Mesenchymal Stem Cells in Regenerative Medicine: From Basic Science to Clinical Translation
This article provides a comprehensive exploration of mesenchymal stem cells (MSCs) for researchers and drug development professionals.
Mesenchymal Stem Cells in Regenerative Medicine: From Basic Science to Clinical Translation
Abstract
This article provides a comprehensive exploration of mesenchymal stem cells (MSCs) for researchers and drug development professionals. It covers the foundational biology of MSCs, including their defining characteristics, sources, and therapeutic mechanisms such as immunomodulation and paracrine signaling. The review details methodological approaches for isolation and characterization, current clinical applications across various diseases, and the significant challenges in the field, including efficacy optimization and manufacturing heterogeneity. It further examines advanced strategies like genetic engineering and cell-free therapies to overcome these hurdles, culminating in an analysis of the clinical trial landscape, regulatory approvals, and evidence-based validation of MSC-based therapies.
The Biology of Mesenchymal Stem Cells: Defining a Therapeutic Powerhouse
Historical Discoveries and Key Milestones in MSC Research
The field of mesenchymal stem cell (MSC) research represents one of the most dynamic and transformative areas in regenerative medicine. From their initial identification as simple fibroblast-like cells to their current status as therapeutic agents with complex immunomodulatory capabilities, MSCs have undergone a remarkable evolution in scientific understanding. This whitepaper traces the critical discoveries and methodological advances that have shaped MSC research, providing scientists and drug development professionals with a comprehensive historical framework. The journey of MSC science reflects broader trends in cell biology, where initial focus on differentiation potential has progressively shifted toward paracrine-mediated mechanisms and clinical translation. Understanding this historical context is essential for appreciating current challenges and future directions in MSC-based therapeutics, particularly as the field moves toward more standardized and efficacious clinical applications [1] [2].
The Pioneering Era: Initial Discovery and Characterization
The foundational period of MSC research established the basic biological properties of these cells and set the stage for all subsequent investigations.
Early Discoveries (1960s-1970s)
The conceptual origins of MSCs date to the 1960s when Soviet scientist A. J. Friedenstein and his team conducted groundbreaking research demonstrating that bone marrow transplantation could yield osteoblast differentiation in vivo. Their experiments identified progenitor cells for both osteoblasts and hematopoietic cells, establishing the existence of a stromal component with regenerative potential within bone marrow. By 1974, Friedenstein and colleagues had successfully isolated a fibroblast-like cell from bone marrow via adherent culture that exhibited colony-forming units (CFU-F) capable of differentiating into osteoblasts and facilitating the formation of hematopoietic clones. This work established the fundamental principle that bone marrow contained not only hematopoietic elements but also stromal precursors with generative capacity—a revolutionary concept at the time [1].
A critical methodological insight from this period was the development of plastic adherence as a separation technique, which remains a defining characteristic of MSCs to this day. In 1987, Dr. Charbord provided further clarification by demonstrating that bone marrow stromal cells cultured in horse serum displayed notable differences in their uptake of serum proteins compared to bone marrow fibroblasts, establishing that MSCs represent a distinct cellular entity despite morphological similarities to fibroblasts in vitro [1].
Establishing Multipotency (1980s-1990s)
The 1980s witnessed crucial advances in understanding the differentiation potential of MSCs. Research in 1987 established that bone marrow stromal cells maintained differentiation potential even after 20–30 passages, retaining the ability to generate bone tissue after implantation in animal models. The pivotal recognition of MSC multipotency came in 1992 when J.N. Beresford and colleagues established that MSCs could differentiate into both adipocytes and osteoblasts, with differentiation pathways influenced by specific culture conditions and biochemical inducers [1].
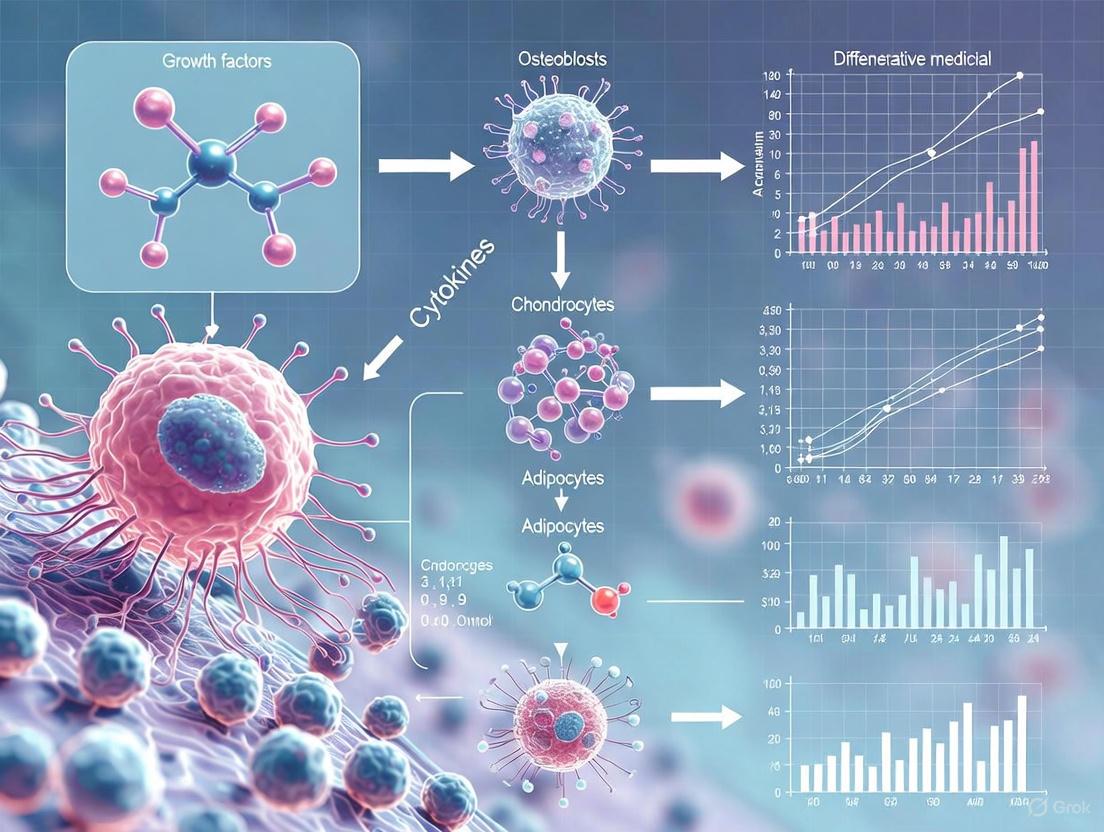
The formal naming of "mesenchymal stem cells" was proposed in 1991 by Dr. Arnold Caplan, who recognized their mesodermal origin and generative potential. This nomenclature systematized the field and provided a conceptual framework for subsequent research. The full demonstration of trilineage differentiation potential—the capacity to differentiate into osteoblasts, chondrocytes, and adipocytes—was definitively established in a landmark 1999 publication in Science, cementing the fundamental identity of MSCs and anticipating their significant contributions to regenerative medicine [1].
Table 1: Key Early Discoveries in MSC Research (1960s-1990s)
| Year | Discovery | Key Researchers | Significance |
|---|---|---|---|
| 1960s | Osteogenic potential of bone marrow transplants | Friedenstein et al. | First evidence of non-hematopoietic progenitor cells in bone marrow |
| 1974 | Isolation of plastic-adherent CFU-F | Friedenstein et al. | Established fundamental isolation method and colony-forming capability |
| 1987 | Distinction between MSCs and fibroblasts | Charbord | Clarified MSC as distinct cellular entity |
| 1991 | Proposal of "mesenchymal stem cell" term | Caplan | Standardized nomenclature and conceptual framework |
| 1992 | Confirmed adipogenic and osteogenic potential | Beresford et al. | Established dual differentiation pathways |
| 1999 | Demonstration of trilineage differentiation | Pittenger et al. | Defined fundamental multipotency of MSCs |
Methodological Advances: Isolation, Characterization and Standardization
The progression of MSC research has been inextricably linked to the development of increasingly sophisticated methodological approaches for isolation, characterization, and culture.
Initial MSC isolation relied exclusively on bone marrow aspiration, but methodological advances have dramatically expanded both sources and techniques. The classic isolation method developed by Friedenstein—plastic adherence in standard culture conditions—remains a cornerstone approach. However, this has been supplemented with specialized techniques for specific tissue sources, including enzymatic digestion (e.g., collagenase for adipose tissue) and mechanical fragmentation (explant methods) [3].
The discovery that MSCs could be isolated from diverse tissue sources represented a critical expansion of the field. In 1991, researchers successfully cultured MSCs from Wharton's jelly portion of the human umbilical cord via a tissue block culture technique. In 2000, a laboratory at the University of Chile isolated mononuclear cells from umbilical cord blood through adherent culture to obtain MSCs. Subsequently, MSCs have been isolated from numerous tissues including adipose tissue, amniotic membrane, gingiva, thymus, placenta, synovium, fetal blood, fetal liver, and fetal lungs [1].
Comparative studies have revealed significant functional differences between MSCs from various sources. For instance, dental pulp-derived MSCs (DPSCs) demonstrate consistently smaller cell size, Nestin positivity, and higher proliferation rates compared to adipose-derived MSCs (ADSCs), while also showing a diminished capacity for adipogenic differentiation. Similarly, ADSCs obtained through different extraction methods (enzymatic digestion versus mechanical fragmentation) exhibit variations in secretome profiles, highlighting how isolation methodology can influence biological properties [3].
Characterization and Standardization
The development of standardized characterization criteria has been essential for advancing MSC research and clinical translation. In 2006, the International Society for Cellular Therapy (ISCT) established minimal criteria for defining human MSCs, creating a unified framework for the field. These criteria include: (1) adherence to plastic under standard culture conditions; (2) specific surface marker expression (≥95% positive for CD105, CD73, and CD90; ≤2% positive for CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR); and (3) capacity for trilineage differentiation into osteogenic, chondrogenic, and adipogenic lineages under in vitro conditions [1] [4].
The functional significance of these surface markers reflects the biological identity of MSCs: CD105 (endoglin) is a type I membrane glycoprotein essential for cell migration and angiogenesis; CD90 (Thy-1) mediates cell-cell and cell-extracellular matrix interactions; and CD73 functions as a 5'-exonuclease that catalyzes the hydrolysis of adenosine monophosphate, playing a role in cell signaling within bone marrow. The negative markers primarily exclude hematopoietic lineages (CD45, CD34), monocyte/macrophage cells (CD14/CD11b), B cells (CD79α/CD19), and potent antigen-presenting cells (HLA-DR) [1].
Diagram Title: MSC Characterization Workflow
Table 2: Standard MSC Characterization Markers and Their Significance
| Marker | Expression | Biological Function | Significance in MSC Identity |
|---|---|---|---|
| CD105 | Positive (≥95%) | Type I membrane glycoprotein; essential for cell migration and angiogenesis | Core MSC marker; critical for regenerative function |
| CD73 | Positive (≥95%) | 5'-exonuclease; catalyzes AMP hydrolysis to adenosine | Core MSC marker; mediates purinergic signaling |
| CD90 | Positive (≥95%) | Cell adhesion molecule; mediates cell-cell and cell-ECM interactions | Core MSC marker; facilitates tissue integration |
| CD45 | Negative (≤2%) | Protein tyrosine phosphatase; marker for all leukocytes | Excludes hematopoietic lineage contamination |
| CD34 | Negative (≤2%) | Cell adhesion factor; marker for hematopoietic stem cells | Excludes hematopoietic stem/progenitor cells |
| HLA-DR | Negative (≤2%) | MHC class II cell surface receptor; antigen presentation | Confirms low immunogenicity; excludes antigen-presenting cells |
Conceptual Evolution: From Differentiation to Paracrine Mechanisms
A fundamental shift in the understanding of MSC therapeutic mechanisms has marked the maturation of the field, moving from a direct differentiation hypothesis to a more complex paracrine model.
The Trophic Shift
By the mid-2000s, research began to challenge the initial assumption that MSCs primarily functioned through direct differentiation and replacement of damaged tissues. Instead, evidence accumulated supporting the concept of "trophism" - that MSCs act as medicinal signaling cells that create a regenerative microenvironment through secreted factors. This paradigmatic shift recognized that MSC therapeutic effects are mediated largely through the release of bioactive molecules including growth factors, cytokines, chemokines, and extracellular vesicles (EVs) that modulate the local cellular environment, promote tissue repair, stimulate angiogenesis, enhance cell survival, and exert anti-inflammatory effects [1] [2].
The recognition of extracellular vesicles as key mediators of MSC effects further refined this paracrine hypothesis. MSC-derived EVs—including exosomes (30-200 nm), microvesicles (100-1000 nm), and apoptotic bodies (0.5-2 microns)—contain diverse biomolecular cargo including metabolites, proteins, nucleic acids (microRNAs, noncoding RNAs), and even organelles such as mitochondria. These EVs function as sophisticated intercellular communication vehicles, delivering therapeutic payloads to recipient cells and demonstrating bioactivity capable of reducing fibrosis, promoting tissue regeneration, and modulating inflammation [5] [2].
Immunomodulatory Capabilities
Parallel to the understanding of trophic mechanisms, research illuminated the profound immunomodulatory capacities of MSCs. MSCs interact with diverse immune cells including T cells, B cells, dendritic cells, and macrophages, modulating immune responses through both direct cell-cell contacts and release of immunoregulatory molecules. These interactions can suppress activation and maturation of innate immune cells while skewing early innate reactions toward an anti-inflammatory phenotype, making MSCs particularly attractive for treating immune-mediated conditions [1] [2].
This immunomodulatory function forms the basis for the first FDA-approved MSC product, Ryoncil (remestemcel-L), approved in December 2024 for treating steroid-refractory acute graft-versus-host disease (SR-aGVHD) in children. This approval validated decades of research into MSC immunobiology and established a regulatory precedent for future MSC-based therapies [6] [7].
Diagram Title: MSC Therapeutic Mechanisms Evolution
Clinical Translation: From Bench to Bedside
The progression of MSCs from laboratory curiosities to clinically implemented therapeutics represents a landmark achievement in regenerative medicine, though this journey has faced significant challenges.
Regulatory Milestones and Approved Therapies
The clinical translation of MSCs began with trials in the 1990s and achieved its most significant regulatory milestone with the December 2024 FDA approval of Ryoncil (remestemcel-L) for pediatric steroid-refractory acute graft-versus-host disease. This approval marked a watershed moment for the field, validating the scientific consensus regarding MSC potential and contributing to renewed activity in MSC clinical development [6] [7].
Globally, multiple MSC therapies have received regulatory approval in various jurisdictions. As of 2025, sixteen MSC therapies have been approved worldwide: ten derived from bone marrow, three from umbilical cord, two from adipose tissue, and one from umbilical cord blood. These approved therapies target conditions including acute graft-versus-host disease, acute myocardial infarction, complex anal fistulas in Crohn's disease, osteoarthritis, and amyotrophic lateral sclerosis [4].
Clinical Trial Landscape
The clinical trial landscape for MSCs has expanded dramatically, reflecting both scientific interest and therapeutic potential. As of October 2024, a query of ClinicalTrials.gov revealed 567 registered studies for "mesenchymal stromal cells" and 1,506 results for "mesenchymal stem cells," including 339 Phase 1, 280 Phase 2, 36 Phase 3, and 7 Phase 4 registered studies. However, this enthusiasm must be balanced against the reality that an overwhelming majority (94%) of registered trials did not report results, highlighting ongoing challenges in clinical translation and data dissemination [2].
The therapeutic applications of MSCs in clinical trials span a remarkable range, including autoimmune diseases (lupus, Crohn's disease, multiple sclerosis), inflammatory disorders (GVHD), neurodegenerative diseases, orthopedic injuries, cardiovascular conditions, and gynecological disorders. Recent trials have demonstrated particular promise in areas where inflammation plays a central role, leveraging the potent immunomodulatory properties of MSCs [1] [8] [4].
Table 3: Clinically Approved MSC Therapies (As of 2025)
| Product Name | Tissue Source | Approval Region | Indication | Year |
|---|---|---|---|---|
| Ryoncil | Bone marrow | United States (FDA) | Pediatric steroid-refractory acute GVHD | 2024 |
| Alofisel | Adipose tissue | European Union | Complex perianal fistulas in Crohn's disease | 2018 |
| Temcell | Bone marrow | Japan | Acute GVHD | 2015 |
| Prochymal | Bone marrow | Canada, New Zealand | Pediatric acute GVHD | 2012, 2015 |
| Cupistem | Adipose tissue | South Korea | Crohn's fistula, Anal fistula | 2012, 2021 |
| Cellgram | Bone marrow | South Korea | Acute myocardial infarction | 2011 |
| Cartistem | Umbilical cord | South Korea | Knee articular cartilage defects | 2012 |
| Neuronata-R | Bone marrow | South Korea | Amyotrophic lateral sclerosis | 2014 |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing MSC research requires specialized reagents and methodological approaches that have been refined through decades of investigation.
Standard Experimental Protocols
Trilineage Differentiation Assay: The fundamental protocol for demonstrating MSC multipotency involves inducing differentiation toward osteogenic, chondrogenic, and adipogenic lineages using specific induction media. For osteogenic differentiation, cells are cultured in DMEM supplemented with 10% FBS, 50μM ascorbic acid-2 phosphate, 10mM β-glycerophosphate, and 0.1μM dexamethasone for 21 days, with mineralization detected by Alizarin Red staining. Adipogenic differentiation uses DMEM with 10% FBS, 1μM dexamethasone, 0.5mM isobutylmethylxanthine, 10μg/ml insulin, and 200μM indomethacin for 14-21 days, with lipid accumulation visualized by Oil Red O staining. Chondrogenic differentiation typically employs pellet culture systems in serum-free DMEM with 1% ITS+ premix, 100nM dexamethasone, 50μg/ml ascorbic acid-2 phosphate, and 10ng/ml TGF-β3 for 21-28 days, with sulfated proteoglycans detected by Alcian Blue or Safranin O staining [3].
Flow Cytometric Immunophenotyping: Standardized characterization of MSC surface markers requires flow cytometric analysis using antibodies against positive markers (CD73, CD90, CD105) and negative markers (CD34, CD45, CD14/CD11b, CD79α/CD19, HLA-DR). Cells are typically harvested using non-enzymatic cell dissociation buffer to preserve surface epitopes, incubated with fluorochrome-conjugated antibodies, and analyzed on a flow cytometer. The ISCT criteria require ≥95% positivity for CD73, CD90, and CD105, and ≤2% positivity for hematopoietic markers [1] [4].
Conditioned Media Collection and Secretome Analysis: For paracrine studies, MSC-conditioned media is collected from subconfluent cultures (typically 70-80% confluence) after 24-48 hours in serum-free conditions to avoid fetal bovine serum contamination. The conditioned media is concentrated using centrifugal filters (3-10 kDa cutoff) and analyzed via ELISA/multiplex arrays for cytokines/growth factors, nanoparticle tracking analysis for extracellular vesicles, and mass spectrometry/microRNA sequencing for comprehensive molecular profiling [5] [3].
Table 4: Essential Research Reagents for MSC Investigation
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Isolation Reagents | Collagenase Type I/II, Ficoll-Paque, RBC lysis buffer, Plastic cultureware | Primary MSC isolation from tissue sources | Tissue-specific enzyme cocktails; adherence separation requires 3-7 days |
| Culture Media | αMEM/DMEM, Fetal Bovine Serum (FBS), L-glutamine, Penicillin/Streptomycin | MSC expansion and maintenance | Serum screening essential for batch consistency; antibiotic-free for therapy |
| Characterization Antibodies | Anti-CD73, CD90, CD105, CD34, CD45, HLA-DR (fluorochrome-conjugated) | Flow cytometric immunophenotyping | Use non-enzymatic detachment to preserve epitopes; include isotype controls |
| Differentiation Inducers | Dexamethasone, IBMX, Indomethacin, Ascorbic acid, TGF-β3, BMPs | Trilineage differentiation assessment | Lineage-specific induction cocktails; differentiation requires 2-4 weeks |
| Secretome Analysis Tools | ELISA kits, Multiplex arrays, Exosome isolation kits, miRNA sequencing reagents | Paracrine mechanism investigation | Serum-free conditioning; protease inhibitors for protein analysis |
Current Challenges and Future Directions
Despite substantial progress, the MSC field faces persistent challenges that must be addressed to fully realize the therapeutic potential of these remarkable cells.
Manufacturing and Standardization Hurdles
A primary challenge in MSC translation remains the inherent variability of primary cell products. MSCs exhibit considerable heterogeneity based on tissue source, donor characteristics (age, health status), isolation method, and culture conditions. This biological variability introduces significant challenges in manufacturing consistent therapeutic products. Additionally, scaling MSC production while maintaining quality presents substantial technical obstacles, as MSCs have a limited number of passages before losing potency or undergoing senescence [6] [2].
Efforts to address these challenges include advances in automation and analytical development that help standardize how MSCs are produced and evaluated. The implementation of robust release criteria and potency assays represents a critical step forward in ensuring consistency and quality. The development of master and working cell banks has allowed for more consistent yields at scale while preserving cellular potency. Additionally, optimized cryopreservation and transport protocols help extend shelf life and simplify logistics for these living therapies [6].
Emerging Frontiers
Several innovative approaches are shaping the future of MSC research and clinical application. iPSC-derived MSCs (iMSCs) offer enhanced consistency, scalability, and reduced donor variability compared to primary MSCs. While not yet FDA-approved, iMSCs are gaining momentum in regenerative medicine trials targeting conditions such as osteoarthritis and graft-versus-host disease [7].
The field is also increasingly exploring cell-free approaches utilizing MSC-derived extracellular vesicles and conditioned media. These strategies potentially offer similar therapeutic benefits with improved safety profiles, easier storage and handling, and potentially fewer regulatory hurdles. MSC-derived EVs are being investigated for applications including COVID-19-related lung injury, chronic wound healing, and neuroinflammation [5] [8].
Genetic engineering of MSCs represents another frontier, with CRISPR-edited lines being tailored for enhanced immunomodulation, targeted delivery, and improved survivability post-transplantation. These approaches may address current limitations in homing efficiency and therapeutic potency [8].
Finally, the discovery of Multilineage-differentiating stress-enduring (Muse) cells within MSC populations has opened new research directions. These endogenous, reparative cells exhibit selective migration to damaged tissues, phagocytic capability, and pluripotent-like differentiation, potentially explaining some of the therapeutic effects observed in MSC administration [5].
The historical journey of MSC research demonstrates a remarkable evolution from basic biological discovery to clinical implementation. The field has progressed from initial observations of bone marrow stromal cells to a sophisticated understanding of multipotent cells with complex immunomodulatory and trophic functions. Key milestones including the standardization of characterization criteria, recognition of paracrine mechanisms, and recent regulatory approvals have established MSCs as legitimate therapeutic agents. However, challenges in manufacturing consistency, clinical efficacy demonstration, and mechanistic understanding remain active areas of investigation. The continued evolution of MSC science—including emerging approaches with iMSCs, engineered cells, and cell-free derivatives—promises to further transform the landscape of regenerative medicine. For researchers and drug development professionals, understanding this historical context provides essential insights for navigating both current challenges and future opportunities in this dynamic field.
In regenerative medicine, the therapeutic potential of Mesenchymal Stem/Stromal Cells (MSCs) has garnered significant attention for their ability to self-renew, differentiate into multiple lineages, and modulate immune responses [1]. However, the initial lack of a universal definition for these cells led to substantial inconsistencies in research findings and clinical trial outcomes. To address this, the International Society for Cell & Gene Therapy (ISCT) established a set of minimal defining criteria for human MSCs, which have become the foundational standard for the field [1]. These criteria ensure that cells characterized as MSCs across different laboratories and clinical studies possess comparable biological properties, thereby enabling the reproducibility of scientific data and the meaningful comparison of clinical results. This standardization is crucial for the rigorous development of MSC-based therapies, facilitating their successful transition from basic science to clinical applications aimed at addressing unmet medical needs [9] [1].
The Core ISCT Defining Criteria
The ISCT standards, established to create a unified framework for the field, specify that MSCs must be defined by a combination of three fundamental criteria [1].
- Plastic Adherence: When cultured under standard conditions, MSCs must adhere to a plastic surface. This is a primary, functional characteristic used to separate MSCs from non-adherent cell populations in the initial isolate, such as hematopoietic cells.
- Specific Surface Marker Expression: MSCs must express a defined set of positive and negative surface antigens, as determined by flow cytometry. To be considered MSCs, a population must exhibit high expression (≥95% positive) of specific markers and similarly high lack of expression (≤2% positive) of others.
- Multilineage Differentiation Potential: Under standard in vitro induction conditions, MSCs must possess the capacity to differentiate into cells of the mesodermal lineage—specifically osteoblasts (bone), adipocytes (fat), and chondrocytes (cartilage). This functional property confirms their stem cell nature.
The table below summarizes these core criteria.
Table 1: Core ISCT Defining Criteria for Human MSCs
| Criterion | Requirement | Key Details |
|---|---|---|
| Plastic Adherence | Must adhere to plastic culture surfaces under standard conditions. | A primary, functional characteristic used for initial isolation. |
| Positive Surface Marker Expression (≥95%) | CD73, CD90, CD105. | CD73 functions as a 5'-exonuclease; CD90 mediates cell-cell and cell-matrix interactions; CD105 is essential for angiogenesis [1]. |
| Negative Surface Marker Expression (≤2%) | CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR. | CD34 is a marker for hematopoietic stem cells; CD45 for white blood cells; CD14/CD11b for monocytes/macrophages; CD79α/CD19 for B cells; HLA-DR is a strongly immunogenic MHC-II molecule [1]. |
| Trilineage Differentiation Potential | Must differentiate into osteoblasts, adipocytes, and chondrocytes in vitro. | Confirmation requires specific staining: Mineral deposits (e.g., Alizarin Red S) for osteogenesis, lipid vacuoles (e.g., Oil Red O) for adipogenesis, and proteoglycans (e.g., Alcian Blue) for chondrogenesis. |
Experimental Protocols for MSC Characterization
This section provides detailed methodologies for verifying the three core ISCT criteria, with a focus on the critical assays for surface marker profiling and differentiation potential.
Surface Marker Analysis by Flow Cytometry
The immunophenotype of MSCs is typically confirmed using flow cytometry. The following protocol outlines the key steps for this analysis.
Workflow for Surface Marker Analysis
Protocol:
- Cell Harvesting: Wash adherent MSC cultures with phosphate-buffered saline (PBS) and detach cells using a trypsin-EDTA solution. Neutralize the trypsin with complete culture medium.
- Cell Preparation: Wash the cell pellet with a flow cytometry staining buffer (e.g., PBS containing 1-2% fetal bovine serum). Filter the cells through a 70μm strainer to obtain a single-cell suspension and perform a cell count.
- Staining: Aliquot approximately 1x10^5 to 5x10^5 cells into separate tubes for unstained, isotype control, and experimental antibody staining. Resuspend cell pellets in staining buffer containing the fluorochrome-conjugated antibodies against the target markers (e.g., CD73, CD90, CD105, CD34, CD45, HLA-DR). Incubate for 30-60 minutes in the dark at 4°C.
- Washing and Analysis: Wash the cells twice with staining buffer to remove unbound antibody. Resuspend the final pellet in a suitable buffer for flow cytometry acquisition.
- Data Interpretation: Analyze the data using flow cytometry software. The cell population is considered positive for a marker if the fluorescence intensity is greater than 99% of the isotype control. The population must meet the ISCT thresholds [1].
Trilineage Differentiation Assays
The functional capacity of MSCs is confirmed by inducing differentiation down osteogenic, adipogenic, and chondrogenic lineages. The diagram below outlines the general workflow, and the table in Section 4 lists the key reagents.
Workflow for Trilineage Differentiation
Protocols:
- Osteogenic Differentiation: Seed MSCs at a defined density (e.g., 2x10^4 cells/cm²). Once cells reach 70% confluency, replace the growth medium with osteogenic induction medium. Culture for 2-4 weeks, refreshing the medium every 3-4 days. To confirm differentiation, fix the cells and stain with 2% Alizarin Red S (pH 4.1-4.3) to detect calcium phosphate deposits, which appear as bright red/orange nodules [10] [1].
- Adipogenic Differentiation: Seed MSCs at a high density (e.g., 2x10^4 cells/cm²). At 100% confluency, stimulate the cells with adipogenic induction medium for 2-3 days, followed by a switch to adipogenic maintenance medium for 1-2 days. Repeat this cycle for 2-3 weeks. To confirm differentiation, fix the cells and stain with Oil Red O working solution to detect intracellular lipid vacuoles, which stain red [10] [1].
- Chondrogenic Differentiation: Pellet 2.5x10^5 MSCs by centrifugation in a conical tube. Culture the pellet in chondrogenic induction medium containing TGF-β (e.g., TGF-β1 or β3) for 3-4 weeks. To confirm differentiation, fix the pellet, embed it in paraffin, section it, and stain with Alcian Blue (pH 2.5) to detect sulfated proteoglycans in the extracellular matrix, which stain blue-green [10] [1].
The Scientist's Toolkit: Essential Research Reagents
The table below details the key reagents and materials required for the characterization of MSCs according to ISCT standards.
Table 2: Essential Research Reagents for MSC Characterization
| Reagent / Material | Function and Application in MSC Research |
|---|---|
| Flow Cytometry Antibodies | Panels for positive (CD73, CD90, CD105) and negative (CD34, CD45, CD11b, CD19, HLA-DR) markers are essential for immunophenotyping and confirming ISCT identity [1]. |
| Osteogenic Induction Medium | Typically contains Dexamethasone, Ascorbic Acid, and β-Glycerophosphate to drive MSC differentiation into osteoblasts and mineral matrix formation [10] [1]. |
| Adipogenic Induction Medium | Typically contains Insulin, Indomethacin, IBMX, and Dexamethasone to stimulate MSC differentiation into adipocytes and lipid accumulation [10] [1]. |
| Chondrogenic Induction Medium | Typically contains TGF-β (e.g., TGF-β1), Insulin-Transferrin-Selenium (ITS), and Ascorbic Acid to promote pellet-based differentiation into chondrocytes and cartilage matrix formation [10] [1]. |
| Histological Stains (Alizarin Red S, Oil Red O, Alcian Blue) | Used for the visual confirmation of successful differentiation: Alizarin Red S for calcium (osteogenesis), Oil Red O for lipids (adipogenesis), and Alcian Blue for proteoglycans (chondrogenesis) [10] [1]. |
| Standard Culture Medium | Typically consists of Dulbecco's Modified Eagle Medium (DMEM) or α-MEM, supplemented with 10% Fetal Bovine Serum (FBS) and 1% Antibiotic-Antimycotic for routine MSC expansion [10]. |
| Trypsin-EDTA Solution | A protease solution used to detach adherent MSCs from plastic culture surfaces for subculturing or preparing cells for analysis [10]. |
While the ISCT criteria provide a minimal definition, it is critical to recognize that MSCs derived from different tissue sources exhibit unique biological properties that can influence their therapeutic application [10] [1].
- Bone Marrow-derived MSCs (BM-MSCs): The most extensively studied type, known for their high differentiation potential and strong immunomodulatory effects [1].
- Adipose Tissue-derived MSCs (AD-MSCs): Easier to harvest in large quantities and yield more cells, with comparable therapeutic properties to BM-MSCs [1].
- Umbilical Cord-derived MSCs (UC-MSCs): Exhibit enhanced proliferation, lower immunogenicity, and longer culture times, making them suitable for allogeneic transplantation [10] [1].
These variations in properties mean that the choice of MSC source is a key strategic decision in both basic research and clinical trial design for regenerative medicine [10].
Mesenchymal stromal cells (MSCs) represent a cornerstone of regenerative medicine, prized for their self-renewal, multipotent differentiation, and potent immunomodulatory capabilities. While the International Society for Cellular Therapy (ISCT) sets minimum criteria for their definition, MSCs derived from different anatomical niches exhibit profound functional and molecular heterogeneity. This technical guide provides an in-depth comparison of MSCs isolated from bone marrow (BM-MSCs), adipose tissue (ADSCs), umbilical cord (UC-MSCs), and dental pulp (DPSCs). We dissect the critical influence of tissue origin on cellular phenotype, proliferation, differentiation potential, and secretome composition, underscoring the necessity of a precise, source-aware approach in both basic research and clinical protocol development. Understanding these differences is paramount for harnessing their full therapeutic potential, as the choice of MSC source is not merely a logistical consideration but a fundamental determinant of biological activity and clinical application.
The tissue microenvironment, or niche, from which MSCs are isolated imprints a distinct identity on the cells, influencing their functional characteristics for therapeutic use [11] [12]. The following table summarizes the core biological and functional properties of MSCs from the four key sources.
Table 1: Functional and Biological Characteristics of MSCs from Different Sources
| Characteristic | Bone Marrow (BM-MSCs) | Adipose Tissue (ADSCs) | Umbilical Cord (UC-MSCs) | Dental Pulp (DPSCs) |
|---|---|---|---|---|
| Isolation & Availability | Invasive harvest; low yield (0.01-0.001% of nucleated cells) [4] | Minimally invasive (e.g., liposuction); high yield [4] | Non-invasive; ethically favorable; readily available [1] [4] | Minimally invasive from medical waste (e.g., third molars) [13] |
| Proliferation & Senescence | Moderate proliferation; higher senescence with age and passage [14] | Moderate proliferation; donor age-dependent [14] | Highest proliferation rate; lowest expression of senescence markers (p53, p21, p16) [4] [14] | High proliferation rate; nestin-positive [13] |
| Tri-Lineage Differentiation | Osteogenic, Chondrogenic, Adipogenic [1] | Osteogenic, Chondrogenic, Adipogenic [1] | Osteogenic, Chondrogenic, Adipogenic [14] | Osteogenic, Chondrogenic; Limited/No Adipogenic [13] |
| Immunophenotype (ISCT) | CD73+, CD90+, CD105+; CD34-, CD45-, HLA-DR- [1] [4] | CD73+, CD90+, CD105+; CD34-, CD45-, HLA-DR- [1] [4] | CD73+, CD90+, CD105+; CD34-, CD45-, HLA-DR- [14] | CD73+, CD90+, CD105+; CD34-, CD45-, HLA-DR- [13] |
| Secretome Profile | Broad range of immunomodulatory and trophic factors [1] | Pro-angiogenic and immunomodulatory factors; specific miRNA sets regulating cell cycle/proliferation [13] | Potent anti-inflammatory (e.g., via Angiopoietin-1) [14] | Specific miRNA sets involved in oxidative stress and apoptosis pathways [13] |
| Key Advantages | Most extensively studied; strong immunomodulation [1] | High cell yield per gram of tissue; ease of harvest [4] | Biologically primitive; high proliferative capacity; low immunogenicity [4] [14] | High accessibility; neural crest origin; high neuro-regenerative potential [13] |
Detailed Experimental Protocols for MSC Characterization
Standardized experimental protocols are critical for the accurate characterization and functional validation of MSCs from any source. The methodologies below are foundational to MSC biology.
Isolation and Culture of Adipose-Derived MSCs (ADSCs)
Objective: To isolate and expand mesenchymal stromal cells from human adipose tissue using two distinct methods: enzymatic digestion and mechanical fragmentation [13].
Materials:
- Tissue Source: Discarded abdominal adipose tissue (e.g., from lipoaspirate).
- Reagents:
- LIPOGEMS system or equivalent for initial tissue processing.
- Basic Medium (BM): αMEM supplemented with 2 mM L-glutamine, 100 IU/ml penicillin, and 0.1 mg/ml streptomycin.
- Enzyme Solution: Collagenase 1A for enzymatic digestion.
- Serum: Fetal Bovine Serum (FBS).
- Trypsin-EDTA for cell detachment.
Protocol:
- Processing: The harvested adipose tissue is processed to remove contaminants like oil and erythrocytes, retaining the intact adipose tissue layer.
- Mechanical Fragmentation (MF):
- A portion of the processed tissue is placed in a culture dish with BM supplemented with 20% FBS.
- Within two weeks, ADSCs migrate from the tissue fragments, adhere to the plastic, and proliferate.
- At 80% confluence, cells are detached with trypsin-EDTA and subcultured for expansion.
- Enzymatic Digestion (Stromal Vascular Fraction - SVF):
- The remaining tissue is washed with DPBS and digested overnight with collagenase 1A at 37°C.
- The digested material is centrifuged, and the cell pellet (the stromal vascular fraction) is plated in BM with 10% FBS.
- At 80% confluence, cells are detached and subcultured.
- Expansion: Cells from both methods are maintained in BM with 10% FBS and used for experiments between passages 4-6.
Trilineage Differentiation Assay
Objective: To confirm the multipotent differentiation capacity of MSCs into osteocytes, adipocytes, and chondrocytes in vitro [13] [1].
Materials:
- Induction Media: Commercially available or laboratory-formulated osteogenic, adipogenic, and chondrogenic differentiation media.
- Staining Reagents:
- Osteogenesis: Alkaline Phosphatase (ALP) stain or Alizarin Red S (for calcium deposition).
- Adipogenesis: Oil Red O (for lipid droplets).
- Chondrogenesis: Safranin O (for proteoglycans) [14].
Protocol:
- Seeding: MSCs are seeded at a standardized density (e.g., 3x10³ cells/well in 48-well plates for osteogenesis and adipogenesis). Chondrogenesis often uses a pelleted micromass culture system.
- Induction: After cell attachment, the standard growth medium is replaced with specific differentiation induction media. Control wells are maintained in standard growth medium.
- Maintenance: Media is changed every 2-3 days for 2-4 weeks.
- Analysis: Differentiation is confirmed by:
- Histochemical Staining: Cells are fixed and stained with lineage-specific dyes (ALP, Oil Red O, Safranin O).
- Gene Expression: Quantitative PCR analysis of lineage-specific markers (e.g., Runx2 for osteogenesis, PPARγ for adipogenesis, SOX9 for chondrogenesis).
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for MSC Isolation, Culture, and Characterization
| Research Reagent | Function/Application | Example in Context |
|---|---|---|
| Collagenase (Type IA) | Enzymatic digestion of tissues (e.g., adipose, umbilical cord) to release stromal cells. | Isolation of ADSCs via the Stromal Vascular Fraction (SVF) method [13]. |
| Fetal Bovine Serum (FBS) | Critical supplement for basal culture media, providing essential growth factors and adhesion proteins for MSC expansion. | Used in basic medium (BM) for the culture of ADSCs and DPSCs [13]. |
| Trypsin-EDTA | Proteolytic enzyme solution used to detach adherent cells from culture plastic for subculturing and propagation. | Standard reagent for passaging all MSC types upon reaching 80% confluence [13]. |
| Defined Induction Media | Media cocktails containing specific factors (e.g., dexamethasone, ascorbate, insulin) to direct MSC differentiation. | Used in trilineage assays to induce osteogenic, adipogenic, and chondrogenic fates [13] [1]. |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Immunophenotyping to confirm MSC identity per ISCT criteria (≥95% positive for CD73, CD90, CD105; ≤2% positive for hematopoietic/endothelial markers). | Essential for the characterization of all MSC populations before experimental use [13] [4] [14]. |
| Cell Culture Tested FN | Coating protein for surfaces; its organization influences stromal cell phenotype and niche engineering. | Used in bioengineered niches to control extracellular matrix presentation and support stem cell maintenance [15]. |
Signaling Pathways and Functional Mechanisms
The therapeutic effects of MSCs are largely mediated through complex paracrine signaling and direct cell-cell interactions, which are influenced by the tissue of origin. The following diagram synthesizes key pathways and functional outcomes, particularly highlighting the immunomodulatory axis.
Discussion: Implications for Research and Therapy
The functional disparities among MSC sources have direct and significant implications for their clinical translation. The recent FDA approval of Ryoncil (remestemcel-L), an allogeneic bone marrow-derived MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD), underscores the therapeutic viability of MSCs [7]. However, the selection of a cell source must be disease-specific. For instance, UC-MSCs, with their potent anti-inflammatory activity mediated by factors like Angiopoietin-1, may be superior for modulating overwhelming immune responses [14]. Conversely, DPSCs, which secrete microRNAs targeting oxidative stress and apoptosis pathways, might offer unique advantages for treating neurodegenerative conditions or dental pulp regeneration [13].
A major challenge in the field is donor heterogeneity and the lack of standardized isolation and expansion protocols. As research advances, new frontiers are emerging, including the use of iPSC-derived MSCs (iMSCs) to overcome limitations of cell source availability and consistency, and the engineering of biomimetic niches that control ECM organization to better maintain stem cell potency ex vivo [7] [15]. Ultimately, treating the stem cell and its microenvironment as an inseparable unit will be key to unlocking the full regenerative potential of MSC-based therapies [11].
Mesenchymal stem cells (MSCs) are adult, multipotent stromal cells with the capacity to differentiate into various cell types of mesodermal origin, most notably osteoblasts, chondrocytes, and adipocytes [16] [1] [17]. This trilineage differentiation potential represents a cornerstone of their application in regenerative medicine, enabling the repair and regeneration of diverse tissues such as bone, cartilage, and fat [1]. Initially discovered in the bone marrow by Friedenstein and colleagues in the 1960s, MSCs have since been isolated from numerous other tissues, including adipose tissue, umbilical cord, placenta, and dental pulp [16] [1]. The International Society for Cellular Therapy (ISCT) has established minimal criteria for defining MSCs, which include: (1) adherence to plastic under standard culture conditions; (2) specific surface marker expression (CD105, CD73, CD90 ≥95%; CD45, CD34, CD14/CD11b, CD79α/CD19, HLA-DR ≤2%); and (3) ability to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [1] [17]. Beyond their differentiation capabilities, MSCs exhibit immunomodulatory properties and secrete bioactive factors that contribute to tissue repair, making them highly attractive for therapeutic development [1]. This whitepaper provides an in-depth technical examination of the molecular regulators, signaling pathways, and experimental methodologies underlying the osteogenic, chondrogenic, and adipogenic differentiation of MSCs, contextualized within the framework of basic science for regenerative medicine research.
Molecular Regulation of Trilineage Differentiation
The commitment of MSCs to a specific lineage is governed by a complex network of transcription factors, signaling pathways, and epigenetic modifications. These molecular drivers often operate in a mutually exclusive manner, where activation of one lineage program simultaneously suppresses alternative fates [17].
Key Transcription Factors and Signaling Pathways
Table 1: Core Transcription Factors Regulating MSC Trilineage Differentiation
| Lineage | Master Transcription Factors | Key Signaling Pathways | Critical Downstream Targets |
|---|---|---|---|
| Osteogenic | Runx2, Osterix (Osx) [16] | Wnt/β-catenin, BMP, FGF-2 [16] | Collagen I, Alkaline Phosphatase, Osteocalcin [16] |
| Chondrogenic | SOX9 [16] | TGF-β, BMP [16] | Collagen II, Aggrecan, SOX5, SOX6 [16] |
| Adipogenic | PPARγ, C/EBPα [17] | Insulin, Glucocorticoids [17] | FABP4, Leptin, Adiponectin [17] |
The osteogenic differentiation of MSCs is primarily regulated by the transcription factor Runt-related transcription factor 2 (Runx2), which is indispensable for osteoblast commitment [16]. Studies on Runx2-deficient mice have demonstrated a complete absence of osteoblasts and bone formation, underscoring its pivotal role [16]. Runx2 operates downstream of multiple signaling pathways, including bone morphogenetic proteins (BMPs) and Wnt/β-catenin signaling, which critically enhance osteoblast differentiation [16]. Osterix (Osx) acts downstream of Runx2, and its deficiency also results in a lack of osteoblast formation [16]. For chondrogenic differentiation, SRY-related high-mobility-group (HMG) box transcription factor 9 (SOX9) is the major regulatory factor involved [16]. SOX9 coordinates the expression of essential extracellular matrix components such as collagen type II and aggrecan, which are fundamental to cartilage structure and function [16]. Transforming growth factor-beta (TGF-β) superfamily members are potent inducers of SOX9 and chondrogenesis [16]. Adipogenic differentiation is coordinated by a cascade of transcription factors, culminating in the activation of peroxisome proliferator-activated receptor gamma (PPARγ) and CCAAT/enhancer-binding protein alpha (C/EBPα) [17]. These factors promote the expression of adipocyte-specific genes, including those encoding fatty acid-binding protein 4 (FABP4), leptin, and adiponectin [17]. The balance between adipogenesis and osteogenesis is particularly critical in bone marrow homeostasis, where an imbalance favoring adipogenesis is associated with bone loss in conditions like osteoporosis [17].
Pathway Interactions and Cross-Regulation
A key feature of MSC lineage commitment is the cross-antagonism between these regulatory pathways. For instance, factors and pathways that stimulate adipogenesis typically inhibit osteogenesis, and vice versa [17]. PPARγ activation not only promotes adipogenesis but also suppresses osteoblast differentiation by inhibiting Runx2 activity [17]. Conversely, Wnt/β-catenin signaling promotes osteogenesis while simultaneously suppressing adipogenesis by downregulating PPARγ [17]. This reciprocal relationship ensures that MSCs commit to a single lineage rather than intermediate states. The molecular basis for this cross-regulation involves direct transcriptional repression, competition for coactivators, and epigenetic modifications that create mutually exclusive chromatin configurations at lineage-specific gene promoters.
Experimental Protocols forIn VitroDifferentiation
Standardized in vitro differentiation protocols are essential for investigating MSC multipotency and for potential therapeutic applications. The following sections detail established methodologies for inducing and assessing trilineage differentiation.
Osteogenic Differentiation Protocol
Induction Medium Composition:
- Base medium: Dulbecco's Modified Eagle Medium (DMEM) - high glucose
- Supplements: 10% Fetal Bovine Serum (FBS)
- Dexamethasone: 100 nM (acts as a synthetic glucocorticoid to promote differentiation)
- Ascorbic acid: 50-100 μM (essential for collagen matrix formation)
- β-glycerophosphate: 10 mM (provides a source of organic phosphate for matrix mineralization) [16]
Procedure:
- Seed MSCs at a density of 5,000-10,000 cells/cm² in standard growth medium.
- At 60-70% confluence, replace growth medium with osteogenic induction medium.
- Refresh the induction medium every 2-3 days for 21-28 days.
- Differentiated osteoblasts will deposit a mineralized extracellular matrix detectable by staining.
Assessment Methods:
- Alizarin Red S Staining: Stains calcium deposits in the mineralized matrix bright orange-red. Quantification can be performed by eluting the dye and measuring absorbance.
- Alkaline Phosphatase (ALP) Activity: Early marker of osteoblast differentiation, measurable using enzymatic assays.
- Gene Expression Analysis: qRT-PCR for osteogenic markers such as Runx2, Osterix, Osteocalcin, and Collagen I [16].
Chondrogenic Differentiation Protocol
Induction Medium Composition:
- Base medium: DMEM - high glucose
- Supplements: 1% ITS+ Premix (Insulin-Transferrin-Selenium)
- Dexamethasone: 100 nM
- Ascorbic acid: 50 μM
- Sodium pyruvate: 100 μg/mL
- Proline: 40 μg/mL
- TGF-β3: 10 ng/mL (key inductive factor for chondrogenesis) [16]
Procedure (Micromass Culture):
- Resuspend MSCs at a high density (5-10 million cells/mL) in induction medium.
- Place 5-10 μL droplets of cell suspension in the center of culture wells and allow cells to adhere for 2-3 hours in a humidified incubator.
- Gently add induction medium to the wells without dislodging the micromass.
- Culture for 21-28 days, refreshing medium every 2-3 days.
- This high-density culture mimics the condensed mesenchyme during embryonic cartilage development.
Assessment Methods:
- Histological Staining: Safranin O or Alcian Blue staining detects sulfated glycosaminoglycans (GAGs) in the cartilage matrix.
- Immunohistochemistry: For collagen type II, the main collagenous component of cartilage.
- Gene Expression Analysis: qRT-PCR for chondrogenic markers including SOX9, Aggrecan, and Collagen II [16].
Adipogenic Differentiation Protocol
Induction Medium Composition:
- Base medium: DMEM - high glucose
- Supplements: 10% FBS
- Dexamethasone: 1 μM
- Isobutylmethylxanthine (IBMX): 0.5 mM (phosphodiesterase inhibitor that increases intracellular cAMP)
- Indomethacin: 200 μM (cyclooxygenase inhibitor that promotes adipogenesis)
- Insulin: 10 μg/mL [17]
Procedure (Two-Step Induction):
- Seed MSCs at 20,000-30,000 cells/cm² and allow to reach 100% confluence.
- Initiate differentiation by adding adipogenic induction medium for 3-5 days.
- Replace with adipogenic maintenance medium (identical to induction medium but without IBMX and indomethacin) for 2-3 days.
- Repeat this cycle 2-3 times over 14-21 days to achieve mature adipocytes with lipid vacuoles.
Assessment Methods:
- Oil Red O Staining: Lipophilic dye that stains intracellular lipid droplets red. Can be quantified after elution.
- Gene Expression Analysis: qRT-PCR for adipogenic markers such as PPARγ, C/EBPα, FABP4 (aP2), and Leptin [17].
Table 2: Standard Staining Methods for Assessing Trilineage Differentiation
| Lineage | Staining Method | Target | Appearance | Time Point |
|---|---|---|---|---|
| Osteogenic | Alizarin Red S | Calcium deposits | Orange-Red | 21-28 days |
| Chondrogenic | Alcian Blue or Safranin O | Glycosaminoglycans (GAGs) | Blue/Green or Orange-Red | 21-28 days |
| Adipogenic | Oil Red O | Intracellular lipid droplets | Red | 14-21 days |
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of MSC differentiation requires a carefully selected set of reagents and tools. The following table compiles essential solutions for studying multipotency.
Table 3: Essential Research Reagents for Studying MSC Trilineage Differentiation
| Reagent Category | Specific Examples | Function in Differentiation |
|---|---|---|
| Induction Factors | Dexamethasone, TGF-β3, BMP-2, IBMX, Indomethacin, Insulin | Activate specific signaling pathways to initiate and drive lineage commitment [16] [17]. |
| Serum & Supplements | Fetal Bovine Serum (FBS), ITS+ Premix (Insulin, Transferrin, Selenium) | Provide essential nutrients, hormones, and attachment factors for cell survival and differentiation [16]. |
| Surface Markers | CD105, CD73, CD90 (Positive); CD45, CD34, HLA-DR (Negative) | Identify and purify MSCs via flow cytometry; confirm cell population purity before differentiation [1] [17]. |
| Staining Kits | Alizarin Red S, Oil Red O, Alcian Blue | Detect and quantify differentiation endpoints (mineralization, lipids, GAGs) [16] [17]. |
| Antibodies | Anti-Collagen I, Anti-Osteocalcin, Anti-Collagen II, Anti-SOX9, Anti-PPARγ | Confirm protein-level expression of lineage-specific markers via immunohistochemistry or Western blot [16] [17]. |
Visualization of Signaling Pathways
The following diagrams, generated using Graphviz DOT language, illustrate the key signaling pathways and molecular relationships governing MSC differentiation.
Osteogenic Signaling Pathway
Chondrogenic Signaling Pathway
Adipogenic Signaling Pathway
MSC Lineage Commitment Relationships
Advanced Research Applications and Methodologies
Contemporary MSC research employs sophisticated technologies to unravel the complexity of differentiation processes and overcome challenges in therapeutic applications.
Transcriptomic Approaches to Differentiation
High-throughput RNA sequencing (RNA-seq) has revolutionized our understanding of the molecular events during MSC differentiation [17]. This approach enables comprehensive profiling of mRNA, microRNA, circular RNA, and long non-coding RNA expression patterns at different time points throughout adipogenesis, osteogenesis, and chondrogenesis [17]. Transcriptome analyses have revealed that the differentiation processes involve complex temporal regulation of gene networks governing cell cycle, metabolism, and extracellular matrix organization. For instance, during osteogenesis, there is sequential activation of genes involved in cell proliferation, followed by matrix maturation and finally mineralization. Similarly, adipogenesis involves coordinated induction of lipid metabolism genes and suppression of osteogenic genes, reflecting the reciprocal relationship between these lineages [17].
Deep Learning for Predicting Differentiation Potential
Recent advances in artificial intelligence have introduced novel approaches for assessing MSC quality and differentiation potential. Convolutional neural networks (CNNs) can predict the multipotency of human MSCs based on cellular morphology with high accuracy (85.98% in one study) [18]. This non-invasive method utilizes bright-field or immunofluorescence images of single cells to classify their differentiation capacity without requiring destructive assays [18]. The implementation of deep learning models such as DenseNet121, VGG19, and InceptionV3 enables researchers to perform quantitative, single-cell characterization of live stem cells, offering significant potential for improved quality control in clinical cell therapies [18]. This approach is particularly valuable for addressing donor-dependent variation in MSC differentiation capacity, which has been a major challenge in clinical applications [18].
Quantitative Lineage Tracing Strategies
Rigorous assessment of MSC differentiation potential at the single-cell level requires sophisticated lineage tracing methodologies [19]. Recent developments include statistical analysis of multicolor lineage tracing and lineage tracing at saturation, which allow researchers to determine multipotency potential with high confidence and assess the fate of all stem cells within a given lineage [19]. These methods provide a framework to resolve whether tissue-specific stem cells are truly multipotent or composed of mixtures of unipotent progenitors—a question of fundamental importance in developmental biology [19]. For MSCs, such approaches could help clarify the heterogeneity within populations and identify subpopulations with enhanced therapeutic potential for specific applications.
The multipotent differentiation potential of MSCs toward osteogenic, chondrogenic, and adipogenic lineages represents a fundamental biological property with tremendous implications for regenerative medicine. The molecular regulation of these processes, centered around master transcription factors Runx2, SOX9, and PPARγ for the respective lineages, involves complex signaling networks that ensure proper lineage commitment. Standardized in vitro protocols enable researchers to direct MSC differentiation for both investigative and therapeutic purposes. Contemporary research employs advanced transcriptomic analyses, deep learning algorithms, and sophisticated lineage tracing strategies to deepen our understanding of these processes and address challenges such as donor variability and population heterogeneity. As basic science continues to elucidate the intricate mechanisms governing MSC multipotency, the translation of this knowledge to clinical applications holds promise for developing effective cell-based therapies for a wide range of degenerative diseases, orthopedic injuries, and other conditions requiring tissue repair and regeneration.
Mesenchymal stem cells (MSCs) have emerged as a highly promising therapeutic strategy in regenerative medicine due to their unique multifunctional capabilities [1]. These non-hematopoietic, multipotent stromal cells possess three fundamental biological properties that underpin their clinical potential: immunomodulation, paracrine activity, and trophic support [20] [21]. Originally identified in bone marrow, MSCs have since been isolated from diverse tissues including adipose tissue, umbilical cord, placental tissue, and dental pulp [1]. The International Society for Cellular Therapy (ISCT) defines MSCs based on three key criteria: adherence to plastic under standard culture conditions; specific surface marker expression (CD73, CD90, CD105 ≥95%; CD34, CD45, CD14, CD19, HLA-DR ≤2%); and tri-lineage differentiation potential into osteocytes, chondrocytes, and adipocytes in vitro [1]. This technical guide provides an in-depth analysis of the core therapeutic mechanisms of MSCs, framed within the context of basic science and translational research applications for scientific and drug development professionals.
Immunomodulatory Mechanisms
Cell-to-Cell Contact-Dependent Immunomodulation
MSCs participate in both innate and adaptive immunity through direct cellular interactions [20]. These contact-dependent mechanisms involve precise molecular engagements with various immune cell populations:
T-cell Regulation: MSCs inhibit naive and memory T-cell responses through upregulation of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), which are critical for T-cell activation and leukocyte recruitment [20]. MSC co-culture with CD4+ T-cells activates the Notch1/forkhead box P3 (FOXP3) pathway, increasing the percentage of CD4+CD25 FOXP3+ regulatory T-cells (Tregs) [20]. Galectin-1, abundantly expressed on MSC surfaces, plays a crucial role in T-cell modulation, as knockdown results in restored CD4+ and CD8+ T-cell proliferation [20]. Programmed death-ligand 1 (PD-L1) and PD-L2 expression on placental MSCs further inhibits T-cell proliferation through cell cycle arrest [20].
B-cell Interactions: Adipose-derived MSCs (A-MSCs) increase survival of quiescent B-cells via contact-dependent mechanisms and facilitate B-cell differentiation independently of T-cells [20]. MSC-mediated inhibition of Caspase 3-mediated B-cell apoptosis occurs through vascular endothelial growth factor (VEGF) upregulation, while proliferation inhibition involves cell cycle arrest in G0/G1 phase mediated by p38 mitogen-activated protein kinase (MAPK) pathways [20].
Innate Immune Cell Engagement: MSC interactions with natural killer (NK) cells result in suppressed granule polarization, indicating differential crosstalk between MSCs and cytotoxic NK cells [20]. MSCs prevent neutrophil apoptosis via ICAM-1-dependent mechanisms, exerting tissue-protective effects [20]. Monocytes phagocytose infused MSCs, inducing phenotypical and functional changes that subsequently modulate adaptive immune responses [20].
Table 1: Cell Contact-Dependent Immunomodulatory Mechanisms
| Immune Cell Type | Molecular Mechanisms | Functional Outcomes |
|---|---|---|
| T-cells | ICAM-1/VCAM-1 upregulation, Notch1/FOXP3 pathway activation, PD-L1/PD-L2 expression | Inhibition of proliferation, increased Treg induction, cell cycle arrest |
| B-cells | VEGF-mediated anti-apoptosis, p38 MAPK pathway activation | Enhanced survival of quiescent cells, cell cycle arrest in G0/G1 phase |
| NK cells | Suppression of granule polarization | Reduced cytotoxic activity |
| Monocytes/Macrophages | Phagocytosis of MSCs, PGE2-mediated switching | Phenotypical and functional changes, M1 to M2 phenotype transition |
| Neutrophils | ICAM-1-dependent anti-apoptosis | Enhanced survival, tissue-protective effects |
Soluble Factor-Mediated Immunomodulation
The MSC secretome contains a diverse repertoire of immunomodulatory molecules that exert potent paracrine effects on immune effector cells [20] [21]:
Cytokine Networks: MSCs secrete transforming growth factor-β1 (TGF-β1), prostaglandin E2 (PGE2), hepatocyte growth factor (HGF), and indoleamine-pyrrole 2,3-dioxygenase (IDO), which collectively inhibit T helper 17 cell (Th17) differentiation while promoting Treg induction [20]. These factors work in concert to inhibit IL-17, IL-22, and IFN-γ production while inducing IL-10 secretion [20]. The IL-25/STAT3/PD-L1 axis has been identified as a key pathway through which MSCs suppress Th17 responses [20].
Extracellular Vesicles: MSC-derived extracellular vesicles (MSC-EVs) and exosomes (30-150 nm diameter) represent important vehicles for immunomodulatory factor delivery [22]. These vesicles contain proteins, mRNAs, and microRNAs that mirror parent MSC immunoregulatory functions while offering advantages including low immunogenicity, enhanced stability, and reduced risks of tumorigenesis or thrombosis compared to whole-cell therapies [22].
Paracrine Signaling and Secretome
Composition and Biological Activity
The MSC paracrine secretome represents a complex mixture of bioactive factors that mediate therapeutic effects without requiring direct cellular differentiation or engraftment [1] [20]:
Growth Factors and Cytokines: MSC secretome includes stem cell factor (SCF), thrombopoietin (TPO), IL-6, TGF-β, FGF, HGF, and VEGF, which collectively promote angiogenesis, support bone marrow niche function, and modulate T-cell-mediated responses [23]. These factors work in concert to create a regenerative microenvironment conducive to tissue repair.
Extracellular Vesicle Cargo: MSC-EVs contain specific protein and nucleic acid cargo that varies depending on MSC tissue source and culture conditions [22]. EV contents include immunomodulatory miRNAs, growth factors, and enzymes that can reprogram recipient cells through horizontal transfer of biological information [22].
Table 2: Key Paracrine Factors in MSC Secretome
| Factor Category | Specific Components | Primary Biological Functions |
|---|---|---|
| Growth Factors | VEGF, FGF, HGF, TGF-β1 | Angiogenesis promotion, fibroblast proliferation, hepatocyte growth, immunomodulation |
| Cytokines | IL-6, IL-10, IL-1RA, SCF, TPO | Hematopoietic support, anti-inflammatory signaling, immunoregulation |
| Lipid Mediators | PGE2 | Macrophage polarization to M2 phenotype, T-cell suppression |
| Enzymes | IDO | Tryptophan catabolism, T-cell proliferation inhibition |
| Extracellular Vesicles | Exosomes, microvesicles | Horizontal transfer of miRNAs, proteins, and lipids to recipient cells |
Tissue Source Variability and Standardization Challenges
The biological functions and characteristics of MSC secretomes vary significantly depending on tissue source, creating both opportunities and challenges for therapeutic development [22]:
Source-Specific Variations: Bone marrow-derived MSCs (BM-MSCs) demonstrate high differentiation potential and strong immunomodulatory effects [1]. Adipose-derived MSCs (AD-MSCs) yield higher cell quantities and exert potent immunomodulatory effects, potentially superior to BM-MSCs for some applications [1] [20]. Umbilical cord-derived MSCs (UC-MSCs) exhibit enhanced proliferation capacity, lower immunogenicity, and minimal risk of initiating allogeneic immune responses [1] [20].
Standardization Deficits: While procedures for MSC isolation, expansion, and therapeutic use have been standardized according to ISCT guidelines, standardized protocols for MSC-EV isolation and purification remain lacking [22]. Significant variations in EV characterization, dose units, and outcome measures across clinical trials underscore the need for harmonized reporting standards [22].
Trophic Support Mechanisms
Hematopoietic Support and Bone Marrow Niche
MSCs provide crucial trophic support for hematopoietic recovery, particularly following hematopoietic stem cell transplantation (HSCT) [23]:
Engraftment Acceleration: Systematic review of 47 clinical studies involving 1,777 patients demonstrated that MSC co-infusion accelerates hematopoietic recovery after HSCT, with particularly consistent benefits for platelet engraftment [23]. MSC recipients showed average neutrophil and platelet engraftment times of 13.96 and 21.61 days, respectively, with approximately 79% of studies reporting enhanced engraftment [23].
Mechanisms of Hematopoietic Support: MSCs contribute to hematopoietic recovery through secretion of cytokines including SCF, TPO, IL-6, and TGF-β, promotion of angiogenesis, support of bone marrow niche integrity, and modulation of T-cell-mediated responses [23]. These effects facilitate engraftment and mitigate graft-versus-host disease (GVHD) in high-risk transplantation settings [23].
Tissue Repair and Regenerative Support
The trophic functions of MSCs extend beyond hematopoietic support to broader tissue repair and regeneration:
Anti-apoptotic Effects: MSCs secrete factors that inhibit programmed cell death in vulnerable cell populations, particularly in ischemic, inflammatory, or mechanically stressed tissues [1] [20]. These anti-apoptotic signals enhance survival of parenchymal cells during injury and recovery phases.
Angiogenic Induction: Through VEGF, FGF, and other angiogenic factor secretion, MSCs promote neovascularization in damaged tissues, restoring perfusion and nutrient delivery to compromised regions [1] [23].
Fibrosis Reduction: MSC trophic factors modulate extracellular matrix remodeling, reducing excessive scar formation while promoting functional tissue restoration [20].
Bacterial Clearance: MSCs enhance phagocytic activity of innate immune cells and may directly secrete antimicrobial peptides, contributing to infection resolution in injured tissues [20].
Experimental Methodologies
MSC-EV Isolation and Characterization Protocols
Standardized methodologies for extracellular vesicle isolation and characterization are critical for research reproducibility and therapeutic development:
Isolation Techniques: Differential centrifugation remains the most common approach, involving sequential centrifugation steps at 300 × g (10 minutes) to remove cells, 2,000 × g (10 minutes) to remove debris, 10,000 × g (30 minutes) to remove larger vesicles, and final ultracentrifugation at 100,000 × g (70 minutes) to pellet EVs [22]. Alternative methods include size-exclusion chromatography, polymer-based precipitation, and immunoaffinity capture.
Characterization Standards: Nanoparticle tracking analysis (NTA) determines particle size distribution and concentration [22]. Flow cytometry confirms surface marker expression (CD63, CD81, CD9) while transmission electron microscopy visualizes vesicle morphology [22]. Western blotting confirms presence of EV-associated proteins (Alix, TSG101) and absence of contaminants (calnexin, GM130).
Immunomodulation Assay Systems
T-cell Proliferation Assays: Peripheral blood mononuclear cells (PBMCs) are labeled with carboxyfluorescein succinimidyl ester (CFSE) and activated with anti-CD3/CD28 antibodies in the presence or absence of MSCs (typically 1:10 to 1:100 MSC:PBMC ratios) [20]. After 3-5 days, CFSE dilution in CD4+ and CD8+ T-cells is measured by flow cytometry to determine proliferation inhibition.
Macrophage Polarization Assays: Human monocytes are differentiated to M1 macrophages with GM-CSF (50 ng/mL) and polarized with IFN-γ (20 ng/mL) plus LPS (100 ng/mL), or to M2 macrophages with M-CSF (50 ng/mL) and IL-4 (20 ng/mL) [20]. MSCs are added in transwell systems or conditioned media is applied. M1 (CD80, CD86, HLA-DR) and M2 (CD206, CD163) marker expression is quantified by flow cytometry after 48 hours.
Table 3: In Vitro Functional Assays for MSC Characterization
| Assay Type | Key Reagents | Readout Parameters | Typical Duration |
|---|---|---|---|
| T-cell Suppression | CFSE, anti-CD3/CD28 antibodies, PBMCs | CFSE dilution, cytokine secretion (IFN-γ, IL-17), Treg induction | 3-5 days |
| Macrophage Polarization | GM-CSF, M-CSF, IFN-γ, LPS, IL-4 | Surface markers (CD80/86, CD206/163), cytokine secretion (TNF-α, IL-10) | 2-3 days |
| IDO Activity | L-tryptophan, kynurenine standard | Kynurenine production (spectrophotometry, 490 nm) | 24-48 hours |
| Angiogenesis Assay | HUVECs, Matrigel, VEGF | Tube formation (branch points, tube length) | 4-18 hours |
| Hematopoietic Support | CD34+ cells, methylcellulose media | CFU-GM, BFU-E, CFU-GEMM colonies | 14 days |
Research Reagent Solutions
Table 4: Essential Research Reagents for MSC Mechanism Studies
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Surface Marker Antibodies | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) | MSC characterization and purity assessment according to ISCT criteria |
| Differentiation Media | Osteogenic: Dexamethasone, β-glycerophosphate, ascorbic acid; Adipogenic: IBMX, indomethacin, insulin; Chondrogenic: TGF-β3, BMP-6 | Tri-lineage differentiation potential verification |
| Cytokine/Chemokine Arrays | TGF-β1, PGE2, IDO, HGF, VEGF detection systems | Secretome analysis and paracrine factor quantification |
| EV Isolation Kits | Ultracentrifugation reagents, size-exclusion columns, polymer-based precipitation kits | Extracellular vesicle isolation and purification |
| Cell Culture Supplements | FBS alternatives (xeno-free), hypoxia-mimetic agents, inflammatory priming cocktails (IFN-γ, TNF-α) | MSC preconditioning to enhance therapeutic potency |
| Flow Cytometry Panels | T-cell (CD4, CD8, CD25, FOXP3), B-cell (CD19, CD20), macrophage (CD80, CD86, CD206) markers | Immunomodulation mechanism analysis |
Clinical Translation and Therapeutic Applications
Current Clinical Evidence
MSC-based therapies have demonstrated potential across diverse clinical applications, supported by accumulating clinical evidence:
Hematopoietic Recovery: Comprehensive systematic review of clinical studies (2000-2025) confirms MSC co-infusion accelerates hematopoietic recovery after transplantation, with platelet engraftment showing the most consistent benefit [23]. MSC therapy demonstrated safety with no major adverse events reported across 47 studies and 1,777 patients [23].
Disease Applications: Clinical trials have explored MSC therapies for autoimmune diseases, inflammatory disorders, neurodegenerative diseases, orthopedic injuries, cardiovascular diseases, and graft-versus-host disease [1] [20]. MSC administration has shown potential efficacy in treating several conditions that resist standard treatment approaches [21].
Dose Optimization Challenges
Clinical translation faces significant dose optimization challenges, particularly for MSC-derived products:
Route-Dependent Dosing: Dose-effect relationships reveal that nebulization therapy achieves therapeutic effects at doses around 10^8 particles, significantly lower than required for intravenous routes, suggesting a narrow and route-dependent effective dose window [22].
Standardization Deficits: Large variations in EV characterization, dose units, and outcome measures across clinical trials underscore the lack of harmonized reporting standards [22]. The field urgently requires standardized dosing frameworks, potency assays, and harmonized clinical protocols to advance safe and effective translation.
The therapeutic potential of MSCs in regenerative medicine is fundamentally underpinned by three core mechanisms: sophisticated immunomodulation through both contact-dependent and soluble factor-mediated pathways, comprehensive paracrine activity via diverse secretome components, and multifaceted trophic support promoting tissue repair and regeneration. The convergence of these mechanisms enables MSCs to coordinate complex tissue responses to injury, inflammation, and degeneration. Current research challenges include standardization of MSC-EV characterization, optimization of dosing parameters across different administration routes, and development of potency assays that reliably predict clinical efficacy. Future directions will likely focus on MSC engineering strategies to enhance homing, increase immunomodulatory potency, and improve therapeutic consistency. As the field advances, understanding the intricate interplay between immunomodulation, paracrine signaling, and trophic support will be essential for developing next-generation MSC-based therapies with enhanced precision and efficacy for clinical applications.
From Bench to Bedside: MSC Applications and Therapeutic Strategies
Standardized Protocols for MSC Isolation, Expansion, and Characterization
Mesenchymal Stromal/Stem Cells (MSCs) have emerged as a cornerstone of regenerative medicine and cell-based therapy due to their unique properties, including self-renewal capacity, multipotent differentiation potential, and immunomodulatory functions [1]. These adult stem cells, first identified in bone marrow, can be isolated from various tissues and possess the ability to modulate the immune system and differentiate into multiple cell lineages, including osteocytes, chondrocytes, and adipocytes [24]. The therapeutic potential of MSCs extends across a broad spectrum of human diseases, from autoimmune and inflammatory disorders to neurodegenerative diseases and orthopedic injuries [1]. Their effects are primarily mediated through the release of bioactive molecules such as growth factors, cytokines, and extracellular vesicles, which play crucial roles in modulating the local cellular environment, promoting tissue repair, angiogenesis, and exerting anti-inflammatory effects [1].
The International Society for Cell and Gene Therapy (ISCT) has established minimum criteria for defining MSCs, which include: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, CD105) while lacking expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR); and (3) capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [1] [25]. These criteria provide a foundational standard for the field, though heterogeneity exists between MSCs from different tissue sources and even between clonal populations from the same source [26].
This technical guide provides comprehensive, standardized protocols for the isolation, expansion, and characterization of MSCs, framed within the context of basic science research to support their therapeutic application in regenerative medicine.
MSCs can be isolated from various somatic and perinatal tissues, each requiring specific isolation techniques. The most common sources include adipose tissue, bone marrow, umbilical cord, and cord blood [27]. The methodology varies depending on the tissue structure and cellular composition, with enzymatic digestion and density gradient centrifugation being the most widely employed techniques [27].
Isolation from Adipose Tissue
Adipose tissue represents a rich source of MSCs, with higher yields compared to bone marrow [1]. Two primary methods have been standardized for isolating adipose-derived MSCs (AD-MSCs):
Standard Isolation Protocol:
- Tissue Processing: Wash approximately 250mL of fat tissue 3-5 times with PBS for 5 minutes each wash, discarding the lower phase until clear [24].
- Enzymatic Digestion: Add collagenase and incubate for 1-4 hours at 37°C on a shaker [24].
- Enzyme Neutralization: Add 10% FBS to neutralize collagenase activity [24].
- Centrifugation: Centrifuge digested fat at 800×g for 10 minutes to separate the stromal vascular fraction (SVF) pellet from floating adipocytes, lipids, and liquid [24].
- Red Blood Cell Lysis: Resuspend SVF pellet in 160mM NH₄Cl and incubate for 10 minutes at room temperature [24].
- Gradient Separation: Layer cells on Percoll or Histopaque gradient and centrifuge at 1000×g for 30 minutes at room temperature [24].
- Cell Filtration: Wash cells twice with PBS, then resuspend cell pellet in PBS and filter sequentially through 100μm and 40μm nylon mesh [24].
- Plating: Resuspend final cell pellet in 40% FBS/DMEM and plate in culture vessels incubated at 37°C, 5% CO₂ [24].
Rapid Isolation Protocol:
- Aspiration: Transfer blood/saline containing adipose tissue into a 50mL conical tube [24].
- Centrifugation: Centrifuge at 400×g for 10 minutes at room temperature [24].
- Erythrocyte Lysis: Resuspend pellet in 160mM NH₄Cl for 5 minutes at room temperature [24].
- Final Processing: Centrifuge at 400×g for 10 minutes, remove supernatant, resuspend pellet in 40% FBS/DMEM, and plate for incubation [24].
Isolation from Umbilical Cord
The umbilical cord, particularly Wharton's jelly, provides a valuable perinatal source of MSCs with enhanced proliferation capacity and lower immunogenicity [27] [1]. The standardized protocol includes:
- Initial Processing: Wash umbilical cords in hypochlorite solution (1:3 dilution), then rinse with PBS [24].
- Short-term Storage: Store umbilical cords in 10% FBS/DMEM-low glucose for up to 12 hours if immediate processing isn't possible [24].
- Enzymatic Digestion: Wash cords three times with PBS, then inject veins and arteries with 3mL of 0.1% collagenase in PBS [24].
- Incubation: Incubate for 20 minutes at 37°C [24].
- Cell Harvesting: Inject 5mL DMEM-low glucose with 10% FBS, then harvest cells by massaging the cord tissue [24].
- Cell Collection: Centrifuge at 300×g for 10 minutes at room temperature, remove supernatant, add culture medium, and plate [24].
- Culture: Incubate at 37°C, 5% CO₂ overnight [24].
Isolation from Cord Blood
Cord blood-derived MSCs are particularly valuable for their neonatal characteristics and accessibility [1]. The isolation protocol involves:
- Sample Preparation: Dilute cord blood with RPMI Medium 1640 at a 3:1 ratio (3 parts cord blood to 1 part RPMI) [24].
- Mononuclear Cell Separation: Isolate mononuclear cells (MNCs) by density gradient centrifugation at 400×g for 30 minutes at room temperature using Ficoll-Paque Premium according to manufacturer's instructions [24].
- Cell Washing: Transfer MNCs to a new centrifuge tube and add PBS at a 1:3 ratio (1 part MNCs to 3 parts PBS) [24].
- Final Processing: Centrifuge at 400×g for 10 minutes at room temperature, remove supernatant, resuspend cells by adding culture medium, and plate [24].
- Culture: Incubate at 37°C, 5% CO₂ overnight [24].
Table 1: Comparison of MSC Sources and Yield Characteristics
| Tissue Source | Isolation Method | Approximate Yield | Advantages | Limitations |
|---|---|---|---|---|
| Adipose Tissue | Enzymatic digestion | High yield (~500,000 cells/g) | Abundant tissue source, minimal morbidity | Requires extensive processing, enzymatic digestion |
| Umbilical Cord | Enzymatic digestion/explant | Moderate to high yield | Perinatal source, high proliferation capacity | Limited availability, ethical considerations in some regions |
| Cord Blood | Density gradient centrifugation | Low to moderate yield | Neonatal source, minimal immunogenicity | Low frequency of MSCs, variable yield |
| Bone Marrow | Density gradient centrifugation/plastic adherence | Low yield (~0.001-0.01% of nucleated cells) | Gold standard, well-characterized | Invasive harvesting, decline in quality with age |
MSC Expansion and Culture Techniques
Proper expansion techniques are critical for generating sufficient cell numbers for therapeutic applications while maintaining MSC functionality and differentiation potential. Standardized protocols ensure consistent results across different laboratories and production facilities.
Culture Vessel Coating
Optimal MSC expansion requires appropriate surface coating to facilitate cell attachment and growth:
- Coating Solution Preparation: Prepare a 5μg/mL working solution in PBS of PRIME-XV MatrIS F or PRIME-XV Human Fibronectin [28].
- Application: Add the diluted product to culture vessel at a final volume per surface area of 0.08mL/cm² [28].
- Incubation: Incubate culture vessels at room temperature for 3 hours or overnight at 2-8°C. Seal with Parafilm to avoid drying if stored at 2-8°C overnight [28].
- Preparation for Use: Aspirate and discard diluted solution from culture vessels before adding mesenchymal stem cells [28].
Table 2: Coating Solution Volumes for Different Culture Vessels
| Culture Vessel | Surface Area (cm²) | Volume of 5μg/mL Attachment Substrate |
|---|---|---|
| 6-well plate | 9.6 | 768 μL/well |
| T-25 flask | 25 | 2 mL/flask |
| T-75 flask | 75 | 6 mL/flask |
Thawing Cryopreserved MSCs
Proper thawing technique is essential for maintaining cell viability and functionality:
- Preparation: Pre-coat tissue culture vessels and pre-warm PRIME-XV MSC Expansion SFM to 37°C for no more than 30 minutes [28].
- Thawing: Rapidly thaw frozen vial of MSCs in a 37°C water bath with gentle swirling until all visible ice has melted (approximately 3 minutes for a 1mL sample) [28].
- Important Note: Do not allow sample to warm above chilled temperatures (0-10°C). Cryovials should be cool to the touch when removed from the water bath [28].
- Dilution: Pipette the entire content of the cryovial into a 15mL conical tube. Carefully add 5-10mL of pre-warmed PRIME-XV MSC Expansion SFM at an approximate rate of 3-5 drops per 10 seconds, gently swirling after each addition [28].
- Plating: Transfer the entire content to a pre-coated tissue culture vessel and incubate at 37°C, 5% CO₂ [28].
- First Medium Change: Aspirate off media and feed cells with pre-warmed PRIME-XV MSC Expansion SFM 24 hours post-thaw [28].
Expansion and Subculture
Maintaining MSC potency through multiple passages requires standardized subculture techniques:
- Preparation: Pre-coat new tissue culture vessels and pre-warm PRIME-XV MSC Expansion SFM to 37°C [28].
- Cell Washing: Remove spent media from culture and gently rinse cells once with PBS (10mL for each T-75 flask) [28].
- Detachment: Add 3mL of room temperature TrypLE Express to each T-75 flask, tilting the flask to disperse evenly over cells [28].
- Incubation: Incubate at 37°C, 5% CO₂, monitoring periodically for cell detachment. Tap the flask side to aid detachment until at least 90% of cells are detached (approximately 5-10 minutes) [28].
- Neutralization: Add 5mL of PRIME-XV MSC Expansion SFM to the flask, disperse cells by pipetting over the entire growth surface, and transfer to a 15mL conical tube [28].
- Centrifugation: Centrifuge at 400×g for 5 minutes and aspirate supernatant [28].
- Cell Counting: Resuspend cell pellet in a small amount of pre-warmed medium and count cells [28].
- Reseeding: Resuspend 4.5-5.0 × 10⁵ cells into 20mL of pre-warmed medium for each pre-coated T-75 flask (approximately 6,000 cells/cm²) [28].
- Culture Maintenance: Remove and discard spent media every two days, and feed cells with pre-warmed medium. Subculture when cells reach 80-90% confluence [28].
Comprehensive MSC Characterization
Thorough characterization is essential for verifying MSC identity, quality, and functional potential. Despite established standards, analysis of clinical trial reports reveals that characterization is often incomplete or variable [26].
Immunophenotyping by Flow Cytometry
Flow cytometric analysis of surface markers remains the primary method for MSC identification according to ISCT criteria:
Table 3: Essential Surface Markers for MSC Characterization
| Marker Category | Specific Markers | Acceptable Expression Range | Functional Significance |
|---|---|---|---|
| Positive Markers | CD73, CD90, CD105 | ≥95% positive | Mesenchymal lineage commitment, adhesion, ectoenzyme activity |
| Negative Markers | CD34, CD45, CD14, CD19, HLA-DR | ≤2% positive | Absence of hematopoietic contamination |
| Additional Optional Markers | CD29, CD44, CD166 | Variable | Adhesion, migration properties |
The immunophenotyping profile confirms the mesenchymal nature of the cells while excluding hematopoietic contaminants. Analysis of clinical trials reveals that only 53.6% of studies reported average values per marker for all cell lots used, while 33.3% included no characterization data at all [26].
Trilineage Differentiation Potential
The capacity for in vitro differentiation into mesodermal lineages represents a fundamental functional characteristic of MSCs. Each lineage requires specific induction cocktails and culture conditions:
Adipogenic Differentiation:
- Induction Media Components: Dexamethasone, isobutylmethylxanthine (IBMX), indomethacin, and insulin [1]
- Differentiation Timeline: 14-21 days
- Validation: Oil Red O staining of lipid vacuoles [26]
Osteogenic Differentiation:
- Induction Media Components: Dexamethasone, ascorbic acid, β-glycerophosphate [1]
- Differentiation Timeline: 21-28 days
- Validation: Alizarin Red S staining of calcium deposits [26]
Chondrogenic Differentiation:
- Induction Media Components: TGF-β, dexamethasone, ascorbic acid, proline, pyruvate [1]
- Differentiation Timeline: 21-28 days
- Validation: Alcian blue or Safranin O staining of proteoglycans [26]
Analysis of published clinical trials shows that osteogenic differentiation was reported in only 29% of papers, adipogenesis in 27%, and chondrogenesis in 20% [26], highlighting a significant gap in functional characterization.
Functional and Potency Assays
Beyond the minimal criteria, additional functional assays provide critical information about MSC therapeutic potential:
Immunomodulatory Assays:
- Mixed lymphocyte reactions (MLR) to assess T-cell suppression [27]
- Cytokine secretion profiling (IDO, PGE2, TGF-β) [1]
- Macrophage polarization assays [1]
Secretome Analysis:
- Multiplex cytokine arrays
- Extracellular vesicle characterization
- Conditioned media analysis
Viability and Proliferation Assessment:
- Population doubling time calculations
- Metabolic activity assays (MTT, XTT)
- Apoptosis assays
Only 8% of clinical trial reports included other functional assays beyond the standard differentiation protocols [26], indicating a substantial opportunity for improvement in comprehensive characterization.
Experimental Workflows and Signaling Pathways
MSC Isolation and Characterization Workflow
Key Signaling Pathways in MSC Biology
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for MSC Studies
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| Culture Media | PRIME-XV MSC Expansion SFM, DMEM, α-MEM | Cell growth and maintenance | Serum-free formulations reduce variability; DMEM with glucose for high metabolic needs |
| Serum Supplements | Fetal Bovine Serum (FBS), Fetal Calf Serum (FCS) | Provides essential growth factors | Batch testing critical for consistency; consider defined serum replacements |
| Dissociation Reagents | TrypLE Express, Collagenase, Trypsin-EDTA | Cell detachment and tissue dissociation | TrypLE less damaging to surface proteins than trypsin |
| Attachment Substrates | PRIME-XV MatrIS F, PRIME-XV Human Fibronectin, Collagen | Facilitates cell adhesion and spreading | Coating essential for some MSC sources; concentration affects differentiation |
| Characterization Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR | Immunophenotyping by flow cytometry | ISCT minimum panel plus additional markers for comprehensive profiling |
| Differentiation Kits | Adipogenic, Osteogenic, Chondrogenic Induction Media | Trilineage differentiation assessment | Quality control for multipotency; standardized kits improve reproducibility |
| Cryopreservation Agents | DMSO, Cryoprotective agents (CPA) | Long-term cell storage | Controlled-rate freezing maintains viability and functionality |
Standardized protocols for MSC isolation, expansion, and characterization are fundamental to advancing both basic science and clinical applications in regenerative medicine. The methodologies outlined in this technical guide provide a robust framework for generating consistent, well-characterized MSC populations suitable for research and therapeutic development. As the field progresses, continued refinement of these protocols—particularly in the areas of functional potency assays and comprehensive characterization—will be essential for realizing the full therapeutic potential of MSC-based therapies. The integration of pharmacokinetic modeling and advanced tracking technologies will further enhance our understanding of MSC behavior in vivo, ultimately leading to more effective and predictable clinical outcomes [29].
The therapeutic application of Mesenchymal Stem Cells (MSCs) has undergone a fundamental paradigm shift over the past decade. Initially valued for their differentiation potential, MSCs are now recognized primarily for their paracrine secretions as the principal mechanism mediating tissue repair and immunomodulation [30]. This secretome, comprising a complex mixture of bioactive factors, includes soluble proteins (growth factors, cytokines, chemokines) and insoluble extracellular vesicles (EVs) that carry proteins, lipids, and nucleic acids [31] [30]. The recognition that MSC-derived conditioned medium (CM) alone can recapitulate many therapeutic effects of whole cells has launched a new era in cell-free regenerative therapies [32] [30]. This whitepaper provides a comprehensive technical guide to harnessing the MSC secretome, with detailed methodologies, signaling pathways, and quantitative analyses for research and therapeutic development.
Secretome Composition and Bioactive Components
The MSC secretome represents a sophisticated communication system that dynamically responds to environmental cues. Its composition varies significantly based on cell source, culture conditions, and environmental stimuli [30].
Table 1: Major Bioactive Components of the MSC Secretome
| Component Category | Key Representatives | Primary Functions |
|---|---|---|
| Growth Factors | VEGF, FGF-2, HGF, IGF-1 [32] | Angiogenesis, cell proliferation, cytoprotection |
| Cytokines/Chemokines | IL-6, IL-10, MCP-1, SDF-1 [32] | Immunomodulation, cell homing, inflammatory response |
| Extracellular Vesicles | Exosomes, microvesicles [33] | Intercellular communication, nucleic acid transfer |
| Lipids & Metabolites | Bioactive lipids, metabolites [30] | Energy regulation, membrane structure, signaling |
The soluble fraction directly influences cellular processes through receptor-mediated signaling, while EVs serve as natural delivery vehicles for functional RNAs (mRNA, miRNA), proteins, and lipids to recipient cells [34]. These EVs can fully fuse with target cell membranes, be internalized, or bind surface receptors to regulate signal transduction [34]. Importantly, preconditioning strategies such as 3D culture, hypoxic conditions, or inflammatory priming can significantly modulate secretome composition to enhance its therapeutic potential for specific applications [30].
Methodologies for Secretome Production and Characterization
Optimized Production Protocols
Standardized Conditioned Media Production from GMSCs [31]:
- Cell Source: Human gingiva-derived MSCs (GMSCs) from discarded dental tissues (IRB-approved)
- Culture Conditions:
- Control: α-MEM with 10% FBS, 1% antibiotics, 2mM L-glutamine
- Xeno-free Induction: Defined xeno-free medium (specific composition optimized for EV production)
- CM Collection: Serum-free conditioning for 48-72 hours from 70-80% confluent cultures
- Concentration: Ultrafiltration using molecular weight cutoff membranes
- EV Separation: 35nm qEVoriginal size exclusion columns for EV isolation from soluble factors
Scalable EV Production Workflow [35]:
- Cell Expansion: Culture MSCs in multilayer flasks or bioreactors under defined conditions
- EV Harvesting: Collect culture supernatant after 48-72 hours
- Clarification: Sequential centrifugation at 300 × g (10 min), 2,000 × g (20 min), and 10,000 × g (30 min) to remove cells and debris
- Concentration: Tangential flow filtration or ultrafiltration
- Purification: Density gradient centrifugation or size-exclusion chromatography
Comprehensive Characterization Techniques
Table 2: Essential Characterization Methods for Secretome Components
| Parameter | Method | Key Specifications | Expected Outcomes |
|---|---|---|---|
| EV Concentration & Size | Nanoparticle Tracking Analysis (NTA) [31] | Laser wavelength: 488nm; Camera: sCMOS; Measurements: 30-100nm range | Particle size distribution, concentration (particles/mL) |
| EV Morphology | Transmission Electron Microscopy (TEM) [31] | Acceleration voltage: 80-120kV; Staining: Uranyl acetate | Spherical, bilayer membrane structure confirmation |
| EV Marker Expression | Western Blot [31] | Antibodies: CD9, CD63, CD81, TSG101; Loading: 20μg protein/lane | Presence of tetraspanins, absence of calnexin |
| Protein Quantification | BCA/ Bradford Assay [31] | Sample dilution: 1:10-1:50; Standard: BSA | Total protein concentration in CM/secretome |
| Functional Cargo | RNA Sequencing/ Proteomics [31] | RNA integrity number >8.0; LC-MS/MS for proteins | miRNA, mRNA, protein cargo identification |
Quantitative Analysis of Secretome Potency
Rigorous quantitative assessment is essential for standardizing secretome-based therapeutics. The following data, derived from optimized GMSC cultures, demonstrates the enhanced potency achievable through culture condition optimization.
Table 3: Quantitative Comparison of Standard vs. Optimized GMSC Secretome
| Parameter | 2D-GMSC Secretome | iGMSC Secretome (Xeno-free) | Fold Change |
|---|---|---|---|
| EV Concentration | Baseline (2.0×10^10 particles/mL) [31] | 3.5×10^10 particles/mL [31] | 1.75× increase |
| IL-10 Secretion | Baseline [31] | Significantly enhanced [31] | Quantitative data not provided |
| TNF-α Suppression (LPS-stimulated) | Baseline [31] | Significantly suppressed [31] | Quantitative data not provided |
| Myogenic TF Induction | Baseline [31] | Potently induced [31] | Quantitative data not provided |
| In Vivo Tongue Regeneration | Moderate regeneration [31] | Promoted rapid tissue repair without fibrosis [31] | Qualitative improvement |
Gene ontology analysis of iGMSCs revealed significant upregulation of genes related to extracellular vesicles and secreted cellular components, with enriched pathways in oxidative phosphorylation, Wnt/β-catenin signaling, Notch signaling, and inflammatory responses compared to 2D-cultured counterparts [31].
Signaling Pathways and Mechanisms of Action
The therapeutic effects of the MSC secretome are mediated through multiple interconnected signaling pathways that regulate fundamental cellular processes.
The MSC secretome exerts its effects through three primary interconnected mechanisms: (1) Immunomodulation via macrophage polarization toward M2 anti-inflammatory phenotypes and T-cell regulation; (2) Tissue regeneration through direct stimulation of myogenic differentiation and angiogenesis; and (3) Cytoprotection through activation of anti-apoptotic pathways [31] [32] [30]. These pathways converge to promote a regenerative microenvironment characterized by reduced inflammation, enhanced progenitor cell differentiation, and diminished fibrosis.
Experimental Models and Functional Validation
In Vitro Functional Assays
Macrophage Polarization Assay [31]:
- Cell Source: Primary macrophages or cell lines (e.g., RAW264.7)
- Stimulation: LPS (100ng/mL) to induce M1 phenotype
- Treatment: Secretome/EV fractions (50-100μg/mL protein concentration)
- Readouts:
- ELISA for IL-10 (M2 marker) and TNF-α (M1 marker)
- Flow cytometry for CD206 (M2) and iNOS (M1)
- RNA analysis for M2/M1 gene signatures
Myogenic Differentiation Assay [31]:
- Cell Source: Murine myoblasts (C2C12) or human skeletal muscle progenitors
- Differentiation Conditions: Switch to 2% horse serum for 3-5 days
- Treatment: Secretome during differentiation phase
- Analysis:
- Immunofluorescence for MyoD, Myogenin, Myosin Heavy Chain
- qRT-PCR for myogenic transcriptional factors
- Fusion index calculation from multinucleated myotubes
In Vivo Validation Models
Rat Tongue Defect Model [31]:
- Animal: Female Sprague-Dawley rats (200-250g)
- Surgery: Creation of standardized tongue muscle defects
- Treatment: Topical application of secretome at excised wound bed
- Assessment:
- Histological analysis of tissue repair/regeneration
- Masson's trichrome staining for fibrosis/scar formation
- Morphometric analysis for shape deformity
- Functional recovery of tongue movement
Hypoxic-Ischemic Brain Injury Model [36]:
- Animal: Rodent models of cerebral hypoxic-ischemic injury
- Treatment: Intranasal or intracerebral administration of GDNF-enriched secretome
- Assessment:
- Immunohistochemistry for neuronal and glial markers
- Cognitive and motor function tests
- Quantification of infarct volume
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Secretome Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Cell Culture Media | α-MEM, DMEM/F12 [31] | MSC expansion and conditioning | Use xeno-free formulations for clinical translation |
| EV Separation Columns | qEVoriginal (35nm) [31] | Size-exclusion chromatography for EV isolation | Preserves EV integrity and function |
| Characterization Antibodies | CD9, CD63, CD81 [31] | EV marker detection via Western blot | Confirm absence of calnexin (negative control) |
| Ultrafiltration Devices | Amicon centrifugal filters [31] | Secretome concentration | Vary molecular weight cutoffs based on application |
| Nanoparticle Tracking | Malvern NanoSight [31] | EV concentration and size distribution | Standardize measurement conditions across experiments |
| Cytokine Arrays | Proteome profiler arrays [32] | Secreted factor screening | Enables comprehensive secretome analysis |
Clinical Translation and Regulatory Considerations
The transition of secretome-based therapies from research to clinical application requires careful attention to manufacturing standardization and quality control. Currently, 64 registered clinical trials are evaluating MSC-EVs for various conditions, including severe COVID-19, ischemic stroke, and complex wound healing [33] [34]. Key considerations for clinical translation include:
- Standardization: Development of Good Manufacturing Practice (GMP)-compliant protocols for consistent secretome production [30]
- Potency Metrics: Establishment of correlation between in vitro potency assays and in vivo efficacy
- Storage and Stability: Optimization of lyophilization protocols for long-term storage without bioactivity loss [31]
- Dosing Strategies: Determination of optimal dosing regimens, routes of administration, and treatment intervals
Engineering approaches, including genetic modification of parent MSCs to overexpress therapeutic factors (e.g., GDNF for neurological applications) and preconditioning strategies (3D culture, hypoxia, inflammatory priming), can further enhance the therapeutic potential of secretome products [36] [30].
The MSC secretome represents a promising cell-free therapeutic platform that harnesses the paracrine power of MSCs while mitigating risks associated with whole-cell transplantation. Through continued refinement of production methodologies, comprehensive characterization, and rigorous functional validation, secretome-based therapies are poised to transform regenerative medicine. The integration of engineering approaches to enhance secretome potency and specificity will further accelerate clinical translation, ultimately enabling new treatment paradigms for a broad spectrum of human diseases.
Clinical Applications in Graft-versus-Host Disease, Orthopedics, and Neurology
Mesenchymal stem cells (MSCs) are non-hematopoietic, multipotent stromal cells characterized by their capacity for self-renewal and differentiation into multiple mesodermal lineages, including osteoblasts, chondrocytes, and adipocytes [1]. The International Society for Cellular Therapy (ISCT) defines MSCs by three key criteria: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, CD105 ≥95%) while lacking expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) ability to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [1]. Originally identified in bone marrow, MSCs have since been isolated from various tissues, including adipose tissue, umbilical cord blood, dental pulp, and placental tissue [1] [37].
The therapeutic potential of MSCs extends beyond differentiation capacity to include profound immunomodulatory properties and paracrine effects through the release of bioactive molecules, including growth factors, cytokines, and extracellular vesicles [1]. These properties make MSCs highly promising candidates for regenerative medicine applications across a spectrum of human diseases. This review examines the clinical applications of MSCs in three distinct therapeutic areas—graft-versus-host disease, orthopedics, and neurology—within the broader context of basic MSC science.
Basic Science of Mesenchymal Stem Cells
Biological Properties and Signaling Pathways
The therapeutic effects of MSCs are mediated through complex signaling pathways and molecular mechanisms. MSCs can modulate immune responses by interacting with various immune cells, including T cells, B cells, dendritic cells, and macrophages, through both direct cell-cell contact and release of immunoregulatory molecules [1]. Key pathways involved in MSC function include:
- JAK-STAT Signaling: IL-6 and IFN-γ regulate immune cell function by activating the Janus kinase 1 (JAK1) signaling pathway, which can be inhibited by selective JAK1 inhibitors such as itacitinib [38].
- ROCK2 Signaling: In chronic graft-versus-host disease, ROCK2 activation upregulates Th17 transcription via STAT3, suppresses regulatory T cells, and regulates actin polymerization to reinforce fibrosis [38].
- TGF-β Signaling: Transforming growth factor beta plays crucial roles in MSC differentiation and immunomodulation, particularly in fibrotic processes and T-regulatory cell function [38].
The following diagram illustrates the key signaling pathways in MSC biology and their cross-talk with immune cells:
MSC Sourcing and Characterization
MSCs can be classified based on their tissue of origin, with each source exhibiting distinct properties:
- Bone Marrow-derived MSCs (BM-MSCs): The most extensively studied type, known for high differentiation potential and strong immunomodulatory effects [1].
- Adipose Tissue-derived MSCs (AD-MSCs): Easier to harvest with higher yields and comparable therapeutic properties to BM-MSCs [1].
- Umbilical Cord-derived MSCs (UC-MSCs): Enhanced proliferation capacity and lower immunogenicity, making them suitable for allogeneic transplantation [1].
- Dental Pulp Stem Cells (DP-SCs): Unique regenerative properties with specific applications in dental medicine [1].
Research Reagent Solutions for MSC Studies
Table 1: Essential Research Reagents for MSC Experimental Workflows
| Reagent Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| Surface Markers | CD73, CD90, CD105 [1] | MSC identification and characterization | Positive selection markers per ISCT criteria |
| Negative Markers | CD34, CD45, CD14, CD19, HLA-DR [1] | Purity assessment and contamination exclusion | Exclusion of hematopoietic lineage cells |
| Differentiation Media | Osteogenic: Dexamethasone, 1,25-dihydroxyvitamin D3 [1] | Lineage-specific differentiation capacity testing | Induction of osteoblast differentiation |
| Cytokines & Growth Factors | IFN-γ, IL-6, TGF-β [38] [1] | Immunomodulatory function assays | Priming MSCs for enhanced immunosuppressive activity |
| Culture Supplements | Fetal bovine serum, defined growth factors [1] | In vitro expansion and maintenance | Support MSC proliferation while maintaining multipotency |
Clinical Application 1: Graft-Versus-Host Disease (GVHD)
Pathophysiology and MSC Mechanisms
Graft-versus-host disease is a life-threatening complication of allogeneic hematopoietic stem cell transplantation that impairs clinical outcomes [38]. GVHD pathophysiology involves complex immune activation:
- Acute GVHD: Characterized by a three-stage "initiation-activation-effector" cascade centered on innate immunity-driven inflammatory responses [38].
- Chronic GVHD: Features immune dysregulation and fibrotic remodeling with abnormal B-cell activation and impaired regulatory T-cell function [38].
MSCs exert therapeutic effects in GVHD through multiple mechanisms:
- Direct inhibition of T-cell proliferation and activation
- Polarization of macrophages toward anti-inflammatory M2 phenotype
- Induction of regulatory T-cells and suppression of pro-inflammatory Th17 cells
- Secretion of paracrine factors that promote tissue repair and reduce inflammation [1]
The following diagram illustrates the pathophysiology of GVHD and MSC mechanisms of action:
Experimental Protocols for GVHD Research
Protocol 1: MSC Suppression of T-cell Proliferation Assay
- Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors by density gradient centrifugation
- Label PBMCs with cell proliferation dye (e.g., CFSE) at 1-5μM for 10 minutes at 37°C
- Activate T-cells using anti-CD3/CD28 antibodies or phytohemagglutinin (PHA)
- Co-culture activated PBMCs with MSCs at ratios from 1:1 to 10:1 (PBMC:MSC)
- Maintain co-cultures for 3-5 days in RPMI-1640 with 10% FBS
- Analyze T-cell proliferation by flow cytometry measuring CFSE dilution
- Quantify cytokine secretion (IFN-γ, TNF-α, IL-10) in supernatant by ELISA
Protocol 2: In Vivo Mouse Model of GVHD
- Use major histocompatibility complex (MHC)-mismatched donor-recipient pairs (e.g., C57BL/6 → BALB/c)
- Irradiate recipients with lethal dose (800-1100 cGy) 24 hours before transplantation
- Infuse donor bone marrow cells (5×10^6) and splenocytes (1-2×10^6) via tail vein
- Administer MSCs (0.5-1×10^6) on day 0 or day +2 post-transplantation
- Monitor clinical GVHD scores based on weight loss, posture, activity, and fur texture
- Assess survival daily and perform histological analysis of target organs (skin, liver, intestine) at endpoint
Clinical Trial Data and Biomarkers
Table 2: Biomarkers in GVHD Pathophysiology and MSC Response Monitoring
| Biomarker Category | Specific Examples | Pathophysiological Role | Response to MSC Therapy |
|---|---|---|---|
| Inflammation-driven | IL-6, IFN-γ, TNF-α [38] | Mediate cytokine storm in aGVHD | Decreased with effective MSC treatment |
| Tissue Damage | REG3α (intestinal), Elafin (skin) [38] | Specific epithelial injury markers | Reduction indicates tissue healing |
| Immunoregulatory | BAFF, Treg populations [38] | B-cell hyperactivity and immune dysregulation in cGVHD | Normalization of balance |
| Fibrosis-related | TGF-β, PDGF, ROCK2 [38] | Drive fibrotic remodeling in cGVHD | Decreased activity with MSC treatment |
Recent clinical advances include the phase 3 REACH3 trial demonstrating ruxolitinib as an evidence-supported option for steroid-refractory cGVHD, with higher response rates and durable disease control compared to best available therapy [39]. Belumosudil and axatilimab have also shown encouraging efficacy and safety in heavily pretreated populations [39]. The BMT CTN 1703 trial demonstrated superior GVHD-free/relapse-free survival for post-transplant cyclophosphamide (PT-Cy)-based GVHD prophylaxis versus tacrolimus/methotrexate [40].
Clinical Application 2: Orthopedic Disorders
MSC Mechanisms in Musculoskeletal Repair
MSCs contribute to orthopedic tissue repair through multiple mechanisms:
- Differentiation Potential: Capacity to differentiate into osteoblasts, chondrocytes, and tenocytes under specific induction conditions [1]
- Paracrine Signaling: Secretion of growth factors (VEGF, FGF, TGF-β) that promote angiogenesis, cell proliferation, and extracellular matrix synthesis [1]
- Immunomodulation: Reduction of inflammation in injured joints through suppression of pro-inflammatory cytokines [41]
- Matrix Remodeling: Secretion of enzymes and enzyme inhibitors that balance extracellular matrix degradation and synthesis [37]
Experimental Protocols for Orthopedic Research
Protocol 1: MSC Osteogenic Differentiation
- Culture MSCs to 70-80% confluence in growth medium
- Switch to osteogenic induction medium containing:
- 10 mM β-glycerophosphate
- 50 μM ascorbic acid-2-phosphate
- 100 nM dexamethasone
- 10% FBS in basal medium
- Change differentiation medium every 3-4 days for 21 days
- Assess mineralization by Alizarin Red S staining (2% solution, pH 4.2) for 10 minutes
- Quantify osteocalcin and osteopontin expression by RT-PCR or immunocytochemistry
- Measure alkaline phosphatase activity using p-nitrophenyl phosphate substrate
Protocol 2: Cartilage Defect Model
- Create full-thickness cartilage defects (3-4mm diameter) in rabbit or porcine knee joints
- Prepare MSC-seeded scaffolds using fibrin or collagen hydrogels at 10-20×10^6 cells/mL
- Implant MSC-scaffold constructs into cartilage defects
- Use cell-free scaffolds and empty defects as controls
- Assess cartilage repair at 8-12 weeks by:
- Macroscopic scoring using ICRS evaluation system
- Histological analysis (Safranin-O, Toluidine Blue staining)
- Mechanical testing of repair tissue
- Immunohistochemistry for collagen type II
Clinical Translation and Outcomes
Table 3: MSC Applications in Orthopedic Disorders: Clinical Evidence
| Condition | MSC Source | Delivery Method | Reported Outcomes | Evidence Level |
|---|---|---|---|---|
| Osteoarthritis | Adipose tissue, Bone marrow [41] | Intra-articular injection | Pain reduction, functional improvement, cartilage protection | Phase I/II trials |
| Bone Non-union | Bone marrow, Umbilical cord [41] | Scaffold-based delivery with bioceramics | Enhanced bone healing, bridging of defects | Case series, limited RCTs |
| Cartilage Defects | Autologous bone marrow [41] | Matrix-induced autologous chondrocyte implantation (MACI) | Improved cartilage quality, integration with native tissue | Registry studies |
| Spinal Fusion | Bone marrow aspirate [41] | Combination with structural grafts | Higher fusion rates, reduced pseudarthrosis | Comparative studies |
Clinical Application 3: Neurological Disorders
MSC Mechanisms in Neurological Repair
MSCs promote neurological recovery through diverse mechanisms:
- Neurotrophic Factor Secretion: Brain-derived neurotrophic factor (BDNF), glial cell line-derived neurotrophic factor (GDNF), and nerve growth factor (NGF) that support neuronal survival and axonal growth [41]
- Immunomodulation: Regulation of microglial activation and polarization toward neuroprotective phenotypes [41]
- Vascular Repair: Enhancement of angiogenesis through VEGF and angiopoietin secretion [42]
- Stimulation of Endogenous Repair: Activation of neural stem cells and progenitor cells through paracrine signaling [41]
Experimental Protocols for Neurological Research
Protocol 1: MSC Secretome Analysis
- Culture MSCs to 70-80% confluence in complete medium
- Wash cells and replace with serum-free medium for 24-48 hours
- Collect conditioned medium and concentrate using 3kD centrifugal filters
- Analyze secretome composition using:
- Proteomic analysis (LC-MS/MS) for protein identification
- Cytokine array for growth factors and cytokines
- Nanoparticle tracking analysis for extracellular vesicle quantification
- Western blot for specific proteins of interest
- Test functional effects of secretome on neuronal cultures or slice cultures
Protocol 2: Stroke Model Testing MSC Efficacy
- Induce middle cerebral artery occlusion (MCAO) in rats or mice
- Administer MSCs (1-2×10^6) via intravenous or intracerebral route 24 hours post-ischemia
- Assess functional recovery using:
- Neurological severity scores (0-18 scale) daily for 14 days
- Rotarod test for motor coordination
- Morris water maze for cognitive function
- Analyze histopathological outcomes at endpoint:
- Infarct volume measurement using TTC staining
- Immunofluorescence for neuronal markers (NeuN), synaptogenesis (synaptophysin), and angiogenesis (CD31)
- Inflammatory cell infiltration (Iba1 for microglia, CD45 for leukocytes)
The following workflow diagram illustrates the experimental approach for evaluating MSC therapies in neurological disorders:
Clinical Applications in Neurological Diseases
Stroke: MSC administration in animal stroke models demonstrates reduced infarct volume, improved functional recovery, and enhanced angiogenesis and neurogenesis [41]. Clinical trials have explored intravenous and intra-arterial delivery routes with emphasis on optimal timing and cell dosing.
Neurodegenerative Diseases: In Parkinson's disease models, MSCs differentiate into dopamine-producing neurons and secrete neurotrophic factors that protect remaining dopaminergic neurons [41]. Alzheimer's disease models show MSC-mediated reduction in amyloid-beta pathology and neuroinflammation.
Multiple Sclerosis: MSCs modulate autoimmune responses, reduce CNS inflammation, and promote remyelination in experimental autoimmune encephalomyelitis (EAE) models [41].
Emerging Technologies and Future Directions
Advanced Therapeutic Strategies
The field of MSC research is rapidly evolving with several emerging technologies:
- 3D Bioprinting and Tissue Engineering: Combination of MSCs with cutting-edge technologies like 3D bioprinting allows precise construction of complex tissue structures, advancing toward functional organ regeneration [42].
- Gene Editing: Integration of MSCs with gene editing techniques enables precise genetic modification for correcting disease-causing mutations and developing personalized therapies [42].
- Extracellular Vesicle Therapeutics: MSC-derived exosomes and extracellular vesicles contain miRNAs, mRNAs, and proteins with high therapeutic potential, offering cell-free alternatives with improved safety profiles [37].
- Priming and Preconditioning: Exposure of MSCs to specific cytokines (e.g., IFN-γ) or 3D culture conditions enhances their therapeutic properties through epigenetic and functional modifications [37].
Technical Considerations and Challenges
Several challenges remain in MSC-based therapies:
- Cell Homing and Engraftment: MSCs struggle to target damaged sites and have short half-lives in vivo [37].
- Senescence: MSCs have limited proliferation cycles, and the secretome from senescent MSCs has reduced therapeutic potential [37].
- Standardization: Great variability in MSC properties between donors, sources, and culture methods [37].
- Safety Concerns: Potential risks include undesired differentiation, tumorigenicity, and pro-inflammatory effects in certain conditions [43].
The International Society for Stem Cell Research (ISSCR) guidelines emphasize the need for rigorous scientific and ethical oversight in stem cell research and clinical translation [43]. These guidelines promote an ethical, practical, and sustainable approach to stem cell research and the development of cell therapies that can improve human health while ensuring patient safety.
Mesenchymal stem cells represent a promising therapeutic modality across diverse clinical applications, including graft-versus-host disease, orthopedic disorders, and neurological conditions. Their multimodal mechanisms of action—encompassing immunomodulation, trophic factor secretion, differentiation capacity, and tissue repair promotion—provide a strong scientific foundation for their therapeutic effects. While challenges remain in optimizing delivery, persistence, and standardization, emerging technologies in 3D bioprinting, gene editing, and extracellular vesicle therapeutics offer exciting avenues for enhancing MSC-based treatments. As research continues to address current limitations and refine therapeutic applications, MSCs hold substantial potential to revolutionize regenerative medicine across these clinically distinct but mechanistically connected fields.
Mesenchymal stem cells (MSCs) have emerged as a cornerstone of regenerative medicine, offering novel therapeutic paradigms for conditions spanning gynecologic health and autoimmune pathology. This whitepaper delineates the foundational science of MSCs, detailing their mechanistic roles in immunomodulation and tissue repair. It provides a critical analysis of their application in specific gynecological disorders and autoimmune diseases, supported by synthesized quantitative data and experimental workflows. The document is structured to serve researchers, scientists, and drug development professionals by integrating current research findings with practical methodological guidance, thereby framing MSC therapeutics within the broader context of basic science and translational research.
Mesenchymal stem cells (MSCs) are multipotent progenitor stromal cells characterized by their self-renewal capacity and ability to differentiate into multiple mesenchymal lineages, including osteoblasts, chondrocytes, and adipocytes [44] [1]. First identified in the bone marrow by Friedenstein and colleagues, MSCs are now known to be widely distributed across various tissues, presenting a unique tool for regenerative medicine [45] [1]. The International Society for Cellular Therapy (ISCT) established minimal criteria for defining MSCs: (1) adherence to plastic under standard culture conditions; (2) positive expression (≥95%) of surface markers CD105, CD73, and CD90, and negative expression (≤2%) of CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR; and (3) ability to differentiate into osteogenic, adipogenic, and chondrogenic lineages in vitro [4] [1]. These standards have been pivotal in standardizing research and bioprocessing protocols for clinical applications [44].
The therapeutic utility of MSCs extends beyond differentiation, heavily relying on their paracrine activity and immunomodulatory functions. MSCs secrete a diverse array of bioactive molecules—including growth factors, cytokines, and chemokines—that modulate the local cellular environment, promote tissue repair, and exert anti-inflammatory effects [44] [1]. Furthermore, their low immunogenicity and ability to migrate to sites of injury and inflammation ("homing") make them attractive for allogeneic transplantation and targeted therapy [44] [10]. The homing process is regulated by chemokines, cytokines, and growth factors, and is dependent on the expression of homing receptors like CXCR4 and activation of integrins [44].
MSC Applications in Gynecological Disorders
The exploration of MSCs in gynecology has advanced rapidly, with therapies derived from diverse sources—including bone marrow, adipose tissue, menstrual blood, umbilical cord, and placenta—undergoing extensive research and clinical trials [4] [46]. Key application areas include intrauterine adhesions (IUA), premature ovarian insufficiency (POI), endometriosis, polycystic ovary syndrome (PCOS), and pelvic floor dysfunction [4] [46].
Premature Ovarian Insufficiency (POI)
POI is a condition characterized by a decline in ovarian function in women under 40, leading to infertility and long-term health risks. MSC-based therapy has shown great promise in restoring ovarian function and fertility in POI animal models [47]. The therapeutic effect is largely mediated through the delivery of exosomes (MSC-EXO), which inhibit apoptosis of ovarian granulosa cells, reduce inflammatory response and fibrosis, and improve vascular function [47]. Sources such as human bone marrow, adipose tissue, umbilical cord, and menstrual blood have all demonstrated efficacy in restoring ovarian function [4] [47]. Notably, MSC-EXO offer advantages including a standardized extraction process, low immunogenicity, minimal tumorigenic risk, and reduced ethical concerns, making them highly suitable for clinical translation [47].
Intrauterine Adhesions (IUA)
IUA, often resulting from endometrial injury, can lead to infertility, amenorrhea, and recurrent pregnancy loss. MSCs contribute to endometrial regeneration and repair through their differentiation potential and paracrine secretions. Preclinical studies in animal models have shown that endometrial mesenchymal stem cells (eMSCs) and menstrual blood-derived MSCs (MenSCs) can effectively repair damaged endometrium [4]. MenSCs, in particular, are easily collected and exhibit a high proliferation rate, making them a promising candidate for individualized therapy [4]. Emerging strategies involve combining MSCs with biomaterial scaffolds, such as hydrogels, to improve cell retention and survival within the uterine cavity, thereby enhancing therapeutic outcomes [46].
Table 1: MSC Applications in Key Gynecological Disorders
| Disorder | Key MSC Mechanisms | Common MSC Sources | Research Phase |
|---|---|---|---|
| Premature Ovarian Insufficiency (POI) | Inhibit granulosa cell apoptosis, reduce inflammation/fibrosis, improve vascularization [47] | Bone Marrow, Umbilical Cord, Adipose Tissue, Menstrual Blood [4] [47] | Preclinical & Clinical Trials [47] |
| Intrauterine Adhesions (IUA) | Endometrial regeneration via differentiation and paracrine factors, anti-fibrosis [4] | Menstrual Blood, Endometrium, Bone Marrow, Umbilical Cord [4] [46] | Preclinical & Clinical Application [4] |
| Endometriosis | Immunomodulation, potential inhibition of lesion establishment [4] | Bone Marrow, Umbilical Cord [4] | Mechanistic Research [4] |
| Polycystic Ovary Syndrome (PCOS) | Improve ovarian morphology, restore hormonal balance [46] | Umbilical Cord, Adipose Tissue [46] | Preclinical Studies [4] [46] |
| Pelvic Floor Dysfunction | Tissue reinforcement, muscle regeneration, nerve repair [4] [46] | Adipose Tissue, Bone Marrow [4] [46] | Preclinical Research [4] |
MSC Applications in Autoimmune and Autoinflammatory Diseases
MSCs have emerged as a promising therapeutic strategy for severe autoimmune and autoinflammatory diseases, conditions often lacking curative treatment options. Their potent immunomodulatory properties allow them to regulate immune responses and reduce inflammation, offering a potential alternative to traditional immunosuppressive drugs, which can lead to tolerance and adverse effects [44] [45].
Immunomodulatory Mechanisms
The immunomodulatory functions of MSCs are primarily mediated through two key mechanisms: direct cell-to-cell contact with immune cells and the release of paracrine factors, including extracellular vesicles (EVs) and a wide array of soluble bioactive molecules [45] [1].
- Direct Cell Contact: MSCs directly interact with various immune cells, including T cells, B cells, natural killer (NK) cells, and dendritic cells (DCs). A critical pathway involves the programmed cell death-ligand 1 (PD-L1) on MSCs engaging with the PD-1 receptor on activated T cells. This interaction delivers an inhibitory signal that suppresses T cell proliferation and promotes the differentiation of regulatory T cells (Tregs), thereby restoring immune balance [45].
- Paracrine Activity: The secretion of molecules such as monocyte chemotactic protein-1 (MCP1), basic fibroblast growth factor-2 (FGF2), vascular endothelial growth factor (VEGF), and hepatocyte growth factor (HGF) plays a prominent role in regulating MSC migration and immunomodulation [44]. These factors can shift macrophages from a pro-inflammatory (M1) to an anti-inflammatory (M2) phenotype, suppress the activation and maturation of DCs, and inhibit the proliferation and antibody production of B cells [45] [1].
Specific Disease Applications
MSCs have been investigated for a range of autoimmune conditions. In rheumatoid arthritis (RA), MSCs can inhibit the proliferation of inflammatory T cells and reduce the production of pro-inflammatory cytokines like TNF-α and IFN-γ [45]. For systemic lupus erythematosus (SLE), MSC transplantation has been shown to ameliorate disease activity by inducing Tregs and suppressing autoreactive B cells [45]. Applications also extend to multiple sclerosis (MS), type 1 diabetes mellitus (T1DM), Crohn's disease, and graft-versus-host disease (GVHD), highlighting the broad potential of MSCs in modulating dysregulated immune responses [44] [45].
Experimental Protocols and Methodologies
Standardized Isolation and Characterization of MSCs
A critical foundation for MSC research is the consistent isolation and characterization of cells according to ISCT standards. The following protocol is adapted from multiple sources detailing methods for bone marrow-derived MSCs (BMSCs) and other tissues [4] [10].
Protocol 1: Isolation and Culture of Human Bone Marrow-Derived MSCs (BMSCs)
- Isolation: Aspirate bone marrow (e.g., from iliac crest). Dilute the aspirate 1:1 in phosphate-buffered saline (PBS) and centrifuge (e.g., 30 min at 3000 rpm) [10].
- Cell Preparation: Isolate the buffy coat (mononuclear cell layer). Wash and plate the cells in culture flasks [10].
- Culture: Use low-glucose Dulbecco's Modified Eagle Medium (LG-DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% antibiotic/antimycotic. Incubate at 37°C with 5% CO₂ [10].
- Expansion: After 3-5 days, remove non-adherent cells. Continuously culture the adherent cells, passaging them upon reaching 70-80% confluence to obtain the desired number of cells [4] [10].
Protocol 2: In Vitro Trilineage Differentiation Assay The multipotent differentiation capacity of MSCs must be confirmed through directed differentiation into osteocytes, adipocytes, and chondrocytes [4] [1].
- Osteogenic Differentiation: Culture MSCs in an induction medium containing dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate for 2-3 weeks. Differentiated osteoblasts can be identified by Alizarin Red S staining, which detects calcium deposits [1].
- Adipogenic Differentiation: Culture MSCs in a medium containing dexamethasone, indomethacin, and insulin for 1-3 weeks. Differentiated adipocytes containing lipid vacuoles can be stained with Oil Red O [1].
- Chondrogenic Differentiation: Pellet culture in a medium containing TGF-β (e.g., TGF-β3), dexamethasone, and ascorbate-2-phosphate for 3-4 weeks. The resulting cartilage pellet, rich in proteoglycans, can be sectioned and stained with Toluidine Blue or Alcian Blue [1].
Isolation of MSC-Derived Exosomes (MSC-EXO)
The therapeutic effects of MSCs are increasingly attributed to their secreted exosomes. Standardized isolation is crucial for research and therapy development [47].
Protocol 3: Extraction of MSC-EXO via Ultracentrifugation
- Conditioned Media Collection: Culture MSCs until 70-80% confluent, then replace medium with exosome-depleted serum media. Collect conditioned media after 24-48 hours [47].
- Initial Centrifugation: Centrifuge the media at 300 × g for 10 min to remove cells.
- Secondary Centrifugation: Centrifuge the supernatant at 2,000 × g for 20 min to remove dead cells and debris.
- Filtration: Filter the supernatant through a 0.22 μm filter.
- Ultracentrifugation: Centrifuge the filtered supernatant at 100,000 × g for 70 min at 4°C to pellet exosomes.
- Washing: Resuspend the pellet in PBS and centrifuge again at 100,000 × g for 70 min. The final pellet contains purified exosomes, which can be resuspended in PBS and stored at -80°C [47].
Table 2: Key Research Reagent Solutions for MSC Work
| Reagent / Material | Function / Application | Example Usage / Specification |
|---|---|---|
| LG-DMEM with FBS | Basal culture medium for MSC expansion [10] | LG-DMEM with 10% (V/V) FBS and 1% (W/V) antibiotic/antimycotic [10] |
| Collagenase Type I/II | Enzymatic digestion of tissues for MSC isolation [10] | Digestion of adipose tissue (Type I) or synovium (Type II) at 37°C [10] |
| Specific Induction Media | Directing MSC differentiation into specific lineages [1] | Contain specific inducing agents (e.g., dexamethasone, TGF-β, IBMX) for osteo-, chondro-, or adipogenesis [1] |
| Flow Cytometry Antibodies | Confirmation of MSC surface marker profile [4] | Positive: CD105, CD73, CD90 (≥95%). Negative: CD45, CD34, HLA-DR (≤2%) [4] [1] |
| IFN-γ (Interferon-gamma) | Pre-conditioning MSCs to enhance immunomodulation [45] | Pretreatment of MSCs to upregulate immunomodulatory factors like PD-L1 [45] |
Visualization of MSC Mechanisms
The following diagrams, generated using Graphviz DOT language, illustrate core concepts in MSC biology, including the homing mechanism and key immunomodulatory pathways.
Diagram 1: MSC Homing to Injury Sites
Diagram 2: MSC Immunomodulatory Mechanisms
MSCs represent a transformative frontier in treating gynecological disorders and autoimmune diseases, underpinned by their robust regenerative and immunomodulatory capacities. The transition from preclinical models to clinical application, however, presents significant challenges that must be addressed by future research. Key hurdles include achieving standardized, large-scale production of MSCs and their derivatives like exosomes, ensuring long-term safety and efficacy, and improving targeted delivery to specific tissues [4] [47].
Future research should focus on optimizing biomaterial scaffolds to enhance MSC retention and survival at injury sites [46]. Furthermore, a deeper understanding of the precise molecular mechanisms, particularly the role of mitochondrial transfer and the contents of the MSC secretome, will be crucial for developing more effective and safer cell-free therapies [45] [47]. As technology and research methodologies advance, MSC-based therapies are poised to play an increasingly prominent role in regenerative medicine, offering hope for treating a broad spectrum of currently intractable conditions.
Within regenerative medicine, mesenchymal stem cells (MSCs) have emerged as a cornerstone therapeutic agent due to their multipotent differentiation potential, immunomodulatory properties, and potent paracrine activity [1] [48]. The therapeutic efficacy of these cells is profoundly influenced by the method of delivery, which governs their biodistribution, engraftment, and ultimate mechanism of action [49] [50]. This review provides an in-depth technical analysis of the three primary administration routes—intravenous injection, local injection, and aerosolized inhalation—examining the underlying scientific principles, methodological protocols, and key applications for each to guide researchers and drug development professionals.
The Scientific Basis of MSC Therapeutics
MSCs are defined by their plastic-adherence, specific surface marker expression (CD73, CD90, CD105; lacking hematopoietic markers CD45, CD34, HLA-DR), and trilineage differentiation capacity [1] [4]. Their therapeutic effects are mediated not only through direct differentiation but significantly through paracrine signaling, via the secretion of growth factors, cytokines, and extracellular vesicles that modulate the immune system, inhibit apoptosis, and promote tissue repair [1] [48] [50]. The choice of administration route is critical, as it determines the microenvironment to which MSCs are exposed, thereby influencing their secretory profile and functional behavior [49].
Intravenous Administration
Principles and Workflow
Systemic intravenous (IV) delivery involves infusing MSCs directly into the venous circulation, allowing for widespread distribution throughout the body. This approach is particularly advantageous for treating systemic or multifocal diseases, as MSCs possess an innate tropism for sites of inflammation and injury [48] [50]. A key mechanistic feature is the pulmonary first-pass effect, where a significant proportion of initially infused cells are sequestered in the lung capillaries before reaching other organs [49].
The diagram below illustrates the journey and fate of MSCs after intravenous infusion.
Experimental Protocol
Title: Intravenous Injection of MSCs for Systemic Delivery
Materials:
- MSCs: Bone marrow or adipose-derived, passage 3-5.
- Vehicle: Sterile phosphate-buffered saline (PBS) or lactated Ringer's solution.
- Equipment: 1-3 mL syringes, 23-27G butterfly needles, cell counting apparatus.
Procedure:
- Cell Preparation: Harvest MSCs at 80-90% confluence using standard trypsinization. Wash and resuspend in the chosen sterile vehicle.
- Dosage Calculation: Prepare a final concentration of 1-10 million cells per kg of recipient body weight in a total volume of 1-10 mL for rodent models. Adjust volume for larger animals and humans.
- Infusion: Access a peripheral vein (tail vein in rodents; cephalic or saphenous in larger animals). Inject the cell suspension slowly over 3-5 minutes to prevent aggregation and embolization.
- Post-Procedure Monitoring: Observe for acute adverse reactions, such as respiratory distress or embolism.
Key Applications:
- Graft-versus-host disease (GvHD) [1] [4]
- Systemic inflammatory disorders [1]
- Neurological conditions (e.g., multiple sclerosis, cerebral ischemia) [50]
Local Injection
Principles and Workflow
Local injection delivers MSCs directly into the target tissue or anatomic compartment, maximizing the local cell concentration and minimizing systemic exposure. This approach is ideal for treating focal defects, such as damaged joints, cardiac tissue post-infarction, or localized areas of inflammation [48] [51]. The primary mechanism involves direct cell-matrix interaction and the localized release of paracrine factors, creating a regenerative microenvironment.
The following diagram outlines the key decision-making process for local injection protocols.
Experimental Protocol
Title: Intra-Articular Injection of MSCs for Knee Osteoarthritis
Materials:
- MSCs: Allogeneic or autologous MSCs from adipose tissue or bone marrow.
- Vehicle: Sterile saline, sometimes combined with hyaluronic acid or platelet-rich plasma (PRP).
- Equipment: 1 mL syringe, 25-27G needle, ultrasound machine for guidance, skin antiseptic.
Procedure:
- Patient/Target Positioning: Position the patient or animal to allow comfortable access to the knee joint, typically with the knee flexed.
- Site Preparation: Identify the injection site (typically the anterolateral or anteromedial joint space). Sterilize the area thoroughly.
- Cell Preparation: Resuspend MSCs at the desired dose (e.g., 10-100 million cells) in a small volume (0.5-5.0 mL) of vehicle.
- Injection: Under aseptic technique (and optionally ultrasound guidance), insert the needle into the joint space. Aspirate slightly to confirm extra-articular placement, then inject the cell suspension slowly.
- Post-Injection: Gently move the joint through its range of motion to distribute the cells. Monitor for local reactions like swelling or pain.
Key Applications:
Aerosolized Inhalation
Principles and Workflow
Aerosolized inhalation administers MSCs or, more commonly, their derived secretome (conditioned medium or exosomes) directly into the respiratory tract via nebulization. This route is non-invasive and targets the lungs with high bioavailability, avoiding first-pass metabolism [49] [52]. It is particularly suited for treating pulmonary diseases, where it leverages local anti-inflammatory, immunomodulatory, and tissue-repair effects [49] [53].
The workflow for nebulizing MSC-derived therapeutics is detailed below.
Experimental Protocol
Title: Nebulized MSC Secretome for Pulmonary Administration
Materials:
- Therapeutic Agent: MSC-conditioned medium (secretome) or purified exosomes.
- Nebulizer: Jet or vibrating mesh nebulizer with a particle size range of 1-5 µm for alveolar deposition.
- Vehicle: Sterile saline (0.9% NaCl).
Procedure:
- Secretome Preparation: Culture MSCs (e.g., human adipose-derived) in serum-free medium until confluent. Collect the supernatant after 48 hours. Centrifuge (300 g for 5 minutes) and filter through a 0.22 µm filter to remove cells and debris. Concentrate ~10 fold using a 3 kDa centrifugal filter unit [49].
- Formulation: Dilute the concentrated secretome or exosomes in sterile saline to the final volume (e.g., 2-5 mL). The particle count for exosomes can range from 1x10^10 to 1x10^11 particles per dose [53].
- Nebulization: Load the formulation into the nebulizer chamber. Administer the aerosol to the patient via a mouthpiece or facemask. A typical session lasts 10-20 minutes, twice daily [49].
- Monitoring: Assess pulmonary function (e.g., SpO₂, FEV1) and monitor for adverse events like cough or bronchospasm.
Key Applications:
- COVID-19-associated ARDS and pneumonia [49]
- Bronchiectasis and other chronic lung diseases [53]
- Acute lung injury and pulmonary fibrosis [52]
Comparative Analysis of Administration Routes
The choice of administration route involves critical trade-offs between targeting efficiency, cell retention, and safety. The table below provides a structured comparison of the technical parameters for the three routes.
Table 1: Quantitative and Qualitative Comparison of MSC Administration Routes
| Parameter | Intravenous | Local Injection | Aerosolized Inhalation |
|---|---|---|---|
| Target Tissues | Systemic; organs with high blood flow (lungs, liver, spleen) [50] | Focal areas (joints, heart, skin) [48] [51] | Lungs and airways [49] [53] |
| Typical Cell Dose (Human) | 1-10 million cells/kg [54] | 10-100 million per site [51] | N/A (Cell-free secretome is standard) |
| Therapeutic Onset | Rapid (systemic paracrine) [1] | Slower (local tissue remodeling) [51] | Rapid (local pulmonary action) [49] |
| Key Advantages | Treats multifocal disease; minimally invasive [48] | High local concentration; avoids pulmonary trap [10] | Non-invasive; targets lungs directly; high safety profile [49] |
| Primary Limitations | Pulmonary entrapment; potential systemic infusion reactions [49] | Invasive; technically demanding; potential for local injury [51] | Limited to pulmonary diseases; formulation stability [52] |
| Efficacy Evidence | Improved fatigue scores; reduced systemic inflammation [54] | Significant improvement in WOMAC/VAS scores in KOA [51] | Reduced ICU stay, improved oximetry in COVID-19 [49] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful MSC administration studies require carefully selected reagents and equipment. The following table catalogs key solutions and their applications in research protocols.
Table 2: Essential Research Reagents and Materials for MSC Administration Studies
| Reagent / Material | Function / Application | Example Usage in Protocols |
|---|---|---|
| LG-DMEM / αMEM Culture Medium | Standard base medium for MSC expansion and maintenance [10]. | Used in the initial culture and passage of BMSCs and SMSCs prior to administration [10]. |
| Fetal Bovine Serum (FBS) | Provides essential growth factors and nutrients for MSC proliferation in vitro [10]. | Supplemented at 10% (V/V) in the primary culture medium for MSC extraction and expansion [10]. |
| Collagenase Type I / II | Enzymatic digestion of tissues to isolate MSCs [10]. | Used for extracting MSCs from adipose tissue (Type I) and synovium (Type II) [10]. |
| Centrifugal Filter Unit (3 kDa MWCO) | Concentrates proteins and vesicles from the MSC secretome for inhalation studies [49]. | Used to achieve ~10-fold concentration of the conditioned medium prior to nebulization [49]. |
| Defined Surface Markers (CD73, CD90, CD105) | Quality control and phenotypic verification of MSCs via flow cytometry [1] [4]. | Used to confirm MSC identity (≥95% expression) before release for therapeutic use [4]. |
| Vibrating Mesh Nebulizer | Generates an aerosol with optimal particle size (1-5 µm) for deep lung delivery [49] [52]. | Device for administering MSC-conditioned medium or exosomes in preclinical and clinical settings [49] [53]. |
The routes of administering MSCs—intravenous, local, and aerosolized—are not merely technical choices but are fundamental to defining therapeutic outcomes. IV delivery offers a systemic solution, local injection ensures precise regional repair, and aerosolized inhalation provides targeted pulmonary treatment with a favorable safety profile. The ongoing refinement of these protocols, including the move toward cell-free secretome therapies, continues to enhance the precision and safety of regenerative medicine. Future research must focus on optimizing biodistribution, standardizing dosage, and conducting rigorous comparative trials to fully unlock the potential of MSC-based therapies.
Overcoming Clinical Hurdles: Engineering Next-Generation MSC Therapies
The therapeutic application of mesenchymal stem/stromal cells (MSCs) represents a cornerstone of modern regenerative medicine, offering promising treatments for conditions ranging from orthopedic injuries to autoimmune diseases. However, the translation of basic science into reliable clinical products faces a fundamental obstacle: heterogeneity. This variability manifests primarily through donor-specific differences and complex manufacturing challenges that significantly impact the biological properties and therapeutic efficacy of MSCs [55] [56]. Understanding and addressing these sources of heterogeneity is critical for advancing MSC research and developing standardized, effective therapies.
Donor variability encompasses differences in MSC properties arising from individual donor characteristics, including age, sex, and genetic background [57] [55]. Simultaneously, manufacturing challenges relate to how isolation, expansion, and preservation techniques can introduce additional variation that affects product quality and consistency [58] [59]. This technical review examines the core sources of heterogeneity, presents experimental approaches for its quantification, and discusses innovative strategies to overcome these challenges, providing researchers with a framework for advancing MSC-based regenerative applications.
Understanding the Multifaceted Nature of MSC Heterogeneity
The biological characteristics of MSCs are significantly influenced by donor-specific factors, creating substantial challenges for standardizing therapies. Research has demonstrated that sex-based differences profoundly affect MSC functionality. A 2023 preprint study revealed that MSCs from male donors exhibited significantly higher metabolic activity and proliferation rates, while female-derived MSCs demonstrated superior osteogenic response, evidenced by increased alkaline phosphatase activity, osteoprotegerin release, and mineral formation in vitro [57].
Donor age represents another critical variable. With aging, MSCs undergo functional decline characterized by cellular enlargement, telomere shortening, accumulation of DNA damage, impaired epigenetic regulation, and elevated levels of reactive oxygen species [55]. These age-related changes reduce MSC density in bone marrow and diminish osteogenic potential while promoting adipogenic differentiation [55]. Additionally, inter-individual variation persists even after accounting for age and sex, with significant differences observed in proliferation capacity, differentiation potential, and immunomodulatory strength among donors of similar demographics [60].
Table 1: Key Donor-Related Variables Impacting MSC Properties
| Variable | Biological Impact | Experimental Evidence |
|---|---|---|
| Donor Sex | Male: Higher proliferation | Metabolic activity significantly higher in male-derived MSCs [57] |
| Female: Enhanced osteogenesis | Increased alkaline phosphatase activity and mineral formation [57] | |
| Donor Age | Reduced osteogenic potential | Decreased bone marrow MSC density and mineralization capacity [55] |
| Increased adipogenic tendency | Shift in differentiation preference toward adipocytes [55] | |
| Cellular senescence markers | Telomere shortening, DNA damage accumulation [55] | |
| Inter-donor Variability | Differential immunomodulation | Varying anti-inflammatory effects in T cell-mediated hepatitis model [60] |
| Proliferation capacity differences | Correlation between proliferation rate and therapeutic efficacy [60] |
Tissue Source and Manufacturing-Induced Heterogeneity
The anatomical source of MSCs introduces another layer of complexity. While MSCs can be isolated from multiple tissues, including bone marrow, adipose tissue, umbilical cord, and dental pulp, each source confers distinct functional characteristics [1] [55]. Bone marrow-derived MSCs (BM-MSCs) remain the most extensively studied, known for their high differentiation potential and strong immunomodulatory effects [1]. Adipose tissue-derived MSCs (AD-MSCs) offer easier harvesting and higher yields, while umbilical cord-derived MSCs (UC-MSCs) exhibit enhanced proliferation capacity and lower immunogenicity, making them suitable for allogeneic transplantation [1].
Manufacturing processes introduce additional variability through culture expansion techniques. Sequential passaging and long-term culture progressively reduce MSC proliferation capacity and therapeutic potency [58]. The duration of cultivation and number of passages significantly differ among manufacturers and institutions, creating further standardization challenges [58]. The choice of culture supplements also critically impacts MSC properties, with fetal bovine serum (FBS) presenting safety concerns including potential adverse immunological reactions and high batch-to-batch variability [58]. These manufacturing-related variables compound inherent donor heterogeneity, creating substantial obstacles to producing consistent therapeutic products.
Experimental Approaches for Quantifying Heterogeneity
Methodologies for Assessing Donor Variability
Rigorous experimental characterization is essential for quantifying and understanding MSC heterogeneity. The International Society for Cell & Gene Therapy (ISCT) has established minimum criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD105, CD73, CD90 ≥95%; CD45, CD34, CD14, CD19, HLA-DR ≤2%), and trilineage differentiation potential [55] [56]. However, these criteria alone are insufficient for addressing functional heterogeneity, necessitating more sophisticated analytical approaches.
Growth Kinetics Analysis provides crucial information about proliferation capacity, a key parameter that correlates with therapeutic efficacy [60]. The experimental protocol involves:
- Seeding MSCs at standardized densities (e.g., 5 × 10³ cells/cm² for primary MSCs)
- Culturing until confluency with regular medium changes
- Harvesting using enzymatic digestion (e.g., TrypLE Select enzyme)
- Cell counting with viability assessment (e.g., Trypan Blue exclusion)
- Calculating population doubling time using the formula: Number of doublings = log₂(counted cells/seeded cells) [59]
Senescence Assessment evaluates cellular aging using Senescence-associated β-galactosidase (SA-β-gal) staining. The protocol entails:
- Fixing cells at various passages (e.g., P2, P5, P10 for MSCs; P8, P12, P16 for iMSCs)
- Incubating with SA-β-gal staining solution (commercially available kits)
- Imaging using standard microscopy (e.g., Leica-DM1 microscope)
- Quantifying positive cells using image analysis software (e.g., ImageJ) [59]
Trilineage Differentiation Assays determine multipotency through directed differentiation:
- Osteogenesis: Culture in DMEM-HG with 100 nM dexamethasone, 10 mM β-glycerophosphate, and 100 μM ascorbic acid for 21 days, with mineralization detected by Alizarin Red S staining [59]
- Adipogenesis: Induction with specific cocktails (typically including insulin, dexamethasone, and indomethacin) with lipid accumulation visualized by Oil Red O staining
- Chondrogenesis: Pellet culture in TGF-β supplemented media with sulfated proteoglycans detected by Alcian Blue staining
Advanced Analytical Techniques
Flow Cytometry enables comprehensive immunophenotyping beyond minimum ISCT criteria. The experimental methodology includes:
- Cell detachment using Triple Select Enzyme
- Staining with MSC phenotyping cocktail antibodies
- Data acquisition on flow cytometer
- Analysis using specialized software (e.g., FlowJo) with representation as log fluorescence intensity versus cell number [59]
Single-Cell RNA Sequencing provides unprecedented resolution of cellular heterogeneity by revealing distinct subpopulations within MSC cultures. Research has identified 12 distinct transcriptional subclusters that vary in proportion across different donors, with these subtle population differences crucially determining functional strength in immunomodulation [60]. This technique enables correlation of specific transcriptional signatures with functional outcomes, potentially identifying predictive biomarkers for therapeutic potency.
Functional Potency Assays measure specific therapeutic capabilities:
- Immunomodulatory Strength: Co-culture with Concanavalin A-stimulated immune cells or animal models of inflammation (e.g., Concanavalin A hepatitis model) with quantification of anti-inflammatory effects [60]
- Secretome Analysis: Characterization of paracrine factor secretion through proteomic analysis of conditioned media
- Angiogenic Potential: Endothelial tube formation assays to assess pro-angiogenic factor secretion
Manufacturing Challenges in MSC Production
Process-Induced Variability and Scalability Issues
The manufacturing of MSCs for clinical applications introduces substantial technical challenges that significantly impact product consistency and quality. The autologous nature of many MSC therapies creates inherent scalability limitations, as each batch is patient-specific and cannot benefit from traditional economies of scale [61]. This personalized approach requires dedicated manufacturing runs for individual patients, dramatically increasing complexity and cost compared to conventional pharmaceuticals.
Supply chain complexities present another critical challenge. The transport of patient-derived cells between collection sites and manufacturing facilities requires meticulous cold chain management to maintain cell viability and prevent contamination [61]. Any delays or temperature excursions during transportation can compromise product quality and therapeutic efficacy. Furthermore, the expansion process necessary to achieve clinical doses introduces replicative senescence and phenotypic drift, with prolonged culture leading to reduced multipotency and metabolic changes that diminish therapeutic properties [59].
The table below summarizes key manufacturing challenges and their impacts on MSC product quality:
Table 2: MSC Manufacturing Challenges and Quality Implications
| Manufacturing Stage | Key Challenges | Impact on MSC Quality |
|---|---|---|
| Cell Sourcing | Donor variability; Tissue source differences | Inherent biological heterogeneity; Variable potency [55] |
| Cell Expansion | Culture-induced senescence; Serial passaging | Reduced proliferation; Loss of stem-like properties [59] |
| Culture Conditions | FBS batch variability; Xenogeneic components | Immunological reactions; Inconsistent performance [58] |
| Scale-Up | Transition to bioreactors; 3D culture systems | Altered secretome; Changes in differentiation potential [58] |
| Quality Control | Functional potency assays; Release criteria | Limited predictive biomarkers; Difficult standardization [58] |
| Storage & Transport | Cryopreservation efficiency; Cold chain maintenance | Reduced viability; Functional impairment [61] |
Quality Control and Standardization Hurdles
Establishing robust quality control systems represents perhaps the most significant manufacturing challenge. The living nature of MSC products necessitates sophisticated potency assays that reliably predict therapeutic performance in vivo [58]. Current quality control typically includes assessment of identity, sterility, viability, purity, and potency, but correlating these parameters with clinical outcomes remains challenging [58]. The absence of universally accepted Critical Quality Attributes (CQAs) that predict therapeutic efficacy further complicates standardization efforts.
Regulatory frameworks for MSC therapies continue to evolve, requiring manufacturers to maintain compliance with Good Manufacturing Practice (GMP) regulations while navigating sometimes ambiguous guidelines [61]. The documentation requirements for chain of identity and chain of custody add additional layers of complexity to an already challenging manufacturing landscape. Furthermore, the transition from research-scale to commercial-scale production often reveals unanticipated interactions between process parameters and product quality, necessitating rigorous process characterization and validation studies.
Emerging Solutions and Standardization Strategies
Innovative approaches are emerging to address MSC heterogeneity and manufacturing challenges. iPSC-derived MSCs (iMSCs) represent a promising alternative to primary MSCs, offering the potential for unlimited expansion without senescence-related modifications [59]. However, recent studies indicate that iMSCs still exhibit batch-to-batch variability in differentiation capacity and extracellular vesicle biological properties, suggesting further refinement is needed [59].
Xeno-free culture systems eliminate animal-derived components that contribute to variability and safety concerns. Studies utilizing xeno-free supplements (XFS) have demonstrated enhanced MSC anti-inflammatory properties through secretion of chondroprotective molecules and therapeutic miRNA encapsulated in extracellular vesicles [59]. Additionally, advanced manufacturing platforms including closed-system bioreactors and automated processing equipment reduce manual manipulation and improve process consistency [61].
Analytical and Process Enhancement Strategies
Enhanced characterization technologies are critical for addressing heterogeneity. Single-cell RNA sequencing enables identification of predictive biomarkers and therapeutic subpopulations, facilitating development of potency markers [60]. Gene ontology analysis of differentially expressed genes has revealed activation in cell cycling and proliferation pathways correlated with stronger anti-inflammatory effects [60].
Process standardization initiatives focus on identifying and controlling critical process parameters. This includes developing defined culture media, standardized passage protocols, and consistent differentiation methods [61]. The implementation of process analytical technologies (PAT) allows real-time monitoring of critical quality attributes, enabling more consistent manufacturing outcomes.
Functional priming strategies enhance MSC therapeutic properties through preconditioning. Exposure to pro-inflammatory cytokines (e.g., IFN-γ, TNF-α) or hypoxic conditions can enhance immunomodulatory capacity and tissue-reparative functions, potentially overcoming inherent donor limitations [56]. Additionally, extracellular vesicle (EV) based therapies derived from MSCs offer cell-free alternatives that maintain therapeutic benefits while reducing risks associated with whole-cell transplantation [59].
Research Reagent Solutions for MSC Studies
Table 3: Essential Research Reagents for MSC Heterogeneity Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Culture Media | Alpha-MEM-GlutaMAX; DMEM-HG | Baseline culture medium for MSC expansion [59] |
| Xeno-Free Supplements | Purstem XFS; Human platelet lysate | Clinical-grade expansion without animal components [59] |
| Differentiation Kits | STEMdiff Mesoderm Induction; Osteo/Chondro/Adipogenic kits | Standardized trilineage differentiation assessment [59] [62] |
| Characterization Antibodies | CD105, CD73, CD90 positive selection; CD45, CD34, CD14 negative selection | Immunophenotyping per ISCT criteria [59] [56] |
| Senescence Detection | Senescence β-Galactosidase Staining Kit | Detection of senescent cells during long-term culture [59] |
| Extracellular Matrix | Fibronectin; Vitronectin; Laminin-111 | Defined substrates for differentiation and migration studies [62] |
| Enzymatic Dissociation | TrypLE Select; Triple Select Enzyme | Gentle cell detachment preserving surface markers [59] |
Addressing donor variability and manufacturing challenges is paramount for advancing MSC-based therapies from basic science to clinical applications. The heterogeneity inherent in MSC biology presents complex obstacles that require multifaceted solutions, including advanced characterization technologies, standardized manufacturing processes, and potentially novel cell sources like iMSCs. As our understanding of the molecular mechanisms underlying MSC heterogeneity improves, so too will our ability to produce more consistent and potent therapeutic products.
Future directions should focus on establishing predictive biomarkers that correlate with therapeutic efficacy, developing closed automated manufacturing systems that minimize process variation, and creating internationally harmonized standards for MSC characterization and quality control. By systematically addressing these challenges, the field can unlock the full potential of MSC-based regenerative medicine, transforming promising basic science into reliable clinical solutions for patients in need.
Improving Cell Survival, Engraftment, and Targeted Homing Post-Transplantation
The therapeutic potential of Mesenchymal Stem Cells (MSCs) in regenerative medicine is vastly limited by a critical post-transplantation bottleneck: extremely low cell survival and engraftment rates. Following transplantation, MSCs encounter a harsh, unfamiliar environment that leads to rapid cell death and inefficient homing to target tissues. Studies reveal that survival of MSCs in liver tissues was less than 5% 4 weeks after transplantation, with massive cell death occurring within the first 24 hours in fibrotic mouse livers and near-complete disappearance within 11 days [63]. This cell attrition represents the major bottleneck in realizing the full therapeutic potential of MSC-based therapies, as their beneficial effects depend critically on the number of viable cells that successfully reach and engraft within injured tissues [63] [64].
The fundamental challenge stems from the dramatic differences between optimized in vitro culture conditions and the stressful in vivo environment. After transplantation, MSCs face multiple stressors including hypoxia, oxidative stress, inflammatory cytokines, and anoikis (detachment-induced apoptosis) [63]. Furthermore, the process of homing to injury sites is inherently inefficient. The therapeutic functions of MSC transplantation rely on either paracrine/immunoregulatory actions (dependent on survival rates in vivo) or hepatic differentiation/fusion functions (dependent on the number of viable MSCs reaching injured liver tissues) [63]. Thus, enhancing MSC engraftment efficiency is paramount for maximizing therapeutic outcomes in regenerative medicine applications.
The Multistep Homing Process: Mechanisms and Barriers
The journey of administered MSCs to target tissues is a complex, multi-step process known as homing. Understanding this cascade is essential for developing strategies to improve its efficiency.
The Homing Cascade
The homing process involves five distinct but interconnected steps [63] [64]:
- Initial Tethering and Rolling: Weak, transient interactions between selectins on endothelial cells and their ligands on MSCs cause the cells to slow down and roll along the vascular endothelium.
- Activation: Chemokines present at the injury site activate G-protein coupled receptors on the rolling MSCs, triggering intracellular signaling that leads to integrin activation.
- Arrest and Firm Adhesion: Activated integrins mediate strong adhesion to immunoglobulin superfamily members on the endothelium, resulting in complete arrest of the MSCs.
- Diapedesis (Transmigration): MSCs crawl to endothelial cell junctions and cross the vascular barrier into the extravascular space using matrix remodelers such as matrix metalloproteinases (MMPs).
- Extravascular Migration: Guided by chemotactic gradients, MSCs migrate through the tissue parenchyma toward the injury site.
Each step in this homing process presents potential points of failure that can drastically reduce the number of MSCs ultimately reaching the target tissue [63].
Visualization of the Homing Process
The following diagram illustrates the multi-step homing cascade of MSCs to injured tissue sites.
Quantifying the Problem: Clinical Evidence of Low Engraftment
The challenge of poor MSC engraftment is substantiated by clinical evidence across multiple disease areas. The table below summarizes key findings from clinical studies that highlight the relationship between MSC survival, engraftment, and therapeutic outcomes.
Table 1: Clinical Evidence of MSC Engraftment Challenges and Outcomes
| Disease Context | Engraftment/Survival Evidence | Therapeutic Outcome | Reference |
|---|---|---|---|
| Liver Diseases (ESLD) | <5% MSC survival at 4 weeks; Massive cell death within 1 day | Improved 3- and 5-year survival in DLC patients | [63] |
| Decompensated Liver Cirrhosis | Low engraftment efficiency | Significant improvement in liver function biomarkers and long-term survival | [63] |
| Acute-on-Chronic Liver Failure | Insufficient delivery to liver | Increased 24-week survival rates; Reduced severe infections | [63] |
| Graft-versus-Host Disease | N/A (Recent FDA approval) | First MSC therapy (Ryoncil) approved for pediatric SR-aGVHD | [7] |
The inconsistency in therapeutic efficacy observed in many MSC clinical trials can be directly attributed to variations in engraftment efficiency. While MSC therapies have demonstrated promising results in conditions such as decompensated liver cirrhosis and acute graft-versus-host disease, the overall clinical translation has been hampered by the inability to ensure sufficient numbers of therapeutic cells reach and persist in target tissues [63] [7].
Strategic Approaches to Enhance MSC Survival and Homing
Four main strategic approaches have been developed to address the challenges of poor MSC survival and homing, each targeting different aspects of the engraftment process.
Preconditioning Strategies
Preconditioning involves exposing MSCs to sublethal stress in vitro to enhance their resilience to the harsh conditions encountered in vivo post-transplantation.
Hypoxic Preconditioning: Culture MSCs under low oxygen conditions (1-5% O₂) for 24-72 hours before transplantation. This activates hypoxia-inducible factor-1α (HIF-1α) signaling, upregulating pro-survival and angiogenic genes, thereby improving MSC resistance to subsequent hypoxic stress in vivo [63].
Cytokine and Drug Pretreatment: Incubate MSCs with specific cytokines or drugs prior to transplantation. Examples include:
- TNF-α pretreatment: Enhances MSC migration capacity by upregulating chemokine receptor expression [63].
- Melatonin pretreatment: Improves MSC survival and paracrine functions through activation of anti-apoptotic pathways [63].
Genetic Modification
Genetic engineering of MSCs to overexpress specific genes enhances their survival, homing, and therapeutic capabilities.
Protocol for CXCR4 Overexpression:
- Isplicate primary MSCs from donor tissue (bone marrow, adipose tissue, or umbilical cord).
- Culture MSCs in appropriate medium until 70-80% confluency.
- Transduce MSCs with lentiviral vectors encoding CXCR4 and a selectable marker (e.g., GFP).
- Select successfully transduced cells using antibiotic selection (e.g., puromycin) or FACS sorting for GFP-positive cells.
- Validate CXCR4 expression by flow cytometry or Western blot before transplantation [63].
This modification enhances homing to injury sites expressing SDF-1, the natural ligand for CXCR4. Other target genes include Akt1 (enhances survival), HGF (improves regenerative potential), and integrin subunits (enhances adhesion) [63].
Cell Surface Engineering
This approach directly modifies the MSC surface to improve targeting and adhesion.
Protocol for Click Chemistry-Mediated Surface Engineering:
- Metabolically label MSCs with azide-modified sugars (Ac4ManNAz) for 2-3 days to incorporate azide groups into surface glycoproteins.
- Conjugate cyclo-RGDfK (or other targeting peptides) to DBCO (dibenzocyclooctyne) groups via NHS ester chemistry.
- Incubate azide-labeled MSCs with DBCO-RGD conjugates for 1-2 hours at room temperature.
- Wash cells thoroughly to remove unbound conjugates before transplantation [64].
This method enhances MSC adhesion to injured endothelium by presenting high densities of integrin-binding RGD peptides on the MSC surface.
Biomaterial-Based Delivery Systems
Biomaterials can protect MSCs during delivery and provide a supportive microenvironment post-transplantation.
Hydrogel Encapsulation Protocol:
- Prepare a sterile solution of biocompatible hydrogel (e.g., alginate, collagen, or PEG-based).
- Mix MSCs with the hydrogel precursor solution at a density of 5-20 × 10⁶ cells/mL.
- Crosslink the hydrogel to encapsulate MSCs using appropriate methods (ionic crosslinking for alginate, thermal gelation for collagen, UV light for PEG).
- Transplant the MSC-laden hydrogel to the target site via injection or surgical implantation.
Hydrogels can be further modified with adhesion peptides (RGD) or controlled release of homing factors (SDF-1) to enhance engraftment [64].
Experimental Workflow for Evaluating Homing and Engraftment
A comprehensive assessment of MSC homing and engraftment requires integrated methodologies spanning from in vitro characterization to in vivo tracking. The following workflow provides a systematic approach for evaluating the effectiveness of homing enhancement strategies.
In Vitro Characterization Methods
Transwell Migration Assay:
- Seed serum-starved MSCs (5 × 10⁴ cells) in the upper chamber of a Transwell insert (5-8 μm pore size).
- Add chemoattractant (e.g., 10-100 ng/mL SDF-1) to the lower chamber.
- Incubate for 6-24 hours at 37°C.
- Remove non-migrated cells from the upper chamber with a cotton swab.
- Fix migrated cells with 4% PFA and stain with 0.1% crystal violet.
- Count migrated cells in 5 random fields under a microscope or extract dye with 10% acetic acid for spectrophotometric quantification at 560 nm [63].
Flow Cytometry for Homing Receptor Expression:
- Harvest MSCs and wash with FACS buffer (PBS + 1% FBS).
- Incubate with antibodies against homing receptors (e.g., anti-CXCR4, anti-Integrins, anti-CD44) for 30 minutes on ice.
- Wash cells and analyze using a flow cytometer.
- Compare receptor expression levels between untreated and engineered MSCs [63] [1].
In Vivo Tracking Methods
Bioluminescence Imaging (BLI) Protocol:
- Engineer MSCs to express luciferase (e.g., Firefly or Gaussia luciferase).
- Administer engineered MSCs to animal models via appropriate route (IV, IP, or local injection).
- Inject animals with luciferin substrate (150 mg/kg, IP) 5-15 minutes before imaging.
- Anesthetize animals and image using an IVIS or similar imaging system.
- Quantify signal intensity in target organs versus background over time (e.g., 1, 3, 7, 14 days post-transplantation) [63].
Quantum Dot Labeling for High-Resolution Tracking:
- Incubate MSCs with CdSe/ZnS core-shell quantum dots (655 nm emission) at 5-20 nM concentration for 4-24 hours.
- Wash cells thoroughly to remove unincorporated quantum dots.
- Administer labeled MSCs to animal models.
- Track cell distribution using fluorescence imaging systems or analyze tissue sections post-sacrifice [64].
Tissue Analysis Methods
Immunohistochemistry for Engrafted MSCs:
- Harvest target tissues at designated time points and fix in 4% PFA.
- Embed in paraffin and section at 5-10 μm thickness.
- Perform antigen retrieval (e.g., citrate buffer, 95°C, 20 minutes).
- Block with 5% normal serum from secondary antibody host species.
- Incubate with primary antibodies against human-specific markers (e.g., anti-human nuclei antigen for human MSCs in mouse models).
- Detect with appropriate fluorescent or enzyme-conjugated secondary antibodies.
- Counterstain with DAPI and image using fluorescence or brightfield microscopy [63].
Quantitative PCR for Human-Specific DNA:
- Extract genomic DNA from mouse tissues harboring human MSCs.
- Perform qPCR with primers specific for human Alu repeats or other human-specific sequences.
- Generate a standard curve using known mixtures of human and mouse DNA.
- Quantify the percentage of human DNA in each sample to estimate MSC engraftment [63].
Table 2: Key Research Reagents for MSC Homing and Engraftment Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Homing Receptor Antibodies | Anti-CXCR4, Anti-Integrin α4/β1, Anti-CD44 | Flow cytometry, Immunostaining | Detection and quantification of homing receptor expression |
| Chemoattractants | SDF-1/CXCL12, HGF, MCP-1 | Transwell migration assays | In vitro assessment of MSC migratory capacity |
| Genetic Modification Tools | Lentiviral vectors (CXCR4, Akt1), CRISPR/Cas9 | Genetic engineering | Enhancement of homing and survival capabilities |
| Cell Tracking Agents | Luciferase reporters, Quantum dots, MRI contrast agents | In vivo cell tracking | Non-invasive monitoring of MSC distribution and persistence |
| Cell Culture Supplements | Melatonin, TNF-α, Hypoxia mimetics (DFO) | Preconditioning strategies | Enhancement of MSC resilience to stress |
| Biomaterial Systems | Alginate hydrogels, RGD-functionalized PEG | Cell delivery platforms | Protection of MSCs and enhancement of retention |
| Cell Surface Markers | CD73, CD90, CD105, CD14, CD34, CD45 | MSC characterization and isolation | Validation of MSC phenotype and purity [1] |
Emerging Technologies and Future Directions
The field of MSC engraftment enhancement is rapidly evolving with several promising technological advances.
Advanced Imaging and AI-Based Prediction
Recent breakthroughs in quantitative phase imaging (QPI) with machine learning enable non-invasive, label-free monitoring of live cells and prediction of stem cell diversity and functional quality based on temporal kinetics [65]. This technology allows researchers to:
- Analyze cellular kinetics of individual stem cells to discover previously undetectable diversity
- Quantitatively evaluate stemness at the single-cell level
- Leverage temporal information to significantly improve prediction accuracy of stem cell function
- Move from snapshot-based identification to dynamic, time-resolved prediction of functional quality [65]
iPSC-Derived MSCs
The emergence of induced pluripotent stem cell-derived MSCs (iMSCs) offers enhanced consistency, scalability, and potentially improved homing capabilities compared to primary MSCs. While not yet FDA-approved, iMSCs are gaining momentum in regenerative medicine trials targeting conditions such as osteoarthritis, tissue repair, and high-risk acute graft-versus-host disease [7].
Clinical Translation and Regulatory Landscape
The clinical translation of MSC therapies has reached significant milestones with recent FDA approvals:
- Ryoncil (remestemcel-L): First MSC therapy approved for pediatric steroid-refractory acute graft-versus-host disease (December 2024) [7]
- Multiple iPSC-based therapies: Receiving FDA IND clearance for various conditions including retinal degeneration, Parkinson's disease, and spinal cord injury [7]
The continued advancement of strategies to enhance MSC survival and homing remains critical for realizing the full potential of these emerging therapies in regenerative medicine.
CRISPR/Cas9 Engineering for Enhanced Immunomodulation and Immune Evasion
Within the broader thesis on the basic science of mesenchymal stem cells (MSCs) in regenerative medicine, a significant challenge persists: the translational gap between their demonstrated therapeutic potential and consistent clinical efficacy. While MSCs possess potent intrinsic immunomodulatory properties and have been introduced as a cornerstone of regenerative medicine for autoimmune and inflammatory disorders, their clinical application is often restricted due to immune rejection and heterogeneity in immunoregulatory responses [66] [67]. The advent of Clustered Regularly Interspaced Short Palindromic Repeats/CRISPR-associated protein 9 (CRISPR/Cas9) technology has revolutionized MSC engineering, enabling precise genetic modifications to enhance their immunological efficacy [66]. This whitepaper explores how CRISPR-mediated editing of MSCs can mitigate immunogenicity, amplify anti-inflammatory functions, and repurpose MSCs for targeted immunotherapy, thereby addressing fundamental biological barriers in regenerative medicine.
The CRISPR/Cas9 system, derived from a bacterial adaptive immune mechanism, provides an unprecedented tool for precise genomic modification. Its core components include a guide RNA (gRNA) that directs the Cas9 nuclease to specific DNA sequences, inducing a double-strand break (DSB) [68]. The cell's subsequent repair mechanisms—nonhomologous end joining (NHEJ) or homology-directed repair (HDR)—enable targeted gene knockout or knock-in, respectively [68]. Beyond the canonical Cas9, an expanding toolkit offers refined applications for MSC engineering, as detailed in Table 1.
Table 1: CRISPR Systems and Their Applications in MSC Engineering
| CRISPR System | Editing/Function | Key Features | Evidence in MSCs |
|---|---|---|---|
| Cas9 | DNA double-strand break (knockout/knock-in) | Most widely used; NGG PAM requirement | Applied for knockout of immunogenicity-related genes (β2M, CIITA) [66] |
| dCas9 (CRISPRi/a) | Transcriptional repression (CRISPRi) or activation (CRISPRa) | Catalytically inactive Cas9 fused to repressors/activators | Used in MSCs to activate anti-inflammatory genes (e.g., IL-10, TSG-6) [66] |
| Cas12a (Cpf1) | DNA cleavage with staggered ends | Distinct PAM (TTTV); shorter gRNAs; sticky-end cuts | Validated in mammalian cells; potential for MSC editing [66] |
| Cas13 | RNA targeting and cleavage | Targets RNA instead of DNA; transient and reversible | High potential for modulation of cytokine or immune transcripts [66] |
The necessity of CRISPR in advancing MSC-based therapies stems from its unparalleled ability to overcome key challenges. It permits for the precise and efficient modification of MSCs to enhance specific therapeutic traits, standardize cell product quality, and, crucially, overcome immunological barriers that hinder their efficacy [66]. This profound capability renders CRISPR an indispensable tool for realizing the therapeutic promise of MSCs in the complex realm of immune-mediated disorders and regenerative medicine [66] [67].
Core Engineering Strategies: Protocols and Data
Engineering "Immune Stealth" MSCs through HLA Disruption
A paramount challenge for allogeneic MSC therapies is host immune recognition and rejection, primarily mediated by Major Histocompatibility Complex Class I (MHC-I) molecules [66] [67].
Detailed Experimental Protocol for β2-Microglobulin (B2M) Knockout:
- gRNA Design: Design one or more sgRNAs targeting the coding sequence of the B2M gene (e.g., within the first few exons). A sample target sequence is
5'-GTAGCGGCTGAATTCAGATG-3'. - Vector Construction: Clone the sgRNA sequence into a CRISPR/Cas9 plasmid backbone (e.g., spCas9) under a U6 promoter. For enhanced efficiency, a dual-guRNA strategy can be employed.
- MSC Transfection: Transfect human umbilical cord MSCs (UC-MSCs) or iPSC-derived MSCs at 70-80% confluence using a nucleofection system optimized for primary cells.
- Clonal Selection: After 48-72 hours, isolate single cells by fluorescence-activated cell sorting (FACS) or limiting dilution into 96-well plates.
- Genotype Validation: Expand clonal lines and validate knockout efficiency.
- Genomic DNA PCR: Amplify the targeted region of the B2M gene.
- T7 Endonuclease I Assay: Survey for indel mutations.
- Sanger Sequencing: Confirm the exact sequence modification in selected clones.
- Flow Cytometry: Confirm the loss of MHC-I (HLA-A,B,C) surface expression using specific antibodies.
Key Data: Studies have demonstrated that CRISPR-mediated deletion of B2M in various MSC sources significantly abrogates HLA class I surface expression [67]. This modification profoundly impacts MSCs' interaction with the host immune system, leading to a marked suppression of T-cell proliferation, activation, and infiltration [66]. For instance, in models of cardiac repair, β2M-deleted UMSCs effectively suppressed CD8+ T cell activation and infiltration, modulated the immune microenvironment by reducing pro-inflammatory mediators like IFN-γ and TNF-α, and consequently enhanced stem cell survival and engraftment [67].
Augmenting Anti-Inflammatory Functions
CRISPR activation (CRISPRa) systems can be deployed to overexpress key immunomodulatory mediators without altering the native genomic sequence.
Detailed Experimental Protocol for TSG-6 Activation using dCas9:
- sgRNA Design: Design sgRNAs to target the promoter region of the TNFAIP6 (TSG-6) gene. These guides should be positioned to recruit transcriptional activators effectively.
- CRISPRa Vector Construction: Utilize a plasmid encoding a nuclease-dead Cas9 (dCas9) fused to a transcriptional activator complex, such as the VP64-p65-Rta (VPR) tripartite activator. Clone the specific TNFAIP6-targeting sgRNAs into this vector.
- MSC Transfection and Selection: Transfect MSCs and select stable pools or clones using a resistance marker (e.g., puromycin) over 1-2 weeks.
- Phenotypic Validation:
- qRT-PCR: Measure TNFAIP6 mRNA levels 5-7 days post-transfection.
- ELISA/Western Blot: Quantify TSG-6 protein secretion in the cell culture supernatant.
- Functional Co-culture Assay: Co-culture engineered MSCs with LPS-activated macrophages and measure the subsequent levels of secreted TNF-α and IL-1β to validate enhanced anti-inflammatory capacity.
Key Data: Engineered MSCs with augmented TSG-6 expression have demonstrated superior efficacy in dampening macrophage-mediated inflammation and promoting a regulatory phenotype, which is critical for treating conditions like rheumatoid arthritis [66].
Table 2: Key Gene Targets for Enhancing MSC Immunomodulation
| Target Gene | Engineering Strategy | Molecular/Functional Outcome | Therapeutic Application |
|---|---|---|---|
| B2M | Knockout (Cas9) | Abrogates MHC-I expression; evades CD8+ T-cell recognition | Universal "off-the-shelf" therapy [66] [67] |
| CIITA | Knockout (Cas9) | Abrogates MHC-II expression; evades CD4+ T-cell recognition | Universal "off-the-shelf" therapy [67] |
| TNFAIP6 (TSG-6) | Overexpression (dCas9-VPR) | Potent anti-inflammatory, protects from TLR4/NF-κB signaling | Rheumatoid Arthritis, IBD [66] |
| IL-10 | Overexpression (dCas9-VPR) | Suppresses pro-inflammatory cytokine secretion; promotes Treg induction | Autoimmune Encephalomyelitis, GVHD [66] |
| TLR4 | Knockout (Cas9) | Reduces responsiveness to pro-inflammatory signals; enhances survival in inflamed sites | Therapy in high-inflammatory milieus [66] |
Engineering Strategy Selection
The Scientist's Toolkit: Essential Research Reagents
Successful CRISPR-mediated engineering of MSCs requires a carefully selected set of reagents and rigorous validation protocols. The following table details the essential components of the research toolkit.
Table 3: Research Reagent Solutions for CRISPR MSC Engineering
| Reagent / Tool Category | Specific Examples & Specifications | Critical Function |
|---|---|---|
| CRISPR Nuclease System | High-fidelity SpCas9 (e.g., HiFi Cas9), dCas9-VPR transcriptional activator | Executes precise DNA cleavage or targeted gene activation without cleavage [66] [68] |
| Delivery Method | Nucleofection (e.g., Lonza 4D-Nucleofector), Lipofection (for MSCs with high transfection efficiency) | Enables efficient intracellular delivery of CRISPR ribonucleoproteins (RNPs) or plasmids [69] |
| gRNA Design & Validation | In silico design tools (e.g., CRISPick, CHOPCHOP), T7 Endonuclease I assay, NGS-based amplicon sequencing | Ensures high on-target activity and identifies potential off-target sites; validates editing efficiency [68] |
| Cell Culture & Selection | Defined MSC culture media (e.g., MEM-α, supplemented with FGF-2), Puromycin/Geneticin (G418) for stable selection | Maintains MSC potency and phenotype during expansion; selects successfully transfected/transduced cells [1] [4] |
| Phenotypic Validation | Flow cytometry antibodies (e.g., anti-HLA-ABC, CD73, CD90, CD105), ELISA kits for cytokine secretion (e.g., TSG-6, IL-10) | Confirms surface marker expression, loss of immunogenic markers, and secretion of therapeutic factors [1] [67] |
| Functional Assays | Mixed Lymphocyte Reaction (MLR), T-cell suppression assay, Macrophage polarization co-culture | Quantifies the immunomodulatory capacity and immune evasion of engineered MSCs in vitro [66] [45] |
Experimental Workflow
CRISPR/Cas9-mediated engineering represents a transformative approach to overcoming the inherent immunological barriers that have limited the clinical translation of mesenchymal stem cells. By enabling the precise creation of "immune stealth" MSCs through B2M and CIITA knockout, and the enhancement of their therapeutic potency via the targeted upregulation of factors like TSG-6 and IL-10, this technology directly addresses core challenges in the basic science of regenerative medicine [66] [67]. The structured experimental protocols and reagent toolkit provided herein offer a foundational roadmap for researchers and drug development professionals to engineer next-generation MSC-based therapies. As the CRISPR toolkit continues to expand with systems like base editors and prime editors, the precision and safety of these genetic modifications will further improve, paving the way for universal, off-the-shelf MSC products capable of treating a wide spectrum of immune-mediated and degenerative diseases without the burden of host rejection.
Strategies to Combat Cellular Senescence and Replicative Aging
Within the broader thesis on the basic science of mesenchymal stem cells (MSCs) in regenerative medicine, understanding and combating cellular senescence represents a pivotal research frontier. MSCs, multipotent stromal cells characterized by their plastic adherence, specific surface marker expression (CD73+, CD90+, CD105+, CD14-, CD34-, CD45-), and tri-lineage differentiation potential, possess immense therapeutic promise [70]. However, their clinical utility is fundamentally constrained by replicative senescence—the irreversible cell cycle arrest occurring after a finite number of divisions—and stress-induced premature senescence [71]. This in-depth technical guide synthesizes current advances in the mechanistic understanding of MSC senescence and outlines targeted strategies to counteract this process, thereby enhancing the efficacy and safety of MSC-based regenerative therapies. The progressive accumulation of senescent MSCs not only diminishes the in vitro expansion potential necessary for therapeutic dosing but also contributes to an aging tissue microenvironment through the senescence-associated secretory phenotype (SASP), ultimately impairing tissue repair and regeneration in vivo [72] [73].
Molecular Mechanisms of MSC Senescence
Primary Drivers of Senescence
Cellular senescence in MSCs is a complex, multifactorial process initiated by various intrinsic and extrinsic stressors. The primary molecular pathways involved are summarized below:
- Replicative Senescence and Telomere Attrition: With each cell division, the ends of chromosomes (telomeres) shorten due to the end-replication problem. Critically short telomeres are recognized as DNA damage, triggering a persistent DNA damage response (DDR) and leading to p53/p21-mediated cell cycle arrest. Oxidative stress accelerates this process by preferentially damaging guanine-rich telomeric sequences [74] [75].
- Oncogene-Induced Senescence (OIS): Hyperactivation of oncogenes such as RAS or RAF drives aberrant proliferation, resulting in replication stress and DDR activation. OIS acts as an innate tumor-suppressive mechanism in MSCs [76].
- Epigenetic Alterations: Senescence involves extensive chromatin remodeling, including loss of heterochromatin marks (e.g., H3K9me3, H3K27me3), derepression of the CDKN2A/p16INK4a locus, and changes in N6-methyladenosine (m6A) RNA methylation, which collectively alter gene expression patterns [74] [75].
- Mitochondrial Dysfunction (MiDAS): Dysfunctional mitochondria exhibit elevated reactive oxygen species (ROS) production, impaired mitophagy, and disrupted metabolic homeostasis, contributing to a reinforced senescent state [76] [74].
- SASP and Paracrine Senescence: Senescent MSCs secrete a plethora of pro-inflammatory factors (IL-6, IL-8, IL-1β), chemokines, growth factors, and matrix metalloproteinases (MMPs). This SASP facilitates immune-mediated clearance of senescent cells but, paradoxically, can also induce senescence in neighboring healthy cells and create a chronic inflammatory microenvironment detrimental to tissue function [77] [76].
The following diagram illustrates the core signaling pathways involved in the initiation and maintenance of cellular senescence:
Functional Consequences of MSC Senescence
The molecular drivers of senescence translate into measurable functional declines critical for regenerative applications:
- Reduced Proliferative Capacity: Senescent MSCs undergo irreversible growth arrest, reaching the Hayflick limit after approximately 14-31 cumulative population doublings in vitro, severely limiting the cell yield for therapies [71].
- Impaired Multipotency: Replicative senescence alters differentiation potential, often skewing MSC fate towards osteogenic lineage at the expense of adipogenic and chondrogenic capacity [71].
- Loss of Homing and Engraftment Efficiency: Aged MSCs exhibit decreased expression of homing receptors (e.g., CXCR4), reducing their migration to injury sites post-transplantation [70].
- SASP-Mediated Tissue Dysfunction: The persistent pro-inflammatory SASP from accumulated MSCs contributes to chronic inflammation (inflammaging), immune dysregulation, and extracellular matrix (ECM) degradation in the host tissue [73].
Therapeutic Strategies to Counteract MSC Senescence
Senolytics and Senomorphics
Senolytics are a class of drugs that selectively induce apoptosis in senescent cells, thereby clearing them from cultures or tissues. Senomorphics suppress the harmful SASP without killing the senescent cell.
Table 1: Key Senolytic and Senomorphic Compounds
| Compound / Strategy | Class / Type | Proposed Mechanism of Action | Experimental Evidence in MSC Context |
|---|---|---|---|
| Dasatinib + Quercetin (D+Q) [77] | Senolytic Cocktail | BCL-2 family inhibition; Tyrosine kinase inhibition | Preclinical studies show reduced SA-β-Gal+ MSCs; improved tissue regeneration in aged models. |
| Fisetin [77] | Senolytic (Natural flavonoid) | PI3K/AKT pathway inhibition; Antioxidant | Demonstrated efficacy in clearing senescent stromal cells; extends healthspan in mouse models. |
| Navitoclax (ABT263) [76] | Senolytic (BCL-2 inhibitor) | BCL-2/BCL-xL inhibition | Reverses immunosuppression in tumor microenvironment; potential for clearing senescent MSCs in bone marrow niche. |
| Metformin [77] [70] | Senomorphic/Senostatic | AMPK activation; Improved mitochondrial function | Used in MSC preconditioning; reduces oxidative stress and inflammatory signaling. |
| Rapamycin [77] [70] | Senomorphic/Senostatic | mTOR inhibition; Enhances autophagy | Shown to delay senescence and maintain stemness in MSC cultures. |
| SRC Exosomes [78] | Senomorphic (Engineered) | Delivery of anti-inflammatory miRNAs (e.g., miR-146a), longevity proteins (e.g., Klotho) | Engineered FOXO3-enhanced MSC exosomes reduced senescence and inflammation in primate model. |
Genetic and Cellular Engineering
Genetic engineering offers precise strategies to enhance MSC resistance to senescence.
- FOXO3 Engineering: Overexpression of the transcription factor FOXO3, a key longevity-associated gene, creates senescence-resistant MSCs (SRCs). These SRCs demonstrated superior survival and function in the harsh inflammatory environment of aged cynomolgus macaques, leading to systemic rejuvenation effects, including improved cognition, bone density, and reproductive health [78].
- CRISPRi-Based Functional Genomics: Genome-wide CRISPR interference (CRISPRi) screens in human adipose-derived MSCs have identified novel senescence regulators. For instance, repression of SAMM50, a mitochondrial outer membrane protein, rejuvenated MSCs by reducing SA-β-Gal activity and positively modulating ECM pathways without altering MSC identity markers [73].
- Telomerase Activation: Ectopic expression of the catalytic subunit of telomerase (hTERT) can extend the replicative lifespan of MSCs by delaying telomere attrition. However, careful safety monitoring is required to avoid oncogenic transformation [75].
Extracellular Vesicle and MSC-Based Therapies
The therapeutic benefits of MSCs are largely mediated by their paracrine secretions, particularly extracellular vesicles (EVs) and exosomes.
- Young MSC-Derived EVs: Systemic administration of EVs isolated from young MSCs or blood plasma can reverse age-related impairments in older recipients. These EVs transfer a cargo of proteins, lipids, and RNAs that alter the transcriptomic profiles of aged tissues towards a more youthful state, improving cognitive function, physical activity, and extending lifespan in rodent models [72] [70].
- MSC Transplantation: The administration of young, healthy MSCs itself has shown pro-longevity effects. Studies in naturally aging and progeroid mice have demonstrated that a single intravenous injection of young, bone marrow-derived MSCs can extend median lifespan by 15% and maximum lifespan by 6%, alongside preservation of bone mineral density [72].
Table 2: Effects of MSC and MSC-EV Administration on Lifespan in Animal Models
| Cell / EV Source | Animal Model | Administration Regimen | Effect on Lifespan | Additional Benefits |
|---|---|---|---|---|
| Bone Marrow MSCs (Young mice) [72] | Aged Balb/C mice | Single IV injection (1x10^6 cells) | ↑ Median: 15%↑ Max: 6% | Preservation of bone mineral density |
| Human Amniotic MSCs [72] | Aged F344 rats | Monthly IV injections till death | ↑ Median: 32%↑ Max: 33% | Maintenance of physical activity and cognitive function |
| Blood Plasma EVs (Young mice) [72] | Aged C57BL/6 mice | Weekly IP injections till death | ↑ Median: 10%↑ Max: 16% | Maintenance of physical activity |
| Muscle-derived Stem Cells [72] | Progeroid (Ercc1−/−) mice | Single IP injection | ↑ Median: 314%↑ Max: 236% | Delay of aging symptoms like kyphosis and muscle wasting |
Experimental Protocols for Senescence Research
Genome-Wide CRISPRi Screening for Senescence Regulators
This protocol identifies novel genes regulating replicative and inflammatory senescence in human MSCs [73].
- Cell Line Engineering: Stably transduce primary human adipose-derived MSCs with a lentivirus expressing dCas9-KRAB (the catalytically dead Cas9 fused to the KRAB transcriptional repression domain).
- sgRNA Library Transduction: Transduce the engineered MSCs at a low MOI with a genome-wide lentiviral sgRNA library (e.g., ~104,535 sgRNAs targeting 18,905 genes + non-targeting controls).
- Replicative Senescence Screening (RSS): Culture the pooled, transduced MSCs for approximately 20 population doublings until significant growth arrest is observed.
- Sequencing and Hit Identification: Isolate genomic DNA from the initial (T0) and final (Tfinal) cell populations. Amplify and sequence the integrated sgRNAs. Calculate a beta score for each gene by comparing sgRNA abundance between T0 and Tfinal. A positive beta score indicates gene enrichment (pro-senescent function), while a negative score indicates depletion (anti-senescent/essential function).
- Validation: Validate top hits (e.g., SAMM50, AK2) using individual sgRNAs in functional assays (SA-β-Gal staining, proliferation assays, surface marker expression).
The workflow for this functional genomic screen is depicted below:
Generating Senescence-Resistant MSCs (SRCs)
This protocol describes the creation of FOXO3-enhanced MSCs with demonstrated efficacy in primates [78].
- Isolation and Culture: Isolate human MSCs from a desired source (e.g., bone marrow, adipose tissue). Confirm identity by flow cytometry for CD73, CD90, CD105 and absence of CD14, CD34, CD45, and HLA-DR.
- Genetic Modification: Transduce early-passage MSCs with a lentiviral vector carrying the human FOXO3 gene under a constitutive or inducible promoter.
- Selection and Expansion: Select successfully transduced cells using an appropriate antibiotic (e.g., Puromycin) and expand the polyclonal SRC population.
- In Vitro Characterization:
- Senescence Challenge: Expose SRCs and wild-type MSCs to senescence-inducing stressors (e.g., high-dose hydrogen peroxide, serial passaging). Quantify senescence markers (SA-β-Gal, p16, p21).
- SASP Profiling: Analyze culture supernatants via ELISA or multiplex immunoassays for SASP factors (IL-6, IL-8, IL-1β).
- Functionality Assays: Compare trilineage differentiation potential, migration capacity, and immunomodulatory function between SRCs and wild-type controls.
- In Vivo Validation: Administer SRCs intravenously to aged animal models (e.g., cynomolgus macaques). Monitor for systemic effects on inflammation, tissue function, and overall health.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating MSC Senescence
| Reagent / Tool | Category | Specific Example(s) | Primary Function in Senescence Research |
|---|---|---|---|
| Senescence-Associated β-Galactosidase (SA-β-Gal) Kit [71] [73] | Histochemical Stain | Commercial kits (e.g., Cell Signaling Technology #9860) | Detection of lysosomal β-galactosidase activity at pH 6.0, a gold-standard biomarker for identifying senescent cells in culture. |
| CRISPRi System [73] | Genetic Tool | dCas9-KRAB + sgRNA library | Enables genome-wide loss-of-function screens to identify novel pro- and anti-senescence genes in human MSCs. |
| SASP Antibody Array / ELISA Panels [77] [76] | Protein Analysis | Proteome Profiler Array (R&D Systems); LEGENDplex kits | Multiplexed quantification of key SASP factors (IL-6, IL-8, CCL2, etc.) secreted by senescent MSCs. |
| Senolytic Compounds [77] [76] | Small Molecules | Dasatinib, Quercetin, Fisetin, Navitoclax (ABT263) | Used to selectively eliminate senescent MSCs from a culture to validate their functional role and for therapeutic development. |
| FOXO3 Expression Vector [78] | Genetic Tool | Lentiviral FOXO3 construct | For generating genetically engineered, senescence-resistant MSCs (SRCs) with enhanced therapeutic durability. |
| Aged MSC Donor Samples [71] | Biological Model | Primary MSCs from young (21-25) vs. elderly (80-92) human donors | Provides a physiologically relevant model to study age-associated gene expression changes and functional decline. |
Targeting cellular senescence in MSCs is no longer a speculative endeavor but a tangible goal with multiple validated strategies. The combined approach of senolytics to clear damaged cells, senomorphics to modulate the microenvironment, and genetic engineering (e.g., FOXO3-SRCs) to create resilient cell products represents a powerful toolkit for enhancing regenerative medicine. The translation of these strategies from bench to bedside will require rigorous safety profiling, particularly for genetically modified cells, and the optimization of delivery methods. Future work should focus on understanding the heterogeneity of senescent MSC populations, developing more precise senescence biomarkers, and integrating biological aging clocks to quantitatively assess the rejuvenation effects of these interventions. By directly addressing the fundamental biology of MSC aging, the field can unlock the full therapeutic potential of these cells for treating age-related diseases and injuries.
The field of regenerative medicine has increasingly recognized that the therapeutic efficacy of mesenchymal stem cells (MSCs) is not solely dependent on the cells themselves but is profoundly influenced by their microenvironment. Biomaterial scaffolds provide a three-dimensional architecture that mimics the native extracellular matrix (ECM), serving not merely as passive delivery vehicles but as bioactive platforms that direct cell fate through structural, mechanical, and chemical cues [79]. These scaffolds address critical limitations of naive MSC transplantation, including poor cell survival, limited retention at injury sites, and insufficient control over differentiation kinetics [79] [80]. The evolution from simple cell carriers to sophisticated, multifunctional systems represents a paradigm shift in tissue engineering strategy, enabling precise spatiotemporal control over the regenerative process.
The integration of MSC biology with advanced biomaterial science has unlocked new potential for treating complex tissue defects that lack intrinsic regenerative capacity. By recapitulating key aspects of the native stem cell niche, engineered scaffolds can enhance MSC viability, direct lineage-specific differentiation, and modulate host immune responses [81]. Furthermore, the combination of scaffold-MSC constructs with complementary therapeutic approaches—including growth factor delivery, genetic engineering, and rehabilitative protocols—creates synergistic effects that significantly outperform individual modalities [82] [83]. This whitepaper provides a comprehensive technical guide to current strategies for optimizing these combinatorial formulations, with a specific focus on translating fundamental MSC biology into enhanced clinical outcomes for tissue regeneration.
Biomaterial Scaffolds for MSC Delivery: Types and Properties
Scaffolds for MSC delivery must satisfy multiple design criteria: biocompatibility, appropriate biodegradation kinetics, mechanical competence matching the target tissue, and porous architecture facilitating cell migration and nutrient diffusion [79] [84]. Different biomaterial classes offer distinct advantages that can be selected based on specific application requirements.
Table 1: Classification of Biomaterial Scaffolds for MSC-Based Therapies
| Scaffold Type | Material Examples | Key Properties | Advantages for MSC Therapy | Primary Applications |
|---|---|---|---|---|
| Natural Polymers | Chitosan, Collagen, Hyaluronic Acid, Alginate | Innate bioactivity, enzymatic degradation, low immunogenicity | Inherent cell adhesion motifs, biocompatibility, tunable physical properties | Injectable gels for minimally invasive delivery; soft tissue regeneration [85] |
| Synthetic Polymers | PLA, PGA, PLGA, PEG | Precise control over mechanical properties, degradation rate, and architecture | Reproducible manufacturing, tunable strength, controlled porosity | 3D-printed and electrospun scaffolds for load-bearing bone and cartilage repair [79] [86] |
| Hydrogels | Chitosan-based, Collagen, PEG, Hyaluronic Acid | High water content, soft elastic properties, injectability | Encapsulation protects MSCs; modular biofunctionalization; stress shielding | Cartilage, neural, and cardiac tissue engineering; drug co-delivery [85] |
| Acellular Biologic Scaffolds | Decellularized tissue ECM (e.g., urinary bladder, small intestine) | Native composition and architecture of ECM proteins and bound factors | Recruits endogenous stem/progenitor cells; provides innate signaling cues | Volumetric muscle loss, tendon repair, organ reconstruction [82] |
Chemical modification strategies significantly enhance the functionality of natural polymer-based scaffolds. For chitosan, common modifications include quaternization to improve water solubility and antimicrobial efficacy, carboxymethylation to enhance bioadhesion and solubility, and sulfonation to introduce anticoagulant and antiviral properties [85]. These functionalizations address inherent limitations while introducing new bioactive capabilities that synergize with MSC therapies. Scaffold fabrication techniques have also advanced considerably, with 3D bioprinting enabling patient-specific geometries, electrospinning producing nanofibrous architectures mimicking natural ECM, and freeze-drying creating highly porous networks ideal for cell infiltration and vascularization [79] [87].
Strategic Functionalization of Scaffolds and MSCs
Physical and Topographical Modification
Surface topography serves as a powerful mechanical cue to direct MSC behavior through contact guidance. Engineered micro- and nanoscale features influence critical cellular processes including adhesion, migration, proliferation, and lineage commitment [86] [81].
Specific dimensional parameters yield predictable cellular responses. For neural regeneration, groove widths of 10-20µm optimally align Schwann cells, while 40µm laminin micropatterns maximize axon growth rate and orientation [86]. Similarly, fiber diameter in electrospun scaffolds significantly influences MSC proliferation, with smaller nanofibers (e.g., <500nm) typically enhancing proliferation rates [86]. These physical cues activate mechanotransduction pathways, including Rho/ROCK signaling and YAP/TAZ nuclear translocation, ultimately regulating transcriptional programs that determine cell fate [81].
Biological and Chemical Functionalization
The bioactivity of scaffolds can be enhanced through the incorporation of signaling molecules that guide MSC behavior. Common strategies include:
- Growth Factor Delivery: Incorporation of BMP-2, VEGF, TGF-β, or FGF to promote osteogenesis, angiogenesis, and chondrogenesis, respectively [79]. Controlled release kinetics are critical to mimic natural healing cascades.
- Genetic Modification of MSCs: Pre-implantation genetic engineering to overexpress osteogenic (e.g., RUNX2), angiogenic (VEGF), or anti-apoptotic genes enhances regenerative capacity [79].
- Plant-Derived Bioactive Compounds: Integration of flavonoids, tannins, and terpenoids provides antimicrobial, antioxidant, and pro-angiogenic activities that address challenges in wound healing [87].
- Peptide Functionalization: Grafting of ECM-derived peptides (e.g., RGD) enhances cell-scaffold integration and can direct specific differentiation pathways [85].
These functionalization strategies can be combined to create synergistic effects. For instance, a scaffold might incorporate topological cues for osteoinduction alongside VEGF for angiogenesis, addressing both bone formation and the vascularization necessary for graft survival [79] [81].
Combination Therapies and Clinical Translation
Integrated Therapeutic Approaches
The combination of scaffold-MSC constructs with adjunct therapies creates powerful multimodal treatments that address multiple aspects of the regenerative process simultaneously.
Table 2: Quantitative Outcomes of Systemic MSC Therapy for Bone Regeneration
| Outcome Measure | Standard Mean Difference (SMD) | 95% Confidence Interval | Number of Studies | Heterogeneity (I²) |
|---|---|---|---|---|
| Bone Mineral Density (BMD) | 3.02 | [1.84, 4.20] | 21 | High |
| Bone Volume/Tissue Volume (BV/TV) | 2.10 | [1.16, 3.03] | 21 | High |
| New Bone Area Percentage | 7.03 | [2.10, 11.96] | 21 | High |
Systemic administration of MSCs demonstrates particular efficacy in bone loss caused by systemic diseases like osteoporosis, with significantly better response in BMD (p=0.05) and BV/TV (p=0.03) compared to other conditions [88]. This highlights the importance of matching delivery strategies to disease pathophysiology.
Regenerative Rehabilitation
The emerging field of regenerative rehabilitation strategically integrates physical rehabilitation with regenerative medicine to enhance functional outcomes. Mechanotransduction—the process by which mechanical stimuli are converted into biochemical signals—represents a key mechanism through which physical modalities enhance MSC-based therapies [82] [83].
In musculoskeletal applications, the combination of stem cell transplantation with muscle loading significantly increases donor cell engraftment in both myopathy and injury models [82]. For neurological applications, electrical stimulation paired with MSC therapy promotes neuroplasticity and circuit reorganization [82] [83]. These combinatorial approaches ensure that regenerated tissue meets functional demands, moving beyond structural repair to meaningful functional recovery.
Experimental Protocols and Methodologies
Standardized Protocols for MSC-Scaffold Evaluation
Protocol 1: In Vitro Evaluation of Functionalized MSCs in 3D Culture
- MSC Expansion: Culture human bone marrow-derived MSCs in α-MEM supplemented with 10% FBS and 1% penicillin/streptomycin at 37°C, 5% CO₂ until 80% confluence (passage 3-5) [79] [80].
- Genetic Modification (if applicable): Transduce MSCs with lentiviral vectors encoding target genes (e.g., BMP-2 for osteogenesis) using MOI 10-50 with 8μg/mL polybrene. Confirm transduction efficiency by qPCR and Western blot [79].
- Cell Seeding on Scaffolds: Sterilize scaffolds (e.g., 5mm diameter×2mm thickness) by UV irradiation. Seed at density of 1×10⁶ cells/scaffold in low-attachment plates. Allow adhesion for 4h before adding culture media [79] [85].
- Osteogenic Induction: Culture in osteogenic medium (DMEM with 10% FBS, 10mM β-glycerophosphate, 50μg/mL ascorbic acid, and 100nM dexamethasone) for 21 days, changing medium every 3 days [79].
- Analysis: Assess osteogenic differentiation by ALP staining (day 7-14), Alizarin Red S mineralization (day 21), and osteogenic gene expression (RUNX2, OPN, OCN) by RT-qPCR [79].
Protocol 2: In Vivo Bone Regeneration Model (Critical-Sized Calvarial Defect)
- Animal Model: Create 5mm critical-sized defects in 8-10 week-old immunocompromised mice (e.g., nude mice) or rats using a trephine drill under anesthesia [88].
- Implant Preparation: Seed 2×10⁶ functionalized MSCs onto 5mm diameter scaffold 24h prior to implantation. Use acellular scaffold and untreated defects as controls.
- Surgical Implantation: Gently place cell-scaffold constructs into defects, ensuring snug fit without compression. Close surgical site in layers [88].
- Postoperative Analysis: At 4-8 weeks post-implantation, harvest calvaria for micro-CT analysis (bone volume/total volume, trabecular number/thickness) and histological processing (H&E, Masson's Trichrome, immunohistochemistry for osteocalcin) [88].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MSC-Scaffold Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| MSC Markers | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) | MSC identification and purification by flow cytometry | Confirmation of MSC phenotype per International Society for Cellular Therapy guidelines [84] [80] |
| Osteogenic Induction Media | Dexamethasone, β-glycerophosphate, Ascorbic acid | In vitro differentiation toward osteoblastic lineage | Standardized formulations allow comparison across studies; optimal concentration varies by MSC source [79] [84] |
| Scaffold Polymers | PLGA, Chitosan, Alginate, Collagen, Hyaluronic Acid | 3D structural support for MSC delivery | Degradation rate should match tissue formation; surface chemistry affects protein adsorption and cell adhesion [79] [85] |
| Genetic Modification Tools | Lentiviral vectors, CRISPR/Cas9 systems, Transfection reagents (e.g., Lipofectamine) | Modifying MSCs to enhance therapeutic potential (e.g., overexpress growth factors) | Optimization of transduction efficiency critical; safety concerns for clinical translation [79] |
| In Vivo Tracking Agents | GFP/luciferase labeling, DIR/DiD fluorescent dyes, MRI contrast agents | Monitoring cell survival, migration, and distribution post-transplantation | Non-invasive imaging enables longitudinal assessment in same subjects; consider label dilution with cell division [88] |
The future of MSC-based regenerative medicine lies in increasingly sophisticated biomaterial platforms that provide dynamic, spatially organized, and patient-specific cues. Emerging trends include four-dimensional (4D) scaffolds that evolve their properties over time in response to environmental stimuli, precision-engineered implants designed using artificial intelligence, and the integration of multiple cell types to recreate complex tissue interfaces [79]. Additionally, the growing understanding of MSC-derived exosomes and microvesicles as paracrine mediators suggests future scaffolds may incorporate these acellular components alongside or instead of whole cells [80].
Despite promising preclinical outcomes, translational challenges remain in manufacturing, immune compatibility, and regulatory pathways. Standardization of cell sources, scaffold fabrication, and functionalization protocols is essential for clinical translation [79] [80]. Furthermore, the field must address donor-specific variability in MSC potency and the implications of cellular senescence for therapeutic efficacy [80]. The convergence of advanced biomaterials with insights from MSC biology, combined with rigorous clinical validation through registered trials, will ultimately unlock the full potential of these technologies to restore tissue structure and function across a spectrum of degenerative conditions and injuries.
Evidence and Efficacy: Analyzing the Clinical Trial and Regulatory Landscape
The field of regenerative medicine has reached a pivotal milestone with the United States Food and Drug Administration's (FDA) first approval of a mesenchymal stem cell (MSC) therapy. This whitepaper provides a comprehensive technical analysis of the regulatory landscape for FDA-approved MSC products, focusing on the recently authorized Ryoncil (remestemcel-L-rknd). Within the broader context of basic MSC science, we examine the therapeutic mechanisms, clinical evidence, manufacturing challenges, and regulatory pathway that culminated in this historic approval for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD). We further explore the implications of this decision for future MSC-based therapies currently in development and provide detailed experimental methodologies and essential research tools that form the foundation of MSC product characterization and potency assessment.
Mesenchymal stem cells (MSCs) are non-hematopoietic, multipotent stromal cells first identified in bone marrow by Soviet scientist A. J. Friedenstein in the 1960s through research demonstrating osteoblastic differentiation potential [1]. According to the International Society for Cellular Therapy (ISCT), MSCs are defined by three key criteria: (1) adherence to plastic under standard culture conditions; (2) specific surface marker expression (CD73, CD90, CD105 ≥95%; CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) tri-lineage differentiation potential into osteocytes, chondrocytes, and adipocytes in vitro [1]. The therapeutic efficacy of MSCs is primarily mediated through paracrine signaling rather than direct differentiation, with cells releasing bioactive molecules including growth factors, cytokines, and extracellular vesicles that modulate immune responses, promote tissue repair, stimulate angiogenesis, and enhance cell survival [1].
MSCs can be isolated from multiple tissue sources, each with distinct characteristics:
- Bone marrow-derived MSCs (BM-MSCs): Most extensively studied, with high differentiation potential and strong immunomodulatory effects [1]
- Adipose tissue-derived MSCs (AD-MSCs): Easier to harvest with higher yields and comparable therapeutic properties [1]
- Umbilical cord-derived MSCs (UC-MSCs): Enhanced proliferation capacity and lower immunogenicity, suitable for allogeneic transplantation [1]
- Dental pulp stem cells (DP-SCs) and placenta-derived MSCs (P-MSCs): Emerging sources with unique regenerative properties for specialized applications [1]
The immunomodulatory capabilities of MSCs emerge through interactions with various immune cells (T cells, B cells, dendritic cells, macrophages) via both direct cell-cell contact and secretion of immunosuppressive molecules including prostaglandin E2 (PGE2), transforming growth factor-β (TGF-β), and indoleamine-2,3-dioxygenase (IDO) [89]. This complex biological foundation underpins their therapeutic application across diverse disease areas, culminating in the first FDA approval of an MSC product after decades of research.
The Regulatory Landscape: FDA-Approved MSC Products
The FDA's "Approved Cellular and Gene Therapy Products" list remains highly selective, with Ryoncil (remestemcel-L-rknd) representing the first and only mesenchymal stromal cell therapy to receive full approval as of December 2024 [90] [91]. This landmark approval signals a new era in cell-based regenerative medicine and establishes important regulatory precedents for future MSC therapies.
Table 1: FDA-Approved Mesenchymal Stem Cell Product
| Product Name | Manufacturer | Biological Material | Indication | Approval Date | Patient Population |
|---|---|---|---|---|---|
| Ryoncil (remestemcel-L-rknd) | Mesoblast, Inc. | Allogeneic bone marrow-derived MSCs | Steroid-refractory acute graft-versus-host disease (SR-aGVHD) | December 18, 2024 | Pediatric patients ≥2 months old [90] |
Comprehensive Product Characterization
Ryoncil is an allogeneic (donor-derived) bone marrow-derived mesenchymal stromal cell therapy with the following key characteristics [90]:
- Source: Isolated from bone marrow of healthy adult donors
- Cell Type: Multipotent mesenchymal stromal cells
- Mechanism: Immunomodulation through paracrine signaling and cell-cell interactions
- Administration: Intravenous infusion
- Dosing Regimen: Twice weekly for four consecutive weeks (total of eight infusions)
The product's approval was supported by Orphan Drug, Fast Track, and Priority Review designations, reflecting the serious, life-threatening nature of SR-aGVHD and the unmet medical need in this patient population [90].
Clinical Evidence and Experimental Design
Pivotal Clinical Trial Methodology
The safety and efficacy of Ryoncil were evaluated in a multicenter, single-arm study enrolling 54 pediatric patients with SR-aGVHD following allogeneic hematopoietic stem cell transplantation [90]. The experimental design incorporated the following key elements:
Patient Population and Eligibility Criteria:
- Pediatric patients (age <1 to 17 years) with grade II–IV SR-aGVHD
- All patients underwent prior allogeneic hematopoietic stem cell transplantation
- Nearly three-quarters met criteria for Minnesota high-risk acute GVHD [89]
Intervention Protocol:
- Patients received intravenous Ryoncil infusions twice weekly for four consecutive weeks
- Each infusion was monitored for potential reactions by treating physicians
- Premedication with corticosteroids and antihistamines was administered prior to each infusion
- Patients showing partial or mixed response at day 28 received additional once-weekly infusions for four additional weeks [90]
Outcome Measures and Assessment Methodology:
- Primary Efficacy Endpoint: Response rate at day 28 post-treatment initiation, evaluated using International Blood and Marrow Transplantation Registry Severity Index Criteria (IBMTR)
- Response Definitions:
- Complete response: Resolution of GVHD symptoms in all organs
- Partial response: Improvement in one organ with no change in another
- Mixed response: Improvement in one organ with worsening in another
- Secondary Endpoints: Duration of response, six-month survival, ability to discontinue immunosuppression [89] [90]
Safety Assessment:
- Comprehensive monitoring for adverse reactions including infections, fever, hemorrhage, edema, abdominal pain, and hypertension
- Specific assessment for hypersensitivity reactions, acute infusion reactions, and potential ectopic tissue formation
- Long-term follow-up for infectious disease transmission and other complications [90]
Clinical Outcomes and Efficacy Data
The pivotal trial demonstrated significant clinical benefits for this high-risk pediatric population:
Table 2: Clinical Efficacy Outcomes from Ryoncil Pivotal Trial
| Outcome Measure | Results | Statistical/Clinical Significance |
|---|---|---|
| Day 28 Complete Response | 30% (16/54 patients) | Complete resolution of GVHD symptoms [90] |
| Day 28 Partial Response | 41% (22/54 patients) | Significant improvement in organ involvement [90] |
| Overall Day 28 Response | 70% (38/54 patients) | Majority achieving clinically meaningful improvement [89] |
| Six-Month Survival | 69% | Remarkable for high-risk population with historically poor prognosis [89] |
| Immunosuppression Discontinuation | >50% within six months | Demonstrated durable response without continued immunosuppression [89] |
The 70% overall response rate was particularly notable given the high-risk patient population and historically poor outcomes with previous treatment options. The trial also reported minimal moderate-to-severe chronic GVHD development (only two cases), suggesting potential disease-modifying effects beyond acute symptom management [89].
Molecular Mechanisms of Action: MSC Signaling Pathways
The therapeutic effects of MSCs in SR-aGVHD are mediated through complex immunomodulatory mechanisms involving multiple signaling pathways and molecular interactions.
MSC Immunomodulatory Signaling Pathway
MSC Immunomodulation in SR-aGVHD
When systemically administered, MSCs are initially trapped in the lungs where they interact with immune cells and respond to inflammatory cytokines through several coordinated mechanisms [89]:
- Secretome Release: Inflammatory cytokines (IFN-γ, TNF-α, IL-1) stimulate MSCs to release anti-inflammatory mediators including PGE2, TGF-β, and IDO [89]
- T Cell Modulation: MSC-derived factors suppress effector T cell proliferation and promote regulatory T cell (Treg) expansion [89]
- Macrophage Polarization: MSC secretions promote polarization of macrophages toward anti-inflammatory M2 phenotype [89]
- Trophic Factor Production: MSCs secrete hepatocyte growth factor (HGF) and vascular endothelial growth factor (VEGF) that directly promote tissue repair and epithelial regeneration [89]
Despite their therapeutic effects, studies indicate that intravenously infused MSCs are rapidly trapped in the lungs and phagocytosed by immune cells, suggesting their actions may be mediated through phagocytic cells that subsequently exert anti-inflammatory effects rather than through direct engraftment at injury sites [89].
In Vitro Potency Assessment Pathway
A critical advancement in Ryoncil development was implementation of a robust potency assay to ensure product consistency, addressing previous challenges with MSC product variability.
In Vitro Potency Assay Workflow
The critical potency assay measures MSC capacity to suppress IL-2 receptor alpha (IL-2Rα) expression on activated T cells in vitro, which correlates with reduced numbers of activated T cells in vivo and predicts clinical response [89]. This assay addressed previous manufacturing challenges: while fewer than 70% of earlier product lots (Prochymal) met potency criteria, all Ryoncil lots used in successful trials met this new potency standard [89].
The Scientist's Toolkit: Essential Research Reagents and Materials
Robust experimental methodologies require specific research tools and quality control measures. The following table outlines essential reagents and materials critical for MSC research and product development.
Table 3: Essential Research Reagents for MSC Product Development
| Research Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| StemRNA Clinical Seed iPSCs | GMP-compliant starting material for iPSC-derived MSC production | Clinical-grade induced pluripotent stem cell clones; FDA Drug Master File (DMF) submitted [7] |
| Potency Assay Components | Quantitative assessment of MSC immunomodulatory function | T cell activation reagents (anti-CD3/CD28), IL-2Rα detection antibodies, flow cytometry validation [89] |
| Cell Culture Media | In vitro expansion and maintenance of MSCs | Serum-free, xeno-free formulations with defined growth factors and cytokines [1] |
| Surface Marker Antibodies | Characterization of MSC identity per ISCT criteria | CD73, CD90, CD105 (positive); CD34, CD45, CD11b, CD19, HLA-DR (negative) [1] |
| Differentiation Induction Media | Demonstration of tri-lineage differentiation potential | Osteogenic, chondrogenic, and adipogenic induction cocktails with specific inducers [1] |
| Cryopreservation Solutions | Long-term storage of MSC products | Defined cryoprotectant formulations (e.g., with DMSO), controlled rate freezing systems [89] |
Regulatory Pathway and Manufacturing Considerations
The approval pathway for Ryoncil involved a complex regulatory journey spanning nearly a decade, with particular attention to manufacturing consistency and potency assays [91]. Key regulatory milestones included:
- 2013-2015: Early-phase clinical trials in pediatric SR-aGVHD [91]
- April 2020: FDA acceptance of Biologics License Application (BLA) with Priority Review [91]
- September 2020: Complete Response Letter requesting additional efficacy data [91]
- 2023-2024: Multiple regulatory interactions focusing on Chemistry, Manufacturing, and Controls (CMC) [91]
- December 18, 2024: Final FDA approval for pediatric SR-aGVHD [90] [91]
Manufacturing challenges specific to MSC products include batch-to-batch variability due to MSC sensitivity to microenvironments, donor source variability, and culture condition differences [91]. The implementation of rigorous potency assays and release criteria was essential for addressing these challenges and demonstrating product consistency [89].
The FDA approval of Ryoncil represents a transformative milestone in regenerative medicine, establishing MSC therapies as a viable treatment modality for serious immune-mediated conditions. This approval validates decades of basic science research into MSC biology and creates a regulatory precedent for future cell-based products. The success of Ryoncil in pediatric SR-aGVHD demonstrates that MSC therapies can address critical unmet medical needs when supported by robust manufacturing controls, validated potency assays, and well-designed clinical trials.
The future of MSC therapeutics includes investigation into multiple new directions:
- Next-Generation MSC Products: iPSC-derived MSCs (iMSCs) offering enhanced consistency and scalability [7]
- Expanded Indications: Ongoing clinical trials for conditions including acute respiratory distress syndrome, multiple sclerosis, osteoarthritis, and aging frailty [91]
- Advanced Manufacturing: Improved bioreactor systems, defined culture media, and enhanced quality control metrics
- Mechanistic Research: Continued investigation into in vivo MSC trafficking, biodistribution, and precise mechanisms of action
As the field advances, the Ryoncil approval provides both a roadmap and foundation for developing MSC therapies that meet rigorous regulatory standards while addressing serious human diseases through innovative cellular mechanisms.
Within the broader thesis on the basic science of mesenchymal stem cells (MSCs) in regenerative medicine, this review synthesizes the current clinical evidence on their safety and efficacy. MSCs are multipotent stromal cells characterized by their self-renewal capacity, differentiation potential into mesodermal lineages, and potent immunomodulatory properties [1] [92]. Defined by the International Society for Cellular Therapy (ISCT), MSCs must adhere to plastic under standard culture conditions, express specific surface markers (CD73, CD90, CD105), and lack expression of hematopoietic markers, while retaining the capacity to differentiate into osteoblasts, adipocytes, and chondrocytes in vitro [1] [93]. Their therapeutic effects are primarily mediated through paracrine signaling via bioactive molecules, including growth factors, cytokines, and extracellular vesicles (EVs), which modulate the local cellular environment, promote tissue repair, and exert anti-inflammatory effects [1] [92]. This systematic review evaluates the consolidated findings from recent meta-analyses and systematic reviews of randomized controlled trials (RCTs) to provide a comprehensive assessment of the safety and efficacy profiles of MSC-based therapies across a spectrum of human diseases.
Methodological Framework for Analysis
Literature Search and Study Selection
The systematic reviews and meta-analyses cited in this paper adhered to rigorous methodological standards. Each followed a pre-registered protocol (typically on PROSPERO) and PRISMA guidelines [94] [93] [95]. Literature searches were conducted across major electronic databases, including PubMed/MEDLINE, Embase, Cochrane Library, and Web of Science. The search strategies incorporated a combination of keywords and Medical Subject Headings (MeSH) related to "mesenchymal stem cells," "clinical trials," and specific disease entities.
Eligibility Criteria and Data Extraction
Eligibility criteria were defined using the PICOS (Population, Intervention, Comparison, Outcome, Study design) framework:
- Population: Patients with specific diseases (e.g., ARDS, acute-on-chronic liver failure, autoimmune diseases, ischemic stroke).
- Intervention: Administration of MSCs or their derived products (e.g., extracellular vesicles), regardless of tissue source (bone marrow, adipose tissue, umbilical cord).
- Comparison: Placebo or conventional standard-of-care therapy.
- Outcomes: Primary efficacy endpoints (e.g., mortality, disease-specific scores) and safety endpoints (adverse events, serious adverse events).
- Study Design: Randomized controlled trials (RCTs) were prioritized in all included reviews [94] [96] [93].
Two independent reviewers screened titles, abstracts, and full-text articles. Data extraction covered study characteristics, patient demographics, intervention details (cell source, dose, route of administration), and outcome measures.
Risk of Bias and Quality Assessment
The quality of the included RCTs was assessed using the Cochrane Risk of Bias tool, evaluating domains such as random sequence generation, allocation concealment, blinding of participants and outcome assessors, incomplete outcome data, and selective reporting [95].
Statistical Analysis
Meta-analyses were performed using statistical software such as RevMan 5.4 and Stata 15.0. For dichotomous outcomes (e.g., mortality, adverse events), the relative risk (RR) with a 95% confidence interval (CI) was calculated. For continuous outcomes (e.g., functional scores), the mean difference (MD) or standardized mean difference (SMD) was used. Heterogeneity was quantified using the I² statistic, with values above 50% indicating substantial heterogeneity. A random-effects model was commonly employed to account for clinical and methodological diversity among the studies [94] [93] [95].
Comprehensive Efficacy and Safety Profiles Across Diseases
The following section details the efficacy and safety outcomes of MSC therapy across various conditions, with summarized data presented in Table 1.
Table 1: Summary of Efficacy and Safety Outcomes of MSC Therapy from Recent Meta-Analyses
| Disease Area | Primary Efficacy Outcome | Effect Size (95% CI) | Safety Outcome (Adverse Events) | Effect Size (95% CI) | References |
|---|---|---|---|---|---|
| Acute Respiratory Distress Syndrome (ARDS) | All-cause mortality (within 1 month) | RR=0.74 (0.63-0.87) p=0.0003 | Serious Adverse Events (SAEs) | RR=0.94 (0.80-1.11) p=0.49 | [94] |
| Acute-on-Chronic Liver Failure | Model for End-Stage Liver Disease (MELD) score (24 weeks) | Significant decrease reported | Adverse Events / Serious Adverse Events | No significant difference | [96] |
| Autoimmune & Rheumatic Diseases | |||||
| - Osteoarthritis (VAS Pain) | Visual Analogue Scale (VAS) | SMD=-1.25 (-2.04 to -0.46) p=0.002 | Adverse Events | RR=1.23 (0.93-1.65) p=0.15 | [93] |
| - Systemic Lupus Erythematosus | Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) | SMD=-2.32 (-3.59 to -1.06) p=0.0003 | Adverse Events | RR=0.83 (0.28-2.51) p=0.76 | [93] |
| - Inflammatory Bowel Disease (IBD) | Clinical Efficacy | RR=2.02 (1.53-2.67) p<0.00001 | Adverse Events | RR=0.99 (0.81-1.22) p=0.96 | [93] [97] |
| Acute Ischemic Stroke | National Institutes of Health Stroke Scale (NIHSS) | SMD=-0.99 (-1.93 to -0.05) | Adverse Events | RR=0.68 (0.40-1.17) | [95] |
Pulmonary Disease: Acute Respiratory Distress Syndrome (ARDS)
A 2025 meta-analysis of 31 studies (1,773 patients) demonstrated that MSC-based therapy significantly reduced all-cause mortality within one month compared to routine therapy [94]. Subgroup analyses revealed that higher cell doses (over 1 × 10⁶ cells/kg or 7 × 10⁷ cells per infusion) were associated with a greater mortality reduction (RR=0.70). Notably, MSC-derived extracellular vesicles and secretomes also showed significant promise (RR=0.63 for mortality) [94]. The therapy was well-tolerated, with no significant differences in adverse events or serious adverse events between the treatment and control groups [94].
Hepatic Disease: Acute-on-Chronic Liver Failure (ACLF)
In ACLF, MSC infusion was effective and safe. A meta-analysis of RCTs showed that patients receiving MSCs had significantly decreased Model for End-Stage Liver Disease (MELD) scores at both 4 and 24 weeks, indicating improved liver function [96]. Reciprocally, albumin (ALB) levels increased, and secondary indicators like international normalized ratio (INR) and alanine aminotransferase (ALT) levels also improved significantly. Critically, MSC treatment did not increase the incidence of adverse events or serious adverse events [96].
Autoimmune and Rheumatic Diseases
A comprehensive 2025 meta-analysis of 42 RCTs (2,183 participants) evaluated MSC transplantation across eight autoimmune and rheumatic diseases, including rheumatoid arthritis (RA), osteoarthritis (OA), systemic lupus erythematosus (SLE), and inflammatory bowel disease (IBD) [93].
- Osteoarthritis: MSC transplantation from various sources (bone marrow, umbilical cord, adipose tissue) significantly improved pain scores on the Visual Analogue Scale [93].
- Systemic Lupus Erythematosus: MSC treatment led to a significant reduction in disease activity as measured by the SLEDAI score [93].
- Inflammatory Bowel Disease: MSC therapy was effective in improving clinical outcomes for IBD. A separate review highlighted its particular efficacy in treating Crohn's disease-related complications, such as perianal fistulas, with healing rates of up to 83% in MSC-treated patients [97]. A pooled analysis showed durable responses, with healing rates of 67.7%, 37.5%, and 46.2% for perianal, rectovaginal, and ileopouch fistulas, respectively, at 12 months [97].
Across all these autoimmune conditions, MSC transplantation did not increase the incidence of adverse events, confirming its favorable safety profile in this patient population [93] [97].
Neurological Disease: Acute Ischemic Stroke
A meta-analysis of 9 RCTs (316 patients) found that MSC transplantation significantly reduced neurological deficits, as measured by the National Institutes of Health Stroke Scale (NIHSS) [95]. However, no significant differences were observed in the Barthel Index (BI) or Modified Rankin Score (mRS), which measure activities of daily living and global disability, respectively. There was no increase in adverse events in the MSC group, suggesting the therapy is safe for stroke patients, though its impact on functional independence requires further study [95].
Core Mechanistic Pathways of MSC Action
The therapeutic effects of MSCs are not primarily due to direct differentiation and engraftment but are mediated through complex paracrine and immunomodulatory mechanisms. The key pathways are illustrated in Figure 1.
Diagram 1: Core Mechanistic Pathways of Mesenchymal Stem Cell (MSC) Action
Figure 1: MSC Therapeutic Mechanisms. MSCs exert effects via paracrine signaling (release of EVs, growth factors, and cytokines) and direct immunomodulation (interacting with and suppressing various immune cells). These interconnected processes collectively promote tissue repair and regeneration [1] [92].
Experimental Models for Validating MSC Mechanisms
In vitro and in vivo models are crucial for dissecting these mechanisms.
- In Vitro Co-culture Systems: MSCs are co-cultured with specific immune cells (e.g., T cells, macrophages) to study direct cell-cell contact and paracrine-mediated suppression. Functional readouts include T-cell proliferation assays (e.g., CFSE dilution) and cytokine profiling of supernatants (e.g., IL-10, TGF-β, IFN-γ) [1].
- Animal Disease Models: Preclinical models are indispensable. For ARDS, the intratracheal lipopolysaccharide (LPS) instillation model in rodents is used to assess MSC efficacy on lung injury and inflammation. For stroke, the middle cerebral artery occlusion (MCAO) model in rodents is standard. Outcomes include infarct volume measurement (via TTC staining or MRI), functional neurological scores, and immunohistochemical analysis for cell survival, angiogenesis, and inflammation [94] [95].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for MSC-Based Therapy Development
| Reagent/Material Category | Specific Examples | Primary Function in R&D |
|---|---|---|
| MSC Source & Culture | Bone Marrow Aspirate, Adipose Tissue, Umbilical Cord Wharton's Jelly, Commercial GMP-grade MSCs | Source material for isolating and expanding MSCs for research and clinical application. |
| Cell Culture Media & Supplements | α-MEM / DMEM-F12, Fetal Bovine Serum (FBS) / Human Platelet Lysate (hPL), Antibiotic-Antimycotic, L-Glutamine, Trypsin/EDTA | Supports in vitro MSC expansion, maintenance of multipotency, and prevents contamination. |
| Flow Cytometry Antibodies | Anti-human CD73, CD90, CD105, CD44, CD45, CD34, CD14, CD19, HLA-DR | Validation of MSC identity and purity per ISCT criteria (positive and negative marker expression) [1]. |
| Differentiation Kits | Osteogenic (Dexamethasone, β-glycerophosphate, Ascorbate), Adipogenic (Dexamethasone, IBMX, Indomethacin), Chondrogenic (TGF-β, Ascorbate) | Functional confirmation of MSC trilineage differentiation potential in vitro [1]. |
| Extracellular Vesicle Isolation Kits | Total Exosome Isolation Reagent, Ultracentrifugation systems, Size-Exclusion Chromatography columns | Isolation and purification of MSC-derived EVs for mechanistic studies and therapeutic development [94]. |
| Animal Model Reagents | Lipopolysaccharide (LPS, for ARDS), Middle Cerebral Artery Occlusion Filaments (for Stroke), Collagen (for Arthritis) | Induction of specific disease phenotypes in preclinical animal models for efficacy testing. |
Regulatory and Clinical Translation Landscape
The field is transitioning from experimental research to clinically approved therapies. In December 2024, the FDA approved Ryoncil (remestemcel-L), an allogeneic bone marrow-derived MSC product, for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD), marking a significant milestone as the first FDA-approved MSC therapy [7]. This approval underscores the viability of MSC-based products. Furthermore, the regulatory landscape is evolving with the entry of induced pluripotent stem cell (iPSC)-derived MSCs (iMSCs) into clinical trials, offering potential for enhanced consistency and scalability [7]. Regulatory designations like Regenerative Medicine Advanced Therapy (RMAT) and Fast Track are being utilized to accelerate the development of promising stem cell therapies [7].
This systematic review consolidates robust evidence from recent meta-analyses demonstrating that MSC-based therapies are a generally safe and effective treatment approach across a diverse range of conditions, including ARDS, liver failure, autoimmune diseases, and neurological disorders. The efficacy is evidenced by significant improvements in disease-specific metrics and mortality in some indications, without an associated increase in adverse events. The therapeutic mechanisms are multifaceted, relying on paracrine signaling and immunomodulation rather than direct cell replacement. Despite the promising data and recent regulatory approvals, challenges remain. These include optimizing protocols for cell source, dose, and timing of administration, and understanding the long-term effects. Future larger and more rigorous RCTs, potentially incorporating next-generation products like iMSCs and defined EV preparations, are warranted to fully validate the efficacy of MSC-based therapies and solidify their role in regenerative medicine.
Mesenchymal stem cells (MSCs) have emerged as a highly promising tool in regenerative medicine due to their self-renewal capacity, multilineage differentiation potential, and immunomodulatory properties [1]. Originally identified in bone marrow, MSCs have since been isolated from a variety of tissues, including adipose tissue, umbilical cord, placental tissue, and dental pulp [1] [4]. The therapeutic potential of MSCs from different tissue origins has been widely explored in preclinical models and clinical trials for a diverse range of human diseases, from autoimmune and inflammatory disorders to neurodegenerative diseases and orthopedic injuries [1].
The International Society for Cellular Therapy (ISCT) has established minimal criteria for defining MSCs: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, and CD105 ≥95%) while lacking expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [1] [4]. Despite these common defining characteristics, MSCs from different tissue sources exhibit significant heterogeneity in their biological properties, differentiation potential, and therapeutic efficacy [98] [4] [99].
This comparative analysis examines the efficacy of MSCs derived from different tissue origins, focusing on their characteristic properties, therapeutic mechanisms, and clinical applications within the broader context of regenerative medicine research.
MSCs can be classified based on their tissue of origin, with each source possessing distinct biological advantages and limitations. The behavior and therapeutic potential of MSCs are regulated by intrinsic and extrinsic factors, including microenvironmental cues, epigenetic modifications, and cytokine signaling [1].
Table 1: Characteristics of MSC Sources from Different Tissues
| Tissue Source | Key Markers | Advantages | Limitations | Differentiation Potential |
|---|---|---|---|---|
| Bone Marrow (BM-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- [1] | Most extensively studied, high differentiation potential, strong immunomodulatory effects [1] | Invasive harvest, limited cell number, decline in quality with donor age [4] | Osteogenic, chondrogenic, adipogenic [1] |
| Adipose Tissue (AD-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- [1] | Easier harvest, higher yield, comparable therapeutic properties, faster proliferation [1] [100] | Donor variability influenced by BMI [101] | Strong adipogenic, osteogenic, chondrogenic [102] |
| Umbilical Cord (UC-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- [1] | Enhanced proliferation, lower immunogenicity, suitable for allogeneic transplantation [1] [4] | Perinatal source only [4] | Osteogenic, chondrogenic, adipogenic [4] |
| Placenta (P-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- [4] | Superior proliferative capacity, pronounced immunosuppressive effects [4] | Complex composition, challenging isolation [4] | Osteogenic, chondrogenic, adipogenic [4] |
| Menstrual Blood (MenSCs) | CD29+, CD73+, CD90+, CD105+, CD45-, CD34- [4] | Easy non-invasive collection, high proliferation rate [4] | Limited to cycling women, relatively new cell source [4] | Osteogenic, chondrogenic, adipogenic [4] |
Bone Marrow-Derived MSCs (BM-MSCs)
BM-MSCs represent the most extensively studied and characterized MSC population. They must be obtained through invasive methods such as bone marrow aspiration, and their number in the bone marrow is limited (approximately 0.01-0.001%) [4]. Typically, BM-MSCs require expansion in culture to obtain adequate cell numbers for therapeutic applications. While autologous BM-MSCs do not trigger immune-related rejection, allogeneic BM-MSCs may cause immune complications, and their quality is influenced by donor age and overall health [4].
Adipose-Derived MSCs (AD-MSCs)
AD-MSCs have gained significant attention due to their abundant availability, with up to 1 billion cells potentially generated from 300g of adipose tissue obtained through liposuction [4]. Compared to BM-MSCs, harvesting AD-MSCs is less invasive, offers faster proliferation rates, and is primarily performed on adipose tissue from the abdomen and thighs [4]. AD-MSCs offer distinct advantages in bone regeneration and skin healing [4]. Several randomized controlled trials have demonstrated their efficacy in orthopedic applications, particularly for cartilage repair and knee osteoarthritis [100] [101].
Umbilical Cord-Derived MSCs (UC-MSCs)
UC-MSCs are typically isolated from Wharton's jelly and contain a high concentration of MSCs [4]. Compared to BM-MSCs, UC-MSCs exhibit significantly higher proliferative and migratory capacities, are produced in greater quantities, and are characterized by high safety, low immunogenicity, high purity, and low application risk [4]. The highest concentration of MSCs and the highest derivation rate are isolated from Wharton's jelly in the umbilical cord [4].
Placental MSCs (P-MSCs) and Menstrual Blood Stem Cells (MenSCs)
The placenta represents a rich source of MSCs, with its structure consisting of the amnion, chorionic frondosum, and basal decidua, all enriched with MSCs [4]. P-MSCs may have superior proliferative capacity compared to umbilical cord MSCs and exhibit more pronounced immunosuppressive effects on dendritic cells and T cells [4]. However, the complex composition of the placenta makes it challenging to isolate pure and safe MSCs.
Menstrual blood stem cells (MenSCs), first reported in 2007, represent a relatively new addition to stem cell therapy [4]. Under optimal culture conditions, MenSCs from young, healthy women can double their proliferation every 20 hours, which is twice the rate observed in bone marrow MSCs [4]. This high proliferation rate results in increased expression of embryonic trophic factors and the extracellular matrix in MenSCs [4].
Therapeutic Efficacy Across Medical Applications
Orthopedic Applications and Cartilage Repair
AD-MSCs have demonstrated significant potential in cartilage tissue engineering due to their accessibility, high proliferation rate, and chondrogenic differentiation capacity [102]. In a prospective, randomized, open, and blinded endpoint study comparing AD-MSCs versus hyaluronic acid for early knee osteoarthritis, MRI results revealed significant and progressive cartilage regeneration in the AD-MSC group [100]. Specifically, medial femoral cartilage lesion volume decreased by 50.06 mm³ in the AD-MSC group, whereas the HA group showed an increase of 36.44 mm³ [100]. Synovial thickness also declined significantly in the AD-MSC group at 3 and 6 months, and the AD-MSC group achieved superior and sustained improvements in WOMAC pain, stiffness, and function scores throughout the 6-month follow-up [100].
A systematic review of AD-MSCs and stromal vascular fraction (SVF) for pain relief in Kellgren-Lawrence grade II-III knee osteoarthritis demonstrated that AD-MSC therapies provide prolonged pain relief and enhanced joint function up to 24 months post-treatment, with superior outcomes in cartilage regeneration compared to SVF [101]. The chondrogenic properties of AD-MSCs make them particularly beneficial for patients younger than 62 years [101].
Table 2: Clinical Efficacy of MSC Sources in Various Medical Applications
| Medical Application | Most Promising MSC Source | Key Efficacy Findings | Reference |
|---|---|---|---|
| Knee Osteoarthritis | Adipose-derived | Cartilage lesion volume reduced by 50.06 mm³ vs increase of 36.44 mm³ with HA; sustained pain relief up to 24 months | [100] [101] |
| Myocardial Infarction | Adipose-derived (for anti-apoptosis); Umbilical cord (for angiogenesis) | AD-MSCs exerted better cardioprotective function and stronger anti-apoptotic effect; UC-MSCs had greater pro-angiogenesis activity | [98] |
| Graft-versus-Host Disease | Bone marrow-derived | First MSC therapy approved by US FDA for pediatric GVHD; modulates allogeneic immune cell responses | [99] |
| Crohn's Disease Fistulas | Adipose-derived | Expanded allogeneic AD-MSCs (Cx601) showed efficacy for complex perianal fistulas in phase 3 trial | [99] |
| Gynecological Diseases | Various (UC, AD, MenSC) | Applications in uterine adhesions, endometriosis, premature ovarian insufficiency with notable efficacy | [4] |
Cardiovascular Applications
In myocardial infarction treatment, a comparative study of UC-MSCs and AD-MSCs revealed differences in their therapeutic strengths [98]. RNA sequencing analysis revealed differences in gene expression related to angiogenesis and apoptosis pathways between UC-MSCs and AD-MSCs [98]. UC-MSCs presented greater pro-angiogenesis activity than AD-MSCs in vitro and in vivo [98]. Both UC-MSCs and AD-MSCs improved cardiac function, decreased infarction area, and inhibited cardiomyocyte apoptosis while promoting angiogenesis post-myocardial infarction in mice [98]. Notably, AD-MSCs exerted a better cardioprotective function than UC-MSCs and demonstrated a stronger anti-apoptotic effect on residual cardiomyocytes [98]. This suggests that the protection of residual cell survival may play a more prominent role than angiogenesis in MSC-based therapy for acute myocardial infarction.
Immunomodulatory Applications
The immunomodulatory properties of MSCs have been exploited for treating immune-related conditions such as graft-versus-host disease (GVHD) and Crohn's disease. Bone marrow-derived MSCs have been approved for pediatric GVHD in the United States, marking the first MSC therapy approved by the U.S. Food and Drug Administration [99]. MSCs can modulate immune responses by interacting with various immune cells, such as T cells, macrophages, and dendritic cells, through both direct cell-cell interactions and the release of immunoregulatory molecules [1]. Additionally, expanded allogeneic adipose-derived MSCs (Cx601) have shown efficacy for complex perianal fistulas in Crohn's disease in a phase 3 randomized, double-blind controlled trial [99].
Gynecological Applications
In gynecology, MSCs from diverse sources—including bone marrow, adipose tissue, menstrual blood, umbilical cord, umbilical cord blood, and placenta—have undergone extensive research and clinical trials [4]. Due to their self-renewal, multidirectional differentiation, and immunomodulatory capabilities, MSCs offer promising prospects for treating various gynecological diseases, such as uterine adhesions, endometriosis, premature ovarian insufficiency, polycystic ovary syndrome, pelvic floor dysfunction, and gynecological tumors [4]. Notably, MSC therapies for uterine adhesions and early-onset ovarian failure have progressed to clinical application, demonstrating notable efficacy [4].
Experimental Methodologies for MSC Characterization
Flow Cytometry Analysis
Flow cytometry is essential for determining the surface marker expression profiles of MSCs from different sources, confirming they meet ISCT criteria [98]. The standard protocol involves:
- Cell Preparation: Harvest MSCs at passage 3-5 and wash with phosphate-buffered saline (PBS) [98].
- Antibody Staining: Incubate cells with fluorochrome-conjugated antibodies against CD14, CD19, CD34, CD45, CD73, CD90, CD105, and HLA-DR, with isotype-matched antibodies as negative controls [98].
- Analysis: Analyze stained cells using a flow cytometer (e.g., Accuri C6 Plus, BD) and process data with specialized software (e.g., Flow Jo V10) [98].
- Interpretation: MSCs should express CD73, CD90, and CD105 (≥95% positive) while lacking expression of hematopoietic markers (≤2% positive) [98].
Trilineage Differentiation Assays
The differentiation potential of MSCs is evaluated after culturing them in specific differentiation media according to established protocols [98].
Adipogenic Differentiation:
- Culture MSCs in adipogenic induction medium (e.g., Gibco) for 14 days [98]
- Confirm differentiation by Oil Red O staining of lipid vacuoles [98]
Osteogenic Differentiation:
- Culture MSCs in osteogenic induction medium (e.g., Gibco) for 21 days [98]
- Verify differentiation by Alizarin Red S staining of calcium deposits [98]
Chondrogenic Differentiation:
- Culture MSCs in chondrogenic induction medium in pellet or micromass culture for 21-28 days [98]
- Assess differentiation by Alcian Blue or Safranin O staining of proteoglycans [1]
Transcriptome Sequencing Analysis
RNA sequencing provides comprehensive insights into the molecular differences between MSCs from various sources:
- RNA Extraction: Isolate high-quality total RNA from MSCs [98]
- Library Preparation and Sequencing: Construct libraries and perform sequencing on platforms such as Illumina [98]
- Differential Expression Analysis: Use tools like DESeq R package to identify differentially expressed genes (DEGs) with criteria such as p-value < 0.05 and fold change > 2 or < 0.5 [98]
- Pathway Analysis: Perform KEGG enrichment analysis to identify pathways enriched in DEGs [98]
- Functional Characterization: Employ methods like ssGSEA in GSVA to calculate pathway scores and characterize functional differences between MSC types [98]
Functional Assays for Therapeutic Potential
Tube Formation Assay (Angiogenesis):
- Seed HUVECs diluted with conditioned medium from MSCs in Matrigel-coated wells [98]
- After 8 hours of incubation, quantify capillary-like structures by measuring total tube length, number of nodes, and number of junctions using ImageJ software [98]
Matrigel Plug Assay (In Vivo Angiogenesis):
- Mix MSCs with Liquid Matrigel and inject subcutaneously into mice [98]
- Harvest plugs after 14 days and analyze vascularization [98]
Animal Disease Models:
- For myocardial infarction: Perform coronary artery ligation in mice and inject MSCs directly into myocardium after surgery [98]
- Assess functional improvement over time (e.g., 28 days post-infarction) using echocardiography and histological analysis [98]
Visualization of MSC Characterization Workflow
Diagram 1: Comprehensive Workflow for Comparative MSC Characterization. This diagram outlines the standardized experimental approach for isolating, characterizing, and functionally validating MSCs from different tissue sources, culminating in comparative efficacy analysis.
Signaling Pathways and Therapeutic Mechanisms
MSCs exert their therapeutic effects through multiple mechanisms, primarily via paracrine secretion of bioactive molecules rather than direct differentiation and engraftment [99]. These mechanisms include:
Paracrine Signaling
MSCs release a diverse range of bioactive molecules, including growth factors, cytokines, chemokines, and extracellular vesicles (EVs) [1] [99]. These components play crucial roles in modulating the local cellular environment, promoting tissue repair, angiogenesis, and cell survival, and exerting anti-inflammatory effects [1]. The concept of the "paracrine effect" has become widely accepted, where MSCs mediate tissue repair and immune modulation through the secretion of these factors [1]. MSC-derived EVs have shown bioactivity capable of treating fibrosis, promoting tissue regeneration, and reducing inflammation [99].
Immunomodulatory Pathways
MSCs interact with various immune cells, such as T cells, B cells, dendritic cells, and macrophages, modulating the immune response through both direct cell-cell interactions and the release of immunoregulatory molecules [1]. MSC-derived soluble factors suppress activation and maturation of innate immune cells and skew early innate reactions toward an anti-inflammatory phenotype [99]. These immunomodulatory effects have become a key factor in developing MSC-based treatments for rheumatoid arthritis, Crohn's disease, and graft-versus-host disease [1].
Diagram 2: MSC Therapeutic Mechanisms and Signaling Pathways. This diagram illustrates the primary mechanisms through which MSCs from different sources exert their therapeutic effects, including paracrine signaling, immunomodulation, and multilineage differentiation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MSC Characterization and Functional Analysis
| Reagent/Category | Specific Examples | Research Application | Function in MSC Research |
|---|---|---|---|
| Surface Marker Antibodies | CD73, CD90, CD105, CD14, CD19, CD34, CD45, HLA-DR [98] | Flow cytometry characterization | Confirm MSC phenotype according to ISCT criteria [98] |
| Differentiation Media | Adipogenic, Osteogenic, Chondrogenic Induction Media (e.g., Gibco) [98] | Trilineage differentiation assays | Induce and validate multipotent differentiation capacity [98] |
| Extracellular Matrix | Matrigel [98] | Tube formation assay, 3D culture | Provide substrate for angiogenesis studies and 3D modeling [98] |
| Cell Culture Supplements | Fetal Bovine Serum (FBS), DMEM medium [98] | Cell expansion and maintenance | Support MSC growth and propagation in culture [98] |
| Molecular Biology Kits | RNA extraction kits, cDNA synthesis kits, qPCR reagents [98] | Gene expression analysis | Quantify differentiation markers and therapeutic genes [98] |
| Animal Models | BALB/C nude mice, C57BL/6 mice [98] | In vivo therapeutic testing | Evaluate MSC efficacy in disease-specific contexts [98] |
| Imaging Reagents | Oil Red O, Alizarin Red S, Alcian Blue [98] | Histological validation | Visualize and quantify differentiation endpoints [98] |
| Sequencing Platforms | Illumina platforms [98] | Transcriptome analysis | Comprehensive molecular profiling of different MSC sources [98] |
The comparative analysis of MSC sources reveals a complex landscape of biological properties and therapeutic potentials. While all MSCs share fundamental characteristics as defined by ISCT criteria, their tissue origin significantly influences their functional capabilities and clinical applications. Bone marrow-derived MSCs represent the most characterized population but face limitations in harvest invasiveness and donor age-related quality decline. Adipose tissue provides an abundant source of MSCs with strong chondrogenic potential, making them particularly valuable for orthopedic applications. Umbilical cord-derived MSCs offer enhanced proliferative capacity and lower immunogenicity, suitable for allogeneic transplantation. Placental and menstrual blood-derived MSCs represent promising but less characterized sources with unique biological properties.
The therapeutic efficacy of different MSC sources varies across medical applications, with AD-MSCs demonstrating superiority in cartilage repair and cardioprotection, UC-MSCs showing enhanced angiogenic potential, and BM-MSCs establishing efficacy in immunomodulatory applications such as GVHD. These differences highlight the importance of matching MSC source to specific clinical indications rather than seeking a universally superior source.
Future research should prioritize standardized protocols, mechanistic studies elucidating source-specific therapeutic actions, and large-scale comparative clinical trials. The emerging fields of MSC-derived extracellular vesicles and enrichment of specific subpopulations like Muse cells represent promising avenues for enhancing therapeutic efficacy while potentially overcoming the challenges associated with cellular heterogeneity. As the field advances, precision medicine approaches that select optimal MSC sources based on their functional strengths for specific disease contexts will likely maximize therapeutic outcomes in regenerative medicine.
Dose-Effect Relationships in MSC and MSC-Derived Extracellular Vesicle Trials
Mesenchymal stem cells (MSCs) have emerged as a cornerstone of regenerative medicine due to their multipotent differentiation capacity, immunomodulatory properties, and trophic factor secretion [1]. These non-hematopoietic stem cells can be isolated from various tissues including bone marrow, adipose tissue, umbilical cord, and placental tissue [1]. According to the International Society for Cellular Therapy (ISCT), MSCs are defined by their adherence to plastic, specific surface marker expression (CD73, CD90, CD105), and capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [1]. The therapeutic paradigm has recently evolved from whole-cell therapies to include cell-free alternatives, particularly MSC-derived extracellular vesicles (MSC-EVs), which offer comparable therapeutic effects with reduced risks [103] [104]. MSC-EVs, including exosomes and microvesicles, are nano-sized membrane-bound structures that carry bioactive molecules and mediate intercellular communication [105]. Understanding dose-effect relationships is crucial for clinical translation, as optimal dosing varies significantly based on administration route, tissue source, and target pathology [103].
Current Clinical Trial Landscape: Quantitative Analysis of Dosing Parameters
Global Clinical Trial Findings on MSC-EV Dosing
A comprehensive statistical summary of global clinical trials registered between 2014 and 2024 provides critical insights into MSC-EV dosing strategies. Analysis of 66 eligible trials from ClinicalTrials.gov, the Chinese Clinical Trial Registry, and the Cochrane Register of Studies revealed significant variations in dosing parameters [103].
Table 1: MSC-EV Dosing Strategies by Administration Route in Clinical Trials
| Administration Route | Typical Dose Range | Therapeutic Indications | Notable Findings |
|---|---|---|---|
| Intravenous Infusion | Variable, typically higher doses | Multi-system diseases, GVHD, inflammatory disorders | Requires higher particle counts; potential systemic exposure concerns |
| Aerosolized Inhalation | ~10⁸ particles | Respiratory diseases (ARDS, COVID-19, lung injury) | Significantly lower effective dose compared to IV; targeted delivery |
| Local Injection | Tissue-specific dosing | Orthopedic injuries, dermatological conditions, localized regeneration | Direct site application; minimal systemic distribution |
The data demonstrate that administration route significantly influences effective dosing, with nebulization therapy achieving therapeutic effects at doses approximately 10⁸ particles, substantially lower than intravenous routes [103]. This suggests a route-dependent effective dose window that must be carefully considered in trial design. The analysis also identified large variations in EV characterization, dose units, and outcome measures across trials, underscoring the lack of harmonized reporting standards [103].
Source-Dependent Potency Variations
MSC therapeutic potency varies significantly based on tissue source, influencing dose-response relationships:
Table 2: MSC Source-Dependent Therapeutic Properties
| MSC Source | Differentiation Potential | Immunomodulatory Capacity | Clinical Advantages |
|---|---|---|---|
| Bone Marrow (BM-MSCs) | High osteogenic differentiation | Strong immunomodulatory effects | Most extensively studied; proven track record |
| Adipose Tissue (AD-MSCs) | Moderate multi-lineage potential | Comparable to BM-MSCs | Easier harvesting; higher yields |
| Umbilical Cord (UC-MSCs) | Enhanced proliferation capacity | Superior immunomodulation | Lower immunogenicity; suitable for allogeneic use |
| Wharton's Jelly (WJ-MSCs) | Neural differentiation preference | Enhanced under hypoxia | Youthful cell source; high expansion potential |
Recent investigations into hypoxia-preconditioned Wharton's Jelly MSCs demonstrated superior efficacy in suppressing T-cell proliferation compared to bone marrow sources, emphasizing the importance of source selection and preconditioning strategies in dose optimization [106].
Experimental Protocols for Dose-Response Investigations
Standardized MSC-EV Isolation and Characterization
Protocol 1: MSC-EV Isolation via Differential Ultracentrifugation
- MSC Culture Expansion: Plate MSCs at 5,000-8,000 cells/cm² in complete media (α-MEM supplemented with 10% FBS and 1% penicillin/streptomycin) [1]
- Serum Deprivation: Replace with EV-depleted serum 48-72 hours prior to collection to reduce contaminating vesicles
- Conditioned Media Collection: Collect media after 24-72 hours based on experimental requirements [106]
- Centrifugation Steps:
- 300 × g for 10 minutes to remove cells
- 2,000 × g for 20 minutes to remove cell debris
- 10,000 × g for 30 minutes to remove apoptotic bodies
- 100,000 × g for 70 minutes to pellet EVs
- Wash with PBS and repeat ultracentrifugation [103]
- Resuspension: Resuspend EV pellet in PBS or appropriate buffer and store at -80°C
Characterization Parameters:
- Nanoparticle Tracking Analysis (NTA): Size distribution and concentration [103]
- Transmission Electron Microscopy: Morphological validation [103]
- Flow Cytometry: Surface marker detection (CD63, CD81, CD9) [103]
- Protein Quantification: BCA assay for standardization [104]
Dose-Response Assessment in Immunomodulation Models
Protocol 2: T-cell Proliferation Inhibition Assay [106]
- CD3+ T-cell Isolation: Isolate from peripheral blood mononuclear cells (PBMNCs) using magnetic-activated cell sorting (MACS)
- Cell Seeding: Plate at varying densities (2×10⁶, 5×10⁶, and 10×10⁶ cells/ml) to assess cell density effects
- CCM Treatment: Apply culture-conditioned media at different concentrations (25%, 50%, 100%) to determine optimal inhibitory concentration
- Hypoxia Preconditioning: Culture MSCs under hypoxic conditions (1% O₂) for 24 hours in a tri-gas incubator to enhance potency [106]
- Proliferation Assessment:
- MTS Assay: Measure metabolic activity at 24-72 hours
- Flow Cytometry: Evaluate CD4+/CD8+ T-cell ratios and activation markers (CD25, CD69)
- Data Analysis: Calculate inhibition percentages and determine IC₅₀ values for different MSC sources
This protocol revealed that CCM collected at 48 hours at 50% concentration exerted the most pronounced inhibitory effect on CD3+ T-cell proliferation, particularly at a density of 5×10⁶ cells/ml [106]. Hypoxia preconditioning significantly enhanced immunomodulatory effects, with WJ-MSCs demonstrating superior efficacy [106].
Figure 1: Experimental Workflow for MSC-EV Dose-Response Studies
Mechanisms of Action: Dose-Dependent Therapeutic Effects
Paracrine Signaling and EV-Mediated Communication
The therapeutic effects of MSCs are primarily mediated through paracrine signaling rather than direct differentiation and engraftment [104]. MSC-EVs serve as crucial messengers in this process, transferring bioactive molecules including microRNAs, proteins, and lipids to recipient cells [105]. Dose-dependent effects manifest through:
- Anti-inflammatory Effects: MSC-EVs polarize macrophages toward the M2 anti-inflammatory phenotype and reduce pro-inflammatory cytokine production (TNF-α, IL-1β, IL-6) in a dose-dependent manner [105]
- Immunomodulation: EVs suppress T-cell proliferation and modulate dendritic cell maturation, with efficacy correlating with vesicle concentration [106] [107]
- Angiogenesis Promotion: Pro-angiogenic miRNAs (e.g., miR-126, miR-210) in MSC-EVs stimulate endothelial cell proliferation and tube formation at optimal doses [104]
- Anti-apoptotic Effects: MSC-EV treatment reduces caspase-3/7 activity and promotes cell survival pathways in dose-responsive patterns [105]
Figure 2: MSC-EV Mechanism of Action and Therapeutic Effects
Critical Signaling Pathways in Dose-Response Relationships
Multiple signaling pathways contribute to the dose-dependent therapeutic effects of MSCs and MSC-EVs:
- TGF-β/Smad Pathway: Regulation of T-cell differentiation and suppression of inflammatory responses [1]
- Wnt/β-catenin Signaling: Enhancement of tissue repair processes and stem cell proliferation [1]
- PI3K/Akt Pathway: Promotion of cell survival and inhibition of apoptosis [104]
- NF-κB Modulation: Downregulation of pro-inflammatory cytokine production [107]
- HIF-1α Activation: Enhanced regenerative capacity through hypoxia preconditioning [106]
The activation thresholds and saturation points of these pathways determine optimal dosing windows, with excessive doses potentially leading to paradoxical effects or reduced efficacy [103] [106].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for MSC-EV Dose-Response Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Mesenchymal Stem Cells | Therapeutic agent source | Select appropriate tissue source (BM, AD, UC) based on target pathology [108] |
| EV-Depleted Fetal Bovine Serum | Cell culture supplement | Essential for EV production without contaminating vesicles [104] |
| Ultracentrifugation Equipment | EV isolation | Gold standard method; alternatives include size-exclusion chromatography, precipitation [103] |
| Nanoparticle Tracking Analyzer | EV quantification | Provides particle size distribution and concentration [103] |
| Flow Cytometer with Nanoscale Capability | EV characterization | Detection of surface markers (CD9, CD63, CD81) [104] |
| Hypoxia Chamber | MSC preconditioning | Enhances therapeutic potency (1-3% O₂) [106] |
| Luminex/Multiplex Assay Kits | Cytokine profiling | Quantification of inflammatory mediators in dose-response studies [106] |
| 3D Culture Systems | Tissue modeling | More physiologically relevant platforms for efficacy testing [109] |
The establishment of robust dose-effect relationships for MSC and MSC-EV therapies remains challenging due to source variability, isolation method differences, and administration route dependencies [103]. Current evidence supports route-specific dosing, with aerosolized inhalation requiring significantly lower doses (~10⁸ particles) than intravenous administration for therapeutic efficacy [103]. The field requires standardized dosing frameworks, potency assays, and harmonized clinical protocols to advance the safe and effective translation of these therapies [103]. Future research should focus on engineering approaches to enhance EV targeting and loading, manufacturing standardization for consistent product quality, and comprehensive biomarker identification for patient stratification and response monitoring [104] [107]. As the field evolves, precise understanding of dose-effect relationships will be paramount for transforming regenerative medicine from promising concept to clinical reality.
Mesenchymal stem cells (MSCs) are non-hematopoietic, multipotent stromal cells characterized by a triad of defining properties: adherence to plastic under standard culture conditions, specific surface marker expression (CD105, CD90, CD73), and capacity for trilineage differentiation into osteocytes, chondrocytes, and adipocytes in vitro [110] [1]. First identified in bone marrow by Friedenstein and colleagues in the 1970s, MSCs have since been isolated from diverse tissue sources including adipose tissue, umbilical cord blood, dental pulp, and placental tissue [110] [1]. The therapeutic profile of MSCs extends beyond differentiation capacity to include potent immunomodulatory functions through interactions with T cells, B cells, dendritic cells, and macrophages, plus the secretion of bioactive molecules that promote tissue repair and angiogenesis [1]. These properties have positioned MSCs as attractive candidates for treating conditions ranging from autoimmune diseases and orthopedic injuries to neurodegenerative disorders [1].
The traditional paradigm of MSC therapy centered on the administration of living cells that would engraft at injury sites, differentiate into target tissues, and directly participate in regeneration. However, accumulating evidence reveals that MSC therapeutic effects are predominantly mediated through paracrine signaling rather than direct cellular replacement [111]. This fundamental understanding has catalyzed a significant shift from whole-cell therapies toward acellular, secretome-based approaches, representing a transformative advancement in regenerative medicine strategy.
The Paradigm Shift: From Whole-Cell to Cell-Free Therapeutics
Limitations of Whole-Cell MSC Therapies
While whole-cell MSC therapies have demonstrated promising results across various disease models, several critical limitations hinder their clinical translation and scalability. Safety concerns include potential immunogenic reactions despite MSC's low immunogenicity, and risks of ectopic tissue formation or tumorigenicity, particularly with spontaneous transformation observed in long-term cultures of certain MSC types [110]. Logistical challenges present substantial barriers, including the need for strict viability control during transportation and storage, requiring cryopreservation with complex protocols [112] [111]. Donor-dependent variability in potency and the necessity for tissue matching in some applications further complicate standardized treatment protocols [110].
Perhaps most significantly, research indicates that engraftment rates of administered MSCs at injury sites are typically minimal and transient, suggesting that long-term cellular integration is not the primary mechanism of therapeutic action [111]. Instead, the beneficial effects appear to be mediated predominantly through paracrine factors secreted by these cells, which has redirected therapeutic focus toward the soluble mediators themselves.
The Secretome: Definition and Composition
The MSC secretome represents the complete repertoire of bioactive molecules released by MSCs, comprising both soluble components and extracellular vesicles (EVs) [112]. This complex biological product includes growth factors (VEGF, HGF, IGF-1, bFGF), cytokines and chemokines (IL-10, TSG-6), lipids, and microRNAs, as well as extracellular vesicles such as exosomes and microvesicles that carry proteins, nucleic acids, and other signaling molecules [112] [111].
The composition of the secretome is dynamic and influenced by multiple factors, including the MSC tissue source (bone marrow, adipose, umbilical cord), donor characteristics, and culture conditions [112] [111]. Umbilical cord-derived MSCs, particularly from Wharton's jelly, demonstrate a secretory profile favoring immunomodulation and tissue repair, while bone marrow-derived MSCs may exhibit age-related functional decline in their secretome composition [111].
Table 1: Key Components of the MSC Secretome and Their Functions
| Component Category | Specific Examples | Primary Functions |
|---|---|---|
| Pro-angiogenic Factors | VEGF, HGF, IGF-1 | Promote blood vessel formation and endothelial cell survival |
| Anti-apoptotic Molecules | bFGF, TGF, GM-CSF | Inhibit programmed cell death and support cell survival |
| Anti-inflammatory Mediators | IL-10, TSG-6, HO-1 | Modulate immune responses, suppress pro-inflammatory cytokines |
| Extracellular Vesicles | Exosomes, Microvesicles | Transfer proteins, lipids, miRNAs between cells; mediate distant effects |
Comparative Analysis: Secretome vs. Whole-Cell Approaches
Therapeutic Mechanisms
Whole-cell MSCs and their secretomes operate through distinct yet overlapping mechanistic pathways. Whole-cell therapies theoretically provide the advantage of direct cellular interactions through cell-to-cell contact and the potential for direct differentiation into target tissues, though this occurs minimally in practice [111]. Additionally, living MSCs can sense and dynamically respond to their microenvironment, adjusting their secretory profile in real-time to local inflammatory and damage signals [112].
In contrast, secretome-based therapies function exclusively through paracrine signaling, delivering a concentrated bolus of bioactive molecules that modulate immune responses, promote neuronal survival, regulate opioid receptor expression, and reprogram glial cell activity [112]. The extracellular vesicle component enables the transfer of complex molecular cargoes, including miRNAs that can durably alter gene expression in recipient cells [111]. This multifaceted mechanism of action is particularly advantageous for treating complex conditions like chronic pain, which involves both neuroimmune activation and central sensitization processes [112].
Advantages and Limitations
The transition to secretome-based therapies addresses several critical limitations of whole-cell approaches while introducing new considerations for clinical translation.
Table 2: Comparative Analysis of Whole-Cell vs. Secretome-Based Therapies
| Parameter | Whole-Cell Therapies | Secretome-Based Therapies |
|---|---|---|
| Immunogenicity | Low but present risk; potential immune reactions | Minimal; acellular nature reduces immunogenicity [112] |
| Tumorigenic Risk | Theoretical concern of ectopic tissue formation or transformation [110] | No risk of tumor formation or uncontrolled differentiation [112] |
| Standardization | High variability between donors and cultures | Easier to standardize, batch, and quality control [112] |
| Storage & Stability | Requires cryopreservation; viability concerns | Lyophilization possible; long-term storage without cryoprotectants [111] |
| Manufacturing | Complex expansion; sterility challenges | Scalable production; compatible with GMP automation [111] |
| Dosing | Based on cell numbers; inconsistent engraftment | Based on protein/content quantification; more precise [112] |
| Regulatory Pathway | Complex cellular product regulations | Simpler biologic/pharmaceutical framework |
| Theoretical Mechanisms | Direct differentiation + paracrine effects | Exclusive paracrine activity |
| Clinical Administration | Potential for pulmonary entrapment (IV route) | Wider safety margin for different administration routes |
Despite these advantages, secretome therapies face their own challenges. Standardization of production methods remains problematic, with variability in secretome composition based on MSC source, culture conditions, and stimulation protocols [112]. The lack of large-scale clinical trials and undefined regulatory pathways for these complex biologics present additional hurdles to widespread clinical adoption [112]. Furthermore, the short half-life of some soluble factors may necessitate repeated administrations or advanced delivery systems to maintain therapeutic effects.
Technical and Methodological Considerations
Secretome Production and Characterization
Standardized protocols for secretome production are essential for clinical translation. The general workflow begins with MSC isolation and expansion from selected tissue sources under defined culture conditions, often using serum-free media to minimize batch variability [111]. For secretome collection, MSCs are typically cultured until 70-80% confluence, then washed and incubated with fresh basal medium for 24-72 hours. The conditioned medium is collected and subjected to sequential centrifugation steps: 300-500 × g to remove cells, 2,000-3,000 × g to remove debris, and 10,000-20,000 × g to pellet large EVs [111]. For exosome isolation, ultracentrifugation at 100,000-120,000 × g or tangential flow filtration methods are employed [111].
Advanced characterization techniques include nanoparticle tracking analysis for vesicle size distribution, western blot for EV markers (CD63, CD81, TSG101), electron microscopy for morphological assessment, and proteomic/miRNA profiling for comprehensive compositional analysis [111]. Potency assays specific to intended therapeutic applications must be developed to ensure batch-to-batch consistency.
Experimental Models and Assessment Methodologies
Preclinical validation of secretome efficacy employs sophisticated disease models and rigorous assessment methodologies. For chronic pain applications, common models include spared nerve injury (neuropathic pain), complete Freund's adjuvant-induced inflammation (inflammatory pain), and monoiodoacetate-induced osteoarthritis (degenerative pain) [112]. Secretome treatments are administered via intraperitoneal, intravenous, or local routes at varying dosages (typically 50-200 μg protein content) and frequencies.
Assessment includes behavioral testing (mechanical allodynia using von Frey filaments, thermal hyperalgesia), molecular analyses (cytokine profiling, Western blot for pain-related markers), and immunohistochemical evaluation of glial activation and neuronal survival [112]. In neonatal disease models like bronchopulmonary dysplasia and necrotizing enterocolitis, secretome administration demonstrates reduced inflammation, enhanced tissue repair, and improved survival outcomes, with umbilical cord-derived MSC secretomes showing particular potency [111].
Table 3: Essential Research Reagents for Secretome Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| MSC Culture Media | αMEM, DMEM/F12 with FGF-2 | MSC expansion and maintenance [110] |
| Separation Technologies | Tangential Flow Filtration, Ultracentrifugation | Secretome concentration and EV isolation [111] |
| EV Characterization | Antibodies to CD63, CD81, TSG101 | Western blot validation of EV markers [111] |
| Nanoparticle Tracking | NanoSight NS300 | Size distribution and concentration of EVs [111] |
| Proteomic Analysis | Mass spectrometry, ELISA arrays | Comprehensive secretome profiling [112] |
| Functional Assays | Tube formation (angiogenesis), T-cell suppression | Potency and mechanism validation [112] [1] |
Clinical Translation and Future Directions
Current Clinical Evidence
Emerging clinical evidence supports the therapeutic potential of MSC secretome across various conditions. For chronic pain management, preliminary clinical studies report analgesic efficacy in osteoarthritis, chronic low back pain, and post-surgical pain, with a favorable safety profile and reduced opioid requirements [112]. In neurological applications, secretome-based approaches show promise for stroke recovery and neurodegenerative diseases, leveraging the neuroprotective and immunomodulatory factors [112]. Neonatal applications demonstrate safety and tolerability in preterm infants with bronchopulmonary dysplasia and necrotizing enterocolitis, with signs of clinical benefit observed in early-stage trials [111].
The therapeutic effects observed in these diverse conditions stem from conserved mechanisms of action, primarily through modulation of neuroimmune interactions and glial cell reprogramming, which addresses core pathophysiological processes across multiple disease states [112].
Technical Challenges and Future Perspectives
Despite promising results, several technical challenges must be addressed to advance secretome therapies. Standardization remains a critical hurdle, requiring development of reference materials and potency assays that correlate with clinical outcomes [112]. Manufacturing scalability needs innovation in bioreactor systems and closed-processing technologies to ensure consistent production of clinical-grade secretome [111]. Delivery optimization demands advanced formulation strategies, including hydrogels or controlled-release systems to extend secretome half-life at target sites [112].
Future development paths include engineering approaches to enhance secretome potency through MSC preconditioning (e.g., hypoxic, inflammatory) or genetic modification to enrich specific therapeutic factors [111]. The regulatory landscape for these complex biologics continues to evolve, requiring clear guidance on characterization, quality control, and clinical trial design specific to secretome-based products [112].
The shift from whole-cell to secretome-based therapies represents a paradigm transformation in regenerative medicine, aligning with a more precise understanding of MSC mechanisms of action. Secretome therapies offer distinct advantages in safety, standardization, and scalability while maintaining the multifaceted therapeutic benefits of their cellular counterparts. As research continues to elucidate the optimal conditions for secretome production, characterization, and delivery, these cell-free approaches are poised to overcome critical limitations that have hindered the clinical translation of whole-cell therapies. With ongoing advances in manufacturing technologies and quality control, MSC secretome-based products hold significant promise as next-generation biologics for diverse applications in chronic pain, neurodegenerative diseases, neonatal disorders, and beyond, potentially bridging critical gaps in current treatment paradigms for conditions with significant unmet medical needs.
Conclusion
The field of MSC-based regenerative medicine is at a pivotal juncture. While the foundational science is robust and the safety profile is well-established, consistent clinical efficacy remains the primary challenge. The future lies in overcoming heterogeneity through standardized manufacturing, leveraging advanced engineering with tools like CRISPR to create enhanced, off-the-shelf products, and rigorously validating therapeutic strategies in well-designed clinical trials. The promising shift towards defined, cell-free therapies using the MSC secretome and extracellular vesicles may offer more scalable and controllable treatment options. For MSC therapies to fully realize their potential and transition into routine clinical practice, a collaborative focus on resolving these critical bottlenecks in manufacturing, delivery, and validation is essential.
References
- 1. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 2. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/abs/pii/S1525001625000930]
- 3. Comparative analysis of human Mesenchymal Stromal Cells ... [https://biologydirect.biomedcentral.com/articles/10.1186/s13062-025-00697-w]
- 4. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 5. Comparison of MSCs and Muse cells: the possible use for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12222320/]
- 6. The resurgence of mesenchymal stem cell therapies [https://www.clinicaltrialsarena.com/sponsored/the-resurgence-of-mesenchymal-stem-cell-therapies/]
- 7. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 8. Mesenchymal Stem Cell News | Trials and Therapies [https://drakrtripuraskinandcosmetologyclinic.com/mesenchymal-stem-cell-news-breakthroughs-trials-and-emerging-therapies-in-2025/]
- 9. Defining minimal criteria for peer-reviewed reporting of ... [https://www.sciencedirect.com/science/article/pii/S1465324925007443]
- 10. Mesenchymal Stem Cells for Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6721852/]
- 11. Stem-Cell Niches in Health and Disease [https://pubmed.ncbi.nlm.nih.gov/40643502/]
- 12. Cell origin and microenvironment: The players of ... [https://pubmed.ncbi.nlm.nih.gov/39765135/]
- 13. Comparative analysis of human Mesenchymal Stromal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616983/]
- 14. Comparative Analysis of Human Mesenchymal Stem Cells ... [https://www.mdpi.com/1422-0067/14/9/17986]
- 15. Bioengineered niches that recreate physiological ... [https://www.nature.com/articles/s41467-024-50054-0]
- 16. New Insights into Osteogenic and Chondrogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3676919/]
- 17. Adipogenesis, Osteogenesis, and Chondrogenesis of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00561/full]
- 18. Predicting multipotency of human adult stem cells derived ... [https://www.nature.com/articles/s41598-022-25423-8]
- 19. Quantitative lineage tracing strategies to resolve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4911926/]
- 20. Mesenchymal Stem Cell Immunomodulation: Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7751844/]
- 21. Mesenchymal Stem Cell Immunomodulation: Mechanisms ... [https://www.sciencedirect.com/science/article/abs/pii/S0165614720301450]
- 22. Trends in mesenchymal stem cell-derived extracellular ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1625787/full]
- 23. Mesenchymal stem cell infusion to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500263X]
- 24. Protocol for Mesenchymal Stem Cell Isolation [https://fujifilmbiosciences.fujifilm.com/protocol-for-mesenchymal-stem-cell-isolation]
- 25. Human mesenchymal stem cells - current trends and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4413017/]
- 26. Characterisation of mesenchymal stromal cells in clinical trial ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02435-1]
- 27. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 28. Protocol for Mesenchymal Stem Cell Expansion [https://fujifilmbiosciences.fujifilm.com/protocol-for-mesenchymal-stem-cell-expansion]
- 29. Quantitative Detection and Modeling the In Vivo Kinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5746161/]
- 30. Mesenchymal stem cell secretome for regenerative medicine [https://www.sciencedirect.com/science/article/pii/S2090123224001814]
- 31. Secretome enriched with small extracellular vesicles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150548/]
- 32. Paracrine mechanisms in adult stem cell signaling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2667788/]
- 33. The tiny giants of regeneration: MSC-derived extracellular ... [https://pubmed.ncbi.nlm.nih.gov/40746857/]
- 34. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 35. Mesenchymal stem cell-derived extracellular vesicles [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1626996/full]
- 36. Recapitulation of in vivo-like paracrine signals of human ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961215005256]
- 37. Mesenchymal Stem Cells: What We Have Learned and How ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762337/]
- 38. Frontiers | Current Status, Challenges, and Integration Pathways of... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1690221/abstract]
- 39. Advances in treatment of chronic graft-versus-host disease [https://pubmed.ncbi.nlm.nih.gov/41247639/]
- 40. Graft-versus-host disease prophylaxis shapes T cell ... [https://www.medrxiv.org/content/10.1101/2025.02.25.25322901v1]
- 41. Stem Cell Research: The Future of Regenerative Medicine ... [https://www.dvcstem.com/post/stem-cell-research]
- 42. Stem cells in regenerative medicine: Unlocking therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2667099225000283]
- 43. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 44. Mesenchymal Stem Cells in the Pathogenesis and Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10671211/]
- 45. Recent advances in the role of mesenchymal stem cells as ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1525380/full]
- 46. Mesenchymal stem cells: Guardians of women's health [https://www.sciencedirect.com/science/article/pii/S2352320424001895]
- 47. Current status and future prospects of mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560345/]
- 48. Clinical application of mesenchymal in stem ... cell regenerative [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03054-0]
- 49. Nebulization of Mesenchymal Stem Cells Secretome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12165292/]
- 50. Frontiers | Mesenchymal for stem in... cells regenerative medicine [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.1068114/full]
- 51. Efficacy and safety of single versus repeated injections of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04638-2]
- 52. Treatment of pulmonary diseases and its clinical challenges [https://www.sciencedirect.com/science/article/pii/S0168365925000197]
- 53. Case Report: successful treatment of severe bronchiectasis ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1690559/full]
- 54. Intravenous Administration of Human-Derived ... [https://pubmed.ncbi.nlm.nih.gov/40869710/]
- 55. The heterogeneity of mesenchymal stem cells: an important ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03587-y]
- 56. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 57. DONOR VARIABILITY IN HUMAN MESENCHYMAL STEM ... [https://pubmed.ncbi.nlm.nih.gov/38014316/]
- 58. Manufacturing Cell and Gene Therapies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10961620/]
- 59. Batch variability and anti-inflammatory effects of iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11999995/]
- 60. 107 Mesenchymal Stem/Stromal Cells INTER-DONOR ... [https://www.sciencedirect.com/science/article/pii/S146532492400152X]
- 61. Manufacturing autologous cell therapies [https://www.patheon.com/us/en/insights-resources/blog/autologous-cell-therapy-manufacturing-challenges-and-best-practices.html]
- 62. Enhancing human pluripotent stem cell differentiation to ... [https://www.sciencedirect.com/science/article/pii/S2589004225007138]
- 63. Enhancing mesenchymal stem cell survival and homing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10478247/]
- 64. Mesenchymal Stromal Cell Homing: Mechanisms and ... [https://www.sciencedirect.com/science/article/pii/S2589004219301415]
- 65. Quantitative phase imaging with temporal kinetics predicts ... [https://www.nature.com/articles/s41467-025-61846-3]
- 66. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574024/]
- 67. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04723-6]
- 68. Revolution of Biotechnology with CRISPR [https://www.nature.com/articles/s12276-025-01452-x]
- 69. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 70. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 71. Aging and Replicative Senescence Have Related Effects on ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0005846]
- 72. Mesenchymal stem cells and their derivatives as potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011939/]
- 73. Identification of replicative aging and inflammatory aging ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03683-7]
- 74. The drug discovery and therapeutic nano-strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605296/]
- 75. Cellular senescence: from homeostasis to pathological ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1534263/full]
- 76. Reprogramming cellular senescence and aging clocks for ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02459-8]
- 77. Targeting Cellular Senescence for Healthy Aging: Advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456441/]
- 78. Rewriting destiny—gene-hacked stem cells ignite a ... [https://www.nature.com/articles/s41419-025-07958-6]
- 79. Functionalized mesenchymal stem cells for enhanced bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577075/]
- 80. Mesenchymal stem cell perspective: cell biology to clinical ... [https://www.nature.com/articles/s41536-019-0083-6]
- 81. Engineering multifunctional surface topography to regulate ... [https://www.sciencedirect.com/science/article/pii/S0142961225000559]
- 82. Regenerative Rehabilitation: Combining Stem Cell Therapies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5488706/]
- 83. Regenerative rehabilitation: Mechanisms, clinical ... [https://www.sciencedirect.com/science/article/pii/S2950575525000395]
- 84. The use of mesenchymal stem cells in tissue engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC2634175/]
- 85. Applicatoin of chitosan-based hydrogel in oral tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10930554/]
- 86. The Influence of the Surface Topographical Cues of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8328695/]
- 87. Harnessing Plant Bioactive Compounds in Biomaterial ... [https://www.mdpi.com/2227-9059/13/10/2414]
- 88. Systemic therapy of MSCs in bone regeneration: a systematic ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02456-w]
- 89. Ryoncil (remestemcel-L-rknd): the first approved cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12543205/]
- 90. FDA Approves First Mesenchymal Stromal Cell Therapy to ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-mesenchymal-stromal-cell-therapy-treat-steroid-refractory-acute-graft-versus-host]
- 91. February 2025 - FDA's Approval of Ryoncil [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/02/12/na-lra-watchdog-update-february-2025]
- 92. Mesenchymal stem cells in treating human diseases [https://pubmed.ncbi.nlm.nih.gov/40841367/]
- 93. Efficacy and safety of mesenchymal stromal cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04184-x]
- 94. Efficacy and safety of mesenchymal stem/stromal cells and ... [https://pubmed.ncbi.nlm.nih.gov/41023747/]
- 95. Efficacy and safety of mesenchymal stem cells in patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823675/]
- 96. Efficacy and safety of mesenchymal stem cell therapy in ... [https://pubmed.ncbi.nlm.nih.gov/40254564/]
- 97. SAFETY AND EFFICACY OF MESENCHYMAL STEM ... [https://www.sciencedirect.com/science/article/pii/S1465324925001707]
- 98. The therapeutic efficacy comparison of MSCs derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077008/]
- 99. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 100. Cartilage Regeneration Potential in Early Osteoarthritis of ... [https://www.mdpi.com/1422-0067/26/17/8476]
- 101. Efficacy of adipose-derived stem cells and stromal vascular ... [https://www.sciencedirect.com/science/article/pii/S0972978X25000947]
- 102. Adipose-Derived Stem Cells for Cartilage Tissue Engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC12132534/]
- 103. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 104. Extracellular vesicle-based drug overview [https://www.nature.com/articles/s41392-025-02312-w]
- 105. Umbrella review of mesenchymal stem cell-derived ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1655623/full]
- 106. Dose-response immunomodulatory effects of ... [https://www.sciencedirect.com/science/article/pii/S2352320425001981]
- 107. Mesenchymal stromal cell extracellular vesicles as immune ... [https://www.sciencedirect.com/science/article/pii/S0166223625001948]
- 108. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 109. Enhancing regenerative medicine: the crucial role of stem ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1269577/full]
- 110. Mesenchymal stem cell and regenerative medicine - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636724/]
- 111. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 112. Cell-Free Therapies for Chronic Pain: The Rise of ... [https://www.mdpi.com/2076-3425/15/12/1263]