Modeling Amyloid-Beta Deposition with iPSC Technology: From Disease Mechanisms to Therapeutic Discovery
Human induced pluripotent stem cells (iPSCs) have revolutionized the study of Alzheimer's disease (AD), enabling researchers to model amyloid-beta (Aβ) deposition in a patient-specific context.
Modeling Amyloid-Beta Deposition with iPSC Technology: From Disease Mechanisms to Therapeutic Discovery
Abstract
Human induced pluripotent stem cells (iPSCs) have revolutionized the study of Alzheimer's disease (AD), enabling researchers to model amyloid-beta (Aβ) deposition in a patient-specific context. This article explores how iPSC-derived neurons, glia, and 3D organoids recapitulate key aspects of Aβ pathology, including the formation of seeding-active oligomers and plaque-associated axonal spheroids. We detail the integration of CRISPR/Cas9 gene editing for manipulating AD-related genes and the use of these models for high-throughput drug screening. The content also addresses critical challenges in model fidelity and standardization, while highlighting the validation of iPSC findings against human postmortem data. This resource provides a comprehensive overview for scientists and drug development professionals seeking to leverage iPSC technology for AD research and therapy development.
Understanding Aβ Seeds and Early Deposition Mechanisms in Patient-Specific Models
The Central Role of Aβ Seeds in Alzheimer's Pathogenesis
For over three decades, the amyloid cascade hypothesis has positioned amyloid-β (Aβ) at the center of Alzheimer's disease (AD) pathogenesis, though not without controversy [1] [2]. Recent clinical successes with Aβ-targeting immunotherapies have revitalized this hypothesis, confirming Aβ's crucial role in AD progression [1] [2]. However, these treatments provide only modest clinical benefits, supporting a two-stage disease model: an early phase driven primarily by Aβ aggregation, followed by a later phase that progresses somewhat independently of Aβ accumulation [1]. This understanding has shifted research focus from terminal amyloid plaques to Aβ seeds—highly bioactive, prion-like assemblies that initiate and propagate the pathogenic cascade [1]. These seeds represent the smallest pathogenic units in Aβ aggregation, acting as templates that corrupt native Aβ monomers into pathological aggregates [1]. Evidence now confirms that Aβ seeds can transmit between humans through medical procedures, raising both therapeutic potential and biosafety concerns [1] [3]. This whitepaper examines the central role of Aβ seeds in Alzheimer's pathogenesis, with particular emphasis on how induced pluripotent stem cell (iPSC) technologies are revolutionizing our ability to study these pathogenic entities.
Molecular Nature and Mechanisms of Aβ Seeds
The Biochemical Identity of Aβ Seeds
The precise molecular nature of Aβ seeds remains elusive, representing a significant challenge in the AD field [1]. Multiple Aβ aggregate forms demonstrate seeding capability, though with varying efficiency. Intracerebral Aβ aggregation can be induced by:
- Small, soluble Aβ seeds from brain parenchyma
- Aβ seeds isolated from various cellular compartments and intracellular membranes
- Purified Aβ fibrils from AD brain tissue
- Aggregated synthetic Aβ peptides [1]
While soluble oligomeric Aβ species appear to have particularly high seeding potency, no single specific conformation can currently be assigned to Aβ seeds [1]. What distinguishes these seeds is their remarkable resilience—they can persist in the living brain for months following exogenous injection, successfully evading endogenous degradation and clearance mechanisms [1]. This persistence underscores their pathogenic significance and represents a key therapeutic challenge.
Prion-like Propagation Mechanisms
Aβ misfolding propagates through the brain via a prion-like mechanism where seeding-active nuclei template the misfolding and aggregation of naïve Aβ monomers into higher aggregation states [1]. This process follows a nucleation-dependent polymerization model beginning with a lag phase during which seeding-active nuclei form, though detectable Aβ deposition has not yet occurred [1]. Consistent with this model, pre-amyloid Aβ seeds have been detected in transgenic mouse models overexpressing amyloid precursor protein (APP) [1]. The critical importance of targeting these early seeds is demonstrated by experiments showing that acute immunotherapy in pre-depositing APP transgenic mice significantly reduces Aβ deposition and associated neurodegeneration later in life [1].
Table 1: Characteristics of Different Aβ Aggregates in Alzheimer's Pathogenesis
| Aggregate Type | Size/State | Seeding Potency | Detection Methods | Therapeutic Relevance |
|---|---|---|---|---|
| Aβ Seeds | Small, soluble oligomers | Very high | PMCA, RT-QuIC, seeding assays | Primary target for preventive therapies |
| Soluble Oligomers | Medium soluble aggregates | High | MSD immunoassays, Western blot | Target of Lecanemab immunotherapy |
| Insoluble Fibrils | Large aggregates | Moderate | Amyloid PET, immunohistochemistry | Target of Donanemab immunotherapy |
| Mature Plaques | Terminal deposits | Low | Histology, amyloid PET | Late-stage pathological hallmark |
Seeding Activity Across Disease Stages
Aβ aggregates from early amyloid stages demonstrate significantly higher seeding potency compared to those from later stages [1]. The seeding-active oligomers crucial for initial Aβ aggregation are termed "on-pathway" to distinguish them from "off-pathway" oligomers not involved in the aggregation process [1]. Importantly, soluble Aβ oligomers are present in both brain tissue and cerebrospinal fluid of early-stage AD patients, though their seeding activity at this early stage requires further characterization [1]. The heightened seeding activity of early aggregates may explain why therapeutic interventions targeting Aβ are most effective when administered early in the disease course.
Modeling Aβ Pathology Using Induced Pluripotent Stem Cells
Fundamentals of iPSC-Based AD Modeling
iPSC technology enables generation of human neurons containing the precise genome of cell donors, permitting creation of disease models from individuals with disease-associated genotypes [4]. This approach offers several key advantages:
- Provides unlimited supply of human neurons and glia expressing endogenous levels of disease proteins
- Enables study of patient-specific genetic backgrounds without overexpression artifacts
- Allows differentiation into specific vulnerable neuronal subtypes and glial cells
- Facilitates investigation of early pathogenic events in human cells [4] [5]
However, limitations exist, particularly regarding cellular maturity. The reprogramming process erases epigenetic signatures of aging—a significant consideration for age-related diseases like AD [4]. Despite this, iPSCs remain the only means to obtain unlimited patient-specific neurons and glia for mechanistic studies.
Recapitulating AD Pathologies in iPSC-Derived Models
iPSC-derived neurons from both familial and sporadic AD patients successfully recapitulate key disease pathologies. Neurons derived from fAD (PSEN1 mutations) and sAD patients show:
- Increased phosphorylation of TAU protein at multiple sites
- Elevated extracellular Aβ1-40 and Aβ1-42 levels
- Significantly increased Aβ1-42/Aβ1-40 ratios in fAD lines
- Increased active GSK3B, a physiological TAU kinase
- Significant upregulation of APP synthesis and cleavage
- Elevated sensitivity to oxidative stress induced by amyloid oligomers [5]
Notably, one of the first studies comparing fAD and sAD iPSC-derived neurons found no evident phenotypic differences except in secreted Aβ1-40 levels, demonstrating iPSC technology's suitability for modeling both AD forms [5].
Advanced 3D Organoid Models
Recent advances have developed more physiologically relevant vascularized neuroimmune organoids containing multiple cell types affected in AD brains: neurons, microglia, astrocytes, and blood vessels [6]. These complex models successfully recapitulate multiple AD pathologies when exposed to sAD brain extracts, including:
- Aβ plaque-like aggregates
- Tau tangle-like aggregates
- Neuroinflammation
- Elevated microglial synaptic pruning
- Synapse and neuronal loss
- Impaired neural network activity [6]
Importantly, these pathologies manifest within four weeks of exposure to AD brain extracts, compared to the months required in conventional organoid models [6]. This accelerated timeline makes these models particularly valuable for therapeutic screening.
Experimental Systems for Investigating Aβ Seeds
Detection and Characterization Methods
Significant challenges exist in studying Aβ seeds due to their presence at levels below detectability by routine methods [1]. Several specialized approaches have been developed:
Seeding Detection Assays:
- Protein Misfolding Cyclic Amplification (PMCA): Amplifies minute quantities of seeds to detectable levels
- Real-Time Quaking-Induced Conversion (RT-QuIC): Detects seeding activity through amyloid formation kinetics
- Transgenic Mouse Bioassays: Measure acceleration of amyloid pathology following inoculation with seed-containing extracts [1] [3]
Extraction Protocols: The method of Aβ extraction significantly impacts seeding activity. Gentle soaking protocols that minimize physical disruption produce "S extracts" containing readily diffusible Aβ species that demonstrate potent seeding activity and neuritotoxicity [3]. These extracts contain a broad range of Aβ assembly sizes and account for essentially all bioactivity present in homogenized extracts [3].
In Vivo Seeding Experiments
Animal studies demonstrate that intracerebral inoculation with Aβ-containing brain homogenates or extracts accelerates Aβ deposition in genetically modified mouse models [3]. Key findings include:
- A single inoculation with AD brain S extracts significantly perturbs learned behavior in AppNL-F/NL-F mice
- Accelerated cerebral amyloid deposition appears 10 months post-inoculation
- Accompanying pathologies include microgliosis, astrocytosis, neuronal dystrophy, and synaptic loss
- Control brain extracts induce none of these effects [3]
These results confirm that diffusible Aβ species from AD brains possess both acute toxicity and seeding activity that can be experimentally transmitted [3].
Table 2: Experimental Models for Studying Aβ Seeds
| Model System | Key Features | Applications | Limitations |
|---|---|---|---|
| iPSC-Derived 2D Neuronal Cultures | Patient-specific genetic background, human physiology | Mechanistic studies, high-throughput screening | Limited cellular complexity, immature phenotypes |
| Vascularized Neuroimmune Organoids | Multiple CNS cell types, 3D architecture, vascularization | Modeling complex pathologies, therapeutic testing | Technical complexity, variability between organoids |
| Transgenic Mouse Models | Intact brain environment, behavioral readouts | In vivo seeding studies, pathology progression | Species differences, overexpression artifacts |
| Biochemical Assays (RT-QuIC/PMCA) | High sensitivity, quantitative detection | Seed detection and quantification, strain characterization | Does not capture cellular context |
Therapeutic Implications and Future Directions
Targeting Aβ Seeds for Therapy
The central role of Aβ seeds in initiating pathogenesis makes them attractive therapeutic targets. Several approaches show promise:
Immunotherapies: Recent successes with anti-Aβ immunotherapies represent a significant milestone, though their mechanisms continue to be refined [2] [7]. Lecanemab preferentially binds soluble Aβ protofibrils, while Donanemab targets deposited plaques [1] [2]. The finding that acute immunotherapy in pre-depositing mice reduces later pathology suggests that early targeting of Aβ seeds may represent the optimal therapeutic strategy [1].
Small Molecule Inhibitors: Compounds like CT1812 show promise for treating multiple dementia types by displacing toxic protein aggregates (both Aβ and α-synuclein) from synapses [7]. Phase 2 trials are currently evaluating its efficacy in early AD patients [7].
Biosafety Considerations
The prion-like transmission of Aβ seeds raises important biosafety concerns. Evidence of iatrogenic cerebral Aβ pathology in humans has been reported following administration of cadaver-sourced human growth hormone or dura mater grafts containing Aβ [3]. These observations emphasize the need to prevent accidental transmissions via medical and surgical procedures and highlight the importance of appropriate safety protocols when handling seed-containing samples [1].
iPSC-Based Drug Discovery Platform
iPSC models are increasingly integrated into drug discovery pipelines. Several clinical trials have been initiated based on iPSC research findings, including trials of bosutinib, ropinirole, and ezogabine for ALS, and WVE-004 and BIIB078 for ALS/FTD [8]. The combination of iPSC models with targeted mass spectrometry provides unprecedented insights into protein regulation, including:
- Protein isoform expression
- Relative levels of cleavage fragments
- Aggregated species
- Functionally critical post-translational modifications [4]
This approach enables determination of how closely iPSC-derived models recapitulate disease profiles observed in human brain [4].
Experimental Protocols for Key Methodologies
Preparation of Diffusible Aβ-Enriched Extracts from Human Brain
Principle: Gently extract diffusible Aβ species from brain tissue while minimizing disruption of larger aggregates [3].
Procedure:
- Dissect gray matter and mince into small chunks using a McIlwain chopper
- Soak minced tissue in five volumes of ice-cold base artificial cerebrospinal fluid (aCSF) plus protease inhibitors at 4°C for 30 minutes with gentle mixing
- Centrifuge at 2,000 × g at 4°C for 10 minutes to remove cellular debris
- Collect upper 90% of supernatant and centrifuge at 200,000 × g for 110 minutes at 4°C
- Remove upper 90% of this second supernatant (designated as S extract)
- Dialyze against 100-fold excess fresh aCSF buffer with three changes over 72 hours using 2K MWCO dialysis cassettes
- Aliquot and store at -80°C until use
Validation: Characterize extracts for Aβ content using MSD immunoassays with m266 capture antibody and 2G3 detection antibody [3].
iPSC-Derived Neuronal Differentiation for AD Modeling
Principle: Generate cortical neurons from human iPSCs to study Aβ and tau pathology [5].
Procedure:
- Maintain iPSCs in pluripotency medium on feeder cells or Matrigel
- Induce neural differentiation using dual SMAD inhibition (SB43152 and Noggin)
- Pattern toward cortical fate using retinoid acid and Wnt inhibitors
- Expand neural progenitor cells (NPCs) in FGF2-containing medium
- Differentiate NPCs into mature cortical neurons by FGF2 withdrawal and addition of BDNF, GDNF, and cAMP
- Maintain neuronal cultures for 8-12 weeks to allow maturation and spontaneous pathology development
- Analyze cultures for AD pathologies:
- Extracellular Aβ levels by ELISA
- Tau phosphorylation by Western blotting
- Synaptic markers by immunocytochemistry
- Electrophysiological properties by multi-electrode arrays
Vascularized Neuroimmune Organoid Generation
Principle: Create 3D organoids containing neurons, microglia, astrocytes, and blood vessels for comprehensive AD modeling [6].
Procedure:
- Generate NPCs, primitive macrophage progenitors (PMPs), and vascular progenitors (VPs) from iPSCs
- Combine 30,000 NPCs, 12,000 PMPs, and 7,000 VPs to form organoids by spontaneous assembly
- Culture in proliferation medium with bFGF for 5 days to promote cellular expansion
- Transition to differentiation medium containing IL-34, VEGF, and neurotrophic factors
- Maintain organoids long-term (4+ weeks) with regular medium changes
- Treat with AD brain extracts to induce pathologies (typically 4-week exposure)
- Analyze resulting pathologies:
- Aβ and tau aggregates by immunohistochemistry
- Synaptic density by synaptophysin/PDS95 staining
- Microglial phagocytosis by synaptic marker internalization
- Neural network activity by calcium imaging
Essential Research Reagents and Tools
Table 3: Key Research Reagents for Investigating Aβ Seeds Using iPSC Models
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| iPSC Lines | fAD (PSEN1/APP mutations), sAD, isogenic controls | Disease modeling, genetic studies | Provide patient-specific genetic background for in vitro models |
| Differentiation Kits | Neural induction media, patterning factors | Generation of disease-relevant cell types | Direct pluripotent stem cell differentiation to neural lineages |
| Aβ Detection Antibodies | m266 (capture), 2G3 (detection), 4G8, 6E10 | Aβ quantification, plaque detection | Recognize specific Aβ epitopes in immunoassays and imaging |
| Tau Phospho-Antibodies | AT8 (pS202/pT205), AT100 (pT212/pS214) | Tau pathology assessment | Detect hyperphosphorylated tau species in pathological aggregates |
| Cell Type Markers | PAX6/NESTIN (NPCs), CD43/CD235 (PMPs), CD31 (endothelial) | Cell identity validation | Confirm specific cell populations in mixed cultures and organoids |
| Seeding Assay Components | Recombinant Aβ monomer, thioflavin T, reaction buffers | Aβ seed detection | Enable amplification and detection of minute seed quantities |
| Cytokines/Growth Factors | IL-34 (microglia survival), VEGF (vascularization), BDNF (neuronal maturation) | Specialized culture support | Maintain specific cell types in complex co-culture systems |
Visualizing Aβ Seed Pathogenesis and Research Workflows
Aβ Seed Pathogenesis Cascade
Figure 1: The central role of Aβ seeds in Alzheimer's disease pathogenesis. The cascade begins with amyloid precursor protein (APP) processing and Aβ monomer generation. Aβ seed formation represents a critical early event that enables prion-like spread throughout the brain, leading to oligomer formation, plaque deposition, and downstream pathological consequences including tau pathology, neuroinflammation, and synaptic dysfunction, ultimately resulting in neuronal loss.
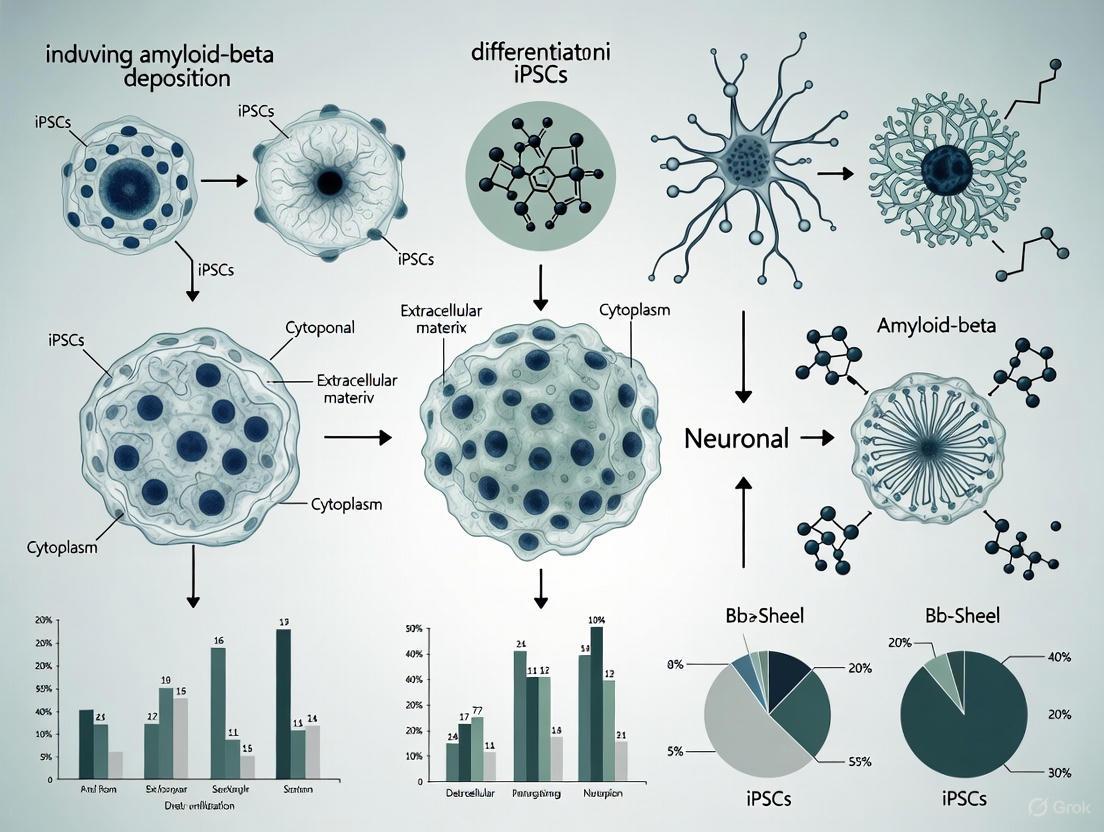
iPSC Modeling of Aβ Pathology
Figure 2: Experimental workflows for modeling Aβ seed pathology using iPSC-based systems. Two-dimensional models (top) follow a sequential process from iPSC generation through therapeutic screening. Three-dimensional vascularized neuroimmune organoid models (bottom) incorporate additional complexity including vascularization and multiple cell type integration, enabling more comprehensive pathology assessment following exposure to AD brain extracts containing Aβ seeds.
Aβ seeds represent the earliest detectable molecular drivers of Alzheimer's pathogenesis, acting as critical instigators of the destructive cascade that culminates in dementia. Their prion-like propagation mechanisms, remarkable resilience to degradation, and ability to transmit between individuals underscore their central role in disease initiation and progression. The emergence of sophisticated iPSC-based models—particularly vascularized neuroimmune organoids that recapitulate multiple AD pathologies within a human cellular environment—provides unprecedented opportunities to dissect seed-mediated pathogenesis and develop targeted therapeutic strategies. As research continues to elucidate the precise molecular nature of these enigmatic seeds and optimize human cellular models for their study, we move closer to effective interventions that can disrupt the earliest events in Alzheimer's pathogenesis, potentially preventing the devastating consequences of this disease.
iPSC Models for Studying Familial vs. Sporadic Alzheimer's Disease
Alzheimer's disease (AD) represents a profound public health challenge, with an estimated 7.1 million Americans currently living with symptoms and projections suggesting this will grow to 13.9 million by 2060 [7]. As the most common cause of dementia, AD pathology is characterized by the accumulation of amyloid-beta (Aβ) plaques and neurofibrillary tau tangles, leading to progressive cognitive decline [9]. Research has traditionally been hampered by models that fail to fully replicate human physiology and pathology. The advent of human induced pluripotent stem cell (iPSC) technology has revolutionized AD research by enabling the generation of patient-derived neural cells that recapitulate human-specific disease mechanisms [10] [11].
iPSCs are particularly valuable for modeling the distinct pathogenic processes underlying familial AD (FAD) and sporadic AD (SAD). FAD accounts for less than 1% of all AD cases and is caused by fully penetrant autosomal dominant mutations in genes such as APP, PSEN1, and PSEN2 [9] [11]. In contrast, SAD represents the vast majority of cases and involves complex interactions between genetic risk factors, aging, and environmental influences, with APOE ε4 being the strongest genetic risk factor, increasing late-onset AD risk by approximately three-fold for heterozygous carriers and 15-fold for homozygous carriers [9]. This technical guide examines how iPSC models are being leveraged to study amyloid-beta deposition across these AD forms, providing researchers with methodologies, applications, and future directions for this transformative technology.
Fundamental Differences Between Familial and Sporadic AD
The pathological distinction between FAD and SAD informs the design and interpretation of iPSC-based disease models. While both forms share hallmark Aβ and tau pathology, their underlying drivers and temporal progression differ significantly.
Table 1: Key Characteristics of Familial vs. Sporadic AD
| Characteristic | Familial AD (FAD) | Sporadic AD (SAD) |
|---|---|---|
| Prevalence | <1% of all cases [11] | >95% of all cases [9] |
| Age of Onset | Early-onset (<60 years) [11] | Late-onset (>60 years) [9] |
| Inheritance | Autosomal dominant | Complex, polygenic |
| Primary Genetic Drivers | Mutations in APP, PSEN1, PSEN2 [9] | APOE ε4 allele and numerous risk genes (TREM2, BIN1, CLU, etc.) [9] [11] |
| Aβ Pathology Mechanism | Increased Aβ42 production or Aβ42/40 ratio [12] [11] | Impaired Aβ clearance and multiple pathways [9] |
| iPSC Modeling Approach | Introduce known pathogenic mutations | Focus on risk variants and polygenic contributions |
FAD mutations directly alter Aβ processing, typically by increasing the production of the more amyloidogenic Aβ42 peptide or the Aβ42/Aβ40 ratio [11]. The seminal iPSC study of FAD by Yagi et al. demonstrated that neurons derived from patients with PS1 (A246E) and PS2 (N141I) mutations showed increased Aβ42 secretion, effectively recapitulating the molecular pathogenesis observed in patients [12]. In contrast, SAD involves more complex mechanisms, with genetic risk factors like APOE4 potentially impairing Aβ clearance rather than production [9]. Many SAD risk genes, including TREM2, CD33, and ABCA7, are highly expressed in glial cells (microglia and astrocytes), highlighting the importance of non-neuronal cells in SAD pathogenesis [9] [11].
iPSC Modeling Strategies for Alzheimer's Disease
Core iPSC Generation and Differentiation
The fundamental workflow for creating iPSC-based AD models begins with somatic cell reprogramming, followed by differentiation into disease-relevant neural cell types.
The core reprogramming process typically uses the OSKM factors (Oct4, Sox2, Klf4, and c-Myc) to convert patient somatic cells into iPSCs [11]. These iPSCs can then be differentiated into various neural lineages using established protocols. Critical advancements include improved differentiation methods for generating human astrocytes and microglia, which better recapitulate human-specific biology compared to rodent cells [11]. The National Alzheimer's Disease iPS Cell Bank managed by the UCI Alzheimer's Disease Research Center exemplifies institutional efforts to share these critical resources across the research community [13].
Genetic Engineering with CRISPR/Cas9
CRISPR/Cas9 gene editing has become an indispensable tool for creating precise iPSC models of AD, particularly for generating isogenic control lines where disease-causing mutations are introduced into healthy iPSCs or corrected in patient-derived iPSCs [14]. This powerful approach enables researchers to study the specific effects of genetic alterations against identical genetic backgrounds.
The CRISPR/Cas9 system consists of two main components: a Cas9 nuclease that cleaves target DNA and a single-guide RNA (sgRNA) that directs Cas9 to specific genomic sequences [14]. When applied to AD research, this technology enables targeted manipulation of pathogenic loci in genes such as APP, PSEN1, PSEN2, and APOE [14]. For example, Kwart et al. used CRISPR/Cas9 to alter Aβ production in mouse models with mutant APP, successfully reducing toxic Aβ peptides without impairing brain function [14]. The technology also facilitates multiplex gene editing by combining multiple sgRNAs in a single experiment, allowing simultaneous investigation of several genetic factors involved in AD pathogenesis [14].
Experimental Models and Methodologies
2D Monoculture and Co-culture Systems
Initial iPSC-based AD models primarily utilized 2D monocultures of neurons to study cell-autonomous disease mechanisms. The foundational study by Yagi et al. established that FAD-iPSC-derived neurons with PS1 and PS2 mutations demonstrated increased Aβ42 secretion and sharp response to γ-secretase inhibitors and modulators, validating this approach for drug screening applications [12]. However, the recognition that non-neuronal cells play crucial roles in AD pathogenesis has driven the development of more complex co-culture systems.
Table 2: Experimental Model Systems for iPSC-Based AD Research
| Model System | Components | Key Applications | Limitations |
|---|---|---|---|
| 2D Monoculture | Single cell type (e.g., neurons) | Study of cell-autonomous mechanisms, high-content screening | Lacks cellular interactions, oversimplified |
| 2D Co-culture | Multiple cell types (e.g., neurons + astrocytes) | Investigation of cell-cell interactions, neuroinflammation | Limited tissue architecture, artificial interfaces |
| 3D Neural Organoids/Neurospheres | Self-organizing 3D structures with multiple neural cell types | Modeling tissue-level organization, complex cell interactions, amyloid plaque formation | Heterogeneity, necrotic cores, variable reproducibility |
| Assembled 3D Neurospheres | Defined ratios of iPSC-derived neurons, astrocytes, microglia | Controlled studies of specific cellular contributions, drug testing | Requires complex assembly, may lack native organization |
3D Organoid and Neurosphere Models
Three-dimensional model systems represent a significant advancement in iPSC-based AD modeling, as they better recapitulate the complex tissue architecture and cell-cell interactions of the human brain. Neural organoids are self-assembled three-dimensional aggregates that generate brain-like structures and recapitulate disease features from molecular to functional levels not fully reproduced by other culture systems [15].
A sophisticated 3D iPSC-derived neurosphere system developed by researchers incorporates neurons, astrocytes, and microglia to model cellular responses to chronic amyloidosis [16]. In this model, microglia demonstrated efficient phagocytosis of Aβ and significantly reduced neurotoxicity, mitigating amyloidosis-induced oxidative stress and neurodegeneration [16]. Furthermore, single-nuclei RNA sequencing revealed that the presence of microglia was essential for Aβ to upregulate AD-like gene expression signatures in astrocytes, including key genes such as APOE, CLU, LRP1, and VIM [16].
Live Human Brain Slice Cultures
Complementing iPSC-based models, live human brain slice cultures (HBSCs) provide a unique platform for validating findings in mature human tissue. Recent research using HBSCs has revealed divergent actions of physiological and pathological Aβ on synapses in live human brain tissue [17]. This approach has demonstrated that pharmacological manipulation of physiological Aβ in either direction results in loss of synaptophysin puncta, whereas treatment with pathological Aβ-containing AD brain extract causes post-synaptic Aβ uptake and pre-synaptic puncta loss without affecting synaptic transcripts [17].
Key Research Reagents and Experimental Tools
Table 3: Essential Research Reagents for iPSC-Based AD Modeling
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Factors | OSKM (Oct4, Sox2, Klf4, c-Myc) | Conversion of somatic cells to pluripotent state [11] |
| Gene Editing Tools | CRISPR/Cas9, sgRNAs | Introduction or correction of disease-associated mutations [14] |
| Neural Differentiation Media | Various specialized formulations | Direction of iPSC differentiation to neurons, astrocytes, microglia [16] |
| Cell Type Markers | MAP2, NeuN (neurons); GFAP (astrocytes); Iba1, P2RY12 (microglia) | Identification and validation of specific cell types [17] [16] |
| AD Pathological Assays | ELISAs for Aβ40, Aβ42, tau; Immunostaining for plaques and tangles | Quantification of disease-relevant biomarkers and pathology [12] [17] |
| Functional Assays | Calcium imaging (GCaMP6f), electrophysiology, oxidative stress sensors (roGFP1) | Assessment of neuronal activity, network function, and cellular stress [17] [16] |
Methodological Protocols for Key Experiments
Generating FAD iPSC Models with Known Mutations
To establish FAD iPSC models, researchers typically begin with dermal fibroblasts or blood samples from patients carrying known pathogenic mutations in APP, PSEN1, or PSEN2 [12] [13]. The standardized protocol involves:
- Reprogramming: Introduce the OSKM factors via non-integrating methods to generate iPSCs, with validation of pluripotency markers [11].
- Neural Differentiation: Differentiate iPSCs into neural progenitor cells (NPCs) using dual SMAD inhibition, then further differentiate into mature neurons using combinations of BDNF, NT-3, and cAMP [12] [16].
- Pathological Validation: Measure Aβ42 secretion and Aβ42/40 ratio via ELISA, expecting significant increases compared to control lines [12].
- Drug Response Testing: Expose neurons to γ-secretase inhibitors (e.g., DAPT) and modulators to validate the model's responsiveness, with FAD lines typically showing sharp concentration-dependent responses [12].
Establishing 3D Neurosphere Models with Chronic Amylosis
For the generation of 3D neurosphere models that replicate chronic amyloid exposure:
- Neurosphere Formation: Plate neural progenitor cells in AggreWell plates to initiate 3D aggregation, then transfer to orbital shakers for continued differentiation and maturation [16].
- Microglia Incorporation: Differentiate microglia separately and add to mature neurospheres, allowing infiltration for 7-10 days [16].
- Aβ Oligomer Treatment: Supplement culture media with synthetic Aβ1-42 oligomers for 3-5 weeks to model chronic amyloidosis [16].
- Functional Assessment: Monitor neuronal activity using GCaMP6f calcium imaging, oxidative stress with roGFP1, and neuronal death via lactate dehydrogenase release or live-dead assays [16].
- Transcriptional Analysis: Perform single-nuclei RNA sequencing to profile Aβ and microglia-driven transcriptional changes across different cell types [16].
CRISPR/Cas9 Gene Editing of APOE in iPSCs
For investigating the role of the major genetic risk factor APOE:
- sgRNA Design: Design sgRNAs targeting sequences near the APOE ε2/ε3/ε4 determinant residues (amino acids 112 and 158) [9] [14].
- Electroporation: Deliver Cas9 protein and sgRNAs as ribonucleoprotein complexes into iPSCs via electroporation [14].
- Isogenic Line Selection: Isolate single-cell clones and validate APOE genotype by sequencing, ensuring isogenicity with parent line [14].
- Phenotypic Characterization: Differentiate edited iPSCs into astrocytes and neurons to assess APOE secretion, Aβ aggregation, and neuronal vulnerability [9].
Current Applications and Future Directions
iPSC models of AD have become indispensable tools for both basic research and drug development. Bibliometric analysis reveals a steady increase in publications over 14 years, with research trends focusing on inflammation, astrocytes, microglia, apolipoprotein E (ApoE), and tau [10]. The United States leads in research contributions, followed by China, with prominent researchers including Li-Huei Tsai from the Massachusetts Institute of Technology [10].
These models are increasingly being used to:
- Elucidate cell-type-specific contributions to Aβ pathology [9] [16]
- Investigate the mechanistic roles of AD risk genes identified through GWAS studies [9]
- Screen and validate candidate therapeutics in human-relevant systems [12] [14]
- Model patient-specific responses to potential treatments [10]
Future directions for the field include addressing current limitations such as model heterogeneity, cellular immaturity, and the absence of aging components [15] [11]. Emerging strategies include the incorporation of additional cell types like vascular cells, development of more reproducible organoid systems, and integration of multi-omics approaches to comprehensively characterize disease mechanisms. As these technologies continue to mature, iPSC-based models hold considerable promise for advancing our understanding of AD pathogenesis and accelerating the development of effective therapeutics for both familial and sporadic forms of this devastating disorder.
The study of complex diseases, such as Alzheimer's disease (AD), requires models that accurately capture genetic susceptibility. Polygenic Risk Scores (PRS) have emerged as a powerful tool for quantifying an individual's genetic predisposition by aggregating the effects of numerous genetic variants across the genome [18]. When combined with advanced in vitro models like those utilizing human induced pluripotent stem cells (hiPSCs), PRS provides a framework for stratifying biological risk and investigating molecular mechanisms underlying disease pathology. This integration is particularly potent in Alzheimer's research, where hiPSC-derived astrocytes and neurons enable the direct study of how genetic susceptibility influences cellular responses to pathological insults like amyloid-beta (Aβ) deposition [19] [20].
The power of PRS lies in its ability to move beyond single-gene effects to model the complex, polygenic nature of most common diseases. PRS are calculated as the sum of an individual's risk alleles for a phenotype, weighted by effect size estimates derived from genome-wide association studies (GWAS) [18]. This individual-level genetic propensity score can then be used to stratify samples for experimental studies, including those using hiPSC-derived cell lines, to contrast biological processes between individuals at high and low genetic risk [18].
Computational Methodology for Polygenic Risk Score Calculation
Foundation of Polygenic Risk Scores
Polygenic Risk Scores provide an estimate of an individual's common genetic liability to a phenotype [18]. The standard PRS calculation involves summing risk alleles across many genetic variants, weighted by their effect sizes as estimated from large-scale GWAS. Formally, for an individual, the PRS is computed as:
[ PRSj = \sum{i=1}^{M} wi \times G{ij} ]
Where (PRSj) is the polygenic risk score for the (j)-th individual, (wi) is the weight (effect size) of the (i)-th single nucleotide polymorphism (SNP) from base GWAS data, (G_{ij}) is the genotype of the (i)-th SNP for the (j)-th individual (coded as 0, 1, or 2 copies of the effect allele), and (M) is the total number of SNPs included in the score [18].
Quality Control Procedures for PRS Analysis
Robust PRS analysis requires stringent quality control of both base (GWAS summary statistics) and target (individual genotype) data. Key quality control measures include [18]:
- Base Data Quality Checks: Heritability check ((h_{snp}^2 > 0.05)), verification of effect allele identification, and standard GWAS quality control including genotyping rate > 0.99, minor allele frequency (MAF) > 1%, and imputation info score > 0.8.
- Target Data Requirements: Minimum sample size of 100 individuals, genotyping rate > 0.99, sample missingness < 0.02, heterozygosity P > 1×10⁻⁶, MAF > 1%, and careful handling of population structure.
- Data Harmonization: Ensuring consistent allele coding and strand orientation between base and target datasets to prevent spurious results.
Table 1: Key Quality Control Parameters for PRS Analysis
| Data Type | QC Parameter | Threshold | Rationale |
|---|---|---|---|
| Base & Target | Genotyping rate | > 0.99 | Minimizes missing data |
| Base & Target | Minor allele frequency | > 1% | Filters rare variants |
| Base & Target | Imputation quality | > 0.8 | Ensures well-imputed SNPs |
| Base Data | Chip heritability | > 0.05 | Ensures sufficient genetic signal |
| Target Data | Sample size | ≥ 100 | Provides adequate power |
Advanced PRS Integration: Risk Factor PRS (RFPRS)
Recent methodologies have extended beyond disease-specific PRS to incorporate genetic susceptibility for risk factors. The Risk Factor Polygenic Risk Score (RFPRS) approach integrates genetic propensity for both disease and its risk factors, potentially enhancing predictive power [21]. This integrated RFDiseasemetaPRS combines information from multiple PRSs:
- Construction of Multiple RFPRSs: Generating PRS for various heritable risk factors (e.g., blood biochemistry, body composition, blood pressure) with SNP heritability > 10% [21].
- Association Screening: Testing associations between RFPRSs and a wide spectrum of diseases to identify significant relationships.
- Meta-Score Development: Combining disease PRS with relevant RFPRSs to create RFDiseasemetaPRS, which has demonstrated improved prediction performance for numerous diseases compared to standard PRS alone [21].
Experimental Integration: PRS with iPSC-Derived Cellular Models
hiPSC-Derived Astrocyte Model of Amyloid-Beta Pathology
The integration of PRS with hiPSC models enables the investigation of genetic risk in a human-relevant system. Key methodological aspects include:
- Astrocyte Differentiation: hiPSCs are differentiated into long-term neuroepithelial-like stem cells, which are then plated on poly-L-ornithine and laminin-coated surfaces in astrocyte differentiation medium containing growth factors (bFGF, heregulin, activin A, IGF-1, CNTF) for 30-66 days [19].
- Neuronal Differentiation: Parallel differentiation of hiPSCs into neurons using neuronal differentiation media with sequential media formulations to promote maturation over 30-66 days [19].
- Amyloid-Beta Exposure: Astrocytes are exposed to sonicated Aβ42 fibrils (200 nM for 2 days) to model pathological protein accumulation, followed by culture in Aβ-free medium for various durations (6-33 days) to study persistence effects [19] [20].
Table 2: Key Research Reagent Solutions for iPSC-Amyloid Beta Studies
| Reagent/Category | Specific Example | Function/Application |
|---|---|---|
| hiPSC Line | Cntrl9 II cell line | Source for differentiated astrocytes and neurons |
| Differentiation Matrix | Poly-L-ornithine & Laminin | Surface coating for cell attachment and differentiation |
| Astrocyte Differentiation Factors | bFGF, Heregulin, Activin A, IGF-1, CNTF | Direct stem cell differentiation toward astrocytic lineage |
| Aβ Preparation | HiLyte Fluor 555 labeled Aβ42 monomers | Generation of sonicated fibrils for cellular uptake studies |
| Cell Culture Media | Advanced DMEM/F12 + supplements | Maintenance of differentiated astrocytes |
Functional Assessment of Aβ-Accumulating Astrocytes
Intracellular Aβ accumulation in astrocytes produces measurable functional consequences:
- Synaptic Dysregulation: Neurons co-cultured with Aβ-exposed astrocytes show significantly decreased frequency of excitatory post-synaptic currents, while conditioned media from these astrocytes induces synaptic hyperactivation [19].
- Sustained Cellular Stress: Aβ-containing astrocytes maintain markers of cellular reactivity and exhibit organelle abnormalities, including endoplasmic reticulum and mitochondrial swelling, even 10 weeks after initial exposure [20].
- Altered Secretory Profile: Aβ-accumulating astrocytes show modified cytokine secretion, including increased CCL2/MCP-1, and form pathological lipid structures, indicating broad metabolic disruption [20].
Visualizing Integrated Workflows and Pathways
The following diagrams illustrate key experimental workflows and conceptual relationships in integrated PRS-iPSC research.
Integrated PRS-iPSC Experimental Workflow
Aβ-Induced Astrocyte Dysfunction Pathways
RFPRS Integration Strategy
Data Presentation and Analytical Outcomes
Quantitative Assessment of PRS Predictive Performance
Table 3: Performance Metrics for Standard PRS vs. RFDiseasemetaPRS
| Disease Category | Number of Diseases | Nagelkerke's Pseudo-R² | Odds Ratio per 1 SD | Net Reclassification Improvement |
|---|---|---|---|---|
| Standard PRS Only | 70 diseases | Reference | Reference | Reference |
| RFDiseasemetaPRS | 31 diseases | Improved | Improved | Positive NRI values |
| Performance Gain | 44.3% of diseases | Significant increase | Significant increase | Better risk classification |
Experimental Outcomes of Aβ-Loaded Astrocytes
Table 4: Functional Consequences of Aβ Accumulation in hiPSC-Derived Astrocytes
| Experimental Measure | Control Astrocytes | Aβ-Exposed Astrocytes | Functional Significance |
|---|---|---|---|
| Neuronal Co-culture: EPSC Frequency | Normal pattern | Significantly decreased | Impaired synaptic support |
| Conditioned Media Effect on Neurons | Normal activation | Synaptic hyperactivation | Secreted factor alteration |
| Aβ Retention Duration | No accumulation | >10 weeks in LAMP1+ organelles | Long-term pathology |
| Cytokine Secretion Profile | Baseline levels | Elevated CCL2/MCP-1 | Chronic neuroinflammation |
| Organelle Integrity | Normal morphology | ER & mitochondrial swelling | Metabolic dysfunction |
Discussion: Implications for Drug Development and Personalized Medicine
The integration of polygenic risk modeling with hiPSC-based experimental systems represents a paradigm shift in how researchers can capture genetic susceptibility for complex diseases like Alzheimer's. The methodology enables:
- Stratified Experimental Models: Using PRS to select hiPSC donors at genetic extremes creates more biologically relevant models for therapeutic screening.
- Mechanistic Insight: The combination of genetic risk profiling with functional cellular assays reveals how polygenic susceptibility manifests in pathological processes like Aβ accumulation in astrocytes.
- Enhanced Predictive Power: RFDiseasemetaPRS approaches demonstrate that incorporating risk factor genetics alongside disease genetics improves prediction accuracy for a substantial proportion of diseases [21].
For drug development professionals, these approaches enable more targeted therapeutic strategies. The experimental evidence that Aβ-loaded astrocytes maintain long-term pathology and alter neuronal function provides specific cellular targets for intervention. Furthermore, the ability to stratify individuals by genetic risk enables development of more personalized therapeutic approaches, potentially targeting different biological pathways in high-risk versus low-risk populations.
The consistent observation that astrocytes store rather than degrade ingested Aβ [19] [20], resulting in sustained cellular stress and dysfunction, highlights the potential for targeting astrocyte-mediated clearance mechanisms as a therapeutic strategy. Combined with PRS-based patient stratification, this could enable preemptive interventions for individuals identified as high genetic risk before widespread neurodegeneration occurs.
Recapitulating Early Amyloid Pathology in Human Neurons
The pursuit of effective therapeutic interventions for Alzheimer's disease (AD) has been persistently hampered by the limited predictive validity of traditional model systems. Despite promising results in rodent models, countless candidate therapeutics have failed to benefit human patients, signaling a critical need for more human-relevant disease models [9]. The advent of human induced pluripotent stem cell (iPSC) technology has revolutionized this landscape by providing unprecedented access to living human neurons and glial cells for pathological investigation. iPSC-derived models now serve as an essential bridge between animal studies and clinical trials, offering a platform that captures human-specific physiology and genetic diversity [22] [10].
The core pathological hallmark of AD—the accumulation of amyloid-β (Aβ) peptides—begins years before clinical symptoms emerge. Recapitulating these early stages of amyloid pathology in human neurons is therefore critical for understanding disease initiation and identifying therapeutic windows for intervention. This technical guide details established and emerging methodologies for modeling early amyloid pathology using human iPSC-derived neural cells, providing researchers with the experimental frameworks needed to advance our understanding of AD pathogenesis.
The Cellular Symphony in Amyloid Pathology: Beyond Neurons
While neuronal production of Aβ has been the historical focus of AD research, contemporary genetic and pathological evidence underscores the essential contributions of non-neuronal cell types to disease progression. Genome-wide association studies have identified numerous AD risk genes predominantly expressed in glial cells, shifting the research paradigm toward a more integrated view of AD pathophysiology [9].
Astrocytes: The Double-Edged Sword of Aβ Clearance and Storage
Astrocytes, crucial for maintaining brain homeostasis, exhibit a complex relationship with Aβ pathology. Human iPSC-derived astrocytes actively engulf large amounts of aggregated Aβ through phagocytic mechanisms. However, rather than effectively degrading this material, they store it within LAMP1-positive organelles for extended periods—at least 10 weeks in culture systems [20]. This incomplete processing has profound consequences for astrocyte function and neuronal health:
- Sustained cellular stress: Astrocytes with intracellular Aβ deposits exhibit persistent reactivity markers and an altered cytokine profile, particularly increased secretion of CCL2/MCP-1 [20].
- Organelle dysfunction: Aβ accumulation induces endoplasmic reticulum swelling, mitochondrial abnormalities, and the formation of pathological lipid structures [20].
- Synaptic impact: When co-cultured with Aβ-bearing astrocytes, neurons show significantly decreased frequency of excitatory post-synaptic currents, indicating impaired synaptic function [19].
- Contradictory signaling: Conditioned media from Aβ-exposed astrocytes paradoxically induces neuronal hyperactivity, suggesting the release of soluble factors that alter neuronal excitability [19].
Microglia: Inflammatory Mediators and Oxidative Stress Contributors
Microglia, the brain's resident immune cells, play pivotal roles in neuroinflammation and oxidative stress in AD. Human microglial models demonstrate elevated production of reactive oxygen species (ROS) when exposed to Aβ42, contributing to the oxidative damage observed in AD brains [23]. Recent advances in machine learning coupled with confocal microscopy have enabled sophisticated quantification of these ROS responses, providing new avenues for evaluating potential therapeutic compounds like cannabidiol for their anti-inflammatory properties [23].
Neuronal Senescence: The Emerging Pathway in AD Pathogenesis
Beyond traditional degeneration mechanisms, neurons exposed to Aβ enter a state of cellular senescence, termed "neurescence." Aβ42 oligomers significantly upregulate senescence markers (p21, PAI-1, SA-β-gal) in multiple human neuronal models, including SK-N-SH cells, SH-SY5Y cells, and neural stem cell-derived neurons [24]. This senescent state is characterized by:
- DNA damage response: Increased levels of 8-OHdG staining, histone variant H2AX phosphorylation (γ-H2AX), and genomic DNA lesions [24].
- SIRT1 suppression: Aβ exposure markedly suppresses sirtuin-1 (SIRT1), a critical regulator of aging, and exogenous SIRT1 expression alleviates Aβ-induced senescence phenotypes [24].
- Pharmacological rescue: Aspirin has been shown to rescue Aβ-induced cellular senescence至少部分通过其 regulation of SIRT1, suggesting potential therapeutic pathways [24].
Table 1: Key Cellular Contributors to Amyloid Pathology in Human iPSC Models
| Cell Type | Primary Role in Aβ Pathology | Functional Consequences | Key Experimental Markers |
|---|---|---|---|
| Neurons | Aβ production via APP processing; Vulnerability to oligomeric Aβ | Senescence induction; Synaptic dysfunction; Altered electrophysiology | p21, PAI-1, SA-β-gal; CDKN2D, ETS2 [24] [25] |
| Astrocytes | Aβ phagocytosis and storage; Trophic support | Incomplete degradation; Chronic reactivity; Altered cytokine secretion | GFAP; CCL2/MCP-1; LAMP1 [20] [19] |
| Microglia | Immune activation; ROS production | Neuroinflammation; Oxidative stress; Phagocytic clearance | ROS (CellROX); IL-1β, IL-6, TNF-α [23] |
Experimental Framework: Methodologies for Modeling Amyloid Pathology
Generation of AD-Relevant Neural Cells from Human iPSCs
The successful recapitulation of early amyloid pathology begins with robust differentiation protocols for generating relevant neural cell types:
Forebrain Neuronal Differentiation:
- Utilize dual-SMAD inhibition in monolayer culture to direct differentiation toward cortical fates [22].
- Employ neuronal differentiation medium containing neurobasal medium with B27 supplement, CultureOne supplement, GlutaMAX, and ascorbic acid [24].
- Allow maturation for 30+ days in vitro to obtain functionally mature neurons capable of forming synaptic connections [19].
Astrocytic Differentiation:
- Differentiate long-term neuroepithelial-like stem cells in Advanced DMEM/F12 supplemented with bFGF, heregulin, activin A, IGF-1, and CNTF [19].
- Culture for 30-66 days in vitro to achieve mature astrocytic properties, including phagocytic capability and cytokine secretion [19].
- Confirm functionality through phagocytosis assays and responsiveness to inflammatory stimuli.
Aβ Preparation and Exposure Protocols
Aβ42 Fibril Preparation:
- Dissolve synthetic Aβ42 peptides in hexafluoroisopropanol (HFIP) and dry overnight at room temperature [24].
- Resuspend in DMSO and dilute in phenol-red free DMEM/F12 medium to 100 μM concentration.
- Incubate at 4°C for 24 hours to form oligomers, or extend incubation to 4 days at 37°C with shaking to form fibrils [24] [19].
- Sonicate fibrils at 20% amplitude (1s on/off pulses for 1 minute) immediately before use to facilitate cellular uptake [19].
Cell Exposure Paradigms:
- For acute effects: Treat cells with 100-200 nM sonicated Aβ for 24-48 hours [24] [19].
- For long-term pathology modeling: Implement pulse-chase experiments with 2-day Aβ exposure followed by extended culture in Aβ-free medium (up to 10 weeks) to study retention and chronic effects [20].
Co-culture Systems for Cell-Cell Interaction Studies
To model the complex interactions between different brain cell types in AD:
- Establish neuronal cultures first (30 days maturation), then add astrocytes at a 1:10 ratio (astrocyte:neuron) [19].
- Maintain co-cultures in neuronal differentiation medium #2 (1:1 mix of neuronal differentiation medium and neurobasal medium with supplements) [19].
- Analyze effects after 7-33 days of co-culture depending on experimental endpoints.
Table 2: Quantitative Assessments of Aβ Effects in Human iPSC-Derived Neural Cells
| Experimental Measure | Control Conditions | Aβ-Exposed Conditions | Experimental Details |
|---|---|---|---|
| Aβ Retention in Astrocytes | Minimal intracellular Aβ | Persistent LAMP1+ inclusions after 10 weeks | 200 nM sonicated Aβ-fibrils, 2d exposure [20] |
| Senescence Markers in Neurons | Baseline p21, PAI-1 expression | Significant upregulation | 100 nM Aβ42 oligomers, 48h exposure [24] |
| Excitatory Post-synaptic Current Frequency | Normal synaptic activity | Significantly decreased | Co-culture with Aβ-exposed astrocytes [19] |
| ROS Production in Microglia | Baseline CellROX signal | Significantly increased | 100 nM Aβ42, 24h exposure [23] |
| SIRT1 Expression in Neurons | Normal SIRT1 levels | Markedly suppressed | 100 nM Aβ42 oligomers, 48h exposure [24] |
Advanced Methodologies: Screening and Discovery Platforms
iPSC-Based Compound Screening and Therapeutic Discovery
The use of iPSC-derived neurons has enabled new approaches to pharmaceutical screening:
- High-Content Phenotypic Screening: Rapid neuronal induction protocols allow screening of compound libraries for Aβ-lowering effects with nearly 100% pure neuronal cultures [26].
- Synergistic Combination Therapy: Identification of anti-Aβ cocktail (bromocriptine, cromolyn, and topiramate) that shows synergistic effects in reducing Aβ levels in familial and sporadic AD patient-derived neurons [26].
- Drug Repurposing Platforms: iPSC-based screening of existing pharmaceutical compounds can identify new applications for AD treatment, accelerating therapeutic development [26].
Machine Learning and Image Analysis in AD Research
Advanced computational methods are enhancing the quantification and interpretation of AD-related phenotypes:
- Convolutional Neural Networks (CNN): Deep learning models can predict ROS responses in microglia based on CellROX fluorescence images, enabling high-throughput screening of compound effects [23].
- Decision Tree Classification: Transcriptomic profiling identifies marker pairs (CDKN2D/ETS2) that accurately distinguish senescent neurons with 99% accuracy and 100% specificity [25].
- Eigengene Approaches: Integration of senescence gene panels (SenMayo, CSP, SIP) enables identification of "neurescent" cells from single-nucleus RNA sequencing data [25].
Table 3: Key Research Reagent Solutions for iPSC-Based Amyloid Pathology Studies
| Reagent/Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| iPSC Differentiation Kits | Neural induction media; Patterning factors | Generation of disease-relevant cell types (forebrain neurons, astrocytes, microglia) | [22] [9] |
| Aβ Peptides | Aβ42 monomers (AnaSpec); HiLyte Fluor 555 labeled Aβ42 | Preparation of oligomeric and fibrillar Aβ for exposure studies | [24] [19] |
| Senescence Detection Kits | SA-β-gal assay; p21/PAI-1 antibodies | Identification of senescent neurons ("neurescence") | [24] [25] |
| Cellular Stress Indicators | CellROX Green/Live-act mCherry | Detection of reactive oxygen species in live cells | [23] |
| Lysosomal Markers | LAMP1 antibodies | Tracking intracellular Aβ storage in astrocytes | [20] |
| Electrophysiology Systems | Multi-electrode arrays; Patch clamp | Functional assessment of neuronal and synaptic activity | [19] |
| Cytokine/Chemokine Assays | CCL2/MCP-1 ELISAs; Multiplex cytokine panels | Quantifying inflammatory responses in glial cells | [20] |
Signaling Pathways in Aβ-Induced Pathology
The following diagram illustrates key signaling pathways involved in Aβ-induced neuronal senescence and cellular dysfunction:
Aβ-Induced Senescence Pathway
Experimental Workflow for Modeling Amyloid Pathology
This diagram outlines a comprehensive experimental workflow for recapitulating early amyloid pathology using human iPSC-derived models:
iPSC Amyloid Modeling Workflow
The development of robust protocols for recapitulating early amyloid pathology in human iPSC-derived neural cells represents a transformative advancement in Alzheimer's disease research. These models successfully capture key aspects of AD pathophysiology—including Aβ accumulation, neuronal senescence, glial activation, and synaptic dysfunction—within a genetically human context. The methodologies outlined in this technical guide provide researchers with comprehensive frameworks for establishing these models, enabling more physiologically relevant studies of disease mechanisms and therapeutic interventions.
As the field progresses, increasing model complexity through multi-cellular systems and organoid approaches will further enhance the physiological relevance of these platforms. Combined with advanced analytical techniques such as machine learning and high-content screening, human iPSC-based models promise to accelerate the development of effective therapies for Alzheimer's disease by bridging the critical gap between animal studies and human clinical response.
Advanced iPSC Platform Development for Aβ Pathology and Drug Screening
The study of complex neurological processes, such as amyloid-beta (Aβ) deposition in Alzheimer's Disease (AD), requires model systems that accurately recapitulate human neurobiology. Induced pluripotent stem cell (iPSC) technology has revolutionized this field by enabling the generation of patient-specific neural cells and tissues. This technical guide provides an in-depth comparison of three primary iPSC-derived neural modeling systems—two-dimensional (2D) cultures, neurospheres, and brain organoids—within the specific context of Aβ pathology research. These systems offer varying levels of biological complexity, from basic cellular monolayers to sophisticated three-dimensional (3D) structures that mimic the human brain's cellular diversity, spatial organization, and functional connectivity [27] [28]. For AD research, particularly the study of Aβ deposition and clearance, the choice of model system significantly impacts the physiological relevance of findings and their translational potential for drug development.
Comparative Analysis of Neural Modeling Platforms
The selection of an appropriate neural model depends on the specific research questions, with each platform offering distinct advantages and limitations for studying Aβ pathology.
Table 1: Quantitative Comparison of Neural Modeling Systems for Amyloid-Beta Research
| Model Characteristic | 2D Cultures | Neurospheres | Brain Organoids |
|---|---|---|---|
| Structural Complexity | Low (monolayer) | Intermediate (3D spheroid) | High (3D, self-organizing) |
| Cellular Diversity | Limited (typically 1-2 cell types) | Moderate (multiple neural cell types) | High (diverse neurons, glia, progenitors) [27] |
| Spatial Architecture | Absent | Limited organization | Recapitulates embryonic brain regions [28] |
| Physiological Relevance to Aβ Pathology | Basic cell-autonomous mechanisms | Improved cell-cell interactions | Human-relevant cell-cell interactions & tissue microenvironment [27] |
| Throughput for Drug Screening | High | Moderate | Moderate to Low [28] |
| Technical Reproducibility | High | Moderate | Variable (batch-to-batch heterogeneity) [28] |
| Modeling Aβ Deposition & Clearance | Limited to intracellular processes | Improved extracellular modeling | Captures extracellular aggregation & complex cell interactions [29] [28] |
| Suitability for BBB Interaction Studies | Limited (can model monolayers) | Limited | Enhanced (especially in vascularized or assembloid models) [27] [29] |
Table 2: Application-Specific Assessment for Aβ Research
| Research Application | Recommended Model | Justification |
|---|---|---|
| High-Throughput Compound Screening | 2D Cultures | Superior throughput and reproducibility for initial screens [28] |
| Mechanistic Studies of Aβ Toxicity | 2D Cultures / Neurospheres | Controlled environment for dissecting specific pathways |
| Aβ Aggregation & Plaque Formation | Brain Organoids | 3D microenvironment promotes in vivo-like extracellular aggregation [28] |
| Cell-Type Specific Contributions to Aβ Pathology | Brain Organoids | Diverse cellular repertoire enables study of neuron-glia interactions |
| Blood-Brain Barrier (BBB) & Aβ Clearance | BBB-specific Organoids / Assembloids | Models neurovascular unit interactions; demonstrates isoform-dependent Aβ clearance [29] |
| Genetic (APOE) Risk Factor Studies | Isogenic Brain Organoids | Controlled genetic background isolates isoform-specific effects on Aβ pathology [29] |
Experimental Protocols for Model Generation
Protocol 1: Generation of Cortical Brain Organoids for Aβ Pathology Modeling
This guided protocol generates region-specific cortical organoids suitable for studying Aβ deposition mechanisms.
Key Reagents:
- Basal Medium: DMEM/F12 [29]
- Neural Induction Supplements: N-2 Supplement, B-27 Supplement (serum-free) [29]
- Small Molecule Patterning Factors: SMAD inhibitors (e.g., Dorsomorphin, SB431542) [28], Retinoic Acid [29]
- Growth Factors: FGF-2 (basic fibroblast growth factor) [29]
- Extracellular Matrix: Matrigel or Geltrex for embedding [28]
Procedure:
- iPSC Maintenance: Culture human iPSCs on a Matrigel-coated surface in mTESR1 medium, passaging as clumps using EDTA or enzymatic dissociation to maintain pluripotency [29].
- Embryoid Body (EB) Formation: Dissociate iPSCs to single cells using Accutase and aggregate 9,000 cells per well in a 96-well U-bottom low-attachment plate in neural induction medium (DMEM/F12, N2, B27, FGF-2) supplemented with SMAD inhibitors [28].
- Neural Induction: Culture EBs for 5-7 days, with medium changes every other day, to form neuroepithelium.
- Matrigel Embedding and Guided Cortical Patterning: On day 7, individually embed EBs in Matrigel droplets. Transfer to orbital shaker and culture in neuronal differentiation medium (DMEM/F12, N2, B27) with dual SMAD inhibition and FGF-2 to promote telencephalic fate for an additional 7-10 days [28].
- Terminal Differentiation and Maturation: After 15-18 days total, transition organoids to a terminal differentiation medium (DMEM/F12, N2, B27, BDNF, GDNF) and culture for up to 3 months on an orbital shaker, with medium changes twice weekly, to promote neuronal maturation and network formation [28].
Protocol 2: Establishing a BBB Assay Using iPSC-Derived Cells for Aβ Clearance Studies
This protocol details the creation of a blood-brain barrier (BBB) model to investigate Aβ transcytosis, a critical clearance pathway [29].
Key Reagents:
- Basal Media: DMEM/F12, Knock-out DMEM [29]
- Specialized Media: Unconditioned Medium (UM), Human Endothelial Serum-Free Medium (hECSR) [29]
- Critical Factors: Retinoic Acid [29]
Procedure for Differentiating BMEC-like cells:
- iPSC Expansion: Culture and expand iPSCs on Matrigel in mTESR1 medium [29].
- Mesodermal Induction (6 days): Singularize iPSCs with Accutase and plate at 30,000 cells/cm². Induce differentiation by replacing mTESR1 with Unconditioned Medium (UM). Change UM daily for 6 days [29].
- Endothelial Patterning (2 days): On day 6, switch to hECSR medium supplemented with 10 µM retinoic acid to specify a brain microvascular endothelial cell (BMEC) fate. Culture for 48 hours [29].
- Cell Purification and Seeding: On day 8, purify BMEC-like cells using a CD271+ neural crest microbead kit or similar endothelial selection method. Seed the purified cells onto collagen IV-coated Transwell filters for permeability and transcytosis assays [29].
Aβ Transcytosis Assay:
- Seed purified BMEC-like cells onto collagen IV-coated Transwell inserts and culture until a tight monolayer forms, confirmed by Trans-Endothelial Electrical Resistance (TEER) measurement.
- Add fluorescently labeled or otherwise detectable Aβ peptides (e.g., Aβ40 or Aβ42) to the upper (brain) chamber.
- Measure the rate of Aβ appearance in the lower (blood) chamber over time using an appropriate detection method (e.g., fluorescence, ELISA).
- To investigate specific pathways, inhibit key transporters like LRP1 or p-glycoprotein with pharmacological inhibitors and compare Aβ flux to untreated controls [29].
Signaling Pathways and Workflows in Organoid Modeling
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for iPSC-Based Neural Modeling and Aβ Research
| Reagent Category | Specific Examples | Function in Research |
|---|---|---|
| Base Media | DMEM/F12, Knock-out DMEM, Essential 6 Medium [29] | Foundation for all culture and differentiation media. |
| Induction & Patterning Factors | SMAD Inhibitors (Dorsomorphin, SB431542), Retinoic Acid, FGF-2 [29] [28] | Direct pluripotent stem cell fate toward specific neural and regional identities. |
| Culture Supplements | N-2 Supplement, B-27 Supplement, BSA, Lipid Concentrate [29] | Provide essential nutrients, hormones, and lipids for cell survival and specialization. |
| Extracellular Matrices | Matrigel, Geltrex, Collagen IV [29] [28] | Provide structural support and biochemical cues to mimic the native cellular microenvironment. |
| Dissociation Enzymes | Accutase, Collagenase/Dispase [29] | Gentle dissociation of cells for passaging and downstream analysis. |
| Differentiation Factors | BDNF, GDNTF [28] | Promote neuronal maturation, survival, and synaptic connectivity in later stages. |
| Genome Editing Tools | CRISPR/Cas9 systems, Isogenic iPSC lines [30] [29] | Create precise disease models and isogenic controls to study specific genetic risk factors like APOE. |
| Analysis Kits & Assays | CellTiter-Glo 3D, ELISA kits for Aβ, TEER Measurement equipment [31] [29] | Assess viability, quantify Aβ peptides, and measure barrier integrity in 3D models and BBB assays. |
Alzheimer's disease (AD) research has entered a transformative phase with the recognition that neuroglial cells—microglia and astrocytes—are not passive bystanders but active contributors to disease pathogenesis. Genome-wide association studies (GWAS) have identified numerous AD risk genes highly expressed in microglia and astrocytes, highlighting their potential role in amyloid-β (Aβ) metabolism and clearance [32] [9] [33]. While microglia possess phagocytic capacity and have been implicated in Aβ clearance, accumulating evidence suggests their contribution to AD pathogenesis is more complex than initially anticipated [32]. Similarly, astrocytes, the most abundant glial cells in the brain, play crucial roles in maintaining brain homeostasis but become dysfunctional in AD, affecting Aβ production and clearance [33].
The limitations of traditional mouse models in fully recapitulating human AD pathology, combined with the failure of promising therapeutics in human clinical trials, have underscored the need for more physiologically relevant human cellular models [9]. The advent of induced pluripotent stem cell (iPSC) technology has revolutionized AD research by providing a renewable source of human brain cells, including microglia and astrocytes [34] [22]. This technical guide explores the latest methodologies for generating and utilizing iPSC-derived microglia and astrocytes to study their complex roles in Aβ clearance, providing researchers with comprehensive protocols and analytical frameworks for advancing our understanding of AD pathophysiology.
Microglia in Aβ Clearance: Dual Roles in Protection and Pathogenesis
Developmental Ontogeny and Generation of iPSC-Derived Microglia
Microglia originate from yolk sac erythromyeloid progenitors (EMP) generated during primitive hematopoiesis, a developmental pathway that must be recapitulated for authentic iPSC differentiation [34]. A robust two-step protocol generates human microglial-like cells (iMGLs) from iPSCs in approximately five weeks [34]. The initial stage involves differentiating iPSCs to hematopoietic progenitors (iHPCs) representing early primitive hematopoietic cells, which are then cultured in serum-free differentiation medium containing critical cytokines—CSF-1, IL-34, and TGFβ1—to drive microglial commitment [34].
The resulting iMGLs closely resemble human fetal and adult microglia at the transcriptomic level, expressing canonical microglial genes including P2RY12, GPR34, C1Q, TREM2, and PROS1 [34]. Functional characterization confirms that iMGLs secrete cytokines in response to inflammatory stimuli, migrate, undergo calcium transients, and robustly phagocytose CNS substrates [34]. This protocol typically yields 30-40 million iMGLs from one million iPSCs, enabling scalable experiments including high-content screening applications [34].
Molecular Mechanisms of Microglial Aβ Clearance
Microglia interact with different forms of Aβ through distinct molecular mechanisms. Soluble Aβ is taken up through macropinocytosis and LDL receptor-related proteins (LRPs)-mediated pathways, while fibrillar Aβ interacts with cell surface innate immune receptor complexes that initiate intracellular signaling cascades stimulating phagocytosis [35]. Key receptors and signaling molecules involved in these processes include:
Table 1: Key Molecular Mediators of Microglial Aβ Clearance
| Molecule | Function in Aβ Clearance | Experimental Evidence |
|---|---|---|
| TREM2 | Recognizes Aβ oligomers and fibrils; regulates phagocytosis; promotes microglial clustering around plaques | TREM2 deficiency enhances Aβ pathology; agonistic antibodies enhance phagocytosis [32] |
| SYK | Downstream signaling molecule necessary for Aβ uptake | SYK inhibition impairs microglial Aβ phagocytosis [32] |
| CD33 | Negatively regulates Aβ uptake by suppressing TREM2 signaling | CD33 overexpression reduces Aβ phagocytosis [32] |
| Axl/Mertk | Recognize phosphatidylserine co-deposited with amyloid plaques | TAM receptor family members facilitate Aβ clearance [32] |
| Piezo1 | Mechanosensing receptor recognizing plaque stiffness | Contributes to Aβ phagocytosis by sensing physical properties [32] |
| Scavenger Receptors | Multiple receptors (MSR1, CD36, SR-BI, RAGE) with Aβ binding capacity | Involvement in Aβ binding and internalization [32] |
The role of microglia in Aβ clearance appears to be context-dependent, varying with disease progression, genetic background, and experimental conditions [32]. Surprisingly, some microglial depletion experiments have resulted in unchanged or even decreased Aβ accumulation, challenging conventional views of their exclusively protective function [32]. This paradox may be explained by recent findings that microglia can promote parenchymal amyloid accumulation in early disease stages through mechanisms such as intracellular Aβ aggregation and release of pro-aggregation factors [32].
Signaling Pathways in Microglial Aβ Clearance
The following diagram illustrates the major receptors and signaling pathways involved in microglial Aβ clearance, highlighting potential therapeutic targets:
Astrocytes in Aβ Metabolism: Beyond Passive Support Cells
Generation and Characterization of iPSC-Derived Astrocytes
Human iPSC-derived astrocytes can be differentiated from long-term neuroepithelial-like stem (ltNES) cells through sequential treatment with specific growth factors including bFGF, heregulin, activin A, IGF-1, and CNTF [36]. The resulting astrocytes express characteristic markers and perform essential functions including trophic support, synapse formation, neurotransmission regulation, calcium homeostasis, and immune response control [33].
Notably, healthy hiPSC-derived astrocytes secrete β-amyloid (Aβ) and play important roles in APP processing, suggesting they have the potential to contribute to Aβ accumulation in AD brains [33]. Astrocytes derived from early-onset AD patients carrying the PSEN1ΔE9 mutation display AD hallmarks including increased Aβ and reactive oxygen species (ROS) production, altered inflammatory responses, and dysregulated calcium homeostasis compared to isogenic control astrocytes [33].
Astrocyte Dysfunction in AD Pathogenesis
In AD, astrocytes undergo profound molecular, morphological, and functional alterations that arise at early stages and exacerbate as disease evolves [33]. Key aspects of astrocyte dysfunction include:
Table 2: Astrocyte Dysfunctions in Alzheimer's Disease
| Dysfunction Category | Specific Alterations | Consequences |
|---|---|---|
| Aβ Metabolism | Increased Aβ secretion; impaired Aβ clearance | Contributes to amyloid accumulation; reduced plaque clearance |
| Lipid/Cholesterol Metabolism | Disrupted cholesterol biosynthesis and transport; APOE4-associated defects | Impaired neuronal support; enhanced Aβ aggregation |
| Inflammatory Response | Elevated proinflammatory cytokine secretion; C3 complement activation | Enhanced neuroinflammation; synaptic pruning defects |
| Calcium Homeostasis | Dysregulated calcium signaling | Disrupted neuron-astrocyte communication |
| Oxidative Stress | Increased ROS production | Neuronal damage; cellular stress |
APOE genotype profoundly influences astrocyte function in AD. Astrocytes are the major cell type expressing and producing Apolipoprotein E (APOE) in the brain, and the APOE4 variant confers the greatest genetic risk for late-onset AD [33]. iPSC-derived astrocytes carrying the APOE4 variant produce and secrete less APOE protein compared to APOE3 astrocytes, are less efficient at clearing extracellular Aβ, and show impaired lipid/cholesterol metabolism and increased inflammatory responses [33]. When co-cultured with neurons, APOE4 astrocytes provide less support for neuronal survival and synaptogenesis while exacerbating neuroinflammation [33].
Experimental Evidence of Astrocyte-Mediated Aβ Clearance Dysfunction
A critical study demonstrated that astrocytes exposed to sonicated Aβ42 fibrils develop intracellular Aβ deposits that severely impact their ability to support neuronal function [36]. Electrophysiological recordings revealed significantly decreased frequency of excitatory post-synaptic currents in neurons co-cultured with Aβ-exposed astrocytes, while conditioned media from these astrocytes had the opposite effect, resulting in synaptic hyperactivation [36]. This suggests that factors secreted from control, but not from Aβ-exposed astrocytes, benefit neuronal wellbeing, and that reactive astrocytes with Aβ inclusions fundamentally alter neuronal network activity [36].
Advanced iPSC-Based Model Systems for Studying Aβ Clearance
Monoculture vs. Co-culture Systems
Reductionist monoculture systems have provided valuable insights into cell-autonomous functions of microglia and astrocytes, but co-culture models better approximate the cellular crosstalk occurring in the AD brain:
- Microglia-Neuron Co-cultures: iMGLs can be co-cultured with iPSC-derived neurons to study synaptic pruning mechanisms and neuroinflammatory responses to Aβ pathology [34].
- Astrocyte-Neuron Co-cultures: Control astrocytes support neuronal survival and synaptogenesis, while Aβ-exposed astrocytes lead to decreased excitatory post-synaptic currents and compromised neuronal viability [36].
- Microglia-Astrocyte-Neuron Tri-cultures: Advanced tri-culture systems demonstrate that astrocyte-secreted interleukin-3 (IL-3) reprograms microglia, enhancing their capacity to cluster and clear Aβ and Tau aggregates [33]. Inflammatory conditions in tri-cultures also increase production of complement protein C3 through reciprocal astrocyte-microglia signaling [33].
3D Organoid and Cerebral Organoid Models
3D cerebral organoids generated from iPSCs represent a significant advancement, modeling early AD-like pathology in a more physiologically relevant context [15] [37]. These self-assembled structures recapitulate aspects of complex pathophysiology, including neuronal network dysfunction and accumulation of pathogenic proteins [15]. When exposed to Aβ, cerebral organoids show deposition in their outer layers, suppressed neural activity, and increased apoptotic signaling [37]. Notably, oxytocin demonstrated protective effects in these models, reducing Aβ deposition and apoptosis while enhancing microglial phagocytosis via OXTR and TREM2 upregulation [37].
Transplantation Models
iMGLs transplanted into transgenic mice and human brain organoids resemble microglia in vivo, providing a chimeric model system to study human microglial function in a more complex environment [34]. Similarly, transplantation of human astrocytes into AD model mouse brains offers unique opportunities to analyze human astrocyte dysfunction in vivo [33]. These chimeric approaches combine the strengths of in vitro and in vivo systems, allowing for investigation of human glial cell function within the context of a living brain.
Methodologies for Functional Assessment of Aβ Clearance
Experimental Protocols for Aβ Phagocytosis and Clearance Assays
Microglial Phagocytosis Assay:
- Generate iMGLs using the two-step differentiation protocol [34].
- Label Aβ42 monomers with HiLyte Fluor 555 and aggregate into insoluble fibrils by incubation on a shaker at 1500 rpm, 37°C for 4 days [36].
- Sonicate Aβ42 fibrils at 20% amplitude, 1s on/off pulses for 1 minute before use to facilitate cellular uptake [36].
- Expose iMGLs to 200 nM sonicated Aβ-F for 48 hours in serum-free differentiation medium.
- After exposure, wash cells and culture in Aβ-free medium for varying durations (2-33 days) to study persistence and consequences of Aβ uptake [36].
- Fix cells and immunostain for microglial markers (Iba1, P2RY12, TREM2) and Aβ to quantify internalization.
- Analyze using flow cytometry, high-content imaging, or confocal microscopy.
Astrocyte-Mediated Aβ Clearance Assay:
- Differentiate iPSCs to astrocytes via ltNES cells using astrocyte differentiation medium supplemented with bFGF, heregulin, activin A, IGF-1, and CNTF [36].
- Culture astrocytes for 30-66 days in vitro to ensure maturity.
- Expose astrocytes to 200 nM sonicated Aβ-F for 2 days [36].
- For co-culture experiments, add control or Aβ-exposed astrocytes (2000 cells/cm²) to 30-day-old neuronal cultures at a 1:10 astrocyte to neuron ratio [36].
- Maintain co-cultures in neuronal differentiation medium for 7-33 days before analysis.
- Assess neuronal function via electrophysiological recordings (excitatory post-synaptic currents), immunocytochemistry, and viability assays.
Research Reagent Solutions for iPSC-Glial Research
Table 3: Essential Research Reagents for iPSC-Glial Studies
| Reagent/Category | Specific Examples | Function in Research |
|---|---|---|
| Differentiation Factors | CSF-1, IL-34, TGFβ1, bFGF, heregulin, activin A, IGF-1, CNTF | Direct iPSC differentiation to microglia and astrocyte lineages |
| Critical Antibodies | Iba1, P2RY12, TREM2, GFAP, CD45, CD11b, Aβ antibodies | Cell identification, characterization, and quantification |
| Aβ Preparation Reagents | Synthetic Aβ42 monomers, aggregation buffers, sonication equipment | Generation of physiologically relevant Aβ species |
| Functional Assay Reagents | HiLyte Fluor 555 labeled Aβ42, calcium indicators, phagocytosis dyes | Quantification of Aβ uptake and cellular responses |
| Cell Culture Matrices | Poly-L-ornithine, laminin, specialized serum-free media | Provision of appropriate microenvironment for glial cells |
The development of sophisticated iPSC-derived glial models has fundamentally advanced our understanding of Aβ clearance mechanisms in Alzheimer's disease. The evidence clearly demonstrates that microglia and astrocytes play complex, dynamic, and sometimes paradoxical roles in AD pathogenesis—contributing to both Aβ clearance and accumulation depending on disease stage, genetic context, and cellular environment [32] [33]. The recognition that microglia may promote parenchymal amyloid accumulation in early disease stages, while astrocytes with intracellular Aβ deposits impair neuronal function, challenges simplistic neuroprotective versus neurotoxic dichotomies [36] [32].
Future research should focus on elucidating the precise mechanisms driving functional changes in microglia and astrocytes throughout disease progression, with particular attention to the stage-specific effects of therapeutic interventions. The integration of gene-editing technologies, multi-omics approaches, and increasingly complex multicellular model systems will be critical for deciphering the intricate interplay between human glial cells and Aβ pathology [15] [9] [33]. As these models continue to mature, they offer renewed hope for identifying novel therapeutic strategies that selectively enhance beneficial glial functions while mitigating detrimental effects, ultimately contributing to the development of effective treatments for Alzheimer's disease.
The integration of CRISPR/Cas9 gene editing with human induced pluripotent stem cell (iPSC) technology has revolutionized the study of Alzheimer's disease pathogenesis, particularly the mechanisms underlying amyloid-beta (Aβ) deposition. This powerful combination enables researchers to create genetically accurate human cellular models that recapitulate key aspects of AD pathology in a controlled laboratory setting. CRISPR/Cas9 provides unprecedented precision in introducing disease-relevant mutations into iPSCs, which can then be differentiated into the various neuronal and glial cell types affected in AD [38] [39]. These engineered cells offer a physiologically relevant human platform for investigating the molecular mechanisms driving Aβ aggregation, screening potential therapeutic compounds, and developing personalized medicine approaches for this devastating neurodegenerative disorder [39] [9].
The core of this approach lies in its ability to model both familial and sporadic AD forms by targeting specific genes implicated in disease pathogenesis. For familial AD, researchers can introduce mutations in the APP, PSEN1, and PSEN2 genes, which directly affect Aβ production and aggregation properties [38] [9]. For the more common sporadic AD, the technology enables investigation of risk factors such as APOE4 and other recently identified genetic variants [39] [9]. This technical guide provides a comprehensive resource for researchers aiming to utilize CRISPR/Cas9 in iPSCs to advance our understanding of amyloid-beta deposition mechanisms and identify novel therapeutic strategies for Alzheimer's disease.
Alzheimer's Disease Genetic Targets for CRISPR Editing
Key Genes and Their Pathogenic Roles
Table 1: Primary Genetic Targets for CRISPR/Cas9 Editing in Alzheimer's Disease Research
| Gene Target | Role in AD Pathogenesis | Effect of Mutations/Risk Variants | CRISPR Editing Applications |
|---|---|---|---|
| APP (Amyloid Precursor Protein) | Precursor to amyloid-beta peptides through sequential cleavage by β- and γ-secretases [40] | Mutations increase total Aβ production or ratio of Aβ42/Aβ40, enhancing aggregation propensity [9] | Introduce FAD mutations; modulate expression levels; create knockout lines [38] |
| PSEN1/PSEN2 (Presenilin 1/2) | Catalytic components of γ-secretase complex that generates Aβ from APP [9] | Mutations alter γ-secretase activity, increasing Aβ42/Aβ40 ratio and promoting aggregation [9] | Correct pathogenic mutations; create knockout cell lines; study secretase function [38] [39] |
| APOE (Apolipoprotein E) | Lipid carrier involved in Aβ clearance and aggregation [9] | APOE4 allele increases AD risk 3-fold (heterozygous) to 15-fold (homozygous) compared to APOE3 [9] | Convert APOE4 to APOE3; study isoform-specific effects on Aβ metabolism [39] |
| BACE1 (Beta-secretase 1) | Enzyme that performs initial cleavage of APP in amyloidogenic pathway [38] | Overexpression increases Aβ production; inhibition reduces plaque formation [38] | Knockdown or knockout to reduce Aβ production; study compensatory mechanisms [38] |
The selection of appropriate genetic targets is fundamental to modeling Alzheimer's disease pathology using CRISPR/Cas9-edited iPSCs. The genes listed in Table 1 represent well-validated targets that play direct roles in Aβ production, clearance, and aggregation. APP and the presenilin genes (PSEN1/PSEN2) are particularly important for modeling familial AD, as mutations in these genes directly alter Aβ generation and properties [9]. APOE editing enables investigation of the most significant genetic risk factor for sporadic AD, with the APOE4 allele dramatically increasing disease susceptibility compared to the common APOE3 variant [9]. Additional emerging targets include TREM2, CD33, and ABCA7, which are primarily expressed in microglia and modulate neuroinflammatory responses that influence Aβ pathology [39].
CRISPR/Cas9 Workflow for iPSC Gene Editing
The following diagram illustrates the comprehensive workflow for generating and validating CRISPR/Cas9-edited iPSC lines for amyloid-beta research:
Diagram 1: Comprehensive workflow for generating CRISPR/Cas9-edited iPSCs for Alzheimer's disease research, covering from initial design to final phenotypic validation.
Experimental Protocols and Methodologies
CRISPR Design and Delivery
Guide RNA Design and Validation: Design guide RNAs (gRNAs) using specialized software such as Integrated DNA Technologies (IDT) software or CRISPOR [41]. For gene knockout strategies, design two gRNAs targeting both sides of the genomic region to be deleted, enabling large deletions up to 15 kb [41]. For precise nucleotide changes or molecular tag insertions (knock-in), design a single gRNA with the cutting site located as close as possible to the insertion point (within 10 bp for optimal efficiency) [41]. To enhance editing efficiency and reduce off-target effects, utilize high-fidelity Cas9 variants (e.g., Alt-R HiFi Cas9 Nuclease V3) and incorporate chemical modifications into gRNAs (e.g., Alt-R CRISPR-Cas9 crRNA XT) to improve stability against cellular nucleases [41]. Validate gRNA cutting efficiency before full experiments using T7E1 assay or computational tools such as TIDE or ICE [41].
Donor Template Design for Knock-in: For homology-directed repair (HDR)-mediated knock-in, design single-stranded DNA donors with two phosphorothioate bond modifications at both 5'- and 3'-ends to enhance stability [41]. Flank the insert (e.g., nucleotide change or molecular tag) with homology arms of at least 30 nucleotides on each side, placing the desired modification in the middle of the donor sequence [41]. Incorporate silent CRISPR-Cas9 blocking mutations in the PAM sequence or gRNA target sequence to prevent re-cleavage of successfully edited alleles [41]. For tracking purposes, consider adding a fluorophore (e.g., Alexa Fluor 660) at the 5' extremity to enable enrichment of transfected cells [41].
iPSC Culture and Transfection: Maintain hiPSCs in feeder-free conditions, passaging cells twice per week as small aggregates for at least two weeks before transfection [41]. Use qualified Matrigel (0.05 mg/mL) or similar extracellular matrix to coat culture vessels, which should be prepared at least 1 hour before cell passaging [41]. For transfection, use dissociated hiPSCs at very low passage that have been recently verified for genomic integrity [41]. Prepare CRISPR-Cas9 ribonucleoprotein (RNP) complexes by combining high-fidelity Cas9 nuclease with synthesized gRNAs according to manufacturer instructions [41]. Deliver RNP complexes using electroporation systems optimized for stem cells, which typically achieves higher efficiency than lipid-based methods for iPSCs.
Selection and Validation of Edited Clones
Isolation of Edited Clones: Following transfection, use fluorescence-activated cell sorting (FACS) to isolate successfully transfected cells, leveraging fluorescent tags incorporated into the gRNA (e.g., ATTO 488) or donor DNA [41]. Plate sorted cells at clonal density (500-1000 cells/cm²) in essential 8 medium or similar iPSC maintenance medium supplemented with ROCK inhibitor (Y-27632) to enhance single-cell survival [41]. Allow 7-14 days for clonal colony formation, with medium changes every other day [41]. For alternative approaches, the ArrayEdit method enables high-content analysis of arrayed hESC colonies in multiwell plates, facilitating efficient editing without destruction of initial edited samples [42].
Molecular Validation of Edits: Pick 20-30 individual clones for expansion and genomic DNA extraction. For knockout lines, perform PCR amplification across the targeted region and analyze by electrophoresis for size changes indicative of deletions [41]. For point mutations or small insertions, use restriction fragment length polymorphism (RFLP) analysis if a silent restriction site was incorporated into the donor design, otherwise proceed directly to Sanger sequencing [41]. Confirm bi-allelic editing through sequencing chromatogram analysis or quantitative methods. Validate absence of off-target edits by examining top predicted off-target sites using T7E1 assay or sequencing [41]. Perform karyotyping to ensure genomic integrity is maintained following editing procedures [41].
Pluripotency and Differentiation Capacity Assessment: After confirming genetic edits, verify that edited iPSCs maintain pluripotency markers (OCT4, NANOG, SOX2, TRA-1-60) through immunocytochemistry or flow cytometry [41]. Confirm differentiation potential by directing edited iPSCs toward neural progenitor cells (NPCs) using dual SMAD inhibition protocols [43] [44]. Assess neuronal maturation and function through electrophysiological measurements, including sodium current development, resting membrane potential, and synaptic activity, which typically emerge after 3-4 weeks of differentiation [44].
Phenotypic Characterization of Aβ Pathology
Neuronal Differentiation and Maturation: Differentiate validated iPSC lines into cortical neurons using established protocols [44]. Monitor neuronal maturation through morphological assessments (soma area, neurite length, branching complexity) and electrophysiological properties [44]. Key developmental milestones include: growth cone maturation peaking around day 9, functional synapse formation emerging after day 23, and progressive increase in sodium current density and synaptic activity through day 38 [44].
Aβ-related Phenotypic Assays: Quantify Aβ secretion in conditioned media using ELISA, specifically measuring Aβ40 and Aβ42 isoforms to calculate the critical Aβ42/Aβ40 ratio [9]. Detect intracellular Aβ oligomers and aggregates using conformation-specific antibodies [1]. Assess amyloid plaque formation in 3D cortical organoid cultures, which typically require extended differentiation periods (2-6 months) to develop robust Aβ pathology [38] [9]. Evaluate downstream pathological events including tau hyperphosphorylation, neuroinflammatory responses, and synaptic dysfunction [39] [40].
Table 2: Key Research Reagents for CRISPR-iPSC Alzheimer's Disease Modeling
| Reagent Category | Specific Products | Application Notes |
|---|---|---|
| CRISPR Components | Alt-R HiFi Cas9 V3 (IDT), chemically modified crRNAs (Alt-R XT) | High-fidelity editing with reduced off-target effects; enhanced gRNA stability [41] |
| iPSC Culture | StemMACS iPS-Brew, mTeSR1, Matrigel (0.05 mg/mL), Gentle Cell Dissociation Reagent | Feeder-free maintenance; enzymatic passaging as aggregates [41] |
| Neural Differentiation | N2/B27 supplements, BDNF, GDNF, cAMP, SMAD inhibitors (dorsomorphin, SB431542) | Efficient neural induction and maturation [43] [44] |
| Aβ Detection | Aβ40/Aβ42 ELISAs, oligomer-specific antibodies (A11, OC), thioflavin S | Quantification of Aβ species; detection of aggregates and plaques [1] [9] |
| Cell Sorting & Isolation | FACS instruments with 488nm and 633nm lasers, anti-pluripotency antibodies, viability dyes | Isolation of edited clones; purification of specific cell populations [41] |
Aβ Seeding and Propagation Mechanisms
The prion-like propagation of amyloid-beta represents a critical mechanism in Alzheimer's disease progression that can be effectively modeled using CRISPR-edited iPSCs. Aβ misfolding spreads through the brain via a seeding mechanism in which small, seeding-active nuclei template the misfolding and aggregation of naïve Aβ monomers into higher aggregation states [1]. Evidence suggests that soluble Aβ oligomers constitute the most seeding-active species, crucial for the initial stages of Aβ aggregation [1]. These seeding-competent oligomers, termed "on-pathway" oligomers, represent the smallest pathogenic units in the aggregation cascade [1].
CRISPR-edited iPSCs enable precise investigation of how mutations in APP, PSEN1, and PSEN2 influence Aβ seeding propensity and strain characteristics. Studies have demonstrated that intracerebral Aβ aggregation can be induced by various seed forms, including small soluble Aβ seeds from brain parenchyma, Aβ seeds isolated from cellular compartments, purified Aβ fibrils, and aggregated synthetic Aβ [1]. Notably, Aβ seeds can persist in the living brain for months, resisting degradation and clearance mechanisms [1]. iPSC-derived neurons and glial cells provide an ideal system for dissecting the cellular mechanisms of Aβ seed uptake, propagation, and clearance, with CRISPR editing enabling precise attribution of specific genetic factors to these processes.
Applications in Disease Modeling and Drug Discovery
Advanced Disease Modeling Approaches
The combination of CRISPR/Cas9 and iPSC technologies enables creation of sophisticated Alzheimer's disease models that recapitulate key aspects of human pathology. These include:
2D Co-culture Systems: Develop co-culture models containing iPSC-derived neurons, astrocytes, and microglia to investigate cell-type-specific contributions to Aβ pathology [9]. Such systems have revealed that microglia carrying AD risk genes (e.g., TREM2 variants) exhibit impaired Aβ clearance and enhanced pro-inflammatory responses [39] [9]. CRISPR editing enables isogenic control generation where only the disease-relevant mutation differs between otherwise identical cells.
3D Organoid Models: Generate cerebral organoids that better mimic the cellular complexity and tissue architecture of the human brain [38] [9]. These 3D systems develop Aβ plaque-like structures and tau pathology over extended culture periods (several months), providing a more physiologically relevant platform for studying Aβ deposition mechanisms [38]. CRISPR editing allows introduction of multiple AD-related genetic risk factors to create models with accelerated or enhanced pathology.
Personalized Disease Modeling: Create patient-specific models by generating iPSCs from individuals with specific genetic backgrounds or clinical presentations, then using CRISPR to correct or introduce mutations to establish causal relationships [39] [9]. This approach enables investigation of how different genetic backgrounds influence Aβ pathology and therapeutic responses.
Drug Screening and Therapeutic Development
CRISPR-edited iPSCs provide a powerful platform for Alzheimer's drug discovery through several applications:
Target Validation: Use CRISPR-based gene editing to validate novel therapeutic targets by knocking out candidate genes in iPSC-derived neural cells and assessing effects on Aβ pathology [38] [39]. For example, BACE1 knockout has been shown to reduce Aβ production, supporting its therapeutic potential [38].
High-Throughput Compound Screening: Implement high-content screening platforms using iPSC-derived neurons with built-in reporters for Aβ pathology or neuronal health [39] [42]. These systems have identified compounds that modulate β- and γ-secretase activity, reduce Aβ oligomer formation, or enhance Aβ clearance [39].
Biomarker Discovery: Identify novel biomarkers by analyzing secreted factors, extracellular vesicles, and metabolic profiles from CRISPR-edited iPSC-derived neural cells with defined genetic alterations [1] [9]. Such biomarkers could enable earlier diagnosis and patient stratification for clinical trials.
Technical Challenges and Limitations
Despite the significant promise of CRISPR/Cas9-edited iPSCs for Alzheimer's research, several technical challenges remain:
Off-Target Effects: CRISPR/Cas9 can induce unintended genetic modifications at sites with sequence similarity to the target site [38] [45]. Mitigation strategies include using high-fidelity Cas9 variants, careful gRNA design with minimal off-target potential, and comprehensive off-target assessment through whole-genome sequencing [41] [45].
Delivery Efficiency: Achieving efficient CRISPR delivery to iPSCs while maintaining high cell viability remains challenging [45]. Electroporation of RNP complexes currently represents the most effective approach, but efficiency varies between iPSC lines and requires optimization [41].
Model Maturity: iPSC-derived neurons typically exhibit fetal-like characteristics and may not fully recapitulate the aging-related aspects of Alzheimer's pathology [38] [9]. Ongoing efforts to accelerate neuronal aging through progerin expression, oxidative stress, or extended culture periods aim to address this limitation [9].
Pathological Complexity: While iPSC models recapitulate certain aspects of Aβ pathology, they often lack the full complexity of amyloid plaque formation and associated neuroinflammation seen in human brain [38]. The development of more complex 3D models and co-culture systems continues to address this challenge [38] [9].
The integration of CRISPR/Cas9 gene editing with iPSC technology has transformed our approach to studying amyloid-beta deposition in Alzheimer's disease. This powerful combination enables creation of human cellular models with precise genetic alterations that recapitulate key aspects of AD pathology. The methodologies outlined in this technical guide provide a framework for researchers to effectively target APP, PSEN1/2, and APOE genes, validate genetic edits, and perform phenotypic characterization of Aβ-related pathology. As these technologies continue to advance, they promise to accelerate our understanding of Alzheimer's disease mechanisms and facilitate the development of novel therapeutic strategies targeting amyloid-beta deposition and its downstream consequences.
High-Content Screening Platforms for Aβ-Targeting Therapeutics
High-content screening (HCS) represents an advanced methodological approach that combines automated microscopy with multi-parametric imaging and computational analysis to extract quantitative data from biological systems at the single-cell level [46] [47]. In the context of Alzheimer's disease (AD) research, HCS platforms have become indispensable tools for evaluating therapeutic compounds targeting amyloid-beta (Aβ) pathology, particularly when integrated with human induced pluripotent stem cell (iPSC)-derived neural models. These platforms enable researchers to simultaneously monitor multiple parameters including Aβ deposition, cellular morphology, synaptic integrity, and stress response pathways in a high-throughput manner, generating rich multivariate datasets that provide comprehensive insights into compound efficacy and mechanisms of action [46] [47].
The integration of HCS with iPSC technology has revolutionized AD therapeutic development by providing human-relevant experimental models that recapitulate key aspects of disease pathology. iPSC-derived neural cells exhibit intracellular Aβ oligomer accumulation and associated cellular stress responses that mirror pathological features observed in AD patients [48]. When combined with HCS, these models create a powerful platform for screening Aβ-targeting therapeutics, allowing for the assessment of multiple phenotypic endpoints simultaneously while maintaining physiological relevance. This approach has become particularly valuable with the recent regulatory approvals of anti-Aβ monoclonal antibodies including Aducanumab, Lecanemab, and Donanemab, which target different forms of aggregated Aβ and have demonstrated the clinical viability of Aβ-targeting strategies [49].
Core Components of HCS Platforms for Aβ Research
Instrumentation and Detection Systems
Modern HCS platforms for Aβ research incorporate several integrated systems that work in concert to enable quantitative imaging and analysis. Automated microscopy systems form the foundation of these platforms, with capabilities for rapid image acquisition across multiple fluorescence channels. These are typically coupled with environmental control modules that maintain physiological conditions during live-cell imaging, which is essential for monitoring dynamic processes such as Aβ aggregation and cellular responses over extended time periods [47]. The detection systems are optimized for sensitivity and resolution, enabling the visualization of subcellular structures and protein aggregates that are critical for assessing Aβ pathology and therapeutic interventions.
Advanced HCS platforms incorporate confocal imaging capabilities to enhance spatial resolution and reduce out-of-focus light, which is particularly important for thick samples such as 3D cerebral organoids. Additionally, laser-based microplate cytometers provide complementary approaches for high-throughput analysis of cellular populations, with violet laser-excited reagents (405 nm) enabling the use of a broader spectrum of fluorescent dyes for multiplexed assays [47]. These systems are integrated with sophisticated image acquisition software that coordinates hardware components, manages experimental protocols, and initiates the automated analysis workflows that are essential for processing the large datasets generated in HCS campaigns.
Analytical Software and Data Processing
The analysis of HCS data requires specialized computational approaches to extract meaningful information from complex multivariate datasets. Current analytical pipelines employ machine learning algorithms and deep learning convolutional neural networks (CNNs) that can be trained to identify and quantify specific pathological features such as Aβ plaques and associated neuroinflammatory responses [50]. These automated analysis systems have demonstrated exceptional precision (>95%) for detecting Aβ areas and microglial cells in complex biological samples, significantly outperforming traditional manual counting methods in both speed and consistency [50].
For data processing, dimension reduction strategies are often applied to manage the complexity of multiparametric HCS data, though these approaches must be carefully validated as they can potentially lower the degree of discrimination between experimental conditions [46]. Alternative analysis methods include cell population summarization using percentile values at the well level, which has been shown to maintain a high degree of classification accuracy while simplifying data interpretation [46]. The implementation of standardized data processing pipelines enables systematic review of alternative analysis strategies and facilitates comparison across different experimental batches and research laboratories, enhancing the reproducibility of HCS-based Aβ research.
iPSC-Derived Neural Models for Aβ Screening
Differentiation Strategies for Neural Cell Types
The generation of physiologically relevant neural models from human iPSCs requires well-established differentiation protocols that recapitulate key aspects of central nervous system development. Current approaches can be broadly categorized into 2D monolayer differentiation and 3D cerebral organoid methods, each offering distinct advantages for Aβ research [51]. For HCS applications, 2D models typically provide better standardization and compatibility with automated imaging systems, while 3D organoids offer enhanced physiological complexity with more natural cell-cell interactions and tissue organization.
A widely adopted protocol for neural differentiation involves dual SMAD inhibition using small molecule inhibitors such as Noggin and SB431542, which promotes efficient conversion of iPSCs to neuroepithelial cells and subsequent formation of neural rosettes within approximately 11 days [51]. These neural rosettes function as reservoirs of neural stem cells (NSCs) that can be isolated and expanded before differentiation into mature neuronal and glial cell types. For astrocyte differentiation, established protocols typically employ a combination of growth factors including fibroblast growth factor-basic (bFGF), heregulin, activin A, insulin-like growth factor 1 (IGF-1), and ciliary neurotropic factor (CNTF) in defined media formulations [36]. Neuronal differentiation is commonly achieved using sequential media conditions that promote neuronal maturation, resulting in cultures that express characteristic neuronal markers and exhibit functional electrophysiological properties [36] [51].
Modeling Aβ Pathology in iPSC-Derived Neural Cells
iPSC-derived neural models have proven invaluable for studying Aβ-associated pathology in a human-relevant system. These models consistently demonstrate accumulation of intracellular Aβ oligomers in both neurons and astrocytes, mirroring observations from AD patient brains [48]. This intracellular Aβ accumulation is associated with significant cellular stress responses, including endoplasmic reticulum stress and oxidative stress, which contribute to neuronal dysfunction and can be quantitatively assessed using HCS approaches [48].
A particularly relevant model for HCS applications involves exposing iPSC-derived astrocytes to sonicated Aβ42 fibrils, which leads to intracellular deposit formation and subsequent functional impairment [36]. In co-culture systems with neurons, these Aβ-laden astrocytes exhibit compromised supportive function, resulting in decreased frequency of excitatory post-synaptic currents—a key functional metric of neuronal health that can be correlated with HCS data [36]. Importantly, the pathological manifestations in these models show differential drug responsiveness, with interventions such as docosahexaenoic acid (DHA) treatment demonstrating the ability to alleviate cellular stress responses, thereby validating their utility for therapeutic screening [48].
Table 1: Key Stress Phenotypes in iPSC-Derived Neural Models of Aβ Pathology
| Cellular Phenotype | Manifestation in Aβ-Exposed Cells | Detection Method in HCS |
|---|---|---|
| Intracellular Aβ Accumulation | Increased oligomeric Aβ in neurons and astrocytes | Immunofluorescence with Aβ antibodies |
| ER Stress | Upregulation of ER stress markers (e.g., BiP, CHOP) | Reporter constructs or immunostaining |
| Oxidative Stress | Elevated reactive oxygen species | CellROX or similar redox-sensitive dyes |
| Synaptic Deficits | Decreased excitatory post-synaptic current frequency | Synaptic marker staining (e.g., PSD-95, synapsin) |
| Altered Astrocyte Function | Impaired neuronal support capacity | Morphological analysis and cytokine secretion |
HCS Assay Development for Aβ-Targeting Therapeutics
Fluorescent Detection of Aβ Species
The detection and quantification of Aβ aggregates in HCS applications relies on specialized fluorescent probes with distinct binding specificities for different Aβ conformations. Traditional dyes such as thioflavin T (ThT) and Congo Red derivatives provide general detection of amyloid structures but typically lack specificity for distinct Aβ polymorphs [52]. Recent advances in probe development have enabled more selective detection of specific Aβ aggregates through high-throughput screening of diverse chemical libraries against multiple synthetic fibril polymorphs [52].
Innovative screening approaches leveraging protein-adaptive differential scanning fluorimetry (paDSF) have identified novel fluoroprobes with improved selectivity for specific Aβ fibril subtypes [52]. These screening campaigns utilize diverse dye collections such as the Aurora library of 300+ chemically diverse compounds, enabling the discovery of under-represented chemotypes including coumarin and polymethine scaffolds with unique binding properties for Aβ aggregates [52]. The development of these improved detection reagents enhances the specificity of HCS assays for evaluating Aβ-targeting therapeutics, particularly for compounds designed to selectively engage specific pathogenic Aβ conformations.
Multiparametric Assay Design
Comprehensive evaluation of Aβ-targeting therapeutics requires assay designs that simultaneously monitor multiple pathological and physiological parameters. Well-optimized HCS assays typically incorporate markers for Aβ load, cellular viability, synaptic density, inflammatory responses, and organelle health in a multiplexed format [50] [47]. This multiparametric approach enables the assessment of both therapeutic efficacy and potential toxicity in a single experimental setup, providing a more complete picture of compound activity.
For Aβ-specific endpoints, HCS assays commonly employ combinations of Aβ-selective dyes or immunofluorescence detection with antibodies against different Aβ species (monomeric, oligomeric, fibrillar) [52] [47]. These are typically combined with cell health indicators such as viability dyes, apoptosis markers (e.g., TUNEL assay), and oxidative stress sensors (e.g., CellROX reagents) to evaluate potential toxic effects [47]. Additionally, neuronal health and function can be assessed through measurements of neurite morphology, synapse number, and mitochondrial function using targeted fluorescent probes [47]. The integration of these diverse endpoints creates a comprehensive profiling system for Aβ-targeting compounds, enabling structure-activity relationship studies and mechanism of action investigations at the cellular level.
Table 2: Essential Research Reagent Solutions for HCS of Aβ-Targeting Therapeutics
| Reagent Category | Specific Examples | Primary Application in HCS |
|---|---|---|
| Aβ Detection Dyes | Thioflavin T, Aβ-selective coumarin dyes [52] | Quantification of Aβ aggregate burden |
| Cell Health Indicators | CellROX reagents, HCS LIVE/DEAD kits [47] | Assessment of oxidative stress and viability |
| Neuronal Markers | β-III-tubulin, MAP2 antibodies, synapsin probes [47] | Evaluation of neuronal integrity and synapses |
| Nuclear Stains | Hoechst 33342, HCS NuclearMask stains [47] | Cell counting and nuclear morphology analysis |
| Secretase Reporters | BACE1 FRET substrates, γ-secretase activity probes | Monitoring APP processing enzyme activity |
| Inflammatory Marker | Iba1 for microglia, GFAP for astrocytes [50] | Assessment of neuroinflammatory responses |
Experimental Protocols for HCS of Aβ Therapeutics
Aβ Exposure and Co-culture Model Setup
The establishment of physiologically relevant Aβ pathology models for HCS applications requires standardized protocols for Aβ preparation and cellular exposure. For studies investigating intracellular Aβ accumulation, a well-validated approach involves exposing iPSC-derived astrocytes to sonicated Aβ42 fibrils (200 nM) for 48 hours in astrocyte differentiation medium, followed by washing and maintenance in Aβ-free medium for varying recovery periods depending on the specific experimental endpoints [36]. The sonication step is critical for generating fibril fragments that can be efficiently internalized by cells, and is typically performed at 20% amplitude with 1 second on/off pulses for 1 minute using a Vibra Cell sonicator or equivalent system [36].
For neuronal co-culture models, iPSC-derived neurons are first cultured for approximately 30 days to allow maturation before the addition of control or Aβ-exposed astrocytes at a ratio of 1:10 (astrocytes:neurons) [36]. These co-cultures are maintained in neuronal differentiation medium and can be analyzed at various timepoints (e.g., 7-33 days after astrocyte addition) depending on the specific parameters being investigated. This model system recapitulates key aspects of AD pathology, including decreased frequency of excitatory post-synaptic currents in neurons co-cultured with Aβ-exposed astrocytes, providing a functional correlate to imaging-based HCS data [36].
Automated Imaging and Analysis Workflow
The HCS workflow for Aβ therapeutic screening involves a standardized sequence of steps from sample preparation to data analysis. Initially, cells are seeded in optical-grade multiwell plates at optimized densities and subjected to experimental treatments including Aβ-targeting therapeutics. Following treatment periods, cells are typically fixed and stained with multiplexed fluorescence panels targeting relevant endpoints, though live-cell imaging approaches can also be employed for dynamic assessments [47].
Automated image acquisition is performed using HCS platforms such as the ArrayScan XTI HCA Reader or similar systems, with settings optimized for each fluorescence channel and multiple fields captured per well to ensure statistical robustness [47]. For Aβ plaque quantification, deep learning-based approaches have demonstrated exceptional performance, with CNN models trained on human-made annotations of Aβ pathology achieving >95% precision in detecting Aβ areas in whole slide images [50]. These automated analysis systems significantly outperform manual counting methods in both speed and consistency, while also providing capabilities for detecting more subtle phenotypic changes that might be overlooked in traditional analyses.
HCS Workflow for Aβ-Targeting Therapeutics: This diagram illustrates the integrated experimental and computational pipeline for screening Aβ-targeting therapeutics using iPSC-derived neural models and high-content screening platforms.
Data Analysis and Interpretation
Quantitative Analysis of Aβ Pathology
The quantitative assessment of Aβ pathology in HCS experiments employs both intensity-based measurements and object-based analyses to capture different aspects of Aβ accumulation and aggregation. Intensity-based measurements provide information about overall Aβ burden within cells or regions of interest, while object-based analyses enable the quantification of discrete Aβ-positive inclusions, such as intracellular aggregates or extracellular deposits [50]. For more sophisticated analyses, deep learning algorithms can be trained to classify different types of Aβ aggregates based on morphological features, providing insights into the structural diversity of Aβ pathology and its modulation by therapeutic interventions.
Advanced analytical approaches also enable the investigation of spatial relationships between Aβ pathology and other cellular features. For example, the association between Aβ deposits and microglial cells can be quantified through proximity analysis, which has revealed important insights into neuroinflammatory responses in AD [50]. In cortical biopsies from iNPH patients, higher Aβ coverage has been identified as a significant predictor of dementia development, while microglial densities and Aβ-associated microglia did not show significant correlation with cognitive outcome, highlighting the complex relationship between Aβ pathology and downstream effects [50]. These sophisticated analytical capabilities enhance the biological insights that can be derived from HCS data, moving beyond simple quantification of Aβ load to more mechanistically informative assessments.
Multivariate Data Analysis Strategies
The analysis of multiparametric HCS data requires specialized statistical approaches to extract meaningful patterns from complex datasets. Dimension reduction techniques such as principal component analysis (PCA) are commonly employed to visualize high-dimensional data in lower-dimensional space, though these approaches must be applied judiciously as they can potentially reduce discrimination between experimental conditions [46]. Alternative strategies include cell population summarization using percentile values, which has been shown to maintain classification accuracy while simplifying data structure [46].
For more sophisticated pattern recognition, machine learning classification algorithms can be trained to identify distinct phenotypic responses to therapeutic interventions based on multiparametric HCS data. These approaches can reveal subtle effects that might be overlooked in univariate analyses and can help identify biomarkers of drug response [46] [50]. The implementation of standardized data analysis pipelines facilitates systematic comparison across different experimental batches and research groups, enhancing the reproducibility and reliability of HCS-based screening data for Aβ-targeting therapeutics.
Integration with Therapeutic Development Pipelines
Mechanism of Action Studies for Aβ-Targeting Therapeutics
HCS platforms provide powerful tools for elucidating the mechanisms of action of Aβ-targeting therapeutics at the cellular level. Different classes of Aβ-targeting compounds exhibit distinct mechanisms including Aβ production inhibition (e.g., BACE1 inhibitors), Aβ aggregation prevention, and A42 clearance promotion (e.g., monoclonal antibodies) [49]. HCS assays can distinguish between these mechanisms by monitoring different Aβ species and cellular responses, providing critical information for lead optimization and candidate selection.
Monoclonal antibodies against Aβ represent a particularly important class of therapeutics that have recently achieved regulatory approval. These antibodies including Aducanumab, Lecanemab, and Donanemab target different forms of aggregated Aβ with distinct epitope specificities: Aducanumab binds Aβ fibrils and plaques (epitope amino acids 3-7), Lecanemab targets soluble protofibrils and aggregates (epitopes 1-16 and 21-29), while Donanemab recognizes N-terminal pyroglutamate-modified Aβ present in mature plaques [49]. HCS platforms can evaluate the functional consequences of these different targeting strategies by assessing their effects on Aβ clearance, neuroinflammatory responses, and neuronal health, providing insights that complement biochemical and biophysical characterization.
Predictive Modeling and Lead Optimization
The rich multiparametric data generated by HCS platforms enables the development of predictive models that can guide lead optimization for Aβ-targeting therapeutics. Quantitative structure-activity relationship (QSAR) models can be built by correlating compound structural features with multiparametric HCS readouts, identifying chemical motifs associated with desirable efficacy and safety profiles [52] [53]. Additionally, mechanistic computational models of Aβ aggregation dynamics can be parameterized using HCS data, creating in silico tools for predicting the effects of therapeutic interventions on Aβ pathology progression [53].
These computational approaches incorporate mass-action kinetics to capture the transitions between different Aβ species (monomers, oligomers, protofibrils, fibrils) and can be coupled with optimal control frameworks to identify dosing strategies that maximize therapeutic efficacy while minimizing adverse effects [53]. For anti-Aβ antibodies, these models have been used to simulate treatment effects and optimize intervention timing, with simulations suggesting that Donanemab achieves the most significant reduction in fibrillar Aβ among currently approved antibodies [53]. The integration of HCS data with these computational models creates a powerful framework for accelerating the development of improved Aβ-targeting therapeutics.
Aβ Pathology and Therapeutic Targeting: This diagram illustrates the pathway of Aβ aggregation from APP processing through to neuronal dysfunction, highlighting key points for therapeutic intervention by different classes of Aβ-targeting compounds.
Emerging Technologies and Applications
The field of HCS for Aβ-targeting therapeutics continues to evolve with emerging technologies that promise to enhance screening capabilities and biological relevance. 3D screening models using cerebral organoids represent a particularly promising direction, offering more physiologically relevant cellular environments and tissue organization for assessing Aβ pathology and therapeutic interventions [51]. These 3D models recapitulate key aspects of in vivo brain architecture and cell-cell interactions, potentially providing more predictive data for clinical outcomes, though they present technical challenges for HCS including light penetration and image analysis complexity.
Advanced label-free imaging techniques such as multiphoton microscopy and stimulated Raman scattering microscopy are being integrated into HCS platforms, enabling longitudinal monitoring of Aβ pathology without the potential artifacts introduced by fluorescent labels [52]. Additionally, multiplexed spectral imaging approaches facilitate the simultaneous detection of multiple Aβ species and cellular markers in the same sample, providing more comprehensive profiling of therapeutic effects [52]. These technological advances, combined with continued improvements in automated image analysis through deep learning, will further enhance the utility of HCS platforms for developing next-generation Aβ-targeting therapeutics.
High-content screening platforms integrated with iPSC-derived neural models have established themselves as essential tools in the development of Aβ-targeting therapeutics for Alzheimer's disease. These systems enable multiparametric assessment of compound effects on Aβ pathology, cellular health, and neuronal function in human-relevant experimental models, providing critical data for lead optimization and candidate selection. The recent regulatory approvals of anti-Aβ monoclonal antibodies have validated the therapeutic potential of Aβ-targeting approaches, while also highlighting the need for continued refinement of screening platforms to identify compounds with improved efficacy and safety profiles.
Future advances in HCS technology, particularly the integration of more physiologically complex 3D models and label-free imaging approaches, promise to further enhance the predictive power of these platforms. Combined with sophisticated computational modeling and analysis approaches, HCS-based screening strategies will continue to play a central role in the development of next-generation Aβ-targeting therapeutics, ultimately contributing to improved treatment options for Alzheimer's disease patients.
Addressing Technical Limitations and Enhancing Model Fidelity
Overcoming Challenges in Organoid Maturation and Cellular Heterogeneity
The use of induced pluripotent stem cell (iPSC)-derived brain organoids has revolutionized the modeling of human neurodevelopment and neurological disorders, including Alzheimer's disease (AD). These three-dimensional structures recapitulate defining features of the developing human brain that are inaccessible to conventional models, providing an unprecedented platform for probing the pathophysiological processes of dementia [54] [15]. However, two fundamental challenges—achieving functionally mature organoids and controlling their cellular heterogeneity—remain significant bottlenecks, particularly for modeling adult-onset conditions like AD which require the mature processing of amyloid-β (Aβ) peptides [54] [1]. This technical guide outlines current strategies and methodologies to overcome these limitations within the context of amyloid-beta deposition research.
The Maturation Bottleneck in Alzheimer's Disease Research
A major constraint in brain organoid technology is their characteristic developmental arrest at fetal-to-early postnatal stages, even after extended culture periods exceeding six months [54]. This immaturity severely limits their utility in modeling adult neurological disorders because the organoids fail to recapitulate postnatal transcriptional signatures and mature pharmacodynamic responses essential for valid drug screening [54].
For Alzheimer's disease research specifically, this maturation deficit is particularly problematic. The amyloid cascade hypothesis places Aβ at the center of AD pathogenesis, with evidence suggesting the disease progresses in two phases: an early phase driven by Aβ aggregation and a later phase that progresses independently of massive Aβ deposition [1]. Critically, the most seeding-active Aβ species—small soluble oligomers considered crucial for the initial stage of aggregation—emerge during early pathological processes [1]. Without achieving sufficient maturity, organoids cannot faithfully model the complex molecular events in Aβ pathogenesis, including the formation of bioactive Aβ seeds that propagate throughout the brain via prion-like mechanisms [1].
Multidimensional Framework for Assessing Organoid Maturity
Evaluating organoid maturation requires a multimodal approach that moves beyond isolated readouts to integrated assessment frameworks. The table below outlines key benchmarks and corresponding techniques for comprehensive maturity evaluation.
Table 1: Multidimensional Assessment of Brain Organoid Maturity
| Assessment Dimension | Key Benchmarks | Technical Methods |
|---|---|---|
| Structural Architecture | Cortical lamination (SATB2, TBR1, CTIP2 layers); Synaptic maturation (SYB2, PSD-95); Barrier formation (glia limitans) | Immunofluorescence/Immunohistochemistry (IF/IHC); Confocal microscopy; Electron microscopy (EM) [54] |
| Cellular Diversity | Neuronal populations (NEUN, MAP2); Astrocytes (GFAP, S100β); Oligodendrocytes (MBP); Neurotransmitter identity (VGLUT1, GAD65/67) | IF/IHC; Fluorescence-activated cell sorting (FACS); Single-cell RNA sequencing (scRNA-seq) [54] |
| Functional Maturation | Synchronized network activity (γ-band oscillations); Synaptic transmission; Gliotransmission | Multielectrode arrays (MEAs); Patch clamp; Calcium imaging [54] [55] |
| Molecular & Metabolic Profiling | Transcriptomic signatures; Metabolic activity; Maturity-stage specific gene expression | scRNA-seq; Bulk RNA sequencing; Metabolic assays [54] |
Advanced electrophysiological assessment techniques, particularly using ultra-high-density CMOS microelectrode arrays (MEAs) with up to 236,880 electrodes, now enable detailed analysis of network connectivity, propagation dynamics, and frequency features at single-cell resolution [55]. These systems can introduce novel quantitative endpoints such as propagation velocity and propagation area for assessing network functionality and pharmacological responses in organoids [55].
Strategies to Accelerate Functional Maturation
Several innovative approaches have emerged to overcome the maturation barrier in brain organoids, moving beyond simple extended culture periods.
Microenvironment Modulation and Bioengineering
Extended conventional 3D culture exacerbates metabolic stress and hypoxia-induced necrosis, creating asynchronous tissue maturation with electrophysiologically active superficial layers juxtaposed with degenerating cores [54]. Emerging strategies focus on decoupling maturation milestones from rigid temporal frameworks through:
- Vascularization: Co-culture with endothelial cells or induction of vascular programs to enhance nutrient and oxygen diffusion, preventing central necrosis and supporting larger tissue volumes [54].
- Electrical Stimulation: Application of defined electrical activity patterns to promote neuronal network maturation and synaptic refinement, mimicking experience-dependent development [54].
- Microfluidic Systems: Perfusion-based culture platforms that improve metabolite clearance and provide more physiological microenvironmental cues [54] [56].
Assembloid Approaches for Circuit Complexity
To model complex neurodegenerative processes like Aβ propagation, region-specific organoids can be fused to create assembloids that recapitulate inter-regional connectivity. For example, midbrain-striatal assembloids have been successfully generated and maintained for extended periods, enabling the study of network-level dysfunction and pathological spread between vulnerable brain regions [55]. These models demonstrate enhanced functional connectivity and more mature network properties compared to single-region organoids.
Addressing Cellular Heterogeneity and Reproducibility
Significant protocol-to-protocol and cell line-to-cell line variability complicates the comparative analysis of organoid models, necessitating robust quality control measures [57] [58].
Standardized Quality Metrics and Selection Criteria
Research has identified the Feret diameter (the longest distance between any two points of the organoid) as a reliable single parameter for characterizing brain organoid quality, with a threshold of 3050 μm demonstrating high predictive value for organoid performance [58]. This morphological parameter correlates with transcriptional profiles and cellular composition, providing a straightforward quality control metric.
Computational analyses have revealed that the abundance of unintended mesodermal differentiation represents a major confounder in unguided brain organoid differentiation protocols [58]. High-quality organoids consistently display lower presence of mesenchymal cells, which negatively correlate with proper neural differentiation. The proportion of mesenchymal cells also positively correlates with organoid Feret diameter, providing both morphological and molecular criteria for quality assessment [58].
Protocol and Cell Line Standardization
Systematic analysis of brain organoids across multiple protocols and cell lines has enabled more reproducible model generation. Studies comparing dorsal forebrain, ventral forebrain, midbrain, and striatal protocols from multiple iPSC lines have established references for cell-type recapitulation and identified early gene expression signatures that predict protocol-driven organoid generation [57]. These resources provide benchmarks for selecting appropriate protocols and cell lines for specific research applications, including Aβ deposition studies.
Experimental Protocols for AD-Relevant Organoid Models
Cerebral Organoid Generation for Aβ Studies
The following protocol generates cortical organoids suitable for studying amyloid-β pathology:
- Day 0: Seed iPSCs (e.g., 201B7 line) at density of 9.0 × 10³ cells per well in EB seeding medium using AggreWell plates to promote embryoid body formation [55].
- Days 2-4: Add 100 μL of EB formation medium to each well [55].
- Day 5: Replace medium with induction medium and incubate for 2 days [55].
- Day 7: Embed organoids in Matrigel (Corning, 354277) and incubate in expansion medium for 3 days [55].
- Day 10 onward: Transition to maturation medium and culture on orbital shaker (e.g., COSH6, AS ONE Corporation) with medium changes every 3-4 days [55].
- Month 3+: Long-term maturation: Switch to BrainPhys Neuronal Medium (STEMCELL Technologies, 05792) for maintenance, enabling extended culture to promote functional maturation [55].
For midbrain organoids relevant to vulnerable regions in AD, protocols utilizing the STEMdiff Midbrain Organoid Differentiation Kit (STEMCELL Technologies, 100-1096) with extended culture periods of 4+ months in BrainPhys medium have demonstrated robust functional maturation [55].
Functional Assessment of Network Maturation
Advanced functional characterization of organoids can be performed using ultra-high-density CMOS microelectrode arrays:
- Preparation: Transfer mature organoids to recording chamber of UHD-CMOS MEA system [55].
- Acquisition: Record field potentials from up to 236,880 electrodes across 32.45 mm² sensing area with appropriate sampling rate (e.g., 20 kHz) [55].
- Analysis:
The Scientist's Toolkit: Essential Reagents and Systems
Table 2: Key Research Reagent Solutions for Brain Organoid Research
| Reagent/System | Function | Example Products |
|---|---|---|
| Stem Cell Culture Media | Maintain pluripotency and support expansion of iPSCs | mTeSR Plus Medium (STEMCELL Technologies) [55] |
| Organoid Differentiation Kits | Generate region-specific organoids with optimized protocols | STEMdiff Cerebral Organoid Kit; STEMdiff Midbrain Organoid Kit (STEMCELL Technologies) [55] |
| Extracellular Matrices | Provide 3D structural support for organoid formation | Matrigel (Corning, 354277); Synthetic hydrogels [59] |
| Neuronal Maintenance Media | Support long-term maturation and functional development | BrainPhys Neuronal Medium (STEMCELL Technologies, 05792) [55] |
| Electrophysiology Systems | Assess functional maturation and network activity | Ultra-high-density CMOS Microelectrode Arrays [55] |
Visualizing Maturation Challenges and Solutions
The diagram below illustrates the core challenges in organoid maturation and the strategic solutions being implemented to overcome them, specifically in the context of Alzheimer's disease research.
Diagram 1: Roadmap for Advanced AD Organoid Models
The convergence of advanced bioengineering strategies with standardized quality control metrics is paving the way for a new generation of brain organoid models with enhanced maturity and reduced heterogeneity. For Alzheimer's disease research, these developments are particularly crucial, as they enable more faithful recapitulation of Aβ seeding and aggregation processes that drive pathogenesis. As organoid technology continues to evolve, integrating these approaches will be essential for creating clinically predictive models that can accelerate the development of effective therapeutics for neurodegenerative diseases.
Mitigating CRISPR/Cas9 Off-Target Effects and Improving Editing Efficiency
The application of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 technology in induced pluripotent stem cell (iPSC)-based disease modeling represents a transformative approach for studying neurodegenerative disorders, particularly Alzheimer's disease (AD). The ability to precisely introduce familial AD (fAD) mutations or correct risk alleles in iPSCs enables the creation of human-relevant neuronal models to study amyloid-beta (Aβ) deposition mechanisms [9]. However, the reliability of these models depends entirely on the precision and efficiency of genome editing. Off-target effects—unintended genetic modifications at sites other than the intended target—pose a significant threat to experimental validity, potentially confounding the interpretation of Aβ-associated phenotypes [60] [61]. Similarly, poor editing efficiency can necessitate extensive screening to obtain properly edited clones, delaying critical experiments. This technical guide provides a comprehensive framework for optimizing CRISPR-Cas9 specificity and efficiency, with particular emphasis on protocols relevant to iPSC-derived neuronal cultures for amyloid-beta research.
Understanding and Detecting CRISPR-Cas9 Off-Target Effects
Mechanisms of Off-Target Activity
The Cas9 nuclease, derived from Streptococcus pyogenes (SpCas9), is guided to its genomic target by a complex formed between a single-guide RNA (sgRNA) and the Cas9 protein. Off-target effects occur when this complex binds and cleaves DNA at sites with significant sequence similarity to the intended target, primarily due to mismatch tolerance between the sgRNA and genomic DNA [62]. Several key factors influence this tolerance:
- Mismatch Position: Mismatches are more easily tolerated in the 5' end of the gRNA (PAM-distal region) compared to the seed region (PAM-proximal region), where single mismatches can prevent Cas9 activation [61] [62].
- Mismatch Quantity: While off-target activity is most common with 1-3 mismatches, cleavage has been reported at sites with up to 6 mismatches [63].
- Non-Canonical PAM Sequences: While SpCas9 primarily recognizes a 5'-NGG-3' PAM sequence, off-target binding and cleavage can occur at sites with non-canonical PAMs such as 5'-NAG-3' [63].
- Cellular Environment: Factors including chromatin accessibility, epigenetic states, and sgRNA secondary structure significantly influence off-target potential, though these are insufficiently considered by standard prediction algorithms [60] [62].
Advanced Detection Methodologies
Comprehensive off-target assessment requires a multi-faceted approach, combining computational prediction with empirical validation. The table below summarizes key detection methods, their principles, and applications relevant to iPSC research.
Table 1: Methods for Detecting CRISPR/Cas9 Off-Target Effects
| Method | Principle | Advantages | Limitations | iPSC Applicability |
|---|---|---|---|---|
| In Silico Prediction (CCTop, Cas-OFFinder) | Computational nomination of off-target sites based on sequence homology to the sgRNA [60]. | Fast, inexpensive, accessible via web interfaces. | Biased toward sgRNA-dependent sites; insufficient consideration of chromatin environment [60]. | Useful for initial sgRNA screening prior to experimental use. |
| GUIDE-seq | Captures double-strand breaks (DSBs) via integration of double-stranded oligodeoxynucleotides (dsODNs), followed by sequencing [60] [63]. | Highly sensitive, low false-positive rate, genome-wide. | Requires efficient dsODN delivery, which can be toxic in some cell types [63]. | Can be challenging in hard-to-transfect iPSCs; optimal in differentiated progenitors. |
| Digenome-seq | Digests purified genomic DNA with Cas9-sgRNA ribonucleoprotein (RNP) complexes in vitro, followed by whole-genome sequencing (WGS) [60] [63]. | Highly sensitive; does not require living cells. | Expensive; requires high sequencing coverage; cell-free system lacks nuclear context [60]. | Suitable for initial off-target profiling before iPSC editing. |
| BLISS | Captures DSBs in situ using dsODNs with a T7 promoter sequence [60]. | Directly captures DSBs in situ; requires low cell input. | Only identifies off-target sites present at the time of detection [60]. | Applicable to precious iPSC-derived neurons where cell numbers may be limited. |
| DISCOVER-seq | Utilizes the DNA repair protein MRE11 as bait to perform chromatin immunoprecipitation followed by sequencing (ChIP-seq) [60]. | Highly sensitive; high precision in cells; exploits endogenous repair machinery. | Potential for false positives [60]. | Works well in iPSCs and their differentiated derivatives. |
Strategic Optimization to Minimize Off-Target Effects
sgRNA Engineering for Enhanced Specificity
The design and composition of the sgRNA are among the most critical factors determining editing specificity. Multiple optimization strategies have proven effective:
- Truncated sgRNAs: Using shorter sgRNA sequences (typically 17-18 nucleotides instead of 20) can reduce off-target effects by decreasing the energy of sgRNA-DNA binding, making the system less tolerant to mismatches [61].
- GC Content Optimization: Maintaining GC content in the sgRNA sequence between 40% and 60% stabilizes the DNA:RNA duplex at the on-target site while destabilizing off-target binding [61].
- Chemical Modifications: Incorporating specific chemical modifications, such as 2'-O-methyl-3'-phosphonoacetate at sites in the ribose-phosphate backbone of sgRNAs, can significantly reduce off-target cleavage while maintaining high on-target activity [61] [64].
- The "GG20" Strategy: Replacing the GX19 sgRNAs at the 5' end with two guanines (creating ggX20 sgRNAs) has been shown to significantly lessen the off-target effect and boost specificity [61].
High-Fidelity Cas9 Variants and Orthologs
Protein engineering has yielded Cas9 variants with dramatically improved specificity profiles, making them particularly valuable for sensitive applications like iPSC-based disease modeling.
Table 2: High-Fidelity Cas9 Variants and Orthologs
| Engineered Nuclease | Engineering Strategy | Key Features | Therapeutic/Research Applications |
|---|---|---|---|
| SpCas9-HF1 (High-Fidelity variant 1) | Four mutations (N497A, R661A, Q695A, Q926A) that reduce non-specific interactions with the DNA phosphate backbone [61]. | Retains on-target activity comparable to wild-type SpCas9 with >85% of sgRNAs tested; demonstrated reduced off-target activity [61]. | Widely used in iPSC gene editing for disease modeling; suitable for introducing fAD mutations. |
| eSpCas9 (enhanced SpCas9) | Mutations (K848A, K1003A, R1060A) that alter positive charges in the DNA binding groove, increasing energy barrier for off-target binding [61]. | Features a proofreading mechanism that traps mutants in an inactive state when bound to mismatched targets [61]. | Recommended for precise genome engineering in stem cells and neuronal derivatives. |
| SaCas9 | Cas9 ortholog from Staphylococcus aureus with natural different PAM requirement (5'-NNGRRT-3') [61]. | Smaller size facilitates delivery; longer PAM requirement naturally reduces the number of potential off-target sites in the genome [61]. | Useful for targeting genomic regions lacking standard SpCas9 PAM sites; valuable for in vivo applications. |
| Cas9 Nickase | Mutation of one nuclease domain (RuvC or HNH) to create a single-strand DNA break (nick) rather than a DSB [61]. | Paired nickase strategy (using two sgRNAs) creates staggered DSBs, dramatically reducing off-target mutations compared to wild-type Cas9 [61]. | Ideal for applications requiring high fidelity, such as introducing point mutations relevant to AD research. |
Delivery Method Optimization
The method and form in which CRISPR components are delivered significantly impact both efficiency and specificity:
- Ribonucleoprotein (RNP) Complexes: Direct delivery of pre-assembled Cas9 protein-sgRNA complexes reduces the time window for off-target activity, as these complexes are rapidly degraded in cells. RNP delivery also avoids the potential for random integration of plasmid DNA [64].
- Inducible Systems: Doxycycline-inducible Cas9 systems (iCas9) enable temporal control of nuclease expression, allowing researchers to limit Cas9 exposure and reduce the cumulative probability of off-target events [64].
- Advanced Nanodelivery: Recent advances in delivery vehicles, such as lipid nanoparticle spherical nucleic acids (LNP-SNAs), have demonstrated enhanced editing efficiency with reduced toxicity. These structures carry CRISPR tools wrapped in a protective shell of DNA, facilitating more efficient cellular uptake and targeted delivery [65].
Maximizing Editing Efficiency in iPSC Systems
Experimental Protocol for High-Efficiency Gene Editing in iPSCs
The following optimized protocol, adapted from recent literature, enables highly efficient gene knockout in iPSCs, achieving stable INDEL efficiencies of 82-93% for single-gene knockouts and over 80% for double-gene knockouts [64].
Protocol: Optimized Gene Knockout in iPSCs Using an Inducible Cas9 System
Step 1: Cell Line Engineering and Culture
- Generate a doxycycline-inducible SpCas9-expressing iPSC line (iCas9) by inserting the doxycycline-spCas9-puromycin cassette into a safe-harbor locus such as AAVS1.
- Culture iPSCs in Pluripotency Growth Medium on Matrigel-coated plates at 37°C with 5% CO₂.
- For editing induction, pre-treat cells with 1-2 μg/mL doxycycline for 24 hours before nucleofection to activate Cas9 expression.
Step 2: sgRNA Design and Preparation
- Design sgRNAs using computational tools (CCTop or Benchling algorithms), prioritizing those with high predicted on-target activity and minimal off-target potential.
- Opt for chemically synthesized and modified sgRNAs (CSM-sgRNAs) incorporating 2'-O-methyl-3'-thiophosphonoacetate at both 5' and 3' ends to enhance intracellular stability.
- Validate sgRNA efficacy through Western blotting to confirm protein knockout, as INDEL frequency alone may not always correlate with functional knockout.
Step 3: Nucleofection Optimization
- Dissociate doxycycline-treated iCas9 iPSCs using EDTA and pellet by centrifugation.
- Combine 5 μg of CSM-sgRNA with nucleofection buffer (P3 Primary Cell 4D-Nucleofector X Kit) for every 8 × 10⁵ cells.
- Electroporate using the CA137 program on a Lonza 4D-Nucleofector.
- For multiple gene knockouts, co-electroporate with two or three sgRNAs at the same weight ratio to a total of 5 μg.
Step 4: Repeated Nucleofection and Clonal Selection
- Conduct a second nucleofection 3 days after the first using identical parameters to increase editing efficiency in the cell population.
- After 5-7 days, assess INDEL efficiency using the ICE (Inference of CRISPR Edits) algorithm or TIDE (Tracking of Indels by Decomposition) analysis of Sanger sequencing data.
- For clonal isolation, single-cell sort edited cells and expand for genotyping and functional validation.
Advanced Editing Systems for Precision Modifications
Beyond standard knockout approaches, newer CRISPR systems offer enhanced capabilities for precise genetic manipulation:
- Prime Editing: This system uses a catalytically impaired Cas9 fused to a reverse transcriptase and a specialized prime editing guide RNA (pegRNA). It can mediate all 12 possible base-to-base conversions, small insertions, and deletions without requiring double-strand breaks or donor DNA templates, significantly reducing off-target effects associated with traditional HDR [61].
- Base Editing: DNA base editors combine a Cas9 nickase with a deaminase enzyme to directly convert one DNA base to another without creating a DSB, enabling highly efficient and precise point mutations with minimal indel formation.
The following diagram illustrates the strategic decision-making process for selecting the appropriate CRISPR tool based on the research objective, particularly in the context of Alzheimer's disease research using iPSCs.
The Scientist's Toolkit: Essential Reagents for CRISPR-iPSC Experiments
Table 3: Essential Research Reagents for CRISPR/iPSC Experiments
| Reagent/Category | Specific Examples | Function/Application | Considerations for Aβ Deposition Research |
|---|---|---|---|
| Cas9 Expression Systems | iCas9 (doxycycline-inducible SpCas9), SpCas9-HF1, eSpCas9 [64] [61]. | Provides the nuclease activity for DNA cleavage. | Inducible systems allow temporal control; high-fidelity variants reduce confounding off-target mutations in AD-relevant genes. |
| sgRNA Modifications | CSM-sgRNA (2'-O-methyl-3'-thiophosphonoacetate) [64]. | Enhances sgRNA stability and specificity; reduces off-target effects. | Improved stability is crucial for efficient editing in hard-to-transfect iPSC-derived neurons and glia. |
| Delivery Tools | 4D-Nucleofector System (Lonza), Lipofectamine CRISPR-MAX, LNP-SNAs [64] [65]. | Introduces CRISPR components into cells. | LNP-SNAs show promise for in vivo editing but are emerging for iPSC use; nucleofection is current gold standard for iPSCs. |
| Detection & Validation | ICE Analysis, TIDE Analysis, GUIDE-seq, Western Blot [64] [60]. | Assesses editing efficiency and validates knockout at protein level. | Western blot essential to confirm loss of AD-related proteins (e.g., APP, presenilin) despite high INDEL rates. |
| iPSC Differentiation Kits | Commercial neuronal differentiation kits, Forebrain neuron protocols. | Generates relevant cell types (neurons, astrocytes, microglia) for Aβ studies. | Select protocols that generate cell types relevant to Aβ metabolism (cortical neurons, astrocytes). |
| Control Cell Lines | Isogenic control lines, Wild-type iPSCs. | Provides proper experimental controls for phenotypic comparisons. | Critical for distinguishing edit-specific phenotypes from background genetic variation in Aβ secretion and aggregation studies. |
The reliability of iPSC-based models for studying amyloid-beta deposition in Alzheimer's disease hinges on the precision and efficiency of genetic modifications. By implementing the strategies outlined in this guide—including careful sgRNA design, utilization of high-fidelity Cas9 variants, optimized delivery methods, and comprehensive off-target assessment—researchers can significantly enhance the validity of their experimental systems. The ongoing development of more precise editing tools, such as prime editors and base editors, coupled with advanced delivery platforms like LNP-SNAs, promises to further elevate the capabilities of CRISPR-based iPSC research. As these technologies continue to mature, they will undoubtedly accelerate our understanding of the molecular mechanisms underlying Alzheimer's pathology and facilitate the development of targeted therapeutic interventions.
Standardizing Aβ Oligomer Preparation and Characterization
The study of amyloid-β oligomers (AβOs) has become a central focus in Alzheimer's disease (AD) research, as these soluble, non-fibrillar aggregates are hypothesized to be the proximate neurotoxic agents responsible for synaptic dysfunction and neurodegeneration [66] [67] [68]. Unlike mature amyloid fibrils which form insoluble plaques, AβOs are metastable, structurally heterogeneous, and exist in low concentrations, presenting significant challenges for their reproducible preparation and characterization [67] [68]. This technical variability has hampered progress in understanding their precise roles in AD pathogenesis and developing targeted therapies.
The emergence of human induced pluripotent stem cell (iPSC) technologies has revolutionized Alzheimer's disease research by providing physiologically relevant human models [22] [9]. iPSC-derived neurons and glial cells recapitulate key aspects of AD pathology, including Aβ production, tau phosphorylation, and neuroinflammatory responses [9] [19]. When modeling amyloid-beta deposition using iPSC-derived systems, researchers frequently apply exogenous Aβ oligomers to study their effects on neuronal function, synaptic integrity, and glial responses [19]. Standardized preparation of these oligomers is therefore essential for generating reproducible, interpretable data across different laboratories and experimental systems.
This guide provides detailed methodologies for producing well-defined Aβ oligomer preparations and characterizing their properties using orthogonal analytical techniques, with particular emphasis on applications in iPSC-based AD models.
Aβ Oligomer Preparation Methods
Photo-Induced Cross-Linking of Unmodified Proteins (PICUP)
The PICUP methodology enables "freezing" of metastable oligomer equilibria through covalent cross-linking, allowing for production of stable, defined oligomer populations [68].
Detailed Protocol:
- Peptide Preparation: Dissolve Aβ40 or Aβ42 to 90 μM in 6 mM NaOH/9 mM Na₂HPO₄. First dissolve peptide in 50 μL of 60 mM NaOH with gentle agitation, then add 225 μL water, followed by 225 μL of 20 mM Na₂HPO₄, pH 7.4.
- Sonication and Clarification: Sonicate the Aβ solution for 1 minute, then centrifuge at 16,000 × g for 10 minutes. Aliquot supernatant into 0.2-mL clear, thin-walled PCR tubes (18 μL/tube).
- Cross-Linking Reaction: Add 1 μL of 60 mM ammonium persulfate (APS) and 1 μL of 3 mM Tris(2,2'-bipyridyl)dichlororuthenium(II) hexahydrate (Ru(Bpy)) to each reaction tube.
- Irradiation: Immediately irradiate tubes for 1 second using a 200-W incandescent lamp in a camera bellows apparatus.
- Reaction Quenching: Immediately add 20 μL of 5% β-mercaptoethanol in 2× sample buffer to terminate the reaction.
- Pooling and Storage: Multiple reactions can be pooled and stored at -20°C for subsequent purification [68].
Critical Parameters:
- Peptide purity and source significantly impact reproducibility
- Fresh preparation of APS and Ru(Bpy) solutions is essential
- Reaction time must be strictly controlled to prevent over-cross-linking
- Oxygen exclusion minimizes side reactions
Isolation of Defined Oligomers via SDS-PAGE and Alkaline Extraction
Following PICUP, defined oligomer species can be isolated using preparative SDS-PAGE coupled with alkaline extraction:
- Preparative SDS-PAGE: Load cross-linked oligomers onto a 10-20% Tricine gel (1-mm thick) alongside unstained molecular weight markers. Electrophorese at 100V until stacking is complete, then at 120V until the dye front reaches the gel bottom.
- Visualization: Stain gel with SimplyBlue Coomassie stain with gentle agitation for 1 hour, followed by destaining in water.
- Gel Excision: Excise gel bands corresponding to desired oligomer states (dimer, trimer, tetramer, etc.) using a clean scalpel.
- Alkaline Extraction: Mince gel slices thoroughly using a disposable pellet pestle. Add 500 μL of 0.1 M ammonium hydroxide per 100 mg of gel material.
- Elution: Rotate samples at 20-24 rpm for 4 hours at room temperature.
- Clarification: Centrifuge at 16,000 × g for 10 minutes and collect supernatant containing extracted oligomers.
- Desalting and Concentration: Remove SDS using commercial removal resins (e.g., SDSOut) and concentrate using centrifugal filters with appropriate molecular weight cutoffs [68].
Preparation of Oligomers for iPSC Studies
For physiological studies using iPSC-derived cells, additional considerations are necessary:
- Endotoxin Removal: Use endotoxin-free water and buffers throughout preparation
- Sterilization: Filter sterilize using low-protein-binding 0.22-μm filters
- Vehicle Control: Prepare identical buffers without Aβ for control treatments
- Concentration Validation: Quantify using Aβ-specific ELISA after preparation
- Stability Assessment: Monitor oligomer integrity over time under storage conditions
Table 1: Critical Parameters for Aβ Oligomer Preparation
| Parameter | PICUP Method | Non-Crosslinked Preparation | Importance |
|---|---|---|---|
| Aβ Concentration | 90 μM | 0.5-86 μM (concentration-dependent assembly) | Determines oligomer size distribution [68] [69] |
| Buffer Conditions | 6 mM NaOH/9 mM Na₂HPO₄ | PBS or cell culture media | Impacts aggregation kinetics and oligomer stability |
| Incubation Time | Immediate (cross-linked) | Hours to days | Affects oligomer maturity and structural properties |
| Temperature | Room temperature (during cross-linking) | 4°C to 37°C | Influences assembly pathways and rates |
| Agitation | Minimal | Variable (affects aggregation) | Can promote or inhibit specific oligomer forms |
Characterization Techniques
Comprehensive characterization of Aβ oligomer preparations requires multiple orthogonal techniques to assess size distribution, structural features, and biological activity.
Size and Morphological Analysis
Western Blotting:
- Use 4-12% Bis-Tris gels for optimal resolution of low molecular weight oligomers
- Transfer to nitrocellulose membranes for immunodetection
- Probe with 6E10 antibody (1:2000 dilution) for Aβ detection [70]
- Include anti-APOE antibody (1:4000) if studying APOE interactions
- Visualize using enhanced chemiluminescence
Electron Microscopy:
- Apply 5 μL of sample to freshly glow-discharged carbon-coated grid
- Adsorb for 2 minutes, blot excess with filter paper
- Wash with deionized water before staining with 1% uranyl acetate for 15 seconds
- Blot excess stain and air-dry grid
- Image using transmission electron microscope operating at 120 kV and 30,000× magnification [70]
Spectral Characterization
Intrinsic Fluorescence Spectroscopy: Aβ40 exhibits concentration-dependent autofluorescence changes during oligomerization:
- Tyrosine Emission: Monomers show emission maximum at ~350 nm (tyrosinate form). During oligomerization, this shifts to 302 nm as tyrosine residues become shielded from aqueous environment [69]
- Aggregation-Induced Emission: Soluble Aβ oligomers develop novel emission in visible spectral region (~500 nm), providing label-free detection method [69]
- Critical Concentrations: Distinct spectral changes occur at cac1 = 0.5 μM and cac2 = 19 μM, corresponding to different aggregation phases [69]
Experimental Parameters for Spectral Analysis:
- Use excitation at 245 nm for maximal tyrosine emission changes
- For visible AIE detection, use excitation at 290-300 nm
- Correct for buffer background and cuvette autofluorescence
- Perform serial dilution studies to establish concentration dependence
Table 2: Analytical Methods for Aβ Oligomer Characterization
| Method | Information Provided | Sample Requirements | Key Findings in Aβ Research |
|---|---|---|---|
| PICUP-SDS-PAGE | Oligomer size distribution, cross-linking efficiency | 10-50 μg protein | Aβ42 forms higher-order oligomers than Aβ40 [68] |
| EM | Morphology, fibril content, aggregate size | 5-10 μL at ~5-50 μM | Reveals polymorphic nature of oligomers [70] |
| Intrinsic Fluorescence | Oligomer concentration, tyrosine environment | 0.5-100 μM in PBS | Blue shift from 350→302 nm indicates aggregation; visible AIE at >19 μM [69] |
| ELISA | Oligomer-specific epitopes, concentration | Varies by assay | Detection in biological fluids; ~90% sensitivity/75% specificity for some assays [67] [71] |
| FCS | Hydrodynamic radius, aggregation state | Low nM concentrations | Identified cac1=0.5 μM and cac2=19 μM for Aβ40 [69] |
Applications in iPSC-Based Alzheimer's Disease Models
Standardized Aβ oligomer preparations are essential tools for investigating disease mechanisms in human iPSC-derived models, which better recapitulate human neurobiology than traditional cell lines or animal models [22] [9].
Modeling Neuronal Dysfunction
iPSC-derived forebrain neurons exposed to defined Aβ oligomers exhibit key features of AD pathology:
- Decreased frequency of excitatory post-synaptic currents [19]
- Altered synaptic transmission and plasticity
- Neuronal hyperexcitability at early stages
- Progressive synaptic loss and neurodegeneration
Experimental Workflow for Neuronal Studies:
- Differentiate iPSCs to forebrain neurons using dual-SMAD inhibition [22]
- Culture for 30-60 days to achieve mature synaptic networks
- Treat with characterized Aβ oligomers (1-500 nM range)
- Assess electrophysiological properties by patch-clamp recording
- Analyze synaptic density by immunocytochemistry (PSD95, synapsin)
- Quantify neuronal viability and apoptosis markers
Astrocyte-Mediated Mechanisms
Human iPSC-derived astrocytes play crucial roles in Aβ clearance and neuronal support functions:
Astrocyte Phagocytosis and Storage:
- Astrocytes ingest large amounts of aggregated Aβ via phagocytosis
- Incomplete degradation leads to intracellular Aβ storage [19]
- Stored Aβ induces cellular stress and alters astrocyte function
- Stressed astrocytes transfer Aβ to neighboring cells via tunneling nanotubes [19]
Impact on Neuronal Support:
- Aβ-laden astrocytes show impaired support of neuronal function
- Co-culture with Aβ-exposed astrocytes decreases frequency of excitatory post-synaptic currents in neurons [19]
- Conditioned media from Aβ-exposed astrocytes induces neuronal hyperactivation [19]
- Secreted factors from stressed astrocytes alter synaptic function
Complex Co-culture Systems
Advanced iPSC models incorporating multiple cell types better mimic the brain microenvironment:
Tri-culture Systems:
- Incorporate iPSC-derived neurons, astrocytes, and microglia
- Enable study of cell-type-specific responses to Aβ oligomers
- Model neuroinflammatory components of AD
- Reveal intercellular spread of pathology
Blood-Brain Barrier Models:
- Include endothelial cells, pericytes, and astrocytes
- Assess Aβ oligomer transport across BBB
- Study neurovascular dysfunction in AD
Research Reagent Solutions
Table 3: Essential Reagents for Aβ Oligomer Research
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Aβ Peptides | Aβ(1-40), Aβ(1-42), Aβ(pE3-42) | Primary substrates for oligomer formation | Source and purity critical; validate by mass spectrometry |
| Cross-linking Reagents | Ammonium persulfate, Ru(Bpy) | Stabilize metastable oligomers via PICUP | Prepare fresh solutions for each use [68] |
| Separation Media | 10-20% Tricine gels, size exclusion matrices | Separate oligomers by size | Tricine gels offer superior resolution for small proteins [68] |
| Detection Antibodies | 6E10, 4G8, OC, A11 | Identify specific oligomer conformations | 6E10 detects residues 1-17 of Aβ [70] |
| Cell Culture Reagents | iPSC differentiation kits, laminin, poly-ornithine | Generate human neurons and glia for testing | Ensure lot-to-lot consistency for reproducible results [22] |
| Fluorescence Probes | Thioflavin T, intrinsic tyrosine fluorescence | Monitor aggregation state | Intrinsic fluorescence enables label-free detection [69] |
Experimental Workflows
The following diagrams illustrate key experimental workflows for standardized Aβ oligomer preparation and application in iPSC models.
Aβ Oligomer Preparation and Characterization Workflow
iPSC-Based AD Model Validation Workflow
Standardized preparation and comprehensive characterization of Aβ oligomers are fundamental prerequisites for rigorous Alzheimer's disease research using human iPSC models. The methods detailed in this guide, particularly the PICUP-based approach for generating defined oligomer populations and the orthogonal characterization strategies, provide a framework for producing reproducible, well-defined Aβ oligomer preparations. When applied to increasingly sophisticated iPSC-derived neural systems, including neurons, astrocytes, and complex co-cultures, these standardized tools will enable more physiologically relevant studies of Aβ-induced neurotoxicity and accelerate the development of targeted therapeutic interventions for Alzheimer's disease.
Ensuring Reproducibility Across iPSC Lines and Differentiation Protocols
The use of induced pluripotent stem cell (iPSC) technology has positioned itself as a transformative approach for modeling Alzheimer's disease (AD) and studying amyloid-β (Aβ) deposition in human neurons. However, without due consideration, the thousands of new human iPSC lines generated in the past decade inevitably affect the reproducibility of iPSC-based experiments [72]. Differences between donor individuals, genetic stability, and experimental variability contribute to iPSC model variation by impacting differentiation potency, cellular heterogeneity, morphology, and transcript abundance [72]. Such effects can confound reproducible disease modeling, particularly for studying the amyloid-β pathway, which is central to AD pathophysiology [73]. This technical guide addresses the core challenges and solutions for ensuring reproducibility in iPSC-based amyloid-β research, providing researchers with standardized approaches for generating reliable, comparable data across laboratories and experimental timelines.
The substantial impact on resulting differentiated cells can overwhelm any biological variation of interest, especially where effect sizes are small [72]. The primary sources of variability include:
Genetic Background: Heterogeneity at the iPSC stage is mainly driven by the genetic background of the donor, more than by any other non-genetic factor [72]. Through systematic generation and phenotyping of hundreds of iPSC lines, the Human Induced Pluripotent Stem Cells Initiative (HipSci) reported that 5-46% of the variation in iPSC cell phenotypes is due to inter-individual differences [72]. iPSC lines derived from the same individual are more similar to each other than to iPSC lines from different individuals, as highlighted by inter-individual variation detected in gene expression and expression quantitative trait loci (eQTLs) [72].
Cellular Heterogeneity: This refers to cell type diversity within the experimental cellular population, arising from the presence of multiple cell types and diversity in morphology, maturation and functionality within each cell type present [72]. This is particularly relevant for amyloid-β research, where the ratio of Aβ42 to Aβ40 production has pathological significance, and cellular heterogeneity can dramatically influence experimental outcomes [74] [73].
Somatic Mutations: These acquired genetic alterations can either pre-exist in the somatic cells or be acquired during reprogramming and culture handling [72]. Subclonal mutations (present in only a fraction of cells) can become selected for during extended culture, potentially influencing amyloid-β processing phenotypes.
iPSC derivation and differentiation are multistep processes where small variations at each step can accumulate and generate significantly different outcomes [72]. Key technical sources include:
Reprogramming Methods: Differences between mRNA reprogramming, viral vectors, or episomal approaches can influence the resulting iPSC characteristics [74].
Differentiation Protocol Variations: Minor differences in small molecules, growth factors, culture conditions, and initial cell seeding density can significantly alter the resulting cell populations [75] [76]. For example, the efficiency and reproducibility of sensory neuron differentiation depends on genetic variations in cell lines, initial density, culture conditions at the start of the experiment, and minor differences in small molecules and coating conditions [75].
Protocol Duration and Maturation State: The maturity of iPSC-derived cells can substantially impact disease-relevant phenotypes. Most current iPSC differentiation protocols produce immature or fetal-like cells [72], which may not fully recapitulate late-onset disease processes like amyloid-β deposition in Alzheimer's disease.
Table 1: Quantitative Impact of Different Variability Sources on iPSC Phenotypes
| Variability Source | Impact Level | Key Affected Parameters | Potential Impact on Aβ Research |
|---|---|---|---|
| Genetic Background | 5-46% of phenotypic variation [72] | Gene expression, eQTLs, DNA methylation, differentiation potential | Altered Aβ42/Aβ40 ratios, tau phosphorylation patterns [74] |
| Differentiation Protocol | Significant differences in neuronal subtypes and function [75] | Neuronal subtype ratios, electrophysiological properties, marker expression | Varied Aβ production and secretion profiles [74] |
| Donor Age & Health Status | Modified disease phenotype recapitulation [75] | Cellular stress responses, metabolic activity, gene expression | Differential response to amyloid-β induced toxicity |
| Culture Duration | Altered maturity and stability [19] | Synaptic maturity, network activity, protein aggregation | Variable amyloid-β aggregation and clearance kinetics |
Strategic Approaches to Enhance Reproducibility
iPSC Line Selection and Quality Control
Clonal iPSC Lines: Clonal iPSC lines originate from a single reprogrammed cell, creating a population of genetically identical cells [77]. This uniformity reduces variability within groups, minimizes confounding factors, and enhances reproducibility. For amyloid-β research, this is particularly important when studying subtle differences in Aβ secretion patterns between control and patient lines [74]. Clonal lines also enable more precise genome editing for introducing AD-related mutations or creating isogenic controls.
Comprehensive Quality Control: Implementation of rigorous quality control measures is essential. This should include:
Master Cell Banks: Establishing quality-controlled master cell banks (MCBs) ensures consistency of input hiPSCs across experiments and differentiations [76]. This practice minimizes drift in iPSC characteristics over time and between experimental batches.
Protocol Standardization and Optimization
Stirred Suspension Systems: For cardiac differentiation, optimized bioreactor protocols in stirred suspension systems have demonstrated improved reproducibility across batches compared to monolayer differentiations [76]. While developed for cardiomyocytes, similar principles may apply to neural differentiations for amyloid-β research. These systems provide better control over cell aggregation, nutrient distribution, and pH buffering capacity [76].
Standardized Differentiation Protocols: For sensory neuronal differentiation, closely matching protocols and reagents between laboratories significantly reduces variability in gene expression patterns [78]. Principal component analysis of transcriptomics indicates that cell type and donor line influence expression more than the lab in which iPSCs were differentiated when protocols are closely matched [78].
Accelerated Differentiation Approaches: Some newer protocols, such as the "Anatomic" protocol for sensory neurons, offer accelerated differentiation while maintaining functional maturity [75]. Reducing differentiation time can minimize opportunities for variability to accumulate during the process.
Table 2: Comparison of Differentiation Protocol Optimization Strategies
| Strategy | Key Features | Advantages | Evidence of Improved Reproducibility |
|---|---|---|---|
| Stirred Suspension Bioreactors | Continuous monitoring of O2, CO2, pH; optimized EB size [76] | Improved scalability, reduced well-to-well variation, more mature functional properties | Higher purity (~94% vs variable), less inter-batch variability, higher viability after cryopreservation (>90%) [76] |
| Small Molecule-Based Differentiation | Use of CHIR99021, IWR-1, dual SMAD inhibition [51] [76] | More cost-effective than growth factors, less lot-to-lot variation | Consistent differentiation across multiple lines (25 differentiations of 14 lines) [76] |
| Inducible Transcription Factor Expression | NGN2 overexpression for neuronal differentiation [74] | Rapid, synchronized differentiation; reduced cellular heterogeneity | More uniform neuronal populations; reduced batch effects |
| Protocol Matching Between Labs | Standardized reagents, timing, and technical methods [78] | Reduced technical artifacts; comparable data across sites | Significant reduction in gene expression variability between laboratories [78] |
Experimental Design and Analytical Frameworks
Robust Experimental Design for Amyloid-β Research
Isogenic Controls: Creating isogenic control lines (derived from the same individual but engineered to differ at only one specific locus) is particularly valuable for amyloid-β research, where multiple genetic factors can influence Aβ production and clearance [72]. These controls help isolate the specific effects of AD-related mutations from background genetic variation.
Multi-Line Comparisons: Including multiple iPSC lines from different genetic backgrounds in amyloid-β studies helps distinguish genotype-specific effects from general phenotypes. For example, research has demonstrated that ApoE4 genotype is associated with increased Aβ production by AD iPSC-neurons [74], which might be missed in studies using limited genetic backgrounds.
Longitudinal Phenotyping: Given that amyloid-β pathology develops over time, longitudinal assessment of Aβ species production (Aβ40, Aβ42, Aβ43) and tau phosphorylation in mature neurons provides more physiologically relevant data than single timepoint measurements [74].
Analytical Approaches to Account for Variation
Bioinformatic Normalization Methods: Statistical approaches can identify and account for unwanted technical variation:
- Principal Component Analysis: Identifies major sources of variation in transcriptomic data [72]
- Probabilistic Estimation of Expression Residuals (PEER): Identifies hidden factors that explain much of the expression variability [72]
- Removal of Unwanted Variation (RUV): Normalization method that identifies and removes unwanted sources of variation within omics readouts [72]
Cross-Laboratory Reference Lines: Establishing "Rosetta lines" - iPSC lines that are commonly used within all experiments by multiple laboratories - enables researchers to address experimental variation between different laboratories' results [72]. These reference lines facilitate direct comparison of data generated across different sites and protocols.
Applications in Amyloid-β Pathway Research
Modeling Amyloid-β Pathology with Enhanced Reproducibility
The amyloid-β pathway is central to Alzheimer's disease pathophysiology, with Aβ accumulation considered an early event in the disease cascade [73]. When applying reproducibility-enhanced iPSC methodologies to Aβ research, several key considerations emerge:
Correlation with Brain Tissue: Studies comparing iPSC-neurons to neuropathologically characterized donor brain tissues have found positive correlations for certain Aβ species in familial AD (e.g., Aβ43 in fAD iPSC-neurons and matched brain tissues) but less substantial correlation in sporadic AD [74]. This highlights the importance of selecting appropriate models for different AD forms.
Genetic Background Effects: The ApoE4 genotype demonstrates how genetic background influences Aβ phenotypes in iPSC models. Research shows the ApoE4 genotype is associated with increased Aβ production by AD iPSC-neurons [74], illustrating how patient stratification can enhance reproducibility within experimental groups.
Multi-Cellular Systems: Incorporating astrocytes into iPSC-based amyloid-β models reveals important cellular interactions. Aβ-exposed astrocytes show impaired ability to support neuronal function, with decreased frequency of excitatory post-synaptic currents in co-cultured neurons [19]. Such complex cellular interactions may be essential for modeling full disease pathophysiology.
Functional Assessment of Amyloid-β Related Phenotypes
Electrophysiological Characterization: Patch clamp recording of iPSC-derived neurons co-cultured with Aβ-exposed astrocytes reveals significant functional alterations, including decreased frequency of excitatory post-synaptic currents [19], providing functional readouts beyond molecular measurements.
Tau Phosphorylation Assessment: Pathologic tau phosphorylation is increased in AD and fAD iPSC-neurons compared to controls and positively correlates with the relative abundance of longer-length Aβ species [74], enabling multiparametric assessment of AD-related pathology.
High-Content Screening Compatibility: Optimized differentiation protocols yield neurons amenable to high-throughput technologies, including automated patch clamp, calcium imaging, and multielectrode array (MEA) techniques [75], facilitating drug discovery applications.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Reproducible iPSC-Based Amyloid-β Research
| Reagent/Category | Specific Examples | Function in Experimental Pipeline | Considerations for Reproducibility |
|---|---|---|---|
| Base iPSC Lines | KOLF2.1J [77], WTC-Cas9 [76] | Well-characterized clonal lines for foundational studies | Genetic stability over passages (>25 passages); comprehensive genomic characterization |
| Neural Induction Supplements | Noggin, SB431542 [51] | Dual SMAD inhibition for efficient neural induction | Consistent sourcing; quality verification between lots |
| Small Molecule Inducers | CHIR99021 (Wnt activator), IWR-1 (Wnt inhibitor) [76] | Directed differentiation toward neural/cardiac lineages | Concentration optimization; temporal precision in application |
| Neuronal Maturation Factors | BDNF, NT-3, GDNF [74] [75] | Promote functional maturation of neurons | Consistent combination and concentration across experiments |
| Amyloid-β Detection Reagents | Aβ40, Aβ42, Aβ43 ELISAs [74] | Quantification of Aβ species production | Same antibody lots for longitudinal studies; standardized normalization methods |
| Cell Type-Specific Markers | TNNT2 (cardiomyocytes) [76], Tuj1/TUBB3 (neurons) [75] | Quality assessment of differentiation efficiency | Consistent antibody validation; standardized quantification methods |
Signaling Pathways and Experimental Workflows
Key Signaling Pathways in Neural Differentiation and Amyloid-β Processing
Diagram 1: Key Pathways in iPSC Neural Differentiation and Amyloid-β Pathology. This workflow illustrates the sequential stages of neural differentiation from iPSCs and the subsequent amyloid-β processing pathway that is central to Alzheimer's disease research.
Experimental Workflow for Reproducible iPSC-Based Amyloid-β Studies
Diagram 2: Experimental Workflow for Reproducible iPSC-Based Amyloid-β Research. This diagram outlines a standardized workflow from iPSC line selection through data analysis, highlighting critical quality control checkpoints that ensure experimental reproducibility.
Ensuring reproducibility across iPSC lines and differentiation protocols is fundamental for advancing amyloid-β research and developing effective therapeutic strategies for Alzheimer's disease. By implementing rigorous quality control measures, standardizing differentiation protocols, utilizing clonal lines, and applying appropriate analytical frameworks, researchers can significantly enhance the reliability and comparability of their findings. The integration of these strategies will strengthen the validity of iPSC-based models of amyloid-β deposition, accelerating both our understanding of disease mechanisms and the development of targeted interventions. As the field progresses, continued emphasis on reproducibility standards will be essential for translating iPSC-based discoveries into clinical applications.
Benchmarking iPSC Findings Against Clinical and Neuropathological Data
Correlating iPSC-Derived Aβ Phenotypes with Human Brain Proteomics
The integration of human induced pluripotent stem cell (iPSC) models with advanced proteomic technologies represents a transformative approach for studying amyloid-beta (Aβ) deposition in Alzheimer's disease (AD). While the amyloid cascade hypothesis has long positioned Aβ at the center of AD pathogenesis, recent evidence suggests that AD progresses in two phases: an early phase driven by Aβ aggregation and a later phase that progresses at least partly independently of Aβ [1]. This understanding has shifted research focus from Aβ plaques to Aβ seeds—small, soluble, seeding-active nuclei that propagate throughout the brain and drive the initial stages of AD pathogenesis [1]. iPSC-derived models, particularly cerebral organoids, now enable the study of these critical early events in human-specific systems that recapitulate patient-specific genetic backgrounds [79] [80]. When combined with mass spectrometry-based proteomics, these models provide unprecedented opportunities to identify the protein networks and key driver proteins underlying Aβ-associated pathology, bridging the gap between genetic risk and functional proteomic consequences in human-relevant systems [81] [82].
iPSC Models for Studying Aβ Deposition
Cerebral Organoids as Human-Relevant Model Systems
Cerebral organoids derived from human iPSCs have emerged as powerful tools for modeling AD pathology because they recapitulate complex cell-cell interactions and develop disease-relevant phenotypes within a human genetic context. Unlike rodent models that capture environmental complexity but lack human-specific disease features, cerebral organoids form extracellular Aβ aggregates and subsequent tauopathy, including tau hyperphosphorylation, thereby effectively recapitulating AD progression [79]. These models are particularly valuable for studying genetic susceptibility as they exclude the influence of environmental factors experienced throughout life, allowing researchers to isolate genetic effects on disease pathogenesis [79].
The application of hiPSC technology in AD research has grown substantially since 2010, with publication rates stabilizing at approximately 80 papers annually in recent years, reflecting increasing adoption by the research community [80]. The United States leads in contributions to this field, followed by China, with prominent researchers including Li-Huei Tsai from the Massachusetts Institute of Technology driving methodological advances [80].
Modeling Genetic Risk with Polygenic Risk Scores
The integration of polygenic risk scores (PRS) with iPSC models enables stratification of genetic susceptibility to AD. Recent research has developed optimized PRS that predict AD dementia and Aβ positivity independent of apolipoprotein E (APOE) status [79]. When cerebral organoids were generated from individuals with high versus low PRS, those from the high PRS group exhibited increased Aβ insolubility and elevated phosphorylated tau (p-tau) levels, providing biological validation of the relevance of polygenic risk in driving AD pathology [79]. This approach demonstrates how genetic risk stratification can be combined with cerebral organoid models to study the molecular mechanisms underlying Aβ deposition.
Table 1: Key Characteristics of iPSC-Derived Cerebral Organoid Models for Aβ Research
| Feature | Description | Utility in Aβ Research |
|---|---|---|
| Cellular Diversity | Contains various brain cell types (neurons, astrocytes, microglia) | Enables study of cell-type-specific responses to Aβ pathology |
| Aβ Aggregation | Forms extracellular Aβ aggregates | Models early stages of amyloid plaque formation |
| Tau Phosphorylation | Develops hyperphosphorylated tau | Captures downstream effects of Aβ accumulation |
| Genetic Background | Retains donor-specific genetic signatures | Enables study of patient-specific vulnerabilities |
| Polygenic Risk Modeling | Recapitulates differences based on AD polygenic risk scores | Connects genetic risk factors with functional phenotypes |
Proteomic Technologies for Aβ Phenotype Analysis
Mass Spectrometry-Based Proteomics
Mass spectrometry (MS) has become an indispensable technology for protein analysis in AD research, enabling researchers to detect, identify, and quantify molecules based on their mass-to-charge ratio (m/z) [83]. Modern MS platforms can detect analytes at concentrations in the attomolar range (10⁻¹⁸), providing the sensitivity necessary to study low-abundance proteins in complex biological samples [83]. All mass spectrometers contain three basic components: an ion source, a mass analyzer, and an ion detector [83]. The system operates under an extreme vacuum (10⁻⁶ to 10⁻⁸ torr) to remove gas molecules and contaminating non-sample ions that could alter ion paths or produce non-specific reaction products [83].
Key MS applications in AD proteomics include:
- Determining protein structure, function, folding, and interactions
- Identifying proteins from the mass of their peptide fragments
- Detecting specific post-translational modifications throughout complex biological mixtures
- Quantifying proteins (relative or absolute) in a given sample [83]
Quantitative Proteomic Workflows
Several quantitative proteomic workflows have been developed, each with distinct advantages and limitations for studying Aβ-related phenotypes:
Tandem Mass Tag (TMT) MS enables multiplexed quantification of over 10,000 proteins across up to 35 samples simultaneously when combined with peptide fractionation via two-dimensional liquid chromatography [82]. This approach provides high proteome coverage, extensive multiplexing, and minimal missing data, though it requires expensive labeling reagents and its quantification can be affected by ratio suppression due to coeluting peptides [82].
Data-Independent Acquisition (DIA) MS has rapidly evolved as an alternative workflow, using faster Orbitrap and time-of-flight instruments capable of identifying thousands of proteins in a single liquid chromatography-MS run [82]. Recent introductions of asymmetric track lossless (Astral) analyzers have increased proteome coverage to approximately 10,000 proteins with less than 1 µg protein loading [82].
Parallel Reaction Monitoring (PRM) represents a targeted MS approach suitable for validation studies, providing exceptional specificity and quantitative accuracy for precise measurement of tens to hundreds of proteins from minimal starting material [82].
Affinity-Based Proteomic Platforms
Affinity-based platforms including Olink and SomaScan complement traditional MS methods by offering signal amplification to detect low-abundance proteins. Olink employs dual antibody-based probes to detect more than 5,400 proteins from approximately 6 µL of sample, while SomaScan uses DNA aptamers to measure up to 11,000 proteins with selected kits, requiring only about 50 µL of sample [82]. These platforms are particularly valuable for biomarker studies requiring analysis of large patient cohorts in automated microwell plate settings [82].
Table 2: Comparison of Major Proteomic Technologies for Aβ Research
| Technology | Principle | Throughput | Sensitivity | Key Applications in Aβ Research |
|---|---|---|---|---|
| TMT-MS | Isobaric labeling with multiplexing | High (up to 35 samples/batch) | Moderate to high (requires ~1µg protein) | Discovery proteomics, deep proteome coverage |
| DIA-MS | Data-independent acquisition | Moderate to high | High (<1µg protein) | Untargeted discovery, single-shot proteomics |
| PRM-MS | Targeted quantification | Low to moderate | Very high | Validation of candidate biomarkers |
| Olink | Proximity extension assay | High | Very high (6µL sample) | Biomarker screening in biofluids |
| SomaScan | Aptamer-based binding | High | High (50µL sample) | Large cohort biomarker studies |
Experimental Workflows for Integration
Generating and Characterizing iPSC-Derived Cerebral Organoids
The workflow begins with iPSC generation from donor fibroblasts or peripheral blood mononuclear cells, followed by directed differentiation into cerebral organoids using established protocols [79] [80]. These organoids mature over several months, during which they spontaneously develop AD-relevant pathologies including Aβ aggregation and tau hyperphosphorylation, particularly when derived from individuals with high genetic risk for AD [79].
Key characterization steps include:
- Aβ solubility analysis to measure the transition from soluble to insoluble aggregates
- Phosphorylated tau quantification using immunoassays or phosphoproteomics
- Morphological assessment of neuronal and glial populations
- Functional analyses of network activity and synaptic function
Proteomic Profiling of iPSC Models
For proteomic analysis, cerebral organoids are typically processed through protein extraction, digestion, and purification before MS analysis. The specific workflow varies depending on the proteomic technology selected:
For TMT-based proteomics, proteins are digested and labeled with isobaric tags, then fractionated by two-dimensional liquid chromatography before MS analysis [84]. This approach was used to profile more than 10,000 proteins across 66 mouse brains in recent studies, demonstrating its applicability to complex neural tissues [84].
For phosphoproteomic analysis, an additional enrichment step is incorporated to capture phosphopeptides, enabling quantification of phosphorylation sites that are crucial for understanding tau pathology and signaling networks in AD [84].
Data Integration and Network Analysis
Multiscale proteomic modeling approaches integrate genetic and proteomic data to construct protein causal networks and identify key driver proteins (KDPs) involved in AD progression [81]. These analyses have revealed detailed protein interaction structures, including AD-associated subnetworks that capture glia-neuron interactions [81]. For example, AHNAK was identified as a top KDP in a glia-neuron network and subsequently validated in iPSC-based AD models, where its downregulation reduced both pTau and Aβ levels [81].
Additional integrative approaches include:
- Protein quantitative trait locus (pQTL) analysis to link genetic risk factors with protein expression changes [82]
- Cross-species comparisons between human tissues and AD mouse models to identify shared pathways in amyloid pathology [84]
- Multi-omics integration of proteomic data with transcriptomic and genomic datasets [82]
Key Research Findings and Validation
Conserved Proteomic Signatures in AD
Proteomic studies of postmortem AD brain tissues have revealed consensus protein alterations that are consistently observed across multiple cohorts and studies. A recent integration of more than 30 whole proteome datasets from AD brains identified 866 consensus proteins based on the magnitude of protein changes and associated statistical significance [82]. When compared with the brain proteome of AD mouse models, 654 of these proteins were detected in mice, with 108 consistently altered in both 5xFAD and APP-KI models [82]. These 108 proteins originate from diverse cell types, with microglia contributing the largest proportion (approximately 40%), followed by neurons and astrocytes [82]. Pathway analysis revealed upregulated processes related to amyloid matrisome, cell migration, complement/coagulation, cytoskeleton organization, and immune response [82].
Human-Mouse Model Comparisons
Comparative proteomic analyses between human AD tissues and mouse models have quantified their similarity and identified important limitations. In a comprehensive study, two commonly used amyloidosis models (5xFAD and APP-KI) replicated only 30% of human protein alterations, while additional genetic incorporation of tau and splicing pathologies increased this similarity to 42% [84]. This analysis also revealed proteome-transcriptome inconsistency in both AD and 5xFAD mouse brains, with inconsistent proteins enriched within the amyloid plaque microenvironment (amyloidome) [84]. Further investigation demonstrated that amyloid formation delays the degradation of amyloidome components, including Aβ-binding proteins and autophagy/lysosomal proteins, providing a potential explanation for the discrepancy between transcript and protein levels [84].
Protein Network Alterations in AD
Network-based analyses of AD proteomes have identified key driver proteins that potentially orchestrate larger functional modules in AD pathogenesis. One study constructed a protein causal network by integrating genetic and proteomic data, revealing an AD-associated subnetwork that captures glia-neuron interactions [81]. This approach moves beyond simple differential expression analysis to identify proteins that occupy strategic positions within dysregulated networks, potentially serving as more effective therapeutic targets. Experimental validation of one such key driver, AHNAK, in iPSC-based models confirmed its functional role in modulating both Aβ and tau pathologies [81].
Table 3: Research Reagent Solutions for iPSC-Proteomics Integration
| Category | Specific Tools/Reagents | Application in Aβ Research |
|---|---|---|
| iPSC Culture | Reprogramming factors, Defined media, Matrices | Generation and maintenance of patient-specific iPSCs |
| Differentiation | Neural induction media, Morphogens, Small molecules | Directed differentiation to cerebral organoids |
| Proteomic Sample Prep | Lysis buffers, Protease inhibitors, Digestion enzymes | Protein extraction and preparation for MS analysis |
| Mass Spectrometry | TMT labels, LC columns, MS instruments | Protein identification and quantification |
| Affinity Reagents | Olink panels, SomaScan kits, Antibodies | Targeted protein quantification and validation |
| Data Analysis | Bioinformatics pipelines, Network modeling software | Proteomic data processing and network analysis |
The integration of iPSC-derived cerebral organoids with advanced proteomic technologies creates a powerful framework for elucidating the molecular mechanisms driving Aβ deposition in Alzheimer's disease. This approach enables researchers to study human-specific protein networks in genetically defined models, bridging the gap between genetic risk factors and functional proteomic consequences. Key advantages include the ability to model patient-specific genetic backgrounds, capture cell-type-specific responses to Aβ pathology, and identify key driver proteins within dysregulated networks. As proteomic technologies continue to advance, with improvements in sensitivity, throughput, and spatial resolution, their combination with increasingly sophisticated iPSC-based models will undoubtedly yield deeper insights into Aβ biology and accelerate the development of targeted therapeutic interventions for Alzheimer's disease.
The validation of therapeutic efficacy for Alzheimer's disease (AD) requires a continuous pipeline that bridges human-relevant preclinical models and clinical trials. Induced pluripotent stem cell (iPSC) technology has emerged as a transformative platform for studying amyloid-β (Aβ) pathology, addressing critical limitations of traditional animal models which often fail to replicate human neuropathology accurately [38]. The complex nature of AD, with its diverse genetic, molecular, and clinical manifestations, necessitates models that capture human-specific disease mechanisms. iPSC-derived models provide a unique human physiological context for investigating Aβ deposition, with research publications in this area steadily increasing since 2015, demonstrating growing scientific engagement [80]. These models are particularly valuable for their ability to retain donor-specific genetic signatures, including APOE ε4 risk alleles and mutations in APP, PSEN1, and PSEN2 genes, enabling study of patient-specific phenotypes and personalized therapeutic approaches [38] [80].
The transition from iPSC-based screening to clinical validation represents a critical pathway in AD drug development. This whitepaper provides a comprehensive technical guide to establishing an integrated workflow for validating therapeutic efficacy against Aβ pathology, detailing experimental methodologies, analytical approaches, and clinical translation strategies for researchers and drug development professionals.
Establishing Physiologically Relevant iPSC Models for Aβ Research
iPSC Model Selection and Differentiation Protocols
The selection of appropriate iPSC models depends on the specific research objectives. For familial AD, lines carrying pathogenic mutations in APP, PSEN1, or PSEN2 are utilized, while sporadic AD models employ lines from patients with appropriate genetic risk factors or CRISPR-Cas9 engineered isogenic controls [38]. Several differentiation protocols have been established for generating neural cell types relevant to Aβ pathology:
Cerebral Organoid Generation: Human cerebral organoids (hCOs) are generated using standardized protocols that guide iPSCs through stages of neural induction, patterning, and maturation. A typical protocol involves embedding iPSCs in Matrigel droplets and maintaining them in neural induction media for 4-6 days, followed by transfer to differentiation media on an orbital shaker for 60-100 days to achieve mature organoids with cortical layer organization [37]. These 3D structures recapitulate key aspects of human brain development, including the formation of neural rosettes, cortical layers, and diverse cell populations.
Neurosphere Culture System: The 3D neurosphere model provides a robust platform for chronic amyloidosis studies. Neural progenitor cells (NPCs) derived from iPSCs are plated in AggreWell 800 plates to initiate neurosphere formation [16]. After 7 days in vitro (DIV), neurospheres are transferred to orbital shakers for subsequent differentiation and maturation. This system spontaneously generates neurons and astrocytes, with microglia added separately through co-culture protocols [16]. Neurospheres are typically maintained for 60 days to achieve appropriate maturation before experimental manipulation.
Microglia Co-culture Protocol: Microglia are essential for modeling neuroinflammatory components of AD. iPSC-derived microglia (hiMG) are generated separately and added to mature neurospheres or organoids, where they infiltrate the tissue over 7-10 days [16]. This approach enables investigation of neuron-glia interactions in Aβ clearance and neuroinflammation.
Model Validation and Quality Control
Rigorous validation of iPSC-derived models is essential for experimental reliability. Key quality control measures include:
- Immunocytochemistry: Confirmation of cell type-specific markers including MAP2 and NeuN for neurons, GFAP for astrocytes, Iba1 and P2RY12 for microglia, and synaptophysin for presynaptic terminals [17] [16].
- Functional Assessment: Measurement of spontaneous synaptic activity and evoked action potentials using whole-cell patch clamp recordings [17]. Calcium imaging using GCaMP6f and measurement of oxidative stress with roGFP1 provide additional functional validation [16].
- Biomarker Secretion: Analysis of endogenous Aβ1-40, Aβ1-42, and tau secretion into culture media using ELISA, with levels normalized to total protein content [17].
- Transcriptional Profiling: Single nuclei RNA sequencing (snRNA-seq) to verify appropriate cell type populations and maturation states through cluster analysis of marker gene expression [16].
Table 1: Quality Control Markers for iPSC-Derived AD Models
| Cell Type | Structural Markers | Functional Assays | Secreted Biomarkers |
|---|---|---|---|
| Neurons | MAP2, NeuN, Synaptophysin | Calcium oscillations, MEA recordings | Neurogranin |
| Astrocytes | GFAP, AQP4, SLC1A3 | Glutamate uptake | - |
| Microglia | Iba1, CX3CR1, PTPRC | Phagocytosis assays | TREM2, pro-inflammatory cytokines |
| Organoids | Cortical layer organization | Network activity (MEA) | Aβ1-40, Aβ1-42, tau |
Therapeutic Screening in iPSC-Based Aβ Models
Induction of Aβ Pathology
Multiple approaches exist for modeling Aβ pathology in iPSC systems:
Chronic Aβ Oligomer Exposure: Application of synthetic Aβ1-42 oligomers (3-10 μM) to mature cultures for varying durations (48 hours to 5 weeks) to induce AD-like pathology [37] [16]. Oligomers are prepared by dissolving synthetic Aβ1-42 peptides in hexafluoroisopropanol (HFIP), followed by evaporation and resuspension in DMSO, then culture media. The solution is incubated at 4°C for 24 hours to form oligomers, with structural characterization using Western blot or atomic force microscopy.
Endogenous Aβ Pathology in Familial AD Lines: iPSCs carrying APP, PSEN1, or PSEN2 mutations spontaneously develop Aβ pathology when differentiated into neuronal lineages, particularly after extended culture (60-100 days) [38] [80]. These models recapitulate increased Aβ1-42/Aβ1-40 ratios and deposition without external manipulation.
Aβ Seed Seeding: Application of seeding-active Aβ assemblies derived from AD patient brain extracts or concentrated cerebrospinal fluid to accelerate aggregation [1]. This approach models prion-like propagation of Aβ pathology observed in human disease.
Efficacy Endpoint Assessment
Comprehensive assessment of therapeutic efficacy requires multi-parametric endpoint analysis:
Aβ Deposition and Clearance: Quantitative immunohistochemistry for Aβ using antibodies such as 6E10, with image analysis to quantify deposition area and intensity [37]. Aβ levels in culture media measured by ELISA provide complementary soluble Aβ metrics.
Neuronal Function Assessment: Multielectrode array (MEA) recordings to evaluate network-level neuronal activity, including mean firing rate, burst frequency, and synchrony [37]. Single-cell calcium imaging using GCaMP6f to monitor calcium oscillations and neuronal responsiveness [16].
Apoptosis and Cell Viability: Caspase-3 activation measured by immunostaining or Western blot, complemented by LDH release assays for cytotoxicity assessment [37].
Microglial Phagocytosis: Immunostaining for Iba1 with Aβ to quantify microglial recruitment to Aβ deposits [37]. Flow cytometry analysis of pHrodo-labeled Aβ uptake by microglia, with quantification of TREM2 expression by RT-qPCR [37] [16].
Transcriptional Profiling: snRNA-seq to characterize therapy-induced changes in gene expression patterns across different cell types, with particular focus on AD-associated genes such as APOE, CLU, LRP1, and VIM [16].
Table 2: Key Endpoints for Therapeutic Efficacy Screening in iPSC Models
| Pathological Process | Assessment Method | Quantitative Metrics |
|---|---|---|
| Aβ Pathology | Aβ immunostaining, ELISA | Deposition area, intensity, soluble Aβ levels |
| Neuronal Health | Caspase-3 staining, LDH release | Apoptotic cell count, cytotoxicity percentage |
| Synaptic Function | MEA recordings, calcium imaging | Firing rate, burst frequency, oscillation frequency |
| Neuroinflammation | Microglial staining, cytokine ELISA | Phagocytosis index, cytokine concentrations |
| Cellular Transcriptomics | snRNA-seq | Differential gene expression, pathway enrichment |
Mechanistic Validation of Candidate Therapeutics
Target Engagement and Pathway Modulation
Understanding therapeutic mechanisms requires rigorous assessment of target engagement and downstream pathway modulation:
Oxytocin-Mediated Protection: A study investigating oxytocin (OXT) in cerebral organoids demonstrated concentration-dependent protection against Aβ toxicity (0.1-1.0 μM) [37]. Pretreatment with OXT for 24 hours before Aβ exposure attenuated Aβ deposition and caspase-3-mediated apoptosis. OXT enhanced microglial recruitment to Aβ deposits and upregulated TREM2 expression, with co-expression of oxytocin receptors (OXTR) on Iba1-positive microglia confirming direct target engagement. Functional assays showed that OXT restored Aβ-impaired calcium oscillations and neuronal network activity.
Microglial Phagocytosis Enhancement: Research using 3D neurosphere models demonstrated that microglia play a central role in Aβ clearance, with iPSC-derived microglia (hiMG) efficiently phagocytosing Aβ and reducing neurotoxicity [16]. snRNA-seq analysis revealed that microglia presence was essential for Aβ-dependent upregulation of astrocytic APOE expression, suggesting a mechanism for microglial-astrocyte crosstalk in AD pathogenesis. This neuroprotective effect was associated with unique gene expression profiles in astrocytes and neurons, including modulation of known AD-associated genes.
CRISPR/Cas9 Genetic Validation: CRISPR/Cas9 enables precise genetic manipulation to validate therapeutic targets in iPSC models [38]. The technology allows creation of isogenic controls through correction of pathogenic mutations (e.g., in APP, PSEN1, PSEN2) or introduction of risk variants (e.g., APOE ε4). Guide RNAs (gRNAs) targeting specific loci are designed with Cas9 nuclease or base-editing systems, with efficiency optimized through delivery method selection (electroporation, viral vectors) and clonal selection. Successful gene editing is confirmed by Sanger sequencing, with off-target effects assessed through whole-genome sequencing.
Signaling Pathway Mapping
Therapeutic efficacy against Aβ pathology often involves modulation of complex signaling pathways. The following diagram illustrates key pathways implicated in Aβ clearance and neuroprotection, integrating findings from multiple iPSC studies:
The diagram above integrates findings from iPSC studies on oxytocin-mediated protection [37] and microglial phagocytosis [16], illustrating how therapeutic targeting of these pathways can promote Aβ clearance and neuroprotection.
Clinical Trial Validation and Biomarker Translation
Clinical Trial Endpoints and Biomarker Correlations
Successful candidates from iPSC screens advance to clinical trials with endpoints that should align with preclinical findings:
Anti-Amyloid Monoclonal Antibodies: Recent approvals of anti-Aβ monoclonal antibodies (lecanemab, donanemab) demonstrate the clinical translation of Aβ-targeting approaches [85]. These therapies consistently demonstrate robust amyloid clearance on PET imaging (≈25-30% reduction) and modest slowing of clinical decline (≈25-30% on CDR-SB over 18 months) in early symptomatic AD [85]. Clinical trials incorporate biomarker assessments including amyloid-PET, CSF Aβ42/40 ratio, plasma pTau181, and pTau217, which provide objective measures of target engagement [85] [86].
Amyloid-Related Imaging Abnormalities (ARIA): A critical safety consideration for anti-Aβ therapies is ARIA, observed more frequently in APOE ε4 carriers [85]. Clinical trials implement rigorous MRI monitoring protocols, with APOE genotyping recommended before treatment initiation. The incidence of ARIA-E (edema) is typically <5% for third-generation antibodies like trontinemab, with most cases being radiographically mild and asymptomatic [86].
Emerging Clinical Trial Designs: Next-generation clinical trials incorporate innovative designs to enhance efficiency. The TRAVELLER pre-screening study uses brief clinical assessments and plasma biomarkers (Elecsys pTau217 test) for broader community outreach and more diverse trial enrollment [86]. Phase III trials for trontinemab (TRONTIER 1 and 2) in early symptomatic AD employ CDR-SB as the primary endpoint after 18 months, with secondary endpoints assessing cognition, function, behavioral symptoms, and quality of life [86].
Table 3: Clinical Trial Endpoints for Aβ-Targeting Therapies
| Endpoint Category | Specific Measures | Clinical Significance |
|---|---|---|
| Clinical Efficacy | CDR-SB, ADAS-Cog, iADRS | Cognitive and functional decline |
| Biomarker Efficacy | Amyloid-PET centiloids, CSF pTau181/217, Neurogranin | Target engagement, downstream effects |
| Safety Monitoring | ARIA-E, ARIA-H incidence | Treatment-associated adverse events |
| Patient Selection | APOE genotyping, amyloid-PET/CSF positivity | Appropriate candidate identification |
Biomarker Translation from iPSC Models to Clinical Applications
Biomarkers validated in iPSC models can inform clinical trial design and patient selection:
pTau217 as a Predictive Biomarker: Roche's Elecsys pTau217 plasma immunoassay demonstrates high accuracy in detecting amyloid pathology, performing comparably to PET scans [86]. This blood-based test has potential for rule-in and rule-out identification of amyloid pathology across care settings, greatly improving patient access and decreasing time to diagnosis.
Microglial Biomarkers: iPSC studies identifying TREM2 upregulation as a marker of enhanced microglial phagocytosis [37] inform clinical biomarker development. TREM2 levels in CSF may provide insights into therapeutic mechanisms in clinical trials, particularly for therapies designed to enhance microglial function.
Multi-analyte Biomarker Panels: iPSC models enable correlation of cellular responses with biomarker signatures, facilitating development of multi-analyte panels for clinical use. Analysis of KLK-6, NCAM-1, neurogranin, and TDP-43 release from human brain slice cultures demonstrates variation with brain region, donor age, and sex [17], highlighting the importance of considering these factors in clinical biomarker interpretation.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents for iPSC-based AD Therapeutic Screening
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| iPSC Lines | Familial AD (APP, PSEN1/2 mutations), isogenic controls | Disease modeling, genetic validation |
| Differentiation Kits | Neural induction media, patterning factors | Generation of neurons, glia, organoids |
| Aβ Assays | Synthetic Aβ1-42, ELISA kits, aggregation standards | Pathology induction, quantification |
| Cell Type Markers | Anti-MAP2, GFAP, Iba1, Synaptophysin antibodies | Cell identification, validation |
| Functional Assays | GCaMP6f, roGFP1, MEA systems | Neuronal activity, oxidative stress |
| Gene Editing Tools | CRISPR/Cas9 systems, gRNA design tools | Genetic manipulation, target validation |
| Omics Platforms | snRNA-seq, proteomics, bioinformatics | Mechanistic studies, biomarker discovery |
The continuous pipeline from iPSC screens to clinical trials represents a transformative approach for validating therapeutic efficacy against Aβ pathology in Alzheimer's disease. iPSC models provide human-relevant platforms for initial target validation and mechanism elucidation, while advanced clinical trial designs with biomarker-rich endpoints enable confirmation of human efficacy. Critical to this pipeline is the alignment of preclinical and clinical endpoints, particularly for Aβ clearance, neuronal protection, and inflammatory modulation. As the field advances, the integration of multi-omics data from iPSC models with clinical biomarker profiles will further enhance our ability to predict therapeutic success and develop effective interventions for this devastating disorder.
Comparative Analysis of iPSC Models with Animal and Postmortem Findings
Abstract Innovative human-induced pluripotent stem cell (iPSC) models are reshaping Alzheimer's disease (AD) research by providing a critical bridge between traditional animal models and postmortem human brain findings. This whitepaper provides a technical guide on how iPSC-derived neurons, glia, and organoids recapitulate human-specific amyloid-beta (Aβ) pathology. We present a comparative analysis of model system fidelity, detailed experimental protocols for modeling Aβ-related phenomena, and visualization of key signaling pathways implicated in Aβ toxicity. The integration of iPSC technology is accelerating the identification of therapeutic targets and the validation of drug efficacy in a human-relevant context.
Alzheimer's disease remains without adequate treatment, largely due to the insufficient predictive power of existing non-human models [80]. The cornerstone of AD pathology, the amyloid-beta (Aβ) peptide, plays a central role, yet studying its behavior in models that fail to replicate human brain physiology has been a major hurdle [87]. Animal models, particularly transgenic mice overexpressing mutant human genes, have provided essential insights but lack the genetic diversity and often the full spectrum of human AD pathology, such as extensive neuronal loss [88] [9]. Postmortem human brain studies are irreplaceable for identifying end-stage pathological changes but offer no ability to interrogate dynamic disease mechanisms [89].
The advent of human induced pluripotent stem cell (hiPSC) technology offers a novel, patient-specific approach to studying AD [80]. iPSCs can be differentiated into all major brain cell types, including forebrain neurons, astrocytes, and microglia, allowing for the study of Aβ pathology in the context of human genetics and cell biology [22] [9]. This technical guide details how iPSC models complement and enhance findings from animal and postmortem studies, with a specific focus on their application in Aβ deposition research for drug discovery.
Comparative Fidelity of Model Systems in Recapitulating Human AD Pathology
Different model systems capture distinct aspects of Alzheimer's disease. The following table summarizes their key characteristics and limitations in the context of Aβ research.
Table 1: Comparative Analysis of AD Model Systems for Amyloid-Beta Research
| Model System | Key Advantages | Major Limitations in Aβ Research | Representative Aβ-related Phenotypes |
|---|---|---|---|
| Animal Models (e.g., Transgenic Mice) | Intact neural circuitry; enables behavioral and in vivo studies [9]. | Fail to fully recapitulate human tau pathology and widespread neuronal loss; rely on non-physiological overexpression of AD genes [88] [9]. | Amyloid plaque deposition; some synaptic dysfunction; glial activation [9]. |
| Postmortem Human Brain Studies | Gold standard for identifying final disease pathology in humans; source of human Aβ for study [87] [89]. | Static snapshot; cannot model disease initiation or progression; confounding factors of agonal state and postmortem delay [89]. | Amyloid plaques; neurofibrillary tangles; neuritic pathology; proteomic signatures of pathology [89]. |
| iPSC-Derived Models (2D & 3D) | Patient-specific genetic background; human-specific Aβ species and metabolism; suitable for longitudinal studies and high-throughput screening [22] [26]. | Lack complex brain architecture; model developmental or early-stage pathology; challenges with cellular maturity and heterogeneity [22] [15]. | Increased Aβ42/Aβ40 ratio; phospho-tau accumulation; endolysosomal dysfunction; synaptic defects; vulnerability to Aβ oligomers [88] [89] [90]. |
iPSC models specifically address a critical gap: the ability to study the effects of patient-derived Aβ in live human neurons. For instance, a key strength is their capacity to model the Aβ42/Aβ40 ratio, a crucial biochemical metric altered by familial AD (FAD) mutations in APP, PSEN1, and PSEN2 [88] [9]. iPSC-derived neurons from patients with these mutations consistently demonstrate an increased Aβ42/Aβ40 ratio, a phenotype that is difficult to faithfully reproduce in non-human cells [88]. Furthermore, transcriptomic analyses reveal that iPSC-derived cortical neurons from sporadic AD (sAD) patients share significant overlap with differentially expressed genes identified in postmortem AD brain tissue, validating their relevance for modeling complex disease processes [90].
Experimental Workflows: From Model Generation to Phenotypic Analysis
Establishing an iPSC Model for Aβ Research
The foundational workflow involves generating and differentiating patient-specific iPSCs into disease-relevant cell types.
Key Protocols for Investigating Aβ Pathology
Several critical experimental protocols are used to investigate Aβ using iPSC models and postmortem tissue.
1. Differentiation of Cortical Neurons via SMAD Inhibition: A widely used protocol involves the dual-SMAD inhibition method (using small molecules like SB431542 and LDN193189) to direct iPSCs toward a neural fate [88] [22]. This efficient, monolayer-based protocol generates a heterogeneous population of forebrain neurons, including glutamatergic and GABAergic subtypes, suitable for studying Aβ production and toxicity.
2. Extraction of Bioactive Aβ from Postmortem Brain: To study the effects of human-derived Aβ, brain tissue is processed using specific extraction methods [87].
- Method I (Readily Diffusible Aβ): Thin cortical slices are soaked in artificial cerebrospinal fluid (aCSF) containing protease inhibitors. This method isolates highly bioactive, soluble Aβ species that remain in the supernatant after centrifugation.
- Method III (Isolation of Pure Aβ Dimers): Brain homogenates are denatured in SDS, followed by size-exclusion chromatography (e.g., using a Superdex 75 column) to separate and collect specific oligomeric forms like Aβ dimers, which have shown disease-relevant activity [87].
3. iPSC-Based Compound Screening: iPSC-derived neurons enable human-specific drug discovery. One established workflow involves [26]:
- Rapid neuronal induction from a large bank of FAD and sAD iPSC lines.
- High-throughput screening of compound libraries, measuring Aβ levels in the culture media via ELISA or similar immunoassays.
- Hit validation and identification of synergistic drug combinations (e.g., bromocriptine, cromolyn, and topiramate) in multiple patient-derived lines.
- Further mechanistic investigation of validated hits.
Table 2: Key Research Reagent Solutions for iPSC-based Aβ Studies
| Reagent / Resource | Function in Experiment | Specific Examples / Notes |
|---|---|---|
| Small Molecule Inhibitors | Directing neural differentiation; modulating signaling pathways. | Dual-SMAD inhibitors (SB431542, LDN193189) for neural induction [88] [22]. mTOR inhibitors (e.g., Rapamycin) for reversing axonal pathology [89]. |
| Cell Culture Media & Supplements | Supporting the growth and maintenance of iPSCs and specialized neural cells. | mTeSR (iPSC maintenance); N2 & B27 supplements (neuronal differentiation and survival) [87]. |
| Differentiation & Patterning Factors | Specifying regional neuronal fates and glial subtypes. | Retinoic Acid, Sonic Hedgehog (SHH) for ventral fates; TGF-β family inhibitors for dorsal/forebrain fates [22]. Growth factors (BDNF, GDNF, NT-3) for neuronal maturation. |
| Antibodies for Characterization | Identifying cell types and assessing AD pathology. | Anti-MAP2, β-III-Tubulin (neurons); GFAP (astrocytes); IBA1 (microglia); PLD3 (axonal spheroids) [89]; Anti-Aβ (6E10, 4G8); Anti-phospho-Tau (AT8) [87]. |
| Assay Kits | Quantifying biomarkers and functional outputs. | ELISA/MSD kits for Aβ40, Aβ42; CellTiter-Glo for viability; ATP-based assays for metabolic activity. |
| Specialized Equipment | Enabling advanced imaging and proteomic analysis. | IncuCyte live-cell imaging system for longitudinal tracking [87]; STED microscope for super-resolution imaging [89]; FPLC system for protein separation [87]. |
Signaling Pathways in Aβ Pathology: Insights from Integrated Models
Recent research integrating postmortem brain proteomics with iPSC models has uncovered novel, reversible mechanisms of Aβ-induced pathology. A prominent finding is the role of the PI3K/AKT/mTOR pathway in axonal spheroid formation around amyloid plaques [89].
The mechanistic insight from this integrated approach is powerful: proteomic analysis of human postmortem brains identified mTOR activation within axonal spheroids, and this finding was functionally validated using iPSC-derived neurons, which showed that mTOR inhibition could ameliorate the pathology [89]. This exemplifies how combining postmortem and iPSC models can reveal druggable pathways.
The comparative analysis solidifies the role of iPSC models as an indispensable component of modern AD research, particularly for Aβ-focused studies. They do not replace animal or postmortem studies but rather complement them by providing a dynamic, human-specific experimental platform that bridges molecular findings from brain tissue with functional validation in a living system. The future of this field lies in increasing model complexity through the use of isogenic cell lines (generated via CRISPR-Cas9), more sophisticated 3D organoid systems that better mimic brain cytoarchitecture [15], and the integration of multi-omics technologies. These advancements will further enhance the predictive validity of iPSC-based drug screening and deepen our understanding of the fundamental mechanisms driving Aβ pathology in the human brain.
Assessing Predictive Value for Drug Development Success
The high failure rate of clinical trials for Alzheimer's disease (AD) underscores the critical need for preclinical models with greater predictive validity. Induced pluripotent stem cell (iPSC) technology, which enables the generation of patient-derived neurons and glia, is emerging as a transformative tool for modeling amyloid-beta (Aβ) pathology and de-risking drug development. This whitepaper assesses the predictive value of iPSC models in AD drug discovery. We synthesize recent data from large-scale phenotypic screens, evaluate the recapitulation of core disease features, and provide detailed protocols for implementing these models. The evidence indicates that iPSC-based platforms can bridge the translational gap, effectively triaging clinical candidates and illuminating mechanisms of sporadic AD, thereby accelerating the development of successful therapeutics.
Alzheimer's disease drug development has been plagued by a high attrition rate, with numerous compounds showing promise in traditional animal models failing in human clinical trials [91]. A significant challenge has been the limited ability of existing models, particularly those based on non-human physiology or non-physiological overexpression of familial AD (FAD) genes, to fully capture the complex, patient-specific pathogenesis of the disease [10] [92]. The advent of human induced pluripotent stem cell (hiPSC) technology offers a novel approach to this problem [10]. By reprogramming somatic cells from patients, researchers can generate a virtually limitless supply of human neurons and glial cells that retain the complete genetic background of the donor, including risk alleles such as APOEε4 [93] [91]. This allows for the creation of personalized disease models that recapitulate individual patient phenotypes, providing a human-relevant system for probing disease mechanisms and screening therapeutic candidates [10]. This whitepaper assesses the growing body of evidence demonstrating the predictive value of iPSC models, specifically in the context of Aβ-targeting drug discovery, and provides a technical guide for their implementation.
The Foundation: How iPSC Models Recapitulate Amyloid-β Pathology
iPSC-derived neurons from both FAD and sporadic AD (SAD) patients have been shown to faithfully model key aspects of Aβ pathology. The core strength of these models lies in their ability to replicate the amyloidogenic processing of APP under endogenous genetic regulation.
- Familial AD Models: iPSC lines generated from patients with mutations in the APP, PSEN1, and PSEN2 genes consistently demonstrate altered APP processing. These mutations lead to an increased Aβ42/Aβ40 ratio, a fundamental pathological event in AD, through mechanisms that enhance the production of the longer, more amyloidogenic Aβ42 peptide and disrupt γ-secretase function [94] [91]. For instance, iPSC lines carrying a PSEN1 (F177S) mutation provide a platform to study very early-onset AD and the concomitant effects of other genetic variants, such as those in the MAPT gene [94].
- Sporadic AD Models: Perhaps more significantly, iPSC models are now successfully capturing pathology in SAD, which constitutes over 95% of all cases. These models recapitulate Aβ accumulation and associated neuronal toxicity, providing a system to study the complex interplay of polygenic risk factors and environmental influences in the majority of patients [91]. The ability to model SAD is a critical advance, as the pathophysiological relevance of models based solely on rare FAD mutations has been increasingly questioned [92].
The following dot code visualizes the amyloidogenic pathway and key therapeutic intervention points modeled in iPSC systems.
Quantitative Evidence: Validating the Predictive Power of iPSC Models
The true predictive value of a preclinical model is measured by its ability to accurately reflect clinical trial outcomes. Recent large-scale studies provide compelling quantitative evidence for iPSC models in this regard.
Large-Scale Screening in Sporadic ALS as a Proof-of-Concept
A landmark study in amyotrophic lateral sclerosis (ALS), a neurodegenerative disease with similar modeling challenges, powerfully demonstrated this principle. Researchers conducted a population-wide phenotypic screen using motor neurons derived from an iPSC library of 100 sporadic ALS (SALS) patients [92]. The screen assessed the efficacy of over 100 drugs that had previously been tested in ALS clinical trials. The results were striking: 97% of these drugs failed to mitigate neurodegeneration in the SALS iPSC model, a finding that directly reflects the high failure rate of these compounds in human trials [92]. This study validates that iPSC models can recapitulate critical sporadic disease features and serve as a highly effective triaging tool, weeding out non-efficacious candidates before they enter costly clinical trials.
Application and Growth in Alzheimer's Disease Research
In the AD field, bibliometric analysis shows a steady increase in publications utilizing hiPSC models over the past 14 years, indicating growing adoption and validation within the research community [10]. The United States and China are the leading contributors, with research trends focusing on key areas like inflammation, astrocytes, microglia, and ApoE, alongside Aβ and tau [10]. This expanding body of work is building the foundational data needed to fully quantify the predictive value of iPSC models for AD therapeutics.
Table 1: Key Quantitative Findings from Recent iPSC Model Studies
| Study Focus | Key Quantitative Finding | Implication for Predictive Value | Source |
|---|---|---|---|
| Sporadic ALS Drug Screening | 97% of clinically tested drugs failed to rescue neurodegeneration in a 100-patient iPSC model. | iPSC models can accurately reflect clinical trial failure rates, validating their use for preclinical triage. | [92] |
| AD iPSC Research Output | 531 research articles published between 2010-2024, with a significant rise post-2015. | The field is rapidly maturing, with a growing evidence base to support the use of these models. | [10] |
| NIH Drug Development Pipeline | 25+ new NIH-developed drug candidates are in clinical trials, many targeting pathways studied in iPSCs (e.g., inflammation, APOE). | iPSC research aligns with and informs the priorities of major funding and regulatory bodies. | [7] |
A Technical Guide: Key Protocols for iPSC-Based Drug Screening
To achieve predictive results, robust and standardized experimental protocols are essential. Below is a detailed workflow for a high-content screening assay designed to assess drug efficacy in iPSC-derived neurons.
Detailed Protocol: High-Content Screening for Neuroprotection
Objective: To quantify the protective effects of drug candidates against Aβ-induced cytotoxicity and neurite degeneration in iPSC-derived cortical neurons.
Workflow Overview:
- iPSC Expansion and Quality Control: Maintain and expand control and AD patient-derived iPSCs under feeder-free conditions. Perform rigorous quality control, including karyotyping, pluripotency marker staining (e.g., OCT4, SOX2, NANOG), and trilineage differentiation potential assays [92] [94].
- Neural Induction and Cortical Neuron Differentiation: Adapt a well-established, high-purity spinal motor neuron or cortical neuron differentiation protocol [92]. A typical 5-stage protocol involves:
- Stage 1: Neural induction using dual SMAD inhibition (e.g., LDN-193189, SB431542).
- Stage 2: Neural progenitor cell (NPC) expansion.
- Stage 3: Cortical patterning (e.g., using retinoids).
- Stage 4: Terminal differentiation into neurons.
- Stage 5: Neuronal maturation (≥60 days for full maturity and robust pathology).
- Cell Culture and Assay Setup: Plate differentiated neurons at a defined density in 96-well or 384-well imaging plates. Ensure cultures are highly enriched for neurons (e.g., >90% Tuj1+ cells) with minimal contamination by astrocytes and microglia [92].
- Compound Treatment: Pre-treat cultures with the drug candidate library for 24 hours prior to the introduction of an Aβ oligomer preparation or other stressor. Include controls: vehicle (DMSO), a positive control for health (e.g., neurotrophic factors), and a negative control for death (e.g., staurosporine). Use at least n=6 replicates per condition.
- Longitudinal Live-Cell Imaging: Monitor neuronal health daily for 3-7 days using an automated live-cell imaging system. Transfer plates to a microscope stage with an environmental chamber (37°C, 5% CO₂). Acquire images in multiple channels (e.g., brightfield, red fluorescence for a viability dye, green fluorescence for a neurite marker) from at least 9 non-overlapping fields per well.
- Quantitative Image Analysis: Use automated image analysis software (e.g., CellProfiler, IN Carta) to extract quantitative data. Key parameters include:
- Neuronal Survival: Count of Tuj1+ cells normalized to time zero.
- Neurite Integrity: Total neurite length per image or per neuron.
- Axonal Degeneration: Measure of neurite fragmentation (e.g., number of breaks per unit length).
- Somatic Health: Mean cell body area.
- Data Analysis and Hit Identification: Normalize data to positive and negative controls. Perform statistical analysis (e.g., one-way ANOVA with post-hoc test) to compare treatment groups to diseased controls. A "hit" is typically defined as a compound that significantly (p < 0.01) improves survival and/or neurite integrity by more than a predefined threshold (e.g., 50% rescue) [92].
The following dot code outlines this multi-stage experimental workflow.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for iPSC-based AD Drug Screening
| Reagent / Solution | Function / Application | Technical Notes |
|---|---|---|
| iPSC Lines | Foundation for generating patient-specific neurons and glia. | Source from repositories or generate in-house via non-integrating episomal reprogramming of patient fibroblasts [92]. |
| Neural Induction Media | Directs pluripotent stem cells toward a neural fate. | Often uses dual SMAD inhibition (LDN-193189, SB431542) for efficient, synchronized induction [91]. |
| Neuronal Maturation Media | Supports long-term survival and synaptic development of neurons. | Contains neurotrophic factors (BDNF, GDNF), cAMP, and ascorbic acid for maturation over 60+ days [92] [91]. |
| Aβ Oligomer Preparation | Pathological insult to model AD-related toxicity in vitro. | Prepare synthetic Aβ42 peptides or isolate from cell culture media; characterize oligomer size via SEC/Western blot [91]. |
| Cell Health/Viability Assays | Quantify cytotoxicity and neuroprotection. | Use multiplexed assays: ATP content (viability), Caspase-3/7 activity (apoptosis), LDH release (necrosis) [92]. |
| High-Content Imaging Systems | Automated, longitudinal imaging of neuronal morphology. | Systems like ImageXpress Pico or Incucyte enable kinetic tracking of survival and neurite degeneration [92]. |
| Phenotypic Analysis Software | Extracts quantitative features from image data. | Software like IN Carta or CellProfiler automates measurement of neurite length, branch points, and soma count [92]. |
Enhancing Predictive Power: Integrating CRISPR and Advanced Models
The predictive validity of iPSC models can be significantly enhanced by integrating them with CRISPR/Cas9 gene editing technology. Two primary approaches are employed:
- Isogenic Control Generation: CRISPR is used to correct disease-causing mutations (e.g., in PSEN1) in patient-derived iPSCs or to introduce these mutations into healthy control iPSCs. This creates genetically matched pairs of cell lines, allowing researchers to attribute observed phenotypic differences solely to the specific genetic alteration, thereby controlling for background genetic variability [93] [91].
- Target Validation and Pathway Engineering: CRISPR/Cas9 can be used to knock out or modulate genes of interest (e.g., APOE, TREM2) in iPSC-derived microglia and astrocytes to study their specific role in Aβ clearance and neuroinflammation, providing deeper mechanistic insights for drug targets [93] [95].
Furthermore, the development of 3D brain organoid models from iPSCs represents a significant leap forward. These organoids can better recapitulate the tissue-level complexity of the brain, including cell-cell interactions and the spontaneous formation of Aβ plaques and neurofibrillary tangles over extended culture periods, offering a more physiologically relevant system for therapeutic testing [10] [91].
iPSC technology has fundamentally shifted the paradigm for preclinical AD research. The quantitative evidence, particularly from analogous neurodegenerative fields like ALS, strongly supports the predictive value of these human-centric models for assessing drug development success [92]. By accurately recapitulating key aspects of Aβ pathology in both familial and sporadic forms of AD and providing a platform for high-content, human-specific drug screening, iPSC models are poised to significantly de-risk the drug development pipeline.
Future advancements will hinge on the standardization of protocols across laboratories, the incorporation of complex multi-cellular systems like organoids, and the integration of multi-omics data with artificial intelligence to identify predictive biomarkers of drug response [96]. As these technologies mature and the scale of iPSC biobanks expands, the vision of personalized medicine for AD—where the most effective therapeutic strategy is identified for an individual patient based on their own cellular phenotype—moves closer to reality [93] [7]. The strategic application of iPSC models is a critical step toward delivering effective, disease-modifying therapies for Alzheimer's disease.
Conclusion
iPSC technology has fundamentally transformed Alzheimer's disease research by providing unprecedented access to patient-specific models of amyloid-beta pathology. These systems successfully recapitulate critical disease mechanisms, from the initial formation of Aβ seeds to complex neuron-glia interactions in 3D environments. The integration of CRISPR gene editing allows for precise manipulation of AD-related genes, creating powerful platforms for target validation and drug discovery. However, realizing the full potential of these models requires addressing persistent challenges in standardization, maturation, and validation. Future research must focus on developing more complete model systems that capture the aging brain environment, improving the scalability of these platforms for high-throughput applications, and strengthening the translational pipeline connecting in vitro findings to clinical outcomes. As these technologies continue to evolve, iPSC-based models of Aβ deposition will play an increasingly central role in identifying novel therapeutic targets and developing personalized intervention strategies for Alzheimer's disease.
References
- 1. Amyloid‐β Seeds in Alzheimer's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583922/]
- 2. Amyloid β-based therapy for Alzheimer's disease [https://www.nature.com/articles/s41392-023-01484-7]
- 3. Experimental evidence that readily diffusible forms of Aβ from ... [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-025-02032-w]
- 4. Mass spectrometry analysis of tau and amyloid‐beta in iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8613538/]
- 5. Neurons derived from sporadic Alzheimer's disease iPSCs ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-017-0317-z]
- 6. Alzheimer's disease patient brain extracts induce multiple ... [https://www.nature.com/articles/s41380-025-03041-w]
- 7. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 8. Drug discovery research with the iPSC models of ... [https://www.sciencedirect.com/science/article/pii/S0168010225001683]
- 9. Modeling Alzheimer's disease with iPSC-derived brain cells [https://www.nature.com/articles/s41380-019-0468-3]
- 10. Human induced pluripotent stem cell models for Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11962003/]
- 11. induced pluripotent stem cell-based disease modeling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6624934/]
- 12. Modeling familial Alzheimer's disease with induced ... [https://pubmed.ncbi.nlm.nih.gov/21900357/]
- 13. Induced Pluripotent Stem Cell Core [https://mind.uci.edu/adrc/ips-cell-core/]
- 14. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches ... [https://www.mdpi.com/2076-3921/14/7/781]
- 15. iPSC-derived neural organoids in dementia research [https://www.sciencedirect.com/science/article/pii/S0168010225001634]
- 16. A 3D human iPSC-derived multi-cell type neurosphere system ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03433-3]
- 17. Divergent actions of physiological and pathological ... [https://www.nature.com/articles/s41467-025-58879-z]
- 18. A guide to performing Polygenic Risk Score analyses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7612115/]
- 19. Intracellular deposits of amyloid-beta influence the ability of human iPSC-derived astrocytes to support neuronal function | Journal of Neuroinflammation | Full Text [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-022-02687-5]
- 20. Long-term effects of amyloid-beta deposits in human iPSC-derived astrocytes - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1044743123000337]
- 21. Integration of risk factor polygenic risk score with disease ... [https://www.nature.com/articles/s42003-024-05874-7]
- 22. Induced pluripotent stem cells as a discovery tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4833689/]
- 23. A predictive machine learning model for cannabinoid effect ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0320219]
- 24. Alzheimer's Amyloid-β Accelerates Human Neuronal Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9249263/]
- 25. Identification of markers for neurescence through ... [https://www.nature.com/articles/s41514-025-00235-y]
- 26. iPSC-Based Compound Screening and In Vitro Trials ... [https://www.sciencedirect.com/science/article/pii/S2211124717315899]
- 27. Brain organoids: a new paradigm for studying human ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1699814/full]
- 28. Human brain organoids: an innovative model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417440/]
- 29. iPSC-derived blood-brain barrier modeling reveals APOE isoform-dependent interactions with amyloid beta | Fluids and Barriers of the CNS [https://link.springer.com/article/10.1186/s12987-024-00580-2]
- 30. Human-Induced Pluripotent Stem Cell Models for Amyloid Cardiomyopathy: From Mechanistic Insights to Therapeutic Discovery [https://www.mdpi.com/2308-3425/12/11/434]
- 31. Nondestructive, quantitative viability analysis of 3D tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10985731/]
- 32. Unraveling the complex role of microglia in Alzheimer's ... [https://inflammregen.biomedcentral.com/articles/10.1186/s41232-025-00383-4]
- 33. hiPSC-based models to decipher the contribution of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10039591/]
- 34. iPSC-derived human microglia-like cells to study neurological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5482419/]
- 35. The role of microglia in amyloid clearance from the AD brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC3653296/]
- 36. Intracellular deposits of amyloid-beta influence the ability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9809017/]
- 37. Human iPSC-derived cerebral organoids reveal oxytocin ... [https://www.sciencedirect.com/science/article/pii/S2352320425001464]
- 38. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291668/]
- 39. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1612868/full]
- 40. Targeting Amyloid-β Proteins as Potential Alzheimer's ... [https://www.mdpi.com/1424-8247/18/11/1731]
- 41. FACS-assisted CRISPR-Cas9 genome editing of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9490201/]
- 42. High-Content Analysis of CRISPR-Cas9 Gene-Edited ... [https://www.sciencedirect.com/science/article/pii/S2213671115003653]
- 43. Neural differentiation from pluripotent stem cells: The role ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3927010/]
- 44. Characteristic analyses of a neural differentiation model ... [https://www.nature.com/articles/s41598-017-12452-x]
- 45. CRISPR/Cas9-Based therapeutics as a promising strategy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009953/]
- 46. Comparison of Multivariate Data Analysis Strategies for ... [https://www.sciencedirect.com/science/article/pii/S2472555222077565]
- 47. High-Content Analysis (Quantitative Imaging) Information [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/cell-imaging-information/high-content-analysis-information.html]
- 48. Modeling Alzheimer's Disease with iPSCs Reveals Stress ... [https://www.sciencedirect.com/science/article/pii/S193459091300012X]
- 49. Therapeutic Advances in Targeting the Amyloid-β Pathway for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564542/]
- 50. Deep learning assisted quantitative analysis of Aβ and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11487103/]
- 51. Human iPSC-Derived Neural Models for Studying Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8930932/]
- 52. High-throughput discovery of fluoroprobes that recognize ... [https://www.nature.com/articles/s41557-025-01889-7]
- 53. Data-driven modeling of amyloid-β targeted antibodies for ... [https://www.nature.com/articles/s41540-025-00610-1]
- 54. Navigating Brain Organoid Maturation: From Benchmarking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383812/]
- 55. Advanced neural activity mapping in brain organoids via ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1634582/full]
- 56. Advancements, Strategies, and Challenges in Organoid- ... [https://www.sciencedirect.com/science/article/pii/S2095809925006083]
- 57. Quantitative profiling of human brain organoid cell diversity ... [https://www.sciencedirect.com/science/article/pii/S2211124725009398]
- 58. Deciphering brain organoid heterogeneity by identifying ... [https://www.nature.com/articles/s42003-025-08855-6]
- 59. Examining the Market for Organoid Culture Systems in 2025 [https://eureka.patsnap.com/report-examining-the-market-for-organoid-culture-systems-in-2025]
- 60. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 61. Recent Advancements in Reducing the Off-Target Effect of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10802171/]
- 62. Off-target interactions in the CRISPR-Cas9 Machinery [https://www.sciencedirect.com/science/article/pii/S2405580825002213]
- 63. Methods for Optimizing CRISPR-Cas9 Genome Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4976696/]
- 64. Optimization of gene knockout approaches and sgRNA ... [https://www.nature.com/articles/s41598-025-24184-4]
- 65. Scientists just made CRISPR three times more effective [https://www.sciencedaily.com/releases/2025/09/250907024543.htm]
- 66. A genetically encoded selection for amyloid-β oligomer binders [https://pubmed.ncbi.nlm.nih.gov/40664790/]
- 67. Methods for the Specific Detection and Quantitation of ... [https://pubmed.ncbi.nlm.nih.gov/27163804/]
- 68. Preparation of Stable Amyloid β-Protein Oligomers of Defined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5767166/]
- 69. Intrinsic visible emission of amyloid-β oligomers [https://pubs.rsc.org/en/content/articlehtml/2025/cp/d5cp01547b]
- 70. Aβ oligomer characterization [https://bio-protocol.org/exchange/minidetail?id=9778230&type=30]
- 71. New Clinical Practice Guideline for Blood-Based Biomarkers [https://aaic.alz.org/releases-2025/clinical-practice-guideline-blood-based-biomarkers.asp]
- 72. Addressing variability in iPSC-derived models of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6994963/]
- 73. The Amyloid-β Pathway in Alzheimer's Disease [https://www.nature.com/articles/s41380-021-01249-0]
- 74. β-Amyloid species production and tau phosphorylation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11333826/]
- 75. How to differentiate induced pluripotent stem cells into ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03696-2]
- 76. Efficient and reproducible generation of human iPSC ... [https://www.nature.com/articles/s41467-024-50224-0]
- 77. Why Clonal iPSC Lines? [https://www.jax.org/news-and-insights/jax-blog/2025/june/clonal-ipsc-lines]
- 78. Transcriptional signatures in iPSC-derived neurons are ... [https://www.sciencedirect.com/science/article/pii/S1873506121004050]
- 79. Polygenic risk score of Alzheimer's disease is associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441735/]
- 80. Human induced pluripotent stem cell models for ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1548701/full]
- 81. Multiscale proteomic modeling reveals protein networks ... [https://www.sciencedirect.com/science/article/pii/S0092867425010311]
- 82. Proteomic landscape of Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257826/]
- 83. Overview of Mass Spectrometry for Protein Analysis [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-mass-spectrometry.html]
- 84. Human and mouse proteomics reveals the shared ... [https://www.nature.com/articles/s41467-025-56853-3]
- 85. Anti-Amyloid Monoclonal Antibodies for Alzheimer's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470750/]
- 86. Roche presents new insights in Alzheimer's disease ... [https://www.roche.com/media/releases/med-cor-2025-07-28]
- 87. Methods for the isolation and analysis of Aβ from postmortem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9909698/]
- 88. Modeling Alzheimer's disease with human iPS cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6689423/]
- 89. Subcellular proteomics and iPSC modeling uncover ... [https://www.nature.com/articles/s43587-025-00823-3]
- 90. iPSC-derived cortical neurons to study sporadic Alzheimer ... [https://www.sciencedirect.com/science/article/pii/S0378427421009152]
- 91. Potential use of iPSCs for disease modeling, drug screening ... [https://cmbl.biomedcentral.com/articles/10.1186/s11658-023-00504-2]
- 92. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 93. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417523/]
- 94. Generation of human induced pluripotent stem cell line ... [https://www.sciencedirect.com/science/article/pii/S1873506125001096]
- 95. A manifesto for Alzheimer's disease drug discovery in the era ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00872-7]
- 96. Drug discovery research with the iPSC models of ... [https://pubmed.ncbi.nlm.nih.gov/41213329/]