hiPSC Models in Alzheimer's Disease: Bridging the Gap Between Familial and Sporadic Pathologies for Drug Discovery
This article provides a comprehensive analysis of human induced pluripotent stem cell (hiPSC) models for both familial (FAD) and sporadic (SAD) Alzheimer's disease.
hiPSC Models in Alzheimer's Disease: Bridging the Gap Between Familial and Sporadic Pathologies for Drug Discovery
Abstract
This article provides a comprehensive analysis of human induced pluripotent stem cell (hiPSC) models for both familial (FAD) and sporadic (SAD) Alzheimer's disease. Tailored for researchers, scientists, and drug development professionals, it explores the foundational biology of AD, detailing established and emerging methodologies for generating neurons, microglia, and astrocytes from patient-derived hiPSCs. The content further addresses critical challenges in model optimization, including achieving cellular maturity and recapitulating sporadic disease. Finally, it examines the application of these models in high-throughput drug screening and validation, highlighting their growing role in de-risicking clinical trials and advancing personalized therapeutic strategies for neurodegenerative disorders.
Decoding Alzheimer's Heterogeneity: Etiology and Pathophysiology in Familial vs. Sporadic Forms
Alzheimer's disease (AD) presents a genetic landscape of striking contrast, characterized by rare, highly penetrant monogenic drivers in familial forms (FAD) and a complex polygenic risk architecture in sporadic forms (SAD). This dichotomy represents a critical framework for understanding disease etiology and developing targeted therapeutic interventions. While FAD accounts for less than 1-5% of all cases and typically presents with early onset (before age 65), SAD constitutes the overwhelming majority (95%) of AD cases and usually manifests later in life [1] [2]. Despite their differing genetic foundations, both forms share core neuropathological features, including extracellular amyloid-β (Aβ) plaques and intracellular neurofibrillary tangles composed of hyperphosphorylated tau protein [1]. Advances in genetic technologies, particularly genome-wide association studies (GWAS) and next-generation sequencing, have progressively refined our understanding of this architecture, revealing both expected divisions and surprising overlaps between these AD forms [3]. For research and drug development, this distinction is paramount, as it necessitates different modeling approaches: FAD can be recapitulated through specific pathogenic mutations, whereas SAD requires accounting for the cumulative burden of numerous risk variants and their interaction with environmental factors.
Monogenic Drivers in Familial Alzheimer's Disease (FAD)
Familial Alzheimer's Disease follows an autosomal dominant inheritance pattern and is primarily caused by highly penetrant, pathogenic mutations in three genes: APP (amyloid precursor protein), PSEN1 (presenilin 1), and PSEN2 (presenilin 2). These mutations are sufficient to cause disease, often with onset before age 65 [1].
Causative Genes and Pathogenic Mechanisms
The table below summarizes the key features of the three major FAD genes.
Table 1: Monogenic Drivers in Familial Alzheimer's Disease
| Gene | Chromosome Location | Protein Function | Number of Known Pathogenic Mutations | Mechanistic Consequence of Mutation | Prevalence in FAD |
|---|---|---|---|---|---|
| APP | 21q.21 | Amyloid precursor protein; cleaved to produce Aβ peptide | >50 [1] | Alters APP processing, increasing total Aβ production or aggregation-prone Aβ42/Aβ43 species [1] | ~10-15% of monogenic cases [4] |
| PSEN1 | 14q.29.2 | Catalytic subunit of γ-secretase complex | >350 (some of unclear pathogenicity) [1] | Disrupts γ-secretase activity, increasing ratio of longer, aggregation-prone Aβ42/Aβ40 peptides [1] | ~80% of monogenic cases [1] |
| PSEN2 | 1q.31-q42 | Catalytic subunit of γ-secretase complex | ~30 [1] | Alters γ-secretase activity, increasing Aβ42/Aβ40 ratio; effect is more variable than PSEN1 [1] | ~5% of monogenic cases [1] |
Mutations in these genes converge on a common pathophysiological pathway: the altered processing of APP and the consequent accumulation of amyloidogenic Aβ peptides, forming the biochemical foundation of the amyloid cascade hypothesis [1] [5]. This hypothesis posits that amyloid deposition is an initial, causative event in a cascade that leads to tau pathology, neurodegeneration, and cognitive decline. The discovery of a protective mutation in APP (A673T) in the Icelandic population, which reduces amyloidogenic peptide formation by approximately 40%, provides compelling genetic support for this hypothesis [1].
Experimental Protocols for Monogenic FAD Research
Protocol 1: Cellular Modeling of FAD using hiPSCs
- hiPSC Generation: Derive hiPSCs from fibroblasts or peripheral blood mononuclear cells (PBMCs) of FAD patients carrying specific APP, PSEN1, or PSEN2 mutations using non-integrating reprogramming methods (e.g., Sendai virus or episomal vectors) [6] [5].
- Genome Editing for Isogenic Controls: Use CRISPR/Cas9 to correct the pathogenic mutation in patient-derived hiPSCs or introduce it into control hiPSC lines to generate genetically matched, isogenic control lines—a critical step for attributing phenotypes specifically to the mutation [5].
- Neuronal Differentiation: Differentiate hiPSCs into cortical neurons using dual-SMAD inhibition protocols (e.g., using small molecule inhibitors for TGF-β and BMP signaling). This typically involves generating neural progenitor cells (NPCs) followed by terminal differentiation over 8-12 weeks [5].
- Phenotypic Analysis:
- Aβ Profiling: Measure levels of Aβ40, Aβ42, and the Aβ42/Aβ40 ratio in conditioned media using ELISA or mass spectrometry. FAD models typically show an increased Aβ42/Aβ40 ratio [5].
- Pathological Assessment: Immunocytochemistry for amyloid plaque-like aggregates and hyperphosphorylated tau (e.g., using antibodies against p-tau181, p-tau231) [5].
- Functional Assays: Perform electrophysiology (e.g., multi-electrode arrays) to assess neuronal network dysfunction and calcium imaging to measure aberrant neuronal activity [5].
Protocol 2: In Vivo Validation in Animal Models
- Model Selection: Utilize transgenic mice overexpressing human FAD mutant genes (e.g., 5xFAD, APP/PS1 models). The 5xFAD model expresses five FAD mutations (Swedish (K670N/M671L), Florida (I716V), and London (V717I) in APP, and M146L and L286V in PSEN1) under the neuron-specific Thy1 promoter [5].
- Longitudinal Phenotyping: Monitor animals for the development of Aβ plaques (e.g., via in vivo imaging or post-mortem immunohistochemistry with antibodies like 6E10), cognitive deficits (e.g., Morris water maze, contextual fear conditioning), and synaptic loss.
- Intervention Studies: Test potential therapeutics by administering compounds and assessing their impact on pathology and behavior.
Polygenic Risk in Sporadic Alzheimer's Disease (SAD)
Sporadic Alzheimer's Disease, representing over 95% of cases, does not exhibit a simple Mendelian inheritance pattern. Instead, its genetic architecture is complex and polygenic, involving a combination of common risk variants with small effect sizes, rare variants with moderate to large effects, and the influential APOE genotype [2] [3].
TheAPOELocus and GWAS-Derived Risk Loci
The apolipoprotein E (APOE) ε4 allele is the most potent genetic risk factor for SAD. Compared to the common ε3 allele, the ε4 allele confers a ~3-4 fold increased risk for heterozygotes and a 12-15 fold increased risk for homozygotes, while the ε2 allele is protective [1] [5]. The APOE genotype is estimated to explain 20-25% of the heritability of SAD. Beyond APOE, large-scale GWAS meta-analyses, such as those by the International Genomics of Alzheimer's Project (IGAP) and the European Alzheimer & Dementia Biobank (EADB), have identified over 90 genomic regions associated with AD risk [3]. The table below summarizes the primary categories of genetic risk factors in SAD.
Table 2: Key Genetic Risk Factors in Sporadic Alzheimer's Disease
| Risk Category | Representative Genes/Loci | Strength of Effect (Odds Ratio) | Primary Implicated Cell Type / Pathway |
|---|---|---|---|
| Major Risk Locus | APOE ε4 allele | 3-4 (heterozygous), 12-15 (homozygous) [5] | Lipid metabolism, Aβ clearance, innate immunity |
| Common Risk Variants (GWAS) | BIN1, CLU, ABCA7, CR1, PICALM, TREM2, CD33, SORL1 [3] | 1.05 - 1.25 per allele | Myeloid cells/immunity, endocytosis, lipid metabolism |
| Rare Coding Variants (Large Effect) | TREM2 (R47H), SORL1, ABCA7 [3] | 2 - 5 (e.g., TREM2 R47H ~3-5) [3] | Myeloid cells/immunity, endosomal trafficking |
Notably, the common risk variants identified through GWAS are not randomly distributed but are significantly enriched in regulatory elements active in myeloid cells (e.g., microglia), implicating neuroinflammation and innate immunity as central processes in SAD etiology [1] [3].
Polygenic Risk Scores and Shared Genetic Architecture
A Polygenic Risk Score (PRS) aggregates the effects of many common risk alleles (both risk-increasing and protective) into a single numeric score, estimating an individual's genetic predisposition to a disease. Research has demonstrated a significant overlap in the genetic architecture across different AD classifications. A pivotal study found that a PRS derived from late-onset AD (LOAD) GWAS was associated with risk not only in sporadic LOAD but also in familial LOAD (fLOAD) and sporadic early-onset AD (sEOAD) [7] [8]. The highest association was observed in sEOAD (OR = 2.27), followed by fLOAD (OR = 1.75) and sLOAD (OR = 1.40), indicating that the burden of common risk variants is associated with familial clustering and an earlier age of onset [7] [8]. Furthermore, in autosomal dominant early-onset AD (eADAD) caused by APP/PSEN1/PSEN2 mutations, the PRS was not associated with disease risk but was associated with cerebrospinal fluid biomarker levels (ptau181/Aβ42), suggesting it may modulate the age at onset or disease penetrance [7] [8].
Experimental Protocols for Polygenic SAD Research
Protocol 1: Constructing and Applying a Polygenic Risk Score
- Base Data: Obtain summary statistics from a large-scale AD GWAS meta-analysis (e.g., from IGAP or EADB) [3].
- Clumping and Thresholding: Prune single-nucleotide polymorphisms (SNPs) for linkage disequilibrium (LD) to ensure independence. Generate scores at multiple p-value thresholds (e.g., PT < 0.001, 0.05, 0.1, 0.5, 1) to determine the most predictive set of variants for the target dataset.
- Score Calculation: In the target genotype dataset, for each individual, calculate the PRS as the sum of risk alleles they carry, weighted by the effect size (log(odds ratio)) from the base GWAS. The formula is: ( PRS = \sum{i} (\betai \times Gi) ), where ( \betai ) is the effect size of SNP i and ( G_i ) is the genotype dosage (0, 1, 2) [7].
- Validation: Test the association between the PRS and disease status in the target cohort using logistic regression, adjusting for covariates like age, sex, and genetic principal components.
Protocol 2: Modeling Polygenic Risk in hiPSC Cohorts
- Cohort Selection: Assemble a diverse hiPSC bank from dozens to hundreds of cognitively assessed healthy elderly and SAD patients, with whole-genome sequencing data available [6].
- Stratification by PRS: Calculate PRS for each hiPSC line and stratify lines into "High-PRS" (e.g., top quartile) and "Low-PRS" (e.g., bottom quartile) groups.
- Differentiation and Multi-cell Culture: Differentiate hiPSCs into relevant brain cell types (neurons, astrocytes, microglia). For more physiological models, generate 2D co-cultures or 3D cerebral organoids containing multiple cell types [6] [5].
- Phenotypic Interrogation: Challenge the models (e.g., with Aβ oligomers, inflammatory stimuli) and assay for SAD-relevant phenotypes: transcriptomic profiles, Aβ and tau pathology, phagocytic capacity of microglia, and neuronal network activity.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Reagents for Investigating AD Genetic Architecture
| Reagent / Solution | Function / Application | Example Use Case |
|---|---|---|
| hiPSCs (patient-derived) | Foundation for in vitro disease modeling; retain donor-specific genetic background. | Generating neuronal and glial cells to study patient-specific pathophysiology [6] [5]. |
| CRISPR/Cas9 System | Precision genome editing for introducing or correcting mutations. | Creating isogenic control lines for FAD studies or introducing risk variants into low-PRS control lines [5]. |
| Differentiation Kits (Neuronal, Microglial) | Standardized protocols to generate specific brain cell types from hiPSCs. | Producing consistent, reproducible cultures of neurons and microglia for pathway and functional analysis [5]. |
| Anti-Aβ & Anti-p-Tau Antibodies | Detection and quantification of key AD pathologies via immunofluorescence, ELISA, and Western blot. | Staining for amyloid plaques (e.g., 6E10) and neurofibrillary tangles (e.g., AT8 for p-tau) in hiPSC-derived cultures or tissue [5]. |
| Cytokine & Chemokine Panels | Profiling inflammatory mediators secreted by glial cells. | Measuring neuroinflammatory responses in microglia and astrocyte cultures derived from High-PRS vs. Low-PRS lines [6]. |
| Multi-Electrode Arrays (MEAs) | Functional assessment of neuronal network activity and synchronization. | Detecting hyperexcitability or network dysfunction in FAD- or SAD-patient neurons [5]. |
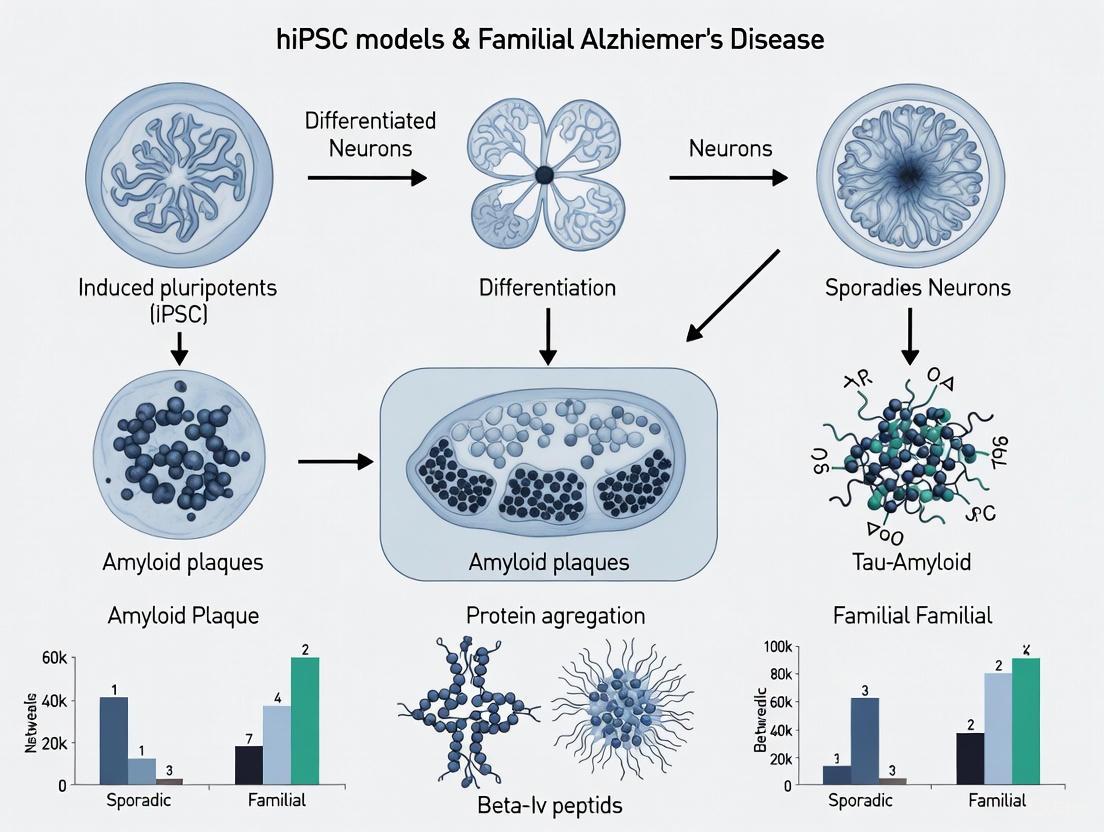
Visualizing Genetic Architecture and Research Workflows
The following diagrams illustrate the core genetic concepts and experimental approaches discussed in this whitepaper.
Genetic Architecture of FAD vs. SAD
hiPSC Modeling Workflow for FAD and SAD
The genetic architecture of Alzheimer's disease is defined by a clear dichotomy between monogenic drivers in FAD and polygenic risk in SAD, yet modern research reveals a shared pathophysiological ground and significant overlap in their underlying genetic risk factors. This understanding directly informs the use of hiPSC models in research and drug development. For FAD, the strategy involves precise modeling of specific pathogenic mutations with isogenic controls to dissect causal mechanisms. For SAD, the approach requires cohort-based studies that capture polygenic risk, focusing on the interplay between multiple risk variants, with a particular emphasis on non-neuronal cell types like microglia. As the field moves forward, integrating genetic findings from diverse ancestries, exploring the role of somatic mutations, and leveraging complex hiPSC-based systems like organoids and microfluidic chips will be crucial for bridging the gap between genetic insight and effective, personalized therapeutic interventions.
Alzheimer's disease (AD) is a progressive neurodegenerative disorder and the most common cause of dementia globally, characterized by a devastating decline in memory and cognitive function. The pathological diagnosis of AD relies on the presence of three core hallmarks: amyloid-β (Aβ) plaques, neurofibrillary tangles (NFTs), and sustained neuroinflammatory responses [9] [10]. For decades, research has been hampered by the inability to model the human brain's complexity and the distinct characteristics of sporadic versus familial AD. The advent of human induced pluripotent stem cell (hiPSC) technology has revolutionized this landscape, enabling the generation of patient-specific brain cells that recapitulate both familial and sporadic disease pathologies in vitro [11] [5] [6]. This whitepaper provides an in-depth technical analysis of the three core pathological hallmarks and details how hiPSC models are elucidating their roles in AD pathogenesis.
Amyloid-β Plaques
Pathological Basis
Amyloid-β plaques are extracellular deposits primarily composed of Aβ peptides, which are generated through the sequential proteolytic cleavage of the Amyloid Precursor Protein (APP) by β-secretase (BACE1) and γ-secretase complexes [5]. The γ-secretase complex, which includes Presenilin 1 (PSEN1) and Presenilin 2 (PSEN2), produces Aβ peptides of varying lengths, with Aβ42 being more aggregation-prone due to its hydrophobicity [5]. In the dominant amyloid cascade hypothesis, an imbalance between Aβ production and clearance leads to the accumulation of Aβ oligomers and ultimately the formation of insoluble plaques, triggering a pathogenic cascade that results in synaptic dysfunction, neuroinflammation, and neuronal death [5] [12].
Insights from hiPSC Models
hiPSC-derived neurons from patients with familial AD (fAD), such as those with APP gene duplications (APPDp) or PSEN1 mutations, faithfully replicate key aspects of amyloid pathology. These models demonstrate significantly higher levels of secreted Aβ(1–40) and increased Aβ42/Aβ40 ratios compared to neurons from non-demented controls [11] [5]. Crucially, hiPSC models have also proven valuable for studying sporadic AD (sAD), with neurons from some sAD patients exhibiting amyloidogenic phenotypes similar to fAD models, including elevated Aβ and large RAB5-positive early endosomes, suggesting convergent pathological mechanisms [11]. Furthermore, isogenic hiPSC lines, where AD-related mutations are introduced via CRISPR/Cas9, allow for controlled studies of specific genetic contributions.
Table 1: Amyloid-β Pathology in hiPSC-Derived Neurons
| hiPSC Model Type | Key Amyloid-Related Phenotypes | Significance |
|---|---|---|
| Familial AD (APPDp) | ↑ APP mRNA, ↑ Secreted Aβ(1–40), ↑ RAB5+ early endosomes [11] | Confirms causative role of APP dosage in amyloidosis |
| Familial AD (PSEN1 ΔE9) | ↑ Aβ secretion, altered inflammatory response [13] | Demonstrates mutation-specific effects on γ-secretase function |
| Sporadic AD (sAD) | Elevated Aβ, phospho-Tau, active GSK-3β in a subset of patients [11] | Proves sporadic cases can exhibit amyloid-driven phenotypes |
Neurofibrillary Tangles
Pathological Basis
Neurofibrillary tangles (NFTs) are intraneuronal aggregates consisting of hyperphosphorylated forms of the microtubule-associated protein tau [9]. In its normal state, tau promotes the assembly and stabilization of microtubules, which are critical for maintaining cell structure and facilitating axonal transport [9] [10]. In AD, tau becomes abnormally phosphorylated at multiple sites, which reduces its affinity for microtubules and promotes its self-assembly into paired helical filaments (PHFs) and eventually NFTs [9] [14]. This process compromises microtubule integrity, impairs axonal transport, and is strongly correlated with neuronal loss and cognitive decline [9] [10].
Insights from hiPSC Models
hiPSC-derived neurons have been instrumental in probing the relationship between amyloid and tau pathology. Neurons from both fAD (APPDp) and sAD patients show significantly elevated levels of phospho-tau (Thr231) and active glycogen synthase kinase-3β (aGSK-3β), a key kinase that phosphorylates tau [11]. A critical experiment using these models revealed that β-secretase (BACE) inhibition, but not γ-secretase inhibition, significantly reduced levels of phospho-Tau(Thr231) and aGSK-3β [11]. This finding suggests a direct relationship between APP proteolytic processing (but not necessarily the Aβ peptide itself) and the activation of pathways leading to tau phosphorylation in human neurons, offering a new perspective on the amyloid-tau nexus.
Neuroinflammation
Pathological Basis
Neuroinflammation is now recognized as a third core hallmark of AD, driven primarily by the activation of glial cells in the central nervous system [9] [14]. Microglia, the brain's resident immune cells, and astrocytes become reactive in response to damage signals like Aβ oligomers and NFTs [9]. This activation triggers the release of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6), chemokines, and reactive oxygen species (ROS) [9] [14]. While an acute inflammatory response can be protective, chronic glial activation creates a toxic environment that drives neurodegeneration. Genome-wide association studies (GWAS) have solidified the role of neuroinflammation by identifying numerous AD risk genes that are highly expressed in microglia and astrocytes (e.g., TREM2, APOE) [9] [5] [13].
Insights from hiPSC Models
hiPSC technology enables the generation of all major brain cell types, allowing for the creation of sophisticated co-culture systems to study neuroinflammation.
- Astrocyte Dysfunction: hiPSC-derived astrocytes carrying the APOE4 allele—the strongest genetic risk factor for sAD—display impaired Aβ clearance, disrupted cholesterol metabolism, and heightened pro-inflammatory responses compared to their APOE3 counterparts [13]. When co-cultured with neurons, APOE4 astrocytes provide less synaptic support and exacerbate neuroinflammation [13].
- Microglial Activation: Tri-culture systems incorporating hiPSC-derived neurons, astrocytes, and microglia model immune cross-talk. In such models, microglia respond to Aβ and tau aggregates, but their function is modulated by other cells. For instance, astrocyte-derived * interleukin-3 (IL-3)* can reprogram microglia to enhance their capacity to cluster and clear Aβ and Tau aggregates [13].
- Complement System: Tri-culture models have shown that under inflammatory conditions, reciprocal signaling between astrocytes and microglia drives the overproduction of the complement protein C3, a key player in synapse elimination, with this effect being amplified in AD cultures [13].
Table 2: Glial Dysfunction in hiPSC Models of Alzheimer's Disease
| Cell Type | AD-Associated Dysfunction | hiPSC Model Insights |
|---|---|---|
| Astrocytes | ↓ Aβ clearance, ↑ inflammation, ↓ synaptic support, metabolic disruption [13] | APOE4 astrocytes are intrinsically pro-inflammatory and less supportive of neurons [13]. |
| Microglia | Chronic activation, altered phagocytosis, pro-inflammatory cytokine release [9] [5] | In tri-cultures, microglia can be "reprogrammed" by astrocyte signals to improve aggregate clearance [13]. |
Experimental Protocols for hiPSC-Based AD Research
Neuronal Differentiation and Phenotypic Analysis
A standardized protocol for generating and analyzing neurons from hiPSCs involves the following key steps [11]:
- hiPSC Generation and Culture: Fibroblasts from fAD, sAD, and non-demented control donors are reprogrammed into hiPSCs using non-integrating methods (e.g., Sendai virus) expressing OCT4, SOX2, KLF4, and c-MYC. Multiple clonal lines are maintained and validated for pluripotency markers and karyotypic stability.
- Neural Induction and Progenitor Expansion: hiPSCs are differentiated into neural progenitor cells (NPCs) via embryoid body formation or dual SMAD inhibition. NPCs are purified using fluorescence-activated cell sorting (FACS) with surface markers (CD184+/CD15+/CD44−/CD271−) and expanded in culture.
- Neuronal Differentiation and Purification: NPCs are differentiated for 3-5 weeks into heterogeneous neuronal cultures. Neurons are then purified to near homogeneity (>90%) using FACS for CD24+/CD184−/CD44− immunoreactivity.
- Phenotypic Analysis:
- Biochemical Assays: ELISA or MSD assays on cell lysates and media to quantify Aβ species (Aβ40, Aβ42) and phosphorylated tau (e.g., Thr231).
- Immunocytochemistry: To visualize and quantify intracellular proteins like MAP2, βIII-tubulin, RAB5, and phospho-tau.
- Electrophysiology: Whole-cell patch-clamp recording to confirm functional neuronal properties, including action potential generation and synaptic activity.
Advanced Co-culture Systems
To model neuroinflammation, more complex 2D and 3D systems are employed [13]:
- Tri-culture System: hiPSC-derived neurons, astrocytes, and microglia are combined in a defined ratio.
- Treatment and Analysis: Cultures are exposed to aggregated Aβ or pro-inflammatory cytokines. The culture medium is analyzed for secreted factors (cytokines, complement proteins), and cells are fixed for immunostaining to analyze glial activation, phagocytosis of Aβ, and neuronal health.
Visualizing Pathological Pathways and Experimental Workflows
Diagram 1: Core AD pathology cascade.
Diagram 2: hiPSC modeling workflow.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for hiPSC-based Alzheimer's Disease Research
| Reagent / Tool | Function in Research | Example Application |
|---|---|---|
| hiPSC Lines | Patient-specific disease modeling | Isogenic lines with edited APOE or PSEN1 alleles to study specific mutations [5] [13]. |
| Neural Differentiation Kits | Directing cell fate to neural lineages | Commercial kits (e.g., STEMdiff) for consistent generation of NPCs and neurons. |
| FACS Antibodies | Purification of specific cell populations | Anti-CD24, CD184, CD44, CD15 for isolating neurons and NPCs [11]. |
| Aβ ELISA/MSD Kits | Quantifying Aβ peptides from media | Measuring Aβ40/Aβ42 ratio in neuronal culture supernatants [11]. |
| Phospho-Tau Antibodies | Detecting tau pathology | Immunostaining or Western Blot for p-Tau (Thr231) [11]. |
| Cytokine Profiling Arrays | Assessing neuroinflammatory states | Quantifying TNF-α, IL-6, IL-1β from co-culture media [9] [13]. |
| γ-/β-Secretase Inhibitors | Probing amyloidogenic pathway | Testing effect on Aβ production and downstream tau phosphorylation [11]. |
| CRISPR/Cas9 Systems | Genome editing for functional studies | Creating isogenic controls or introducing risk variants (e.g., APOE4) [13]. |
The amyloid cascade hypothesis (ACH), which posits amyloid-β (Aβ) accumulation as the initiating trigger of Alzheimer's disease (AD), has dominantly influenced research and drug development for decades. The advent of human induced pluripotent stem cell (hiPSC) technology provides a revolutionary platform for reevaluating this hypothesis using patient-derived neurons. This whitepaper synthesizes current evidence from hiPSC models, demonstrating how they elucidate shared and distinct pathophysiological endotypes across familial (fAD) and sporadic (sAD) forms of the disease. We detail critical experimental protocols, present quantitative data, and visualize core signaling pathways, offering a refined, hiPSC-informed perspective on AD pathogenesis and therapeutic targeting.
The amyloid cascade hypothesis, formally articulated in 1992, proposes that AD pathogenesis is initiated by an imbalance in Aβ production and clearance, leading to Aβ aggregation into oligomers and plaques. This, in turn, is hypothesized to trigger tau pathology, neuroinflammation, synaptic dysfunction, and eventual neuronal loss [15]. Despite its longevity, the hypothesis faces significant challenges, including the poor correlation between amyloid plaque burden and cognitive decline, and the limited clinical efficacy of anti-amyloid therapies [16] [17].
hiPSC technology, pioneered by Shinya Yamanaka, enables the generation of patient-specific neurons, astrocytes, and microglia, offering a human-relevant system to model AD [6] [18]. Bibliometric analysis reveals a steady increase in hiPSC-AD publications over the past 14 years, with research trends focusing on inflammation, astrocytes, microglia, apolipoprotein E (ApoE), and tau [6]. This resource allows for the direct interrogation of the ACH in a human neuronal context, capturing patient-specific genetic backgrounds and the complexity of sAD, which constitutes the majority of cases.
hiPSC Models Differentiate and Refine Amyloid-Associated Mechanisms
hiPSC models have been instrumental in moving beyond a simplistic view of the ACH, revealing subtler dysregulations in amyloid precursor protein (APP) processing and its downstream consequences.
Familial AD Models: Beyond Aβ42
In fAD, caused by mutations in PSEN1, PSEN2, or APP, hiPSC-derived neurons have validated the shift in γ-secretase activity toward the production of longer, more aggregation-prone Aβ peptides (e.g., Aβ42) [19] [20]. However, multi-omics studies on hiPSC-derived neurons harboring PSEN1A79V, PSEN2N141I, and APPV717I mutations reveal that common disease endotypes extend far beyond Aβ. These include:
- Dedifferentiation: A reversion to a less-differentiated cellular state.
- Synaptic Signaling Dysregulation: Repression of genes critical for synaptic function.
- Mitochondrial Repression: Downregulation of oxidative phosphorylation and metabolic pathways.
- Inflammation: Activation of pro-inflammatory pathways [20]. This indicates that fAD mutations trigger a broad pathogenic network where altered Aβ production is one component of a multifaceted cellular crisis.
Sporadic AD Models: Polygenic Risk and Cellular Vulnerability
Modeling sAD requires capturing its polygenic nature. Recent resources like the IPMAR Resource have created a collection of over 100 hiPSC lines from donors with extremes of global AD polygenic risk scores (PRS) and complement pathway-specific PRS [21]. This allows researchers to study the molecular consequences of genetic risk in a controlled in vitro setting. Furthermore, a groundbreaking study using wild-type murine neurons identified a unique subpopulation that spontaneously recapitulates fAD phenotypes, including inefficient γ-secretase activity, endo-lysosomal abnormalities, and increased vulnerability to toxic insults [19]. This suggests that sAD may involve the selective vulnerability of specific neuronal populations due to intrinsic variability in proteostatic mechanisms, rather than a deterministic genetic mutation.
Experimental Protocols for hiPSC-Based AD Research
Protocol 1: Generating and Differentiating Cortical Neurons from hiPSCs
This protocol is adapted from methodologies used in foundational hiPSC-AD studies [20].
- Reprogramming: Dermal fibroblasts from patients and non-demented controls are reprogrammed into hiPSCs using non-integrating methods (e.g., episomal vectors) to minimize genomic alterations.
- Neural Induction: hiPSCs are co-cultured with PA6 stromal cells to induce neural differentiation. To enhance neural induction, cultures are treated with 5 μM dorsomorphin (a BMP inhibitor) and 10 μM SB431542 (a TGF-β inhibitor) for the first 6 days.
- Neural Stem Cell (NSC) Expansion: On day 12, NSCs are isolated by Fluorescence-Activated Cell Sorting (FACS) using a cell surface signature (CD24+/CD184+/CD44−/CD271−). NSCs are expanded in NSC growth medium supplemented with 20 ng/mL human basic Fibroblast Growth Factor (bFGF-2).
- Neuronal Differentiation: Upon reaching 80% confluence, the medium is switched to neuron differentiation medium (lacking bFGF-2) for 3 weeks to promote terminal differentiation into cortical neurons.
- Neuronal Purification: Differentiated cultures are dissociated and magnetically purified using anti-PE conjugated magnetic beads after incubation with antibodies against CD184 and CD44. The supernatant, containing purified CD184−/CD44− neurons, is collected for downstream applications [20].
Protocol 2: Fluorescence Imaging and FACS of Neurons with Altered γ-Secretase Activity
This protocol enables the identification and isolation of neurons with inherent vulnerabilities [19].
- Biosensor Expression: Primary wild-type or hiPSC-derived neurons are transduced with an adeno-associated virus (AAV) packaging a FRET-based γ-secretase biosensor (e.g., C99 Y-T) under a neuron-specific promoter (e.g., human synapsin, hSyn).
- Confocal Microscopy & FRET Imaging: Live neurons are imaged using a confocal microscope equipped with environmental control (CO2 and temperature). The biosensor is excited with a 405 nm laser, and emissions are detected simultaneously at 460–480 nm (donor, mTurquoise-GL) and 520–540 nm (acceptor, YPet). The FRET ratio (YPet/mTurquoise-GL) is calculated on a cell-by-cell basis, with a lower ratio indicating diminished γ-secretase endopeptidase-like activity.
- Fluorescence-Activated Cell Sorting (FACS): For live-cell sorting, neurons are stained with Propidium Iodide (PI) to exclude dead cells. Neurons expressing the biosensor are excited with a 405 nm laser, and emissions are collected in the 425–475 nm and 500–550 nm channels. The designated 20% of neurons with the lowest FRET ratios (diminished activity) and the 20% with the highest ratios (control) are sorted into separate populations for subsequent molecular and functional analyses [19].
Quantitative Data and Comparative Analysis
Table 1: Key hiPSC Lines for Modeling Genetic Risk in Alzheimer's Disease
| Resource Name | Description of hiPSC Lines | Key Genetic Features | Associated Data |
|---|---|---|---|
| IPMAR Resource [21] | >100 lines from donors with extremes of polygenic risk. | • 34 lines: High global PRS (Late-Onset AD)• 29 lines: High global PRS (Early-Onset AD)• 27 lines: Low global PRS (Control)• 19 lines: Extremes of complement pathway PRS | Clinical, longitudinal, and genetic datasets. Available via EBiSC and DPUK. |
| FAD Multi-omics Study [20] | Isogenic and patient-derived lines. | • PSEN1A79V (fAD)• PSEN2N141I (fAD)• APPV717I (fAD)• Non-demented controls (NDC) | RNA-seq, ATAC-seq, and proteomic data on purified neurons. |
Table 2: Phenotypic Characterization of Neuronal Subpopulations with Altered γ-Secretase Activity [19]
| Assay Type | Parameter Measured | Neurons with Low γ-Secretase Activity | Control Neurons (High Activity) |
|---|---|---|---|
| Biochemical | Aβ42/Aβ40 ratio | ↑ Increased | Normal |
| Cellular Imaging | Endo-lysosomal morphology | Abnormally enlarged | Normal |
| Functional Assay | Viability after oxidative stress (DTDP) | ↓ Significantly decreased | More resistant |
| Functional Assay | Viability after excitotoxicity (Glutamate) | ↓ Significantly decreased | More resistant |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for hiPSC-based AD Mechanistic Studies
| Reagent / Kit | Function / Application | Example Use Case |
|---|---|---|
| Dorsomorphin & SB431542 [20] | Small molecule inhibitors for highly efficient neural induction from hiPSCs. | Directing hiPSCs toward a neural lineage during co-culture with PA6 cells. |
| FRET-based γ-secretase biosensor (C99 Y-T) [19] | Visualizing and quantifying endogenous γ-secretase activity in live neurons. | Identifying neuronal subpopulations with inherently inefficient γ-secretase function via live-cell imaging or FACS. |
| Magnetic Cell Sorting Kits (e.g., anti-PE beads) [20] | Purifying specific cell populations (e.g., neurons) from heterogeneous cultures. | Isolating CD184-/CD44- neurons from differentiated hiPSC cultures for clean omics analysis. |
| Human Aβ38 & Aβ42 ELISA Kits [19] | Quantifying specific Aβ peptide species from conditioned media or cell lysates. | Confirming a pathological shift in Aβ production in FAD lines or sorted neuronal populations. |
| LysoPrime Green & Propidium Iodide (PI) [19] | Staining acidic organelles (endo-lysosomes) and identifying dead cells, respectively. | Assessing endo-lysosomal morphology and quantifying cell viability in health and after insult. |
Visualizing Pathways and Workflows
Diagram 1: The Expanded Amyloid Cascade in hiPSC Models. hiPSC studies show FAD mutations initiate a cascade that extends beyond Aβ to fundamental cellular dysfunctions.
Diagram 2: hiPSC Experimental Workflows for sAD and fAD. Complementary approaches for modeling polygenic risk and investigating intrinsic neuronal vulnerability.
hiPSC models have provided an indispensable, human-relevant platform for a rigorous re-evaluation of the amyloid cascade hypothesis. The evidence compels a move from a linear, Aβ-centric view to a complex model where amyloid dysregulation is one critical node within a broader network of cellular pathology. Key insights include the identification of common molecular endotypes across genetic forms of AD and the existence of vulnerable neuronal subpopulations in sporadic contexts. Future research must leverage large-scale hiPSC resources, such as those capturing polygenic risk, and continue to develop more complex co-culture and organoid systems to unravel the interplay between amyloid, tau, glial cells, and neuroinflammation. This hiPSC-refined understanding is crucial for developing therapeutics that target the core cellular vulnerabilities in AD, moving beyond the sole removal of amyloid.
The pathogenesis of neurodegenerative diseases, particularly Alzheimer's disease (AD), has historically focused on neuronal pathology. However, emerging research highlights the critical roles of glial cells—microglia and astrocytes—as active contributors to disease mechanisms. This whitepaper examines how these resident immune cells transition from homeostatic supporters to pathogenic drivers in neurodegenerative processes, with a specific focus on insights gained from human induced pluripotent stem cell (hiPSC) models. The integration of hiPSC technology has been crucial for dissecting cell-intrinsic pathologies, revealing distinct glial phenotypes in familial versus sporadic AD, and identifying novel therapeutic targets. By leveraging patient-specific hiPSCs, researchers can now model the complex interplay of genetics and cellular pathology, providing unprecedented opportunities for drug development and personalized medicine approaches in neurological disorders.
The central nervous system (CNS) operates through sophisticated interactions between neurons and glial cells, with microglia and astrocytes serving as essential components of the neuroimmune interface. Microglia, the resident immune macrophages of the CNS, and astrocytes, the predominant homeostatic support cells, collectively maintain brain homeostasis through surveillance, metabolic support, synaptic regulation, and inflammatory modulation [22] [23]. In Alzheimer's disease (AD) and other neurodegenerative conditions, these glial cells undergo functional transformation, contributing to neuroinflammation, synaptic dysfunction, and protein aggregation pathologies.
The advent of human induced pluripotent stem cell (hiPSC) technology has revolutionized our ability to model these complex glial-neuronal interactions in patient-specific contexts. Bibliometric analysis reveals a steady increase in hiPSC-AD publications over the past 14 years, with the United States and China leading research contributions [6]. Current research trends have particularly focused on neuroinflammation, astrocytes, microglia, apolipoprotein E (ApoE), and tau pathology, highlighting the growing recognition of glial mechanisms in AD pathogenesis [6]. This whitepaper synthesizes current understanding of microglial and astrocytic pathophysiology in neurodegenerative disease, with emphasis on findings from hiPSC models that distinguish sporadic from familial disease mechanisms.
Pathological Transformation of Microglia
Physiological Functions and Phenotypic Heterogeneity
Under homeostatic conditions, microglia exhibit a highly ramified morphology with extensive branching processes that continuously surveil the CNS microenvironment. These dynamic sentinel cells perform essential functions including phagocytosis of cellular debris, clearance of pathological protein aggregates, and regulation of synaptic plasticity through direct interactions with neurons [22] [24]. Microglia display remarkable heterogeneity and phenotypic plasticity, transitioning along a functional spectrum in response to microenvironmental cues. The traditional M1 (pro-inflammatory)/M2 (anti-inflammatory) classification has been superseded by recognition of disease-specific activation states identified through single-cell transcriptomics [22].
Microglial activation states are tightly regulated by complex receptor networks that sense environmental changes. Key receptors include Triggering Receptor Expressed on Myeloid Cells 2 (TREM2), immunomodulatory receptors (CD33), pattern recognition receptors (Toll-like receptors, NLRs), scavenger receptors (SR-A, CD36), and TAM family tyrosine kinases (Tyro3, Axl, MerTK) [24]. These receptors enable microglia to detect damage-associated molecular patterns (DAMPs), pathogen-associated molecular patterns (PAMPs), and neurodegenerative disease-related proteins such as amyloid-β (Aβ) and tau.
Mechanisms in Neurodegenerative Pathogenesis
In Alzheimer's disease, microglia demonstrate dual roles that can both ameliorate and exacerbate pathology. Initially, microglia attempt to clear Aβ deposits through phagocytic activity, with TREM2 playing a critical role in promoting microglial survival, proliferation, and phagocytic function [24]. However, genetic variants in microglia-associated genes, including TREM2, CD33, and MS4A, significantly elevate AD risk and impair these protective functions [22]. The R47H mutation in TREM2, for instance, diminishes microglial capacity to phagocytose Aβ, contributing to plaque accumulation [24].
Sustained microglial activation leads to the production of pro-inflammatory cytokines (IL-1β, TNF-α) and chemokines that establish chronic neuroinflammation, ultimately driving synaptic loss and neuronal damage [24]. Microglia also contribute to neurodegeneration through immunometabolic reprogramming, with disruptions in glucose, lipid, and amino acid metabolism influencing their functional states [22]. Recent research has identified ferroptosis—an iron-dependent form of cell death—as a particularly vulnerable pathway in microglia, with iron overload inducing inflammatory phenotypes and contributing to neurotoxicity [25].
Table 1: Key Microglial Receptors in Alzheimer's Disease Pathogenesis
| Receptor | Primary Ligands | Signaling Pathways | Functional Role in AD |
|---|---|---|---|
| TREM2 | Aβ, ApoE, apoptotic cells | DAP12/SYK | Phagocytosis, cell survival, metabolic regulation |
| CD33 | Sialic acid residues | Unknown | Inhibits phagocytosis; risk gene for AD |
| TLR4 | Aβ, LPS | NF-κB, MAPK | Pro-inflammatory activation |
| CX3CR1 | Fractalkine (CX3CL1) | Various | Microglia-neuron communication; neuroprotection |
| CD36 | Aβ, oxidized LDL | NF-κB, NLRP3 inflammasome | Aβ uptake; pro-inflammatory response |
Astrocytic Contributions to Disease Progression
Homeostatic Functions and Reactive Transformation
Astrocytes constitute the most abundant glial cell type in the CNS and perform diverse homeostatic functions essential for neuronal health. These include regulation of ionic balance (particularly K⁺ and Ca²⁺), metabolic support through the glutamate-glutamine cycle and lactate shuttle, neurotransmitter recycling, synaptic modulation, and blood-brain barrier maintenance [23]. Under pathological conditions, astrocytes undergo reactive transformation characterized by morphological changes (hypertrophy, process swelling), molecular alterations (increased GFAP expression), and functional reprogramming.
Reactive astrocytes are broadly categorized into neurotoxic (A1) and neuroprotective (A2) phenotypes, though this classification represents a simplification of a continuous functional spectrum [23]. The A1 phenotype is induced by activated microglia releasing IL-1α, TNF-α, and C1q, leading to production of inflammatory mediators and loss of normal homeostatic functions. Conversely, A2 astrocytes upregulate neurotrophic factors and anti-inflammatory cytokines that support neuronal survival and tissue repair [23].
Pathogenic Mechanisms in Neurodegeneration
In Alzheimer's disease, astrocytes respond to Aβ deposition by releasing pro-inflammatory factors that exacerbate neuroinflammation [23]. Astrocyte dysfunction also contributes to AD pathology through metabolic disturbances, including lipid droplet accumulation, mitochondrial dysfunction, and oxidative stress imbalance [23]. Recent research has identified a failed astrocyte stress response to Aβ as an early inducer of amyloid and tau pathology through activation of δ-secretase, a stress-induced protease implicated in both amyloidogenic and tau-related proteolytic processing [26].
Experimental models demonstrate that astrocytes with diminished stress response capabilities (via SORCS2 deficiency) exhibit heightened sensitivity to Aβ-induced stress, resulting in massive amyloid and tau pathologies [26]. These findings position astrocyte distress as a potential mechanism linking amyloid and tau comorbidities in AD. Additional astrocytic contributions to neurodegeneration include disruption of synaptic function through impaired glutamate clearance and release of synaptotoxic factors, as well as blood-brain barrier dysfunction that compromises CNS integrity [23].
Table 2: Astrocyte Dysfunctions in Neurodegenerative Diseases
| Pathogenic Mechanism | Functional Consequences | Associated Diseases |
|---|---|---|
| A1 Reactive Polarization | Neuroinflammation, synaptotoxicity, oxidative stress | AD, PD, ALS |
| Metabolic Reprogramming | Lipid droplet accumulation, mitochondrial dysfunction, oxidative stress | AD, PD, MS |
| Glutamate Dysregulation | Excitotoxicity, synaptic impairment | AD, ALS, epilepsy |
| Blood-Brain Barrier Disruption | Enhanced CNS permeability, immune cell infiltration | AD, MS, stroke |
| δ-secretase Activation | Enhanced Aβ and tau proteolytic processing | AD |
hiPSC Models for Dissecting Sporadic versus Familial Alzheimer's Disease
hiPSC Technology Platform
Human induced pluripotent stem cell (hiPSC) technology has emerged as a transformative platform for disease modeling, enabling generation of patient-specific neurons, glia, and three-dimensional organoid systems that recapitulate human physiology and pathology [6] [27]. The technology involves reprogramming somatic cells (typically fibroblasts or blood cells) into pluripotent stem cells through expression of defined transcription factors, followed by differentiation into disease-relevant cell types [6]. This approach allows researchers to investigate intrinsic cellular pathologies independent of confounding factors such as peripheral immunity or aging environments.
HiPSC models offer particular advantages for studying glial cells in neurodegenerative diseases, as they retain donor-specific genetic and molecular signatures, enabling modeling of patient-specific phenotypes [6]. The ability to differentiate hiPSCs into purified populations of microglia-like cells and astrocytes has facilitated investigation of cell-autonomous contributions to disease pathogenesis, as well as cell-cell interactions in more complex co-culture systems [28].
Modeling Familial versus Sporadic AD
A significant application of hiPSC technology involves distinguishing pathological mechanisms between familial (autosomal dominant) and sporadic (polygenic) forms of Alzheimer's disease. Familial AD models typically utilize hiPSCs from patients with mutations in APP, PSEN1, or PSEN2 genes, which directly impact Aβ production and processing. In contrast, modeling sporadic AD requires capture of the complex polygenic risk architecture through several approaches:
Polygenic Risk Score Stratification: Researchers have created hiPSC collections capturing extremes of global AD polygenic risk, including lines from high-risk late-onset AD (34 lines), high-risk early-onset AD (29 lines), and low-risk control donors (27 lines) [21]. This IPMAR Resource (iPSC Platform to Model Alzheimer's Disease Risk) enables systematic investigation of how polygenic risk converges on specific cellular phenotypes.
Pathway-Specific Genetic Risk: Some resources focus on specific pathways, such as complement system biology, with hiPSC lines selected for extremes of complement pathway-specific genetic risk (9 high-risk AD, 10 low-risk controls) [21].
Endophenotype Analysis: hiPSC models reveal distinct glial-intrinsic phenotypes across neurodegenerative diseases. In multiple sclerosis, for example, hiPSC-derived cultures from people with primary progressive MS (PPMS) contain fewer oligodendrocytes and show increased expression of immune and inflammatory genes in oligodendrocyte lineage cells and astrocytes, matching glial profiles from MS postmortem brains [28].
These approaches demonstrate that hiPSC models can capture disease-relevant cellular phenotypes independent of extrinsic factors, providing platforms for dissecting fundamental disease mechanisms and screening therapeutic interventions.
Experimental Protocols for hiPSC-Based Glial Research
hiPSC Differentiation to Glial Cells
Protocol: Generation of Microglia-Enriched Cultures from hiPSCs
- Maintenance of hiPSCs: Culture hiPSCs on Matrigel-coated plates in mTeSR Plus medium with daily medium changes until 70-80% confluency.
- Mesodermal Induction: Dissociate hiPSCs with Accutase and transfer to low-attachment plates in differentiation medium containing BMP4, VEGF, SCF, and IL-3 to form embryoid bodies.
- Myeloid Progenitor Expansion: After 10 days, transfer embryoid bodies to Matrigel-coated plates in medium containing M-CSF, IL-3, and GM-CSF to promote hematopoietic progenitor expansion.
- Microglial Differentiation: Harvest floating progenitors and culture in medium containing IL-34, GM-CSF, and TGF-β to induce microglial fate for 14-21 days.
- Characterization: Analyze cells for expression of microglial markers (IBA1, TMEM119, P2RY12) using flow cytometry and immunocytochemistry.
Protocol: Astrocyte Differentiation from hiPSCs
- Neural Induction: Differentiate hiPSCs to neural progenitor cells (NPCs) using dual SMAD inhibition (LDN193189, SB431542) for 10-14 days.
- NPC Expansion: Culture NPCs in neural expansion medium containing EGF and FGF2 for 2-3 passages.
- Astrocyte Differentiation: Switch NPCs to astrocyte differentiation medium (DMEM/F12, N2 supplement, 1% FBS) for 30-45 days.
- Astrocyte Maturation: Culture in CNTF, BMP4, or LIF-containing medium for additional 14-21 days to promote maturation.
- Characterization: Verify astrocyte identity using markers (GFAP, S100β, AQP4) and functional assays (glutamate uptake, calcium imaging).
Functional Assays for Glial Phenotyping
Microglial Phagocytosis Assay
- Incubate hiPSC-derived microglia with pHrodo Red-conjugated Aβ42 fibrils (1 µg/mL) for 2 hours
- Fix cells with 4% PFA and counterstain with DAPI
- Quantify phagocytosed Aβ using fluorescence microscopy or flow cytometry
- Include control wells with cytochalasin D (phagocytosis inhibitor)
Astrocyte Neurotoxicity Assay
- Culture hiPSC-derived astrocytes in serum-free medium for 24 hours to collect conditioned medium
- Apply astrocyte-conditioned medium to hiPSC-derived cortical neurons
- Assess neuronal viability after 48 hours using MTT assay or Live/Dead staining
- Measure LDH release as indicator of cytotoxicity
Multi-electrode Array (MEA) for Network Activity
- Plate hiPSC-derived neurons and astrocytes (1:1 ratio) on MEA plates
- Record spontaneous electrical activity for 10 minutes weekly
- Analyze firing rate, burst frequency, and network synchronization
- Challenge with glutamate or Aβ to assess functional responses
Research Reagent Solutions
Table 3: Essential Research Reagents for hiPSC Glial Research
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Reprogramming Systems | CytoTune iPSC Sendai Reprogramming Kit, Episomal vectors | Footprint-free reprogramming of somatic cells to hiPSCs |
| Differentiation Kits | STEMdiff Astrocyte Differentiation Kit, Microglia Differentiation Kit | Standardized differentiation protocols for glial cells |
| Cell Type Markers | Anti-GFAP (astrocytes), Anti-IBA1/TMEM119 (microglia), Anti-MBP (oligodendrocytes) | Identification and purification of specific glial cell types |
| Cytokines/Growth Factors | IL-34, M-CSF (microglia), CNTF, BMP4 (astrocytes) | Directional differentiation and maintenance of glial phenotypes |
| Functional Assay Kits pHrodo Aβ Phagocytosis Assay, Glutamate Uptake Assay Kit | Quantification of glial-specific functional capacities | |
| Single-Cell RNA Seq | 10x Genomics Chromium System, SMART-seq reagents | Transcriptional profiling of glial heterogeneity |
Signaling Pathways in Glial Pathogenesis
Microglial Receptor Signaling Network
Microglial Receptor Signaling: This diagram illustrates key receptor-mediated pathways in microglial activation. TREM2 signaling through DAP12/SYK promotes phagocytosis and cell survival, while TLR4 and CD36 activate inflammatory responses and pyroptosis through NF-κB and NLRP3 inflammasome pathways, respectively.
Astrocyte Dysfunction in Neurodegeneration
Astrocyte Dysfunction Pathways: This diagram summarizes molecular pathways driving astrocyte dysfunction in neurodegeneration. Aβ and microglial signals promote the neurotoxic A1 phenotype, while SORCS2 deficiency enables δ-secretase activation, linking amyloid and tau pathologies. Metabolic dysfunction contributes directly to neuronal death.
Future Directions and Therapeutic Implications
The expanding knowledge of glial pathophysiology in neurodegenerative diseases has opened new avenues for therapeutic development. Several promising strategies are emerging:
Microglia-Targeted Therapies: Approaches include TREM2 agonism to enhance phagocytic function, CD33 antagonism to reduce inhibitory signaling, and modulation of immunometabolic pathways to reprogram microglial phenotypes [22] [24]. Targeting microglial ferroptosis represents another novel strategy for neuroprotection [25].
Astrocyte-Directed Interventions: Potential therapies include modulation of astrocyte polarization toward neuroprotective A2 phenotypes, metabolic reprogramming to address bioenergetic deficits, and inhibition of pathogenic pathways such as δ-secretase activation [23] [26].
Gene Therapy Approaches: CRISPR-based and viral vector-mediated interventions could correct glial-specific genetic risk factors or enhance protective functions in both microglia and astrocytes.
Advanced hiPSC Applications: Future research will leverage multi-omics integration, three-dimensional organoid systems, and machine learning approaches to decipher the complex spatiotemporal dynamics of glial responses across disease stages [27]. These technologies will enhance prediction of therapeutic responses and identification of patient-specific treatment strategies.
The continued refinement of hiPSC models that accurately capture the genetic diversity of sporadic Alzheimer's disease will be essential for translating glial biology into effective clinical interventions. By focusing on the expanding roles of microglia and astrocytes in disease pathogenesis, researchers and drug development professionals can identify novel therapeutic targets that address the multifaceted nature of neurodegenerative processes.
Alzheimer's disease (AD) is a devastating neurodegenerative disorder that represents the most common cause of dementia worldwide. While early-onset familial AD (FAD) accounts for less than 5% of cases and is caused by fully penetrant mutations in APP, PSEN1, and PSEN2 genes, the overwhelming majority of cases are sporadic late-onset AD (LOAD) with a complex, polygenic etiology [5] [2]. The heritability of LOAD is estimated to be as high as 80%, underscoring the critical importance of genetic risk factors in disease pathogenesis [29]. For nearly three decades, genome-wide association studies (GWAS) have served as a powerful, hypothesis-free approach for identifying genetic variants that contribute to LOAD risk. Since the initial discovery of APOE as the strongest genetic risk factor for sporadic AD in 1993, GWAS has identified numerous additional susceptibility loci, revealing novel biological pathways and potential therapeutic targets [30] [29]. This review synthesizes current knowledge of GWAS-identified genetic risk factors for sporadic AD, with particular emphasis on their functional validation using human induced pluripotent stem cell (hiPSC) models, which offer unprecedented opportunities for studying AD pathogenesis in human-derived neurons and glial cells.
The APOE Locus: The Preeminent Genetic Risk Factor for Sporadic AD
APOE Genotype and AD Risk Spectrum
The APOE ε4 allele remains the strongest genetic risk factor for sporadic Alzheimer's disease, while the APOE ε2 allele provides the strongest genetic protection, as confirmed by multiple large-scale GWAS and meta-analyses [30]. The three common APOE alleles (ε2, ε3, and ε4) encode protein isoforms that differ at amino acid positions 112 and 158, resulting in significant functional consequences for AD pathogenesis [31]. The population distribution of these alleles creates a remarkable risk spectrum, with APOE ε4 homozygotes facing up to a 15-fold increased risk of developing AD compared to the most common ε3/ε3 genotype, while APOE ε2 carriers enjoy significantly reduced risk [5] [31]. This dose-dependent effect of APOE ε4 underscores its central role in AD pathophysiology.
Table 1: APOE Genotype and Associated Alzheimer's Disease Risk
| Genotype | Prevalence in General Population | Relative Risk for AD | Key Characteristics |
|---|---|---|---|
| ε2/ε2 | ~1% | 0.13 OR | Strongest protection, associated with longevity |
| ε2/ε3 | ~11% | 0.39 OR | Protective effect relative to ε3/ε3 |
| ε3/ε3 | ~60% | Reference (1.0) | Most common genotype |
| ε3/ε4 | ~23% | ~3-fold increase | Intermediate risk |
| ε4/ε4 | ~2% | 8-15-fold increase | Highest genetic risk for sporadic AD |
Differential Pathological Mechanisms of APOE Isoforms
APOE isoforms differentially impact multiple AD-related pathological processes beyond their well-established effects on amyloid-β metabolism and clearance. APOE4 significantly increases Aβ aggregation and deposition, reduces Aβ clearance, exacerbates tau pathology and neurofibrillary tangle formation, amplifies neuroinflammatory responses, and disrupts blood-brain barrier integrity [30] [31]. In contrast, APOE2 demonstrates protective effects across these same pathways. The recently identified APOE3-Christchurch (R136S) mutation, discovered in a woman resistant to autosomal dominant AD despite carrying a PSEN1 E280A mutation, appears to inhibit Aβ oligomerization and disrupt APOE binding to heparan sulfate proteoglycans and LDL receptor family members, providing insights into potential protective mechanisms [30]. These isoform-specific effects highlight the complex multifactorial nature of APOE's contribution to AD pathogenesis.
GWAS-Identified Genetic Risk Loci Beyond APOE
Evolution of GWAS Findings in Alzheimer's Disease
GWAS of Alzheimer's disease began in 2007 with initial studies that primarily confirmed the overwhelming association of APOE with disease risk [29]. These early studies, though limited in sample size and genotyping density, established GWAS as a valuable approach for identifying AD susceptibility genes. Technological advances and international collaborations have dramatically expanded GWAS scope and power, with current studies incorporating hundreds of thousands of participants and millions of genetic variants. The largest recent GWAS meta-analysis, published in 2022, identified 75 risk loci for AD, including 42 new loci not previously associated with the disease [32]. This expanding genetic landscape reveals the extraordinary polygenic nature of sporadic AD and implicates diverse biological pathways in disease pathogenesis.
Table 2: Key GWAS-Identified Risk Loci for Sporadic Alzheimer's Disease
| Gene/Locus | Year Identified | Primary Function | Contribution to AD Pathogenesis |
|---|---|---|---|
| BIN1 | 2010 | Membrane trafficking, endocytosis | Modulates tau pathology, influences amyloid processing |
| CLU | 2009 | Chaperone, complement pathway | Aβ clearance, synaptic function, inflammation |
| ABCA7 | 2011 | Lipid transporter, phagocytosis | Aβ clearance, microglial function |
| PICALM | 2009 | Clathrin-mediated endocytosis | Aβ internalization, blood-brain barrier integrity |
| CR1 | 2009 | Complement activation | Inflammation, synaptic pruning |
| SORL1 | 2013 | APP trafficking, endosomal function | Aβ production, endosomal dysfunction |
| TREM2 | 2012 | Microglial signaling, phagocytosis | Neuroinflammation, plaque encapsulation |
| MS4A | 2011 | Immune signaling, calcium homeostasis | B-cell function, microglial activation |
| CD33 | 2011 | Sialic acid binding, innate immunity | Microglial phagocytosis, inflammation |
| EPHA1 | 2011 | Tyrosine kinase receptor, cell signaling | Immune response, synaptic plasticity |
Functional Categorization of Risk Genes and Pathways
The GWAS-identified risk genes can be broadly categorized into several biological pathways, with immune response and microglial function representing the most prominent category. Genes such as TREM2, CR1, ABCA7, and MS4A cluster within this pathway, highlighting the critical importance of neuroinflammation in AD pathogenesis [32]. A second major category includes genes involved in endosomal trafficking and protein sorting, including BIN1, PICALM, and SORL1, which influence APP processing and Aβ generation [29]. Lipid metabolism and transport represent a third significant pathway, with APOE serving as the cornerstone but joined by other lipid-related genes. Additional pathways include synaptic function, protein degradation, and vascular biology, reflecting the multifactorial nature of AD pathophysiology [32]. The preponderance of immune-related genes identified by GWAS has fundamentally shifted AD research toward greater emphasis on neuroimmune mechanisms.
hiPSC Models for Functional Validation of GWAS Findings
hiPSC Technology: Advantages and Applications in AD Research
Human induced pluripotent stem cell (hiPSC) technology has emerged as a transformative approach for studying sporadic Alzheimer's disease, addressing critical limitations of traditional animal models that often fail to fully recapitulate human-specific pathophysiology [6] [5]. By reprogramming somatic cells from individuals with specific genetic backgrounds into pluripotent stem cells, researchers can generate patient-derived neurons, astrocytes, microglia, and other brain cell types that retain the donor's complete genetic risk profile [6]. This platform enables: (1) isogenic comparison of risk variants by genome editing, (2) investigation of cell-type-specific effects, (3) modeling of human-specific disease processes, and (4) screening of therapeutic compounds in a human genetic context. Bibliometric analysis reveals rapidly growing application of hiPSC models in AD research, with annual publications increasing significantly since 2015 and research trends focusing on inflammation, astrocytes, microglia, APOE, and tau [6].
Experimental Workflow for hiPSC-Based Functional Validation
Key Methodologies for hiPSC-Based AD Research
Patient Recruitment and hiPSC Line Generation
The initial step involves careful selection of donors representing specific genetic backgrounds, typically including individuals carrying high-risk alleles (e.g., APOE ε4/ε4), protective alleles (e.g., APOE ε2/ε2), and appropriate controls (e.g., APOE ε3/ε3) [6]. Skin biopsies or blood samples are collected, and somatic cells (typically fibroblasts or peripheral blood mononuclear cells) are reprogrammed into hiPSCs using non-integrating Sendai virus or episomal vectors expressing the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) [6]. Multiple clonal lines are established and rigorously characterized for pluripotency markers (OCT4, NANOG, SSEA-4), karyotypic normality, and differentiation potential before experimental use.
Genome Editing for Isogenic Comparisons
CRISPR/Cas9-mediated genome editing enables creation of isogenic hiPSC lines that differ exclusively at specific risk variants, allowing researchers to isolate the functional consequences of individual polymorphisms [5]. Common strategies include: (1) introducing protective mutations into high-risk genetic backgrounds (e.g., converting APOE4 to APOE3), (2) introducing risk variants into neutral genetic backgrounds, and (3) knocking out risk genes to establish their necessity for observed phenotypes. Precise editing is verified by Sanger sequencing, off-target effects are assessed by whole-genome sequencing, and multiple independently edited clones are characterized to control for clonal variation.
Neural Differentiation and Co-culture Systems
hiPSCs are differentiated into relevant neural cell types using established protocols. Cortical neurons are generated through dual SMAD inhibition, while astrocytes are differentiated through neural progenitor expansion and glial induction [33]. Microglial precursors are generated using specific cytokine cocktails and matured in the presence of IL-34 and CSF-1. For more complex modeling, 2D co-culture systems and 3D cerebral organoids are established to investigate cell-cell interactions. These systems recapitulate key AD pathological features, including Aβ accumulation, tau phosphorylation, and neuroinflammatory responses in a human genetic context [5].
Signaling Pathways Implicated by GWAS in Sporadic AD
Table 3: Key Research Reagent Solutions for hiPSC-Based AD Modeling
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| hiPSC Lines | APOE3/3, APOE4/4, APOE2/2 hiPSCs; isogenic edited lines | Isogenic comparison of genetic risk variants | Verify pluripotency, karyotype stability, genetic background |
| Differentiation Kits | Commercial neural induction kits; astrocyte differentiation media | Generation of relevant neural cell types | Optimize protocol efficiency; assess functional maturity |
| Genome Editing Tools | CRISPR/Cas9 systems; base editors; prime editors | Introduction of specific risk/protective variants | Monitor off-target effects; use multiple independent clones |
| Cell Type Markers | Anti-MAP2 (neurons); Anti-GFAP (astrocytes); Anti-IBA1 (microglia) | Characterization of differentiated cells | Use multiple markers; confirm functional properties |
| Pathological Assays | ELISA for Aβ42/40; Western for p-Tau; Phos-tag gels | Quantification of AD-related pathologies | Standardize culture conditions; use appropriate controls |
| Functional Assays | Multi-electrode arrays; calcium imaging; synaptic dye uptake | Assessment of neuronal network activity | Control for cell density; use appropriate analysis methods |
| Co-culture Systems | Transwell inserts; microfluidic devices; 3D organoid platforms | Modeling cell-cell interactions | Optimize cell ratios; validate system reproducibility |
GWAS has fundamentally expanded our understanding of the genetic architecture of sporadic Alzheimer's disease, moving beyond APOE to identify numerous susceptibility loci that converge on distinct biological pathways. The integration of these GWAS findings with hiPSC-based disease models represents a powerful approach for functional validation and mechanistic exploration of how these genetic variants contribute to disease pathogenesis. Current evidence strongly supports a central role for immune-related processes, lipid metabolism, and endosomal trafficking in AD pathophysiology, with APOE serving as a critical node connecting these pathways. Future research directions should include: (1) development of more complex multi-cell type systems to better model in vivo interactions, (2) integration of additional AD risk factors such as aging and environmental influences, (3) application of single-cell omics technologies to identify cell-type-specific effects of risk variants, and (4) leveraging hiPSC-based models for high-throughput therapeutic screening. The continued synergy between large-scale genetic studies and human cellular models holds exceptional promise for elucidating the fundamental mechanisms underlying sporadic AD and developing effective, genetically-informed therapeutic strategies.
Building Better Brain Models: hiPSC Differentiation, Co-cultures, and 3D Systems
The generation of human induced pluripotent stem cells (hiPSCs) from somatic cells represents a cornerstone of modern biomedical research, providing an unparalleled tool for disease modeling and therapeutic development. Within Alzheimer's disease (AD) research, this technology has enabled the creation of patient-specific neural models that capture the complex genetic architecture of both familial and sporadic disease forms [6] [34]. The reprogramming of somatic cells to a pluripotent state fundamentally rewrites cellular identity through epigenetic remodeling, reversing the process of developmental specialization [35]. This technical guide examines contemporary reprogramming methodologies and donor selection strategies, with particular emphasis on their application in developing physiologically relevant hiPSC models for AD research. The critical interplay between reprogramming techniques and careful donor selection enables researchers to create platforms that accurately recapitulate the polygenic nature of common AD, thereby facilitating drug discovery and mechanistic studies [36] [37].
Molecular Mechanisms of Somatic Cell Reprogramming
Historical Foundations and Key Discoveries
The conceptual foundation for cellular reprogramming was established through pioneering nuclear transfer experiments by John Gurdon in 1962, demonstrating that the somatic cell nucleus retains the genetic completeness required for embryonic development [34] [35]. This discovery of epigenetic plasticity was later validated through cell fusion experiments showing that mouse and human embryonic stem cells (ESCs) could reprogram somatic cells within heterokaryons [34]. The field transformed in 2006 when Shinya Yamanaka identified a minimal set of transcription factors—Oct4, Sox2, Klf4, and c-Myc (OSKM)—sufficient to reprogram mouse fibroblasts to pluripotency [6] [34] [18]. The subsequent generation of human iPSCs by Yamanaka and James Thomson's groups in 2007 established the core technology now widely applied in disease modeling [34].
Epigenetic Remodeling During Reprogramming
Reprogramming somatic cells to pluripotency involves profound epigenetic reorganization that occurs in distinct phases. The early phase is characterized by stochastic silencing of somatic genes and initial activation of early pluripotency-associated genes, while the late phase involves more deterministic activation of the core pluripotency network [34]. Critical epigenetic modifications include:
- DNA Demethylation: Promoter regions of key pluripotency genes (OCT4, SOX2) are heavily methylated in somatic cells but undergo demethylation during reprogramming, facilitated by agents like 5-azacytidine that enhance reprogramming efficiency [38].
- Histone Modification: Somatic cells typically exhibit hypoacetylated histone H4 and specific methylation patterns (H3K9me) that must be reversed to a pluripotent state. Histone deacetylase inhibitors like valproic acid and modulation of H3K79 methylation by Dot1L improve reprogramming efficiency [38] [34].
- Mesenchymal-to-Epithelial Transition (MET): Reprogramming requires MET, accomplished by suppressing EMT mediators (TGFβ1, TGFβR2, Smad) and activating E-cadherin through epigenetic regulation of relevant promoters [38].
The following diagram illustrates the key molecular transitions during somatic cell reprogramming:
Mathematical Models of Reprogramming
The stochastic nature of early reprogramming has been formalized through mathematical models that predict efficiency and kinetics. The model f(Cd, k) describes reprogramming as a function of cell divisions (Cd) and cell-intrinsic reprogramming rate (k) [38]. This framework explains how factors like p53/p21 inhibition accelerate reprogramming by increasing division rates, thereby making stochastic events occur earlier. Another model, V(S) = f (gene regulatory architecture, culture conditions), conceptualizes reprogramming as overcoming "energy barriers" between cellular states [38].
Reprogramming Techniques and Methodologies
Factor-Based Reprogramming Strategies
Multiple approaches have been developed for delivering reprogramming factors to somatic cells, each with distinct advantages and limitations for AD research applications:
- Integrating Viral Vectors: Early reprogramming methods used retroviruses or lentiviruses to deliver OSKM factors, providing high efficiency but risking insertional mutagenesis and transgene reactivation [34].
- Non-Integrating Methods: Episomal vectors, Sendai virus, and mRNA transfection offer non-integrating alternatives that generate footprint-free iPSCs, essential for clinical applications and accurate disease modeling [34].
- Chemical Reprogramming: Fully chemical reprogramming using seven small-molecule compounds was demonstrated in 2013, providing a completely non-genetic approach [34].
Enhancing Reprogramming Efficiency
Several strategies have been identified to improve the efficiency and quality of iPSC generation:
- Small Molecule Enhancers: Vitamin C enhances reprogramming by facilitating histone demethylase Jhdm1a/1b function, which suppresses senescence regulator Ink4a/Arf [38].
- Senescence Bypass: Disruption of the p53 network and other senescence pathways significantly enhances iPSC production efficiency [38].
- microRNA-mediated Reprogramming: microRNAs like the 302-367 cluster can remove epigenetic repressors from pluripotency gene promoters and enable reprogramming without additional transcription factors [38].
Donor Selection Strategies for Alzheimer's Disease Research
Genetic Considerations for AD Modeling
Donor selection represents a critical consideration for generating clinically relevant hiPSC models of Alzheimer's disease. AD exists along a spectrum from rare autosomal-dominant familial forms (FAD) to common sporadic cases (sAD) with complex genetic architecture:
- Familial AD Donors: Characterized by highly penetrant mutations in APP, PSEN1, or PSEN2 genes, suitable for modeling monogenic disease mechanisms [39].
- Sporadic AD Donors: Involve polygenic risk influenced by APOE genotype and numerous other genetic variants identified through genome-wide association studies [36].
Polygenic Risk Score-Based Donor Selection
The IPMAR resource (iPSC Platform to Model Alzheimer's Disease Risk) exemplifies a sophisticated donor selection strategy that captures extremes of polygenic risk for common AD [36] [21] [37]. This resource includes:
- 90 iPSC lines with extremes of global AD polygenic risk: 34 from high-risk late-onset AD donors, 29 from high-risk early-onset AD donors, and 27 from low-risk cognitively healthy controls [36].
- 19 iPSC lines with complement pathway-specific polygenic risk: 9 from high-risk AD donors and 10 from low-risk controls [36].
- Comprehensive associated data: All lines have associated clinical, longitudinal, and genetic datasets available through cell and data repositories [21].
Table 1: IPMAR Resource Donor Stratification Based on Polygenic Risk Scores
| Donor Category | Number of iPSC Lines | Mean Global PRS (SD) | Mean Complement PRS (SD) | Age of Onset (SD) |
|---|---|---|---|---|
| Late-Onset AD (High Global PRS) | 34 | 2.2 (±0.5) | N/A | 72 (±6) |
| Early-Onset AD (High Global PRS) | 29 | 2.1 (±0.4) | N/A | 51 (±3) |
| Healthy Controls (Low Global PRS) | 27 | -1.9 (±0.4) | N/A | N/A |
| AD (High Complement PRS) | 9 | N/A | 2.4 (±0.3) | 71 (±6) |
| Healthy Controls (Low Complement PRS) | 10 | N/A | -1.9 (±0.2) | N/A |
APOE Genotype Considerations
The APOE ε4 allele remains the most significant genetic risk factor for sporadic AD, with odds ratios between 3.62 and 34.3 depending on population [36]. Donor selection should carefully consider APOE genotype alongside polygenic risk scores to accurately model the genetic complexity of AD.
Experimental Workflows and Protocols
IPSC Generation and Quality Control Protocol
The generation of the IPMAR resource exemplifies a robust workflow for creating genetically stratified iPSC banks:
- Donor Selection: Identify donors from well-characterized cohorts using polygenic risk scoring from genome-wide association data [36].
- Somatic Cell Collection: Obtain peripheral blood mononuclear cells (PBMCs) or skin fibroblasts from selected donors, prioritizing recent donations [36].
- Reprogramming: Transform somatic cells using non-integrating methods to generate footprint-free iPSCs.
- Quality Control: Perform comprehensive characterization including pluripotency marker expression, karyotyping, and differentiation potential [36].
- Banking and Distribution: Cryopreserve validated lines and make them available through repositories like EBiSC and DPUK [37].
Vascularized Neuroimmune Organoid Generation
Advanced disease modeling employs complex 3D organoid systems that incorporate multiple cell types affected in AD:
- Progenitor Generation: Derive neural progenitor cells (NPCs), primitive macrophage progenitors (PMPs), and vascular progenitors (VPs) from hiPSCs [40].
- 3D Co-culture: Combine NPCs, PMPs, and VPs at optimized ratios (30,000:12,000:7,000) to facilitate self-organization into organoids [40].
- Maturation Culture: Maintain organoids in neural differentiation medium supplemented with IL-34, VEGF, and other factors to support neuronal, microglial, and vascular maturation [40].
- Disease Modeling: Expose organoids to AD brain extracts to induce multiple pathologies including Aβ plaques, tau tangles, and neuroinflammation within four weeks [40].
Table 2: Essential Research Reagents for hiPSC-based Alzheimer's Disease Modeling
| Reagent Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Induction of pluripotency in somatic cells |
| Small Molecule Enhancers | Vitamin C, Valproic acid, 5-azacytidine | Improve reprogramming efficiency through epigenetic modulation |
| Differentiation Factors | IL-34, VEGF, bFGF, BMP4 | Direct differentiation toward neural, vascular, and microglial lineages |
| Cell Type Markers | PAX6/NESTIN (NPCs), CD235/CD43 (PMPs), CD31 (endothelial) | Characterization and validation of progenitor populations |
| Pathology Assays | Aβ and tau antibodies, synaptic markers, inflammation cytokines | Detection and quantification of AD-related pathologies |
Applications in Alzheimer's Disease Research and Drug Development
Disease Modeling Applications
HiPSC models derived through careful reprogramming and donor selection enable numerous research applications:
- Mechanistic Studies: Investigating the molecular consequences of polygenic risk in human neurons and glia, particularly pathways involving inflammation, complement, and apolipoprotein E [6] [36].
- Pathological Recapitulation: Modeling key AD pathologies including amyloid plaque-like aggregates, tau tangle-like formations, neuroinflammation, synaptic loss, and neuronal death [40].
- Patient Stratification: Identifying distinct molecular subtypes of AD based on genetic risk profiles, enabling personalized therapeutic approaches [36].
Drug Discovery and Validation
HiPSC platforms provide human-relevant systems for therapeutic development:
- High-Throughput Screening: Vascularized neuroimmune organoids enable medium-throughput evaluation of candidate compounds using relevant human cellular environments [40].
- Therapeutic Validation: Testing FDA-approved drugs like Lecanemab in organoid models has demonstrated significant reduction of amyloid burden and revealed potential vascular inflammation side effects [40].
- CRISPR Screening: Combining hiPSCs with CRISPR/Cas9 enables functional validation of genetic risk factors and identification of novel therapeutic targets [39].
The following diagram illustrates the integrated workflow from donor selection to drug discovery:
The integration of refined reprogramming techniques with genetically informed donor selection strategies has transformed our approach to Alzheimer's disease modeling. hiPSC technology now enables researchers to capture the complex polygenic nature of sporadic AD through resources like IPMAR, while advanced differentiation protocols generate increasingly sophisticated models like vascularized neuroimmune organoids. These platforms recapitulate key AD pathologies in human cells and provide valuable systems for drug discovery and validation. As reprogramming methods continue to evolve toward greater efficiency and fidelity, and as our understanding of AD genetics expands, hiPSC-based models will play an increasingly central role in deciphering disease mechanisms and developing effective therapeutics for this devastating neurodegenerative disorder.
The ability to direct the differentiation of human induced pluripotent stem cells (hiPSCs) into specific neural cell types—cortical neurons, astrocytes, and microglia—has revolutionized Alzheimer's disease (AD) research. These patient-derived cells provide unprecedented opportunities to model both sporadic (SAD) and familial (FAD) Alzheimer's disease in vitro, enabling researchers to study disease mechanisms, screen therapeutic compounds, and investigate the complex cell-cell interactions that drive neurodegeneration [6] [5]. The differentiation protocols for generating these neural cells represent a cornerstone of modern neurodegenerative disease modeling, allowing for the creation of isogenic cell lines that capture patient-specific genetic backgrounds and disease phenotypes.
For AD research, hiPSC models are particularly valuable because they address critical limitations of traditional rodent models, which often fail to fully recapitulate human disease pathology and have not successfully predicted therapeutic outcomes in human clinical trials [5]. The development of robust differentiation protocols enables researchers to generate the key brain cell types involved in AD pathogenesis, including neurons vulnerable to amyloid-β and tau pathology, astrocytes that contribute to metabolic support and inflammatory responses, and microglia that play crucial roles in synaptic pruning and clearance of protein aggregates [41] [5]. This technical guide provides comprehensive methodologies for generating these essential neural cell types within the context of Alzheimer's disease research using hiPSC models.
Core Signaling Pathways Governing Neural Cell Fate
The differentiation of hiPSCs into neural lineages is controlled by a core set of evolutionarily conserved signaling pathways that direct cells toward specific neural fates. Understanding and manipulating these pathways is essential for generating pure populations of cortical neurons, astrocytes, and microglia.
Key Developmental Signaling Pathways
BMP Signaling plays a critical role in the binary fate decision between neural and epidermal ectoderm. BMP antagonists (Noggin, Chordin, Follistatin) are essential neural inducers that block BMP signaling, promoting neural fate acquisition while inhibiting alternative lineages [42] [43]. During neural differentiation of mouse ES cells, BMP4 treatment significantly inhibits neural commitment while upregulating non-neural markers like Id1, demonstrating its potent anti-neuralizing activity [43]. BMP signaling also promotes astrocyte differentiation in later developmental stages, particularly through SMAD-mediated transcriptional activation [42].
Notch Signaling maintains neural progenitor renewal and inhibits neuronal commitment through activation of downstream effectors like HES1, HES5, and BLBP [44] [42]. In the human developing neocortex, asymmetric Notch activation occurs in self-renewing daughter cells following basal radial glial cell divisions, independently of basal fibre inheritance [44]. Notch signaling also promotes astroglial fates while preventing oligodendrocyte formation during later gliogenic phases [42].
Wnt Signaling exhibits stage-dependent effects, promoting proliferation of early neural progenitor cells while supporting neurogenesis in later stages [42]. The canonical Wnt pathway involves β-catenin stabilization and translocation to the nucleus, where it complexes with TCF/LEF transcription factors to activate target genes. Wnt signaling induces neuronal and astroglial differentiation while suppressing oligodendroglial differentiation [42].
Other Critical Pathways include Sonic Hedgehog (Shh) for dorsoventral patterning, FGF for promoting neural induction through Smad1 phosphorylation, and STAT3 which promotes astrocyte differentiation particularly in combination with BMP and Notch signaling [42]. STAT3 activation occurs through phosphorylation following cytokine receptor engagement (LIF, CNTF, IL-6), leading to dimerization, nuclear translocation, and binding to target gene promoters [42].
Figure 1: Core Signaling Pathways in Neural Fate Determination. Multiple signaling pathways interact to regulate neural cell fate decisions. BMP antagonists promote neural induction, while Notch signaling maintains progenitor pools. Wnt and other pathways exhibit stage-specific effects on proliferation versus differentiation.
Quantitative Analysis of Neural Progenitor Division Modes
Live imaging studies of human basal radial glial cells (bRGs) in fetal tissue and cerebral organoids have revealed distinct division modes that influence neurogenesis. The following table summarizes the quantitative analysis of bRG division modes from a study investigating 1,101 dividing bRG cells in cerebral organoids:
Table 1: Quantitative Analysis of Basal Radial Glial Cell Division Modes in Human Cerebral Organoids
| Division Mode | Daughter Cell Fates | Relative Frequency | Key Features | Experimental Evidence |
|---|---|---|---|---|
| Symmetric Amplifying | Two SOX2+ progenitor cells | Abundant | Expands progenitor pool | Live imaging of 1,101 dividing bRGs [44] |
| Direct Neurogenic | Differentiating cells (EOMES+ or NEUN+) | Frequent, especially in OSVZ | Bypasses intermediate progenitors | Correlative live-fixed imaging [44] |
| Asymmetric Self-Renewing | One SOX2+ and one differentiating cell | Observed | Maintains progenitor population | Notch activation in self-renewing daughters [44] |
| Symmetric Self-Consuming | Two differentiating daughters | Less common | Depletes progenitor pool | Fate mapping in developing neocortex [44] |
The abundance of symmetric amplifying divisions and frequent self-consuming direct neurogenic divisions in human bRG cells suggests an alternative route to the asymmetric self-renewing divisions that dominate in mouse apical radial glial progenitor cells [44]. These division modes are remarkably conserved between human fetal tissue and cerebral organoids, supporting the value of organoid systems for modeling early human neurogenesis in both healthy development and disease contexts like Alzheimer's [44].
hiPSC Differentiation to Cortical Neurons
Principles of Cortical Neuron Specification
The generation of cortical neurons from hiPSCs relies on recapitulating developmental processes through sequential manipulation of key signaling pathways. Cortical neuron differentiation typically occurs through dual-SMAD inhibition, which promotes neural induction by concurrently blocking both BMP and TGF-β signaling pathways [5] [43]. This approach efficiently directs hiPSCs toward a neural fate while suppressing non-neural lineages. The resulting neural progenitor cells can then be patterned toward cortical fates using small molecules and growth factors that mimic embryonic cortical development.
The differentiation process produces various cortical neuron subtypes in a temporal sequence that mirrors in vivo development, with deep-layer neurons appearing first, followed by upper-layer neurons [5]. This progression is governed by both intrinsic genetic programs and extrinsic cues that can be manipulated to enrich for specific neuronal populations relevant to Alzheimer's disease research, particularly those vulnerable to neurodegeneration.
Detailed Cortical Neuron Differentiation Protocol
Stage 1: Neural Induction (Days 0-10)
- Culture hiPSCs at 70-80% confluence in mTeSR or equivalent medium
- Begin dual-SMAD inhibition using 100nM LDN-193189 (BMP inhibitor) and 10μM SB431542 (TGF-β inhibitor) in neural induction medium
- Change medium daily for 10 days
- Observe formation of neural rosettes by day 7-10
Stage 2: Cortical Patterning (Days 10-30)
- Pattern neural progenitor cells toward cortical fate using 1μM IWR-1 (Wnt inhibitor) to promote forebrain identity
- Add 100ng/mL FGF2 to support neural progenitor expansion
- Passage cells as needed using Accutase
- Monitor expression of cortical markers (PAX6, FOXG1, TBR2)
Stage 3: Neuronal Differentiation (Days 30-90)
- Withdraw FGF2 and switch to neuronal differentiation medium containing B27 supplement
- Add 20ng/mL BDNF, 20ng/mL GDNF, and 1mM cAMP to support neuronal maturation
- Maintain cultures for 60-90 days to allow full maturation and synaptic development
- Assess neuronal function using electrophysiology and calcium imaging
Stage 4: Characterization and Validation
- Immunostaining for cortical markers: βIII-tubulin (neurons), MAP2 (mature neurons), CTIP2 (deep-layer neurons), BRN2 (upper-layer neurons)
- RNA analysis for cortical layer-specific genes
- Functional assessment through patch-clamp electrophysiology
- Validation of synaptic activity using immunostaining for PSD-95 and synapsin
Table 2: Critical Reagents for Cortical Neuron Differentiation from hiPSCs
| Reagent Category | Specific Compounds | Concentration | Function | Mechanism of Action |
|---|---|---|---|---|
| SMAD Inhibitors | LDN-193189 | 100nM | BMP pathway inhibition | Blocks BMP type I receptors ALK2/3 |
| SB431542 | 10μM | TGF-β pathway inhibition | Inhibits TGF-β type I receptors ALK4/5/7 | |
| Wnt Pathway Modulators | IWR-1 | 1μM | Forebrain patterning | Wnt pathway inhibition through tankyrase stabilization |
| Growth Factors | FGF2 | 100ng/mL | Neural progenitor expansion | Activates FGF receptor signaling |
| BDNF | 20ng/mL | Neuronal maturation | Binds TrkB receptor, promotes survival | |
| GDNF | 20ng/mL | Neuronal support | Enhances dopaminergic and cortical neuron survival | |
| Other Supplements | B27 | 1X | Neuronal health | Provides antioxidants and fatty acids |
| cAMP | 1mM | Neuronal maturation | Activates PKA signaling, enhances maturation |
hiPSC Differentiation to Astrocytes
Principles of Astrocyte Specification
Astrogenesis typically follows neurogenesis during brain development, with the transition from neuronal to glial production being regulated by both intrinsic and extrinsic factors [42] [5]. Key signaling pathways promoting astrocyte differentiation include Notch, BMP, and CNTF/LIF/IL-6 families which activate JAK-STAT signaling [42]. In hiPSC differentiation systems, this temporal sequence is maintained, with efficient astrocyte generation requiring extended maturation periods of several months to achieve functional properties resembling primary human astrocytes.
Astrocytes generated from hiPSCs are particularly valuable for Alzheimer's disease research due to their multiple roles in AD pathogenesis, including their contribution to neuroinflammation, their function in Aβ clearance, their support of neuronal metabolic needs, and their role in maintaining synaptic homeostasis [41] [5]. The ability to generate astrocytes from both FAD and SAD hiPSC lines enables investigation of cell-autonomous and non-cell-autonomous mechanisms in AD progression.
Detailed Astrocyte Differentiation Protocol
Stage 1: Neural Progenitor Cell Generation (Days 0-20)
- Generate neural progenitor cells (NPCs) using dual-SMAD inhibition as described in cortical neuron protocol
- Expand NPCs in neural expansion medium containing FGF2 and EGF
- Confirm NPC identity using immunostaining for SOX2, NESTIN, and PAX6
Stage 2: Gliogenic Committment (Days 20-60)
- Passage NPCs using Accutase and plate at high density
- Switch to gliogenic induction medium containing 10% FBS or 1μM BMP4
- Alternatively, use CNTF (10ng/mL) or LIF (10ng/mL) to promote astroglial fate
- Culture for 30-40 days with medium changes every 2-3 days
Stage 3: Astrocyte Maturation (Days 60-180)
- Maintain cells in astrocyte maturation medium containing 1% FBS, N2 supplement, and BMP4
- Passage cells as needed using trypsin-EDWA
- Extended maturation (up to 180 days) improves functional properties
- Some protocols use 3D culture or rotary bioreactors to enhance maturation
Stage 4: Characterization and Validation
- Immunostaining for astrocyte markers: GFAP, S100β, AQP4, EAAT1/GLAST
- Functional assessment of glutamate uptake using glutamate assay
- Calcium imaging to evaluate calcium signaling dynamics
- RNA sequencing to confirm transcriptional profile matching primary astrocytes
- Phagocytosis assays using pHrodo-labeled Aβ or synaptic material
Figure 2: Astrocyte Differentiation Workflow from hiPSCs. The differentiation process extends over approximately 180 days, progressing through neural progenitor, gliogenic commitment, and maturation stages with key signaling molecules directing each transition toward functional astrocytes.
hiPSC Differentiation to Microglia
Principles of Microglia Specification
Microglia differ from other neural cell types in their developmental origin, deriving from yolk sac erythro-myeloid progenitors rather than neuroectoderm [45] [41]. These primitive macrophages colonize the developing brain early in embryogenesis and undergo maturation in response to CNS environmental cues [41]. hiPSC differentiation protocols for microglia must therefore recapitulate this unique developmental trajectory, typically progressing through hematopoietic progenitor intermediates before final microglial maturation.
In Alzheimer's disease research, microglia are particularly important due to their roles in Aβ clearance, synaptic pruning, and neuroinflammation [41] [5]. Recent genetic studies have identified numerous AD risk genes that are highly expressed in microglia, highlighting their crucial contribution to disease pathogenesis [5]. The ability to generate authentic human microglia from hiPSCs enables investigation of these genetic risk factors and development of more physiologically relevant models of neuroinflammation in AD.
Detailed Microglia Differentiation Protocol
Stage 1: Hematopoietic Progenitor Generation (Days 0-10)
- Culture hiPSCs in mTeSR until 80% confluent
- Transition to serum-free hematopoietic induction medium containing 100ng/mL BMP4, 50ng/mL VEGF, and 20ng/mL SCF
- Change medium daily for 10 days
- Observe emergence of floating hematopoietic progenitor cells
Stage 2: Myeloid Progenitor Differentiation (Days 10-20)
- Collect floating hematopoietic progenitors and replate in low-attachment plates
- Culture in myeloid specification medium containing 100ng/mL M-CSF, 25ng/mL IL-3, and 50ng/mL GM-CSF
- Maintain for 10-14 days with medium changes every 3-4 days
- Confirm CD45+/CD43+ myeloid progenitor identity using flow cytometry
Stage 3: Microglial Maturation (Days 20-40)
- Transfer myeloid progenitors to microglial maturation medium containing 100ng/mL IL-34, 10ng/mL GM-CSF, and 5ng/mL TGF-β
- Culture for 14-21 days to allow microglial maturation
- Alternatively, co-culture with developing neural organoids for enhanced maturation
- Monitor morphological changes from amoeboid to ramified morphology
Stage 4: Characterization and Validation
- Flow cytometry for microglial markers: TMEM119, P2RY12, CX3CR1, TREM2
- Functional assessment of phagocytosis using pHrodo-labeled Aβ or latex beads
- Cytokine secretion profiling in response to inflammatory stimuli (LPS, Aβ)
- Transcriptional analysis to confirm microglial signature
- Morphological analysis of process complexity and dynamic surveillance
Table 3: Microglia Differentiation Reagents and Key Markers
| Stage | Critical Factors | Concentration | Target Markers | Functional Assays |
|---|---|---|---|---|
| Hematopoietic Progenitor | BMP4, VEGF, SCF | 100ng/mL, 50ng/mL, 20ng/mL | CD34, CD43, CD45 | Colony formation |
| Myeloid Specification | M-CSF, IL-3, GM-CSF | 100ng/mL, 25ng/mL, 50ng/mL | CD45, CD11b, CD14 | Proliferation capacity |
| Microglial Maturation | IL-34, TGF-β, GM-CSF | 100ng/mL, 5ng/mL, 10ng/mL | TMEM119, P2RY12, CX3CR1 | Phagocytosis, cytokine release |
| Functional Validation | - | - | TREM2, IBA1 | Aβ clearance, synaptic pruning |
The Scientist's Toolkit: Essential Research Reagents
Successful differentiation of neural cell types from hiPSCs requires carefully selected reagents and materials. The following table provides a comprehensive overview of essential research tools for directing neural fate, with particular emphasis on their applications in Alzheimer's disease research.
Table 4: Essential Research Reagent Solutions for Neural Cell Differentiation and Alzheimer's Disease Modeling
| Reagent Category | Specific Examples | Applications | Key Functions | Considerations for AD Research |
|---|---|---|---|---|
| Small Molecule Inhibitors | LDN-193189, SB431542, DMH1, IWR-1 | Neural induction, patterning | SMAD inhibition, Wnt modulation | Consistency across FAD/SAD lines |
| Growth Factors & Cytokines | FGF2, EGF, BMP4, IL-34, M-CSF, CNTF | Lineage specification, maturation | Receptor signaling activation | Batch-to-batch variability |
| Cell Surface Markers | CD44, CD184, CD15, CD24, CD271, CD45 | Cell sorting, purification | Isolation of specific populations | Purity requirements for assays |
| Extracellular Matrix | Matrigel, Laminin, Poly-L-Ornithine | Cell adhesion, differentiation | Structural support, signaling | Impact on disease phenotypes |
| Characterization Antibodies | SOX2, PAX6, TBR2 (progenitors); βIII-tubulin, MAP2 (neurons); GFAP, S100β (astrocytes); TMEM119, P2RY12 (microglia) | Lineage validation | Cell type identification | Specificity for human epitopes |
| Functional Assay Reagents pHrodo-labeled Aβ, FM dyes, Glutamate assay kits, ELISA kits | Functional validation | Phagocytosis, synaptic function, metabolism | Disease-relevant readouts | |
| Gene Editing Tools | CRISPR/Cas9 systems, PiggyBac transposon | Isogenic controls, reporter lines | Genetic manipulation | Introduction of FAD mutations |
Applications in Alzheimer's Disease Research
The differentiation protocols outlined in this guide enable the generation of essential cellular tools for Alzheimer's disease research using hiPSCs. These models are particularly valuable for investigating the distinct mechanisms underlying sporadic and familial AD, modeling cell-type-specific contributions to disease pathogenesis, and developing more physiologically relevant drug screening platforms.
Modeling Sporadic vs. Familial Alzheimer's Disease
hiPSC models derived from SAD patients capture the complex genetic heterogeneity of the disease, including the influence of risk alleles like APOE4, while FAD models with mutations in APP, PSEN1, or PSEN2 enable investigation of specific disease-causing mechanisms [6] [5]. The ability to generate isogenic controls through gene editing—introducing pathogenic mutations into healthy lines or correcting mutations in patient lines—provides powerful experimental tools for dissecting disease mechanisms while controlling for genetic background effects [5].
Advanced Model Systems: Co-cultures and Organoids
Beyond monocultures, researchers are developing increasingly complex models that incorporate multiple neural cell types to better capture the cellular interactions occurring in the AD brain [41] [5]. These include:
- Neuron-astrocyte co-cultures to model neuroglial interactions and astrocyte-mediated neurotoxicity or protection
- Neuron-microglia co-cultures to investigate neuroinflammatory mechanisms and phagocytic clearance of Aβ and tau
- Tri-culture systems containing neurons, astrocytes, and microglia to model the "tripartite synapse" and complex cell interactions
- Brain organoids with integrated microglia to study tissue-level organization and disease processes in a 3D environment
These advanced models enable researchers to investigate critical aspects of AD pathogenesis, including neuroinflammation, synaptic pruning, Aβ clearance, and cell-type-specific vulnerabilities, providing more physiologically relevant systems for drug discovery and mechanistic studies [41] [5].
The protocols and methodologies outlined in this technical guide provide researchers with comprehensive tools for generating the key neural cell types involved in Alzheimer's disease pathogenesis. The ability to differentiate hiPSCs into cortical neurons, astrocytes, and microglia—and to combine them in increasingly complex co-culture systems—enables the creation of physiologically relevant human models for studying both sporadic and familial AD. These cellular models represent essential tools for unraveling disease mechanisms, identifying novel therapeutic targets, and screening potential treatments, ultimately contributing to the development of effective interventions for this devastating neurodegenerative disorder.
Human induced pluripotent stem cell (hiPSC) technology has revolutionized Alzheimer's disease (AD) research by providing patient-specific models that recapitulate human physiology and pathology. The pathogenesis of AD involves complex interactions between multiple cell types in the central nervous system (CNS), creating an urgent need for advanced culture systems that extend beyond single-cell-type models [2]. Research trends have increasingly focused on inflammation, astrocytes, microglia, and apolipoprotein E (ApoE), highlighting the importance of intercellular communication in disease progression [6]. This technical guide explores advanced co-culture and tri-culture platforms that enable researchers to study these dynamic interactions within physiologically relevant environments, offering crucial insights for both familial AD (fAD) and the more prevalent but less understood sporadic AD (sAD), which accounts for over 95% of cases [2].
Tri-Culture Systems: Recapitulating Neuro-Glial Interactions
hiPSC-Derived Neuron-Astrocyte-Microglia Tri-culture
The integration of neurons, astrocytes, and microglia in a single culture system represents a significant advancement for modeling the neuroinflammatory components of AD pathology. A recently developed cryopreservation-compatible protocol enables standardized study of dynamic intercellular relationships [46].
Table 1: Key Components of hiPSC-Derived Tri-culture System
| Component | Description | Functional Significance in AD |
|---|---|---|
| Neurons | hiPSC-derived cortical neurons | Primary cells affected by Aβ and tau pathology; model synaptic loss and neuronal death |
| Astrocytes | hiPSC-derived astrocyte lineage | Regulate synaptic function, release inflammatory mediators, contribute to Aβ metabolism |
| Microglia | hiPSC-derived microglial cells | Brain resident immune cells; mediate neuroinflammation, phagocytose Aβ aggregates |
Protocol: Establishing Tri-culture from hiPSCs
- Cell Line Selection: Utilize hiPSCs from both fAD (with APP, PSEN1, or PSEN2 mutations) and sAD patients to enable comparative studies [2].
- Genetic Engineering: Transduce iPSCs with cell type-specific factors for directed differentiation.
- Sequential Differentiation:
- Differentiate hiPSCs to neural progenitor cells (NPCs)
- Generate intermediate cryopreserved stocks of each cell population
- Differentiate NPCs to cortical neurons, astrocytes, and microglia using specific media formulations
- Tri-culture Assembly: Combine the three cell types in defined ratios optimized for neuronal health and glial interactions.
- Functional Validation: Confirm system functionality through calcium imaging, cytokine secretion profiling, and phagocytosis assays [46].
Figure 1: Experimental workflow for establishing hiPSC-derived tri-culture systems
Applications in Alzheimer's Disease Research
This tri-culture platform enables investigation of critical AD-specific processes:
- Astrocyte-induced microglial activation in response to fAD neuronal signals
- Microglial-dependent synaptic pruning and its contribution to cognitive decline
- Clusterin (CLU) modulation of astrocyte reactivity and microglial synaptic remodeling [46]
- APOE isoform-specific effects on neuroinflammation and Aβ clearance
Advanced Co-culture Systems for Specialized Functions
Oligodendrocyte-Neuron Co-culture for Myelination Studies
Myelination deficits contribute to cognitive impairment in AD. A direct co-culture protocol using three-dimensional (3D) nanomatrix plates enables controlled study of neuron-oligodendrocyte interactions and myelination patterns [47].
Protocol: 3D Oligodendrocyte-Neuron Co-culture
- 3D Scaffold Preparation: Coat plates with 3D nanofiber networks to mimic extracellular matrix
- Neuronal Differentiation: Differentiate hiPSCs into cortical neurons directly on 3D nanofibers
- Oligodendrocyte Differentiation: Generate oligodendrocyte precursor cells (OPCs) from hiPSCs
- Cell Isolation: Detach and isolate hiPSC-derived oligodendrocyte lineage cells
- Co-culture Establishment: Seed oligodendrocyte lineage cells onto established neuronal cultures in the 3D microenvironment [47]
Table 2: Comparison of 2D vs 3D Co-culture Systems for Myelination Studies
| Parameter | 2D Co-culture | 3D Nanofiber Co-culture |
|---|---|---|
| Myelination Efficiency | Moderate | Enhanced |
| Structural Complexity | Limited | Physiologically relevant architecture |
| Long-term Stability | 2-3 weeks | 4+ weeks |
| Drug Screening Compatibility | High | Moderate |
| Imaging Accessibility | Excellent | Technically challenging |
Cardiomyocyte Co-culture Systems for Drug Toxicity Screening
Though developed for cardiotoxicity assessment, hiPSC-derived cardiomyocyte (hiPSC-CM) co-culture methodologies provide valuable paradigms for ensuring cellular functionality in complex culture systems, with relevance to AD model validation [48].
Functional Validation of Signaling Pathways
- ErbB2 Pathway Analysis: Confirm expression and functionality through phosphorylation of AKT and Erk1/2
- Real-time Functional Monitoring: Employ impedance and field potential measurements to assess cellular health
- Multiparameter Endpoints: Combine calcium cycling, contractility, and electrophysiological measurements [48]
Signaling Pathways in Advanced Culture Systems
Complex culture systems require thorough characterization of relevant signaling pathways to ensure physiological relevance. The following diagram illustrates key pathways implicated in AD that can be studied using these advanced platforms:
Figure 2: Key signaling pathways relevant to hiPSC model functionality and drug screening
Research Reagent Solutions for Advanced Culture Systems
Table 3: Essential Research Reagents for hiPSC Co-culture and Tri-culture Platforms
| Reagent Category | Specific Examples | Function | Application in AD Research |
|---|---|---|---|
| Cell Culture Media | Plating media; Maintenance media; Neural induction media; Astrocyte differentiation media; Microglial differentiation media | Support cell survival, proliferation, and specific differentiation | Enable generation of disease-relevant cell types from fAD and sAD hiPSCs |
| Extracellular Matrix | Gelatin; Fibronectin; Basement membrane extracts (e.g., ATCC CellMatrix); 3D nanofiber scaffolds | Provide structural support and biochemical cues that mimic native microenvironment | Enhance maturation and physiological relevance of neuronal and glial cultures |
| Characterization Antibodies | Cardiac troponin I (cardiomyocytes); Myomesin; β-III-tubulin (neurons); GFAP (astrocytes); IBA1 (microglia) | Cell type identification and purity assessment | Quality control for culture systems; confirmation of cell-type specific pathology |
| Cell Signaling Reagents | Neuregulin-1β (NRG); Phospho-specific antibodies (p-AKT, p-ERK); Caspase activation assays | Pathway activation and functional assessment | Monitor neuroprotective vs neurotoxic signaling in AD models |
| Functional Assays | Real-time cell analysis (RTCA) systems; Calcium imaging kits; LDH cytotoxicity assays; ATP content assays | Multiparameter assessment of cell health and function | Quantify Aβ toxicity, synaptic dysfunction, and drug efficacy |
Methodological Considerations for Alzheimer's Disease Research
Stratification of Familial vs. Sporadic AD Models
The application of co-culture and tri-culture systems must account for fundamental differences between fAD and sAD:
- fAD Models: Utilize hiPSCs with known pathogenic mutations (APP, PSEN1, PSEN2) to study deterministic genetic factors
- sAD Models: Employ hiPSCs from patients without known mutations but confirmed AD pathology; require larger sample sizes to account for heterogeneity
- Isogenic Controls: Use CRISPR-edited isogenic cell lines to isolate effects of specific genetic risk factors (e.g., APOE ε4) [6] [2]
Protocol Optimization for Disease Modeling
- Challenge: Standardized methods for multi-lineage co-culture remain limited in the field [46]
- Solution: Implement systematic quality control measures including:
- Regular assessment of cardiomyocyte purity and contractility (for cardiotoxicity assessment) [48]
- Validation of neuronal activity through multielectrode array (MEA) recordings
- Confirmation of glial activation states through cytokine profiling
Advanced co-culture and tri-culture systems represent the frontier of hiPSC-based Alzheimer's disease research, enabling unprecedented investigation of cell-type-specific contributions to disease pathogenesis. By recapitulating the multi-cellular environment of the human brain, these platforms address critical limitations of traditional mono-culture systems and animal models, particularly for the complex, multifactorial sporadic AD. The methodologies outlined in this technical guide provide researchers with robust frameworks for implementing these sophisticated models, accelerating both basic science discoveries and therapeutic development for this devastating neurodegenerative disorder.
The study of Alzheimer's disease (AD) has long been constrained by the limitations of existing models. Traditional two-dimensional (2D) cell cultures lack the architectural complexity and cell-cell interactions of native brain tissue, while animal models fail to fully recapitulate human-specific disease pathology and are limited by species differences [49] [50]. This is particularly problematic for sporadic AD (sAD), which represents over 95% of all cases and involves complex interactions between genetic and environmental factors that cannot be easily modeled in genetically modified animals [40]. The emergence of three-dimensional (3D) brain organoids derived from human induced pluripotent stem cells (hiPSCs) represents a transformative approach that bridges these critical gaps in neuroscience research.
Brain organoids are 3D multicellular structures that mimic the structural and functional complexities of the human brain through self-organization and differentiation of pluripotent stem cells under specific in vitro conditions [51] [50]. These miniaturized encephalic models capture key aspects of human brain development and disease progression that were previously inaccessible for direct investigation. For AD research specifically, brain organoids offer an unprecedented platform for modeling the multifaceted pathology including β-amyloid and tau protein aggregation, neuroinflammation, and aging processes in a human-relevant system [49]. The technology enables generation of both familial AD (fAD) models through genetic manipulation and sporadic AD (sAD) models that capture the complex aetiology of the most prevalent form of the disease [6] [40].
The integration of hiPSC technology with 3D organoid culture has created powerful patient-specific models that retain donor-specific genetic and molecular signatures, enabling researchers to dissect the mechanistic diversity underlying AD and paving the way for personalized therapeutic strategies [6]. This review comprehensively examines the current state of brain organoid technology, its application in deciphering AD pathology, and the advanced methodological innovations that are enhancing the physiological relevance and translational potential of these remarkable models.
Methodological Foundations: Generating Physiologically Relevant Brain Organoids
Core Differentiation Strategies and Regional Patterning
The generation of brain organoids relies on two principal methodologies: self-organization and directed differentiation. The self-organization approach, pioneered by Lancaster and Knoblich, exploits the intrinsic developmental programming of human pluripotent stem cells (hPSCs) to spontaneously form neuroectodermal structures with minimal external guidance [51] [50]. This method typically involves embedding hPSC aggregates in Matrigel droplets and culturing them in neural induction media, resulting in whole-brain organoids containing multiple brain regions [50]. While this approach generates remarkable heterogeneity and recapitulates early developmental processes, it often yields variable results with inconsistent regional specification.
In contrast, the directed differentiation approach applies precise temporal sequences of exogenous morphogens to guide regional specification along the anterior-posterior and dorso-ventral axes of the neural tube [50]. This method employs specific patterning factor cocktails to generate region-specific organoids such as cortical, hippocampal, hypothalamic, or midbrain organoids. The application of dual-SMAD inhibition (blocking both TGF-β and BMP signaling) efficiently converts hPSCs to neuroectodermal identity, while subsequent treatments with Wnt activators, SHH, FGF8, or other morphogens drive specific regional fates [50]. This approach offers greater consistency and reproducibility, making it particularly valuable for modeling region-specific vulnerabilities in AD, such as hippocampal and cortical degeneration.
Table 1: Key Patterning Factors for Generating Region-Specific Brain Organoids
| Brain Region | Key Patterning Factors | Application Timing | Resulting Cell Types |
|---|---|---|---|
| Cortical | Wnt/Nodal antagonists (Dkk1, LeftyA), BMPRIA-Fc | Early stages (days 0-5) | Cortical neurons, glial cells |
| Hippocampal | Wnt signaling, BMP treatment | Intermediate stages | Dentate gyrus neurons, CA1-CA3 pyramidal neurons |
| Midbrain | SHH activation, FGF8, dose-dependent insulin | Early and intermediate stages | Dopaminergic neurons |
| Ventral Telencephalon | Early SHH activation | Early stages | GABAergic neurons |
| Hypothalamic | SHH activation, TGF-β inhibition | Early stages | Neuroendocrine neurons |
Advanced Protocol: Generating Vascularized Neuroimmune Organoids for sAD Modeling
A cutting-edge protocol for generating vascularized neuroimmune organoids capable of recapitulating multiple sAD pathologies was recently described [40]. This comprehensive method involves several critical stages:
Progenitor Cell Generation: Neural progenitor cells (NPCs), primitive macrophage progenitors (PMPs), and vascular progenitors (VPs) are independently derived from hPSCs using established protocols. NPC identity is confirmed by co-expression of PAX6 and NESTIN, while PMPs express CD235 and CD43 markers [40].
3D Co-culture Assembly: Progenitor cells are combined in precise ratios (30,000 NPCs, 12,000 PMPs, and 7,000 VPs) and spontaneously assemble into organoids. The initial "Proliferation stage" (5 days) uses fibroblast growth factor (bFGF) to promote cellular expansion [40].
Maturation Phase: Organoids are transitioned to a neural differentiation medium containing IL-34 and VEGF to support neuronal, microglial, and vascular maturation during the extended "Differentiation stage" [40].
sAD Pathology Induction: To model sAD, organoids are exposed to postmortem brain extracts from sAD patients, which contain proteopathic seeds (Aβ and tau) that induce aggregation of endogenous proteins. Remarkably, this method recapitulates multiple AD pathologies within four weeks, compared to the 3-6 months typically required for fAD organoid models [40].
This advanced protocol represents a significant leap forward by incorporating multiple cell types affected in AD—neurons, astrocytes, microglia, and vascular cells—within a single 3D system, creating a more physiologically relevant environment for studying disease mechanisms and therapeutic interventions.
Application to Alzheimer's Disease Research: Bridging Models and Mechanisms
Modeling Familial versus Sporadic Alzheimer's Disease
Brain organoids have demonstrated exceptional utility in modeling both familial and sporadic forms of AD, each requiring distinct methodological approaches. For familial AD (fAD), researchers introduce known pathogenic mutations (e.g., in APP, PSEN1, or PSEN2) into hiPSCs via genome editing or utilize hiPSCs from genetic carriers. These fAD models consistently recapitulate key pathological features including Aβ plaque-like aggregates and hyperphosphorylated tau accumulation, typically emerging after 3-6 months in culture [40].
For sporadic AD (sAD), modeling approaches are more complex due to the polygenic and environmentally influenced nature of the disease. The vascularized neuroimmune organoid system exposed to sAD brain extracts has proven particularly effective, demonstrating the induction of multiple AD pathologies including Aβ plaque-like aggregates, tau tangle-like aggregates, neuroinflammation, elevated microglial synaptic pruning, synapse/neuronal loss, and impaired neural network activity [40]. Proteomics analysis of these organoids revealed disrupted AD-related pathways, providing insights into the multifaceted mechanisms underlying sAD pathogenesis.
A powerful patient-specific approach led by Young-Pearse et al. generated hiPSC lines from over 50 participants of the Religious Orders Study and Rush Memory and Aging Project (ROS/MAP) who had extensive longitudinal clinical data, genetic profiling, and postmortem neuropathology [52]. This resource demonstrated that different genetic backgrounds in humans generate different profiles of Aβ and tau in stem cell-derived neurons, and these molecular profiles showed predictive value for clinical outcomes, highlighting the potential for personalized disease modeling and drug response prediction [52].
Recapitulating Hallmark Alzheimer's Pathologies
Brain organoids have successfully replicated the major pathological hallmarks of AD, providing unprecedented opportunities to study disease mechanisms and progression:
Aβ Pathology: Both fAD organoids and sAD brain extract-treated organoids develop Aβ plaque-like aggregates with species profiles that correlate with cognitive decline trajectories observed in human patients [40] [52]. The Aβ42/Aβ40 ratio, a crucial diagnostic biomarker in patients, is also recapitulated in organoid models [49].
Tau Pathology: Organoids exhibit hyperphosphorylated tau and tau tangle-like structures that mirror the neurofibrillary pathology observed in postmortem AD brains [40]. Specific tau species generated in organoid systems have been associated with tangle deposition levels and cognitive decline in human donors [52].
Neuroinflammation: The incorporation of microglia in advanced organoid models enables study of neuroinflammatory processes central to AD pathogenesis. AD organoids demonstrate microglial activation, cytokine release, and elevated synaptic pruning, reflecting the neuroimmune dysregulation observed in patients [49] [40].
Synaptic and Neuronal Dysfunction: Organoid models recapitulate the synapse loss and neuronal degeneration that underpin cognitive decline in AD. Multi-electrode array recordings of organoids have revealed impaired neural network activity following induction of AD pathology [40].
Table 2: Alzheimer's Disease Pathologies Recapitulated in Brain Organoid Models
| AD Pathology | Organoid Model Features | Model Type | Timeframe for Development |
|---|---|---|---|
| Aβ Aggregation | Aβ plaque-like aggregates, altered Aβ42/Aβ40 ratio | fAD organoids, sAD brain extract-treated organoids | 4 weeks (sAD extract) to 3-6 months (fAD) |
| Tau Pathology | Hyperphosphorylated tau, tangle-like structures | fAD organoids, sAD brain extract-treated organoids | 4 weeks (sAD extract) to 3-6 months (fAD) |
| Neuroinflammation | Microglial activation, cytokine release, synaptic pruning | Vascularized neuroimmune organoids | 4 weeks |
| Synaptic/Neuronal Loss | Decreased synaptic markers, neuronal death | fAD organoids, sAD brain extract-treated organoids | 1-6 months |
| Network Dysfunction | Impaired neural network activity | Mature cortical organoids, vascularized neuroimmune organoids | 4 weeks to 6+ months |
Drug Discovery and Therapeutic Validation
Brain organoids provide a valuable platform for preclinical drug testing and validation. The physiological relevance of organoid models addresses the critical translational gap between animal studies and human clinical trials. For example, treatment of sAD brain extract-exposed vascularized neuroimmune organoids with Lecanemab, an FDA-approved anti-Aβ antibody, resulted in significant reduction of amyloid burden, demonstrating the utility of this system for evaluating therapeutic efficacy [40]. Interestingly, this treatment also revealed elevated vascular inflammation as a potential side effect, highlighting the ability of complex organoid models to detect unexpected therapeutic consequences [40].
The patient-specific organoid approach developed by Young-Pearse et al. offers particular promise for predicting individual responses to AD therapeutics [52]. Their system enables testing of whether drugs like Aducanumab might be more effective in specific genetic subgroups of AD patients, potentially paving the way for personalized treatment approaches that match therapeutics to individual disease profiles.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful generation and analysis of brain organoids requires a comprehensive suite of specialized reagents and tools. The table below details essential research solutions for AD modeling using brain organoids.
Table 3: Essential Research Reagent Solutions for Alzheimer's Disease Brain Organoid Research
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Stem Cell Sources | hiPSCs from fAD patients, sAD patients, isogenic controls | Provides genetically defined foundation for organoid generation | Donor diversity critical for population relevance; multiple lines recommended |
| Extracellular Matrix | Matrigel, synthetic hydrogels | Provides 3D scaffolding for organoid growth and organization | Batch variability in Matrigel; synthetic alternatives offer consistency |
| Neural Induction Factors | TGF-β inhibitors (SB431542), BMP inhibitors (Noggin, LDN193189) | Directs pluripotent stem cells toward neural lineage | Dual-SMAD inhibition establishes robust neuroectodermal commitment |
| Patterning Morphogens | Wnt agonists/antagonists, SHH, FGF8, BMPs | Specifies regional identity along AP and DV axes | Concentration and timing critically determine regional fate |
| Maturation Factors | BDNF, GDNF, NT-3, cAMP | Promotes neuronal maturation, synapse formation | Extended maturation (6+ months) enables advanced features |
| Microglia Support | IL-34, CSF-1, TGF-β | Supports microglial survival and function in neuroimmune organoids | Essential for modeling neuroinflammation in AD |
| Vascularization Factors | VEGF, FGF2 | Promotes endothelial network formation | Critical for nutrient perfusion and blood-brain barrier modeling |
| AD Pathology Inducers | sAD brain extracts, synthetic Aβ fibrils, tau seeds | Induces AD-like pathology in organoids | sAD extracts provide patient-derived pathological triggers |
Advanced Imaging and Analysis Technologies for Organoid Characterization
The complex 3D architecture of brain organoids necessitates advanced imaging technologies that can resolve structural and dynamic processes without compromising viability. Traditional methods like brightfield microscopy provide basic visualization but lack the resolution for detailed subcellular analysis [53]. Fluorescence microscopy techniques (confocal, light-sheet) enable specific labeling but are limited by phototoxicity, photobleaching, and the challenges of antibody penetration in thick tissues [53] [54].
Emerging label-free imaging technologies are revolutionizing organoid analysis by enabling long-term, high-resolution monitoring without fluorescent labels. Holotomography (HT), a 3D extension of quantitative phase imaging, provides subcellular resolution (155 nm lateral, 947 nm axial) and allows quantitative measurement of organoid volume, protein concentration, and dry mass [53]. This approach has been successfully used for continuous time-lapse imaging of organoids for up to 120 hours, capturing dynamic processes including growth patterns and drug responses without phototoxic effects [53].
Machine learning approaches are further enhancing label-free imaging capabilities. The LabelFreeTracker system uses U-Net neural networks trained on bright-field and fluorescence images to visualize nuclei and membranes in 3D organoids from bright-field images alone, enabling automated quantification of cell movement, shape changes, proliferation, and lineage tracing without the need for fluorescent reporter engineering [54].
For functional analysis, multi-electrode arrays (MEAs) and calcium imaging enable monitoring of neural network activity in organoids, providing crucial functional readouts to complement structural and molecular analyses [49]. These technologies have detected spontaneous excitatory postsynaptic currents at 4 months and mature network activity in organoids cultured for more than 6 months [50].
Current Challenges and Future Directions
Despite remarkable progress, several challenges remain in the brain organoid field. The lack of complete vascularization limits nutrient perfusion and organoid size, typically constraining organoids to 3-4 mm in diameter and resulting in hypoxic cores with cell death [51]. The absence of blood-brain barrier (BBB) functionality and peripheral immune components further reduces physiological relevance [49]. Additionally, organoids generally reflect earlier developmental stages rather than mature adult brain tissue, though extended culture periods (up to 694 days) have shown transitions toward postnatal molecular signatures [50].
Technical challenges include batch-to-batch variability in organoid generation and the high cost and complexity of prolonged cultures. From an analytical perspective, the cellular heterogeneity within organoids presents challenges for data interpretation, necessitating sophisticated single-cell analysis approaches.
Future developments are focusing on several key areas:
Enhanced Vascularization: Integrating functional vascular networks through incorporation of vascular progenitors and fluidic systems to improve nutrient delivery and maturation [40] [55].
Multi-regional Connectivity: Using assembloid approaches to fuse region-specific organoids and model circuit-level interactions between different brain areas affected in AD [56].
Standardization and Scaling: Developing standardized protocols and bioreactor systems for consistent, large-scale organoid production suitable for high-throughput drug screening [51].
Integration with Artificial Intelligence: Combining organoid technology with AI-driven digital twins to create predictive models of individual disease trajectories and treatment responses [49].
Organoid Intelligence: Exploring the potential of brain organoids for biological computing and learning studies, creating novel platforms for understanding cognition and neural computation [51].
The convergence of these technologies promises to enhance the translational value of brain organoids, potentially transforming them into indispensable tools for AD drug discovery, personalized medicine, and ultimately, improving patient outcomes.
Experimental Workflows and Signaling Pathways
The following diagrams illustrate key processes in brain organoid generation and Alzheimer's disease modeling, based on protocols and mechanisms described in the search results.
The advent of human induced pluripotent stem cell (hiPSC) technology has revolutionized preclinical research for complex neurodegenerative disorders like Alzheimer's disease (AD). By enabling the generation of patient-derived neurons, astrocytes, microglia, and cerebral organoids, hiPSC models provide a human-specific platform for investigating disease mechanisms and screening therapeutic compounds [6] [5]. These models are particularly valuable for capturing the genetic diversity and multifactorial pathology of AD, which existing animal models often fail to fully recapitulate [6] [5]. Research using hiPSC models has steadily increased over the past 14 years, with the United States and China emerging as leading contributors to this growing field [6].
Alzheimer's disease manifests primarily in two forms: familial AD (fAD), caused by deterministic mutations in genes such as APP, PSEN1, and PSEN2; and sporadic AD (sAD), which accounts for >95% of cases and involves a complex interplay of genetic risk factors and environmental influences [57] [5]. While fAD models benefit from well-defined genetic drivers that consistently produce amyloid-β pathology, modeling sAD presents greater challenges due to its heterogeneity and lack of single causative mutations [57]. Nevertheless, hiPSC-derived neural models from both fAD and sAD patients have demonstrated key disease-relevant phenotypes, including increased Aβ42 secretion, altered Aβ42:40 ratios, tau hyperphosphorylation, oxidative stress, and neurite degeneration [58] [57] [59]. The development of increasingly complex co-culture systems and 3D organoid models now enables researchers to study cell-type-specific contributions and intercellular dynamics in AD pathogenesis [60] [5].
Table 1: Key Characteristics of hiPSC Models for Alzheimer's Disease Research
| Feature | Familial AD (fAD) Models | Sporadic AD (sAD) Models |
|---|---|---|
| Genetic Basis | Known mutations in APP, PSEN1, or PSEN2 [58] [5] | Polygenic risk factors (e.g., APOE4, TREM2) [57] [5] |
| Disease Penetrance | Complete, autosomal dominant [5] | Incomplete, multifactorial [57] |
| Age of Onset | Early-onset (<60 years) [5] | Late-onset (>70 years) [5] |
| Key Pathological Features | Increased Aβ42 production or Aβ42:40 ratio [58] | Variable Aβ pathology; impaired clearance [57] |
| Model Consistency | High phenotypic consistency across lines [58] | High patient-to-patient variability [57] |
| Primary Applications | Pathway analysis, compound screening [58] | Risk factor analysis, personalized medicine [57] |
High-Throughput Screening in hiPSC-Derived AD Models
Platform Development and Validation
The implementation of high-throughput screening (HTS) in hiPSC-derived AD models requires careful optimization at multiple levels, from cell production to phenotypic assessment. A critical first step involves establishing robust differentiation protocols that yield highly pure populations of relevant neural cell types. For cortical modeling, dual SMAD inhibition using Noggin and SB431542 efficiently generates PAX6+ neural precursor cells within 11 days, which can subsequently differentiate into functionally mature cortical neurons [60]. These cultures can be further enriched through manual selection of neural rosettes or fluorescence-activated cell sorting (FACS) using specific neural surface markers [60].
For HTS applications, protocol efficiency and reproducibility are paramount. A five-stage spinal motor neuron differentiation protocol has been adapted for large-scale screening, generating cultures with >92% purity (ChAT+, MNX1/HB9+, Tuj1+) and minimal contamination from astrocytes (<0.12%) and microglia (<0.04%) [61]. Such highly enriched cultures provide a valuable reductionist system for assessing cell-autonomous disease mechanisms while minimizing confounding variables in compound screening [61].
Phenotypic validation of disease-relevant features is essential before embarking on large-scale screening campaigns. In sAD models, this includes documenting reduced neuronal survival, accelerated neurite degeneration, altered Aβ secretion, tau pathology, and transcriptional dysregulation consistent with post-mortem AD brain signatures [57] [61] [59]. Longitudinal live-cell imaging pipelines equipped with cell-type-specific reporters enable quantitative tracking of these degenerative processes over time, providing robust endpoints for evaluating compound efficacy [61].
Screening Paradigms and Hit Identification
HTS in hiPSC-derived AD models can follow either phenotype-based or target-based approaches. Phenotypic screening offers the advantage of identifying compounds that modify disease-relevant processes without requiring prior knowledge of specific molecular targets. For example, screens measuring protection against Aβ-induced toxicity, reduction in tau hyperphosphorylation, or reversal of neurite degeneration have identified promising therapeutic candidates [61].
Target-based screening focuses on specific molecular pathways implicated in AD pathogenesis. Current research trends have particularly emphasized inflammation, astrocyte and microglia function, apolipoprotein E (ApoE) biology, and tau pathology as promising target areas [6]. The emergence of CRISPR/Cas9 gene editing enables precise introduction of fAD mutations or sAD risk factors into control hiPSC lines, creating isogenic pairs that differ only at the disease-relevant locus [5]. These engineered systems provide highly controlled backgrounds for screening campaigns focused on specific genetic drivers.
The scale of contemporary HTS in hiPSC models is exemplified by recent work in amyotrophic lateral sclerosis (ALS), where a library of 100 sALS lines was used to evaluate over 100 clinical-stage compounds [61]. This approach found that less than 5% of drugs tested showed efficacy across sALS donors, remarkably mirroring the high failure rate of ALS clinical trials [61]. Similarly structured screening initiatives are now underway for AD, leveraging lessons from these pioneering efforts in other neurodegenerative conditions.
Table 2: Key Components for HTS in hiPSC-Derived Alzheimer's Models
| Component | Specifications | Application in HTS |
|---|---|---|
| Cell Source | Patient-derived hiPSCs (fAD, sAD, controls); isogenic lines [57] [5] | Donor-matched disease modeling; genetic control |
| Differentiation Format | 2D monolayers; 3D organoids; co-culture systems [60] [57] | Pathway analysis; cell-cell interactions |
| Differentiation Markers | PAX6 (neural precursors); Tuj1 (neurons); GFAP (astrocytes); CD11B (microglia) [61] | Quality control; purity assessment |
| Disease Phenotypes | Aβ42 secretion; tau phosphorylation; neurite degeneration; cell survival [58] [57] [61] | Primary screening endpoints |
| Screening Readouts | ELISA/MSD (Aβ); immunofluorescence (tau, neurites); live-cell imaging (survival) [58] [61] | Quantitative phenotyping |
| Validation Methods | Transcriptomics; electrophysiology; secondary assays [61] [59] | Hit confirmation |
Diagram 1: High-Throughput Screening Workflow for hiPSC-Based AD Models. This flowchart outlines the key steps in implementing a screening campaign using hiPSC-derived neural models, from cell line generation through hit identification.
Lead Optimization Strategies for AD Therapeutics
Hit-to-Lead Progression
The hit-to-lead (H2L) phase represents a critical bridge between initial screening hits and optimized lead compounds with demonstrated efficacy and favorable drug-like properties [62]. During this stage, confirmed hits—typically exhibiting binding affinities in the micromolar range (10⁻⁶ M)—undergo limited optimization to improve potency (often to nanomolar range, 10⁻⁹ M), selectivity, and preliminary pharmacokinetic properties [62].
The H2L process begins with hit confirmation, where initial screening results are verified through dose-response characterization, orthogonal assay testing, and assessment of synthetic tractability [62]. For AD therapeutics, this typically involves evaluating compounds across multiple disease-relevant endpoints in hiPSC-derived models, including Aβ modulation, tau pathology, neuronal survival, and neurite integrity [61]. Promising hit clusters are then selected for hit expansion through the synthesis or acquisition of structural analogs to establish preliminary structure-activity relationships (SAR) [62].
Modern H2L campaigns increasingly leverage integrated approaches combining high-throughput experimentation (HTE) with computational prediction. Recent advances have demonstrated how comprehensive reaction datasets (e.g., 13,490 Minisci-type C-H alkylation reactions) can train deep graph neural networks to accurately predict reaction outcomes, enabling efficient diversification of hit structures [63]. Such approaches have generated virtual libraries containing >26,000 molecules, from which strategically selected compounds were synthesized and achieved remarkable potency improvements—up to 4500-fold over the original hit [63].
Multi-Dimensional Optimization
Successful lead optimization requires balancing multiple compound properties simultaneously. Key considerations for AD therapeutics include:
- Blood-brain barrier (BBB) penetration: Critical for CNS-targeting drugs, assessed through P-glycoprotein interaction screening and permeability assays [62]
- Metabolic stability: Evaluation of compound half-life and metabolic susceptibility in hepatic microsome systems [62]
- Selectivity profiling: Screening against related targets to minimize off-target effects [62]
- In vitro safety pharmacology: Assessment of cytotoxicity, P450 enzyme inhibition, and human serum albumin binding [62]
For AD programs specifically, optimization must also address the complex pathophysiology of the disease. The limited success of single-target approaches has spurred interest in multi-target strategies and combination therapies. A notable example from ALS research identified a promising therapeutic combination (baricitinib, memantine, and riluzole) through systematic combinatorial testing in sALS models [61]. Similarly, for sAD, where multiple pathways are simultaneously dysregulated, such multi-target approaches may offer superior efficacy compared to single-agent interventions.
Diagram 2: Lead Optimization Strategy for AD Therapeutics. This diagram illustrates the multi-parameter optimization process during hit-to-lead progression, highlighting key properties that must be balanced to identify promising lead compounds.
Experimental Protocols for hiPSC-Based AD Modeling and Screening
Neural Differentiation and Disease Modeling
Cortical Neuron Differentiation from hiPSCs
- Maintain hiPSCs in feeder-free conditions using mTeSR1 medium on Matrigel-coated plates until 70-80% confluent [60]
- Initiate neural induction using dual SMAD inhibition: supplement medium with 100 ng/mL Noggin (or 500 nM LDN-193189) and 10 μM SB431542 [60]
- Culture for 11 days, changing medium daily, until neural rosettes appear [60]
- Manually pick rosettes and plate on poly-ornithine/laminin-coated surfaces in neural maintenance medium (NMM) containing Neurobasal, B27, N2, 20 ng/mL bFGF, and 20 ng/mL EGF [60]
- Passage neural precursors using Accutase and expand for 2-3 passages before terminal differentiation [60]
- Differentiate into cortical neurons by switching to NMM without bFGF/EGF but supplemented with 20 ng/mL BDNF, 20 ng/mL GDNF, 1 mM dibutyryl-cAMP, and 200 μM ascorbic acid for 4-6 weeks [60]
- Validate differentiation through immunocytochemistry for cortical markers (TBR1, CTIP2) and neuronal markers (MAP2, Tuj1) [60]
sAD Model Development with Environmental Risk Factors
- Differentiate cortical neurons from sAD patient-derived hiPSCs as described above [59]
- At day 30 of differentiation, expose cultures to Alzheimerogens:
- Assess transcriptomic changes via RNA sequencing and compare to post-mortem AD brain signatures [59]
- Validate pathological phenotypes including Aβ secretion (ELISA), tau phosphorylation (Western blot), and synaptic integrity (immunocytochemistry) [59]
High-Content Screening for Neuroprotective Compounds
Longitudinal Live-Cell Imaging of Neuronal Health
- Differentiate motor neurons or cortical neurons in 96-well or 384-well imaging plates using optimized protocols [61]
- Transduce with cell-type-specific reporter: Use lentiviral vectors expressing GFP under control of the HB9 promoter (motor neurons) or TBR1 promoter (cortical neurons) [61]
- At day 35-42 of differentiation, treat with compound library using automated liquid handling [61]
- Acquire images every 24 hours for 7-14 days using automated high-content imaging systems [61]
- Quantify neuronal health parameters:
- Normalize data to vehicle-treated controls and calculate fold-change in survival and neurite integrity [61]
Compound Screening Cascade for AD Therapeutics
- Primary screening: Test compounds at 10 μM in triplicate using survival and neurite integrity as primary endpoints [61]
- Hit confirmation: Retest active compounds in dose-response (1 nM - 30 μM) across 3-5 independent differentiations [61]
- Secondary assays:
- Aβ modulation: Measure Aβ40, Aβ42, and sAPPβ levels in conditioned media via ELISA or MSD [58] [57]
- Tau pathology: Quantify phosphorylated tau (AT8, PHF1 epitopes) via immunofluorescence [57]
- Transcriptomic profiling: Perform RNA-seq to identify pathway modulation [61] [59]
- Functional assessment: Evaluate electrophysiological properties using multi-electrode arrays [61]
- Selectivity screening: Counter-screen against related targets (e.g., other kinases, GPCRs) and assess cytotoxicity in non-neuronal cell types [62]
Table 3: Research Reagent Solutions for hiPSC-Based AD Screening
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, C-MYC (Yamanaka factors) [6] | Generation of hiPSCs from somatic cells |
| Neural Induction Agents | Noggin, SB431542, LDN-193189 [60] | Dual SMAD inhibition for neural specification |
| Neural Maturation Factors | BDNF, GDNF, NGF, NT-3, dibutyryl-cAMP [60] | Promote neuronal survival, maturation, and synaptic development |
| Cell-Type-Specific Markers | PAX6 (neural precursors), Tuj1 (neurons), GFAP (astrocytes), IBA1 (microglia) [60] [61] | Quality control and purity assessment |
| Disease-Relevant Assays | Aβ ELISAs, phospho-tau antibodies, synaptic markers [58] [57] | Quantification of AD pathological hallmarks |
| Gene Editing Tools | CRISPR/Cas9 systems, siRNA, antisense oligonucleotides [5] | Genetic manipulation for target validation and isogenic line generation |
Navigating Model Limitations: Maturity, Reproducibility, and SAD Recapitulation
The application of human induced pluripotent stem cell (hiPSC)-derived neurons in modeling Alzheimer's disease (AD) represents one of the most promising avenues for understanding human-specific disease mechanisms and developing novel therapeutics. However, these models face a fundamental challenge: hiPSC-derived neurons typically exist in a fetal-like state that fails to fully recapitulate the mature physiological properties of adult human brain neurons [64] [5]. This immaturity barrier is particularly problematic for modeling late-onset neurodegenerative disorders like sporadic AD, where age-related pathological processes unfold over decades [5]. The "maturity challenge" thus constitutes a critical bottleneck that must be overcome to enhance the translational relevance of hiPSC-based AD models.
The distinction between familial AD (FAD) and sporadic AD (SAD) further compounds this challenge. FAD models utilizing hiPSCs with mutations in APP, PSEN1, or PSEN2 may demonstrate pathological features like amyloid-β accumulation even in relatively immature neurons [5]. In contrast, SAD modeling requires recapitulating complex gene-environment interactions that likely manifest only in fully mature neuronal circuits, necessitating advanced maturation techniques to observe relevant phenotypes [6] [5]. This technical guide provides a comprehensive framework for addressing neuronal immaturity, with specific application to both FAD and SAD research.
Comprehensive Characterization of Neuronal Maturation: Establishing Essential Benchmarks
A systematic approach to characterizing hiPSC-derived neuron maturation requires multimodal assessment spanning morphological, functional, and network-level properties. Establishing standardized benchmarks is essential for comparing results across studies and validating model systems for AD research.
Morphological Maturation Parameters
Morphological development provides the structural foundation for neuronal function. During extended culture periods (up to 300 days in vitro), hiPSC-derived cortical neurons exhibit progressive increases in somal area (from approximately 208 μm² to 557 μm²) and primary dendrite width (from 2.96 μm to 7.86 μm) [65]. These changes correlate with the development of more complex arborization patterns and the emergence of pyramidal-like morphology with distinct apical and basal dendrites resembling native cortical neurons [65]. Sholl analysis demonstrates increasing dendritic complexity with culture time, characterized by greater numbers of intersections at increasing distances from the soma [66].
Electrophysiological Maturation Markers
Functional maturation is most directly assessed through electrophysiological measurements. Whole-cell patch-clamp recordings reveal progressive changes in intrinsic membrane properties and excitability during extended culture periods [64] [66]. The following table summarizes key electrophysiological parameters and their developmental trajectories:
Table 1: Electrophysiological Maturation Parameters of hiPSC-Derived Neurons
| Parameter | Immature State | Mature State | Functional Significance | Measurement Technique |
|---|---|---|---|---|
| Resting Membrane Potential | Relatively depolarized | More hyperpolarized (stable) | Improved ion channel expression and function | Current-clamp recordings |
| Input Resistance (Rᵢ) | High (~1-2 GΩ) | Lower (~200-500 MΩ) | Increased membrane surface area, channel density | Voltage response to hyperpolarizing current |
| Membrane Capacitance (Cₘ) | Low | Higher | Increased membrane surface area | Voltage clamp measurements |
| Action Potential Properties | Broader, smaller amplitude | Sharper, larger amplitude | Mature Na⁺/K⁺ channel expression and kinetics | Depolarizing current pulses |
| Firing Patterns | Single spikes | Repetitive, regular firing | Development of mature ion channel complements | 0.5-1 s depolarizing current pulses |
| Synaptic Currents | Sparse or absent | Robust spontaneous postsynaptic currents | Functional synapse formation | Voltage-clamp recordings |
Data synthesized from [64] [66] [65]
At the network level, multi-electrode arrays (MEAs) enable non-invasive monitoring of developmental progression. Initial sparse spiking activity evolves into complex network behaviors including synchronized burst firing (SBF) over culture periods of 20-30 weeks [65]. This progression reflects the functional integration of neurons into coordinated circuits—a critical milestone for modeling network dysfunction in AD.
Molecular and Synaptic Maturation Markers
Molecular profiling reveals shifts in receptor subunit composition and synaptic protein expression during maturation. Cortical neurons transition from co-expressing both excitatory (VGlut1) and inhibitory (GABA) markers at early stages (day 21) to predominantly excitatory phenotypes (VGlut1 only) by later stages (day 40) [67]. GABAA receptor subunits show altered expression patterns, with developmental changes in subunit composition affecting receptor function and pharmacological properties [66]. The emergence of long-term potentiation (LTP), a canonical cellular mechanism of learning and memory, provides a critical functional benchmark that typically requires 5-6 weeks of maturation [66] [67].
Experimental Workflows for Functional Maturation Assessment
Comprehensive evaluation of hiPSC-derived neuronal maturation requires integrated experimental workflows that systematically assess development across multiple dimensions.
Figure 1: Integrated Workflow for Neuronal Maturation Assessment. This workflow outlines the temporal progression of hiPSC-derived neuronal maturation and key assessment methods at each stage, culminating in applications for Alzheimer's disease modeling.
Detailed Patch-Clamp Protocol for Functional Characterization
The patch-clamp technique remains the gold standard for evaluating intrinsic neuronal properties and synaptic function. Below is a detailed methodology adapted from recent studies [64] [66]:
Materials and Setup:
- Recording System: MultiClamp 700B amplifier or equivalent with digitizer
- Micromanipulators: Motorized or hydraulic for precise electrode positioning
- Recording Chamber: Temperature-controlled (32-37°C) with perfusion system
- Pipette Solution (mM): 120 K-gluconate, 10 KCl, 10 HEPES, 4 MgATP, 0.3 NaGTP, 10 Na-phosphocreatine (pH 7.3 with KOH)
- Extracellular Solution (mM): 140 NaCl, 5 KCl, 2 CaCl₂, 1 MgCl₂, 10 HEPES, 10 glucose (pH 7.4 with NaOH)
Current-Clamp Protocol for Intrinsic Properties:
- Establish whole-cell configuration with appropriate seal resistance (>1 GΩ)
- Measure resting membrane potential in zero-current mode
- Apply hyperpolarizing current steps (-20 to -100 pA, 500 ms) to calculate input resistance (Rᵢ) from steady-state voltage response
- Apply depolarizing current steps (+10 to +200 pA, 500 ms) to evoke action potentials
- Analyze action potential properties: threshold, amplitude, half-width, afterhyperpolarization
- Determine firing patterns in response to prolonged depolarization (regular, adapting, bursting)
Voltage-Clamp Protocol for Synaptic Properties:
- Hold cells at -70 mV to detect spontaneous excitatory postsynaptic currents (sEPSCs)
- Hold cells at 0 mV to detect spontaneous inhibitory postsynaptic currents (sIPSCs)
- Apply glutamate or GABA receptor antagonists (CNQX/AP-5 or bicuculline) to confirm receptor specificity
- For evoked responses, use extracellular stimulation while recording postsynaptic currents
Data Analysis:
- Calculate membrane capacitance (Cₘ) from current responses to voltage steps
- Determine action potential kinetics using differentiation of voltage traces
- Analyze synaptic event frequency, amplitude, and kinetics using detection algorithms (e.g., MiniAnalysis, Clampfit)
Multi-Electrode Array (MEA) Protocol for Network Assessment
MEA recordings provide non-invasive, long-term monitoring of network development [64] [65]:
Culture Preparation:
- Plate hiPSC-derived neurons on commercially available MEA plates (e.g., 60-electrode arrays) pre-coated with poly-L-ornithine/laminin
- Maintain cultures in BrainPhys neuronal medium supplemented with appropriate neurotrophic factors (BDNF, GDNF)
- Include co-culture with human astrocytes (10-20% of total cells) to enhance maturation and long-term viability
Recording Parameters:
- Sample rate: 20-50 kHz per electrode
- Bandpass filter: 200-3000 Hz for spike detection
- Recordings: 10-30 minutes per session, weekly or biweekly assessments
- Environmental control: Temperature (37°C), CO₂ (5%) during extended recordings
Data Analysis Metrics:
- Mean firing rate: Average spikes per second across active electrodes
- Synchronized burst firing (SBF): Detect using burst detection algorithms (e.g., Max Interval method)
- Network bursting: Percentage of electrodes participating in coordinated bursts
- Inter-spike interval: Distribution of intervals between consecutive spikes
Advanced Maturation Strategies for Alzheimer's Disease Research
Prolonged Culture and Co-culture Systems
Extended culture durations of 20-30 weeks are necessary for hiPSC-derived cortical neurons to develop mature electrophysiological properties and pharmacological responses [65]. Co-culture with human astrocytes significantly enhances neuronal survival during extended culture and promotes morphological and functional maturation through secreted factors and direct contact [65]. For AD modeling specifically, incorporating microglia and other glial cells becomes crucial, as recent genetic findings highlight non-neuronal cell types in SAD pathogenesis [5].
3D Culture and Brain Organoid Systems
Three-dimensional brain organoids offer enhanced maturation potential compared to 2D cultures by better recapitulating the tissue microenvironment [64]. The self-organization of multiple cell types in organoids supports more advanced neuronal maturation and circuit formation. For FAD modeling, 3D systems demonstrate accelerated Aβ aggregation and tau pathology, while for SAD, they may better model the complex cell-cell interactions implicated in disease progression [5].
Pharmacological and Molecular Manipulation
Strategic manipulation of signaling pathways can accelerate maturation. The BDNF and GDNF treatment paradigm (10 ng/mL each) promotes neuronal maturation and synaptic development in hiPSC-derived cortical cultures [66]. Additionally, manipulating inhibitory signaling using GABAA receptor antagonists like picrotoxin can unmask mature plasticity mechanisms such as LTP in relatively young cultures [67].
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 2: Research Reagent Solutions for Neuronal Maturation Studies
| Reagent/Category | Specific Examples | Function/Application | Key References |
|---|---|---|---|
| Neurotrophic Factors | BDNF, GDNF (10 ng/mL each) | Promote neuronal survival, maturation, and synaptic development | [66] |
| Maturation Media | BrainPhys Neuronal Medium | Optimized formulation to support neuronal function and network activity | [66] [65] |
| Electrophysiology Reagents | K-gluconate internal solution, CNQX, AP-5, bicuculline | Assess intrinsic properties, synaptic transmission, and receptor function | [64] [66] |
| Cell Type Markers | β-tubulin III, MAP2, VGlut1, GAD67 | Identify neuronal identity, maturation stage, and neurotransmitter phenotype | [67] [65] |
| Synaptic Markers | Synaptophysin, PSD-95, Bassoon | Visualize and quantify synapse formation and maturation | [65] |
| Pluripotency Validators | TRA-1-60, SSEA-4, Oct4 | Confirm complete reprogramming and pluripotent state prior to differentiation | [68] [69] |
Application to Alzheimer's Disease Research: Familial vs. Sporadic Models
The maturity challenge manifests differently in FAD versus SAD modeling approaches, requiring tailored strategies for each application.
Familial AD Modeling Considerations
FAD models utilizing hiPSCs with mutations in APP, PSEN1, or PSEN2 may exhibit disease-relevant phenotypes even at relatively immature stages, including increased Aβ42/Aβ40 ratios and elevated phospho-tau levels [5]. However, full manifestation of neuronal vulnerability and network dysfunction likely requires advanced maturation. The use of 3D culture systems and prolonged culture (≥3 months) enhances the development of pathological features such as amyloid aggregation and neuritic dystrophy in FAD models [5].
Sporadic AD Modeling Considerations
SAD modeling presents greater challenges due to the complex interplay of genetic risk factors and age-related processes. Key strategies include:
Genetic Risk Factor Incorporation:
- Focus on APOE genotype (ε4 allele as major risk factor)
- Incorporate GWAS-identified risk genes (TREM2, CD33, CLU) through gene editing or patient-specific hiPSCs
- Utilize isogenic cell lines to isolate effects of specific risk variants
Enhanced Maturation for Age-Related Phenotypes:
- Extend culture periods to 6-12 months to observe late-onset phenotypes
- Incorporate multiple brain cell types (microglia, astrocytes) to model cell-autonomous vs. non-autonomous effects
- Apply progeria-related factors or oxidative stress to mimic aspects of aging
Functional Assessment for SAD Endophenotypes:
- Focus on network hyperexcitability and synaptic dysfunction as early pathological features
- Assess endolysosomal function and axonal transport deficits
- Measure calcium signaling dysregulation as a functional integrator of multiple risk pathways
Overcoming the fetal-like state of hiPSC-derived neurons requires a multifaceted approach combining extended culture timelines, advanced culture systems, and comprehensive functional validation. The maturation strategies outlined in this technical guide provide a roadmap for generating more physiologically relevant models of both familial and sporadic Alzheimer's disease. As these methods continue to evolve, they promise to enhance the translational predictive power of hiPSC-based platforms for drug discovery and pathophysiological investigation, ultimately bridging the gap between in vitro models and the complex reality of human brain aging and neurodegeneration.
The advent of human induced pluripotent stem cell (hiPSC) technology has revolutionized the study of Alzheimer's disease (AD), enabling investigators to deconstruct disease mechanisms within patient-specific human neural cells. However, this powerful approach is accompanied by two significant sources of biological variability that can confound experimental results: inherent genetic differences between human donors and technical artifacts introduced during cellular reprogramming. For a complex, polygenic disorder like sporadic Alzheimer's disease (sAD), where disease manifests from the interplay of numerous genetic risk factors and environmental influences, distinguishing true disease phenotypes from background "noise" becomes methodologically paramount [36] [2]. Similarly, in familial AD (fAD) research, while causative mutations are known, understanding variable penetrance and expression requires careful control of genetic background. This technical guide examines the sources and impacts of this variability and provides a framework of experimental strategies to control for these factors, thereby enhancing the reliability and translational relevance of hiPSC-based AD models.
Donor-to-Donor Genetic Heterogeneity
The genetic architecture of Alzheimer's disease fundamentally differs between its familial and sporadic forms, directly influencing the strategy for donor selection and the interpretation of donor-derived models.
Familial AD (fAD) accounts for less than 5% of cases and is typically caused by fully penetrant autosomal-dominant mutations in genes such as APP, PSEN1, and PSEN2 [36] [5]. The disease etiology in these cases is primarily driven by these single-gene mutations, which often lead to altered Amyloid-β (Aβ) production or the Aβ42/Aβ40 ratio [5].
Sporadic AD (sAD), constituting over 95% of all cases, is polygenic and complex. Its heritability is estimated between 60% and 80%, contributed to by a combination of common and rare genetic variants [36] [2]. The apolipoprotein ε4 allele (APOE ε4) is the strongest genetic risk factor, with odds ratios ranging from 3.62 to 34.3 depending on population and zygosity [36]. Beyond APOE, genome-wide association studies (GWAS) have associated more than 70 common and rare genetic variants with sAD heritability, implicating biological pathways such as immune responses, complement activation, endocytosis, and lipid transport [36]. This polygenicity means that each sAD patient possesses a unique combination of genetic risk variants, leading to substantial phenotypic heterogeneity between donors.
Table 1: Key Genetic Factors in Alzheimer's Disease Pathogenesis
| Gene/Pathway | Association Type | Biological Implication | Prevalence/Impact |
|---|---|---|---|
| APP, PSEN1, PSEN2 | Familial AD (Causative) | Altered Amyloid-β production/aggregation | <5% of AD cases [2] |
| APOE ε4 | Sporadic AD (Strong Risk) | Lipid transport, Aβ clearance | Odds Ratio: 3.62-34.3 [36] |
| Complement Pathway | Sporadic AD (Polygenic Risk) | Immune response, synaptic pruning | Captured in Polygenic Risk Scores [36] |
| TREM2, ABCA7 | Sporadic AD (GWAS Risk) | Microglial function, lipid metabolism | Modest individual effect, significant in combination [5] |
Variability from Cellular Reprogramming
The process of reprogramming somatic cells (e.g., fibroblasts, PBMCs) into hiPSCs can introduce technical artifacts that constitute a second major source of variability, independent of the donor's disease status.
- Reprogramming Method Selection: Non-integrating methods are now standard to minimize the risk of genomic alterations. Among these, Sendai virus (SeV) and episomal vector reprogramming are most common. A 2025 comparative analysis found that while the source material (fibroblasts, LCLs, PBMCs) did not significantly impact success rates, the SeV method yielded significantly higher reprogramming success rates compared to the episomal method [70].
- Genomic Instability: Early-passage hiPSCs can exhibit a higher number of copy number variants (CNVs), potentially due to replication stress during reprogramming. These CNVs can lead to genetic mosaicism, though rapid selection often occurs during propagation, causing later-passage iPSCs to be more genetically stable [71]. Exome sequencing studies have also identified fixed point mutations in hiPSC lines not present in the parent fibroblasts, with a predicted load of approximately six coding mutations per iPSC genome. Notably, these mutations are often enriched in genes implicated in cancer [71].
Table 2: Comparison of Non-Integrating hiPSC Reprogramming Methods
| Parameter | Sendai Virus (SeV) | Episomal Vectors |
|---|---|---|
| Mechanism | CytoTune kit; transduction with 4 SeV vectors (hOCT4, hSOX2, hKLF4, hC-MYC) [70] | Nucleofection with OriP/EBNA1 vectors (hOCT3/4, hSOX2, hKLF4, hL-MYC, LIN28) [70] |
| Genomic Integration | Non-integrating, diluted out over passages [70] | Non-integrating, but requires electroporation [70] |
| Relative Success Rate | Significantly higher [70] | Lower than SeV [70] |
| Key Starting Cells | Fibroblasts, PBMCs [70] | Fibroblasts, LCLs [70] |
| Primary Concern | Residual viral presence requires testing [70] | Lower efficiency can necessitate more clones [70] |
Strategic Approaches to Control Variability
Donor Selection and Cohort Design
A genetically-informed donor selection strategy is the first and most critical step in mitigating the confounding effects of donor-to-donor heterogeneity.
- The Polygenic Risk Score (PRS) Framework: The PRS aggregates the effects of all known AD-associated genetic variants into a single quantitative measure of an individual's genetic susceptibility [36]. This tool can predict an individual's risk of developing AD with approximately 84% accuracy [36]. Selecting donors from the extremes of the PRS distribution allows for the creation of more phenotypically coherent experimental cohorts.
- The IPMAR Resource Model: The iPSC Platform to Model Alzheimer's Disease Risk (IPMAR) exemplifies this strategic approach. It comprises:
- 90 iPSC lines with extremes of global AD PRS: 34 from high-risk late-onset AD (LOAD) donors, 29 from high-risk early-onset AD (EOAD) donors, and 27 from low-risk, cognitively healthy controls [36].
- 19 iPSC lines with extremes of complement pathway-specific PRS: 9 from high-risk AD donors and 10 from low-risk controls [36].
- Isogenic Control Lines: For both fAD and sAD research, genome editing (e.g., CRISPR-Cas9) is used to correct or introduce disease-associated mutations in hiPSCs. This creates genetically matched isogenic control lines, effectively isolating the phenotypic impact of a specific genetic variant from the background genetic noise of the donor [5].
Experimental and QC Workflows
A rigorous, standardized workflow from reprogramming through differentiation and analysis is essential to manage variability.
Diagram 1: The hiPSC generation and validation workflow includes key quality control checkpoints to ensure genomic integrity and pluripotency [36] [70].
A Toolkit for Robust Experimental Design
Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for hiPSC AD Modeling
| Reagent/Resource | Function/Description | Example/Note |
|---|---|---|
| Sendai Virus Vectors | Non-integrating delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC). | CytoTune Sendai Reprogramming Kit [70] |
| Episomal Vectors | Non-integrating, plasmid-based reprogramming factor delivery. | OriP/EBNA1 vectors with hOCT3/4, hSOX2, hKLF4, hL-MYC [70] |
| Polygenic Risk Score (PRS) | Quantifies individual's genetic susceptibility for donor stratification. | Aggregates >70 known AD-associated variants [36] |
| IPMAR Resource | A predefined collection of iPSC lines capturing extremes of AD polygenic risk. | Available via EBiSC cell repository and DPUK data repository [36] |
| Isogenic Control Lines | Genetically matched controls created via genome editing (e.g., CRISPR-Cas9). | Critical for isolating variant effects from background noise [5] |
| ROCK Inhibitor (Y-27632) | Enhances survival of hiPSCs after passaging and thawing. | Used in culture medium for 20-24 hours post-thaw [70] |
Statistical Design and Reproducibility
To ensure robust and reproducible findings, the experimental design must account for multiple variables.
- Adequate Sample Size (N): Given the substantial genetic and technical variability, studies must utilize a sufficiently large number of independent hiPSC lines (N) per experimental group to achieve statistical power. Relying on a small number of lines (e.g., n<3) risks identifying line-specific artifacts rather than true disease-related phenotypes [36].
- N > 1 Design: The "N" in a well-designed hiPSC study refers to the number of biologically independent donor lines, not the number of technical replicates or differentiated wells from a single line. Experiments should be designed with an N sufficiently large to power statistical comparisons between groups of lines.
- Batch-Controlled Differentiation: Differentiate multiple hiPSC lines from different experimental and control groups simultaneously to control for batch effects in the differentiation process and subsequent functional assays.
Diagram 2: An experimental design that combines a large cohort of genetically-stratified donors with isogenic controls, processed in multiple batches to ensure robust and reproducible findings [36].
The intrinsic genetic heterogeneity of human populations and the technical challenges of cellular reprogramming present formidable, yet surmountable, obstacles in hiPSC-based AD research. By adopting a strategic framework that includes genetically informed donor selection using tools like Polygenic Risk Scores, leveraging large, well-characterized iPSC resources such as IPMAR, implementing rigorous quality control throughout the cellular workflow, and employing robust experimental designs with adequate sample sizes and isogenic controls, researchers can effectively control for variability. This disciplined approach is paramount for distinguishing true disease-relevant pathophysiology from experimental noise, thereby accelerating the discovery of novel therapeutic targets for both sporadic and familial Alzheimer's disease.
Within the broader thesis on human induced pluripotent stem cell (hiPSC) models for Alzheimer's disease (AD) research, a critical challenge emerges: while familial AD (fAD) models leveraging known pathogenic mutations have advanced our understanding, they represent only 1-5% of cases. The overwhelming majority of AD is sporadic (sAD), characterized by complex polygenic architecture and environmental influences that have remained notoriously difficult to model experimentally. The limitations of traditional rodent models in capturing human-specific disease heterogeneity—driven by genetic diversity, epigenetic modifications, and environmental factors—have necessitated models that recapitulate patient-specific pathologies [18]. hiPSC technology addresses this fundamental challenge by enabling the generation of patient-derived neurons, glia, and organoids that retain donor-specific genetic and molecular signatures, thereby providing a transformative approach to dissect the mechanistic diversity underlying sAD [18].
The emergence of sophisticated polygenic risk scoring methodologies, combined with controlled environmental insult paradigms, now enables researchers to engineer sAD pathology in vitro with unprecedented fidelity. This technical guide outlines the core principles and methodologies for constructing these next-generation sAD models, bridging the critical gap between monocentric fAD models and the complex reality of sporadic disease. By capturing the genetic complexity and environmental interactions that drive sAD, these approaches promise to accelerate therapeutic discovery for the most prevalent form of this devastating neurodegenerative disorder.
Core Principles: Deconstructing Sporadic Alzheimer's Complexity
The Polygenic Architecture of Sporadic Alzheimer's Disease
Sporadic AD is fundamentally polygenic, with heritability estimates ranging from 60-80% driven by the combined effects of many common genetic variants, each with small effect sizes. Genome-wide association studies (GWAS) have identified dozens of candidate causal genes, many highly expressed in microglia and astrocytes [72]. Unlike monogenic fAD driven by deterministic mutations in genes such as APP, PSEN1, and PSEN2, sAD risk emerges from the aggregate contribution of hundreds to thousands of genetic variants distributed across the genome.
The polygenic risk score (PRS) has emerged as a powerful quantitative tool to capture this distributed genetic risk. PRS calculates an individual's cumulative genetic susceptibility by summing risk alleles weighted by their effect sizes derived from large-scale GWAS [73]. However, conventional genome-wide PRS lacks cellular specificity, potentially diluting critical cell-type-specific risk signals. Emerging cell-type-specific AD polygenic risk scores (ADPRS) address this limitation by focusing on genes specifically expressed in particular cell types, revealing that microglial and astrocytic genetic risks impact distinct disease processes [72].
Environmental Insults as Disease Modifiers
Environmental factors interact with genetic susceptibility to modify sAD risk and progression timeline. These insults include:
- Metabolic dysfunction: Insulin resistance, diabetes, and cardiovascular factors
- Inflammatory exposures: Systemic inflammation, infection, and immune activation
- Toxicant exposure: Heavy metals, air pollutants, and occupational neurotoxicants
- Lifestyle factors: Diet, exercise, cognitive engagement, and sleep patterns
These environmental modifiers do not typically initiate pathology in genetically resilient individuals but can significantly accelerate disease progression in genetically susceptible backgrounds through mechanisms including neuroinflammation, oxidative stress, protein misfolding, and impaired proteostasis.
The Critical Role of Glial Cells in Sporadic Pathology
Single-cell transcriptomic analyses have revealed that many AD risk genes are specifically expressed in microglia and astrocytes, highlighting the central role of non-neuronal cells in sAD pathogenesis [72]. Microglial ADPRS associates with neuritic plaques, microglial activation, neurofibrillary tangles (tau), and cognitive decline, while astrocytic ADPRS primarily affects diffuse and neuritic plaques (amyloid-β) [72]. This cell-type-specific risk pattern emerges early in the disease process, with microglial ADPRS associating with both amyloid-β and tau pathology even in cognitively unimpaired elderly individuals [72].
Methodological Framework: Engineering Sporadic Pathology In Vitro
Donor Selection and Polygenic Risk Stratification
The foundation of robust sAD modeling begins with careful donor selection and genetic risk stratification:
Cohort Selection: Donors should be selected from large cohorts (n>6,000) with comprehensive phenotypic data, including research-diagnosed early or late-onset AD cases and elderly cognitively healthy controls who have lived through the age of risk for disease development (>85 years) [74] [21]. The IPMAR Resource exemplifies this approach, comprising hiPSC lines from over 100 donors selected from extremes of global AD polygenic risk [21].
Polygenic Risk Quantification:
- Perform genome-wide genotyping using standardized arrays
- Impute to reference panels for maximal genetic coverage
- Calculate PRS using effect sizes from latest AD GWAS meta-analyses
- Stratify donors into risk percentiles (e.g., high-risk = >90th percentile, low-risk = <10th percentile)
Pathway-Specific Risk Scoring: For investigating specific biological mechanisms, calculate pathway-defined PRS (pPRS) focusing on variants within genomic pathways of interest (e.g., complement system, TGF-β signaling) [73]. This approach increases power to detect gene-environment interactions by reducing dilution from variants unrelated to the pathway of interest [73].
hiPSC Generation, Quality Control, and Differentiation
Reprogramming Methodology:
- Use non-integrating episomal vectors to avoid genomic integration
- Implement automated robotics platforms to maximize output and uniformity [61]
- Conduct rigorous quality control including genomic integrity, pluripotency confirmation, and trilineage differentiation potential
Comprehensive Quality Control:
- Karyotyping to confirm genomic integrity
- Pluripotency marker confirmation (OCT4, NANOG, SOX2, TRA-1-60)
- Trilineage differentiation potential (ectoderm, mesoderm, endoderm)
- Identity matching with donor fibroblasts
- Mycoplasma testing
Cell-Type-Specific Differentiation:
Table 1: Core Differentiation Protocols for Alzheimer's Disease Relevant Cell Types
| Cell Type | Key Transcription Factors | Maturation Time | Characterization Markers | AD-Relevant Functions |
|---|---|---|---|---|
| Cortical Neurons | NGN2, NeuroD1 | 6-8 weeks | MAP2, βIII-tubulin, Synapsin | Aβ production, tau pathology, neuronal death |
| Microglia | PU.1, IRF8 | 4-6 weeks | IBA1, TMEM119, P2RY12 | Aβ clearance, neuroinflammation, synaptic pruning |
| Astrocytes | NFIA, NFIB, SOX9 | 8-12 weeks | GFAP, S100β, EAAT1 | Cholesterol metabolism, synaptic support, Aβ metabolism |
| Blood-Brain Barrier | BMEC progenitors | 3-4 weeks | Claudin-5, ZO-1, Glut1 | Barrier function, nutrient transport |
For motor neuron differentiation relevant to neurodegenerative disease modeling, adapt established five-stage protocols with extensively optimized maturation conditions [61]. These protocols should generate high-purity cultures (>92% motor neurons) co-expressing choline acetyltransferase (ChAT), motor neuron and pancreas homeobox 1 (MNX1/HB9), and β-tubulin III (Tuj1) [61].
Introducing Environmental Insults: Standardized Paradigms
Metabolic Challenge Protocol:
- Prepare high-glucose medium (45 mM) supplemented with 500 μM palmitic acid
- Expose cultures for 72 hours, followed by 24-hour recovery in standard medium
- Include insulin (100 nM) during challenge to model insulin resistance
- Measure extracellular glucose, lactate production, and mitochondrial respiration
Inflammatory Priming Protocol:
- Prepare cytokine mixture: IL-1β (10 ng/mL), TNF-α (20 ng/mL), IFN-γ (25 ng/mL)
- Apply for 48 hours to microglia-containing co-cultures
- For chronic low-grade inflammation, use LPS (10 ng/mL) for 7 days
- Monitor NF-κB activation, cytokine secretion, and phagocytic function
Oxidative Stress Induction:
- Apply menadione (5-20 μM) for 4 hours to induce mitochondrial ROS
- Alternatively, use buthionine sulfoximine (BSO; 100 μM) for 24 hours to deplete glutathione
- Measure ROS production, glutathione levels, and oxidative damage markers
Experimental Readouts and Validation: Capturing Disease-Relevant Phenotypes
Functional Assays for Microglial and Astrocytic Responses
Phagocytic Assay:
- Incubate cultures with pHrodo-red conjugated Aβ42 (1 μM) for 4 hours
- Quantify internalized fluorescence via flow cytometry or high-content imaging
- Normalize to cell number using nuclear stains
- Include control wells with cytochalasin D (5 μM) to inhibit phagocytosis
Migratory/Surveillance Capacity:
- Seed microglia in insert, remove insert, and image migration into cell-free area
- Capture time-lapse images every 10 minutes for 24 hours
- Quantify migration distance, velocity, and directional persistence
- Use scratch assay or microfluidic platforms for compartmentalized co-cultures
Cytokine Secretion Profiling:
- Collect conditioned medium after 24-hour treatment
- Analyze using multiplex ELISA (IL-6, IL-1β, TNF-α, TGF-β, CCL2)
- Normalize to total cellular protein
- Compare baseline and stimulated secretion patterns
Alzheimer's Disease Pathological Hallmarks
Aβ Measurements:
- Extract cell lysates in Guanidine-HCl buffer
- Measure Aβ40 and Aβ42 levels using MSD or ELISA platforms
- Calculate Aβ42/Aβ40 ratio as indicator of pathogenic processing
- For extracellular Aβ, analyze conditioned medium concentrated 10x
Tau Pathology Assessment:
- Fix cultures and immunostain for total tau (HT7) and phospho-tau (AT8, AT100, PHF1)
- Quantify neuritic intensity, dystrophy, and bead-like varicosities
- For soluble tau species, perform Western blot of Sarkosyl-soluble fractions
- Implement FRET-based biosensors for real-time tau aggregation monitoring
Neuronal Health and Function:
- Capture longitudinal live-cell images daily using automated microscopy
- Quantify neurite length, branching complexity, and fragmentation
- Measure spontaneous electrical activity using multi-electrode arrays
- Assess cell death via propidium iodide uptake or caspase-3 activation
Validating Clinical Relevance
Donor Survival Correlation: For motor neuron models, correlate neurite degeneration metrics with actual donor survival times to establish clinical relevance [61]. In SALS models, accelerated neurite degeneration should correlate with donor survival, validating the pathophysiological relevance [61].
Transcriptomic Alignment: Compare in vitro gene expression signatures with postmortem brain tissue datasets. SALS motor neurons should show significant differential expression consistent with postmortem spinal cord tissues from patients [61].
Pharmacological Validation: Test established medications with known clinical efficacy (e.g., riluzole for ALS). The model should reproduce expected efficacy, rescuing cellular phenotypes and reversing transcriptomic abnormalities [61] [75].
Applications in Therapeutic Development
Drug Screening and Validation
Large-scale phenotypic screening using hiPSC models from 100+ sporadic disease patients enables robust therapeutic discovery [61]. Key considerations:
Primary Screening Endpoints:
- Neuronal survival (high-content imaging)
- Neurite integrity and complexity
- Pathological protein accumulation
- Glial activation state
Secondary Validation:
- Dose-response in multiple high-PRS lines
- Specificity assessment in low-PRS controls
- Functional rescue (electrophysiology, calcium imaging)
- Transcriptomic/pathway analysis
Combinatorial Testing: Identify synergistic drug combinations through systematic pairing of effective single agents. In SALS models, combinatorial testing identified baricitinib, memantine and riluzole as a promising therapeutic combination [61].
Clinical Trial Stratification Biomarkers
Cell-type-specific ADPRS can inform clinical trial design by identifying individuals most likely to respond to specific interventions. For example, the epilepsy drug levetiracetam may slow brain atrophy specifically in individuals who do not carry the Alzheimer's risk gene, APOE ε4 [76]. hiPSC-derived models from trial participants can serve as living biomarkers to predict treatment response.
Research Reagent Solutions: Essential Tools for Sporadic AD Modeling
Table 2: Key Research Reagents for Engineering Sporadic AD Pathology
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| hiPSC Lines | IPMAR Resource (n=109 lines) [21], Answer ALS (n=1,000 lines) [61] | Capture polygenic risk spectrum | Select lines with associated clinical, longitudinal, and genetic datasets |
| Differentiation Kits | STEMdiff Motor Neuron Kit, PSC-Derived Microglia Kit | Generate relevant cell types | Optimize for high purity and maturity; validate with multiple markers |
| Cytokines/Stimulants | IL-1β, TNF-α, IFN-γ, LPS, Aβ42 oligomers | Induce inflammatory states | Use human recombinant proteins; dose with time-course optimization |
| Reporters | HB9-turboGFP (motor neurons), TREM2-GFP (microglia) | Cell-type-specific monitoring | Use non-integrating viral delivery for transient expression |
| Assay Kits | MSD Aβ Triplex, Luminex Neurological Panel | Quantify biomarkers | Validate with positive and negative controls; establish linear range |
| Small Molecules | CT1812 (sigma-2 receptor antagonist) [76], BACE inhibitors | Target validation and screening | Include multiple chemical scaffolds; assess blood-brain barrier penetration |
The integration of polygenic risk stratification with environmental challenge paradigms in hiPSC models represents a transformative approach for engineering sporadic Alzheimer's pathology. These systems move beyond deterministic monogenic models to capture the complex genetic and environmental interactions that drive the most common forms of neurodegenerative disease. By leveraging cell-type-specific genetic risk scores and physiologically relevant insult paradigms, researchers can now model the continuum of sporadic AD with unprecedented fidelity.
The resulting models show exceptional promise for therapeutic development, having demonstrated capacity to replicate clinical trial outcomes and identify novel therapeutic combinations [61]. As these platforms continue to evolve through increased cohort sizes, improved cellular complexity (including multicellular organoid systems), and more sophisticated environmental exposure modeling, they will increasingly become the standard for preclinical validation in the pursuit of effective treatments for sporadic Alzheimer's disease.
The study of Alzheimer's disease (AD) has been transformed by human induced pluripotent stem cell (hiPSC) technology, which enables the generation of patient-derived neurons, glia, and brain organoids that retain donor-specific genetic and molecular signatures [6] [18]. This advancement is particularly crucial for modeling the complex spectrum of AD, which encompasses both rare familial forms (fAD) driven by deterministic mutations in genes such as APP, PSEN1, and PSEN2, and common sporadic forms (sAD) influenced by polygenic risk and environmental factors [36] [19]. Traditional rodent models, while valuable, often lack human-specific disease features and cannot fully capture the substantial genetic heterogeneity of human AD [6] [36]. hiPSC models address this critical limitation by providing a human-relevant system that recapitulates patient-specific pathologies, thereby enabling researchers to dissect the mechanistic diversity underlying AD and paving the way for personalized therapeutic strategies [6] [18].
Innovative phenotyping technologies are now pushing the boundaries of what can be studied in hiPSC models. Live-cell imaging, advanced transcriptomics, and sophisticated functional assays together provide an unprecedented, multi-dimensional view of disease mechanisms. These approaches allow for the direct observation of dynamic cellular processes, the mapping of complete molecular profiles, and the quantitative assessment of cellular functions—all within a human genetic context. This technical guide explores how these cutting-edge phenotyping methods are being applied to hiPSC-based AD research, providing detailed methodologies and resources to empower researchers in the field.
Live-Cell Imaging for Dynamic Tracking of Alzheimer's Disease Pathogenesis
Live-cell imaging transcends traditional endpoint assays by enabling the direct, real-time observation of dynamic pathological processes in living neurons. This approach is invaluable for capturing transient cellular states and heterogeneous responses that are often averaged out in population-level analyses.
FRET-Based Biosensors for Monitoring Endogenous γ-Secretase Activity
Experimental Protocol: To monitor endogenous γ-secretase activity in live neurons, researchers have developed a FRET-based biosensor system [19].
- Biosensor Design and Expression: Utilize genetically encoded biosensors such as the C99 Y-T biosensor, which is based on the FRET pair mTurquoise-GL (donor) and YPet (acceptor). This biosensor incorporates the C99 substrate of γ-secretase. Deliver the biosensor cDNA into primary cortical neurons (e.g., from E14-16 mouse embryos or human iPSC-derived neurons) via adeno-associated virus (AAV) under the control of a neuron-specific promoter like human synapsin (hSyn) at 5-7 days in vitro (DIV) [19].
- Imaging Setup: Conduct imaging sessions at 12-15 DIV. Use an Olympus FV3000RS Confocal Laser Scanning Microscope or equivalent system equipped with environmental control (37°C, 5% CO2). For FRET imaging, excite the donor (mTurquoise-GL) with a 405 nm laser and simultaneously collect emission signals at 460–480 nm (donor emission) and 520–540 nm (acceptor emission, FRET signal) [19].
- Data Acquisition and Analysis: Acquire time-lapse images to track changes in γ-secretase activity. Calculate the FRET ratio (YPet/mTurquoise-GL emission ratio) on a cell-by-cell basis using ImageJ and generate pseudo-color FRET images in MATLAB. This ratio is inversely correlated with γ-secretase activity—a higher FRET ratio indicates lower cleavage activity [19].
- Cell Sorting of Distinct Populations: Following imaging, use Fluorescence Activated Cell Sorting (FACS) to isolate neuronal subpopulations based on their FRET ratios. Employ a BD FACSAria II Cell Sorter or similar instrument. Gate neurons to exclude dead cells (e.g., using Propidium Iodide staining), then sort the top 20% of neurons with the highest YPet/mTurquoise-GL ratios (low γ-secretase activity) and the bottom 20% with the lowest ratios (high γ-secretase activity) for downstream biochemical and functional analyses [19].
Phenotyping Neuronal Vulnerability and Lysosomal Dysfunction
Experimental Protocol: The unique neuronal subpopulations identified by FRET-based sorting can be further characterized for downstream pathological phenotypes.
- Lysosomal Staining: Treat sorted neuronal populations with LysoPrime Green (1 µM) to label acidic organelles. Incubate for 30 minutes at 37°C, then image using confocal microscopy with 488 nm excitation and 500–540 nm emission detection. Quantify lysosomal size, number, and morphology [19].
- Vulnerability Assays: Challenge sorted neurons with toxic insults to assess differential susceptibility. Treat cultures with:
- Excitotoxicity: 50-100 µM L-glutamate for 1-2 hours.
- Oxidative Stress: 10-50 µM 4,4’-dithiodipyridine (DTDP) for 1-2 hours.
- Lysosomal Stress: 1-5 mM L-Leucyl-L-Leucine methyl ester (LLOMe) for 2-6 hours [19].
- Cell Viability Measurement: After challenge, assess cell death using Propidium Iodide (PI, 1 µg/mL). Image with 561 nm excitation and 600–680 nm emission detection. Quantify the percentage of PI-positive cells in each sorted population to determine relative vulnerability [19].
Table 1: Key Research Reagents for Live-Cell Imaging in AD Models
| Reagent/Assay | Function/Application | Example Specifications |
|---|---|---|
| C99 Y-T FRET Biosensor | Reports endogenous γ-secretase activity in live neurons | AAV-hSyn-C99 Y-T; FRET pair: mTurquoise-GL/YPet [19] |
| LysoPrime Green | Stains acidic organelles (lysosomes) for live imaging | 1 µM, 30 min incubation; Ex/Em: 488/500-540 nm [19] |
| Propidium Iodide (PI) | Cell viability marker for live-cell imaging | 1 µg/mL; Ex/Em: 561/600-680 nm [19] |
| Pharmacological Agents | Induce cellular stress to probe vulnerability | Glutamate (50-100 µM), DTDP (10-50 µM), LLOMe (1-5 mM) [19] |
Diagram 1: Live-cell imaging and sorting workflow for profiling neuronal subpopulations based on γ-secretase activity.
Spatial and Single-Cell Transcriptomics for Mapping Molecular Landscapes
Transcriptomic technologies have evolved from bulk RNA sequencing to high-resolution spatial and single-cell methods, enabling the precise mapping of molecular changes to specific cell types and anatomical contexts within complex tissues.
Spatial Transcriptomics for Contextualizing Gene Expression
Experimental Protocol: Spatial transcriptomics (ST) bridges the gap between cellular gene expression and tissue architecture, which is critical for understanding AD pathology in relation to hallmarks like amyloid plaques [77] [78].
- Technology Selection: Choose between imaging-based (img-ST) and sequencing-based (seq-ST) approaches based on resolution and transcriptome coverage needs:
- Img-ST (e.g., MERFISH, seqFISH, Xenium): Offers subcellular resolution (e.g., ~220 nm with Stereo-seq) but requires pre-selection of a gene panel (typically 100-6,000 genes). Ideal for hypothesis-driven studies focusing on specific pathways [78].
- Seq-ST (e.g., 10x Visium, Slide-seq): Captures the entire transcriptome without pre-selection but at lower spatial resolution (10-50 μm). Optimal for discovery-based studies [78].
- Tample Preparation: Fresh-frozen or optimally fixed brain tissue sections (e.g., 10-20 μm thickness) from AD models or post-mortem human brains are mounted onto specialized ST slides. For img-ST, tissues are hybridized with gene-specific, barcoded probe libraries. For seq-ST, tissues are permeabilized to allow mRNA capture on spatially barcoded oligonucleotide arrays [78].
- Data Acquisition and Imaging: For img-ST, perform multiple rounds of hybridization and fluorescence imaging (e.g., using a Vizgen MERSCOPE or 10x Genomics Xenium platform). For seq-ST, after on-slide cDNA synthesis, libraries are prepared for next-generation sequencing [78].
- Integration with Neuroimaging: For a multi-modal analysis, spatially registered maps from ST can be directly integrated with neuroimaging data, such as diffusion tensor imaging (DTI) from MRI. This "spatial imaging-transcriptomics" paradigm allows correlation of transcriptomic signatures with in vivo imaging phenotypes, like fractional anisotropy, to uncover the molecular basis of microstructural changes in the AD brain [77].
APOE Isoform-Specific Transcriptomic and Epigenomic Profiling
Experimental Protocol: To dissect the cell-autonomous effects of the major AD genetic risk factor APOE in microglia, a xenotransplantation model combined with multi-omics profiling can be employed [79].
- iPSC-Derived Microglia Generation and Transplantation: Differentiate isogenic hiPSC lines (differing only at the APOE locus: E2/E2, E3/E3, E4/E4, and APOE-KO) into microglial precursors. Transplant these human microglia into the brains of immunodeficient AppNL-G-F AD model mice at 1-2 months of age [79].
- Tissue Harvest and Cell Isolation: At 12 months post-transplantation (when Aβ pathology is extensive), perfuse mice and dissect brain regions of interest. Dissociate brain tissue and isolate the transplanted human microglia using Fluorescence-Activated Cell Sorting (FACS) with human-specific antibodies (e.g., CD11b + hCD45+) [79].
- Multi-Omics Library Preparation:
- RNA-seq: Extract total RNA from sorted microglia (e.g., using a kit like the Qiagen RNeasy Plus Micro Kit). Prepare sequencing libraries (e.g., with the SMART-Seq v4 Ultra Low Input RNA Kit) for transcriptome profiling [79].
- ATAC-seq: From the same cell sorts, use the transposase-based Assay for Transposase-Accessible Chromatin with high-throughput sequencing (ATAC-seq) to profile genome-wide chromatin accessibility. Use 5,000-50,000 cells per sample for robust library preparation [79].
- Bioinformatic Analysis: Process raw sequencing data through standard pipelines (e.g., STAR for RNA-seq, ENCODE ATAC-seq pipeline). Perform differential expression (DE) analysis (e.g., with DESeq2) and differential accessibility (DA) analysis to identify genes and regulatory elements altered by APOE genotype. Integrate findings with AD GWAS data using tools like MAGMA for genetic enrichment analysis [79].
Table 2: Core Transcriptomic and Functional Assays for hiPSC-Based AD Research
| Assay Category | Key Technology | Primary Application in AD Research | Key Outcome Measures |
|---|---|---|---|
| Spatial Transcriptomics | MERFISH, 10x Xenium, 10x Visium | Map gene expression in plaque-associated niches; characterize microglial states [78] | Cell-type-specific spatial localization; differential gene expression relative to pathology |
| Single-Cell/Nuclei RNA-seq | 10x Genomics Chromium | Profile cellular heterogeneity and identify novel cell states in AD brains and models [78] | Cell-type proportions; differentially expressed genes; trajectory inference |
| Epigenomics | ATAC-seq | Map chromatin accessibility landscapes in specific cell types (e.g., APOE genotype effects in microglia) [79] | Differentially accessible chromatin regions; transcription factor motif enrichment |
| Integrated Multi-omics | RNA-seq + ATAC-seq | Correlate transcriptomic changes with altered regulatory elements in isogenic cell models [79] | Coordinated gene expression and chromatin changes; mechanistic insights into genetic risk |
Diagram 2: Multi-omics profiling workflow for defining APOE isoform-specific functions in human microglia.
Functional Assays for Quantifying Cellular Phenotypes
Beyond molecular profiling, functional assays are essential for quantifying the downstream cellular consequences of AD-related genetic variants and pathologies, linking molecular changes to tangible phenotypic deficits.
Polygenic Risk Stratification in hiPSC Cohorts
Experimental Protocol: Modeling the polygenic nature of sAD requires large, genetically characterized hiPSC cohorts.
- Donor Selection and iPSC Generation: Select donors from well-phenotyped cohorts based on extreme polygenic risk scores (PRS) and disease status. For example, the IPMAR resource includes 109 lines: 63 from high-PRS AD patients (34 LOAD, 29 EOAD), 27 from low-PRS cognitively healthy controls, and 19 with extremes of complement pathway-specific PRS [36] [21].
- Differentiation and Functional Screening: Differentiate these iPSCs into relevant cell types (neurons, astrocytes, microglia) or 3D organoids. Subject the differentiated cultures to a panel of functional assays tailored to interrogate AD-relevant pathways, such as Aβ secretion, tau phosphorylation, phagocytosis, and inflammatory responses [36].
- Data Integration: Correlate functional assay outcomes with donor PRS, APOE genotype, and clinical data to identify cellular phenotypes that are driven by polygenic risk and to discover potential subgroups of patients who share common functional deficits, paving the way for personalized therapeutic approaches [36].
CRISPR/Cas9 for Genetic Manipulation and Functional Validation
Experimental Protocol: CRISPR/Cas9 gene editing enables precise genetic manipulations in hiPSCs to establish causal relationships between genetic variants and cellular phenotypes [39].
- sgRNA Design and Complex Formation: Design single-guide RNAs (sgRNAs) targeting the gene of interest (e.g., APOE, APP, PSEN1, BACE1). Complex the sgRNA with Cas9 nuclease protein. For base editing or knock-in, include a repair template [39].
- Delivery into hiPSCs: Deliver the CRISPR/Cas9 complex into hiPSCs via electroporation or nucleofection. For difficult-to-transfect cells, use ribonucleoprotein (RNP) complexes for higher efficiency and reduced off-target effects [39].
- Selection and Validation: Isolate clonal lines following delivery. Validate successful editing through Sanger sequencing, PCR, and Western blotting. Perform extensive quality control, including karyotyping and pluripotency marker staining, to ensure genomic integrity and stemness [39].
- Functional Phenotyping: Differentiate the isogenic edited lines (e.g., APOE3 vs. APOE4) into the desired cell type and subject them to functional assays. This enables direct comparison of phenotypes, such as Aβ phagocytosis capacity in microglia or synaptic activity in neurons, while controlling for the genetic background [79] [39].
Table 3: hiPSC Cohort Models for Familial vs. Sporadic Alzheimer's Disease
| hiPSC Model Type | Genetic Characteristics | Key Advantages | Representative Resources |
|---|---|---|---|
| Familial AD (fAD) | Deterministic mutations in APP, PSEN1, PSEN2 [19] [39] | Strong, penetrant phenotype; established causality; ideal for studying amyloid pathway | Isogenic lines with PSEN1 M146V, APP Swedish, etc. |
| Sporadic AD (sAD) - Polygenic | High vs. Low Polygenic Risk Score (PRS); may include APOE ε4 [36] | Captures genetic complexity of common AD; enables stratification by polygenic burden | IPMAR Resource (109 lines) [36] |
| Isogenic (CRISPRed) | Single gene/variant edited into common background (e.g., APOE ε3 to ε4) [79] [39] | Controls for genetic background; isolates specific variant effects | APOE2/2, E3/3, E4/4, KO isogenic sets [79] |
| Pathway-Specific sAD | High vs. Low risk in specific biological pathways (e.g., complement) [36] | Links polygenic risk to specific biological mechanisms; identifies patient subgroups | IPMAR Complement PRS lines (19 lines) [36] |
The application of human induced pluripotent stem cell (hiPSC) technology in Alzheimer's disease (AD) research represents a paradigm shift in our ability to model human-specific disease processes in vitro. Research reveals a steady increase in hiPSC-AD publications over 14 years, with the United States and China leading scientific contributions [6]. This growth underscores the critical need for standardized methodologies to ensure research rigor and reproducibility, particularly when distinguishing between sporadic (sAD) and familial (fAD) disease forms.
While fAD models benefit from defined genetic mutations (e.g., in APP, PSEN1, PSEN2), sAD models must capture complex polygenic risk profiles and environmental influences. The IPMAR Resource, a collection of over 100 hiPSC lines, exemplifies a standardized approach by capturing extremes of global AD polygenic risk and complement pathway-specific genetic risk from well-characterized donors [21]. Such resources highlight how rigorous quality control and standardization are fundamental to generating clinically relevant, reproducible models of human disease.
Best Practices for hiPSC Line Generation and Characterization
Somatic Cell Source Selection and Reprogramming
The initial choice of somatic cell source directly influences reprogramming efficiency, genomic stability, and experimental outcomes. Table 1 compares the primary cell sources used for hiPSC generation.
Table 1: Somatic Cell Sources for hiPSC Generation
| Cell Source | Reprogramming Efficiency | Invasiveness of Collection | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Dermal Fibroblasts | Moderate | Invasive (skin biopsy) | High genomic stability; reliable expansion and banking [80] | Slower reprogramming; invasive procedure |
| Peripheral Blood Mononuclear Cells (PBMCs) | Comparable to fibroblasts | Minimally invasive | Readily available; suitable for translational studies [80] | Requires specific culture conditions |
| Urinary Epithelial Cells | Robust | Completely non-invasive | Easily repeatable sampling; enables multiple lines from same donor [80] | --- |
| Keratinocytes | Higher than fibroblasts | Low (hair pluck) | --- | Yields fewer starting cells |
Pluripotency induction requires meticulous attention to vector selection. While early protocols used integrating retroviral/lentiviral vectors, best practices now favor integration-free methods (episomal vectors, synthetic mRNA, Sendai virus) to minimize risks of insertional mutagenesis and enhance clinical safety [80]. Reprogramming efficiency remains low (<0.1% to several percent) and is influenced by donor age, cell type, and epigenetic profile, with younger donor cells typically reprogramming more efficiently [80].
Comprehensive Quality Control and Pluripotency Verification
Rigorous quality control is non-negotiable for establishing validated hiPSC lines. The following verifications must be performed:
- Pluripotency Marker Expression: Confirm expression of canonical markers (OCT4, NANOG, SOX2) via PCR, immunocytochemistry, or flow cytometry [80].
- Functional Pluripotency Assay: Demonstrate differentiation capacity into all three germ layers (ectoderm, mesoderm, endoderm) through directed differentiation, generating representative cell types like neurons, cardiomyocytes, and myocytes [80].
- Genomic Integrity Monitoring: Regularly evaluate chromosomal stability and epigenetic patterns, as reprogramming can introduce abnormalities that compromise differentiation potential [80].
The International Society for Stem Cell Research (ISSCR) emphasizes the importance of selecting appropriate PSC starting material and ensuring quality at every stage—from cell banking and ancillary materials to drug product manufacturing [81]. Adherence to these standards provides a foundation for reproducible research.
Standardized Culture and Differentiation for AD Modeling
Culture System Selection and Maintenance
hiPSC culture requires tightly controlled microenvironmental conditions to maintain viability and pluripotency. While early systems used feeder layers of mitotically inactivated mouse embryonic fibroblasts, feeder-free systems with extracellular matrix coatings (Matrigel, recombinant laminin) are now preferred for enhanced reproducibility and minimized xenogeneic contamination [80].
Chemically defined media formulations (mTeSR1, E8) supplemented with essential growth factors (e.g., FGF2) and differentiation pathway inhibitors (e.g., TGF-β/activin A) enable greater standardization for translational applications [80]. Long-term cryopreservation using cryoprotectants like 10% DMSO allows stable reconstitution of lines, though continuous genomic monitoring during extended passaging is essential due to inherent instability risks [80].
Neural Differentiation and AD Model Validation
For AD modeling, standardized neural differentiation protocols must generate consistent populations of excitatory neurons, astrocytes, and microglia that recapitulate disease-relevant pathology. The ISSCR Best Practices provide essential guidance on raw material use and regulatory considerations for such differentiation processes [81].
Key validation steps for hiPSC-derived AD models include:
- fAD Model Validation: Confirm elevated Aβ42/Aβ40 ratios, endo-lysosomal abnormalities, and increased neuronal vulnerability in fAD lines [19] [82].
- sAD Model Validation: Verify transcriptomic and proteomic profiles consistent with sAD polygenic risk, including complement pathway dysregulation in high-risk lines [21].
- Pathological Hallmark Recapitulation: Demonstrate β-amyloid deposition, tau hyperphosphorylation, and neurofibrillary tangle accumulation where applicable [80].
Computational Tools for Quantitative Structural Analysis
Advanced computational tools are increasingly essential for standardized, quantitative assessment of hiPSC-derived cellular models. These tools overcome limitations of subjective manual scoring, particularly for analyzing structurally disorganized cells common in disease models.
Table 2: Computational Tools for Analyzing hiPSC-Derived Cells
| Tool Name | Primary Function | Key Features | Application in Disease Modeling |
|---|---|---|---|
| SarcGraph (Enhanced) | Detects and analyzes sarcomeres and z-discs in hiPSC-CMs | Deep learning-based classifier; ensemble graph-scoring; reduces false positives in immature cells [83] [84] | Quantifies structural disorganization in diseased cardiomyocytes |
| SarcTrack | Segmentation and tracking of individual sarcomeres | Enables study of contraction rate and sarcomere shortening at individual sarcomere level [83] [84] | Analyzes contractile dysfunction in disease models |
| ZlineDetection | Detects z-discs in mature cells with aligned structures | Quantifies z-disc alignment and sarcomere length [83] [84] | Assesses structural maturity in cardiac models |
| SarcOptiM | Tracks sarcomere length | Uses Fast Fourier Transforms; available as ImageJ plugin [83] [84] | Measures structural changes in response to interventions |
The enhanced SarcGraph framework exemplifies computational standardization, incorporating a deep learning-based z-disc classifier that significantly reduces false positive sarcomere detections in immature cells and improves myofibril chain detection in mature samples [84]. This approach enables extraction of biologically meaningful structural features at scale, providing an alternative to subjective manual scoring.
Research Reagent Solutions for AD Modeling
Table 3: Essential Research Reagents for hiPSC Alzheimer's Disease Modeling
| Reagent/Category | Function | Example Applications |
|---|---|---|
| PLD3 Antibody | Protein bait for proximity labeling of axonal spheroids | Selective isolation of PAAS proteome in postmortem AD brains [82] |
| C99 Y-T Biosensor | FRET-based recording of endogenous γ-secretase activity | Visualizing cell-by-cell heterogeneity in γ-secretase activity in live neurons [19] |
| mTOR Inhibitors | Pharmacological modulation of PI3K/AKT/mTOR pathway | Testing reversibility of axonal spheroid pathology in iPSC-derived neurons [82] |
| AAV-hSyn Vectors | Cell-specific biosensor delivery | Neuron-specific expression of FRET biosensors under human synapsin promoter [19] |
| LysoPrime Green | Fluorescent labeling of acidic organelles | Visualizing endo-lysosomal abnormalities in AD models [19] |
| Matrigel/Laminin | Extracellular matrix for feeder-free culture | Maintaining hiPSC pluripotency and supporting neural differentiation [80] |
Experimental Workflow for Investigating Disease Mechanisms
The following diagram illustrates a standardized workflow for investigating axonal pathology mechanisms in AD using integrated hiPSC modeling and proteomic approaches:
Integrated Workflow for AD Axonal Pathology Investigation
This workflow, adapted from a 2025 Nature Aging study, demonstrates how proximity labeling proteomics in postmortem human brains can identify key pathways (e.g., mTOR signaling) that are subsequently validated and manipulated in human iPSC-derived neurons [82]. This integrated approach revealed that mTOR inhibition ameliorates plaque-associated axonal spheroid pathology in both iPSC-derived neurons and mouse models [82].
Addressing Key Challenges in sAD versus fAD Modeling
Genetic Complexity and Polygenic Risk Modeling
While fAD models incorporate specific deterministic mutations, sAD modeling requires capturing polygenic risk. The IPMAR Resource addresses this challenge by selecting hiPSC lines with extremes of global AD polygenic risk scores (PRS) from well-characterized donors, including high-risk late-onset AD (n=34), high-risk early-onset AD (n=29), and low-risk control (n=27) lines [21]. This approach enables researchers to study the complex interplay of multiple genetic risk factors in sAD pathogenesis.
Phenotypic Heterogeneity and Single-Cell Analysis
Both fAD and sAD models exhibit significant cell-to-cell heterogeneity, which can be leveraged to understand differential neuronal vulnerability. A 2025 study discovered a unique subpopulation of wild-type neurons that recapitulates fAD phenotypes, including diminished γ-secretase activity, endo-lysosomal abnormalities, and increased vulnerability to toxic insults [19]. This heterogeneity can be analyzed at single-cell resolution using FRET-based biosensors (e.g., C99 Y-T biosensor) and fluorescence-activated cell sorting (FACS) to isolate neuronal subpopulations with distinct functional characteristics [19].
Implementing rigorous quality control and standardization protocols throughout the hiPSC workflow—from somatic cell selection and reprogramming to differentiation, characterization, and computational analysis—is fundamental for generating reproducible, clinically relevant models of both familial and sporadic Alzheimer's disease. Adherence to ISSCR best practices [81], utilization of well-characterized resources like the IPMAR collection [21], and adoption of standardized computational tools [83] [84] will accelerate the translation of hiPSC-based findings into therapeutic advancements for this devastating disorder. As the field progresses, continued refinement of these standards will enhance our ability to model complex disease mechanisms and develop effective, personalized interventions.
Bench to Bedside: Validating hiPSC Models and Informing Clinical Translation
Alzheimer's disease (AD) research has historically relied on animal models, particularly transgenic mice, which have provided foundational insights but suffer from critical limitations in recapitulating the full spectrum of human disease pathology. These models are predominantly based on mutations associated with familial AD (fAD), which represents less than 1% of all cases, creating a significant translational gap for the sporadic AD (sAD) that constitutes over 95% of the disease burden [85]. The accumulating failures of clinical trials and the controversial approval of amyloid-targeting therapies with limited clinical benefits have underscored the urgent need for more physiologically relevant models that better mirror human disease mechanisms [85]. Human induced pluripotent stem cell (hiPSC) technology has emerged as a transformative approach that enables the generation of patient-specific neurons, glia, and brain organoids that retain donor-specific genetic and molecular signatures [6] [18]. This technical guide examines how hiPSC models recapitulate key AD phenotypes, with particular emphasis on their application for distinguishing and modeling the distinct pathological mechanisms underlying sporadic and familial Alzheimer's disease.
hiPSC Models for Sporadic vs. Familial Alzheimer's Disease
The etiology of Alzheimer's disease fundamentally shapes the modeling strategy. hiPSC models provide a unique platform to investigate both familial and sporadic forms within a human-relevant context.
Familial AD (fAD) results from autosomal dominant mutations in genes such as APP, PSEN1, and PSEN2, leading to aggressive early-onset disease. hiPSC models derived from fAD patients or engineered to contain these mutations consistently demonstrate robust amyloid-β pathology, including increased Aβ42/Aβ40 ratios and elevated total Aβ levels [86]. These models have been instrumental in validating the amyloid cascade hypothesis and investigating downstream pathological events.
Sporadic AD (sAD) involves complex polygenic risk factors, environmental influences, and aging-related processes. Modeling sAD has historically presented greater challenges, but hiPSC approaches now capture this complexity through several innovative strategies. The IPMAR Resource exemplifies one approach, establishing over 100 hiPSC lines capturing extremes of global AD polygenic risk, including high-risk late-onset AD (34 lines), high-risk early-onset AD (29 lines), and low-risk control (27 lines) [21]. These lines are selected from extensive cohorts of research-diagnosed cases and elderly cognitively healthy controls who have lived through the age of risk (>85 years), providing associated clinical, longitudinal, and genetic datasets [21]. Additional models focus on pathway-specific genetic risk, such as complement pathway polymorphisms [21].
Table 1: Key Characteristics of Familial vs. Sporadic AD hiPSC Models
| Characteristic | Familial AD Models | Sporadic AD Models |
|---|---|---|
| Genetic Basis | Monogenic mutations (APP, PSEN1/2) | Polygenic risk scores (PRS), APOE genotype, pathway-specific risk |
| Disease Onset | Early-onset (typically <65 years) | Late-onset (typically >65 years) |
| Pathological Hallmarks | Strong Aβ pathology, synaptic dysfunction, hyperphosphorylated tau | Variable pathology, mitochondrial dysfunction, oxidative stress |
| Modeling Approach | Patient-derived hiPSCs or isogenic lines with introduced mutations | Large cohort-derived hiPSCs with high/low polygenic risk, APOE isogenic lines |
| Key Advantages | Strong phenotype penetrance, clear genetic causality | Captures human genetic diversity, relevant to majority of cases |
| Primary Applications | Pathogenic mechanism studies, initial drug screening | Personalized medicine, gene-environment interactions, risk modifier identification |
Recapitulating Core Alzheimer's Pathologies in hiPSC Models
Amyloid-β Pathology and Processing
hiPSC-derived neurons from both fAD and sAD patients successfully recapitulate key aspects of amyloid pathology central to AD. fAD models with APP or PSEN1 mutations consistently demonstrate altered APP processing with increased Aβ42/Aβ40 ratios, a well-established driver of amyloid aggregation [86]. These models have been essential for investigating gamma-secretase function and testing targeted therapeutics. Notably, sAD models also exhibit amyloid pathology, though often with more variable expression patterns that may better reflect the heterogeneity of human disease. The consistency of amyloid phenotypes across independently generated hiPSC lines with diverse genetic backgrounds confirms the robustness of this approach for capturing disease-relevant biology [86].
Tau Pathology and Neurofibrillary Tangles
Beyond amyloid pathology, hiPSC models recapitulate crucial features of tau dysfunction. Neurons derived from both fAD and sAD patients develop hyperphosphorylated tau, a key precursor to neurofibrillary tangle formation [86]. These tau abnormalities manifest in multiple hiPSC models, including those from fAD patients with PSEN1 mutations and sAD patients with varying genetic risk profiles [86]. The presence of tau pathology in hiPSC models is particularly significant given that most transgenic mouse models fail to develop robust neurofibrillary tangles, highlighting the enhanced pathological relevance of human cellular models [85].
Mitochondrial Dysfunction and Oxidative Stress
Transcriptomic analyses of hiPSC-derived neurons from AD patients have identified consistent dysregulation in mitochondrial genes, implicating oxidative stress as a major driver of disease pathology [86]. Integrative analysis of multiple datasets reveals fourteen key mitochondria-related genes that show significant dysregulation in both postmortem brain tissues and hiPSC-derived neurons from AD patients [86]. These mitochondrial abnormalities manifest as impaired electron transport chain function, increased reactive oxygen species (ROS) production, disrupted calcium homeostasis, and defective mitophagy. The consistency of these findings across both fAD and sAD models suggests mitochondrial dysfunction represents a central convergence point in AD pathogenesis, potentially preceding other pathological features.
Neuroinflammation and Glial Contributions
Advanced hiPSC models now incorporate glial cells, including astrocytes and microglia, to more completely model the neuroinflammatory components of AD. Co-culture systems demonstrate that AD hiPSC-derived neurons promote pro-inflammatory activation in microglia, which in turn exacerbates neuronal damage. Bibliometric analysis reveals inflammation, astrocytes, microglia, and apolipoprotein E (ApoE) as emerging research trends in the hiPSC field, reflecting growing recognition of non-cell autonomous mechanisms in AD pathogenesis [6] [18]. The inclusion of patient-specific microglia with different ApoE isoforms represents a particularly promising approach for investigating how genetic risk modifiers influence neuroinflammatory responses.
Table 2: Key AD Phenotypes Recapitulated in hiPSC Models
| Phenotype Category | Specific Pathologies Observed | Assessment Methods | Significance |
|---|---|---|---|
| Amyloid Pathology | Altered Aβ42/Aβ40 ratio, increased total Aβ, amyloid plaque formation (in organoids) | ELISA, immunocytochemistry, Western blot | Validates disease relevance, supports amyloid hypothesis |
| Tau Pathology | Hyperphosphorylated tau, pre-tangle formations, disrupted microtubule stability | Immunocytochemistry, Western blot, FRET-based biosensors | Connects amyloid and tau pathologies, models later disease stages |
| Mitochondrial Dysfunction | Elevated ROS, impaired ETC function, disrupted Ca2+ homeostasis, fragmented morphology | MitoStress Test, ROS dyes, TMRM, mitoTracker | Identifies early pathogenic events, therapeutic targets |
| Synaptic Deficits | Reduced synapse number, impaired synaptic transmission, decreased spine density | Electrophysiology, immunocytochemistry (synaptophysin/PSD-95) | Correlates with cognitive decline, functional readout |
| Neuroinflammation | Activated microglia, reactive astrocytes, cytokine secretion | Cytokine array, immunocytochemistry, phagocytosis assays | Models non-cell autonomous mechanisms, biomarker source |
| Network Abnormalities | Hyperexcitability, aberrant oscillatory activity, impaired synchrony | MEA, calcium imaging, patch-clamp electrophysiology | Functional correlate of cognitive impairment, translational bridge |
Experimental Workflows and Methodologies
hiPSC Generation and Neuronal Differentiation
The foundation of robust AD modeling begins with careful hiPSC generation and differentiation. For fAD, multiple approaches are employed: (1) derivation of hiPSCs from patients with known pathogenic mutations; (2) introduction of specific mutations into control hiPSCs using CRISPR/Cas9 gene editing to create isogenic pairs that differ only at the disease-relevant locus. For sAD, the strategy involves (1) establishing hiPSC lines from well-characterized cohorts with extensive clinical and genetic data; (2) selecting lines representing extremes of polygenic risk scores; (3) focusing on specific genetic risk factors like APOE genotype through isogenic editing [21].
Neuronal differentiation typically employs dual-SMAD inhibition protocols using small molecules (SB431542, LDN193189) to direct neural induction, followed by patterning toward forebrain identities using additional small molecules (IWR-1, CHIR99021). Mature neuronal cultures are typically maintained for 8-12 weeks to allow full development of AD-relevant phenotypes, with regular assessment of neuronal markers (MAP2, NeuN) and synaptic maturity (synaptophysin, PSD-95) [86].
Phenotypic Screening and Validation Assays
Comprehensive phenotypic characterization employs multiple complementary approaches. Transcriptomic analysis begins with RNA extraction from hiPSC-derived neurons, followed by library preparation and sequencing. Differential gene expression analysis identifies consistently dysregulated pathways, with mitochondrial dysfunction emerging as a prominent feature across both fAD and sAD models [86]. For functional assessment, mitochondrial stress tests using Seahorse Analyzers measure basal respiration, ATP production, and spare respiratory capacity, while reactive oxygen species are quantified using CM-H2DCFDA or MitoSOX dyes [86].
Amyloid-β pathology is typically quantified through ELISA measurements of Aβ40 and Aβ42 in conditioned media, with calculation of the critical Aβ42/Aβ40 ratio [86]. Tau phosphorylation is assessed through Western blot or immunocytochemistry using phospho-specific antibodies (e.g., AT8 for p-tau Ser202/Thr205). Electrophysiological function is evaluated through multi-electrode arrays (MEAs) that detect network-level hyperactivity, a feature observed in both AD models and human patients [86].
Diagram 1: Experimental Workflow for hiPSC-based AD Modeling
Table 3: Essential Research Reagents for hiPSC-based AD Modeling
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| hiPSC Lines | IPMAR Resource lines (high/low polygenic risk) [21], fAD mutation lines (APP, PSEN1/2), APOE isogenic lines | Capturing genetic diversity, establishing disease relevance |
| Neural Induction | SMAD inhibitors (SB431542, LDN193189), B27 supplement, N2 supplement | Directing neural differentiation, supporting neuronal survival |
| Differentiation Factors | BDNF, GDNF, NT-3, cAMP, ascorbic acid | Promoting neuronal maturation, synaptic development |
| Phenotype Assays | Aβ ELISA kits, mitochondrial stress test kits, calcium indicators (Fluo-4, Fura-2), ROS sensors (CM-H2DCFDA) | Quantifying key AD pathologies, functional assessment |
| Antibodies | Anti-Aβ (6E10, 4G8), anti-phospho-tau (AT8, AT100), anti-MAP2, anti-synaptophysin, anti-PSD-95 | Immunodetection of pathological markers, neuronal characterization |
| Gene Editing Tools | CRISPR/Cas9 systems, donor vectors for homologous recombination | Creating isogenic controls, introducing specific mutations |
Signaling Pathways in Alzheimer's Pathology
The pathological processes in Alzheimer's disease involve complex interactions between multiple signaling pathways that are increasingly well-modeled in hiPSC systems. Mitochondrial dysfunction emerges as a central node, with consistent transcriptomic alterations in mitochondrial genes across both fAD and sAD models [86]. These mitochondrial defects lead to increased oxidative stress, which in turn exacerbates amyloid and tau pathology through multiple mechanisms, including activation of kinase pathways that promote tau hyperphosphorylation.
Diagram 2: Key Pathogenic Pathways in Alzheimer's Disease
Neuroinflammatory pathways represent another critical component, with patient-specific microglia and astrocytes contributing to disease progression through cytokine secretion and altered neuron-glia interactions. The emergence of hiPSC models that incorporate these glial cells enables more complete investigation of these non-cell-autonomous mechanisms, particularly how genetic risk factors like APOE genotype influence neuroinflammatory responses [6] [18].
hiPSC technology has fundamentally advanced our ability to model Alzheimer's disease by providing human-relevant systems that recapitulate key pathological features of both familial and sporadic forms. The face validity of these models is demonstrated through their consistent manifestation of amyloid and tau pathology, mitochondrial dysfunction, synaptic deficits, and neuroinflammatory signatures that mirror the human disease. The strategic application of these models to compare isogenic lines differing only at specific risk loci, alongside panels of lines capturing polygenic risk extremes, provides unprecedented opportunity to dissect the distinct and overlapping mechanisms driving different AD forms. As these models continue to evolve through incorporation of more complex cellular communities, improved maturation protocols, and integration with multi-omics technologies, they promise to accelerate the identification of novel therapeutic targets and biomarkers urgently needed to address the growing global burden of Alzheimer's disease.
The high failure rate of Alzheimer's disease (AD) clinical trials, despite promising preclinical results in animal models, underscores a critical lack of predictive validity in conventional drug screening platforms [5]. This challenge is particularly acute when distinguishing therapeutic responses in sporadic AD (sAD), which accounts for over 95% of cases, from familial AD (fAD) driven by fully penetrant autosomal dominant mutations [36] [5]. Human induced pluripotent stem cell (hiPSC) technology presents a paradigm shift by enabling the creation of patient-derived neural models that retain individual genetic backgrounds and disease-specific phenotypes [6] [87].
The core premise of hiPSC-based predictive validity lies in deploying human-pathophysiological-relevant models early in the drug discovery pipeline. This approach fundamentally "humanizes" preclinical screening by introducing patient-specific genetic context before clinical trials, potentially de-risking drug development and improving success rates [87]. This technical guide examines the current state of hiPSC models for AD drug screening, focusing on methodologies, validated applications, and emerging best practices for enhancing predictive validity in both sporadic and familial AD contexts.
HiPSC Model Systems: From Monocultures to Complex Organoids
Neural Differentiation Strategies
Robust neuronal differentiation from hiPSCs is foundational to AD modeling. Current protocols primarily utilize dual-SMAD inhibition (blocking both BMP and TGF-β signaling) to efficiently direct pluripotent cells toward neural ectoderm lineage progenitors, significantly enriching cultures for neural progenitor cells (NPCs) [87]. These NPCs can be stably expanded and subsequently differentiated into functionally specialized cortical neurons, astrocytes, and oligodendrocytes.
- Neural Progenitor Cell-Based Differentiation: HiPSCs form embryoid body-like aggregates followed by neural rosette structures that are manually or enzymatically selected to establish homogeneous, expandable NPC populations. These NPCs can be maintained long-term while retaining differentiation potential [87].
- Small Molecule-Driven Direct Differentiation: Protocols using GSK-3β, TGFβ, and Notch inhibitors, plus LIF3, enable high-efficiency derivation of multipotent neural stem cells directly from hiPSCs, yielding forebrain, midbrain, and hindbrain neuronal and glial subtypes [87].
- Neural Organoid Generation: Three-dimensional self-assembling organoids recapitulate complex tissue architecture and cell-cell interactions not achievable in 2D systems. Recent advances incorporate gene-editing technologies and co-assembly of organoids with specific cell types to enhance pathological relevance [88].
Modeling Sporadic versus Familial Alzheimer's Disease
Table 1: HiPSC Model Configurations for AD Subtypes
| AD Subtype | Genetic Characteristics | Modeling Approach | Key Advantages |
|---|---|---|---|
| Familial AD (fAD) | Autosomal dominant mutations in APP, PSEN1, PSEN2 [5] | Introduction of known mutations via CRISPR/Cas9 in control lines [39] | Controlled genetic background; clear phenotype-genotype correlation |
| Sporadic AD (sAD) | Polygenic risk involving >70 common/rare variants [36] | Patient-derived iPSCs with polygenic risk score stratification [36] | Captures human genetic diversity; models complex gene-environment interactions |
| APOE4-Associated Risk | APOE ε4 allele (3-15x increased risk) [5] | Isogenic APOE line comparison (ε2, ε3, ε4) [39] | Focuses on major genetic risk factor; reveals allele-specific pathological mechanisms |
The IPMAR Resource exemplifies the modern approach to sAD modeling, comprising 109 iPSC lines selected from extremes of global AD polygenic risk, including high-risk late-onset AD, high-risk early-onset AD, and low-risk cognitively healthy controls [36]. This resource captures the substantial genetic diversity underlying common AD, enabling researchers to stratify patients based on specific genetic risk profiles for personalized therapeutic development.
Measuring Functional Outcomes: Electrophysiological and Circuit-Level Phenotypes
A critical advancement in hiPSC-based screening is the move beyond molecular readouts to functional metrics that more closely reflect cognitive deficits. Long-term potentiation (LTP), a cellular correlate of learning and memory, represents one such translationally relevant endpoint [89].
Microelectrode Array (MEA) Platform for LTP Assessment
A validated functional assay employs hiPSC-derived cortical neurons and primary astrocytes co-cultured on patterned microelectrode arrays where surface chemistry creates circuit connections between electrodes to model LTP [89]. This system demonstrates significant reduction in LTP maintenance when exposed to Amyloid-Beta 42 (Aβ42) oligomers, effectively modeling the mild cognitive impairment (MCI) stage of AD before significant neuronal loss occurs [89].
Diagram 1: Functional LTP Screening Workflow for Predictive Drug Assessment
The experimental protocol for this system involves:
- Cell Culture: hiPSC-derived cortical neurons are plated on patterned MEAs and maintained for 28-35 days to ensure mature synaptic connections [89].
- Baseline Recording: Pre-treatment LTP is measured following high-frequency stimulation (HFS) to establish baseline synaptic plasticity.
- Pathological Challenge: Application of soluble Aβ42 oligomers (dimmers, trimers, dodecamers) at concentrations that impair LTP without causing significant cell death [89].
- Therapeutic Testing: Co-administration of experimental compounds with Aβ42 oligomers or subsequent treatment after LTP impairment.
- Functional Assessment: LTP maintenance is measured at 1-hour post-treatment, with recovery toward baseline indicating therapeutic efficacy [89].
This platform has demonstrated predictive validity with known AD therapeutics including Donepezil, Memantine, Rolipram, and Saracatinib, all of which showed protection against Aβ42-induced LTP impairment [89].
Successful Clinical Translation: From hiPSC Screens to Clinical Trials
Several candidate therapeutics identified using hiPSC-based screening platforms have advanced to clinical trials, demonstrating the predictive validity of this approach:
Table 2: Clinical Trial Candidates Emerging from hiPSC Research
| Therapeutic Candidate | Target Condition | hiPSC-Based Evidence | Clinical Trial Status |
|---|---|---|---|
| Bosutinib | ALS/AD | Reduction of pathological protein accumulation in patient-derived neurons [75] | Clinical trials initiated |
| Ropinirole | ALS/AD | Enhanced autophagic clearance of aggregated proteins in iPSC-derived neurons [75] | Clinical trials initiated |
| Ezogabine | ALS | Modulation of neuronal hyperexcitability in patient-derived motor neurons [75] | Clinical trials initiated |
| WVE-004 | ALS/FTD | Target engagement and biomarker modulation in relevant cellular models [75] | Clinical trials initiated |
| BIIB078 | ALS/FTD | Efficacy in patient-derived neurons bearing specific genetic mutations [75] | Clinical trials initiated |
These examples highlight how phenotype-based screening in human iPSC-derived models can identify and validate therapeutic candidates with greater translational potential than traditional target-based approaches [75] [89]. The incorporation of artificial intelligence into hiPSC-based screening platforms further enhances the identification of novel therapeutic candidates and predictive patterns [75].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for hiPSC-Based AD Modeling
| Reagent/Platform | Function | Application in AD Research |
|---|---|---|
| Dual-SMAD Inhibitors | Directs neural differentiation | Efficient generation of neural progenitor cells from hiPSCs [87] |
| Polygenic Risk Score (PRS) | Quantifies genetic susceptibility | Stratification of sporadic AD patients for cohort selection [36] |
| CRISPR/Cas9 System | Precision genome editing | Creation of isogenic lines; introduction or correction of AD-related mutations [39] |
| Patterned MEA Chips | Measures network-level electrophysiology | Functional assessment of LTP as a cognitive correlate [89] |
| 3D Organoid Culture Systems | Models tissue complexity | Recapitulation of amyloid plaques, tau pathology, and neuroinflammation [88] |
| Aβ42 Oligomers | Induces AD-related pathophysiology | Experimental challenge for modeling synaptic dysfunction [89] |
Technical Considerations and Best Practices
Ensuring Experimental Rigor
- Donor Selection and Stratification: For sAD studies, select donors based on polygenic risk scores rather than just disease status to capture genetic complexity. The IPMAR resource demonstrates this with 63 high-PRS AD lines and 27 low-PRS controls [36].
- Biological and Technical Replication: Account for genetic background variability by using multiple donor lines (biological replicates) and within-line replicates (technical replicates) [90].
- Incorporation of Isogenic Controls: For fAD studies, create CRISPR-corrected isogenic lines from patient-derived iPSCs to control for genetic background [39].
- Functional Endpoints: Prioritize physiologically relevant endpoints like LTP maintenance, network synchronization, and calcium signaling over solely molecular readouts [89].
Addressing Current Limitations
While hiPSC models offer remarkable advantages, several challenges remain:
- Maturation State: iPSC-derived neurons often reflect developmental stages rather than aged adult neurons. Incorporating progerin expression or extended culture periods can partially address this limitation [87].
- Model Complexity: Simple monocultures lack the multicellular interactions of the brain. Co-culture systems and 3D organoids that include microglia, astrocytes, and vascular components better recapitulate the brain microenvironment [5] [88].
- Scalability: High-content functional screening requires adaptation to higher throughput formats while maintaining physiological relevance [87].
Diagram 2: Multi-Tiered Model Validation for Enhanced Predictive Power
HiPSC-based models for Alzheimer's disease have transitioned from simple proof-of-concept systems to sophisticated platforms capable of predicting clinical trial outcomes. The key to enhancing predictive validity lies in selecting physiologically relevant model systems (appropriate for sAD versus fAD), implementing functional endpoints that mirror clinical manifestations, and rigorously validating these models against known clinical compounds. As the field advances, integrating multi-omics approaches, complex organoid systems, and machine learning analytics with hiPSC platforms will further bridge the gap between preclinical discovery and clinical success, ultimately accelerating the development of effective Alzheimer's therapeutics.
The development of effective therapeutics for sporadic neurodegenerative diseases represents one of the most significant challenges in modern medicine. Amyotrophic lateral sclerosis (ALS), particularly its sporadic form (SALS), has witnessed groundbreaking advances through the application of large-scale induced pluripotent stem cell (iPSC) models. This case study examines a landmark screening initiative that utilized a 100-patient SALS iPSC library to identify a promising combinatorial therapy [61]. The methodologies, validation paradigms, and therapeutic discovery framework established in this ALS research provide a transformative blueprint for advancing sporadic Alzheimer's disease (AD) research, addressing critical gaps in modeling its complex etiology and accelerating the development of targeted interventions.
Neurodegenerative diseases such as Alzheimer's disease and amyotrophic lateral sclerosis present a dual challenge in biomedical research: the majority of cases are sporadic with unknown etiology, and available models have historically failed to recapitulate human pathophysiology accurately. While familial forms linked to specific genetic mutations have been modeled in animals, these account for only a small percentage of cases, and translational failure rates exceed 97% in ALS therapeutic development [61]. The emergence of human induced pluripotent stem cell (hiPSC) technology promised to overcome these limitations by enabling the generation of patient-derived neurons that retain the complete genetic background of donors. However, until recently, no appropriately powered studies had demonstrated reduced survival of SALS motor neurons compared to controls—a fundamental pathological hallmark [61]. This case study analyzes how a large-scale, population-wide iPSC screening approach for SALS has successfully overcome these limitations and explores its direct application to sporadic Alzheimer's disease research.
The ALS Blueprint: Large-Scale iPSC Screening
iPSC Library Design and Patient Cohort
The foundational element of the ALS breakthrough was the establishment of a comprehensively characterized iPSC library capturing the clinical, genetic, and biological heterogeneity of the SALS population [61].
Table 1: SALS iPSC Library Donor Demographics and Clinical Characteristics
| Characteristic | Distribution | Significance |
|---|---|---|
| Cohort Size | 100 SALS patients, 25 healthy controls | Enables population-wide significance |
| ALS Subtypes | 76 classic ALS, 13 lower motor neuron-predominant, 3 upper motor neuron-predominant, 5 suspected PLS | Captures clinical heterogeneity |
| Disease Course Metrics | Documented onset age, site of onset, ALSFRS-R progression, survival time | Correlates in vitro phenotypes with donor outcomes |
| Genetic Background | European ancestry (95%), pathogenic variants identified in some "sporadic" cases | Controls for population stratification |
The library was generated through automated reprogramming of donor fibroblasts using non-integrating episomal vectors, followed by rigorous quality control including genomic integrity verification, pluripotency confirmation, and trilineage differentiation potential assessment [61].
Motor Neuron Differentiation and Phenotypic Screening Platform
A critical innovation was the development of a robust, standardized motor neuron differentiation and phenotyping pipeline capable of modeling neurodegeneration—a key pathological hallmark of ALS.
Experimental Protocol: Motor Neuron Differentiation and Validation
- Differentiation Method: Adapted five-stage protocol from established spinal motor neuron differentiation methods with optimized maturation and screening conditions [61]
- Purity Validation: Cultures contained 92.44 ± 1.66% motor neurons (co-expressing ChAT, MNX1/HB9, and Tuj1), 97.66 ± 0.99% Tuj1+ neurons, minimal astrocytes (0.12 ± 0.01% GFAP+), and microglia (0.04 ± 0.02% CD11B+) [61]
- Phenotypic Assessment: Longitudinal live-cell imaging with motor neuron-specific HB9-turboGFP reporter enabled daily monitoring of survival and neurite degeneration [61]
- Key Phenotypes: SALS motor neurons exhibited significantly reduced survival and accelerated neurite degeneration that correlated with donor survival [61]
Transcriptomic Validation and Disease Relevance
Beyond cellular phenotypes, the model demonstrated molecular relevance through transcriptomic profiling. SALS motor neurons showed significant differential expression consistent with postmortem spinal cord tissues from ALS patients, validating the pathophysiological relevance of the model [61]. This transcriptional dysregulation was reversed by pharmacological intervention with riluzole, further strengthening the biological significance of the findings.
Drug Screening and Combinatorial Therapeutic Discovery
The validated platform was deployed for systematic therapeutic evaluation, mirroring the clinical translation pipeline.
Table 2: Drug Screening Outcomes in SALS iPSC Model
| Screening Category | Number Tested | Positive Hits | Key Findings |
|---|---|---|---|
| Drugs Previously in ALS Trials | >100 | <5% | 97% failure rate reflected clinical trial outcomes |
| Single-Agent Therapeutics | Multiple | Riluzole, Memantine, Baricitinib | Each showed significant but partial efficacy |
| Combinatorial Therapy | Multiple combinations | Riluzole + Memantine + Baricitinib | Significantly increased SALS motor neuron survival |
Experimental Protocol: Drug Screening Approach
- Primary Screening: Compounds tested across multiple SALS lines for rescue of survival deficit
- Validation: Positive hits confirmed in secondary phenotypic assays
- Combination Testing: Effective single agents tested in pairwise and three-way combinations
- Mechanistic Studies: Transcriptomic and functional analyses of rescue effects
The most significant outcome was the identification of a three-drug combination—baricitinib (a JAK inhibitor), memantine (an NMDA receptor antagonist), and riluzole (the current ALS standard of care)—that significantly increased SALS motor neuron survival across the heterogeneous donor population [61]. This represents the first therapeutic candidate validated across SALS donors to encompass heterogeneity in drug efficacy within the patient population.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for Large-Scale iPSC Screening
| Reagent/Platform | Function | Application in ALS Study |
|---|---|---|
| Non-integrating Episomal Vectors | Footprint-free reprogramming | Generation of clinically relevant iPSCs without genetic modification |
| Motor Neuron Differentiation Kit | Directed differentiation | Consistent generation of high-purity motor neurons (92.44%) |
| HB9-turboGFP Reporter | Motor neuron-specific labeling | Longitudinal tracking of survival and neurite dynamics |
| Longitudinal Live-Cell Imager | Continuous phenotypic monitoring | Daily assessment of neurodegeneration metrics |
| Single-Cell RNA-Seq Platform | Transcriptomic profiling | Identification of disease signatures and pathway analysis |
| Automated Robotics Platform | High-throughput processing | Enables large-scale screening across 100+ lines |
Translating the ALS Blueprint to Alzheimer's Disease
The methodologies and validation frameworks established in the ALS iPSC screening initiative offer a direct strategic roadmap for addressing analogous challenges in sporadic Alzheimer's disease research.
Building a Comprehensive Sporadic AD iPSC Library
Current AD research faces similar limitations in modeling sporadic cases, which constitute over 95% of patients. The ALS blueprint suggests key considerations for sporadic AD iPSC library development:
Library Design Principles:
- Cohort Size and Diversity: Recruitment of 100+ sporadic AD patients capturing the full spectrum of clinical presentation, APOE genotypes, and polygenic risk scores [37]
- Clinical Annotation: Comprehensive donor phenotyping including cognitive trajectories, neuroimaging biomarkers, and CSF profiles
- Control Strategy: Age-matched controls with low polygenic risk scores and normal cognitive aging [37]
- Genetic Characterization: Whole-genome sequencing to identify relevant risk variants and control for population stratification
The recently established "iPSC Platform to Model Alzheimer's disease Risk" (IPMAR) resource, generating stem cells from 100 individuals selected for extremes of AD polygenic risk scores, represents an initial step in this direction [37]. This resource will be made available worldwide to facilitate studies on how genetic risk variants impact brain cell health and function.
Developing Relevant AD Cellular Phenotypes and Assays
A critical challenge in AD iPSC modeling has been the development of robust, disease-relevant phenotypes that manifest within experimentally feasible timeframes. The ALS experience suggests:
Potential AD Phenotypic Assays:
- Neuronal Vulnerability: Selective vulnerability of glutamatergic and cholinergic neurons
- Axonal Degeneration: Neurite retraction and synaptic loss measurements
- Proteinopathy: Aβ accumulation and tau phosphorylation using sensitive biosensors
- Network Dysfunction: MEA-based functional assessment of neuronal networks
Advanced model systems such as 3D organoid cultures and organ-chip technologies that incorporate multiple cell types (including microglia and endothelial cells) may enhance pathological maturation [91]. The spinal cord-chip model developed for ALS, which combined iPSC-derived motor neurons with endothelial-like cells and incorporated media flow to enhance maturation, demonstrated ALS-specific dysregulation of glutamatergic and synaptic signaling [91]. Similar blood-brain-barrier chip models for AD could provide crucial insights into neurovascular contributions to disease.
Transcriptomic Convergence Across Diseases
Single-cell RNA sequencing approaches have revealed early convergent signatures in ALS that transcend genetic heterogeneity. A cross-comparison of human iPSC motor neuron models of familial and sporadic ALS revealed early, MN-resolved transcriptomic disease signatures that were concordant with postmortem MNs and predictive across human and mouse models [92] [93]. This approach, which accounted for genetic and experimental variability through repeated differentiations and multiple sequencing platforms, identified dysregulated genes that were consistently altered across both familial and sporadic cases.
Application of similar methodologies to AD could identify core pathogenic pathways operational across diverse genetic backgrounds. The relaxation of statistical thresholds to identify subtly dysregulated genes, as employed in the ALS study, may be particularly valuable for detecting early pathogenic changes in AD [93].
Drug Screening and Validation Strategies
The ALS screening paradigm demonstrates the critical importance of testing candidate therapeutics across a genetically diverse iPSC library to account for heterogeneous treatment responses.
AD Drug Screening Implementation:
- Primary Phenotypic Screening: Aβ toxicity, tau phosphorylation, neurite degeneration, or network hyperexcitability
- Compound Libraries: Previously failed AD therapeutics, mechanism-based compounds, FDA-approved libraries
- Combination Therapies: Focus on multi-target approaches addressing AD multifactoriality
- Stratification Analysis: Identification of patient subgroups with enhanced drug responsiveness
The confirmation in ALS that 97% of drugs previously failed in clinical trials also failed to show efficacy in the SALS iPSC model validates this approach for de-risking therapeutic development [61]. Similar systematic reevaluation of failed AD compounds in patient-derived models could identify subsets worth re-purposing or inform combination strategies.
Technical Implementation and Methodological Considerations
Standardization and Quality Control
The successful execution of large-scale iPSC screening requires rigorous standardization and quality control protocols:
Key Quality Metrics:
- Genomic Stability: Regular karyotyping and whole-genome sequencing to monitor mutations
- Line Identity: STR profiling to confirm donor identity
- Pluripotency Verification: Expression of canonical markers and trilineage differentiation potential
- Differentiation Efficiency: Consistent production of target cell types across lines and batches
- Batch Effects: Implementation of randomized plating and processing to minimize technical artifacts
Data Integration and Analytical Approaches
The integration of multimodal data streams represents both a challenge and opportunity in large-scale iPSC studies:
Data Integration Framework:
- Clinical Covariates: Age, sex, disease progression metrics, neuroimaging data
- Genetic Data: Polygenic risk scores, APOE genotype, whole-genome sequencing
- Cellular Phenotypes: Survival, morphology, functional parameters
- Molecular Profiles: Transcriptomic, epigenetic, proteomic signatures
Advanced analytical approaches including machine learning and pathway enrichment analyses can identify patterns across these diverse data modalities and reveal patient-specific pathogenic mechanisms.
The large-scale iPSC screening platform developed for sporadic ALS represents a transformative approach to neurodegenerative disease modeling and therapeutic discovery. Its successful application to ALS—demonstrating clinically relevant phenotypes, transcriptomic fidelity, accurate prediction of clinical trial failures, and identification of a novel combinatorial therapy—provides a validated blueprint for sporadic Alzheimer's disease research.
Implementation of this blueprint in AD requires (1) establishment of comprehensively characterized sporadic AD iPSC libraries capturing population heterogeneity, (2) development of robust, disease-relevant phenotypic assays manifesting within experimentally accessible timeframes, (3) application of single-cell transcriptomic approaches to identify convergent pathways across genetic backgrounds, and (4) systematic therapeutic screening with emphasis on combinatorial approaches and stratified responses.
The growing iPSC market, projected to reach US$4.69 billion by 2033, reflects increasing investment and technological advancement in this field [94] [95]. Integration of emerging technologies such as organ-chip systems, automated high-content screening, and artificial intelligence with iPSC-based platforms will further enhance their predictive validity and throughput [75] [91]. By adopting the lessons from ALS iPSC screening, the Alzheimer's research community can accelerate the development of effective, personalized therapeutics for this devastating disorder.
Alzheimer's disease (AD) remains a debilitating neurodegenerative disorder without adequate treatment, characterized by progressive cognitive decline and dementia [6] [18]. The research community faces a fundamental challenge: current models individually fail to fully replicate the complex human physiology and pathology of AD. Sporadic Alzheimer's disease (sAD) accounts for over 95% of cases with an etiology that remains poorly understood, while familial AD (fAD), representing less than 5% of cases, is driven by specific autosomal dominant mutations [2]. This etiological divide necessitates research models that can address both distinct and shared disease mechanisms.
The limitations of existing approaches are significant. Rodent models, while invaluable for capturing systemic complexity and behavioral outputs, lack particular human-specific disease features and have shorter lifespans that may not fully support the development of neurodegeneration [6] [2]. Post-mortem human brain tissue provides ultimate biological relevance but represents only the end-stage of the disease process, offering limited insights into early pathogenic events. Within this landscape, human induced pluripotent stem cell (hiPSC) technology has emerged as a transformative approach, enabling the generation of patient-derived neurons, glia, and organoids that retain donor-specific genetic and molecular signatures [6] [18].
This technical guide outlines structured methodologies for integrating hiPSC models with traditional animal studies and post-mortem data, creating a powerful synergistic framework that leverages the unique strengths of each approach while mitigating their individual limitations, with particular emphasis on addressing the distinct challenges of sporadic and familial Alzheimer's disease.
Biological Validation: Establishing Pathophysiological Concordance
Transcriptomic Alignment Across Model Systems
A critical first step in model integration involves establishing transcriptomic concordance between hiPSC-derived cells and their in vivo counterparts. Research demonstrates that hiPSC-derived neurons most closely resemble fetal brain tissue, which may limit their direct comparison to adult post-mortem samples [96]. However, methodological advances are addressing this challenge.
Table 1: Transcriptomic Concordance Between hiPSC Models and Post-Mortem Tissue in Schizophrenia Research (Adapted from [97])
| Analysis Approach | Key Finding | Implication for AD Research |
|---|---|---|
| Uncorrected Analysis | Limited disease signal detection | Highlights need for analytical refinement |
| Cell Type Composition Correction | Boosted disease signal significantly | Suggests accounting for neuronal/glial proportions |
| Covariate Adjustment | Increased concordance with post-mortem data | Reduces technical and biological noise |
| Validation Cohort | 94 RNA-Seq samples (47 NPCs, 47 neurons) | Supports statistical power requirements |
The workflow for establishing transcriptomic alignment involves rigorous bioinformatic pipelines that account for multiple sources of variation. Reducing the stochastic effects of differentiation by correcting for cell type composition has been shown to significantly boost disease signal and increase concordance with post-mortem datasets [97]. This approach is particularly relevant for AD research, where cell-type specific vulnerabilities (e.g., glutamatergic neurons, astrocytes, microglia) contribute differentially to disease pathogenesis.
Pathological Hallmark Recapitulation
A core strength of hiPSC models lies in their ability to recapitulate key AD pathological features, albeit with limitations. Research utilizing hiPSC-derived neurons from patients with fAD mutations (e.g., in PSEN1, PSEN2, APP) has demonstrated increased production of amyloid-beta (Aβ) isoforms, particularly the pathogenic Aβ42/Aβ40 ratio [2]. However, the spontaneous formation of amyloid plaques and neurofibrillary tangles – hallmark pathologies of post-mortem AD brains – has been challenging to achieve in two-dimensional hiPSC cultures.
Advanced three-dimensional organoid systems now enable more robust modeling of AD pathology. These systems demonstrate Aβ aggregation and phosphorylated tau accumulation over extended culture periods (often exceeding 6 months), providing a platform for studying the temporal sequence of AD pathogenesis [2]. The integration of microglia and other glial cells in these systems further enhances their physiological relevance, as neuroinflammation is increasingly recognized as a critical contributor to AD progression [6] [18].
For animal model integration, hiPSC-derived neural progenitor cells can be transplanted into rodent brains to create chimeric models that combine human neurons with an in vivo environment. These chimeric models allow researchers to study human neuronal pathology in the context of a living organism, including interactions with a functional immune system and exposure to systemic factors [2]. This approach is particularly valuable for studying sAD, where environmental and systemic factors likely interact with genetic predispositions.
Technical Integration: Methodological Frameworks for Data Correlation
Cross-System Assay Standardization
To enable meaningful comparisons across model systems, standardized assays must be implemented to measure conserved biological endpoints. Key pathological processes in AD – including oxidative stress, synaptic dysfunction, and aberrant neuronal network activity – can be quantified across hiPSC models, animal systems, and in some cases, post-mortem tissue.
Table 2: Standardized Assays for Cross-Model Comparison in AD Research
| Pathological Process | hiPSC Model Assays | Animal Model Assays | Post-Mortem Measures |
|---|---|---|---|
| Oxidative Stress | ROS indicators, Transcriptomics [96] | In vivo ROS sensors, Lipid peroxidation assays | Oxidative damage markers (8-OHdG, HNE) |
| Synaptic Deficits | Electrophysiology, Immunocytochemistry [96] | Electrophysiology, Behavioral assays | Synaptic protein levels (synaptophysin, PSD-95) |
| Network Dysfunction | MEA recordings, Calcium imaging [98] | EEG, fMRI, Calcium imaging | - |
| Inflammation | Cytokine release, Microglial activation [6] | PET imaging, Cytokine measures | Microglial activation markers, Cytokines |
Recent advances in hiPSC-based modeling now enable more direct technical integration. For example, the development of PIEZO1-HaloTag hiPSC lines allows precise visualization of endogenous mechanosensitive channel localization and activity across diverse cell types and organoids using advanced imaging techniques [99]. This chemogenetic platform facilitates the monitoring of channel activity with temporal resolution approaching that of patch clamp electrophysiology, enabling correlations between molecular-scale imaging in hiPSC-derived cells and functional measurements in animal models.
High-Content Analysis Workflows
The integration of automated high-content analysis platforms addresses a critical challenge in hiPSC research: the quantitative and reproducible assessment of cellular phenotypes. For AD research, where subtle morphological changes may precede overt pathology, these approaches are particularly valuable.
The IAPSCI (image analysis pipeline for single-channel images) workflow enables robust segmentation of hiPSCs solely on phase-contrast single-channel images, overcoming limitations associated with analyzing cells with highly variable morphology [100]. When combined with HipDynamics, an R-based software solution that reduces the dimension of time to a single data point, researchers can integrate live imaging data with endpoint datasets while retaining the dynamics of cellular responses [100].
Similar approaches have been applied to model AMD (Age-related Macular Degeneration) using hiPSC-derived retinal pigment epithelium (RPE) cells on Electric Cell–substrate Impedance Sensing (ECIS) microelectrode arrays [101]. This tissue-on-a-chip approach combined with reproducible electrical wounding assays enables quantitative, real-time monitoring of cellular repair processes – a methodology directly transferable to AD research for studying neuronal damage response.
Analytical Approaches: Computational Frameworks for Data Integration
Bibliometric-Informed Research Design
Bibliometric analysis of the hiPSC-AD research landscape reveals emerging trends and collaborative opportunities that can guide integrated research strategies. An analysis of 531 articles on hiPSC models of AD published between 2010 and 2024 identifies key focus areas including inflammation, astrocytes, microglia, apolipoprotein E (ApoE), and tau [6] [18]. These findings highlight pathways amenable to cross-model validation and suggest priority areas for resource allocation.
The steady increase in publications over 14 years, with the United States leading in contributions followed by China, reflects growing recognition of hiPSC models' value in AD research [6] [18]. The stabilization of annual publications at approximately 80 papers in recent years indicates field maturation, suggesting that integration with complementary approaches represents the next frontier for advancement.
Power Analysis and Cohort Design Considerations
A critical consideration in designing integrated studies is statistical power, particularly given the substantial resources required for multi-modal approaches. Research indicates that for studies of complex genetic disorders like sAD, maximizing the number of individuals in hiPSC cohorts – even at the expense of replicate hiPSC clones – generally provides greater statistical power [97]. This design principle mirrors approaches already well-established in genetics and should inform the allocation of resources across model systems.
For fAD research, where specific mutations drive pathology, smaller hiPSC cohorts may suffice, potentially enabling more intensive characterization across multiple model systems. In both cases, careful matching of cohort characteristics (e.g., age, sex, genetic background) across hiPSC, animal, and post-mortem studies enhances the validity of cross-system comparisons.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for Integrated hiPSC Studies
| Reagent/Platform | Function | Application in Integrated Studies |
|---|---|---|
| PIEZO1-HaloTag hiPSCs [99] | Chemogenetic platform for visualizing endogenous mechanosensitive channels | Correlate subcellular localization with functional measures in animal models |
| ECIS Microelectrode Arrays [101] | Real-time impedance sensing for barrier function and cell migration | Quantitative comparison of cellular repair processes across models |
| IAPSCI Pipeline [100] | Image analysis for single-channel phase-contrast images | Standardized morphological analysis across experimental systems |
| HipDynamics Software [100] | Dimensionality reduction for live imaging data | Temporal dynamics analysis comparable to electrophysiological recordings |
| CRISPR Engineering [99] | Precise genetic modification of hiPSCs | Introduce fAD mutations or correct sAD risk variants for isogenic controls |
| CiteSpace & VOSviewer [6] | Bibliometric analysis tools | Identify emerging research trends and collaborative opportunities |
Experimental Protocols: Detailed Methodologies for Key Experiments
Protocol: Transcriptomic Alignment Analysis
This protocol outlines the steps for establishing transcriptomic concordance between hiPSC-derived neural cells and post-mortem brain tissue, adapted from methodologies described in [97].
- Sample Preparation: Generate RNA-seq data from hiPSC-derived neural progenitor cells (NPCs) and neurons (minimum 6 weeks differentiation). Include matched post-mortem brain samples from comparable brain regions (e.g., prefrontal cortex).
- Quality Control and Batch Correction: Implement rigorous quality control including genotype concordance analysis using VerifyBamID to detect sample mislabeling or contamination. Account for batch effects in both tissue culture and RNA-seq processing.
- Cell Type Composition Analysis: Estimate cell type proportions in both hiPSC-derived and post-mortem samples using reference-based deconvolution algorithms (e.g., CIBERSORTx) with brain-specific reference signatures.
- Differential Expression Analysis: Conduct differential expression analysis comparing disease versus control states within each model system, incorporating cell type composition as a covariate in the statistical model.
- Cross-System Concordance Assessment: Evaluate overlap in differentially expressed genes across model systems using hypergeometric tests. Perform pathway enrichment analysis on shared gene sets to identify conserved biological processes.
Protocol: High-Content Phenotypic Screening
This protocol details the implementation of automated high-content analysis for quantifying AD-relevant cellular phenotypes, integrating approaches from [101] and [100].
- Platform Establishment: Culture hiPSC-derived neurons or cerebral organoids on compatible imaging platforms (e.g., ECIS arrays or multi-well plates for high-content screening).
- Live-Cell Imaging: Conduct time-lapse imaging over defined periods (e.g., 24-72 hours) using phase-contrast and/or fluorescence microscopy, maintaining physiological conditions (37°C, 5% CO₂).
- Image Analysis Pipeline: Apply the IAPSCI workflow for robust segmentation of single-channel images:
- Load images and perform illumination correction
- Apply advanced thresholding with morphological operations
- Identify primary objects using a combination of intensity and shape criteria
- Measure morphological features (e.g., neurite length, soma size, branching complexity)
- Temporal Data Reduction: Process time-series data using HipDynamics to reduce dimensionality while preserving dynamic information, generating composite phenotypic signatures for each cell line.
- Cross-Model Comparison: Compare hiPSC-derived phenotypic signatures with analogous measures from animal models (e.g., dendritic morphology from Golgi-stained tissue) and post-mortem human samples.
The integration of hiPSC models with animal studies and post-mortem data represents a powerful paradigm for advancing Alzheimer's disease research. By leveraging the unique strengths of each approach – the human relevance and genetic tractability of hiPSCs, the systemic and behavioral comprehensiveness of animal models, and the ultimate biological validity of post-mortem tissue – researchers can construct a more complete understanding of AD pathogenesis than any single approach could provide.
This multi-modal framework is particularly crucial for addressing the distinct challenges posed by sporadic and familial AD. For fAD, integrated approaches enable researchers to determine how specific mutations converge on shared pathological pathways. For sAD, these strategies facilitate the exploration of how polygenic risk factors and environmental influences interact to drive disease. As the field progresses, leveraging the experimental and analytical frameworks outlined in this guide will accelerate the development of urgently needed therapeutic strategies for this devastating disorder.
The escalating global burden of Alzheimer's disease (AD), coupled with the high failure rate of single-target therapeutic agents, has necessitated a paradigm shift in drug discovery. This whitepaper delineates an integrated framework for identifying therapeutic candidates, leveraging human induced pluripotent stem cell (hiPSC) models to bridge the critical gap between traditional preclinical models and human pathophysiology. The central thesis posits that hiPSC-based models, which faithfully recapitulate the distinct etiologies of sporadic (sAD) and familial AD (fAD), provide an indispensable platform for rationally designing both combinatorial drugs and personalized medicine strategies. We detail the application of these models for target identification, validation, and the evaluation of multi-target-directed ligands (MTDLs) and combination therapies (CTs). Furthermore, we provide a comprehensive toolkit of experimental protocols, quantitative data summaries, and visualization aids to equip researchers with the methodologies necessary to advance the next generation of Alzheimer's therapeutics.
Alzheimer's disease is a progressive neurodegenerative disorder and the leading cause of dementia worldwide, characterized by progressive cognitive decline and pathological hallmarks including amyloid-beta (Aβ) plaques and neurofibrillary tangles composed of hyperphosphorylated tau [6] [2]. A critical distinction in AD etiology lies between the rare, early-onset familial AD (fAD), driven by autosomal dominant mutations in genes such as APP, PSEN1, and PSEN2, and the common sporadic AD (sAD), which accounts for over 95% of all cases and involves complex interactions between genetic risk factors (e.g., APOE ɛ4), aging, and environment [2]. This etiological divergence has profound implications for therapeutic development.
For decades, preclinical research has relied heavily on animal models, most of which are based on fAD mutations. While instrumental, these models fail to fully capture the heterogeneity and specific pathophysiology of human sAD [6] [102]. Consequently, many promising therapeutic candidates have failed in clinical translation. The advent of human induced pluripotent stem cell (hiPSC) technology has revolutionized this landscape. hiPSCs, generated by reprogramming patient somatic cells (e.g., from skin or blood) into a pluripotent state, can be differentiated into various neural cell types, including neurons, astrocytes, and microglia [102]. This enables the generation of patient-specific and disease-specific models that retain the donor's genetic background, providing a human-relevant system to dissect disease mechanisms and screen therapeutic interventions [6] [103].
hiPSC Models for Sporadic vs. Familial Alzheimer's Disease
hiPSC models offer a unique platform to delineate the specific pathological mechanisms and therapeutic vulnerabilities of sAD and fAD.
- Familial AD (fAD) Models: Isogenic hiPSC lines, where disease-causing mutations (e.g., in PSEN1 or APP) are introduced into healthy control lines or corrected in patient-derived lines, are a powerful tool. These genetically matched pairs allow researchers to isolate the functional impact of a specific mutation in a controlled genetic background, enabling precise dissection of pathogenic mechanisms like altered Aβ production or tau hyperphosphorylation [103].
- Sporadic AD (sAD) Models: hiPSCs derived from sAD patients capture the complex polygenic risk and epigenetic landscape of the disease. These models are crucial for studying the role of risk factors like APOE ɛ4 and for investigating the interplay between genetics and environmental stressors in the most prevalent form of AD [2]. Research using these models has revealed stress phenotypes associated with intracellular Aβ and differential drug responsiveness, highlighting the need for personalized therapeutic approaches [2].
The table below summarizes the key characteristics of these models.
Table 1: Characteristics of hiPSC Models for Familial and Sporadic AD
| Feature | Familial AD (fAD) hiPSC Models | Sporadic AD (sAD) hiPSC Models |
|---|---|---|
| Genetic Basis | Monogenic; known mutations in APP, PSEN1, PSEN2 | Polygenic; complex risk factors (e.g., APOE ɛ4) |
| Representativeness | Accounts for <5% of AD cases [2] | Accounts for >95% of AD cases [2] |
| Modeling Approach | Isogenic pairs for precise mutation study [103] | Patient-derived lines capturing genetic heterogeneity |
| Key Applications | Mechanistic studies of Aβ and tau pathology | Studying gene-environment interactions, personalized drug screening |
| Research Trends | Well-established modeling strategies | Emerging focus; identified as a critical research gap [6] |
Advanced hiPSC-Derived Model Systems
Moving beyond simple 2D cultures, advanced protocols now enable the creation of more physiologically relevant models:
- Two-Dimensional (2D) Co-cultures: Defined protocols exist to differentiate hiPSCs into specific neural lineages, including excitatory and inhibitory neurons, midbrain dopaminergic neurons (relevant for co-pathologies), astrocytes, and microglia [102]. Co-culturing these cell types allows for the study of cell-cell interactions in AD pathogenesis, such as neuroinflammation.
- Three-Dimensional (3D) Organoids and Tri-cultures: Cerebral organoids and engineered 3D microfluidic systems can recapitulate the complex cellular architecture and cell-cell interactions of the human brain. For instance, a 3D tri-culture model incorporating neurons, astrocytes, and microglia demonstrated AD-specific phenotypes like microglial recruitment, axonal fragmentation, and nitric oxide release [102]. These systems provide a more holistic view of disease processes.
Therapeutic Approaches: From Combination Therapy to Personalized Medicine
The multifactorial nature of AD, particularly sAD, suggests that modulating a single target is insufficient. HiPSC models are ideally suited to develop and test two complementary strategies: combination therapy and personalized medicine.
Combinatorial Drug Therapy
Combination Therapy (CT) involves using two or more drugs with distinct mechanisms of action to achieve synergistic or additive effects. The current standard of care for AD is a CT targeting both the cholinergic and glutamatergic systems [104].
- Evidence for Combination Therapy: A fixed-dose combination of memantine (an NMDAR antagonist) and donepezil (a cholinesterase inhibitor, ChEI) is approved for moderate to severe AD. Real-world observational studies and clinical trials have shown that this CT can slow the rate of cognitive and functional decline, reduce neurobehavioral symptoms, and delay nursing home admission compared to ChEI monotherapy or no treatment [104]. The efficacy is more pronounced when started early [104].
- Multi-Target-Directed Ligands (MTDLs): An alternative to administering multiple drugs is designing single chemical entities that act on multiple targets simultaneously. A prominent example is Memoquin, a compound developed through MTDL design to target pathways related to Aβ aggregation, oxidative stress, and cholinesterase activity [104]. Another strategy involves designing hybrid molecules that combine the pharmacophores of memantine and galantamine, aiming to confer synergistic neuroprotection by targeting NMDA receptors and nicotinic acetylcholine receptors, respectively [104].
Table 2: Key Evidence for Combination Therapy in Alzheimer's Disease
| Combination Therapy | Study Design | Key Findings | Reference |
|---|---|---|---|
| ChEI + Memantine | 4-year, real-world observational study (n=382) | Slowed cognitive and functional decline vs. ChEI monotherapy | [104] |
| Donepezil + Memantine | 24-week RCT, moderate to severe AD (n=404) | Significant improvement in cognition (SIB), function (ADCS-ADL), and clinician's global assessment (CIBIC+) vs. donepezil alone | [104] |
| ChEI + Memantine | Long-term observational study (n=943) | Significantly extended time to nursing home admission | [104] |
| Galantamine + Memantine | Preclinical in vitro study | Sub-active concentrations of each drug provided full neuroprotection against NMDA-induced toxicity, suggesting synergy | [104] |
Personalized Medicine in AD
Personalized medicine aims to tailor therapeutic strategies to individual patient characteristics. HiPSC technology is a cornerstone of this approach in AD research [105] [103].
- Patient Stratification: hiPSC lines derived from a diverse cohort of sAD and fAD patients can reveal population-specific and individual-specific drug responses. This helps in identifying biomarkers that predict therapeutic efficacy and in stratifying patient populations for clinical trials [103].
- From Proteomics to Proteoformics: While pharmacogenomics focuses on how genes affect drug response, the field is advancing toward proteoformics. A "canonical" protein can exist in multiple proteoforms due to genetic variations, alternative RNA splicing, and post-translational modifications [105]. Different proteoforms can have dramatically different functions and responses to drugs. Therefore, developing protein drugs or biomarkers targeted at specific proteoforms, rather than the canonical protein, represents the future of precision medicine, enabling more accurate diagnostics and targeted therapies [105].
Experimental Protocols for hiPSC-Based Therapeutic Discovery
This section provides detailed methodologies for key experiments in the drug discovery pipeline.
Protocol 1: Generating an hiPSC-Derived Tri-culture Model of Neuroinflammation
Purpose: To create a 3D in vitro model that recapitulates neuron-astrocyte-microglia interactions in AD-related neuroinflammation [102].
Materials:
- hiPSCs from healthy controls and AD patients.
- Neural induction medium (e.g., with dual-SMAD inhibitors).
- Maturation media for astrocytes (e.g., containing CNTF, LIF) and microglia (e.g., containing IL-34, GM-CSF).
- 3D microfluidic platform or low-attachment plates for organoid formation.
Procedure:
- Neural Induction: Differentiate hiPSCs into neural precursor cells (NPCs) using a validated protocol, such as dual-SMAD inhibition.
- Neuronal/Astrocytic Differentiation: Differentiate NPCs into a mixed population of neurons and astrocytes in a 3D matrix within a microfluidic device or as free-floating organoids.
- Microglia Differentiation: Differentiate hiPSCs into microglia precursors using a yolk-sac mimicking protocol with cytokines like BMP4, IL-3, and subsequently IL-34 and M-CSF.
- Tri-culture Assembly: Introduce the derived microglia into the neuronal-astrocytic 3D culture system.
- Phenotypic Validation: Challenge the model with Aβ oligomers or post-mortem AD brain extracts. Assess outcomes such as:
- Microglial migration and morphology (Iba1 staining).
- Pro-inflammatory cytokine release (ELISA).
- Neuronal damage (e.g., axonal fragmentation via tau/MAP2 staining).
- Nitric oxide production.
Protocol 2: High-Content Screening of MTDLs using hiPSC-Derived Neurons
Purpose: To quantitatively evaluate the efficacy of Multi-Target-Directed Ligands (MTDLs) in reversing AD-related phenotypes.
Materials:
- Isogenic hiPSC-derived neurons (e.g., with and without PSEN1 mutation).
- MTDL candidate (e.g., Memoquin).
- Immunocytochemistry reagents for Aβ, p-tau, and synaptic markers (e.g., PSD-95, Synapsin).
- High-content imaging system.
Procedure:
- Cell Culture: Plate hiPSC-derived neurons in 96-well or 384-well imaging plates.
- Compound Treatment: Treat cells with a dose range of the MTDL candidate. Include positive controls (e.g., known secretase inhibitors) and vehicle controls.
- Fixation and Staining: At a predetermined endpoint, fix cells and immunostain for key AD biomarkers (Aβ, p-tau) and synaptic markers.
- Image Acquisition and Analysis: Automatically acquire images on a high-content imager. Use analysis software to quantify:
- Intracellular Aβ intensity and aggregate size.
- Phospho-tau intensity and localization.
- Synaptic puncta density and size.
- Data Analysis: Calculate Z-scores and dose-response curves to determine the potency and efficacy of the MTDL in modulating multiple pathological pathways simultaneously.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for hiPSC-based AD Research
| Reagent/Solution | Function/Application | Example |
|---|---|---|
| Isogenic hiPSC Panels | Precisely isolate the impact of a specific mutation; essential for target validation and lead discovery. | Panels with mutations in APP, PSEN1, or APOE; available from repositories like The Jackson Laboratory [103]. |
| Disease-Relevant Cell Lines | Model patient-specific pathophysiology and for personalized drug screening. | hiPSCs derived from sAD patients with varying APOE genotypes or other risk factors [2]. |
| Neural Differentiation Kits | Standardized, efficient generation of neurons, astrocytes, or microglia from hiPSCs. | Kits for cortical neurons, midbrain dopaminergic neurons, or microglia [102]. |
| 3D Culture Matrices | Support the formation of complex 3D structures like cerebral organoids or engineered tissues. | Synthetic hydrogels (e.g., PEG-based), Basement Membrane Extract (BME). |
| Analysis Software | Quantify complex cellular phenotypes from imaging data. | Sarc-Graph (for sarcomere analysis in cardiotoxicity studies) [106], CONTRAX (for contractile function) [107], high-content analysis software (e.g., CellProfiler). |
Visualizing Workflows and Signaling Pathways
Diagram: hiPSC-Based Therapeutic Discovery Pipeline
Diagram: Key Pathogenic Pathways in Alzheimer's Disease
The integration of hiPSC models for both sporadic and familial Alzheimer's disease into the therapeutic discovery pipeline marks a transformative advance. These models provide the necessary human physiological context to deconvolute the disease's complexity, validate novel targets, and rationally design combinatorial and personalized therapeutic strategies. As the field progresses, key areas for development include the standardization of hiPSC differentiation protocols, the enhancement of 3D model complexity to include vascular and immune components, and the integration of multi-omics data (genomics, proteoformics) with high-content phenotypic screening. By adopting this comprehensive and human-relevant framework, researchers are poised to identify and validate the next generation of therapeutic candidates with a higher probability of clinical success, ultimately moving closer to effective interventions for this devastating disorder.
Conclusion
hiPSC technology has fundamentally transformed Alzheimer's disease research by providing experimentally versatile, human-specific models that capture critical aspects of both familial and sporadic forms. These models successfully bridge a long-standing translational gap, offering a more physiologically relevant platform for deconstructing disease mechanisms and screening therapeutics. Future progress hinges on overcoming challenges related to cellular maturation, model standardization, and the complex integration of polygenic risk. The convergence of hiPSCs with cutting-edge tools like genome editing, 3D organoids, artificial intelligence, and multi-omics profiling is paving the way for a new era of personalized medicine. This will not only accelerate the identification of novel drug targets but also ultimately enable the development of more effective, patient-specific treatments for Alzheimer's disease.
References
- 1. Genetic architecture of Alzheimer's disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7409822/]
- 2. Spontaneous and familial models of Alzheimer's disease [https://www.sciencedirect.com/science/article/abs/pii/S0024320523005532]
- 3. Step by step: towards a better understanding of the genetic ... [https://www.nature.com/articles/s41380-023-02076-1]
- 4. Recent Advances and Future Directions in Alzheimer's ... [https://pubmed.ncbi.nlm.nih.gov/40869138/]
- 5. Modeling Alzheimer's disease with iPSC-derived brain cells [https://www.nature.com/articles/s41380-019-0468-3]
- 6. Human induced pluripotent stem cell models for Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11962003/]
- 7. Polygenic risk score of sporadic late-onset Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5803427/]
- 8. Polygenic risk score of sporadic late-onset Alzheimer's ... [https://pubmed.ncbi.nlm.nih.gov/28943286/]
- 9. Neuroinflammatory Signaling in the Pathogenesis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9199559/]
- 10. A deep dive into the pathological hallmarks of Alzheimer's ... [https://pubmed.ncbi.nlm.nih.gov/41175916/]
- 11. Probing sporadic and familial Alzheimer's disease using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3338985/]
- 12. Recent advances in Alzheimer's disease: mechanisms ... [https://www.nature.com/articles/s41392-024-01911-3]
- 13. hiPSC-based models to decipher the contribution of human ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-023-00612-9]
- 14. Neuroinflammation in the pathogenesis of Alzheimer's ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2014.00112/full]
- 15. | News-Medical Amyloid Cascade Hypothesis [https://www.news-medical.net/life-sciences/Amyloid-Cascade-Hypothesis.aspx]
- 16. the Validating Through the Revised Criteria of... Amyloid Cascade [https://pubmed.ncbi.nlm.nih.gov/40359457/]
- 17. Who is benefiting from the amyloid of Alzheimer’s? | STAT hypothesis [https://www.statnews.com/2025/02/11/amyloid-hypothesis-alzheimers-research-lecanemab-aduhelm/]
- 18. Frontiers | Human induced pluripotent stem cell models for... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1548701/full]
- 19. A unique subpopulation of wild-type neurons recapitulating ... [https://www.nature.com/articles/s41419-025-07934-0]
- 20. Integrative multiomics reveals common endotypes across ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-024-01659-6]
- 21. Modeling common Alzheimer's disease with high and low ... [https://www.sciencedirect.com/science/article/pii/S2213671125001742]
- 22. The role of microglia in neurodegenerative diseases [https://www.sciencedirect.com/science/article/abs/pii/S0161589025001853]
- 23. Astrocyte in Neurological Disease: Pathogenesis and Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271643/]
- 24. Pathogenesis and therapeutic applications of microglia ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1508023/full]
- 25. The role of microglia in neurodegenerative diseases [https://pubmed.ncbi.nlm.nih.gov/40307457/]
- 26. Astrocytes distress triggers brain pathology through ... [https://www.nature.com/articles/s41467-025-65536-y]
- 27. Editorial: Advancing neurodevelopmental disorder models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12647108/]
- 28. Patient iPSC models reveal glia-intrinsic phenotypes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11560525/]
- 29. An Overview of Genome-Wide Association Studies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5563735/]
- 30. APOE and Alzheimer's Disease: Advances in Genetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8096522/]
- 31. ApoE in Alzheimer's disease - Molecular Neurodegeneration [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-022-00574-4]
- 32. New insights into the genetic etiology of Alzheimer's ... [https://www.nature.com/articles/s41588-022-01024-z]
- 33. Astrocytic APOE4 genotype-mediated negative impacts on ... [https://www.sciencedirect.com/science/article/pii/S2213671123003016]
- 34. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 35. Somatic cell reprogramming and transitions between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3032267/]
- 36. Modeling common Alzheimer's disease with high and low ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365843/]
- 37. First Large-Scale Stem Cell Bank Enables Worldwide ... [https://www.isscr.org/isscr-news/first-large-scale-stem-cell-bank-enables-worldwide-studies-on-genetic-risk-for-alzheimers-disease]
- 38. Reprogramming somatic cells to pluripotency [https://pmc.ncbi.nlm.nih.gov/articles/PMC3903711/]
- 39. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches ... [https://www.mdpi.com/2076-3921/14/7/781]
- 40. Alzheimer's disease patient brain extracts induce multiple ... [https://www.nature.com/articles/s41380-025-03041-w]
- 41. Crosstalk Between Astrocytes and Microglia: An Overview [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01416/full]
- 42. Dynamic signaling for neural stem cell fate determination - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2675157/]
- 43. Acquisition of neural fate by combination of BMP blockade ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10522999/]
- 44. A cell fate decision map reveals abundant direct ... [https://www.nature.com/articles/s41556-024-01393-z]
- 45. Microglia–Astrocyte Interaction in Neural Development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10417796/]
- 46. Protocol for generating a human iPSC-derived tri-culture ... [https://pubmed.ncbi.nlm.nih.gov/41134673/]
- 47. Three-dimensional co-culture platform of human induced ... [https://www.sciencedirect.com/science/article/pii/S2666166723001223]
- 48. Use of Human Induced Pluripotent Stem Cell-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4568555/]
- 49. The translational power of Alzheimer's-based organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119642/]
- 50. Human 3D brain organoids: steering the ... [https://www.nature.com/articles/s41420-023-01523-w]
- 51. Emerging brain organoids: 3D models to decipher, identify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11869974/]
- 52. New brain model sheds patient-specific light on Alzheimer's ... [https://www.hsci.harvard.edu/news/new-brain-model-sheds-patient-specific-light-ad]
- 53. Long-term three-dimensional high-resolution imaging of ... [https://www.nature.com/articles/s12276-024-01312-0]
- 54. Label-free cell imaging and tracking in 3D organoids [https://www.sciencedirect.com/science/article/pii/S2666386425001213]
- 55. Advanced 3D Imaging and Organoid Bioprinting for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11031334/]
- 56. building higher-order complexity and neural circuitry models [https://www.sciencedirect.com/science/article/pii/S0167779925000460]
- 57. Modelling Sporadic Alzheimer's Disease Using Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6267251/]
- 58. Modeling familial Alzheimer's disease with induced ... [https://pubmed.ncbi.nlm.nih.gov/21900357/]
- 59. iPSC-derived cortical neurons to study sporadic Alzheimer ... [https://www.sciencedirect.com/science/article/pii/S0378427421009152]
- 60. Human iPSC-Derived Neural Models for Studying Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8930932/]
- 61. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 62. Hit to lead [https://en.wikipedia.org/wiki/Hit_to_lead]
- 63. Expediting hit-to-lead progression in drug discovery ... [https://www.nature.com/articles/s41467-025-66324-4]
- 64. Challenges in Physiological Phenotyping of hiPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7479826/]
- 65. Physiological maturation and drug responses of human ... [https://www.nature.com/articles/srep26181]
- 66. Multifactorial approach is needed to unravel the maturation ... [https://www.nature.com/articles/s41598-024-81140-4]
- 67. Article A functional hiPSC-cortical neuron differentiation ... [https://www.sciencedirect.com/science/article/pii/S2213671121005907]
- 68. Stem Cell Surface Marker Expression Defines Late Stages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4922850/]
- 69. Validating human induced pluripotent stem cell-specific ... [https://www.sciencedirect.com/science/article/pii/S1465324924006108]
- 70. Human iPSC Reprogramming Success: The Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 71. Reprogramming's unintended consequences [https://www.nature.com/articles/nrg2975]
- 72. Cell-type-specific Alzheimer's disease polygenic risk ... [https://www.nature.com/articles/s41467-023-43132-2]
- 73. Pathway polygenic risk scores (pPRS) for the analysis of gene ... [https://pubmed.ncbi.nlm.nih.gov/40763299/]
- 74. Modeling common Alzheimer's disease with high and low ... [https://pubmed.ncbi.nlm.nih.gov/40614728/]
- 75. Drug discovery research with the iPSC models of ... [https://www.sciencedirect.com/science/article/pii/S0168010225001683]
- 76. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 77. A spatial imaging-transcriptomics paradigm for deciphering ... [https://pubmed.ncbi.nlm.nih.gov/40742809/]
- 78. Microglia networks within the tapestry of alzheimer's disease ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00897-y]
- 79. The APOE isoforms differentially shape the transcriptomic ... [https://www.nature.com/articles/s41467-025-60099-4]
- 80. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 81. The ISSCR Launches Roadmap for Developing Pluripotent ... [https://www.isscr.org/isscr-news/the-isscr-launches-best-practices]
- 82. Subcellular proteomics and iPSC modeling uncover ... [https://www.nature.com/articles/s43587-025-00823-3]
- 83. Quantifying HiPSC-CM structural organization at scale with ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013436]
- 84. Quantifying HiPSC-CM structural organization at scale with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520406/]
- 85. Lost in translation: Inconvenient truths on the utility of ... [https://elifesciences.org/articles/90633]
- 86. Mapping key mitochondrial genes in Alzheimer's disease ... [https://www.nature.com/articles/s41598-025-27019-4]
- 87. Human Pluripotent Stem Cell-Derived Models and Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8193821/]
- 88. iPSC-derived neural organoids in dementia research [https://www.sciencedirect.com/science/article/pii/S0168010225001634]
- 89. Validation of a functional human AD model with four AD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11142300/]
- 90. Recommendations, guidelines, and best practice for the ... [https://www.sciencedirect.com/science/article/pii/S2772408523001072]
- 91. An organ-chip model of sporadic ALS using iPSC-derived ... [https://www.sciencedirect.com/science/article/pii/S193459092500222X]
- 92. Cross-comparison of human iPSC-derived motor neuron ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7897311/]
- 93. Cross-Comparison of Human iPSC Motor Neuron ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/33382996/]
- 94. Induced Pluripotent Stem Cells (iPSCs) Market Prospects ... [https://www.businesswire.com/news/home/20251111238841/en/Induced-Pluripotent-Stem-Cells-iPSCs-Market-Prospects-2025-2033-Industry-Gains-Traction-with-Rising-Investments-and-Collaborations---ResearchAndMarkets.com]
- 95. Induced Pluripotent Stem Cells Market Report 2025–2033 [https://syg.ma/@renubresearch/induced-pluripotent-stem-cells-market-report-2025-2033-cell-type-country]
- 96. New considerations for hiPSC-based models of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6109625/]
- 97. Transcriptional signatures of schizophrenia in hiPSC ... [https://www.nature.com/articles/s41467-017-02330-5]
- 98. Cell-specific models of hiPSC-CMs developed by the ... [https://www.nature.com/articles/s41598-024-63413-0]
- 99. Visualizing PIEZO1 localization and activity in hiPSC- ... [https://www.nature.com/articles/s41467-025-59150-1]
- 100. A Novel Automated High-Content Analysis Workflow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5030730/]
- 101. Real-time quantitative monitoring of hiPSC-based model of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4456427/]
- 102. Emerging hiPSC Models for Drug Discovery in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8347370/]
- 103. Advancing Therapeutic Discovery: Through hiPSC-Derived ... [https://www.genengnews.com/sponsored/advancing-therapeutic-discovery-through-hipsc-derived-systems/]
- 104. Combination Drug Therapy for the Management of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7246721/]
- 105. Personalized Drug Therapy: Innovative Concept Guided With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10950891/]
- 106. Sarc-Graph: Automated segmentation, tracking, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8523047/]
- 107. Tracking single hiPSC-derived cardiomyocyte contractile ... [https://www.nature.com/articles/s41467-024-49755-3]