Hydrogel Scaffolds for Stem Cell Delivery: Engineering the Microenvironment for Enhanced Regenerative Therapy
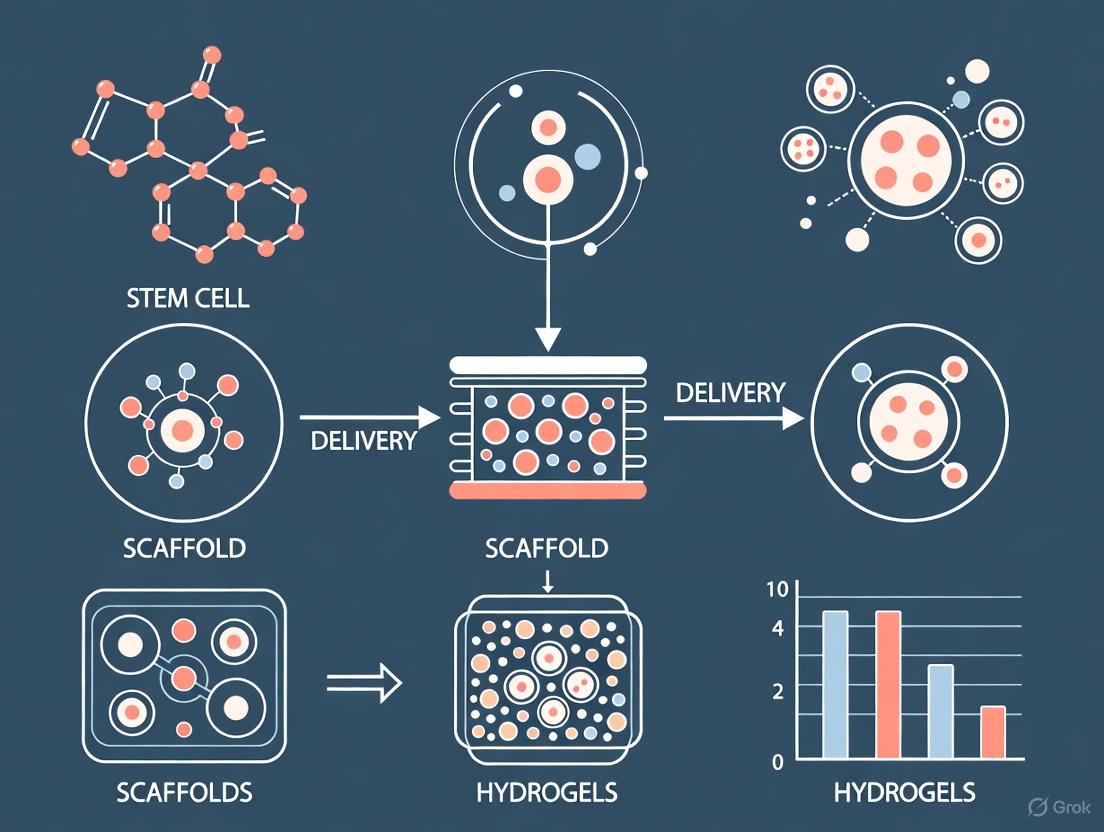
This article provides a comprehensive analysis of hydrogel-based scaffolds as advanced delivery systems for stem cells in regenerative medicine.
Hydrogel Scaffolds for Stem Cell Delivery: Engineering the Microenvironment for Enhanced Regenerative Therapy
Abstract
This article provides a comprehensive analysis of hydrogel-based scaffolds as advanced delivery systems for stem cells in regenerative medicine. Tailored for researchers and drug development professionals, it explores the foundational principles of hydrogel design, including tunable mechanical properties and biomimicry of the native extracellular matrix. The scope extends to methodological advances in 3D bioprinting and application-specific formulations for musculoskeletal, neural, and dermal repair. It further addresses critical challenges in cell viability, immunogenicity, and manufacturing, while evaluating preclinical and clinical validation strategies. By synthesizing current research and future trajectories, this review serves as a strategic guide for overcoming translational barriers and harnessing the full potential of cell-laden hydrogels.
The Hydrogel-Stem Cell Nexus: Principles of a Biomimetic Microenvironment
The extracellular matrix (ECM) is far more than a passive scaffold for cells; it is a dynamic, instructive microenvironment that actively regulates cell behavior, fate, and function [1] [2]. For stem cell research, particularly in the development of delivery methods and scaffolds, recreating this complex niche is paramount to controlling stem cell survival, retention, and therapeutic efficacy post-transplantation [3]. Hydrogels—three-dimensional networks of hydrophilic polymers that imbibe large quantities of water—have emerged as the leading platform for mimicking the native ECM [2]. They provide a physiologically relevant 3D environment that can be engineered with tunable biochemical and biophysical properties, offering a superior alternative to traditional two-dimensional culture systems and enabling significant advances in stem cell delivery for regenerative medicine [1] [3].
Key Properties of the Native ECM to Be Replicated
To design effective hydrogels, one must first understand the key properties of the native ECM that govern cell behavior. These can be categorized into three main groups:
- Biochemical Composition: The ECM is composed of a complex mixture of proteins (e.g., collagens, elastin, fibronectin, laminin) and polysaccharides (e.g., hyaluronic acid) [1] [4]. These components provide specific cell-adhesion motifs and act as reservoirs for growth factors.
- Structural Properties: The ECM possesses a distinct architecture, often fibrous, with defined pore sizes and topography that influence cell migration, nutrient diffusion, and tissue organization [1].
- Mechanical Properties: Tissues exhibit unique mechanical behaviors, including specific stiffness (elastic modulus), viscoelasticity (a combination of solid- and fluid-like behavior), and non-linear stress-strain relationships [1] [5]. Cells sense these mechanical cues through a process called mechanotransduction.
The following table summarizes target properties for engineering hydrogels.
Table 1: Key Native ECM Properties and Their Roles in Guiding Cell Behavior
| ECM Property Category | Specific Parameters | Impact on Cell Behavior |
|---|---|---|
| Biochemical | Presence of adhesion motifs (e.g., RGD) | Supports cell attachment, survival, and prevents anoikis [2] |
| Tissue-specific composition (e.g., laminin) | Directs tissue-specific differentiation and function [6] | |
| Structural | Pore size and porosity | Governs cell migration, nutrient diffusion, and waste removal [3] |
| Fiber topography and (an)isotropy | Influences cell polarity, migration, and cytoskeletal organization [1] | |
| Mechanical | Stiffness (Elastic Modulus) | Directs stem cell lineage commitment [3] |
| Viscoelasticity | Affects cell spreading, proliferation, and mechanosensing [1] [5] |
Designing Biomimetic Hydrogels: From Concept to Application
The rational design of hydrogels involves the strategic incorporation of specific biochemical and biophysical cues to replicate the native ECM microenvironment. The logical workflow for designing such hydrogels is outlined below.
Incorporating Biochemical Cues
To make synthetic hydrogels bioactive, they must be functionalized with molecules that facilitate cell adhesion and signaling.
- Cell-Adhesive Peptides: The most common strategy is incorporating the arginine-glycine-aspartate (RGD) peptide sequence, a universal integrin-binding domain found in many ECM proteins like fibronectin [2] [4]. This is essential for the survival of anchorage-dependent cells.
- Proteoglycan Mimetics: Molecules like heparin and chondroitin sulfate can be incorporated to mimic the function of native ECM proteoglycans. They sequester and release growth factors (e.g., VEGF, BMP-2), providing localized biochemical signaling to encapsulated stem cells [3] [2].
- Engineered Proteins: Advanced strategies involve designing novel biofunctional components. For example, a genetically engineered Link module (LinkCFQ) can be used to crosslink hyaluronan and gelatin, creating an ECM-inspired hydrogel with high biocompatibility and degradability [7].
Tuning Structural and Mechanical Properties
The physical parameters of a hydrogel are critical determinants of stem cell fate.
- Mechanical Properties: Hydrogel stiffness is a primary regulator of mesenchymal stromal cell (MSC) differentiation. Softer hydrogels (1–10 kPa) promote neurogenic and adipogenic lineages, while stiffer matrices (25–40 kPa) favor osteogenic commitment [3]. Furthermore, the viscoelasticity (the ability to dissipate energy, like native tissues) of hydrogels has been shown to significantly impact cell spreading and proliferation [1] [5].
- Structural Properties: Parameters like polymer molecular weight, concentration, and crosslinking density determine the hydrogel's pore size and fiber architecture [1]. This microstructure governs the diffusion of nutrients and oxygen, as well as the migration of cells within the 3D construct [3].
Table 2: Targeting Mechanical Properties for Stem Cell Differentiation
| Target Cell Fate | Optimal Hydrogel Stiffness | Key ECM Components to Mimic |
|---|---|---|
| Adipogenic / Neurogenic | 1 - 10 kPa | Soft adipose tissue / brain ECM [3] |
| Musculoskeletal | 25 - 40 kPa | Stiffer collagenous matrix of bone [3] |
| Cartilaginous | Variable (Viscoelastic) | Collagen II, Hyaluronic Acid networks [2] |
Experimental Protocols and Workflows
Protocol 1: Fabrication and Characterization of a Biofunctionalized PEG-Based Hydrogel
This protocol details the creation of a synthetic hydrogel functionalized with RGD peptides to support MSC encapsulation.
Research Reagent Solutions Table 3: Essential Materials for PEG-RGD Hydrogel Formation
| Reagent / Material | Function in the Protocol |
|---|---|
| 4-Arm PEG-Acrylate (PEG-AC) | Synthetic polymer backbone that forms the hydrogel network via crosslinking. |
| RGD-Adhesive Peptide (e.g., GCGYGRGDSPG) | Contains the integrin-binding RGD sequence and a cysteine residue for covalent conjugation. |
| Protease-Degradable Crosslinker (e.g., KCGPQG↓IWGQCK) | Forms degradable bonds within the hydrogel, allowing cell-mediated remodeling. |
| Triethanolamine (TEA) Buffer, pH 8 | Creates a basic environment for the Michael-type addition reaction. |
| Mesenchymal Stem Cells (MSCs) | Primary cells to be encapsulated and studied. |
Part A: Conjugation of RGD Peptide to PEG-AC
- Prepare Reaction Mixture: Dissolve 4-arm PEG-AC (100 mg) in 1 mL of 0.1 M TEA buffer, pH 8.
- Add Peptide: Add a molar excess of the cysteine-terminated RGD peptide (e.g., 1.2x molar ratio per acrylate group) to the PEG solution.
- React: Allow the reaction to proceed for 2 hours at room temperature under gentle agitation, protected from light.
- Purify: Dialyze the resulting PEG-RGD macromer against deionized water for 48 hours to remove unreacted peptide. Lyophilize and store at -20°C.
Part B: Encapsulation of MSCs and Hydrogel Formation
- Prepare Precursor Solution: Dissolve the purified PEG-RGD macromer and the protease-degradable crosslinker in a cell-compatible buffer (e.g., PBS). Sterilize the solution by passing it through a 0.22 µm filter.
- Cell Suspension: Trypsinize, count, and centrifuge the MSCs. Resuspend the cell pellet in a small volume of culture medium to create a concentrated cell suspension.
- Mixing: Gently mix the cell suspension with the sterile hydrogel precursor solution to achieve a final density of 5-10 million cells/mL.
- Gelation: Pipet the cell-polymer mixture into the desired mold (e.g., a silicone mold or multi-well plate). Incubate at 37°C for 20-45 minutes to allow for complete crosslinking and hydrogel formation.
- Culture: After gelation, carefully add culture medium to cover the hydrogel and place the construct in a cell culture incubator (37°C, 5% CO₂).
Characterization Workflow:
- Mechanical Testing: Use a rheometer to measure the storage (G') and loss (G'') moduli of the hydrogel to confirm its stiffness and viscoelastic properties.
- Cell Viability Assay: At 24 hours post-encapsulation, assess cell viability using a Live/Dead assay kit following the manufacturer's instructions.
Protocol 2: Forming and Assessing a Human Tissue-Derived ECM Hydrogel
This protocol utilizes decellularized ECM from human tissues to create a biologically complex scaffold [6].
Part A: Preparation of ECM Hydrogel from Decellularized Powder
- Source ECM: Obtain decellularized ECM powder from a certified supplier (e.g., human skin, bone, fat, or birth tissue) [6].
- Digest: Suspend the ECM powder at a concentration of 10-30 mg/mL in a pepsin solution (0.1 M HCl) and stir for 48-72 hours at 4°C until the solution becomes viscous and homogeneous.
- Neutralize: Neutralize the digest with 0.1 M NaOH and add a 10x concentrated PBS solution and culture medium to achieve physiological pH and salt concentration. Keep the neutralized ECM solution on ice to prevent premature gelation.
Part B: Gelation Kinetics and Stability Analysis
- Gelation Time: Transfer the neutralized ECM solution to a pre-chilled rheometer plate and initiate a time sweep at 37°C. The gelation point (tgel) is defined as the time when the storage modulus (G') crosses over and exceeds the loss modulus (G'') [6].
- Compressive Modulus: Form cylindrical ECM hydrogels and allow them to set at 37°C. Using a universal testing machine, perform unconfined compression tests on the hydrated gels at a constant strain rate. Calculate the compressive modulus from the linear region of the resulting stress-strain curve.
- Stability Study: Weigh pre-formed ECM hydrogels (Wi), incubate them in PBS or culture medium at 37°C, and record their wet weight (Wf) over 4 weeks. Calculate the percentage of mass remaining as (Wf / Wi) * 100.
Advanced Material Platforms and Future Directions
The field is moving beyond simple homogeneous gels toward more sophisticated, functional platforms.
- ECM-Mimetic Hydrogel Nanocomposites: Incorporating nanomaterials (e.g., carbon nanotubes, gold nanoparticles) can enhance mechanical strength, introduce electrical conductivity, and create stimuli-responsiveness (e.g., to magnetic fields or light) for advanced applications in bioelectronics and 4D bioprinting [4].
- "Smart" and Shape-Memory Hydrogels: These materials can change their properties in response to physiological stimuli (e.g., pH, enzymes) or recover a pre-defined shape after injection. This is highly relevant for minimally invasive delivery of stem cells and for creating complex 3D structures in situ [3] [8].
- Decellularized ECM (dECM) Hydrogels: dECM hydrogels, derived from actual human tissues, preserve the complex, tissue-specific biochemical composition of the native ECM. Studies show that hydrogels derived from different human tissues (e.g., skin, birth) have distinct physicochemical properties and differentially support stem cell metabolic activity, underscoring the importance of selecting the appropriate tissue source for specific regenerative applications [6].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for ECM-Mimetic Hydrogel Research
| Category & Reagent | Key Function in Hydrogel Design |
|---|---|
| Synthetic Polymers | |
| Poly(Ethylene Glycol) (PEG) | Biologically inert "blank slate" backbone; highly tunable mechanical properties [2] [4]. |
| Poly(Acrylamide) (PAm) | Allows precise control over substrate stiffness for mechanobiology studies [2]. |
| Natural Polymers | |
| Hyaluronic Acid (HA) | Major ECM glycosaminoglycan; promotes cell migration and proliferation [2] [7]. |
| Collagen Type I | Most abundant ECM protein; offers innate bioactivity and self-assembling properties [1] [6]. |
| Functionalization Agents | |
| RGD Peptide | Critical integrin-binding ligand for enabling cell adhesion to synthetic hydrogels [2] [4]. |
| Heparin | Glycosaminoglycan mimetic; binds and sequesters growth factors for localized delivery [3] [2]. |
| Crosslinking Enzymes | |
| Microbial Transglutaminase (MTG) | Catalyzes stable isopeptide bonds between proteins; used in biofabrication [7]. |
| Advanced Materials | |
| Decellularized ECM (dECM) | Provides a tissue-specific complex mixture of native ECM proteins and factors [6]. |
| Self-Assembling Peptides (e.g., RADA16) | Form nanofibrous structures mimicking native ECM architecture [5]. |
Hydrogels, three-dimensional (3D) cross-linked polymer networks capable of absorbing and retaining large amounts of water, have emerged as fundamental biomaterials in regenerative medicine and tissue engineering [9] [10]. Their high water content, biocompatibility, and tunable physical and chemical properties make them exceptionally suitable for creating supportive microenvironments for stem cell delivery and tissue regeneration [3]. Based on their origin, hydrogel polymers are broadly classified into natural, synthetic, and hybrid categories, each offering distinct advantages and limitations for designing stem cell delivery scaffolds [9] [11]. Natural polymers provide inherent bioactivity and cellular recognition, synthetic polymers offer mechanical robustness and high tunability, while hybrid systems aim to synergistically combine the benefits of both [9]. The selection of the core material class directly influences critical scaffold properties such as mechanical strength, degradation kinetics, and bioactivity, thereby dictating the success of the stem cell therapy by modulating cell viability, retention, and function post-transplantation [3].
Core Material Classes: Properties and Characteristics
The distinct properties of natural, synthetic, and hybrid hydrogels determine their specific applicability in stem cell delivery. The table below provides a comparative summary of these core material classes.
Table 1: Comparative Analysis of Natural, Synthetic, and Hybrid Hydrogel Polymers for Stem Cell Delivery
| Feature | Natural Polymer Hydrogels | Synthetic Polymer Hydrogels | Hybrid (Natural/Synthetic) Hydrogels |
|---|---|---|---|
| Example Polymers | Alginate, Chitosan, Gelatin Methacrylate (GelMA), Hyaluronic Acid, Collagen [9] [11] [10] | Polyethylene Glycol (PEG), Polyvinyl Alcohol (PVA), Polyacrylamide (PAAm) [9] [10] | PVA/Sodium Alginate, PEG-graft-Chitosan, Alginate-CMC-GelMA composites [9] [12] [10] |
| Key Advantages | High biocompatibility, inherent biodegradability, presence of cell-adhesive motifs (e.g., RGD), intrinsic bioactivity [9] [11] | Excellent mechanical strength, high durability, slow degradation rate, highly tunable properties (e.g., stiffness, degradation) [9] [3] | Combines biocompatibility of natural polymers with mechanical strength and tunability of synthetic polymers; enables advanced properties like self-healing and conductivity [9] |
| Key Limitations | Poor mechanical properties, high batch-to-batch variability, rapid and unpredictable degradation rates [9] [11] | Lack of intrinsic bioactivity, potential for inflammatory responses due to degradation by-products, limited cell-interactive functions [9] [11] | Increased complexity in synthesis and characterization; optimization of component interactions is challenging [9] |
| Stem Cell Function Influence | Support high cell viability and direct stem cell fate through native biochemical cues [3] [13]. | Provide controlled mechanical cues (e.g., matrix stiffness) to guide stem cell differentiation [3]. | Allows for simultaneous tuning of biochemical and mechanical signals to precisely modulate stem cell behavior [9] [3]. |
Application Notes in Stem Cell Delivery and Tissue Engineering
The application of these material classes is exemplified in specific tissue engineering contexts, demonstrating their critical role in advancing regenerative medicine.
Mesenchymal Stromal Cell (MSC) Delivery for Musculoskeletal Repair: Hydrogel-based delivery systems are a promising strategy to enhance the therapeutic efficacy of MSCs [3]. Bioactive natural polymers like chitosan and hyaluronic acid mimic the native extracellular matrix (ECM), supporting MSC viability and paracrine signaling. Furthermore, the mechanical properties of hydrogels can be tuned to guide MSC differentiation; for instance, stiffer matrices (25–40 kPa) promote osteogenic commitment, which is crucial for bone tissue engineering [3].
3D Bioprinting of Stem Cell-Laden Constructs: In extrusion-based 3D bioprinting, bioinks must balance printability, stability, and biocompatibility [12]. Hybrid hydrogel systems are particularly advantageous. A notable example is a composite bioink of Alginate, Carboxymethyl Cellulose (CMC), and GelMA, which leverages a dual-crosslinking mechanism (ionic with CaCl₂ for Alginate and covalent with UV for GelMA) to achieve excellent printability and long-term mechanical stability, supporting enhanced cell proliferation for gradient tissue regeneration [12].
Neural Stem/Progenitor Cell (NSPC) Delivery for Traumatic Brain Injury (TBI): Biomaterial scaffolds like hydrogels are essential for repairing the complex microenvironment of TBI [14]. Chitosan-based hydrogels, known for their non-toxicity, biodegradability, and biocompatibility, can be used to deliver NSPCs or bioactive molecules to the injury site. They provide structural support, modulate local inflammation, and guide axonal regeneration, thereby enhancing the potential for functional recovery [14].
Detailed Experimental Protocol: Formulation and Evaluation of a Hybrid Hydrogel Bioink
This protocol details the synthesis and characterization of a tri-component hybrid bioink (Alginate-CMC-GelMA) for extrusion-based bioprinting of stem cell-laden constructs, based on established methodologies [12].
Research Reagent Solutions
Table 2: Essential Materials and Reagents for Hybrid Bioink Formulation
| Item Name | Function / Role in the Protocol |
|---|---|
| Sodium Alginate (Alg) | Natural polysaccharide polymer; provides shear-thinning behavior and enables ionic cross-linking for structural integrity [12]. |
| Carboxymethyl Cellulose (CMC) | Natural polymer derivative; enhances viscosity and improves the rheological properties and printability of the bioink [12]. |
| Gelatin Methacrylate (GelMA) | Photo-crosslinkable natural polymer; provides thermoresponsive behavior and cell-adhesive RGD motifs, supporting long-term stability and biocompatibility [12]. |
| Photoinitiator (e.g., LAP) | Initiates radical polymerization upon UV light exposure, leading to covalent cross-linking of the GelMA network [12]. |
| Calcium Chloride (CaCl₂) Solution | Ionic cross-linker for alginate chains; enables rapid initial stabilization of the printed structure [12]. |
| Primary Cells (e.g., MSCs) | The biological payload; encapsulated within the bioink to create living tissue constructs [3] [12]. |
Step-by-Step Methodology
Part A: Polymer Solution Preparation
- Prepare Alginate and CMC Solution: Dissolve 4g of sodium alginate and 10g of carboxymethyl cellulose in 100mL of sterile, cell-culture grade phosphate-buffered saline (PBS). Stir continuously at room temperature until the polymers are fully dissolved and a homogeneous, viscous solution is formed.
- Prepare GelMA Solution: Separately, dissolve GelMA at the desired concentration (e.g., 8%, 12%, or 16% w/v) in PBS at 37°C. Add a photoinitiator (e.g., 0.25% w/v Lithium phenyl-2,4,6-trimethylbenzoylphosphinate - LAP) and ensure it is completely dissolved while protecting the solution from light.
- Formulate Hybrid Bioink: Combine the Alginate-CMC solution with the GelMA solution in a 1:1 volume ratio. Mix them thoroughly but gently at a temperature above the gelation point of Gelatin (e.g., 37°C) to avoid premature setting. The final formulation is designated as 4% Alg–10% CMC–GelMA.
Part B: Rheological and Printability Assessment
- Rheological Testing: Perform rotational and oscillatory rheometry on the bioink.
- Flow Sweep Test: Measure viscosity over a shear rate range (e.g., 0.1 to 100 s⁻¹) to confirm shear-thinning behavior, which is essential for extrudability.
- Amplitude Sweep Test: Determine the linear viscoelastic region (LVE) and yield stress, which correlates to the minimum extrusion pressure required.
- Temperature Ramp Test: Monitor storage (G′) and loss (G″) moduli while cooling from 37°C to 15°C to characterize thermoresponsive gelation.
- Thixotropy Test: Apply alternating low and high shear strains to assess the bioink's self-recovery capability after extrusion.
- Printability Evaluation: Load the bioink into a sterile cartridge and perform extrusion printing using a calibrated bioprinter. Assess printability by quantifying the fiber diameter, filament uniformity, and ability to form stable 3D structures (e.g., a grid). A dimensionless printability value (Pr) can be calculated from these parameters.
Part C: Cell Encapsulation, Bioprinting, and Post-Printing Analysis
- Cell Mixing: Gently mix a suspension of MSCs with the prepared hybrid bioink at a temperature of 37°C to achieve a final desired cell density (e.g., 1-10 million cells/mL). Avoid introducing air bubbles.
- Extrusion Bioprinting: Print the cell-laden bioink under sterile conditions using optimized parameters (e.g., nozzle diameter, pressure, print speed, and bed temperature of 15°C).
- Dual Cross-Linking:
- Ionic Cross-linking: Immediately after deposition, mist the printed construct with a sterile 100-200 mM CaCl₂ solution.
- Photo-Cross-linking: Following ionic stabilization, expose the entire construct to UV light (e.g., 365 nm wavelength) for a determined time (e.g., 30-60 seconds) to cross-link the GelMA network.
- Post-Printing Culture and Evaluation:
- Transfer the cross-linked constructs to cell culture media.
- Mechanical Stability Test: Perform an oscillatory time sweep test over 21 days to monitor the evolution of the storage modulus (G′) and assess long-term stability.
- Biocompatibility Assay: At predetermined time points (e.g., days 1, 7, 14), assess cell viability using a Live/Dead assay and quantify metabolic activity using an AlamarBlue or MTS assay.
Diagram 1: Hybrid bioink workflow from formulation to analysis.
Pathway and Decision Logic for Material Selection
The selection of an appropriate hydrogel class for a specific stem cell delivery application is guided by the key functional requirements of the target tissue. The following decision logic outlines this process.
Diagram 2: Decision logic for hydrogel class selection.
The field of stem cell research is undergoing a paradigm shift, moving beyond a purely biochemical perspective to embrace the critical role of physical cues in directing cell fate. The mechanical properties of the extracellular matrix (ECM)—particularly stiffness and elasticity—are now recognized as powerful directives that govern stem cell behavior, including differentiation, proliferation, and morphogenesis [15] [16]. This application note details how researchers can harness these mechanical cues within hydrogel-based scaffold systems to precisely control stem cell fate for regenerative medicine and drug development applications. The fundamental principle underlying this approach is mechanotransduction, the process by which cells convert mechanical stimuli from their environment into biochemical signals [17] [16]. When stem cells adhere to a substrate, they exert contractile forces through their cytoskeleton. The resistance they encounter, determined by the substrate's stiffness, triggers intracellular signaling cascades that ultimately lead to specific transcriptional programs and lineage commitment [17]. By engineering hydrogels with tunable mechanical properties, we can therefore create artificial niches that guide stem cells toward desired phenotypes without relying exclusively on soluble factors.
Core Concepts: Stiffness as a Fate Determinant
The Stiffness-Differentiation Relationship
A foundational discovery in mechanobiology is that mesenchymal stem cells (MSCs) sense matrix stiffness and differentiate accordingly. The following table summarizes the well-established relationship between substrate stiffness and lineage specification for MSCs.
Table 1: Matrix Stiffness as a Determinant of MSC Differentiation Lineage
| Target Tissue | Approximate Stiffness Range | Primary Differentiation Outcome | Key Regulatory Pathways/Proteins |
|---|---|---|---|
| Neural Tissue | 0.1 - 1 kPa [17] | Neurogenic differentiation [17] | Not Specified |
| Muscle Tissue | 8 - 17 kPa [17] | Myogenic differentiation [17] | Not Specified |
| Adipose Tissue | ~2 - 10 kPa [18] | Adipogenic differentiation [18] | Low YAP/TAZ activity [18] |
| Bone Tissue | >34 kPa [17] | Osteogenic differentiation [17] [18] | High YAP/TAZ activity [18] |
This relationship is not merely a passive response but is governed by sophisticated mechanotransduction pathways. Yes-associated protein (YAP) and its transcriptional coactivator with PDZ-binding motif (TAZ) are key nuclear effectors. On stiff matrices, YAP/TAZ translocate to the nucleus to promote the expression of osteogenic genes, whereas on soft matrices, they remain cytoplasmic, permitting adipogenesis [18]. Inhibition of YAP has been shown to significantly downregulate osteogenic markers even in stiff 3D-bioprinted constructs, confirming its central role [18].
Key Mechanotransduction Pathways
The journey from a mechanical cue to a change in cell fate involves a well-defined signaling cascade. The following diagram illustrates the core mechanotransduction pathway initiated by hydrogel stiffness.
Diagram 1: Core mechanotransduction pathway from matrix stiffness to cell fate (based on [17] [16] [18])
Advanced Material Systems and Protocols
Protocol: Fabricating Stiffness-Tuned Alginate-Gelatin (Alg-Gel) Hydrogels for 3D Bioprinting
This protocol describes the synthesis of Alg-Gel composite hydrogels with decoupled stiffness and porosity for 3D bioprinting applications, adapted from a 2020 study [18].
Objective: To create 3D-bioprinted hydrogel constructs with defined stiffness to study MSC differentiation in a controlled microenvironment.
Materials:
- Sodium Alginate (120–190 kDa, 39% guluronic acid)
- Gelatin (Type B, 40–100 kDa)
- Ultrapure Water
- Calcium Chloride (CaCl₂) Solution (2.5% w/v for crosslinking)
- Mouse MSCs (e.g., isolated from C57BL/6 mice)
- MesenCult Expansion Medium
- Osteogenic/Adipogenic (O/A) Induction Medium (for differentiation assays)
- 3D Bioprinter with temperature-controlled printhead and crosslinking system
Procedure:
- Hydrogel Preparation:
- Prepare Alg-Gel precursor solutions according to Table 2 to achieve different stiffness levels. For example, to make the "1A3G" formulation, dissolve 1g of sodium alginate and 3g of gelatin in 100 mL of ultrapure water.
- Stir the mixture in a sealed container at 60°C for 12 hours until fully dissolved.
- Sterilize the solution by pasteurization or filtration.
- Store the sterile Alg-Gel bioink at 4°C until use.
Cell Harvesting and Encapsulation:
- Culture and expand MSCs in MesenCult Expansion Medium.
- Trypsinize MSCs at ~80% confluence and resuspend in the sterile, cold Alg-Gel bioink to a final density of 5-10 × 10^6 cells/mL. Maintain the bioink-cell suspension on ice to prevent premature gelation.
3D Bioprinting and Crosslinking:
- Load the cell-laden bioink into a temperature-controlled printhead cartridge (maintained at ~18-22°C).
- Print the constructs into a desired 3D architecture (e.g., a grid structure) directly into a bath of 2.5% CaCl₂ solution.
- Allow the printed constructs to crosslink in the CaCl₂ bath for 10-15 minutes to ensure ionic gelation of the alginate.
Post-Printing Culture and Differentiation:
- Carefully transfer the crosslinked constructs to cell culture plates.
- Culture the constructs in either standard growth medium (DMEM) or O/A Induction Medium. Refresh the medium every 2-3 days.
- The constructs can be cultured for up to 21 days for differentiation analysis.
Validation and Analysis:
- Mechanical Testing: Confirm the Young's modulus of each hydrogel formulation using a compression test, selecting the first 10% of the stress-strain curve for calculation [18].
- Viability: Assess cell viability at 24 and 72 hours post-printing using Live/Dead staining. Viability should exceed 95% [19].
- Differentiation Assay: After 14-21 days, fix constructs and co-stain for alkaline phosphatase (ALP, osteogenic marker) and Oil Red O (lipid droplets, adipogenic marker). Perform qPCR to analyze gene expression of ALP and LPL (lipoprotein lipase) as early as day 3 [18].
- Pathway Inhibition: To confirm the role of YAP/TAZ, treat a set of constructs with a YAP inhibitor (e.g., Verteporfin) and observe the downregulation of differentiation markers [18].
Innovative System: Shell-Hardened Macroporous Hydrogels for Bone Regeneration
For challenging applications like bone regeneration, where mechanical integrity must be maintained during degradation, advanced hydrogel designs are required. A 2025 study introduced a macroporous hydrogel with spatiotemporally programmed mechanical properties [19].
Design Principle: A soft-templating technique using liquid-liquid phase separation between polyethylene glycol (PEG) and dextran creates a macroporous structure. Preassembled, acryl-modified lysozyme nanofibers self-assemble at the liquid-liquid interface, forming a rigid, protein-fiber-coated shell around each pore [19].
Experimental Workflow:
- Phase Separation: Create a phase-separated mixture of PEG and dextran in water. The dextran phase forms non-percolating droplets that act as soft templates for macropores.
- Interfacial Self-Assembly: Add acryl-modified lysozyme nanofibers to the system. The fibers migrate to and stabilize the PEG-dextran interface.
- Copolymerization: Incorporate polymerizable monomers (e.g., acrylamide), degradable and non-degradable PEG crosslinkers (PEG-ACLT and PEG-ACA), and an acrylated RGD peptide into the PEG phase.
- Gelation and Encapsulation: Initiate free-radical polymerization under blue light (405 nm) with a photoinitiator (Lap) to form the final hydrogel. Encapsulate stem cells by adding their suspension to the dextran phase prior to polymerization [19].
Key Advantages:
- The macroporous structure (pores ~50 μm) prevents contact inhibition during cell proliferation.
- The rigid pore shell provides sustained mechanical cues for osteodifferentiation, protecting cells from mechanical loads even as the softer hydrogel matrix degrades.
- Tunable degradation is achieved by adjusting the ratio of degradable to non-degradable PEG crosslinkers, potentially synchronizing with new tissue deposition.
- This system has demonstrated efficacy in bone regeneration in both rabbit and porcine models [19].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Mechanobiology Studies
| Item Name | Function/Application | Example Use Case |
|---|---|---|
| Polyacrylamide (PAA) | Synthetic hydrogel for 2D and 3D culture with widely tunable stiffness (2 Pa - 55 kPa) [20]. | Fundamental studies on stiffness-mediated fate decisions [21] [17]. |
| Alginate-Gelatin (Alg-Gel) | Composite bioink for 3D bioprinting; stiffness tuned via concentration and ionic crosslinking [18]. | 3D-bioprinted constructs for studying MSC differentiation in a controlled porosity environment [18]. |
| PEG-based Crosslinkers | (e.g., PEG-ACLT (degradable) and PEG-ACA (non-degradable)): Create hydrogel networks with programmable mechanics and degradation [19]. | Fabricating hydrogels with spatiotemporally controlled mechanical properties [19]. |
| Acrylated RGD Peptide | Synthetic peptide grafted into hydrogels to facilitate integrin-mediated cell adhesion [19]. | Providing essential biochemical adhesion cues in synthetic hydrogels that lack natural cell-binding domains [19]. |
| YAP/TAZ Inhibitor | (e.g., Verteporfin): Pharmacological inhibitor to probe the role of the YAP/TAZ pathway in mechanotransduction. | Validating the necessity of YAP/TAZ signaling in stiffness-directed differentiation [18]. |
The precise engineering of hydrogel stiffness and architecture provides a powerful, non-biological method for directing stem cell fate. The protocols and material systems outlined here—from straightforward stiffness-tuned Alg-Gel bioinks for 3D bioprinting to sophisticated shell-hardened macroporous hydrogels—offer researchers a toolkit to recreate critical aspects of the native stem cell niche. As the field progresses, the integration of other mechanical properties like viscoelasticity [17] [20] and the use of piezoelectric materials to provide endogenous electrical stimulation in response to mechanical loading [22] will further enhance the complexity and fidelity of these artificial microenvironments. By mastering these mechanical directives, scientists and drug developers can advance the development of more effective and predictive in vitro models and accelerate the translation of stem cell-based therapies for regenerative medicine.
Within the field of regenerative medicine, the efficacy of stem cell-based therapies is profoundly influenced by the design of the delivery scaffold. A critical triad of architectural properties—porosity, topography, and nutrient diffusion—dictates the success of these constructs by directly modulating key cellular processes, including viability, adhesion, proliferation, and differentiation [23] [24]. This Application Note delineates the quantitative relationships between these scaffold parameters and stem cell behavior, providing validated experimental protocols to guide the development of advanced hydrogel-based delivery systems for research and therapeutic applications.
Background and Significance
Stem cell-laden hydrogels function as synthetic extracellular matrices (ECMs), providing a three-dimensional (3D) microenvironment that instructs cellular fate. The architecture of this microenvironment is not a passive backdrop but an active instructor of cell behavior [3] [25]. Porosity and pore interconnectivity are fundamental for the diffusion of nutrients and oxygen, as well as the removal of metabolic waste, which are essential for maintaining cell viability throughout the scaffold volume [23] [24]. Simultaneously, the topographical orientation of scaffold fibers—whether random or aligned—provides "contact guidance" cues that direct cell morphology, migration, and tissue-specific organization [26]. Mastering the interplay of these properties is therefore crucial for creating scaffolds that not only support stem cell survival but also guide functional tissue regeneration.
Data Presentation and Analysis
Influence of Pore Architecture on Cellular Processes
The following table summarizes the effects of specific pore architectural parameters on stem cell behavior and scaffold functionality, as established in current literature.
Table 1: Influence of Scaffold Pore Architecture on Stem Cell Behavior and Scaffold Function
| Architectural Parameter | Targeted Tissues & Cell Behaviors | Impact on Scaffold Function & Cellular Response |
|---|---|---|
| Pore Size [23] | • Bone: 300-600 µm• Cartilage: 100-200 µm• Skin & General Tissue: 50-150 µm | • Regulates cell infiltration, migration, and spatial organization.• Larger pores enhance vascularization; specific sizes can promote lineage commitment. |
| High Interconnectivity [23] [24] | • All tissues, especially thick constructs. | • Ensures efficient nutrient/waste exchange, preventing necrotic cores.• Enables uniform cell distribution and colony formation. |
| Aligned Topography [26] | • Neural, Muscular, Tendon/Ligament (Anisotropic tissues). | • Provides "contact guidance" for directional cell growth and matrix deposition.• Enhances mechanical strength in the direction of alignment. |
Hydrogel Composition and Resulting Physicochemical Properties
The properties of a hydrogel scaffold are directly determined by its composition and crosslinking method. The table below compares common hydrogel systems used in stem cell delivery.
Table 2: Comparison of Hydrogel Systems for Stem Cell Delivery
| Hydrogel System | Gelation Mechanism | Key Advantages | Limitations / Challenges |
|---|---|---|---|
| Polysaccharide-Based (e.g., Chitosan, Alginate) [27] [28] | Ionic (e.g., Ca²⁺), Schiff base, Physical crosslinking. | Excellent biocompatibility; biodegradable; tunable mechanical properties. | Batch-to-batch variability (natural sources); limited bioactivity without modification. |
| Synthetic (e.g., PEG derivatives) [29] [25] | Chemical crosslinking (e.g., photo-polymerization). | High reproducibility; precise control over mechanical properties. | Often lacks intrinsic bioactivity; requires functionalization (e.g., with RGD peptides). |
| Hybrid/Composite [3] [25] | Combination of multiple mechanisms. | Couples bioactivity of natural polymers with tunable mechanics of synthetic polymers. | Optimization of multiple components can be complex. |
| Stimuli-Responsive "Smart" Hydrogels [3] [25] | pH, temperature, enzymatic activity. | Enables controlled release of cells/bioactive factors in response to local physiological cues. | Requires careful design to match the specific stimuli at the target site. |
Experimental Protocols
Protocol: Fabrication of Aligned Fibrous Scaffolds via Electrospinning
Principle: A high-voltage electrostatic field is applied to a polymer solution to generate a charged jet, which is collected on a rotating mandrel. The speed of the mandrel determines the degree of fiber alignment [26].
Materials:
- Polymer (e.g., PCL, PLGA, or a blended natural/synthetic polymer)
- Suitable solvent (e.g., chloroform, DMF)
- Electrospinning apparatus (syringe pump, high-voltage power supply, collector)
- Rotating mandrel collector
Procedure:
- Solution Preparation: Dissolve the polymer in the appropriate solvent at a concentration of 5-15% (w/v). Stir until a homogeneous solution is achieved.
- Apparatus Setup: Load the solution into a syringe. Set the flow rate to 0.5-2.0 mL/h. Set the tip-to-collector distance to 10-20 cm. Connect the high-voltage power supply (10-20 kV).
- Fiber Collection: For aligned fibers, set the rotating mandrel speed to a high velocity (≥1300 rpm or ≥3.0 m/s) [26]. For random fibers, use a stationary or slowly rotating (∼300 rpm) flat collector.
- Post-processing: Dry the collected fibrous scaffolds under vacuum for 24 hours to remove residual solvent.
Validation:
- Characterization: Use scanning electron microscopy (SEM) to confirm fiber morphology and alignment. Analyze SEM images with software (e.g., ImageJ) to determine average fiber diameter and orientation distribution.
Protocol: Fabrication of Porous Hydrogels via Particulate Leaching
Principle: A sacrificial porogen (e.g., salt crystals) of a defined size is mixed with a polymer solution. After the polymer solidifies, the porogen is dissolved, leaving behind a porous network [23].
Materials:
- Hydrogel precursor (e.g., methacrylated alginate, gelatin, or PEG)
- Salt crystals (NaCl) sieved to specific size ranges (e.g., 150-250 µm, 250-425 µm)
- Crosslinking initiator (e.g., photo-initiator Irgacure 2959 for UV crosslinking)
- Deionized water
Procedure:
- Porogen Mixing: Mix the sieved salt particles with the hydrogel precursor solution at a predetermined weight ratio (e.g., 70-90% porogen) to achieve the desired porosity.
- Crosslinking: Transfer the mixture into a mold. For photopolymerizable hydrogels, expose to UV light (λ = 365 nm, intensity = 5-10 mW/cm²) for 3-10 minutes.
- Porogen Leaching: Immerse the crosslinked hydrogel in a large volume of deionized water. Change the water 3-5 times daily for 2-3 days to completely dissolve the salt.
- Hydration & Storage: Rinse the porous hydrogel with PBS and store at 4°C until use.
Validation:
- Characterization: Use SEM to visualize pore size, morphology, and interconnectivity. Measure the equilibrium swelling ratio to assess porosity.
Protocol: Evaluating Nutrient Diffusion and Cell Viability in 3D Constructs
Principle: This protocol assesses the functional outcome of scaffold porosity by monitoring the diffusion of a fluorescent glucose analog (2-NBDG) and quantifying live/dead cell distribution throughout the scaffold.
Materials:
- Cell-laden porous scaffold
- Fluorescent glucose analog (2-NBDG)
- Live/Dead viability/cytotoxicity kit (e.g., Calcein AM / Propidium Iodide)
- Confocal laser scanning microscope (CLSM)
- Image analysis software (e.g., ImageJ, Imaris)
Procedure:
- Scaffold Seeding: Encapsulate human adipose-derived stem cells (hADSCs) or other relevant stem cells within the hydrogel at a density of 1-5 million cells/mL during the fabrication process [27].
- Culture: Maintain the cell-laden constructs in standard culture conditions for the duration of the experiment.
- Diffusion Assay: At the desired time point (e.g., day 1, 3, 7), incubate scaffolds in culture medium containing 2-NBDG (e.g., 100 µM) for 1-2 hours.
- Viability Staining: Rinse scaffolds with PBS and incubate with Calcein AM (2 µM) and Propidium Iodide (4 µM) in PBS for 30-45 minutes.
- Imaging: Image the entire scaffold thickness using CLSM. Acquire Z-stacks from the top to the bottom of the scaffold.
Analysis:
- Diffusion Profile: Plot the fluorescence intensity of 2-NBDG as a function of scaffold depth. A uniform profile indicates effective diffusion.
- Viability Quantification: Calculate the percentage of live cells (Calcein AM positive) and dead cells (Propidium Iodide positive) in multiple regions, including the core of the scaffold. High core viability (>80%) indicates sufficient nutrient diffusion [27].
Signaling Pathways and Conceptual Workflows
Scaffold Architecture to Cell Fate Signaling Pathway
The following diagram illustrates the mechanotransduction signaling pathway through which architectural cues from the scaffold are converted into biochemical signals that direct stem cell fate.
Diagram Title: Scaffold Architecture to Cell Fate Signaling Pathway
Integrated Experimental Workflow for Scaffold Evaluation
This workflow outlines the key steps for designing, fabricating, and characterizing a stem cell-laden hydrogel scaffold.
Diagram Title: Integrated Scaffold Evaluation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Hydrogel-Based Stem Cell Research
| Category / Item | Function / Application | Example Formulations / Notes |
|---|---|---|
| Natural Polymers | Provide biocompatibility and bioactivity; mimic the native ECM. | Hyaluronic Acid (HA): Major ECM component; can be modified (e.g., Ald-HA) for crosslinking [27].Chitosan/Na-Alginate: Forms gentle ionic-crosslinked gels; versatile for cell encapsulation [27] [28]. |
| Synthetic Polymers | Offer precise control over mechanical and chemical properties. | Poly(ethylene glycol) (PEG): "Gold standard" for highly tunable, bio-inert hydrogels; requires functionalization with adhesion peptides (e.g., RGD) [29] [25]. |
| Crosslinkers & Initiators | Enable hydrogel formation and control gelation kinetics. | Photo-initiators (Irgacure 2959): For UV-induced gelation of methacrylated polymers.Divalent Cations (CaCl₂): For ionic crosslinking of alginate.Oxidizing Agents (NaIO₄): To create aldehyde groups on polysaccharides for Schiff base crosslinking [27] [28]. |
| Bioactive Additives | Enhance biological function and guide stem cell fate. | RGD Peptide: Promotes integrin-mediated cell adhesion.Growth Factors (BMP-2, VEGF): Can be encapsulated to direct osteogenesis or vascularization [3] [25]. |
| Characterization Tools | Assess scaffold physical properties and biological response. | Scanning Electron Microscopy (SEM): For pore size, morphology, and fiber diameter.Rheometer: For measuring storage (G') and loss (G") moduli.Confocal Microscopy: For 3D cell viability, distribution, and differentiation analysis. |
The transition from traditional two-dimensional (2D) cell culture to three-dimensional (3D) microenvironment modeling represents a fundamental paradigm shift in regenerative medicine and stem cell research. While 2D cultures on plastic surfaces have been the standard methodology for decades, they fail to recapitulate the complex architecture and signaling environments found in native tissues [30]. This limitation has profound implications for stem cell biology, particularly in the context of therapeutic applications where the microenvironment directly controls cell fate and function [31].
The native stem cell niche is a specialized, physiologically 3D microenvironment that immediately surrounds cells in living tissue, providing structural, biochemical, mechanical, and stimulatory cues necessary for appropriate functioning during homeostasis and in response to physiological change [31]. When stem cells are removed from this 3D context, they exhibit altered functionality, phenotype, and responsiveness to environmental cues, creating significant challenges for clinical translation [31]. The development of hydrogel-based delivery systems has emerged as a promising strategy to overcome these limitations by providing biomimetic 3D platforms that recapitulate key features of the native extracellular matrix (ECM), supporting cell viability, retention, and function upon transplantation [3].
Fundamental Limitations of 2D Culture Systems
Traditional 2D culture systems, while convenient and cost-effective, introduce artificial constraints that dramatically alter cellular behavior. The fundamental differences between 2D and 3D environments are summarized in Table 1.
Table 1: Comparative Analysis of 2D vs. 3D Cell Culture Systems
| Parameter | 2D Culture Systems | 3D Culture Systems |
|---|---|---|
| Spatial Architecture | Flat, monolayer growth with unnatural polarization | Physiologically relevant 3D organization with natural cell-cell interactions |
| Cell Morphology | Forced spreading and flattening | Natural, unconstrained shape and volume |
| Nutrient/Gas Exchange | Direct, uniform access | Gradient-dependent, mimicking in vivo conditions |
| Mechanical Cues | Rigid, non-compliant substrates | Tunable stiffness matching native tissues |
| Gene Expression Profiles | Altered, non-physiological patterns | In vivo-like expression patterns |
| Drug Response | Often inaccurate prediction of efficacy | Clinically relevant drug sensitivity |
| Stem Cell Differentiation | Directed primarily by soluble factors only | Integrated cues from matrix, mechanics, and topology |
Cells cultured in 2D systems lack the complex architectural context found in living tissues, leading to altered morphology, polarity, and signaling pathways [30]. This artificial environment generates data with limited predictive value for in vivo responses, particularly regarding drug efficacy and stem cell differentiation potential [30]. The forced polarization of cells on 2D substrates creates an unnatural mechanical environment that strongly influences cytoskeletal organization and mechanotransduction pathways, which cannot be decoupled from other experimental parameters [32].
Perhaps most critically for stem cell research, 2D culture environments fail to support the balanced differentiation and self-renewal behavior characteristic of native stem cell niches. The spatial positioning, cell-ECM interactions, and mechanical cues that collectively regulate stem cell fate in vivo are largely absent in traditional 2D systems [31].
The Critical Importance of 3D Microenvironments for Stem Cell Function
Recapitulating Native Stem Cell Niches
Three-dimensional microenvironments provide essential cues that regulate fundamental stem cell behaviors, including self-renewal, differentiation, and paracrine signaling. The 3D niche comprises multiple integrated components that collectively influence cell fate:
Diagram 1: Components of the 3D stem cell microenvironment. The integrated nature of these cues directs stem cell fate decisions.
The extracellular matrix (ECM) in 3D environments not only provides structural and organizational guidance for tissue development but also actively defines and maintains cellular phenotype and drives cell fate decisions [31]. Cells within 3D matrices are surrounded by a complex architecture of proteins, polysaccharides, and proteoglycans that undergo dynamic change through assembly, remodeling, and degradation events. Adhesion to specific ECM components via integrins, cadherins, and discoidin domain receptors activates signaling programs sensitive to the composition and orientation of the ECM [31].
The Impact of Geometry and Mechanical Cues in 3D
Advanced 3D culture systems have revealed the profound influence of geometrical and mechanical cues on stem cell behavior. In pioneering research using 3D microniches to control individual human mesenchymal stem cell volume and shape, studies demonstrated that actin filament organization, focal adhesions, nuclear shape, YAP/TAZ localization, cell contractility, and lineage selection are all sensitive to cell volume and geometry [32].
The mechanical properties of the 3D microenvironment, particularly matrix stiffness, have been shown to direct stem cell differentiation along specific lineages. For example, softer hydrogels with elastic moduli in the range of 1–10 kPa promote adipogenic or neurogenic differentiation, whereas stiffer matrices ranging from 25 to 40 kPa favor osteogenic commitment [3]. This mechanosensitivity underscores the importance of substrate stiffness in guiding stem cell fate decisions, with 3D environments providing the necessary context for these mechanical signals to be properly interpreted.
Table 2: Matrix Stiffness and Corresponding Stem Cell Differentiation Outcomes
| Matrix Stiffness Range | Primary Lineage Commitment | Representative Native Tissues |
|---|---|---|
| 0.1-1 kPa | Neural | Brain tissue, neural matter |
| 1-10 kPa | Adipogenic, Neurogenic | Adipose tissue, spinal cord |
| 10-25 kPa | Musculoskeletal | Muscle, connective tissue |
| 25-40 kPa | Osteogenic | Pre-mineralized bone, cartilage |
| >40 kPa | Highly mineralized tissues | Mature bone, calcified tissues |
Furthermore, pore architecture within 3D hydrogels significantly affects nutrient diffusion, waste elimination, and cell migration—all essential for maintaining a viable and functionally active stem cell population in situ [3]. Complementing these internal features, hydrogel surface geometry—including roughness, curvature, and micro- or nano-topography—plays a critical role in modulating stem cell adhesion, proliferation, and lineage commitment [3].
Hydrogel-Based 3D Microenvironments for Stem Cell Delivery
Hydrogels as Biomimetic Platforms
Hydrogels have emerged as ideal platforms for creating 3D microenvironments for stem cell delivery due to their unique properties that closely mimic the physical and biochemical characteristics of native ECM. These water-swollen, crosslinked polymer networks provide biocompatibility, tunable mechanical strength, and the ability to encapsulate and release cells or bioactive molecules [3]. The combination of mesenchymal stromal cells (MSCs) and hydrogels has gained considerable attention in regenerative medicine, offering a synergistic approach to enhance tissue regeneration [3].
Injectable hydrogels, including those based on natural polymers such as alginate, collagen, gelatin, or hyaluronic acid, enable minimally invasive administration, in situ gelation, and conformation to irregular defect geometries. This ensures precise stem cell localization, retention, and protection within injured tissues [3]. Synthetic variants such as polyethylene glycol (PEG) and polyvinyl alcohol (PVA) offer improved mechanical tunability and reproducibility, though often at the expense of bioactivity. Composite hydrogels combining natural and synthetic components aim to leverage the advantages of both material classes [3].
Advanced Hydrogel Design Strategies
Recent advances in hydrogel design include the development of "smart" hydrogels responsive to physiological stimuli, enabling controlled release of encapsulated cells or bioactive molecules in response to local cues [3]. These dynamic hydrogels can prolong therapeutic action, support tissue remodeling, and potentially provide on-demand modulation of stem cell activity.
A promising strategy to further refine hydrogel bioactivity involves engineering matrices with controlled surface or volumetric charge to non-covalently sequester nucleic acids (microRNA, mRNA, plasmid DNA). Such gene-activated hydrogels can prolong local factor residence, protect labile cargos from degradation, and enable cell-responsive release, thereby extending and amplifying stem cell paracrine activity in vivo [3].
Hydrogels derived from decellularized ECM have also gained increasing attention as stem cell carriers. These biomaterials closely mimic the native biochemical composition and architecture of tissues, thereby providing a bioactive microenvironment that promotes cell adhesion, survival, and lineage-specific differentiation [3]. However, the intrinsic mechanical weakness and batch-to-batch variability of pure ECM hydrogels may limit their translational application, leading to the development of bio-hybrid systems combining ECM components with synthetic polymers [3].
Experimental Protocol: Establishing a Simplified 3D Collagen Hydrogel System for Stem Cell Culture
This protocol describes the establishment of a cost-effective and mechanically robust 3D collagen hydrogel system suitable for stem cell culture, enabling physiologically relevant in vitro modeling of cell-matrix interactions. The system utilizes rat tail type I collagen to form a stable 3D network that supports stem cell viability and function, providing a simplified alternative to complex bioprinting methods [33].
The fundamental principle involves the self-assembling fibrillogenesis of type I collagen under neutral pH and physiological temperature (37°C) to form an interwoven 3D network with tunable stiffness and porosity. This scaffold provides a supportive microenvironment for stem cell proliferation and differentiation while maintaining crucial biomechanical cues absent in 2D systems [33].
Diagram 2: Workflow for 3D collagen hydrogel preparation. Sequential mixing with maintained order is critical for uniform gel formation.
Materials and Reagent Preparation
Table 3: Essential Research Reagents for 3D Collagen Hydrogel System
| Reagent/Component | Specifications | Function in Protocol |
|---|---|---|
| Rat Tail Type I Collagen | 5 mg/ml concentration, sterile | Primary matrix-forming polymer providing structural foundation |
| 10x Phosphate Buffered Saline (PBS) | Sterile, isotonic | Provides physiological ionic strength for fibrillogenesis |
| 0.1 mol/L Sodium Hydroxide (NaOH) | Sterile filtered | Neutralizes acidic collagen solution to initiate gelation |
| Complete Culture Medium | With serum and supplements | Maintains cell viability during gel formation |
| Cell Suspension | 85-95% confluency, 1.3 × 10^6 cells/ml | Cellular component for encapsulation |
| Type I Collagenase | 1 mg/ml in DMEM/F-12 | Enzymatic digestion for cell recovery from hydrogels |
| 24-Well Plates | Standard tissue culture treated | Molds for uniform gel column formation |
Step-by-Step Methodology
Component Preparation
- Pre-cool the mouse tail type I collagen solution (5 mg/ml) on ice
- Prepare cell suspension at 85-95% confluency (approximately 8 × 10^6 cells), trypsinize, and resuspend in 6 ml complete culture medium
- Ensure all reagents are sterile and at appropriate temperatures
Sequential Mixing (Critical Order)
- Add 42 μl of 10x PBS to each well of a 24-well plate
- Add 18 μl of 0.1 mol/L NaOH to each well
- Add 300 μl of mouse tail type I collagen (5 mg/ml) to each well
- Add 1 ml of cell suspension in complete medium
- Mix by pipetting up and down exactly five times
- Note: Maintain this exact order—premature addition of NaOH to acidic collagen results in uneven gel formation
Gelation and Incubation
- Transfer the 24-well plate to a 37°C incubator with 5% CO2
- Incubate for 10 minutes for complete gel formation
- Validate successful gelation by semi-transparent appearance with pale orange color and pH of 7.3–7.4
Cell Adaptation Period
- Allow cells to adapt to the 3D gel environment for 6–8 hours
- Maintain standard culture conditions during this stabilization period
Experimental Applications
- Proceed with planned experiments including viability assessment, differentiation studies, or mechanical testing
- For cell recovery: Digest gels with 1 mg/ml collagenase solution at 37°C with gentle shaking for 20 minutes
Quality Control and Validation
- Structural Integrity: The resultant gel should maintain structural stability for 24 hours during culture and remain stable for up to 4 days
- Morphological Assessment: Scanning electron microscopy should reveal a consistent nanofiber network with uniform porosity
- Cell Viability: Assess via live/dead staining; >90% viability should be maintained at 24 hours
- Mechanical Properties: The gel should resist deformation under mechanical loading up to 30 mmHg pressure
Applications in Regenerative Medicine and Disease Modeling
The implementation of 3D microenvironment systems has demonstrated significant potential across multiple regenerative medicine applications. In musculoskeletal diseases, MSC-laden hydrogels have shown enhanced therapeutic effects, with the 3D environment supporting both differentiation capacity and paracrine factor secretion [34]. For neural disorders, injectable microgel scaffolds have been developed to support neural progenitor cell transplantation and vascularization after stroke, addressing critical limitations in cell survival and integration within ischemic microenvironments [35].
In spinal cord injury treatment, hydrogels serve as both delivery systems and scaffolds, providing structural support while inhibiting the progression of secondary injury through localized delivery of bioactive factors [36]. The 3D architecture enables unidirectional growth of nerve cells while delivering therapeutic agents in situ, demonstrating how dimensional context directly influences regenerative outcomes.
The application of 3D models extends beyond regenerative medicine to disease modeling and drug discovery. Cancer research has particularly benefited from 3D culture systems that accurately mimic tumor microenvironments, providing insights into morphological and cellular changes associated with disease progression and enabling more predictive drug screening platforms [30].
The shift from 2D to 3D microenvironments represents more than a technical advancement—it constitutes a fundamental requirement for meaningful stem cell research and therapeutic development. The evidence consistently demonstrates that the dimensional context in which cells are cultured profoundly influences their behavior, gene expression, differentiation potential, and therapeutic efficacy. As regenerative medicine advances toward clinical applications, embracing the complexity of 3D microenvironments will be essential for developing truly effective stem cell-based therapies.
The continued refinement of hydrogel-based 3D culture systems, including the development of stimuli-responsive matrices, decellularized ECM platforms, and tunable synthetic hybrids, promises to further enhance our ability to mimic native stem cell niches. These advanced platforms will not only accelerate therapeutic development but also deepen our fundamental understanding of stem cell biology within its proper physiological context.
Fabrication and Translation: From 3D Bioprinting to Targeted Tissue Regeneration
Three-dimensional (3D) bioprinting has emerged as a revolutionary additive manufacturing technology for fabricating complex, cell-laden tissue constructs with the potential to address critical challenges in regenerative medicine and drug development. This technology enables the precise spatial patterning of living cells, biomaterials, and biological molecules to create tissue-like structures that mimic native extracellular matrix (ECM) environments [37]. The convergence of 3D bioprinting with stem cell research has created a powerful paradigm for producing patient-specific tissue models and regenerative scaffolds, leveraging the multi-lineage differentiation potential and self-renewal capacity of stem cells [38]. More recently, four-dimensional (4D) bioprinting has expanded these capabilities by introducing dynamic, time-dependent transformations in printed structures in response to specific stimuli, offering new avenues for creating more biologically relevant tissues [39].
This article details advanced protocols and application notes for the fabrication of stem cell-laden constructs, framed within the broader context of developing improved stem cell delivery systems. We provide a comprehensive scientific toolkit containing optimized bioink formulations, detailed procedural protocols, and standardized evaluation metrics tailored for researchers and drug development professionals working at the intersection of biofabrication and regenerative medicine.
Bioprinting Technology Landscape
The selection of an appropriate bioprinting technology is fundamental to project success, as each method offers distinct advantages and limitations regarding resolution, cell viability, and compatible materials. The following table summarizes the key characteristics of major bioprinting platforms:
Table 1: Comparison of Bioprinting Technologies
| Bioprinter Type | Resolution | Cell Viability | Speed | Cost | Suitable Bioink Viscosities | Key Applications |
|---|---|---|---|---|---|---|
| Extrusion-Based [39] [40] | 50-1000 μm [40] | 40-90% [39] | Slow [39] | Medium [39] | 30 mPa·s to >6×10⁷ mPa·s [39] [40] | Bone, cartilage, muscle, vascular tissues [41] [37] |
| Inkjet-Based [37] [39] | High [39] | 80-95% [39] | Fast [39] | Low [39] | 3.5-12 mPa·s [39] | Skin, thin tissues, neuronal networks [37] |
| Laser-Assisted [37] [42] | High [39] | >85% [39] | Medium [39] | High [39] | 1-300 mPa·s [39] | High-precision patterning, vascular structures [37] |
| Stereolithography/DLP [43] [42] | High [39] | >85% [39] | Fast [39] | Low [39] | No limitation [39] | Complex 3D architectures, dentin, neovascular structures [44] |
Technology Selection Guidelines
Extrusion-based bioprinting remains the most widely used approach for creating dense, cell-laden constructs for tissue regeneration, particularly advantageous for printing high-viscosity bioinks and high cell densities [40] [42]. Its versatility makes it suitable for fabricating constructs for skeletal and locomotor systems such as bone, cartilage, and skeletal muscle [41]. Inkjet bioprinting offers superior cell viability and speed but is limited to low-viscosity bioinks, making it ideal for thin tissues and precise cellular patterning [37] [39]. Laser-assisted bioprinting provides nozzle-free operation and excellent viability but at higher equipment costs [42]. Digital Light Processing (DLP) technologies, including stereolithography, enable high-resolution fabrication of complex structures through photopolymerization, with recent advances demonstrating the creation of stem cell spheroids within hydrogel constructs [44] [42].
Bioink Design and Formulation
Bioinks represent the cornerstone of successful bioprinting, requiring careful balancing of mechanical, structural, and biological properties to support both printability and cell functionality. The concept of the "biofabrication window" describes the compromise between printability and cell viability that must be optimized for each application [40].
Essential Bioink Properties
Ideal bioinks must possess several key characteristics: Shear-thinning behavior to reduce viscosity under extrusion stress and protect cells during printing; Yield stress to prevent spreading after deposition; Self-healing capability to recover viscosity post-extrusion; controlled Crosslinking kinetics for stabilization; and appropriate Degradability with non-toxic byproducts [43] [40]. These properties collectively ensure that bioinks can be smoothly extruded while maintaining structural fidelity and supporting long-term cell survival and function.
Bioink Formulations for Stem Cell Delivery
Table 2: Advanced Bioink Formulations for Stem Cell Delivery
| Bioink Composition | Crosslinking Method | Mechanical Properties | Stem Cell Compatibility | Key Applications | Performance Highlights |
|---|---|---|---|---|---|
| GelMA-Sodium Alginate-Bioactive Glass (BGM) [45] | Ionic (Ca²⁺) + Photocrosslinking | Enhanced compressive modulus | mBMSCs, DPSCs [45] [44] | Periodontal tissue, bone regeneration | Significantly improved osteogenic differentiation and apatite formation [45] |
| GelMA-Dextran Emulsion [44] | Photocrosslinking | Tunable mechanical support | DPSCs, MSC spheroids [44] | Dentin, neovascular structures | Enables in-situ stem cell spheroid formation with enhanced differentiation [44] |
| Hyaluronic Acid-GelMA [37] | Photocrosslinking | Cartilage-like mechanical properties | MSCs [37] | Cartilage reconstruction | Direct reconstruction of cartilage in sheep models [37] |
| Decellularized ECM (dECM) Bioinks [38] | Thermal | Tissue-specific biochemical cues | hiPSCs, various stem cells [38] | Organ-specific models | Provides tissue-specific niche for enhanced differentiation [38] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Bioprinting Applications
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Gelatin Methacryloyl (GelMA) [40] [45] | Photocrosslinkable hydrogel base with inherent cell adhesion motifs | Various bloom strengths; typically modified with methacrylic anhydride [40] |
| Sodium Alginate [43] [45] | Ionic-crosslinkable polysaccharide for rapid stabilization | Often combined with GelMA or other polymers to improve printability [45] |
| Poly(ethylene glycol) Diacrylate (PEGDA) [37] [39] | Synthetic, biologically inert "blank slate" polymer | Highly tunable mechanical properties; requires bioactive functionalization [40] |
| Bioactive Glass Microspheres (BGM) [45] | Osteogenic and angiogenic bioactive filler | SiO₂-CaO-P₂O₅ composition enhances bioactivity and mechanical properties [45] |
| Photoinitiator 2959 [45] | UV-activated crosslinking initiator for cytocompatible polymerization | Critical concentration optimization required for cell viability [45] |
| Matrix Metalloproteinase (MMP)-Sensitive Peptides [40] | Enables cell-mediated hydrogel remodeling | Essential for stem cell migration and matrix invasion [40] |
Experimental Protocols
Protocol 1: Fabrication of Bioactive Composite Scaffolds for Periodontal Regeneration
This protocol details the fabrication of GelMA-SA-BGM composite scaffolds laden with mesenchymal stem cells and growth factors for complex tissue regeneration, based on the work of [45].
Materials Preparation:
- Synthesize GelMA using standard methacrylation protocols [45]
- Prepare bioactive glass microspheres (BGM) with composition 60% SiO₂, 36% CaO, 4% P₂O₅ via sol-gel method [45]
- Dissolve GelMA (10% w/v) and sodium alginate (4% w/v) in PBS at 37°C
- Suspend BGM (2% w/v) in the polymer solution and mix thoroughly
- Add photoinitiator (PI-2959, 0.5% w/v) to the bioink
- Isolate and expand mouse bone marrow mesenchymal stem cells (mBMSCs) or human dental pulp stem cells (DPSCs) [45] [44]
Bioprinting Procedure:
- Mix the bioink with mBMSCs or DPSCs at a density of 5×10⁶ cells/mL
- Add growth factors (BMP-2 for osteogenesis, PDGF for soft tissue repair) at 100 ng/mL each
- Load the cell-laden bioink into a temperature-controlled extrusion cartridge (maintained at 22-25°C)
- Print through a 22G-27G nozzle (200-400 μm diameter) at 5-15 kPa pressure
- Deposit layers onto a print bed maintained at 10°C
- Apply ionic crosslinking with 2% CaCl₂ solution for 5 minutes post-printing
- Perform photocurring with UV light (365 nm, 5-10 mW/cm²) for 60 seconds to achieve final stabilization
Culture and Evaluation:
- Maintain constructs in osteogenic media (DMEM with 10% FBS, β-glycerophosphate, ascorbic acid, and dexamethasone) [45]
- Assess cell viability using Live/Dead staining at 1, 3, and 7 days post-printing
- Evaluate osteogenic differentiation via ALP activity at 7 days and Alizarin Red staining at 21 days
- For in vivo evaluation, implant in Beagle dog periodontal defects for 8 weeks followed by histological analysis [45]
Protocol 2: DLP Bioprinting for In-Situ Stem Cell Spheroid Formation
This protocol describes a advanced DLP-based approach for creating stem cell spheroids within high-performance hydrogel constructs, adapted from [44].
Materials Preparation:
- Prepare GelMA solution (15% w/v) in PBS
- Dissolve dextran (20% w/v) in culture media
- Isolate and concentrate dental pulp stem cells (DPSCs) or mesenchymal stem cells (MSCs)
Spheroid Formation and Bioprinting:
- Create cell/dextran microdroplets by mixing DPSCs (10×10⁶ cells/mL) with dextran solution
- Emulsify the cell/dextran mixture within the GelMA precursor solution
- Load the emulsion into a DLP bioprinter reservoir
- Project 405 nm light with 20 mW/cm² intensity in 5-10 second exposures per 100 μm layer
- Culture the printed constructs in standard growth media
- Allow dextran to leach out over 24-48 hours, creating cavities that promote cell aggregation and spheroid formation
Characterization:
- Monitor spheroid formation over 3-7 days using phase-contrast microscopy
- Assess stemness maintenance via immunostaining for Nestin, Oct4, and Sox2
- Evaluate differentiation potential by transferring to appropriate inductive media
- For in vivo evaluation, implant in dentin regeneration models and assess for vascularized tissue formation after 4 weeks [44]
Diagram 1: Comprehensive workflow for stem cell bioprinting, covering critical stages from bioink design to functional evaluation.
Evaluation and Optimization Methods
Assessing Geometrical Fidelity and Cell Viability
Maintaining high post-printing cell viability while achieving desired structural fidelity represents a central challenge in bioprinting. The following table summarizes key evaluation parameters and their optimization strategies:
Table 4: Critical Evaluation Metrics and Optimization Approaches
| Evaluation Parameter | Optimal Range | Measurement Techniques | Optimization Strategies |
|---|---|---|---|
| Cell Viability [42] | >80% (short-term), >70% (long-term) | Live/Dead assay, Calcein AM/Propidium Iodide [45] [42] | Optimize nozzle diameter, pressure, crosslinking duration; incorporate shear-thinning modifiers [40] [42] |
| Geometrical Fidelity [46] | <10% deviation from design [46] | Optical Coherence Tomography (OCT), micro-CT [46] | Implement iterative feedback bio-printing (IFBP); optimize bioink viscosity and gelation kinetics [46] |
| Mechanical Properties [40] | Tissue-matched modulus | Compression testing, rheology | Adjust polymer concentration, crosslinking density, composite reinforcement [40] [45] |
| Metabolic Activity [45] | Continuous increase over 7+ days | AlamarBlue assay, glucose consumption | Ensure appropriate bioink degradability, porosity, and nutrient diffusion [40] [45] |
| Lineage-Specific Differentiation [45] [44] | Marker expression 2-3x baseline | qPCR, immunostaining, histology | Incorporate bioactive cues (BGM, growth factors); control spheroid size [45] [44] |
Iterative Feedback Bio-Printing for Quality Control
The Iterative Feedback Bio-Printing (IFBP) approach leverages Optical Coherence Tomography (OCT) for non-destructive, 3D quantification of printed scaffolds, enabling significant improvements in geometrical fidelity. This method involves:
- Printing an initial set of calibration scaffolds with varying design parameters
- 3D imaging and quantitative analysis using OCT to characterize actual pore size, strut size, and volume porosity
- Establishing linear correlation models between designed and printed parameters
- Adjusting design parameters based on empirical formulas to compensate for systematic deviations
- Re-printing with optimized parameters to achieve geometrical mismatches below 7% (compared to 30-40% without optimization) [46]
This approach has demonstrated significant improvements in biological outcomes, including enhanced cell viability, proliferation, and tissue-specific function (e.g., hepatocyte markers CYP3A4 and albumin in liver models) [46].
Diagram 2: 4D bioprinting pathways showing how external stimuli trigger structural and biological transformations in printed constructs over time.
Applications in Stem Cell Research and Regenerative Medicine
Tissue-Specific Applications
Periodontal Tissue Regeneration: The GelMA-SA-BGM composite bioink has demonstrated significant regeneration of gingival tissue, periodontal ligament, and alveolar bone in Beagle dog models. Scaffolds laden with mBMSCs and growth factors (BMP-2 and PDGF) achieved reconstructed periodontal structures within 8 weeks post-implantation [45].
Dentin and Vascularized Tissue Regeneration: DLP-bioprinted GelMA-dextran constructs supporting DPSC spheroid formation have shown capability to regenerate dentin and neovascular-like structures in vivo. The in-situ spheroid formation enhances stem cell differentiation potential and supports complex tissue morphogenesis [44].
Cartilage Reconstruction: Extrusion-printed HA-GelMA scaffolds laden with MSCs have successfully demonstrated direct reconstruction of cartilage in sheep models, with enhanced expression of cartilage-specific genes and improved mechanical properties resembling native tissue [37].
Cardiac Tissue Engineering: 3D-bioprinted endothelialized myocardium patches have been fabricated using GelMA hydrogels containing HUVECs and cardiac progenitor cells. These constructs exhibited functional properties, including spontaneous contraction and formation of vessel-like structures, showing promise for myocardial repair [37] [38].
Emerging Frontiers: 4D Bioprinting and Organ-on-Chip Applications
Four-dimensional bioprinting introduces dynamic temporal dimension to biofabrication, creating structures that evolve their shape or functionality in response to environmental stimuli. This approach leverages smart materials that respond to temperature, pH, light, or magnetic fields to achieve post-printing morphological changes [39]. These4D systems are particularly valuable for creating self-assembling tissue structures and adapting to in vivo environments after implantation.
The integration of 3D-bioprinted tissues with microfluidic systems has advanced the development of sophisticated organ-on-chip models for drug development and disease modeling. These systems enable precise control over biochemical and mechanical microenvironments, allowing for high-fidelity modeling of human physiology and disease pathways while reducing reliance on animal models [39].
The convergence of 3D/4D bioprinting technologies with advanced stem cell biology has created unprecedented opportunities for fabricating functional tissue constructs with complex architectural and biological features. The protocols and formulations detailed in this application note provide a robust foundation for researchers developing next-generation stem cell delivery systems and tissue models. As bioink designs continue to evolve toward greater biomimicry and intelligence, and as bioprinting technologies offer enhanced resolution and viability, the field moves closer to achieving the ultimate goal of fabricating clinically relevant tissues and organs for regenerative medicine and drug development applications.
Injectable Hydrogels for Minimally Invasive Delivery and In Situ Gelation
Injectable hydrogels represent a transformative class of biomaterials in regenerative medicine, offering a minimally invasive approach for stem cell delivery and tissue regeneration. These three-dimensional, water-swollen polymeric networks can be administered as liquids or shear-thinning gels through standard needles or catheters, subsequently forming stable gels in situ that closely mimic the native extracellular matrix (ECM) [47] [48]. This capability provides significant advantages over pre-formed scaffolds, including reduced patient discomfort, lower procedural costs, and the ability to conform perfectly to irregular tissue defects, making them particularly valuable for delivering delicate therapeutic cargo like stem cells [47] [3].
The significance of these materials is especially pronounced in the context of stem cell therapies. While mesenchymal stromal cells (MSCs) show remarkable promise for tissue repair due to their multipotent differentiation capacity and paracrine signaling functions, their therapeutic efficacy is often limited by rapid cell death, washout from injection sites, and insufficient microenvironmental support after transplantation [3]. Hydrogel-based delivery systems address these critical challenges by providing a protective, biomimetic environment that supports MSC viability, retention, and function [3]. By carefully engineering physical, chemical, and biological properties, researchers can create injectable hydrogels that not only serve as passive cell carriers but actively modulate stem cell behavior to enhance regenerative outcomes across diverse tissue contexts.
Classification and Gelation Mechanisms of Injectable Hydrogels
Injectable hydrogels can be broadly classified based on their crosslinking mechanisms and responsiveness to various stimuli. Understanding these classifications is fundamental to selecting appropriate systems for specific biomedical applications, particularly for stem cell delivery where gelation conditions must preserve cellular viability and function.
Crosslinking Mechanisms
Table 1: Classification of Injectable Hydrogels by Crosslinking Mechanism
| Crosslinking Type | Interactions/Bonding | Stimuli Examples | Advantages | Limitations |
|---|---|---|---|---|
| Physical | Non-covalent (electrostatic, H-bonding, hydrophobic) | Temperature, pH, ion concentration | Reversible, self-healing, high biocompatibility | Mechanically weaker, potential premature dissolution |
| Chemical | Covalent (click chemistry, Michael addition, Schiff base) | Light, enzymatic activity, pH | Enhanced mechanical stability, controlled degradation | Potential cytotoxicity from crosslinkers/reactions |
| Dual Crosslinking | Combination of physical and covalent | Tandem stimuli (e.g., guest-host + light) | Sequential control, optimized injection & stability | More complex synthesis and formulation |
The crosslinking strategy fundamentally defines the structural and functional properties of injectable hydrogels. Physically crosslinked systems rely on reversible, non-covalent interactions that enable self-healing and shear-thinning behavior, allowing the material to flow under stress and recover its structure afterward [48] [49]. These systems are particularly valuable for cell delivery as they typically avoid potentially cytotoxic crosslinking agents. In contrast, chemically crosslinked hydrogels form irreversible covalent networks that offer enhanced mechanical stability and prolonged retention at the target site, though the crosslinking chemistry must be carefully selected to maintain biocompatibility [48]. More advanced systems now employ dual-crosslinking approaches that combine the advantages of both mechanisms. For instance, a hyaluronic acid-based system utilizes initial guest-host interactions for injectability and localized retention, followed by secondary covalent crosslinking to achieve final mechanical properties tailored for specific therapeutic applications [49].
Stimuli-Responsive Systems
Table 2: Classification of Stimuli-Responsive Injectable Hydrogels
| Stimulus Type | Representative Materials | Gelation Mechanism | Applications in Stem Cell Delivery |
|---|---|---|---|
| Physical | |||
| Temperature | PLGA-PEG-PLGA, PEG-PLA, methylcellulose [47] | Thermal-induced sol-gel transition | Cell encapsulation, drug delivery |
| Shear Stress | Hyaluronic acid guest-host systems [49] | Shear-thinning and self-healing | Minimally invasive delivery through catheters |
| Chemical | |||
| pH | PEG-diacrylate/acrylic acid/alginate [47] | pH-dependent crosslinking | Wound dressings, targeted drug release |
| Ionic Concentration | Alginate-based composites [47] | Divalent cation crosslinking | Cell scaffolds, drug delivery |
| Biological | |||
| Enzymatic | MMP-responsive peptides [48] [50] | Enzyme-cleavable crosslinks | Cell-responsive degradation, targeted therapy |
| Multi-Responsive | Combination systems | Multiple trigger mechanisms | Enhanced control over gelation and function |
Stimuli-responsive or "smart" hydrogels represent an advanced category that reacts to specific environmental triggers through physical or chemical changes. These systems provide dynamic interactions with their biological environment, allowing precise spatial and temporal control over therapeutic actions [48]. For stem cell delivery, this responsiveness can be harnessed to create microenvironments that actively support cellular functions. For example, enzyme-responsive hydrogels can degrade in response to cell-secreted matrix metalloproteinases (MMPs), facilitating stem cell migration and tissue integration [50]. Similarly, shear-thinning systems enable smooth delivery through fine needles with minimal cell damage, followed by rapid structural recovery to retain cells at the implantation site [49].
Quantitative Properties of Hydrogel Systems
The therapeutic efficacy of injectable hydrogels for stem cell delivery depends critically on their quantitative physical and biological properties. These parameters must be carefully tuned to match both the delivery requirements and the specific regenerative application.
Table 3: Quantitative Properties of Representative Injectable Hydrogel Systems
| Hydrogel System | Storage Modulus (G') | Gelation Time | Degradation Timeline | Cell Viability | Key Applications |
|---|---|---|---|---|---|
| Alg/CMC/GelMA Bioink [51] [12] | Tunable via composition | Temperature & UV-controlled | >21 days stability | Enhanced proliferation at 4% Alg–10% CMC–16% GelMA | Gradient tissue regeneration |
| Ald-HA/Suc-CS Polysaccharide [27] | Tailorable mechanical properties | Fast gelation at physiological temperature | Controlled degradation rate | Near 100% hADSC viability at 14 days | Cartilage regeneration, KOA treatment |
| Hyaluronic Acid GH/DC [49] | GH: <1 kPa, DC: ~41 kPa | Tandem crosslinking | Prolonged with dual-crosslinking | Compatible with cell delivery | Myocardial infarction, LV remodeling |
| GelMA/str-ZnO Composite [50] | Increased with str-ZnO concentration | MMP-responsive | Sustained (28+ days retention) | Supports BMSCs and chondrocytes | Osteoarthritis, cartilage ECM homeostasis |
The data illustrates how specific formulations achieve properties tailored for their intended applications. The Alg/CMC/GelMA bioink system demonstrates long-term mechanical stability essential for extended tissue regeneration processes, while the Ald-HA/Suc-CS polysaccharide hydrogel maintains exceptional cell viability crucial for stem cell-based therapies [51] [12] [27]. The hyaluronic acid-based system shows how mechanical properties can be dramatically enhanced through dual-crosslinking strategies, achieving stiffness values necessary for mechanically demanding environments like myocardial tissue [49]. The GelMA/str-ZnO composite exemplifies how incorporation of functional nanoparticles can modulate both rheological behavior and biological functionality, enabling sustained therapeutic release alongside structural support [50].
Experimental Protocols
Protocol 1: Development of Alg/CMC/GelMA Bioink for Extrusion Bioprinting
This protocol outlines the systematic development of a ternary hydrogel bioink for extrusion-based bioprinting, with specific application for stem cell delivery and gradient tissue regeneration [51] [12].
Materials and Reagents:
- Alginate (Alg, 4% w/v)
- Carboxymethyl cellulose (CMC, 10% w/v)
- Gelatin methacrylate (GelMA, 8%, 12%, and 16% concentrations)
- Photoinitiator (e.g., LAP)
- Calcium chloride (CaCl₂) crosslinking solution
- Phosphate buffered saline (PBS)
- Mesenchymal stem cells
Equipment:
- Rotational rheometer
- Extrusion-based bioprinter with UV curing system
- Sterile tissue culture facilities
- Scanning electron microscope
Methodology:
Bioink Preparation:
- Prepare separate solutions of Alg, CMC, and GelMA in PBS or culture media.
- Combine polymers at the specified ratios (4% Alg–10% CMC–GelMA) under sterile conditions.
- Mix thoroughly but gently to avoid introducing air bubbles.
- For cell-laden bioinks, resuspend stem cells in the polymer solution at the desired density (typically 1-20×10^6 cells/mL).
Rheological Characterization:
- Perform oscillatory rheology to determine viscoelastic properties:
- Amplitude sweep: Identify linear viscoelastic region (LVR) and yield stress.
- Frequency sweep: Measure structural relaxation time and moduli crossover.
- Thixotropy test: Assess recovery after shear by applying low (0.1% strain, 60s) and high (500% strain, 10s) oscillatory shear deformation cycles.
- Temperature ramp: Monitor G' and G'' during temperature changes (4-37°C) to simulate printing conditions.
- Perform oscillatory rheology to determine viscoelastic properties:
Printability Assessment:
- Quantify printability using dimensionless ratios (e.g., printability value Pr) and fiber diameter measurements.
- Optimize printing parameters (pressure, speed, nozzle diameter) based on rheological data.
- Assess filament continuity, shape fidelity, and structural stability of printed constructs.
Crosslinking and Scaffold Formation:
- Utilize dual-crosslinking approach:
- Primary crosslinking: Ionic crosslinking with CaCl₂ solution.
- Secondary crosslinking: UV photopolymerization (e.g., 365 nm, 5-10 mW/cm²) with photoinitiator.
- Determine optimal crosslinking time for each mechanism to balance cell viability and structural integrity.
- Utilize dual-crosslinking approach:
Biological Validation:
- Evaluate cell viability using live/dead staining at 1, 7, and 14 days post-printing.
- Assess cell morphology and distribution within printed constructs.
- Analyze tissue-specific differentiation markers relevant to target application.
Figure 1: Experimental workflow for developing and validating ternary bioink for stem cell delivery.
Protocol 2: Formulation of MMP-Responsive GelMA/str-ZnO Hydrogel for Cartilage Regeneration
This protocol details the preparation and characterization of a smart hydrogel system for co-delivery of miRNA and stem cells to modulate extracellular matrix homeostasis in osteoarthritis treatment [50].
Materials and Reagents:
- Gelatin methacrylate (GelMA)
- Streamlined zinc oxide nanoparticles (str-ZnO)
- Polyethyleneimine (PEI, 1.2 kDa)
- miR-17-5p
- Photoinitiator (Irgacure 2959)
- Collagenase II (for degradation studies)
- Bone marrow mesenchymal stem cells (BMSCs)
Equipment:
- FTIR spectrometer
- Zeta potential analyzer
- Oscillatory rheometer
- Fluorescence imaging system
- SEM with elemental mapping capability
Methodology:
Synthesis of str-ZnO@PEI Complex:
- Prepare str-ZnO nanoparticles via non-aqueous ammonolysis using anhydrous zinc acetate.
- Complex str-ZnO with branched-PEI (1.2 kDa) at optimal 10:1 molar ratio through SN2 reaction facilitated by epichlorohydrin.
- Characterize complexation by FTIR (amine band at 1628 cm⁻¹) and zeta potential measurements.
miRNA Loading:
- Combine str-ZnO@PEI with miR-17-5p at 5:1 mass ratio for complete encapsulation.
- Verify loading by gel electrophoresis (absence of free miRNA bands).
- Assess complex stability at 4°C for up to 7 days.
Hydrogel Formulation:
- Dissolve GelMA in PBS containing photoinitiator (0.5% w/v).
- Incorporate str-ZnO@PEI/miR-17 complexes into GelMA solution with gentle mixing.
- Confirm uniform dispersion by elemental mapping of Zn and SEM imaging.
Mechanical and Rheological Characterization:
- Perform oscillatory rheology to measure storage modulus (G') with increasing str-ZnO concentration.
- Note: G' increases with str-ZnO concentration until agglomeration occurs at 2% concentration.
- Evaluate shear-thinning behavior and recovery for injectability assessment.
Degradation and Release Kinetics:
- Assess MMP-responsive degradation in collagenase II solution (simulating OA environment).
- Monitor cumulative release of str-ZnO@PEI/miR-17 complexes over 7 days (target: ~66% release).
- Evaluate miRNA release profile at lysosomal pH (pH 5) over 48 hours.
In Vitro Biological Evaluation:
- Encapsulate BMSCs in hydrogel and assess viability over 21 days.
- Analyze chondrogenic differentiation through specific marker expression (SOX9, aggrecan).
- Evaluate ECM synthesis and catabolic factor inhibition (MMP13, ADAMTS5).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Injectable Hydrogel Development
| Category | Specific Reagents | Function/Purpose | Key Considerations |
|---|---|---|---|
| Natural Polymers | Alginate, Chitosan, Hyaluronic Acid, Gelatin [47] [27] | Biomimetic scaffold foundation, cell adhesion | Batch-to-batch variability, potential immunogenicity |
| Synthetic Polymers | PEG, PVA, PLGA-PEG-PLGA [47] [3] | Tunable mechanics, reproducibility | Lack innate biofunctionality, require modification |
| Functional Modifiers | Methacrylate groups, Aldehyde groups, Succinyl groups [12] [27] | Enable crosslinking, property modulation | Modification degree affects gelation & biocompatibility |
| Crosslinkers | CaCl₂ (ionic), UV/Light (covalent), Enzymes [51] [48] | Network formation, stability control | Crosslinking kinetics crucial for cell viability |
| Bioactive Cues | RGD peptides, Growth Factors (VEGF, BMP-2), miRNAs [3] [50] | Direct cell behavior, enhance regeneration | Controlled release kinetics, stability in hydrogel |
| Characterization Tools | Rheometers, SEM, FTIR, Cell viability assays [51] [12] [50] | Material property assessment, biological validation | Multiple complementary techniques required |
Signaling Pathways in Hydrogel-Mediated Stem Cell Therapy
The therapeutic effects of stem cell-laden hydrogels involve complex signaling cascades that regulate cell survival, differentiation, and tissue regeneration. Understanding these pathways is essential for rational hydrogel design.
Figure 2: Key signaling pathways activated by functional hydrogels to direct stem cell behavior and tissue regeneration.
The diagram illustrates how engineered hydrogels activate multiple signaling pathways to coordinate regenerative processes. The Ihh/PTHrP pathway, activated by zinc ion release from str-ZnO nanoparticles, promotes BMSC recruitment and chondrogenic differentiation [50]. Simultaneously, mechanotransduction pathways (YAP/TAZ, RHO-ROCK) respond to hydrogel stiffness and topography, directing stem cell fate decisions and ECM production [3]. Integrin-mediated signaling, enhanced by RGD peptides and other adhesive motifs, further supports cell survival and tissue-specific differentiation. These coordinated signals ultimately restore tissue homeostasis through balanced anabolism and catabolism, functional integration with native tissue, and resolution of inflammatory responses.
Injectable hydrogels for minimally invasive delivery and in situ gelation represent a rapidly advancing frontier in stem cell delivery and regenerative medicine. The continued refinement of these systems—particularly through smart responsive designs, enhanced biomechanical compatibility, and advanced fabrication techniques—holds significant promise for addressing complex clinical challenges across diverse tissue contexts. As research progresses toward more sophisticated biomimetic systems and standardized protocols, injectable hydrogels are poised to become indispensable tools in the translational pipeline, ultimately bridging the gap between laboratory innovation and clinical application in stem cell-based therapies.
Osteochondral defects, characterized by damage to both the articular cartilage and the underlying subchondral bone, present a significant clinical challenge in orthopedics due to the poor intrinsic healing capacity of cartilage tissue and the complex, graded architecture of the osteochondral unit [52] [53]. These defects, often resulting from trauma, osteoarthritis, or other degenerative conditions, lead to pain, reduced mobility, and a decreased quality of life [52]. Conventional treatments, including microfracture surgery, autologous chondrocyte implantation (ACI), and osteochondral allografts, frequently provide only short-term relief and are hampered by limitations such as donor site morbidity, limited graft availability, and the formation of inferior fibrocartilage that integrates poorly with the native tissue [52] [54]. The critical need for innovative therapeutic strategies that can simultaneously promote the regeneration of both the cartilage and bone layers in a coordinated manner has driven the advancement of tissue engineering approaches [52] [53].
Within this field, nano-hydrogel systems have emerged as a leading biomaterial for constructing biomimetic scaffolds [52] [53]. These three-dimensional, water-swollen polymeric networks can be engineered to mimic the native extracellular matrix (ECM) of osteochondral tissues [52]. Their nano-scale features, high surface area, and tunable physical and chemical properties make them ideal candidates for supporting cell adhesion, proliferation, and differentiation [52]. Furthermore, their versatility allows for functionalization and the controlled delivery of therapeutic agents, such as growth factors, cytokines, and cells, significantly enhancing their regenerative potential [52] [54]. This application note details the current status, key protocols, and research tools for utilizing nano-hydrogel-based strategies for osteochondral regeneration, framed within the broader context of stem cell delivery methods.
Current Status and Key Quantitative Findings
A recent systematic review evaluating 41 studies on nano-hydrogel preparations for osteochondral repair confirms their strong potential, highlighting customizable mechanical and biological properties, high biocompatibility, tunable degradation, and enhanced tissue integration in both in vitro and in vivo models [52] [55]. The design of these scaffolds varies to address the anisotropy of the osteochondral unit, encompassing single-phase, bilayered, trilayered, and gradient structures, and can be formulated as either injectable or pre-formed implants [52]. The polymers used originate from natural, synthetic, or hybrid sources [52].
Despite the promising results, the evidence base is currently limited by significant study heterogeneity, a moderate risk of bias in existing literature, and a lack of standardized outcome measures and protocols, which complicates direct comparison and clinical extrapolation [52]. Future work must focus on long-term validation, functional outcome measures, and the development of smart, adaptive materials to support clinical translation [52].
The table below summarizes quantitative data from recent key studies to facilitate comparison of material properties and performance outcomes.
Table 1: Key Quantitative Findings from Osteochondral Regeneration Studies
| Scaffold System / Strategy | Key Composition | Mechanical Properties | Biological Outcomes (In Vivo) | Source |
|---|---|---|---|---|
| Strengthened Hybrid Hydrogel | Poly(N-acryloyl 2-glycine) (PACG) and Methacrylated Gelatin (GelMA) | Tensile Strength: 1.1 MPaCompressive Strength: 12.4 MPaYoung's Modulus: 320 kPaCompression Modulus: 837 kPa | Enhanced repair of articular cartilage and new subchondral bone formation in a defect model. | [53] |
| Soft-Hard Hybrid Scaffold | Bioactive Hydrogel (Kartogenin, BMSCs) + Biodegradable Mg Alloy | Cartilage-layer: Replicated mechanical properties of native hyaline cartilage.Bone-layer: Mechanical response comparable to trabecular bone. | Promoted simultaneous regeneration of cartilage and subchondral bone; improved interface stability; upregulation of osteogenic and chondrogenic genes. | [56] |
| Injectable Anisotropic Construct | Semi-IPN Hydrogel with Chondroitin Sulfate Nanoparticles (ChS-NPs) and Nanohydroxyapatite (nHA) | Anisotropic construct with a smooth gradation in mechanical properties from the chondral to subchondral zone. | Designed to mimic native interfacial tissue and restore functional osteochondral tissue in osteoarthritis. | [53] |
| General Nano-Hydrogel Systems | Various natural, synthetic, and hybrid polymers. | High tunability to match native tissue mechanics (Compressive modulus of cartilage: 1.36-39.2 MPa; bone: 4.4-229 MPa). | High biocompatibility, tunable degradation rates, and enhanced tissue integration reported across multiple animal models (rats, rabbits). | [52] [53] |
Detailed Experimental Protocols
Protocol: Fabrication and Characterization of a Strengthened PACG-GelMA Nano-Hydrogel
This protocol outlines the synthesis and evaluation of a high-strength hydrogel composite for load-bearing osteochondral defects [53].
I. Materials Synthesis
- Synthesis of PACG Pre-polymer: Synthesize cleavable poly(N-acryloyl 2-glycine) via controlled radical polymerization. Purify the product via dialysis and lyophilization.
- Preparation of GelMA: Methacrylate gelatin according to established protocols. Dissolve the final product in PBS to create a stock solution.
- Hydrogel Fabrication: Mix the PACG pre-polymer and GelMA solution at a predetermined optimal ratio (e.g., 1:1 by weight). Add the photo-initiator (Irgacure 2959) at 0.5% w/v. Pipette the solution into a mold and expose to UV light (e.g., 365 nm, 5 mW/cm²) for 5-10 minutes to form a crosslinked network.
II. Mechanical Characterization
- Compressive Testing: Using a universal mechanical tester, perform unconfined compression tests on cylindrical hydrogel samples (e.g., 8mm diameter x 4mm height) at a constant strain rate (e.g., 1 mm/min). Calculate the compressive strength and compressive modulus from the resulting stress-strain curve.
- Tensile Testing: Mold samples into dog-bone shapes. Perform tensile tests at a constant crosshead speed. Record the tensile strength and Young's modulus (elastic modulus).
III. In Vitro Biological Evaluation
- Cell Seeding: Seed Bone Marrow Stromal Cells (BMSCs) or human Adipose-derived Stem Cells (ASCs) onto the sterilized hydrogel surface at a density of 50,000 cells/cm².
- Chondrogenic/Osteogenic Differentiation: Culture cells in appropriate differentiation media. For chondrogenesis, use media supplemented with TGF-β3, ITS, and ascorbate. For osteogenesis, use media supplemented with dexamethasone, β-glycerophosphate, and ascorbate.
- Analysis: After 21-28 days, assess differentiation via:
- Gene Expression: qPCR analysis for chondrogenic (e.g., SOX9, AGGREcan, COL2A1) and osteogenic (e.g., RUNX2, OSTEOCALCIN, ALP) markers.
- Histology: Section samples and stain with Alcian Blue (for proteoglycans in cartilage) and Alizarin Red (for calcium deposits in bone).
IV. In Vivo Efficacy Assessment
- Animal Model: Establish a full-thickness osteochondral defect model (e.g., in rabbit femoral condyle or rat trochlea).
- Implantation: Randomize animals into groups: (1) Defect implanted with the PACG-GelMA hydrogel, (2) Defect left empty, (3) Defect treated with a standard control material.
- Outcome Measures: At 8 and 12 weeks post-implantation, euthanize animals and analyze the joints via:
- Macroscopic Evaluation: Assess tissue appearance and integration.
- Histological Scoring: Use standardized scoring systems (e.g., ICRS or O'Driscoll score) on Safranin-O/Fast Green and Hematoxylin & Eosin (H&E) stained sections to evaluate cartilage repair, matrix structure, and subchondral bone restoration.
Diagram 1: Hydrogel fabrication and testing workflow.
Protocol: Implantation of a Soft-Hard Hybrid Scaffold
This protocol describes the methodology for assessing a composite scaffold integrating a bioactive hydrogel with a biodegradable magnesium alloy for coordinated osteochondral regeneration [56].
I. Scaffold Preparation
- Fabrication of Mg Alloy Base: Fabricate a porous magnesium alloy scaffold using 3D printing or space-holder methods to match the mechanical response of trabecular bone.
- Preparation of Bioactive Hydrogel: Dissolve a natural polymer (e.g., gelatin, hyaluronic acid) in PBS. Incorporate kartogenin (KGN) and suspend BMSCs or ASCs at a concentration of 10-20 million cells/mL.
- Assembly: Compress the cell-laden bioactive hydrogel into the pores of the pre-formed Mg scaffold, creating an integrated soft-hard hybrid construct.
II. Surgical Implantation in an Osteochondral Defect Model
- Animal Anesthesia and Preparation: Anesthetize a large preclinical animal (e.g., a sheep or goat) and prepare the knee joint for aseptic surgery.
- Defect Creation: Perform an arthrotomy to expose the femoral condyle. Create a critical-sized osteochondral defect (e.g., 6mm diameter) using a drill.
- Implantation: Implant the hybrid scaffold press-fit into the defect, ensuring the hydrogel-cartilage side is flush with the articular surface. Include control groups (empty defect, sham surgery).
- Closure and Post-op Care: Close the joint capsule, fascia, and skin in layers. Administer post-operative analgesics and allow animals to bear weight ad libitum.
III. Post-Sacrifice Analysis
- Micro-Computed Tomography (μCT): Scan explanted condyles at high resolution to quantify bone regeneration within the defect, including bone volume/total volume (BV/TV) and trabecular number/thickness.
- Histological and Immunohistochemical Analysis:
- Process undecalcified sections for histological staining (Toluidine Blue, Safranin-O for proteoglycans; H&E for general structure).
- Perform immunohistochemistry for Collagen Type II to confirm hyaline-like cartilage formation.
- Biomechanical Push-out Test: Assess the integration strength between the regenerated tissue and the native bone using a mechanical tester to measure the force required to push the regenerated tissue core out of the defect.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Osteochondral Tissue Engineering
| Research Reagent / Material | Function and Rationale | Example Application |
|---|---|---|
| Methacrylated Gelatin (GelMA) | A photo-crosslinkable biopolymer derived from collagen; provides natural cell-adhesion motifs and tunable mechanical properties. | Serves as the primary hydrogel matrix for cell encapsulation and support in composite scaffolds [53]. |
| Kartogenin (KGN) | A small molecule drug that promotes chondrocyte differentiation from stem cells. | Incorporated into the hydrogel phase to specifically drive chondrogenesis and cartilage matrix production [56]. |
| Biodegradable Magnesium (Mg) Alloy | Provides mechanical support comparable to trabecular bone; degrades over time, releasing ions that promote osteogenesis and angiogenesis. | Used as the rigid, osteogenic base in soft-hard hybrid scaffold designs [56]. |
| Nanohydroxyapatite (nHA) | A nanocrystalline form of the natural mineral component of bone; enhances osteoconductivity and mechanical strength of hydrogels. | Incorporated into the "bone" layer of bilayered or gradient hydrogels to promote bone regeneration [53]. |
| Adipose-Derived Stromal/Stem Cells (ASCs) | Multipotent stem cells with the ability to differentiate into chondrocytes and osteoblasts; readily available from patient adipose tissue. | Seeded into scaffolds as a key cellular component for regenerating both cartilage and bone tissues [54]. |
| Chondroitin Sulfate Nanoparticles (ChS-NPs) | Nanoparticles derived from a major glycosaminoglycan in cartilage; can provide bioactive signals and modify material properties. | Used to functionalize hydrogels to enhance their chondrogenic potential and mimic the cartilage ECM [53]. |
| Transforming Growth Factor-Beta 3 (TGF-β3) | A cytokine that is a potent inducer of chondrogenesis in mesenchymal stem cells. | A standard component of in vitro chondrogenic differentiation media used to precondition cells within scaffolds [54]. |
Signaling Pathways and Molecular Mechanisms
The regeneration of the osteochondral unit is orchestrated by the activation of specific signaling pathways that guide stem cell differentiation towards chondrogenic and osteogenic lineages. Key pathways involved in the success of scaffold-based therapies are illustrated below.
Diagram 2: Key signaling pathways in osteochondral regeneration.
Traumatic Brain Injury (TBI) is a major cause of chronic neurological deficits and mortality worldwide, with dynamic pathological processes leading to primary mechanical damage and a protracted secondary injury phase characterized by neuroinflammation, excitotoxicity, and the formation of a inhibitory glial scar [14]. The resultant loss of brain parenchyma and formation of a cystic cavity create a microenvironment that is profoundly hostile to natural regeneration and the survival of transplanted therapeutic cells [57] [58]. This application note examines the confluence of stem cell therapy and advanced biomaterial scaffolds as a promising strategy to overcome these barriers. By providing a permissive, three-dimensional microenvironment, biomaterial scaffolds enhance the delivery, survival, and integration of stem cells, thereby facilitating neural tissue reconstruction and functional recovery post-TBI [59] [14].
Biomaterial Scaffold Design for the TBI Microenvironment
The ideal scaffold for TBI repair must be biocompatible, biodegradable, and mimic the unique physical and biochemical properties of the native brain extracellular matrix (ECM) [14]. Post-TBI, the brain's mechanical stiffness undergoes significant changes, with healthy tissue (~1 kPa) softening in scarred areas (to nearly ~50 Pa) [57]. This dynamic mechanical landscape has informed the development of tailored hydrogels.
Table 1: Key Biomaterial Classes for Neural Tissue Engineering in TBI
| Material Class | Examples | Key Properties | Primary Functions in TBI Repair |
|---|---|---|---|
| Natural Polymers | Chitosan, Collagen, Hyaluronic acid, Alginate, Gelatin [59] [60] [14] | Innate biocompatibility, bioactivity, often biodegradable. | Mimic native ECM; provide structural support; enhance cell adhesion and survival. |
| Synthetic Polymers | Poly(L-lactic acid) (PLLA), Polycaprolactone (PCL), Polyethylene glycol (PEG) [59] | Tunable mechanical properties, degradation rates, and consistency. | Offer design control for stiffness and architecture; create reproducible scaffolds. |
| Conductive Polymers | Polypyrrole, Polyaniline, Polythiophene [59] | Conduct electrical impulses. | Enhance neurite outgrowth and neuronal activity; improve nerve signal transmission. |
| Dynamic Hydrogels | Dynamic Stiffness Hydrogels (DSH), Dynamic Network Hydrogels (DNH) [57] | Stiffness that changes in response to stimuli; reversible, viscoelastic networks. | Model pathological stiffness changes in vitro; improve integration as fillers in vivo. |
A critical advancement is the design of electrically charged hydrogels. One study engineered a porous cryogel with a balanced 1:1 ratio of cationic and anionic monomers (C1A1 hydrogel). This specific charge profile was found to be most effective for the attachment, growth, and differentiation of neural stem cells (NSCs) [58]. When implanted into a TBI model, the VEGF-immersed C1A1 hydrogel promoted host-derived vascular network formation and supported the stepwise transplantation and differentiation of NSCs, leading to tissue reconstruction [58].
Detailed Experimental Protocols
This protocol outlines the synthesis of a cationic-anionic cryogel for neural tissue engineering.
I. Materials
- Monomers: 3-(Acryloylaminopropyl)-trimethylammonium chloride (APTMA, cationic), 2-Acrylamido-2-methylpropane sulfonic acid, sodium salt (NaMPS, anionic).
- Crosslinker: N,N'-methylenebisacrylamide (BIS).
- Initiators: Ammonium persulfate (APS) and N,N,N',N'-Tetramethylethylenediamine (TEMED).
- Equipment: Glass mold plates, cooling bath, hole punch, autoclave, scanning electron microscope (SEM), tensile testing machine.
II. Stepwise Methodology
- Solution Preparation: Prepare a 1 M monomer solution in deionized water with a 1:1 molar ratio of APTMA to NaMPS. Add BIS crosslinker at 4 mol% relative to the total monomer concentration.
- Oxygen Removal: Purge the solution with argon gas for 20 minutes to remove dissolved oxygen, which inhibits polymerization.
- Cryogelation: Add 0.1% (v/v) TEMED and 0.4% (w/v) APS to initiate polymerization. Immediately inject the solution into a pre-cooled glass mold maintained at -16°C in a cooling bath. Allow polymerization to proceed at -16°C for 12-24 hours.
- Post-processing: Thaw the polymerized gel at room temperature and immerse in a large volume of PBS for 7 days, refreshing the PBS daily to remove unreacted chemicals.
- Sterilization and Shaping: Autoclave the gel sheet at 120°C for 20 minutes. Use a hole punch to create gel disks of the desired diameter for cell culture or implantation.
- Characterization:
- Porosity and Morphology: Analyze the freeze-dried gel microstructure using SEM.
- Mechanical Properties: Measure the compressive Young's modulus to ensure it matches brain tissue stiffness (~0.1 - 1 kPa).
- Surface Charge: Determine the zeta potential using a particle size analyzer.
This protocol describes a combinatorial strategy to enhance the therapeutic efficacy of NSCs for TBI.
I. Materials
- Hydrogel: Schiff base hydrogel formed by conjugating carboxymethyl chitosan and phenylaldehyde-functionalized polyethylene glycol (PEG).
- Cells: Neural Stem Cells (NSCs) isolated from C57BL/6J mice.
- Stimulation Equipment: Therapeutic ultrasound device.
- Animal Model: C57BL/6J mouse model of controlled cortical impact (TBI).
II. Stepwise Methodology
- Hydrogel Encapsulation: Suspend NSCs in the liquid precursor of the carboxymethyl chitosan-Schiff base hydrogel. Allow the hydrogel to crosslink around the cells, forming a 3D encapsulating scaffold.
- In Vitro Ultrasound Stimulation: Apply controlled ultrasound stimulation to the NSC-laden hydrogels in culture. Parameters (e.g., frequency, intensity, duration) must be optimized to promote neural lineage differentiation and neurotrophic factor secretion without damaging cells.
- In Vivo Implantation: In the TBI mouse model, carefully implant the NSC-encapsulated hydrogel construct into the lesion cavity.
- Post-operative Assessment:
- Behavioral Analysis: Monitor motor and cognitive recovery over several weeks using tests like the rotarod, Morris water maze, or neurological severity scores.
- Histological and Molecular Analysis: At endpoint, analyze brain tissues for neural tissue regeneration, differentiation of transplanted NSCs (via immunostaining for neuronal markers), and expression of growth factors.
Signaling Pathways in Biomaterial-Mediated Neural Repair
The therapeutic effects of biomaterial-stem cell constructs are mediated through the modulation of key signaling pathways that promote a regenerative microenvironment.
Diagram Title: Key Signaling Pathways in Biomaterial-Mediated Neural Repair
The scaffold itself and the encapsulated stem cells secrete neurotrophic factors (e.g., BDNF, GDNF), which activate pathways such as ERK/Stat6/MERTK to promote cell survival and VGLUT1/VGLUT2-mediated glutamate signaling to support synaptic plasticity [59]. Concurrently, the scaffold modulates the inflammatory response by influencing IL-1R1 signalling, reducing secondary injury [59]. These coordinated actions create a conducive environment for neurite outgrowth, neurogenesis, and angiogenesis, culminating in functional neural circuit integration.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Neural Tissue Engineering
| Reagent/Material | Function/Application | Examples from Research |
|---|---|---|
| Carboxymethyl Chitosan | Forms biocompatible, injectable hydrogels via Schiff base reaction; supports NSC delivery. | Hydrogel for NSC encapsulation combined with ultrasound stimulation [60]. |
| Cationic/Anionic Monomers (APTMA, NaMPS) | Creates hydrogels with defined surface charge to optimize NSC adhesion and differentiation. | C1A1 hydrogel (1:1 charge ratio) for stepwise neuronal tissue reconstruction [58]. |
| Alginate/PVA Aqueous Two-Phase System (ATPS) | Creates phase-separated, microporous microgels (PSMM) for high-density NPC encapsulation. | Injectable micropore-forming scaffold for enhanced NPC survival and vascularization [35]. |
| Polyethylene Glycol (PEG) | Synthetic polymer used as a backbone for hydrogels; offers tunable mechanical properties. | PEG-based hydrogels used in dynamic stiffness hydrogels (DSH) for TBI modeling [57]. |
| Neurotrophic Factors (VEGF, BDNF) | Bioactive molecules that promote angiogenesis (VEGF) and neuronal survival/differentiation (BDNF). | VEGF-immersed hydrogels to promote host-derived vascular network formation [58]. |
| Gas-Shearing Microfabrication Device | Enables ultrahigh-throughput production of uniform microgels for cell delivery. | Used to fabricate phase-separated microporous microgels (PSMM) [35]. |
The integration of sophisticated biomaterial scaffolds with stem cell therapies represents a paradigm shift in the approach to TBI repair. By moving beyond standalone cell injections, researchers can now create defined microenvironments that actively participate in the regenerative process. Future directions will likely focus on the development of even "smarter" biomaterials that can dynamically respond to the evolving injury milieu, the use of patient-specific iPSC-derived cells to avoid immune rejection, and the combination of scaffolds with controlled-release systems for drugs and genetic material [14] [61]. As these technologies mature, they hold the transformative potential to restore function and improve the quality of life for millions affected by traumatic brain injury.
Chronic wounds, driven by an increasing incidence of diabetes and an aging population, represent a significant global health burden, costing healthcare systems tens of billions of dollars annually and causing severe morbidity [62] [13]. The complex wound healing process—progressing through hemostasis, inflammation, proliferation, and remodeling—is often disrupted in chronic states, leading to a hostile microenvironment of excessive inflammation, impaired angiogenesis, and cellular senescence [63] [64]. While stem cell-based therapies, particularly using Mesenchymal Stromal Cells (MSCs), have shown remarkable promise due to their multipotency, immunomodulatory capacity, and pro-angiogenic secretome, their clinical translation has been hampered by low cell survival, poor retention, and transient engraftment upon direct injection into wound sites [3] [63] [64].
Hydrogel scaffolds have emerged as a transformative delivery strategy to overcome these limitations. These biomimetic, three-dimensional (3D) polymer networks closely mimic the native extracellular matrix (ECM), providing a protective and instructive microenvironment for encapsulated cells [3] [65]. This application note details how engineered hydrogel scaffolds enhance MSC-based therapies for wound healing, providing structured data, experimental protocols, and key resource information to support preclinical research and development.
Hydrogel Design Principles for Enhanced MSC Function
The therapeutic efficacy of MSC-laden hydrogels is dictated by their tunable physicochemical properties, which can be engineered to modulate specific MSC behaviors and fate.
- Biophysical Cues: Hydrogel stiffness (elastic modulus) is a critical mechanoregulator of MSC differentiation. Softer hydrogels (1–10 kPa) promote adipogenic or neurogenic commitment, while stiffer matrices (25–40 kPa) favor osteogenesis [3]. Furthermore, pore architecture and surface topography directly influence nutrient diffusion, waste removal, cell migration, and cytoskeletal organization, all of which are essential for maintaining a viable and functionally active MSC population [3].
- Biochemical Cues: The incorporation of bioactive molecules, such as Arg-Gly-Asp (RGD) peptides for cell adhesion, or growth factors like VEGF and FGF-2, augments MSC functionality by activating integrin-mediated signaling and enhancing the secretion of regenerative cytokines [3]. Using decellularized ECM to form hydrogels provides a naturally bioactive microenvironment that promotes lineage-specific differentiation [3].
- Advanced Formulations: "Smart" or stimuli-responsive hydrogels that gel in response to physiological triggers (e.g., temperature, pH) enable minimally invasive injection and conformal filling of irregular wounds [3] [65]. Composite or hybrid systems, such as those combining ECM components with synthetic polymers like polyethylene glycol (PEG), aim to leverage the bioactivity of natural materials with the mechanical robustness and reproducibility of synthetics [3].
Table 1: Key Hydrogel Properties and Their Impact on MSC Behavior in Wound Healing
| Hydrogel Property | Target Range/Type for Wound Healing | Impact on MSC Function & Healing Process |
|---|---|---|
| Elastic Modulus | 1 - 10 kPa [3] | Promotes soft tissue regeneration; prevents fibrotic differentiation. |
| Porosity & Pore Size | > 48 μm (microporous) [35] | Enhances cell infiltration, vascular ingrowth, and nutrient diffusion. |
| Source Material | Natural (e.g., Hyaluronic Acid, Collagen, Alginate); Synthetic (e.g., PEG); Hybrid [3] [63] | Natural polymers offer bioactivity; synthetic polymers offer tunability; hybrids combine advantages. |
| Bioactive Functionalization | RGD peptides, Laminin, VEGF, FGF-2 [3] | Enhances cell adhesion, survival, and paracrine signaling; directs specific differentiation. |
| Degradation Rate | Tunable to match tissue regeneration speed (weeks) [3] | Ensures timely space creation for new tissue while providing temporary support. |
| Delivery Format | Injectable, in-situ crosslinking [3] [65] | Allows minimally invasive application and conforms to complex wound geometries. |
Quantitative Preclinical and Clinical Outcomes
The therapeutic benefit of MSC-laden hydrogels is demonstrated by accelerated wound closure, enhanced angiogenesis, and improved quality of healing in animal models and early-stage clinical trials.
Table 2: Efficacy Outcomes of MSC-Laden Hydrogels in Preclinical and Clinical Studies
| Study Model / Type | Key Intervention | Reported Efficacy Outcomes | Source / Citation |
|---|---|---|---|
| Systematic Review (Human) | AD-MSCs (various deliveries) | Reduced pain, shorter healing times, improved cosmesis in peripheral arterial disease, diabetic wounds, venous ulcers. | [62] |
| Randomized Clinical Trial | Human fibroblasts/keratinocytes (Graftskin) vs. control | 56% complete healing vs. 38% in control (p=0.0042); median time to closure: 65 vs. 90 days (p=0.0026). | [62] |
| In Vivo (Rat Stroke Model) | NPCs in micropore-forming microgel scaffold | Significant enhancement in NPC survival, differentiation, and long-term neurological recovery. | [35] |
| Systematic Review (Animal) | Hydrogels loaded with Cell-Conditioned Medium (H-CM) | Superior wound contraction and tissue regeneration compared to hydrogel or CM alone. | [66] |
| In Vivo (Murine Diabetic Model) | Pharmacologically preconditioned AD-MSCs | Upregulation of VEGF & HIF-1α; promoted angiogenesis and accelerated wound closure. | [64] |
Detailed Experimental Protocol: Fabrication and In Vivo Evaluation of an MSC-Laden Hydrogel
This protocol outlines the methodology for creating and testing a cell-laden, injectable hydrogel in a murine diabetic wound model, synthesizing established practices from the literature [3] [63] [64].
Materials Preparation
- Hydrogel Polymer: Select a biocompatible polymer such as methacrylated hyaluronic acid (MeHA) or gelatin (GelMA). Prepare a sterile solution at a defined concentration (e.g., 3-5% w/v) in PBS.
- Crosslinking System: For photo-crosslinkable hydrogels, use a photoinitiator (e.g., LAP, Irgacure 2959) at a cytocompatible concentration (e.g., 0.05% w/v). For ionic crosslinking (e.g., alginate), prepare a sterile calcium sulfate (CaSO₄) slurry or calcium chloride (CaCl₂) solution.
- Mesenchymal Stem Cells (MSCs): Culture and expand human AD-MSCs or BM-MSCs in standard medium. Preconditioning with cytokines (e.g., IL-1β, TNF-α) or under hypoxic conditions (1-5% O₂) for 24-48 hours prior to encapsulation can enhance their therapeutic potency [64].
- Animal Model: Utilize a genetically diabetic mouse (e.g., db/db) or a mouse with streptozotocin (STZ)-induced diabetes. Anesthetize and create one or multiple full-thickness excisional wounds on the dorsum.
Hydrogel Preparation and Cell Encapsulation
- Cell Harvesting: Detach MSCs using a gentle enzyme (e.g., TrypLE), wash, and resuspend them in the hydrogel precursor solution at the desired density (e.g., 5-20 million cells/mL).
- Mixing: Gently mix the cell-polymer suspension with the crosslinker or photoinitiator to ensure homogeneity without introducing bubbles.
- Injection and Gelation:
- For in-situ gelation: Draw the cell-hydrogel mixture into a sterile syringe. Carefully inject the mixture into the wound bed or directly onto the wound, covering the entire area.
- For photo-crosslinking: After application, expose the wound to visible or UV light (e.g., 365 nm, 5-10 mW/cm²) for 1-3 minutes to initiate crosslinking and form a stable gel.
- Dressing: Apply a sterile, non-occlusive dressing over the gelled hydrogel to protect the wound.
In Vivo Assessment and Analysis
- Wound Closure Kinetics: Capture digital images of the wounds at regular intervals (e.g., days 0, 3, 7, 10, 14). Use image analysis software (e.g., ImageJ) to calculate the wound area and percentage of wound closure over time.
- Histological and Immunofluorescence Analysis: At predetermined endpoints, euthanize the animals and harvest the wound tissue.
- Processing: Fix tissue in 4% PFA, dehydrate, embed in paraffin, and section.
- Staining: Perform Hematoxylin and Eosin (H&E) for general morphology and Masson's Trichrome for collagen deposition.
- Immunostaining: Stain sections with antibodies against CD31 (to quantify angiogenesis/new blood vessels), α-SMA (to identify myofibroblasts and mature vessels), and Cytokeratin (to assess re-epithelialization).
- Statistical Analysis: Compare results against control groups (e.g., untreated wounds, blank hydrogel, injected MSCs alone) using appropriate statistical tests (e.g., one-way ANOVA with post-hoc test), with a significance threshold of p < 0.05.
MSC Hydrogel Mechanism of Action
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing MSC-Laden Hydrogels for Wound Healing
| Reagent / Material | Function / Role | Examples & Notes |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Therapeutic agent; source of regenerative paracrine factors and differentiated cells. | Adipose-derived (AD-MSCs, high yield), Bone Marrow-derived (BM-MSCs), Umbilical Cord-derived (UC-MSCs, high proliferative rate) [62] [13]. |
| Hydrogel Polymers | 3D scaffold material; provides mechanical support and biochemical cues. | Natural: Hyaluronic Acid, Collagen, Alginate, Fibrin. Synthetic: Polyethylene Glycol (PEG), Polyvinyl Alcohol (PVA). ECM-derived: Decellularized tissues [3] [63]. |
| Bioactive Peptides/Growth Factors | Functionalization agents; enhance cell adhesion and direct cellular responses. | RGD peptide (cell adhesion), VEGF (angiogenesis), FGF-2 (fibroblast proliferation), BMP-2 (bone formation) [3]. |
| Crosslinkers / Initiators | Induce hydrogel formation from liquid precursors. | Ca²⁺ solutions (for alginate), Photoinitiators (LAP for UV/blue light), Enzymes (e.g., Horseradish Peroxidase) [3] [65]. |
| Preconditioning Agents | Enhance MSC resilience and paracrine activity prior to encapsulation. | Cytokines (IL-1β, TNF-α, IFN-γ), Hypoxia (1-5% O₂), Drugs (e.g., Caffeic acid, α-ketoglutarate) [64]. |
Hydrogel Scaffold Engineering Strategy
Hydrogel scaffolds represent a paradigm shift in stem cell delivery, transforming MSCs from a standalone therapeutic with limited efficacy into a robust and controlled regenerative medicine product. By providing a biomimetic 3D niche, these systems directly address the critical challenges of cell viability, retention, and function in the hostile wound environment. The future of this field lies in the clinical translation of increasingly sophisticated "smart" hydrogels—those capable of responding dynamically to wound cues (e.g., pH, enzyme activity) for on-demand drug release [3], and the development of xeno-free, GMP-compliant formulations to meet regulatory standards. The integration of hydrogel scaffolds with other engineering strategies, such as MSC preconditioning and genetic modification, promises to further synergize and enhance therapeutic outcomes, ultimately offering more effective and personalized solutions for patients suffering from chronic wounds.
The field of regenerative medicine is undergoing a significant transformation, moving away from whole-cell therapies toward sophisticated cell-free approaches that harness the therapeutic power of mesenchymal stem cell (MSC) secretions. Traditionally, the therapeutic benefits of MSCs were attributed primarily to their ability to engraft and differentiate at injury sites. However, recent research has revealed that less than 1% of administered MSCs survive beyond one week in vivo, indicating that their remarkable healing properties must stem from alternative mechanisms [67]. This discovery has shifted scientific focus toward the paracrine activity of MSCs—specifically, their secretome, which comprises all factors secreted into the extracellular space, including soluble proteins and extracellular vesicles (EVs) such as exosomes [67] [68].
The MSC secretome acts as a comprehensive bioactive cocktail that regulates key biological processes including immunomodulation, angiogenesis, and tissue repair [67]. This cell-free approach provides considerable advantages over traditional cell-based therapies by mitigating risks associated with whole-cell transplantation, such as immune compatibility issues, tumorigenicity, emboli formation, and infection transmission [67] [69]. Furthermore, secretome-based products offer superior practicality with easier storage, handling, and shelf-life stability, positioning them as ready-to-use biologic pharmaceuticals that can be standardized for dosage, safety, and potency [67] [70].
Quantitative Analysis of MSC Secretome Applications
The therapeutic potential of the MSC secretome and its derivatives has been demonstrated across a vast spectrum of disease models. The tables below summarize key quantitative data regarding clinical trial progress and specific therapeutic applications.
Table 1: Registered Clinical Trials for MSC-Derived Extracellular Vesicles (EVs) as of 2025 (Selected Examples) [69]
| NCT Number | Condition | Phase | Enrollment | Status |
|---|---|---|---|---|
| NCT05354141 | Acute Respiratory Distress Syndrome | 3 | 970 | Recruiting |
| NCT04223622 | Osteoarthritis | N/A | 36 | Completed |
| NCT05261360 | Knee Injury | 2 | 30 | Recruiting |
| NCT06598202 | Amyotrophic Lateral Sclerosis | 1/2 | 38 | Recruiting |
| NCT05669144 | Myocardial Infarction | 1/2 | 20 | Unknown |
| NCT05813379 | Skin Rejuvenation | 1/2 | 20 | Recruiting |
| NCT04173650 | Dystrophic Epidermolysis Bullosa | 1/2 | 10 | Recruiting |
| NCT05787288 | COVID-19 Pneumonia | 1 | 240 | Recruiting |
Table 2: Preclinical Therapeutic Applications of MSC Secretome and Conditioned Media [67]
| Pathology | Donor Cells | Key Findings (in models) |
|---|---|---|
| Lung Injury | Bone Marrow MSCs | Improved pathophysiology biomarkers [67]. |
| Myocardial Infarction | Adipose-derived Stem Cells (ADSCs) | As effective as corresponding MSC transplantation [67]. |
| Cerebral Ischemia/Stroke | Bone Marrow MSCs | Sufficient to significantly improve biomarkers [67]. |
| Skin Wound Healing | Adipose-derived Stem Cells (ADSCs) | Promoted repair and regeneration [67] [71]. |
| Alzheimer’s Disease | Dental Pulp Stem Cells | Demonstrated therapeutic potential [67]. |
| Parkinson’s Disease | Wharton's Jelly MSCs | Showed beneficial effects [67]. |
| Spinal Cord Injury | Bone Marrow MSCs | Promoted repair and functional recovery [67]. |
| Liver Fibrosis | Umbilical Cord Perivascular Cells | Showed anti-fibrotic effects [67]. |
Experimental Protocols for Secretome and Exosome Production
Standardized protocols are critical for the reproducible production of high-quality MSC secretome and exosomes. The following sections detail key methodological workflows.
Protocol 1: Production of MSC Conditioned Media (CM)
Objective: To collect the complete secretome (soluble factors and vesicles) from MSC cultures for therapeutic or analytical use [70].
Materials:
- Cell Source: MSCs (e.g., from bone marrow, adipose tissue, or umbilical cord).
- Culture Vessels: Cell factories or multilayer flasks for large-scale production.
- Basal Medium: Serum-free, xeno-free medium (e.g., DMEM/F12).
- Collection Tubes: Sterile, low-protein-binding tubes.
- Centrifugation Equipment: Refrigerated centrifuges.
Workflow:
- Cell Culture and Expansion: Isolate and expand MSCs under standard conditions (37°C, 5% CO₂) using serum-containing media. Perform quality control checks to ensure cell viability, surface marker expression (CD105+, CD73+, CD90+, CD45-, CD34-, CD14-, HLA-DR-), and tri-lineage differentiation potential [67] [70].
- Serum Deprivation: Once MSCs reach 70-80% confluence, wash the monolayer thoroughly with phosphate-buffered saline (PBS) to remove all serum constituents. Replace the medium with a defined, serum-free basal medium.
- Conditioning Phase: Incubate the cells in the serum-free medium for 24-48 hours. The duration should be optimized to maximize yield while minimizing cellular stress and the release of apoptotic factors [70].
- CM Collection: Collect the medium into sterile tubes.
- Clarification: Centrifuge the collected medium at 2,000 × g for 20 minutes at 4°C to remove cell debris. Follow with a second centrifugation at 10,000 × g for 30 minutes at 4°C to pellet larger vesicles and apoptotic bodies.
- Concentration and Storage: The clarified CM can be used directly, concentrated using tangential flow filtration or ultrafiltration, and stored at -80°C [70].
Protocol 2: Isolation and Purification of Exosomes
Objective: To isolate and purify the exosome fraction from MSC-conditioned media [70] [72].
Materials:
- Ultracentrifuge: Preparative ultracentrifuge with fixed-angle or swinging-bucket rotors.
- Ultracentrifuge Tubes: Polypropylene or polycarbonate bottles/tubes.
- PBS: Sterile, particle-free phosphate-buffered saline.
- Filter: 0.22 µm PVDF syringe filter.
- Characterization Equipment: Nanoparticle Tracking Analysis (NTA), Transmission Electron Microscopy (TEM), Western Blot apparatus.
Workflow:
- Pre-processed CM: Start with CM that has been pre-cleared of cells and debris (Protocol 1, Steps 5-6).
- Ultracentrifugation: Transfer the CM to ultracentrifuge tubes. Pellet exosomes and small vesicles by ultracentrifugation at 100,000 × g for 70-120 minutes at 4°C [70].
- Wash: Carefully discard the supernatant. Resuspend the pellet in a large volume of cold, sterile PBS. This wash step removes soluble protein contaminants.
- Second Ultracentrifugation: Repeat the ultracentrifugation step (100,000 × g, 70-120 min, 4°C) to re-pellet the washed exosomes.
- Final Resuspension: Completely discard the supernatant and resuspend the final exosome pellet in a small volume of PBS or a suitable buffer (e.g., 50-200 µL). Filter through a 0.22 µm filter if sterility is required.
- Characterization and Storage: Quantify and characterize the exosomes using NTA for size distribution, TEM for morphology, and Western Blot for markers (e.g., CD63, CD81, TSG101). Store at -80°C [69] [70].
Advanced Delivery and Engineering Strategies
Enhancement of Secretome Potency
The therapeutic potency of the native MSC secretome can be significantly enhanced through various "priming" or "licensing" strategies that modulate the MSC microenvironment [71] [70]:
- Inflammatory Priming: Pre-treatment of MSCs with pro-inflammatory cytokines like IFN-γ and TNF-α upregulates the expression of key immunomodulatory molecules such as Indoleamine 2,3-dioxygenase (IDO) and Prostaglandin E2 (PGE2), enhancing their immunosuppressive capacity [71].
- Hypoxic Preconditioning: Culturing MSCs under low oxygen tension (e.g., 1-5% O₂) mimics their native niche and upregulates the secretion of pro-angiogenic and pro-survival factors like VEGF and HGF [71].
- 3D Culture Systems: Growing MSCs as spheroids or in dynamic 3D bioreactors, as opposed to traditional 2D monolayers, enhances cell-cell contact and leads to a secretome with a higher concentration of therapeutic factors and improved regenerative potential [70] [73].
Hydrogel-Based Delivery Systems for Sustained Release
A major challenge in secretome therapy is the rapid clearance of soluble factors and exosomes from the target site. To address this, hydrogel-based delivery systems have been developed to provide localized and sustained release, thereby enhancing therapeutic efficacy [34] [73] [74].
Hydrogels are water-swollen, three-dimensional polymer networks that mimic the native extracellular matrix. They can be engineered from natural (e.g., alginate, collagen, hyaluronic acid) or synthetic (e.g., polyethylene glycol - PEG) polymers [73]. These systems protect the encapsulated secretome or exosomes from degradation and rapid clearance, effectively creating a local "bioreactor" at the injury site.
Table 3: Research Reagent Solutions for Hydrogel-Based Secretome Delivery
| Reagent/Material | Function/Description | Example Application |
|---|---|---|
| Methacrylated Hyaluronic Acid (MeHA) | A photocrosslinkable, bioactive polymer that forms hydrogels with tunable mechanical properties. | Serves as an injectable, biodegradable scaffold for exosome delivery in cartilage repair [73]. |
| Chitosan | A natural polysaccharide derived from chitin that forms thermosensitive or ionic-crosslinked gels. | Used to create hydrogels that provide sustained release of exosomes for bone and wound healing [74]. |
| Poly(N-isopropylacrylamide) - pNIPAM | A temperature-responsive polymer; cells adhere and grow at 37°C and detach as intact sheets below 32°C. | Foundation for creating scaffold-free cell sheets for transplantation [75]. |
| Decellularized ECM (dECM) Hydrogels | Hydrogels derived from processed natural tissues, providing a complex, tissue-specific biochemical milieu. | Bio-hybrid dECM-synthetic polymer hydrogels enhance MSC retention and regenerative capacity [73]. |
| Platelet Lysate (PL) | A xeno-free, human-derived source of growth factors and proteins, used as a hydrogel component or culture supplement. | Ensures GMP-compliant, clinical-grade production of MSC-laden hydrogels [73]. |
The following diagram illustrates the workflow for creating and utilizing a secretome- or exosome-laden hydrogel for tissue regeneration.
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Reagents for MSC Secretome and Exosome Research
| Reagent / Kit | Primary Function in Research |
|---|---|
| CD63/CD81/CD9 Antibodies | Detection of classical exosome surface tetraspanin markers via Western Blot or flow cytometry for vesicle characterization [72]. |
| TSG101 Antibody | Detection of an exosome marker associated with the ESCRT pathway, used for vesicle characterization [72]. |
| Nanoparticle Tracking Analyzer (NTA) | Instrument for determining the size distribution and concentration of exosomes in suspension (e.g., Malvern Nanosight) [69]. |
| Transmission Electron Microscope (TEM) | High-resolution imaging tool for visualizing the characteristic cup-shaped morphology of exosomes [69]. |
| Ultracentrifuge | Essential equipment for the differential centrifugation method of exosome isolation from conditioned media [70]. |
| Size-Exclusion Chromatography (SEC) Columns | Purification of exosomes from soluble proteins based on size, often yielding high-purity vesicles with retained biological activity [67] [70]. |
| Recombinant Human IFN-γ | A cytokine used to prime MSCs, enhancing the immunomodulatory profile of the resulting secretome [71]. |
| Serum-Free, Xeno-Free Media | Chemically defined media for producing clinical-grade secretome and exosomes, avoiding contamination with animal-derived proteins [70]. |
| 3D Culture Bioreactors | Systems (e.g., spinner flasks, hydrogels) for expanding MSCs in three dimensions to enhance secretome yield and potency [70] [73]. |
| Proteomic Array Kits | Multiplexed assays (e.g., cytokine arrays) for comprehensive analysis of soluble factors present in the MSC secretome [68]. |
Overcoming Translational Hurdles: Viability, Immunogenicity, and Scalability
The therapeutic potential of stem cells in regenerative medicine is often limited by the harsh realities of the transplantation microenvironment. Upon delivery, cells encounter a hostile landscape characterized by hypoxia, nutrient deprivation, inflammatory cytokines, and oxidative stress, leading to massive cell death and compromised function [76] [77]. This hostile microenvironment significantly contributes to the low cell survival rates (often as low as 1-20%) and poor engraftment that plague the clinical translation of stem cell therapies [65] [77]. This Application Note details strategies, with a focus on biomaterial scaffolds and preconditioning protocols, designed to shield cells from these initial stresses, thereby enhancing their survival, retention, and ultimate therapeutic potency.
Engineering Solutions for Potency Preservation
Biomaterial Scaffolds as Synthetic Niches
Biomaterial scaffolds, particularly hydrogels, can be engineered to mimic the native extracellular matrix (ECM), providing both structural support and biochemical cues that promote cell survival and function.
- Design Principles for Hydrogels: An ideal hydrogel for stem cell delivery should be injectable for minimally invasive application, biocompatible to avoid immune rejection, and possess tunable physical properties (e.g., stiffness, porosity, degradability) that match the target tissue [65]. Crucially, they can be functionalized with bioactive molecules to direct cell fate.
- Evidence of Efficacy: A recent study demonstrated the success of a synthetic thermoresponsive terpolymer scaffold composed of N-isopropylacrylamide (NiPAAm), vinylphenylboronic acid (VPBA), and polyethylene glycol monomethyl ether monomethacrylate (PEGMMA). This scaffold supported the maintenance of pluripotency and robust proliferation of human pluripotent stem cells (hPSCs). When functionalized with RGD peptides, vitronectin, and fibronectin, it significantly enhanced cardiac differentiation efficiency, resulting in a ∼65% expression of the cardiac-specific marker cTnT, outperforming traditional matrices like Matrigel [78].
- Mechanisms of Action: These synthetic hydrogels protect cells by creating a physical barrier against inflammatory onslaught, facilitating the delivery of oxygen and nutrients, and providing adhesive motifs that inhibit anoikis (a form of cell death due to detachment) [14] [65].
Microenvironment Preconditioning Strategies
Preconditioning involves exposing stem cells in vitro to sub-lethal levels of stress, thereby activating endogenous cytoprotective mechanisms and "priming" them for the challenges they will face in vivo [76] [77].
- Cytokine Preconditioning: Pre-treating Mesenchymal Stem Cells (MSCs) with specific cytokines can enhance their resilience and paracrine activity. For instance:
- Interferon-γ (IFN-γ) and TNF-α promote macrophage polarization toward the pro-healing M2 phenotype by upregulating CCL2 and IL-6 [76].
- Transforming Growth Factor-β1 (TGF-β1) preconditioning enhances the survival and engraftment of bone marrow-derived MSCs (BMSCs), significantly reducing wound healing time in murine models [76].
- IL-1β preconditioning enhances MSCs migration by upregulating matrix metalloproteinase-3 (MMP-3) expression [76].
- Disease Microenvironment Preconditioning (DMP): A more sophisticated approach involves preconditioning cells with serum or other body fluids from diseased patients or animals, or with a cocktail of small molecules that mimic the disease milieu. This process strengthens the cells' ability to acclimatize and respond efficiently to the hostile microenvironment post-transplantation [77].
- Pharmacological Preconditioning: Compounds like α-ketoglutarate, a key metabolic intermediate with antioxidant properties, have been shown to improve Adipose-derived Stem Cell (ADSC) survival in burn models by increasing the expression of VEGF and HIF-1α, which promote angiogenesis [76].
Table 1: Summary of Microenvironment Preconditioning Strategies
| Preconditioning Type | Example Agents | Key Effects on Stem Cells | Documented Outcome |
|---|---|---|---|
| Cytokine Preconditioning | IFN-γ, TNF-α, TGF-β1, IL-1β | Enhanced immunomodulation; improved survival and migration; increased angiogenic potential | Accelerated wound healing in murine models; promoted M2 macrophage polarization [76] |
| Disease Microenvironment (DMP) | Patient-derived serum/plasma | Improved adaptation to inflammation, hypoxia, and oxidative stress | Enhanced survival, integration, and functional efficacy in cardiovascular and neurodegenerative disease models [77] |
| Pharmacological Preconditioning | α-ketoglutarate, Caffeic Acid | Enhanced antioxidant defense; increased secretion of pro-angiogenic factors | Improved ADSC survival and accelerated wound closure in a chemically induced burn model [76] |
Advanced Screening and Quality Control
Ensuring the potency of stem cell lines before transplantation is critical. High-throughput screening (HTS) and deep learning (DL) models have emerged as powerful tools for quality control.
- Functional Screening with AI: Conventional assays for evaluating MSC function are often low-throughput and lack clinical relevance. To address this, a deep learning-based framework was developed that uses live-cell microscopic images of MSC populations to classify cell lines based on the expression of multilineage differentiating stress-enduring (MUSE) markers, which are associated with high therapeutic efficacy. An optimized DenseNet121 model achieved an accuracy of 0.922 and an AUC of 0.975, providing a convenient and non-invasive method for functional screening [79].
- High-Throughput 3D Screening Platforms: The development of automated 3D cell culture platforms, integrated with high-throughput imaging and machine-learning analysis, allows for the quantitative screening of stem cell behavior and drug responses in a more physiologically relevant environment [80].
Detailed Experimental Protocols
Protocol: Cytokine Preconditioning of MSCs for Enhanced Potency
This protocol outlines the steps to precondition MSCs with a cytokine cocktail to improve their resilience and therapeutic function for in vivo delivery.
I. Materials
- Human Mesenchymal Stem Cells (hMSCs), passage 3-5
- Standard MSC growth medium (e.g., α-MEM with 10% FBS)
- Preconditioning medium: Serum-free basal medium
- Recombinant human cytokines: IFN-γ, TNF-α, TGF-β1
- Phosphate Buffered Saline (PBS), sterile
- Cell culture flasks/plates
- CO₂ incubator (37°C, 5% CO₂)
II. Procedure
- Cell Culture: Culture and expand hMSCs in standard growth medium until they reach 70-80% confluence.
- Preparation of Preconditioning Medium:
- Preconditioning Phase:
- Wash the hMSCs twice with sterile PBS to remove residual serum.
- Carefully aspirate the PBS and add the preconditioning medium containing the cytokine cocktail to the cells.
- Incubate the cells for 24 hours under standard culture conditions (37°C, 5% CO₂) [77].
- Harvesting Preconditioned Cells:
- After 24 hours, aspirate the preconditioning medium.
- Wash the cells gently with PBS to remove cytokines.
- Harvest the cells using a standard trypsinization protocol.
- Centrifuge the cell suspension, aspirate the supernatant, and resuspend the cell pellet in an appropriate buffer (e.g., saline or transplantation medium) for immediate use.
- Validation (Optional but Recommended):
- Validate the preconditioning effect by analyzing the expression of markers related to immunomodulation (e.g., TSG-6, PGE2) or stress resistance (e.g., HIF-1α, antioxidant enzymes) via RT-qPCR or flow cytometry [76].
Protocol: Functionalization of a Thermo-Responsive Synthetic Hydrogel
This protocol describes the functionalization of a NiPAAm-based terpolymer scaffold with bioactive peptides to enhance stem cell adhesion and differentiation.
I. Materials
- Synthetic thermoresponsive terpolymer (e.g., poly(NiPAAm-co-VPBA-co-PEGMMA)) [78]
- RGD peptide sequence (e.g., GRGDS)
- Vitronectin or fibronectin
- Cold, deionized (DI) water
- Coupling buffer (e.g., MES buffer, pH 5.5)
- Crosslinker (e.g., EDC/NHS chemistry may be utilized for covalent attachment)
- Cell culture plates
II. Procedure
- Polymer Solution Preparation:
- Dissolve the terpolymer powder in cold DI water (4°C) to a final concentration of 1-5% (w/v). The polymer will dissolve readily at temperatures below its Lower Critical Solution Temperature (LCST) [78].
- Sterilize the solution by passing it through a 0.22 µm filter.
- Biofunctionalization:
- Add the bioactive molecules (RGD peptide, vitronectin, or fibronectin) directly to the sterile polymer solution. A recommended starting concentration for RGD is 0.1-1.0 mM [78].
- Mix gently to ensure even distribution without creating bubbles.
- Coating and Gelation:
- Add the functionalized polymer solution to the cell culture plates.
- Incubate the plates at 37°C for 30-60 minutes. The thermoresponsive nature of the polymer will cause it to undergo a sol-gel transition, forming a stable, bioactive hydrogel layer on the surface.
- Cell Seeding:
- Once the hydrogel has formed, gently wash it with cold cell culture medium to remove any unbound molecules and equilibrate the pH.
- Seed the stem cell suspension directly onto the pre-warmed, functionalized hydrogel surface.
- Validation:
- The efficacy of the functionalized scaffold can be validated by assessing cell attachment efficiency, proliferation, and differentiation potential compared to non-functionalized controls. For example, flow cytometry or immunofluorescence for cardiac markers like cTnT can confirm enhanced cardiomyocyte differentiation [78].
Signaling Pathways and Workflows
The following diagrams illustrate the core concepts of hostile microenvironment challenges and the strategic solutions discussed in this note.
Diagram 1: Stem Cell Potency Challenge and Solution Overview.
Diagram 2: Signaling in Preconditioned MSCs.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Potency Preservation Research
| Reagent / Material | Function / Application | Example from Research |
|---|---|---|
| Synthetic Terpolymer (NiPAAm-based) | Forms a thermoresponsive, tunable synthetic scaffold for 2D/3D cell culture that facilitates non-invasive cell harvesting. | Poly(NiPAAm-co-VPBA-co-PEGMMA) supported hPSC pluripotency and cardiac differentiation [78]. |
| Bioactive Peptides (RGD) | Functionalizes synthetic scaffolds to promote integrin-mediated cell adhesion, survival, and differentiation. | RGD incorporation significantly enhanced cell expansion and cardiac differentiation efficiency on terpolymer scaffolds [78]. |
| Recombinant Cytokines (IFN-γ, TGF-β1) | Key agents for preconditioning MSCs to enhance their immunomodulatory profile, survival, and engraftment post-transplantation. | Preconditioning with IFN-γ and TGF-β1 improved MSC resistance to inflammatory stress and wound healing capacity [76] [77]. |
| Deep Learning Model (DenseNet121) | A convolutional neural network for high-throughput, non-invasive quality control and functional prediction of MSC lines based on morphology. | Classified MSC lines by potency (MUSE markers) with 92.2% accuracy from live-cell images [79]. |
| Natural Polymer Hydrogels (Chitosan, HA) | Provides a biocompatible, biomimetic scaffold for cell delivery. Can be modified for injectability and bioactivity. | Chitosan hydrogels noted for non-toxicity, biodegradability, and providing a hydrated microenvironment for implanted cells [14] [65]. |
The quest to direct stem cell fate for regenerative medicine relies on the ability to replicate the dynamic nature of the native extracellular microenvironment. Stimuli-responsive "smart" hydrogels have emerged as powerful platforms to achieve this temporal and spatial control, transitioning biomaterials from passive scaffolds to active participants in stem cell manipulation [81] [82]. These advanced materials can be engineered to respond to specific external or internal stimuli—including light, electrical fields, magnetic fields, and ultrasound—enabling precise delivery of biochemical and biophysical cues to encapsulated stem cells [81] [83]. By integrating these responsive capabilities, researchers can create sophisticated controlled-release systems for growth factors, drugs, and genetic material, and dynamically alter scaffold properties to guide stem cell adhesion, proliferation, and differentiation [81] [84]. This application note details the core principles, key protocols, and essential reagents for leveraging stimuli-responsive hydrogels in stem cell delivery and tissue engineering, providing a practical framework for researchers developing next-generation regenerative therapies.
Application Notes: Key Stimuli and System Design
The design of a smart hydrogel system begins with selecting an appropriate stimulus based on the target application, desired depth of penetration, and level of spatiotemporal control required. The most widely researched exogenous stimuli for stem cell control are light, electrical, and magnetic fields.
Table 1: Comparison of Key Stimuli for Smart Hydrogel Systems
| Stimulus | Spatiotemporal Control | Tissue Penetration | Common Hydrogel Components | Primary Stem Cell Applications |
|---|---|---|---|---|
| Light | High (can be focused) | Low to Moderate (UV-Vis); Better (NIR) | PEG with photolabile linkers (e.g., nitrobenzyl ether, coumarin) [81] | Patterned differentiation, controlled growth factor release, 4D patterning [81] [83] |
| Electrical | Moderate to High | High | Conductive polymers (e.g., PEDOT:PSS), carbon nanomaterials, MXenes [85] [86] | Neural and cardiac tissue engineering, guided neurite outgrowth [81] [86] |
| Magnetic | Moderate (remote actuation) | High | Magnetic nanoparticles (e.g., Fe₃O₄) embedded in polymer networks (e.g., alginate, collagen) [81] [82] | Remote-controlled mechanostimulation, targeted drug/cell delivery [81] |
| Ultrasound | Moderate | High | Microbubble-incorporated hydrogels, sonosensitive polymers [81] | Remote-controlled drug release, non-invasive activation in deep tissues [81] |
Design Principles for Stem Cell Delivery
When engineering smart hydrogels as stem cell delivery scaffolds, several key principles must be considered. The mechanical properties of the hydrogel, such as stiffness and elasticity, should mimic the target native tissue to provide appropriate mechanotransductive cues [81] [86]. The degradation profile must be tunable and synchronized with new tissue formation, often achieved using hydrolytically or enzymatically labile crosslinks [84] [83]. Furthermore, the incorporation of bioactive motifs, such as RGD peptides for cell adhesion or specific protease cleavage sites for cell-mediated remodeling, is critical for supporting stem cell viability and function [81] [86]. For injectable applications, shear-thinning and in situ self-healing properties are highly desirable, allowing for minimally invasive delivery and immediate restoration of scaffold integrity at the target site [87] [86].
Experimental Protocols
Protocol: Fabrication of a Photoresponsive PEG-Based Hydrogel for Spatially Controlled Stem Cell Differentiation
This protocol describes the synthesis of a polyethylene glycol (PEG) hydrogel incorporated with a photolabile nitrobenzyl ether crosslinker, enabling light-patterned presentation of biochemical cues to direct human mesenchymal stem cell (hMSC) fate [81].
Materials:
- PEG-diPDA: PEG-diphotodegradable acrylate (photolabile crosslinker)
- LAP photoinitiator: Lithium phenyl-2,4,6-trimethylbenzoylphosphinate
- RGDSP peptide: Cell-adhesive peptide sequence
- BMP-2 mimetic peptide: Osteoinductive factor
- 365 nm UV light source with photomask or digital micromirror device
- hMSCs (passage 3-5)
Procedure:
- Hydrogel Precursor Solution Preparation: Dissolve 10 mM PEG-diPDA and 2 mM LAP photoinitiator in sterile PBS. Add 1 mM RGDSP peptide to promote cell adhesion.
- hMSC Encapsulation: Trypsinize, count, and resuspend hMSCs in the precursor solution at a density of 5-10 million cells/mL. Mix gently but thoroughly.
- Hydrogel Polymerization: Pipet 50-100 µL of the cell-precursor suspension into a sterile mold. Expose to 5 mW/cm² of 365 nm UV light for 60 seconds to form a soft, cell-laden hydrogel.
- Spatial Patterning of Bioactive Cues: Place a photomask defining the desired pattern over the hydrogel or use a digital micromirror device. Apply a second UV exposure (10 mW/cm² for 120 seconds) to selectively degrade the hydrogel network in illuminated regions.
- Presentation of Differentiation Cues: Immediately incubate the patterned hydrogel in a solution containing 50 µg/mL BMP-2 mimetic peptide conjugated to a cysteine-terminated linker for 60 minutes. The peptide will conjugate exclusively to the photopatterned regions via thiol-ene click chemistry.
- Cell Culture and Analysis: Culture the constructs in a basal medium without strong differentiation inducers. After 14 days, assay for osteogenic differentiation via alkaline phosphatase (ALP) staining and qPCR for osteogenic markers (e.g., RUNX2, OCN). Differentiation will be confined to the photopatterned regions [81].
Protocol: Developing an Injectable, Conductive Hydrogel for Neural Stem Cell Delivery
This protocol outlines the creation of a shear-thinning, conductive hydrogel based on hyaluronic acid and a conductive polymer, designed to support neural stem cell (NSC) delivery and enhance neurite outgrowth through electrical stimulation [87] [86].
Materials:
- GMHA: Glycidyl methacrylate-modified hyaluronic acid
- PEDOT:PSS: Poly(3,4-ethylenedioxythiophene) polystyrene sulfonate conductive nanoparticles
- LAP photoinitiator
- Neural Stem Cells (NSCs) derived from human induced pluripotent stem cells (iPSCs)
Procedure:
- Conductive Hydrogel Ink Synthesis:
- Dissolve GMHA in PBS at 3% (w/v).
- Blend in PEDOT:PSS suspension to a final concentration of 0.3% (w/v) and mix thoroughly via vortexing.
- Add LAP photoinitiator to a final concentration of 0.1% (w/v). Protect the solution from light.
- Rheological Characterization:
- Perform rheology to confirm shear-thinning behavior. Viscosity should decrease significantly with increasing shear rate and recover rapidly upon removal of shear.
- NSC Encapsulation and Injection:
- Resuspend NSCs in the GMHA/PEDOT:PSS ink at 10 million cells/mL.
- Load the cell-hydrogel composite into a 1 mL syringe fitted with a 22G needle.
- Extrude the hydrogel smoothly into a cell culture well or a neural defect model.
- In Situ Crosslinking: After injection, expose the construct to 5 mW/cm² of 405 nm blue light for 90 seconds to crosslink the GMHA, forming a stable, conductive network.
- Electrical Stimulation Protocol:
- Culture the constructs for 3 days to allow cell recovery.
- Apply a biphasic electrical stimulation regimen (100 mV/mm, 1 Hz, 1 hour per day for 5 days) using embedded electrodes.
- Assessment of Neural Differentiation:
Table 2: Key Functional Outcomes of Featured Hydrogel Systems
| Hydrogel System | Stimulus Applied | Observed Material Change | Resulting Stem Cell Response | Validation Methods |
|---|---|---|---|---|
| Photoresponsive PEG [81] | 365 nm UV Light (patterning) | Localized hydrogel degradation & peptide tethering | Spatially confined osteogenic differentiation of hMSCs | ALP activity, qPCR (RUNX2, OCN), immunofluorescence |
| Conductive GMHA/PEDOT:PSS [85] [86] | Electrical Field (100 mV/mm) | Generation of an electrical field within the 3D scaffold | Enhanced NSC neurite outgrowth and neuronal maturation | Immunostaining (β-III-tubulin), neurite length quantification, PCR for neural markers |
| Magnetic Alginate Composite [81] [82] | Oscillating Magnetic Field | Cyclic mechanical deformation of the hydrogel matrix | Chondrogenic differentiation of MSCs via mechanotransduction | Histology (Safranin-O), GAG/DNA assay, collagen type II immunofluorescence |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Smart Hydrogel Research
| Reagent / Material | Function / Role | Example Application Notes |
|---|---|---|
| PEG-diacrylate (PEGDA) [81] | Synthetic polymer backbone; provides a bioinert, tunable base for hydrogel formation. | Functionalize with photolabile groups (e.g., nitrobenzyl ether) or peptides. Low batch-to-batch variability. |
| Gelatin Methacryloyl (GelMA) [83] [86] | Photocrosslinkable natural polymer; combines biocompatibility of gelatin with controllable polymerization. | Ideal for cell-laden scaffolds. Stiffness is tuned by UV exposure time and concentration. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) [81] | Cytocompatible photoinitiator; generates radicals under UV or blue light to initiate crosslinking. | Superior to Irgacure 2959 due to higher water solubility and efficiency at longer wavelengths (405 nm). |
| PEDOT:PSS [85] [86] | Conductive polymer dispersion; imparts electronic conductivity to hydrogels for electrical stimulation. | Blend with natural polymers (e.g., HA, alginate). Can be modified to improve stability. |
| Photolabile Crosslinkers (e.g., PEG-diPDA, nitrobenzyl ether) [81] | Enable light-triggered hydrogel degradation or cleavage of tethered molecules. | Use with 365 nm UV for cleavage. Ideal for creating dynamic patterns of biochemical cues. |
| RGDSP Cell-Adhesion Peptide [81] [86] | Promotes integrin-mediated cell attachment to otherwise non-adhesive hydrogels (e.g., pure PEG). | Critical for supporting survival of encapsulated stem cells. Can be tethered covalently. |
| Magnetic Nanoparticles (Fe₃O₄) [81] [82] | Provide magneto-responsiveness for remote mechanical stimulation or targeted delivery. | Coat with silica or polymers to enhance biocompatibility and prevent aggregation. |
Stimuli-responsive smart hydrogels represent a paradigm shift in stem cell delivery and tissue engineering, moving from static supports to dynamic, communicative matrices. The protocols and systems detailed here—utilizing light, electrical, and other stimuli—provide researchers with robust methodologies to spatially and temporally control the stem cell microenvironment. As the field progresses, the integration of multiple responsive functions, the optimization of biosafety, and advancements in scalable production technologies will be critical for translating these sophisticated biomaterial systems from the laboratory to the clinic, ultimately enabling more effective and personalized regenerative therapies [81] [82] [83].
Mesenchymal stromal cell (MSC)-based therapies represent a promising frontier in regenerative medicine and drug development. However, the therapeutic efficacy of MSCs is often limited by poor survival rates, low engraftment efficiency, and limited secretory activity following transplantation, particularly within the challenging microenvironment of injured tissues [64] [88]. To address these limitations, preconditioning strategies have emerged as a critical step in pre-transplantation processing to enhance MSC resilience and functionality. Preconditioning involves the ex vivo exposure of MSCs to sublethal stimuli that mimic the in vivo stress conditions they will encounter post-transplantation [88]. This process activates intrinsic protective mechanisms and enhances the cells' pro-regenerative capacities. This Application Note provides detailed protocols and frameworks for three key preconditioning strategies—cytokine exposure, hypoxia, and pharmacological agents—with particular emphasis on their application in conjunction with advanced delivery systems like hydrogels and scaffolds.
Preconditioning Strategies: Mechanisms and Comparative Analysis
Preconditioning enhances MSC function through various molecular mechanisms, ultimately improving their survival, paracrine activity, and homing ability. The table below summarizes the core mechanisms, key signaling pathways, and functional outcomes for each strategy.
Table 1: Comparative Analysis of MSC Preconditioning Strategies
| Preconditioning Strategy | Key Molecular Mechanisms | Key Signaling Pathways | Primary Functional Outcomes |
|---|---|---|---|
| Cytokine Preconditioning | HIF-1α stabilization; Upregulation of pro-survival & immunomodulatory genes; Enhanced exosome cargo loading [89] [90] [64] | PI3K/AKT; NF-κB; MAPK/ERK [90] [64] | Enhanced immunomodulation; Improved migration & homing; Polarization of macrophages to M2 phenotype [89] [64] |
| Hypoxic Preconditioning | HIF-1α stabilization; Metabolic reprogramming (glycolysis ↑); Increased expression of pro-angiogenic factors [91] [92] [64] | HIF-1α / VEGF; PI3K/AKT [91] [92] | Enhanced secretion of angiogenic factors (VEGF); Improved cell survival & proliferation; Increased production & efficacy of EVs [91] [92] |
| Pharmacological Preconditioning | Activation of antioxidant & anti-inflammatory pathways; Enhanced mitochondrial membrane potential [64] [88] [93] | Nrf2/Sirt3/FoxO3a; GSTO1-mediated antioxidant activity [92] [88] | Protection against oxidative stress; Enhanced paracrine secretion (VEGF, SDF-1); Improved angiogenesis & wound closure [64] [93] |
The following diagram illustrates the central signaling pathway shared by hypoxia and cytokine preconditioning, leading to enhanced MSC therapeutic functions.
Detailed Experimental Protocols
Protocol 1: Cytokine Preconditioning for Enhanced Immunomodulation
This protocol details the preconditioning of human umbilical cord blood MSCs (hUCB-MSCs) with a cytokine combination to boost their anti-inflammatory potential, particularly for treating inflammatory conditions like psoriasis [89].
3.1.1 Research Reagent Solutions
Table 2: Essential Reagents for Cytokine Preconditioning
| Item | Specification / Function | Example Source / Catalog No. |
|---|---|---|
| Human MSCs | Human Umbilical Cord Blood (hUCB-MSCs); Confirm expression of CD73, CD90, CD105 and lack of CD14, CD34, CD45, HLA-DR. | Commercially sourced (e.g., Invitrogen). |
| Basal Medium | α-MEM or DMEM. | Gibco (e.g., α-MEM #12571063). |
| Culture Supplement | Serum-free supplement to ensure defined conditions. | Helios UltraGRO-Advanced (#HPCFDCGL50). |
| Recombinant Cytokines | IL-17, IL-22, TNF-α; Key inflammatory cytokines that prime MSC immunomodulatory response. | PeproTech, R&D Systems. |
| Phosphate Buffered Saline (PBS) | For washing steps. | Gibco. |
3.1.2 Step-by-Step Procedure
- Cell Seeding: Plate early-passage (P3-P5) hUCB-MSCs at approximately 80% confluence in standard culture plates using a complete medium composed of α-MEM supplemented with 5% UltraGRO-Advanced.
- Starvation (Optional but Recommended): 24 hours after seeding, replace the complete medium with a serum-free or supplement-free basal medium (e.g., α-MEM only) for 2-4 hours to synchronize the cell cycle and reduce background signaling.
- Cytokine Stimulation: Replace the medium with a fresh serum-free medium containing the preconditioning cytokine cocktail.
- Final Concentrations: 20 ng/mL IL-17, 20 ng/mL IL-22, and 20 ng/mL TNF-α [89].
- Control Group: Include a control group of MSCs cultured in a serum-free medium without cytokines.
- Incubation: Incubate the cells for 24-48 hours in a standard humidified incubator at 37°C with 5% CO₂.
- Post-Preconditioning Processing: After incubation, carefully collect the conditioned medium for subsequent isolation of exosomes or the secretome.
- For cell transplantation, detach the preconditioned MSCs using a standard trypsinization protocol. Wash the cell pellet twice with PBS to remove any residual cytokines before incorporation into hydrogels or in vivo administration.
Protocol 2: Hypoxic Preconditioning to Boost Paracrine Function
This protocol enhances the production and therapeutic efficacy of MSC-derived extracellular vesicles (EVs) through controlled oxygen deprivation [91] [92].
3.2.1 Research Reagent Solutions
Table 3: Essential Reagents for Hypoxic Preconditioning
| Item | Specification / Function | Example Source / Catalog No. |
|---|---|---|
| Hypoxia Chamber/Workstation | A tri-gas incubator or sealed chamber to precisely maintain low O₂ environment. | Baker Ruskinn, BioSpherix. |
| Gas Mixture | 5% CO₂, balanced with N₂ to achieve 1-5% O₂. | Commercial gas supplier. |
| O₂ Monitor | Continuous verification of chamber O₂ concentration. | - |
| MSCs | Human Umbilical Cord MSCs (hUC-MSCs) or Bone Marrow MSCs (BM-MSCs). | - |
| EV Isolation Reagents | Ultracentrifugation reagents or commercial EV isolation kits. | - |
3.2.2 Step-by-Step Procedure
- Cell Preparation: Culture MSCs in T175 flasks until they reach 80-90% confluence.
- Hypoxia Induction:
- Normoxic Control: Maintain control MSCs in a standard incubator with 21% O₂ and 5% CO₂ at 37°C for the same duration.
- Validation of Hypoxic Response: Post-incubation, validate preconditioning efficacy by analyzing the stabilization of HIF-1α via Western blot (Primary Antibody: CST #14179) [92].
- EV Collection and Isolation:
- After hypoxia exposure, wash cells with PBS and culture in an EV-production medium (e.g., supplement-free basal medium) for another 24 hours under the same oxygen conditions.
- Collect the conditioned medium and isolate EVs via sequential ultracentrifugation: 2,000 × g for 20 min (to remove dead cells and debris), followed by 100,000 × g for 70 min at 4°C to pellet EVs [92].
- Wash the EV pellet in PBS and re-pellet at 100,000 × g for 70 min. Resuspend the final EV pellet in PBS or a suitable buffer for storage at -80°C.
- Characterization: Characterize isolated EVs using Nanoparticle Tracking Analysis (NTA) for size/concentration, Transmission Electron Microscopy (TEM) for morphology, and Western blot for surface markers (CD9, CD63, CD81) [92].
Protocol 3: Pharmacological Preconditioning for Oxidative Stress Resistance
This protocol uses pharmacological agents to prime MSCs for enhanced survival in the oxidative stress-rich environments typical of damaged tissues [64] [93].
3.3.1 Research Reagent Solutions
Table 4: Essential Reagents for Pharmacological Preconditioning
| Item | Specification / Function | Example Source / Catalog No. |
|---|---|---|
| Pharmacological Agents | Caffeic acid, α-ketoglutarate, Lipopolysaccharide (LPS); Activate cytoprotective pathways. | Sigma-Aldrich. |
| Antioxidants | N-acetyl-L-cysteine (NAC), α-lipoic acid; Scavenge ROS and support redox homeostasis. | Sigma-Aldrich. |
| Cell Viability Assay | CCK-8 kit for quantifying MSC proliferation and survival. | APEx BIO (#K1018). |
| ELISA Kits | For quantifying secreted factors (e.g., VEGF, BDNF, SDF-1). | R&D Systems. |
3.3.2 Step-by-Step Procedure
- Agent Preparation: Prepare stock solutions of the chosen pharmacological agent in a suitable solvent (e.g., DMSO or PBS) and filter-sterilize.
- Dose Optimization: Conduct a dose-response experiment to identify the optimal, non-toxic concentration that elicits a protective response.
- Preconditioning Treatment: Treat MSCs at 70-80% confluence with the optimized concentration of the pharmacological agent in a complete growth medium.
- Incubation: Incubate the cells for 24 hours in a standard humidified incubator (37°C, 5% CO₂).
- Post-Treatment Processing: After treatment, the conditioned medium can be collected as a drug-preconditioned secretome. For cell therapy, wash the MSCs thoroughly with PBS to remove traces of the pharmacological agent before subsequent use.
- Validation: Assess preconditioning success by measuring:
Integration with Hydrogel-Based Delivery Systems
The full therapeutic potential of preconditioned MSCs is realized when combined with advanced delivery systems. Hydrogels provide a protective 3D microenvironment that maintains the enhanced state of preconditioned MSCs and facilitates localized delivery [73] [3].
Key Integration Workflow:
- Precondition: Apply one of the above protocols to enhance MSC functionality ex vivo.
- Encapsulate: Post-preconditioning, immediately mix the MSC pellet with the hydrogel precursor solution (e.g., methacrylated gelatin (GelMA), hyaluronic acid, or fibrin).
- Cross-link: Induce gelation (via temperature, light, or ionic cross-linking) to form a 3D scaffold containing the preconditioned MSCs.
- Implant/Transplant: Apply the MSC-laden hydrogel construct to the wound or injury site.
Hydrogel Design Parameters for Preconditioned MSCs:
- Mechanical Properties: Tune stiffness (elastic modulus) to guide differentiation (1-10 kPa for adipogenic/neurogenic; 25-40 kPa for osteogenic) [73] [3].
- Bioactive Cues: Incorporate peptides (e.g., RGD) and growth factors (e.g., VEGF) to synergize with the preconditioned MSC secretome [73].
- Degradation Kinetics: Engineer degradation rates to match the timeline of tissue repair and MSC-mediated secretion [3].
Troubleshooting and Quality Control
| Issue | Potential Cause | Solution |
|---|---|---|
| Poor MSC Survival Post-Preconditioning | Excessive stimulus intensity or duration. | Optimize cytokine/drug concentration and exposure time; ensure O₂ levels are not <1% for hypoxia [91] [64]. |
| Inconsistent EV Yield | Inconsistent cell confluency prior to EV production; inefficient isolation. | Standardize cell confluence at 80-90%; use consistent ultracentrifugation protocols [92]. |
| Low Efficacy of Preconditioned MSCs in Hydrogels | Hydrogel matrix hinders nutrient/waste exchange or secretome diffusion. | Optimize hydrogel porosity and degradation rate; use injectable hydrogels for minimally invasive delivery [73] [3]. |
| Failure to Upregulate Target Proteins (e.g., HIF-1α) | Faulty hypoxia chamber; degraded cytokines/drugs. | Regularly calibrate O₂ sensors; use fresh aliquots of preconditioning agents [91] [92]. |
Addressing Immunogenicity and Batch-to-Batch Variability in Natural Polymers
The utilization of natural polymers as scaffolds for stem cell delivery represents a frontier in regenerative medicine, offering inherent biocompatibility and bioactivity that synthetic materials often struggle to match. These polymers—including polysaccharides like alginate, chitosan, and hyaluronic acid, and proteins such as collagen, silk, and fibrin—are components of or share similarities with the native extracellular matrix (ECM) [94] [95]. This biomimicry facilitates cell recognition, adhesion, and signaling, making them ideal candidates for creating a supportive microenvironment for transplanted stem cells [96]. Their innate biological properties can directly support stem cell viability, guide differentiation, and modulate immune responses, which are critical functions for successful tissue regeneration [95] [96].
However, two significant challenges impede the clinical translation and reliable application of natural polymer-based scaffolds: immunogenicity and batch-to-batch variability. Immunogenicity refers to the potential of a material to provoke an undesirable immune response, which can lead to inflammation, scaffold degradation, and ultimately, the failure of the therapeutic implant [95]. While natural polymers are generally considered low in immunogenicity compared to their synthetic counterparts, they are not inherently inert. For instance, certain polymers like chitosan can activate specific immune pathways, such as toll-like receptor (TLR)/MyD88, leading to the upregulation of pro-inflammatory cytokines [95]. Batch-to-batch variability, on the other hand, arises from the complex and often heterogeneous biological sources of these polymers. Differences in extraction methods, source species, age, and environmental factors can lead to inconsistencies in molecular weight, purity, chemical composition, and physical properties between production lots [94] [96]. This variability poses a major hurdle for manufacturing scaffolds with reproducible mechanical and biological properties, which is a prerequisite for regulatory approval and clinical success [3] [73].
Addressing these challenges is not merely a matter of improving material quality; it is fundamental to advancing the entire field of stem cell delivery. A predictable and controlled host response, coupled with a reproducible scaffold performance, is essential for developing safe and effective regenerative therapies. This Application Note provides a structured overview of the sources of these challenges, outlines standardized protocols for their assessment, and proposes strategic mitigation frameworks to guide researchers in the development of reliable natural polymer-based stem cell delivery systems.
Understanding the Challenges
The immunogenic potential of a natural polymer is not a single property but an interplay of its biological origin, molecular structure, and the presence of residual contaminants. Understanding these sources is the first step toward effective mitigation.
- Residual Endogenous Components: Polymers isolated from animal or human tissues (e.g., collagen, hyaluronic acid) may carry residual non-polymer components such as lipids, nucleic acids, and cellular proteins from the source material. These contaminants can act as damage-associated molecular patterns (DAMPs) or xeno-antigens, triggering innate and adaptive immune responses through pattern recognition receptors (PRRs) like Toll-like Receptors (TLRs) on immune cells [95] [97]. For example, residual endotoxins in marine-derived alginate are a common concern.
- Innate Polymer Bioactivity: The polymer molecules themselves possess innate biological motifs that can directly interact with the immune system. Chitin, the precursor to chitosan, is recognized by immune receptors such as FIBCD1 and NKR-P1, potentially upregulating cytokines and activating natural killer (NK) cell cytotoxicity [95]. Similarly, cellulose has been shown to induce TLR2-mediated NF-κB activation, a key pathway in inflammatory responses [95].
- Structural and Physical Properties: The higher-order structure of the polymer, including its molecular weight, fibril organization, and surface topography, can influence immune cell behavior. Fibrillar structures and specific molecular weight fractions may be interpreted by the immune system as "non-self" or as signs of tissue damage, thereby eliciting an inflammatory response [95].
The following diagram illustrates the primary signaling pathways through which natural polymers can trigger an immune response.
Causes of Batch-to-Batch Variability
The biological origin of natural polymers is the root cause of their inconsistent properties. This variability can manifest in multiple critical parameters that directly impact scaffold performance and stem cell behavior.
- Source Heterogeneity: Factors such as the species, age, diet, and specific tissue from which the polymer is sourced (e.g., bovine collagen from different herds or alginate from different seaweed harvests) can lead to fundamental differences in polymer chains, such as amino acid or monosaccharide sequence and chain length [95].
- Extraction and Purification Methods: The processes used to isolate the polymer from raw biomass are often complex and difficult to control with perfect reproducibility. Variations in temperature, pH, reaction time, and the purity of enzymes or chemicals used can alter the degree of deacetylation (in chitosan), the ratio of mannuronic to guluronic acid (in alginate), or the level of collagen cross-linking [94] [95].
- Post-Isolation Processing: Techniques like sterilization (e.g., gamma irradiation, ethylene oxide), lyophilization, and milling can further modify polymer properties, including molecular weight degradation and surface chemistry, introducing another layer of variability [95].
The table below summarizes the key variable parameters and their direct impact on scaffold function.
Table 1: Impact of Batch-to-Batch Variability on Scaffold Properties
| Variable Parameter | Impact on Scaffold Properties | Consequence for Stem Cell Therapy |
|---|---|---|
| Molecular Weight | Degradation kinetics, mechanical strength (e.g., stiffness, elasticity), viscosity of pre-gel solutions [94] [95] | Altered stem cell differentiation (e.g., osteogenesis vs. adipogenesis guided by matrix stiffness) [3] [96] |
| Purity / Contaminants | Immunogenicity, unwanted cellular signaling, toxicity [95] | Activation of immune cells, reduced stem cell viability, unpredictable paracrine secretion [95] [63] |
| Chemical Composition | Cross-linking density, ligand density for cell adhesion, water absorption capacity [94] [95] | Variability in cell adhesion, spreading, and survival post-encapsulation [96] |
| Physical Structure | Fibril size, porosity, pore interconnectivity [95] [98] | Differences in nutrient diffusion, cell migration, and neovascularization within the scaffold [98] |
Assessment Protocols
To control immunogenicity and variability, robust and standardized assessment protocols are essential. The following sections provide detailed methodologies for quantitative evaluation.
Protocol for In Vitro Immunogenicity Profiling
This protocol is designed to screen natural polymer batches for their potential to activate immune responses using human macrophage-like cells.
1. Research Reagent Solutions
Table 2: Essential Reagents for Immunogenicity Assessment
| Reagent | Function / Rationale |
|---|---|
| THP-1 human monocyte cell line | A standardized model that can be differentiated into macrophage-like cells, reducing donor-to-donor variability compared to primary cells. |
| Phorbol 12-myristate 13-acetate (PMA) | Differentiates THP-1 monocytes into adherent, macrophage-like cells. |
| Polymer test extracts | Sterile extracts of the natural polymer scaffolds prepared in complete cell culture medium (e.g., 1-10 mg/mL, incubated for 24-72 hours at 37°C). |
| Lipopolysaccharide (LPS) | A potent TLR4 agonist used as a positive control for immune activation. |
| ELISA Kits for TNF-α, IL-1β, IL-6, IL-10 | For quantitative measurement of key pro-inflammatory and anti-inflammatory cytokines in the cell culture supernatant. |
| Flow cytometry antibodies (CD80, CD86, HLA-DR) | To quantify the surface expression of co-stimulatory and antigen-presentation molecules on macrophages, indicating their activation state. |
| qPCR reagents for primers (TNF, IL1B, IL6, ARG1) | To assess the transcriptional upregulation of immune genes, providing an early and sensitive measure of activation. |
2. Experimental Workflow
- Step 1: Cell Differentiation: Culture THP-1 cells in RPMI-1640 medium supplemented with 10% FBS. Seed cells in 24-well plates at a density of 2.5 x 10^5 cells per well and treat with 100 ng/mL PMA for 48 hours to induce differentiation into macrophages. Replace medium with fresh, PMA-free medium and rest cells for 24 hours before stimulation.
- Step 2: Polymer Stimulation: Prepare sterile extracts of each polymer batch. Apply the polymer extracts to the differentiated THP-1 macrophages. Include a negative control (culture medium only) and a positive control (100 ng/mL LPS). Incubate for 6 hours (for mRNA analysis) and 24 hours (for protein and surface marker analysis).
- Step 3: RNA Isolation and qPCR Analysis: After 6 hours, lyse cells and extract total RNA. Synthesize cDNA and perform qPCR using pre-validated primers for pro-inflammatory markers (TNF, IL1B, IL6) and alternative activation markers (ARG1). Calculate fold-change in gene expression using the 2^(-ΔΔCt) method normalized to housekeeping genes (e.g., GAPDH, ACTB) and relative to the negative control.
- Step 4: Protein-Level Analysis (ELISA): After 24 hours, collect cell culture supernatants and centrifuge to remove debris. Use commercial ELISA kits according to manufacturer instructions to quantify the secretion of TNF-α, IL-1β, IL-6, and IL-10. Measure absorbance using a microplate reader and interpolate concentrations from a standard curve.
- Step 5: Immune Phenotyping (Flow Cytometry): After 24 hours, gently detach macrophages using a cell scraper. Stain cells with fluorescently labeled antibodies against CD80 (activation marker), CD86 (activation marker), and HLA-DR (MHC class II). Use isotype-matched antibodies as controls. Analyze stained cells on a flow cytometer and report results as Mean Fluorescence Intensity (MFI) or percentage of positive cells.
3. Data Interpretation A polymer batch with low immunogenicity potential should show minimal upregulation of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) and activation markers (CD80, CD86) compared to the negative control, with a profile significantly lower than the LPS-positive control. A shift toward an anti-inflammatory state, indicated by IL-10 secretion and ARG1 expression, may be desirable for certain regenerative applications.
Protocol for Quantifying Batch Consistency
This protocol outlines a suite of physicochemical tests to establish a consistency profile for each incoming polymer batch.
1. Research Reagent Solutions
- Size Exclusion Chromatography (SEC) columns and standards
- Nuclear Magnetic Resonance (NMR) solvents (e.g., D2O)
- Enzymatic assay kits (e.g., for endotoxin/LAL test)
- Rheometer
2. Experimental Workflow and Acceptance Criteria
Table 3: Physicochemical Tests for Batch Consistency
| Test Method | Parameter Measured | Protocol Summary | Acceptance Criterion |
|---|---|---|---|
| Size Exclusion Chromatography (SEC) | Molecular Weight Distribution | Dissolve polymer at 1-5 mg/mL in appropriate solvent (e.g., acetate buffer for chitosan). Inject onto SEC system with multi-angle light scattering (MALS) and refractive index (RI) detectors. | ±15% of baseline Mw/Mn (weight-average/number-average molecular weight) of a pre-qualified Master Batch. |
| Monosaccharide/Amino Acid Analysis | Chemical Composition | For polysaccharides: Hydrolyze polymer with strong acid (e.g., TFA), then analyze released monosaccharides via HPAEC-PAD or HPLC. For proteins: Perform acid hydrolysis and analyze via amino acid analyzer. | M/G ratio (alginate) ±10%; Deacetylation degree (chitosan) ±5%; Amino acid profile ±10% of Master Batch. |
| 1H-Nuclear Magnetic Resonance (NMR) | Chemical Structure & Purity | Dissolve polymer in deuterated solvent (e.g., D2O). Acquire 1H-NMR spectrum. Identify characteristic peaks and integrate to calculate ratios (e.g., M/G ratio). | NMR fingerprint must match Master Batch profile. No new, significant unidentified peaks. |
| Endotoxin/LAL Test | Pyrogen Contaminants | Use a commercial Limulus Amebocyte Lysate (LAL) assay kit (chromogenic or gel-clot) following manufacturer's protocol on a polymer extract. | < 0.25 EU/mL in final scaffold extract, per FDA guideline for medical devices. |
| Rheometry | Viscoelastic Properties | For hydrogels: Characterize storage modulus (G') and loss modulus (G") under oscillatory shear at 37°C. Report the plateau G' value. | G' (Storage Modulus) ±20% of the value measured for scaffolds fabricated from the Master Batch. |
The following diagram maps this multi-parameter workflow for systematic batch quality control.
Mitigation Strategies
A proactive approach that combines material engineering, rigorous sourcing, and advanced manufacturing can significantly mitigate the challenges of immunogenicity and variability.
Strategies to Minimize Immunogenicity
- Advanced Purification and Decellularization: For polymers derived from animal tissues, implementing rigorous decellularization and purification protocols is crucial. This involves a combination of detergents, enzymes (e.g., nucleases), and solvent extractions to remove cellular debris, lipids, and nucleic acids that act as primary immunogens [95]. The efficiency of this process should be verified by quantifying residual DNA (e.g., < 50 ng/mg dry weight) and protein content.
- Chemical Modification: Masking or altering immunogenic epitopes on the polymer chain can reduce immune recognition.
- PEGylation: Covalently attaching poly(ethylene glycol) (PEG) chains to the polymer surface can create a steric shield, reducing protein adsorption and immune cell recognition [94].
- Cross-linking: Specific cross-linking strategies can alter the polymer's tertiary structure, potentially burying immunogenic motifs. However, the choice of cross-linker (e.g., genipin vs. glutaraldehyde) must be considered for its own cytotoxicity and potential to create neoantigens [95].
- Combinatorial Approaches Using Synthetic Polymers: Developing composite or hybrid hydrogels that blend natural polymers with highly reproducible synthetic polymers like poly(ethylene glycol) (PEG) or poly(vinyl alcohol) (PVA) can leverage the bioactivity of the natural component while diluting its immunogenic potential and improving mechanical control [3] [73]. Synthetic components can provide a bioinert backbone, while natural polymers can be incorporated at lower, more controlled doses to provide specific cell-adhesion motifs.
Strategies to Reduce Batch-to-Batch Variability
- Strict Source Control and Standardization: Establish qualified suppliers and specify the biological source in extreme detail (e.g., species, age, tissue location). For plant-derived polymers, controlled growth conditions and harvest times should be mandated.
- Good Manufacturing Practice (GMP) and Standardized Protocols: Transitioning from lab-scale extraction to GMP-compliant production processes is essential for clinical translation. This involves defining and tightly controlling all critical process parameters (CPPs)—such as temperature, pH, reaction time, and reagent purity—during extraction, purification, and sterilization [3] [73].
- Implementing a Quality-by-Design (QbD) Framework: Instead of merely testing final batches, a QbD approach proactively builds quality into the product design and manufacturing process. This involves:
- Defining a Target Product Profile (TPP) for the scaffold (e.g., desired stiffness, degradation rate).
- Identifying the Critical Quality Attributes (CQAs) of the polymer (e.g., molecular weight, degree of deacetylation, endotoxin level) that impact the TPP.
- Establishing the Design Space for the manufacturing process—the range of CPPs that consistently produce polymer meeting all CQAs.
- Implementing continuous Process Analytical Technology (PAT) to monitor CPPs in real-time for immediate corrective action.
Application in Stem Cell Delivery
For a stem cell delivery scaffold, the ultimate test of successful mitigation is its performance in supporting stem cell function. The following in vitro assay is critical for validating a polymer batch.
Protocol: Functional Validation via Mesenchymal Stromal Cell (MSC) Encapsulation
- Objective: To assess the viability, morphology, and paracrine function of MSCs encapsulated within the hydrogel scaffold, confirming the material supports therapeutic potential.
- Materials: Master and test batch hydrogels, human Bone Marrow-derived MSCs (hBM-MSCs), cell culture medium, live/dead viability/cytotoxicity kit (e.g., Calcein-AM/Ethidium homodimer-1), ELISA kits for VEGF and TGF-β1.
- Method:
- Hydrogel Preparation and Cell Encapsulation: Mix passage 4-6 hBM-MSCs with the polymer precursor solution at a density of 5-10 x 10^6 cells/mL. Induce gelation (e.g., via ionic cross-linking for alginate, thermal for collagen) to form 3D cell-laden constructs.
- Viability and Morphology Assessment (Day 1, 3, 7): At each time point, incubate constructs in live/dead stain for 30-45 minutes. Image using confocal microscopy. Analyze images to calculate percentage live cells. Note cell morphology (e.g., rounded vs. spread), as this indicates biocompatibility and integrin-mediated adhesion.
- Paracrine Function Analysis (Day 3): Collect conditioned medium from the constructs after 24 hours of incubation. Centrifuge to remove debris and analyze for secretion of key regenerative factors like Vascular Endothelial Growth Factor (VEGF) and Transforming Growth Factor-beta (TGF-β1) using ELISA. Compare the secretory profile of MSCs in the test batch to those in the Master Batch scaffold.
- Success Criteria: A suitable polymer batch will support:
- High Cell Viability: >80% viability over 7 days in culture.
- Appropriate Morphology: Cell spreading indicative of positive integrin engagement with the matrix.
- Robust Paracrine Activity: VEGF and TGF-β1 secretion levels comparable to or greater than those in the Master Batch, confirming the scaffold does not suppress the therapeutic function of MSCs [3] [63] [73].
The path to clinical translation of natural polymer-based stem cell delivery systems is paved with the challenges of immunogenicity and batch-to-batch variability. These issues are not insurmountable but require a disciplined, multi-faceted approach. By understanding the molecular and structural sources of these challenges, implementing rigorous and quantitative assessment protocols, and adopting strategic mitigation frameworks like advanced purification, hybrid material design, and QbD, researchers can significantly enhance the reliability and safety of their biomaterial scaffolds. The consistent production of functional scaffolds that direct stem cell fate predictably is the ultimate goal, enabling the development of robust and effective regenerative therapies.
The regeneration of load-bearing soft tissues—such as tendon, ligament, and vascular conduits—presents a unique challenge in tissue engineering. These tissues are routinely subjected to significant repetitive tensile forces, requiring engineered constructs that are not only biocompatible and supportive of stem cell function but also mechanically robust and durable [3] [99]. Conventional hydrogels often fail to provide the necessary mechanical strength and resilience for such applications, creating a critical "mechanical gap" between the scaffold's performance and the native tissue's requirements [99]. This Application Note details protocols and design strategies for developing advanced hydrogel scaffolds that bridge this gap, focusing on systems that have demonstrated superior mechanical performance while effectively supporting mesenchymal stromal cell (MSC) function for regenerative applications. By combining sustainable biomaterials like lignin with efficient crosslinking chemistry and strategic reinforcement, these scaffolds meet the dual demands of biological functionality and mechanical competence for load-bearing tissue regeneration.
Key Material Properties of Robust Hydrogel Scaffolds
The following table summarizes target properties for hydrogels intended for load-bearing soft tissue engineering, based on recent research findings.
Table 1: Target Properties for Load-Bearing Hydrogel Scaffolds
| Property Category | Specific Property | Target Value / Ideal Characteristic | Significance for Load-Bearing Tissues |
|---|---|---|---|
| Mechanical Performance | Ultimate Tensile Strength | > 80 kPa [99] | Withstands physiological tensile loads without failure. |
| Elongation at Break | Up to ~175% [99] | Provides necessary flexibility and strain tolerance. | |
| Fatigue Resistance | Sustained performance over >100 cycles [99] | Ensures durability under repetitive mechanical stress. | |
| Physicochemical Properties | Swelling Capacity | ~260% [99] | Maintains hydrated microenvironment while resisting excessive swelling that weakens structure. |
| Degradation Rate | Tunable to align with tissue healing timeline [3] | Provides temporary support until new tissue matures. | |
| Structural Properties | Porosity | 3D Interconnected Porous Network [99] | Facilitates cell migration, nutrient diffusion, and vascularization. |
| Pore Architecture | Bimodal distribution (Mesopores 2-50 nm & Micropores <2 nm) [99] | May enhance bioactivity and nutrient exchange. | |
| Biological Performance | Cytocompatibility | >85% cell viability after 96 hours [99] | Ensures scaffold supports cell survival and proliferation. |
| Bioactivity | Provision of cell-instructive cues [3] [65] | Directs desired stem cell behavior (e.g., differentiation, immunomodulation). |
Experimental Protocols
Protocol: Synthesis of Mechanically Robust Lignin-Based Tubular Hydrogels
This protocol describes the fabrication of tubular hydrogel scaffolds from organosolv lignin (OL) and polyvinyl alcohol (PVA), crosslinked with epichlorohydrin (ECH), for applications requiring mechanical resilience [99].
Materials:
- Polymers: Organosolv Lignin (OL), Polyvinyl Alcohol (PVA)
- Crosslinker: Epichlorohydrin (ECH)
- Solvent: Deionized Water
- Base Catalyst: Sodium Hydroxide (NaOH) solution
- Reinforcement (Optional): Polypropylene mesh
- Molding Setup: Glass rod and test tube for tubular conformation.
Procedure:
- Solution Preparation: Prepare separate aqueous solutions of OL (5% w/v) and PVA (10% w/v). Heat and stir as needed to achieve complete dissolution.
- Mixing: Combine the OL and PVA solutions in a 1:1 weight ratio. Mix thoroughly to achieve a homogeneous polymer blend.
- Crosslinking:
- Place the mixture in an ice bath.
- Add ECH crosslinker to the polymer blend to a final concentration of 5% v/v (identified as optimal).
- Adjust the pH to ~12 using NaOH solution to initiate the nucleophilic substitution reaction.
- Stir the reaction mixture for 24 hours at room temperature to form a covalently crosslinked network.
- Tubular Scaffold Fabrication:
- Pour the reacted hydrogel precursor into a mold consisting of a glass rod (to define the inner lumen) placed concentrically within a test tube (to define the outer diameter).
- For reinforced constructs, carefully place a polypropylene mesh around the inner glass rod before pouring the precursor.
- Cure the hydrogel in the mold at 60°C for 2 hours to complete the crosslinking and set the tubular geometry.
- Post-Processing and Sterilization:
- Carefully demold the tubular hydrogel.
- Wash extensively with deionized water to remove any unreacted chemicals and neutralize the pH.
- Sterilize the scaffolds using gamma irradiation or ethylene oxide gas prior to in vitro or in vivo studies.
Protocol: Formulation of an Alginate/Hyaluronic Acid (HA) Thiol-Yne Click-Hydrogel
This protocol outlines the synthesis of a highly stable and mechanically strong hydrogel via thiol-yne click chemistry, suitable for injectable delivery and load-bearing soft tissue support [100].
Materials:
- Alkyne-Modified Hyaluronic Acid (HA)
- Thiol-Modified Alginate
- Photoinitiator: e.g., Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP)
- UV Light Source (365 nm, ~5-10 mW/cm²)
Procedure:
- Polymer Solution Preparation: Dissolve the alkyne-modified HA and thiol-modified alginate in a physiologically compatible buffer (e.g., PBS) at the desired concentration to create separate precursor solutions.
- Precursor Mixing: Combine the HA-alkyne and alginate-thiol solutions in a stoichiometric ratio (typically 1:1 thiol-to-yne) to ensure complete crosslinking.
- Photoinitiation and Gelation:
- Add the LAP photoinitiator to the mixed polymer solution at a standard concentration (e.g., 0.05% w/v).
- Pipette the solution into a mold or syringe.
- Expose the solution to UV light (365 nm) for a defined period (e.g., 5-10 minutes) to initiate the rapid, radical-mediated thiol-yne click reaction, resulting in gelation.
- Characterization: The resulting hydrogel can be characterized for its mechanical properties via rheometry or uniaxial tensile testing, demonstrating superior stability and mechanical performance for soft tissue engineering.
Protocol: Encapsulation and Culture of MSCs in Hydrogel Scaffolds
This standard protocol ensures high cell viability and function post-encapsulation, a critical step for creating a therapeutic cell-delivery system [3] [65].
Materials:
- Mesenchymal Stem Cells (MSCs) (e.g., from bone marrow or umbilical cord)
- Complete MSC Culture Medium (e.g., DMEM with 10% FBS and 1% Penicillin/Streptomycin)
- Sterile Hydrogel Precursor Solution (e.g., from Protocols 3.1 or 3.2)
- Cell Dissociation Reagent (e.g., Trypsin-EDTA)
- Centrifuge Tubes
Procedure:
- Cell Harvesting: Culture MSCs to 80-90% confluence. Wash with PBS, detach using a cell dissociation reagent, and collect the cell pellet by centrifugation.
- Cell Resuspension: Gently resuspend the concentrated cell pellet in a small volume of the sterile, cytocompatible hydrogel precursor solution to achieve the desired final cell density (e.g., 1-5 million cells/mL).
- Encapsulation:
- For in situ forming hydrogels (e.g., the click-hydrogel from Protocol 3.2), transfer the cell-laden precursor solution to a mold and induce gelation (e.g., via UV exposure).
- For pre-formed scaffolds (e.g., the tubular hydrogel from Protocol 3.1), seed the cell suspension onto the scaffold and allow for cell attachment.
- Culture and Maintenance:
- After gelation/seeding, transfer the constructs to culture plates.
- Add complete MSC culture medium.
- Culture the MSC-laden hydrogels in a standard humidified incubator (37°C, 5% CO₂), changing the medium every 2-3 days.
- Assessment: Monitor cell viability, morphology, and metabolic activity using standard assays like Live/Dead staining, MTT, or AlamarBlue.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Developing MSC-Laden Hydrogels for Load-Bearing Tissues
| Reagent / Material | Function and Rationale | Example from Protocols |
|---|---|---|
| Organosolv Lignin | Sustainable biopolymer that enhances mechanical strength, provides antioxidant activity, and improves structural stability of the hydrogel network [99]. | Protocol 3.1 |
| Thiol-Modified Alginate | Forms stable, covalent crosslinks via efficient click chemistry; contributes to mechanical robustness and injectability of the hydrogel [100]. | Protocol 3.2 |
| Alkyne-Modified HA | Provides bioactive cues for cell adhesion and proliferation; modified for rapid, controlled crosslinking via click chemistry [100]. | Protocol 3.2 |
| Epichlorohydrin (ECH) | Bifunctional crosslinker that creates strong ether linkages between polymer chains (e.g., lignin and PVA), defining the hydrogel's mechanical properties [99]. | Protocol 3.1 |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | A cytocompatible photoinitiator that generates radicals under UV light to initiate crosslinking reactions for cell encapsulation under mild conditions [100]. | Protocol 3.2 |
| Polypropylene Mesh | Provides macroscopic reinforcement to tubular hydrogel constructs, significantly enhancing tensile strength and fatigue resistance for load-bearing applications [99]. | Protocol 3.1 |
Signaling Pathways and Experimental Workflows
Hydrogel-Stem Cell Mechanotransduction Signaling
This diagram illustrates the key signaling pathways through which the mechanical and biochemical properties of a hydrogel scaffold direct MSC behavior toward tissue regeneration.
Experimental Workflow for Scaffold Development & Testing
This diagram outlines the logical sequence and key decision points in the process of developing and validating a robust hydrogel scaffold for load-bearing tissue engineering.
The transition of stem cell-based therapies from promising research to widely available clinical and commercial products is critically dependent on overcoming manufacturing challenges. This document details the application notes and protocols essential for scaling up the production of stem cell-laden hydrogel constructs under Good Manufacturing Practice (GMP) standards. Adherence to these principles ensures that therapeutic products are not only biologically effective but also consistently safe, pure, and potent for clinical application. The following sections provide a structured framework for navigating the path from laboratory-scale innovation to scalable, commercially viable manufacturing processes.
Application Notes: Core Principles for Scalable GMP Manufacturing
Scaling up stem cell-hydrogel therapies requires a paradigm shift from manual, open-process research methods to automated, closed-system manufacturing. The following notes outline the critical operational and quality considerations.
Note 1.1: Defining a GMP-Compliant Raw Material Strategy
The foundation of a GMP process is the consistent quality of all input materials. For hydrogel-based therapies, this presents a significant challenge, particularly with naturally derived polymers.
- Challenge: Natural hydrogels (e.g., collagen, fibrinogen) often exhibit batch-to-batch variability and carry risks of xenogenic contamination [3].
- Solution: Prioritize the use of xeno-free, synthetic, or defined components.
- Synthetic Polymers: Polyethylene glycol (PEG) and polyvinyl alcohol (PVA) offer superior lot-to-lot consistency, tunable mechanical properties, and reduced risk of immunogenicity [3] [83].
- Platelet Derivatives: As human-sourced alternatives to fetal bovine serum, platelet lysates and other derivatives are increasingly used as GMP-compliant, clinically acceptable components for cell culture and hydrogel formulation [3].
- Documentation: All materials must be accompanied by a Certificate of Analysis (CoA) to ensure they meet pre-defined specifications for identity, purity, and functionality.
Note 1.2: Implementing a Closed and Controlled Scalable Expansion Process
Traditional 2D cell culture in flasks or multi-tray stacks is not viable for commercial-scale production due to extensive manual handling, high contamination risk, and poor reproducibility [101].
- Challenge: Scaling adherent mesenchymal stromal cell (MSC) cultures while maintaining cell quality and morphology.
- Solution: Adopt single-use, closed-system bioreactors designed for adherent cells.
- Technology: Integrable multiplate bioreactors (e.g., Integrity Xpansion system) mimic the 2D growth environment of stack plates but within a single, compact, and instrument-controlled vessel [101].
- Benefits:
- Reduced Footprint: One 180-plate bioreactor can replace 18 multitray stacks, reducing facility space by >60% [101].
- Process Control: Integrated sensors for pH, dissolved oxygen (DO), and temperature allow for real-time monitoring and control, enhancing process reproducibility [101].
- Reduced Operational Complexity: Replaces thousands of daily aseptic operations with a single closed process, significantly lowering labor costs and contamination risk [101].
Table 1: Economic Impact of Scaling with Single-Use Bioreactors
| Manufacturing Parameter | Traditional Multi-tray Stacks | Single-Use Multiplate Bioreactor | Impact |
|---|---|---|---|
| Aseptic Operations (per 3,000 patients/year) | ~2,000 per day | Minimal (closed system) | ~40% reduction in operational expenses [101] |
| Facility Cleanroom Class | Class B | Class C | ~50% reduction in capital expenditure [101] |
| Estimated Operator Requirement | 300 | ~150 | Labor costs halved [101] |
Note 1.3: Advancing Hydrogel Fabrication with 4D Bioprinting and AI
Next-generation manufacturing leverages smart materials and data-driven design to create dynamic tissue constructs.
- 4D Bioprinting: This technique combines 3D bioprinting with stimuli-responsive ("smart") hydrogels that change shape or function over time in response to physiological triggers (e.g., temperature, pH) [83]. This is ideal for creating dynamic scaffolds that better integrate with host tissue.
- AI-Driven Design: Machine learning (ML) and artificial intelligence (AI) algorithms can predict optimal hydrogel formulations (e.g., polymer composition, crosslinking density) for desired mechanical strength, degradation rates, and drug release profiles, drastically reducing experimental trial-and-error [83].
Experimental Protocols
This section provides a detailed, step-by-step methodology for a key unit operation in the manufacturing process: the scalable production of MSCs within a GMP-compliant, closed-system bioreactor.
Protocol 2.1: Scalable Expansion of Adherent MSCs in a Single-Use Multiplate Bioreactor
Objective: To achieve high-density expansion of adherent MSCs in a closed, controlled, and scalable system, generating a cell batch suitable for subsequent encapsulation in hydrogels for therapeutic use.
Principle: This protocol utilizes a single-use bioreactor with multiple, thin, gas-permeable plates to provide a large surface area for cell growth. Media circulation is optimized to minimize shear stress while ensuring adequate nutrient delivery and waste removal. The process is monitored in real-time to determine the optimal harvest point.
Materials:
- Cell Source: Master Cell Bank of human MSCs (e.g., adipose-derived or bone marrow-derived).
- Bioreactor: Integrity Xpansion multiplate bioreactor or equivalent [101].
- GMP-Grade Media: Xeno-free, serum-free mesenchymal stem cell growth medium.
- Supplement: GMP-compliant platelet lysate or defined growth factor cocktail.
- Reagents: Trypsin/EDTA solution or equivalent GMP-compliant detachment reagent, Phosphate Buffered Saline (PBS).
- Equipment: Biosafety cabinet, calibrated pipettes, sterile connection device (e.g., welder), peristaltic pump, cell counter.
Procedure:
Pre-culture and Inoculum Preparation:
- Thaw a vial from the working cell bank and expand MSCs in 2D culture flasks using GMP-grade media until sufficient cell numbers are achieved for bioreactor inoculation.
- Harvest cells using a standard trypsinization procedure. Quench the enzyme with excess media, centrifuge, and resuspend the cell pellet in fresh, pre-warmed media to a defined concentration.
- Perform a cell count and viability assessment (e.g., via Trypan Blue exclusion). Viability must be >90% to proceed.
Bioreactor Setup and Inoculation:
- Place the single-use bioreactor into its control unit within the incubator.
- Aseptically connect the media bag and inoculation bag to the bioreactor's ports using a sterile tube welder.
- Using a peristaltic pump, transfer the cell suspension into the bioreactor to initiate the culture. Ensure an even distribution of cells across the plates by following the manufacturer's recommended circulation protocol.
Process Monitoring and Control:
- Set and maintain critical process parameters for the entire run:
- Temperature: 37°C
- pH: 7.2 - 7.4 (controlled by CO₂ gassing or buffer)
- Dissolved Oxygen (DO): 20-50%
- Monitor cell growth and morphology in real-time using an integrated imaging system (e.g., Ovizio) [101]. Track key metrics like cell density and confluence.
- Perform scheduled off-line sampling from a designated sample port to monitor metabolites (e.g., glucose, lactate) and confirm cell counts.
- Set and maintain critical process parameters for the entire run:
Harvesting:
- Initiate harvest when cells reach 80-90% confluence, as determined by the integrated imaging system.
- Drain the spent culture media from the system.
- Wash the cell layers with pre-warmed PBS to remove residual serum and metabolites.
- Add a GMP-compliant detachment reagent and circulate it through the bioreactor to dissociate the cells from the plates.
- Re-circulate the cell suspension and transfer it out into a harvest bag. Rinse the plates with fresh media to maximize cell recovery.
- Centrifuge the harvested cell suspension to pellet the cells and resuspend in the final formulation buffer for immediate use in hydrogel encapsulation or cryopreservation.
Post-process Analysis:
- Determine the Total Cell Yield and Viability.
- Perform quality control (QC) tests, which may include:
- Flow Cytometry: To confirm MSC surface marker profile (CD73+, CD90+, CD105+, CD45-, CD34-) [102].
- Sterility Test: Using BacT/ALERT or direct inoculation.
- Endotoxin Test: Limulus Amebocyte Lysate (LAL) assay.
The following workflow diagram summarizes the key stages of this scalable expansion process.
Protocol 2.2: Formulation of a GMP-Compliant, MSC-Laden Hydrogel
Objective: To encapsulate the harvested MSCs within a tunable, xeno-free hydrogel matrix that supports cell viability and function, and is suitable for clinical administration (e.g., injectable).
Principle: This protocol utilizes a PEG-based hydrogel crosslinked via a bio-orthogonal, cytocompatible reaction (e.g., Michael-type addition between thiols and vinyl sulfones). The hydrogel precursors are functionalized with RGD peptides to promote cell adhesion and can be mixed with cells to form a uniform 3D network upon crosslinking.
Materials:
- Cells: Harvested MSCs from Protocol 2.1.
- Polymer Precursors:
- 4-arm PEG-Vinyl Sulfone (PEG-VS)
- PEG-dithiol (crosslinker)
- RGD-functionalized PEG peptide (e.g., GCGYGRGDSPG)
- Buffer: Triethanolamine (TEOA) buffer, pH 8.0, or other GMP-compliant cytocompatible buffer.
- Equipment: Sterile biosafety cabinet, vortex mixer, microcentrifuge tubes, syringes and luer-lock connectors.
Procedure:
- Precursor Preparation: Dissolve PEG-VS and PEG-dithiol separately in TEOA buffer to a final concentration of 4% (w/v). Sterile-filter both solutions.
- RGD Functionalization: Dissolve the RGD-peptide in buffer and add it to the PEG-VS solution at a molar ratio that ensures not all VS groups are consumed. Allow this reaction to proceed for 15-20 minutes to create a cell-adhesive PEG-VS precursor.
- Cell-Polymer Mixing: Centrifuge the harvested MSCs and resuspend them at twice the desired final density in the crosslinker (PEG-dithiol) solution.
- Gelation: In a 1:1 ratio, combine the cell-loaded crosslinker solution with the RGD-functionalized PEG-VS solution. Mix gently but thoroughly by pipetting or using a double-syringe connector. The gel will form within minutes at room temperature.
- Curing and Assessment: Transfer the gel to a 37°C incubator for 30 minutes to complete the crosslinking. The resulting MSC-laden hydrogel is ready for in-process quality control or packaging.
Table 2: The Scientist's Toolkit: Essential Reagents for GMP Hydrogel Formulation
| Reagent / Material | Function / Rationale | GMP-Compliant Consideration |
|---|---|---|
| 4-arm PEG-Vinyl Sulfone | Synthetic polymer backbone; provides tunable mechanical properties and minimal batch variability. | Source from a supplier that provides Drug Master Files (DMFs) and full traceability. |
| PEG-dithiol Crosslinker | Forms stable, cytocompatible crosslinks with PEG-VS via Michael addition. | Ensure high purity and absence of toxic impurities. |
| RGD Adhesion Peptide | Promotes integrin-mediated cell adhesion, enhancing MSC survival and function within the hydrogel [3]. | Use synthetic peptides with a defined sequence and CoA. |
| Triethanolamine Buffer | Provides a suitable pH environment for the crosslinking reaction without cytotoxic byproducts. | USP-grade or equivalent. |
Visualization of Strategic Pathways
The journey from research to commercial product requires navigating a defined strategic pathway, balancing biological innovation with rigorous manufacturing and regulatory planning. The following diagram illustrates this critical path.
Bench-to-Bedside Evidence: Preclinical Models, Clinical Trials, and Efficacy Analysis
The transition from promising in vitro results to successful clinical applications represents a critical juncture in regenerative medicine. For stem cell-based therapies, particularly those utilizing advanced delivery methods like scaffolds and hydrogels, demonstrating efficacy in clinically relevant animal models is a mandatory step. These preclinical models are indispensable for evaluating the therapeutic potential, safety, and mechanistic action of mesenchymal stromal cell (MSC)-laden hydrogel constructs. They provide a complex physiological environment to assess how these engineered systems modulate the healing process in pathologies such as ischemic stroke, chronic wounds, and neurodegenerative disorders. This application note synthesizes key quantitative outcomes from recent preclinical studies, provides detailed experimental protocols for replication, and visualizes the core signaling pathways involved, serving as a strategic guide for researchers and drug development professionals in the field.
Quantitative Preclinical Outcomes
The following tables summarize the efficacy of MSC-hydrogel therapies across different animal models of human disease, highlighting key parameters such as cell retention, functional recovery, and tissue regeneration.
Table 1: Preclinical Outcomes of MSC-Laden Hydrogels in Neurological Disease Models
| Disease Model | Animal Species | Hydrogel System | Key Quantitative Outcomes | Proposed Mechanism | Citation |
|---|---|---|---|---|---|
| Ischemic Stroke | Rodent (Rat/Mouse) | Carrier-based hydrogels (e.g., Hyaluronic acid, PEG) | - Significantly higher MSC survival and retention at lesion site vs. bolus injection- ~45% reduction in infarct volume- ~30% improvement in neurological function scores (e.g., mNSS) | Enhanced paracrine signaling; immunomodulation; reduced apoptosis; axonal reorganization | [103] |
| Alzheimer's Disease (AD) | Transgenic Mice (e.g., APP/PS1) | Not Specified (Review Focus) | - Reduction in amyloid-β plaque load- Improvement in spatial memory (e.g., Morris water maze performance) | Modulation of neuroinflammation; clearance of pathological proteins | [104] |
| Parkinson's Disease (PD) | Rodent, Non-Human Primate | Not Specified (Review Focus) | - Functional recovery in motor tasks (e.g., apomorphine-induced rotation)- Increased survival of transplanted dopaminergic neurons | Dopaminergic neuron replacement; trophic factor support | [104] |
Table 2: Preclinical Outcomes of MSC-Laden Hydrogels in Peripheral Tissue Injury Models
| Disease Model | Animal Species | Hydrogel System | Key Quantitative Outcomes | Proposed Mechanism | Citation |
|---|---|---|---|---|---|
| Diabetic Wound Healing | Rodent (Mouse/Rat) | Natural polymer hydrogels (e.g., Collagen, Alginate) | - Reduction in wound healing time by ~30-40%- >50% increase in capillary density (angiogenesis)- Increased collagen deposition and improved collagen alignment | Enhanced MSC secretion of VEGF, SDF-1; macrophage polarization to M2 phenotype; improved re-epithelialization | [64] |
| Myocardial Infarction | Porcine, Rodent | Injectable decellularized ECM hydrogels, PEG | - ~25% improvement in ejection fraction- Significant reduction in scar tissue area- Increased border zone vascularity | Attenuation of adverse remodeling; cardiomyocyte survival; angiogenesis | [3] |
| Cartilage Repair | Porcine, Rodent | Composite ECM-Synthetic hydrogels | - Superior regeneration of hyaline-like cartilage vs. empty defect- High integration with native tissue- Improved mechanical properties of repaired tissue | Support of chondrogenic differentiation; provision of biomechanical cues | [3] |
Detailed Experimental Protocols
Protocol: Fabrication of a Preclinical MSC-Laden Hydrogel for Wound Healing
This protocol outlines the steps for creating a cytokine-preconditioned MSC-laden collagen-based hydrogel for use in a murine diabetic wound model [64].
I. Materials
- Primary Cells: Human Umbilical Cord MSCs (HUC-MSCs) or Bone Marrow-derived MSCs (BMSCs).
- Hydrogel Polymer: Type I Collagen solution (e.g., from rat tail tendon).
- Preconditioning Agent: Recombinant Human TGF-β1 cytokine.
- Culture Reagents: MSC expansion medium (e.g., DMEM/F12, 10% FBS, 1% Penicillin/Streptomycin), PBS, trypsin/EDTA.
- Animals: Diabetic (e.g., db/db) mice, 8-12 weeks old.
- Equipment: Sterile biosafety cabinet, cell culture incubator (37°C, 5% CO2), centrifuge.
II. Methodology
Step 1: Preconditioning of MSCs
- Culture HUC-MSCs to 80% confluence in standard expansion medium.
- Replace the medium with fresh medium containing a defined concentration of TGF-β1 (e.g., 10 ng/mL).
- Incubate the cells for 24-48 hours under standard culture conditions (37°C, 5% CO2).
- After incubation, wash the cells with PBS and proceed to harvesting.
Step 2: Harvesting and Preparing the MSC Suspension
- Aspirate the preconditioning medium and wash the cell layer with PBS.
- Add sufficient trypsin/EDTA to cover the cells and incubate until cells detach.
- Neutralize the trypsin with complete medium and collect the cell suspension.
- Centrifuge the suspension at 300 x g for 5 minutes. Aspirate the supernatant and resuspend the cell pellet in an appropriate volume of PBS or serum-free medium.
- Perform a cell count and adjust the concentration to 1 x 10^7 cells/mL for hydrogel encapsulation.
Step 3: Hydrogel Preparation and Cell Encapsulation
- On ice, mix the sterile collagen solution with the predetermined volume of cell suspension to achieve a final cell density of 5 x 10^6 cells/mL within the hydrogel and a final collagen concentration of 5 mg/mL. Gently mix to avoid bubble formation.
- To induce gelation, add neutralization solution (e.g., a mixture of NaOH and HEPES-buffered saline) as per the manufacturer's instructions. The mixture will become viscous.
- Quickly transfer the cell-hydrogel mixture to the wound bed or a pre-chilled mold.
Step 4: In Vivo Implantation in a Diabetic Mouse Model
- Anesthetize the db/db mouse and create a full-thickness excisional wound (e.g., 8 mm diameter) on the dorsum.
- Carefully pipette 100 µL of the pre-gel solution (containing 500,000 preconditioned MSCs) directly into the wound bed, ensuring even coverage.
- Allow the hydrogel to solidify for 1-2 minutes at room temperature before applying a sterile semi-occlusive dressing.
- Monitor wounds every second day for closure rate and collect tissue samples at predetermined endpoints for histological and molecular analysis.
Protocol: Establishing a Transgenic Rodent Model for Neurodegenerative Disease
This protocol describes the general approach for utilizing transgenic animal models to test MSC-hydrogel therapies for Alzheimer's Disease [104].
I. Materials
- Animals: Transgenic mice (e.g., APP23, Tg2576, PS2APP) expressing human mutant genes associated with AD (e.g., APP, PSEN1).
- Genotyping Kits: DNA extraction kit, PCR reagents, primers specific for the transgene.
II. Methodology
- Animal Acquisition and Colony Maintenance: Acquire breeding pairs from a reputable repository. Maintain the colony under specific pathogen-free (SPF) conditions with a 12-hour light/dark cycle.
- Genotyping: At weaning (3-4 weeks of age), perform ear clipping for unique identification and DNA collection. Extract genomic DNA and perform PCR analysis with transgene-specific primers to identify positive transgenic animals and wild-type littermate controls.
- Baseline Phenotyping: At the age of interest (e.g., 6 months for early pathology), conduct baseline behavioral tests (e.g., Morris water maze for spatial memory, open field for anxiety and locomotion) to confirm disease phenotype.
- Therapy Administration: Anesthetize the animal and secure it in a stereotaxic frame. Using a micro-syringe pump, inject a low volume (e.g., 2-5 µL) of the MSC-laden hydrogel construct stereotaxically into the target brain region (e.g., hippocampus or lateral ventricle).
- Post-operative Monitoring and Analysis: Allow the animal to recover and monitor daily for well-being. Repeat behavioral tests at defined intervals post-treatment. At the study endpoint, perfuse the animal transcardially with PBS followed by 4% PFA. Extract brains for subsequent immunohistochemical (e.g., for Aβ plaques, tau tangles, synaptic markers) and biochemical analyses.
Signaling Pathways and Experimental Workflows
The therapeutic effect of MSC-laden hydrogels is mediated by complex signaling pathways. The diagram below illustrates the key mechanisms by which MSCs, supported by a hydrogel scaffold, facilitate wound healing.
Diagram 1: Signaling Mechanisms of MSC-Laden Hydrogels in Wound Healing. This workflow illustrates how the construct modulates the three phases of healing via paracrine signaling and direct differentiation, leading to controlled inflammation, tissue regeneration, and reduced scarring [64].
The general workflow for conducting a preclinical efficacy study, from hydrogel design to outcome analysis, is standardized. The following diagram outlines this critical path.
Diagram 2: Preclinical Evaluation Workflow for MSC-Hydrogel Therapies. This pathway outlines the key stages from biomaterial preparation and cell processing to in vivo testing and final analysis in a clinically relevant animal model [3] [64].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Preclinical MSC-Hydrogel Studies
| Research Reagent | Function/Application | Specific Examples |
|---|---|---|
| Mesenchymal Stromal Cells (MSCs) | Therapeutic agent; source of paracrine factors and differentiated cells. | Human Umbilical Cord MSCs (HUC-MSCs), Bone Marrow-derived MSCs (BMSCs), Adipose-derived MSCs (ADSCs) [64]. |
| Natural Polymer Hydrogels | Biomimetic 3D cell delivery scaffold; provides structural support. | Type I Collagen, Hyaluronic Acid, Fibrin, Alginate [3] [64]. |
| Synthetic Polymer Hydrogels | Tunable, reproducible scaffold with defined mechanical properties. | Polyethylene Glycol (PEG), Polyvinyl Alcohol (PVA) [3]. |
| Decellularized ECM Hydrogels | Highly bioactive scaffold mimicking native tissue microenvironment. | Porcine or bovine-derived myocardial, dermal, or cartilage ECM [3]. |
| Preconditioning Agents | Enhance MSC resilience, paracrine activity, and therapeutic function prior to transplantation. | Cytokines (TGF-β1, IFN-γ, IL-1β), Pharmacological agents (α-ketoglutarate, Caffeic acid) [64]. |
| Stimuli-Responsive Hydrogels | "Smart" materials enabling controlled release of cells/drugs in response to physiological cues (pH, enzymes). | Enzyme-degradable (MMP-sensitive) peptides, temperature-sensitive polymers (e.g., Poloxamers) [3]. |
| Transgenic Animal Models | Preclinical models that recapitulate genetic and pathological features of human diseases. | APP/PS1 mice (Alzheimer's), db/db mice (Diabetic Wounds) [104] [64]. |
The translation of regenerative medicine from laboratory research to clinical application represents a significant frontier in modern medicine. Within this field, stem cell-based therapies, particularly those utilizing mesenchymal stromal cells (MSCs), have emerged as a promising strategy for treating conditions ranging from musculoskeletal defects to cardiac injury [3]. However, the therapeutic efficacy of MSCs is often compromised by poor cell survival, rapid washout from the target site, and insufficient integration within the hostile injury microenvironment [3] [64]. To address these challenges, biomaterial scaffolds, especially hydrogels, have been developed as advanced delivery systems that enhance cell retention, viability, and function [3] [105]. This application note provides a structured framework for analyzing data from early-phase clinical trials investigating these innovative therapies, with a specific focus on feasibility, safety, and preliminary efficacy endpoints. The guidance is framed within the context of a broader thesis on stem cell delivery methods, underscoring the pivotal role of scaffold design in therapeutic success.
Quantitative Data Synthesis from Early-Phase Trials
Early-phase trials for scaffold-based stem cell therapies must establish a foundation for later-stage studies. The following tables synthesize key quantitative metrics for feasibility, safety, and efficacy from recent clinical research.
Table 1: Feasibility and Safety Profile in Early-Phase Clinical Trials
| Metric Category | Specific Parameter | Reported Outcome / Typical Benchmark | Relevant Indication(s) |
|---|---|---|---|
| Manufacturing Feasibility | Rate of successful product manufacture | >95% success rate using GMP-compliant, xeno-free components [3] | Broadly applicable |
| Final cell viability post-encapsulation | Typically required to be >70-80% pre-implantation [3] | Broadly applicable | |
| Procedure Feasibility | Success rate of scaffold delivery | High for injectable systems; conforms to irregular defect geometries [3] | Bone, Cardiac, Dermal |
| In-situ gelation time | Tunable from seconds to minutes for injectable hydrogels [3] | Broadly applicable | |
| Short-Term Safety | Treatment-Emergent Adverse Events (TEAEs) | Majority mild-to-moderate; comparable to control groups [106] | Advanced Heart Failure |
| Serious Adverse Events (SAEs) | Not attributed to MSC-hydrogel product in multiple trials [3] [106] | Advanced Heart Failure, Bone Defects | |
| Long-Term Safety | Ectopic tissue formation | Not reported in reviewed studies [3] [105] | Bone, Musculoskeletal |
| Systemic immunogenicity | Low, due to immunomodulatory properties of MSCs [105] | Broadly applicable |
Table 2: Preliminary Efficacy Endpoints in Specific Indications
| Therapeutic Area | Primary Efficacy Endpoint | Reported Outcome | Cell Delivery System |
|---|---|---|---|
| Advanced Heart Failure [106] | Left Ventricular Ejection Fraction (LVEF) | Improvement of 2-5% in MSC groups vs. control | Intramyocardial/Intracoronary injection |
| Minnesota Living with Heart Failure Questionnaire (MLHFQ) | Score improvement (~10 points) noted | Intramyocardial/Intracoronary injection | |
| 6-Minute Walk Test (6MWT) | Increased distance (20-50 meters) | Intramyocardial/Intracoronary injection | |
| Bone Fracture/Non-Union [105] | Radiographic bone union | Significant improvement vs. control in pilot trials | Injectable gels, 3D-printed scaffolds |
| Defect bridging on CT scan | Accelerated time to bridging | Injectable gels, 3D-printed scaffolds | |
| Diabetic Wound Healing [64] | Wound closure rate | Significant acceleration vs. standard care | Hydrogel scaffolds |
| Complete wound closure time | Reduction in time to full re-epithelialization | Hydrogel scaffolds |
Experimental Protocols for Key Analyses
Robust experimental protocols are essential for generating reliable data in early-phase trials. The following section details key methodologies.
Protocol for Assessing Feasibility of Hydrogel-Stem Cell Product Manufacturing
Objective: To standardize the manufacture and quality control of a sterile, functional MSC-laden hydrogel product. Materials: See "The Scientist's Toolkit" in Section 5. Procedure:
- MSC Expansion: Culture MSCs (from bone marrow, adipose tissue, or umbilical cord) under standard conditions. Use only cells between passages 3-5 to ensure potency and minimize senescence [105].
- Harvest and Mixing: At ~80% confluence, harvest cells via trypsinization. Count and resuspend the MSC pellet in a sterile, pre-gel solution (e.g., a functionalized PEG precursor or natural polymer like collagen or HA) to achieve a target concentration of 5-20 million cells/mL [3] [107].
- Viability Assessment (Pre-gel): Mix a small aliquot of the cell-polymer suspension with a viability stain (e.g., Trypan Blue). Cell viability must exceed 80% before proceeding.
- Product Formation: For injectable systems, load the cell-polymer mixture into a dual-barrel syringe system. Gelation is initiated upon mixing the precursor components, either immediately before or after injection, depending on the cross-linking mechanism (e.g., photo-initiation, ionic, thermal) [3] [108].
- Quality Control (QC):
- Sterility: Perform tests per pharmacopeia guidelines on a sample from each batch.
- Identity: Confirm MSC phenotype via flow cytometry for surface markers (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-) [105].
- Potency: Conduct an in vitro assay, such as osteogenic differentiation for bone applications or T-cell suppression for immunomodulation, to confirm biological activity [105].
Protocol for In Vivo Safety and Biodistribution Tracking
Objective: To evaluate the local and systemic safety, as well as the retention and persistence, of implanted MSC-laden hydrogels in a preclinical model. Materials: Luciferase or GFP-transfected MSCs, In Vivo Imaging System (IVIS), Histology reagents, Serum cytokine assay kits. Procedure:
- Cell Labeling: Use genetically engineered MSCs expressing a reporter gene (e.g., luciferase for bioluminescence) for sensitive tracking.
- Implantation: Administer the MSC-laden hydrogel into the target site (e.g., a critical-sized bone defect, myocardium) in an appropriate animal model. Include control groups (scaffold only, cells only, sham).
- Clinical Observation: Monitor animals daily for signs of distress, pain, or abnormal behavior for the study duration.
- Biodistribution Imaging (Weekly):
- Anesthetize animals injected with luciferase-expressing MSCs.
- Inject the substrate (D-luciferin) intraperitoneally.
- Acquire images using IVIS to quantify the bioluminescent signal, which correlates with viable cell mass and location [105].
- Serum Analysis (Terminal):
- Collect blood samples at study endpoint.
- Analyze serum for systemic inflammatory cytokines (e.g., IL-6, TNF-α) and troponins (for cardiac studies) to assess systemic inflammatory response or off-target damage [106].
- Histopathological Analysis:
- Harvest the target organ and key off-target organs (e.g., liver, lung, spleen).
- Process tissues for sectioning and staining with H&E.
- Score sections for local inflammation, fibrosis, foreign body response, and any evidence of ectopic tissue formation.
Protocol for Preliminary Efficacy Assessment in a Bone Defect Model
Objective: To quantitatively assess the bone regenerative capacity of an MSC-laden hydrogel in a critical-sized defect. Materials: Micro-CT scanner, Biomechanical tester, Histology reagents for bone (e.g., Alizarin Red, von Kossa). Procedure:
- Surgery and Implantation: Create a critical-sized segmental defect (e.g., 8mm in rat femur). Implant the test article (MSC-laden hydrogel) into the defect. Compare against empty defect, hydrogel-only, and standard-of-care (e.g., autograft) groups.
- Longitudinal Radiographic Analysis (4, 8, 12 weeks):
- Biomechanical Testing (Terminal, 12 weeks):
- Harvest the healed bone and dissect it free of soft tissue.
- Perform a torsion test to failure using a biomechanical testing system.
- Calculate the ultimate torque and stiffness of the regenerated bone. Compare these values to those of native, unoperated bone to determine the percentage of mechanical recovery [107].
- Histomorphometry (Terminal):
- Process explanted bones for undecalcified histology.
- Stain sections with von Kossa (for mineral) and Alizarin Red (for calcium).
- Quantify the percentage of the defect area that is positively stained for new bone formation.
Signaling Pathways and Experimental Workflows
Understanding the mechanistic pathways and standardizing workflows is critical for trial design and data interpretation.
Diagram 1: Key signaling pathways through which hydrogel scaffolds influence mesenchymal stem cell (MSC) fate. The hydrogel provides both mechanical (stiffness, RGD peptides) and biochemical (BMP-2, Wnt ligands) cues that activate intracellular signaling cascades (YAP/TAZ, BMP/Smad, β-catenin), leading to the upregulation of the master transcription factor RUNX2 and subsequent osteogenic differentiation. Concurrently, MSCs exert therapeutic effects via paracrine secretion of factors that promote angiogenesis and immunomodulation [3] [105].
Diagram 2: A standardized workflow for early-phase clinical trials investigating MSC-hydrogel therapies. The process begins with robust preclinical validation and the development of a Good Manufacturing Practice (GMP)-compliant production process, culminating in a data-driven decision point for advancing the therapy to larger efficacy trials [3] [106].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for MSC-Hydrogel Therapy Development
| Item Category | Specific Example | Function / Rationale | Key Reference |
|---|---|---|---|
| Hydrogel Polymers (Natural) | Hyaluronic Acid (HA), Chitosan, Collagen, Decellularized ECM | Provides innate bioactivity, biocompatibility, and cell-adhesive motifs; mimics native tissue environment. | [3] [14] [109] |
| Hydrogel Polymers (Synthetic) | Polyethylene Glycol (PEG), Polyacrylamide (PAAm) | Offers highly tunable mechanical properties, controlled degradation, and reduced batch-to-batch variability. | [3] [108] |
| Biofunctionalization Agents | RGD Peptides, Acrylated RGD, BMP-2, VEGF | Confers specific bioactivity to guide cell adhesion, differentiation, and tissue-specific regeneration. | [3] [108] [105] |
| Crosslinkers | 4-armed PEG Acrylate (PEG-ACLT), 4-armed PEG Acrylamide (PEG-ACA) | Determines hydrogel network formation, stiffness, and degradation kinetics (ester-based vs. non-degradable). | [108] |
| Cell Tracking Reagents | Luciferase Reporter Genes, GFP, Cell Viability Stains (Calcein AM) | Enables non-invasive in vivo cell tracking (biodistribution, persistence) and in vitro viability assessment. | [105] |
| Characterization Kits | ELISA/Luminex for Cytokines, ALP Assay Kit, Alizarin Red S | Quantifies MSC secretory profile (paracrine function) and osteogenic differentiation potential. | [105] [109] |
The efficacy of cell-based therapies is profoundly influenced by the delivery system used to transport therapeutic cells to the target site. Conventional methods, primarily using saline solutions, often suffer from low cell retention and rapid dispersion from the implantation site. This application note provides a comparative analysis of an advanced hydrogel-based delivery system against conventional saline-based delivery for mesenchymal stem cells (MSCs) in bone fracture healing, detailing quantitative outcomes, experimental protocols, and essential research tools.
The following table summarizes the key quantitative findings from a direct comparison of hydrogel and saline carriers in a rat long bone fracture model, highlighting the superior performance of the hydrogel system across multiple parameters. [110]
Table 1: Comparative Quantitative Outcomes of Hydrogel vs. Saline MSC Carriers
| Parameter | Assessment Method | Group C (Saline) | Group H (Hydrogel) | Significance |
|---|---|---|---|---|
| MSC Survival (Signal Duration) | Fluorescence Imaging (Post-fracture) | Lasted <2 weeks | Lasted until 2 weeks | Longer in Group H |
| MSC Signal Intensity | Fluorescence Imaging (Radiance Efficiency) | Lower | Higher in each period | Higher in Group H |
| Early Chemokine Expression (2 weeks) | Western Blot | Baseline | ↑ SDF-1, ↑ MCP-1 | Significantly higher in Group H |
| Late Osteogenesis (6 weeks) | Western Blot (BMP-2, TGF-β1) | No significant difference | No significant difference | No inter-group difference |
| Bone Volume (BV) | Micro-CT (6 weeks) | Baseline | Higher | Significantly higher in Group H |
| Percentage Bone Volume (PBV) | Micro-CT (6 weeks) | Baseline | Higher | Significantly higher in Group H |
| Bone Mineral Density (BMD) | Micro-CT (6 weeks) | Baseline | Higher | Significantly higher in Group H |
Experimental Protocols
Protocol 1: Carrier Preparation and MSC Encapsulation
This protocol describes the preparation of hydrogel and saline carriers for MSC delivery. [110]
- Objective: To prepare a sterile, cell-compatible hydrogel carrier and a standard saline carrier for MSCs.
- Materials:
- Hydrogel polymer (e.g., Methacrylated Gelatin (GelMA), Polyethylene Glycol (PEG))
- Photoinitiator (e.g., Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP))
- Phosphate Buffered Saline (PBS) or Normal Saline (0.9% NaCl)
- Expanded and characterized MSCs (e.g., from rat bone marrow)
- Cell culture medium
- UV light source (for photocrosslinkable hydrogels)
- Sterile tubes, pipettes, and syringes
- Procedure:
- Hydrogel Precursor Solution: Dissolve the hydrogel polymer in PBS to a desired concentration (e.g., 5-10% w/v). Ensure sterility.
- Photoinitiator Addition: Mix in a photoinitiator (e.g., 0.1% w/v LAP) under low-light conditions.
- Cell Suspension: Centrifuge MSC culture, aspirate the medium, and resuspend the cell pellet.
- For Hydrogel (Group H): Resuspend the MSC pellet in a small volume of the hydrogel precursor solution to achieve the target cell density (e.g., 1-5 million cells/mL). Keep the cell-polymer mix on ice to prevent premature gelation. [110]
- For Saline (Group C): Resuspend the MSC pellet in normal saline to the same cell density. [110]
- Crosslinking (for Hydrogel): Load the cell-laden hydrogel precursor into a syringe. For photocrosslinking, expose the material to UV light (e.g., 365 nm, 5-10 mW/cm²) for a specified duration (e.g., 30-60 seconds) to form a stable gel. Alternatively, use ionically or thermally crosslinked systems per manufacturer instructions.
Protocol 2: In Vivo Fracture Model and Cell Delivery
This protocol outlines the surgical procedure for creating a long bone fracture in a rat model and administering the MSC-carrier constructs. [110]
- Objective: To establish a standardized long bone fracture model and compare the efficacy of different MSC carriers via direct local injection.
- Materials:
- Wistar rats (e.g., 8-12 weeks old)
- Anesthetic (e.g., Isoflurane)
- Surgical tools (scalpel, forceps, retractors)
- Bone fracture fixation system (e.g., intramedullary pinning)
- Sterile syringes and needles (e.g., 27G)
- Prepared MSC-carrier constructs (from Protocol 1)
- Procedure:
- Anesthesia and Preparation: Anesthetize the rat and shave the surgical site (e.g., hind limb). Disinfect the area with alternating betadine and alcohol swabs.
- Surgical Exposure: Make a skin incision and carefully dissociate the muscle tissue to expose the femoral shaft.
- Fracture Creation: Perform a standardized osteotomy (e.g., using a oscillating saw) to create a critical-sized segmental defect in the femur, or create a closed fracture model. [110]
- Stabilization: Stabilize the fracture using an appropriate internal fixation method like an intramedullary pin or an external fixator. [110]
- Carrier Injection: Using a sterile syringe, inject the prepared MSC-hydrogel precursor or MSC-saline suspension directly into the fracture site. Ensure the hydrogel precursor is injected prior to gelation if using in-situ forming systems. [110]
- Wound Closure: Suture the muscle layer and skin closed.
- Post-operative Care: Monitor animals and administer analgesics as per institutional animal care guidelines.
Protocol 3: Post-Analysis and Endpoint Assessment
This protocol describes the methods for analyzing MSC retention, protein expression, and bone healing at specified endpoints. [110]
- Objective: To quantify MSC survival, chemokine expression, and ultimate bone regeneration.
- Materials:
- In vivo imaging system (IVIS) for fluorescence
- Micro-Computed Tomography (Micro-CT) system
- Western blot equipment
- Antibodies against SDF-1, MCP-1, BMP-2, TGF-β1
- Tissue homogenizer
- Procedure:
- MSC Survival Tracking:
- If MSCs are labeled with a fluorescent marker (e.g., GFP, DiR), image live animals at multiple time points (e.g., day 1, 3, 7, 14) post-surgery using an IVIS system. [110]
- Quantify the total flux or radiance efficiency at the fracture site to compare signal intensity and duration between groups. [110]
- Protein Expression Analysis (2 weeks):
- Euthanize a subset of animals at 2 weeks post-operation.
- Harvest the fracture callus tissue and homogenize it in RIPA buffer with protease inhibitors.
- Perform Western blot analysis on the protein lysates to assess the expression levels of early chemokines (SDF-1, MCP-1). [110]
- Micro-CT Evaluation (6 weeks):
- At the 6-week endpoint, harvest the intact femurs.
- Scan the bones using a micro-CT system at a defined isotropic resolution (e.g., 10-20 μm).
- Reconstruct the 3D images and use analysis software to calculate morphometric parameters: Bone Volume (BV), Percentage Bone Volume (PBV; BV/TV), and Bone Mineral Density (BMD). [110]
- Late Osteogenesis Marker Analysis (6 weeks):
- Analyze a separate set of 6-week callus samples via Western blot for osteogenesis-related proteins (BMP-2, TGF-β1). [110]
- MSC Survival Tracking:
Signaling Pathways and Experimental Workflow
The following diagrams illustrate the key signaling pathways influenced by the delivery system and the overall experimental workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Hydrogel-based Cell Delivery Research
| Item | Function/Description | Example Materials |
|---|---|---|
| Hydrogel Polymers | 3D scaffold that encapsulates cells, provides mechanical support, and enables sustained release. | Gelatin Methacryloyl (GelMA), Hyaluronic Acid (HA), Poly(Ethylene Glycol) (PEG), Fibrin, Chitosan [111] [112] [113] |
| Crosslinkers & Initiators | Facilitate the formation of the hydrogel's 3D network from a liquid precursor. | Photoinitiators (e.g., LAP), Calcium Chloride (for alginate), Enzymes (e.g., Transglutaminase) [112] |
| Therapeutic Cells | The active biological component for regenerative therapy. | Mesenchymal Stem Cells (MSCs from bone marrow, adipose, umbilical cord) [110] [13] |
| Characterization Equipment | Analyzes drug/cell release kinetics, mechanical properties, and degradation profile of the hydrogel. | UV-Vis Spectrophotometer, Rheometer, High-Performance Liquid Chromatography (HPLC) [111] |
| In Vivo Imaging System | Tracks the survival, retention, and location of labeled cells in live animals over time. | Fluorescence Imager (e.g., IVIS Spectrum) [110] |
| Micro-CT Scanner | Provides high-resolution 3D imaging and quantitative analysis of bone morphology and mineralization. | Skyscan, Scanco Medical systems [110] |
| Protein Analysis Tools | Detects and quantifies expression levels of specific proteins (chemokines, growth factors) in tissue samples. | Western Blot apparatus, Specific Antibodies (SDF-1, MCP-1, BMP-2) [110] |
The field of regenerative medicine is increasingly divided into two distinct yet complementary therapeutic paradigms: cell-based therapies and cell-free (secretome) approaches. Cell-based therapies involve the administration of living cells, such as Mesenchymal Stem Cells (MSCs), to repair damaged tissues through direct differentiation and paracrine signaling [114]. In contrast, cell-free therapies utilize the conditioned medium or secretome derived from these cells, which contains a multitude of bioactive molecules, growth factors, and extracellular vesicles (EVs) that mediate therapeutic effects without the risks associated with whole-cell transplantation [115]. Understanding the relative efficacy and safety profiles of these approaches is critical for clinical translation, particularly within the context of advanced delivery systems like hydrogels and tissue scaffolds.
The therapeutic landscape has evolved significantly from early cell-based approaches. While MSCs were initially valued for their multipotent differentiation potential, recent perspectives emphasize their paracrine activity as the primary mechanism of action [114]. The secretome contains epidermal growth factor (EGF), basic fibroblast growth factor (bFGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), hepatocyte growth factor (HGF), keratinocyte growth factor (KGF), and insulin-like growth factor (IGF) that collectively accelerate tissue regeneration [102]. This paradigm shift toward cell-free alternatives addresses critical challenges in cell-based therapy, including tumorigenicity risk, immune rejection, and storage/logistical complications [115].
Comparative Analysis of Therapeutic Profiles
The choice between cell-based and cell-free approaches requires careful consideration of their respective efficacy and safety profiles. The table below provides a structured comparison of key characteristics:
Table 1: Efficacy and Safety Comparison of Cell-Based and Cell-Free Therapies
| Parameter | Cell-Based Therapies | Cell-Free (Secretome) Therapies |
|---|---|---|
| Mechanism of Action | Direct differentiation; Paracrine signaling; Cell-cell contact [114] | Trophic signaling; Extracellular vesicle-mediated transfer of bioactive molecules [115] |
| Therapeutic Components | Living MSCs, Muse cells, immune cells [102] [114] | Growth factors, cytokines, exosomes, microvesicles, miRNAs [115] |
| Biodistribution | Variable engraftment; Potential pulmonary entrapment; Limited to damaged sites (Muse cells) [102] [116] | Superior tissue penetration; Cross blood-brain barrier; Systemic distribution [115] |
| Immunogenicity | Low but present; Allogeneic rejection risk [114] | Negligible; No HLA-mediated immune response [115] |
| Tumorigenicity Risk | Low but measurable (MSCs); Theoretical concern for malignant transformation [116] | Minimal; No replicative capacity [115] |
| Regulatory Complexity | High (cell viability, function, safety) [116] | Moderate (biomolecule characterization, potency) [115] |
| Storage & Stability | Cryopreservation required; Limited shelf life [116] | Lyophilization possible; Extended shelf life [115] |
| Dosing Precision | Cell number-based; Variable potency [114] | Protein/vesicle concentration-based; More standardized [115] |
Emerging Cell Types: Muse Cells
A notable advancement in cell-based therapy is the identification of Multilineage-differentiating stress enduring (Muse) cells. These endogenous, reparative cells exhibit pluripotent-like characteristics and are found in various tissues, including as a subpopulation in MSCs [102]. Unlike conventional MSCs, intravenously injected Muse cells selectively home to damaged tissues by sensing the universal damage signal sphingosine-1-phosphate, where they phagocytose damaged/apoptotic cells and directly differentiate into tissue-specific cells to repair three-dimensional structure [102]. Critically, clinical trials have demonstrated that HLA-mismatched donor Muse cells escape immune rejection and survive long-term in recipient tissues without immunosuppressant treatment, offering significant safety advantages over traditional MSCs [102].
Integration with Scaffold and Hydrogel Delivery Systems
The therapeutic efficacy of both cell-based and cell-free approaches can be significantly enhanced through integration with advanced delivery systems, particularly hydrogels. These water-swollen, crosslinked polymer networks provide a three-dimensional microenvironment that recapitulates key features of the native extracellular matrix, supporting cell viability, retention, and function upon transplantation [3].
Table 2: Hydrogel Design Parameters for Cell-Based and Cell-Free Therapies
| Hydrogel Property | Impact on Cell-Based Therapy | Impact on Cell-Free Therapy |
|---|---|---|
| Mechanical Stiffness | Guides differentiation (1-10 kPa for neurogenesis; 25-40 kPa for osteogenesis) [3] | Modulates release kinetics; Affects host tissue integration |
| Degradation Profile | Must align with tissue regeneration timeline [3] | Controls factor release duration; Should match therapeutic window |
| Porosity & Architecture | Affects nutrient diffusion, waste elimination, cell migration [3] | Influences host cell infiltration and vascularization |
| Bioactive Cues (RGD, Growth Factors) | Enhances cell adhesion, activates integrin signaling [3] | Can be engineered to sequester and release therapeutic factors |
| Injectable Formulation | Minimally invasive administration; Conforms to defect geometry [3] | Enables precise localization of therapeutic factors |
| Stimuli-Responsiveness | Enables controlled cell release in response to physiological cues [3] | Allows on-demand release of bioactive factors |
For cell-based approaches, MSC-laden hydrogels have demonstrated enhanced tissue repair across diverse pathological contexts, including musculoskeletal, cardiovascular, gastrointestinal, dermal, and neural injuries [3]. The hydrogel microenvironment supports MSC viability and function while preventing washout from the injury site. Similarly, for cell-free therapies, hydrogels can be engineered to encapsulate and controllably release the secretome components, including exosomes and growth factors, providing sustained therapeutic exposure at the target site [3].
Advanced "smart" hydrogel designs incorporate environmental triggers (e.g., pH, temperature, enzymatic activity) to enable controlled release of encapsulated cells or bioactive molecules [3]. These systems can prolong therapeutic action and support tissue remodeling. Additionally, composite hydrogels combining natural polymers (e.g., alginate, collagen, hyaluronic acid) with synthetic variants (e.g., polyethylene glycol) leverage the bioactivity of natural materials with the mechanical tunability of synthetic polymers [3].
Experimental Protocols and Assessment Methodologies
Protocol: Assessment of MSC Secretome Composition and Bioactivity
Objective: To isolate, characterize, and evaluate the therapeutic potential of MSC-derived secretome, including extracellular vesicles (EVs) and soluble factors.
Materials:
- Research Reagent Solutions:
- DMEM/F12 serum-free medium: For secretome collection without serum contamination
- Protease and phosphatase inhibitors: Preserve protein and phosphoprotein integrity
- Exosome Isolation Kit: For EV purification (e.g., precipitation-based or size-exclusion chromatography)
- BCA Protein Assay Kit: Quantify total protein content
- ELISA Kits: Specific for VEGF, FGF, IGF-1, TGF-β1 quantification
- NanoSight NS300: Nanoparticle tracking analysis for vesicle size and concentration
- Transwell migration assay: Evaluate chemotactic properties
- Endothelial tube formation assay: Assess pro-angiogenic potential
Methodology:
- Cell Culture and Secretome Collection:
- Culture MSCs (umbilical cord, adipose, or bone marrow-derived) to 80% confluence
- Replace with serum-free medium and culture for 24-48 hours
- Collect conditioned medium and centrifuge at 2,000 × g for 30 minutes to remove cells and debris
- Concentrate using 3 kDa molecular weight cut-off filters
Extracellular Vesicle Isolation:
- Process conditioned medium using exosome isolation kit per manufacturer's instructions
- Characterize EVs by nanoparticle tracking (size distribution: 30-200 nm) and Western blotting for CD63, CD81, TSG101 markers
- Quantify particle concentration and protein content
Functional Bioactivity Assays:
- Angiogenesis Assay: Seed human umbilical vein endothelial cells (HUVECs) on Matrigel; add secretome samples; quantify tube length and branch points after 6-18 hours
- Anti-apoptotic Assay: Induce apoptosis in target cells with H₂O₂; treat with secretome; measure caspase-3/7 activity and cell viability
- Immunomodulation Assay: Activate peripheral blood mononuclear cells with lipopolysaccharide; co-culture with secretome; quantify cytokine levels (IL-10, TNF-α) via ELISA
Protocol: Evaluation of Cell-Based Therapies in 3D Hydrogel Systems
Objective: To assess the viability, functionality, and therapeutic efficacy of MSCs or Muse cells encapsulated within hydrogel delivery systems.
Materials:
- Research Reagent Solutions:
- Methacrylated gelatin (GelMA) or Hyaluronic Acid (HAMA): Photocrosslinkable hydrogel precursors
- Photoinitiator (LAP or Irgacure 2959): For UV-induced crosslinking
- CellTracker dyes (CMFDA, CMTMR): For long-term cell tracking
- AlamarBlue or MTT reagent: Assess metabolic activity and viability
- Live/Dead viability/cytotoxicity kit: Distinguish live vs. dead cells
- Histology reagents (formalin, paraffin, sectioning equipment): For structural analysis
- Immunofluorescence staining antibodies: For cell-specific markers
Methodology:
- Hydrogel Preparation and Cell Encapsulation:
- Prepare 5-10% (w/v) GelMA or HAMA solution in PBS with 0.1% photoinitiator
- Trypsinize, count, and resuspend MSCs or Muse cells in hydrogel precursor solution at 5-20 × 10⁶ cells/mL
- Pipette 50-100 μL of cell-hydrogel mixture into molds and crosslink with UV light (365 nm, 5-10 mW/cm²) for 30-60 seconds
- Culture constructs in complete medium, changing every 2-3 days
Viability and Function Assessment:
- Live/Dead Staining: At days 1, 3, 7, and 14, incubate constructs with calcein-AM (2 μM) and ethidium homodimer-1 (4 μM) for 30-45 minutes; image with confocal microscopy
- Metabolic Activity: Incubate with AlamarBlue (10% v/v) for 2-4 hours; measure fluorescence (560/590 nm)
- Gene Expression Analysis: Extract RNA from hydrolyzed constructs; perform RT-qPCR for lineage-specific markers (SOX9, RUNX2, PPARγ) and paracrine factors (VEGF, HGF, TGF-β)
In Vivo Transplantation and Analysis:
- Implant MSC-laden hydrogels subcutaneously in immunodeficient mice or disease models
- Harvest constructs at 2, 4, and 8 weeks for histology (H&E, Masson's trichrome) and immunohistochemistry (human-specific antibodies)
- Assess biodistribution using in vivo imaging if cells are pre-labeled with luciferase or fluorescent reporters
Safety Assessment Frameworks
Robust safety assessment is essential for both cell-based and cell-free therapies, with particular considerations for each approach. Regulatory agencies like the FDA and EMA require comprehensive evaluation of multiple critical parameters before clinical translation [116].
Table 3: Safety Assessment Parameters for Cell-Based and Cell-Free Therapies
| Safety Parameter | Cell-Based Assessment Methods | Cell-Free Assessment Methods |
|---|---|---|
| Tumorigenicity | Soft agar colony formation; In vivo tumor formation in immunodeficient mice [116] | N/A (lacks replicative capacity) |
| Immunogenicity | Mixed lymphocyte reaction; HLA typing; Cytokine release assays [116] | Complement activation; Cytokine profiling |
| Biodistribution | qPCR for species-specific DNA; In vivo imaging (PET, MRI) [116] | Fluorescent dye labeling; Radioisotope tracking |
| Toxicity Profile | Clinical pathology; Histopathology of major organs [116] | Standard toxicology studies; Organ function tests |
| Product Quality | Sterility, identity, potency, viability, genetic stability [116] | Bioburden, endotoxin, potency, stability |
For cell-based therapies, a critical safety consideration is the oncogenic potential, which can be assessed using a combination of in vitro methods and in vivo models in immunocompromised animals [116]. Additionally, biodistribution patterns must be thoroughly evaluated using quantitative PCR and imaging techniques (PET, MRI) to monitor cell fate over time [116]. Immunogenicity studies are essential to understand how transplanted cells interact with the recipient's immune system, including assessment of potential immune activation or rejection.
For cell-free therapies, while risks associated with whole cells are eliminated, comprehensive characterization of the secretome composition is essential. This includes quantification of individual components, stability studies, and assessment of potential off-target effects [115]. The batch-to-batch consistency must be rigorously controlled, and potency assays developed to ensure predictable therapeutic effects [115].
Signaling Pathways and Mechanisms of Action
The therapeutic mechanisms of cell-based and cell-free therapies involve complex signaling pathways that modulate inflammation, promote tissue repair, and stimulate regeneration. The diagram below illustrates the key pathways involved in MSC and secretome-mediated tissue repair:
Diagram 1: Mechanisms of Action in Cell-Based and Cell-Free Therapies
For cell-based approaches, MSCs exert their effects through multiple mechanisms, including direct differentiation into tissue-specific cells, paracrine signaling via soluble factors, and cell-cell contact mediating immunomodulation [114]. Additionally, MSC-derived extracellular vesicles facilitate EV-mediated communication through transfer of miRNAs and other regulatory molecules that alter gene expression in recipient cells [115].
In contrast, cell-free therapies primarily work through the soluble factors and extracellular vesicles present in the secretome. These components activate growth factor signaling pathways, modulate cytokine networks, deliver mRNA for protein synthesis, and provide regulatory miRNAs that promote cellular rejuvenation [115]. A key mechanism involves macrophage polarization from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype, creating a tissue environment conducive to regeneration [102].
The choice between cell-based and cell-free therapeutic approaches depends on multiple factors, including the specific clinical application, safety considerations, manufacturing capabilities, and regulatory pathways. Cell-based therapies offer the potential for structural integration and long-term tissue regeneration, particularly through advanced cell types like Muse cells that demonstrate superior engraftment and differentiation capacity [102]. However, they present greater challenges in terms of safety assessment, storage, and regulatory approval.
Cell-free therapies provide a compelling alternative with favorable safety profiles, reduced regulatory complexity, and enhanced stability [115]. Their ability to cross biological barriers like the blood-brain barrier makes them particularly attractive for neurological applications [115]. However, they may lack the sustained therapeutic effect of living cells and require more frequent administration.
The future of regenerative medicine likely lies in hybrid approaches that combine the advantages of both paradigms. This could involve using cell-free therapies for acute conditions or as initial treatment, followed by cell-based approaches for long-term structural repair. Additionally, advanced delivery systems like smart hydrogels can be engineered to optimize the performance of both cell-based and cell-free therapies, providing controlled release and enhanced localization at the target site [3].
Further research should focus on standardizing characterization methods, developing potency assays, and establishing clear regulatory frameworks for both therapeutic modalities. As the field evolves, the integration of these approaches with advanced biomaterials and delivery systems will undoubtedly expand their clinical applications and therapeutic potential.
Regulatory Landscapes and Standardization Challenges for Hydrogel-Based Products
Hydrogel-based products are increasingly pivotal in advanced therapeutic strategies, particularly for stem cell delivery. These three-dimensional, water-swollen polymer networks provide a biomimetic microenvironment that supports stem cell viability, retention, and function upon transplantation [3]. However, their intricate polymer structures and dynamic biological interactions present significant regulatory and standardization challenges. The translation of these sophisticated biomaterials from research to clinical application requires navigating complex regulatory frameworks that vary globally, while simultaneously establishing robust, reproducible characterization protocols. This document outlines the current regulatory considerations for hydrogel-based stem cell products and provides detailed experimental protocols for standardized characterization, serving as a practical resource for researchers and developers in the field.
Regulatory Frameworks for Hydrogel-Based Products
Regulatory bodies classify hydrogel-based products depending on their primary mode of action, composition, and intended use. For stem cell delivery applications, they are often regulated as combination products, where the hydrogel acts as a delivery scaffold (medical device component) for the biological entity (stem cells) [3] [117].
Classification by Region
The regulatory pathway and requirements can differ significantly across major markets. The following table summarizes the key regulatory considerations in the United States, European Union, and India.
Table 1: Regional Regulatory Landscapes for Hydrogel-Based Biomedical Products
| Region & Regulatory Body | Classification & Pathway | Key Standards & Considerations |
|---|---|---|
| United States (US FDA) | Class I, II, or III medical device, or as a combination product (device + biologic) [117]. | Biocompatibility (ISO 10993) [118], sterility, proof-of-concept data, quality control for raw materials, and comprehensive preclinical testing [3]. |
| Europe (EU MDR) | Class I, IIa, IIb, or III under Medical Device Regulation (MDR). | Requires a notified body, strict risk assessment, clinical evaluation, and post-market surveillance. Compliance with general safety and performance requirements (Annex I of MDR) is mandatory [117]. |
| India (CDSCO) | Classified as a medical device under the Central Drugs Standard Control Organization (CDSCO) [117]. | Adherence to standards set by the Indian government, which are increasingly aligned with international norms, though specific pathways are less detailed in the available literature [117]. |
Key Standardization Challenges
Despite established frameworks, several challenges persist in standardizing hydrogel-based products for stem cell delivery:
- Batch-to-Batch Variability: Natural polymer-based hydrogels (e.g., collagen, alginate) can exhibit variations between production batches, affecting performance and complicating regulatory approval [118] [25]. Implementing rigorous quality control over raw materials and manufacturing processes is critical.
- Complex and Dynamic Properties: Hydrogels are not inert; their mechanical properties, degradation kinetics, and interaction with cells are dynamic [25]. Regulators require evidence that these properties are consistently characterized and controlled [3].
- Scalability and Manufacturing: Translating lab-scale hydrogel fabrication to Good Manufacturing Practice (GMP)-compliant, large-scale production presents significant hurdles in maintaining sterility, purity, and function [3].
- Benchmarking and Phantom Development: The development of reliable hydrogel-based standards and phantoms is critical for validating and optimizing new imaging and characterization techniques used in quality control and preclinical testing [119].
Essential Characterization Protocols for Hydrogel-Based Stem Cell Carriers
A standardized characterization workflow is fundamental for research reproducibility, product development, and regulatory submissions. The following protocols detail key experiments to profile hydrogel properties relevant to stem cell delivery.
Protocol 1: Microarchitectural Analysis via Scanning Electron Microscopy (SEM)
Principle: SEM provides high-resolution, nanometer-scale visualization of the hydrogel surface topography, pore structure, and fiber morphology, which directly influence cell migration, aggregation, and nutrient diffusion [120].
Materials:
- Hydrogel sample (cell-free, critical point dried)
- Conductive coating (gold or carbon)
- Scanning Electron Microscope
Procedure:
- Sample Preparation: Synthesize hydrogel and freeze at -80°C. Lyophilize to preserve the native microarchitecture by removing water without collapsing the porous structure [120].
- Mounting and Coating: Mount the dried hydrogel on an SEM stub using conductive tape. Sputter-coat the sample with a thin layer (~10-20 nm) of gold or carbon to render it conductive [120].
- Imaging and Analysis: Transfer the sample to the SEM chamber. Image at an accelerating voltage of 5-15 kV. Capture multiple micrographs from different areas and batches to ensure representative analysis.
- Quantification: Use image analysis software (e.g., ImageJ) to measure:
- Pore Size: Determine the average Feret's diameter of at least 100 pores.
- Porosity Percentage: Calculate the area fraction of void space relative to the total area.
- Fiber Diameter: Measure the width of polymeric strands at multiple points.
Reporting Standards: Report mean values ± standard deviation for all quantified parameters from a minimum of n=3 independent hydrogel batches.
Protocol 2: Rheological Profiling of Mechanical Properties
Principle: Rheometry quantifies the viscoelastic properties of hydrogels, which are known to direct stem cell fate decisions such as differentiation. It measures the storage modulus (G', elasticity) and loss modulus (G", viscosity) [25].
Materials:
- Rheometer with a parallel plate geometry
- Hydrogel precursor solution
Procedure:
- Instrument Setup: Load the precursor solution onto the rheometer Pelt plate pre-set to the gelation temperature (e.g., 37°C for many bio-hydrogels). Lower the upper plate to a defined gap (e.g., 500 μm), ensuring no slip at the interface.
- Time Sweep Experiment: Initiate gelation (e.g., via UV light for photocurable gels, or temperature change) while applying a small, constant oscillatory strain (e.g., 1%) and an angular frequency (e.g., 1 rad/s). Monitor G' and G" over time until the moduli plateau, indicating complete gelation. The crossover point of G' and G" is the gelation point [25].
- Amplitude Sweep: At the end of gelation, apply a range of oscillatory strains (e.g., 0.1% to 100%) at a fixed frequency to determine the linear viscoelastic region (LVER).
- Frequency Sweep: Within the LVER, apply a range of angular frequencies (e.g., 0.1 to 100 rad/s) to characterize the mechanical stability of the hydrogel network across different timescales.
Reporting Standards: Report the plateau G' and G" values from the time sweep, the gelation time, and the G' value from the frequency sweep at a physiologically relevant frequency (e.g., 1 rad/s).
Table 2: Target Mechanical Properties for Stem Cell Delivery in Various Tissues
| Target Tissue | Target Elastic Modulus (G') | Rationale |
|---|---|---|
| Adipose or Neural Tissue [3] | 1 - 10 kPa | Softer matrices promote adipogenic or neurogenic differentiation. |
| Musculoskeletal Tissue [3] | 25 - 40 kPa | Stiffer matrices favor osteogenic commitment. |
| General Injectable Carrier | G' > G" | Ensures solid-like behavior to prevent premature dissolution upon injection. |
Protocol 3: In Vitro Biocompatibility and Cell Function Assessment
Principle: This protocol evaluates hydrogel cytotoxicity and its ability to support key stem cell functions, including viability, proliferation, and self-renewal, within the 3D microenvironment.
Materials:
- Mesenchymal Stromal Cells (MSCs) or other relevant stem cells.
- Cell-laden hydrogel constructs.
- Cell culture reagents: culture medium, live/dead viability assay kit (e.g., calcein-AM/ethidium homodimer-1), PrestoBlue/MTT assay kit, reagents for immunohistochemistry (e.g., primary antibodies against stem cell markers like OCT4).
Procedure:
- Hydrogel Cell Encapsulation: Trypsinize and concentrate cells. Resuspend the cell pellet in the hydrogel precursor solution at the desired density (e.g., 1-5 million cells/mL). Cast the cell-polymer mixture into molds and induce gelation.
- Viability and Proliferation:
- Live/Dead Staining: At defined time points (e.g., days 1, 3, 7), incubate constructs with calcein-AM (for live cells) and ethidium homodimer-1 (for dead cells) for 30-45 minutes. Image using confocal microscopy and quantify the live cell percentage.
- Metabolic Activity: At each time point, transfer constructs to a new well with culture medium containing PrestoBlue reagent. Incubate for 1-4 hours, measure fluorescence/absorbance, and compare to a standard curve to estimate cell number.
- Self-Renewal Capacity Assessment:
- Gene Expression Analysis: Extract RNA from constructs and perform qRT-PCR for core pluripotency markers (e.g., OCT4, SOX2, NANOG).
- Immunohistochemistry: Fix constructs, section, and stain for stem cell markers. Positive staining indicates maintenance of an undifferentiated state.
- Pathway Analysis: As demonstrated in PG hydrogel studies, transcriptome sequencing can identify activated self-renewal pathways (e.g., non-canonical Wnt signaling) [121].
Reporting Standards: Include representative images from live/dead and immunohistochemistry stains. Provide quantitative data for metabolic activity and gene expression as mean ± SD from n≥3 independent experiments.
The Scientist's Toolkit: Essential Research Reagents
The following table lists key materials commonly used in the development and testing of hydrogels for stem cell delivery.
Table 3: Key Research Reagent Solutions for Hydrogel-Based Stem Cell Delivery
| Reagent / Material | Function & Application | Examples & Notes |
|---|---|---|
| Natural Polymers | Provide innate bioactivity and biocompatibility; mimic the native ECM. | Collagen [25], Gelatin Methacryloyl (GelMA) [121], Fibrin [120], Hyaluronic Acid (HA) [25]. |
| Synthetic Polymers | Offer high tunability, mechanical strength, and reproducibility. | Polyethylene Glycol (PEG) [118] [25], Polyacrylamide (PAAm) [119], Polyvinyl Alcohol (PVA) [25]. |
| Photoinitiators | Generate radicals under light to crosslink photocurable polymers. | Irgacure 2959 (for UV light) [119]; must be cytocompatible at working concentrations. |
| Bioactive Peptides | Functionalize synthetic hydrogels to enable cell adhesion. | RGD (arginine-glycine-aspartic acid) peptide [3] [25] to promote integrin-mediated cell binding. |
| Crosslinking Agents | Create stable chemical bonds between polymer chains. | N,N'-methylenebisacrylamide (for PAAm) [119]; Glutaraldehyde; enzymes like Transglutaminase (for specific natural polymers). |
Workflow and Signaling Pathway Visualization
Hydrogel Characterization and Regulatory Pathway Workflow
The following diagram outlines the key stages from hydrogel development to regulatory submission, integrating the characterization protocols outlined above.
Diagram 1: Hydrogel Development Workflow
Hydrogel-Stem Cell Signaling Interaction
Hydrogel properties directly influence stem cell fate through mechanotransduction and biochemical signaling. This diagram summarizes key pathways involved in maintaining self-renewal, as evidenced in studies with porous GelMA hydrogels [121].
Diagram 2: Stem Cell Signaling Pathway
Conclusion
Hydrogel scaffolds represent a paradigm shift in stem cell delivery, moving beyond passive carriers to active, tunable microenvironments that critically enhance therapeutic efficacy. The integration of advanced biofabrication, smart material science, and a deepened understanding of stem cell biology is key to overcoming current challenges in cell viability, functional integration, and manufacturing. Future progress hinges on the development of self-assembling and multifunctional 'smart' hydrogels capable of dynamic, spatiotemporal control over the healing process. Continued interdisciplinary collaboration, coupled with robust preclinical and clinical validation, is essential to fully realize the potential of these technologies, paving the way for a new generation of effective, standardized, and clinically accessible regenerative therapies.
References
- 1. Revisiting the biophysical aspects of extracellular-matrix ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d5bm00210a]
- 2. Hydrogels as Extracellular Matrix Analogs - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6318624/]
- 3. Mesenchymal stromal cell-laden hydrogels in tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464487/]
- 4. Extracellular-Matrix-Mimetic Hydrogels by Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155247/]
- 5. A Comparison of the Mechanical Properties of ECM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12023840/]
- 6. A Comprehensive Comparison of Human ECM Properties ... [https://www.mdpi.com/2079-4983/14/7/363]
- 7. Extracellular matrix-inspired hydrogel of hyaluronan and ... [https://www.nature.com/articles/s43246-022-00309-4]
- 8. Shape memory hydrogels in tissue engineering [https://www.sciencedirect.com/science/article/pii/S2452199X25003627]
- 9. Advances in the application of natural/synthetic hybrid hydrogels in tissue engineering and delivery systems: A comprehensive review - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0378517325001590]
- 10. Fundamental Concepts of Hydrogels: Synthesis, Properties, and Their Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7697203/]
- 11. Advances in natural polymer-based hydrogels: synthesis, applications, and future directions in biomedical and environmental fields | Discover Polymers [https://link.springer.com/article/10.1007/s44347-025-00017-5]
- 12. A comprehensive protocol for hydrogel-based bioink design [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb00737b]
- 13. Cell-engineered technologies for wound healing and ... [https://www.nature.com/articles/s44385-025-00042-w]
- 14. Biomaterials and stem cells targeting the microenvironment for ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01521e]
- 15. Getting physical: Material mechanics is an intrinsic cell cue [https://www.sciencedirect.com/science/article/pii/S193459092300173X]
- 16. Intrinsic Mechanical Cues and Their Impact on Stem Cells ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.761871/full]
- 17. Unlocking the therapeutic potential of cellular mechanobiology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577691/]
- 18. Stiffness-mediated mesenchymal stem cell fate decision in 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7382973/]
- 19. with programmed spatiotemporal Hydrogels for... mechanical cues [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003706/]
- 20. Effects of hydrogel stiffness and viscoelasticity on organoid ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01131-7]
- 21. A Review on the Design of Hydrogels With Different Stiffness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8822157/]
- 22. Frontiers | Bioelectric cues from piezoelectric materials in stem - cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1707436/full]
- 23. The Overview of Porous, Bioactive Scaffolds as Instructive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7407612/]
- 24. Recent Advances in 3D Bioprinting of Porous Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470888/]
- 25. Current hydrogel advances in physicochemical and ... [https://www.nature.com/articles/s41392-021-00830-x]
- 26. Topographic Orientation of Scaffolds for Tissue Regeneration [https://www.mdpi.com/2313-7673/7/3/131]
- 27. Injectable biodegradable polysaccharide-based hydrogels for ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb00287g]
- 28. Research Progress of Sodium Alginate-Based Hydrogels in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469324/]
- 29. Hydrogel scaffolds for tissue engineering: Progress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3963751/]
- 30. Perspective of 3D culture in medicine: transforming ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1491669/full]
- 31. The Natural and Engineered 3D Microenvironment as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2738762/]
- 32. 3D microniches reveal the importance of cell size and shape [https://www.nature.com/articles/s41467-017-02163-2]
- 33. Development of a simplified and scalable hydrogel-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123143/]
- 34. Hydrogels empowered mesenchymal stem cells and the ... [https://www.sciencedirect.com/science/article/pii/S104366182500043X]
- 35. Injectable micropore-forming microgel scaffold for neural ... [https://www.nature.com/articles/s41467-025-64240-1]
- 36. Research progress of hydrogels as delivery systems and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1111882/full]
- 37. An Introduction to 3D Bioprinting: Possibilities, Challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6266989/]
- 38. 3D bioprinting using stem cells | Pediatric Research [https://www.nature.com/articles/pr2017252]
- 39. Hydrogel-based 3D bioprinting: A comprehensive review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7414424/]
- 40. Bioprinting 101: Design, Fabrication, and Evaluation of Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7480731/]
- 41. 3D bioprinting of cell-laden constructs for regenerative ... [https://www.sciencedirect.com/science/article/pii/S2666138121000219]
- 42. A review on cell damage, viability, and functionality during 3D ... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-022-00429-5]
- 43. Hydrogels for 3D bioprinting in tissue engineering and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10339415/]
- 44. 3D bioprinting of high-performance hydrogel with in-situ ... [https://www.sciencedirect.com/science/article/pii/S2452199X24004365]
- 45. 3D Bioprinting of a Bioactive Composite Scaffold for Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10377653/]
- 46. Iterative feedback bio-printing-derived cell-laden hydrogel ... [https://www.nature.com/articles/s41598-018-21274-4]
- 47. In situ Forming Injectable Hydrogels for Drug Delivery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6003852/]
- 48. Unlocking the potential of stimuli-responsive injectable ... [https://www.frontiersin.org/journals/biomaterials-science/articles/10.3389/fbiom.2025.1641339/full]
- 49. Injectable Shear-Thinning Hydrogels for Minimally Invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5123705/]
- 50. Streamlined metal-based hydrogel facilitates stem cell ... [https://www.nature.com/articles/s41467-025-59725-y]
- 51. A comprehensive protocol for hydrogel-based bioink design [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb00737b]
- 52. The current status of nano-hydrogel preparations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259566/]
- 53. Multifunctional hydrogels: advanced therapeutic tools for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10403923/]
- 54. The Emerging Use of ASC/Scaffold Composites for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.893992/full]
- 55. The current status of nano-hydrogel preparations for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1611522/full]
- 56. A soft-hard hybrid scaffold for osteochondral regeneration ... [https://www.sciencedirect.com/science/article/pii/S0142961225004120]
- 57. Dynamic Hydrogel‐Based Strategy for Traumatic Brain Injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11717553/]
- 58. Engineering of an electrically charged hydrogel implanted ... [https://www.nature.com/articles/s41598-023-28870-z]
- 59. Exploration of biomaterial and stem cell-based strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574274/]
- 60. Carboxymethyl chitosan hydrogel synergistically regulates ... [https://www.sciencedirect.com/science/article/pii/S2590049825000840]
- 61. Stem cell therapies for neurological disorders [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-024-01987-1]
- 62. The Efficacy of Stem Cells in Wound Healing: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10931571/]
- 63. Hydrogel Scaffolds to Deliver Cell Therapies for Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8126987/]
- 64. Engineering strategies to enhance the research progress of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04471-7]
- 65. Designing biofunctional hydrogels for stem cell biology and ... [https://www.sciencedirect.com/science/article/abs/pii/S1226086X23005403]
- 66. Advancing wound healing by hydrogel-based dressings ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03976-x]
- 67. Mesenchymal Stem Cell Secretome: Toward Cell-Free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618501/]
- 68. Mesenchymal stem cells secretome: The cornerstone of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7789121/]
- 69. The tiny giants of regeneration: MSC-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310703/]
- 70. Updated protocols for cell lysate, secretome, and exosome ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000568]
- 71. Current Strategies and Therapeutic Applications of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11206583/]
- 72. RETRACTED ARTICLE: A paradigm shift in cell-free approach ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-02980-6]
- 73. Mesenchymal stromal cell-laden hydrogels in tissue ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1670649/full]
- 74. Different exosomes are loaded in hydrogels for the ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1545636/full]
- 75. Scaffold-free cell-based tissue engineering therapies [https://www.nature.com/articles/s41536-021-00133-3]
- 76. Engineering strategies to enhance the research progress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220656/]
- 77. Disease microenvironment preconditioning: An evolving ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925006915]
- 78. Synthetic thermoresponsive scaffolds for the expansion and ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04674b?page=search]
- 79. High throughput screening of mesenchymal stem cell lines ... [https://www.nature.com/articles/s41598-022-21653-y]
- 80. 3D cell cultures toward quantitative high-throughput drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0165614722000797]
- 81. Stimuli‐Responsive Biomaterials: Scaffolds for Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11468740/]
- 82. Stimuli-responsive smart materials: Bridging the gap ... [https://www.sciencedirect.com/science/article/abs/pii/S2405886625000314]
- 83. Advancements in Hydrogels: A Comprehensive Review of ... [https://www.mdpi.com/2073-4360/17/15/2026]
- 84. Hydrogel Conjugation: Engineering of Hydrogels for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300585/]
- 85. Research progress onconductive hydrogels and their ... [https://pubs.rsc.org/en/content/articlelanding/2025/ta/d5ta01456e]
- 86. Multidimensional exploration of hydrogels as biological ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1576524/full]
- 87. Recent advances and challenges of injectable hydrogels in ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500642X]
- 88. Recent advances in pre-conditioned mesenchymal stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03374-9]
- 89. Study of the Therapeutic Effect of Cytokine-Preconditioned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383953/]
- 90. preconditioning strategies for MSC-derived extracellular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 91. Hypoxia-induced metabolic reprogramming in mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183037/]
- 92. Enhanced therapeutic effects of hypoxia-preconditioned ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04166-z]
- 93. The Preservation of the Therapeutic Efficacy of the Secretome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473753/]
- 94. Natural and Synthetic Polymers for Biomedical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11055061/]
- 95. Bioactive potential of natural biomaterials [https://www.nature.com/articles/s41392-021-00512-8]
- 96. Using Polymeric Materials to Control Stem Cell Behavior ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5538808/]
- 97. Therapeutic synthetic and natural materials for ... [https://pubs.rsc.org/en/content/articlehtml/2024/cs/d3cs00805c]
- 98. Assessing cell migration in hydrogels: An overview of ... [https://www.sciencedirect.com/science/article/pii/S2590006422003350]
- 99. Engineering Lignin‐Based Tubular Hydrogel Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548947/]
- 100. Robust alginate/hyaluronic acid thiol–yne click-hydrogel ... [https://pubs.rsc.org/en/content/articlelanding/2020/bm/c9bm01494b]
- 101. Scaling Up Stem Cells [https://www.bioprocessintl.com/single-use/scaling-up-stem-cells]
- 102. Comparison of MSCs and Muse cells: the possible use for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12222320/]
- 103. A review: Carrier-based hydrogels containing bioactive ... [https://www.sciencedirect.com/science/article/pii/S2452199X25000143]
- 104. An update on mammalian and non-mammalian animal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977071/]
- 105. Functionalized mesenchymal stem cells for enhanced bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577075/]
- 106. A comprehensive review of clinical trials and Progress in stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514481/]
- 107. Engineering a stem cell-embedded bilayer hydrogel with ... [https://www.sciencedirect.com/science/article/pii/S2452199X25001033]
- 108. Hydrogels with programmed spatiotemporal mechanical ... [https://www.nature.com/articles/s41467-025-59016-6]
- 109. Hydrogel-Based Scaffolds: Advancing Bone Regeneration ... [https://www.mdpi.com/2310-2861/11/3/175]
- 110. Comparison of the effects of hydrogel and normal saline as ... [https://pubmed.ncbi.nlm.nih.gov/40629444/]
- 111. Hydrogels as Drug Delivery Systems: A Review of Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7762425/]
- 112. Tissue engineering: Hydrogel scaffolds and mechanical ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868625003021]
- 113. Innovative modification strategies and emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066444/]
- 114. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 115. Review Stem cell-free therapy for healthy brain aging [https://www.sciencedirect.com/science/article/pii/S0753332225008704]
- 116. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 117. Regulation of hydrogel-based products for biomedical ... [https://www.sciencedirect.com/science/article/abs/pii/B9780443292606000032]
- 118. How Hydrogel Works — In One Simple Flow ( 2025 ) [https://www.linkedin.com/pulse/how-hydrogel-works-one-simple-flow-2025-trend-analysts-s-ugbof]
- 119. Development of hydrogel-based standards and phantoms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10753126/]
- 120. A Beginner's Guide to the Characterization of Hydrogel ... [https://www.mdpi.com/2310-2861/8/9/535]
- 121. Topical delivery of cultivated limbal stem cells via porous ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925005206]