GMP Manufacturing for Clinical-Grade Stem Cells: Protocols, Challenges, and Future Directions
This article provides a comprehensive guide to Good Manufacturing Practice (GMP) protocols for producing clinical-grade stem cells, tailored for researchers, scientists, and drug development professionals.
GMP Manufacturing for Clinical-Grade Stem Cells: Protocols, Challenges, and Future Directions
Abstract
This article provides a comprehensive guide to Good Manufacturing Practice (GMP) protocols for producing clinical-grade stem cells, tailored for researchers, scientists, and drug development professionals. It covers the foundational principles of GMP and its critical importance in cell therapy, details step-by-step methodological protocols for isolation, expansion, and characterization, addresses common troubleshooting and optimization strategies for manufacturing challenges, and explores validation frameworks and comparative analyses of different stem cell sources and culture systems. The content synthesizes current best practices and regulatory considerations to support the translation of stem cell research from the laboratory to clinical applications.
The Pillars of GMP: Building a Foundation for Clinical-Grade Stem Cell Production
Defining GMP and Its Critical Role in Cell Therapy Safety and Efficacy
Good Manufacturing Practice (GMP) represents a system for ensuring that products are consistently produced and controlled according to quality standards appropriate to their intended use. For cell therapies, classified as Advanced Therapy Medicinal Products (ATMPs) in Europe and as human cells, tissues, or cellular and tissue-based products (HCT/Ps) in the United States, compliance with GMP is mandatory for clinical application [1] [2]. The fundamental principle of GMP in this field is that safety and efficacy cannot be assured by final product testing alone but must be built into the manufacturing process through rigorous controls at every stage [3]. This is particularly critical for cell therapies, which consist of living, dynamic biological entities that cannot be sterilized or filtered at the final product stage, making process control paramount to patient safety [4].
Core GMP Principles for Cell Therapy Manufacturing
Quality Management Systems
A comprehensive Quality Management System (QMS) forms the foundation of GMP, encompassing all aspects of production from starting materials to final product release. This system requires that all activities are thoroughly documented and audited regularly to maintain product consistency and compliance with regulatory standards [3]. The QMS provides the framework for defining responsibilities, procedures, and controls to ensure that every product batch meets predefined specifications for quality, purity, and identity.
Facility and Environmental Control
GMP facilities for cell therapy must be designed to higher standards than conventional laboratories, with proper cleanroom classifications (Grade A, B, C, and D) based on air purity and particle counts [3] [4]. Environmental control, monitoring, and maintenance are critical to prevent contamination and determine operational efficiency. These facilities incorporate multi-level aseptic protection solutions, including clean rooms, laminar flow hoods, and closed cultivation systems to restrain airborne particles and avoid product contamination [4].
Process Validation and Control
All manufacturing processes must be validated and controlled according to standard operating procedures. This includes critical materials management, sample collection, processing, culturing, storage, quality control testing, and product release [3]. Process controls must demonstrate that the manufacturing process consistently yields a product meeting its quality attributes, with particular attention to aseptic processing since terminal sterilization is not possible for living cell products [1].
GMP-Compliant Manufacturing Processes and Protocols
Starting Materials and Reagents
A fundamental GMP requirement is the use of clinical-grade reagents free from animal contaminants. Traditional fetal bovine serum (FBS) has been largely replaced by xenogeneic-free alternatives such as human platelet lysate (hPL) or completely defined, serum-free media to eliminate risks of immunogenicity and transmission of infectious agents [5] [6] [1]. For example, a 2025 study demonstrated that FPMSCs (infrapatellar fat pad-derived mesenchymal stem cells) exhibited enhanced proliferation rates when cultured in MSC-Brew GMP Medium compared to standard MSC media, showing lower doubling times across passages [6].
Table 1: Comparison of GMP-Compliant Culture Media for MSC Expansion
| Media Formulation | Composition | Performance Results | Manufacturer |
|---|---|---|---|
| MSC-Brew GMP Medium | Animal component-free | Lower doubling times, higher colony formation | Miltenyi Biotec |
| MesenCult-ACF Plus Medium | Animal component-free | Supports MSC expansion and maintenance | StemCell Technologies |
| X-VIVO-15 | Serum-free with cytokines | Used in HSC gene therapy protocols | Lonza |
| Supplementation with human platelet lysate (hPL) | Human-derived growth factors | Superior to FBS for AT-MSC expansion in bioreactors | Various |
Automated Manufacturing Platforms
To ensure reproducibility and scale-up capability, automated closed-system platforms have been developed for GMP-compliant cell manufacturing, including the Quantum Cell Expansion System (Terumo BCT), CliniMACS Prodigy (Miltenyi Biotec), Cocoon Platform (Lonza), and Xuri Cell Expansion System W25 (Cytiva) [4]. These systems minimize manual open manipulations, reduce contamination risk, and provide a controlled environment for consistent cell expansion. For instance, the Quantum system reduced needed passages by half and open manipulations from 54,400 to 133 steps compared to flask-based propagation of BM-MSCs [4].
Table 2: Automated Platforms for GMP-Compliant Cell Manufacturing
| Platform | Technology | Scale/Capacity | Reported Output |
|---|---|---|---|
| Quantum Cell Expansion System | Hollow fiber bioreactor | 21,000 cm² (equiv. to 120 T-175 flasks) | 100-276 × 10⁶ BM-MSCs in 7-day expansion |
| CliniMACS Prodigy | Integrated cell processing with ACC | Culture vessel dependent | 29-50 × 10⁶ MSCs at P0 from mobilized blood |
| Cocoon Platform | Automated cell therapy manufacturing | Patient-scale | Designed for individualized therapies |
| Xuri W25 System | Wave-induced motion bioreactor | Scalable from 100 mL to 25 L | Compatible with suspension cell culture |
Protocol: GMP-Compliant MSC Expansion
The following protocol outlines the key steps for GMP-compliant expansion of mesenchymal stem/stromal cells (MSCs) based on current methodologies [6] [1]:
- Tissue Acquisition and Donor Screening: Source tissue (e.g., bone marrow, adipose tissue, umbilical cord) must be obtained with appropriate informed consent and donor eligibility determination, including screening for relevant communicable disease agents (RCDADs) [7] [1].
- Cell Isolation: Process tissue using enzymatic digestion (e.g., 0.1% collagenase for 2 hours at 37°C for adipose tissue) or density gradient separation in a closed system [5] [6].
- Primary Culture: Seed cells at density of 1,000-4,000 cells/cm² in GMP-compliant, animal component-free medium supplemented with appropriate growth factors [1].
- Cell Expansion: Culture cells to 80-90% confluency in multilayered flasks or bioreactors. Use animal component-free dissociation reagents for passaging. Limit population doublings to prevent senescence (typically <20 doublings) [1].
- Harvest and Formulation: Harvest cells using gentle detachment methods. Formulate in final infusion solution with appropriate cryoprotectant if needed.
- Cryopreservation: Cryopreserve in controlled-rate freezing system with defined cryoprotectant (e.g., DMSO at appropriate concentration) [4].
- Quality Control Testing: Perform comprehensive testing including viability, identity, potency, and sterility before product release.
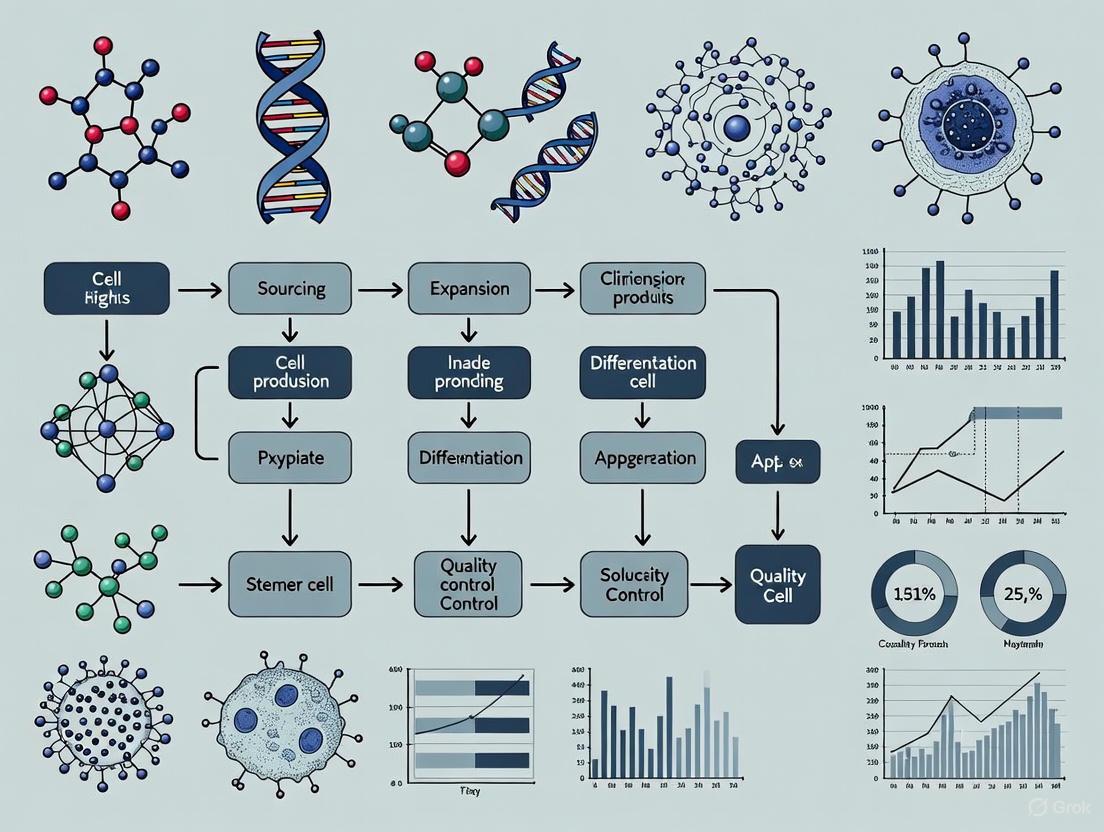
Diagram 1: GMP-Compliant MSC Manufacturing Workflow. This diagram outlines the critical stages in the production of clinical-grade mesenchymal stem/stromal cells, from tissue acquisition to final product release.
Quality Control and Product Characterization
Identity, Purity, and Potency Assays
According to International Society for Cellular Therapy (ISCT) guidelines, MSCs must demonstrate: (I) plastic adherence; (II) expression of CD105, CD73, and CD90 (>95% positive) and lack of expression of CD45, CD34, CD14, CD11b, CD79α, and HLA-DR (<2% positive); and (III) ability to differentiate into adipocytes, chondrocytes, and osteoblasts in vitro [4] [1]. Additional testing for immunomodulatory activity and genomic stability is recommended to ensure product safety and functionality [4]. A 2025 study on GMP-manufactured FPMSCs reported post-thaw viability >95% (exceeding the >70% requirement) and maintained sterility and stem cell marker expression even after 180 days of storage [6].
Safety Testing
Comprehensive safety testing includes sterility (bacteria, fungi), mycoplasma, endotoxin, and adventitious virus testing [6] [1]. In-process controls and final product testing must demonstrate absence of microbial contamination. Additional safety assessments may include karyotype analysis, in vitro potential for malignant transformation, and in vivo toxicity studies in immunodeficient animals, as demonstrated in a 2017 study of GMP-manufactured interferon γ-primed MSCs which showed no evidence of toxicity [8].
Regulatory Framework and Global Perspectives
GMP requirements for cell therapies vary across regulatory jurisdictions, though all emphasize a risk-based approach with increasing stringency through clinical development phases [2]. In the United States, the FDA regulates HCT/Ps under 21 CFR 1271, with phase 1 products reviewed under IND applications, while phase 2 and 3 products require manufacturing site registration [2]. In the European Union, the EMA requires manufacturing authorization for all clinical trial stages, with certification by a qualified person (QP) [2]. Canada takes a flexible risk-based approach, with GMP assessment conducted through Clinical Trial Application reviews for all development phases [2].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential GMP-Compliant Reagents for Cell Therapy Manufacturing
| Reagent/Material | Function | GMP-Compatible Examples |
|---|---|---|
| Cell Culture Media | Supports cell growth and expansion | MSC-Brew GMP Medium, MesenCult-ACF Plus, X-VIVO-15 |
| Dissociation Reagents | Cell passaging and harvesting | TrypLE Select, TrypZean, GMP-grade collagenase |
| Culture Supplements | Enhance growth and maintain cell properties | Human platelet lysate (e.g., PLT-Max, Stemulate) |
| Cryopreservation Media | Maintain cell viability during frozen storage | Defined cryoprotectant solutions with DMSO |
| Cell Separation Reagents | Isolate target cell populations | Ficoll-Paque PREMIUM, CliniMACS reagents |
| Process Additives | Improve efficiency of specific steps | LentiBOOST, protamine sulfate (for transduction) |
GMP implementation is fundamental to ensuring the safety and efficacy of cell-based therapies. By establishing robust quality systems, employing standardized manufacturing processes with defined reagents, and implementing comprehensive quality control testing, developers can deliver consistent, high-quality cell products for clinical applications. The field continues to evolve with advancements in automated platforms, improved culture systems, and harmonized regulatory approaches that collectively support the translation of promising cell therapies from research to clinical practice.
Core Components of a GMP Quality Management System (QMS)
A Good Manufacturing Practice (GMP)-compliant Quality Management System (QMS) is a structured framework of documented procedures and controls essential for the consistent production of clinical-grade stem cell products. For researchers developing Advanced Therapy Medicinal Products (ATMPs), implementing a robust QMS is not merely a regulatory formality but a fundamental component of ensuring product safety, identity, purity, potency, and efficacy. This application note details the core components of a GMP QMS, provides practical protocols for implementation within stem cell research, and discusses emerging regulatory considerations for decentralized manufacturing.
The transition of stem cell therapies from research to clinical application is governed by stringent regulatory frameworks. The European Commission's ATMP Regulation classifies stem-cell-based products for human use as pharmaceuticals, bringing them under the purview of GMP guidelines [9]. Unlike conventional drugs, stem cell therapies comprise living, fragile biological entities that cannot be standardized identically to a chemical pill, making a robust, risk-based QMS paramount for controlling variability and ensuring patient safety [9].
A GMP-compliant QMS provides the foundation for consistent production, risk mitigation, and regulatory compliance throughout the product lifecycle. Its core principles are often summarized as the "Five Ps": People, Processes, Procedures, Products, and Premises [10]. Adherence to these principles minimizes risks such as contamination, mislabeling, and process failures, which are critical when manufacturing patient-specific autologous therapies [10] [11].
Core Components of a GMP-Compliant QMS
A comprehensive QMS for clinical-grade stem cell manufacturing is built upon several interconnected pillars. The table below summarizes the fundamental components and their primary objectives.
Table 1: Core Components of a GMP-Compliant QMS for Stem Cell Manufacturing
| QMS Component | Primary Objective | Key Documentation & Outputs |
|---|---|---|
| Quality Management | To oversee the entire system, ensuring product quality and facilitating continual improvement [12] [13]. | Quality Manual, Quality Policy, Management Review Records, Quality Risk Management (QRM) files [14] [13]. |
| Personnel & Training | To ensure all staff are qualified, trained, and adhere to hygiene protocols to prevent errors and contamination [15] [13]. | Organizational Charts, Job Descriptions, Training Plans & Matrices, Training Records, Competency Assessments, Hygiene SOPs [15] [13]. |
| Premises & Equipment | To provide and maintain a controlled environment and qualified equipment suitable for stem cell manufacturing [15] [16]. | Facility & Cleanroom Validation Records, Equipment Logs, Calibration & Maintenance Records, Cleaning Validation Reports [15] [16]. |
| Documentation & Record Keeping | To provide documented evidence that all GMP activities have been performed correctly. "If it isn't documented, it didn't happen." [15] | Standard Operating Procedures (SOPs), Batch Manufacturing Records (BMRs), Deviation Reports, Logbooks [12] [15]. |
| Process & Procedure Control | To ensure manufacturing processes are defined, validated, and controlled to consistently yield products meeting specifications [10] [15]. | Validated Manufacturing Protocols, Process Flow Diagrams, Critical Process Parameter (CPP) monitoring records [15]. |
| Raw Material & Supplier Management | To guarantee the quality of ancillary materials (AMs) and starting materials, which directly impacts final product safety and efficacy [17] [15]. | Approved Supplier List, Supplier Audit Reports, Raw Material Specifications, Incoming Inspection Records [17] [15]. |
| Quality Control (QC) & Testing | To monitor, sample, and test raw materials, in-process samples, and final products to ensure they meet quality standards [15] [13]. | QC Test Methods & Protocols, Specifications, Certificates of Analysis (CoA), Stability Study Data [13]. |
| Deviations, CAPA, and Change Control | To manage unplanned events, identify root causes, implement corrective actions, and control modifications to validated systems [12] [15]. | Deviation Reports, CAPA Records, Change Control Requests, Effectiveness Verification Reports [12] [15]. |
The following workflow diagram illustrates the logical relationships and interdependencies between these core components within an effective QMS.
Diagram 1: GMP QMS Component Relationships
Practical Implementation and Experimental Protocols
Protocol: Ancillary Material (AM) Qualification for Stem Cell Culture
The quality of ancillary materials (AMs)—such as cell isolation reagents, culture media, and cytokines—is widely recognized as having a direct impact on the safety and efficacy of the final cell therapy product [17]. Their qualification is a critical GMP activity.
1. Principle To establish the source, identity, purity, biological safety, and general suitability of an AM for its intended use in the manufacturing process of a clinical-grade stem cell product, following a risk-based approach as guided by USP <1043> and Ph. Eur. 5.2.12 [17].
2. Materials and Reagents Table 2: Research Reagent Solutions for AM Qualification
| Item | Function / Purpose | Critical Quality Attribute |
|---|---|---|
| Ancillary Material (AM)(e.g., GMP-grade FBS) | Provides essential growth factors and nutrients for stem cell expansion. | Identity, Purity, Sterility, Viral Safety, Endotoxin Level. |
| Characterization Assay Kits(e.g., Flow Cytometry, ELISA) | Confirm AM identity and detect specific impurities or contaminants. | Specificity, Accuracy, Precision. |
| Sterility Testing Media(e.g., Fluid Thioglycollate Medium) | Detects microbial contamination in the AM. | Growth Promotion. |
| Endotoxin Testing Kit(e.g., LAL Assay) | Quantifies bacterial endotoxin levels. | Confirmed validity and sensitivity. |
| Cell Line for Bio-functionality Testing(e.g., Reference hPSC Line) | Assesses the impact of the AM on stem cell phenotype and function. | Stable Karyotype, Validated Phenotype. |
3. Methodology
- Step 1: Supplier Qualification & Documentation Review. Audit the AM supplier or request a GMP Master File from them. Obtain and review the Certificate of Analysis (CoA) for the specific lot, and ensure full traceability of the material's origin [17] [15].
- Step 2: Identity and Purity Testing. Perform testing to confirm the AM's identity (e.g., using spectroscopic or chromatographic methods) and purity. Test for impurities and contaminants relevant to the source (e.g., bovine viruses in serum, host cell proteins in recombinant proteins) [17].
- Step 3: Safety Testing. Conduct sterility testing (according to pharmacopoeial methods), mycoplasma testing (if applicable), and endotoxin testing. The endotoxin limit should be justified based on the final product's route of administration and dose [9].
- Step 4: Performance/Bio-functionality Testing. Using a well-characterized stem cell line, evaluate the AM's performance against a predefined reference standard or a research-grade equivalent. Key parameters include:
- Cell Viability and Growth Kinetics: Perform daily cell counts and viability assays (e.g., Trypan Blue exclusion) over a minimum of three passages.
- Phenotype Maintenance: Analyze stem cell markers (e.g., Tra-1-60, SSEA-4 for pluripotency) via flow cytometry at each passage.
- Differentiation Potential: Conduct directed differentiation assays (e.g., to ectoderm, mesoderm, and endoderm lineages) to confirm the AM does not impair pluripotency.
- Step 5: Stability Testing. Establish the AM's shelf-life under recommended storage conditions by repeating critical identity, purity, safety, and functionality tests at predetermined time points.
4. Data Analysis and Acceptance Criteria Compare all test results against predefined specifications. The AM lot is deemed qualified only if it meets all acceptance criteria for identity, purity, safety, and functionality. Any out-of-specification (OOS) result must be investigated through a formal deviation and CAPA process.
Protocol: Process Validation for Stem Cell Expansion
Process validation provides documented evidence that the stem cell expansion process consistently produces a product meeting its predetermined quality attributes.
1. Principle To demonstrate, through rigorous and documented experimentation, that the proposed manufacturing process for stem cell expansion is robust, reproducible, and capable of consistently yielding a product that complies with its quality target product profile (QTPP) [15].
2. Methodology (Three-Lot Validation Approach)
- Stage 1: Process Design. Define the QTPP and identify Critical Quality Attributes (CQAs) of the final cell product (e.g., viability, identity, potency, sterility). Using risk assessment, link CQAs to Critical Process Parameters (CPPs) of the expansion process (e.g., seeding density, media exchange frequency, passaging method, oxygen tension). Design a scalable process and establish control strategies for these CPPs.
- Stage 2: Process Qualification.
- Equipment Qualification: Ensure all equipment (e.g., bioreactors, incubators, centrifuges) used in the process has undergone Installation, Operational, and Performance Qualification (IQ/OQ/PQ) [15].
- Process Performance Qualification (PPQ): Execute a minimum of three consecutive consecutive full-scale GMP batches using the defined process and the qualified equipment. The batches must be manufactured by trained personnel in the GMP facility using qualified AMs.
- Stage 3: Continued Process Verification. Implement ongoing monitoring of the validated process during routine production to ensure it remains in a state of control.
3. Data Collection and Acceptance Criteria During PPQ, extensive data must be collected for each batch. The table below outlines key validation data points.
Table 3: Key Data Points for Stem Cell Expansion Process Validation
| Process Stage | Parameter Monitored | Acceptance Criteria |
|---|---|---|
| Starting Material | Donor Cell Viability, Identity | Viability > X%, Confirmed donor identity. |
| In-Process Controls | Cell Doubling Time, Metabolite Levels (e.g., Glucose), Phenotype (Flow Cytometry) | Consistent doubling time, Metabolite levels within range, Phenotype purity > Y%. |
| Final Product Release | Total Cell Number, Viability, Identity, Potency, Sterility, Endotoxin | Cell number > Z, Viability > 80%, Identity confirmed, Potency assay met, Sterile, Endotoxin < threshold. |
Special Considerations for Stem Cell Therapies and Emerging Trends
Navigating the Regulatory Landscape for Ancillary Materials
A common challenge for researchers is the qualification of AMs not manufactured under GMP. It is a misconception that only "GMP-grade" AMs can be used in clinical trials. Regulatory guidance allows for a risk-based approach, particularly for early-phase trials [17]. The responsibility for AM qualification lies with the therapy manufacturer, who can leverage supplier documentation (e.g., ISO 13485 certification) and perform additional testing to establish suitability [17]. Claims of "cell-therapy-grade" are market-driven and not a recognized regulatory standard [17].
The Rise of Decentralized Manufacturing
For autologous stem cell therapies, decentralized manufacturing at or near the point of care (POCare) is an emerging paradigm to overcome logistical hurdles and reduce costs [11]. This model involves manufacturing in multiple, geographically dispersed sites (e.g., academic health centers) under the oversight of a central "Control Site" [11]. The Control Site holds the regulatory license, maintains the central product file, and ensures consistency and comparability across the entire network through a robust, integrated QMS [11]. Regulatory bodies like the MHRA, FDA, and EMA are developing frameworks to accommodate this shift, emphasizing the need for automated, closed-system technologies to minimize process variability [11].
Implementing a comprehensive, GMP-compliant QMS is a non-negotiable requirement for translating stem cell research from the laboratory to the clinic. Its core components—from quality management and personnel training to meticulous documentation and robust process control—form an interdependent ecosystem designed to ensure product quality and patient safety. As the field evolves with trends like decentralized manufacturing, the principles of GMP and a robust, adaptable QMS will remain the cornerstone of safe and effective stem cell therapy development.
Understanding Regulatory Landscapes and Global Standards (FDA, EMA, ISO)
The transition of stem cell-based therapies from research to clinical application is a complex process governed by stringent regulatory frameworks. These frameworks, established by bodies like the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the International Organization for Standardization (ISO), ensure that cell therapies are safe, efficacious, and of high quality. For researchers and drug development professionals, navigating this multifaceted regulatory landscape is critical for the successful development and approval of clinical-grade stem cell products. This document outlines the core principles of Good Manufacturing Practices (GMP), risk management, and key regulatory requirements, providing a foundation for compliance in stem cell research and manufacturing.
Core Regulatory and Standardization Bodies
United States Food and Drug Administration (FDA)
The FDA regulates stem cell products primarily as Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/Ps) under 21 CFR Part 1271 [18]. The level of regulatory oversight is tiered and risk-based. Products that are minimally manipulated and intended for homologous use do not require pre-market approval. However, most stem cell products, particularly those that are more than minimally manipulated or intended for non-homologous use, are regulated as biological products and require an Investigational New Drug (IND) application for clinical trials and eventual Biologics License Application (BLA) approval [18].
A key requirement is that establishments involved in the manufacture of HCT/Ps must register with the FDA and list their products [19]. The FDA also enforces Current Good Manufacturing Practice regulations to ensure quality [20]. In January 2025, the FDA issued new draft guidance clarifying requirements for in-process controls under 21 CFR § 211.110, supporting the use of advanced manufacturing technologies while emphasizing a risk-based approach and the need for in-process testing to ensure batch uniformity [21].
Table: Key FDA Regulations for Stem Cell Products
| Regulation | Title | Key Focus |
|---|---|---|
| 21 CFR Part 1271 | Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/Ps) | Registration, listing, donor eligibility, and current good tissue practice (GTP) |
| 21 CFR Part 211 | Current Good Manufacturing Practice for Finished Pharmaceuticals | GMP requirements for drug products, including quality control and facility controls |
| 21 CFR Part 600 | Biological Products: General | Additional requirements for biological products |
International Organization for Standardization (ISO)
ISO standards provide internationally recognized frameworks for quality and risk management. For medical devices, including some combination products or equipment used in cell therapy manufacturing, ISO 14971 specifies a process for risk management throughout the entire product lifecycle [22]. The standard requires manufacturers to identify hazards, estimate and evaluate associated risks, implement risk control measures, and monitor the effectiveness of controls [23].
Another critical standard is ISO 13485, which specifies requirements for a Quality Management System (QMS) for organizations involved in the design and manufacture of medical devices. A QMS certified to ISO 13485 demonstrates a commitment to consistent quality and meeting regulatory requirements [17]. Furthermore, ISO 9001 defines requirements for a general QMS, demonstrating an organization's ability to consistently provide products that meet customer and regulatory requirements [17].
European Medicines Agency (EMA) and Other Global Bodies
The EMA regulates stem cell therapies through the Advanced Therapy Medicinal Products (ATMP) regulation. While the provided search results focus on FDA and ISO, it is important to note that the EMA's requirements are equally rigorous. The European Pharmacopoeia (Ph. Eur.) provides critical guidance on raw materials, which are referred to as ancillary materials in cell therapy manufacturing [17]. Furthermore, the International Society for Stem Cell Research (ISSCR) provides influential, regularly updated guidelines for stem cell research and clinical translation. The ISSCR emphasizes fundamental principles such as integrity of the research enterprise, primacy of patient welfare, and transparency [24].
GMP Manufacturing Protocols for Clinical-Grade Stem Cells
Ancillary Material (AM) Qualification
Ancillary Materials are components, reagents, and materials used during the manufacture of a cell therapy product but not intended to be part of the final product [17]. Examples include cell isolation reagents, culture media, and cryopreservation media. The quality of AMs directly impacts the safety, efficacy, and consistency of the final cell therapy product.
Manufacturers must qualify all AMs, a process of establishing the source, identity, purity, biological safety, and general suitability for use [17]. This follows a risk-based approach, as there is no single "cell-therapy grade" universally mandated. Guidance can be found in United States Pharmacopeia (USP) Chapter <1043> and Ph. Eur. General Chapter 5.2.12 [17].
Table: Ancillary Material Qualification Framework
| Quality Attribute | Description | Common Test Methods |
|---|---|---|
| Identity | Confirmation of the material's identity | Certificate of Analysis (CoA), spectroscopic methods |
| Purity | Freedom from contaminants (e.g., endotoxins, bioburden) | LAL testing, microbial enumeration, sterility testing |
| Potency | Biological activity relevant to its function | Functional assays, growth promotion tests |
| Safety | Freedom from adventitious agents | Viral safety testing, in vitro/vivo adventitious agent tests |
Risk Management in Manufacturing
A proactive risk management process, as defined by ISO 14971, is integral to GMP compliance. The process involves risk analysis, evaluation, control, and production, and post-production monitoring [22]. Risk control options for medical devices, which can be analogously applied to manufacturing processes, include [22]:
- Inherent safety by design: e.g., using closed-system processing to reduce contamination risk.
- Protective measures: e.g., incorporating in-process safety testing and controls.
- Information for safety: e.g., providing comprehensive documentation and standard operating procedures (SOPs).
This risk-based approach is also echoed in the FDA's cGMP regulations and recent guidance, which allows for flexibility in defining "significant phases" for in-process testing, provided the determination is justified by scientific rationale [21].
Current GMP Guidelines and Advanced Manufacturing
The FDA's cGMP regulations (21 CFR Parts 210 and 211) establish the minimum standards for methods, facilities, and controls used in drug manufacturing [20]. A significant recent development is the FDA's January 2025 draft guidance on complying with 21 CFR § 211.110, which addresses in-process controls and supports the adoption of advanced manufacturing technologies [21].
Advanced manufacturing includes innovative technologies that enhance drug quality and production, such as continuous manufacturing and real-time quality monitoring using Process Analytical Technology (PAT) [21]. The guidance advises that while process models are beneficial, they should be paired with in-process testing or examination, as the FDA has not yet identified any model that can reliably adapt to all unplanned disturbances during production [21].
Experimental Protocols for Regulatory Compliance
Protocol: Qualification of a New Ancillary Material (Serum-Free Medium)
1.0 Objective To establish the safety, identity, purity, and functional performance of a new serum-free medium for use in the manufacturing of a clinical-grade mesenchymal stem cell (MSC) product.
2.0 Scope This protocol applies to all raw materials intended for use as Ancillary Materials in GMP-compliant cell therapy manufacturing.
3.0 Materials and Equipment
- Test article: Serum-free medium (SFM) batch.
- Reference standard: A previously qualified medium or a research-grade equivalent for comparison.
- Cells: Master Cell Bank of human MSCs.
- Equipment: CO2 incubator, biosafety cabinet, cell counter, flow cytometer, endotoxin testing kit, sterility test kits.
4.0 Methodology 4.1 Identity Testing: Compare the physical appearance (color, clarity) and osmolality of the test article against the manufacturer's specifications. 4.2 Purity and Safety Testing:
- Sterility Test: Inoculate the test article into fluid thioglycollate medium and soybean-casein digest medium per USP <71>.
- Mycoplasma Test: Perform a validated PCR-based or culture-based method.
- Endotoxin Test: Use a Limulus Amebocyte Lysate (LAL) assay to ensure levels are below the specified limit (e.g., <0.5 EU/mL). 4.3 Functional Performance Testing:
- Cell Growth and Proliferation: Seed MSCs at a defined density in the test SFM and a control medium. Perform cell counts and viability assessments (e.g., via Trypan Blue exclusion) over 3-5 passages. Calculate population doubling times.
- Cell Phenotype Maintenance: After expansion in the test SFM, analyze cells by flow cytometry for standard MSC surface markers (CD73, CD90, CD105) and absence of hematopoietic markers (CD34, CD45).
- Differentiation Potential: Differentiate expanded MSCs into adipocytes, osteocytes, and chondrocytes using standard differentiation kits. Assess differentiation via staining (Oil Red O, Alizarin Red, Alcian Blue, respectively).
5.0 Acceptance Criteria The test article meets all acceptance criteria if it passes sterility and mycoplasma tests, has endotoxin levels below the specified limit, supports MSC expansion with stable viability and phenotype, and maintains trilineage differentiation potential comparable to the control.
Protocol: Risk Analysis for a Cell Processing Step (Enzymatic Passaging)
1.0 Objective To perform a risk analysis for the enzymatic passaging step in MSC manufacturing to identify and control potential hazards.
2.0 Methodology (per ISO 14971)
- Risk Analysis: Identify foreseeable hazards associated with using a recombinant trypsin replacement enzyme.
- Hazard: Residual enzyme activity in the final cell product.
- Hazardous Situation: Administration of the cell product to a patient, leading to unintended tissue digestion or immune reaction.
- Risk Evaluation: Estimate the severity of harm (e.g., moderate tissue damage) and probability of occurrence. The initial risk level is deemed unacceptable and requires mitigation.
- Risk Control: Implement a risk control measure.
- Measure: Introduce a defined, validated washing step with a serum-containing medium or a specific enzyme inhibitor after cell detachment to ensure no residual enzyme activity remains.
- Verification: Perform a validated assay to detect and quantify residual enzyme activity in the final cell product to verify the effectiveness of the washing step.
3.0 Output A risk management file entry documenting the hazard, initial risk assessment, the implemented control measure, and the verification data confirming residual enzyme levels are below the acceptable limit.
The Scientist's Toolkit: Research Reagent Solutions
Navigating the regulatory requirements for ancillary materials is a critical task. The following table details key material categories and their functions in stem cell manufacturing workflows.
Table: Essential Materials for Clinical-Grade Stem Cell Manufacturing
| Material Category | Key Function | Regulatory & Quality Considerations |
|---|---|---|
| Cell Isolation Kits | To isolate specific cell types (e.g., MSCs, HSCs) from tissue or blood sources. | Components (e.g., antibodies) must be qualified. Prefer closed-system, GMP-manufactured kits to reduce contamination risk and streamline validation [17]. |
| Cell Culture Media | To support the growth, expansion, and maintenance of stem cells in vitro. | Formulation must be consistent and free of animal-derived components (xeno-free). Supplier should provide a detailed TSE/BSE statement and Certificate of Analysis [17]. |
| Cell Dissociation Reagents | To detach adherent cells from culture surfaces for passaging or harvest. | Enzymatic reagents must be tested for sterility and purity. A validated washing/inactivation step is critical to ensure no residual activity in the final product. |
| Cryopreservation Media | To preserve cell products at ultra-low temperatures for storage and transport. | Formulation should use defined, clinically acceptable cryoprotectants (e.g., DMSO). The final DMSO concentration in the product must be safe for human administration. |
| Cell Differentiation Kits | To direct stem cells toward specific lineages (e.g., cardiomyocytes, neurons). | Kit components must be qualified for clinical use. The differentiation process must be robust, reproducible, and yield a well-characterized cell population. |
Workflow and Relationship Visualizations
Regulatory Pathway for a Stem Cell Product
The following diagram outlines the key stages and major regulatory milestones in the development of a clinical-grade stem cell therapy.
Ancillary Material Qualification Workflow
This flowchart details the step-by-step process for qualifying an ancillary material for use in GMP manufacturing.
The Critical Importance of Ancillary Material (AM) Qualification and Risk Assessment
The transition of stem cell research from the laboratory to the clinic represents one of the most significant challenges in modern regenerative medicine. Within the context of Good Manufacturing Practice (GMP) for clinical-grade stem cells, ancillary materials—reagents and components used in manufacturing but not intended for inclusion in the final product—present a critical variable affecting both product safety and efficacy [17]. The qualification and risk assessment of these materials constitute a foundational element of quality assurance for Advanced Therapeutic Medicinal Products (ATMPs) [25]. Unlike traditional pharmaceuticals, cell and gene therapy products cannot undergo terminal sterilization, making the quality and safety of every input material paramount to the final product's therapeutic profile [26]. This application note details the structured framework necessary for AM qualification, providing both the regulatory context and practical protocols to ensure compliance and patient safety throughout the clinical development lifecycle.
Regulatory Framework for Ancillary Materials
Global Guidelines and Definitions
The regulatory landscape for AMs is defined by several key pharmacopeia documents and guidelines, which, while not legally binding, establish the current industry standards for quality and safety. A fundamental challenge lies in the varied terminology, where "ancillary materials" (US) and "raw materials" (EU) often refer to the same components [17] [25]. These materials include cell isolation reagents, culture and cryopreservation media, cytokines, growth factors, and disposable plasticware [17].
Globally, there is no mandated "cell therapy grade" for AMs, and claims of such are market-driven rather than reflecting an accepted regulatory standard [17]. Instead, regulators expect a risk-based qualification strategy tailored to the specific material's use and the stage of clinical development [17] [26]. The following table summarizes the core regulatory documents governing AMs.
Table 1: Key Global Regulatory Guidelines for Ancillary Materials
| Guideline | Issuing Body | Geographic Scope | Core Focus |
|---|---|---|---|
| USP <1043> "Ancillary Materials for Cell, Gene and Tissue-Engineered Products" [25] [26] | United States Pharmacopeia | Primarily US, globally influential | Risk classification system and general qualification guidance for AMs. |
| Ph. Eur. 5.2.12 "Raw Materials for the Production of Cell-Based and Gene Therapy Medicinal Products" [17] [25] | European Directorate for the Quality of Medicines & HealthCare | European Union | Stringent requirements for biological origin materials, production within a suitable QMS, and sterility. |
| IPRP Report "General Considerations for Raw Materials..." [25] | International Pharmaceutical Regulators Programme | International (including US, EU, Japan, Canada) | Quality Management Systems, supplier approval, and transparency of origin and traceability. |
| ISO 20399:2022(E) [25] | International Organization for Standardization | International | Framework outlining the roles and responsibilities of AM suppliers and users. |
The Risk-Based Approach to AM Qualification
A risk-based approach (RBA) is the cornerstone of AM management, aligning with fundamental GMP principles and regulatory guidance such as ICH Q9 [27]. This systematic process involves identifying potential hazards, assessing their impact, and implementing appropriate control measures to focus resources on areas of highest risk to product quality and patient safety [17] [27].
USP <1043> provides a widely adopted framework, categorizing AMs into a four-tiered risk classification to guide the level of qualification needed [26]. The classification is based on the material's source, complexity, and criticality to the manufacturing process [25] [26].
Table 2: USP <1043> Ancillary Material Risk Classification Tier
| Tier | Risk Level | Description | Example Materials |
|---|---|---|---|
| 1 | Lowest | Materials of high purity with a well-defined chemical structure, low risk of adventitious agents. | Inorganic salts, simple buffers [26]. |
| 2 | Low | Materials of known structure, but with potential for minor impurities; often not of human or animal origin. | Sugares, amino acids, recombinant proteins [25] [26]. |
| 3 | Moderate | Materials of unknown structure or materials of animal or human origin that have been purified. | Growth factors, cytokines, human serum albumin [25] [26]. |
| 4 | Highest | Materials of human or animal origin with minimal processing, presenting a high risk of contamination. | Serum, trypsin, primary cells [26]. |
The following workflow diagram illustrates the systematic process for risk assessment and management of AMs.
Implementing an AM Qualification Program
Material Qualification and Supplier Management
The qualification process translates risk assessment into actionable controls. The ultimate responsibility for AM qualification lies with the cell therapy manufacturer, but a close partnership with the supplier is essential for efficiency [17]. The process involves several key steps:
Supplier Qualification and Quality Agreements: Conduct thorough due diligence on potential AM suppliers. This should include, where possible, an on-site audit of the manufacturing facility to assess their Quality Management System (QMS) [26]. Establishing a robust quality agreement is critical. This agreement should mandate advanced notification of any changes to the AM, as such changes can significantly impact the manufacturing process and final product [17] [26].
Documentation and Traceability: Request and maintain comprehensive regulatory support documentation from the supplier. Essential documents include:
- Certificate of Analysis (CoA): Verifies product identity, purity, and quality against specifications.
- Certificate of Compliance (CoC): States adherence to a quality standard like GMP or ISO.
- TSE/BSE Statement: Confirms the material is free from transmissible spongiform encephalopathy agents.
- Certificate of Origin (COO): Provides traceability for materials, especially those of human or animal origin [25] [26]. For clinical phases, suppliers like ACROBiosystems offer extensive Level 2 documentation packages exceeding 1000 pages, which include detailed analytical method validation reports and Standard Operating Procedures (SOPs) [25].
Material Sourcing and Control: For critical materials, managing the supply source is vital. A single-source material requires maintaining a safety stock and a formal supply agreement to ensure continuity. If multiple sources are available, they must be evaluated and qualified early in development [26]. All materials must be stored, tracked, and labeled correctly to prevent mix-ups and ensure their quality is maintained until use.
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the appropriate grade of materials is a key decision in the translational pathway. The following table outlines common reagent categories and examples used in GMP-compliant stem cell research and manufacturing.
Table 3: Essential Reagent Solutions for Clinical-Grade Stem Cell Research
| Reagent Category | Function | GMP-Grade Example(s) |
|---|---|---|
| Basal Media | Provides essential nutrients for cell growth and maintenance. | Essential 8 [28], StemFit Basic03/Basic04 CT [29], Nutristem [28] |
| Differentiation Media | Directs pluripotent stem cells toward specific lineages. | StemFit for Differentiation [29], StemXVivo Chondrogenic Media [30] |
| Growth Factors/Cytokines | Signalling molecules that control cell fate, proliferation, and differentiation. | GMP FGF, GMP EGF (Bio-techne) [28], bFGF, Activin A [29] |
| Cell Dissociation Reagents | Enzymatic or non-enzymatic passaging of adherent cells. | StemPro Accutase [28], GMP EDTA [28] |
| Extracellular Matrices (ECM) | Provides a substrate for cell attachment and growth. | Recombinant Vitronectin (VTN-N) [28], Laminin-521 (LN521) [28] |
| Small Molecule Inhibitors | Enhances cell survival after passaging or thawing. | GMP ROCK inhibitor (Revitacell) [28] |
| Serum-Free Supplements | Chemically defined replacements for fetal bovine serum (FBS). | CTS B27, CTS N2 [28] |
Case Study: GMP-Grade Neural Progenitor Derivation
Experimental Protocol
The following protocol, adapted from a published study, demonstrates the practical application of AM qualification in deriving long-term neuroepithelial-like stem cells (lt-NES) from clinical-grade human embryonic stem cells (hESCs) under GMP-compliant conditions [28].
Objective: To robustly derive and bank lt-NES cells from multiple clinical-grade hESC lines using exclusively GMP-grade ancillary materials.
Materials:
- Cell Lines: Clinical-grade hESC lines (e.g., MasterShef series from UK Stem Cell Bank) [28].
- Culture Vessels: Aggrewell 800 plates (Stem Cell Technologies), standard cell culture-treated plates [28].
- Key GMP-Grade Reagents: Refer to Table 3 in Section 3.2 for specific examples used in this workflow.
Methodology:
hESC Pre-Culture: Maintain hESCs on recombinant VTN-N Vitronectin in GMP Essential 8 medium. Passage using GMP EDTA, ensuring colonies are detached as small clumps [28].
Embryoid Body (EB) Formation:
- Dissociate undifferentiated hESCs to single cells using StemPro Accutase.
- Resuspend 3 x 10^6 cells in 1.5 mL of Essential 6 medium supplemented with Revitacell.
- Transfer the cell suspension to one well of an Aggrewell 800 plate pre-treated with E6 + Revitacell. Centrifuge at 2000×g to aggregate cells.
- After 24 hours, carefully replace the medium entirely with fresh E6. Perform a 50% medium change daily from day 2 to day 4 [28].
Neural Induction and Rosette Selection:
- On day 5, detach EBs from the Aggrewell plate and collect them using a reversible strainer.
- Plate EBs onto a culture dish coated with GMP-grade Laminin 521 (10 µg/mL in DPBS+/+).
- Culture in GMP N2 media (CTS DMEM-F12 + CTS N2 + CTS B27 + Glutamax), changing the media daily for 3-5 days to induce neural differentiation.
- Once neural rosettes appear, select them using the STEMdiff Neural Rosette Selection Reagent for 45-60 minutes at 37°C. Gently detach and collect the purified rosette clusters [28].
lt-NES Establishment and Expansion:
- Centrifuge the collected rosettes and resuspend in N2 media supplemented with 10 ng/mL each of GMP FGF and GMP EGF (N2 EF media) plus Revitacell.
- Plate at high density onto Laminin 521-coated plates (e.g., one well of a 48-well plate). Critical Step: High cell density is required for survival and proliferation.
- Feed daily with GMP N2 EF media. Once confluent, passage using accutase for 1 minute at 37°C, and continue expanding with a split ratio of approximately 1:1 [28].
The following workflow diagram summarizes this GMP-grade differentiation protocol.
Outcome and Analysis
This GMP-adapted protocol successfully demonstrated the robust and reproducible derivation of lt-NES from several clinical-grade hESC lines [28]. The resulting lt-NES cells were multipotent, bankable, and karyotypically stable, retaining the capacity for high neurogenic potential and differentiation into various neuronal subtypes [28]. This case highlights the feasibility of translating research protocols to GMP-compliant processes by systematically replacing research-grade reagents with qualified GMP-grade AMs, thereby creating a flexible tool to speed up translation to clinic for neurological therapies.
The path from research to clinically applicable stem cell therapies is paved with rigorous quality control, at the heart of which lies the meticulous qualification and risk assessment of ancillary materials. A successful strategy is not defined by simply selecting "GMP-grade" labels but by implementing a holistic, risk-based program that encompasses thorough supplier qualification, comprehensive documentation, and stringent material control. As the regulatory landscape evolves, the principles outlined in this document—alignment with global pharmacopeia standards, proactive risk management, and robust supplier partnerships—provide a sustainable framework for ensuring the safety, quality, and efficacy of revolutionary stem cell-based medicines.
In the field of clinical-grade stem cell research, the controlled environment is as critical as the biological protocol itself. Current Good Manufacturing Practice (cGMP) cleanrooms provide the foundational infrastructure necessary to ensure that advanced therapeutic medicinal products (ATMPs) are manufactured with the highest standards of safety, quality, and efficacy. These specialized environments are designed to maintain extremely low levels of airborne particles and microbial contamination, thereby protecting sensitive cell cultures from pollutants that could compromise their integrity [31]. For stem cell therapies, where the product is often both the treatment and the drug, the cleanroom facility becomes an extension of the manufacturing process, directly influencing the critical quality attributes of the final cellular product.
The transition from research-grade to clinically-applicable stem cell products necessitates adherence to cGMP standards, which differ from basic Good Manufacturing Practices (GMP) through their emphasis on employing current, state-of-the-art technologies and systems [32]. Regulatory bodies including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) mandate cGMP compliance for stem cell products intended for human administration, with facilities subject to rigorous inspection and validation requirements [33]. This application note details the essential facility requirements, design principles, and validation protocols for establishing cGMP-compliant cleanrooms specifically tailored to the unique demands of clinical-grade stem cell research and manufacturing.
Core Principles of cGMP Cleanroom Design
Classification and Zoning
cGMP cleanrooms operate on a zoning principle that establishes progressively cleaner environments from peripheral areas to critical processing zones. This graded approach to contamination control is fundamental to protecting stem cell products during their most vulnerable processing stages.
- Grade Definitions: Cleanrooms are classified into grades A-D according to EU GMP guidelines, corresponding to ISO 14644 classes 5-8 [34]. Grade A (ISO 5) represents the highest cleanliness level for high-risk operations like open-container processing and aseptic filling, while Grades B-D provide background environments with decreasing stringency [34].
- Activity-Specific Zoning: Stem cell manufacturing processes must be mapped to appropriate cleanroom classifications. Hematopoietic stem cell gene therapy requires aseptic processing in Grade A environments [35], while the derivation and expansion of neural progenitor cells may be conducted in Grade B or C backgrounds [28].
- Dynamic Classifications: cGMP guidelines recognize two distinct operational states: "at rest" (unoccupied but operational) and "in operation" (occupied with processes underway) [36]. This distinction acknowledges that personnel presence and activities inevitably impact environmental conditions.
Table 1: cGMP Cleanroom Classifications and Applications in Stem Cell Research
| EU GMP Grade | ISO Classification | Maximum Particles/m³ ≥0.5μm | Typical Applications in Stem Cell Research |
|---|---|---|---|
| A | ISO 5 | 3,520 [33] | Aseptic filling, open vial operations, critical open processes |
| B | ISO 6-7 | 35,200-352,000 [33] | Background environment for Grade A operations, cell processing |
| C | ISO 7 | 352,000 [33] | Component preparation, buffer and media preparation |
| D | ISO 8 | 3,520,000 [33] | Support areas, washing and staging areas, gowning rooms |
Pressure Cascade and Airflow Control
A fundamental principle in cGMP cleanroom design is the establishment of pressure differentials that create a directional airflow from cleaner to less clean areas, preventing the ingress of contaminants.
- Pressure Differential Model: Cleaner zones maintain higher pressure than adjacent less-clean areas, with typical differentials of 10–15 Pa between adjacent rooms [34]. This pressure cascade ensures air flows from critical processing areas toward support spaces, carrying potential contaminants away from product exposure sites.
- Airflow Patterns: Unidirectional airflow (UDAF), formerly known as laminar airflow, provides a consistent, parallel stream of HEPA-filtered air across critical zones, sweeping contaminants away from the product and processing area [34]. Non-unidirectional (turbulent) airflow is acceptable in less critical areas where product is not directly exposed.
- Air Change Rates: Proper air change rates are essential for maintaining cleanliness classifications, with higher grades requiring more frequent air changes. Grade A/B areas typically require significantly higher air change rates than Grade C/D areas, though specific rates should be determined through risk assessment and validation studies [34].
Table 2: Pressure Differential and Airflow Requirements
| Parameter | Grade A | Grade B | Grade C | Grade D |
|---|---|---|---|---|
| Min. Pressure Differential | 10-15 Pa relative to background [34] | 10-15 Pa relative to adjacent less clean areas [34] | 10-15 Pa relative to adjacent less clean areas [34] | Positive pressure relative to corridor [34] |
| Airflow Pattern | Unidirectional [34] | Non-unidirectional or mixed [34] | Non-unidirectional [34] | Non-unidirectional [34] |
| Air Change Rate (typical) | N/A (LAF device) | Significantly higher than lower grades [34] | Moderate [34] | Lower [34] |
Material and Personnel Flow
Controlling the movement of people, materials, and equipment is essential for maintaining cleanroom integrity and preventing cross-contamination.
- Unidirectional Flow: cGMP cleanrooms must adhere to unidirectional flow principles, where people, raw materials, and equipment move sequentially from "less clean" to "more clean" zones [34]. There should be no crossover or backtracking that could compromise cleaner areas.
- Segregated Pathways: Separate entry airlocks for people and materials enhance contamination control [34]. Dedicated gowning rooms should include step-over benches to facilitate proper attire donning while minimizing particle transfer [34].
- Process Flow Design: The facility layout should logically sequence operations from material receipt through to final product packaging, minimizing the need for intermediate material storage or backtracking. High-risk processes should be geographically separated from potentially contaminating activities [34].
Facility Design Specifications
Architectural Finishes and Materials
cGMP regulations mandate specific material requirements for cleanroom surfaces to enable effective cleaning and disinfection while minimizing particle generation.
- Wall Systems: Surfaces must be smooth, waterproof, easy-to-clean, and rigid to minimize contamination risk [36]. Preferred materials include fiber-reinforced plastic (FRP), uPVC, and high-quality stainless steel, all of which offer chemical resistance to harsh disinfectants [32].
- Flooring: Heat-welded vinyl with integral coved bases is standard, providing a seamless, smooth surface that prevents microbial buildup [32]. Static-dissipative options are available for environments where electrostatic discharge could damage sensitive equipment or affect processes [37].
- Ceilings: Cleanroom-rated ceiling systems should feature coved junctions with walls and flush-mounted lighting to eliminate corners where dust could collect [32]. The entire assembly must be airtight and compatible with regular decontamination procedures.
- Door Design: Doors must be seamless, easily cleanable, and resistant to cleaning agents [36]. Sliding doors are discouraged due to their inherent gaps and recesses that challenge effective cleaning [36]. Interlocking door systems prevent the simultaneous opening of adjacent spaces, maintaining pressure differentials [32].
Table 3: Surface Material Requirements for cGMP Cleanrooms
| Surface Type | Material Options | Key Properties | Maintenance Considerations |
|---|---|---|---|
| Walls | FRP, uPVC, Powder-coated steel, Stainless steel [32] | Smooth, non-shedding, chemical resistant [32] | Compatible with sporicidal agents, resistant to abrasion |
| Floors | Heat-welded vinyl, Static-dissipative vinyl, Epoxy [32] | Seamless, covable, chemical resistant [32] | Withstand frequent cleaning, non-slip surface |
| Ceilings | Cleanroom-rated grid systems with gasketed panels | Flush-mounted, airtight, cove corners [32] | Integrated lighting, accessible for maintenance |
| Doors | Interlocking, seamless [37] | Easy to clean, no recesses [36] | Interlock systems to maintain pressure [32] |
HVAC and Filtration Systems
The heating, ventilation, and air conditioning (HVAC) system forms the engineering core of any cGMP cleanroom, responsible for maintaining all critical environmental parameters.
- Air Filtration: HEPA filters are standard for cGMP cleanrooms, providing 99.97% efficiency in removing particles ≥0.3 micrometers [38]. For the most critical applications, ultra-low particulate air (ULPA) filters may be employed for even higher efficiency. Filter integrity testing is essential, with penetration not exceeding 0.03% [38].
- Air Handling Units: These systems must deliver filtered air at precise temperatures, humidity levels, and velocities while maintaining specified pressure differentials [36]. Redundant systems or backup power supplies are often necessary for critical environments to ensure uninterrupted operation.
- Monitoring and Control: Automated building management systems continuously monitor and log environmental parameters including temperature, humidity, and pressure differentials [32]. These systems typically incorporate audible and visual alarms to promptly alert staff to deviations from established parameters.
Monitoring and Control Systems
Comprehensive monitoring provides the data necessary to demonstrate continuous compliance with cGMP standards.
- Particle Monitoring: Continuous particle counting is required in Grade B and Grade A environments [37]. Laser particle counters measure both viable and non-viable particulates at specified locations and frequencies, with data logged for regulatory review.
- Environmental Parameters: Temperature and humidity must be continuously monitored and maintained within validated ranges appropriate for the specific stem cell processes being conducted [36].
- Microbial Monitoring: Active air sampling and surface monitoring detect viable organisms, with settle plates used to assess airborne microbial contamination over time [36]. Personnel monitoring through contact plates assesses gowning effectiveness.
Cleanroom Qualification Protocol
The qualification of cGMP cleanrooms follows a rigorous lifecycle approach encompassing multiple stages of verification and validation. This systematic process ensures the facility consistently operates according to design specifications and regulatory requirements.
Qualification Stages
User Requirements Specification (URS): This foundational document analyzes the need for the cleanroom and justifies its implementation, identifying contamination risks to products, processes, and people [36]. The URS includes statutory requirements, business considerations, and anticipated future needs.
Design Qualification (DQ): Verifies that the proposed cleanroom design is fit for its intended purpose through conceptual, basic, and detailed design stages [36]. DQ bridges the URS and construction phases, ensuring the design will meet all specified requirements before procurement and building commence.
Factory Acceptance Testing (FAT)/Site Acceptance Testing (SAT): FAT ensures equipment meets specifications before shipment, while SAT confirms installation complies with the design and operates as expected [36]. These tests verify installation completeness and performance parameters, including classification testing in accordance with ISO 14644-1 [36].
Installation Qualification (IQ): Documents that the cleanroom has been built and installed according to approved specifications and drawings [36]. IQ includes verification of as-built conditions, HVAC calibration, HEPA filter integrity test data review, critical equipment calibration status, and initial microbial contamination measurements [36].
Operational Qualification (OQ): Demonstrates that the fully functional cleanroom operates within specified parameters under "at-rest" conditions [36]. OQ testing includes:
- Airflow velocity and volume measurements
- Air pressure difference tests
- Filter integrity testing (DOP testing)
- Airflow visualization studies (smoke tests)
- Recovery testing
- Temperature and humidity uniformity mapping
- Lighting level verification
- Noise and vibration level checks
Performance Qualification (PQ): Confirms that the cleanroom consistently maintains required operational performance under "in-operation" conditions with typical personnel presence and manufacturing processes [36]. PQ involves:
- Cleanroom classification at in-operation state
- Determination of microbial contamination levels during simulated operations
- Verification of clean-up times and recovery rates
- Testing of worst-case operational scenarios
- Demonstration of operational robustness over a sustained period
Experimental Protocol: Cleanroom Recovery Test
Purpose: To determine the time required for a cleanroom to recover from a simulated particle generation event and return to its specified cleanliness classification.
Principle: Introducing an artificial aerosol challenge to the cleanroom and measuring the time required for particle counts to reduce to specified limits after the aerosol generation ceases.
Materials:
- Aerosol generator (capable of producing polydisperse particles)
- Laser particle counter(s) with data logging capability
- Environmental monitoring system
- Stopwatch or automated timer
Procedure:
- Ensure cleanroom is operational under standard conditions with HVAC system functioning normally.
- Place particle counter in location representative of critical zones.
- Generate aerosol challenge until particle counts exceed classification limit by at least 10-fold.
- Simultaneously cease aerosol generation and start timing.
- Record particle counts at predetermined intervals (e.g., every 30 seconds).
- Continue monitoring until particle counts have returned to the baseline levels specified for the cleanroom classification.
- Repeat test in multiple locations for comprehensive assessment.
Acceptance Criteria: The cleanroom must recover to specified cleanliness levels within the validated time frame, typically demonstrating a 100:1 reduction in particle counts within several minutes for higher classification areas.
Stem Cell Research Application
Facility Adaptation for Stem Cell Processing
Stem cell research and manufacturing present unique challenges that require specific adaptations to standard cGMP cleanroom designs.
- Closed System Processing: Whenever possible, stem cell processing should employ closed systems that minimize product exposure to the immediate environment. When processing occurs in closed systems with aseptic validation, it may be performed in ISO-7 (Class 10,000) environments rather than the more stringent ISO-5 (Class 100) required for open manipulations [33].
- Incubation Facilities: Cell culture incubators represent potential contamination sources and should be located in Grade C environments at minimum. Their placement must allow for adequate airflow around the equipment while maintaining accessibility for monitoring and maintenance.
- Cryopreservation Areas: Facilities must include appropriate space for controlled-rate freezing and secure storage of cryopreserved cell products. Liquid nitrogen storage presents asphyxiation risks that must be addressed through proper room ventilation and oxygen monitoring.
- Material Flow for Cell Culture: The pathway for media, supplements, and culture vessels must maintain sterility from preparation through to final use. Dedicated pass-through autoclaves and vaporized hydrogen peroxide (VHP) chambers can facilitate material transfer between classified areas.
Case Study: GMP-Grade Neural Progenitor Cell Derivation
The implementation of a GMP-compliant protocol for deriving long-term neuroepithelial stem cell progenitors (lt-NES) from clinical-grade human embryonic stem cells demonstrates the practical application of cGMP cleanroom principles [28].
Process Overview:
- Undifferentiated hESCs are dissociated into single cells using StemPro Accutase in a Grade B background environment with Grade A biological safety cabinet.
- Cells are suspended in GMP Essential 6 medium and transferred to Aggrewell plates for embryoid body formation.
- After 5 days, embryoid bodies are plated onto GMP-grade recombinant Laminin 521-coated vessels in Grade C environment.
- Neural induction proceeds for 3-5 days with daily media changes using GMP N2 media formulations.
- Neural rosettes are selected using STEMdiff Neural Rosette Selection Reagent.
- Selected rosettes are expanded in N2 media supplemented with GMP-grade FGF and EGF to establish lt-NES cultures.
Critical Facility Considerations:
- All reagents must be GMP-grade, including recombinant enzymes, growth factors, and matrix components [28].
- Cell processing between open and closed systems determines the required cleanroom classification for each step [33].
- Environmental monitoring must demonstrate consistent control throughout the extended culture period, which may span several weeks.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: GMP-Grade Reagents for Clinical-Grade Stem Cell Research
| Reagent Category | Specific Examples | Function | GMP-Grade Source Examples |
|---|---|---|---|
| Basal Media | Essential 8, Essential 6, X-VIVO-15 [28] | Support growth and maintenance of stem cells | Thermo Fisher Scientific CTS [28] |
| Growth Factors | FGF, EGF, SCF, TPO, Flt3-L [35] [28] | Direct stem cell proliferation and differentiation | Bio-Techne GMP-grade [28] |
| Dissociation Agents | StemPro Accutase, GMP EDTA [28] | Cell passaging and single-cell suspension | Thermo Fisher Scientific GMP-grade [28] |
| Extracellular Matrices | Recombinant Laminin 521, Vitronectin [28] | Provide substrate for cell attachment and signaling | Biolamina, Thermo Fisher Scientific CTS [28] |
| Supplements | N2, B27, Revitacell [28] | Enhance cell survival and differentiation | Thermo Fisher Scientific CTS [28] |
| Cell Culture Supplements | LentiBOOST, protamine sulfate [35] | Enhance transduction efficiency in gene therapy | Commercial GMP-grade sources [35] |
The design and implementation of cGMP-compliant cleanrooms for clinical-grade stem cell research requires meticulous attention to architectural finishes, HVAC systems, monitoring capabilities, and qualification protocols. By adhering to the principles and practices outlined in this application note, researchers and manufacturers can create controlled environments that protect the integrity of stem cell products throughout their manufacturing lifecycle. The facility itself becomes an essential tool in ensuring the safety, purity, and efficacy of advanced stem cell therapies, ultimately supporting their successful translation from research concepts to clinically impactful treatments for patients.
From Donor to Dose: A Step-by-Step GMP Manufacturing Workflow
Within the framework of Good Manufacturing Practice (GMP) for clinical-grade stem cells, the initial steps of donor selection and tissue acquisition are critical. These foundational processes determine the safety, quality, and ultimate efficacy of the final cell-based medicinal product. This document outlines standardized, ethically grounded protocols for the sourcing and collection of starting materials, specifically addressing mesenchymal stem cells (MSCs) from the infrapatellar fat pad and hematopoietic stem cells (HSCs) for allogeneic transplantation and gene therapy. Adherence to these protocols ensures compliance with regulatory standards and lays the groundwork for successful translational research [39] [7].
Ethical Donor Selection
Ethical donor selection balances the clinical needs of the recipient with the safety and autonomy of the donor, with particular care required when the donor is a minor.
Clinical and Ethical Considerations for Allogeneic HSC Donors
For allogeneic Hematopoietic Stem Cell Transplantation (allo-HSCT), stem cells may be obtained from mobilized peripheral blood, bone marrow, or umbilical cord blood [40]. The selection process must prioritize the safety of both donor and recipient.
Key Ethical Principles:
- Informed Consent: Donors must receive accurate information regarding potential adverse events and the health burden of donation [40] [41].
- Risk-Benefit Analysis: Donation should be excluded when excessive risks to the donor are foreseeable, and the recipient's risks must be outweighed by the expected benefits [40].
- Management of Conflict of Interest: A distinct living donor advocacy team is recommended, especially for minor donors, to ensure the decision is free of coercion and that the donor's interests are protected [41]. This is crucial as parental authority in such cases involves a natural conflict of interest between the well-being of the sick child and the healthy donor child [41].
Donor Eligibility Determination: This is based on review of medical records, a physical exam, and clinical laboratory testing for Relevant Communicable Disease Agents and Diseases (RCDADs). Required tests typically include screening for HIV, Hepatitis B & C, HTLV, Treponema pallidum, and others as per regulations (FDA 21 CFR 1271) [7].
Sourcing of MSC Donor Tissue
MSCs can be isolated from various tissues, with the infrapatellar fat pad (IFP) representing a less invasive source compared to bone marrow. IFP tissue is often available as surgical waste from procedures like anterior cruciate ligament (ACL) reconstruction, reducing patient morbidity [39] [6].
Protocol Approvals and Informed Consent:
- The collection protocol must be approved by an institutional research ethics review committee [39] [6].
- Written informed consent must be obtained from patients after screening against defined inclusion and exclusion criteria [39] [6].
Table 1: Example Donor Demographics for Infrapatellar Fat Pad Sourcing
| Sample ID | Age | Sex | Body Mass Index |
|---|---|---|---|
| FPMSC-8 | 22 | M | 26.0 |
| FPMSC-11 | 24 | M | 20.5 |
| FPMSC-13 | 20 | F | 38.3 |
Source: Adapted from [6]
Tissue Acquisition and Initial Processing Workflows
The acquisition process varies by tissue source but must consistently adhere to aseptic techniques and Good Tissue Practices (GTP).
Umbilical Cord Blood for iPSC Generation
Cord blood is a common starting material for generating clinical-grade induced pluripotent stem cell (iPSC) banks [7]. The acquisition workflow involves multiple critical checkpoints to ensure GMP compliance.
Key Steps:
- Informed Consent: Must cover the intended use of donated tissue, benefits, risks, confidentiality, and voluntary participation, and must be approved by an Institutional Review Board (IRB) [7].
- Tissue Recovery: Performed by trained specialists in a hospital setting using aseptic techniques compliant with GTP [7].
- Shipping and Receiving: The cord blood unit is packaged and shipped to the manufacturing facility using validated procedures. Upon receipt, the tissue is stored appropriately and transferred to a designated cell therapy area [7].
- Quarantine and Release: The initial manufacturing steps are performed under quarantine until donor screening and testing results are received, reviewed by a qualified person (e.g., a medical director) and the Quality Assurance (QA) group, and the tissue is formally released [7].
Infrapatellar Fat Pad (IFP) Processing for MSC Isolation
The protocol for isolating MSCs from IFP tissue involves mechanical and enzymatic processing to derive a primary cell population.
- Tissue Harvesting: IFP tissue (10-20 g) is acquired using an arthroscopic shaver and sterile collection chamber during ACL reconstructive surgery.
- Mechanical Processing: The tissue is cut into approximately 1 mm³ pieces.
- Enzymatic Digestion: The minced tissue is digested with 0.1% collagenase in serum-free media for 2 hours at 37°C.
- Cell Separation: The digested tissue is centrifuged at 300 ×g for 10 minutes. The supernatant is removed, and the cell pellet is washed with PBS and filtered through a 100 μm filter.
- Primary Culture: The filtered cells are centrifuged again, and the resulting pellet is resuspended in standard MSC media (e.g., MEM α supplemented with 10% FBS and gentamicin) for initial culture.
- Cryopreservation: Cells are typically cryopreserved at the end of the first passage using a cryoprotectant like DMSO.
Experimental Protocols for GMP-Compliant Cell Expansion and Characterization
GMP-Compliant Expansion of MSCs
Transitioning from research-grade to clinical-grade MSCs requires the use of defined, animal component-free media to eliminate risks of contamination and immunogenicity [39] [6].
Subculture Protocol:
- Thawing: Cryopreserved FPMSCs are thawed and seeded in standard or animal component-free media.
- Passaging: Cells are passaged at 80-90% confluency and seeded at a density of 5 × 10³ cells/cm².
- Media Comparison: The performance of different GMP-compliant media (e.g., MesenCult-ACF Plus Medium vs. MSC-Brew GMP Medium) should be evaluated against standard MSC media [39] [6].
Quantitative Assessment of Cell Proliferation and Potency:
- Cell Doubling Time: Calculated over multiple passages using the formula:
Doubling Time = (duration * ln(2)) / ln(final concentration / initial concentration)[39] [6]. Cells are counted at each passage using a hemacytometer. - Colony Forming Unit (CFU) Assay: To assess clonogenic potential (potency). Cells are seeded at low densities (e.g., 20, 50, 100, and 500 cells per dish) and grown for 10 days. Colonies are then fixed with formalin, stained with Crystal Violet, and imaged for counting [39] [6].
Table 2: Quantitative Results from GMP Media Comparison on FPMSCs
| Assessment Metric | Standard MSC Media | MesenCult-ACF Plus | MSC-Brew GMP Medium |
|---|---|---|---|
| Doubling Time | Higher | Intermediate | Lower (indicating enhanced proliferation) |
| Colony Formation | Standard | Intermediate | Higher (indicating enhanced potency) |
| Post-Thaw Viability | >70% (minimum requirement) | >95% | >95% (maintained for up to 180 days) |
| Sterility | Compliant | Compliant | Compliant |
| Marker Expression | Maintained | Maintained | Maintained |
Source: Summarized from [39] [6]
Quality Control and Release Criteria
A comprehensive QC strategy is essential for product release. The following assays were validated for GMP-FPMSCs derived from multiple donors [39] [6]:
- Viability: Assessed using Trypan Blue exclusion, with results >95% (>70% required for release).
- Sterility: Tested using the Bact/Alert system.
- Purity and Identity:
- Stability: Post-thaw viability and sterility are checked after extended storage (e.g., up to 180 days) to determine shelf-life.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials used in the featured GMP-compliant experiments for MSC expansion.
Table 3: Essential Reagents for GMP-Compliant MSC Culture
| Reagent / Material | Function / Application | Example Product (Supplier) |
|---|---|---|
| Animal Component-Free Media | Defined culture medium eliminating risks of animal-derived contaminants; essential for clinical-grade cell expansion. | MSC-Brew GMP Medium (Miltenyi Biotec) [39] [6] |
| Defined Culture Supplements | Serum-free supplements providing growth factors and nutrients for consistent cell growth. | MesenCult-ACF Plus Medium (StemCell Technologies) [39] [6] |
| Cell Dissociation Reagents | Enzymatic passaging of adherent cells; non-animal origin versions are required for GMP. | Not specified in results, but TrypLE or similar is typical. |
| Characterization Kits | Standardized antibody panels for confirming MSC identity and purity via flow cytometry. | BD Stemflow Human MSC Analysis Kit (BD Biosciences) [39] [6] |
| Cryopreservation Medium | Protects cell viability during freeze-thaw cycles; typically contains DMSO and a protein base. | Not specified in results, but commercial GMP-grade DMSO solutions are available. |
The translation of stem cell research from the laboratory to the clinic necessitates the implementation of Good Manufacturing Practice (GMP) standards throughout the entire cell manufacturing process. Isolation, as the first critical step, significantly influences the safety, purity, potency, and overall quality of the final cell-based therapeutic product. GMP-compliant isolation techniques are designed to minimize variability, exclude animal-derived components, and ensure sterility, thereby reducing risks of contamination and immunogenicity. This document details the core enzymatic and non-enzymatic methodologies, providing standardized protocols and data-driven comparisons for researchers developing clinical-grade stem cell manufacturing pipelines.
The choice between enzymatic and non-enzymatic isolation is fundamental, impacting cell yield, viability, phenotype, and regulatory compliance. The table below summarizes the key characteristics of these approaches.
Table 1: Comparison of GMP-Compliant Enzymatic and Non-Enzymatic Isolation Techniques
| Feature | Enzymatic Isolation | Non-Enzymatic Isolation |
|---|---|---|
| Basic Principle | Uses enzymes (e.g., collagenase) to digest the extracellular matrix and release cells [42]. | Relies on mechanical forces (mincing, agitation) and/or cell migration from tissue explants [43] [44]. |
| Primary Output | Stromal Vascular Fraction (SVF) or a suspension of individual cells [42]. | Tissue fragments for explant culture or mechanically derived tissue SVF (tSVF) [45]. |
| Typical Cell Yield | Generally higher initial cell yield [42]. | Lower initial cell yield, reliant on subsequent outgrowth [43]. |
| Cell Viability | Can be lower if enzymatic digestion is overly aggressive; requires optimization [43]. | Typically high, as it avoids exposure to harsh enzymes [43]. |
| Process Duration | Shorter, single-process step (hours) [46]. | Longer, requires cell outgrowth over days to weeks [43]. |
| Key Advantages | High yield, scalability, defined process duration. | Simpler, lower cost, avoids enzymatic reagent variability and potential residue. |
| Key Challenges | Risk of enzyme-induced cell damage/surface marker alteration; requires GMP-grade enzymes and rigorous validation; higher cost [42] [43]. | Lower and less consistent yield; potential for selective cell population expansion; longer process. |
| GMP Compliance Focus | Sourcing GMP-grade enzymes; validating digestion parameters (concentration, time); demonstrating removal of enzyme residues [43]. | Ensuring aseptic tissue processing; standardizing explant size and culture initiation; validating mechanical dissociation parameters [45]. |
The following workflow diagram illustrates the decision-making process and fundamental steps for selecting and implementing a GMP-compliant isolation technique.
Detailed Experimental Protocols
Protocol 1: Enzymatic Isolation of Infrapatellar Fat Pad-Derived MSCs (FPMSCs)
This protocol, adapted from a 2025 study, details the GMP-compliant enzymatic isolation of MSCs from the infrapatellar fat pad, a less invasive and clinically promising tissue source [46] [39] [6].
Materials and Reagents
- Tissue Source: Human infrapatellar fat pad (IFP) tissue (10-20 g), obtained as surgical waste during anterior cruciate ligament reconstructive surgery with informed consent [39] [6].
- Digestion Enzyme: GMP-grade Collagenase (Type not specified in protocol) [39] [6].
- Basal Medium: MEM α [39] [6].
- Process Aids: Phosphate-Buffered Saline (PBS), 100 µm cell strainer.
- GMP-Compliant Culture Medium: MSC-Brew GMP Medium (Miltenyi Biotec) was identified as optimal for proliferation and potency [46].
Step-by-Step Procedure
- Tissue Pre-processing: Aseptically mince the IFP tissue into fragments of approximately 1 mm³ using surgical scalpels [39] [6].
- Enzymatic Digestion: Transfer the tissue fragments into a digestion solution containing 0.1% collagenase in serum-free media. Incubate for 2 hours at 37°C with continuous agitation [39] [6].
- Reaction Termination & Filtration: Add complete medium to neutralize the enzyme. Pass the resulting cell suspension through a 100 µm cell strainer to remove undigested tissue debris [39] [6].
- Cell Pellet Collection: Centrifuge the filtrate at 300 × g for 10 minutes. Carefully decant the supernatant, which contains adipocytes and digestion solution [39] [6].
- Cell Washing: Resuspend the cell pellet in PBS and centrifuge again at 300 × g for 10 minutes [39] [6].
- Primary Culture: Resuspend the final cell pellet (the Stromal Vascular Fraction, SVF) in MSC-Brew GMP Medium and seed into appropriate culture vessels [46] [39] [6].
- Cryopreservation (Optional): At the end of the first passage, cells can be cryopreserved using a controlled-rate freezer in a cryopreservation solution, such as one containing 10% DMSO, to create a Master Cell Bank [39] [6].
Protocol 2: Enzymatic Isolation of Wharton's Jelly-derived MSCs (WJ-MSCs)
This protocol provides optimized parameters for the enzymatic isolation of WJ-MSCs from umbilical cord tissue, a source known for its high proliferation potential and low immunogenicity [43].
Materials and Reagents
- Tissue Source: Human umbilical cord tissue (>20 cm length), collected post-cesarean section with informed consent and transported at 2-10°C within 24 hours [43].
- Digestion Enzyme: GMP-grade Collagenase NB6 (Nordmark Biochemicals) [43].
- GMP-Compliant Culture Medium: NutriStem (Biological Industries) supplemented with 2% or 5% human platelet lysate (hPL) showed similar efficacy for cell expansion [43].
Step-by-Step Procedure
- Tissue Pre-processing: Decontaminate the umbilical cord with 0.5% povidone-iodine solution. Dissect to expose and remove blood vessels, then mince the Wharton's jelly into 1-4 mm³ fragments [43].
- Optimized Enzymatic Digestion: Digest the tissue fragments with 0.4 PZ U/mL Collagenase NB6 for 3 hours at 37°C [43].
- Cell Collection: Neutralize the enzyme with complete medium and collect the cell suspension via centrifugation.
- Primary Culture: Seed the digested cells at an optimal density. The study noted a positive correlation between the weight of umbilical cord tissue used and the yield of P0 WJ-MSCs [43].
- Culture Observation: WJ-MSCs isolated via this enzymatic method demonstrated faster initial outgrowth compared to the explant method [43].
Protocol 3: Non-Enzymatic (Explant) Isolation of Mucosal Cells
This protocol demonstrates a GMP-compliant, animal-component-free method for isolating epithelial cells and fibroblasts from buccal mucosa biopsies, utilizing a physical (non-enzymatic) explant approach and automated dissociation [44].
Materials and Reagents
- Tissue Source: Human buccal mucosa pinch biopsies.
- Dissociation Solution: TrypLE (a non-animal recombinant enzyme preparation suitable for GMP) [44].
- Serum Substitute: Pooled Human Platelet Lysate (HPL), available as a GMP-compliant product [44].
- Culture Medium: DMEM supplemented with HPL.
- Specialized Equipment: Octodissociator (for standardized mechanical dissociation) [44].
Step-by-Step Procedure
- Tissue Separation: Incubate the biopsy in neutral protease for ~16 hours at 4°C to separate the epithelial sheet from the underlying lamina propria [44].
- Fibroblast Isolation (from Lamina Propria):
- Mechanically dissociate the lamina propria using the Octodissociator with a standardized program (e.g., "hskin1")
- Seed the resulting cell suspension in DMEM with HPL on fibronectin-coated plates to enhance initial adhesion [44].
- Epithelial Cell Isolation (from Epithelial Sheet):
- Cryopreserve the separated epithelial sheet to allow for the concurrent development of a feeder layer.
- Thaw and digest the sheet using TrypLE, with dissociation assisted by the Octodissociator (program "37TDK1") [44].
- Co-culture Setup: Culture the digested epithelial cells on a feeder layer of growth-arrested autologous buccal fibroblasts (arrested with 10 µM Mitomycin C for 2 hours) in medium containing 5% HPL and 5 µM Y-27632 (ROCK inhibitor), which significantly improved cell viability and growth [44].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues critical reagents and their functions for establishing GMP-compliant isolation processes.
Table 2: Essential Reagents for GMP-Compliant Cell Isolation
| Reagent / Solution | Function in Isolation Process | GMP-Compliant Example |
|---|---|---|
| Collagenase NB6 | GMP-grade enzyme for digesting collagen in extracellular matrix to release cells from tissues like umbilical cord [43]. | Collagenase NB6 GMP (Nordmark Biochemicals) [43]. |
| MSC-Brew GMP Medium | A serum-free, xeno-free medium formulated for the expansion and culture of MSCs under GMP conditions [46] [47]. | MSC-Brew GMP Medium (Miltenyi Biotec) [46]. |
| Human Platelet Lysate (HPL) | A source of growth factors and cytokines used as a serum replacement in culture media to support cell growth and avoid animal derivatives [44]. | GMP-compliant pooled HPL from qualified vendors [44]. |
| TrypLE Select | A recombinant, non-animal derived enzyme solution used to dissociate adherent cells, serving as a GMP-compliant alternative to trypsin [44]. | TrypLE Select (Gibco) [44]. |
Critical process parameters and their optimized values from the cited studies are summarized below for direct comparison and protocol design.
Table 3: Summary of Optimized Isolation Parameters from Recent studies
| Tissue Source | Isolation Method | Key Optimized Parameters | Outcome Metrics |
|---|---|---|---|
| Wharton's Jelly [43] | Enzymatic | Enzyme: 0.4 PZ U/mL Collagenase NB6Time: 3 hoursCulture Medium: NutriStem + 2-5% hPL | Higher yield of P0 WJ-MSCs; faster outgrowth than explant method. |
| Infrapatellar Fat Pad [39] [6] | Enzymatic | Enzyme: 0.1% CollagenaseTime: 2 hoursCulture Medium: MSC-Brew GMP Medium | Enhanced proliferation & colony formation; >95% post-thaw viability. |
| Buccal Mucosa [44] | Explant / Non-Enzymatic | Dissociation: OctodissociatorCulture Additive: 5% HPL + 5µM Y-27632Feeder Layer: Autologous fibroblasts | High viability (96%); achieved sufficient cell numbers for tissue engineering. |
The following diagram synthesizes the key steps and quality control checkpoints for a generalized GMP-compliant enzymatic isolation workflow, from tissue acquisition to the final cell product.
The transition to xeno-free, chemically defined media is a critical step in developing robust Good Manufacturing Practice (GMP) protocols for clinical-grade stem cells. Traditional culture systems often rely on components of animal origin, such as serum and mouse embryonic fibroblast (MEF) feeders, which introduce significant risks including pathogen contamination, batch-to-batch variability, and immunogenic reactions in recipients [48]. For cell therapies intended for human use, the use of animal-origin components necessitates extensive and costly viral safety testing [49]. The regulatory definition of xeno-free extends beyond the absence of serum to encompass all raw materials, requiring that no components are sourced from other species at any point in the manufacturing process [49].
Implementing xeno-free systems is not merely a regulatory checkbox but a fundamental requirement for scalable and safe manufacturing. GMP guidelines emphasize the importance of a robust quality management system (QMS) with thorough documentation, qualification procedures for all materials, and validation of processes [49]. For stem cell therapies, this means utilizing cell culture media and bioreactor systems that are both chemically defined and produced under GMP-compliant conditions. These systems provide the consistency needed for scaling from laboratory research to industrial-scale production, ensuring that every cell product batch meets stringent safety and efficacy standards for clinical applications [50].
Xeno-Free Media Systems
Essential Components and Formulations
Xeno-free media are chemically defined formulations that provide all necessary nutrients, minerals, and growth factors required for stem cell self-renewal and proliferation without using animal-derived components. These media typically include essential components such as DMEM/F12 base, L-ascorbic acid, sodium selenium, transferrin, and critical growth factors like basic Fibroblast Growth Factor (bFGF) and Transforming Growth Factor-beta (TGF-β1) or its functional equivalent Nodal [48]. The precise formulation is crucial for maintaining pluripotency while supporting expansion. For instance, bFGF has been identified as a critical additive for maintaining human pluripotent stem cell (hPSC) self-renewal in feeder-free cultures, typically used at concentrations between 40-100 ng/ml [48].
Unlike research-use-only (RUO) media, GMP-compliant xeno-free media must be produced under stringent quality controls. The International Council for Harmonisation (ICH) and regional guidelines like those from the FDA and European Medicines Agency (EMA) provide frameworks for qualifying raw materials and starting materials [49]. This involves comprehensive testing for identity, purity, and biological safety profiles, including screening for adventitious agents. Suppliers must provide detailed documentation, and manufacturers should conduct audits to ensure compliance throughout the supply chain [49].
Commercial Xeno-Free Media Solutions
Several companies offer GMP-compliant, xeno-free media specifically designed for clinical-grade stem cell expansion. The table below summarizes key commercial solutions:
Table 1: Commercial GMP-Compliant Xeno-Free Media for Stem Cell Expansion
| Product Name | Target Cell Types | Key Characteristics | Regulatory Support |
|---|---|---|---|
| NutriStem hPSC XF [50] | Human pluripotent stem cells (hPSC) | Xeno-free, serum-free, supports long-term growth and differentiation | DMF available, manufactured under cGMP |
| Essential 8 [48] | Induced pluripotent stem cells (iPSC) | Chemically defined, consists of 8 essential components | Suitable for manufacturing transition |
| MSC NutriStem XF [50] | Human mesenchymal stem/stromal cells (hMSC) | Xeno-free, supports high proliferation rates | DMF available, cGMP manufactured |
| 4Cell Nutri-T Medium [50] | T cells, TIL, CAR-T, PBMC | Serum-free, xeno-free, optimized for immunotherapies | cGMP production, DMF available |
These commercial media systems facilitate the transition from research to clinical applications by providing complete regulatory support, including Drug Master Files (DMF) that can be referenced in investigational new drug (IND) applications [50]. The selection of an appropriate media should be based on the specific cell type, expansion requirements, and regulatory strategy for the intended clinical application.
Media Optimization Workflow
The process of developing and optimizing xeno-free media involves systematic evaluation of components and their effects on cell growth and functionality. The following diagram illustrates the key decision points in media optimization:
Scalable Bioreactor Technologies
Bioreactor Systems for Stem Cell Expansion
Traditional two-dimensional (2D) static culture systems present significant limitations for clinical-scale stem cell production, including high labor requirements, space constraints, and inconsistent gradient formation of media components and metabolic wastes [48]. To address these challenges, the field has moved toward dynamic suspension culture systems that enable three-dimensional (3D) expansion of stem cells as aggregates or on microcarriers. These systems provide superior control over critical process parameters such as pH, dissolved oxygen (DO), temperature, and nutrient concentration, leading to more consistent and efficient cell expansion [48].
Multiple bioreactor platforms have been adapted for stem cell culture, each with distinct advantages:
- Stirred-tank bioreactors: Offer excellent scalability and process control, suitable for microcarrier-based culture
- Vertical-wheel bioreactors: Provide low-shear mixing ideal for sensitive stem cell populations
- Rocking-motion bioreactors: Combine simplicity with improved mass transfer over static systems
- Fixed-bed bioreactors: Enable high-density cell growth with minimal shear stress
The selection of an appropriate bioreactor system depends on multiple factors including the specific cell type, growth characteristics (single-cell vs. aggregate culture), target production scale, and available infrastructure for process monitoring and control.
Process Parameters and Monitoring
Successful scale-up in bioreactor systems requires careful optimization and control of multiple parameters. The table below outlines key process parameters and their typical ranges for stem cell expansion:
Table 2: Critical Process Parameters for Stem Cell Bioreactor Cultures
| Parameter | Optimal Range | Monitoring Method | Impact on Cell Growth |
|---|---|---|---|
| Dissolved Oxygen | 20-50% | Optical or electrochemical probes | Affributes differentiation, proliferation, and metabolic activity |
| pH | 7.2-7.4 | In-line pH probe | Influences enzyme activity and cell metabolism |
| Temperature | 37°C ± 0.5°C | Resistance temperature detectors | Critical for maintenance of pluripotency |
| Agitation Rate | Cell type-dependent | Impeller rotation monitoring | Controls mixing while minimizing shear stress |
| Glucose Concentration | Maintain 2-4 mM | Off-line analysis or biosensors | Prevents nutrient limitation or waste accumulation |
| Metabolites (Lactate) | Monitor accumulation | Off-line analysis | Indicator of metabolic state and culture health |
Advanced monitoring technologies are increasingly being implemented in stem cell bioprocessing. These include:
- In-line sensors: For real-time measurement of pH, DO, and temperature
- Automated sampling systems: For off-line analysis of nutrients, metabolites, and cell quality attributes
- Process analytical technologies (PAT): For monitoring critical quality attributes in real-time
- Biomass sensors: For non-invasive monitoring of cell growth and density
These technologies enable the implementation of quality by design (QbD) principles, where the process design space is defined and controlled to ensure consistent product quality [49].
Integrated Bioreactor System
Modern scalable bioreactor systems integrate multiple components to maintain optimal culture conditions. The relationship between these system components can be visualized as follows:
Application Notes and Protocols
Protocol: Scaling Up iPSC Expansion in Xeno-Free Suspension Culture
This protocol describes a standardized method for scaling up induced pluripotent stem cell (iPSC) expansion in xeno-free, defined media using stirred-tank bioreactors, suitable for generating clinical-grade cells for therapeutic applications.
Materials Required
- Table 4: Research Reagent Solutions for iPSC Expansion lists essential materials
- Sterile, single-use stirred-tank bioreactor (e.g., 1L-10L working volume)
- pH and dissolved oxygen (DO) probes, calibrated
- Temperature control system
- Agitation system with marine-style impeller
- Gas mixing system (air, O₂, N₂, CO₂)
Table 3: Research Reagent Solutions for iPSC Expansion
| Reagent/Consumable | Function | Example Product |
|---|---|---|
| Xeno-Free Media | Provides nutrients and growth factors for maintenance and expansion | NutriStem hPSC XF [50] |
| Defined Matrix | Provides substrate for adherent culture or microcarriers | Recombinant Laminin-521 |
| Passaging Reagent | Enables gentle cell dissociation for subculture | Enzyme-free passaging solution |
| Microcarriers | Provides surface for adherent growth in suspension | Collagen-coated polystyrene microcarriers |
| Cell Viability Assay | Assesses cell health and expansion efficiency | Flow cytometry with Annexin V/PI |
Procedure
Bioreactor Preparation
- Assemble the bioreactor system according to manufacturer's instructions, ensuring all components are sterile
- Add xeno-free culture media (e.g., NutriStem hPSC XF) to the bioreactor vessel, typically 60-70% of working volume
- If using microcarriers, add at appropriate density (e.g., 15-20 g/L for Cytodex 3) and allow hydration for at least 4 hours
- Calibrate pH and DO probes according to manufacturer specifications
- Set initial process parameters: temperature 37°C, DO 40%, pH 7.2, agitation 40-60 rpm
Inoculation
- Harvest iPSCs from 2D culture using enzyme-free dissociation reagent
- Determine cell viability and concentration using automated cell counter
- Transfer cell suspension to bioreactor via sterile sample port to achieve target seeding density (typically 2-4 × 10⁵ cells/mL)
- Adjust final volume with pre-warmed media to desired working volume
Process Monitoring and Control
- Monitor pH and DO continuously, implementing control loops to maintain setpoints
- Adjust gas flow rates (O₂, N₂, CO₂, air) automatically to maintain DO at 40% and pH at 7.2
- Take daily samples for off-line analysis: cell count, viability, glucose consumption, lactate production
- Assess pluripotency markers (OCT4, NANOG, SOX2) every 3-4 days via flow cytometry
- Monitor cell morphology and aggregation patterns using microscopy
Feeding Strategy
- Implement continuous perfusion or daily batch feeding based on glucose consumption rates
- For perfusion cultures, maintain cell retention using spin filters or alternating tangential flow (ATF) systems
- For batch feeding, replace 50-70% of media volume daily once glucose levels decrease below 2 mM
Harvesting
- When target cell density is reached (typically 2-4 × 10⁶ cells/mL), terminate culture
- For microcarrier cultures, separate cells from microcarriers using appropriate enzymatic treatment
- Concentrate cells using continuous-flow centrifugation or depth filtration
- Wash cells with xeno-free buffer solution
- Perform final quality control assessments: viability (>90%), pluripotency markers (>85% positive), sterility, and karyotype
Troubleshooting
- Low viability: Check for excessive shear stress (reduce agitation) or nutrient limitation (increase feeding)
- Poor growth: Verify quality of starting cell population and concentration of critical growth factors
- Spontaneous differentiation: Confirm maintenance of proper culture conditions and cell passaging before overconfluence
- Cell aggregation issues: Optimize inoculation density and agitation parameters
Protocol: Monitoring Pluripotency During Bioreactor Expansion
Regular assessment of pluripotency is essential during scaled-up stem cell expansion to ensure maintenance of undifferentiated state and therapeutic potential.
Materials
- Flow cytometer with appropriate lasers and filters
- Antibodies against pluripotency markers (OCT4, SOX2, NANOG, SSEA4, TRA-1-60)
- Isotype controls for flow cytometry
- Fixation and permeabilization buffers
- RNA extraction kit for gene expression analysis
Procedure
- Sample Collection
- Aseptically remove 10-20 mL of culture suspension from bioreactor
- Count cells and assess viability
- Aliquot 1-2 × 10⁶ cells for flow cytometry and 0.5-1 × 10⁶ cells for RNA analysis
Flow Cytometry Analysis
- Fix cells with 4% paraformaldehyde for 15 minutes at room temperature
- For intracellular markers (OCT4, SOX2, NANOG), permeabilize cells with 0.1% Triton X-100 for 10 minutes
- Incubate with primary antibodies against pluripotency markers for 30 minutes at 4°C
- Wash and incubate with fluorescently-labeled secondary antibodies if necessary
- Analyze using flow cytometry, comparing to appropriate isotype controls
- Document percentage of positive cells for each marker
Gene Expression Analysis
- Extract total RNA using appropriate kit
- Synthesize cDNA using reverse transcriptase
- Perform quantitative PCR (qPCR) for pluripotency genes (POUSF1, NANOG, SOX2)
- Normalize to housekeeping genes (GAPDH, HPRT1)
- Compare expression levels to reference undifferentiated stem cells
Data Interpretation
- Cultures should maintain >85% expression of key pluripotency markers by flow cytometry
- Pluripotency gene expression should not decrease more than 2-fold compared to reference
- Investigate any significant decreases in marker expression and consider adjusting culture parameters
Regulatory Considerations for GMP Compliance
Transitioning from research-use-only (RUO) to GMP-compliant manufacturing requires careful planning and implementation of quality systems. GMP guidelines emphasize a robust quality management system (QMS) with comprehensive documentation, validation protocols, and thorough supplier qualification [49]. The FDA guidelines for vendor qualification require clear specifications, verification through audits, and ongoing monitoring throughout the contract period [49].
For stem cell manufacturing, particular attention must be paid to the qualification of raw materials and starting materials. According to ICH guidelines, starting materials are intended to become part of the active biological substance in the final therapeutic product [49]. This includes the cell lines themselves, viral vectors for genetic modification, and critical growth factors. All materials should be sourced from qualified vendors with appropriate documentation, and companies should aim to avoid animal-origin components whenever possible to reduce the risk of transmitting adventitious agents [49].
Documentation requirements for GMP compliance include:
- Standard Operating Procedures (SOPs) for all critical processes
- Batch records documenting each manufacturing run
- Certificate of Analysis for all raw materials
- Validation protocols for equipment and processes
- Stability studies for both intermediate and final cell products
- Quality control testing results for identity, purity, potency, and sterility
The implementation of a QMS often follows the Plan-Do-Check-Action (PDCA) cycle, emphasizing continual improvement through repeated cycles of planning, implementation, checking outcomes, and refining processes [49]. This systematic approach ensures that stem cell manufacturing processes remain in a state of control and consistently produce cells that meet their predefined quality attributes.
In the development of clinical-grade stem cell therapies, comprehensive cell characterization is a cornerstone of ensuring product safety, identity, and biological function. For Advanced Therapy Medicinal Products (ATMPs) governed by Good Manufacturing Practice (GMP) regulations, characterization is not merely a research activity but a rigorous quality control requirement [51] [52]. The biological nature of the active substances in cell therapies introduces unique challenges, as these products represent autonomous viable systems capable of persisting in the body long-term, potentially causing serious adverse effects if not properly characterized [52].
An orthogonal approach—using multiple independent methods to assess the same quality attribute—has become the standard for comprehensive product characterization, helping to eliminate false negative or false positive results and providing a more complete understanding of product properties and heterogeneity [52]. This application note details the essential assays for characterizing the critical quality attributes (CQAs) of identity, purity, viability, and potency within a GMP-compliant framework for clinical-grade stem cell research and development.
Critical Quality Attributes (CQAs) and the Orthogonal Approach
For cell therapy products, leading regulatory agencies including the FDA, EMA, and WHO typically define functional CQAs as identity, potency, purity, and viability [52]. These attributes must be monitored throughout the manufacturing process, from the intermediate products to the final formulation.
Table 1: Orthogonal Methods for Assessing Critical Quality Attributes
| Quality Attribute | Definition | Key Analytical Methods | Regulatory Purpose |
|---|---|---|---|
| Identity | Verification of origin and unique cell population [52] [53]. | Flow cytometry, STR analysis, karyotyping, DNA sequencing [52] [53]. | Confirms cell lineage and genetic stability; prevents misidentification [53]. |
| Purity | Freedom from contaminants and unrelated cell types [53]. | Sterility testing, mycoplasma testing, endotoxin assays, flow cytometry for residual markers [51] [53]. | Ensures product safety by detecting microbial or process-related impurities [51]. |
| Viability | Ability of cells to remain alive and functional [53]. | Automated cell counting (e.g., NucleoCounter), flow cytometry with viability dyes, metabolic assays [54] [53]. | Reflects manufacturing process robustness and impacts product efficacy [54]. |
| Potency | Specific biological function or therapeutic activity [51]. | Directed differentiation, cytokine secretion assays, in vivo animal models [51] [55] [39]. | Measures the therapeutic mechanism of action; a lot-release criterion [51]. |
The relationship between these CQAs and the testing strategy is logically structured as follows:
Detailed Assay Methodologies
Identity Assays
Identity confirmation requires a multi-level approach spanning genotypic, phenotypic, and morphological characteristics [52]. For autologous products, this includes proving the cells originated from a specific patient, while for allogeneic therapies, identity must include determination of major histocompatibility complex antigens to prevent rejection [52].
Flow Cytometry for Phenotypic Identity
Purpose: To identify and quantify specific cell populations based on surface and intracellular markers [52] [39].
Detailed Protocol:
- Sample Preparation: Harvest cells using gentle dissociation reagents (e.g., enzyme-free cell dissociation buffers). Wash cells twice with PBS containing 1% bovine serum albumin (BSA).
- Antibody Staining: Resuspend approximately 1×10^6 cells in 100 µL of flow cytometry staining buffer. Add fluorochrome-conjugated antibodies against target markers (e.g., CD73, CD90, CD105 for MSCs; OCT4, NANOG for iPSCs) and appropriate isotype controls [39]. Incubate for 30 minutes in the dark at 4°C.
- Fixation (if intracellular staining): For intracellular markers like OCT4, fix cells with 4% paraformaldehyde for 20 minutes, then permeabilize with 0.1% Triton X-100 for 10 minutes before antibody addition.
- Data Acquisition: Analyze samples using a flow cytometer (e.g., BD FACS Fortessa) equipped with appropriate lasers and filters. Collect a minimum of 10,000 events per sample.
- Gating Strategy: Exclude debris based on forward and side scatter properties. Identify viable cells using a viability dye (e.g., propidium iodide). Analyze fluorescence intensity compared to isotype controls [39].
Acceptance Criteria: For human MSCs, ≥95% of cells must express CD73, CD90, and CD105, while ≤2% must be negative for hematopoietic markers CD45, CD34, CD14, CD19, and HLA-DR [39].
Purity and Safety Assays
Purity encompasses both freedom from microbial contamination and absence of unwanted cell types in the final product.
Sterility and Mycoplasma Testing
Purpose: To ensure products are free from bacterial, fungal, and mycoplasma contamination [51] [53].
Detailed Protocol:
- Sample Collection: Aseptically collect 1-5 mL of cell culture supernatant or resuspended cell product.
- Sterility Testing (according to Ph. Eur. 2.6.1): Inoculate samples into both fluid thioglycollate medium (FTM) and soybean-casein digest medium (SCDM). Incubate FTM at 30-35°C and SCDM at 20-25°C for 14 days.
- Mycoplasma Testing (according to Ph. Eur. 2.6.7): Inoculate samples into both broth and agar media. Incubate under aerobic and anaerobic conditions for 28 days. Include positive controls (e.g., M. orale, M. pneumoniae).
- Rapid Molecular Alternatives: Nucleic acid amplification techniques (NAT) or PCR-based methods can provide faster results for process monitoring [53].
Acceptance Criteria: No evidence of microbial growth in sterility tests after 14 days, and no mycoplasma colonies after 28 days of incubation [53].
Viability Assays
Accurate viability assessment is fundamental during manufacturing and reflects process robustness [54].
Automated Viable Cell Counting
Purpose: To provide a robust, reproducible method for determining viable cell concentration and total viability, reducing analyst-dependent variability [54].
Detailed Protocol (Validated per ICH Q2(R1)):
- Sample Preparation: Obtain a representative sample of the cell suspension. For adherent cells, detach using a standardized method and ensure a single-cell suspension.
- Staining: Mix 50 µL of cell suspension with 50 µL of ready-to-use reagent containing propidium iodide (PI) in a prefilled ViaCassette. PI is incorporated by permeable (non-viable) cells and binds to DNA [54].
- Measurement: Insert the cassette into an automated cell counter (e.g., NucleoCounter NC-100). The instrument automatically captures fluorescence images and analyzes them to determine total and non-viable cell counts.
- Calculation: Viable cell count is calculated as the difference between total and non-viable cells. Percentage viability = (Viable cell count/Total cell count) × 100 [54].
- Method Validation: The method should be validated for specificity, linearity, accuracy, and precision according to ICH Q2(R1) guidelines [54].
Acceptance Criteria: Viability should typically be >70% for clinical applications, with optimal products achieving >90% viability [39]. The automated method should demonstrate high precision (<10% coefficient of variation) [54].
Potency Assays
Potency assays measure the specific biological activity attributable to the product's therapeutic effect and are considered a lot-release criterion by regulatory agencies [51].
In Vitro Differentiation Assay
Purpose: To demonstrate the functional capacity of stem cells to differentiate into relevant lineages, confirming their potency [51] [55].
Detailed Protocol for Trilineage Differentiation (Mesenchymal Stem Cells):
- Osteogenic Differentiation:
- Seed MSCs at 2×10^4 cells/cm² in growth medium.
- After 24 hours, replace with osteogenic induction medium (e.g., MSC Osteogenic Differentiation Medium) containing dexamethasone, ascorbic acid, and β-glycerophosphate.
- Culture for 21 days, changing medium twice weekly.
- Fix with 70% ethanol and stain with 2% Alizarin Red S to detect calcium deposits.
Adipogenic Differentiation:
- Seed MSCs at 2×10^4 cells/cm² in growth medium.
- After 24 hours, replace with adipogenic induction medium (e.g., MSC Adipogenic Differentiation Medium) containing dexamethasone, indomethacin, and IBMX.
- Culture for 14-21 days, changing medium twice weekly.
- Fix with 10% formalin and stain with Oil Red O to detect lipid vacuoles.
Chondrogenic Differentiation:
- Pellet 2.5×10^5 MSCs by centrifugation at 300×g for 10 minutes.
- Maintain pellet in chondrogenic induction medium (e.g., MSC Chondrogenic Differentiation Medium) containing TGF-β3 for 21-28 days.
- Fix with 10% formalin, embed in paraffin, section, and stain with Alcian Blue to detect proteoglycans.
Acceptance Criteria: Successful differentiation is confirmed by positive staining for all three lineages compared to undifferentiated controls maintained in growth medium.
The workflow for implementing these key assays in a GMP environment is systematic:
Case Study: GMP-Compliant Characterization of Infrapatellar Fat Pad MSCs
A recent study demonstrated the complete characterization of mesenchymal stem cells derived from infrapatellar fat pad (FPMSCs) under GMP-compliant conditions [39]. The table below summarizes the quantitative results from their characterization assays:
Table 2: Characterization Results for GMP-Compliant FPMSCs
| Test Category | Specific Assay | Result | Acceptance Criteria |
|---|---|---|---|
| Viability | Post-thaw viability | >95% | >70% [39] |
| Identity | Flow cytometry for CD73, CD90, CD105 | ≥95% positive | ≥95% positive [39] |
| Identity | Flow cytometry for CD45, CD34 | ≤2% positive | ≤2% positive [39] |
| Purity/Safety | Sterility (Bact/Alert) | No growth | No growth [39] |
| Purity/Safety | Mycoplasma | Negative | Negative [39] |
| Purity/Safety | Endotoxin | Within specifications | Within specifications [39] |
| Potency | Colony Forming Unit (CFU) | Higher in optimized media | Enhanced potency [39] |
| Stability | Shelf-life (post-thaw) | Up to 180 days | Maintained specifications [39] |
The study highlighted the importance of optimized culture conditions, showing that FPMSCs exhibited enhanced proliferation rates and higher colony formation when cultured in specific GMP-compliant media (MSC-Brew GMP Medium) compared to standard MSC media [39]. This comprehensive characterization approach supported the clinical readiness of these cells for potential therapeutic applications.
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 3: Key Reagents and Equipment for GMP Cell Characterization
| Item | Function | Example Products/Catalog Numbers |
|---|---|---|
| GMP-compliant Cell Culture Media | Supports cell expansion while maintaining genetic stability under defined conditions | MSC-Brew GMP Medium [39], MesenCult-ACF Plus Medium [39] |
| Flow Cytometry Antibody Panels | Identifies specific cell surface markers for identity and purity assessment | BD Stemflow Human MSC Analysis Kit (CD73, CD90, CD105, CD45) [39] |
| Automated Cell Counter | Provides precise, reproducible viability and cell count measurements | NucleoCounter NC-100 with ViaCassette reagents [54] |
| Cell Separation System | Isoles specific cell populations from heterogeneous samples | CliniMACS Prodigy System [56] |
| Mycoplasma Testing Kits | Detects mycoplasma contamination to ensure product safety | PCR-based or culture-based GMP-compliant kits [53] |
| Differentiation Media Kits | Assesses multipotent differentiation capacity for potency testing | Osteogenic, Adipogenic, Chondrogenic Differentiation Media Kits [39] |
Comprehensive characterization of identity, purity, viability, and potency through an orthogonal testing approach is fundamental to the successful development and manufacturing of clinical-grade stem cell therapies. The assays and protocols detailed in this application note, when implemented within a GMP-compliant quality system, provide the necessary framework to ensure product safety, consistency, and efficacy. As the field advances, the integration of automated methods and standardized protocols will be crucial for the broader clinical translation of stem cell-based ATMPs.
Final Formulation, Cryopreservation, and Cold Chain Logistics
For clinical-grade stem cell therapies, the processes of final formulation, cryopreservation, and cold chain logistics represent a critical continuum that determines therapeutic success. These interdependent stages ensure that cellular products maintain their identity, potency, viability, and safety from the manufacturing facility to the patient bedside. Within the framework of Good Manufacturing Practice (GMP), this journey requires meticulously controlled and validated protocols to mitigate risks associated with cellular degradation, contamination, and functional drift. The complexity of managing living biological products demands an integrated approach that addresses both technical challenges in cryobiology and logistical challenges in distribution, all while maintaining comprehensive regulatory compliance and documentation.
Final Formulation of Stem Cell Products
Objectives and Critical Parameters
The final formulation step transitions expanded stem cells into a product suitable for cryopreservation and eventual administration. This process aims to achieve a standardized, well-characterized cell suspension with defined concentration, viability, and excipient composition. Key objectives include:
- Defined Cellular Composition: Achieving target cell concentration and ensuring high viability post-thaw.
- Cryoprotectant Addition: Incorporating protective agents while minimizing cellular stress.
- Container Closure: Transferring the final product into appropriate cryogenic vials or infusion bags.
- Quality Verification: Performing in-process controls to verify pre-cryopreservation quality attributes.
Cryoprotectant Strategies and DMSO Management
Dimethyl sulfoxide (DMSO) remains the most widely used cryoprotectant for stem cell products, despite its inherent cytotoxic and osmotic challenges. As a central player in cryobiology, DMSO's efficacy must be balanced against its toxicity [57]. The addition of cryoprotectant solution increases extracellular osmolality to approximately 1400 mOsm for 10% DMSO, compared with approximately 260–320 mOsm for most culture media [57]. This creates a significant osmotic imbalance that drives the exchange of water for cryoprotectant molecules, potentially causing osmotic shock if not properly managed.
Table 1: Cryoprotectant Formulations for Clinical-Grade Stem Cells
| Formulation Component | Concentration Range | Function | Clinical Considerations |
|---|---|---|---|
| Dimethyl Sulfoxide (DMSO) | 5-10% | Penetrating cryoprotectant; reduces intracellular ice formation | Osmotic stress; biochemical toxicity; exothermic reaction upon hydration [57] |
| Hydroxyethyl Starch (HES) | 6% [58] | Non-penetrating cryoprotectant; reduces extracellular ice formation | Bulking agent; improves post-thaw recovery |
| Ethylene Glycol | 5% [58] | Alternative penetrating cryoprotectant | Can be used in combination with DMSO [58] |
| Human Serum Albumin | 2.5-5% | Protein stabilizer; reduces mechanical stress | Defined pharmaceutical-grade sources required |
| Dextran 40 | 2.5-5% | Colloidal stabilizer; modulates osmotic pressure | Alternative to HES in some formulations |
| Sucrose/Trehalose | 50-100mM | Non-penetrating stabilizer; stabilizes membranes | Helps in osmotic balancing |
For therapeutic applications, DMSO exposure time should be limited to 30 minutes or less prior to freezing to minimize toxicity [57]. The cryoprotectant solution should be added slowly and in a controlled manner to avoid osmotic shock, with pre-cooled reagents used to counteract the exothermic reaction that occurs when DMSO mixes with aqueous solutions [57].
Automation in Final Formulation
The traditional manual approach to final formulation introduces significant user-dependent variability, making automation increasingly essential for manufacturing scalability and product consistency. Automated systems address several critical needs:
- Reduction of Open Process Steps: Minimizing contamination risk through functionally closed systems [57].
- Process Control and Traceability: Ensuring consistent cryoprotectant addition rates and providing electronic data capture [57].
- Scalability and Reproducibility: Enabling standardized processing across multiple batches [57].
- Personnel Protection: Reducing operator exposure to cryoprotectant chemicals.
Ideal automated systems for final formulation should incorporate single-use disposable fluid paths, precise temperature control, and industry-standard computation for data integrity [57].
Cryopreservation Methodologies
Controlled-Rate Freezing Protocols
Controlled-rate freezing represents the gold standard for clinical-grade stem cell cryopreservation, employing precise cooling profiles to maximize cell viability. The following workflow outlines a standardized approach for pluripotent stem cell cryopreservation:
This protocol, adapted from established methods for human pluripotent stem cells, emphasizes critical control points throughout the process [59]. For clinical applications, all steps must employ defined, xeno-free media and reagents to ensure regulatory compliance.
Cryopreservation of Specific Stem Cell Types
Different stem cell populations require optimized cryopreservation approaches tailored to their biological characteristics:
Human Pluripotent Stem Cells (hPSCs) An efficient protocol for hESCs and iPSCs uses EDTA dissociation to create small cell aggregates that survive cryopreservation with higher efficiency [59]. The cryopreservation medium consists of E8 medium, a fully defined, animal product-free formulation suitable for translational research [59]. The inclusion of Rho-associated protein kinase (ROCK) inhibitor (Y-27632) in the recovery medium significantly improves survival post-thaw [59].
Mesenchymal Stem Cells (MSCs) GMP-compliant protocols for MSCs derived from infrapatellar fat pad (FPMSCs) have demonstrated post-thaw viabilities exceeding 95%, far above the 70% minimum requirement for product release [46]. These cells maintained stem cell marker expression and sterility specifications even after extended cryostorage (up to 180 days), demonstrating protocol robustness [46].
Peripheral Blood Mononuclear Cells (PBMCs) For cryopreserving purified PBMCs, serum-free cryopreservation media such as CryoStor CS10 provide a safe, protective environment during freezing, storage, and thawing processes [60]. Cells are typically frozen at concentrations of 0.5-10 × 10^6 cells/mL using a standard slow rate-controlled cooling protocol (approximately -1°C/minute) [60].
Quality Control and Validation
Comprehensive quality assessment is integral to the cryopreservation process. For clinical-grade StemRNA iPSCs, each clone undergoes rigorous validation including:
- Genetic Integrity Assessment: Combined approach of G-band karyotyping and NGS-based oncogenetic analysis profiling variants in over 400 cancer-related genes [61].
- Pluripotency Verification: Flow cytometry analysis for marker expression and directed differentiation to measure functional pluripotency potential [61].
- Viability and Sterility Testing: Testing for endotoxin, mycoplasma, and other contaminants [61] [46].
Table 2: Post-Thaw Quality Specifications for Clinical-Grade Stem Cells
| Quality Parameter | Minimum Specification | Testing Method | Frequency |
|---|---|---|---|
| Viability | >70% (typically >95% achieved) [46] | Trypan Blue, Flow cytometry | Each batch |
| Sterility | No detectable growth | BacT/Alert, Culture | Each batch |
| Mycoplasma | No detectable contamination | PCR/Culture | Each batch |
| Endotoxin | <0.5 EU/mL | LAL assay | Each batch |
| Identity/Purity | >90% marker expression | Flow Cytometry | Each batch |
| Genetic Stability | Normal karyotype | Karyotyping/NGS | Periodic (e.g., every 5 passages) [59] |
| Differentiation Potential | 3-germ layer formation | Directed differentiation/RT-qPCR | Master Cell Bank |
Cold Chain Logistics and Storage
GMP Storage Facilities
Maintaining product integrity during storage requires facilities operating under Current Good Manufacturing Practice (cGMP) regulations with robust environmental controls, monitoring systems, and segregation protocols [62]. Key requirements include:
- Temperature Monitoring: Continuous monitoring with alarm systems for deviation detection [62].
- Access Control: Security measures to prevent unauthorized access [62] [63].
- Segregation and Quarantine: Dedicated areas for quarantined, approved, and rejected materials with clear labeling [62].
- Documentation and Traceability: Meticulous record-keeping of storage conditions and material movements [62].
GMP warehouses must maintain strict cleanliness and hygiene standards, implement regular pest control measures, and ensure staff are thoroughly trained in GMP regulations and procedures [63].
Transportation and Cold Chain Management
The transport of cryopreserved stem cell products presents unique challenges requiring specialized cold chain logistics. Maintaining temperature control during distribution is critical for product stability.
Cold chain logistics operations must comply with applicable regulations, including 21 CFR part 11 for electronic records and signatures [62]. Good Distribution Practice (GDP) guidelines extend beyond transportation to encompass various aspects of the pharmaceutical supply chain including storage, handling, and documentation procedures [64].
Validation and Qualification
Validation is necessary to confirm that storage and transportation systems produce expected results, as required by GxP rules [64]. Essential pharmaceutical distribution chain components requiring qualification and validation include:
- Storage chambers and cold rooms
- Insulated shipping containers
- Temperature monitoring data loggers
- Transportation vehicles with protective features
Qualification of all elements must precede validation, following standards such as the EU-GMP Guideline Annex 15 [64]. Without proper validation and qualification programs, GDP compliance cannot be achieved [64].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for GMP-Compliant Stem Cell Cryopreservation
| Reagent/Catalog Item | Function | GMP/Clinical Grade Availability |
|---|---|---|
| CryoStor CS10 [60] | Serum-free cryopreservation medium with 10% DMSO | Yes (Defined, xeno-free) |
| StemRNA Clinical Reprogramming Technology [61] | Footprint-free RNA reprogramming for iPSC generation | Yes (Clinical-grade) |
| E8 Medium / TeSR-E8 [59] | Defined, animal product-free culture medium for hPSCs | Yes (Xeno-free formulations) |
| ROCK Inhibitor (Y-27632) [59] | Improves cell survival after thawing and single-cell passaging | Yes (Pharmaceutical grade) |
| Pronase/EDTA for Stem [58] | Enzyme formulation for cell dissociation before cryopreservation | Yes |
| CP-5E Cryopreservation Medium [58] | Combination cryoprotectant (6% HES, 5% DMSO, 5% ethylene glycol) | Yes |
| Matrigel/Vitronectin [59] | Extracellular matrix for cell attachment | Yes (Defined versions available) |
The successful translation of stem cell therapies from research to clinical application hinges on robust, reproducible, and validated protocols for final formulation, cryopreservation, and cold chain logistics. These interdependent processes must be designed and implemented with a thorough understanding of cryobiology principles, regulatory requirements, and practical distribution challenges. By adopting defined, xeno-free reagents, implementing controlled-rate freezing methodologies, maintaining rigorous quality control, and establishing secure cold chains, developers can ensure that cellular therapies maintain their critical quality attributes throughout their journey from production to patient administration. As the field advances, increased automation and digital monitoring will further enhance the reliability and scalability of these essential processes, ultimately supporting the broader availability of regenerative medicine treatments.
Navigating Manufacturing Hurdles: Troubleshooting and Process Optimization
For Advanced Therapy Medicinal Products (ATMPs) like clinical-grade stem cells, mitigating contamination risks is a non-negotiable requirement of Good Manufacturing Practice (GMP) to ensure patient safety and product efficacy. Stem cell manufacturing involves an ex vivo expansion over a relatively long period, which significantly increases the risk of microbiological contamination that can adversely affect product quality and safety [65]. Contamination can lead to severe patient adverse reactions, including fever, chills, infections, irreversible septic shock, and even death [65]. A comprehensive quality control program must therefore be implemented, covering the entire manufacturing process from the source of cells and starting materials to the final cellular medicine [65]. This application note details the essential testing strategies—sterility, mycoplasma, and endotoxin testing—required for the release of clinical-grade stem cell products, providing standardized protocols and acceptance criteria framed within GMP requirements for mesenchymal stem cells (MSCs) and other stem cell-based ATMPs.
Establishing Testing Frameworks and Release Criteria
A robust microbiological quality control program for stem cell ATMPs should implement testing at critical phases of production, including the Master Cell Bank (MCB), Working Cell Bank (WCB), and the final cellular medicine [65]. The framework must define strict release criteria that the final product must meet before it can be deemed safe for clinical administration.
Table 1: Summary of Essential Microbiological Release Tests for Clinical-Grade Stem Cell Products
| Test Type | Recommended Method | Pharmacopoeia Reference | Acceptance Criteria for Release | Application Point |
|---|---|---|---|---|
| Sterility | Direct Inoculation or Membrane Filtration [65] | Ph. Eur. 2.6.1 [66] | No growth of aerobic/anaerobic bacteria or fungi after 14 days incubation [67] [65] | Final Product, MCB, WCB |
| Mycoplasma | Validated Nucleic Acid Amplification Test (NAT) [68] | Ph. Eur. 2.6.7 [68] | Negative result by validated NAT/PCR method [67] [68] | Final Product, MCB, WCB |
| Endotoxin | Kinetic Chromogenic LAL Test [66] | Ph. Eur. 2.6.14 [66] | < 5.0 EU/mL [67] or a calculated limit (e.g., 39 EU/mL for specific products) [66] | Final Product, MCB, WCB |
These tests are integral to a broader quality system. The manufacturing process itself must occur in a GMP-accredited facility, and all starting materials and reagents must be certified as sterile and endotoxin-free [65]. Furthermore, a Gram stain is often performed on the final product just before release as a rapid, though not comprehensive, check for contamination; a positive result typically prevents the product from being administered [65]. The validation of each analytical technique is crucial to demonstrate the sensitivity, limit of detection, and robustness of the method for the specific cell product being tested [65].
Experimental Protocols for Essential Quality Control Tests
Sterility Testing by Direct Inoculation
Sterility testing is a mandatory release test for parenteral administration to ensure the absence of viable microorganisms.
- Principle: The test is designed to detect the presence of viable aerobic/anaerobic bacteria and fungi by inoculating the sample into culture media and observing for growth [65].
- Materials:
- Thioglycollate Penase Broth (TPB): For detecting anaerobic and aerobic bacteria.
- Tryptic Soy Penase Broth (TSPB): For detecting fungi and aerobic bacteria.
- Test Samples: 1 mL of intermediate product (supernatant) or final cell suspension.
- Procedure:
- Aseptically inoculate 1 mL of the test sample into each of the two media (TPB and TSPB). The volume of the product should not exceed 10% of the medium volume [65].
- Incubate the inoculated TPB at 35°C and TSPB at 22°C for 14 days [65].
- Observe the media for turbidity, which indicates microbial growth, on days 3, 4, 5, 7, and 14 [67].
- Include negative controls (e.g., 1 mL of 0.9% sterile NaCl) for each medium [65].
- Interpretation: The product meets the test criteria if no turbidity (growth) is observed in any of the test media after the 14-day incubation period. Growth promotion tests should be performed regularly to validate the efficacy of the media [65].
Mycoplasma Detection by Validated Real-Time PCR
Mycoplasma contamination is a widespread problem in cell culture, and its absence is a critical release criterion. Nucleic Acid Amplification Techniques (NAT), like real-time PCR, offer a fast and sensitive alternative to traditional culture methods.
- Principle: This protocol uses a validated real-time PCR assay to detect mycoplasma DNA, in compliance with Ph. Eur. 2.6.7 [68].
- Materials:
- MycoSEQ Mycoplasma Detection Assay (Thermo Fisher) or equivalent validated PCR kit.
- Real-Time PCR System (e.g., QuantStudio5).
- Sample: Cell pellet or supernatant containing at least 5×10^5 cells [65].
- Procedure:
- Sample Inactivation: Inactivate DNases by heating the sample to 95°C for 10 minutes [65].
- DNA Extraction: Extract genomic DNA using a dedicated kit (e.g., MB DNA from Minerva Biolabs), ensuring sensitivity for mycoplasma genomes [65].
- PCR Setup: Prepare the reaction mix according to the kit's instructions.
- Amplification: Run the real-time PCR protocol as validated. A typical validation ensures the method's sensitivity, specificity, and robustness, and confirms the removal of any matrix-derived interference from the cell product [68].
- Interpretation: A negative result is required for product release. The validation study must demonstrate that the assay can reliably detect mycoplasma in the presence of the stem cell product matrix [68].
Endotoxin Testing by Kinetic Chromogenic LAL Assay
The Limulus Amebocyte Lysate (LAL) test is the standard for detecting bacterial endotoxins, which are pyrogenic components of gram-negative bacteria.
- Principle: Endotoxins activate a clotting enzyme in the LAL, which can be measured kinetically using a chromogenic substrate [66].
- Materials:
- Endosafe PTS (Charles River) or equivalent kinetic chromogenic LAL test system.
- LAL Reagent Water.
- Sample: Final cell product suspension.
- Procedure:
- Determine Endotoxin Limit and MVD: Calculate the Maximum Valid Dilution (MVD) based on the endotoxin limit for the product. For an injectable, the limit is often 5.0 EU/mL [67], though it can be calculated based on dose (e.g., 39 EU/mL for a specific BM-MNC product) [66].
- Sample Preparation: Dilute the sample to fall within the validated range of the assay. For a BM-MNC product, 1:10 and 1:100 dilutions have been successfully validated [66].
- Assay Execution: Perform the test according to the manufacturer's instructions and the validated method described in Ph. Eur. 2.6.14 [66].
- Include Controls: Run a positive product control (PPC) to confirm the sample does not contain interfering factors that inhibit or enhance the reaction [66].
- Interpretation: The product passes if the measured endotoxin concentration is below the established limit (e.g., < 5.0 EU/mL). The assay must be validated to show that the sample matrix does not interfere with the test [66].
The Scientist's Toolkit: Essential Reagents and Materials
The successful implementation of GMP-compliant quality control tests relies on the use of qualified reagents and equipment. The following toolkit lists key solutions referenced in the protocols.
Table 2: Research Reagent Solutions for Contamination Testing
| Reagent/Material | Function/Application | Example Product/Reference |
|---|---|---|
| Animal Component-Free GMP Media | Provides a consistent, safe environment for MSC expansion, reducing contamination risks and batch variability. | MSC-Brew GMP Medium (Miltenyi Biotec) [39] [6] |
| Sterility Test Media | Culture media designed to support the growth of a broad spectrum of aerobic/anaerobic bacteria and fungi. | Thioglycollate Penase Broth (TPB), Tryptic Soy Penase Broth (TSPB) [65] |
| Mycoplasma Detection Kit | Validated PCR-based kit for the sensitive and specific detection of mycoplasma DNA in cell products. | MycoSEQ Mycoplasma Detection Assay (Thermo Fisher) [68], VenorGeM PCR Kit (Minerva Biolabs) [65] |
| Endotoxin Test System | Automated system for performing kinetic chromogenic LAL tests for precise endotoxin quantification. | Endosafe PTS (Charles River) [66] |
| GMP-Grade Small Molecules | Ancillary reagents (e.g., ROCK inhibitors) used in stem cell workflows to improve cell survival and differentiation. | Bio-Techne GMP Small Molecules [69] |
The implementation of rigorously validated sterility, mycoplasma, and endotoxin testing protocols is fundamental to the GMP-compliant manufacture of clinical-grade stem cells. By adhering to pharmacopoeia methods and establishing a comprehensive quality control program that spans from cell bank to final product, manufacturers can significantly mitigate contamination risks. This application note provides a foundational framework and detailed protocols that researchers and drug development professionals can adapt and validate within their own facilities. As the regulatory landscape for ATMPs continues to evolve, a commitment to stringent microbiological quality control remains the cornerstone of ensuring patient safety and the successful translation of stem cell therapies from the bench to the clinic.
In the field of clinical-grade stem cell research, batch-to-batch consistency is not merely an operational goal but a fundamental requirement for regulatory approval and therapeutic efficacy. For researchers and drug development professionals, overcoming variability represents one of the most significant challenges in translating promising stem cell research into clinically viable therapies. The pleiotropic nature of biological medicinal products, including stem cell-derived products, introduces substantial complexity for quality control, as these products comprise multiple bioactive ingredients that must remain consistent across manufacturing batches [70].
Variability in stem cell manufacturing can originate from multiple sources, including donor variability (genetic background, age, sex, epigenetic state), culture conditions (media composition, matrix coating), reagent inconsistency (especially poorly validated antibodies or growth factors), and protocol differences (seeding density, passage number, timing of media changes) [71]. Even subtle differences in handling conditions, such as pipetting technique or time outside the incubator, can introduce significant variability that compromises experimental results and therapeutic outcomes.
This Application Note outlines a systematic framework for controlling variability through Good Manufacturing Practice (GMP) principles, standardized protocols, and robust quality control measures. By implementing these strategies, research institutions and manufacturing facilities can achieve the high degree of batch-to-batch consistency required for clinical translation and regulatory approval of stem cell-based therapies.
A comprehensive understanding of variability sources is essential for developing effective control strategies. In stem cell research, variability manifests in both biological attributes (potency, differentiation capacity) and process parameters (yield, viability) across different manufacturing batches.
For cellular secretomes—a promising cell-free therapeutic approach—the challenge is particularly pronounced. These biological products contain a complex mixture of bioactive substances, including proteins, peptides, different lipid species, and extracellular vesicles, which must maintain consistent composition and potency across batches to ensure reproducible therapeutic effects [70]. The concerted action of all these ingredients is often required to exert the intended biological effects, justifying the use of secretome as a whole rather than purified biomolecules [70].
The regulatory landscape further emphasizes the importance of consistency. GMP standards describe the minimum criteria that manufacturers must meet throughout the manufacture and distribution of drug substances or products [72]. Manufacturing to GMP standards requires compliance with all relevant standards and rigorous quality control testing to ensure that medicines maintain constant high quality, are appropriate for their intended use, and meet the requirements of marketing authorization or clinical trial authorization [72].
Table 1: Major Sources of Variability in Stem Cell Manufacturing
| Variability Category | Specific Sources | Impact on Product Quality |
|---|---|---|
| Biological Sources | Donor genetic background, age, sex, epigenetic state [71] | Affects differentiation potential, proliferation rate, therapeutic potency |
| Process-Related Sources | Media composition, matrix coating, seeding density [71] | Influences cell morphology, marker expression, functional characteristics |
| Reagent Variability | Lot-to-lot differences in growth factors, cytokines, antibodies [71] | Causes inconsistent differentiation outcomes and experimental results |
| Operational Differences | Passage number, timing of media changes, handling techniques [71] | Affects cell viability, metabolic state, and performance in functional assays |
| Environmental Factors | Temperature fluctuations, CO2 levels, incubation times [71] | Impacts cell health, growth rates, and genetic stability |
Systematic Approach to Process Validation
Process validation provides a structured framework for ensuring consistent manufacturing performance. According to regulatory guidelines, process validation involves a series of activities taking place over the lifecycle of the product and process, with activities organized into three distinct stages [73].
Stage 1 - Process Design: This initial stage focuses on defining the commercial manufacturing process based on knowledge gained through development and scale-up activities. The goal is to design a process suitable for routine commercial manufacturing that can consistently deliver a product meeting its quality attributes [73]. During this stage, manufacturers should build comprehensive process knowledge and understanding, utilizing tools such as Design of Experiment (DOE) studies to reveal relationships between component characteristics or process parameters and the quality of in-process material or final product [73].
Stage 2 - Process Qualification: This stage evaluates the process design to determine if the process is capable of reproducible commercial manufacturing [73]. Process qualification involves rigorous assessment of the manufacturing process under controlled conditions to demonstrate consistent performance and to establish that all predetermined specifications are met consistently.
Stage 3 - Continued Process Verification: This ongoing stage provides assurance during routine production that the process remains in a state of control [73]. Manufacturers should implement ongoing programs to collect and analyze product and process data, which can identify process or product problems or opportunities for process improvements.
The FDA encourages an integrated team approach to process validation that includes expertise from a variety of disciplines (e.g., engineering, production, quality control, and quality assurance) [73]. This collaborative approach ensures comprehensive evaluation of all process aspects and facilitates robust process design and control.
Diagram 1: Process Validation Lifecycle Approach
GMP-Compliant Manufacturing Strategies
Core GMP Principles for Consistency
Implementing GMP-compliant manufacturing requires strict adherence to established principles and procedures. GMP standards describe the minimum criteria that pharmaceutical manufacturers must meet throughout the manufacture and distribution of the drug substance or drug product [72]. In Europe, for example, any medicines manufactured for use on the continent must be manufactured in line with GMP, and compliance with these standards is verified through audit before regulatory authorities grant a manufacturing license [72].
Key GMP principles essential for batch-to-batch consistency include:
- Precisely followed Standard Operating Procedures (SOPs) [16]
- Strict Quality Control (QC) and Quality Assurance (QA) systems [16]
- Rigorous personnel training and proficiency testing [16]
- Meticulous documentation and record keeping [16]
- Comprehensive testing of final products according to FDA guidance and requirements [16]
These principles ensure that stem cell products maintain constant high quality, are appropriate for their intended use, and meet the requirements of the marketing authorization or clinical trial authorization [72].
Material Standardization Strategies
Standardizing starting materials and reagents is fundamental to reducing batch-to-batch variability. Several key strategies have emerged as best practices in stem cell manufacturing:
GMP-Grade Reagents: Utilizing GMP-grade reagents minimizes variability by enforcing batch-to-batch consistency and comprehensive quality control measures [71]. These reagents undergo rigorous testing and validation to ensure they meet strict specifications for use in clinical manufacturing.
Feeder-Free Systems: While early stem cell expansion relied on animal feeder cells, modern protocols increasingly opt for feeder-free substrates, which eliminate batch inconsistency and associated contamination risks [71]. This approach provides greater control over the culture environment and reduces a significant source of variability.
Xeno-Free Media: By removing all animal-derived components, xeno-free media minimizes biological contaminants and supports compatibility with clinical translation [71]. This strategy reduces the risk of introducing undefined variables and enhances product consistency and safety.
Master Cell Banks (MCBs): Establishing well-characterized MCBs provides a standardized starting material for manufacturing processes. GMP-grade MCB production services are available for various cell types, including mesenchymal stem cells (MSCs) and iPSC-derived MSCs (iMSCs), offering controlled expansion under GMP-grade conditions to yield therapeutic-scale cell quantities with high consistency [74].
Quality Control and Analytical Development
Establishing Comprehensive Quality Control Parameters
Implementing robust quality control measures is essential for detecting and controlling batch-to-batch variability. A pre-defined set of physico-chemical-biological tests, collectively referred to as product specification criteria, represents a crucial part of the control strategy to ensure the efficacy and consistency of biological products [70]. These specifications are established by the manufacturer based on data obtained during product development, characterization, manufacturing consistency, process development, pre-clinical studies, and stability tests [70].
Quality control parameters for stem cell products typically include:
- Sterility testing to exclude microbial contamination [70]
- Tests for uniformity of dosage units [70]
- Moisture content analysis for lyophilized drug products [70]
- Qualitative descriptions of physical state, color of lyophilisate, and clarity of reconstituted product [70]
- Physical assessments of other quality attributes, such as pH and osmolality [70]
- Functional potency assays that determine biological properties related to pharmacological action [70]
For cellular secretomes, quality control should include quantification of key ingredients, such as cytokines, lipids, and extracellular vesicles, and functional assessment of potency using relevant bioassays [70].
Stability Studies and Shelf-Life Determination
Stability studies are a vital component of pharmaceutical development and supporting documentation for regulatory submissions [72]. These studies involve placing samples in their container closure system into environmentally controlled chambers to determine how the product changes over time when subjected to specific environmental conditions [72]. During the study, samples are periodically assessed through physicochemical and microbiological tests according to a predefined study protocol [72].
When designing stability studies, several factors must be considered:
- Formal registration stability studies must be performed on multiple batches to assess potential batch-to-batch variability [72]
- Studies should evaluate the impact of product packaging on stability [72]
- Sample quantities must be sufficient to cover all testing and account for potential repeat testing and investigation of atypical results [72]
- Studies must simulate expected storage conditions to establish accurate shelf life [72]
The International Council for Harmonisation (ICH) provides guidelines for testing the stability of biological products, intended to demonstrate that the drug product meets its specification throughout its intended shelf life [70]. For complex biological products like secretomes, a single stability-indicating test is usually insufficient, and a set of product-specific tests is necessary to assess stability profiles of all relevant components [70].
Experimental Data and Case Studies
Quantitative Assessment of Batch Consistency
Recent studies have demonstrated the feasibility of achieving high batch-to-batch consistency in complex biological products. Research on GMP-compliant production of therapeutic stressed peripheral blood mononuclear cell-derived secretomes (PBMCsec) showed that inter-batch differences in bioactive components and secretome properties were small despite considerable variations in protein concentrations and potencies between individual donor secretomes [70].
Table 2: Batch Consistency in GMP-Compliant PBMC Secretome Production
| Parameter Assessed | Method of Analysis | Inter-Batch Variability | Stability Over 6 Months |
|---|---|---|---|
| Cytokine Composition | Multiplex immunoassays | Low variability in key regenerative cytokines | Stable at temperatures up to +5°C |
| Lipid Content | Mass spectrometry | Consistent profile across batches | Maintained composition in lyophilized form |
| Extracellular Vesicles | Nanoparticle tracking analysis | Minimal batch-to-batch differences | Particle count and size distribution stable |
| Pro-angiogenic Potency | Tube formation assay | High consistency in functional activity | Potency retained in lyophilized product |
| Protein Concentration | Spectrophotometric methods | Higher donor-to-donor than batch-to-batch variation | Stable under recommended storage conditions |
Stability testing of PBMCsec demonstrated that analytical and functional properties remained stable when lyophilisates were stored at temperatures up to +5°C for 6 months [70]. This research established that consistent production of cell-derived, yet cell-free secretome as a biological medicinal product is achievable through GMP-compliant processes [70].
Experimental Protocol: Consistency Assessment for Stem Cell-Derived Products
Objective: To evaluate batch-to-batch consistency of stem cell-derived products through comprehensive physicochemical and functional analyses.
Materials and Equipment:
- Multiple batches of the stem cell product (minimum of 3 batches)
- Qualified cell culture facility with standardized equipment
- Analytical instruments (HPLC, mass spectrometer, flow cytometer)
- Materials for functional assays (tube formation, gene expression)
- Reference standards for quantitative analyses
Procedure:
Sample Preparation:
- Reconstitute or prepare samples according to established protocols
- Ensure consistent handling across all batches
- Document any deviations from standard procedures
Physicochemical Characterization:
- Determine protein concentration using standardized spectrophotometric methods
- Analyze cytokine profile via multiplex immunoassays
- Characterize lipid composition using mass spectrometry
- Quantify extracellular vesicles through nanoparticle tracking analysis
Functional Potency Assessment:
- Perform tube formation assay to assess pro-angiogenic potential
- Conduct cell-based protein and reporter gene assays
- Evaluate specific biological activities functionally related to the product's therapeutic indication
Data Analysis:
- Calculate mean and standard deviation for each parameter across batches
- Perform statistical analysis to determine significance of inter-batch differences
- Compare results against predetermined acceptance criteria
Stability Assessment:
- Store samples under recommended conditions
- Repeat key analyses at predetermined timepoints
- Monitor for changes in product characteristics over time
Acceptance Criteria: Batch-to-batch variability should not exceed predetermined limits based on product development data and intended therapeutic application. Functional potency should remain within specified ranges to ensure consistent biological activity.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing effective batch consistency strategies requires utilizing appropriate reagents and materials designed to minimize variability. The following table outlines key solutions available to researchers pursuing GMP-compliant stem cell manufacturing.
Table 3: Essential Research Reagent Solutions for Batch Consistency
| Reagent Category | Specific Product Examples | Function in Ensuring Consistency |
|---|---|---|
| GMP-Grade Cell Culture Media | Xeno-free, defined composition media [71] | Provides consistent nutrient composition while eliminating animal-derived components that introduce variability |
| Feeder-Free Culture Systems | Defined matrix coatings, synthetic substrates [71] | Eliminates batch variability associated with feeder cells and provides standardized growth surfaces |
| Characterized Cell Banks | GMP-grade Master Cell Banks (MCBs), Working Cell Banks (WCBs) [74] | Provides standardized, well-characterized starting material with comprehensive quality control documentation |
| Quality-Control Tested Growth Factors | GMP-grade cytokines, differentiation factors [71] | Ensures consistent potency and activity in directing stem cell differentiation and maintenance |
| Standardized Differentiation Kits | validated protocols with quality-controlled reagents | Reduces technical variability in generating specific cell types from pluripotent stem cells |
Risk Management and Regulatory Considerations
Implementing Risk-Based Approaches
Modern regulatory guidelines encourage the adoption of risk-based decision making throughout the product lifecycle [73]. Rather than categorizing attributes and parameters as simply critical or non-critical, the perception of criticality as a continuum rather than a binary state is more useful when implementing a lifecycle approach to process validation [73].
All attributes and parameters should be evaluated in terms of their roles in the process and impact on the product or in-process material, with the degree of control commensurate with their risk to the process and process output [73]. Higher risk attributes or parameters warrant a higher degree of control to ensure consistent product quality.
Risk analysis tools can be used to screen potential variables for Design of Experiment (DOE) studies, helping to minimize the total number of experiments conducted while maximizing knowledge gained [73]. This efficient approach to process understanding facilitates the identification and control of key sources of variability.
Diagram 2: Risk Management Process for Variability Control
Regulatory Framework and Compliance
Compliance with regulatory requirements is essential for clinical translation of stem cell therapies. Process validation for finished pharmaceuticals is a legally enforceable requirement under section 501(a)(2)(B) of the Food, Drug, and Cosmetic Act, which states that drugs must be manufactured in conformity with current good manufacturing practice [73].
The CGMP regulations require that manufacturing processes be designed and controlled to assure that in-process materials and the finished product meet predetermined quality requirements and do so consistently and reliably [73]. This includes establishing control procedures "to monitor the output and to validate the performance of those manufacturing processes that may be responsible for causing variability in the characteristics of in-process material and the drug product" [73].
Global regulatory harmonization continues to evolve, with upcoming changes to ICH standards aimed at consolidating stability guidelines into a cohesive document that addresses core stability principles across different product types, including advanced therapies and biologics [72]. These updates will include the integration of modern risk management principles and the adoption of new technologies that support predictive modeling and enhanced stability strategies [72].
Achieving consistent batch-to-batch performance in stem cell manufacturing requires a systematic, science-based approach encompassing process understanding, control strategy implementation, and continuous verification. By adopting the strategies outlined in this Application Note—including robust process validation, material standardization, comprehensive quality control, and risk-based decision making—researchers and manufacturers can significantly reduce variability and enhance product consistency.
The field continues to evolve with emerging opportunities for further enhancing batch consistency:
- Advanced analytical technologies enabling more comprehensive characterization of complex products
- Process analytical technologies (PAT) facilitating real-time monitoring and control
- Automated and closed processing systems reducing human-derived variability
- Predictive modeling based on comprehensive process data
- Harmonized global standards for advanced therapy medicinal products
As demonstrated by successful case studies, consistent GMP-compliant production of complex biological products is achievable through meticulous attention to process design, qualification, and verification [70]. By implementing these strategies, the stem cell research community can accelerate the translation of promising therapies from bench to bedside while ensuring consistent quality, safety, and efficacy.
Addressing Cell Stress and Senescence During Expansion
In the transition of stem cell therapies from research to clinical application, the expansion process under Good Manufacturing Practice (GMP) conditions presents a major challenge. A critical obstacle is the management of cell stress and senescence during in vitro culture, which can compromise the safety, potency, and quality of the final cell product [75]. Mesenchymal stem cells (MSCs) are promising for cell-based therapies but repeated passaging and suboptimal culture conditions can induce replicative senescence and the adoption of a pro-inflammatory senescence-associated secretory phenotype (SASP), characterized by the secretion of cytokines like IL-6 and IL-8 [75] [76]. This application note details standardized, GMP-compliant protocols for the expansion of human MSCs, with a specific focus on monitoring and mitigating cellular stress and senescence to ensure the production of high-quality cells for clinical use.
Monitoring Senescence and Stress: Key Assays and Metrics
Rigorous in-process controls are essential for identifying the emergence of senescent cells. The following table summarizes the key assays for evaluating cellular senescence and health during expansion.
Table 1: Key Assays for Monitoring Cell Stress and Senescence
| Assay Type | Measured Parameter(s) | Significance in Senescence & Stress Monitoring | Typical Results in Stressed/Senescent Cells |
|---|---|---|---|
| Senescence-Associated β-Galactosidase (SA-β-gal) Staining [75] [76] | Percentage of SA-β-gal positive cells | A hallmark of cellular senescence; detects lysosomal β-galactosidase activity at pH 6.0. | Significant increase in stained cells [76]. |
| Flow Cytometry for MSC Surface Markers [39] [75] | Expression of CD73, CD90, CD105; absence of CD45. | Purity and identity; senescence can alter marker expression. | Downregulation of markers like CD146 and CD105 [75]. |
| Growth Kinetics Analysis [39] | Population Doubling (PD) time, Cumulative PDs. | Proliferative capacity; increased doubling time indicates stress/senescence. | Lower cumulative PDs and higher doubling times [75]. |
| Colony-Forming Unit (CFU) Assay [39] | Number of colonies formed from single cells. | Clonogenic potential, an indicator of stem cell "potency." | Reduced colony-forming efficiency. |
| Gene Expression Analysis (qPCR) [75] | Expression of senescence genes (p53, p16), SASP factors (IL-6, IL-8), lineage markers. | Molecular signature of senescence and differentiation. | Upregulation of p53, p16, IL-6, and IL-8 [76]. |
| Telomere Length Analysis [75] | Mean telomere length. | Replicative history and stress; shortened telomeres are associated with senescence. | Decrease in telomere length with passaging [75]. |
GMP-Compliant Experimental Protocols
Isolation and Baseline Expansion of Mesenchymal Stem Cells
This protocol is adapted from established procedures for infrapatellar fat pad-derived MSCs (FPMSCs) and can be modified for other tissue sources like dental pulp (DPSCs) or alveolar bone marrow (aBMMSCs) [39] [75].
- Tissue Acquisition and Ethics: Obtain tissue (e.g., infrapatellar fat pad, dental pulp) following surgical procedures with informed consent and approval from the institutional ethics review committee [39].
- Enzymatic Digestion: Mince the tissue into approximately 1 mm³ pieces. Digest using a GMP-grade enzyme cocktail such as 0.1% collagenase type I or a mixture of collagenase/dispase in serum-free media for 1-2 hours at 37°C with agitation [39] [75].
- Cell Isolation and Plating: Neutralize the digestion reaction, filter the cell suspension through a 100 μm filter, and centrifuge. Resuspend the cell pellet in an animal component-free, GMP-compliant expansion medium (e.g., MSC-Brew GMP Medium) and plate in culture flasks [39].
- Primary Culture and Passaging: Culture at 37°C with 5% CO₂. Change media every 2-3 days. Upon reaching 80-90% confluency, passage cells using a GMP-grade dissociation reagent like CTS TrypLE Select. Consistently use a ROCK inhibitor (e.g., Y-27632 or GMP-grade RevitaCell Supplement) in the medium for the first 18-24 hours post-passage to reduce anoikis and improve cell survival [39] [77]. For expansion, seed cells at a density of 5 × 10³ cells/cm² [39].
Protocol for Evaluating Culture Media Impact on Senescence
To assess the effect of different media on cellular stress, a comparative study should be performed.
- Experimental Setup: After the first passage, split cells from a single donor into multiple culture conditions. Test at least two different animal component-free, GMP-compliant media (e.g., MSC-Brew GMP Medium and MesenCult-ACF Plus Medium) against a standard FBS-containing medium as a control [39].
- Long-Term Expansion and Sampling: Culture cells over multiple passages (e.g., up to passage 10), strictly maintaining consistent seeding densities and passaging intervals [75]. At each passage (e.g., P3, P6, P10), sample cells for the assays listed in Table 1.
- Data Collection: Calculate population doubling time at each passage. At predetermined passages (e.g., P3 and P10), perform SA-β-gal staining, flow cytometry for MSC markers, and CFU assays [39] [75]. For gene expression analysis, harvest RNA and perform qPCR for senescence and SASP markers.
Protocol for Investigating the cGAS-STING Signaling Pathway in Senescence
The cGAS-STING pathway is a key regulator of inflammation and senescence and can be investigated as a potential target for mitigation [76].
- Induction of Senescence: Culture NP cells or MSCs with 10 ng/mL interleukin-1β (IL-1β) for 48 hours to induce a premature senescent state [76].
- Gene Silencing: Transfect cells with cGAS-targeting small interfering RNA (siRNA) using a GMP-compatible transfection system prior to IL-1β exposure. A non-targeting siRNA should be used as a control [76].
- Phenotypic Assessment: After 48 hours of IL-1β treatment, assess senescence via SA-β-gal staining and the expression of SASP factors (IL-6, IL-8, TNF-α) by ELISA or Western blotting [76].
Results and Data Interpretation
Impact of Culture Media on Senescence and Proliferation
Data from comparative media studies should be quantified and presented for clear decision-making. The table below summarizes expected outcomes.
Table 2: Comparative Analysis of Media Formulations on MSC Properties
| Parameter | Standard FBS Media | MesenCult-ACF Plus Medium | MSC-Brew GMP Medium |
|---|---|---|---|
| Average Doubling Time | Reference Value | Lower than standard media [39] | Lowest doubling time, indicating enhanced proliferation [39] |
| CFU Capacity | Reference colonies | Higher than standard media [39] | Highest number of colonies, indicating enhanced potency [39] |
| Senescence (SA-β-gal+ cells) | High at late passage | Reduced compared to FBS media | Lowest levels at equivalent passages |
| Marker Stability (e.g., CD105) | Downregulation with passaging [75] | Better retention than FBS media | High, stable expression (>95% positive) across passages [39] |
| GMP Compliance | No | Yes | Yes |
The Role of the cGAS-STING Pathway
Experimental data will likely demonstrate that IL-1β treatment significantly increases the percentage of SA-β-gal-positive cells and upregulates SASP factors (IL-6, IL-8, TNF-α). This should be correlated with increased expression of cGAS, p53, and p16 [76]. Silencing cGAS is expected to reverse these effects, resulting in a lower percentage of senescent cells and reduced SASP expression, even in the presence of IL-1β [76]. This confirms the pathway's critical role in stress-induced senescence.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key GMP-Compliant Reagents for MSC Expansion
| Reagent Category | Example Product | Function & Importance |
|---|---|---|
| Xeno-Free Basal Media | MSC-Brew GMP Medium [39] | Defined, animal origin-free formulation for consistent expansion; supports high proliferation and maintains marker expression. |
| Xeno-Free Media Supplements | MesenCult-ACF Plus Supplement [39] | Chemically defined or human-sourced supplements to create a complete xeno-free medium. |
| Dissociation Reagent | CTS TrypLE Select [77] | Animal origin-free, recombinant enzyme for cell passaging; stable at room temperature and clinically compliant. |
| ROCK Inhibitor | RevitaCell Supplement (CTS) [77] | Improves cell survival after passaging and cryopreservation; contains a highly specific ROCK inhibitor with antioxidants. |
| Extracellular Matrix | Recombinant Vitronectin (CTS) [77] | Defined, recombinant coating matrix for cell attachment; eliminates variability and safety risks of animal-derived matrices. |
| Cell Separation | EasySep Human T Cell Isolation Kit [78] | For immune cell isolation in co-culture studies or potency assays (e.g., immunomodulation). |
| Cryopreservation Medium | CryoStor CS10 [78] | GMP-manufactured, defined cryopreservation solution designed to minimize cell stress and death during freeze-thaw cycles. |
Signaling Pathways and Experimental Workflows
cGAS-STING Pathway in Cellular Senescence
Figure 1: cGAS-STING Pathway in Senescence. Cytosolic DNA from damage activates cGAS, leading to cGAMP production and STING activation, which drives NF-κB-mediated SASP expression and cellular senescence [76].
Experimental Workflow for Senescence Assessment
Figure 2: Senescence Assessment Workflow. Process from cell isolation through expansion and sampling to multi-assay senescence evaluation.
Implementation for Clinical Manufacturing
Integrating these protocols ensures a robust strategy for managing cell stress. Key implementation steps include:
- Media Selection: Prioritize GMP-compliant, animal component-free media that demonstrate superior performance in maintaining low doubling times, high clonogenicity, and stable phenotype, as validated by internal studies [39].
- Process Consistency: Maintain consistent seeding densities, passaging schedules, and quality checks to minimize unpredictable stress.
- In-Process Monitoring: Incorporate SA-β-gal staining and flow cytometry as routine quality control checkpoints at critical passages during master cell bank generation and production runs.
- Mitigation Strategy: If senescence is detected, investigate culture conditions. The use of ROCK inhibitors post-passaging is a proven intervention to reduce immediate stress [77]. Further research into modulating specific pathways like cGAS-STING may offer future strategies [76].
By adopting these standardized application notes and protocols, researchers and manufacturers can enhance the quality, consistency, and therapeutic potential of clinically manufactured stem cells.
The transition from research to clinical application in stem cell therapies necessitates the replacement of traditional, xenogenic culture supplements with clinically suitable alternatives. Fetal Bovine Serum (FBS) has been the long-standing supplement for mesenchymal stem cell (MSC) expansion. However, its use in clinical settings raises concerns regarding pathogen transmission, immunogenic reactions, and ethical considerations [79]. Human Platelet Lysate (HPL) has emerged as a powerful, human-derived alternative that not only mitigates these risks but also demonstrates superior performance in promoting MSC proliferation [80] [81]. This Application Note provides a comparative analysis of FBS and HPL, supported by quantitative data, and outlines detailed, GMP-aligned protocols for implementing HPL in MSC culture systems to enhance the manufacturing of clinical-grade cell therapies.
Comparative Analysis: FBS vs. HPL
The following tables summarize the key characteristics and performance metrics of FBS and HPL based on systematic reviews and meta-analyses.
Table 1: Characteristic Comparison of FBS and HPL
| Feature | Fetal Bovine Serum (FBS) | Human Platelet Lysate (HPL) |
|---|---|---|
| Origin | Bovine (animal) [79] | Human (allogeneic or autologous) [79] |
| Composition | Complex, undefined mixture; batch-to-batch variability [79] [82] | Rich in human growth factors (PDGF, bFGF, TGF-β, IGF-1, VEGF) [79] |
| GMP/Clinical Suitability | Not ideal; risk of xenogenic immunization and zoonotic transmission [79] | Preferred alternative; compliant with GMP principles when properly sourced and tested [79] |
| Typical Working Concentration | 10% [80] [83] [81] | 5-10% [80] [83] [81] |
| Regulatory Status | Subject to increasing restrictions for clinical applications [81] | Accepted as a clinical-grade supplement; requires viral testing of source material [79] |
Table 2: Quantitative Performance Meta-Analysis of BMSCs and ASCs
| Performance Metric | 10% FBS (Reference) | 5-10% HPL | Significance |
|---|---|---|---|
| Population Doubling (PD) | Baseline | Higher | HPL significantly increases the number of cell doublings [80] [81] |
| Doubling Time (DT) | Baseline | Lower | HPL significantly reduces the time required for cells to double [80] [81] |
| Proliferation Rate | Baseline | Enhanced | Consistent finding across multiple studies for both Bone Marrow and Adipose-derived MSCs [80] [81] [79] |
| Cell Morphology | Fibroblastic, spindle-shaped | Fibroblastic, spindle-shaped (unchanged) [83] [79] | |
| Immunophenotype (CD73+, CD90+, CD105+) | Maintained | Maintained [83] [79] | |
| Trilineage Differentiation Potential | Maintained | Maintained (osteogenic, adipogenic, chondrogenic) [83] [79] |
Experimental Protocols
Protocol: Expansion of Human MSCs using HPL-Supplemented Medium
This protocol is adapted for the robust expansion of human Bone Marrow-MSCs (BMSCs) in a GMP-oriented, xeno-free system [83].
A. Materials (Research Reagent Solutions)
| Item | Function | Example & Catalog Number |
|---|---|---|
| Basal Medium | Provides essential nutrients and salts. | α-MEM (e.g., Sigma-Aldrich, M8042) [83] |
| HPL Supplement | Provides human-derived growth factors and adhesion molecules. | PLTMax Human Platelet Lysate (e.g., Sigma-Aldrich, SCM141) [83] |
| Heparin | Prevents coagulation of fibrinogen present in HPL. | Heparin (e.g., Sigma-Aldrich, H3149), 2 U/mL [83] |
| L-Glutamine | Essential amino acid for cell metabolism. | L-Glutamine (e.g., Sigma-Aldrich, A8185), 2 mM [83] |
| Antibiotic-Antimycotic | Prevents bacterial and fungal contamination. | Penicillin-Streptomycin Solution [83] |
| Recombinant bFGF | Enhances proliferation and stemness. | Human recombinant basic FGF (e.g., Sigma-Aldrich, F0291), 8 ng/mL [83] |
| Cell Dissociation Reagent | Enzymatically detaches adherent cells for passaging. | StemPro Accutase (e.g., Thermo Fisher, A1110501) [28] |
| Rock Inhibitor | Improves cell survival after passaging or thawing. | GMP ROCK Inhibitor (e.g., RevitaCell) [28] |
B. Methodology
Medium Preparation
- Prepare complete culture medium by supplementing α-MEM basal medium with:
- Filter-sterilize the complete medium using a 0.22 µm filter. The medium can be stored at 4°C for up to 2 weeks.
Cell Seeding and Culture
- Thaw a vial of BMSCs and resuspend the cells in complete medium containing a ROCK inhibitor (e.g., 1:100 RevitaCell) to enhance post-thaw viability [28].
- Seed cells at a density of 3,000 - 5,000 cells/cm² on standard tissue culture plastic flasks.
- Incubate cells at 37°C in a humidified atmosphere with 5% CO₂.
- Perform a complete medium change every 2-3 days.
Cell Passaging
- Once cells reach 70-80% confluence, remove the culture medium.
- Wash the cell layer gently with a balanced salt solution (e.g., DPBS).
- Add pre-warmed Accutase to cover the cell layer and incubate at 37°C for 2-3 minutes [28].
- When cells detach, neutralize the enzyme with an equal volume of complete medium.
- Collect the cell suspension, centrifuge (e.g., 300 x g for 5 minutes), and resuspend the pellet in fresh complete medium.
- Re-seed cells at the recommended seeding density for continued expansion.
Protocol: HPL Production via Freeze-Thaw Lysis
The method of platelet lysis significantly impacts the growth factor release and efficacy of HPL. The freeze-thaw method is widely used and effective [80] [79].
A. Materials
- Pooled human platelet concentrates (from apheresis or buffy coat)
- Freezer (-80°C)
- Water bath (37°C)
- Centrifuge
B. Methodology
- Source Material: Obtain platelet units from qualified blood banks, ensuring donor screening for relevant communicable diseases [79].
- Freezing: Subject the pooled platelet units to freezing at -80°C for a minimum of 12 hours to ensure complete crystallization.
- Thawing: Thaw the frozen platelet units in a 37°C water bath until completely liquid.
- Lysis Cycles: Repeat the freeze-thaw cycle a minimum of 3 times to ensure maximal platelet rupture and growth factor release. Meta-analysis indicates that applying at least 3 cycles correlates with a more significant reduction in cell doubling time compared to FBS [80] [81].
- Clarification: Centrifuge the lysate at a high speed (e.g., 3,000 - 4,000 x g for 30 minutes) to remove platelet membranes and debris.
- Filtration and Storage: Filter the supernatant through a 0.22 µm filter under sterile conditions. Aliquot the final HPL product and store at ≤ -20°C or lower.
Signaling Pathways and Experimental Workflows
HPL Signaling Pathway in MSC Proliferation
The superior proliferative effect of HPL is mediated by a synergistic combination of growth factors that activate key intracellular signaling pathways in MSCs.
Experimental Workflow for Comparative Assessment
This workflow outlines the key steps for a direct, head-to-head comparison of HPL and FBS in MSC culture, generating data on proliferation, phenotype, and function.
The evidence demonstrates that HPL is a superior and clinically translatable alternative to FBS for MSC expansion. It drives faster proliferation while maintaining critical MSC identity and functionality. The transition to HPL is a critical step in developing robust, safe, and efficient GMP manufacturing protocols for cell-based therapies. Adhering to standardized HPL production methods, such as employing multiple freeze-thaw cycles, and using qualified, virus-tested source materials are essential for ensuring batch-to-batch consistency and compliance with regulatory standards for advanced therapeutic medicinal products (ATMPs) [80] [81] [79].
Implementing Closed and Automated Systems to Reduce Human Error
The transition to closed and automated systems represents a paradigm shift in Good Manufacturing Practice (GMP) for clinical-grade stem cell production. This evolution is driven by the critical need to minimize human error and process variability, which are significant challenges in advanced therapeutic medicinal product (ATMP) manufacturing. In conventional manual processes, human error accounts for nearly 40% of major incidents in complex operations, with costly consequences including batch failures, regulatory non-compliance, and compromised patient safety [84]. Automated systems address these vulnerabilities by providing standardized, reproducible processes essential for manufacturing consistency and product quality.
Within stem cell research and therapy development, the implementation of automation technologies has demonstrated remarkable improvements in process robustness and product characterization. This document provides detailed application notes and protocols for implementing these systems, specifically framed within the context of GMP manufacturing for clinical-grade stem cells, to support researchers, scientists, and drug development professionals in enhancing their translational pipelines.
Quantitative Impact of Automation on Manufacturing Metrics
Recent studies across multiple cell therapy applications have quantified the significant benefits of automated, closed-system manufacturing compared to manual, open-process approaches. The following table summarizes key performance indicators from published automated processes:
Table 1: Performance Metrics of Automated Cell Manufacturing Systems
| Process Metric | Manual/Open Process Performance | Automated/Closed System Performance | Reference Cell Type |
|---|---|---|---|
| Process Consistency | High donor-to-donor variability | Consistent yields across donors (16.1-16.4% recovery) [85] | Natural Killer (NK) cells |
| Cell Viability | Variable post-processing viability | Maintained high viability (>88.6%, up to 95.4%) [85] | NK cells |
| Product Purity | Risk of contamination during handling | High purity (CD3-CD56+ cells avg. 98.4%) [85] | NK cells |
| Cell Expansion | Variable expansion rates | Enhanced proliferation rates, lower doubling times [46] | Mesenchymal Stem Cells (MSCs) |
| Sterility Assurance | Multiple open processing steps | Closed system with no microbial growth detected [85] | NK cells |
| Post-Thaw Viability | Variable recovery after cryopreservation | Maintained >95% viability post-thaw [46] | MSCs |
The data demonstrates that automated systems provide substantial improvements in critical quality attributes essential for clinical applications. For example, in NK cell manufacturing, automated processes consistently achieved high purity and efficient T-cell depletion (log depletions of 4.75-6.05), crucial for patient safety [85]. Similarly, automated MSC expansion systems demonstrated enhanced proliferation rates and maintained post-thaw viability exceeding 95%, meeting stringent release criteria for clinical applications [46].
Application Notes: Automated Platforms for Stem Cell Manufacturing
Closed-System Automated Manufacturing Platforms
The CliniMACS Prodigy platform (Miltenyi Biotec) represents a state-of-the-art automated, closed-system technology that has been successfully implemented for various cell therapy manufacturing applications. This system enables end-to-end processing from starting material to final product within a single, integrated platform, significantly reducing human intervention points [86] [85]. The platform has been programmed to perform complex, multi-step manufacturing processes including:
- Cell separation and selection via immunomagnetic labeling
- Culture and transduction processes with precise fluid management
- Product formulation and harvest with integrated sampling capabilities
This integrated approach has proven particularly valuable for haematopoietic stem cell (HSC) gene therapy, where traditional methods require sophisticated ex vivo gene transfer in dedicated GMP facilities. The automated system enables a point-of-care strategy that eliminates the need for extensive local cGMP facility infrastructure, potentially expanding availability to a broader patient population [86].
Implementation Considerations for Stem Cell Applications
Successful implementation of automated systems requires careful consideration of several factors specific to stem cell manufacturing:
- Process Translation: Existing manual protocols must be systematically adapted to automated platforms, which may require optimization of timing, reagent volumes, and incubation parameters [28].
- Quality Control Integration: Automated systems should incorporate in-process monitoring and sampling capabilities to ensure process control and facilitate quality testing throughout manufacturing [85].
- Regulatory Compliance: Automated processes must be designed to meet GMP documentation requirements, with comprehensive validation data demonstrating consistency, reproducibility, and product quality [46] [28].
- Personnel Training: Operators require specialized training for automated system operation, maintenance, and troubleshooting, shifting their role from hands-on manipulation to system supervision and data monitoring [87].
Experimental Protocols: Automated Manufacturing Workflows
Protocol 1: Automated Natural Killer (NK) Cell Manufacturing
This protocol details the automated manufacturing of clinical-grade NK cells using the CliniMACS Prodigy platform, adapted from the process described by Saah et al. (2024) [85].
Materials and Reagents
Table 2: Research Reagent Solutions for Automated NK Cell Manufacturing
| Reagent/Consumable | Function/Purpose | GMP-Grade Designation |
|---|---|---|
| Leukapheresis product | Starting material (peripheral blood mononuclear cells) | Clinical-grade source material |
| CD3 and CD56 MicroBeads | Immunomagnetic cell depletion and enrichment | GMP-grade cell separation reagents |
| IL-2 and IL-15 cytokines | NK cell activation and functional enhancement | GMP-grade cytokines |
| CliniMACS PBS/EDTA Buffer | System buffer for washing and dilution | GMP-grade buffer solution |
| CliniMACS Prodigy NKCT Set | Disposable tubing set for NK cell processing | Sterile, single-use closed system |
| Bact/Alert Culture Bottles | Sterility testing throughout process | Microbiological quality control |
Methodology
System Setup and Priming
- Load the CliniMACS Prodigy NKCT tubing set onto the instrument according to manufacturer instructions.
- Prime the system with CliniMACS PBS/EDTA buffer to remove air and ensure proper fluid path function.
- Program the instrument to execute the three-step NK cell manufacturing process.
Cell Processing
- Load the leukapheresis product into the system under sterile conditions.
- Initiate the automated process:
- Step 1: CD3+ Cell Depletion - The system automatically adds CD3 MicroBeads, incubates, and performs magnetic depletion of T-cells.
- Step 2: CD56+ Cell Enrichment - The system adds CD56 MicroBeads to the CD3-depleted fraction, followed by magnetic enrichment of NK cells.
- Step 3: Cytokine Activation - The enriched CD56+ cells are transferred to the culture chamber and incubated with IL-2 (100 IU/mL) and IL-15 (10 ng/mL) for 12 hours.
Product Harvest and Formulation
- After the activation period, the system automatically washes the cells to remove cytokines and debris.
- The final NK cell product is concentrated into a transfer bag for harvest.
- Integrated sampling ports allow for aseptic removal of samples for quality control testing.
Quality Control Assessment
- Viability: Assess via trypan blue exclusion or flow cytometry with viability dyes (>70% required, typically >88% achieved).
- Purity: Analyze by flow cytometry for CD3-CD56+ cells (typically >98% purity).
- Potency: Evaluate CD69 activation marker expression (typically shows significant upregulation post-activation) and cytotoxicity against target cells.
- Sterility: Perform BacT/Alert testing throughout process with no growth detected.
The entire process requires approximately 25 hours from start to finish, with minimal operator intervention beyond initial setup and final product harvest [85].
Protocol 2: Automated Mesenchymal Stem Cell (MSC) Expansion
This protocol outlines the automated expansion of GMP-compliant mesenchymal stem cells derived from infrapatellar fat pad (FPMSCs), adapted from the optimized culture conditions described in recent research [46].
Materials and Reagents
Table 3: Research Reagent Solutions for Automated MSC Expansion
| Reagent/Consumable | Function/Purpose | GMP-Grade Designation |
|---|---|---|
| MSC-Brew GMP Medium | Animal-free culture medium for MSC expansion | GMP-grade cell culture medium |
| GMP-grade Trypsin/EDTA | Cell detachment and passage | GMP-grade dissociation reagent |
| Recombinant Vitronectin | Culture surface coating for attachment | GMP-grade attachment substrate |
| CryoStem Freeze Medium | Cryopreservation of final cell product | GMP-grade cryopreservation medium |
| Rock Inhibitor (Y-27632) | Enhancement of post-thaw viability | GMP-grade small molecule inhibitor |
Methodology
Isolation and Initial Culture
- Isolate FPMSCs from infrapatellar fat pad tissue following established GMP-compliant protocols.
- Culture primary cells in MSC-Brew GMP Medium in traditional culture vessels until sufficient cells are available for automated system inoculation.
Automated Bioreactor Setup
- Load the automated bioreactor system (such as the CliniMACS Prodigy with appropriate culture chamber) with GMP-grade culture vessels or microcarriers.
- Prime the system with MSC-Brew GMP Medium and equilibrate to 37°C, 5% CO2.
Automated Expansion Process
- Inoculate the system with passage 2-3 MSCs at a density of 3,000-5,000 cells/cm².
- Program the system for automated medium exchange every 48-72 hours with integrated metabolite monitoring.
- Implement automated cell passaging when 70-80% confluence is reached, detected via integrated imaging systems.
- The system automatically adds pre-warmed Trypsin/EDTA for detachment.
- Neutralizes the enzyme with culture medium after detachment.
- Performs cell counting and reseeding at optimal density.
Harvest and Cryopreservation
- Upon reaching target cell numbers or passage limit, initiate automated harvest procedure.
- The system performs final cell counting, viability assessment, and formulation in cryopreservation medium.
- Automated filling of cryocontainers with integrated labeling.
- Programmed rate-controlled freezing with transfer to vapor phase liquid nitrogen storage.
Quality Control Testing
- Viability: >95% viability post-thaw (exceeding the >70% minimum requirement).
- Identity: Flow cytometry confirmation of MSC markers (CD73+, CD90+, CD105+, CD14-, CD19-, CD34-, CD45-, HLA-DR-).
- Potency: Colony-forming unit (CFU) assays demonstrating maintained differentiation potential.
- Sterility: Negative mycoplasma, endotoxin, and sterility testing throughout process.
Studies implementing this approach have demonstrated enhanced proliferation rates with lower doubling times across passages compared to standard MSC media, along with maintenance of stem cell marker expression and all required specifications for product release, even after extended storage (up to 180 days) [46].
Workflow Visualization
The following diagram illustrates the logical workflow and decision points in implementing automated systems for GMP-compliant stem cell manufacturing:
Automated System Implementation Workflow
This implementation workflow emphasizes the systematic approach required for successful integration of automated technologies into GMP stem cell manufacturing. The process begins with comprehensive analysis of existing manual processes to identify specific pain points and quality variabilities, followed by strategic platform selection based on technical requirements and manufacturing goals [87] [84].
The protocol translation phase requires meticulous adaptation of manual processes to automated platforms, often requiring optimization of timing, reagent concentrations, and integration of quality control checkpoints [28]. The qualification phase involves rigorous validation to demonstrate process consistency, product quality, and compliance with regulatory requirements [46] [85]. Successful operational implementation depends on comprehensive staff training to transition personnel from hands-on technicians to system supervisors and data analysts [87].
The implementation of closed and automated systems represents a transformative advancement in GMP manufacturing of clinical-grade stem cells. These technologies directly address the critical challenge of human error reduction while enhancing process consistency, product quality, and manufacturing efficiency. The protocols and application notes presented here demonstrate that automated systems can successfully be applied across diverse cell types, including mesenchymal stem cells, haematopoietic stem cells, and immune effector cells like NK cells.
The quantitative data from recent studies confirms that automated systems deliver superior process consistency, enhanced product purity, and maintained cell viability compared to manual approaches. Furthermore, the closed-system nature of these platforms significantly reduces contamination risks, supporting the manufacturing of safe, clinical-grade cell products.
As the field of regenerative medicine advances toward broader clinical application, the adoption of automated manufacturing technologies will be essential for scaling production, ensuring quality, and meeting regulatory requirements. The integration of human oversight with automated precision creates an optimal manufacturing paradigm that leverages the strengths of both approaches – the consistency and reproducibility of automation with the adaptability and problem-solving capabilities of human expertise [87]. This balanced approach will accelerate the translation of stem cell research from the laboratory to clinical applications, ultimately expanding patient access to these promising therapies.
Proving Product Quality: Validation, Release Criteria, and Comparative Analysis
Establishing Critical Quality Attributes (CQAs) and Product Release Specifications
In the Good Manufacturing Practice (GMP) manufacturing of clinical-grade stem cells, defining Critical Quality Attributes (CQAs) and product release specifications is a foundational requirement of a Quality by Design (QbD) framework [88] [89]. CQAs are physical, chemical, biological, or microbiological properties or characteristics that must be within an appropriate limit, range, or distribution to ensure the desired product quality [90]. These attributes are crucial for the safety and functionality of stem cell-based therapeutics. Establishing well-defined CQAs and stringent release specifications ensures that stem cell products are consistent, reliable, and effective for clinical applications, thereby supporting the translation of regenerative medicine from research to clinical practice [88] [91].
Defining Critical Quality Attributes (CQAs) for Stem Cells
The inherent biological variability of stem cells necessitates a rigorous, multi-parameter approach to quality control. CQAs for stem cell products must comprehensively address identity, purity, potency, viability, and safety [88] [39]. These attributes are directly influenced by Critical Process Parameters (CPPs) during manufacturing, such as seeding density, feeding regime, and the quality of raw materials [88].
The table below summarizes the core CQAs for a clinical-grade stem cell product, linking them to the analytical methods used for their assessment.
Table 1: Essential Critical Quality Attributes (CQAs) and Measurement Methods for Stem Cell Products
| CQA Category | Specific Attribute | Analytical Method | Target Release Specification |
|---|---|---|---|
| Identity | Expression of pluripotency markers (e.g., OCT4, NANOG) | Flow Cytometry [88] [89] | >95% positive for specific markers [88] |
| Identity | Expression of MSC surface markers (CD73+, CD90+, CD105+) | Flow Cytometry [39] | >95% positive, CD45- [39] |
| Purity | Lack of undesifferentiated cell types | Flow Cytometry | Varies based on product type |
| Potency | Specific Growth Rate (SGR) | Cell counting and calculation [88] | ~0.018 hour⁻¹ ± 1.5x10⁻³ [88] |
| Potency | Colony Forming Unit (CFU) Assay | Crystal Violet staining & count [39] | Higher colony formation in optimized media [39] |
| Viability | Cell Viability | Trypan Blue Exclusion [88] [39] | ≥ 95% [88] [39] |
| Safety | Sterility (Mycoplasma, Bacteria) | qPCR / Bact/Alert [39] | No detection [39] |
| Safety | Endotoxin Level | Endotoxin Assay [39] | Below regulatory threshold [39] |
The relationship between CPPs and CQAs is dynamic. For example, research on H9 human embryonic stem cells (hESCs) has demonstrated that CPPs like seeding density and feeding frequency directly impact CQAs such as Specific Growth Rate (SGR) and viability [88]. An optimized protocol using a seeding density of 20,000 cells/cm² with a 100% medium exchange after 48 hours was shown to support robust growth and high viability while maintaining pluripotency [88]. Furthermore, the use of animal component-free, GMP-compliant media formulations is a critical CPP that directly affects the safety and consistency CQAs of the final product [39].
Experimental Protocols for CQA Assessment
Protocol 1: Flow Cytometry for Cell Identity and Purity
This protocol is used to quantify the expression of intracellular pluripotency markers (e.g., OCT4) and surface markers (e.g., for MSCs) to assess identity and purity CQAs [88] [39].
Detailed Methodology:
- Cell Harvesting: Harvest cells using a non-enzymatic agent like Accumax and centrifuge at 500xg for 5 minutes [89].
- Fixation and Permeabilization: Resuspend the cell pellet in PBS and fix with 4% paraformaldehyde for 10 minutes. For intracellular markers (e.g., OCT4), permeabilize cells using a commercial permeabilization buffer [89].
- Staining: Incubate cells with fluorochrome-conjugated antibodies against target markers (e.g., OCT4, CD73, CD90, CD105) and corresponding isotype controls for 30-60 minutes in the dark [89] [39].
- Analysis: Wash cells to remove unbound antibody and analyze on a flow cytometer (e.g., Attune NxT or BD FACS Fortessa). Use software (e.g., FCS Express) to gate on the live cell population and determine the percentage of cells positive for the markers [89] [39].
Protocol 2: Population Doubling Time and Specific Growth Rate (SGR)
This protocol measures cell proliferation, a key potency CQA, by calculating the population doubling time and SGR [88] [39].
Detailed Methodology:
- Seeding: Seed cells at a standardized density (e.g., 5 × 10³ cells/cm² for MSCs [39] or 20,000 cells/cm² for hESCs [88]) in complete culture medium.
- Culture and Harvest: Culture cells until they reach 80-90% confluency. Harvest and count cells using a hemacytometer or automated cell counter, assessing viability via Trypan Blue exclusion [39].
- Calculation: Calculate the doubling time over multiple passages using the formula:
Doubling Time = (duration * ln(2)) / ln(final concentration / initial concentration)[39]. The Specific Growth Rate (SGR) is derived from the slope of the natural log of the cell concentration versus time plot and is expressed in hour⁻¹ [88].
Protocol 3: Colony Forming Unit (CFU) Assay
This functional assay assesses the clonogenic potential, or potency, of a stem cell population, indicating the presence of a robust progenitor cell fraction [39].
Detailed Methodology:
- Low-Density Seeding: Seed cells at very low densities (e.g., 20, 50, 100, and 500 cells) in a culture dish containing the appropriate medium [39].
- Incubation: Culture the cells for 10-14 days without disturbance to allow for colony formation.
- Staining and Quantification: Fix cells with 10% neutral buffered formalin for 30 minutes, wash with PBS, and stain with 10% Crystal Violet for visualization. Count colonies (typically defined as clusters of >50 cells) manually or using imaging software [39].
The following workflow diagram illustrates the logical sequence and decision points in establishing and verifying CQAs for product release.
The Scientist's Toolkit: Key Research Reagent Solutions
The transition from research-grade to GMP-compliant manufacturing requires careful selection of raw materials and reagents. The following table details essential reagents and their functions in establishing and monitoring CQAs.
Table 2: Key GMP-Compliant Reagents for Stem Cell Manufacturing and CQA Assessment
| Reagent/Kit | Function in CQA Context | Specific Example |
|---|---|---|
| Animal Component-Free Media | Ensures cell expansion under xeno-free conditions; critical for safety and consistency CQAs. Supports enhanced proliferation and potency [39]. | MSC-Brew GMP Medium [39]; MesenCult-ACF Plus Medium [39]; StemMACS iPS-Brew XF [89]. |
| GMP-Grade Enzymes | Used for cell passaging; maintains cell viability and phenotype (a purity and identity CQA). | Accumax [89]; GMP-grade Collagenase [39]. |
| Flow Cytometry Kits | Validated kits for standardized assessment of identity CQAs (surface marker expression). | BD Stemflow Human MSC Analysis Kit [39]. |
| Cell Viability Stains | Differentiates live/dead cells for viability CQA. | Trypan Blue [88] [89] [39]. |
| qPCR Kits | Detects microbial contamination for safety CQAs (e.g., Mycoplasma). | Commercial Mycoplasma detection kits [89] [39]. |
Establishing a robust set of CQAs and product release specifications is non-negotiable for the successful clinical translation of stem cell therapies. This requires a systematic approach that integrates QbD principles, employs precise and validated analytical methods, and utilizes GMP-compliant reagents. The protocols and frameworks outlined herein provide a actionable roadmap for researchers and manufacturers to ensure that their stem cell products are consistently safe, pure, potent, and effective, thereby building the foundation for reliable and successful clinical outcomes in regenerative medicine.
The translation of mesenchymal stem cell (MSC)-based therapies from laboratory research to clinical applications requires rigorous protocols that comply with Good Manufacturing Practice (GMP) standards. This ensures the production of safe, efficacious, and quality-controlled cell products for human use [3]. While bone marrow has been the traditional source of MSCs, the infrapatellar fat pad (IFP) presents a promising alternative, often accessed as surgical waste during knee procedures with minimal donor-site morbidity [46] [39]. However, transitioning from research-grade to clinical-grade IFP-derived MSC (FPMSC) production necessitates validated, standardized GMP-compliant processes. This case study details the development and validation of a complete GMP protocol for the isolation, expansion, and storage of FPMSCs, providing a framework for their use in clinical trials and regenerative medicine applications [46].
Materials and Methods
Tissue Source and Donor Eligibility
- Tissue Source: IFP tissue was obtained as waste material from patients undergoing anterior cruciate ligament (ACL) reconstructive surgery [39].
- Ethical Compliance: The protocol was approved by the relevant research ethics review committee. Written informed consent was obtained from all participants prior to inclusion [46].
- Donor Screening: Patients were screened against detailed inclusion and exclusion criteria. Eligible patients underwent surgical excision of 10–20 g of IFP tissue via an arthroscopic portal using an arthroscopic shaver and a sterile in-line collection chamber [39].
Critical Reagents and Research Solutions
The following GMP-grade reagents are essential for ensuring a clinically compliant manufacturing process.
Table 1: Essential GMP-Grade Reagents for FPMSC Manufacturing
| Reagent Name | Function | GMP-Grade Example |
|---|---|---|
| MSC-Brew GMP Medium | Animal component-free expansion medium | Miltenyi Biotec, Cat# 170-076-325 [46] [39] |
| Collagenase | Enzymatic digestion of tissue | 0.1% solution in serum-free media [39] |
| Vitronectin | Culture surface coating | Recombinant VTN-N (e.g., A14700, Life Technologies) [28] |
| Trypan Blue | Cell viability assessment | Used post-thaw and during culture [46] [39] |
| StemPro Accutase | Gentle cell dissociation | Used for passaging (e.g., A1110501, Life Technologies) [28] |
Protocol: GMP-Compliant Isolation and Expansion of FPMSCs
Isolation of FPMSCs
- Tissue Processing: The harvested IFP tissue was cut into approximately 1 mm³ pieces under aseptic conditions [39].
- Enzymatic Digestion: The minced tissue was digested with 0.1% collagenase in serum-free media for 2 hours at 37°C with constant agitation [39].
- Cell Collection: The digested tissue was centrifuged at 300 ×g for 10 minutes. The resulting cell pellet was washed with PBS, filtered through a 100 μm strainer, and centrifuged again [39].
- Initial Plating: The cell pellet was resuspended in a standard MSC medium or directly in a GMP-compliant medium and seeded in a culture vessel [39].
Expansion of FPMSCs
- Subculture: Cells were passaged at 80–90% confluency and seeded at a density of 5 × 10³ cells/cm² [39].
- GMP Media Comparison: The study optimized culture conditions by comparing two animal component-free media: MesenCult-ACF Plus Medium and MSC-Brew GMP Medium, against standard MSC media [46] [39].
- Process Validation: The isolation and expansion process was repeated using cells from four additional donors in a GMP-accredited facility to validate robustness and reproducibility [46].
Analytical Methods and Quality Control Assays
Quality control is paramount in GMP manufacturing. The following assays were used to characterize the final cell product and ensure it met pre-defined release specifications [92].
- Cell Doubling Time: Calculated over three passages using the formula:
Doubling Time = (duration * ln(2)) / ln(final concentration / initial concentration)[39]. - Colony-Forming Unit (CFU) Assay: Cells were seeded at low densities (20, 50, 100, and 500 cells per dish) and cultured for 10 days. Colonies were fixed and stained with Crystal Violet to assess clonogenic potential, a indicator of potency [46] [39].
- Flow Cytometry: Cells at the third passage were analyzed for MSC surface markers using a human MSC analysis kit. Purity was defined by the percentage of cells positive for CD73, CD90, and CD105, and negative for CD45 [46] [39].
- Viability and Sterility Testing:
- Viability: Assessed using Trypan Blue exclusion. A viability of >95% was consistently achieved against a minimum requirement of >70% [46].
- Sterility: Tests for bacterial (e.g., Bact/Alert) and mycoplasma contamination were performed [46].
- Endotoxin: Endotoxin levels were measured to ensure safety [46].
- Stability and Storage: The final cell product was cryopreserved. Stability was assessed post-thaw, with viability and sterility checked after extended storage (up to 180 days) to determine shelf-life [46].
The following workflow diagram illustrates the complete GMP protocol from tissue collection to final product release.
Results and Data Analysis
Quantitative Assessment of Media Performance
The comparison of culture media revealed that MSC-Brew GMP Medium significantly enhanced FPMSC proliferation and potency compared to standard media and another animal-free formulation.
Table 2: Functional Comparison of Culture Media on FPMSCs
| Culture Medium | Doubling Time | Colony Formation | MSC Marker Expression (%) |
|---|---|---|---|
| Standard MSC Media | Higher | Lower | >95% [46] |
| MesenCult-ACF Plus | Intermediate | Intermediate | >95% [46] |
| MSC-Brew GMP Medium | Lower (indicating faster proliferation) | Higher (indicating enhanced potency) | >95% [46] [39] |
Quality Control and Product Release Specifications
The GMP-validation data, encompassing cells from multiple donors, confirmed that the final FPMSC product consistently met all pre-defined release criteria.
Table 3: Final Product Release Specifications and Results
| Quality Attribute | Test Method | Release Specification | Validation Result |
|---|---|---|---|
| Viability | Trypan Blue | >70% | >95% [46] |
| Sterility | Bact/Alert | No contamination | Sterile [46] |
| Mycoplasma | Mycoplasma Assay | Absent | Absent [46] |
| Endotoxin | Endotoxin Assay | Below threshold | Below threshold [46] |
| Phenotype (Identity) | Flow Cytometry | CD45-/CD73+/CD90+/CD105+ | Expression maintained post-thaw [46] |
| Stability | Post-thaw assessment after 180 days | Maintains viability and sterility | Viability and sterility maintained [46] |
Discussion
This case study successfully demonstrates the feasibility of a robust, reproducible, and GMP-compliant protocol for producing clinical-grade FPMSCs. The use of MSC-Brew GMP Medium was critical, as it reliably supported higher proliferation rates and clonogenic capacity, which are essential for generating sufficient cell numbers for therapy while maintaining functional potency [46] [39].
A cornerstone of GMP is quality by design (QbD), where quality is built into the product through rigorous process design and control, rather than merely tested at the end [93]. This study embodies this principle by:
- Defining Critical Process Parameters: Seeding density, passage confluency, and specific enzyme use were standardized [39].
- Establishing Critical Quality Attributes (CQAs): Viability, purity, sterility, and potency were identified as key CQAs and monitored throughout [46] [92].
- Implementing Analytical Method Validation: The test methods used (e.g., flow cytometry, sterility tests) were validated to ensure they consistently produced reliable results confirming the CQAs [92].
The protocol's validation across multiple donors confirms its robustness and is a critical step for regulatory approval. Furthermore, the stability of the cryopreserved final product for up to 180 days provides essential flexibility for clinical logistics [46]. This work serves as a foundational template for the translational application of FPMSCs, paving the way for clinical trials targeting inflammatory joint diseases, osteoarthritis, and other conditions amenable to MSC-based therapies [94].
Mesenchymal stem cells (MSCs) have emerged as a cornerstone of regenerative medicine and cell-based therapeutics, offering significant potential for treating a wide spectrum of diseases due to their multi-lineage differentiation capacity, immunomodulatory properties, and paracrine activity [95]. For clinical applications, the selection of an optimal MSC source is a critical determinant of therapeutic success, particularly within the framework of Good Manufacturing Practice (GMP) protocols required for producing clinical-grade cells [96] [97]. This application note provides a systematic comparison of three principal MSC sources—Bone Marrow (BM), Adipose Tissue (AT), and Umbilical Cord Blood (UCB)—evaluating their biological characteristics, expansion potential, and functional properties to inform strategic decision-making for therapeutic development. We present standardized protocols for their isolation, characterization, and GMP-compliant expansion to support researchers and drug development professionals in translating MSC therapies from bench to bedside.
Biological Characteristics and Phenotype
MSCs from BM, AT, and UCB share fundamental characteristics as defined by the International Society for Cellular Therapy (ISCT) criteria, including fibroblastoid morphology, plastic adherence, and a specific surface antigen profile [95]. They are consistently positive for CD29, CD44, CD73, CD90, CD105, and HLA-ABC, and negative for hematopoietic markers (CD14, CD19, CD34, CD45, CD79a) and HLA-DR [95]. Despite these similarities, subtle differences in their biological properties and gene expression profiles can influence their suitability for specific clinical applications, particularly when cultured in serum-free media (SFM) compliant with GMP standards [98].
Proliferation Capacity and Senescence
A critical differentiator among MSC sources is their expansion potential, a key consideration for generating clinically relevant cell numbers.
Table 1: Proliferation and Senescence Characteristics of MSCs from Different Sources
| Parameter | Bone Marrow (BM) | Adipose Tissue (AT) | Umbilical Cord Blood (UCB) |
|---|---|---|---|
| Culture Longevity | Growth arrest at Passage 11-12 [95] | Growth arrest at Passage 11-12; shortest culture time [95] | Growth arrest at Passage 14-16; significantly longer culture periods [95] |
| Population Doubling Time | Longer PDT [95] | Intermediate PDT [95] | Shortest PDT, indicating highest proliferation rate [95] |
| Clonogenicity (CFU-F Assay) | 16.5 ± 4.4 colonies [95] | 6.4 ± 1.6 colonies [95] | 23.7 ± 5.8 colonies [95] |
| Senescence Markers | High expression of p53, p21, and p16 in late passages [95] | High expression of p53, p21, and p16 in late passages [95] | Significantly lower expression of p53, p21, and p16 [95] |
| Senescence-Associated β-Galactosidase (Passage 6) | ~11% positive cells [95] | ~13% positive cells [95] | Almost no positive cells [95] |
UCB-MSCs demonstrate a clear superiority in proliferation and resistance to senescence, characterized by the highest colony-forming capacity, longest culture duration, and minimal expression of aging-related proteins [95]. This "younger" phenotype makes them particularly suitable for extensive expansion in GMP processes.
Differentiation Potential
The trilineage differentiation potential is a defining functional property of MSCs. While all three sources can differentiate into osteogenic, chondrogenic, and adipogenic lineages, their efficacy varies.
Table 2: Differentiation Potential of MSCs from Different Sources
| Lineage | Bone Marrow (BM) | Adipose Tissue (AT) | Umbilical Cord Blood (UCB) |
|---|---|---|---|
| Osteogenesis | Effective [95] | Effective [95] | Effective [95] |
| Chondrogenesis | Effective [95] | Effective [95] | Effective [95] |
| Adipogenesis | Effective [95] | Effective [95] | Variable; some studies report no adipogenic capacity [99] |
It is noteworthy that the differentiation potential can be influenced by the culture medium, with studies showing that under defined SFM, MSCs from neonatal tissues (like amniotic membrane and chorionic plate) exhibit varying efficiencies in osteogenic and adipogenic differentiation [98].
Secretome and Anti-inflammatory Properties
The therapeutic benefits of MSCs are largely attributed to their paracrine activity. Comparative studies using co-culture models with LPS-activated macrophages demonstrate that UCB-MSCs exhibit superior anti-inflammatory effects, significantly reducing the secretion of pro-inflammatory cytokines such as IL-1α, IL-6, and IL-8 [95]. This effect has been linked, in part, to the secretion of Angiopoietin-1 (Ang-1) by UCB-MSCs [95]. The potency of the secretome also forms the basis for developing exosome-based therapies, with UCB-MSC-released exosomes showing efficacy in promoting wound healing by enhancing skin cell proliferation, migration, and suppressing inflammation [100].
GMP Manufacturing Protocols
Workflow for Clinical-Grade MSC Production
The transition from research-grade to clinical-grade MSCs requires a meticulously controlled and documented process in accordance with GMP guidelines for Advanced Therapy Medicinal Products (ATMPs) [96] [97]. The following workflow outlines the critical stages from donor selection to final product release.
Detailed Experimental Protocols
This standardized protocol can be adapted for BM, AT, or UCB, with source-specific modifications.
I. Materials and Reagents
- Tissue Source: BM aspirate, lipoaspirate (AT), or umbilical cord blood.
- Transport Medium: Cold, sterile Dulbecco's Phosphate Buffered Saline (DPBS) with antibiotics.
- Digestion Solution: GMP-grade Collagenase (e.g., 0.1% for AT and UCB) [95] [39].
- Culture Medium: GMP-compliant, xeno-free medium (e.g., MSC-Brew GMP Medium, MesenCult-ACF Plus Medium, or MSCGM-CD) [39] [98].
- Culture Vessels: T-flasks or multi-layer bioreactors for expansion.
II. Method
- Tissue Collection and Transport: Aseptically collect tissue and transport to the GMP facility in a qualified shipping container with temperature monitoring [96].
- Processing and Isolation:
- Bone Marrow: Isolate mononuclear cells (MNCs) using Ficoll density gradient centrifugation. Seed MNCs directly in culture medium [101].
- Adipose Tissue: Mince tissue into small pieces (~1 mm³). Digest with 0.1% GMP-grade collagenase in serum-free media for 2 hours at 37°C with agitation. Centrifuge (300 ×g, 10 min) to separate the stromal vascular fraction (SVF) pellet from adipocytes. Wash pellet with PBS and filter through a 100 μm filter [39].
- Umbilical Cord Blood: Process using Ficoll density gradient centrifugation to isolate MNCs. Seed MNCs directly in culture medium. Note: Success rate for isolation can be variable [100] [99].
- Initial Culture: Resuspend the cell pellet from any source in pre-warmed GMP-compliant culture medium. Seed cells at a density of 5 × 10³ to 1 × 10⁴ cells/cm² in culture vessels. Maintain at 37°C in a 5% CO₂ humidified incubator [39] [98].
- Medium Changes and Passaging: Perform the first medium change after 72-96 hours to remove non-adherent cells. Thereafter, change medium every 2-3 days. When cultures reach 80-90% confluence, passage cells using a GMP-grade dissociation agent (e.g., TrypLE Express). A standard seeding density for expansion is 5 × 10³ cells/cm² [39] [98].
Protocol: Characterization and Quality Control for GMP Release
All quality control assays must be validated for GMP compliance.
I. Immunophenotyping by Flow Cytometry
- Sample Preparation: Harvest P3-P5 MSCs and wash with FACS buffer (PBS with 0.5% FBS).
- Staining: Incubate cells with fluorescently conjugated antibodies against CD73, CD90, CD105, CD45, CD34, CD14 or CD11b, CD19, and HLA-DR for 1 hour at room temperature, protected from light [95] [100].
- Analysis: Wash cells and analyze on a flow cytometer (e.g., CytoFLEX). A population is considered positive if ≥95% of cells express CD73, CD90, and CD105, and ≤5% express hematopoietic markers [95].
II. Trilineage Differentiation Assay Use a commercially available GMP-compliant differentiation kit or prepare media with GMP-grade components.
- Adipogenic Differentiation: Culture confluent MSCs in adipogenic induction medium for 14-21 days. Fix cells and stain lipid droplets with Oil Red O [98] [100].
- Osteogenic Differentiation: Culture subconfluent MSCs (~50-70%) in osteogenic induction medium for 14-21 days. Fix cells and stain calcium deposits with Alizarin Red S [98] [100].
- Chondrogenic Differentiation: Pellet 2.5 × 10⁵ MSCs in a conical tube and culture in chondrogenic induction medium for 21 days. Fix the pellet, section, and stain proteoglycans with Alcian Blue [98] [100].
III. Proliferation and Senescence Assays
- Population Doubling Time (PDT): Calculate at each passage using the formula:
Doubling Time = (duration * ln2) / ln(final concentration / initial concentration)[39]. - Colony Forming Unit (CFU-F) Assay: Seed low densities of MSCs (e.g., 20-500 cells per dish) and culture for 10-14 days. Fix and stain colonies with Crystal Violet. Count colonies containing >50 cells [95] [39].
- Senescence-Associated β-Galactosidase (SA-β-Gal) Staining: Perform using a commercial kit according to the manufacturer's instructions. Count blue-stained cells as senescent [95].
The Scientist's Toolkit: Essential GMP-Compliant Reagents
Table 3: Key Reagent Solutions for GMP-Compliant MSC Manufacturing
| Reagent Category | Example Products | Function & Importance |
|---|---|---|
| Xeno-Free Culture Media | MSC-Brew GMP Medium (Miltenyi Biotec), MesenCult-ACF Plus Medium (StemCell Technologies), MSCGM-CD (Lonza) [39] [98] | Provides a defined, animal-component-free environment for MSC expansion, eliminating risks of xenogeneic immunogenicity and pathogen transmission. Essential for clinical safety. |
| GMP-Grade Dissociation Agents | TrypLE Express (Thermo Fisher) [98] | A recombinant enzyme alternative to trypsin for cell passaging. Ensures a controlled, animal-origin-free process, enhancing product consistency and safety. |
| Cell Bank Cryopreservation Media | Formulations with Human Serum Albumin (HSA) and DMSO-free cryoprotectants [97] | Protects cell viability and functionality during freeze-thaw. Defined, xeno-free cryomedium reduces lot-to-late variability and improves post-thaw recovery for "off-the-shelf" products. |
| Characterization Kits | BD Stemflow Human MSC Analysis Kit (BD Biosciences) [39] | Provides standardized, validated antibodies and protocols for flow cytometric analysis of MSC surface markers, ensuring consistent identity testing and quality control. |
| Differentiation Kits | Human Mesenchymal Stem Cell Functional Identification Kit (R&D Systems) [98] | Offers GMP-compliant, standardized media for trilineage differentiation, enabling reliable potency assessment and functional validation of the MSC product. |
The comparative analysis presented in this application note underscores that while BM, AT, and UCB-derived MSCs meet the minimal criteria for MSCs, they possess distinct biological and manufacturing profiles. UCB-MSCs offer superior proliferative capacity, delayed senescence, and potent anti-inflammatory paracrine activity, making them a highly attractive source for allogeneic, "off-the-shelf" therapies requiring large-scale expansion [95]. AT represents a highly accessible source with a high frequency of MSCs, suitable for both autologous and allogeneic approaches [102]. BM-MSCs, the historical gold standard, remain a viable option but are limited by invasive harvesting and donor age-related variability [39].
The successful translation of these cell sources into therapies is contingent upon rigorous adherence to GMP manufacturing protocols, from donor selection and xeno-free culture to comprehensive quality control. The choice of MSC source should be strategically aligned with the target clinical indication, desired mechanism of action (e.g., direct differentiation vs. paracrine effects), and the practical constraints of production scalability. By implementing the standardized protocols and quality frameworks outlined herein, researchers and clinicians can advance the development of safe, efficacious, and consistent MSC-based ATMPs.
The transition from research to clinical-grade stem cell manufacturing necessitates rigorous benchmarking of culture media to ensure optimal performance in cell proliferation, potency, and differentiation potential. This application note provides a standardized framework for evaluating culture media using quantitative metrics and detailed protocols. Within the context of Good Manufacturing Practice (GMP) for clinical-grade stem cells, we summarize critical performance data across diverse media formulations, outline step-by-step experimental methodologies for assessment, and visualize key signaling pathways and workflows. Our findings indicate that defined, xeno-free media formulations significantly enhance differentiation consistency and reduce lot-to-lot variation, which is paramount for clinical manufacturing scale-up.
Culture media composition is a critical determinant of stem cell fate, influencing self-renewal, proliferation, and differentiation efficacy. In GMP manufacturing, the shift from ill-defined, serum-containing supplements to chemically defined, xeno-free formulations is essential to minimize immunogenic contamination and ensure batch-to-batch consistency [29] [103]. This document establishes a standardized benchmarking approach to evaluate media performance using quantitative metrics for proliferation and potency, providing researchers and drug development professionals with validated protocols for seamless transition into clinical manufacturing workflows.
Results and Data Presentation
Quantitative Media Performance Benchmarking
The following tables consolidate quantitative data from recent studies on culture media performance for different stem cell types, highlighting key metrics for proliferation and functional potency.
Table 1: Performance of GMP-Grade Stem Cell Media in Proliferation and Differentiation
| Media Type | Cell Type | Key Performance Metrics | Outcome |
|---|---|---|---|
| StemFit for Differentiation (GMP) [29] | Human iPSC/ESC | Chemically defined, animal component-free differentiation | "Unmatched differentiation," high consistency, minimal lot-to-lot variation |
| MSC-Brew GMP Medium [46] | Infrapatellar Fat Pad MSCs (FPMSCs) | Doubling time, Colony Forming Unit (CFU) assay | Lower doubling times across passages, higher colony formation indicating enhanced proliferation and potency |
| DMEM + 15% FBS [104] | Porcine Male Gonocytes | Gonocyte count after 28 days | Greatest number of gonocytes (P < 0.001) |
| DMEM + 5% FBS + 10% KSR [104] | Porcine Male Gonocytes | Colony diameter and number after 28 days | Largest diameter and greatest number of colonies (P < 0.001) |
Table 2: Influence of Media on Mesenchymal Stromal Cell (MSC) Characteristics [105]
| Culture Medium | MSC Yield/1000 MNCs | Growth Index | Effect on Surface Markers | Chondrogenic Differentiation (GAG/DNA) |
|---|---|---|---|---|
| Medium A (DMEM-LG + 10% FCS) | Varied significantly | Varied significantly | Significant influence on CD10, CD90, CD105, CD140b, CD146, STRO-1 | Superior |
| Medium B (αMEM + 10% FCS) | Varied significantly | Varied significantly | Significant influence on CD10, CD90, CD105, CD140b, CD146, STRO-1 | Not Superior |
| Medium C ("Verfaillie" variant) | Varied significantly | Varied significantly | Significant influence on CD10, CD90, CD105, CD140b, CD146, STRO-1 | Not Superior |
| Medium D ("Bernese" variant) | Varied significantly | Varied significantly | Significant influence on CD10, CD90, CD105, CD140b, CD146, STRO-1 | Not Superior |
Signaling Pathways in Stem Cell Fate
Culture media supplements activate specific signaling pathways to direct stem cell fate. The diagram below illustrates the core pathways involved in maintaining pluripotency and driving differentiation, which are critical for assessing media potency.
Experimental Protocols
Protocol: Benchmarking Media for MSC Proliferation and Potency
This protocol outlines the steps for comparing different culture media using bone marrow-derived mesenchymal stromal cells (BM-MSCs), adapted from a published study [105].
3.1.1 Reagents and Equipment
- Cell Source: Human bone marrow aspirates.
- Culture Media: Media A (DMEM-LG + 10% FCS), B (αMEM + 10% FCS), C ("Verfaillie" variant), D ("Bernese" variant) [105].
- Supplements: Fetal Calf Serum (FCS), Penicillin/Streptomycin, growth factors (PDGF-BB, EGF, TGF-β1, FGF-2) as per media formulations.
- Equipment: T75 cm² cell culture flasks, humidified CO₂ incubator (37°C, 6% CO₂), centrifuge.
3.1.2 Step-by-Step Procedure
- Isolation of Mononuclear Cells (MNCs):
- Dilute bone marrow 1:1 with isotonic saline solution containing heparin.
- Isolate MNCs using Ficoll-Paque PLUS density gradient centrifugation.
- Resuspend the MNC pellet in the four different test media at a density of 5 × 10⁵ cells/cm² in T75 flasks.
Cell Expansion and Passaging:
- After 24 hours, discard non-adherent cells.
- Replace the medium every 72 hours.
- Monitor cultures daily via phase-contrast microscopy.
- Upon reaching 80% confluence, detach cells with trypsin/EDTA, count using trypan blue exclusion, and reseed for subsequent passages. Repeat until Passage 4 (P4).
Data Collection and Analysis:
- MSC Yield: Calculate the number of MSCs at P0 per 1000 seeded MNCs.
- Growth Index: Determine at each passage as (number of cells before passage) / (number of cells after passage).
- Surface Marker Analysis: At P4, analyze expression of CD105, CD73, CD90, and absence of hematopoietic markers (CD45, CD34, CD14, CD11b) by flow cytometry.
- Chondrogenic Differentiation: In P4, pellet 5 × 10⁵ cells and induce chondrogenesis for 21-28 days. Quantify glycosaminoglycan (GAG) content using a DMMB assay and normalize to DNA content (PicoGreen assay).
Protocol: Validating GMP-Compliant, Animal Component-Free Media
This protocol describes methods for validating GMP-grade media like StemFit or MSC-Brew for clinical manufacturing [29] [46].
3.2.1 Reagents and Equipment
- Cell Lines: Human iPSCs or MSCs.
- GMP Media: StemFit Basic03/Basic04 CT or MSC-Brew GMP Medium.
- Key Proteins: GMP-grade bFGF, Activin A.
- Equipment: Bioreactors (for scaled-up processes), cryopreservation equipment.
3.2.2 Step-by-Step Procedure
- Cell Thawing and Seeding:
- Rapidly thaw cryopreserved iPSCs or MSCs in a 37°C water bath.
- Seed cells onto GMP-compliant, defined matrices in pre-warmed GMP-grade media.
Maintenance and Passaging:
- Culture cells under standard conditions (37°C, 5% CO₂).
- For iPSCs, passage colonies using EDTA or enzyme-free dissociation reagents when they reach 70-80% confluence.
- For MSCs, passage at 80-90% confluence using trypsin/EDTA.
Assessment of Proliferation and Karyotype:
- Population Doubling Time: Calculate over multiple passages using cell counts.
- Cell Viability: Assess using trypan blue exclusion (>95% viability is required for clinical release [46]).
- Genomic Stability: Perform G-band karyotyping and Next-Generation Sequencing (NGS)-based oncogenetic analysis at predetermined passages (e.g., P10+).
Assessment of Potency and Differentiation:
- Pluripotency Markers (for iPSCs): Confirm expression of OCT4, SOX2, NANOG via flow cytometry or immunocytochemistry.
- Trilineage Differentiation (for MSCs): Direct cells towards osteogenic, adipogenic, and chondrogenic lineages and confirm using lineage-specific stains (Alizarin Red, Oil Red O, Alcian Blue/Safranin O, respectively).
- Functional Differentiation (for iPSCs): Perform directed differentiation into target cells (e.g., neural cells, cardiomyocytes) and characterize using functional assays and marker expression.
The experimental workflow for the above protocols is summarized in the following diagram:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for GMP-Compliant Stem Cell Culture
| Reagent / Material | Function / Description | Example Use-Case |
|---|---|---|
| Chemically Defined Media (e.g., StemFit) [29] | Base medium formulation; xeno-free, chemically defined to ensure consistency and safety. | Maintenance and differentiation of human iPSCs/ESCs for clinical applications. |
| GMP-Grade Growth Factors (e.g., bFGF, Activin A) [29] | Key signaling molecules to direct stem cell fate (self-renewal or differentiation). | Added to defined media to maintain pluripotency (bFGF) or direct differentiation (Activin A). |
| Knockout Serum Replacement (KSR) [104] | Defined serum replacement to reduce batch variability and animal component use. | Used in combination with basal media like DMEM for feeder-free cultures of sensitive stem cells. |
| Human Platelet Lysate (PL) [106] | Animal-free supplement rich in growth factors, supporting high proliferation rates. | Expansion of Mesenchymal Stem Cells (MSCs) as a replacement for Fetal Bovine Serum (FBS). |
| ROCK Inhibitor (Y-27632) [103] | Small molecule that inhibits apoptosis, enhancing survival of dissociated stem cells. | Added to culture medium for 24 hours after passaging to improve single-cell survival and cloning efficiency. |
| GMP-Compliant Dissociation Reagents | Enzymatic or non-enzymatic solutions for cell passaging, manufactured under GMP standards. | Used for detaching adherent stem cell cultures while maintaining cell viability and phenotype. |
Implementation in GMP Manufacturing
Integrating benchmarked media into GMP workflows requires a strategic approach. Prioritize media that are available exclusively as GMP-grade to eliminate protocol requalification during technology transfer [29]. Implement raw material control strategies using GMP-produced supplements like Stemline media and cytokines [107]. Ensure comprehensive quality control (QC) testing for each cell bank, including viability (>95%), sterility, mycoplasma, endotoxin, identity (flow cytometry), and karyotypic stability [61] [46]. Finally, establish a master cell bank using a validated, exclusive stem cell clone to ensure long-term product consistency and regulatory compliance [61].
Stability Studies and Determining Shelf-Life for Final Cell Products
For clinical-grade stem cell therapies, demonstrating product stability throughout the shelf life is a mandatory regulatory requirement to ensure safety, identity, purity, potency, and viability until patient administration [108] [109]. Stability studies provide the scientific data to define appropriate storage conditions, shelf life, and expiration dates, forming a critical part of the Chemistry, Manufacturing, and Controls (CMC) section for Investigational New Drug (IND) applications and marketing authorizations [110] [109]. Unlike traditional pharmaceuticals, cell therapy products (CTPs) are living, dynamic systems that cannot be terminally sterilized and are highly sensitive to environmental stresses during storage and transport [110] [108]. This application note details a risk-based, GMP-compliant framework for designing and executing stability studies for final stem cell products, providing standardized protocols to generate defensible data for regulatory submissions.
Regulatory Framework and Critical Definitions
Foundational Regulations
Stability testing programs must comply with international GMP regulations and guidelines:
- US FDA: 21 CFR 211.166 mandates a written stability testing program with defined sample size, test intervals, storage conditions, and validated methods [109].
- International Council for Harmonisation (ICH): Q1A(R2) to Q1F guidelines provide a global framework for stability testing protocols [109].
- European Medicines Agency (EMA): Requires an ongoing stability program to monitor products over their entire shelf life [109].
A stability-indicating method is an analytical procedure that accurately and reliably measures active ingredients, degradation products, and impurities without interference.
Stability Study Types
- Real-Time Stability Studies: Products are stored under recommended long-term storage conditions and monitored to determine the intended shelf life. This provides the most reliable data but is time-consuming [111] [112].
- Accelerated Stability Studies: Products are stored under exaggerated stress conditions (e.g., elevated temperature) to rapidly predict stability and identify potential degradation pathways [111] [110].
- Ongoing Stability Studies: After market approval or clinical trial initiation, this program monitors products throughout their shelf life to verify that they remain within specifications under labeled storage conditions [109].
Designing the Stability Study Program
Risk-Based Approach to Study Design
A successful stability program begins with a systematic risk assessment addressing product-, process-, and patient-related factors [108]. Key risk considerations include:
- Cell Origin: Autologous vs. allogeneic products present different stability and handling risks.
- Product Formulation: Cryopreserved vs. fresh liquid formulations have vastly different stability profiles and testing requirements.
- Storage Conditions: Sensitivity to temperature deviations, light, and container closure systems must be evaluated.
- Administration Route: This influences sterility and impurity requirements.
Defining Critical Quality Attributes (CQAs) and Stability-Indicating Assays
Stability testing must monitor CQAs most likely to change during storage and impact product quality. For stem cell products, these typically include the attributes outlined in Table 1.
Table 1: Essential Critical Quality Attributes (CQAs) and Stability Testing Methods for Cell Therapy Products
| Quality Attribute | Stability-Indicating Assay | Acceptance Criteria (Example) | Testing Frequency |
|---|---|---|---|
| Viability | Flow cytometry (e.g., 7-AAD), membrane integrity assays | ≥ 70% post-thaw viability | Each time point |
| Potency/Biological Activity | Cell-specific bioassays (e.g., differentiation, cytokine secretion) | Maintain pre-defined potency range vs. reference standard | Key time points (T0, Tmid, Tend) |
| Cell Identity/Purity | Flow cytometry (surface markers), PCR, NGS | ≥ 90% positive for lineage-specific markers | Each time point |
| Safety: Sterility | BacT/ALERT, microbial culture | No microbial growth | Each time point (or validated alternative) |
| Safety: Mycoplasma | PCR-based or culture methods | Not detected | Key time points |
| Safety: Endotoxin | LAL assay | ≤ 5 EU/kg/hr (product-specific) | Each time point |
| Vector Copy Number (for genetically modified cells) | qPCR/digital PCR | Within validated range, no significant increase | Key time points |
The Multi-Attribute Method (MAM), which uses advanced analytics to monitor multiple CQAs simultaneously from a single sample, is emerging as a powerful approach for complex biologics and can be integrated with next-generation sequencing (NGS) for comprehensive genetic stability assessment [113].
Stability Study Protocol and Storage Conditions
A written stability protocol must define [109]:
- Batch Selection and Number: A minimum of three batches representative of the manufacturing process and final product formulation should be placed on stability. Batches should be from different donors (allogeneic) or manufacturing runs.
- Container Closure System: Testing must use the identical primary packaging (vials, bags) intended for the final product.
- Storage Conditions and Test Intervals: Based on ICH guidelines, with time points designed to support the proposed shelf life. Table 2 provides a standard schedule for a cryopreserved cell product.
Table 2: Example Stability Study Schedule for a Cryopreserved Allogeneic Cell Product
| Study Type | Storage Condition | Proposed Shelf Life | Testing Time Points |
|---|---|---|---|
| Real-Time | ≤ -150°C (Vapor phase LN2) | 24 months | 0, 3, 6, 9, 12, 18, 24 months |
| Accelerated | -80°C | Predictive | 0, 1, 2, 3, 6 months |
| Transport Simulation | Dry Ice / Shipping Conditions | N/A | Pre- and post-shipment (e.g., 48h on dry ice) |
For liquid storage products (e.g., stored at 2-8°C), real-time studies should be conducted at the recommended storage temperature, while accelerated studies might include room temperature (e.g., 25°C/60% RH) and elevated temperatures (e.g., 37°C) [110].
The following workflow diagram outlines the key stages in designing and executing a GMP-compliant stability study program.
Detailed Experimental Protocols
Protocol 1: Post-Thaw Viability and Potency Assessment
This protocol is critical for cryopreserved cell products to confirm stability after the freeze-thaw process, a key stress event.
Methodology:
- Thawing: Rapidly thaw a stability sample vial in a 37°C water bath until only a small ice crystal remains.
- Dilution: Slowly dilute the cell suspension 1:10 with pre-warmed, GMP-grade cell culture media containing a protective agent like human serum albumin.
- Viability & Cell Count: Mix a sample of the cell suspension 1:1 with Trypan Blue. Count live (unstained) and dead (blue) cells using an automated cell counter or hemocytometer. Calculate viability:
% Viability = (Live Cell Count / Total Cell Count) * 100. - Potency Assay (Example: Differentiation Capacity): Plate the thawed cells at a specified density (e.g., 10,000 cells/cm²) in differentiation-inducing media (e.g., GMP-grade media supplemented with specific growth factors). Culture for a defined period (e.g., 14-21 days), refreshing media every 2-3 days. Analyze resulting differentiated cells via flow cytometry for lineage-specific markers or quantify a specific secreted functional factor (e.g., IDS enzyme activity for MPSII [35]).
Quality Control: Include a pre-qualified reference standard cell sample in each assay run to control for inter-assay variability.
Protocol 2: Stability-Indicating Identity and Purity Assay via Flow Cytometry
This protocol verifies that the cell population maintains its identity and purity throughout the shelf life.
Methodology:
- Sample Preparation: Aliquot a defined number of cells (e.g., 1x10^6) from the stability time point sample into flow cytometry tubes.
- Staining: Centrifuge cells and resuspend in flow cytometry buffer. Add fluorescently conjugated antibodies against target surface markers (e.g., CD34 for HSCs, CD73/CD90/CD105 for MSCs) and appropriate isotype controls. Incubate for 30 minutes in the dark at 4°C.
- Washing and Fixation: Wash cells twice with buffer to remove unbound antibody. Resuspend in a fixation buffer (e.g., 1-4% paraformaldehyde) if analysis is not immediate.
- Acquisition and Analysis: Acquire data on a flow cytometer calibrated with standard fluorescence beads. Analyze data to determine the percentage of cells positive for the specific identity markers.
Protocol 3: Sterility Testing with Rapid Microbiology Methods
Given the short shelf life of some fresh cell products, rapid methods are advantageous.
Methodology (Using BacT/ALERT Culture System):
- Sample Inoculation: Aseptically transfer a specified volume of the cell product (as per validated method, e.g., 1-5 mL) into both BacT/ALERT iAST (aerobic) and iNST (anaerobic) culture bottles.
- Incubation and Monitoring: Load the bottles into the BacT/ALERT instrument, which incubates them at 35±1.5°C and continuously monitors for CO2 production, a sign of microbial growth.
- Result Interpretation: The system flags positive samples. A sample is considered sterile only if no growth is detected throughout the validated incubation period (e.g., 7-14 days). Any positive result must trigger an Out-of-Specification (OOS) investigation [109].
Data Analysis, Shelf-Life Determination, and Regulatory Documentation
Statistical Analysis and Shelf-Life Calculation
For quantitative CQAs like viability and potency, shelf life is determined by assessing the confidence limits of the regression line fitted to the stability data. The expiration date is the point at which the one-sided 95% confidence limit for the mean intercepts the acceptable lower specification limit [111]. For CQAs with a defined limit (e.g., sterility), shelf life is the duration during which the product consistently meets this limit. Data from accelerated studies can support the proposed shelf life by providing early insights into degradation patterns, often using models like the Arrhenius equation [112].
Handling Out-of-Specification (OOS) Results
Any OOS result obtained during stability testing must be investigated per a predefined OOS procedure [109]. The investigation must determine if the OOS is due to a laboratory error, a stability study execution error, or a true product failure. Failure to adequately investigate OOS stability results is a common finding in FDA Warning Letters [109].
Stability Report and Regulatory Submission
The stability report for a regulatory submission must include [109]:
- Executive Summary with proposed shelf life and storage conditions.
- Detailed Protocol describing all aspects of the study design.
- Complete Data Tables for all batches and all CQAs at every time point.
- Graphical Representations of data trends for key CQAs.
- Statistical Analysis and justification for the proposed shelf life.
- Conclusions linking the data to the proposed shelf life and label claims.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Cell Product Stability Studies
| Reagent/Material | Function in Stability Studies | GMP-Grade Sourcing Example |
|---|---|---|
| Cryopreservation Media | Formulated solutions (e.g., with DMSO) to maintain cell viability and function during freeze-thaw cycles and long-term storage. | Commercial GMP-grade cryomedium. |
| Cell Culture Media & Supplements | Serum-free, xeno-free media and defined growth factors (e.g., FGF, EGF, SCF, TPO) for post-thaw recovery and potency assays [28] [35]. | CTS Essential 8, X-VIVO 15, recombinant cytokines. |
| Flow Cytometry Antibodies | Panels of validated, fluorescently conjugated antibodies for assessing cell identity, purity, and activation status. | GMP-compliant, in-vivo diagnostic grade antibodies. |
| Cell-Based Potency Assay Kits | Validated kits for measuring specific biological functions (e.g., enzyme activity, differentiation capacity). | Custom-developed or commercially available GMP kits. |
| Rapid Microbiology Systems | Automated, validated systems (e.g., BacT/ALERT) for faster sterility testing of short-shelf-life products. | FDA-cleared/CE-marked instruments and culture bottles. |
| Validated PCR Assays | Tests for mycoplasma, adventitious viruses, and vector copy number (for genetically modified cells). | GMP-grade qPCR/dPCR kits and assays. |
The following diagram illustrates the interconnected testing framework for assessing the stability of a final cell product.
A robust, GMP-compliant stability program is non-negotiable for the successful clinical translation of stem cell therapies. It requires early planning, a science-driven risk assessment, and the use of validated, stability-indicating methods. By adopting the structured approach and detailed protocols outlined in this document, researchers and developers can generate high-quality data that convincingly demonstrates product stability, supports regulatory approvals, and, most importantly, ensures the delivery of a safe and potent therapy to patients.
Conclusion
The successful translation of stem cell therapies from research to clinic is fundamentally dependent on robust, reproducible, and compliant GMP manufacturing protocols. This requires an integrated approach, from meticulous raw material qualification and process control to comprehensive product validation. Key takeaways include the industry-wide shift to xeno-free culture systems, the critical need for standardized release criteria based on CQAs, and the increasing adoption of automation to enhance consistency. Future progress hinges on developing more precise potency assays, establishing greater regulatory harmonization across global markets, and continuing to innovate scalable manufacturing technologies. These advancements will be crucial for meeting the growing demand, evidenced by the stem cell manufacturing market's significant projected growth, and for delivering safe and effective therapies to patients worldwide.
References
- 1. of mesenchymal stromal/ Production according to stem ... cells good [https://stemcellres.biomedcentral.com/articles/10.1186/scrt217]
- 2. Considering Cell Therapy Product “Good Manufacturing Practice” Status - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936751/]
- 3. Current Good (cGMP) Facility... | SpringerLink Manufacturing Practice [https://link.springer.com/chapter/10.1007/978-981-16-7589-8_3]
- 4. Automated Manufacturing Processes and Platforms for Large-scale... [https://link.springer.com/article/10.1007/s12015-024-10812-5]
- 5. Overview of current adipose-derived stem (ADSCs) processing... cell [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02006-w]
- 6. Optimizing mesenchymal stem cell therapy: from isolation to GMP-compliant expansion for clinical application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054297/]
- 7. cGMP-Manufactured Human Induced Pluripotent Stem Cells Are Available for Pre-clinical and Clinical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4624993/]
- 8. Profile of Safety Manufactured... Good Manufacturing Practice [https://pubmed.ncbi.nlm.nih.gov/28887912/]
- 9. Regenerative medicine and regulation: what’s GMP got to do with it? | Eurostemcell [https://www.eurostemcell.org/regenerative-medicine-and-regulation-whats-gmp-got-do-it]
- 10. 5 Main Components of GMP : A Comprehensive Guide [https://www.scilife.io/blog/main-components-gmp]
- 11. Implementation of a quality management system for decentralized manufacturing of cell and gene therapy products - technical and regulatory considerations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361990/]
- 12. Top GMP and Guidelines for Best Practices 2025 [https://jafconsulting.com/top-gmp-guidelines-and-best-practices-for-2025/]
- 13. in Quality ... Management System Good Manufacturing Practice [https://www.gmpsop.com/quality-management-system-in-good-manufacturing-practice/]
- 14. -Compliant GMP ( Quality ): Definition... Management System QMS [https://simplerqms.com/quality-management-system-gmp/]
- 15. Key Components of GMP : A Practical ... - JAF Consulting, Inc. [https://jafconsulting.com/key-components-of-gmp-a-practical-implementation-guide/]
- 16. UC Davis Good Manufacturing Practice Laboratory [https://health.ucdavis.edu/stemcellresearch/gmp/]
- 17. Regulatory Support [https://www.stemcell.com/regulatory-support]
- 18. Florida's New Stem Laws: Unburdened by What Has... - JDSupra Cell [https://www.jdsupra.com/legalnews/florida-s-new-stem-cell-laws-unburdened-8674100/]
- 19. and Listing | Registration FDA [https://www.fda.gov/industry/fda-basics-industry/registration-and-listing]
- 20. Current Good Manufacturing Practice (CGMP) Regulations | FDA [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 21. FDA Issues New Guidance on Current Good Manufacturing Practices for Drugs | Advisories | Arnold & Porter [https://www.arnoldporter.com/en/perspectives/advisories/2025/01/fda-guidance-good-manufacturing-practices-for-drugs]
- 22. ISO 14971 - Wikipedia [https://en.wikipedia.org/wiki/ISO_14971]
- 23. ISO 14971: Risk Management for Medical Devices [Guide] [https://www.greenlight.guru/blog/iso-14971-risk-management]
- 24. — Guidelines Society for International Research Stem Cell [https://www.isscr.org/guidelines]
- 25. Standards for GMP in CGT Ancillary Materials Manufacturing [https://www.news-medical.net/whitepaper/20240222/What-are-the-US-and-EU-Compliance-Requirements-for-GMP-ancillary-materials-in-CGT-Manufacturing.aspx]
- 26. CMC considerations for CGT products [https://www.cardinalhealth.com/en/services/manufacturer/biopharmaceutical/drug-development-and-regulatory/resources-for-regulatory-consulting/cmc/cmc-considerations-for-cgt-products.html]
- 27. Risk-Based Approach in GMP - [https://pharmuni.com/2024/11/25/risk-based-approach-in-gmp/]
- 28. GMP-grade neural progenitor derivation and differentiation from clinical-grade human embryonic stem cells | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01915-0]
- 29. Defined stem media offers easy transition to cell ... clinical [https://engineering-update.co.uk/2025/03/11/defined-stem-cell-media-offers-easy-transition-to-clinical-manufacturing/]
- 30. Stem Cell Protocols: R&D Systems [https://www.rndsystems.com/protocol-types/stem-cell-protocols]
- 31. The Ultimate Guide to Cleanroom Standards: ISO vs GMP | Dalkia UK [https://dalkia.co.uk/news-insights/the-ultimate-guide-to-cleanroom-standards-iso-vs-gmp/]
- 32. - Allied cGMP Cleanrooms Cleanrooms [https://alliedcleanrooms.com/cleanrooms/cgmp-cleanrooms/]
- 33. Establishing a stem cell culture laboratory for clinical trials - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3459639/]
- 34. How to Design a GMP-Compliant Cleanroom Layout ( 2025 Pharma...) [https://www.pharmanow.live/pharma-manufacturing/cleanrooms-gmp-cleanroom-layout-guide]
- 35. Design and validation of a GMP for... stem cell manufacturing protocol [https://pmc.ncbi.nlm.nih.gov/articles/PMC11214401/]
- 36. Cleanroom Qualification And Validation In GMP | GMP Insiders [https://gmpinsiders.com/cleanroom-qualification-and-validation/]
- 37. CGMP Cleanroom | American Cleanroom Systems [https://www.americancleanrooms.com/cgmp-cleanroom/]
- 38. FDA Cleanroom Facilities & Equipment: cGMP Requirements - High-Tech Conversions [https://high-techconversions.com/fda-cleanroom-facilities-equipment-cgmp-requirements/]
- 39. Optimizing mesenchymal stem cell therapy: from isolation to GMP-compliant expansion for clinical application | BMC Molecular and Cell Biology | Full Text [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-025-00539-7]
- 40. for Allogenic Hemopoietic Donor Transplantation... Selection Stem Cell [https://pubmed.ncbi.nlm.nih.gov/28680446/]
- 41. A Decision-Making Approach for Children to Ethically Serve as Stem ... [https://link.springer.com/chapter/10.1007/978-3-031-04166-2_12]
- 42. and Enzymatic - non systems for adipose... enzymatic isolation [https://pubmed.ncbi.nlm.nih.gov/26435835/]
- 43. A GMP - compliant method for Wharton’s jelly-derived... manufacturing [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03725-0]
- 44. of mucosal epithelial cells and fibroblasts... GMP compliant isolation [https://www.nature.com/articles/s41598-021-91939-0?error=cookies_not_supported&code=523b6906-6023-4bfd-962e-a1802ab17966]
- 45. GMP Compliant Production of Therapeutic Components of Autologous Adipose Tissue | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-0716-4510-9_24]
- 46. Optimizing mesenchymal stem therapy: from isolation to... cell [https://pubmed.ncbi.nlm.nih.gov/40329219/]
- 47. Frontiers | GMP - compliant , serum-free cultures preserve therapeutic... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1633912/full]
- 48. Chaselection [https://www.chaselection.com/newsinfo/552.html]
- 49. Research Use Only to Good Manufacturing Practices | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/biotech-lab-solutions/biotech-learning-center/ruo-gmp-compliant-biologics.html]
- 50. 专用培养基|限定培养基|德国Sartorius赛多利斯 [https://www.sartorius.com.cn/products/cell-culture-media/specialty-media]
- 51. of human induced pluripotent Characterization : Current... stems cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9929203/]
- 52. View of Orthogonal approach and critical quality attributes for gene and... [https://rrpharmacology.ru/index.php/journal/article/view/738/629]
- 53. Bank Cell Guideline: Testing & Its Protocol Characterization [https://lifesciences.danaher.com/us/en/library/cell-bank-characterization.html]
- 54. Validation of an automated viable cell counting assay for GMP manufacturing of human induced pluripotent stem cells - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1369703X23001481]
- 55. - GMP neural progenitor derivation and differentiation from... grade [https://pubmed.ncbi.nlm.nih.gov/32948237/]
- 56. Establishing a GMP-compliant manufacturing process and phase-appropriate analytics for early development of a FiCAR T-cell product with a novel CAR spacer | Scientific Reports [https://www.nature.com/articles/s41598-025-92736-9]
- 57. De-risking the final , fill and finish step in formulation therapy... cell [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/1847/derisking-the-final-formulation-fill-and-finish-step-in-cell-therapy-manufacturing-considerations-for-an-automated-solution]
- 58. A Simple and Efficient Method of Slow Freezing for... | SpringerLink [https://link.springer.com/protocol/10.1007/7651_2015_211]
- 59. of Human Pluripotent Cryopreservation in Defined... Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4252050/]
- 60. for Cryopreserving PBMCs | Protocol Technologies STEMCELL [https://www.stemcell.com/how-to-cryopreserve-pbmcs.html]
- 61. iPSC Production Service: GMP - Clinical Human iPSCs and... grade [https://www.reprocell.com/clinical-stem-cell-services/gmp-ipsc-production]
- 62. Navigating Biopharma Services: GMP Storage Facilities and Cold Chain Logistics [https://www.tobinscientific.com/blog/navigating-biopharma-services-gmp-storage-facilities-and-cold-chain-logistics]
- 63. Your Guide to GMP Warehousing | Mercury [https://www.shipmercury.com/blog/march-2024/your-guide-to-gmp-warehousing]
- 64. Cold Chain Compliance: Essential Practices & Guidelines [https://www.elpro.com/en/learn/gdp-cold-chain-compliance]
- 65. Standard Requirement of a Microbiological Quality Control Program for the Manufacture of Human Mesenchymal Stem Cells for Clinical Use - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4015505/]
- 66. A practical approach for the validation of sterility, endotoxin and potency testing of bone marrow mononucleated cells used in cardiac regeneration in compliance with good manufacturing practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2753319/]
- 67. Preclinical Regulatory Validation of a 3-Stage Amniotic Mesenchymal... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2478751/]
- 68. A practical approach for gmp-compliant validation of real-time PCR method for mycoplasma detection in human mesenchymal stromal cells as advanced therapy medicinal product - PubMed [https://pubmed.ncbi.nlm.nih.gov/34362616/]
- 69. GMP Small Molecules for Stem Cell Therapy Workflows | Bio-Techne [https://www.bio-techne.com/gmp-products/gmp-small-molecules]
- 70. Reproducibility of GMP -compliant production of therapeutic stressed... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1524-2]
- 71. in tissue engineering: Why standardization matters... | Abcam Stem cells [https://www.abcam.com/en-us/stories/articles/stem-cells-in-tissue-engineering]
- 72. Hand-in-hand: good and stability studies manufacturing practice [https://www.iptonline.com/articles/hand-in-hand-good-manufacturing-practice-and-stability-studies]
- 73. Process Validation Protocol [https://www.webofpharma.com/2022/05/process-validation-protocol.html]
- 74. MCB Generation Services for iMSCs and MSCs: GMP and Clinical Grade [https://www.reprocell.com/clinical-stem-cell-services/gmp-imsc-and-msc-production]
- 75. Isolation and prolonged expansion of oral mesenchymal stem ... cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-017-0705-0]
- 76. The regulatory mechanism of cyclic GMP -AMP synthase on... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11265083/]
- 77. Pluripotent Stem Cell Culture Scale-Out - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK571710/]
- 78. ImmunoCult™: GMP - Manufactured Medium and T Cell Activators [https://www.stemcell.com/immunocult-for-t-cell-therapy-manufacturing]
- 79. Human platelet lysate to substitute fetal in hMSC... bovine serum [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02489-4]
- 80. Systematic review and meta-analysis on the use of human platelet... [https://pubmed.ncbi.nlm.nih.gov/35379348/]
- 81. Systematic review and meta-analysis on the use of human platelet... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02815-1]
- 82. , ultra-low IgG, US origin 500 mL | thermofisher.com Fetal Bovine Serum [https://www.thermofisher.com/order/catalog/product/16250078]
- 83. PLTMax® Human Platelet Lysate ( hPL ): A Superior Serum -Free... [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/stem-cell-culture/pltmax-human-platelet-lysate-mesecnhymal-stem-cell]
- 84. How Automation Can Prevent IT Outages Caused by Human Error [https://cloudsoft.io/blog/outages-human-error-automation]
- 85. Automated and closed clinical - grade ... manufacturing protocol [https://www.nature.com/articles/s41598-024-76791-2?error=cookies_not_supported&code=36e05581-e2e7-4548-b42e-09ba7e577e01]
- 86. Semi- automated manufacturing of lentivirus... closed system [https://pmc.ncbi.nlm.nih.gov/articles/PMC5080442/]
- 87. Automation vs. Human Error: The Hidden Battle in Manufacturing [https://www.orcalean.com/article/automation-vs.-human-error:-the-silent-war-on-your-factory-floor]
- 88. Understanding cell culture dynamics: a tool for defining protocol... [https://pubmed.ncbi.nlm.nih.gov/33757391/]
- 89. Quantifying human pluripotent stem cell attributes with population balance modeling | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04668-w]
- 90. A Step-By-Step Guide to Developing GMP SOPs [https://goaudits.com/blog/gmp-standard-operating-procedures/]
- 91. Design and validation of a GMP stem cell manufacturing protocol for MPSII hematopoietic stem cell gene therapy - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2329050124000871]
- 92. What is analytical method validation in GMP [https://www.gmpsop.com/what-is-analytical-method-validation-in-gmp/]
- 93. GLP and GMP Approaches to Method Validation — Going the Same Way? [https://www.spectroscopyonline.com/view/glp-and-gmp-approaches-method-validation-going-same-way]
- 94. Human infrapatellar mesenchymal stem cells show... fat pad [https://www.nature.com/articles/s41598-022-07569-7?error=cookies_not_supported&code=478267cd-ba26-4b6b-b71c-95b129d45c27]
- 95. of Human Mesenchymal Comparative from... Analysis Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3794764/]
- 96. Frontiers | Optimization of Mesenchymal Stromal Cell (MSC) Manufacturing Processes for a Better Therapeutic Outcome [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.918565/full]
- 97. Current good manufacturing practice considerations for mesenchymal stromal cells as therapeutic agents - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9934414/]
- 98. of mesenchymal Comparative derived from... analysis stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-1104-x]
- 99. (PDF) Comparative of Mesenchymal Analysis from Stem ... Cells Bone [https://www.academia.edu/21835471/Comparative_Analysis_of_Mesenchymal_Stem_Cells_from_Bone_Marrow_Umbilical_Cord_Blood_or_Adipose_Tissue]
- 100. of GMP blood mesenchymal manufacturing ... umbilical cord stem [https://www.ntno.org/v09p0095.htm]
- 101. Production of mesenchymal stromal/stem cells according to good manufacturing practices: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3707032/]
- 102. GMP-compliant human adipose tissue-derived mesenchymal stem cells for cellular therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/25138723/]
- 103. Optimizing stem cell culture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3348118/]
- 104. and supplements affect Culture , colony-formation... media proliferation [https://pubmed.ncbi.nlm.nih.gov/35633612/]
- 105. Different culture affect growth characteristics, surface marker... media [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-14-223]
- 106. Frontiers | Culture Supplements Derived from Human Platelet... Medium [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2017.00066/full]
- 107. Stem Cells [https://www.sigmaaldrich.com/US/en/products/cell-culture-and-analysis/cell-lines-and-specialty-cell-culture/stem-cells]
- 108. Cell therapy: cGMP facilities and manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3666518/]
- 109. FDA 483s and Warning Letters concerning Stability Testing - GMP Journal [https://www.gmp-journal.com/current-articles/details/fda-483s-and-warning-letters-concerning-stability-testing.html]
- 110. GMP Stability & Release Testing for Biologics [https://www.goprolytix.com/prolytix-resources/addressing-gmp-stability-testing-and-gmp-release-testing-challenges-for-advanced-biotherapeutics/]
- 111. Know: Product Shelf Life Determination [https://foodindustryhub.com/knowledge-centre/know-product-shelf-life-determination/]
- 112. Testing Explained: Principles, Shelf & Best Practices... Life Methods [https://www.jymachinetech.com/shelf-life-testing-explained-principles-methods-best-practices-2025/]
- 113. Genetic Stability Testing Using NGS and MAM: Optimizing CHO Cell Line Development [https://www.genedata.com/resources/learn/details/blog/cho-cell-lines-characterization-with-ngs]