Modeling Alzheimer's Risk: Investigating APOE Isoform-Specific Effects in Human iPSC-Derived Neurons and Brain Cell Types
Human induced pluripotent stem cells (hiPSCs) have emerged as a transformative platform for investigating the mechanistic roles of Apolipoprotein E (APOE) isoforms in Alzheimer's Disease (AD) and other neurodegenerative conditions.
Modeling Alzheimer's Risk: Investigating APOE Isoform-Specific Effects in Human iPSC-Derived Neurons and Brain Cell Types
Abstract
Human induced pluripotent stem cells (hiPSCs) have emerged as a transformative platform for investigating the mechanistic roles of Apolipoprotein E (APOE) isoforms in Alzheimer's Disease (AD) and other neurodegenerative conditions. This article synthesizes current research utilizing isogenic hiPSC models to dissect how APOE2, E3, and E4 differentially influence neuronal health, synaptic function, amyloid-β pathology, and blood-brain barrier integrity. We explore foundational APOE biology, methodological advances in stem cell differentiation and genome editing, troubleshooting of experimental challenges, and validation through comparison with clinical observations and animal models. This comprehensive analysis provides researchers and drug development professionals with critical insights for developing targeted therapeutic strategies based on APOE genotype.
APOE Isoforms and Neurobiology: Establishing the Genetic Framework for Alzheimer's Disease
APOE Genotype as the Strongest Genetic Risk Factor for Late-Onset Alzheimer's Disease
The apolipoprotein E (APOE) gene is the most significant genetic risk factor for late-onset Alzheimer's disease (LOAD). Among its three common isoforms, the APOE ε4 allele dramatically increases AD risk in a dose-dependent manner, while the APOE ε2 allele confers protection compared to the neutral APOE ε3 allele. This whitepaper delves into the molecular and cellular mechanisms through which APOE isoforms influence AD pathogenesis, with a particular emphasis on insights gained from human induced pluripotent stem cell (hiPSC) models. We review how APOE isoforms differentially regulate amyloid-β (Aβ) aggregation and clearance, tau pathology, neuroinflammation, lipid metabolism, and synaptic function. Furthermore, we summarize current therapeutic strategies targeting APOE pathways and provide a detailed toolkit for researchers, including standardized experimental protocols and reagents for modeling APOE in hiPSC-derived neural cells.
Alzheimer's disease (AD) is a progressive neurodegenerative disorder and the most common cause of dementia worldwide. The APOE ε4 allele is the strongest genetic risk factor for LOAD, with individuals carrying one copy of ε4 having a 3-4 fold increased risk, and homozygotes facing a 12-15 fold increase compared to non-carriers [1] [2]. Conversely, the APOE ε2 allele is associated with a reduced risk of AD [2]. The APOE protein is a lipid-transport protein that is highly expressed in the brain, primarily by astrocytes and, to a lesser extent, by microglia [3] [4]. It plays a critical role in brain lipid homeostasis, synaptic integrity, and neuronal repair. The three APOE isoforms differ only by single amino acid substitutions at positions 112 and 158, yet these differences have profound impacts on protein structure and function, influencing AD risk through a complex interplay of Aβ-dependent and Aβ-independent mechanisms [2] [5].
The emergence of hiPSC technology has revolutionized the study of AD, allowing for the generation of patient-specific neural cells, including neurons, astrocytes, and microglia. This provides a critical humanized platform to investigate the isoform-specific effects of APOE in a physiologically relevant context, bridging the gap between animal models and human clinical disease [6].
APOE Genetics and Risk Quantification
Allelic Variants and Population Frequency
The human APOE gene is located on chromosome 19 and encodes three major alleles—ε2, ε3, and ε4—with a worldwide frequency of approximately 8.4%, 77.9%, and 13.7%, respectively [2]. These alleles give rise to three protein isoforms that differ at two key amino acid positions:
- APOE2: Cysteine-112, Cysteine-158
- APOE3: Cysteine-112, Arginine-158
- APOE4: Arginine-112, Arginine-158 [2]
Table 1: APOE Isoform Characteristics and Associated AD Risk
| APOE Isoform | Amino Acid Positions (112/158) | Relative AD Risk (vs. APOE3/3) | Approximate Allele Frequency |
|---|---|---|---|
| APOE2 | Cysteine/Cysteine | 0.6 (Reduced) | ~8% |
| APOE3 | Cysteine/Arginine | 1.0 (Neutral) | ~78% |
| APOE4 | Arginine/Arginine | 3-4 (Heterozygote), 12-15 (Homozygote) | ~14% |
Data synthesized from [1] [2] [5]
Dose-Dependent Effect of APOE4
The association between APOE4 and AD risk is dose-dependent. A large meta-analysis established that compared to the common ε3/ε3 genotype, the odds ratio for AD increases to 3.2 for ε3/ε4 heterozygotes and rises to 14.9 for ε4/ε4 homozygotes [2]. APOE4 is also associated with an earlier age of onset of AD [7] [2]. The protective effect of APOE2 is similarly dose-dependent, with ε2/ε3 heterozygotes showing reduced risk and ε2/ε2 homozygotes exhibiting the strongest protection [2] [5].
Molecular and Cellular Mechanisms of APOE in AD
APOE isoforms influence AD pathogenesis through a multitude of mechanisms, which can be broadly categorized into Aβ-dependent and Aβ-independent pathways.
Aβ-Dependent Mechanisms
APOE isoforms differentially regulate Aβ metabolism, including its aggregation, deposition, and clearance.
- Amyloid Plaque Deposition: Human studies using amyloid PET imaging and post-mortem analysis consistently show that APOE4 carriers exhibit a significantly increased amyloid plaque burden compared to non-carriers, following an isoform-dependent pattern (E4 > E3 > E2) [3] [2]. The presence of APOE is required for the formation of amyloid plaques, as its absence in mouse models dramatically reduces Aβ deposition [3] [8].
- Aβ Clearance: APOE facilitates the cellular clearance of Aβ through receptor-mediated endocytosis. APOE4 is less effective than other isoforms in promoting Aβ clearance, potentially due to its impaired binding to certain receptors like LRP1 and its rapid degradation, which leads to its reduced levels in the brain [4] [2].
- Aβ Aggregation: In vitro studies suggest that APOE4 accelerates the fibrillization of Aβ into neurotoxic plaques compared to APOE2 and APOE3 [2].
Aβ-Independent Mechanisms
Significant evidence indicates that APOE4 contributes to AD pathology through mechanisms that operate independently of Aβ.
- Synaptic Dysfunction and Toxicity: APOE4 is associated with synaptic deficits both in humans and in animal models. APOE4-targeted replacement (TR) mice exhibit impairments in spatial learning, reduced dendritic spine density, and simpler dendritic arborization in the hippocampus and cortex, even in the absence of amyloid plaques [7] [8]. A recent mechanistic study revealed that APOE4 directly binds to the presynaptic protein VAMP2 with higher affinity than APOE3, thereby impairing the assembly of the SNARE complex and subsequent synaptic vesicle release, providing a direct molecular link to synaptic dysfunction [9].
- Tau Pathology: APOE4 exacerbates tau-mediated neurodegeneration and neurofibrillary tangle pathology. The interaction between APOE and tau appears to be independent of Aβ, and APOE4 drives a neuroinflammatory response that enhances tau pathology [4].
- Neuroinflammation: APOE isoforms differentially regulate the innate immune response in the brain. APOE4 tends to drive a pro-inflammatory state in microglia and astrocytes, which may contribute to neurodegeneration [3]. The interaction between APOE and microglial TREM2 is crucial for microglial function and response to neurodegeneration [3] [5].
- Endolysosomal Dysfunction: Enlarged endosomes represent an early pathological feature in AD neurons. Recent research using primary neurons indicates that APOE4 impairs endolysosomal function, leading to reduced degradative capacity and predisposing neurons to cholesterol accumulation over time [10].
- Cerebrovascular Deficits and Lipid Metabolism: APOE4 is associated with cerebral amyloid angiopathy (CAA) and impaired cerebrovascular function [2]. It also disrupts normal brain lipid homeostasis, leading to changes in neuronal lipid composition that can affect membrane integrity, synaptic signaling, and energy metabolism [4] [2]. APOE4 makes neurons more vulnerable to lipid peroxidation and subsequent ferroptotic cell death [4].
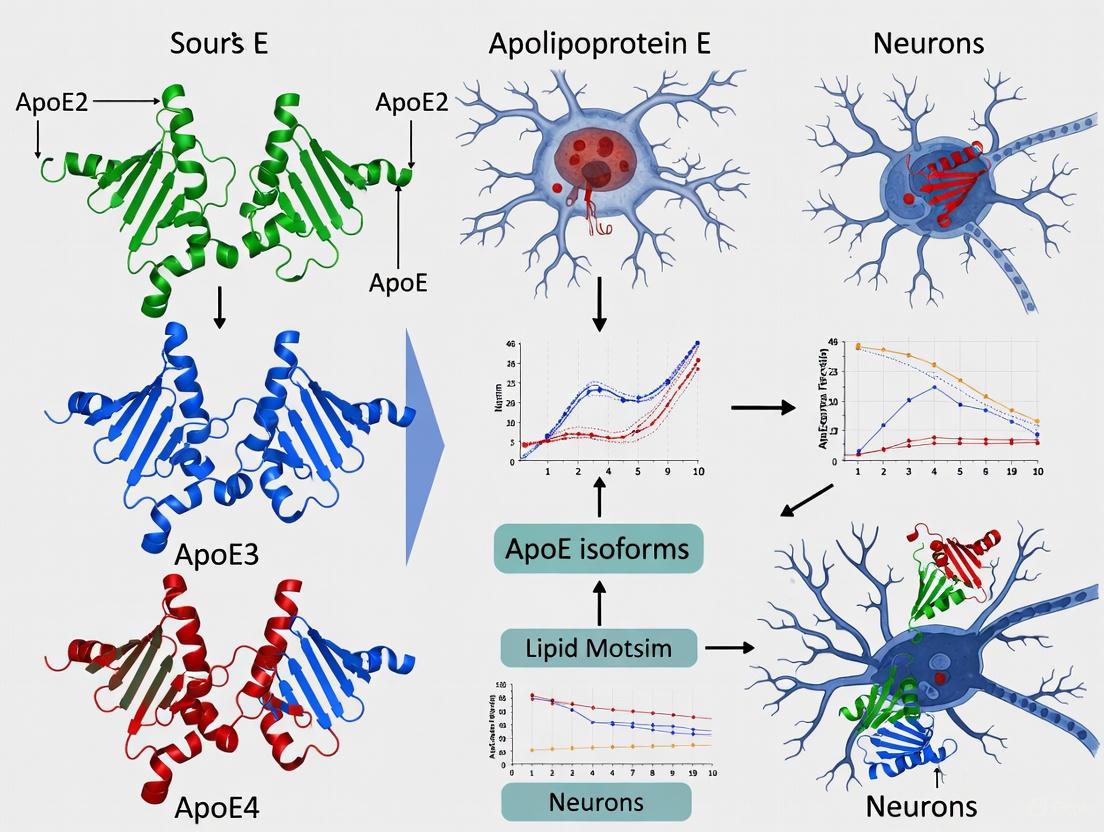
Diagram 1: APOE4 pathogenic mechanisms in Alzheimer's disease. The APOE4 isoform (red) drives pathology through multiple parallel pathways, including both amyloid-β-dependent and independent processes, which collectively contribute to disease progression.
APOE Research in hiPSC-Derived Models
hiPSC technology provides a powerful platform for studying the cell-type-specific effects of APOE isoforms in a human genetic background.
hiPSC Differentiation Protocols for Neural Cells
Table 2: Key hiPSC Differentiation Protocols for Neural Cells
| Target Cell Type | Key Patterning Factors/Signals | Key Markers | Primary Application in APOE/AD Research |
|---|---|---|---|
| Cortical Neurons | Dual-SMAD inhibition (e.g., Noggin, SB431542); BDNF, GDNF [6] | MAP2, TBR1, CTIP2 | Study synaptic toxicity, tau pathology, and electrophysiological deficits. |
| Midbrain Dopaminergic Neurons | SHH, WNT, FGF8; Floor-plate based protocol [6] | TH, LMX1A, FOXA2, NURR1 | Model relevant for Parkinson's disease dementia and Lewy body dementia, also APOE-related risks. |
| Astrocytes | CNTF, LIF, NFIA; OR SOX9 overexpression [6] | GFAP, S100β | Investigate APOE secretion, lipid metabolism, and neuroinflammatory responses. |
| Microglia | BMP4, IL-3, IL-6, M-CSF, IL-34 [6] | P2RY12, TMEM119, IBA1 | Model neuroinflammation, Aβ phagocytosis, and TREM2-APOE interactions. |
2D vs. 3D Model Systems
- 2D Monocultures and Co-cultures: Simplified systems where a single cell type or a defined mix of cells (e.g., neurons and astrocytes) is differentiated. Ideal for high-throughput screening and mechanistic studies in a controlled environment [6].
- 3D Organoids and Tri-culture Systems: Cerebral organoids are self-organizing 3D structures that recapitulate some aspects of the brain's cellular diversity and complexity. Advanced 3D systems can incorporate neurons, astrocytes, and microglia to better model cell-cell interactions and disease pathology, such as microglial recruitment and neurotoxicity in an AD context [6].
Experimental Protocols for hiPSC-based APOE Research
Protocol: Generating and Differentiating APOE-isoform hiPSCs
This protocol outlines the generation of an APOE-isoform specific hiPSC model and differentiation into cortical neurons.
hiPSC Generation and Genotyping:
- Generate hiPSCs from patient fibroblasts or peripheral blood mononuclear cells (PBMCs) carrying specific APOE genotypes (ε2/ε2, ε3/ε3, ε4/ε4) using non-integrating reprogramming methods (e.g., Sendai virus or episomal vectors) [6].
- Confirm pluripotency (e.g., expression of OCT4, SOX2, NANOG) and perform karyotyping.
- Genotype the APOE locus to confirm the isoform status of the hiPSC lines.
Cortical Neuron Differentiation via Dual-SMAD Inhibition:
- Neural Induction: Culture hiPSCs until they reach 70-80% confluence. Treat with neural induction medium containing SMAD inhibitors (e.g., 10 µM SB431542 and 100 nM LDN-193189) for 10-14 days to generate neural progenitor cells (NPCs). Medium should be changed daily [6].
- NPC Expansion: Dissociate the neural rosettes and plate the NPCs on a suitable substrate (e.g., Matrigel). Expand NPCs in NPC medium containing FGF2.
- Neuronal Differentiation: Withdraw FGF2 and culture NPCs in neuronal differentiation medium supplemented with BDNF (20 ng/mL) and GDNF (20 ng/mL) for over 28 days to promote terminal differentiation into cortical neurons [6].
- Characterization: Validate neuronal identity by immunocytochemistry for MAP2, β-III-tubulin, and synapsin. Assess functionality via electrophysiology (patch-clamp).
Protocol: Assessing APOE4-induced Synaptic Defects via SNARE Complex Assembly
This protocol is based on a recent study investigating the presynaptic mechanism of APOE4 [9].
Treatment of Neuronal Cultures:
- Use primary hippocampal neurons from APOE knockout mice or human APOE-TR hiPSC-derived neurons.
- At Days In Vitro (DIV) 7, treat cultures with 10 µM of recombinant human APOE3 or APOE4 protein for 24 hours [9].
Co-immunoprecipitation (Co-IP) and Western Blot:
- Harvest treated cells and lyse in IP buffer.
- Incubate lysates with an anti-APOE antibody (e.g., ab1906) overnight at 4°C.
- Add Protein A/G beads for 2 hours, wash complexes, and elute proteins.
- Analyze eluates and total lysates by Western blotting using antibodies against VAMP2, SNAP-25, syntaxin-1, and APOE to assess SNARE complex components and interactions [9].
Functional Assay: Synaptic Vesicle Release with FM4-64 Dye:
- Load mature neuronal cultures (e.g., from APOE3-TR or APOE4-TR mice) with FM4-64 dye by stimulating with high K+ solution.
- Wash the cultures extensively to remove excess dye.
- Image the synapses using live-cell microscopy. Stimulate the neurons again and measure the destaining kinetics (fluorescence loss) as an indicator of synaptic vesicle exocytosis [9].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for APOE and hiPSC Neuroscience Research
| Reagent / Tool Category | Specific Examples | Function / Application |
|---|---|---|
| hiPSC Lines | APOE-genotyped patient-derived hiPSCs; CRISPR-edited isogenic APOE hiPSC lines (e.g., ε3/ε3 vs ε4/ε4) | Provide a physiologically relevant human model system to study isoform-specific effects on a controlled genetic background. |
| Differentiation Kits & Factors | SMAD inhibitors (LDN-193189, SB431542); BDNF, GDNF; SHH, Purmorphamine; IL-34, M-CSF | Direct efficient differentiation of hiPSCs into specific neural lineages (neurons, astrocytes, microglia). |
| Critical Antibodies | Anti-APOE (e.g., ab1906); Anti-MAP2; Anti-β-III-Tubulin; Anti-GFAP; Anti-VAMP2/Synaptobrevin-2; Anti-SNAP-25 | Characterize cell identity, protein expression, localization, and interactions (via ICC, Western Blot, Co-IP). |
| Recombinant Proteins | Recombinant human APOE3 and APOE4 (lipidated and non-lipidated) | Used for direct treatment of cultures to study acute, isoform-specific effects on neurons and glia. |
| Specialized Assays | FM4-64 dye (synaptic vesicle release); DQ-BSA (lysosomal degradation); ELISA/MSD for Aβ and phospho-tau | Functional readouts for synaptic function, endolysosomal activity, and AD-relevant biomarkers. |
Therapeutic Implications and Future Directions
Understanding the multifaceted roles of APOE has opened several promising therapeutic avenues.
- APOE-directed Therapeutics: Strategies include using anti-sense oligonucleotides (ASOs) to reduce APOE4 expression, developing APOE structure correctors to convert the APOE4 protein into a more APOE3-like conformation, and gene therapy to deliver the protective APOE2 allele to at-risk individuals [4].
- Leveraging Protective Variants: The study of naturally occurring protective variants like APOE Christchurch and the COLBOS variant of REELIN has revealed new mechanisms of resilience, such as reduced binding to heparan sulfate proteoglycans (HSPGs), which is associated with diminished tau pathology [4]. Mimicking these effects pharmacologically is an active area of research.
- Lipid Metabolism and Ferroptosis: Given APOE4's role in disrupting lipid metabolism and promoting lipid peroxidation, therapies targeting the ferroptosis pathway (e.g., ferrostatin-1) or enhancing lipid efflux are being explored [4].
- Immunomodulation: Targeting the APOE-TREM2 axis in microglia to modulate neuroinflammation and enhance clearance of pathological proteins represents another promising strategy [3] [5].
The APOE genotype remains the cornerstone of genetic risk for late-onset Alzheimer's disease. Its influence extends far beyond amyloid-β, impacting tau pathology, synaptic integrity, neuroinflammation, and cellular metabolism. The integration of hiPSC-derived models has been instrumental in elucidating these human-specific, cell-type-specific mechanisms in a controlled genetic environment. The future of AD therapy will likely include personalized approaches based on APOE status, with treatments aimed at mitigating the detrimental effects of APOE4 or harnessing the protective mechanisms of APOE2. Continued research using these advanced models is crucial for translating these mechanistic insights into effective disease-modifying treatments.
Structural and Functional Differences Between APOE2, E3, and E4 Isoforms
Apolipoprotein E (ApoE) is a 34-kDa glycoprotein that plays a critical role in lipid metabolism, serving as a principal cholesterol carrier in the brain and periphery [11] [12]. The APOE gene exists as three major polymorphic alleles—ε2, ε3, and ε4—encoding protein isoforms that differ by single amino acid substitutions yet exhibit profoundly different functional impacts [11] [13]. Within the context of induced pluripotent stem cell (iPSC) neuronal research, understanding these isoforms is paramount, as APOE4 represents the strongest genetic risk factor for sporadic Alzheimer's disease (AD), increasing risk by 3-fold in heterozygotes and up to 15-fold in homozygotes compared to the neutral APOE3 isoform, while APOE2 appears protective [14] [15] [13]. This technical guide comprehensively details the structural and functional differences between these isoforms, with specific emphasis on their implications for neurodegenerative disease research utilizing human iPSC-derived models.
Genetic and Protein Structure
Allelic Variation and Evolutionary Origins
The human APOE isoforms arose from sequential mutations over millions of years. APOE4 is the ancestral form, with the T61R mutation occurring in the human lineage after the primate-human split [16] [12]. Approximately 220,000 years ago, a Cys112Arg substitution in the APOE4 gene created the APOE3 allele, followed by an Arg158Cys substitution in APOE3 around 80,000 years ago that created the APOE2 allele [12]. These evolutionary changes resulted in the three major human isoforms characterized by specific amino acid combinations at positions 112 and 158, within the receptor-binding region of the N-terminal domain [11] [13].
Table 1: Fundamental Characteristics of Human APOE Isoforms
| Isoform | Amino Acid Position 112 | Amino Acid Position 158 | Worldwide Allele Frequency | AD Risk Relative to E3/E3 |
|---|---|---|---|---|
| APOE2 | Cysteine | Cysteine | 8.4% [12] | Reduced ~40% [13] |
| APOE3 | Cysteine | Arginine | 77.9% [12] | Neutral (reference) |
| APOE4 | Arginine | Arginine | 13.7% [12] | Heterozygous: 3-4× [14]; Homozygous: 12-15× [14] [13] |
Structural Conformations
ApoE is structured into two primary domains: an N-terminal domain (residues 1-167) containing the receptor-binding region (residues 136-150), and a C-terminal domain (residues 206-299) encompassing the lipid-binding site (residues 244-272), connected by a protease-sensitive hinge region [17] [14]. The single amino acid substitutions differentially affect the protein's conformation through domain interaction, a phenomenon particularly relevant to APOE4.
APOE4's structure (Arg112, Arg158) facilitates a pathological domain interaction where the Arg112 in the N-terminal domain interacts with Glu255 in the C-terminal domain, creating a more compact, unstable structure [17] [16]. This conformation alters the protein's lipid binding capacity, receptor interactions, and increases oligomerization propensity [13]. In contrast, APOE3 (Cys112, Arg158) and APOE2 (Cys112, Cys158) do not exhibit this domain interaction, with APOE2 showing impaired receptor binding due to the Cys158 substitution [11] [12].
Functional Consequences in the Central Nervous System
Lipid Metabolism and Synaptic Function
ApoE serves as the principal cholesterol carrier in the brain, mainly produced by astrocytes and, to a lesser extent, by microglia and stressed neurons [11] [13]. The isoforms differentially modulate lipid transport, with APOE4 exhibiting impaired lipid binding capacity and reduced ability to support synaptic maintenance and repair [13]. iPSC-derived astrocytes carrying APOE4 demonstrate impaired Aβ uptake and intracellular cholesterol accumulation compared to isogenic APOE3 counterparts [15].
Amyloid-β Pathology
APOE4 potently influences amyloid-β metabolism through multiple mechanisms, enhancing both production and impairing clearance of Aβ peptides [18]. Research using iPSC-derived cerebral organoids demonstrates that organoids from AD patients have increased levels of Aβ and phosphorylated tau compared to healthy subject-derived organoids, with APOE4 specifically exacerbating tau pathology [19]. APOE4 promotes APP expression and enhances BACE1 transcription and activity, thereby increasing amyloidogenic processing of APP [18]. Simultaneously, APOE4 inhibits insulin-degrading enzyme (IDE) and neprilysin (NEP) expression, critical proteases for Aβ degradation, and impairs cellular clearance through disrupted endolysosomal trafficking and autophagy [18].
Tau Phosphorylation and Neurodegeneration
Beyond amyloid pathology, APOE4 exacerbates tau-mediated neurodegeneration. Cerebral organoids from AD patients carrying APOE4/4 show significantly greater apoptosis and decreased synaptic integrity compared to other genotypes [19]. APOE4 enhances tau phosphorylation through activation of oxidative stress pathways, disruption of lipid metabolism, and inflammatory signaling [18]. Isogenic conversion of APOE4 to APOE3 in iPSC-derived cerebral organoids from AD patients attenuates tau pathology and neurodegeneration, confirming the isoform-specific effect [19].
Neuroinflammation
APOE isoforms differentially regulate neuroinflammatory responses. Transcriptional profiling of iPSC-derived microglia-like cells reveals that APOE4 alters expression of immune response genes and reduces Aβ phagocytosis capacity [15]. APOE4 increases ROS production, activates the NLRP3 inflammasome, and modulates TREM2 signaling pathways, collectively amplifying neuroinflammatory states that contribute to neurodegeneration [18].
Energy Metabolism
APOE4 disrupts cerebral energy homeostasis, with carriers exhibiting impaired glucose metabolism detectable by FDG-PET imaging [14]. iPSC-based studies demonstrate that APOE4 competes for insulin receptors, inhibits key metabolic enzymes, and promotes lipid accumulation, leading to mitochondrial dysfunction and oxidative stress [18]. These metabolic disturbances appear early in the disease process and contribute to synaptic dysfunction and neurodegeneration.
Table 2: Functional Consequences of APOE Isoforms in CNS Cell Types
| Cellular Function | APOE2 | APOE3 | APOE4 |
|---|---|---|---|
| Lipid Binding & Cholesterol Transport | Moderate efficiency [13] | High efficiency [11] | Reduced efficiency; Cholesterol accumulation in astrocytes [15] |
| Aβ Clearance | Moderate [13] | Normal [18] | Impaired; Reduced phagocytosis by microglia [15] [18] |
| Tau Pathology | Not associated [13] | Baseline [19] | Exacerbated phosphorylation & aggregation [18] [19] |
| Synaptic Integrity | Protective effect [13] | Normal maintenance [19] | Decreased synaptophysin & PSD95; Increased synapse loss [19] |
| Neuroinflammation | Anti-inflammatory [13] | Moderate response [15] | Enhanced pro-inflammatory activation of microglia [15] [18] |
| Energy Metabolism | Not well characterized | Normal glucose metabolism [14] | Impaired mitochondrial function; Insulin resistance [14] [18] |
Experimental Models and Methodologies
iPSC-Derived Neuronal Models
The development of human iPSC models has revolutionized the study of APOE isoforms in a genetically defined, human-relevant system. Key methodological approaches include:
Isogenic iPSC Line Generation: CRISPR/Cas9 genome editing enables creation of isogenic iPSC lines differing only at APOE loci, controlling for background genetic variation [15]. The editing process involves introducing Cys112Arg substitution to convert APOE3 to APOE4, or the reverse to convert APOE4 to APOE3, with verification by Sanger sequencing and whole exome sequencing to confirm absence of off-target mutations [15].
Cerebral Organoid Differentiation: Cerebral organoids generated through embryoid body formation followed by neuroectodermal induction in Matrigel scaffolds recapitulate 3D cortical architecture with ventricular zones containing neural progenitors and outer layers with mature neurons and astrocytes [19]. These organoids demonstrate appropriate temporal development, with deep cortical layer neurons (Ctip2+) emerging by week 4 and superficial layer neurons (Satb2+) appearing by week 12, alongside astrocyte maturation and migration [19].
Phenotypic Assessment in iPSC Models
Comprehensive characterization of APOE isoform-specific effects in iPSC models includes:
Transcriptomic Profiling: RNA-sequencing of iPSC-derived neurons, astrocytes, and microglia reveals hundreds of differentially expressed genes between APOE3 and APOE4 genotypes, with neuronal signatures showing enrichment for synaptic function pathways and microglial signatures revealing immune response alterations [15]. Co-expression network analysis identifies genes co-regulated with APOE, with enrichment for lipid metabolism, immune response, and AD-associated pathways [15].
Pathological Assessment: Cerebral organoids analyzed at multiple timepoints (weeks 4, 8, 12) demonstrate APOE4-associated phenotypes including increased apoptosis (cleaved caspase-3 immunoreactivity), decreased synaptic markers (synaptophysin, PSD95), and elevated phosphorylated tau [19]. APOE4 also exacerbates Aβ-related pathology in AD patient-derived organoids [19].
Functional Assays: iPSC-derived astrocytes and microglia are assessed for Aβ phagocytosis capacity, cholesterol accumulation, and inflammatory cytokine secretion, with APOE4 consistently impairing homeostatic functions [15].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for APOE Isoform Studies in iPSC Models
| Reagent/Category | Specific Examples | Research Application | Function in APOE Research |
|---|---|---|---|
| Isogenic iPSC Lines | CRISPR/Cas9-edited APOE3/3, APOE4/4 [15] | Controlled genotype-phenotype studies | Enables comparison of isoform effects in identical genetic backgrounds |
| Differentiation Kits | Commercial neural induction kits; Neurogenin2 expression systems [15] | Generation of specific neural cell types | Produces neurons, astrocytes, microglia for cell-type-specific analyses |
| 3D Culture Systems | Matrigel scaffolds; Rotary orbital culture systems [19] | Cerebral organoid generation | Recapitulates complex tissue architecture and cell-cell interactions |
| APOE Detection Antibodies | Isoform-specific antibodies; Total APOE antibodies [19] | Protein expression quantification | Measures APOE secretion, cellular localization, and isoform-specific effects |
| Synaptic Markers | Anti-synaptophysin; Anti-PSD95 [19] | Synaptic integrity assessment | Quantifies APOE4-associated synaptic loss and therapeutic rescue |
| Pathology Assays | Aβ ELISAs; Phospho-tau antibodies (AT8, etc.); Cleaved caspase-3 antibodies [19] | Neurodegeneration pathway analysis | Evaluates amyloid, tau, and apoptotic pathology in isoform-specific models |
| Lipid Staining Dyes | Filipin; Bodipy-cholesterol; Oil Red O [15] | Cholesterol accumulation visualization | Detects APOE4-associated lipid metabolism defects |
| Transcriptomic Tools | RNA-sequencing platforms; Single-cell RNA-seq kits [15] | Genome-wide expression profiling | Identifies APOE-regulated pathways across neural cell types |
The structural differences between APOE isoforms, particularly the domain interaction unique to APOE4, propagate through multiple functional pathways to profoundly influence Alzheimer's disease risk and progression. Human iPSC-based models including cerebral organoids now provide unprecedented opportunities to study these isoform-specific effects in a genetically controlled, human-relevant system. The experimental methodologies and reagents outlined in this review provide a foundation for investigating APOE biology and developing isoform-targeted therapeutic strategies. Future research leveraging these approaches will be essential for elucidating the precise mechanisms by which APOE isoforms differentially contribute to neurodegeneration and for developing personalized medicine approaches for APOE-related Alzheimer's disease risk.
The apolipoprotein E (APOE) gene, located on chromosome 19, is the strongest genetic risk factor for late-onset Alzheimer's disease (AD). Its three common alleles—APOE2, APOE3, and APOE4—differ by single nucleotide polymorphisms resulting in amino acid substitutions at residues 112 and 158, and confer dramatically different AD risk profiles [20]. The APOE4 allele substantially increases AD risk in a dose-dependent manner, with heterozygous carriers facing a 3-4 fold increased risk and homozygous carriers facing a 9-15 fold increased risk compared to the most common APOE3 allele [20]. In contrast, the APOE2 allele demonstrates protective effects, reducing AD risk by approximately 40% and delaying disease onset [21] [20]. This whitepaper examines the molecular mechanisms underlying these differential risk profiles within the context of induced pluripotent stem cell (iPSC) neuronal research, providing a technical resource for researchers and drug development professionals working in neurodegenerative disease.
Table 1: APOE Genotype and Alzheimer's Disease Risk Profile
| Genotype | Relative Risk for AD | Compared To | Key Clinical Associations |
|---|---|---|---|
| APOE2/2 | 0.13x (87% reduction) | APOE3/3 | Strongest protection, delayed onset [21] |
| APOE2/3 | ~0.5x (50% reduction) | APOE3/3 | Moderate protection [21] |
| APOE3/3 | 1.0x (reference) | - | Most common genotype, neutral risk [20] |
| APOE3/4 | 3-4x increased risk | APOE3/3 | Earlier onset by 5-10 years [22] |
| APOE4/4 | 9-15x increased risk | APOE3/3 | Earlier onset, potential distinct genetic form of AD [23] [20] |
Molecular Mechanisms of APOE Isoform Function
Protein Structure and Lipid Binding
The APOE protein is a 34 kDa glycoprotein comprising 299 amino acids with two primary structural domains: an N-terminal receptor-binding domain (residues 1-167) and a C-terminal lipid-binding domain (residues 206-299) [20]. The isoforms differ at two critical positions: APOE2 (Cys112, Cys158), APOE3 (Cys112, Arg158), and APOE4 (Arg112, Arg158) [14] [20]. These structural variations significantly impact APOE's binding affinity to lipids and receptors, particularly the low-density lipoprotein receptor (LDLR) [24]. APOE2 exhibits reduced binding affinity to LDLR compared to APOE3 and APOE4, which paradoxically contributes to its protective function by limiting lipid uptake and preventing lysosomal stress [24].
Lysosomal Function and Lipid Homeostasis
Recent research has revealed that APOE isoforms differentially impact lysosomal function through their interactions with LDLR. APOE4, with its high binding affinity to LDLR, promotes excessive uptake of lipidated APOE particles into lysosomes of astrocytes and neurons, leading to lysosomal stress and lipofuscin accumulation [24]. Lipofuscin, an autofluorescent pigment resulting from lipid peroxidation, is a hallmark of lysosomal dysfunction and cellular aging. The order of lipofuscin accumulation follows APOE4 > APOE3 > APOE2, directly correlating with AD risk [24]. APOE2's reduced binding to LDLR limits lysosomal lipid loading, thereby protecting against dysfunction. This mechanism is supported by the observation that the APOE3-Christchurch mutation, which similarly reduces LDLR binding, provides remarkable protection against AD despite high amyloid burden [24].
Brain Energy Metabolism
APOE isoforms differentially regulate brain energy homeostasis, particularly in aging neurons facing glucose hypometabolism. APOE3 facilitates neuronal utilization of long-chain fatty acids as an alternative energy source through interaction with the sortilin receptor [25]. This metabolic flexibility is crucial for neuronal survival when glucose availability declines. In contrast, APOE4 disrupts sortilin-mediated lipid uptake, creating an energy deficit in neurons and increasing their vulnerability to degeneration [25]. This APOE4-induced impairment in alternative fuel utilization represents a key non-amyloid mechanism contributing to AD pathogenesis.
Neuroinflammation and Immune Response
Substantial evidence indicates that APOE4 promotes pro-inflammatory states across neurodegenerative diseases. A comprehensive proteomic analysis of cerebrospinal fluid and plasma revealed that APOE4 carriers exhibit a distinct inflammatory signature characterized by enrichment of viral processes, T-cell signaling, and pro-inflammatory pathways including Toll-like receptor, TNF, and IL-17 signaling [26]. This signature was consistent across AD, Parkinson's disease, and frontotemporal dementia, suggesting APOE4 confers a fundamental biological vulnerability through immune modulation rather than disease-specific mechanisms [26].
Experimental Models and Methodologies
APOE "Switch" Mouse Model
A groundbreaking approach to studying APOE isoform effects involves the inducible APOE4-to-APOE2 "switch" mouse model (APOE4s2) [27]. This knock-in model contains a floxed coding region of human APOE4 followed by exon 4 of human APOE2, allowing temporal induction of allele switching through tamoxifen-activated Cre recombinase.
Table 2: Key Research Reagent Solutions for APOE Isoform Studies
| Research Tool | Application | Key Utility in APOE Research |
|---|---|---|
| APOE4s2 "Switch" Mice [27] | In vivo functional studies | Enables temporal control of APOE4 to APOE2 transition in adult mice |
| iPSC-Derived Human Neurons [25] | Human cellular models | Provides human-specific genetic background for studying isoform effects |
| Homogeneous Time-Resolved Fluorescence (HTRF) [24] | Protein-protein interaction | Quantifies lipAPOE-LDLR binding affinities |
| Surface Plasmon Resonance (SPR) [24] | Binding kinetics | Measures real-time binding affinity between APOE isoforms and LDLR |
| Single-cell RNA-seq [27] [28] | Transcriptomic profiling | Identifies cell-type-specific responses to APOE isoforms |
| ATAC-seq [28] | Epigenomic profiling | Maps chromatin accessibility changes in microglia with different APOE isoforms |
Experimental Protocol: APOE Allelic Switching and Phenotypic Assessment
- Animal Crossing: APOE4s2 mice are crossed with ROSA26-CreERT1 Cre drivers to generate floxed ROSA26-CreERT1(APOE4s2G) mice
- Switch Induction: 2-month-old APOE4s2G mice receive tamoxifen to activate Cre recombinase, inducing transition from APOE4 to APOE2 expression
- Efficiency Validation:
- qPCR: APOE mRNA expression analysis in liver and brain tissues confirms transition from APOE4 to APOE2 mRNA
- Mass Spectrometry: Proteomic analysis verifies replacement of ApoE4 protein with ApoE2 (92-99% efficiency in plasma)
- Phenotypic Assessment:
- Metabolic profiling: Plasma lipid measurements after Western diet challenge
- Cognitive testing: Behavioral assays in 5xFAD background mice
- Neuropathology: Amyloid burden, gliosis, and plaque-associated ApoE quantification [27]
Human iPSC-Derived Brain Cell Models
Protocol: Studying APOE-Mediated Lipid Metabolism in Human Neurons
- iPSC Differentiation: Generate astrocytes and neurons from human iPSCs carrying specific APOE genotypes
- Metabolic Stress Induction: Culture cells under glucose-deficient conditions to simulate aging-related metabolic stress
- Lipid Utilization Assessment:
- Treat cells with fluorescently-labeled long-chain fatty acids
- Measure fatty acid uptake in the presence of APOE3 vs. APOE4
- Evaluate sortilin receptor function through inhibition experiments
- Functional Rescue Experiments: Test metabolic rescue using bezafibrate to restore fatty acid oxidation [25]
Xenotransplantation of Human Microglia
Protocol: Microglial APOE Isoform Function in Amyloid Response
- Microglia Generation: Differentiate iPSC-derived human microglia with defined APOE genotypes (APOE2/0, APOE3/0, APOE4/0)
- Transplantation: Introduce human microglia into brains of AppNL-G-F mouse model of Alzheimer's disease
- Cell Isolation: At 12 months, isolate microglia by FACS using human-specific antibodies (CD11b + hCD45+)
- Multi-Omics Profiling:
- RNA-seq: Transcriptomic analysis to identify differentially expressed genes
- ATAC-seq: Epigenomic landscape assessment through chromatin accessibility mapping [28]
Signaling Pathways and Molecular Interactions
Diagram 1: APOE Isoform Signaling Pathways and Functional Consequences. This diagram illustrates the molecular mechanisms through which different APOE isoforms influence cellular processes relevant to Alzheimer's disease pathogenesis. APOE2's reduced binding to LDLR limits lysosomal lipid loading and prevents lipofuscin accumulation. APOE3 enables normal lipid metabolism through sortilin interaction, maintaining energy homeostasis. APOE4 enhances LDLR binding leading to lysosomal dysfunction, disrupts sortilin-mediated lipid utilization, and promotes neuroinflammation, collectively increasing neuronal vulnerability.
Diagram 2: Experimental Workflow for APOE Isoform Research in iPSC-Derived Models. This diagram outlines integrated experimental approaches for studying APOE isoform biology using human iPSC-derived cell models, combining in vitro systems with in vivo xenotransplantation and multi-omics analyses to identify therapeutic targets.
Therapeutic Implications and Future Directions
APOE-Targeted Therapeutic Strategies
Research elucidating the differential risk profiles of APOE isoforms has revealed several promising therapeutic approaches. APOE2-mimetic strategies represent a promising approach, with studies showing that astrocyte-specific switching from APOE4 to APOE2 in adult mice improves cognition, decreases amyloid pathology, reduces gliosis, and lowers plaque-associated ApoE [27]. Small molecule interventions targeting APOE4-induced metabolic deficits have also shown promise, with bezafibrate restoring fatty acid metabolism in APOE4-expressing neurons [25]. Additionally, liver X receptor agonists that reduce polyunsaturated fatty acid levels can inhibit lipofuscin accumulation and lysosomal degeneration in mouse models, offering another potential therapeutic avenue [24].
Personalized Medicine Approaches
The profound differences in AD risk mediated by APOE genotype underscore the importance of genotype-tailored prevention strategies [23]. APOE4 status modifies the relationship between numerous non-genetic risk factors and dementia, with stronger associations found for specific factors in carriers versus non-carriers [23]. Furthermore, the recent recognition that APOE4 homozygosity may represent a distinct genetic form of Alzheimer's disease [23] highlights the need for precision medicine approaches that consider APOE status in both clinical trial design and therapeutic development.
The dramatic differential risk profiles between APOE4 and APOE2 alleles—with APOE4 increasing AD risk 3-15 fold while APOE2 is protective—stem from fundamental differences in their effects on lysosomal function, lipid metabolism, energy homeostasis, and neuroinflammation. iPSC-based neuronal models combined with innovative experimental approaches like inducible allele switching and xenotransplantation have provided unprecedented insights into these mechanisms. These advances illuminate promising therapeutic strategies focused on converting APOE4 toxicity to APOE2-like protection, enhancing lysosomal function, and restoring metabolic flexibility. As our understanding of APOE biology continues to evolve, it creates exciting opportunities for developing targeted interventions that may fundamentally alter Alzheimer's disease treatment and prevention.
The Central Role of APOE in Brain Lipid Transport and Cholesterol Homeostasis
Apolipoprotein E (APOE) is a critical lipid transport protein in the central nervous system (CNS), serving as the primary coordinator of cholesterol homeostasis and lipid redistribution within the brain. As the strongest genetic risk factor for late-onset Alzheimer's disease (AD), APOE exists as three major isoforms—APOE2, APOE3, and APOE4—that differentially influence brain physiology and disease pathogenesis. The brain is the most cholesterol-rich organ, containing approximately 30% of the body's cholesterol, yet it cannot import cholesterol from the periphery due to the blood-brain barrier. Instead, the brain relies entirely on local synthesis and sophisticated transport mechanisms, with APOE playing the central role in lipid trafficking and redistribution between cells. This whitepaper examines the structural and functional basis of APOE's role in brain lipid homeostasis, with particular emphasis on implications for iPSC-based neuronal models and therapeutic development.
Structural Basis of APOE Function
Domain Organization and Lipid Binding Properties
APOE is a 299-amino acid glycoprotein characterized by two distinct structural and functional domains separated by a protease-sensitive loop [29]. The N-terminal domain (residues 1-191) forms a four-helix bundle structure and contains the receptor-binding region (residues 136-150), while the C-terminal domain (residues 192-299) mediates primary lipid binding interactions [29] [4]. This two-domain organization enables APOE to exist in alternate lipid-free and lipid-associated states, functioning as a dynamic lipid carrier [29].
- Receptor Binding Domain: The N-terminal region contains the low-density lipoprotein receptor (LDLR) binding site, with critical basic residues between positions 136-150 that mediate interaction with LDLR family members [29] [4].
- Lipid Binding Domain: The C-terminal region (residues 244-272) features high hydrophobicity and mediates binding to phospholipids, cholesterol, and other lipids [4]. This domain drives APOE self-association in the lipid-free state and facilitates lipoprotein particle formation [29].
- Isoform-Specific Structural Variations: The three major APOE isoforms differ by single amino acid substitutions at positions 112 and 158, which profoundly influence structure and function [4]:
- APOE3: Cysteine112, Arginine158 (considered reference isoform)
- APOE2: Cysteine112, Cysteine158 (reduced receptor binding)
- APOE4: Arginine112, Arginine158 (domain interaction, altered lipid binding)
Table 1: APOE Isoform Characteristics and Functional Consequences
| Isoform | Amino Acid Positions | Structural Features | LDLR Binding | AD Risk |
|---|---|---|---|---|
| APOE2 | Cys112, Cys158 | Altered salt bridge network | ~1% of APOE3 [29] | Protective [4] |
| APOE3 | Cys112, Arg158 | Reference structure | Normal (reference) | Neutral [4] |
| APOE4 | Arg112, Arg158 | Domain interaction, molten globule state [4] | Comparable to APOE3 [4] | High risk [4] |
Lipoprotein Particle Formation in CNS
In the brain, APOE is primarily secreted by astrocytes as discoidal lipoprotein particles resembling high-density lipoproteins (HDL) in the periphery [3]. These particles typically range from 8-20 nm in diameter, with the most common size being approximately 12.5 nm [3]. Structural studies using cryo-electron microscopy reveal that APOE forms antiparallel dimers within these lipoprotein particles, creating a structural framework for lipid incorporation and transport [3]. The lipidation state of APOE significantly influences its structure and receptor binding properties, with lipid-associated APOE exhibiting enhanced receptor binding capacity compared to lipid-free APOE [29].
APOE Isoforms in Neuronal Lipid Homeostasis
Cholesterol Transport and Metabolism
The maintenance of brain cholesterol homeostasis is crucial for neuronal function, as cholesterol is an essential component of cell membranes, contributes to synaptic integrity, and facilitates signal transduction. APOE serves as the principal carrier of cholesterol in the CNS, mediating its delivery to neurons via receptor-mediated endocytosis [4]. The differential effects of APOE isoforms on cholesterol homeostasis have profound implications for neuronal health and function:
- Receptor Binding Affinities: APOE isoforms exhibit markedly different binding affinities for members of the LDL receptor family. Surface plasmon resonance studies demonstrate that lipidated APOE3 and APOE4 bind LDLR with high affinity (16 nM and 9 nM, respectively), while APOE2 shows substantially weaker binding (approximately 800 nM) [4]. These differences significantly impact lipid delivery efficiency to neurons.
- Cellular Lipid Uptake: The APOE4 isoform demonstrates preferential binding to specific lipid species, including monosialotetrahexosylganglioside (GM1), with higher affinity than cholesterol [30]. This altered binding preference may contribute to cholesterol dysregulation in APOE4 carriers and promote amyloid-β oligomer aggregation, a key event in AD pathogenesis [30].
- Endolysosomal Processing: Recent investigations in primary neuronal models reveal that APOE4 impacts endolysosomal function in an age-dependent manner. With prolonged time in culture (serving as an aging proxy), APOE4-expressing neurons demonstrate reduced degradative capacity and decreased numbers of active lysosomal compartments [10]. When supplied with cholesterol, aged APOE4 neurons show a predisposition to accumulate cholesterol within the endolysosomal system, potentially disrupting cellular homeostasis [10].
Signaling Pathways and Receptor Interactions
APOE mediates its effects through interaction with multiple receptors in the CNS, activating diverse signaling pathways that influence neuronal function, survival, and plasticity. The major APOE receptors in the brain belong to the LDL receptor family and include LDLR, LRP1, VLDLR, and ApoER2 [4].
Diagram 1: APOE Receptor Interactions and Signaling Pathways (Max Width: 760px)
The diagram above illustrates the two major pathways through which APOE and its receptors influence neuronal function: (1) the lipid uptake pathway mediated primarily by LDLR and LRP1, and (2) the Reelin signaling pathway activated through VLDLR and ApoER2 binding. The Reelin pathway is particularly important for brain development, synaptic plasticity, and neuronal migration [4].
Experimental Approaches for iPSC Neuron Research
Methodologies for Investigating APOE Biology
The study of APOE isoforms in human neurons has been revolutionized by induced pluripotent stem cell (iPSC) technologies, enabling the investigation of isoform-specific effects in genetically defined human neuronal systems. Key methodological approaches include:
APOE Genotyping and Isoform Expression Analysis
- Protocol: Genomic DNA extraction from iPSCs followed by APOE genotyping using PCR-RFLP or sequencing-based methods targeting residues 112 and 158. Confirm APOE expression at mRNA and protein levels in differentiated neurons using RT-qPCR and Western blotting [4].
- Application: Establish isogenic APOE iPSC lines expressing different APOE isoforms (E2/E3/E4) to control for genetic background effects when investigating isoform-specific phenotypes.
Lipid Uptake and Trafficking Assays
- Protocol: Differentiate iPSCs to cortical neurons using established protocols (e.g., dual SMAD inhibition). Incubate neurons with fluorescently labeled cholesterol (e.g., Bodipy-Cholesterol) or phospholipids complexed with recombinant APOE isoforms. Measure uptake kinetics using live-cell imaging and quantify intracellular distribution [30] [10].
- Application: Compare lipid internalization rates and subcellular localization between APOE isoforms. APOE4-expressing neurons typically show altered endocytic trafficking and delayed lysosomal processing.
Endolysosomal Function Assessment
- Protocol: Differentiate iPSCs to neurons and culture for extended periods (≥60 days) to model age-related effects. Assess endolysosomal pH using pH-sensitive dyes (e.g., LysoSensor), degradative capacity with DQ-BSA assay, and lysosomal enzyme activity [10].
- Application: APOE4 neurons demonstrate reduced degradative ability and decreased active lysosomal compartments with prolonged culture time, reflecting age-dependent dysfunction.
Lipidomic Profiling
- Protocol: Extract lipids from iPSC-derived neurons and analyze using LC-MS/MS. Focus on gangliosides (particularly GM1), cholesterol esters, and phospholipids. Monitor APOE-lipid interactions using microscale thermophoresis (MST) [30].
- Application: APOE4 shows preferential binding to GM1 over cholesterol, potentially explaining lipid trafficking alterations in APOE4 carriers.
Table 2: Quantitative Receptor Binding Affinities of APOE Isoforms
| APOE Isoform | LDLR Binding (Kd) | Relative Binding Efficiency | Lipid Preference | Experimental Method |
|---|---|---|---|---|
| APOE2 | ~800 nM [4] | ~1% of APOE3 [29] | Altered specificity | Surface plasmon resonance [4] |
| APOE3 | 16 nM [4] | Reference (100%) | Balanced lipid binding | Surface plasmon resonance [4] |
| APOE4 | 9 nM [4] | Comparable to APOE3 | Preferential GM1 binding [30] | Surface plasmon resonance [4] |
APOE and Neuronal Endolysosomal Pathology
Research using primary neuronal cultures and iPSC-derived models has revealed that APOE4 significantly impacts endolysosomal function, particularly under aging-relevant conditions:
Diagram 2: Temporal Progression of APOE4-Induced Endolysosomal Alterations (Max Width: 760px)
The time-dependent emergence of APOE4-related endolysosomal dysfunction highlights the importance of modeling neuronal aging in iPSC systems. While young APOE4 neurons may show minimal phenotypic differences, prolonged culture reveals significant impairments in degradative capacity and lipid handling [10]. This has critical implications for experimental design in iPSC-based AD modeling, suggesting that extended maturation periods are necessary to capture APOE4-specific pathologies.
Research Reagent Solutions
Table 3: Essential Research Tools for APOE Lipid Transport Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| APOE Sources | Recombinant human APOE isoforms (E2, E3, E4); Conditioned media from APOE-expressing astrocytes | Lipid binding and uptake assays; Neuronal treatment studies | Ensure proper lipidation state; Lipid-free vs. lipid-associated APOE has different properties [29] |
| Lipid Probes | Bodipy-cholesterol, Bodipy-GM1, NBD-phospholipids, DQ-BSA | Tracking lipid uptake, trafficking, and degradation | Use complexed with APOE or liposomes; Consider fluorescent quenching approaches [30] [10] |
| Neuronal Markers | MAP2, NeuN, Tau, Synapsin-1 | Characterization of iPSC-derived neurons | Validate neuronal maturity and subtype specification (cortical vs. other regions) |
| Endolysosomal Markers | EEA1 (early endosomes), Rab7 (late endosomes), LAMP1 (lysosomes), Cathepsin D | Assessing endolysosomal morphology and function | Combine with functional assays (pH, degradation activity) [10] |
| Receptor Binding Tools | Recomceptor LDLR/LRP1 extracellular domains; Receptor antibodies | Surface plasmon resonance; Receptor binding assays | Account for isoform-specific binding differences; APOE2 has markedly reduced LDLR binding [4] |
APOE serves as the central coordinator of lipid transport and cholesterol homeostasis in the brain, with isoform-specific structural differences dictating functional consequences for neuronal health. The APOE4 isoform, the strongest genetic risk factor for late-onset Alzheimer's disease, exhibits altered lipid binding preferences, impaired receptor interactions, and promotes endolysosomal dysfunction in an age-dependent manner. iPSC-based neuronal models provide powerful experimental systems for investigating these isoform-specific effects in human cells, particularly when combined with sophisticated lipid trafficking assays and appropriate aging protocols. Understanding the precise molecular mechanisms through which APOE isoforms influence neuronal lipid homeostasis will enable the development of targeted therapeutic strategies for APOE-related neurodegenerative disorders.
APOE Isoform Effects on Amyloid-β Aggregation, Clearance, and Plaque Deposition
Apolipoprotein E (APOE) is the strongest genetic risk modifier for late-onset Alzheimer's disease (AD), with its three major isoforms—APOE2, APOE3, and APOE4—exerting profound effects on disease susceptibility and pathological progression [31] [13]. The primary physiological function of apoE is to mediate lipid transport in the brain and periphery, but it also significantly influences key AD pathological processes, particularly those involving amyloid-β (Aβ) [31] [13]. Inheritance of the APOE4 allele considerably increases AD risk in a dose-dependent manner, while the APOE2 allele confers protection relative to the common APOE3 allele [32] [13]. These differential risk profiles are intimately linked to how each isoform modulates the aggregation, clearance, and deposition of Aβ peptides in the brain. Understanding these isoform-specific mechanisms provides critical insights into AD pathogenesis and reveals potential therapeutic targets for this devastating neurodegenerative disorder.
APOE Isoforms: Structure, Function, and Expression
Structural Characteristics and Receptor Interactions
The APOE gene, located on chromosome 19, encodes a 299-amino acid glycoprotein that circulates as a 34-kDa glycosylated protein [3] [14]. The three major apoE isoforms differ by single amino acid substitutions at positions 112 and 158:
- APOE2: Cysteine112, Cysteine158
- APOE3: Cysteine112, Arginine158
- APOE4: Arginine112, Arginine158 [31] [32]
These single amino acid substitutions lead to significant structural alterations that profoundly influence protein function, stability, and receptor binding [31]. ApoE comprises two major structural domains: an N-terminal domain (residues 1-167) containing the receptor-binding region (residues 136-150), and a C-terminal domain (residues 206-299) containing the lipid-binding region (residues 244-272), connected by a hinge region [31] [13] [14]. The domain interaction between the N- and C-terminal regions is a key structural difference among isoforms, with apoE4 exhibiting a unique preference for such interactions that contribute to its pathological effects [13].
ApoE exerts its physiological effects by binding to several receptors from the low-density lipoprotein (LDL) receptor family, including LDLR, LRP1, VLDLR, and ApoER2 (also known as LRP8), as well as heparan sulfate proteoglycans (HSPGs) and the triggering receptor expressed on myeloid cells 2 (TREM2) [31] [32] [3]. These receptor interactions exhibit remarkable isoform specificity, which significantly impacts Aβ metabolism and clearance.
Table 1: ApoE Receptor Binding Specificities and Functions
| Receptor | Isoform-Specific Binding | Lipidation Required | Primary Functions in AD |
|---|---|---|---|
| LDLR | Lipidated apoE: apoE2 << apoE3 = apoE4 [32] | Yes [32] | Mediates lipoprotein and Aβ clearance [31] [32] |
| LRP1 | Lipidated apoE: apoE2 < apoE3 = apoE4 [32] | Likely not required [32] | Mediates Aβ clearance; signal transduction; neurotrophic effects [31] [32] |
| VLDLR | Non-lipidated apoE: apoE2 = apoE3 = apoE4 [32] | No [32] | Mediates reelin signaling; lipoprotein clearance [31] [32] |
| ApoER2 | Non-lipidated apoE: apoE2 << apoE3 = apoE4 [32] | No [32] | Regulates reelin signaling; synaptic receptor trafficking [31] [32] |
| HSPG | Non-lipidated apoE: apoE2 < apoE3 < apoE4 [32] | No [32] | Facilitates lipoprotein and Aβ clearance; co-receptor for LRP1 [31] |
| TREM2 | Both lipidated and non-lipidated apoE: apoE2 = apoE3 = apoE4 [32] | No [32] | Mediates microglial phagocytosis of Aβ; maintains disease-associated microglia phenotype [32] |
Expression Patterns and Lipidation Status
In the central nervous system (CNS), apoE is primarily produced and secreted by astrocytes, with additional contributions from microglia and, under certain pathological conditions, neurons [31] [3] [13]. Peripheral and CNS pools of apoE are separated by the blood-brain barrier, with no exchange of apoE-containing lipoproteins between these compartments [32] [13]. The lipidation status of apoE significantly influences its function, with lipidated apoE representing the predominant form in the human CNS [33]. However, poorly- or non-lipidated apoE increases Aβ pathology and AD risk in both mouse models and humans [33].
ApoE isoform expression follows a distinct pattern, with apoE2 demonstrating greater stability and higher expression levels compared to apoE3 and apoE4. Human studies show that cortical apoE levels are highest in APOE2 carriers and lowest in APOE4 carriers [32], a pattern replicated in APOE-targeted replacement (APOE-TR) mice, where APOE2-TR mice exhibit higher levels of apoE in interstitial fluid and brain lysate than APOE3-TR mice, followed by APOE4-TR mice [32].
Differential Effects of APOE Isoforms on Aβ Aggregation
Modulation of Aβ Oligomerization and Fibrillation
ApoE isoforms differentially influence the aggregation kinetics of Aβ, with apoE4 promoting earlier and more abundant amyloid deposition compared to apoE3 and apoE2 [33] [13]. Recent single-molecule imaging studies reveal that all apoE isoforms associate with Aβ during the early stages of aggregation but dissociate as fibrillation proceeds [33]. These dynamic interactions significantly influence the size, composition, and pathogenicity of Aβ aggregates throughout the aggregation process.
Biophysical studies demonstrate that apoE binding to Aβ slows the oligomer growth and maintains a faster diffusion rate for Aβ peptides over time [34]. This inhibitory effect on oligomerization occurs in an isoform-dependent manner, with apoE4 exhibiting reduced capacity to prevent the formation of neurotoxic Aβ oligomers compared to apoE2 and apoE3 [34] [35]. The formation of soluble apoE/Aβ complexes represents a crucial mechanism modulating Aβ aggregation, with apoE4 forming less stable complexes with Aβ compared to apoE3, particularly in lipidated forms [35].
Table 2: Quantitative Effects of ApoE Isoforms on Aβ Aggregation and Deposition
| Parameter | APOE2 | APOE3 | APOE4 | References |
|---|---|---|---|---|
| Brain Aβ Deposition | Reduced | Intermediate | Significantly increased | [33] [3] |
| Soluble Oligomeric Aβ | Decreased | Intermediate | Increased | [35] |
| ApoE-Aβ Co-aggregate Size (Non-lipidated) | ~500-900 nm | ~500-900 nm | ~500-900 nm | [33] |
| ApoE-Aβ Co-aggregate Size (Lipidated) | ~200-250 nm | ~200-250 nm | ~200-250 nm | [33] |
| Rate of Aβ Fibril Formation (with lipidated apoE) | Slowed | Intermediate | Accelerated | [33] |
| Stability of ApoE/Aβ Complex | High | High (SDS-stable) | Low (SDS-labile) | [35] |
Co-aggregation and Plaque Formation
ApoE significantly co-deposits with Aβ in amyloid plaques in AD brains [33] [3]. The extent of co-aggregation varies by isoform, with apoE4 showing preferential association with Aβ deposits. Recent research utilizing single-molecule pull-down (SiMPull) technology demonstrates that apoE-Aβ co-aggregates account for approximately 50% of the mass of diffusible Aβ aggregates detected in the frontal cortices of APOE4 homozygotes [33]. These co-aggregates exhibit distinct physicochemical properties based on apoE lipidation status, with non-lipidated apoE forming larger co-aggregates with Aβ compared to lipidated apoE [33].
The isoform-specific effects on Aβ aggregation correlate with AD risk, as APOE4 carriers exhibit increased Aβ deposition, earlier amyloid positivity in life, and a faster-growing Aβ burden compared to non-carriers [33]. The presence of apoE is required for initial plaque formation during early stages of Aβ accumulation, potentially through its influence on Aβ fibrillogenesis and microglial uptake of Aβ [3].
Mechanisms of Aβ Clearance Modulated by APOE Isoforms
Receptor-Mediated Clearance Pathways
ApoE isoforms differentially regulate Aβ clearance through receptor-mediated pathways, with apoE4 being less efficient than apoE2 and apoE3 in facilitating Aβ removal [31] [13]. The major receptors involved in apoE-dependent Aβ clearance include LDLR, LRP1, and HSPGs [31] [32]. The binding affinity of apoE isoforms to these receptors directly influences their efficiency in Aβ clearance, with apoE4 exhibiting impaired receptor interactions compared to other isoforms.
The lipidation status of apoE critically affects its function in Aβ clearance, with lipidated apoE demonstrating enhanced efficiency in promoting Aβ clearance compared to poorly lipidated forms [33] [35]. ApoE4 is more prone to lipidation defects, contributing to its reduced capacity to facilitate Aβ clearance [35]. Additionally, apoE competes with Aβ for binding to clearance receptors, with apoE4 potentially exacerbating Aβ accumulation by outcompeting Aβ for receptor binding sites [33].
Glymphatic Clearance and Proteolytic Degradation
Beyond receptor-mediated pathways, apoE isoforms influence glymphatic clearance and proteolytic degradation of Aβ. The glymphatic system, a brain-wide perivascular network, facilitates the clearance of soluble proteins and metabolites from the CNS, and its function is impaired in AD [13]. ApoE isoforms differentially affect glymphatic function, with apoE4 associated with reduced clearance efficiency compared to other isoforms [13].
Several Aβ-degrading enzymes, including neprilysin and insulin-degrading enzyme, participate in Aβ proteolysis, and their activity appears to be modulated by apoE isoforms [13]. ApoE4 is associated with reduced expression and activity of these enzymes, further contributing to Aβ accumulation [13].
Experimental Approaches for Studying APOE-Aβ Interactions
Methodologies for Assessing ApoE-Aβ Complex Formation
Various experimental approaches have been developed to investigate the molecular interactions between apoE and Aβ, each with specific advantages and limitations:
1. Fluorescence Cross-Correlation Spectroscopy (FCCS): This single-molecule technique allows real-time observation of apoE-Aβ interactions in solution. Using alternating laser excitation FCCS (ALEX-FCCS), researchers can monitor the diffusion time of freely diffusing Aβ and its complexes with apoE, providing insights into oligomerization kinetics and complex stoichiometry [34]. This method revealed that apoE binding maintains a faster diffusion rate for Aβ over time, slowing its oligomerization [34].
2. Single-Molecule Pull-Down (SiMPull): This assay enables characterization of individual aggregates within heterogeneous populations. Aβ aggregates are captured using surface-tethered antibodies and imaged via two-color total internal reflection fluorescence (TIRF) microscopy after adding detector antibodies for Aβ and apoE [33]. This technique allows quantification of aggregate size, shape, and composition, revealing that apoE co-aggregates with Aβ in early aggregation stages but dissociates as fibrillation proceeds [33].
3. Co-immunoprecipitation (Co-IP) and Western Blotting: These traditional biochemical methods assess apoE-Aβ complex formation under various conditions. The stringency of detection methods significantly affects results, with SDS-PAGE potentially disrupting less stable complexes (particularly apoE4-Aβ) [35]. The inclusion of reducing agents (β-mercaptoethanol, DTT) can disrupt both SDS-stable apoE3/Aβ and apoE4/Aβ complexes [35].
4. Surface Plasmon Resonance (SPR): This technique quantitatively measures binding affinities between apoE isoforms and Aβ peptides. SPR studies have demonstrated isoform-specific differences in apoE binding to Aβ, with lipidated apoE3 showing more stable complex formation with Aβ compared to apoE4 [35].
Research Reagent Solutions for APOE-Aβ Studies
Table 3: Essential Research Reagents for Studying APOE-Aβ Interactions
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| ApoE Proteins | Recombinant human apoE2, apoE3, apoE4; Lipidated vs. non-lipidated forms; Astrocyte-secreted apoE [33] [35] | In vitro aggregation assays; Receptor binding studies; Cellular uptake experiments | Lipidation status critically affects function; Source (recombinant vs. cell-secreted) influences physiological relevance |
| Aβ Peptides | Aβ(1-40), Aβ(1-42); Fluorescently-labeled (Atto 647N, Alexa Fluor); Pre-formed oligomers [34] [33] | Aggregation kinetics; Co-aggregation studies; Cellular toxicity assays | Peptide preparation method significantly affects aggregation state; Labeling position influences biological activity |
| Detection Antibodies | 6E10 (Aβ detection); EPR19392 (apoE detection); Isoform-specific apoE antibodies [33] | SiMPull; Immunoprecipitation; Immunohistochemistry; Western blotting | Antibody specificity crucial for accurate detection; Combination of multiple antibodies enhances validation |
| Cellular Models | APOE-TR mice; Primary astrocytes/microglia from TR mice; Human iPSC-derived neurons/glia [7] [32] [3] | Cellular uptake studies; Inflammatory response assessment; Drug screening | APOE-TR mice lack full AD pathology; iPSC models capture human genetic background but vary in differentiation efficiency |
| ApoE Receptors | Recombinant LDLR, LRP1, HSPG; Receptor-specific antibodies; Receptor-deficient cells [31] [32] | Receptor binding assays; Clearance pathway identification; Competitive inhibition studies | Receptor interactions are cell-type specific; Multiple receptors often involved in redundant pathways |
Implications for Therapeutic Development
ApoE-Targeted Therapeutic Strategies
The isoform-specific effects of apoE on Aβ aggregation and clearance present promising opportunities for therapeutic intervention. Several strategic approaches have emerged:
1. ApoE Structure Correctors: Small molecules designed to disrupt the pathogenic domain interaction in apoE4, converting its structure and function to be more apoE3-like [13]. These compounds have shown promise in cell culture models, abolishing detrimental effects of apoE4 in cultured neurons [36].
2. ApoE Mimetic Peptides: Short peptides that mimic the receptor-binding region of apoE, enhancing Aβ clearance without isoform-specific detrimental effects [13]. These peptides have demonstrated efficacy in animal models, reducing Aβ pathology and improving cognitive function.
3. Immunotherapy Targeting ApoE-Aβ Complexes: Antibodies specifically targeting pathological apoE-Aβ complexes, particularly those involving apoE4 [33]. Selective removal of non-lipidated apoE4-Aβ co-aggregates has been shown to enhance clearance of toxic Aβ by glial cells and reduce secretion of inflammatory markers and membrane damage [33].
4. ApoE Lipidation Enhancers: Approaches to improve apoE lipidation, particularly for apoE4, including liver X receptor (LXR) agonists and ATP-binding cassette (ABC) transporter activators [13]. Enhanced lipidation promotes Aβ clearance and reduces aggregation.
Integration with iPSC-Based Disease Modeling
The integration of APOE isoform studies with induced pluripotent stem cell (iPSC) technology provides a powerful platform for investigating human-specific disease mechanisms and screening therapeutic compounds. iPSC-derived neurons, astrocytes, and microglia from genotyped donors allow researchers to:
- Model human-specific pathophysiology in controlled genetic backgrounds
- Study cell-type-specific effects of apoE isoforms in relevant human CNS cells
- Screen therapeutic compounds for efficacy in humanized systems
- Investigate inflammatory responses in microglia with different APOE genotypes
Recent advances in iPSC differentiation protocols have enabled the generation of authentic brain cell types that recapitulate key aspects of AD pathology, providing valuable tools for validating findings from animal models and primary cell cultures [3].
APOE isoforms differentially influence Aβ aggregation, clearance, and plaque deposition through multiple interconnected mechanisms. APOE4 enhances AD risk by promoting Aβ aggregation into toxic oligomers and plaques while impairing clearance pathways, whereas APOE2 confers protection through opposite effects. The lipidation status of apoE significantly modulates these interactions, with lipidated apoE generally facilitating Aβ clearance while non-lipidated forms may promote pathogenic aggregation. Understanding these isoform-specific mechanisms at the molecular level provides critical insights for developing targeted therapies aimed at mitigating the detrimental effects of APOE4 while harnessing the protective mechanisms of APOE2. Future research integrating human iPSC models with advanced biophysical techniques will further elucidate these complex interactions and accelerate the development of effective APOE-targeted therapeutics for Alzheimer's disease.
Connections Between APOE and Tau Pathology, Neuroinflammation, and Synaptic Dysfunction
Apolipoprotein E (APOE), a lipid transport protein, exists in three major isoforms—APOE2, APOE3, and APOE4—with the APOE4 allele representing the strongest genetic risk factor for late-onset Alzheimer's disease (AD), conferring up to a 10-15-fold increased risk in homozygous individuals [37]. While historically investigated for its role in amyloid-β (Aβ) pathology, contemporary research increasingly demonstrates that APOE4 exerts multifaceted pathogenic effects across several core AD pathways. This technical review synthesizes current evidence on how APOE4 directly and indirectly influences tau pathology, drives chronic neuroinflammation, and precipitates synaptic dysfunction, with particular emphasis on insights gained from human induced pluripotent stem cell (iPSC) models. Understanding these interconnected mechanisms is paramount for developing targeted therapeutic strategies for APOE4-associated neurodegeneration.
APOE4 and Tau Pathology
The relationship between APOE4 and tau pathology extends beyond its established role in amyloid accumulation, representing a core pathogenic pathway independently linked to neurodegeneration and cognitive decline.
Direct Exacerbation of Tau Pathogenesis
Evidence from human iPSC-derived cerebral organoid models demonstrates that APOE4 significantly aggravates tau pathology. Cerebral organoids derived from AD patients carrying APOE ε4/ε4 show increased levels of phosphorylated tau compared to those with APOE ε3/ε3 genotype [19]. Importantly, this APOE4-related effect on tauopathy is observed in cerebral organoids from both healthy subjects and AD patients, suggesting its influence operates independently of disease status [19]. Isogenic conversion of APOE4 to APOE3 in these model systems attenuates tau pathology, providing causal validation of APOE4's role in tau hyperphosphorylation [19].
Mechanistically, APOE4 appears to accelerate early seeding of amyloid pathology, which subsequently facilitates tau spreading [38]. The presence of APOE4 also alters the relationship between tau pathology and synaptic density, with studies showing the associations between synaptic density and tau pathology are significantly regulated by APOE ε4 genotype [38]. This suggests APOE4 may lower the threshold for tau-mediated synaptic toxicity.
Biomarker Correlations
Postmortem brain studies reveal significant negative correlations between synaptic protein levels (including SV2A and synaptophysin) and phospho-tau concentrations, with these relationships being particularly pronounced in APOE ε4 carriers [39] [40]. Reductions in synaptic vesicle protein 2A (SV2A) are more severe in AD patients carrying APOE ε4, and these reductions correlate strongly with both Aβ and phospho-tau levels [39] [40]. This indicates that APOE4 amplifies the detrimental effects of tau pathology on synaptic integrity.
Table 1: Quantitative Effects of APOE4 on Tau and Synaptic Pathology in Human Studies
| Study Model | Tau Pathology Measure | Effect of APOE4 | Technical Approach |
|---|---|---|---|
| iPSC-derived cerebral organoids [19] | Phosphorylated tau levels | Significant increase in AD-E4 vs. AD-E3 organoids | Immunostaining, Western blot |
| Cognitively impaired participants [38] | Tau pathology mediation on synaptic density | APOE4 genotype regulates association between tau and synaptic density | PET imaging ([18F]SynVesT-1) |
| Postmortem human brain [39] [40] | Correlation with synaptic protein SV2A | Stronger negative correlation in APOE4 carriers | Mass spectrometry, IHC staining |
| Human brain-derived extracellular vesicles [40] | Phospho-tau levels in BDEVs | Significant negative correlation with SV2A in APOE4 carriers | LC-MS/MS proteomics |
APOE4 and Neuroinflammation
APOE4 fundamentally alters neuroimmune function, establishing a chronic pro-inflammatory state that contributes to neurodegeneration through multiple non-cell-autonomous mechanisms.
Glial Cell Dysregulation
Microglia and astrocytes, the primary immune cells of the central nervous system, express the majority of brain APOE and become progressively dysfunctional under APOE4 conditions [41] [42]. APOE4 disrupts their normal immunomodulatory functions, promoting a chronic inflammatory state that accelerates neurodegeneration [41]. Specifically, APOE4 exacerbates Aβ and tau burden-associated inflammation, creating a vicious cycle where pathology and neuroinflammation mutually reinforce each other [42].
Cell-specific APOE expression facilitates cross-talk between microglial and astroglial subsets, performing a diverse range of functions that become dysregulated in APOE4 carriers [42]. Under disease conditions, these immune cells show progressive dysfunction in regulating metabolic and immunoregulatory pathways, shifting from homeostatic functions toward pro-inflammatory states that damage neurons [41].
Systemic Inflammatory Signature
Recent large-scale proteomic profiling has revealed a conserved APOE ε4-associated pro-inflammatory immune signature persistent across brain, cerebrospinal fluid (CSF), and plasma, irrespective of specific neurodegenerative disease [26]. This signature is characterized by enrichment in pro-inflammatory immune and infection pathways, including T cell, B cell, and inflammatory signaling cascades such as Toll-like receptor (TLR), tumor necrosis factor (TNF), interleukin-17 (IL-17), JAK/STAT, and NF-κB pathways [26].
Immune cell subtype enrichment analysis demonstrates that APOE ε4-associated proteins are most enriched in nonclassical and intermediate monocytes, memory CD8 T cells, Tregs, memory CD4 T cells, natural killer (NK) cells, and γδ T cells [26]. This systemic inflammatory phenotype suggests APOE4 confers a fundamental biological vulnerability to neurodegeneration through immune modulation rather than disease-specific mechanisms.
Figure 1: APOE4-Induced Neuroinflammatory Signaling Pathways. APOE4 triggers glial cell dysregulation, activating multiple inflammatory signaling cascades and immune cell responses that drive chronic neuroinflammation and neurodegeneration.
APOE4 and Synaptic Dysfunction
Synaptic loss represents the strongest pathological correlate of cognitive decline in AD, and APOE4 significantly exacerbates this process through multiple interconnected mechanisms.
Synaptic Density and Protein Alterations
Quantitative neuroimaging studies using synaptic PET tracers demonstrate that APOE ε4 allele carriers exhibit significant synaptic loss in the medial temporal lobe compared to non-carriers [38]. This APOE4-associated synaptic depletion is mediated to different extents by both Aβ and tau pathology, with analyses suggesting these AD biomarkers partially explain the effect of APOE ε4 on synaptic density [38].
At the molecular level, APOE4 is associated with pronounced reductions in key synaptic proteins. Postmortem studies show significantly lower levels of synaptic vesicle protein 2A (SV2A) in AD patients, particularly in the hippocampus and entorhinal cortex, with APOE ε4 carriers showing further reductions compared to non-carriers [39] [40]. SV2A levels in brain-derived extracellular vesicles (BDEVs) and brain tissues positively correlate with synaptophysin levels and negatively correlate with Aβ and phospho-tau levels [40]. Reductions in SV2A are associated with decreased levels of other crucial synaptic proteins, including synaptotagmins, GAP43, and SNAP25, suggesting widespread disruption of the synaptic machinery in APOE4 carriers [40].
Metabolic Dysregulation at Synapses
Emerging research indicates that APOE4 impairs neuronal energy metabolism, indirectly disrupting synaptic function. Neurons exposed to APOE3 protein can utilize long-chain fatty acids as an alternative energy source when glucose is scarce, a critical adaptive mechanism in the aging brain [25]. However, this metabolic flexibility is impaired by APOE4, which disrupts the interaction with the sortilin receptor, preventing lipid uptake by neurons [25].
This metabolic disruption is particularly detrimental at synapses, which have high energy demands. The inability to switch to lipid metabolism when glucose availability declines likely compromises synaptic vesicle cycling, neurotransmitter release, and postsynaptic signaling, ultimately contributing to synaptic degeneration in APOE4 carriers [25].
Table 2: APOE4 Effects on Synaptic Integrity Across Experimental Models
| Experimental System | Key Synaptic Findings | Functional Consequences |
|---|---|---|
| Human iPSC-derived cerebral organoids [19] | Decreased synaptophysin and PSD95 in AD organoids; APOE4 exacerbates synaptic integrity loss | Increased apoptosis and neurodegeneration |
| Cognitively impaired human participants [38] | Significant synaptic loss in medial temporal lobe of APOE4 carriers | Mediated by Aβ and tau pathology |
| Postmortem human brain [39] [40] | Reduced SV2A, synaptophysin, synaptotagmins, GAP43, SNAP25 in APOE4 carriers | Correlated with cognitive impairment |
| Human stem cell-derived neurons [25] | Impaired lipid metabolism under glucose scarcity | Synaptic energy deficiency |
| Human brain organoids [43] | Disrupted neural network function with heightened excitability and synchronicity | Altered network formation during development |
iPSC-Based Modeling of APOE4 Mechanisms
Human induced pluripotent stem cell (iPSC) models have emerged as powerful tools for elucidating APOE4-specific pathogenic mechanisms in a human-relevant, controlled genetic background.
Cerebral Organoid Models
iPSC-derived cerebral organoids recapitulate complex aspects of human brain development and disease pathology, providing unique insights into APOE4 effects in a three-dimensional, multicellular environment. Cerebral organoids from AD patients carrying APOE ε4/ε4 show greater apoptosis and decreased synaptic integrity compared to those with APOE ε3/ε3 genotype [19]. Transcriptomic analysis reveals that AD patient-derived cerebral organoids are associated with enhancement of stress granules and disrupted RNA metabolism, pathways exacerbated by APOE4 [19].
A critical advantage of this model system is the ability to perform isogenic controls—converting APOE4 to APOE3 in the same genetic background—which has demonstrated that APOE4-related degenerative phenotypes can be attenuated by gene correction [19]. This approach provides causal evidence for APOE4's role in AD pathogenesis and offers a platform for therapeutic screening.
Neurodevelopmental Impacts
Recent evidence from brain organoid models indicates that APOE4 influences cortical neurodevelopment, altering the establishment of functional neural networks [43]. APOE4 reduces cortical neurons and increases glia by promoting gliogenic transcriptional programs, while increasing proliferation and differentiation of GABAergic progenitors, resulting in persistent increases in GABAergic neurons [43].
Multi-electrode array recordings in assembloids reveal that APOE4 disrupts neural network function, resulting in heightened excitability and synchronicity [43]. These developmental alterations may establish vulnerable neural circuits that predispose to degeneration later in life, suggesting APOE4 effects extend beyond aging to influence initial brain construction.
Experimental Protocol: Cerebral Organoid Generation from iPSCs
Workflow Overview:
- iPSC Maintenance: Maintain human iPSCs with APOE ε3/ε3 or ε4/ε4 genotype on Matrigel-coated plates in mTeSR Plus medium, passing with EDTA when 70-80% confluent.
- Embryoid Body (EB) Formation: Dissociate iPSCs with Accutase and aggregate 9,000 cells per well in ultra-low attachment 96-well plates in media containing BMP4, TGF-β inhibitor, and ROCK inhibitor.
- Neuroepithelial Expansion: Transfer EBs to Matrigel droplets on day 5, culture in neural induction media for 7 days to form neuroepithelial buds.
- Organoid Maturation: Transfer organoids to orbital shaker on day 12 in neuronal differentiation medium, maintain under rotary conditions for 8-12 weeks with weekly medium changes.
- Analysis: Process organoids for immunohistochemistry, protein extraction, or RNA sequencing at appropriate timepoints [19].
Key Quality Controls:
- Verify pluripotency markers (SSEA4, Nanog, TRA-1-60) in starting iPSCs
- Confirm normal karyotype after reprogramming
- Monitor ventricular zone formation with SOX2+ neural progenitors at week 4
- Verify sequential emergence of deep (Ctip2+) and superficial (Satb2+) cortical layers
- Confirm presence of GFAP+ astrocytes with mature morphology by week 12 [19]
Figure 2: iPSC-Derived Cerebral Organoid Workflow for Modeling APOE4 Pathogenesis. The experimental pipeline for generating and analyzing cerebral organoids that recapitulate APOE4-specific phenotypes including tau pathology, synaptic deficits, and network dysfunction.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating APOE4 Mechanisms
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| iPSC Lines | Isogenic APOE ε3/ε3 vs. ε4/ε4 lines; AD patient-derived iPSCs | Cerebral organoid modeling, neuronal differentiation | Causal validation of APOE4 effects through isogenic correction [19] |
| Synaptic PET Tracers | [18F]SynVesT-1, [18F]SynVesT-2, [11C]UCB-J | In vivo synaptic density quantification | APOE4 carriers show medial temporal lobe synaptic loss [38] [39] |
| Antibodies for Synaptic Proteins | Anti-SV2A, anti-synaptophysin, anti-PSD95 | Immunohistochemistry, Western blot | SV2A reduction in AD hippocampus correlated with APOE4 [39] [40] |
| Proteomic Platforms | SomaScan, LC-MS/MS | CSF, plasma, and tissue proteome profiling | APOE4-associated inflammatory signature across diseases [26] |
| Metabolic Modulators | Bezafibrate, fatty acid supplements | Restoring lipid metabolism | Improved neuronal fuel utilization in APOE4 models [25] |
| Single-Cell RNAseq | 10x Genomics, Smart-seq2 | Cell-type-specific transcriptomics | APOE4 effects on gliogenesis and neurodevelopment [43] |
The evidence reviewed herein establishes that APOE4 contributes to Alzheimer's pathogenesis through integrated effects on tau phosphorylation, neuroimmune function, and synaptic integrity. Rather than operating through isolated mechanisms, APOE4 establishes a pathogenic ecosystem where tau pathology, chronic inflammation, and synaptic dysfunction mutually reinforce each other, ultimately driving neurodegeneration. The emergence of human iPSC-based models, particularly cerebral organoids, has been instrumental in elucidating these connections while controlling for genetic background.
Future research directions should prioritize the development of APOE4-selective therapeutics that target the specific mechanisms outlined in this review, including modulators of lipid metabolism [25], anti-inflammatory approaches that counter the APOE4-specific immune signature [26], and interventions that bolster synaptic resilience. Furthermore, the discovery that APOE4 influences neurodevelopmental processes [43] suggests potential early-life intervention opportunities. As our understanding of APOE4 pathophysiology continues to evolve, leveraging these human-specific model systems will be crucial for developing precision medicine approaches for APOE4-associated neurodegeneration.
hiPSC Technology and Genome Editing: Building Precision Models for APOE Research
Generating Isogenic hiPSC Lines with Defined APOE Genotypes Using CRISPR/Cas9
Apolipoprotein E (APOE) is a protein with crucial functions in lipid metabolism and neurobiology, representing the strongest genetic risk factor for late-onset Alzheimer's disease (AD) [44] [11]. The three major human isoforms—APOE2, APOE3, and APOE4—differ by only one or two amino acids at positions 112 and 158, yet these minor variations profoundly impact protein structure and disease risk [12] [11]. APOE4 increases AD risk up to 12-fold in homozygous individuals, while APOE2 appears protective against the disease [44] [12]. This striking differential risk profile has made understanding APOE isoform-specific effects a critical focus in neurodegenerative disease research.
The emergence of human induced pluripotent stem cell (hiPSC) technology has revolutionized the study of APOE biology in disease-relevant human cell types. However, genetic background variability in patient-derived hiPSCs can confound the specific effects of APOE isoforms. The generation of isogenic hiPSC lines—where APOE alleles are precisely edited against an identical genetic background—provides a powerful solution to this challenge [45] [19]. This technical guide outlines robust methodologies for creating and validating isogenic hiPSC lines with defined APOE genotypes using CRISPR/Cas9 genome editing, enabling precise dissection of APOE isoform-mediated effects in human cellular models of Alzheimer's disease and related disorders.
APOE Isoforms: Structural and Functional Basis for Gene Editing
Genetic and Structural Basis of APOE Isoforms
The APOE gene is located on chromosome 19 in a cluster with APOC1 and APOC2, consisting of four exons and three introns totaling 3597 base pairs [12]. The APOE protein comprises 299 amino acids folded into two structural domains: an N-terminal domain (residues 1-191) forming a four-helix bundle that contains the receptor-binding region, and a C-terminal domain (residues 206-299) containing the lipid-binding region, connected by a hinge region [12] [11]. The three major isoforms differ at critical positions:
- APOE3 (most common, neutral risk): Cysteine at 112, Arginine at 158
- APOE4 (highest AD risk): Arginine at both 112 and 158
- APOE2 (protective against AD): Cysteine at both 112 and 158 [12] [11]
The single amino acid substitutions in APOE4 (C112R) and APOE2 (R158C) profoundly alter protein structure and function. APOE4 exhibits a unique "domain interaction" where Arg-112 facilitates a salt bridge formation between Arg-61 and Glu-255, drawing the N- and C-terminal domains closer together [46] [11]. This structural alteration changes APOE4's lipid binding properties, receptor interaction, and stability compared to APOE3 and APOE2.
Functional Consequences of APOE Isoforms in the Brain
In the central nervous system, APOE is primarily produced by astrocytes and microglia, serving as the principal cholesterol carrier in the brain [12] [11]. APOE isoforms differentially impact multiple cellular processes relevant to AD pathogenesis:
Table 1: Functional Differences Between APOE Isoforms in Neural Cells
| Cellular Process | APOE2 | APOE3 | APOE4 |
|---|---|---|---|
| Receptor Binding | Reduced LDLR binding | Normal binding | Normal binding |
| Lipid Transport | Impaired | Normal | Altered distribution |
| Aβ Clearance | Protective effect | Baseline | Impaired |
| Tau Phosphorylation | Reduced | Baseline | Increased |
| Synaptic Integrity | Protective | Baseline | Disrupted |
| Endolysosomal Function | Normal | Normal | Impaired [47] |
| Neuronal Vulnerability | Reduced | Baseline | Increased |
APOE4 is associated with multiple AD-related pathological phenotypes in human models, including increased Aβ production, elevated tau phosphorylation, GABAergic neuron degeneration, synaptic loss, and impaired endolysosomal function [46] [19] [47]. Importantly, converting APOE4 to APOE3 in isogenic hiPSC lines rescues these pathological phenotypes, demonstrating the specific effects of the APOE4 isoform and validating gene editing as a therapeutic strategy [46] [19].
Experimental Design and Workflow for Generating Isogenic APOE hiPSC Lines
Strategic Planning for APOE Genome Editing
The generation of isogenic APOE hiPSC lines requires careful strategic planning. Two primary approaches can be employed:
- Isogenic Line Generation: Creating all three APOE isoform lines (E2/E2, E3/E3, E4/E4) from a single parental hiPSC line with a defined APOE genotype
- Isogenic Conversion: Converting a specific APOE allele (typically APOE4) to another allele (typically APOE3) in patient-derived lines to create isogenic pairs [46] [19]
The latter approach was successfully employed by Zhao et al., who demonstrated that isogenic conversion of APOE4 to APOE3 in AD patient-derived cerebral organoids attenuated APOE4-related phenotypes including tau pathology and neurodegeneration [19]. This strategy controls for both the disease background and the genetic background, allowing specific attribution of phenotypes to the APOE4 allele.
Detailed Workflow for CRISPR/Cas9-Mediated APOE Editing
The following workflow outlines the key steps for generating and validating isogenic APOE hiPSC lines:
Key Considerations for Each Step:
gRNA Design: Design single guide RNAs (sgRNAs) targeting sequences near amino acid positions 112 and 158 in exon 4 of APOE. The sgRNAs should ideally target sequences within 10-20 base pairs of the intended edit to maximize HDR efficiency [48] [45].
Donor Template Construction: Create a single-stranded oligodeoxynucleotide (ssODN) donor template containing the desired nucleotide changes with 60-90 bp homology arms on each side. For APOE4 to APOE3 conversion, this requires changing codon 112 from CGC (Arg) to TGC (Cys) [46].
CRISPR/Cas9 Delivery: Use ribonucleoprotein (RNP) complexes comprising purified Cas9 protein and synthetic sgRNA, delivered via electroporation. RNP delivery minimizes off-target effects and reduces exposure time to nucleases [48].
Clonal Isolation: Employ a two-step clonal isolation protocol beginning with mechanical picking of individual colonies followed by enzymatic dissociation and expansion, achieving efficiencies of >2% precisely edited colonies [45].
Research Reagents and Experimental Solutions
Table 2: Essential Research Reagents for APOE Genome Editing in hiPSCs
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Parental hiPSC Lines | WTC hiPSC line [48], Patient-derived APOE4/4 hiPSCs [19] | Provides genetic background for editing; available from repositories like Coriell Institute |
| CRISPR Components | Cas9 protein, Synthetic sgRNAs, ssODN donor templates [48] | Facilitates precise genome editing through homology-directed repair |
| Cell Culture Reagents | Essential 8 Medium, Matrigel, Recombinant Vitronectin [48] [19] | Maintains hiPSC pluripotency and supports clonal expansion |
| Delivery Systems | Neon Transfection System, Amaxa Nucleofector [48] | Enables efficient RNP complex delivery into hiPSCs |
| Selection Markers | Fluorescent reporters (GFP), Antibiotic resistance genes [48] | Enriches for successfully edited cells (optional) |
| Characterization Antibodies | Anti-SSEA4, Anti-Nanog, Anti-TRA-1-60 [19] | Verifies pluripotency after editing |
| Differentiation Reagents | Neural induction media, Astrocyte differentiation supplements [19] | Enables functional validation in relevant cell types |
Quality Control and Validation of Edited hiPSC Lines
Genotypic Validation and Pluripotency Assessment
Comprehensive validation of edited hiPSC lines is essential before experimental use. The following protocol outlines key quality control measures:
Genotypic Validation:
- Perform Sanger sequencing of the targeted APOE region to confirm precise nucleotide changes without unintended mutations [45]
- Validate both 5' and 3' genomic breakpoints to ensure correct editing [49]
- Sequence cDNA synthesized from mRNA to confirm expression of the correct APOE transcript [49]
- Perform western blotting to verify expression of the expected APOE protein isoform (e.g., 86 kDa fragment for EML4-ALK fusion validation provides a reference for protein validation approaches) [49]
Pluripotency and Genomic Integrity:
- Verify expression of pluripotency markers (Nanog, Sox2, TRA-1-60, TRA-1-81) through immunostaining [19]
- Confirm normal karyotype through chromosomal analysis (G-banding) [19]
- Demonstrate trilineage differentiation potential by assessing formation of endodermal (Sox17), mesodermal (Brachyury), and ectodermal (Nestin/Sox2) cells [19]
- Test teratoma formation capacity in immunodeficient mice as a gold standard for pluripotency [46]
Functional Validation in Differentiated Cell Types
Following genotypic validation, isogenic APOE hiPSC lines must be functionally assessed in relevant differentiated cell types:
Neuronal Differentiation:
- Differentiate hiPSCs into cortical neurons using established protocols, achieving >90% purity (MAP2+ cells) [46]
- Assess APOE expression and secretion patterns in neurons; APOE4 neurons typically show ~60% reduced secreted APOE compared to APOE3 [46]
- Evaluate AD-relevant phenotypes including Aβ secretion, tau phosphorylation, and synaptic integrity [46] [19]
Cerebral Organoid Formation:
- Generate 3D cerebral organoids containing multiple neural cell types using established protocols [19]
- Analyze organoids for ventricle-like structures with Sox2+ neural progenitors and Tuj1+ neuroblasts by week 4 [19]
- Assess sequential emergence of cortical layers (Ctip2+ deep layer neurons by week 4, Satb2+ superficial layer neurons by week 12) [19]
- Evaluate astrocyte development (GFAP+ cells) with immature morphology at week 4 and mature morphology by week 12 [19]
Applications in Disease Modeling and Therapeutic Development
Modeling APOE Isoform-Specific Phenotypes in Neural Cells
Isogenic APOE hiPSC lines enable precise dissection of isoform-specific effects in human neural cells. Key findings from studies utilizing this approach include:
Table 3: Quantitative Phenotypic Differences in Isogenic APOE hiPSC Models
| Phenotypic Measure | APOE2/2 | APOE3/3 | APOE4/4 | Experimental Context |
|---|---|---|---|---|
| Secreted ApoE (ng/mL) | ~110% | 100% (reference) | ~40% | Neuronal culture [46] |
| Aβ40 Secretion | ~80% | 100% (reference) | >200% | Neuronal culture [46] |
| Phospho-Tau Levels | ~80% | 100% (reference) | ~150% | Neuronal culture [46] |
| Neuronal Apoptosis | Reduced | Baseline | Increased | Cerebral organoids [19] |
| Synaptic Integrity | Protected | Baseline | Impaired | Cerebral organoids [19] |
| Endolysosomal Function | Normal | Normal | Impaired after prolonged culture | Primary neurons [47] |
RNA-sequencing of isogenic APOE microglia xenotransplanted into mouse models of AD has revealed widespread transcriptomic and epigenomic differences, with the most significant changes observed between APOE2 and APOE4 isoforms [44]. Specifically, APOE4 is associated with impaired microglial proliferation, migration, and immune responses, while APOE2 shows enhanced phagocytic capabilities [44].
Therapeutic Screening and Target Validation
Isogenic APOE hiPSC lines provide valuable platforms for therapeutic development:
Small Molecule Screening:
- APOE4 structure correctors that convert APOE4 to an APOE3-like conformation can be tested for their ability to rescue AD-related phenotypes [46]
- Treatment with such correctors has been shown to ameliorate APOE4-associated detrimental effects, providing proof of concept for this therapeutic approach [46]
Gene Therapy Validation:
- Isogenic lines enable clean testing of gene therapies aimed at modulating APOE expression or function
- The demonstration that APOE4 knockout neurons behave similarly to APOE3 neurons supports APOE4-targeted knockdown approaches [44] [46]
Pathway-Specific Drug Testing:
- Transcriptomic analyses reveal APOE isoform-specific pathway alterations that can be targeted therapeutically [44]
- Vitamin D receptor signaling, enhanced in APOE2 microglia, represents one such potential therapeutic pathway [44]
Technical Considerations and Troubleshooting
Optimization of Genome Editing Efficiency
Successful generation of isogenic APOE hiPSC lines requires optimization of several technical parameters:
Improving HDR Efficiency:
- Synchronize hiPSCs in M-phase using cell cycle inhibitors to enhance HDR rates [48]
- Use small molecule HDR enhancers such as SCR7 or RS-1 during editing
- Employ double-stranded DNA donors with longer homology arms (800-1000 bp) for more complex edits
Minimizing Off-Target Effects:
- Use high-fidelity Cas9 variants (e.g., eSpCas9, SpCas9-HF1) to reduce off-target editing [48]
- Perform whole-genome sequencing to identify and exclude lines with unintended mutations
- Use computational prediction tools to design sgRNAs with minimal off-target potential
Clonal Selection and Expansion:
- Implement fluorescence-activated cell sorting (FACS) to enrich for successfully edited cells when using fluorescent reporters [48]
- Use mechanical picking for initial clonal isolation to maintain genomic stability [45]
- Expand multiple independent clones (minimum 3-5) for each edit to control for clonal variation
Experimental Design Considerations
When designing experiments with isogenic APOE hiPSC lines, several factors require consideration:
Appropriate Differentiation Protocols:
- Select differentiation protocols that yield cell types relevant to APOE biology (astrocytes, microglia, neurons)
- Include appropriate timepoints for phenotype manifestation; some APOE4-related endolysosomal defects only emerge after prolonged culture [47]
Inclusion of Proper Controls:
- Always include both the parental line and the isogenic corrected line as controls
- Consider including APOE-knockout lines to distinguish between loss-of-function and gain-of-toxic-function mechanisms [44] [46]
Validation in Multiple Cellular Contexts:
- Assess phenotypes in both 2D cultures and 3D organoid models to capture different aspects of APOE biology [46] [19]
- Consider cell-type specific effects, as APOE4 impacts different neural cell types (astrocytes, microglia, neurons) through distinct mechanisms [47]
The generation of isogenic hiPSC lines with defined APOE genotypes represents a powerful approach for delineating isoform-specific effects in human cellular models of Alzheimer's disease. By controlling for genetic background variability, these models enable precise attribution of phenotypic differences to APOE genotype, accelerating both mechanistic understanding and therapeutic development for APOE-related neurological disorders.
Differentiation Protocols for Neurons, Astrocytes, and Brain Microvascular Endothelial Cells
The advent of human induced pluripotent stem cell (iPSC) technology has revolutionized the study of the human brain, providing an unprecedented window into neurological development and disease. This is particularly transformative for research focused on apolipoprotein E (apoE), the strongest genetic risk factor for sporadic Alzheimer's disease (AD) and other dementias [13] [20]. The ability to differentiate human iPSCs into specific brain cell types—including neurons, astrocytes, and brain microvascular endothelial cells (BMECs)—offers a physiologically relevant human system to dissect the isoform-specific effects of apoE (E2, E3, E4) on cellular function and pathology [50] [51]. These in vitro models enable researchers to move beyond animal models, which often fail to fully recapitulate human-specific apoE biology, and to probe disease mechanisms in a controlled, human genetic background. This technical guide provides detailed, established protocols for generating these critical brain cell types from human iPSCs, with a specific emphasis on their application in apoE research, including the generation of isogenic APOE-knockout lines for controlled functional studies [52] [53]. The integration of these differentiated cells into co-culture systems and complex 3D organoids is further empowering scientists to model the intricate cell-cell interactions within the neurovascular unit and to elucidate how apoE isoforms modulate brain homeostasis in health and disease [54] [53].
Successful differentiation requires carefully selected reagents. The table below summarizes key solutions used in the protocols featured in this guide.
Table 1: Key Research Reagent Solutions for iPSC Differentiation
| Reagent Category | Specific Example(s) | Function in Differentiation |
|---|---|---|
| Basement Membrane Matrix | Corning Matrigel Growth Factor Reduced (GFR) [54] [50] | Provides a substrate that supports pluripotent stem cell attachment and growth, and is used for plating neural rosettes and organoids. |
| Stem Cell Maintenance Medium | mTeSR1 [54] [55] | A defined, serum-free medium used to maintain human iPSCs in a pluripotent state. |
| Neural Induction Medium | STEMdiff Neural Induction Medium [55]; DMEM/F12 with N2 supplement, MEM-NEAA, and heparin [50] | Directs the differentiation of iPSCs toward a neural progenitor cell (NPC) fate. |
| Dissociation Reagents | Accutase [53]; ReLeSR [54]; Papain Dissociation System [53] | Enzymatic or chemical solutions used to gently dissociate iPSC colonies or 3D tissues into single cells or small clumps for passaging or analysis. |
| Astrocyte Differentiation Medium | DMEM/F12 with N2 supplement, BMP-4 (or FBS) [50] | Promotes the gliogenic switch, driving neural progenitor cells to differentiate into astrocytes. |
| Endothelial Cell Medium | Human Endothelial-SFM, supplemented with B27, Retinoic Acid, and bFGF [54] [56] | Supports the maturation and maintenance of brain microvascular endothelial cells with barrier properties. |
| Cerebral Organoid Medium | STEMdiff Cerebral Organoid Kit (Medium A, B, C, D, E) [53] | A sequential medium system that guides the self-organization of iPSCs into 3D cerebral organoids. |
| ROCK Inhibitor | Y-27632 [54] [53] | Improves cell survival after dissociation and plating by inhibiting apoptosis. |
| Coating Proteins for BMECs | Collagen IV & Fibronectin [54] | Creates a defined, biologically relevant surface that promotes the attachment and polarization of BMECs. |
Quantitative Data from iPSC-Derived Brain Cell Models
The utility of iPSC-derived models is demonstrated by quantitative data on their physiological functions, many of which are directly relevant to apoE biology.
Table 2: Functional Metrics of iPSC-Derived Brain Cell Models
| Cell Type / Model | Key Functional Assay | Reported Metric | Relevance to ApoE Research |
|---|---|---|---|
| Brain Microvascular Endothelial Cells (BMECs) | Transendothelial Electrical Resistance (TEER) | 2,000 - 8,000 Ω·cm² in defined media [56]; averages of 2,000-4,000 Ω·cm² [54] | Confirms barrier integrity; allows study of apoE's role in BBB maintenance and lipoprotein transport. |
| Astrocytes | Apolipoprotein E Secretion | Robust increase from Day 20 of differentiation, sustained through maturation (Day 45) [50] | Direct measurement of astrocytic apoE production, enabling isoform-specific comparison of secretion levels. |
| Astrocytes | Glutamate Uptake | Significantly higher in iPSC-derived astrocytes vs. HEK293FT cells [50] | Validates astrocyte functionality; apoE4 has been linked to impaired synaptic support. |
| Astrocytes | Aβ Phagocytosis | Impaired uptake in APOE4 vs. isogenic APOE3 astrocytes [51] | Models a key apoE4-linked deficit in clearing amyloid-β, a primary AD pathology. |
| Neurons (in co-culture) | Neuronal Survival & Synaptogenesis | Reduced support from APOE4/ε4 astrocytes compared to APOE3/ε3 astrocytes [50] | Demonstrates the isoform-specific, non-cell-autonomous neurotrophic support governed by apoE. |
| Cerebral Organoids | Lipid Accumulation | Increased lipid droplets in APOE4 and APOE-/- organoids [53] | Connects apoE status to neuronal cholesterol biosynthesis and astrocytic lipid storage, key pathways in AD. |
Detailed Differentiation Methodologies
Generation of Cerebral Organoids for Brain Modeling
Cerebral organoids provide a 3D model to study apoE in a complex, multi-cell-type environment. The following workflow details a standardized protocol.
Protocol Details:
- Day 0: Harvest human iPSCs using Accutase to create a single-cell suspension. Seed 15,000 cells per well in a 96-well U-bottom ultra-low-attachment plate in Medium A (from the STEMdiff Cerebral Organoid Kit) supplemented with 10 μM Y-27632 (ROCK inhibitor) to enhance survival [53].
- Days 2 & 4: Add 100 μL of fresh Medium A to each well without disturbing the forming embryoid bodies (EBs) [53].
- Day 5: Carefully transfer individual EBs to a low-attachment 48-well plate containing Medium B to initiate neural induction [53].
- Days 7-10: Once EBs have expanded and begun to show neural epithelium, embed each EB in a 20 μL droplet of Matrigel to provide a supportive scaffold for complex tissue growth [53].
- Subsequent Culture: Transfer the Matrigel-embedded organoids to a 6-well low-attachment plate with Medium C + D for 3 days. Finally, move them to an orbital shaker in a dish with Medium E for long-term maturation. After 4 weeks, transition to a neuronal maturation medium, with organoids typically ready for analysis by Day 90 [53]. For APOE studies, organoids can be generated from isogenic iPSC lines where the APOE gene has been knocked out via CRISPR-Cas9 [52] [53] or that carry different APOE genotypes (ε3/ε3, ε4/ε4) [53].
Differentiation of iPSCs to Astrocytes
Astrocytes are the primary producers of apoE in the brain, making their differentiation critical.
Protocol Details:
- Neural Progenitor Cell (NPC) Generation: Begin by culturing iPSC clumps in suspension for 5-7 days in neural induction medium to form neurospheres. Plate these neurospheres on a Matrigel-coated surface to form neural rosettes, which express markers like Nestin and PAX6. Rosettes are then dissociated and expanded as a monolayer of NPCs [50].
- Astrocyte Differentiation: A critical factor is the passage number of NPCs. For astrocyte differentiation, use later-passage NPCs (e.g., passage 6 or higher), as this promotes a gliogenic switch. Differentiate these NPCs by culturing in media containing factors like fetal bovine serum (FBS) or BMP-4 [50].
- Maturation and Validation: Astrocytic markers emerge over time. S100β-positive cells can be detected as early as day 15, while the population becomes nearly 100% positive for both S100β and GFAP by day 45 [50]. Validate astrocyte functionality through glutamate uptake assays [50]. Crucially, apoE secretion significantly increases from day 20 onward, indicating functional maturation [50]. This protocol can be applied to iPSCs from donors with different APOE genotypes to study intrinsic isoform effects [50], or to isogenic APOE-knockout lines [52] to probe the fundamental role of apoE in astrocyte biology.
Differentiation of iPSCs to Brain Microvascular Endothelial Cells (BMECs)
BMECs form the critical barrier of the BBB, and their differentiation has been refined to achieve high fidelity.
Protocol Details:
- Defined Differentiation: Recent protocols emphasize fully defined, serum-free conditions to improve consistency [56]. This involves a two-step process where iPSCs are first differentiated toward a mesodermal lineage and then specified to an endothelial fate.
- Key Components: The differentiation medium typically includes Retinoic Acid (RA), which is crucial for inducing BBB properties, and basic Fibroblast Growth Factor (bFGF) [54] [56]. The base medium is often Human Endothelial-SFM, supplemented with B27 [54].
- Purification and Seeding: After differentiation, cells are dissociated and seeded onto filters or plates coated with an extracellular matrix. A common and effective coating is a mixture of human collagen IV and fibronectin (e.g., 400 μg/mL and 100 μg/mL, respectively) [54].
- Validation: The gold standard for validating BMEC barrier function is the measurement of Transendothelial Electrical Resistance (TEER). Using defined protocols, TEER values consistently exceeding 2,000 Ω·cm², and often reaching over 4,000 Ω·cm², can be achieved across multiple cell lines [56]. These cells also express functional efflux transporters (e.g., P-gp) and exhibit receptor-mediated transcytosis [55]. For apoE research, this model is essential for studying how different isoforms affect BBB integrity and the transport of lipoproteins and therapeutic agents into the brain.
ApoE Signaling Pathways in Brain Cell Types
ApoE exerts its effects through complex, cell-type-specific signaling pathways. The following diagram synthesizes key pathways identified in iPSC-based studies.
Pathway Descriptions:
- Lipid Metabolism and Cholesterol Biosynthesis: ApoE is a major lipid carrier. In neurons, APOE deficiency leads to a cell-autonomous upregulation of cholesterol biosynthesis genes [53]. APOE4 astrocytes show impaired cholesterol efflux and accumulation of lipid droplets [53] [51].
- Neurotrophic Support and Synaptogenesis: APOE4 astrocytes are less effective than APOE3 astrocytes in supporting neuronal survival and synaptogenesis in co-culture, indicating a loss of neurotrophic function [50].
- Amyloid-β Pathology: APOE4 glial cells (astrocytes and microglia) are impaired in their ability to clear extracellular Aβ, contributing to its accumulation [51]. Isogenic APOE4 neurons also secrete higher levels of Aβ42 compared to APOE3 neurons [51].
- Intracellular Signaling: scRNA-seq of cerebral organoids revealed that APOE deficiency activates the EIF2 signaling pathway, which is associated with cellular stress and can alter organoid cellular composition. This effect can be alleviated with an integrated stress response inhibitor (ISRIB) [53]. APOE deletion also leads to activation of the Wnt/β-catenin pathway, concurrent with reduced expression of its inhibitor, SFRP1, in glial cells [53].
Discussion and Concluding Remarks
The differentiation protocols detailed in this guide provide a robust foundation for establishing human cellular models to investigate the multifaceted roles of apoE in the brain. The quantitative data and functional validations confirm that these iPSC-derived cells—neurons, astrocytes, BMECs, and their assemblies in organoids—recapitulate critical aspects of in vivo biology relevant to apoE function, from lipid metabolism and synaptic support to barrier integrity. The integration of these tools with CRISPR-Cas9 gene editing to create isogenic APOE-knockout and allele-converted lines is a particularly powerful strategy [52] [51]. It allows for the precise dissection of apoE isoform effects against a uniform genetic background, controlling for the confounding variability inherent in patient-derived lines.
Future directions in this field will likely involve the further refinement of these protocols to achieve even greater maturity and longevity of the cultures, especially for modeling late-onset processes of neurodegenerative diseases. Furthermore, the creation of more complex multi-culture systems, such as coupling iPSC-derived BMECs with astrocytes and neurons in microfluidic "BBB-on-a-chip" models, will enable the study of apoE-mediated crosstalk within the entire neurovascular unit [54] [55]. Finally, the application of these cellular models in high-content drug screening holds immense promise for identifying novel therapeutics that can mitigate the pathogenic effects of APOE4. By providing standardized, detailed methodologies, this guide aims to equip researchers with the technical knowledge to leverage these transformative models, thereby accelerating our understanding of apoE biology and the development of effective treatments for Alzheimer's disease and related dementias.
Modeling Blood-Brain Barrier Function and Amyloid-β Clearance in iPSC-Derived Systems
The blood-brain barrier (BBB) is a sophisticated cellular interface that meticulously regulates the exchange of substances between the bloodstream and the central nervous system (CNS), maintaining the delicate homeostasis required for optimal brain function. BBB dysfunction is increasingly recognized as a critical factor in the pathogenesis of Alzheimer's disease (AD), particularly in the dysregulation of amyloid-β (Aβ) metabolism and clearance [57]. The advent of induced pluripotent stem cell (iPSC) technology has revolutionized the study of this complex neurovascular unit, enabling researchers to create human-specific models that recapitulate key aspects of BBB function and dysfunction.
Central to both AD risk and BBB function is the apolipoprotein E (APOE) gene, the strongest genetic risk factor for late-onset Alzheimer's disease. The three common APOE isoforms—APOE2, APOE3, and APOE4—differentially influence Aβ aggregation, clearance, and multiple cellular pathways within the BBB [13] [20]. APOE4 increases AD risk up to 15-fold in homozygotes compared to the neutral APOE3 isoform, while APOE2 confers significant protection [13] [20]. Understanding how these isoforms operate within iPSC-derived BBB models provides critical insights into AD mechanisms and therapeutic development.
This technical guide examines the current methodologies for modeling BBB function and Aβ clearance using iPSC-derived systems, with particular emphasis on how APOE isoforms influence these processes. We provide detailed protocols, quantitative comparisons, and visualization tools to advance research in this rapidly evolving field.
Blood-Brain Barrier Biology and Amyloid-β Clearance Pathways
BBB Cellular Architecture and Function
The BBB is a highly specialized multicellular structure composed primarily of brain microvascular endothelial cells (BMECs), pericytes, and astrocytes, which collectively form a selective barrier between the blood and brain parenchyma [58]. BMECs constitute the core physical barrier, characterized by elaborate tight junctions comprising proteins such as claudin-5 (CLDN5), occludin, and zonula occludens-1 (ZO-1) that limit paracellular diffusion [57] [58]. These specialized junctions require the majority of molecular transport to occur through transcellular pathways regulated by membrane transporters [58].
Pericytes, embedded within the vascular basement membrane, play crucial roles in BBB induction, regulation, and maintenance through direct communication with BMECs [58]. Astrocytes extend end-feet processes that extensively cover the extraluminal surface of BMECs and pericytes, contributing to BBB integrity and function through the regulation of transporter expression and localization [58]. The coordinated interaction of these cellular components enables the BBB to maintain CNS homeostasis while selectively transporting essential nutrients and removing waste products, including Aβ peptides [57].
Amyloid-β Clearance Mechanisms at the BBB
Aβ clearance across the BBB is primarily mediated by specific transporter proteins expressed on BMECs. The balance between efflux and influx transporters determines the net flux of Aβ between the brain and periphery [57]. Key transporters include:
- LRP1 (low-density lipoprotein receptor-related protein 1): Mediates Aβ efflux from brain to blood
- P-glycoprotein (P-gp): Promotes Aβ efflux from brain to blood
- RAGE (receptor for advanced glycation end-products): Mediates Aβ influx from blood to brain
In Alzheimer's disease, this delicate balance is disrupted, with studies demonstrating decreased expression of LRP1 and P-gp efflux transporters alongside increased expression of RAGE influx transporter, creating conditions favorable for Aβ accumulation [57].
Table 1: Key Amyloid-β Transporters at the Blood-Brain Barrier
| Transporter | Primary Function | Expression Change in AD | Role in Aβ Homeostasis |
|---|---|---|---|
| LRP1 | Aβ efflux | Decreased | Reduced clearance from brain |
| P-glycoprotein | Aβ efflux | Decreased | Reduced clearance from brain |
| RAGE | Aβ influx | Increased | Enhanced entry into brain |
| ABCB1 | Efflux of various compounds | Polymorphisms affect deposition | Indirect influence on Aβ levels |
APOE Isoforms and Their Structural Differences
Human APOE exists as three major isoforms—APOE2, APOE3, and APOE4—that differ by amino acid substitutions at positions 112 and 158 [13] [31]. APOE3 (Cys112, Arg158) is considered the neutral variant, while APOE2 (Cys112, Cys158) is protective, and APOE4 (Arg112, Arg158) confers significant AD risk [13]. These single amino acid substitutions profoundly impact APOE structure and function: APOE4 exhibits a unique structural alteration characterized by domain interaction between the N- and C-terminal regions, while APOE2 shows reduced receptor binding affinity due to conformational changes [31] [59].
These structural differences translate to functional consequences at the BBB. APOE isoforms demonstrate differential binding affinities to key receptors involved in Aβ clearance, particularly LRP1, with APOE4 exhibiting impaired binding compared to APOE3 [31]. Additionally, APOE isoforms vary in their lipidation status and stability, with APOE4 being less stable and more prone to degradation [31].
Diagram 1: APOE receptor interactions in Aβ clearance. APOE isoforms differentially bind to receptors LRP1 and LDLR, influencing amyloid-β clearance pathways.
iPSC-Derived BBB Models: Methodologies and Applications
Differentiation of iPSCs into BBB Cellular Components
The generation of functional BBB models from iPSCs requires the directed differentiation of multiple neural cell types. Below we outline core protocols for deriving BBB constituents:
3.1.1 iPSC to Brain Microvascular Endothelial Cell (BMEC) Differentiation
Day 0-2: Mesoderm Induction
- Culture iPSCs to ~80% confluence in essential 8 medium or equivalent
- Switch to differentiation medium containing BMP4 (10-20 ng/mL) and CHIR99021 (3-6 µM) to drive mesodermal commitment
- Change medium daily for 2 days
Day 3-5: Endothelial Specification
- Transition to medium supplemented with VEGF (50-100 ng/mL) and FGF2 (20-40 ng/mL) to promote endothelial differentiation
- Change medium daily for 3 days
Day 6-8: Barrier Maturation
- Replace with endothelial cell medium containing retinoic acid (1-5 µM) to enhance barrier properties
- Culture for 2-3 days with daily medium changes
- Purify BMEC population using CD31+ magnetic bead selection or similar methodology
3.1.2 iPSC to Pericyte Differentiation
Day 0-4: Neural Crest Induction
- Culture iPSCs to ~80% confluence
- Activate TGF-β signaling with SB431542 (10 µM) and inhibit BMP signaling with LDN193189 (100-200 nM)
- Add CHIR99021 (3 µM) to stabilize β-catenin
- Change medium every other day
Day 5-10: Mesenchymal Commitment
- Switch to medium containing PDGF-BB (50 ng/mL) and TGF-β1 (5 ng/mL) to promote pericyte specification
- Change medium every 2-3 days
- Verify differentiation via NG2 and PDGFR-β expression
3.1.3 iPSC to Astrocyte Differentiation
Day 0-10: Neural Progenitor Cell (NPC) Induction
- Utilize dual SMAD inhibition with SB431542 (10 µM) and LDN193189 (100 nM)
- Change medium every other day until neural rosettes form
Day 11-60: Astrocyte Specification
- Culture NPCs in medium containing CNTF (10 ng/mL), BMP4 (10 ng/mL), and FGF2 (10 ng/mL)
- Change medium twice weekly for 6-8 weeks
- Confirm astrocyte identity via GFAP and S100β expression
Advanced BBB Model Systems
3.2.1 2D Transwell Co-culture Models The most established iPSC-BBB model utilizes Transwell inserts with BMECs seeded on the membrane, while pericytes and astrocytes are cultured in the basolateral chamber. This setup allows for:
- Paracellular permeability assessment via TEER measurement and tracer flux
- Transporter activity quantification using specific substrates/inhibitors
- Receptor expression and function analysis
3.2.2 3D Microfluidic Organ-on-a-Chip Models More advanced models incorporate microfluidic platforms that better recapitulate the physiological BBB environment by:
- Providing shear stress (typically 1-4 dyne/cm²) through continuous perfusion
- Enabling 3D cellular architecture and cell-cell interactions
- Supporting real-time barrier function monitoring
- Allowing directional transport studies under flow conditions
3.2.3 BBB Organoid Models Recent developments include the generation of self-organizing BBB organoids that:
- Contain multiple CNS cell types in spatially relevant organizations
- Exhibit native tissue-like features including selective barrier properties
- Show complex electrical activity and cerebrospinal fluid production
- Enable study of cell-cell signaling in a more physiological context [60]
Diagram 2: iPSC differentiation workflow for BBB models. Schematic overview of differentiation protocols to generate BBB cellular components from human induced pluripotent stem cells.
APOE Isoform-Dependent Effects on BBB Function and Aβ Clearance
Quantitative Analysis of APOE Isoform Effects
Recent studies using isogenic iPSC-derived BBB models have revealed profound isoform-specific effects of APOE on Aβ clearance and deposition. The table below summarizes key quantitative findings:
Table 2: APOE Isoform-Specific Effects in iPSC-Derived BBB Models
| Parameter | APOE2 | APOE3 | APOE4 | Experimental System | Citation |
|---|---|---|---|---|---|
| Aβ40 Transport | Increased clearance | Baseline | Significantly impeded clearance | iPSC-derived BMECs | [61] |
| Aβ42 Transport | Increased transport | Baseline | Not reported | iPSC-derived BMECs | [61] |
| Extracellular Aβ Deposition | Least deposition | Intermediate | Heightened deposition | iPSC-derived pericyte-like cells | [61] |
| Amyloid Plaque Load | Significant reduction | Intermediate | Increased | In vivo mouse models | [20] |
| Aβ Oligomer Stabilization | Reduced stabilization | Intermediate | Enhanced stabilization | Biochemical assays | [20] |
| LRP1/P-gp Dependent Transport | Preserved function | Baseline | Impaired function | iPSC-derived BMECs | [61] |
Mechanistic Insights into APOE-Mediated Aβ Clearance
The differential effects of APOE isoforms on Aβ clearance can be attributed to several key mechanisms:
4.2.1 Receptor-Mediated Clearance Pathways APOE isoforms demonstrate differential binding affinities to key receptors involved in Aβ clearance. APOE4 exhibits impaired binding to LRP1 compared to APOE3, resulting in reduced Aβ clearance efficiency [31]. This receptor interaction dependency was demonstrated in studies showing that APOE-mediated Aβ transport by BMEC-like cells is dependent on LRP1 and p-glycoprotein pathways [61].
4.2.2 Blood-Brain Barrier Integrity While isogenic BMEC-like cells with different APOE genotypes showed similar trans-endothelial electrical resistance (TEER) and tight junction integrity under baseline conditions [61], the response to pathological insults may differ significantly. APOE4 has been associated with increased BBB leakage in clinical studies, suggesting compromised barrier function under stress conditions [61].
4.2.3 Lipidation and Stability Differences APOE isoforms exhibit distinct lipidation profiles and protein stability. APOE4 is less stable and more prone to degradation compared to other isoforms, potentially contributing to its impaired function in Aβ clearance [31]. The lipidation status significantly influences APOE's ability to bind and transport Aβ peptides.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for iPSC-BBB and Aβ Clearance Studies
| Category | Reagent/Assay | Specific Example | Application/Function | Technical Notes |
|---|---|---|---|---|
| iPSC Culture | Maintenance Medium | Essential 8 Medium | Undifferentiated iPSC culture | Feeder-free culture |
| Extracellular Matrix | Matrigel | iPSC attachment substrate | Dilute in DMEM/F12 | |
| BBB Differentiation | Small Molecules | CHIR99021 (GSK-3β inhibitor) | Mesoderm induction | Optimize concentration for each line |
| Growth Factors | VEGF, FGF2, BMP4 | Endothelial specification | Use research-grade cytokines | |
| Differentiation Factor | Retinoic Acid | Barrier maturation | Light-sensitive, prepare fresh | |
| Barrier Assessment | TEER Measurement | EVOM3 Voltohmmeter | Barrier integrity quantification | Measure multiple locations |
| Permeability Tracers | Sodium fluorescein, Dextrans | Paracellular permeability | Use multiple sizes | |
| APOE/Aβ Analysis | APOE Genotyping | PCR-RFLP, Sequencing | APOE isoform determination | Confirm with protein analysis |
| Aβ ELISA | V-PLEX Aβ Peptide Panel | Aβ40/Aβ42 quantification | Measure both media and lysates | |
| Immunocytochemistry | Anti-Aβ, Anti-APOE antibodies | Localization and expression | Optimize fixation and permeabilization | |
| Functional Assays | Transporter Assays | LRP1 inhibitors (RAP) | Receptor-specific function | Use multiple concentrations |
| Efflux Assays | P-gp substrates (Rhodamine 123) | Transporter activity | Include specific inhibitors |
Experimental Protocols for Assessing APOE-Isoform Specific Effects
APOE Isoform-Dependent Aβ Transport and Clearance Assay
Objective: Quantify differences in Aβ transport across iPSC-derived BMECs expressing different APOE isoforms.
Materials:
- Isogenic iPSC-derived BMECs with APOE2/3/4 genotypes
- Serum-free endothelial cell medium
- Fluorescently-labeled or radio-labeled Aβ peptides (Aβ40, Aβ42)
- LRP1 inhibitor (Receptor-Associated Protein, RAP)
- P-glycoprotein inhibitor (Elacridar or similar)
- 24-well Transwell plates (0.4 μm pore size)
- ELISA kits for Aβ quantification
Procedure:
- Differentiate iPSCs into BMECs using the protocol in Section 3.1.1
- Seed BMECs (1.0×10⁵ cells/insert) on Transwell filters and culture for 3-5 days until TEER >1500 Ω×cm²
- Pre-treat BMECs with or without transporter inhibitors (LRP1 inhibitor: 500 nM RAP; P-gp inhibitor: 1 μM Elacridar) for 2 hours
- Add fluorescent/radiolabeled Aβ (100 nM) to either apical or basolateral chamber for directional transport studies
- Incubate at 37°C for 2, 4, and 6 hours
- Collect samples from both chambers at each time point
- Quantify Aβ levels using fluorescence, radioactivity, or ELISA
- Calculate permeability coefficients (Papp) and efflux/influx ratios
Data Analysis:
- Compare transport rates between APOE isoforms
- Assess inhibitor sensitivity to determine pathway specificity
- Normalize data to TEER values and cell viability
APOE-Dependent Aβ Deposition in Pericyte-like Cells
Objective: Evaluate the effect of APOE isoforms on Aβ deposition using iPSC-derived pericyte-like cells.
Materials:
- Isogenic iPSC-derived pericyte-like cells with APOE2/3/4 genotypes
- Pericyte medium supplemented with PDGF-BB
- Synthetic Aβ42 peptides (prepared as oligomers or fibrils)
- Thioflavin T or Congo Red for amyloid detection
- Immunofluorescence reagents for Aβ and pericyte markers
Procedure:
- Differentiate iPSCs into pericyte-like cells following Section 3.1.2 protocol
- Seed pericyte-like cells on coverslips in 24-well plates (5.0×10⁴ cells/well)
- Treat cells with 1 μM prepared Aβ42 for 48 hours
- Fix cells with 4% paraformaldehyde for 15 minutes
- Stain with Thioflavin T (1%) for 30 minutes or perform immunocytochemistry for Aβ
- Counterstain with pericyte markers (NG2, PDGFR-β) and DAPI
- Image using fluorescence or confocal microscopy
- Quantify amyloid deposition using image analysis software
Data Analysis:
- Quantify amyloid area per field across APOE genotypes
- Assess colocalization with pericyte markers
- Compare deposition patterns between APOE isoforms
iPSC-derived BBB models have emerged as powerful tools for investigating the intricate relationship between APOE isoforms, blood-brain barrier function, and amyloid-β clearance in Alzheimer's disease. The development of isogenic APOE iPSC lines has been particularly transformative, enabling researchers to isolate isoform-specific effects against identical genetic backgrounds.
The accumulating evidence clearly demonstrates that APOE isoforms differentially regulate multiple aspects of BBB function and Aβ metabolism, with APOE4 impairing clearance mechanisms while APOE2 appears to enhance protective pathways. These models have revealed that APOE-mediated effects occur through multiple interdependent mechanisms, including receptor binding affinity, protein stability, lipidation status, and inflammatory signaling.
Future advancements in this field will likely focus on developing more complex multicellular models that better recapitulate the human neurovascular unit, incorporating microglia and neurons alongside traditional BBB components. The integration of microfluidic platforms that provide physiological shear stress and enable real-time monitoring of barrier function will further enhance the physiological relevance of these models. Additionally, the application of gene editing technologies to introduce protective APOE variants like the Christchurch mutation will provide new insights into therapeutic strategies for APOE4-mediated AD risk.
As these models continue to evolve, they will play an increasingly vital role in drug discovery and validation, enabling high-throughput screening of compounds designed to mitigate APOE4-associated deficits in Aβ clearance and BBB function. The ultimate goal remains the translation of these findings into effective therapeutics for Alzheimer's disease that target the specific pathogenic mechanisms associated with different APOE genotypes.
This technical guide details critical functional assays for investigating the effects of apolipoprotein E (ApoE) isoforms in human induced pluripotent stem cell (iPSC)-derived neurons. ApoE, a lipid transport protein, exists as three common isoforms (ApoE2, ApoE3, ApoE4) with the ApoE4 isoform constituting the strongest genetic risk factor for late-onset Alzheimer's disease, while ApoE2 appears protective [13]. ApoE isoforms differentially modulate synaptic integrity, neuronal survival, and lipid homeostasis in the central nervous system [62] [13]. The assays herein—neuronal survival, synaptogenesis, and lipid metabolism analysis—are essential for delineating the isoform-specific pathophysiological mechanisms in iPSC-neuron models, providing a framework for target discovery and therapeutic development for Alzheimer's disease and related dementias.
Neuronal Survival Assays
Assessing neuronal survival is fundamental to understanding ApoE-mediated neuroprotection and toxicity. ApoE4 expression is linked to increased neurodegeneration and synaptic loss, whereas ApoE2 may promote neuronal resilience [13].
Key Assays and Quantitative Readouts
Table 1: Core Assays for Quantifying Neuronal Survival
| Assay Name | Measured Parameters | Technology Platform | Key ApoE4-Related Phenotypes |
|---|---|---|---|
| Live/Dead Staining | Ratio of live (calcein-AM+) to dead (propidium iodide+) cells | Fluorescence microscopy / HCA | Increased neuronal death in ApoE4/4 cultures vs. ApoE3/3 or ApoE2/2 [13] |
| Caspase-3 Activity | Cleaved caspase-3 (immunofluorescence); caspase-3/7 activity (luminescence) | Plate reader, WB, IF | Elevated baseline apoptosis in ApoE4 neurons under stress (e.g., oxidative, Aβ) [13] |
| MTT / Cell Titer-Glo | Metabolic activity (MTT); ATP content (Cell Titer-Glo) | Absorbance / Luminescence plate reader | Reduced metabolic activity in ApoE4 neurons; can correlate with viability loss |
| Lactate Dehydrogenase (LDH) Release | LDH enzyme activity in culture medium | Absorbance plate reader | Higher LDH release indicates increased membrane damage and cytotoxicity in ApoE4 models |
Detailed Experimental Protocol: High-Content Analysis of Neuronal Viability
Principle: This protocol uses automated fluorescence microscopy to simultaneously quantify live neurons, dead cells, and total neuronal population in ApoE isoform-defined iPSC-neuron cultures.
Materials:
- ApoE Genotyped iPSC-Neurons: Isogenic iPSC lines with APOE ε2/ε2, ε3/ε3, and ε4/ε4 genotypes.
- Staining Reagents: Calcein-AM (2 µM), Propidium Iodide (PI, 1.5 µM), Hoechst 33342 (5 µg/mL).
- Imaging Equipment: High-content imaging system.
Procedure:
- Culture: Plate iPSC-derived cortical neurons (Day 35+ of differentiation) at 50,000 cells/well in a poly-D-lysine coated 96-well plate. Maintain cultures for 7 days pre-assay.
- Treatment: Apply experimental conditions (e.g., Aβ oligomers, oxidative stress inducers, or control medium) for 24-48 hours.
- Staining: Incubate with Calcein-AM, PI, and Hoechst 33342 in pre-warmed neural basal medium for 30 minutes at 37°C.
- Image Acquisition: Image 9-15 fields per well using a 10x or 20x objective.
- Quantification: Use analysis software to:
- Count total nuclei.
- Identify Calcein-AM positive cells as live neurons.
- Identify PI-positive cells as dead cells.
- Data Analysis: Calculate:
- % Live Neurons = (Calcein-AM+ cells / Total nuclei) × 100
- % Cell Death = (PI+ cells / Total nuclei) × 100
- Compare results across ApoE isoform lines and treatment conditions.
Synaptogenesis and Synaptic Function Assays
Synapses are primary targets of ApoE pathophysiology. ApoE localizes at synaptic terminals and isoforms differentially regulate synapse formation, stability, and function [63]. ApoE4 induces hyperexcitability and synaptic loss, while ApoE3 supports synaptogenesis [63].
Key Assays and Quantitative Readouts
Table 2: Core Assays for Quantifying Synaptogenesis and Function
| Assay Name | Measured Parameters | Technology Platform | Key ApoE4-Related Phenotypes |
|---|---|---|---|
| Immunofluorescence Synaptic Puncta | Density of pre- (vGlut1, Synapsin) and post-synaptic (PSD-95) markers | Confocal microscopy / HCA | Reduced density and co-localization of pre/postsynaptic markers in ApoE4 neurons [63] |
| Live-Cell Calcium Imaging | Neuronal firing rate, synchrony, calcium transient frequency | Fluo-4 AM dye; fluorescent microscope | Astrocytic ApoE4 induces hyperexcitability; Neuronal ApoE3 promotes efficient firing [63] |
| Electrophysiology | Spontaneous postsynaptic currents (sPSCs), miniature PSCs (mPSCs) | Patch clamp | Altered frequency/amplitude of sPSCs/mPSCs, indicating impaired synaptic transmission |
| Western Blot / ELISA | Protein levels of synaptic markers (Synapsin, PSD-95) | Western Blot, ELISA | Decreased levels of key synaptic proteins in ApoE4 neuronal lysates |
Detailed Experimental Protocol: Synaptic Puncta Analysis by High-Content Imaging
Principle: Quantify synaptic density and maturity by immunostaining for pre- and post-synaptic proteins and measuring their co-localization.
Materials:
- Primary Antibodies: Mouse anti-PSD-95 (Post-synaptic), Guinea pig anti-VGlut1 (Pre-synaptic).
- Secondary Antibodies: Alexa Fluor 568 anti-mouse, Alexa Fluor 647 anti-guinea pig.
- Other Reagents: Neuronal marker (e.g., Chicken anti-MAP2), DAPI.
Procedure:
- Culture & Fix: Plate ApoE-isoform iPSC-neurons. At maturity (e.g., DIV 40-50), fix cells with 4% PFA for 15 minutes.
- Permeabilization/Blocking: Permeabilize with 0.1% Triton X-100 and block with 5% normal goat serum for 1 hour.
- Antibody Staining:
- Incubate with primary antibodies (PSD-95, VGlut1, MAP2) diluted in blocking buffer overnight at 4°C.
- Wash and incubate with species-appropriate fluorescent secondary antibodies for 1 hour at room temperature.
- Counterstain with DAPI.
- Image Acquisition: Acquire high-resolution z-stack images using a confocal microscope with a 63x oil objective.
- Image Analysis:
- Use software to create a neuronal mask based on MAP2 staining.
- Identify PSD-95 and VGlut1 puncta within the mask using intensity and size thresholding.
- Calculate puncta density (puncta/µm of neurite).
- Perform co-localization analysis to identify "mature synapses" and report as a percentage of total PSD-95 puncta.
Signaling Pathway: ApoE Modulation of Synaptic Function
The diagram below illustrates how different ApoE isoforms from astrocytes and neurons differentially influence neuronal excitability and synaptic integrity, integrating findings from live calcium imaging and synaptic puncta analysis [63].
Lipid Metabolism Analysis
Lipids are fundamental components of synaptic membranes and myelin; their metabolism is profoundly regulated by ApoE isoforms [62] [64]. ApoE4 is associated with dysregulated lipid metabolism in microglia and neurons, leading to impaired transport, defective efflux, and lipid droplet accumulation [44].
Key Assays and Quantitative Readouts
Table 3: Core Assays for Analyzing Neuronal Lipid Metabolism
| Assay Name | Measured Parameters | Technology Platform | Key ApoE4-Related Phenotypes |
|---|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Quantification of 1000+ lipid species (e.g., phospholipids, sphingolipids, cholesterol esters) | LC-MS/MS | Altered phospholipid composition; reduced PUFA-containing species; increased ceramides in ApoE4 cells [62] [64] |
| Filipin Staining | Free cholesterol accumulation in cells | Fluorescence microscopy | Perinuclear cholesterol accumulation in ApoE4 neurons due to endosomal trapping [13] |
| Cholesterol Efflux Assay | Rate of cholesterol export from neurons to ApoE acceptors | Radiolabeled/fluorescent cholesterol, plate reader | Impaired cholesterol efflux to ApoE4 lipoproteins vs. ApoE3 [13] |
| Oil Red O / BODIPY Staining | Neutral lipid droplet accumulation | Fluorescence microscopy / HCA | Increased lipid droplets in ApoE4 microglia and astrocytes under stress [44] |
Detailed Experimental Protocol: Lipidomics Sample Preparation from iPSC-Neurons
Principle: Extract and quantify the global lipid profile from ApoE-isoform neurons to identify isoform-specific lipid metabolic signatures.
Materials:
- ApoE Genotyped iPSC-Neurons.
- Lipid Extraction Solvents: HPLC-grade methanol, methyl-tert-butyl ether (MTBE), chloroform.
- Internal Standards: SPLASH LipoGrade stable isotope-labeled lipid mix.
- Equipment: Benchtop centrifuge, sonicator, LC-MS/MS system.
Procedure:
- Cell Quenching and Harvest: Rapidly aspirate medium from 6-well plates and wash with ice-cold PBS. Quench metabolism by adding 1 mL of ice-cold methanol. Scrape cells and transfer suspension to a glass tube.
- Lipid Extraction (MTBE/Methanol/Water method):
- Add 3.75 mL of MTBE and 1.25 mL of methanol containing internal standards to the sample.
- Sonicate for 30 minutes in an ice-cold water bath.
- Add 1.5 mL of water to induce phase separation. Centrifuge at 2,000 x g for 10 minutes.
- Collect the upper organic (MTBE) phase containing the lipids into a new glass tube.
- Sample Evaporation and Reconstitution: Dry the organic phase under a gentle stream of nitrogen. Reconstitute the dried lipid extract in 200 µL of dichloromethane:methanol (1:1, v/v) for LC-MS analysis.
- LC-MS/MS Analysis:
- Chromatography: Use a C18 reversed-phase column with a 15-minute gradient from 60% mobile phase A (acetonitrile:water, 60:40 with 10 mM ammonium formate) to 100% mobile phase B (isopropanol:acetonitrile, 90:10 with 10 mM ammonium formate).
- Mass Spectrometry: Operate in both positive and negative electrospray ionization modes with data-dependent acquisition (DDA) or parallel reaction monitoring (PRM).
- Data Analysis: Use lipidomics software to identify and quantify lipid species. Normalize to internal standards and protein content. Perform multivariate statistics to find lipids differentially abundant across ApoE genotypes.
Experimental Workflow: Integrated Lipid Metabolism Analysis
The diagram below outlines a comprehensive workflow for assessing lipid metabolism in ApoE iPSC-neuron models, from cell culture to data interpretation.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for ApoE iPSC-Neuron Research
| Reagent / Resource | Function / Application | Example & Notes |
|---|---|---|
| Isogenic ApoE iPSC Lines | Controls for genetic background; isolates ApoE isoform effects. | Key resource available from repositories (e.g., CIRM, Allen Cell Collection). Ensure genomic validation of ApoE allele knock-in. |
| ApoE Isoform-Specific Antibodies | Differentiate ApoE isoforms in WB, IF; detect intracellular ApoE. | Clone: WUE-4 (Novus Biologicals, NB110-60531) for WB/IF [63]. |
| Synaptic Markers Antibody Panel | Quantify pre- and post-synaptic density and maturity. | Pre-synaptic: vGlut1 (Synaptic Systems); Post-synaptic: PSD-95 (Cell Signaling). Validate for IF in human neurons. |
| Live-Cell Calcium Dyes | Measure neuronal activity and network synchrony. | Fluo-4 AM (Invitrogen) for kinetic imaging. ApoE4 cultures show hyperexcitability [63]. |
| Lipidomics Internal Standards | Enable absolute quantification of lipid species in LC-MS. | SPLASH LipoGrade Mix (Avanti Polar Lipids) contains deuterated lipids across multiple classes. |
| Recombinant Human ApoE Proteins | Study acute effects of ApoE isoforms in neuronal cultures. | Available from multiple vendors (e.g., Sigma-Aldrich). Critical: Check lipidation status (lipid-poor vs. reconstituted lipoproteins). |
| Cholesterol Efflux Assay Kits | Standardized measurement of cholesterol transport. | Commercially available kits (e.g., Abcam) use fluorescent cholesterol. ApoE4 as an acceptor shows impaired efflux [13]. |
Co-culture Systems to Study Cell-Cell Interactions in the Neurovascular Unit
The neurovascular unit (NVU) represents a highly specialized functional interface between the circulatory and central nervous systems, acting as a critical guardian of brain homeostasis. This dynamic structure consists of brain microvascular endothelial cells (BMECs) forming the blood-brain barrier (BBB), surrounded by and interacting with pericytes, astrocytes, microglia, and neurons [65] [66]. The intricate signaling between these cellular components regulates BBB integrity, cerebral blood flow, nutrient transport, and waste clearance—processes fundamental to maintaining optimal neural function. Research has firmly established that NVU dysfunction is a hallmark of numerous neurological conditions, including Alzheimer's Disease (AD), where the apolipoprotein E (APOE) ε4 allele stands as the strongest genetic risk factor for the late-onset sporadic form [31] [20] [14].
The development of in vitro co-culture systems has become indispensable for disentangling the complex autocrine, paracrine, and juxtacrine signaling within the human NVU. These models provide a controlled, reproducible platform to investigate cellular interactions that are exceptionally challenging to parse in vivo, especially in humans [67]. For researchers focusing on APOE isoforms and their mechanistic roles in neurodegenerative disease, incorporating isogenic human induced pluripotent stem cell (iPSC)-derived models represents a particularly powerful approach. These systems allow for the direct comparison of different APOE genotypes (APOE2, APOE3, APOE4) on NVU function within an otherwise identical genetic background, thereby isolating the specific effects of these alleles on pathways such as amyloid-β clearance, neuroinflammation, and metabolic coupling [68] [66]. This technical guide outlines the core principles, methodologies, and applications of contemporary NVU co-culture systems, with a specific emphasis on their utility in APOE research.
Core Components of the Neurovascular Unit
A physiologically relevant NVU co-culture model must incorporate its principal cellular constituents, each contributing unique and essential functions.
Brain Microvascular Endothelial Cells (BMECs): These cells form the physical barrier of the BBB, characterized by continuous tight junctions (TJs) and adherens junctions (AJs) that severely restrict paracellular diffusion. They also express a sophisticated array of influx and efflux transporters that regulate transcellular molecular passage [65] [69]. BMECs can be sourced from primary human isolates (e.g., the hCMEC/D3 cell line) or, with increasing prevalence, differentiated from human iPSCs, which often demonstrate superior barrier properties [65] [68].
Pericytes: These cells are embedded within the vascular basement membrane and play critical roles in BBB development, maintenance, and regulation of cerebral blood flow. iPSC-derived pericyte-like cells have been shown to secrete APOE, with the isoform influencing amyloid deposition—APOE4 exacerbates, while APOE2 reduces, extracellular amyloid accumulation [68].
Astrocytes: The most abundant glial cells, astrocytes extend end-feet processes that ensheath cerebral capillaries. They provide crucial trophic support to endothelial cells, directly contributing to the induction and maintenance of barrier properties [65]. Astrocytes are a primary source of APOE in the central nervous system [31] [14].
Neurons: Neuronal activity is coupled to vascular responses, a process known as neurovascular coupling. The presence of neurons or neural stem cells (NSCs) in co-culture systems has been demonstrated to enhance barrier integrity and promote the maturation of astrocytic end-feet [70] [67].
Microglia: As the resident immune cells of the CNS, microglia contribute to neuroinflammation and are implicated in AD pathogenesis. They also represent a secondary source of APOE in the brain [31] [66].
Table 1: Key Cellular Constituents of the Neurovascular Unit and Their Primary Functions
| Cell Type | Primary Functions in the NVU | Relevance to APOE Biology |
|---|---|---|
| Brain Microvascular Endothelial Cells (BMECs) | Forms the physical and metabolic blood-brain barrier; expresses tight junctions and specialized transporters. | APOE4 impairs amyloid-β clearance via LRP1; disrupts intracellular iron homeostasis [68] [71]. |
| Pericytes | Regulates BBB development, stability, and capillary blood flow. | APOE4 genotype associated with increased extracellular amyloid deposition [68]. |
| Astrocytes | Provides trophic support; forms end-feet contact with vasculature; modulates immune response. | Major producer of APOE in the CNS; supports lipid transport and neuronal repair [31] [14]. |
| Neurons/Neural Stem Cells (NSCs) | Controls neurovascular coupling; enhances barrier integrity through signaling. | APOE isoforms differentially affect tau pathology, synaptic plasticity, and neurodegeneration [20] [67]. |
| Microglia | Mediates CNS immune response and clearance of debris. | Contributes to APOE production; APOE4 heightens neuroinflammatory response [31] [66]. |
Establishing a Human iPSC-Derived Tri-culture NVU Model
The following diagram outlines the general workflow for establishing a tri-culture NVU model using isogenic human iPSCs, a method highly suited for APOE isoform research.
Detailed Experimental Protocol
1. Differentiation of Isogenic iPSCs into NVU Components
- BMEC-like cells: Utilize established differentiation protocols involving sequential exposure to unconditioned medium (DMEM/F12 supplemented with KnockOut Serum Replacement, non-essential amino acids, and β-mercaptoethanol) for 6 days, followed by endothelial cell specification in human endothelial serum-free medium (hECSR) supplemented with basic fibroblast growth factor (bFGF, 20 ng/mL) and retinoic acid (RA, 10 µM) for 2 days [68]. The use of isogenic iPSC lines (e.g., APOE2/2, APOE3/3, APOE4/4) is critical for isolating APOE genotype-specific effects.
- Astrocytes and Neural Stem Cells (NSCs): Differentiate iPSCs into NSCs using dual-SMAD inhibition, which can subsequently be matured into astrocytes or maintained as NSCs. For tri-culture, NSCs are often used as they can represent neuronal influence and enhance barrier function [66] [67].
2. Co-culture Assembly in a Transwell System
- Coat the apical side of a Transwell filter (e.g., 0.4 µm pore size) with a matrix of collagen IV (1 mg/mL) and fibronectin (0.5 mg/mL).
- Seed the differentiated BMEC-like cells onto the coated filter at a high density (e.g., (1.0 \times 10^6 \, \text{cells/cm}^2)).
- Plate astrocytes and/or NSCs in the basolateral chamber of the Transwell plate at a density of approximately (5.0 \times 10^4 \, \text{cells/cm}^2) in a neuroglial differentiation medium [66].
- Culture the assembled system for 2-4 days to allow the establishment of stable cell-cell interactions and barrier maturation.
3. Key Assays for Functional Validation
- Barrier Integrity: Quantify the integrity of the BMEC monolayer by measuring Transendothelial Electrical Resistance (TEER) using a volt-ohm meter. A competent BBB model should typically achieve TEER values significantly higher than a monoculture (e.g., 1500-3000 Ω×cm²). TEER should be monitored regularly [65] [66].
- Permeability Assays: Assess paracellular leakage by tracking the flux of fluorescent tracer molecules (e.g., sodium fluorescein, 376 Da; dextrans, 4-70 kDa) from the apical to the basolateral compartment.
- Transporter Activity: Evaluate the functional expression of key efflux transporters, such as P-glycoprotein (P-gp), using specific substrates/inhibitors.
- Molecular Phenotyping: Confirm the expression of characteristic markers via immunofluorescence (e.g., ZO-1 for tight junctions, β-III-tubulin for neurons, GFAP for astrocytes) and qPCR.
Table 2: Quantitative Functional Comparisons in a Representative iPSC-Derived Tri-culture Model
| Parameter | BMEC Monoculture | BMEC + Astrocyte Co-culture | BMEC + Astrocyte + Neuron Tri-culture | Notes |
|---|---|---|---|---|
| Transendothelial Electrical Resistance (TEER) | Baseline (e.g., ~1000 Ω×cm²) | Increased ~1.5-fold [65] | Highest TEER (~2-fold increase over monoculture) [65] [66] | Tri-culture most closely mimics in vivo barrier tightness. |
| Amyloid-β 42 (Aβ42) Clearance (Brain-to-Blood) | Baseline | N/D | APOE2: IncreasedAPOE3: IntermediateAPOE4: Decreased [68] | APOE4 impedes clearance, contributing to amyloid pathology. |
| Extracellular Amyloid Deposition (in Pericytes) | N/A | N/A | APOE2: LowestAPOE3: IntermediateAPOE4: Highest [68] | Consistent with protective/risk profiles of APOE isoforms. |
APOE Signaling Pathways in the NVU
The differential effects of APOE isoforms on NVU function are mediated through their interactions with specific cell-surface receptors, orchestrating a complex signaling network that influences AD-related pathologies. The following diagram summarizes the key pathways involved.
The core mechanism involves APOE lipoprotein particles binding to members of the low-density lipoprotein (LDL) receptor family, including LRP1, LDLR, ApoER2, and VLDLR [31]. These receptors are differentially expressed across NVU cell types. The isoform-specific amino acid substitutions (e.g., Arg112 and Arg158 in APOE4) alter the protein's structure, stability, and receptor-binding affinity, leading to divergent downstream consequences [31] [20]. For instance, impaired clearance of amyloid-β (Aβ) by BMECs, a process dependent on LRP1, is a well-established detrimental pathway associated with the APOE4 isoform [68]. Furthermore, recent research using iPSC-derived brain endothelial cells indicates that APOE4 can cell-autonomously disrupt endosome maturation and iron homeostasis, revealing novel pathways by which this risk allele compromises NVU function [71].
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in establishing a reliable NVU co-culture model depends on the consistent use of high-quality, well-defined reagents. The following table catalogues key solutions and materials used in the protocols cited herein.
Table 3: Essential Research Reagents and Materials for NVU Co-culture Models
| Reagent/Material | Function/Application | Example from Search Results |
|---|---|---|
| Isogenic Human iPSC Lines | Genetically identical cells differing only at the APOE locus (E2/E2, E3/E3, E4/E4) to isolate allele-specific effects. | Commercially available lines (e.g., from Alstem) used to derive all NVU cell types [68]. |
| Transwell Hanging Inserts | Semi-permeable membrane supports that create separate "blood" (apical) and "brain" (basolateral) compartments for co-culture. | Used in tri-culture models with hCMEC/D3 endothelial cells, 1321N1 astrocytes, and SH-SY5Y neurons [65]. |
| Collagen IV & Fibronectin | Extracellular matrix proteins for coating culture surfaces to support adhesion and maturation of BMEC-like cells. | Used at 1 mg/mL and 0.5 mg/mL, respectively, to coat surfaces for iPSC-derived BMEC-like cells [68] [66]. |
| Retinoic Acid (RA) | Small molecule additive to endothelial cell culture medium that enhances barrier properties by promoting tight junction formation. | Used at 10 µM during the final stage of BMEC differentiation and in the apical medium of established cultures [68]. |
| hECSFM / B-27 Supplement | Endothelial serum-free medium and a defined supplement providing hormones, lipids, and antioxidants crucial for endothelial and neural cell health. | Constituents of the endothelial cell (EC) medium for BMEC-like cells [68] [66]. |
| Basic Fibroblast Growth Factor (bFGF) | Mitogen and survival factor used in the maintenance and differentiation of both NSCs and endothelial cells. | Added at 10-20 ng/mL in NSC expansion media and BMEC differentiation media [68] [67]. |
Advanced co-culture systems that faithfully replicate the human neurovascular unit are no longer a luxury but a necessity in translational neuroscience research. By integrating isogenic human iPSC-derived cells, these models provide an unparalleled platform for deconstructing the cell-type-specific mechanisms by which APOE isoforms modulate NVU function and contribute to Alzheimer's disease pathogenesis. The protocols and insights outlined in this guide provide a foundation for implementing these powerful models, enabling researchers to probe the multifaceted roles of APOE in amyloid clearance, tau pathology, neuroinflammation, and metabolic dysfunction at the brain's primary vascular interface. The continued refinement of these systems, including the incorporation of fluid flow (shear stress) and the integration of additional cell types like microglia, promises to further deepen our understanding and accelerate the discovery of novel therapeutic strategies for AD and other neurodegenerative disorders.
High-Content Screening Platforms for Drug Discovery Targeting APOE Pathways
Apolipoprotein E (APOE) polymorphism represents the strongest genetic risk factor for sporadic, late-onset Alzheimer's disease (AD), impacting more than half of all AD cases [13]. The APOE ε4 allele increases AD risk in a gene dose-dependent manner by up to 15-fold in homozygotes, while the APOE ε2 allele confers protective effects relative to the common ε3 allele [72] [13]. These isoforms differ at amino acid positions 112 and 158 (apoE2: Cys112/Cys158; apoE3: Cys112/Arg158; apoE4: Arg112/Arg158), resulting in structural and functional differences that profoundly impact AD pathogenesis through multiple mechanisms [13]. Given that over 95% of AD cases are sporadic or late-onset, APOE-targeted therapeutic strategies offer the potential to benefit a substantial patient population [73] [13]. The complexity of APOE biology and its involvement in diverse pathological pathways necessitates sophisticated screening platforms that can capture these multifactorial effects in physiologically relevant models.
High-Content Screening Platforms for APOE-Targeted Drug Discovery
Core Components of High-Content Screening Platforms
High-content screening (HCS) is a powerful quantitative image-based approach that enables high-throughput assessment of hundreds to thousands of chemical or genetic perturbations on cellular phenotypes, often at single-cell resolution [74]. Modern HCS platforms integrate several core components: (1) physiologically relevant biological models such as induced pluripotent stem cell (iPSC)-derived cerebral organoids; (2) specific staining protocols using fluorescent dyes, molecular probes, or antibodies; (3) automated imaging systems with multiwell plate handling robotics; and (4) sophisticated data analysis pipelines for multiparametric phenotypic quantification [74]. These platforms are particularly valuable for APOE-targeted drug discovery because they can capture the complex, multifactorial effects of APOE isoforms on diverse pathological processes, including Aβ aggregation, tau phosphorylation, synaptic dysfunction, neuroinflammation, and calcium dysregulation [73].
Cerebral Organoid Platforms for APOE Research
The development of iPSC-derived cerebral organoids (iCOs) has revolutionized AD modeling by recapitulating key pathological features of the human brain in a three-dimensional context. Park et al. established a robust network-based drug-screening platform that integrates mathematical modeling with the pathological features of AD using iCOs, including CRISPR-Cas9-edited isogenic APOE lines [73]. This platform employed 1,300 organoids from 11 participants to build a high-content screening system for testing blood-brain barrier-permeable FDA-approved drugs [73]. The organoids demonstrated key AD pathological features, including elevated Aβ1-42, Aβ1-40, total tau, and phosphorylated tau secretion in PiB+ iCOs (derived from patients with positive amyloid PET scans) compared to PiB- iCOs, with these levels significantly correlating with actual brain Aβ deposition measured by PiB-PET SUVR [73]. Importantly, APOE ε4 carrier iCOs secreted more pathogenic proteins than APOE ε4 non-carriers, confirming the isoform-specific effects on AD pathology [73].
Figure 1: Workflow of High-Content Screening Platform Using Human Cerebral Organoids for APOE-Targeted Drug Discovery
Key APOE Pathways Amenable to High-Content Screening
APOE isoforms impact multiple pathological pathways in AD, each of which can be quantified using high-content screening approaches:
Amyloid-β Pathology: APOE ε4 significantly exacerbates Aβ deposition and plaque formation while impairing Aβ clearance. High-content assays can quantify Aβ burden using immunostaining with antibodies such as 6E10 and morphological analysis of plaque size and distribution [72] [13].
Tau Pathophysiology: APOE ε4 promotes tau phosphorylation and tangle formation. Screening approaches employ phospho-tau-specific antibodies (e.g., AT8) to quantify neurofibrillary tangle pathology and neuronal integrity [72] [75].
Synaptic Dysfunction: APOE isoforms differentially affect synaptic density and function. High-content platforms can quantify pre- and postsynaptic markers (e.g., PSD-95, synapsin) and dendritic complexity [73] [13].
Neuroinflammation: APOE ε4 enhances neuroinflammatory responses in microglia and astrocytes. Screening assays measure morphological changes in glial cells and secretion of proinflammatory cytokines [44] [13].
Calcium Homeostasis: APOE ε4 iCOs demonstrate abnormal calcium regulation with higher calcium fluorescence and more calcium peaks, measurable via live-cell calcium imaging [73].
Table 1: Key APOE Pathways and High-Content Screening Approaches
| Pathway | Biological Significance | HCS Readouts | Validation Assays |
|---|---|---|---|
| Aβ Aggregation & Clearance | APOE4 increases Aβ deposition and plaque formation [72] [13] | Aβ immunostaining, plaque size/number quantification [73] | ELISA for Aβ40/42, PiB-PET correlation [73] |
| Tau Phosphorylation & Aggregation | APOE4 promotes tau hyperphosphorylation and tangle formation [72] [75] | Phospho-tau immunostaining, neuronal morphology [73] | Western blot for tau species, neuronal death assays [73] |
| Synaptic Density & Function | APOE4 reduces synaptic markers and impairs synaptic plasticity [73] [13] | Quantification of pre/postsynaptic markers, dendritic complexity [73] | RNA-seq for synaptic genes, electrophysiology [73] |
| Neuroinflammatory Response | APOE4 enhances proinflammatory microglial activation [44] [13] | Microglial morphology, cytokine profiling, phagocytosis assays [44] | RNA-seq of immune pathways, cytokine ELISAs [44] |
| Calcium Homeostasis | APOE4 disrupts calcium signaling, leading to hyperexcitability [73] | Live-cell calcium imaging, oscillation frequency analysis [73] | Calcium dye fluorescence, peak detection algorithms [73] |
Experimental Protocols for APOE-Targeted Drug Screening
Cerebral Organoid Generation and Maintenance
The generation of iPSC-derived cerebral organoids follows a guided differentiation protocol with timed supplementation of specific growth factors to yield multiple neuronal subtypes at consistent proportions [73]. The step-by-step methodology includes:
iPSC Generation and Quality Control: Generate iPSCs from patient fibroblasts or peripheral blood mononuclear cells using non-integrating Sendai virus or episomal vectors. Quality control includes verification of pluripotency markers (Oct4, Tra1-60, Sox2), alkaline phosphatase staining, and karyotype analysis to ensure genomic integrity [73].
Cerebral Organoid Differentiation: Adapt the guided differentiation protocol as described by Park et al. [73]. Briefly, aggregate iPSCs into embryoid bodies in low-attachment plates using media containing ROCK inhibitor Y-27632. Induce neural ectoderm formation with dual SMAD inhibition using LDN-193189 and SB-431542 for 10-12 days. Pattern neuroepithelial buds toward forebrain identity using BDNF, GDNF, and TGF-β inhibitors. Maintain organoids in spinning bioreactors or orbital shakers for long-term maturation (60+ days) to allow development of complex neuronal networks and spontaneous electrical activity [73].
Isogenic APOE Line Generation: Utilize CRISPR-Cas9 genome editing to introduce specific APOE alleles (ε2, ε3, ε4) into control iPSC lines, creating isogenic pairs that differ only at the APOE locus, thus controlling for background genetic variability [73].
High-Content Screening Assay Protocol
The screening protocol developed by Park et al. provides a robust framework for APOE-targeted drug discovery [73]:
Organoid Plating and Drug Treatment: Plate uniform-sized organoids (200-300 μm diameter) in 96-well or 384-well imaging plates pre-coated with poly-D-lysine. Treat with candidate compounds across a concentration range (typically 1 nM-10 μM) for 7-14 days, with medium changes every 2-3 days.
Multiplexed Staining: Fix organoids with 4% paraformaldehyde and permeabilize with 0.3% Triton X-100. Implement multiplexed staining with the following panel:
- Nuclei: Hoechst 33342 (1 μg/mL)
- Neurons: Anti-βIII-tubulin (1:500) with Alexa Fluor 488 secondary
- Astrocytes: Anti-GFAP (1:1000) with Alexa Fluor 568 secondary
- Pathological Aβ: Anti-Aβ (6E10, 1:500) with Alexa Fluor 647 secondary
- Phosphorylated tau: Anti-p-tau (AT8, 1:250) with Alexa Fluor 594 secondary
Automated Image Acquisition: Use high-content imaging systems (e.g., CellInsight, ImageXpress) with 10× and 20× objectives to acquire z-stack images (5-7 slices with 10 μm interval) at multiple fields per well. Maintain consistent exposure times across plates and batches.
Image Analysis and Feature Extraction: Process images using automated analysis pipelines (e.g., CellProfiler, Harmony software) with the following analysis modules:
- 3D organoid segmentation based on βIII-tubulin staining
- Nuclear detection and counting within the organoid mask
- Aβ aggregate identification and quantification (count, size, intensity)
- p-tau puncta detection and intensity measurement
- Neuronal process tracing and complexity analysis
- Astrocyte activation assessment based on GFAP intensity and morphology
Multiparametric Hit Identification: Normalize data to positive (disease model) and negative (healthy control) controls. Calculate Z-scores for each parameter and employ multivariate analysis to identify compounds that normalize multiple pathological features simultaneously.
Table 2: Key Research Reagent Solutions for APOE-Targeted High-Content Screening
| Reagent Category | Specific Examples | Function in HCS Workflow | Application in APOE Research |
|---|---|---|---|
| iPSC Lines | Patient-derived iPSCs, CRISPR-edited isogenic APOE lines (E3/E4) [73] | Disease modeling with human genetic background | Study APOE isoform-specific effects in controlled genetic context |
| Differentiation Kits | Neural induction media, patterning factors (BDNF, GDNF) [73] | Generate cerebral organoids with consistent cellular composition | Produce 3D models recapitulating AD pathology |
| Antibodies for Phenotyping | Anti-βIII-tubulin, MAP2, GFAP, Sox2 [73] | Cell type identification and quantification | Verify neuronal/glial composition in organoids |
| Pathology Markers | Anti-Aβ (6E10), anti-phospho-tau (AT8) [73] | Quantification of AD pathological hallmarks | Measure APOE-modulated Aβ and tau pathology |
| Calcium Indicators | Fluo-4 AM, Cal-520 AM [73] | Live-cell imaging of neuronal activity | Detect APOE4-associated calcium dysregulation |
| Cell Death Assays Propidium iodide, TUNEL, caspase kits [73] | Quantification of neuronal vulnerability | Assess neuroprotective effects of candidate drugs | |
| Lipidation Assays | Filipin, Nile red, cholesterol probes [13] | Visualization of lipid metabolism | Study APOE-mediated lipid transport dysfunction |
APOE-Targeted Therapeutic Screening Case Study: A03 Compound
A targeted screening approach identified A03, a small-molecule APOE4-targeted therapeutic candidate that normalizes sirtuin 1 (SirT1) levels [75]. The screening methodology included:
High-Throughput Screening Setup: Utilize murine neuroblastoma N2a cells stably transfected with APOE4 (N2a-E4), which show significantly lower SirT1 levels compared to APOE3-transfected cells [75].
Primary Screening Assay: Implement a customized SirT1 AlphaLISA assay to screen compound libraries for SirT1 enhancers. The assay measures SirT1 protein levels in response to compound treatment in APOE4-expressing cells [75].
Secondary Validation: Confirm hits in multiple cell models, including human glioblastoma cells transiently transfected with APOE4 (A172-E4). Evaluate selectivity by measuring effects on related sirtuins (e.g., SirT2) and assess functional outcomes such as increased soluble amyloid precursor protein α (sAPPα) levels [75].
In Vivo Validation: Test promising candidates in APOE4-targeted replacement mice crossed with 5XFAD amyloid model (E4FAD mice). Administer compounds via oral gavage for 56 days and assess cognitive improvement using Novel Object Recognition testing, followed by biochemical analysis of SirT1 levels in hippocampal tissue [75].
This approach successfully identified A03, which demonstrated brain penetrance, increased SirT1 levels in the hippocampus, and improved cognition in the E4FAD mouse model without observed toxicity [75].
APOE Signaling Pathways and Screening Strategies
Figure 2: APOE Signaling Pathways and Corresponding High-Content Screening Strategies
High-content screening platforms utilizing human iPSC-derived models represent a transformative approach for APOE-targeted drug discovery. The integration of cerebral organoids with isogenic APOE editing, multiparametric imaging, and computational analysis provides an unprecedented opportunity to identify therapeutics that address the multifaceted role of APOE in AD pathogenesis. Future developments will likely include the incorporation of microfluidic systems to enhance throughput, the integration of multi-omics data for deeper mechanistic insights, and the implementation of more complex assembloid models containing multiple brain cell types to better capture cell-autonomous and non-cell-autonomous effects of APOE isoforms [44] [74]. As these platforms continue to evolve, they offer significant promise for developing precision medicine approaches that can effectively target APOE-related pathways in diverse patient populations.
Addressing Experimental Challenges in hiPSC-Based APOE Modeling
Ensuring Consistent Differentiation Efficiency Across Multiple APOE Genotypes
The apolipoprotein E (APOE) gene, particularly its ε4 allele, represents the strongest genetic risk factor for sporadic Alzheimer's disease (AD), while the ε2 allele confers protective effects [76] [77]. In the burgeoning field of induced pluripotent stem cell (iPSC) research, ensuring consistent differentiation efficiency across these genotypes is paramount for reliable disease modeling and drug development. The inherent biological differences between APOE isoforms—including their divergent effects on energy metabolism, lipid homeostasis, and neuronal development—can significantly impact differentiation outcomes and introduce unwanted variability [78] [46] [51]. This technical guide provides a comprehensive framework for standardizing differentiation protocols across multiple APOE genotypes, enabling researchers to generate more reproducible and physiologically relevant human neuronal models for studying AD mechanisms and therapeutic interventions.
Establishing a Genetically Controlled Framework for APOE Research
The Imperative for Isogenic iPSC Lines
The gold standard for controlling genetic variability in APOE research involves using APOE-isogenic iPSC lines. These lines are genetically identical except for the specific APOE alleles at the endogenous APOE locus, typically created using CRISPR/Cas9 genome editing techniques [76] [77]. Multiple studies have demonstrated that comparing results from completely different genetic backgrounds (non-isogenic lines) can lead to confounding interpretations due to background genetic effects. The isogenic approach allows researchers to attribute observed phenotypic differences directly to the APOE genotype rather than to unrelated genetic variations [46] [51].
Commercially available isogenic iPSC lines, such as the BIONi010-C series (EBiSC), include:
- BIONi010-C2: APOE3/3
- BIONi010-C4: APOE4/4
- BIONi010-C6: APOE2/2
- BIONi010-C3: APOE knockout (KO) [76] [77]
These validated lines provide an essential foundation for consistent differentiation across genotypes. The inclusion of an APOE-KO line is particularly valuable for determining whether APOE4 effects represent a gain-of-toxic-function (APOE4 specific phenotypes) versus loss-of-function (phenotypes shared with APOE-KO) mechanisms [78] [46].
Core Principles for Maintaining Genotypic Integrity
Maintaining genotypic consistency throughout differentiation requires:
- Regular genotyping: Confirm APOE status at passage points before differentiation initiation and post-differentiation
- Karyotypic stability monitoring: Ensure normal chromosomal counts throughout culture expansion
- Pluripotency marker verification: Confirm expression of Nanog, Sox2, TRA-1-60, and TRA-1-81 before differentiation [46]
- Mycoplasma testing: Routine screening for contamination
Quantitative Differentiation Parameters Across APOE Genotypes
Neuronal Differentiation Efficiency and Phenotypic Variation
Table 1: APOE Genotype-Specific Differentiation Outcomes in Neuronal Cultures
| Parameter | APOE2 | APOE3 | APOE4 | APOE-KO | Measurement Method |
|---|---|---|---|---|---|
| Differentiation Efficiency | 90 ± 1.5% | 90 ± 1.5% | 90 ± 1.5% | Similar to E2/E3 | MAP2+ cells [46] |
| Neurite Outgrowth | Reference | Risk-neutral | Enhanced | Similar to E2/E3 | Morphometric analysis [51] |
| Synapse Formation | Reference | Baseline | Increased | N/D | Synaptophysin staining [51] |
| Tau Phosphorylation | Decreased | Baseline | Significantly increased | Resembles E3 | Western blot (AT8, AT180, PHF1) [46] |
| Aβ42 Secretion | Decreased | Baseline | >2-fold increase | Similar to E3 | ELISA [46] |
| Full-length ApoE Secretion | Reference | Baseline | ~60% reduction | None detected | Western blot [46] |
Metabolic and Functional Parameters in Differentiated Cells
Table 2: Metabolic and Functional Characteristics by APOE Genotype
| Cell Type | Parameter | APOE2 | APOE3 | APOE4 | APOE-KO |
|---|---|---|---|---|---|
| Neurons | Mitochondrial ATP Production | Baseline | Baseline | Significantly enhanced | Resembles E3 [78] |
| Neurons | Basal Respiration | Baseline | Baseline | Increased | Resembles E3 [78] |
| Astrocytes | Mitochondrial ATP Production | Baseline | Baseline | Reduced | Similar to E2 [76] [77] |
| Astrocytes | Glycolytic ATP Production | Baseline | Baseline | Reduced | Similar to E2 [76] [77] |
| Astrocytes | Glycolytic Capacity | Baseline | Baseline | Enhanced | Similar to E2 [76] [77] |
| Astrocytes | Mitochondrial Respiration | Baseline | Baseline | Elevated | Similar to E2 [76] [77] |
| BBB Models | Aβ42 Clearance | Enhanced | Baseline | Impaired | N/D [79] |
Standardized Differentiation Protocols for Consistent Results
Neural Induction and Maintenance Protocol
The following protocol, adapted from multiple studies [46] [76] [77], ensures consistent neural differentiation across APOE genotypes:
Day 0-6: Neural Induction
- Culture iPSCs at 30,000 cells/cm² in unconditioned medium (UM)
- UM Composition:
- Change medium daily
- On day 3, switch to Neural Induction Medium 2 (same as above without Dorsomorphin)
Day 7+: Neural Progenitor Cell (NPC) Expansion
- Passage cells to poly-L-ornithine (15 μg/mL) and laminin (10 μg/mL) coated plates
- Culture in Neural Stem Cell Maintenance Medium (NSMM):
- Passage every 6-7 days at 90-100% confluency
- For first five passages, add 2 μM Thiazovivin to NSMM
- After five passages, add 5 ng/mL FGF and 5 ng/mL EGF
Neuronal Differentiation and Maturation
Terminal Neuronal Differentiation (Day 28+)
- Plate NPCs at appropriate density (50,000-100,000 cells/cm²) on poly-L-ornithine/laminin coated surfaces
- Culture in neuronal maturation medium:
- Neurobasal medium
- 1× B27 supplement
- 2 mM GlutaMAX
- 20 ng/mL BDNF
- 20 ng/mL GDNF
- 1 mM cAMP
- 200 nM ascorbic acid [46]
- Change medium every 2-3 days
- Maintain for 4-8 weeks for full maturation
- Assess purity by MAP2 immunostaining (target >90% MAP2+ cells)
Astrocytic Differentiation Protocol
From NPCs to Immature Astrocytes
- Plate NPCs onto fibronectin (1 mg/mL) coated plates at 135,000 cells/well (6-well plate)
- Culture in astrocyte differentiation medium:
- Change medium every 2-3 days
- Differentiate for 4-6 weeks to achieve mature astrocytic phenotype
Quality Control and Validation Metrics
Essential Quality Control Checkpoints
- Pluripotency verification pre-differentiation: Confirm >90% expression of Oct4, Nanog, Sox2
- Neural progenitor validation: Verify >85% expression of Sox2, nestin, Pax6, FoxG1
- Neuronal purity assessment: Achieve >90% MAP2+ cells with appropriate neuronal morphology
- Astrocytic validation: Confirm >80% GFAP+ cells with characteristic astrocyte morphology
- APOE secretion validation: Quantify full-length APOE and fragment levels by Western blot
- Functional validation: Document expected APOE genotype-specific phenotypes (e.g., increased p-tau in APOE4 neurons)
Troubleshooting Common Genotype-Specific Issues
APOE4-Specific Challenges:
- Reduced APOE secretion: APOE4 neurons typically secrete ~60% less full-length APOE than APOE3; focus on intracellular phenotypes or overexpress APOE4 if studying secreted effects [46]
- Increased fragmentation: APOE4 shows higher fragment-to-full-length ratio; include protease inhibitors in lysis buffers
- Enhanced metabolic activity: Account for increased mitochondrial ATP production in experimental design [78]
APOE2 Considerations:
- Protective phenotypes: Use as a comparative control for APOE4-specific pathologies
- Similarity to APOE-KO: In some assays, APOE2 resembles APOE-KO; interpret results in context of gain vs. loss of function [76] [77]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for APOE iPSC Differentiation Studies
| Reagent Category | Specific Examples | Function | Genotype-Specific Considerations |
|---|---|---|---|
| CRISPR/Cas9 Tools | SpCas9, sgRNAs targeting APOE locus | Generating isogenic lines | Verify complete sequencing of edited locus |
| Cell Culture Matrix | Vitronectin, Poly-L-ornithine, Laminin, Fibronectin | Substrate for cell attachment and differentiation | Consistent coating density across genotypes |
| Neural Induction Supplements | CHIR99021, SB431542, Dorsomorphin, Compound E | Directing neural lineage specification | Uniform concentration across all genotypes |
| Cell Culture Media | mTESR+, Advanced DMEM/F12, Neurobasal | Maintenance and differentiation | Identical lots for comparative studies |
| Differentiation Factors | hLIF, BDNF, GDNF, CNTF, BMP4 | Promoting specific neural lineages | Concentration optimization may be needed |
| Metabolic Assays | Seahorse XF Analyzer reagents, mitochondrial dyes | Assessing bioenergetic profiles | Account for genotype-specific baseline differences [78] [76] |
| APOE Detection Reagents | APOE isoform-specific antibodies, ELISA kits | Quantifying APOE expression and secretion | Antibodies must distinguish isoforms without cross-reactivity |
Experimental Workflows and Signaling Pathways
APOE Isoform Differentiation and Analysis Workflow
APOE-Sortilin Signaling Pathway in Neuronal Metabolism
Achieving consistent differentiation efficiency across APOE genotypes requires meticulous attention to genetic controls, standardized protocols, and genotype-specific validation. The implementation of isogenic iPSC panels, coupled with the rigorous quality control measures and optimized differentiation protocols outlined in this guide, provides a robust foundation for reproducible research into APOE-mediated mechanisms in Alzheimer's disease and other neurological conditions. As the field advances, continued refinement of these approaches will enhance our understanding of how APOE isoforms contribute to neuronal function and dysfunction, ultimately accelerating the development of targeted therapeutic interventions for APOE4-associated disease risk.
Standardizing Functional Maturation of iPSC-Derived Neurons and Astrocytes
The standardization of functionally mature human induced pluripotent stem cell (iPSC)-derived neurons and astrocytes represents a pivotal challenge in modeling Alzheimer's disease (AD) and understanding the isoform-specific effects of apolipoprotein E (APOE). As the strongest genetic risk factor for late-onset AD, the APOE ε4 allele confers significantly increased risk, while the APOE ε2 allele is protective [31]. Human iPSC models provide a unique platform to investigate these effects in a physiologically relevant human cellular context, overcoming the limitations of animal models that fail to fully recapitulate human-specific disease pathologies [80]. However, the value of these models is entirely dependent on the functional maturity of the differentiated cells, which must accurately mimic the properties of adult human brain cells to yield meaningful insights into disease mechanisms.
The maturation status of iPSC-derived neural cells profoundly influences key physiological processes relevant to APOE biology, including lipid metabolism, synaptic plasticity, and neuroinflammatory responses. Immature neuronal networks may not adequately demonstrate the APOE isoform-dependent effects on synaptic function and neuronal viability that are crucial for understanding AD pathogenesis [50]. Similarly, the maturation state of iPSC-derived astrocytes directly impacts their ability to support neuronal function, regulate the extracellular environment, and model the complex interplay between APOE isoforms and amyloid beta pathology [81] [82]. This technical guide outlines standardized approaches for generating and validating functionally mature iPSC-derived neurons and astrocytes, with specific emphasis on their application to APOE research.
Quantitative Benchmarks for Functional Maturation
Temporal Maturation Profiles of iPSC-Derived Neural Cells
Table 1: Key maturation milestones and temporal dynamics in iPSC-derived neural cultures
| Cell Type | Maturation Stage | Time Point | Key Markers & Functional Properties | APOE-Relevance |
|---|---|---|---|---|
| Cortical Neurons | Early immature | Day 21 | Co-expression of VGlut1 & GABA; No sustained LTP [83] | Limited APOE isoform differential effects |
| Cortical Neurons | Late mature | Day 40+ | Solely VGlut1+; Sustained LTP for >1h; Spontaneous synaptic activity [83] | APOE4 shows impaired synaptogenesis vs. APOE3 [50] |
| Astrocytes (LSF Protocol) | Precursor stage | ~60 days | S100β > GFAP; Basic glutamate uptake [82] | Suboptimal for modeling APOE-lipidation |
| Astrocytes (LSF Protocol) | Mature | 5 months | High GFAP/S100β; Complex morphology; Domain organization [82] | APOE4 particles less lipidated vs. APOE3 [50] |
| Astrocytes (SSC Protocol) | Moderately mature | 2 months | Mixed maturity; Lower GFAP expression [82] | Variable APOE secretion effects |
Electrophysiological Benchmarks for Neuronal Maturation
Table 2: Functional electrophysiological parameters of mature iPSC-derived neurons
| Parameter | Immature Neurons | Mature Neurons | Measurement Technique | Significance for APOE Research |
|---|---|---|---|---|
| Resting Membrane Potential | ~-45 to -50 mV | -58.2 ± 1.0 mV [84] | Whole-cell patch clamp | Neuronal health and viability in APOE models |
| Action Potential Amplitude | <50 mV | 66.5 ± 1.3 mV [84] | Whole-cell patch clamp | Network functionality across APOE genotypes |
| Spontaneous Synaptic Activity | Rare or absent | Present in 74% of neurons (16.03 ± 0.82 pA) [84] | Patch clamp or MEA | Synaptic deficits in APOE4 models |
| Sustained Firing Capacity | Single spikes or brief bursts | Mature trains (11.9 ± 0.5 Hz) [84] | Current injection | Neuronal resilience in APOE2 models |
| Long-Term Potentiation (LTP) | Absent without GABA blockade | Persists >1 hour [83] | Multi-electrode array | Synaptic plasticity mechanisms |
Experimental Protocols for Directed Differentiation and Maturation
Standardized Cortical Neuron Differentiation Protocol
The following protocol, adapted from Hickman and colleagues [83], generates pure excitatory cortical neuronal cultures capable of long-term potentiation without astrocyte co-culture:
Days 1-7: Neural Induction
- Begin with high-quality human iPSCs at 80-90% confluence.
- Apply dual SMAD inhibition using LDN193189 (100-200nM) and SB431542 (10μM) in neural induction medium.
- Culture in defined, xeno-free conditions to eliminate variability from serum or animal components.
- Key quality control: Formation of neuroepithelial morphology with extended processes.
Days 8-21: Cortical Patterning and Regional Specification
- Introduce DKK-1 (Wnt antagonist) and DMH-1 (BMP inhibitor) to promote telencephalic specification.
- Withdraw DKK-1 and introduce cyclopamine (SHH inhibitor) to specify dorsal cortical fate.
- Critical validation point: >90% of cells should express PAX6 and OTX2, confirming cortical identity.
Days 22-40: Functional Maturation
- Culture in trophic support medium containing BDNF (20ng/ml), GDNF (20ng/ml), cAMP (1μM), ascorbic acid (200μM), and laminin (2μg/ml).
- Replace half of the medium volume 3 times per week to maintain nutrient and factor concentrations.
- Functional validation: At day 40, immunocytochemistry should show >95% β-III tubulin+ neurons with exclusive VGlut1 expression (no GABA), indicating pure excitatory phenotype [83].
Astrocyte Differentiation: Comparison of Methodologies
The selection of astrocyte differentiation protocol significantly impacts maturation status and functionality, with important implications for APOE modeling:
Long, Serum-Free (LSF) Protocol [82]:
- Duration: 5 months total differentiation time
- Methodology: Neural induction via dual SMAD inhibition (11 days) → Neurosphere formation in suspension (2 months) → Terminal differentiation with CNTF and BMP4 (7 days)
- Outcome: High GFAP/S100β expression (76% GFAP+), complex morphology, non-overlapping domains
- Advantages: High maturity; suitable for modeling mature astrocyte functions including APOE lipidation
- Disadvantages: Labor-intensive; low yield; potential for reactive state
Short, Serum-Containing (SSC) Protocol [82]:
- Duration: 2 months total differentiation time
- Methodology: Neural precursor generation → Astrocyte commitment with CHIR99021, purmorphamine, and bFGF → Terminal maturation with 1% FBS
- Outcome: Moderate GFAP expression, simpler morphology
- Advantages: Faster; higher yield; compatible with neuronal differentiation from same precursors
- Disadvantages: Lower maturity; serum introduces variability
Co-culture Systems for Enhanced Maturation
Akerman and colleagues demonstrated that cortical iPSC-astrocytes derived from a common progenitor pool exert pro-maturational effects on iPSC-derived cortical neurons [81]:
Optimal Co-culture Configuration:
- Differentiate neurons and astrocytes from the same cortical progenitor population to maintain regional specificity.
- Establish neuronal cultures first, then add astrocytes at a 60:40 neuron:astrocyte ratio after 2-3 weeks of neuronal differentiation.
- Maintain in neural basal medium with B27 supplement, without additional growth factors.
- Functional outcomes: Enhanced synaptic activity, increased action potential firing, spontaneous network activity, and accelerated maturation compared to neuronal monocultures.
Signaling Pathways Governing Neural Maturation
The differentiation and maturation of iPSC-derived neurons and astrocytes involves precisely orchestrated signaling pathways that can be visualized in the following workflow:
Figure 1: Signaling pathway workflow for standardized neuronal and astrocyte maturation. The directed differentiation of functionally mature cortical neurons and astrocytes requires sequential activation and inhibition of specific signaling pathways, with precise timing critical for achieving reproducible results across different iPSC lines.
APOE Isoform-Specific Functional Assessments
Evaluating APOE-Mediated Effects in Mature Neural Cultures
Functionally mature iPSC-derived neural cultures enable the investigation of APOE isoform-specific effects relevant to Alzheimer's disease pathogenesis:
Neuronal Vulnerability Assessments:
- Co-culture APOE ε3/ε3 or APOE ε4/ε4 astrocytes with wild-type neurons to isolate non-cell autonomous effects [50]
- Quantify neuronal survival over 14-21 days in serum-free conditions
- Assess dendritic complexity and spine density via MAP2 immunostaining
- Expected outcome: APOE ε4/ε4 astrocytes provide less neurotrophic support, resulting in ~30-40% reduced neuronal viability compared to APOE ε3/ε3 astrocytes [50]
Synaptogenesis Assays:
- Measure co-localization of pre-synaptic (Synapsin) and post-synaptic (PSD-95) markers in neurons co-cultured with APOE variant astrocytes
- Perform whole-cell patch clamp recordings to quantify spontaneous excitatory post-synaptic currents (sEPSCs)
- Expected outcome: Neurons co-cultured with APOE ε4/ε4 astrocytes show significantly reduced synaptic density and frequency of sEPSCs [50]
APOE Lipidation Status:
- Analyze APOE particle size distribution using native PAGE followed by Western blotting
- Categorize particles as large (>669 kDa), medium (440-669 kDa), or small (<440 kDa)
- Expected outcome: APOE4 particles show significantly reduced lipidation compared to APOE3, particularly in the medium particle fraction [50]
Blood-Brain Barrier Modeling with APOE Variants
Recent advances in iPSC-derived blood-brain barrier (BBB) models reveal APOE isoform-dependent interactions with amyloid beta:
BBB Amyloid Clearance Assay:
- Differentiate isogenic APOE2/2, APOE3/3, and APOE4/4 iPSCs to brain microvascular endothelial-like cells (BMEC-like cells)
- Measure "brain-to-blood" transport of Aβ40 and Aβ42 across BMEC-like cell monolayers
- Key finding: APOE4 significantly impedes Aβ40 clearance, while APOE2 enhances Aβ42 transport compared to APOE3 [79]
- Mechanism: APOE-mediated amyloid transport depends on LRP1 and p-glycoprotein pathways
Vascular Amyloid Deposition:
- Differentiate isogenic APOE iPSCs to pericyte-like cells
- Quantify extracellular Aβ42 deposition following exposure to synthetic Aβ42
- Key finding: APOE4 pericyte-like cells show heightened extracellular amyloid deposition, while APOE2 displays minimal deposition [79]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents for standardized neural differentiation and APOE research
| Reagent Category | Specific Reagents | Function | Concentration | Considerations for APOE Research |
|---|---|---|---|---|
| Small Molecule Inhibitors | LDN193189, SB431542, DMH-1, Cyclopamine | Neural induction, patterning | 100-200nM LDN, 10μM SB [83] | Critical for reproducible cortical fate |
| Growth Factors & Cytokines | BDNF, GDNF, bFGF, EGF, CNTF, BMP4 | Neuronal survival, astrocyte maturation | 20ng/ml BDNF/GDNF [83] | Batch-to-batch variability affects reproducibility |
| Extracellular Matrix | Laminin, Poly-L-ornithine, Matrigel | Cell adhesion, process outgrowth | 2-20μg/ml [83] [84] | Impact on neuronal maturation and network formation |
| APOE Genotyping | PCR primers, sequencing | Confirm APOE isoform status | N/A | Essential for isogenic line validation |
| Lipid Transport Assays | Native PAGE, Antibodies | APOE lipidation status | N/A | APOE4 shows reduced lipidation [50] |
| Electrophysiology | Multi-electrode arrays, Patch clamp | Functional network assessment | N/A | Gold standard for maturity validation |
The standardization of functionally mature iPSC-derived neurons and astrocytes represents a transformative advancement for investigating APOE isoform-specific effects in Alzheimer's disease. The protocols and validation benchmarks outlined in this technical guide provide a framework for generating reproducible human neural cultures that recapitulate critical aspects of brain physiology, including synaptic plasticity, neuronal-glia interactions, and APOE-mediated lipid metabolism. As the field progresses, the integration of these standardized maturation approaches with emerging technologies such as cerebral organoids and microfluidic systems will further enhance our ability to model the complex interplay between APOE genotypes and AD pathogenesis in a human-relevant context. Importantly, the consistent application of these maturation standards across laboratories will accelerate the discovery of APOE-mediated disease mechanisms and the development of targeted therapeutic interventions for Alzheimer's disease and other neurodegenerative disorders.
Technical Considerations for Amyloid-β Transport and Deposition Assays
The accumulation of amyloid-β (Aβ) in the brain is a cardinal pathological hallmark of Alzheimer's disease (AD), and its interplay with apolipoprotein E (ApoE) isoforms represents a critical area of investigation. Technical assays for evaluating Aβ transport and deposition provide the foundation for understanding disease mechanisms and developing therapeutic interventions. These assays are particularly relevant in the context of ApoE isoforms in iPSC neuron research, where isoform-specific effects on Aβ metabolism—with ApoE4 increasing AD risk and ApoE2 conferring protection—can be systematically modeled [14] [20]. The accurate quantification of diverse Aβ aggregates and the assessment of their transit across the blood-brain barrier (BBB) are technically challenging yet essential for advancing this field.
Aβ exists in multiple structural forms—monomers, soluble oligomers, protofibrils, and fibrils—each exhibiting distinct biochemical properties and degrees of neurotoxicity [85] [86]. Soluble Aβ oligomers are considered highly neurotoxic due to their ability to disrupt synaptic function and impair long-term potentiation [85]. Understanding ApoE's isoform-dependent influence on Aβ aggregation and clearance requires robust technical approaches capable of distinguishing these species within complex biological systems like iPSC-derived neuronal cultures.
Amyloid-β Aggregation Cascade and ApoE Interactions
The aggregation of Aβ follows a stepwise cascade, beginning with monomeric peptides that misfold and assemble into small, soluble oligomers containing a beta-hairpin structure [85] [86]. These oligomers further aggregate into protofibrils, which represent an intermediate stage between oligomers and mature fibrils. Ultimately, these species organize into fibrillar structures characterized by extensive beta-sheet content, culminating in the formation of insoluble plaques [85]. The location of aggregates—whether intracellular, membrane-bound, or extracellular—also significantly influences their toxic potential [86].
ApoE isoforms differentially influence this aggregation process. ApoE4 has a stronger stabilizing effect on Aβ oligomers compared to ApoE3, while ApoE2 more effectively lowers Aβ oligomer levels [20]. These isoform-specific interactions directly impact Aβ deposition and clearance mechanisms, making them crucial considerations when designing transport and deposition assays for iPSC neuron models.
Table 1: Amyloid-β Species in the Aggregation Cascade
| Aβ Species | Size/Structure | Key Characteristics | Neurotoxicity | Detection Considerations |
|---|---|---|---|---|
| Monomers | 4-5 kDa, unstructured | Natural processing product of APP; exists as Aβ40, Aβ42, and other variants | Low | Accessible epitopes; can be specifically quantified with well-selected antibodies |
| Soluble Oligomers | Small, soluble aggregates | Contain beta-hairpin structure; highly mobile | High (disrupt synaptic function) | Epitopes may become partially hidden; requires specific buffer conditions |
| Protofibrils | Intermediates between oligomers and fibrils | Transitional structures | Moderate to High | Preferentially bound by antibodies like lecanemab |
| Fibrils | Large aggregates with extensive beta-sheet content | Form insoluble precipitates | Lower (chronic impact) | N- and C-terminal epitopes often hidden within aggregate structure |
| Plaques | Insoluble extracellular deposits | Contain dense fibrillar networks; hallmark pathological feature | Chronic (via inflammation) | Require strong acids (formic acid) for solubilization before detection |
Amyloid-β Transport Mechanisms at the Blood-Brain Barrier
The BBB plays a pivotal role in regulating Aβ levels in the brain through receptor-mediated transport systems. Low-density lipoprotein receptor-related protein 1 (LRP1) is a key efflux transporter responsible for moving Aβ from the brain to the circulation [87]. The trafficking route of LRP1 is influenced by the avidity of its interaction with cargo molecules, creating distinct pathways with different functional outcomes [87].
Mid-avidity binding promotes PACSIN2-mediated transcytosis, enabling rapid, degradation-free transport of LRP1 cargo across endothelial cells. In contrast, high-avidity binding triggers clathrin-mediated endocytosis through PICALM and Rab5-dependent sorting, frequently leading to lysosomal degradation and reduced membrane-bound LRP1 availability [87]. In Alzheimer's disease, LRP1 expression decreases with age and is nearly undetectable in AD patients and animal models, impairing Aβ clearance capacity [87].
ApoE isoforms interact differently with LDL receptor family members, creating isoform-specific effects on Aβ clearance. ApoE3 and ApoE4 demonstrate similar high binding affinities to LDLR, whereas ApoE2 exhibits substantially weaker binding affinity [31]. The impaired function of LRP1 in AD and its interaction with ApoE isoforms underscores the importance of incorporating BBB transport assays in iPSC neuron research.
Quantitative Assays for Amyloid-β Deposition
ELISA-Based Detection and Quantification
Enzyme-Linked Immunosorbent Assay (ELISA) remains a widely utilized method for quantifying Aβ levels in biological samples, including brain homogenates and cell culture supernatants from iPSC neuron models. The structural complexity of Aβ aggregates presents significant challenges for accurate detection, as portions of the peptide may become hidden within aggregate structures [85] [86].
Critical considerations for ELISA-based quantification include:
Antibody Selection: Careful selection of antibodies targeting accessible epitopes specific to the aggregation state of interest is essential. Antibodies recognizing N-terminal regions may detect a broader range of Aβ species, while C-terminal specific antibodies can distinguish Aβ40 from Aβ42 [85]. Using a combination of antibodies that recognize different regions of Aβ may enhance sensitivity and specificity.
Sample Preparation: The preparation of homogenates must enable effective separation of soluble, membrane-bound, and insoluble Aβ species [86]. Buffers without detergent will mainly contain soluble Aβ, while detergent-containing buffers (e.g., Triton-X100) dissolve membranes allowing detection of membrane-associated Aβ. Insoluble Aβ fibrils require strong acids like formic acid for solubilization before detection [86].
Protease Inhibition: To minimize protein degradation, protease inhibitors should be added to homogenization buffers, and homogenization should be performed consistently across samples to minimize variation [86].
PET Imaging Quantification
Positron Emission Tomography (PET) imaging allows non-invasive assessment of amyloid plaque deposition in the brain. Quantitative analysis of amyloid PET images provides standardized uptake value ratios (SUVRs) that indicate the degree of amyloid deposition [88]. Several automated quantification software packages are available, including PMOD and Heuron, which show comparable performance in quantifying amyloid deposits despite differences in absolute SUVR values [88].
Key technical aspects for PET quantification include:
Reference Region Selection: The cerebellar gray matter is commonly used as a reference region for quantitative analysis, though the pons is also used for certain tracers like 18F-flutemetamol [88].
Cutoff Values: SUVR cutoff values for amyloid positivity vary depending on the quantification method, with reported values of approximately 1.40 for PMOD and 1.45 for Heuron when using cerebellar gray matter as reference [88].
Table 2: Comparison of Amyloid-β Quantification Methods
| Method | Principle | Sensitivity | Species Detected | Throughput | Key Applications | Limitations |
|---|---|---|---|---|---|---|
| ELISA | Antibody-based recognition of Aβ epitopes | High (pM-nM range) | Dependent on antibody specificity; can be optimized for specific forms | Medium to High | Quantification in solutions, homogenates, cell culture media | Epitope masking in aggregates; requires specific sample preparation |
| PET Imaging | Radioligand binding to amyloid plaques in living brain | Macroscopic deposition | Primarily fibrillar/plaque Aβ | Low | Longitudinal studies in clinical and preclinical models | Limited resolution; does not distinguish oligomers from fibrils |
| Immuno-cytochemistry/ histochemistry | Antibody staining in fixed cells/tissues | Variable | Dependent on antibody and epitope accessibility | Low | Spatial distribution in cells (iPSC neurons) and tissues | Qualitative/semi-quantitative; fixation affects epitopes |
| Western Blot | Size separation and antibody detection | Medium | Can separate monomers from small oligomers by size | Low | Distinguishing aggregate sizes in soluble fractions | Difficult for large aggregates; semi-quantitative |
Experimental Protocols for Key Assays
Protocol: ELISA for Specific Aβ Species in iPSC Neuron Cultures
This protocol outlines the steps for quantifying different Aβ species from iPSC-derived neuronal cultures, considering ApoE isoform effects.
Materials and Reagents:
- iPSC-derived neurons with defined ApoE genotypes
- Cell culture medium appropriate for neuronal maintenance
- Protease inhibitor cocktail
- Homogenization buffers: PBS (soluble fraction), Triton-X buffer (membrane-associated fraction), formic acid (insoluble fraction)
- Aβ ELISA kits with appropriate specificity (e.g., specifically detecting oligomers or total Aβ)
- Microplate reader capable of 450 nm measurement
Procedure:
Sample Collection: Collect conditioned media from iPSC neuron cultures (e.g., at different differentiation time points). Centrifuge at 3,000 × g for 10 minutes to remove cellular debris.
Cell Homogenization:
- For soluble Aβ: Lyse cells in PBS buffer with protease inhibitors. Centrifuge at 100,000 × g for 1 hour at 4°C. Collect supernatant.
- For membrane-associated Aβ: Resuspend pellet in Triton-X buffer (e.g., 1% Triton-X100 in PBS). Incubate on ice for 30 minutes. Centrifuge at 100,000 × g for 1 hour at 4°C. Collect supernatant.
- For insoluble Aβ: Solubilize remaining pellet in 70% formic acid. Incubate for 2 hours on ice. Neutralize with 1M Tris base (1:20 dilution) before ELISA.
ELISA Procedure:
- Follow manufacturer's instructions for the specific ELISA kit.
- Include standard curves for appropriate quantification.
- Assess samples in duplicate or triplicate.
- Incubate with detection antibody and substrate, then measure absorbance.
Data Analysis:
- Calculate Aβ concentrations from standard curves.
- Normalize to total protein content or cell number.
- Compare Aβ levels across ApoE genotypes and experimental conditions.
Troubleshooting:
- If signals are weak, consider concentrating samples or using more sensitive ELISA kits.
- High background may indicate insufficient washing or antibody cross-reactivity.
Protocol: Assessing LRP1-Mediated Aβ Transport in BBB Models
This protocol describes an in vitro assay to evaluate ApoE isoform effects on LRP1-mediated Aβ transport using iPSC-derived endothelial cells.
Materials and Reagents:
- iPSC-derived brain endothelial cells
- Transwell inserts (3μm pore size)
- Fluorescently-labeled Aβ peptides
- LRP1 inhibitors (e.g., RAP)
- ApoE isoforms (commercially available or purified)
- Transport buffer (e.g., HBSS)
- Plate reader capable of fluorescence detection
Procedure:
BBB Model Setup:
- Culture iPSC-derived endothelial cells on Transwell inserts until they form a tight monolayer (confirm with TEER measurement).
- Differentiate cells with appropriate media to enhance BBB properties.
Transport Assay:
- Prepare transport buffer containing fluorescent Aβ (e.g., 100nM) with or without specific ApoE isoforms.
- Add donor solution to the apical (luminal) compartment.
- Collect samples from the basolateral (abluminal) compartment at various time points (e.g., 30, 60, 120 minutes).
- Measure fluorescence in collected samples to quantify transported Aβ.
Inhibition Studies:
- Pre-treat cells with LRP1 inhibitor RAP (500nM) for 30 minutes before transport assay.
- Compare transport rates with and without inhibition to determine LRP1-specific contribution.
Data Analysis:
- Calculate apparent permeability coefficients (Papp).
- Compare transport efficiency across different ApoE isoform conditions.
- Normalize data to control conditions.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Amyloid-β Transport and Deposition Assays
| Reagent/Material | Function/Application | Key Considerations | Example Uses |
|---|---|---|---|
| ApoE Isoforms (E2, E3, E4) | Study isoform-specific effects on Aβ aggregation and clearance | Source (recombinant vs. endogenous); lipidation status | Adding to cell culture to modulate Aβ metabolism; in vitro aggregation assays |
| LRP1 Modulators (e.g., RAP) | Inhibit LRP1 function to assess its role in Aβ transport | Specificity for LRP1 vs. other receptors; concentration optimization | Transport assays in BBB models to determine LRP1-specific contribution |
| Aβ Antibodies (N-terminal, C-terminal, oligomer-specific) | Detection and quantification of specific Aβ forms | Epitope accessibility in different aggregate forms; specificity | ELISA setup; immunostaining of iPSC neurons; Western blot |
| Triton-X100 Detergent | Solubilization of membrane-associated Aβ | Concentration optimization; potential interference with assays | Sample preparation for membrane-bound Aβ fraction |
| Formic Acid | Solubilization of insoluble Aβ aggregates and plaques | Requires neutralization before analysis; handling safety | Processing insoluble Aβ fractions from brain homogenates or cell lysates |
| Protease Inhibitor Cocktails | Prevent Aβ degradation during sample processing | Broad-spectrum vs. specific inhibitors; compatibility with assays | Added to homogenization buffers for all sample preparations |
| BBB Transport Model Components (Transwell inserts, endothelial cells) | Create in vitro BBB for transport studies | Barrier integrity confirmation (TEER measurement); cell source | LRP1-mediated Aβ transport assays with ApoE variants |
The technical landscape for assessing Aβ transport and deposition continues to evolve, offering increasingly sophisticated methods for investigating ApoE isoform effects in iPSC neuron models. The integration of complementary techniques—from highly sensitive ELISA configurations to advanced imaging approaches—provides a comprehensive toolkit for unraveling the complex relationship between ApoE genetics and Aβ pathology. As these assays become more refined, they will undoubtedly accelerate our understanding of Alzheimer's disease mechanisms and support the development of targeted therapeutics for individuals carrying specific ApoE alleles.
Controlling for Genetic Background Effects Through Isogenic Line Validation
In the field of Alzheimer's disease (AD) research, the apolipoprotein E (APOE) ε4 allele stands as the strongest genetic risk factor for sporadic, late-onset cases. The use of human induced pluripotent stem cells (iPSCs) has emerged as a powerful tool for modeling AD, enabling the study of patient-specific neurons and glia in vitro. However, a significant challenge in attributing phenotypic differences directly to a variant of interest, such as APOE4, is the confounding influence of the vast genetic variation between individual human donors. Isogenic line validation, the process of generating genetically identical cell lines that differ only at the specific allele of interest, provides a critical solution to this problem. This technical guide outlines the necessity, methodologies, and applications of isogenic controls, with a specific focus on dissecting the multifaceted roles of APOE isoforms in iPSC-derived neuronal models.
The Critical Need for Isogenic Controls in iPSC Research
Research utilizing patient-derived iPSCs is inherently complicated by the presence of a unique and complex genetic background in every donor. When comparing iPSC lines from different individuals—for instance, a healthy control with the APOE3/ε3 genotype to an AD patient with the APOE4/ε4 genotype—observed phenotypic differences cannot be confidently attributed to the APOE variant alone. The entirety of other genetic differences between the two donors serves as a major confounding variable [89] [19].
This "genetic background effect" is a well-documented phenomenon across model organisms. Studies have shown that the same mutation can produce quantitatively different, and sometimes even contradictory, phenotypes when placed on different genetic backgrounds [89]. For example, in Drosophila, the role of certain genes in longevity could not be replicated when the experiments were repeated in different wild-type genetic backgrounds, underscoring the profound impact of genetic modifiers [89]. In the context of late-onset disorders like AD, where in vitro phenotypes are often subtle, controlling for this background variation is not merely beneficial but essential for establishing a direct causal relationship [90].
Isogenic cell lines, where the genetic background is held constant, eliminate this confounding variable. By correcting the disease-associated mutation (e.g., APOE4) to the reference sequence (e.g., APOE3) in a patient-derived iPSC line, or by introducing the risk variant into a healthy control line, researchers create a perfectly matched pair. Any phenotypic differences observed between these isogenic lines can then be definitively linked to the specific APOE allele, significantly enhancing the validity and interpretability of experimental results.
Methodologies for Generating Isogenic iPSC Lines
The creation of isogenic iPSC lines relies on precise genome editing technologies. The following section details the core workflow and the key reagents required.
Core Genome Editing Workflow
The process begins with the selection of a donor iPSC line, which is then subjected to genome editing using engineered nucleases. The workflow involves multiple steps of cloning, screening, and validation to ensure the generation of a clonal, isogenic cell line with the desired genotype and stable karyotype. The diagram below illustrates this multi-stage process.
Key Technologies and Reagent Solutions
The following table summarizes the essential reagents and their functions in the genome editing pipeline for generating isogenic iPSC lines.
Table 1: Research Reagent Solutions for Isogenic Line Generation
| Reagent / Tool | Function in Experiment | Key Considerations |
|---|---|---|
| Zinc Finger Nucleases (ZFNs) | Early technology for creating targeted double-strand breaks in DNA (e.g., for APOE or α-synuclein point mutations) [90]. | Can be difficult and expensive to design for new targets. |
| CRISPR/Cas9 System | Current standard for genome editing; uses a guide RNA (gRNA) to direct Cas9 nuclease to a specific genomic locus for cleavage. | Requires careful gRNA design to minimize off-target effects. |
| Donor DNA Template | Contains the desired corrected sequence (e.g., APOE3); used by the cell's homology-directed repair (HDR) pathway. | Typically designed with silent mutations to prevent re-cleavage. |
| Isogenic Validated iPSCs | The final product; a clonal cell line with the desired mutation and a verified normal karyotype and pluripotency. | Essential starting material for all downstream differentiation experiments. |
Experimental Design and Validation of Isogenic Lines
Once a potential isogenic clone is generated, a rigorous validation protocol is essential to confirm its identity and quality before its use in functional experiments.
Genotypic and Phenotypic Validation Workflow
The validation of a newly generated isogenic iPSC clone is a multi-faceted process that ensures the edit is correct and the cell line remains stable and pluripotent. The process involves confirming the DNA sequence, checking for unintended edits, and verifying the fundamental properties of the stem cells, as outlined in the workflow below.
Key Validation Assays and Outcomes
Table 2: Core Validation Assays for Isogenic iPSC Lines
| Validation Stage | Methodology | Expected Outcome for a Validated Line |
|---|---|---|
| Genotypic Confirmation | Sanger sequencing of the edited APOE locus. | DNA sequence confirms the intended base change (e.g., Arg112 to Cys112 for APOE4-to-E3 correction) with no random insertions/deletions. |
| Off-Target Analysis | Whole-genome sequencing or targeted sequencing of predicted off-target sites. | No unintended mutations in coding or regulatory regions compared to the parental line. |
| Pluripotency Check | Immunocytochemistry for stem cell markers (e.g., SSEA4, Nanog, TRA-1-60) [19]. | High expression of pluripotency markers in the undifferentiated state. |
| Functional Pluripotency | In vitro trilineage differentiation followed by immunostaining for markers of endoderm (Sox17), mesoderm (Brachyury), and ectoderm (Nestin/Sox2) [19]. | Successful differentiation into cell types representing all three germ layers. |
| Genomic Stability | Karyotype analysis (G-banding) [19]. | Normal, stable karyotype (46 chromosomes) without major rearrangements. |
Application in APOE Isoform Functional Analysis
The power of the isogenic approach is demonstrated by its ability to clarify the specific, background-independent effects of APOE isoforms on AD-related pathologies in human cellular models.
Phenotypic Rescue in Cerebral Organoids
A seminal study utilizing isogenic correction of APOE4 to APOE3 in AD patient-derived iPSCs revealed the direct role of this allele in exacerbating disease phenotypes in 3D cerebral organoids. The organoids derived from APOE4/4 AD patients showed increased apoptosis and decreased synaptic integrity. Importantly, isogenic conversion of APOE4 to APOE3 attenuated these AD-related phenotypes, including reducing apoptosis and tau pathology, thereby demonstrating a direct causal role for APOE4 in these degenerative pathways [19].
Dissecting Cell-Type-Specific Effects
Isogenic lines allow for the precise dissection of how APOE genotypes function in different neural cell types. For example, while APOE is predominantly expressed by astrocytes and microglia, its expression and function in neurons under pathological conditions can be specifically studied using isogenic models. Research has shown that the loss of the AD risk gene SORL1 induces a neuron-specific reduction in APOE and clusterin (CLU) levels, and that this regulation is linked to TGF-β/SMAD signaling [91]. Using isogenic lines ensures that such cell-type-specific regulatory mechanisms are not obscured by background genetic variation.
Quantitative Data from Isogenic Model Studies
The following table summarizes key quantitative findings from studies that utilized isogenic controls to investigate APOE-dependent effects.
Table 3: Phenotypic Comparisons in Isogenic APOE iPSC Models
| Phenotype Measured | Experimental Model | Key Isogenic Comparison Finding | Citation |
|---|---|---|---|
| Apoptosis (Cleaved Caspase-3) | Cerebral Organoids | APOE4/4 AD organoids showed significantly higher levels vs. isogenic APOE3/3 corrected lines. | [19] |
| Tau Phosphorylation | Cerebral Organoids | APOE4 exacerbated tau pathology; severity was reduced in isogenic APOE4-to-E3 corrected lines. | [19] |
| Synaptic Integrity (PSD95/Synaptophysin) | Cerebral Organoids | Synaptic markers were decreased in AD organoids; APOE4 had a synergistic effect with AD status. | [19] |
| APOE and CLU Expression | iPSC-derived Neurons | Loss of SORL1 induced a neuron-specific reduction in APOE and CLU, a finding validated in isogenic models. | [91] |
| Endolysosomal Function | Primary Neurons from ApoE mice | ApoE4 neurons showed reduced degradative ability and fewer active lysosomes only after prolonged time in culture. | [10] |
The integration of isogenic line validation into the experimental workflow is no longer an optional luxury but a fundamental requirement for rigorous mechanistic studies using human iPSCs. This is particularly true for the field of Alzheimer's disease research focused on APOE isoforms, where subtle, cell-type-specific effects are critical to understanding pathogenesis and developing therapeutics. By controlling for the massive confounding variable of genetic background, isogenic models empower researchers to:
- Definitively assign causality to the APOE4 allele for specific cellular phenotypes.
- Uncover novel, cell-type-specific pathways regulated by APOE.
- Provide a genetically clean system for high-content drug screening and target validation.
As genome editing technologies continue to advance, the generation of isogenic lines will become more efficient and accessible, ultimately accelerating our understanding of APOE biology and the development of precision medicine for Alzheimer's disease and other complex disorders.
Optimizing Lipid Particle Analysis and APOE Lipidation Status Assessment
In the study of neurodegenerative diseases, particularly Alzheimer's Disease (AD), the apolipoprotein E (APOE) gene represents the strongest genetic risk factor, with its ε4 allele significantly increasing susceptibility to late-onset AD [72] [13]. The central function of apoE, a lipid transport protein primarily produced by astrocytes in the brain, is critically dependent on its lipidation status—the process by which lipids bind to the apoE protein to form functional lipoprotein particles [92] [13]. Research using human induced pluripotent stem cell (iPSC)-derived models has demonstrated that the APOE4 isoform is less effectively lipidated than APOE2 and APOE3, leading to impaired cholesterol transport and increased pathological features associated with AD [50] [92]. This technical guide provides comprehensive methodologies for analyzing lipid particles and assessing APOE lipidation status within the context of iPSC-derived neuronal models, enabling researchers to investigate the fundamental role of lipid metabolism in neurodegenerative disease pathogenesis.
Quantitative Landscape of Lipid Alterations in Disease Models
Table 1: Key Lipidomic Alterations in APOE4 Models and Neurodegenerative Conditions
| Lipid Class | Experimental Model | Change in APOE4/AD | Functional Significance | Citation |
|---|---|---|---|---|
| Cholesterol Esters (CE) | APOE4 iAstrocytes | ↑ Accumulation | Impaired cholesterol transport; AD-associated | [93] |
| Triacylglycerides (TG) | APOE4 iAstrocytes | ↑ Accumulation | Lipid metabolism dysfunction | [93] |
| Total Cholesterol | NPC1-inhibited human astrocytes | ↑ 4-fold | Lysosomal cholesterol trafficking deficit | [92] |
| Sphingomyelins (SM) | iMicroglia vs iNeurons | ↑ in microglia | Cell-type specific lipotypes | [93] |
| Phosphatidylserine (PS) | iMicroglia vs iNeurons | ↑ in microglia | Cell-type specific lipotypes | [93] |
| APOE4 Lipidation | iPSC-derived astrocytes | ↓ Relative to APOE2/3 | Impaired lipid efflux capacity | [50] [92] |
Table 2: Functional Consequences of APOE Isoform Differences in Cellular Models
| Parameter | APOE2 | APOE3 | APOE4 | Experimental Context |
|---|---|---|---|---|
| Aβ42 Transport at BBB | ↑ Increased | Intermediate | ↓ Decreased | iPSC-derived BMEC-like cells [79] |
| Extracellular Aβ Deposition | ↓ Reduced | Intermediate | ↑ Increased | iPSC-derived pericyte-like cells [79] |
| Cholesterol Efflux | ↑ (67% reduction) | ↑ (62% reduction) | ↓ Ineffective | NPC1-inhibited fibroblasts [92] |
| Cell Survival | Protective | Protective | ↓ Impaired | NPC1-inhibition model [92] |
| Neurite Outgrowth | N/A | ↑ Greater | ↓ Impaired | Post-injury recovery [13] |
Methodologies for Lipid Particle Analysis and APOE Characterization
Comprehensive Lipidomic Profiling of iPSC-Derived Brain Cells
Cell Culture and Differentiation:
- Utilize established protocols to differentiate control iPSC lines (e.g., BIONi037-A) into glutamatergic iNeurons, iAstrocytes, and iMicroglia [93].
- Validate cell fate and purity using immunocytochemistry for cell-type-specific markers: MAP2 for neurons, aquaporin 4 (AQP4) for astrocytes, and Iba1 for microglia [93].
- Culture cells to appropriate maturity, noting that apoE secretion from iPSC-derived astrocytes significantly increases after 20 days of differentiation, with robust levels maintained by day 45 [50].
Lipid Extraction and Analysis:
- Employ comprehensive, quantitative shotgun lipidomic analysis capable of quantifying >1,000 lipid species across 16 different lipid classes [93].
- Key lipid classes to monitor include: phosphatidylcholine (PC), phosphatidylethanolamine (PE), lysophospholipids (LPC, LPE), sphingomyelins (SM), phosphatidylserine (PS), ceramides (CER), diacylglycerides (DG), triacylglycerides (TG), cholesterol esters (CE), and free fatty acids (FAs) [93].
- For intracellular lipid assessment, use fluorescent probes: filipin for free cholesterol and bodipy493/503 for neutral lipid droplets [92]. Quantify accumulation via fluorescence microscopy or flow cytometry.
Data Integration and Sharing:
- Utilize resources like the Neurolipid Atlas (https://neurolipidatlas.com/) for comparative analysis of neurolipidomics data across different disease models and brain regions [93].
- This open-access data common allows exploration of cell-type-specific lipid profiles and disease-associated alterations, facilitating benchmarking against established datasets.
APOE Lipidation Status Assessment
APOE Particle Size Characterization:
- Collect conditioned media from iPSC-derived astrocytes (day 45-55 of differentiation) under serum-free conditions [50].
- Concentrate extracellular media using centrifugal filters with appropriate molecular weight cutoffs.
- Analyze apoE particle size using Native-PAGE followed by Western blotting with anti-apoE antibodies [50].
- Categorize apoE immunoreactivity into three groups: large particles (>669 kDa), medium particles (440-669 kDa), and small particles (<440 kDa) [50].
- Compare the distribution pattern across isogenic iPSC-derived astrocytes with different APOE genotypes (APOE2/2, APOE3/3, APOE4/4).
Lipidation-Dependent Functional Assays:
- Cholesterol efflux assays: Treat NPC1-inhibited cells (using U18666A) with recombinant apoE isoforms and measure cholesterol reduction via filipin staining or mass spectrometry [92]. APOE2 and APOE3 typically reduce intracellular cholesterol by 60-70%, while APOE4 shows significantly less efficacy [92].
- Amyloid beta transcytosis assays: Using iPSC-derived brain microvascular endothelial cell-like cells (BMEC-like cells) in Transwell systems, assess "brain-to-blood" Aβ40 and Aβ42 transport capabilities in the presence of different apoE isoforms [79].
- Extracellular amyloid deposition: Culture iPSC-derived pericyte-like cells with different APOE genotypes with Aβ42 and quantify deposition, noting that APOE4 typically increases deposition while APOE2 decreases it relative to APOE3 [79].
Experimental Models for Lipid Dysregulation
NPC1 Inhibition Model:
- Induce intracellular cholesterol accumulation by treating human fibroblasts or iPSC-derived astrocytes with U18666A (3-5 μg/mL), a potent inhibitor of the lysosomal transporter NPC1 [92].
- Treat for 2-6 days, monitoring cholesterol accumulation over time through filipin staining and co-localization with LAMP1 for lysosomal localization [92].
- Evaluate compensatory responses through Western blotting for ABCA1 (cholesterol efflux transporter) and HMGCR (cholesterol synthesis enzyme) [92].
Lipidation Enhancement Strategies:
- Test therapeutic interventions using synthetic lipopeptides designed to enhance APOE4 lipidation [92].
- Combine recombinant APOE4 with lipopeptides and assess rescue of cholesterol efflux function, reduction in intracellular cholesterol, and normalization of AD-related proteins (APP, BACE, C-terminal fragments) [92].
- Confirm enhanced lipidation through Native-PAGE analysis showing increased proportion of large, lipidated APOE4 particles [92].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Lipid Particle Analysis and APOE Research
| Reagent/Cell Line | Specification | Research Application | Key Function |
|---|---|---|---|
| Isogenic iPSC Lines | APOE2/2, APOE3/3, APOE4/4 | All experiments | Genetically-controlled APOE expression |
| BIONi037-A iPSC Line | Control line | Cell differentiation | Reference background |
| U18666A | NPC1 inhibitor | Cholesterol accumulation model | Induces lysosomal cholesterol trafficking deficits |
| Recombinant APOE | Isoforms E2, E3, E4 | Functional rescue studies | Cholesterol efflux assessment |
| Anti-APOE antibody | Western blot, Native-PAGE | APOE detection | Lipidation status analysis |
| Filipin | Fluorescent dye | Cholesterol visualization | Free cholesterol staining |
| Bodipy493/503 | Neutral lipid dye | Lipid droplet quantification | Neutral lipid accumulation assessment |
| Collagen IV | Coating substrate | BBB transwell models | BMEC differentiation support |
Signaling Pathways and Experimental Workflows
APOE Lipidation and Cholesterol Trafficking Pathway
Experimental Workflow for APOE Lipidation Analysis
Technical Considerations and Data Interpretation
When interpreting lipid particle analysis data, researchers should note that iPSC-derived brain cells recapitulate in vivo lipotypes, with neurons, astrocytes, and microglia exhibiting distinct lipid profiles that mirror primary cell isolates [93]. For instance, astrocytes typically show the highest cholesterol ester stores, consistent with their role as cholesterol suppliers in the brain [93]. The functional consequences of reduced APOE4 lipidation manifest in multiple pathways: impaired Aβ clearance at the blood-brain barrier, increased extracellular amyloid deposition, dysfunctional cholesterol transport, and reduced neuronal support capacity [50] [79] [92]. Recent therapeutic approaches focus on enhancing APOE4 lipidation through synthetic lipopeptides, which can restore cholesterol efflux function and normalize AD-related protein abnormalities [92]. These findings highlight the central role of proper lipid metabolism in neuronal health and the potential for lipidation-enhancing strategies as therapeutic interventions for APOE4-associated neurodegenerative diseases.
Troubleshooting Blood-Brain Barrier Integrity Measurements in vitro
The blood-brain barrier (BBB) is a complex, dynamic interface that critically maintains central nervous system (CNS) homeostasis by regulating the exchange of substances between the bloodstream and the brain [94] [95]. Within the context of apolipoprotein E (APOE) isoform research, particularly using induced pluripotent stem cell (iPSC)-derived neurons, accurately modeling and assessing BBB integrity is paramount. APOE isoforms (E2, E3, E4) hold significant implications for Alzheimer's Disease risk and pathophysiology, with evidence suggesting these risks are mediated, in part, through BBB-specific mechanisms [68]. Research utilizing isogenic human iPSC lines has demonstrated that while APOE genotype may not directly impact all fundamental BBB properties in brain microvascular endothelial cell-like cells (BMEC-like cells), it significantly influences critical processes such as amyloid-beta (Aβ) clearance and deposition [68]. This technical guide details the core methodologies for measuring BBB integrity in vitro, provides troubleshooting strategies for common pitfalls, and frames these techniques within the specific experimental considerations of APOE isoform research.
Core Principles of BBB Integrity
The BBB's selective permeability is primarily governed by brain microvascular endothelial cells (BMECs), which are characterized by continuous tight junctions (TJs), minimal pinocytic activity, and specialized transport systems [94] [58]. These TJs, composed of proteins such as claudin-5, occludin, and ZO-1, create a high-resistance paracellular barrier [94] [96]. Pericytes and astrocytes are integral components of the neurovascular unit (NVU), providing essential cues for the induction and maintenance of barrier properties [94] [58]. In APOE-focused studies, it is crucial to recognize that the BBB is not a static barrier but a dynamic interface whose function can be modulated by genetic background. For instance, APOE4 has been linked to impaired "brain-to-blood" Aβ40 transport and increased vascular amyloid deposition in iPSC-derived pericyte-like models, independent of changes to baseline TJ integrity [68].
Table 1: Key Functional Metrics for Assessing BBB Integrity In Vitro
| Metric | What It Measures | Typical In Vivo Values | Common In Vitro Targets |
|---|---|---|---|
| Transendothelial Electrical Resistance (TEER) | Ionic permeability/ Tight junction integrity | 1,500 - 8,000 Ω·cm² [96] | >200 Ω·cm² (minimal); >500-1000 Ω·cm² (good) [97] |
| Solute Permeability Coefficient (P) | Macromolecule paracellular leakage | Varies by solute size/charge | Low values for high MW molecules (e.g., 10⁻⁷ cm/s for 70 kDa dextran) [97] |
| Tight Junction Protein Localization | Junctional complex organization & expression | Continuous, linear distribution at cell borders | Assessed via immunofluorescence for Claudin-5, Occludin, ZO-1 [96] |
| Efflux Transporter Activity | Functional activity of P-gp, BCRP | Active efflux of specific substrates | E.g., Calcein-AM assay for P-gp; reduced accumulation indicates activity [94] |
Critical Measurement Techniques and Protocols
Transendothelial Electrical Resistance (TEER)
TEER is the gold-standard, non-destructive method for quantifying the ionic permeability of a BBB monolayer, directly reflecting the tightness of TJs [95].
Detailed Protocol:
- Apparatus: Use an epithelial volt-ohm meter with a pair of compatible electrodes (e.g., chopstick or cup electrodes). Ensure the equipment is sterilized before use.
- Measurement: For Transwell inserts, place the electrodes in both the apical (luminal) and basolateral (abluminal) compartments. The electrodes must not touch the membrane to avoid damage.
- Calculation: Record the resistance (R, in Ω) and subtract the value of a blank insert (Rblank, in Ω) containing only culture medium. Multiply this net resistance by the surface area (A, in cm²) of the insert membrane: TEER = (R - Rblank) × A. The unit is Ω·cm².
- Frequency: Monitor TEER regularly (e.g., daily) throughout the culture period to track barrier formation and stability.
Troubleshooting TEER:
- Low or Stagnant TEER:
- Cell Source & Differentiation: Confirm the quality and purity of your BMEC-like cells. For iPSC-derived cells, validate differentiation efficiency with endothelial markers (e.g., CD105, vWF) and ensure a high confluence (>97%) [68] [97].
- Lack of NVU Cues: Incorporate pericytes and astrocytes in co-culture or conditioned media to enhance TJ formation [94] [96]. APOE4-carrying pericytes may exhibit pro-amyloidogenic phenotypes, which could indirectly influence barrier induction [68].
- Absence of Flow: Implement dynamic flow conditions using microfluidic systems. Physiological shear stress (estimated 1-2 Pa in human brain capillaries) upregulates TJ protein expression and significantly improves barrier resistance [98] [58].
- High Variability Between Replicates:
- Inconsistent Seeding: Standardize cell seeding density and ensure a homogeneous cell suspension.
- Edge Effects: Avoid using outer wells of culture plates for critical experiments due to higher evaporation rates.
- Electrode Handling: Clean and calibrate electrodes consistently before each measurement.
Solute Permeability Assays
These assays measure the paracellular flux of molecular tracers, complementing TEER data by assessing barrier integrity against larger molecules.
Detailed Protocol: Sodium Fluorescein (NaFl, 376 Da) or FITC-Dextran Permeability [99] [97]
- Tracer Solution: Prepare the tracer molecule (e.g., 0.1 mg/mL NaFl or 1 mg/mL FITC-dextran of a specific molecular weight, such as 4kDa or 70kDa) in the cell culture medium or a physiological buffer like Ringer's solution with 1% BSA. Pre-warm to 37°C.
- Application: Add the tracer to the apical (luminal) compartment. For a 24-well Transwell insert (~0.3 cm²), 200-300 µL is typical.
- Sampling: At designated time points (e.g., 30, 60, 90, 120 minutes), collect a small aliquot (e.g., 50-100 µL) from the basolateral compartment. Replace the volume with fresh, pre-warmed tracer-free medium to maintain hydrostatic pressure.
- Quantification: Measure the fluorescence of the samples using a microplate reader (Ex/Em for NaFl: ~485/520 nm). Calculate the concentration from a standard curve.
- Calculation: The apparent permeability coefficient (Papp) is calculated as: Papp = (dQ/dt) / (A × C₀) where dQ/dt is the steady-state flux rate (mol/s), A is the membrane surface area (cm²), and C₀ is the initial tracer concentration in the donor chamber (mol/mL).
Troubleshooting Permeability Assays:
- Unexpectedly High Permeability:
- Validate TJ Integrity: Confirm that high TEER values were established prior to the assay. Use immunofluorescence to check for continuous, linear TJ protein localization.
- Check for Cytotoxicity: Ensure the tracer or its vehicle is not toxic to the cells. Perform a viability assay if necessary.
- Account for Efflux Transporters: Sodium fluorescein is a substrate for some efflux transporters. Apparent high permeability could be due to active transport. Consider using inhibitors or tracers that are not known substrates to isolate paracellular transport [94].
- High Background Noise:
- Control for Adsorption: Include a blank insert (no cells) to account for tracer binding to the membrane and plate. This blank value should be subtracted.
- Avoid Contamination: Take care not to pipette from the basolateral compartment into the apical one during sampling.
Figure 1: Workflow for performing and troubleshooting solute permeability assays.
Immunofluorescence and Protein Analysis
Visualizing the organization and expression levels of TJ proteins is essential for validating barrier maturity and investigating structural defects.
Detailed Protocol: Immunofluorescence for Tight Junctions
- Fixation: Wash cells with PBS and fix with 4% paraformaldehyde for 15-20 minutes at room temperature.
- Permeabilization and Blocking: Permeabilize cells with 0.1-0.25% Triton X-100 in PBS for 10 minutes, then block with 3-5% bovine serum albumin (BSA) or normal serum for 1 hour to reduce non-specific binding.
- Staining: Incubate with primary antibodies (e.g., against ZO-1, Claudin-5, Occludin) diluted in blocking buffer overnight at 4°C. Wash thoroughly with PBS, then incubate with fluorophore-conjugated secondary antibodies and a nuclear counterstain (e.g., DAPI) for 1 hour at room temperature, protected from light.
- Imaging: Acquire images using a confocal microscope. Analyze the images for continuous, honeycomb-like staining at the cell borders. Discontinuous, fragmented, or cytoplasmic localization indicates poor TJ formation.
Troubleshooting Immunofluorescence:
- High Background: Optimize antibody concentrations and increase the number and duration of washes after primary and secondary antibody incubation.
- Weak or No Signal: Confirm antibody specificity and compatibility with your cell source (e.g., human iPSC-derived BMECs). Check the fixation and permeabilization steps.
APOE-Isoform Specific Considerations and Advanced Models
When modeling APOE-related pathologies, standard 2D Transwell models may be insufficient. The functional consequences of APOE isoforms often manifest in complex interactions within the NVU and under physiologically relevant conditions.
Key Findings from APOE BBB Research:
- Amyloid Clearance: BMEC-like cells showed isoform-dependent differences in Aβ transport. APOE4 protein impeded Aβ40 clearance, while APOE2 enhanced Aβ42 transport, a process dependent on LRP1 and p-glycoprotein pathways [68].
- Pericyte Contribution: APOE4 pericyte-like cells demonstrated heightened extracellular Aβ42 deposition, whereas APOE2 cells showed the least deposition, aligning with clinical observations of vascular amyloid load [68].
- Experimental Implications: Simply confirming similar baseline TEER and TJ protein expression across isogenic APOE lines is not sufficient. Functional assays for amyloid transport and deposition in co-culture models are necessary to capture the pathophysiological phenotype.
Implementing Advanced Models:
- Microfluidic BBB-on-a-Chip: These platforms incorporate dynamic fluid flow and shear stress, which are critical for inducing a mature BBB phenotype [98] [58]. They allow for controlled co-culture of iPSC-derived BMECs, pericytes, and astrocytes in a spatially relevant architecture, ideal for studying how APOE isoforms affect barrier function under near-physiological conditions and for performing real-time permeability assays.
- 3D Bioprinted Models: This emerging technology offers unparalleled control over the spatial arrangement of different NVU cell types and ECM components, enabling the creation of more anatomically correct models to study APOE-mediated effects [96].
Figure 2: APOE isoform effects on key BBB pathways related to amyloid pathology. APOE genotype influences amyloid-beta clearance in BMECs and extracellular deposition in pericytes [68].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Research Reagent Solutions for In Vitro BBB Modeling
| Category | Specific Item / Example | Function / Application | Considerations for APOE Research |
|---|---|---|---|
| Cell Sources | iPSC lines (Isogenic APOE2/2, E3/3, E4/4) [68] | Genetically controlled basis for BMEC & pericyte differentiation. | Critical. Use isogenic lines to isolate APOE effects from genetic background noise. |
| Culture Media | Endothelial Serum-Free Medium with bFGF & RA [68] [97] | Differentiation & maintenance of BMEC-like cells. | Retinoic acid (RA) enhances barrier properties. |
| Permeability Tracers | Sodium Fluorescein (NaFl, 376 Da), FITC-Dextrans (e.g., 4, 40, 70 kDa) [99] [97] | Measuring paracellular permeability of small to large molecules. | Use a range of sizes. Be aware some (e.g., NaFl) can be efflux transporter substrates. |
| Functional Assay Kits | Calcein-AM | Substrate for P-glycoprotein (P-gp) efflux activity. | APOE4 can alter transporter function; monitor activity [94] [68]. |
| Antibodies | Anti-Claudin-5, Anti-Occludin, Anti-ZO-1 [96] | Immunofluorescence assessment of tight junctions. | Confirm species reactivity for human iPSC-derived cells. |
| Key Chemicals | Retinoic Acid [97] | Potent inducer of BBB properties in vitro. | Standardize concentration and exposure time. |
| Specialized Platforms | Microfluidic Organ-on-a-Chip [98] [100] | Incorporating physiological shear stress & complex co-cultures. | Essential for revealing subtle, physiologically relevant APOE phenotypes. |
Bridging hiPSC Findings with Clinical Observations and Animal Models
Correlating iPSC Findings with Human Neuroimaging and Biomarker Data
The apolipoprotein E (APOE) gene, the strongest genetic risk factor for sporadic Alzheimer's disease (AD), exists in three common isoforms: APOE2, APOE3, and APOE4. These isoforms confer varying degrees of risk, with APOE4 significantly increasing AD risk and APOE2 being protective relative to the most common APOE3 variant [68] [14]. Human induced pluripotent stem cell (iPSC) technology has emerged as a powerful platform for modeling AD, enabling the study of human neurons and glia carrying specific APOE isoforms in a controlled environment. However, a critical challenge lies in validating that pathological mechanisms discovered in iPSC models accurately reflect the disease processes observed in the human brain. This technical guide details strategies and methodologies for correlating key findings from iPSC-based models of APOE-driven pathology with data obtained from human neuroimaging and biomarker studies, thereby strengthening the translational relevance of in vitro discoveries.
Key APOE Isoform-Driven Phenotypes in iPSC Models and their Human Correlates
iPSC-derived models recapitulate core AD-related pathologies influenced by APOE genotype. The table below summarizes major phenotypic findings from these models and their corresponding correlates in human clinical data.
Table 1: Correlating iPSC-Derived APOE Phenotypes with Human Biomarkers and Imaging
| iPSC-Derived Phenotype (APOE4 vs. APOE2/3) | Experimental Protocol Summary | Human Correlate (Neuroimaging/Biomarker) |
|---|---|---|
| Impaired Amyloid-β (Aβ) Clearance at the Blood-Brain Barrier (BBB) | Isogenic iPSC-derived brain microvascular endothelial cells (BMECs) were used in "brain-to-blood" Aβ transport assays. Recombinant APOE protein isoforms were applied to assess their specific effect on Aβ transport pathways involving LRP1 and p-glycoprotein [68]. | Positron Emission Tomography (Amyloid-PET): APOE4 carriers show higher amyloid burden and faster Aβ deposition rates [14] [101].Cerebrospinal Fluid (CSF): APOE4 carriers have lower CSF Aβ42 levels, consistent with impaired clearance and sequestration in plaques [14]. |
| Increased Aβ Deposition in Pericytes | Isogenic iPSC-derived brain pericyte-like cells were cultured and assessed for extracellular Aβ deposition. APOE4 pericyte-like cells showed heightened deposition compared to isogenic APOE2 and APOE3 lines [68]. | Pathology & Imaging: Accelerated degeneration of brain pericytes and increased vascular amyloid deposition are observed in APOE4 carriers [68]. |
| Dysregulated Microglial Transcriptome/Epigenome | iPSC-derived human microglia of defined APOE genotypes were transplanted into the brains of AD model mice (AppNL-G-F). After 12 months, microglia were isolated via FACS for RNA-seq and ATAC-seq analysis [28]. | Post-mortem Tissue: Human APOE4 carrier brains show pro-inflammatory changes and enrichment of microglial activation states associated with neurodegeneration [28] [102]. |
| Altered Neuronal Viability & Neuroinflammation | Human astrocytes, immortalized microglia (HMC3), and neuroblastoma cells (SH-SY5Y) were treated with 20 nM recombinant APOE2, E3, or E4 protein for 24 hours. Cell viability (MTS assay) and inflammatory markers (e.g., IL-1β, TNFα, IL-6) were quantified [102]. | Fluorodeoxyglucose-PET (FDG-PET): APOE4 carriers exhibit pronounced glucose hypometabolism in temporoparietal cortex and precuneus, indicating neuronal dysfunction [14]. |
Methodologies for iPSC-Based APOE Phenotyping
Differentiation of Isogenic iPSCs into Neural and Neurovascular Cells
A cornerstone of this research is the use of isogenic iPSC lines, where the APOE genotype is the only variable, minimizing confounding effects from genetic background [68].
- iPSC Culture and Maintenance: Culture iPSCs on Matrigel-coated plates in mTESR1 medium, with daily medium changes [68].
- Brain Microvascular Endothelial Cell (BMEC) Differentiation: Differentiate iPSCs using a defined, serum-free protocol. Cells are first cultured in unconditioned medium (UM) for six days, followed by 48 hours in human Endothelial Serum-Free Medium (hECSR) supplemented with basic fibroblast growth factor (bFGF), B-27, and retinoic acid to promote endothelial maturation and barrier properties [68].
- Brain Pericyte-like Cell Differentiation: Differentiate iPSCs into a neural crest stem cell population using Essential 6 medium supplemented with dorsomorphin, SB431542, CHIR99021, bFGF, and heparin. Enrich for CD271+ neural crest cells using magnetic-activated cell sorting (MACS) and expand them in Essential 6 medium with 10% FBS [68].
- Microglia Differentiation: Differentiate iPSCs into microglia using specialized protocols. For xenotransplantation studies, these microglia can be transplanted into the brains of immunodeficient AD model mice to study their response to amyloid pathology in vivo [28].
Functional Assays for BBB and Amyloid Phenotyping
- Aβ Transport Assay: To assess "brain-to-blood" Aβ clearance, plate differentiated BMEC-like cells on Transwell filters. Apply fluorescently labeled or otherwise detectable Aβ peptides (e.g., Aβ1-40) to the apical ("brain") chamber and measure the rate of appearance in the basolateral ("blood") chamber over time using ELISA or similar techniques. This assay can be performed in the presence of recombinant APOE isoforms or receptor blockers to dissect specific pathways [68].
- Trans-endothelial Electrical Resistance (TEER): Use an epithelial volt-ohm meter to measure TEER across the BMEC-like cell monolayer as a quantitative indicator of barrier integrity [68].
- Extracellular Aβ Deposition Assay: Culture iPSC-derived pericyte-like cells and quantify the amount of Aβ that deposits in the extracellular matrix over time using immunofluorescence or ELISA [68].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for iPSC-based APOE and AD Research
| Reagent / Resource | Function and Application in APOE Research |
|---|---|
| Isogenic Human iPSC Lines (APOE2/2, E3/3, E4/4, KO/KO) | Provides a genetically controlled system to isolate the effects of APOE isoforms on cellular phenotypes without the confounding influence of background genetics [68] [80]. |
| Recombinant Human APOE Protein (Isoforms E2, E3, E4) | Used to treat cultures of neurons, glia, or endothelial cells to directly probe isoform-specific effects on signaling, inflammation, and Aβ metabolism [102]. |
| Matrigel | A basement membrane matrix used as a substrate for coating culture vessels to support the attachment and growth of iPSCs and some differentiated cell types [68]. |
| Retinoic Acid | A small molecule used during the differentiation of iPSCs to BMEC-like cells to enhance the development of robust barrier properties, including high TEER [68]. |
| CRISPR/Cas9 Gene Editing System | Used for two primary purposes: 1) to create isogenic iPSC lines by editing the APOE locus in a parental line, and 2) to correct or introduce disease-relevant mutations in patient-derived iPSCs for functional studies [103]. |
| LRP1 and p-glycoprotein pathway modulators | Pharmacological inhibitors or antibodies used in transport assays (e.g., with BMEC-like cells) to dissect the specific contribution of these pathways to APOE-isoform dependent Aβ clearance [68]. |
Signaling Pathways and Experimental Workflows
APOE Isoform Signaling in Microglia and Astrocytes
The following diagram illustrates the isoform-specific signaling mechanisms in glial cells, linking them to pathological outcomes relevant to AD.
Integrated Workflow for Correlative Studies
This workflow outlines the sequential process from iPSC modeling to clinical correlation, providing a roadmap for translational research projects.
The strategic correlation of iPSC-derived cellular phenotypes with in vivo neuroimaging and biomarker data is essential for validating the pathophysiological relevance of discoveries made with APOE-isogenic models. The consistent observation that APOE4 impairs Aβ clearance in iPSC-BMEC models aligns with human amyloid-PET data showing earlier and greater plaque deposition in APOE4 carriers [68] [14]. Similarly, the pro-inflammatory and neurotoxic signatures of APOE4 glia and neurons in vitro correspond to the glucose hypometabolism and neuroinflammation detected in patients [14] [102]. As iPSC models increase in complexity—incorporating multi-cell type systems, 3D organoids, and fluid flow—these correlations will become increasingly robust, solidifying the role of iPSC technology in bridging molecular mechanisms with clinical manifestations of Alzheimer's disease and accelerating the development of targeted therapies.
APOE4-Specific Impairments in Neuronal Support by Human Astrocytes
The APOE4 allele stands as the most significant genetic risk factor for late-onset Alzheimer's disease (AD). Although expressed in various cell types, APOE in the brain is produced predominantly by astrocytes, which are critical for neuronal support through lipid transport, metabolic regulation, and immune signaling. This whitepaper synthesizes recent findings from human iPSC-based models demonstrating that the APOE4 isoform confers astrocyte-specific dysfunctions that disrupt their normal support functions, leading to increased neuronal vulnerability. Key impairments are observed in immunometabolic coupling, response to amyloid-β, and energy metabolism, providing a mechanistic basis for APOE4-associated AD risk and highlighting potential therapeutic targets within astrocyte-neuron interaction networks.
Apolipoprotein E (APOE) is a lipid transporter crucial for shuttling cholesterol and other lipids in the brain to maintain neuronal membranes, support synaptic growth, and facilitate injury repair [104]. The three common human isoforms—APOE2, APOE3, and APOE4—differ by only one or two amino acids, yet these differences profoundly alter their structure and function. The APOE4 allele increases the risk of developing AD by 3-4 fold in heterozygous carriers and up to 15-fold in homozygotes compared to the common, risk-neutral APOE3 allele, while APOE2 is considered protective [76] [19].
In the central nervous system, astrocytes are the primary producers of APOE [104]. These glial cells provide multiple forms of support to neurons, including regulating neuronal metabolism, supplying neurotransmitters, maintaining synaptic connectivity, and modulating immune responses via cytokine signaling [104]. A growing body of evidence indicates that APOE4 alters fundamental astrocyte functions, reducing their ability to support neuronal health and leaving neurons more vulnerable to stress and disease insults such as amyloid-β (Aβ) accumulation, a key pathological protein in AD [104]. This review examines the specific impairments in neuronal support conferred by APOE4 in human astrocytes, drawing on recent advances in iPSC-derived models that provide a human-relevant system for investigating these mechanisms.
Core Mechanisms of APOE4-Driven Astrocyte Dysfunction
Immunometabolic Alterations in Response to Amyloid-β
When challenged with amyloid-β, APOE4 astrocytes exhibit a maladaptive immunometabolic response characterized by disrupted cytokine signaling and altered energy metabolism. Research using conditioned media from APOE3 versus APOE4 astrocyte cultures reveals that media from Aβ-challenged APOE4 astrocytes causes neurons to significantly increase their basal mitochondrial and glycolytic metabolic rates compared to neurons treated with media from APOE3 astrocytes [104]. This suggests a compensatory increase in neuronal metabolic stress when supported by reactive APOE4 astrocytes.
These metabolic changes in neurons correlate with specific alterations in APOE4 astrocyte function, including:
- Increased glycolytic ATP production in APOE4 astrocytes following Aβ exposure [104]
- Lack of appropriate cytokine secretion in response to Aβ challenge [104]
- Astrocytic cytokine signatures that can predict basal metabolism of treated neurons [104]
The maladaptive immunometabolic response of APOE4 astrocytes is driven in part by preferential utilization of the cRel transcription factor, a component of the NF-κB pathway. Inhibiting cRel translocation in APOE4 astrocytes abrogates inflammatory-induced glycolytic shifts and mitigates pro-inflammatory cytokine production [105].
Intrinsic Bioenergetic Deficits in APOE4 Astrocytes
APOE4 expression alters the fundamental energy metabolism of astrocytes, potentially undermining their ability to meet neuronal metabolic demands. Studies using APOE-isogenic human iPSC-derived astrocytes (iAstrocytes) have revealed genotype-dependent metabolic alterations:
Table 1: Metabolic Parameters in APOE-Isogenic Human iAstrocytes
| Metabolic Parameter | APOE2 iAstrocytes | APOE3 iAstrocytes | APOE4 iAstrocytes |
|---|---|---|---|
| Mitochondrial ATP Production | Similar to APOE3 | Baseline | Reduced [76] |
| Glycolytic ATP Production | Similar to APOE3 | Baseline | Reduced [76] |
| Glycolytic Capacity | Similar to APOE3 | Baseline | Enhanced [76] |
| Mitochondrial Respiration | Similar to APOE-KO | Baseline | Elevated [76] |
| Proton Leak | Lower than APOE4 | Baseline | Elevated [76] |
Notably, despite showing increased glycolytic capacity and mitochondrial respiration, APOE4 iAstrocytes produce less total ATP than other variants, indicating reduced metabolic efficiency [76]. Mass spectrometry-based metabolomic analysis has identified various energy and glucose metabolism-related pathways that are differentially regulated in APOE4 astrocytes, including mitochondrial electron transport chain and glycolysis [76]. The substantial metabolic differences observed between APOE4 and APOE-knockout astrocytes suggest that APOE4 acts through a gain-of-function mechanism rather than mere loss of function [76].
Transcriptional and Epigenetic Reprogramming
APOE4 expression in astrocytes drives distinct transcriptional repertoires at single-cell resolution, promoting heterogenous reactive states with potentially detrimental consequences for neuronal support. Following pro-inflammatory challenge, APOE4-expressing astrocytes acquire transcriptionally distinct subpopulations characterized by enrichment in:
- Metal cation buffering genes (Mt1, Mt2) [105]
- NF-κB signaling pathways [105]
- Interferon response genes [105]
- Glycolysis/Gluconeogenesis pathways [105]
Spatial transcriptomic analysis reveals that these APOE4-associated astrocyte subtypes show increased expression at the spot-level in brain tissue following inflammatory challenge, with regional enrichment in borders, white matter tracks, and internal capsule areas [105]. This transcriptional reprogramming is driven in part by preferential utilization of the cRel transcription factor in APOE4 astrocytes, creating a maladaptive immunometabolic response that may contribute to neuronal dysfunction [105].
Quantitative Data Synthesis
Table 2: APOE4-Specific Astrocyte Impairments and Functional Consequences
| Astrocyte Function | APOE4-Specific Alteration | Experimental System | Impact on Neuronal Support |
|---|---|---|---|
| Response to Aβ | Lack of cytokine secretion; Increased glycolytic ATP production | Primary mouse astrocytes [104] | Increased neuronal metabolic stress |
| Glycolytic Function | Enhanced glycolysis but reduced glycolytic ATP production | Human iAstrocytes [76] | Reduced metabolic support efficiency |
| Mitochondrial Function | Elevated respiration with increased proton leak | Human iAstrocytes [76] | Compromised energy metabolism |
| Inflammatory Response | Preferential cRel/NF-κB utilization; Enhanced pro-inflammatory cytokines | Mouse model & human iAstrocytes [105] | Increased neuroinflammatory environment |
| Developmental Influence | Promotes gliogenesis at expense of neurogenesis | Human cortical organoids [106] | Altered neuronal network formation |
Experimental Models and Methodologies
iPSC-Derived Astrocyte Models
The generation of human iPSC-derived astrocytes (iAstrocytes) from APOE-isogenic lines has provided a powerful platform for investigating APOE genotype-specific effects without the confounding influence of genetic background differences. A standard differentiation protocol involves:
- Neural Induction: Using dual SMAD inhibition with small molecules (CHIR99021, SB431542, Dorsomorphin, and Compound E) for 7 days to convert iPSCs to neural progenitor cells (NPCs) [76]
- NPC Maintenance: Culture in neural stem cell maintenance medium on poly-L-ornithine/laminin-coated surfaces [76]
- Astrocyte Differentiation: Exposure to BMP4, CNTF, and LIF for 30-40 days to generate mature, functional astrocytes [76]
These iAstrocytes express characteristic astrocyte markers (GFAP, S100β) and demonstrate typical astrocyte functions, allowing for the investigation of APOE genotype-dependent differences in energy metabolism, inflammatory responses, and neuronal support functions [76].
Cerebral Organoid and Assembled Model Systems
Three-dimensional cerebral organoids and assembled systems provide more physiologically relevant models for studying astrocyte-neuron interactions in a complex microenvironment. Key methodologies include:
- Cerebral Organoid Generation: Embryonic body formation followed by neuroepithelial expansion in Matrigel scaffold and maturation under rotary conditions [19]
- Regional Patterning: Cortical organoids (excitatory neurons) and ganglionic eminence organoids (inhibitory neurons) can be generated separately and assembled [106]
- Multi-electrode Array Recording: Functional assessment of neural network activity in fused organoids (assembloids) [106]
These 3D models recapitulate APOE4-related phenotypes including increased apoptosis, decreased synaptic integrity, and exacerbated tau pathology [19], as well as altered network excitability and synchronicity [106].
Metabolic Assays and Functional Readouts
Key methodologies for assessing astrocyte metabolic function and neuronal support include:
- Seahorse ATP Rate Assay: Simultaneous measurement of mitochondrial and glycolytic ATP production rates in live cells [76]
- Extracellular Flux Analysis: Assessment of glycolytic function and mitochondrial respiration through sequential injection of metabolic modulators [104]
- Genetically-Encoded Nanosensor FLIM Analysis: Measurement of lactate dynamics and other metabolic intermediates [76]
- Cytokine Profiling: Multiplex immunoassays to characterize secreted cytokine signatures [104]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating APOE4 in Astrocyte Models
| Reagent / Tool | Function / Application | Example Use in APOE4 Research |
|---|---|---|
| APOE-Isogenic iPSC Lines | Controlled genetic background for APOE isoform comparison | Generation of iAstrocytes with defined APOE genotype [76] |
| Dual SMAD Inhibitors | Induction of neural differentiation | Conversion of iPSCs to neural progenitor cells [76] |
| Recombinant Aβ42 | Modeling Alzheimer's disease pathology | Challenge astrocyte cultures to assess inflammatory response [104] |
| Seahorse XFe24 Analyzer | Real-time metabolic profiling | Measurement of glycolytic and mitochondrial function [104] [76] |
| cRel Inhibitors | NF-κB pathway modulation | Testing mechanistic role of cRel in APOE4 astrocyte phenotype [105] |
| Cytokine Multiplex Assays | Inflammatory signaling profiling | Characterization of astrocyte secretome following stimulation [104] |
| Human Microglia Xenotransplantation Model | In vivo assessment of human microglial function | Study APOE isoform effects in AD context [44] |
Signaling Pathways and Experimental Workflows
APOE4 Astrocyte Immunometabolic Signaling Pathway
Diagram 1: APOE4 drives maladaptive immunometabolic responses in astrocytes through cRel activation, leading to neuronal stress.
Experimental Workflow for APOE4 Astrocyte-Neuron Coculture Studies
Diagram 2: Experimental workflow for studying APOE4 astrocyte effects on neuronal support using conditioned media approaches.
Discussion and Future Perspectives
The evidence from human iPSC-based models consistently demonstrates that APOE4 confers specific impairments in astrocyte functions essential for neuronal support. These include maladaptive immunometabolic responses, compromised bioenergetic efficiency, and altered transcriptional programs that collectively create an environment conducive to neurodegeneration. The APOE4 astrocyte phenotype is characterized not by a simple loss of function but rather by a gain of dysfunctional properties that actively contribute to neuronal stress [76].
Notably, many of these APOE4-associated deficits manifest primarily or are significantly exacerbated in the presence of challenges such as Aβ exposure or inflammatory stimuli [104]. This suggests that APOE4 carriers may possess a reduced threshold for maintaining neuronal homeostasis under physiological stress, potentially explaining their increased vulnerability to AD. Furthermore, emerging evidence indicates that APOE4 influences neurodevelopmental processes, altering the balance of excitatory and inhibitory neurons and increasing network excitability [106]. These developmental effects may establish a vulnerable baseline that, combined with age-dependent astrocyte dysfunction, predisposes to neurodegeneration.
Future research should focus on:
- Identifying therapeutic approaches to normalize APOE4 astrocyte metabolism
- Exploring gene editing strategies to convert APOE4 to APOE3 in human astrocytes
- Developing small molecule inhibitors targeting cRel/NF-κB signaling in APOE4 astrocytes
- Investigating the interaction between astrocyte APOE4 and microglial dysfunction in AD pathogenesis
The advancement of more complex in vitro models, including triculture systems incorporating astrocytes, neurons, and microglia [107], will provide deeper insights into how cell-type-specific APOE4 effects interact to drive AD pathology. These human-relevant models offer promising platforms for both understanding disease mechanisms and screening potential therapeutic interventions targeting APOE4-related astrocyte dysfunction.
Isoform-Dependent Effects on Amyloid-β Clearance Across the Blood-Brain Barrier
The apolipoprotein E (APOE) gene, the strongest genetic risk factor for late-onset Alzheimer's disease (AD), exists as three major isoforms—APOE2, APOE3, and APOE4—that differentially influence the clearance of amyloid-β (Aβ) across the blood-brain barrier (BBB). This technical review synthesizes current evidence demonstrating that APOE4 expression disrupts Aβ efflux mechanisms at the BBB, leading to accelerated Aβ accumulation and increased AD risk. In contrast, APOE2 enhances clearance pathways and confers protection. Within the context of APOE research using induced pluripotent stem cell (iPSC)-derived neurons and glia, this whitepaper details the molecular mechanisms, summarizes critical quantitative findings, and outlines essential experimental protocols for investigating these isoform-specific effects. Understanding these pathways is paramount for developing novel therapeutic strategies aimed at mitigating Aβ pathology in AD.
Alzheimer's disease is the leading cause of dementia worldwide, with over 95% of cases classified as sporadic, late-onset AD (LOAD). The APOE gene remains the strongest and most prevalent genetic risk factor for LOAD, with its three common isoforms exerting differential effects on disease risk [13] [108]. The APOE4 allele significantly increases AD risk in a gene dose-dependent manner, with homozygotes facing up to a 15-fold increased risk compared to the most common APOE3 allele. Conversely, the APOE2 allele is protective, reducing AD risk by approximately half [13]. While these isoforms differ by only single amino acid substitutions at positions 112 and 158, these changes profoundly alter the protein's structure and function, particularly in relation to Aβ metabolism and clearance [108].
Accumulating evidence from human studies indicates that APOE genotype dramatically influences cerebral Aβ deposition. Cognitively normal APOE4/ε4 individuals show significantly lower CSF Aβ42 concentrations and higher Pittsburgh Compound B (PIB) retention on PET imaging, indicating greater amyloid burden, compared to APOE3/ε3 and APOE2/ε3 carriers [109]. This review examines the mechanistic basis for these clinical observations, focusing specifically on how APOE isoforms differentially regulate Aβ clearance across the BBB—a process estimated to account for the elimination of more than 85% of CNS-produced Aβ [68] [79].
Molecular Mechanisms of APOE Isoform-Dependent Aβ Clearance
Receptor-Mediated Clearance Pathways at the BBB
The BBB serves as a critical interface for maintaining CNS homeostasis and provides the principal route for Aβ elimination from the brain. APOE isoforms differentially influence Aβ clearance through specific receptor-mediated pathways, primarily involving the low-density lipoprotein receptor-related protein 1 (LRP1) and the very-low-density lipoprotein receptor (VLDLR) [110] [111].
Table 1: Key Receptors in APOE-Mediated Aβ Clearance
| Receptor | Function in Aβ Clearance | APOE Isoform Specificity |
|---|---|---|
| LRP1 | Primary efflux transporter for free Aβ; rapid clearance pathway | Preferentially binds apoE2 and apoE3; apoE4 binding is diminished |
| VLDLR | Alternative clearance pathway for Aβ-apoE complexes; slower endocytotic rate | Primary receptor for apoE4 and Aβ-apoE4 complexes |
| LRP1/VLDLR | Combined pathway for efficient clearance | Used by apoE2 and apoE3 complexes, but not apoE4 complexes |
Research by Deane et al. demonstrated that lipid-poor apoE4 redirects Aβ clearance from the rapid LRP1 pathway to the slower VLDLR pathway [110] [111]. When Aβ binds to apoE4, the resulting complex is internalized predominantly via VLDLR, which has a substantially slower endocytotic rate compared to LRP1. In contrast, apoE2 and apoE3, as well as their complexes with Aβ, are cleared via both VLDLR and LRP1, resulting in substantially faster clearance rates than Aβ-apoE4 complexes [110]. This receptor switching mechanism underlies the impaired Aβ clearance associated with APOE4.
Figure 1: APOE Isoform-Dependent Receptor Pathways for Aβ Clearance. ApoE2 and ApoE3 complexes with Aβ utilize the LRP1 receptor for rapid clearance, while ApoE4 complexes are redirected to the slower VLDL receptor pathway.
The Role of APOE Lipidation Status
The lipidation status of apoE significantly influences its function in Aβ clearance. Lipidated apoE (lipo-apoE) isoforms are cleared from the brain at substantially slower rates (2- to 3-fold slower) than their lipid-poor counterparts [110] [111]. Astrocyte-secreted lipo-apoE4 exhibits the greatest retention rate in the brain and the slowest efflux across the BBB compared to other apoE isoforms or Aβ peptides alone [111]. This impaired clearance is further exacerbated by the finding that lipo-apoE4 impedes the "brain-to-blood" Aβ40 transport capabilities of brain microvascular endothelial cells (BMECs), while APOE2 enhances Aβ42 transport in model systems [68] [79].
Co-aggregation of APOE with Aβ
Recent single-molecule imaging studies reveal that all apoE isoforms associate with Aβ during early aggregation stages, forming transient co-aggregates that subsequently dissociate as fibrillation proceeds [33]. These apoE-Aβ co-aggregates account for approximately 50% of the mass of diffusible Aβ aggregates detected in the frontal cortices of APOE4 homozygotes. APOE4 carriers exhibit significantly more diffusible Aβ aggregates than APOE3 carriers, suggesting that apoE4 not only impairs clearance but may also stabilize pathogenic Aβ species [33]. The lipidation state of apoE influences the size of these co-aggregates, with non-lipidated apoE forming larger early-stage co-aggregates (~500-900 nm) compared to lipidated apoE (~200-250 nm) [33].
Quantitative Analysis of APOE Isoform Effects on Aβ Kinetics
Clearance Rates and Brain Retention
Table 2: Comparative Clearance Kinetics of Aβ and APOE Isoforms at the BBB
| Ligand | BBB Transport Rate Constant (k, min⁻¹ × 10³) | Relative Retention in Brain | Half-Time for Clearance (min) |
|---|---|---|---|
| Free Aβ40 | 4.1 [111] | 1.0 (Reference) | - |
| Free Aβ42 | 2.4 [111] | 1.7x higher than Aβ40 | - |
| Lipid-poor apoE2 | 2.4 [111] | 3.8x higher than Aβ40 | - |
| Lipid-poor apoE3 | 2.4 [111] | 3.8x higher than Aβ40 | - |
| Lipid-poor apoE4 | 1.7 [111] | 9.5x higher than Aβ40 | - |
| Lipo-apoE2 | 0.9 [111] | 11.7x higher than Aβ40 | - |
| Lipo-apoE3 | 1.0 [111] | - | - |
| Lipo-apoE4 | 0.5 [111] | 15.9x higher than Aβ40 | - |
The data demonstrate a clear isoform-dependent pattern, with apoE4 exhibiting the slowest clearance and highest brain retention, particularly in its lipidated form. Lipo-apoE4 has an 8.3-fold lower transport rate across the BBB than free Aβ40 and a 2.6-fold lower rate than lipo-apoE2 [111]. This impaired clearance directly correlates with increased Aβ deposition in both human studies and animal models.
Biomarker Correlations in Human Studies
Table 3: APOE Genotype Effects on Biomarkers of Aβ Deposition in Cognitively Normal Individuals
| APOE Genotype | CSF Aβ42 (pg/mL) | % with CSF Aβ42 <500 pg/mL | PIB-PET Positivity | Clinical AD Risk |
|---|---|---|---|---|
| ε2/ε3 | 755.7 [109] | Lowest proportion | Lowest proportion | Reduced (~50% lower) [13] |
| ε3/ε3 | 695.6 [109] | Low | Low | Reference |
| ε3/ε4 | 619.6 [109] | Intermediate | Intermediate | Increased |
| ε4/ε4 | 437.4 [109] | Highest proportion | Highest proportion | Highly increased (up to 15x) [13] |
Human biomarker studies consistently show that APOE4 carriers exhibit lower CSF Aβ42 levels, which reflects sequestration of Aβ into brain amyloid plaques [109]. The prevalence of abnormal amyloid biomarkers follows a clear APOE allele-dependent pattern (ε4/ε4 > ε3/ε4 > ε3/ε3 > ε2/ε3), directly corresponding to known AD risk profiles [109].
Experimental Models and Methodologies
iPSC-Derived Blood-Brain Barrier Models
The development of human iPSC-derived BBB models has provided powerful tools for investigating APOE isoform-specific effects in a human-relevant system. These models utilize isogenic iPSC lines where APOE alleles have been precisely edited using CRISPR/Cas9 technology to produce APOE2/APOE2, APOE3/APOE3, and APOE4/APOE4 lines, minimizing confounding effects from genetic background [68] [51] [79].
Key Differentiation Protocol for BMEC-like Cells:
- Culture Expansion: iPSCs are singularized with Accutase and expanded to 30,000 cells/cm² prior to differentiation initiation [68] [79].
- Unconditioned Media Stage: Cells are maintained in unconditioned medium (UM) with daily changes for 6 days [68] [79].
- Endothelial Induction: UM is replaced with human endothelial serum-free medium (hECSR) supplemented with 20 ng/mL basic fibroblast growth factor (bFGF), 2% B-27, and 10 μM retinoic acid for 48 hours [68] [79].
- Characterization: Resulting BMEC-like cells should exhibit high trans-endothelial electrical resistance (TEER) and express characteristic tight junction proteins (claudin-5, occludin, ZO-1) [68] [79].
Key Differentiation Protocol for Pericyte-like Cells:
- Neural Crest Induction: iPSCs are differentiated in Essential 6 medium supplemented with 1 μM dorsomorphin, 10 μM SB431542, 1 μM CHIR99021, 10 μg/L bFGF, and 22.5 mg/L heparin to generate neural crest stem cells [68] [79].
- Cell Enrichment: CD271+ cells are enriched using neural crest stem cell microbeads and seeded at 10,000 cells/cm² [68] [79].
- Pericyte Expansion: Cells are expanded for 6 days in Essential 6 medium supplemented with 10% FBS [68] [79].
Figure 2: Workflow for Generating iPSC-Derived BBB Models for APOE-Aβ Interaction Studies. This diagram illustrates the parallel differentiation of iPSCs into brain microvascular endothelial-like cells and pericyte-like cells for functional assays.
Critical Functional Assays
Aβ Transcytosis Assay:
- BMEC-like cells are cultured on collagen IV-coated Transwell inserts [79].
- Fluorescently labeled Aβ (Aβ40 or Aβ42) is added to the apical ("blood") or basolateral ("brain") chamber.
- Transport is quantified by measuring tracer appearance in the opposite chamber over time using fluorescence or ELISA [79].
- Specific receptor pathways can be inhibited using RAP (receptor-associated protein) for LRP1, or specific antibodies for VLDLR [110] [111].
In Vivo Microdialysis for Aβ Clearance:
- This technique measures the concentration and clearance of soluble Aβ in brain interstitial fluid (ISF) of mouse models [109].
- Mice expressing human APOE isoforms are used (e.g., PDAPP/TRE model) [109].
- A microdialysis probe is implanted into the hippocampus or cortex, and ISF is collected at regular intervals [109].
- Aβ levels are quantified using ELISA, and clearance rates are calculated from disappearance curves after administering γ-secretase inhibitor to block Aβ production [109].
Single-Molecule Pull-Down (SiMPull) for ApoE-Aβ Co-aggregates:
- This assay characterizes individual aggregates at different stages of aggregation [33].
- Aβ42 is captured using surface-tethered 6E10 antibody [33].
- Samples are imaged using two-color total internal reflection fluorescence (TIRF) microscopy after adding detector antibodies for Aβ (Alexa-Fluor-647-labeled 6E10) and apoE (Alexa-Fluor-488-labeled EPR19392) [33].
- Colocalization analysis determines the size, composition, and abundance of apoE-Aβ co-aggregates [33].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Investigating APOE-Aβ Interactions at the BBB
| Reagent/Cell Line | Specification | Application | Key Findings Enabled |
|---|---|---|---|
| Isogenic iPSC Lines | APOE2/2, APOE3/3, APOE4/4 (Alstem) [68] [79] | BBB differentiation; neuronal/glial co-cultures | APOE4 increases Aβ secretion in neurons and impairs Aβ uptake in astrocytes [51] |
| Recombinant apoE Proteins | Lipid-poor and lipidated isoforms [110] [111] | Transport assays; binding studies | apoE4 impedes Aβ40 transport; apoE2 enhances Aβ42 clearance [68] [79] |
| Receptor Inhibitors | RAP (LRP1 inhibitor); receptor-specific antibodies [110] [111] | Pathway mechanistic studies | apoE4 redirects clearance from LRP1 to VLDLR pathway [110] |
| Detection Antibodies | 6E10 (Aβ); EPR19392 (apoE) [33] | SiMPull; co-aggregation analysis | All apoE isoforms form early co-aggregates with Aβ [33] |
| Collagen IV-Coated Transwells | 0.4 μm pore size [79] | BBB permeability and transport assays | APOE genotype affects Aβ transcytosis without altering TEER [79] |
Implications for Therapeutic Development
The isoform-dependent effects of APOE on Aβ clearance present multiple avenues for therapeutic intervention. Strategies include:
- APOE4-Targeted Therapies: Converting apoE4 to apoE3-like structure or function through small molecules or gene editing [108] [51].
- Receptor Pathway Modulation: Enhancing LRP1-mediated clearance or blocking the deleterious effects of apoE4-VLDLR interactions [110].
- Lipidation Enhancement: Promoting apoE lipidation through ABCA1 agonists to improve its function, particularly for apoE4 [13].
- Co-aggregate Disruption: Selectively targeting pathological apoE-Aβ co-aggregates, particularly non-lipidated apoE4-Aβ species [33].
Recent work has demonstrated that selectively removing non-lipidated apoE4-Aβ co-aggregates enhances clearance of toxic Aβ by glial cells and reduces inflammatory marker secretion and membrane damage, highlighting a promising path for AD therapeutics [33].
APOE isoforms differentially regulate Aβ clearance across the BBB through distinct receptor-mediated pathways, with apoE4 impairing clearance through redirecting Aβ to the slower VLDLR pathway and promoting co-aggregation with Aβ. The development of human iPSC-derived BBB models has provided robust experimental systems for investigating these mechanisms in a human-relevant context and for screening potential therapeutic compounds. Targeting the specific pathological interactions between apoE4 and Aβ represents a promising strategy for developing effective therapies for Alzheimer's disease that could benefit the majority of patients with the late-onset, sporadic form of this devastating condition.
Comparative Analysis of Lipid Metabolism and Synaptic Support Functions
Apolipoprotein E (ApoE) is a critical lipid transport protein in the central nervous system, with its three major isoforms—ApoE2, ApoE3, and ApoE4—exerting profound and isoform-dependent effects on neuronal health. Within the context of sporadic Alzheimer's disease and other neurodegenerative disorders, these isoforms differentially regulate lipid metabolism and synaptic integrity. The advent of human induced pluripotent stem cell (iPSC) technologies has provided a physiologically relevant platform to dissect these mechanisms in a human genetic background. This review synthesizes findings from iPSC-derived models, including neurons, astrocytes, and cerebral organoids, to provide a comparative analysis of how ApoE isoforms modulate lipid homeostasis and synaptic support functions, offering insights for future therapeutic strategies.
In the brain, apolipoprotein E is predominantly produced by astrocytes and serves as the principal carrier of cholesterol and other lipids to neurons [3] [50]. This lipid transport is fundamental for maintaining synaptic integrity, facilitating injury repair, and supporting overall neuronal homeostasis [50] [112]. The three major human ApoE isoforms differ by single amino acid substitutions: ApoE3 (cysteine-112, arginine-158), the most common allele; ApoE4 (arginine-112, arginine-158), the strongest genetic risk factor for late-onset Alzheimer's disease; and ApoE2 (cysteine-112, cysteine-158), which is associated with a protective effect [3] [36]. ApoE4 increases the risk of Alzheimer's disease approximately 3-fold in heterozygotes and 12-fold in homozygotes compared to ApoE3 [3]. Beyond Alzheimer's, ApoE4 is also a recognized risk factor for Dementia with Lewy Bodies and Parkinson's disease dementia, underscoring its broad role in neurodegeneration [113]. This review leverages evidence from human iPSC-based models to compare the isoform-specific functions of ApoE in lipid metabolism and its consequent impact on synaptic support.
ApoE Isoforms and Lipid Metabolism in iPSC-Derived Models
Lipid metabolism is a central process disrupted by ApoE isoforms, with ApoE4 consistently associated with detrimental alterations.
Table 1: Impact of ApoE Isoforms on Lipid Metabolism in iPSC Models
| ApoE Isoform | Lipidation Status | Key Lipid Phenotypes | Experimental Model | Citation |
|---|---|---|---|---|
| ApoE3 | Well-lipidated | Efficient lipid transport; Lower lipid droplet accumulation | iPSC-derived astrocytes; Cerebral organoids | [50] [113] |
| ApoE4 | Poorly lipidated | Reduced lipid transport; Increased lipid droplets & cholesterol esters; Disrupted organelle lipid | iPSC-derived astrocytes; Cerebral organoids | [50] [113] [112] |
| ApoE2 | N/A* | Protective; Rescues lipid phenotypes in ApoE-deficient models | Cerebral organoids with exogenous ApoE2 | [113] |
| ApoE-KO | N/A | Increased fatty acid utilization; Massive lipid droplet accumulation; Synaptic loss | Isogenic ApoE-KO cerebral organoids | [113] |
*N/A: Not specifically reported in the cited studies for this parameter.
Human iPSC-derived astrocytes carrying the APOE ε4/ε4 genotype secrete lipoprotein particles that are significantly less lipidated than those secreted by APOE ε3/ε3 astrocytes [50]. This deficient lipidation is a fundamental defect that impairs ApoE4's ability to transport lipids effectively [112]. Consequently, cerebral organoids with APOE ε4/ε4 or those with complete APOE knockout exhibit a marked accumulation of lipid droplets and cholesterol esters [113]. Lipidomic analyses of ApoE-deficient organoids further reveal increased fatty acid utilization, pointing to a profound dysregulation of overall lipid homeostasis [113]. The provision of exogenous ApoE2 or ApoE3, but not ApoE4, can partially rescue these lipid metabolic defects in ApoE-deficient organoids, highlighting the functional deficiency of the ApoE4 isoform [113].
ApoE Isoforms and Synaptic Support Functions
The dysregulation of lipid metabolism directly impacts the ability of astrocytes to support neuronal synapses.
Table 2: Synaptic Support Functions of ApoE Isoforms in iPSC Models
| ApoE Isoform | Neuronal Viability | Synaptogenesis & Synaptic Integrity | Experimental Model | Citation |
|---|---|---|---|---|
| ApoE3 | Supports neuronal survival | Effectively promotes synaptogenesis; Maintains synaptic protein levels | Co-culture of iPSC-derived astrocytes & neurons; Cerebral organoids | [50] [19] |
| ApoE4 | Reduced support for survival | Less effective in supporting synaptogenesis; Exacerbates synapse loss in disease | Co-culture of iPSC-derived astrocytes & neurons; AD patient-derived organoids | [50] [19] |
| ApoE2 | N/A | Protective (associated with delayed disease onset) | Population studies | [3] |
| ApoE-KO | N/A | Synaptic loss accompanied by lipid dysregulation | Isogenic ApoE-KO cerebral organoids | [113] |
Functional assays demonstrate that human iPSC-derived astrocytes with the APOE ε3/ε3 genotype are capable of promoting neuronal survival and synaptogenesis when co-cultured with neurons. In stark contrast, APOE ε4/ε4 astrocytes are significantly less effective in supporting these critical neurotrophic functions [50]. In complex cerebral organoid models, APOE4 exacerbates synapse loss and neurodegeneration, particularly in organoids derived from Alzheimer's disease patients [19]. This suggests that ApoE4 compromises the ability of glial cells to provide adequate lipid and metabolic support to synapses, especially under pathological stress. The detrimental effects of ApoE4 on synapses are not limited to Alzheimer's pathology; ApoE4 also exacerbates α-synuclein accumulation, which is directly linked to synaptic dysfunction in Lewy body diseases [113].
Detailed Experimental Protocols from Key Studies
Generation and Differentiation of Human iPSCs into Cerebral Organoids
This protocol is adapted from studies that utilized cerebral organoids to model ApoE-related pathology [113] [19].
- Day 0: Embryoid Body (EB) Formation. Human iPSCs are dissociated into a single-cell suspension using Accutase. Approximately 15,000 cells are seeded per well in a U-bottom ultra-low-attachment 96-well plate in EB formation medium, supplemented with a ROCK inhibitor (Y-27632, 10 µM) to enhance cell survival.
- Day 2 & 4: EB Maintenance. Add 100 µL of fresh EB formation medium to each well without disturbing the forming EBs.
- Day 5: Neural Induction. Transfer individual EBs to a low-attachment 48-well plate containing neural induction medium. Culture for 3-5 days without agitation.
- Day ~7-9: Matrigel Embedding. Embed each EB in 20 µL of Matrigel droplets to provide a scaffold for neuroepithelial expansion. Transfer the embedded EBs to neural expansion medium in low-attachment plates and culture for 3 days.
- Day ~12+: Long-term Maturation. Transfer the organoids to an orbital shaker for long-term culture in neuronal maturation medium. The medium is replaced regularly. Organoids develop over 8-12 weeks, generating complex tissues with neural progenitor zones, mature neurons, and astrocytes.
Co-culture of Human iPSC-Derived Astrocytes and Neurons
This protocol is used to specifically assess the neurotrophic capacity of astrocytes in an isoform-dependent manner [50].
- Step 1: Astrocyte Differentiation. Differentiate iPSC-derived neural progenitor cells (NPCs) into astrocytes by maintaining them in gliogenic medium for over 45 days. Astrocyte maturity is confirmed by immunostaining for markers such as GFAP, S100β, AQP4, and Vimentin. Functional maturity can be assessed via a glutamate uptake assay.
- Step 2: Neuronal Differentiation. Differentiate a separate batch of NPCs (at low passage numbers) into neurons by withdrawing growth factors. Neuronal identity is confirmed by immunostaining for markers like MAP2.
- Step 3: Co-culture Establishment. Plate the differentiated astrocytes and neurons together in a defined co-culture medium, or seed neurons onto a established layer of astrocytes.
- Step 4: Functional Assessment. After an appropriate co-culture period (e.g., 7-14 days), assay for neuronal health and synapse formation. Key endpoints include:
- Neuronal Survival: Quantify viable neurons or measure apoptotic markers (e.g., cleaved caspase-3).
- Synaptogenesis: Immunostain for pre-synaptic (e.g., Synaptophysin) and post-synaptic (e.g., PSD95) markers and quantify their puncta density and co-localization.
Visualization of ApoE Workflows and Pathways
The following diagrams illustrate the core experimental workflows and pathophysiological pathways discussed in this review.
Diagram 1: iPSC Model Generation Workflow
Diagram 2: ApoE4 Pathogenic Cascade
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for iPSC-Based ApoE and Lipid Metabolism Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| STEMdiff Cerebral Organoid Kit | Provides optimized media for robust, reproducible cerebral organoid generation. | Modeling brain development and disease in 3D [113] [19]. |
| Anti-ApoE Antibodies | Detection and quantification of ApoE protein (e.g., via Western Blot, ELISA). | Measuring ApoE secretion and lipidation status from iPSC-astrocytes [50]. |
| Isogenic APOE iPSC Lines | Controls for genetic background; generated via CRISPR/Cas9 to convert APOE4 to APOE3 or create KO. | Defining ApoE4-specific effects independent of donor variability [19]. |
| Lipid Dyes (e.g., BODIPY) | Staining and visualization of neutral lipids and lipid droplets in fixed or live cells. | Quantifying lipid accumulation in ApoE4 or ApoE-KO organoids [113]. |
| Native-PAGE | Analysis of lipoprotein particle size and lipidation status without denaturation. | Comparing the size and lipidation of ApoE3 vs. ApoE4 particles from astrocytes [50]. |
| Synaptic Markers (Synaptophysin, PSD95) | Immunostaining for pre- and post-synaptic proteins to quantify synapse density and integrity. | Assessing synaptic loss in cerebral organoids or co-culture systems [19]. |
Evidence from human iPSC-derived models conclusively demonstrates that the ApoE4 isoform is fundamentally impaired in its ability to maintain lipid homeostasis and provide synaptic support compared to ApoE3 and ApoE2. The core deficit of poor lipidation underlies a cascade of pathogenic events, including lipid droplet accumulation, dysfunctional lipid transport to neurons, and an increased burden of pathological proteins like α-synuclein and phosphorylated tau, ultimately leading to synaptic failure and neurodegeneration. The isogenic conversion of APOE4 to APOE3 in patient-derived cells rescues multiple disease phenotypes, validating ApoE4 as a compelling therapeutic target [19]. Future research should focus on developing "ApoE structure correctors" and strategies to enhance the lipidation and function of the ApoE4 protein, with the goal of restoring its natural neuroprotective and synaptotrophic functions in patients.
Validation of APOE2 Protective Mechanisms in Human iPSC-Derived Cell Systems
The apolipoprotein E (APOE) gene, the strongest genetic risk factor for late-onset Alzheimer's disease (AD), exists in three common isoforms: APOE2, APOE3, and APOE4. Whereas APOE4 significantly increases AD risk, the APOE2 allele confers pronounced protection, reducing lifetime disease risk by approximately 40% [114]. The precise mechanisms underlying APOE2's protective effects have remained elusive. However, the advent of human induced pluripotent stem cell (iPSC) technologies has revolutionized this investigative landscape. The generation of isogenic human iPSC lines, which differ exclusively at the APOE locus, provides a genetically controlled system to delineate the cell-type-specific, protective functions of APOE2. This whitepaper synthesizes current evidence from iPSC-derived models—including neurons, astrocytes, microglia, and specialized blood-brain barrier (BBB) cell types—to validate the multi-faceted mechanisms of APOE2 protection. These mechanisms encompass enhanced amyloid-β (Aβ) clearance, reduced Aβ production and deposition, modulation of neuroinflammation, and the restoration of bioenergetic and lipid homeostasis. The insights garnered from these human cell systems are not only clarifying a long-standing enigma in AD research but are also establishing a robust platform for the identification and validation of novel, mechanism-driven therapeutic targets.
In the central nervous system, APOE is produced primarily by astrocytes and microglia and plays a crucial role in lipid transport and homeostasis [12]. The three isoforms, APOE2, APOE3, and APOE4, differ by only one or two amino acids at positions 112 and 158, yet these minor changes profoundly alter the protein's structure and function [12]. APOE4 is the strongest genetic risk factor for late-onset AD, with homozygotes facing a greater than 10-fold increased risk. In stark contrast, APOE2 homozygotes have an exceptionally low likelihood of developing AD [114].
Historically, research has disproportionately focused on the deleterious effects of APOE4. While this has yielded valuable insights, understanding the inherent protection conferred by APOE2 is equally critical. It represents a natural, protective phenotype that, if understood and therapeutically mimicked, could benefit a broad population of at-risk individuals. Human iPSC-derived cell systems, particularly those utilizing isogenic lines, now provide the necessary genetic precision and human-relevant context to dissect these mechanisms without the confounding variables of interspecies differences or human genetic diversity [114]. This technical guide details the experimental approaches and findings that are validating APOE2's protective role across various cellular contexts of Alzheimer's disease pathology.
Key Mechanistic Insights from iPSC Models
Amyloid-β Pathology and Clearance
The protective effect of APOE2 is strongly linked to the reduction of key AD pathologies, beginning with amyloid-β. iPSC-derived neural cultures harboring familial AD (fAD) mutations demonstrate that the conversion from APOE3 to APOE2 significantly reduces the secretion of Aβ peptides [114]. This reduction is potentially driven by a mechanism related to non-amyloidogenic processing of the amyloid precursor protein (APP), suggesting APOE2 actively steers processing toward a less pathogenic pathway [114].
Beyond production, Aβ clearance is a critical point of APOE isoform modulation. Research using iPSC-derived brain microvascular endothelial cell-like cells (BMEC-like cells) to model the BBB has revealed that recombinant APOE2 protein increases the "brain-to-blood" transport of amyloid-beta 1–42 (Aβ42) [68]. Conversely, APOE4 significantly impedes the clearance of amyloid-beta 1–40 (Aβ40) [68]. These processes are dependent on LRP1 and p-glycoprotein pathways, mirroring known in vivo mechanisms. Furthermore, in iPSC-derived pericyte-like cells, APOE4 is associated with heightened extracellular Aβ42 deposition, while APOE2 displays the least deposition, aligning with the clinical observation of reduced vascular amyloid in APOE2 carriers [68].
Table 1: APOE Isoform-Specific Effects on Amyloid-β Pathology in iPSC Models
| Cellular Model | Experimental Readout | APOE2 Effect | APOE3 Effect (Reference) | APOE4 Effect |
|---|---|---|---|---|
| Neural Cultures [114] | Aβ Secretion | ↓ Reduction | Baseline | ↑ Increase |
| BMEC-like Cells [68] | Aβ42 Transport | ↑ Increase | Baseline | ↓ Decrease |
| BMEC-like Cells [68] | Aβ40 Transport | No significant change | Baseline | ↓↓ Strong Decrease |
| Pericyte-like Cells [68] | Extracellular Aβ42 Deposition | ↓↓ Strong Reduction | Baseline | ↑↑ Strong Increase |
Neuroinflammation and Microglial Function
Microglia, the brain's resident immune cells, are pivotal in the AD response, and their function is profoundly shaped by APOE genotype. Recent research profiling the transcriptomic and epigenomic landscapes of human iPSC-derived microglia xenotransplanted into AD mouse models has identified widespread differences dependent on the APOE isoform [44].
The most significant differences were observed between the protective APOE2 and risk-inducing APOE4 isoforms. APOE2 microglia exhibited a unique genetic signature associated with increased phagocytic capability, suggesting a more efficient clearance of pathological proteins like Aβ. In contrast, APOE4 microglia showed impairments in key immune response pathways [44]. A direct comparison of APOE4 to APOE2 microglia revealed 1,639 differentially expressed genes, underscoring the extensive impact of the isoform on microglial phenotype [44]. These findings indicate that APOE2 may confer protection by promoting a microglial state that is more responsive, phagocytically active, and less prone to a chronic, damaging inflammatory response.
Table 2: APOE Isoform Effects on Neuroinflammation and Metabolism in Cellular Models
| Phenotype Category | Experimental Model | APOE2 Signature | APOE4 Signature |
|---|---|---|---|
| Microglial Phenotype [44] | iPSC-derived Microglia (RNA-seq/ATAC-seq) | ↑ Phagocytic capabilityRobust immune response | ↓ Impaired proliferation/migrationDysregulated immune response |
| Neuroinflammation [115] | Knock-in Rat Model (Cytokines) | ↓ Lower levels of IL-13, IL-4, IL-5 (vs. APOE4) | ↑ Higher levels of IL-13, IL-4, IL-5 (vs. APOE2) |
| Brain Metabolism [116] | Gene-targeted Mouse Brain | Robust glucose & ketone body metabolism | Deficient glucose uptake & metabolism |
Lipid Metabolism and Bioenergetics
APOE is a master regulator of lipid metabolism, and its isoforms differentially impact this critical homeostatic process. Analysis of cerebral organoids derived from APOE-deficient and isogenic iPSC lines revealed that APOE deletion leads to a cell-type-specific disruption of lipid homeostasis, including upregulated cholesterol biosynthesis in excitatory neurons and excessive lipid accumulation in astrocytes [53]. These phenotypes are relevant to the protective mechanism of APOE2, as APOE4 cerebral organoids show altered cholesterol metabolism compared to their APOE3 counterparts [53].
Furthermore, studies in targeted replacement mice have shown that brain energy metabolism is differentially modulated by APOE isoforms. APOE2 brains exhibit a more robust profile in the uptake and metabolism of glucose, the brain's primary fuel, and ketone bodies, a secondary energy source [116]. This bioenergetic robustness, potentially mediated by the PPAR-γ/PGC-1α signaling pathway, may translate to enhanced synaptic function and resilience, thereby reducing AD risk [116].
Detailed Experimental Protocols for Key assays
This protocol generates a human BBB model for studying Aβ transport.
- Key Reagents: Matrigel, mTESR1 medium, Accutase, Knock-out Serum Replacement, DMEM/F12, Human Endothelial Serum-Free Medium (hECSR), basic fibroblast growth factor (bFGF), B-27 Supplement, retinoic acid.
- Procedure:
- Culture & Expansion: Maintain iPSCs on Matrigel-coated plates with mTESR1 medium. For differentiation, singularize cells with Accutase and plate at a density of 30,000 cells/cm².
- Induction (6 days): Replace medium with Unconditioned Medium (UM). UM is composed of DMEM/F12, Knock-out Serum Replacement, MEM non-essential amino acids, GlutaMAX, and β-mercaptoethanol. Change UM daily for 6 days.
- Maturation (2 days): On day 6, switch to hECSR medium supplemented with 20 ng/mL bFGF, 2% B-27, and 10 µM retinoic acid. Culture for 48 hours.
- Analysis: BMEC-like cells can be assessed for barrier integrity (Trans-Endothelial Electrical Resistance, TEER), tight junction protein expression, and Aβ transport assays.
This functional assay directly quantifies isoform-specific differences in Aβ clearance.
- Key Reagents: Recombinant human APOE2, APOE3, and APOE4 proteins, fluorescently labeled or unlabeled Aβ peptides, BMEC-like cells.
- Procedure:
- Cell Preparation: Differentiate iPSCs to BMEC-like cells as described in Protocol 1 and seed them on Transwell filters to form a confluent monolayer.
- Treatment & Transport: Add Aβ peptides to the apical ("brain") compartment in the presence or absence of recombinant APOE proteins. To probe mechanism, inhibitors of key pathways (e.g., LRP1 or p-glycoprotein inhibitors) can be co-applied.
- Quantification: Incubate for a set period (e.g., several hours). Sample media from the basolateral ("blood") compartment and quantify the amount of transported Aβ using ELISA or similar techniques.
- Data Analysis: Compare transport rates across APOE isoform conditions. APOE2 is typically associated with increased Aβ42 transport compared to APOE3 and APOE4 [68].
This protocol creates a complex 3D model to study cell-type-specific effects in a native-like environment.
- Key Reagents: STEMdiff Cerebral Organoid Kit, Low-attachment plates, Matrigel, Neuronal Maturation Medium.
- Procedure:
- Embryoid Body (EB) Formation (Day 0): Dissociate iPSCs to a single-cell suspension and seed into a U-bottom ultra-low-attachment 96-well plate in Medium A with a Rho kinase inhibitor.
- Neural Induction (Days 2-5): Feed EBs with additional Medium A on days 2 and 4. On day 5, transfer EBs to a low-attachment plate in Medium B.
- Matrigel Embedding & Expansion (Days 7-10): After 3-5 days in Medium B, embed individual EBs in Matrigel droplets and culture in Medium C+D.
- Maturation (>Day 10): Transfer organoids to an orbital shaker and maintain in neuronal maturation medium for several months to allow for advanced cellular differentiation and maturation.
- Analysis: Organoids can be dissociated for single-cell RNA sequencing, analyzed for lipid content, or sectioned for immunohistochemistry to assess amyloid pathology, neuroinflammation, and neural differentiation.
Signaling Pathways and Experimental Workflows
APOE Modulated Amyloid Processing Pathway
iPSC Experimental Workflow for APOE2 Validation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for APOE-iPSC Research
| Reagent / Resource | Function / Application | Example Source / Citation |
|---|---|---|
| Isogenic iPSC Lines | Genetically controlled model to isolate APOE isoform effects; available as APOE2/2, APOE3/3, APOE4/4, and APOE-KO. | Alstem [68]; CRISPR/Cas9-edited lines [114] |
| BMEC Differentiation Kit | Generates brain microvascular endothelial cell-like cells for BBB and Aβ transport studies. | Custom protocol using hECSR medium + retinoic acid [68] |
| Cerebral Organoid Kit | Generates 3D cerebral organoids for studying cell-type-specific interactions and lipid metabolism. | STEMdiff Cerebral Organoid Kit [53] |
| Recombinant APOE Protein | Used in treatment assays to directly test the effect of specific isoforms on cellular pathways. | Commercially available human APOE2, E3, E4 proteins [68] |
| LRP1 / p-gp Inhibitors | Pharmacological tools to validate the specific pathways involved in APOE-mediated Aβ clearance. | Small molecule inhibitors (e.g., RAP for LRP1) [68] |
Human iPSC-derived cell systems have unequivocally validated APOE2's protection against Alzheimer's disease pathologies through a concert of mechanisms operating across different cell types. The combined evidence demonstrates that APOE2 reduces Aβ secretion by shifting APP processing, enhances its clearance across the BBB, minimizes its deposition in pericytes, promotes a neuroprotective microglial phenotype, and helps maintain healthy lipid and energy metabolism.
The future of this field lies in building more complex, multi-cellular systems to investigate how these cell-autonomous mechanisms integrate within the neurovascular unit. Furthermore, the application of multi-omics technologies—transcriptomics, epigenomics, and lipidomics—to these isogenic models will uncover novel downstream effectors of APOE2 protection. These validated human cellular models and the mechanistic insights they provide are indispensable for the pharmaceutical industry, offering a robust, genetically precise platform for high-throughput screening of therapeutics designed to mimic the protective APOE2 phenotype, ultimately paving the way for promising new strategies in Alzheimer's disease prevention and treatment.
Integrating hiPSC Data with GWAS Findings and Post-Mortem Brain Studies
The integration of human induced pluripotent stem cell (hiPSC) models with genome-wide association studies (GWAS) and post-mortem brain (PMB) analyses represents a transformative approach in neuroscience research, particularly for elucidating the mechanisms of complex neurodegenerative and psychiatric disorders. This methodological synergy enables researchers to bridge the critical gaps between genetic risk associations, molecular pathways, and functional cellular phenotypes. Within this framework, the apolipoprotein E (APOE) gene serves as a paradigmatic example, with its isoforms (ε2, ε3, ε4) conferring differential risk for Alzheimer's disease (AD) and other neurodegenerative conditions. The ε4 allele is the strongest genetic risk factor for late-onset AD, while the ε2 allele appears protective [117] [118]. This technical guide provides a comprehensive framework for designing, executing, and interpreting studies that integrate these complementary approaches, with specific emphasis on APOE isoform research in hiPSC-derived neuronal models.
Scientific Rationale for Methodological Integration
Each methodological approach—hiPSC modeling, GWAS, and PMB analysis—offers distinct advantages and suffers from characteristic limitations that can be mitigated through strategic integration. GWAS identifies statistical associations between genetic variants and disease risk across large populations but provides limited insight into biological mechanisms or cell-type-specific effects [119] [120]. Post-mortem brain studies offer a direct window into the end-stage neuropathology of disease but cannot establish causality or separate primary from compensatory mechanisms [118]. hiPSC models enable the study of patient-specific genetic backgrounds in living human neurons and glia, allowing for controlled experimental manipulation and direct observation of cellular phenotypes; however, they typically reflect developmental or early pathological stages rather than mature disease states [121].
The convergence of these methods creates a powerful cyclical framework for scientific discovery: GWAS identifies risk loci, PMB analyses reveal associated molecular and cellular changes in affected tissue, and hiPSC models establish causal relationships and functional mechanisms in a human cellular context. For APOE research, this integration has been particularly fruitful, revealing isoform-specific effects on neuronal apoptosis, energy metabolism, endolysosomal function, and immune activation that would remain obscured by any single approach [117] [78] [26].
Methodological Foundations
Genome-Wide Association Studies (GWAS)
GWAS identifies genetic variants associated with diseases or traits by analyzing genome-wide single nucleotide polymorphisms (SNPs) in large case-control cohorts. Current standards for well-powered GWAS require sample sizes in the tens to hundreds of thousands to detect variants with small effect sizes typical for complex disorders [119]. For APOE-related research, special consideration must be given to the strong linkage disequilibrium in the APOE genomic region, which extends to adjacent genes like TOMM40, requiring sophisticated statistical approaches to dissect independent effects [118].
Key Analytical Methods:
- Stratified LD Score Regression (sLDSC): Tests for enrichment of heritability in specific functional categories or cell-type-specific gene sets [119].
- MAGMA (Multi-marker Analysis of GenoMic Annotation): Performs gene-based and gene-set analyses using GWAS summary statistics, testing for association between a set of genes and the phenotype of interest [120].
- Polygenic Risk Scoring (PRS): Calculates an individual's genetic liability for a trait by aggregating the effects of many risk-associated variants [121].
Post-Mortem Brain Studies
PMB research provides critical insights into the neuropathological endpoints of disease processes. For optimal molecular preservation, post-mortem intervals should be minimized (typically ≤8 hours) [118]. Regional specificity is essential, as pathological changes and gene expression patterns vary significantly across brain areas, with the temporal cortex and hippocampus being particularly relevant for AD research [118] [122].
Advanced PMB Methodologies:
- Single-nucleus RNA sequencing (snRNA-seq): Enables transcriptomic profiling at single-cell resolution, revealing cell-type-specific changes in gene expression [122].
- Proteomic profiling: Mass spectrometry-based approaches quantify protein abundance and post-translational modifications in PMB tissue [26].
- Multiplexed immunofluorescence: Allows simultaneous visualization of multiple protein markers within their spatial context, preserving architectural information [122].
hiPSC-Derived Neural Models
hiPSCs are generated through reprogramming of somatic cells (typically fibroblasts or blood cells) using defined factors, then differentiated into specific neural lineages through established protocols [123]. For APOE research, both neuronal and glial differentiation are critical, as APOE is primarily expressed by astrocytes in the brain but also impacts neuronal function [78].
Essential Differentiation Protocols:
- Cortical neuronal differentiation: Generates excitatory neurons resembling those in the cerebral cortex, vulnerable in AD [117].
- Oligodendrocyte differentiation: Enables study of myelination processes, relevant for both AD and schizophrenia research [120].
- Astrocyte differentiation: Critical for APOE studies, as astrocytes are the primary source of APOE in the brain [78].
Experimental Design Considerations:
- Isogenic controls: CRISPR/Cas9 genome editing to generate APOE-isogenic lines (ε2/ε2, ε3/ε3, ε4/ε4) on identical genetic backgrounds, controlling for confounding genetic variation [78] [123].
- Maturation state: Extended differentiation periods (90-120 days) or pro-maturation factors may be required to observe age-associated phenotypes [10].
- Multi-lineage co-cultures: Better model cell-cell interactions than monocultures [122].
Integrated Analytical Frameworks
Trait-Cell Type Mapping Strategies
Two complementary computational frameworks integrate GWAS with single-cell transcriptomic data to identify disease-relevant cell types:
Table 1: Comparison of Trait-Cell Type Mapping Strategies
| Strategy | Description | Key Methods | Advantages | Limitations |
|---|---|---|---|---|
| SC-to-GWAS | Identifies specifically expressed genes (SEGs) for cell types, then tests for GWAS enrichment | Cepo→sLDSC, Cepo→MAGMA-GSEA | Robust statistical framework, controls for background enrichment | Dependent on SEG quality, may miss subtle effects |
| GWAS-to-SC | Starts with trait-associated genes, computes disease relevance scores per cell based on expression | mBAT-combo→scDRS | Direct integration at single-cell level, captures coordinated expression | Sensitive to gene list quality, may be confounded by technical variation |
The Cepo algorithm for identifying SEGs has demonstrated superior performance in trait-cell type mapping compared to other metrics, despite not necessarily ranking classical marker genes highest [119]. This suggests that effective mapping requires gene sets that capture broader functional specialization beyond canonical markers.
Cross-Species Validation
Mouse scRNA-seq data can provide initial insights for trait-cell type mapping, with validation in human datasets being essential for biological relevance [119]. Consistency between species increases confidence in identified associations, while discrepancies highlight species-specific biology.
Multimodal Data Integration
Advanced statistical methods including multi-omics factor analysis, integrative non-negative matrix factorization, and neural network-based approaches enable simultaneous analysis of GWAS, transcriptomic, proteomic, and epigenetic datasets to identify coherent biological modules across data types [26].
Experimental Findings in APOE Research
APOE Isoform-Specific Cellular Phenotypes in hiPSC Models
hiPSC studies have revealed numerous APOE isoform-dependent effects in human neurons and glia:
Table 2: APOE Isoform-Specific Phenotypes in hiPSC-Derived Neural Models
| Phenotype Category | APOE2 Effect | APOE3 Effect | APOE4 Effect | Study System |
|---|---|---|---|---|
| Neuronal Apoptosis | Significant protection against H2O2-induced apoptosis [117] | Moderate protection against H2O2-induced apoptosis [117] | No protective effect; higher concentrations toxic [117] | iPSC-derived cortical neurons |
| Energy Metabolism | Baseline mitochondrial ATP production [78] | Baseline mitochondrial ATP production [78] | Enhanced mitochondrial ATP production and basal respiration [78] | APOE-isogenic iN cells |
| Endolysosomal Function | Normal degradative ability [10] | Normal degradative ability [10] | Reduced degradative ability with prolonged culture; cholesterol accumulation [10] | Primary neurons from ApoE-targeted mice |
| Signaling Pathways | Regulates Akt/FoxO3a/Bim signaling under oxidative stress [117] | Regulates Akt/FoxO3a/Bim signaling under oxidative stress [117] | Deficient regulation of Akt/FoxO3a/Bim pathway [117] | iPSC-derived cortical neurons |
Molecular Signatures Across Compartments
Large-scale proteomic studies have identified an APOE ε4-associated signature consistent across brain tissue, cerebrospinal fluid (CSF), and plasma, characterized by pro-inflammatory immune pathways and enrichment in monocytes, T cells, and natural killer cells [26]. This signature appears independent of specific proteinopathies (amyloid-β, tau, TDP-43, α-synuclein), suggesting APOE4 creates a general vulnerability state rather than specifically driving one pathology.
Cell-Type-Specific Transcriptomic Changes
snRNA-seq of PMB tissue reveals that AD-associated transcriptomic changes are highly APOE genotype-dependent [122]:
- APOE2 carriers: Upregulated synaptic and myelination pathways despite AD pathology, preserving synapses and myelin at protein level
- APOE3 homozygotes: Downregulated synaptic and myelination pathways, with reduced corresponding proteins
- APOE4 carriers: Complex pattern with reduced synaptic pathways but upregulated myelination pathways in oligodendrocytes, yet with variable protein-level effects
Technical Protocols
Generation of APOE-Isogenic hiPSC Lines
CRISPR/Cas9 Genome Editing Protocol:
- Design gRNAs targeting sequences flanking the APOE coding region or specific SNP locations
- Electroporate hiPSCs with Cas9-gRNA ribonucleoprotein complex and donor template containing desired APOE allele
- Isolate single-cell clones and expand for genotyping
- Validate correct editing through Sanger sequencing, karyotyping, and pluripotency marker staining
- Differentiate multiple edited clones to neural lineages to confirm consistent phenotype [78] [123]
hiPSC-Derived Cortical Neuron Differentiation
Protocol for Apoptosis Studies:
- Maintain hiPSCs in mTeSR or Essential 8 medium on Matrigel-coated plates
- Neural induction using dual SMAD inhibition (LDN193189, SB431542) for 10-12 days
- Pattern toward cortical fate using retinoic acid and patterning factors
- Expand neural progenitor cells in FGF2-containing medium
- Differentiate for 45-60 days in neurobasal medium with BDNF, GDNF, and cAMP
- Treat with recombinant APOE isoforms (0-100 nM) for 24 hours before H2O2 challenge (50-200 μM, 24 hours) [117]
Functional Assays for APOE Isoform Effects
Neuronal Apoptosis Assessment:
- Quantify activated caspase-3/7 using luminescent assays
- Analyze DNA fragmentation via TUNEL staining
- Assess mitochondrial membrane potential with TMRE or JC-1 dyes
- Measure Annexin V/propidium iodide staining by flow cytometry [117]
Metabolic Phenotyping:
- Measure mitochondrial respiration using Seahorse XF Analyzer
- Quantify ATP production rates (glycolytic vs. mitochondrial)
- Assess mitochondrial content and morphology via MitoTracker staining and electron microscopy [78]
Endolysosomal Function:
- Evaluate endosomal morphology using EEA1 and Rab7 immunostaining
- Assess lysosomal proteolysis with DQ-BSA substrate
- Measure cholesterol accumulation via filipin staining [10]
Visualization of Experimental Workflows and Signaling Pathways
Integrated APOE Research Workflow
Integrated APOE Research Workflow Diagram
APOE Isoform-Specific Signaling in Neuronal Apoptosis
APOE Signaling in Neuronal Apoptosis
Research Reagent Solutions
Table 3: Essential Research Reagents for APOE-hiPSC Studies
| Reagent Category | Specific Examples | Application | Key Considerations |
|---|---|---|---|
| hiPSC Lines | APOE-isogenic hiPSCs (ε2/ε2, ε3/ε3, ε4/ε4); Patient-derived hiPSCs from genetically stratified cohorts | All functional studies | Verify pluripotency; use multiple clones per genotype; monitor karyotypic stability |
| Differentiation Kits | Commercial neural induction kits; Defined media components (BDNF, GDNF, NT-3, cAMP) | Generation of specific neural cell types | Batch consistency; use same differentiation lot across experiments |
| APOE Proteins | Recombinant human ApoE isoforms (E2, E3, E4); Lipidated ApoE preparations | Treatment studies to isolate isoform effects | Ensure proper lipidation state; validate protein activity and purity |
| Antibodies | Anti-ApoE (isoform-specific); Neural markers (MAP2, Tuj1); Glial markers (GFAP, S100β); Synaptic markers (PSD95, Synapsin) | Immunocytochemistry, Western blot | Validate specificity for intended applications; optimize working concentrations |
| Assay Kits | Caspase-3/7 activity assays; Mitochondrial stress test kits; Lysosomal function probes | Functional phenotyping | Establish baseline ranges for each hiPSC line; include relevant controls |
| CRISPR Tools | Cas9 nucleases; gRNAs targeting APOE locus; HDR templates with desired alleles | Isogenic line generation | Verify complete sequencing of edited region; screen for off-target effects |
Interpretation Guidelines and Limitations
Contextualizing hiPSC Findings
hiPSC-derived neural models typically reflect fetal or early postnatal developmental stages rather than mature adult brain tissue [121]. This limitation is particularly relevant for age-associated disorders like AD, though extended culture periods, pro-aging factors, and genetic aging acceleration strategies can partially address this concern. Observations in hiPSC models should be interpreted as revealing predisposition mechanisms rather than modeling full disease states.
Reconciling Discrepant Findings
Discrepancies between hiPSC, PMB, and animal model findings should be carefully analyzed rather than dismissed. For example, APOE4-associated metabolic enhancements observed in hiPSC-derived neurons [78] might represent early compensatory mechanisms that precede eventual metabolic decline in aged brain tissue. Temporal dynamics of phenotypic emergence must be considered when integrating findings across experimental systems.
Statistical Considerations
Appropriate sample sizes for hiPSC studies must account for both inter-individual and intra-clonal variability. For isogenic comparisons, a minimum of 3-5 independent clones per genotype is recommended, with biological replicates from different differentiations. Power calculations should be based on pilot studies of the specific phenotypic assays being employed.
The integration of hiPSC models with GWAS and PMB analyses represents a powerful framework for elucidating the functional mechanisms underlying genetic associations in neurological and psychiatric disorders. The APOE paradigm demonstrates how this multidisciplinary approach can reveal isoform-specific effects on diverse cellular processes including apoptosis regulation, energy metabolism, immune activation, and endolysosomal function. Future methodological advances will likely include improved maturation of hiPSC-derived neural cells, more sophisticated multi-lineage co-culture systems, and enhanced computational methods for cross-modal data integration. This integrated approach promises to accelerate the translation of genetic discoveries into mechanistic insights and ultimately, targeted therapeutic strategies for neurodegenerative disorders.
Conclusion
Human iPSC-based modeling has fundamentally advanced our understanding of APOE isoform-specific effects in Alzheimer's disease pathogenesis. The consistent findings across multiple laboratories—demonstrating APOE4-associated impairments in neuronal support, synaptogenesis, amyloid-β clearance, and blood-brain barrier function—provide a robust platform for therapeutic development. The ability to recapitulate key features of AD pathology in isogenic human cell systems offers unprecedented opportunities for drug screening and personalized medicine approaches. Future research should focus on developing more complex multicellular models, including brain organoids and microfluidic systems, to better capture the interplay between different cell types in the brain. Additionally, longitudinal studies tracking APOE-related changes throughout neuronal maturation and aging will be crucial for understanding the progressive nature of AD. These hiPSC-based approaches hold particular promise for developing genotype-stratified therapies that could fundamentally alter how we treat Alzheimer's disease based on an individual's APOE profile.
References
- 1. Alzheimer's genes: Are you at risk? [https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers-genes/art-20046552]
- 2. Apolipoprotein E and Alzheimer disease: risk, mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3726719/]
- 3. Current insights into apolipoprotein E and the immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11578782/]
- 4. Apolipoprotein E in Alzheimer's disease [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00843-y]
- 5. 2: protective APOE and therapeutic implications for... mechanism [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-020-00413-4]
- 6. Emerging hiPSC Models for Drug Discovery in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8347370/]
- 7. Alzheimer's Disease Genetic Risk Factor APOE-ε4 Also Affects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5839141/]
- 8. Apolipoprotein E in synaptic plasticity and Alzheimer's disease... [https://pubmed.ncbi.nlm.nih.gov/25358504/]
- 9. 4 Regulates APOE Function by... | Research Square Synaptic [https://www.researchsquare.com/article/rs-380304/v1]
- 10. Neuronal endolysosomal alterations induced by ... [https://www.sciencedirect.com/science/article/pii/S0021925825023294]
- 11. Apolipoprotein E: Structure and Function in Lipid Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4253862/]
- 12. Apolipoprotein E [https://en.wikipedia.org/wiki/Apolipoprotein_E]
- 13. ApoE in Alzheimer's disease - Molecular Neurodegeneration [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-022-00574-4]
- 14. the role of apolipoprotein E in brain energy metabolism ... [https://www.nature.com/articles/s41398-025-03550-w]
- 15. APOE4 causes widespread molecular and cellular alterations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6023751/]
- 16. Evolution of human apolipoprotein E (APOE) isoforms [https://www.sciencedirect.com/science/article/pii/S1568163717300806]
- 17. Structural differences between apoE3 and apoE4 may be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3384159/]
- 18. The multifaceted roles of apolipoprotein E4 in Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238274/]
- 19. APOE4 exacerbates synapse loss and neurodegeneration ... [https://www.nature.com/articles/s41467-020-19264-0]
- 20. Multi-functional role of apolipoprotein E in ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1535280/full]
- 21. APOE R176C (ApoE2) [https://www.alzforum.org/mutations/apoe-r176c-apoe2]
- 22. Rethinking Alzheimer's: Why this common gene variant is bad ... [https://med.stanford.edu/news/insights/2025/09/rethinking-alzheimers-gene-variant-apoe4.html]
- 23. The role of APOE ε4 in modulating the relationship ... [https://pubmed.ncbi.nlm.nih.gov/41083880]
- 24. APOE2 reduces risk of Alzheimer's disease by protection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399190/]
- 25. Why APOE4 raises Alzheimer's risk [https://www.mdc-berlin.de/news/press/why-apoe4-raises-alzheimers-risk]
- 26. APOE ε4 carriers share immune-related proteomic ... [https://www.nature.com/articles/s41591-025-03835-z]
- 27. APOE4 to APOE2 allelic switching in mice improves ... [https://www.nature.com/articles/s41593-025-02094-y]
- 28. The APOE isoforms differentially shape the transcriptomic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106835/]
- 29. Apolipoprotein E: from lipid transport to neurobiology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3022415/]
- 30. Apolipoprotein E (APOE) regulates the transport of ... [https://www.sciencedirect.com/science/article/pii/S0021925825026304]
- 31. Apolipoprotein E in Alzheimer's disease: molecular insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12023563/]
- 32. APOE2: protective mechanism and therapeutic implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7640652/]
- 33. Co-aggregation with Apolipoprotein E modulates the ... [https://www.nature.com/articles/s41467-024-49028-z]
- 34. Binding of Apolipoprotein E Inhibits the Oligomer Growth of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636854/]
- 35. Soluble apoE/Aβ complex: mechanism and therapeutic target ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/1750-1326-9-2]
- 36. Apolipoprotein E (APOE) Isoforms and Neurobiology of ... [https://link.springer.com/rwe/10.1007/978-3-031-73368-0_155]
- 37. REVIEW Apolipoprotein E and Alzheimer's disease [https://www.sciencedirect.com/science/article/pii/S2211383521003944]
- 38. APOE ε4 is associated with decreased synaptic density in ... [https://pubmed.ncbi.nlm.nih.gov/38477490/]
- 39. associations with Aβ, tau, synaptic proteins and APOE ε4 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459057/]
- 40. associations with Aβ, tau, synaptic proteins and APOE ε4 [https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-025-00508-2]
- 41. APOE mediated neuroinflammation and neurodegeneration in ... [https://pubmed.ncbi.nlm.nih.gov/35232622/]
- 42. Review APOE mediated neuroinflammation and ... [https://www.sciencedirect.com/science/article/pii/S1044532322000112]
- 43. APOE4 impacts cortical neurodevelopment and alters network ... [https://pubmed.ncbi.nlm.nih.gov/40541173/]
- 44. The APOE isoforms differentially shape the transcriptomic ... [https://www.nature.com/articles/s41467-025-60099-4]
- 45. Generation of Isogenic Human iPS Cell Line Precisely ... [https://pubmed.ncbi.nlm.nih.gov/26059412/]
- 46. Gain of toxic Apolipoprotein E4 effects in Human iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5948154/]
- 47. Neuronal endolysosomal alterations induced by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357307/]
- 48. Systematic gene tagging using CRISPR / Cas in human stem cells to... 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC5638588/]
- 49. an EML4-ALK fusion NSCLC cell line [https://www.nature.com/articles/d42473-019-00011-z]
- 50. APOE ε4/ε4 diminishes neurotrophic function of human iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5886091/]
- 51. APOE4 Causes Widespread Molecular and Cellular ... [https://www.sciencedirect.com/science/article/pii/S0896627318303805]
- 52. Generation and validation of APOE knockout human iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8190508/]
- 53. APOE deficiency impacts neural differentiation and cholesterol ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03444-y]
- 54. iPS Cell Differentiation into Brain Microvascular Endothelial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10285505/]
- 55. A novel human induced pluripotent stem cell blood-brain ... [https://www.nature.com/articles/s41598-018-19522-8]
- 56. A Simplified, Fully Defined Differentiation Scheme for ... [https://www.sciencedirect.com/science/article/pii/S2213671119301754]
- 57. Relationship Between Amyloid-β Deposition and Blood– ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2021.695479/full]
- 58. Mechanobiology of the blood-brain barrier during ... [https://www.nature.com/articles/s41467-025-61888-7]
- 59. Apolipoprotein E isoforms and lipoprotein metabolism [https://pubmed.ncbi.nlm.nih.gov/25328986/]
- 60. Cutting-edge advances in modeling the blood–brain barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373415/]
- 61. iPSC-derived blood-brain barrier modeling reveals APOE ... [https://pubmed.ncbi.nlm.nih.gov/39394110/]
- 62. Regulation of synaptic function and lipid metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296456/]
- 63. Astrocytic and Neuronal Apolipoprotein E Isoforms ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.734001/full]
- 64. Neuronal Lipid Metabolism: Multiple Pathways Driving ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2018.00010/full]
- 65. A human-derived neurovascular unit in vitro model to study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9762047/]
- 66. Human isogenic cells of the neurovascular unit exert ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-023-00471-y]
- 67. In Vitro Modeling of the Neurovascular Environment by ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0106346]
- 68. iPSC-derived blood-brain barrier modeling reveals APOE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11468049/]
- 69. Microfluidic models of the neurovascular unit: a translational ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-023-00490-9]
- 70. Implementation of the neuro-glia-vascular unit through co ... [https://www.sciencedirect.com/science/article/pii/S0165027023002480]
- 71. Article ApoE4 disrupts intracellular trafficking and iron ... [https://www.sciencedirect.com/science/article/pii/S2213671125002115]
- 72. Apolipoprotein E as a Therapeutic Target in Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC5526196/]
- 73. A logical network-based drug-screening platform ... - Nature [https://www.nature.com/articles/s41467-020-20440-5]
- 74. High-content screening in drug discovery: A brief guide [https://alitheagenomics.com/blog/high-content-screening-in-drug-discovery-a-brief-guide]
- 75. A small molecule ApoE4-targeted therapeutic candidate ... [https://www.nature.com/articles/s41598-018-35687-8]
- 76. APOE genotype-dependent differences in human astrocytic ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1603657/full]
- 77. APOE genotype-dependent differences in human astrocytic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434100/]
- 78. APOE4 Increases Energy Metabolism in APOE-Isogenic ... [https://pubmed.ncbi.nlm.nih.gov/39056789/]
- 79. iPSC-derived blood-brain barrier modeling reveals APOE ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-024-00580-2]
- 80. Using human induced pluripotent stem cells (hiPSCs) to ... [https://www.sciencedirect.com/science/article/pii/S0969996120300632]
- 81. Pro-maturational Effects of Human iPSC-Derived Cortical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7363746/]
- 82. Comparison of two protocols for the generation of iPSC ... [https://biologicalproceduresonline.biomedcentral.com/articles/10.1186/s12575-023-00218-x]
- 83. A functional hiPSC-cortical neuron differentiation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8758945/]
- 84. A simplified protocol for differentiation of ... [https://www.nature.com/articles/mp201756]
- 85. Key considerations for ELISA-based quantification of ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1645952/full]
- 86. Key considerations for ELISA-based quantification of diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521455/]
- 87. Rapid amyloid - β clearance and cognitive recovery through multivalent... [https://www.nature.com/articles/s41392-025-02426-1?error=cookies_not_supported&code=e283f8a0-36f7-4b83-b945-41400dec70ae]
- 88. Comparison of automated quantification of amyloid ... [https://www.nature.com/articles/s41598-023-36986-5]
- 89. Unpredictable Effects of the Genetic Background ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6829147/]
- 90. Generation of Isogenic Pluripotent Stem Cells Differing ... [https://www.sciencedirect.com/science/article/pii/S0092867411006611]
- 91. Cell-type-specific regulation of APOE and CLU levels in ... [https://www.sciencedirect.com/science/article/pii/S2211124723010057]
- 92. ApoE4 requires lipidation enhancement to resolve cellular ... [https://www.nature.com/articles/s41598-025-96531-4]
- 93. The Neurolipid Atlas: a lipidomics resource for ... [https://www.nature.com/articles/s42255-025-01365-z]
- 94. 3D in vitro blood–brain barrier models - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537694/]
- 95. A blood-brain barrier overview on structure, function, impairment, and... [https://pubmed.ncbi.nlm.nih.gov/33208141/]
- 96. Advances in 3D bioprinting for modeling the blood-brain ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1703403/full]
- 97. Blood-Brain Barrier (BBB) Permeability and Transport ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7889748/]
- 98. Recent advances in 3D models for multiparametric blood ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d4tb02499k]
- 99. Blood-brain barrier (BBB) permeability assay. [https://bio-protocol.org/exchange/minidetail?id=823573&type=30]
- 100. Launch of the CEN Workshop 'Guidelines for Blood-Brain ... [https://www.cencenelec.eu/news-events/news/2025/workshop/2025-05-20-biscuit/]
- 101. APOE C130R (ApoE4) [https://www.alzforum.org/mutations/apoe-c130r-apoe4]
- 102. Isoform-Specific Effects of Apolipoprotein E on Markers ... [https://www.mdpi.com/1467-3045/43/1/18]
- 103. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 104. Apolipoprotein E ε4 modulates astrocyte neuronal support ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10903110/]
- 105. APOE4 drives transcriptional heterogeneity and maladaptive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9934552/]
- 106. APOE4 impacts cortical neurodevelopment and alters network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277819/]
- 107. Astrocyte induction of disease-associated microglia is ... [https://www.sciencedirect.com/science/article/pii/S2211124725005480]
- 108. Review Apolipoprotein E isoform-dependent effects on the ... [https://www.sciencedirect.com/science/article/abs/pii/S1388198121001086]
- 109. Human apoE isoforms differentially regulate brain amyloid-β ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3192364/]
- 110. apoE isoform–specific disruption of amyloid β peptide ... [https://www.jci.org/articles/view/36663]
- 111. apoE isoform–specific disruption of amyloid β peptide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2582453/]
- 112. Review Apolipoprotein E in lipid metabolism and ... [https://www.sciencedirect.com/science/article/pii/S1043276023000929]
- 113. Apolipoprotein E regulates lipid metabolism and α-synuclein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8500881/]
- 114. APOE2 mitigates disease-related phenotypes in an isogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8501163/]
- 115. Analysis of early effects of human APOE isoforms on ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01832-2]
- 116. Human ApoE Isoforms Differentially Modulate Brain Glucose ... [https://pubmed.ncbi.nlm.nih.gov/29967007/]
- 117. Isoform-Specific Effects of Apolipoprotein E on Hydrogen ... [https://pubmed.ncbi.nlm.nih.gov/34769014/]
- 118. APOE mRNA and Protein Expression in Postmortem Brain are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2829359/]
- 119. Benchmarking methods integrating GWAS and single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12140538/]
- 120. iPSC-modelling reveals genetic associations and ... [https://www.nature.com/articles/s41398-025-03509-x]
- 121. New considerations for hiPSC-based models of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6109625/]
- 122. APOE genotype determines cell-type-specific pathological ... [https://www.sciencedirect.com/science/article/abs/pii/S0896627325001357]
- 123. Integration of CRISPR-engineering and hiPSC-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7484226/]