In Vivo Stem Cell Tracking: Imaging Techniques for Monitoring Therapeutic Efficacy and Safety
Stem cell therapies hold immense clinical potential for treating conditions from cardiovascular disease to neurological disorders.
In Vivo Stem Cell Tracking: Imaging Techniques for Monitoring Therapeutic Efficacy and Safety
Abstract
Stem cell therapies hold immense clinical potential for treating conditions from cardiovascular disease to neurological disorders. However, their clinical translation is hampered by an inability to non-invasively monitor transplanted cells in living subjects. This article provides a comprehensive overview of in vivo stem cell imaging techniques for researchers and drug development professionals. It explores the foundational principles of cell labeling, details the methodology and applications of major imaging modalities like MRI, PET, SPECT, and optical imaging, addresses key technical challenges and optimization strategies, and offers a comparative analysis for validating and selecting the appropriate imaging approach. The integration of these imaging technologies is crucial for elucidating stem cell fate, optimizing therapeutic protocols, and accelerating the safe transition of stem cell therapies from the laboratory to the clinic.
The Why and How: Foundational Principles of Stem Cell Tracking
The Critical Need for In Vivo Monitoring in Stem Cell Therapies
The field of stem cell therapies is reaching a pivotal juncture, with several treatments achieving significant regulatory milestones. Between 2023 and 2025, the FDA approved therapies like Omisirge for accelerating neutrophil recovery, Lyfgenia for sickle cell disease, and in late 2024, Ryoncil as the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease [1]. Simultaneously, the global clinical trial landscape for pluripotent stem cells (PSCs) has expanded, encompassing over 115 trials and more than 1,200 patients dosed by December 2024 [1]. This rapid clinical translation underscores an urgent and critical need: the development of reliable in vivo monitoring systems to track the fate, function, and efficacy of administered stem cells. In vivo monitoring is not merely a research tool but a fundamental component for ensuring patient safety, validating therapeutic mechanisms, and meeting the rigorous oversight demanded by international guidelines such as those from the International Society for Stem Cell Research (ISSCR) [2]. Without precise tracking, the scientific community cannot adequately address central questions about cell survival, migration, engraftment, and potential off-target effects, which are essential for the responsible advancement of regenerative medicine.
Key Monitoring Modalities: Principles and Applications
A range of sophisticated imaging and tracking modalities has been developed, each with unique principles, advantages, and limitations. The choice of modality depends on the specific research question, balancing requirements for spatial resolution, temporal resolution, depth of penetration, and quantifiability. The table below provides a structured comparison of the primary methodologies used for in vivo stem cell tracking.
Table 1: Core In Vivo Stem Cell Tracking Modalities
| Modality | Core Principle | Key Applications | Spatial Resolution | Penetration Depth | Key Quantitative Metric |
|---|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) [3] | Detects changes in T2 relaxation caused by internalized superparamagnetic iron oxide nanoparticles (SPIONs) | Tracking cell migration to injury sites; long-term engraftment studies | High (10-100 µm) | Unlimited | SPION density via voxel-based analysis of T2-weighted signal intensity |
| Positron Emission Tomography (PET) [3] | Detects gamma photons from positron-emitting radioisotopes (e.g., 18F-FDG, 64Cu) labeling cells | Real-time distribution and homing; cell viability via metabolic tracers | Low (1-2 mm) | Unlimited | Tracer uptake quantified as Standardized Uptake Value (SUV) in Region-of-Interest (ROI) |
| Bioluminescence Imaging (BLI) [3] | Detects photon emission from luciferase-expressing cells after substrate (luciferin) administration | Longitudinal cell survival and proliferation studies; high-throughput screening | Very Low (3-5 mm) | Limited (1-2 cm) | Photon flux (photons/second) measured by software like Living Image |
| Photoacoustic Imaging (PAI) [3] | Laser-pulsed contrast agents (e.g., gold nanorods) generate ultrasonic waves via thermoelastic expansion | Superficial structure imaging; tracking in highly vascularized tissues | Moderate (10-500 µm) | Limited (3-4 cm) | Signal amplitude correlating with density of labeled cells |
| Quantum Dots (QDs) [3] | Fluorescent semiconductor nanoparticles excited by external light source | High-resolution histological tracking; multicolor cell fate mapping | Very High (sub-cellular) | Very Limited | Fluorescence intensity analyzed via spectral unmixing |
Integrated Multi-Modality Imaging
No single modality provides a perfect solution; therefore, integrated approaches are increasingly employed to overcome individual limitations. For instance, a common strategy involves using PET/MRI with hybrid tracers like 64Cu-SPIONs [3]. This combination leverages the high sensitivity of PET for initial cell localization with the superior anatomical resolution and soft-tissue contrast of MRI for precise spatial mapping. Successful signal synchronization requires sophisticated voxel-wise co-registration algorithms and image fusion software (e.g., Amide, OsiriX) to align signal intensities temporally and spatially [3]. This multi-modality paradigm is becoming the gold standard for pre-clinical validation, providing a more comprehensive and reliable dataset on stem cell behavior in living organisms.
Detailed Experimental Protocols for Key Modalities
Protocol: MRI Tracking with SPIONs
Objective: To track the in vivo migration and persistence of human Mesenchymal Stem Cells (hMSCs) in a rodent model of cerebral ischemia using Magnetic Resonance Imaging.
Materials:
- Cells: Human MSCs (e.g., from Lonza, passages 3-5).
- Labeling Agent: Superparamagnetic Iron Oxide Nanoparticles (SPIONs), e.g., Ferucarbotran.
- Transfection Agent: Protamine sulfate.
- Imaging Instrument: 7-Tesla or higher preclinical MRI scanner.
Methodology:
- Cell Labeling:
- Culture hMSCs to ~80% confluence in standard growth media.
- Incubate cells with a serum-free medium containing SPIONs (e.g., 50 µg Fe/mL) and protamine sulfate (1.5 µg/mL) for 4-6 hours at 37°C under 5% CO₂ [3].
- Remove labeling medium, wash cells three times with PBS to eliminate excess nanoparticles, and trypsinize for harvesting.
- Cell Transplantation:
- Induce cerebral ischemia in the rodent model using standard methods (e.g., transient middle cerebral artery occlusion).
- At the desired time post-injury, inject 1x10⁶ SPION-labeled hMSCs in 5 µL of PBS stereotactically into the ipsilateral striatum or via intracarotid injection [3].
- In Vivo MRI Acquisition:
- Anesthetize the animal and place it in the MRI scanner with a dedicated rodent head coil.
- Acquire T2-weighted fast spin-echo sequences or T2*-weighted gradient-echo sequences. SPIONs create localized magnetic field inhomogeneities, appearing as hypointense (dark) signals on these scans [3].
- Perform baseline imaging pre-injection and follow up at multiple time points (e.g., days 1, 3, 7, 14 post-transplantation).
- Data Quantification:
- Analyze MRI data using software like ImageJ or custom algorithms.
- Perform voxel-based analysis to quantify the hypointense volume and signal intensity in the region of interest, which correlates with the local density and distribution of SPION-labeled cells [3].
- Correlate signal changes over time with behavioral or histological outcomes.
Protocol: Bioluminescence Imaging (BLI) for Cell Survival
Objective: To longitudinally monitor the survival and proliferation of induced Pluripotent Stem Cell (iPSC)-derived neural progenitor cells in an immunodeficient mouse model.
Materials:
- Cells: iPSC-derived neural progenitor cells genetically modified to stably express firefly luciferase (FLuc) reporter gene.
- Substrate: D-Luciferin, potassium salt (15 mg/mL in PBS).
- Imaging Instrument: In vivo imaging system (IVIS) equipped with a highly sensitive CCD camera.
Methodology:
- Cell Preparation and Transplantation:
- Harvest luciferase-expressing neural progenitor cells.
- Transplant 1x10⁶ cells in 2 µL per site via stereotactic injection into the target brain region (e.g., striatum or hippocampus) [3].
- Image Acquisition:
- At each imaging time point (e.g., weekly), intraperitoneally inject the mouse with D-luciferin (150 mg/kg body weight) [3].
- After 10-12 minutes (to allow for systemic distribution and substrate conversion), anesthetize the animal and place it in the imaging chamber.
- Acquire a photographic image followed by a bioluminescence image using an exposure time of 1-60 seconds, depending on signal strength.
- Data Quantification:
- Use integrated software (e.g., Living Image) to quantify the total photon flux.
- Define a Region of Interest (ROI) over the injection site and measure the radiance in units of photons per second per steradian per square centimeter (p/s/sr/cm²) [3].
- Plot radiance over time to generate a kinetic curve of cell survival and proliferation. A decreasing signal indicates cell death, while an increasing signal suggests proliferation.
Table 2: Key Reagent Solutions for Stem Cell Tracking
| Research Reagent / Material | Function / Application | Critical Considerations |
|---|---|---|
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) [3] | MRI contrast agent; internalized by cells for in vivo magnetic tracking. | Potential signal dilution upon cell division; degradation over time requires calibration; use of transfection agents (e.g., protamine) can enhance uptake. |
| Firefly Luciferase (FLuc) Reporter Gene [3] | Genetic label for bioluminescence imaging; enables monitoring of cell viability and location. | Requires genetic modification; signal is dependent on substrate (luciferin) bioavailability and cell metabolism; limited by tissue penetration depth. |
| Gold Nanorods [3] | Photoabsorbing contrast agent for Photoacoustic Imaging; converts light to sound. | Imaging efficacy is wavelength-dependent; allows for deeper tissue imaging than fluorescence. |
| Quantum Dots (QDs) [3] | Fluorescent nanoparticles for high-resolution histological tracking and multicolor imaging. | Potential cytotoxicity; susceptible to photobleaching over time; ideal for ex vivo or superficial in vivo applications. |
| 64Cu-SPION Conjugates [3] | Hybrid tracer for dual-modality PET/MRI imaging. | Enables correlative imaging with high sensitivity (PET) and high resolution (MRI); requires careful management of tracer dose and stability. |
| StemRNA Clinical iPSC Seed Clones [1] | GMP-compliant, master cell bank for deriving consistent, clinically relevant cell types. | Submission of a Drug Master File (DMF) to FDA streamlines regulatory submissions for therapy developers. |
Emerging Technologies and Future Directions
The field of stem cell monitoring is rapidly evolving beyond traditional tracking to include predictive functional assessment. A groundbreaking approach published in 2025 integrates quantitative phase imaging (QPI) with machine learning to forecast hematopoietic stem cell (HSC) diversity and functional quality [4]. This label-free technique analyzes temporal kinetic data—such as dry mass, sphericity, and division patterns—from individual live cells during ex vivo expansion. By applying a machine learning algorithm to this data, researchers can predict future stem cell function, such as lineage bias and long-term self-renewal capacity, based on past cellular behavior [4]. This represents a paradigm shift from static, snapshot identification to dynamic, predictive forecasting of stem cell potency.
Furthermore, advanced spectroscopic methods like Broadband Coherent Anti-Stokes Raman Scattering (BCARS) microscopy allow for quantitative, label-free characterization of stem cell lineage commitment. BCARS can chemically map hundreds of cells with high spatial resolution, revealing population heterogeneity by detecting intrinsic biochemical markers like lipids for adipocytes and minerals for osteoblasts [5]. These non-invasive technologies not only enhance the quality control of cell products prior to transplantation but also hold the potential to be adapted for in vivo sensing, paving the way for a new era of precision in regenerative medicine.
The successful clinical translation of stem cell therapies is inextricably linked to our ability to reliably monitor these living drugs within the patient. As evidenced by recent FDA approvals and the expanding clinical trial landscape, the field is maturing rapidly, making robust in vivo tracking a non-negotiable component of therapeutic development. The existing toolkit—spanning MRI, PET, BLI, and multi-modality approaches—provides powerful means to address critical questions of safety and efficacy. Meanwhile, emerging technologies like QPI-driven machine learning and advanced spectroscopy promise to further revolutionize the field by moving from simple location tracking to predictive functional assessment. Adherence to evolving international guidelines and the integration of these sophisticated monitoring protocols will ensure that the immense promise of stem cell therapies is realized safely, effectively, and ethically.
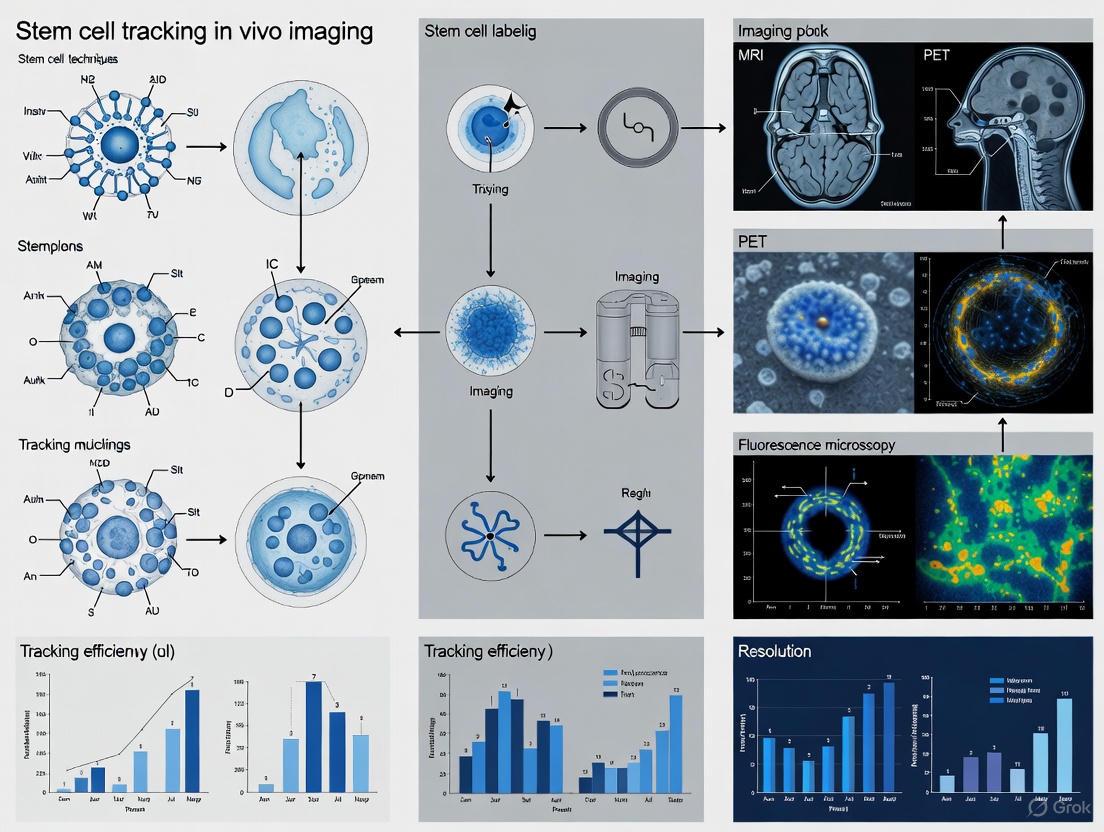
Visualized Workflows
Multi-Modality Cell Tracking Workflow
QPI-ML Predictive Analysis Pipeline
Tracking Cell Homing, Survival, Distribution, and Engraftment
The efficacy of stem cell therapies is fundamentally dependent on the successful journey of administered cells—their distribution throughout the body, targeted homing to sites of injury, subsequent survival in a hostile microenvironment, and long-term engraftment within the host tissue. Advanced in vivo imaging techniques are therefore indispensable for monitoring these dynamic processes non-invasively and longitudinally. These methodologies provide critical, quantitative data on cell fate, thereby accelerating the development and validation of regenerative therapies [6] [7]. This document outlines core protocols and application notes for tracking these critical cellular events, framed within the context of stem cell tracking for research and therapeutic development.
The selection of an appropriate imaging modality is a critical first step in experimental design, as each technology offers a unique balance of strengths and limitations. Key performance metrics include spatial resolution, temporal resolution, sensitivity, and depth penetration. The table below provides a comparative summary of major in vivo cell tracking techniques.
Table 1: Comparison of Key In Vivo Cell Tracking Modalities
| Tracking Modality | Spatial Resolution | Sensitivity (Cell Number) | Tracking Duration | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) [6] [7] | 25-100 µm | 10⁵ - 10⁶ | Weeks to Months | High anatomical detail; No ionizing radiation | Low sensitivity; Signal dilution from cell division |
| Positron Emission Tomography (PET) [6] [7] | 1-2 mm | 10² - 10⁴ | Hours to Days (dictated by radioisotope half-life) | Very high sensitivity; Quantitative biodistribution data | Radiation exposure; Poor anatomical context (requires CT/MRI fusion) |
| Bioluminescence Imaging (BLI) [6] | 3-5 mm | 10² - 10⁴ | Unlimited (with substrate re-administration) | High sensitivity; Low background; Low cost | Limited tissue penetration; Semi-quantitative |
| Photoacoustic Imaging (PAI) [6] | 10-500 µm | N/A | Unlimited (with stable labels) | Good depth-to-resolution ratio; Functional imaging | Limited clinical translation for cell tracking |
| Computed Tomography (MicroCT) [7] | 10-100 µm | 10⁴ - 10⁵ | Months (with stable contrast agents) | High-resolution 3D anatomy; Quantitative | Generally lower sensitivity for cell tracking; Radiation dose |
The performance of cell therapies is often quantified by key metrics. For instance, studies have shown that the survival of Mesenchymal Stem Cells (MSCs) in liver tissues can be less than 5% four weeks after transplantation, with a large number of cells dying within the first day [8]. Improving these metrics is a major focus of ongoing research.
Table 2: Key Quantitative Metrics in Cell Therapy Efficiency
| Parameter | Typical Challenge/Value | Implication |
|---|---|---|
| Cell Survival in Liver Tissue [8] | < 5% at 4 weeks post-transplantation | Indicates massive cell attrition, a major bottleneck for therapy efficacy. |
| Early Cell Death [8] | Large-scale death within 1 day post-transplantation | Highlights the extreme sensitivity of cells to the in vivo environment after transplantation. |
| MSC Engraftment in Fibrotic Liver [8] | Surviving MSCs nearly completely disappear by 11 days | Underscores the need for strategies to enhance cell survival and retention. |
Experimental Protocols for Key Tracking Methodologies
MRI-Based Tracking with Superparamagnetic Iron Oxide Nanoparticles (SPIONs)
This protocol details the labeling of stem cells with SPIONs for non-invasive tracking using MRI, allowing for the visualization of cell migration and distribution within anatomical context [6] [7].
Workflow Overview:
Materials:
- Stem Cells: (e.g., Mesenchymal Stem Cells, Neural Stem Cells).
- Labeling Agent: SPIO or USPIO nanoparticles (e.g., Ferucarbotran).
- Transfection Agent: Protamine sulfate (optional, to enhance uptake).
- Cell Culture Medium: Appropriate medium for the cell type.
- Imaging Instrument: Preclinical MRI system (e.g., 7T or higher).
Procedure:
- Cell Culture: Expand stem cells under standard conditions to 70-80% confluence.
- Labeling:
- Prepare a labeling medium by supplementing standard culture medium with SPIONs at a concentration of 25-100 µg Fe/mL.
- For difficult-to-label cells, add a transfection agent like protamine sulfate (0.5-1.5 µg/mL) to facilitate nanoparticle internalization.
- Incubate cells with the labeling medium for 12-48 hours.
- Washing and Harvesting:
- Remove the labeling medium and wash the cells thoroughly with PBS (3-5 times) to eliminate any non-internalized nanoparticles.
- Trypsinize the cells and resuspend in a suitable buffer (e.g., saline) for transplantation. Perform a cell count and viability assessment (e.g., Trypan Blue exclusion).
- Quality Control:
- Validate labeling efficiency by performing Prussian Blue staining on an aliquot of cells to confirm intracellular iron presence.
- Ensure labeled cells maintain normal viability, proliferation, and differentiation capacity.
- Transplantation: Administer the SPION-labeled cells into the animal model via the intended route (e.g., intravenous, intra-organ).
- In Vivo MRI:
- Anesthetize the animal and place it in the MRI scanner.
- Acquire T2-weighted or T2*-weighted sequences, where SPIONs create a hypointense (dark) signal.
- Conduct serial imaging over days or weeks to track cell migration and persistence.
- Data Analysis:
- Use software tools (e.g., ImageJ, OsiriX) to quantify the hypointense signal volume and its change over time.
- Correlate signal voids with anatomical location.
- Validation:
- After the final imaging time point, euthanize the animal and harvest tissues for histology.
- Confirm the presence of SPION-labeled cells using Perls' Prussian Blue staining co-localized with specific cell markers.
Radionuclide-Based Tracking for Biodistribution and Homing
This protocol uses radionuclides like ¹¹¹In to label cells for tracking with Single-Photon Emission Computed Tomography (SPECT), providing highly sensitive, quantitative data on whole-body biodistribution and homing to target tissues [7].
Workflow Overview:
Materials:
- Stem Cells: (e.g., MSCs, dendritic cells).
- Radiotracer: ¹¹¹In-oxyquinoline (¹¹¹In-oxine).
- Radiation Safety Equipment: Shields, dosimeters, dedicated lab space.
- Imaging Instrument: Preclinical SPECT/CT scanner.
- Gamma Counter: For ex vivo tissue analysis.
Procedure:
- Cell Preparation: Harvest cells and wash thoroughly. Resuspend the cell pellet (e.g., 10⁶ - 10⁷ cells) in a small volume (e.g., 100 µL) of saline or PBS without phenol red.
- Radiolabeling:
- Add ¹¹¹In-oxine (100-500 µCi) to the cell suspension and incubate for 15-20 minutes at 37°C with gentle agitation.
- The lipophilic ¹¹¹In-oxine complex diffuses across the cell membrane, where ¹¹¹In dissociates and binds to intracellular components.
- Washing and QC:
- Add excess cell medium to stop the reaction and pellet the cells by centrifugation.
- Carefully remove the supernatant (contains free radiotracer) and wash the cells twice with fresh medium.
- Resuspend the final cell pellet in transplantation buffer.
- Measure the radioactivity in the cell pellet and the combined washes to calculate labeling efficiency, which should typically be >70%.
- Cell Viability Check: Perform a rapid viability assay (e.g., Trypan Blue) post-labeling to ensure the process has not induced significant toxicity.
- Transplantation and Imaging:
- Inject the radiolabeled cells into the animal model.
- Acquire SPECT/CT images at multiple time points (e.g., 1h, 24h, 48h, 72h post-injection). The CT scan provides anatomical reference for the functional SPECT data.
- Quantitative Analysis:
- Use region-of-interest (ROI) analysis on the fused SPECT/CT images to quantify the percentage of injected dose per gram of tissue (%ID/g) in target organs (e.g., tumor, liver, spleen, lungs).
- Ex Vivo Validation:
- Euthanize the animal after the final scan and harvest major organs.
- Weigh the tissues and measure their radioactivity using a gamma counter to obtain a precise, high-sensitivity biodistribution profile.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful cell tracking relies on a suite of specialized reagents and materials. The table below details essential components for the protocols described.
Table 3: Essential Reagents and Materials for Cell Tracking Experiments
| Reagent/Material | Function/Application | Example Specifics |
|---|---|---|
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) [6] [7] | MRI contrast agent. Internalized by cells, causing detectable darkening (T2 contrast) on MRI scans. | Ferucarbotran; Size: 50-500 nm; Incubation concentration: 25-100 µg Fe/mL. |
| ¹¹¹In-Oxyquinoline (¹¹¹In-oxine) [7] | Radiotracer for SPECT imaging and quantitative biodistribution studies. | Half-life: 2.8 days; Emits gamma photons; Used for labeling cells like MSCs and leukocytes. |
| Transfection Agents [6] | Enhance cellular uptake of labeling agents like SPIONs. | Protamine sulfate; Used at 0.5-1.5 µg/mL in labeling medium. |
| Luciferase Reporter Genes [6] | Genetic label for bioluminescence imaging (BLI). Cells express the enzyme luciferase. | Requires transfection (viral vectors); Substrate: D-luciferin; Provides high-sensitivity, longitudinal data on cell viability/location. |
| Quantum Dots (QDs) [6] [7] | Fluorescent nanoparticles for high-resolution optical imaging and histology. | Semiconductor nanocrystals (2-5 nm); High resistance to photobleaching; Emission spectra are narrow and tunable. |
| Gold Nanorods [6] | Contrast agents for Photoacoustic Imaging (PAI). Absorb light and generate ultrasonic waves. | Strong absorption in the Near-Infrared (NIR) region; Allows for deeper tissue imaging. |
| Dual-Modality Tracers [6] | Allow cell tracking with two complementary techniques (e.g., PET and MRI). | Example: ⁶⁴Cu-SPION conjugates; Enable high-sensitivity detection (PET) with high anatomical resolution (MRI). |
In the field of regenerative medicine, stem cell therapy has emerged as a promising intervention for a wide range of diseases, including neurological, cardiovascular, and hematological disorders, through mechanisms such as cell replacement, paracrine factor secretion, and immune regulation [9] [10]. However, the clinical translation of these therapies faces a significant challenge: the inability to non-invasively monitor the transplanted cells in living subjects. The in vivo pharmacokinetic and pharmacodynamic profiles of stem cell therapy remain largely unclear, creating a critical knowledge gap in understanding stem cell fate, function, and efficacy [11] [10].
Molecular imaging bridges this gap by enabling longitudinal, non-invasive visualization of stem cell biological behaviors post-transplantation [9]. The fundamental approaches for stem cell tracking are categorized into two distinct strategies: direct and indirect labeling. Direct labeling involves incorporating detectable markers (fluorescent dyes, magnetic nanoparticles, or radiolabeled compounds) directly into cells prior to transplantation [12] [10]. In contrast, indirect labeling uses reporter genes transduced into stem cells, which are then visualized upon injection of specific probes [9] [12]. This dichotomy in strategy represents a core methodological consideration that influences every aspect of experimental design and data interpretation in stem cell research.
Core Principles: Direct versus Indirect Labeling
Direct Labeling Methodology
Direct labeling introduces labeling agents into cells through physical co-incubation or transfection methods before transplantation [12]. These agents become stably incorporated or attached to cellular components, allowing immediate detection post-transplantation. The method is technically straightforward and does not involve genetic modification of the target cells, reducing concerns about genetic responses and adverse events [9].
The underlying mechanism relies on transporting tracers into cells via endocytosis, transporter systems, or physical transfection, followed by intracellular retention through metabolic trapping or membrane anchoring [12]. For instance, 18F-FDG is taken up and retained in cells via glucose transporters and hexokinase-mediated phosphorylation, while 111In-oxine and 99mTc-HMPAO passively diffuse across cell membranes and are retained intracellularly [9]. Lipophilic compounds like hexadecyl-4-124I-iodobenzoate (124I-HIB) anchor efficiently into cellular membranes through simple incubation [9].
Indirect Labeling Methodology
Indirect labeling represents a genetically engineered approach where stem cells are modified to express reporter genes that produce detectable proteins or receptors [9] [12]. These reporter genes are integrated into the cellular genome using viral vectors, CRISPR/Cas9, or other gene-editing technologies, enabling permanent labeling that is passed to progeny cells [12] [13].
The imaging process requires administration of a specific probe or substrate that interacts with the reporter gene product. For example, cells expressing the herpes simplex virus type 1 thymidine kinase (HSV1-tk) reporter gene can be visualized after injecting radiolabeled substrates like 9-(4-[18F]fluoro-3-(hydroxymethyl)butyl)guanine ([18F]FHBG) [10]. Similarly, cells engineered with luciferase genes become detectable upon administration of luciferin substrate, generating bioluminescent signals [13].
Comparative Analysis: Strategic Advantages and Limitations
Table 1: Fundamental Characteristics of Direct and Indirect Labeling Methods
| Parameter | Direct Labeling | Indirect Labeling |
|---|---|---|
| Basic Principle | Physical incorporation of labels into cells [9] | Genetic engineering with reporter genes [9] |
| Typical Labels | Radionuclides (18F-FDG, 111In-oxine), SPIO, fluorescent dyes [9] [12] | Reporter genes (HSV1-tk, luciferase, GFP), receptor proteins [9] [13] |
| Cell Modification | No genetic modification required [9] | Permanent genetic modification necessary [12] |
| Signal Duration | Short-term (hours to days) [9] [12] | Long-term (weeks to months) [12] [10] |
| Signal & Cell Viability | Signal persists regardless of cell viability [12] | Signal correlates with viable, functional cells [11] |
| Proliferation Tracking | Label dilution with cell division [9] [12] | Stable inheritance by daughter cells [12] |
| Differentiation Monitoring | No specific differentiation insight [12] | Can use tissue-specific promoters [10] |
| Clinical Translation | Simpler regulatory pathway (no genetic modification) [9] | Complex regulatory pathway (genetic modification) [11] |
Table 2: Imaging Modalities and Their Applications in Stem Cell Tracking
| Imaging Modality | Direct Labeling Agents | Indirect Reporter Systems | Sensitivity | Spatial Resolution | Temporal Resolution |
|---|---|---|---|---|---|
| PET | 18F-FDG, 64Cu-PTSM, 124I-HIB [9] | HSV1-tk, sodium iodide symporter (NIS) [9] [10] | High (picomolar) [9] | 1-2 mm [9] | Minutes to hours [12] |
| SPECT | 111In-oxine, 99mTc-HMPAO [9] | NIS, other reporter genes [9] | High (picomolar) [9] | 1-2 mm [9] | Minutes to hours [12] |
| MRI | Superparamagnetic iron oxide (SPIO) [9] [11] | Ferritin, β-galactosidase [13] | Low (micromolar) [11] | 25-100 μm [11] | Minutes [11] |
| Optical Imaging | Fluorescent dyes (Cy dyes, Alexa Fluor) [14] [13] | Luciferase, fluorescent proteins (GFP, RFP) [10] [13] | High (femtomolar for bioluminescence) [13] | 2-3 mm (surface), >1 cm (deep tissue) [13] | Seconds to minutes [12] |
The strategic selection between direct and indirect labeling involves careful consideration of their respective advantages and limitations. Direct labeling offers immediate visualization post-transplantation, technical simplicity, and avoids genetic modification of cells [9]. However, this approach suffers from several fundamental constraints: signal dilution through cell division, inability to distinguish between living and dead cells, and limited long-term monitoring capability due to radiodecay or label efflux [9] [12]. For instance, 124I-HIB-labeled adipose-derived stem cells could only be tracked for 9 days in normal myocardium and 3 days in infarcted myocardium [9].
Indirect labeling addresses many limitations of direct approaches by providing permanent genetic labeling that is inherited by progeny cells, enabling long-term monitoring throughout the experiment duration [12] [10]. Since reporter gene expression requires viable, functionally active cells, the signal directly correlates with cell viability [11]. Furthermore, tissue-specific promoters can be incorporated to monitor differentiation status [10]. The primary limitations include potential immunogenicity of reporter proteins, more complex implementation requiring genetic engineering expertise, and variable transduction efficiency [11].
Experimental Protocols and Methodologies
Protocol 1: Direct Labeling with Radiolabeled Compounds
Objective: To track short-term distribution and homing of stem cells using direct radiolabeling.
Materials:
- Stem cells (e.g., mesenchymal stem cells, adipose-derived stem cells)
- Radiolabeling agent (e.g., 18F-FDG, 124I-HIB, 64Cu-PTSM)
- Cell culture medium and incubation equipment
- Radiation safety equipment
- PET/SPECT imaging system
Procedure:
- Cell Preparation: Harvest stem cells at 70-80% confluency using standard trypsinization procedures. Wash cells with PBS and resuspend in appropriate medium at concentration of 1-5 × 10^6 cells/mL [9].
- Labeling Incubation: Incubate cells with radiolabeling agent (e.g., 18F-FDG, 37-74 MBq/10^6 cells) for 30-60 minutes at 37°C with gentle agitation [9].
- Washing: Centrifuge cells at 300 × g for 5 minutes and carefully remove supernatant containing unincorporated radiotracer. Repeat washing step twice with fresh medium to ensure complete removal of excess label [9].
- Quality Control: Measure radioactivity associated with cells using gamma counter. Determine labeling efficiency (typically 5-20% for 18F-FDG) and cell viability via trypan blue exclusion [9].
- Transplantation: Resuspend labeled cells in appropriate transplantation medium. Administer to experimental subject via predetermined route (intravenous, intramyocardial, etc.) [9].
- Imaging: Perform serial PET/SPECT imaging immediately post-transplantation and at predetermined timepoints. For 18F-FDG (t1/2 = 110 min), imaging is typically limited to first 6-8 hours [9].
Critical Considerations:
- Optimize labeling conditions to maintain cell viability (>90% post-labeling)
- Account for radionuclide physical half-life in experimental timeline
- Include controls for potential radiotracer leakage from dead cells
- For 124I-HIB (t1/2 = 4.2 days), tracking up to 9 days is feasible in normal tissue [9]
Protocol 2: Indirect Labeling with Reporter Genes
Objective: To monitor long-term viability, proliferation, and distribution of stem cells using reporter gene imaging.
Materials:
- Stem cells
- Reporter gene construct (e.g., triple fusion reporter: fluorescent protein/luciferase/HSV1-tk)
- Gene delivery system (lentiviral vectors, CRISPR/Cas9)
- Appropriate substrate (e.g., luciferin for bioluminescence, [18F]FHBG for PET)
- In vivo imaging system (bioluminescence, PET, or fluorescence)
Procedure:
- Genetic Modification:
- For viral transduction: Incubate stem cells with lentiviral vectors carrying reporter gene at appropriate MOI (typically 10-100) for 24-48 hours [13].
- For CRISPR/Cas9 integration: Transfect stem cells with plasmid containing reporter gene flanked by homology arms for specific genomic integration [13].
- Selection and Expansion: Apply selection pressure (e.g., antibiotics for resistance markers) for 1-2 weeks. Isolate single-cell clones and expand reporter-positive populations [13].
- Validation:
- Confirm reporter expression via fluorescence microscopy or flow cytometry for fluorescent proteins.
- Validate functionality using substrate incubation (luciferin for bioluminescence assay).
- Assess stem cell properties (differentiation potential, surface markers) to ensure genetic modification hasn't altered fundamental characteristics [13].
- Transplantation: Administer validated reporter-expressing cells to experimental subjects via appropriate route [10].
- Longitudinal Imaging:
- For bioluminescence imaging: Inject D-luciferin (150 mg/kg intraperitoneally), image 10-20 minutes post-injection under anesthesia [13].
- For PET imaging: Inject reporter-specific probe (e.g., [18F]FHBG for HSV1-tk, 7.4 MBq intravenous), image 1-2 hours post-injection [10].
- Schedule imaging sessions at regular intervals (days to weeks) to monitor cell fate.
Critical Considerations:
- Monitor for potential immune responses against reporter proteins
- Validate stable reporter expression throughout experiment duration
- Use tissue-specific promoters to monitor differentiation (e.g., neuronal promoters for neural stem cells) [10]
- Triple fusion reporters enable multimodal imaging (fluorescence, bioluminescence, PET) [10]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Stem Cell Tracking
| Reagent Category | Specific Examples | Primary Function | Applications |
|---|---|---|---|
| Direct Labeling Agents | 18F-FDG, 111In-oxine, 99mTc-HMPAO [9] | Short-term cell labeling for nuclear imaging | Tracking initial cell distribution and homing [9] |
| Magnetic Nanoparticles | Superparamagnetic iron oxide (SPIO), ferumoxytol [11] [10] | Cell labeling for MRI contrast | High-resolution anatomical localization [11] |
| Fluorescent Probes | Cy dyes, Alexa Fluor dyes, FITC [14] [13] | Direct fluorescence labeling | In vitro validation, histological analysis, in vivo surface imaging [14] |
| Reporter Gene Constructs | HSV1-tk, luciferase, GFP/RFP [9] [13] | Genetic cell labeling | Long-term viability and proliferation monitoring [10] |
| Reporter Substrates | [18F]FHBG, luciferin [10] [13] | Activation of reporter systems | PET and bioluminescence imaging of reporter genes [10] |
| Gene Delivery Systems | Lentiviral vectors, CRISPR/Cas9 [12] [13] | Stable integration of reporter genes | Creating constitutively expressing cell lines [13] |
Strategic Implementation and Decision Framework
Choosing between direct and indirect labeling strategies requires systematic consideration of research objectives, technical constraints, and biological questions. The following decision framework provides guidance for selecting the appropriate methodology:
Implementation Considerations:
Hybrid Approaches: Combined direct and indirect labeling can provide complementary information. For example, direct labeling with SPIO nanoparticles enables precise anatomical localization via MRI, while reporter genes allow long-term viability assessment [13].
Multimodal Imaging: Triple fusion reporter genes (e.g., combining fluorescent protein, luciferase, and PET reporter) enable correlation of multiple imaging modalities, enhancing data robustness [10].
Clinical Translation Pathway: For preclinical studies with clinical translation as the ultimate goal, consider regulatory pathways early. Direct labeling has simpler regulatory approval process, while indirect labeling faces additional hurdles due to genetic modification [11].
Troubleshooting Common Issues:
- For low signal in direct labeling: optimize labeling conditions (concentration, incubation time, temperature)
- For reporter gene silencing: use different promoters or gene integration methods
- For high background: adjust washing procedures (direct) or optimize substrate clearance time (indirect)
The strategic dichotomy between direct and indirect labeling methods represents a fundamental consideration in stem cell tracking research. Direct labeling offers simplicity and immediate applicability for short-term distribution studies, while indirect labeling provides powerful tools for long-term monitoring of cell viability, proliferation, and differentiation. The choice between these approaches ultimately depends on specific research questions, technical capabilities, and regulatory considerations.
As stem cell therapies continue to advance toward clinical application, molecular imaging through appropriate labeling strategies will play an increasingly critical role in understanding stem cell fate and function. Future developments will likely focus on improved multimodal approaches, more sensitive reporters, and clinical translation of these tracking methodologies. By strategically implementing either direct or indirect labeling—or combinations thereof—researchers can significantly enhance our understanding of stem cell biology and accelerate the development of effective regenerative therapies.
In the field of stem cell tracking for regenerative medicine, in vivo imaging is crucial for monitoring the distribution, migration, and survival of transplanted cells. Direct labeling stands as a fundamental approach for these studies, prized for its straightforward implementation compared to genetically-encoded indirect methods. This technique involves incorporating a labeling agent—such as a radionuclide, fluorescent dye, or magnetic nanoparticle—into cells prior to their transplantation [15] [9]. While this method offers significant advantages in simplicity and immediate applicability, it is inherently constrained by two major challenges: the dilution of the signal over time due to cell division and the potential for false positives caused by label leakage from dead cells. This application note details the principles, protocols, and critical considerations for employing direct labeling in stem cell tracking, providing researchers with a framework to optimize its use while mitigating its inherent limitations.
Core Principles and Key Challenges
The Mechanism of Direct Labeling
Direct cell labeling methods function by introducing a contrast agent or tracer into stem cells ex vivo. After the labeling procedure, these cells are administered to a recipient, enabling their detection through various imaging modalities [15]. The label is typically incorporated into cells through processes such as endocytosis, transporter-mediated uptake, or simple diffusion across the cell membrane, where it may be metabolically trapped [12]. This process allows for explicit detection and monitoring of the distribution of these cells in target organs [15].
Fundamental Limitations
The primary limitations of direct labeling stem from the biological orthogonality of the tracer and cell viability. The tracer itself does not replicate with the cell and is not passed on to daughter cells during division. This leads to two critical issues:
- Signal Dilution: With each cell division, the concentration of the labeling agent per cell is halved, leading to a progressive weakening of the detectable signal. This ultimately restricts long-term monitoring capabilities [9]. Furthermore, the labeled material can be asymmetrically distributed between progeny cells [15].
- False Positives: If a labeled cell dies, the contrast agent can be released into the extracellular space. It may then be phagocytosed by host macrophages or other non-target cells, or simply remain as background signal. This results in an imaging signal that no longer corresponds to the location or viability of the originally transplanted therapeutic cells [12].
The following diagram illustrates the workflow of direct labeling and the emergence of its key challenges over time.
Quantitative Comparison of Direct Labeling Agents
The choice of labeling agent dictates the compatible imaging modality and influences the duration and reliability of tracking. The table below summarizes key characteristics of commonly used agents.
Table 1: Properties of Common Direct Labeling Agents for Stem Cell Tracking
| Labeling Agent | Imaging Modality | Key Feature | Typical Tracking Duration | Primary Cause of Signal Loss |
|---|---|---|---|---|
| Fluorescent Dyes (e.g., DiR) [15] | Optical Imaging | High sensitivity, real-time data | Days to a few weeks | Photobleaching, cell division, leakage |
| Quantum Dots (QDs) [15] | Optical Imaging | High resolution, multiplexing capability | Several weeks | Potential long-term toxicity, cell division |
| Polymer Dots (Pdots) [16] | Optical Imaging (NIR) | High brightness, low cytotoxicity | ~7 days (as demonstrated) | Cell division, clearance |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) [15] [9] | Magnetic Resonance Imaging (MRI) | High spatial resolution, deep tissue penetration | 1-2 weeks (e.g., 8 weeks shown in SCI model [15]) | Cell division, iron metabolism |
| 18F-FDG [9] | Positron Emission Tomography (PET) | High sensitivity, quantitative | Hours (t1/2 = 110 min) | Radiodecay, leakage |
| 99mTc-HMPAO [9] | Single-Photon Emission Computed Tomography (SPECT) | Clinical availability | Hours (t1/2 = 6 h) | Radiodecay, leakage |
| 111In-oxine [9] | SPECT | Longer half-life than 99mTc | Several days (t1/2 = 2.8 d) | Radiodecay, leakage |
| 124I-HIB [9] | PET | Membrane-anchored, longer tracking | Up to 9 days (demonstrated in normal myocardium) | Radiodecay, cell death |
Detailed Experimental Protocols
Protocol: Labeling Stem Cells with Near-Infrared Fluorescent Polymer Dots
This protocol is adapted from studies using semiconducting polymer dots (Pdots) for high-brightness cell tracking, which demonstrated effective monitoring of stem cell distribution for up to seven days in vivo [16].
4.1.1 Research Reagent Solutions
Table 2: Essential Materials for Pdots Labeling
| Item | Function/Description | Example/Note |
|---|---|---|
| NIR-Emitting Pdots | Fluorescent probe for tracking. | e.g., DFDBT/NIR800 blend, emission at 800 nm [16]. |
| Cell-Penetrating Peptide (CPP) | Enhates cellular uptake of Pdots. | e.g., TAT peptide (GRKKRRQRRRPQ) [16]. |
| Poly(styrene-co-maleic anhydride) (PSMA) | Functional copolymer for nanoparticle coating and stabilization. | Mn = 1700 [16]. |
| Stem Cell Line | Target cells for labeling and tracking. | e.g., Mesenchymal Stem Cells (MSCs). |
| Appropriate Cell Culture Medium | Maintains cell viability during labeling. | Serum-free recommended during labeling. |
| Phosphate Buffered Saline (PBS) | Washing and dilution buffer. | |
| Flow Cytometer | Quantifying labeling efficiency and brightness. | |
| In Vivo Imaging System (IVIS) | Non-invasive tracking of labeled cells in animal models. |
4.1.2 Step-by-Step Procedure
Pdots Preparation and Functionalization:
- Prepare Pdots using the nano-precipitation method. Mix the semiconducting polymers (e.g., DFDBT and NIR800) with the functional copolymer PSMA in THF.
- Vigorously inject the THF solution into ultrapure water and stir to allow nanoparticle self-assembly.
- Remove the organic solvent via dialysis or nitrogen purging.
- Conjugate the TAT cell-penetrating peptide to the surface of the Pdots via the amine-reactive chemistry of the PSMA copolymer. Purify the TAT-Pdots using size-exclusion chromatography or dialysis.
Cell Culture:
- Maintain stem cells (e.g., MSCs) in their recommended growth medium under standard culture conditions (37°C, 5% CO2).
- Harvest cells at 70-80% confluency using a standard trypsinization procedure. Wash cells once with PBS.
Cell Labeling:
- Resuspend the cell pellet in serum-free medium at a concentration of 1-5 x 10^6 cells/mL.
- Add the prepared TAT-Pdots solution to the cell suspension. The optimal working concentration should be determined empirically (e.g., 5-20 nM final Pdots concentration).
- Incubate the cell-Pdots mixture for 2-4 hours at 37°C with gentle agitation every 30 minutes.
Washing and Validation:
- After incubation, centrifuge the cell suspension (e.g., 300 x g for 5 minutes) and carefully remove the supernatant containing unincorporated Pdots.
- Wash the cells with PBS at least three times to ensure complete removal of free Pdots.
- Resuspend the labeled cells in PBS or complete medium for immediate use.
- Quantify Labeling Efficiency: Analyze an aliquot of the labeled cells using a flow cytometer. Compare the fluorescence intensity to unlabeled control cells. The protocol aims for a brightness increase of ~4 orders of magnitude [16].
- Assess Cell Viability: Perform a viability assay (e.g., trypan blue exclusion) post-labeling to ensure the procedure has not induced significant toxicity.
In Vivo Administration and Imaging:
- Transplant the Pdots-labeled stem cells into your animal model via the desired route (e.g., intravenous injection through the tail vein).
- Anesthetize the animals and image them using an in vivo imaging system (IVIS) with appropriate filters for NIR fluorescence (e.g., excitation 745 nm, emission 800 nm).
- Acquire images at predetermined time points (e.g., 1 hour, 1 day, 4 days, 7 days post-transplantation) to track cell distribution and persistence.
Protocol: Magnetic Resonance Imaging with SPIONs
This protocol outlines the labeling of stem cells with superparamagnetic iron oxide nanoparticles (SPIONs) for tracking via MRI, a method that has been used to monitor cells for up to 8 weeks in models of spinal cord injury [15].
4.2.1 Step-by-Step Procedure
- Cell Culture: Harvest and wash the target stem cells as described in section 4.1.2.
- SPIONs Labeling:
- Resuspend the cell pellet in culture medium containing SPIONs (e.g., Ferucarbotran). The typical iron concentration used ranges from 50 to 200 µg Fe/mL.
- To enhance labeling efficiency, add a transfection agent (e.g., poly-L-lysine) to the mixture according to the manufacturer's instructions.
- Incubate the cells for 12-24 hours under standard culture conditions.
- Washing and Validation:
- After incubation, wash the cells thoroughly with PBS 3-5 times to remove any unincorporated nanoparticles.
- Confirm labeling efficiency via Prussian Blue staining for iron.
- Verify that stem cell viability and differentiation potential remain uncompromised post-labeling.
- In Vivo Administration and MRI:
- Transplant the SPIONs-labeled cells into the target tissue (e.g., intracardiac injection for myocardial infarction models or intraspinal injection for SCI models).
- Perform MRI scans at multiple time points using T2/T2*-weighted sequences. The labeled cells will appear as hypointense (dark) signal areas against the brighter background tissue [15].
Critical Interpretation of Data and Mitigating Pitfalls
The primary challenge in direct labeling is distinguishing true positive signals from false positives arising from label leakage. The diagram below outlines the decision process for data interpretation and validation.
To minimize misinterpretation, researchers should:
- Establish a Baseline: Understand the expected pharmacokinetics and biodistribution of the free label itself.
- Use Multiple Modalities: Correlate findings with a second, independent imaging technique where possible.
- Mandatory Post-Mortem Analysis: As shown in the diagram, histological validation is essential. Correlate the in vivo signal with ex vivo tissue analysis using specific cell markers and label-specific stains (e.g., Prussian Blue for iron) to confirm the cellular source of the signal [15] [17].
- Track Signal Kinetics: A rapidly disseminating or shifting signal, especially one accumulating in clearance organs like the liver and spleen, is a strong indicator of label leakage rather than viable cell migration [9].
Direct labeling remains a powerful and accessible technique for short- to medium-term tracking of stem cells in vivo, offering a straightforward path to answer critical questions about initial cell homing and early distribution. Its simplicity and relatively low technical barrier make it an excellent starting point for many preclinical studies. However, the inherent limitations of signal dilution upon cell division and the pervasive risk of false positives due to label leakage demand a cautious and critical approach to data interpretation. By selecting the appropriate label for the experimental timeframe and biological question, following optimized protocols to ensure cell health, and—most importantly—implementing rigorous histological validation, researchers can effectively leverage the simplicity of direct labeling while mitigating its drawbacks. For studies requiring long-term tracking or monitoring of cell proliferation, indirect reporter gene-based methods may be a more suitable, albeit more complex, alternative [12] [9].
In the field of stem cell tracking and regenerative medicine, understanding the long-term fate, proliferation, and differentiation of therapeutic cells is paramount. While direct labeling methods, which involve loading cells with contrast agents, are straightforward, they suffer from a critical limitation: the label dilutes with each cell division, causing the signal to fade and preventing long-term observation [18] [11]. Indirect reporter gene labeling overcomes this fundamental barrier. This technique involves genetically engineering cells to stably incorporate a reporter gene into their genome. The expression product of this gene—be it an enzyme, a receptor, or a transporter—can then interact with an externally administered probe to generate a detectable signal for non-invasive imaging [18] [19]. Because the reporter gene is integrated into the cell's DNA, it is passed on to all progeny, providing a heritable and permanent mark for long-term lineage tracing. This allows researchers to monitor the survival, migration, and differentiation of stem cells over weeks or months in living subjects, offering unparalleled insights into their in vivo biology and therapeutic efficacy [10] [19].
The following diagram illustrates the core principle of how indirect reporter gene labeling enables long-term lineage tracing, contrasting it with the limitation of direct labeling.
Molecular Principles and Key Reporter Gene Systems
The functionality of indirect reporter gene labeling hinges on the molecular biology of the reporter genes themselves. A typical construct consists of a regulatory response element (which controls when and where the gene is turned on) and the reporter gene itself, which produces a measurable signal [20]. When a therapeutic cell, such as a stem cell, is engineered to express such a construct, its activation leads to the production of a reporter protein. This protein then interacts with a compatible imaging probe, leading to signal generation that can be detected by various imaging modalities [18].
Reporter genes are broadly classified into three categories based on their mechanism of action: enzyme-based, receptor-based, and transporter-based systems [19]. Each class offers distinct advantages and is compatible with different imaging technologies. The choice of reporter depends on factors such as sensitivity, clinical translatability, and the need for multiplexing. The table below summarizes the key performance metrics of common biological activity methods, highlighting the position of reporter gene assays among other techniques.
Table 1: Performance Comparison of Biological Activity Assay Methods
| Classification | Detection Method | Limit of Detection (LOD) | Dynamic Range | Intra-batch CV (%) |
|---|---|---|---|---|
| Cell-based Activity Methods | Cell Proliferation Inhibition | ~10⁻⁹ – 10⁻¹² M | Varies (e.g., cell ratio dependent) | Below 10% |
| Cytotoxicity Assay | ~100 cells per test well | 10–90% cell death | Below 10% | |
| Transgenic Cell-based Methods | Reporter Gene Assay (RGA) | ~10⁻¹² M | 10² – 10⁶ relative light units | Below 10% |
| New Technology-based Methods | Surface Plasmon Resonance (SPR) | ~10⁻⁹ M | Wide (10⁴ – 10⁶) | ~1–5% |
| Homogeneous Time-Resolved Fluorescence (HTRF) | ~10⁻¹² M | Moderate (10² – 10⁴) | ~2–8% |
Data adapted from a 2025 review on biological activity methods [20]. CV: Coefficient of Variation.
Table 2: Key Reporter Gene Systems for In Vivo Imaging
| Reporter Gene Class | Reporter Name | Mechanism of Action | Imaging Modality | Example Imaging Probe |
|---|---|---|---|---|
| Enzyme | Herpes Simplex Virus Type 1 Thymidine Kinase (HSV1-tk) | Phosphorylates and traps probes inside cells | PET, SPECT | ¹²⁴I-FIAU, ¹⁸F-FHBG |
| Transporter | Sodium Iodide Symporter (NIS, SLC5A5) | Concentrates anions from extracellular space | PET, SPECT | ¹²⁴I⁻, ⁹⁹mTcO₄⁻ |
| Receptor | Dopamine D2 Receptor (D2R) | Binds specific ligands on cell surface | PET, SPECT | ¹⁸F-Fallypride |
| Light-Producing Enzyme | Firefly Luciferase (Fluc) | Catalyzes light-emitting reaction with substrate | Bioluminescence Imaging | D-luciferin |
| Fluorescent Protein | Green/Red Fluorescent Protein (GFP, RFP) | Fluoresces upon light excitation | Fluorescence Imaging | None (endogenous) |
Information synthesized from multiple sources on reporter gene technology [18] [19].
Detailed Experimental Protocols
Protocol 1: Constructing a Stable Reporter Cell Line Using CRISPR/Cas9
The stability and reliability of lineage tracing data are highly dependent on the quality of the reporter cell line. CRISPR/Cas9-mediated gene editing allows for the rapid and precise insertion of a reporter gene cassette into a specific, defined genomic locus, known as a "safe harbor." This method ensures consistent and predictable transgene expression, which is critical for quantitative longitudinal studies [20].
Workflow Overview:
- Guide RNA (gRNA) and Donor Vector Design: Design gRNAs that target a safe harbor locus, such as the AAVS1 or ROSA26 locus. Synthesize a donor vector containing your reporter gene of choice (e.g., Fluc, eGFP) flanked by homology arms complementary to the target site.
- Cell Transfection/Transduction: Co-transfect/co-transduce the target cells (e.g., mesenchymal stem cells, T cells) with the plasmid or mRNA encoding the Cas9 nuclease, the gRNA, and the donor vector.
- Selection and Clonal Expansion: After transfection, apply the appropriate selection antibiotic (e.g., Puromycin) for 7-14 days to eliminate non-transfected cells. Subsequently, seed the cells at a very low density to allow for the isolation and expansion of single-cell-derived clones.
- Validation of Integration: Screen the expanded clones for successful reporter gene integration. Use polymerase chain reaction (PCR) to confirm the correct 5' and 3' junction fragments. Further validate the clone with the strongest and most consistent signal via Western blot (to confirm reporter protein expression) and Sanger sequencing (to confirm the integrity of the integrated sequence).
Protocol 2: In Vivo Lineage Tracing of Stem Cells in a Murine Model
This protocol describes the use of an inducible Cre/loxP system for spatiotemporal control of reporter gene activation, enabling precise lineage tracing of specific stem cell populations in live mice [21].
Workflow Overview:
- Animal Model Preparation: Cross-breed two genetically engineered mouse lines: a) a driver mouse expressing CreER recombinase under a tissue-specific promoter (e.g., K14-CreER for skin stem cells), and b) a reporter mouse harboring a LoxP-STOP-LoxP (LSL) cassette upstream of a reporter gene (e.g., GFP, LacZ) at the ROSA26 locus [21] [22].
- Tamoxifen Induction for Sparse Labeling: To achieve clonal, single-cell resolution, administer a low dose of tamoxifen (e.g., 1-5 mg per 25 g body weight, intraperitoneally) to adult mice. Tamoxifen binds to CreER, causing its translocation to the nucleus where it excises the STOP cassette, thereby permanently activating the reporter gene in a sparse, random subset of stem cells [21].
- Long-Term In Vivo Imaging: Anesthetize the mouse and image it using the appropriate modality at regular intervals (e.g., weekly).
- For Fluorescence/Bioluminescence Imaging: Use a cooled CCD camera system. For bioluminescence, inject the substrate (e.g., D-luciferin, 150 mg/kg intraperitoneally) 10 minutes prior to imaging [18] [19].
- For PET/SPECT Imaging: Administer the radiolabeled probe (e.g., ¹⁸F-FHBG for HSV1-tk) intravenously. After a suitable uptake period (e.g., 60 minutes), anesthetize the animal and acquire a static scan [19].
- Data Analysis and Lineage Tree Reconstruction: Coregister images from different time points. Use software to track the spatial location, expansion, and migration of labeled clones over time. The hierarchical relationships between cells can be reconstructed into a lineage tree to visualize the progeny of a single labeled progenitor.
The following diagram maps out this integrated experimental workflow, from genetic engineering to in vivo analysis.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of indirect reporter gene labeling requires a suite of well-characterized reagents. The table below details key materials and their functions in a typical lineage tracing experiment.
Table 3: Essential Research Reagents for Reporter Gene-Based Lineage Tracing
| Reagent Category | Specific Example | Function in the Experiment |
|---|---|---|
| Reporter Genes | Firefly Luciferase (Fluc), HSV1-thymidine kinase (HSV1-tk), Green Fluorescent Protein (GFP) | Serves as the genetic marker; its expression produces a protein that generates the detectable signal for tracking cells and their progeny. |
| Inducible Systems | CreER, Tet-On/Off (rtTA/tTA) | Provides spatiotemporal control over reporter gene expression, allowing researchers to initiate labeling at a precise time during development or in response to a stimulus. |
| Editing Tools | CRISPR/Cas9 system (Cas9 nuclease, gRNA) | Enables precise, site-specific integration of the reporter gene construct into the host cell genome, ensuring stable and consistent expression. |
| Imaging Probes | D-luciferin (for Fluc), ¹⁸F-FHBG (for HSV1-tk), ¹²⁴I⁻ (for NIS) | The substrate or ligand that interacts with the reporter protein to produce a signal (e.g., light or radioactivity) detectable by imaging equipment. |
| Cell Lineage Labels | Multicolor Confetti reporter, Brainbow cassette | Allows for the simultaneous tracking of multiple clones within the same organism by stochastically assigning one of several fluorescent colors to a cell and its descendants. |
Application Notes and Technical Considerations
Application in Stem Cell Therapy Monitoring
Indirect reporter gene labeling is indispensable for the preclinical development of stem cell therapies. It allows researchers to answer critical questions about the in vivo behavior of transplanted cells. For instance, in models of myocardial infarction, stem cells engineered with a triple-fusion reporter gene (e.g., combining Fluc, GFP, and HSV1-tk) have been tracked using bioluminescence imaging (BLI) and PET to confirm their engraftment, survival, and proliferation in the infarcted heart [10]. Similarly, in neurological disorders, the fate of transplanted human neural stem cells and their role in promoting brain repair has been elucidated using this technology [11]. The ability to longitudinally monitor the same cohort of animals reduces inter-subject variability and provides robust data on therapeutic cell kinetics.
Pitfalls and Optimization Strategies
- Immunogenicity: Reporter genes of non-human origin (e.g., Fluc, HSV1-tk) can elicit an immune response that leads to the elimination of the labeled cells, confounding long-term data. Strategy: Use human-derived reporter genes (e.g., human mitochondrial thymidine kinase 2 [hTK2], human deoxycytidine kinase [hdCK]) where possible to minimize immune recognition [19].
- Signal Dilution in Differentiating Cells: As stem cells differentiate, the promoter driving the reporter gene may become silenced, leading to signal loss that is not due to cell death. Strategy: Drive reporter expression with a ubiquitous and constitutive promoter (e.g., EF1α, CAG) to ensure expression in all progeny, regardless of differentiation state.
- Position Effect Variegation: Random integration of the reporter construct can lead to variable expression levels due to influences from surrounding chromatin. Strategy: Use CRISPR/Cas9 to target safe harbor loci (e.g., AAVS1, ROSA26), which provide a more predictable and consistent expression environment [20].
- Phototoxicity and Tissue Attenuation (Optical Imaging): Extended exposure to excitation light in fluorescence imaging can damage cells, and light scattering limits imaging in deep tissues. Strategy: For long-term live imaging, use bioluminescence or red-shifted fluorescent proteins, and optimize imaging intervals and exposure times to minimize photodamage [23].
The advancement of stem cell therapies hinges on the ability to non-invasively monitor administered cells in vivo. Molecular imaging serves as a powerful tool for examining complex cellular processes, understanding disease mechanisms, and evaluating the kinetics of cell therapies [24]. For researchers and drug development professionals, defining the ideal imaging agent is paramount. Such an agent must harmonize three core principles: biocompatibility (minimal impact on cell viability, function, and the host organism), specificity (accurate targeting and distinction from background signals), and sensitivity (detection of low cell numbers at high resolution) [24] [11]. This Application Note delineates these parameters within the context of stem cell tracking, providing structured data and detailed protocols to guide experimental design.
Core Principles of an Ideal Imaging Agent
The performance of an imaging agent is evaluated against a set of interdependent criteria. The table below summarizes the key characteristics of an ideal agent for stem cell tracking.
Table 1: Key Characteristics of an Ideal Imaging Agent for Stem Cell Tracking
| Characteristic | Description | Importance in Stem Cell Tracking |
|---|---|---|
| High Sensitivity | Ability to detect a small number of labeled cells [11]. | Enables monitoring of initial cell engraftment and long-term survival at low cell densities. |
| High Specificity | Clear distinction of the signal from the labeled cells against the biological background [24]. | Accurately determines cell location, migration, and homing to target tissues. |
| Excellent Biocompatibility | Non-toxic to the cell and the host, with no alteration of cell biology (e.g., viability, proliferation, differentiation potential) [24] [11]. | Ensures that the therapeutic effect is not compromised and that observed effects are due to the therapy, not the label. |
| Capacity for Long-Term Monitoring | The label is retained within the cell and remains detectable for the duration of the study [24]. | Allows for longitudinal studies in the same subject, tracking the entire fate of the administered cells. |
| Quantification Capability | The signal intensity should correlate with the number of labeled cells [25]. | Provides quantitative data on cell survival and proliferation over time. |
Comparative Analysis of Imaging Modalities
No single imaging modality excels in all categories; each presents a unique balance of strengths and weaknesses. The choice of modality depends on the specific research question, whether it is short-term homing or long-term viability and proliferation [11].
Table 2: Comparison of Imaging Modalities for Stem Cell Tracking
| Imaging Modality | Typical Spatial Resolution | Typical Penetration Depth | Key Advantages | Key Disadvantages & Biocompatibility Considerations |
|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | 1 mm [26] / 25-100 µm [25] | 50 cm [26] | High spatial resolution; excellent soft-tissue contrast; deep penetration [24] [26]. | Low sensitivity, requiring high labeling agent load (e.g., SPIOs); potential impact of SPIOs and magnetic fields on stem cell biology (e.g., altered differentiation) [11]. |
| Positron Emission Tomography (PET) | 5 mm [26] / 1-2 mm [25] | 50 cm [26] | Very high sensitivity (picomolar); quantitative; deep penetration [24] [25]. | Use of ionizing radiation; limited spatial resolution; radiotracer half-life limits duration of tracking (hours to days) [24] [25]. |
| Optical Imaging (Bioluminescence/Fluorescence) | 1 mm [26] / 1 µm [25] | 1-2 mm [26] | High sensitivity; low cost; ease of use; suitable for reporter genes [25] [26]. | Limited tissue penetration due to light scattering; primarily suitable for small animals [25]. |
| Photoacoustic Tomography (PAT) | 0.1 mm [26] | 10 cm [26] | Good resolution at depth; high functional and chemical sensitivity [26]. | Relatively new technology; requires coupling medium; limited clinical translation [25] [26]. |
| Ultrasound (US) | 0.3 mm [26] | 10 cm [26] | Real-time imaging; high speed; deep penetration; safe and inexpensive [26]. | Low intrinsic sensitivity and chemical specificity for cell tracking; often requires contrast agents like microbubbles [26]. |
Experimental Protocols for Agent Evaluation
Protocol 1: Direct Labeling of Mesenchymal Stem Cells (MSCs) with Superparamagnetic Iron Oxide Nanoparticles (SPIONs) for MRI
This protocol details the direct labeling of MSCs with SPIONs, a common approach for tracking cell delivery and short-term homing with MRI [24] [25].
Research Reagent Solutions
| Item | Function |
|---|---|
| Human Mesenchymal Stem Cells (MSCs) | Primary cell type for therapy and tracking studies [24]. |
| SPIONs (e.g., Ferucarbotran) | MRI contrast agent; shortens T2 relaxation time, creating dark contrast on T2-weighted images [25]. |
| Protamine Sulfate | Transfection agent; enhances cellular internalization of SPIONs via endocytosis [25]. |
| Cell Culture Medium (e.g., DMEM) | Provides nutrients and environment for maintaining cells during labeling. |
| Philips iU22 or GE Logiq E9 US System | For initial guidance of cell delivery, if required [27] [11]. |
| High-Field MRI Scanner (≥7T) | For high-resolution in vivo tracking of SPION-labeled cells [26]. |
Methodology:
- Cell Culture: Culture human MSCs in standard medium until 70-80% confluent [24].
- Labeling Complex Formation: Incubate SPIONs (e.g., 50-100 µg Fe/mL) with protamine sulfate (e.g., 5-10 µg/mL) in serum-free medium for 30-60 minutes at 37°C to form the labeling complex [25].
- Cell Labeling: Replace the culture medium with the SPION-protamine complex solution. Incubate cells for 4-24 hours under standard culture conditions (37°C, 5% CO₂) [25].
- Washing and Harvesting: After incubation, wash cells thoroughly with phosphate-buffered saline (PBS) to remove excess particles. Harvest cells using standard trypsinization procedures [24].
- Quality Control: Determine labeling efficiency and iron load per cell using techniques like Prussian Blue staining or mass spectrometry [11]. Validate that labeling does not adversely affect cell viability (e.g., >95% via trypan blue exclusion) and key functions such as differentiation potential [11].
- In Vivo Imaging: Administer the labeled MSCs (e.g., via intramyocardial injection). Acquire T2*-weighted MRI sequences to track the cells as hypointense (dark) signals [25].
Protocol 2: Reporter Gene Imaging of Stem Cell Viability Using Bioluminescence
This protocol employs genetic engineering to express a reporter gene (luciferase), enabling long-term monitoring of cell viability and location via bioluminescence imaging (BLI) [25] [11].
Research Reagent Solutions
| Item | Function |
|---|---|
| Stem Cell Line (e.g., Neural Stem Cells) | Genetically modifiable cells for long-term tracking studies [11]. |
| Lentiviral Vector with Luciferase Reporter | Mediates stable integration of the luciferase gene into the host cell genome [25]. |
| D-Luciferin (Firefly substrate) | Enzyme substrate; produces bioluminescent light (photons) upon interaction with luciferase [25]. |
| In Vivo Imaging System (IVIS) | Highly sensitive CCD camera for detecting low-light bioluminescence signals from live animals [25]. |
| Living Image Software | For quantifying photon flux (photons/second) as a measure of cell viability and number [25]. |
Methodology:
- Genetic Modification: Transduce stem cells with a lentiviral vector encoding the firefly luciferase (Fluc) reporter gene under a constitutive promoter. Select stable populations using an appropriate antibiotic (e.g., puromycin) [25].
- Validation: Confirm reporter gene expression and function in vitro by adding D-luciferin (e.g., 150 µg/mL) to culture media and detecting bioluminescence.
- Cell Transplantation: Administer the engineered stem cells into the target organ of an animal model (e.g., rat model of brain injury) [11].
- In Vivo Imaging: At designated time points, inject the animal intraperitoneally with D-luciferin (e.g., 150 mg/kg). Anesthetize the animal and place it in the IVIS chamber. Acquire images 10-20 minutes post-injection, using a 1-second to 5-minute acquisition time [25].
- Quantification and Analysis: Use software (e.g., Living Image) to define a region of interest (ROI) and quantify the total photon flux. Correlate signal intensity with cell viability and number [25] [11].
Decision Framework and Advanced Concepts
Choosing an Imaging Strategy
The decision between direct labeling and reporter gene imaging is fundamental. Direct labeling (e.g., with SPIONs, radionuclides, or quantum dots) is ideal for tracking the initial delivery and short-term homing of cells, as the signal is strong and immediate. However, the signal does not indicate cell viability and dilutes with cell division [24] [11]. Reporter gene imaging, while requiring genetic modification, is superior for long-term monitoring as the signal is directly tied to viable, functioning cells and is not diluted upon proliferation [11].
Mechanism of a Novel Bio-Responsive Imaging Agent
Innovative agents are being developed to detect specific pathophysiological conditions. The following diagram illustrates the mechanism of a dual 31P/19F-MR bio-responsive polymer probe designed to detect reactive oxygen species (ROS), which are abundant in inflammation and cancer [28].
The "ideal" imaging agent for stem cell tracking is context-dependent, defined by the specific therapeutic question. While direct labeling agents like SPIONs offer a practical solution for monitoring cell delivery, reporter genes provide unparalleled insight into long-term cell fate. The future of the field lies in the development of multimodal agents [24] [25] and smart, bio-responsive probes [28] that combine high sensitivity and specificity with the ability to report on the functional state of both the administered cells and their microenvironment. By adhering to the core principles of biocompatibility, specificity, and sensitivity, researchers can robustly track stem cells and accelerate the translation of regenerative therapies from the bench to the bedside.
The Imaging Toolkit: Modalities, Protocols, and Real-World Applications
The administration of exogenous stem cells offers significant promise for regenerating damaged organs, particularly in the context of cardiovascular disease and ischemic stroke [29] [30]. However, the failure of many cellular therapies in clinical trials can be attributed to uncertainties regarding stem cell fate post-transplantation, including their survival, migration, and engraftment at target sites [29] [31]. Non-invasive monitoring is therefore critical for optimizing therapeutic protocols. Among the available imaging modalities, Magnetic Resonance Imaging (MRI) provides high anatomical resolution and unlimited depth penetration, making it an ideal platform for tracking cells in vivo [32]. When combined with Superparamagnetic Iron Oxide Nanoparticles (SPIONs) as contrast agents, MRI enables the serial, non-invasive monitoring of accurately delivered cell therapeutics, offering profound insights into their biodistribution and persistence [29] [33]. This application note details the methodologies and protocols for utilizing SPIONs to track stem cells, framed within the broader thesis of advancing in vivo imaging techniques for regenerative medicine.
SPIONs as Contrast Agents
Mechanism of Action and Physicochemical Properties
SPIONs are composed of an iron oxide core, typically magnetite (Fe₃O₄) or maghemite (γ-Fe₂O₃), coated with a biocompatible polymer such as dextran, carboxydextran, or siloxanes [33] [34] [35]. Their superparamagnetic property means they become highly magnetic under an external magnetic field but retain no residual magnetism once the field is removed, which prevents aggregation and facilitates their use in biological systems [31]. As MRI contrast agents, SPIONs primarily act as potent T2 agents, creating strong local magnetic field inhomogeneities that dephase nearby water protons, resulting in a pronounced signal void (hypointensity) on T2- and T2*-weighted MR images [29] [33] [34]. This "blooming artifact" amplifies the detectable area beyond the physical volume of the nanoparticles themselves, significantly enhancing MRI sensitivity and allowing for the detection of single or small clusters of labeled cells [32].
Table 1: Commercially Available and Representative SPION Formulations for Cell Labeling
| Brand/Name | Coating Material | Hydrodynamic Size (nm) | Classification | Primary Application/Target | Relaxivity, r2 (mM⁻¹s⁻¹) |
|---|---|---|---|---|---|
| Ferumoxides (Feridex, Endorem) | Dextran | 120-180 | SPIO | Liver, Stem Cell Labeling | ~160 [33] |
| Ferucarbotran (Resovist) | Carboxydextran | ~60 | SPIO | Liver, Stem Cell Labeling | N/A |
| Ferumoxytol (Feraheme) | Carboxymethyl-dextran | ~30 | USPIO | Macrophage, Blood Pool | N/A |
| Sinerem (AMI-227) | Dextran | 15-30 | USPIO | Blood Pool, Lymph Node | N/A |
| ProMag (MPIO) | Polystyrene | 1000-1730 | MPIO | Cell Labeling | N/A |
| VivoTrax | Moldable | ~28 | SPIO | MPI/MRI Cell Tracking | N/A |
The surface engineering of SPIONs is paramount to their in vivo performance. The coating determines the particles' colloidal stability, circulation half-life, and ability to overcome biological barriers [35]. Furthermore, surface functionalization with cations or transfection agents facilitates the efficient internalization of SPIONs into non-phagocytic stem cells, such as mesenchymal stem cells (MSCs) and neural stem cells (NSCs) [29] [33].
Quantitative Performance of SPIONs
The effectiveness of SPIONs for cell tracking is quantified by their relaxivity (r2) and the achievable cellular iron load. These factors directly influence the minimum number of cells detectable by MRI.
Table 2: Quantitative Metrics of Selected SPIONs for Stem Cell Labeling
| SPION Type / Formulation | Core Diameter (nm) | Overall Size (nm) | Zeta Potential (mV) | Typical Iron Load (pg Fe/Cell) | Approximate Detection Limit (Cells) |
|---|---|---|---|---|---|
| Ferumoxides-PLL [33] | 6.2 | N/A | -42 | 41.5 | ~10³ [32] |
| N-dodecyl-PEI2k/SPIO [33] | N/A | 54.7 | +40 | 7.1 | N/A |
| CMCS-SPIONs [33] | 6-10 | 55.4 | -21.4 | 26.7 | N/A |
| IONP-6PEG-HA [33] | 10 | 75 | -9.1 | ~14,590 | N/A |
| Synomag-D (in cells) [36] | N/A | N/A | N/A | N/A | 1,000 (MPI) |
| ProMag (MPIO) (in cells) [36] | N/A | >1000 | N/A | N/A | 250 (MPI) |
Experimental Protocols for Stem Cell Labeling and Tracking
SPION Labeling of Stem Cells
Efficient labeling of stem cells is a prerequisite for successful tracking. The following protocols describe two established methods: magnetofection and magnetoelectroporation (MEP).
Diagram: Workflow for SPION Labeling of Stem Cells. Two primary methods, Magnetofection and Magnetoelectroporation (MEP), are used to internalize SPIONs into cells ex vivo prior to transplantation and imaging.
Protocol: Magnetofection with Transfection Agents
This method uses cationic transfection agents to form complexes with anionic SPIONs, promoting adsorptive endocytosis.
SPION Complex Preparation:
- In a sterile tube, combine clinical-grade SPIONs (e.g., Ferumoxides, 100-200 µg Fe/mL) with a transfection agent such as protamine sulfate (0.5-1 µg/mL) or poly-L-lysine (PLL) in serum-free culture media.
- Vortex gently and incubate the mixture for 15-30 minutes at room temperature to allow complex formation [29] [33].
Cell Labeling:
- Harvest the target stem cells (e.g., Mesenchymal Stem Cells - MSCs) and plate at 50-80% confluency.
- Replace the culture media with the prepared SPION-transfection agent complex.
- Incubate cells for 24-48 hours at 37°C and 5% CO₂ [29].
Post-Labeling Processing:
- Gently wash the cells 3-5 times with PBS to remove any extracellular iron complexes.
- Verify labeling efficiency via Prussian Blue staining for intracellular iron.
- Confirm cell viability (e.g., >95%) using Trypan Blue exclusion assay before transplantation [31].
Protocol: Magnetoelectroporation (MEP)
MEP offers a rapid, transfection-agent-free alternative, using low-voltage electrical pulses to enhance SPION uptake.
Cell Preparation:
- Harvest and count stem cells. Centrifuge to form a pellet (e.g., 1-5 million cells).
- Resuspend the cell pellet in an electroporation buffer containing SPIONs at a high concentration (e.g., 500 µg Fe/mL - 1 mg Fe/mL) [29].
Electroporation:
- Transfer the cell-SPION suspension to an electroporation cuvette.
- Apply a series of low-voltage, short-duration pulses (e.g., 5-10 pulses of 150-300 V for 1-10 ms). Specific parameters must be optimized for the cell type [29][citation:15 from PMC779145].
- The entire process is completed in a matter of minutes.
Post-Labeling Processing:
- Immediately transfer the cells to pre-warmed complete culture media.
- Proceed with washing, viability checks, and efficiency validation as described in Section 3.1.1.
In Vivo MRI Tracking Protocol
After transplanting labeled cells into the target organ (e.g., intramyocardial, intracerebral, or intravenous injection), in vivo MRI is performed for longitudinal tracking.
Diagram: MRI Acquisition Pathways for SPION Detection. SPION-labeled cells can be visualized using standard T2/T2-weighted sequences (negative contrast) or specialized positive contrast sequences that help mitigate ambiguity from background hypointensities.*
Recommended MRI Hardware: Preclinical (7T-11.7T) or Clinical (3T) MRI scanners. Use dedicated surface coils for optimal signal-to-noise ratio.
Pulse Sequence Selection and Parameters:
- Primary Sequence: T2*-Weighted Gradient Echo (GRE) - This is the most sensitive sequence for detecting SPION-induced signal voids.
- Typical Parameters (for 3T): TR/TE = 300-600/15-30 ms, Flip Angle = 15°-30°, Matrix = 256x256, Slice Thickness = 1-2 mm.
- Confirmatory Sequence: T2-Weighted Fast Spin Echo (FSE/TSE) - Less sensitive to background inhomogeneities, providing better anatomical context.
- Optional: Positive Contrast Sequences - To improve specificity, techniques like IRON or Susceptibility Gradient Mapping (SGM) can be employed to generate hyperintense signals from the SPIONs [34].
- Primary Sequence: T2*-Weighted Gradient Echo (GRE) - This is the most sensitive sequence for detecting SPION-induced signal voids.
Image Analysis:
- Qualitative: Identify regions of signal void (hypointensity) co-localized with the injection site or migration pathways.
- Quantitative: Measure the volume of hypointensity or changes in T2/T2* relaxation times in the region of interest. Note that this provides an estimate of local iron content, not direct cell number, due to factors like label dilution and variable iron load [34] [36].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for SPION-Based Cell Tracking
| Item Category | Specific Examples | Function & Application Note |
|---|---|---|
| SPION Contrast Agents | Ferumoxides (Feridex/Endorem), Ferucarbotran (Resovist), VivoTrax, Custom-synthesized SPIONs (e.g., PLL-coated) | Generate contrast for MRI detection. Choice depends on core size, coating, and required cellular iron load. |
| Transfection Agents | Protamine Sulfate, Poly-L-Lysine (PLL), Lipofectamine | Facilitate SPION internalization into non-phagocytic cells via magnetofection. Protamine sulfate is commonly used in clinical protocols. |
| Viability/Cytotoxicity Assays | Trypan Blue Exclusion Assay, MTT/XTT Assay, LDH Assay | Essential for confirming that the labeling process does not adversely affect stem cell viability, proliferation, or differentiation capacity. |
| Labeling Efficiency Stains | Prussian Blue (for iron), Immunofluorescence Staining | Used to visually confirm and quantify the intracellular presence of SPIONs post-labeling. |
| In Vivo Imaging Tools | MRI with T2*/GRE sequences, Positive Contrast Software (e.g., IRON, SGM), Magnetic Particle Imaging (MPI) Scanner | MPI is an emerging modality that directly images SPIOs with high sensitivity and quantifiability, overcoming some MRI limitations [36]. |
Discussion and Future Perspectives
While SPION-enhanced MRI is a powerful tool for stem cell tracking, several challenges persist. A significant limitation of direct SPION labeling is that the MRI signal reflects the presence of the iron label, not necessarily cell viability; the label can be retained in macrophages after cell death, leading to false-positive signals [29] [32]. Furthermore, the contrast agent dilutes with each cell division, limiting long-term tracking of proliferating cells [29]. The "blooming artifact", while boosting sensitivity, can obscure fine anatomical details and complicates accurate quantification of cell numbers [34] [32].
Future directions aim to overcome these hurdles. The development of MRI reporter genes could enable the monitoring of only living, functional cells and track cell proliferation indefinitely [29]. Emerging imaging technologies like Magnetic Particle Imaging (MPI) offer direct, positive contrast quantification of SPIONs without background tissue signal, showing promise for highly sensitive cell tracking with detection limits as low as 250 cells in preclinical models [36]. Finally, the design of "smart" or responsive contrast agents that activate only upon specific cellular events, such as enzyme activity, could provide functional insights beyond mere location [37]. The integration of these advanced techniques with the high anatomical resolution of MRI will be instrumental in validating and optimizing stem cell therapies for clinical application.
The efficacy of stem cell therapy (SCT) is heavily dependent on the ability to monitor transplanted cells in vivo. Non-invasive imaging provides crucial information on cell survival, distribution, and engraftment, which is essential for validating treatment efficacy and optimizing protocols. [38] [39] Among available modalities, radionuclide imaging, specifically Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT), stands out for its unparalleled sensitivity, capable of detecting trace amounts of radiolabeled cells deep within the body. [40] [39]
For researchers and drug development professionals, these techniques offer a powerful tool to resolve contradictory results from clinical trials by providing quantitative data on cell delivery and persistence. [39] [41] This application note details the protocols and quantitative advantages of PET and SPECT within the context of stem cell therapy development.
Comparative Analysis of Imaging Modalities
While various imaging techniques are employed in stem cell research, their sensitivity, spatial resolution, and applicability for long-term tracking vary significantly. The table below provides a quantitative comparison of the primary modalities.
Table 1: Comparison of Stem Cell Imaging Modalities
| Imaging Modality | Detection Sensitivity | Spatial Resolution | Quantitative Capability | Primary Use in Stem Cell Tracking |
|---|---|---|---|---|
| PET | High (10⁻¹¹ - 10⁻¹² mol/L) [40] | 1-2 mm [39] | Excellent | Tracking cell biodistribution, persistence, and kinetics. [41] |
| SPECT | High (10⁻¹⁰ - 10⁻¹¹ mol/L) | 1-2 mm [39] | Good | Cell homing and short-term localization studies. [38] [39] |
| MRI | Low (10⁻³ - 10⁻⁵ mol/L) | 25-100 µm [39] | Moderate | Anatomical localization of magnetically labeled cells; requires high cell numbers. [39] |
| Optical Imaging | High (Bioluminescence) | Limited (3-5 mm) [39] | Semi-Quantitative | Preclinical tracking in small animals; limited by tissue depth. [39] |
PET offers superior sensitivity and quantitative accuracy compared to SPECT, though its radiopharmaceuticals are often more costly and have shorter half-lives. [40] SPECT remains highly valuable due to the longer half-lives of its isotopes, which can be better suited for tracking over several days. [40]
Experimental Protocols for Radionuclide Cell Labeling
Direct Radiolabeling of Stem Cells for Short-Term Tracking
Direct labeling involves incorporating a radiotracer into cells ex vivo prior to administration. This method is ideal for short-term tracking of initial cell homing and distribution. [38] [41]
Protocol: Direct Labeling with 18F-FDG or 111In-Oxine
- Cell Preparation: Expand and culture the therapeutic stem cells (e.g., MSCs, hematopoietic stem cells) to 70-80% confluence.
- Radiotracer Incubation:
- Resuspend cells in a buffered saline solution at a concentration of 1-5 x 10^7 cells/mL.
- Add the radiotracer (e.g., 18F-FDG (3.7-37 MBq) or 111In-oxine (7.4-18.5 MBq)) and incubate for 15-30 minutes at 37°C. [39]
- Washing and Purification: Centrifuge the cell suspension and carefully remove the supernatant containing unincorporated radiotracer. Wash the cell pellet twice with sterile PBS.
- Viability and Labeling Efficiency Check:
- Perform a trypan blue exclusion assay to ensure cell viability remains >90% post-labeling. [38]
- Use a gamma counter to measure activity in the cell pellet and supernatants to calculate labeling efficiency.
- Cell Administration: Resuspend the labeled cells in an appropriate infusion solution and administer to the subject via the intended route (e.g., intravenous, intracoronary).
- Image Acquisition:
Reporter Gene Imaging for Long-Term Cell Fate
For long-term monitoring of cell survival, proliferation, and persistence, indirect labeling with a reporter gene system is required. [38] [41] This approach involves genetically engineering cells to express a reporter protein that can interact with an injected radiotracer.
Protocol: PET Imaging with HSV1-tk Reporter Gene
- Genetic Engineering: Stably transduce stem cells with a viral vector (e.g., lentivirus) carrying the Herpes Simplex Virus type 1 thymidine kinase (HSV1-tk) reporter gene. A common construct also includes a fluorescent protein (e.g., GFP) for subsequent FACS purification. [38]
- Cell Sorting and Validation: Use Fluorescence-Activated Cell Sorting (FACS) to isolate a pure population of reporter-positive cells. Validate reporter gene expression and ensure normal cell function and differentiation capacity post-transduction.
- Cell Administration and Imaging:
- Administer the engineered cells to the subject.
- For imaging, inject the specific PET tracer for HSV1-tk, such as [18F]FHBG (9-(4-[18F]-fluoro-3-hydroxymethylbutyl)guanine).
- Perform PET scans at serial time points (days to weeks). The signal intensity will be proportional to the number of viable, reporter-expressing cells. [39]
Figure 1: Experimental workflow for tracking stem cells in vivo using direct and indirect radionuclide imaging methods.
The Scientist's Toolkit: Essential Reagents and Materials
Successful radionuclide imaging requires a suite of specialized reagents and equipment. The following table outlines key solutions for your research.
Table 2: Key Research Reagent Solutions for Radionuclide Imaging
| Item Name | Function/Description | Application Example |
|---|---|---|
| ¹⁸F-FDG ([18F]Fluorodeoxyglucose) | Glucose analogue radiotracer; accumulates in cells with high metabolic activity. | Direct labeling of stem cells for short-term PET tracking. [39] |
| ¹¹¹In-Oxine | Lipophilic complex that diffuses into cells; 111In remains trapped after oxine degrades. | Direct labeling for SPECT imaging and longer-term (days) tracking. [38] [39] |
| HSV1-tk Reporter System | Reporter gene; phosphorylates specific radiotracer probes, trapping them inside transduced cells. | Long-term fate monitoring of engineered stem cells via PET. [38] [39] |
| Fluorescence-Activated Cell Sorter (FACS) | Cell sorting technology that uses fluorescent labels to purify a specific cell population. | Isolation of stem cell populations stably expressing a fluorescent reporter gene (e.g., GFP). [38] |
| Good Manufacturing Practice (GMP) Grade Materials | Raw materials and processes meeting stringent quality control standards for clinical use. | Essential for the production of radiopharmaceuticals and cell products intended for human clinical trials. [41] [42] |
Critical Considerations for Research and Translation
Cytotoxicity and Functional Impact
The toxicity of contrast agents and radiotracers must be rigorously evaluated before use in SCT. [38] Key considerations include:
- Radiation Damage: Doses that are too high can impair proliferative activity and cause DNA damage in stem cells. [38] For example, 89Zr-oxine can impair the proliferation and survival of regulatory T cells (Tregs). [41]
- Viability Assessment: Employ assays like trypan blue exclusion, MTT, or resazurin to measure cell viability and metabolic activity post-labeling. [38]
- Functional Validation: Ensure that the labeling process does not alter the stem cells' differentiation capacity or therapeutic function. [39] [41]
Regulatory and Clinical Translation Pathways
Integrating imaging into cell therapy trials involves navigating regulatory frameworks. [41] [2]
- FDA Approval Pathway: Radiopharmaceuticals require extensive testing, cGMP production, and a lengthy approval process. [41] Initial human research often starts with a Radioactive Drug Research Committee (RDRC) application. [41]
- Combination Product Consideration: When an investigational cell therapy is used with an imaging probe, both products must meet safety and efficacy standards. [41] [2]
- Ethical Compliance: All research must adhere to guidelines, such as those from the International Society for Stem Cell Research (ISSCR), which emphasize rigorous independent peer review, oversight, and informed consent. [2]
Figure 2: Key hurdles and a phased pathway for translating a radionuclide imaging protocol from research to clinical use.
Optical imaging, particularly fluorescence and bioluminescence imaging, has become a cornerstone technology in preclinical research, enabling the non-invasive, real-time visualization of biological processes in living animals [43]. For stem cell research, these modalities are indispensable for tracking the fate, distribution, and functional efficacy of transplanted cells in vivo [7] [44]. Fluorescence imaging detects light emitted by fluorescent probes or proteins after excitation with an external light source, while bioluminescence imaging relies on the enzymatic reaction between a luciferase enzyme and its substrate to produce light internally [44]. This application note details standardized protocols and key methodological considerations for employing these techniques in the context of stem cell tracking, framed within the broader objective of advancing regenerative medicine and therapeutic development.
Comparative Analysis of Imaging Modalities
The choice between fluorescence and bioluminescence imaging depends on the specific requirements of the study, as each modality offers distinct advantages and faces particular limitations [43] [44].
Table 1: Comparison of Fluorescence and Bioluminescence Imaging for Stem Cell Tracking
| Feature | Fluorescence Imaging | Bioluminescence Imaging |
|---|---|---|
| Signal Origin | External light excitation of fluorophores [43] | Internal enzymatic reaction (luciferase + substrate) [44] |
| Background Signal | Yes, due to tissue autofluorescence [43] | Negligible, as no external light is required [44] |
| Sensitivity | High, but limited by background [43] | Extremely high (e.g., AkaLuc detects ~1,000 cells) [45] |
| Tissue Penetration | Limited by light scattering and absorption [43] | Generally superior for deep-tissue detection [45] |
| Spatial Resolution | High (micrometer scale) in superficial tissues [23] | Lower, suitable for whole-body localization [44] |
| Quantification | Can be complex due to variable probe concentration and tissue optics [46] | More straightforward, correlates with cell viability and number [44] |
| Genetic Encoding | Yes (e.g., GFP, mCherry, mRFPruby) [23] | Yes (e.g., Firefly luciferase, AkaLuc) [45] |
| Typical Applications | Cell tracking, molecular pathway activity, surgical guidance [46] [23] | Monitoring cell viability, tumor growth, and minimal residual disease [45] |
The following workflow diagram illustrates the decision-making process for selecting and implementing an appropriate optical imaging strategy for stem cell tracking.
Experimental Protocols
Protocol for Bioluminescence Imaging of Minimal Residual Disease
This protocol, adapted from a recent study on triple-negative breast cancer, enables sensitive detection of rare stem cells or therapy-resistant persister cells surviving treatment [45].
A. Generation of Bioluminescent Reporter Cells
- Lentiviral Transduction: Construct a bicistronic lentiviral dual-reporter vector encoding a luciferase (e.g., AkaLuc for high sensitivity [45] or Firefly luciferase) and a fluorescent protein (e.g., mCherry) for downstream validation.
- Stem Cell Transduction: Transduce the target stem cells (e.g., KB1P organoids [45] or mesenchymal stem cells) with the lentiviral vector.
- Selection and Enrichment: Use fluorescence-activated cell sorting (FACS) to isolate a pure population of reporter-positive cells based on mCherry fluorescence. Perform two rounds of sorting to ensure high stability of expression [45].
B. Validation of Reporter Function In Vitro
- Sensitivity Assay: Seed a serial dilution of reporter cells (e.g., from 5 to 10,000 cells) in a black-walled, clear-bottom 96-well plate.
- Substrate Addition: Add the appropriate luciferase substrate (e.g., AkaLumine-HCl for AkaLuc [45] or D-luciferin for Firefly luciferase) to the culture medium.
- Signal Detection: Immediately measure bioluminescence signal using a cooled CCD camera system (e.g., IVIS Spectrum or AMI HT [47]). The AkaLuc/AkaLumine system can detect as few as 5 cells in vitro, offering a 100-fold increase in sensitivity over traditional Firefly luciferase/luciferin [45].
C. In Vivo Imaging of Stem Cells
- Animal Preparation: Anesthetize mice using isoflurane (2-3% in oxygen).
- Substrate Administration: Administer the luciferase substrate via intraperitoneal injection (e.g., 15 mg/mL AkaLumine-HCl in PBS [45]).
- Image Acquisition: Place animals in the imaging chamber of the optical system and acquire a sequence of images. Typical acquisition times range from 1 second to 5 minutes, depending on signal strength [47].
- Data Quantification: Use analysis software (e.g., Living Image, Aura) to quantify the total flux (photons/second) within a defined region of interest.
Table 2: Key Reagents and Equipment for Bioluminescence Imaging
| Item | Specification/Function | Example |
|---|---|---|
| Reporter Gene | Genetic source of bioluminescence | AkaLuc, Firefly luciferase (FLuc) [45] |
| Substrate | Enzyme cofactor for light production | AkaLumine-HCl, D-luciferin [45] |
| Imaging System | Sensitive camera for photon detection | IVIS Spectrum, AMI HT [47] |
| Analysis Software | Quantifies bioluminescence signal | Living Image, Aura [47] |
Protocol for Longitudinal Fluorescence Imaging of Stem Cells
This protocol is designed for long-term tracking of stem cell location and behavior, incorporating strategies to minimize phototoxicity [23].
A. Stem Cell Labeling
- Genetic Labeling (Recommended for long-term tracking):
- Exogenous Labeling (For short-term tracking):
B. In Vivo Imaging and Cell Tracking
- Animal Immobilization: For long-term imaging of specific structures, secure the area of interest. In some models, this can involve immobilizing a limb using surgical glue on a coverslip [23].
- Microscope Setup: Use a confocal or two-photon microscope equipped with an environmental chamber (maintaining 37°C and 5% CO₂). A 20x objective (e.g., Zeiss Plan-Apochromat 20x/0.8) is often suitable for cellular resolution [23].
- Image Acquisition Parameters:
- Wavelength: Use long wavelengths (e.g., red/far-red) to minimize light scattering and photodamage [23].
- Time-lapse Settings: Set appropriate intervals (e.g., every 20 minutes) and z-stack depths to capture cell dynamics while minimizing light exposure [23].
- Laser Power: Use the lowest possible laser power that yields a detectable signal.
- Cell Lineage Analysis: Utilize computer-assisted cell tracking software (e.g., as described in Parhyale leg regeneration studies [23]) to trace cell lineages and movements over time.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful optical imaging experiments require careful selection of reagents and instruments. The following table catalogs key solutions for stem cell tracking studies.
Table 3: Research Reagent Solutions for Optical Imaging
| Category | Item | Function & Application |
|---|---|---|
| Reporter Genes | AkaLuc [45] | Ultra-sensitive luciferase for detecting minimal residual disease (e.g., ~1,000 cells). |
| Firefly Luciferase (FLuc) [44] | Standard luciferase for general bioluminescence imaging. | |
| H2B-mRFPruby [23] | Histone-bound red fluorescent protein for nuclear labeling and long-term cell tracking. | |
| Fluorescent Probes | Near-Infrared (NIR) Dyes (e.g., Cy5) [43] | Reduce tissue absorption and autofluorescence for deeper imaging. |
| Indocyanine Green (ICG) [46] | FDA-approved NIR dye for assessing tissue perfusion and sentinel lymph nodes. | |
| Quantum Dots [7] | Semiconductor nanocrystals with bright, stable fluorescence for cell labeling. | |
| Substrates | AkaLumine-HCl [45] | Synthetic substrate for AkaLuc, enabling high-intensity bioluminescence. |
| D-Luciferin [44] | Natural substrate for Firefly luciferase. | |
| Imaging Instruments | IVIS Spectrum [47] | Preclinical imager for 2D/3D fluorescence and bioluminescence. |
| Confocal Microscope [23] | Provides high-resolution cellular and subcellular fluorescence imaging. | |
| Critical Assay Kits | Cell Viability Assay | Confirm reporter labeling does not impair stem cell function. |
| FACS Sorting Reagents [45] | Isolate a pure population of reporter-expressing cells. |
Fluorescence and bioluminescence imaging provide powerful, complementary tools for advancing stem cell research in preclinical models. Adherence to standardized protocols, such as the community-driven REFLECT guidelines for fluorescence imaging [46], and the selection of appropriate reagents and sensitive reporters like AkaLuc [45] are critical for generating reproducible, quantitative, and biologically meaningful data. As these technologies continue to evolve with brighter probes, more sensitive detectors, and sophisticated analytical algorithms, their role in elucidating stem cell dynamics and accelerating the development of cell-based therapies will become increasingly indispensable.
The field of regenerative medicine has been transformed by the integration of stem cell therapies, offering new hope for treating a wide spectrum of diseases, from neurological afflictions like Parkinson's and Alzheimer's to cardiac complications and bone regeneration challenges [48]. The core premise of these therapies hinges on the remarkable capacity of stem cells to differentiate into specialized cell types and replace dysfunctional tissues. However, harnessing this transformative power requires meticulous monitoring of stem cell behavior post-transplantation to ensure both safety and efficacy [48] [49]. Without robust tracking systems, navigating stem cell therapy becomes akin to "flying blind," making it difficult to verify if cells are migrating to target tissues, proliferating appropriately, or differentiating correctly, while also obscuring potential side effects like tumor formation [48] [49].
Multimodal imaging addresses this critical need by amalgamating the strengths of different imaging modalities to compensate for their individual limitations. While unimodal approaches like fluorescence imaging provide molecular specificity and real-time monitoring, they often grapple with issues like limited tissue penetration depth [48]. Conversely, other techniques offer high-resolution anatomical details or insights into metabolic processes but lack the specificity of fluorescence. A harmonized imaging approach provides a comprehensive amalgamation of anatomical, functional, and molecular data, which is indispensable for understanding the multifaceted environments that stem cells navigate within the body [48]. This integrated strategy not only refines therapeutic protocols by informing dosage and administration routes but also acts as insurance against data loss or misinterpretation, ensuring a more accurate assessment of stem cell fate and function [48].
Core Imaging Modalities and Their Synergies
Multimodal imaging leverages complementary technologies to build a complete picture of stem cell behavior. The table below summarizes the key modalities used in contemporary stem cell tracking research.
Table 1: Key Imaging Modalities for Stem Cell Tracking
| Modality | Key Strengths | Primary Limitations | Common Labeling Methods | Tracking Duration |
|---|---|---|---|---|
| Fluorescence Imaging | High spatial resolution, real-time monitoring, multi-fluorescence detection (multiplexing) [48] | Limited tissue penetration, photobleaching [48] | Fluorescent proteins (e.g., GFP), fluorescent dyes, nanoparticles [48] | Short to long-term (depends on method) [48] |
| Photoacoustic (PA) Imaging | High sensitivity & spatial resolution, good tissue penetration [49] | Requires contrast agents for most stem cells [49] | Gold nanoparticles (nanorods, clusters) [49] | Mid to long-term [49] |
| Magnetic Resonance Imaging (MRI) | No radiation, excellent soft tissue contrast [48] | High cost, lower sensitivity, potentially long acquisition times [50] [48] | Iron oxide nanoparticles, quantitative MRI parameters (R1, R2*) [50] | Mid to long-term [48] |
| Positron Emission Tomography (PET) | High sensitivity, deep tissue imaging, quantitative metabolic data [48] | Use of radioactive tracers, high cost, lower spatial resolution [48] | Radiolabeled compounds (e.g., ^18^F-FDG) | Short-term (depends on tracer half-life) [48] |
| Optical Coherence Tomography (OCT) | High-resolution cross-sectional imaging, non-invasive [49] | Unable to differentiate donor from native cells without contrast agents [49] | Gold nanoparticles for contrast enhancement [49] | Long-term [49] |
| Bioluminescence (BL) Imaging | Very high sensitivity, no external light source required [48] | Low spatial resolution, requires genetic modification [48] | Genetic labeling (e.g., luciferase expression) [48] | Mid to long-term [48] |
The synergy in multimodal imaging comes from pairing modalities that compensate for each other's weaknesses. For instance, a combined Photoacoustic Microscopy and Optical Coherence Tomography (PAM-OCT) system leverages the high optical contrast of PAM with the superior micro-anatomical depth resolution of OCT [49]. Similarly, while quantitative MRI (qMRI) provides reproducible metrics related to tissue microstructure like myelin or iron content, its specificity is limited; thus, combining it with diffusion MRI (dMRI) can help disentangle microstructural differences [50]. The integration of fluorescence with MRI or PET creates a platform where real-time cellular events can be contextualized within high-resolution anatomical or metabolic frameworks [48].
Detailed Experimental Protocol: Multimodal Stem Cell Tracking with PAOFM
This protocol details the procedure for longitudinal tracking of human induced pluripotent stem cells differentiated to retinal pigment epithelium (hiPSC-RPE) using a multimodal platform integrating Photoacoustic Microscopy, Optical Coherence Tomography, and Fluorescence Microscopy (PAOFM), powered by chain-like gold nanoparticle cluster (GNC) nanosensors [49].
Research Reagent Solutions and Essential Materials
Table 2: Key Research Reagents and Materials
| Item Name | Function/Application | Key Characteristics |
|---|---|---|
| Human iPSC-RPE Cells | Target cell for transplantation and tracking [49] | Differentiated from human induced pluripotent stem cells, model for retinal degenerative diseases. |
| Ultraminiature GNC-RGD | Contrast agent for PAM and OCT imaging [49] | Chain-like cluster of 3-5 gold nanoparticles (7-8 nm diameter), absorption peak in NIR, functionalized with RGD peptides [49]. |
| CALNN and Cystearnine Peptides | Used as linkers in GNC fabrication [49] | Facilitate the clustering of individual spherical gold nanoparticles. |
| Femtosecond Pulsed Laser System | Fabrication of GNCs via pulsed laser ablation (PLA) [49] | Provides a "green synthesis" method for highly pure, colloidal-stable GNPs without chemical precursors [49]. |
| PAOFM Integrated Imaging System | Core imaging platform for in vivo tracking [49] | Custom system combining Photoacoustic Microscopy, Optical Coherence Tomography, and Fluorescence Microscopy. |
| Laser Burn Model (Rabbit) | In vivo model of RPE damage and degeneration [49] | Creates a clinically relevant injury site to monitor targeted migration of transplanted hiPSC-RPE cells. |
Step-by-Step Methodology
Part I: Synthesis and Characterization of GNC Contrast Agents
- Fabrication of Gold Nanoparticles (GNPs): Generate spherical, colloidal GNPs with an average diameter of 5 nm using a femtosecond pulsed laser ablation (PLA) method in deionized water. This physical method yields non-toxic, highly pure nanoparticles free from capping or stabilizing agents [49].
- Assembly of GNCs: Cluster 3-5 individual GNPs into chain-like structures (GNCs) using CALNN and cysteamine peptides as linkers. This assembly shifts the optical absorption spectrum into the Near-Infrared (NIR) window, which is optimal for in vivo imaging due to reduced light absorption by hemoglobin and other tissues [49].
- Surface Functionalization: Conjugate the GNCs with Arg-Gly-Asp (RGD) peptides. The RGD peptide sequence promotes integrin-mediated binding to cells, enhancing cellular uptake and labeling efficiency [49].
- Characterization: Verify the size, morphology, and stability of the GNC-RGD using Transmission Electron Microscopy (TEM) and zeta potential measurements. Confirm the NIR absorption peak via spectroscopy [49].
Part II: Cell Labeling and Transplantation
- Cell Culture: Maintain and expand hiPSC-RPE cells under standard culture conditions appropriate for the cell line.
- Labeling with GNC-RGD: Incubate hiPSC-RPE cells with the fabricated GNC-RGD nanosensors. The nanoparticles are internalized by the cells, providing a strong PA contrast signal.
- Validation of Labeling: Use in vitro microscopy to confirm successful labeling and ensure that cell viability and functionality (e.g., differentiation potential) are not adversely affected.
- Animal Model Preparation: Generate a model of RPE degeneration in rabbits using a laser to create controlled burn lesions. This creates a target site for monitoring cell migration.
- Cell Transplantation: Inject the GNC-RGD-labeled hiPSC-RPE cells into the subretinal space of the rabbit model [49].
Part III: Longitudinal In Vivo Multimodal Imaging
- System Calibration: Prior to imaging, calibrate the integrated PAOFM system to ensure co-registration of signals from all three modalities.
- Image Acquisition:
- PAM: Illuminate the eye with a pulsed laser at the NIR absorption wavelength of the GNCs. The labeled cells will absorb the light, generate thermal expansion, and produce acoustic waves detected by an ultrasonic transducer to reveal their location [49].
- OCT: Simultaneously, use OCT to obtain high-resolution, cross-sectional images of the retinal layers. This provides the anatomical context for locating the PAM signal and assessing tissue integrity [49].
- FM: If the GNC-RGD possesses fluorescent properties or co-labeling is used, employ fluorescence microscopy for additional validation and high-sensitivity surface imaging [49].
- Data Co-registration and Analysis: Overlay the PAM signal (indicating cell location) onto the OCT structural images. Quantify the number and distribution of labeled cells at the site of injury over time.
- Longitudinal Monitoring: Repeat the non-invasive PAOFM imaging sessions at regular intervals (e.g., weekly or monthly) for an extended period, up to 6 months, to track cell migration, persistence, and the therapeutic effect on retinal structure [49].
Diagram 1: Experimental workflow for multimodal stem cell tracking with PAOFM, showing the integrated steps from contrast agent synthesis to longitudinal imaging.
Quantitative Data and Comparative Analysis
The efficacy of a multimodal approach is demonstrated through quantifiable data on imaging performance and cellular behavior. The tables below summarize key quantitative findings from the featured protocol and a comparison of labeling strategies.
Table 3: Quantitative Performance of PAOFM Imaging for Stem Cell Tracking
| Parameter | Result / Value | Implication / Significance |
|---|---|---|
| GNC Size (post-disassembly) | 7-8 nm diameter [49] | Enables potential renal excretion, improving biocompatibility and safety profile [49]. |
| GNC Absorption Peak | Near-Infrared (NIR) regime [49] | Red-shifted absorption avoids hemoglobin interference, enabling high signal-to-background ratio in vivo [49]. |
| Tracking Duration | Up to 6 months [49] | Demonstrates capability for long-term, longitudinal assessment of cell fate. |
| Zeta Potential of GNC | ≈ -41 mV [49] | Indicates high colloidal stability in solution. |
| Spatial Resolution | Exceptional (PAM & OCT are high-resolution modalities) [49] | Allows precise localization of cells within tissue structures. |
Table 4: Comparison of Stem Cell Labeling Methods for Fluorescence-Based Tracking
| Labeling Method | Key Advantages (Pros) | Key Limitations (Cons) | Tracking Duration |
|---|---|---|---|
| Genetic (e.g., GFP) | Long-term tracking, expression passed to progeny [48] | Potential impact on cell function, time-consuming genetic modification [48] | Long-term [48] |
| Fluorescent Dye | High fluorescence intensity, relatively simple [48] | Photobleaching, potential cell toxicity, label dilution upon cell division [48] | Short to mid-term [48] |
| Nanoparticles (e.g., GNC) | High stability, minimal photobleaching, tunable properties [48] [49] | Potential impact on cell function, complexity of synthesis [48] | Mid to long-term [48] |
The integration of multimodal imaging platforms, such as PAOFM, represents a paradigm shift in stem cell therapy research. By synergistically combining the high contrast of PAM, the micro-anatomical resolution of OCT, and the specificity of FM, these platforms enable non-invasive, longitudinal, and high-resolution tracking of stem cells in vivo [49]. This comprehensive data collection is crucial for validating the safety and efficacy of cellular therapies, understanding fundamental cell biology post-transplantation, and optimizing clinical protocols.
Future developments in this field will likely focus on the refinement of contrast agents for enhanced sensitivity and biocompatibility, further integration of artificial intelligence for image analysis and diagnosis, and the miniaturization of imaging systems for broader clinical application [51]. As these technologies mature, multimodal imaging will undoubtedly become an indispensable cornerstone of translational stem cell research, bridging the gap between laboratory discovery and effective clinical therapeutics.
Within the context of stem cell tracking for in vivo imaging, nanoparticles have emerged as indispensable tools, leveraging their unique magnetic and optical properties to non-invasively monitor cell fate, migration, and engraftment. The convergence of nanotechnology with stem cell biology addresses a pressing need in regenerative medicine and drug development: the ability to longitudinally track therapeutic cells within a living organism. This application note details how engineered nanoparticles serve as versatile contrast agents, providing researchers with methodologies to elucidate the in vivo dynamics of stem cells through magnetic resonance imaging (MRI) and optical imaging modalities. The multifunctionality of these nanoscale agents not only enhances imaging contrast but also opens avenues for therapeutic applications, creating a powerful platform for theranostics in preclinical research.
Magnetic Nanoparticles as Contrast Agents
Properties and Mechanisms
Magnetic nanoparticles (MNPs), particularly superparamagnetic iron oxide nanoparticles (SPIOs and USPIOs), function as negative (T2) contrast agents in Magnetic Resonance Imaging (MRI). Their superparamagnetic property causes local magnetic field inhomogeneities, leading to a rapid dephasing of proton spins and a consequent decrease in signal intensity (T2 relaxation) in the regions where they are located [7] [52]. This effect enables the sensitive detection of small cell clusters labeled with these nanoparticles. For positive (T1) contrast, gadolinium-based nanoparticles (e.g., Gd₂O₃) are employed. Gadolinium ions (Gd³⁺) possess seven unpaired electrons that efficiently enhance the longitudinal relaxation rate (T1) of water protons, resulting in a bright, positive signal on T1-weighted MRI scans [53]. The key parameter quantifying the efficacy of T1 agents is longitudinal relaxivity (r1), while for T2 agents, it is transverse relaxivity (r2).
Table 1: Characteristics of Magnetic Nanoparticle Contrast Agents
| Nanoparticle Type | Core Material | Typical Size Range | Imaging Modality | Relaxivity (r1 or r2) | Primary Mechanism |
|---|---|---|---|---|---|
| SPIOs/USPIOs | Iron Oxide (Fe₃O₄) | 5-500 nm [7] | T2-Weighted MRI | High r2 [52] | Induces magnetic field inhomogeneity, shortening T2 |
| Gadolinium NPs | Gd₂O₃ | ~2-3 nm [53] | T1-Weighted MRI | r1 = 33.4 s⁻¹mM⁻¹ [53] | Dipolar interaction with water protons, shortening T1 |
| Manganese NPs | MnO | Varies | T1-Weighted MRI | r1 = 13.5 s⁻¹mM⁻¹ [53] | Similar to Gd, but with lower relaxivity |
Experimental Protocol: MRI Tracking of Stem Cells Labeled with SPIOs
This protocol details the ex vivo labeling of mesenchymal stem cells (MSCs) with SPIOs for subsequent in vivo tracking via MRI.
Research Reagent Solutions:
- SPIO Nanoparticles: Commercially available, dextran-coated Ferucarbotran (Resovist) or similar.
- Transfection Agent: Poly-L-lysine (PLL) or other cationic agents to facilitate nanoparticle uptake (concentration to be optimized).
- Mesenchymal Stem Cell Culture: Human MSCs derived from bone marrow or adipose tissue.
- Cell Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS) and 1% Penicillin-Streptomycin.
- Phosphate Buffered Saline (PBS): For washing cells.
- Trypsin-EDTA: For cell detachment.
Procedure:
- Cell Culture: Culture MSCs in T-75 flasks using complete culture medium until 70-80% confluent. Maintain standard culture conditions (37°C, 5% CO₂).
- Labeling Complex Formation: Incubate SPIOs (e.g., at a final iron concentration of 25-50 µg/mL) with a transfection agent (e.g., PLL at 0.75 µg/mL) in serum-free medium for 30-60 minutes at room temperature to form SPIO-transfection agent complexes [7].
- Cell Labeling:
- Wash the MSCs twice with pre-warmed PBS.
- Add the SPIO-complex solution to the cells in a serum-free medium.
- Incubate the cells for 2-24 hours under standard culture conditions [7].
- Post-Labeling Processing:
- Remove the labeling medium and wash the cells thoroughly with PBS at least three times to remove any non-internalized nanoparticles.
- Detach the cells using trypsin-EDTA and resuspend in complete medium or PBS for counting.
- Viability and Efficacy Assessment:
- Determine cell viability using a Trypan Blue exclusion assay.
- Confirm iron uptake via Perl's Prussian Blue staining [54].
- In Vivo Transplantation and Imaging:
- Transplant the labeled MSCs (e.g., 1x10⁵ cells in PBS) into the target organ (e.g., rat brain striatum) of an animal model using a stereotactic injector [54].
- Perform MRI on the animal using a high-field scanner (e.g., 7T or higher for small animals). Use T2-weighted sequences (e.g., spin-echo or gradient-echo) where the labeled cells will appear as hypointense (dark) regions [7].
Diagram 1: Workflow for stem cell MRI tracking using SPIOs.
Optical Nanoparticles as Contrast Agents
Properties and Mechanisms
Optical nanoparticles provide high-sensitivity contrast for fluorescence imaging, a modality invaluable for preclinical research due to its ease of use and potential for real-time imaging. Key agents include quantum dots (QDs) and semiconducting polymer nanoparticles (SPNs). QDs are inorganic semiconductor nanocrystals (2-5 nm) characterized by broad absorption spectra, narrow, tunable emission bands, and exceptional resistance to photobleaching compared to conventional fluorescent dyes [7] [55]. SPNs, derived from self-assembling conjugated polymers, offer exceptional brightness per particle, fast radiative rates, and excellent photostability, making them superior for long-term tracking studies [55]. The primary mechanism involves the absorption of photons, promotion of electrons to an excited state, and subsequent emission of lower-energy photons upon electron relaxation.
Table 2: Characteristics of Optical Nanoparticle Contrast Agents
| Nanoparticle Type | Composition | Typical Size Range | Emission Range | Key Advantage |
|---|---|---|---|---|
| Quantum Dots (QDs) | CdSe/ZnS core/shell | 2-5 nm [7] | Tunable, VIS-NIR | High quantum yield, narrow emission, photostability [7] |
| Semiconducting Polymer Nanoparticles (SPNs) | Conjugated Polymers (e.g., MEH-PPV, PCPDTBT) | 60-150 nm [55] | VIS-NIR-II | Exceptional brightness, excellent photostability, biocompatibility [55] |
| Cy5.5 Dye-Loaded Nanoparticles | Organic dye in chitosan/other polymer matrix | ~100-200 nm [56] | ~695-710 nm | Well-established chemistry, suitable for NIR imaging [56] |
Experimental Protocol: Stem Cell Labeling via Bioorthogonal Chemistry for Optical Tracking
This protocol describes a surface-labeling technique using bioorthogonal click chemistry, which offers high specificity and reduced risk of altering core cell functions compared to some internalization methods [56].
Research Reagent Solutions:
- Metabolic Precursor: Tetra-acetylated N-azidoacetyl-d-mannosamine (Ac₄ManNAz).
- Imageable Nanoparticles: Bicyclo[6.1.0]nonyne-modified glycol chitosan nanoparticles (BCN-CNPs) loaded with Cy5.5 [56].
- Stem Cell Culture: As in Protocol 2.1.
- Cell Culture Medium, PBS, Trypsin-EDTA.
Procedure:
- Metabolic Glycoengineering:
- Culture stem cells to 50-60% confluence.
- Treat the cells with Ac₄ManNAz (e.g., 50 µM) in complete culture medium for 2-3 days. This metabolic precursor introduces exogenous azide (-N₃) groups onto the cell surface glycoproteins [56].
- Preparation of Clickable Nanoparticles: Use pre-synthesized BCN-modified glycol chitosan nanoparticles (BCN-CNPs) loaded with the near-infrared fluorescent dye Cy5.5 [56].
- Bioorthogonal Labeling:
- Wash the Ac₄ManNAz-treated cells twice with PBS.
- Incubate the cells with BCN-CNP-Cy5.5 (e.g., 100 µg/mL) in serum-free medium for 1-2 hours at 37°C. The BCN group on the nanoparticle undergoes a rapid, copper-free cycloaddition "click" reaction with the azide groups on the cell surface [56].
- Post-Labeling Processing:
- Remove the labeling solution and wash the cells thoroughly with PBS.
- The labeled nanoparticles are rapidly internalized via cell membrane turnover.
- Validation:
- Analyze labeling efficiency using flow cytometry or confocal microscopy.
- Confirm cell viability and normal differentiation potential.
- In Vivo Transplantation and Imaging:
Diagram 2: Stem cell optical tracking workflow using bioorthogonal chemistry.
Multimodal and Genetically Encoded Approaches
Advancing Tracking with Multimodal Nanoparticles
Multimodal nanoparticles integrate two or more contrast mechanisms into a single platform, overcoming the limitations of individual imaging modalities. A prominent example is the combination of MRI and optical imaging. For instance, SPNs have been co-loaded with iron oxide nanoparticles, creating a single agent that provides the high spatial resolution and deep tissue penetration of MRI with the high sensitivity and molecular insights of fluorescence imaging [55]. This allows for precise anatomical localization of stem cells via MRI and detailed cellular-level analysis via optical techniques ex vivo or in intraoperative settings.
Genetically Encoded Contrast Agents
For long-term stem cell tracking across multiple cell generations, genetically encoded reporters are ideal. A novel approach involves engineering stem cells to express bacterial nanocompartments, such as encapsulins from Quasibacillus thermotolerans. These nanocompartments include a shell protein and a ferroxidase cargo protein that catalyzes the formation of ferric oxide nanoparticles inside the shell, functioning as an endogenous, genetically programmed T2 contrast agent for MRI [54]. When combined with a fluorescent protein like GFP, this system enables multimodal (MRI/optical) tracking without repeated nanoparticle administration.
Experimental Protocol Outline: Creating a Genetically Encoded MR Reporter Cell Line
- Genetic Construct Design: Clone the genes for the encapsulin shell and ferroxidase cargo protein into a lentiviral vector alongside a separate gene for a fluorescent protein (e.g., GFP), linked by a viral 2A peptide for simultaneous expression [54].
- Lentiviral Production: Generate lentiviral particles carrying the genetic construct.
- Stem Cell Transduction: Transduce the target stem cells (e.g., immortalized human MSCs) with the lentiviral particles.
- Selection and Expansion: Select successfully transduced cells using antibiotic resistance (e.g., puromycin) and expand the stable cell line.
- Iron Supplementation: Culture the engineered cells in medium supplemented with ferric ammonium citrate (e.g., 0.5 mM) to provide the iron substrate for biomineralization and contrast generation [54].
- Validation: Confirm iron oxide formation and MRI contrast capability in cell pellets using a preclinical MRI scanner and via Perls staining [54]. These cells can now be transplanted and tracked long-term without further labeling.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Nanoparticle-Based Stem Cell Tracking
| Reagent / Material | Function / Application | Example / Notes |
|---|---|---|
| Superparamagnetic Iron Oxide Nanoparticles (SPIOs/USPIOs) | Ex vivo cell labeling for in vivo tracking via T2-weighted MRI. | Ferucarbotran; often used with transfection agents like poly-L-lysine [7]. |
| Gadolinium Oxide (Gd₂O₃) Nanoparticles | Ex vivo or in vivo use as a T1 contrast agent for bright-contrast MRI. | Requires surface coating (e.g., with PAA, PEG) for colloidal stability and biocompatibility [53]. |
| Semiconducting Polymer Nanoparticles (SPNs) | High-performance fluorescent probes for sensitive optical imaging in the NIR window. | Noted for exceptional brightness and photostability [55]. |
| Metabolic Precursors (e.g., Ac₄ManNAz) | Enables bioorthogonal labeling by introducing chemical receptors (azides) onto cell surfaces [56]. | |
| Click-Chemistry Compatible Nanoparticles (e.g., BCN-CNPs) | Specifically targets and labels cells pre-treated with metabolic precursors via copper-free click reaction [56]. | Can be loaded with various imaging agents (dyes, iron oxide, gold). |
| Lentiviral Vectors for Encapsulin Systems | Creates stable, genetically modified stem cell lines for endogenous production of MRI contrast [54]. | Allows long-term, multimodal tracking without repeated labeling. |
| Transfection Agents (e.g., Poly-L-lysine) | Enhances cellular uptake of nanoparticles during ex vivo labeling protocols [7]. | Critical for efficient loading of non-functionalized nanoparticles. |
Cardiovascular disease (CVD), particularly ischemic heart disease, remains the leading global cause of mortality, accounting for over 17 million deaths annually and projected to rise to more than 23 million by 2030 [57] [58]. Myocardial infarction (MI) triggers a cascade of events leading to irreversible cardiomyocyte loss and adverse remodeling, often progressing to heart failure. Unlike certain lower vertebrates, the adult mammalian heart possesses very limited innate regenerative capacity, creating a significant unmet clinical need that conventional therapies cannot fully address [58] [59].
Stem cell-based regenerative therapies represent a promising frontier for repairing damaged cardiac tissue. The primary vision for Cardiovascular Regenerative Medicine (CaVaReM) is to develop treatments that can restore cardiac function through mechanisms including direct cardiomyocyte replacement, stimulation of angiogenesis, and potent paracrine signaling [58]. Realizing this potential requires not only advanced cell-based products but also sophisticated methods to monitor transplanted cells in living subjects. Non-invasive molecular imaging has therefore become an indispensable tool for validating the efficacy of these therapies by enabling researchers to track the location, survival, and functional integration of administered cells [60] [10].
Stem Cell Types for Myocardial Repair
Various stem cell types have been investigated for cardiac repair, each with distinct advantages, limitations, and mechanisms of action. The table below summarizes the key cell types under investigation.
Table 1: Stem Cell Types for Cardiac Repair
| Cell Type | Origin | Key Advantages | Major Limitations | Primary Mechanisms of Action |
|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone marrow, adipose tissue, umbilical cord | Immunomodulatory properties, low immunogenicity, strong paracrine signaling [58] [24] [59] | Limited differentiation into functional cardiomyocytes, poor long-term engraftment [59] | Paracrine secretion of growth factors, anti-inflammatory effects, angiogenesis promotion [57] [59] |
| Induced Pluripotent Stem Cell-Derived Cardiomyocytes (iPSC-CMs) | Reprogrammed somatic cells (e.g., skin, blood) | Patient-specific, no ethical concerns, potential for true remuscularization [57] [59] | Risk of arrhythmias, tumorigenicity potential, requires extensive pre-differentiation [59] | Direct integration into host myocardium, electrical coupling, contractile force contribution [59] |
| Embryonic Stem Cell-Derived Cardiomyocytes (ESC-CMs) | Blastocyst inner cell mass | High differentiation capacity, robust cardiomyocyte yield | Ethical concerns, immunorejection risk, tumorigenicity (teratoma formation) [58] | Direct replacement of contractile cells, paracrine effects |
| Cardiac Progenitor Cells (CPCs) | Heart tissue | Cardiac lineage commitment, endogenous origin, lower arrhythmia risk | Very limited availability, difficult to expand in culture [58] | Differentiation into endothelial cells and smooth muscle cells, paracrine signaling |
Among these, MSCs and iPSC-CMs have emerged as the most promising candidates for clinical application. MSCs function primarily through indirect mechanisms, secreting a panel of trophic factors that modulate the immune response, reduce fibrosis, and promote angiogenesis [59]. In contrast, iPSC-CMs offer the potential for direct remuscularization by replacing lost contractile tissue and electrically integrating with the host myocardium [59].
In Vivo Imaging Modalities for Stem Cell Tracking
Monitoring the fate of transplanted cells is crucial for optimizing therapeutic efficacy and safety. Molecular imaging technologies provide non-invasive, longitudinal insights into cell survival, distribution, and engraftment.
Table 2: Imaging Modalities for Stem Cell Tracking
| Imaging Modality | Detection Mechanism | Spatial Resolution | Tissue Penetration | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | Magnetic field effects on labeled cells (e.g., SPIOs) [61] | High (25-100 µm) [60] | Unlimited | Excellent anatomical detail, no ionizing radiation, serial imaging capability [60] [61] | Low sensitivity for cell detection, signal dilution with cell division, potential background artifacts [60] [24] |
| Positron Emission Tomography (PET) | Detection of positron-emitting radiotracers | Low (1-2 mm) [60] | Unlimited | Very high sensitivity, quantitative capabilities, clinical translation [60] [61] | Ionizing radiation, limited spatial resolution, short tracer half-life [60] [61] |
| Single-Photon Emission Computed Tomography (SPECT) | Detection of gamma-emitting radionuclides | Low (1-2 mm) [60] | Unlimited | Relatively high sensitivity, lower cost than PET [60] | Lower sensitivity than PET, ionizing radiation, limited spatial resolution [60] |
| Bioluminescence Imaging (BLI) | Luciferase enzyme reaction with substrate (e.g., luciferin) [61] | Very Low (3-5 mm) | Limited (1-2 cm) [60] | High sensitivity, low cost, no background autofluorescence [60] [61] | Requires genetic modification, limited tissue penetration, semi-quantitative [60] [61] |
| Fluorescence Imaging | Light emission after excitation of fluorophores | Low (2-3 mm) | Limited (1-2 cm) | High sensitivity, real-time imaging, multiple probes | Background autofluorescence, limited tissue penetration, light scattering [60] [61] |
Labeling Strategies for Stem Cell Tracking
The imaging modalities above rely on two primary approaches to label stem cells for in vivo tracking:
Direct Labeling: Cells are incubated with contrast agents (e.g., superparamagnetic iron oxide nanoparticles (SPIOs) for MRI, radiotracers for PET, or quantum dots for fluorescence) before transplantation [61] [24]. This approach is technically straightforward but suffers from label dilution as cells divide and the inability to distinguish between living and dead cells, as the contrast agent may persist in tissues after cell death [60] [24].
Reporter Gene Labeling: Stem cells are genetically engineered to express reporter genes (e.g., luciferase for BLI, herpes simplex virus thymidine kinase (HSV-tk) for PET, or ferritin for MRI) [60] [61] [10]. This method provides a self-renewing signal that is dependent on cell viability and is not diluted upon cell division, enabling long-term monitoring and lineage tracing [60] [10]. A significant advancement is the development of triple-fusion reporter genes that allow simultaneous tracking with multiple modalities (e.g., fluorescence, bioluminescence, and PET) from a single genetic construct [10].
Experimental Protocols for Stem Cell Therapy Assessment
Protocol: MSC Preparation and Intramyocardial Delivery in a Rodent MI Model
This protocol outlines the key steps for evaluating the therapeutic potential of MSCs in a preclinical model of myocardial infarction.
Step 1: Myocardial Infarction Model Establishment
- Anesthetize adult rats or mice using isoflurane (2-4% in oxygen).
- Perform endotracheal intubation and connect to a mechanical ventilator.
- Execute a left thoracotomy to expose the heart.
- Permanently ligate the left anterior descending (LAD) coronary artery using 7-0 prolene suture to induce myocardial infarction.
- Confirm successful infarction by visual observation of blanching in the left ventricular anterior wall.
Step 2: MSC Harvesting and Expansion
- Isolate human or rodent MSCs from bone marrow or adipose tissue.
- Culture and expand MSCs in complete medium (DMEM supplemented with 10% FBS, 1% penicillin/streptomycin) at 37°C with 5% CO₂.
- Passage cells at 80-90% confluence, typically every 3-5 days.
- Use cells at passages 3-6 for transplantation to maintain phenotypic stability.
Step 3: Cell Labeling for Tracking (Optional)
- For MRI tracking: Incubate 1×10⁶ MSCs with 50 µg/mL SPIO particles for 24 hours [61].
- For PET tracking: Incubate cells with 18F-FDG (37-74 MBq) for 30-60 minutes before transplantation [24].
- For reporter gene labeling: Transduce MSCs with lentiviral vectors encoding luciferase or other reporter genes 72-96 hours before transplantation [10].
Step 4: Intramyocardial Cell Delivery
- One week post-MI, re-anesthetize and re-open the thoracic cavity of the subject.
- Resuspend 1×10⁶ MSCs in 50-100 µL of sterile PBS.
- Using a 30-gauge Hamilton syringe, perform multiple (3-5) intramyocardial injections (10-20 µL per injection) around the infarct border zone.
- Monitor heart rhythm during injection for potential arrhythmias.
Step 5: In Vivo Imaging and Functional Assessment
- For BLI: Inject D-luciferin (150 mg/kg, i.p.) and acquire images 10-20 minutes post-injection using a CCD camera system [61].
- For MRI: Perform cardiac-gated T2*-weighted sequences at specific time points (e.g., days 1, 7, 14, 28 post-transplantation) to track SPIO-labeled cells [61].
- For functional assessment: Conduct echocardiography pre-transplantation and at weekly intervals post-transplantation to measure left ventricular ejection fraction, end-systolic volume, and end-diastolic volume.
Protocol: iPSC-CM Transplantation and Multimodal Imaging
This protocol describes the use of patient-specific iPSC-derived cardiomyocytes for myocardial repair, with an emphasis on advanced tracking techniques.
Step 1: iPSC Generation and Cardiomyocyte Differentiation
- Generate human iPSCs by reprogramming somatic cells (e.g., dermal fibroblasts) using non-integrating Sendai virus vectors encoding OCT4, SOX2, KLF4, and c-MYC [57].
- Maintain iPSCs in feeder-free culture using mTeSR1 medium on Matrigel-coated plates.
- Differentiate iPSCs into cardiomyocytes using a directed monolayer differentiation protocol with sequential activation and inhibition of the WNT signaling pathway using CHIR99021 and IWP2, respectively.
- Purify cardiomyocytes using glucose-free metabolic selection media or fluorescence-activated cell sorting (FACS) for cardiomyocyte-specific markers.
Step 2: Reporter Gene Engineering
- Introduce a triple-fusion reporter gene (e.g., combining firefly luciferase, GFP, and herpes simplex virus thymidine kinase) into the iPSCs using CRISPR/Cas9-mediated gene editing, targeting a safe-harbor locus (e.g., AAVS1) [10].
- Validate reporter expression and ensure normal differentiation capacity and electrophysiological properties of the engineered iPSC-CMs.
Step 3: In Vitro Characterization of iPSC-CMs
- Perform flow cytometry to quantify expression of cardiac troponins (cTnT, cTnI), α-actinin, and connexin 43.
- Assess electrophysiological properties using multi-electrode array (MEA) or patch-clamp techniques.
- Evaluate calcium handling using Fluo-4 AM or similar calcium-sensitive dyes.
Step 4: Cell Transplantation and Multimodal Imaging
- Transplant 5-10×10⁶ iPSC-CMs as single cells or 3D engineered tissue patches into the infarcted heart of immunodeficient mice or rats.
- For BLI: Image weekly after D-luciferin injection to monitor cell survival and proliferation [10].
- For PET: Administer [¹⁸F]FHBG (a substrate for HSV-tk) to specifically detect viable iPSC-CMs at various time points [10].
- Co-register BLI and PET signals with cardiac MRI to correlate cell location and survival with functional and anatomical improvements.
Signaling Pathways in Myocardial Repair
Stem cells promote cardiac repair through activation of multiple interconnected signaling pathways. The diagram below illustrates the key molecular mechanisms involved.
Diagram 1: Signaling Pathways in Stem Cell-Mediated Myocardial Repair. This diagram illustrates the key mechanisms through which transplanted stem cells, particularly MSCs and iPSC-CMs, promote cardiac repair. MSC-mediated effects are predominantly paracrine (yellow nodes), secreting factors that promote angiogenesis, reduce apoptosis, recruit progenitor cells, and modulate inflammation. iPSC-CMs primarily contribute through direct mechanisms (green nodes), including electrical integration and direct contractile force. These pathways collectively lead to improved cardiac function (blue node).
Experimental Workflow for Stem Cell Tracking in Cardiac Repair
The comprehensive evaluation of stem cell therapies requires an integrated approach combining cell preparation, transplantation, multimodal imaging, and functional assessment.
Diagram 2: Experimental Workflow for Stem Cell Therapy Assessment. This workflow outlines the key stages in evaluating stem cell therapies for cardiac repair, from cell preparation through intervention to comprehensive analysis. The process emphasizes the integration of multimodal imaging with functional assessment to establish correlations between cell fate and therapeutic outcomes.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of stem cell tracking experiments requires carefully selected reagents and materials. The table below details essential components for cardiovascular stem cell research.
Table 3: Essential Research Reagents for Cardiac Stem Cell Tracking
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Stem Cell Sources | Human MSCs, iPSCs, iPSC-CMs, CPCs | Therapeutic cell product for transplantation | Select based on mechanism: MSCs for paracrine effects, iPSC-CMs for remuscularization [58] [59] |
| Reporter Genes | Firefly luciferase (FLuc), HSV-thymidine kinase (HSV-tk), GFP, RFP | Enable long-term cell tracking via BLI, PET, fluorescence | Triple-fusion reporters allow multimodal imaging from a single construct [60] [10] |
| Direct Labeling Agents | SPIOs, ¹⁸F-FDG, ⁶⁴Cu, Quantum Dots, NIR fluorophores | Provide contrast for MRI, PET, fluorescence imaging | Consider half-life (radiotracers) and dilution effects from cell division [61] [24] |
| Cell Delivery Materials | Hamilton syringes (30-gauge), catheter-based infusion systems, biomaterial scaffolds | Enable precise cell administration to target cardiac tissue | Biomaterials can enhance cell retention and survival post-transplantation [59] |
| Molecular Probes & Substrates | D-luciferin (for BLI), [¹⁸F]FHBG (for PET) | Activate or bind to reporter systems for signal generation | Optimize dosing and timing for peak signal detection [61] [10] |
| Differentiation Factors | CHIR99021 (WNT activator), IWP2 (WNT inhibitor), growth factors | Direct stem cell differentiation toward cardiomyocyte lineage | Sequential WNT manipulation efficiently generates iPSC-CMs [59] |
| Immunomodulatory Reagents | Immunosuppressants (e.g., tacrolimus), HLA-editing tools | Prevent rejection of allogeneic cell transplants | CRISPR/Cas9-mediated HLA disruption enhances immune compatibility [59] |
The integration of advanced stem cell therapies with sophisticated in vivo imaging technologies represents a powerful approach for addressing the significant clinical challenge of myocardial repair. While substantial progress has been made in identifying promising cell candidates like MSCs and iPSC-CMs, and in developing sensitive tracking methods such as reporter gene imaging, the field continues to face challenges related to cell engraftment, survival, and functional integration [59]. Future directions will likely focus on combinatorial approaches utilizing biomaterial scaffolds, repeated cell administration, and refined patient selection criteria to improve therapeutic outcomes [59]. As molecular imaging technologies continue to evolve, they will play an increasingly vital role in bridging the gap between preclinical validation and successful clinical translation, ultimately fulfilling the promise of cardiovascular regenerative medicine for patients with ischemic heart disease.
Stem cell-based regenerative medicine presents a promising frontier for treating neurological disorders, with neural stem cells (NSCs) offering potential for cell replacement and functional recovery in conditions such as stroke and brain injury [11]. A significant challenge in clinical translation is the need to non-invasively monitor the fate and efficacy of transplanted cells within the living brain. Molecular imaging addresses this critical need by enabling longitudinal tracking of NSC engraftment, survival, and integration, thereby illuminating the mechanisms of functional improvement and optimizing therapeutic protocols [11] [10]. This application note details the integration of advanced in vivo imaging methodologies with NSC therapy development, providing structured data and protocols to support researchers in this field.
Table 1: In Vivo Imaging Modalities for Neural Stem Cell Tracking
| Imaging Modality | Labelling Strategy | Spatial Resolution | Molecular Sensitivity | Key Applications in NSC Tracking |
|---|---|---|---|---|
| MRI | Direct (e.g., SPIO nanoparticles) | Excellent (µm range) [11] | Low [11] | Short-term homing, real-time delivery guidance, structural integration [11] [62] |
| PET | Indirect (Reporter genes, e.g., HSV1-tk) [11] | Good (mm range) | High [11] | Long-term viability, cell proliferation, and functional biology [11] [10] |
| Bioluminescence Imaging (BLI) | Indirect (Reporter genes, e.g., Firefly luciferase) [63] | Low | Very High | Serial monitoring of cell survival and proliferation in small animals [11] [63] |
| Ultrasound | Indirect (Reporter genes for surface markers) [11] | Moderate | Low | Monitoring transplanted cells using targeted microbubbles [11] |
Table 2: Hydrogel Scaffold Properties and NSC Proliferation Metrics
| Parameter | Soft Hydrogel (1,800 Pa) | Stiff Hydrogel (5,800 Pa) | Cell-Only Control |
|---|---|---|---|
| Matrix Elasticity (G′) | 1,800 Pa [63] | 5,800 Pa [63] | Not Applicable |
| In Vivo NSC Proliferation (Up to Day 21) | Most vigorous [63] | Less vigorous [63] | Intermediate |
| Kinetics of Luciferase Activity | Standard time-to-peak | Slow time-to-peak after D-luciferin administration [63] | Standard time-to-peak |
| Detection Limit (In Vitro, MRI with SPIO) | Not Applicable | Not Applicable | ~1,000 MSCs [11] |
Experimental Protocols
Protocol: In Vivo Tracking of NSC Viability Using Bioluminescence Imaging
This protocol utilizes reporter gene imaging to monitor the survival and proliferation of human neural stem cells (F3-effluc) encapsulated in a gelatin-polyethylene glycol-tyramine (GPT) hydrogel in nude mice [63].
I. Materials
- Cells: F3 human neural stem cell line, genetically engineered to express enhanced firefly luciferase (F3-effluc) [63].
- Hydrogel: GPT conjugate, Horseradish Peroxidase (HRP), Hydrogen Peroxide (H₂O₂) [63].
- Imaging Substrate: D-luciferin, potassium salt.
- Equipment: In vivo imaging system (e.g., IVIS spectrum), Advanced Rheometer.
II. Methods
- GPT Hydrogel Preparation (200 µL) [63]:
- Prepare two solutions:
- Solution A: 3% (w/w) GPT polymer dissolved in HRP stock solution.
- Solution B: 3% (w/w) GPT polymer dissolved in H₂O₂ solution (concentration 0.0038% to 0.0075% w/w for elasticity control).
- Rapidly mix 100 µL of Solution A and 100 µL of Solution B to form the hydrogel via enzyme-mediated cross-linking.
- Prepare two solutions:
Cell Encapsulation and Transplantation:
- Mix F3-effluc cells with the GPT polymer solution prior to cross-linking.
- Inject the cell-hydrogel mixture subcutaneously or into the target organ of anesthetized nude mice.
Bioluminescence Image Acquisition and Analysis:
- Intraperitoneally inject D-luciferin (150 mg/kg) into the mice.
- Acquire serial images at multiple time points (e.g., daily for the first week, then weekly) to monitor proliferation.
- Analyze the bioluminescence signal intensity and kinetics, noting the delayed time-to-peak in stiffer hydrogels [63].
Validation:
- Upon study completion, perform Ki-67-specific immunostaining on explanted hydrogels to confirm proliferating cells [63].
Protocol: Direct Labeling of Mesenchymal Stem Cells with SPIO for MRI Tracking
This protocol describes direct labeling for short-term monitoring of stem cell delivery and homing, noting potential impacts on cell biology [11].
I. Materials
- Cells: Human Mesenchymal Stem Cells (MSCs).
- Labeling Agent: Superparamagnetic Iron Oxide (SPIO) nanoparticles.
- Equipment: High-field MRI scanner, cell culture incubator.
II. Methods
- SPIO Labeling of MSCs:
- Incubate MSCs with SPIO nanoparticles in culture medium according to manufacturer's instructions.
- Note: Exposure to magnetic fields post-labeling can enhance the total iron load per cell and optimize imaging properties but may inhibit colony-forming ability and affect differentiation [11].
Cell Delivery and MRI:
Functional and Behavioral Correlation:
- Correlate MRI data with structural and functional MRI (e.g., resting-state fMRI) and sensorimotor behavior tests to assess therapeutic success and plastic reorganization [62].
Protocol: In Vitro Differentiation of Human Neural Stem Cells
This supporting protocol details the directed differentiation of NSCs into neuronal and glial lineages for in vitro characterization [64].
I. Materials
- Cell Culture Vessels: Coated with CELLstart, Geltrex matrix, or poly-L-ornithine/laminin [64].
- Media:
- Expansion Medium: StemPro NSC SFM Complete Medium with KnockOut D-MEM/F-12, StemPro Neural Supplement, EGF (20 ng/mL), and bFGF (20 ng/mL) [64].
- Neuronal Differentiation Medium: Neurobasal Medium supplemented with B-27 Serum-Free Supplement (2%) and GlutaMAX [64].
- Astrocyte Differentiation Medium: D-MEM with N-2 Supplement (1%), GlutaMAX, and 1% FBS [64].
- Oligodendrocyte Differentiation Medium: Neurobasal Medium with B-27 Supplement, GlutaMAX, and T3 (30 ng/mL) [64].
II. Methods
- Coating Culture Vessels: Coat plates with the appropriate substrate (e.g., Geltrex matrix diluted 1:100 in cold D-MEM/F-12) for at least 1 hour at room temperature before use [64].
- NSC Expansion: Culture NSCs in Expansion Medium on coated vessels until they reach 70-80% confluence.
- Directed Differentiation:
- For Neurons: Plate NSCs on coated vessels and culture in Neuronal Differentiation Medium for 14-21 days, with medium changes every 2-3 days.
- For Astrocytes: Plate NSCs and culture in Astrocyte Differentiation Medium for 10-14 days.
- For Oligodendrocytes: Plate NSCs and culture in Oligodendrocyte Differentiation Medium for 10-14 days.
- Immunostaining: Fix differentiated cells and immunostain for lineage-specific markers (e.g., MAP2 for neurons, GFAP for astrocytes, GalC for oligodendrocytes) to confirm successful differentiation [64].
Visualizations
NSC Therapy Workflow
Stem Cell Tracking Pathways
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for NSC Engraftment Studies
| Category | Item | Function and Application |
|---|---|---|
| Cell Culture | StemPro NSC SFM | A defined, serum-free medium for the expansion and maintenance of human neural stem cells [64]. |
| B-27 & N-2 Supplements | Serum-free supplements essential for neuronal and glial differentiation and survival [64]. | |
| Geltrex Matrix / Laminin | Extracellular matrix proteins used to coat culture vessels, providing a substrate that supports NSC attachment and differentiation [64]. | |
| In Vivo Tracking | SPIO Nanoparticles | Superparamagnetic iron oxide particles for direct labeling of cells, enabling detection by MRI [11]. |
| D-Luciferin | The substrate for firefly luciferase, administered in vivo to generate a bioluminescence signal from cells expressing the luciferase reporter gene [63]. | |
| Scaffolding | GPT Hydrogel | An injectable, in situ-crosslinkable hydrogel scaffold that provides a 3D supportive niche for implanted NSCs, enhancing survival and allowing control over mechanical properties [63]. |
Overcoming Technical Hurdles: Challenges and Optimization Strategies
Addressing Signal Dilution from Cell Division in Direct Labeling
In the field of stem cell tracking for regenerative medicine, in vivo imaging is crucial for monitoring the fate, migration, and survival of transplanted cells. Direct labeling methods, which involve introducing a labeling agent into cells prior to transplantation, are widely used due to their simplicity and absence of genetic modification [9]. However, a significant limitation of these methods is signal dilution caused by cell division, where the labeling agent is distributed among daughter cells, leading to a progressive decrease in signal intensity that can impede long-term monitoring [9] [65]. This application note details protocols and strategies to mitigate this challenge, enabling more reliable long-term tracking of stem cells in vivo.
The Problem: Signal Dilution in Direct Labeling
Direct cell labeling is a straightforward technique where stem cells are incubated with a contrast agent or tracer ex vivo before being administered to a recipient [9]. While this approach is powerful, the label dilutes with each cell division. The amount of label per cell decreases, and it may be distributed asymmetrically to the progeny [9]. Furthermore, labels can be lost by cells through natural excretion processes or, in the case of radionuclides, radioactive decay [9]. This decay in signal intensity does not necessarily correlate with cell death, complicating the interpretation of viability and distribution data in long-term studies. The following diagram illustrates this core problem and its consequences for quantitative imaging.
Strategic Approaches to Mitigate Signal Dilution
Researchers can adopt several strategic approaches to overcome the limitation of signal dilution, each with its own advantages and considerations. The choice of strategy depends on the specific requirements of the study, such as the desired tracking duration and the available imaging instrumentation.
Table 1: Strategic Approaches for Mitigating Signal Dilution
| Strategy | Mechanism | Advantages | Considerations |
|---|---|---|---|
| Use of Non-Dividing Cells | Transplantation of quiescent or terminally differentiated cells reduces the rate of label dilution. | Simplifies data interpretation; signal loss more directly correlates to cell death. | Not applicable for studies requiring proliferation or differentiation dynamics. |
| Covalent Tethering | Using labels that form stable covalent bonds with intracellular components (e.g., proteins), reducing passive loss [66]. | Minimizes non-dilutive signal loss; enhances signal retention per cell. | Does not prevent dilution from cell division; requires specialized chemistry. |
| Signal Amplification | Employing labeling agents or imaging techniques that generate a strong signal per unit of label. | Allows detection of lower label concentrations; extends tracking window. | May require specialized imaging equipment (e.g., high-sensitivity detectors). |
| Proliferation-Sensitive Agents | Using agents that are retained upon cell division or whose retention is linked to specific metabolic activity. | Can provide information on both cell location and proliferative status. | Complex agent design and validation; not yet widely available. |
Research Reagent Solutions
Selecting the appropriate labeling reagent is paramount for a successful tracking study. The ideal reagent should provide a strong initial signal and be well-retained within the cell.
Table 2: Key Reagents for Direct Stem Cell Labeling
| Reagent | Function & Mechanism | Key Considerations |
|---|---|---|
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | MRI contrast agent internalized via endocytosis; creates dark contrast on T2-weighted images [65]. | Biocompatible; may require transfection agents (e.g., protamine sulfate) for enhanced uptake. Signal quantification requires voxel-based analysis [65]. |
| 124I-Hexadecyl Iodobenzoate (124I-HIB) | Lipophilic PET tracer that anchors into cellular membranes [9]. | Enables tracking for up to 9 days in normal tissue; relatively long half-life of 124I (4.2 days) allows longer studies [9]. |
| 64Cu-DOTA-Hexadecyl Benzoate (64Cu-DOTA-HB) | Lipophilic PET tracer chelated with DOTA for stable complexation of 64Cu [9]. | 64Cu has a relatively long half-life (12.7 h); DOTA chelator is clinically available [9]. |
| NHS-Ester Dyes (e.g., Alexa Fluor series) | Forms a stable amide bond with primary amines (-NH2) on surface and intracellular proteins [66]. | Covalent bonding minimizes label loss; suitable for high-resolution fluorescence imaging. High-density labeling enables visualization of fine structures [66]. |
| Quantum Dots (QDs) | Semiconductor nanoparticles for fluorescence imaging; produce intense, stable emissions [65]. | Signal analyzed via spectral unmixing; potential toxicity and photobleaching require consideration [65]. |
Detailed Experimental Protocols
Protocol 1: Direct Radiolabeling with 124I-HIB for PET Tracking
This protocol is adapted from studies tracking adipose-derived stem cells (ADSCs) in myocardial infarction models, allowing monitoring for several days [9].
Workflow Overview:
Materials:
- Stem cells (e.g., ADSCs)
- 124I-HIB solution
- Cell culture medium and PBS
- Centrifuge
Procedure:
- Cell Preparation: Harvest stem cells at 70-90% confluency using standard methods (e.g., trypsinization). Wash and count cells.
- Labeling: Resuspend cell pellet in a small volume (e.g., 1-2 mL) of pre-warmed serum-free medium. Add 124I-HIB solution (e.g., 37-74 kBq per 10^6 cells). Incubate for 2-4 hours at 37°C with gentle agitation.
- Washing: Centrifuge the cell suspension (e.g., 300 x g for 5 min). Carefully remove the supernatant (contains unincorporated radiotracer) and wash the cell pellet with PBS. Repeat this wash step three times to ensure removal of free 124I-HIB.
- Quality Control: Resuspend the labeled cells in an appropriate administration medium. Perform a viability assay (e.g., trypan blue exclusion) and a functional assay to confirm the labeling process has not impaired the cells' therapeutic properties.
- Transplantation and Imaging: Transplant the required number of labeled cells into the subject. Acquire PET images at predetermined time points (e.g., 2 hours, 1, 3, 5, 7, and 9 days post-transplantation).
- Data Analysis: Draw regions of interest (ROIs) around the transplantation site and a reference background region. Quantify the radioactivity as percentage of injected dose per gram of tissue (%ID/g) or as a percentage of the signal from the first imaging time point [9].
Protocol 2: Covalent Membrane Labeling with NHS-Ester Dyes
This protocol uses NHS-ester chemistry for high-density, stable labeling of membrane proteins, ideal for tracking cell morphology and short-term interactions with high-resolution microscopy [66].
Materials:
- Stem cells in suspension (e.g., DC2.4 dendritic cells)
- Alexa Fluor 647 NHS-ester (or similar)
- DMSO (anhydrous)
- HEPES-buffered saline (HBS) or PBS (ice-cold)
- Centrifuge
Procedure:
- Dye Preparation: Dissolve the Alexa Fluor 647 NHS-ester in anhydrous DMSO to create a stock solution (e.g., 10 mM). Prepare the working solution by diluting the stock in ice-cold HBS or PBS immediately before use.
- Labeling: Harvest cells and wash twice with ice-cold buffer. Resuspend the cell pellet at a density of 1-10 x 10^6 cells/mL in ice-cold buffer. Add the dye working solution to the cell suspension (final dye concentration ~10-100 µM). Incubate on ice for 5-30 minutes, protecting the tube from light. The cold temperature minimizes dye internalization.
- Quenching and Washing: Add a large excess (e.g., 10x volume) of ice-cold complete medium (containing serum proteins, which will quench the reaction) to the labeling mixture. Centrifuge to pellet cells and remove the supernatant. Wash the cells three times with ice-cold PBS to remove any unreacted dye.
- Validation: Confirm extracellular labeling using a trypan blue quenching test [66]. Resuspend a small aliquot of labeled cells in PBS and image. Then, add trypan blue (0.4%) and image again. A significant reduction (>50%) in fluorescence intensity confirms successful extracellular membrane labeling.
- Transplantation and Imaging: Transplant cells for in vivo tracking or plate for in vitro live-cell imaging. The covalent bond provides stable labeling, enabling visualization of cell shapes, membrane fibers, and dynamic interactions for several hours [66].
Data Analysis and Interpretation
Accurate quantification of imaging data is essential. For radionuclide-based tracking, ROI analysis is used to measure signal decay over time. It is critical to differentiate signal loss due to radionuclide decay, cell death, and label dilution from cell division. Using a long-lived isotope and establishing a baseline for biological half-life are key. For MRI, software like ImageJ is used for voxel-based analysis of SPION density, though artifacts from iron degradation must be considered [65]. Fluorescence data from NHS-ester dyes or QDs require background subtraction and, for in vivo applications, compensation for tissue attenuation.
Signal dilution from cell division is an inherent challenge in direct stem cell labeling. However, by strategically selecting long-lived or stably-bound reagents like 124I-HIB, 64Cu-DOTA-HB, or NHS-ester dyes and following robust labeling protocols, researchers can significantly extend the in vivo tracking window. These methods provide invaluable insights into stem cell survival, migration, and engraftment, accelerating the development of safe and effective regenerative therapies.
Mitigating False Positives from Phagocytosis of Dead Cells
Within the context of stem cell therapy research, in vivo cell tracking is indispensable for monitoring transplanted cell fate. A significant confounder in this process is the generation of false positive signals due to the phagocytosis of dead or dying labeled cells by immune cells such as macrophages. This phenomenon can lead to a profound misinterpretation of cell biodistribution, persistence, and homing, as the signal originates from the phagocyte rather than the therapeutic cell. This application note details protocols and strategies to identify, mitigate, and account for these false positives, thereby enhancing the reliability of cell tracking data in preclinical research. The core challenge lies in distinguishing the signal from viable, functionally engrafted stem cells from the background noise of immune-mediated clearance.
Background and Mechanisms
The Source of False Positives: Phagocytic Clearance
The innate immune system rapidly clears dead and dying cells. When stem cells labeled with contrast agents (e.g., iron oxide nanoparticles, fluorescent markers) undergo apoptosis or necrosis post-transplantation, they are recognized and engulfed by phagocytes, primarily macrophages. The internalized label subsequently resides within the macrophage, creating a false signal that can be mistaken for a surviving stem cell [67] [68] [69]. This is a particular challenge with direct labeling methods, where the contrast agent is not diluted by cell division and can persist long after the original cell has died [67].
Key Phagocytic Pathways and Checkpoints
Recent research has identified specific molecular pathways that regulate phagocytosis. Notably, the tetraspanin CD37 has been identified as a novel phagocytic checkpoint on macrophages. Tumor-derived Macrophage Migration Inhibitory Factor (MIF) binds to CD37, promoting the phosphorylation of CD37Y13 and recruiting SHP1. This cascade inhibits AKT signaling, ultimately suppressing phagocytosis. Conversely, targeting CD37 with a specific antibody (e.g., naratuximab) blocks this inhibitory pathway, promoting phagocytosis [70]. Understanding such pathways is crucial, as modulating them can influence the rate at which dead cells are cleared, potentially impacting the background false positive signal.
Table 1: Key Molecules in Phagocytic Checkpoint Signaling
| Molecule | Role in Phagocytosis | Potential Impact on False Positives |
|---|---|---|
| CD37 | Phagocytic checkpoint receptor on macrophages; its engagement inhibits phagocytosis. | A target for mitigation; blocking CD37 promotes clearance of dead cells, potentially increasing short-term false positives. |
| MIF | Tumor-derived ligand that binds CD37, initiating an anti-phagocytic signaling cascade. | High MIF levels may suppress macrophage activity, reducing clearance of dead cells and prolonging their signal. |
| SHP1 | Phosphatase recruited by phosphorylated CD37; part of the downstream inhibitory signaling. | A key node in the intracellular signaling pathway that suppresses phagocytosis. |
| AKT | Signaling protein whose activity is inhibited by the CD37/SHP1 pathway. | AKT inhibition impairs the phagocytic capability of macrophages. |
The following diagram illustrates the signaling pathway through which the CD37 checkpoint regulates phagocytosis, based on findings from [70]:
Imaging Modalities and False Positive Challenges
No single imaging modality is immune to false positives from phagocytosis; however, their characteristics and the nature of the signal differ. The table below summarizes the primary modalities used in stem cell tracking and their specific vulnerabilities.
Table 2: Cell Tracking Modalities and Vulnerability to False Positives
| Imaging Modality | Labeling Method | Primary False Positive Challenge |
|---|---|---|
| Magnetic Resonance Imaging (MRI) | Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Signal void (T2/T2* effect) from macrophages that have ingested dead labeled cells is indistinguishable from that of live cells. Difficult to quantify [68] [71]. |
| Magnetic Particle Imaging (MPI) | Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Linearly quantitative signal for iron. However, signal from macrophages that have phagocytosed labeled cells is identical to signal from live stem cells [72] [71]. |
| Optical Imaging | Fluorescent dyes, Bioluminescent reporter genes | Phagocytosis of fluorescent labels by macrophages leads to signal from incorrect cell type. Bioluminescence (requiring ATP) is more specific to viable cells [67] [69]. |
| Multimodal Imaging | Combination (e.g., SPIONs + Fluorophore) | Co-registration of signals can help confirm location but does not inherently distinguish phagocytosed labels. Allows cross-validation [67]. |
Magnetic Particle Imaging (MPI) demonstrates significant advantages for quantification, as its signal is linearly quantitative to the amount of iron oxide present, independent of tissue depth [72] [71]. However, this quantitative power does not inherently discriminate between iron in stem cells and iron in macrophages. One study successfully tracked MNP-loaded THP-1 monocytes in real-time, achieving a 95% detection rate of inserted cells in a phantom model [72]. This high sensitivity underscores the need for complementary strategies to confirm that the signal originates from the intended cells.
Experimental Protocols for Mitigation
Protocol: Using a Phagocytosis Assay to Quantify False Positives
This protocol leverages a live-cell imaging approach to directly observe and quantify the phagocytosis of dead, labeled stem cells by macrophages, providing a baseline metric for false positive potential [73] [74].
1. Preparation of Target Cells (Stem Cells):
- Culture and expand the stem cells of interest (e.g., Mesenchymal Stem Cells - MSCs).
- Labeling: Incubate cells with a fluorescent cell tracker (e.g., CFSE) according to manufacturer instructions. Alternatively, label with SPIONs for correlative MRI/MPI studies.
- Induction of Cell Death: Induce apoptosis in a portion of the labeled stem cells using a validated method (e.g., exposure to hydrogen peroxide or staurosporine). Confirm cell death via flow cytometry (Annexin V/PI staining).
- Control: Keep a portion of labeled stem cells viable.
2. Preparation of Phagocytes:
- Isolate primary macrophages from donor blood or use a macrophage cell line (e.g., RAW 264.7).
- Label macrophages with a different, spectrally distinct fluorescent cell tracker (e.g., CellTrace Far Red).
3. Co-culture and Live-Cell Imaging:
- Plate macrophages in a 96-well glass-bottom plate.
- Add the pre-treated (dead or viable) labeled stem cells to the macrophage culture at a defined ratio (e.g., 5:1, stem cells to macrophages).
- Place the plate in an automated, environmentally controlled live-cell imaging microscope (e.g., Olympus ScanR system).
- Acquire time-lapse images over 3-6 hours.
4. Image Analysis with AI-based Segmentation:
- Use a pre-trained neural network like AIstain (a U-Net-based model) for accurate, label-free segmentation and identification of macrophages in the phase-contrast channel [73] [74].
- Quantify the fluorescence from the stem cell label (e.g., CFSE) within the boundaries of the segmented macrophages.
- A macrophage positive for the stem cell label is counted as a false positive event.
- Quantification: Calculate the percentage of phagocytic macrophages and the average number of ingested cells per macrophage over time.
Protocol: Validating Cell Viability Post-Transplantation Using MPI and Bioluminescence
This protocol uses a dual-modality approach to differentiate between the robust, ATP-dependent signal of bioluminescence (specific to viable cells) and the iron-based signal of MPI (which persists regardless of cell viability) [67] [71].
1. Stem Cell Engineering and Labeling:
- Stably transduce stem cells with a luciferase reporter gene (for bioluminescence imaging) and a fluorescent protein (e.g., GFP) for post-mortem validation.
- Dual-Labeling: Incubate the engineered cells with SPIONs (e.g., Synomag or Resovist) at an iron concentration of 0.5 mmol/L for several hours [72].
- Wash cells thoroughly to remove excess, unincorporated nanoparticles.
2. In Vivo Experimentation:
- Transplant the dual-labeled stem cells into your animal disease model.
- Acquire longitudinal images using both MPI and Bioluminescence (BLI) at multiple time points post-transplantation (e.g., day 1, 3, 7, 14).
3. Image Co-registration and Analysis:
- Co-register the MPI and BLI images with an anatomical scan (e.g., CT or MRI).
- Viability Assessment: At each time point, a strong, co-localized MPI and BLI signal indicates the presence of viable, engrafted stem cells.
- False Positive Identification: A persistent or increasing MPI signal in a location where the BLI signal has decayed or disappeared indicates a site where dead stem cells have been cleared and their iron load has potentially been phagocytosed by host macrophages.
4. Ex Vivo Validation:
- At the endpoint, harvest organs for ex vivo MPI and BLI imaging to determine the final biodistribution with high sensitivity [71].
- Perform histology on target tissues. Use:
- Perls' Prussian Blue stain to localize iron.
- Immunofluorescence for GFP (to identify the transplanted cells) and a macrophage marker (e.g., CD68 or IBA1) [68].
- The confirmation of iron (Prussian Blue+) within CD68+ cells that are GFP- provides definitive evidence of a false positive signal.
The workflow for this dual-modality validation protocol is outlined below:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagents for Mitigating False Positives
| Item | Function/Application | Example Products/Sources |
|---|---|---|
| pHrodo BioParticles Conjugates | Phagocytosis assay reagent; fluorescence dramatically increases in acidic phagolysosomes, providing a direct readout of phagocytosis. | pHrodo Red or Deep Red Conjugates (Invitrogen) [73]. |
| SPIONs for MPI/MRI | Magnetic labels for cell tracking. Enable deep-tissue, quantitative imaging. | Resovist, Synomag (Micromod) [72] [71]. |
| Luciferase Reporter Kits | For engineering cells to express luciferase, enabling BLI as a viability-specific readout. | Luciferase vectors, D-luciferin substrate (various suppliers). |
| Anti-CD37 Antibody | Research tool to modulate the CD37 phagocytic checkpoint pathway. | Naratuximab (for research use) [70]. |
| AI-Based Segmentation Software | For accurate, label-free analysis of live-cell imaging data in phagocytosis assays. | AIstain (U-Net model for Olympus ScanR) [73] [74]. |
| FluoroBrite DMEM Medium | Low-fluorescence live-cell imaging medium, essential for reducing background in fluorescent phagocytosis assays. | Gibco Thermo Fisher Scientific [73]. |
Mitigating false positives from phagocytosis is not a matter of applying a single technique but of adopting a strategic, multi-layered approach. Key recommendations include: (1) understanding the phagocytic mechanisms relevant to your model; (2) employing dual-modality imaging, preferably combining a viability-sensitive technique (like BLI) with an anatomical/deep-tissue tracer (like MPI/MRI); and (3) using definitive ex vivo histology to confirm the cellular source of the in vivo signal. By integrating these protocols and considerations into stem cell tracking studies, researchers can significantly improve the accuracy of their data interpretation, leading to more reliable conclusions about the true fate and efficacy of cellular therapeutics.
Ensuring Labeling Does Not Impair Stem Cell Viability or Function
Within the field of stem cell therapy, the ability to track transplanted cells in vivo is crucial for understanding their biodistribution, engraftment, and long-term fate. A fundamental challenge in this process is that the labeling procedure itself must not compromise the core biological properties of the stem cells—their viability, proliferative capacity, and differentiation potential. Impairment of these functions undermines the therapeutic efficacy the tracking aims to evaluate, creating a critical bottleneck in translational research. This application note details standardized protocols and analytical methods designed to ensure that stem cell labeling for imaging, particularly with nanoparticles, preserves cellular integrity and function.
Key Considerations for Labeling Stem Cells
The choice of labeling strategy is a balance between achieving sufficient signal for detection and maintaining cell health. The following factors must be optimized for any new labeling protocol:
- Contrast Agent Toxicity: The chemical composition, concentration, and potential for leaching of toxic ions (e.g., from radionuclides or gadolinium chelates) must be evaluated [39].
- Labeling Efficiency and Stability: The protocol must ensure high and consistent uptake of the contrast agent while minimizing the risk of the label being released and taken up by non-target cells after transplantation, which leads to false-positive signals [11] [39].
- Impact on Cell Physiology: The label should not alter stem cell metabolism, induce premature differentiation, trigger apoptosis, or inhibit proliferation and migratory capacity [75].
The following table summarizes findings from key studies on the effects of different labeling agents on stem cell viability and function.
Table 1: Comparative Effects of Different Labeling Agents on Stem Cell Viability and Function
| Labeling Agent / Method | Cell Type Tested | Key Findings on Viability/Function | Citation |
|---|---|---|---|
| Gold Nanoparticles (GNPs) (20 nm, glucose-coated) | PLX-PAD (Stromal Cells), T-Cells | Minimal impairment to viability/proliferation; T-cells showed slight functional impairment only at high concentrations (≥0.70 mg/mL) and long incubation (120 min). | [75] |
| Superparamagnetic Iron Oxide (SPIO) | Human Mesenchymal Stem Cells (MSCs) | SPIO labeling combined with magnetic field exposure inhibited colony-forming ability and altered gene expression under adipogenic/osteogenic differentiation. | [11] |
| ESIONPs-GSH (T1-T2 MRI contrast) | Bone Marrow MSCs (BMSCs) | Biocompatible, with negligible effects on proliferation and differentiation of BMSCs post-labeling. | [76] |
| 111In-oxine (Radionuclide) | CD34+ Hematopoietic Progenitor Cells | Impaired proliferation and differentiation capacity observed. | [39] |
Detailed Experimental Protocols
Protocol 1: Optimizing Gold Nanoparticle (GNP) Labeling
This protocol, adapted from a systematic investigation, outlines the steps for optimizing GNP labeling for cell tracking [75].
The logical flow for establishing an optimized GNP labeling protocol is as follows.
Materials and Reagents
Table 2: Research Reagent Solutions for GNP Labeling
| Item | Function / Description | Example / Note |
|---|---|---|
| Gold Nanoparticles (GNPs) | Contrast agent for cell tracking. | 20 nm spherical, glucose-coated for enhanced uptake [75]. |
| Cell Culture Medium | Maintains cell health during labeling. | Serum-free or complete medium appropriate for the specific stem cell type. |
| Centrifuge | Washes cells to remove unincorporated GNPs. | - |
| Flame Atomic Absorption System (FAAS) | Quantifies gold content per cell to measure uptake. | Critical for protocol optimization [75]. |
| Cell Viability Assay | Assesses membrane integrity and metabolic activity. e.g., Trypan Blue exclusion, MTT/XTT assays. | |
| Colony-Forming Unit (CFU) Assay | Evaluates stem cell self-renewal capacity post-labeling. | Cells are seeded at low density and colonies are counted after 14 days [77]. |
Step-by-Step Procedure
- Cell Preparation: Seed the target stem cells (e.g., MSCs, immune cells) at an appropriate density and allow them to adhere and grow to ~70-80% confluency under standard culture conditions (37°C, 5% CO₂).
- GNP Solution Preparation: Prepare a stock solution of sterile, biocompatible GNPs (e.g., 20 nm glucose-coated) in the cell culture medium. Serially dilute this stock to create a range of working concentrations (e.g., 0.1, 0.35, 0.70, 1.0 mg/mL).
- Labeling Incubation: Replace the culture medium on the cells with the GNP-containing media. Incubate the cells for a range of time periods (e.g., 15, 30, 60, 120 minutes) at 37°C with 5% CO₂.
- Washing: After incubation, carefully remove the GNP-containing medium. Wash the cell monolayer gently but thoroughly with PBS or fresh culture medium 2-3 times to remove all non-internalized GNPs.
- Harvesting Cells: Use a standard cell dissociation reagent (e.g., trypsin/EDTA) to harvest the labeled cells. Neutralize the trypsin with complete medium and collect the cell suspension.
- Quantification of Uptake: Pellet the cells by centrifugation. Use Flame Atomic Absorption Spectroscopy (FAAS) to lyse the cell pellet and precisely measure the gold content, which can be normalized to the cell number [75].
- Viability and Functional Assays: Immediately after labeling, perform viability counts (e.g., trypan blue exclusion). For long-term functional assessment, perform colony-forming unit (CFU) assays and differentiation assays (osteogenic, adipogenic, chondrogenic) following established protocols [77].
Protocol 2: Viability-Monitoring with T1-T2 Switchable MRI Agents
This protocol utilizes a novel contrast agent to track cell viability post-transplantation via MRI [76].
Mechanism of Action
The contrast agent ESIONPs-GSH is sensitive to reactive oxygen species (ROS) elevated during cell death. The mechanism for MRI signal switching is outlined below.
Materials and Reagents
- ESIONPs-GSH Contrast Agent: An extremely small iron oxide nanoparticle coated with ROS-sensitive glutathione (GSH) and amphipathic ADPS molecules [76].
- MRI Scanner: For in vivo tracking of transplanted cells.
- Materials for BMSC Culture and Transplantation: Standard reagents for maintaining bone marrow mesenchymal stem cells and for the animal model of choice.
Step-by-Step Procedure
- Contrast Agent Preparation: Synthesize and characterize the ESIONPs-GSH agent according to established methods, ensuring monodisperse particles that function as a T1 contrast agent [76].
- Stem Cell Labeling: Incubate Bone Marrow Mesenchymal Stem Cells (BMSCs) with a pre-optimized, biocompatible concentration of ESIONPs-GSH.
- Washing and Validation: Wash the cells thoroughly to remove excess contrast agent. Validate labeling efficiency and confirm the T1-weighted MRI signal in vitro.
- Cell Transplantation: Transplant the labeled BMSCs into the target organism (e.g., a mouse model) at the desired site (e.g., subcutaneous, intramyocardial).
- Longitudinal MRI Monitoring: Image the animals at various time points post-transplantation using a clinical or preclinical MRI scanner. Monitor for a spatial signal switch from T1 hyperintensity (bright, indicating live cells) to T2 hypointensity (dark, indicating cell death and nanoparticle aggregation) [76].
Concluding Recommendations
Ensuring that stem cell labeling does not impair viability or function is a non-negotiable prerequisite for reliable in vivo tracking research. Researchers should:
- Systematically Optimize: Always perform dose and time-course experiments for any new label or cell type, using quantitative uptake and functional assays.
- Validate Function: Go beyond simple viability stains. Conduct CFU assays and lineage-specific differentiation assays post-labeling to confirm retention of stemness.
- Choose the Right Modality: Select a labeling strategy that balances sensitivity, resolution, and minimal toxicity for the specific research question, whether it's short-term homing (direct labeling) or long-term viability (reporter genes or smart agents) [11] [39].
- Leverage Advanced Agents: Consider next-generation "smart" contrast agents, like ESIONPs-GSH, which provide functional information on cell viability alongside location, adding a critical dimension to tracking studies [76].
Optimizing Cellular Uptake and Retention of Contrast Agents
The efficacy of stem cell therapies is profoundly influenced by the ability to monitor transplanted cells non-invasively over time. A critical determinant for the success of tracking technologies, particularly for clinical imaging modalities like MRI and CT, is the efficient and sustained labeling of stem cells with contrast agents. The cellular uptake and subsequent retention of these agents are not passive processes but are governed by a complex interplay of nanoparticle properties and cellular mechanisms. Optimizing these parameters is essential for achieving high signal-to-noise ratios, enabling long-term monitoring of cell fate, and ultimately validating the therapeutic potential of stem cell-based treatments. This document outlines targeted strategies and detailed protocols to enhance the labeling efficiency of stem cells for in vivo tracking.
Quantitative Insights: Nanoparticle Properties and Performance
The physicochemical properties of nanoparticles directly dictate their interactions with stem cells. The following table summarizes key attributes and their quantified impact on cellular uptake and retention, providing a basis for rational contrast agent design.
Table 1: Influence of Nanoparticle Properties on Cellular Uptake and Retention
| Particle Property | Impact on Uptake/Retention | Quantitative Findings & Experimental Evidence |
|---|---|---|
| Size | Dictates the primary internalization pathway and efficiency. | • ~70 nm PLAG-encapsulated Au nanoclusters showed 3x higher endocytosis compared to smaller, non-encapsulated forms over 24h in HeLa cells [78].• Hybrid PLGA-lipid Gd nanoparticles under 200 nm demonstrated superior cellular uptake in pancreatic cancer cell lines [79]. |
| Surface Functionalization | Actively engages with cellular transporters to boost internalization. | • Albumin-functionalized PLGA-lipid Gd NPs showed the highest cellular uptake in MiaPaca2 and Panc1 cells, followed by adenosine- and glutamine-coated NPs [79]. |
| Biodegradability & Structural Dynamics | Governs long-term retention and potential exocytosis. | • Degradable poly-L-arginine (PLAG) matrix allowed de-aggregation of internalized Au NPs, leading to ~3.5 times faster exocytosis compared to non-degradable equivalents [78]. |
| Aggregation/De-aggregation | Utilizes size changes to optimize different lifecycle stages. | • Aggregation of small NPs into larger structures enhances endocytosis. Subsequent de-aggregation upon biodegradation facilitates improved excretion, minimizing long-term intracellular retention and potential toxicity [78]. |
Experimental Protocols for Optimized Labeling
Protocol: Surface Functionalization of PLGA-Lipid Nanoparticles for Enhanced Uptake
This protocol details the synthesis of hybrid Gd-loaded nanoparticles functionalized with targeting ligands to exploit metabolic pathways in target cells [79].
- Objective: To synthesize albumin-, adenosine-, or glutamine-functionalized PLGA-lipid Gd nanoparticles to enhance contrast agent uptake in stem cells.
- Materials:
- Poly(D,L-lactide-co-glycolide) (PLGA) 50:50
- Gd-DOTAMA(C18H37)2 (or similar amphiphilic Gd chelate)
- DSPE-PEG(2000)-methoxy
- DPPE-PEG(2000)-NHS
- Bovine Serum Albumin (BSA), Adenosine, Fmoc-Gln(Trt)-OH (for glutamine)
- Polyvinyl Alcohol (PVA)
- Dichloromethane (DCM), N,N'-Dimethylformamide (DMF)
- HEPES-buffered saline
- Procedure:
- Formation of Oil-in-Water Emulsion:
- Dissolve 25 mg PLGA and 3.2 mg Gd-DOTAMA in DCM (organic phase).
- Prepare an aqueous solution of 2% PVA.
- Emulsify the organic phase into the aqueous PVA solution using a probe sonicator (e.g., 100 W for 2 minutes on ice).
- Nanoparticle Hardening:
- Stir the emulsion overnight at room temperature to evaporate the organic solvent and allow nanoparticle hardening.
- Surface Functionalization:
- Activation: Incorporate DPPE-PEG(2000)-NHS into the initial organic phase or add to the hardened NP suspension to provide active NHS ester groups.
- Conjugation: Incubate the NHS-activated NPs with the desired ligand (BSA, adenosine, or glutamine derivative) in HEPES buffer (pH ~7.3) for 4-6 hours under gentle agitation.
- Purification: Purify the functionalized nanoparticles by repeated centrifugation and washing or via dialysis against HEPES-buffered saline to remove unreacted ligands and PVA.
- Formation of Oil-in-Water Emulsion:
- Validation: Characterize NPs using Dynamic Light Scattering (DLS) for size and zeta potential, and NMR relaxometry for Gd relaxivity. Confirm enhanced uptake via MRI signal enhancement in vitro or inductively coupled plasma mass spectrometry (ICP-MS) for Gd quantification [79].
Protocol: Evaluating Uptake and Retention Kinetics Using Aggregating/De-aggregating Systems
This protocol leverages size-changing nanoparticles to maximize uptake and then facilitate clearance, optimizing both labeling and safety profiles [78].
- Objective: To quantify the enhancement in endocytosis and exocytosis using biodegradable nanoparticle systems that aggregate and de-aggregate.
- Materials:
- ~1.7 nm Gold Nanoclusters (Au NCs)
- Biodegradable polymer (e.g., Poly-L-arginine, PLAG)
- Cell culture of interest (e.g., HeLa cells, stem cells)
- Appropriate cell culture media and reagents
- ICP-MS or spectrophotometer for Au quantification
- Procedure:
- Synthesis of Aggregated NPs: Encapsulate the small Au NCs within the PLAG matrix to form aggregated nanoparticles of approximately 70 nm diameter.
- Uptake Experiment:
- Culture cells and expose them to either the encapsulated Au NPs or an equivalent amount of non-aggregated, non-degradable Au NPs of similar initial size.
- Incubate for a set period (e.g., 24 hours).
- Wash cells thoroughly to remove non-internalized nanoparticles.
- Lyse cells and quantify the total intracellular gold content using ICP-MS.
- Retention/Exocytosis Experiment:
- After the uptake period and washing, replenish the culture medium with fresh, nanoparticle-free medium.
- Incubate the cells for a defined exocytosis period (e.g., 24-72 hours).
- At designated time points, collect the culture medium and lyse the cells.
- Quantify the gold content in both the cell lysate and the excreted medium to calculate the percentage of contrast agent retained versus excreted.
- Expected Outcome: Cells treated with the biodegradable, aggregating NPs will show significantly higher initial Au uptake and a substantially higher rate and amount of Au excreted over time compared to cells treated with non-degradable NPs [78].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Contrast Agent Uptake and Retention Studies
| Research Reagent | Function & Application |
|---|---|
| Poly-L-arginine (PLAG) | A biodegradable polymer used to encapsulate small nanoclusters, forming larger aggregates that enhance endocytosis and subsequently degrade to facilitate exocytosis [78]. |
| Hybrid PLGA-Phospholipid Polymers | Provides a stable, biocompatible nanoparticle core. The phospholipid layer improves circulation time and enables facile surface functionalization via PEG spacers with active groups (e.g., NHS ester) [79]. |
| Ligands (Albumin, Adenosine, Glutamine) | Target specific cellular uptake pathways. Albumin targets micropinocytosis; adenosine targets nucleoside transporters (ENTs/CNTs); glutamine targets amino acid transporters, all highly active in many stem and cancer cells [79]. |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | A classic MRI contrast agent for cell tracking. Internalized via endocytosis, they create a strong T2/T2* contrast, allowing sensitive detection of labeled stem cells in vivo [80] [81]. |
| Macrocyclic Gd(III) Complexes | The preferred choice for T1-weighted MRI contrast due to superior kinetic stability, minimizing the release of toxic free Gd³⁺ ions. Used as a core agent in responsive and nanoparticle-based probes [82] [83]. |
Workflow and Pathway Visualizations
Optimization Strategy Workflow
The following diagram illustrates the logical pathway for optimizing contrast agent uptake and retention, from nanoparticle design to experimental validation.
Cellular Pathway of Functionalized Nanoparticles
This diagram maps the journey of a functionalized nanoparticle from administration to internalization and excretion, highlighting key cellular mechanisms.
Strategies for Long-Term Monitoring and Lineage Tracing
Lineage tracing remains an indispensable methodology for understanding cell fate, tissue formation, and human development. It encompasses any experimental design aimed at establishing hierarchical relationships between cells, delineating all progeny produced by a single cell or group of cells over time [84] [85]. A successful lineage-tracing experiment must fulfill three core requirements: (1) careful assessment of the initially marked cells to clearly define the starting population, (2) use of markers that remain exclusively in the original cells and their progeny without diffusion to neighbors, and (3) sufficient marker stability without toxicity during the entire tracing period [85]. This framework is crucial for stem cell research, where understanding the potential of a single cell to produce diverse progeny is fundamental. Modern studies are increasingly multimodal, incorporating advanced microscopy, state-of-the-art sequencing, and computational tools to handle the resulting complex datasets [84]. This application note details current strategies and protocols for long-term stem cell monitoring and lineage tracing, providing researchers with practical methodologies for implementation in vivo.
Current Lineage Tracing Technologies
Genetic Labeling Systems
Site-Specific Recombinase (SSR) Systems: The Cre-loxP system is a cornerstone of imaging-based lineage tracing. In this system, Cre recombinase excises a STOP codon flanked by loxP sites, activating a fluorescent reporter gene. The specificity is controlled by driving Cre expression with cell-type-specific promoters. Sparse labeling approaches, such as titrating the dose of Tamoxifen in inducible CreERT2 models, allow for the labeling of limited numbers of cells within a population, enabling clonal analysis [84].
Dual Recombinase Systems: Combining Cre-loxP with analogous technologies like Dre-rox creates dual recombinase systems. These systems offer enhanced experimental flexibility, allowing for expression following recombination of either Cre or Dre, both Cre and Dre, or Cre in the absence of Dre. Such systems have been used to determine the origin of regenerative cells in remodelled bone and to investigate the cellular origins of alveolar epithelial stem cells post-injury [84].
Multicolour Lineage Tracing: The introduction of multicolour reporter cassettes like "Brainbow" and "R26R-Confetti" represented a major advance. These cassettes use stochastic Cre-loxP-mediated excision/inversion to express up to four different fluorescent proteins, allowing clonal analysis at the single-cell level. They have been applied across diverse tissues, including hematopoietic, epithelial, kidney, and skeletal cells, and are increasingly used in live-imaging studies [84].
Table 1: Key Genetic Tools for Lineage Tracing
| Tool Name | Type | Key Feature | Example Applications |
|---|---|---|---|
| Cre-loxP | Site-Specific Recombinase | Excision of STOP cassette to activate reporter [84] | Clonal analysis; ubiquitous application [84] |
| Dre-rox | Site-Specific Recombinase | Heterospecific to Cre-loxP; can be used in combination [84] | Distinguishing homogeneous tissue layers (e.g., in bone) [84] |
| R26R-Confetti | Multicolour Reporter | Stochastic expression of 1 of 4 fluorescent proteins [84] | Intravital imaging of clonal dynamics [84] [21] |
| Tet-OFF/Tet-ON | Inducible Expression System | Doxycycline-controlled gene expression [21] | Gene overexpression or knockdown in traced clones [21] |
| H2B-GFP Pulse-Chase | Label-Retaining System | Identifies slow-cycling cells [85] | Hair follicle stem cell identification [85] |
Imaging and Non-Imaging Modalities
Non-Invasive Imaging for Tracking: Multiple modalities enable the in vivo tracking of stem cells post-transplantation. These include Magnetic Resonance Imaging (MRI) using superparamagnetic iron oxide nanoparticles (SPIONs), Positron Emission Tomography (PET) with radioisotopes, and bioluminescence imaging using luciferase-expressing cells [86]. Quantitative phase imaging (QPI) is an emerging label-free technique that, when combined with machine learning, can predict hematopoietic stem cell diversity by analyzing cellular kinetics like dry mass and division patterns [4].
Non-Imaging Tracking Methods: Sequencing-based technologies leverage naturally occurring somatic mutations or intentionally introduced genomic barcodes as inherited signatures to reconstruct lineage relationships [85]. Furthermore, the "carbon dating" technique utilizes historical atmospheric Carbon-14 levels to retrospectively birthdate cells in human tissues, providing insights into human neurogenesis [85].
Table 2: Modalities for Long-Term Stem Cell Tracking
| Modality | Measurement Principle | Key Parameters Quantified | Limitations |
|---|---|---|---|
| MRI with SPIONs | T2 relaxation time shortening by iron oxides [86] | SPION density and distribution; cell location [86] | Signal loss from nanoparticle degradation; artifacts [86] |
| PET/SPECT | Detection of gamma photons from radioisotope decay [86] | Tracer uptake correlating to cell distribution/density [86] | Radiotracer half-life and toxicity; background signal [86] |
| Bioluminescence Imaging | Photon emission from luciferase-luciferin reaction [86] | Photon flux (photons/sec) indicating viability/location [86] | Limited tissue penetration; light scattering [86] |
| Quantitative Phase Imaging (QPI) | Label-free measurement of optical path length delay [4] | Cellular dry mass, sphericity, division kinetics [4] | Requires specialized instrumentation and analysis [4] |
| scRNA-seq | Single-cell transcriptome sequencing [86] | Gene expression profiles; differentiation trajectories [86] | Technical noise (dropout events); destructive method [86] |
Detailed Experimental Protocols
Protocol: In Vivo Lineage Tracing of Stem Cells with Genetic Manipulation
This protocol combines the Cre and Tet inducible systems for simultaneous lineage tracing and genetic manipulation of single stem cells in live mice, followed by long-term monitoring via two-photon microscopy [21].
I. Materials
- Mouse Lines: Inducible CreER driver line (e.g., K14-CreER for skin), LSL-tTA allele, mTomato-LSL-mGFP Cre reporter allele, TetO-responsive reporter (e.g., TetO-H2BGFP), TetO-responsive gain/loss-of-function allele [21].
- Reagents: Tamoxifen, Doxycycline, Phosphate Buffered Saline (PBS).
- Equipment: Two-photon laser scanning fluorescent microscope, Flow cytometer, Microinjection system.
II. Methods
Step 1: Mouse Cross and Genotyping
- Cross the appropriate mouse lines to generate experimental animals carrying all required alleles: the CreER driver, mTomato-LSL-mGFP, LSL-tTA, and the TetO transgenes.
- Confirm genotypes by PCR.
Step 2: Sparse, Clonal Labeling and Genetic Manipulation
- Administer a low, titrated dose of Tamoxifen (via intraperitoneal injection or oral gavage) to adult mice to stochastically activate CreER. This results in two distinct clone types in the tissue:
- "Normal" clones: Express membrane-bound GFP (mG) after Cre-mediated excision of the tdTomato (mT) STOP cassette.
- "Genetically altered" clones: Also express the tTA transgene after Cre-mediated recombination. tTA drives expression of both a fluorescent nuclear reporter (e.g., H2B-GFP) and the gene of interest from TetO promoters [21].
- To control the timing of genetic manipulation, administer or withhold Doxycycline in the diet/drinking water to control TetO-driven expression (for TetOFF systems).
Step 3: Long-Term In Vivo Imaging
- Anesthetize the mouse and place it on the microscope stage.
- Using a two-photon microscope, image the same, predefined region of interest over multiple sessions (e.g., weekly for several weeks).
- Identify and document the location, size, and morphology of mGFP-labeled (normal) and H2B-GFP-labeled (altered) clones.
- Track clonal dynamics, including cell division, migration, and differentiation, by comparing images across time points.
Step 4: Tissue Harvest and End-Point Analysis
- At the endpoint, harvest the tissue.
- Process for flow cytometry to quantify population sizes or for immunohistochemistry to analyze differentiation markers and tissue architecture at the single-cell level.
Protocol: Lineage Tracing of Regeneration-Associated Macrophages
This protocol details the steps for isolating and transplanting macrophage subpopulations from injured skeletal muscle of donor mice into injured recipient mice for in vivo lineage tracing [87].
I. Materials
- Mice: Congenic CD45.1+ donor mice, CD45.2+ recipient mice.
- Reagents: Cardiotoxin, Collagenase D, Dispase II, Fluorescently-labeled antibodies for FACS.
- Equipment: Flow cytometer with cell sorter, Microinjection system.
II. Methods
Step 1: Muscle Injury and Cell Isolation
- Induce skeletal muscle injury in CD45.1+ donor mice via intramuscular cardiotoxin injection.
- After 3-5 days, euthanize the mice and harvest the injured skeletal muscle.
- Mechanically mince and enzymatically digest the tissue using a cocktail of Collagenase D and Dispase II.
- Prepare a single-cell suspension and stain with fluorescent antibodies against cell surface markers (e.g., CD45, CD11b, F4/80) to identify macrophage subpopulations.
Step 2: Fluorescence-Activated Cell Sorting (FACS)
- Use a flow cytometer with cell sorting capability to isolate specific, regeneration-associated macrophage subpopulations from the CD45.1+ donor cell suspension.
Step 3: Transplantation
- Pre-injure the skeletal muscle of CD45.2+ recipient mice with cardiotoxin.
- Intramuscularly transplant the FACS-isolated CD45.1+ macrophage subpopulation into the pre-injured site of the recipient mouse.
Step 4: Phenotyping Transplanted Cells
- At designated time points post-transplantation, harvest the recipient muscle tissue.
- Create a single-cell suspension and stain with antibodies for flow cytometry analysis.
- Identify the transplanted CD45.1+ cells and their progeny, and phenotype them using markers for various macrophage states to trace their fate during the regeneration process [87].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Lineage Tracing Experiments
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Tamoxifen | Induces nuclear translocation of CreERT2, activating recombination [21]. | Dose must be titrated for sparse, clonal labeling [21]. |
| Doxycycline | Binds to tTA/rtTA to control (TetOFF) or induce (TetON) gene expression from TetO promoters [21]. | Administered in food/water for sustained control. |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | MRI contrast agent internalized by cells for in vivo tracking [86]. | Potential cytotoxicity; signal dilutes with cell division [86]. |
| Nucleoside Analogues (BrdU, EdU) | Incorporated into DNA during synthesis to label proliferating cells [84] [85]. | Cytotoxic at high doses/time; diluted with proliferation [85]. |
| Carbocyanine Dyes (DiI, DiO) | Lipophilic dyes that integrate into cell membranes for short-term tracing [85]. | Water-insoluble, preventing diffusion; diluted with division [85]. |
| Luciferin | Substrate for luciferase enzyme; produces bioluminescence for in vivo imaging [86]. | Requires genetic modification of cells; limited by tissue penetration [86]. |
| Collagenase/Dispase | Enzyme cocktail for digesting tissues to obtain single-cell suspensions [87]. | Concentration and time must be optimized for each tissue type [87]. |
| Fluorescent Antibody Panels | Label cell surface and intracellular proteins for identification and phenotyping via flow cytometry [87] [88]. | Requires validation for specific applications and species. |
Data Analysis and Computational Tools
Modern lineage tracing generates complex datasets that require sophisticated computational tools for analysis. For image-based data, high-content analysis platforms like ImageJ/Fiji can be used to extract quantitative morphological descriptors (e.g., cell area, shape, fluorescence intensity) from individual cells [88]. These descriptors can be analyzed with dimensionality reduction algorithms, such as Uniform Manifold Approximation and Projection (UMAP) or t-distributed Stochastic Neighbor Embedding (t-SNE), to identify subpopulations of cells based on phenotypic similarities [4] [88].
When integrating temporal kinetic data from live imaging, machine learning algorithms can be trained on parameters such as division rate, inter-division time, and changes in dry mass to predict future stem cell function, such as differentiation potential or self-renewal capacity [4]. For sequencing-based lineage tracing, computational pipelines are used to identify and track naturally occurring somatic mutations or introduced barcodes over time to reconstruct lineage trees [85].
Navigating the Trade-offs Between Sensitivity, Resolution, and Penetration
The central challenge in non-invasive stem cell tracking lies in navigating the inherent and often inverse relationships between three key imaging parameters: sensitivity, spatial resolution, and penetration depth. Sensitivity refers to the ability to detect a small number of labeled cells against background noise, while spatial resolution defines the smallest distance at which two cells can be distinguished as separate entities. Penetration depth determines how deep into tissue the imaging signal can be effectively captured. These trade-offs are not merely technical constraints but fundamental considerations that dictate which imaging modality is appropriate for specific research questions in stem cell therapy development. No single imaging technology currently excels in all three domains simultaneously, necessitating careful selection based on the specific requirements of the experimental or clinical scenario.
The pursuit of optimal stem cell tracking methodologies has driven the development of increasingly sophisticated imaging technologies, each with characteristic strengths and limitations. For researchers tracking stem cells in living organisms, the ideal modality would combine the sensitivity to detect single cells, the resolution to pinpoint their exact location, and the penetration capability to track them anywhere in the body. In practice, however, enhancing one parameter typically comes at the expense of another. For instance, techniques offering exceptional cellular resolution often suffer from limited penetration depth, while modalities with excellent penetration may lack the sensitivity for single-cell detection. Understanding these trade-offs is essential for designing robust experimental protocols and accurately interpreting in vivo stem cell tracking data.
Comparative Analysis of Imaging Modalities
Table 1: Quantitative Comparison of Stem Cell Imaging Modalities
| Imaging Modality | Sensitivity (Cell Detection Limit) | Spatial Resolution | Penetration Depth | Key Trade-offs |
|---|---|---|---|---|
| Ultrasound with Microbubbles [89] | Single-cell level demonstrated | 8-10 µm (with microfluidic probe) [90] | Unlimited (clinical use demonstrated) | Resolution limited by wavelength; Requires contrast agent |
| Magnetic Particle Imaging (MPI) [72] | <10 cells (theoretical) | ~1 mm (pre-clinical systems) | Unlimited (pre-clinical demonstration) | Excellent sensitivity but currently limited resolution; Radiation-free |
| Photoacoustic Microscopy (PAM) [49] | High (nanoparticle-enhanced) | Several micrometers | ~1 mm in soft tissue | Combines optical resolution with ultrasound depth penetration |
| Magnetic Resonance Imaging (MRI) [30] | ~10⁴ cells (in vivo) | 25-100 µm (pre-clinical) | Unlimited (clinical use) | Poor sensitivity despite excellent penetration and resolution |
| Optical Imaging | High (in superficial tissues) | 1-10 µm | <1 mm (limited by scattering) | Excellent resolution and sensitivity but poor penetration |
Table 2: Contrast Agents and Their Applications in Stem Cell Tracking
| Contrast Agent | Compatible Modalities | Stem Cell Application | Key Characteristics |
|---|---|---|---|
| Lipid-shelled Microbubbles [89] | Ultrasound | Macrophage labeling | Enables single-cell detection; FDA-approved formulation available |
| Chain-like Gold Nanoparticle Clusters (GNC) [49] | Photoacoustic, OCT, Fluorescence | hiPSC-RPE cell tracking | 7-8 nm size enables renal excretion; Improved biocompatibility |
| Magnetic Nanoparticles (MNPs) [72] | MPI, MRI | Monocyte (THP-1) tracking | Enables quantitative cell number determination; Linear signal correlation |
| Synomag/Resovist [72] | MPI | Cell migration studies | Commercial availability; Excellent MPI performance |
| Ultraminiature GNC-RGD [49] | Multimodal imaging | Retinal pigment epithelium regeneration | Red-shifted absorption avoids hemoglobin overlap |
The quantitative comparison reveals how different technologies navigate the fundamental trade-offs in stem cell imaging. Ultrasound with microbubble labeling achieves remarkable single-cell sensitivity while maintaining unlimited penetration depth, though its spatial resolution remains constrained by acoustic wavelength limitations [89]. In contrast, Magnetic Particle Imaging (MPI) offers exceptional sensitivity with a theoretical detection limit of fewer than ten cells and quantitative tracking capabilities, but currently suffers from limited spatial resolution in the millimeter range [72]. Photoacoustic approaches represent a hybrid solution, combining optical contrast with ultrasonic detection to achieve micrometer-scale resolution at depths of approximately 1 mm in soft tissues [49].
The selection of appropriate contrast agents further modulates these fundamental trade-offs. Microbubbles dramatically enhance the scattering cross-section of labeled cells by several orders of magnitude, enabling their detection against tissue background despite the relatively low intrinsic contrast of cellular components [89]. Gold nanoparticle clusters can be engineered for optimal near-infrared absorption, providing enhanced contrast while maintaining biocompatibility and renal clearance pathways [49]. Magnetic nanoparticles for MPI enable real-time quantitative tracking of cell numbers with high temporal resolution, addressing a significant limitation of other modalities [72].
Detailed Experimental Protocols
Protocol: Microbubble Labeling for Ultrasound Stem Cell Tracking
Principle: This protocol utilizes the inherent phagocytic capability of stem cells and immune cells to incorporate lipid-shelled microbubbles, enhancing their ultrasound scattering cross-section by several orders of magnitude and enabling single-cell detection [89].
Materials:
- Cell culture (RAW264.7 macrophages, primary bone marrow-derived macrophages, or human dendritic cells)
- Definity microbubbles (Lantheus Medical Imaging) or equivalent lipid-shelled microbubbles
- Cell culture medium (appropriate for cell type)
- Petri dishes with glass bottoms for imaging
- Ultrasound system with high-frequency transducers (≥20 MHz)
- Surgical glue for in vivo immobilization (if needed)
Procedure:
- Cell Culture and Preparation: Culture stem cells or progenitor cells to 70-80% confluence in appropriate medium. For primary cells, confirm appropriate differentiation using surface marker expression (e.g., CD11b and F4/80 for BMDMs; CD14, CD11b, CD68 for human macrophages) [89].
- Microbubble Incubation: Introduce microbubbles (10¹⁰ bubbles/mL concentration) into the culture medium. Invert petri dishes to enhance contact between buoyant microbubbles and cells, facilitating labeling via phagocytosis.
- Incubation Time Optimization: Incubate for 2-6 hours based on cell type. RAW264.7 macrophages show optimal labeling after 4 hours (75.7% ± 9.3% labeling efficiency). Primary bone marrow-derived macrophages may achieve 100% labeling efficiency after 4 hours [89].
- Washing and Viability Assessment: Gently wash cells three times with fresh medium to remove non-internalized microbubbles. Assess cell viability using trypan blue exclusion or equivalent method.
- Functional Validation: Verify that labeled cells retain normal migration capability using transwell migration assays. Confirm that phenotype and cytokine secretion profiles remain unaltered following microbubble incorporation [89].
- In Vivo Administration and Imaging: Administer labeled cells intravenously. Image using nonlinear ultrasound modalities at low mechanical indices (MI < 0.3) to prevent microbubble destruction while maintaining cell viability and function.
Troubleshooting Tips:
- If labeling efficiency is low, increase microbubble concentration or extend incubation time
- If cell viability decreases post-labeling, reduce microbubble concentration or incubation time
- For in vivo tracking, use nonlinear imaging techniques to distinguish microbubble signals from tissue background
Microbubble Labeling and Tracking Workflow
Protocol: Gold Nanocluster Labeling for Multimodal Stem Cell Imaging
Principle: This protocol employs ultraminiature chain-like gold nanoparticle clusters (GNC) for longitudinal tracking of stem cells using combined photoacoustic microscopy, optical coherence tomography, and fluorescence imaging [49].
Materials:
- Human induced pluripotent stem cells differentiated to retinal pigment epithelium (hiPSC-RPE) or other stem cell types
- Ultraminiature GNC-RGD (7-8 nm diameter after disassembly)
- Pulsed laser ablation system for GNC fabrication (if synthesizing in-house)
- CALNN and cysteamine peptides for GNC stabilization
- Multimodal imaging system (PAM-OCT-fluorescence)
- Rabbit model of RPE degeneration (for validation studies)
Procedure:
- GNC Fabrication and Characterization: Synthesize GNC using pulsed laser ablation method. Cluster 3-5 individual colloidal GNPs (average diameter 7-8 nm) using CALNN and cysteamine peptides. Verify size distribution and stability (zeta potential ≈ -41 mV) [49].
- Surface Functionalization: Conjugate RGD peptides to GNC surface to enhance cellular uptake and targeting.
- Stem Cell Labeling: Incubate hiPSC-RPE cells with GNC-RGD at optimized concentration. Determine optimal incubation time and concentration to achieve sufficient labeling without cytotoxicity.
- Biocompatibility Assessment: Evaluate labeled cell viability, proliferation, and differentiation capacity. Confirm that GNC-RGD does not alter stem cell function or regenerative potential.
- Multimodal Imaging: Transplant labeled cells into target tissue (e.g., subretinal space in rabbit model). Image using combined PAM-OCT-fluorescence system at regular intervals over extended periods (up to 6 months) [49].
- Image Co-registration and Analysis: Correlate photoacoustic signals with structural OCT data and fluorescent markers to validate cell location, distribution, and migration patterns.
Key Advantages:
- Enables longitudinal tracking over months due to nanoparticle stability
- Combines deep penetration of ultrasound with high resolution of optical techniques
- Renal-excretable size (7-8 nm) improves safety profile
- Multimodal validation enhances data reliability
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Stem Cell Tracking
| Reagent/Category | Specific Examples | Function in Stem Cell Tracking | Compatible Modalities |
|---|---|---|---|
| Microbubble Contrast Agents | Definity (FDA-approved), Custom lipid-shelled MBs with C4F10/C3F8 gases | Enhance ultrasound scattering cross-section; Enable single-cell detection | Ultrasound (B-mode, Nonlinear modes) |
| Gold Nanoparticles | Ultraminiature GNC-RGD, Chain-like gold nanoparticle clusters, Gold nanorods | Provide strong optical absorption for photoacoustic contrast; Surface functionalization for targeting | Photoacoustic, OCT, Fluorescence, micro-CT |
| Magnetic Nanoparticles | Resovist, Synomag (SynP50, SynC30), Iron oxide MNPs | Enable cell detection via magnetic properties; Quantitative cell number determination | MPI, MRI |
| Nanobiosensors | CRISPR/Cas13a FRET beacons, MoS2 nanopores, dCas9-SunTag scaffolds | Monitor differentiation status in real-time; Detect miRNA dynamics | Fluorescence, Electrical readout |
| Stem Cell Lines | hiPSC-RPE, RAW264.7 macrophages, THP-1 monocytes, Primary BMDMs | Disease modeling; Cell therapy development; Track immune cell recruitment | Multimodal compatible |
| Animal Models | Rabbit RPE degeneration model, Rodent tumor models (e.g., 4T1 breast cancer) | Validate tracking methodologies in pathophysiologically relevant contexts | All in vivo modalities |
Decision Framework and Future Directions
Imaging Modality Selection Framework
Emerging technologies are progressively overcoming the traditional limitations in sensitivity, resolution, and penetration. Nanobiosensors represent a particularly promising direction, with CRISPR/Cas13a FRET beacons enabling real-time monitoring of microRNA dynamics during stem cell differentiation at single-cell resolution [91]. Similarly, monolayer molybdenum disulfide (MoS2) nanopores allow single-molecule precision in measuring transcriptional bursting during lineage commitment [91]. These approaches provide unprecedented insights into the molecular events preceding phenotypic changes during stem cell differentiation.
The integration of multiple modalities continues to advance, with systems like PAOFM (photoacoustic microscopy-optical coherence tomography-fluorescence microscopy) demonstrating the power of combining complementary strengths [49]. Such integrated systems provide both structural information (OCT) and functional or molecular data (photoacoustic/fluorescence), enabling comprehensive assessment of stem cell location, viability, and functional integration into host tissues. Additionally, the development of renal-excretable nanoparticles addresses critical safety considerations for clinical translation, balancing optimal imaging characteristics with biocompatibility [49].
Future developments will likely focus on closed-loop systems that not only monitor stem cell behavior but also actively modulate the cellular environment based on real-time feedback. The combination of advanced imaging technologies with artificial intelligence-driven analytics promises to enhance our ability to track stem cells with increasing precision, ultimately accelerating the development of safe and effective stem cell-based therapies.
Validation and Clinical Translation: Comparing Modalities and Assessing Efficacy
Stem cell therapies hold tremendous potential for treating a wide range of conditions, including tumors, injury, inflammation, and cardiovascular diseases [67]. However, the clinical translation of these therapies relies heavily on the ability to monitor stem cell movement, differentiation, and survival after transplantation [92]. Real-time, unbiased, long-term tracking of stem cell homing, differentiation, proliferation, and survival in vivo is essential for evaluating treatment efficacy and biosafety [67]. No single imaging modality can simultaneously meet all requirements of noninvasiveness, high penetration, and high resolution [67]. This application note provides a detailed comparison of three major imaging modalities—MRI, PET/SPECT, and optical imaging—for stem cell tracking, including their principles, applications, advantages, limitations, and detailed experimental protocols.
Imaging Modality Comparison
Table 1: Technical comparison of major imaging modalities for stem cell tracking
| Parameter | MRI | PET/SPECT | Optical Imaging |
|---|---|---|---|
| Spatial Resolution | Excellent (μm-mm) [67] | Limited (mm-cm) [93] | Good (mm) for deep tissue [67] |
| Tissue Penetration Depth | Unlimited [67] | Unlimited [67] | Limited (mm-cm) [67] |
| Detection Sensitivity | Low (μM-mM) [94] | Very High (pM-nM) [95] | High (nM) [96] |
| Quantitative Accuracy | High for anatomy [94] | High for quantification [97] | Moderate [98] |
| Temporal Resolution | Moderate (minutes-hours) [94] | Good (seconds-minutes) [97] | Excellent (real-time) [67] |
| Molecular Imaging Capability | Moderate [94] | Excellent [95] | Excellent [98] |
| Clinical Translation | Widespread [67] | Widespread [95] | Emerging [98] |
| Cost | High [96] | High [96] | Low [96] |
| Ionizing Radiation | No [67] | Yes [67] | No [67] |
Table 2: Comparison of stem cell labeling approaches across imaging modalities
| Labeling Method | MRI | PET/SPECT | Optical Imaging |
|---|---|---|---|
| Direct Labeling | SPIONs, USPIONs [95] | 18F-FDG, 64Cu, 89Zr [92] | Fluorescent dyes, QDs, AuNPs [92] |
| Indirect Labeling | Reporter genes (e.g., ferritin) [67] | Reporter genes (e.g., HSV-tk) [92] | Luciferase, GFP, RFP [67] |
| Labeling Duration | Limited (signal dilution) [67] | Short (radioactive decay) [67] | Long (stable expression) [67] |
| Effect on Cell Viability | Generally safe [95] | Radiation toxicity concerns [92] | Phototoxicity concerns [92] |
Magnetic Resonance Imaging (MRI)
Principle and Applications
MRI is a noninvasive, radiation-free imaging modality with high anatomical resolution and unlimited imaging depth, enabling whole-body scanning of living organisms [67]. Conventional MRI generates signals through excitation of water protons in a constant magnetic field [67]. For stem cell tracking, cells are labeled with contrast agents that change relaxation times of nearby water protons [67]. Superparamagnetic iron oxide nanoparticles (SPIONs) and ultrasmall superparamagnetic iron oxide nanoparticles (USPIONs) are widely used as T2 contrast agents, creating dark contrast on T2-weighted images [95] [92]. MRI provides excellent soft tissue contrast and is suitable for monitoring NPs throughout complex biological environments [96].
Detailed Experimental Protocol
SPION Labeling of Stem Cells
Materials:
- Superparamagnetic Iron Oxide Nanoparticles (SPIONs)
- Stem cells (e.g., mesenchymal stem cells)
- Protamine sulfate or other transfection agents
- Cell culture medium and reagents
- MRI scanner (preclinical or clinical)
- Image analysis software (e.g., ImageJ)
Procedure:
- Cell Culture: Maintain stem cells in appropriate culture medium under standard conditions.
- SPION Preparation: Prepare SPIONs according to manufacturer's protocol. Sterilize by filtration.
- Labeling Optimization: Determine optimal SPION concentration (typically 25-100 μg Fe/mL) and incubation time (4-24 hours) for specific cell type.
- Transfection Enhancement: To enhance cellular internalization, add transfection agents such as protamine sulfate (1.5 μg/mL) to SPION solution [92].
- Incubation: Incubate cells with SPION-containing medium for predetermined time.
- Washing: Remove SPION-containing medium and wash cells 3× with PBS to remove extracellular nanoparticles.
- Viability Assessment: Perform trypan blue exclusion test or MTT assay to confirm cell viability post-labeling.
- Transplantation: Administer labeled cells to subject via appropriate route (intravenous, intramyocardial, etc.).
MRI Acquisition Parameters
Preclinical System (e.g., 7T/9.4T Scanner):
- Pulse Sequence: T2-weighted fast spin echo or gradient echo
- TR/TE: 2000-3000/40-80 ms (T2-weighted)
- Matrix Size: 256×256
- Slice Thickness: 0.5-1 mm
- Averages: 4-8
- Acquisition Time: 10-20 minutes
Data Analysis:
- Signal Quantification: Use voxel-based analysis to assess SPION density in specific regions [92].
- Background Subtraction: Account for artifacts and signal interference from adjacent tissues [92].
- Cell Quantification: Generate calibration curve relating signal intensity to cell number using phantom studies.
Positron Emission Tomography/Single Photon Emission Computed Tomography (PET/SPECT)
Principle and Applications
PET and SPECT are nuclear medicine techniques that provide exceptional sensitivity for molecular imaging [95]. PET detects pairs of gamma photons emitted by positron-emitting radionuclides, while SPECT detects single gamma photons [98]. Both modalities excel at tracking the distribution and metabolic activity of radiolabeled stem cells in vivo [92]. Recent advancements in dedicated systems like the NeuroEXPLORER have demonstrated high quantitative precision across a wide range of imaging conditions [97]. The integration of these modalities with MRI in PET/MRI and SPECT/MRI systems combines the strengths of different imaging techniques, allowing for more accurate detection [95].
Detailed Experimental Protocol
Radiolabeling of Stem Cells
Materials:
- Radioisotopes (18F-FDG, 64Cu, 89Zr for PET; 111In for SPECT)
- Stem cells
- Radiolabeling facility with appropriate shielding
- Radiation detection equipment
- PET or SPECT scanner
- Image reconstruction software
Procedure:
- Radioisotope Preparation: Obtain radioisotopes from certified supplier with appropriate specific activity.
- Labeling Method Selection: Choose direct labeling (incubation with radiotracer) or indirect labeling (reporter gene approach).
- Direct Labeling:
- Incubate cells with 18F-FDG (3.7-37 MBq/106 cells) or alternative radiotracer for 30-60 minutes at 37°C [92].
- Wash cells 3× with PBS to remove unincorporated radioactivity.
- Measure cell-associated radioactivity using gamma counter.
- Reporter Gene Labeling:
- Quality Control: Assess radiochemical purity (>95%) and cell viability post-labeling.
- Transplantation: Inject radiolabeled cells intravenously or directly into target tissue.
PET/SPECT Image Acquisition
PET Acquisition Parameters:
- Scan Duration: 10-30 minutes (static); 60-90 minutes (dynamic)
- Energy Window: 435-650 keV (for 18F)
- Reconstruction Algorithm: Filtered back projection or maximum likelihood estimation [92]
- Attenuation Correction: CT-based or segmentation-based
SPECT Acquisition Parameters:
- Collimator: Low-energy high-resolution or pinhole for small animals
- Energy Window: Photopeak ±10% (e.g., 140±14 keV for 99mTc)
- Projections: 64-128 over 360°
- Reconstruction: Iterative reconstruction (OSEM) with attenuation and scatter correction
Data Analysis:
- Region-of-Interest (ROI) Analysis: Draw ROIs on target tissues and reference regions.
- Quantification: Calculate standardized uptake values (SUVs) for PET or percentage injected dose per gram (%ID/g) for both modalities.
- Kinetic Modeling: For dynamic studies, apply appropriate compartmental models to derive physiological parameters.
Optical Imaging
Principle and Applications
Optical imaging techniques visualize physiological and pathological activities at molecular and cellular levels with high sensitivity and specificity [67]. Modalities include fluorescence imaging, bioluminescence imaging (BLI), and photoacoustic imaging (PAI) [67]. These techniques are particularly valuable for monitoring stem cell viability, proliferation, and differentiation in preclinical models [92]. Near-infrared fluorescence (NIR) imaging, especially in the second near-infrared window (NIR-II, 1000-1700 nm), exhibits improved tissue penetration compared to visible light imaging [67].
Detailed Experimental Protocol
Bioluminescence Imaging of Stem Cells
Materials:
- Stem cells expressing luciferase reporter gene
- D-luciferin substrate (for firefly luciferase)
- In vivo imaging system (IVIS) with cooled CCD camera
- Anesthesia equipment (isoflurane system)
- Sterile surgical tools for cell implantation
Procedure:
- Reporter Cell Preparation:
- Genetically modify stem cells to express luciferase using lentiviral or retroviral transduction.
- Validate reporter expression using in vitro bioluminescence assay.
- Clone and expand high-expressing cells.
- Cell Transplantation:
- Anesthetize animal using isoflurane (2-3% for induction, 1-2% for maintenance).
- Administer cells via appropriate route (intravenous, intracranial, intramyocardial, etc.).
- Substrate Administration:
- Inject D-luciferin intraperitoneally (150 mg/kg in PBS) 10-15 minutes before imaging [92].
- For coelenterazine-dependent luciferases (e.g., Renilla), administer 0.5-5 μg per mouse intravenously.
- Image Acquisition:
- Anesthetize animal and place in imaging chamber.
- Set acquisition parameters: exposure time (1-300 seconds), binning, f/stop.
- Acquire series of images at different time points post-transplantation.
- Data Analysis:
- Quantify total photon flux (photons/second) within regions of interest.
- Normalize to background signal from control animals.
- Create kinetic curves of cell viability and proliferation over time.
Fluorescence Imaging with Nanoprobes
Materials:
- Fluorescent probes (organic dyes, quantum dots, NIR dyes)
- Fluorescence imaging system
- Appropriate filter sets
Procedure:
- Cell Labeling:
- Incubate stem cells with fluorescent probes (e.g., DiD, DiR, Qtracker) according to manufacturer's protocol.
- For quantum dots, use concentration of 5-20 nM for 2-4 hours.
- Wash cells 3× with PBS to remove excess dye.
- Validation:
- Confirm labeling efficiency using flow cytometry or fluorescence microscopy.
- Assess potential toxicity using proliferation assays.
- In Vivo Imaging:
- Anesthetize animal and position in imaging system.
- Set appropriate excitation and emission filters for specific fluorophore.
- Acquire images at multiple time points post-transplantation.
- Data Analysis:
- Use spectral unmixing techniques to separate specific signal from background autofluorescence [92].
- Quantify fluorescence intensity in regions of interest.
- For tomographic approaches, reconstruct 3D distribution of labeled cells.
Multimodal Imaging Approaches
Multimodal imaging combines the strengths of different imaging modalities to overcome their individual limitations [67]. For stem cell tracking, this approach enables comprehensive assessment of cell location, viability, and function [67]. Common multimodal strategies include PET/MRI, SPECT/MRI, and optical/MRI [95] [98].
Diagram 1: Multimodal imaging integrates complementary modalities and contrast agents
PET/MRI with Hybrid Contrast Agents
Recent developments include dual-purpose contrast agents that work with both PET and MRI simultaneously [99]. One approach uses cleverly designed molecules that combine gadolinium (for MRI) and radioactive fluorine-18 (for PET) [99]. The synthesis involves swapping nonradioactive fluorine atoms in MRI contrast agents for radioactive fluorine-18 atoms, a process that can be completed in less than 30 minutes using automated synthesis [99]. This enables simultaneous acquisition of high-resolution anatomical information (MRI) and highly sensitive molecular detection (PET).
Detailed Protocol: Multimodal Stem Cell Tracking
Materials:
- Multimodal contrast agent (e.g., 64Cu-SPION conjugates)
- PET/MRI scanner
- Image fusion software (e.g., Amide or OsiriX)
Procedure:
- Agent Preparation: Prepare multimodal contrast agent according to established protocols.
- Cell Labeling: Label stem cells with multimodal agent using optimized concentration and incubation time.
- Validation: Confirm labeling efficiency and cell viability through in vitro assays.
- Image Acquisition:
- Position subject in PET/MRI scanner.
- Acquire simultaneous or sequential PET and MRI data.
- For MRI: Use T1-weighted and T2-weighted sequences.
- For PET: Acquire static or dynamic scans as required.
- Data Fusion:
- Use algorithms to integrate PET and MRI data for voxel-wise co-registration [92].
- Apply spatial alignment and signal intensity normalization across modalities.
- Analysis:
- Correlate anatomical location (MRI) with functional information (PET).
- Quantify cell number and distribution using both signals for validation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents and materials for stem cell tracking experiments
| Reagent/Material | Function | Example Applications |
|---|---|---|
| SPIONs/USPIONs | T2 contrast agent for MRI; shortens transverse relaxation time of water protons [95] | Magnetic labeling of stem cells for MRI tracking [92] |
| 64Cu, 18F, 89Zr | Positron-emitting radioisotopes for PET imaging [92] | Radiolabeling of cells or nanoparticles for PET tracking [95] |
| Luciferase Reporter | Bioluminescent enzyme that generates light upon substrate addition [67] | Genetic labeling of stem cells for BLI tracking of viability [92] |
| Quantum Dots | Semiconductor nanoparticles with stable, intense fluorescence [92] | Fluorescent labeling for long-term cell tracking [67] |
| Transfection Agents | Enhance cellular internalization of contrast agents [92] | Improve SPION uptake during labeling procedures [92] |
| Dual-Modality Probes | Single agents detectable by multiple imaging modalities [98] | PET/MRI imaging with hybrid molecules [99] |
| Image Analysis Software | Quantification and visualization of imaging data [92] | ROI analysis, 3D reconstruction, signal quantification |
Each imaging modality offers distinct advantages for stem cell tracking: MRI provides high spatial resolution and excellent soft tissue contrast, PET/SPECT offers unparalleled sensitivity for quantitative molecular imaging, and optical techniques enable real-time monitoring of cellular processes with high specificity. The choice of modality depends on specific research questions, balancing spatial resolution, sensitivity, penetration depth, and clinical translatability. Multimodal approaches that combine complementary techniques represent the future of stem cell tracking, providing comprehensive information about cell location, viability, and function. Recent advances in contrast agents, including dual-purpose probes for PET/MRI, are paving the way for more accurate and informative stem cell tracking studies that will accelerate clinical translation of stem cell therapies.
Correlating Cell Presence with Therapeutic Functional Outcomes
This application note establishes a framework for correlating in vivo cell presence with therapeutic functional outcomes, a critical challenge in advanced therapy development. We present integrated methodologies combining non-invasive tracking technologies with functional assessments to quantitatively link biodistribution, persistence, and cellular kinetics to clinical efficacy. By leveraging recent advances in imaging technologies and machine learning, these protocols enable researchers to move beyond simple detection toward predictive assessment of therapeutic function. The approaches detailed herein support the optimization of cell-based therapies across diverse applications including oncology, regenerative medicine, and hematologic disorders.
The therapeutic efficacy of cellular therapeutics is fundamentally dependent on successful engraftment, targeted migration, and sustained functional persistence within the host environment. However, significant translational barriers remain, with low engraftment rates and limited long-term efficacy hampering clinical development [100]. Traditional endpoint analyses provide only snapshot data, failing to capture the dynamic cellular behaviors that ultimately determine therapeutic success.
Emerging technologies now enable researchers to establish quantitative relationships between cell presence and functional outcomes through two complementary approaches: (1) Longitudinal tracking of labeled cells using non-invasive imaging modalities, and (2) Predictive profiling of cellular kinetics using label-free methods that forecast functional potential. This application note provides detailed protocols for implementing these approaches across diverse therapeutic contexts, with structured data presentation and standardized methodologies to enhance reproducibility across research institutions.
Quantitative Imaging for Cell Tracking and Correlation with Outcomes
In Vivo Tracking Modalities and Applications
Non-invasive imaging technologies enable longitudinal monitoring of cell fate through direct labeling with contrast agents or genetic engineering with reporter genes. The selection of appropriate modality depends on resolution requirements, sensitivity, and compatibility with target tissue environments.
Table 1: In Vivo Cell Tracking Modalities and Technical Specifications
| Modality | Spatial Resolution | Temporal Resolution | Detection Limit (Cell Number) | Key Applications | Key Reagents |
|---|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | 25-100 μm | Minutes to hours | 10^3-10^5 (with SPIO) | Neurological diseases, myocardial infarction, muscular dystrophy | SPIO/USPIO nanoparticles (dextran-coated) |
| MicroCT | 10-100 μm | Minutes | 10^3-10^5 (with SPIO) | Muscular dystrophy, stem cell homing to muscle tissue | SPIO nanoparticles |
| SPECT | 1-2 mm | Minutes to hours | 10^2-10^4 | Atherosclerosis, inflammatory diseases, mesenchymal stem cell trafficking | 111In-oxine, 99mTc-HMPAO |
| PET | 1-2 mm | Seconds to minutes | 10^2-10^4 | Oncology, metabolic imaging, cell proliferation | 18F-FDG, 89Zr-oxine, 64Cu-PTSM |
| Quantum Dots | Limited by light diffusion | Seconds to minutes | Single cell (in vitro) | Intravital microscopy, multicolor imaging, lymph node mapping | CdSe/ZnS core-shell nanocrystals |
These modalities have demonstrated clinical relevance across multiple disease contexts. In neurological applications, SPIO-labeled neural stem cells successfully migrated to ischemic brain regions in rodent models, with MRI confirming targeted localization to lesion sites [7]. Similarly, in cardiology, radionuclide-labeled mesenchymal stem cells showed specific homing to infarcted myocardium within 24 hours post-administration, with persistence detected at 7 days follow-up [7].
Protocol: SPIO Labeling for MRI/MicroCT Tracking
Purpose: To label therapeutic cells with superparamagnetic iron oxide nanoparticles for non-invasive tracking using MRI or microCT imaging platforms.
Materials:
- Superparamagnetic iron oxide nanoparticles (SPIOs, 50-500 nm) or ultrasmall SPIOs (USPIOs, 5-50 nm)
- Cell culture medium appropriate for target cell type
- Transfection agents (e.g., poly-L-lysine, lipofectamine) - optional
- Magnetic separation columns
- Prussian blue staining kit
- Cell viability assay kit
Procedure:
- Cell Preparation: Culture cells to 70-80% confluence under standard conditions.
- SPIO Preparation: Dilute SPIO stock solution in serum-free medium to achieve final iron concentration of 25-100 μg/mL.
- Labeling Incubation: Incubate cells with SPIO-containing medium for 12-48 hours at 37°C, 5% CO₂.
- Wash and Recovery: Remove SPIO medium, wash cells 3× with PBS, and culture in fresh complete medium for 4-24 hours.
- Magnetic Separation: Pass cells through magnetic column to remove unincorporated nanoparticles.
- Quality Control:
- Determine labeling efficiency via Prussian blue staining (>80% recommended)
- Confirm cell viability (>90% recommended) using trypan exclusion or MTT assay
- Verify functional competence through cell-specific functional assays
- Administration: Administer labeled cells to animal model via appropriate route.
- Imaging: Perform serial MRI/microCT imaging at predetermined time points.
Technical Notes:
- For difficult-to-label cells, incorporate transfection agents at optimized concentrations
- Determine optimal labeling duration and concentration for each cell type
- Include unlabeled controls to distinguish background signals
- For microCT, the high spatial resolution enables 3D visualization and quantification of cell distribution [7]
Predictive Profiling Through Cellular Kinetics
Quantitative Phase Imaging for Functional Prediction
Quantitative phase imaging (QPI) represents a paradigm shift from static snapshots to dynamic forecasting of functional potential through non-invasive, label-free monitoring of cellular kinetics. This approach enables correlation of temporal behavior with therapeutic functional outcomes without the potential confounding effects of labeling procedures.
In hematopoietic stem cell (HSC) applications, QPI-driven machine learning analyzed 11 kinetic parameters from 11,512 cell images to identify distinct functional clusters [4]. This approach revealed remarkable diversity within phenotypically pure HSC populations, with proliferation rates varying from <4 cells to >20 cells after 96 hours expansion, and morphological outputs ranging from cells with dry masses <100 pg to >200 pg [4].
Table 2: QPI Kinetic Parameters Correlated with Functional Outcomes
| Kinetic Parameter | Measurement Method | Correlation with Functional Outcome | Application Context |
|---|---|---|---|
| Proliferation Rate | Cell count over time | HSCs producing >20 cells in 96h showed enhanced repopulation capacity | Hematopoietic stem cell transplantation |
| Dry Mass | Quantitative phase shift measurement | Cells >200 pg associated with differentiated phenotypes | Stem cell quality assessment |
| Division Gap | Time between first and second divisions | Intervals >5h indicated asymmetric divisions | Stemness evaluation |
| Sphericity | Morphological computational analysis | High sphericity + low velocity = immature HSCs (Cluster 3) | Murine and human HSC classification |
| Length/Width Ratio | Morphological computational analysis | Elongated cells (high ratio) showed lower stem cell potential | Human cord blood CD34+ cell sorting |
Protocol: QPI with Machine Learning Prediction
Purpose: To dynamically monitor single-cell kinetics and predict functional outcomes using quantitative phase imaging and machine learning classification.
Materials:
- Ptychographic quantitative phase imaging system
- U-bottom 96-well culture plates
- Single-cell expansion culture system
- Time-lapse imaging chamber with environmental control
- Computational resources for machine learning analysis
Procedure:
- Cell Preparation: Sort single cells (e.g., CD201+CD150+CD48−KSL for murine HSCs) into 96-well U-bottom plates.
- Time-Lapse QPI: Acquire phase images every 10-30 minutes for 96 hours under controlled conditions (37°C, 5% CO₂).
- Feature Extraction: Quantify kinetic parameters including:
- Dry mass
- Sphericity
- Velocity
- Length/width ratio
- Division timing and symmetry
- Proliferation rate
- Dimensionality Reduction: Perform Uniform Manifold Approximation and Projection (UMAP) to visualize high-dimensional data.
- Cluster Identification: Apply clustering algorithms (e.g., DBSCAN) to identify distinct behavioral populations.
- Functional Validation: Correlate kinetic profiles with in vivo repopulation capacity or lineage differentiation potential.
- Model Training: Train machine learning classifiers to predict functional outcomes from kinetic parameters.
Technical Notes:
- Maintain consistent environmental conditions throughout imaging
- Ensure adequate temporal resolution to capture division events
- Validate predictions with functional assays for each application
- The meniscus compensation in ptychographic QPI enables aberration-free imaging even in U-bottom wells [4]
Signaling Pathways and Functional Correlations
CAR T-cell Signaling Complexes and Clinical Outcomes
In engineered cell therapies, proximal signaling events directly correlate with therapeutic efficacy and adverse events. Quantitative multiplex co-immunoprecipitation (QMI) profiling of CAR T-cells has identified specific protein interaction networks associated with clinical outcomes.
Analysis of 41BB-CD3ζ CAR T-cell products revealed that a CRS-associated signaling module enriched for interactions among CD28, FYB, and SRC family kinases (LCK, FYN) correlated with cytokine release syndrome severity [101]. Machine learning classifiers trained on these QMI features could retrospectively identify CRS samples with high accuracy, enabling pre-infusion risk assessment [101].
Signaling Modules in CAR T-cell Therapies
Protocol: Signaling Network Profiling via QMI
Purpose: To profile proximal protein interaction networks in therapeutic cells and correlate interaction patterns with clinical outcomes.
Materials:
- Antibody array for 21 key signaling proteins
- Co-immunoprecipitation reagents
- Quantitative detection system
- Bioinformatic analysis pipeline
Procedure:
- Cell Stimulation: Activate therapeutic cells (e.g., CAR T-cells via CD19 engagement).
- Protein Extraction: Lyse cells at predetermined time points post-stimulation.
- Multiplex Co-immunoprecipitation: Profile ~200 binary interactions among target signaling proteins.
- Quantitative Analysis: Measure interaction strengths using standardized detection methods.
- Network Construction: Build correlation networks and cluster interactions into functional modules.
- Clinical Correlation: Associate module behavior with patient outcomes (e.g., CRS, efficacy).
- Classifier Development: Train predictive models using top QMI features.
Technical Notes:
- Standardize stimulation conditions across batches
- Include reference samples for normalization
- Validate findings in independent cohorts
- This approach enables pre-infusion risk assessment for adverse events [101]
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Cell Tracking and Functional Correlation
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Contrast Agents | SPIO/USPIO nanoparticles (50-500 nm) | MRI cell tracking, magnetic separation | Dextran coating improves solubility; size affects clearance |
| Radiotracers | 111In-oxine, 18F-FDG | PET/SPECT tracking, biodistribution studies | 111In has 2.8-day half-life for longer tracking |
| Fluorescent Tags | Quantum dots (CdSe/ZnS) | Intravital microscopy, multicolor imaging | Resistance to photobleaching; potential cytotoxicity |
| Cell Sorting Reagents | CD201, CD150, CD48, Sca1 antibodies | HSC isolation for functional studies | Combination defines functional subsets |
| Culture Systems | Single-cell expansion platforms | Clonal analysis, kinetic profiling | Maintain stemness during expansion |
| Signaling Profiling | QMI antibody arrays | Protein interaction network mapping | Requires specialized computational analysis |
| iPSC Reprogramming | REPROCELL StemRNA Clinical Seed iPSCs | GMP-compliant iPSC generation | Regulatory documentation available via DMF |
Integrated Workflow for Correlation Studies
A comprehensive approach to correlating cell presence with functional outcomes requires integration of multiple technologies from pre-administration profiling to longitudinal tracking and endpoint analysis.
Integrated Workflow for Correlating Cell Presence with Functional Outcomes
The correlation of cell presence with therapeutic functional outcomes requires a multifaceted approach that integrates dynamic cellular profiling with longitudinal tracking technologies. The protocols detailed in this application note provide a standardized framework for establishing these critical correlations across diverse therapeutic contexts. By implementing these methodologies, researchers can advance from simply detecting cell presence to predicting functional efficacy, ultimately enhancing the development and optimization of cellular therapeutics. As the field evolves, continued refinement of these approaches will further strengthen the predictive power of pre-administration assessments and in vivo monitoring technologies.
Within the broader context of stem cell tracking and in vivo imaging research, quantitative imaging serves as the cornerstone for validating therapeutic efficacy and understanding fundamental biological processes. The transition from merely determining cell location to precisely quantifying cell numbers represents a critical advancement in the field. This progression enables researchers to move beyond qualitative observations to obtain robust, numerical data on stem cell retention, proliferation, and engraftment following transplantation [10] [102]. These quantitative metrics are indispensable for optimizing delivery methods, dosing regimens, and ultimately, clinical outcomes in regenerative medicine.
The significance of precise cell quantification is particularly evident in clinical trials for conditions such as ischemic stroke, where stem cell therapy shows promise but outcomes vary significantly based on cell delivery and survival parameters [30]. Advanced imaging techniques provide the necessary tools to dissect these variables, offering non-invasive, longitudinal insights that were previously inaccessible. This protocol details the methodologies bridging cell localization and counting, with direct application to stem cell therapy development.
Comparative Analysis of Quantitative Imaging Modalities
The selection of an appropriate imaging modality is paramount and depends heavily on the specific research question, balancing factors such as resolution, sensitivity, depth penetration, and the capacity for quantification. Molecular imaging techniques, including Positron Emission Tomography (PET) and Magnetic Resonance Imaging (MRI), allow for non-invasive, longitudinal tracking of stem cell pharmacokinetics and pharmacodynamics in vivo [10]. These modalities can be complemented by advanced microscopy methods that provide high-resolution data at the cellular and subcellular levels.
Table 1: Key Imaging Modalities for Cell Localization and Tracking
| Imaging Modality | Spatial Resolution | Temporal Resolution | Primary Applications in Stem Cell Tracking | Key Advantages | Inherent Limitations for Quantification |
|---|---|---|---|---|---|
| Clinical PET | 1-2 mm | Minutes to Hours | Tracking biodistribution, cell homing, and early survival [10] [103]. | High sensitivity (picomolar), quantitative potential, deep tissue penetration. | Limited spatial resolution, radiation exposure, signal dilution from cell division. |
| Clinical MRI | 25-100 µm | Minutes | Monitoring cell localization and migration over weeks [30] [15]. | Excellent anatomical detail, no ionizing radiation, deep tissue penetration. | Lower sensitivity compared to PET, potential for ambiguous signal from iron particles. |
| Single-Molecule Localization Microscopy (SMLM) | ~10-20 nm (lateral) | Seconds to Minutes | Mapping nanoscale organization of molecules within cells [104] [105]. | Extremely high spatial resolution, single-molecule sensitivity. | Limited to superficial tissue or ex vivo samples, complex data processing. |
| Quantitative Phase Imaging (QPI) | N/A (Label-free) | Minutes to Hours | Non-invasive monitoring of cell growth, morphology, and kinetics [4]. | Label-free, provides biophysical metrics (dry mass, density). | Indirect measure of cell state, requires validation with other methods. |
For pure cell counting applications, especially in histology, object-based colocalization analysis (OBCA) has emerged as a powerful tool. This method segments individual cells as "objects" within an image, allowing for automated quantification of cells expressing specific markers. A recent study demonstrated that semi-automated and automated OBCA techniques show strong correlation with manual counting (R² = 0.7764–0.9954) while drastically reducing analysis time, making them indispensable for large datasets [106].
Experimental Protocols
Protocol 1: Validating Automated Cell Counting in Histological Samples
This protocol outlines the steps to validate automated colocalized cell counting against the manual gold standard, using immune cells in arachnoid tissue as a model system [106].
1. Sample Preparation and Staining
- Tissue Acquisition: Obtain human arachnoid tissue samples (e.g., from neurosurgical procedures for syringomyelia) and embed in paraffin [106].
- Multiplex Immunohistochemistry (MP-IHC): Deparaffinize tissue sections and perform multiplex staining.
- Use primary antibodies for immune cell markers: anti-CD4 (helper T-cells), anti-CD8 (cytotoxic T-cells), anti-CD20 (B-cells), and a combination of anti-CD68 and anti-IBA1 (macrophages).
- Use appropriate fluorescently-conjugated secondary antibodies (e.g., Alexa Fluor 488, 647, 594).
- Nuclear Counterstaining: Include DAPI staining to identify all cell nuclei.
- Image Acquisition: Image stained sections using a fluorescence slide-scanning microscope (e.g., Zeiss Axio Imager.Z2) with a 20x objective. Stitch image tiles to create whole-specimen composites for analysis [106].
2. Image Pre-processing for Analysis
- Using ImageJ or similar software, convert individual channel images to 16-bit.
- Adjust brightness and contrast uniformly across all samples if staining intensity is low.
- Create composite images by merging the DAPI channel (green) with each immune marker channel (red). For multi-marker cells (e.g., DAPI/CD68/IBA1), merge all three channels [106].
3. Cell Counting: Manual vs. Automated
- Manual Counting: Have two independent observers count colocalized cells (defined as cells co-stained for DAPI and an immune marker) in the composite images. This serves as the "gold standard" [106].
- Semi-Automated & Automated Counting: Use OBCA software (e.g., custom pipelines in ImageJ or commercial solutions). The software will:
- Segment images to distinguish background from cellular objects based on intensity thresholding.
- Identify centroids of each stained object.
- Determine colocalization when centroids of different markers (e.g., DAPI and CD8) are within a predefined distance [106].
4. Data Analysis and Validation
- Compare automated and semi-automated counts to manual counts using correlation analysis (e.g., Pearson correlation) and statistical tests (e.g., t-test).
- Validate that the correlation is strong (R² > 0.75) and that the methods significantly reduce analysis time without sacrificing biological accuracy [106].
Protocol 2: In Vivo Stem Cell Tracking using Reporter Gene Imaging
This protocol describes how to track and localize stem cells in vivo using a reporter gene system, which is ideal for long-term monitoring of cell survival and proliferation [10].
1. Reporter Gene Engineering
- Select a Reporter Gene: Choose a gene suitable for your imaging modality. A common choice is a triple-fusion reporter gene combining Herpes Simplex Virus thymidine kinase (HSV-tk) for PET imaging, firefly luciferase for bioluminescence imaging, and a fluorescent protein (e.g., red fluorescent protein) for histological validation [10].
- Genetic Modification: Introduce the reporter gene construct into your stem cells (e.g., human induced pluripotent stem cell-derived cardiomyocytes) using CRISPR/Cas9 gene editing or lentiviral transduction to create a stable cell line [10].
2. Cell Transplantation and Image Acquisition
- Animal Model: Use an appropriate disease model (e.g., myocardial infarction in rats).
- Cell Delivery: Transplant the engineered stem cells (e.g., via intramyocardial injection).
- Longitudinal Imaging:
- PET Imaging: At multiple time points post-transplantation, inject the radiotracer 9-(4-[18F]fluoro-3-(hydroxymethyl)butyl)guanine ([18F]FHBG), which is phosphorylated and trapped by the HSV-tk enzyme. Acquire PET images to localize and quantify the signal from the transplanted cells [10].
- Bioluminescence Imaging (BLI): Inject the substrate D-luciferin and acquire optical images to detect the light emission from firefly luciferase, providing a complementary readout on cell location and viability [10].
3. Image Analysis and Quantification
- Co-registration: Fuse PET images with anatomical CT or MRI scans to precisely localize the signal within the target organ.
- Signal Quantification: Draw regions of interest (ROIs) around the target area and calculate standardized uptake values (SUVs) for PET data or total flux (photons/second) for BLI data. This provides a quantitative measure of signal strength over time, which correlates with the number of viable, reporter-expressing cells [10].
Table 2: Research Reagent Solutions for Stem Cell Tracking
| Reagent / Material | Function / Application | Specific Example | Considerations for Use |
|---|---|---|---|
| Triple-Fusion Reporter Gene | Enables multi-modal imaging (PET, BLI, fluorescence) of the same cell population [10]. | HSV1-tk / Fluc / Rfp | Requires genetic modification of cells; ensures reporter expression does not alter stem cell function. |
| Radiotracer ([18F]FHBG) | PET probe that accumulates in cells expressing the HSV-tk reporter gene [10]. | 9-(4-[18F]fluoro-3-(hydroxymethyl)butyl)guanine | Short half-life (110 min) requires on-site cyclotron; ideal for short-term tracking. |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Direct label for MRI tracking; creates hypointense signals on T2/T2*-weighted images [15]. | Ferumoxytol | Signal can be diluted with cell division and may be phagocytosed by macrophages upon cell death. |
| Multiplex IHC Antibody Panel | Allows simultaneous detection of multiple cell types and markers in fixed tissue [106]. | Anti-CD4, CD8, CD20, CD68, IBA1 | Requires spectral unmixing or careful fluorophore selection to avoid bleed-through. |
| Quality Control Maps (QCM) | Algorithm for real-time assessment of Single-Molecule Localization Microscopy (SMLM) data quality [104]. | N/A | Parameter-free, robust algorithm that enables smart microscopy by adjusting acquisition in real-time. |
Integrated Workflow from Localization to Quantification
A comprehensive stem cell tracking study integrates multiple techniques to move from gross localization to precise quantification, both in vivo and ex vivo. The workflow begins with non-invasive in vivo imaging to monitor global cell fate, followed by high-resolution validation for precise counting and molecular analysis.
This integrated approach is powerful for answering complex questions. For instance, a study might use PET imaging with a reporter gene to track the overall survival of cardiomyocytes derived from induced pluripotent stem cells in a rat infarct model over several weeks [10]. At the study endpoint, the heart is harvested, sectioned, and stained. High-resolution confocal microscopy or SMLM can then be used to visualize the grafted cells and their integration with host tissue. Finally, automated cell counting on these sections provides the ground-truth quantification of final cell numbers, which can be correlated with the non-invasive PET signal intensity measured earlier [10] [106]. This validates the in vivo imaging data and provides a complete picture from localization to precise enumeration.
Discussion
The field of quantitative imaging for stem cell research is rapidly evolving, with several advanced technologies enhancing both localization accuracy and counting precision. Single Molecule Localization Microscopy (SMLM) is pushing the boundaries of spatial resolution, but its use in depth has been limited by optical aberrations. Innovative solutions like the soSMARt method, which combines single-objective light-sheet microscopy with adaptive optics and real-time drift correction, now enable volumetric SMLM with nanometric resolution throughout entire cells [105]. This allows for quantitative analysis of molecular distributions in 3D, far beyond the coverslip surface.
Furthermore, label-free techniques like Quantitative Phase Imaging (QPI) are emerging as powerful tools for predicting stem cell fate and quality. By analyzing cellular kinetics—such as dry mass, sphericity, and division patterns—QPI coupled with machine learning can classify hematopoietic stem cells based on their functional potential, a diversity that snapshot analyses cannot resolve [4]. This approach moves quantification from simple cell counting to predictive, functional assessment based on dynamic temporal data.
Despite these advancements, challenges remain. No single modality provides a perfect solution; the ideal strategy often involves a multimodal approach that leverages the strengths of different techniques [102]. For instance, combining the high sensitivity of PET for initial localization and tracking with the high resolution of microscopy for final validation and counting provides a comprehensive quantitative profile. As imaging technologies and analytical algorithms continue to improve, the ability to precisely localize and count stem cells in vivo will be crucial for translating regenerative therapies from the laboratory to the clinic, ensuring that these therapies are not only delivered but also effective.
The translation of stem cell therapies from promising preclinical data to successful clinical applications has been hampered by inconsistent and often puzzling clinical trial outcomes. A pivotal factor in deciphering these mixed results is the inability to directly observe the fate and function of administered cells within the living body. In vivo imaging has thus emerged as an indispensable discipline, providing a non-invasive window into the dynamic behaviors of stem cells post-transplantation. By visualizing critical parameters such as cell survival, migration patterns, and engraftment efficiency, imaging technologies offer a mechanistic bridge between therapeutic administration and clinical readout, transforming our capacity to interpret trial data [10].
This document provides a structured overview of current imaging modalities, detailing their respective protocols and applications. It is structured to serve as a practical resource for researchers and drug development professionals, enabling the strategic integration of imaging into clinical trial design to deconvolute complex therapeutic responses and accelerate the development of effective stem cell-based treatments.
Modality Comparison and Clinical Application
The selection of an appropriate imaging modality is a critical first step in trial design, balancing factors such as resolution, sensitivity, depth penetration, and quantitative capability. The following tables summarize the key characteristics and clinical trial contexts for the most prominent technologies.
Table 1: Technical Specifications and Capabilities of Key Imaging Modalities
| Imaging Modality | Spatial Resolution | Tissue Penetration | Key Measurable Parameters | Primary Limitations |
|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | 25-100 µm | Unlimited | Anatomical location of labeled cells, tissue morphology and structure | Low sensitivity, potential signal dilution from cell division, background interference [107] [10] |
| Positron Emission Tomography (PET) | 1-2 mm | Unlimited | Metabolic activity, cell viability, reporter gene expression, distribution density | Use of ionizing radiation, limited temporal resolution due to radiotracer half-life [107] [10] |
| Bioluminescence Imaging (BLI) | N/A (2-3 mm in practice) | 1-2 cm | Cell viability and proliferation (longitudinal), bioluminescent flux (photons/second) | Requires genetic modification, low spatial resolution, limited to small animal models [107] |
| Quantitative Phase Imaging (QPI) | Sub-micrometer | In vitro only | Cell dry mass, sphericity, velocity, division kinetics | Not suitable for in vivo tracking; limited to predictive quality control [108] |
| Photoacoustic Imaging (PAI) | ~50 µm | Several centimeters | Spatial distribution of labeled cells via ultrasonic wave detection | Signal attenuation from tissue scattering, requires specific laser wavelengths for contrast agents [107] |
Table 2: Imaging Correlates for Interpreting Common Clinical Trial Challenges
| Clinical Trial Observation | Recommended Imaging Approach | Data Output for Interpretation | Implied Biological Mechanism |
|---|---|---|---|
| Initial symptom improvement followed by rapid decline | PET with [18F]FDG or Reporter Gene Imaging | Rapid loss of signal at engraftment site post-transplantation | Poor long-term cell survival or rapid cell death after initial engraftment [10] |
| Therapeutic effect in unexpected anatomical locations | MRI with SPIONs or Direct Radionuclide Labeling (PET) | Signal accumulation in non-target organs or secondary disease sites | Off-target migration (homing to non-therapeutic tissues) or entrapment in filtering organs [107] [10] |
| High patient-to-patient variability in efficacy | Pre-treatment QPI or Post-treatment PET/MRI | Correlation of pre-treatment cellular kinetic profiles or post-treatment engraftment efficiency with clinical outcome | Underlying heterogeneity in stem cell potency or differential engraftment efficiency among recipients [108] |
| Lack of efficacy despite predicted mechanism | Multimodal Imaging (e.g., PET/MRI) | Evidence of successful engraftment and cell survival without functional improvement (e.g., no change in glucose metabolism) | Failure of cells to execute therapeutic function (e.g., lack of differentiation or insufficient paracrine signaling) despite survival [10] |
Experimental Protocols
This section provides detailed, actionable protocols for key imaging methodologies relevant to clinical trial analysis.
Direct Magnetic Resonance Imaging (MRI) Tracking of Stem Cells
This protocol describes the procedure for labeling and tracking stem cells with Superparamagnetic Iron Oxide Nanoparticles (SPIONs) to monitor their in vivo localization using MRI [107].
- Primary Application: Determining the anatomical distribution and retention of cells at the target site and in non-target organs over time.
- Key Reagents:
- Superparamagnetic Iron Oxide Nanoparticles (SPIONs): Core contrast agent for generating T2 contrast.
- Protamine Sulfate: Transfection agent to enhance cellular internalization of SPIONs.
Step-by-Step Procedure:
- Cell Labeling: a. Harvest and wash stem cells to remove serum. b. Incubate cells with SPIONs (e.g., at 50-100 µg Fe/mL) in serum-free medium, optionally supplemented with a transfection agent like protamine sulfate (1.5-5 µg/mL), for 4-24 hours at 37°C [107]. c. Wash cells thoroughly with PBS to remove excess, unincorporated nanoparticles. d. Confirm labeling efficiency and cell viability via Prussian Blue staining and a viability assay (e.g., Trypan Blue exclusion).
Cell Transplantation: a. Administer the labeled cells (e.g., ~1-5 x 10^6 cells) into the patient or animal model via the intended clinical route (e.g., intravenous, intramyocardial). b. Retain an aliquot of labeled cells for in vitro validation.
Image Acquisition: a. Perform baseline MRI scans pre-transplantation. b. Image subjects at predetermined time points (e.g., 24h, 7d, 28d post-transplantation) using a clinical MRI system. c. Acquire T2-weighted or T2*-weighted sequences, where SPIONs create hypointense (dark) signal artifacts.
Data Analysis and Quantification: a. Co-register post-transplantation images with the baseline scan. b. Manually or semi-automatically identify and count hypointense voxels in the region of interest. c. Use software tools (e.g., ImageJ, OsiriX) to quantify the volume or area of signal void. d. Correlate the hypointense signal regions with anatomical location to determine cell distribution. Note that signal quantification is indirect and requires careful calibration to account for artifacts and signal interference from adjacent tissues [107].
Reporter Gene-Based Monitoring with Positron Emission Tomography (PET)
This protocol leverages genetic engineering to enable long-term, highly sensitive tracking of stem cell survival and proliferation, overcoming the label dilution limitation of direct labeling [107] [10].
- Primary Application: Longitudinal assessment of cell viability and biodistribution, particularly in trials where long-term engraftment is critical.
- Key Reagents:
- Reporter Gene Construct (e.g., HSV-sr39tk, D2R): Encodes a protein that selectively traps or binds a PET probe.
- PET Radiotracer (e.g., [18F]FHBG for tk, [18F]FESP for D2R): The reporter probe used for imaging.
Step-by-Step Procedure:
- Genetic Modification of Stem Cells: a. Engineer stem cells to stably express a PET-sensitive reporter gene (e.g., herpes simplex virus type 1 thymidine kinase - HSV1-tk). This can be achieved using lentiviral vectors or CRISPR/Cas9-mediated gene editing for targeted integration [107]. b. Expand the transduced cells and validate reporter gene expression and function via in vitro assays (e.g., [3H]Penciclovir uptake assay for tk).
Cell Transplantation: Administer the genetically modified cells into the subject as per the trial protocol.
Image Acquisition: a. At each imaging time point, synthesize the specific PET radiotracer (e.g., 9-(4-[18F]fluoro-3-hydroxymethylbutyl)guanine, [18F]FHBG, for HSV1-tk). b. Intravenously inject the radiotracer into the subject. c. After a suitable uptake period (e.g., 1-2 hours), perform a PET/CT scan according to standard clinical protocols. The CT scan provides anatomical co-registration.
Data Analysis and Quantification: a. Reconstruct PET images using computational algorithms such as filtered back projection (FBP) or maximum likelihood expectation maximization (MLEM) [107]. b. Draw regions of interest (ROIs) around the target tissue and reference background tissue. c. Quantify radiotracer uptake as Standardized Uptake Value (SUV) or percent injected dose per gram of tissue (%ID/g). d. The magnitude of radiotracer uptake within the ROI is directly correlated with the number of viable, reporter-expressing cells. A decline in signal over time indicates cell loss.
In Vitro Predictive Potency Assessment via Quantitative Phase Imaging (QPI)
This protocol uses label-free, high-content imaging to analyze the temporal kinetics of individual stem cells during expansion, predicting their in vivo functional potential prior to transplantation [108].
- Primary Application: Quality control and potency assessment of cell batches to minimize product heterogeneity, a potential source of variable clinical outcomes.
- Key Reagents:
- Single-HSC Ex Vivo Expansion Culture System: Specialized medium and conditions for maintaining stem cell function in vitro.
Step-by-Step Procedure:
- Cell Preparation and Imaging: a. Sort single phenotypically defined stem cells (e.g., murine CD201+CD150+CD48-KSL cells or human Lin-CD34+CD38-CD45RA-CD90+CD201+ cells) into 96-well U-bottom plates. b. Culture cells in an ex vivo expansion system and place in a time-lapse QPI microscope system. c. Acquire images every 5-20 minutes for several days (e.g., 96 hours) [108].
Kinetic Feature Extraction: a. Use automated tracking software to follow individual cells and their progeny over time. b. Extract quantitative parameters for each cell, including: - Dry Mass: A measure of biomass. - Sphericity: A measure of roundness. - Velocity: Rate of movement. - Division Gap: Time interval between consecutive cell divisions. - Proliferation Rate: Number of cells produced over the culture period [108].
Data Analysis and Prediction Modeling: a. Perform dimensionality reduction (e.g., Uniform Manifold Approximation and Projection, UMAP) on the multi-parametric kinetic data to identify distinct cellular clusters. b. Train a machine learning classifier (e.g., random forest, support vector machine) to correlate the in vitro kinetic profiles of individual cells with their known in vivo repopulation potential or differentiation bias, as determined by parallel transplantation experiments. c. Apply the validated model to predict the functional quality of new, untested stem cell batches based on their QPI kinetics alone.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Stem Cell Tracking and Analysis
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| SPIONs (Superparamagnetic Iron Oxide Nanoparticles) | MRI contrast agent for direct cell labeling and tracking. | Biocompatibility, potential impact on stem cell differentiation capacity, signal dilution with cell division [107] [10]. |
| Reporter Genes (e.g., Luciferase, HSV-tk, GFP) | Enables bioluminescence, PET, or fluorescence imaging of viable, genetically modified cells. | Requires genetic manipulation; ensures stable, long-term expression without silencing; considers safety for clinical translation [107] [10]. |
| Radiotracers (e.g., [18F]FDG, [18F]FHBG, 64Cu) | PET probes for imaging cell metabolism or reporter gene expression. | Short half-life necessitates on-site cyclotron for some tracers; requires radiation safety protocols [107] [10]. |
| Quantum Dots (QDs) / Gold Nanoparticles | Fluorescent or photoacoustic contrast agents for high-resolution optical imaging. | Potential cytotoxicity; photobleaching (QDs); intracellular uptake efficiency must be optimized [107]. |
| scRNA-seq Barcoding Kits | Allows single-cell transcriptomic analysis to correlate cell fate with imaging data. | High cost; complex bioinformatic analysis required; integrates imaging data with molecular phenotyping [107]. |
Visualizing Workflows and Pathways
The following diagrams illustrate the logical flow of two primary imaging strategies and the experimental setup for predictive potency assessment.
Stem Cell Imaging Decision Pathway
Predictive Potency Workflow
Multimodal Correlation Analysis
Bench-to-bedside translation, often termed Translational Research (TR), aims to bridge the gap between basic scientific discoveries and their application in clinical practice to improve patient outcomes [109] [110]. In the context of stem cell therapies, this process is pivotal for harnessing the potential of regenerative medicine. Despite promising preclinical results, the clinical efficacy of stem cell therapies has often fallen short of expectations, underscoring a critical need to understand and overcome the barriers in their translational pathway [111] [10]. Molecular imaging has emerged as an indispensable tool in this endeavor, enabling the non-invasive, longitudinal monitoring of transplanted cells in vivo [111] [15]. By visualizing the fate, distribution, and function of stem cells, molecular imaging provides crucial insights that help deconstruct the complexities of cell therapy, thereby facilitating the optimization of protocols and enhancing therapeutic efficacy [10] [24]. This application note delineates the current successes, persistent barriers, and detailed methodologies in the translational pipeline of stem cell therapies, with a focused lens on the role of in vivo imaging.
The Translational Pipeline: From T0 to T4
The continuum of clinical and translational science has been formally divided into discrete stages, labeled T0 through T4, which encapsulate the entire journey from fundamental discovery to population health impact [112].
- T0 (Pre-Translation): This initial phase involves basic discovery research conducted at the laboratory bench. It includes the identification of fundamental physiological processes, disease mechanisms, and potential therapeutic targets, such as the isolation and characterization of novel stem cell populations [112].
- T1 (Translation to Humans): T1 translation involves moving discoveries from the laboratory into human application for the first time. This stage encompasses early-phase clinical trials (Phase I and II) to assess the safety, tolerability, and preliminary efficacy of a new therapy. In stem cell research, this includes first-in-human studies of cell transplantation [112].
- T2 (Translation to Patients): In this stage, evidence for the clinical application of a discovery is established. This involves later-phase clinical trials (Phase III) to determine efficacy and generate the evidence base required for the development of clinical practice guidelines [112].
- T3 (Translation to Practice): T3 translation focuses on the dissemination and implementation of evidence-based guidelines into routine clinical practice within academic healthcare systems. It addresses the gap between knowing what works and ensuring it is used correctly in patient care [112].
- T4 (Translation to Population Health): The final stage seeks to translate clinical knowledge into broader public health impact through disease prevention and health promotion programs. This involves altering community and population behaviors to improve global wellness and reduce the burden of disease [112].
The following diagram illustrates this multi-stage translational pathway and the role of imaging within it:
Current Successes in Stem Cell Therapy and Imaging
Stem cell therapies have demonstrated significant clinical potential across a spectrum of diseases. Key successes include their application in autoimmune, neurological, and cardiovascular conditions, supported by advanced molecular imaging techniques.
Clinical Therapeutic Successes
- Graft-versus-Host Disease (GVHD): A phase III trial of Remestemcel-L, a bone marrow-derived MSC product, showed a 70.4% overall response rate at day 28 in pediatric patients with steroid-refractory acute GVHD, demonstrating durable benefit [113].
- Cardiovascular Disease: The PARACCT trial reported that allogeneic MSCs help reduce scar formation and enhance ejection fraction in patients recovering from myocardial infarction [113].
- Inflammatory Bowel Disease (IBD): Preclinical studies highlight the ability of MSCs to modulate immune responses; MSC treatment reduces colitis severity by inducing macrophage polarization toward an anti-inflammatory state through the secretion of interleukin-10 (IL-10) [113].
- Neurological Disorders: MSC-derived exosomes have been shown to slow motor neuron degeneration in animal models of amyotrophic lateral sclerosis (ALS). Ongoing clinical trials, such as MASTERS-2, are investigating intravenous MSC therapy to promote neurogenesis and angiogenesis in stroke patients [113].
Advanced Imaging Applications
Molecular imaging has been successfully deployed to monitor these therapies. For instance, using a triple fusion reporter gene (red fluorescent protein, firefly luciferase, and herpes simplex virus thymidine kinase) allows for tracking transplanted cardiomyocytes derived from induced pluripotent stem cells with fluorescence imaging, bioluminescence imaging, and PET [10]. Furthermore, combined [18F]FDG and [18F]FHBG PET can track the differentiation of transplanted stem cells and monitor the recovery of cardiac function in myocardial infarction [10].
Table 1: Key Clinical Successes in Stem Cell Therapy
| Therapeutic Area | Cell Type | Key Findings/Clinical Evidence | Role of Molecular Imaging |
|---|---|---|---|
| Graft-versus-Host Disease (GVHD) | Bone Marrow-MSCs (Remestemcel-L) | 70.4% response rate in pediatric steroid-refractory patients in a Phase III trial [113]. | Not specified in context. |
| Myocardial Infarction | Allogeneic MSCs | Reduced scar formation and improved ejection fraction (PARACCT trial) [113]. | PET/MRI tracks cell survival and cardiac function improvement [10]. |
| Inflammatory Bowel Disease | MSCs | Preclinical models show reduced colitis severity via macrophage polarization (IL-10) [113]. | Preclinical BLI and SPECT monitor homing to inflamed colon [111]. |
| Stroke & Neurodegeneration | MSCs and derived exosomes | Slowed motor neuron degeneration in ALS models; clinical trials ongoing (e.g., MASTERS-2) [113]. | PET detects reduced β-amyloid in Alzheimer's models post-MSC transplant [10]. |
Major Barriers to Translation
Despite promising successes, the translation of stem cell therapies from bench to bedside faces several significant barriers, which have been identified through both preclinical and clinical imaging studies.
Limited Cell Engraftment and Survival
A primary barrier is the dramatic loss of transplanted cells shortly after delivery. Molecular imaging studies across cardiovascular and neurological diseases have consistently shown that less than 5% of intravenously or intracoronarily delivered stem cells successfully engraft in the target tissue [111]. The majority of cells are sequestered in non-target organs, particularly the lungs, liver, and spleen [111] [24]. The mode of delivery significantly impacts initial retention, with intramyocardial injection showing higher retention (≈11%) compared to intracoronary (≈2.6%) or intravenous (≈3.2%) delivery [111].
Poor Control of Cell Differentiation and Function
Ensuring that transplanted stem cells differentiate into the desired functional cell types and integrate properly into the host tissue remains a formidable challenge. While reporter gene imaging allows for tracking cell survival, monitoring specific differentiation and functional maturation in vivo requires more sophisticated, tissue-specific reporter systems that are not yet widely available [10].
Immunogenicity and Host Response
While mesenchymal stem cells (MSCs) are considered immunoprivileged, allogeneic transplantation can still elicit host immune responses that lead to the rejection of transplanted cells over time. Furthermore, the immune-modulatory functions of MSCs can have dual roles in oncology, sometimes promoting and other times inhibiting tumor progression, a complexity that necessitates careful monitoring [24].
Tumorigenicity of Pluripotent Stem Cell Derivatives
The risk of tumor formation, particularly teratomas from residual undifferentiated pluripotent stem cells (ESCs and iPSCs), is a major safety concern that hinders clinical translation. Molecular imaging is being explored to detect early markers of oncogenic transformation, but reliable and sensitive strategies for long-term safety monitoring are still under development [111].
Table 2: Major Barriers Identified via Molecular Imaging
| Barrier | Imaging Evidence | Impact on Therapeutic Efficacy |
|---|---|---|
| Low Cell Engraftment & Survival | BLI and SPECT show <5% cell retention in target tissue; majority in lungs/liver [111]. | Directly limits the number of cells available for tissue repair and paracrine signaling. |
| Uncontrolled Cell Fate | Lack of robust in vivo imaging methods to track specific differentiation and functional integration [10]. | Compromises the ability to form functional, integrated tissue and restore organ function. |
| Host Immune Response | Immune-mediated clearance of allogeneic cells observed in longitudinal tracking studies [24]. | Reduces long-term engraftment and necessitates immunosuppression or patient-specific cells. |
| Tumorigenic Potential | Reporter genes could potentially be designed to detect early teratoma formation in PSC-derived grafts [111]. | Poses a significant safety risk, requiring extensive preclinical testing and long-term monitoring. |
Detailed Experimental Protocols
To address the barriers outlined above, robust and reproducible experimental protocols are essential. The following sections provide detailed methodologies for key procedures in stem cell tracking.
Protocol 1: Direct Labeling of MSCs with Superparamagnetic Iron Oxide Nanoparticles (SPIONs) for MRI Tracking
Application: This protocol is used for the short-term (up to 2 weeks) non-invasive tracking of mesenchymal stem cells (MSCs) post-transplantation in animal models to assess initial homing and biodistribution [15] [24].
Principle: SPIONs are internalized by cells and act as strong T2/T2* contrast agents in Magnetic Resonance Imaging (MRI), causing a localized signal void (dark contrast) at the site of labeled cell accumulation [15] [67].
Materials:
- Cells: Human Umbilical Cord Mesenchymal Stem Cells (hUC-MSCs) or Bone Marrow-MSCs (BM-MSCs) [15] [113].
- Labeling Agent: Dextran-coated SPIONs (e.g., Ferucarbotran).
- Culture Medium: Standard MSC growth medium (e.g., DMEM/F12 supplemented with 10% FBS and 1% Penicillin/Streptomycin).
- Transfection Agent: (Optional) Poly-L-lysine to enhance labeling efficiency.
- Staining Solution: Prussian Blue stain for iron detection.
Procedure:
- Cell Culture: Culture hUC-MSCs to 70-80% confluence in T-75 flasks under standard conditions (37°C, 5% CO₂).
- Labeling Medium Preparation: Prepare the labeling medium by adding SPIONs to the culture medium at a final iron concentration of 50-100 µg/mL. If needed, add poly-L-lysine (0.75 µg/mL) to facilitate nanoparticle uptake [15].
- Incubation: Replace the standard culture medium with the SPION-containing labeling medium. Incubate the cells for 12-24 hours.
- Washing: Remove the labeling medium and wash the cells thoroughly 3 times with phosphate-buffered saline (PBS) to remove any extracellular iron particles.
- Harvesting: Harvest the labeled cells using a standard trypsinization procedure.
- Validation (Prussian Blue Staining):
- Fix an aliquot of labeled cells (≈1x10⁵) with 4% paraformaldehyde for 10 minutes.
- Incubate with a 1:1 mixture of 4% potassium ferrocyanide and 4% hydrochloric acid for 20 minutes.
- Counterstain with Nuclear Fast Red for 5 minutes.
- Observe under a microscope; intracellular iron will appear as blue granules.
- Transplantation: Resuspend the validated, SPION-labeled MSCs in sterile PBS at the desired concentration (e.g., 4x10⁴ cells/µL) for transplantation into the target organ (e.g., intramyocardial or intraspinal injection) [15].
- In Vivo MRI Tracking: Perform MRI on the animal model at multiple time points (e.g., 1 day, 1 week, 2 weeks post-transplantation) using a T2*-weighted gradient-echo sequence to detect hypointense signals indicative of labeled cell presence.
Protocol 2: Indirect Labeling with a Reporter Gene for Multimodal Imaging
Application: Long-term monitoring of stem cell survival, proliferation, and location using bioluminescence imaging (BLI) and positron emission tomography (PET) [111] [10].
Principle: Cells are genetically engineered to stably express a fusion reporter gene (e.g., Firefly Luciferase - FLuc for BLI, and Herpes Simplex Virus Thymidine Kinase - HSV-tk for PET). The signal is dependent on cell viability and is passed to daughter cells, enabling long-term tracking [10] [67].
Materials:
- Cells: Induced Pluripotent Stem Cell-derived Cardiomyocytes (iPSC-CMs) or MSCs.
- Reporter Construct: Plasmid or viral vector (lentivirus/adenovirus) encoding a triple fusion reporter gene (e.g., FLuc, HSV-tk, and a fluorescent protein like RFP).
- Substrates: D-luciferin (for BLI); [18F]FHBG (9-(4-[18F]fluoro-3-(hydroxymethyl)butyl)guanine) for PET.
- Culture Medium: Appropriate medium for the cell type.
- Selection Antibiotic: e.g., Puromycin, if the vector contains a resistance gene.
Procedure:
- Cell Transduction:
- Culture iPSC-CMs to 50-60% confluence.
- Transduce the cells with the reporter gene-containing lentivirus at a pre-optimized Multiplicity of Infection (MOI) in the presence of a transduction enhancer (e.g., Polybrene).
- Incubate for 24-48 hours.
- Selection and Expansion:
- Replace the medium with fresh growth medium containing the appropriate selection antibiotic (e.g., 1 µg/mL puromycin).
- Maintain selection pressure for 5-7 days to eliminate non-transduced cells, then expand the stably transduced polyclonal population.
- In Vitro Validation:
- Bioluminescence: Incubate an aliquot of cells with D-luciferin (150 µg/mL) and image using a cooled CCD camera system to confirm FLuc activity.
- Fluorescence: Use fluorescence microscopy to confirm expression of the fluorescent protein (e.g., RFP).
- Transplantation: Transplant the validated, reporter-expressing cells into the target organ of immunocompromised animal models (e.g., myocardial infarction model).
- In Vivo Multimodal Imaging:
- BLI: Inject the animal intraperitoneally with D-luciferin (150 mg/kg). Acquire images 10-15 minutes post-injection under anesthesia. BLI provides a sensitive, 2D assessment of overall cell survival and location [111].
- PET/CT: Inject the animal intravenously with the PET tracer [18F]FHBG (100-200 µCi). After a 60-minute uptake period, perform a static PET scan followed by a low-dose CT scan for anatomical co-registration. PET provides quantitative, 3D information on the spatial distribution of viable cells [10].
The workflow for this multimodal imaging approach is detailed below:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Stem Cell Tracking
| Reagent / Tool | Function / Application | Key Characteristics |
|---|---|---|
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Direct labeling agent for MRI cell tracking [15] [67]. | T2/T2* contrast agent; causes signal drop on MRI; biodegradable; limited by dilution upon cell division. |
| Near-Infrared (NIR) Fluorophores (e.g., DiR, IR-786) | Direct labeling for optical fluorescence imaging [15] [24]. | Reduced tissue autofluorescence; deeper tissue penetration (up to 10 cm); suitable for intraoperative guidance. |
| Reporter Gene Systems (e.g., Firefly Luciferase - FLuc) | Indirect labeling for bioluminescence imaging (BLI) of cell viability [111] [10]. | High sensitivity; low background; requires substrate (D-luciferin); signal proportional to live cell number. |
| Reporter Gene Systems (e.g., HSV-tk) | Indirect labeling for PET imaging of cell location and survival [10]. | High sensitivity and quantitative 3D tomography; requires radioactive substrate ([18F]FHBG); translatable to clinic. |
| Quantum Dots (QDs) | Direct labeling for multiplexed fluorescence imaging [15] [24]. | Semiconductor nanocrystals; bright, photostable; multiple colors with single excitation; potential cytotoxicity concerns. |
| Zirconium-89 (89Zr) | Radiolabel for direct cell labeling and long-term PET tracking [24]. | Long half-life (3.3 days); suitable for tracking over several days to a week; requires chelator for cell labeling. |
Bench-to-bedside translation of stem cell therapies is a complex, multi-stage process fraught with challenges, most notably poor cell engraftment and survival. Molecular imaging has proven to be an invaluable scientific partner in this journey, providing non-invasive, longitudinal data that is critical for understanding the in vivo behavior and therapeutic mechanisms of stem cells. The integration of direct and indirect labeling strategies with multimodal imaging platforms (e.g., BLI, PET, MRI) offers a comprehensive toolkit to dissect these complexities. As the field progresses, the continued refinement of these imaging technologies, coupled with advances in cell engineering and biomaterials, will be paramount in overcoming existing barriers, ensuring patient safety, and ultimately fulfilling the immense clinical promise of stem cell-based regenerative medicine.
The transition of stem cell therapies from laboratory research to clinical applications necessitates a paradigm shift in how therapeutic efficacy is defined and measured. While the initial focus of in vivo tracking has rightly been on confirming the successful delivery and initial localization of transplanted cells, this provides a incomplete picture of therapeutic success. True efficacy is determined by the functional integration of these cells into the host tissue, where they perform appropriate physiological roles. The emerging consensus in regenerative medicine indicates that a comprehensive assessment must extend beyond mere cell presence to evaluate cell viability, phenotypic differentiation, functional activity, and ultimately, the restoration of tissue function [15] [114]. This protocol details a multimodal imaging framework designed to address this critical need, enabling researchers to correlate traditional biodistribution data with sophisticated metrics of functional integration.
The limitation of tracking methodologies that rely solely on localization is particularly evident in clinical trials for conditions such as myocardial infarction and neurological disorders, where modest functional improvements have been reported despite confirmed cell delivery [114] [115]. These outcomes suggest that cells may fail to survive long-term, migrate to incorrect niches, or differentiate inappropriately. Therefore, defining efficacy requires a multifaceted approach that interrogates not only "where the cells are" but more importantly, "what the cells are doing" within the host environment. The protocols outlined herein leverage the latest advancements in molecular imaging, reporter gene technology, and label-free quantitative assessment to provide a more comprehensive evaluation of stem cell therapy efficacy, ultimately accelerating the development of more reliable and effective treatments.
Core Imaging Modalities for Tracking and Functional Assessment
A combination of imaging modalities is essential to overcome the limitations inherent in any single technology. The table below summarizes the key characteristics of primary modalities used for stem cell tracking and functional evaluation.
Table 1: Core Imaging Modalities for Stem Cell Tracking and Functional Assessment
| Modality | Principle | Key Probes/Reporters | Spatial Resolution | Tissue Penetration | Primary Tracking Application | Functional Integration Metrics |
|---|---|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | Detection of contrast agents affecting magnetic field homogeneity | SPIONs (e.g., Feridex), Gd3+, 19F compounds [15] [115] | >25 μm [115] | No limit | Cell localization, migration, and biodistribution over weeks [114] | Anatomical integration, tissue morphology, and vascularization (via contrast-enhanced MRI) |
| Positron Emission Tomography (PET) | Detection of gamma rays from radionuclide decay | 18F-FDG, 18F-FHBG, Reporter genes (e.g., HSV1-tk) [15] [116] | >1 mm [115] | No limit | Short-term cell trafficking and reporter gene expression | Cell metabolism (18F-FDG), specific gene expression/differentiation (reporter genes) [116] |
| Optical Imaging | Detection of visible or near-infrared light | Fluorescent dyes (DiR, CM-DiI), Quantum Dots, Luciferase reporter genes [15] [114] | >2 mm [115] | <1 cm (limited) [115] | High-resolution cell visualization in superficial tissues or post-mortem validation | Dynamic monitoring of cell proliferation and viability (via bioluminescence) |
| Quantitative Phase Imaging (QPI) | Label-free measurement of light phase shifts induced by cells | N/A (Label-free) [4] | Sub-micrometer | Limited to ex vivo or superficial in vivo | N/A for in vivo tracking, but excellent for ex vivo single-cell analysis | Single-cell kinetics, division patterns, dry mass, and morphology predictive of stemness [4] |
Detailed Experimental Protocols
Protocol 1: Multimodal Tracking of MSC Differentiation in Myocardial Infarction
This protocol describes a methodology for monitoring the differentiation of transplanted Mesenchymal Stem Cells (MSCs) into a cardiomyogenic lineage and the subsequent recovery of cardiac function in a rat myocardial infarction (MI) model, using a combination of PET and CT imaging [116].
Reagent Preparation
- Stem Cells: Isolate and culture Bone Marrow-derived MSCs (BMSCs) from donor rats.
- Reporter Gene Construct: Generate a lentiviral vector containing the Herpes Simplex Virus Type 1 thymidine kinase (HSV1-tk) reporter gene under the control of the cardiac-specific α-myosin heavy chain (α-MHC) promoter.
- Cell Transfection: Transduce BMSCs with the α-MHC-HSV1-tk lentiviral vector to create stable cell lines. Include a control group of non-transfected BMSCs.
- Animal Model: Induce myocardial infarction in rats via permanent ligation of the left anterior descending coronary artery. A sham-operated group should undergo the same surgical procedure without artery ligation.
Experimental Workflow
- Cell Transplantation: One week post-MI, directly inject ~1-2 million α-MHC-HSV1-tk-transfected BMSCs (in saline) into the peri-infarct border zone of the left ventricle. Include control groups (MI model with no cells, MI with non-transfected cells).
- Metabolic Imaging of Cardiac Function (18F-FDG PET):
- At multiple time points post-transplantation (e.g., days 3, 16, 30, and 45), fast animals for 4-6 hours to shift cardiac metabolism to glucose.
- Inject 18F-FDG (~3.7-7.4 MBq) intravenously via a tail vein.
- After a 45-minute uptake period under anesthesia, acquire static PET images of the thorax.
- Data Analysis: Draw regions of interest (ROIs) over the infarcted and non-infarcted myocardium. Calculate the percentage of injected dose per gram of tissue (% ID/g) to quantify glucose metabolism recovery [116].
- Reporter Gene Imaging of Cell Differentiation (18F-FHBG PET/CT):
- 24 hours after each 18F-FDG scan, inject the HSV1-tk reporter probe 9-(4-18F-fluoro-3-hydroxymethylbutyl)guanine (18F-FHBG) intravenously.
- After a 60-90 minute uptake period, acquire fused PET/CT images.
- Data Analysis: Quantify 18F-FHBG uptake (% ID/g) in the heart. An increasing signal over time indicates activation of the α-MHC promoter, serving as a surrogate metric for cardiomyogenic differentiation of the transplanted BMSCs [116].
- Validation: At the study endpoint, perform histopathological and immunohistochemical analysis of heart tissues for validation. Stain for cardiac markers (e.g., cardiac Troponin I, GATA-4) and the HSV1-tk reporter to confirm the differentiation of transplanted cells.
Diagram 1: Multimodal imaging workflow for tracking MSC differentiation and cardiac function recovery.
Protocol 2: Label-Free Functional Prediction of HSC Potency via QPI
This protocol leverages quantitative phase imaging (QPI) and machine learning to non-invasively predict the functional quality and diversity of hematopoietic stem cells (HSCs) based on their temporal kinetic behavior during ex vivo expansion [4].
Reagent and Instrument Preparation
- Stem Cells: Isolate phenotypically defined murine or human HSCs. For mouse, use CD201+CD150+CD48−KSL cells; for human, use Lin-CD34+CD38-CD45RA-CD90+CD201+ cells from cord blood.
- Culture System: Utilize a previously established single-cell ex vivo expansion culture system that maintains HSC function [4].
- Imaging System: A ptychographic QPI microscope capable of long-term, label-free, time-lapse imaging of live cells in culture plates is required.
Experimental Workflow
- Single-Cell Sorting: Sort individual HSCs into each well of a 96-well U-bottom plate containing expansion media.
- Time-Lapse QPI Acquisition:
- Place the culture plate in the QPI microscope within a controlled environmental chamber (37°C, 5% CO2).
- Acquire time-lapse images of each well every 5-15 minutes for a minimum of 36 hours and up to several days.
- Single-Cell Kinetic Feature Extraction:
- Use automated cell tracking and segmentation software to analyze the QPI image sequences for each cell.
- Extract a panel of quantitative kinetic and morphological parameters for each cell, including:
- Dry Mass: A measure of biomass.
- Division Rate/Timing: Interval between divisions (e.g., Division Gap).
- Morphology: Sphericity, length/width ratio.
- Motility: Velocity and displacement.
- Division Patterns: Frequency of normal vs. abnormal cytokinesis.
- Machine Learning and Classification:
- Perform dimensionality reduction (e.g., UMAP) on the extracted multi-parameter dataset from thousands of cell images.
- Cluster cells based on their kinetic profiles to identify distinct behavioral phenotypes.
- Correlate these kinetic clusters with functional outcomes from parallel experiments, such as in vivo repopulation capacity or maintenance of stem cell surface markers in long-term culture.
- Model Validation: The QPI-driven prediction model must be validated against gold-standard functional assays (e.g., transplantation and spleen colony-forming assays) to confirm that specific kinetic signatures are predictive of high stemness.
Diagram 2: QPI and machine learning workflow for predicting HSC functional quality.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Stem Cell Tracking and Functional Analysis
| Item Name | Function/Application | Key Characteristics | Example Use Case |
|---|---|---|---|
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Direct cell labeling for MRI tracking [15] [114] | Creates hypointense (dark) signals on T2/T2*-weighted MRI; biocompatible; allows tracking for several weeks. | Monitoring MSC biodistribution in spinal cord injury or myocardial infarction models [15] [114]. |
| Reporter Gene Systems (e.g., HSV1-tk) | Genetic cell labeling for PET or bioluminescence imaging [15] [116] | Reports on cell viability and specific gene expression; enables long-term tracking if integrated. | Monitoring cardiomyogenic differentiation via a cardiac-specific (α-MHC) promoter driving HSV1-tk expression [116]. |
| Near-Infrared (NIR) Fluorophores (e.g., DiR) | Direct cell labeling for optical imaging [15] | Reduced tissue autofluorescence and deeper tissue penetration compared to visible light fluorophores. | Short-term tracking of MSC migration to tumor sites in small animal models [15]. |
| Quantum Dots (QDs) | Direct cell labeling for multiplexed optical imaging [15] [114] | High brightness, photostability, and narrow emission spectra for simultaneous tracking of multiple cell populations. | Distinguishing different stem cell populations injected into the same animal using different QD wavelengths [15]. |
| Quantitative Phase Imaging (QPI) Microscope | Label-free analysis of single-cell kinetics [4] | Non-invasive; requires no contrast agents or genetic modification; measures biomass and morphology. | Predicting HSC functional diversity and stemness based on division patterns and dry mass during expansion [4]. |
Data Analysis and Integration for Efficacy Assessment
The final and most critical phase is the integrated analysis of data from all modalities to define a composite metric of functional integration. This involves:
Temporal Correlation of Signals: Overlaying and comparing data streams from different modalities across time points is essential. For instance, in the cardiac model, a sustained increase in the 18F-FHBG signal (indicating differentiation) should temporally correlate with or precede the improvement in 18F-FDG uptake (indicating metabolic recovery of the tissue) [116]. A dissociation between these signals—e.g., cells localize but do not differentiate or improve function—provides crucial insight into therapy failure.
Quantification and Thresholding: Establishing quantitative thresholds for success is necessary for objective assessment. This could include:
- A specific fold-increase in reporter probe uptake (e.g., 18F-FHBG) over baseline.
- A statistically significant improvement in a functional imaging parameter (e.g., myocardial 18F-FDG uptake) compared to control groups.
- A minimal percentage of transplanted cells exhibiting a specific kinetic signature (e.g., "Cluster 4" morphology in QPI) predictive of high potency.
Validation with Gold Standards: The non-invasive imaging metrics must be rigorously validated against endpoint histological and functional analyses. This includes immunohistochemistry for cell-specific markers, PCR for donor-specific genes, and physiological measurements of tissue function. This step grounds the imaging findings in biological reality and strengthens the predictive value of the defined efficacy metrics.
By adopting this comprehensive, multi-parametric framework, researchers can move beyond the simplistic question of "Are the cells there?" and begin to answer the more profound and clinically relevant question: "Are the cells functioning as intended to repair the tissue?"
Conclusion
In vivo imaging has transformed from a supportive technique to a cornerstone of stem cell therapy development, providing the critical ability to non-invasively monitor cell fate in real time. The synergy between advanced labeling strategies—from robust direct labels to sophisticated reporter genes—and a suite of complementary imaging modalities enables a multidimensional view of therapeutic cell behavior. While challenges such as long-term quantitation and ensuring biological inertness remain, the trajectory points toward increased use of multimodal approaches and smarter contrast agents, particularly nanoparticles. For researchers and clinicians, the strategic application of these imaging tools is no longer optional but essential for validating mechanisms, optimizing dosing and delivery routes, and ultimately demonstrating the safety and efficacy required for successful clinical translation. The future of stem cell therapies will be increasingly visualized, quantified, and guided by the powerful lens of molecular imaging.
References
- 1. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 2. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 3. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOoqhikqUW6GWCUUBFWmOyusLEuIpZS7Dlf4pTu2fsMyqUm-MILHl]
- 4. Quantitative phase imaging with temporal kinetics predicts ... [https://www.nature.com/articles/s41467-025-61846-3]
- 5. Quantitative, Label-Free Characterization of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4074749/]
- 6. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOooa3BdUsUHZxJ0Uou2sMiSY0scwjjuyPU8k3F7nNKFQUlR4sX_J]
- 7. Stem Cell Tracking by Nanotechnologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2869236/]
- 8. Enhancing mesenchymal stem cell survival and homing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10478247/]
- 9. Stem Cell Monitoring with a Direct or Indirect Labeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5135688/]
- 10. Future direction: molecular imaging-based stem cell research [https://link.springer.com/article/10.1007/s00259-025-07067-8]
- 11. In vivo imaging for stem cell therapy - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3072214/]
- 12. Noninvasive strategies of cell-tracking in vivo [https://www.sciencedirect.com/science/article/abs/pii/S0165993624000980]
- 13. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOopH1xEe3tqvI6LV37L0NPJsBfsTDMN0-0sF2EgdR3bTwHBphU6m]
- 14. What are the 2 methods for labelling antibodies? - tracer cro [https://www.tracercro.com/resources/blogs/what-are-the-2-methods-for-labelling-antibodies/]
- 15. In Vivo Stem Cell Imaging Principles and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10686800/]
- 16. In vivo dynamic cell tracking with long-wavelength ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961220303859]
- 17. In Vivo Tracking Techniques for Cellular Regeneration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3579215/]
- 18. Multimodality reporter gene imaging [https://www.thno.org/v08p2954.htm]
- 19. Non-invasive Reporter Gene Imaging of Cell Therapies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7264441/]
- 20. Advancements in the application of reporter gene cell lines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460214/]
- 21. In vivo genetic alteration and lineage tracing of single stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7408291/]
- 22. Lineage Tracing and Molecular Real-Time Imaging of ... [https://www.mdpi.com/2079-6374/12/9/703]
- 23. Long-term live imaging, cell identification and cell tracking ... [https://elifesciences.org/articles/107534]
- 24. Noninvasive in vivo cell tracking using molecular imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC7789123/]
- 25. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOor3wzmt5KJmcVWUtmx-l7v0dUb75McuUrnSfCCSJmvaRoD_7LfT]
- 26. Imaging Biomaterial-Tissue Interactions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5837919/]
- 27. A Comparison of the Sensitivity of Contrast-Specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9498646/]
- 28. Bio-responsive polymers for dual 31 P/ 19 F-magnetic ... [https://www.nature.com/articles/s43246-024-00623-z]
- 29. Imaging of stem cells using MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3037795/]
- 30. Clinical trials and advanced MRI techniques with stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505762/]
- 31. Tracking Transplanted Stem Cells Using Magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4564577/]
- 32. A primer on in vivo cell tracking using MRI [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1193459/full]
- 33. Superparamagnetic Iron Oxide Nanoparticles as MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3741608/]
- 34. Detection and Quantification of Magnetically Labeled Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2680943/]
- 35. Superparamagnetic iron oxide nanoparticles for MR ... [https://www.sciencedirect.com/science/article/abs/pii/S1471489214000940]
- 36. Advances in magnetic particle imaging: evaluating ... [https://www.frontiersin.org/journals/imaging/articles/10.3389/fimag.2025.1610258/full]
- 37. A responsive MRI contrast agent to monitor functional cell ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811906005751]
- 38. Stem Cell Imaging: Tools to Improve Cell Delivery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4736428/]
- 39. Comparison of Imaging Techniques for Tracking Cardiac Stem ... [https://jnm.snmjournals.org/content/48/12/1916]
- 40. Radiopharmaceuticals for PET and SPECT Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC9103893/]
- 41. Practical considerations for clinical translation of PET ... [https://www.nature.com/articles/s44303-025-00127-6]
- 42. Radiochemistry for positron emission tomography [https://www.nature.com/articles/s41467-023-36377-4]
- 43. An update on recent advances in fluorescent materials for ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03102h]
- 44. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOopM71tociW39Y_-gUW0cCMS9szwUYiVwQUFxT4FCeX41vK1gC-1]
- 45. Enhanced bioluminescence imaging of tumor cells ... [https://www.nature.com/articles/s41523-025-00795-y]
- 46. Reflect: reporting guidelines for preclinical, translational ... [https://www.nature.com/articles/s44303-025-00125-8]
- 47. Optical Imaging - Biomedical Research Imaging Center [https://www.med.unc.edu/bric/preclinical-molecular-imaging/pmi-equipment/optical-systems/]
- 48. Fluorescence-Based Mono- and Multimodal Imaging for In ... [https://www.mdpi.com/2218-273X/13/12/1787]
- 49. Multimodal Imaging-Guided Stem Cell Ocular Treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11804834/]
- 50. Assessing quantitative MRI techniques using multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289042/]
- 51. Comparison between multimodal foundation models and ... [https://www.sciencedirect.com/science/article/pii/S2211568425000968]
- 52. A Mini-Review on the Multimodal Applications of ... [https://www.sciencedirect.com/science/article/pii/S2790676025000317]
- 53. Current Status and Future Aspects of Gadolinium Oxide ... [https://www.mdpi.com/2079-4991/15/17/1340]
- 54. Generation of hTERT-immortalized human mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619327/]
- 55. Semiconducting Polymer Nanoparticles as Multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447056/]
- 56. In vivo stem cell tracking with imageable nanoparticles that ... [https://www.sciencedirect.com/science/article/abs/pii/S014296121730385X]
- 57. Stem Cell Therapies in Cardiovascular Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6203676/]
- 58. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 59. Stem cell-based therapy in cardiac repair after myocardial ... [https://www.sciencedirect.com/science/article/abs/pii/S0022282823002134]
- 60. New imaging probes to track cell fate: reporter genes in stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5665705/]
- 61. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOopGh8k8dNNSWDy0gsXty5YW2YWvxcLMkoBh1njTNxfZpYo6EWdf]
- 62. - In NMR vivo [https://www.sf.mpg.de/research/hoehn]
- 63. bioluminescence In for viable human vivo ... imaging neural stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4452629/]
- 64. Differentiating Neural Stem Cells into Neurons & Glial Cells [https://www.thermofisher.com/us/en/home/references/protocols/neurobiology/neurobiology-protocols/differentiating-neural-stem-cells-into-neurons-and-glial-cells.html]
- 65. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOopavsrEF1diqDyoc_PUExW31-6icrvm6pfGWdgh0yApVuYADro3]
- 66. Unveiling cellular communications through rapid pan- ... [https://www.nature.com/articles/s41467-025-58779-2]
- 67. Optical and MRI Multimodal Tracing of Stem Cells In Vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC10751174/]
- 68. Macrophage tracking with USPIO imaging and T2 mapping ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11589617/]
- 69. Nanoparticles for Stem Cell Tracking and the Potential ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.662406/full]
- 70. Targeting CD37 promotes macrophage-dependent ... [https://www.nature.com/articles/s41467-025-61348-2]
- 71. Quantitative Magnetic Particle Imaging Monitors the ... [https://www.thno.org/v06p0291.htm]
- 72. Counting cells in motion by quantitative real-time magnetic ... [https://www.nature.com/articles/s41598-024-54784-5]
- 73. Protocol for performing and analyzing a live-cell imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12282420/]
- 74. AIstain: Enhancing microglial phagocytosis analysis ... [https://www.sciencedirect.com/science/article/pii/S2667237525002437]
- 75. In-vitro Optimization of Nanoparticle-Cell Labeling ... [https://www.nature.com/articles/srep15400]
- 76. In Vivo MRI tracking of bone mesenchymal stem cell ... [https://www.sciencedirect.com/science/article/abs/pii/S1748013224004079]
- 77. Comparison between manual and automated methods for ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1556697/full]
- 78. Quantification of optimizing cellular uptake and excretion ... [https://www.sciencedirect.com/science/article/pii/S1748013225001914]
- 79. Cellular Uptake of Hybrid PLGA-Lipid Gadolinium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183577/]
- 80. Use of Nanoparticle Contrast Agents for Cell Tracking with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5481820/]
- 81. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOor00rAeg9iLLM6zeivpkHZc5Yo4srwtich18Pr4vKammNez6bcL]
- 82. Recent advances in bioresponsive macrocyclic gadolinium(III ... [https://pubs.rsc.org/en/content/articlehtml/2025/dt/d5dt00191a]
- 83. Editorial: Magnetic resonance imaging contrast agents [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634343/]
- 84. Next generation lineage tracing and its applications ... [https://www.nature.com/articles/s41540-025-00542-w]
- 85. The Theory and Practice of Lineage Tracing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4618107/]
- 86. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOoqd3E0H2PGvKze_b0VWZ8CcAZdWH3z-tJCknLlaaVDapc1sxTrT]
- 87. Protocol for in vivo lineage tracing of regeneration ... [https://www.sciencedirect.com/science/article/pii/S2666166725002503]
- 88. Imaging and Tracking Stem Cells: A High Content ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3960299/]
- 89. Imaging of macrophage accumulation in solid tumors with ... [https://www.nature.com/articles/s41467-025-61624-1]
- 90. Protocol Extension in 2025 [https://www.nature.com/nprot/articles?type=protocol-extension&year=2025]
- 91. Nanobiosensors for monitoring of stem-cell differentiation ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1652480/full]
- 92. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOopi_kdyA6NiVtX0mtQhTx1O48huLteUHlBL6L4nBhoZ6kY0K1s-]
- 93. A review of state-of-the-art resolution improvement ... [https://ejnmmiphys.springeropen.com/articles/10.1186/s40658-025-00724-9]
- 94. At the crossroads of techniques and contrast agents ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525000931]
- 95. Multimodal imaging in cancer detection: the role of SPIONs ... [https://pubmed.ncbi.nlm.nih.gov/40531182/]
- 96. Advances in multimodal imaging techniques in nanomedicine [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03255e]
- 97. Moving Beyond Standard Evaluations [https://jnm.snmjournals.org/content/66/1/150]
- 98. Multimodality Molecular Imaging with Combined Optical and ... [https://jnm.snmjournals.org/content/49/2/169]
- 99. New dual-purpose contrast agent revolutionizes PET and ... [https://www.news-medical.net/news/20240805/New-dual-purpose-contrast-agent-revolutionizes-PET-and-MRI-integration-for-enhanced-diagnosis-A-Research.aspx]
- 100. Overview of Cellular Therapeutics Clinical Trials: Advances ... [https://www.mdpi.com/1422-0067/26/12/5770]
- 101. CD28 signaling complexes are correlated with patient ... [https://pubmed.ncbi.nlm.nih.gov/41260903/]
- 102. Stem cells therapy molecular tracking — the special focus ... [https://journals.viamedica.pl/rpor/article/view/108578]
- 103. Non-invasive In-Vivo Imaging of Stem Cells after Transplantation in Cardiovascular Tissue [https://www.thno.org/v03p0561.htm]
- 104. Real-time quantitative control of single-molecule ... [https://www.sciencedirect.com/science/article/pii/S0006349525001092]
- 105. In-depth single molecule localization microscopy using ... [https://www.nature.com/articles/s41467-025-62198-8]
- 106. Optimizing Colocalized Cell Counting Using Automated and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11926031/]
- 107. Methodologies for Tracking Stem Cells In Vivo [https://www.jangocell.com/methodologies-tracking-stem-cells-in-vivo/?srsltid=AfmBOopIJNJvf8r6-BOCKdPownDE7OvBRmChGCagqXtJ1uDXO7O8qE1Q]
- 108. Quantitative phase imaging with temporal kinetics predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12260078/]
- 109. Beyond Bench and Bedside: Disentangling the Concept of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4293498/]
- 110. Translational research: From benchside to bedside [https://www.sciencedirect.com/science/article/abs/pii/S0020138308001101]
- 111. STEM CELL IMAGING: FROM BENCH TO BEDSIDE - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4024441/]
- 112. Clinical and Translational Science: From Bench‐Bedside to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5439613/]
- 113. From bench to bedside: translating mesenchymal stem cell ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1639439/full]
- 114. Stem cell labeling for noninvasive delivery and tracking in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3096938/]
- 115. Stem Cell Tracking Technologies for Neurological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5613625/]
- 116. In vivo imaging to monitor differentiation and therapeutic ... [https://www.nature.com/articles/s41598-017-06571-8]