Generating Kidney Organoids from iPSCs: A Comprehensive Guide for Disease Modeling and Drug Development
Kidney organoids derived from human induced pluripotent stem cells (iPSCs) have emerged as a transformative platform for modeling renal development and disease.
Generating Kidney Organoids from iPSCs: A Comprehensive Guide for Disease Modeling and Drug Development
Abstract
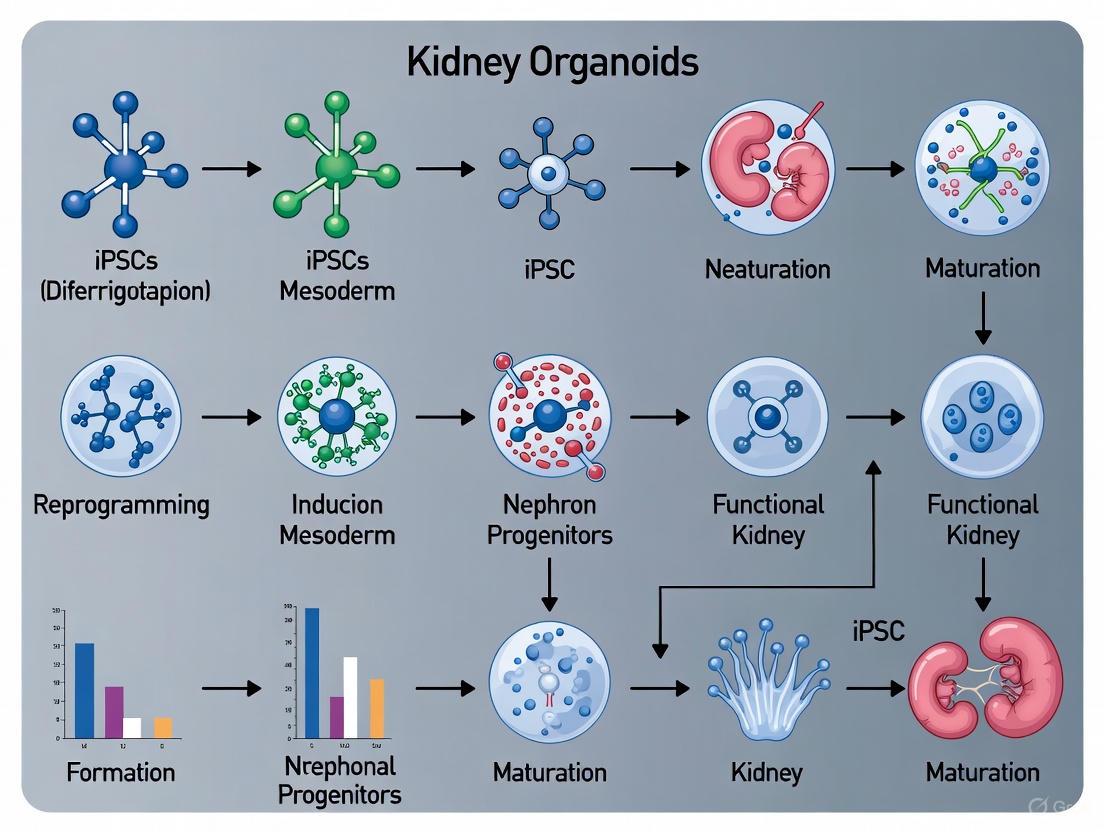
Kidney organoids derived from human induced pluripotent stem cells (iPSCs) have emerged as a transformative platform for modeling renal development and disease. This article provides a comprehensive overview for researchers and drug development professionals, covering the foundational principles of kidney organogenesis and iPSC biology. It details step-by-step differentiation protocols, explores their direct application in modeling hereditary diseases and nephrotoxicity, and addresses critical challenges such as cellular immaturity and off-target cells. Furthermore, it outlines advanced validation techniques using single-cell transcriptomics and functional assays, positioning kidney organoids as a powerful, human-relevant system for advancing mechanistic studies and therapeutic discovery.
The Foundation of Kidney Organoids: From iPSC Technology to Developmental Principles
Ethical and Practical Advantages of iPSCs
Induced pluripotent stem cells (iPSCs) represent a pivotal innovation in regenerative medicine, offering a path to bypass the significant ethical controversies associated with embryonic stem cells (ESCs). The generation of ESCs requires the destruction of human embryos, raising profound ethical questions regarding the commencement of life and the moral status of the embryo [1] [2]. iPSC technology elegantly circumvents this issue by reprogramming adult somatic cells (e.g., from skin or blood) back into a pluripotent state, eliminating the need for embryos entirely [2]. This provides a less morally contentious source of pluripotent cells, aligning scientific progress with key ethical considerations [1] [2].
Beyond their ethical advantage, iPSCs offer substantial practical benefits for research and therapy. They enable the creation of patient-specific cell lines, which are invaluable for personalized disease modeling and can dramatically lower the risk of immune rejection in cell transplantation therapies [1] [2]. This contrasts with allogeneic ESC-derived cells, which face major immunological rejection challenges unless extensive HLA-matched donor banks are established [1].
Table 1: Key Comparisons Between iPSCs and Embryonic Stem Cells (ESCs)
| Feature | Induced Pluripotent Stem Cells (iPSCs) | Embryonic Stem Cells (ESCs) |
|---|---|---|
| Cell Source | Adult somatic cells (e.g., skin, blood) | Inner cell mass of a blastocyst-stage embryo [1] |
| Ethical Status | Avoids embryo destruction; considered ethically less contentious [2] | Involves destruction of human embryos; raises significant ethical debate [1] [2] |
| Immunological Compatibility | Can be generated from the patient for autologous use, minimizing rejection [1] | Typically allogeneic, requiring immunosuppression or HLA-matched banks [1] |
| Research & Therapeutic Applications | Disease modeling, drug screening, personalized cell therapy [1] | Disease modeling, drug screening, cell therapy (with limitations) [1] |
Protocols for Kidney Organoid Generation from iPSCs
The generation of kidney organoids from human iPSCs relies on protocols that mimic embryonic kidney development through stepwise manipulation of key signaling pathways. Below is a consolidated protocol based on established methods [3] [4].
Key Materials:
- Human iPSCs: Maintained in mTeSR1 medium on Geltrex-coated plates [3].
- Key Reagents: CHIR99021 (a GSK-3β inhibitor and WNT pathway agonist), FGF9, Heparin, Activin A [3].
- Basal Medium: Advanced RPMI 1640 supplemented with Glutamax [3].
Detailed Stepwise Protocol
- Maintenance of iPSCs: Culture human iPSCs in mTeSR medium on Geltrex-coated plates. For passaging, use Gentle Cell Dissociation Reagent and maintain cells in small clumps [3].
- Induction of Intermediate Mesoderm: Differentiate iPSCs using 5–8 µM CHIR99021 in Advanced RPMI 1640 medium for 72–96 hours. This critical step activates the WNT pathway to specify the intermediate mesoderm lineage [3].
- Specification of Metanephric Cap Mesenchyme: Replace the medium with Activin A differentiation medium, containing 10 ng/ml Activin A, 200 ng/ml FGF9, and 1 µg/ml heparin, and culture for 24 hours [3].
- Formation of Kidney Progenitor Aggregates: Dissociate the cells using Accutase and re-aggregate them in a fresh medium containing 3 µM CHIR99021, 200 ng/ml FGF9, and 1 µg/ml heparin. For 3D organoid formation, transfer the cell suspension to a low-attachment 96-well U-bottom plate and culture for 5 days. This allows the cells to self-assemble into aggregates [3].
- Maturation of Kidney Organoids: Continue culturing the aggregates in a basal differentiation medium (without FGF9 and heparin) to promote spontaneous differentiation into tubules and glomerular-like structures. The entire process typically requires 18-25 days to form structured organoids [3] [4].
Applications in Disease Modeling
Kidney organoids derived from iPSCs provide a powerful platform for modeling human renal diseases, offering significant advantages over traditional 2D cultures and animal models. Their 3D, multicellular architecture allows for the study of complex disease mechanisms involving multiple cell types [4].
Modeling Autosomal Dominant Polycystic Kidney Disease (ADPKD)
ADPKD, caused by mutations in PKD1 or PKD2 genes, has been successfully modeled using iPSC-derived kidney organoids [5] [4].
- Protocol: Introduce biallelic loss-of-function mutations into the PKD1 or PKD2 genes in a control iPSC line using CRISPR-Cas9 genome editing. Differentiate these isogenic mutant iPSCs into kidney organoids alongside unedited controls [5].
- Phenotype: After about 35 days in culture, mutant organoids spontaneously develop fluid-filled cysts within the tubules, phenocopying the hallmark of ADPKD, while isogenic control organoids do not [4].
- Model Enhancement: Cystogenesis efficiency can be dramatically improved (from ~6% to ~75%) by growing the organoids in suspension culture using low-attachment plates instead of adherent culture conditions [4]. This system has been used to investigate the role of the extracellular matrix and has shown that embedding organoids in collagen droplets can reduce cyst formation [5].
Modeling Podocytopathies
Podocyte-specific diseases, such as those linked to podocalyxin (PODXL) mutations, can also be modeled.
- Protocol: Generate PODXL −/− iPSCs and corresponding isogenic controls via CRISPR-Cas9, then differentiate them into kidney organoids [5].
- Phenotype: Organoids with the knockout display defective podocyte formation, including failures in basal junctional assembly and microvilli formation, mirroring findings in PODXL-deficient mice and informing the mechanisms of human congenital nephrotic syndrome [5].
Table 2: Kidney Disease Models Using iPSC-Derived Organoids
| Disease Modeled | Genetic Target | Method of Modeling | Key Phenotype in Organoids |
|---|---|---|---|
| Autosomal Dominant Polycystic Kidney Disease (ADPKD) | PKD1, PKD2 | CRISPR-Cas9 knockout in control iPSCs [5] [4] | Tubular cyst formation [5] [4] |
| Podocytopathy (e.g., FSGS, Nephrotic Syndrome) | PODXL | CRISPR-Cas9 knockout in control iPSCs [5] | Defects in podocyte foot process assembly and junctional migration [5] |
| Drug-Induced Kidney Injury | N/A (Wild-type organoids) | Treatment with nephrotoxins (e.g., Cisplatin, Gentamicin) [4] | Specific expression of injury markers (KIM-1) in tubular cells; Caspase-3 activation [4] |
The Scientist's Toolkit: Essential Reagents and Materials
Successful generation and application of kidney organoids require a suite of specialized reagents.
Table 3: Essential Research Reagents for Kidney Organoid Generation and Application
| Reagent / Material | Function / Purpose | Example Usage in Protocol |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; activates WNT signaling to induce intermediate mesoderm [3] [4]. | Used at 5-8 µM for initial differentiation (3-4 days) [3]. |
| FGF9 & Heparin | Promotes survival and specification of kidney progenitor cells (metanephric mesenchyme) [3]. | Used at 200 ng/ml (FGF9) with 1 µg/ml heparin after CHIR99021 treatment [3]. |
| Low-Attachment Plates | Facilitates 3D self-assembly of cells into organoids and improves cystogenesis in disease modeling [5] [3]. | Used for 3D aggregation and maturation of kidney progenitor cells [3]. |
| CRISPR-Cas9 System | Genome editing tool for introducing disease-causing mutations or correcting them in iPSCs [5] [4]. | Used to create isogenic mutant lines (e.g., PKD1/PKD2 KO) for disease modeling [5]. |
| DMOG (Dimethyloxallyl Glycine) | HIF-1α stabilizer; promotes vascularization and cell survival under hypoxia in organoids [3]. | Treated at 10 µM to enhance endothelial network formation [3]. |
| Cisplatin | Chemotherapeutic agent and nephrotoxin; used to model acute kidney injury in organoids [4]. | Used at ~10 µM to induce tubular cell injury and apoptosis for toxicity studies [3] [4]. |
The development of the mammalian kidney is a classic model of reciprocal tissue interactions, driven by reciprocal signaling between two key embryonic progenitor tissues: the metanephric mesenchyme (MM) and the ureteric bud (UB) [6] [7]. The UB, an epithelial outgrowth from the Wolffian duct, invades the MM, a population of mesoderm-derived cells. This invasion initiates a sophisticated developmental program wherein the UB undergoes iterative branching morphogenesis to form the collecting duct system, while the MM, in response to signals from the UB, condenses and undergoes mesenchymal-to-epithelial transition (MET) to form the nephrons, the functional filtration units of the kidney [6] [8].
Recapitulating these interactions in vitro is the cornerstone of generating kidney organoids from induced pluripotent stem cells (iPSCs). These organoids provide an unprecedented platform for disease modeling, drug toxicity screening, and exploring the principles of regenerative medicine [7]. The fidelity of these models hinges on successfully mimicking the complex, stage-specific crosstalk that occurs between the MM and UB during embryonic development. This document details the core signaling pathways, provides protocols for generating UB and MM lineages, and explores advanced assembloid models that capture the essence of kidney organogenesis for research applications.
Key Signaling Pathways in MM-UB Crosstalk
The dialogue between the MM and UB is mediated by a well-orchestrated set of signaling pathways. The diagrams below summarize the core signaling interactions and the critical pathway that drives nephron formation.
Figure 1: Core Signaling in Kidney Organogenesis. The MM secretes GDNF, which binds to the RET receptor on the UB epithelium, inducing branching morphogenesis. In response, the UB secretes signals like WNT9b and FGFs, which promote survival of the MM and induce the WNT4-mediated MET critical for nephron formation [6] [7] [8].
Figure 2: The WNT4 Autocrine Loop for Nephrogenesis. A key event in nephron formation is the autoinduction of WNT4 within the MM. UB-derived WNT9b triggers the expression of WNT4 in the MM, which then acts as an autocrine signal to drive the subsequent steps of MET, leading to the formation of a nephron [8].
Quantitative Data on MM-UB Interactions
Table 1: Key Quantitative Findings from MM and UB Interaction Studies
| Finding | Quantitative Result | Experimental Model | Significance |
|---|---|---|---|
| Branching Efficiency | UB branching can occur without MM contact, but requires MM for vectorial elongation and stalk tapering [6]. | Isolated rat UB culture & recombination with MM [6]. | MM provides essential contact-dependent cues for proper 3D architecture. |
| Functional Maturation | Co-cultured UB+MM tissue expressed OAT1, Na-Pi2, AVP receptor, resembling E19 kidney [6]. | Rat UB+MM recombinant [6]. | Contact with MM promotes functional maturation of proximal tubule and collecting duct segments. |
| Progenitor Induction Efficiency | Protocol achieves ~90% efficiency in generating PAX2+/GATA3+ pronephric intermediate mesoderm [9]. | Human pluripotent stem cell (hPSC) differentiation [9]. | Highly efficient starting point for generating UB organoids. |
| Collecting Duct Purity | UB organoids differentiate into CD organoids containing >95% principal and intercalated cells [9]. | hPSC-derived UB organoids (scRNA-seq) [9]. | Enables high-fidelity modeling of the collecting system. |
| Patterning Correction | MM can normalize "branchless" UB morphology induced by growth factors like FGF7/heregulin [6]. | Dysmorphic UB cultured with MM [6]. | MM has a "quality control" or sculpting role, ensuring robust branching patterns. |
Table 2: Protocols for Deriving Kidney Lineages from Human Pluripotent Stem Cells (hPSCs)
| Protocol Step | Objective | Key Signaling Factors & Media | Duration | Outcome / Markers |
|---|---|---|---|---|
| 1. Primitive Streak Induction | Specify mesendodermal fate. | CHIR99021 (WNT agonist), FGF2, BMP4, Activin A [9]. | 30 hours [9]. | >95% TBXT+ cells [9]. |
| 2. Intermediate Mesoderm (IM) Specification | Generate anterior/pronephric IM. | Retinoic Acid (RA), FGF2, LDN193189 (BMP inhibitor), A83-01 (TGF-β inhibitor) [10] [9]. | 48 hours [9]. | ~90% PAX2+/GATA3+ cells; LHX1+, HOXB7+ [9]. |
| 3. Nephric Duct (ND) Spheroid Formation | Promote 3D organization and early UB lineage commitment. | Aggregate cells; culture with RA, FGF9, GDNF [10] [9]. | 4 days [9]. | Spheroids expressing PAX2, GATA3, RET, EMX2 [9]. |
| 4. UB Organoid & Branching Morphogenesis | Initiate branching morphogenesis. | Embed ND spheroids in extracellular matrix (e.g., Matrigel) [10] [9]. | 7 days [10]. | Branched, RET+ tip-domain structures [9]. |
| 5. Collecting Duct (CD) Differentiation | Generate functional principal and intercalated cells. | Mature in specialized medium; for ICs, induce FOXI1 expression [9]. | 7-10 days [10]. | Functional ENaC+ principal cells and V-ATPase+ intercalated cells [9]. |
| MM / Nephron Progenitor Differentiation | Generate nephron-forming MM. | CHIR99021, then FGF9 with or without BMP7 [7]. | 7-10 days [7]. | SIX2+ nephron progenitors; WT1+, PAX2+ structures [7]. |
Advanced Model Systems: Kidney Assembloids
While individual UB or nephron organoids are valuable, the most physiologically relevant models combine these lineages to form kidney progenitor assembloids (KPAs). These systems more faithfully recapitulate the spatial patterning and reciprocal interactions of the developing kidney [11].
In a KPA, hPSC-derived induced ureteric progenitor cells (iUPCs) and induced nephron progenitor cells (iNPCs) are combined. The iUPCs self-organize into a central, branching UB-like structure, while the iNPCs form renal vesicles (RVs) and nascent nephrons that polarize around and fuse with the central "collecting duct" [11]. This self-organization mirrors the in vivo process of nephron formation and connection to the excretory system. These assembloids show dramatically improved cellular complexity and maturity, and have been successfully used to model human autosomal dominant polycystic kidney disease (ADPKD), recapitulating cyst formation and complex cell-cell interactions in vivo [11].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Kidney Organoid and Assembloid Research
| Reagent / Tool | Function in Protocol | Key Example(s) |
|---|---|---|
| Small Molecule Inhibitors/Activators | Direct cell fate by modulating key signaling pathways. | CHIR99021 (GSK3β inhibitor, activates WNT); LDN193189 (BMP inhibitor); A83-01 (TGF-β inhibitor) [10] [9]. |
| Growth Factors | Provide mitogenic and patterning signals for progenitor expansion and differentiation. | FGF2/FGF9 (IM specification, NPC maintenance); GDNF (UB growth/branching); BMP7 (supports MM survival) [6] [7] [9]. |
| Extracellular Matrix (ECM) | Provides a 3D scaffold that supports tissue organization and morphogenesis. | Growth Factor-Reduced Matrigel [6] [9]. |
| Reporter Cell Lines | Enables tracking and purification of specific progenitor populations. | GATA3-mScarlet (labels pronephric IM, ND, and UB lineages) [9]. |
| Gene Editing Tools | For disease modeling and functional studies. | CRISPR-Cas9 (e.g., for generating PKD2-/- models in assembloids) [11]. |
Troubleshooting and Protocol Optimization
A common challenge in kidney organoid differentiation is the appearance of off-target cell types, such as chondrocytes, which can proliferate with extended culture [12]. Recent research has shown that this can be mitigated by modifying the standard protocol.
- Problem: Appearance of Alcian Blue-positive cartilage in organoids after day 18-25 of culture, correlated with increased expression of SOX9, COL2A1, and ACAN [12].
- Solution: Extend the supplementation of FGF9 in the culture medium. Maintaining FGF9 for one additional week (e.g., until day 12 of the protocol) significantly reduces chondrocyte formation without adversely affecting renal structures like glomeruli and tubules [12].
- Rationale: FGF9 is crucial for normal kidney development and has been shown to suppress chondrocyte differentiation in other systems, helping to maintain renal progenitor identity [12].
Application in Disease Modeling
The primary application of these sophisticated organoid and assembloid systems is the modeling of human kidney diseases. iPSCs derived from patients with genetic disorders can be differentiated into kidney lineages to study disease mechanisms in vitro.
- Polycystic Kidney Disease (PKD): The KPA platform has been successfully used to model ADPKD. Genome-edited PKD2-/- human KPAs grown in vivo robustly recapitulate the cystic phenotype, revealing complex interactions between cyst-lining epithelium, stroma, and macrophages [11].
- Chronic Disease Modeling: Kidney organoids (iTubuloids) can be subjected to repetitive injury, such as multiple rounds of hypoxia, to model chronic kidney disease. After one injury, organoids recover efficiently, but after three rounds, they express markers of maladaptive repair (SAA1, SAA2, S100A8/A9), mimicking the progression to chronic disease [13].
The process of kidney organogenesis, centered on the reciprocal induction between the MM and UB, provides the essential blueprint for generating in vitro models of the kidney. By meticulously applying developmental principles, researchers can now direct hPSCs through the intermediate mesoderm stage to form self-organizing UB organoids, nephron-containing MM organoids, and, most powerfully, assembloids that combine these lineages. These models, which are becoming increasingly structurally complex and functionally mature, offer a powerful path for mechanistic studies of kidney development, accurate disease modeling, and high-throughput toxicology screening, thereby accelerating the pace of discovery in nephrology.
The generation of kidney organoids from induced pluripotent stem cells (iPSCs) recapitulates the complex process of embryonic kidney development, providing an unprecedented platform for disease modeling, drug screening, and regenerative medicine research. Central to this process are three key signaling pathways—WNT, FGF, and BMP—that act in concert to orchestrate the spatial and temporal differentiation of nephron progenitors into segmented nephron structures [14]. These pathways form an integrated signaling network that directs the patterning of the proximal-distal axis of the nephron, ultimately yielding specialized renal cell types including podocytes, proximal tubules, and distal tubules [15]. Understanding and manipulating these pathways is fundamental to generating high-fidelity kidney organoids that accurately model human kidney physiology and disease. This application note details the specific roles of WNT, FGF, and BMP signaling in kidney organoid differentiation, providing structured protocols, quantitative data, and practical reagent solutions to empower researchers in optimizing their organoid generation workflows.
Pathway Functions and Experimental Manipulation
The following table summarizes the core functions, key ligands, and experimental manipulation strategies for each critical signaling pathway in kidney organoid differentiation.
Table 1: Key Signaling Pathways in Kidney Organoid Differentiation
| Pathway | Primary Roles in Kidney Organogenesis | Key Ligands & Receptors | Activation Methods | Inhibition Methods |
|---|---|---|---|---|
| WNT/β-catenin | Initiates nephrogenesis; drives PTA formation; controls PD axial patterning; dosage determines proximal/distal fate [15] [16]. | WNT9B, WNT4 [16] [14]; Receptor: Frizzled, LRP5/6 [16] | CHIR99021 (GSK3β inhibitor) [14] [17] [18] | IWP-2, DKK1 [16] |
| BMP | Supports MM survival/proliferation; integrates with WNT/FGF to tune PD patterning; required for proximal fate [15] [14]. | BMP2, BMP4, BMP7 [19] [14]; Receptors: ALK2, ALK3, ALK6, BMPR2 [19] | Recombinant BMP proteins (e.g., BMP2, BMP4, BMP7) [14] [18] | DMH1, LDN-193189, Noggin, Gremlin [15] [19] |
| FGF | Promotes UB branching and NPC differentiation; sustains NPC population; crucial for distal nephron and loop of Henle maturation [15] [12] [14]. | FGF8, FGF9 [15] [14]; Receptors: FGFR1, FGFR2 [12] | Recombinant FGF proteins (e.g., FGF9, FGF2) [12] [14] [18] | BGJ398, AZD4547 |
Experimental Workflow for Signaling Pathway Modulation
The sequential and combinatorial manipulation of WNT, BMP, and FGF signaling is critical for directing the differentiation of iPSCs through key developmental stages toward functional kidney organoids. The diagram below illustrates a generalized experimental workflow, which can be modified to achieve specific patterning outcomes.
Protocol: Generating Proximal-Biased Kidney Organoids
Recent research highlights the critical challenge of generating mature proximal tubule cells in kidney organoids, which are essential for modeling tubular injury and drug toxicity. The following protocol details a method to generate proximal-biased (PB) organoids by modulating signaling pathways to mimic in vivo development [20].
- Key Principle: Transient PI3K inhibition during early nephrogenesis activates Notch signaling, shifting nephron axial differentiation toward proximal precursor states that mature into functional proximal convoluted tubule cells [20].
- Differentiation Baseline: Begin with a standard kidney organoid differentiation protocol, such as a modified Takasato protocol, to generate nephron progenitor aggregates [15] [20].
- Intervention Window: Apply a PI3K inhibitor (e.g., LY294002) at the pretubular aggregate (PTA) to early renal vesicle (RV) transition stage, typically around differentiation days 10-12 [20].
- Mechanistic Insight: PI3K inhibition drives cells through a JAG1+/HNF1B+ medial fate, culminating in the expansion of HNF4A+ proximal tubule precursors. This bypasses an abnormal triple-positive (HNF1B+/HNF4A+/JAG1+) cell state commonly observed in standard organoid protocols [20].
- Outcome Validation: Successful differentiation yields organoids with homogenous proximal tubule structures broadly expressing solute carriers (SLCs). These organoids demonstrate functional albumin and dextran transport and exhibit characteristic KIM1/HAVCR1 upregulation and SOX9 induction upon nephrotoxic injury [20].
Protocol: Inducing Distal Nephron Fate and Plasticity
The plasticity of nephron patterning can be exploited to generate distal nephron segments, including the thick ascending loop of Henle.
- Key Principle: A WNTON/BMPOFF state established during axial symmetry breaking establishes a distal nephron identity [15].
- Intervention: At the PTA/RV stage (e.g., differentiation day 10), maintain WNT signaling (e.g., via CHIR99021) while simultaneously inhibiting BMP signaling (e.g., with DMH-1 or LDN-193189) [15].
- Maturation: The imposed distal identity can mature into thick ascending loop of Henle cells by endogenously activating FGF signaling [15].
- Fate Switching: Remarkably, distal-fated nephron cells devoid of FGF signaling can revert to a proximal cell state. This transformation is itself dependent on BMP signal transduction, demonstrating high plasticity and tunability [15].
Quantitative Data and Phenotypic Outcomes
The effects of signaling pathway modulation can be quantified by measuring changes in key marker genes and cellular outcomes. The following table compiles experimental data from recent studies.
Table 2: Quantitative Outcomes of Pathway Modulation in Kidney Organoids
| Experimental Condition | Key Marker Changes | Phenotypic Outcome | Reference |
|---|---|---|---|
| WNTON / BMPOFF | ↑ HNF1B, ↑ POU3F3, ↑ TFAP2A | Enhanced distal nephron fate specification; maturation into thick ascending loop of Henle cells [15]. | [15] |
| BMPON / FGFOFF (in distal-fated cells) | ↓ Distal markers, ↑ HNF4A, ↑ JAG1 | Fate switching from distal to proximal nephron cell states [15]. | |
| Transient PI3Ki (Proximal Biasing) | Expansion of HNF4A+ precursors; ↑ Expression of SLC transporters | Proximal-biased organoids with enhanced maturity and nephrotoxin response [20]. | [20] |
| FGF9 Extension (Day 5 to Day 12) | ↓ SOX9, ↓ COL2A1, ↓ ACAN | Significant reduction in off-target chondrocyte population; improved renal purity [12]. | [12] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Manipulating Key Signaling Pathways
| Reagent | Primary Function | Application in Kidney Organoid Differentiation |
|---|---|---|
| CHIR99021 | Potent and selective GSK-3 inhibitor; activates canonical WNT/β-catenin signaling [14] [17]. | Used in initial primitive streak induction and subsequent patterning stages. Dosage and timing are critical for proximal/distal patterning [15] [18]. |
| Recombinant FGF9 | Ligand for FGF receptors; key mesoderm inducer and NPC maintenance factor [14] [17]. | Critical for intermediate mesoderm induction and sustaining nephron progenitors. Extended treatment (up to day 12) reduces off-target chondrogenesis [12]. |
| Recombinant BMP4/BMP7 | Ligands for BMP receptors; involved in mesoderm patterning and MM survival [14] [18]. | Used in conjunction with FGF9 for IM induction (BMP4) and for supporting MM (BMP7). Essential for establishing proximal nephron fate [15] [14]. |
| DMH-1 | Selective inhibitor of BMP type I receptor ALK2 [15]. | Used to create a "BMPOFF" state during patterning to promote distal nephron fates [15]. |
| LY294002 | Potent and selective PI3K inhibitor [20]. | Applied transiently at PTA/RV stage to drive proximal tubule development via Notch activation [20]. |
Integrated Pathway Logic and Crosstalk
The WNT, FGF, and BMP pathways do not function in isolation but form a complex, integrated signaling network. The logic of their interactions is fundamental to achieving specific organoid patterning goals.
Mastery of the WNT, FGF, and BMP signaling pathways is indispensable for the precise engineering of kidney organoids from iPSCs. As research progresses, the move beyond simple activation and inhibition toward fine-tuned, spatiotemporal control of these pathways will be crucial. This includes optimizing the precise dosage, sequence, and duration of pathway modulation to enhance the maturation and functionality of organoids. Furthermore, integrating these strategies with advanced culture systems such as bioreactors, microfluidic chips, and vascularization techniques will help overcome current limitations. The protocols and data outlined herein provide a foundational framework for researchers to manipulate these core pathways, thereby generating more physiologically relevant kidney organoids for robust disease modeling and drug screening applications.
The Self-Organizing Potential of Pluripotent Stem Cells into 3D Renal Structures
The generation of three-dimensional kidney organoids from pluripotent stem cells (PSCs), including induced pluripotent stem cells (iPSCs), represents a transformative advancement in nephrology research. These organoids are in vitro models that recapitulate key aspects of kidney development, structure, and function, providing a promising platform for investigating disease mechanisms, performing drug screening, and developing regenerative therapies [7] [18]. The self-organization of PSCs into renal structures mirrors embryonic kidney development, where sequential signaling cues drive the differentiation of intermediate mesoderm into nephron progenitors that subsequently form intricate, segmented nephron-like structures [7] [14]. Within the context of disease modeling research, patient-specific iPSC-derived kidney organoids offer unprecedented opportunities to study genetic kidney diseases such as polycystic kidney disease and congenital anomalies of the kidney and urinary tract (CAKUT) [7] [14]. Despite remarkable progress, challenges remain in achieving full structural and functional maturation, necessitating continued refinement of differentiation protocols and integration of bioengineering strategies to enhance physiological relevance [21] [22].
Key Signaling Pathways in Kidney Organoid Development
The self-organization of pluripotent stem cells into kidney organoids recapitulates embryonic kidney development, which is orchestrated by precisely timed signaling interactions. Understanding these pathways is essential for optimizing differentiation protocols and generating physiologically relevant 3D renal structures for disease modeling.
Figure 1. Key signaling pathways directing kidney organoid differentiation from pluripotent stem cells. The diagram illustrates the sequential developmental stages and the primary signaling molecules required at each transition point, based on established differentiation protocols [7] [18] [14].
The differentiation process follows a conserved developmental trajectory, beginning with the induction of posterior primitive streak through WNT activation via GSK3β inhibitors such as CHIR99021 [7] [14]. Subsequent patterning into intermediate mesoderm requires fibroblast growth factor 9 (FGF9) and, in some protocols, bone morphogenetic protein 7 (BMP7) [7] [14]. The metanephric mesenchyme stage is characterized by the emergence of nephron progenitor cells (NPCs) expressing key transcription factors including SIX2, WT1, PAX2, and OSR1, which are maintained and expanded through continued FGF9 exposure [7] [18]. These NPCs ultimately undergo mesenchymal-to-epithelial transition (MET) to form nephron-like structures containing glomerular, proximal tubular, and distal tubular segments [7] [14]. The temporal integration of these signaling pathways regulates the formation of nephrons, with WNT signaling (WNT4, WNT9b) being essential for MET and nephron induction, while Notch signaling contributes to nephron segmentation and fate specification [7] [14].
Comparative Analysis of Kidney Organoid Differentiation Protocols
Several research groups have established core protocols for generating kidney organoids from human pluripotent stem cells (hPSCs), each with distinct advantages and limitations for disease modeling applications. The table below summarizes the key characteristics of four principal methodologies.
Table 1: Comparison of Major Kidney Organoid Differentiation Protocols
| Protocol | Cell Source | Key Signaling Molecules | Efficiency of NPC Generation | Major Cellular Components | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Taguchi et al. [18] | Mouse ESC/hiPSCs | BMP4, Activin A, FGF2, CHIR, Retinoic Acid | 20–70% | Wt1/nephrin+ glomeruli; cadherin6+ proximal tubules; E-cadherin+ distal tubules | Foundational step toward kidney reconstruction | Requires coculture with mouse embryonic spinal cords; lower efficiency; immaturity |
| Morizane et al. [18] | hESCs/hiPSCs | CHIR99021, Activin A, FGF9 | 80–90% | Multi-segmented nephron structures with podocytes, proximal tubules, loops of Henle, and distal tubules | Uses fully defined medium; higher efficiency; suitable for chemical screening | Differentiation efficiency affected by hPSC line variability; no collecting duct structures |
| Freedman et al. [18] | hESCs/hiPSCs | CHIR99021 (GSK3β inhibition only) | Not specified | Segmented nephron structures with proximal tubules, podocytes, and endothelial cells | No exogenous FGF2, Activin, or BMP; low cost; high throughput; simple steps | Organoids random in size; no collecting duct structure; more off-target cells |
| Little's Team [18] | iPSC/hESC | CHIR99021, FGF9 | Not specified | Multiple nephrons surrounded by endothelial and stromal populations | Higher cell yield; low cost; specifies intermediate mesoderm before aggregate formation | Immaturity comparable to other protocols |
Each protocol employs a multi-step approach that mirrors kidney development. The Morizane protocol generates NPCs through 8-9 days of differentiation, beginning with induction of late primitive streak via WNT signaling regulation, followed by exposure to activin A to form posterior intermediate mesoderm, and finally treatment with FGF9 to generate NPCs [18]. These NPCs can then form kidney organoids in 96-well plates suitable for chemical screening. In contrast, the Freedman protocol utilizes a two-step approach that forms spheroids first followed by GSK3β inhibition, requiring no exogenous addition of FGF2, activin, or BMP [18]. Little's team employs a suspension culture method that increases final cell yield by 3-4 folds compared to static culture, thereby reducing costs while maintaining transcriptional equivalence of renal cell types [18].
Advanced Protocol: Monocyte-Enhanced Kidney Organoid Differentiation
Recent research has revealed that incorporating immune cell components, particularly monocytes, can significantly improve the efficiency and quality of kidney organoid differentiation. The following protocol integrates monocyte co-culture to enhance organoid development for disease modeling applications.
Materials and Reagents
Table 2: Essential Research Reagents for Monocyte-Enhanced Kidney Organoid Differentiation
| Reagent/Category | Specific Examples | Function in Protocol |
|---|---|---|
| Base Cell Line | Human Episomal iPSC Line (e.g., ThermoFisher Gibco A18945) | Starting cellular material for organoid differentiation |
| Basal Medium | Advanced RPMI 1640 with L-Glutamine | Foundation for differentiation media formulations |
| Key Signaling Molecules | CHIR99021 (GSK3β inhibitor, 10 μM), Noggin (5 ng/mL), Activin A (10 ng/mL) | Sequential induction of primitive streak, intermediate mesoderm, and nephron progenitors |
| Monocyte Isolation | Classical Monocyte Isolation Kit (Miltenyi Biotec) | Isolation of CD14+CD16– monocytes from human peripheral blood |
| Monocyte Culture | M-CSF (20 ng/mL), IFNγ (20 ng/mL) + LPS (20 ng/mL), IL-4 (20 ng/mL) | Monocyte differentiation and polarization into M1/M2 macrophages |
| Apoptosis/Autophagy Modulation | Rapamycin (mTOR inhibitor) | Activation of autophagy to prevent CHIR-induced apoptosis |
| Analysis Reagents | Cell counting kit 8, Autophagy detection kit, Antibodies for cleaved Caspase 3, PARP-1, TBX6, OSR1, Nephrin, E-Cadherin | Assessment of cell survival, autophagy, and differentiation markers |
Step-by-Step Procedure
Day -7 to Day 0: Monocyte Preparation
- Isolate human CD14+CD16– monocytes from peripheral blood buffy coats using a Classical Monocyte Isolation Kit according to manufacturer's instructions.
- For functionality testing, treat monocytes with 20 ng/mL M-CSF for 7 days to differentiate into macrophages, then polarize using either:
- M1 polarization: 20 ng/mL IFNγ + 20 ng/mL LPS for 24 hours
- M2 polarization: 20 ng/mL IL-4 for 24 hours
- Verify polarization success by assessing expression of IL-6, IL-10, and TNFα.
Day 0: iPSC Seeding
- Culture human iPSCs in StemFlex medium on Geltrex-coated cell culture plates.
- Seed iPSCs at a density of 0.75 × 10^6 cells/cm² for differentiation.
Day 1-4: Mesoderm Induction
- Replace culture medium with Basal Medium (Advanced RPMI 1640 with 200 μM L-Glutamine and 0.5% KnockOut Serum Replacement) supplemented with 10 μM CHIR99021 and 5 ng/mL noggin.
- Refresh the medium after 2 days with the same components.
- Optional rapamycin treatment: Add rapamycin during this stage to activate autophagy and reduce CHIR-induced apoptosis.
Day 4-7: Intermediate Mesoderm Formation
- Change to Basal Medium supplemented with 10 ng/mL Activin A.
- Culture for 3 days with medium refreshment on day 5-6.
Day 7-9+: Organoid Formation and Monocyte Co-culture
- Begin indirect co-culture with prepared monocytes or iPSC-derived macrophages using a transwell system.
- Continue culture with appropriate kidney organoid differentiation medium (specific factors depend on base protocol used – Morizane et al. recommended).
- Refresh medium every 2-3 days and monitor organoid development.
- Harvest organoids for analysis between days 24-26.
Critical Protocol Notes
- Monocytes prevent CHIR-induced apoptosis through release of extracellular vesicles and induction of autophagy, significantly improving organoid differentiation efficiency [23].
- The co-culture system should use functionally validated monocytes that have demonstrated proper differentiation and polarization capacity.
- Rapamycin treatment alone improves iPSC survival during CHIR treatment but does not enhance differentiation; monocytes provide both survival and differentiation benefits [23].
- This protocol can be adapted for both adherent culture and 3D organoid formation formats.
Engineering Innovations for Enhanced Organoid Maturation
Recent bioengineering approaches have addressed key limitations in kidney organoid technology, particularly regarding structural maturity, reproducibility, and scalability for disease modeling research. These innovations include sophisticated culture platforms, bioprinting technologies, and vascularization strategies.
Advanced Culture Platforms
The UniMat (Uniform and Mature organoid culture platform) represents a significant advancement in organoid culture technology. This system features a 3D geometrically-engineered, permeable membrane that provides both geometrical constraints for uniformity and unrestricted supply of soluble factors for maturation [22]. Fabricated from electrospun polycaprolactone (PCL) and Pluronic F108 nanofibers, the UniMat creates a porous, hydrophilic environment that enhances nutrient exchange and gas permeability while promoting cell aggregation through its V-shaped microwell design [22]. When used for kidney organoid culture, the UniMat platform achieves approximately 87% efficiency in generating nephron-like structures with improved uniformity and enhanced maturation, including increased expression of nephron transcripts, more in vivo-like cell-type balance, and better long-term stability [22].
3D Bioprinting Applications
Extrusion-based 3D bioprinting has emerged as a powerful tool for scalable production of kidney organoids. This technology enables automated fabrication of self-organizing kidney organoids with high reproducibility in cell number and viability [24] [25]. The process involves creating a wet cell paste from differentiated nephron progenitor cells, which is then loaded into a bioprinter for precise deposition onto Transwell filters [25]. Bioprinting facilitates rapid generation of organoids (approximately one micromass every 3 seconds) with minimal size variation (coefficient of variation 1-4%) and allows scaling from 6-well to 96-well formats for high-throughput drug screening [25]. Modifications to printing parameters can manipulate organoid biophysical properties, including size, cell number, and conformation, with specific configurations substantially increasing nephron yield per starting cell number [25].
Figure 2. Workflow for 3D bioprinting of kidney organoids and their research applications. The process begins with nephron progenitor cells, which are processed into a cell paste for bioprinting, followed by extended culture to form mature structures suitable for various research applications [24] [25].
Vascularization and Structural Complexity
Enhancing vascularization remains a critical challenge in kidney organoid maturation. Millifluidic culture systems that cultivate kidney organoids under flow conditions have demonstrated expansion of endogenous endothelial progenitor pools and production of vascular networks with perfusable lumens surrounded by mural cells [18]. Additionally, protocols for generating ureteral organoids from PSCs have been developed, combining induced stromal progenitors with ureteric bud epithelia to create ureter-like spherical organoids [26]. These advancements in modeling different renal components contribute to more physiologically relevant systems for disease modeling and therapeutic screening.
Applications in Disease Modeling and Drug Development
Kidney organoids derived from iPSCs have demonstrated significant utility in modeling genetic kidney diseases and screening for nephrotoxic compounds, providing valuable platforms for both basic research and pharmaceutical development.
Genetic Disease Modeling
iPSC-derived kidney organoids offer particular promise for studying genetic kidney diseases such as polycystic kidney disease (PKD) and congenital anomalies of the kidney and urinary tract (CAKUT) [7] [14]. By using patient-specific iPSCs, researchers can generate organoids that recapitulate key pathological features of these diseases, enabling investigation of disease mechanisms and high-throughput screening of potential therapeutics [7]. For example, organoids with PKD-associated mutations develop cyst-like structures that can be quantified and manipulated to test intervention strategies [7] [22]. Similarly, disease modeling using organoids generated from patients with TBX18 mutations has successfully replicated pathological features associated with ureteral developmental defects [26].
Nephrotoxicity Screening
The pharmaceutical industry has embraced kidney organoids for preclinical nephrotoxicity screening, addressing a critical need in drug development. Bioprinted organoids in 96-well formats have been validated for compound testing, demonstrating reproducible responses to known nephrotoxins [25]. For instance, treatment with aminoglycoside antibiotics or the chemotherapeutic agent doxorubicin produces dose-dependent injury responses in specific renal cell types within organoids [25]. Organoids exposed to doxorubicin show specific activation of caspase 3 and loss of MAFB staining within podocytes, along with upregulation of the kidney injury molecule KIM1 (HAVCR1) [25]. These models provide more human-relevant toxicity data compared to traditional 2D renal cell cultures or animal models, potentially improving drug safety prediction.
The self-organizing potential of pluripotent stem cells into 3D renal structures has established a powerful platform for kidney disease modeling research. Through continued refinement of differentiation protocols, integration of immune components, and application of bioengineering innovations, kidney organoids are becoming increasingly physiologically relevant and technically reproducible. The ongoing development of more complex systems incorporating vascularization, ureteral components, and improved maturation will further enhance their utility in both basic research and translational applications. As these technologies continue to evolve, iPSC-derived kidney organoids promise to accelerate our understanding of renal development and disease mechanisms while improving the efficiency and safety of drug development pipelines.
Protocols and Applications: A Stepwise Guide to Generating and Utilizing Kidney Organoids
The advent of three-dimensional kidney organoid technology represents a transformative advance in nephrology, offering an unprecedented in vitro platform to study human kidney development, model disease, and screen therapeutics [7]. Kidney organoids, primarily derived from human pluripotent stem cells (PSCs), including induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs), are capable of self-organizing into nephron-like structures that recapitulate key aspects of early kidney development [7] [27]. This application note provides a comparative analysis of four pioneering differentiation protocols—Taguchi, Morizane, Takasato, and Freedman—framed within the context of generating kidney organoids from iPSCs for disease modeling research. We summarize quantitative data in structured tables, detail methodological workflows, and visualize signaling pathways to serve as a practical resource for researchers and drug development professionals.
Core Protocol Comparison
The stepwise differentiation of human PSCs to kidney organoids is designed to recapitulate embryonic kidney development, progressing through primitive streak, intermediate mesoderm, and metanephric mesoderm stages before forming self-organizing, three-dimensional renal tissues [7] [27]. Below, we compare the defining characteristics of four foundational protocols.
Table 1: Key Characteristics of Kidney Organoid Differentiation Protocols
| Protocol | Starting Cell Format | Key Inducing Factors | Major Renal Progenitors Generated | Time to Nephron Structures | Reported Efficiency |
|---|---|---|---|---|---|
| Taguchi et al. | Embryoid bodies | CHIR99021, FGF2, Retinoic Acid | Metanephric mesenchyme (MM) only | ~20 days | High efficiency for MM [7] |
| Morizane et al. | Monolayer | CHIR99021, FGF9, BMP7 | Primarily MM, some ureteric epithelium | 10-12 days for progenitor populations; ~25 days for organoids [28] [29] | ~90% efficiency for MM [27] |
| Takasato et al. | Monolayer → 3D aggregate | CHIR99021, FGF9, BMP7 (varies) | MM, ureteric epithelium, interstitial, endothelial progenitors | 18-21 days for segmented nephrons [7] [27] [20] | Diverse renal lineages [27] |
| Freedman et al. | hPSC-derived epiblast spheroids in Matrigel | CHIR99021, FGF9, BMP7 | Nephron tubules, glomeruli, endothelial cells [27] | Not explicitly stated in provided context | Generates renal tubules, glomeruli, endothelial cells [27] |
Table 2: Functional Outputs and Limitations of Kidney Organoid Protocols
| Protocol | Nephron Segments Present | Off-Target Cell Types Reported | Documented Functional Assays | Noted Limitations |
|---|---|---|---|---|
| Taguchi et al. | Glomeruli, renal tubules | Not specified in provided context | Forms nephrons when combined with Wnt signals [7] | Lacks collecting ducts and other renal lineages [27] |
| Morizane et al. | Podocytes, tubular epithelia | Neuronal clusters, muscle cells [29] | Response to nephrotoxicants (cisplatin, gentamicin) [27] | Limited heterogeneity; contains off-target cells [29] |
| Takasato et al. | Glomeruli, proximal tubules, distal tubules, loops of Henle | Neuronal clusters, melanocyte-like cells [29] | Megalin/cubilin-mediated endocytosis; cisplatin response [27] [20] | 10-20% non-renal cells; immature proximal tubules [29] [20] |
| Freedman et al. | Renal tubules, glomeruli | Not specified in provided context | Not specified in provided context | Not specified in provided context |
Detailed Methodologies
Taguchi and Nishinakamura Protocol
This protocol employs an embryoid body-based approach guided by insights from mouse embryology to generate metanephric mesenchyme [7] [27].
Key Steps:
- Embryoid Body Formation: Aggregate iPSCs to form embryoid bodies in low-adhesion plates.
- Posterior Primitive Streak Induction: Treat embryoid bodies with CHIR99021 (a GSK3β inhibitor and WNT agonist) for 4 days.
- Intermediate Mesoderm Induction: Culture with FGF2 and retinoic acid for further differentiation.
- Metanephric Mesenchyme Specification: Cells express markers of metanephric mesenchyme (e.g., SIX2, PAX2, WT1).
- Nephron Formation: Combine induced metanephric mesenchyme cells with mouse dorsal spinal cord or activate WNT signaling using CHIR99021 to induce nephron formation, resulting in glomerular and tubular structures [7] [27].
Critical Notes: This protocol focuses exclusively on generating the metanephric mesenchyme and its nephron derivatives, without inducing collecting duct, renal interstitial, or endothelial cells [27]. The resulting nephrons can become vascularized when transplanted under a mouse renal capsule [27].
Morizane and Bonventre Protocol
This monolayer-based protocol emphasizes generating a homogeneous nephron progenitor population with high efficiency [7] [29].
Key Steps:
- Primitive Streak Induction: Culture iPSCs as a monolayer and activate WNT signaling with CHIR99021 for 3-4 days to induce posterior primitive streak.
- Intermediate Mesoderm Induction: Pattern posterior primitive streak toward intermediate mesoderm using FGF9 and BMP7 for several days.
- Nephron Progenitor Expansion: Maintain and expand nephron progenitor populations with FGF9.
- 3D Aggregation and Differentiation: Dissociate cells and aggregate into 3D spheroids in low-adhesion plates or transwell filters. Continue culture for ~18 days to allow self-organization into nephron structures [7] [28] [29].
Critical Notes: This protocol generates kidney organoids relatively quickly and cost-effectively, making it well-suited for large-scale assays such as drug screening [28]. Single-cell RNA-seq analysis reveals this protocol produces a high proportion of podocytes but also contains off-target neuronal and muscle cells [29].
Takasato Protocol
This comprehensive protocol simultaneously induces multiple renal progenitor populations to generate kidney organoids containing nephrons connected to collecting ducts and surrounded by renal interstitium and endothelial networks [27].
Key Steps:
- Monolayer Differentiation (7 days):
- Days 1-4: Induce posterior primitive streak in iPSC monolayer using CHIR99021.
- Days 4-7: Differentiate posterior primitive streak into intermediate mesoderm using FGF9.
- 3D Culture (18 days):
- Monolayer Differentiation (7 days):
Critical Notes: This protocol generates the broadest diversity of renal cell types, including glomerular podocytes (expressing PODXL, NPHS1), proximal tubules (LTL+, SLC3A1+), distal tubules, and collecting duct cells, as well as renal interstitial cells and an endothelial network [7] [27]. However, proximal tubule maturation remains incomplete, with low expression of key solute carriers under standard conditions [20]. A recent refinement using transient PI3K inhibition during early nephrogenesis can shift differentiation toward proximal tubule fates, creating "proximal-biased" organoids with enhanced functional maturity [20].
Freedman Protocol
This approach utilizes a unique starting point with hPSC-derived epiblast spheroids embedded in Matrigel to generate kidney organoids.
Key Steps:
- Epiblast Spheroid Formation: Create hPSC-derived epiblast spheroids by sandwiching hPSCs between two layers of dilute Matrigel.
- Epithelial-to-Mesenchymal Transition: Spheroids undergo EMT to form a monolayer.
- Mesenchymal-to-Epithelial Transition: Cells are reaggregated, prompting MET and resulting in formation of renal tubules, glomeruli, and endothelial cells [27].
Critical Notes: This method generates nephron structures including glomeruli and renal tubules along with endothelial cells, but detailed characterization of all renal lineages produced is not provided in the available context [27].
Signaling Pathways in Kidney Organoid Differentiation
The differentiation of kidney organoids relies on precise temporal activation of key developmental signaling pathways. The following diagram illustrates the core signaling events and their temporal sequence across major differentiation protocols.
The directed differentiation of kidney organoids recapitulates embryonic kidney development through sequential activation of conserved signaling pathways [7] [27]. Canonical WNT signaling, typically activated by the GSK3β inhibitor CHIR99021, drives the initial specification of posterior primitive streak, which represents the progenitor population for all mesoderm, including kidney lineages [7] [27]. Subsequently, FGF9 signaling promotes patterning of the posterior primitive streak toward intermediate mesoderm, with some protocols incorporating BMP7 to enhance this process [7] [27] [30]. Continued FGF9 signaling supports the maintenance and expansion of nephron progenitor populations within the metanephric mesenchyme [7]. Finally, a secondary WNT signal, potentially through CHIR99021 activation or endogenous WNT production, triggers mesenchymal-to-epithelial transition and nephron formation [7] [27]. Additional pathways including BMP, Notch, and retinoic acid signaling contribute to nephron segmentation and cell fate specification in a protocol-dependent manner [7] [20].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Kidney Organoid Differentiation
| Reagent/Category | Protocol Applications | Function in Differentiation |
|---|---|---|
| CHIR99021 | Taguchi, Morizane, Takasato, Freedman | GSK3β inhibitor that activates canonical WNT signaling; induces posterior primitive streak [7] [27] |
| FGF9 (Fibroblast Growth Factor 9) | Morizane, Takasato, Freedman | Patterns posterior primitive streak to intermediate mesoderm; maintains nephron progenitors [7] [27] [30] |
| BMP7 (Bone Morphogenetic Protein 7) | Morizane, Takasato (some variations) | Enhances intermediate mesoderm induction; supports progenitor survival/proliferation [7] |
| FGF2 (Basic Fibroblast Growth Factor) | Taguchi | Promotes intermediate mesoderm induction in embryoid body protocol [27] |
| Retinoic Acid | Taguchi | Promotes intermediate mesoderm induction in embryoid body protocol [27] |
| Matrigel | Freedman | Provides 3D extracellular matrix environment for epiblast spheroid formation and differentiation [27] |
| Transwell Filters | Takasato, Morizane (some applications) | Provides air-media interface for 3D organoid culture, enhancing tissue organization [27] [30] |
Applications in Disease Modeling and Limitations
Disease Modeling Applications
Kidney organoids generated using these protocols have been widely applied to model genetic kidney diseases such as polycystic kidney disease (PKD), congenital anomalies of the kidney and urinary tract (CAKUT), and nephrotic syndrome [7] [31]. Patient-specific iPSC-derived organoids offer a unique platform for analyzing disease pathophysiology and performing therapeutic screening [7] [31]. For instance, organoids with HNF1B deletion, linked to congenital kidney defects, have been used to validate experimental systems for studying renal developmental biology [30]. Similarly, organoids have been employed to model ciliopathic renal phenotypes and podocyte injury [31].
Functional Assessment and Toxicity Screening
Kidney organoids demonstrate clinically relevant functions, particularly in nephrotoxicity testing. Proximal tubules within organoids display megalin- and cubilin-mediated endocytosis and respond to nephrotoxicants like cisplatin by undergoing specific apoptosis [27]. This response is attributed to the presence of basolateral organic cation transporter 2 (OCT2) and copper transporter 1 (CTR1) that mediate cisplatin uptake [27]. The development of "proximal-biased" organoids with enhanced expression of solute carriers has further improved the utility of organoids for studying proximal nephrotoxicity and tubulopathies [20].
Current Limitations and Refinement Strategies
Despite their promise, kidney organoids face several limitations. They generally represent fetal rather than adult kidney tissue, with incomplete maturation and lack of full nephron segmentation [7] [28] [20]. Organoids typically contain 10-20% non-renal cell types, including neuronal and muscle cells, which reflect incomplete lineage specification [29]. Vascularization is limited under standard culture conditions, though co-culture with endothelial cells or transplantation into immunodeficient mice can enhance vascular integration [7]. Recent innovations aim to address these limitations through bioengineering strategies such as microfluidic organ-on-a-chip platforms, 3D bioprinting, and optimized differentiation protocols that reduce off-target cells and enhance functional maturation [7] [31] [20].
The Taguchi, Morizane, Takasato, and Freedman protocols each offer distinct approaches to kidney organoid generation, with trade-offs in cellular diversity, protocol complexity, and applicability to specific research questions. The Taguchi protocol provides a focused model of metanephric mesenchyme and nephron formation, while the Takasato protocol generates the broadest spectrum of renal cell types, including nephrons connected to collecting ducts. The Morizane protocol balances efficiency and reproducibility, making it suitable for larger-scale applications. Continued refinement of these protocols through bioengineering, single-cell technologies, and signaling pathway manipulation will further enhance the physiological relevance and translational potential of kidney organoids for disease modeling and drug discovery.
The generation of kidney organoids from human induced pluripotent stem cells (hiPSCs) represents a transformative approach in biomedical research, offering unprecedented opportunities for studying renal development, disease modeling, and drug screening. This protocol is framed within a broader thesis on leveraging hiPSC-derived kidney organoids for disease modeling research, providing researchers and drug development professionals with a detailed roadmap for in vitro nephrogenesis. The fundamental strategy involves recapitulating key milestones of embryonic kidney development through directed differentiation, which proceeds through three critical phases: primitive streak induction, intermediate mesoderm patterning, and nephron progenitor formation [32]. Each of these stages must be precisely controlled through specific signaling pathway activation to generate kidney organoids containing functional nephron structures.
The kidney develops from the intermediate mesoderm, which gives rise to two key progenitor populations: the metanephric mesenchyme (MM) and the ureteric bud (UB). The MM contains self-renewing nephron progenitor cells (NPCs) that express critical transcription factors including SIX2, WT1, PAX2, and OSR1 [7]. These NPCs ultimately form all epithelial components of the nephron except the collecting duct through a process of mesenchymal-to-epithelial transition (MET) [7]. Successful duplication of this process in vitro requires meticulous control of developmental signaling pathways, including WNT, BMP, FGF, and RA signaling, at specific timepoints and concentrations [33]. The protocols outlined below synthesize established methodologies from leading research groups to provide a comprehensive framework for generating kidney organoids with robust nephron structures for research applications.
Developmental Biology Principles
Embryonic Origins of Kidney Structures
Understanding the embryonic origins of renal structures is essential for designing effective differentiation protocols. The adult kidney derives from the metanephros, which begins development through reciprocal inductive signaling between two key embryonic tissues: the ureteric bud (UB) and the metanephric mesenchyme (MM) [7]. The UB evaginates from the posterior portion of the Wolffian duct and undergoes repeated branching to form the collecting duct system, while the MM contains nephron progenitor cells that differentiate into all nephron segments including glomeruli, proximal tubules, loops of Henle, and distal tubules [7] [34]. This developmental process is orchestrated by precisely timed signaling interactions, with WNT signaling (particularly WNT9b and WNT4) being essential for MET and nephron induction [7]. BMP7 supports MM survival and proliferation, while FGF signaling (especially FGF8 and FGF9) promotes cell differentiation and UB branching [7]. Notch signaling contributes to nephron segmentation and fate specification, ensuring the proper formation of distinct nephron regions [7].
Developmental Timeline and Signaling
Table: Key Developmental Stages and Their In Vitro Recapitulation
| Developmental Stage | In Vivo Timing (Human) | Key Signaling Pathways | Major Markers | In Vitro Equivalent |
|---|---|---|---|---|
| Primitive Streak | Week 2-3 | WNT, Nodal/Activin, BMP | Brachyury (T), MIXL1 | CHIR99021 treatment |
| Intermediate Mesoderm | Week 3-4 | WNT, FGF, BMP | OSR1, PAX2, LHX1 | FGF9 ± BMP7 treatment |
| Metanephric Mesenchyme | Week 4-5 | FGF9, WNT, RA | SIX2, WT1, SAL11 | 3D aggregation + FGF9 |
| Nephron Formation | Week 5+ | WNT, Notch, FGF | NPHS1, LTL, ECAD | Spontaneous in organoids |
Experimental Protocols
Primitive Streak Induction
The initial step in kidney organoid differentiation involves guiding hiPSCs toward primitive streak identity, which represents the developmental stage preceding mesoderm formation. This is typically achieved through transient activation of the canonical WNT signaling pathway using GSK3β inhibitors.
Detailed Protocol:
- Culture hiPSCs to approximately 70-80% confluence in feeder-free conditions using essential stem cell maintenance medium such as mTeSR or StemFlex.
- Initiate differentiation by switching to a basal medium such as Advanced RPMI 1640 supplemented with 1-2% GlutaMax and 1-2% penicillin-streptomycin.
- Add CHIR99021 at optimized concentrations ranging from 3-12 µM (typically 8-10 µM for most cell lines) for 24-48 hours [7] [18]. The optimal concentration and duration must be determined empirically for specific hiPSC lines, as prolonged WNT activation promotes more posterior fates [34].
- Monitor morphological changes including the transition from compact colonies to more dispersed, elongated cells with mesenchymal appearance.
- Confirm successful induction by assessing expression of primitive streak markers Brachyury (T) and MIXL1 via immunocytochemistry or qPCR, typically visible within 24-48 hours.
Critical Considerations:
- The concentration and duration of CHIR99021 treatment significantly influence the resulting cell fate, with longer exposures promoting posterior primitive streak fates that give rise to kidney lineages [34].
- Cell density at differentiation initiation critically affects efficiency, with optimal results typically achieved at 70-80% confluence.
- Batch-to-batch variability in CHIR99021 activity necessitates quality control measures for reproducible results.
Intermediate Mesoderm Patterning
Following primitive streak induction, cells must be guided toward intermediate mesoderm identity, the direct precursor to kidney lineages. This stage requires precise manipulation of WNT, FGF, and BMP signaling.
Detailed Protocol:
- Following primitive streak induction (typically 24-48 hours), replace medium containing CHIR99021 with fresh basal medium.
- Add patterning factors including FGF9 (50-100 ng/mL) with or without BMP7 (10-50 ng/mL) for 3-5 days [7] [18]. Some protocols incorporate retinoic acid (RA) at this stage to support posterior IM patterning [18].
- Consider aggregate formation by transferring cells to low-attachment plates or using forced aggregation methods to promote 3D organization, which enhances IM patterning.
- Monitor for IM markers including OSR1, PAX2, and LHX1 via immunostaining or qPCR, typically emerging within 2-3 days of patterning factor addition.
- Assess morphology characterized by compact, epithelial-like clusters emerging within the more dispersed mesenchymal population.
Critical Considerations:
- The transition from primitive streak to IM represents a critical fate decision point, with anterior IM giving rise to ureteric bud lineages and posterior IM forming metanephric mesenchyme [32].
- The combination of FGF9 with BMP7 enhances the efficiency of IM induction in some protocols, while others achieve successful differentiation with FGF9 alone [18].
- The duration of WNT activation during the previous stage influences the response to patterning factors, with appropriate posteriorization being essential for kidney lineage specification.
Nephron Progenitor Formation and Organoid Generation
The final differentiation step involves expanding and maintaining nephron progenitor populations, followed by 3D organoid formation to support self-organization into nephron structures.
Detailed Protocol:
- After IM patterning (typically 4-6 days total differentiation), continue culture with FGF9 (50-100 ng/mL) to support nephron progenitor expansion.
- Transfer to 3D culture by forming aggregates in low-adhesion plates or embedding in extracellular matrix such as Matrigel to promote tissue-level organization [34].
- Maintain in 3D culture for 10-21 days, with medium changes every 2-3 days using renal organoid medium typically containing FGF9 alone or in combination with other factors such as BMP4, RA, or CHIR99021 at lower concentrations [18].
- Monitor nephron formation evidenced by the emergence of distinct morphological regions including cyst-like structures, tubular extensions, and dense glomerular clusters.
- Validate organoid identity through immunostaining for nephron progenitor markers (SIX2, CITED1), podocyte markers (WT1, NPHS1, PODXL), proximal tubule markers (LTL, CUBN), and distal tubule markers (ECAD, SLC12A1) [7].
Critical Considerations:
- The efficiency of NPC generation varies significantly between protocols, with Morizane's protocol reporting 80-90% SIX2+ cells compared to 20-70% in Taguchi's approach [18].
- Organoids generated using standard protocols typically exhibit fetal-like characteristics, resembling first-trimester human kidney more than adult tissue [34].
- Significant protocol-dependent variability exists in off-target cell types, with some protocols generating 10-20% non-renal cells [18].
Research Reagent Solutions
Table: Essential Reagents for Kidney Organoid Differentiation
| Reagent Category | Specific Examples | Function | Typical Concentrations |
|---|---|---|---|
| WNT Agonists | CHIR99021 | GSK3β inhibitor inducing primitive streak and posterior mesoderm | 3-12 µM (stage-dependent) |
| Growth Factors | FGF9 | Supports IM patterning and nephron progenitor maintenance | 50-100 ng/mL |
| Morphogens | BMP4, BMP7 | Promotes mesoderm formation and IM patterning | 10-50 ng/mL |
| Retinoids | Retinoic Acid (RA) | Patterns IM and supports nephron segmentation | 0.1-1 µM |
| Basal Media | Advanced RPMI 1640 | Base medium for differentiation | 100% |
| 3D Culture | Matrigel, AggreWell | Provides scaffold for 3D organization | Varies by system |
Signaling Pathway Diagrams
Diagram Title: Kidney Organoid Differentiation Workflow
Diagram Title: Signaling Pathways in Kidney Organogenesis
Protocol Variations and Comparative Analysis
Several research groups have established distinct but overlapping protocols for kidney organoid generation, each with specific advantages and limitations. The table below summarizes key protocol variations from leading research groups, enabling researchers to select approaches most appropriate for their specific applications.
Table: Comparative Analysis of Kidney Organoid Differentiation Protocols
| Protocol Parameter | Taguchi et al. | Morizane et al. | Freedman et al. | Little Group |
|---|---|---|---|---|
| Initial Primitive Streak Induction | BMP4 (24h) → Activin A + FGF2 (48h) | CHIR99021 (monolayer) | Spheroid formation → CHIR99021 | CHIR99021 (suspension) |
| IM Patterning | BMP4 + high CHIR (10µM, 6 days) → Activin A + BMP4 + CHIR (3µM) + RA (2 days) | CHIR99021 → Activin A → FGF9 | Single-step CHIR99021 without exogenous FGF2/Activin/BMP | Modified CHIR99021 and growth factor timing |
| NPC Generation Efficiency | 20-70% SIX2+ cells | 80-90% SIX2+ cells | Not specified | Not specified |
| 3D Culture Method | Coculture with mouse spinal cord | Aggregation in low-adhesion plates | Matrigel sandwich | Suspension culture |
| Key Cell Types Generated | Glomeruli, proximal and distal tubules | Multi-segmented nephrons (podocytes, PT, LoH, DT) | Podocytes, proximal tubules, endothelial cells | Multiple nephrons with endothelial and stromal cells |
| Unique Advantages | Forms glomerular structures | Defined medium, high NPC efficiency | Simple, cost-effective, high-throughput | High cell yield, reduced costs |
| Major Limitations | Requires non-human tissue, lower efficiency | Line-dependent variability, no collecting duct | Random organoid size, no collecting duct | Immaturity similar to other protocols |
Technical Considerations and Troubleshooting
Optimization Strategies
Successful kidney organoid generation requires careful optimization of several parameters. Key considerations include:
- hiPSC Line Variability: Different hiPSC lines exhibit substantial variation in differentiation efficiency. Preliminary testing with multiple lines or CRISPR-edded isogenic controls is recommended for critical applications [18].
- Temporal Precision: The timing of growth factor addition is critical, with even 4-6 hour deviations potentially altering differentiation outcomes. Establish strict medium change schedules.
- 3D Culture Configuration: The method of 3D aggregation significantly influences organoid development. Forced aggregation using microwell plates (e.g., AggreWell) improves uniformity compared to spontaneous aggregation [35].
- Maturation Limitations: Standard protocol-generated organoids typically resemble first-trimester fetal kidney [34]. Enhanced maturation may require extended culture, specialized culture conditions such as air-liquid interface [35], or transplantation into animal hosts.
Quality Assessment Metrics
Rigorous quality control is essential for generating reproducible, high-quality kidney organoids. Key assessment metrics include:
- Molecular Characterization: Immunofluorescence analysis for segment-specific markers (podocytes: NPHS1, WT1; proximal tubule: LTL; distal tubule: ECAD) at day 18-21 of differentiation.
- Structural Assessment: Light microscopic evaluation for the presence of distinct glomerular-like bodies connected to tubular structures.
- Purity Evaluation: Quantification of off-target cell types (typically 10-20% in most protocols) using specific neural and muscle markers [18].
- Functional Assessment: For advanced applications, evaluate tubular function through dextran uptake assays or glomerular function through albumin retention.
Applications in Disease Modeling and Drug Development
Kidney organoids generated using these protocols serve as valuable tools for modeling genetic kidney diseases, including polycystic kidney disease (PKD) and congenital anomalies of the kidney and urinary tract (CAKUT) [7]. The patient-specific nature of hiPSC-derived organoids enables creation of personalized disease models that recapitulate individual genetic backgrounds. For drug development applications, kidney organoids provide human-relevant systems for nephrotoxicity screening and efficacy testing, addressing limitations of animal models and traditional 2D culture systems [36]. Recent advances in organoid culture, including microfluidic systems [7] and air-liquid interface approaches [35], further enhance the physiological relevance and scalability of these models for preclinical research.
The advent of kidney organoids derived from induced pluripotent stem cells (iPSCs) has revolutionized the study of human renal diseases in a controlled, accessible in vitro environment. These three-dimensional structures recapitulate key aspects of kidney development, architecture, and function, providing researchers with unprecedented opportunities to model hereditary and acquired kidney diseases [7] [14]. For diseases like polycystic kidney disease (PKD), Alport syndrome, and acute kidney injury (AKI), kidney organoids have emerged as powerful platforms for elucidating pathological mechanisms, validating genetic findings, and screening potential therapeutic compounds [4] [37]. This application note details successful protocols and case studies demonstrating how iPSC-derived kidney organoids are advancing our understanding of these conditions, providing researchers with practical methodologies for implementing these models in their investigative workflows.
Kidney Organoid Generation from iPSCs
The foundation of effective disease modeling lies in the robust differentiation of iPSCs into kidney organoids. The following protocol, adapted from established methods, outlines the key steps for generating kidney organoids containing segmented nephron-like structures [7] [14].
Protocol: Directed Differentiation of iPSCs into Kidney Organoids
Key Reagents Required:
- Human iPSCs (healthy or patient-derived)
- CHIR99021 (GSK3β inhibitor)
- Recombinant Human FGF9
- Recombinant Human BMP7
- Matrigel or Geltrex
- Advanced RPMI 1640 Medium
Procedure:
Intermediate Mesoderm Induction (Days 0-4):
- Culture iPSCs to 70-80% confluence in a defined, feeder-free system.
- Initiate differentiation by switching to advanced RPMI 1640 medium containing 8-12 µM CHIR99021.
- Culture for 4 days, changing medium every 48 hours. CHIR99021 activates WNT signaling, driving cells toward a posterior primitive streak and intermediate mesoderm fate [7] [14].
Nephron Progenitor Cell Specification (Days 4-9):
- On day 4, replace medium with advanced RPMI 1640 containing FGF9 (200 ng/mL).
- Culture for 5 days with medium changes every 2-3 days. FGF9 supports the maintenance and expansion of nephron progenitor populations [7].
3D Aggregation and Nephron Formation (Days 9-26):
- On day 9, dissociate cells into single cells using Accutase.
- Resuspend cells in differentiation medium containing FGF9 and transfer to low-attachment plates or specialized platforms like the UniMat system to promote 3D aggregation [22].
- Culture for 14-18 days, allowing for self-organization into nephron-like structures. Medium should be changed every 3-4 days.
Quality Control:
- Monitor for the emergence of tubular and glomerular-like structures.
- Validate differentiation by immunostaining for segment-specific markers: PODXL (podocytes), LTL (proximal tubules), CDH1 (distal tubules) [22].
- Use single-cell RNA sequencing to assess cell type composition and purity if available [7].
Table 1: Key Markers for Characterizing Kidney Organoid Differentiation
| Nephron Segment | Marker | Expected Expression Pattern |
|---|---|---|
| Podocytes | PODXL, NPHS1, WT1 | Glomerular-like structures |
| Proximal Tubule | LTL, CUBN, SLC3A1 | Tubular structures with brush border |
| Distal Tubule | CDH1, SLC12A1 | Tubular structures |
| Stromal Cells | FOXD1, PDGFRβ | Interstitial areas |
Disease Modeling Applications
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
ADPKD, caused primarily by mutations in PKD1 or PKD2 genes, leads to progressive cyst formation and renal function decline. iPSC-derived kidney organoids have successfully modeled key aspects of ADPKD pathogenesis, including cystogenesis and the "second hit" hypothesis [38] [4].
Experimental Workflow for ADPKD Modeling:
The following diagram illustrates the complete workflow for generating and analyzing ADPKD kidney organoids:
Protocol: Modeling Cystogenesis in ADPKD Organoids
Genetic Manipulation:
Organoid Generation:
- Differentiate both mutant and control iPSCs into kidney organoids using the protocol in Section 2.1.
Cyst Induction:
- On day 18-21 of differentiation, supplement medium with 10-20 µM forskolin (an adenylate cyclase activator) or 10 µM nifedipine (an L-type calcium channel blocker) to stimulate cyst formation [38].
- Treat for 10-14 days, refreshing compounds every 2-3 days.
Phenotypic Analysis:
- Quantify cyst number and size using brightfield or phase-contrast microscopy.
- Employ automated image analysis platforms like OrganoID for high-throughput quantification [39].
- Assess intracellular cAMP levels via ELISA.
- Evaluate renin expression in cystic epithelium via immunostaining or RNA analysis, as ectopic renin expression is a hallmark of ADPKD organoids [38].
Key Findings:
- ADPKD organoids recapitulate elevated cAMP levels and abnormal calcium signaling central to cyst pathogenesis [38].
- Cyst formation often requires a "second hit" beyond genetic mutation, mimicked by forskolin or nifedipine treatment [38].
- Aberrant activation of the renin-angiotensin-aldosterone system (RAAS) has been observed in ADPKD organoids, with ectopic renin expression detected in the cystic epithelium [38].
Alport Syndrome
Alport Syndrome results from mutations in COL4A3, COL4A4, or COL4A5 genes, encoding type IV collagen chains essential for glomerular basement membrane (GBM) integrity [40]. While modeling the structural GBM defects in organoids remains challenging, they offer potential for studying disease mechanisms and screening therapeutic interventions.
Protocol: Modeling Alport Syndrome in Kidney Organoids
iPSC Generation:
- Generate iPSCs from Alport Syndrome patients with confirmed COL4A3, COL4A4, or COL4A5 mutations.
- Create gene-corrected isogenic controls using CRISPR/Cas9.
Organoid Differentiation:
- Differentiate patient and control iPSCs into kidney organoids using the standard protocol.
Phenotypic Characterization:
- Analyze GBM composition and structure by transmission electron microscopy for hallmark GBM thickening and lamellation.
- Perform immunostaining for collagen α3, α4, and α5 chains.
- Assess podocyte injury markers (WT1, SYNPO, NPHS1) and proteinuria-associated proteins.
Drug Testing:
- Treat organoids with RAAS blockers (e.g., ramipril), SGLT2 inhibitors (e.g., dapagliflozin), or novel investigational compounds.
- Monitor for changes in marker expression and morphological improvements.
Key Insights:
- Alport Syndrome organoids can potentially model early developmental aspects of the disease, though full recapitulation of advanced GBM pathology remains challenging [40].
- These organoids provide platforms for testing RAAS blockade and emerging therapies like SGLT2 inhibitors, endothelin receptor antagonists, and gene therapy approaches [40].
Acute Kidney Injury
Kidney organoids effectively model drug-induced AKI, demonstrating segment-specific toxicity and cellular injury responses that mirror in vivo pathology [7] [4].
Protocol: Modeling AKI in Kidney Organoids
Organoid Generation:
- Generate kidney organoids from iPSCs using standard protocols.
Toxin Exposure:
- On day 18-24 of differentiation, treat organoids with nephrotoxic agents:
- Gentamicin (1-2 mM) for proximal tubule injury
- Cisplatin (10-50 µM) for tubular damage
- Culture with toxins for 24-72 hours.
- On day 18-24 of differentiation, treat organoids with nephrotoxic agents:
Damage Assessment:
- Quantify expression of injury biomarkers KIM-1 (proximal tubules) and NGAL via immunostaining or qPCR.
- Assess apoptosis via cleaved caspase-3 staining.
- Evaluate functional impairment using dextran uptake assays.
Key Findings:
- AKI organoids show specific, segmental injury patterns with proximal tubules particularly vulnerable to gentamicin and cisplatin [4].
- Injury markers like KIM-1 are specifically upregulated in tubular epithelial cells after toxin exposure, mimicking in vivo responses [4].
- These models enable high-throughput screening of nephroprotective compounds.
Table 2: Quantitative Assessment of Disease Phenotypes in Kidney Organoid Models
| Disease Model | Induction Method | Key Readouts | Typical Response |
|---|---|---|---|
| ADPKD | 10-20 µM Forskolin for 10-14 days | Cyst number and diameter | 75-87% of organoids develop cysts under optimized conditions [38] [22] |
| Alport Syndrome | Patient-derived iPSCs with COL4A3/4/5 mutations | GBM abnormalities, collagen chain expression | Variable penetration based on mutation type [40] |
| Acute Kidney Injury | 10-50 µM Cisplatin for 24-72 hours | KIM-1 expression, caspase-3 activation | Specific proximal tubule injury; >50% increase in KIM-1+ cells [4] |
Advanced Technologies Enhancing Disease Modeling
Bioengineering Platforms
Advanced culture systems like the UniMat platform address critical limitations in organoid maturation and reproducibility. UniMat employs a 3D geometrically-engineered permeable membrane that provides physical constraints for uniform organoid growth while enabling efficient nutrient and gas exchange [22]. This system significantly enhances organoid uniformity, maturation, and scalability, producing kidney organoids with more in vivo-like cell-type balance and enhanced vascularization [22].
AI-Powered Image Analysis
The OrganoID platform utilizes deep learning to automatically recognize, label, and track individual organoids in brightfield and phase-contrast microscopy images [39]. This tool enables high-throughput, precise quantification of organoid count, size, and complex morphological changes in response to experimental manipulations, dramatically improving analysis efficiency and accuracy for drug screening applications.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Kidney Organoid Disease Modeling
| Reagent/Category | Function | Example Applications |
|---|---|---|
| CRISPR/Cas9 Systems | Introduction or correction of disease-associated mutations | Generating isogenic pairs for ADPKD (PKD1/PKD2) and Alport Syndrome (COL4A3/4/5) [38] [4] |
| Small Molecule Inducers | Mimic "second hit" in cystogenesis or induce specific injury | Forskolin (cAMP activation) and nifedipine (calcium channel blockade) for ADPKD; cisplatin for AKI [38] [4] |
| Differentiation Modulators | Direct lineage specification | CHIR99021 (WNT activation) for mesoderm induction; FGF9 for nephron progenitor maintenance [7] [14] |
| Extracellular Matrices | Provide 3D structural support | Matrigel for initial iPSC culture; agarose hydrogel for low-attachment in UniMat system [22] |
| AI-Based Analysis Tools | Automated quantification of organoid morphology | OrganoID for tracking organoid count, size, and shape changes in high-throughput screens [39] |
iPSC-derived kidney organoids have emerged as powerful, physiologically relevant models for studying PKD, Alport Syndrome, and AKI. The protocols and applications detailed herein provide researchers with practical frameworks for implementing these innovative systems in their investigations. While challenges remain in achieving full functional maturation and vascular integration, ongoing advances in bioengineering, gene editing, and analytical technologies continue to enhance the fidelity and utility of these models. As the field progresses, kidney organoids promise to accelerate our understanding of renal disease mechanisms and facilitate the development of novel therapeutic strategies.
The high incidence of drug-induced nephrotoxicity (DIN) remains a significant concern in drug discovery and development, accounting for approximately 19-25% of acute renal failure cases [41] [42]. The renal proximal tubule epithelial cells (RPTECs) are the primary site for drug accumulation and reabsorption, making them particularly vulnerable to toxic injury through mechanisms including mitochondrial dysfunction, impaired tubular transport, and increased oxidative stress [41]. Traditional two-dimensional (2D) cell cultures and animal models have limitations in accurately predicting human-specific drug responses, leading to high attrition rates in clinical trials [43].
The emergence of kidney organoids derived from human induced pluripotent stem cells (iPSCs) represents a transformative platform for nephrotoxicity assessment. These three-dimensional (3D) structures recapitulate human kidney complexity with greater fidelity than traditional models, offering significant advantages in predicting drug responses and enabling personalized disease modeling [44]. This application note details functional assays for assessing nephrotoxicity, drug uptake, and injury marker expression within the context of iPSC-derived kidney organoids, providing researchers with standardized protocols for evaluating renal toxicity in physiologically relevant systems.
Key Functional Assays for Nephrotoxicity Assessment
Assessment of Transporter Function
The proper polarization and transporter expression of renal proximal tubule cells are crucial for accurate drug toxicity evaluation [42]. The integrated biomimetic array chip (iBAC) platform enables the construction of a high-throughput human renal proximal tubule model that exhibits improved epithelial polarization and membrane transporter activity compared to static Transwell cultures [42].
Table 1: Quantitative Parameters for Transporter Function Assays
| Functional Parameter | Experimental Probe | Inhibitor Control | Measurement Method | Key Findings |
|---|---|---|---|---|
| P-glycoprotein (P-gp) Efflux Activity | Rhodamine 123 (2 μM) | Verapamil (10 μM) | Apparent permeability (Papp) measurement | hRPTECs on iBAC showed significantly higher efflux function compared to static cultures [42] |
| Organic Anion Transport | DiOC2 (10 μM) | Ko143 (10 μM) | Apparent permeability (Papp) measurement | Functional activity demonstrated polarization-dependent transport [42] |
| Protein Endocytosis | Fluorescein-conjugated dextran | N/A | Fluorescence quantification | Kidney spheroids displayed proximal tubule-specific functional properties [45] |
| Gamma-Glutamyltransferase (GGT) Activity | Gamma-glutamyl-p-nitroanilide | N/A | Spectrophotometric activity assay | Immortalized human renal cells showed increased GGT activity compared to hPTECs [45] |
Injury Marker Expression Analysis
Emerging biomarkers offer significant advantages over traditional methods for detecting renal injury earlier and with greater accuracy [46]. The integration of these biomarkers with artificial intelligence-driven models has the potential to enhance diagnostic precision in personalized nephrology [46].
Table 2: Nephrotoxicity Biomarkers and Detection Methods
| Biomarker Category | Specific Marker | Detection Method | Significance | Application in Organoids |
|---|---|---|---|---|
| Early Injury Markers | Neutrophil gelatinase-associated lipocalin (NGAL) | ELISA, Immunostaining | Increases within hours of kidney injury [46] | Real-time assessment of kidney health [46] |
| Kidney injury molecule-1 (KIM-1) | ELISA, qPCR | Allows earlier and more targeted interventions [46] | Non-invasive diagnostic tool in organoid media [46] | |
| Tubular Injury Markers | Soluble urokinase plasminogen activator receptor (suPAR) | ELISA, Immunoassay | Linked to disease progression and endothelial dysfunction [46] | Prognostic indicator for disease modeling [46] |
| Cystatin C | Immunoassay | Less affected by muscle mass or metabolic fluctuations [46] | Improved sensitivity over creatinine-based assessment [46] | |
| Oxidative Stress Markers | Glutathione (GSH) content | High content screening (HCS) | Measures cellular redox state [41] | Multiparametric toxicity assessment [41] |
| Complex Injury Panels | Multi-omics approaches (proteomics, transcriptomics) | RNA sequencing, Mass spectrometry | Reveals molecular signatures of early disease [46] | Comprehensive profiling of organoid responses [46] |
Cellular Health and Viability Endpoints
Multi-parametric high content screening (HCS) approaches allow simultaneous measurement of multiple cell health markers in kidney-relevant in vitro models to better predict drug-induced nephrotoxicity [41].
Table 3: Cellular Health and Viability Assays
| Viability Parameter | Assessment Method | Experimental Details | Significance in Nephrotoxicity |
|---|---|---|---|
| Cell Viability | Dye exclusion/retention, Enzyme/ion leakage | Membrane integrity assays | Determines compound cytotoxicity [47] |
| Mitochondrial Membrane Potential (MMP) | Tetramethylrhodamine methyl ester (TMRM) staining | HCS automated imaging | Indicator of mitochondrial dysfunction [41] |
| Mitochondrial Mass | Nonyl acridine orange (NAO) staining | HCS automated imaging | Assesses mitochondrial content and health [41] |
| Phospholipidosis (PLD) | HCS staining | Fluorescent phospholipid probes | Detects phospholipid accumulation [41] |
| ATP Content | Luciferase-based assay | Cell lysis and quantification | Measures metabolic activity and cell health [41] |
| Apoptosis/Necrosis | Caspase activation, Propidium iodide uptake | Flow cytometry, HCS | Distinguishes modes of cell death [47] |
Experimental Protocols
Protocol for Transporter Function Assessment
Materials:
- Integrated biomimetic array chip (iBAC) [42]
- Primary human renal proximal tubule epithelial cells (hRPTECs) [42]
- Serum-free culture medium
- Rhodamine 123 (2 μM) or DiOC2 (10 μM) [42]
- Verapamil (10 μM) or Ko143 (10 μM) for inhibitor controls [42]
- Microplate reader with fluorescence detection (Ex = 495 nm, Em = 535 nm) [42]
Procedure:
- Seed hRPTECs on iBAC at density of 2 × 10^5 cells/cm^2 and culture for 5-7 days to establish polarized monolayer [42].
- Confirm barrier function by measuring transepithelial electrical resistance (TEER) using specialized resistance meter [42].
- Prepare serum-free culture medium containing fluorescent substrates (Rhodamine 123 or DiOC2) with or without corresponding inhibitors.
- Perfuse substrate-containing medium through the microchannel of the bottom layer at 2 circles/min using iBAC Rocker [42].
- Add blank serum-free culture medium to the intermediate reservoir.
- After two hours of dynamic absorption, collect samples from both compartments.
- Quantify fluorescence levels using microplate reader to determine apparent permeability (Papp) [42].
- Calculate transporter activity by comparing Papp values with and without inhibitors.
Protocol for Nephrotoxicity Assessment Using High Content Screening
Materials:
- iPSC-derived kidney organoids or hRPTECs [41] [42]
- 96-well or 384-well microplates suitable for automated imaging
- Cell health markers: GSH content, PLD, MMP, mitochondrial mass probes [41]
- Fixation solution (4% paraformaldehyde)
- Permeabilization buffer (0.1% Triton X-100)
- Blocking solution (1% BSA in PBS)
- Primary and secondary antibodies for injury markers (NGAL, KIM-1) [46]
- High content imaging system with environmental control
Procedure:
- Plate kidney organoids or cells in 3D culture matrix in microplates and culture for 5-7 days to establish mature phenotypes.
- Treat with test compounds for 24-72 hours with appropriate vehicle controls and reference nephrotoxicants.
- For chronic exposure studies (up to 14 days), use multi-parametric HCS approach [41].
- Incubate with cell health marker dyes for 30-60 minutes according to manufacturer's protocols.
- Fix cells with 4% paraformaldehyde for 15 minutes at room temperature.
- Permeabilize with 0.1% Triton X-100 for 10 minutes.
- Block with 1% BSA for 30 minutes.
- Incubate with primary antibodies against injury markers (NGAL, KIM-1) overnight at 4°C [46].
- Incubate with fluorescently-labeled secondary antibodies for 1 hour at room temperature.
- Image using high content imaging system with 20x or 40x objectives.
- Analyze images using automated algorithms to quantify fluorescence intensity, morphological changes, and marker expression.
Protocol for Functional Kidney Spheroid Generation
Materials:
- Mixed immortalized renal cell lines [45]
- Extracellular matrix (Matrigel or collagen type I) [45]
- Spheroid-forming unit (SFU) protocol equipment [45]
- Renal epithelial culture medium with BMP7 supplementation [45]
- Rotation culture system
Procedure:
- Culture mixed immortalized renal cells in renal epithelial medium with BMP7 to maintain progenitor characteristics [45].
- Seed cells using hanging-drop method to form initial aggregates [45].
- Transfer aggregates to rotation culture using SFU protocol for 7 days to promote maturation [45].
- Confirm expression of renal lineage markers (proximal tubule, loop of Henle, distal tubules, podocytes) via immunostaining and qPCR [45].
- Validate functional maturity through dextran uptake assays and GGT activity measurements [45].
- Use for nephrotoxicity studies by exposing to compounds and assessing injury markers and viability endpoints.
Research Reagent Solutions
Table 4: Essential Research Reagents for Kidney Organoid Functional Assays
| Reagent Category | Specific Product | Function/Application | Key Features |
|---|---|---|---|
| Cell Sources | Primary hRPTECs (Lonza) | Gold standard for proximal tubule models [42] | Maintain transporter expression, proper polarization |
| iPSC-derived renal progenitors | Patient-specific disease modeling [43] | Recapitulate genetic background, personalized responses | |
| Culture Systems | Integrated biomimetic array chip (iBAC) | Microfluidic platform for tubular culture [42] | Applies physiological fluid shear stress (0.22 dyne/cm²) |
| Extracellular matrix (Matrigel, Collagen I) | 3D scaffold for organoid formation [45] | Supports self-organization and polarization | |
| Functional Probes | Rhodamine 123 | P-glycoprotein efflux transporter substrate [42] | Assesses polarized drug transport capability |
| Fluorescein-conjugated dextran | Protein endocytosis assessment [45] | Measures proximal tubule-specific reabsorption function | |
| Biomarker Detection | NGAL ELISA kits | Early injury marker quantification [46] | Detects subclinical nephrotoxicity before functional decline |
| KIM-1 antibodies | Tubular injury immunostaining [46] | Specific marker for proximal tubule damage | |
| Cell Health Dyes | GSH content probes | Oxidative stress assessment [41] | Quantifies cellular redox state in multiparametric HCS |
| MitoMass and MMP dyes | Mitochondrial function evaluation [41] | Assesses mitochondrial health and membrane integrity |
Workflow and Pathway Diagrams
Nephrotoxicity Assessment Workflow
Signaling Pathways in Kidney Organoid Maturation
The integration of functional assays using iPSC-derived kidney organoids and advanced microphysiological systems represents a paradigm shift in nephrotoxicity assessment. The protocols outlined in this application note provide researchers with standardized methods for evaluating drug uptake, transporter function, and injury marker expression in physiologically relevant models. These approaches enable more accurate prediction of human-specific drug responses earlier in the development pipeline, potentially reducing late-stage attrition due to nephrotoxicity. As kidney organoid technology continues to evolve with improvements in reproducibility, vascularization, and functional maturation, these functional assays will play an increasingly critical role in both drug safety assessment and personalized medicine applications.
High-Throughput Drug Screening and the Promise for Personalized Medicine
High-throughput drug screening (HTS) constitutes the predominant paradigm for novel drug discovery, enabling the rapid testing of thousands of chemical compounds for therapeutic potential [48]. In the evolving landscape of personalized medicine, the convergence of HTS with induced pluripotent stem cell (iPSC) technology represents a transformative approach. The generation of kidney organoids from human iPSCs provides a physiologically relevant, human-derived model system that recapitulates the complexity of the kidney, comprising various cell types organized in nephron-like architectures [49] [50]. These patient-specific organoids serve as powerful platforms for disease modeling and drug evaluation, offering a path toward tailored therapies for kidney diseases such as autosomal dominant polycystic kidney disease (ADPKD) and drug-induced nephrotoxicity [50] [51]. This application note details the integration of iPSC-derived kidney organoids into quantitative HTS (qHTS) pipelines, providing detailed protocols and analytical frameworks to advance preclinical drug discovery and toxicity assessment for personalized medicine applications.
High-Throughput Screening Approaches: A Comparative Analysis
Drug screening methodologies have evolved beyond traditional target-based and phenotype-based approaches. Pharmacotranscriptomics-based drug screening (PTDS) has emerged as a distinct class, detecting gene expression changes following drug perturbation on a large scale [48] [52]. When combined with artificial intelligence, PTDS can analyze the efficacy of drug-regulated gene sets, signaling pathways, and complex diseases, making it particularly suitable for screening complex interventions like Traditional Chinese Medicine [48]. The table below summarizes the core screening approaches used in modern drug discovery.
Table 1: Comparative Analysis of High-Throughput Drug Screening Approaches
| Screening Approach | Core Principle | Typical Readouts | Key Applications | Notable Advantages |
|---|---|---|---|---|
| Phenotypic Screening (qHTS) [49] [51] | Observes phenotypic changes (e.g., viability, 3D morphometry) in response to compound exposure across multiple concentrations. | Cell viability (GF-AFC, CTG), 3D cyst growth, automated morphometric analysis. | Nephrotoxicity screening, therapeutic assessment, drug repurposing (e.g., for ADPKD) [51]. | Identifies bioactive compounds without prior knowledge of a specific molecular target; generates concentration-response curves for potency/efficacy estimation. |
| Pharmacotranscriptomics (PTDS) [48] [52] | Detects global gene expression changes in cells after drug perturbation. | Genome-wide transcriptome data (via microarray, RNA-seq). | Pathway-based drug discovery, mechanism of action analysis for complex drugs (e.g., TCM) [48]. | Provides deep mechanistic insights; uses AI to connect pathway modulation to therapeutic outcomes. |
| Pathway-Based Screening [48] | A subset of PTDS focusing on the activity of specific signaling pathways. | Enrichment of gene sets related to specific pathways (e.g., WNT, TGF-β). | Targeted drug discovery, combination therapy design. | Contextualizes drug effects within known biological networks; facilitates rational polypharmacology. |
Protocol: A Workflow for High-Throughput Screening Using Kidney Organoids
Generation and Maturation of iPSC-Derived Kidney Organoids
Principle: Human iPSCs are directed to differentiate into 3D kidney organoids that mimic the cellular composition and segmented structures of the native kidney, including podocytes and tubular epithelia [49] [50].
Materials:
- Source Cells: Human iPSCs (e.g., BJFF.6 hiPSCs) [49].
- Culture Medium: StemFit Basic04 (for iPSC maintenance) and advanced RPMI supplemented with 1% GlutaMAX (for differentiation) [49].
- Differentiation Factors: CHIR 99021 (GSK-3β inhibitor), Dorsomorphin, Activin A, recombinant human FGF9 [49].
- Culture Vessels: Geltrex-coated plates for 2D culture; ultra-low attachment 96-well or 1536-well spheroid microplates (e.g., Akura 96 Spheroid Microplates) for 3D organoid formation [49] [51].
Procedure:
- Maintenance of iPSCs: Culture human iPSCs on Geltrex-coated 6-well plates in StemFit Basic04 complete medium, passaging weekly with Accutase. For passaging, supplement the medium with a ROCK inhibitor (Y-27632) [49].
- Differentiation into Nephron Progenitor Cells (NPCs):
- Seed iPSCs at a density of 6,000 cells per well in a Geltrex-coated 24-well plate.
- Day 0-4: Induce differentiation by adding CHIR 99021 (5.5 µM) and Dorsomorphin (200 nM) in advanced RPMI/GlutaMAX medium.
- Day 4-7: Add Activin A (10 ng/mL).
- Day 7-8: Add recombinant human FGF9 (10 ng/mL) [49].
- 3D Organoid Formation:
- On Day 8, detach the NPCs using Accutase to create a single-cell suspension.
- Transfer the suspension to ultra-low attachment 96-well plates at a concentration of 50,000 cells per well to form 3D spheroids.
- Day 8-10: Continue differentiation by adding CHIR (2.5 µM) and FGF9 (10 ng/mL).
- Day 10-14: Add FGF9 alone (10 ng/mL) [49].
- Organoid Maturation: Culture the kidney organoids in advanced RPMI supplemented with 1% GlutaMAX, with medium changes three times per week. For screening, use organoids cultured for ~49 days or longer to achieve a more mature phenotype, including expression of key drug transporters (e.g., SLC22 family) [49].
Quantitative High-Throughput Screening (qHTS) and Phenotypic Assessment
Principle: Kidney organoids are exposed to compound libraries in a qHTS format, which generates concentration-response curves directly from the primary screen, allowing for the assessment of compound potency and efficacy [51]. Phenotypic readouts include cell viability and high-content 3D morphometric analysis.
Materials:
- Compound Library: FDA-approved drug library (e.g., Tocriscreen FDA-approved library) or custom collections, prepared in DMSO [49] [51].
- Viability Assay Reagents: GF-AFC substrate (for live-cell protease activity) and CellTiter-Glo (CTG) reagent (for ATP quantification) [51].
- Immunofluorescence Staining Reagents: Primary antibodies (e.g., anti-CDH1, anti-Podocalyxin), secondary antibodies, blocking buffer (BB/ADB), and tissue clearing reagents [49].
- Imaging Equipment: Automated high-content imaging systems capable of 3D confocal imaging.
Procedure:
- Compound Exposure:
- At day 49 of organoid differentiation, add compounds from the screening library. A typical screening concentration is 10 µM, with exposure lasting 7 days (e.g., from day 49 to day 56), with medium changes three times per week [49].
- For nephrotoxicity modeling, co-expose organoids to a nephrotoxicant like cisplatin (5 µM) and candidate therapeutic compounds [49].
- Viability and Proliferation Assessment (qHTS in 1536-well format):
- After 48 hours of compound treatment, perform a two-step viability readout:
- First, add the GF-AFC substrate and measure fluorescence (excitation/emission ~400/505 nm) to assess viable cell mass.
- Second, add the luminescent CTG reagent to quantify cellular ATP levels [51].
- After 48 hours of compound treatment, perform a two-step viability readout:
- 3D Phenotypic Profiling (Cyst Growth Assay):
- For disease-specific models (e.g., ADPKD), culture
Pkd1-null cells in a 3D matrix to form cysts. - Treat with compounds identified from the initial viability screen.
- Measure cyst growth and number over time to confirm disease-modifying effects independent of general cytotoxicity [51].
- For disease-specific models (e.g., ADPKD), culture
- Whole-Mount 3D Immunofluorescence and Imaging:
- Fix organoids in 4% PFA for 1 hour.
- Permeabilize and block in blocking buffer (1% BSA, 5% donkey serum, 1% Triton X-100 in PBS) for 1 hour.
- Incubate with primary antibodies overnight at 4°C, followed by secondary antibodies.
- Perform tissue clearing to enable deep imaging.
- Acquire 3D images using an automated confocal microscope [49].
- Machine-Learning-Based Morphometric Analysis:
- Use automated segmentation and classification algorithms to quantify nephron segment-specific features from the 3D image data (e.g., tubule diameter, cyst volume, segment proportions) [49].
The following workflow diagram summarizes the key steps of this protocol:
Data Analysis and QC in qHTS
Principle: The analysis of qHTS data involves fitting statistical models, most commonly the Hill equation (HEQN), to concentration-response data to estimate parameters for ranking compounds by bioactivity [53]. However, parameter estimation can be highly variable if the experimental design does not adequately define the asymptotes of the concentration-response curve.
Hill Equation (Logistic Form):
Ri = E0 + (E∞ - E0) / [1 + exp{-h(logCi - logAC50)}]
Where Ri is the measured response at concentration Ci, E0 is the baseline response, E∞ is the maximal response, AC50 is the concentration for half-maximal response, and h is the Hill slope parameter [53].
Key Quality Control Considerations:
- Parameter Estimate Uncertainty: AC50 estimates are precise only when the tested concentration range defines at least one of the two HEQN asymptotes. Estimates can span several orders of magnitude when this condition is not met, leading to poor reproducibility [53].
- Assay Replication: Increasing sample size (experimental replicates) improves the precision of AC50 and Emax estimates, as shown in the simulated data below [53].
- Activity Call Reliability: Use classification approaches with reliable performance across diverse response profiles to minimize false positives and negatives. Not all substances produce sigmoidal curves, and some non-monotonic responses may reflect real biology not captured by the HEQN [53].
Table 2: Impact of Sample Size on Parameter Estimation in Simulated qHTS Data (Adapted from [53])
| True AC50 (µM) | True Emax (%) | Sample Size (n) | Mean [95% CI] for AC50 Estimates | Mean [95% CI] for Emax Estimates |
|---|---|---|---|---|
| 0.001 | 50 | 1 | 6.18e-05 [4.69e-10, 8.14] | 50.21 [45.77, 54.74] |
| 0.001 | 50 | 3 | 1.74e-04 [5.59e-08, 0.54] | 50.03 [44.90, 55.17] |
| 0.001 | 50 | 5 | 2.91e-04 [5.84e-07, 0.15] | 50.05 [47.54, 52.57] |
| 0.1 | 25 | 1 | 0.09 [1.82e-05, 418.28] | 97.14 [-157.31, 223.48] |
| 0.1 | 25 | 3 | 0.10 [0.03, 0.39] | 25.53 [5.71, 45.25] |
| 0.1 | 25 | 5 | 0.10 [0.05, 0.20] | 24.78 [-4.71, 54.26] |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table catalogues critical reagents and their functions for establishing a robust kidney organoid screening platform.
Table 3: Essential Research Reagents for Kidney Organoid Screening
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Human iPSCs [49] [50] | Renewable source for generating patient-specific kidney organoids. | BJFF.6 hiPSCs; quality controlled lines with proven differentiation potential. |
| Ultra-Low Attachment Plates [49] | Facilitate 3D spheroid and organoid formation by preventing cell adhesion. | Akura 96 Spheroid Microplates (InSphero). |
| Small Molecule Inducers [49] | Direct differentiation of iPSCs along the nephron lineage. | CHIR 99021 (WNT activation), Dorsomorphin, Activin A, FGF9. |
| Viability Assay Reagents [51] | Multiplexed assessment of cell health and proliferation in HTS formats. | GF-AFC (measures live-cell protease activity), CellTiter-Glo (measures ATP content). |
| Tissue Clearing Reagents [49] | Enable deep-tissue imaging by rendering the organoid optically transparent. | Used prior to automated 3D imaging for high-resolution morphometry. |
| FDA-Approved Drug Library [49] [51] | Collection of compounds for drug repurposing screens. | Tocriscreen FDA-approved drugs library; ~8,000 compounds for qHTS. |
| Primary Antibodies [49] | Label specific cell types and structures in organoids for phenotypic analysis. | Anti-CDH1 (tubules), Anti-Podocalyxin (podocytes). |
| QC Assay Kits [54] | Ensure quality and genetic fidelity of source cells and final organoids. | STR profiling, karyotyping, mycoplasma testing, differentiation potential assays. |
Signaling Pathways in Kidney Disease and Drug Action
Understanding the key signaling pathways active in kidney organoids and their associated diseases is critical for rational drug design and interpreting screening results. The following diagram illustrates pathways frequently targeted in kidney disease drug discovery, such as ADPKD.
Overcoming Challenges: Strategies to Enhance Organoid Maturation and Fidelity
Kidney organoids derived from human induced pluripotent stem cells (iPSCs) represent a transformative platform for studying renal development, disease modeling, and drug screening. However, a significant challenge remains the cellular immaturity of these in vitro models, which limits their physiological relevance and translational application. This Application Note details standardized protocols and analytical frameworks for benchmarking kidney organoids against native human fetal and adult kidney tissues, leveraging single-cell technologies to quantify and improve organoid maturation.
Benchmarking Kidney Organoid Composition and Maturity
Single-Cell Census Reveals Prototypical Renal Cell Types
Comprehensive single-cell RNA sequencing (scRNA-seq) analyses confirm that kidney organoids self-assemble into a diversity of renal cell types. When benchmarked against human tissue, organoid cell types show greatest transcriptional similarity to first-trimester fetal kidney, indicating a developmentally arrested state [29] [55]. The tables below summarize the cellular composition and maturity scores of typical kidney organoids.
Table 1: Cellular Composition of Kidney Organoids Based on scRNA-Seq Analysis
| Cell Class | Representative Markers | Presence in Organoids | Similarity to Human Tissue |
|---|---|---|---|
| Podocytes | NPHS2, NPHS1, WT1, PODXL | 14-29% of cells [29] | Fetal (8-17 weeks) [55] |
| Proximal Tubule | LRP2, LTL, SLC3A1 | Protocol-dependent [29] | Fetal (8-17 weeks) [55] |
| Distal Nephron | CDH1, GATA3, AQP2 | Present [55] | Fetal distal tubule [55] |
| Loop of Henle | SLC12A1 | Present [29] [55] | Fetal [55] |
| Nephron Progenitors | PAX2, LHX1, SIX2 | Present (Immature) [55] | Fetal mesenchyme [55] |
| Stromal Cells | FOXD1, SULT1E1, DCN | Multiple subsets [55] | Fetal stromal cells [55] |
Table 2: Identified Off-Target Cell Populations in Untreated Organoids
| Off-Target Cell Type | Representative Markers | Reported Prevalence | Strategy for Reduction |
|---|---|---|---|
| Neuronal Cells | SOX2, STMN2, TUBB3 | ~11% of cells [29] | BDNF/NTRK2 inhibition [29] |
| Muscle Cells | MYOG, MYLPF | Protocol-dependent [29] | Transplantation [55] |
| Melanocyte-like Cells | PMEL, MLANA | Present in some protocols [29] | Transplantation [55] |
Key Limitations in Organoid Maturation
Critical limitations identified through benchmarking include:
- Incomplete Nephron Segmentation: Organoids lack defined distal convoluted tubules (DCT) and collecting duct (CD) segments with principal and intercalated cells found in adult kidney [55].
- Transcriptional Immaturity: While organoids contain prototypical renal cell types, their global gene expression profiles align more closely with fetal than adult tissues [29] [55].
- Presence of Off-Target Cells: All current protocols generate 10-21% non-renal cell types, including neuronal, muscle, and melanocyte-like populations [29].
Experimental Protocols for Characterization and Improvement
Protocol 1: Single-Cell RNA Sequencing for Benchmarking
Objective: To comprehensively characterize the cellular identity, purity, and maturity of kidney organoids by comparing them to reference datasets from human fetal and adult kidney.
Materials:
- Single-cell suspension from day 25-29 kidney organoids (≥10,000 cells)
- Reference scRNA-seq datasets from human fetal (8-17 week) and adult kidney
- DropSeq or 10x Genomics platform reagents
- Computational resources for data analysis (R, Python, Seurat, Scanpy)
Procedure:
- Organoid Dissociation: Mechanically and enzymatically dissociate kidney organoids into single-cell suspensions using collagenase IV (1-2 mg/mL) and Accutase. Pass cells through a 40-μm strainer and confirm viability >80% [29] [55].
- Single-Cell Library Preparation: Process cells using the chosen high-throughput scRNA-seq platform (e.g., 10x Genomics) according to manufacturer instructions. Target a sequencing depth of ~50,000 reads per cell [29].
- Data Integration and Clustering: Process raw sequencing data with standard pipelines (Cell Ranger). Integrate organoid data with public or newly generated fetal and adult kidney reference datasets using mutual nearest neighbors (MNN) batch correction [29].
- Cell Type Annotation: Perform graph-based clustering and annotate cell types using known marker genes (Table 1).
- Maturity Assessment: Use random forest classifiers to project organoid cells onto fetal and adult reference maps to quantify similarity [55]. Perform differential expression analysis to identify immature versus mature gene signatures.
Protocol 2: Inhibition of BDNF/NTRK2 Signaling to Reduce Neuronal Off-Target Cells
Objective: To significantly reduce the prevalence of off-target neuronal populations in kidney organoids, thereby improving purity, based on findings that this pathway is active during organoid differentiation [29].
Materials:
- iPSCs committed to posterior intermediate mesoderm (day 3-4 of differentiation)
- ATR-002 (NTRK2 inhibitor) or other selective BDNF/NTRK2 pathway inhibitor
- Base differentiation medium (Advanced RPMI 1640)
- Small molecule inhibitors (CHIR99021, FGF9, Heparin)
Procedure:
- Organoid Differentiation: Differentiate iPSCs into kidney organoids using a established protocol (e.g., Takasato or Morizane method) [29].
- Inhibitor Treatment: From the point of 3D aggregation (approximately day 4-7), supplement the differentiation medium with a selective NTRK2 inhibitor (e.g., ATR-002 at 1 μM). Refresh the medium with the inhibitor every 48 hours until day 18-25 [29].
- Validation and Analysis: Harvest organoids and quantify the reduction in neuronal cells (typically ~90%) via:
- Immunofluorescence: Stain for neuronal markers (e.g., TUBB3, STMN2) and renal markers (e.g., NPHS1, LRP2).
- scRNA-seq: Confirm reduction in neuronal cluster abundance and assess for any unintended effects on kidney differentiation [29].
Protocol 3: Organoid Transplantation for Enhanced Maturation
Objective: To improve organoid maturation and reduce off-target cells by transplanting organoids under the kidney capsule of immunodeficient mice, providing a more physiological microenvironment [55].
Materials:
- Mature kidney organoids (day 25-30)
- NOD-scid IL2Rgamma[null] (NSG) mice, 8-12 weeks old
- Sterile surgical equipment (forceps, scissors, suture)
- Anesthesia system (Isoflurane)
Procedure:
- Organoid Preparation: Harvest mature organoids and keep in cold base medium until transplantation.
- Surgical Transplantation: Anesthetize the mouse and make a small flank incision. Gently expose the kidney. Using a fine glass pipette or needle, place 3-5 organoids under the renal capsule [55].
- Post-Operative Care: Return the mouse to its cage and monitor for 4-6 weeks.
- Graft Analysis: After 4-6 weeks, harvest the kidney and analyze the transplanted organoids.
- Histology: Fixed tissue sections for H&E and immunofluorescence staining for mature renal markers (e.g., PODXL, LRP2, AQP2).
- scRNA-seq: Process grafts to quantify changes in cell composition, specifically noting the diminished off-target populations and evidence of enhanced maturation [55].
Signaling Pathways in Kidney Development and Organoid Differentiation
The in vitro differentiation of iPSCs into kidney organoids recapitulates key developmental signaling pathways that drive the specification of renal lineages from the intermediate mesoderm. The following diagram illustrates the core pathway.
Figure 1: Key Signaling Pathways in Kidney Organoid Differentiation. The stepwise differentiation of iPSCs into kidney organoids is directed by the sequential activation of core developmental signaling pathways. The process begins with WNT activation to induce a posterior primitive streak fate, followed by FGF9 signaling to pattern the intermediate mesoderm. Sustained FGF9 supports the metanephric mesenchyme and nephron progenitor populations, with a subsequent WNT pulse driving the mesenchymal-to-epithelial transition that forms segmented nephrons [14].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Kidney Organoid Differentiation and Characterization
| Reagent/Category | Example Product | Function in Protocol |
|---|---|---|
| WNT Pathway Activator | CHIR99021 (GSK3β inhibitor) | Induces primitive streak and posterior intermediate mesoderm; critical for nephrogenesis [14] [56]. |
| Growth Factors | Recombinant Human FGF9 | Patterns and maintains intermediate mesoderm and nephron progenitor populations [14] [56]. |
| Extracellular Matrix | Cultrex Basement Membrane Extract, Type 2 | Provides a 3D scaffold for organoid self-organization and growth [57]. |
| Cell Dissociation Agent | Accutase / TrypLE | Gently dissociates organoids into single cells for scRNA-seq or subculture [57]. |
| Inhibitors for Purity | ATR-002 (NTRK2 inhibitor) | Suppresses off-target neuronal differentiation by blocking BDNF/NTRK2 signaling [29]. |
| Antibodies for Validation | Anti-PODXL, Anti-NPHS1, Anti-LRP2, Anti-TUBB3 | Validates renal cell type identity and purity via immunofluorescence [29] [55]. |
A significant challenge in the differentiation of kidney organoids from induced pluripotent stem cells (iPSCs) is the consistent appearance of off-target, non-renal cell populations. These undesirable cells, primarily neurons and myocytes, can represent 10-20% of the total cells in an organoid and typically appear around 18 days of culture, complicating the interpretation of disease modeling data and reducing the physiological relevance of the model [12]. This Application Note details evidence-based strategies to minimize these off-target populations, with a particular focus on protocol modifications that enhance the purity of renal lineages for more reliable research outcomes.
Understanding Off-Target Populations in Kidney Organoids
During standard differentiation protocols, iPSCs can give rise to cell types not native to the kidney. Single-cell RNA sequencing analyses have confirmed the presence of clusters expressing neural and muscular markers, indicating a divergence from the intended renal differentiation path [12]. The appearance of these cells is attributed to the inherent complexity of directing stem cell fate and the presence of signaling environments that can support multiple lineage specifications simultaneously. Minimizing these populations is crucial for producing higher-quality kidney organoids that can be maintained longer in culture, thereby improving their maturation potential for more accurate disease modeling and drug screening applications [12] [7].
Quantitative Assessment of Off-Target Cells
The following table summarizes key findings from the literature regarding the prevalence and characteristics of off-target cell types in kidney organoids.
Table 1: Characterization of Off-Target Cell Populations in Kidney Organoids
| Off-Target Cell Type | Reported Prevalence | Key Identified Markers | Typical Onset in Culture |
|---|---|---|---|
| Neurons | 10-20% of total cells [12] | Neural-specific class III beta-tubulin (TUJ-1) [58] | Around day 18 [12] |
| Myocytes | 10-20% of total cells [12] | Desmin [58] | Around day 18 [12] |
| Chondrocytes | Observed in prolonged culture [12] | COL2A1, SOX9, ACAN [12] | Between days 18 and 25 [12] |
Core Strategy: Protocol Modification with Extended FGF9 Treatment
Rationale and Mechanistic Insight
Fibroblast Growth Factor 9 (FGF9) is a critical morphogen in native kidney development, promoting the survival and expansion of nephron progenitor populations [7]. Beyond its pro-renal role, FGF9 has been demonstrated to possess an inhibitory effect on alternative differentiation pathways, including chondrogenesis [12]. Extending exposure to FGF9 capitalizes on this dual function, thereby favoring renal lineage commitment over off-target fates.
The diagram below illustrates the signaling logic and experimental workflow for this strategy.
Detailed Experimental Protocol
Objective: To reduce the emergence of neuronal and muscle populations in iPSC-derived kidney organoids by extending the duration of FGF9 supplementation.
Key Reagent Solutions: Table 2: Essential Research Reagents for Protocol Implementation
| Reagent | Function/Application in Protocol |
|---|---|
| FGF9 (Recombinant Human) | Key signaling molecule for renal lineage specification and suppression of off-target differentiation [12]. |
| CHIR99021 (GSK3β Inhibitor) | Canonical WNT pathway activator for initial induction of primitive streak and intermediate mesoderm [7]. |
| BMP7 (Recombinant Human) | Used in some protocols alongside FGF9 to pattern intermediate mesoderm [7]. |
| Low-Adhesion Plates | For 3D spheroid formation and subsequent organoid culture. |
Step-by-Step Workflow:
Initial Differentiation and Aggregation: Differentiate iPSCs into kidney organoids according to your established base protocol (e.g., Takasato or Morizane method [7]). This typically involves:
- Primitive Streak Induction: Treat iPSCs with CHIR99021 for 3-4 days to activate WNT signaling and specify posterior primitive streak.
- Intermediate Mesoderm Patterning: Pattern the primitive streak cells into intermediate mesoderm using FGF9 and, optionally, BMP7.
- 3D Aggregation: Dissociate the cells and aggregate them into 3D spheroids in low-adhesion plates to initiate self-organization.
Modified FGF9 Treatment Regimen:
- Control Protocol: Maintain organoids in culture medium as described in the base protocol, where FGF9 supplementation is typically stopped around day 5 of differentiation.
- Experimental Protocol: Supplement the culture medium with FGF9 (e.g., 50-200 ng/mL, concentration should be optimized for your cell line and base protocol) for 1 additional week, continuing treatment until approximately day 12 of differentiation [12].
Organoid Maturation and Analysis:
- After the extended FGF9 treatment, continue to culture the organoids under standard conditions until the desired endpoint (e.g., day 25-30).
- Assess the efficiency of off-target population reduction using the analytical methods outlined in Section 5.
Validation and Analysis Methods
To confirm the reduction of neuronal and muscle cells, the following analytical approaches are recommended:
Immunofluorescence (IF) Staining:
- Targets for Off-Target Cells: Stain for neuronal marker TUJ-1 and muscle marker Desmin [58]. A successful protocol will show a significant reduction in the area and intensity of staining for these markers.
- Targets for Renal Structures: Co-stain for renal markers to ensure protocol modifications do not compromise target differentiation. Key markers include NPHS1 (podocytes, glomeruli), LTL (proximal tubules), and ECAD (tubules) [12] [7].
Gene Expression Analysis (qPCR):
- Quantify the expression levels of lineage-specific markers.
- Off-Target Marker Panels: Analyze transcripts for neuronal (e.g., TUBB3) and myogenic (e.g., MYOD1, DES) genes.
- Renal Marker Panels: Analyze transcripts for renal lineage genes (e.g., SIX2, WT1, NPHS1) to verify renal identity is maintained or enhanced [12].
Histological Staining:
- Use stains like Alcian Blue to identify other common off-target populations, such as cartilage, which can appear in prolonged cultures and is also suppressed by extended FGF9 treatment [12].
Kidney organoids derived from induced pluripotent stem cells (iPSCs) have emerged as a transformative platform for studying renal development, disease modeling, and drug nephrotoxicity screening [7]. These three-dimensional structures recapitulate key aspects of kidney development, forming nephron-like structures including glomerular and tubular segments [7]. However, conventional static culture methods severely limit organoid viability and maturation, primarily due to inadequate nutrient delivery and waste removal that leads to necrotic core formation [59] [60]. This technological gap represents a critical bottleneck in harnessing the full potential of kidney organoids for research and therapeutic applications.
Advanced culture systems incorporating bioreactors and millifluidic technologies address these limitations by providing dynamic microenvironments that enhance viability, promote structural maturation, and improve experimental reproducibility [59] [61]. These systems mimic physiological conditions through controlled fluid flow, nutrient perfusion, and mechanical stimulation, ultimately generating organoids with greater physiological relevance for disease modeling and drug screening applications [59] [61]. This Application Note details protocols and analytical methods for implementing these advanced culture technologies specifically for kidney organoid research.
System Comparisons and Selection Criteria
Table 1: Comparison of Advanced Culture Systems for Kidney Organoids
| System Type | Key Features | Scalability | Shear Stress | Primary Applications | Reported Benefits |
|---|---|---|---|---|---|
| Spinning Bioreactors | Rotational culture, homogeneous mixing | High (batch culture) | Low to moderate | Large-scale organoid production, expansion | 3-5.2x faster proliferation [61] |
| Millifluidic Chips | Continuous laminar flow, chamber-based | Medium throughput | Very low | Long-term culture, enhanced differentiation | Significantly reduced necrotic core [60] |
| Microfluidic Organ-on-Chip | Precise microenvironment control, integrated sensors | Lower throughput | Can be high | Disease modeling, drug toxicity testing | Improved structural organization [59] |
| Automated Bioreactor Platforms | Standardized, controlled culture conditions | High | Controlled | High-throughput screening, reproducible production | Improved batch-to-batch consistency [62] |
Operational Principles and Design Considerations
The fundamental advantage of dynamic culture systems lies in their ability to overcome diffusion limitations inherent in static cultures. In millifluidic systems, computational modeling predicts significantly enhanced oxygen concentrations throughout organoids, with particularly dramatic improvements in core regions that would otherwise become necrotic [60]. For example, computational fluid dynamics simulations of midbrain organoids demonstrated that millifluidic culture could raise oxygen levels in core regions above critical thresholds for cell viability, effectively eliminating necrotic cores [60].
Spinning bioreactors operate on different principles, creating homogeneous fluid distributions that ensure uniform exposure to nutrients, oxygen, and signaling molecules throughout the culture vessel [61]. The miniaturized spinning bioreactor (RPMotion) has been specifically optimized for epithelial organoid culture, including kidney lineages, demonstrating 3-5.2-fold increased proliferation rates compared to static controls while maintaining organ-specific phenotypes [61].
Microfluidic systems offer the most precise environmental control, enabling researchers to recreate biomechanical cues such as fluid shear stress – a particularly relevant parameter for kidney organoids given the physiological flow conditions in native nephrons [59]. These systems can be fabricated using 3D printing technologies, with polydimethylsiloxane (PDMS) being the most common material due to its gas permeability and biocompatibility [63].
Implementation Protocols
Bioreactor-Based Kidney Organoid Generation
Table 2: Protocol for Simple Bioreactor-Based Kidney Organoid Generation from iPSCs
| Step | Process Parameters | Duration | Key Quality Controls |
|---|---|---|---|
| iPSC Maintenance | Culture in mTeSR1 on Vitronectin XF-coated plates | Until 80% confluency | Pluripotency marker expression, morphology |
| Mesoderm Induction | CHIR99021 (GSK3β inhibitor) in basal medium | 4 days | Primitive streak marker expression |
| Intermediate Mesoderm Patterning | FGF9 ± BMP7 supplementation | 3-5 days | PAX2, OSR1 expression |
| 3D Aggregation | Transfer to low-attachment plates, 8,000-9,000 cells/well | 24-48 hours | Uniform embryoid body formation |
| Nephron Differentiation | FGF9, CHIR99021 in spinning bioreactor | 14 days | Tubular structure emergence (day 8) |
| Maturation | Continuous culture in spinning bioreactor | Up to 29 days | Optimal morphology at day 14 [30] |
This protocol, adapted from published methods [30], generates kidney organoids with tubular structures visible by day 8 and optimal tissue morphology at day 14. Comparison with fetal human kidney samples suggests that day-14 organoids most closely resemble late capillary loop stage nephrons [30]. The bioreactor environment significantly enhances the efficiency and reproducibility of organoid formation while reducing reagent costs compared to conventional methods.
Millifluidic Chip Culture for Enhanced Organoid Maturation
For established kidney organoids (typically day 10-14 of differentiation), transfer to millifluidic systems enables long-term culture with enhanced viability and maturation:
- Organoid Transfer: Pre-formed kidney organoids are carefully transferred to millifluidic chambers pre-coated with GelTrex or similar basement membrane matrix [60].
- System Priming: Culture chambers are filled with renal differentiation medium (N2B27 base supplemented with BDNF, GDNF, cAMP, ascorbic acid, and TGF-β3) [60].
- Flow Establishment: Peristaltic pumps are activated at defined flow rates (typically 200-250 μL/min for millifluidic chambers of 2-4 mL volume) to establish continuous laminar flow [60].
- Long-term Maintenance: Medium is refreshed every 3-5 days, with organoids maintained for up to 29 days or longer for maturation studies [64].
- Monitoring: Organoids are regularly assessed for viability, size progression, and morphological changes.
Computational modeling confirms that this millifluidic approach maintains oxygen concentrations throughout organoids above critical thresholds, preventing the necrotic core formation commonly observed in static cultures [60]. The system also enhances differentiation efficiency, likely due to improved metabolic maturation under flow conditions.
Analytical Methods for Quality Assessment
Rigorous quality assessment is essential for validating kidney organoids cultured in advanced systems. The following analytical approaches provide comprehensive characterization:
- Proteomic Analysis: Mass spectrometry-based proteomics can quantify over 6,700 proteins in organoids, revealing maturation-dependent changes including decreased podocyte markers (NPHS1, SYNPO) and increased extracellular matrix proteins (COL1A1, FN1) over time [64].
- Single-Cell RNA Sequencing: This method identifies cell type composition and differentiation trajectories, demonstrating that most proteome changes localize to podocytes, tubular, and stromal cells [64].
- Immunofluorescence Validation: Confocal microscopy of key markers including nephrin (podocytes), LTL (proximal tubules), ECAD (distal tubules), and WT1 (glomerular epithelium) confirms structural organization [7] [64].
- Functional Assays: Albumin uptake assays test proximal tubule function, while response to cytokine stressors like TNFα demonstrates physiological relevance through inflammatory activation [64].
Research Reagent Solutions
Table 3: Essential Research Reagents for Kidney Organoid Culture in Advanced Systems
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Induction Molecules | CHIR99021 (GSK3β inhibitor) | WNT activation, mesoderm induction | Concentration optimization critical [7] |
| Patterning Factors | FGF9, BMP7 | Intermediate mesoderm patterning, nephron progenitor maintenance | Used sequentially or in combination [7] |
| Maturation Cocktails | BDNF, GDNF, cAMP, TGF-β3 | Enhanced neuronal and tubular maturation | Particularly beneficial in millifluidic systems [60] |
| Extracellular Matrices | GelTrex, Matrigel | 3D structural support, biomechanical cues | Reduced concentration required in perfusion systems [63] |
| Basal Media | N2B27 supplement | Defined culture environment | Supports multiple renal lineages [60] |
Signaling Pathways in Kidney Organoid Development
Figure 1: Signaling Pathway Timeline in Kidney Organoid Differentiation
Experimental Workflow Integration
Figure 2: Integrated Workflow from iPSCs to Application-Ready Organoids
Applications in Disease Modeling and Drug Development
The enhanced viability and maturation achieved through advanced culture systems significantly expand the applications of kidney organoids in disease modeling and drug development. Organoids cultured under these improved conditions demonstrate relevant pathophysiological responses, such as increased expression of inflammatory markers (C3, VCAM1) following TNFα exposure – replicating key aspects of human proteinuric kidney disease [64]. This capability makes them particularly valuable for modeling genetic kidney disorders like polycystic kidney disease and congenital anomalies of the kidney and urinary tract (CAKUT) [7].
For drug development applications, the improved reproducibility and scalability of bioreactor-cultured organoids support high-throughput nephrotoxicity screening and therapeutic evaluation [62] [61]. The integration of organoids with microfluidic systems creates opportunities for studying complex disease processes and multi-organ interactions, further enhancing their predictive value for human physiology and toxicology [59].
Advanced culture systems incorporating bioreactors and millifluidic technologies represent a significant advancement in kidney organoid research, directly addressing the critical limitations of conventional static culture methods. The protocols and methodologies detailed in this Application Note provide researchers with practical frameworks for implementing these systems, enabling the generation of kidney organoids with enhanced viability, maturation, and physiological relevance. As these technologies continue to evolve, they promise to further bridge the gap between in vitro models and human kidney physiology, accelerating progress in disease modeling, drug screening, and regenerative medicine applications.
The generation of kidney organoids from induced pluripotent stem cells (iPSCs) presents a transformative opportunity for disease modeling and regenerative medicine. However, a significant challenge remains the lack of integrated, functional vasculature, which limits organoid maturation, size, and physiological relevance. This application note details two synergistic strategies to overcome this limitation: the in vitro co-culture of iPSC-derived kidney organoids with endothelial cells to create pre-vascularized constructs, and their subsequent in vivo transplantation to promote functional anastomosis with the host circulation. These protocols are essential for researchers aiming to create more sophisticated and predictive kidney models for studying disease mechanisms and drug responses.
Key Research Reagent Solutions
The following table catalogues essential materials and reagents used in the vascularization and transplantation of kidney organoids.
Table 1: Essential Research Reagents for Vascularization and Transplantation
| Reagent / Material | Function / Application | Examples & Key Details |
|---|---|---|
| Human Umbilical Vein Endothelial Cells (HUVECs) | A common endothelial cell source for co-culture, enabling the formation of vascular networks within organoids [65] [66]. | Easy-to-harvest; used in creating liver, bone, and cardiac tissue constructs [65]. |
| iPSCs from Patients and Donors | Foundation for generating patient-specific kidney organoids for personalized disease modeling [67]. | Used to derive podocytes for modeling recurrent Focal Segmental Glomerulosclerosis (FSGS) [67]. |
| Extracellular Matrix (ECM) Hydrogels | Provides a 3D scaffold that supports cell self-organization and vascular network formation [65] [66]. | Matrigel is used to facilitate the self-assembly of vascularized endothelial cell–pancreatic islet organoids [66]. |
| Pro-Angiogenic Growth Factors | Directs differentiation and stimulates the formation and stabilization of blood vessels [65]. | Vascular Endothelial Growth Factor (VEGF) is crucial for angiogenesis; Angiopoietin-1 (Ang-1) promotes vascular maturation and stability [68]. |
| Normothermic Machine Perfusion (NMP) System | An ex vivo platform for maintaining and delivering organoids to a decellularized organ scaffold, enabling engraftment [56] [69]. | Used to infuse human kidney organoids into porcine kidneys, demonstrating feasibility for ex vivo cell-based therapies [56] [69]. |
Quantitative Data on Organoid Differentiation and Vascularization
The initial conditions for organoid generation, specifically the number of cells used to form the initial 3D spheroids, significantly impact the resulting organoid's cellular composition and degree of maturation.
Table 2: Impact of Seeding Density on Kidney Organoid Differentiation
| Seeding Density (PIM-committed Cells) | Relative Proportion of Podocyte-, Endothelial-, and Tubular-like Cells | Proportion of Stromal-like Cells | Key Transcriptional Features |
|---|---|---|---|
| 500 & 8,000 cells | Larger proportion [56] | Less abundancy [56] | Higher expression of podocyte markers (TCF21, NPHS2, MAFB) and mitochondrial biogenesis regulator PGC1A [56]. |
| 100,000 & 250,000 cells | Smaller proportion [56] | More abundancy [56] | Lower expression of maturation-associated markers [56]. |
Quantitative assessments of vascularization success include measuring the extent of vascular network formation and its functional benefits.
Table 3: Functional Outcomes of Organoid Vascularization
| Assay Type | Measured Parameter | Outcome of Successful Vascularization |
|---|---|---|
| Glucose-Stimulated Insulin Secretion (GSIS) | Insulin secretion capacity | Co-culture of pancreatic islet organoids with HUVECs significantly enhanced insulin secretion in response to high glucose stimulation [66]. |
| Cell Viability Staining (e.g., Calcein-AM/PI) | Percentage of live cells | Vascularized co-culture prolonged the survival of pancreatic islet organoids during in vitro culture [66]. |
| F-Actin Redistribution (FAR) Assay | Quantitative podocyte injury | A novel method to detect injury caused by circulating permeability factors in FSGS models; used with iPSC-derived podocytes [67]. |
Experimental Protocols
Protocol 1: Co-culture for Pre-vascularizing Kidney Organoids
This protocol outlines the process of generating pre-vascularized kidney organoids through co-culture with endothelial cells, leveraging self-organization principles.
Title: Pre-vascularized Kidney Organoid Workflow
Detailed Procedure:
iPSC Culture and PIM Commitment:
- Culture iPSCs on vitronectin-coated plates in Essential 8 medium.
- To induce posterior intermediate mesoderm (PIM) commitment, treat the cell monolayer with 8 μM CHIR99021 in Advanced RPMI 1640 basal medium for 3 days [56].
- Subsequently, treat the cells with 200 ng/mL FGF9, 1 μg/mL heparin, and 10 ng/mL activin A for 24 hours [56].
3D Spheroid Formation:
- On the day of spheroid formation (designated day 0), treat PIM-committed monolayers with 5 μM CHIR99021 for 1 hour while maintaining FGF9 signaling [56].
- Dissociate the monolayer into single cells and seed them in V-bottom 96-well plates to allow for self-aggregation. For optimal differentiation, use seeding densities between 500 and 8,000 cells per well [56].
Co-culture with Endothelial Cells:
- Combine the formed kidney organoid spheroids with Human Umbilical Vein Endothelial Cells (HUVECs). The specific ratio may require optimization, but a common approach is to mix the cell types during the spheroid formation step or to seed endothelial cells around the pre-formed organoids [65] [66].
- Culture the co-culture in a specialized medium that supports both renal and endothelial cell types.
3D Embedding and Differentiation:
- Embed the co-cultured spheroids in an ECM hydrogel, such as Matrigel, which facilitates self-assembly and vascular network formation [66].
- Maintain the embedded constructs in free-floating culture conditions for up to 16 days to allow for further differentiation and maturation into vascularized kidney organoids [56].
Protocol 2: In Vivo Transplantation via Normothermic Machine Perfusion
This protocol describes an advanced method for transplanting organoids into a whole-organ scaffold using normothermic machine perfusion (NMP), which promotes engraftment and further maturation.
Title: Organoid Transplantation via NMP
Detailed Procedure:
Organ and NMP System Preparation:
Organoid Infusion:
- Harvest the pre-vascularized kidney organoids and prepare them as a suspension in an appropriate carrier medium.
- Infuse the organoid suspension into the organ's arterial circuit while it is being maintained on the NMP system. This allows the organoids to be distributed throughout the organ's vascular architecture [56] [69].
Engraftment and Transplantation:
- Continue perfusion for several hours to allow the infused organoids to engraft within the host organ scaffold.
- Following the ex vivo perfusion period, the organ containing the engrafted human organoids can be transplanted into an animal model for in vivo studies. Research has confirmed the presence of human cells after this procedure, validating the feasibility of the approach [56] [69].
Application in Disease Modeling: A Case Study in FSGS
The integration of these vascularization strategies powerfully enables personalized disease modeling. A prime example is the study of idiopathic nephrotic syndrome and recurrent focal segmental glomerulosclerosis (FSGS) after kidney transplantation.
Mechanism of Action: The protocol involves generating iPSCs from both patients with FSGS and their respective kidney donors [67]. These iPSCs are differentiated into podocytes, the key cells affected in this disease. To model recurrence, donor-derived iPSC-podocytes are exposed to plasma from the corresponding patient, which may contain circulating permeability factors (CPF) that cause podocyte injury [67].
Key Assay: Podocyte injury is quantitatively assessed using a F-actin redistribution (FAR) assay, a novel method that measures cytoskeletal disruption [67]. This personalized in vitro model allows researchers to cross-match donor podocytes with patient factors, assessing individual susceptibility to FSGS recurrence and providing a platform for screening potential therapeutic interventions [67].
The convergence of kidney organoid technology with advanced genome editing represents a transformative approach in nephrology research. Kidney organoids derived from induced pluripotent stem cells (iPSCs) self-organize into three-dimensional structures containing glomerular, tubular, and stromal compartments, recapitulating key aspects of human kidney development and disease [7] [70]. When combined with CRISPR/Cas9-mediated generation of reporter lines, these systems enable unprecedented resolution for tracing cell lineage decisions, optimizing differentiation protocols, and modeling disease mechanisms [71] [70]. This Application Note details methodologies for creating and applying reporter lines in kidney organoid research, providing structured protocols and analytical frameworks for researchers pursuing disease modeling and drug development.
Kidney Organoid Generation from iPSCs
Fundamental Principles and Protocols
The generation of kidney organoids from iPSCs follows a stepwise differentiation process that recapitulates embryonic kidney development, progressing through primitive streak, intermediate mesoderm, and metanephric mesenchyme stages [7] [70]. This process is orchestrated through sequential activation of key signaling pathways:
Figure 1: Signaling pathway progression in kidney organoid differentiation.
Core differentiation protocols typically involve an initial priming step using CHIR99021 (a GSK3β inhibitor) to activate WNT signaling and direct cells toward posterior primitive streak [7] [70]. This is followed by treatment with FGF9 and, in some protocols, BMP7 to pattern the intermediate mesoderm [7]. Cells are then aggregated into 3D spheroids and cultured in low-adhesion conditions to promote self-organization into nephron-like structures containing podocytes (expressing NPHS1, PODXL), proximal tubules (LTL+), and distal segments [7].
Key Research Reagent Solutions
Table 1: Essential reagents for kidney organoid generation and genetic engineering
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Small Molecule Inducers | CHIR99021, BMP7, FGF9 | Direct differentiation through developmental stages | CHIR99021 concentration and timing critically influence efficiency [7] |
| Gene Editing Components | Cas9 protein, sgRNA, ssODN donor templates | Precise genome editing | Ribonucleoprotein (RNP) delivery reduces off-target effects [72] |
| Reporter Constructs | Fluorescent proteins (BFP, mNeon, GFP), Cre/LoxP systems | Cell lineage tracing and live imaging | Homology-independent methods can improve knock-in efficiency [73] |
| Enhancement Reagents | Nedisertib (DNA-PK inhibitor), Nocodazole | Improve HDR efficiency | Nedisertib (0.25 μM) increased precise editing by 24% in BEL-A cells [72] |
| Validation Tools | scRNA-seq, Immunostaining, MALDI-MSI | Characterize organoid composition | MALDI-MSI provides lipidomic profiles without tissue dissociation [74] |
CRISPR/Cas9 Methodology for Reporter Line Generation
Protocol: Efficient Knock-in via Homology-Directed Repair
This protocol enables precise insertion of reporter genes into specific loci in iPSCs, facilitating lineage tracing in kidney organoids.
Materials:
- iPSCs with confirmed pluripotency and normal karyotype
- Cas9 protein (3 μg per reaction)
- Target-specific sgRNA (1:2.5 ratio with Cas9)
- Single-stranded oligodeoxynucleotide (ssODN) donor template (100 pmol)
- Nucleofection system (e.g., Amaxa 4D-Nucleofector with DZ100 program)
- Nedisertib (0.25 μM in DMSO)
- Cell culture media for iPSC maintenance and organoid differentiation
Procedure:
Design Phase (Days 1-2):
- Design sgRNA to target genomic locus of interest immediately adjacent to desired insertion site
- Design ssODN donor template containing:
- Homology arms (36-91 nucleotides flanking cut site)
- Reporter gene (e.g., fluorescent protein)
- Necessary regulatory elements
Nucleofection Preparation (Day 3):
- Harvest and count iPSCs, preparing 5×10⁴ cells per nucleofection reaction
- Pre-mix Cas9 protein and sgRNA at 1:2.5 ratio in RNP complex, incubate 10-15 minutes at room temperature
- Add ssODN donor template to RNP complex
Nucleofection (Day 3):
- Use DZ100 program on Amaxa 4D-Nucleofector
- Resuspend cell pellet in RNP/ssODN mixture
- Transfer to nucleocuvette and nucleofect
- Immediately recover cells in pre-warmed medium
HDR Enhancement (Day 3-4):
- Add Nedisertib (0.25 μM) to culture medium 2 hours post-nucleofection
- Maintain Nedisertib for 24-48 hours to enrich HDR efficiency
Recovery and Expansion (Days 4-10):
- Culture transfected cells in iPSC maintenance medium
- Monitor fluorescence if reporter includes visible marker
- Expand edited cells for validation and differentiation
Troubleshooting Tips:
- Low editing efficiency: Optimize sgRNA design and verify RNP complex quality
- Poor cell viability: Reduce Cas9 concentration or optimize nucleofection parameters
- Insufficient clone recovery: Include a viability-enhancing reagent like ROCK inhibitor
Quantitative Assessment of Editing Efficiency
Table 2: Optimization parameters for CRISPR-Cas9 editing in stem cells
| Parameter | Optimal Condition | Effect on Editing Efficiency | Effect on Viability |
|---|---|---|---|
| Cas9 Concentration | 3 μg/reaction | Higher concentrations increase editing but may reduce viability | 88% viability maintained at optimal concentration [72] |
| gRNA:Cas9 Ratio | 1:2.5 | Balanced ratio maximizes on-target cleavage | Extreme ratios (high or low) can decrease viability by >15% |
| ssODN Donor | 100 pmol/reaction | Sufficient donor template improves HDR rate | Minimal impact on viability |
| Nedisertib Concentration | 0.25 μM | Increases precise editing by 24% | Maintains 74% viability [72] |
| Cell Number | 5×10⁴ cells/reaction | Optimal cell density improves recovery | Higher densities reduce transfection efficiency |
Lineage Tracing Applications in Kidney Organoids
Protocol: Multicolor Lineage Tracing in Kidney Organoids
This protocol employs CRISPR/Cas9 to introduce heritable genetic barcodes enabling high-resolution tracking of cell fate decisions during kidney organoid development.
Materials:
- iPSCs with integrated inducible Cas9 system
- Lentiviral vectors containing barcode library
- Doxycycline or other Cas9 inducers
- Organoid differentiation reagents
- Single-cell RNA sequencing platform
- Bioinformatics pipeline for barcode analysis
Procedure:
Barcode Library Design and Delivery (Days 1-7):
- Design a sgRNA library targeting synthetically introduced, transcriptionally silent genomic barcode arrays
- Package sgRNA library into lentiviral vectors at low MOI (<0.3) to ensure single barcode integration per cell
- Transduce iPSCs and select with appropriate antibiotics for stable integrants
Induction of Diverse Barcodes (Days 8-10):
- Add doxycycline (1-2 μg/mL) to induce Cas9 expression for 48-72 hours
- Cas9 generates unique insertion-deletion mutations (indels) in barcode arrays, creating diverse genetic signatures
Kidney Organoid Differentiation (Days 11-25):
- Differentiate barcoded iPSCs into kidney organoids using established protocols
- Allow cellular proliferation and differentiation to propagate barcodes to descendant cells
Single-Cell Analysis (Days 26-30):
- Dissociate organoids to single-cell suspension
- Perform single-cell RNA sequencing to capture both:
- Transcriptomic data for cell identity
- Barcode sequences for lineage relationships
Lineage Tree Reconstruction (Days 31-35):
- Use computational tools to cluster cells with shared barcodes
- Reconstruct lineage relationships based on barcode similarity
- Overlay transcriptional identities onto lineage framework
Applications:
- Mapping nephron progenitor differentiation trajectories
- Identifying bipotential precursors in kidney development
- Tracing clonal expansion in disease models
- Validating organoid differentiation efficiency
Workflow Integration Diagram
Figure 2: Workflow for CRISPR-based lineage tracing in kidney organoids.
Advanced Applications in Disease Modeling
Protocol: Modeling Genetic Kidney Diseases with Isogenic Reporter Lines
This protocol creates patient-specific disease models by introducing disease-causing mutations into reporter lines, enabling direct observation of pathological processes in kidney organoids.
Materials:
- Patient-derived iPSCs or wild-type iPSCs
- CRISPR/Cas9 components for introducing specific mutations
- Reporter constructs for tagging cell-type-specific markers
- Nephrotoxic compound library (for secondary screens)
- Functional assays (albumin uptake, ciliary staining, etc.)
Procedure:
Reporter Line Generation (Weeks 1-4):
- Introduce fluorescent reporter into lineage-specific gene (e.g., PODXL for podocytes or LTL for proximal tubules) using HDR protocol
- Validate reporter specificity and function in kidney organoids
Disease Mutation Introduction (Weeks 5-8):
- Using the same reporter line, introduce patient-specific mutation via HDR
- Generate isogenic control lines by similarly targeted but wild-type editing
- Confirm mutation status by sequencing and functional validation
Phenotypic Screening (Weeks 9-12):
- Differentiate reporter lines into kidney organoids
- Monitor disease-relevant phenotypes (e.g., cyst formation for PKD, barrier integrity for glomerulopathies)
- Use reporter expression to isolate specific cell types for molecular analyses
Therapeutic Intervention (Weeks 13-16):
- Treat diseased organoids with candidate therapeutic compounds
- Quantify phenotypic rescue using reporter expression and morphological changes
- Perform transcriptomic/proteomic analyses on sorted cell populations
Case Study: Polycystic Kidney Disease Modeling
- Generated kidney organoids with PKHD1 mutations using CRISPR/Cas9
- Observed accelerated cyst formation in mutant organoids compared to isogenic controls
- Used proximal tubule reporter to demonstrate tubular origin of cysts
- Screened compound library identifying candidates that reduce cyst formation [70]
The integration of CRISPR/Cas9-generated reporter lines with kidney organoid technology provides a powerful platform for elucidating lineage relationships, optimizing differentiation protocols, and modeling disease mechanisms. The methodologies detailed in this Application Note enable researchers to track cell fate decisions with high resolution, create precise disease models with isogenic controls, and perform quantitative assessments of differentiation efficiency. As kidney organoid systems continue to mature through improved vascularization, patterning, and functional maturation, CRISPR-based lineage tracing will remain an essential tool for validating these advances and expanding the utility of organoids in both basic research and drug development pipelines.
Validation and Benchmarking: Ensuring Organoid Faithfulness to Human Kidney Biology
The generation of kidney organoids from human induced pluripotent stem cells (hiPSCs) presents a transformative approach for modeling human development, disease, and drug screening. However, the complexity and heterogeneity of these three-dimensional structures necessitate robust, high-resolution validation methods. Single-cell RNA sequencing (scRNA-seq) has emerged as the gold standard for validating organoid quality, providing an unbiased cellular census that assesses composition, identity, and reproducibility at the transcriptome level [75] [43]. This technology enables researchers to move beyond bulk analysis and limited marker staining, offering a comprehensive, data-driven evaluation of how well organoids recapitulate the target tissue—the human kidney.
The power of scRNA-seq lies in its ability to deconstruct organoids into their constituent cell types, quantify their proportions, identify rare or off-target populations, and benchmark their maturity against native human fetal and adult tissues [55]. By profiling hundreds of thousands of single cells, researchers can address critical questions about organoid faithfulness, ensuring they serve as reliable surrogates in biomedical research. This application note details the protocols and methodologies for leveraging scRNA-seq to validate and quality-control kidney organoids derived from hiPSCs.
Core Single-Cell RNA Sequencing Technologies
Several scRNA-seq protocols are available, each with distinct advantages in throughput, transcript coverage, and applications. The choice of protocol significantly influences the resolution of the organoid census.
Table 1: Comparison of Key scRNA-seq Protocols Relevant to Organoid Analysis
| Protocol | Isolation Strategy | Transcript Coverage | UMI | Amplification Method | Key Features for Organoid Research |
|---|---|---|---|---|---|
| Drop-Seq [76] | Droplet-based | 3'-end | Yes | PCR | High-throughput, low cost per cell; ideal for profiling thousands of cells from complex organoids. |
| inDrop [76] | Droplet-based | 3'-end | Yes | IVT* | Uses hydrogel beads; cost-effective for large-scale experiments. |
| Smart-Seq2 [76] | FACS | Full-length | No | PCR | High sensitivity for low-abundance transcripts; superior for detecting splice variants and RNA editing. |
| CEL-Seq2 [76] | FACS | 3'-only | Yes | IVT | Linear amplification reduces bias; suitable for lower-throughput, high-precision studies. |
| SPLiT-Seq [76] | Not required | 3'-only | Yes | PCR | Uses combinatorial indexing; no need for physical single-cell isolation, enabling massive scalability. |
IVT: In vitro transcription *FACS: Fluorescence-activated cell sorting
For most kidney organoid validation studies, droplet-based methods like Drop-Seq and 10x Genomics Chromium (which builds on similar principles) are preferred due to their ability to profile tens of thousands of cells simultaneously, capturing the full spectrum of cellular heterogeneity [76] [77]. However, for investigations requiring full-length transcript information, such as isoform usage in developing nephrons, plate-based full-length methods like Smart-Seq2 are more appropriate.
Essential Workflow for Organoid Dissociation and Library Preparation
The initial and most critical wet-lab step is the creation of a high-quality single-cell or single-nucleus suspension from kidney organoids.
- Single-Cell Suspension: This involves the enzymatic and mechanical dissociation of the 3D organoid structure. A typical protocol might use a combination of collagenase and trypsin to digest extracellular matrix, followed by gentle pipetting or passage through a fine needle. It is crucial to work on ice and use chilled buffers to minimize the transcriptional stress response that dissociation can induce [77]. Viability should be confirmed using dyes like trypan blue, and the cell concentration should be adjusted to the requirements of the chosen scRNA-seq platform (e.g., 500-20,000 cells/μL for 10x Genomics) [77].
- Single-Nucleus RNA-seq (snRNA-seq): This is a powerful alternative, especially for tissues that are difficult to dissociate or for frozen organoid samples. snRNA-seq profiles the RNA within the nucleus, which can provide a different expression profile bias compared to whole cells but is highly effective for classifying cell types and states in complex tissues [77].
- Library Preparation and Sequencing: Following the manufacturer's protocol for the chosen platform (e.g., 10x Genomics), cells are encapsulated into droplets with barcoded beads, enabling mRNA capture, reverse transcription, and cDNA amplification. The resulting libraries are then sequenced using a paired-end strategy, with a recommended depth of about 20,000 reads per cell to confidently quantify gene expression [77].
Workflow for scRNA-seq of Kidney Organoids
Key Quality Assessments via scRNA-seq
Defining Cellular Composition and Identifying Off-Target Cells
A primary application of scRNA-seq is conducting a precise census of cell types within a kidney organoid. Unsupervised clustering of the single-cell transcriptome data reveals distinct populations corresponding to podocytes, proximal tubules, distal nephron segments, and interstitial cells [55]. A critical finding from these analyses is the common presence of off-target cells—populations not native to the kidney, such as neuronal cells (expressing SOX2, STMN2), muscle-like cells (expressing MYOG), and melanocytes [75] [55].
The proportion of these off-target cells can vary significantly between different iPSC lines and differentiation protocols. scRNA-seq enables the quantification of this variability, providing a key quality metric. For instance, one study profiling over 450,000 cells from kidney organoids derived from four iPSC lines found that while nephron cell classes were reproducible, the proportion of off-target cells was a major source of line-to-line variability [55]. This data is crucial for optimizing differentiation protocols to enhance organoid purity.
Table 2: Common Cell Types and Off-Target Populations Identified in Kidney Organoids via scRNA-seq
| Cell Category | Specific Cell Type / Population | Key Marker Genes | Typical Proportion in Organoids |
|---|---|---|---|
| On-Target Kidney | Podocytes | NPHS2, NPHS1, WT1 | Variable (~5-20%) |
| Proximal Tubule (PT) | LRP2 | Variable (~10-25%) | |
| Thick Ascending Limb (TAL) | SLC12A1 | Variable (~5-15%) | |
| Distal Nephron | GATA3, AQP2 | Variable (~5-15%) | |
| Nephron Progenitor Cells (NPC) | PAX2, LHX1 | Can be high in immature organoids | |
| Off-Target | Neuronal-like | SOX2, STMN2 | Highly variable (can be >10%) |
| Muscle-like | MYOG | Highly variable | |
| Melanocyte-like | PMEL | Highly variable |
Benchmarking against Native Tissue and Assessing Maturation
scRNA-seq allows for the direct comparison of organoid transcriptomes with those of human fetal and adult kidney cells. Computational integration and classification algorithms (e.g., random forest) show that kidney organoid cells are most similar to first and second-trimester fetal kidneys, confirming their immature state [75] [55]. This benchmarking identifies deficiencies in maturity and missing populations. For example, many kidney organoid protocols historically failed to generate a mature, segmented collecting duct with principal cells (AQP2+) and intercalated cells [75].
Furthermore, ligand-receptor analysis of scRNA-seq data from differentiating organoids can pinpoint signaling pathways that drive the development of off-target lineages. For instance, the BDNF-NTRK2 pathway was identified as active in off-target neurons. The inhibition of NTRK2 with K252a during differentiation successfully reduced neuronal contamination by 90%, demonstrating how scRNA-seq data can directly guide protocol improvement [75].
Analytical Framework for Organoid Validation
Application to Kidney Organoid Disease Modeling
The ultimate test for a kidney organoid is its utility in modeling human disease. scRNA-seq is instrumental in validating that disease phenotypes are accurately recapitulated. In autosomal dominant polycystic kidney disease (ADPKD) models, CRISPR/Cas9 knockout of PKD1 or PKD2 in hiPSCs leads to cyst formation in kidney organoids. scRNA-seq can confirm that the cystic cells originate from specific tubular segments and reveal the altered transcriptional pathways driving cystogenesis [75] [43].
Similarly, for modeling acute kidney injury (AKI), organoids can be exposed to nephrotoxins like cisplatin. scRNA-seq analysis not only verifies the induction of injury biomarkers (e.g., HAVCR1 in proximal tubules, NGAL in distal tubules) but also identifies the specific subpopulations of tubular cells that are most vulnerable to damage, providing deeper mechanistic insights than bulk assays [75]. This granular level of validation is essential for building confidence in organoid-based disease models and employing them in high-throughput drug screening.
Table 3: Key Research Reagent Solutions for scRNA-seq of Kidney Organoids
| Item | Function / Application | Example Products / Assays |
|---|---|---|
| Dissociation Enzymes | Breakdown of extracellular matrix to create single-cell suspensions. | Collagenase, Trypsin-EDTA, Accutase, Liberase. |
| Viability Stain | Distinguishing live from dead cells prior to library prep. | Trypan Blue, Propidium Iodide (PI), 7-AAD. |
| Dead Cell Removal Kit | Removal of apoptotic cells to improve data quality. | Magnetic bead-based kits (e.g., from Miltenyi Biotec). |
| scRNA-seq Kit | Core reagent kit for single-cell partitioning, barcoding, and library construction. | 10x Genomics Chromium Next GEM Single Cell 3' Reagent Kits, Parse Biosciences Evercode Whole Transcriptome Kit. |
| Nuclei Isolation Kit | For extraction of nuclei from frozen or hard-to-dissociate organoids. | 10x Genomics Nuclei Isolation Kit, Covaris truChIP Chromatin Shearing Kit. |
| Bioanalyzer/TapeStation | Quality control of RNA and final sequencing libraries. | Agilent Bioanalyzer 2100, Agilent TapeStation. |
| Next-Generation Sequencer | High-throughput sequencing of prepared libraries. | Illumina NovaSeq, NextSeq. |
Single-cell RNA sequencing has firmly established itself as an indispensable tool in the quality control pipeline for kidney organoid research. It provides an unparalleled, unbiased resolution to validate cellular identity, assess reproducibility across iPSC lines, benchmark maturity, and confirm disease phenotypes. As organoid protocols continue to evolve towards greater complexity and maturity—for example, by incorporating collecting duct lineages and vascularization—scRNA-seq will remain the critical gold standard for validation, ensuring these powerful models faithfully serve the advancement of kidney research and drug discovery.
Within the field of nephrology, kidney organoids derived from human induced pluripotent stem cells (iPSCs) have emerged as a transformative platform for studying human development, disease mechanisms, and drug responses in vitro [18] [34]. A critical question, however, surrounds their fidelity to native human kidney tissues across developmental stages. Evaluating this fidelity is a prerequisite for validating organoids as accurate models for adult kidney diseases, which affect hundreds of millions globally [18] [34].
Single-cell RNA sequencing (scRNA-seq) has become the gold standard for this rigorous comparison, enabling unbiased characterization of cellular heterogeneity, lineage relationships, and transcriptional maturity [29] [78]. This Application Note synthesizes current protocols and analytical frameworks for comparing kidney organoid transcriptomes to fetal and adult human kidney references. We provide a detailed experimental workflow, summarize key quantitative findings in structured tables, and outline essential reagent solutions to guide researchers in validating their own organoid models for disease modeling research.
Comparative Analysis of Kidney Organoid Transcriptomes
Key Findings from Single-Cell Transcriptomic Studies
Comprehensive scRNA-seq analyses have revealed critical insights into the composition and maturity of kidney organoids. A landmark study by Wu et al. (2018) compared two widely used directed differentiation protocols—Takasato and Morizane—by analyzing 83,130 cells from 65 organoids against fetal and adult human kidney transcriptomes [29]. The data indicate that while both protocols generate a diverse range of kidney cell types, the derived cells are immature and resemble first-trimester fetal kidney more closely than adult tissue [29] [34]. Furthermore, a significant proportion of cells (10–20%) are non-renal, including neuronal and muscle cell types [29] [18].
Table 1: Quantitative Comparison of Kidney Organoid Protocols via scRNA-Seq (adapted from Wu et al.)
| Protocol Feature | Takasato Protocol | Morizane Protocol |
|---|---|---|
| Representative Nephron Structures | Glomeruli, properly segmented tubules [29] | Multisegmented nephron structures [18] |
| Podocyte Proportion | ~11% (iPSC-derived) [34] | ~28.5% (iPSC-derived) [29] [34] |
| Tubular Epithelium Proportion | Higher than Morizane [29] | Lower than Takasato [29] |
| Off-Target Cell Proportion | ~21% (neuronal, melanocyte-like) [29] | ~11%-14.3% (neuronal, muscle) [29] [34] |
| Presence of Ureteric Bud/Collecting Duct | Small amount of UB-like regions [34] | Not typically reported [18] |
Benchmarking Maturity Against Native Tissues
Bulk RNA-seq comparisons have confirmed that kidney organoids are most similar to first-trimester and second-trimester fetal kidneys, expressing primitive multipotent markers like SIX2 that are absent in the fully differentiated adult nephron [34]. A more recent transcriptome-wide analysis of tubuloids—epithelial organoids derived from adult nephrectomies, fetal kidneys, or iPSC-derived kidney organoids—provides further refinement of these maturity signatures.
Table 2: Transcriptomic Signatures of Kidney Organoids and Tubuloids
| Model System | Proximal Tubule Marker Expression | Collecting Duct Signature | Key Transcriptional Hallmarks |
|---|---|---|---|
| Adult Human Kidney | Strongest expression [79] | N/A (reference tissue) | Full maturity and functional markers |
| iPSC-derived Kidney Organoids | Higher than adult tubuloids [79] | Low or absent [18] [79] | Fetal/primitive progenitor signatures (e.g., SIX2, PAX2) [34] |
| Adult-Derived Tubuloids | Weaker than iPSC organoids [79] | Enriched [79] | Signatures of aging and inflammation [79] |
| Fetal-Derived Tubuloids | Intermediate [79] | Enriched [79] | Enhanced ureteric tip progenitor signatures [79] |
Experimental Protocols for Transcriptomic Comparison
Core Workflow: From Organoid Generation to scRNA-Seq Analysis
The following diagram outlines the integrated experimental and computational pipeline for assessing organoid fidelity.
Detailed Methodologies
Protocol 1: Kidney Organoid Differentiation from hiPSCs
The following diagram summarizes the key signaling pathways and steps for generating kidney organoids via two common protocols.
Key Steps for the Takasato Protocol (Nephron Progenitor Focus) [29] [18]:
- Primitive Streak Induction: Treat iPSCs with a high dose of the WNT agonist CHIR99201 (e.g., 10 µM) and BMP4 for 24-48 hours to induce a mesodermal lineage [18].
- Posterior Intermediate Mesoderm (PIM) Specification: Continue culture with lower dose CHIR99201 (e.g., 3 µM) alongside Activin A, BMP4, and Retinoic Acid for several days [18].
- Nephron Progenitor Formation: Further differentiate PIM with CHIR99201 (e.g., 1 µM) and FGF9 to generate metanephric mesenchyme expressing markers like SIX2, PAX2, and WT1 [18].
- 3D Organoid Maturation: Dissociate cells and aggregate in 3D culture to promote self-organization into nephron structures containing podocytes, proximal tubules, and distal tubules over ~18-26 total days [29].
Key Steps for the Morizane Protocol [29] [18]:
- Primitive Streak Induction: Treat iPSCs with CHIR to induce late primitive streak.
- Posterior Intermediate Mesoderm Specification: Expose to Activin A to form posterior intermediate mesoderm.
- Nephron Progenitor Formation: Treat with FGF9 to generate NPCs with high efficiency (80-90% expressing SIX2, SALL1, WT1, PAX2) [18].
- 3D Organoid Maturation: Transfer NPCs to 3D culture on low-adherence 96-well plates to form spherical organoids with segmented nephrons [18].
Protocol 2: Single-Cell RNA Sequencing of Organoids
Organoid Dissociation and Cell Preparation [29] [80]:
- Harvesting: Gently collect day 18-26 organoids and wash in cold PBS.
- Enzymatic Dissociation: Incubate organoids in a dissociation enzyme (e.g., TrypLE Select, Accutase, or collagenase) at 37°C for 10-20 minutes with gentle pipetting to create a single-cell suspension.
- Viability and Counting: Pass cells through a cell strainer (e.g., 40 µm), centrifuge, and resuspend. Assess viability and count cells (e.g., using Trypan Blue exclusion). Aim for >90% viability.
- Optional Fluorescence-Activated Cell Sorting (FACS): For enriching specific populations like endothelial cells (ECs), stain the single-cell suspension with a fluorescent antibody (e.g., anti-human CD31) and sort the positive population [80].
scRNA-seq Library Preparation and Sequencing [29] [78]:
- Platform Selection: Use high-throughput droplet-based systems like 10X Genomics Chromium or DropSeq.
- Library Construction: Follow the manufacturer's protocol for single-cell encapsulation, cell lysis, reverse transcription, cDNA amplification, and library construction. The goal is to capture transcripts from thousands of individual cells.
- Sequencing: Sequence libraries on an Illumina platform to a sufficient depth (e.g., 50,000 reads per cell).
Protocol 3: Bioinformatic Analysis and Benchmarking
Data Preprocessing and Clustering [29]:
- Alignment and Quantification: Align sequencing reads to a reference genome (e.g., GRCh38) using tools like Cell Ranger (10X Genomics) or STAR. Generate a gene expression matrix (genes x cells).
- Quality Control: Filter out low-quality cells based on thresholds for unique gene counts, total transcripts, and high mitochondrial read percentage.
- Normalization and Scaling: Normalize data for sequencing depth and scale for downstream analysis using Seurat or Scanpy.
- Dimensionality Reduction and Clustering: Perform Principal Component Analysis (PCA) on highly variable genes. Use graph-based clustering on significant PCs and visualize cells in 2D using t-distributed Stochastic Neighbor Embedding (t-SNE) or Uniform Manifold Approximation and Projection (UMAP). This reveals transcriptionally distinct cell populations.
Comparative Analysis [29] [79]:
- Cell Type Annotation: Annotate clusters by cross-referencing their top differentially expressed genes with known markers from the literature and reference datasets (e.g., from fetal and adult kidney).
- Integration with Reference Datasets: Integrate the organoid scRNA-seq dataset with publicly available or in-house scRNA-seq datasets from human fetal and adult kidneys. This allows direct comparison and assessment of similarity.
- Differential Expression and Pathway Analysis: Identify genes and pathways that are differentially active between organoid cell types and their native counterparts.
- Pseudotemporal Ordering: Use tools like Monocle to reconstruct lineage relationships and infer differentiation trajectories within the organoid data, revealing transcription factor networks associated with fate decisions [29].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Kidney Organoid and Transcriptomics Workflows
| Reagent / Tool | Function / Purpose | Example Use in Protocol |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; activates WNT signaling to induce mesoderm and posteriorize intermediate mesoderm [18]. | Used in initial stages of both Takasato and Morizane protocols [29] [18]. |
| FGF9 (Fibroblast Growth Factor 9) | Promotes survival and proliferation of nephron progenitor cells (NPCs) [18]. | Critical component for NPC generation in Morizane protocol and later stages of Takasato protocol [18]. |
| BMP4 (Bone Morphogenetic Protein 4) | A morphogen involved in mesoderm induction and patterning [18]. | Used in the initial differentiation phase of the Taguchi/Takasato protocol [18]. |
| Activin A | A TGF-β family member used to direct differentiation towards intermediate mesoderm [18]. | Key component in the Morizane protocol for posterior intermediate mesoderm formation [18]. |
| Retinoic Acid | Signaling molecule that patterns the intermediate mesoderm and supports nephron segmentation [18]. | Used in the Takasato protocol for posterior intermediate mesoderm formation [18]. |
| Anti-human CD31 Antibody | Cell surface marker for endothelial cells; used for fluorescence-activated cell sorting (FACS) [80]. | Enrichment of endothelial cells from dissociated organoids for targeted scRNA-seq analysis [80]. |
| 10X Genomics Chromium System | Microfluidic platform for high-throughput single-cell RNA sequencing library preparation [78]. | Generation of barcoded scRNA-seq libraries from thousands of single organoid cells [29] [78]. |
| BDNF/NTRK2 Inhibitor | Inhibits the BDNF-NTRK2 signaling pathway, which is aberrantly active in off-target neuronal cells in organoids [29]. | Refinement protocol: Adding inhibitor reduces neuronal contamination by 90% without impairing kidney differentiation [29]. |
Rigorous comparison of kidney organoid transcriptomes to native fetal and adult tissues is no longer optional but a fundamental standard for validating in vitro models. The integrated application of robust differentiation protocols, scRNA-seq technology, and sophisticated bioinformatic benchmarking provides an unprecedented ability to quantify the fidelity—and limitations—of kidney organoids. While current models capture many aspects of the fetal kidney, challenges remain in achieving full maturation, reducing off-target cells, and incorporating missing components like a functional vasculature and collecting duct system [29] [18] [81]. The continued refinement of these models, guided by detailed transcriptional blueprints, is essential to fully realizing their potential for accurately modeling human kidney diseases and advancing therapeutic discovery.
Within the field of renal research, the generation of kidney organoids from induced pluripotent stem cells (iPSCs) presents a transformative approach for modeling human disease. However, the translational potential of these models is critically dependent on their reproducibility. Substantial biological and technical variability can obscure disease phenotypes and compromise drug discovery efforts [82] [83]. This application note details the principal sources of variability in iPSC-derived kidney organoid research and provides structured protocols and benchmarks to enhance the rigor and reproducibility of these essential in vitro models.
Biological and Technical Variability
The reproducibility of iPSC-derived kidney organoids is challenged by multiple interdependent factors.
- Genetic Heterogeneity: Unlike inbred animal models, human iPSC lines carry the inherent genetic diversity of their donors. This can confound the identification of disease-specific phenotypes, particularly for complex disorders [82].
- iPSC Culture and Derivation Practices: As iPSC technology has become more established, a concerning decline in the reporting of quality control (QC) assessments has been observed. Inconsistent culture practices, passaging methods, and incomplete characterization of starting cell lines introduce significant technical artifacts [82].
- Differentiation Protocol Inconsistencies: Kidney organoid differentiation is a multi-step process sensitive to variations in reagent lots, cell seeding density, and the timing of growth factor additions [82] [7]. Minor protocol modifications are often under-reported, hindering cross-laboratory replication.
A comprehensive analysis of 58 studies using iPSC-derived neural cells to model intellectual and developmental disabilities revealed a median quality score of 16 out of 23, highlighting a widespread issue of incomplete methodological reporting [82].
The Immaturity of Organoid Systems
It is crucial to recognize that current kidney organoid models are inherently immature, resembling embryonic rather than adult kidney tissue [11] [83] [7]. This immaturity limits their utility for modeling late-onset kidney diseases. Furthermore, organoids often lack a fully integrated collecting duct system and exhibit limited vascularization, which restricts their functional capacity [11] [7]. Acknowledging that "organoids are not organs" is a fundamental first step in critically evaluating the data they produce [83].
Best Practices for Enhancing Reproducibility
Strategies for Robust Experimental Design
To mitigate the impact of variability, researchers should adopt the following strategies.
- Employ Isogenic Controls: For monogenic diseases, using CRISPR-Cas9 to correct the disease-causing mutation in patient-derived iPSCs, or to introduce it into control lines, provides the most rigorous control for genetic background. Analysis shows low rates of unwanted changes in gene-edited human PSCs, especially with modern, high-fidelity editing systems [82].
- Utilize Multiple Cell Lines: When isogenic controls are not feasible, the use of multiple patient-derived and control lines (ideally from non-affected family members) helps to distinguish genuine disease phenotypes from background genetic noise [82].
- Implement Comprehensive QC: A rigorous and standardized QC pipeline must be applied at every stage of the organoid generation process, from the pluripotent stem cell stage through to the final differentiated product [82].
Table 1: Essential Quality Control Benchmarks for Kidney Organoid Differentiation
| Stage | QC Category | Specific Assay | Key Readouts/Parameters |
|---|---|---|---|
| iPSC | Molecular & Cellular | Karyotyping / Genetic Analysis | G-banded karyotyping, SNP microarray, CNV analysis, mycoplasma testing [82] |
| Immunostaining / RT-qPCR | Pluripotency markers (OCT4, Nanog, SSEA3/4) [82] | ||
| Technical | Cell Line Metadata | Cell source, reprogramming method, donor demographics, passage number [82] | |
| Progenitor | Molecular & Cellular | RNA Sequencing / RT-qPCR | Progenitor markers (SIX2, WT1, PAX2, OSR1) [11] [7] |
| Immunostaining | Protein expression of progenitor markers | ||
| Technical | Culture Practices | Media composition, extracellular matrix, seeding density, passage number [82] | |
| Organoid | Molecular & Cellular | RNA Sequencing / RT-qPCR | Segmented nephron markers (NPHS1, PODXL, LTL, ECAD) [7] |
| Immunostaining | Structural formation of glomeruli, tubules, and stroma | ||
| Functional | Imaging & Morphometrics | Quantification of organoid size, cyst formation, nephron patterning [11] |
Advanced Model Systems: The Kidney Progenitor Assembloid
Recent innovations, such as the kidney progenitor assembloid (KPA), offer new avenues to improve reproducibility and structural fidelity. This system involves the separate differentiation of iPSCs into induced nephron progenitor cells (iNPCs) and ureteric progenitor cells (iUPCs), which are then combined in a defined ratio to self-assemble [11].
This approach yields a spatially patterned organoid with nephrons surrounding a central collecting duct system, dramatically improving cellular complexity, maturation, and physiological function compared to conventional organoids [11]. The KPA platform has demonstrated exceptional potential for faithfully recapitulating complex diseases like autosomal dominant polycystic kidney disease (ADPKD) [11].
The workflow for generating these assembloids is summarized below:
Detailed Protocols
Protocol: Stirred Suspension Bioreactor Differentiation
Adapting differentiation protocols from static monolayer to stirred suspension systems can significantly enhance yield, reduce batch-to-batch variation, and improve functional maturation, as demonstrated in cardiac differentiation [84]. The following is a generalized workflow adaptable for kidney progenitor differentiation.
Key Principle: Stirred bioreactors provide a homogeneous environment, improving nutrient distribution, gas exchange, and consistent cell aggregation, which directly addresses major sources of technical variability [84].
Workflow:
- Input Cell Quality Control: Begin with quality-controlled master cell banks. Validate pluripotency marker expression (e.g., >70% SSEA4+ via FACS) and ensure normal karyotype [84].
- Embryoid Body (EB) Formation: Seed high-quality iPSCs into a stirred bioreactor system to allow for spontaneous EB aggregation.
- Size Monitoring: Monitor EB diameter daily. Initiate differentiation when the majority of EBs reach a target diameter of ~100 µm to ensure optimal factor penetration [84]. EBs that are too large (>300 µm) differentiate inefficiently.
- Directed Differentiation: Activate the key signaling pathway (e.g., WNT via CHIR99021) for a defined period.
- Pathway Inhibition: After a defined gap, inhibit the pathway (e.g., using IWR-1) to drive specification.
- Maturation and Harvest: Continue culture in maturation media with periodic media changes.
Table 2: Benchmarking Suspension vs. Monolayer Differentiation
| Parameter | Stirred Suspension Bioreactor | Static Monolayer |
|---|---|---|
| Scalability | Highly scalable from mL to L volumes [84] | Poor scalability, limited by surface area |
| Yield (cells/mL) | ~1.2 million [84] | Lower and more variable |
| Purity | High (~94% TNNT2+ in cardiac model) [84] | Variable between batches and wells |
| Inter-Batch Variability | Lower | Higher [84] |
| Functional Maturity | More mature functional properties observed [84] | Less mature |
Protocol: Computational Composition Analysis with CellMap
Bulk RNA-seq is cost-effective but masks cellular heterogeneity. Computational deconvolution tools like CellMap can characterize the cellular composition of kidney organoids from bulk transcriptomics data, providing a high-resolution, reproducible QC metric [85].
- Principle: CellMap uses non-negative least squares (NNLS) regression to decompose a bulk RNA-seq sample into cell type proportions based on pre-defined cell type expression profiles derived from single-cell or single-nucleus RNA-seq datasets [85].
- Procedure:
- Generate Reference Profiles: Build cell type-specific expression profiles (e.g., for podocytes, proximal tubule cells, distal tubule cells, stromal cells, off-target neurons) from publicly available or in-house scRNA-seq datasets of human kidney or kidney organoids.
- Sequence Your Organoids: Perform bulk RNA-seq on your differentiated kidney organoid samples.
- Deconvolution Analysis: Use the CellMap tool to estimate the proportion of each cell type present in the bulk organoid sample.
- Application: This method allows for robust batch-to-batch comparison, assessment of differentiation protocol reproducibility, and verification of the absence of significant off-target cell types [85].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Kidney Organoid Generation
| Reagent / Material | Function & Importance | Example Use |
|---|---|---|
| CHIR99021 | A GSK3β inhibitor that activates canonical WNT signaling. Critical for initial induction of primitive streak and intermediate mesoderm [7]. | Used in the first step of most kidney organoid protocols to direct mesodermal fate [7]. |
| FGF9 (Fibroblast Growth Factor 9) | Supports the survival, maintenance, and expansion of the metanephric mesenchyme and nephron progenitor cells [7]. | Added after WNT activation to pattern intermediate mesoderm and maintain nephron progenitors [11] [7]. |
| BMP7 (Bone Morphogenetic Protein 7) | Supports MM survival and proliferation during kidney development [7]. | Included in some protocols alongside FGF9 to enhance progenitor cell yield [7]. |
| Extracellular Matrix (e.g., Matrigel) | Provides a 3D scaffold that supports cell polarization, self-organization, and survival, mimicking the in vivo basement membrane [83] [86]. | Used to embed progenitor cells or EBs to facilitate 3D organoid formation and maturation. |
| R-spondin | Agonist of the WNT signaling pathway by binding to LGR receptors. Enhances WNT signaling specificity and strength [83]. | Used in tissue-derived organoid cultures and can be incorporated into PSC-derived protocols to stabilize progenitor states. |
| Stirred Bioreactor System | Provides a controlled, homogeneous environment for cell culture. Improves differentiation efficiency, yield, and consistency by enhancing nutrient/waste exchange [84]. | For scalable and reproducible generation of EBs and subsequent differentiation into kidney lineages. |
Signaling Pathways in Kidney Organogenesis
The successful differentiation of iPSCs into kidney organoids requires the precise, sequential activation of key developmental signaling pathways. The following diagram outlines the core pathways involved in this process:
Defining Quality Control Metrics for Consistent and Reliable Organoid Generation
The generation of kidney organoids from induced pluripotent stem cells (iPSCs) has emerged as a transformative technology for modeling renal development, disease, and drug toxicity. However, the inherent variability in self-organization processes poses a significant challenge to their reliability and broad adoption in research and drug development. Quality control (QC) is therefore not merely a supplementary step but a fundamental requirement to ensure that generated organoids consistently possess the necessary structural, cellular, and functional attributes to serve as valid experimental models. This application note provides a standardized framework of QC metrics and detailed protocols, framed within the context of a broader thesis on using iPSC-derived kidney organoids for disease modeling research. By implementing these standardized assessments, researchers can significantly enhance the reproducibility and predictive power of their kidney organoid studies.
Defining Key Quality Control Metrics for Kidney Organoids
A comprehensive QC strategy for kidney organoids should employ a hierarchical approach, beginning with non-invasive, rapid assessments and progressing to more in-depth molecular and functional analyses [87]. The following metrics are critical for a thorough evaluation.
Morphology and Size Assessment
Purpose: To perform an initial, non-invasive evaluation of organoid formation and overall health. Methodology: Bright-field imaging is used to assess key morphological features. Key Metrics:
- Morphology: Optimal organoids exhibit a dense overall structure with well-defined, smooth borders. Suboptimal features include poor compaction, degradation over time (cell shedding), and the presence of protruding or internal cystic cavities [87].
- Size and Growth Profile: Consistent size within and across batches is a key indicator of reproducible growth. Diameter should be tracked over time; drastic deviations often signal underlying issues. Necrotic cores, indicative of diffusion limitations, commonly appear in organoids exceeding 400 µm in diameter [87] [88].
Table 1: Scoring System for Morphology and Size Assessment
| QC Criterion | Score 0 (Poor) | Score 3 (Adequate) | Score 5 (Excellent) |
|---|---|---|---|
| Surface Integrity | Severe degradation/cell loss | Minor surface irregularities | Smooth, well-defined border |
| Structural Compactness | Very loose, fragmented | Moderately dense | Dense, spherical structure |
| Cystic Structures | Large or multiple cysts | Minor, non-protruding cysts | Absent |
| Size Uniformity (CV) | >30% | 15-30% | <15% |
| Diameter (at day 20) | <150 µm or >400 µm | 150-250 µm or 300-400 µm | 250-300 µm |
Cellular Composition and Cytoarchitectural Organization
Purpose: To verify the presence and correct spatial arrangement of key renal cell types, confirming successful differentiation and patterning. Methodology: Immunofluorescence staining and confocal microscopy at specific time points (e.g., day 20-30 of differentiation) [7] [34]. Key Metrics:
- Cellular Composition: The presence and proportion of podocytes (expressing NPHS1, PODXL), proximal tubule cells (LTL+), distal tubule cells (ECAD+), and stromal cells (FOXD1+) should be confirmed [7]. A lower proportion of off-target cells (e.g., neurons, myocytes) indicates more precise differentiation.
- Cytoarchitectural Organization: The organoid should exhibit distinct nephron-like structures, including glomerular-like formations with surrounding tubules. The presence of well-developed, polarized tubular structures with clear lumens is a marker of advanced maturation [7] [34].
Table 2: Scoring System for Cellular Composition and Organization
| QC Criterion | Score 0 (Poor) | Score 3 (Adequate) | Score 5 (Excellent) |
|---|---|---|---|
| Podocyte (NPHS1+) Presence | <5% | 5-15% | >15% |
| Proximal Tubule (LTL+) Presence | <10% | 10-25% | >25% |
| Off-Target Cells | >30% | 15-30% | <15% |
| Glomerular Structure Formation | Absent | Rudimentary structures | Multiple, well-defined glomeruli |
| Tubular Organization | Disorganized cell clusters | Short, poorly polarized tubules | Elongated, polarized tubules with clear lumens |
Functional and Transcriptomic Assessment
Purpose: To evaluate the functional maturity and transcriptional fidelity of kidney organoids relative to native human tissue. Methodology:
- Functional Assessment: Uptake assays (e.g., albumin endocytosis in LTL+ tubules) demonstrate proximal tubule functionality [7].
- Transcriptomic Similarity: RNA-sequencing followed by analysis with quantitative algorithms (e.g., Organ-Specific Gene Expression Panels) can calculate a percentage similarity to fetal or adult human kidney transcriptomes [89].
Diagram 1: Hierarchical kidney organoid QC workflow.
Detailed Protocols for Key QC Experiments
Protocol 1: Initial Morphological QC via Live Imaging
Principle: Real-time, non-invasive monitoring of organoid growth and morphology to ensure consistency and identify early failures [90]. Materials:
- Equipment: Automated live-cell imaging system (e.g., Tecan Spark Cyto) or inverted microscope with camera.
- Software: Image analysis software (e.g., ImageJ, CellProfiler). Procedure:
- Image Acquisition: At defined intervals (e.g., days 5, 10, 15, 20), acquire bright-field images of the entire organoid culture plate well.
- Image Analysis: Use software to automatically identify and outline individual organoids.
- Parameter Quantification: For each organoid, measure:
- Area (µm²) and Diameter (µm).
- Circularity: (4π × Area) / Perimeter². A value close to 1.0 indicates a perfect circle.
- Number of organoids per well to assess aggregation efficiency.
- Data Interpretation: Compare the distribution of size and circularity against established batch controls. Organoids falling outside two standard deviations of the mean for key parameters should be flagged for exclusion.
Protocol 2: Immunofluorescence for Cellular Composition
Principle: To validate the presence and spatial organization of key renal cell types using specific antibodies. Materials:
- Fixative: 4% Paraformaldehyde (PFA).
- Permeabilization/Blocking Buffer: PBS with 0.3% Triton X-100 and 5% normal donkey serum.
- Primary Antibodies: Anti-NPHS1 (podocytes), Anti-LTL (proximal tubules, conjugated to FITC), Anti-ECAD (distal tubules), Anti-SIX2 (nephron progenitors).
- Secondary Antibodies: Fluorophore-conjugated antibodies raised against appropriate host species.
- Mounting Medium: with DAPI. Procedure:
- Fixation: Fix organoids in 4% PFA for 30-60 minutes at room temperature.
- Permeabilization and Blocking: Incubate organoids in blocking buffer for 2-4 hours at room temperature.
- Primary Antibody Incubation: Incubate organoids with primary antibody cocktails diluted in blocking buffer for 24-48 hours at 4°C.
- Washing: Wash 3x with PBS over 6 hours.
- Secondary Antibody Incubation: Incubate with secondary antibodies (and LTL if not directly conjugated) diluted in blocking buffer for 24 hours at 4°C, protected from light.
- Washing and Mounting: Wash 3x with PBS, mount on glass slides, and image using a confocal microscope.
- Analysis: Quantify the percentage area positive for each marker and assess co-localization and structural organization.
Protocol 3: Transcriptomic Similarity Analysis
Principle: To quantitatively assess the transcriptional similarity of kidney organoids to native human kidney tissue [89]. Materials:
- RNA Extraction Kit: Suitable for 3D cultures (e.g., with mechanical disruption).
- RNA-Sequencing Services: Platform for library prep and sequencing.
- Bioinformatic Tool: Web-based Similarity Analytics System (W-SAS) or similar algorithm [89]. Procedure:
- RNA Extraction: Pool 10-15 organoids per biological replicate. Extract total RNA following the kit protocol, including a DNase I digestion step.
- RNA-Sequencing: Assess RNA quality (RIN > 8.0). Prepare RNA-seq libraries and sequence on an appropriate platform (e.g., Illumina) to a depth of at least 20 million reads per sample.
- Data Analysis:
- Preprocessing: Generate normalized expression values (e.g., TPM, FPKM).
- Similarity Calculation: Input the normalized expression matrix into the W-SAS platform, selecting the kidney-specific gene panel.
- Output: The system returns a quantitative similarity score (%) between the organoid sample and the target human kidney tissue.
- Interpretation: A higher percentage indicates greater transcriptional fidelity. This score provides an objective, standardized benchmark for optimizing differentiation protocols.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Kidney Organoid QC
| Item Category | Specific Example | Function in QC Protocol |
|---|---|---|
| Culture System | Air-liquid interface (AirLiwell) platform [35] | Enhances standardization, prevents organoid fusion, improves oxygenation, and reduces hypoxia-induced necrosis. |
| Imaging System | Automated live-cell imager (e.g., Tecan Spark Cyto) [90] | Enables non-invasive, quantitative monitoring of organoid growth, morphology, and number over time. |
| Extracellular Matrix | Synthetic hydrogels [88] | Defined, reproducible alternative to variable, animal-derived Matrigel for supporting 3D organoid growth. |
| Key Differentiation Factors | CHIR99021 (WNT agonist), FGF9, BMP7 [7] [34] | Critical for directing iPSCs through primitive streak, intermediate mesoderm, and metanephric mesenchyme stages. |
| Validation Antibodies | Anti-NPHS1, Anti-LTL, Anti-ECAD, Anti-SIX2 [7] [34] | Essential markers for confirming the presence of podocytes, proximal tubules, distal tubules, and nephron progenitors via immunostaining. |
| Bioinformatic Tool | Web-based Similarity Analytics System (W-SAS) [89] | Provides a quantitative score (%) of organoid similarity to human kidney based on RNA-seq data. |
Diagram 2: Key signaling pathway in kidney organoid differentiation.
The consistent generation of high-quality kidney organoids is paramount for robust disease modeling and drug screening. The QC framework presented here—integrating morphological, cellular, and transcriptional metrics within a structured, hierarchical workflow—provides a tangible path toward achieving this goal. By adopting these standardized protocols and leveraging the essential tools outlined, researchers can significantly reduce variability, make objective quality assessments, and ultimately enhance the reliability and translational relevance of their kidney organoid research.
Conclusion
Kidney organoids generated from iPSCs represent a robust and increasingly sophisticated model that faithfully mirrors key aspects of human kidney development and disease. While challenges related to full maturation, vascular integration, and protocol standardization persist, the field is rapidly advancing through innovations in bioengineering, genomic tools, and single-cell analytics. The convergence of these technologies is paving the way for more accurate human disease modeling, high-fidelity drug screening, and the long-term goal of generating functional renal tissues for regenerative therapy. As these models continue to evolve, they hold the immense potential to fundamentally reshape our approach to understanding and treating kidney diseases.
References
- 1. Research and therapy with induced pluripotent stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6873767/]
- 2. The Ethical Advantages of iPSCs [https://necstgen.com/ethical-advantages-ipscs/]
- 3. HIF-1α promotes kidney organoid vascularization and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03528-9]
- 4. Kidney Organoids as Disease Models: Strengths, ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.563981/full]
- 5. Applications of kidney organoids derived from human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6030416/]
- 6. The instructive role of metanephric mesenchyme in ureteric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2781331/]
- 7. Kidney Organoids: Current Advances and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12653128/]
- 8. Epithelial transformation of metanephric mesenchyme in ... [https://www.nature.com/articles/372679a0]
- 9. Human ureteric bud organoids recapitulate branching ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9957856/]
- 10. Directed differentiation of ureteric bud and collecting duct ... [https://www.nature.com/articles/s41596-023-00847-2]
- 11. Spatially patterned kidney assembloids recapitulate ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925003285]
- 12. FGF9 treatment reduces off-target chondrocytes from iPSC- ... [https://www.nature.com/articles/s41536-025-00428-9]
- 13. IPSC-DERIVED KIDNEY ORGANOIDS OUTPERFORM ... [https://anzsnevents.com/22555/]
- 14. Kidney Organoids: Current Advances and Applications [https://www.mdpi.com/2075-1729/15/11/1680]
- 15. Axial nephron fate switching demonstrates a plastic system ... [https://www.nature.com/articles/s41467-025-63290-9]
- 16. Wnt signaling in kidney: the initiator or terminator? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7591426/]
- 17. Human pluripotent stem cell-derived kidney organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC10915962/]
- 18. Progress of Induced Pluripotent Stem Cell-Derived Renal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11908814/]
- 19. Human iPSCs as Model Systems for BMP-Related Rare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10487005/]
- 20. Controlling nephron precursor differentiation to generate ... [https://www.nature.com/articles/s41467-025-63107-9]
- 21. Unlocking the full potential of human pluripotent stem cell ... [https://www.sciencedirect.com/science/article/pii/S0085253825003278]
- 22. Scalable production of uniform and mature organoids in a ... [https://www.nature.com/articles/s41467-024-53073-z]
- 23. Monocytes prevent apoptosis of iPSCs and promote ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03739-8]
- 24. 3D bioprinting of human iPSC-Derived kidney organoids ... [https://www.sciencedirect.com/science/article/pii/S2405886624000095]
- 25. Cellular extrusion bioprinting improves kidney organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7855371/]
- 26. In vitro generation of a ureteral organoid from pluripotent ... [https://www.nature.com/articles/s41467-025-60693-6]
- 27. Generating kidney organoids from human pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5113819/]
- 28. Protocol for Large-Scale Production of Kidney Organoids ... [https://www.sciencedirect.com/science/article/pii/S2666166720301374]
- 29. Comparative analysis and refinement of human PSC-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6324730/]
- 30. A Simple Bioreactor-Based Method to Generate Kidney ... [https://www.sciencedirect.com/science/article/pii/S2213671118302819]
- 31. Kidney organoids: a pioneering model for kidney diseases [https://www.sciencedirect.com/science/article/abs/pii/S1931524422001463]
- 32. A strategy for generating kidney organoids: Recapitulating ... [https://www.sciencedirect.com/science/article/pii/S0012160616302408]
- 33. Recreating kidney progenitors from pluripotent cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6219987/]
- 34. Disease Modeling with Kidney Organoids [https://www.mdpi.com/2072-666X/13/9/1384]
- 35. Generation of Individualized, Standardized, and Electrically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346388/]
- 36. iPSC-derived and Patient-Derived Organoids: Applications ... [https://www.sciencedirect.com/science/article/pii/S2666027X24000501]
- 37. Human induced pluripotent stem cell-derived kidney ... [https://www.sciencedirect.com/science/article/pii/S2468451121000866]
- 38. Advances and Challenges in Modeling Autosomal Dominant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852630/]
- 39. OrganoID: A versatile deep learning platform for tracking and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9645660/]
- 40. evolving treatment strategies in Alport syndrome [https://link.springer.com/article/10.1007/s00467-025-07046-z]
- 41. Chronic Exposure Nephrotoxicity | Cyprotex... - Evotec Assay [https://www.evotec.com/en/nephrotoxicity/chronic-exposure-nephrotoxicity-assay]
- 42. Evaluation and Functional Assessment of Human... Nephrotoxicity [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496563/]
- 43. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 44. Advancements, Strategies, and Challenges in Organoid- ... [https://www.sciencedirect.com/science/article/pii/S2095809925006083]
- 45. Effective reconstruction of functional organotypic kidney spheroid for... [https://www.nature.com/articles/s41598-019-53855-2?error=cookies_not_supported&code=53cdf4fe-eeb3-4117-a0ae-8b9a9c613a0c]
- 46. Emerging Biomarkers and Advanced Diagnostics in Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110191/]
- 47. Testing Services - Creative Bioarray Nephrotoxicity [https://dda.creative-bioarray.com/nephrotoxicity.html]
- 48. Advances in high-throughput drug screening based on ... [https://www.sciencedirect.com/science/article/pii/S2090123225006897]
- 49. Advancing preclinical drug evaluation through automated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11304660/]
- 50. with iPS Cells - PMC Modeling Kidney Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC4689367/]
- 51. A high-throughput screening platform for Polycystic Kidney ... [https://www.nature.com/articles/s41598-020-61082-3]
- 52. Advances in high-throughput drug screening based on ... [https://pubmed.ncbi.nlm.nih.gov/40945847/]
- 53. Quantitative high-throughput screening data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375054/]
- 54. Essential Guidelines for Manufacturing and Application of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11170116/]
- 55. Single cell census of human kidney organoids shows ... [https://www.nature.com/articles/s41467-019-13382-0]
- 56. Systematic production of human kidney organoids ... - Nature [https://www.nature.com/articles/s41551-025-01542-1]
- 57. Understanding patient-derived tumor organoid growth through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11324155/]
- 58. Tissue-engineered neuromuscular organoids [https://www.nature.com/articles/s42003-025-08484-z]
- 59. Organoids-on-a-chip: microfluidic technology enables culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11933005/]
- 60. Millifluidic culture improves human midbrain organoid vitality ... [https://pubs.rsc.org/en/content/articlehtml/2018/lc/c8lc00206a]
- 61. Accelerated production of human epithelial organoids in a ... [https://www.sciencedirect.com/science/article/pii/S2667237524002935]
- 62. U.S. Patent for Scalable, Standardized Organoid Culture ... [https://www.moleculardevices.com/newsroom/news/us-patent-for-scalable-standardized-organoid-culture-method]
- 63. Retinal organoids on-a-chip: a 3D printed micro-millifluidic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8387452/]
- 64. An integrated organoid omics map extends modeling ... [https://www.nature.com/articles/s41467-023-39740-7]
- 65. Vascularization via Spheroids and Organoids in 3D Bioprinting [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071597/]
- 66. A Protocol for the In Vitro Culturing of Vascularized ... [https://www.mdpi.com/2306-5354/12/11/1222]
- 67. Personalized disease recurrence modeling using iPSC- ... [https://pubmed.ncbi.nlm.nih.gov/40036883/]
- 68. Quantitative Analysis of Factors Regulating Angiogenesis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8614798/]
- 69. Systematic production of human kidney organoids for ... [https://pubmed.ncbi.nlm.nih.gov/41174010/]
- 70. Combining Kidney Organoids and Genome Editing ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2020.00010/full]
- 71. The application of iPSC-derived kidney organoids and ... [https://www.sciencedirect.com/science/chapter/edited-volume/abs/pii/B9780323857673000074]
- 72. Optimizing CRISPR methodology for precise gene editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580712/]
- 73. CRISPR-Based Knock-In for Cell Lineage Tracing [https://link.springer.com/protocol/10.1007/7651_2025_669]
- 74. Assessment of hiPSC-derived kidney organoids from ... [https://www.sciencedirect.com/science/article/pii/S2405844025024661]
- 75. Single-cell RNA sequencing and kidney organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276109/]
- 76. Navigating single-cell RNA-sequencing: protocols, tools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085826/]
- 77. Establishing single cell RNA transcriptomics: a brief guide [https://frontiersinzoology.biomedcentral.com/articles/10.1186/s12983-025-00579-x]
- 78. Kidney and Organoid Single Cell Transcriptomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC6609508/]
- 79. Comparative Analysis of Human Kidney Organoid and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12338369/]
- 80. Single cell transcriptomics of human kidney organoid ... [https://www.nature.com/articles/s41536-025-00418-x]
- 81. Advances and challenges toward developing kidney ... [https://www.sciencedirect.com/science/article/pii/S1934590923002564]
- 82. Balancing serendipity and reproducibility: Pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8190574/]
- 83. Organoids are not organs: Sources of variation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10277837/]
- 84. Efficient and reproducible generation of human iPSC ... [https://www.nature.com/articles/s41467-024-50224-0]
- 85. Characterizing the composition of iPSC derived cells from ... [https://www.nature.com/articles/s41598-022-22115-1]
- 86. Organoids | Nature Reviews Methods Primers [https://www.nature.com/articles/s43586-022-00174-y]
- 87. Towards a quality control framework for cerebral cortical ... [https://www.nature.com/articles/s41598-025-14425-x]
- 88. Examining the Market for Organoid Culture Systems in 2025 [https://eureka.patsnap.com/report-examining-the-market-for-organoid-culture-systems-in-2025]
- 89. Development of a quantitative prediction algorithm for ... [https://www.nature.com/articles/s41467-021-24746-w]
- 90. Improving organoid reproducibility through real-time imaging [https://www.tecan.com/tecan-journal/improving-organoid-reproducibility-through-real-time-imaging]