Karyotype Monitoring in Stem Cells: A Comprehensive Guide to Detecting and Managing Genetic Instability for Research and Therapy
Genetic instability in stem cells, particularly induced pluripotent stem cells (iPSCs), poses a significant challenge to their research validity and therapeutic safety.
Karyotype Monitoring in Stem Cells: A Comprehensive Guide to Detecting and Managing Genetic Instability for Research and Therapy
Abstract
Genetic instability in stem cells, particularly induced pluripotent stem cells (iPSCs), poses a significant challenge to their research validity and therapeutic safety. This article provides researchers, scientists, and drug development professionals with a comprehensive overview of the causes, consequences, and monitoring solutions for karyotypic abnormalities. We explore the foundational biology of genetic instability, detail current and emerging karyotyping methodologies, offer troubleshooting strategies for culture optimization, and present a comparative analysis of validation techniques. By synthesizing the latest research and regulatory perspectives, this guide aims to equip professionals with the knowledge to ensure genomic integrity in stem cell applications, from basic research to clinical translation.
The Unstable Core: Understanding the Causes and Consequences of Genetic Instability in Stem Cells
FAQs: Core Concepts and Best Practices
Q1: What is the fundamental difference between chromosomal aberrations and copy number variations (CNVs) in the context of stem cell genetic instability?
Chromosomal aberrations are large-scale abnormalities that can be observed under a microscope using traditional karyotyping methods. They include changes in chromosome number (aneuploidy) and large structural rearrangements such as translocations, inversions, and large deletions/duplications, typically larger than 5-10 megabases (Mb) [1]. In contrast, Copy Number Variations (CNVs) are sub-microscopic changes in the DNA sequence, defined as DNA segments of one kilobase or larger that are present at a variable copy number compared to a reference genome [2]. These smaller alterations (often ranging from 1 Kb to several Mb) require higher-resolution molecular techniques for detection but can have dramatic effects on gene expression and tumorigenic potential in stem cells [3].
Q2: Why is regular genetic monitoring absolutely essential for maintaining stem cell cultures in research and drug development?
Stem cells grown in culture are exposed to strong selection pressures that often result in genomic alterations [4]. These genetic changes can confer a selective advantage to subpopulations of cells, allowing them to rapidly take over the culture within very few passages. The consequences are severe and multifaceted:
- Compromised Research Validity: Genetic aberrations affect differentiation capacity, stem cell identity, and cellular behavior, jeopardizing the accuracy and reproducibility of basic research and disease modeling [1] [4].
- Tumorigenicity Risk: Aneuploidy and structural variations are hallmarks of cancer. Genetically abnormal stem cells may generate more aggressive teratomas and pose significant safety risks for therapeutic applications [4] [5].
- Regulatory Compliance: Stem cells intended for translational research or clinical use must meet rigorous genetic characterization release criteria. Regulatory bodies like the FDA emphasize comprehensive cytogenetic analysis for Investigational New Drug (IND) applications [1].
Q3: When should researchers perform genetic stability checks on their stem cell cultures?
Regular characterization is recommended at specific critical points to ensure culture integrity [1]:
- Establishment of a new cell line or upon acquisition from external sources
- Before establishing a master cell bank
- At the start of significant experimental protocols
- At regular intervals during prolonged culture (recommended every 10 passages)
- Before publishing results or concluding major experiments
- Prior to any clinical application
Q4: Can digital PCR (dPCR) replace traditional karyotype analysis for comprehensive genetic assessment?
No, dPCR should be viewed as complementary to karyotype analysis rather than a replacement [1]. While dPCR is faster and can detect small-scale genetic changes in known targets (point mutations, specific copy number variations), it cannot detect unknown abnormalities or identify large-scale structural abnormalities such as balanced translocations and aneuploidies. The most common aberrations found in genetically unstable cells—aneuploidy and large-scale structural rearrangements—would be missed by relying solely on dPCR, potentially compromising research findings and safety [1].
Troubleshooting Guides
Issue 1: Inconclusive or Suboptimal Karyotyping Results
Problem: Poor chromosome spreading, weak banding patterns, or inability to obtain sufficient metaphase cells for G-banded karyotype analysis.
| Possible Cause | Recommended Solution |
|---|---|
| Suboptimal cell culture conditions | Ensure cells are in log-phase growth and healthy. Use pre-warmed media and avoid over-confluence. |
| Incorrect mitotic arrest timing | Optimize colchicine/colcemid concentration and exposure time (typically 1-4 hours). Too short: insufficient metaphases; too long: over-contracted chromosomes. |
| Inadequate hypotonic treatment | Freshly prepare hypotonic solution (e.g., potassium chloride) and optimize incubation time (usually 15-30 minutes at 37°C). |
| Poor slide preparation | Ensure slides are clean and use controlled dropping technique. Adjust humidity and temperature during spreading. Age slides appropriately before staining. |
Protocol: Standard G-Banded Karyotyping for Stem Cells [1]
- Culture Preparation: Grow stem cells to 60-80% confluence in log-phase growth.
- Mitotic Arrest: Add colcemid to culture medium (final concentration 0.1 µg/mL) and incubate for 1-4 hours at 37°C.
- Harvesting: Trypsinize cells and collect by centrifugation.
- Hypotonic Treatment: Resuspend cell pellet in pre-warmed 0.075M KCl and incubate for 15-30 minutes at 37°C.
- Fixation: Gradually add fresh methanol:acetic acid (3:1) fixative while gently vortexing. Repeat centrifugation and fixation 2-3 times.
- Slide Preparation: Drop cell suspension onto clean, wet slides and air dry.
- G-Banding: Age slides, then treat with trypsin and stain with Giemsa or Leishman's stain.
- Analysis: Examine 15-20 metaphase spreads under microscope for chromosomal abnormalities >5-10 Mb.
Issue 2: Discrepant Findings Between Different Genetic Assessment Methods
Problem: Karyotype analysis appears normal but other methods (e.g., aCGH, RNA-Seq) suggest genetic abnormalities, or vice versa.
| Possible Cause | Recommended Solution |
|---|---|
| Resolution limitations | Karyotyping detects >5-10 Mb changes. Use higher-resolution methods (aCGH, SNP array) for submicroscopic CNVs. |
| Mosaicism below detection threshold | Karyotyping examines 15-20 cells; abnormalities in <10-20% of population may be missed. Increase the number of cells analyzed or use DNA-based methods. |
| Method-specific blind spots | Karyotyping detects balanced translocations; aCGH cannot. Use orthogonal methods for comprehensive assessment. |
| Culture heterogeneity | Subpopulations with different genetic profiles may exist. Isclone single-cell clones for pure populations. |
Protocol: High-Resolution aCGH for CNV Detection in Stem Cells [3]
- DNA Isolation: Extract high-quality genomic DNA from stem cells using phenol-chloroform or column-based methods. Assess purity (A260/280 ratio ~1.8).
- DNA Labeling: Denature 500 ng of test DNA and sex-matched reference DNA, then label with Cy3-dUTP and Cy5-dUTP respectively using random primers.
- Hybridization: Combine labeled samples with Cot-1 DNA and hybridization buffer. Apply to 135K StemArray microarray and hybridize at 42°C for 72 hours.
- Washing and Scanning: Wash slides stringently and scan at 2µm resolution using a microarray scanner.
- Data Analysis: Extract and normalize data using specialized software (e.g., NimbleScan). Call aberrations using segmentation algorithms (e.g., FASST2) with minimum of 4 probes, log2 ratio ≥0.3 for gains, ≤-0.3 for losses.
Issue 3: Detecting Genetic Abnormalities in Differentiated Cell Populations
Problem: Standard e-Karyotyping methods become noisy when analyzing differentiated cells due to gene expression changes.
Solution: Implement eSNP-Karyotyping, which utilizes allelic bias in RNA-Seq data rather than overall expression levels [6].
Protocol: eSNP-Karyotyping for Detecting Chromosomal Aberrations [6]
- RNA Sequencing: Extract high-quality RNA and prepare sequencing libraries. Sequence to sufficient depth (recommended 15-20 million mapped reads).
- SNP Calling: Identify single nucleotide polymorphisms from RNA-Seq data using GATK HaplotypeCaller.
- SNP Filtering: Filter SNPs with coverage <20 reads and minor allele frequency <0.2 to eliminate technical artifacts.
- Allelic Ratio Analysis: For each SNP, calculate the ratio of reads between the more-expressed allele and less-expressed allele.
- Aberration Detection: Order SNPs by chromosomal location and identify regions with statistically significant deviations from the expected 1:1 allelic ratio using moving average plots and t-tests with FDR correction.
Technical Data and Method Comparisons
Comparison of Genetic Instability Assessment Methods
| Method | Resolution | Key Strengths | Key Limitations | Best Applications |
|---|---|---|---|---|
| G-Banded Karyotyping [1] | 5-10 Mb | Gold standard; detects balanced and unbalanced large abnormalities; provides whole-genome view | Requires live, dividing cells; labor-intensive; low resolution | Routine monitoring; regulatory compliance; initial characterization |
| aCGH [3] [4] | 15 Kb - 1 Mb | High resolution for CNVs; automated; no cell culture required | Cannot detect balanced rearrangements or polyploidy | Identifying submicroscopic CNVs; detailed characterization |
| SNP Array [4] | 20 Kb - 1 Mb | Detects CNVs + loss of heterozygosity (LOH); can detect polyploidy | Cannot detect balanced translocations | Population diversity studies; LOH detection |
| RNA-Seq eSNP-Karyotyping [6] | Gene-level | Uses existing expression data; no reference sample needed; detects gains/losses | Requires heterozygous SNPs; depends on expression | Analysis of differentiated cells; secondary use of RNA-Seq data |
| Whole Genome Sequencing [4] | Single-base | Highest resolution; detects all variant types | Expensive; computationally intensive; complex analysis | Comprehensive characterization; research studies |
Common Recurrent Genetic Abnormalities in Cultured Stem Cells
| Chromosomal Region | Type of Abnormality | Associated Genes | Functional Consequences |
|---|---|---|---|
| Trisomy 12 [3] [6] | Aneuploidy | Multiple genes | Enhanced self-renewal, competitive growth advantage |
| Trisomy 17 [3] | Aneuploidy | Multiple genes | Culture adaptation, potential tumorigenicity |
| 20q11.21 amplification [6] [5] | CNV gain | BCL2L1 (Bcl-xL) | Anti-apoptotic, survival advantage |
| 3q13.13 amplification [3] | CNV gain (~595 Kb) | DPPA2, DPPA4 | Pluripotency marker amplification, possible selective advantage |
| 16q23.3 deletion [3] | CNV loss (~285 Kb) | CDH13 | Increased growth, reduced apoptosis (tumor suppressor loss) |
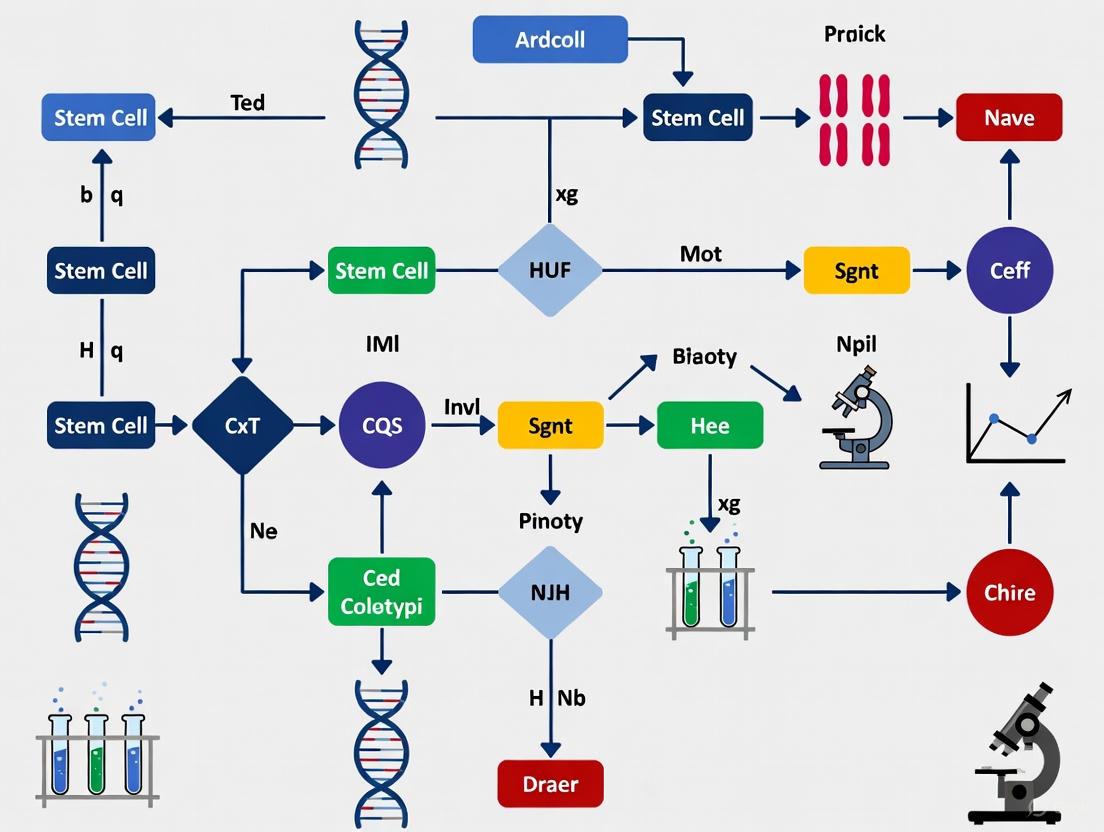
Visualized Workflows and Pathways
Genetic Instability Monitoring Workflow
Method Selection Decision Pathway
Research Reagent Solutions
Essential Materials for Genetic Instability Assessment
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Mitotic Arrest Agents | Colchicine, Colcemid, Demecolcine | Arrests cells in metaphase for chromosome analysis in karyotyping [1] |
| Hypotonic Solutions | 0.075M Potassium Chloride | Swells cells to separate chromosomes for better spreading [1] |
| Fixatives | Methanol:Acetic Acid (3:1) | Preserves chromosome structure and morphology for analysis [1] |
| Staining Reagents | Giemsa stain, Leishman's stain | Creates G-banding patterns for chromosome identification [1] |
| aCGH Microarrays | 135K StemArray, Whole-genome arrays | High-resolution platform for detecting copy number variations [3] |
| DNA Labeling Kits | Cy3-dUTP, Cy5-dUTP labeling kits | Fluorescent labeling for comparative genomic hybridization [3] |
| SNP Array Platforms | Illumina, Affymetrix arrays | Genotype analysis and loss of heterozygosity detection [4] |
| NGS Library Prep Kits | RNA-Seq, WGS library preparation | Preparation of sequencing libraries for high-resolution analysis [6] |
| Bioinformatics Tools | GATK HaplotypeCaller, NimbleScan, Nexus Copy Number | Data analysis for variant calling and aberration detection [3] [6] |
Stem cell cultures are vital tools for studying development, disease, and creating cell-based therapies. However, their genetic integrity is constantly threatened by reprogramming stress and the pressures of in vitro culture. These stressors can induce genetic abnormalities that compromise research validity, disease modeling accuracy, and patient safety in therapeutic applications [1]. This technical support center outlines the primary drivers of this instability and provides actionable troubleshooting guides to help researchers maintain genetically stable cell lines.
Understanding the Stressors: FAQs on Drivers of Instability
FAQ 1: What are the fundamental types of stress that lead to genetic instability?
- Reprogramming Stress: The process of converting somatic cells into induced pluripotent stem cells (iPSCs) forces a massive transcriptional rewiring. This process can disrupt cellular metabolism, leading to NADH reductive stress, where an accumulation of NADH drives harmful metabolic reprogramming and increases reactive oxygen species (ROS) production [7].
- Culture-Induced Stress: The in vitro environment is inherently stressful. Key stressors include:
- Proteostatic Stress: The high demand for protein synthesis in rapidly dividing cultures can overwhelm the endoplasmic reticulum (ER), leading to ER stress and the unfolded protein response (UPR). Persistent UPR activation can trigger apoptosis [8].
- Oxidative Stress: Metabolic imbalances in culture can generate excess ROS, causing DNA damage and genomic lesions [8].
- Suboptimal Culture Conditions: Factors like high cell density, over-confluence during passaging, and enzymatic dissociation can inflict mechanical and chemical stress, selectively favoring the growth of abnormal cells [9] [10].
FAQ 2: What are the most common genetic abnormalities acquired in culture?
The most frequent abnormalities are aneuploidies (gains or losses of whole chromosomes) and large-scale structural rearrangements such as translocations, inversions, and duplications or deletions larger than 5-10 megabases. Chromosome region 9p21 is a known hotspot for such aberrations [1].
FAQ 3: How do metabolic stresses like NADH reductive stress connect to genetic damage?
NADH reductive stress is often a consequence of mitochondrial dysfunction, nutrient overload, or hypoxia. It serves as a central mediator in disease pathways by enhancing ROS production and reducing ATP levels. The resulting oxidative stress can directly damage DNA, while the energy deficit can impair crucial DNA repair mechanisms, creating a permissive environment for mutations to arise and persist [7].
Troubleshooting Common Culture Problems
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Excessive Differentiation (>20%) [9] | Old culture medium; over-confluent cultures; prolonged time outside incubator. | Use fresh medium (<2 weeks old); remove differentiated areas before passaging; passage before over-confluence; limit plate handling to <15 minutes. |
| Low Cell Attachment After Passaging [9] [10] | Over-sensitive to passaging reagent; low initial seeding density; incorrect cultureware. | Reduce incubation time with passaging reagent; plate 2-3x more cell aggregates; ensure use of non-tissue culture-treated plates with Vitronectin XF. |
| Poor Neural Induction Efficiency [10] | Low-quality hPSCs; incorrect plating density; single-cell suspension. | Use high-quality, undifferentiated hPSCs; plate cell clumps (not single cells) at 2–2.5 x 10⁴ cells/cm²; consider 10 µM ROCK inhibitor at passage. |
| Unexpected Cell Death/ Cytotoxicity [10] | Normal post-transduction effect during reprogramming; overly confluent at passaging. | Continue culture per protocol; if passaging overly confluent cells, use a ROCK inhibitor (e.g., Y27632) to improve survival. |
| Inconsistent Experimental Results [1] | Undetected genetic abnormalities in stem cell line; phenotype drift. | Implement regular genetic monitoring (e.g., karyotyping); establish a robust quality control system with standardized protocols. |
Genetic Monitoring: Protocols and Schedules
Regular genetic characterization is non-negotiable for ensuring culture integrity. G-banded karyotyping is the gold standard for detecting large-scale abnormalities [1].
| Key Event or Milestone | Monitoring Action |
|---|---|
| Acquisition or Derivation of a new cell line | Perform initial karyotyping to establish a genomic profile. |
| Initial Biobanking for future use/distribution | Confirm genetic identity and stability before creating a master cell bank. |
| Start of a Critical Experimental Protocol | Verify genetic integrity to ensure a valid starting point. |
| During Long-Term Culture (In-Process Control) | Monitor genomic stability at regular intervals (e.g., every 10 passages). |
| Conclusion of Experiments / Prior to Publication | Confirm the genetic identity and integrity of the cell line used. |
Note: While digital PCR (dPCR) is useful for detecting known, small-scale mutations, it cannot replace karyotyping, as it will miss unknown abnormalities and large-scale structural changes like translocations [1].
The Scientist's Toolkit: Essential Research Reagents
| Reagent / Material | Function & Application |
|---|---|
| ROCK Inhibitor (Y27632) [10] | Improves survival of single cells and cryo-recovered cells by inhibiting apoptosis; used during passaging and thawing. |
| Essential 8 Medium [10] | A defined, feeder-free culture medium designed for the maintenance and expansion of human PSCs. |
| Vitronectin (VTN-N) [10] | A defined, recombinant substrate used for feeder-free culture of human PSCs, providing an attachment surface. |
| ReLeSR / Gentle Cell Dissociation Reagent [9] | Non-enzymatic reagents for passaging PSCs as cell aggregates, minimizing mechanical and enzymatic stress. |
| Geltrex / Matrigel [10] | A basement membrane matrix extract used as a substrate to coat cultureware for plating and maintaining various cell types, including NSCs. |
| B-27 Supplement [10] | A serum-free supplement essential for the long-term survival and growth of neuronal cells in culture. |
| Collagenase/Dispase Enzymes [11] | Enzymatic cocktails used for the gentle dissociation of tissues to isolate primary cells. |
| Cryo-SFM Plus [12] | An advanced cryopreservation medium designed to maintain high cell viability and integrity during frozen storage. |
Visualizing Stress Pathways and Experimental Workflows
Cellular Stress Signaling Pathways
Genetic Integrity Monitoring Workflow
Human pluripotent stem cells (hPSCs), including both embryonic and induced pluripotent stem cells, are invaluable tools for developmental studies, disease modeling, and regenerative medicine. However, long-term culture of these cells is associated with the accumulation of karyotypic abnormalities that may change their developmental potential, malignant capacity, and therapeutic safety. The genomic integrity of hPSC lines requires routine monitoring, as reprogramming and prolonged in vitro cultivation can induce genetic instability. Research has revealed that chromosomal aberrations in hPSCs occur in a non-random, sporadic manner, with particularly recurrent abnormalities involving chromosomes 1, 12, 17, 20, and X. These recurrent changes are observed in both research-grade and clinically-oriented stem cell lines, raising significant concerns for their application in translational medicine and drug development.
Cataloging the Recurrent Chromosomal Hotspots
Large-scale studies on thousands of hPSC samples have identified that the most common karyotypic abnormalities involve partial or whole gains of chromosomes 12, 17, 20, and X. These recurrent abnormalities provide a selective advantage to the cells in culture, leading to their outcompetition of karyotypically normal cells over successive passages.
Comprehensive Table of Recurrent Aberrations
Table 1: Recurrent chromosomal aberrations in human pluripotent stem cells
| Chromosome | Specific Abnormality | Frequency | Key Genes Involved | Functional Consequences |
|---|---|---|---|---|
| 12 | Trisomy 12 (whole-chromosome gain) | High | Numerous pluripotency-associated genes | Enhanced self-renewal, reduced differentiation potential |
| 17 | Trisomy 17, gain of 17q25 | High | TP53 | Altered apoptosis, selective growth advantage |
| 20 | Gain of 20q11.21 | Very High | BCL2L1 (BCL-XL) | Anti-apoptotic effect, proliferation advantage |
| 1 | Trisomy 1q | Moderate | Multiple oncogenes | Increased proliferation rates |
| X | Trisomy X (in female lines) | Moderate | X-linked regulators | Altered differentiation capacity |
The recurrence of these specific abnormalities across independent cell lines and laboratories suggests strong selective pressures in culture conditions that favor cells with these genetic changes. These alterations frequently involve genes that provide survival advantages, such as anti-apoptotic genes or genes that enhance proliferation rates.
Technical FAQs: Addressing Researcher Questions on Aberration Detection
Q1: What is the detection limit for mosaicism in hPSC cultures using standard karyotyping methods? Conventional G-banding karyotyping can typically detect mosaicism at levels of approximately 10-20%. More sensitive methods like digital PCR (dPCR) can detect lower levels of mosaicism for specific known targets, but cannot identify unknown or structural abnormalities. Recognition of this detection limit is crucial for developing strategies for routine laboratory practice and regulation for the use of hPSCs in regenerative medicine [13].
Q2: How do culture conditions affect the acquisition of chromosomal abnormalities in hPSCs? Studies involving over 100 continuous passages have demonstrated that single-cell passaging and feeder-free conditions are associated with a higher incidence of cytogenetic changes. hPSCs cultured as single-cells displayed increased rates of cell proliferation and persistence of pluripotency markers in differentiation assays. This emphasizes the need to meticulously evaluate the effects of new media types, substrates, and passaging methods on hPSC stability, particularly for cultures intended for clinical use [13].
Q3: Why do karyotypically abnormal hPSCs often overtake cultures? Karyotypically abnormal hPSCs can bypass developmental restrictions that limit the growth of normal cells. Research has identified a series of bottlenecks that restrict the growth of karyotypically normal hPSCs when seeded as single-cells. A large proportion of normal cells die shortly after plating, and those that survive often fail to re-enter the cell cycle. In contrast, karyotypically abnormal hPSCs successfully bypass these bottlenecks, providing them with a competitive advantage in standard culture conditions [13].
Q4: What are the safety concerns regarding these recurrent abnormalities? The recurrent abnormalities identified in hPSCs are also frequently observed in human cancers, raising significant safety concerns for using these cells in therapeutic applications. Specifically, gains of chromosomes 12, 17, and 20, as well as duplication of 20q11.21 containing the BCL2L1 anti-apoptotic gene, are associated with increased growth rates and survival advantages reminiscent of cancer cells [13].
Methodologies for Detecting Chromosomal Aberrations
Multiple complementary techniques are available for detecting chromosomal abnormalities in hPSCs, each with distinct advantages, limitations, and appropriate applications in quality control pipelines.
Comparative Table of Detection Methods
Table 2: Techniques for detecting chromosomal aberrations in stem cells
| Method | Resolution | Key Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| G-banding Karyotyping | ~5-10 Mb | Comprehensive genome view, detects balanced/unbalanced rearrangements, gold standard | Requires skilled interpretation, needs actively dividing cells | Routine quality control, regulatory compliance |
| FISH | 50-500 kb | Targeted analysis, works on interphase cells, quantitative | Limited to pre-selected targets | Confirming specific suspected abnormalities |
| SNP Arrays | <50 kb | Genome-wide coverage, detects copy number variations and UPD | Cannot detect balanced rearrangements | High-resolution screening of genomic imbalances |
| aCGH | <50 kb | Genome-wide coverage, sensitive for copy number changes | Cannot detect balanced rearrangements or low-level mosaicism | Comprehensive copy number analysis |
| RNA-Seq eSNP-Karyotyping | Variable | Uses existing transcriptome data, no separate DNA analysis needed | Limited to expressed regions, requires sufficient coverage | Integrated analysis when RNA-Seq data is available |
| KaryoLite BoBs | Arm-level | High-throughput, cost-effective, simple data analysis | Limited to chromosome arm-level resolution | Rapid screening of common aneuploidies |
Experimental Protocol: G-Banded Karyotyping for hPSCs
Regular karyotyping is essential for monitoring hPSC genomic integrity. The following protocol outlines the standard procedure for G-banded karyotype analysis:
Cell Preparation and Harvest:
- Culture hPSCs to 60-80% confluence in appropriate conditions.
- Add mitotic arresting agent (colchicine, colcemid, or demecolcine) to actively dividing cells for 4-6 hours.
- Dissociate cells using enzyme-free dissociation buffer or gentle enzymatic treatment.
- Transfer cell suspension to centrifuge tubes and pellet cells at 1000 rpm for 8 minutes.
Hypotonic Treatment and Fixation:
- Resuscell pellet in pre-warmed 0.075M KCl hypotonic solution and incubate at 37°C for 20 minutes.
- Add freshly prepared methanol:acetic acid (3:1) fixative slowly while gently mixing.
- Centrifuge and repeat fixation twice with fresh fixative.
- Drop cell suspension onto clean, wet microscope slides and air dry.
G-Banding and Analysis:
- Age slides overnight at 60°C or use chemical aging methods.
- Treat slides with trypsin solution followed by Leishman's stain [14] [1].
- Examine under high-resolution microscope and capture images of 20+ metaphase spreads.
- Arrange chromosomes into karyogram using specialized software.
- Analyze for numerical and structural abnormalities according to ISCN nomenclature.
Diagram: Karyotyping workflow for genetic monitoring
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful karyotype monitoring requires specific reagents and materials designed for stem cell culture and cytogenetic analysis. The following table outlines essential solutions for establishing a robust genetic monitoring pipeline.
Table 3: Essential research reagents for karyotype analysis
| Reagent/Material | Function | Example Application | Technical Notes |
|---|---|---|---|
| KaryoLite BoBs | High-throughput molecular karyotyping using BAC probes on beads | Rapid screening of common aneuploidies in multiple cell lines | Detects arm-level abnormalities with 100 ng DNA input [15] |
| Leishman's Stain | G-banding chromosome staining for microscopic analysis | Conventional karyotyping following standard protocols | Provides characteristic banding patterns for chromosome identification [14] |
| Colcemid | Mitotic arresting agent | Metaphase chromosome preparation | Optimize concentration and exposure time for optimal chromosome spreading |
| mTeSR1 Medium | Defined, feeder-free culture medium | Maintenance of hPSCs prior to karyotype analysis | Provides consistent culture conditions minimizing selective pressures [16] |
| Matrigel Matrix | Extracellular matrix for cell attachment | Feeder-free culture substrate for hPSCs | Batch-to-batch variation may affect culture stability |
| Sendai Virus Vectors | Non-integrating reprogramming method | Generation of iPSC lines | Associated with higher genetic instability compared to episomal vectors [16] |
| Episomal Vectors | Non-viral reprogramming method | Generation of integration-free iPSC lines | Lower frequency of copy number alterations compared to viral methods [16] |
Troubleshooting Guide: Addressing Common Experimental Challenges
Researchers frequently encounter specific technical challenges when monitoring chromosomal stability in hPSCs. The following troubleshooting guide addresses the most common issues and provides evidence-based solutions.
Problem: Inadequate metaphase spreads for karyotyping Possible Causes and Solutions:
- Insufficient cell division: Ensure cells are in log-phase growth before harvesting. Optimize culture conditions to promote proliferation.
- Suboptimal hypotonic treatment: Adjust KCl concentration and incubation time based on cell type. Test different durations (15-25 minutes).
- Poor slide preparation: Adjust humidity, temperature, and dropping height during slide preparation. Ensure fixative is freshly prepared.
Problem: Inconsistent detection of low-level mosaicism Possible Causes and Solutions:
- Limited sample size: Increase the number of metaphases analyzed from 20 to 50+ to improve detection sensitivity.
- Methodological limitations: Employ orthogonal methods such as FISH to confirm suspected mosaicism detected by karyotyping.
- Suboptimal culture sampling: Sample multiple culture vessels and different passage numbers to comprehensively assess mosaicism.
Problem: Culture adaptation and emergence of abnormal clones Possible Causes and Solutions:
- Selective pressure in culture: Avoid over-trypsinization and extreme dilution cloning. Use bulk passaging methods when possible.
- Suboptimal culture conditions: Regular quality control of culture reagents. Avoid frequent changes in media formulation or substrate.
- Extended passaging: Establish early passage master cell banks and limit experimental use to lower passage numbers.
Diagram: Method selection for chromosomal analysis
Quality Control Recommendations and Regulatory Considerations
Establishing a systematic approach to karyotypic monitoring is essential for maintaining hPSC quality and ensuring regulatory compliance, particularly for cells intended for therapeutic applications.
Strategic Timing for Karyotype Analysis
Regular karyotyping should be performed at specific milestones in the stem cell culture lifecycle [1]:
- At the acquisition or derivation of a new cell line
- During initial biobanking and master cell bank establishment
- At the start of experimental protocols or differentiation studies
- As an in-process control every 10 passages during extended culture
- At the conclusion of major experiments prior to publication
- Before creating working cell banks for distribution
Addressing Regulatory Requirements
For stem cells intended for clinical applications, regulatory bodies like the FDA emphasize comprehensive cytogenetic analysis using validated methods. Investigational New Drug (IND) applications and Biologics License Applications (BLA) require detailed information on genetic stability, including data from cytogenetic testing. G-banded karyotyping remains widely recognized across the stem cell community and by regulatory bodies as the "gold standard" measurement for genetic stability, providing a comprehensive visual overview of the entire chromosome complement [1].
The recurrent chromosomal aberrations affecting chromosomes 1, 12, 17, 20, and X represent a significant challenge in hPSC research and application. Understanding these hotspots, their functional consequences, and methods for their detection is essential for producing robust, reproducible research and developing safe therapeutic products. By implementing systematic karyotype monitoring protocols at critical culture milestones, employing appropriate detection methods based on specific research needs, and understanding the technical challenges associated with cytogenetic analysis, researchers can better ensure the genetic integrity of their stem cell lines. This comprehensive approach to genomic monitoring supports both basic research quality and the translational pathway for stem cell-based therapies.
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common genetic abnormalities found in human pluripotent stem cells (hPSCs) during routine culture?
hPSCs, including both embryonic and induced pluripotent stem cells, are prone to acquiring recurrent genetic abnormalities during prolonged in vitro culturing. The most frequently observed aberrations are specific chromosomal gains and mutations in key tumor suppressor genes [17] [18].
- Common Chromosomal Gains: Recurrent aneuploidies often involve gains of whole chromosomes or specific chromosomal arms. The most prevalent include chromosomes 20, 1q, 12, 17, and 8 [17] [18] [19]. For instance, gain of 20q11.21 is one of the most frequently reported anomalies in hPSC cultures [19].
- Common Gene Mutations: Pathogenic single nucleotide variants (SNVs) are often found in cancer-associated genes. The most commonly mutated gene is TP53, a critical tumor suppressor. Other less frequent mutations occur in genes like EGFR and CDK12 [17].
FAQ 2: How do genetic abnormalities directly impact the differentiation potential of hPSCs?
Culture-acquired genetic alterations can significantly compromise the utility of hPSCs by affecting their fundamental properties, including their capacity to differentiate into specialized cell types [18]. Abnormalities can alter the efficiency of differentiation protocols and the functionality of the resulting differentiated cells [19]. For example, studies have shown that cell lines with specific genetic aberrations can exhibit altered proliferation and differentiation capacities, which would negatively impact their use in generating specific cell types for research or therapy [17].
FAQ 3: What is the link between culture-adapted hPSCs and increased tumorigenic risk?
Prolonged culture can lead to "culture adaptation," where hPSCs with specific genetic aberrations that confer a growth advantage (like anti-apoptotic mutations) outcompete normal cells [17]. These culture-adapted cells are not just genetically different; they also display more aggressive tumorigenic potential.
- From Teratoma to Teratocarcinoma: While normal hPSCs typically form benign teratomas, culture-adapted cells with specific aberrations have been shown to form more malignant, teratocarcinoma-like tumors. These immature tumors contain undifferentiated, cancerous cells in addition to the differentiated tissues found in teratomas, representing a significantly higher safety risk [17].
- Aggressive Tumor Growth: The genetic aberrations acquired during culture are closely linked to an increase in "tumorigenic aggressiveness" [17].
FAQ 4: Can genetic testing predict the formation of abnormal tissues in animal models?
Yes, specific types of genetic tests can be highly predictive. Research has shown that analyzing Copy Number Variants (CNVs) is a more reliable predictor of abnormal tissue formation after transplantation of iPSC-derivatives into immunodeficient mice than looking for single nucleotide variants (SNVs) [20].
- Low Predictivity of SNVs: The presence of SNVs or small deletions in cancer-related genes showed no strong positive correlation with abnormal tissue formation, with an overall predictivity of only 29% [20].
- High Predictivity of CNVs: In contrast, a copy number higher than 3 in a genomic region was strongly correlated with abnormal tissue formation, with an overall predictivity of 86%. This suggests that CNV analysis is a powerful tool for risk assessment in preclinical safety evaluations [20].
Troubleshooting Guide: Identifying and Managing Genetic Abnormalities
Problem: Suspected genetic overgrowth in your hPSC culture. Solution: Implement a regular and rigorous genomic quality control (QC) strategy.
Step 1: Routine Monitoring
Regular testing is crucial because a genetically abnormal clone can completely overtake a culture in as little as five passages [19].
- Action: Perform routine karyotyping at regular intervals (e.g., every 10-15 passages) and after critical manipulations like reprogramming or gene editing [19].
- Method Selection: The table below compares common QC methods.
| Method | Key Function | Key Advantage | Primary Limitation |
|---|---|---|---|
| G-banding Karyotyping [19] | Detects large-scale chromosomal aberrations (≥5-10 Mb). | Genome-wide view; can detect balanced translocations. | Low resolution; requires living, dividing cells. |
| SNP Array Analysis [19] | Detects copy number variants (CNVs) and loss of heterozygosity (LOH). | Higher resolution (~350 kb); detects CN-LOH. | Cannot detect balanced translocations. |
| Whole Exome/Genome Sequencing [17] | Identifies single nucleotide variants (SNVs) and small insertions/deletions. | Base-pair resolution of coding (exome) or entire (genome) sequences. | More expensive; data analysis is complex. |
Step 2: Interpretation of Results
Compare your QC data against known recurrent abnormalities.
- Action: If analysis reveals a known high-risk aberration (e.g., gain of 1q, 12p, 17q, or 20q; or a TP53 mutation), the cell line should be discarded for clinical purposes and used for research only with extreme caution [17] [19].
- Quantitative Data: The table below summarizes the frequency and functional impact of the most common abnormalities.
| Genetic Abnormality | Approximate Frequency in Studies | Impact on Pluripotency | Impact on Tumorigenicity |
|---|---|---|---|
| Gain of 20q/20q11.21 [17] [18] [19] | Very common (e.g., 8.6% of lines in one study [18]) | Confers growth advantage; linked to anti-apoptotic gene BCL2L1 [17]. | Increases tumorigenic aggressiveness [17]. |
| Gain of 1q [18] [19] | Very common (e.g., 7.2% of tests [18]) | Associated with feeder-free and high-density culture [18]. | Increases tumorigenic aggressiveness [17]. |
| TP53 mutations [17] [16] | Very common (e.g., >30% of samples in one analysis [17]) | Provides selective growth advantage in culture [17]. | Strongly linked to cancer; dramatically increases risk [17]. |
| Trisomy 8 [18] | Less common (e.g., 2.9% of tests [18]) | Confers a growth advantage in culture. | Increases tumorigenic aggressiveness [17]. |
Step 3: Preventive Measures
- Culture Practices: Avoid extended passaging and minimize stress by using gentle, defined passaging methods. Be aware that some aberrations, like 1q gain, are associated with specific culture conditions like feeder-free systems [18].
- Banking: Create early-passage master cell banks and perform comprehensive QC (karyotyping and SNP array) on the banked cells to ensure a baseline of genetic normality.
Experimental Protocols for Key Assays
Protocol 1: SNP Array Analysis for High-Resolution CNV Detection
This protocol provides a practical guide for using SNP arrays for quality control, based on the method described by [19].
1. DNA Extraction:
- Isolate high-quality genomic DNA from hPSCs using a commercial kit (e.g., QIAamp DNA Blood Mini Kit). Ensure DNA integrity and concentration.
2. Array Processing:
- Process the DNA on a commercial SNP array platform (e.g., Illumina Global Screening Array).
- The protocol uses allele-specific primer extension (ASPE) and single-base extension (SBE) on fluorescence-labeled BeadChips to genotype hundreds of thousands of SNPs across the genome.
3. Data Analysis with GenomeStudio:
- Load the scanned data into Illumina's GenomeStudio software with the cnvPartition plug-in.
- Key QC Metrics:
- Call Rate: The percentage of successfully genotyped SNPs. An acceptable call rate is typically >95% [19].
- CNV Detection: The software algorithm (cnvPartition) will automatically call CNVs (gains and losses) and regions of Loss of Heterozygosity (LOH) based on deviations from expected signal intensities and allele frequencies.
4. Interpretation:
- Visually inspect the genome-wide plots for large-scale aberrations.
- Cross-reference any called CNVs with databases of known recurrent hPSC aberrations (e.g., 20q11.21, 1q).
Protocol 2: The Teratoma Assay for Assessing Pluripotency and Tumorigenicity
The teratoma assay is the gold-standard in vivo test for pluripotency and a key assessment of tumorigenic potential [17] [21].
1. Cell Preparation:
- Harvest undifferentiated hPSCs. A common injection dose is 1x10^6 to 2x10^6 cells per site [16].
- Resuspend the cell pellet in an appropriate buffer, often mixed with an extracellular matrix like Matrigel to enhance engraftment.
2. Animal Transplantation:
- Inject the cell suspension subcutaneously, intramuscularly, or under the testis capsule of immunodeficient mice (e.g., NOD/SCID mice). The subcutaneous dorsal flank is a common site [16].
3. Observation and Tumor Harvest:
- Monitor mice for tumor formation over 8-16 weeks [16].
- Excise the resulting teratoma and fix it in formalin for histological processing.
4. Histological Analysis:
- Embed the fixed teratoma in paraffin and section it.
- Stain sections with Hematoxylin and Eosin (H&E).
- Examine the tissue for the presence of differentiated structures representing all three embryonic germ layers:
- Ectoderm (e.g., neural rosettes, pigmented cells, keratinocytes)
- Mesoderm (e.g., cartilage, bone, muscle, adipose tissue)
- Endoderm (e.g., gut-like epithelial structures, respiratory epithelium)
Signaling Pathways and Logical Relationships
Teratoma Formation Mechanism
The following diagram summarizes the key factors and mechanisms that contribute to teratoma formation from transplanted hPSCs, integrating genetic, cellular, and host-related factors.
The Scientist's Toolkit: Essential Research Reagents & Materials
This table lists key materials and reagents essential for the experiments and quality control procedures discussed in this guide.
| Item | Specific Example(s) | Function in Experiment/QC |
|---|---|---|
| Reprogramming Vectors | Sendai Virus (CytoTune-iPS), Episomal Vectors [16] | Non-integrating methods to generate integration-free iPSCs from somatic cells. |
| hPSC Culture Medium | mTeSR1 [16] | Defined, feeder-free medium for the maintenance of undifferentiated hPSCs. |
| DNA Extraction Kit | QIAamp DNA Blood Mini Kit [19] | Isolates high-quality genomic DNA for downstream genetic analysis (e.g., SNP array, sequencing). |
| SNP Array Platform | Illumina Global Screening Array [19] | High-resolution platform for genome-wide detection of CNVs and LOH. |
| Analysis Software | GenomeStudio with cnvPartition [19] | Software for analyzing SNP array data to automatically call CNVs and assess quality metrics. |
| Immunodeficient Mice | NOD/SCID mice [16] [21] | In vivo host for the teratoma assay, preventing immune rejection of transplanted human cells. |
| Extracellular Matrix | Matrigel [16] | Used as a scaffold mixed with hPSCs for transplantation to support engraftment and teratoma formation. |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why do we observe a rapid takeover of cultures by genetically variant human pluripotent stem cells (hPSCs)?
A1: The rapid overgrowth, or selective advantage, occurs when genetically variant hPSC populations have intrinsic properties that differ from wild-type cells. Research indicates these variants often exhibit a higher proliferative rate or a more favorable response to the specific culture environment. Computational modeling has identified three critical process parameters that drive this phenomenon when variants are present: total culture density, initial proportion of variant cells, and the degree of variant cell overgrowth [22].
Q2: During which stages of iPS cell generation and differentiation are we most likely to see the emergence of genetically variant cells?
A2: Genomic alterations can occur at multiple stages. One systematic investigation observed a total of ten copy number alterations (CNAs) and five single-nucleotide variations (SNVs) across the phases of reprogramming, differentiation, and passaging. The study found that the reprogramming method matters; iPS cells generated using the Sendai virus (SV) method showed a higher frequency of CNAs and SNVs during the reprogramming phase compared to those generated with episomal vectors (Epi) [23].
Q3: What are the critical consequences of this selective advantage for manufacturing cell-based products?
A3: The primary consequence is the potential impact on Critical Quality Attributes (CQAs) of the final product. Genetic variations can alter the differentiation potential of hPSCs or cause phenotypic variation in the resulting differentiated cells. For products that specify a maximum allowable proportion of variant cells, understanding and controlling the growth dynamics between wild-type and variant populations is essential for ensuring product quality, safety, and efficacy [22].
Q4: What key signaling pathways are often disrupted in cells that gain a selective advantage?
A4: While specific pathways can vary, the TP53 tumor suppressor pathway is frequently implicated. Studies on iPS cell genomic instability have identified TP53 mutations as a key vulnerability, underscoring the need for careful genomic scrutiny. Furthermore, gene expression analysis has revealed upregulation of chromosomal instability-related genes in late-passage cells that exhibit genomic instability, pointing to broader disruptions in cell cycle control and DNA damage response pathways [23].
Experimental Protocols for Monitoring Selective Advantage
Protocol 1: Longitudinal Genomic Instability Assessment during iMS Cell Differentiation
This protocol is designed to trace genomic alterations from the initiation of iPS cells through to induced Mesenchymal Stromal/Stem (iMS) cell differentiation [23].
Key Steps:
- Reprogramming: Generate integration-free iPS cell lines from human dermal fibroblasts using either Sendai virus (SV) vectors (CytoTune-iPS 2.0 kit) or non-viral episomal plasmid vectors.
- Characterization: Validate iPS cell colonies through Alkaline Phosphatase (ALP) staining, immunocytochemistry for pluripotency markers (e.g., Oct3/4, Nanog, Tra-1-81), and teratoma formation assays.
- Differentiation: Differentiate validated iPS cells into iMS cells using appropriate differentiation media and conditions.
- Passaging: Maintain and passage both iPS cells and derived iMS cells according to standard protocols (e.g., manual passaging every 5-7 days for iPS cells).
- Genomic Analysis: At each key phase (reprogramming, passaging, differentiation), perform comprehensive genomic analysis. The cited study used:
- Chromosomal Microarray Analysis (CMA) for Copy Number Alterations (CNAs).
- Next-Generation Sequencing (NGS) for Single Nucleotide Variations (SNVs).
- Conventional chromosome analysis.
Objective: To define the genomic scenarios and identify the specific stages (reprogramming, passaging, or differentiation) where genetically variant clones emerge and persist.
Protocol 2: Computational Modeling of Variant-Wild-Type Growth Dynamics
This methodology uses a computational model to mathematically describe and predict the growth dynamics between genetically variant and wild-type hPSCs in co-culture systems [22].
Key Steps:
- Model Formulation: Develop a mathematical model that describes the growth behaviors of wild-type and variant hPSCs, both in individual and co-culture systems.
- Parameter Identification: Use the model to identify Critical Process Parameters (CPPs). The cited research pinpointed three key CPPs:
- Total culture density.
- The initial proportion of variant cells within the culture system.
- The specific overgrowth rate of the variant cells.
- Model Validation: Calibrate and validate the model's predictions against empirical data from actual co-culture experiments.
- Scenario Prediction: Use the validated model to run simulations predicting how variability in the CPPs (like different seeding densities or initial variant proportions) affects the prevalence of both cell populations over time.
Objective: To identify opportunities for manufacturing process control by predicting the conditions that favor variant overgrowth, allowing for proactive process adjustments.
Quantitative Data on Genomic Instability
Table 1: Frequency of Genomic Alterations in iPS Cells During Reprogramming and Differentiation [23]
| Reprogramming Method | Phase | Cell Lines with Copy Number Alterations (CNAs) | Cell Lines with Single Nucleotide Variations (SNVs) |
|---|---|---|---|
| Sendai Virus (SV) | Reprogramming | 100% (All lines) | Information Not Specified |
| Episomal Vectors (Epi) | Reprogramming | 40% | Information Not Specified |
| Sendai Virus (SV) | Passaging & Differentiation | Observed | Exclusively Observed in SV-derived cells |
| Episomal Vectors (Epi) | Passaging & Differentiation | Observed | None Detected |
Table 2: Critical Process Parameters Driving Selective Advantage of Variant hPSCs [22]
| Critical Process Parameter (CPP) | Impact on Critical Quality Attribute (CQA) |
|---|---|
| Total Culture Density | Impacts the overall growth dynamics and competition for resources between variant and wild-type cells. |
| Initial Proportion of Variant Cells | A higher starting proportion can lead to a more rapid dominance of the culture by the variant population. |
| Variant Cell Overgrowth Rate | The intrinsic growth rate advantage of the variant clone is a direct driver of its prevalence in the culture. |
Research Reagent Solutions
Table 3: Essential Reagents for Investigating Selective Advantage in Stem Cells
| Research Reagent | Function / Application | Example from Literature |
|---|---|---|
| CytoTune-iPS 2.0 Sendai Reprogramming Kit | For integrating reprogramming factors (Oct4, Sox2, Klf4, c-Myc) via Sendai virus vector to generate iPS cells. | Used to create SV-iPS cells for genomic instability studies [23]. |
| Episomal iPS Reprogramming Vectors | For non-viral, integration-free reprogramming using plasmids encoding factors (Oct4, Sox2, Klf4, l-Myc, Lin28A, shp53). | Used to create Epi-iPS cells for comparative genomic analysis [23]. |
| mTeSR1 Medium | A defined, feeder-free culture medium for the maintenance and expansion of human pluripotent stem cells. | Used for culturing established iPS cell colonies [23]. |
| Chromosomal Microarray Analysis (CMA) | A high-resolution technique for genome-wide detection of copy number variations (CNVs) and copy-neutral loss of heterozygosity. | Used to identify copy number alterations (CNAs) in iPS and iMS cells [23]. |
| Next-Generation Sequencing (NGS) | A high-throughput sequencing technology for comprehensive detection of single nucleotide variations (SNVs) and other sequence-level changes. | Used to identify single-nucleotide variations (SNVs) during passaging and differentiation [23]. |
Visualizing Concepts and Workflows
Diagram 1: Selective advantage in stem cell culture.
Diagram 2: Mechanisms for selective advantage.
The Karyotyping Toolkit: From Gold-Standard G-Banding to Cutting-Edge Genomic Technologies
G-banding, or Giemsa banding, is a fundamental cytogenetic technique and the gold-standard method for obtaining a whole-genome overview of chromosomal integrity in a single assay. It is particularly vital in stem cell research, where genomic instability can arise during reprogramming, in vitro cultivation, and differentiation. Genetically abnormal clones can overtake a human pluripotent stem cell (hPSC) culture in less than five passages, making routine monitoring essential for valid research and safe clinical applications [19]. By providing a macroscopic analysis of the genome, G-banding allows researchers to identify significant chromosomal abnormalities that could compromise experimental results and therapeutic potential [24] [25].
Frequently Asked Questions (FAQs)
What is the core principle behind G-banding?
G-banding is a DNA staining technique that investigates the structure of condensed chromosomes. The Giemsa stain binds specifically to the phosphate groups of DNA, attaching more readily to regions rich in adenine-thymine (A-T) base pairs. These regions appear as dark bands. Conversely, less condensed chromatin, which tends to be richer in guanine-cytosine (G-C), incorporates less stain and appears as light bands. The result is a unique, chromosome-specific pattern of light and dark bands called a karyogram [26] [24] [25].
Why is G-banding considered the gold standard?
G-banding remains the gold standard because it provides a whole-genome overview in a single assay and is the only method that can detect balanced structural aberrations, such as reciprocal translocations and inversions, which do not involve a change in DNA copy number. This is crucial for a comprehensive assessment of genomic stability [19].
What are the most common chromosomal aberrations found in hPSCs using G-banding?
Studies of induced pluripotent stem cells (iPSCs) have shown a pattern of recurrent, culture-acquired abnormalities. In one karyotypic analysis of 65 iPSC lines, the overall frequency of abnormalities was 23%. The most frequent recurrent aberrations were gains of chromosome 20 or 20q, and gains of the 1q arm [18]. These recurrent changes are thought to provide a selective growth advantage in culture [18] [25].
Table 1: Recurrent Karyotype Abnormalities in iPSCs (from a study of 65 lines) [18]
| Abnormality | Type | Percentage of Unique Aberrant Lines |
|---|---|---|
| Trisomy 20 / i(20q) | Whole or partial chromosome gain | 38.5% |
| 1q duplication / translocation-duplication | Partial chromosome gain | 30.8% |
| Trisomy 8 | Whole chromosome gain | 15.4% |
| Balanced translocation | Structural rearrangement | 23.1% |
What is the main limitation of G-banding?
The primary limitation of G-banding is its limited resolution, typically detecting only larger-scale aberrations of 5–10 Mb or greater [24] [19] [25]. This means smaller genetic alterations, such as the common and clinically significant 20q11.21 amplification in hPSCs, often fall below its detection limit [25]. Furthermore, the technique requires living, actively dividing cells and significant expertise to perform and interpret accurately [24] [19].
Troubleshooting Guide
Problem 1: Poor Chromosome Spreading and Morphology
- Issue: Overlapping or poorly spread metaphase chromosomes, or insufficient metaphase cells for analysis.
- Possible Causes and Solutions:
- Incorrect colcemid concentration or exposure time: Optimize the concentration and duration of colcemid treatment to arrest a sufficient number of cells in metaphase without over-condensing the chromosomes. A typical protocol uses 0.04 μg/mL colcemid for 2 hours [19].
- Low mitotic index: Ensure cells are in a log phase of growth and healthy before harvesting. Use cells at an appropriate confluence.
- Suboptimal hypotonic treatment: The hypotonic solution (e.g., 0.075M KCl) swells the cells, helping to spread the chromosomes. Adjust the incubation time and temperature (e.g., 37°C for 60 minutes) for optimal results [19].
- Fixation issues: Use a fresh, chilled methanol:acetic acid fixative (3:1 ratio) and ensure the fixation steps are performed correctly to preserve chromosome structure [24].
Problem 2: Weak or Blurry G-Banding Patterns
- Issue: Bands lack contrast, appear fuzzy, or are indistinct, making chromosome identification difficult.
- Possible Causes and Solutions:
- Incomplete trypsin digestion: Over-digestion with trypsin leads to pale, "ghost-like" chromosomes. Under-digestion results in uniformly dark, non-banded chromosomes. Precisely calibrate the trypsin incubation time for your specific cell type and conditions [24].
- Suboptimal Giemsa staining: Ensure the Giemsa stain is fresh and properly filtered. Optimize the staining time and concentration.
- Aged microscope slides: Use freshly prepared slides. Slides that have been stored for too long may produce poor banding.
- Poor-quality metaphase spreads: Refer to solutions in Problem 1 to improve chromosome morphology.
Problem 3: Inconsistent Results Between Analyses
- Issue: Variable detection of abnormalities or differing karyotype interpretations.
- Possible Causes and Solutions:
- Cell culture-induced instability: Be aware that chromosomal aberrations can arise and expand during passaging. Karyotype at consistent, early passages and monitor frequently. A genetically abnormal clone can overtake a culture very rapidly [19].
- Technical subjectivity: G-banding interpretation requires a high level of expertise. Ensure analysis is performed by a trained cytogeneticist and that a sufficient number of metaphases (e.g., at least 20) are evaluated [19].
- Methodological variability: Strictly adhere to a standardized laboratory protocol for cell harvesting, slide preparation, and banding to improve reproducibility.
Detailed Experimental Protocol for G-Banding Karyotyping of hPSCs
The following workflow details the key steps for preparing metaphase chromosomes for G-banding analysis from human pluripotent stem cells.
- Cell Culture and Mitotic Arrest: Grow hPSCs to a healthy, sub-confluent state in log-phase growth. Add colcemid (a mitotic spindle inhibitor) to the culture medium at a final concentration of 0.04 μg/mL and incubate for 2 hours at 37°C. This arrests dividing cells at metaphase, when chromosomes are most condensed [19].
- Cell Harvest and Hypotonic Treatment: Harvest cells using trypsin or Accutase to create a single-cell suspension. Centrifuge and subject the cell pellet to a hypotonic solution (commonly 0.075M KCl, sometimes mixed with sodium citrate). Incubate at 37°C for 60 minutes. This causes the cells to swell, which helps spread the chromosomes upon slide preparation [19].
- Fixation: Centrifuge the cells and carefully remove the hypotonic solution. Resuspend the pellet in a freshly prepared, chilled fixative solution (3:1 methanol to acetic acid). Repeat the centrifugation and resuspension in fresh fixative several times (typically 3-4) to thoroughly clean and fix the cells [24] [19].
- Slide Preparation: Drop the fixed cell suspension onto clean, wet microscope slides from a height of about 30-50 cm. Allow the slides to air dry. Proper technique is critical for achieving well-spread metaphase chromosomes. Examine slides under a phase-contrast microscope to assess chromosome spread and density [24].
- Aging and Banding: Age the slides, either by incubating at 60°C overnight or at 90°C for about one hour. Treat the slides briefly with a trypsin solution to digest chromosomal proteins. The time and concentration must be carefully optimized. Stain the slides with a filtered Giemsa stain for 5-10 minutes, then rinse and air dry [24].
- Analysis and Reporting: Analyze the G-banded metaphase spreads under a bright-field microscope at 100x oil immersion. A minimum of 20 metaphase cells should be structurally evaluated. Chromosomes are identified by their characteristic banding patterns and arranged into a karyogram. The final report is generated according to the International System for Human Cytogenetic Nomenclature (ISCN) [24] [19].
Comparison of Karyotyping Methods
While G-banding is the gold standard for a macroscopic overview, other technologies offer complementary capabilities. The table below compares key methods used in hPSC research.
Table 2: Comparison of Common Karyotyping Methods in Stem Cell Research [26] [19] [25]
| Method | Resolution | Key Advantages | Key Limitations | Best For |
|---|---|---|---|---|
| G-Banding | 5 - 10 Mb | Gold standard; detects balanced structural rearrangements; whole-genome view. | Low resolution; requires live, dividing cells; subjective. | Initial, macroscopic genome screening. |
| SNP Array | ~350 kb - 2 Mb | High resolution; detects CNVs, CN-LOH; automated analysis. | Cannot detect balanced translocations. | High-resolution CNV and LOH detection. |
| Array CGH (e.g., KaryoStat+) | >1 - 2 Mb | Whole-genome coverage for CNVs; improved resolution over G-banding. | Cannot detect balanced rearrangements or CN-LOH. | Sensitive, genome-wide CNV screening. |
| ddPCR | Single gene/region | Extremely sensitive; absolute quantification; detects low-level mosaicism. | Targeted analysis only (e.g., 24 hotspots); not a whole-genome method. | Validating and monitoring specific, common aberrations (e.g., 20q11.21). |
| Next-Generation Sequencing (NGS) | 1 bp (but limited for large SVs) | Single-base resolution; detects SNVs and CNVs. | High cost; complex data analysis; may miss large SVs. | Most comprehensive detection of SNVs and CNVs. |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for G-Banding Karyotyping [24] [19]
| Reagent / Material | Function | Notes for Experimental Success |
|---|---|---|
| Colcemid | A mitotic inhibitor that disrupts spindle formation, arresting cells in metaphase. | Concentration and incubation time are critical to obtain sufficient metaphase spreads without over-condensing chromosomes. |
| Hypotonic Solution (KCl) | Causes cells to swell, separating the chromosomes for clearer analysis. | Must be pre-warmed and used immediately after preparation for consistent results. |
| Methanol:Acetic Acid Fixative | Preserves the chromosomal structure and removes cytoplasmic debris. | Must be prepared fresh and kept cold for optimal fixation. |
| Trypsin | Digestive enzyme used in controlled amounts to treat slides, enabling the Giemsa stain to produce banding patterns. | The most sensitive step; requires precise calibration for clear, high-contrast bands. |
| Giemsa Stain | DNA-specific dye that binds preferentially to A-T rich regions, creating the characteristic light and dark banding pattern. | Should be filtered before use to remove particulates that can cause uneven staining. |
| Microscope Slides | Surface for metaphase chromosome spreading. | Must be clean and often used slightly wet ("breathing" on them) to facilitate chromosome spreading during dropping. |
Frequently Asked Questions (FAQs)
What are the core differences between aCGH and SNP arrays in detecting CNVs?
Answer: While both are high-resolution array technologies, their primary differences lie in the type of genetic variants they detect and their underlying principles.
- Array Comparative Genomic Hybridization (aCGH): This technique is designed specifically to detect copy number variations (CNVs) by performing a competitive hybridization between a test and a reference DNA sample, both labeled with different fluorescent dyes (e.g., Cyanine 3 and Cyanine 5) [27]. It provides a direct, quantitative measure of DNA copy number differences between the two samples but cannot detect copy-number neutral events like loss of heterozygosity (LOH) or identify ploidy status.
- Single Nucleotide Polymorphism (SNP) Arrays: SNP arrays can also detect CNVs but do so by comparing the intensity of sample hybridization to a reference set, not through a direct competitive hybridization [1]. A key advantage is their ability to simultaneously detect CNVs, LOH, and uniparental disomy (UPD) because they genotype hundreds of thousands of specific SNP loci across the genome.
What is the typical resolution and detection limit of these array technologies?
Answer: The resolution is determined by the number and density of probes on the array. Higher-density arrays offer greater resolution for detecting smaller aberrations.
- Common Array Formats:
- Mosaicism Detection: Genomic aberrations smaller than 10 Mb can be successfully detected in samples with as low as 10% mosaicism using optimized aCGH protocols [27]. This is significantly more sensitive than traditional G-banded karyotyping, which typically detects mosaicism at levels exceeding 10-20% [28].
My aCGH data shows a "wave effect." What causes this and how can it be mitigated?
Answer: A wavy pattern of hybridization intensities along the chromosome is a known technical artifact [27].
- Primary Causes:
- GC content bias: Probes with high GC content can hybridize differently.
- DNA isolation bias: Inefficiencies during DNA extraction can contribute.
- Solutions:
When should I use aCGH or SNP array over other techniques like karyotyping or FISH?
Answer: The choice of technique depends on your research question, required resolution, and the need for genome-wide versus targeted analysis. The following table compares key characteristics:
| Feature | G-banded Karyotyping | FISH (20q11.21 example) | aCGH | SNP Array |
|---|---|---|---|---|
| Resolution | >5-10 Mb [28] [1] | ~0.55-4.6 Mb (for 20q11.21) [28] | High (probe-dependent) [27] | High (probe-dependent) [1] |
| Primary Use | Genome-wide, large structural changes [1] | Targeted, submicroscopic CNVs [28] | Genome-wide CNV detection [27] | Genome-wide CNV, LOH, and ploidy [1] |
| Best for Detecting | Aneuploidy, translocations, large inversions/deletions [28] | Low-level mosaicism, specific recurrent CNVs (e.g., BCL2L1) [28] | Submicroscopic CNVs across the entire genome [27] | CNVs, regions of homozygosity (LOH), UPD [1] |
| Throughput | Low | Low | Medium to High | Medium to High |
For stem cell research, the ISSCR standards recommend routine genetic monitoring. Karyotyping provides a baseline for large-scale integrity, while aCGH and SNP arrays are essential for high-resolution, genome-wide screening of culture-acquired CNVs that karyotyping will miss [28] [29].
What are the critical quality control metrics for a successful aCGH experiment?
Answer: Rigorous QC is essential for generating reliable and reproducible data. Key metrics to check after probe labeling and hybridization include:
Table: Essential aCGH Quality Control Metrics
| Metric | Description | Ideal Value |
|---|---|---|
| DNA Yield | Total amount of labeled DNA generated. | >5.0 µg (for 4x180k arrays) [27] |
| Dye Incorporation | pmol of dye incorporated per reaction. | Cy3: ≥300 pmol; Cy5: ≥200 pmol [27] |
| Specific Activity | pmol of dye incorporated per µg of DNA. | Cy3: ≥60 pmol/µg; Cy5: ≥40 pmol/µg [27] |
| Signal Intensity | Overall fluorescence intensity measurement. | >200 [27] |
| Background Noise | Standard deviation of negative control probes. | <25 [27] |
| Signal-to-Noise Ratio | Ratio of probe signal to background noise. | >30 [27] |
| Derivative Log Ratio (DLR) | Measure of variation of signal around the mean. | <0.2 [27] |
Troubleshooting Guides
Problem: Low Signal-to-Noise Ratio
A low signal-to-noise ratio can obscure true genetic alterations and lead to inaccurate data interpretation.
- Potential Causes and Solutions:
- Cause: Poor DNA quality.
- Solution: Check DNA purity via spectrophotometry (A260/280 >1.8; A260/230 2.0-2.2) and integrity via gel electrophoresis. Re-purify if necessary [27].
- Cause: Inefficient labeling reaction.
- Solution: Adhere strictly to labeling protocol incubation times and temperatures. Do not shorten the denaturation or primer extension steps [27].
- Cause: Suboptimal hybridization conditions.
- Solution: Ensure the correct buffer stringency, temperature, and amount of Cot-1 DNA are used [27].
- Cause: High background noise.
- Solution: Protect Cyanine dyes from light during all steps. Check that the array itself is not contaminated [27].
- Cause: Poor DNA quality.
Problem: Dye Bias in aCGH
Dye bias occurs when one fluorescent dye (e.g., Cy3 or Cy5) consistently shows higher intensity than the other, independent of actual copy number changes.
- Potential Causes and Solutions:
- Cause: Inefficient or unequal dye incorporation.
- Solution: Check dye incorporation and specific activity metrics via NanoDrop. Ensure labeling reactions for both test and reference samples are performed identically and with fresh reagents [27].
- Cause: Environmental factors.
- Solution: Be aware that Cy5 is more sensitive to ozone degradation than Cy3. Perform hybridizations in a controlled environment, and consider using an ozone scrubber if necessary [27].
- Confirmatory Test: Perform a "dye swap" experiment, where the dyes used to label the reference and test DNA are switched. A true genetic anomaly will be consistent, while a dye-specific artifact will reverse with the dyes [27].
- Cause: Inefficient or unequal dye incorporation.
Problem: Detecting Mosaicism in hPSC Cultures
Subpopulations of genetically distinct cells (mosaicism) can be missed if the detection method lacks sensitivity.
- Guidance:
- Understand Sensitivity Limits: No technique can detect mosaicism at 0%. Digital PCR (dPCR) is highly sensitive for known targets, while arrays can detect ~10% mosaicism for smaller aberrations [28] [27].
- Use Orthogonal Techniques: No single method is perfect. A combined approach is most effective. The following diagram illustrates a recommended testing strategy for comprehensive genomic stability monitoring in hPSCs:
Problem: High Derivative Log Ratio (DLR)
A high DLR value (>0.2) indicates excessive noise in the array data, reducing confidence in CNV calls.
- Potential Causes and Solutions:
- Cause: Poor DNA quality or integrity.
- Solution: This is the most common cause. Re-check DNA quality and use high molecular weight DNA for all labeling reactions [27].
- Cause: Inefficient labeling.
- Solution: Verify that the labeling reaction produced sufficient DNA yield and dye incorporation, as outlined in the QC table above [27].
- Cause: Bubbles or scratches on the array.
- Solution: Handle arrays carefully during hybridization and washing steps. Ensure the hybridization chamber is properly sealed [27].
- Cause: Poor DNA quality or integrity.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for aCGH and Genetic Monitoring
| Reagent / Kit | Function | Key Consideration |
|---|---|---|
| CGH Labeling Kit (e.g., CYTAG TotalCGH) | Incorporates fluorescent dyes (Cy3/Cy5) into test and reference DNA via random priming. | Choose based on needs: SNP compatibility, or low input (e.g., 50 ng) with kits like CYTAG SuperCGH [27]. |
| Cot-1 DNA | Blocks non-specific hybridization of repetitive DNA sequences, reducing background noise. | The amount used is critical to prevent "wave effect" artifacts [27]. |
| Purification Columns (e.g., silica membrane-based) | Removes unincorporated dyes, enzymes, and salts after the labeling reaction. | Included in many commercial kits. Alternative purification methods include ethanol precipitation [27]. |
| Microarray Platform | The slide containing thousands of immobilized DNA probes for hybridization. | Select format based on required resolution (60K vs. 180K) and number of samples per run [27]. |
| Digital PCR (dPCR) Assay | A highly sensitive targeted method to quantify specific, recurrent CNVs (e.g., 20q11.21). | Not a substitute for karyotyping or arrays, but an excellent complementary tool for monitoring common hPSC abnormalities [29]. |
Troubleshooting Guides and FAQs
Wet Lab and Library Preparation
Q1: My NGS run failed during initialization with a "W1 pH out of range" error. What should I do?
This error on the Ion PGM System indicates the pH of the W1 solution is out of range or the volume is insufficient. First, check that at least 200 mL of solution remains in the W1 bottle and that all sippers and bottles are securely attached. Press "Start" to restart the measurement. If the error persists, discard the solution in the W1 bottle, prepare a fresh solution with 350 µL of 100 mM NaOH, and restart the initialization process. If issues continue, detach and clean the reagent bottles, check for line blockages, and inspect the chip port for standing solution, replacing the chip if necessary [30].
Q2: How can I address library preparation failures that lead to low cluster density or poor sequencing yield?
Library preparation issues often stem from suboptimal DNA quality, quantity, or fragmentation. Verify the quantity and quality of your input DNA using fluorometric methods. Ensure the library preparation protocol, including fragmentation and adapter ligation, is meticulously followed. For GC-rich or difficult templates, use polymerases optimized for high-GC content and consider PCR additives. Incorporating unique dual indexes during library preparation can help identify and filter index-hopped reads in multiplexed samples, providing higher confidence in your results [31] [32].
Instrumentation and Run Monitoring
Q3: The instrument displays a "Chip Not Detected" error on my Ion S5 system. What are the likely causes?
This error typically arises from a clamp not being fully closed, a chip that is not properly seated, or a damaged chip. Open the chip clamp, remove the chip, and inspect for physical damage or signs of moisture outside the flow cell. If damaged, replace it with a new chip. Ensure the chip is correctly positioned, close the clamp firmly, and run the Chip Check again. If the error persists, the issue may lie with the chip socket, and you should contact Technical Support [30].
Q4: My sequencer shows connectivity issues with the server. How can I resolve this?
For "No Connectivity to Torrent Server" errors on Ion S5 systems, first disconnect and then re-connect the Ethernet cable. Confirm that your router and network are operational. If the problem is not resolved, a system restart may be necessary. From the Main Menu, select Tools > Shut Down, wait 30 seconds, and then power the instrument back on. If connectivity alarms continue, contact Technical Support [30].
Data Analysis and Variant Calling
Q5: My data analysis reveals a high number of false-positive variant calls, particularly indels in homopolymer regions. How can I improve specificity?
This is a common challenge with some sequencing technologies. To improve variant calling accuracy:
- Increase Sequencing Depth: Ensure sufficient coverage (e.g., >100x for heterogeneous samples) to distinguish true low-frequency variants from errors [33].
- Apply Bioinformatics Filters: Use quality scores (Q-scores), strand bias filters, and remove variants located in homopolymer stretches or other problematic genomic regions [33] [34].
- Utilize Unique Dual Indexes: This allows for the computational identification and removal of reads that have experienced index hopping, a common source of sample cross-contamination [31].
- Benchmark with Proficiency Testing: Leverage insights from proficiency testing programs, which highlight that homopolymer regions and genes with high GC-content are frequent sources of false positives and require special attention during assay validation [32].
Q6: What are the primary sources of uncertainty in NGS variant calling, and how can they be mitigated?
Uncertainty in NGS data arises from several sources, including sequencing errors, misalignments, and amplification biases. Key mitigation strategies are summarized in the table below [33] [34].
Table 1: Common Sources of Uncertainty in NGS Data and Mitigation Strategies
| Source of Uncertainty | Description | Mitigation Strategy |
|---|---|---|
| Sequencing Errors | Platform-specific errors (e.g., indels in homopolymers for Ion Torrent, substitutions for Illumina) [33]. | Apply base quality recalibration and platform-specific error correction algorithms. |
| Alignment Ambiguity | Reads misaligned, especially in repetitive regions or for indels [33]. | Use optimized aligners; perform manual review of aligned reads in a genomic viewer. |
| Amplification Bias | Duplicated reads from PCR over-amplification skew variant allele frequencies [33]. | Use PCR-free library prep where possible; mark/remove duplicate reads. |
| Low Coverage | Regions with insufficient reads prevent confident variant calling [34]. | Design experiments to ensure adequate mean coverage and uniform coverage distribution. |
Stem Cell Research-Specific Considerations
Q7: Within the context of stem cell genetic instability research, how does NGS complement traditional karyotyping?
NGS and karyotyping provide complementary information for comprehensive genomic stability assessment. While traditional G-banded karyotyping is excellent for detecting large-scale chromosomal abnormalities (>5-10 Mb) such as aneuploidy, translocations, and inversions, it cannot resolve smaller structural variants [35] [36]. NGS, particularly whole-genome sequencing, provides base-pair resolution, enabling the detection of single-nucleotide variants (SNVs), small indels, and copy number variations (CNVs) below the detection limit of karyotyping. This is crucial for identifying mutations in known plasticity genes or oncogenes. Furthermore, targeted NGS panels can be designed to routinely monitor specific loci known to be unstable in pluripotent stem cells, such as the 20q11.21 amplification, which is a common recurrence and provides a growth advantage but is undetectable by standard karyotyping [35].
Experimental Protocols for Key NGS Methods
Protocol 1: Targeted Resequencing for Monitoring Common Stem Cell Genetic Variants
This protocol is designed for the routine monitoring of known genetic variants in human pluripotent stem cell (hPSC) cultures, focusing on regions prone to instability like 20q11.21.
- Panel Design: Design or select a targeted sequencing panel that includes common genetic instability loci in hPSCs (e.g., TP53, 20q11.21, 12p). The total target size will vary based on the number of regions [31].
- Library Preparation: Using 50-100 ng of genomic DNA from your hPSC line, perform library construction. This involves DNA fragmentation, adapter ligation, and PCR amplification. For multiplexing, use unique dual indexes to tag each library, allowing multiple samples to be pooled and sequenced in one run [31].
- Sequencing: Pool the indexed libraries and sequence on an appropriate NGS platform (e.g., Illumina MiSeq or Ion Torrent PGM). Aim for a high depth of coverage (>500x) to confidently detect low-level mosaicism [33].
- Data Analysis:
- Alignment: Map the sequenced reads to a human reference genome (e.g., hg38) using a suitable aligner like BWA or Bowtie2 [33].
- Variant Calling: Use a variant caller (e.g., GATK) to identify SNPs and indels against the reference.
- CNV Analysis: Perform copy number variant analysis using tools that assess read depth across the targeted regions to identify amplifications or deletions [35].
Protocol 2: Whole-Genome Sequencing for Comprehensive Genomic Characterization
Use this protocol for a base-pair resolution overview of your stem cell genome, ideal for characterizing new cell lines or investigating unexplained phenotypic changes.
- Library Preparation: Construct a sequencing library from 100 ng - 1 µg of high-quality gDNA. For the most uniform coverage, a PCR-free library preparation method is recommended to avoid amplification biases [33].
- Sequencing: Sequence the library on a high-throughput platform (e.g., Illumina NovaSeq) to achieve a minimum of 30x coverage across the genome. Use paired-end sequencing (e.g., 2x150 bp) to improve alignment accuracy and structural variant detection [31] [33].
- Data Analysis:
- Primary Analysis: Perform base calling and demultiplexing to generate FASTQ files [37].
- Secondary Analysis: Align reads to a reference genome to create BAM files, then call variants (SNPs, indels, CNVs, SVs) to produce a VCF file [33] [37].
- Tertiary Analysis: Annotate variants and filter them against population databases. Focus on variants in genes associated with growth and differentiation, cancer, or known hPSC instability loci [33].
The following diagram illustrates the core bioinformatics workflow from raw sequencing data to variant calls, which is common to both targeted and whole-genome sequencing protocols.
NGS Variant Discovery Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for NGS-Based Stem Cell Genomic Monitoring
| Item | Function | Application in Stem Cell Research |
|---|---|---|
| NGS Library Prep Kit | Converts genomic DNA into a sequenceable library by fragmenting DNA and ligating platform-specific adapters [31]. | The starting point for all NGS workflows; essential for preparing libraries from hPSC genomic DNA. |
| Unique Dual Indexes | Short DNA sequences added to each library fragment, allowing multiple samples to be pooled (multiplexed) and sequenced simultaneously, then computationally separated [31]. | Enables cost-effective monitoring of multiple hPSC lines or timepoints by pooling up to 384 samples in a single run. |
| Targeted Sequencing Panel | A pre-designed set of probes to capture and enrich specific genomic regions of interest for sequencing [31]. | Allows focused, cost-effective sequencing of known instability loci (e.g., 20q11.21, TP53) in routine hPSC quality control. |
| Control Ion Sphere Particles | Quality control particles included with Ion S5 kits used to monitor instrument performance and template preparation [30]. | Critical for ensuring the sequencing run itself is performing optimally before using data for hPSC characterization decisions. |
| High-Fidelity Polymerase | A DNA polymerase with proofreading activity to minimize errors introduced during PCR amplification steps in library prep [33]. | Reduces artifactual mutations in sequencing data, ensuring variants called are true biological variants in the stem cell line. |
Understanding and Overcoming Data Analysis Bottlenecks
NGS data analysis involves multiple steps where errors and biases can be introduced. The following diagram maps common issues and their solutions throughout the typical workflow.
Common NGS Data Analysis Pitfalls & Solutions
In the field of stem cell research, maintaining genomic integrity is paramount. Low-frequency mosaicism—the presence of multiple genetically distinct cell populations within a single stem cell line—poses a significant challenge for quality control in both research and therapeutic applications. These mosaic variants often exist at very low variant allele frequencies (VAF) , sometimes below 1%, making them difficult to detect with conventional genomic analysis methods [38]. Digital droplet PCR (ddPCR) has emerged as a powerful tool for identifying these rare variants with exceptional sensitivity and precision, providing researchers with a critical method for ensuring the genetic stability of stem cell cultures [25]. This technical support center provides comprehensive guidance for implementing ddPCR in stem cell karyotype monitoring research.
Frequently Asked Questions (FAQs): ddPCR for Mosaicism Detection
Q1: What makes ddPCR more sensitive than traditional PCR or NGS for detecting low-frequency mosaicism?
ddPCR achieves superior sensitivity through sample partitioning, where each reaction is divided into approximately 20,000 nanoliter-sized droplets [38]. This partitioning allows individual DNA molecules to be amplified in isolation, effectively enriching low-abundance targets that would be obscured in a bulk reaction. While next-generation sequencing (NGS) typically detects variants down to approximately 1% variant allele frequency (VAF), ddPCR can reliably identify variants at 0.1% VAF or lower [38]. In research specifically detecting the GNAQ mutation, the demonstrated detection limit for standard ddPCR was 0.25%, which could be further enhanced to 0.1% when combined with peptide nucleic acid (PNA) technology [39].
Q2: How does ddPCR fit into a stem cell research workflow for genetic quality control?
ddPCR serves as a highly targeted complement to broader genomic screening methods in stem cell research. While array-based karyotyping or NGS provides a genome-wide overview, ddPCR offers ultra-sensitive, specific validation for known recurrent abnormalities [25]. For instance, the common 20q11.21 amplification found in cultured human pluripotent stem cells (hPSCs) can be detected at low levels using ddPCR, even when array-based methods show normal karyotype [25]. This makes ddPCR ideal for ongoing monitoring of known risk loci in stem cell banks.
Q3: What are the key limitations of ddPCR that researchers should consider?
The primary limitation of ddPCR is its targeted nature—it requires prior knowledge of the exact genetic variant being detected [38] [40]. This makes it unsuitable for discovery of novel variants or whole-genome screening. Additionally, designing effective ddPCR assays requires careful optimization of variant-specific probes, typically utilizing minor groove binder or locked nucleic acid technologies for high specificity [38]. NGS remains the preferred method for unbiased detection of novel genetic changes.
Q4: How do I calculate the copies/μL in my original stock solution from ddPCR results?
Accurate calculation requires accounting for all dilution factors in your experimental setup. The AnalysisSuite Software can perform these calculations when you input the appropriate dilution factors. For example:
- If you add 1 μL of a 1:10 diluted sample to a reaction with a final volume of 16 μL
- The dilution factor is: (1/16) × (1/10) = 0.00625 (1:160) [41]
Inputting this dilution factor into the software will automatically calculate the copies/μL in your starting stock solution.
Q5: What are the advantages of using ddPCR for mosaic mutation detection in stem cell therapy development?
For stem cell therapy applications, ddPCR offers significantly lower cost and faster turnaround time compared to high-depth NGS [38]. It requires only a very small amount of input DNA (as little as 1 ng from FFPE tissue has been successfully used) [38], which is particularly valuable when working with precious stem cell samples. The absolute quantification capability without need for standard curves and excellent reproducibility make it ideal for tracking mosaic variant levels across different cell passages or differentiation stages.
Troubleshooting Common Experimental Issues
Issue 1: Poor Separation Between Positive and Negative Droplet Populations
- Potential Cause: Suboptimal probe design or concentration.
- Solution: Validate probes using positive control DNA when available. Optimize probe and primer concentrations through titration experiments. For SNP detection, ensure you're using appropriate chemistry such as minor groove binder probes which provide better discrimination between wild-type and mutant alleles [38].
Issue 2: Inconsistent Results at Very Low Variant Allele Frequencies (<0.1%)
- Potential Cause: Stochastic effects due to limited template molecules.
- Solution: Increase the amount of input DNA to raise the number of template molecules analyzed, while ensuring you remain within the digital range (where some partitions contain no template) [41] [39]. For extremely rare variants (<0.1%), consider implementing a pre-amplification step such as PNA-clamping PCR prior to ddPCR analysis [39].
Issue 3: Software Analysis Challenges
- Potential Cause: Improper threshold setting or sample overloading.
- Solution: Manually verify and adjust fluorescence thresholds in the analysis software if automatic setting is inadequate. Ensure samples are sufficiently diluted to be in the "digital range" where some droplets are positive and others negative [41]. Use recommended browsers (Google Chrome v4.0+ or Firefox) for the analysis software [41].
Quantitative Data Comparison of Detection Methods
Table 1: Comparison of Genomic Detection Methods for Mosaicism
| Method | Theoretical Detection Limit | Practical Detection Limit for Mosaicism | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Sanger Sequencing | ~20% VAF [38] | ~20% VAF | Low cost, simple interpretation | Low sensitivity, not quantitative |
| Next-Generation Sequencing (NGS) | Varies with read depth | ~1% VAF with 300-500× coverage [38] [39] | Unbiased, genome-wide detection | Higher cost, longer turnaround, bioinformatics complexity |
| ddPCR | ~0.008% [38] | 0.1-0.25% [38] [39] | Ultra-sensitive, absolute quantification, fast, cost-effective | Requires prior knowledge of variant, limited multiplexing |
| PNA-ddPCR | ~0.1% (3 copies) [39] | 0.1% with enhanced specificity [39] | Exceptional sensitivity for known variants | Additional optimization required, qualitative at extreme low limits |
Table 2: Documented Detection Limits for Specific Mosaic Mutations Using ddPCR
| Disease/Condition | Gene | Mutation | Sample Type | Detection Limit | Citation |
|---|---|---|---|---|---|
| Focal Brain Malformations | MTOR | Various somatic mutations | Brain tissue | 0.3% VAF [38] | PMC10360090 |
| McCune-Albright Syndrome | GNAS | p.R201H | Peripheral blood leukocytes | 0.2% (0.005% with nested PNA-PCR) [42] | ESPE Abstracts |
| Sturge-Weber Syndrome | GNAQ | c.548G>A | Brain tissue, blood, saliva | 0.25% (0.1% with PNA-ddPCR) [39] | Nature Sci Rep |
| Hemophilia A | F8 | Various mutations | Blood | <1% for 97% of positions [40] | Research Square |
Experimental Protocols for Detecting Mosaic Mutations
Protocol 1: Standard ddPCR for Recurrent Mosaic Mutations in Stem Cell Cultures
This protocol is adapted from methods used to detect low-frequency somatic mutations in brain malformation research [38] and applied to stem cell monitoring.
Materials Needed:
- ddPCR Supermix for Probes (no dUTP)
- Target-specific FAM-labeled mutant probe and HEX/VIC-labeled wild-type probe
- Droplet generator and reader
- Thermal cycler compatible with ddPCR
- Restriction enzymes (if needed to reduce genomic DNA viscosity)
Step-by-Step Method:
- DNA Extraction and Quantification: Extract high-quality genomic DNA from stem cell cultures using standard methods. Accurately quantify DNA using fluorometry for precise copy number determination.
- Reaction Setup: Combine DNA (recommended starting amount: 10-100 ng) with ddPCR supermix, primers (final concentration: 900 nM each), and mutant/wild-type probes (final concentration: 250 nM each) in a total volume of 20-22 μL.
- Droplet Generation: Transfer the reaction mixture to a droplet generation cartridge. Generate approximately 20,000 droplets using the droplet generator [38].
- PCR Amplification: Transfer droplets to a 96-well plate and seal. Perform PCR amplification with optimized cycling conditions:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing/Extension: 55-60°C (probe-specific) for 60 seconds
- Enzyme deactivation: 98°C for 10 minutes
- Hold at 4°C
- Droplet Reading: Place plate in droplet reader, which measures fluorescence in each droplet individually.
- Data Analysis: Use manufacturer's software to calculate variant allele frequency based on the ratio of mutant-positive to wild-type-positive droplets, applying Poisson statistics to account for random partitioning [38].
Protocol 2: Enhanced Sensitivity PNA-ddPCR for Ultra-Rare Variants
This protocol combines peptide nucleic acid (PNA) clamping with ddPCR for improved detection of very low-frequency mosaicism (<0.1%), adapted from methods used in Sturge-Weber syndrome research [39].
Materials Needed:
- PNA oligomer complementary to wild-type allele
- Standard ddPCR reagents (as in Protocol 1)
- Additional PCR reagents for pre-amplification
Step-by-Step Method:
- PNA Clamping PCR: Set up a preliminary PCR reaction containing:
- Genomic DNA (up to 100 ng)
- PNA oligomer (concentration requires optimization, typically 0.5-2 μM)
- Standard PCR primers, dNTPs, and polymerase
- PNA Clamping Cycling Conditions:
- The PNA clamp binds preferentially to wild-type sequences during annealing, inhibiting their amplification while allowing mutant sequences to amplify preferentially.
- ddPCR Analysis: Dilute the PNA clamping PCR product and use as input for standard ddPCR analysis (as described in Protocol 1).
- Result Interpretation: The combination of PNA clamping and ddPCR can lower detection limits to 0.1% or lower, enabling identification of extremely rare mosaic variants [39].
Workflow Visualization
Research Reagent Solutions
Table 3: Essential Reagents and Materials for ddPCR Mosaicism Detection
| Reagent/Material | Function | Application Notes |
|---|---|---|
| ddPCR Supermix for Probes | Provides optimized buffer, enzymes, and dNTPs for probe-based digital PCR | Select no-dUTP version unless contamination prevention is required |
| TaqMan Mutation Detection Probes | Sequence-specific detection of wild-type and mutant alleles | Use MGB or LNA technology for enhanced specificity; FAM for mutant, HEX/VIC for wild-type |
| Droplet Generation Oil & Cartridges | Creates water-in-oil emulsion partitions | Critical for consistent droplet formation; use manufacturer-recommended consumables |
| PNA Oligomers | Wild-type sequence clamping for enhanced sensitivity | Designed to complement wild-type sequence around mutation site; inhibits wild-type amplification |
| Positive Control DNA | Assay validation and optimization | Synthetic oligonucleotides or known positive sample DNA; essential for establishing detection thresholds |
| DNA Quantification Standards | Accurate DNA concentration measurement | Fluorometric methods preferred over spectrophotometry for genomic DNA |
Frequently Asked Questions (FAQs)
Q1: At which passages should I routinely karyotype my stem cell cultures? A comprehensive study of 65 hiPSC lines recommends a baseline frequency, with data suggesting that 17.3% of cell lines from patients and a rising percentage in lines from healthy donors exhibited chromosomal aberrations. Karyotyping should be performed during initial culture characterization (passages 5 to 40, with a median of 17) and repeated at later passages, as the frequency of abnormal lines can increase over time [18].
Q2: What are the most common genetic abnormalities I might encounter? Recurrent, culture-acquired aberrations account for the majority of genetic changes. The table below summarizes the most frequent abnormalities you should monitor for [18].
Table 1: Recurrent Karyotypic Abnormalities in hiPSCs
| Type of Aberration | Specific Chromosomal Changes | Approximate Frequency Among Abnormal Lines |
|---|---|---|
| Recurrent Gains | Trisomy 20 / 20q gain | 38.5% |
| 1q arm duplication | 30.8% | |
| Trisomy 8 | 15.4% | |
| Recurrent Losses | Losses of chromosomes 10, 18, and 22 | Less common than gains |
| Structural Rearrangements | Unbalanced translocations involving 1q, 15, and 18 | Observed in a subset of abnormal lines |
Q3: My cells are differentiating excessively. Could this be linked to genetic instability? Yes, excessive and spontaneous differentiation can be a sign of culture stress, which is a known driver of genetic instability [18]. Before passaging, ensure you remove areas of differentiation. Other common culture issues that can stress cells and should be avoided include [9]:
- Using old culture medium (ensure it is less than 2 weeks old when stored at 2-8°C).
- Allowing cultures to overgrow.
- Keeping culture plates out of the incubator for extended periods (>15 minutes).
- Plating cell aggregates at too high a density.
Q4: Are newer technologies better than traditional karyotyping for routine checks? Each method has strengths and limitations, and a combination is often best for a comprehensive view [43].
- Karyotyping (G-banding) is excellent for detecting large-scale numerical and structural abnormalities but has limited resolution.
- Chromosomal Microarray (e.g., CytoScanHD) can identify subtle, sub-microscopic copy number variations (e.g., a 1.7 Mbps gain) that karyotyping might miss [43].
- Droplet Digital PCR (ddPCR) provides ultra-sensitive, quantitative validation of specific mutations identified by other methods and is more accurate than conventional qPCR for avoiding false positives [43].
Troubleshooting Guides
Problem: Sudden Change in Cell Morphology or Growth Rate
Potential Cause: Emergence of a culture-adapted clone with a selective advantage, often due to a recurrent chromosomal aberration.
Action Plan:
- Immediate Action: Immediately karyotype the culture. If possible, isolate and analyze individual clones.
- Confirmatory Testing: If karyotype is normal, perform a higher-resolution analysis (e.g., microarray) to check for submicroscopic changes, particularly on chromosome 20q11.21, which harbors cancer-related genes like ASXL1 [43].
- Prevention for Future:
- Reduce Culture Stress: Optimize passaging techniques to avoid single-cell dissociation when possible, as this can favor the outgrowth of clones with 20q gains [18].
- Monitor More Frequently: Increase the frequency of your genetic monitoring for several passages after any significant change in protocol or observed stress.
Problem: Low Cell Attachment or Survival After Passaging
Potential Cause: This could be a sign of general culture health issues or cellular stress, which can precede genetic instability.
Action Plan [9]:
- Check Technical Factors:
- Plate 2-3 times the number of cell aggregates initially.
- Work quickly after dissociation to minimize the time aggregates are in suspension.
- Ensure you are using the correct plate type (non-tissue culture-treated for Vitronectin XF; tissue culture-treated for Matrigel).
- Optimize Passaging:
- If aggregate size is too small (<50 μm), decrease incubation time with the passaging reagent by 1-2 minutes and minimize pipetting manipulation.
- If colonies are difficult to dislodge, increase incubation time with the passaging reagent by 1-2 minutes.
- Genetic Check: If problems persist across multiple attempts, karyotype the culture to rule that out as a contributing factor.
Experimental Protocols for Genetic Monitoring
Protocol 1: Routine G-Banding Karyotype Analysis
This protocol outlines the general process for preparing metaphase chromosomes for karyotypic analysis, a cornerstone of genetic stability assessment [43].
Key Reagents & Materials:
- Cell Culture Suspension: Actively dividing hiPSCs.
- Colchicine Solution: To arrest cells in metaphase.
- Hypotonic Solution (e.g., Potassium Chloride): To swell the cells and spread chromosomes.
- Carnoy's Fixative (3:1 Methanol:Glacial Acetic Acid): To fix cell morphology.
- Giemsa Stain: For chromosome banding.
- Microscope Slides and Coverslips.
Methodology:
- Metaphase Arrest: Add colchicine to the culture medium to a final concentration of 40 ng/mL and incubate for 3 hours at 37°C [44].
- Cell Harvesting: Gently dissociate cells to a single-cell suspension and transfer to a centrifuge tube.
- Hypotonic Treatment: Centrifuge cells, resuspend in a pre-warmed hypotonic solution, and incubate for 20 minutes at 37°C.
- Fixation: Perform multiple rounds of centrifugation, carefully remove the supernatant, and resuspend the cell pellet in fresh Carnoy's fixative. Repeat 2-3 times.
- Slide Preparation: Drop the fixed cell suspension onto clean, cold microscope slides and allow to air dry.
- Staining and Analysis: Stain slides with Giemsa and analyze under a microscope with an automated scanning system. At least 20 metaphase spreads should be analyzed per sample [44] [43].
Protocol 2: Validation of Specific Mutations via Droplet Digital PCR (ddPCR)
For validated, high-confidence mutations identified from sequencing, ddPCR provides a highly sensitive and quantitative method for tracking their frequency in a population [43].
Key Reagents & Materials:
- Genomic DNA: Extracted from hiPSCs or hiPSC-derived cells.
- ddPCR Supermix: For probe-based digital PCR.
- FAM and HEX-labeled Probe Assays: Specific for the mutant and wild-type alleles, respectively.
- DG8 Cartridges and Gaskets: For droplet generation.
- Droplet Reader Oil and PCR Plate Sealer.
- QX200 Droplet Reader and Quantasoft Software.
Methodology:
- Assay Design: Design and validate TaqMan probe assays for the specific mutation of interest and the corresponding wild-type sequence.
- Reaction Setup: Combine genomic DNA, ddPCR supermix, and mutant/wild-type probes. Include appropriate negative and positive controls.
- Droplet Generation: Use the QX200 Droplet Generator to partition the reaction mixture into approximately 20,000 nanoliter-sized droplets.
- PCR Amplification: Perform endpoint PCR on the droplet emulsion.
- Droplet Reading and Analysis: Use the QX200 Droplet Reader to count the fluorescence (FAM+/HEX+) in each droplet. The software will calculate the absolute concentration (copies/μL) of the mutant and wild-type sequences in the original sample.
The Scientist's Toolkit: Essential Reagents for Monitoring
Table 2: Key Research Reagent Solutions for Karyotype Monitoring
| Reagent/Material | Function | Example Application |
|---|---|---|
| H2B-Dendra2 Protein | A photoactivatable fluorescent protein used to label nuclei and track target cells for single-cell genomics [45]. | Investigating de novo chromosomal abnormality (CA) formation in live cells. |
| DACT-1 | A small-molecule dye used for photolabelling and cell tracking, bypassing the need for genetic manipulation [45]. | Alternative to Dendra2 for live-cell imaging and sorting of cells with nuclear atypia. |
| Carnoy's Fixative | A histological fixative (typically 3:1 ethanol:acetic acid) that preserves chromosome structure [46]. | Preparing metaphase chromosome spreads for karyotype analysis. |
| Colchicine | A mitotic inhibitor that disrupts spindle formation, arresting cells in metaphase [44]. | Accumulating a sufficient number of cells in metaphase for chromosome analysis. |
| Oligo-FISH Probe Libraries | Bioinformatically designed oligonucleotide pools for fluorescence in situ hybridization [47]. | High-resolution chromosome painting and identification of structural variations. |
| CytoScanHD Chip | A high-density microarray used for chromosomal microarray analysis (CMA) [43]. | Detecting submicroscopic copy number variants and loss of heterozygosity. |
Workflow Diagram: Genetic Instability Monitoring Pathway
The following diagram illustrates a comprehensive workflow for monitoring and responding to genetic instability in stem cell cultures, integrating both routine checks and advanced analysis.
Mitigating Risk: Strategic Approaches to Minimize Instability and Optimize Culture Conditions
Troubleshooting Guides and FAQs
FAQ: How Do Culture Conditions Affect the Genomic Stability of Stem Cells?
Why are culture conditions like passaging method and feeder systems critical for genomic stability? Long-term culture of human pluripotent stem cells (hPSCs) can lead to recurrent genomic abnormalities and copy number variations, which are highly influenced by culture conditions [48]. Enzymatic single-cell passaging has been shown to be highly deleterious to the hPSC genome, with karyotype abnormalities and copy number variations occurring very rapidly, sometimes within five passages after switching hESCs to enzymatic dissociation [48]. Subchromosomal abnormalities often precede or accompany karyotype abnormalities and are associated with increased occurrence of DNA double-strand breaks [48]. Feeder-free protocols and high-density cell culture have been associated with specific abnormalities such as 1q gain [18].
What are the most common genomic abnormalities observed in stem cell cultures? Recurrent abnormalities can account for more than 90% of all genetic alterations in hPSCs [18]. The most common recurrent abnormalities include:
- Gains of chromosomes or chromosomal segments 20/20q, 1q, 12, and 17
- Less common gains of chromosomes X and 8
- Losses of chromosomes 10, 18, and 22 [18]
In one study of 65 iPSC lines, karyotype abnormalities were identified in 23% of analyses, with trisomy 20 and 1q duplications being particularly prevalent [18].
How quickly can genomic abnormalities emerge in culture? Genomic alterations are not restricted to long-term culture but can occur very rapidly. Research has demonstrated that karyotype abnormalities and copy number variations can be detected within five passages after switching hESCs to enzymatic dissociation [48]. Prolonged passaging can result in up to 80% of cell lines exhibiting aberrations [18].
Troubleshooting Guide: Addressing Culture-Induced Genomic Instability
Problem: Unexpected differentiation or morphological changes in culture Potential Causes and Solutions:
- Cause: Overgrowth or suboptimal passaging interval leading to cellular stress.
- Solution: Monitor cultures daily for morphological changes indicating differentiation; less than 10% of iPSCs should exhibit a differentiated morphology [49]. Passage cells at 50-75% confluency, typically every 4-7 days [50].
- Cause: Inconsistent aggregate size during passaging.
- Solution: Maintain optimal aggregate size of 50-200 μm during passaging to ensure proper attachment to the matrix [50].
Problem: Detection of genomic abnormalities during routine quality control Potential Causes and Solutions:
- Cause: Use of enzymatic single-cell passaging methods.
- Solution: Transition to aggregate passaging methods, which allow for long-term expansion of human ES and iPS cells while maintaining an expected karyotype [50]. Enzyme-free dissociation reagents like Gentle Cell Dissociation Reagent (GCDR) or ReLeSR can be used to generate appropriately sized aggregates [50].
- Cause: Extended culture duration without genetic monitoring.
- Solution: Implement regular genetic analysis using appropriate detection methods. For cells passaged as single cells, conduct more frequent genetic analysis to ensure the karyotype is as expected [50].
Problem: Decreased cell viability after passaging Potential Causes and Solutions:
- Cause: Over-dissociation creating single cells rather than aggregates.
- Solution: When using enzyme-free passaging, create a uniform suspension of aggregates approximately 50-200 μm in size; do not create a single-cell suspension [50]. Avoid over-pipetting during passaging, as single cells will not establish colonies after seeding [49].
- Cause: Inadequate handling after passaging.
- Solution: After plating aggregates, leave them to settle for 24 hours prior to the first medium change [50]. Move the plate in several quick, short, back-and-forth and side-to-side motions to evenly distribute cell aggregates, as uneven distribution may result in increased differentiation [51].
Quantitative Data on Culture-Induced Genomic Instability
Table 1: Frequency of Karyotype Abnormalities in iPSC Cultures
| Study Parameter | Findings |
|---|---|
| Overall frequency of abnormal cell lines | 21% (13 out of 62 cell lines) [18] |
| Abnormalities in lines from healthy donors | Increased from 2/10 to 4/10 after re-karyotyping at later passages [18] |
| Abnormalities in lines from patients with genetic disorders | 9/52 unique lines (17.3%) [18] |
| Cell lines with recurrent aberrations | 78.6% (11 out of 14 aberrant cell clones) [18] |
| Trisomy 20 frequency | 8.6% of all tests, 38.5% of unique aberrant lines [18] |
| 1q duplication frequency | 7.2% of all tests, 30.8% of unique aberrant lines [18] |
Table 2: Comparison of Karyotyping Methods for Genomic Monitoring
| Karyotyping Assay | Estimated Turnaround Time | Resolution | Key Advantages | Key Limitations |
|---|---|---|---|---|
| G-banding (Staining) | 3-4 weeks | 5-10 Mb | Detects balanced and unbalanced abnormalities | Lower resolution [26] |
| Whole Genome Sequencing | 6-8 weeks | 1 bp | Highest resolution, comprehensive | Cost-prohibitive, may miss large structural changes [26] |
| Array-Based Methods (KaryoStat) | 3-4 weeks | 1-2 Mb | Whole-genome coverage, good for unbalanced abnormalities | Cannot detect balanced abnormalities [26] |
| hPSC Genetic Analysis Kit (qPCR) | 1 week | 9 targeted hot spots | Rapid, cost-effective for common abnormalities | Limited to predefined targets [26] |
| iCS-digital PSC (ddPCR) | 1 week | 24 targeted hot spots | Rapid, sensitive for common hotspots | Limited genome coverage [26] |
Experimental Protocols for Culture Condition Audits
Protocol 1: Enzyme-Free Aggregate Passaging Using ReLeSR
Purpose: To passage human pluripotent stem cells as aggregates while minimizing genomic instability [51] [50].
Materials:
- Cultured hPSCs in mTeSR Plus or similar medium
- ReLeSR enzyme-free dissociation reagent
- D-PBS without Ca++ and Mg++
- Appropriate cell culture matrix (e.g., Vitronectin XF, Matrigel)
- 6-well culture plates
- Cell scraper
- 15 mL conical tube
Procedure:
- Coat new culture plates with appropriate matrix at least 1 hour before passaging.
- Wash cells with 1 mL/well of D-PBS and aspirate completely.
- Add 1 mL/well of ReLeSR and aspirate within 1 minute, leaving a thin film of liquid.
- Incubate at 37°C for 4-8 minutes. Monitor dissociation progress microscopically.
- Add 1 mL/well of culture medium.
- Gently detach colonies by scraping with a cell scraper.
- Transfer detached cell aggregates to a 15 mL conical tube.
- Gently pipette the aggregate mixture to achieve uniform aggregates of 50-200 μm in size.
- Plate the aggregate mixture at desired density onto coated wells.
- Distribute evenly by moving the plate in quick, short motions and do not disturb for 24 hours [51] [50].
Quality Control Notes:
- Optimal dissociation time varies by cell line; determine empirically when using a new line.
- Avoid creating single-cell suspensions.
- Change medium daily or every other day until next passaging [51].
Protocol 2: Transitioning from Single-Cell to Aggregate Cultures Using GCDR
Purpose: Convert monolayer single-cell cultures to aggregate cultures to enhance genomic stability [50].
Materials:
- Single-cell hPSC culture
- Gentle Cell Dissociation Reagent (GCDR)
- D-PBS without Ca++ and Mg++
- Appropriate culture medium
- 1000 μL pipette tips
- Cell scraper
Procedure:
- Wash cells with D-PBS and aspirate.
- Add GCDR and incubate at 15-25°C for 4-8 minutes.
- Carefully aspirate GCDR without shaking/tapping the plate.
- Add culture medium.
- Tilt plate to approximately 45° angle and gently score a crosshatched pattern in the monolayer using a pipette tip.
- Scrape gently with cell scraper to detach remaining colonies.
- Transfer detached aggregates to a 15 mL conical tube.
- Gently pipette to break up aggregates to optimal size (50-200 μm).
- Plate aggregates and maintain without disturbance for 24 hours [50].
Decision Framework for Passaging Method Selection
The following workflow outlines the process for selecting appropriate passaging methods based on research objectives and stability concerns:
Research Reagent Solutions for Genomic Stability Monitoring
Table 3: Essential Reagents for Culture Condition Audits and Genomic Monitoring
| Reagent/Category | Specific Examples | Function/Purpose | Considerations |
|---|---|---|---|
| Enzyme-Free Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent (GCDR) | Passaging hPSCs as aggregates to minimize genomic stress | Maintain aggregate size of 50-200 μm; avoid single-cell formation [51] [50] |
| Culture Matrices | Vitronectin XF, Corning Matrigel, Cell Basement Membrane | Provide extracellular scaffolding for cell attachment in feeder-free systems | Coating concentration and time affect cell attachment and growth [51] [49] |
| Culture Media | mTeSR Plus, TeSR-E8, Pluripotent Stem Cell SFM XF/FF | Defined formulations supporting pluripotency | Some media specifically formulated for single-cell passaging [50] [49] |
| Genomic Analysis Kits | hPSC Genetic Analysis Kit, Genomic DNA Purification Kit | Quality control and genetic stability assessment | Choose based on required resolution and turnaround time [50] [26] |
| ROCK Inhibitor | Y-27632 | Enhance cell survival after single-cell passaging | Use for first 24 hours only; longer exposure may alter cellular metabolism [50] |
| Feeder Cells | Irradiated Mouse Embryonic Fibroblasts (MEFs), Human Foreskin Fibroblasts (HFFs) | Support hPSC growth through secreted factors and direct contact | Mitotically inactivated; risk of transmitting animal pathogens [49] [52] |
Implementation Recommendations
For researchers conducting culture condition audits, the following evidence-based practices are recommended:
Establish Baseline Genomic Status: Perform comprehensive karyotyping at the initiation of any new culture system using a method appropriate for your resolution requirements [26].
Implement Regular Monitoring: Schedule genetic analyses at regular intervals, with frequency determined by passaging method—more frequently for single-cell cultures (every 5-10 passages) than aggregate cultures (every 10-15 passages) [50].
Validate Culture Transitions: When transitioning between culture systems (e.g., feeder to feeder-free, enzymatic to aggregate passaging), monitor genomic stability particularly closely during the first 5-10 passages, as this period shows highest vulnerability to genomic alterations [48] [18].
Document Culture History: Maintain detailed records of passaging methods, dissociation reagents, culture densities, and any observed morphological changes to correlate with genomic stability data.
Utilize Multiple Assessment Methods: Combine different monitoring approaches, such as periodic high-resolution karyotyping with more frequent targeted assays for common abnormalities (e.g., 20q11.21, 1q gains) to balance comprehensive assessment with practical constraints [26].
Troubleshooting Guide: Managing Selective Pressure in Stem Cell Cultures
Problem 1: Observation of Rapid Culture Takeover by a Specific Cell Population
- Symptoms: A morphologically distinct subpopulation of cells begins to dominate the culture within a few passages, leading to decreased heterogeneity.
- Underlying Cause: This is a classic sign of a bottleneck effect where a genetically abnormal clone has a survival or proliferation advantage under standard culture conditions, leading to its selective outgrowth. Studies have shown that an aberrant clone can completely overtake a culture in less than five passages [19]. Common recurrent chromosomal aberrations provide a fitness advantage in vitro [18].
- Solutions:
- Implement Regular Karyotyping: Perform G-banding analysis regularly (e.g., every 10 passages) to detect large-scale chromosomal abnormalities. This is the gold-standard method for a genome-wide overview and can detect structural aberrations like translocations [19].
- Incorporate High-Resolution Genomic Analysis: Use Single-Nucleotide Polymorphism (SNP) array analysis to identify smaller copy number variations (CNVs) or copy-neutral loss of heterozygosity (CN-LOH) that are below the detection limit of G-banding. This method can detect abnormalities larger than 350 kb with high sensitivity [19].
- Bank Cells Early: Create a master cell bank at the earliest possible passage after cell line derivation and characterization. Use low-passage cells for critical experiments to minimize culture-acquired adaptations.
- Monitor Known Hotspots: Specifically check for recurrent abnormalities involving gains of chromosomes 20/20q, 1q, 12, and 17, or losses of chromosomes 10, 18, and 22, as these are frequently selected for in culture [18] [19].
Problem 2: Decreased Differentiation Efficiency or Altered Differentiation Potential
- Symptoms: The stem cell line fails to efficiently differentiate into target lineages, or the resulting differentiated cells exhibit unexpected phenotypes or functions.
- Underlying Cause: Culture-acquired genetic alterations can significantly impact critical cell properties, including differentiation capacity and pluripotency maintenance [18]. For example, gains of chromosome 12 or 17q have been associated with altered differentiation potential [19].
- Solutions:
- Validate Genomic Integrity Pre-Differentiation: Perform a round of genomic quality control (e.g., via SNP array) on the pluripotent stem cells before initiating a major differentiation experiment.
- Use a Control Cell Line: Always include a well-characterized control stem cell line (e.g., H9 or H7) in differentiation experiments to control for protocol-specific issues [53].
- Optimize Passaging Confluence: Avoid routine passaging at very high confluencies, as this can be a selective pressure. Passage cells upon reaching ~85% confluency for optimal health [53].
Problem 3: Poor Cell Survival After Single-Cell Passaging
- Symptoms: Significant cell death occurs when cells are passaged as single cells, leading to long recovery times and potential selective bottlenecks.
- Underlying Cause: The physical stress of single-cell dissociation favors the survival of clones that are more resistant to anoikis (cell detachment-induced apoptosis). Specific aberrations, like the gain of 20q, are known to favor survival after single-cell passaging [18].
- Solutions:
- Use ROCK Inhibitor: Include a ROCK inhibitor (e.g., Y-27632) in the culture medium for 18-24 hours after passaging to improve the survival of single cells [53].
- Consider Aggregate Passaging: If the experimental workflow allows, use manual passaging or non-enzymatic reagents (like ReLeSR) to passage cells in small, uniform aggregates rather than as single cells, which is less stressful [9].
- Optimize Split Ratios: Carry cells at a range of split ratios to prevent consistently passaging at high confluencies, which can lead to poor survival and selection [53].
Frequently Asked Questions (FAQs)
Q1: What is the "bottleneck effect" in the context of stem cell culture? A: The bottleneck effect occurs when a selective pressure in the culture environment, such as passaging, cryopreservation, or the culture conditions themselves, gives a survival or growth advantage to a specific subpopulation of cells. This can lead to the rapid dominance of a genetically abnormal clone, reducing the overall genetic diversity of the culture and potentially compromising its functionality and safety for research or therapy [18] [19].
Q2: Why are certain chromosomal abnormalities, like gain of 1q or 20q, so frequently reported in hPSC cultures? A: These recurrent abnormalities are not random; they confer a selective advantage under standard in vitro culture conditions. For instance, the 1q gain has been associated with feeder-free protocols and high-density cell culture, while the 20q11.21 amplification favors survival after single-cell passaging. The genes located in these regions often promote cell growth, inhibit apoptosis, or enhance attachment, allowing affected cells to outcompete their normal counterparts [18] [19].
Q3: How often should I check my stem cell lines for genomic instability? A: There is no one-size-fits-all answer, but a robust quality control plan is essential. Key timepoints for genomic analysis include:
- After establishing a new cell line (following reprogramming or gene editing).
- Before creating a master cell bank.
- At the start of a major differentiation experiment.
- Routinely during maintenance cultivation, e.g., every 10-20 passages, or if morphological changes or reduced performance are observed.
Q4: What is the advantage of using SNP array analysis over traditional G-banding karyotyping? A: While G-banding is excellent for detecting large structural and numerical changes across the entire genome, SNP array analysis offers higher resolution, capable of identifying smaller copy number variations (down to ~350 kb) and copy-neutral loss of heterozygosity (CN-LOH). However, a key limitation of SNP arrays is that they cannot detect balanced translocations, which is why a combination of both methods provides the most comprehensive assessment [19].
Q5: My culture has become overgrown by a differentiated population. Is this a genetic bottleneck? A: Not necessarily in the genetic sense. This is more likely a culture condition issue, where the cells are being maintained in suboptimal conditions that promote spontaneous differentiation. However, if a karyotypically abnormal clone emerges, it may also exhibit a differentiated morphology. To address this, ensure your culture medium is fresh and not expired, remove differentiated areas manually before passaging, and avoid leaving cells outside the incubator for extended periods [9].
Recurrent Chromosomal Aberrations in hPSCs
The following table summarizes common, culture-acquired chromosomal aberrations identified through karyotype and SNP array analyses, which are indicative of strong selective pressure [18] [19].
Table 1: Common Recurrent Aberrations and Their Proposed Selective Advantages
| Chromosomal Abnormality | Frequency in Studies | Associated Selective Pressure or Advantage |
|---|---|---|
| Trisomy 20 / 20q gain | Very high (e.g., 38.5% of aberrant lines in one study) | Favors survival after single-cell passaging [18]. |
| 1q duplication/gain | Very high (e.g., 30.8% of aberrant lines) | Associated with feeder-free and high-density culture protocols [18]. |
| Trisomy 8 | Common (e.g., 15.4% of aberrant lines) | A recurrent anomaly that provides a growth advantage in vitro [18]. |
| Trisomy 12 | Common | Well-established recurrent aberration linked to proliferation boost. |
| Trisomy 17 / 17q gain | Common | Another recurrent anomaly that provides a growth advantage in vitro. |
| Trisomy X | Common | Can confer a selective advantage in female cell lines. |
Experimental Protocol: SNP Array Analysis for Genomic Quality Control
This protocol provides a practical guide for using Illumina's GenomeStudio software to analyze SNP array data for detecting chromosomal aberrations in hPSCs, based on the method outlined by [19].
1. DNA Extraction and SNP Array Processing
- Extraction: Isolate genomic DNA from hPSCs using a kit such as the QIAamp DNA Blood Mini Kit. Ensure DNA quality and quantity meet the requirements for the array platform.
- Array Processing: Process the DNA on a suitable SNP array platform (e.g., Illumina's Global Screening Array). This involves hybridizing fragmented, fluorescently labeled DNA to the array chip, followed by washing and scanning, typically performed by a core facility or commercial service.
2. Data Analysis in GenomeStudio
- Software Setup: Use Illumina's GenomeStudio V2.0.5 with the cnvPartition plug-in (v3.2.0 or higher) for CNV calling.
- Quality Control Metrics: Assess the quality of the data. The Call Rate (percentage of successfully genotyped SNPs) should be >95% to be considered acceptable. A low call rate can indicate poor-quality DNA or technical issues [19].
- CNV Detection: The cnvPartition algorithm will automatically segment the genome and call CNVs. Visually inspect the whole-genome plot for obvious regions of gain (copy number >2) or loss (copy number <2). Pay close attention to known recurrent regions like 20q11.21.
3. Interpretation and Validation
- Correlate with Known Aberrations: Compare detected CNVs against databases of known recurrent hPSC aberrations.
- Confirm with Orthogonal Method: For any novel or unexpected finding, confirm the result with an orthogonal method, such as G-banding karyotyping (to rule out balanced translocations) or digital PCR for a specific region.
- Action: If a confirmed abnormality is found in a research cell line, document it thoroughly. For lines intended for therapy, the culture should be terminated, and a new batch should be revived from an earlier, validated stock.
The workflow for this quality control process is summarized in the diagram below.
The Scientist's Toolkit: Essential Reagents for Genomic Quality Control
Table 2: Key Research Reagents and Tools for Monitoring Genetic Stability
| Item / Reagent | Function / Application | Example / Note |
|---|---|---|
| SNP Microarray Kit | High-resolution detection of copy number variations (CNVs) and loss of heterozygosity (LOH). | Illumina Global Screening Array [19]. |
| GenomeStudio with cnvPartition | Software for analyzing SNP array data to automatically call CNVs and assign genotypes. | Critical for researchers with minimal bioinformatics expertise [19]. |
| G-banding Karyotyping Service | Gold-standard method for genome-wide detection of large structural and numerical chromosomal abnormalities. | Essential for identifying balanced translocations, which SNP arrays miss [19]. |
| ROCK Inhibitor | Improves cell survival after single-cell passaging, reducing a key selective pressure. | Y-27632; use for 18-24 hours post-passaging [53]. |
| Non-Enzymatic Passaging Reagent | Allows passaging cells in clumps, reducing stress and selective pressure compared to single-cell methods. | ReLeSR or Gentle Cell Dissociation Reagent [9]. |
| Defined, Feeder-Free Culture System | Provides a consistent and controlled environment, reducing undefined stressors that can drive selection. | Essential 8 Medium on VTN-N [53]. |
Frequently Asked Questions
What is the 20q11.21 amplification and why is it a major concern in hPSC research?
The 20q11.21 amplification is a specific copy number variant (CNV) found in approximately 20-26% of human pluripotent stem cell (hPSC) lines worldwide [54] [55]. This abnormality provides cells with a significant survival advantage, allowing them to rapidly overtake cultures. The concern stems from its prevalence and the fact that the same amplification is found in about 20% of human cancers, raising important safety questions for therapeutic applications [54] [56].
Which specific gene drives the selective advantage and through what mechanism?
The gene BCL2L1, which encodes the anti-apoptotic protein BCL-XL, has been identified as the driver of this selective advantage [57]. The amplification leads to overexpression of BCL-XL, which enhances cell survival by conferring resistance to apoptosis. This provides mutated cells with a powerful growth advantage, particularly under standard culture stresses like passaging, thawing, and single-cell dissociation [54] [57].
How quickly can a 20q11.21-amplified subpopulation take over a culture?
Cells with the 20q11.21 amplification can completely overtake a culture in less than five passages [19]. Competition assays have demonstrated that when 20q11.21-amplified cells are mixed with normal cells at a 1:9 ratio, this ratio reverses to 9:1 by passage 10 [57].
What impact does this amplification have on differentiation capacity?
The effects on differentiation are lineage-specific. Some studies report decreased differentiation potential toward neural lineages [54] [55], while others have found enhanced differentiation capacity for certain lineages like retinal pigment epithelium (RPE) [58]. This suggests the impact may depend on the specific differentiation protocol and target cell type.
Does the presence of 20q11.21 in hPSCs automatically make their derivatives tumorigenic?
Not necessarily. Research on RPE differentiation found that 20q11.21-containing RPE cells displayed a mature phenotype and exhibited no malignant transformation capacity in vitro [58]. However, studies with neural precursors derived from 20q11.21-amplified hPSCs did produce tumors in SCID mice [54]. The tumorigenic risk likely depends on the specific differentiated cell type and additional genetic factors.
Detection and Monitoring Strategies
Comparison of Detection Methods
| Method | Resolution | Detection Capability | Time Required | Best Use Cases |
|---|---|---|---|---|
| Karyotyping (G-banding) | 5-10 Mb [19] | Large chromosomal abnormalities; misses small CNVs [19] | Several days to weeks [55] | Initial cell line characterization; detecting large structural changes [55] |
| SNP Array | ~350 kb [19] | CNVs, copy-neutral LOH; cannot detect balanced translocations [19] | 1-3 days | High-resolution screening; identification of common recurrent aberrations [19] |
| Digital PCR | Single gene level [55] | Specific targeted anomalies below 5Mb; quantitative [55] | 1-3 days [55] | Frequent in-process testing; monitoring for specific known abnormalities like 20q11.21 [55] |
| FISH (Fluorescence In Situ Hybridization) | Single gene level | Visual confirmation of specific amplifications; can detect mosaicism [57] | 1-2 days | Confirming specific abnormalities identified by other methods [55] |
Quantitative Data on 20q11.21 Prevalence and Impact
| Parameter | Reported Value | Context/Source |
|---|---|---|
| Prevalence in hPSC lines | 20-26% [54] [55] | International Stem Cell Initiative analysis [54] |
| Prevalence in colorectal cancer | 7-9% [56] | TCGA genomic series [56] |
| Minimal amplicon size | 0.56 Mb [54] | Contains 13 genes [54] |
| Key driver gene | BCL2L1 (BCL-XL) [57] | Confirmed through gain-and-loss-of-function studies [57] |
| Recommended testing frequency | Every 5-10 passages [55] | Prevents culture takeover by abnormal cells [55] |
| Growth rate advantage | 3-7 fold increase [57] | Varies with seeding density [57] |
Experimental Protocols
Protocol 1: Digital PCR Detection of 20q11.21 Amplification
Purpose: To routinely detect 20q11.21 amplifications present at low frequencies in hPSC cultures.
Materials:
- Genomic DNA from hPSCs (QIAamp DNA Blood Mini Kit or equivalent)
- TaqMan Copy Number Assays for target genes (BCL2L1, ID1, HM13)
- Reference assay (located in non-amplified region)
- Digital PCR system and compatible consumables
- Appropriate master mix for digital PCR
Procedure:
- Extract genomic DNA using standardized protocols, ensuring high quality and purity.
- Dilute DNA to working concentration (typically 10-20 ng/μL).
- Prepare digital PCR reaction mix according to manufacturer's instructions including target and reference assays.
- Partition samples into thousands of individual reactions using your digital PCR system.
- Amplify using the following cycling conditions:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing/Extension: 60°C for 1 minute
- Analyze results using system software to determine copy number variation.
- Interpret results: Ratio >1.2 suggests presence of amplification [55].
Technical Notes: Digital PCR can detect the 20q11.21 amplification present in as low as 5-10% of cells in a mosaic culture [55]. This method is particularly valuable for regular monitoring due to its sensitivity, speed, and cost-effectiveness compared to other methods.
Protocol 2: Competitive Growth Assay to Measure Selective Advantage
Purpose: To quantify the growth advantage conferred by the 20q11.21 amplification.
Materials:
- Wild-type hPSCs (control)
- 20q11.21-amplified hPSCs
- Fluorescent cell tracker (e.g., GFP-labeled control cells)
- Standard hPSC culture equipment and reagents
Procedure:
- Mix GFP-labeled wild-type hPSCs with unlabeled 20q11.21-amplified hPSCs at a 9:1 ratio.
- Plate the mixed population at standard density (8×10⁴ cells/cm²) and culture under normal conditions.
- Passage cells every 5-7 days, maintaining detailed records of passage numbers.
- At each passage, analyze the ratio of GFP-positive to GFP-negative cells using fluorescence microscopy or flow cytometry.
- Continue monitoring for at least 10 passages.
- Calculate the growth advantage based on the shift in population ratios over time [57].
Expected Results: The 20q11.21-amplified cells will typically reverse the initial 9:1 ratio to approximately 1:9 by passage 10, demonstrating their strong selective advantage [57].
Data Visualization
Detection Strategy Workflow
BCL-XL Mediated Survival Advantage Mechanism
Research Reagent Solutions
| Reagent/Tool | Specific Function | Application Notes |
|---|---|---|
| BCL-XL Inhibitor (ABT-263) | Selective BCL-XL inhibition [57] | Suppresses growth advantage of 20q11.21 cells at 250 nM [57] |
| shRNA for BCL2L1 | Knockdown of BCL2L1 expression [57] | Reduces BCL-XL protein to normal levels [57] |
| TaqMan Copy Number Assays | Quantitative CNV detection [55] | Target genes: BCL2L1, ID1, HM13 [57] |
| Global Screening Array v3.0 | SNP array analysis [19] | Detects CNVs >350 kb; call rate >95% required [19] |
| Anti-BCL-XL Antibodies | Protein level quantification [57] | Western blot validation of overexpression [57] |
Troubleshooting Guide
Problem: Suspected mosaic culture with low-frequency 20q11.21 amplification
Solution: Implement digital PCR testing rather than standard karyotyping. Digital PCR can detect the abnormality when present in as little as 5-10% of the population, while karyotyping often requires at least 20-30% abnormal cells for detection [55] [19].
Problem: Rapid culture takeover by fitter cells despite regular passaging
Solution:
- Increase testing frequency to every 5 passages
- Avoid excessive single-cell passaging
- Maintain higher seeding densities where possible
- Consider using BCL-XL inhibitors in research settings (not for therapeutic applications) [55] [57]
Problem: Inconsistent differentiation results between different batches of the same cell line
Solution: Test for 20q11.21 amplification, as it can alter differentiation propensity in a lineage-specific manner. Neural differentiation is particularly susceptible to impairment, while other lineages like RPE may show enhanced differentiation [54] [58].
Problem: Need to eliminate 20q11.21-amplified cells from valuable culture
Solution: Treatment with BCL-XL inhibitor ABT-263 at 250 nM can selectively reduce the growth advantage of amplified cells, allowing normal cells to recover. However, complete elimination may require single-cell cloning and extensive characterization [57].
Implementing a Multi-Method Quality Control Pipeline for Comprehensive Coverage
Troubleshooting Guides for Karyotype Analysis
Guide 1: Resolving Inconclusive Karyotyping Results
Issue or Problem Statement A researcher obtains ambiguous or suboptimal results from a G-banded karyotyping experiment, making it difficult to identify chromosomal abnormalities in their stem cell line.
Symptoms or Error Indicators
- Poor chromosome spreading on the metaphase slide, with overlapping chromosomes [1]
- Faint or indistinct G-banding patterns, preventing accurate chromosome identification [1]
- Inability to achieve the required resolution (typically 5-10 Mb) for detecting significant abnormalities [1]
Environment Details
- Cell type: Human pluripotent stem cells (hPSCs) [1] [26]
- Culture conditions: Long-term cultured hPSCs [26]
- Technique used: G-banded karyotype analysis [1]
Possible Causes
- Suboptimal cell culture techniques exacerbating genetic abnormalities [1]
- Insufficient mitotic arrest during metaphase preparation [1]
- Inadequate hypotonic treatment or fixation during slide preparation [1]
- Over-condensed or under-condensed chromosomes due to timing issues [1]
Step-by-Step Resolution Process
- Verify Cell Culture Quality: Ensure cells are actively dividing and free from contamination before analysis. Use healthy, log-phase cultures [1]
- Optimize Colcemid Exposure: Titrate colcemid concentration (0.01-0.1 µg/mL) and exposure time (1-4 hours) to achieve optimal chromosome condensation without excessive contraction [1]
- Adjust Hypotonic Treatment: Fine-tune potassium chloride exposure (15-30 minutes at 37°C) to improve chromosome spreading without causing rupture [1]
- Modify Fixation Protocol: Ensure fresh 3:1 methanol:acetic acid fixative is used, with multiple changes to remove cellular debris [1]
- Control Humidity During Dropping: Maintain 40-50% humidity for optimal chromosome spreading when preparing slides [1]
Escalation Path or Next Steps If problems persist after optimization:
- Send samples to a specialized cytogenetics service provider for independent verification [1]
- Implement orthogonal validation method such as array-based karyotyping or ddPCR for specific hotspots [26]
Validation or Confirmation Step
- Examine slide for minimum of 20 well-spread metaphase cells with 350-450 band resolution [1]
- Confirm detection of known common abnormalities like 20q11.21 amplification [26]
Additional Notes or References
- G-banding has limitations for detecting abnormalities <5Mb; consider complementary techniques for comprehensive coverage [1]
- Regular karyotyping is recommended every 10 passages for stem cell cultures [1]
Guide 2: Addressing Discrepancies Between Different Karyotyping Methods
Issue or Problem Statement A researcher finds conflicting results when comparing data from G-banding karyotyping and higher-resolution methods like ddPCR or array-based techniques.
Symptoms or Error Indicators
- G-banding shows normal karyotype while other methods detect subchromosomal abnormalities [26]
- Digital PCR identifies specific copy number variations not visible through conventional cytogenetics [1] [26]
- Inconsistent findings between methods creating uncertainty about stem cell line genetic integrity [26]
Environment Details
- Quality control pipeline for stem cell banking or pre-clinical research [1]
- Methods compared: G-banding vs. ddPCR, array-based karyotyping, or NGS [26]
- Specific concern: Common hPSC abnormalities like 20q11.21 amplification [26]
Possible Causes
- Resolution limitations of G-banding (>5-10 Mb) versus higher-resolution methods [1] [26]
- ddPCR targeting specific known hotspots while G-banding provides genome-wide but lower-resolution view [1] [26]
- Mosaicism levels below detection threshold of G-banding (>10%) [1]
- Technical artifacts in specific methodology (e.g., array hybridization issues) [26]
Step-by-Step Resolution Process
- Method Capability Assessment:
Experimental Verification:
- Repeat G-banding analysis with increased number of metaphase cells (50+)
- Validate ddPCR findings with alternative method (e.g., array-based karyotyping) [26]
Data Correlation:
- Map identified abnormalities to chromosomal bands for cross-method comparison
- Confirm if detected abnormalities are known hPSC hotspots (e.g., 20q11.21, 12p13.31) [26]
Historical Reference Check:
- Compare with previous passage data to identify emerging abnormalities
- Review literature on common method-specific artifacts [26]
Escalation Path or Next Steps For critical applications (e.g., clinical use):
- Engage independent laboratory for verification using same methodology [1]
- Consult regulatory guidelines for required methods in IND applications [1]
Validation or Confirmation Step
- Establish consensus result through majority of methods
- Confirm biological significance through functional assays if discrepancies remain
Additional Notes or References
- Multi-method approach recommended for comprehensive genetic assessment [1] [26]
- FDA guidelines emphasize comprehensive cytogenetic analysis using validated methods for stem cell products [1]
Frequently Asked Questions (FAQs)
FAQ 1: Method Selection and Implementation
Q: What is the recommended frequency for karyotyping stem cell cultures, and does this differ by research phase?
A: Regular karyotyping is essential for monitoring stem cell genomic integrity. The recommended frequency is every 10 passages during routine culture [1]. Additionally, specific checkpoints require karyotyping: when establishing primary donor materials, upon acquisition or derivation of a new cell line, during initial biobanking, at the start of experimental protocols, as an in-process control, and before concluding experiments or publication [1]. For critical applications like cell therapy products, more frequent monitoring may be necessary to comply with FDA guidelines for Investigational New Drug applications [1].
Q: Can newer methods like digital PCR completely replace traditional G-banding karyotyping?
A: No, dPCR should be viewed as complementary to rather than a replacement for karyotype analysis [1]. While dPCR is faster and can detect small-scale genetic changes like point mutations and copy number variations in known targets, it cannot detect unknown abnormalities or identify large-scale structural abnormalities such as translocations [1]. The most common aberrations found in genetically unstable cells include aneuploidy and large-scale structural rearrangements that require visualization through G-banding [1]. A balanced approach incorporating orthogonal techniques provides the most holistic view of genetic stability [1].
Q: What are the key considerations when choosing between different karyotyping methods?
A: Selection depends on multiple factors including the type of genetic abnormalities you need to detect, required resolution, research stage, and regulatory compliance needs [1] [26]. G-banding provides a comprehensive visual overview of the entire chromosome complement but has limited resolution (5-10 Mb) [1]. Array-based methods offer better resolution (1-2 Mb) but cannot detect balanced abnormalities [26]. Digital PCR provides excellent resolution for specific hotspots but lacks whole-genome coverage [26]. Next-generation sequencing offers high resolution but can be cost-prohibitive [26]. Consider your specific needs for abnormality detection, resolution requirements, and budget constraints when selecting methods.
FAQ 2: Technical and Interpretation Challenges
Q: What are the most common genomic abnormalities we should specifically monitor for in human pluripotent stem cells?
A: hPSCs show recurrent genomic abnormalities that require vigilant monitoring. The 20q11.21 amplification is particularly common, detected in more than 20% of worldwide cultured hPSCs and representing 22.9% of recurrent structural variants [26]. Cells with this gain have a selective advantage and can completely overtake a culture within a few passages [26]. Other common abnormalities include trisomy of chromosomes 12, 17, 8, and X [1] [26]. These abnormalities often fall below the size detection limit of conventional G-banding, necessitating complementary methods like ddPCR or array-based detection for comprehensive monitoring [26].
Q: How does the choice of reprogramming method affect genomic instability in derived iPSCs?
A: Reprogramming method significantly impacts genomic instability. Recent research demonstrates that iPS cells generated using the Sendai virus (SV) method exhibit higher frequencies of copy number alterations and single-nucleotide variations compared with those generated with episomal vectors (Epi) [23]. Specifically, all SV-iPS cell lines exhibited CNAs during the reprogramming phase, while only 40% of Epi-iPS cells showed such alterations [23]. Additionally, SNVs were observed exclusively in SV-derived cells during passaging and differentiation [23]. Gene expression analysis also revealed upregulation of chromosomal instability-related genes in late-passage SV-iPSCs [23].
Q: What constitutes adequate sample size and reporting standards for karyotyping experiments?
A: For G-banded karyotyping, analysis of a minimum of 20 metaphase cells is standard practice to detect mosaicism levels above 10% [1]. However, for critical applications or when investigating potential low-level mosaicism, examining additional cells may be necessary. The analysis should include both the total number of chromosomes and structural examination of each chromosome. Reporting should specify the number of cells analyzed, resolution achieved (band level), detailed description of any abnormalities using standard International System for Human Cytogenomic Nomenclature, and any limitations of the analysis [1].
Quantitative Data Comparison of Karyotyping Methods
Table 1: Comparison of Key Karyotyping Method Characteristics
| Method | Resolution | Turnaround Time | Key Advantages | Key Limitations |
|---|---|---|---|---|
| G-banding | 5-10 Mb [1] [26] | 3-4 weeks [26] | Detects balanced and unbalanced abnormalities; provides visual chromosome overview; gold standard accepted by regulatory bodies [1] | Requires live, proliferating cells; labor-intensive; limited resolution [1] |
| Array-based Karyotyping | 1-2 Mb [26] | 3-4 weeks [26] | Whole-genome coverage; higher resolution than G-banding; does not require cell culture [26] | Cannot detect balanced abnormalities; cannot identify ring chromosomes [26] |
| Digital Droplet PCR | Single gene level [26] | 1 week [26] | High sensitivity for targeted hotspots; quantitative; fast turnaround [26] | Limited to known targets; no whole-genome coverage [1] [26] |
| Next-Generation Sequencing | 1 bp [26] | 6-8 weeks [26] | Highest resolution; can detect point mutations and small indels [26] | Cost-prohibitive; may miss large structural changes; complex data analysis [26] |
Table 2: Common hPSC Genomic Abnormalities and Detection Capabilities
| Genomic Abnormality | Frequency in hPSCs | G-banding Detection | Array Detection | ddPCR Detection |
|---|---|---|---|---|
| 20q11.21 amplification | >20% [26] | Limited (often below detection) [26] | Yes (with >1Mb resolution) [26] | Excellent (targeted) [26] |
| Trisomy 12 | Common [1] | Excellent [1] | Excellent [26] | Only if targeted [26] |
| Trisomy 8 | Common [1] | Excellent [1] | Excellent [26] | Only if targeted [26] |
| Balanced translocations | Variable [1] | Excellent [1] | Cannot detect [26] | Cannot detect [1] |
| Small CNVs (<5Mb) | Variable [26] | Limited [1] | Good [26] | Excellent if targeted [26] |
Experimental Workflows and Methodologies
G-banding Karyotyping Protocol
Principle: G-banded karyotype analyses are prepared from mitotic cells arrested in metaphase when chromosomes are most condensed and visible. The Giemsa staining technique specifically binds to phosphate groups of DNA, attaching to regions with high adenine-thymine bonding to create dark bands, while less condensed chromatin (rich with guanine and cytosine) appears as light bands [1].
Detailed Methodology:
- Cell Culture and Harvest: Use actively dividing cells treated with mitotic arresting agents like colchicine, colcemid, or demecolcine to arrest cells in metaphase [1]
- Hypotonic Treatment: Apply hypotonic solutions to increase cell volume, swelling cells and allowing chromosomes to spread apart [1]
- Fixation: Use methanol-acetic acid solution to fix cells [1]
- Slide Preparation: Drop cell suspension onto slides for chromosome spreading [1]
- Staining: Stain with Leishman's Stain which binds to DNA, highlighting regions rich in A-T pairs [1]
- Analysis: Under microscope, Leishman-banded chromosomes display unique "bar code" of light and dark bands for each chromosome. Cytogeneticists arrange these images into a karyogram to identify microscopic genetic abnormalities (>5-10Mb) [1]
Digital Droplet PCR Karyotyping Protocol
Principle: Digital droplet PCR uses massive sample partitioning to absolutely quantify nucleic acids, with probes designed to hotspot regions in DNA known to be problematic where genomic abnormalities commonly occur [26].
Detailed Methodology:
- Sample Preparation: Combine DNA from sample cells with primers, probes, and ddPCR supermix [26]
- Droplet Generation: Load samples onto droplet generating machine creating ~20,000 monodispersed PCR-ready droplets [26]
- PCR Amplification: Transfer droplets to 96-well plate for PCR amplification in compatible thermal cycler [26]
- Droplet Reading: Analyze droplets in droplet reader using two-color detection system for multiplexed analysis [26]
- Data Analysis: Positive droplets containing at least one copy of target exhibit increased fluorescence. The fraction of positive droplets is fitted to Poisson distribution to determine absolute initial copy number of target DNA [26]
Workflow Diagrams
Multi-Method QC Pipeline Diagram
Multi-Method QC Pipeline for Stem Cell Genetic Monitoring
Karyotyping Method Selection Algorithm
Karyotyping Method Selection Decision Tree
Research Reagent Solutions
Table 3: Essential Reagents and Materials for Stem Cell Karyotyping
| Reagent/Material | Function/Purpose | Examples/Specifications |
|---|---|---|
| Mitotic Arrest Agents | Arrest cells in metaphase for chromosome analysis [1] | Colchicine, colcemid, demecolcine (typically 0.01-0.1 µg/mL) [1] |
| Hypotonic Solutions | Swell cells and separate chromosomes for spreading [1] | Potassium chloride (0.075M) for 15-30 minutes at 37°C [1] |
| Fixatives | Preserve chromosome morphology and prepare for staining [1] | Fresh 3:1 methanol:acetic acid solution [1] |
| DNA Stains | Create banding patterns for chromosome identification [1] | Giemsa stain, Leishman's Stain (highlight A-T rich regions) [1] |
| Cell Culture Media | Maintain stem cell pluripotency and genetic stability [23] | mTeSR1 for iPSCs; fibroblast medium for feeder cells [23] |
| Reprogramming Vectors | Generate integration-free iPSCs with minimal genomic instability [23] | Sendai virus vectors; episomal plasmid vectors [23] |
| qPCR/dPCR Reagents | Detect specific chromosomal abnormalities in known hotspots [26] | iCS-digital PSC 24 probes kit; TaqMan probe-based assays [26] |
| Array Hybridization Kits | Detect copy number variations across whole genome [26] | KaryoStat, KaryoStatS+ arrays [26] |
Chromosomal instability is a well-documented challenge in stem cell research. Human pluripotent stem cells (hPSCs) in culture are susceptible to acquiring genetic abnormalities that can compromise experimental results and therapeutic applications [59]. These culture-acquired genetic changes can alter growth rates, differentiation potential, and cellular functionality, ultimately affecting the reproducibility and reliability of research data [59]. This guide provides a structured framework for interpreting karyotyping results and implementing appropriate actions when abnormalities are detected in your stem cell cultures.
Understanding Karyotype Analysis and Its Limitations
Karyotype analysis is a fundamental cytogenetic tool for evaluating chromosomal stability and structural integrity in stem cells [60]. The standard G-banding technique provides a comprehensive visual overview of the entire chromosome complement, enabling detection of genetic abnormalities at a single-cell level [1]. However, it's crucial to understand that traditional karyotyping has a resolution limit of approximately 5-10 Mb, meaning smaller genetic alterations may go undetected [26] [3].
Table 1: Detection Capabilities of Karyotyping Methods
| Method | Resolution | Detectable Abnormalities | Key Limitations |
|---|---|---|---|
| G-banding | 5-10 Mb | Aneuploidies, translocations, inversions, large duplications/deletions [1] | Requires live, proliferating cells; cannot detect point mutations or small CNVs [1] |
| SNP Array | 350 kb - 1 Mb | Copy number variations (CNVs), copy-neutral loss of heterozygosity (CN-LOH) [61] | Cannot detect balanced translocations; limited ability to identify sub-clonal populations [61] |
| ddPCR | Target-specific | Known hotspot mutations (e.g., 20q11.21, TP53 variants) [26] | Targeted approach only; no whole-genome coverage [26] |
| Next-Generation Sequencing | 1 bp | Point mutations, small insertions/deletions, CNVs [26] | Cost-prohibitive for routine use; may miss large structural changes [26] |
Common Karyotypic Abnormalities in Stem Cell Cultures
Research over the past two decades has revealed a consistent pattern of recurrent genetic changes in hPSCs. The most common abnormalities include:
- Gains of chromosomes 12, 17, X, or 1 [61]
- Amplification of 20q11.21 - occurring in more than 20% of cultured hPSCs worldwide [26]
- Single nucleotide variants in TP53 [59]
These variants typically confer selective growth advantages, allowing abnormal cells to rapidly overtake a culture—sometimes within 5-10 passages [59] [61]. Cells with the 20q11.21 amplification, for instance, can completely dominate a culture within a few passages [26].
Action Framework for Specific Abnormalities
Major Aneuploidies (Trisomy 12, 17, X, etc.)
Interpretation: These abnormalities represent significant genomic alterations that dramatically affect cell behavior and differentiation capacity.
Recommended Actions:
- Immediate cessation of experimental use for critical applications
- Bank replacement with earlier passage vials confirmed to be normal
- Documentation of the passage number and culture conditions when the abnormality emerged
- Investigation of culture conditions that may have contributed to genomic stress
Subkaryotypic Abnormalities (e.g., 20q11.21 Amplification)
Interpretation: This common amplification falls below the detection limit of conventional G-banding but can be identified using higher-resolution methods like SNP arrays or ddPCR [26]. It provides cells with a selective growth advantage and reduces differentiation capacity.
Recommended Actions:
- Confirm with orthogonal method (e.g., ddPCR if initially detected by array)
- Evaluate experimental impact based on your research goals
- Consider controlled use for non-therapeutic, basic research with appropriate caveats in publications
- Implement more frequent monitoring for lines maintained despite abnormalities
Low-Level Mosaicism (<10% Abnormal Cells)
Interpretation: G-banding karyotyping typically cannot detect mosaicism below 10% [1]. Higher-resolution methods may identify lower-level abnormal populations.
Recommended Actions:
- Increase monitoring frequency to approximately every 5 passages
- Optimize culture conditions to reduce selective pressures
- Perform single-cell cloning to isolate genetically normal subpopulations
- Consider pre-emptive banking of early-passage stocks
Systematic Response Protocol
Decision Framework for Responding to Karyotypic Abnormalities
Preventive Monitoring Schedule
Implementing a proactive monitoring schedule is essential for early detection of genetic abnormalities. The International Society for Stem Cell Research (ISSCR) provides specific recommendations for timing genetic assessment [62] [59]:
Table 2: Recommended Monitoring Schedule for Stem Cell Cultures
| Timing | Assessment Type | Rationale |
|---|---|---|
| Master/Working Cell Bank Creation | Comprehensive genomic characterization [59] | Establish baseline genetic status before large-scale use |
| Every 10 Passages | Routine monitoring (G-banding or higher-resolution method) [1] | Detect culture-acquired changes before they dominate the population |
| After Major Manipulations (reprogramming, gene editing, cloning) | Targeted genetic assessment [59] | Identify stress-induced abnormalities |
| Pre-Experimental Use | Application-appropriate validation | Ensure genetic integrity at experiment start point [1] |
| At Protocol Completion | Final genetic status confirmation [1] | Document line integrity for publication |
Research Reagent Solutions Toolkit
Table 3: Essential Reagents for Karyotype Analysis and Monitoring
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| Mitotic Arrest Reagents | Colcemid (demecolcine), Nocodazole, Colchicine [60] | Arrests cells in metaphase for chromosome analysis |
| Hypotonic Solutions | 0.075 M KCl, Sodium citrate [60] | Swells cells to spread chromosomes apart for clearer visualization |
| Fixatives | Methanol:Acetic Acid (3:1) [60] | Preserves chromosomal structure for analysis |
| Staining Reagents | Giemsa stain (G-banding), Q-banding, C-banding alternatives [60] | Creates banding patterns for chromosome identification |
| DNA Analysis Kits | SNP arrays (Illumina), ddPCR kits (Stem Genomics iCS-digital PSC) [61] [26] | Enables high-resolution detection of subkaryotypic abnormalities |
| Cell Handling Reagents | Trypsin-EDTA, PBS, complete culture medium [60] | Maintains cell viability and preparation for analysis |
Frequently Asked Questions (FAQs)
How often should I perform karyotyping on my stem cell cultures? Best practice is to perform karyotyping at early passages, before major manipulations such as gene editing, and at routine intervals during long-term culture (e.g., every 10 passages) [60]. The ISSCR recommends monitoring for genetic changes at multiple timepoints: before experiments, during experiments (approximately every 10 passages), after major culture bottlenecks, and whenever alterations in growth characteristics are observed [59].
Can karyotype analysis detect all types of genetic abnormalities? No. Karyotyping is excellent for detecting large chromosomal changes such as aneuploidy, translocations, or deletions above ~5-10 Mb [60]. Smaller genetic alterations, including point mutations, microdeletions, or the common 20q11.21 amplification often require complementary methods such as SNP arrays, FISH, ddPCR, or next-generation sequencing for comprehensive genomic assessment [26] [60].
What are the most common abnormalities observed in stem cells during long-term culture? Recurrent abnormalities include trisomy 12, trisomy 8, trisomy 17, isochromosome 17q, and amplification of 20q11.21 in human pluripotent stem cells [61] [60]. These changes can influence proliferation and differentiation, with the 20q11.21 amplification occurring in more than 20% of cultured hPSCs worldwide [26].
My G-banding results appear normal, but my cells show altered growth characteristics. What should I do? If no karyotypic abnormalities are apparent but cells show altered properties, assess the cells for presence of recurrent copy number variants not readily detected by karyotype analysis (e.g., 20q11.21 for hPSCs) and point mutations (e.g., in TP53 for hPSCs) [59]. Consider using higher-resolution methods such as SNP array or targeted ddPCR.
Are newer methods like ddPCR a substitute for traditional karyotype analysis? No. While ddPCR is faster and can detect small-scale genetic changes in known targets, it cannot detect unknown abnormalities or identify large-scale structural abnormalities such as translocations [1]. The two most common aberration types in genetically unstable cells—aneuploidy and large-scale structural rearrangements—require karyotyping for detection. ddPCR should be viewed as complementary to, not a replacement for, karyotype analysis [1].
Effective management of karyotypic abnormalities in stem cell cultures requires both rigorous monitoring protocols and informed decision-making when issues arise. By implementing the guidelines outlined in this document—including regular assessment schedules, appropriate response protocols based on abnormality type and research context, and complementary use of detection technologies—researchers can maintain the genetic integrity of their cell lines and ensure the reliability of their research outcomes. Consistent documentation and sharing of genetic findings further strengthens the collective knowledge base and promotes reproducibility across the stem cell research community.
Benchmarking Karyotyping Methods: A Critical Analysis of Sensitivity, Resolution, and Regulatory Fit
For researchers and drug development professionals working with stem cells, monitoring genetic instability is not just a best practice—it is a critical necessity for ensuring experimental reproducibility and clinical safety. Chromosomal abnormalities arise frequently in human pluripotent stem cell (hPSC) cultures, with studies indicating that up to 30-35% of cultures analyzed by G-banding harbor a genetic abnormality [28]. These culture-acquired changes can confer selective growth advantages to variant cells, potentially altering cell phenotypes and compromising the validity of research data and the safety of clinical applications [1] [28].
This technical guide provides a comparative analysis of the resolution and detection capabilities of various karyotyping platforms. It is structured to help you select the appropriate genetic monitoring strategy for your stem cell research, troubleshoot common experimental issues, and understand the technical specifications of each method within the broader context of maintaining genomic integrity in stem cell banks.
## Platform Comparison: Resolution and Detection Capabilities
### Technical Specifications of Karyotyping Methods
The following table summarizes the key performance metrics of the primary karyotyping platforms used in stem cell research.
Table 1: Comparative Analysis of Karyotyping Platforms
| Karyotyping Assay | Theoretical Resolution | Effective Detection Limit (Abnormality Size) | Mosaicism Detection Sensitivity | Key Abnormalities Detected |
|---|---|---|---|---|
| G-banded Karyotyping | ~400-550 bands [28] | 5-10 Mb [1] [26] [36] | >10-20% [28] [36] | Aneuploidies, balanced/unbalanced translocations, large inversions, duplications/deletions >5-10 Mb [1] [36] |
| Array-Based Karyotyping (aCGH/SNP) | Varies by probe density (e.g., 1-2 Mb for KaryoStat) [26] | ~1 Mb (can be lower with high-density designs) [63] | Varies; generally higher than G-banding | Unbalanced abnormalities only (deletions, duplications, aneuploidy); cannot detect balanced translocations or inversions [26] |
| FISH (Targeted) | Single gene/locus [28] | As low as 0.55 Mb (e.g., 20q11.21 amplification) [28] | ~5-10% (by analyzing 200+ interphase cells) [28] | Specific, known abnormalities (e.g., gains/losses at 20q11.21, aneuploidy for specific chromosomes) |
| Digital PCR (ddPCR) | Single exon [26] | Target-specific; excels at small, known CNVs [26] | Highly sensitive for low-level mosaicism of targeted areas [26] | Copy number variations (CNVs) at pre-defined genomic hotspots (e.g., 24 common hPSC abnormality regions) [26] |
| Next-Generation Sequencing (NGS) | 1 base pair (theoretical) [26] | ~40-50 bp (in practice, for small CNVs) [63] | Varies with sequencing depth | Can detect a wide range of unbalanced abnormalities; bioinformatic challenge for balanced rearrangements [26] |
### Interpreting the Data: Strengths and Limitations in Practice
- G-banding offers a genome-wide, unbiased view of chromosomal structure but can miss submicroscopic changes. A common and problematic amplification in hPSCs at 20q11.21 (ranging from 0.55 to 4.6 Mb) often falls below its detection threshold [26] [28].
- Array-based methods provide superior resolution for detecting copy number changes but are blind to balanced structural rearrangements that do not alter gene dosage, such as reciprocal translocations or inversions [26].
- Targeted methods (FISH, ddPCR) deliver high sensitivity for specific, known abnormalities and are excellent for routine monitoring of common culture-acquired defects. However, they offer no information about the rest of the genome [26] [28].
- NGS holds the promise of ultimate resolution but can be cost-prohibitive and computationally intensive. Its ability to detect large balanced structural changes can also be limited without specialized bioinformatics [26] [63].
## Frequently Asked Questions (FAQs) & Troubleshooting
### Platform Selection and Interpretation
Q1: My G-banded karyotype result is normal, but my hPSCs are exhibiting unusually rapid proliferation. What could be wrong?
A normal G-banded result rules out large-scale chromosomal abnormalities (>5-10 Mb). However, the observed phenotypic change could be driven by a smaller, culture-acquired abnormality. The most likely culprit is the 20q11.21 amplification, which is found in over 20% of hPSC cultures and confers a selective growth advantage but is often too small to be detected by G-banding [26] [28].
- Recommended Action: Follow up with a higher-resolution assay targeted at this specific region, such as the 20q11.21 (BCL2L1) FISH test or a ddPCR kit designed for hPSC genomic hotspots [26] [28].
Q2: When should I use FISH instead of, or in addition to, G-banded karyotyping?
FISH is a complementary technique best used in these scenarios:
- Targeted Screening: To check for a specific, common abnormality known to be undetectable by karyotyping (e.g., 20q11.21 amplification) [28].
- Confirming a Suspected Abnormality: To validate a potential rearrangement suspected from a karyotype [1].
- High-Sensitivity Mosaicism Detection: When you need to rule out a low-level abnormal subpopulation. FISH can reliably detect mosaicism at levels of 5-10%, whereas karyotyping typically requires the abnormal clone to represent 10-20% of the culture [28].
Q3: What is the most common cause of a failed karyotyping experiment ("no growth")?
The success of traditional karyotyping is highly dependent on pre-analytical sample quality. The most common causes of failure are:
- Low Sample Cellularity: A nucleated cell count of ≤7x10³/µL is significantly associated with unsuccessful karyotyping [64].
- Sample Type: Peripheral blood (PB) samples have a much higher rate of failure (41.9% for high-cellularity PB) compared to bone marrow (BM) samples (3.9% for high-cellularity BM) in hematological malignancies. This principle translates to stem cell culture; the sample must contain enough healthy, actively dividing cells [64].
- Poor Cell Health or Suboptimal Culture Conditions: The cells must be alive and actively proliferating at the time of sample collection to yield metaphase chromosomes for analysis [1].
### Experimental Protocol and Best Practices
Q4: What is the recommended frequency for karyotyping my hPSC cultures?
The International Society for Stem Cell Research (ISSCR) recommends genetic monitoring at key stages [28]:
- Upon acquisition or derivation of a new cell line.
- Before establishing a master or working cell bank.
- Before starting critical experiments.
- Approximately every 10 passages during ongoing culture.
- After major culture bottlenecks (e.g., cloning, genetic modification).
- At the conclusion of experiments or if significant changes in cell behavior are observed.
Q5: How can I optimize my cell culture to improve karyotyping success?
The process of chromosome preparation is sensitive and requires optimized conditions. The workflow below outlines the key steps for a successful harvest, with critical parameters highlighted.
Karyotyping Harvest Workflow & Key Parameters
## The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Kits for Karyotyping workflows
| Item / Assay | Function / Application | Example Use-Case in Stem Cell Research |
|---|---|---|
| Mitotic Arrest Agents (Colcemid) | Arrests cells in metaphase, allowing for the accumulation of condensed chromosomes for analysis [1]. | Standard step in the preparation of G-banded karyotypes from hPSC cultures. |
| Giemsa Stain | DNA-specific dye that binds preferentially to AT-rich regions, creating the characteristic light-and-dark G-banding pattern for chromosome identification [1] [26]. | The standard stain used for G-banded karyotype analysis. |
| 20q11.21 FISH Probe Kit | Fluorescently labeled probes targeting the BCL2L1 gene locus (20q11.21) and a control region to detect amplifications via fluorescence in situ hybridization (FISH) [28]. | High-resolution, targeted screening for the most common culture-acquired abnormality in hPSCs. |
| hPSC Genetic Analysis ddPCR Kit | A multiplexed digital droplet PCR assay targeting common genomic hotspots for abnormality in hPSCs (e.g., 24 regions) [26]. | Fast, sensitive, and quantitative monitoring of known CNV hotspots without the need for whole-genome analysis. |
| Array-Based Karyotyping Kit (e.g., KaryoStat) | A microarray containing thousands of oligonucleotide probes used for genome-wide copy number variation (CNV) analysis [26] [63]. | A comprehensive, higher-resolution alternative to G-banding for detecting unbalanced genomic abnormalities. |
| Whole Genome Amplification (WGA) Kit | Amplifies nanograms of genomic DNA to micrograms, required for array-based and NGS-based karyotyping methods [65] [26]. | Preparing sufficient DNA from a limited cell sample for high-resolution molecular karyotyping. |
No single karyotyping platform is perfect. A strategic, multi-layered approach is often the most effective way to ensure the genomic integrity of stem cell cultures.
- Establish a Baseline with G-banding: Use this comprehensive, gold-standard method for initial characterization of new lines and at banking points to rule out large structural and numerical abnormalities [1] [28].
- Monitor High-Risk Passages with Targeted Assays: Integrate FISH for 20q11.21 or a multiplexed ddPCR assay into your routine quality control schedule (e.g., every 10 passages) to catch the most common, small abnormalities that confer a selective advantage [26] [28].
- Resolve Ambiguities with Higher Resolution: If phenotypic changes suggest a genetic problem but G-banding is normal, employ array-based karyotyping or NGS to uncover smaller copy number variations across the genome [66] [63].
- Prioritize Sample Quality: Regardless of the method chosen, the success of any karyotyping experiment hinges on starting with healthy, actively dividing cells processed in a timely manner [64].
By understanding the resolution, limitations, and appropriate application of each platform, researchers can build a robust genetic monitoring strategy that safeguards their research and accelerates the safe development of stem cell-based therapies.
In stem cell research and regenerative medicine, ensuring genomic stability of cell lines is paramount. Karyotype analysis serves as a crucial quality control check, as chromosomal abnormalities can arise during cell reprogramming, differentiation, and prolonged passaging. These aberrations may compromise experimental results, lead to erroneous conclusions, and pose significant safety risks for clinical applications. While G-banding karyotyping has been the traditional cytogenetic workhorse for decades, its resolution limitations can miss clinically significant aberrations that are readily detected by modern molecular cytogenetic techniques like the KaryoStat HD Assay and droplet digital PCR (ddPCR). This case study demonstrates a streamlined, high-resolution workflow that combines these advanced technologies to safeguard the genetic integrity of stem cell lines, providing researchers with the sensitivity needed to detect subtle yet critical chromosomal changes invisible to conventional G-banding.
Technical Limitations of Standard G-Banding Analysis
G-banding karyotype analysis, while widely used, has inherent technical limitations that can impact its effectiveness in detecting chromosomal aberrations in stem cell cultures.
- Resolution Limit: The primary constraint of G-banding is its resolution. Even with optimal chromosome morphology, this technique can only reliably detect aberrations larger than 5–10 Mb [24]. This means smaller deletions, duplications, or copy number variations (CNVs) go undetected.
- Metaphase Requirement: G-banding analysis is exclusively performed on metaphase chromosomes, which requires cells to be actively dividing and arrested in metaphase [24]. This presents a significant drawback, as it only reflects the chromosomal status of the small fraction of cells that are in metaphase at the time of harvesting—which can represent as few as 0.01% of the total cell population [67]. Consequently, the analysis may miss aberrations present in the majority of interphase cells.
- Subjectivity and Expertise: Scoring G-banded samples is a manual process that requires significant expertise. The accurate identification of chromosomal bands and the detection of subtle rearrangements are highly dependent on the skill and experience of the cytogeneticist, introducing an element of subjectivity [24].
- Inability to Detect Cryptic Aberrations: Certain types of chromosomal rearrangements, such as cryptic translocations or inversions, are notoriously difficult to detect with G-banding because they do not alter the overall banding pattern significantly. Studies have shown that in diseases like acute lymphoblastic leukemia (ALL), G-banding with normal karyotype (CN-ALL) can miss a substantial number of aberrations. One study found cryptic alterations in 34% of CN-ALL cases using higher-resolution FISH techniques [68].
The following table summarizes the key capabilities and limitations of G-banding:
Table: Capabilities and Limitations of G-Banding Karyotype Analysis
| Aspect | Capability/Limitation |
|---|---|
| Resolution | >5–10 Mb [24] |
| Cell Requirement | Requires metaphase cells; cannot analyze interphase nuclei [24] |
| Detectable Aberrations | Numerical abnormalities, large structural rearrangements (translocations, inversions, insertions, deletions) [24] |
| Undetectable Aberrations | Submicroscopic aberrations (<5–10 Mb), cryptic translocations, low-level mosaicism [24] [68] |
| Expertise Required | High; requires trained cytogeneticists [24] |
To overcome the limitations of G-banding, several molecular cytogenetic techniques have been developed. The table below compares G-banding with the KaryoStat HD Assay and ddPCR.
Table: Comparison of Karyotyping Techniques
| Technique | Resolution | Key Advantages | Key Limitations | Best Use Case |
|---|---|---|---|---|
| G-Banding | >5–10 Mb [24] | Inexpensive; provides genome-wide view of metaphase structure; detects balanced rearrangements. | Low resolution; requires cell culture and metaphase spreads; highly subjective. | Initial screening for large aneuploidies and gross structural rearrangements. |
| KaryoStat HD Assay | 25–50 kb [69] [70] | High sensitivity (>99%); detects CNVs, AOH, and contamination; standardized analysis. | Cannot detect truly balanced translocations; requires specific scanner (GeneChip 3000). | Comprehensive, genome-wide quality control for pluripotent stem cell banks. |
| ddPCR | Single copy variation | Absolute quantification; high sensitivity for low-frequency mutations; no standard curves needed. | Targeted analysis (requires prior knowledge of sequence); limited genome-wide scope. | Validating and monitoring specific, known oncogenic mutations or CNVs. |
The KaryoStat HD Assay Workflow
The KaryoStat HD Assay is a microarray-based solution designed for high-resolution detection of chromosomal abnormalities. The protocol is completed in approximately 2.5 to 3 days [69] [70]. The workflow is as follows:
The assay utilizes over 2.6 million markers across the genome, providing coverage for all OMIM and RefSeq genes. Its key analytical outputs include:
- Copy Number (CN) Analysis: Reliably detects gains and losses as small as 25–50 kb [69] [70].
- Absence of Heterozygosity (AOH): Identifies regions of AOH with a resolution of >1 Mb, which can suggest uniparental disomy or consanguinity [70].
- Genotyping (Sample ID): The included single-nucleotide polymorphisms (SNPs) allow for sample identity tracking and detection of cross-contamination [69].
The Role of Droplet Digital PCR (ddPCR)
While the KaryoStat HD Assay provides a comprehensive genome-wide snapshot, droplet digital PCR (ddPCR) offers a highly sensitive and precise method for targeted validation and longitudinal monitoring. In an integrated workflow, ddPCR is used to:
- Validate Specific Findings: Confirm subtle copy number variations or specific point mutations identified by the KaryoStat HD Assay.
- Monitor Low-Level Mosaicism: Track the frequency of a specific aberration over multiple cell passages with extreme precision, as ddPCR can quantify rare variants down to <0.1% allele frequency.
- Routine Quality Control: Once a known, recurrent aberration is identified in a cell line (e.g., a specific TP53 mutation), ddPCR can be used as a cost-effective, rapid test to screen for that specific variant in future batches.
Integrated Experimental Protocol for Stem Cell Genomic Monitoring
This protocol outlines a comprehensive strategy for detecting chromosomal aberrations in pluripotent stem cell (PSC) lines by integrating KaryoStat HD and ddPCR assays.
Stage 1: Cell Culture and Sample Preparation
- Cell Line: Human induced PSCs (iPSCs).
- Culture Conditions: Maintain iPSCs in mTeSR1 medium on Matrigel-coated plates. Culture cells to ~80% confluency.
- Sample Collection:
- For KaryoStat HD Assay: Harvest cells and extract high-quality genomic DNA using the DNeasy Blood & Tissue Kit. Assess DNA purity and quantity (A260/A280 ~1.8).
- For ddPCR: Harvest a separate aliquot of cells for RNA/DNA extraction depending on the target (e.g., DNA for copy number analysis, RNA for gene expression fusions).
- For KaryoStat HD Assay: Harvest cells and extract high-quality genomic DNA using the DNeasy Blood & Tissue Kit. Assess DNA purity and quantity (A260/A280 ~1.8).
Stage 2: Genome-Wide Screening with KaryoStat HD Assay
- Follow the manufacturer's instructions included in the KaryoStat HD Assay Plus kit (Catalog Number 905405) [69].
- Restriction Digestion and Ligation: Digest 250 ng of gDNA and ligate adaptors.
- PCR Amplification: Amplify the ligated DNA using a provided primer.
- Fragmentation and Labeling: Fragment the PCR product and label with biotin.
- Hybridization: Mix the labeled target and hybridize to the KaryoStat HD array for 16 hours at 50°C.
- Washing and Staining: Use the GeneChip Fluidics Station for automated washing and staining.
- Scanning: Scan the array using the GeneChip Scanner 3000.
- Data Analysis:
- Analyze the scanned data with the Chromosomal Analysis Suite (ChAS) software.
- Identify regions of copy number gain/loss and absence of heterozygosity (AOH) against a human reference genome.
- Flag any aberration >25 kb for further investigation.
Stage 3: Targeted Validation and Monitoring with ddPCR
- Assay Design: Design primer/probe sets for regions identified by KaryoStat HD (e.g., a specific gene deletion) or for common aberrations in stem cells (e.g., TP53 mutations).
- Reaction Setup:
- Prepare the ddPCR reaction mix containing sample DNA, primers, probe, and ddPCR Supermix.
- Generate droplets using a QX200 Droplet Generator.
- PCR Amplification:
- Transfer the droplets to a 96-well plate.
- Perform PCR amplification on a thermal cycler using optimized cycling conditions.
- Droplet Reading and Analysis:
- Read the plate on a QX200 Droplet Reader.
- Analyze the data using QuantaSoft software.
- Determine the target concentration (copies/μL) and calculate copy number variation or mutant allele frequency based on Poisson statistics.
Troubleshooting Guide and FAQs
Q1: Our KaryoStat HD data shows a small, novel copy number variant (CNV). How can we confirm it is real and not an artifact?
- A1: This is a perfect use case for ddPCR. Design primer/probe sets that flank the predicted breakpoint of the CNV and a reference assay for a stable region elsewhere in the genome. Use ddPCR to perform a CNV assay on the original DNA sample. The absolute quantification and high precision of ddPCR will independently confirm the presence and the exact copy number of the variant.
Q2: We have a stem cell line that appears normal by G-banding but shows aberrant differentiation. What is the best approach?
- A2: Proceed directly to the KaryoStat HD Assay. Its high resolution can uncover submicroscopic aberrations in key differentiation genes that G-banding misses. One study found that G-banding failed to detect ~34% of abnormalities later found with molecular cytogenetics [68]. The AOH feature of KaryoStat HD can also reveal regions of potential uniparental disomy that could silence imprinted genes critical for development.
Q3: How can we monitor for low-level oncogenic mutations that might arise during extended passaging?
- A3: Implement a ddPCR-based monitoring program. For known recurrent mutations (e.g., in TP53), design mutation-specific ddPCR assays. This method is exceptionally sensitive for detecting rare mutant molecules in a background of wild-type DNA, allowing you to track the emergence and expansion of a mutant clone long before it becomes the dominant population.
Q4: What is the best way to store and handle reagents for the KaryoStat HD Assay?
- A4: Proper storage is critical for assay performance [69] [71].
- Store at 2–8°C: Arrays, Module 2 (Pre-Lab TE Buffer and Water), Module 4 (Main Lab Stain, Holding Buffer, Beads, Water).
- Store at -5 to -30°C: Module 1 (Pre-Lab Restriction, Ligation, Amplification), Module 3 (Main Lab Fragmentation, Labeling, Hybridization).
- Store at room temperature: Module 5 (Main Lab Elution Buffer), Purification Wash Buffer, Wash Buffers A and B.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Essential Reagents and Kits for Advanced Karyotype Analysis
| Product/Assay | Function | Key Features |
|---|---|---|
| KaryoStat HD Assay Plus (Thermo Fisher) | High-resolution, genome-wide detection of CNVs and AOH [69] [70]. | >2.6 million markers; detects 25–50 kb aberrations; includes arrays, reagents, and analysis software. |
| QX200 Droplet Digital PCR System (Bio-Rad) | Absolute quantification of nucleic acids for targeted validation and monitoring. | High sensitivity for rare variants; no standard curve required; ideal for CNV and mutation detection. |
| Chromosomal Analysis Suite (ChAS) | Software for analyzing data from KaryoStat arrays [70]. | User-friendly interface; automated aberration calling; no need for advanced cytogenetics expertise. |
| GeneChip Scanner 3000 | Mandatory scanner for reading KaryoStat arrays [69] [70]. | 7G scanner for high-intensity imaging of GeneChip probe arrays. |
| STEMdiff Mesenchymal Progenitor Kit | Used for differentiating iPSCs into mesenchymal stromal cells in research settings [16]. | Defined, serum-free system for standardized differentiation. |
Relying solely on G-banding for karyotypic assessment of stem cells presents a significant risk due to its low resolution. An integrated approach, using the KaryoStat HD Assay for comprehensive, genome-wide screening followed by ddPCR for sensitive, targeted validation and monitoring, provides a powerful solution. This robust workflow enables researchers to identify cryptic aberrations, validate findings with confidence, and proactively monitor genomic integrity, thereby ensuring the safety and reliability of stem cells for advanced research and therapeutic development.
Frequently Asked Questions
Q1: What is the lowest level of mosaicism that traditional karyotyping (G-banding) can reliably detect? Traditional karyotyping has a detection limit of approximately 5-10% for mosaic abnormalities. Sensitivity depends heavily on the number of metaphase cells analyzed. To exclude mosaicism with 95% confidence, specific sampling is required [72]:
- 30 metaphases → excludes 10% mosaicism
- 50 metaphases → excludes 6% mosaicism Analyzing over 500 metaphases would be necessary to confidently exclude mosaicism at a level below 1%, which is typically impractical for routine laboratory practice [72].
Q2: How does the sensitivity of ddPCR compare to FISH and qPCR for detecting mosaic variants? Droplet Digital PCR (ddPCR) is generally the most sensitive targeted technique, capable of detecting very low levels of mosaicism (below 1%) by absolutely quantifying DNA copy number without relying on a standard curve [73] [74]. Fluorescence In Situ Hybridization (FISH) and quantitative PCR (qPCR) are less sensitive than ddPCR for low-level mosaicism. These methods can miss abnormal cells when they constitute less than 5-10% of the total cell population [72].
Q3: My karyotyping results were normal, but I still suspect genetic variation in my stem cell culture. Why might this be? A normal karyotype does not guarantee a genetically pure culture. Commonly employed methods like karyotyping, FISH, and qPCR can miss variants present in up to 10% of cells [72]. Furthermore, karyotyping has a resolution limit of 5-10 Mb, meaning small but clinically significant copy-number variants (e.g., the common 20q11.21 amplification in hPSCs) can be undetectable [72] [26].
Q4: When should I use NGS instead of a targeted method like ddPCR? The choice depends on your goal:
- Use Next-Generation Sequencing (NGS) when you need whole-genome coverage to discover unknown or novel abnormalities. NGS is more sensitive than karyotyping or array-based methods and can detect mosaicism at lower variant allele frequencies than Sanger sequencing [74] [26].
- Use ddPCR when you are monitoring specific, known hotspots of genetic variation (e.g., common trisomies or the 20q11.21 amplicon). It offers the highest sensitivity and precise quantification for targeted applications [26].
Q5: What is a major pitfall in selecting a sample for mosaic variant detection? The choice of tissue is critical. Mosaicism can be tissue-restricted. Analyzing DNA from blood or saliva may yield a false negative if the mosaic variant is only present in another affected tissue (e.g., bone, skin, or brain) [74]. Always select the affected tissue for analysis whenever possible.
Troubleshooting Guides
Issue 1: Low Sensitivity in Detecting Low-Frequency Mosaic Events
- Problem: Abnormal cells are present in the culture but are not being detected by the current method.
- Solution:
- Switch to a more sensitive method: For targeted detection, adopt ddPCR. For genome-wide discovery, use NGS with high sequencing depth [73] [74].
- Increase sampling: If sticking with karyotyping, increase the number of metaphases scored. Be aware that scoring over 500 cells to detect <1% mosaicism is often not feasible for routine work [72].
- Validate across techniques: Confirm findings from one method (e.g., a potential low-level finding from NGS) with an orthogonal, highly sensitive method like ddPCR [26].
Issue 2: Inconsistent Results Between Different Genetic Stability Assays
- Problem: Karyotyping reports a normal result, but a qPCR or ddPCR assay indicates a copy-number variant.
- Solution:
- Understand resolution limits: This is a common occurrence. Karyotyping cannot detect changes smaller than 5-10 Mb. The commonly amplified 20q11.21 region in hPSCs is often below this detection limit but is readily picked up by PCR-based methods [72] [26].
- Trust the higher-resolution method: In such conflicts, the result from the higher-resolution technique (ddPCR, NGS) is more likely to be correct for the specific target analyzed.
- Contextualize the finding: Determine if the identified genetic change is a known, culture-adapted variant (e.g., gains of chromosomes 1, 12, 17, or 20) that confers a selective growth advantage [72].
Comparison of Technical Methods
The table below summarizes the key characteristics of different mosaicism detection techniques.
Table 1: Comparison of Methods for Detecting Mosaicism in Stem Cell Cultures
| Method | Best-Case Detection Limit for Mosaicism | Effective Resolution | Genome Coverage | Key Advantage | Key Disadvantage |
|---|---|---|---|---|---|
| Karyotyping (G-banding) | 5-10% [72] | 5-10 Mb [72] [26] | Whole Genome | Visualizes entire chromosome structure | Low resolution and throughput; labor-intensive |
| FISH | 5-10% [72] | Single probes (~1-500 kb) | Targeted | Visualizes abnormalities in single cells | Requires prior knowledge of target; low multiplexing |
| qPCR | ~10% [72] | Single assays | Targeted | Rapid and cost-effective for known targets | Relies on standard curves; less sensitive than ddPCR |
| Array-based Karyotyping | >1 Mb [26] | 1-2 Mb [26] | Whole Genome | High-throughput for CNVs | Cannot detect balanced rearrangements |
| ddPCR | <1% (as low as 0.1-0.01% in optimized assays) [73] [74] | Single assays | Targeted | Highest sensitivity & absolute quantification | Limited to known targets |
| Next-Generation Sequencing (NGS) | 1-5% (Varies with depth) [74] | Single Base Pair [26] | Whole Genome | Discovers novel variants genome-wide | Higher cost and complex data analysis |
Experimental Protocols
Protocol 1: Digital Droplet PCR (ddPCR) for Mosaic CNV Detection
This protocol is adapted for detecting common copy number variations (e.g., 20q11.21 amplification) in human pluripotent stem cells (hPSCs) [26].
Sample Preparation:
- Extract genomic DNA from your hPSC sample using a standard kit (e.g., QIAamp DNA Mini Kit).
- Dilute the DNA to a working concentration (e.g., 50-100 ng/µL).
- Prepare a 20 µL reaction mix containing:
- 1X ddPCR Supermix (for probes)
- 900 nM of each forward and reverse primer
- 250 nM of each FAM and HEX-labeled probe
- ~50 ng of sample DNA
- Include a wild-type control and a no-template control (NTC).
Droplet Generation:
- Load the reaction mix into a droplet generator.
- This device partitions the sample into approximately 20,000 nanodroplets.
PCR Amplification:
- Transfer the droplets to a 96-well plate.
- Seal the plate and run a standard TaqMan PCR protocol on a thermal cycler.
- Example cycling conditions: 95°C for 10 min (enzyme activation), then 40 cycles of 94°C for 30 sec (denaturation) and 60°C for 1 min (annealing/extension).
Droplet Reading and Analysis:
- Place the plate into a droplet reader.
- The reader measures the fluorescence (FAM and HEX) in each droplet.
- Use the manufacturer's software (e.g., QuantaSoft) to analyze the data.
- Positive droplets (containing the target) will show high fluorescence. Negative droplets (lacking the target) will show low background fluorescence.
- The software uses Poisson statistics to calculate the absolute concentration of the target DNA in copies/µL.
Protocol 2: qPCR Assay for Common hPSC Aneuploidies
This provides a rapid, accessible method for routine screening [72].
Primer and Probe Design:
- Design TaqMan primers and probes to target commonly amplified regions in hPSCs (e.g., on chromosomes 1, 12, 17, 20).
- Include a reference assay for a stable locus on a non-target chromosome (e.g., chromosome 7).
qPCR Setup and Run:
- Prepare reactions with your DNA sample, primers/probes, and a master mix (e.g., TaqMan Genotyping Master Mix).
- Run the qPCR on a real-time cycler using standard conditions.
Data Analysis:
- Use the ΔΔCq method to calculate relative copy number.
- A lower Cq value for the target compared to the reference in a test sample versus a control sample indicates a potential copy number gain.
Decision Workflow for Method Selection
The following diagram outlines a logical process for selecting the most appropriate detection method based on your experimental goals.
Method Selection Workflow
Research Reagent Solutions
Essential materials and kits for implementing the discussed techniques.
Table 2: Key Research Reagents for Mosaicism Detection
| Reagent / Kit | Function | Example Use Case |
|---|---|---|
| iCS-digital PSC 24 probe kit (Stem Genomics) | ddPCR kit with 24 pre-designed probes | Targeted screening for the most common CNV hotspots in hPSCs [26]. |
| KaryoStat+/KaryoStatS+ Assay (Thermo Fisher) | Array-based karyotyping | Genome-wide detection of copy number variations with >1 Mb resolution [26]. |
| QIAamp DNA Mini Kit (QIAGEN) | Genomic DNA extraction | High-quality DNA preparation from various cell and tissue samples [73]. |
| TaqMan Genotyping Master Mix (Thermo Fisher) | qPCR reaction mix | Robust amplification for copy number analysis via qPCR. |
| ddPCR Supermix for Probes (Bio-Rad) | ddPCR reaction mix | Stable emulsion formation and precise quantification in droplet digital PCR [26]. |
In stem cell research and therapy development, ensuring genomic integrity is paramount. The potential for genomic instability in stem cells, including the emergence of copy number alterations (CNAs) and single-nucleotide variations (SNVs), poses a significant risk for tumorigenesis and represents a major challenge for clinical translation [75] [16]. Orthogonal validation, the practice of confirming results using multiple, methodologically independent techniques, is a critical strategy to ensure the accuracy and reliability of genetic data. This technical support guide explores the powerful synergy of combining three key technologies—karyotyping, next-generation sequencing (NGS), and droplet digital PCR (ddPCR)—for comprehensive genomic monitoring in stem cell research.
Frequently Asked Questions (FAQs) & Troubleshooting
1. Why is a single genetic analysis method insufficient for characterizing stem cell lines?
No single technology provides a complete picture of a stem cell's genomic landscape. Each has inherent limitations in resolution, scope, and sensitivity. Relying on one method alone risks missing critical anomalies, which is unacceptable for therapeutic applications where patient safety is the priority.
- Karyotyping offers a genome-wide, cytogenetic view but at a low resolution (typically detecting alterations >5-10 Mb) [16].
- NGS can identify point mutations and small indels across the exome or genome, and specific panels can detect some CNAs, but it may miss low-frequency variants due to limited sequencing depth and can be confounded by sequencing artifacts [76] [77].
- ddPCR provides ultra-sensitive, absolute quantification of specific, known mutations but is not a discovery tool, as it requires prior knowledge of the target sequence [78].
2. We observed a normal karyotype but are concerned about specific oncogenic mutations. What is the recommended validation path?
A normal karyotype is reassuring for the absence of large-scale chromosomal aberrations but does not rule out point mutations or very small insertions/deletions. In this scenario, the following orthogonal workflow is recommended:
- Step 1: Broad Screening with NGS. Use a targeted NGS panel covering known oncogenes and tumor suppressor genes (e.g., TP53) relevant to your cell type to screen for potential mutations [16] [79].
- Step 2: Confirmatory Quantification with ddPCR. For any putative mutations identified by NGS, especially those at low variant allele frequencies (VAF < 5%), design a specific ddPCR assay. ddPCR excels at confirming and precisely quantifying low-level variants due to its high sensitivity and resistance to PCR artifacts [78] [77].
- Troubleshooting Tip: If the NGS-reported VAF is very low (<1%) and ddPCR does not confirm the variant, it may have been a sequencing error. Techniques like Blocker Displacement Amplification (BDA) coupled with Sanger sequencing can also be used for orthogonal confirmation of very low-frequency NGS calls [77].
3. Our NGS data suggests a potential copy number variation (CNV) in a key genomic region. How can we validate this finding?
NGS-based CNA calling can sometimes generate false positives due to coverage biases. Orthogonal confirmation is essential.
- Primary Orthogonal Method: Karyotyping or FISH. If the suspected CNV is large (several megabases), traditional karyotyping can be used for confirmation. For smaller CNVs, fluorescence in situ hybridization (FISH) with locus-specific probes provides a highly specific cytogenetic validation [16].
- Alternative/Complementary Method: ddPCR. For CNVs affecting a specific gene of interest, ddPCR can be an excellent quantitative tool. By comparing the copy number of the target gene to a reference gene (known two copies) in a duplex reaction, ddPCR can independently confirm and quantify the CNV with high precision [78].
4. During quality control of a new induced pluripotent stem cell (iPSc) line, what is the optimal orthogonal validation strategy?
The generation of iPS cells is prone to introducing genomic alterations. A comprehensive, multi-layered approach is advised [16]:
- Initial Screening: Perform karyotyping to rule out gross chromosomal abnormalities and NGS (whole exome or genome) to identify point mutations and small indels.
- Focus on Critical Regions: Pay special attention to mutations in genes associated with genomic stability (e.g., TP53) and oncogenes, which are commonly acquired during reprogramming [16].
- Quantitative Confirmation: Use ddPCR to validate any identified, potentially damaging mutations in cancer-related genes to establish their precise VAF, which is crucial for assessing clonality and risk.
The table below summarizes the core strengths and limitations of each technique for clear comparison.
Table 1: Comparison of Genomic Analysis Techniques for Stem Cell Monitoring
| Technology | Optimal Use Case | Key Strengths | Inherent Limitations |
|---|---|---|---|
| Karyotyping | Detecting large-scale aneuploidies, translocations, and deletions/duplications > 5-10 Mb. | Genome-wide view, detects balanced rearrangements, established gold standard for cytogenetics. | Low resolution, requires metaphase cells, labor-intensive. |
| NGS | Unbiased discovery of SNVs, small indels, and CNAs across many genes or the entire genome. | High resolution, highly multiplexed, provides sequence-level detail. | Can miss low-VAF variants (<1-5%), data analysis complexity, potential for false positives. |
| ddPCR | Ultra-sensitive quantification and validation of known, specific mutations or CNVs. | Absolute quantification without standards, high precision, excellent for detecting rare variants (<0.1% VAF). | Not a discovery tool, low multiplexing capability, requires pre-defined targets. |
Essential Experimental Protocols
Protocol 1: Orthogonal Validation of a PutativeTP53Mutation Identified by NGS
Background: NGS analysis of an iPS cell line at passage 15 identified a missense variant in the TP53 gene with a VAF of 8%. This protocol outlines steps for orthogonal confirmation using ddPCR.
Materials:
- DNA Sample: High-quality genomic DNA from the iPS cell line in question.
- ddPCR Supermix: For probe-based digital PCR (e.g., Bio-Rad ddPCR Supermix for Probes).
- Assays: A custom TaqMan assay designed for the specific TP53 mutation and a reference assay for a wild-type sequence or a different reference gene.
- Droplet Generator & Reader: A compatible ddPCR system (e.g., Bio-Rad QX200) [78].
Method:
- Reaction Setup: Prepare a 20 µL reaction mix containing ddPCR Supermix, the target and reference assays, and ~20 ng of genomic DNA.
- Droplet Generation: Transfer the reaction mix to a droplet generator cartridge. Following the manufacturer's instructions, generate approximately 20,000 nanoliter-sized droplets.
- PCR Amplification: Carefully transfer the emulsified droplets to a 96-well PCR plate. Seal the plate and run a standard thermal cycling protocol optimized for the assays.
- Droplet Reading: After PCR, place the plate in a droplet reader. The reader will flow droplets one-by-one and measure the fluorescence in two channels (e.g., FAM and HEX).
- Data Analysis: Use the associated software to analyze the data. The software will cluster droplets as mutant-positive, wild-type-positive, double-positive, or negative. It will then apply Poisson statistics to calculate the absolute concentration (copies/µL) and VAF of the mutant allele in the original sample [78].
Interpretation: A VAF confirmed by ddPCR close to the NGS-reported VAF (e.g., 8%) validates the presence of the mutation. A VAF of ~50% suggests a heterozygous mutation in all cells, while a lower VAF may indicate a subclonal population.
Protocol 2: Monitoring Genomic Instability Across iPS Cell Generation and Differentiation
Background: This protocol, adapted from a systematic investigation, outlines how to track genomic alterations from fibroblast reprogramming through to differentiated mesenchymal stromal/stem cells (iMS cells) using a combination of techniques [16].
Materials:
- Cell Samples: Source fibroblasts, multiple clones of derived iPS cells (at early and late passages), and the resulting iMS cells (at multiple passages).
- Genomic DNA from all cell samples.
- Platforms: Karyotyping equipment, NGS platform (e.g., for whole exome sequencing), and ddPCR system.
Method:
- Longitudinal Sampling: Collect samples at key phases: parental fibroblasts, iPS cell clones post-reprogramming, iPS cells at late passage (e.g., >P20), iMS cells after differentiation, and iMS cells at late passage.
- Cytogenetic Analysis (Karyotyping): Perform G-band karyotyping on metaphase cells from iPS and iMS cell samples to monitor for gross chromosomal changes [16].
- Deep Sequencing (NGS): Subject genomic DNA from all sample timepoints to whole exome or genome sequencing to identify SNVs and CNAs that arise during the process. Note: Sendai virus (SV) reprogramming methods may show a higher frequency of CNAs and SNVs compared to episomal vector (Epi) methods [16].
- Targeted Validation (ddPCR): For any mutations identified in key genes (e.g., TP53), use ddPCR as described in Protocol 1 to confirm the finding and track the VAF of the mutation across different passages and stages of differentiation.
Interpretation: This multi-phase approach allows you to pinpoint when specific genomic alterations occurred (e.g., during reprogramming, differentiation, or extended culture) and monitor their clonal dynamics.
Research Reagent Solutions
The table below lists key reagents and materials essential for implementing these orthogonal validation protocols.
Table 2: Essential Research Reagents for Orthogonal Genomic Validation
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| TaqMan ddPCR Assays | For target-specific amplification and fluorescent detection in digital PCR. | Custom-designed assays from Bio-Rad or Integrated DNA Technologies (IDT) for known mutations. |
| ddPCR Supermix | Optimized reaction mix for droplet-based digital PCR. | Bio-Rad ddPCR Supermix for Probes. |
| NGS Library Prep Kits | For preparing sequencing libraries from genomic DNA. | Kits such as Illumina's TruSeq DNA PCR-Free or hybrid-capture panels for targeted sequencing. |
| Cell Culture Reagents | For maintaining and expanding stem cell lines for analysis. | Defined media like mTeSR1 for iPS cells, MesenCult-ACF for MSC differentiation [16]. |
| Chromosomal Microarray Kit | For high-resolution detection of CNAs and loss of heterozygosity (LOH). | An alternative to NGS for CNA detection, offering high sensitivity. |
| gBlocks Gene Fragments | Synthetic double-stranded DNA used as positive controls for ddPCR assay validation. | Ordered from IDT; contains the exact mutant sequence to validate custom ddPCR assays [77]. |
Workflow Visualization
The following diagram illustrates the decision-making process and synergistic relationship between karyotyping, NGS, and ddPCR in a comprehensive stem cell monitoring strategy.
Frequently Asked Questions (FAQs)
FAQ 1: What are the key differences in CMC (Chemistry, Manufacturing, and Controls) requirements between an IND and a BLA for a cell therapy product?
For an IND application, the primary goal is to ensure safety for initial human trials. The CMC information should be sufficient to demonstrate that the product is adequately characterized and controlled for phase-appropriate clinical testing [80] [81]. The focus is on the description of the manufacturing process, raw material controls, and preliminary data on identity, purity, potency, and safety.
In contrast, a BLA requires a comprehensive data package to demonstrate that the product is safe, pure, and potent for widespread marketing [82] [81]. This includes complete, validated manufacturing and control processes, extensive stability data, and evidence that the product is consistently produced to predefined quality specifications under full Good Manufacturing Practice (GMP) compliance.
FAQ 2: Why is karyotype monitoring critical for stem cell-based therapies, and what are the most common chromosomal aberrations we should track?
Human pluripotent stem cells (hPSCs) are prone to genomic instability during reprogramming, gene editing, and in vitro cultivation [19]. A genetically abnormal clone can overtake a culture in less than five passages [19]. These aberrations can impact differentiation potential, the functionality of derived cells, and the safety of cell replacement therapies [19].
Recurrent culture-acquired aberrations are well-documented. The table below summarizes the most frequent ones to monitor.
Table 1: Recurrent Karyotypic Abnormalities in hPSCs
| Abnormality Type | Specific Chromosomal Regions/Chromosomes | Reported Frequency |
|---|---|---|
| Recurrent Gains | Chromosomes 20, 1q, 12, 17, 8, X [18] [19] | Gains of chromosome 20 and 1q are among the most common [18]. |
| Recurrent Losses | Chromosomes 10, 18, 22 [18] [19] | Frequently observed in large-scale studies [18]. |
FAQ 3: Our potency assay results are inconsistent between runs. What could be causing this, and how can we improve robustness for our BLA?
Inconsistent potency assays are often due to variables in the bioassay system itself. Key parameters to control and document include [83]:
- Cell Passage Number and Viability: Using cells outside a validated passage range or with low viability.
- Reference Standard (RS) Handling: Improper storage, reconstitution, or use of an unqualified RS.
- Critical Reagents: Variability in media, serum, or other key components between lots.
- Assay Protocol: Inconsistent timing, temperature, or cell seeding density.
To improve robustness for a BLA, you must advance from a "fit-for-purpose" to a fully validated assay [83]. This involves:
- Formal Qualification/Validation: Systematically evaluating accuracy, precision (repeatability and intermediate precision), linearity, range, and specificity [83].
- Creating a Master Cell Bank: Producing a large, characterized cell bank under GMP guidance to ensure a consistent, long-term supply of assay cells [83].
- Detailed SOPs and Documentation: Implementing a comprehensive Standard Operating Procedure and workbook to ensure any qualified operator can execute the method reliably [83].
FAQ 4: We are preparing for a pre-BLA meeting with the FDA. What are the most common CMC deficiencies that lead to complete response letters (CRLs)?
An analysis of FDA CRLs from 2020–2024 found that 74% of rejections cited quality or manufacturing issues [84]. Common CMC deficiencies include [84]:
- Analytical Gaps: Lack of adequate assay validation, particularly for potency, or tech transfer inadequacies.
- Insufficient Process Control: Failure to demonstrate a robust, reproducible, and well-controlled manufacturing process at commercial scale.
- Facility Issues: Concerns about the manufacturing facility or process raised during pre-approval inspections.
- Incomplete Comparability Data: Inadequate data to support that the product remains unchanged after a manufacturing process change.
Troubleshooting Guides
Issue 1: Detection of a Mosaic or Sub-Clonal Chromosomal Abnormality
Problem: Your routine G-banding or SNP array analysis detects an abnormal cell population alongside normal cells, making it difficult to decide on the next steps.
Solution:
- Confirm with a Complementary Method: Use a second, independent technique to verify the finding. G-banding is excellent for detecting mosaics in individual metaphases, while SNP arrays provide high-resolution data on the entire population [19].
- Quantify the Abnormality: If using G-banding, score a larger number of metaphases (e.g., 50-100) to determine the exact percentage of abnormal cells [19].
- Assess the Aberration:
- If it's a known recurrent, selective aberration (e.g., 20q11.21 gain), the clone has a growth advantage. It is highly recommended to discard the culture and go back to a low-passage, fully characterized master bank [19].
- If the abnormality is non-recurrent and at a low level, you may attempt to "cure" the culture by single-cell cloning and pick karyotypically normal clones. However, this requires extensive re-characterization.
- Document Everything: Record the passage number, method of detection, and percentage of abnormal cells. This is critical for regulatory filings and investigating the root cause.
Issue 2: Failure in Assay Validation for Potency
Problem: Your potency assay fails validation parameters, such as poor precision (high %CV) or a lack of parallelism between the reference standard and test sample curves.
Solution: Table 2: Troubleshooting Bioassay Validation Failures
| Validation Failure | Potential Root Cause | Corrective Action |
|---|---|---|
| High %CV (Poor Precision) | Unstable critical reagents; inconsistent cell culture health or passage number; variable manual pipetting. | Create large, single-use aliquots of reagents; strictly control cell culture conditions and passage window; automate liquid handling where possible [83]. |
| Lack of Parallelism | The reference standard and test sample have different biological mechanisms of action; the assay format is not suitable. | Re-evaluate the fundamental biology of the product and the assay design. A non-parallel curve may indicate the assay is not measuring the intended activity [83]. |
| Failed Specificity | Matrix components or excipients in the drug product interfere with the assay signal. | Modify the sample dilution or buffer; include a relevant blank or control to subtract background interference [83]. |
| Poor Robustness | The assay is highly sensitive to small, uncontrolled changes in parameters (e.g., incubation time, temperature). | Perform a Design of Experiment (DoE) study to identify critical parameters and establish acceptable operating ranges for them [83]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Karyotype Monitoring and Quality Control
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| Colcemid | Arrests cells in metaphase, the stage of cell division where chromosomes are condensed and visible for karyotyping [19]. |
| SNP Microarray Kit | High-resolution platform for genome-wide detection of copy number variations (CNVs) and loss of heterozygosity (LOH) that are too small for G-banding to detect [18] [19]. |
| GMP-Grade Master Cell Bank | A large, well-characterized stock of cells used as a starting point for bioassays. Ensures consistency and reproducibility of assay results over many years and across development phases [83]. |
| Reference Standard (RS) | A qualified sample of the drug product or a representative material with a defined potency. Serves as the benchmark for comparing the activity of test samples in potency assays [83]. |
| Quality DNA Extraction Kit | Essential for obtaining high-molecular-weight, pure DNA for SNP array analysis. A low call rate (<95-98%) due to poor DNA quality can invalidate results [19]. |
Experimental Protocols
Protocol 1: High-Resolution Karyotype Monitoring Using SNP Array Analysis
This protocol supplements traditional G-banding by detecting sub-microscopic chromosomal changes [19].
Workflow Overview:
Detailed Methodology:
- DNA Extraction: Extract high-quality genomic DNA from hPSCs using a commercial kit (e.g., QIAamp DNA Blood Mini Kit). Ensure DNA concentration and purity (A260/280 ratio) meet the requirements of your chosen SNP array platform [19].
- Array Processing: Process the DNA on a selected SNP array platform (e.g., Illumina Global Screening Array). This involves labeling the DNA, hybridizing it to the array, washing, and scanning according to the manufacturer's instructions [19].
- Data Analysis in GenomeStudio:
- Load the scanned data into Illumina's GenomeStudio software with the cnvPartition plug-in.
- Check the call rate for each sample. A call rate >95-98% is generally considered acceptable and indicates high-quality data [19].
- Use the cnvPartition algorithm to identify regions of copy number variation (CNV). The software will assign a confidence score for each CNV call.
- Interpretation: Focus on CNVs that are large (>1-5 Mb) and have high confidence scores. Compare the findings to databases of known, recurrent hPSC aberrations (see Table 1). Small, low-confidence calls or known benign variants may be disregarded.
Protocol 2: Phase-Appropriate Bioanalytical Assay Development
This workflow outlines the stages for developing a potency assay from research use to BLA submission [83].
Workflow Overview:
Detailed Methodology:
- Stage 1: Fit-for-Purpose (for IND-enabling studies)
- Goal: Develop an assay that is biologically relevant and provides reliable results for early decision-making.
- Process: Optimize key parameters (cell concentration, drug dilution, incubation time) to achieve a reproducible dose-response curve. Demonstrate initial accuracy and reproducibility, sufficient to support early safety studies [83].
- Documentation: A detailed research report is sufficient.
Stage 2: Qualification (for Phase 2 studies)
- Goal: Establish intermediate precision, accuracy, and robustness to support dose optimization and process development.
- Process: Execute a minimum of 3-8 experiments to define preliminary acceptance criteria for specificity, accuracy, precision, and parallelism (see FAQ 3 for metrics) [83].
- Critical Step: Create a Master Cell Bank under GMP-quality oversight to ensure long-term assay consistency [83].
- Documentation: A formal qualification report is required.
Stage 3: Validation (for BLA submission)
- Goal: Demonstrate the assay is reproducible, robust, and suitable for lot release and stability testing.
- Process: Perform 6-12 experiments under full GMP/GLP compliance. Formally validate all ICH Q2(R2) parameters (specificity, accuracy, precision, etc.) [83].
- Documentation: A pre-approved validation protocol and a comprehensive validation report are mandatory. All work is conducted with detailed SOPs and subject to Quality Assurance audit [83].
Conclusion
Karyotype monitoring is not a mere formality but a critical, non-negotiable component of quality control in stem cell research and therapy development. A proactive, multi-layered strategy that combines foundational understanding of instability mechanisms with a tailored, multi-method monitoring pipeline is essential to mitigate risks. The future of safe clinical translation hinges on the adoption of more sensitive, accessible, and standardized genomic integrity assessments. As technologies like NGS and ddPCR become more integrated into routine practice, the field must converge on robust regulatory guidelines that keep pace with scientific advancement, ensuring that stem cell-based therapies are both effective and safe for patients.
References
- 1. The Barcode of Genetic Health: Karyotyping in Stem Cell ... [https://www.wicell.org/blog/the-barcode-of-genetic-health-karyotyping-in-stem-cell-cultures/]
- 2. Cancer Copy Number Variants (CNVs): A Guide for Clinical ... [https://pages.bionano.com/cancer-copy-number-variants]
- 3. High-Resolution Genomic Profiling of Chromosomal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3337514/]
- 4. Analyzing the genomic integrity of stem cells - StemBook - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK133286/]
- 5. Chromosomal Instability and Karyotype Correction in ... [https://link.springer.com/article/10.1134/S1022795419100090]
- 6. Analysis of chromosomal aberrations and recombination ... [https://www.nature.com/articles/ncomms12144]
- 7. NADH reductive stress drives metabolic reprogramming [https://www.sciencedirect.com/science/article/pii/S0962892425001576]
- 8. Endoplasmic reticulum stress: molecular mechanism and ... [https://www.nature.com/articles/s41392-023-01570-w]
- 9. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 10. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/hk/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 11. Primary Cell Culture Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/primary-cell-culture-market]
- 12. Human Primary Cell Culture Market Size & Forecast, 2025 ... [https://www.coherentmarketinsights.com/industry-reports/human-primary-cell-culture-market]
- 13. PSC Genomic Integrity and Stability | Cell Quality [https://www.stemcell.com/psc-cell-quality/genomic-integrity]
- 14. A protocol for karyotyping and genetic editing of induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11930342/]
- 15. High-throughput karyotyping of human pluripotent stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3502865/]
- 16. Tracing genomic instability in induced mesenchymal ... [https://www.nature.com/articles/s12276-025-01439-8]
- 17. The Tumorigenic Potential of Human Pluripotent Stem - PMC Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9397652/]
- 18. Chromosomal Aberrations in Induced Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387029/]
- 19. Chromosomal quality control in hPSCs: A practical guide to ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1599923/full]
- 20. (Open Access) Correlation Between Genetic Abnormalities in Induced... [https://scispace.com/papers/correlation-between-genetic-abnormalities-in-induced-mq7kxd98]
- 21. Effects of histocompatibility and host immune responses on the... [https://link.springer.com/article/10.1007/s00281-011-0266-8]
- 22. Modeling the selective growth advantage of genetically ... [https://www.sciencedirect.com/science/article/pii/S1465324924000288]
- 23. Tracing genomic instability in induced mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046023/]
- 24. G Banding - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/g-banding]
- 25. Advancements in Karyotyping & the Impact on Cell-based ... [https://www.editco.bio/blog/advancements-in-karyotyping-and-the-impact-on-cell-based-research]
- 26. What Is Karyotyping? Methods and Their Significance [https://www.synthego.com/blog/karyotyping-cell-research/]
- 27. Tips for Successful aCGH [https://www.enzo.com/note/tips-for-successful-acgh/]
- 28. Frequently Asked Questions on hPSC Characterization ... [https://www.stemcell.com/hpsc-services-faq.html]
- 29. Find out how to karyotype your hPSC cells on a budget [https://www.stemgenomics.com/blog/genomic-stability-control-arguments-to-justify-the-costs/]
- 30. Support- NGS Sequencing Troubleshooting [https://www.thermofisher.com/in/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-support/ngs-support-troubleshooting.html]
- 31. Next-generation Sequencing Glossary | NGS terminology [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/tutorials/glossary.html]
- 32. (PDF) Next - Generation Somatic and Germline Assay... Sequencing [https://www.academia.edu/122097506/Next_Generation_Sequencing_Somatic_and_Germline_Assay_Troubleshooting_Guide_Derived_From_Proficiency_Testing_Data]
- 33. From next-generation resequencing reads to a high-quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5234474/]
- 34. NGS Data Analysis Bottlenecks: Common Pitfalls & Proven ... [https://www.genomebeans.com/blog/ngs-data-analysis-bottlenecks-common-pitfalls-and-how-to-overcome-them]
- 35. Submit Your Interest for hPSC Characterization Services [https://www.stemcell.com/forms/hpsc-services-quote.html]
- 36. Try a karyotype service optimized for human stem cells [https://www.stemgenomics.com/range-of-assays/genomic-stability-karyotyping-assays/g-banding-karyotyping/]
- 37. Glossary of NGS — deepTools 2.0.1 documentation terms [https://deeptools.readthedocs.io/en/2.0.1/content/help_glossary.html]
- 38. Utility of droplet digital polymerase chain reaction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10360090/]
- 39. Ultra–sensitive droplet digital PCR for detecting a low– ... [https://www.nature.com/articles/srep22985]
- 40. Detection of mosaics in hemophilia A by deep Ion Torrent ... [https://www.sciencedirect.com/science/article/pii/S247503792202088X]
- 41. Digital PCR Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/digital-pcr-support/digital-pcr-support-troubleshooting.html]
- 42. Droplet Digital PCR is a Useful Method for Detection of Mosaic ... [https://abstracts.eurospe.org/hrp/0092/hrp0092fc3.4]
- 43. Assessment of Genetic Stability in Human Induced ... [https://www.mdpi.com/1422-0067/25/2/1101]
- 44. Analysis of complex chromosomal structural variants ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1605461/full]
- 45. Origins of chromosome instability unveiled by coupled ... [https://www.nature.com/articles/s41586-025-09632-5]
- 46. Optimization of Chromosome Preparation and Karyotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346318/]
- 47. Thriving or Withering? Plant Molecular Cytogenetics in the ... [https://www.mdpi.com/1422-0067/26/14/7013]
- 48. Temporal Analysis of Genome Alterations Induced by Single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4333508/]
- 49. Stem Cell Culture Guide [https://www.atcc.org/resources/culture-guides/stem-cell-culture-guide]
- 50. Aggregate Passaging for ES and iPS Cell Maintenance [https://www.stemcell.com/aggregate-passaging-hpsc-maintenance.html]
- 51. Protocol for Passaging Human Pluripotent Stem Cells Non ... [https://www.stemcell.com/enzyme-free-passaging-of-hpscs-using-relesr.html]
- 52. Feeder Layer Cell Actions and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4533020/]
- 53. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 54. Gains of 20q11.21 in human pluripotent stem cells - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10828824/]
- 55. Why you should care about 20q chromosomal abnormality [https://www.stemgenomics.com/blog/why-you-should-care-about-20q-chromosomal-abnormality/]
- 56. Chromosome 20q11.21 Amplifications in Colorectal Cancer [https://cgp.iiarjournals.org/content/18/3_Suppl/487]
- 57. BCL-XL Mediates the Strong Selective Advantage of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3841249/]
- 58. Gain of 20q11.21 in human pluripotent stem cells enhances ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04196-7]
- 59. Section 3: Genomic Characterization [https://www.isscr.org/basic-research-standards/genomic-characterization]
- 60. Karyotype Analysis Protocol [https://www.creative-biolabs.com/stem-cell-therapy/karyotype-analysis.htm]
- 61. Chromosomal quality control in hPSCs: A practical guide to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259632/]
- 62. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 63. Comprehensive performance comparison of high-resolution ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-017-3658-x]
- 64. Pre-analytical parameters associated with unsuccessful ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6376323/]
- 65. Comparative Analysis of Two NGS-Based Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11353422/]
- 66. HIGH-RESOLUTION GENOMIC ARRAYS FACILITATE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2613764/]
- 67. Cytogenetic heterogeneity and their serial dynamic ... [https://pubmed.ncbi.nlm.nih.gov/25974687/]
- 68. High rates of submicroscopic aberrations in karyotypically ... [https://molecularcytogenetics.biomedcentral.com/articles/10.1186/s13039-015-0153-4]
- 69. KaryoStat™ HD Assay Plus 24 assays | Request for Quote [https://www.thermofisher.com/order/catalog/product/905405]
- 70. KaryoStat Assays for Assessing Genomic Stability of PSC ... [https://www.thermofisher.com/us/en/home/life-science/stem-cell-research/induced-pluripotent-stem-cells/pluripotent-stem-cell-detection/karyostat-arrays-genomic-stability.html]
- 71. KaryoStat™ HD Assay Plus - ABI Applied Biosystems [https://www.fishersci.fi/shop/products/karyostat-hd-assay-plus/17153019]
- 72. Detecting Genetic Mosaicism in Cultures of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5106530/]
- 73. Choosing the Best Tissue and Technique to Detect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10815810/]
- 74. Mosaicism in clinical genetics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8751420/]
- 75. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 76. Comparison of the Data of a Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8756135/]
- 77. Confirming putative variants at ≤ 5% allele frequency ... [https://www.nature.com/articles/s41598-021-91142-1]
- 78. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 79. Artificial intelligence and systems biology analysis in stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476622/]
- 80. FDA IND CMC Requirements for Biologics: A 2025 ... [https://scxcmc.com/fda-ind-cmc-requirements-for-biologics/]
- 81. How to prepare early for regulatory submissions from IND ... [https://www.biolifesolutions.com/resource-center/insights-blog/how-to-prepare-early-for-regulatory-submissions-from-ind-to-bla/]
- 82. The Biologics License Application (BLA) Process Explained [https://www.thefdagroup.com/blog/2014/07/test-the-biologics-license-application-bla-process/]
- 83. Selecting Bioanalytical Assays for FDA Approved Clinical ... [https://www.marinbio.com/company/selecting-bioanalytical-assays-fda-clinical-trials-commercialization/]
- 84. Why Strong Technical + Regulatory Alignment Matters [https://synergbiopharma.com/why-strong-technical-regulatory-alignment-matters/]