Genomic Integrity Assessment via Karyotyping
Purpose: To identify chromosomal abnormalities acquired during in vitro culture expansion.
Materials:
- Colcemid solution (10μg/mL)
- Hypotonic solution (0.075M KCl)
- Fixative (3:1 methanol:glacial acetic acid)
- Giemsa stain
- Microscope with 100x oil immersion objective
Methodology:
- Culture cells to 60-70% confluence in T-25 flasks.
- Add colcemid to final concentration 0.1μg/mL and incubate for 2-4 hours at 37°C.
- Trypsinize cells and transfer to conical tube, centrifuge at 200×g for 5 minutes.
- Resuspend pellet in pre-warmed 0.075M KCl hypotonic solution and incubate 15 minutes at 37°C.
- Add fixative dropwise while vortexing gently, then centrifuge at 200×g for 5 minutes.
- Repeat fixation step twice more with fresh fixative.
- Drop cell suspension onto clean, wet slides and allow to air dry.
- Stain with Giemsa for 8-10 minutes, rinse gently with distilled water, and air dry.
- Analyze 20-50 metaphase spreads per sample for chromosomal abnormalities.
Interpretation: Document numerical and structural abnormalities. Establish threshold for acceptable abnormalities based on product class and clinical indication.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Oncogenic Risk Assessment
| Reagent/Category | Specific Examples | Function | Application Context |
|---|---|---|---|
| Genome Editing Systems | CRISPR-Cas9 (High-fidelity variants), TALEN proteins, Zinc Finger Nucleases | Site-specific genomic modification | GSH targeting, safe transgene integration |
| Viral Delivery Systems | Lentiviral vectors (self-inactivating), Adenovirus-associated vectors (AAV) | Gene delivery with reduced genotoxic risk | Transient expression, non-integrating approaches |
| Cell Selection Markers | Puromycin resistance, Neomycin resistance, Fluorescent proteins (GFP, RFP) | Selection of successfully modified cells | Enrichment of properly engineered populations |
| DNA Repair Modulators | HDR enhancers (RS-1, L755507), NHEJ inhibitors (SCR7) | Direction of DNA repair toward precise outcomes | Enhanced precision of genome editing |
| Apoptosis Inducers | AP1903 (iCasp9), ganciclovir (HSV-TK) | Safety switches for elimination of problematic cells | Emergency ablation of transplanted cells |
| Pluripotency Detection | Antibodies to TRA-1-60, SSEA-4, OCT4 | Identification of residual undifferentiated cells | Final product quality control |
| Senescence Markers | SA-β-galactosidase substrate, p16/ p21 antibodies | Detection of cellular aging | Monitoring of culture expansion limits |
Signaling Pathways and Experimental Workflows
Diagram 1: Comprehensive Tumorigenicity Risk Mitigation Workflow. This integrated approach spans from initial cell sourcing through long-term monitoring, incorporating multiple safety layers at each development stage.
Diagram 2: DNA Damage Response Pathways in Stem Cell Genomic Stability. This pathway illustrates cellular mechanisms for maintaining genomic integrity following genotoxic insults, highlighting critical decision points that determine repair fidelity versus transformation risk.
The historical trajectory of stem cell applications reveals an evolving paradigm where safety and efficacy are increasingly recognized as interdependent qualities. The strategic integration of genomic stability considerations throughout product development represents a maturing of the field toward clinically robust solutions. Future directions will likely focus on predictive computational models for oncogenic risk, enhanced synthetic biology approaches for containment strategies, and standardized regulatory frameworks for long-term genomic surveillance [55].
As the field advances, collaborative efforts to refine manufacturing, harmonize global standards, and prioritize patient-specific risk stratification will be critical to advancing these transformative approaches [55]. By reconciling therapeutic innovation with genomic integrity, safety-engineered stem cell applications herald a paradigm shift toward precision regenerative medicine, offering curative potential while preempting secondary oncogenesis [55].
The field of regenerative medicine and precision oncology has been fundamentally reshaped by the progressive integration of stem cell biology. The historical evolution of stem cell applications, beginning with hematopoietic stem cell transplantation, has expanded into a sophisticated paradigm of precision medicine, leveraging stem cells not only as therapeutic agents but also as engineered platforms for drug delivery and disease modeling [27]. A cornerstone of this evolution is the shift from autologous to allogeneic cell therapies, which promise standardized, "off-the-shelf" treatments for a broad patient population [56]. However, the immunologic disparity between donor and recipient presents a significant barrier, primarily host-mediated immune rejection and graft-versus-host disease (GvHD), which can limit therapeutic efficacy and safety [57] [56]. This whitepaper provides an in-depth technical guide to the mechanisms of allogeneic rejection and the experimental approaches being developed to overcome these immune barriers, framing them within the ongoing advancement of precision medicine.
Immune Rejection Mechanisms in Allogeneic Cell Therapies
Allogeneic rejection is a multi-faceted immune response orchestrated by the recipient's immune system against donor-derived cells. A precise understanding of the underlying mechanisms is critical for developing effective countermeasures.
- Host vs. Graft Reaction: The recipient's immune system, particularly CD8+ T cells, recognizes foreign Human Leukocyte Antigen (HLA) molecules on the surface of donor cells via T cell receptors (TCRs). This recognition triggers cytotoxic killing of the therapeutic cells, leading to their rapid clearance and treatment failure [58] [56]. Furthermore, pre-existing HLA donor-specific antibodies can mediate rejection, similar to what is observed in solid organ transplantation [56].
- Graft vs. Host Disease: Conversely, donor T cells present within the therapeutic product can recognize the recipient's tissues as foreign and mount an immune attack, a potentially life-threatening complication [59] [56].
- NK Cell-Mediated Killing: Strategies that eliminate HLA expression to evade T cells can inadvertently make donor cells vulnerable to natural killer (NK) cell attack. NK cells detect the "missing self" – the absence of "self" HLA molecules – and initiate cytotoxicity [58]. Overcoming this requires preserving or engineering the expression of non-classical HLA molecules like HLA-E, which engage inhibitory receptors on NK cells to signal "self" [58].
Table 1: Key Immune Effector Cells in Allogeneic Rejection
| Immune Cell Type | Primary Recognition Mechanism | Consequence for Allogeneic Cell Product |
|---|---|---|
| CD8+ T Cell | TCR recognition of foreign HLA class I (HLA-A, B, C) | Cytotoxic killing and rejection of donor cells [58] |
| NK Cell | Detection of absent or altered HLA expression ("Missing Self") | Lysis of donor cells lacking inhibitory ligand expression [58] |
| Macrophage | Phagocytosis via opsonic receptors or missing "Don't Eat Me" signals | Phagocytosis of donor cells [58] |
Engineering Approaches to Overcome Allogeneic Rejection
The field has developed a suite of sophisticated engineering strategies to create allogeneic cell products that evade host immunity. These can be broadly categorized into gene editing and non-editing technologies.
Gene Editing for HLA Ablation
The direct knockout of HLA molecules is a primary strategy to prevent T-cell-mediated rejection.
- Experimental Protocol for HLA Knockdown: A 2025 study detailed a one-step lentiviral method to generate hypoimmunogenic CAR-NK cells.
- Design of shRNAs: shRNAs are bioinformatically designed to target conserved regions of HLA-ABC heavy chains or the common subunit β2-microglobulin (B2M). Specificity is crucial; shRNAs must have ≥2 mismatches with HLA-E to preserve its expression and avoid NK cell activation [58].
- Vector Construction: A single lentivector is constructed to express the HLA-targeting shRNA (e.g., shRNA #1 for HLA-ABC), a chimeric antigen receptor, and an immune checkpoint modulator like PD-L1 or single-chain HLA-E (SCE) [58].
- Cell Transduction and Validation: NK cells are activated and transduced with the lentivector. Successful knockdown is validated via flow cytometry for surface HLA-ABC and HLA-E. Functional assays, such as co-culture with allogeneic CD8+ T cells, confirm resistance to T-cell-mediated killing [58].
The following diagram illustrates the logical workflow and components of this engineering strategy.
Exploiting Immune Checkpoints and Modulatory Molecules
Beyond ablation, engineered expression of immunomodulatory molecules can actively inhibit host immune responses.
- PD-L1 Overexpression: PD-L1 on donor cells engages the PD-1 receptor on activated host T cells, delivering an inhibitory signal that suppresses T-cell function and promotes tolerance [58]. This not only prevents rejection but also reduces exhaustion in the engineered cells, enhancing their anti-tumor potency [58].
- HLA-E and CD47 Expression: As noted, forced expression of HLA-E inhibits NK cell activity via the NKG2A receptor [58]. Similarly, overexpression of CD47, a "don't eat me" signal, blocks phagocytosis by host macrophages [58].
Table 2: Engineered Immune Modulators for Evading Rejection
| Molecule | Engineered Function | Target Host Immune Cell | Mechanism of Action |
|---|---|---|---|
| PD-L1 | Immune Checkpoint Inhibitor | T Cells | Binds PD-1 on T cells, inhibiting their activation and cytotoxic function [58] |
| HLA-E | Non-classical HLA Molecule | NK cells and a subset of T cells | Engages inhibitory NKG2A receptor, preventing "missing-self" killing [58] |
| CD47 | "Don't Eat Me" Signal | Macrophages | Binds SIRPα, transducing a signal that inhibits phagocytosis [58] |
The choice of starting cell material can inherently reduce immunogenicity.
- Umbilical Cord Blood (UCB) Cells: UCB-derived T and NK cells are more antigen-naïve and exhibit reduced alloreactivity compared to adult peripheral blood cells. They also show lower expression of exhaustion markers and produce fewer pro-inflammatory cytokines, lowering the risk and severity of GvHD [59].
- Induced Pluripotent Stem Cells (iPSCs): iPSCs can be differentiated into immune effector cells and genetically edited to create hypoimmunogenic master cell lines. A significant advantage is the feasibility of multi-locus gene editing while in the pluripotent state, enabling the generation of standardized, off-the-shelf products with reduced immunogenicity [59] [27].
- Regulatory T Cells (Tregs): Instead of evading immunity, polyclonal or antigen-specific Tregs can be administered to actively suppress the host immune response and promote tolerance, showing promise in clinical trials for GvHD and solid organ transplantation [60].
Detailed Experimental Protocol: Generating Hypoimmunogenic CAR-NK Cells
The following protocol, adapted from a 2025 Nature Communications paper, details the key steps for creating allogeneic NK cells resistant to rejection [58].
Objective: To generate allogeneic CAR-NK cells capable of evading host T and NK cell-mediated rejection through selective HLA knockdown and PD-L1 expression.
Materials:
- Source Cells: NK cells isolated from healthy donor peripheral blood or umbilical cord blood.
- Lentiviral Vector: Construct encoding an anti-HLA-ABC shRNA (e.g., shRNA #1), a CAR (e.g., anti-CD19), and PD-L1 or single-chain HLA-E (SCE).
- Culture Reagents: IL-2, IL-15, and NK cell expansion media.
- Transduction Enhancer: Retronectin or similar reagent.
- Assessment Tools: Flow cytometry antibodies for HLA-ABC, HLA-E, PD-L1, and the CAR transduction marker.
Methodology:
- NK Cell Isolation and Activation: Isolate NK cells from PBMCs using negative selection magnetic beads. Activate the cells by culturing in media supplemented with IL-2 (100-200 U/mL) and IL-15 (10-50 ng/mL) for 24-48 hours.
- Lentiviral Transduction: Pre-coat non-tissue culture treated plates with retronectin (10 µg/mL). Add the lentiviral vector to the plates, then seed the activated NK cells at a low multiplicity of infection (MOI ~5). Centrifuge the plate to enhance viral contact (spinoculation). Incubate at 37°C for 24 hours.
- Cell Expansion and Selection: Replace the transduction media with fresh expansion media containing IL-2 and IL-15. Expand the transduced NK cells for 10-14 days, maintaining a cell density of 0.5-1 x 10^6 cells/mL. Cells can be sorted based on the CAR marker or PD-L1 expression to enrich for the modified population.
- In Vitro Functional Validation:
- T-cell Killing Assay: Co-culture engineered NK cells with allogeneic, activated CD8+ T cells from an HLA-mismatched donor. Measure NK cell survival using flow cytometry or a cytotoxicity assay (e.g., LDH release) after 24-48 hours. Engineered NK cells should show significantly higher survival compared to non-transduced controls.
- NK cell Killing Assay: Use a standard chromium-51 release assay or flow-based killing assay to test the susceptibility of engineered NK cells to lysis by allogeneic host NK cells. Cells expressing HLA-E or PD-L1 should demonstrate resistance to NK cell-mediated killing.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing Allogeneic Cell Therapies
| Reagent / Tool | Category | Function in Experimental Protocol |
|---|---|---|
| CliniMACS Plus System | Cell Isolation | Magnetic bead-based clinical-scale separation of Tregs or other cell subsets [60] |
| Lentiviral Vector | Gene Delivery | Stable integration of genetic payloads (CAR, shRNA, immune modulators) into target cells [58] |
| CRISPR/Cas9 System | Gene Editing | Precise knockout of endogenous genes (e.g., TCR, HLA) to reduce immunogenicity [59] [56] |
| shRNA (e.g., #1, #13) | Gene Knockdown | Targeted knockdown of HLA-ABC without affecting HLA-E expression [58] |
| Recombinant IL-2 | Cell Culture | Critical cytokine for ex vivo expansion and maintenance of T cells and NK cells [60] [58] |
| Single-Chain HLA-E (SCE) | Engineered Molecule | A single-polypeptide version of HLA-E that provides a potent "self" signal to inhibit NK cells [58] |
| Rapamycin | Small Molecule | mTOR inhibitor used in Treg expansion and Tconv reprogramming to enhance stability and function [60] |
The journey of stem cells from basic biological curiosities to the core of next-generation precision medicine is exemplified by the sophisticated engineering of allogeneic cell therapies. Overcoming immune rejection is not a single hurdle but a series of challenges posed by T cells, NK cells, and the broader immune environment. The convergence of gene-editing technologies, immune checkpoint biology, and innovative cell sourcing provides a powerful toolkit to design stealth therapeutic cells. As these strategies mature, the establishment of comprehensive cell banks featuring a wide array of HLA profiles and fully engineered hypoimmunogenic lines will be crucial for translating the promise of universal, off-the-shelf cell therapies into a widespread clinical reality, ultimately reshaping the treatment of cancer, autoimmune disorders, and beyond [57] [27].
The historical evolution of stem cell applications in precision medicine is a narrative of remarkable scientific achievement, transitioning from foundational laboratory discoveries to groundbreaking clinical interventions. This journey has been propelled by an increasing understanding of diverse stem cell types, including embryonic stem cells (ESCs), adult stem cells (ASCs), and induced pluripotent stem cells (iPSCs), each offering unique therapeutic potential [13]. These cells form the cornerstone of regenerative medicine, with the capacity to differentiate into various cell types and repair damaged tissues, offering hope for conditions ranging from neurodegenerative disorders to cardiovascular ailments [13] [23]. However, the path from bench to bedside is fraught with complexity. The very properties that make stem cells transformative—their living, dynamic nature—also present unparalleled manufacturing challenges. Scaling these sophisticated biological products for widespread clinical impact, while rigorously adhering to Current Good Manufacturing Practice (cGMP), constitutes the most significant hurdle in realizing the full potential of precision medicine today. This guide addresses the critical manufacturing complexities and compliance requirements essential for translating stem cell science into reliable, scalable, and safe therapeutics for patients.
The Evolving Stem Cell Landscape: From Bench to Bedside
The field has progressed from early research on pluripotency and differentiation to a robust clinical trial landscape. As of late 2024, a major review identified 115 global clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products, primarily targeting indications in ophthalmology, neurology, and oncology [18]. This growth is supported by regulatory milestones, including recent FDA approvals of stem cell-based products, which signal a maturing industry [18]. The therapeutic promise of stem cells is now undeniable, but its broad realization is inextricably linked to overcoming the dual challenges of manufacturing scalability and stringent quality control.
Table: Recent FDA-Approved Stem Cell-Based Therapies (2023-2025)
| Product Name (Approval Date) | Cell Type / Basis | Indication | Key Manufacturing & Clinical Considerations |
|---|---|---|---|
| Omisirge (Apr 2023) [18] | Cord Blood-Derived Hematopoietic Progenitor Cells (Allogeneic) | Accelerate neutrophil recovery in patients with hematologic malignancies | Nicotinamide-modified stem cell graft; addresses manufacturing consistency for allogeneic use. |
| Lyfgenia (Dec 2023) [18] | Autologous Hematopoietic Stem Cells (with genetic modification) | Sickle cell disease with history of vaso-occlusive events | Complex autologous process involving patient cell collection, ex vivo gene modification, and reinfusion. |
| Ryoncil (Dec 2024) [18] | Allogeneic Bone Marrow-Derived Mesenchymal Stem Cells (MSCs) | Pediatric steroid-refractory acute Graft vs. Host Disease (SR-aGVHD) | First FDA-approved MSC therapy; demonstrates scalable allogeneic platform for multiple patients from a single donor. |
Navigating Core Manufacturing Complexities
The journey from a research protocol to a commercially viable stem cell therapy is paved with intricate manufacturing hurdles. These challenges are magnified when moving from small-scale research to industrial-level production.
Process Design: Autologous vs. Allogeneic Paradigms
The choice between autologous (patient-specific) and allogeneic (donor-derived, off-the-shelf) therapies dictates the entire manufacturing workflow [61].
- Autologous Processes: These are highly personalized. Starting material is collected from the patient, necessitating a dedicated and segregated batch for each individual. This creates inherent complexities in logistics, chain of identity management, and batch-to-batch variability, making it difficult to achieve traditional pharmaceutical economies of scale [61] [62].
- Allogeneic Processes: A single donation from a healthy donor is used to manufacture a master cell bank, which can then be expanded to create hundreds or thousands of doses [61]. This model offers immediate product availability and is more cost-effective, but it requires massive scale-up in bioreactors and introduces the challenge of managing immunological rejection, often requiring gene editing or immunosuppression [61].
The Scalability Bottleneck: From Manual to Automated Systems
A significant barrier to commercialization is the reliance on labor-intensive, open-handling steps in early-stage process development. These manual processes are error-prone, variable, and difficult to scale [61] [62]. The industry is therefore shifting towards closed, automated systems.
- Benefits of Automation: Closed automated systems significantly reduce contamination risk, lower labor costs, improve process reproducibility, and enhance operator safety [61].
- Implementation Challenges: Despite their promise, these technologies face constraints. They can lose accuracy with very small volumes (critical for autologous therapies), and for allogeneic production, ensuring scalability while maintaining cell quality and function is a key hurdle [61]. Furthermore, newer devices must be validated for cGMP compliance, which requires substantial investment and expertise [61].
Analytical and Quality Control Testing
Ensuring the safety, purity, potency, and identity of the final stem cell product is non-negotiable. This requires a robust battery of in-process testing and release criteria. The industry faces a challenge in developing potency assays that truly reflect the biological mechanism of action of the therapy, particularly for stem cells whose function may be multimodal (e.g., immunomodulation, trophic factor secretion). As one industry expert notes, "reliable quality systems with QC strategies and method suitability will ensure quality and regulatory compliance are achieved" [62]. The high cost and complexity of these QC tests contribute significantly to the overall treatment cost [62].
A Framework for cGMP Compliance in Stem Cell Manufacturing
Achieving cGMP compliance is not merely a regulatory checkbox but a foundational element for producing safe and effective therapies. cGMP provides the framework for ensuring that products are consistently produced and controlled according to quality standards.
Foundational cGMP Principles
- Documentation and Traceability: Every material, step, and decision in the manufacturing process must be thoroughly documented. For autologous therapies, maintaining an unambiguous chain of identity from patient to product and back is critical.
- Facility and Equipment Control: Manufacturing facilities must be designed with appropriate airflow, segregation, and cleaning protocols to prevent cross-contamination and microbial ingress. Equipment must be qualified, calibrated, and maintained.
- Supplier and Material Management: All raw materials, reagents, and consumables must be qualified for their intended use. Sourcing from vendors that provide Drug Master Files (DMFs) can streamline regulatory submissions by providing comprehensive data on material quality and manufacturing [18].
The Control Strategy: Embracing Quality by Design (QbD)
A proactive approach to quality involves building it into the process from the beginning, a concept known as Quality by Design (QbD). This involves:
- Defining Critical Quality Attributes (CQAs): These are the physical, chemical, biological, and microbiological properties or characteristics that must be within an appropriate limit, range, or distribution to ensure the desired product quality (e.g., cell viability, identity, potency, sterility).
- Identifying Critical Process Parameters (CPPs): These are the process parameters whose variability impacts the CQAs and therefore must be monitored or controlled to ensure the process produces the desired quality.
- Establishing a Control Strategy: This is a planned set of controls, derived from current product and process understanding, that ensures process performance and product quality. As noted by a pharmaceutical expert, "Quality risk assessment, along with QbD tools, will help establish the control strategy for new processes" [62].
Experimental Workflows and Process Optimization
Translating a research protocol into a cGMP-compliant manufacturing process requires meticulous planning and optimization. Below is a generalized workflow for manufacturing an allogeneic stem cell therapy, highlighting critical stages where control is paramount.
Diagram: cGMP Workflow for Allogeneic Stem Cell Therapy Manufacturing
Key Experimental Protocols for Process Characterization
To ensure the process in the diagram is robust, specific experimental protocols must be employed.
Protocol 1: Optimizing Cell Expansion in Bioreactors
- Objective: To determine the optimal set of Critical Process Parameters (CPPs) for scaling up stem cell expansion while maintaining Critical Quality Attributes (CQAs).
- Methodology: Use Design of Experiments (DoE) to systematically vary parameters such as pH, dissolved oxygen (DO), feeding schedule, and agitation speed in a benchtop bioreactor. Monitor cell growth kinetics, metabolism (e.g., glucose consumption, lactate production), and daily samples for CQAs (e.g., viability, identity markers, karyotype).
- Outcome Analysis: Establish a design space where the process consistently yields cells meeting all pre-defined CQA specifications. This validated model becomes the basis for your commercial manufacturing process.
Protocol 2: Validating a Closed-System Cell Processing Unit
- Objective: To demonstrate that a new automated, closed-system processing unit is equivalent or superior to the open manual process it is replacing.
- Methodology: Perform a side-by-side comparison study using the same donor starting material. Split the sample and process one half with the traditional manual method and the other with the automated system.
- Outcome Analysis: Compare key output metrics including total cell yield, viability, purity, processing time, and sterility. The automated system must demonstrate non-inferiority in cell quality and a significant reduction in open-processing time to justify its implementation in a GMP setting.
The Scientist's Toolkit: Essential Research Reagent Solutions
A robust manufacturing process relies on high-quality, well-characterized reagents. The table below details key materials essential for stem cell therapy development and production.
Table: Research Reagent Solutions for Stem Cell Therapy Manufacturing
| Item | Function & Rationale |
|---|---|
| GMP-Grade iPSC Master Cell Bank | A clonal, fully characterized master cell bank, such as those filed under a Drug Master File (DMF), serves as a consistent and regulatable starting material for allogeneic therapies, ensuring traceability and quality [18]. |
| Chemically Defined, Xeno-Free Culture Media | Eliminates lot-to-lot variability and the risk of zoonotic pathogen transmission, which is critical for process consistency and patient safety. Essential for cGMP compliance. |
| Cell Separation Kits (e.g., MACS) | Magnetic-activated cell sorting kits allow for the specific isolation of target cell populations (e.g., CD34+ hematopoietic stem cells) from a heterogeneous starting mixture, ensuring product purity [63]. |
| Gene Editing Systems (e.g., CRISPR-Cas9) | Enables precise genetic modification for therapies requiring gene correction (e.g., Lyfgenia) or to enhance therapeutic properties (e.g., immune evasion in allogeneic products) [13] [61]. |
| Critical Reagents for QC Assays | Includes standardized kits and reference materials for sterility, mycoplasma, endotoxin, flow cytometry, and potency assays. These reagents must be qualified for their intended use in lot release testing. |
The future of stem cell manufacturing is being shaped by several key trends aimed at overcoming current complexities. The shift toward allogeneic, "off-the-shelf" therapies is a primary strategy to improve scalability and reduce costs [61]. Furthermore, the industry is moving towards greater process automation and standardization to enhance reproducibility and efficiency [61] [63]. The adoption of modular and decentralized manufacturing models, including point-of-care production, aims to reduce turnaround times and improve patient access, though they present their own challenges in quality control standardization [62]. Finally, advanced analytical technologies like in-line sensors and multi-omics are being integrated to enable real-time quality monitoring and smarter control strategies.
In conclusion, scaling stem cell therapies for widespread impact is a multifaceted challenge that demands deep scientific expertise and rigorous engineering principles. Success hinges on the seamless integration of advanced biology with robust, automated manufacturing platforms, all underpinned by an unwavering commitment to cGMP compliance. By adopting a Quality by Design approach, strategically investing in automation and closed systems, and fostering collaboration across academia, industry, and regulators, the field can overcome these manufacturing complexities. This will ultimately fulfill the historic promise of stem cell research: to deliver personalized, regenerative medicines to the patients who need them, reliably and at scale.
Stem cell applications in precision medicine have evolved from foundational research into a revolutionary frontier in modern medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries [13]. As this field progresses toward clinical translation, ensuring product quality through robust potency assays and release criteria has become indispensable for confirming that cellular therapies exhibit consistent biological activity linked to their intended clinical mechanism of action [64] [65]. Potency assays serve as quantitative measures of a product-specific biological activity that is functionally linked to relevant biological properties and, ideally, the product's in vivo mechanism of action [66]. In the context of Advanced Therapy Medicinal Products (ATMPs), these assays represent a fundamental aspect of quality control, ideally serving as biomarkers of efficacy in vivo [64].
The historical journey of stem cell investigation, tracing back to pivotal contributions from late 19th and early 20th century scientists, has established the groundwork for contemporary stem cell research [13]. With recent breakthroughs including embryonic stem cell isolation and induced pluripotent stem cell discovery, the field has progressed to clinical applications requiring rigorous quality standards [13]. The complexity of stem cell-based products, coupled with their living nature and frequent patient-specific manufacturing, necessitates sophisticated testing strategies to ensure that each product lot meets predefined specifications for safety, purity, identity, and potency before clinical use [66]. This technical guide examines the critical importance of potency assays and release criteria within the evolving landscape of stem cell-based precision medicine, providing researchers and drug development professionals with methodologies and frameworks for ensuring product quality and consistency.
The Regulatory and Scientific Framework for Potency Testing
Defining Potency in Cellular Therapies
According to regulatory guidelines, potency represents the quantitative measure of a biological activity specific to a product that is linked to relevant biological properties [66]. For cellular therapies, this biological activity should reflect the intended therapeutic effect and ideally correlate with clinical response. Unlike small molecule drugs with well-defined chemical structures, stem cell therapies derive their therapeutic effects from complex, often multifunctional biological activities, making potency assessment particularly challenging [64] [66]. The International Society for Stem Cell Research (ISSCR) emphasizes that stem cell-based interventions must undergo rigorous and independent expert review of safety and efficacy before clinical application, with potency testing serving as a critical component of this evaluation [67].
The fundamental purpose of potency testing extends beyond lot release to include ensuring product consistency across manufacturing lots, confirming manufacturing process validation, and providing critical data for comparability assessments following manufacturing changes [66]. As the field advances toward more complex stem cell-based products, including genetically modified cells and combination therapies, the role of potency assays becomes increasingly important for demonstrating product quality throughout the product lifecycle.
Challenges in Potency Assay Development
Developing robust potency assays for stem cell therapies presents unique challenges that distinguish them from traditional pharmaceuticals:
- Limited Product Quantity: Most cellular therapies are patient-specific, with limited final product available for testing [66]
- Time Constraints: Cellular therapies often have short shelf lives, requiring rapid testing between production completion and patient administration [66]
- Product Complexity: Stem cell products frequently contain multiple cell types with complex, sometimes synergistic mechanisms of action [66]
- Biological Variability: Donor genetic and physiological heterogeneity contributes to product variability [66]
- Multifunctional Activity: Many stem cell products exhibit multiple biological activities, making selection of a single potency endpoint challenging [64]
These challenges necessitate careful consideration during assay design and validation to ensure that potency measurements truly reflect the product's biological activity while remaining feasible within manufacturing constraints.
Establishing Comprehensive Release Criteria for Stem Cell Products
Fundamental Release Criteria for Cellular Therapies
All cellular therapy products must demonstrate safety, purity, identity, and potency before human use [66]. Release criteria encompass objective standards based on clinical trial and manufacturing data that evaluate these critical quality attributes during production and at lot release. For stem cell products, particularly mesenchymal stromal cells (MSCs), specific release criteria have been established by international organizations including the International Society for Cell and Gene Therapy (ISCT) [68].
Table 1: Fundamental Release Criteria for Stem Cell Therapies
| Quality Attribute | Testing Method | Acceptance Criteria Examples |
|---|---|---|
| Viability | Flow cytometry with vital dyes | Typically ≥70-80% viable cells |
| Identity/Purity | Flow cytometry for surface markers | Expression of CD90, CD73, CD105 (>95%); lack of hematopoietic markers (CD45, CD34, CD14) (<5%) [69] |
| Sterility | BacT/ALERT, Gram stain | No microbial growth detected |
| Mycoplasma | PCR or culture methods | No mycoplasma detected |
| Potency | Functional assays specific to mechanism of action | Significant biological activity above negative control |
| Endotoxin | LAL assay | ≤5 EU/kg body weight |
These criteria form the foundation for product release, with specific acceptance criteria established during process development and refined based on clinical experience.
Advanced Characterization and Novel Biomarkers
While classical surface markers (CD90, CD73, CD105) remain fundamental for MSC identification, research has identified additional biomarkers that may provide more robust release criteria and functional relevance. Studies on clinical-grade adipose-derived MSCs have validated non-classical markers including CD36, CD163, CD271, CD200, CD273, CD274, CD146, CD248, and CD140B that may potentially discriminate MSCs from other cell types and provide novel information for manufacturing quality control [69]. These markers exhibit variability among different cell isolates from diverse donors and may be informative during manufacturing, particularly for freshly prepared, previously frozen, or proliferative state MSCs [69].
The evolving understanding of stem cell biology continues to refine release criteria, with emerging technologies enabling more sophisticated characterization approaches. As stated by Caplan, MSCs increasingly function as "Medicinal Signaling Cells" whose paracrine action rather than differentiation capacity induces regeneration, highlighting the importance of characterizing secretory profiles alongside traditional markers [68].
Methodologies for Potency Assay Development and Validation
Potency Assay Design Considerations
Designing appropriate potency assays requires careful consideration of the product's mechanism of action, clinical indication, and manufacturing constraints. The assay should quantitatively measure a biological activity that is therapeutically relevant and ideally linked to the product's in vivo mechanism of action [65] [66]. For stem cell products with multiple mechanisms of action, a matrix of potency assays may be necessary to fully characterize product functionality [64].
The development of potency assays typically progresses through stages, beginning with identifying the critical biological activity during preclinical development and culminating in validated assays prior to Phase III clinical trials [66]. A well-designed potency assay should demonstrate specificity, accuracy, precision, linearity, range, and robustness following validation according to regulatory guidelines [65].
Experimental Protocols for Key Potency Assays
Immunomodulatory Potency Assay for MSCs
For MSCs with immunomodulatory functions, potency can be assessed through their capacity to suppress immune cell activation or promote anti-inflammatory environments. A recently developed assay measures the anti-inflammatory capacity of MSCs in an M1 macrophage-dominated inflammatory environment [65]:
Protocol Overview:
- Establish inflammatory model: Differentiate THP-1 monocytes into M1-polarized macrophages using phorbol esters and interferon-gamma
- Coculture system: Coculture MSCs with M1-polarized macrophages at optimized ratios (determined to be 1:5 to 1:10 in published studies)
- Stimulation: Activate the coculture with lipopolysaccharide or other inflammatory stimuli
- Readout: Quantify interleukin-1 receptor antagonist (IL-1RA) secretion by ELISA as a measure of anti-inflammatory potency
- Validation: Confirm successful macrophage differentiation via CD36 and CD80 marker expression, and proinflammatory TNF-α release
This assay demonstrated guideline-concordant selectivity, accuracy, and precision over a relevant concentration range, with batch release testing of 71 consecutively manufactured MSC batches showing low failure rates and high comparability between donors [65].
Cytotoxic Potency Assay for Immune Effector Cells
For cytotoxic T lymphocytes, NK cells, or CAR-modified cells, potency is frequently measured through direct cytotoxic activity against target cells:
Protocol Overview:
- Effector cell preparation: Expand and activate cytotoxic cells using IL-2 and/or IL-7/IL-15
- Target cell selection: Use tumor cell lines or primary cells expressing target antigens
- Coculture setup: Combine effector and target cells at varying effector-to-target ratios
- Cytotoxicity measurement:
- Traditional methods: 51Chromium release assay measuring isotope release from dying target cells
- Modern approaches: Flow cytometry with dead/live cell dyes or measurement of endogenous proteins (LDH)
- Surrogate markers: Quantify degranulation markers (CD107a) or inflammatory cytokines (IFN-γ, TNF-α) following target cell contact [64]
Molecular Assays for Potency Assessment
Emerging approaches utilize gene expression profiling and microRNA analysis to assess potency of cellular therapies [66]. These molecular assays offer potential for comprehensive characterization of cellular products:
Protocol Overview:
- RNA isolation: Extract high-quality RNA from cellular product
- Gene expression profiling: Utilize microarray or RNA-sequencing to assess expression of potency-related genes
- Data analysis: Identify expression signatures correlated with biological activity
- Validation: Confirm predictive value of signature through functional assays
Preliminary studies have shown that microRNA expression patterns can distinguish different types of stem cells and leukocytes, suggesting potential application in potency testing [66].
Diagram 1: Potency assay workflows for different cell types. Critical measurement endpoints are highlighted in green.
Advanced Technologies and Emerging Approaches
Novel Analytical Platforms
The field of potency testing continues to evolve with advancements in analytical technologies enabling more precise and predictive assessments:
- Single-cell RNA sequencing: Provides unprecedented resolution for characterizing cellular heterogeneity within products [13]
- CRISPR technology: Enables precise genome editing for creating reporter cell lines for potency assessment [13]
- Microarray gene expression profiling: Facilitates identification of potency signatures correlated with biological activity [66]
- Multiplex cytokine profiling: Allows comprehensive characterization of secretory profiles for immunomodulatory cells
- High-content imaging: Enables morphological and functional assessment at single-cell resolution
These technologies offer opportunities to develop potency assays that more accurately predict clinical performance while providing insights into product biology.
Integration of Potency Assays with Precision Medicine Approaches
The evolution of stem cell applications in precision medicine has created opportunities to align potency testing with individualized therapeutic approaches. Next-generation sequencing (NGS) technologies enable detailed characterization of tumor biology and stem cell differentiation pathways, facilitating the development of patient-specific potency models [27]. The integration of NGS with stem cell platforms allows researchers to identify patient-specific targets and predict therapeutic responses, potentially enabling more personalized potency assessment strategies [27].
For induced pluripotent stem cell (iPSC)-derived therapies, potency assays must account for both the differentiation efficiency and functional maturity of the resulting cells. The growing clinical trial landscape for iPSC-derived products, including therapies for ophthalmologic, neurologic, and oncologic indications, underscores the need for robust potency assays tailored to these advanced therapies [18].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Potency Assay Development
| Reagent Category | Specific Examples | Function in Potency Assessment |
|---|---|---|
| Cell Culture Media | RPMI-1640, DMEM/F12, X-VIVO 15 | Maintain cell viability and function during assay |
| Cytokines/Growth Factors | IL-2, IL-7, IL-15, IFN-γ, M-CSF | Activate and differentiate cells for functional assessment |
| Antibodies for Flow Cytometry | CD3, CD4, CD8, CD14, CD19, CD56, CD73, CD90, CD105 | Cell phenotyping and purity assessment |
| ELISA Kits | IFN-γ, TNF-α, IL-1RA, Granzyme B | Quantify secretory activity and immune modulation |
| Viability Assays | 7-AAD, Propidium Iodide, Calcein AM | Assess cell health and function |
| Target Cell Lines | K562, Jurkat, THP-1, A549 | Provide standardized targets for functional assays |
| Molecular Biology Reagents | RNA extraction kits, cDNA synthesis kits, qPCR reagents | Gene expression analysis for potency signatures |
| Reference Standards | WHO International Standards, in-house reference panels | Assay calibration and cross-lot comparability |
These essential materials form the foundation for developing and implementing robust potency assays, with careful selection and qualification critical for assay performance.
Implementation Strategy: From Development to Validation
Systematic Potency Assay Implementation
Successfully implementing potency assays requires a structured approach that aligns with product development phases:
Phase I: Target Product Profile Analysis
- Identify critical quality attributes based on mechanism of action
- Define desired product profile and key biological activities
- Establish preliminary potency endpoints
Phase II: Assay Design and Development
- Select appropriate assay format (in vitro, in vivo, molecular)
- Optimize assay conditions and parameters
- Establish preliminary acceptance criteria
- Assess assay feasibility and robustness
Phase III: Assay Qualification
- Demonstrate specificity, precision, and linearity
- Establish analytical range and detection limits
- Evaluate intermediate precision and reproducibility
- Define system suitability criteria
Phase IV: Assay Validation
- Conduct full validation per regulatory guidelines
- Establish final acceptance criteria based on clinical data
- Implement for lot release and stability testing
This systematic approach ensures that potency assays are scientifically sound, technically feasible, and regulatory compliant throughout product development.
Case Study: Successful Potency Assay Implementation
The development of a potency assay for ABCB5+ MSCs demonstrates a successful implementation approach [65]. This assay measured IL-1RA secretion in an M1 macrophage coculture model and addressed key challenges through:
- Systematic ratio optimization: Testing wide MSC/macrophage ratios to identify optimal conditions for near-maximal stimulation
- Comprehensive validation: Demonstrating guideline-concordant selectivity, accuracy, and precision
- Manufacturing integration: Implementing for batch release of 71 consecutively manufactured MSC batches
- Clinical correlation: Establishing absolute maximum IL-1RA levels per MSC for future comparison with clinical efficacy
This approach resulted in a therapeutically relevant, straightforward, robust, and reproducible potency assay that effectively supported product development [65].
Diagram 2: Potency assay implementation pathway aligned with product development phases.
As stem cell applications continue to evolve within precision medicine, potency assay strategies must advance accordingly. The future landscape will likely include:
- Multi-parameter potency matrices that capture the complex biological activities of stem cell products
- Advanced analytical technologies including single-cell omics and high-content imaging for deeper product characterization
- Mechanistically-driven assays based on improved understanding of in vivo mechanisms of action
- Patient-specific potency models incorporating individual patient characteristics and disease states
- Real-time potency monitoring through innovative process analytical technologies
The continued development of robust potency assays and release criteria remains essential for realizing the full potential of stem cell therapies in precision medicine. By establishing scientifically rigorous and clinically relevant quality standards, researchers and drug development professionals can ensure that these revolutionary therapies deliver on their promise to transform treatment for debilitating diseases and injuries.
From Trials to Treatment: Clinical Validation and Regulatory Pathways
The journey of stem cell therapies from foundational laboratory research to validated clinical applications represents one of the most significant progressions in modern precision medicine. This evolution is characterized by a critical transition from preclinical validation to clinical efficacy, requiring rigorous demonstration of both safety and therapeutic potential. The historical context of stem cell applications reveals a field that has progressively matured from early experimental concepts into a discipline defined by robust clinical trials and regulatory oversight [23] [13]. As the field advances, the integration of innovative technologies like artificial intelligence and systems biology (SysBio) is accelerating this translational pathway, enabling more predictive preclinical models and refined clinical trial designs [70]. This whitepaper analyzes the landmark studies and methodological frameworks that have established the current standards for demonstrating safety and efficacy in stem cell research, providing drug development professionals with a comprehensive resource for navigating this complex landscape.
Analysis of Landmark Clinical Trials and Regulatory Milestones
Recent FDA Approvals and Late-Stage Clinical Programs
The regulatory landscape for stem cell therapies has seen significant milestones between 2023-2025, marking a turning point in clinical translation. These approvals and advanced trials demonstrate the evolving evidence standards required for regulatory endorsement.
Table 1: Recently FDA-Approved Stem Cell Therapies (2023-2025)
| Therapy Name | Cell Type | Indication | Approval Date | Key Efficacy Outcomes |
|---|---|---|---|---|
| Ryoncil (remestemcel-L) | Allogeneic bone marrow-derived MSCs | Pediatric steroid-refractory acute graft-versus-host disease | December 2024 | Modulation of immune response and inflammation in life-threatening condition [18] |
| Omisirge (omidubicel-onlv) | Cord blood-derived hematopoietic progenitor cells | Hematologic malignancies (cord blood transplantation) | April 2023 | Accelerated neutrophil recovery and reduced infection risk post-myeloablative conditioning [18] |
| Lyfgenia (lovotibeglogene autotemcel) | Autologous hematopoietic stem cells (gene-modified) | Sickle cell disease (age ≥12) | December 2023 | 88% achieved complete resolution of vaso-occlusive events (6-18 months post-treatment) [18] |
Table 2: Promising Late-Stage Clinical Trials (2024-2025)
| Therapy/Program | Cell Type | Indication | Trial Phase | Key Efficacy Findings |
|---|---|---|---|---|
| VX-880 (Zimislecel) | Stem cell-derived islet cells | Type 1 Diabetes | Phase 1/2/3 (pivotal) | 11 of 12 patients reduced or eliminated exogenous insulin use; achieved HbA1C below 7.0% and time-in-range above 70% [71] |
| Fertilo | iPSC-derived ovarian support cells | In vitro oocyte maturation | Phase III (first iPSC-based in U.S.) | Reduced hormonal burden on patients; resulted in first live birth [18] |
| OpCT-001 | iPSC-derived therapy | Retinal degeneration (retinitis pigmentosa, cone-rod dystrophy) | Phase I/IIa | First iPSC-based therapy for primary photoreceptor diseases [18] |
| FT819 | iPSC-derived CAR T-cell therapy | Systemic lupus erythematosus (including lupus nephritis) | Phase I (RMAT designated) | Off-the-shelf allogeneic approach for autoimmune disease [18] |
Quantitative Efficacy Outcomes from Recent Meta-Analyses
Recent systematic reviews and meta-analyses provide compelling quantitative evidence for stem cell efficacy across multiple conditions, offering insights into magnitude of therapeutic effects.
Table 3: Efficacy Outcomes from Recent Meta-Analyses of Stem Cell Clinical Trials
| Condition | Number of Trials/Participants | Primary Efficacy Endpoint | Outcome Measure | Statistical Significance |
|---|---|---|---|---|
| Acute/Subacute Ischemic Stroke | 13 trials (n=872 patients) | mRS score 0-1 at 1 year | Risk Ratio: 1.74 | p=0.020; I²=0% [72] |
| Acute/Subacute Ischemic Stroke | 13 trials (n=872 patients) | mRS score 0-2 at 90 days | Risk Ratio: 1.31 | p=0.044; I²=0% [72] |
| Acute Myocardial Infarction | 15 trials (n=1,218 participants) | Long-term LVEF improvement | Mean Difference: 2.63% | p=0.02 [73] |
| Acute Myocardial Infarction | 15 trials (n=1,218 participants) | Long-term relative infarct size | Standardized Mean Difference: -0.63 | p<0.0001 [73] |
Safety profiles across these analyses have been generally favorable. For ischemic stroke, no significant differences were observed in serious adverse events or mortality between cell therapy and control groups [72]. In myocardial infarction, stem cell therapy was associated with fewer adverse events than controls and no cardiac-related cancer cases were reported, though longer follow-up was recommended to assess potential oncogenic risks [73].
Advanced Preclinical Methodologies and Experimental Protocols
Single-Cell Analysis and Live-Cell Imaging Approaches
Modern preclinical assessment employs sophisticated single-cell resolution technologies that provide unprecedented insights into stem cell behavior and therapeutic mechanisms. Quantitative single-cell approaches have become fundamental for understanding the molecular control of cell fates, utilizing high-throughput molecular readouts and continuous, noninvasive observation of cell behavior over time [74]. These methodologies enable researchers to move beyond population averages and account for the inherent heterogeneity in stem cell populations, which is critical for predicting in vivo behavior and potential therapeutic effects.
Key methodological frameworks include:
- Time-lapse imaging microscopy: Allows continuous observation of individual cells throughout differentiation processes, providing kinetic data on division patterns, migration, and fate decisions
- High-throughput single-cell molecular profiling: Techniques including single-cell RNA sequencing (scRNA-seq) enable comprehensive transcriptomic analysis of individual cells within heterogeneous populations
- Automated lineage tracing: Computational approaches that track progeny of individual stem cells to establish lineage relationships and differentiation pathways
Quantitative Assessment of Stem Cell-Derived Organoids and Tissues
A critical challenge in preclinical development has been the quantitative assessment of stem cell-derived products. Recent advances have addressed this through computational approaches that systematically evaluate the quality and maturity of stem cell-derived organoids and cells. The Web-based Similarity Analytics System provides a quantitative calculation system to assess organ-specific similarity based on organ-specific gene expression panels (Organ-GEP) [75].
The experimental workflow for this quantitative assessment involves:
- RNA-seq analysis of hPSC-derived organoids/cells
- Processing of raw RNA-seq data (TPM, FPKM/RPKM values)
- Calculation of organ similarity using specialized algorithms (LuGEP for lung, StGEP for stomach, HtGEP for heart)
- Generation of quantitative similarity score (%) indicating degree of resemblance to target human organ
This methodology represents a significant advancement over traditional qualitative assessments based on limited marker analysis, providing researchers with standardized metrics for quality control and optimization of differentiation protocols [75].
Systems Biology and Artificial Intelligence Integration
The integration of systems biology (SysBio) and artificial intelligence (AI) represents a transformative approach to overcoming translational barriers in stem cell therapy. SysBioAI analysis enables holistic examination of complex biological systems by employing advanced computational and mathematical modeling to integrate diverse molecular interactions between genes, proteins, and cellular pathways [70]. This approach has proven particularly valuable for:
- Analysis of large-scale multi-omics datasets from stem cell products and clinical trial outcomes
- Identification of patient-specific response biomarkers to predict treatment efficacy
- Optimization of manufacturing processes and product characterization
- Enabling the "Iterative Circle of Refined Clinical Translation" through continuous learning from clinical data
The practical implementation of SysBioAI has demonstrated success in related fields such as chimeric antigen receptor (CAR)-T cell therapy, including automated manufacturing, safety and efficacy monitoring, and predictive approaches for improving cell fitness and clinical efficacy [70]. Application of these approaches to stem cell therapy addresses crucial limitations that have hampered clinical translation, including product heterogeneity, incomplete mechanistic understanding, and limited predictive power of traditional trial designs.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Reagents and Solutions for Stem Cell Translation
| Reagent/Solution | Function | Application Context |
|---|---|---|
| REPROCELL StemRNA Clinical iPSC Seed Clones | GMP-compliant, quality-controlled starting material for iPSC therapies | Clinical trial material generation; FDA Drug Master File submitted [18] |
| Organ-Specific Gene Expression Panels (Organ-GEP) | Quantitative assessment of organoid similarity to human tissues | Quality control of differentiated cells/organoids; protocol optimization [75] |
| CRISPR/Cas9 Gene Editing Systems | Precise genetic modification of stem cells | Disease modeling; therapeutic cell engineering; safety enhancements [13] |
| Advanced 3D Culture Matrices | Mimic native tissue microenvironment for organoid development | Organoid generation; disease modeling; drug screening [75] |
| Single-Cell RNA Sequencing Reagents | High-resolution transcriptomic profiling of heterogeneous populations | Cell product characterization; potency assay development; mechanism of action studies [74] [13] |
| cGMP-compliant Cell Culture Media | Support expansion and differentiation under regulatory standards | Manufacturing of clinical-grade cell products [23] [18] |
The landscape of stem cell therapy development is evolving toward increasingly sophisticated approaches that leverage integrated data analysis and precision medicine principles. The convergence of SysBio and AI is enabling a more comprehensive understanding of stem cell behavior and therapeutic mechanisms, moving beyond reductionist approaches to embrace biological complexity [70]. Future directions focus on patient-specific response prediction, product optimization through iterative analysis, and development of personalized regenerative therapies tailored to individual patient characteristics and disease states. As the field advances, the continued refinement of preclinical models, quantitative assessment tools, and clinical trial designs will accelerate the translation of stem cell discoveries into validated therapies that fulfill the promise of precision regenerative medicine. The landmark trials and methodological advances analyzed in this whitepaper provide both a foundation and framework for this continued evolution, highlighting the critical pathway from preclinical validation to demonstrated clinical efficacy and safety.
The field of stem cell applications in precision medicine has evolved from foundational biological discovery to transformative clinical reality. This journey has been accompanied by the parallel development of sophisticated regulatory frameworks designed to ensure safety and efficacy while fostering innovation. The historical progression from embryonic stem cell (ESC) isolation in the 1980s to the groundbreaking discovery of induced pluripotent stem cells (iPSCs) in 2006 has fundamentally expanded therapeutic possibilities while addressing ethical considerations [13] [17]. As the science has advanced, regulatory agencies have adapted existing pathways and created new ones, such as the Regenerative Medicine Advanced Therapy (RMAT) designation, to address the unique challenges presented by regenerative medicine products [76]. This guide provides researchers, scientists, and drug development professionals with a comprehensive technical overview of navigating the core FDA regulatory processes—Investigational New Drug (IND) applications, Biologics License Applications (BLA), and RMAT designation—within the context of modern stem cell-based precision medicine.
Historical Evolution of Stem Cell Applications in Medicine
The integration of stem cell biology into therapeutic development represents one of the most significant medical revolutions of the past half-century. The field has matured through distinct phases:
Foundational Era (Late 19th - Late 20th Century): Early contributions from Boveri, Häcker, Maximow, and Cohnheim established core principles of stem cell biology, with the first identification of ESCs in 1981 marking a critical turning point [13]. Human ESC isolation in 1998 opened new therapeutic possibilities but also introduced persistent ethical controversies that would shape regulatory discourse [17].
Reprogramming Revolution (2006-Present): Shinya Yamanaka's discovery that somatic cells could be reprogrammed into iPSCs using defined transcription factors (OCT4, SOX2, KLF4, c-MYC) addressed ethical concerns and enabled patient-specific therapeutic strategies [13] [17]. This breakthrough fundamentally expanded the scale and scope of personalized regenerative medicine.
Translational Expansion (2010s-Present): The clinical translation of stem cell therapies accelerated with advancing understanding of different stem cell types—embryonic, adult, and induced pluripotent—each with distinct differentiation capabilities and therapeutic applications [23] [13]. The 21st Century Cures Act of 2016 established the RMAT designation to specifically support development of regenerative medicine products targeting unmet medical needs [77] [78].
Current Era (2020s): Characterized by increasingly sophisticated applications of iPSC-derived therapies across ophthalmology, neurology, oncology, and metabolic disorders, with growing emphasis on precision medicine approaches [18] [13] [17]. As of 2025, over 115 global clinical trials involving 83 distinct pluripotent stem cell-derived products have been documented, dosing over 1,200 patients with more than 10¹¹ cells [18].
Core Regulatory Framework and Pathways
Investigational New Drug (IND) Application
The IND application represents the formal gateway to initiating clinical investigations of biological products in human subjects. For stem cell therapies, INDs are submitted to the FDA's Center for Biologics Evaluation and Research (CBER), specifically the Office of Therapeutic Products (OTP) [79]. An IND becomes effective 30 days after submission unless the FDA places it on clinical hold [18].
Key components of an IND application for stem cell therapies include:
- Preclinical Data: Evidence from in vitro and animal studies demonstrating proof-of-concept, mechanism of action, and preliminary safety assessment [79]
- Clinical Protocol: Detailed study design for the initial clinical trial, including patient selection criteria, dosing regimen, and safety monitoring procedures
- Chemistry, Manufacturing, and Controls (CMC): Comprehensive description of the manufacturing process, quality control testing, and product characterization [79]
- Pharmacovigilance Plan: Strategies for safety monitoring and reporting during clinical development
Biologics License Application (BLA)
The BLA represents the comprehensive marketing application for biological products, submitted after sufficient clinical evidence of safety and efficacy has been generated. For gene therapies and many stem cell products, BLAs are reviewed by CBER's OTP [79]. The standard review timeline is 10 months, though this can be reduced to 6 months for products granted Priority Review [79].
Critical elements of a successful BLA for stem cell therapies include:
- Clinical Data: Results from Phase I-III trials demonstrating safety and efficacy in the target population [79]
- CMC Information: Detailed manufacturing process validation, facility information, and stability data [79]
- Labeling: Draft prescribing information and product labeling
- Risk Evaluation and Mitigation Strategies (REMS): Plans for managing known or potential safety risks
- Long-Term Follow-Up Data: Particularly important for stem cell therapies with potential for delayed adverse events such as tumorigenicity [18]
Regenerative Medicine Advanced Therapy (RMAT) Designation
Established under the 21st Century Cures Act, RMAT designation provides an expedited development pathway for promising regenerative medicine therapies. A drug is eligible for RMAT designation if it meets the following criteria [77]:
- Qualifies as a regenerative medicine therapy (cell therapy, therapeutic tissue engineering product, human cell and tissue product, or combination products)
- Intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition
- Preliminary clinical evidence indicates potential to address unmet medical needs
The benefits of RMAT designation include more frequent FDA interactions, potential priority review, and flexibility in clinical trial design. As of September 2025, the FDA has received almost 370 RMAT designation requests and approved 184, with 13 RMAT-designated products ultimately approved for marketing [78].
Table: Key FDA Regulatory Pathways for Stem Cell Therapies
| Pathway | Purpose | Key Features | Typical Timeline | Success Considerations |
|---|---|---|---|---|
| IND | Permission to begin clinical trials | Requires preclinical safety data, manufacturing information, and clinical protocols | 30-day review period | Robust preclinical package; well-characterized product |
| BLA | Marketing approval for commercial distribution | Comprehensive data on safety, efficacy, and manufacturing | 10 months standard; 6 months priority | Positive pivotal trial results; validated manufacturing process |
| RMAT | Expedited development pathway | Intensive FDA guidance; potential for accelerated approval | 60-day designation review | Preliminary clinical evidence; serious condition with unmet need |
Current Regulatory Landscape and Recent Approvals
The regulatory landscape for stem cell therapies has evolved significantly in recent years, with several notable approvals demonstrating the maturation of the field. As of December 2024, the FDA's Approved Cellular and Gene Therapy Products list remains selective but growing [18].
Recent Stem Cell Therapy Approvals
Ryoncil (remestemcel-L): Approved in December 2024 as the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD) in patients aged ≥2 months. This allogeneic bone marrow-derived MSC product modulates immune response and mitigates inflammation associated with SR-aGVHD [18].
Omisirge (omidubicel-onlv): Approved in April 2023 for patients (12-65 years) with hematologic malignancies undergoing cord blood transplantation. This allogeneic nicotinamide-modified stem cell graft derived from umbilical cord blood accelerates neutrophil recovery and reduces infection risk [18].
Lyfgenia (lovotibeglogene autotemcel): Approved in December 2023 as an autologous cell-based gene therapy for patients aged 12 years and older with sickle cell disease and history of vaso-occlusive events. This one-time treatment involves genetically modifying the patient's own hematopoietic stem cells to produce modified hemoglobin (HbAT87Q) [18].
RMAT-Approved Products
The FDA maintains a public list of RMAT approvals, which as of September 30, 2025, includes several innovative therapies [80]:
Table: Selected RMAT-Approved Products (2024-2025)
| Proprietary Name | Established Name | Applicant | Approval Date | Use |
|---|---|---|---|---|
| ZEVASKYN | Prademagene zamikeracel | Abeona Therapeutics Inc. | 28-APR-2025 | Treatment of wounds associated with recessive dystrophic epidermolysis bullosa (RDEB) |
| SYMVESS | Acellular tissue engineered vessel-tyod | Humacyte Global, Inc. | 19-DEC-2024 | Vascular conduit for extremity arterial injury when urgent revascularization is needed |
| AUCATZYL | Obecabtagene autoleucel | Autolus, Inc. | 08-NOV-2024 | Treatment of adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL) |
| TECELRA | Afamitresgene autoleucel | Adaptimmune LLC | 01-AUG-2024 | Treatment of adult patients with unresectable or metastatic synovial sarcoma |
Emerging Trends in Regulatory Guidance
Recent FDA draft guidance issued in September 2025 highlights evolving regulatory thinking in several key areas [78]:
- Encouraging innovative trial designs for rare diseases, including those comparing multiple investigational agents and utilizing natural history data as historical controls
- Support for multi-site trials with shared data to support individual BLAs when using common manufacturing protocols
- Increased emphasis on patient engagement in endpoint selection and trial design
- Recognition of unique safety considerations requiring long-term safety monitoring, potentially using digital health technologies
- Acceptance of real-world evidence to support accelerated approval applications
Experimental Design and Methodological Frameworks
Stem Cell Characterization and Quality Control
Robust experimental design begins with comprehensive characterization of stem cell populations. Key methodologies include:
Pluripotency Assessment: Evaluation of differentiation potential through in vitro embryoid body formation or in vivo teratoma formation assays, coupled with analysis of pluripotency markers (OCT4, SOX2, NANOG) via immunocytochemistry or flow cytometry [13]
Genetic Stability Monitoring: Karyotype analysis and whole-genome sequencing to detect chromosomal abnormalities that may arise during extended culture periods, particularly important for iPSC lines [18]
Functional Potency Assays: Development of quantitative, cell-based assays that measure biologically relevant functions predictive of clinical efficacy, required for both IND and BLA submissions [79]
Preclinical Proof-of-Concept Studies
Preclinical studies should be designed to provide evidence supporting both safety and potential efficacy:
Disease-Relevant Animal Models: Utilization of immunocompromised rodent models for evaluating engraftment and tumorigenicity, and genetically engineered or disease-induced models for efficacy assessment [13]
Biodistribution Studies: Tracking of administered cells using bioluminescence imaging, PCR-based methods, or other sensitive detection techniques to understand migration patterns and potential off-target localization [79]
Tumorigenicity Assessment: Long-term studies (often 6-12 months) in appropriate animal models to evaluate potential for uncontrolled growth, particularly critical for pluripotent stem cell-derived products [18] [13]
The following diagram illustrates the key experimental workflow from stem cell sourcing through preclinical development:
Clinical Trial Considerations for Stem Cell Therapies
Clinical development of stem cell therapies requires special considerations:
Novel Endpoint Development: For degenerative conditions where traditional endpoints may not capture clinically meaningful benefits, development of novel biomarkers or functional endpoints is often necessary [78]
Immunosuppression Strategies: For allogeneic products, appropriate immunosuppression regimens must be developed and optimized to prevent rejection while minimizing infection risk [17]
Long-Term Follow-Up: Implementation of extended observation periods (often 15 years) to monitor for delayed adverse events, particularly important for integrating gene therapies and pluripotent stem cell-derived products [79]
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful navigation of the regulatory pathway requires careful selection and qualification of research materials. The following table outlines key reagents and their functions in stem cell therapy development:
Table: Essential Research Reagents for Stem Cell Therapy Development
| Reagent Category | Specific Examples | Function | Regulatory Considerations |
|---|---|---|---|
| Reprogramming Factors | Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) | Reprogram somatic cells to iPSCs | Quality and consistency critical; use of integration-free methods preferred [17] |
| Differentiation Inducers | Growth factors, cytokines, small molecules | Direct lineage-specific differentiation | Well-characterized and qualified reagents essential for process consistency [13] |
| Cell Culture Matrices | Matrigel, recombinant laminin, vitronectin | Provide substrate for cell attachment and growth | Xeno-free alternatives preferred for clinical applications [18] |
| Characterization Antibodies | Anti-OCT4, NANOG, SSEA-4, lineage-specific markers | Assessment of pluripotency and differentiation status | Validation for specific applications required [13] |
| Cell Sorting Markers | Fluorescent antibodies for FACS, magnetic beads | Isolation of specific cell populations | Purity and viability critical for therapeutic cell populations [18] |
Strategic Regulatory Planning and Best Practices
Early Engagement and Regulatory Interactions
Successful regulatory navigation begins with early and strategic engagement with FDA. Key interaction points include:
Pre-IND Meetings: Opportunity to obtain FDA feedback on preclinical study designs, CMC plans, and proposed clinical trial designs [79]
INTERACT Meetings: Early, non-binding discussions for innovative products, particularly valuable for novel stem cell-based approaches with limited regulatory precedent [79]
RMAT Designation Requests: Can be submitted concurrently with an IND or as an amendment to an existing IND, with FDA response within 60 calendar days [77]
Chemistry, Manufacturing, and Controls (CMC) Strategy
Robust CMC documentation is critical throughout development. Key considerations include:
Manufacturing Consistency: Demonstration of process control and product consistency across batches, with particular attention to comparability when process changes are implemented [78] [79]
Potency Assays: Development of quantitative, biologically relevant assays that measure therapeutic activity, required for both INDs and BLAs [79]
Scalability Planning: Early consideration of manufacturing scalability, with processes that can transition from research-scale to commercial production while maintaining product quality [79]
Clinical Development Strategies
Efficient clinical development programs for stem cell therapies should incorporate:
Patient Selection Rationale: Clear biological and clinical rationale for patient population selection, with consideration for both scientific and regulatory perspectives [78]
Endpoint Alignment: Early engagement with patient communities and regulatory agencies to ensure endpoints are clinically meaningful and trial designs are feasible [78]
Risk Management: Comprehensive safety monitoring plans that address both anticipated and theoretical risks associated with stem cell-based products [78]
The following diagram illustrates the integrated regulatory pathway from preclinical development through marketing approval:
The regulatory landscape for stem cell therapies continues to evolve in parallel with scientific advances. Several emerging trends are likely to shape future development:
Precision Medicine Integration: Increasing personalization of stem cell therapies, including patient-specific iPSC approaches, will require regulatory flexibility while maintaining standards for safety and efficacy [13] [17]
Advanced Manufacturing Technologies: Automation, closed-system processing, and real-time quality monitoring will enhance product consistency and scalability [79]
Novel Analytical Methods: Advanced characterization techniques including single-cell RNA sequencing, proteomic profiling, and functional potency assays will enable more comprehensive product understanding [13]
Global Regulatory Harmonization: Increasing alignment between international regulatory bodies may streamline development programs for global markets [76]
The successful navigation of FDA regulatory pathways for stem cell therapies requires strategic planning, robust science, and proactive regulatory engagement. By understanding the historical context, current requirements, and emerging trends outlined in this guide, researchers and drug development professionals can more effectively advance promising stem cell-based therapies through the development pipeline and ultimately to patients in need.
The field of regenerative medicine has undergone a profound transformation, evolving from the foundational use of hematopoietic stem cells in bone marrow transplants to sophisticated platforms capable of generating patient-specific cell types for personalized therapies. This historical journey represents a paradigm shift from a one-size-fits-all approach to precision medicine, where treatments are tailored to individual genetic makeup, disease characteristics, and therapeutic needs [13] [27]. Central to this evolution are critical strategic decisions regarding cell sourcing—specifically the choice between autologous versus allogeneic approaches and between induced pluripotent stem cells (iPSCs) versus embryonic stem cells (ESCs). These decisions carry significant implications for therapeutic efficacy, safety profiles, manufacturing complexity, and clinical scalability [81]. As of late 2025, the global clinical landscape includes over 115 clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products, with more than 1,200 patients dosed and no class-wide safety concerns identified, underscoring the accelerating translation of these technologies into clinical applications [18]. This technical analysis provides a comprehensive comparison of these foundational approaches, examining their relative effectiveness within the broader context of advancing precision medicine through stem cell research.
Core Technological Platforms: Understanding the Stem Cell Classes
Pluripotent Stem Cells: iPSCs vs. ESCs
Pluripotent stem cells represent the cornerstone of modern regenerative medicine due to their unique capacity to differentiate into virtually any cell type in the body. The two primary classes—iPSCs and ESCs—share the fundamental property of pluripotency but differ significantly in their origins and associated considerations.
Embryonic Stem Cells (ESCs) are derived from the inner cell mass of blastocyst-stage embryos [13] [27]. Their use has been historically controversial due to the ethical implications of embryo destruction, which has led to strict regulatory frameworks in many countries [23] [13]. Despite these challenges, ESCs remain valuable research tools due to their well-established differentiation protocols and extensive characterization over decades of study.
Induced Pluripotent Stem Cells (iPSCs), first generated by Takahashi and Yamanaka in 2006, are adult somatic cells reprogrammed into a pluripotent state through the introduction of specific transcription factors (OCT4, SOX2, KLF4, and c-MYC) [82]. This breakthrough created an ethically neutral alternative to ESCs while enabling the generation of patient-specific cell lines for personalized medicine applications [82] [27]. The reprogramming process involves extensive transcriptional and epigenetic remodeling, progressing through distinct phases where somatic identity is suppressed and pluripotency networks are stabilized [82]. Early iPSC generation methods raised safety concerns due to integrating viral vectors, prompting the development of safer non-integrating approaches including episomal plasmids, synthetic mRNAs, and Sendai virus vectors [82].
Table 1: Key Characteristics of Pluripotent Stem Cell Platforms
| Feature | Induced Pluripotent Stem Cells (iPSCs) | Embryonic Stem Cells (ESCs) |
|---|---|---|
| Origin | Reprogrammed adult somatic cells (e.g., skin fibroblasts, blood cells) | Inner cell mass of blastocyst-stage embryos [13] [27] |
| Pluripotency Status | Pluripotent [82] | Pluripotent [13] |
| Key Advantages | Avoids ethical controversies; enables patient-specific modeling; autologous applications possible [82] [27] | Established differentiation protocols; extensive research history; "gold standard" pluripotency [13] |
| Key Limitations | Genetic/epigenetic abnormalities risk; variability in differentiation outcomes; tumorigenicity concerns [82] | Ethical controversies; immune rejection in allogeneic applications; limited genetic diversity [23] [13] |
| Immunogenicity | Autologous: Minimal rejection [82] | Allogeneic: Requires immunosuppression or immune matching [81] |
| Regulatory Status | Clinical trials ongoing (e.g., Parkinson's, retinal diseases) [82] [18] | Limited clinical application due to ethical restrictions [13] |
Therapeutic Delivery Models: Autologous vs. Allogeneic
The strategic decision between autologous and allogeneic cell therapy models represents a critical juncture in therapeutic development, with each approach offering distinct advantages and challenges across manufacturing, clinical application, and commercial considerations.
Autologous cell therapies involve collecting cells from a patient, potentially modifying them ex vivo, and reinfusing them into the same individual. This approach eliminates the risk of immune rejection and avoids graft-versus-host disease (GvHD), making it particularly valuable for long-term engraftment [81]. However, autologous therapies face significant challenges related to manufacturing complexity, as each batch is patient-specific, requiring rigorous chain-of-identity management and resulting in high costs and logistical burdens [81]. Additionally, the time required for manufacturing (weeks) may be prohibitive for patients with rapidly progressing diseases, and cell quality can be compromised in patients who have undergone extensive prior treatments or whose cells are affected by the disease process itself [81].
Allogeneic cell therapies utilize cells from healthy donors to create "off-the-shelf" products that are readily available for treatment. This approach enables规模化生产, batch consistency, and potentially lower costs per dose [81]. These therapies are particularly advantageous for acute conditions where treatment timing is critical. However, allogeneic approaches face the significant challenge of immune rejection, potentially requiring immunosuppression or genetic engineering to overcome host immune responses [81]. The risk of GvHD also necessitates careful donor-recipient matching, particularly for human leukocyte antigen (HLA) compatibility [81].
Table 2: Comparative Analysis of Autologous vs. Allogeneic Delivery Models
| Characteristic | Autologous Model | Allogeneic Model |
|---|---|---|
| Cell Source | Patient's own cells [81] | Healthy donor(s) [81] |
| Immune Compatibility | High (minimal rejection risk) [81] | Variable (requires matching/immunosuppression) [81] |
| GvHD Risk | None [81] | Present (requires management) [81] |
| Manufacturing Model | Patient-specific ("service-based") [81] | "Off-the-shelf" [81] |
| Production Scalability | Low (individual batches) [81] | High (large batches) [81] |
| Cost Structure | High per dose [81] | Lower per dose (at scale) [81] |
| Treatment Timeline | Weeks (manufacturing delay) [81] | Immediate availability [81] |
| Cell Quality | Variable (dependent on patient health) [81] | Consistent (healthy donors) [81] |
| Regulatory Complexity | High (batch-to-batch variability) [81] | Moderate (standardized products) [81] |
| Ideal Application | Chronic conditions, immunogenic concerns [81] | Acute conditions, mass-market treatments [81] |
Experimental and Methodological Approaches
Key Experimental Workflows
The development of effective stem cell therapies relies on standardized yet continuously evolving experimental workflows. These methodologies encompass everything from initial cell line generation to final product administration, with specific protocols varying based on the chosen technological platform.
iPSC Generation and Differentiation Workflow: The creation of clinical-grade iPSCs begins with somatic cell acquisition (typically dermal fibroblasts or peripheral blood mononuclear cells) from patients or donors under strict informed consent and ethical guidelines [82]. These cells undergo reprogramming using non-integrating methods such as episomal plasmids, Sendai virus vectors, or synthetic mRNA [82]. The resulting iPSC clones are rigorously characterized for pluripotency markers (OCT4, SOX2, NANOG), genomic integrity (karyotyping, whole-genome sequencing), and differentiation potential (embryoid body formation) [82] [83]. For therapeutic applications, iPSCs are differentiated into specific lineages using standardized protocols incorporating precise temporal sequences of growth factors and small molecules [82]. The final cell products undergo comprehensive quality control testing for viability, purity, potency, sterility, and freedom from contaminants before cryopreservation or administration [83].
Allogeneic MSC Therapy Manufacturing: Mesenchymal stem cells (MSCs) for allogeneic applications are typically isolated from bone marrow, adipose tissue, or umbilical cord tissue from healthy screened donors [23] [84]. These cells undergo extensive in vitro expansion using defined culture media under Good Manufacturing Practice (GMP) conditions [84]. Throughout the expansion process, cells are monitored for maintenance of phenotypic markers (CD73+, CD90+, CD105+, CD45-) and differentiation capacity into osteogenic, adipogenic, and chondrogenic lineages [84]. The final product is formulated into doses that can be cryopreserved for "off-the-shelf" use [84]. Recent advances have explored iPSC-derived MSCs (iMSCs) to enhance consistency and scalability compared to primary MSCs [18].
Figure 1: Therapeutic Manufacturing Workflows
The Scientist's Toolkit: Essential Research Reagents
Stem cell research and therapy development require specialized reagents and tools to ensure reproducible, high-quality results. The following table outlines key components of the stem cell researcher's toolkit.
Table 3: Essential Research Reagents for Stem Cell Research
| Reagent Category | Specific Examples | Research Function |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [82] | Reprogram somatic cells to iPSCs |
| Cell Culture Media | Defined pluripotency maintenance media; lineage-specific differentiation kits | Support stem cell growth and direct differentiation |
| Small Molecule Inhibitors/Activators | CHIR99021 (GSK3β inhibitor), Valproic acid (HDAC inhibitor) [82] | Enhance reprogramming efficiency; direct differentiation |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG; lineage-specific markers | Verify pluripotency and differentiation status |
| Gene Editing Tools | CRISPR/Cas9 systems [82] [13] | Genetic correction; introduce reporter genes |
| Cell Sorting Markers | Fluorescent antibodies for FACS; magnetic bead separation | Purify specific cell populations |
| Quality Control Assays | Karyotyping; mycoplasma testing; endotoxin assays [83] | Ensure product safety and genetic stability |
Quantitative Effectiveness and Clinical Translation
Comparative Effectiveness Metrics
Evaluating the relative effectiveness of different stem cell approaches requires examination of multiple parameters across clinical, manufacturing, and commercial dimensions. The following table synthesizes key quantitative and qualitative metrics for each platform based on current clinical data and research findings.
Table 4: Comparative Effectiveness Metrics Across Stem Cell Platforms
| Effectiveness Metric | Autologous iPSCs | Allogeneic iPSCs | Allogeneic ESCs | Allogeneic MSCs |
|---|---|---|---|---|
| Time to Treatment | Months [81] | Immediate (cryopreserved) [81] | Immediate (cryopreserved) [81] | Immediate (cryopreserved) [81] |
| Manufacturing Success Rate | Variable (patient factors) [81] | High (donor selection) [81] | High (established lines) | High [84] |
| Immune Rejection Risk | Very Low [82] [81] | Moderate (requires matching) [81] | Moderate (requires matching) [81] | Low (immunoprivileged) [81] |
| Tumorigenicity Risk | Present (genomic instability) [82] | Present (genomic instability) [82] | Present (teratoma formation) [83] | Very Low [23] |
| Regulatory Approvals | Limited (emerging) [18] | Limited (emerging) [18] | Very Limited (ethical barriers) [13] | Yes (Ryoncil for GVHD) [18] |
| Therapeutic Durability | Potentially long-term [81] | Variable (immune rejection) [81] | Variable (immune rejection) [81] | May require redosing [84] |
| Relative Cost per Dose | Very High [81] | Moderate (at scale) [81] | Moderate (at scale) | Moderate [84] |
Clinical Translation Landscape
The clinical translation of stem cell therapies has achieved significant milestones in recent years, with regulatory approvals and advanced clinical trials demonstrating the viability of various approaches. As of December 2024, the global clinical landscape includes 115 clinical trials involving 83 distinct pluripotent stem cell-derived products, with over 1,200 patients dosed and no class-wide safety concerns identified [18]. Recent FDA approvals highlight the advancing clinical translation of stem cell therapies:
- Ryoncil (remestemcel-L): Approved in December 2024 as the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD), representing a significant advance for allogeneic cell therapy [18].
- Lyfgenia (lovotibeglogene autotemcel): Approved in December 2023 as an autologous cell-based gene therapy for sickle cell disease, demonstrating the viability of autologous approaches for genetic disorders [18].
- Omisirge (omidubicel-onlv): Approved in April 2023 for patients with hematologic malignancies undergoing cord blood transplantation, illustrating the continued evolution of allogeneic hematopoietic stem cell therapies [18].
The iPSC clinical pipeline has expanded significantly, with therapies now targeting ophthalmological, neurological, and cardiovascular conditions [82] [18]. Notably, Fertilo became the first iPSC-based therapy to receive FDA IND clearance for Phase III trials in February 2025, representing a milestone for the field [18]. Additionally, ongoing clinical trials include OpCT-001 (iPSC-derived therapy for retinal degeneration), FT819 (iPSC-derived CAR T-cell therapy for lupus), and multiple iPSC-derived neural progenitor cell therapies for Parkinson's disease, spinal cord injury, and ALS [18].
The comparative analysis of autologous versus allogeneic and iPSC versus ESC approaches reveals a complex landscape with no universal superior solution. Each platform offers distinct advantages that must be weighed against specific research objectives and clinical requirements. The historical progression of stem cell applications in precision medicine demonstrates an evolving understanding of how to strategically deploy these different technological platforms to address specific therapeutic challenges.
Autologous iPSC approaches offer the compelling advantage of immune compatibility and potential for long-term engraftment without immunosuppression, making them particularly valuable for chronic conditions and disorders where immune rejection poses significant risks [82] [81]. However, their high costs, manufacturing complexities, and extended production timelines currently limit widespread application [81]. Allogeneic approaches, including both ESC and iPSC-derived products, provide the scalability and immediacy necessary for treating acute conditions and developing commercially viable therapies, though they require careful management of immune responses [81]. The emergence of HLA-matched iPSC banks represents a promising strategy to combine the advantages of allogeneic scalability with reduced immunogenicity [82].
The future trajectory of stem cell applications in precision medicine will likely see increased integration of gene editing technologies to enhance safety and efficacy, continued refinement of differentiation protocols to improve purity and functionality, and development of sophisticated delivery systems to ensure cell survival and integration [82] [85]. Additionally, combining stem cell platforms with advanced biomaterials and tissue engineering approaches will further expand their therapeutic potential [85]. As the field continues to evolve, strategic selection between autologous and allogeneic and between iPSC and ESC platforms will remain fundamental to advancing personalized regenerative treatments that address the unique genetic and clinical characteristics of individual patients.
Stem cell therapy represents a groundbreaking frontier in modern medicine, offering unprecedented potential to transform the treatment landscape for debilitating conditions like graft-versus-host disease (GVHD) and hematologic malignancies [13]. The historical evolution of these therapies within precision medicine reflects a journey from foundational hematopoietic stem cell transplants to sophisticated cellular products engineered for specific therapeutic applications.
This whitepaper examines approved stem cell-based therapies and their role in managing GVHD and blood cancers, focusing on mechanistic insights, clinical efficacy, and manufacturing considerations. The integration of these therapies into the precision medicine paradigm highlights a shift toward personalized treatments that leverage the unique biological properties of stem cells to target specific disease pathways and patient profiles [13].
Approved Stem Cell Therapies: Clinical Landscape
The therapeutic application of stem cells has expanded significantly beyond traditional hematopoietic stem cell transplantation (HSCT) to include advanced products with specialized functions.
Table 1: Approved Stem Cell-Based Therapies for GVHD and Hematologic Malignancies
| Therapy Name | Therapy Type | Indication | Mechanism of Action |
|---|---|---|---|
| RYONCIL (remestemcel-L) | Allogeneic MSC Therapy | Steroid-refractory acute GVHD | Immunomodulation via T-cell suppression and anti-inflammatory signaling [86] |
| CASGEVY (exagamglogene autotemcel) | Cell Therapy (CRISPR-Cas9 modified) | Blood and immune system disorders | Genetic modification of hematopoietic stem cells to restore functional hemoglobin production [87] |
| Various Hematopoietic Stem Cell Transplant Protocols | HSCT | Hematologic malignancies (AML, MDS, ALL) | Myeloablation followed by donor cell infusion to reconstitute healthy blood and immune systems [88] |
The efficacy of these therapies is well-established in clinical settings. For steroid-refractory acute GVHD, mesenchymal stem cell (MSC) administration significantly improves overall response rates (Risk Ratio: 1.13, 95% CI: 1.03-1.23, P = 0.007) and complete response rates (Risk Ratio: 1.43, 95% CI: 1.19-1.70, P < 0.001) based on meta-analyses of randomized controlled trials [86]. Furthermore, MSC treatment reduces the incidence of chronic GVHD (Hazard Ratio: 0.60, 95% CI: 0.42-0.86, P = 0.005) and improves failure-free survival (Hazard Ratio: 0.72, 95% CI: 0.54-0.95, P = 0.022) [86].
Mechanistic Insights: How Stem Cell Therapies Work
Mesenchymal Stem Cells in GVHD Management
MSCs demonstrate potent immunomodulatory capabilities through multiple interconnected mechanisms. These adult stem cells regulate key immune populations—including T and B lymphocytes, natural killer cells, and dendritic cells—by influencing their proliferation, activation, and maturation [86]. The therapeutic effect in GVHD occurs through:
- Cellular Interaction: Direct cell-to-cell contact leading to T-cell apoptosis via the FAS/FAS-ligand pathway
- Soluble Factor Secretion: Release of anti-inflammatory molecules including prostaglandin E2, indoleamine 2,3-dioxygenase, and hepatocyte growth factor
- Trophic Effects: Production of extracellular vesicles and exosomes containing microRNAs that modulate recipient cell function [13] [86]
MSCs also promote the expansion of regulatory T cells (Tregs) and help rebalance the Th1/Th2 ratio, creating a more tolerogenic immune environment [86]. This multifaceted mechanism enables MSCs to target the dysregulated immune response in GVHD without causing broad immunosuppression.
Diagram 1: MSC immunomodulation mechanisms in GVHD (Title: MSC Immunomodulation in GVHD)
Hematopoietic Reconstruction in Malignancies
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) represents a dual-edged therapeutic approach for hematologic malignancies. The procedure involves myeloablative conditioning to eliminate malignant cells, followed by infusion of donor hematopoietic stem cells to reconstitute a healthy blood and immune system [88]. The therapeutic effect derives from both the intensity of the conditioning regimen and the graft-versus-leukemia (GVL) effect, where donor immune cells recognize and eliminate residual malignant cells [88].
Precision medicine approaches now enable better patient selection for allo-HSCT based on genetic risk stratification. In acute myeloid leukemia (AML), for instance, transplantation is prioritized for intermediate- and adverse-risk groups per European LeukemiaNet classification, with curative potential reaching approximately 40-50% depending on risk category [88].
Advanced Prophylaxis and Treatment Protocols
GVHD Prophylaxis Strategies
Effective GVHD prophylaxis has revolutionized transplantation outcomes. Post-transplant cyclophosphamide (PTCy) has emerged as a particularly effective strategy, demonstrating significant reductions in both acute and chronic GVHD incidence [89] [90].
Table 2: GVHD Prophylaxis Regimens and Outcomes
| Prophylaxis Regimen | Acute GVHD Reduction | Chronic GVHD Reduction | Key Clinical Benefits |
|---|---|---|---|
| PTCy-based regimens | 29% grade II-IV at day +100 [89] | 7% cumulative incidence at 2 years [88] | Lower treatment failure rates (28% vs 44% with ATG) [89] |
| CNI + Methotrexate | Higher risk vs PTCy (HR: 2.69 for grade II-IV) [88] | Increased risk vs PTCy (HR: 1.34) [88] | Traditional approach with established efficacy |
| Sirolimus + Cyclophosphamide + Cyclosporine | No significant increase vs standard [90] | Significant reduction (3% vs 33% moderate-severe) [90] | Improved GVHD-free relapse-free survival |
The immunologic basis for PTCy efficacy lies in its selective targeting of alloreactive T-cells. When administered during the specific window of T-cell activation post-transplant (typically days +3 and +4), cyclophosphamide induces apoptosis in rapidly dividing alloreactive T-cells while sparing regulatory T-cells and resting lymphocytes, thereby preserving the graft-versus-leukemia effect while minimizing GVHD [90].
Experimental Workflows: From Laboratory to Clinic
The development pathway for stem cell therapies requires rigorous standardization and quality control measures to ensure safety and efficacy.
Diagram 2: Stem cell therapy development workflow (Title: Stem Cell Therapy Development Workflow)
Manufacturing and Regulatory Framework
cGMP Considerations for MSC Production
Producing clinical-grade MSCs requires strict adherence to current Good Manufacturing Practice (cGMP) standards to ensure product quality, safety, and reproducibility [91]. The manufacturing process faces unique regulatory challenges related to the heterogeneous nature of MSC cultures and complex production workflows.
Key cGMP considerations include:
- Donor Selection: Choice between autologous (patient's own cells) versus allogeneic (donor-derived) sources, with implications for immune compatibility and logistics [91]
- Cell Source Selection: Isolation from bone marrow, umbilical cord, or adipose tissue, each with distinct biological characteristics and regulatory considerations [91]
- Culture Media Composition: Movement away from fetal bovine serum toward defined, xeno-free media supplements like human platelet lysate to reduce contamination risks [91]
- Process Standardization: Control of critical parameters including plating density, passage number, and confluency to ensure batch-to-batch consistency [91]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Stem Cell Therapy Research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Gibco CTS Rotea Counterflow Centrifugation System | Closed system for cell processing | Enables leukopak processing, PBMC separation, cell washing with high viability [87] |
| Gibco CTS Dynacellect Magnetic Separation System | Automated cell isolation and bead removal | Provides high cell purity, recovery, and viability; GMP-compliant [87] |
| Gibco CTS Xenon Electroporation System | Non-viral transfection via electroporation | Modular, large-scale system for T-cell, NK-cell engineering [87] |
| Defined, xeno-free culture media | MSC expansion without animal components | Reduces contamination risk; enhances batch consistency [91] |
| Human platelet lysate (hPL) | Serum alternative for cell culture | Defined human-derived supplement replacing fetal bovine serum [91] |
Automation plays a crucial role in addressing manufacturing challenges. Automated systems minimize human intervention, reducing contamination risks and improving process consistency essential for regulatory compliance and patient safety [87]. These technologies enable scalable production while maintaining the stringent quality standards required for clinical applications.
Emerging Approaches and Future Directions
The field of stem cell therapy continues to evolve with several promising developments:
- Novel Drug Combinations: Recent clinical trials demonstrate that combining sirolimus with cyclophosphamide and cyclosporine reduces moderate to severe chronic GVHD to just 3% compared to 33% with previous standard regimens [90]
- Precision Patient Selection: Refined risk stratification using molecular and cytogenetic features helps identify patients most likely to benefit from transplantation, with specific criteria established for AML, MDS, and ALL [88]
- Advanced Cell Engineering: Emerging technologies including CRISPR-based gene editing in hematopoietic stem cells and T-cell receptor engineering enable more targeted approaches with improved safety profiles [13] [87]
- Biomarker-Driven Therapy: Research focuses on identifying predictive biomarkers for treatment response, potentially allowing personalized selection of stem cell products based on patient-specific factors [86]
The future integration of stem cell therapies within precision medicine will likely involve increased personalization of both the cellular products themselves and the associated prophylactic regimens, optimized based on individual patient characteristics and disease biology.
Stem cell therapies for GVHD and hematologic malignancies represent a significant advancement in precision medicine, offering targeted mechanisms of action with demonstrated clinical efficacy. The continued evolution of these approaches—from improved prophylaxis regimens like PTCy to standardized GMP manufacturing—highlight the dynamic nature of this therapeutic领域.
As research progresses, the integration of emerging technologies like gene editing, automation, and biomarker identification will further enhance the precision and effectiveness of stem cell applications. These developments reinforce the critical role of stem cell therapies in the expanding arsenal of precision medicine approaches for complex hematologic conditions.
Conclusion
The historical evolution of stem cell applications solidifies their indispensable role in precision medicine. The journey from foundational discoveries to sophisticated engineering has transformed stem cells from a biological curiosity into a powerful platform for creating patient-specific models and targeted therapies. While significant challenges in safety, manufacturing, and regulation persist, the convergence of stem cell science with CRISPR gene editing, single-cell RNA sequencing, and advanced bioengineering provides a clear roadmap for the future. The ongoing integration of these technologies promises to unlock a new era of truly individualized regenerative and oncological treatments, moving beyond disease management to potential cures and fundamentally reshaping the landscape of biomedical research and clinical practice.
References
- 1. Two decades of embryonic stem cells: a historical overview [https://pmc.ncbi.nlm.nih.gov/articles/PMC6396646/]
- 2. Immortal: An oral history of stem cell discovery [https://morgridge.org/feature/immortal/]
- 3. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 4. The History of Stem Cell Medical Advancement [https://beikecelltherapy.com/stem-cell-treatment-timeline/]
- 5. Stem cells: a comprehensive review of origins and emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9404248/]
- 6. Stem Cells: A Historical Review about Biological, Religious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8105090/]
- 7. Comparison of the Biological Characteristics ... [https://www.nature.com/articles/s41598-018-23396-1]
- 8. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 9. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 10. Translation of Human iPSCs: From Clinical Trial in a Dish to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5086255/]
- 11. Drug discovery research with the iPSC models of ... [https://pubmed.ncbi.nlm.nih.gov/41213329/]
- 12. Induced Pluripotent Stem Cells (iPSCs) Market Prospects ... [https://www.businesswire.com/news/home/20251111238841/en/Induced-Pluripotent-Stem-Cells-iPSCs-Market-Prospects-2025-2033-Industry-Gains-Traction-with-Rising-Investments-and-Collaborations---ResearchAndMarkets.com]
- 13. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 14. Adult Stem Cells: Explained (2025) [https://www.dvcstem.com/post/adult-stem-cells]
- 15. Editorial: Advances in perinatal stem cells research and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1725523/full]
- 16. Advances in perinatal stem cells research and applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635932/]
- 17. A new kind of stem cell is revolutionizing regenerative ... [https://www.asbmb.org/asbmb-today/science/040125/stem-cells-revolutionize-regenerative-medicine]
- 18. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 19. Advances in Perinatal Stem Cells Research and Applications [https://www.frontiersin.org/research-topics/68833/advances-in-perinatal-stem-cells-research-and-applications/magazine]
- 20. Stem Cells and Organoid Technology in Precision ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.573562/full]
- 21. Next generation lineage tracing and its applications ... [https://www.nature.com/articles/s41540-025-00542-w]
- 22. Future regenerative medicine developments and their ... [https://www.sciencedirect.com/science/article/pii/S0753332222015207]
- 23. Stem Cell Research: The Future of Regenerative Medicine ... [https://www.dvcstem.com/post/stem-cell-research]
- 24. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 25. Stem Cell Research Controversy: A Deep Dive (2025) [https://www.dvcstem.com/post/stem-cell-research-controversy]
- 26. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 27. The role of stem cells in precision medicine: next-generation ... [https://jenci.springeropen.com/articles/10.1186/s43046-025-00328-5]
- 28. Regenerative Medicine Innovation Project (RMIP) [https://www.nih.gov/regenerative-medicine-innovation-project-rmip]
- 29. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 30. Mesenchymal stem cells in treating human diseases [https://pubmed.ncbi.nlm.nih.gov/40841367/]
- 31. Mesenchymal stromal cell extracellular vesicles as immune ... [https://www.sciencedirect.com/science/article/pii/S0166223625001948]
- 32. Immunomodulatory properties of mesenchymal stem cells ... [https://link.springer.com/article/10.1007/s11626-025-01109-z]
- 33. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 34. Mesenchymal stromal cell-laden hydrogels in tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464487/]
- 35. Oncolytic viruses for cancer: what's been going on in 2025? [https://www.labiotech.eu/in-depth/oncolytic-virus-therapy-cancer-2025/]
- 36. Oncolytic virotherapy: basic principles, recent advances ... [https://www.nature.com/articles/s41392-023-01407-6]
- 37. Viral warfare: unleashing engineered oncolytic viruses to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1618751/full]
- 38. Recent advances of engineered oncolytic viruses-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10763442/]
- 39. Advances in cancer immunotherapy and future directions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596039/]
- 40. Visualizing quantitative microscopy data: History and challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819578/]
- 41. Disease-in-a-Dish: The Contribution of Patient-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7978494/]
- 42. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 43. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 44. Editorial: Role of induced pluripotent stem cells (iPSCs) in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1734717/full]
- 45. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 46. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 47. Drug Discovery Services [https://www.ncardia.com/applications/discovery-services]
- 48. Developments and Opportunities for 3D Bioprinted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8287496/]
- 49. 3D bioprinting bone/cartilage organoids - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451290/]
- 50. Advancing organoid development with 3D bioprinting [https://www.accscience.com/journal/OR/1/1/10.36922/OR025040004]
- 51. A roadmap for the implementation of 3D-printed organs in ... [https://www.sciencedirect.com/science/article/pii/S2666998625001607]
- 52. Trends & Strategies Shaping the $4.6+ Billion Induced [https://www.globenewswire.com/news-release/2025/11/10/3184731/0/en/Trends-Strategies-Shaping-the-4-6-Billion-Induced-Pluripotent-Stem-Cells-iPSCs-Market-2025-2033-Expanding-Applications-in-Drug-Discovery-and-Disease-Modeling.html]
- 53. New 3D bioprinting technique may improve production of ... [https://news.mit.edu/2025/new-3d-bioprinting-technique-may-improve-production-engineered-tissue-0917]
- 54. Genome Stability Program [https://hillmanresearch.upmc.edu/research/programs/ccsg/genome-stability]
- 55. Preventing secondary primary malignancies (SPMs) in CAR-T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542518/]
- 56. Allogeneic Cellular Therapy – Diagnostic Challenges and ... [https://www.cap.org/member-resources/articles/allogeneic-cellular-therapy-diagnostic-challenges-and-opportunities-for-laboratory-practice]
- 57. The immune boundaries for stem cell based therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC3828859/]
- 58. Selective HLA knockdown and PD-L1 expression prevent ... [https://www.nature.com/articles/s41467-025-63863-8]
- 59. Allogeneic CART progress: platforms, current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198129/]
- 60. Regulatory T cell therapies: from patient data to biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615433/]
- 61. The Next Frontier: Industrializing Cell Therapy Manufacturing [https://www.isctglobal.org/telegrafthub/blogs/isct-head-office1/2025/10/07/the-next-frontier-industrializing-cell-therapy-man]
- 62. 2025 cell and gene challenges: Thoughts from our editorial ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617532-2025-cell-and-gene-challenges-Thoughts-from-our-editorial-board/]
- 63. World's Top 40 Companies in Stem Cell Concentration ... [https://www.sphericalinsights.com/blogs/world-s-top-40-companies-in-stem-cell-concentration-system-2025-watchlist-statistical-report-2024-2035]
- 64. Potency assays and biomarkers for cell-based advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288881/]
- 65. Potency assay to predict the anti-inflammatory capacity of a ... [https://www.sciencedirect.com/science/article/pii/S1465324924000501]
- 66. Potency analysis of cellular therapies: the emerging role of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-5-24]
- 67. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 68. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 69. Identification and validation of multiple cell surface markers of ... [https://pubmed.ncbi.nlm.nih.gov/27515308/]
- 70. Artificial intelligence and systems biology analysis in stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476622/]
- 71. Exciting updates from Vertex stem cell-based therapy ... [https://breakthrought1d.ca/exciting-updates-from-vertex-stem-cell-based-therapy-clinical-trials/]
- 72. Efficacy and safety of stem cell therapy for acute and ... [https://www.nature.com/articles/s41598-025-04405-6]
- 73. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207128/]
- 74. Quantitative Single-Cell Approaches to Stem Cell Research [https://www.sciencedirect.com/science/article/pii/S1934590914004664]
- 75. Development of a quantitative prediction algorithm for ... [https://www.nature.com/articles/s41467-021-24746-w]
- 76. The Evolving Regulatory Landscape in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10162454/]
- 77. Regenerative Medicine Advanced Therapy Designation [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/regenerative-medicine-advanced-therapy-designation]
- 78. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 79. BLA Filing Process for Gene Therapy Products: 2025 Guide [https://insights.forgebiologics.com/bla-filing-process-for-gene-therapy-products-2025-guide]
- 80. CBER Regenerative Medicine Advanced Therapy (RMAT) ... [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/cber-regenerative-medicine-advanced-therapy-rmat-approvals]
- 81. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 82. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 83. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 84. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 85. Stem cells in regenerative medicine: Unlocking therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2667099225000283]
- 86. A meta-analysis of randomized controlled trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623177/]
- 87. Guide to Cell Therapy GMP Manufacturing for Autologous ... [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 88. New Approaches Combat GVHD and Improve ... [https://www.onclive.com/view/new-approaches-combat-gvhd-and-improve-transplantation-outcomes-in-hematologic-malignancies]
- 89. EBMT 2025 Highlight: Real-World GVHD Prophylaxis [https://www.onclive.com/view/ebmt-2025-highlight-real-world-gvhd-prophylaxis-insights-from-the-geth-tc-group-study]
- 90. New drug regimen prevents both chronic and acute graft ... [https://www.fredhutch.org/en/news/spotlight/2025/11/crd-oshima-jclinoncol.html]
- 91. Current good manufacturing practice considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9934414/]