GMP Compliance in Patient-Specific Stem Cell Therapies: From Foundational Principles to Commercial Manufacturing
This article provides a comprehensive guide to Good Manufacturing Practice (GMP) compliance for researchers and drug development professionals navigating the complex transition from laboratory research to clinical manufacturing of patient-specific...
GMP Compliance in Patient-Specific Stem Cell Therapies: From Foundational Principles to Commercial Manufacturing
Abstract
This article provides a comprehensive guide to Good Manufacturing Practice (GMP) compliance for researchers and drug development professionals navigating the complex transition from laboratory research to clinical manufacturing of patient-specific stem cell therapies. Covering foundational ethical principles and regulatory frameworks, the content details practical methodologies for facility design, quality systems, and process automation. It addresses critical troubleshooting strategies for donor variability and process transfer challenges, while outlining phase-appropriate validation approaches for analytical methods and product characterization. With the global cell and gene therapy market projected to reach $97 billion by 2033, this resource offers essential insights for developing compliant, scalable manufacturing processes that ensure patient safety and therapeutic efficacy.
Ethical Foundations and Regulatory Frameworks for Stem Cell Therapy Manufacturing
The translation of patient-specific stem cell therapies from research to clinical application is guided by a framework of core ethical principles. Rigor, oversight, and transparency are not merely ancillary concerns but foundational requirements for ensuring scientific integrity, patient safety, and public trust in Advanced Therapy Medicinal Products (ATMPs) [1] [2]. These principles are operationalized through adherence to Good Manufacturing Practice (GMP), which provides a quality assurance system for the entire manufacturing process [3]. This document outlines practical application notes and protocols for integrating these ethical pillars into the GMP-compliant development of patient-specific stem cell therapies, providing a roadmap for researchers, scientists, and drug development professionals.
Foundational Ethical Principles
The International Society for Stem Cell Research (ISSCR) guidelines establish a set of widely shared ethical principles for stem cell research and clinical translation [1] [4]. These principles form the ethical bedrock upon which specific manufacturing protocols are built.
- Integrity of the Research Enterprise: The primary goals are to advance scientific understanding and generate robust evidence for addressing unmet medical needs. This requires independent peer review, oversight, and accountability at every stage, from basic research to clinical trials [1] [4].
- Primacy of Patient Welfare: The welfare of patients and research subjects is paramount. This principle mandates that clinical testing must never allow the promise for future patients to override the welfare of current research subjects [1] [4]. Providing unproven stem cell-based interventions outside of formal, regulated research settings is a breach of professional ethics [1] [2].
- Respect for Patients and Research Subjects: Researchers and clinicians must empower potential research participants to exercise valid informed consent. Patients must be accurately informed about the risks and the current state of evidence for novel interventions [1] [4].
- Transparency: Researchers must promote the timely exchange of accurate scientific information, including the publication of both positive and negative results. This extends to communicating with patient communities and the public about the state of the art, including uncertainties [1] [4].
- Social and Distributive Justice: The benefits of clinical translation should be distributed justly and globally. This includes addressing unmet medical needs, ensuring fair subject selection in clinical trials, and working to make new therapies accessible [1] [4].
Application of Ethical Principles in GMP Manufacturing
The ethical principles of rigor, oversight, and transparency are implemented through specific, actionable GMP standards in the manufacturing process for patient-specific stem cell therapies.
Rigor in Process and Analytics
Rigor is demonstrated through validated, reproducible manufacturing processes and analytical methods. This ensures that every product batch meets pre-defined quality attributes, which is critical for patient safety and product efficacy.
Table 1: Key Quality Attributes and Validated Analytical Methods for hiPSC Manufacturing
| Quality Attribute | Validated Analytical Method | Key Validation Parameters | Importance for Patient-Specific Therapies |
|---|---|---|---|
| Viable Cell Count | Automated image cytometer (e.g., NucleoCounter NC-100) [5] | Specificity, linearity, accuracy, precision (intra-/inter-operator reproducibility) [5] | Ensures accurate dosing; reflects manufacturing process robustness [5] |
| Cell Identity/Purity | Flow Cytometry | Specificity, accuracy, precision | Confirms the presence of target cell types and absence of unintended lineages (e.g., residual pluripotent cells) |
| Potency | Cell-specific functional assay (e.g., enzymatic activity, in vivo model) [6] | Specificity, linearity, range, accuracy | Measures the biological activity critical for the intended therapeutic effect |
| Sterility | Microbial culture & Mycoplasma testing | Specificity, limit of detection | Ensures the product is free from microbial contamination |
Oversight Through Defined Workflows and Controls
Oversight is embedded into the manufacturing workflow through institutional review, regulatory compliance, and multiple in-process control (IPC) checkpoints. A specialized Embryo Research Oversight (EMRO) process is required for research involving human embryos or the generation of sensitive models like stem cell-based embryo models (SCBEMs) [1] [2]. The ISSCR explicitly prohibits the transplantation of SCBEMs into a uterus or their culture to the point of potential viability (ectogenesis) [1] [7].
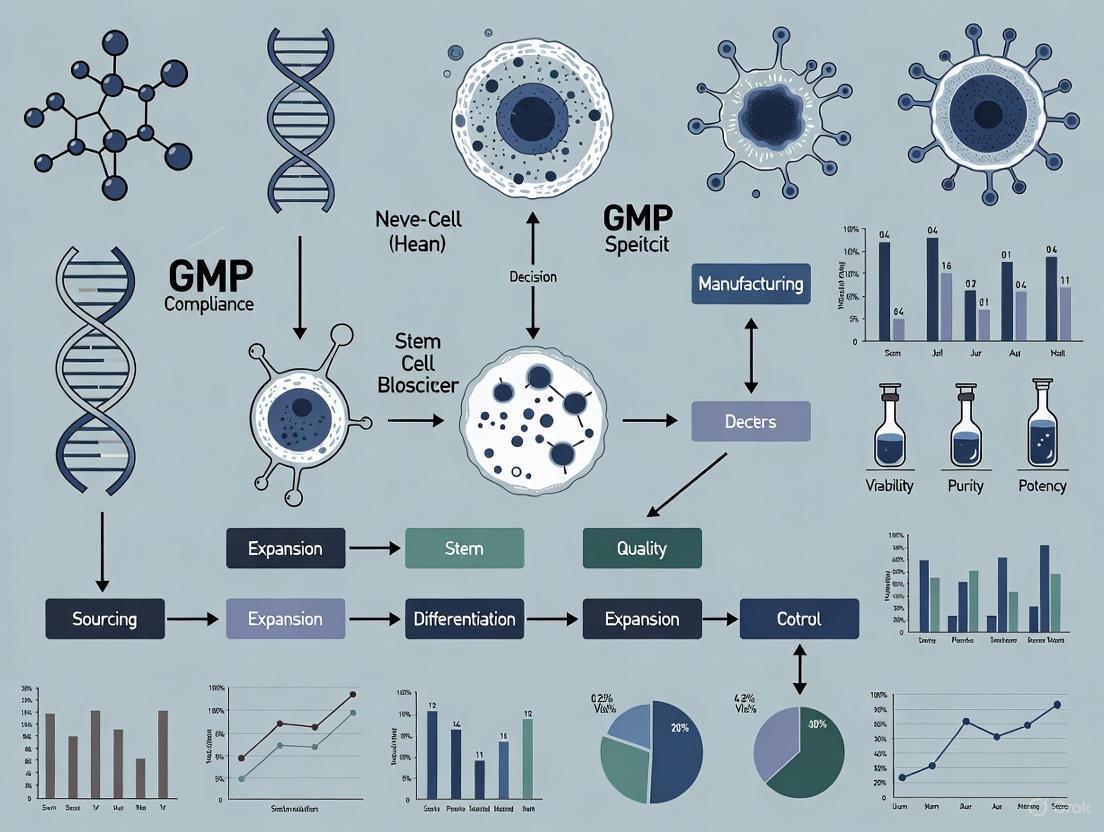
The following workflow diagram illustrates the integration of ethical and GMP oversight points in a typical autologous cell therapy manufacturing process, from patient material collection to product release.
Transparency in Documentation and Reporting
Transparency is maintained through comprehensive and traceable documentation, which is a cornerstone of GMP. This includes:
- Batch Records: Detailed, step-by-step documentation of the entire manufacturing process for each patient-specific batch [3].
- Raw Material Traceability: Full traceability of all reagents and raw materials, including their sourcing and quality testing [3].
- Deviation and Incident Reporting: A system for documenting and investigating any deviation from established procedures [3].
- Data Sharing: Commitment to publishing clinical trial results, regardless of outcome, to contribute to the collective scientific knowledge [1] [4].
Experimental Protocols
Protocol: Validation of an Automated Viable Cell Counting Method for hiPSCs
This protocol is critical for ensuring rigor in a key quality control test during the GMP manufacturing of human induced pluripotent stem cells (hiPSCs), a common starting material for patient-specific therapies [5].
1.0 Objective: To validate an automated viable cell counting method (e.g., NucleoCounter NC-100) for specificity, linearity, range, accuracy, and precision in accordance with ICH Q2(R1) and EudraLex cGMP guidelines [5].
2.0 Materials:
- hiPSC Culture: A well-characterized hiPSC line, maintained under defined conditions.
- Automated Cell Counter: NucleoCounter NC-100 or equivalent.
- Reagents: Proprietary cassettes with immobilized Propidium Iodide (PI).
- Reference Method Instrument: Flow cytometer.
3.0 Methodology:
- 3.1 Sample Preparation: Generate hiPSC samples with a wide range of viabilities (e.g., 50-95%). This can be achieved by subjecting cells to various stress conditions (e.g., heat, nutrient deprivation).
- 3.2 Specificity: Demonstrate that the method can specifically distinguish between viable and non-viable cells via PI staining, which is incorporated only by permeabilized (dead) cells.
- 3.3 Linearity and Range: Serially dilute samples of known high viability and measure the viable cell concentration with the automated counter. The method's range of reliability is established where results show a linear relationship (R² > 0.98) with expected concentrations [5].
- 3.4 Accuracy: Compare the viable cell count results from the automated method against the results from the reference method (flow cytometry) for the same set of samples. The mean difference should be within pre-defined acceptance criteria (e.g., <10%).
- 3.5 Precision:
- Intra-operator precision: A single analyst performs multiple counts on the same sample.
- Inter-operator precision: Different qualified analysts perform counts on the same sample set. The relative standard deviation (RSD) for both should be within acceptable limits (e.g., <15%).
4.0 Data Analysis: The validation report must include all raw data, calculations for linearity, accuracy, and precision, and a conclusion on the method's suitability for its intended use in GMP manufacturing.
Protocol: Stability Study of Leukapheresis Product for Autologous Therapy
This protocol ensures oversight and rigor in handling the patient's starting material, which is critical for the success of autologous therapies like CAR-T cells [8].
1.0 Objective: To define the optimal storage conditions and maximum hold time for a leukapheresis product (LP) prior to the initiation of manufacturing.
2.0 Materials:
- Leukapheresis Products: Fresh LPs from healthy donors or patients.
- Storage Equipment: Temperature-monitored refrigerators (2-8°C) and room temperature (15-25°C) environments.
- Analytical Equipment: Flow cytometer, automated cell counter.
3.0 Methodology:
- 3.1 Storage: Aliquot a single LP and store portions at both cool temperature (CT: 2-8°C) and room temperature (RT: 15-25°C).
- 3.2 Sampling: Collect samples from each condition at defined timepoints (e.g., 0, 25, 49, 73, 121 hours).
- 3.3 Testing: At each timepoint, assess:
- Viability: Percentage of viable CD45+ leukocytes, CD3+ T cells, CD4+ T cells, CD8+ T cells, etc., using flow cytometry with a viability dye.
- Cell Composition: Frequencies of key leukocyte subpopulations (monocytes, B cells, T cells, NK cells).
- Appearance: Visual inspection for color change or aggregation.
- 3.4 Acceptance Criteria: Stability is defined as the time during which average viability for critical cell types remains ≥90% and cell composition remains consistent without statistically significant change from baseline (T0) [8].
4.0 Data Analysis: Plot viability and cell composition data over time for both storage conditions. The maximum hold time is determined by the latest timepoint where all acceptance criteria are met. Data from one study indicated stability for at least 25 hours at RT and 73 hours at CT [8].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for GMP-Compliant Stem Cell Therapy Manufacturing
| Reagent/Material | Function | GMP Considerations |
|---|---|---|
| StemRNA Clinical Seed iPSCs [9] | A standardized, clonal master hiPSC line used as a starting material for deriving therapeutic cells. | Submission of a Drug Master File (DMF) to regulators provides comprehensive data on donor screening, GMP manufacturing, and quality controls, streamlining IND filings [9]. |
| Lentiviral Vector [6] [8] | A vector for the stable introduction of a therapeutic transgene (e.g., a corrective gene or CAR) into patient cells. | The manufacturing process must be GMP-compliant. The vector must be tested for safety (e.g., replication-competent lentivirus, sterility, potency) [6]. |
| Transduction Enhancers (LentiBOOST, Protamine Sulfate) [6] | Chemicals that improve the efficiency of lentiviral transduction. | Reducing the quantity of costly viral vector required while maintaining high transduction efficiency. Must be qualified for GMP use [6]. |
| Cell Separation Reagents (e.g., CD4/CD8 Enrichment) [8] | To isolate specific cell populations (e.g., T cells) from a leukapheresis product for further processing. | Use of closed-system, GMP-grade reagents and equipment (e.g., CliniMACS) is required to ensure sterility and process consistency [8]. |
| Validated Cell Culture Media | To support the growth and maintenance of stem cells or their derivatives. | Must be xeno-free or chemically defined where possible. Sourced from qualified suppliers with full traceability and certificate of analysis [5] [3]. |
The path to delivering safe and effective patient-specific stem cell therapies is inextricably linked to the steadfast application of the ethical principles of rigor, oversight, and transparency. These principles are given practical form through stringent GMP compliance, which governs every facet of manufacturing—from the quality of the starting materials and the validation of analytical methods to the comprehensive documentation of the process. As the field advances with emerging technologies, such as complex stem cell-based embryo models, a proactive and adaptive ethical and regulatory framework, as exemplified by the updated ISSCR guidelines, is essential [1] [7]. By embedding these core principles into their work, researchers and drug developers can ensure the scientific integrity of their products, uphold the highest standards of patient welfare, and maintain the public trust necessary for the continued progress of regenerative medicine.
For developers of patient-specific stem cell therapies, navigating the U.S. regulatory landscape is a critical component of translational research. The Center for Biologics Evaluation and Research (CBER) within the FDA regulates biological products, including cell and gene therapy products, under the Federal Food, Drug and Cosmetic Act and the Public Health Service Act [10]. These therapies are classified as Advanced Therapy Medicinal Products (ATMPs) and must adhere to a rigorous framework to ensure patient safety, product quality, and therapeutic efficacy [3] [11]. A fundamental understanding of the distinctions between Good Manufacturing Practice (GMP) and Good Tissue Practice (GTP) is essential for designing compliant manufacturing processes. GMP provides the comprehensive system for ensuring product quality, while GTP requirements focus specifically on preventing the introduction and transmission of communicable diseases by human cells, tissues, and cellular and tissue-based products (HCT/Ps) [12]. This application note details the specific requirements and provides protocols to facilitate compliance for patient-specific stem cell therapy development.
Regulatory Framework: CBER, GMP, and GTP
The Role of FDA CBER
CBER is responsible for regulating biological products for human use. This includes stem cell therapies, which are often evaluated as somatic cell therapy products [10]. For medical devices that are integral to the collection or manufacturing process of these biologics—such as blood collection and processing devices—CBER also maintains regulatory jurisdiction [13] [14]. This oversight ensures that the entire ecosystem surrounding a cell therapy product, from the starting material to the final product, is held to a consistent standard of quality and safety.
GMP Requirements in Detail
Current Good Manufacturing Practice (CGMP) regulations represent the minimum requirements for ensuring that drugs—including finished pharmaceuticals like stem cell therapies—are manufactured with consistent strength, purity, and quality [15]. The core CGMP regulations for finished pharmaceuticals are detailed in 21 CFR Part 211, while general GMP principles are in 21 CFR Part 210 [15] [12]. These regulations are not merely guidelines but are enforceable standards, and compliance is mandatory for product approval and marketing [15] [3].
Table: Key CGMP Regulations for Cell Therapy Products
| 21 CFR Part | Regulatory Focus | Key Requirements for Cell Therapy Manufacturing |
|---|---|---|
| Part 211 (Finished Pharmaceuticals) | Comprehensive quality standards for drug products [12]. | Organization & Personnel, Buildings & Facilities, Equipment, Control of Components & Containers, Production & Process Controls, Laboratory Controls, Records & Reports [12]. |
| Part 600 (Biological Products) | Establishment standards for biological products [12]. | Personnel, Physical Establishment, Equipment, Records, Retention Samples, Reporting of Deviations [12]. |
| Part 1271 (HCT/Ps) | Good Tissue Practice (GTP) requirements for preventing contamination [12]. | Donor Eligibility, Current GTP, Registration & Listing (Note: Part 1271 is specifically for GTP, not GMP) [12]. |
For cell therapies, GMP compliance requires a meticulous, well-documented approach from the initial cell acquisition through to the final product release. Key considerations outlined in the regulations and supporting literature include [3] [11] [12]:
- Organization and Personnel: A qualified quality control unit must be established with the responsibility and authority to approve or reject all components, drug product containers, closures, in-process materials, packaging, labeling, and the final drug product.
- Buildings and Facilities: Designed with adequate space and cleanroom classifications (e.g., ISO 7 or better) to prevent contamination or mix-ups. Air filtration, ventilation, and environmental monitoring are critical.
- Production and Process Controls: Written procedures must be established and followed, with strict control over aseptic processing, equipment calibration, and in-process testing. Yields must be calculated and deviations investigated.
- Laboratory Controls: Requirements for testing and release for distribution, stability testing, and reserve samples. This includes rigorous testing for sterility, mycoplasma, endotoxin, and cell identity, viability, and potency.
GTP vs. GMP: A Comparative Analysis
While GMP provides the overarching quality framework for the final drug product, Good Tissue Practice (GTP) requirements under 21 CFR Part 1271 focus specifically on the handling of human cells, tissues, and cellular and tissue-based products (HCT/Ps) to prevent the introduction, transmission, and spread of communicable diseases [12]. For an autologous stem cell therapy, both sets of regulations apply. GTP governs the donor screening and testing (even for autologous donors), and the handling of cells as HCT/Ps, while GMP governs the subsequent manufacturing of those cells into a finished drug product.
Table: GTP vs. GMP Requirements for Patient-Specific Stem Cell Therapies
| Aspect | Good Tissue Practice (GTP) Focus | Good Manufacturing Practice (GMP) Focus |
|---|---|---|
| Primary Objective | Prevent communicable disease transmission [12]. | Ensure safety, identity, strength, quality, and purity of the drug product [15]. |
| Scope | Donor eligibility, procurement, storage, and handling of HCT/Ps [12]. | Entire manufacturing process from receipt of raw materials to finished product release [15] [12]. |
| Donor Eligibility | Required: donor screening and testing [12]. | Not applicable to GMP as a standalone requirement; donor eligibility is a GTP function. |
| Facility Control | Focus on preventing cross-contamination between HCT/Ps [12]. | Comprehensive control of entire facility, including cleanroom standards, environmental monitoring, and pest control [12]. |
| Process Validation | Not explicitly required under GTP. | Required under GMP (21 CFR 211.100, 211.113) to ensure process reproducibility and control of microbiological contamination [12]. |
| Personnel | Training relevant to tasks performed on HCT/Ps [12]. | Established organizational structure with a dedicated quality unit; extensive GMP training [12]. |
GMP Compliance for Patient-Specific Therapies: Key Considerations
Manufacturing patient-specific stem cell therapies under GMP presents unique challenges. The following considerations, derived from current regulatory guidance and scientific literature, are critical for success [16] [11] [17]:
- Autologous vs. Allogeneic Source: Autologous therapies use the patient's own cells, which eliminates concerns of immune rejection but introduces significant logistical hurdles. These include individualized batch production, tracking, and testing, often under tight time constraints for acute conditions. Allogeneic "off-the-shelf" products offer scalability but require careful assessment of donor-specific immune responses [11].
- Donor and Cell Source: The donor's age, gender, health status, and tissue source (e.g., bone marrow, adipose tissue, umbilical cord) can significantly impact the properties and therapeutic efficacy of the final MSC product. This biological variability must be accounted for in process development and quality control [11].
- Cell Expansion and Culture Media: The expansion process (isolation method, plating density, passage number) must be standardized and validated. The use of undefined media supplements like fetal bovine serum (FBS) is discouraged due to risks of contamination and variability. GMP-compliant, xenogeneic-free alternatives, such as human platelet lysate (hPL) or chemically defined media, are essential for clinical-grade production [11].
- Product Fitness and Cryopreservation: Most "off-the-shelf" therapies are cryopreserved. The cryopreservation process and the choice of cryoprotectant (preferably xenogeneic-free and DMSO-free) can significantly impact cell viability, functionality, and in vivo persistence post-thaw. These effects must be thoroughly characterized [11].
- Process Automation and Closed Systems: Implementing automated, closed-system technologies is key to reducing manual errors, preventing contamination, enhancing process consistency, and enabling scalability. Automated systems for cell separation, washing, concentration, and genetic modification are increasingly available and vital for GMP compliance [17].
Experimental Protocols for GMP-Compliant Manufacturing
Protocol: GMP-Compliant Expansion of Mesenchymal Stromal Cells (MSCs)
This protocol outlines a standardized process for the expansion of clinical-grade MSCs, aligning with cGMP considerations highlighted in recent research [11].
I. Objective: To isolate and expand human MSCs from bone marrow aspirate under GMP-compliant conditions for use in clinical trials.
II. Materials and Reagents
- Starting Material: Bone marrow aspirate from qualified donor.
- Culture Media: Xeno-free, serum-free MSC expansion medium.
- Supplement: GMP-grade human platelet lysate (hPL).
- Dissociation Reagent: GMP-grade recombinant trypsin-like enzyme.
- Consumables: Single-use, sterile cell culture flasks/vessels, pipettes, and centrifugation tubes.
III. Methodology
- Cell Isolation and Seeding:
- Dilute bone marrow aspirate 1:1 with PBS containing 1% human serum albumin.
- Isolate mononuclear cells using density gradient centrifugation (e.g., Ficoll-Paque) or an automated, closed-system cell processing device.
- Wash cells twice with PBS/albumin and count viable cells using an automated cell counter.
- Seed cells at a density of 5x10^3 cells/cm² in culture vessels pre-filled with complete culture medium (base medium supplemented with 5% hPL).
- Cell Culture and Expansion:
- Incubate cultures at 37°C, 5% CO₂.
- Perform a complete medium exchange every 2-3 days.
- Monitor cells daily for morphology, confluence, and any signs of contamination.
- Cell Passaging:
- Once cells reach 70-80% confluence, remove culture medium and wash with PBS.
- Add dissociation reagent and incubate until cells detach.
- Neutralize the enzyme with complete medium and collect the cell suspension.
- Centrifuge, resuspend, and perform a viable cell count.
- Re-seed cells at the same initial density (5x10^3 cells/cm²) for continued expansion. Do not exceed passage 6 to maintain genomic stability.
- Cell Harvest and Cryopreservation:
- Upon achieving the target cell number, harvest cells as in step 3.
- Resuspend the final cell pellet in a GMP-compliant cryoprotectant solution (e.g., containing 5-10% DMSO and human serum albumin) at a pre-defined concentration.
- Fill controlled-rate freezing bags or vials and cryopreserve using a programmed freezer.
- Transfer to a GMP-managed liquid nitrogen storage system.
IV. Quality Control Testing
- Identity: Flow cytometry analysis for positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) MSC surface markers.
- Viability: >80% viability post-thaw, assessed by trypan blue exclusion or flow-based methods.
- Potency: Assay tailored to mechanism of action (e.g., immunosuppression assay using T-cell proliferation).
- Safety: Sterility (bacteria/fungi), mycoplasma, and endotoxin testing per pharmacopoeial methods. Karyotyping at initial master cell bank and at end of production.
Protocol: Process Validation for Aseptic Manufacturing
I. Objective: To validate the aseptic manufacturing process for a patient-specific stem cell therapy, demonstrating a sterility assurance level (SAL) of 10^-3 or better.
II. Materials
- Sterile culture media and reagents.
- Environmental monitoring equipment (settling plates, air samplers, contact plates).
- Process simulation (media fill) containers identical to product containers.
- Tryptic Soy Broth (TSB) and Fluid Thioglycollate Medium (FTM).
III. Methodology
- Simulation Setup:
- Perform the media fill simulation using TSB in the actual GMP manufacturing suite.
- The simulation must mimic the entire aseptic process, including all manual manipulations, durations, and interventions, from the inoculation of the starting material (simulated with TSB) to the final container closure.
- Use the same equipment and personnel as in the actual manufacturing process.
- Execution:
- A minimum of three separate runs should be performed, each representing a worst-case scenario (e.g., maximum number of operator interventions, longest process duration).
- Incubate all media-filled containers at 20-25°C for 14 days and at 30-35°C for 7 days.
- Observe containers for microbial growth at regular intervals.
- Acceptance Criteria:
- The process is considered validated if no more than 1 out of 3000-5000 units (depending on batch size) shows contamination, which corresponds to the target SAL.
- Any contaminated unit must be investigated to identify the root cause (e.g., environmental monitoring data, personnel practices).
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagent Solutions for GMP Cell Therapy Manufacturing
| Reagent/Material | Function | GMP-Compliant Considerations |
|---|---|---|
| Xeno-Free Cell Culture Medium | Provides nutrients for cell growth and expansion. | Must be chemically defined, devoid of animal-derived components, and manufactured under a quality system. Supports batch-to-batch consistency [11]. |
| Human Platelet Lysate (hPL) | Serum substitute that provides growth factors and adhesion proteins. | Must be sourced from certified human donors, tested for pathogens, and processed to remove platelets and cellular debris. A GMP-grade alternative to FBS [11]. |
| Cell Dissociation Reagents | Enzymatically detaches adherent cells for passaging. | Recombinant, non-animal derived enzymes (e.g., trypsin replacements) are preferred. Must be sterile and supplied with a Certificate of Analysis [17]. |
| Cryopreservation Medium | Protects cells from ice-crystal damage during freeze-thaw. | Formulations should be DMSO-free or use low concentrations. All components must be pharmaceutical-grade and the final mixture sterile-filtered [11]. |
| Cell Separation Reagents | Isolates target cell populations (e.g., T-cells, MSCs) from heterogeneous mixtures. | Antibody cocktails and magnetic beads must be clinically approved, supplied in sterile, single-use vials, and used within closed-system automated instruments [17]. |
Workflow and Regulatory Pathway Visualizations
Regulatory Pathway for CBER Submission
GMP Manufacturing Workflow for Autologous Therapy
Successfully bringing a patient-specific stem cell therapy from research to clinic under the purview of FDA CBER demands a proactive and integrated understanding of GMP and GTP regulations. The regulatory framework, centered on 21 CFR Parts 211, 210, 600, and 1271, is designed to be dynamic, evolving with scientific progress to ensure rigorous safety and quality standards without stifling innovation [15] [3] [12]. By embedding GMP principles into the earliest stages of process development—through careful consideration of cell source, raw materials, process automation, and robust quality control—researchers and drug developers can build a solid foundation for clinical translation. Adherence to these detailed application notes and protocols will help in navigating this complex landscape, ultimately accelerating the delivery of safe and effective transformative therapies to patients.
The field of stem cell research and therapy has witnessed remarkable advancements over the past decade, progressing from foundational laboratory studies to approved clinical treatments for previously untreatable conditions. This rapid evolution has necessitated the development of robust international standards and harmonization efforts to ensure scientific rigor, patient safety, and ethical integrity across global research and clinical applications. The International Society for Stem Cell Research (ISSCR) serves as the preeminent global organization establishing guidelines that address the international diversity of cultural, political, legal, and ethical issues associated with stem cell research and its translation to medicine [1].
The primary societal mission of basic biomedical research and its clinical translation is to alleviate and prevent human suffering caused by illness and injury. This collective effort depends on public support and contributions from many stakeholders, including scientists, clinicians, patients, research participants, industry members, regulators, and governmental officials [1]. Global harmonization of regulatory frameworks has become increasingly crucial as cell and gene therapies demonstrate therapeutic potential, with nearly 50 therapies approved in the United States alone as of 2025 [18]. These harmonization efforts aim to streamline development processes, reduce costs, facilitate international collaborations, and ultimately hasten patient access to life-saving treatments across geographical boundaries [19].
Current International Regulatory Landscape
ISSCR Guidelines Framework
The ISSCR Guidelines for Stem Cell Research and Clinical Translation underwent a targeted update in 2025, maintaining fundamental principles while responding to scientific advances. The guidelines maintain and underscore widely shared principles in science that call for rigor, oversight, and transparency in all areas of practice [1]. The 2025 update specifically refined recommendations for stem cell-based embryo models (SCBEMs) in response to scientific and oversight developments in this rapidly evolving area [7].
Table: Key Revisions in ISSCR 2025 Guidelines Update
| Aspect Updated | Previous Approach | 2025 Revision |
|---|---|---|
| Terminology | Classification as "integrated" or "non-integrated" models | Inclusive term "SCBEMs" |
| Oversight Requirements | Varied by model type | All 3D SCBEMs require clear rationale, defined endpoint, and appropriate oversight |
| Transplantation Restrictions | Specific prohibitions | Reiterated prohibition on uterine transplantation in living hosts |
| Culture Limitations | Not explicitly addressed | Prohibits ex vivo culture to point of potential viability (ectogenesis) |
The ISSCR Standards for Human Stem Cell Use in Research, released in 2023, provide additional guidance designed to enhance reproducibility and rigor of stem cell research through minimum characterization and reporting criteria for scientists working with human stem cells [20]. These standards include a "Reporting Practices for Publishing Results with Human Pluripotent and Tissue Stem Cells" checklist to help scientists, reviewers, and journal editors assess manuscripts for inclusion of critical details relevant to stem cell work [20].
Global Regulatory Variations
Regulatory frameworks governing cell and gene therapies vary significantly across the globe, shaped by unique regional medical, ethical, safety, and economic considerations [19]. These variations affect how therapies are developed, approved, and brought to market, impacting the speed and availability of innovative treatments.
Table: Regional Regulatory Approaches for Advanced Therapies
| Region | Regulatory Body | Key Initiatives/Pathways | Notable Characteristics |
|---|---|---|---|
| United States | Food and Drug Administration (FDA) | Regenerative Medicine Advanced Therapy (RMAT), Fast Track | Progressive policies under 21st Century Cures Act |
| European Union | European Medicines Agency (EMA) | PRIME (PRIority MEdicines) | Enhanced support for promising medicines targeting unmet needs |
| United Kingdom | Medicines and Healthcare products Regulatory Agency (MHRA) | Innovative Licensing and Access Pathway (ILAP) | Accelerated time to market post-Brexit |
| Japan | Pharmaceuticals and Medical Devices Agency (PMDA) | Accelerated approval system | Leader in regenerative therapy approval in Asia |
| Canada | Health Canada | Advanced Therapeutic Products Pathway | Flexible regulatory oversight adapting to novel therapies |
| Australia | Therapeutic Goods Administration (TGA) | Priority Review Pathway, Provisional Approval | Expedited approval for serious conditions |
| China | National Medical Products Administration (NMPA) | Accelerated approval pathways | Recent reforms for transparent review process |
The lack of regulatory harmonization poses multifaceted challenges for global pharmaceutical companies, including duplicative clinical trials, increased development costs, and elongated timelines to market entry [19]. This fragmentation is particularly problematic for cell and gene therapies, which often target rare diseases with small patient populations, making multiple separate trials to meet different regional standards both inefficient and ethically questionable [19].
GMP Compliance in Patient-Specific Stem Cell Therapies
Fundamental GMP Principles
Good Manufacturing Practice (GMP) compliance represents a critical component in the translation of stem cell research into clinically applicable therapies. GMP standards ensure that stem cell-based products are consistently produced and controlled according to quality standards appropriate for their intended use. For patient-specific therapies, this involves implementing rigorous quality control systems throughout the entire manufacturing process, from somatic cell acquisition to final therapeutic product administration.
The investigational medicinal product (IMP) manufacturing process for hematopoietic stem cell gene therapy typically involves harvesting hematopoietic stem cells expressing CD34 from apheresis of mobilized peripheral blood, isolation of CD34+ cells, pre-stimulation, ex vivo transduction with lentiviral vectors, and various quality control checks before administration to the patient [21]. The complexity of these processes demands comprehensive documentation, environmental monitoring, and quality assurance systems to prevent contamination, cross-contamination, and errors.
GMP Manufacturing Protocol: Hematopoietic Stem Cell Gene Therapy
The following detailed protocol outlines a GMP-compliant manufacturing process for hematopoietic stem cell gene therapy (HSCGT) based on established methodologies [21].
Materials and Equipment
Table: Essential Reagents and Materials for GMP HSCGT Manufacturing
| Category | Specific Reagents/Materials | Function/Purpose |
|---|---|---|
| Cell Source | Patient peripheral blood CD34+ cells | Starting material for genetic modification |
| Mobilization Agents | G-CSF, Plerixafor | Mobilize stem cells to peripheral blood |
| Cell Separation | CliniMACSplus instrument with magnetic beads | Isolation of CD34+ cells |
| Culture Media | Serum-free X-VIVO-15 | Base medium for cell culture |
| Media Supplements | Human albumin serum (HAS) | Protein supplement, cryoprotectant |
| Cytokines/Growth Factors | Flt3-L, SCF, TPO, IL-3 | Promote cell survival, proliferation, and maintenance of stemness |
| Transduction Enhancers | LentiBOOST, Protamine sulfate | Improve transduction efficiency |
| Vector | GMP-grade lentiviral vector | Gene delivery vehicle |
| Quality Assessment | Flow cytometry, CFU assays, Vector copy number (VCN) analysis | Assess cell phenotype, functionality, and transduction efficiency |
Step-by-Step Manufacturing Process
Patient Cell Mobilization and Collection
- Administer granulocyte-colony stimulating factor (G-CSF) and plerixafor to mobilize hematopoietic stem cells from bone marrow to peripheral blood
- Perform leukapheresis to collect mobilized cells under aseptic conditions
- Transport collected cells to manufacturing facility in temperature-controlled shipping container
CD34+ Cell Isolation
- Process apheresis product using CliniMACSplus instrument with magnetic bead separation for CD34+ cell selection
- Determine cell count, viability, and purity via flow cytometry analysis
- Cryopreserve cells if not proceeding immediately to transduction
Pre-stimulation and Culture
- Thaw and wash cryopreserved CD34+ cells if applicable
- Resuspend cells in pre-stimulation media: X-VIVO-15 supplemented with 1% HAS, Flt3-L (100ng/mL), SCF (100ng/mL), TPO (100ng/mL), and IL-3 (10ng/mL)
- Incubate cells at 37°C, 5% CO₂ for 24-48 hours
Lentiviral Transduction
- Calculate required lentiviral vector quantity based on cell count and target multiplicity of infection (MOI)
- Prepare transduction media: X-VIVO-15 with 1% HAS, cytokines, and transduction enhancers (LentiBOOST at 1:100 dilution and protamine sulfate at 4μg/mL)
- Combine cells with lentiviral vector in appropriate culture vessel (bag or flask)
- Perform two sequential transductions at 24-hour intervals with incubation at 37°C, 5% CO₂
Post-transduction Culture and Harvest
- After final transduction, wash cells to remove excess vector and replenish with fresh culture media
- Continue culture for 24-48 hours to allow transgene expression
- Harvest cells, perform final formulation in cryopreservation media
- Fill final product into appropriate infusion bags
Cryopreservation and Storage
- Controlled-rate freezing to -80°C followed by transfer to vapor phase liquid nitrogen for long-term storage
- Maintain chain of identity and chain of custody throughout process
GMP Manufacturing Workflow for Patient-Specific Stem Cell Therapies
Critical Quality Control Assessments
Implementing robust quality control measures throughout the manufacturing process is essential for ensuring final product safety, purity, and potency. The following parameters should be monitored:
- Cell Viability and Count: Assess via trypan blue exclusion or automated cell counters at multiple process stages
- Cell Phenotype: Confirm CD34+ purity and absence of contaminants via flow cytometry
- Transduction Efficiency: Evaluate vector copy number (VCN) per cell using digital PCR
- Biological Function: Perform colony-forming unit (CFU) assays to assess differentiation potential
- Sterility: Test for bacterial/fungal contamination (BacT/ALERT), mycoplasma, and endotoxin
- Potency: Measure functional enzyme activity or transgene expression
Recent Advances and Clinical Applications
Approved Stem Cell Therapies and Clinical Progress
The stem cell therapy landscape has matured significantly between 2023-2025, with several therapies receiving regulatory approval and many advancing through clinical trials [9]. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products targeting indications in ophthalmology, neurology, and oncology, with over 1,200 patients dosed and no significant safety concerns reported [9].
Table: Recently Approved Stem Cell-Based Therapies (2023-2025)
| Therapy Name | Approval Date | Cell Type | Indication | Key Clinical Outcomes |
|---|---|---|---|---|
| Omisirge | April 17, 2023 | Cord blood-derived hematopoietic progenitor cells | Hematologic malignancies undergoing cord blood transplantation | Accelerates neutrophil recovery, reduces infection risk |
| Lyfgenia | December 8, 2023 | Autologous cell-based gene therapy | Sickle cell disease with history of vaso-occlusive events | 88% achieved complete resolution of vaso-occlusive events (6-18 months) |
| Ryoncil | December 18, 2024 | Allogeneic bone marrow-derived MSCs | Pediatric steroid-refractory acute graft versus host disease | First MSC therapy approval for SR-aGVHD |
| Fertilo | FDA IND clearance February 2025 | iPSC-derived ovarian support cells | Support ex vivo oocyte maturation | Phase III trial, first live birth reported |
Emerging Technologies and Approaches
Several emerging technologies are shaping the future of stem cell therapy manufacturing and clinical application:
iPSC-Derived MSCs (iMSCs): Offering enhanced consistency and scalability compared to primary MSCs, iMSCs are gaining momentum in regenerative medicine trials targeting conditions such as osteoarthritis and tissue repair [9].
Off-the-Shelf Allogeneic Products: Development of universal donor cell lines aims to overcome limitations of patient-specific therapies, including production time and cost [18].
Point-of-Care Manufacturing: Automated, closed-system platforms enable decentralized manufacturing within treatment institutions, reducing logistical burdens and potentially improving access [18].
Enhanced Gene Editing: CRISPR/Cas9 and other precision gene editing technologies allow for more targeted genetic modifications in stem cell therapies.
Global Harmonization Initiatives
Current Harmonization Efforts
Global harmonization of cell and gene therapy regulations has gained significant momentum, with multiple initiatives aimed at aligning regulatory requirements across regions. The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) has endorsed a proposal to develop guidance on manufacturing changes for cell and gene therapies, known as Advanced Therapy Medicinal Products (ATMPs) [22]. This initiative, led by the Biotechnology Innovation Organization (BIO), addresses the critical issue of comparability when manufacturing processes are modified.
The comparability challenge is particularly complex for ATMPs, which range from relatively simple mRNA-based products to highly complex cell-based therapies like CAR-T cells and stem-cell derived products [22]. The proposed guidelines aim to establish global standards for demonstrating comparability following manufacturing changes, reducing redundant efforts and regulatory delays across different countries.
Benefits of Harmonized Regulations
The harmonization of regulatory frameworks across regions offers substantial benefits:
Accelerated Patient Access: Aligned approval standards and procedures reduce redundancy and minimize delays, facilitating smoother transition of therapies from clinical trials to market [19].
Enhanced International Collaboration: Unified standards enable multi-center trials with consistent requirements, promoting global sharing of data and resources [19].
Reduced Development Costs: Streamlined operations and leveraged efficiencies lower financial barriers, particularly important in resource-intensive regenerative medicine [19].
Predictable Market Conditions: Harmonized regulations reduce regulatory risk, encouraging investment in innovative therapies [19].
Global Harmonization Framework for Advanced Therapies
Implementation Challenges and Future Directions
Addressing Implementation Barriers
Despite progress in standardization and harmonization, significant challenges remain in implementing these frameworks globally:
Financial Barriers: The high costs of cell and gene therapies (ranging from ~$275,000 to >$4 million in the U.S.) present substantial challenges to broad implementation and equitable access [18].
Infrastructure Limitations: Complex manufacturing and administration requirements limit use to large academic centers, particularly impacting lower- to middle-income countries (LMICs) [18].
Regulatory Discrepancies: Differing requirements across regions necessitate duplicate trials and create logistical challenges for global development programs [19].
Manufacturing Complexity: The personalized nature of many stem cell therapies creates supply chain challenges and limits scalability [18].
Strategies for Enhanced Global Implementation
Several strategies are emerging to address these challenges and promote wider adoption of stem cell therapies:
Alternative Manufacturing Models: Point-of-care manufacturing utilizing automated, closed platforms can increase production efficiency and reduce error while maintaining quality [18].
Academic-Industry Partnerships: Collaboration between academic researchers, pharmaceutical companies, and non-profit entities can help develop sustainable models for therapy development and distribution [18].
Innovative Payment Structures: Alternative financing models, including outcome-based agreements and installment payments, can address the challenge of high upfront costs [18].
Capacity Building: Programs to establish manufacturing infrastructure and train specialized personnel in underserved regions can promote more equitable global access [1].
The field continues to evolve rapidly, with the ISSCR maintaining an agile approach to guideline updates through targeted revisions in response to scientific advances [7]. This responsive framework ensures that international standards remain relevant and effective in promoting ethical, practical, and sustainable approaches to stem cell research and clinical translation.
Risk-Based Approaches for Early-Phase Clinical Trials and Commercial Manufacturing
Within the development of patient-specific stem cell therapies, the application of a risk-based approach to Good Manufacturing Practice (GMP) compliance is fundamental to navigating the journey from early-phase clinical trials to commercial manufacturing. This philosophy, endorsed by regulatory agencies like the FDA, allows developers to focus resources on areas most critical to patient safety and product quality [23] [24]. For advanced therapies, which are often characterized by high complexity and a lack of terminal sterilization, integrating risk management from the outset is not just beneficial—it is essential for ensuring both regulatory compliance and the delivery of safe, effective treatments [25] [23].
This document outlines practical, phase-appropriate strategies for implementing risk-based GMP systems, providing structured protocols and visual guides to support researchers, scientists, and drug development professionals in this innovative field.
Phase-Appropriate Application of Risk-Based GMP
The core principle of a risk-based approach is that the level of control and documentation should be commensurate with the stage of development and the potential risks to product quality and patient safety [26] [24]. The following table summarizes the key differences in applying GMP principles during early-phase development versus commercial manufacturing for patient-specific stem cell therapies.
Table: Risk-Based GMP Considerations Across Development Phases
| Aspect | Early-Phase Clinical Trials (Phase I-IIa) | Commercial Manufacturing (Phase III & Beyond) |
|---|---|---|
| Primary Focus | Patient safety, proof-of-concept, and process learning [26] [23]. | Consistent product quality, efficacy, and commercial viability. |
| Stability Studies | "Fit-for-purpose" data to support storage and clinical use duration; one representative batch may be sufficient [26]. | Full ICH-compliant stability programs to define shelf life; multiple batches required [26]. |
| Process Validation | Emphasis on controlling Critical Process Parameters (CPPs) and monitoring Critical Quality Attributes (CQAs) for early process consistency [23]. | Full, formal process validation required to demonstrate the process consistently produces product meeting its pre-defined specifications. |
| Specifications | Preliminary, based on limited data and focused on safety attributes (e.g., sterility, viability, identity) [26]. | Comprehensive and justified by substantial data from multiple GMP batches. |
| Documentation | Phase-appropriate, with a focus on traceability and data integrity for critical steps [27]. | Extensive and rigorous documentation system, fully aligned with updated Chapter 4 EU GMP guidelines and data integrity principles (ALCOA++) [27]. |
| Facility & Equipment | Flexible, adaptable systems that can handle process changes; closed and automated systems to minimize contamination risk [23] [17]. | Fixed, validated, and scalable processes with qualified equipment in a dedicated, controlled environment. |
A proactive risk management framework is the cornerstone of operations in early-phase development [23]. From procuring raw materials to defining product release specifications, each unit operation is strategically evaluated throughout the product development lifecycle. This ensures that resources are directed toward high-risk areas, such as sterility, cell viability, and dose determination, while allowing for greater flexibility in lower-risk areas to foster innovation and efficiency [23] [24].
Experimental Protocols for a Risk-Based Approach
Protocol: Risk Assessment for Raw Materials in Cell Therapy Manufacturing
1. Objective: To establish a systematic methodology for identifying, assessing, and controlling risks associated with raw and ancillary materials used in the production of patient-specific stem cell therapies.
2. Materials:
- List of all raw materials, reagents, and supplements (e.g., growth factors, cytokines, culture media).
- Supplier qualification data.
- Risk Assessment Tool (e.g., Failure Mode and Effects Analysis - FMEA template).
3. Methodology: a. Risk Identification: * Form a cross-functional team (Quality, Process Development, Manufacturing). * Brainstorm potential failure modes for each material (e.g., supplier variability, endotoxin contamination, presence of animal-derived components, stability issues).
4. Documentation: The risk assessment, including the rationale for all scores and defined control strategies, must be documented and approved within the Quality System.
Protocol: Phase-Appropriate Stability Study for an Autologous Stem Cell Product
1. Objective: To generate "fit-for-purpose" stability data for an investigational autologous stem cell therapy to support the proposed storage conditions and use period for an early-phase (Phase I/II) clinical trial.
2. Materials:
- Representative batch(es) of the final drug product in its intended container closure system.
- Qualified stability chambers set to specified storage conditions (e.g., vapor phase of liquid nitrogen, controlled-rate freezer).
- Fit-for-purpose and validated analytical methods for testing.
3. Methodology: a. Study Design: * Utilize a bracketing or matrixing approach if justified [26]. * Store samples under long-term storage conditions and potential accelerated or stress conditions to understand degradation pathways. * Plan testing time points to cover the clinical use period (e.g., time-zero, midpoint, and end-of-use period).
4. Data Analysis & Reporting: * The data should support the proposed shelf life and storage conditions described in the Investigational New Drug (IND) application [26]. * A stability protocol must be written, and all data must be traceable and reliable [26].
Workflow Diagram: Risk-Based Manufacturing of Patient-Specific Therapies
The following diagram illustrates the integrated, risk-managed workflow for manufacturing a patient-specific stem cell therapy, from cell collection to patient infusion.
Autologous Therapy Manufacturing Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful development and manufacturing of cell-based therapies depend on using well-characterized materials. The following table details key reagent solutions and their critical functions in the process.
Table: Essential Reagents for Stem Cell Therapy Manufacturing
| Reagent / Material | Function | GMP Considerations |
|---|---|---|
| Cell Culture Media | Provides essential nutrients for cell growth, viability, and expansion. | Use of xeno-free, chemically defined GMP-grade formulations to ensure consistency and reduce risk of contamination [17]. |
| Growth Factors & Cytokines | Directs stem cell differentiation, expansion, and maintains potency. | High purity and well-documented sourcing. Requires stringent testing for identity, potency, and purity [25]. |
| Cell Separation Reagents | Isulates target cell populations from a heterogenous starting material (e.g., leukapheresis product). | Use in closed, automated systems (e.g., counterflow centrifugation, magnetic separation) to ensure sterility and reproducibility [17]. |
| Genetic Modification Tools | (If applicable) For introducing new genetic material (e.g., CRISPR/Cas9 components, viral vectors). | Comprehensive characterization and testing for safety (e.g., absence of replication-competent viruses). Documentation of lineage and manufacturing process is critical [25]. |
| Cryopreservation Media | Allows for long-term storage of final drug product and intermediate cell banks. | Formulated with GMP-grade cryoprotectants (e.g., DMSO). Requires validation of the freeze-thaw process to ensure post-thaw viability and function [25]. |
For researchers and drug development professionals working on patient-specific stem cell therapies, establishing a robust system for documentation and traceability is not merely a regulatory hurdle; it is the foundational element that ensures product quality, patient safety, and the scientific integrity of the entire development process. Advanced Therapy Medicinal Products (ATMPs), which include cell and gene therapies, fall under pharmaceutical law, making compliance with Good Manufacturing Practice (GMP) mandatory [3] [28]. The biological nature of these living therapies introduces unique challenges—each starting material and reagent is effectively part of the final product [28]. Consequently, a seamless, well-documented quality system that bridges research and clinical translation is essential for transforming a promising laboratory discovery into a regulated, clinically viable therapy.
Foundational Principles: GMP and the Regulatory Landscape
What is GMP and Why is it Non-Negotiable?
Good Manufacturing Practice (GMP) is a quality assurance system that ensures products are consistently produced and controlled according to state-of-the-art quality standards appropriate to their intended use [3]. In the context of ATMPs, GMP encompasses all aspects of the manufacturing process, including:
- Premises and equipment
- Staff training
- Operational processes
- Packaging and storage conditions
- Overarching quality assurance and comprehensive documentation systems [3]
The primary mission is to protect patients by ensuring that every product batch is safe, pure, potent, and reliable. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) require that ATMP manufacture adheres to GMP guidelines, and full marketing approval is contingent upon the successful submission of a Biologics License Application (BLA) or equivalent, which is heavily reliant on exhaustive documentation [9] [28].
The Documentation Hierarchy in a GMP Environment
A robust GMP documentation system is layered, with each level serving a distinct purpose. The following diagram illustrates the logical relationships and flow within a GMP documentation system.
Diagram 1: The hierarchical structure of GMP documentation, from overarching regulations to specific records.
This hierarchy ensures that every action is traceable back to an approved procedure and, ultimately, to regulatory requirements. Key documents include:
- Policy Manuals: Top-level documents describing overall laboratory management and organization [29].
- Standard Operating Procedures (SOPs): Provide detailed, specific requirements for laboratory activities [29].
- Test Methods and Specifications: Step-wise directions for test procedures and their pass/fail criteria [29].
- Records and Raw Data: Laboratory notebooks, testing sheets, and analytical printouts that provide evidence of what was actually done [29].
Application Note: A Practical Framework for GMP-Compliant iPSC Banking
Generating a clinical-grade induced pluripotent stem cell (iPSC) bank is a critical first step in manufacturing patient-specific therapies. The following section outlines a standardized protocol for establishing a GMP-compliant master cell bank, complete with essential quality control metrics.
Experimental Protocol: GMP-Compliant iPSC Line Generation and Banking
Objective: To generate, characterize, and bank a clonal, GMP-compliant iPSC master cell line from a qualified somatic cell source for use in manufacturing patient-specific therapies.
Starting Material: Somatic cells (e.g., from cord blood CD34+ cells or patient biopsy) from a qualified and consented donor [30].
Key Reagent Solutions: Table 1: Essential GMP-Compliant Reagents for iPSC Generation and Culture
| Reagent / Material | Function | GMP-Compliant Example / Consideration |
|---|---|---|
| Reprogramming Vectors | Introduction of reprogramming factors. | Use of non-integrating, episomal vectors to avoid genomic modification [30]. |
| GMP-compliant Culture Medium | Supports iPSC growth and maintenance. | Defined, xeno-free media (e.g., StemMACS iPS-Brew XF) [30]. |
| Cell Culture Substrate | Surface for cell attachment and growth. | Defined substrates like iMatrix-511 [30]. |
| Passaging Reagent | Detaches cells for sub-culturing. | Enzymatic, animal-origin-free reagents like Accutase [30]. |
| Rho-associated kinase (ROCK) inhibitor | Improves cell survival after passaging. | Use of Y-27632 at 10 µM [30]. |
Methodology:
- Reprogramming: Transfect the qualified somatic cell source with the non-integrating reprogramming vector system. Use a validated electroporation device and protocol [30].
- Clonal Isolation and Expansion: Culture transfected cells under GMP-compliant conditions. Manually pick emerging iPSC colonies based on characteristic morphology and expand them clonally. Use a ROCK inhibitor (e.g., 10 µM Y-27632) during passaging to enhance survival [30].
- Master Cell Bank (MCB) Creation: Once a clonal line is expanded, cryopreserve a large number of vials at an early passage as the MCB. Use controlled-rate freezing and validated cryostorage conditions. The entire process must be documented in a detailed batch record [30].
Quality Control and Release Specifications for iPSC Master Cell Banks
A comprehensive set of quality control (QC) tests must be performed on the MCB prior to its release for further differentiation. The results must meet pre-defined specifications, documented in a Certificate of Analysis (CoA).
Table 2: Example QC Release Specifications for a GMP-Compliant iPSC Master Cell Bank
| QC Test Category | Specific Test / Assay | Release Specification | Rationale |
|---|---|---|---|
| Identity | Short Tandem Repeat (STR) Profiling | Match with donor somatic cells | Confirms lineage and absence of cross-contamination [30]. |
| Potency / Pluripotency | Flow Cytometry (SSEA-4, TRA-1-60) | >90% positive for pluripotency markers | Verifies functional pluripotent state [30]. |
| Viability & Sterility | Viability (Trypan Blue exclusion) | >90% post-thaw viability | Ensures product fitness. |
| Mycoplasma Testing (qPCR) | Negative | Prevents contamination [30]. | |
| Safety | Sterility (Bacterial/Fungal culture) | No growth observed | Ensures aseptic processing [3]. |
| In Vitro Tumorigenicity (Soft Agar Assay) | No colony formation | Assesses oncogenic potential [30]. | |
| Purity / Genetic Integrity | Karyotype (G-banding) | Normal (46, XX or XY) | Confirms genomic stability at a macroscopic level [30]. |
| Whole-Genome Sequencing (WGS) | Low overall mutation load, absence of pathogenic variants in oncogenes/tumor suppressors | Identifies sub-microscopic genetic variants; neonatal cord blood-derived lines have shown a low mutation load [30]. |
Traceability in Practice: From Ancillary Materials to Final Product
Traceability is the golden thread that runs through the entire product lifecycle. It requires that the origin and history of every component and process step can be precisely determined.
Managing Ancillary Materials (AMs)
Ancillary materials (AMs) are critical reagents used in the manufacturing process, such as cell culture media, cytokines, and enzymes. Since they contact the cells, their quality is integral to the final ATMP [28]. A secure supply chain with comprehensive documentation is vital.
Required Documentation for GMP-Compliant AMs:
- Certificate of Analysis (CoA): Confirms the product meets defined quality and performance standards [28].
- Certificate of Origin (CoO): Details the source of all raw materials [28].
- TSE Certificate: Certifies that animal-derived products minimize the risk of Transmissible Spongiform Encephalopathy [28].
- Drug Master File (DMF): A confidential, detailed file submitted to the FDA by the supplier. An Investigational New Drug (IND) application sponsor can reference a DMF via a Letter of Authorization (LoA) from the supplier, streamlining the regulatory review [9] [28].
Recommendation: Transition from research-grade to GMP-compliant AMs early in the R&D/pre-clinical phases. Changing AMs later necessitates costly and time-consuming comparative studies to demonstrate product consistency [28].
The Product Journey and Chain of Identity
For patient-specific therapies, maintaining a secure "chain of identity" from the patient donor to the final infused product is paramount. The workflow below visualizes this traceability and documentation flow.
Diagram 2: The product journey and critical traceability points for a patient-specific stem cell therapy.
Building a robust quality system founded on comprehensive documentation and traceability is a strategic imperative for successfully translating patient-specific stem cell therapies from the research bench to the clinic. By integrating GMP principles early, securing a well-documented supply chain for ancillary materials, and implementing a hierarchical documentation system, developers can navigate the complex regulatory landscape with confidence. This disciplined approach not only safeguards patient safety and ensures regulatory compliance but also generates the high-quality, reproducible data essential for proving the efficacy and commercial viability of these transformative advanced therapies.
Practical Implementation of GMP Systems and Manufacturing Processes
For manufacturers of patient-specific stem cell therapies, the cleanroom facility is a critical cornerstone of product quality, patient safety, and regulatory compliance. Adherence to Good Manufacturing Practice (GMP) is a legal requirement for Advanced Therapy Medicinal Products (ATMPs), which include stem cell-based therapies [3] [25]. The cleanroom provides the controlled environment necessary to prevent microbiological contamination, cross-contamination between patient batches, and to ensure the consistent production of a viable, living product that cannot be terminally sterilized [25].
Cleanrooms are classified according to the International Organization for Standardization (ISO) 14644-1 standard, which defines the maximum permissible concentration of airborne particles per cubic meter of air [31] [32]. The classification system ranges from ISO 1 (cleanest) to ISO 9 (least clean) [33]. This document will focus on the classifications most relevant to stem cell therapy production, typically spanning ISO 5 to ISO 8, and outline the integrated environmental controls and material flow required to maintain their aseptic conditions.
Cleanroom Classification and Particle Limits
The following table summarizes the key particle count requirements for ISO classes 5 through 8, which are the primary classes involved in the manufacturing of stem cell therapies. Particle counts are cumulative [34].
Table 1: ISO 14644-1 Cleanroom Classification Standards and Particle Concentration Limits (maximum particles per m³) [33] [31] [32]
| ISO Class | FED STD 209E Equivalent | ≥ 0.5 µm | ≥ 1 µm | ≥ 5 µm |
|---|---|---|---|---|
| ISO 5 | Class 100 | 3,520 | 832 | 29 |
| ISO 6 | Class 1,000 | 35,200 | 8,320 | 293 |
| ISO 7 | Class 10,000 | 352,000 | 83,200 | 2,930 |
| ISO 8 | Class 100,000 | 3,520,000 | 832,000 | 29,300 |
Different stages of the stem cell manufacturing process require different levels of environmental control. For example, open manipulations critical to product quality, such as the final formulation of the cell therapy product, must be performed in an ISO 5 environment, often provided by a laminar flow biosafety cabinet located within an ISO 7 or ISO 8 cleanroom [25] [31]. The surrounding room functions as a buffer zone, maintaining a higher air pressure to protect the critical zone from contamination ingress.
Table 2: GMP Grade Equivalents and Typical Applications in Stem Cell Therapy
| GMP Grade (EU) | Equivalent ISO Classification | Typical Applications in Stem Cell Therapy |
|---|---|---|
| Grade A | ISO 5 (in operation) | Critical processing zones (e.g., biosafety cabinets for cell manipulation, filling) |
| Grade B | ISO 7 (in operation) | Background environment for Grade A zones (e.g., aseptic preparation and filling rooms) |
| Grade C | ISO 7 / ISO 8 (in operation) | Preparation of less critical solutions, cleanroom gowning areas |
| Grade D | ISO 8 (at rest) | Handling of cleaned components, warehousing for sterilized materials |
Environmental Control Systems
HEPA Filtration and Airflow Principles
High-Efficiency Particulate Air (HEPA) filtration is the definitive technology for achieving the required air cleanliness. A true HEPA filter must capture at least 99.97% of particles 0.3 micrometers in diameter, the Most Penetrating Particle Size (MPPS) [35] [32]. Some facilities may employ Ultra-Low Penetration Air (ULPA) filters, which capture 99.999% of particles down to 0.12 microns, for stricter control [32].
The effectiveness of HEPA filtration is realized through two primary airflow strategies:
- Laminar (Unidirectional) Airflow: Air moves in a single direction at a uniform velocity (typically 0.45 m/s ±20%), creating parallel streamlines that sweep particles away from the critical processing zone. This is essential for ISO 5 (Grade A) environments [32].
- Turbulent (Non-unidirectional) Airflow: Clean, HEPA-filtered air is introduced in a way that creates mixing and dilution to control contamination. This is common in ISO 7 and ISO 8 (Grade B/C) background rooms and requires a higher number of air changes per hour to achieve cleanliness [32].
Key Design and Operational Parameters
Table 3: Cleanroom Design Requirements by ISO Classification [36] [31] [34]
| Parameter | ISO 5 / Grade A | ISO 7 / Grade B | ISO 8 / Grade C/D |
|---|---|---|---|
| Air Changes Per Hour (ACH) | 240 - 480 (approx.) | 60 - 90 (approx.) | 10 - 25 (approx.) |
| Ceiling HEPA Filter Coverage | 90 - 100% | 7 - 15% | 4 - 5% |
| Typical Airflow Pattern | Laminar | Turbulent | Turbulent |
| Typical Filtration | HEPA or ULPA | HEPA | HEPA |
Additional critical environmental parameters that must be continuously monitored and controlled include:
- Pressure Differentials: Cleanrooms maintain a cascading pressure gradient, with the cleanest rooms (e.g., ISO 5) at the highest positive pressure relative to adjacent less-clean areas. This prevents inflow of contaminated air. A differential of 1 to 20 mmHg pressure is typical [33].
- Temperature and Humidity: Tight control is required to prevent particle generation and microorganism proliferation, and to ensure staff comfort. The HVAC system must maintain these within specified limits (e.g., 20-24°C, 45-60% RH) [33] [25].
- Recovery: The cleanroom must rapidly return to its specified classification after a contamination event, such as door opening or personnel activity [33].
Material Flow and Personnel Movement
In GMP facilities, the flow of materials and personnel is designed to be logical and unidirectional to prevent cross-contamination, which is a significant risk when manufacturing patient-specific therapies [25].
Material Flow Protocol
- Introduction: All raw materials, reagents, and equipment must enter through a designated receiving and quarantine area.
- Decontamination: Materials are transferred to a staging area for decontamination. Outer packaging is removed and wiped down with a suitable disinfectant.
- Transfer into Cleanroom: Decontaminated materials are passed into the cleanroom through a double-sided pass-through hatch or airlock. Materials should never be introduced directly into a higher-grade cleanroom from an uncontrolled corridor.
- Internal Movement: Within the cleanroom, materials should move from areas of lower cleanliness (e.g., ISO 8) to higher cleanliness (e.g., ISO 7, then ISO 5).
- Waste Exit: All waste materials must be sealed in approved, non-shedding bags and removed via a dedicated exit path or pass-through to prevent cross-contamination with incoming materials.
Personnel Gowning and Entry Protocol
Personnel are a primary source of contamination. A strict, sequential gowning procedure is mandatory.
Validation and Monitoring Protocols
Cleanroom validation is a multiphase process to ensure the facility is designed, installed, and operates according to its specified ISO classification and GMP requirements [33].
Validation Phases
- Design Qualification (DQ): Documented verification that the proposed design is suitable for the intended purpose.
- Installation Qualification (IQ): Documented verification that the facility is built and installed according to the approved design and specifications. Testing is performed "as-built" (empty and without personnel).
- Operational Qualification (OQ): Documented verification that the facility operates as intended throughout all anticipated operating ranges. Testing is performed "at-rest" (with equipment installed but without personnel activity).
- Performance Qualification (PQ): Documented verification that the facility consistently performs as intended under routine production conditions. Testing is performed "in-operation" (with equipment and personnel present) [33].
Key Test Methodologies
Table 4: Cleanroom Validation Tests and Methodologies
| Test Parameter | Test Method | Acceptance Criteria | Frequency |
|---|---|---|---|
| Airborne Particle Count | Use of a discrete particle counter to measure concentration of particles at specified sizes. | Meets maximum limits for target ISO class per ISO 14644-1 [33]. | Every 6-12 months, continuous monitoring for Grade A. |
| HEPA Filter Integrity Leak Test | Introduction of a polydisperse aerosol (e.g., PAO, DOP) upstream of the filter and scanning the downstream face and seals with a probe. Leakage must be ≤ 0.01% [33] [32]. | Meets ISO 14644-3 standards. | Every 24 months. |
| Airflow Velocity & Volume | Use of an anemometer to measure velocity at HEPA filter face. Volume is calculated (T = A x V). Air changes per hour (ACH) are derived. | Velocity and ACH meet design specifications for target ISO class (e.g., 20 ACH for ISO 8) [36] [33]. | Every 12 months. |
| Airflow Visualization / Smoke Pattern Test | A smoke generator is used to release a visible stream of smoke near filters and critical zones to visualize airflow direction and uniformity. | Smoke must show unidirectional flow in laminar zones and not reverse or stagnate in critical areas [33]. | Every 12-24 months. |
| Pressure Differential | Use of a calibrated magnehelic gauge or electronic pressure transducer to measure the pressure difference between adjacent rooms. | Maintains specified cascade (e.g., ≥ 10-15 Pa between successive grades) [33]. | Continuously monitored. |
| Recovery Test | Introduction of an aerosol to artificially elevate particle count, followed by timing how long it takes for the room to recover to its specified class limit. | Time to recover is within specified limits (e.g., minutes from ISO 7 to ISO 5) [33]. | After initial qualification and post-modification. |
| Viable (Microbial) Monitoring | Settling plates (passive air sampling), active air samplers, and surface contact plates (e.g., swabs) are used to collect samples, which are then incubated to quantify microbial growth. | Action levels based on EU GMP Annex 1 or internal standards. | Daily/weekly for plates, continuous for active air samplers in Grade A. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 5: Key Reagent Solutions and Materials for Cleanroom Environmental Monitoring
| Item | Function / Application | Key Consideration for GMP |
|---|---|---|
| Nutrient Agar Contact Plates | Used for surface monitoring of viable microorganisms on equipment and personnel gloves. | Growth medium must be validated for its intended use. Incubation time and temperature are specified in SOPs. |
| Tryptic Soy Agar (TSA) Settling Plates | Plates exposed to air to passively monitor airborne microbial contamination (settling by gravity). | Exposure time is standardized (e.g., 4 hours). Plates are incubated aerobically. |
| Liquid Growth Media for Air Samplers | Used in active air samplers that draw a known volume of air to quantitatively assess microbial load. | Media choice and sampling volume are validated. |
| Aerosol Challenge Agent (e.g., PAO, DOP) | A polydisperse aerosol of Polyalphaolefin (PAO) or Diocyl Phthalate (DOP) used to challenge HEPA filters during integrity testing. | The material must generate particles in the MPPS range (0.1 - 0.3 µm). Material safety data must be reviewed [32]. |
| Isopropyl Alcohol (IPA) Solutions | A common cleanroom disinfectant for wiping down surfaces and equipment. | Used at a specified concentration (e.g., 70%) and prepared with sterile water for injection (WFI). |
| Sterile, Non-Shedding Wipes | Used in conjunction with disinfectants for cleaning surfaces. Must not shed particles or fibers. | Material compatibility with disinfectants must be assessed. |
| Particle Counter Calibration Standard | A suspension of particles of known, uniform size used to calibrate airborne particle counters. | Traceable to a national standard. Calibration is performed at defined intervals per quality system. |
For the successful and compliant manufacture of patient-specific stem cell therapies, a robust facility design is non-negotiable. This requires a holistic, risk-based approach that integrates the correct cleanroom classification, precise environmental controls (HEPA filtration, pressure, temperature, humidity), and rigorously enforced, unidirectional flows for materials and personnel. Continuous validation and monitoring, as dictated by ISO standards and GMP regulations, provide the documented evidence necessary to ensure the living cellular product is manufactured in a consistently controlled and safe environment, thereby protecting the patient and ensuring product efficacy.
The manufacturing of patient-specific stem cell therapies represents a frontier in personalized medicine, yet its complexity poses significant challenges for Good Manufacturing Practice (GMP) compliance. The individual nature of autologous therapies necessitates a manufacturing paradigm where each patient batch is a unique product, requiring meticulous control to ensure safety, identity, and purity [37]. Traditional open manual processes are particularly susceptible to two critical vulnerabilities: the risk of microbial contamination and the inherent variability introduced by human operators. These challenges can compromise product quality, lead to batch failures, and ultimately delay life-saving treatments for patients [38] [39].
Closed automated systems offer a transformative solution by integrating sterile barriers, software controls, and automated unit operations to create a controlled manufacturing environment. This approach is central to modern GMP, which mandates that production be consistent and controlled to quality standards appropriate for their intended use [3] [25]. For "living medicines" like stem cell therapies, where the product cannot be terminally sterilized, the adoption of closed automation is not merely an efficiency improvement but a fundamental component of a robust contamination control strategy and a critical enabler for scalable, compliant manufacturing [25] [40].
Quantitative Comparison of Automated Cell Processing Systems
Selecting the appropriate automated system requires a careful analysis of performance data. The following table summarizes key parameters for several commercially available technologies, providing a basis for initial evaluation in the context of a specific therapy and process flow.
Table 1: Performance Metrics of Representative Automated Cell Processing Systems
| System | Core Technology | Cell Recovery | Input Volume | Input Cell Capacity | Cell Processing Time |
|---|---|---|---|---|---|
| Rotea System [38] | Counterflow Centrifugation | 95% | 30 mL – 20 L | 10 x 10⁹ | 45 min |
| Sepax [38] | Electric centrifugation motor and pneumatic piston drive | 70% | 30 mL – 3 L | 10–15 x 10⁹ | 90 min |
| LOVO [38] | Spinning Membrane Filtration | 70% | 30 mL – 22 L | 3 x 10⁹ | 60 min |
| ekko [38] | Acoustic Cell Processing | 89% | 1–2 L | 1.6 x 10⁹ | 40 min |
| CliniMACS Prodigy [38] [40] | Magnetic Separation | 85% | 1–2 L | 3 x 10⁹ | N/A |
These systems can be broadly categorized. Modular closed systems are optimized for individual unit operations (e.g., centrifugation, magnetic separation), offering flexibility to mix-and-match best-in-class instruments from different suppliers. In contrast, integrated closed systems are fully automated, all-in-one platforms designed as end-to-end solutions for producing a specific patient's cell product [38]. The choice between them depends on the need for process versatility versus the desire for a simplified, single-vendor workflow.
Impact on GMP Compliance: Contamination and Variability
Mitigating Contamination Risk
In GMP manufacturing, ensuring product sterility is paramount. Open systems, which require direct operator manipulation and expose the product to the ambient environment, carry a high risk of microbial contamination and cross-contamination between patient samples [38] [25]. Closed automated systems address this by physically isolating the product within a sterile fluidic pathway. This design principle significantly reduces the reliance on aseptic technique and the stringent, expensive cleanroom classifications (e.g., Grade A/B) typically required for open processes. In many cases, closed systems can operate effectively in a Grade C or controlled non-classified environment, enhancing facility flexibility while maintaining a high sterility assurance level [38].
Evidence from GMP manufacturing runs underscores this benefit. A study on the production of allogeneic natural killer (NK) cells from cord blood using a closed, semi-automated process reported robust performance across 36 manufacturing runs without noted contamination events, enabling production within a Class C cleanroom [40]. This is a direct result of minimizing open handlings and human intervention, the primary vectors for introducing microbial and particulate contaminants [39].
Reducing Operator-Induced Variability
The multi-step, manual processes common in early-stage therapy development are highly vulnerable to human error and procedural inconsistencies. This leads to batch-to-batch variability, making it difficult to demonstrate the process robustness and product consistency demanded by regulators [38] [17].
Automation directly addresses this by standardizing execution. Software-driven protocols ensure that critical steps like cell washing, concentration, and reagent addition are performed with precise timing, volumes, and forces every time [17]. This process standardization is crucial for CMC (Chemistry, Manufacturing, and Controls) documentation and for establishing a validated, reproducible manufacturing process [39]. Furthermore, automation alleviates the burden on technical staff, allowing them to be reallocated from repetitive, high-risk tasks to higher-value oversight and quality control functions [41]. This is particularly impactful given the industry's challenge with high operator turnover rates, which can approach 70% within 18 months and perpetuate variability [39].
Application Note: CD34+ Hematopoietic Stem Cell Enrichment in a Closed System
Objective
To establish a reliable, GMP-compliant protocol for the enrichment of CD34+ hematopoietic stem cells (HSCs) from human umbilical cord blood (UCB) using the CliniMACS Prodigy system, ensuring high cell recovery and purity for subsequent differentiation into therapeutic cell products.
Background
UCB is a valuable source of HSCs for allogeneic cell therapy. The initial isolation of CD34+ cells is a critical first unit operation that impacts the quality and yield of the entire manufacturing process. Performing this step in a closed, automated system reduces contamination risk and improves process consistency compared to manual magnetic-activated cell sorting (MACS) [40].
Materials and Reagents
Table 2: Key Research Reagent Solutions for CD34+ Enrichment
| Item | Function | Specific Example |
|---|---|---|
| CliniMACS PBS/EDTA Buffer | Washing and dilution buffer to maintain cell viability and prevent clumping. | Miltenyi Biotech |
| Human Serum Albumin (HSA) | Added to buffer as a protein supplement to protect cells during processing. | 0.5% HSA in PBS/EDTA |
| CliniMACS CD34 Reagent | FcR-blocking and CD34-specific antibody conjugated to magnetic microbeads for cell selection. | Miltenyi Biotech |
| Intravenous Immunoglobulin (IgG) | Used for Fc receptor blocking to reduce non-specific cell labeling. | Griffols Deutschland GmbH |
| Elution Medium | Cell culture medium used to collect the positively selected CD34+ cell fraction. | Proprietary Basal Growth Medium [40] |
Methodology
Workflow Overview: CD34+ HSC Enrichment from Cord Blood
Step-by-Step Protocol:
UCB Unit Receipt and Pre-processing:
- Receive fresh UCB unit at the manufacturing facility. Transport should be temperature-controlled (15–25°C) and avoid X-ray screening [40].
- Verify unit eligibility based on pre-defined criteria (e.g., ≥ 3.5E06 total CD34+ cells for GMP batches).
- Collect pre-process data: unit weight/volume, total nucleated cell count, and CD34+ cell count.
System Setup and Priming:
- Within a Grade C cleanroom, load the sterile, single-use tubing set (e.g., TS310 for Prodigy) onto the CliniMACS Prodigy instrument.
- Follow the software-guided (e.g., V1.4) setup and priming procedure using CliniMACS PBS/EDTA Buffer supplemented with 0.5% HSA [40].
Cell Labeling and Loading:
- Transfer the UCB unit into the system's sample bag.
- Add FcR blocking reagent (5% IgG solution) to the sample to minimize non-specific binding.
- Add the CliniMACS CD34 Reagent. The system may automatically mix and incubate the sample for a defined period to allow antibody binding.
Automated Processing:
- Initiate the "LP-34 Enrichment" protocol on the Prodigy software.
- The system automatically performs the following sequence:
- Transfers the labeled cell suspension through a pre-programmed series of washes to remove unbound reagents and platelets.
- Passes the cell suspension through a magnetic column that retains the labeled CD34+ cells.
- Washes the column to remove unlabeled, non-target cells (negative fraction).
- Elutes the magnetically retained CD34+ cells from the column after removal from the magnetic field, collecting them in a final bag.
Product Collection and Quality Control:
- The resulting eluate (approximately 80 mL) contains the enriched CD34+ HSCs.
- Aseptically collect a 1 mL sample from the eluate for immediate quality control testing.
- The remaining product is transferred to the next process step (e.g., expansion culture) or cryopreserved.
Performance Data and Outcomes
Analysis of 36 manufacturing runs demonstrated the robustness of this method. The table below stratifies performance based on the starting CD34+ cell content of the UCB unit.
Table 3: Performance of CliniMACS Prodigy in CD34+ Cell Enrichment (N=36) [40]
| Starting CD34+ Cell Content | Number of Runs | Average CD34+ Cell Recovery | Average Purity |
|---|---|---|---|
| Low (< 4.50E06 cells) | 11 | 68.18% | 57.48% |
| Medium (4.50-7.00E06 cells) | 13 | 68.46% | 62.11% |
| High (> 7.00E06 cells) | 12 | 71.94% | 69.73% |
The data confirms that the system delivers consistent cell recovery across a wide range of input qualities. Factors such as UCB age, total nucleated cell count, and platelet or red blood cell content were found to have no significant impact on performance, highlighting the process's robustness and suitability for GMP manufacturing [40].
Application Note: Closed System Harvest and Concentration of NK Cells
Objective
To harvest and concentrate natural killer (NK) cells from a large-scale culture into a final formulation buffer, ready for cryopreservation, using a closed automated system to maximize cell yield and viability while minimizing operator intervention.
Background
Following the expansion and differentiation of NK cells from HSCs in bioreactors, the culture volume is large (often 2-5 liters), and the cells are dilute. A critical downstream step is to gently harvest and concentrate these cells into a small volume for final product formulation. Performing this as a closed, automated unit operation is essential for maintaining sterility and process consistency [40].
Methodology
Workflow Overview: NK Cell Harvest and Concentration
Step-by-Step Protocol:
Harvest and System Setup:
- Connect the harvest line from the bioreactor (e.g., Xuri cellbag) to the input line of the CliniMACS Prodigy system equipped with a centrifugation tubing set in a closed, aseptic manner.
- Load the appropriate formulation buffer (e.g., cryopreservation medium) into a designated bag on the system.
Automated Concentration Process:
- Select the "Harvest and Concentration" protocol on the Prodigy touchscreen interface.
- The system automatically performs the following:
- Transfers the cell culture harvest from the bioreactor into its integrated centrifuge.
- Spins the cells under controlled conditions to form a pellet.
- Removes and diverts the spent culture supernatant to a waste bag.
- Gently resuspends the cell pellet in a defined, small volume of formulation buffer.
Final Product Collection:
- The concentrated cell product (typically reduced to a volume of 50-100 mL) is transferred into a final product bag.
- The system automatically mixes the bag to ensure a homogeneous cell suspension.
Quality Control and Release:
- A sample is taken for pre-release QC tests, including:
- Cell Count and Viability: Using an automated cell counter (e.g., via trypan blue exclusion).
- Identity/Purity: Flow cytometry analysis for NK cell markers (e.g., CD45+CD56+), confirming purity remains high (e.g., >80%) [40].
- Potency: A functional cytotoxicity assay may be performed.
- Sterility: Sampling for sterility testing according to pharmacopoeial methods.
- A sample is taken for pre-release QC tests, including:
Performance Data and Outcomes
The harvest and concentration process was evaluated across 29 batches with varying culture volumes.
Table 4: Performance of Automated Harvest and Concentration for NK Cells [40]
| Culture Volume | Number of Batches | Average Cell Yield | NK Cell Purity Post-Concentration |
|---|---|---|---|
| Low (< 2 L) | 7 | 74.59% | >80% |
| Medium (2–5 L) | 14 | 82.69% | >80% |
| High (> 5 L) | 8 | 83.74% | >80% |
The data shows high and consistent cell yield, with a modest ~20% cell loss, and maintained high NK cell purity. Impurity levels (B and T cells) remained low or undetectable, confirming the process effectively handles different production scales without compromising critical quality attributes [40].
The integration of closed automated systems is a cornerstone of modern GMP compliance for patient-specific stem cell therapies. As demonstrated in the application notes, these technologies directly address the core challenges of contamination risk and operator variability by providing a controlled, reproducible manufacturing environment. The quantitative performance data confirms that systems like the CliniMACS Prodigy can deliver the robustness, consistency, and documentation required for clinical and commercial manufacturing. For researchers and developers, early adoption of these platforms in process development is a critical strategic decision. It facilitates a smoother technology transfer to GMP facilities, strengthens the CMC package for regulatory submissions, and paves the way for scaling out production to make these transformative therapies accessible to a greater number of patients.
In the development of patient-specific stem cell therapies, the transition from Research Use Only (RUO) to Good Manufacturing Practice (GMP)-compliant reagents represents a critical juncture in translating laboratory research into clinical applications. This transition is not merely a regulatory checkbox but a fundamental requirement for ensuring the safety, identity, purity, and efficacy of advanced therapy medicinal products (ATMPs) [3]. For stem cell therapies, where products consist of living cells, the quality of raw materials directly impacts the biological properties of the final therapeutic product [42] [43]. The inherent variability and potential immunogenicity of stem cell-based products necessitate a rigorously controlled manufacturing environment from the earliest stages of development.
The fundamental distinction between RUO and GMP materials lies not necessarily in their chemical composition, but in the quality systems governing their production, documentation, and testing [44]. RUO reagents are intended for non-clinical laboratory research where the primary focus is experimental feasibility, while GMP-grade materials must adhere to stringent regulations that ensure consistent production and control according to quality standards appropriate for human use [45]. This application note provides a structured framework for navigating this critical transition within the context of GMP compliance for manufacturing patient-specific stem cell therapies.
Key Distinctions Between RUO and GMP Reagents
Understanding the fundamental differences between RUO and GMP-grade materials is essential for successful transition planning. The distinction extends beyond the physical reagents to encompass the entire quality system governing their production.
Table 1: Core Differences Between RUO and GMP-Grade Reagents
| Attribute | RUO (Research Use Only) | GMP (Good Manufacturing Practice) |
|---|---|---|
| Intended Use | Non-clinical laboratory research [45] | Manufacturing, testing, or treatment of human clinical or diagnostic products [45] |
| Regulatory Status | Not for human use; not subject to strict regulatory control [45] [44] | Must comply with regional regulations (e.g., FDA 21 CFR 211, EMA GMP) for human use [42] [46] |
| Quality Systems | Produced using good laboratory procedures without formalized quality systems [44] | Manufactured under a state-of-the-art Quality Management System (QMS) with rigorous change control [42] |
| Documentation | Limited certificates of analysis; often lacks full traceability [47] | Comprehensive documentation including batch-specific Certificates of Analysis, full traceability, and manufacturing records [42] [45] |
| Testing & Validation | Variable purity and functionality testing; no formal validation [47] | Strictly defined and validated testing for identity, purity, potency, and safety (e.g., endotoxin, sterility) [45] |
| Consistency | Potential for batch-to-batch variability [45] | High batch-to-batch consistency ensured by controlled processes and raw materials [42] |
| Supplier Qualification | Typically not required | Mandatory vendor qualification, including audits and quality agreements [42] |
A critical concept is that "GMP grade" is not simply a product specification but a reflection of the quality system under which the material is produced [42]. No general legal requirement for GMP exists for all raw materials; instead, their use in a therapeutic product is controlled by the manufacturer, who must qualify and document their suitability for human use [42].
Strategic Framework for Transitioning to GMP-Compliant Reagents
Risk-Based Assessment and Prioritization
A strategic, risk-based approach is essential for a efficient and effective transition. This begins with a comprehensive inventory of all materials used in the manufacturing process and a assessment of their criticality.
Table 2: Risk Assessment and Mitigation Strategy for Critical Raw Materials
| Material Category | Risk Considerations | Mitigation Strategies |
|---|---|---|
| Starting Materials (e.g., donor cells, viral vectors) [42] | Direct impact on active biological substance; potential for introducing adventitious agents [43]. | Rigorous donor screening and eligibility determination [43]. Complete understanding of cell line history and viral safety [42]. Use of GMP Master Cell Banks [48]. |
| Culture Media & Supplements | Direct contact with cells; potential source of contaminants (e.g., mycoplasma, viruses). | Select GMP-grade, fully defined, xeno-free formulations. Test for adventitious agents and performance [43]. |
| Growth Factors & Cytokines | Impact cell differentiation, proliferation, and final product function; potential immunogenicity. | Use GMP-grade recombinant factors with documented traceability and absence of animal components [42]. |
| Vectors for Genetic Modification (e.g., plasmids, mRNA) | Direct impact on genetic integrity and safety of the final product [48]. | Use integration-free, GMP-manufactured vectors [43]. Full characterization of identity and purity [42]. |
| Materials of Animal Origin (e.g., serum, trypsin) | High risk of introducing viral and prion contaminants [42]. | Avoidance is the best strategy. If unavoidable, use certified animal origin-free products or materials with viral testing/inactivation data [42]. |
| Processing Reagents (e.g., separation matrices, buffers) | Potential for leaching of harmful substances or introduction of impurities. | Risk-assess based on contact with product and removal during purification. Use GMP-grade with toxicology data where applicable. |
The Scientist's Toolkit: Essential GMP-Compliant Materials for Stem Cell Therapy
Transitioning a stem cell therapy process requires systematically replacing all RUO materials with GMP-compliant alternatives. The table below outlines key reagent solutions essential for clinical-grade manufacturing.
Table 3: Essential GMP-Compliant Reagents for Stem Cell Therapy Manufacturing
| Reagent Solution | Function in Manufacturing Process | Critical GMP Considerations |
|---|---|---|
| GMP Master Cell Bank [48] [43] | Provides the foundational, well-characterized cell source for all production batches. | Donor eligibility, informed consent for clinical/commercial use, comprehensive characterization (karyotyping, pluripotency), and freedom from adventitious agents [48] [43]. |
| Defined, Xeno-Free Culture Medium [43] | Supports the growth and maintenance of stem cells without undefined components. | Serum-free and animal origin-free formulation; raw material traceability and quality testing; consistency in performance [42] [43]. |
| Clinical-Grade Recombinant Growth Factors | Directs stem cell differentiation and proliferation toward the desired therapeutic cell type. | GMP manufacturing; certificate of analysis with data on identity, purity, potency, and endotoxin levels; non-animal derived [42]. |
| GMP-Grade Reprogramming Factors (e.g., mRNA) [48] | For generating induced Pluripotent Stem Cells (iPSCs) without genomic integration. | Integration-free method; absence of residual vector; well-defined and characterized [48] [43]. |
| Detachment & Dissociation Reagents | Passaging and harvesting cells during the expansion and differentiation process. | Defined, animal-origin free composition; supported by regulatory filings (e.g., Drug Master File) [44]. |
| Formulation Buffers & Cryopreservation Media | Final formulation and storage of the cell therapy product. | Composition and quality of all ingredients; sterility and endotoxin testing; validated stability profile [42]. |
Experimental Protocol: Qualification of a GMP-Compliant Raw Material
This protocol outlines a systematic approach for qualifying a new GMP-grade raw material, such as a critical growth factor, and integrating it into a stem cell differentiation process.
Protocol: Analytical and Functional Qualification of a GMP-Growth Factor
Objective: To qualify a GMP-grade growth factor as a direct replacement for an RUO-grade material in a defined differentiation protocol, ensuring it meets analytical specifications and maintains or improves biological performance.
Materials and Equipment:
- GMP-grade growth factor (test material) with Certificate of Analysis (CoA)
- Existing RUO-grade growth factor (control material)
- GMP-compliant stem cell Master Cell Bank
- Defined, xeno-free basal differentiation medium
- Sterile, tissue culture-treated plates
- Flow cytometer with appropriate antibodies for target cell markers
- Cell viability analyzer (e.g., trypan blue exclusion or automated cell counter)
- QC equipment for in-testing (endotoxin, sterility)
Methodology: Step 1: Documentation Review and Supplier Qualification
- Obtain and review the full Device Master File (if available) and CoA for the GMP-grade material from the supplier [42]. Verify that the supplier has been qualified through an audit or site visit [42].
- Confirm critical quality attributes from the CoA: appearance, identity (e.g., mass spectrometry), purity (e.g., >98% by HPLC), potency (e.g., ED50 in a bioassay), endotoxin level (<1 EU/μg), and sterility [45].
Step 2: Analytical Comparability Testing
- Reconstitute both the GMP-test and RUO-control materials according to their respective instructions.
- Perform side-by-side analytical tests, which may include:
- SDS-PAGE: To confirm protein identity and purity and detect any degradation or impurity profiles.
- Reverse-Phase HPLC: To compare chromatographic profiles and assess molecular integrity.
- Endotoxin Testing: Use a LAL assay to confirm the level meets the specification for its intended use.
Step 3: In vitro Functional Bioassay
- Thaw a vial of the GMP-compliant Master Cell Bank and expand cells to the required number under GMP-like conditions.
- Seed cells at a defined density in multiple plates for differentiation.
- Experimental Groups:
- Group A (Test): Differentiation medium supplemented with the GMP-grade growth factor.
- Group B (Control): Differentiation medium supplemented with the RUO-grade growth factor.
- Group C (Basal): Differentiation medium only (negative control).
- Differentiate cells according to the established protocol, harvesting samples at key time points (e.g., day 7, day 14, terminal differentiation).
Step 4: Performance Endpoint Analysis
- Flow Cytometry: Analyze the expression of specific surface markers for the target differentiated cell type (e.g., CD45+CD56+ for NK cells [48]). Compare the percentage of positive cells and marker intensity between Groups A and B.
- Cell Viability and Yield: Measure total cell count and viability at the end of the differentiation process.
- Functional Potency Assay: Perform a functional assay relevant to the cell type (e.g., cytokine release upon stimulation for immune cells, phagocytosis activity for macrophages). The functionality of the final cell product is a critical release parameter [3].
Step 5: Data Analysis and Decision
- Use statistical analysis (e.g., t-test for pairwise comparison) to determine if the performance of the GMP-grade material is non-inferior to the RUO-grade control.
- A successful qualification is demonstrated when the GMP-grade material produces a target cell population with comparable purity, viability, and functional potency to the control, while meeting all its analytical specifications.
Workflow Visualization: Raw Material Qualification Process
The following diagram illustrates the logical workflow and decision points for qualifying a new GMP-compliant raw material.
Regulatory and Quality Considerations
Documentation and Traceability
A cornerstone of GMP is comprehensive documentation. The EU GMP Chapter 4 (draft 2025) emphasizes a "life cycle approach" to documentation within a pharmaceutical quality system (PQS) [27]. Essential documents include:
- Standard Operating Procedures (SOPs): For all manufacturing and testing operations [42].
- Batch Manufacturing Records: Provide a complete history of each production batch [46].
- Certificates of Analysis: Batch-specific for all raw materials, confirming they meet pre-defined specifications [42].
- Traceability Documentation: Allows tracking of every component, including raw materials, back to its origin [42] [3]. This is crucial for investigating deviations or adverse events.
Quality Management System (QMS) and the PDCA Cycle
A robust QMS is the overarching framework that ensures GMP compliance. It often implements the Plan-Do-Check-Act (PDCA) cycle for continuous improvement [42]:
- Plan: Establish objectives and processes for material qualification and supplier management.
- Do: Implement the processes, including procuring and testing materials.
- Check: Monitor and measure processes against policies and objectives, and report the results.
- Act: Take actions to continually improve process performance based on the data collected [42].
The transition from RUO to GMP-compliant reagents is a complex but indispensable process in the development of safe and effective patient-specific stem cell therapies. Success hinges on early and strategic planning, a thorough risk-based assessment of all raw materials, and a rigorous qualification process underpinned by a robust Quality Management System. By adopting the structured framework and protocols outlined in this application note, developers can navigate this critical transition more efficiently, mitigating downstream risks and building a solid foundation for regulatory submissions and successful clinical translation.
The manufacturing of patient-specific stem cell therapies represents one of the most complex challenges in modern biopharmaceutical production. These living products cannot be terminally sterilized and often possess inherent biological variability that must be controlled to ensure consistent safety and efficacy profiles. Quality by Design (QbD) is a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and control based on sound science and quality risk management [49]. For stem cell therapies, this means building quality into the product from the earliest stages of development rather than relying solely on end-product testing.
The International Society for Stem Cell Research (ISSCR) maintains guidelines that underscore the need for rigor, oversight, and transparency in all areas of stem cell research and clinical translation [1]. Implementing QbD principles directly supports these requirements by providing a structured framework for identifying and controlling critical factors that impact product quality. This approach is particularly vital as the field advances, with the first FDA-approved mesenchymal stem cell product (Ryoncil) receiving approval in 2024 for pediatric steroid-refractory acute graft-versus-host disease [9], establishing new benchmarks for manufacturing quality.
Fundamental QbD Framework and Terminology
Core QbD Elements
A comprehensive QbD implementation for stem cell therapies consists of five interconnected elements that form a complete quality management system:
- Quality Target Product Profile (QTPP): A prospective summary of the quality characteristics of the stem cell therapy necessary to ensure the desired product quality, taking into account safety and efficacy [49]. The QTPP forms the basis for design and development of the product.
- Critical Quality Attributes (CQAs): Physical, chemical, biological, or microbiological properties or characteristics of the stem cell product that must be within an appropriate limit, range, or distribution to ensure the desired product quality [49] [50].
- Critical Process Parameters (CPPs): Process parameters whose variability impacts CQAs and therefore must be monitored or controlled to ensure the process produces the desired product quality [50].
- Critical Material Attributes (CMAs): Physical, chemical, biological, or microbiological properties or characteristics of input materials that must be within appropriate limits or distributions to ensure the desired product quality [49].
- Control Strategy: A planned set of controls, derived from current product and process understanding, that ensures process performance and product quality [49].
QbD Visual Framework
The following diagram illustrates the logical relationships and workflow between these core QbD elements in stem cell therapy manufacturing:
QbD Element Relationships in Stem Cell Manufacturing
This framework demonstrates how QTPP drives the identification of CQAs, which in turn guides the determination of which material attributes and process parameters are critical. Process Analytical Technology (PAT) provides real-time monitoring of both CQAs and CPPs, feeding data back to inform the control strategy [50].
Defining Critical Quality Attributes for Stem Cell Therapies
CQA Identification and Categorization
For stem cell therapies, CQAs are derived from the QTPP and represent the biological, chemical, and physical attributes most critical to product safety and efficacy. The criticality of an attribute is determined primarily by the severity of harm to the patient should the product fall outside the acceptable range for that attribute [49]. Based on recent advancements in stem cell manufacturing, CQAs can be categorized into three distinct classes as implemented in an advanced QbD framework for mesenchymal stem/stromal cell (MSC) manufacturing [51]:
Table 1: Categorization of Critical Quality Attributes for Stem Cell Therapies
| CQA Category | Definition | Examples for Stem Cell Therapies |
|---|---|---|
| Functional CQAs (fCQAs) | Attributes related to the therapeutic mechanism of action and biological function | - Immunomodulatory potency- Differentiation potential- Secretome profile- Migratory capacity |
| Manufacturing CQAs (mCQAs) | Attributes ensuring consistent production and product stability | - Viability post-cryopreservation- Cell doubling time- Genomic stability- Identity/purity markers |
| In-Process CQAs (iCQAs) | Attributes monitored during manufacturing to ensure process control | - Metabolic rates- Morphology indicators- Surface marker expression- Culture confluence |
Establishing CQA Acceptance Criteria
Establishing scientifically justified acceptance criteria for CQAs requires extensive characterization and understanding of the relationship between product attributes and clinical performance. The following table summarizes quantitative CQA ranges demonstrated in recent GMP manufacturing studies:
Table 2: Exemplary CQA Ranges and Acceptance Criteria from Recent Stem Cell Manufacturing Studies
| Critical Quality Attribute | Measurement Method | Target Range | Justification |
|---|---|---|---|
| Cell Viability | Flow cytometry with viability dyes | ≥ 80% | Maintains therapeutic potency and ensures adequate viable cell dose [21] |
| Vector Copy Number (for gene-modified therapies) | qPCR/digital PCR | 1.0-3.0 copies/cell | Balances therapeutic efficacy with genotoxicity risk [21] |
| Immunophenotype Purity | Flow cytometry for CD73/CD90/CD105 positive (≥95%) and CD45/CD34 negative (≤5%) | ≥ 95% positive for identity markers≤ 5% positive for hematopoietic markers | Complies with ISCT MSC definition criteria and ensures product identity [52] |
| Differentiation Potential | Tri-lineage differentiation with quantitative staining | Osteogenic: ≥ 2-fold increase in mineralizationAdipogenic: ≥ 30% lipid-containing cellsChondrogenic: Positive proteoglycan staining | Confirms functional potency and stemness characteristics [53] |
| Microbiological Safety | USP sterility testing, mycoplasma PCR, endotoxin LAL | Sterile, mycoplasma-free, endotoxin < 5 EU/kg | Meets pharmacopeial standards for patient safety [54] |
| Karyotypic Stability | G-banding karyotype analysis | Normal diploid karyotype (46, XX or XY) | Ensures genetic integrity after extensive in vitro expansion [55] |
Establishing Critical Process Parameters
Risk-Based Approach to CPP Identification
Critical Process Parameters are identified through a systematic risk assessment evaluating the potential impact of each process parameter on CQAs. Parameters with significant impact on CQAs are designated as CPPs and must be carefully controlled within predetermined ranges [50]. The manufacturing process for hematopoietic stem cell gene therapy provides a robust example of this approach, where CPP identification has enabled reproducible GMP manufacturing [21].
Comprehensive CPP Ranges for Stem Cell Manufacturing
The following table consolidates CPPs and their acceptable ranges from recent GMP-compliant stem cell manufacturing platforms:
Table 3: Critical Process Parameters and Their Ranges in Stem Cell Manufacturing
| Manufacturing Stage | Critical Process Parameter | Target Range | Impact on CQAs |
|---|---|---|---|
| Cell Isolation | Enzyme concentration (e.g., collagenase) | 0.1-0.5% (w/v) | Impacts cell viability, surface marker preservation, and recovery yield |
| Cell Expansion | Seeding density | 1,000-5,000 cells/cm² for MSCs0.5-2.0×10^6 cells/mL for suspension | Affects proliferation rate, differentiation potential, and senescence |
| Cell Expansion | Medium exchange frequency | Every 48-72 hours | Maintains nutrient levels, removes waste, affects metabolic stress |
| Genetic Modification | Multiplicity of infection (MOI) | 12.5-100 (with transduction enhancers) | Directly impacts transduction efficiency and vector copy number [21] |
| Genetic Modification | Transduction enhancer concentration (LentiBOOST/protamine sulfate) | Manufacturer-specified optimal range | Increases transduction efficiency 3-fold while reducing vector requirements [21] |
| Cell Harvest | Detachment time | 5-15 minutes at 37°C | Affects membrane integrity, viability, and post-thaw recovery |
| Cryopreservation | Cooling rate | -1°C/min to -40°C, then -10°C/min to -120°C | Critical for maintaining viability and functionality post-thaw |
| Cryopreservation | Cryoprotectant concentration (DMSO) | 5-10% (v/v) | Balances cryoprotection with potential toxicity effects |
Experimental Protocols for CQA and CPP Determination
Protocol: Design of Experiments for CPP Definition
Objective: Systemically determine the relationship between process parameters and CQAs to establish proven acceptable ranges for CPPs.
Materials:
- GMP-compliant cell culture medium (e.g., X-VIVO-15 with 1% human albumin serum) [21]
- Cytokines and growth factors (Flt3-L, SCF, TPO, IL-3) at GMP-grade [21]
- Bioreactor or multilayer cell culture vessels
- Process Analytical Technology tools (e.g., bioanalyzers, metabolite analyzers)
Methodology:
- Factor Selection: Identify potential CPPs through prior knowledge and risk assessment (e.g., seeding density, medium composition, feeding schedule).
- Experimental Design: Implement a fractional factorial design to efficiently screen multiple parameters simultaneously.
- Process Modeling: Develop mathematical models describing the relationship between CPPs and CQAs using response surface methodology.
- Design Space Definition: Establish the multidimensional combination of CPPs that ensures CQAs remain within target ranges.
- Control Strategy Implementation: Define monitoring systems and control limits for each CPP within the design space.
Validation: Execute three consecutive validation runs at manufacturing scale demonstrating consistent CQA profiles within predefined specifications.
Protocol: Transduction Efficiency Optimization for HSC Gene Therapy
Objective: Maximize transduction efficiency while maintaining appropriate vector copy number and cell viability for hematopoietic stem cell gene therapy applications.
Materials:
- GMP-grade lentiviral vector (e.g., IDS.ApoEII LV for MPSII therapy) [21]
- Human CD34+ cells isolated via CliniMACSplus system [21]
- Transduction enhancers: LentiBOOST and protamine sulfate
- Serum-free medium: X-VIVO-15 with 1% HSA
- Cytokine cocktail: Flt3-L, SCF, TPO, IL-3
Methodology:
- Cell Preparation: Thaw cryopreserved CD34+ cells and pre-stimulate for 24-48 hours in cytokine-supplemented medium.
- Transduction Setup: Aliquot cells into multiple culture conditions varying:
- MOI (12.5, 25, 50, 100)
- TE combinations (none, LentiBOOST only, protamine sulfate only, both)
- Vector incubation time (6-24 hours)
- Efficiency Assessment:
- Analyze transduction efficiency via flow cytometry for transgene expression
- Determine vector copy number by qPCR on genomic DNA
- Assess cell viability and proliferation capacity
- Functional Assessment:
- Perform colony-forming unit (CFU) assays to evaluate hematopoietic potential
- Measure intracellular enzyme activity (e.g., IDS activity for MPSII therapy)
- Data Analysis: Identify optimal conditions balancing high transduction efficiency (>70%) with appropriate VCN (1.0-3.0) and maintained cell viability (>80%).
Expected Outcomes: Implementation of this protocol typically demonstrates a 3-fold improvement in transduction efficiency with TE inclusion while reducing vector quantity requirements [21].
Process Analytical Technology Implementation
PAT Integration in Stem Cell Manufacturing
Process Analytical Technology (PAT) refers to systems for real-time monitoring of CPPs and CQAs during the manufacturing process [50]. For stem cell therapies, PAT implementation is essential due to the living nature of the product and inability to perform terminal sterilization. The advanced QbD framework for MSC manufacturing successfully integrated PAT for real-time quality monitoring and control throughout scale-up [51].
The following diagram illustrates a PAT-integrated manufacturing workflow for stem cell therapies:
PAT-Integrated Stem Cell Manufacturing Workflow
PAT Tools and Applications
In-line Monitoring Tools:
- Bioanalyzers: Real-time assessment of metabolite levels (glucose, lactate, glutamate)
- Flow cytometry systems: Automated immunophenotyping and viability assessment
- Microscopy with image analysis: Confluence monitoring and morphological assessment
- Biomarker sensors: Detection of secreted factors indicating differentiation status
Implementation Strategy:
- Identify CQAs amenable to real-time monitoring
- Select appropriate analytical technologies matching process timing constraints
- Establish correlation between PAT measurements and reference methods
- Define control limits and response protocols for out-of-specification PAT readings
- Integrate PAT data with manufacturing execution systems for automated control
Essential Research Reagent Solutions
The successful implementation of QbD principles requires carefully selected reagents and materials that comply with regulatory requirements. The following table details essential research reagent solutions for stem cell therapy development:
Table 4: Essential Research Reagent Solutions for QbD Implementation in Stem Cell Therapy Development
| Reagent Category | Specific Examples | Function in QbD Implementation | Regulatory Considerations |
|---|---|---|---|
| GMP-compliant Culture Media | TeSR-AOF for pluripotent stem cells, StemSpan-AOF for HSCs, MesenCult-ACF Plus for MSCs [53] | Provides consistent, animal origin-free base for manufacturing processes; reduces lot-to-lot variability | ISO 20399, USP <1043>, ICH Q7 compliance; extensive safety testing documentation [53] |
| Cell Activation/Expansion Reagents | ImmunoCult T cell activators, StemSpan supplements with cytokines | Enables controlled expansion while maintaining functional potency; critical for process consistency | GMP-compliant manufacturing; regulatory documentation for IND/CTA submissions [53] |
| Cryopreservation Media | CryoStor CS10 [53] | Maintains cell viability and functionality post-thaw; critical for product stability | Serum- and animal component-free formulation; GMP-compliant |
| GMP-compliant iPSC Lines | REPROCELL StemRNA Clinical Seed iPSCs [55], Catalent's off-the-shelf iPSC banks [9] | Provides standardized, characterized starting materials; reduces source variability | Comprehensive testing (sterility, mycoplasma, endotoxin, viral screening); FDA DMF submission [9] |
| Transduction Enhancers | LentiBOOST, protamine sulfate [21] | Improves transduction efficiency 3-fold while reducing vector requirements; critical CPP | GMP-grade availability; toxicity profiling required |
Implementing a systematic Quality by Design approach is no longer optional but essential for successful development and regulatory approval of patient-specific stem cell therapies. By establishing scientifically-derived Critical Quality Attributes and Critical Process Parameters, manufacturers can build quality into their products from the earliest development stages rather than relying on end-product testing alone. The integration of Process Analytical Technology enables real-time quality assurance and forms the basis for an effective control strategy.
As the stem cell therapy field advances with recently approved products and an expanding clinical trial landscape [9], the application of QbD principles becomes increasingly critical for demonstrating product consistency, manufacturing robustness, and ultimately, ensuring patient safety. The frameworks, protocols, and parameters outlined in this application note provide a foundation for researchers and drug development professionals to implement these principles in their own stem cell therapy development programs.
The translation of patient-specific stem cell therapies from academic research laboratories to Good Manufacturing Practice (GMP) facilities represents a critical pathway for bringing regenerative medicine treatments to patients. This process, known as technology transfer, involves moving research processes into a controlled, regulated environment capable of producing clinical-grade materials. Successful technology transfer requires meticulous planning, rigorous documentation, and adaptation of research protocols to meet stringent regulatory requirements for safety, purity, and potency [25]. The International Society for Stem Cell Research (ISSCR) emphasizes that maintaining widely shared principles in science that call for rigor, oversight, and transparency provides assurance that stem cell research is conducted with scientific and ethical integrity [1]. This application note examines key considerations and presents protocols supporting effective technology transfer within the framework of GMP compliance for manufacturing patient-specific stem cell therapies.
Regulatory Framework and Quality Systems
Foundational Regulatory Requirements
Technology transfer activities must operate within a well-defined regulatory framework that governs the production of advanced therapy medicinal products. GMP compliance is non-negotiable in cell therapy manufacturing as it ensures patient safety, regulatory approval, and product consistency by enforcing strict quality control at every production stage [56]. Regulatory bodies including the FDA (21 CFR Part 210 & 211) and EMA require extensive documentation and process validation before granting approval for cell and gene therapies [57] [56]. A risk-based quality system approach forms the foundation for compliance, addressing facilities, equipment, materials, and documentation controls [25].
Critical Quality Attributes for Stem Cell Therapies
Establishing and monitoring Critical Quality Attributes (CQAs) is essential for maintaining product quality throughout technology transfer and manufacturing. CQAs are measurable properties that define product quality, safety, and efficacy [56]. For patient-specific stem cell therapies, key CQAs must be rigorously defined and controlled throughout the manufacturing process.
Table 1: Critical Quality Attributes for Patient-Specific Stem Cell Therapies
| Quality Attribute | Target Specification | Analytical Method |
|---|---|---|
| Cell Viability | >80% (post-thaw) | Flow cytometry, dye exclusion [58] [59] |
| Cell Purity/Identity | >90% target cell population | Flow cytometry, molecular profiling [58] |
| Potency | Meets pre-defined functional assay criteria | Functional assays (e.g., differentiation, cytokine secretion) [58] |
| Sterility | No microbial, fungal, or mycoplasma contamination | Sterility testing, mycoplasma testing [25] [56] |
| Genetic Stability | Normal karyotype, no unwanted mutations | Karyotyping, DNA sequence verification [58] |
Technology Transfer Process: Key Stages and Considerations
Pre-Transfer Planning
The technology transfer process begins with comprehensive planning and gap analysis to identify differences between research and GMP environments. This stage includes documenting the research process in extreme detail, identifying critical process parameters, and establishing acceptance criteria for the transferred process. The ISSCR guidelines emphasize the importance of transparency and timely exchange of accurate scientific information during this collaborative phase [1]. Facility design considerations are paramount, with clean rooms classified according to air purity requirements (Class A-D) and strict controls for temperature, humidity, and pressure [25].
Process Adaptation and Qualification
Adapting research protocols to GMP-compliant processes often requires substituting research-grade reagents with GMP-grade materials, implementing closed systems to reduce contamination risk, and establishing in-process controls. Automation solutions can significantly enhance process consistency; for example, automated cell processing systems like the Gibco CTS Rotea Counterflow Centrifugation System offer closed processing with high cell recovery and viability [17]. Process qualification activities demonstrate that the adapted process consistently produces material meeting all pre-defined CQAs and is robust enough for clinical manufacturing.
Case Study: Technology Transfer of an Autologous iPSC-Derived Therapy
This case study examines the technology transfer of an autologous induced pluripotent stem cell (iPSC)-derived dopaminergic neural progenitor cell therapy for Parkinson's disease from an academic research laboratory to a GMP facility. The therapy involves reprogramming patient somatic cells to iPSCs, differentiating them to neural progenitor cells, and formulating the final product [9]. The technology transfer was conducted following a structured approach with defined milestones and quality controls.
Table 2: Technology Transfer Timeline and Key Milestones
| Phase | Duration | Key Activities | Deliverables |
|---|---|---|---|
| Pre-Transfer Planning | 3 months | Process documentation, gap analysis, reagent sourcing | Technology transfer plan, quality agreements |
| Process Adaptation | 5 months | reagent qualification, protocol optimization, draft batch records | Adapted SOPs, qualified materials list |
| Engineering Runs | 2 months | Equipment qualification, process simulation, staff training | Equipment validation documents, trained personnel |
| Process Performance Qualification | 3 months | Three consecutive successful batches, analytical testing | PPQ report, validated methods, CQA verification |
| Documentation Finalization | 1 month | Compilation of all documents for regulatory submission | Complete CMC section for IND application |
Experimental Protocols
Protocol 1: GMP-Compliant iPSC Generation and Characterization
This protocol outlines the critical steps for generating clinical-grade iPSCs under GMP conditions, a foundational process for patient-specific stem cell therapies.
Materials:
- GMP-grade reprogramming vectors or mRNA
- GMP-grade cell culture media and supplements
- Matrigel Matrix or GMP-approved recombinant laminin-521
- Sterile, single-use bioreactors or multilayer flasks
- Quality control assay reagents
Procedure:
- Cell Source Collection: Obtain patient skin biopsy or blood sample under aseptic conditions. Transport to GMP facility maintaining appropriate temperature conditions and chain of custody documentation.
- Somatic Cell Isolation: Isolate fibroblasts or peripheral blood mononuclear cells using GMP-compliant dissociation reagents and density gradient centrifugation.
- Reprogramming: Use integration-free, GMP-grade reprogramming vectors to generate iPSCs. Perform transduction in a closed system where possible.
- iPSC Expansion and Cloning: Culture emerging iPSC colonies on GMP-approved substrates. Mechanically pick colonies or use single-cell passaging with GMP-grade ROCK inhibitor.
- Banking: Create Master Cell Bank and Working Cell Bank following GMP principles. Cryopreserve in controlled-rate freezer with appropriate documentation.
- Characterization: Perform comprehensive testing including:
- Pluripotency marker analysis (flow cytometry for Tra-1-60, SSEA4, OCT4, SOX2)
- Trilineage differentiation potential (embryoid body formation)
- Karyotype analysis
- Short tandem repeat (STR) profiling for identity confirmation
- Mycoplasma testing and sterility testing
Quality Controls:
- Document all procedures using controlled batch records
- Monitor critical process parameters including cell viability, doubling time, and morphology
- Ensure all testing meets pre-defined acceptance criteria before bank release
Protocol 2: Neural Differentiation and Final Product Formulation
This protocol describes the GMP-compliant differentiation of iPSCs to dopaminergic neural progenitor cells and final product formulation.
Materials:
- GMP-grade neural differentiation media components
- GMP-approved growth factors (FGF, BMP inhibitors, SHH)
- Single-use bioreactor or cell factory systems
- Formulation buffer (GMP-grade saline with appropriate excipients)
Procedure:
- iPSC Preparation: Thaw vial from Working Cell Bank and expand iPSCs to required number while maintaining pluripotent state.
- Neural Induction: Initiate differentiation using dual SMAD inhibition protocol with GMP-grade small molecules.
- Midbrain Patterning: Pattern neural progenitor cells to floor plate fate using GMP-grade SHH and FGF8.
- Dopaminergic Differentiation: Further differentiate to dopaminergic neural progenitor cells using combination of growth factors.
- Harvest and Formulation: Harvest cells using GMP-grade enzymatic or mechanical dissociation. Wash and resuspend in formulation buffer at target concentration.
- Final Fill: Aseptically fill into final product containers. Cryopreserve in vapor phase liquid nitrogen.
Quality Controls:
- In-process controls for cell count, viability, and morphology
- Flow cytometry for neural progenitor markers (NESTIN, SOX1, SOX2) and dopaminergic markers (FOXA2, LMX1A, OTX2)
- Potency assay measuring dopamine secretion in vitro
- Final product testing for sterility, mycoplasma, endotoxin, and cell viability
Process Workflow and Critical Control Points
The following diagram illustrates the complete workflow for the technology transfer and manufacturing process, highlighting critical control points and quality checks.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful technology transfer requires careful selection and qualification of reagents and materials that meet regulatory requirements. The following table details essential materials and their GMP-compliant alternatives used in the featured case study.
Table 3: Research Reagent Solutions for GMP-Compliant Stem Cell Manufacturing
| Material Category | Research Grade Example | GMP-Compliant Alternative | Critical Function |
|---|---|---|---|
| Reprogramming Vectors | Lentiviral vectors (research grade) | GMP-grade non-integrating episomal vectors or mRNA | Introduction of pluripotency factors without genomic integration [9] |
| Culture Substrate | Matrigel (research grade) | Recombinant laminin-521 (GMP-grade) | Defined substrate for pluripotent stem cell attachment and growth [17] |
| Cell Culture Media | Research-grade basal media with FBS | Xeno-free, GMP-grade media with defined components | Support cell growth while minimizing contamination risk [56] |
| Differentiation Factors | Research-grade growth factors | GMP-grade recombinant proteins (FGF, BMP, SHH) | Direct lineage-specific differentiation with lot-to-lot consistency [17] |
| Dissociation Reagents | Research-grade trypsin/EDTA | GMP-grade recombinant trypsin or enzyme-free dissociation | Cell passaging while maintaining viability and functionality [58] |
Analytical Methods and Quality Control Strategies
Quantitative Single-Cell Approaches
Advanced analytical methods are essential for comprehensive characterization of stem cell products. Quantitative single-cell approaches enable detailed assessment of cellular heterogeneity, which is critical for understanding product consistency and potency. Techniques such as single-cell RNA sequencing, high-content imaging, and flow cytometry provide multidimensional data on cell identity, function, and purity [60]. Implementing these methods during technology transfer helps identify critical quality attributes and establish meaningful release criteria.
In Vivo Kinetics and Tracking Methods
For cell therapies, understanding in vivo behavior is an important aspect of product characterization. Quantitative detection methods including PCR-based assays (detection limit: 100 cells/gram tissue), flow cytometry (detection limit: 1,000 cells), and optical imaging (detection limit: 1,000 cells) provide valuable data on cell distribution, persistence, and potential migration to non-target tissues [59]. While primarily used in preclinical studies, these methods inform product characterization and help design appropriate safety monitoring strategies for clinical trials.
Successful technology transfer of patient-specific stem cell therapies from academic labs to GMP facilities requires systematic approach that balances scientific innovation with regulatory compliance. Key success factors include early and comprehensive planning, careful attention to documentation, rigorous process understanding, and implementation of appropriate quality controls. The case study and protocols presented herein provide a framework for navigating this complex process. As the field advances with an increasing number of stem cell therapies entering clinical trials and receiving regulatory approval [9], establishing robust, scalable technology transfer processes becomes increasingly critical for making these innovative treatments available to patients in need while maintaining the highest standards of safety and efficacy.
Addressing Manufacturing Challenges and Scaling Patient-Specific Therapies
Managing Donor Variability in Autologous Cell Starting Materials
The development of autologous cell therapies represents a paradigm shift in personalized medicine. However, the inherent variability in donor-derived cellular starting materials introduces significant challenges for the standardization and manufacturing of these products under Good Manufacturing Practice (GMP) regulations [61]. Unlike traditional pharmaceuticals, the "raw material" for autologous therapies is the patient's own cells, which are highly variable due to factors such as disease status, prior treatments, and individual biological differences [61] [62]. This variability can profoundly impact both upstream and downstream manufacturing processes, potentially affecting critical quality attributes (CQAs) of the final drug product [61]. This Application Note provides a structured framework for understanding, quantifying, and managing donor variability to ensure consistent production of safe, efficacious, and GMP-compliant patient-specific stem cell therapies.
Variability in cellular starting materials originates from multiple sources, which can be categorized as patient-specific, collection-related, or process-related.
Patient-Specific Factors
The health and biological characteristics of the donor are primary drivers of variability. Key factors include:
- Disease Severity and Type: The specific cancer or disease, its stage, and the patient's place in the treatment protocol significantly influence cell quality and suitability for manufacturing [61] [62]. For example, patients with Chronic Lymphocytic Leukemia (CLL) often present with lymphocytosis, while lymphoma patients may exhibit lymphopenia, directly impacting the collected cell populations [62].
- Prior Treatments: Chemotherapy, radiation, and immunotherapy can have significant impacts on patient cells, affecting their quantity, quality, and functionality for genetic modification and expansion [61].
- Demographics and Physiology: Patient age, genetic and epigenetic factors, underlying health conditions, medications, and environmental exposures all contribute to the overall quality of the cellular starting material [61].
Collection-Related Factors
The process of collecting starting material introduces another layer of variability:
- Apheresis Procedures: Differences in apheresis protocols, collection devices, operator training, and the type and concentration of anticoagulants used can affect the quality of the collected leukapheresis product [61] [62].
- Collection Efficiency: This can be impacted by patient-specific factors such as pre-apheresis CD3+ cell counts, hematocrit level, platelet level, and vascular access quality [61] [62].
- Logistics: The time between apheresis and manufacturing initiation, along with shipping conditions, can affect cell viability and functionality [61].
Process-Related Factors
Post-collection handling and processing steps contribute additional variability:
- Cryopreservation and Thawing: The choice of cryopreservation media, freezing rates, storage conditions, and thawing methods can influence post-thaw recovery and cell viability [61] [62].
- Cell Culture and Expansion: Factors related to cell culture conditions, including media composition and incubation parameters, contribute to variations in the final product [61].
- Quality Controls: Different facilities may implement varying regulatory or quality controls, leading to inconsistencies in raw material assessment and processing [61].
A Risk-Based Approach for Managing Variability
A systematic, risk-based approach is essential for managing donor variability while maintaining GMP compliance. The core strategy involves identifying the most critical starting material attributes, defining associated CQAs, and implementing control strategies at each process step.
Quantitative Data on Donor Variability and Its Impact
Understanding the magnitude of variability and its potential effects requires careful measurement and documentation of key parameters. The following tables summarize critical data points for assessing and managing donor variability.
Table 1: Key Pre-Collection Variables and Their Impact on Mononuclear Cell Products
| Variable Category | Specific Parameters | Measurable Impact on Product | Potential Manufacturing Consequences |
|---|---|---|---|
| Patient Demographics | Age, clinical indication [62] | Total mononuclear cell count, CD3+ cell percentage [62] | Varying expansion potential, transduction efficiency [62] |
| Disease Status | Disease type (e.g., CLL, ALL, Lymphoma) [62] | Lymphocytosis (CLL) vs. Lymphopenia (Lymphoma) [62] | Lower manufacturing success rates for specific indications (e.g., lymphoma) [62] |
| Prior Treatment | Chemotherapy, radiation, immunotherapy [61] | Cell quantity, quality, and functionality [61] | Reduced suitability for genetic modification and clinical-scale expansion [61] |
Table 2: Approved Autologous CAR T-Cell Therapies: Doses and Presentation
| T Cell Drug Product | Dose (CAR-Positive Viable T Cells) | Primary Container | Fill Volume per Container |
|---|---|---|---|
| Brexucabtagene autoleucel (Tecartus) | 2 × 10⁶ per kg body weight, max. 2 × 10⁸ [63] | Cryogenic infusion bag [63] | ~68 mL [63] |
| Axicabtagene ciloleucel (Yescarta) | 2 × 10⁶ per kg body weight, max. 2 × 10⁸ [63] | Cryogenic infusion bag [63] | ~68 mL [63] |
| Tisagenlecleucel (Kymriah) | 0.6–6.0 × 10⁸ [63] | Cryogenic infusion bag [63] | 10–50 mL [63] |
| Idecabtagene vicleucel (Abecma) | 3.0–4.6 × 10⁸ [63] | Cryogenic infusion bag [63] | Within validated range [63] |
Table 3: Core Analytical Methods for Characterizing Cellular Starting Materials
| Analytical Method | Key Measured Parameters | Role in Managing Variability |
|---|---|---|
| Flow Cytometry | Cell composition (e.g., CD3+, CD4+, CD8+), purity, contaminant populations (monocytes, granulocytes) [62] | Identifies non-T cell contaminants that can inhibit T cell proliferation or induce apoptosis [62] |
| Cell Counting & Viability | Total nucleated cell count, viability (e.g., by trypan blue exclusion) [61] | Essential for adjusting process parameters and final drug product dose [61] |
| In-process Potency Assays | Cytokine secretion, cytotoxic activity, transduction efficiency [61] | Provides early indication of batch success and helps define CQAs [61] |
Experimental Protocols for Variability Assessment and Control
Protocol: Standardized Assessment of Leukapheresis Material
Objective: To consistently characterize incoming leukapheresis material and identify potential variability that may impact manufacturing.
Materials:
- Leukapheresis product
- Research Reagent Solutions:
- Ficoll-Paque Premium: Density gradient medium for mononuclear cell separation [62].
- DPBS, without Ca²⁺/Mg²⁺: Phosphate-buffered saline for cell washing and dilution.
- Trypan Blue Solution (0.4%): For viable cell counting.
- Flow Cytometry Antibody Panel: Anti-CD3, CD4, CD8, CD14, CD19, CD56, and viability dye.
Procedure:
- Sample Preparation: Aseptically remove a representative sample from the leukapheresis bag. Record total product volume.
- Cell Counting and Viability:
- Dilute a 20 µL sample 1:10 with PBS.
- Mix 20 µL of diluted sample with 20 µL of 0.4% Trypan Blue.
- Load onto a hemocytometer and count total and viable nucleated cells.
- Calculate total nucleated cell count and viability percentage.
- Mononuclear Cell Separation (if required for analysis):
- Dilute the leukapheresis product 1:1 with PBS.
- Carefully layer 15 mL of diluted product over 15 mL of Ficoll-Paque in a 50 mL conical tube.
- Centrifuge at 400 × g for 30 minutes at room temperature with the brake off.
- Carefully collect the mononuclear cell layer at the interface and wash twice with PBS.
- Immunophenotyping by Flow Cytometry:
- Aliquot 1 × 10⁶ cells into FACS tubes.
- Stain with pre-titrated antibodies for 30 minutes at 4°C in the dark.
- Wash cells twice with FACS buffer (PBS + 2% FBS).
- Resuspend in fixation buffer and acquire data on a flow cytometer.
- Analyze the percentages of T cells (CD3+), helper T cells (CD3+CD4+), cytotoxic T cells (CD3+CD8+), monocytes (CD14+), B cells (CD19+), and NK cells (CD3-CD56+).
Data Analysis: Compare the cell composition, viability, and total cell count against established acceptance criteria for your manufacturing process. Material falling outside these criteria may require process adjustments.
Protocol: Process Flexibility and Adjustment for Variable Growth Kinetics
Objective: To accommodate variable T cell expansion rates through in-process monitoring and feed adjustment.
Materials:
- Isolated T cells
- Research Reagent Solutions:
- GMP-grade T Cell Culture Medium: Base medium (e.g., X-VIVO 15, TexMACS) supplemented with human serum albumin or FBS.
- GMP-grade T Cell Activator: e.g., Anti-CD3/CD28 beads or soluble antibodies.
- Cytokines: Recombinant human IL-2, IL-7, or IL-15.
- Cell Counting Reagents: As in Protocol 5.1.
Procedure:
- T Cell Activation and Culture:
- Seed T cells at a density of 1 × 10⁶ cells/mL in activation medium containing the T cell activator and appropriate cytokines.
- Incubate at 37°C, 5% CO₂.
- In-process Monitoring:
- Day 2-3: Perform daily cell counts and viability assessments. Monitor cell size and blast formation by microscopy.
- If growth kinetics are slow (< 1.5-fold increase in cell number by day 3), consider supplementing with additional cytokines (e.g., IL-2) or adjusting the cell density.
- If excessive activation or cell death is observed, consider partial medium exchange to remove waste products.
- Process Adjustment Points:
- Feed Strategy: Use real-time cell count data to adjust feed volumes or frequency. Automated systems can facilitate this [17].
- Harvest Decision: Base the harvest day on achieving target cell numbers or a specific expansion fold, rather than a fixed timeline. This accommodates variable doubling times.
This flexible, data-driven approach allows the process to be tailored to the specific growth characteristics of each donor's cells.
Integrated Workflow for Managing Variability in GMP Manufacturing
A holistic approach, integrating control strategies from donor to final product, is essential for GMP compliance. The following diagram outlines a comprehensive workflow designed to mitigate variability at each stage.
Research Reagent Solutions for Variability Management
The consistent use of high-quality, well-characterized reagents is fundamental to managing variability in autologous cell therapy manufacturing. The following table details essential materials and their functions.
Table 4: Essential Research Reagent Solutions for Managing Donor Variability
| Reagent / Material | Function | Importance for Managing Variability |
|---|---|---|
| GMP-grade Cell Culture Media | Provides nutrients and environment for cell growth and expansion [17]. | Formulated for consistency; reduces lot-to-lot variability compared to research-grade media. Supports robust growth across diverse donor cells. |
| GMP-grade Cytokines (e.g., IL-2) | Stimulates T-cell proliferation and survival [63]. | Critical for optimizing expansion of cells with variable growth kinetics. Quality ensures consistent performance across all batches. |
| Cell Separation Kits (e.g., Ficoll, CD3/CD28 beads) | Isolates target cell populations (e.g., PBMCs, T-cells) [62] [17]. | Standardizes the initial input population, reducing the impact of contaminating cells (e.g., monocytes, granulocytes) that can inhibit T-cell processes [62]. |
| GMP-grade Cryopreservation Media | Protects cells during freeze-thaw processes [63]. | Minimizes cell loss and preserves function post-thaw, countering the variable sensitivity of donor cells to cryopreservation stress [61]. |
| Vector / Transduction Reagent | Mediates genetic modification (e.g., CAR gene insertion) [63]. | High-quality, consistent reagents are essential for achieving reproducible transduction efficiency across donor cells with varying susceptibility to genetic modification [61]. |
| Automated Cell Processing Systems | Integrated, closed systems for cell washing, concentration, and separation [64] [17]. | Reduces operator-dependent variability and contamination risk. Provides flexibility to adapt processing parameters to different incoming cell materials [17]. |
The advancement of patient-specific stem cell therapies represents a frontier in modern medicine, offering potential cures for a range of debilitating diseases. However, the manufacturing of these autologous therapies—produced from a patient's own cells—faces significant scalability challenges within the constraints of Good Manufacturing Practice (GMP). Unlike traditional pharmaceuticals or allogeneic "off-the-shelf" cell products, personalized manufacturing requires the simultaneous production of thousands of individual batches, each meeting identical quality and safety standards [65] [66].
This application note details a structured framework for overcoming scalability limitations through process optimization, focusing on the integration of automation, decentralized manufacturing models, and quality by design (QbD) principles. The strategies and protocols described herein are designed to help researchers and drug development professionals navigate the complex journey from preclinical development to commercial-scale GMP manufacturing.
Scalability Challenges in Personalized Therapies
Scalability for autologous cell therapies is achieved through "scale-out"—running many identical, small-scale processes in parallel—rather than the "scale-up" model used for large-batch production [67]. This presents unique hurdles:
- Process Variability: The biological starting material (patient cells) is inherently variable, complicating the establishment of a standardized, robust process [66].
- Logistical Complexity: Coordinating cell collection, transport, manufacturing, and re-implantation across multiple geographies and timelines is a monumental task [68].
- Cost of Goods (COGs): Labor-intensive, manual processes using expensive raw materials can lead to COGs that exceed the therapy's reimbursable value [67].
- Regulatory Hurdles: Demonstrating product consistency and quality across numerous individual batches manufactured at different sites requires a sophisticated Quality Management System (QMS) [66].
Table 1: Key Scalability Challenges and Their Impact
| Challenge | Impact on Manufacturing | Consequence for Commercialization |
|---|---|---|
| Inherent Variability of Starting Material | Difficulty in process standardization; risk of batch failure. | Inconsistent product quality and efficacy. |
| Manual, Open Handling Steps | Labor-intensive; high contamination risk; difficult to replicate across sites. | High COGs; limited production capacity. |
| Complex Supply Chain & Logistics | Risk of cell viability loss during transport; strict vein-to-vein timelines. | Limited patient access; logistical failures. |
| Demonstrating Multi-Site Comparability | Need for extensive validation studies across different manufacturing locations. | Regulatory delays; barriers to global market access. |
Strategic Framework for Scalable GMP Manufacturing
Adoption of Closed and Automated Systems
Transitioning from open, manual processes to closed automated systems is a cornerstone of scalable personalized manufacturing. Automation significantly reduces the risk of contamination, decreases labor costs and timelines, and improves process reproducibility [65]. A key consideration is selecting technologies that balance flexibility with reliability.
- Technology Selection: The market offers "one solution" automated platforms that perform all manufacturing steps in a fully closed system, as well as modular platforms designed for specific steps [65].
- Implementation Focus: Prioritize automation for steps that are labor-intensive, prone to variability, or create bottlenecks in throughput (e.g., cell separation, washing, and final product formulation) [68].
Quantitative data from a clinical lab demonstrates that integrating a sample preparation system with a flow cytometer can reduce operator hands-on time for a standard wash assay by approximately 75%, from 32 minutes to just 8 minutes [69]. This level of efficiency is critical for scale-out.
Table 2: Impact of Automation on Key Process Parameters
| Process Parameter | Manual Process | Automated, Closed System | Improvement |
|---|---|---|---|
| Average Hands-on Time per Batch | 32 minutes | 8 minutes | 75% reduction [69] |
| Risk of Contamination | High (open handling) | Low (closed system) | Significant reduction [65] |
| Process Reproducibility | Operator-dependent | Standardized | Major improvement [65] [68] |
| Analytical Throughput | ~43 samples processed in 4 hours | ~90 samples processed in 4 hours | ~110% increase [69] |
Implementing a Decentralized Point-of-Care Manufacturing Model
Decentralized manufacturing is an emerging paradigm where products are manufactured at multiple sites under central management, often at or near the point of care (POCare) [66]. This model directly addresses scalability and logistics challenges for autologous therapies.
- Regulatory Framework: Regulatory bodies are developing frameworks for this model. The UK's MHRA has created new licenses for "manufacturer’s license (Point of Care, POC)," where a central "Control Site" supervises decentralized manufacturing and holds the POCare Master File [66].
- Quality Management System (QMS): A robust QMS is essential. The Control Site ensures consistency across all manufacturing nodes through standardized platforms, centralized training, and oversight of quality assurance [66].
- Enabling Technology: This model relies on closed-system automated technologies and rapidly deployable, modular manufacturing units (e.g., "GMP-in-a-box") that minimize infrastructure requirements and process variability at each site [66].
Process Standardization and Quality by Design (QbD)
A successful scale-out strategy depends on a highly standardized and well-characterized process.
- Target Product Profile (TPP): Begin development with the TPP in mind. This living document aligns manufacturing requirements with product specifications, defining minimal, target, and ideal criteria for commercial success [67].
- Quality by Design (QbD): Implement QbD principles to build quality into the process from the start. This involves identifying Critical Quality Attributes (CQAs) and using tools like Design of Experiments (DoE) to understand the impact of process parameters on CQAs, thereby creating a robust and scalable process [67] [68].
- Analytical Standardization: Use standardized instruments and assays across all manufacturing and QC sites. For example, flow cytometers with features like "Universal Setup" allow easy transfer of user-defined assays from one instrument to another, ensuring data comparability and consistency of results globally [69].
Experimental Protocol: Optimization of a Scalable GMP-Compliant Transduction Process
The following protocol provides a detailed methodology for optimizing the lentiviral transduction of hematopoietic stem cells (HSCs), a critical step in many gene therapy manufacturing processes. This protocol is based on a validated GMP process for an investigational HSC gene therapy for Mucopolysaccharidosis type II (MPSII) [21].
Objective
To establish a robust, scalable, and efficient transduction protocol for hCD34+ cells using GMP-grade lentiviral vector (LV) and transduction enhancers (TEs), achieving high vector copy number (VCN) and transduction efficiency while maintaining cell viability and multipotency.
Materials and Reagents
Table 3: Essential Research Reagent Solutions for GMP-Compliant Transduction
| Reagent / Solution | Function / Role in Process | GMP Consideration |
|---|---|---|
| GMP-grade Lentiviral Vector | Delivery of therapeutic gene to target HSCs. | Must be produced under GMP standards [21]. |
| Serum-Free Media (X-VIVO-15) | Base medium for cell culture and transduction. | Defined, xeno-free formulation supports regulatory compliance. |
| Cytokine Cocktail (Flt3-L, SCF, TPO, IL-3) | Pre-stimulation of HSCs to promote cell cycle entry, which is essential for LV transduction. | Use GMP-grade cytokines. |
| Human Albumin Solution (HAS) | Supplement to culture media; enhances cell viability. | Use GMP-grade 1% HSA [21]. |
| Transduction Enhancers (LentiBOOST & Protamine Sulfate) | Increase transduction efficiency, allowing for a reduction in the required vector quantity [21]. | GMP-grade equivalents must be sourced for clinical manufacturing. |
| Cryopreservation Solution | Long-term storage of the final drug product. | Formulated with DMSO and other excipients under GMP. |
Equipment
- Class II Biological Safety Cabinet
- CO2 Incubator (37°C, 5% CO2)
- Centrifuge
- Automated Cell Counter
- CFU assay materials (MethoCult medium)
- qPCR system for VCN analysis
- Enzyme activity assay kit
Method
Step 1: Cell Thaw and Pre-stimulation
- Thaw cryopresened human CD34+ cells (hCD34+) in a 37°C water bath.
- Slowly dilute the cell suspension in pre-warmed serum-free media (X-VIVO-15) supplemented with 1% HSA and cytokines (Flt3-L, SCF, TPO, IL-3).
- Perform a cell count and viability assessment (e.g., via Trypan Blue exclusion).
- Seed cells at a density of 1-2 x 10^6 cells/mL in an appropriate culture vessel (e.g., a G-Rex bioreactor or cell culture bag).
- Incubate cells for 24-48 hours at 37°C, 5% CO2 to pre-stimulate.
Step 2: Lentiviral Transduction
- After pre-stimulation, harvest cells and centrifuge.
- Prepare the transduction medium: fresh serum-free media with cytokines, 1% HSA, the required MOI of GMP-grade LV, and TEs (LentiBOOST and protamine sulfate at optimized concentrations) [21].
- Resuspend the cell pellet in the transduction medium at a higher density (e.g., 5-10 x 10^6 cells/mL) to promote virus-cell contact.
- Seed the cell-virus mixture into a new culture vessel. For a scalable, closed process, use gas-permeable cell culture bags.
- Perform the first transduction for 8-24 hours at 37°C, 5% CO2.
- Optionally, perform a second transduction by repeating steps 1-5 with fresh transduction medium.
Step 3: Post-Transduction Culture and Harvest
- Following transduction, centrifuge cells to remove the vector-containing medium.
- Resuspend cells in fresh, pre-warmed growth medium (serum-free media with cytokines and 1% HSA) and transfer to a new culture vessel.
- Continue culture for 24-72 hours to allow for transgene expression before final harvest.
- Harvest the cells, perform a final cell count and viability check, and formulate into the final drug product for cryopreservation.
Analytical and QC Testing
- Vector Copy Number (VCN): Perform qPCR on genomic DNA from a sample of the final product to confirm the average number of vector integrations per cell [21].
- Transduction Efficiency: Assess using flow cytometry for reporter genes or by measuring intracellular enzyme activity (e.g., IDS activity for MPSII) [21].
- Cell Viability and Potency: Use a colony-forming unit (CFU) assay to confirm the multipotent differentiation potential of the transduced HSCs [21].
- Sterility Testing: Perform mandatory mycoplasma, bacterial, and fungal sterility tests on the final product.
Workflow Diagram: Scalable GMP Manufacturing Process
The diagram below illustrates the integrated workflow for a scalable, decentralized manufacturing process for personalized stem cell therapies, from cell collection to patient infusion.
Scalable Decentralized Manufacturing Workflow
Overcoming the scalability limitations in personalized stem cell therapy manufacturing is a multifaceted challenge that requires a holistic approach. As detailed in this application note, a successful strategy integrates:
- Technological Innovation: The adoption of closed, automated systems to reduce variability and contamination risk.
- Operational Model Shift: The implementation of a decentralized POCare manufacturing framework, supported by a robust, centralized QMS.
- Scientific Rigor: The application of QbD principles from the earliest stages of process development to create a robust and well-understood process.
By adopting these strategies, researchers and developers can de-risk the path to commercialization, enhance patient access, and ensure that these transformative therapies can be manufactured consistently, safely, and at a viable cost. The future of personalized medicine depends on building scalable, GMP-compliant manufacturing pathways today.
The manufacturing of patient-specific stem cell therapies represents a frontier in regenerative medicine, but its complexity presents significant challenges for consistent, scalable, and compliant production. Current Good Manufacturing Practice (cGMP) compliance requires robust, reproducible processes with minimal operator-dependent variability [70]. This application note details integrated automation solutions for two critical unit operations in stem cell therapy manufacturing: counterflow centrifugation for cell processing and electroporation for genetic modification. By implementing closed, automated systems for these procedures, manufacturers can address key bottlenecks in production workflow, enhance product quality, and maintain regulatory compliance throughout the development of patient-specific therapies.
Automated Counterflow Centrifugation
Counterflow centrifugation (CFC), also referred to as counterflow centrifugal elutriation, is an advanced cell processing technology that enables continuous separation, washing, and concentration of cells. Unlike traditional batch centrifugation which processes samples in discrete steps, counterflow centrifugation maintains a continuous flow of cells and buffer, reducing processing time and handling while improving cell viability and recovery [71].
In CFC systems, cells are introduced into a spinning chamber where they experience two opposing forces: centrifugal force pushing them outward and fluid dynamic drag force moving them inward. By precisely balancing these forces through control of flow rates and rotation speed, cells can be separated based on size, density, and sedimentation characteristics. This technology is particularly valuable for processing sensitive primary cells used in stem cell therapies, including hematopoietic stem cells, mesenchymal stromal cells (MSCs), and induced pluripotent stem cells (iPSCs) [71] [72].
Key System Specifications: The Gibco CTS Rotea Counterflow Centrifugation System exemplifies modern automated CFC technology designed for cGMP environments. This versatile system applies proven counterflow centrifugation methods to a broad range of cell processing applications in cell therapy development and manufacturing [73]. The system's closed architecture and single-use disposable kits minimize contamination risk while providing exceptional flexibility for various cell processing applications including CAR-T therapy, stem cell therapy, and PBMC isolation [73].
Automated Electroporation Systems
Electroporation is a non-viral transfection technique that uses electrical pulses to create temporary pores in cell membranes, allowing payloads such as DNA, RNA, or proteins to enter cells [74]. This physical delivery method achieves high transfection efficiency even with hard-to-transfect primary cells, including stem cells and immune cells [74]. Electroporation can deliver larger payloads (>7 kb) than cationic lipid-based or viral methods and is generally easier and less costly than viral transfection [74].
Advanced electroporation systems now feature flow electroporation technology, where cells flow through a processing chamber where discrete volumes are electroporated then collected continually. This innovation enables genetic engineering at large scale, moving from single cuvette experiments to commercial-scale production [75].
Key System Specifications: Both the MaxCyte ExPERT platform and Thermo Fisher Scientific CTS Xenon Electroporation System represent state-of-the-art automated electroporation technologies. The CTS Xenon System offers reliably high transfection performance in volumes of up to 25 mL in less than 25 minutes with exceptional cell viability and recovery [74]. The system accommodates single-use electroporation chambers—1 mL SingleShot chamber for batch processing and 5-25 mL MultiShot cartridge for continuous processing—enabling scalability from process development to GMP manufacturing [74].
Quantitative Performance Data
Counterflow Centrifugation Performance Metrics
Table 1: Performance Metrics of Automated Counterflow Centrifugation Systems
| Parameter | Gibco CTS Rotea System | Traditional Manual Centrifugation |
|---|---|---|
| Processing Time | 30-45 minutes per sample | 60-120 minutes per sample |
| Cell Recovery Rate | Typically >85% | Highly variable (60-90%) |
| Cell Viability | Consistently >90% | Variable (70-95%) |
| Contamination Risk | Reduced via closed system | Higher due to open processing |
| Operator Hands-on Time | <15 minutes | 45-90 minutes |
| Volume Reduction Capacity | Up to 200:1 concentration | Limited to ~10:1 concentration |
| Process Consistency | High (automated parameters) | Variable (operator-dependent) |
Data compiled from [71] and [72].
Electroporation Performance Metrics
Table 2: Performance Metrics of Automated Electroporation Systems
| Parameter | CTS Xenon System | MaxCyte ExPERT Platform | Traditional Electroporation |
|---|---|---|---|
| Transfection Efficiency | 61-85% gene editing efficiency [74] | Routinely >90% for multiple cell types [75] | Highly variable (30-70%) |
| Cell Viability | Usually >70%, within 10% of untransfected controls [74] | High viability with maximal cell recovery [75] | Often <50% for difficult cells |
| Processing Volume Range | 1mL to 25mL [74] | Thousands to billions of cells [75] | Typically <500μL |
| Processing Time | <25 minutes for 25mL [74] | Rapid processing with quick setup | 30-60 minutes including setup |
| Scalability | Seamless from development to manufacturing [74] | Single platform from concept to commercialization [75] | Limited scalability |
| cGMP Compliance | Designed for GMP manufacturing with compliance software [74] | Enables cGMP-compliant workflows [75] | Research use only |
Application Protocols
Protocol 1: Automated Cell Processing Using Counterflow Centrifugation for Stem Cell Therapy Manufacturing
This protocol details the use of automated counterflow centrifugation for washing and concentrating mesenchymal stromal cells (MSCs) prior to formulation as a patient-specific therapy.
Materials and Equipment:
- Gibco CTS Rotea Counterflow Centrifugation System or equivalent automated CFC system
- Sterile single-use processing kit
- Cell suspension (e.g., expanded MSCs in culture medium)
- Appropriate wash buffer (e.g., PBS without Ca2+/Mg2+)
- Sterile collection bags or tubes
- cGMP-compliant cell culture facility
Procedure:
- System Preparation: Install the single-use processing kit according to manufacturer instructions. Prime the system with wash buffer to remove air and verify proper fluid path function.
- Parameter Setup: Program the system operating parameters based on cell type:
- Rotation Speed: 2,000-3,000 RPM for MSCs
- Buffer Flow Rate: 100-200 mL/min
- Processing Temperature: 2-8°C
- Sample Loading: Aseptically connect the cell suspension bag to the system. For MSCs at passage 4-6, typical input volume is 500mL-1L at 0.5-1×10^6 cells/mL.
- Processing Phase: Initiate the automated processing sequence. The system will:
- Continuously introduce cell suspension into the spinning chamber
- Wash cells with 5-10 volumes of buffer
- Concentrate cells while removing processing media components
- Maintain temperature control throughout the process
- Cell Collection: Once processing completes, cells are automatically transferred to the collection bag. Typical output is 10-20mL at 25-50×10^6 cells/mL.
- System Purge: Follow manufacturer instructions for proper system shutdown and disposal of single-use components.
Quality Control Assessment:
- Determine cell concentration and viability using automated cell counters
- Assess sterility through Gram stain and microbial culture
- Verify identity through flow cytometry for MSC markers (CD73+, CD90+, CD105+, CD45-)
- Evaluate functionality through differentiation assays (osteogenic, adipogenic, chondrogenic)
This automated process reduces hands-on time by approximately 70% compared to manual centrifugation while improving cell recovery and consistency [71] [72].
Protocol 2: Automated Electroporation for Genetic Modification of Stem Cells
This protocol describes the use of flow electroporation for efficient genetic modification of induced pluripotent stem cells (iPSCs) while maintaining cGMP compliance throughout the manufacturing process.
Materials and Equipment:
- CTS Xenon Electroporation System or MaxCyte ExPERT Platform
- Appropriate single-use electroporation chamber or cassette
- Electroporation buffer (specific to cell type)
- Cells for transfection (e.g., iPSCs at 80-90% confluence)
- Payload material (DNA, RNA, or protein)
- Recovery media with appropriate supplements
Procedure:
- Cell Preparation: Harvest iPSCs using gentle dissociation reagent. Wash and resuspend in electroporation buffer at optimal density:
- iPSCs: 1-2×10^7 cells/mL
- Final Volume: Adjust based on chamber capacity (1-25mL)
- Payload Preparation: Prepare nucleic acid or protein payload in appropriate buffer. For CRISPR-Cas9 editing, prepare ribonucleoprotein (RNP) complexes by incubating sgRNA with Cas9 protein for 10-20 minutes at room temperature.
- Sample Mixing: Combine cells with payload material at optimal ratio:
- DNA: 5-20μg per 1×10^6 cells
- RNP Complexes: 10-50pmol per 1×10^6 cells
- System Setup: Install appropriate sterile electroporation chamber. Load sample mixture into chamber assembly according to manufacturer instructions.
- Electroporation Parameters: Program system with optimized parameters:
- Voltage: Cell type-specific (e.g., 1350V for iPSCs)
- Pulse Width: 10-30ms
- Pulse Number: 1-3 pulses
- Interval: 5-10 seconds between pulses
- Processing: Initiate electroporation protocol. The automated system delivers programmed electrical pulses while monitoring parameters in real-time.
- Rest and Recovery: Immediately transfer electroporated cells to pre-warmed recovery media. Incubate at 37°C for 10-15 minutes before transferring to culture vessels for expansion.
Post-Transfection Analysis:
- Assess cell viability at 24 hours post-electroporation (expect >70% for optimized protocols)
- Evaluate transfection efficiency at 48-72 hours using flow cytometry or imaging
- For gene editing applications, analyze editing efficiency at 72-96 hours using T7E1 assay or next-generation sequencing
- Monitor cell proliferation and functionality to ensure maintenance of stemness properties
This automated electroporation process enables high-efficiency genetic modification while maintaining cGMP compliance through closed processing and comprehensive documentation [75] [74].
Integrated Workflow Visualization
Figure 1: Integrated automated workflow for patient-specific stem cell therapies. The diagram illustrates the sequential processing steps from starting material to final product, with continuous cGMP compliance monitoring and automated data recording throughout the manufacturing process.
Research Reagent Solutions
Table 3: Essential Research Reagents for Automated Cell Processing Systems
| Reagent Category | Specific Examples | Function | cGMP Compliance Status |
|---|---|---|---|
| Electroporation Buffers | CTS Xenon Electroporation Buffer, MaxCyte Electroporation Buffer | Optimized conductivity and composition for efficient molecular delivery with maintained cell viability | CTS buffers meet USP <1043> and EP 5.2.12 requirements [74]; MaxCyte buffer is animal-derived component free [75] |
| Cell Culture Media | Gibco CTS OpTmizer Pro SFM, Xeno-Free MSC Expansion Media | Support cell growth and maintenance while meeting regulatory requirements for raw materials | Serum-free, xeno-free formulations available with CTS grade for clinical manufacturing [70] [73] |
| Growth Factors & Cytokines | PeproGMP Cytokines, Recombinant Human Proteins | Direct cell differentiation, expansion, and functionality in defined culture systems | GMP-manufactured with comprehensive documentation for regulatory filings [70] [73] |
| Cell Dissociation Reagents | Enzyme-free dissociation buffers, Trypsin alternatives | Gentle cell detachment while maintaining surface receptor integrity | Defined formulations without animal components reduce contamination risk [70] |
| Cryopreservation Media | Defined cryoprotectant solutions | Maintain cell viability and functionality during freeze-thaw cycles | Formulated without DMSO or with reduced concentrations to minimize toxicity [72] |
Regulatory Considerations for cGMP Compliance
Implementing automated solutions for stem cell therapy manufacturing requires careful attention to regulatory requirements across multiple jurisdictions. Key considerations include:
Raw Material Qualification: All raw materials must be properly qualified with assessment of lot-to-lot variability, testing for residuals on the final cell product, and additional safety testing as needed [70]. The manufacturer must qualify whether suppliers can provide necessary traceability, characterization, and regulatory filing support documentation [70].
Closed System Validation: Automated systems claiming closed processing must demonstrate effective containment and prevention of contamination through appropriate validation studies. This includes testing for maintenance of sterility throughout the processing workflow [74] [72].
Software Compliance: Automated systems with digital controls must comply with 21 CFR Part 11 requirements for electronic records and electronic signatures when used in GMP manufacturing [74]. Systems should provide audit trails, user access controls, and data integrity protections.
Process Analytical Technologies: Implementation of in-process monitoring and controls is essential for demonstrating process consistency and product quality. Automated systems should incorporate capabilities for real-time monitoring of critical process parameters [70] [71].
Quality Control Testing: Comprehensive characterization of critical quality attributes including purity, potency, and safety must be established as release criteria [70]. The International Society for Cell & Gene Therapy (ISCT) has updated criteria to include tissue-source origin and functional assays assessing immunomodulatory capability and trophic factor secretion [70].
The integration of automated counterflow centrifugation and electroporation systems addresses critical challenges in manufacturing patient-specific stem cell therapies. These technologies enable reproducible processing with minimal operator intervention, reduced contamination risk, and improved product consistency—all essential elements for cGMP compliance. As the field advances toward more complex stem cell-based products, continued innovation in automation platforms will be essential for scaling production while maintaining the rigorous quality standards required for clinical application. The protocols and data presented herein provide a framework for implementation of these technologies within a regulatory-compliant manufacturing environment for patient-specific stem cell therapies.
The successful development and manufacturing of patient-specific stem cell therapies, such as autologous CAR-T cell therapies and induced pluripotent stem cell (iPSC)-derived products, depend on a robust and well-managed supply chain for ancillary materials (AMs) [17]. AMs are critical reagents and components—including cell isolation reagents, culture media, growth factors, and differentiation-inducing small molecules—used in the manufacturing process but not intended to be part of the final therapeutic product [76] [77]. The quality and availability of these materials directly impact the safety, purity, potency, and identity of the final cell therapy product, making their consistent supply a cornerstone of Good Manufacturing Practice (GMP) compliance [76] [25].
This application note provides a structured framework for the qualification and supply chain management of AMs, outlining specific protocols and risk-based approaches to ensure consistent quality and availability throughout the clinical development of patient-specific stem cell therapies.
Ancillary Material Qualification: A Risk-Based Framework
Ancillary material qualification is the process of establishing the source, identity, purity, biological safety, and general suitability of a given AM for its intended use in manufacturing [76]. Given the absence of specific, definitive regulations for AMs, the United States Pharmacopeia (USP) chapter <1043> provides a foundational guideline for developing appropriate qualification programs using a risk-based approach [76] [77].
USP <1043> Tiered Risk Classification
USP <1043> classifies AMs into four tiers based on risk, which determines the extent of qualification required. The classification considers the material's intrinsic characteristics and its potential impact on the final cell product.
Table 1: USP <1043> Ancillary Material Risk Classification and Qualification Requirements
| Risk Tier | Risk Level & Description | Key Qualification Activities |
|---|---|---|
| Tier 1 | Low-risk, highly qualified materials (e.g., salts, sugars) [76] | Cross-reference Drug Master File (DMF); obtain Certificate of Analysis (CoA); assess removal from final product and lot-to-lot variability [76]. |
| Tier 2 | Moderate-risk materials | All Tier 1 activities, plus confirmation of critical CoA results and additional characterization as needed [76]. |
| Tier 3 | High-risk materials (e.g., animal-derived components, growth factors) [76] | All Tier 1 & 2 activities, plus extensive characterization and adventitious agent testing [76]. |
| Tier 4 | High-risk, minimally qualified materials (e.g., novel cytokines) [76] | All activities for Tiers 1-3, plus potential collaboration with supplier to upgrade the AM manufacturing process to cGMP standards [76]. |
The following workflow outlines the sequential process for qualifying an ancillary material, from initial risk assessment to final approval for GMP use.
Critical Reagents for Stem Cell Therapy Manufacturing
The manufacturing of patient-specific stem cell therapies relies on a suite of specialized reagents. Selecting the appropriate grade and qualifying these reagents early is critical for process consistency and regulatory compliance.
Table 2: Key Research Reagent Solutions for Stem Cell Therapy Manufacturing
| Reagent Category | Specific Examples | Function in Manufacturing Process |
|---|---|---|
| Cell Culture Media | Serum-free culture media, supplements | Supports the expansion and maintenance of stem cells and T-cells under defined conditions [77] [17]. |
| Growth Factors & Cytokines | Recombinant proteins (e.g., G-CSF, interleukins) | Directs stem cell differentiation or promotes ex vivo cell expansion and activation [77]. |
| Small Molecules | Synthetic inhibitors, pathway agonists | Precisely controls differentiation, reprogramming, and cell signaling pathways; offers high purity and scalability [77]. |
| Cell Isolation Reagents | Antibody cocktails, magnetic beads | Isulates specific cell populations (e.g., T-cells from leukapheresis product, specific stem cell subtypes) from a heterogenous starting material [76] [17]. |
| Gene Editing Reagents | CRISPR-Cas9 systems, mRNA, plasmids | Facilitates genetic modification of cells, as in CAR-T therapy [17]. |
| Cryopreservation Media | Formulated solutions with DMSO | Preserves cell viability and function during long-term storage and transport [76]. |
Experimental Protocols for Ancillary Material Qualification
Protocol: Qualification of a Growth Factor for Stem Cell Differentiation
This protocol details the steps to qualify a growth factor used to direct the differentiation of iPSCs into a specific lineage, classifying it as a USP <1043> Tier 3 or 4 material due to its high potential impact on the final product's safety and efficacy.
1.0 Objective To establish the purity, identity, potency, and functional suitability of a growth factor for use in the differentiation stage of a stem cell therapy manufacturing process.
2.0 Materials and Equipment
- Test growth factor (at least three independent lots)
- Reference standard (where available)
- Qualified iPSC master cell bank
- Basal differentiation media
- Cell culture plates and equipment
- Flow cytometer with appropriate antibodies
- SDS-PAGE and HPLC systems
- LAL assay kit for endotoxin testing
3.0 Methodology
3.1 Supplier Documentation and DMF Review
- Request and audit the supplier's complete documentation package, including the Certificate of Analysis (CoA) and, if available, the Drug Master File (DMF) [76].
- Verify that the material is manufactured under a quality management system, ideally cGMP, and is animal-origin free [77].
3.2 Identity and Purity Testing
- Identity: Confirm using mass spectrometry (if critical) or SDS-PAGE against a reference standard.
- Purity: Analyze by HPLC-SEC to determine monomeric purity and quantify high-molecular-weight aggregates and fragments. Specifications should be ≥95% monomeric protein.
- Endotoxin: Test using a kinetic chromogenic Limulus Amebocyte Lysate (LAL) assay. The acceptance criterion is typically <0.1 EU/μg.
3.3 Potency and Functional Bioassay
- Cell-Based Potency Assay: Differentiate a qualified iPSC line using a standardized protocol with the test growth factor.
- Analysis: At the process endpoint, harvest cells and analyze the percentage of target cells (e.g., dopaminergic neurons for a Parkinson's disease therapy) using flow cytometry.
- Acceptance Criterion: The differentiation efficiency achieved with the test material should not vary by more than ±15% from the efficiency achieved with a pre-qualified reference standard.
3.4 Lot-to-Lot Variability Assessment
- Perform the functional bioassay (section 3.3) using three separate lots of the growth factor.
- The differentiation efficiency across the three lots should meet the pre-defined acceptance criteria and show a standard deviation of less than 10%.
4.0 Data Analysis and Acceptance Criteria Compile all data and compare against pre-defined specifications. The growth factor is qualified for GMP manufacturing only if it meets all identity, purity, potency, and consistency criteria.
Protocol: Managing a Critical Raw Material Supply Chain
This protocol provides a methodology for establishing a resilient supply chain for a single-source, critical raw material.
1.0 Objective To ensure the continuous and qualified supply of a critical ancillary material by implementing a dual-supplier strategy and rigorous change control process.
2.0 Methodology
2.1 Supplier Qualification and Quality Agreements
- Audit: Conduct an on-site audit of the primary supplier's facilities and quality systems [76] [78].
- Quality Agreement: Execute a formal quality agreement that stipulates the supplier must provide advanced notification of any intended changes to the material's manufacturing process or specifications [76].
- Documentation: Secure a long-term supply agreement and ensure access to the DMF for regulatory submissions [76].
2.2 Establishment of a Qualified Second Source
- Identify and Qualify: Proactively identify and qualify a secondary supplier for the same material, following the qualification protocol in 3.1.
- Bridging Study: Perform a comprehensive comparability study (analytical testing and functional bioassay) to demonstrate equivalence between the primary and secondary source materials.
2.3 Inventory Management
- Maintain a strategic stockpile of the qualified material sufficient for a predefined number of manufacturing runs (e.g., 6-12 months of production) to buffer against supply chain disruptions.
3.0 Change Control Implementation
- Any change in supplier or material version triggers a formal change control process.
- The new lot must pass all qualification testing, and a side-by-side comparability study must be completed using the current GMP master cell bank before the new material is released for GMP use.
A Strategic Partnership Model for Supply Chain Management
Effective supply chain management requires close collaboration between cell therapy manufacturers (Users) and their reagent suppliers. A clear division of responsibilities is essential for efficiency and regulatory compliance.
Table 3: User and Supplier Accountabilities for Ancillary Material Qualification
| Qualification Activity | Supplier Accountability | User (Manufacturer) Accountability |
|---|---|---|
| Provide CoA, CoC, CoO | Primary | Review |
| Performance in intended application | Primary | |
| Conduct risk assessment | Primary | |
| Confirm critical CoA results | Primary | |
| Characterization testing | Support | Primary |
| Assess lot-to-lot variation | Primary | |
| Assess residual material in final product | Primary | |
| Stability studies | Support | Primary |
| Supplier audit | Primary | |
| Prepare and submit DMF | Primary | |
| Notify user of manufacturing changes | Primary | [76] |
The following diagram illustrates the interconnected relationships and material flows between the key entities in a resilient supply chain for stem cell therapy manufacturing.
As the stem cell therapy field advances, with an increasing number of products like Ryoncil (remestemcel-L) and iPSC-derived therapies entering clinical trials and gaining FDA approval, the demand for high-quality, well-characterized ancillary materials will continue to grow [9]. A proactive, science-based, and collaborative approach to ancillary material qualification and supply chain management is not merely a regulatory hurdle but a fundamental enabler of patient safety and therapeutic success. By implementing the risk-based frameworks, experimental protocols, and partnership models outlined in this application note, researchers and drug development professionals can build a foundation of quality and compliance from the laboratory bench to commercial-scale GMP manufacturing.
Batch-to-Batch Consistency Strategies Amid Biological Diversity
For developers of patient-specific stem cell therapies, achieving batch-to-batch consistency amid inherent biological diversity represents a fundamental challenge in Good Manufacturing Practice (GMP) compliance. The autologous nature of these therapies means that the starting biological material—the patient's own cells—varies significantly between individuals in terms of viability, proliferation capacity, and responsiveness to manufacturing processes [79]. These inherent variations introduce substantial challenges in producing standardized, consistent therapeutic products. Furthermore, additional critical raw materials such as plasmids, viral vectors, and lipids also exhibit batch-to-batch variability, creating a complex balancing act where manufacturing processes must constantly adjust to achieve standardized outputs [79].
The consequences of inconsistent batches extend beyond quality concerns to direct impacts on patient safety and therapeutic efficacy. Batch effects can introduce technical variations that compromise data integrity, potentially leading to misleading outcomes, irreproducible results, and in extreme cases, incorrect clinical decisions [80]. In one documented case, batch effects introduced through a change in RNA-extraction solution resulted in incorrect classification outcomes for 162 patients, 28 of whom subsequently received incorrect or unnecessary chemotherapy regimens [80]. This underscores the critical importance of robust batch consistency strategies throughout the manufacturing workflow.
Foundational Framework: GMP Principles for Managing Variability
Quality by Design in Raw Material Selection and Control
The foundation for managing biological diversity begins with rigorous raw material control under a GMP framework. According to regulatory guidelines, raw materials used in cell therapy manufacturing must align with specific quality standards and regulatory requirements set forth by authorities such as the FDA and EMA [81] [3]. The selection process should prioritize materials that demonstrate consistent performance characteristics and comprehensive documentation, including Certificates of Analysis (CoA), Certificates of Origin (CoO), and Safety Data Sheets (SDS) [81].
A critical consideration is the source and purity of materials, with particular emphasis on minimizing animal-derived components that can introduce risks such as contamination, transmission of infectious agents, and potential immune reactions in patients [81]. The growing emphasis on xenogeneic-free materials reflects an industry shift toward safer, more controlled manufacturing environments. As outlined in USP Chapter <1043>, comprehensive risk assessments, characterization, and qualification of ancillary materials are essential to ensure their suitability and compatibility with cell therapy processes [81].
Strategic Partnership Between Material Users and Suppliers
Effective management of batch consistency requires close collaboration between raw material users and suppliers, as outlined in the ISO-20399 standard [81]. This cooperative relationship ensures transparency and shared responsibility for quality outcomes. The standard provides clear recommendations for distributing responsibilities between suppliers and users across various activities essential for quality assurance.
Table: ISO-20399 Recommended Responsibilities for Raw Material Management
| Activity | Supplier Responsibility | User Responsibility |
|---|---|---|
| Provide documented evidence of raw material safety | ||
| Assess stability of raw material/ancillary material | ||
| Inform user of changes impacting raw material | ||
| Provide CoA, CoO, and SDS for raw material | ||
| Conduct characterization testing of raw material | ||
| Execute quality and supply agreement | ||
| Conduct risk-based supplier qualification process | ||
| Qualify performance in intended application | ||
| Assess effect of lot-to-lot variation on final product |
This shared responsibility model significantly contributes to successful quality outcomes by ensuring both parties actively participate in critical quality assurance activities [81]. Without such collaboration, manufacturers risk technical support gaps from suppliers and potential quality inconsistencies.
Technical Strategies for Enhancing Process Consistency
Automation and Closed System Technologies
Automation represents a cornerstone technology for reducing variability in cell therapy manufacturing. Automated systems minimize human intervention, thereby reducing the risk of errors and contamination that are crucial for maintaining the integrity of patient-specific therapies [17]. By ensuring that each batch is produced under uniform conditions, automation enhances consistency and quality—essential elements for both regulatory compliance and patient safety [17].
Specific automated technologies offering significant benefits include:
- Closed Cell Processing Systems: Systems like the Gibco CTS Rotea Counterflow Centrifugation System provide closed processing with low output volumes, process flexibility, and high cell recovery/viability for applications including leukopak processing, PBMC separation, and cell wash/concentration [17].
- Automated Magnetic Separation Systems: Systems such as the Gibco CTS Dynacellect Magnetic Separation System offer closed, automated isolation and bead removal with high throughput scalability, maintaining high cell purity, recovery, and viability while being GMP-compliant [17].
- Modular Electroporation Systems: Technologies like the Gibco CTS Xenon Electroporation System provide closed, modular, large-scale electroporation capabilities for non-viral transfection and electroporation of T-cells and NK-cells in GMP-compliant workflows [17].
The integration of these automated systems into manufacturing workflows reduces operator variability and hands-on time, leading to more consistent inter-batch outcomes while minimizing contamination risks [17].
Advanced Bioreactor Systems for Scalable 3D Culture
Traditional two-dimensional (2D) planar culture systems present significant challenges for scalable, consistent stem cell manufacturing, including limitations in scalability, substantial cell loss during processing, and unwanted batch-to-batch variability [82]. The implementation of three-dimensional (3D) suspension bioreactor systems addresses these challenges by enabling uniform culture conditions throughout the manufacturing process.
Recent advances in Vertical Wheel (VW) bioreactor technology demonstrate impressive results in scaling up human induced pluripotent stem cell-derived islet production while maintaining consistency [82]. When scaling from 0.1 L to 0.5 L reactors, this technology achieved a 12-fold increase in islet equivalent count (from 15,005 to 183,002 IEQ) without compromising islet structure or function [82]. The single-vessel, single-batch process eliminated the need for 2D planar culture and disruptive cell disaggregation-aggregation steps, resulting in more consistent outcomes with minimal variability and reduced cell loss [82].
Table: Quantitative Outcomes of Bioreactor Scale-Up for SC-Islet Production
| Parameter | 0.1 L Bioreactor | 0.5 L Bioreactor | Improvement Factor |
|---|---|---|---|
| Islet Equivalent Count (IEQ) | 15,005 | 183,002 | 12.2x |
| β-cell Composition | ~63% (CPPT+NKX6.1+ISL1+) | ~63% (CPPT+NKX6.1+ISL1+) | No change |
| Glucose Responsive Insulin Release | 3.9-6.1-fold increase | 3.9-6.1-fold increase | No change |
| Cluster Size Uniformity | Maintained | Maintained | No change |
| Transcriptional Maturity | Similar to adult islets | Similar to adult islets | No change |
The implementation of aphidicolin (APH), a potent cell growth inhibitor, further enhanced process consistency by reducing cell proliferation variability and minimizing off-target cell populations without the need for physical disaggregation-aggregation steps [82]. This approach demonstrates how strategic process design can effectively manage biological variability while maintaining product quality.
Protocol: Enhanced Lentiviral Transduction for Hematopoietic Stem Cells
Background and Principle
This optimized protocol for hematopoietic stem cell gene therapy (HSCGT) manufacturing demonstrates key principles for maintaining batch consistency amid biological variability. The method incorporates transduction enhancers (TEs) to improve transduction efficiency while reducing vector requirements, thereby enhancing process consistency and cost-effectiveness [21]. The protocol has been validated under GMP-compliant conditions for clinical application in treating Mucopolysaccharidosis type II (MPSII) and can be adapted for other HSCGT applications.
Materials and Equipment
- Biological Materials: Cryopreserved human CD34+ cells (hCD34) isolated from leukapheresis via magnetic bead separation using CliniMACSplus instrument [21]
- Culture Media: Serum-free X-VIVO-15 supplemented with 1% human albumin serum (HAS) [21]
- Cytokines: fms-related tyrosine kinase 3 ligand (Flt3-L), stem cell factor (SCF), thrombopoietin (TPO), and interleukin-3 (IL-3) [21]
- Transduction Enhancers: LentiBOOST and protamine sulfate [21]
- Lentiviral Vector: GMP-grade IDS.ApoEII LV (or alternative therapeutic vector) [21]
- Equipment: GMP-compliant cell culture equipment, biosafety cabinet, CO2 incubator, flow cytometer for analysis
Step-by-Step Procedure
Cell Thaw and Pre-stimulation
- Thaw cryopreserved hCD34+ cells rapidly at 37°C
- Wash cells to remove cryopreservation medium
- Resuspend cells in X-VIVO-15 medium supplemented with cytokine cocktail (Flt3-L, SCF, TPO, IL-3)
- Culture cells at density of 0.5-1×10^6 cells/mL for 24-48 hours in a 37°C, 5% CO2 incubator
Transduction Enhancement Setup
- Prepare working concentrations of LentiBOOST and protamine sulfate according to manufacturer recommendations
- Test vector concentrations across a range (e.g., 12.5, 25, 50, and 100 MOI) with and without TEs to determine optimal conditions
Lentiviral Transduction
- Aliquot pre-stimulated cells into transduction vessels
- Add appropriate concentration of TEs (LentiBOOST and protamine sulfate)
- Add lentiviral vector at predetermined MOI
- Mix gently and incubate for 16-24 hours at 37°C, 5% CO2
- Repeat transduction a second time for enhanced efficiency
Post-transduction Processing
- Wash cells to remove excess vector and TEs
- Culture cells in fresh medium with cytokines for expansion as needed
- Assess transduction efficiency and cell viability
Quality Control Assessments
- Perform colony-forming unit (CFU) assays by seeding transduced or mock-transduced cells in methylcellulose medium
- Count burst-forming unit-erythroid (BFU-E), CFU granulocyte, macrophage (GM), and CFU granulocyte, erythrocyte, monocyte, megakaryocyte (GEMM) colonies after 14 days
- Analyze vector copy number (VCN) via PCR on pooled CFU colonies and cells from liquid culture
- Measure intracellular transgene expression (e.g., IDS activity for MPSII application)
Critical Parameters and Troubleshooting
- TE Toxicity Management: TEs alone may cause 40-50% decrease in colony numbers across all colony types. This toxicity is mitigated when TEs are combined with LV at appropriate concentrations [21].
- Optimal MOI Determination: At MOI of 12.5, TEs increase transduction efficiency from 33.3% to 94.1% for BFU-Es and from 55.6% to 94.1% for CFU-GM colonies. Higher MOIs (e.g., 100) with TEs may show significant toxicity [21].
- Efficiency Validation: TEs typically increase VCN by 2.5- to 2.9-fold for pooled CFU colonies and cells grown in 14-day liquid culture, with intracellular transgene activity increasing by approximately 4.8-fold in pooled CFU colonies [21].
Analytical Framework: Batch Effect Detection and Correction
Statistical Methods for Batch Effect Correction
Despite robust process controls, batch effects may still occur in analytical data, potentially obscuring true biological signals and compromising interpretation. Several statistical methods have been developed to identify and correct for these technical variations:
- Combat: Utilizes an empirical Bayes framework to adjust for known batch variables, particularly effective for structured bulk RNA-seq data with clearly defined batch information [83].
- SVA (Surrogate Variable Analysis): Estimates hidden sources of variation that may represent batch effects and removes them from statistical models, useful when batch variables are unknown or partially observed [83].
- limma removeBatchEffect: Applies linear modeling-based correction, frequently integrated into differential expression workflows when batch variables are known and additive [83].
- Harmony: Aligns cells in a shared embedding space to reduce batch-driven clustering in single-cell or spatial RNA-seq data while preserving biological variation [83].
Table: Comparison of Batch Effect Correction Methods
| Method | Strengths | Limitations | Best Applications |
|---|---|---|---|
| Combat | Simple, widely used; adjusts known batch effects using empirical Bayes | Requires known batch info; may not handle nonlinear effects | Bulk RNA-seq with defined batches |
| SVA | Captures hidden batch effects; suitable when batch labels are unknown | Risk of removing biological signal; requires careful modeling | Complex studies with unknown covariates |
| limma removeBatchEffect | Efficient linear modeling; integrates with DE analysis workflows | Assumes known, additive batch effect; less flexible | Bulk RNA-seq with known batch effects |
| Harmony | Preserves biological variation; compatible with single-cell workflows | Computational intensity for large datasets | Single-cell RNA-seq, spatial transcriptomics |
Validation Metrics for Batch Correction
Successful batch effect correction requires rigorous validation using both visual and quantitative approaches:
- Visual Assessment: Dimensionality reduction techniques like PCA or UMAP should show samples grouping by biological identity rather than batch after successful correction [83].
- Quantitative Metrics:
- Average Silhouette Width (ASW): Measures clustering tightness and separation
- Adjusted Rand Index (ARI): Assesses similarity between clustering results
- Local Inverse Simpson's Index (LISI): Evaluates batch mixing and cell identity preservation
- k-nearest neighbor Batch Effect Test (kBET): Tests for residual batch effects [83]
These validation approaches should be implemented to ensure that correction methods effectively remove technical variation while preserving biologically relevant signals.
Essential Reagents and Materials for Consistent Manufacturing
The successful implementation of consistency strategies requires carefully selected reagents and materials that meet stringent quality standards. The following toolkit represents essential components for robust stem cell therapy manufacturing:
Table: Research Reagent Solutions for Consistent Stem Cell Manufacturing
| Reagent Category | Specific Examples | Function | Consistency Considerations |
|---|---|---|---|
| GMP-Grade Small Molecules | Aphidicolin (APH), Small molecule inducers | Control cell differentiation, inhibit proliferation | Synthetic origin ensures high purity and low batch-to-batch variation [77] |
| Cytokines/Growth Factors | FGFbasic-TS, Flt3-L, SCF, TPO, IL-3 | Promote cell growth, differentiation, maintenance | GMP-grade with demonstrated stability (e.g., FGFbasic-TS stable 3 days vs. 1 day for competitors) [81] [21] |
| Transduction Enhancers | LentiBOOST, Protamine sulfate | Improve lentiviral transduction efficiency | Reduce vector requirements while maintaining high efficiency [21] |
| Cell Culture Media | X-VIVO-15, Serum-free formulations | Support cell growth and maintenance | Xenogeneic-free formulations minimize contamination risks [81] [21] |
| Bioreactor Systems | Vertical Wheel Bioreactors | Enable scalable 3D culture with uniform conditions | Maintain consistent cluster size with minimal variability during scale-up [82] |
Achieving batch-to-batch consistency amid biological diversity requires an integrated approach spanning raw material control, process automation, advanced culture technologies, and robust analytical methods. The strategic implementation of GMP principles throughout the manufacturing workflow provides a foundation for managing inherent variability while maintaining product quality and safety. As the field of patient-specific stem cell therapies continues to evolve, these consistency strategies will play an increasingly critical role in ensuring that innovative treatments can transition successfully from research to clinical application, ultimately delivering safe and effective therapies to patients in need.
The protocols and frameworks presented here demonstrate that through careful process design, strategic technology implementation, and comprehensive quality control, manufacturers can overcome the challenges posed by biological diversity to produce consistent, therapeutically valuable cell products.
Analytical Method Validation and Product Characterization for Regulatory Compliance
The manufacturing of patient-specific stem cell therapies represents a frontier in modern medicine, offering potential treatments for a range of conditions where conventional approaches are inadequate [25]. Unlike traditional pharmaceuticals, these are living, dynamic products that cannot be terminally sterilized or fully characterized by testing the final product alone [25] [3]. This inherent complexity makes the role of a robust quality control (QC) system, founded on Current Good Manufacturing Practice (cGMP) principles and guided by the ICH Q2(R1) guideline for analytical method validation, absolutely critical for ensuring patient safety and product efficacy [15] [84]. Adherence to cGMP is not merely a regulatory hurdle; it is an integral part of the quality assurance system, ensuring that products are consistently produced and controlled to the quality standards appropriate for their intended use [15] [85]. This application note details the practical integration of ICH Q2(R1) validation parameters within a cGMP-compliant QC framework, specifically tailored for the unique challenges of manufacturing patient-specific stem cell therapies.
cGMP Regulatory Framework for Cell Therapy QC
In the United States, the FDA mandates that the methods, facilities, and controls used in the manufacturing, processing, and packing of drug products, which include Advanced Therapy Medicinal Products (ATMPs) like stem cell therapies, comply with cGMP regulations [15]. The core objective is to ensure that a product is safe for use and that it possesses the ingredients and strength it claims to have [15]. For cell-based products, the QC laboratory is a focal point for regulatory scrutiny because the decision to release or reject a batch is based on its test results [86].
Key cGMP Requirements for the QC Laboratory
The cGMP regulations for quality control laboratories, as outlined in 21 CFR 211.160, require that all laboratory methods used for the assessment of components, in-process materials, and finished products must be scientifically sound and appropriate [86]. Key requirements include:
- Equipment Qualification and Calibration: All equipment must be properly qualified for its intended use and undergo regular maintenance and calibration to ensure the validity of generated results [87].
- Comprehensive Documentation: Laboratory records must be "current, permanent, legible, accurate, clear, consistent, and complete" [87]. Any work not documented is considered not performed.
- Out-of-Specification (OOS) Investigations: A formal system must be in place for the management and investigation of OOS results [86].
- Stability Testing: A written stability testing program must be in place to determine the expiration date of the product, which is particularly challenging for short-lived cell therapies [25] [86].
- Personnel Training: An adequate number of qualified personnel must be available, and an active cGMP training program must be maintained to ensure staff are competent in their assigned functions [87].
Table 1: Essential cGMP Systems for a Quality Control Laboratory
| cGMP System | Key Requirements | Application to Stem Cell Therapy QC |
|---|---|---|
| Quality System | Quality Assurance Unit, Standard Operating Procedures (SOPs), Change Control, Self-Inspections [87] [86] | Ensures overall compliance and provides a framework for all quality activities [25]. |
| Laboratory Controls | Scientifically sound specifications, validated test methods, equipment qualification, data integrity [86] | Applied to testing raw materials, in-process samples, and the final cell product [25]. |
| Documentation System | Batch records, laboratory notebooks, logbooks, raw data storage, audit trails [87] [85] | Provides traceability for each patient-specific batch from donor to recipient [25] [3]. |
| Personnel & Training | Defined organization, position descriptions, training programs, summaries of training [87] | Critical for ensuring staff are trained in aseptic manipulation and specific analytical techniques [25]. |
ICH Q2(R1) Guideline and Analytical Method Validation
The ICH Q2(R1) guideline, titled "Validation of Analytical Procedures," provides a harmonized framework for validating analytical methods to ensure their reliability, reproducibility, and robustness [84]. Its purpose is to align the criteria for analytical procedures among regulatory bodies, thereby facilitating mutual acceptance of data and streamlining market access for pharmaceutical products [84]. For stem cell therapies, where the "product" is living cells, demonstrating that analytical methods are validated is a cornerstone of proving product quality.
Key Validation Parameters According to ICH Q2(R1)
The guideline defines a set of key validation characteristics that should be considered based on the type of analytical procedure [84]. A comprehensive understanding of these parameters is essential for developing QC assays for cell therapies.
- Specificity: The ability of the method to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradants, or matrix components [84]. For a flow cytometry assay identifying a specific stem cell surface marker, specificity would ensure the antibody binds only to the intended target.
- Accuracy: The closeness of agreement between the value which is accepted as a conventional true value or an accepted reference value and the value found. This is often established by spiking a known number of cells into a sample and assessing recovery.
- Precision: Expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions. It includes repeatability (intra-assay), intermediate precision (inter-day, inter-analyst), and reproducibility (inter-laboratory).
- Detection Limit (LOD) & Quantitation Limit (LOQ): The lowest amount of analyte in a sample that can be detected (LOD) or quantitatively determined with suitable precision and accuracy (LOQ). This is critical for detecting low levels of microbial contamination or residual reagents.
- Linearity and Range: The linearity of an analytical procedure is its ability to elicit test results that are directly proportional to the concentration of analyte in the sample. The range is the interval between the upper and lower concentrations for which linearity, accuracy, and precision have been established.
- Robustness: A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., temperature, pH, incubation time) and provides an indication of its reliability during normal usage [84].
Table 2: Summary of ICH Q2(R1) Validation Parameters and Typical Targets for Stem Cell Assays
| Validation Parameter | Definition | Example Target for a Cell-Based Potency Assay |
|---|---|---|
| Specificity | Ability to measure analyte specifically in the presence of other components | No interference from culture media components or dead cells. |
| Accuracy | Closeness of measured value to true value | ±70-150% recovery of spiked analyte or cells (matrix-dependent). |
| Precision (Repeatability) | Agreement under same operating conditions over a short interval | ≤20-25% Relative Standard Deviation (RSD) for biological assays. |
| Linearity | Test results are directly proportional to analyte concentration | R² ≥ 0.95 over the specified range of the assay. |
| Range | Interval between upper and lower levels of analyte demonstrating linearity, accuracy, and precision | e.g., 70-130% of the expected potency. |
| Robustness | Resilience to deliberate, small changes in method parameters | The method provides consistent results with minor variations in incubation time (±5%) or temperature (±2°C). |
| LOD/LOQ | Lowest amount of analyte that can be detected/quantified | LOD for mycoplasma detection: < 10 CFU/mL. |
Experimental Protocols for Critical QC Assays
The following protocols are designed to be performed within a cGMP-compliant laboratory environment, following approved SOPs and with all data recorded in bound laboratory notebooks or electronic systems [87].
Protocol: Validation of a Flow Cytometry Assay for Cell Identity (Specificity, Precision)
Objective: To validate a flow cytometry method for identifying a specific cell surface marker (e.g., CD90 for mesenchymal stem cells) by assessing specificity, precision, and linearity.
Materials:
- Single-cell suspension of the stem cell therapy product.
- Fluorescently conjugated antibody against target antigen and isotype control.
- Flow cytometry staining buffer (e.g., PBS with 2% FBS).
- Flow cytometer, calibrated daily using standard beads.
Methodology:
- Sample Preparation: Aliquot 1x10^5 cells into three separate tubes. Label them as Test, Isotype Control, and Unstained.
- Staining: Add the recommended volume of specific antibody to the Test tube and an equivalent volume of isotype control antibody to the Isotype Control tube. Leave the Unstained tube as is. Incubate for 30 minutes in the dark at 4°C.
- Washing: Add 2 mL of staining buffer to each tube, centrifuge at 300 x g for 5 minutes, and carefully decant the supernatant. Repeat once.
- Resuspension and Analysis: Resuspend the cell pellets in 0.5 mL of staining buffer. Analyze immediately on the flow cytometer, collecting a minimum of 10,000 events per sample.
- Validation Experiments:
- Specificity: Compare the histogram of the Test sample to the Isotype Control and Unstained controls. A clear, distinct positive population in the Test sample confirms specificity.
- Precision (Repeatability): Prepare and analyze six replicates of the same cell sample in a single assay session. Calculate the %RSD of the percentage of positive cells.
- Intermediate Precision: Repeat the assay on three different days, with two different analysts. Use ANOVA to assess the variance between days and analysts.
Protocol: Cell-Based Potency Assay (Accuracy, Linearity, Robustness)
Objective: To validate an in vitro differentiation assay that measures the ability of stem cells to form osteocytes as a measure of potency.
Materials:
- Test stem cell population.
- Validated osteogenic differentiation media and control media.
- Alizarin Red S stain for calcium deposition.
- Plate reader.
Methodology:
- Cell Seeding: Seed cells in a 24-well plate at a density known to be sub-confluent (e.g., 2x10^4 cells/cm²) in growth media. Use a minimum of 6 wells per condition.
- Differentiation Induction: After 24 hours, replace the growth media in the test wells with osteogenic induction media. Replace media in control wells with control media. Refresh media every 3-4 days.
- Termination and Staining: After 21 days, wash wells with PBS, fix cells with 70% ethanol for 1 hour, and stain with Alizarin Red S solution for 20 minutes.
- Quantification: Wash extensively with distilled water to remove non-specific stain. Elute the bound stain with 10% cetylpyridinium chloride and measure the absorbance at 562 nm.
- Validation Experiments:
- Accuracy (Recovery): Spike a known number of pre-validated, highly potent cells into a sample of low-potency cells. Calculate the recovery of the potency signal.
- Linearity and Range: Seed a series of cell densities (e.g., from 0.5x10^4 to 8x10^4 cells/cm²) and establish the linear range of the resulting absorbance signal.
- Robustness: Deliberately vary key parameters, such as the concentration of a critical media component (e.g., β-glycerophosphate ±10%) or the staining time (±10%). Assess the impact on the final absorbance reading.
Diagram 1: Analytical Method Validation Workflow.
The Scientist's Toolkit: Essential Research Reagent Solutions
The quality of reagents and materials is paramount in a cGMP environment. Each material must be qualified upon receipt, and primary and back-up suppliers must be approved [87].
Table 3: Essential Reagents and Materials for cGMP-Compliant Stem Cell QC
| Reagent/Material | Function | Critical Quality Attributes | cGMP Compliance Consideration |
|---|---|---|---|
| Cell Culture Media | Supports cell growth and maintenance. | Formulation, osmolality, pH, endotoxin level. | Must be sterile, and sourced from qualified vendors with Certificate of Analysis (CoA). Raw materials should be tested for identity [25] [87]. |
| Growth Factors & Cytokines | Directs cell differentiation and proliferation. | Biological activity (potency), purity, sterility. | Require rigorous identity and potency testing. Stability data under storage conditions is essential [25]. |
| Fluorochrome-Conjugated Antibodies | Cell identification and characterization via flow cytometry. | Specificity, fluorescence intensity, lot-to-lot consistency. | Validation of each new lot is required against a previous lot or a control cell line to confirm performance [87]. |
| Reference Standards | System suitability control for analytical methods. | Defined identity, purity, and potency. | Must be fully characterized, properly stored, and secured. Periodic re-evaluation is required to ensure continued suitability [87]. |
| PCR Kits (e.g., for Mycoplasma) | Detection of microbial contaminants. | Sensitivity (LOD), specificity, robustness. | Must be validated for the specific cell matrix. Short shelf-life products require strict inventory control [25] [86]. |
The successful translation of patient-specific stem cell therapies from research to clinic hinges on a robust, scientifically sound, and regulatory-compliant quality control system. This requires the seamless integration of cGMP principles—which govern the entire manufacturing and testing environment—with the technical rigor of ICH Q2(R1) for validating the analytical methods themselves [15] [84]. The dynamic nature of these living products demands a risk-based approach where quality is built into the process through validated methods, rigorous documentation, and highly trained personnel [25] [87]. By adopting the frameworks and protocols outlined in this application note, developers of these advanced therapies can ensure they generate reliable, meaningful quality data. This not only fulfills regulatory expectations but, more importantly, builds a foundation of trust in the safety and efficacy of these transformative medicines for patients.
Within current Good Manufacturing Practice (cGMP) facilities manufacturing patient-specific stem cell therapies, the cell count is more than a simple quantification—it is a critical potency test that directly indicates the therapeutic dose [88]. For Advanced Therapy Medicinal Products (ATMPs) like human induced pluripotent stem cells (hiPSCs), achieving therapeutically relevant doses requires large-scale cell expansion, making a fast and reliable cell counting method essential for process monitoring [89]. Conventional manual counting using a hemocytometer is heavily dependent on the operator's expertise and is time-consuming, posing a significant bottleneck and variability risk in a cGMP environment [89] [90].
Automation of this critical step, through fluorescence imaging-based or image cytometer-based systems, has emerged as a solution to enhance precision and rapidity [89] [91]. However, implementing any new analytical method in a cGMP workflow requires formal validation to ensure it is fit for its intended purpose. This application note details the validation of an automated cell counting method, focusing on the core parameters of specificity, linearity, accuracy, and precision, providing researchers and drug development professionals with a structured framework for compliance.
Validation Parameters and Experimental Design
The validation of analytical methods for ATMPs must comply with regulatory guidelines, primarily the International Council for Harmonisation (ICH) Q2(R1) guidance and the European Pharmacopoeia [89] [88]. The objective is to demonstrate that the automated method is comparable to, or superior than, the compendial method—typically the manual Bürker hemocytometer [88].
Table 1: Core Validation Parameters and Their Definitions
| Parameter | Regulatory Definition | Validation Objective |
|---|---|---|
| Accuracy | The closeness of agreement between an accepted reference value and the value found. | Demonstrate that the automated count results agree with the reference (manual) method. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample. | Quantify the method's repeatability (intra-assay precision) and reproducibility (inter-operator precision). |
| Specificity | The ability to assess the analyte unequivocally in the presence of other components. | Confirm the method can accurately distinguish and count target cells (e.g., viable hiPSCs) in a mixture. |
| Linearity | The ability to obtain test results that are directly proportional to the concentration of the analyte. | Establish that the method provides proportional results across a specified range of cell concentrations. |
| Range | The interval between the upper and lower concentrations of analyte for which it has been demonstrated that the analytical procedure has a suitable level of precision, accuracy, and linearity. | Define the operational cell concentration range for which the method is valid. |
Experimental Workflow for Validation
The validation process follows a logical sequence, beginning with accuracy assessment against the reference method, followed by precision, specificity, and linearity evaluations.
Detailed Experimental Protocols
Protocol 1: Assessing Accuracy
Principle: Accuracy is evaluated by comparing cell count results from the automated method with those from the reference manual method (Bürker hemocytometer) across a range of samples [88].
Materials:
- Cell suspension of hiPSCs or other relevant therapeutic cell type.
- Automated cell counter (e.g., Fluorescence imaging-based NucleoCounter NC-100 system) [89].
- Bürker hemocytometer and microscope.
- Appropriate viability stain (e.g., Trypan Blue for manual method; proprietary fluorescent stains like acridine orange/DAPI for automated systems) [88] [91].
Procedure:
- Prepare a homogeneous cell suspension from a master batch of hiPSCs.
- Serially dilute the cell suspension to obtain at least 5 different concentrations covering the expected working range (e.g., from 1x10^5 to 2x10^6 cells/mL) [88].
- For each dilution, perform cell counting in triplicate using both the automated system and the Bürker hemocytometer.
- For the Bürker method, load 10 µL of cell suspension onto the chamber and count the cells in the four large corner squares according to standard procedures [88]. Calculate the concentration.
- For the automated method, follow the manufacturer's instructions for sample loading and analysis.
Data Analysis:
- Calculate the average count for each dilution and method.
- Perform linear regression analysis, plotting automated method results (y-axis) against the reference method results (x-axis).
- The coefficient of determination (R²) should be >0.95, and the slope should be close to 1 to demonstrate agreement [89].
Protocol 2: Evaluating Precision (Repeatability and Reproducibility)
Principle: Precision is assessed by analyzing the variation in results from multiple measurements of the same sample by the same operator (repeatability) and by different operators (reproducibility) [89] [88].
Materials:
- A single, homogeneous batch of hiPSC suspension at a target concentration.
Procedure:
- Repeatability (Intra-assay Precision): A single, trained operator analyzes the same homogeneous cell sample at least 10 times in a single session using the automated system.
- Reproducibility (Inter-operator Precision): Two or more operators independently prepare and analyze aliquots from the same homogeneous cell sample using the same automated system. Each operator should perform the analysis at least 3 times.
Data Analysis:
- For all measurements, calculate the average cell concentration and the standard deviation (SD).
- Determine the Coefficient of Variation (CV%) using the formula: CV% = (Standard Deviation / Mean) x 100.
- Acceptance Criterion: For viable cell counts, the CV% should typically be <5% for intra-assay precision and <10% for inter-operator precision [88].
Table 2: Example Precision Data for an Automated Cell Counter
| Sample | Operator | Mean Concentration (cells/mL) | Standard Deviation | CV% | Acceptance Met? |
|---|---|---|---|---|---|
| hiPSC Batch A | Op1 (Repeatability, n=10) | 1.52 x 10^6 | 0.04 x 10^6 | 2.6% | Yes (<5%) |
| hiPSC Batch A | Op1 vs. Op2 (Reproducibility, n=6) | 1.49 x 10^6 | 0.11 x 10^6 | 7.4% | Yes (<10%) |
Protocol 3: Determining Specificity
Principle: Specificity confirms that the method can accurately discriminate and quantify viable cells in the presence of non-viable cells and debris [91].
Materials:
- Cell suspension with a known, high viability (>90%).
- Sample of the same cells intentionally rendered non-viable (e.g., by heat treatment or ethanol fixation).
Procedure:
- Prepare two samples: one with high-viability cells and one with predominantly non-viable cells.
- Mix the two samples in known ratios (e.g., 90:10, 70:30, 50:50 viable:non-viable) to create test samples with defined viabilities.
- Analyze each mixture using the automated cell counter, which typically uses a fluorescent stain (e.g., acridine orange for viable cells, DAPI for non-viable cells) to differentiate between the two populations [91].
- Record the viability percentage and total cell count for each mixture.
Data Analysis:
- Compare the measured viability from the automated system against the expected viability based on the mixing ratio.
- The method is specific if the measured viabilities show a strong linear relationship (R² > 0.95) with the expected values and accurately reflect the prepared ratios.
Protocol 4: Establishing Linearity and Range
Principle: This test demonstrates that the automated method provides results directly proportional to the true cell concentration over a declared operating range [88].
Materials:
- Concentrated cell suspension.
Procedure:
- Prepare a series of at least 5 dilutions from a concentrated cell stock. The dilution range should be broad, for example from 1:8 to 1:128, to cover scenarios from low to high cell density [88].
- Count each dilution in triplicate using the automated system.
- Record the measured concentration for each dilution.
Data Analysis:
- Plot the measured concentration (y-axis) against the expected concentration (x-axis, based on dilution factor).
- Perform linear regression analysis. The range is considered linear if the R² value is ≥ 0.98 and the residuals show no systematic pattern.
- The "range" is defined as the interval between the lowest and highest concentrations for which these linearity criteria are met.
The Scientist's Toolkit: Essential Reagents and Materials
Successful validation and implementation of an automated cell counting method require specific reagents and systems designed for cGMP compliance.
Table 3: Key Research Reagent Solutions for Automated Cell Counting Validation
| Item | Function & Description | cGMP-Compliant Consideration |
|---|---|---|
| Fluorescence-Based Automated Counter (e.g., NucleoCounter NC-100) | System that uses fluorescent dyes (e.g., Acridine Orange/DAPI) and image analysis to automatically count and discriminate viable and non-viable cells [89]. | Preferred for validated processes due to higher precision, reduced operator dependency, and software compliance with 21 CFR Part 11 [89] [88]. |
| Proprietary Fluorescent Stains/Cassettes | Pre-packaged, ready-to-use reagents and disposable cassettes containing the vital fluorescent dyes for cell staining and counting. | Sourced from the instrument manufacturer with appropriate Certificate of Analysis (CoA) to ensure quality, consistency, and traceability [89]. |
| Disposable Counting Chambers (e.g., Fast Read 102) | Single-use, plastic slides that eliminate the need for cleaning and prevent cross-contamination [88]. | Ideal for cleanroom environments; they avoid the waste disposal issues associated with traditional dyes like Trypan Blue [88]. |
| Standardized Cell Reference Material | Cells with known and stable characteristics used as a control to periodically verify instrument performance. | Critical for ongoing method verification; should be well-characterized and sourced from a qualified GMP-compliant bank. |
| cGMP-Compliant Culture Media | Media used for expanding and suspending cells prior to counting. | All raw materials, including media, must be qualified and meet quality standards for ATMP manufacturing [92]. |
Implementation in cGMP Manufacturing
Integrating a validated automated cell counter into a cGMP workflow for patient-specific stem cell therapies enhances control over critical quality attributes. The relationship between the counting method and other manufacturing systems is crucial for overall product quality.
The validated cell count acts as a critical in-process control (IPC) during upstream processing, providing data on cell number and viability—key potency and quality attributes. This data directly informs decisions about harvest timing and the final therapeutic dose, ensuring batch-to-batch consistency and compliance with the overarching Quality Management System (QMS) [92].
The validation of automated cell counting methods is a cornerstone of robust, cGMP-compliant manufacturing for patient-specific stem cell therapies. By systematically addressing specificity, linearity, accuracy, and precision, as outlined in this application note, manufacturers can replace operator-dependent, variable manual methods with precise, reliable, and efficient automated systems. This transition is pivotal for scaling up production, ensuring the delivery of accurate and therapeutically relevant cell doses, and ultimately, upholding the safety and efficacy of advanced stem cell therapies. The protocols and parameters described provide a clear roadmap for researchers and developers to achieve regulatory compliance and enhance manufacturing quality control.
For stem cell therapies to transition from research to clinically applicable treatments, rigorous product characterization is a non-negotiable requirement of Good Manufacturing Practice (GMP). This process provides the critical data that confirms product quality, consistency, and safety throughout development and manufacturing [25]. Characterization is defined as the "determination of physiochemical properties, biological activity, immunochemical properties, purity and impurities" of a biological product [93]. In the context of GMP compliance for patient-specific stem cell therapies, a systematic Quality by Design (QbD) approach is mandated, beginning with a hypothesis on the product's Mechanism of Action (MOA) and the definition of a Target Product Profile (TPP) [93]. This framework establishes the foundation for identifying Critical Quality Attributes (CQAs)—the physical, chemical, biological, or microbiological properties that must be controlled within appropriate limits to ensure the desired product quality, safety, and efficacy [93]. This document details the application notes and experimental protocols for characterizing the five core CQAs: Identity, Purity, Potency, Viability, and Tumorigenicity.
Regulatory Framework and Critical Quality Attributes (CQAs)
The legal requirements for Cell-based Medicinal Products (CBMPs) are established under various regional regulations, such as Regulation 1394/2007/EEC in Europe and guidance from the U.S. Food and Drug Administration (FDA) [94] [25]. A risk-based approach is fundamental throughout the product development lifecycle. The initial risk analysis identifies potential hazards linked to the product, its manufacturing process, and its clinical use, forming the basis for a comprehensive risk management plan [25]. The characterization scheme must be tailored to the specific product, with the understanding that not all tests can be performed on each batch, especially for autologous therapies with short shelf-lives. In such cases, rigorous process validation and in-process testing compensate for the lack of full batch-release testing [25].
Table 1: Categories of Acceptance Criteria for Cell Therapies [93]
| Category | Regulatory Reference | Definition | Examples |
|---|---|---|---|
| Identity | 21CFR610.14 | Assays that identify the product for proper labeling and distinguish it from other products. | Cell surface/intracellular markers, gene expression, secreted molecules, peptide sequences. |
| Purity | 21CFR600.3 | Tests for residual materials from manufacturing and contaminating cell types. | Residual beads, enzymes, reagents; presence of unwanted cell populations. |
| Potency | 21CFR600.3 | A measure of biological activity demonstrating the product's capacity to affect a given result. | Differentiation assays, cytokine secretion, enzymatic activity, gene expression. |
| Safety | - | Tests mainly for adventitious agents. | Sterility, mycoplasma, endotoxin, immunogenicity, tumorigenicity. |
| Other | - | Includes other critical quality tests. | Appearance, dose, viability, and cell counts. |
The following workflow diagram illustrates the systematic QbD approach to product characterization and its integration with GMP manufacturing.
Detailed Characterization Protocols
Identity Testing
3.1.1 Application Note: Identity testing confirms the unique characteristics of the stem cell product, ensuring it is what it claims to be. This is crucial for patient-specific therapies to prevent misadministration and for batch-to-batch consistency in allogeneic products. For induced pluripotent stem cells (iPSCs), identity confirmation spans from the initial somatic cell source to the final differentiated product [94] [55].
3.1.2 Experimental Protocol: Flow Cytometry for Cell Surface Markers
- Objective: To quantify the expression of specific markers to confirm cell type identity (e.g., pluripotency markers for iPSCs, lineage-specific markers for differentiated cells).
- Materials:
- Single-cell suspension of the stem cell product.
- Fluorescently conjugated antibodies against target markers (e.g., TRA-1-60, SSEA-4 for iPSCs; CD73, CD90, CD105 for MSCs).
- Isotype control antibodies.
- Flow cytometry buffer (e.g., PBS with 1-2% FBS).
- Fixation solution (if required).
- Flow cytometer.
- Method:
- Cell Preparation: Harvest and wash cells to create a single-cell suspension. Determine cell count and viability.
- Staining: Aliquot approximately 1x10^6 cells per test tube. Centrifuge and resuspend pellet in 100 µL of flow buffer containing the predetermined optimal concentration of antibody. Include isotype controls for background subtraction.
- Incubation: Incubate for 30-60 minutes in the dark at 4°C.
- Washing: Wash cells twice with 2 mL of flow buffer to remove unbound antibody.
- Fixation: If required, resuspend cells in 200-500 µL of fixation buffer.
- Acquisition: Analyze samples on the flow cytometer. Collect a minimum of 10,000 events per sample.
- Analysis: Use flow cytometry software to gate on viable cells and analyze the percentage of cells positive for the target markers compared to isotype controls. A defined acceptance criterion (e.g., >90% positive for key markers) must be established.
Purity Testing
3.2.1 Application Note: Purity encompasses both process-related impurities (residual materials from manufacturing like enzymes, beads, or vectors) and product-related impurities (unwanted cell types). For iPSC-derived therapies, a key purity concern is the presence of residual undifferentiated pluripotent cells, which poses a significant tumorigenic risk [93] [95].
3.2.2 Experimental Protocol: qPCR for Residual Vector Detection
- Objective: To detect and quantify residual reprogramming vectors in clinical-grade iPSCs, ensuring their absence or level is below a pre-defined safety threshold [94].
- Materials:
- Genomic DNA extracted from the iPSC master cell bank.
- TaqMan qPCR assay specific for the vector sequence (e.g., Sendai virus genes, Epstein-Barr virus origin of replication for episomal vectors).
- Standard curve prepared from a serially diluted plasmid containing the target sequence.
- qPCR reagents (master mix, nucleotides, polymerase).
- Real-time PCR instrument.
- Method:
- DNA Extraction: Extract high-quality genomic DNA from a known number of cells (e.g., 1x10^6). Quantify DNA concentration and purity (A260/A280 ratio).
- Reaction Setup: Prepare qPCR reactions in triplicate for each sample, standard, and no-template control (NTC). A typical 20 µL reaction contains 1X TaqMan master mix, 1X assay mix, and 50-100 ng of genomic DNA.
- Thermocycling: Run the plate on the real-time PCR instrument using the following standard conditions: Hold: 50°C for 2 min, 95°C for 10 min; 40 Cycles: 95°C for 15 sec, 60°C for 1 min.
- Analysis: Generate a standard curve from the serial dilution and use it to determine the absolute copy number of the residual vector in the sample DNA. Report the result as vector copies per diploid genome or per µg of genomic DNA.
Potency Assay
3.3.1 Application Note: The potency assay is a quantitative measure of the biological activity of the cell product, linked to its relevant Mechanism of Action. It is considered the most critical CQA as it serves as an indicator of product efficacy. A matrix of assays is often recommended due to the difficulty in selecting a single test that fully predicts clinical response [93].
3.3.2 Experimental Protocol: In Vitro Trilineage Differentiation Assay
- Objective: To demonstrate the functional capacity of iPSCs to differentiate into cell types of the three germ layers (ectoderm, mesoderm, endoderm), confirming their pluripotent potency.
- Materials:
- Undifferentiated iPSCs.
- Commercial trilineage differentiation kits or validated in-house media formulations.
- Tissue culture plates.
- Fixation and staining solutions.
- Antibodies for germ layer-specific markers: β-III Tubulin (ectoderm), Brachyury (mesoderm), Sox17 (endoderm).
- Method:
- Cell Seeding: Seed dissociated iPSCs into multiple culture plates or chamber slides.
- Differentiation: Upon reaching appropriate confluence, replace the maintenance medium with specific differentiation media according to the kit or protocol instructions for each germ layer lineage. Maintain cells in differentiation media for 10-21 days, with regular medium changes.
- Analysis: After the differentiation period, analyze the cells.
- Immunocytochemistry: Fix cells and stain with antibodies against the germ layer-specific markers. Use fluorescence microscopy to confirm the presence of each cell type.
- qRT-PCR: Isolve RNA and perform qRT-PCR to quantify the expression of lineage-specific genes relative to undifferentiated iPSCs.
- Reporting: The assay is deemed successful if a significant proportion of cells (e.g., >30% as determined by flow cytometry) express the relevant markers for each germ layer, demonstrating the pluripotent potency of the starting population.
Viability and Cell Counting
3.4.1 Application Note: Viability and cell count are "Other" category tests that are essential for determining the dose to be administered to a patient. Accurate dosing is critical for both safety and efficacy. The method must be robust, reproducible, and able to distinguish between live and dead cells.
3.4.2 Experimental Protocol: Automated Cell Counting with Viability Staining
- Objective: To accurately determine the total cell count and the percentage of viable cells in the final product for dose formulation and release.
- Materials:
- Single-cell suspension of the final product.
- Trypan Blue or Acridine Orange/Propidium Iodide (AO/PI) stain.
- Automated cell counter (e.g., Vi-CELL) or hemocytometer.
- Method:
- Sample Preparation: Mix the cell suspension thoroughly. For automated counters, mix a defined volume of cell suspension with an equal volume of dye.
- Loading: Load the mixture into a disposable slide or chamber.
- Analysis: Insert the slide into the automated cell counter. The instrument will automatically capture images, count total cells, and identify dead cells (which take up the dye). For manual counting, load the chamber and count live (unstained) and dead (blue-stained) cells in specific squares.
- Calculation:
- Viability (%) = (Number of Viable Cells / Total Number of Cells) × 100
- Total Viable Cells = (Total Cell Count) × (Viability % / 100)
- Cell Concentration (cells/mL) = Total Viable Cells / Volume
Tumorigenicity Testing
3.5.1 Application Note: Tumorigenicity is the single greatest safety concern for therapies involving pluripotent stem cells due to their innate capacity for unlimited self-renewal [95]. Testing must be designed to detect the potential of the product to form tumors in vivo. This is a critical component of the non-clinical safety studies required before first-in-human trials [25].
3.5.2 Experimental Protocol: In Vivo Tumorigenicity Assay in Immunodeficient Mice
- Objective: To assess the tumor-forming potential of the final stem cell product in an in vivo model.
- Materials:
- Final formulated cell therapy product.
- Control cells: Undifferentiated iPSCs (positive control), human fibroblasts (negative control).
- Immunodeficient mice (e.g., NOD-scid gamma (NSG) mice).
- Matrigel (optional, to enhance engraftment).
- In vivo imaging system (e.g., bioluminescence, if cells are engineered).
- Method:
- Cell Preparation: Prepare cells at the required concentration for injection. A common test article is the final differentiated product, but it is also critical to test the undifferentiated iPSC master cell bank.
- Animal Injection: Divide mice into groups (test article, positive control, negative control). Inject a high dose of cells (e.g., 1x10^7 cells) subcutaneously or intramuscularly into each mouse. For orthotopic models, cells are injected into the relevant organ.
- Observation and Monitoring: Monitor mice regularly for up to 6 months for signs of distress and palpable tumor formation. If using bioluminescent cells, image animals weekly to monitor cell growth.
- Necropsy and Histopathology: At the end of the study, euthanize all animals and perform a gross necropsy. Excise and weigh the injection site and major organs. Tissues are fixed, sectioned, and stained with Hematoxylin and Eosin (H&E) for histological examination by a pathologist to identify any teratoma or tumor formation.
- Reporting: The assay is successful if the positive control group forms teratomas/tumors and the negative control does not. The final product is considered to have a lower tumorigenic risk if no tumors are observed in the test article group over the study period.
Table 2: Summary of Key Characterization Assays and Standards
| CQA | Key Analytical Methods | Typical Acceptance Criteria | Relevant Standards |
|---|---|---|---|
| Identity | Flow Cytometry, PCR, Gene Expression | >90% expression of target markers; Genetic match to donor (autologous) | ISCT minimal criteria for MSCs; ICH Q6B [52] |
| Purity | qPCR, Flow Cytometry, Residual DNA/Enzyme assays | Residual undifferentiated cells <0.1%; Residual vector below detection limit | European Pharmacopoeia, USP [94] [25] |
| Potency | Trilineage Differentiation, ELISA, Functional Co-cultures | Significant upregulation of lineage genes; Specific biological activity level | 21CFR600.3; Requires matrix of assays [93] |
| Viability | Automated Cell Counting, AO/PI Staining | >70% viability (product-specific) | FACT Common Standards [96] |
| Tumorigenicity | In Vivo Assay (e.g., in NSG mice), Soft Agar Assay | No tumor formation at injection site over study duration | Non-clinical safety study guidelines [25] |
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents and materials critical for the successful characterization of GMP-compliant stem cell therapies.
Table 3: Key Research Reagent Solutions for Product Characterization
| Reagent/Material | Function in Characterization | Application Example |
|---|---|---|
| GMP-Grade iPSC Master Cell Bank | Provides a standardized, well-characterized, and safe starting material for generating clinical-grade cell therapies. | Serves as the source for deriving differentiated cells for therapy; ensures traceability and consistency [94] [55]. |
| Validated Antibody Panels | Used in flow cytometry and immunocytochemistry to detect specific cell surface and intracellular markers for identity and purity analysis. | Confirming pluripotency (SSEA-4, OCT4) or lineage-specific differentiation (β-III Tubulin, Brachyury) [93]. |
| qPCR/TaqMan Assays | Enable highly sensitive and quantitative detection of specific DNA or RNA sequences for identity, purity, and potency testing. | Detecting residual reprogramming vectors; measuring gene expression changes during differentiation [94]. |
| Trilineage Differentiation Kits | Provide standardized, optimized media and protocols to reliably direct stem cell differentiation toward the three germ layers. | Serving as a key component of the potency assay for pluripotent stem cells [93]. |
| Cell Counting Reagents (e.g., AO/PI) | Fluorescent dyes that distinguish between live and dead cells for accurate viability and cell count measurements. | Used in automated cell counters (e.g., Vi-CELL) for final product dose formulation and release [93]. |
| GMP-Compliant Culture Media & Supplements | Support the growth and maintenance of cells during process development and manufacturing without introducing impurities. | Ensuring the final product is manufactured under defined and controlled conditions [25] [55]. |
Comprehensive product characterization is the cornerstone of GMP compliance and the successful translation of patient-specific stem cell therapies. The protocols outlined for Identity, Purity, Potency, Viability, and Tumorigenicity testing provide a framework for generating the necessary evidence that a therapy is safe, pure, potent, and effective. As the field evolves, the development of universally accepted standards, as promoted by organizations like the ISSCR and FACT, will be crucial for harmonizing these practices globally [97] [96]. Adhering to a rigorous, QbD-driven characterization strategy is not merely a regulatory hurdle but a fundamental scientific and ethical obligation to ensure the well-being of patients participating in clinical trials and receiving these transformative medicines.
Sterility Testing and Microbial Safety for Short Shelf-Life Products
This application note provides a comprehensive framework for implementing rapid sterility testing methods to ensure microbial safety of short shelf-life products, with specific application to patient-specific stem cell therapies. These advanced therapy medicinal products (ATMPs) present unique challenges due to their living cellular nature, inability to undergo terminal sterilization, and extremely limited shelf lives ranging from hours to days. The document outlines regulatory considerations, validated rapid microbiological methods (RMMs), detailed experimental protocols, and implementation strategies aligned with current Good Manufacturing Practice (cGMP) requirements for cellular therapeutics. By adopting these risk-based approaches, manufacturers can significantly reduce vein-to-vein time while maintaining the highest standards of patient safety and regulatory compliance.
Patient-specific stem cell therapies represent one of the most challenging categories of short shelf-life products from a microbial safety perspective. These living cellular products cannot be terminally sterilized and often have shelf lives of 48-72 hours, making conventional 14-day sterility testing described in USP <71> completely impractical [25] [98]. The regulatory framework recognizes these constraints through documents such as the revised USP <1071>, which provides guidance on risk-based approaches for rapid microbiological methods [99] [100]. Manufacturing occurs in cGMP facilities that must adhere to stringent requirements for environmental controls, equipment validation, and quality systems as defined in 21 CFR Parts 210, 211, and 1271 [101]. The living nature of these cellular products introduces multiple risk factors including potential for microbiological contamination, loss of cell function or viability, and unpredictable biological behavior, necessitating innovative approaches to sterility assurance that balance patient safety with practical manufacturing constraints [25] [3].
Regulatory Framework and Compliance Considerations
Current Regulatory Landscape
The United States Pharmacopeia (USP) has significantly updated its guidance to address the unique needs of short shelf-life products. The revised USP <1071>, scheduled for implementation in August 2025, introduces a risk-based approach specifically designed for rapid microbiological methods in sterile short-life products [99]. Key updates include redefinition of rapid method applications, introduction of probability calculations for contamination risk assessment, removal of detection limits as critical operational parameters, and expanded guidance on validation and proficiency testing [99]. This revised chapter specifically affects related documents including USP <1117> on Microbiological Best Laboratory Practices and USP <1046> on Cell-Based Advanced Therapies, creating a cohesive framework for ATMP manufacturers [99].
The Food and Drug Administration recognizes that alternative microbiological methods may be used for sterility testing when properly validated according to USP <1223> [100]. For cell-based products, additional regulations under 21 CFR Part 1271 governing human cells, tissues, and cellular and tissue-based products apply, creating a multi-layered regulatory structure that addresses both conventional pharmaceutical standards and biological product considerations [101].
Risk-Based Approach to Compliance
A fundamental principle underlying modern sterility testing for short shelf-life products is the risk-based approach, which considers multiple factors including product attributes, manufacturing conditions, and patient impact [100]. The risk assessment should evaluate whether non-sterile components are used, the number and complexity of aseptic manipulations, environmental control levels, and administration route/volume [100]. This approach enables manufacturers to justify their sterility testing strategy based on solid scientific rationale and quality-by-design principles rather than one-size-fits-all requirements.
Comparative Analysis of RMM Technologies
Table 1: Comparison of Rapid Sterility Testing Technologies for Short Shelf-Life Products
| Technology | Method Type | Detection Time | Limit of Detection | Key Advantages | Sample Volume | Regulatory Status |
|---|---|---|---|---|---|---|
| Solid Phase Cytometry (SCANRDI) | Non-growth-based | 3-4 hours | Single cell | Detects VBNC microorganisms; unaffected by antimicrobials | Filterable volumes | FDA-approved drug applications exist [100] |
| Isothermal Microcalorimetry (calScreener+) | Growth-based | 1-3 days | <5 CFU | Detects metabolic heat; facilitates contaminant recovery | Low volume (no filtration) | Recognized in USP <1071> [98] |
| Nucleic Acid Amplification (RiboNAT) | Non-growth-based | 7 hours | Targets rRNA | Reduces false positives; higher sensitivity | Filterable volumes | Complies with USP <1223> [102] |
| Traditional Growth-Based (USP <71>) | Growth-based | 14 days | Varies | Compendial method; established history | 100mL recommended | Gold standard [103] |
| Growth-Based Rapid Methods | Growth-based | 6-7 days | Varies | Reduced time vs. USP <71> | Varies by product | USP <71> compliant [103] |
Technology Selection Considerations
Each rapid microbiological method offers distinct advantages and limitations for specific applications in stem cell therapy manufacturing. Solid phase cytometry systems excel in detecting viable but non-culturable (VBNC) microorganisms that might be missed by growth-based methods, making them particularly valuable for products with inherent antimicrobial properties [100]. Isothermal microcalorimetry provides direct measurement of microbial metabolism through heat production, enabling real-time detection while maintaining the ability to recover contaminants for further investigation [98]. Nucleic acid amplification methods offer exceptional speed but may require additional steps to distinguish between viable and non-viable microorganisms [102].
The product matrix significantly influences technology selection. Cell therapies with high cell densities present challenges for filtration-based methods, favoring technologies like isothermal microcalorimetry that can handle complex matrices without sample preparation [98]. Similarly, sample volume requirements must be considered, as many ATMPs are available only in small quantities, making low-volume methods particularly advantageous.
Experimental Protocols and Methodologies
Protocol 1: Solid Phase Cytometry for Sterility Testing
Principle: This non-growth-based method uses fluorescent labeling of esterase activity in viable microorganisms followed by laser scanning and microscopic verification [100].
Materials and Reagents:
- SCANRDI instrument system (bioMérieux)
- Viability stains (fluorescent esters)
- Sterile membrane filtration units
- Appropriate culture media for recovery attempts (e.g., chocolate agar)
- Phosphate buffered saline (PBS) or suitable diluent
Procedure:
- Sample Preparation: Aseptically transfer 100-500μL of cell therapy product into sterile PBS. For products with potential antimicrobial activity, include neutralizers in the diluent.
- Filtration: Filter the sample through a 0.45μm sterile membrane under aseptic conditions.
- Staining: Apply fluorescent viability stain to the membrane and incubate for predetermined time (typically 60-90 minutes).
- Scanning: Place membrane in SCANRDI instrument for laser scanning. The system detects fluorescent events indicating viable microorganisms.
- Verification: Trained technicians perform microscopic verification of detected events using fluorescence microscopy to distinguish microorganisms from auto-fluorescent particles.
- Result Interpretation: Samples with no verified microbial cells after microscopic examination are considered sterile.
- Optional Recovery: For positive results, transfer membrane to enriched chocolate agar and incubate at 30-35°C for 20-72 hours to attempt microbial recovery for identification.
Validation Parameters: According to USP <1223>, validate for limit of detection, specificity, robustness, ruggedness, and equivalency to compendial method [100].
Protocol 2: Isothermal Microcalorimetry for Cell Therapy Products
Principle: This growth-based method detects heat flow from microbial metabolism in real-time, providing continuous monitoring of contamination [98].
Materials and Reagents:
- calScreener+ instrument (Symcel)
- USP <71> recommended culture media (Fluid Thioglycollate Medium and Tryptic Soy Broth)
- Sterile ampoules or vials compatible with the instrument
- Reference microbial strains (USP <71> panel plus Cutibacterium acnes)
- Biological safety cabinet for aseptic processing
Procedure:
- Sample Preparation: Aseptically transfer 0.5-2mL of cell therapy product into sterile calScreener+ vials. Include positive controls with <5 CFU of reference strains.
- Media Addition: Add recommended culture media according to manufacturer's instructions, maintaining appropriate oxygen conditions for aerobes and anaerobes.
- Loading: Place vials into calibrated instrument chambers maintained at recommended temperatures (20-25°C for TSB, 30-35°F for FTM).
- Data Acquisition: Initiate continuous monitoring of heat flow. The system automatically records metabolic heat production in real-time.
- Detection Algorithm: Software algorithms identify contamination events based on heat flow patterns exceeding threshold values.
- Results Interpretation: Negative results can be reported when no detectable heat flow occurs within validated timeframes (typically 24-72 hours).
- Contaminant Recovery: For positive detection, the non-destructive nature allows immediate subculture for identification.
Method Suitability: Test with actual cell therapy products spiked with <5 CFU of relevant microorganisms including bacteria, yeast, and mold [98].
Protocol 3: Nucleic Acid Amplification-Based Rapid Sterility Testing
Principle: This method detects microbial contamination through amplification of ribosomal RNA (rRNA) targets using reverse transcriptase real-time PCR (RT-rtPCR) [102].
Materials and Reagents:
- RiboNAT Rapid Sterility Test kit or equivalent
- Nucleic acid extraction reagents
- RT-rtPCR instrumentation and consumables
- Positive extraction controls
- PCR-grade water
- Lysis buffers for difficult-to-lyse microorganisms
Procedure:
- Sample Processing: Filter product through sterile membrane (0.45μm) to concentrate potential contaminants.
- Cell Lysis: Apply lysis buffer to membrane to release microbial rRNA. Include mechanical disruption if needed for robust lysis.
- Nucleic Acid Extraction: Purify rRNA using validated extraction methods. Include controls for extraction efficiency.
- Reverse Transcription: Convert rRNA to cDNA using reverse transcriptase and target-specific or random primers.
- Amplification: Perform real-time PCR with broad-range microbial primers or multiplexed pathogen-specific assays.
- Detection: Monitor amplification in real-time. Samples crossing threshold within validated timeframe indicate contamination.
- Confirmatory Testing: Consider orthogonal testing for positive results to rule out amplification artifacts.
Validation Parameters: Establish limit of detection for representative microorganisms, specificity, robustness, and inhibition controls [102].
Implementation Strategy for cGMP Compliance
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Essential Reagents and Materials for Rapid Sterility Testing
| Reagent/Material | Function | Application Notes | Quality Requirements |
|---|---|---|---|
| Viability Stains | Fluorescent labeling of esterase activity in viable cells | Critical for solid phase cytometry; requires optimization for different matrices | USP/EP grade; certificate of analysis required |
| Culture Media | Supports microbial growth in growth-based methods | Must follow USP <71> formulations; may require supplementation for fastidious organisms | Sterility tested; growth promotion tested per USP <71> |
| Nucleic Acid Extraction Kits | Isolation of microbial RNA/DNA | Must efficiently lyse diverse microorganisms; remove inhibitors | PCR-grade; validated for sensitivity with representative organisms |
| Reference Microorganisms | Method validation and controls | USP <71> panel plus environmentally relevant isolates | Certified reference materials from recognized collections |
| Membrane Filters | Sample concentration | 0.45μm pore size; compatible with staining procedures | Sterilized by validated methods; non-inhibitory |
| Neutralizing Agents | Counteract antimicrobial properties | Required for products with preservatives or inherent antimicrobial activity | Validated for effectiveness; non-toxic to microorganisms |
Quality Systems and Documentation
Implementation of rapid sterility testing methods requires robust quality systems including comprehensive documentation, change control procedures, and investigation protocols. All rapid methods must undergo rigorous validation following USP <1223> guidelines, demonstrating comparable or superior performance to the compendial method [100]. The validation package should include data on limit of detection, specificity, precision, robustness, and ruggedness specific to the product matrix.
Out-of-specification results require thorough investigation following cGMP principles. Investigations should include review of batch records, environmental monitoring data, personnel monitoring results, and equipment maintenance records [100]. While identification of contaminating microorganisms is valuable for root cause analysis, cGMP regulations recognize that investigations may be successful without speciation when supported by other evidence [100].
Visualization of Method Selection and Implementation Workflow
Rapid Sterility Testing Method Selection Workflow
The implementation of rapid sterility testing methods for short shelf-life stem cell therapies represents a critical advancement in regenerative medicine manufacturing. By adopting the technologies and protocols outlined in this document, manufacturers can significantly reduce vein-to-vein time while maintaining rigorous safety standards. The field continues to evolve with emerging technologies promising even faster detection times, with some platforms targeting 48-hour detection by 2025 [98]. Successful implementation requires careful technology selection based on product-specific characteristics, thorough validation following regulatory guidelines, and integration within a comprehensive quality system. As the regulatory landscape continues to adapt to the unique challenges of advanced therapies, manufacturers should maintain awareness of evolving standards and engage early with regulatory agencies to ensure compliance while advancing patient access to these transformative therapies.
Phase-Appropriate Validation Strategies from Phase I to Commercial Manufacturing
The development of patient-specific stem cell therapies presents unique manufacturing and regulatory challenges due to their complex nature, often involving living cells, limited batch sizes, and challenging contamination control. A phase-appropriate approach to Good Manufacturing Practice (GMP) compliance is crucial for navigating the journey from early clinical trials to commercial marketing authorization successfully. This strategy applies the appropriate level of controls and validation at each stage of development, balancing risk management with practical feasibility [104].
The fundamental principle of phase-appropriate compliance recognizes that product and process knowledge increases throughout the product lifecycle. Initially, in Phase I, the focus is on ensuring patient safety while allowing sufficient flexibility for process refinement. As development progresses to Phase II and III, manufacturing consistency and characterization become increasingly important, culminating in a fully validated commercial process [104]. This structured approach is particularly vital for advanced therapy medicinal products (ATMPs), including stem cell-based therapies, where the science is advancing faster than regulatory guidance can be established [104].
The Three-Stage Process Validation Framework
Process validation for pharmaceutical manufacturing, including stem cell therapies, follows a three-stage framework as outlined by regulatory authorities. This lifecycle approach ensures quality is built into the manufacturing process from development through commercial production [105] [106].
Stage 1: Process Design
Process Design constitutes the research and development phase where the manufacturing process is defined and developed based on knowledge gained through experimentation and risk assessment [105]. The key elements of this stage include:
Development of Quality Target Product Profile (QTPP): A prospective summary of the quality characteristics necessary for the stem cell therapy to achieve the intended safety and efficacy profile [106].
Identification of Critical Quality Attributes (CQAs): Quality attributes of the final cell therapy product that must be controlled within appropriate limits to ensure the product achieves its intended safety, purity, potency, and efficacy [106].
Definition of Critical Process Parameters (CPPs): Process parameters whose variability impacts CQAs and therefore must be monitored or controlled to ensure the process produces the desired product quality [106].
Risk Assessment: Systematic evaluation of potential risks to product quality, focusing attention on the most significant factors [106].
During Process Design, experiments that generate material for clinical trials must be conducted under cGMP conditions, though full GMP implementation may be introduced in a phase-appropriate manner in early-stage trials [107] [106]. The output of this stage includes a development report, risk assessment, control strategy document, and final manufacturing process description that form the foundation for process qualification [106].
Stage 2: Process Qualification
Process Qualification evaluates the process designed in Stage 1 to ensure it is capable of reproducible commercial manufacturing at the intended scale [105]. This stage includes:
Facility Qualification: Ensuring buildings and facilities adhere to local regulations and pharmaceutical manufacturing requirements, including appropriate cleanroom classifications and environmental monitoring [105] [25].
Equipment Qualification: Verification that all equipment is properly installed, operational, and performing within required parameters [25].
Process Performance Qualification (PPQ): Documented evidence that the manufacturing process, as designed, can consistently produce products meeting predetermined specifications and quality attributes [106].
Process Qualification requires rigorous documentation through protocols and reports that demonstrate the manufacturing process's reliability and robustness before commercial distribution [106]. For cell therapies, this includes qualification of aseptic processing operations, which cannot be terminally sterilized [25].
Stage 3: Continued Process Verification
Continued Process Verification involves ongoing monitoring during commercial production to ensure the process remains in a state of control [105]. Key activities include:
Process Monitoring: Regular sampling and analysis of critical process parameters and quality attributes at various manufacturing steps [106].
Data Analysis and Review: Statistical analysis of process data to detect trends, process drift, or potential deviations [106].
Process Updates: Implementing process improvements and adjustments based on accumulated knowledge and monitoring data [105].
This stage employs a risk-based approach to determine monitoring frequency and extent, focusing on process aspects most critical to product quality [106]. The goal is to detect and address process variation before it impacts product quality, ensuring consistent production of safe and effective stem cell therapies throughout the product lifecycle.
Phase-Specific Implementation Strategies
Phase I Clinical Trial Requirements
For initial clinical trials, the implementation of GMP principles should be risk-based and phase-appropriate, focusing on ensuring patient safety while acknowledging limited process knowledge [104] [107]. Key considerations include:
Basic Quality Systems: Establishment of fundamental quality systems, including documentation, change control, and deviation management [104].
Safety-Focused Testing: Product release testing prioritizing safety parameters, including sterility, endotoxin, and identity [104] [25].
Process Controls: Implementation of critical process controls based on initial risk assessment and limited manufacturing experience [104].
Characterization: Preliminary product characterization, with understanding that specifications may evolve as product knowledge increases [104].
At this stage, a pharmaceutical quality system (PQS) in accordance with ICH Q12 should be established, though it may be less comprehensive than required for commercial production [104]. The primary goal is to generate sufficient safety data while maintaining flexibility for process improvement.
Phase II and III Clinical Trial Requirements
As development progresses to later-phase trials, manufacturing consistency and product characterization become increasingly important [104]. Requirements include:
Enhanced Process Controls: Tightening of process parameter ranges based on knowledge gained from Phase I experience [104].
Expanded Product Characterization: More comprehensive characterization of critical quality attributes, including potency assays that correlate with clinical activity [104].
Improved Documentation: More detailed batch records, standard operating procedures, and manufacturing documentation [104].
Scale-Up Considerations: Demonstration of manufacturing consistency at a scale representative of commercial production [104].
The transition between phases represents a key decision point where manufacturing processes should be sufficiently defined to ensure consistent production of clinical trial material across multiple sites and batches [104].
Commercial Manufacturing Requirements
Commercial manufacturing requires a fully validated process and comprehensive quality system to ensure consistent production of safe and effective products [105]. Key elements include:
Complete Process Validation: Successful completion of all three stages of process validation [106].
Robust Quality System: Comprehensive pharmaceutical quality system encompassing all aspects of manufacturing and quality control [25].
Stable Process and Methods: Established manufacturing process and analytical methods with demonstrated robustness [104].
Supply Chain Controls: Qualified suppliers and controlled raw materials to ensure consistent product quality [25].
Commercial manufacturing must comply with full GMP requirements as specified in relevant regulations and guidance documents [25]. The process should be well-characterized and controlled, with established ranges for critical process parameters that ensure consistent product quality.
Experimental Protocols and Case Studies
Case Study: GMP-Compliant CAR T-Cell Manufacturing
A recent study established a GMP-compliant manufacturing process for a novel autologous CD19-targeted CAR T-cell product (19-FiCART) intended for adult patients with high-risk B-cell lymphoma [8]. The manufacturing protocol illustrates phase-appropriate approach for early clinical development.
Starting Material Stability Assessment
Objective: Define optimal storage conditions and maximum hold time between leukapheresis and manufacturing initiation [8].
Methodology:
- Fresh, healthy donor-derived leukapheresis products (LPs) were stored at two temperature conditions: room temperature (RT; 15-25°C) and cool temperature (CT; 2-8°C)
- Cellular composition and viability were monitored over a 5-day period using flow cytometry and viability staining
- Parameters assessed included white blood cell counts, lymphocyte subpopulations (T-cells, B-cells, NK cells, NKT cells, monocytes), and apoptosis markers
Results Summary: Table: Leukapheresis Product Stability Under Different Storage Conditions
| Parameter | Room Temperature (15-25°C) | Cool Temperature (2-8°C) |
|---|---|---|
| Max Hold Time with >90% Viability | 49 hours | 73 hours |
| Monocyte Stability | Rapid decline after 49 hours | Stable throughout 121-hour study |
| T-cell Stability | Moderate decline after 73 hours | Stable throughout 121-hour study |
| Appearance Changes | Darker red color after 121 hours (RBC fragmentation) | No significant change |
| Apoptotic Cells | Lower levels (1.2% ± 1.6% at 121 hours) | Higher levels (4.9% ± 2.0% at 121 hours) |
This study established that LPs remained stable for at least 25 hours at RT and 73 hours at CT, providing critical data for defining hold times in the manufacturing process [8].
CAR T-Cell Manufacturing Process
The established 12-day semi-automated manufacturing process included CD4/CD8-positive cell enrichment and lentiviral transduction [8]. Key unit operations included:
- CD4/CD8 Enrichment: Using clinical-grade magnetic separation systems
- T-cell Activation: Through CD3/CD28 stimulation
- Lentiviral Transduction: To introduce the CAR construct
- Ex Vivo Expansion: Culture in GMP-compliant media for 12 days
- Formulation: Preparation of final drug product
The process consistently yielded more than 2 × 10^9 highly viable CAR+ T cells, sufficient for clinical application, and demonstrated potent anti-tumor activity in preclinical models [8].
Quality Control Strategy for Early Clinical Development
A phase-appropriate analytics strategy was implemented for in-process control and batch characterization [8]. The testing strategy included:
Table: Quality Control Testing Strategy for CAR T-Cell Products
| Testing Stage | Test Methods | Phase I Focus | Phase III/Commercial Focus |
|---|---|---|---|
| Starting Material (Leukapheresis) | Cell count, viability, flow cytometry | Identity, viability, cell composition | Same plus additional safety markers |
| In-Process Controls | Cell count, viability, transduction efficiency | Key parameters only | Comprehensive panel including vector copy number |
| Drug Substance/Product Release | Sterility, mycoplasma, endotoxin, potency, identity | Safety-focused (sterility, endotoxin, identity) | Full release panel including potency, purity, impurities |
| Characterization | Cytokine secretion, tumor killing assays, memory phenotype | Preliminary assessment | Comprehensive profiling |
This tiered approach ensures patient safety while allowing for method development and refinement as the product advances through clinical development [8].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of phase-appropriate validation strategies requires carefully selected reagents, equipment, and systems designed for GMP compliance. The following toolkit highlights essential components for stem cell therapy manufacturing:
Table: Essential Tools and Reagents for GMP-Compliant Stem Cell Therapy Manufacturing
| Category | Specific Examples | Function | GMP Considerations |
|---|---|---|---|
| Cell Processing Systems | Gibco CTS Rotea Counterflow Centrifugation System | Closed cell processing, washing, concentration | GMP-compliant, reduced contamination risk [17] |
| Cell Separation Systems | Gibco CTS Dynacellect Magnetic Separation System | Automated cell isolation, bead removal | Closed system, high cell purity and viability [17] |
| Genetic Modification Systems | Gibco CTS Xenon Electroporation System | Non-viral transfection, cell engineering | GMP-compliant, modular design [17] |
| Cell Culture Media | GMP-grade culture media, cytokines, growth factors | Cell expansion, maintenance | Chemically defined, xeno-free formulations [108] |
| Analytical Tools | Flow cytometry, PCR, sterility testing systems | Product characterization, release testing | Validated methods, GMP-compliant platforms [8] |
| Software Systems | CTS Cellmation software | Process monitoring, data integrity | 21 CFR Part 11 compliance [17] |
These tools enable the implementation of closed, automated manufacturing processes that reduce contamination risk and improve process consistency, which is particularly important for autologous therapies where scale-out rather than scale-up is required [17].
Workflow and Process Diagrams
Phase-Appropriate Validation Strategy Workflow
Diagram Title: Three-Stage Process Validation Lifecycle
This diagram illustrates the interconnected three-stage approach to process validation, showing how activities progress from initial process design through commercial production verification, with each stage building upon the previous one.
Stem Cell Therapy Manufacturing Workflow
Diagram Title: Cell Therapy Manufacturing with Process Controls
This workflow depicts a generalized stem cell therapy manufacturing process, highlighting critical unit operations and corresponding in-process control points that ensure product quality throughout manufacturing.
Implementing phase-appropriate validation strategies is essential for the successful development and commercialization of patient-specific stem cell therapies. By aligning validation activities with product development stage, manufacturers can efficiently utilize resources while ensuring patient safety and maintaining regulatory compliance. The framework presented in this document provides a structured approach to process validation that evolves from initial process design through commercial production, with increasing rigor and documentation requirements at each stage.
As the field of stem cell therapy continues to advance, with over 2,000 cell and gene therapies in clinical pipelines as of 2024, adherence to these principles will be crucial for delivering safe and effective treatments to patients [104]. The case studies and practical implementation strategies outlined here provide researchers and drug development professionals with actionable guidance for navigating the complex regulatory landscape while advancing innovative therapies through clinical development to commercial reality.
Conclusion
Achieving GMP compliance for patient-specific stem cell therapies requires an integrated approach spanning ethical frameworks, robust manufacturing systems, strategic troubleshooting, and rigorous validation. The foundational principles of rigor, oversight, and transparency must guide every manufacturing decision, while automated closed systems and quality by design approaches address critical scalability and consistency challenges. As the field advances toward allogeneic and in vivo approaches, the lessons learned from autologous therapy manufacturing will remain invaluable. Success demands early consideration of manufacturability, phase-appropriate compliance strategies, and continuous adaptation to evolving regulatory expectations. By embracing these comprehensive GMP principles, researchers and developers can accelerate the translation of promising stem cell research into safe, effective, and accessible therapies for patients in need.
References
- 1. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 2. ISSCR releases new global guidelines for stem cell research [https://www.eurostemcell.org/isscr-releases-new-global-guidelines-stem-cell-research]
- 3. Regenerative medicine and regulation: what's GMP got to ... [https://www.eurogct.org/regenerative-medicine-and-regulation-whats-gmp-got-do-it]
- 4. 1. Fundamental Ethical Principles [https://www.isscr.org/guidelines/fundamental-ethical-principles]
- 5. Validation of an automated viable cell counting assay for ... [https://www.sciencedirect.com/science/article/abs/pii/S1369703X23001481]
- 6. Design and validation of a GMP stem cell manufacturing ... [https://pubmed.ncbi.nlm.nih.gov/38946936/]
- 7. The ISSCR Releases Targeted Update to the Guidelines ... [https://www.isscr.org/isscr-news/the-isscr-releases-targeted-update-to-the-guidelines-for-stem-cell-research-and-clinical-translation]
- 8. Establishing a GMP-compliant manufacturing process and ... [https://www.nature.com/articles/s41598-025-92736-9]
- 9. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 10. Center for Biologics Evaluation and Research (CBER) [https://www.fda.gov/about-fda/fda-organization/center-biologics-evaluation-and-research-cber]
- 11. Current good manufacturing practice considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9934414/]
- 12. Current Good Manufacturing Practice [https://www.aabb.org/regulatory-and-advocacy/regulatory-affairs/regulatory-for-cellular-therapies/biological-products/current-good-manufacturing-practice]
- 13. Devices Regulated by the Center for Biologics Evaluation ... [https://www.fda.gov/vaccines-blood-biologics/premarket-notification-510k-process-cber-regulated-products/devices-regulated-center-biologics-evaluation-and-research]
- 14. What medical devices does CBER regulate? [https://www.fda.gov/industry/fda-basics-industry/what-medical-devices-does-cber-regulate]
- 15. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 16. focusing on induced pluripotent stem cell (iPSC)-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11583560/]
- 17. Guide to Cell Therapy GMP Manufacturing for Autologous ... [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 18. How to democratize cell and gene therapy: A global ... [https://www.sciencedirect.com/science/article/pii/S1525001625002709]
- 19. Global Harmonization of Cell and Gene Therapy Regulations [https://www.pharmafocusamerica.com/strategy/bridging-boundaries-toward-global-harmonization]
- 20. The ISSCR Releases Global Standards to Enhance Rigor ... [https://www.isscr.org/isscr-news/the-isscr-releases-global-standards-to-enhance-rigor-and-reproducibility-of-stem-cell-research]
- 21. Design and validation of a GMP stem cell manufacturing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11214401/]
- 22. BIO Group to Suggest Global Guidelines for Regulating ... [https://www.scbio.org/bio-group-to-suggest-global-guidelines-for-regulating-cell-and-gene-therapies/]
- 23. Navigating Operational Complexities in Phase I GMP Cell Therapy... [https://news.cuanschutz.edu/gates/operational-complexity-in-phase-i-gmp-cell-therapy-manufacturing]
- 24. Risk-Based Approach in GMP - [https://pharmuni.com/2024/11/25/risk-based-approach-in-gmp/]
- 25. Cell therapy: cGMP facilities and manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3666518/]
- 26. Development GMPs for Stability (Part IV) | Pharmaceutical... Early [https://www.pharmtech.com/view/early-development-gmps-stability-part-iv]
- 27. Chapter 4 - new Requirements for GMP Documentation? [https://www.gmp-compliance.org/gmp-news/ema-chapter-4-new-requirements-for-gmp-documentation]
- 28. Amsbio's Guide to GMP [https://www.amsbio.com/gmp/guide-to-gmp/]
- 29. Typical GMP documentation in a quality control laboratory [https://www.gmpsop.com/typical-gmp-documentation-in-a-quality-control-laboratory/]
- 30. GMP-compliant iPS cell lines show widespread plasticity in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11386223/]
- 31. Clean Room Classifications & ISO Standards [https://www.americancleanrooms.com/cleanroom-classifications/]
- 32. Cleanroom HEPA Filters: Your Complete Guide [https://csitesting.com/cleanroom-hepa-filters/]
- 33. Cleanroom Validations Process Explained [https://www.pristinecleanbags.com/cleanroom-validation/?srsltid=AfmBOoqVMJiDPmObtx78NBxYlphWU-rvyYXHsxH1gsZRUmYRdOl2sDd6]
- 34. What is an ISO 8 Cleanroom? Definition and Requirements [https://alliedcleanrooms.com/iso-8-cleanrooms-definition-and-requirements/]
- 35. HEPA Filters in Cleanrooms [https://www.cleanroomsolutions.com/blog/posts/hepa-filters-in-cleanrooms]
- 36. What Is An ISO-8 Cleanroom Classification? [https://www.americancleanrooms.com/what-is-iso-8-cleanroom-classification/]
- 37. Manufacturing autologous cell therapies [https://www.patheon.com/us/en/insights-resources/blog/autologous-cell-therapy-manufacturing-challenges-and-best-practices.html]
- 38. Closed System Automation for Cell Therapy [https://www.thermofisher.com/blog/behindthebench/closed-system-automation-cell-therapy/]
- 39. Closed-Loop Manufacturing Is The Cell Therapy ... [https://www.cellandgene.com/doc/closed-loop-manufacturing-is-the-cell-therapy-revolution-we-need-0001]
- 40. Closed-system manufacturing of therapeutic NK cells using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238007/]
- 41. Why manual bottle filling puts biomanufacturers at risk [https://www.susupport.com/blogs/knowledge/operator-burden-why-manual-bottle-filling-puts-biomanufacturers-at-risk]
- 42. Research Use Only to Good Manufacturing Practices [https://www.thermofisher.com/us/en/home/biotech-lab-solutions/biotech-learning-center/ruo-gmp-compliant-biologics.html]
- 43. cGMP-Manufactured Human Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4624993/]
- 44. GMP Grade vs. Reagent Grade [https://listlabs.com/gmp-explained-gmp-vs-reagent/]
- 45. The Critical Differences Between RUO and GMP Reagents [https://www.linkedin.com/pulse/from-bench-clinic-critical-differences-4g63c]
- 46. FDA Good Manufacturing Practices (GMP): 2025 Guide [https://pharmuni.com/2025/11/06/fda-good-manufacturing-practices-complete-year-guide-for-compliance-and-quality/]
- 47. Can You Use Research-Grade Reagents in GMP ... [https://synapse.patsnap.com/article/can-you-use-research-grade-reagents-in-gmp-manufacturing]
- 48. GMP iPSC Production Service: Clinical-grade Human ... [https://www.reprocell.com/clinical-stem-cell-services/gmp-ipsc-production]
- 49. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 50. Qbd Cqa Cpp Pat Understanding Process [https://www.nnit.com/insights/articles/qbd-cqa-cpp-pat-understanding-process]
- 51. Advanced Quality by Design (QbD) Approach to Large ... [https://www.sciencedirect.com/science/article/pii/S1465324925003718]
- 52. Stem Cell Clinics in the United States: Explained (2025) [https://www.dvcstem.com/post/stem-cells-usa]
- 53. Cell Therapy Development - Areas of Interest [https://www.stemcell.com/tissue-and-cell-types/cell-therapy-research.html]
- 54. Good Manufacturing Practice for Cell & Cell-Based Therapies [https://www.roosterbio.com/blog/good-manufacturing-practice-for-cell-and-cell-based-therapies-facilities-quality-control/]
- 55. Off-the-Shelf GMP-Compliant iPS Cells for Application in ... [https://www.sciencedirect.com/science/article/pii/S1465324925005663]
- 56. GMP compliance in Cell Therapy & AAV manufacturing [https://greenelephantbiotech.com/blog/gmp-compliance-in-cell-therapy-aav-manufacturing/]
- 57. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 58. Process Steps in Cell Therapy Manufacturing [https://www.cellandgene.com/topic/cell-therapy-manufacturing]
- 59. Quantitative Detection and Modeling the In Vivo Kinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5746161/]
- 60. Quantitative Single-Cell Approaches to Stem Cell Research [https://www.sciencedirect.com/science/article/pii/S1934590914004664]
- 61. Managing Raw Material Variability for Autologous Cell ... [https://www.biopharminternational.com/view/managing-raw-material-variability-for-autologous-cell-therapies]
- 62. Addressing Variability in Donor Tissues and Cells - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK544028/]
- 63. Formulation Considerations for Autologous T Cell Drug Products [https://pmc.ncbi.nlm.nih.gov/articles/PMC8400304/]
- 64. Automated manufacturing of cell therapies [https://www.sciencedirect.com/science/article/pii/S0168365925001701]
- 65. The Next Frontier: Industrializing Cell Therapy Manufacturing [https://www.isctglobal.org/telegrafthub/blogs/isct-head-office1/2025/10/07/the-next-frontier-industrializing-cell-therapy-man]
- 66. Implementation of a quality management system for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361990/]
- 67. Process Development Considerations for Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4572896/]
- 68. Smarter Ways to Scale in Cell and Gene Therapy ... [https://www.patheon.com/us/en/insights-resources/blog/smarter-pathways-to-scale-in-cell-and-gene-therapy-manufacturing.html]
- 69. GMP Manufacturing and Quality Control [https://www.bdbiosciences.com/en-us/solutions/drug-discovery-development/gmp-manufacturing-quality-control]
- 70. Acceleration of Translational Mesenchymal Stromal Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8076909/]
- 71. Advances in automated cell washing and concentration [https://www.sciencedirect.com/science/article/pii/S1465324921002292]
- 72. #09 Delivering Efficiency and Quality to Cell Therapy ... [https://www.terumo.com/technology/stories/09]
- 73. Cell & Gene Therapy Solutions [https://www.thermofisher.com/es/en/home/clinical/cell-gene-therapy.html]
- 74. CTS Xenon Electroporation System Features [https://www.thermofisher.com/us/en/home/clinical/cell-gene-therapy/cell-therapy/cell-therapy-manufacturing-solutions/xenon-electroporation-system/features.html]
- 75. Our Electroporation Technology [https://maxcyte.com/our-technology/]
- 76. Qualifying Ancillary/Raw Materials for Cell Therapy [https://www.stemcell.com/ancillary-material-qualification.html]
- 77. GMP Ancillary Materials: Importance for Stem Cell Therapy ... [https://www.tocris.com/resources/tocris-blog/gmp-ancillary-materials-importance-stem-cell-therapy-manufacture]
- 78. How to ensure quality and compliance in clinical supply ... [https://www.gmpsop.com/compliance-in-clinical-supply-chain-management/]
- 79. How To Reduce Batch-to-Batch Variation In Cell Therapy ... [https://www.cellandgene.com/doc/how-to-reduce-batch-to-batch-variation-in-cell-therapy-manufacturing-0001]
- 80. Assessing and mitigating batch effects in large-scale omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447944/]
- 81. Key considerations for raw material selection in cell ... [https://www.ptglab.com/news/blog/key-considerations-for-raw-material-selection-in-cell-therapy-manufacturing/?srsltid=AfmBOorHvQrSo5t5zUl2njtFh7d2mMYDbaH3kb0JZgiz9tP0ok5Af1Bz]
- 82. Scale up manufacturing approach for production of human ... [https://www.nature.com/articles/s41536-025-00409-y]
- 83. Why You Must Correct Batch Effects in Transcriptomics Data? [https://www.metwarebio.com/transcriptomics-batch-effect-correction/]
- 84. Understanding the ich ( Q ) 2 R 1 guideline [https://www.linkedin.com/pulse/understanding-ich-q2r1-guideline-priyadarshana-asolkar-cipgc]
- 85. Current Good Manufacturing Practices (cGMP) [https://www.qualityze.com/blogs/cGMP-role-in-quality]
- 86. cGMP and GLP Regulations for Quality Control Labs [https://www.complianceonline.com/resources/cgmp-and-glp-regulations-for-quality-control-labs.html]
- 87. The Laboratory Control System: Fulfilling cGMP ... [https://www.biopharminternational.com/view/laboratory-control-system-fulfilling-cgmp-requirements]
- 88. Validation of analytical methods in GMP: the disposable Fast ... [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-10-112]
- 89. Validation of an automated cell counting method for cGMP ... [https://www.sciencedirect.com/science/article/pii/S2215017X22000091]
- 90. Validation of an automated cell counting method for cGMP ... [https://pubmed.ncbi.nlm.nih.gov/35198419/]
- 91. Validation of an automated viable cell counting assay for ... [https://ui.adsabs.harvard.edu/abs/2023BioEJ.19608953P/abstract]
- 92. Manufacturing & Controls for Advanced Therapy Medical ... [https://www.eurogct.org/research-pathways/research-and-innovation/fundamental-research/manufacturing-phase/manufacturing]
- 93. Characterization and analysis of cell therapies [https://www.thermofisher.com/blog/behindthebench/characterization-and-analysis-of-cell-therapies/]
- 94. Quality and Regulatory Requirements for the Manufacture ... [https://pubmed.ncbi.nlm.nih.gov/39821060/]
- 95. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 96. Standards | FACT [https://www.factglobal.org/standards/]
- 97. 5. Standards in Stem Cell Research [https://www.isscr.org/guidelines/standards-in-stem-cell-research]
- 98. Faster and More Confident Rapid Sterility Testing of Cell ... [https://symcel.com/science-blog/faster-and-more-confident-rapid-sterility-testing]
- 99. Revision of USP chapter <1071> on rapid methods and its ... [https://www.gmp-compliance.org/gmp-news/revision-of-usp-chapter-1071-on-rapmethods-and-its-effect-on-other-usp-chapters]
- 100. Non-Growth-Based Alternative Sterility Testing - bioMerieux [https://www.biomerieux.com/corp/en/education/resource-hub/pharma-quality-control/white-papers/non-growth-based-alternative-sterility-testing.html]
- 101. What is GMP? [https://www.kumc.edu/research/midwest-stem-cell-therapy-center/facility/what-does-gmp-mean.html]
- 102. Cut Sterility Test Time from Days to Hours [https://www.rapidmicrobiology.com/news/cut-sterility-test-time-from-days-to-hours]
- 103. Nelson Labs Launches Rapid Product Sterility Testing [https://www.nelsonlabs.com/news/nelson-labs-launches-innovative-rapid-sterility-testing/]
- 104. Phase-appropriate Compliance for Cell and Gene Therapies [https://www.biopharminternational.com/view/phase-appropriate-compliance-for-cell-and-gene-therapies]
- 105. Stages Process Validation Explained [https://www.nnit.com/insights/articles/stages-process-validation-explained]
- 106. QbD Validation Strategies: The Process Design Phase Part 1 [https://www.bioprocessonline.com/doc/qbd-validation-strategies-the-process-design-phase-0001]
- 107. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 108. GMP‐Compliant Process for the Manufacturing of an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365392/]