iPSC Disease Modeling for Rare Genetic Disorders: From Patient Cells to Precision Therapies
This article provides a comprehensive resource for researchers and drug development professionals on utilizing induced pluripotent stem cells (iPSCs) to model rare genetic diseases.
iPSC Disease Modeling for Rare Genetic Disorders: From Patient Cells to Precision Therapies
Abstract
This article provides a comprehensive resource for researchers and drug development professionals on utilizing induced pluripotent stem cells (iPSCs) to model rare genetic diseases. It covers the foundational rationale for iPSC use, given that over 80% of rare diseases have a genetic origin and fewer than 10% have approved therapies. The content details methodological advances in reprogramming, 2D/3D differentiation, and organoid generation, illustrated with case studies across neurological, renal, and cardiovascular disciplines. It further addresses critical troubleshooting aspects, such as managing genomic instability and optimizing cell maturation, and evaluates the validation and comparative power of iPSC models against traditional methods. Finally, it discusses the integration of these models into drug discovery pipelines and their growing utility in the wake of regulatory shifts like the FDA Modernization Act 2.0.
The Imperative for iPSCs in Tackling the Rare Disease Challenge
Rare diseases, though individually uncommon, collectively represent a significant global health challenge affecting hundreds of millions of people worldwide. These conditions are characterized by their diversity, complexity, and the substantial diagnostic and therapeutic gaps that plague the rare disease community. With the recent declaration of rare diseases as a global health priority by the World Health Assembly, there is renewed impetus to address the unmet needs of this population [1]. This whitepaper examines the current landscape of rare diseases, focusing on their collective prevalence, phenotypic and genotypic diversity, and the critical shortage of effective treatments. Against this backdrop, we explore the emerging role of induced pluripotent stem cell (iPSC) technology as a transformative platform for rare disease research and therapeutic development.
The Scale and Impact of Rare Diseases
Global Prevalence and Definition
While definitions vary globally, rare diseases are universally recognized by their low prevalence, with estimates ranging from 40-50 cases per 100,000 people depending on the jurisdiction [2]. The collective burden, however, is substantial, as shown in Table 1.
Table 1: Global Rare Disease Burden and Characteristics
| Metric | Global Statistics | References |
|---|---|---|
| Total Number of Distinct Rare Diseases | 7,000 - 10,000 | [3] [4] |
| Global Prevalence | 263 - 446 million people (3.5% - 5.9% of world population) | [1] [3] [2] |
| Diseases with Genetic Origin | Approximately 80% | [3] [4] |
| Diseases with Pediatric Onset | 50% - 75% | [2] |
| Diseases with Approved Therapies | Less than 10% | [3] [4] [5] |
The recent adoption of the first-ever rare diseases resolution by the World Health Assembly marks a landmark recognition of this public health issue, urging countries to integrate rare diseases into national health planning and accelerate research and innovation [1].
Socioeconomic and Healthcare Burden
The impact of rare diseases extends far beyond prevalence statistics, creating profound challenges for patients, healthcare systems, and societies:
- Diagnostic Odyssey: Patients typically experience diagnostic delays of 5-7.6 years, consulting with an average of 8 physicians and receiving 2-3 misdiagnoses before obtaining a correct diagnosis [2]. In Europe, 25% of patients wait between 5 and 30 years from symptom onset to diagnosis [2].
- Economic Impact: Rare diseases exert a significant financial burden on healthcare systems globally, with per-patient-per-year healthcare costs up to 10 times greater than for more common diseases [3] [4]. Orphan drugs are reported to be as high as 13.8 times more expensive than conventional medications [2].
- Psychosocial Consequences: The various disabilities arising from these conditions lead to significant physical, emotional, and financial hardship for patients and families [1]. Stigma, discrimination, and social isolation are commonly reported by both patients and caregivers [2].
The Therapeutic Gap and Research Challenges
Despite affecting hundreds of millions globally, the rare disease community faces a vast therapeutic gap, with fewer than 10% of diagnosed rare diseases having suitable drug treatments [3] [4] [5]. This gap stems from multiple fundamental research challenges:
- Small Patient Populations: Limited numbers of patients for clinical studies complicate traditional research approaches and drug development pathways [6].
- Limited Biological Samples: Access to patient-derived biological materials for research is often severely restricted [6].
- Inadequate Disease Models: Many rare diseases lack physiologically relevant models that accurately recapitulate human disease pathophysiology [6].
- Economic Disincentives: The small market opportunity for each individual rare disease provides limited commercial incentive for biopharmaceutical investment [2].
The recent FDA Modernization Act 2.0, which allows therapeutics to be tested in cell-based assays without mandatory animal testing, has created new opportunities for innovative approaches to rare disease research, particularly favoring human-relevant models like iPSCs [3] [4].
iPSC-Based Disease Modeling: A Path Forward
Foundations of iPSC Technology for Rare Diseases
Induced pluripotent stem cells (iPSCs) are adult somatic cells that have been reprogrammed to a pluripotent state, capable of differentiating into virtually any cell type in the human body [7]. For rare diseases, approximately 80% of which have genetic origins, patient-derived iPSCs and their isogenic controls represent unique model systems for mechanistic studies and therapeutic development [3] [4].
Table 2: Key Research Reagent Solutions for iPSC-Based Rare Disease Modeling
| Research Reagent | Function in Rare Disease Research |
|---|---|
| Reprogramming Factors | Introduce pluripotency (e.g., via Sendai virus or mRNA) to convert patient somatic cells to iPSCs. |
| Differentiation Kits | Direct iPSCs toward specific lineages (e.g., neuronal, cardiac, renal) affected by rare diseases. |
| Gene Editing Tools | Create isogenic controls (CRISPR-Cas9) or introduce specific mutations into control iPSC lines. |
| Extracellular Matrix | Provide physiological scaffolding for 2D culture or 3D organoid formation (e.g., Matrigel). |
| Cytokines/Growth Factors | Pattern iPSC differentiation toward specific tissue fates through controlled signaling exposure. |
The utility of iPSC-based models spans multiple research applications, including disease mechanism elucidation, drug screening and toxicity studies, and the development of personalized therapeutic approaches [3] [4] [7].
Experimental Design and Workflow
A robust iPSC-based disease modeling workflow requires careful experimental design, particularly regarding the number of biological replicates needed to achieve statistically significant results. Recent empirical evidence using RNA sequencing data from Lesch-Nyhan disease models suggests that optimal results are obtained with iPSC lines from 3-4 unique individuals per group, with 2 lines per individual recommended without statistical corrections for multiple lines from the same donor [8].
The workflow begins with obtaining patient somatic cells (typically through skin biopsy or blood draw), followed by reprogramming using defined factors to generate iPSCs. These iPSCs are then expanded and characterized before being directed toward disease-relevant cell types using specific differentiation protocols. The resulting models enable various research applications, including mechanistic studies, drug screening, and personalized medicine approaches [8] [3] [4].
Applications in Specific Rare Diseases
iPSC-based models have demonstrated particular utility for studying rare diseases affecting tissues and organs that are difficult to access in patients. Notable examples include:
- Juvenile Nephronophthisis (NPH): Researchers developed the first human NPH disease models using patient-derived iPSCs and gene-edited iPSCs differentiated into kidney organoids. These models demonstrated that NPHP1-deficient cells exhibit abnormal cell proliferation, primary cilia abnormalities, and renal cyst formation - key disease phenotypes that were reversed upon NPHP1 reintroduction [3] [4].
- RDH12-associated Retinitis Pigmentosa: Retinal organoids derived from patient iPSCs carrying dominant RDH12 mutations showed reduced photoreceptor numbers, shortened photoreceptor length, and disruptions in the vitamin A pathway, replicating features of the human disease [3] [4].
- Lesch-Nyhan Disease: Transcriptomic analysis of iPSC models revealed disease-relevant changes in gene expression patterns, providing insights into underlying molecular mechanisms [8].
Integrating iPSC Models with Advanced Computational Approaches
The convergence of iPSC technology with advanced computational methods represents the next frontier in rare disease research. In silico technologies - including mechanistic models, machine learning, and digital twins - offer scalable tools for disease characterization, drug discovery, and virtual trials that complement experimental approaches [6]. These computational methods are particularly valuable for rare diseases, where limited patient numbers constrain traditional research.
This integrated approach enables a bidirectional workflow where standardized data from iPSC models parameterize computational models, and model predictions subsequently guide the next round of experimental investigation. This creates a virtuous cycle that maximizes the utility of scarce patient-derived materials and accelerates therapeutic development [6].
Addressing Diversity and Equity in Rare Disease Research
Despite technological advances, significant challenges remain in ensuring equitable representation in rare disease research. Patients from historically marginalized communities face additional barriers to diagnosis and care, and are often underrepresented in research studies [5]. This lack of diversity has implications for the generalizability of findings and the effectiveness of therapies across populations.
Recent initiatives like the Rare Disease Diversity Coalition (RDDC) are working to address these disparities through systemic change focused on diversity in research and clinical trials, improving the patient and caregiver journey, and advocating for supportive legislation [5]. The development of updated demographic categories that better capture global diversity in rare disease patient registries represents another step toward more inclusive research practices [9].
A 2025 probability-based national survey in the United States found that 8% of U.S. adults report living in a household affected by rare disease, with an additional 7% living with undiagnosed illnesses [10]. These households are more likely to adopt innovative healthcare technologies, including telehealth (63% vs. 45% in non-rare disease households) and AI tools for health information (38% vs. 21%), demonstrating their role as early adopters in the healthcare ecosystem [10].
The global burden of rare diseases represents a critical challenge and opportunity for the biomedical research community. While the therapeutic gap remains substantial, emerging technologies like iPSC-based disease models offer unprecedented opportunities to understand disease mechanisms and develop new treatments. The recent policy recognition of rare diseases as a global health priority, combined with scientific advances in stem cell biology and computational medicine, creates a fertile environment for progress.
Future directions for the field include developing more sophisticated differentiation protocols to generate mature cell types that better reflect adult disease states, improving 3D organoid systems to capture tissue-level complexity, and strengthening international collaboration to share resources and data. As these efforts advance, iPSC-based approaches are poised to play an increasingly central role in narrowing the therapeutic gap for the hundreds of millions affected by rare diseases worldwide.
Rare diseases present a formidable challenge to the global healthcare system. With an estimated 7,000–10,000 distinct rare diseases identified, their collective prevalence is substantial, affecting between 263–446 million individuals worldwide [4]. Approximately 80% of these conditions have a genetic origin, yet less than 10% have approved therapies, creating a significant therapeutic gap [4]. Traditional research models, including animal studies and immortalized cell lines, have proven insufficient for addressing these conditions due to species-specific differences, limited availability of patient biological samples, and inability to recapitulate human pathophysiology accurately [11]. The emergence of induced pluripotent stem cell (iPSC) technology has introduced a powerful platform that directly addresses these challenges through patient-specific, scalable, and physiologically relevant human disease models.
iPSCs are adult somatic cells that have been reprogrammed to a pluripotent state, capable of differentiating into virtually any cell type in the human body [12]. This breakthrough technology, first developed by Takahashi and Yamanaka in 2006, has since evolved into a sophisticated tool for disease modeling, drug discovery, and therapeutic development [12]. For rare genetic disorders specifically, iPSC-based models offer unique advantages that are transforming our approach to understanding disease mechanisms and developing effective treatments.
Core Advantages of iPSC Technology
Patient-Specificity
The genetic makeup of iPSCs mirrors that of the donor, making them exceptionally valuable for studying genetic rare diseases. Researchers can generate iPSCs directly from patients with rare genetic conditions, creating cell lines that carry the exact mutations responsible for the disease [11] [7]. This patient-specificity enables several critical applications:
Accurate Disease Modeling: iPSCs derived from patients with known genetic mutations allow researchers to study disease mechanisms in a human genetic context. For example, in a study of Lesch-Nyhan disease (caused by mutations in the HPRT1 gene), patient-derived iPSCs provided crucial insights into disease-relevant changes in gene expression [8].
Isogenic Controls: Through CRISPR/Cas9 gene editing, researchers can correct disease-causing mutations in patient-derived iPSCs to create genetically matched control lines [12] [13]. This powerful approach allows for precise comparison between diseased and corrected cells, eliminating the confounding effects of genetic background variability. This methodology has been successfully applied in disease modeling for Parkinson's disease, where the A53T SNCA mutation was corrected in patient-derived iPSCs for mechanistic studies [12].
Personalized Therapeutic Screening: Patient-specific iPSC models enable drug testing on the exact genetic background of an individual, allowing for personalized assessment of therapeutic efficacy and toxicity [7].
A significant challenge in rare disease research is the limited availability of biological samples from affected patients. iPSC technology fundamentally addresses this limitation through:
Indefinite Expansion: Once established, iPSC lines can be expanded indefinitely in culture, providing a renewable source of biological material for research [14]. This is particularly crucial for rare diseases, where patient numbers are small and primary tissue samples are extremely scarce.
High-Throughput Applications: Differentiated iPSC-derived cells can be scaled for drug discovery efforts, including high-throughput screening campaigns. These cells can be plated in 384- or 1536-well formats, imaged automatically, and analyzed using high-content imaging systems to extract rich phenotypic data at scale [14].
Biobanking: iPSCs from patients with rare genotypes/phenotypes can be stored in biobanks as a resource for genotype/phenotype correlation analyses, study of rare mutations, and development of precision medicine applications [11].
Table 1: Scalability Applications of iPSC Technology in Rare Disease Research
| Application | Scale | Utility | Example |
|---|---|---|---|
| Drug Screening | 384- to 1536-well plates | High-throughput compound testing | Identification of compounds rescuing neuronal function in neurodegenerative diseases [14] |
| Biobanking | Multiple cell lines from various patients | Resource for rare disease research | Storage of patient-specific iPSCs for genotype/phenotype studies [11] |
| Clinical Translation | GMP-manufactured cell batches | Therapeutic development | Manufacturing of clinical-grade iPSC-derived products for transplantation [15] |
Physiological Relevance
iPSC-derived models offer unprecedented physiological relevance compared to traditional in vitro systems:
Human Biology: iPSC-derived cells maintain human genotype and often demonstrate complex functional behaviors that immortalized lines cannot replicate, such as spontaneous contraction in cardiomyocytes or synaptic firing in neurons [14].
2D vs. 3D Model Systems: iPSCs can be differentiated into both two-dimensional monolayer cultures and three-dimensional organoids, each offering distinct advantages for disease modeling. While 2D cultures are cost-effective and easily manageable for initial drug assessment, 3D organoids offer a more natural environment with cell-to-cell and cell-to-extracellular matrix interactions that better mimic human organ/tissue architecture [11].
Disease-Relevant Phenotypes: iPSC-derived models successfully replicate key disease features. For instance, in Juvenile Nephronophthisis (NPH), NPHP1-deficient iPSCs exhibited abnormal cell proliferation, abnormalities in primary cilia, and renal cyst formation in iPSC-derived kidney organoids – all clinically relevant phenotypes [4]. Similarly, in a rare form of autosomal dominant retinitis pigmentosa (RDH12-AD), retinal organoids exhibited reduced photoreceptor number, shortened photoreceptor length, and disruptions in the vitamin A pathway, reflecting the disease course seen in patients [4].
Experimental Design and Methodologies
Establishing Robust iPSC-Based Rare Disease Models
Creating reliable iPSC models for rare diseases requires careful experimental design. A 2025 study on Lesch-Nyhan disease used gene expression profiles determined by RNA sequencing to empirically evaluate the impact of the number of unique individuals and replicate iPSC lines needed for robust results [8]. The findings provide crucial guidance for the field:
Optimal Line Numbers: The best results were obtained with iPSC lines from 3-4 unique individuals per group, with 2 lines per individual [8]. This approach helps account for both inter-individual genetic variability and technical reproducibility.
Technical Variance Management: The study revealed that when all lines were produced in parallel using the same methods, most variance in gene expression came from technical factors unrelated to the individual from whom the iPSC lines were prepared [8]. This highlights the importance of standardizing reprogramming and differentiation protocols.
Analytical Considerations: Results for detecting disease-relevant changes in gene expression depended on the analytical method employed, emphasizing the need for appropriate statistical approaches in experimental design [8].
iPSC Reprogramming and Differentiation Workflows
The fundamental process of creating iPSC-based disease models involves multiple critical steps, each requiring specific reagents and quality control measures:
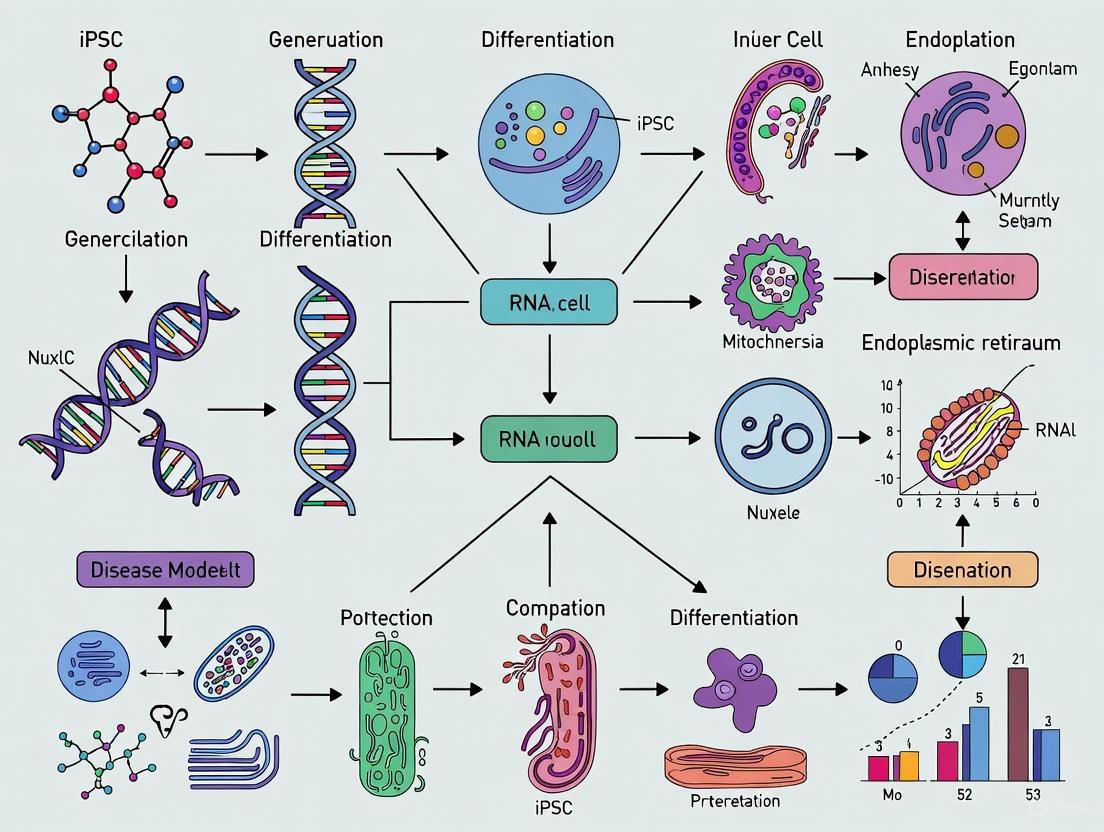
Diagram 1: iPSC Modeling Workflow
Table 2: Essential Research Reagents for iPSC-Based Rare Disease Modeling
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Dedifferentiation of somatic cells to pluripotent state | Non-integrating delivery methods (episomal plasmids, mRNA) preferred for clinical translation [12] |
| Extracellular Matrices | Laminin-521, Matrigel | Provide structural support and biochemical cues for cell growth and differentiation | Laminin-521 used in clinical-grade process development [16] |
| Differentiation Factors | Tissue-specific growth factors, small molecules | Direct lineage-specific differentiation | BMP4, activin A for germ layer specification; protocol-specific factors for target tissues [11] |
| Gene Editing Tools | CRISPR/Cas9 systems | Create isogenic controls through precise genetic modification | Enables correction of disease-causing mutations in patient-derived iPSCs [12] [13] |
| Analytical Tools | Single-cell RNA sequencing, high-content imaging | Quality control and phenotypic assessment | scRNA-seq used to demonstrate consistency of cellular outcomes [16] |
Advanced 3D Model Development
For many rare diseases, 3D organoid models provide superior physiological relevance compared to traditional 2D cultures. The general procedure for generating organoids involves:
Germ Layer Specification: iPSCs are directed toward a specific embryonic germ layer (ectoderm, mesoderm, or endoderm) using selected factors that activate cell differentiation commitment, such as WNT, BMP4, and activin A [11].
Tissue-Specific Differentiation: Cells are differentiated into the target tissue/organ through the addition of tissue-specific growth factors and small molecules [11].
3D Structure Formation: Cells are embedded in an ECM gel or aggregated in a 3D structure using scaffold-forming external biomaterials to allow self-organization [11].
This approach has been successfully applied to model rare neurological disorders, such as Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV), using dorsal root ganglia (DRG) organoids derived from patient-specific iPSCs [13]. These organoids revealed that NTRK1 mutations disrupt the balance of neuronal and glial differentiation in human DRG during development, providing crucial insights into disease mechanisms [13].
Applications in Rare Disease Research and Drug Development
Disease Mechanism Elucidation
iPSC-based models have enabled groundbreaking insights into the pathophysiology of numerous rare diseases:
Juvenile Nephronophthisis (NPH): Using patient-derived iPSCs and kidney organoids, researchers demonstrated that NPHP1 deficiency leads to abnormal cell proliferation, primary cilia abnormalities, and renal cyst formation. Importantly, reintroduction of NPHP1 expression reversed cyst formation, confirming the gene's role in disease pathogenesis and validating the model system [4].
Neurexin 1 (NRXN1)-Related Disorders: To study the influence of the same mutation in different genetic backgrounds, researchers developed "village editing" – CRISPR/Cas9 gene editing in a cell village format – generating NRXN1 knockouts in iPSC lines from 15 donors with varying polygenic risk scores for schizophrenia. This approach demonstrated that genetic background deeply influences gene expression changes in NRXN1 knockout neurons [13].
Usher Syndrome and Marfan Syndrome: Comprehensive reviews highlight how iPSC-based models have advanced understanding of these rare conditions, offering valuable insights into disease mechanisms and potential for discovering new therapies [4].
Drug Discovery and Toxicity Testing
iPSC-based models are increasingly integrated into drug development pipelines for rare diseases:
Cardiac Safety Screening: iPSC-derived cardiomyocytes are now used routinely to screen for drug-induced arrhythmia risk and have been integrated into regulatory safety initiatives like CiPA (Comprehensive in vitro Proarrhythmia Assay) [14].
Phenotypic Screening: iPSC-derived neurons from patients with Alzheimer's, Parkinson's, and ALS are used in phenotypic screens that have identified compounds capable of rescuing neuronal function in vitro [14]. Similar approaches are being applied to rare diseases.
Drug Repurposing: iPSC-derived hepatocyte-like cells have been used to model familial hypercholesterolemia, revealing that cardiac glycosides reduced ApoB secretion – identifying a potential drug repurposing opportunity [14].
The regulatory landscape is also evolving to support these applications. The FDA Modernization Act 2.0 allows therapeutics to be tested in cell-based assays without the need for animal testing for progression to clinical trials, which is likely to further drive interest in iPSC-based models for rare disease studies [4].
Current Challenges and Future Directions
Despite the considerable promise of iPSC technology, several challenges remain to be addressed:
Maturation Limitations: Many iPSC differentiation protocols yield cells with fetal-like phenotypes, which may not fully recapitulate late-onset disease aspects [14]. Developing novel technologies to precisely control the maturation of specific cell types is crucial for both drug screening and mechanistic studies [4].
Standardization and Reproducibility: Protocols for iPSC culture and differentiation are improving but still not uniform across laboratories. Efforts to benchmark electrophysiological performance or gene expression signatures are underway but not yet universal [14].
Technical Demands and Cost: iPSC models are technically demanding to create and maintain, with media, reagents, and culture time contributing to significant costs, particularly for HTS-scale assays [14] [7].
Model Complexity: While 3D organoids better recapitulate tissue architecture, they often lack proper vascularization, resulting in necrosis and apoptosis of some cells [11]. They also show considerable variation from batch to batch, limiting reproducibility [11].
Future advancements are likely to focus on enhancing model complexity through the development of assembloids (connecting organoids of different lineages), improving vascularization, and integrating immune system components. Additionally, the combination of iPSC technology with artificial intelligence and machine learning for automated colony morphology classification and differentiation outcome prediction will enhance standardization, quality control, and reproducibility in iPSC manufacturing [12].
iPSC-based model systems represent a transformative approach for rare disease research, addressing fundamental limitations of traditional models through their unique combination of patient-specificity, scalability, and physiological relevance. As the technology continues to evolve with improvements in gene editing, differentiation protocols, and analytical techniques, iPSCs are poised to accelerate our understanding of rare disease mechanisms and the development of effective treatments. For the 94% of rare diseases that currently lack approved therapies, these advances offer renewed hope for patients and researchers alike [4]. The ongoing collaboration between clinicians, geneticists, and stem cell biologists will be essential to fully realize the potential of iPSC technology in overcoming the challenges of rare disease research.
Rare diseases, often perceived as a collection of isolated medical curiosities, represent a significant and cumulative global health challenge. While individually defined by their low prevalence—affecting fewer than 5 in 10,000 people in Europe or fewer than 200,000 people in the United States—they are collectively common [17]. Recent epidemiological studies estimate that there are between 7,000 and 10,000 distinct rare diseases, cumulatively affecting 263–446 million individuals worldwide, which corresponds to a global prevalence of 3.5–6% [3]. This substantial burden is further magnified by a critical therapeutic gap; less than 10% of these diseases have approved therapies, leaving the vast majority of patients without effective treatment options [3] [17]. Moreover, rare diseases exert a significant financial strain on healthcare systems, as the per-patient-per-year healthcare cost can be up to 10 times greater than that of more common diseases [3].
The exploration of this therapeutic chasm is tightly linked to the fundamental genetic origin of these conditions. Approximately 80% of rare diseases have a genetic basis, with a majority being monogenic—caused by defects in a single gene [3] [17]. This high degree of genetic determinism, while complicating the clinical landscape, provides a clear scientific entry point for research. It creates an ideal scenario for modeling diseases in vitro, as the pathogenic trigger can often be traced to a specific, identifiable genetic variant. The discovery of induced pluripotent stem cell (iPSC) technology has therefore revolutionized the field, offering a patient-specific, scalable, and physiologically relevant preclinical model system to elucidate disease mechanisms and screen potential therapeutics [3] [18]. This whitepaper details how the genetic architecture of rare diseases makes iPSCs an unparalleled model system for accelerating research and drug development.
The Genetic Landscape of Rare Diseases
The following table summarizes the key epidemiological and genetic characteristics that define the challenge of rare diseases and highlight the rationale for iPSC-based modeling.
Table 1: Epidemiological and Genetic Landscape of Rare Diseases
| Aspect | Global Statistics | Implication for Disease Modeling |
|---|---|---|
| Total Number of Diseases | 7,000 - 10,000 distinct conditions [3] | Vast diversity requires scalable and flexible research models. |
| Cumulative Prevalence | 263 - 446 million people affected (3.5-6% global prevalence) [3] | Significant collective health impact justifies major research investment. |
| Genetic Origin | ~80% are genetic, mostly monogenic [3] [17] | Provides a direct and traceable target for mechanistic studies. |
| Therapeutic Gap | >90% of rare diseases lack an approved therapy [3] | Highlights a critical unmet medical need and a large field for drug discovery. |
| Economic Burden | Per-patient costs can be up to 10x higher than common diseases [3] | Underlines the economic incentive for developing effective treatments. |
The Imperative for Advanced Model Systems
The predominance of genetic drivers in rare diseases necessitates biological models that can accurately recapitulate human pathophysiology. Traditional approaches, including animal models and immortalized cell lines, have provided valuable insights but are often hampered by substantial limitations. Animal models may not fully replicate human disease due to anatomic, embryonic, and metabolic differences between species, leading to difficulties in translating therapeutic discoveries to clinical trials [17]. Immortalized cell lines, on the other hand, are often not an accurate reflection of primary patient cells and cannot model the developmental context of many congenital disorders [17].
The high genetic component of rare diseases creates a precise and testable hypothesis: that introducing a patient-specific mutation into a pluripotent cell capable of differentiation will result in a cellular model that manifests key aspects of the disease phenotype. This is the fundamental promise of iPSC technology. By capturing an individual's entire genomic background, including modifiers and polymorphisms, patient-derived iPSCs offer a unique system to study not only the primary genetic lesion but also the complex interplay of genetic factors that influence disease severity and presentation [17] [19]. This is particularly crucial for the nearly 50% of rare diseases that manifest in children and are a leading cause of infant mortality [17].
iPSC Technology: A Primer for Rare Disease Research
Historical Development and Core Methodology
The field of cellular reprogramming was built upon foundational work demonstrating the reversibility of cell fate. John Gurdon's seminal somatic cell nuclear transfer (SCNT) experiments in 1962 showed that a nucleus from a differentiated somatic cell could support the development of an entire organism, proving that genetic information remains intact during differentiation [18]. This concept of epigenetic reversibility was later catalyzed into a practical technology by Shinya Yamanaka and colleagues, who discovered in 2006 that the forced expression of four transcription factors—Oct4, Sox2, Klf4, and Myc (OSKM)—could reprogram mouse somatic cells into induced pluripotent stem cells [17] [18]. This breakthrough was rapidly extended to human cells in 2007 by both Yamanaka's group (using OSKM) and James Thomson's group (using OCT4, SOX2, NANOG, and LIN28) [20] [18].
The core experimental protocol for generating patient-derived iPSCs involves several key steps, which can be achieved through clinically compliant processes [20] [21]:
- Somatic Cell Isolation: Fibroblasts from skin biopsies or mononuclear cells from peripheral blood are the most common starting materials. For example, researchers at Nationwide Children's Hospital successfully used skin fibroblasts from patients with prune belly syndrome and posterior cloaca to generate iPSC lines [21].
- Reprogramming Factor Delivery: The genes encoding the reprogramming factors are introduced into the somatic cells. While early methods used integrating retroviral vectors, current best practices employ non-integrating methods such as episomal plasmids [20], Sendai virus, or mRNA transfection to minimize the risk of genomic alterations.
- Pluripotency Induction and Culture: Following transduction, cells are cultured under conditions that promote the emergence and expansion of iPSC colonies, which are identified by their characteristic compact, embryonic stem cell-like morphology.
- Validation and Characterization: Established clones are rigorously tested for pluripotency. Key assays include:
- Immunocytochemistry for pluripotency-associated proteins (e.g., OCT4, SOX2, NANOG) [21].
- Transcriptomic analysis to confirm the activation of pluripotency networks.
- In vitro differentiation into cells of all three germ layers (ectoderm, mesoderm, and endoderm) [21].
- Karyotyping to ensure genomic integrity [21].
Key Research Reagents and Tools for iPSC Modeling
The standardized workflow for iPSC generation and disease modeling relies on a suite of essential reagents and tools, as detailed below.
Table 2: Essential Research Reagent Toolkit for iPSC-Based Rare Disease Modeling
| Reagent/Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| Reprogramming Vectors | Episomal plasmids (e.g., pEB-Tg), Sendai virus, mRNA cocktails [20] | Non-integrating delivery of OSKM/L transcription factors to initiate reprogramming. |
| Cell Culture Media | Priming medium (IMDM/Ham's F12 base), essential supplements (Lipids, BSA, ITS-X) [20] | Supports expansion of somatic cells (e.g., CD34+ cells) and the reprogramming process. |
| Cytokines & Growth Factors | rhSCF, rhFlt3-ligand, rhThrombopoietin, IL-3 [20] | Enhances reprogramming efficiency when used during somatic cell expansion. |
| Pluripotency Validation Antibodies | Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA-4 | Immunocytochemical confirmation of successful reprogramming to a pluripotent state. |
| Genome Editing Tools | CRISPR/Cas9 systems (e.g., SpCas9), HDR donors, sgRNAs [17] [19] | Creation of isogenic controls via precise genetic correction or introduction of mutations. |
| Lineage-Specific Differentiation Kits | Commercially available kits for neurons, cardiomyocytes, hepatocytes, etc. | Directs iPSCs toward disease-relevant cell types for phenotypic analysis. |
The Strategic Fit: Genetic Rare Diseases and iPSC Models
Unprecedented Access to Affected Cell Types
A paramount challenge in researching many rare genetic diseases is the inability to safely access and study the affected human tissues, such as neurons, cardiomyocytes, or specific renal cell types. iPSC technology directly overcomes this barrier. By differentiating patient-derived iPSCs into the relevant affected cell types, researchers can generate an unlimited supply of living human cells that carry the disease-causing mutation for in-depth analysis [17]. For instance, studies on Juvenile Nephronophthisis (NPH), a genetic kidney disease, have utilized patient-derived iPSCs differentiated into kidney organoids. These organoids successfully recapitulated disease-specific phenotypes, including abnormal cell proliferation and renal cyst formation, providing a novel human model for mechanistic studies [3]. Similarly, iPSC-derived retinal organoids have been used to model a rare form of autosomal dominant retinitis pigmentosa, revealing a reduction in photoreceptor number and disrupted retinol biosynthesis over time [3].
Isogenic Controls and the Power of CRISPR Gene Editing
The combination of iPSC technology with CRISPR/Cas9 genome editing represents a particularly powerful approach for rare disease research. A central challenge in interpreting disease phenotypes in patient-derived cells is controlling for the immense genetic variability between human individuals. To address this, researchers can use CRISPR/Cas9 to correct the disease-causing mutation in a patient-derived iPSC line, thereby generating an isogenic control line that is genetically identical except for the pathogenic variant [3] [19]. The reverse is also possible: introducing a specific mutation into a healthy control iPSC line.
This workflow allows for ultra-precise causal inference. Any phenotypic differences observed between the diseased and the corrected isogenic control lines can be confidently attributed to the specific genetic mutation under investigation, as the confounding effect of background genetic variation is eliminated. For example, in the NPH kidney organoid model, the reintroduction of the corrected NPHP1 gene was shown to reverse cyst formation, directly demonstrating the gene's role in the pathological phenotype [3]. This pairing of iPSCs and CRISPR provides a level of experimental control that is unattainable with patient biopsies or animal models.
From 2D Cultures to 3D Organoid Systems
The initial application of iPSCs in disease modeling primarily involved two-dimensional (2D) monocultures. While valuable, these systems lack the cellular complexity and tissue-level architecture of human organs. The field has since evolved to develop three-dimensional (3D) organoids, which are self-organizing structures that mimic the multicellular composition and spatial organization of native tissues [17] [18].
The following diagram illustrates the integrated workflow from patient cell to 2D and 3D disease models, highlighting key steps and technology integrations.
Organoids have been successfully generated for a wide range of tissues, including the cerebrum, retina, inner ear, stomach, liver, and kidney [17]. For rare diseases, these 3D models offer a more physiologically relevant context to study complex pathological processes like cyst formation in kidney diseases, photoreceptor degeneration in retinal diseases, and interneuron migration defects in neurodevelopmental disorders [3] [17]. The fusion of organoids modeling different brain regions has even enabled the study of interneuron migration defects in Timothy syndrome, a rare neurodevelopmental disorder, providing insights with broader implications for autism spectrum disorder [17].
Applications in Drug Discovery and Development
The therapeutic deficit in rare diseases creates an urgent need for efficient drug discovery pipelines. iPSC-derived disease models are increasingly being deployed in high-throughput screening (HTS) platforms to identify novel therapeutic compounds. These human cell-based assays provide a more physiologically relevant and predictive system compared to traditional immortalized cell lines or animal models [18]. Furthermore, the FDA Modernization Act 2.0, which now allows cell-based assays to be used for investigational new drug applications without mandatory animal testing, is likely to drive further interest in iPSC-based models for rare disease drug development [3].
Beyond small-molecule screening, iPSCs also form the foundation for a new generation of cell replacement therapies. For rare diseases characterized by specific cellular loss or dysfunction, such as certain forms of blindness or muscular degeneration, iPSCs can be differentiated in vitro into the required cell type and then transplanted back into the patient (autologous therapy) or a matched recipient (allogeneic therapy) [3] [17]. While this application faces challenges related to safety, manufacturing, and efficacy, early-stage clinical trials, such as those using iPSC-derived retinal pigment epithelium for macular degeneration, provide hope for the future of regenerative medicine for rare disorders [17].
The convergence of two key facts—that approximately 80% of rare diseases are genetic in origin, and that human iPSCs can be differentiated into virtually any affected cell type—has created an unparalleled synergy for biomedical research. iPSC-based models directly address the core challenges of rare disease research: the inaccessibility of human tissues, the lack of relevant animal models, and the critical need for patient-specific therapeutic strategies. By providing a scalable, patient-derived, and genetically tractable platform, iPSC technology has moved rare disease research from the periphery to the forefront of precision medicine. As differentiation protocols become more sophisticated, genome editing more precise, and high-throughput screening more automated, the role of iPSCs will only expand, accelerating the path from genetic understanding to effective therapies for the millions of patients affected by these conditions.
Rare genetic diseases collectively affect an estimated 263–446 million people worldwide, yet approximately 94% of these conditions lack approved therapies, creating a significant unmet medical need. Traditional research approaches have been hampered by two fundamental constraints: the scarcity of patient samples and the poor predictive validity of animal models that often fail to recapitulate human disease pathophysiology. This whitepaper examines how induced pluripotent stem cell (iPSC) technology is revolutionizing rare disease research by overcoming these historical hurdles. We present a comprehensive technical framework encompassing optimized study designs, advanced differentiation protocols, and integrated computational approaches that enable robust disease modeling and drug discovery. The validated methodologies and experimental workflows detailed herein provide researchers with a strategic roadmap for advancing therapeutic development for rare genetic disorders.
Rare diseases present a formidable research challenge due to their low individual prevalence, genetic heterogeneity, and limited availability of biological samples. With 80% having a genetic origin and less than 10% having approved therapies, these conditions represent a significant frontier in biomedical science [4] [3]. Traditional research paradigms relying on animal models have proven inadequate for many rare diseases due to fundamental species-specific differences in physiology and genetics that limit their translational relevance [22]. The emergence of iPSC technology has initiated a paradigm shift in rare disease research, enabling the generation of patient-specific cellular models that faithfully recapitulate human disease mechanisms.
Induced pluripotent stem cells, first developed by Takahashi and Yamanaka in 2006, allow for the reprogramming of adult somatic cells into a pluripotent state capable of differentiating into virtually any cell type [12]. This breakthrough has created unprecedented opportunities for studying rare genetic disorders in human cells, facilitating both mechanistic studies and drug discovery efforts. The subsequent refinement of iPSC technologies, including non-integrating reprogramming methods, CRISPR-Cas9 gene editing, and advanced differentiation protocols, has further enhanced their utility for modeling rare diseases [12] [23]. This whitepaper provides a comprehensive technical guide to leveraging iPSC-based systems to overcome the traditional bottlenecks in rare disease research.
Establishing Robust iPSC Study Designs for Rare Diseases
Determining Optimal Experimental Scale
A critical consideration in iPSC-based rare disease research is determining the appropriate number of cell lines and donors required to generate statistically robust and reproducible results. Empirical studies using Lesch-Nyhan disease as a model have provided valuable insights into optimal study design, revealing that best results were obtained with iPSC lines from 3-4 unique individuals per group, with 2 lines per individual [24] [8]. This finding challenges earlier recommendations that advocated for studying a single iPSC line from at least 4 unrelated individuals and demonstrates that technical variance can outweigh inter-individual variance when standardized protocols are implemented.
For diseases with particularly heterogeneous presentations or genetic backgrounds, larger sample sizes may be necessary. A groundbreaking study on sporadic amyotrophic lateral sclerosis (ALS) demonstrated the power of large-scale approaches by establishing an iPSC library from 100 patients, enabling population-wide phenotypic screening and identification of therapeutic candidates effective across diverse genetic backgrounds [25]. This scale represents a significant advance beyond traditional rare disease studies, which typically included only 1-3 unique cases, often with just 1-2 sublines per case [24].
Table 1: Recommended iPSC Line Numbers for Rare Disease Studies
| Study Type | Recommended Unique Donors | Recommended Lines Per Donor | Key Considerations |
|---|---|---|---|
| Proof-of-Concept | 3-4 | 2 | Balance statistical power with practical constraints [24] |
| Population-Based Screening | 10+ | 1-2 | Capture clinical and genetic heterogeneity [25] |
| Drug Discovery | 5-8 | 2 | Identify compounds effective across multiple genetic backgrounds [25] |
| Mechanistic Studies | 3-4 | 2-3 | Control for technical variability while maintaining biological relevance [24] |
Addressing Technical Variability
A key finding from optimized iPSC studies is that when all lines are produced in parallel using the same methods, most variance in gene expression profiles comes from technical factors unrelated to the individual from whom the iPSC lines were prepared [24] [8]. This highlights the critical importance of standardizing reprogramming, differentiation, and analytical protocols across all samples in a study. Implementing automated robotics platforms for reprogramming and differentiation can significantly enhance uniformity and reduce batch effects, as demonstrated in the large-scale ALS study where fibroblasts were reprogrammed with non-integrating episomal vectors using an automated system [25].
Statistical approaches also play a crucial role in managing technical variability. Studies have shown that results for detecting disease-relevant changes in gene expression depend on the analytical method employed and whether statistical procedures are used to address multiple iPSC lines from the same individual [24]. Mixed-effects models that account for the nested structure of the data (multiple lines per donor) often provide the most appropriate analytical framework for iPSC studies.
Advanced iPSC Modeling Platforms and Methodologies
Two-Dimensional versus Three-Dimensional Modeling Systems
iPSC-based modeling platforms have evolved from simple two-dimensional (2D) monocultures to complex three-dimensional (3D) organoid systems that better recapitulate tissue architecture and cellular interactions. Both approaches offer distinct advantages and are suited to different research applications.
Table 2: Comparison of 2D and 3D iPSC-Based Modeling Systems
| Characteristic | 2D Models | 3D Organoid Models |
|---|---|---|
| Throughput | High-throughput screening compatible [23] | Medium-throughput, improving with automation [22] |
| Complexity | Reduced system, minimal cell-cell interactions | Recapitulates tissue architecture, cellular heterogeneity [4] |
| Differentiation Efficiency | Typically high, homogeneous | Variable between organoids, protocol-dependent |
| Physiological Relevance | Limited tissue context | Enhanced; exhibits functional tissue units [22] |
| Applications | Initial drug screening, electrophysiology, mechanistic studies [23] | Disease modeling requiring tissue context, developmental studies [4] |
The selection between 2D and 3D systems should be guided by research objectives. For high-throughput drug screening or detailed electrophysiological studies, 2D models offer practical advantages. For investigating diseases with complex tissue pathology or developmental origins, 3D organoids provide superior physiological relevance. Recent advances in organoid technology have enabled the generation of kidney organoids to model Juvenile Nephronophthisis [4] [3] and retinal organoids to study inherited retinitis pigmentosa [4] [3], demonstrating the utility of these systems for rare disease research.
Integrating Gene Editing for Isogenic Controls
CRISPR-Cas9 genome editing has become an essential tool in iPSC-based disease modeling, enabling the creation of isogenic control lines that are genetically identical to patient-derived iPSCs except for the disease-causing mutation [12] [23]. This approach powerfully controls for individual genetic background effects, allowing researchers to confidently attribute observed phenotypes to specific mutations. Two primary strategies are employed:
- Disease Correction: Repairing the disease-causing mutation in patient-derived iPSCs to generate genetically matched controls [12]
- Disease Introduction: Introducing specific mutations into healthy control iPSCs to establish causal relationships between genotypes and phenotypes [23]
The generation of isogenic controls has proven particularly valuable for studying rare diseases where access to multiple patients with identical mutations is limited. For example, in Parkinson's disease research, CRISPR has been used to correct the A53T SNCA mutation in patient-derived iPSCs, creating isogenic lines that enabled clear dissection of disease mechanisms [12]. Similarly, gene editing has been employed to investigate Emery-Dreifuss muscular dystrophy type 1 (EDMD1) by introducing EMD mutations into control lines [23].
Technical Workflows for iPSC-Based Disease Modeling
iPSC Generation and Quality Control Workflow
Diagram 1: iPSC Line Generation and Validation Workflow
The initial generation and validation of iPSC lines represents a critical foundation for reliable disease modeling. Best practices include:
Reprogramming Method Selection: Use non-integrating methods such as episomal plasmids, Sendai virus vectors, or synthetic mRNAs to avoid insertional mutagenesis and ensure clinical translatability [12]. The large-scale ALS study utilized non-integrating episomal vectors reprogrammed using an automated robotics platform to maximize output and uniformity [25].
Comprehensive Pluripotency Assessment: Employ multiple validation methods including immunostaining for pluripotency markers (SSEA3, SSEA4, TRA1-60, TRA1-81, NANOG), gene expression profiling of pluripotency genes, and PluriTest pluripotency scores derived from RNA sequencing data [24].
Genomic Integrity Monitoring: Perform karyotype analysis of a minimum of 20 metaphase cells at 400 band resolution to exclude relevant abnormalities, and conduct regular monitoring for genomic mutations that may arise during culture [24].
Trilineage Differentiation Potential: Verify differentiation capacity using established protocols such as the STEMdiff Trilineage Differentiation Kit, with immunostaining for ectoderm (PAX6, NESTIN), endoderm (SOX17, FOXA2), and mesoderm (brachyury, NCAM) markers [24].
Mutation Confirmation: Confirm the presence of disease-causing mutations through RT-PCR and visualization in RNA sequencing read alignments using tools such as the Integrative Genomics Viewer [24].
Directed Differentiation and Phenotypic Screening Pipeline
Diagram 2: Differentiation and Phenotypic Screening Pipeline
The differentiation of iPSCs into disease-relevant cell types followed by comprehensive phenotyping represents the core of iPSC-based disease modeling. Key technical considerations include:
Protocol Optimization: Adapt established differentiation protocols to maximize purity and maturation. The ALS study utilized a five-stage protocol adapted from established spinal motor neuron differentiation methods with extensively optimized maturation and screening conditions capable of discriminating between healthy control and diseased motor neurons [25]. This protocol generated cultures with 92.44% ± 1.66% motor neurons, demonstrating the high purity achievable with optimized methods.
Longitudinal Live-Cell Imaging: Implement automated live-cell imaging systems to monitor cell health and degeneration over time. The ALS study developed a robust pipeline using daily live-cell imaging with a virally delivered non-integrating motor neuron-specific reporter (HB9-turbo) to quantitatively assess motor neuron survival and neurite degeneration [25]. This approach enabled the identification of significant survival deficits in patient-derived neurons that correlated with donor survival.
Multi-Omics Profiling: Integrate transcriptomic, epigenomic, and proteomic analyses to comprehensively characterize molecular phenotypes. RNA sequencing provides a wealth of information regarding the condition of the cells and has standardized metrics for quality control [24]. Studies should target sufficient sequencing depth (e.g., 50 million paired-end reads) and implement strategies to mitigate technical batch effects by processing all samples in a single batch when possible [24].
Functional Validation: Include electrophysiological assessments, calcium imaging, or other functional assays appropriate to the cell type being studied. In the ALS model, pharmacological testing with riluzole not only rescued motor neuron survival but also reversed electrophysiological abnormalities, demonstrating functional restoration [25].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for iPSC-Based Rare Disease Modeling
| Category | Specific Tools | Application | Technical Notes |
|---|---|---|---|
| Reprogramming Systems | Episomal plasmids, Sendai virus vectors, synthetic mRNAs [12] | Footprint-free iPSC generation | Non-integrating methods preferred for clinical translation |
| Gene Editing Tools | CRISPR-Cas9 systems [12] [23] | Isogenic control generation, mutation correction | Enables causal relationship establishment between genotype and phenotype |
| Differentiation Kits | STEMdiff Trilineage Differentiation Kit [24] | Pluripotency validation, directed differentiation | Standardized protocols enhance reproducibility |
| Quality Control Assays | Karyotyping, immunostaining, RNA sequencing [24] | Line validation, pluripotency confirmation | Regular genomic integrity monitoring essential |
| Phenotyping Platforms | Live-cell imaging systems, electrophysiology platforms, multi-omics technologies [25] | Disease phenotype characterization | Longitudinal assessment captures progressive phenotypes |
| Analytical Tools | RNAseq analysis pipelines, variant interpretation algorithms [24] [6] | Data integration, pathogenicity prediction | Computational methods enhance diagnostic accuracy |
Integrated Computational-Experimental Approaches
The integration of in silico technologies with iPSC-based experimental models represents a powerful frontier in rare disease research. Computational approaches can enhance the design and interpretation of iPSC studies through several key applications:
Variant Interpretation: AI-enhanced pipelines leverage whole-genome and exome sequencing combined with phenotype extraction from electronic health records to improve diagnostic accuracy for rare diseases [6]. Tools such as REVEL, MutPred, and SpliceAI provide scalable assessment of variant pathogenicity, though performance on ultra-rare variants remains challenging [6].
Drug Repurposing: Network-based algorithms and virtual screening platforms can identify potential therapeutic candidates from existing compound libraries, significantly accelerating drug discovery for rare diseases [6]. This approach is particularly valuable given that approximately 94% of rare diseases lack approved treatments [3].
Clinical Trial Simulation: Pharmacokinetic models and virtual trial platforms help optimize clinical trial designs for small patient populations, addressing a fundamental challenge in rare disease therapeutic development [6]. These approaches support model-informed drug development and facilitate regulatory submissions.
The convergence of iPSC-based experimental models with in silico technologies creates a powerful framework for rare disease research, enabling more efficient use of limited patient-derived materials and enhancing the predictive validity of preclinical studies.
iPSC-based disease modeling has fundamentally transformed the research landscape for rare genetic disorders, providing solutions to the historical challenges of sample scarcity and inadequate animal models. Through optimized study designs incorporating 3-4 unique donors with 2 lines per individual, advanced differentiation protocols generating highly pure cell populations, and integration of gene editing for isogenic controls, researchers can now generate robust, reproducible disease models that faithfully recapitulate human pathophysiology. The convergence of these experimental approaches with computational technologies and the implementation of large-scale iPSC libraries enables comprehensive disease modeling and therapeutic discovery even for ultra-rare conditions. As these technologies continue to evolve, they promise to accelerate the development of effective treatments for the millions of patients affected by rare genetic diseases worldwide.
Building Better Models: From Somatic Cell to Complex Organoid
The foundation of robust induced pluripotent stem cell (iPSC)-based disease modeling lies in the selection of an appropriate somatic cell source for reprogramming. This choice directly influences reprogramming efficiency, the quality of the resulting iPSC lines, and their subsequent applicability in mechanistic studies and drug discovery [26]. For research into rare genetic disorders, where patient samples are often scarce and precious, this decision is paramount. This technical guide provides an in-depth comparison of three primary somatic cell sources: dermal fibroblasts, peripheral blood mononuclear cells (PBMCs), and urinary epithelial cells. We evaluate these sources within the specific context of building reproducible and clinically relevant in vitro models for rare diseases, focusing on practical methodologies, quantitative performance metrics, and integration into a scalable research pipeline.
The initial step in iPSC generation is the isolation of somatic cells from a donor. The chosen cell source impacts the reprogramming trajectory, the epigenetic landscape of the iPSCs, and the overall experimental timeline [26] [27]. Below, we detail the three most common starting materials.
Dermal Fibroblasts: Historically the first cell type used for iPSC generation, fibroblasts are typically obtained via skin punch biopsy [26]. This method provides a high yield of genomically stable cells that can be readily expanded and banked, making them a reliable source [26] [27]. However, the collection procedure is invasive, requires medical personnel, and may result in minor patient discomfort or scarring.
Peripheral Blood Mononuclear Cells (PBMCs): PBMCs, isolated from whole blood samples, offer a less invasive alternative to skin biopsy [26]. Blood collection is a routine clinical procedure, allowing for easier serial sampling from the same donor. PBMCs demonstrate comparable reprogramming efficiency to fibroblasts and are increasingly favored in translational studies [26] [28]. A key consideration is the need for stimulation to activate proliferation in certain blood cell populations before reprogramming can be initiated.
Urinary Epithelial Cells: Cells isolated from urine samples, including renal epithelial cells and urine-derived stem cells (USCs), represent a completely non-invasive, patient-friendly, and easily repeatable method of sample acquisition [26] [29]. Urine-derived cells can be collected without any clinical procedure, facilitating the generation of multiple iPSC lines from the same donor within a short timeframe [26] [29]. Notably, due to their epithelial origin, these cells reprogram more efficiently and rapidly than fibroblasts, as the process eliminates the need for a mesenchymal-to-epithelial transition (MET) [29]. One study reported a transduction rate of 80% and the emergence of distinct iPSC colonies expressing pluripotency markers within 7 days, compared to 28 days for some mesenchymal cell-derived lines [29].
Table 1: Comparative Analysis of Somatic Cell Sources for iPSC Generation
| Parameter | Dermal Fibroblasts | Peripheral Blood Mononuclear Cells (PBMCs) | Urinary Epithelial Cells |
|---|---|---|---|
| Collection Method | Skin punch biopsy [26] | Venipuncture (blood draw) [26] | Non-invasive urine collection [26] [29] |
| Invasiveness | Invasive | Minimally invasive | Non-invasive |
| Reprogramming Efficiency | Variable, can be low [26] | Comparable to fibroblasts [26] | High; more efficient and rapid than fibroblasts [29] |
| Key Advantages | High genomic stability, reliable, well-established protocols [26] [27] | Minimally invasive collection, accessible, suitable for serial sampling [26] | Completely non-invasive, high patient compliance, rapid reprogramming, no MET required [26] [29] |
| Key Limitations | Invasive collection, potential for scarring, requires clinical personnel for collection [26] | Requires stimulation for some cell types, finite expansion potential ex vivo [28] | Lower initial cell yield, requires optimization for consistent culture [29] |
| Ideal Use Case | Foundational research, biobanking, when maximum genomic stability is prioritized | Large-scale cohort studies, longitudinal monitoring, hematological disorders | Pediatric studies, fragile patients, serial sampling, urological and renal disease modeling |
Experimental Protocols for Cell Isolation and Reprogramming
Isolation and Culture of Primary Cells
Dermal Fibroblasts: A skin punch biopsy (3-4 mm) is cleaned to remove adipose tissue and minced into ~1 mm³ pieces. Explants are placed on a culture dish and maintained in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10-20% Fetal Bovine Serum (FBS) and 1% penicillin/streptomycin. Fibroblasts migrate from the explants over 1-3 weeks and are expanded through serial passaging using trypsin/EDTA [26] [27].
Peripheral Blood Mononuclear Cells (PBMCs): Whole blood is collected in anticoagulant tubes (e.g., EDTA or heparin). PBMCs are isolated via density-gradient centrifugation using Ficoll-Paque. The mononuclear cell layer is carefully extracted, washed, and resuspended in a suitable medium, such as RPMI-1640 with 10% FBS. For reprogramming, cells may be stimulated with cytokines (e.g., SCF, IL-3, IL-6) or mitogens to promote proliferation [26] [28].
Urinary Epithelial Cells / Urine-Derived Stem Cells (USCs): A mid-stream urine sample (50-200 ml) is collected in a sterile container. Cells are collected by centrifugation and resuspended in a specialized culture medium, such as Keratinocyte Serum-Free Medium (KSFM) or REGM, supplemented with growth factors (e.g., EGF, BPE). The cell pellet is resuspended and plated. Medium is changed periodically to selectively favor the growth of USCs or epithelial cells over contaminating cells [29]. The isolated cells exhibit high proliferative capacity and can be expanded for subsequent reprogramming.
Reprogramming to Pluripotency
Reprogramming involves resetting the epigenetic and transcriptional state of a somatic cell to a pluripotent state, typically via the introduction of key transcription factors. The original Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) remain a standard combination [26] [27]. The delivery method is critical for the safety and quality of the resulting iPSCs.
Table 2: Common Reprogramming Methods for iPSC Generation
| Method | Mechanism | Advantages | Disadvantages | Suitability for Rare Disease Modeling |
|---|---|---|---|---|
| Retroviral/Lentiviral Vectors | Genomic integration of transgenes [26] [27] | High efficiency, robust [27] | Risk of insertional mutagenesis, transgene reactivation [26] [27] | Lower suitability due to safety concerns for future therapies; useful for basic research [26] |
| Sendai Virus | RNA virus-based, non-integrating, replication-incompetent [26] [27] | High efficiency, non-integrating, can be cleared from cells [27] | Requires diligence to confirm viral clearance, biosafety level considerations [27] [28] | High suitability; widely used for generating clinical-grade iPSCs [28] |
| Episomal Vectors | Non-integrating plasmid DNA with Epstein-Barr virus elements [27] | Non-integrating, cost-effective [27] | Lower reprogramming efficiency, requires daily transfection for some protocols [27] | Good suitability; balance of safety and accessibility [26] [29] |
| Synthetic mRNA | Direct delivery of reprogramming factor mRNAs [28] | Non-integrating, high efficiency, no vector to clear [28] | Can trigger innate immune response, requires multiple transfections [28] | Excellent suitability; emerging as a leading method for footprint-free iPSCs [28] |
Emerging Protocol: Synthetic RNA Reprogramming of PBMCs A recent advanced protocol demonstrates the generation of iPSCs from PBMCs using synthetic RNA [28]. The process involves mixing the PBMC suspension, reprogramming medium (e.g., StemFit AK03N without bFGF), synthetic RNAs encoding the reprogramming factors (e.g., StemRNA 3rd Gen Reprogramming Kit), a transfection reagent, and iMatrix-511, then seeding them together in a single step. This approach allows RNA delivery from the entire cell surface, enhancing efficiency. Co-transfection with MDM4 mRNA, a suppressor of p53 function, has been shown to significantly boost reprogramming efficiency in PBMCs by mitigating stress-induced p53 activation [28]. iPSC-like colonies typically emerge around 14 days post-transfection and can be picked and expanded under standard feeder-free conditions.
The Scientist's Toolkit: Essential Reagents for iPSC Workflows
Table 3: Key Research Reagent Solutions for iPSC Generation and Culture
| Reagent / Kit Name | Function | Application Context |
|---|---|---|
| StemRNA 3rd Gen Reprogramming Kit (REPROCELL) | Synthetic mRNAs for OCT4, SOX2, KLF4, c-MYC, LIN28, and miR-302/367 cluster for footprint-free reprogramming [28] | Primary reprogramming of fibroblasts and PBMCs [28] |
| iMatrix-511 (Laminin-511 E8 fragment) | Recombinant human protein substrate for feeder-free culture; supports iPSC attachment, survival, and self-renewal [28] | Coating culture vessels for both reprogramming and maintenance of established iPSCs [28] |
| StemFit AK03N / Essential 8 (E8) Medium | Chemically defined, xeno-free medium formulations optimized for iPSC growth; contain essential growth factors like FGF2 and TGF-β/Activin A [26] [28] | Maintenance of pluripotency during routine culture and in some reprogramming protocols [26] |
| Yamanaka Factor Lentivirus / Sendai Virus | Viral particles for delivering OCT4, SOX2, KLF4, and c-MYC to somatic cells. | Standard, high-efficiency reprogramming of various somatic cell types. |
| mTeSR1 / mTeSR Plus | Chemically defined, serum-free media widely used for the maintenance of human iPSCs in feeder-free conditions. | Routine culture and expansion of established iPSC lines. |
Quality Control and Characterization of Generated iPSCs
Rigorous quality control is imperative to confirm the successful generation of high-quality iPSCs, especially for modeling rare diseases where phenotypic accuracy is crucial.
- Pluripotency Marker Analysis: Expression of canonical pluripotency-associated transcription factors and surface antigens (e.g., OCT4, SOX2, NANOG, TRA-1-60, SSEA-4) must be confirmed. This is typically done via immunocytochemistry, flow cytometry, or PCR-based assays [26].
- Genomic Integrity Assessment: Reprogramming can introduce chromosomal abnormalities or mutations. Karyotyping and whole-genome sequencing should be performed to ensure genomic integrity [26] [30]. One study noted that iPSCs maintain donor-specific epigenetic patterns, and while the relationship between genetic and epigenetic variation is strongest in iPSCs, epigenetic variation increases upon differentiation [30].
- Functional Pluripotency Assay: The gold standard is in vivo teratoma formation in immunodeficient mice, where iPSCs should form differentiated tissues from all three germ layers (ectoderm, mesoderm, endoderm). A more practical in vitro alternative is directed differentiation into representatives of the three germ layers, followed by analysis of lineage-specific markers [26].
The selection of a somatic cell source for iPSC generation is a strategic decision that balances practical collection logistics, reprogramming efficiency, and the specific requirements of the rare disease under investigation. Dermal fibroblasts remain a robust, genomically stable option. PBMCs offer a minimally invasive path suitable for large-scale studies. Urinary epithelial cells stand out for their completely non-invasive collection and high reprogramming efficiency, making them ideal for vulnerable patient populations and longitudinal studies. As reprogramming technologies, particularly non-integrating methods like synthetic mRNA, continue to advance, the barrier to generating high-fidelity iPSC models from even the most accessible cell sources will continue to diminish. This progress promises to accelerate the use of patient-specific iPSCs in elucidating the pathogenesis of rare genetic disorders and developing novel therapeutic strategies.
Appendix: Workflow and Signaling Diagrams
IPSC Generation Workflow: This diagram illustrates the workflow for generating iPSC-based disease models from three patient cell sources.
MET Bypass in Reprogramming: This diagram shows the key difference in reprogramming mesenchymal versus epithelial cells, highlighting the MET bypass that makes urinary cells more efficient. MET = Mesenchymal-to-Epithelial Transition.
The advent of induced pluripotent stem cell (iPSC) technology has revolutionized biomedical research, offering unprecedented opportunities for disease modeling, drug screening, and regenerative medicine. For rare genetic disorders research, where patient samples are scarce and disease mechanisms are often poorly understood, iPSCs provide a uniquely powerful platform for generating patient-specific cellular models [4]. The foundation of this technology rests on reprogramming somatic cells to a pluripotent state by reactivating endogenous transcriptional networks governing self-renewal and differentiation potential [18].
A critical consideration in iPSC generation is the choice of reprogramming method, particularly regarding genomic integration of exogenous genetic material. Early approaches utilizing integrating viral vectors, while efficient, carried risks of insertional mutagenesis and altered cellular behavior, posing significant concerns for both basic research and clinical applications [26] [31]. Consequently, integration-free methods have been developed to mitigate these risks while maintaining high reprogramming efficiency.
This technical guide provides an in-depth evaluation of two leading integration-free reprogramming methods—episomal vectors and Sendai virus—within the context of iPSC disease modeling for rare genetic disorders. We examine their molecular mechanisms, practical implementation, and comparative performance characteristics to inform researchers and drug development professionals in selecting appropriate reprogramming strategies for their specific research objectives.
Molecular Mechanisms of Integration-Free Reprogramming
Somatic cell reprogramming to pluripotency involves profound reorganization of epigenetic landscapes, gene expression networks, and cellular metabolism. The process typically occurs in two broad phases: an initial stochastic phase where somatic genes are silenced and early pluripotency-associated genes are activated, followed by a more deterministic phase where late pluripotency genes are activated and a stable pluripotent state is established [18]. Throughout this process, cells undergo metabolic reprogramming from oxidative phosphorylation to glycolysis and mesenchymal-to-epithelial transition (MET), particularly when fibroblasts serve as the starting population [18].
The Yamanaka factors (OCT4, SOX2, KLF4, MYC) function as pioneer factors that initiate chromatin remodeling at pluripotency loci, while simultaneously repressing somatic cell-specific transcriptional programs [26]. OCT4 and SOX2 play particularly crucial roles in activating the core pluripotency network, while MYC enhances chromatin accessibility and promotes global transcriptional amplification [18].
Episomal Vector Mechanisms
Episomal vectors are plasmid-based systems that utilize elements from the Epstein-Barr (EB) virus for extrachromosomal maintenance and replication. These vectors contain the origin of viral replication (oriP) and EB nuclear antigen 1 (EBNA1) gene, which together enable nuclear retention and once-per-cell-cycle replication of the plasmid without integration into the host genome [32]. The EBNA1 protein facilitates nuclear import and retention of the vector through binding to oriP, while also contributing to transcriptional activation of other reprogramming factors [32].
A key advantage of episomal vectors is their natural loss over time during cell division (at a rate of approximately 5% per cell cycle), eventually yielding iPSC lines free of exogenous genetic material without requiring additional manipulation [32]. Vectors incorporating the spleen focus-forming virus U3 (SFFV) promoter, which exhibits strong activity in hematopoietic cells, have demonstrated enhanced reprogramming efficiency for blood-derived cells [33].
Table 1: Key Components of Episomal Reprogramming Systems
| Component | Function | Variations/Improvements |
|---|---|---|
| oriP/EBNA-1 | Enables episomal replication and nuclear retention | Fundamental to all EBV-based episomal systems |
| SFFV U3 promoter | Strong promoter activity in hematopoietic cells | Enhances PBMC reprogramming efficiency |
| 2A "self-cleaving" peptides | Enables equimolar expression of multiple genes from single transcript | E2A, P2A, T2A sequences link OCT4-SOX2 |
| BCL-XL | Anti-apoptotic factor enhances cell survival during reprogramming | Particularly valuable for difficult-to-reprogram cells |
| SV40LT | Immortalizing factor that enhances reprogramming efficiency | Used in some systems but raises safety concerns |
Sendai Virus Mechanisms
Sendai virus is a non-integrating RNA virus belonging to the paramyxovirus family that replicates in the cytoplasm of infected cells without transitioning through a DNA intermediate [34]. The cytoplasmic replication mechanism fundamentally prevents genomic integration, making it a safe choice for generating integration-free iPSCs [32]. The virus exhibits high infectivity for numerous cell types, including difficult-to-transfect cells such as peripheral blood mononuclear cells (PBMCs) [34].
Sendai virus-based reprogramming systems deliver the Yamanaka factors as separate viral particles or as a polystronic construct, allowing control over the stoichiometry of reprogramming factor expression [34]. Like episomal vectors, Sendai virus is gradually diluted out of cells during repeated passaging, though the clearance process may require extended culture time or temperature-sensitive mutants that facilitate more rapid elimination at non-permissive temperatures [34].
Figure 1: Workflow of Integration-Free iPSC Reprogramming. Both episomal vector and Sendai virus methods progress through distinct reprogramming phases before yielding integration-free iPSCs.
Technical Comparison of Integration-Free Methods
Efficiency and Performance Characteristics
Reprogramming efficiency varies considerably between methods and depends on multiple factors, including cell source, donor characteristics, and technical execution. The table below summarizes key performance metrics for episomal vector and Sendai virus reprogramming systems based on current literature.
Table 2: Performance Comparison of Integration-Free Reprogramming Methods
| Parameter | Episomal Vectors | Sendai Virus |
|---|---|---|
| Reprogramming Efficiency | ~20-30 colonies/1×10^6 PBMCs [33]; >100-fold improvement with optimized vectors [33] | High efficiency; 1 kit can generate up to 60,000 colonies from 2×10^6 fibroblasts [34] |
| Time to iPSC Colony Emergence | 3-4 weeks | 2-3 weeks |
| Genomic Integration Risk | Low but occasional integration reported [31] | No integration (cytoplasmic replication) [35] |
| Clearance Timeline | Gradual loss over passages; ~70 days without intervention [31] | Temperature-sensitive mutants accelerate clearance; otherwise gradual dilution |
| Cost Considerations | Low cost after initial setup [33] | Higher reagent cost but can be aliquoted for multiple experiments [34] |
| Primary Cell Sources | PBMCs, fibroblasts [33] | PBMCs, fibroblasts, other difficult-to-transfect cells [32] |
Method-Specific Optimization Strategies
Episomal Vector Optimization
Critical advances in episomal vector technology have centered on optimizing the stoichiometry of reprogramming factor expression. Research demonstrates that expressing OCT4 and SOX2 as a polycistronic transcript linked by the E2A sequence (OS) ensures their equimolar expression, significantly enhancing reprogramming efficiency [33]. Similarly, delivering MYC and KLF4 on separate vectors rather than as a fusion construct enables a higher and more gradual increase in the MYC to KLF4 ratio during reprogramming, resulting in dramatic (~100-fold) improvements in efficiency [33].
The combination of optimized episomal vectors (OS + M + K + B, where B represents BCL-XL) has demonstrated reprogramming efficiency comparable to Sendai virus but at a fraction of the cost, making it an attractive option for large-scale iPSC generation efforts [33]. Additional enhancement strategies include:
- Sodium butyrate supplementation: Inhibition of histone deacetylases (HDACs) facilitates epigenetic remodeling during reprogramming [33]
- Hypoxic culture conditions (5% O₂): Reduces oxidative stress and enhances reprogramming efficiency
- Chemical cocktails: Including CHIR99021 (GSK3β inhibitor), A83-01 (TGF-β inhibitor), and ascorbic acid further enhance efficiency [31]
Sendai Virus Optimization
Sendai virus systems benefit from high innate transduction efficiency, but several optimization strategies can further enhance performance:
- Aliquoting and storage: Sendai virus maintains >50% activity even after three freeze-thaw cycles, enabling cost-effective partitioning of single kits for 24-48 reprogramming experiments [34]
- Spin transduction: Brief centrifugation following viral exposure increases transduction efficiency [34]
- Reduced viral quantities: As little as 1/100 of a standard CytoTune 2.0 kit can successfully generate iPSCs from tested lines [34]
- Butyrate supplementation: Enhances Sendai virus-mediated reprogramming in defined feeder-free culture systems [34]
Figure 2: Key Optimization Strategies for Episomal Vector and Sendai Virus Reprogramming.
Experimental Protocols
Episomal Vector Reprogramming Protocol for PBMCs
This protocol outlines the optimized method for reprogramming peripheral blood mononuclear cells using episomal vectors, based on established procedures with demonstrated high efficiency [33].
Pre-reprogramming Culture Phase
- Isolate PBMCs from fresh or frozen blood samples using density gradient centrifugation.
- Culture PBMCs in erythroid medium for 6 days to expand erythroid progenitors [33].
- Use Stemline-based serum-free erythroid medium supplemented with erythropoietin, SCF, and IL-3.
Nucleofection and Reprogramming Phase
- On day 6, harvest expanded cells and nucleofect with episomal vector combination (OS + M + K + B) using appropriate nucleofection system.
- Plate transfected cells onto Matrigel- or Geltrex-coated plates in erythroid medium.
- Culture in hypoxia (5% O₂) for enhanced reprogramming efficiency.
- Gradually transition to iPSC induction medium over 3-5 days.
- Supplement with sodium butyrate (0.2-0.8 mM) from days 6-14 post-transfection to enhance reprogramming [33].
iPSC Colony Selection and Expansion
- First iPSC colonies typically appear between 18-25 days post-nucleofection.
- Manually pick well-defined colonies between days 25-30.
- Expand colonies in feeder-free conditions using mTeSR or E8 medium.
- Passage using EDTA or enzyme-free dissociation methods to preserve viability.
- Confirm episomal vector loss by PCR for EBNA-1 around passage 10-12.
Sendai Virus Reprogramming Protocol
This protocol describes efficient Sendai virus-mediated reprogramming, optimized for high-throughput applications and minimal reagent usage [34].
Viral Transduction
- Plate 1×10⁴ to 5×10⁴ freshly passaged somatic cells per well of a 24-well plate.
- Transduce with Sendai virus vectors (CytoTune iPS 2.0 Sendai Kit) 2 hours after plating using synchronized timing for multiple samples.
- Use virus aliquots diluted 1:50 to 1:100 of manufacturer's recommended concentration for cost efficiency [34].
- Consider spin transduction (1000-2000 × g for 30-90 minutes) for difficult-to-transfect cells to enhance infection efficiency.
Culture and Medium Transitions
- Culture transduced cells in somatic cell medium for 48 hours post-transduction.
- Evaluate morphological changes at day 2 as an early indicator of successful transduction.
- Transition to iPSC induction medium (e.g., mTeSR with 1 mM nicotinamide and 0.2 mM sodium butyrate).
- Implement 2-day feeding schedule with medium removal every 6 days to reduce costs and labor [34].
- Plate directly onto Matrigel-coated plates in reprogramming medium without pre-coating medium change to streamline process.
Colony Expansion and Backup
- First colonies typically appear within 14-21 days.
- For clonal expansion, split cells onto 48-well plates after first passage for single-colony development.
- Use EDTA/PBS passaging method (without neutralization or centrifugation) for efficient iPSC expansion [34].
- Cryopreserve backup pools at multiple stages: after first split, at day 20, and during colony expansion.
Applications in Rare Genetic Disease Modeling
Advantages for Rare Disease Research
iPSC technology offers particular advantages for rare genetic disease research, where patient populations are small, biological samples are scarce, and research funding is often limited. Approximately 80% of rare diseases have a genetic origin, making patient-derived iPSCs uniquely valuable model systems [4]. Key applications in rare disease research include:
- Patient-specific disease modeling: iPSCs capture the complete genetic background of individual patients, including modifier genes and polymorphisms that may influence disease expression [4]
- Isogenic control generation: CRISPR/Cas9 gene editing enables correction of disease-causing mutations in patient-derived iPSCs, creating perfectly matched controls [4]
- Drug screening and toxicity testing: iPSC-derived differentiated cells enable high-throughput compound screening for therapeutic development [26]
- Pathogenesis elucidation: iPSC models facilitate investigation of molecular and cellular disease mechanisms in relevant cell types [8]
Successful Applications in Specific Rare Diseases
iPSCs generated via integration-free methods have successfully modeled numerous rare genetic disorders, providing insights into disease mechanisms and enabling therapeutic development:
- Lesch-Nyhan disease: Caused by HPRT1 mutations, modeled using iPSCs to identify disease-relevant transcriptomic changes [8]
- Juvenile Nephronophthisis: Patient-derived iPSCs and kidney organoids revealed abnormal cell proliferation, ciliary defects, and cyst formation reversible with NPHP1 reintroduction [4]
- RDH12-retinitis pigmentosa: iPSC-derived retinal organoids replicated photoreceptor degeneration and functional deficits observed in patients [4]
- Usher syndrome: iPSC models enable investigation of molecular mechanisms underlying combined hearing and vision loss [4]
- Marfan syndrome: iPSCs carrying FBN1 mutations replicate disease features in vitro for mechanistic studies [4]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Integration-Free Reprogramming
| Reagent Category | Specific Examples | Function and Application Notes |
|---|---|---|
| Reprogramming Vectors | pCXLE-episomal vectors (OS, M, K, B) [33]; CytoTune Sendai Virus [34] | Delivery of reprogramming factors; optimal vector combinations enhance efficiency |
| Cell Culture Media | mTeSR1, TeSR-E8 [31] [34]; Stemline erythroid medium [33] | Support pluripotent stem cell growth and reprogramming; defined formulations enhance reproducibility |
| Small Molecule Enhancers | Sodium butyrate [33] [34]; CHIR99021 [31]; A83-01 [31]; Ascorbic acid [31] | Enhance reprogramming efficiency through epigenetic modulation and signaling pathway inhibition |
| Extracellular Matrices | Matrigel, Geltrex, recombinant laminin-521 [34] | Provide substrate for iPSC attachment and growth in feeder-free systems |
| Cell Dissociation Reagents | Accutase, EDTA solution [34] | Gentle cell dissociation for passaging while maintaining viability |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 | Confirm pluripotency marker expression through immunocytochemistry or flow cytometry |
Integration-free reprogramming methods represent critical tools for establishing clinically relevant iPSC models of rare genetic diseases. Both episomal vectors and Sendai virus systems offer distinct advantages—episomal vectors provide a cost-effective, non-viral approach suitable for large-scale initiatives, while Sendai virus delivers high efficiency across diverse cell sources, including challenging primary cells like PBMCs.
The continuing refinement of these technologies, particularly through optimized factor stoichiometry and enhanced culture conditions, has dramatically improved efficiency and reliability. For rare disease research, where patient materials are precious and often limited, selecting the appropriate reprogramming method is paramount to successful disease modeling, drug discovery, and ultimately therapeutic development for these underserved conditions.
The application of induced pluripotent stem cells (iPSCs) has fundamentally transformed the landscape of rare genetic disease research. By enabling the generation of patient-specific disease-relevant cells, iPSC technology provides unprecedented access to human pathophysiology. This technical guide details current methodologies for directing iPSCs into neurons, cardiomyocytes, and renal cells—cell types critically affected in a multitude of rare disorders. With approximately 80% of rare diseases having a genetic origin and fewer than 10% having approved therapies, the development of robust, reproducible differentiation protocols is paramount for both mechanistic studies and therapeutic development [4]. The following sections provide a comprehensive overview of differentiation strategies, signaling pathways, and practical tools essential for researchers engaged in modeling rare diseases.
Core Differentiation Protocols
Directed Differentiation to Cortical Neurons
The generation of cortical neurons enables the study of numerous neurological and neurodevelopmental rare diseases, such as subtypes of Usher syndrome and Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV) [4] [13].
Detailed Methodology:
- Starting Culture: Maintain human iPSCs in feeder-free conditions using Essential 8 (E8) medium on defined matrices like laminin-521 or vitronectin to minimize variability [36].
- Neural Induction: Transition aggregates to neural induction medium containing dual SMAD signaling pathway inhibitors (e.g., LDN-193189 for BMP inhibition and SB-431542 for TGF-β inhibition) for 7-10 days to promote neural ectoderm fate.
- Neural Patterning: To specify cortical excitatory neuronal fates, add small molecules like IWP-2 (a Wnt inhibitor) and retinoic acid to pattern the neural epithelium towards a forebrain identity.
- Terminal Differentiation & Maturation: After 28-35 days, dissociate neural progenitor cells and plate them for terminal differentiation in media containing brain-derived neurotrophic factor (BDNF), neurotrophin-3 (NT-3), and cyclic AMP (cAMP) to promote neuronal maturation and synaptic formation [13]. For advanced modeling, these neurons can be co-cultured with mouse or human glial cells to enhance maturity and functionality.
- Quality Control: Assess efficiency via immunostaining for pan-neuronal markers (βIII-Tubulin), cortical layer markers (e.g., TBR1 for deep layers, BRN2 for upper layers), and synaptic markers (e.g., PSD-95, Synapsin-1). Functional validation can include patch-clamp recordings to confirm action potential generation and synaptic activity.
Guided Differentiation to Cardiac HDCs
A "guided differentiation" approach toward cardiac lineages prioritizes the generation of heterogeneous, rhythmically contracting cell aggregates containing multiple cardiac-relevant cell types, ideal for population-level studies and disease modeling [37].
Detailed Methodology:
- Aggregate Formation: Harvest iPSCs to form 3D aggregates approximately 300 µm in diameter, culturing them in Essential 8 medium supplemented with 10 µM CEPT (a cocktail to improve cell survival) for 24 hours to promote aggregate stability [37].
- Cardiac Mesoderm Induction: Employ temporal Wnt modulation. First, activate Wnt signaling by replacing the medium with "heart medium" (RPMI-1640 supplemented with B-27 minus insulin) containing 6 µM CHIR99021 (a GSK-3β inhibitor) for 24 hours.
- Cardiac Lineage Specification: At day 3 of differentiation, replace the medium with heart medium containing 4 µM IWP-2 (a Wnt inhibitor) for 48 hours to specify cardiac progenitor cells.
- Maturation: From day 5 onwards, maintain the aggregates in base heart medium, refreshing it every 48 hours. Rhythmically contracting aggregates, termed cardiac Heterogeneous Differentiating Cultures (HDCs), typically emerge by day 8-10 and can be harvested for analysis around day 16 [37].
- Characterization: The resulting cardiac HDCs contain cardiomyocytes (marked by TNNT2, MYH6, ACTC1), epicardial cells (SFRP5, WT1), cardiac fibroblasts (TCF21, PDGFRA), endothelial cells (CDH5, PECAM1), and hematopoietic cells. Characterization includes single-cell RNA sequencing, immunofluorescence, patch-clamp recordings for action potentials, and intracellular Ca²⁺ measurements to confirm functionality [37].
Direct Reprogramming to Cardiomyocyte-like Cells
An alternative to pluripotency bypass is the direct reprogramming of somatic cells into functional cardiomyocyte-like cells (hCiCMs) using small molecules, offering a potential scalable, autologous cell source for regenerative therapies [38].
Detailed Methodology:
- Somatic Cell Source: Isolate human urine-derived cells (hUCs) as a non-invasive somatic cell source. Culture hUCs in a 1:1 mixture of DMEM/F12 and keratinocyte serum-free medium supplemented with 5-10% FBS and EGF [38].
- Chemical Induction: Upon reaching confluence, transdifferentiate hUCs using a cocktail of 15 small molecules under xeno-free conditions. The cocktail includes pathways modulators for Wnt, TGF-β, and other signaling pathways critical for cardiac development.
- Maturation and Purity: The reprogramming efficiency can reach ~15% by day 30, with purity exceeding 96% by day 60, as confirmed by the expression of cardiomyocyte markers (cTnT, α-actinin), the presence of sarcomeric structures observed via transmission electron microscopy, and functional assessments including regular calcium transients and ventricular-like action potentials [38].
- Functional Assessment: Perform patch-clamp recordings to confirm action potentials and measure intracellular Ca²⁺ transients to evaluate excitation-contraction coupling. Single-cell RNA sequencing can reveal cardiomyocyte subpopulations and maturation status, often showing similarity to embryonic human heart cells [38].
Differentiation to Renal Organoids
For rare renal diseases like Juvenile Nephronophthisis (NPH), kidney organoids derived from patient-specific iPSCs provide a powerful human model system [4].
Detailed Methodology:
- Renal Progenitor Induction: Differentiate iPSCs aggregates in media containing CHIR99021 at a defined concentration for 3-4 days to induce intermediate mesoderm, the precursor to kidney lineages.
- Kidney Organoid Maturation: Transfer aggregates to a 3D culture system in the presence of FGF9 and heparin to promote the self-organization of nephron structures, including glomeruli-like and tubule-like structures, over 18-25 days.
- Disease Modeling: For disease modeling, utilize iPSCs from patients with NPHP1 mutations. NPHP1-deficient organoids typically exhibit phenotypes such as abnormal cell proliferation, defects in primary cilia, and renal cyst formation, which can be rescued by reintroducing functional NPHP1 expression [4].
- Characterization: Analyze organoids via immunostaining for renal progenitor markers (e.g., SIX2, WT1), podocyte markers (e.g., PODXL), and tubular markers (e.g., E-Cadherin, LTL). Cyst formation is a key quantitative readout for disease phenotyping.
Signaling Pathways and Workflows
The differentiation of iPSCs into specific lineages is governed by the precise temporal manipulation of key evolutionary conserved signaling pathways. The following diagrams outline the core logical workflows and pathways for generating neurons, cardiomyocytes, and renal cells.
Neural Differentiation Pathway
Cardiac Differentiation Pathway
Renal Differentiation Pathway
The following tables consolidate key quantitative metrics from the cited differentiation protocols, providing a reference for expected outcomes and experimental design.
Table 1: Efficiency and Timeline of Featured Differentiation Protocols
| Cell Type | Protocol Type | Key Inducers | Time to Phenotype | Reported Efficiency | Key Characterization Markers |
|---|---|---|---|---|---|
| Cortical Neurons [13] | Directed 2D/3D | Dual SMAD inhibitors, Wnt inhibitors | 28-40 days | Varies by line; high purity possible | βIII-Tubulin, TBR1, BRN2, Synapsin |
| Cardiac HDCs [37] | Guided 3D | CHIR99021, IWP-2 | 16 days | Diverse cardiac lineage cells | TNNT2, SFRP5, TCF21, CDH5 |
| Cardiomyocytes (Chemical Reprogramming) [38] | Direct Reprogramming | Small molecule cocktail | 30-60 days | ~15% (Day 30), >96% purity (Day 60) | cTnT, α-actinin, Sarcomeric structures |
| Kidney Organoids [4] | Directed 3D | CHIR99021, FGF9, Heparin | 18-25 days | Formation of nephron structures | SIX2, WT1, PODXL, E-Cadherin |
Table 2: Key Small Molecules and Growth Factors for iPSC Differentiation
| Reagent Name | Signaling Pathway Target | Primary Function in Differentiation | Example Protocol |
|---|---|---|---|
| CHIR99021 [37] | Wnt/β-catenin (Activator) | Induces mesoderm formation (cardiac, renal) | Cardiac HDCs, Renal Organoids |
| IWP-2 [37] | Wnt (Inhibitor) | Specifies cardiac progenitor fate | Cardiac HDCs |
| LDN-193189 | BMP (Inhibitor) | Promotes neural ectoderm formation | Cortical Neurons |
| SB-431542 | TGF-β/Activin (Inhibitor) | Promotes neural ectoderm formation | Cortical Neurons |
| FGF9 [4] | FGF Signaling | Supports renal progenitor expansion & morphogenesis | Renal Organoids |
| BDNF & NT-3 [13] | Neurotrophin Signaling | Promotes neuronal survival and maturation | Cortical Neurons |
| B-27 Supplement [37] | N/A | Serum-free supplement for cell health and maturation | Cardiac HDCs, Neural Cultures |
The Scientist's Toolkit: Research Reagent Solutions
Successful and reproducible differentiation relies on a foundation of high-quality, well-defined reagents. The following table details essential materials and their functions.
Table 3: Essential Research Reagents for iPSC Culture and Differentiation
| Reagent Category | Specific Product Examples | Critical Function | Technical Notes |
|---|---|---|---|
| Defined Culture Medium | Essential 8 (E8) [36] | Xeno-free medium for maintenance of iPSC pluripotency | Reduces inter-line variability compared to undefined media. |
| Defined Matrix | Laminin-521, Vitronectin [36] | Recombinant substrates for iPSC attachment and growth in feeder-free conditions | Promotes greater uniformity among PSC lines. |
| Small Molecule Libraries | Commercially available libraries (e.g., Tocris, Selleckchem) [38] | Screening for novel inducers and optimizing reprogramming/differentiation | Used to identify effective cocktail combinations. |
| Differentiation Basal Media | RPMI-1640, DMEM/F-12 | Base media for formulation of specialized differentiation media | Often supplemented with B-27 or N-2. |
| Cell Dissociation Reagents | Gentle Cell Dissociation Enzyme, Accutase | Passaging iPSCs and dissociating organoids to single cells | Maintains high cell viability for downstream applications. |
| Characterization Antibodies | Anti-OCT4, NANOG (Pluripotency); Anti-βIII-Tubulin, TNNT2, PODXL (Differentiated) | Confirmation of pluripotency and lineage-specific differentiation | Essential for immunocytochemistry and flow cytometry. |
The continuous refinement of differentiation protocols is critical for enhancing the fidelity of iPSC-based models for rare genetic diseases. Key trends shaping the future of this field include the adoption of defined culture conditions to minimize inter-line variability and improve reproducibility [36], the development of complex 3D models like organoids and assembloids that better recapitulate tissue structure and cell-cell interactions [4] [13], and the integration of CRISPR-Cas9 gene editing to create isogenic control lines, which are essential for attributing phenotypes directly to a specific mutation against a constant genetic background [4] [39]. Furthermore, automated, high-throughput production of iPSC lines is enabling the generation of large, standardized biobanks, facilitating powerful population-level studies [40]. By leveraging the strategies and tools outlined in this guide, researchers can robustly generate disease-relevant cell types, thereby accelerating our understanding of rare disease mechanisms and the development of much-needed therapeutic interventions.
Inherited rare diseases represent a significant challenge in medical research, collectively affecting an estimated 263–446 million people worldwide [41] [3]. Among these conditions, Juvenile Nephronophthisis (NPH) and Retinitis Pigmentosa (RP) stand as prototypical examples of monogenic disorders that lead to progressive organ failure and severe disability. The drug development landscape for such conditions remains stark, with approximately 94% of rare diseases lacking approved treatments [41]. This therapeutic gap stems largely from the limitations of traditional preclinical models, including two-dimensional cell cultures that fail to recapitulate tissue architecture and animal models that often poorly mimic human disease pathology due to species differences [42] [43].
The advent of induced pluripotent stem cell (iPSC) technology has revolutionized rare disease modeling by enabling the generation of patient-specific human tissues in vitro. iPSC-based platforms offer scalable, renewable, physiologically relevant preclinical models that retain the patient's specific genetic background [41]. Approximately 80% of rare diseases have a genetic origin, making patient-derived iPSCs and their isogenic controls uniquely powerful model systems [41] [3]. These technologies have converged with advanced three-dimensional (3D) culture techniques to produce complex in vitro models (CIVMs), particularly organoids that closely mimic the architecture and function of native organs [43] [44].
This technical guide explores the development and application of 3D organoid models for Juvenile Nephronophthisis and Retinitis Pigmentosa, framing these advances within the broader context of iPSC disease modeling for rare genetic disorders research. We provide detailed methodologies, quantitative analyses, and resource guidance to empower researchers and drug development professionals in deploying these transformative technologies.
Disease Background and Modeling Rationale
Juvenile Nephronophthisis (NPH)
Juvenile Nephronophthisis is an autosomal recessive cystic kidney disease and the most common genetic cause of end-stage renal failure in children and young adults [41]. NPH is characterized by corticomedullary cyst formation, tubular basement membrane disruption, and progressive tubulointerstitial nephritis leading to renal fibrosis [41]. The condition typically presents with polyuria, polydipsia, and growth retardation, progressing to end-stage renal disease by approximately 13 years of age [41]. Mutations in at least 25 different genes (NPHP1-NPHP25) have been associated with NPH, with NPHP1 mutations accounting for 20%-40% of cases [41]. These genes predominantly encode proteins localized to primary cilia, basal bodies, or centrosomes, placing NPH within the category of ciliopathies.
Retinitis Pigmentosa (RP)
Retinitis Pigmentosa constitutes a heterogeneous group of inherited retinal dystrophies characterized by progressive photoreceptor degeneration, starting with rod cells and subsequently affecting cone cells [42] [45]. Clinical presentation typically includes night blindness, progressive visual field constriction leading to tunnel vision, and eventual loss of central vision. RP exhibits all inheritance patterns (autosomal dominant, autosomal recessive, X-linked, and mitochondrial), with mutations in over 80 genes implicated in its pathogenesis [46] [45]. The genetic heterogeneity of RP presents significant challenges for therapeutic development, necessitating models that can capture patient-specific pathophysiology.
Table 1: Key Characteristics of Juvenile Nephronophthisis and Retinitis Pigmentosa
| Characteristic | Juvenile Nephronophthisis | Retinitis Pigmentosa |
|---|---|---|
| Primary Affected Tissue | Kidney | Retina |
| Key Pathological Features | Corticomedullary cysts, tubular atrophy, interstitial fibrosis | Photoreceptor degeneration, outer nuclear layer thinning |
| Common Genetic Causes | NPHP1-NPHP25 mutations (cilia-associated proteins) | Mutations in RDH12, RP2, RHO, PDE6B, etc. |
| Inheritance Pattern | Autosomal recessive | Autosomal dominant, autosomal recessive, X-linked |
| Modeling Challenges | Recapitulating cystic changes in kidney tubules | Capturing photoreceptor degeneration and functional deficits |
iPSC-Derived Organoid Models: Methodological Framework
Retinal Organoid Generation and Characterization
The differentiation of iPSCs into retinal organoids follows a multi-stage process that recapitulates key aspects of in vivo retinogenesis [42]. This process can be broadly categorized into three distinct stages spanning approximately 180 days:
Initial Stage (Differentiation Days 30-50): Organoids exhibit a well-defined, luminous outer neuroepithelial margin populated by neuroretinal progenitor cells (NPCs) and retinal ganglion cells (RGCs). RGCs represent the first retinal cell type to undergo differentiation, with their numbers declining after day 90 [42].
Intermediate Stage (Days 80-120): Organoids develop a dark-phase core as the bright margins diminish and early progenitors of cone and rod photoreceptors begin to emerge [42].
Maturation Stage (Days 120-180): The outer edge becomes more prominent as photoreceptor structures commence differentiation, eventually forming laminated structures with distinct nuclear and synaptic layers [42].
The resulting retinal organoids contain most major retinal neuron cell types, including rod and cone photoreceptors, ganglion cells, horizontal cells, bipolar cells, and Müller glia, organized in a stratified architecture that mimics the native retina [42]. These organoids develop ultrastructural features of mature photoreceptors, including an outer limiting membrane, basal bodies with connecting cilia displaying photoreceptor-specific microtubule arrangements, and rudimentary outer segment-like structures [42] [46].
Figure 1: Retinal organoid differentiation workflow. The process recapitulates key stages of in vivo retinogenesis over 180 days, producing stratified retinal tissue with mature photoreceptors. NPCs: neuroretinal progenitor cells; RGCs: retinal ganglion cells.
Kidney Organoid Generation for NPH Modeling
While the search results provide less specific detail on kidney organoid protocols compared to retinal organoids, recent advances have enabled the generation of kidney organoids from patient-derived iPSCs that recapitulate features of NPH [41]. These models have demonstrated abnormal cell proliferation, primary cilia abnormalities, and renal cyst formation – hallmark features of NPH pathophysiology [41]. The kidney organoid system has proven valuable for studying disease mechanisms and testing therapeutic interventions, as evidenced by the rescue of cyst formation following reintroduction of NPHP1 expression [41].
Experimental Modeling of Disease Pathogenesis
RP2-Associated Retinitis Pigmentosa
RP2 mutations cause a severe form of X-linked retinitis pigmentosa (XLRP), accounting for approximately 15% of all cases [46]. RP2 functions as a GTPase-activating protein (GAP) for the small GTPase ARL3, which plays a crucial role in trafficking lipidated proteins (such as transducin, GRK1, and PDE6) to the photoreceptor outer segment [46]. To model this condition, researchers have developed gene-edited isogenic RP2 knockout (RP2 KO) iPSCs and RP2 patient-derived iPSCs to produce 3D retinal organoids [46].
Strikingly, both RP2 KO and RP2 patient-derived organoids showed a peak in rod photoreceptor cell death at day 150 (D150) with subsequent thinning of the organoid outer nuclear layer (ONL) by D180 of culture [46]. This temporal pattern of degeneration closely correlates with rod photoreceptor differentiation, providing a human-relevant model of the disease process. The RP2-deficient organoids developed morphologically normal photoreceptors with inner segments rich in mitochondria and rudimentary outer segment-like structures with connecting cilia, indicating that RP2 ablation does not prevent initial photoreceptor differentiation but rather leads to subsequent degeneration [46].
Table 2: Temporal Progression of Photoreceptor Degeneration in RP2-Deficient Retinal Organoids
| Time Point | Structural Features | Functional/Molecular Markers |
|---|---|---|
| Day 150 | Peak rod photoreceptor cell death | Reduced rhodopsin expression |
| Day 180 | Outer nuclear layer (ONL) thinning | Loss of recoverin-positive cells |
| Day 150-180 | Preservation of inner segments and connecting cilia | ARL13B-positive ciliary structures |
| Mature Organoids | Laminated structure with ONL and INL | Presence of cone arrestin, PKCα, CRALBP |
RDH12-Associated Retinitis Pigmentosa
RDH12 encodes a photoreceptor NADPH-dependent retinal reductase enzyme that converts all-trans-retinal to all-trans-retinol in the visual cycle [45]. Heterozygous variants in RDH12 cause a rare autosomal dominant form of retinitis pigmentosa (RDH12-AD). Retinal organoids generated from a patient with a heterozygous pathogenic frameshift variant (c.759del, p.Phe254Leufs*24) in RDH12 exhibited correct localization of RDH12 to photoreceptor inner segments up to week 44 [45].
However, transmission electron microscopy at week 37 revealed that photoreceptors were less abundant and shorter in length compared to controls [45]. Functional assessments at week 44 demonstrated severe disruptions in visual cone function, retinol biosynthesis, and the vitamin A pathway [45]. This disease model successfully recapitulated the later-onset, milder disease course observed in human patients with RDH12-AD, providing valuable insights into disease etiology and potential therapeutic targets.
Nephronophthisis Modeling in Kidney Organoids
The first human NPH disease models using patient-derived iPSCs, gene-edited iPSCs, and differentiated kidney organoids have demonstrated abnormal cell proliferation, abnormalities in primary cilia, and renal cyst formation [41]. Importantly, reintroduction of NPHP1 expression reversed the cyst formation observed in organoids, validating the model's utility for testing therapeutic interventions [41]. This kidney organoid system provides novel insights into NPH disease mechanisms and opens avenues for therapeutic development.
Therapeutic Testing and Rescue Strategies
Gene Therapy Approaches
Retinal organoids have emerged as valuable platforms for testing gene-based therapeutics. In RP2-deficient retinal organoids, adeno-associated virus (AAV)-mediated gene augmentation with human RP2 rescued the degeneration phenotype, preventing ONL thinning and restoring rhodopsin expression [46]. This demonstration of successful rescue in a human-derived 3D model provides critical preclinical evidence supporting the potential of gene therapy for RP2-associated XLRP.
The organoid system offers particular advantages for testing AAV-based therapies, including the ability to evaluate tropism of different AAV serotypes for human photoreceptors, assess expression levels and patterns of transgenes, and monitor functional rescue in a human cellular environment that recapitulates key aspects of the disease pathophysiology [46].
Pharmacological Interventions
While the search results did not provide specific examples of pharmacological testing in NPH or RP organoid models, the broader field of organoid pharmacology is advancing rapidly. Organoids are increasingly recognized for their potential in drug screening, toxicity assessment, and mechanistic research [44]. Patient-derived organoids (PDOs) establish clinically relevant biomimetic platforms for drug efficacy assessment by faithfully preserving the histopathological features and genetic landscape of native tissues [44]. Their inherent 3D architecture and cellular heterogeneity can accurately simulate individualized treatment responses, significantly improving preclinical prediction ability and reducing dependence on animal experiments [44].
Figure 2: Therapeutic testing pipeline using patient-specific organoids. Multiple intervention strategies can be evaluated for structural, molecular, and functional rescue of disease phenotypes.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagent Solutions for Organoid Modeling
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Stem Cell Sources | Patient-derived iPSCs, Gene-edited isogenic controls [41] [46] | Provide genetically relevant background for disease modeling |
| Differentiation Factors | FGF2, Retinoic Acid [45] | Promote retinal patterning and photoreceptor maturation |
| Cell Type Markers | Recoverin, Rhodopsin, Cone Arrestin [46] | Identify photoreceptors and assess differentiation efficiency |
| Structural Proteins | ARL13B, Polyglutamylated Tubulin (GT335) [46] | Visualize ciliary structures and outer segment development |
| Cell Death Assays | TUNEL staining [45] | Quantify photoreceptor degeneration in disease models |
| Gene Editing Tools | CRISPR/Cas9, gRNAs [47] [46] | Create isogenic controls or introduce disease mutations |
| Viral Vectors | Adeno-associated viruses (AAVs) [46] | Deliver therapeutic genes for rescue experiments |
| Imaging Technologies | Transmission Electron Microscopy [46] [45] | Assess ultrastructural features of photoreceptors and cilia |
Technical Protocols for Key Experiments
Retinal Organoid Differentiation Protocol
Based on the methodologies described across multiple studies [42] [46] [45], the following protocol represents a consensus approach for generating retinal organoids from iPSCs:
iPSC Culture and Quality Control: Maintain iPSCs in feeder-free conditions on Basement Membrane Matrix-coated plates using standard stem cell media. Regularly assess pluripotency markers and karyotype stability.
Embryoid Body Formation: Dissociate iPSCs to single cells using enzyme-based dissociation and transfer to low-attachment plates to promote aggregate formation in neural induction media.
Neural Induction: Culture aggregates in neural induction media containing SMAD signaling inhibitors for 3-4 weeks to promote neural differentiation, with media changes every 2-3 days.
Optic Vesicle Formation: Between days 21-32, manually select and isolate optic vesicle-like structures based on morphological characteristics.
Retinal Organoid Maturation: Transfer isolated optic cups to low-attachment plates and culture in retinal differentiation media supplemented with 10 ng/mL FGF2 for initial patterning, followed by extended maturation with 0.5 µM retinoic acid to promote photoreceptor differentiation.
Long-term Maintenance: Culture organoids for up to 180 days, with careful media changes 2-3 times weekly, to allow for complete photoreceptor maturation and outer segment formation.
CRISPR/Cas9-Mediated Gene Editing in Organoids
For acute genetic manipulation in organoids, the following electroporation-based protocol has been successfully employed [47]:
Guide RNA Design: Design paired gRNAs targeting the same exon with PAM sites spaced 7-11 bp apart to maximize protein disruption probability. Select gRNAs based on activity scores (close to 1) and specificity scores (close to 100%).
Organoid Preparation: Slice organoids to approximately 300µm thickness using a vibratome to enhance nutrient access and enable identification of ventricular-like structures.
Electroporation Mixture Preparation: Combine CRISPR/Cas9 ribonucleoprotein (RNP) complexes with fluorescent reporters in an appropriate electroporation buffer.
Microinjection and Electroporation: Inject the mixture into the ventricular-like cavity of sliced organoids using fine glass capillaries. Apply electrical pulses (typically 5 pulses of 50V for 1ms duration with 100ms intervals) using platinum plate electrodes.
Post-Electroporation Recovery: Immediately transfer electroporated organoids to recovery media containing Rho-associated kinase (ROCK) inhibitor for 24 hours, then return to standard culture conditions.
Efficiency Validation: Assess editing efficiency 3-7 days post-electroporation through fluorescence analysis, PCR-based assays, or immunostaining for target protein loss.
The development of 3D organoid models for Juvenile Nephronophthisis and Retinitis Pigmentosa represents a significant advancement in rare disease research. These iPSC-derived CIVMs faithfully recapitulate key aspects of disease pathophysiology, including photoreceptor degeneration in RP and renal cyst formation in NPH, while providing human-relevant platforms for therapeutic testing. The methodologies and resources outlined in this technical guide provide researchers with a foundation for implementing these sophisticated model systems to advance our understanding of disease mechanisms and accelerate therapeutic development for these devastating rare genetic disorders.
The study of rare genetic disorders presents a significant challenge for biomedical research due to limited patient populations, scarcity of biological samples, and often poorly understood disease mechanisms. With over 7,000 distinct rare diseases identified and approximately 80% having a genetic origin, the cumulative impact is substantial, affecting an estimated 263–446 million people worldwide [4] [3]. Historically, research has relied heavily on animal models, which frequently fail to recapitulate key aspects of human pathophysiology due to species-specific differences in genetics, morphology, and molecular pathways [48]. The advent of induced pluripotent stem cell (iPSC) technology has revolutionized this landscape by providing scalable, renewable, and patient-specific preclinical models that faithfully mirror human disease biology [4] [14].
This technical guide examines the application of iPSC-based models to three distinct categories of rare genetic disorders: Usher syndrome, Marfan syndrome, and BMP-related rare diseases. Through detailed case studies, we explore how patient-specific iPSCs and advanced differentiation protocols enable researchers to recapitulate disease phenotypes in vitro, uncover underlying molecular mechanisms, and identify potential therapeutic targets. The integration of these human-relevant models into drug discovery pipelines represents a paradigm shift in rare disease research, offering a path to address the critical unmet need for effective treatments, as over 90% of rare diseases currently lack approved therapies [4] [3].
iPSC Disease Modeling Fundamentals
Core Principles and Workflows
iPSC-based disease modeling leverages the ability to reprogram patient somatic cells into pluripotent stem cells, which can then be differentiated into the specific cell types affected by a particular disorder. The foundational workflow involves: (1) somatic cell collection from readily accessible tissues like peripheral blood or skin biopsies; (2) reprogramming through the introduction of pluripotency factors; (3) iPSC characterization and quality control; (4) directed differentiation into target cell types; and (5) phenotypic analysis of disease-relevant characteristics [48] [49].
A critical advancement in this field has been the development of isogenic controls through precise genome editing technologies like CRISPR-Cas9. By correcting disease-causing mutations in patient-derived iPSCs or introducing specific mutations into healthy iPSC lines, researchers can create genetically matched control lines that eliminate the confounding effects of genetic background variability [50]. This approach enables systematic evaluation of the causal relationship between genetic mutations and resulting phenotypes, strengthening experimental conclusions and facilitating drug discovery efforts [50] [51].
Advanced Model Systems
While two-dimensional (2D) monocultures provided the initial platform for iPSC-based disease modeling, the field has rapidly advanced toward more physiologically relevant three-dimensional (3D) models. Organoids—self-organizing, 3D tissue structures derived from stem cells—recapitulate aspects of native tissue architecture, cellular heterogeneity, and tissue-specific functions that are absent in traditional 2D cultures [4] [51]. The emergence of assembloids (combining multiple organoid types) and organ-on-chip technologies (integrating microfluidics with 3D cultures) further enhances physiological relevance by modeling inter-cellular and inter-tissue interactions, as well as incorporating biomechanical and other microenvironmental cues [52] [48].
These complex in vitro models (CIVMs) are particularly valuable for rare diseases that affect multiple cell types or involve complex tissue-level pathophysiology. Furthermore, recent regulatory changes, including the FDA Modernization Act 2.0, now recognize the utility of these human-cell-based assays for preclinical testing, potentially reducing the reliance on animal models for drug development [4].
Disease-Specific Case Studies
Usher Syndrome
Usher syndrome represents a family of inherited disorders characterized by the dual sensory impairments of hearing loss and vision loss due to retinitis pigmentosa, sometimes accompanied by vestibular dysfunction [4]. This autosomal recessive condition is both the most common form of deaf-blindness and the most frequent cause of combined hearing and vision loss, with an estimated prevalence of 4-17 per 100,000 people [4]. The disorder is classified into three major clinical types (I, II, and III) based on symptom severity, onset, and progression, with at least nine genetic loci identified across these types.
The proteins encoded by Usher syndrome genes play critical roles in the development and function of hair cells in the inner ear and photoreceptor cells in the retina. These proteins form multiprotein complexes involved in adhesive interactions, mechanoelectrical transduction, and intracellular signaling in sensory cells. Mutations disrupt normal cellular architecture and function, leading to progressive sensory cell degeneration.
iPSC Modeling Approaches
iPSC-based models for Usher syndrome typically focus on generating the two primary affected cell types: photoreceptor cells and auditory hair cells. For retinal modeling, researchers employ stepwise differentiation protocols that recapitulate key stages of retinal development, resulting in retinal organoids containing the major retinal cell types, including photoreceptors [4]. Similarly, protocols for inner ear organoids generate sensory epithelia containing hair cell-like cells that exhibit structural and functional characteristics of native hair cells.
A significant advantage of iPSC models for Usher syndrome is the ability to study the human-specific aspects of sensory cell development and function that cannot be adequately captured in animal models. Furthermore, patient-derived iPSCs enable investigation of genotype-phenotype correlations across different Usher syndrome subtypes and specific mutations, potentially revealing mutation-specific pathogenic mechanisms [4].
Key Research Findings
Recent studies using Usher syndrome iPSC models have provided new insights into the timing and mechanisms of sensory cell degeneration. Retinal organoids derived from patient iPSCs have demonstrated early abnormalities in photoreceptor outer segment development and disrupted protein localization of Usher proteins, even before overt degeneration occurs [4]. These models have also revealed mutation-specific effects on protein stability, ciliary trafficking, and intercellular adhesion.
In inner ear organoids, Usher syndrome mutations lead to structural defects in hair cell bundles and impaired mechanotransduction, mirroring the auditory dysfunction observed in patients. The ability to generate both retinal and vestibular cell types from the same patient iPSC line also enables investigation of why certain Usher syndrome mutations preferentially affect auditory versus vestibular function [4].
Marfan Syndrome
Marfan syndrome is an autosomal dominant connective tissue disorder caused by pathogenic variants in the FBN1 gene, which encodes the extracellular matrix protein fibrillin-1 [49]. This multi-system disorder affects approximately 1 in 5,000 individuals and manifests primarily in the skeletal, ocular, and cardiovascular systems [49]. Characteristic features include aortic root dilatation (potentially leading to dissection), ectopia lentis (lens dislocation), and skeletal abnormalities such as long limbs, tall stature, and arachnodactyly [49].
Fibrillin-1 monomers assemble into microfibrils that provide structural support to elastic tissues and regulate the bioavailability of growth factors from the transforming growth factor beta (TGF-β) and bone morphogenetic protein (BMP) families [49]. The prevailing pathogenic mechanism involves either haploinsufficiency (reduced fibrillin-1 production) or dominant-negative effects of mutant protein, both leading to altered TGF-β signaling and compromised tissue integrity [49]. More than 3,300 different FBN1 variants have been documented, with missense mutations affecting calcium-binding EGF domains being most common [49].
Table 1: Marfan Syndrome Model Characteristics
| Aspect | iPSC-Derived Vascular Smooth Muscle Cells | iPSC-Derived Cardiomyocytes | iPSC-Derived Mesenchymal Progenitors |
|---|---|---|---|
| Key Phenotypes | Impaired contractility, synthetic shift, ECM disorganization | Calcium handling abnormalities, arrhythmias | Enhanced osteogenic potential, reduced adipogenesis |
| Signaling Alterations | Increased TGF-β and ERK1/2 signaling | Altered TGF-β/BMP crosstalk | Dysregulated BMP signaling |
| Functional Assays | Contraction measurements, proteomic analysis | Calcium imaging, patch clamp | Differentiation assays, mineralization tests |
| Therapeutic Insights | Losartan response variable by mutation type | Beta-blocker effects on arrhythmias | Potential for bisphosphonate intervention |
iPSC Modeling Approaches
The generation of patient-specific iPSCs for Marfan syndrome has enabled the in vitro modeling of multiple disease manifestations. Researchers have established 52 distinct human pluripotent stem cell lines for Marfan syndrome to date [49]. These cells are differentiated primarily into vascular smooth muscle cells (VSMCs) and cardiomyocytes to model the life-threatening cardiovascular complications, and into mesenchymal progenitors to investigate skeletal manifestations [49].
Standardized protocols for VSMC differentiation typically involve either neural crest or paraxial mesoderm pathways, reflecting the different developmental origins of smooth muscle in distinct aortic segments [49]. For cardiomyocyte differentiation, well-established methods using activin A and BMP4 yield high-purity populations of beating cells [49]. The resulting cells are characterized through a combination of molecular analyses, functional assays, and, increasingly, 3D tissue engineering approaches to better mimic the native tissue microenvironment [49].
Key Research Findings
iPSC models of Marfan syndrome have successfully recapitulated key disease features observed in patients. VSMCs derived from patient iPSCs demonstrate impaired contractility, a proliferative/synthetic shift in phenotype, and disorganized extracellular matrix [49]. These pathological changes correlate with increased TGF-β and ERK1/2 signaling, consistent with findings from animal models and human tissue studies [49].
Cardiomyocytes from Marfan patients exhibit calcium handling abnormalities and increased susceptibility to arrhythmias, providing a cellular basis for the electrical abnormalities observed in patients [49]. Interestingly, iPSC models have revealed substantial phenotypic variability based on the specific FBN1 mutation, helping to explain the clinical heterogeneity observed among patients with different genotypes [49].
From a therapeutic perspective, iPSC-based models have been used to test drug responses in a patient-specific manner. For instance, the TGF-β antagonist losartan shows variable effectiveness across different FBN1 mutations in iPSC models, potentially informing personalized treatment strategies [49].
BMP-Related Rare Diseases
Bone morphogenetic proteins (BMPs) belong to the TGF-β superfamily and play crucial roles in development, tissue homeostasis, and cell fate determination [52]. Disorders involving BMP signaling include Fibrodysplasia Ossificans Progressiva (FOP), Pulmonary Arterial Hypertension (PAH), and Hereditary Haemorrhagic Telangiectasia (HHT) [52]. These conditions demonstrate how dysregulation of a fundamental signaling pathway can lead to diverse pathological manifestations across different organ systems.
FOP is an ultra-rare genetic disorder (approximately 1 in 1.5-2 million) characterized by progressive heterotopic ossification (bone formation in soft tissues) [52]. Most cases are caused by activating mutations in the ACVR1 gene encoding a BMP type I receptor [52]. PAH involves vascular remodeling and elevated pulmonary arterial pressure, with BMPR2 mutations identified in approximately 70-80% of heritable cases [52]. HHT is a vascular disorder featuring arteriovenous malformations and is frequently associated with mutations in ENG or ACVRL1, both encoding components of the BMP signaling pathway [52].
iPSC Modeling Approaches
iPSC modeling of BMP-related disorders presents unique challenges because BMP signaling plays critical roles in pluripotent stem cell maintenance and differentiation [52]. Gain- or loss-of-function mutations in BMP pathway components can therefore alter the behavior of undifferentiated iPSCs and affect their differentiation efficiency, requiring careful optimization of protocols for each specific mutation [52].
For FOP modeling, iPSCs are differentiated into skeletal progenitor cells and endothelial cells to investigate the cellular origins and mechanisms of heterotopic ossification [52]. For PAH, the focus is on generating pulmonary arterial endothelial cells and pulmonary arterial smooth muscle cells to model vascular remodeling [52]. HHT modeling involves differentiation into endothelial cells and the formation of vascular organoids to study arteriovenous malformation development [52].
Advanced model systems for BMP-related diseases increasingly incorporate complex microenvironmental cues such as biomechanical forces (shear stress, cyclic stretch), hypoxia, and inflammatory cytokines to more faithfully recapitulate disease pathogenesis [52]. These approaches recognize that disease manifestations often require both genetic predisposition and environmental triggers.
Key Research Findings
iPSC models of FOP have provided crucial insights into the cellular mechanisms driving heterotopic ossification. Research using these models has demonstrated that ACVR1 mutations confer dysregulated BMP pathway activation in response to inflammatory stimuli, particularly activin A, which normally inhibits osteogenesis in wild-type cells [52]. This altered signaling promotes enhanced chondrogenic and osteogenic differentiation of skeletal progenitor cells and endothelial-to-mesenchymal transition, contributing to pathologic bone formation [52].
In PAH, iPSC-derived endothelial cells with BMPR2 mutations exhibit impaired barrier function, increased apoptosis, and dysregulated angiogenesis [52]. When exposed to inflammatory cytokines or hypoxia, these cells produce more extracellular matrix and show enhanced proliferation, mirroring the vascular remodeling observed in patients [52]. Interestingly, iPSC models have revealed cell-type-specific effects of BMPR2 mutations, with endothelial cells being more severely affected than smooth muscle cells in some contexts [52].
HHT models using patient-derived iPSCs have uncovered early developmental alterations in vascular network formation and impaired pericyte coverage of endothelial tubes, providing mechanistic insights into the formation of fragile, dilated vessels characteristic of the disorder [52].
Table 2: BMP-Related Rare Diseases: Modeling Approaches and Phenotypes
| Disease | Gene Mutations | Key Cell Types Derived | Disease-Relevant Phenotypes |
|---|---|---|---|
| FOP | ACVR1 (ALK2) | Skeletal progenitors, endothelial cells | Enhanced chondrogenesis/osteogenesis, aberrant activin A response, EndMT |
| PAH | BMPR2, ACVRL1 | Pulmonary arterial endothelial cells, smooth muscle cells | Increased proliferation, apoptosis resistance, inflammatory activation |
| HHT | ENG, ACVRL1 | Endothelial cells, vascular organoids | Vascular network abnormalities, impaired mural cell recruitment |
Technical Approaches and Methodologies
Experimental Workflows and Protocols
The successful application of iPSC technology to rare disease modeling requires robust, standardized workflows spanning cell reprogramming, quality control, differentiation, and phenotypic analysis. For reprogramming, non-integrating methods such as Sendai virus vectors or episomal plasmids are preferred to minimize genomic alterations [49]. Following reprogramming, comprehensive characterization is essential, including assessment of pluripotency markers (OCT4, SOX2, NANOG, SSEA antigens), karyotypic stability, and trilineage differentiation potential [49].
Disease-specific differentiation protocols are continually being refined to enhance efficiency, purity, and maturation. For Marfan syndrome cardiovascular modeling, established protocols generate VSMCs through either neural crest or paraxial mesoderm pathways with efficiencies exceeding 80-90% [49]. For Usher syndrome retinal models, multi-stage differentiation over 30-40 weeks produces retinal organoids with all major retinal cell types, including properly localized phototransduction proteins in photoreceptors [4].
Advanced model systems increasingly incorporate 3D culture platforms, co-culture systems, and biomechanical stimulation to enhance physiological relevance. For BMP-related vascular disorders, exposure of endothelial cells to laminar shear stress significantly improves maturation and promotes the acquisition of artery-specific markers [52]. Similarly, for Marfan syndrome aortopathy models, cyclic stretch of VSMCs in engineered tissues better recapitulates the mechanical environment of the aortic wall [49].
Signaling Pathway Analysis
A key strength of iPSC disease models is the ability to investigate dysregulated signaling pathways in human cells with patient-specific genetic backgrounds. For Marfan syndrome, analysis typically focuses on TGF-β signaling readouts such as phospho-SMAD2/3 levels, though increasing attention is being paid to BMP signaling (phospho-SMAD1/5/8) and ERK1/2 activation [49]. For BMP-related disorders, comprehensive pathway analysis includes not only canonical SMAD signaling but also non-canonical pathways such as MAPK and PI3K-AKT [52].
The following diagram illustrates the key signaling pathways involved in these rare diseases, particularly highlighting the TGF-β/BMP pathway central to Marfan syndrome and BMP-related disorders:
Diagram 1: Signaling pathways in rare diseases. Mutated genes (red) affect TGF-β/BMP signaling, leading to disrupted cellular processes (blue) and associated diseases (green).
Research Reagent Solutions
The following table details essential reagents and tools used in iPSC-based modeling of rare diseases:
Table 3: Essential Research Reagents for iPSC Disease Modeling
| Reagent Category | Specific Examples | Application in Rare Disease Modeling |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC | Generation of patient-specific iPSCs from somatic cells [49] |
| CRISPR-Cas9 Systems | Cas9 nucleases, gRNA vectors | Creation of isogenic controls via precise genome editing [50] [51] |
| Differentiation Kits | Commercial cardiomyocyte, neuronal, hepatocyte kits | Standardized generation of disease-relevant cell types [50] |
| Extracellular Matrix | Matrigel, laminin, fibronectin | Substrate for 2D culture and 3D organoid formation [52] |
| Cytokines/Growth Factors | BMP4, TGF-β, activin A, VEGF | Directed differentiation and pathway stimulation studies [52] [49] |
| Pathway Inhibitors | Losartan, dorsomorphin, SB431542 | Therapeutic testing and mechanistic studies [52] [49] |
| Characterization Antibodies | Anti-OCT4, SSEA-4, cell-type-specific markers | Quality control of pluripotency and differentiation [49] |
iPSC-based disease models have emerged as powerful tools for unraveling the pathophysiology of rare genetic disorders and accelerating therapeutic development. The case studies presented here—covering Usher syndrome, Marfan syndrome, and BMP-related rare diseases—demonstrate how this technology enables researchers to recapitulate disease-specific phenotypes in vitro, uncover novel mechanistic insights, and test potential therapeutic strategies in human cellular systems with patient-specific genetic backgrounds.
As the field advances, key challenges remain, including enhancing the maturation of iPSC-derived cells, improving the complexity and physiological relevance of 3D model systems, and developing standardized protocols to ensure reproducibility across laboratories [4] [51]. The integration of iPSC models with emerging technologies such as single-cell multi-omics, high-content screening, and in silico modeling promises to further enhance their utility for both basic research and drug discovery [6].
For the rare disease community, iPSC technology represents more than just a research tool—it offers hope for addressing the profound unmet therapeutic needs of patients. By providing human-relevant models that bridge the gap between animal studies and clinical trials, iPSC-based approaches have the potential to de-risk drug development and bring effective treatments to patients more rapidly. As these technologies continue to evolve and mature, they will undoubtedly play an increasingly central role in the quest to understand and treat rare genetic disorders.
Navigating Technical Complexities and Enhancing Model Fidelity
Addressing Genomic and Epigenetic Instability in iPSC Cultures
Induced pluripotent stem cells (iPSCs) hold transformative potential for modeling rare genetic disorders and developing regenerative therapies. However, their clinical and research utility is significantly challenged by genomic and epigenetic instability that arises during reprogramming and long-term culture [53] [54]. For rare disease research, where patient-derived cells are invaluable and often scarce, ensuring the genetic and epigenetic fidelity of iPSC models is paramount to generating reproducible and meaningful data. This technical guide examines the sources and types of these instabilities, provides detailed protocols for their detection and mitigation, and outlines a comprehensive quality control framework to support robust iPSC-based disease modeling.
Origins of Genomic Variations in iPSCs
Genetic variations in iPSCs originate from three primary sources: pre-existing variations in parental somatic cells, mutations acquired during the reprogramming process itself, and passage-induced mutations that accumulate during prolonged culture [53]. One study demonstrated that at least half of the copy number variations (CNVs) observed in iPSCs are derived from low-frequency somatic variants present in the parental skin fibroblasts [53]. Meanwhile, research indicates that a substantial proportion of point mutations are acquired during the human iPSC reprogramming process [53].
Epigenetic Barriers in Reprogramming and Culture
The reprogramming of somatic cells to a pluripotent state requires profound epigenetic remodeling, including genome-wide DNA demethylation and histone modification changes [55]. This process is often incomplete, leading to epigenetic abnormalities that can affect iPSC differentiation potential and function. Key epigenetic marks include DNA methylation, which typically silences gene expression when present in promoter regions, and various histone modifications such as H3K4me3 (associated with active transcription) and H3K27me3 (associated with transcriptional repression) [55]. The retention of somatic memory—epigenetic marks characteristic of the cell of origin—can create an epigenetic barrier that influences lineage differentiation bias [55].
Table 1: Primary Sources of Genomic Instability in iPSC Cultures
| Source | Key Characteristics | Common Genetic Changes | Influencing Factors |
|---|---|---|---|
| Pre-existing Variations in Parental Somatic Cells | Low-frequency variants in source tissue become fixed during clonal expansion [53]. | SNVs, CNVs | Age of donor, cell type used for reprogramming (e.g., skin fibroblasts), donor's genetic background [53]. |
| Reprogramming-Induced Mutations | Occur during or immediately after the onset of reprogramming; not present in parental cells [53]. | Point mutations, CNVs (often deletions) [53] | Reprogramming method, stress from factor expression, oxidative stress [53] [54]. |
| Passage-Induced Mutations | Accumulate during prolonged in vitro culture; subject to selective pressure [53]. | Aneuploidy (e.g., trisomy 12, 8, X), specific CNVs (e.g., 20q11.21 amplification) [53] | Culture duration, enzymatic passaging methods, spontaneous mutations conferring growth advantage [53] [56]. |
Types and Hotspots of Genomic Instability
The most frequently observed chromosomal aberrations in iPSCs include trisomy 12, trisomy 8, and gains of the X chromosome [53]. The 20q11.21 amplification represents the most recurrent CNV hotspot, found in both iPSCs and ESCs [53]. This region contains genes associated with pluripotency and anti-apoptosis, such as DNMT3B, ID1, and BCL2L1, providing a selective advantage to cells carrying this duplication [53]. Single nucleotide variants (SNVs) have also been identified through whole genome sequencing, with studies reporting an average of approximately 10 protein-coding mutations per human iPSC line [53].
Figure 1: Origins and Evolution of Genomic Instability in iPSCs. The process from somatic cell to established iPSC line involves multiple stages where genetic variations can be introduced or selected for.
Detection Methods and Monitoring Strategies
Genomic Instability Detection Technologies
A tiered approach utilizing complementary technologies is recommended for comprehensive genomic assessment [53]. Each method varies in resolution, cost, and the specific type of abnormalities it detects, as summarized in Table 2.
Table 2: Methods for Detecting Genomic Instability in iPSCs
| Method | Resolution | Key Applications | Limitations | Recommended Frequency |
|---|---|---|---|---|
| G-banding Karyotyping | ~5-10 Mb | Detection of numerical chromosomal changes (aneuploidy) and large structural rearrangements [53]. | Limited resolution; cannot detect small CNVs or SNVs [53]. | Early passages (P7-P10) and every 10-15 passages thereafter [56]. |
| SNP/Array CGH | ~50-100 kb | Genome-wide detection of CNVs and loss of heterozygosity (LOH) [53]. | Cannot detect balanced translocations/inversions or low-frequency mosaicism [53]. | During master cell bank establishment and periodically for quality control. |
| Whole Genome Sequencing (WGS) | Single nucleotide | Comprehensive detection of SNVs, small indels, CNVs, and structural variants across entire genome [53]. | Higher cost; requires bioinformatics expertise; may detect variants of unknown significance [53]. | For comprehensive characterization of master cell banks and critical study lines. |
Epigenetic Analysis Methods
Evaluating the epigenetic landscape of iPSCs is equally critical, particularly for disease modeling applications. Key methodologies include:
- DNA Methylation Analysis: Bisulfite sequencing provides base-resolution mapping of DNA methylation, revealing the methylation status of pluripotency and differentiation-associated genes [55].
- Chromatin Immunoprecipitation (ChIP): Using antibodies specific to histone modifications (e.g., H3K4me3, H3K27me3) to assess the chromatin state of key regulatory regions [55].
- Teratoma Formation Assay: An in vivo test for developmental potential wherein iPSCs are injected into immunodeficient mice and resulting tumors are assessed for differentiation into all three germ layers [56].
Mitigation Strategies and Experimental Protocols
Culture Conditions to Minimize Instability
The choice of culture system significantly impacts the genomic stability of iPSCs. Feeder-free, chemically defined media such as Essential 8 (E8) medium reduce selective pressures and improve reproducibility compared to serum-containing systems [56]. For passaging, non-enzymatic methods using EDTA-based solutions (e.g., Versene) are recommended over enzymatic dissociation, as they minimize cellular stress and apoptosis [56]. Maintaining optimal seeding density is also crucial—most hiPSC lines should reach 70-80% confluence within 4-5 days when passaged at standard densities [56].
Protocol: Routine iPSC Culture and Passaging
Basic Protocol 1: Propagation of hiPSCs in Feeder-Free Conditions [56]
- Coating: Dilute Matrigel or other extracellular matrix (e.g., Laminin-521) in cold DMEM/F-12. Add to culture vessels and incubate at room temperature for 1 hour.
- Preparation: Pre-warm Essential 8 Medium, DMEM/F-12, and 0.5 mM EDTA (Versene) solution to room temperature.
- Passaging:
- Aspirate medium from iPSC cultures and wash once with DMEM/F-12.
- Add appropriate volume of Versene solution to cover the surface and incubate at 37°C for 5-8 minutes.
- Monitor cells under microscope until edges of colonies begin to detach.
- Aspirate Versene and add Essential 8 Medium. Gently pipette to dislodge cells into small clusters.
- Transfer cell suspension to Matrigel-coated plates containing fresh Essential 8 Medium at appropriate split ratio (typically 1:10 to 1:20).
- Maintenance: Change medium daily. Visually inspect cultures daily for spontaneous differentiation and manually remove differentiated areas if present.
Protocol: Characterization of Pluripotency and Genetic Integrity
Basic Protocol 3: Immunocytochemical Analysis of Pluripotency Markers [56]
- Fixation: Culture iPSCs on Matrigel-coated glass coverslips until 70-80% confluent. Aspirate medium and fix with 4% paraformaldehyde for 15 minutes at room temperature.
- Permeabilization and Blocking: Permeabilize cells with 0.1% Triton X-100 for 10 minutes, then block with 3% bovine serum albumin (BSA) for 1 hour.
- Antibody Staining:
- Incubate with primary antibodies against pluripotency markers (OCT4, SOX2, NANOG, SSEA-4) diluted in blocking buffer overnight at 4°C.
- Wash 3 times with PBS, then incubate with fluorophore-conjugated secondary antibodies for 1 hour at room temperature in the dark.
- Counterstain nuclei with DAPI and mount on glass slides.
- Analysis: Image using fluorescence microscopy. High-quality iPSCs should show >90% positive staining for core pluripotency factors.
Alternate Protocol: Flow Cytometry Analysis [56]
For quantitative assessment, dissociate iPSCs to single cells using Accutase, fix and permeabilize, then stain with antibodies against pluripotency markers for analysis by flow cytometry. This method provides quantitative data on the percentage of cells expressing key pluripotency markers.
Epigenetic Modulation Strategies
Epigenetic modifiers can be employed to improve reprogramming efficiency and potentially reset aberrant epigenetic marks:
Table 3: Epigenetic Modulators in iPSC Generation and Culture
| Epigenetic Target | Chemical Drug | Effect on Reprogramming | Proposed Mechanism |
|---|---|---|---|
| DNA Methylation | 5-Azacytidine (AZA) [55] | Improves efficiency [55] | DNA methyltransferase inhibitor; promotes demethylation and reactivation of pluripotency genes. |
| Histone Acetylation | Valproic Acid (VPA) [55] | Enables iPSC generation with only Oct4 and Sox2 [55] | Histone deacetylase (HDAC) inhibitor; creates more open chromatin state. |
| Histone Acetylation | Butyrate [55] | Significantly improves human iPSC generation efficiency [55] | HDAC inhibitor; more potent than VPA for human cell reprogramming. |
| Histone Methylation | BIX-01294 [55] | Stimulates iPSC generation; can compensate for Sox2 and c-Myc [55] | Inhibitor of G9a histone methyltransferase; reduces H3K9me2 repressive mark. |
Quality Control Framework for iPSC-Based Disease Modeling
Implementing a rigorous quality control framework is essential for generating reliable data from iPSC-based disease models, particularly for rare genetic disorders where reproducibility is critical.
Figure 2: Comprehensive Quality Control Workflow for iPSC Lines. A multi-tiered approach is necessary to ensure the quality and stability of iPSC lines used for disease modeling research.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for iPSC Culture and Characterization
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Defined Culture Media | Essential 8 (E8) Medium [56] | Chemically defined, xeno-free medium for feeder-free iPSC culture. | Simpler formulation than earlier media; supports robust pluripotency. |
| Extracellular Matrices | Matrigel, Geltrex, Laminin-521 [56] | Coating substrate for cell attachment in feeder-free systems. | Matrigel is a complex mixture; defined laminins (e.g., 521) improve consistency. |
| Non-Enzymatic Passaging Reagents | Versene (EDTA) [56] | Gentle, enzyme-free dissociation of iPSC colonies. | Maintains high viability; helps preserve genomic stability compared to enzymes. |
| Pluripotency Markers | Antibodies to OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 [56] | Characterization of pluripotent state via immunostaining or flow cytometry. | Core panel for routine quality control; should show >90% positive staining. |
| Genomic Integrity Assays | G-banding kits, SNP array kits, WGS services [53] [56] | Detection of chromosomal abnormalities and genetic variations. | Tiered approach based on need and resources; karyotyping is a minimum requirement. |
| Vector Clearance Tests | RT-PCR for Sendai virus [56] | Confirm clearance of reprogramming vectors in established iPSC lines. | Critical for ensuring transgene-free status, especially for clinical applications. |
The systematic addressing of genomic and epigenetic instability is fundamental to advancing iPSC-based disease modeling for rare genetic disorders. Through understanding the origins of instability, implementing sensitive detection methods, adopting culture practices that minimize selective pressures, and establishing rigorous quality control frameworks, researchers can significantly enhance the reliability and reproducibility of their iPSC models. As the field progresses, integrating more sophisticated epigenetic editing tools and organoid technologies will further strengthen our ability to model rare diseases with high fidelity, ultimately accelerating the development of targeted therapeutics for these conditions with high unmet medical needs.
Optimizing Differentiation and Maturation Protocols for Disease-Relevant Adult Phenotypes
The application of induced pluripotent stem cell (iPSC) technology in modeling rare genetic disorders represents a transformative approach for pathological analysis and therapeutic development, particularly for conditions where patient samples are exceedingly scarce [57]. However, a significant challenge persists: many iPSC-derived cells exhibit fetal-like characteristics that may not accurately recapitulate the adult phenotypes often required for studying late-onset diseases [58] [59]. The functional maturity of resulting neuronal networks remains one of the most important considerations in establishing optimized and standardized methods for neural differentiation of iPSCs [59]. Optimizing differentiation and maturation protocols is therefore paramount for generating disease-relevant adult phenotypes that can yield mechanistically insightful and therapeutically actionable data.
This technical guide synthesizes current advancements in iPSC differentiation strategies, focusing on protocol optimization for enhanced functional maturity, relevance to adult disease states, and application in rare genetic disorder research. We provide detailed methodologies, quantitative comparisons, and standardized workflows to facilitate the generation of more predictive in vitro models for drug discovery and pathophysiological investigation.
Current Challenges in Achieving Adult Phenotypes
Despite significant advancements in iPSC technology, several limitations persist in recapitulating disease-specific pathological phenotypes and mechanistic pathways. Protocol heterogeneity remains a critical challenge due to differences in cellular/tissue sources, induction methods, and culture conditions [58]. Existing induction protocols still face technical complexities and cannot indefinitely generate all desired human cell types [58]. Furthermore, functional immaturity often plagues iPSC-derived models, with many cells exhibiting embryonic or fetal characteristics rather than the adult phenotypes necessary for modeling late-onset diseases [59]. This limitation is particularly problematic for neurodegenerative disease modeling, where adult neuronal electrophysiological properties are essential for accurate pathophysiological representation.
Optimization Strategies for Enhanced Differentiation and Maturation
Improved Differentiation Protocols
Recent protocol refinements have demonstrated substantial improvements in maturation outcomes across multiple cell lineages. In hematopoietic differentiation, an optimized 2D-multistep monolayer method incorporating aryl hydrocarbon receptor (AhR) hyperactivation generated 7-fold greater efficiency in producing CD34+ progenitors while reducing hands-on time by 40% and cutting reagent costs by half [60]. Key modifications included omitting select medium changes, extending Wnt activation, and adding reagents directly to existing cultures rather than complete medium replacement [60].
For neuronal differentiation, a simplified protocol consistently generated electrophysiologically mature iPSC-derived cortical lineage neuronal networks without requiring astrocyte co-culture or specialized media [59]. This approach produced networks with a consistent 60:40 neuron-to-astrocyte ratio arising from common forebrain neural progenitors, closely mimicking developmental processes [59]. The resulting neurons demonstrated mature electrophysiological properties, including appropriate resting membrane potential (-58.2±1.0 mV), action potential threshold (-50.9±0.5 mV), and spontaneous synaptic activity [59].
Advanced Maturation Techniques
Three-Dimensional Culture Systems
The integration of cerebral organoid technology has propelled iPSC applications to new stages by enabling the development of complex neural structures [58]. Patient-derived or CRISPR-edited cerebral organoids serve as ideal disease models that better recapitulate the cellular diversity and spatial organization of native tissue [58] [18]. These 3D models demonstrate particular utility for rare diseases where structural abnormalities can be reproduced using iPSC-derived cerebral organoids [57].
Co-culture and Microenvironment Optimization
Neuron-astrocyte interactions are critical during neurodevelopment and in the adult brain, with astrocytes substantially improving the functional maturation of human pluripotent stem cell-derived neurons [59]. Whereas some protocols utilize exogenous astrocyte co-culture, more physiological approaches differentiate both cell types from a common neural progenitor, enhancing developmental relevance and reducing variability [59].
Protocol Selection Framework
Table 1: Direct Comparison of Hematopoietic Differentiation Methods
| Method Type | Efficiency (CD34+ cells) | Functional Progenitors | Cost Index | Hands-on Time | Phenotype Recapitulation |
|---|---|---|---|---|---|
| 2D-multistep (optimized) | 7× higher than original | Robust CFU formation; multilineage potential | 50% of original | 40% reduction | Accurate for DS and β-thalassemia |
| 2D-simple | Moderate | Limited lineage specificity | Low | Low | Variable disease specificity |
| 3D-EB multistep | High | Good myeloid potential | High | High | Moderate sensitivity |
| 3D-EB simple | Low | Restricted potential | Moderate | Moderate | Limited disease modeling |
Table 2: Electrophysiological Maturity Metrics in Optimized Neuronal Differentiation
| Parameter | Value (Mean ± SE) | Benchmark for Maturity | Protocol Duration |
|---|---|---|---|
| Resting Membrane Potential | -58.2 ± 1.0 mV | <-55 mV | 8-10 weeks |
| Capacitance | 49.1 ± 2.9 pF | >45 pF | 8-10 weeks |
| Action Potential Threshold | -50.9 ± 0.5 mV | <-50 mV | 8-10 weeks |
| Action Potential Amplitude | 66.5 ± 1.3 mV | >65 mV | 8-10 weeks |
| Neurons Firing APs | ~100% | >95% | 8-10 weeks |
| Spontaneous Synaptic Activity | 74% of cells | >70% | 8-10 weeks |
Signaling Pathway Manipulation for Lineage-Specific Maturation
Precise control of developmental signaling pathways is essential for directing lineage specification and functional maturation. The diagram below illustrates the key signaling pathways targeted in optimized neural differentiation protocols:
Signaling Pathways in Neural Differentiation
The optimized 2D-multistep hematopoietic protocol incorporates AhR hyperactivation using 6-formylindolo[3,2-b]carbazole (FICZ) to drive expansion of hematopoietic progenitor cells, particularly megakaryocyte-erythroid progenitors [60]. For midbrain dopaminergic neuron differentiation—critical for Parkinson's disease modeling—precise temporal control of SHH and Wnt signaling is essential for proper regional specification and functional maturation [61].
Experimental Workflow for Optimized Differentiation
The following diagram outlines a comprehensive workflow for generating mature, disease-relevant phenotypes from iPSCs:
iPSC Differentiation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for iPSC Differentiation
| Reagent Category | Specific Examples | Function in Differentiation | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT3/4, SOX2, KLF4, c-MYC (OSKM) [58] | Induction of pluripotency in somatic cells | Episomal plasmid delivery reduces genomic integration risk [57] |
| Neural Induction Agents | SMAD inhibitors (Noggin, SB431542) [59] | Direct differentiation toward neural lineage | Dual inhibition enhances efficiency and purity |
| Patterning Molecules | SHH, Wnt agonists/antagonists, FGF2 [61] | Regional specification of neural subtypes | Precise temporal control critical for midbrain dopamine neurons |
| Maturation Enhancers | BDNF, GDNF, ascorbic acid, db-cAMP [59] | Promotion of functional maturity | Combination required for electrophysiological maturation |
| Small Molecule Enhancers | CHIR99021 (GSK3β inhibitor), A-83-01 (TGF-β inhibitor) [58] | Enhance reprogramming and differentiation efficiency | Chemical cocktails can replace transcription factors |
| Extracellular Matrix | Laminin, iMatrix-511, Matrigel [57] [59] | Provide structural support and biochemical cues | Influences cell polarity, migration, and differentiation |
Detailed Methodological Protocols
Optimized Neuronal Differentiation Protocol
This protocol generates electrophysiologically mature cortical lineage neurons without specialized media or astrocyte co-culture [59]:
Neural Precursor Cell (NPC) Generation:
- Culture iPSCs on mouse embryonic fibroblasts or in feeder-free conditions with essential 8 medium.
- Dissociate iPSCs with collagenase (100 U/ml for 7 minutes at 37°C).
- Form embryoid bodies (EBs) in non-adherent plates in human ES cell medium on orbital shaker.
- At day 2, transition to neural induction medium (DMEM/F12, 1% N2 supplement, 2 μg/ml heparin).
- At day 7, plate slightly dissociated EBs onto laminin-coated dishes (20 μg/ml).
- Culture in neural induction medium until day 14, then switch to NPC medium.
- Passage at 1:4 ratio when confluent; cells become stable NPCs after passage 5.
Neural Differentiation and Maturation:
- Plate NPCs (passages 5-11) on poly-L-ornithine/laminin-coated coverslips.
- Use neural differentiation medium: Neurobasal medium, 1% N2, 2% B27-RA, MEM/NEAA, BDNF (20 ng/ml), GDNF (20 ng/ml), db-cAMP (1 μM), ascorbic acid (200 μg/ml), and laminin (2 μg/ml).
- For weeks 1-4, perform complete medium changes three times weekly.
- After 4 weeks, change only half the medium volume to preserve secreted factors.
- Functional maturity is achieved between 8-10 weeks post-plating.
Optimized Hematopoietic Differentiation Protocol
This 2D-multistep method incorporates AhR hyperactivation for enhanced hematopoietic progenitor production [60]:
Key Modifications from Original Protocol:
- Omit medium changes on days 2, 3, 7, 10, and 15.
- Add reagents directly to culture wells on days 2, 7, and 10.
- Extend Wnt activation by 2 days.
- Eliminate day-3 increase in bFGF concentration.
Differentiation Process:
- Initiate differentiation with BMP4, VEGF, and Wnt activation.
- Add FICZ (AhR agonist) on specified days to expand hematopoietic progenitors.
- Harvest suspension cells at day 16 without disrupting adherent monolayer.
- Characterize by flow cytometry for CD34, CD43, CD45, and lineage-specific markers.
- Verify function using colony-forming unit (CFU) assays.
Quality Control and Validation Metrics
Rigorous quality assessment is essential for ensuring phenotype relevance and reproducibility. For neuronal differentiation, validate through:
- Immunocytochemistry: MAP2, Synapsin, PSD95 for neurons; GFAP for astrocytes; regional markers (FOXG1, TBR1) for identity confirmation [59].
- Electrophysiology: Whole-cell patch clamp recording to verify mature properties including resting membrane potential, action potential generation, and synaptic activity [59].
- Gene Expression: qPCR for pluripotency factors (OCT3/4, NANOG) during iPSC stage, neural markers during differentiation [57].
For hematopoietic differentiation, employ:
- Flow Cytometry: CD34+ progenitor quantification, CD34+CD45+ and CD34+CD43+ hematopoietic progenitors, lineage commitment markers [60].
- Functional Assays: Colony-forming unit (CFU) assays to evaluate multilineage potential and progenitor frequency [60].
- Molecular Analysis: Gene expression profiling of key hematopoietic regulators.
Optimizing differentiation and maturation protocols for disease-relevant adult phenotypes requires integrated consideration of signaling pathway manipulation, culture system design, and functional validation. The strategies outlined herein provide a framework for generating more physiologically relevant models of rare genetic disorders, enabling more accurate disease modeling, drug screening, and therapeutic development. As iPSC technology continues to evolve, standardized protocols ensuring mature cellular phenotypes will be increasingly crucial for translating basic research into clinical applications for rare diseases.
The use of induced pluripotent stem cells (iPSCs) has revolutionized the modeling of human genetic diseases, offering unprecedented access to patient-specific human cell types for investigating disease mechanisms and developing new treatments. This is particularly transformative for rare genetic disorders and neurological conditions, where access to primary human tissue is severely limited. However, the power of iPSC-based disease modeling is critically dependent on appropriately managing multiple sources of experimental variance. A cornerstone of reproducible iPSC research lies in optimizing study design—specifically, determining the minimum number of independent donor individuals and the number of iPSC lines per donor required to achieve robust and statistically significant results. Underpowered studies plagued by uncontrolled variability diminish the reliability of findings and hinder the translation of preclinical results to clinical applications. This technical guide, framed within the context of rare genetic disorder research, synthesizes current empirical evidence to provide researchers, scientists, and drug development professionals with a framework for designing rigorous and efficient iPSC experiments.
The Challenge of Variance in iPSC Models
iPSC derivation and differentiation are multistep processes where small variations at each stage can accumulate, generating significantly different outcomes [62]. The substantial impact of this variability can overwhelm the biological variation of interest, especially when studying phenotypes with small effect sizes. The primary sources of this variance can be categorized as follows:
Genetic Background: The genetic background of the donor is the most significant source of heterogeneity in iPSC models. Studies have reported that 5-46% of the variation in iPSC cell phenotypes is attributable to inter-individual differences [62]. iPSC lines derived from the same individual are consistently more similar to each other than to lines from different individuals, a pattern observed at the level of gene expression, epigenetic markers, and functional differentiation potential [62] [63].
Technical and Experimental Noise: This includes variability introduced during reprogramming, clone selection, cell culture, and differentiation. Variance can arise from differences in culture batches, reagents, and handling protocols. One study using RNA sequencing on iPSCs modeling Lesch-Nyhan disease found that, when all lines were produced in parallel using the same methods, most variance in gene expression came from technical factors unrelated to the individual donor [8].
Somatic Cell Memory: The potential retention of epigenetic memory from the parent somatic cell type was initially a major concern. However, research comparing genetically matched iPSCs from different tissues (e.g., fibroblasts and blood) has shown that while lines from the same donor are highly similar, donor-specific genetic variation imparts a stronger influence on the iPSC's molecular profile and differentiation potential than the cell type of origin [63].
Quantitative Guidelines for iPSC Study Design
A critical review of recent literature reveals a growing consensus on the optimal number of donors and lines needed to achieve sufficient statistical power. The following table summarizes key quantitative findings from empirical studies.
Table 1: Empirical Recommendations for iPSC Study Design from Key Publications
| Study Focus | Recommended Number of Unique Donors | Recommended Lines Per Donor | Key Findings |
|---|---|---|---|
| Transcriptomics (Lesch-Nyhan disease) [8] | 3-4 per group | 2 | Best results were obtained with iPSC lines from 3-4 unique individuals per group. Using 2 lines per individual improved results without needing statistical corrections for multiple lines from the same donor. |
| Proteomics (iPSC-derived astrocytes) [64] | More donors prioritized | Fewer clones | Including more independent donors has a much larger positive influence on statistical power than adding more clones per donor. Inter-donor variability was significantly larger than inter-clonal variability. |
| Power Analysis (iPSC-derived neurons) [65] | Case-control designs often underpowered | N/A | Analysis showed that published case-control iPSC studies are generally underpowered. Designs using multiple isogenic pairs can increase absolute power up to 60% or require up to 5-fold fewer lines. |
These findings coalesce around several critical principles for experimental design:
- Prioritize Donor Number Over Clone Number: The most consistent finding across multiple studies and data types (transcriptomic, proteomic, functional) is that increasing the number of independent biological donors (n) has the greatest positive impact on statistical power [64]. This is a direct consequence of genetic background being the dominant source of variance.
- A Practical Minimum: For a robust case-control study, a minimum of 3-4 unique donors per experimental group is a widely supported baseline [8].
- Lines Per Donor: Including 2 iPSC lines per donor is recommended to control for clonal variability and technical artifacts arising from the reprogramming process itself, without overly complicating the statistical analysis [8].
- The Isogenic Advantage: For studies investigating the effect of a specific genetic variant, isogenic controls—where the mutation is introduced or corrected in a control background—provide a powerful alternative. This design controls for genetic background noise and can achieve equivalent statistical power with significantly fewer lines, though it may limit generalizability to a diverse patient population [65].
Detailed Experimental Protocols for Robust Study Design
Protocol for a Case-Control Study of a Rare Genetic Disorder
This protocol outlines the steps for a well-powered investigation using patient-derived iPSCs.
Step 1: Donor Recruitment and iPSC Generation
- Cohort Definition: Recruit a minimum of 3-4 patients with a confirmed genetic diagnosis of the disorder and 3-4 genetically matched healthy controls. Secure informed consent and ethical approval.
- Reprogramming: Reprogram somatic cells (e.g., fibroblasts or peripheral blood mononuclear cells) from each donor using a non-integrating method (e.g., Sendai virus or episomal vectors) to minimize genomic alterations.
- Clone Selection: Pick a minimum of 3 clonal lines per donor at random after confirming successful reprogramming (via pluripotency marker expression and teratoma formation or in vitro differentiation potential). Avoid cherry-picking clones based on morphology.
Step 2: Quality Control and Line Expansion
- Quality Control: Perform karyotyping and STR profiling on all clones to confirm genomic integrity and identity. Use SNP arrays to check for copy number variations.
- Line Expansion: Expand and bank a master cell stock for each of the 2 selected lines per donor. This ensures all subsequent experiments use cells from the same passage range.
Step 3: Parallel Differentiation and Phenotyping
- Differentiation: Differentiate all iPSC lines in parallel to the relevant cell type (e.g., cortical neurons for a neurodevelopmental disorder) using a standardized, validated protocol. For each differentiation run, include all lines and batches in a randomized block design to avoid batch effects confounded with group identity.
- Phenotypic Assay: At the appropriate maturation timepoint, perform the key functional assay (e.g., electrophysiology, calcium imaging, proteomic analysis) on the differentiated cells. The experiment should be repeated across multiple independent culture batches to account for technical variance.
Step 4: Data Analysis and Statistics
- Statistical Modeling: Use mixed-effects models for analysis. This allows the inclusion of "Donor" as a random effect, correctly accounting for the non-independence of multiple lines and batches derived from the same individual [65]. This approach prevents inflation of false positive rates.
- Power Analysis: For future studies, use published web tools (e.g., https://jessiebrunner.shinyapps.io/App_PowerCurves/) to estimate statistical power for different iPSC study designs and sample sizes based on pilot data [65].
Protocol for an Isogenic Line Validation Study
This protocol is used to confirm the phenotypic impact of a specific mutation.
Step 1: Line Generation
- Use CRISPR/Cas9 gene editing to introduce the patient-specific point mutation into a well-characterized control iPSC line. Alternatively, correct the mutation in a patient-derived line.
- Generate at least 2-3 independently edited clonal lines for each condition (isogenic mutant and isogenic control) to control for potential off-target effects.
Step 2: Validation
- Sequentially validate clones by Sanger sequencing to confirm the intended edit, karyotyping to ensure genomic integrity, and pluripotency marker staining.
Step 3: Differentiation and Phenotyping
- Differentiate the validated isogenic pairs in parallel, using the same differentiation protocol and batch design as above.
- Perform the phenotypic assays. The reduced genetic noise in this design often allows for clear detection of phenotype with fewer replicates, but the use of multiple independent clones is still critical.
Visualizing Variance and Experimental Design
The following diagram illustrates the primary sources of variance in iPSC studies and the core principles of two common experimental designs.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and their functions critical for successful and reproducible iPSC disease modeling.
Table 2: Essential Reagents and Materials for iPSC Disease Modeling Studies
| Reagent / Material | Function & Importance in Disease Modeling |
|---|---|
| Non-Integrating Reprogramming Vectors (e.g., Sendai virus, episomal plasmids) | To generate footprint-free iPSCs from patient somatic cells, minimizing genetic alterations that could confound disease-related phenotypes. |
| Genetically Defined Control Lines | Essential for case-control studies. Includes healthy control lines matched for sex, ancestry, and ideally, familial background to reduce genetic noise. |
| Isogenic iPSC Pairs | The gold standard for confirming causality of a genetic variant. Created via gene-editing to differ only at the locus of interest, providing a clean genetic background. |
| Standardized Differentiation Kits/Protocols | To ensure consistent, efficient, and reproducible generation of the relevant cell type (e.g., cortical neurons, cardiomyocytes) across all lines and batches. |
| Validated Phenotyping Assays | Functional readouts (e.g., multi-electrode arrays for neuronal activity, Seahorse analyzers for metabolism) that are robust, quantitative, and relevant to the disease pathology. |
| Quality Control Assays | Karyotyping, mycoplasma testing, and pluripotency validation kits are non-negotiable for confirming the integrity and identity of iPSC lines throughout the study. |
The reliability of conclusions drawn from iPSC disease models is inextricably linked to the rigor of the experimental design. For the field of rare genetic disorders, where patient samples are scarce and the imperative for robust data is high, adhering to evidence-based guidelines is paramount. The collective findings synthesized in this guide underscore that statistical power and experimental reproducibility are maximized by prioritizing the number of independent biological donors, typically 3-4 per group, and using a minimum of 2 lines per donor to control for clonal and technical variance. Furthermore, researchers must employ appropriate statistical models that account for the nested structure of iPSC data. By integrating these principles into their workflow—leveraging both carefully designed case-control cohorts and powerful isogenic pairs—scientists can effectively manage experimental variance, thereby accelerating the discovery of meaningful disease mechanisms and potential therapeutic avenues.
The study of ultra-rare neurodevelopmental disorders (NDDs) presents significant scientific challenges, including limited patient populations, scarcity of tissue for analysis, and the frequent absence of representative animal models [66]. Induced pluripotent stem cell (iPSC) technology has emerged as a powerful platform for investigating disease mechanisms by enabling the creation of patient-specific neural cells [67]. However, modeling these disorders effectively requires overcoming substantial technical hurdles, particularly in achieving robust and reproducible differentiation of iPSCs into the relevant neural cell types affected by the disease [36]. This case study examines the strategic approaches for addressing differentiation challenges when modeling an ultra-rare neurodevelopmental disorder, framed within the broader context of iPSC disease modeling for rare genetic disease research.
Background: The iPSC Advantage in Rare Neurodevelopmental Disorders
Rare diseases collectively affect an estimated 263–446 million people worldwide, with approximately 80% having a genetic origin [3]. A substantial proportion of these are neurodevelopmental disorders, which arise from disruptions in the highly coordinated molecular and cellular events of brain development [66] [67]. The key advantage of iPSC-based models lies in their ability to recapitulate a patient's unique genetic signature and the disease-altered trajectory of early brain development, providing a window into pathological processes that begin during prenatal development [67].
For ultra-rare disorders, the challenge of obtaining sufficient sample sizes is particularly acute. Recent research indicates that robust experimental design requires iPSC lines from 3-4 unique individuals per group, with 2 lines per individual recommended to strengthen results [8]. This approach helps address the inherent variability in iPSC models while accounting for the practical constraints of studying extremely rare conditions.
Critical Challenges in Differentiation for Ultra-Rare NDDs
Technical and Biological Variability
A primary obstacle in modeling ultra-rare NDDs is the significant variability observed between iPSC lines, which can obscure disease-specific phenotypes. This variability stems from multiple sources:
- Reprogramming inconsistencies: Differences in epigenetic memory retention and reprogramming efficiency [36]
- Culture condition effects: Undefined culture conditions using fetal bovine serum (FBS) and fibroblast feeders increase inter-line variability [36]
- Genetic background diversity: The same mutation can produce different phenotypic outcomes across genetic backgrounds [13]
Recent studies demonstrate that defined culture conditions significantly reduce inter-line variability, promoting greater uniformity while maintaining pluripotency [36]. This standardization is crucial for distinguishing true disease phenotypes from technical artifacts.
Cell Type-Specific Differentiation Barriers
For many ultra-rare NDDs, the affected cell types may be specific neuronal subtypes or glial cells that are challenging to generate from iPSCs. For instance, studies of Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV) require the generation of dorsal root ganglia (DRG) organoids containing specific sensory neuron populations [13]. Similarly, modeling disorders involving cortical interneurons necessitates prolonged differentiation periods to capture late-born neuronal populations [13].
Strategic Framework for Overcoming Differentiation Challenges
Implementing Defined Culture Systems
Transitioning from undefined to defined culture conditions represents a critical first step in reducing variability. Research analyzing over 100 iPSC and embryonic stem cell lines demonstrated that defined conditions significantly reduce inter-line variability and decrease the expression of somatic cell markers that may persist in undefined conditions [36].
Table 1: Key Components of Defined Culture Systems for Robust Neural Differentiation
| Component | Undefined Conditions | Defined Conditions | Impact on Differentiation |
|---|---|---|---|
| Base Matrix | Fibroblast feeders, Matrigel | Laminin-521, Vitronectin | Reduces batch-to-batch variability in neural differentiation efficiency |
| Media | FBS-containing media | Essential 8 (E8), other defined formulations | Promotes uniform neural induction and patterning |
| Key Signaling Factors | Variable, unknown concentrations | Precise concentrations of bFGF, TGF-β | Enables consistent neural subtype specification |
Advanced Genome Engineering for Isogenic Controls
The creation of isogenic control lines through CRISPR/Cas9 gene editing is essential for controlling for genetic background effects. This approach involves correcting disease-causing mutations in patient-derived iPSCs or introducing specific mutations into control lines [68] [13]. For example, in studying HSAN IV caused by NTRK1 mutations, researchers generated isogenic controls by correcting the patient's mutations using CRISPR-based gene editing, enabling the isolation of phenotype effects specifically attributable to the disease-causing variant [13].
Recent innovations such as "village editing" – performing CRISPR/Cas9 gene editing in a cell village format across multiple donor lines – further enable the investigation of how specific mutations interact with different genetic backgrounds [13]. This approach is particularly valuable for understanding variable expressivity in ultra-rare disorders.
Complex Model Systems: From 2D to 3D
While 2D neuronal cultures have provided valuable insights, 3D model systems often better recapitulate the complexity of human neural development. Organoid and assembloid models enable the study of cell-cell interactions, migration, and tissue-level organization [3] [13].
Table 2: Comparison of iPSC-Based Neural Model Systems
| Model Type | Key Features | Differentiation Timeline | Applications in Ultra-Rare NDDs |
|---|---|---|---|
| 2D Monolayer Neurons | Relatively simple, homogeneous populations, amenable to high-content screening | 4-8 weeks | Electrophysiological studies, high-throughput drug screening |
| Brain Region-Specific Organoids | 3D architecture, multiple cell types, regional identity | 10-20 weeks | Disorders with known regional vulnerability, structural abnormalities |
| Assembloids | Multiple region integration, circuit formation, cell migration | 20-40+ weeks | Disorders affecting connectivity, interneuron migration defects |
For instance, dorsal-ventral assembloids have been used to model the prolonged migration of cortical interneurons, a process that extends into the postnatal period in humans [13]. These models revealed that interneuron chain migration requires both intrinsic neuronal cues and specific interactions with surrounding astrocytes – findings that could not be obtained from 2D systems.
Experimental Workflow for Differentiation Optimization
The following workflow outlines a systematic approach to developing and validating neural differentiation protocols for ultra-rare NDD modeling:
Key Methodological Details
Reprogramming and Quality Control: For ultra-rare disorders, it is essential to bank multiple clones (approximately 120 per donor) and rigorously quality control them through karyotyping, pluripotency tests (PluriTest), and clearance of reprogramming vectors [68]. This ensures the availability of high-quality starting material despite limited donor numbers.
Neural Induction and Subtype Specification: The choice of neural induction method (e.g., dual SMAD inhibition for cortical neurons) must be tailored to the disorder's affected cell types. For example, generating DRG organoids for HSAN IV modeling requires specific patterning factors to direct neural crest differentiation toward sensory neuron fates [13].
Maturation and Functional Validation: Many neurodevelopmental phenotypes manifest only after extended maturation. Protocols must accommodate extended culture periods (up to 390 days in some assembloid models) to capture late-onset phenotypes [13]. Functional validation should include electrophysiological measurements using micro-electrode arrays (MEAs), calcium imaging, and synaptic activity assessments.
Research Reagent Solutions for Ultra-Rare NDD Modeling
Table 3: Essential Research Reagents for iPSC-Based NDD Modeling
| Reagent Category | Specific Examples | Function in Differentiation | Technical Considerations |
|---|---|---|---|
| Reprogramming Systems | Non-integrating Sendai virus, Episomal vectors | Footprint-free reprogramming of patient somatic cells | Sendai virus requires confirmation of clearance; essential for clinical translation |
| Defined Culture Matrices | Laminin-521, Vitronectin | Replace undefined Matrigel and feeder layers | Promote consistent attachment and growth; reduce batch variability |
| Neural Induction Cocktails | Dual SMAD inhibitors (LDN-193189, SB431542) | Direct differentiation toward neural lineage | Concentration and timing critical for regional specification |
| Neural Patterning Factors | Retinoic acid, SHH, BMPs, WNTs | Specify regional identity and neuronal subtypes | Must be optimized for specific disorder-relevant brain regions |
| Gene Editing Tools | CRISPR/Cas9, TALENs | Create isogenic controls; introduce disease mutations | Require thorough off-target assessment and clonal validation |
| Cell Type Characterization Antibodies | PAX6 (neural progenitors), TBR1 (deep layer neurons), CTIP2 | Validate neural differentiation efficiency and identity | Essential for quality control at each differentiation stage |
Overcoming differentiation challenges in ultra-rare neurodevelopmental disorders requires a multifaceted approach centered on standardization, appropriate control strategies, and the implementation of physiologically relevant model systems. The integration of defined culture conditions, robust differentiation protocols, and advanced genome engineering enables researchers to distinguish genuine disease phenotypes from technical artifacts – a critical consideration when patient materials are extremely limited.
Future advances will likely come from continued refinement of differentiation protocols to enhance cellular maturity and diversity, the integration of iPSC models with multi-omics technologies, and the development of more complex assembloid systems that capture circuit-level abnormalities. Furthermore, initiatives to standardize protocols and share rare disease iPSC lines through international collaborations will be essential for accelerating progress in understanding these challenging conditions. As these technologies mature, they offer the promise of not only illuminating disease mechanisms but also identifying therapeutic strategies for conditions that have long eluded effective treatment.
The application of induced pluripotent stem cells (iPSCs) in modeling rare genetic disorders represents a transformative approach in biomedical research. Approximately 80% of rare diseases have a genetic origin, making patient-derived iPSCs and their isogenic controls unique model systems for mechanistic studies and therapeutic development [4]. However, the reliability of these models is fundamentally dependent on the quality of the underlying iPSCs. Genomic instability in iPSCs—including karyotypic abnormalities, copy number variations (CNVs), and single nucleotide polymorphisms—poses a significant challenge, with studies reporting an average of 6-12 protein-coding mutations per iPSC line [69]. For rare disease research, where patient-derived cells are often scarce and difficult to obtain, establishing robust quality control (QC) benchmarks is not merely advantageous but essential for generating physiologically relevant and reproducible data. This technical guide provides a comprehensive framework for quality control in iPSC generation and maintenance, specifically contextualized for rare disease modeling applications.
The Critical Role of QC in Rare Disease Modeling
iPSC-based models have emerged as indispensable tools for studying rare diseases like Juvenile Nephronophthisis, Usher syndrome, and Marfan syndrome [4]. The utility of these models hinges on their ability to accurately recapitulate disease pathophysiology without the confounding variables introduced by technical artifacts or genomic alterations acquired during reprogramming and culture.
Recent studies demonstrate that non-genetic factors such as induction set variations and operator techniques account for 30-70% of differentiation variability, while genetic factors (cell line-specific variations) contribute only 2-30% [70]. This highlights that stringent procedural controls are as critical as genomic assessments. Furthermore, iPSC genomic instability significantly impacts differentiation outcomes; cultures derived from genomically stable iPSCs exhibit reduced variance and improved marker expression profiles during motor neuron differentiation, directly enhancing model reliability for disease modeling [70].
The financial implications of inadequate QC are substantial, with rare disease healthcare costs being up to 10 times greater per patient per year than for more common diseases [4]. Implementing comprehensive QC benchmarks from the outset ensures more efficient use of scarce patient resources and accelerates the path to therapeutic development.
Assessing Pluripotency: Methodologies and Benchmarks
Defining Pluripotency in QC Frameworks
Pluripotency refers to a cell's capacity to differentiate into derivatives of all three germ layers. This functional potential must be rigorously demonstrated through multiple complementary assays. The qualitative assessment of pluripotency has evolved toward quantitative metrics that provide objective benchmarks for comparing iPSC lines across different reprogramming methods and laboratories [71].
Core Pluripotency Assessment Techniques
Table 1: Pluripotency Assessment Methodologies
| Method Category | Specific Techniques | Key Output Metrics | Acceptance Criteria |
|---|---|---|---|
| Gene Expression Analysis | qRT-PCR, RNA-Seq | Expression levels of core pluripotency factors (OCT4, SOX2, NANOG) | >50-fold expression vs. somatic cells [72] |
| Protein Expression Analysis | Immunocytochemistry, Flow Cytometry | Percentage of cells positive for pluripotency markers | >90% positive for OCT4, SOX2, SSEA-4 [73] |
| Functional Capacity Assays | In vitro spontaneous differentiation, In vivo teratoma formation | Presence of ectoderm, mesoderm, and endoderm derivatives | 3 germ layer formation in vitro; structured teratomas in vivo [69] |
| Epigenetic Status | Bisulfite sequencing, ChIP-PCR | Demethylation of pluripotency promoter regions | <30% methylation at OCT4 promoter [72] |
Experimental Protocol: Trilineage Differentiation Assessment
Materials:
- Basal Medium: DMEM/F12 supplemented with 20% KnockOut Serum Replacement, 1% GlutaMAX, 1% Non-Essential Amino Acids, and 0.1 mM β-mercaptoethanol
- Enzymatic Passaging Reagent: Versene or ReLeSR
- Extracellular Matrix: Matrigel or Geltrex
- Fixation Solution: 4% Paraformaldehyde (PFA) in PBS
- Germ Layer-Specific Antibodies: Anti-βIII-tubulin (ectoderm), Anti-α-smooth muscle actin (mesoderm), Anti-AFP (endoderm)
Procedure:
- Preparation: Culture iPSCs to 70-80% confluence in feeder-free conditions using mTeSR1 medium.
- Induction: Dissociate colonies into small clumps using ReLeSR and plate at high density in ultra-low attachment plates containing basal medium.
- Maintenance: Culture embryoid bodies for 14-21 days, changing medium every other day.
- Analysis: Transfer embryoid bodies to adhesion plates, allow outgrowth for 7 days, fix with 4% PFA, and perform immunocytochemistry for germ layer markers.
- Quantification: Image five random fields per biological replicate and quantify the percentage of area positive for each germ layer marker.
Monitoring Genomic Integrity: Approaches and Interpretation
Types of Genomic Abnormalities in iPSCs
iPSCs demonstrate a propensity for genomic instability that can be categorized into three primary classes:
- Karyotype Aberrations: Large-scale chromosomal abnormalities including aneuploidies (particularly trisomy of chromosomes 12, 17, or X) and structural rearrangements. These abnormalities have been extensively documented in both hiPSCs and hESCs [69].
- Copy Number Variations (CNVs): Deletions or amplifications of DNA segments ranging from 1kb to several Mb. Studies demonstrate that hiPSCs contain significantly more CNVs than non-pluripotent samples, with these variations frequently affecting common fragile sites or sub-telomeric regions [69].
- Single Nucleotide Variations (SNVs): Point mutations in coding regions, with whole exome sequencing revealing an average of 6 protein-coding mutations per iPSC line [69].
Genomic Stability Assessment Techniques
Table 2: Genomic Integrity Monitoring Methods
| Technique | Target Abnormalities | Detection Limit | Throughput | Key Applications |
|---|---|---|---|---|
| Karyotype G-banding | Aneuploidies, large structural rearrangements | >5-10 Mb | Low | Routine screening [69] |
| SNP Genotyping | CNVs, Uniparental Disomy (UPD), Loss of Heterozygosity (LOH) | >50 kb | Medium | Essential for UPD detection [69] |
| CGH/SNP Array | Genome-wide CNVs, aneuploidy | >10-50 kb | High | Comprehensive CNV screening [69] |
| Targeted qPCR | Common karyotypic abnormalities (e.g., 20q11.21 gain) | NA | High | Rapid screening of known hotspots [70] |
| Whole Exome/Genome Sequencing | SNVs, small indels, comprehensive variant profiling | Single nucleotide | Medium-High | Research settings, thorough characterization [69] |
Experimental Protocol: Targeted qPCR for Common Karyotypic Abnormalities
Rationale: A targeted RT-qPCR approach provides a cost-effective, rapid method for routine monitoring of the nine most common karyotypic abnormalities in human iPSCs, including gains at 1q, 12p13.31, 17q, 20q11.21, and Xp22.11 [70].
Materials:
- qPCR Assay: Commercial karyotyping PCR panels (e.g., STEMCELL Technologies) or custom-designed primers for common abnormality loci
- Instrument: Real-time PCR system with multiplexing capability
- Reference Genes: Primers for diploid regions on multiple chromosomes
Procedure:
- DNA Extraction: Isolate genomic DNA from iPSCs at approximately 80% confluence using a column-based method.
- qPCR Setup: Prepare reactions according to manufacturer's protocol, including reference samples with known copy numbers.
- Amplification: Run qPCR with appropriate cycling conditions.
- Data Analysis: Calculate copy number using the ΔΔCt method relative to reference genes.
- Interpretation: Cell lines with chromosomal copy numbers <1.5 or >2.5 (<0.7 or >1.3 for chromosome X in male lines) are considered "abnormal" and should be excluded from critical experiments [70].
The Quality Control Workflow: An Integrated Approach
The following diagram illustrates the comprehensive quality control workflow for iPSC generation and characterization, integrating both pluripotency and genomic integrity assessments:
Diagram 1: Comprehensive QC workflow for iPSC generation and characterization, integrating pluripotency and genomic integrity assessments.
Impact of Reprogramming and Culture on QC Outcomes
Reprogramming Method Selection
The choice of reprogramming method significantly influences genomic integrity and success rates. Non-integrating methods are strongly preferred for rare disease modeling due to their reduced risk of genomic alterations:
- Sendai Virus (SeV): Demonstrates significantly higher success rates compared to episomal methods while maintaining non-integrating characteristics [73].
- Episomal Vectors: Effective but with lower efficiency; requires careful monitoring for residual vector persistence.
- mRNA Reprogramming: Avoids genomic integration entirely but requires sophisticated delivery protocols.
Comparative studies show that non-integrating methods have a significantly lower number of CNVs, SNPs, and chromosomal mosaicism relative to integrating lentiviral methods [73].
Culture Conditions and Genomic Stability
Long-term culture of iPSCs presents substantial risks to genomic integrity. Studies demonstrate that iPSC genomic architecture changes over time in culture, directly impacting differentiation capacity and increasing phenotypic variability [70]. Specific culture-related considerations include:
- Passaging Methods: Enzymatic passaging (e.g., Versene, ReLeSR) versus mechanical passaging influences selection pressures on subpopulations.
- Oxygen Tension: Reduced oxygen tension (5% O₂) may reduce oxidative stress and associated DNA damage.
- Culture Substrate: Matrigel versus feeder-free systems can influence growth characteristics and genetic stability.
Routine monitoring is essential, as abnormalities such as 20q11.21 amplification provide a growth advantage that leads to progressive dominance of abnormal clones in culture [69].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for iPQC QC
| Reagent/Material | Function | Example Applications | Technical Notes |
|---|---|---|---|
| Sendai Viral Vectors | Delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC) | Primary cell reprogramming | Non-integrating; diluted out over passages [73] |
| Episomal Vectors | Non-integrating plasmid-based reprogramming | Fibroblast, PBMC reprogramming | Requires nucleofection; lower efficiency than SeV [73] |
| mTeSR1 Medium | Feeder-free maintenance of iPSCs | Routine culture, expansion | Defined medium supporting pluripotency [73] |
| Matrigel/Geltrex | Extracellular matrix for adhesion | Feeder-free culture systems | Provides essential adhesion signals [73] |
| Y-27632 (ROCK inhibitor) | Inhibits apoptosis in single cells | Post-thaw recovery, passaging | Critical for survival after dissociation [73] |
| Karyostat PCR Assay | Detection of common karyotypic abnormalities | Routine genomic screening | Targeted qPCR for 9 common abnormalities [70] |
| STEMdiff Trilineage Differentiation Kit | Directed differentiation to three germ layers | Pluripotency verification | Standardized protocol for consistency [71] |
| Anti-OCT4/SOX2/TRA-1-60 Antibodies | Immunodetection of pluripotency markers | Flow cytometry, immunocytochemistry | Essential for pluripotency confirmation [73] |
Relationship Between QC Failures and Phenotypic Outcomes in Rare Disease Modeling
The following diagram illustrates how specific QC failures manifest as compromised experimental outcomes in rare disease research:
Diagram 2: Relationship between specific QC failures and compromised experimental outcomes in rare disease modeling.
Establishing and maintaining rigorous quality control benchmarks for pluripotency and genomic integrity is fundamental to the successful application of iPSC technology in rare disease research. The framework presented here—encompassing comprehensive assessment of pluripotency through multiple complementary assays, systematic monitoring of genomic integrity using tiered approaches, and understanding the impact of technical variables—provides a foundation for generating reliable, reproducible disease models. As the field advances toward clinical applications and more complex disease modeling, these QC benchmarks will continue to evolve, but the core principles of thorough characterization and continuous monitoring will remain essential for scientific rigor and therapeutic development.
Assessing Model Power and Translational Potential
The advent of induced pluripotent stem cells (iPSCs) has revolutionized biomedical research, offering an unprecedented platform for studying human diseases in vitro. By reprogramming adult somatic cells into a pluripotent state, researchers can generate patient-specific cells capable of differentiating into virtually any cell type, thereby creating powerful models for investigating disease mechanisms and therapeutic interventions [18]. This technology holds particular promise for rare genetic disorders, which collectively affect hundreds of millions worldwide yet mostly lack effective treatments due to limited patient populations and research resources [4] [17]. However, a central question remains: how faithfully do these iPSC-derived models recapitulate the complex pathology of human diseases?
The recapitulation of disease phenotypes in iPSC models is influenced by multiple factors, including the genetic background of donors, reprogramming methods, differentiation protocols, and the cellular microenvironment. Understanding these variables is crucial for researchers and drug development professionals relying on these models for preclinical studies. This technical review examines the current state of iPSC disease modeling, with a specific focus on rare genetic disorders, by evaluating the fidelity of pathological recapitulation, discussing methodological considerations, and presenting advanced approaches to enhance physiological relevance.
Factors Influencing Phenotypic Fidelity in iPSC Models
Genetic and Epigenetic Considerations
The foundation of faithful disease modeling begins with the preservation and accurate representation of disease-causing genetic variants in iPSC systems. Approximately 80% of rare diseases have a genetic origin, making iPSCs particularly valuable for these conditions [4]. Patient-derived iPSCs inherently carry the complete genetic background of the donor, including the primary mutation responsible for the disease and potential genetic modifiers that may influence phenotype expressivity [17]. This genetic completeness enables the investigation of monogenic disorders like Lesch-Nyhan disease (caused by HPRT1 mutations) as well as more complex polygenic conditions [8] [17].
However, genetic fidelity alone does not guarantee pathological recapitulation. The epigenetic landscape of iPSCs and their derivatives significantly influences phenotypic expression. Recent research demonstrates that epigenetic variation is most strongly associated with genetic variation at the iPSC stage, but this relationship weakens following differentiation into specific lineages [30]. This epigenetic divergence may explain why some iPSC-derived cell models fail to fully manifest late-onset disease characteristics. Interestingly, studies have revealed that donor-specific epigenetic patterns persist through reprogramming and can be maintained through differentiation, though to a lesser extent than at the pluripotent stage [30]. This suggests that both genetic and epigenetic signatures contribute to phenotypic fidelity.
The use of isogenic controls—patient-derived iPSCs where the disease-causing mutation has been corrected using gene-editing technologies like CRISPR-Cas9—represents a powerful strategy for controlling for genetic background effects [4] [74]. This approach strengthens causal inference by ensuring that observed phenotypic differences can be directly attributed to the specific genetic variant under investigation rather than unrelated genetic differences between donors [51].
Developmental Maturation and Cellular Environment
A significant challenge in iPSC-based disease modeling is the developmental immaturity of many iPSC-derived cell types. These cells frequently display fetal-like gene expression profiles, electrophysiological activity, or metabolic states, which may limit their ability to accurately model late-onset disorders [51]. For example, iPSC-derived neurons often exhibit transcriptional signatures similar to fetal rather than adult neurons, potentially explaining why some neurodegenerative disease phenotypes are incompletely recapitulated [51] [17].
To address this limitation, researchers have developed various maturation strategies to promote more adult-like states, including:
- Prolonged culture periods extending over several months
- Bioengineering approaches incorporating biomechanical stimulation
- Co-culture systems with supporting cell types (e.g., astrocytes with neurons)
- Small molecule treatments that promote maturation pathways
- Metabolic manipulation to induce cellular aging [51] [17]
The cellular environment also profoundly influences phenotypic expression. Traditional two-dimensional monocultures lack the tissue context and cellular interactions present in vivo. For instance, in Amyotrophic Lateral Sclerosis (ALS) models, neuronal toxicity was not evident in the absence of glial cells carrying SOD1 mutations, highlighting the importance of multi-cellular environments for full pathological manifestation [17].
Quantitative Analysis of iPSC Model Fidelity
Experimental Design Considerations for Robust Modeling
The statistical robustness of iPSC-based disease modeling depends on appropriate experimental design, particularly regarding the number of biological replicates needed to distinguish true disease phenotypes from background variability. Empirical studies using gene expression profiles from RNA sequencing have provided valuable insights into optimal study designs for iPSC research.
Table 1: Optimal Experimental Design for iPSC Disease Modeling Based on RNAseq Analysis
| Factor | Recommended Specification | Impact on Phenotypic Recapitulation |
|---|---|---|
| Number of unique individuals | 3-4 per group | Minimizes effects of genetic background variability while maintaining practical feasibility |
| Number of iPSC lines per individual | 2 lines without statistical corrections | Controls for clonal variability without reducing statistical power |
| Primary source of variance | Technical factors > individual differences | Highlights importance of standardized protocols across lines |
| Analytical method dependence | Varies by detection algorithm | Emphasizes need for multiple complementary assessment methods |
A recent study modeling Lesch-Nyhan disease found that the best results were obtained using iPSC lines from 3-4 unique individuals per group, with 2 lines per individual providing optimal statistical power without requiring corrections for multiple lines from the same donor [8]. Counterintuitively, in studies where all lines were produced in parallel using identical methods, most variance in gene expression came from technical factors unrelated to the individual from whom the iPSC lines were prepared [8]. This finding underscores the importance of standardized protocols in iPSC research to minimize technical variability that could obscure genuine disease phenotypes.
Recapitulation of Disease Phenotypes Across Disorder Categories
iPSC models have demonstrated variable success in recapitulating disease-specific phenotypes across different categories of disorders. The fidelity of pathological manifestation depends on multiple factors, including disease mechanism, affected cell types, and the availability of robust differentiation protocols.
Table 2: Phenotypic Recapitulation in iPSC Models of Rare Diseases
| Disease Category | Example Conditions | Recapitulated Phenotypes | Limitations/Challenges |
|---|---|---|---|
| Neurological Disorders | Lesch-Nyhan disease, Friedreich's ataxia, ALS | Disease-relevant changes in gene expression, neuronal loss, protein aggregation | Developmental immaturity of neurons, lack of circuit-level complexity |
| Renal Disorders | Juvenile Nephronophthisis (NPH), Polycystic Kidney Disease | Abnormal cell proliferation, primary cilia defects, renal cyst formation | Limited structural organization in organoids, variable reproducibility |
| Retinal Disorders | Retinitis Pigmentosa (RDH12-AD), Age-related Macular Degeneration | Photoreceptor degeneration, reduced cell numbers, shortened photoreceptors | Extended differentiation time required, technical challenges in organoid maintenance |
| Cardiometabolic Disorders | Long QT syndrome, Duchenne Muscular Dystrophy | Electrophysiological abnormalities, contractile deficits, metabolic alterations | Immature cardiac electrophysiology, lack of mechanical load in culture |
The application of three-dimensional organoid systems has significantly enhanced phenotypic recapitulation for many diseases. For example, kidney organoids carrying PKD1 or PKD2 mutations display cyst formation reminiscent of patient pathology in Autosomal Dominant Polycystic Kidney Disease (ADPKD) [51]. Similarly, retinal organoids from patients with RDH12-associated retinitis pigmentosa exhibited reduced photoreceptor numbers and shortened photoreceptor length, mirroring key aspects of the human disease [4]. These advancements highlight how structural context and multi-cellular environments contribute to more faithful disease modeling.
Advanced Methodologies for Enhanced Pathological Recapitulation
Protocol for Establishing iPSC Models of Rare Genetic Diseases
Creating robust iPSC models of rare diseases requires meticulous attention to each step of the process, from patient recruitment to phenotypic validation. The following protocol outlines key methodological considerations for establishing faithful disease models:
Patient Recruitment and Sample Collection
- Obtain informed consent following institutional guidelines
- Collect appropriate somatic cells (typically skin fibroblasts or peripheral blood mononuclear cells)
- Record detailed clinical information, including disease severity and developmental stage
- Consider family members, including affected and unaffected individuals, for controls [17]
Reprogramming to Pluripotency
- Select appropriate reprogramming method based on intended applications:
- Non-integrating methods (Sendai virus, episomal plasmids, mRNA) for clinical applications
- Integrating methods (lentivirus) for basic research when higher efficiency is needed
- Characterize multiple clones for each patient using pluripotency markers (e.g., OCT4, SOX2, NANOG)
- Perform karyotyping to ensure genomic integrity [18] [74]
- Select appropriate reprogramming method based on intended applications:
Genetic Validation and Isogenic Control Generation
- Confirm presence of disease-causing mutation via sequencing
- Generate isogenic controls using CRISPR-Cas9 gene editing:
Directed Differentiation to Affected Cell Types
- Select differentiation protocol based on disease relevance
- Optimize protocol efficiency using lineage-specific markers
- Consider multi-lineage differentiation for disorders affecting multiple tissues
- Implement quality control measures for each differentiation batch [17]
Phenotypic Characterization and Functional Validation
The Scientist's Toolkit: Essential Reagents for iPSC Disease Modeling
Table 3: Essential Research Reagents for iPSC-Based Disease Modeling
| Reagent Category | Specific Examples | Function in Disease Modeling |
|---|---|---|
| Reprogramming Factors | OSKM (OCT4, SOX2, KLF4, c-MYC), OSLN (OCT4, SOX2, LIN28, NANOG) | Initiate cellular reprogramming to pluripotent state; various delivery methods available |
| Gene Editing Tools | CRISPR-Cas9 systems, guide RNAs, donor templates | Create isogenic controls, introduce disease mutations, correct pathogenic variants |
| Differentiation Inducers | Small molecules (CHIR99021, SB431542), Growth factors (BMP4, FGF2, VEGF) | Direct lineage-specific differentiation toward affected cell types |
| Characterization Antibodies | Pluripotency markers (OCT4, NANOG, SSEA-4), Lineage-specific markers (TUJ1, CTNT, SOX17) | Validate pluripotent status and differentiation efficiency |
| Organoid Culture Matrices | Matrigel, Laminin-521, Synthetic hydrogels | Provide three-dimensional support for self-organization and tissue maturation |
Visualization of Key Workflows and Signaling Pathways
The following diagrams illustrate critical workflows and relationships in iPSC-based disease modeling, providing visual guidance for experimental planning and interpretation.
Diagram 1: iPSC Disease Modeling Workflow. This diagram outlines the core workflow for establishing iPSC disease models, highlighting the cyclical process of clinical correlation that validates pathological recapitulation.
Diagram 2: Factors Determining Phenotypic Fidelity. This diagram illustrates the multidimensional factors that collectively influence how faithfully iPSC models recapitulate human disease pathology.
iPSC technology has fundamentally transformed our approach to studying rare genetic diseases, providing unprecedented access to patient-specific human cells for pathological investigation and therapeutic development. The fidelity of phenotypic recapitulation in these models depends critically on multiple interconnected factors, including genetic background, epigenetic signatures, developmental maturity, and cellular microenvironment. While challenges remain—particularly in modeling late-onset disorders and achieving full cellular maturation—continuous methodological advancements are steadily enhancing the physiological relevance of iPSC-based disease models.
The integration of three-dimensional organoid systems, co-culture approaches, and bioengineering strategies represents a promising direction for improving pathological recapitulation. These complex models better mimic tissue architecture and multi-cellular interactions, enabling the emergence of disease phenotypes that may not manifest in simpler culture systems. Additionally, the application of gene editing technologies like CRISPR-Cas9 allows for creation of precisely controlled isogenic lines that strengthen causal inference in disease modeling studies.
As the field progresses, standardization of protocols and rigorous benchmarking across laboratories will be essential for maximizing the translational potential of iPSC disease models. With ongoing innovations in differentiation techniques, maturation strategies, and model complexity, iPSC-based approaches are poised to become increasingly faithful representations of human disease pathology, accelerating therapeutic development for rare genetic disorders that have long eluded effective treatment.
Rare genetic disorders, which collectively affect an estimated 263–446 million people worldwide, present significant challenges for research and therapeutic development [3]. Approximately 80% of rare diseases have a genetic origin, yet less than 10% have approved therapies, creating an urgent need for accurate model systems to elucidate disease mechanisms [3] [4]. Induced pluripotent stem cell (iPSC) technology has emerged as a transformative platform for studying these conditions, providing patient-specific cells that can be differentiated into affected cell types. However, a major challenge in iPSC-based disease modeling has been distinguishing true mutation-specific phenotypes from background genetic variation and experimental noise.
Isogenic controls represent the solution to this challenge. These are iPSC lines that are genetically identical except for a specific mutation of interest, created by using gene editing technologies to either introduce a disease-causing mutation into healthy cells or correct the mutation in patient-derived cells [75]. This powerful approach enables researchers to attribute observed differences directly to the genetic variant being studied, rather than to the broader genetic background of the donor. For rare disease research, where patient cohorts are small and genetic heterogeneity is common, isogenic controls provide the scientific rigor necessary to confidently establish genotype-phenotype relationships and advance therapeutic development.
Foundations of Isogenic Control Generation
Conceptual Framework and Methodological Approaches
The fundamental principle behind isogenic controls is the creation of genetically matched cell lines that differ only at the specific locus of interest. This is achieved through a two-pronged strategy that can be applied based on resource availability and research objectives:
- Disease-Correction Approach: Patient-derived iPSCs carrying a pathogenic mutation are corrected using gene editing to create an isogenic control line, while the original mutated line serves as the disease model [75].
- Disease-Introduction Approach: iPSCs from healthy donors are edited to introduce specific disease-causing mutations, with the unedited line serving as the control [75].
The core technological advancement enabling precise genetic manipulation in iPSCs is the CRISPR-Cas9 system, which can be deployed in multiple configurations depending on the experimental needs. The table below summarizes the primary gene editing approaches used for generating isogenic controls.
Table 1: Gene Editing Approaches for Isogenic Control Generation
| Editing Method | Mechanism | Primary Applications | Key Advantages |
|---|---|---|---|
| CRISPR-Cas9 Nuclease with HDR | Creates double-strand breaks repaired via homology-directed repair using donor templates | Introducing specific mutations, gene corrections | High precision with donor template guidance |
| Base Editors | Directly converts one DNA base to another without double-strand breaks | Single-nucleotide changes, SNP corrections | Reduced indel formation, higher efficiency for point mutations |
| Prime Editors | Uses reverse transcriptase to copy edited sequence from pegRNA template | All types of genetic modifications without double-strand breaks | Versatile, minimal off-target effects |
Technical Workflow for Isogenic Control Generation
The generation of genetically validated isogenic controls follows a systematic pipeline with multiple quality checkpoints to ensure experimental integrity. The process requires careful execution at each stage, from initial cell line selection through final clone validation.
Figure 1: Isogenic Control Generation Workflow
Experimental Design and Methodological Implementation
Establishing Robust Experimental Protocols
Successful genetic validation requires standardized protocols that account for the unique challenges of iPSC culture and differentiation. The methodology below outlines a comprehensive approach for using isogenic controls to establish genotype-phenotype relationships:
Phase 1: Cell Culture and Maintenance
- Maintain isogenic iPSC lines in feeder-free culture conditions using defined essential 8 medium
- Passage cells using EDTA-based dissociation to maintain colony morphology
- Regularly test for mycoplasma contamination and authenticate cell lines
- Monitor genomic stability through karyotyping and targeted qPCR assays for common abnormalities such as 20q11.21 amplification [70]
Phase 2: Directed Differentiation
- Employ established differentiation protocols tailored to the disease-relevant cell type
- For neurological disorders: Use dual-SMAD inhibition to generate neural progenitor cells, followed by region-specific patterning factors
- For cardiac diseases: Apply Wnt modulation to direct cells toward cardiomyocyte lineage
- Include quality control checkpoints at each stage using flow cytometry for lineage-specific markers
Phase 3: Phenotypic Analysis
- Conduct functional assays relevant to the disease pathology
- Perform molecular analyses (transcriptomics, proteomics) on paired isogenic lines
- Implement high-content imaging and automated analysis for quantitative phenotypic assessment
- Apply electrophysiological characterization for excitable cells (neurons, cardiomyocytes)
Phase 4: Data Integration and Validation
- Compare phenotypes between isogenic pairs across multiple differentiation batches
- Include additional patient lines to assess generalizability beyond isogenic background
- Use statistical models that account for batch effects and differentiation variability
Research Reagent Solutions for Isogenic Control Experiments
Table 2: Essential Research Reagents for Isogenic Control Studies
| Reagent Category | Specific Examples | Primary Function | Technical Considerations |
|---|---|---|---|
| Reprogramming Systems | Sendai virus vectors, episomal plasmids | Generate iPSCs from somatic cells | Non-integrating systems preferred for clinical applications |
| Gene Editing Tools | CRISPR-Cas9 nucleases, base editors, prime editors | Introduce or correct mutations in iPSCs | High-fidelity Cas variants reduce off-target effects |
| Cell Culture Media | Defined essential 8 medium, differentiation kits | Maintain pluripotency and direct differentiation | Xeno-free formulations enhance reproducibility |
| Characterization Reagents | Flow cytometry antibodies, PCR assays | Validate cell identity and genomic integrity | Standardized panels enable cross-study comparisons |
| Analysis Platforms | Single-cell RNA sequencing, high-content imagers | Phenotypic screening and molecular profiling | Automated systems reduce operator-dependent variability |
Applications in Rare Disease Research and Drug Development
Case Studies Demonstrating Genetic Validation
The integration of isogenic controls has enabled critical advances across multiple rare disease domains by providing unambiguous genetic validation:
Neurological Disorders In Parkinson's disease research, isogenic iPSC lines with mutations in the LRRK2 G2019S gene demonstrated mitochondrial dysfunction and increased vulnerability in dopaminergic neurons [75]. The use of isogenic controls confirmed that these phenotypes were directly attributable to the LRRK2 mutation rather than background genetic variation. Similarly, for Alzheimer's disease, isogenic neurons with APP and PSEN1 mutations successfully reproduced early pathological changes including Aβ deposition and tau phosphorylation [75].
Cardiac Channelopathies In the study of long QT syndrome, isogenic iPSC-derived cardiomyocytes with KCNQ1 or SCN5A mutations have been extensively used for drug risk assessment and mechanism investigation [75]. The isogenic control design enabled researchers to directly link action potential prolongation and arrhythmogenic potential to specific ion channel mutations, providing platforms for personalized drug testing.
Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV) Research using patient-derived iPSCs with NTRK1 mutations revealed a previously unknown disease mechanism involving lineage switching between sensory neurons and glial cells during development [13]. The creation of isogenic controls through CRISPR-mediated correction of the patient's mutation provided definitive evidence that this developmental defect was directly caused by NTRK1 dysfunction [13].
Integration with Drug Discovery Platforms
The combination of isogenic controls with high-throughput screening technologies has created powerful platforms for rare disease drug discovery:
High-Throughput Compound Screening: Isogenic iPSC-derived cells enable screening against disease-relevant phenotypes with built-in controls for background variation [14] [75]. For example, in a Parkinson's disease model with GBA mutations, researchers used CRISPR-edited iPSC neurons to screen for small molecules that could restore GCase enzyme activity and lysosomal function [75].
Toxicity Assessment: Isogenic cardiomyocytes and hepatocytes provide human-relevant systems for evaluating drug safety [14]. The controlled genetic background increases sensitivity for detecting mutation-specific toxicities.
Clinical Trial Stratification: By testing drug responses across multiple isogenic pairs with the same mutation but different genetic backgrounds, researchers can identify genetic modifiers of treatment efficacy, potentially informing patient selection for clinical trials [75].
Technical Challenges and Quality Control Considerations
Addressing Variability in iPSC-Based Models
A significant challenge in iPSC research is the inherent variability that can obscure genuine genotype-phenotype relationships. Recent studies have quantified the sources of this variability to improve experimental design:
Table 3: Sources of Variability in iPSC Differentiation and Their Impact
| Variability Source | Contribution to Overall Variance | Mitigation Strategies |
|---|---|---|
| Technical Factors (Induction Set) | 30-70% | Standardized protocols, automated systems |
| Operator Effects | Significant contributor | Extensive training, automated platforms |
| Cell Line Genetics | 2-30% | Use of isogenic controls, multiple lines |
| Genomic Instability | Significant impact on differentiation | Regular karyotyping, targeted qPCR |
Recent research has demonstrated that non-genetic factors—particularly the induction set and operator—are the predominant sources of variability in iPSC differentiation, outweighing the contribution from cell line genetics [70]. This highlights the critical importance of standardized protocols and appropriate experimental design, including the use of isogenic controls to account for genetic contributions to variability.
Genomic instability represents another significant challenge, with common karyotypic abnormalities such as 20q11.21 gain substantially impacting differentiation capacity [70]. Regular monitoring of genomic integrity through targeted qPCR assays for common abnormalities is essential for maintaining experimental reproducibility.
Optimization Strategies for Enhanced Reproducibility
Several methodological advances have improved the reliability of isogenic control experiments:
Automated Culture Systems: Implementation of automated iPSC maintenance and differentiation reduces operator-dependent variability and enhances reproducibility [70] [76].
Enhanced Characterization: Comprehensive molecular profiling through single-cell RNA sequencing validates differentiation efficiency and cellular composition [77].
Multiple Clone Analysis: Including multiple independently derived clones for each genetic condition controls for potential off-target effects of gene editing.
Long-term Culture Monitoring: Regular assessment of genomic stability throughout extended culture periods prevents the accumulation of genetic abnormalities that could confound results.
Future Directions and Emerging Technologies
Advanced Model Systems and Analytical Approaches
The field of isogenic control-based research is rapidly evolving with several promising technological developments:
Complex In Vitro Models The integration of isogenic controls with three-dimensional organoid and assembloid systems represents a significant advancement for modeling tissue-level phenotypes [3] [51]. For example, dorsal-ventral assembloids have been used to model interneuron migration in human brain development, revealing previously inaccessible aspects of neural circuit formation [13]. Similar approaches applied to isogenic systems will enable more physiologically relevant modeling of rare disease mechanisms.
Multiplexed Editing Approaches New methodologies such as "village editing" enable CRISPR-Cas9 gene editing in a cell village format, allowing researchers to study the same mutation across multiple genetic backgrounds simultaneously [13]. This approach is particularly valuable for understanding how genetic modifiers influence expressivity of rare disease mutations.
Artificial Intelligence and Machine Learning AI-guided differentiation and phenotypic analysis are being increasingly applied to enhance standardization and reproducibility in iPSC research [74] [75]. Machine learning algorithms can predict efficient gRNA designs, optimize differentiation protocols, and analyze complex multidimensional data from isogenic comparisons.
Clinical Translation and Therapeutic Development
The rigorous genetic validation enabled by isogenic controls directly supports the development of therapies for rare genetic disorders:
Target Identification: Confirmed genotype-phenotype relationships provide validated molecular targets for therapeutic intervention.
Clinical Trial Design: Understanding the effect size of specific mutations through isogenic comparisons helps power clinical trials for ultra-rare genetic conditions.
Personalized Medicine: The combination of patient-derived iPSCs with isogenic correction enables the development of personalized treatment approaches matched to individual genetic profiles.
As the field advances, ongoing technological improvements in gene editing efficiency, differentiation protocol standardization, and analytical methods will further enhance the power of isogenic controls to unravel the complexities of rare genetic diseases and accelerate the development of effective treatments.
Isogenic controls represent an indispensable toolset for establishing definitive genotype-phenotype relationships in iPSC-based disease modeling. By controlling for genetic background and technical variability, these carefully engineered cell lines enable researchers to attribute phenotypic differences directly to specific genetic variants with high confidence. For rare disease research, where patient populations are small and genetic heterogeneity is substantial, this approach provides the scientific rigor necessary to advance our understanding of disease mechanisms and develop targeted therapies. As the technologies for generating and characterizing isogenic controls continue to evolve, their integration with complex model systems and high-throughput screening platforms will undoubtedly accelerate the pace of therapeutic discovery for rare genetic disorders.
The high failure rates in drug development, particularly in areas like central nervous system (CNS) disorders where attrition rates reach 90%, underscore a critical translational gap between preclinical models and human therapeutic outcomes [78]. This whitepaper provides a comparative analysis of two primary research models: traditional animal models and human induced pluripotent stem cells (iPSCs). For researchers focused on rare genetic disorders, iPSC-based models present a transformative opportunity to study disease mechanisms within patient-specific genetic contexts, enabling more predictive human biology modeling and accelerating therapeutic development. The integration of iPSC technology with advanced genome editing and complex culture systems is rapidly establishing a new paradigm for rare disease research.
Despite decades of innovation, current preclinical models frequently fail to reliably predict human outcomes, creating a significant translational gap in biomedical research. Fewer than 1 in 10 drug candidates entering clinical trials ultimately reach patients, highlighting the profound limitations of existing systems [78]. This challenge is particularly acute for rare genetic diseases, approximately 80% of which have genetic origins, yet less than 10% have approved therapies [3] [4]. The reliance on animal models and traditional cell culture systems has created a bottleneck in understanding human-specific disease mechanisms, especially for conditions affecting inaccessible tissues like the human brain or heart. The emergence of iPSC technology in 2006-2007 represented a paradigm shift, enabling investigators to create patient-specific cellular models that capture human genetic backgrounds for studying disease mechanisms and therapeutic responses [18].
Induced Pluripotent Stem Cells (iPSCs)
iPSCs are generated by reprogramming adult somatic cells (typically skin fibroblasts or blood cells) back to an embryonic-like pluripotent state through the introduction of specific transcription factors. The original reprogramming factors, known as Yamanaka factors (OSKM), include OCT4, SOX2, KLF4, and c-MYC [18] [79]. This reprogramming process involves profound epigenetic remodeling that erases somatic cell memory and reestablishes pluripotency, enabling the cells to differentiate into virtually any cell type in the human body [18].
The molecular mechanisms of somatic cell reprogramming occur in two primary phases: an early stochastic phase where somatic genes are silenced and early pluripotency genes are activated, followed by a more deterministic late phase where established pluripotency networks are stabilized [18]. This reprogramming capacity demonstrates that cellular differentiation, while stable, is not irreversible—a finding that earned Dr. Shinya Yamanaka and Dr. John Gurdon the 2012 Nobel Prize in Physiology or Medicine [79].
Traditional Animal Models
Animal models range from zebrafish and rodents to canines and pigs, each offering different advantages based on their physiological similarities to humans [80]. Larger animals like pigs generally have more physiological similarities to humans, making them potentially better disease models, but they present practical challenges related to handling, maintenance costs, and ethical considerations [80]. Different species have evolved distinct mechanisms of disease onset, with organ characteristics varying based on evolutionary history and environmental adaptations [80]. For example, mice have heart rates of 300-600 bpm compared to 60-100 bpm in humans, creating significant translational challenges for cardiovascular research [80].
Comparative Analysis: iPSCs vs. Animal Models
Table 1: Comprehensive Comparison of iPSCs and Animal Models for Rare Disease Research
| Feature | iPSC Models | Animal Models |
|---|---|---|
| Human Biological Relevance | High - Directly derived from human patients with complete human genetic background [17] | Variable - Species-specific differences in genetics, physiology, and metabolism [80] |
| Genetic Precision | Excellent - Can introduce specific human disease mutations via CRISPR; create isogenic controls [17] [79] | Limited - Genetic engineering possible but may not recapitulate human genetic context [80] |
| Developmental Modeling | Good for early developmental processes; can model tissue morphogenesis in organoids [17] | Excellent - Intact physiological systems and developmental processes [80] |
| Complex System Integration | Improving with co-culture and organoid systems but still reductionist [17] | Native - Intact organ systems with natural circulatory, immune, and endocrine systems [80] |
| Throughput & Scalability | High - Suitable for high-throughput screening campaigns [78] | Low - Time-consuming and expensive, especially for larger species [80] |
| Regulatory Landscape | Supported by FDA Modernization Act 2.0; FDA roadmap to reduce animal testing [78] [4] | Well-established but evolving; required for many preclinical safety studies [78] |
| Maturity Modeling | Challenging - Cells often maintain fetal-like characteristics; maturation protocols improving [80] [17] | Native - Natural progression through developmental stages to adulthood [80] |
| Cost & Infrastructure | Moderate - Requires specialized cell culture facilities; decreasing costs with automation [40] | High - Especially for larger species requiring specialized facilities and care [80] |
| Temporal Modeling | Limited for aging and late-onset disorders without artificial aging induction [17] | Excellent for natural disease progression and aging studies [80] |
Table 2: Specific Applications in Drug Discovery Workflow
| Drug Discovery Stage | iPSC Applications | Animal Model Applications |
|---|---|---|
| Target Identification | Functional genomics with CRISPR screening in human cells [78] | Pathway analysis in intact physiological systems [80] |
| Hit-to-Lead Optimization | Structure-activity relationships in human-relevant pathways [78] | Pharmacokinetic and efficacy studies in whole organisms [80] |
| Safety & Toxicology | Early cardiotoxicity screening with iPSC-cardiomyocytes; hepatotoxicity assessment [78] | Comprehensive organ system toxicology and off-target effects [80] |
| Clinical Trial Predictive Value | Improving - Human-specific signaling pathways and metabolism [78] | Variable - Poor translation for many disease areas, especially CNS [78] |
Experimental Design and Protocols for iPSC-Based Disease Modeling
Establishing Optimal Study Design Parameters
Robust iPSC-based disease modeling requires careful consideration of experimental design parameters. For rare disease studies, recent empirical evidence using transcriptomic profiling suggests that optimal results are obtained using iPSC lines from 3-4 unique individuals per group, with 2 lines per individual [8]. This approach helps account for both biological and technical variability while remaining practical for rare diseases where patient numbers are limited.
Protocol 1: Generation of Isogenic iPSC Lines Using CRISPR-Cas9
The creation of isogenic control lines is critical for distinguishing disease-specific phenotypes from background genetic variation [17] [79].
- iPSC Culture: Maintain human iPSCs in feeder-free conditions using defined essential 8 medium on vitronectin-coated plates [79].
- Guide RNA Design: Design and validate sgRNAs targeting the specific genetic locus of interest using computational tools to minimize off-target effects [79].
- CRISPR RNP Electroporation: Complex purified Cas9 protein with synthetic sgRNA to form ribonucleoproteins (RNPs). Introduce RNPs and single-stranded DNA donor template (if knock-in) into iPSCs via electroporation [79].
- Clonal Isolation: After recovery, dissociate iPSCs to single cells and plate at clonal density. Isolate individual colonies and expand in 96-well plates [79].
- Genotype Validation: Extract genomic DNA from expanded clones and validate edits by Sanger sequencing, PCR analysis, or next-generation sequencing. Screen for potential off-target edits at predicted sites [79].
- Characterization: Validate pluripotency marker expression (OCT4, NANOG, SOX2) and trilineage differentiation potential of edited clones to ensure maintained pluripotency [79].
Protocol 2: Differentiation of iPSCs to Disease-Relevant Cell Types
Neuronal Differentiation (for neurological disorders):
- Pattern iPSCs toward neural ectoderm using dual SMAD inhibition (SB43152 and LDN193189) for 10-12 days [81] [17].
- Specify toward neuronal subtypes using region-specific patterning factors (e.g., SHH for ventral forebrain, retinoic acid for hindbrain/spinal cord) [17].
- Maturate neurons for 8-12 weeks with neurotrophic factors (BDNF, GDNF, NT-3) for functional maturation [17].
Cardiomyocyte Differentiation (for cardiovascular disorders):
Organoid Generation (for tissue-level modeling):
- Aggregate iPSCs in low-adhesion plates to promote self-organization [17].
- Pattern toward target tissue using staged addition of morphogens with precise concentration gradients [17].
- Embed in extracellular matrix substitutes (Matrigel) to support 3D architecture [17].
- Extended maturation (often 2-6 months) with agitation to enhance nutrient exchange [17].
Protocol 3: Phenotypic Screening in iPSC-Derived Models
Functional Assessment:
- Neuronal function: Multi-electrode arrays (MEA) to measure network activity and synchronization [78].
- Cardiac function: Impedance recording or calcium imaging to assess contractility and rhythmicity [78] [80].
- Metabolic assessment: Seahorse analyzer to measure mitochondrial function and metabolic flux [78].
High-Content Imaging:
Diagram 1: iPSC-Based Disease Modeling Workflow. This workflow illustrates the process from patient sample collection through therapeutic development using iPSC technology.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for iPSC-Based Disease Modeling
| Reagent/Platform | Function | Examples/Notes |
|---|---|---|
| Reprogramming Factors | Convert somatic cells to pluripotent state | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) [18] |
| CRISPR-Cas9 Systems | Precise genome editing for creating isogenic controls | Ribonucleoprotein (RNP) delivery reduces off-target effects [79] |
| Defined Culture Media | Maintain pluripotency or direct differentiation | Essential 8 for maintenance; specialized media for differentiation [79] |
| Extracellular Matrices | Provide structural support for cell growth | Vitronectin, Matrigel, synthetic hydrogels [17] |
| opti-ox Technology | Deterministic reprogramming for consistent differentiation | Enables production of highly pure cell populations (ioCells) [78] |
| Multi-Electrode Arrays | Functional assessment of electrically active cells | Measures neuronal firing patterns or cardiac rhythmicity [78] |
| Automated Platforms | High-throughput screening and consistent culture | NYSCF Array for standardized iPSC production [40] |
| Reference iPSC Lines | Standardized baseline for comparative studies | KOLF2.1J provides genomic stability and consistent differentiation [40] |
iPSC Applications in Rare Genetic Disease Research
iPSC technology has demonstrated particular value in rare genetic disease research, enabling investigation of conditions that were previously difficult to model. Several case studies highlight this application:
Lesch-Nyhan Disease: Caused by mutations in HPRT1 gene, recent transcriptomic studies using patient-derived iPSCs have helped establish optimal experimental designs for detecting disease-relevant changes in gene expression [8].
Juvenile Nephronophthisis (NPH): Researchers developed the first human NPH disease models using patient-derived iPSCs and gene-edited iPSCs differentiated into kidney organoids, demonstrating abnormal cell proliferation, cilia defects, and renal cyst formation reversible with NPHP1 gene correction [3] [4].
RDH12-associated Retinitis Pigmentosa: Patient-derived retinal organoids exhibited reduced photoreceptor numbers and shortened photoreceptor length, replicating the late-onset, milder disease course seen in patients and providing insight into disease mechanisms [4].
LQT3 Syndrome: Patient-derived iPSCs with sodium channel mutations were differentiated into cardiomyocytes that recapitulated the cardiac arrhythmia phenotype and were predictive of patient-specific responses to pharmacotherapy [17].
These examples demonstrate how iPSC models capture human-specific disease pathophysiology that may not be fully recapitulated in animal models, particularly for rare genetic conditions with complex tissue-specific manifestations.
Integrated Approaches: Combining iPSCs and Animal Models
The most powerful research strategies often integrate both iPSC and animal model approaches to leverage their complementary strengths:
Diagram 2: Integrated Drug Discovery Pipeline. This diagram illustrates the synergistic relationship between human genetics, iPSC models for mechanistic studies, and animal models for systemic validation in therapeutic development.
This integrated approach leverages the human relevance of iPSCs for target identification and mechanistic studies with the systemic context of animal models for validation of therapeutic efficacy and safety assessment. For example, candidate drugs identified in iPSC-based screens can be advanced to animal models for pharmacokinetic and whole-organism efficacy studies, while observations from animal models can be further investigated mechanistically using human iPSC-derived cells [80].
The comparative analysis of iPSCs and animal models reveals a complementary rather than competitive relationship in biomedical research. While animal models continue to provide invaluable insights into systemic physiology and complex organismal responses, iPSC-based models offer unprecedented access to human-specific disease mechanisms, particularly for rare genetic disorders. The rapid advancement of iPSC technology—including improved differentiation protocols, 3D organoid systems, and integration with CRISPR genome editing—is accelerating our understanding of human biology and disease pathogenesis.
For rare disease research, iPSCs represent a particularly transformative technology, enabling investigation of conditions that affect small patient populations where traditional research models have been limiting. As regulatory frameworks evolve to embrace human-cell-based models, and as the technologies become more standardized and accessible, iPSCs are poised to play an increasingly central role in the therapeutic development pipeline. The future of predictive human disease modeling lies not in choosing between iPSCs and animal models, but in strategically integrating both approaches to maximize their respective strengths while acknowledging their limitations.
The FDA Modernization Act 2.0, signed into law in December 2022, represents a fundamental transformation in how the U.S. Food and Drug Administration evaluates the safety and efficacy of new therapeutics [82]. This comprehensive legislation explicitly permits the use of specific alternatives to animal testing, including cell-based assays such as human induced pluripotent stem cells (iPSCs), organoids, and organs-on-chips, alongside advanced artificial intelligence (AI) methods [82]. For researchers focused on rare genetic disorders, this policy shift is particularly transformative. It acknowledges that over 80% of rare diseases have a genetic origin and that traditional animal models often fail to accurately predict human responses due to fundamental species differences in genetics, drug metabolism, and disease pathophysiology [4] [3]. The Act establishes a new regulatory framework where human-relevant, iPSC-based models are not merely supplementary tools but can serve as primary evidence in investigational new drug (IND) applications, accelerating the development of treatments for the approximately 94% of rare diseases that currently lack approved therapies [4] [3].
The Scientific and Regulatory Imperative for Change
Limitations of Traditional Animal Models
The longstanding requirement for animal testing, established by the Federal Food, Drug, and Cosmetic Act of 1938, has been increasingly recognized as scientifically problematic for human drug development [82]. Pharmacogenomic differences between animal models and humans result in substantial variation in how drugs are absorbed, distributed, metabolized, and excreted [82]. Enzymes such as cytochrome P450 that are involved in drug metabolism vary in number and function between species, leading to inaccurate predictions of drug behavior in humans [82]. The inbred nature of rodent models creates an additional limitation—while mice of the same strain share approximately 98.6% of their genome, making them effectively clones, humans have vast genetic diversity that leads to significant variation in drug metabolism, targets, and interactions [82]. This genetic diversity means that data from individual animals are more akin to technical replicates rather than biologically representative samples, potentially explaining why 60% of phase I and II clinical trials fail due to lack of efficacy and 30% fail due to toxicity concerns [82].
Policy Evolution: From FDA Modernization Act 2.0 to Implementation
The FDA Modernization Act 2.0 provided the legislative foundation for alternatives to animal testing, but the FDA has subsequently developed additional frameworks to implement this vision. The agency has announced a specific plan to phase out animal testing requirements for monoclonal antibodies and other drugs, replacing them with more human-relevant methods including AI-based computational models, cell lines, and organoid toxicity testing [83]. Commissioner Martin A. Makary described this initiative as a "paradigm shift in drug evaluation" that promises to "accelerate cures and meaningful treatments for Americans while reducing animal use" [83].
More recently, the FDA has introduced complementary new pathways, including the "Plausible Mechanism Pathway" for ultra-rare conditions and the Rare Disease Evidence Principles (RDEP), which further clarify how non-animal data can support drug approval [84] [85]. These frameworks specifically acknowledge the futility of many animal studies for rare diseases and state that the agency will "embrace nonanimal models where possible" [84]. For rare diseases driven by known genetic defects with very small patient populations (generally fewer than 1,000 persons in the U.S.), the RDEP process confirms that substantial evidence of effectiveness can be established through one adequate and well-controlled study plus robust confirmatory evidence, which may include strong mechanistic or biomarker evidence and data from relevant non-clinical models—exactly the type of data generated by iPSC-based assays [85].
iPSC-Based Models as Engine of Rare Disease Research
Technical Foundations of iPSC Disease Modeling
Induced pluripotent stem cells are created from easily collected somatic cell sources, such as skin fibroblasts, leukocytes, or urine, after reprogramming using the four Yamanaka factors (OCT4, SOX2, KLF4, and cMYC) [82]. For rare disease research, this technology enables the creation of patient-specific disease models by reprogramming cells from individuals with specific genetic mutations, allowing scientists to recapitulate disease characteristics in vitro [82]. These models can be further refined through gene editing to create isogenic controls—genetically identical lines that differ only at the disease-causing locus—which enable researchers to distinguish direct mutation effects from background genetic variation [4] [3].
The experimental workflow for iPSC-based disease modeling typically involves several key stages, from cell line establishment through differentiation and phenotypic analysis, with specific quality control checkpoints essential for generating reproducible, reliable data as represented below:
Determining Optimal Experimental Design Parameters
A critical consideration in iPSC-based rare disease research is determining the appropriate number of cell lines and replicates needed to achieve robust, statistically significant results. A 2025 study empirically evaluated this question using RNA sequencing data from iPSC models of Lesch-Nyhan disease (LND), caused by mutations in the HPRT1 gene [8]. The research provides specific guidance on experimental design parameters:
Table 1: Optimal iPSC Line Numbers Based on Empirical Evidence
| Factor | Recommendation | Experimental Impact |
|---|---|---|
| Unique Individuals | 3-4 per group | Captures essential biological variability while remaining practically feasible for rare diseases |
| Lines per Individual | 2 without statistical corrections | Improves results when all lines are produced in parallel using the same methods |
| Major Variance Source | Technical factors (when production methods standardized) | Highlights importance of consistent protocols rather than individual genetic differences |
This study found that in well-controlled experiments where all lines were produced in parallel using standardized methods, most variance in gene expression came from technical factors unrelated to the individual from whom the iPSC lines were prepared [8]. This finding underscores the importance of rigorous protocol standardization in iPSC-based assays intended for regulatory submissions.
Advanced iPSC Applications: From 2D Models to 3D Organoids
iPSC-based rare disease modeling has evolved from simple two-dimensional cultures to complex three-dimensional systems that better recapitulate tissue and organ-level pathophysiology. The following diagram illustrates the progression from patient cell collection through to advanced 3D model systems and their applications in therapeutic development:
Recent research demonstrates the power of these advanced models. For Juvenile Nephronophthisis (NPH), a genetic kidney disease without effective treatments, researchers developed the first human disease models using patient-derived iPSCs and kidney organoids [4] [3]. These organoids exhibited abnormal cell proliferation, abnormalities in primary cilia, and renal cyst formation—all key disease phenotypes—which were reversed upon reintroduction of the NPHP1 gene [4] [3]. Similarly, for a rare form of autosomal dominant retinitis pigmentosa (RDH12-AD), retinal organoids derived from patient iPSCs replicated the late-onset, milder disease course seen in patients, showing reduced photoreceptor numbers and disrupted retinol biosynthesis after 44 weeks of development [3].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of iPSC-based assays for regulatory submissions requires carefully selected reagents and tools. The following table details key solutions and their applications in iPSC-based rare disease research:
Table 2: Essential Research Reagent Solutions for iPSC-Based Rare Disease Modeling
| Reagent Category | Specific Examples | Function in Workflow |
|---|---|---|
| Reprogramming Factors | Synthetic mRNA, Sendai virus, episomal vectors | Introduction of Yamanaka factors (OCT4, SOX2, KLF4, cMYC) for somatic cell reprogramming |
| Gene Editing Tools | CRISPR/Cas9 systems, base editors, prime editors | Creation of isogenic controls and introduction of disease-causing mutations |
| Differentiation Kits | Commercial media, small molecule cocktails | Directed differentiation into specific lineages (neuronal, cardiac, renal, hepatic) |
| Characterization Antibodies | Pluripotency markers (OCT4, NANOG, SOX2), lineage-specific markers | Validation of iPSC quality and differentiation efficiency |
| 3D Culture Matrices | Synthetic hydrogels, basement membrane extracts | Support for organoid formation and tissue-like development |
The selection of appropriate reagents must be guided by the need for reproducibility and quality control, particularly when generating data for regulatory submissions under the new frameworks established by FDA Modernization Act 2.0. Documentation of reagent sources, lot numbers, and detailed protocols becomes essential for demonstrating experimental rigor.
Case Studies: iPSC Models Informing Rare Disease Therapeutics
Neural Disease Modeling Using "Village Editing" Approaches
A novel "village editing" approach—CRISPR/Cas9 gene editing in a cell village format—has been developed to study the influence of genetic background on disease expression [13]. Researchers applied this method to investigate neurexin 1 (NRXN1), a gene linked to schizophrenia, by generating NRXN1 knockouts in iPSC lines from 15 donors with low, neutral, or high polygenic risk scores for the disorder [13]. After differentiating these edited lines into cortical excitatory neurons and performing RNA sequencing, the team found that genetic background deeply influences gene expression changes in NRXN1 knockout neurons [13]. This approach provides a framework for studying gene functions in complex, polygenic disorders and acknowledges the critical role of human genetic diversity in therapeutic development—a key consideration enabled by the FDA's new policy direction.
Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV)
For HSAN IV, a rare autosomal genetic disorder characterized by congenital insensitivity to pain with anhidrosis, researchers established human dorsal root ganglia (DRG) organoids from iPSCs derived from a patient's urine [13]. The patient carried homozygous mutations in the NTRK1 gene, and the team generated an isogenic control by correcting the mutation using CRISPR-based gene editing [13]. Analysis revealed that DRG organoids from HSAN IV patients underwent lineage switching between sensory neurons and glial cells, with a marked reduction of sensory neurons during early neurogenesis and premature initiation of gliogenesis [13]. These findings suggest that NTRK1 mutations disrupt the balance of neuronal and glial differentiation in human DRG development, providing new insights into disease mechanisms and potential therapeutic targets.
Regulatory Alignment: Optimizing iPSC Assays for the New Framework
Implementing Quality Control Standards
To align iPSC-based assays with regulatory expectations under FDA Modernization Act 2.0, researchers should implement rigorous quality control measures throughout their experimental workflows:
- Pluripotency Validation: Comprehensive characterization using flow cytometry for surface markers (TRA-1-60, SSEA4), immunocytochemistry for transcription factors (OCT4, NANOG), and trilineage differentiation potential
- Genetic Stability Monitoring: Regular karyotyping and whole-genome sequencing to identify chromosomal abnormalities or mutations accumulated during culture
- Line Authentication: Short tandem repeat (STR) profiling to confirm cell line identity and prevent cross-contamination
- Mycoplasma Testing: Frequent screening for mycoplasma contamination using PCR-based methods
- Differentiation Efficiency Quantification: Flow cytometry and qPCR analysis of lineage-specific markers to ensure consistent differentiation protocols
Documentation for Regulatory Submissions
When preparing iPSC-based data for regulatory submissions, researchers should maintain comprehensive documentation including:
- Detailed standard operating procedures (SOPs) for all critical processes
- Complete reagent documentation (sources, lot numbers, certificates of analysis)
- Raw data from all characterization experiments
- Statistical analysis plans and power calculations
- Validation data for all assay endpoints
- Evidence of reproducibility across multiple cell lines and differentiations
The FDA's recent draft guidance on "Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations" emphasizes the importance of robust data collection and transparent reporting for studies using novel approaches, particularly when traditional randomized controlled trials are not feasible [86].
The FDA Modernization Act 2.0 represents more than just a regulatory policy change—it establishes a new scientific paradigm that recognizes the superior predictive value of human-based cellular models over traditional animal testing for drug development. For rare disease researchers, this shift creates unprecedented opportunities to advance therapeutics using iPSC-based assays that directly address human pathophysiology and genetic diversity. The subsequent introduction of the Plausible Mechanism Pathway and Rare Disease Evidence Principles further solidifies this direction, providing clearer routes for therapies developed using these human-relevant models to reach patients [84] [85].
Future advancements will likely focus on enhancing the physiological relevance of iPSC models through improved maturation protocols, multi-tissue systems, and immunocompetent co-cultures that better replicate human tissue environments. The integration of AI and machine learning with iPSC data holds particular promise for predicting patient-specific responses and identifying novel therapeutic candidates [82]. As these technologies evolve, the alignment between regulatory policy and scientific innovation established by FDA Modernization Act 2.0 will continue to accelerate the development of effective treatments for rare genetic disorders, ultimately addressing the tremendous unmet need in this space.
The development of treatments for rare genetic disorders represents one of the most significant challenges in modern medicine. With over 7,000 identified rare diseases—approximately 80% of which have genetic origins—and fewer than 10% having approved therapies, there is a substantial unmet medical need [3] [4]. The traditional drug development pipeline, often exceeding a decade and costing billions of dollars, is particularly ill-suited for rare diseases due to small patient populations, geographic dispersion of patients, and limited understanding of disease mechanisms [87] [88].
The advent of induced pluripotent stem cell (iPSC) technology has revolutionized rare disease research by providing patient-specific cellular models that recapitulate pathological features in vitro. iPSCs are generated by reprogramming adult somatic cells through the introduction of transcription factors such as OCT4, SOX2, KLF4, and c-MYC, returning them to a pluripotent state capable of differentiating into virtually any cell type [15] [40]. This breakthrough has enabled researchers to create humanized disease models for conditions that were previously difficult to study, facilitating both mechanistic investigation and drug discovery.
This technical guide examines how iPSC-based models have successfully bridged the gap between laboratory research and clinical applications in rare diseases, highlighting specific success stories, detailed methodologies, and the essential tools that have enabled these advances.
iPSC Disease Modeling Fundamentals
Model Generation and Experimental Design
The generation of clinically relevant iPSC models requires careful experimental design and rigorous characterization. A key consideration is determining the optimal number of cell lines needed to achieve statistically robust results while accounting for biological and technical variability. A 2025 study using Lesch-Nyhan disease (caused by HPRT1 mutations) as a model system empirically demonstrated that using iPSC lines from 3-4 unique individuals per group, with 2 lines per individual, provides the most reliable results for detecting disease-relevant changes in gene expression without requiring statistical corrections for multiple lines from the same individual [8].
The standard workflow for establishing iPSC-based disease models involves several critical stages:
Somatic Cell Acquisition: Dermal fibroblasts or peripheral blood mononuclear cells (PBMCs) are most commonly collected from patients with confirmed genetic diagnoses and appropriately matched healthy controls.
Reprogramming: Using non-integrating methods such as Sendai virus or episomal vectors to deliver Yamanaka factors (OCT4, SOX2, KLF4, c-MYC), somatic cells are reprogrammed into iPSCs.
Characterization: Pluripotency must be confirmed through:
- Expression of pluripotency markers (NANOG, TRA-1-60, SSEA4) via immunocytochemistry
- Trilineage differentiation potential (ectoderm, mesoderm, endoderm) in vitro
- Karyotype analysis to ensure genomic integrity
Differentiation: Directed differentiation into disease-relevant cell types using specific growth factors, small molecules, and culture conditions.
Isogenic Control Generation: CRISPR/Cas9 gene editing corrects disease-causing mutations in patient-derived iPSCs or introduces these mutations into healthy iPSCs, creating genetically matched controls that isolate the effects of specific mutations from background genetic variation [3].
The following diagram illustrates this comprehensive workflow from patient cell collection to functional drug screening:
Advanced Model Systems
While two-dimensional cultures provide valuable insights, complex three-dimensional models better recapitulate tissue architecture and cell-cell interactions. Organoid systems have been successfully established for various rare diseases, including kidney organoids for Juvenile Nephronophthisis (NPHP1-deficient) and retinal organoids for autosomal dominant retinitis pigmentosa (RDH12-AD) [3]. These 3D models manifest disease-specific phenotypes such as renal cyst formation and photoreceptor degeneration, providing robust platforms for therapeutic screening.
Success Stories in Rare Disease Drug Discovery
Neurodegenerative Disorders
iPSC models have proven particularly valuable for neurodegenerative rare diseases, where access to affected human neurons is otherwise impossible. Several candidates identified through iPSC-based screening have advanced to clinical trials:
Table 1: Clinical-Stage Therapeutic Candidates Identified Through iPSC Screening for Neurodegenerative Diseases
| Drug Candidate | Target Condition | Mechanism of Action | Discovery Approach | Clinical Trial Status |
|---|---|---|---|---|
| Bosutinib | Amyotrophic Lateral Sclerosis (ALS) | Kinase inhibition | iPSC-derived motor neuron screening | Clinical trials based on iPSC research [89] |
| Ropinirole | Amyotrophic Lateral Sclerosis (ALS) | Dopamine agonist | iPSC-derived motor neuron screening | Clinical trials based on iPSC research [89] |
| Ezogabine | Amyotrophic Lateral Sclerosis (ALS) | Potassium channel opener | iPSC-derived motor neuron screening | Clinical trials based on iPSC research [89] |
| WVE-004 | ALS/Frontotemporal Dementia | RNA-targeting therapeutic | iPSC model-informed design | Clinical trials initiated [89] |
| BIIB078 | ALS/Frontotemporal Dementia | Antisense oligonucleotide | iPSC model-informed design | Clinical trials initiated [89] |
For ALS, researchers generated iPSCs from patients with various genetic backgrounds (including C9orf72, SOD1, TARDBP, and FUS mutations) and differentiated them into motor neurons. These cells exhibited disease-relevant phenotypes including protein aggregation, oxidative stress, and reduced survival. High-content screening of compound libraries identified existing drugs that ameliorated these pathological features, leading to the clinical evaluation of bosutinib, ropinirole, and ezogabine [89].
Sensory Disorders
Ocular rare diseases have particularly benefited from iPSC-based modeling and drug development. Research on autosomal dominant retinitis pigmentosa (RDH12-AD) utilized patient-specific retinal organoids that demonstrated reduced photoreceptor numbers, shortened photoreceptor segments, and disruptions in retinol biosynthesis and the vitamin A pathway by week 44 of differentiation—faithfully recapitulating the late-onset, mild disease course observed in patients [3]. This model provides a platform for identifying compounds that can stabilize photoreceptor function and survival.
Beyond drug discovery, iPSC-derived retinal pigment epithelial cells have been successfully transplanted in clinical studies for conditions like bullous keratopathy, demonstrating the dual application of iPSC technology for both drug screening and cell replacement therapies [15].
Renal and Metabolic Disorders
Juvenile Nephronophthisis (NPH), a genetic kidney disease without effective treatments, has been modeled using NPHP1-deficient iPSCs and kidney organoids. These models exhibited abnormal cell proliferation, primary cilia abnormalities, and renal cyst formation. Importantly, reintroduction of NPHP1 expression reversed cyst formation, providing proof-of-concept for genetic intervention and a platform for pharmacological screening [3].
In the metabolic domain, drug repurposing screens using iPSC-derived hepatocytes from patients with lysosomal storage disorders have identified compounds that enhance enzyme function or reduce substrate accumulation, offering promising therapeutic avenues.
Detailed Experimental Protocols
High-Content Screening for Neurodegenerative Diseases
The following protocol outlines the essential steps for conducting drug screens using iPSC-derived neurons:
Phase 1: iPSC Differentiation into Motor Neurons
- Culture Maintenance: Maintain iPSCs in essential 8 medium on Geltrex-coated plates until 70-80% confluent.
- Neural Induction: Switch to neural induction medium containing DMEM/F12, N2 supplement, non-essential amino acids, and dual SMAD inhibitors (LDN-193189 100nM, SB431542 10μM) for 10 days.
- Motor Neuron Patterning: Add retinoic acid (0.1μM) and purmorphamine (Sonic Hedgehog agonist, 0.5μM) for 14 days to pattern cells toward caudal and motor neuron fates.
- Maturation: Plate neural progenitors on poly-ornithine/laminin-coated plates in neurobasal medium with BDNF, GDNF, and CNTF (10ng/mL each) for 21-28 days.
- Characterization: Verify motor neuron identity by immunostaining for HB9, ISL1, and ChAT, with quantification of purity (>70% required for screening).
Phase 2: Compound Screening
- Assay Setup: Plate 10,000 cells/well in 384-well imaging plates. At day 28 of maturation, add compounds from screening libraries at 10μM in 0.1% DMSO.
- Viability Assessment: After 72 hours of treatment, measure cell viability using CellTiter-Glo 3D.
- Phenotypic Analysis: Fix cells and immunostain for disease-relevant markers (TDP-43 aggregates for ALS, tau for frontotemporal dementia). Image using high-content imagers (ImageXpress, Operetta).
- Image Analysis: Quantify phenotypic endpoints using automated algorithms (CellProfiler, ImageJ).
- Hit Selection: Define hits as compounds showing >30% protection from disease phenotype with Z' factor >0.4.
Phase 3: Hit Validation
- Dose Response: Retest hits in 8-point dose response (0.1nM-30μM) across 3 independent differentiations.
- Counter-Screening: Assess selectivity in isogenic control lines and additional cell types (cortical neurons, astrocytes).
- Mechanistic Studies: Conduct transcriptomic (RNA-seq) and proteomic analyses to elucidate mechanisms of action.
Organoid-Based Screening for Structural Abnormalities
For diseases with structural phenotypes like renal cyst formation:
- Organoid Generation: Differentiate iPSCs into kidney organoids using CHIR99021 (3-6μM) for 4 days followed with FGF9 (200ng/mL) and Heparin (1μg/mL) for 10 days.
- Disease Phenotype Induction: For cystogenesis assays, transfer organoids to 3D Matrigel droplets and culture for 21-28 days.
- Compound Treatment: Add compounds to culture medium with refreshment every 3 days.
- Phenotypic Quantification: Fix and immunostain organoids for nephron markers (LTL, ECAD, WT1), then image using confocal microscopy. Quantify cyst number and size using volumetric analysis (Imaris software).
- Functional Assessment: For renal organoids, measure albumin uptake and response to vasopressin.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of iPSC-based drug screening requires carefully selected reagents and platforms. The following table details essential tools mentioned in recent successful studies:
Table 2: Essential Research Reagents for iPSC-Based Rare Disease Drug Screening
| Reagent Category | Specific Examples | Function in Workflow | Application Notes |
|---|---|---|---|
| Reprogramming Systems | Sendai virus (CytoTune), episomal vectors | Somatic cell reprogramming to pluripotency | Non-integrating systems preferred for clinical translation |
| Characterization Antibodies | Anti-NANOG, TRA-1-60, SSEA4 | Pluripotency verification | Essential for quality control pre-differentiation |
| Differentiation Kits | STEMdiff Motor Neuron Kit, Intestinal Organoid Kit | Directed differentiation to specific lineages | Improve reproducibility across laboratories |
| Extracellular Matrices | Geltrex, Matrigel, Laminin-521 | Support cell growth and differentiation | Critical for 3D organoid culture and polarised cells |
| Gene Editing Tools | CRISPR/Cas9 systems, donor vectors | Isogenic control generation | Essential for confirming phenotype causality |
| Cell Viability Assays | CellTiter-Glo, Calcein AM | Compound toxicity assessment | Used as counter-screen for specificity |
| High-Content Imaging Systems | ImageXpress, Operetta CLS | Phenotypic quantification | Enable multiparametric analysis at single-cell resolution |
| Multi-omics Platforms | RNAseq, proteomics, metabolomics | Mechanistic investigation | Identify pathways and biomarkers |
Automation has become increasingly important in iPSC-based screening, with institutions like the New York Stem Cell Foundation pioneering automated, standardized production of iPSCs at scale, enabling the generation of biobanks with thousands of high-quality lines for robust statistical analysis [40].
Integration with In Silico Technologies
The combination of iPSC models with advanced computational approaches represents the cutting edge of rare disease research. In silico technologies complement experimental models in several key areas:
Target Identification: Network pharmacology algorithms analyze interactome data to identify novel therapeutic targets, as demonstrated in amyotrophic lateral sclerosis using the PandaOmics platform [6].
Virtual Screening: Molecular docking and quantitative structure-activity relationship (QSAR) models enable in silico screening of compound libraries against targets identified from iPSC transcriptomic data.
Clinical Trial Optimization: For diseases with extremely small patient populations, synthetic control arms and virtual trials help demonstrate efficacy where traditional randomized trials are impractical [6].
The integration of iPSC-derived data with computational models creates a virtuous cycle where experimental results refine in silico predictions, which in turn guide more focused and informative experimental screens.
iPSC-based disease modeling has fundamentally transformed the therapeutic development landscape for rare genetic disorders. The success stories outlined in this guide demonstrate how patient-derived cells can de-risk and accelerate the drug discovery process, moving candidates from bench to bedside with a higher probability of clinical success. The ability to recapitulate disease phenotypes in human cells, screen compound libraries directly on affected cell types, and validate mechanisms in genetically defined systems has addressed critical bottlenecks in rare disease research.
Future advances will likely focus on enhancing model complexity through multi-tissue systems, improving cellular maturation to better represent adult-onset diseases, and deeper integration with computational approaches. As the field moves forward, standardized protocols, automated production, and collaborative biobanking will be essential to maximize the potential of iPSC technology. With these advances, iPSC-based drug screening promises to deliver much-needed therapies for the millions of patients affected by rare genetic diseases worldwide.
Conclusion
iPSC-based disease modeling has fundamentally transformed the approach to rare genetic disorders, offering an unprecedented, human-specific window into pathogenesis and therapeutic discovery. By enabling the creation of patient-derived, physiologically relevant models in 2D and 3D formats, this technology directly addresses the critical bottleneck of sample scarcity. While challenges in standardization, maturation, and functional validation persist, ongoing advancements in gene editing, single-cell sequencing, and organoid technology are rapidly enhancing model precision. The convergence of large-scale iPSC biobanks, automated production platforms, and supportive regulatory frameworks is paving a clear path forward. Future progress hinges on continued international collaboration and the development of even more complex, multi-cellular systems that fully capture the tissue microenvironment, ultimately accelerating the delivery of much-needed therapies for the millions affected by rare diseases worldwide.
References
- 1. Seventy-eighth World Health Assembly – Daily update: 24 ... [https://www.who.int/news/item/24-05-2025-seventy-eighth-world-health-assembly---daily-update--24-may-2025]
- 2. Rare disease emerging as a global public health priority [https://pmc.ncbi.nlm.nih.gov/articles/PMC9632971/]
- 3. Studying rare diseases using induced pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450901/]
- 4. Editorial: Studying rare diseases using induced pluripotent ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/full]
- 5. Rare Needs Representation Too | CHEST Advocates [https://www.chestnet.org/guidelines-and-topic-collections/publications/chest-advocates/rare-needs-representation-too]
- 6. Advancing the frontier of rare disease modeling: a critical ... [https://www.nature.com/articles/s41746-025-02068-1]
- 7. Unlocking Rare Disease Mysteries: The Promise of iPSC ... [https://patientworthy.com/2025/09/13/unlocking-rare-disease-mysteries-the-promise-of-ipsc-based-model-systems/]
- 8. Modeling rare genetic disease with patient-derived induced ... [https://pubmed.ncbi.nlm.nih.gov/40751518/]
- 9. Updated demographics categories to capture the true diversity ... [https://pubmed.ncbi.nlm.nih.gov/40757058/]
- 10. Rare Disease in the U.S. 2025 - SSRS [https://ssrs.com/insights/rare-disease-in-the-us-2025/]
- 11. Advanced Cellular Models for Rare Study: Exploring Neural... Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC10815694/]
- 12. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 13. Modeling Human Neural Development and Disease with ... [https://www.isscr.org/upcoming-programs/poster-award-webinar]
- 14. Stem cell disease modeling: A new era for drug discovery | Abcam [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 15. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 16. Translation of a human induced pluripotent stem cell ... [https://www.medrxiv.org/content/10.1101/2025.04.02.25324702v1]
- 17. Modeling Rare Diseases with Induced Pluripotent Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6033695/]
- 18. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 19. Modeling rare diseases with induced pluripotent stem cell ... [https://www.sciencedirect.com/science/article/abs/pii/S089085081830001X]
- 20. Detailed Characterization of Human Induced Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4919381/]
- 21. Creation of Patient-Derived Induced Pluripotent Stem Cell ... [https://pediatricsnationwide.org/2025/04/22/creation-of-patient-derived-induced-pluripotent-stem-cell-lines-for-studying-rare-pediatric-genitourinary-disorders/]
- 22. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 23. Special Issue : Research in iPSC-Based Disease Models [https://www.mdpi.com/journal/ijms/special_issues/79F01GK40O]
- 24. Modeling rare genetic disease with patient-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317316/]
- 25. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 26. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 27. Current Development of iPSC-Based Modeling in ... [https://www.mdpi.com/1422-0067/26/8/3774]
- 28. MDM4 enables efficient human iPS cell generation from ... [https://www.nature.com/articles/s41598-025-16446-y]
- 29. Exploiting urine-derived induced pluripotent stem cells for ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-01035-4]
- 30. iPSCs and iPSC-derived cells as a model of human ... [https://www.nature.com/articles/s41467-025-56569-4]
- 31. Efficient exogenous DNA-free reprogramming with suicide ... [https://www.nature.com/articles/s12276-019-0282-7]
- 32. Generating Virus-free and Integration-free Induced ... [https://www.thermofisher.com/us/en/home/communities-social/blog/blogs/generating-virus-free-and-integration-free-induced-pluripotent-stem-cells-ipscs.html]
- 33. Enhanced Generation of Integration-free iPSCs from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4911493/]
- 34. A cost-effective and efficient reprogramming platform for ... [https://www.nature.com/articles/srep11319]
- 35. Epigenetic-scale comparison of human iPSCs generated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6222281/]
- 36. Defined culture conditions robustly maintain human stem ... [https://www.nature.com/articles/s42003-025-07658-z]
- 37. Guided Differentiation of Pluripotent Stem Cells into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10370173/]
- 38. Reprogramming of human urine cells into cardiomyocytes ... [https://www.nature.com/articles/s43856-025-00963-y]
- 39. Induced Pluripotent Stem (iPS) Cells & Gene Editing | Cyagen APAC [https://apac.cyagen.com/community/technical-bulletin/Induced-Pluripotent-Stem-iPS-Cells-Gene-Editing.html]
- 40. Reprogramming biology: iPSCs and the future of predictive ... [https://www.jax.org/news-and-insights/2025/november/reprogramming-biology-ipscs-and-the-future-of-predictive-research]
- 41. Studying Rare Diseases Using induced Pluripotent Stem ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/abstract]
- 42. Progress of iPSC-derived retinal organoids in the study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577290/]
- 43. Human-based complex in vitro models: their promise and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1526306/full]
- 44. Review Organoids pharmacology and toxicology [https://www.sciencedirect.com/science/article/pii/S2950489925000351]
- 45. Frontiers | Dominant RDH12-retinitis pigmentosa impairs ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1511066/full]
- 46. Modeling and Rescue of RP2 Retinitis Pigmentosa Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7363745/]
- 47. 切片人皮质类器官的电穿孔用于基因功能研究 [https://www.jove.com/cn/t/67598/electroporation-sliced-human-cortical-organoids-for-studies-gene]
- 48. Induced Pluripotent (iPSC) and Mesenchymal (MSC) Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192707/]
- 49. Human stem cell models for Marfan syndrome [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1498669/full]
- 50. Disease Modeling | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/disease-modeling.html]
- 51. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 52. Human iPSCs as Model Systems for BMP-Related Rare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10487005/]
- 53. Genomic Instability of iPSCs: Challenges Towards Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5346115/]
- 54. Current Challenges of iPSC-Based Disease Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6562607/]
- 55. Epigenetic Modulations of Induced Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3640613/]
- 56. A Protocol for Culture and Characterization of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10506163/]
- 57. A disease-specific iPS cell resource for studying rare and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10485998/]
- 58. Current Development of iPSC -Based Modeling in Neurodegenerative... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027653/]
- 59. A simplified protocol for differentiation of electrophysiologically... [https://www.nature.com/articles/mp201756?error=cookies_not_supported&code=c3005f17-234d-4a73-9a7d-30423633734c]
- 60. Direct Comparison of Four Hematopoietic Differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7486192/]
- 61. iPSC-based cell replacement therapy: from basic research ... [https://www.sciencedirect.com/science/article/pii/S1465324925000532]
- 62. Addressing variability in iPSC-derived models of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6994963/]
- 63. Genetic Variability Overrides the Impact of Parental Cell ... [https://www.sciencedirect.com/science/article/pii/S2213671115003744]
- 64. Systematic assessment of variability in the proteome ... [https://www.sciencedirect.com/science/article/pii/S1873506121003597]
- 65. Power and optimal study design in iPSC-based brain ... [https://www.nature.com/articles/s41380-022-01866-3]
- 66. Patient-derived iPSC modeling of rare neurodevelopmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7962756/]
- 67. Human induced pluripotent stem cells for modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5782822/]
- 68. Precision Health Resource of Control iPSC Lines for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6915802/]
- 69. Genomic integrity of human induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6828592/]
- 70. Examining iPSC derived motor neuron variability and ... [https://www.nature.com/articles/s41598-025-23378-0]
- 71. What is the success rate of induced pluripotent stem cells? [https://int.livhospital.com/success-rate-of-induced-pluripotent-stem-cells/]
- 72. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 73. Human iPSC Reprogramming Success: The Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 74. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 75. CRISPR And iPSC Disease Modeling And Drug Screening [https://www.cellandgene.com/doc/crispr-and-ipsc-disease-modeling-and-drug-screening-0001]
- 76. Induced Pluripotent Stem Cells Production Market 2025 [https://www.custommarketinsights.com/report/induced-pluripotent-stem-cells-production-market/]
- 77. Human iPSC-derived spinal neural progenitors enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373886/]
- 78. Cell-based drug discovery: Why human iPSC-derived ... [https://www.bit.bio/blog/cell-based-drug-discovery-with-human-ipsc-models]
- 79. CRISPR Editing in iPSCs [https://www.synthego.com/ipsc-crispr/]
- 80. Animal Disease Models and Patient-iPS-Cell-Derived In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10045735/]
- 81. Mouse models and induced pluripotent stem cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5539390/]
- 82. FDA Modernization Act 2.0: transitioning beyond animal ... [https://www.jci.org/articles/view/175824]
- 83. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 84. FDA's New “Plausible Mechanism Pathway” and Other ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-plausible-mechanism-pathway-and-other-initiatives-drugs-for-ultra-rare-conditions]
- 85. FDA Advances Rare Disease Drug Development with New ... [https://www.fda.gov/news-events/press-announcements/fda-advances-rare-disease-drug-development-new-evidence-principles]
- 86. Rare Disease Focus: FDA's Trio of Cell and Gene Therapy ... [https://www.ropesgray.com/en/insights/alerts/2025/11/rare-disease-focus-fdas-trio-of-cell-and-gene-therapy-draft-guidances-highlight-expedited-programs]
- 87. From Lab to Clinic: Success Stories of Repurposed Drugs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535746/]
- 88. Rare Disease Management Insights for 2025: Navigating ... [https://www.pm360online.com/rare-disease-management-insights-for-2025-navigating-payer-challenges/]
- 89. Drug discovery research with the iPSC models of ... [https://pubmed.ncbi.nlm.nih.gov/41213329/]