Modeling Parkinson's Disease: How iPSC Technology is Unraveling Pathogenesis and Accelerating Therapy
This article provides a comprehensive overview of induced pluripotent stem cell (iPSC) models and their transformative role in Parkinson's disease (PD) research.
Modeling Parkinson's Disease: How iPSC Technology is Unraveling Pathogenesis and Accelerating Therapy
Abstract
This article provides a comprehensive overview of induced pluripotent stem cell (iPSC) models and their transformative role in Parkinson's disease (PD) research. It covers the foundational principles of recapitulating PD pathology in patient-specific neurons, explores advanced methodological applications in disease modeling and drug screening, addresses key challenges and optimization strategies for robust model systems, and validates iPSC models against traditional preclinical approaches. Aimed at researchers and drug development professionals, this review synthesizes current evidence and highlights the direct clinical translation of these technologies, including recent trial results, to illustrate their potential in creating a new paradigm for understanding and treating PD.
Recapitulating Parkinson's Pathology: From Patient Cells to Disease-Relevant Neurons
The pursuit of effective treatments for Parkinson's disease (PD) has been persistently hampered by the inadequacy of animal models to fully recapitulate human-specific disease pathogenesis. The emergence of induced pluripotent stem cell (iPSC) technology has inaugurated a transformative era in neurodegenerative disease research. This whitepaper delineates the core challenge of modeling PD and elaborates on how patient-specific iPSCs are being leveraged to create human-relevant models for investigating disease mechanisms and advancing drug discovery. We detail experimental methodologies for generating and characterizing iPSC-derived dopaminergic neurons, present quantitative data from recent pioneering clinical trials, and provide a curated toolkit of essential research reagents. By integrating advanced genomic engineering with complex culture systems, iPSC-based models are overcoming traditional species barriers, offering an unprecedented platform for elucidating the human-specific pathophysiology of Parkinson's disease.
Parkinson's disease stands as the second most common neurodegenerative disorder worldwide, affecting millions and posing an escalating societal burden as global populations age [1] [2]. The core pathological hallmark of PD is the progressive loss of dopaminergic (DA) neurons in the substantia nigra pars compacta, leading to the characteristic motor symptoms of tremor, bradykinesia, rigidity, and postural instability [3] [4]. A critical barrier to developing disease-modifying therapies has been the lack of accurate models that capture the human-specific complexities of PD pathogenesis. Traditional animal models, while valuable for studying certain aspects of disease, fail to replicate the unique vulnerabilities of human neurons and the multifaceted interplay of genetic and environmental factors that drive disease progression in humans [3].
The discovery of induced pluripotent stem cells (iPSCs) by Shinya Yamanaka and colleagues established a watershed moment, creating new possibilities for modeling human diseases [5] [3]. iPSCs are generated by reprogramming patient-specific somatic cells back to a pluripotent state through the introduction of key transcription factors, notably OCT4, SOX2, KLF4, and c-MYC [5] [3]. These patient-derived cells offer two profound advantages: they circumvent the ethical concerns associated with human embryonic stem cells (hESCs), and they provide a platform for studying disease processes in the exact genetic background of patients [4]. For a complex, multifactorial disorder like Parkinson's disease, where both genetic susceptibility and environmental exposures contribute to pathogenesis, iPSC technology represents a paradigm shift for creating human-specific disease models that can bridge the translational gap between preclinical research and effective clinical therapeutics [1] [3].
Foundations of iPSC Technology
Generation of Footprint-Free iPSCs
The initial methods for generating iPSCs relied on integrating viral vectors, such as retroviruses or lentiviruses, which carried the risk of insertional mutagenesis and oncogenic transformation, particularly concerning since c-MYC and KLF4 are known oncogenes [3]. To overcome these limitations for both research and clinical applications, significant efforts have been directed at developing non-integrating, "footprint-free" reprogramming methods that leave the genome intact [3]. The following table summarizes the primary approaches:
Table 1: Footprint-Free Reprogramming Methods for iPSC Generation
| Method | Mechanism | Key Features | References |
|---|---|---|---|
| Episomal Plasmids | Non-integrating plasmids that support prolonged transgene expression. | Simple, robust; plasmids are gradually diluted and lost during cell divisions. | [3] |
| Sendai Virus (SeV) | RNA virus that replicates in the cytoplasm without integrating into the host genome. | Highly efficient; virus is gradually diluted and degraded with cell division. | [3] |
| Synthetic mRNA | Modified mRNAs encoding reprogramming factors are transfected into cells. | High efficiency; requires repeated transfections and careful control of immune response. | [3] |
| Recombinant Proteins | Reprogramming factors fused with cell-penetrating peptides (e.g., TAT) are delivered directly. | No genetic material introduced; efficiency can be lower. | [3] |
Characterization and Validation of Pluripotency
Following reprogramming, putative iPSC colonies must be rigorously characterized to confirm their pluripotent state. This involves a multi-faceted approach assessing key markers and functional capacities [5]:
- Morphology: Colonies should exhibit classic embryonic stem cell-like morphology, with a high nucleus-to-cytoplasm ratio and prominent nucleoli.
- Surface Marker Expression: Flow cytometry or immunocytochemistry confirms the expression of characteristic pluripotency antigens such as SSEA-4 and TRA-1-80 [5].
- Pluripotency Potential: The gold standard functional test is the demonstration of differentiation into derivatives of all three germ layers. This can be assessed in vitro via spontaneous formation of embryoid bodies (EBs), with subsequent immunostaining for markers like alpha-fetoprotein (AFP, endoderm), β-III-tubulin (B-III-TUB, ectoderm), and smooth-muscle antibody (SMA, mesoderm) [5]. Alternatively, the in vivo teratoma formation test can be used, wherein iPSCs are injected into immunocompromised mice and the resulting tumors are examined for tissues from all three germ layers [5].
Modeling Parkinson's Disease with iPSC-Derived Neurons
Differentiation into Midbrain Dopaminergic Neurons
A critical step in modeling PD is the efficient and specific differentiation of iPSCs into authentic midbrain-like DA neurons. Protocols have evolved significantly from early methods that involved embryoid body formation or stromal cell co-culture (PA6/SDIA) [4]. The current state-of-the-art leverages knowledge of developmental biology to direct differentiation through a floor-plate intermediate, mimicking the natural origin of these neurons in the embryo [6] [7].
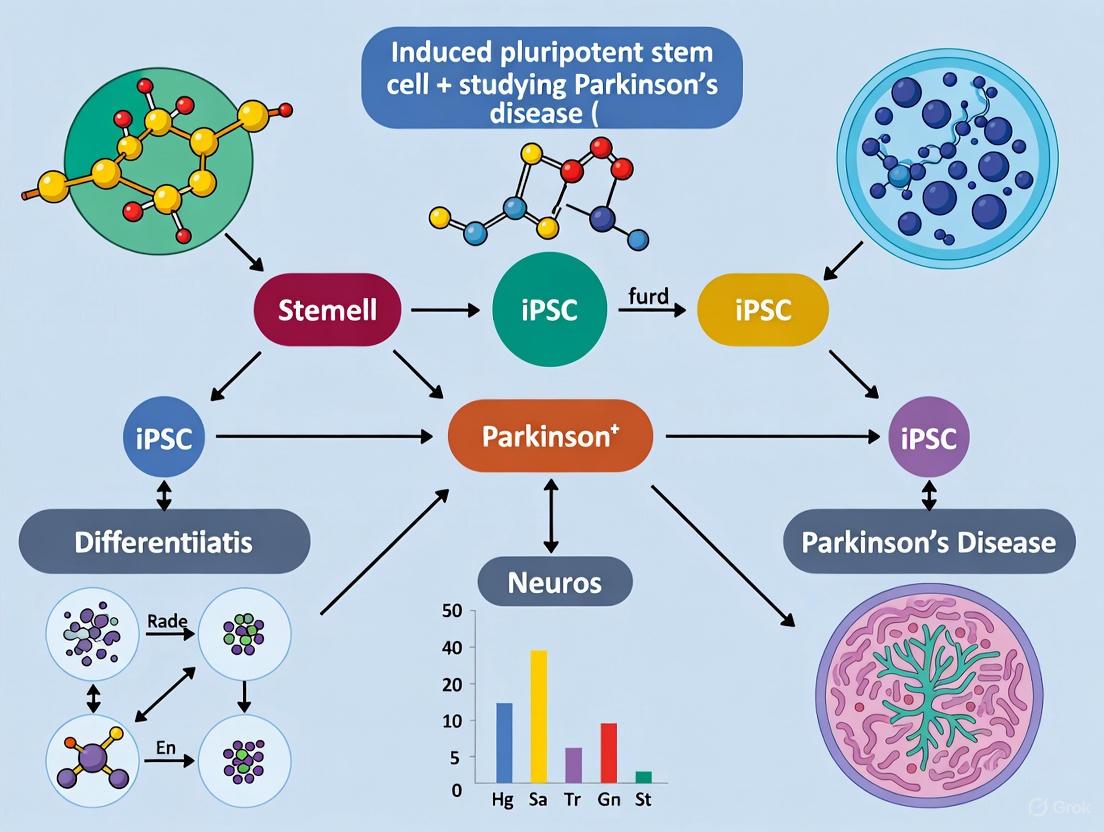
The following diagram illustrates a generalized experimental workflow for the generation and application of iPSC-derived DA neurons for Parkinson's disease research:
Diagram 1: Workflow for iPSC-Derived PD Modeling
Detailed Protocol for DA Neuron Differentiation: A typical protocol involves several key stages [4]:
- Neural Induction and Patterning (Days 1-12): iPSCs are transitioned to neural medium. To specify a midbrain fate, key developmental morphogens are added. Sonic Hedgehog (SHH) is used to ventralize the neural tissue, while FGF8 acts as a caudalizing factor, together patterning the cells toward a midbrain floor-plate identity. This stage can be monitored by the emergence of markers like FOXA2 and LMX1A.
- Progenitor Expansion (Days 12-20): The neural progenitor cells are maintained and expanded in the presence of SHH and FGF8, along with Ascorbic Acid (AA), which promotes progenitor survival and dopaminergic fate.
- Terminal Differentiation (Days 20+): Cells are dissociated and replated. Morphogens are withdrawn, and the culture is switched to a terminal differentiation medium containing neurotrophic factors such as Brain-Derived Neurotrophic Factor (BDNF), Glial Cell Line-Derived Neurotrophic Factor (GDNF), and TGF-β3, as well as cAMP. These factors support the maturation, survival, and phenotypic stability of the emerging DA neurons, which begin expressing tyrosine hydroxylase (TH), the rate-limiting enzyme in dopamine synthesis, and other markers like NURR1 and PITX3.
To enrich for the correct population, fluorescence-activated cell sorting (FACS) can be used to select cells expressing the surface marker CORIN, a floor-plate marker, thereby purifying the DA progenitor pool before final differentiation [6].
Advanced Model Systems: From 2D to 3D and Co-cultures
While 2D monolayers of iPSC-derived DA neurons are valuable, the brain is a complex 3D environment with multiple interacting cell types. To better model PD pathogenesis, the field is advancing toward more sophisticated systems [1] [5]:
- Co-culture Systems: Culturing iPSC-derived neurons alongside iPSC-derived astrocytes or microglia provides critical insights into cell-cell interactions, neuroinflammation, and non-cell-autonomous mechanisms of neurodegeneration [1] [8]. For instance, microglia derived from PD patients may have impaired phagocytosis of alpha-synuclein or may release pro-inflammatory cytokines that exacerbate neuronal damage.
- 3D Organoids: These self-organizing, three-dimensional structures more closely mimic the cellular diversity and spatial organization of the human brain. Brain region-specific organoids can model interregional disease processes and network-level dysfunctions observed in PD [1]. The integration of midbrain-specific organoids with other regions like the cortex or striatum in assembloids is a cutting-edge approach to study circuit-level vulnerabilities.
Phenotypic Analysis and Key Pathogenic Insights
iPSC-derived DA neurons from patients with both familial and sporadic forms of PD have successfully recapitulated key aspects of the disease pathology, validating their use for mechanistic studies. The following table summarizes major phenotypes observed in models based on specific genetic mutations:
Table 2: Key Phenotypes in iPSC-Derived DA Neurons from Familial PD Patients
| Gene/Protein | Mutation | Observed Phenotypes in iPSC-Derived DA Neurons | Citations |
|---|---|---|---|
| α-synuclein (SNCA) | A53T / Triplication | Elevated α-synuclein levels, endoplasmic reticulum stress, nitrosative stress, increased reactive oxygen species, reduced neurite outgrowth. | [3] |
| LRRK2 | G2019S | Elevated α-synuclein, increased susceptibility to oxidative stress (H₂O₂), impaired neurite outgrowth, mitochondrial dysfunction, delayed initiation of mitophagy. | [3] |
| Parkin (PARK2) | Deletions (Exon 3/5) | Mitochondrial dysfunction, increased sensitivity to cellular stress. | [3] |
| PINK1 | Point Mutations | Mitochondrial impairments, similar to Parkin mutations, consistent with their shared pathway in mitophagy. | [3] |
These convergent phenotypes, particularly around mitochondrial health and protein homeostasis, across multiple genetic forms of PD point toward shared downstream pathogenic pathways, offering validated targets for therapeutic intervention.
Clinical Translation and Validation
The ultimate validation of iPSC-based models comes from their successful translation into clinical therapies. Recent landmark clinical trials have demonstrated the safety and potential efficacy of transplanting iPSC-derived dopaminergic progenitors into PD patients, marking a historic milestone for the field.
Table 3: Summary of Recent Stem Cell-Based Clinical Trials for Parkinson's Disease
| Trial Parameter | Kyoto University Trial (iPSC-Derived) | Bemdaneprocel Trial (hESC-Derived) |
|---|---|---|
| Cell Source | Allogeneic iPSCs from HLA-homozygous donor | Human Embryonic Stem Cells (hESCs) |
| Study Phase | Phase I/II | Phase I |
| Patients Enrolled | 7 (for safety), 6 (for efficacy) | 12 |
| Dosing | Low: 2.1-2.6 million cells/hemisphereHigh: 5.3-5.5 million cells/hemisphere | Low: 0.9 million cells/putamenHigh: 2.7 million cells/putamen |
| Immunosuppression | Tacrolimus (15 months) | 1 year (Basiliximab, steroids, tacrolimus) |
| Primary Safety Outcome | No serious adverse events; 73 mild-moderate events. | No adverse events related to cell product; 2 serious AEs (seizure, COVID-19) unrelated to cells. |
| Efficacy Signal (Motor) | MDS-UPDRS Part III OFF score improved by 9.5 pts (20.4%) on average at 24 months. | MDS-UPDRS Part III OFF score improved by 23 pts on average in high-dose cohort at 18 months. |
| Dopamine Production | 18F-DOPA PET Ki values increased by 44.7% in putamen. | Increased 18F-DOPA PET uptake in putamen at 18 months. |
| Reference | [6] | [7] |
These trials confirm that stem cell-derived dopaminergic progenitors can survive engraftment, produce dopamine, and improve motor function in patients without forming tumors, providing a powerful proof-of-concept for the entire iPSC modeling and drug discovery pipeline.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and tools essential for conducting research using iPSC models of Parkinson's disease.
Table 4: Research Reagent Solutions for iPSC-based PD Modeling
| Reagent / Tool Category | Specific Examples | Function / Application |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) | Epigenetic reprogramming of somatic cells to pluripotency. |
| Neural Patterning Factors | Sonic Hedgehog (SHH), FGF8, CHIR99021 (GSK3β inhibitor) | Directs differentiation toward midbrain floor-plate and dopaminergic progenitor fate. |
| Neuronal Maturation Factors | BDNF, GDNF, Ascorbic Acid (AA), TGF-β3, cAMP | Supports survival, maturation, and phenotypic stability of dopaminergic neurons. |
| Cell Sorting Markers | CORIN, LMX1A, FOXA2 | Identification and purification of dopaminergic progenitors via FACS. |
| Characterization Antibodies | Tyrosine Hydroxylase (TH), NURR1, β-III-Tubulin, MAP2 | Immunocytochemical validation of dopaminergic neuronal identity and maturity. |
| Gene Editing Tools | CRISPR-Cas9, gRNA designs | Creation of isogenic control lines; introduction or correction of disease-associated mutations. |
The core challenge of modeling a human-specific neurodegenerative disease like Parkinson's is being met through the continuous refinement of iPSC-based technologies. Future directions will focus on increasing model complexity and physiological relevance. This includes the development of more sophisticated blood-brain barrier (BBB) models to study toxin permeability and drug delivery, the integration of advanced omics technologies (transcriptomics, proteomics, metabolomics) to deconstruct disease pathways, and the application of high-content imaging and electrophysiology to quantify dynamic disease phenotypes in real-time [1] [8]. Furthermore, the combination of iPSCs with gene editing tools like CRISPR-Cas9 allows for the creation of isogenic control lines—genetically identical cells where only the disease-causing mutation has been corrected—which serve as the perfect experimental control for discerning true disease-related phenotypes from background genetic noise [5] [3].
In conclusion, iPSC technology has fundamentally altered the landscape of Parkinson's disease research. By providing a patient-specific, human-relevant platform, it overcomes the longstanding limitations of animal models. The successful differentiation of iPSCs into vulnerable midbrain dopaminergic neurons, the recapitulation of key pathological features in vitro, and the recent triumphant translation into early-stage clinical trials collectively affirm that iPSC models are an indispensable tool for unraveling pathogenesis and accelerating the development of much-needed therapeutic interventions for Parkinson's disease.
The advent of induced pluripotent stem cells (iPSCs) has revolutionized biomedical research, providing an unprecedented platform for studying human development, disease modeling, and developing regenerative therapies. This technology enables the reprogramming of somatic cells back to a pluripotent state, allowing them to differentiate into any cell type in the body. For research on Parkinson's disease (PD) pathogenesis, iPSC technology offers a powerful tool to generate patient-specific dopaminergic neurons, the primary cells affected in PD, facilitating the study of disease mechanisms in a human-relevant context [9] [10]. This technical guide details the fundamental principles, methods, and applications of somatic cell reprogramming, with a specific focus on its critical role in advancing PD research.
Historical Foundation and Core Principles
The conceptual foundation for iPSC technology was laid by pioneering work in nuclear reprogramming. John Gurdon's seminal somatic cell nuclear transfer (SCNT) experiments in 1962 demonstrated that a nucleus from a differentiated somatic cell could be reprogrammed to support the development of an entire organism, proving that the genetic material in somatic cells remains intact and could be reversed to an embryonic state [11]. This established the principle of cellular plasticity – that cell fate is not irreversible but can be altered by factors in the cellular environment.
The direct generation of iPSCs was achieved by Shinya Yamanaka's team in 2006. Through a systematic screening of factors important for maintaining embryonic stem cell (ESC) identity, they identified four key transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as the OSKM or Yamanaka factors)—that were sufficient to reprogram mouse fibroblasts into pluripotent stem cells [12] [11]. This groundbreaking discovery was rapidly followed in 2007 with the successful generation of human iPSCs, both by Yamanaka's group using the OSKM factors and by James Thomson's team using an alternative combination: OCT4, SOX2, NANOG, and LIN28 [12] [11]. These breakthroughs opened the door to creating patient-specific pluripotent cells without the ethical concerns associated with human embryos.
The reprogramming process involves a profound epigenetic remodeling, where the somatic cell's gene expression pattern is erased and replaced with a pluripotency network. This process occurs in phases: an early, stochastic phase where somatic genes are silenced and early pluripotency genes are activated, followed by a more deterministic late phase where the stable pluripotent state is established [11]. A key morphological event during fibroblast reprogramming is the mesenchymal-to-epithelial transition (MET), which is critical for establishing the epithelial characteristics of pluripotent stem cells [11].
Molecular Mechanisms of Reprogramming
The reprogramming of a somatic cell to a pluripotent state is driven by the coordinated action of the Yamanaka factors, which function to dismantle the somatic gene expression program and activate the endogenous pluripotency network.
- Core Pluripotency Factors: OCT4 (encoded by POU5F1) and SOX2 are central transcription factors that form a core regulatory circuit to activate the expression of genes essential for self-renewal and pluripotency, while simultaneously repressing genes involved in differentiation [12] [13]. They play non-redundant roles, and neither can be omitted from the reprogramming cocktail.
- Supporting Factors: KLF4 assists in the activation of pluripotency genes and contributes to the MET process. c-MYC, a potent oncogene, primarily enhances reprogramming efficiency by promoting widespread changes in chromatin structure and boosting cell proliferation, thereby facilitating the access of other factors to their target genes [12] [13]. Due to its tumorigenic potential, c-MYC is often considered dispensable, and safer family members like L-MYC can be used as substitutes [12].
The following diagram illustrates the key molecular stages and signaling pathways involved in the reprogramming process:
Reprogramming Methods and Delivery Systems
A critical aspect of iPSC generation is the method used to deliver the reprogramming factors into the somatic cell. Each method balances reprogramming efficiency with safety concerns, particularly the risk of genomic integration and potential tumorigenesis.
Table 1: Comparison of Primary Reprogramming Factor Delivery Systems
| Delivery System | Genetic Material | Genomic Integration | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Retrovirus | DNA | Yes | High efficiency; Robust reprogramming | Integrates into genome; Reactivation of transgenes [12] [13] |
| Lentivirus | DNA | Yes | Can infect non-dividing cells; High efficiency | Integrates into genome; Complex production [13] |
| Sendai Virus | RNA | No | High efficiency; Non-integrating; Can be diluted out | Viral clearance required; Immunogenic potential [13] |
| Episomal Plasmid | DNA | No (typically) | Non-integrating; Simple production | Low efficiency; Requires repeated transfection [13] |
| Synthetic mRNA | RNA | No | High efficiency; Non-integrating; Controlled timing | Immunogenic; Requires daily transfection [13] |
| Recombinant Protein | Protein | No | Non-integrating; No genetic material | Very low efficiency; Technically challenging [12] |
Beyond the original Yamanaka factors, research has identified numerous alternative reprogramming factors and small molecules that can enhance efficiency and safety. Factors like SALL4, NR5A2, and GLIS1 can substitute for core factors or complement the OSKM combination [12] [13]. Small molecule compounds have been used to replace specific transcription factors; for example, RepSox can replace Sox2 [12]. Furthermore, fully chemical reprogramming using defined small molecule cocktails has been achieved, representing a completely non-genetic approach to generating iPSCs [12] [11]. Epigenetic modulators such as valproic acid (VPA), sodium butyrate, and trichostatin A can significantly enhance reprogramming efficiency by opening chromatin structure and facilitating the activation of pluripotency genes [12] [13].
The Scientist's Toolkit: Essential Reagents for iPSC Generation
Successful reprogramming requires a suite of specialized reagents and tools. The following table details key components of a researcher's toolkit for generating and validating iPSCs.
Table 2: Key Research Reagent Solutions for iPSC Generation
| Reagent Category | Specific Examples | Function in Reprogramming |
|---|---|---|
| Core Reprogramming Factors | OSKM (OCT4, SOX2, KLF4, c-MYC) or OSNL (OCT4, SOX2, NANOG, LIN28) cocktails | Initiate and drive the epigenetic and transcriptional remodeling toward pluripotency [12] [11] |
| Efficiency Enhancers | Valproic Acid (VPA), Sodium Butyrate, Trichostatin A, 5'-azacytidine | Histone deacetylase inhibitors and DNA methyltransferase inhibitors that open chromatin to improve factor access [12] [13] |
| Signaling Pathway Modulators | CHIR99021 (GSK3β inhibitor), A-83-01 (TGF-β receptor inhibitor), PD0325901 (MEK inhibitor) | Enhance reprogramming efficiency by modulating key signaling pathways like WNT and TGF-β [13] |
| Source Somatic Cells | Dermal fibroblasts, Peripheral Blood Mononuclear Cells (PBMCs), Renal epithelial cells from urine | Provide the starting genetic material for reprogramming; choice affects efficiency and practicality [13] |
| Pluripotency Validation | Antibodies against OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 | Used in immunocytochemistry or flow cytometry to confirm protein expression of pluripotency markers [11] |
Application to Parkinson's Disease Research
The ability to generate iPSCs from PD patients and differentiate them into dopaminergic neurons has transformed the landscape of PD research. Patient-specific iPSCs capture the individual's entire genetic background, including mutations in genes like SNCA (encoding α-synuclein) and LRRK2 that are linked to PD, thereby providing a unique humanized model to study the disease [14] [9] [10].
The standard workflow involves:
- Reprogramming: Generating iPSCs from a PD patient's somatic cells (e.g., skin fibroblasts or blood cells) using a non-integrating method like Sendai virus or episomal plasmids for clinical relevance [13].
- Directed Differentiation: Differentiating the iPSCs into midbrain dopaminergic neurons. This is achieved by mimicking embryonic development through the sequential use of small molecules and growth factors that activate specific signaling pathways, such as SMAD inhibition, followed by SHH activation and WNT activation to pattern the cells toward a midbrain fate [15] [10]. Key transcription factors like LMX1A and FOXA2 are critical markers of successful differentiation.
- Disease Modeling and Drug Screening: The resulting dopaminergic neurons can be used to investigate disease-specific phenotypes, such as α-synuclein aggregation (a key component of Lewy bodies), mitochondrial dysfunction, and neuronal vulnerability [14] [9]. These cells serve as a platform for high-throughput drug screening to identify compounds that can mitigate the observed pathological features.
The following diagram outlines this applied workflow for Parkinson's disease research:
Furthermore, the integration of CRISPR-Cas9 genome editing allows for the correction of disease-causing mutations in patient-derived iPSCs, creating isogenic control lines that are genetically identical except for the mutation of interest. This powerful approach enables researchers to conclusively link observed cellular pathologies to specific genetic defects [13]. The emergence of 3D organoid models from iPSCs offers an even more sophisticated system, allowing for the study of dopaminergic neurons in a tissue-like context that includes other cell types, such as glia, potentially revealing novel cell-cell interactions critical to PD pathogenesis [15] [10].
The fundamental technology of reprogramming somatic cells to pluripotence has evolved from a groundbreaking discovery into a robust and essential tool for modern biological research. A deep understanding of the molecular mechanisms, delivery methods, and reagent options is crucial for the effective generation and application of iPSCs. In the specific context of Parkinson's disease research, this technology provides a unparalleled human model system to deconstruct the molecular pathways leading to dopaminergic neuron degeneration. It accelerates the path from basic scientific discovery to therapeutic intervention, enabling mechanistic studies, target validation, and pre-clinical drug screening in a patient-specific context, thereby holding immense promise for unlocking the mysteries of PD and developing much-needed disease-modifying therapies.
The pathological hallmarks of Parkinson's disease (PD), primarily the aggregation of α-synuclein protein and the formation of Lewy bodies, have been notoriously difficult to recapitulate in traditional laboratory models. This challenge has significantly hindered the understanding of disease mechanisms and the development of effective therapies. The advent of induced pluripotent stem cell (iPSC) technology has revolutionized this landscape. By enabling the generation of patient-specific neural cells and complex three-dimensional midbrain organoids, iPSCs provide a human-relevant system to model the intricate pathophysiology of PD in a dish [16] [13]. This technical guide details how these advanced in vitro models are being leveraged to investigate alpha-synuclein aggregation and Lewy body-like inclusions, framing these approaches within the broader thesis that iPSC-based systems are indispensable for elucidating Parkinson's disease pathogenesis.
Modeling Alpha-Synuclein Aggregation
The propensity of alpha-synuclein to misfold and aggregate is a central event in Parkinson's disease. Conventional cell cultures and animal models often fail to replicate the spontaneous and progressive nature of this process within a human neuronal context. iPSC-derived models have overcome this barrier through several innovative strategies.
Genetic Predisposition Models
A primary method involves introducing key genetic risk factors associated with PD into iPSC-derived neurons and organoids.
- GBA1 Mutations: Studies using human midbrain-like organoids (hMLOs) generated from GBA1 knockout isogenic cell lines have demonstrated that the loss of glucocerebrosidase function, especially when coupled with wild-type α-synuclein overexpression, results in a substantial accumulation of detergent-resistant, β-sheet–rich α-syn aggregates [17]. This model directly links a common genetic risk factor to a core pathological phenotype.
- SNCA Triplication: Patient-derived iPSCs carrying a triplication of the SNCA gene (which encodes α-synuclein) provide a model for familial PD. These cells inherently overproduce α-synuclein, leading to its aggregation. Research has shown that impairing glucocerebrosidase function in these patient-derived organoids further promotes the formation of Lewy body-like inclusions, highlighting an interaction between genetic risk factors [17].
Table 1: Genetic Perturbations for Modeling α-Synuclein Aggregation
| Genetic Perturbation | Model System | Key Pathological Outcome |
|---|---|---|
| GBA1-/- + SNCA OE | Isogenic hMLOs | Substantial accumulation of detergent-resistant, β-sheet-rich α-syn aggregates [17] |
| SNCA Triplication | Patient-derived hMLOs | α-syn aggregation; LB-like inclusion formation enhanced by impaired GCase function [17] |
| LRRK2 Mutations | iPSC-derived dopaminergic neurons | Increased susceptibility to proteostatic stress and aggregation (Based on established PD risk genes) |
Optogenetics-Assisted Induction System (OASIS)
To overcome the slow and variable timeline of spontaneous aggregation, researchers have developed an optogenetics-assisted α-synuclein aggregation induction system [18]. This system uses a blue light-sensitive protein domain fused to α-synuclein, allowing for the precise and rapid induction of aggregation in PD hiPSC-derived midbrain dopaminergic neurons and organoids upon light stimulation.
- Protocol Overview:
- Cell Line Generation: Engineer hiPSCs to express a fusion protein of α-synuclein and a photosensitive domain (e.g., cry2olig).
- Neural Differentiation: Differentiate the engineered hiPSCs into midbrain dopaminergic neurons or generate midbrain organoids using established protocols.
- Aggregation Induction: Expose the cultures to blue light pulses (e.g., 1-5 Hz frequency) for a defined period (minutes to hours) to trigger the oligomerization of the fusion protein.
- Phenotype Validation: Confirm aggregation via immunofluorescence using antibodies against phosphorylated α-synuclein and assess neuronal toxicity through viability assays.
- Utility: The OASIS model enables high-throughput, reproducible induction of pathology, making it particularly suitable for primary drug screening and mechanistic studies over short timelines [18].
Figure 1: Experimental workflow for the Optogenetics-Assisted α-synuclein Aggregation Induction System (OASIS), enabling rapid and controlled pathology generation.
Recapitulating Lewy Body-like Inclusions
Lewy bodies are intraneuronal inclusions that represent the definitive pathognomonic sign of Parkinson's disease. Reproducing these complex structures in vitro has been a major goal for the field.
Key Experimental Protocol: Generating hMLOs with Dual Perturbations
The following detailed methodology is adapted from research that successfully generated Lewy body-like inclusions in human midbrain-like organoids (hMLOs) [17].
- Objective: To investigate the combined effect of GBA1 deficiency and α-synuclein overexpression on Lewy body formation.
- Materials and Methods:
- Cell Line Generation:
- Generate GBA1−/− human embryonic stem cells (hESCs) or iPSCs using CRISPR/Cas9 with a guide RNA targeting exon 4 of the GBA1 gene.
- Create a separate isogenic line with a doxycycline-inducible SNCA (α-synuclein) overexpression construct.
- Dual Perturbation Model: Cross these lines or use co-transduction to create a dual-perturbation hPSC line.
- hMLO Generation:
- Dissociate hPSCs and plate them in 96-well culture plates in neuronal induction medium.
- On day 3, switch to floor plate induction medium.
- On day 7, embed the forming organoids in reduced growth factor Matrigel.
- Transfer organoids to an orbital shaker and culture them in tissue growth medium (Neurobasal medium supplemented with growth factors like BDNF, GDNF, and ascorbic acid), with medium changes every 3-4 days.
- For the inducible SNCA line, add doxycycline to the culture medium to trigger α-synuclein overexpression during the maturation phase (e.g., from day 30 onwards).
- Phenotypic Analysis (after ~60-80 days of maturation):
- Immunohistochemistry: Fix hMLOs with 4% PFA, embed in paraffin, and section. Stain sections with antibodies against α-synuclein and ubiquitin. Lewy body-like inclusions are identified as spherically symmetric structures with an eosinophilic core that are positive for both markers.
- Transmission Electron Microscopy (TEM): Fix hMLOs with 2% PFA/3% glutaraldehyde, post-fix with 1% OsO4, and process through dehydration and resin embedding. Ultrathin sections can be used to visualize the dense fibrillar structure of the inclusions.
- Cell Line Generation:
- Key Findings: This protocol reliably produces Lewy body-like inclusions that morphologically resemble those found in post-mortem PD brains and are positive for α-synuclein and ubiquitin [17].
Table 2: Quantitative Analysis of Pathological Phenotypes in iPSC-PD Models
| Pathological Readout | Measurement Technique | Exemplary Finding | Significance |
|---|---|---|---|
| α-Synuclein Aggregation | Immunostaining (pS129-α-syn); FRET/Flow Cytometry | Detergent-resistant, β-sheet-rich aggregates in GBA1−/−/SNCA OE hMLOs [17] | Confirms key pathological protein state |
| Lewy Body-like Inclusions | IHC (H&E, α-syn/Ubiquitin); Transmission Electron Microscopy | Spherical inclusions with eosinophilic core, positive for α-syn and ubiquitin [17] | Recapitulates definitive PD pathology |
| Neuronal Loss | Immunostaining (TH+, NeuN+ cells); Viability Assays | ~40% loss of mDA neurons in OASIS midbrain organoids over 21 days [18] | Models neurodegeneration |
| Dopaminergic Function | HPLC, FSCV, Electrophysiology | Reduced dopamine release; Altered neuronal firing [19] | Links pathology to functional deficits |
| Mitochondrial Dysfunction | Seahorse Assay, JC-1/TMRM Staining | Decreased ATP production; Reduced mitochondrial membrane potential [19] | Captures key downstream cellular stress |
The Scientist's Toolkit: Essential Research Reagents
Successfully modeling PD pathology requires a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for iPSC-based PD Modeling
| Reagent / Tool | Function in Experiment | Specific Examples / Notes |
|---|---|---|
| iPSC Lines | Foundation for disease modeling; provide patient-specific or genetically engineered background. | Patient-derived (e.g., GBA1 N370S, SNCA triplication); Isogenic CRISPR-edited lines (e.g., GBA1−/−) [17]. |
| Neural Differentiation Kits | Direct differentiation of iPSCs into relevant neural cell types. | Commercial kits available for midbrain dopaminergic neurons; Protocols for floorplate-mediated induction [17] [4]. |
| Cerebral Organoid Media | Support the complex 3D growth and maturation of brain-like tissues. | Neuronal induction, floor plate induction, and tissue growth media with supplements (BDNF, GDNF, AA, cAMP) [17]. |
| CRISPR/Cas9 Systems | For precise genome editing to introduce or correct mutations. | Used to generate GBA1−/− lines and other isogenic controls [17] [13]. |
| Optogenetic Constructs | Enable controlled, light-induced protein aggregation. | cry2olig-α-syn fusion gene for OASIS model [18]. |
| Key Antibodies | Critical for identifying and characterizing cells and pathology. | TH (dopaminergic neurons); pS129-α-syn (pathological α-syn); Ubiquitin (LBs); CORIN/FOXA2 (midbrain progenitors) [17] [6]. |
| Small Molecule Modulators | Probe pathways and rescue phenotypes in drug screens. | Rapamycin (induces autophagy, shown to rescue α-syn pathology [19]); Conduritol-β-epoxide (chemical inhibition of GCase [17]). |
The ability to model key pathological hallmarks of Parkinson's disease—specifically, alpha-synuclein aggregation and Lewy body-like inclusions—in iPSC-derived neuronal systems marks a transformative advance in neuroscience research. The integration of patient-specific genetics, CRISPR genome editing, 3D organoid technology, and innovative tools like optogenetics has created tractable and human-relevant models that bridge the gap between traditional models and the complex human disease state. These systems provide an unparalleled platform for deconstructing disease mechanisms, exploring genotype-phenotype relationships, and, most importantly, conducting high-throughput screening for novel therapeutic candidates that can mitigate or prevent the underlying pathology of Parkinson's disease.
Parkinson's disease (PD) is the second most common neurodegenerative disorder, characterized by the progressive loss of dopaminergic neurons in the substantia nigra pars compacta and the presence of Lewy bodies in surviving neurons [20] [3]. The etiological landscape of PD encompasses both sporadic (approximately 85-90% of cases) and familial (approximately 10-15% of cases) forms, though this distinction has become increasingly blurred with advancing genetic research [21]. The emergence of induced pluripotent stem cell (iPSC) technology has revolutionized PD research by enabling the generation of patient-specific neural cells, providing unprecedented opportunities to model disease pathogenesis and investigate the functional consequences of genetic mutations in a human cellular context [16] [13].
Within the framework of iPSC-based disease modeling, four genes have garnered significant research attention: SNCA, LRRK2, GBA, and PINK1. These genes represent different inheritance patterns and molecular mechanisms contributing to PD pathogenesis. SNCA and LRRK2 are primarily associated with autosomal dominant forms, while PINK1 follows autosomal recessive inheritance. GBA mutations are considered the most significant genetic risk factor for PD [22] [23]. This technical guide examines the roles of these key genes in PD pathogenesis through the lens of contemporary iPSC research, providing a comprehensive resource for investigators utilizing these models to unravel disease mechanisms and develop novel therapeutic strategies.
Genetic Foundations of PD: Key Genes and Mutations
Understanding the genetic architecture of Parkinson's disease is fundamental to utilizing iPSC models effectively. The following table summarizes the key characteristics of the four focal genes in this review:
Table 1: Key Genetic Factors in Parkinson's Disease
| Gene | Inheritance Pattern | Protein Function | Common Mutations | Prevalence in PD | Key Cellular Pathways Affected |
|---|---|---|---|---|---|
| SNCA | Autosomal dominant | Synaptic function, neurotransmitter release | A53T, A30P, E46K, gene multiplications | ~0.3% of all PD [24] [21] | α-synuclein aggregation, mitochondrial dysfunction, oxidative stress |
| LRRK2 | Autosomal dominant | Kinase signaling, membrane trafficking | G2019S, R1441C, R1441G | 1-2% of all PD; higher in specific populations [23] | Lysosomal function, mitochondrial homeostasis, neurite outgrowth |
| GBA | Risk factor | Lysosomal enzyme (glucocerebrosidase) | N370S, L444P, E326K | Most common genetic risk factor [22] [23] | Lysosomal-autophagic function, α-synuclein metabolism |
| PINK1 | Autosomal recessive | Mitochondrial quality control | Point mutations, deletions | ~0.3% of all PD [21] | Mitophagy, mitochondrial dysfunction, oxidative stress response |
The prevalence estimates demonstrate that known causal mutations are relatively rare in the overall PD population, with the collective frequency of mutations in established PD genes occurring in less than 2% of patients [21]. However, these genetic variants provide crucial insights into pathogenic mechanisms relevant to both familial and sporadic disease forms. iPSC models have been particularly valuable in exploring these mechanisms while controlling for individual genetic background through the use of isogenic controls generated via CRISPR/Cas9 gene editing [20] [13].
SNCA (α-Synuclein): From Protein Aggregation to Cellular Dysfunction
Genetic and Molecular Background
The SNCA gene encodes α-synuclein, a 144-amino acid protein that is the primary structural component of Lewy bodies, the pathognomonic proteinaceous inclusions found in PD brains [24] [20]. SNCA was the first gene linked to familial PD, with the identification of the A53T missense mutation in a large Italian family [24]. Since this discovery, additional point mutations (A30P, E46K, H50Q, G51D, A53E) as well as gene multiplications (duplications and triplications) have been associated with autosomal dominant PD [20]. The dosage effect observed with SNCA multiplications provides compelling evidence that increased expression of wild-type α-synuclein is sufficient to cause PD, with triplication carriers developing more severe disease than duplication carriers [24] [20].
Pathogenic Mechanisms Elucidated by iPSC Models
iPSC-derived dopaminergic neurons from patients with SNCA triplication have been particularly informative for studying α-synuclein pathogenesis. These cells exhibit a two-fold increase in α-synuclein protein levels and a six-fold increase in mRNA levels, successfully modeling the protein accumulation observed in PD brains [20]. Key pathological features observed in these models include:
- Oxidative Stress: SNCA triplication iPSC-derived dopaminergic neurons demonstrate elevated oxidative stress markers and increased sensitivity to peroxide-induced oxidation. This phenotype can be reversed by knocking out endogenous α-synuclein, confirming the central role of α-synuclein in driving oxidative damage [20].
- Mitochondrial Dysfunction: Transcriptomic analyses of purified SNCA triplication iPSC-derived dopaminergic neurons revealed perturbations in genes associated with mitochondrial function. At the functional level, these cells exhibit morphological changes in mitochondria, decreased mitochondrial membrane potential, and disrupted endoplasmic reticulum-mitochondrial associations that impact Ca²⁺ homeostasis and ATP production [20].
- Lysosomal Dysfunction: Accumulated α-synuclein disrupts RAB1a-mediated hydrolase transport from the Golgi apparatus to lysosomes, reducing lysosomal function. Overexpression of RAB1a restores Golgi structure, improves hydrolase transport and activity, and reduces pathological α-synuclein accumulation [20].
- Nuclear Toxicity: Under conditions of oxidative stress, C-terminal fragments of α-synuclein translocate to the nucleus where they can bind to chromatin and activate DNA damage responses. SNCA triplication iPSC-derived neural progenitor cells demonstrate accelerated senescence and impaired genomic integrity [20].
Experimental Protocols for SNCA Modeling
The following workflow outlines a standard protocol for generating and analyzing SNCA mutant iPSC-derived neuronal models:
Diagram 1: Experimental workflow for SNCA iPSC model generation and analysis
LRRK2: Kinase Function and Converging Pathogenic Pathways
Genetic and Molecular Background
LRRK2 (leucine-rich repeat kinase 2) mutations represent the most common genetic cause of autosomal dominant PD, with the G2019S mutation accounting for approximately 1-2% of all PD cases and higher percentages in specific ethnic populations such as Ashkenazi Jewish and North African Berber descendants [23]. The LRRK2 gene encodes a large multi-domain protein containing both GTPase and kinase activities. The G2019S mutation, located in the kinase domain, enhances kinase activity and is considered a key driver of pathogenesis [20] [23].
Pathogenic Mechanisms Elucidated by iPSC Models
iPSC-derived dopaminergic neurons from LRRK2 G2019S mutation carriers have revealed several consistent pathological phenotypes:
- Elevated α-Synuclein Levels: Similar to SNCA mutant models, LRRK2 G2019S iPSC-derived dopaminergic neurons demonstrate increased α-synuclein accumulation, suggesting a convergence of pathogenic mechanisms on this key protein [3].
- Mitochondrial Dysfunction: LRRK2 G2019S neurons exhibit increased mitochondrial DNA damage and delayed initiation of mitophagy, the selective autophagy of damaged mitochondria [3]. These cells also show abnormalities in mitochondrial morphology and distribution.
- Neurite Outgrowth Deficits: Multiple studies have reported reduced neurite complexity and branching in LRRK2 G2019S iPSC-derived neurons, suggesting disruptions in neuronal connectivity and function [3].
- Lysosomal Impairment: LRRK2 mutations impact lysosomal function by altering the activity of key lysosomal proteins, including transcription factor EB (TFEB), a master regulator of lysosomal biogenesis [20].
Experimental Protocols for LRRK2 Modeling
The standard approach for evaluating LRRK2 pathogenesis in iPSC models includes:
Table 2: Key Assays for LRRK2 Pathogenesis Evaluation
| Assay Category | Specific Assays | Key Readouts | Technical Considerations |
|---|---|---|---|
| Kinase Activity | In vitro kinase assays, Phospho-substrate detection | LRRK2 autophosphorylation, RAB10 phosphorylation | Use specific LRRK2 inhibitors (e.g., LRRK2-IN-1) as controls |
| Neurite Morphology | High-content imaging of neuronal cultures | Neurite length, branching complexity, Sholl analysis | Analyze at multiple time points during maturation |
| Mitochondrial Function | Seahorse extracellular flux analysis, Live imaging with mito-trackers | OCR, ECAR, mitochondrial membrane potential, motility | Combine functional assays with morphological assessment |
| Lysosomal Function LysoTracker staining, Cathepsin activity assays | Lysosomal pH, proteolytic activity, TFEB localization | Monitor acute response to lysosomal stressors (e.g., chloroquine) | |
| Protein Aggregation FRET-based α-synuclein sensors, Filter trap assay | α-synuclein oligomerization, insoluble protein accumulation | Compare baseline levels and stress-induced aggregation |
GBA: Linking Lysosomal Function and Synucleinopathology
Genetic and Molecular Background
GBA mutations, which encoding the lysosomal enzyme glucocerebrosidase (GCase), represent the most common genetic risk factor for PD [22] [23]. While GBA mutations cause Gaucher's disease in a recessive manner, heterozygous mutations significantly increase the risk of developing PD by 5-8 fold [21]. The most common GBA mutations associated with PD are N370S and L444P, though numerous other variants have been identified [22].
Pathogenic Mechanisms Elucidated by iPSC Models
iPSC-derived dopaminergic neurons from GBA mutation carriers have revealed a bidirectional relationship between GCase dysfunction and α-synuclein pathology:
- Reduced GCase Activity: GBA mutant neurons exhibit decreased GCase enzyme activity and impaired lysosomal function, leading to the accumulation of glycosphingolipids that promote α-synuclein aggregation [20] [23].
- α-Synuclein Accumulation: Impaired lysosomal clearance of α-synuclein in GBA mutant neurons leads to increased α-synuclein levels and aggregation, which in turn further inhibits GCase activity, creating a pathogenic feedback loop [20].
- Mitochondrial Dysfunction: Similar to other genetic forms of PD, GBA mutant neurons demonstrate mitochondrial impairments, including reduced membrane potential and altered morphology [20].
PINK1: Mitochondrial Quality Control and Recessive PD
Genetic and Molecular Background
PINK1 (PTEN-induced putative kinase 1) mutations cause autosomal recessive early-onset PD [20]. PINK1 encodes a serine/threonine kinase localized to mitochondria that plays a critical role in mitochondrial quality control. Together with Parkin (encoded by PRKN), PINK1 functions in a pathway to identify and eliminate damaged mitochondria through mitophagy [20] [23].
Pathogenic Mechanisms Elucidated by iPSC Models
iPSC models of PINK1 deficiency have provided crucial insights into mitochondrial pathophysiology in PD:
- Mitophagic Impairment: PINK1 mutant iPSC-derived dopaminergic neurons exhibit defective mitophagy, with impaired recruitment of Parkin to damaged mitochondria and subsequent failure to clear dysfunctional organelles [20] [3].
- Mitochondrial Dysfunction: These cells demonstrate multiple mitochondrial abnormalities, including reduced ATP production, increased oxidative stress, and altered morphology [20].
- Enhanced Vulnerability: PINK1 deficient neurons show increased sensitivity to mitochondrial stressors such as CCCP and rotenone, confirming the importance of PINK1 in mitochondrial stress response [20].
Table 3: Key Research Reagents for iPSC-Based PD Modeling
| Reagent Category | Specific Examples | Application | Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) | iPSC generation from somatic cells | Non-integrating methods (Sendai virus, episomal vectors) preferred [13] |
| Neural Induction Supplements | SB431542, LDN193189, Noggin | Dual SMAD inhibition for neural induction | Critical for efficient neural conversion [13] |
| Midbrain Patterning Factors | SHH, FGF8, CHIR99021 (GSK3β inhibitor) | Dopaminergic neuron specification | CHIR99021 activates Wnt signaling for floor plate induction [3] |
| Neuronal Maturation Factors | BDNF, GDNF, TGF-β3, DBC, ascorbic acid | Dopaminergic neuron maturation & maintenance | Essential for functional maturation and long-term survival [3] |
| Gene Editing Tools | CRISPR/Cas9 systems | Generation of isogenic controls | Critical for controlling for genetic background [20] [13] |
| Key Antibodies | Tyrosine hydroxylase (TH), FOXA2, LMX1A, α-synuclein | Cell characterization and pathology assessment | Validate for human-specific epitopes where available |
| Pathway Reporters | MitoTimer, LC3-GFP, ROS-sensitive dyes | Dynamic assessment of cellular pathways | Enable live-cell imaging of pathological processes |
iPSC-Based Therapeutic Development and Clinical Translation
The therapeutic implications of iPSC-based PD research extend from drug discovery to cell replacement strategies. The pathological mechanisms identified in genetic iPSC models have revealed novel therapeutic targets, including LRRK2 kinase activity, GCase function, and mitochondrial quality control pathways [20] [23]. Furthermore, iPSC-derived dopaminergic neurons provide a human-relevant platform for high-throughput drug screening and validation.
Notably, iPSC technology has advanced to clinical applications for PD. A recent phase I/II trial demonstrated the safety and potential efficacy of allogeneic iPSC-derived dopaminergic progenitors transplanted into the putamen of PD patients [6]. This study reported no serious adverse events over 24 months, increased dopamine production in the putamen (as measured by 18F-DOPA PET), and improvements in motor symptoms in several patients [6]. This pioneering trial establishes a foundation for cell replacement therapies in PD and validates the utility of iPSC-based approaches for developing clinically viable treatments.
iPSC-based modeling has fundamentally advanced our understanding of Parkinson's disease pathogenesis, particularly through the study of key genes such as SNCA, LRRK2, GBA, and PINK1. These models have revealed converging pathogenic pathways—including mitochondrial dysfunction, impaired protein homeostasis, and lysosomal abnormalities—that connect diverse genetic forms of PD and likely extend to sporadic disease. The continued refinement of iPSC differentiation protocols, combined with advanced gene editing and multi-omics approaches, will further enhance the physiological relevance of these models. As the field progresses, iPSC-based studies will play an increasingly central role in validating therapeutic targets, screening candidate compounds, and developing personalized approaches for treating this complex neurodegenerative disorder.
While the loss of dopaminergic neurons in the substantia nigra remains the cardinal pathological feature of Parkinson's disease, emerging research underscores the indispensable role of glial cells in disease pathogenesis. This whitepaper explores how microglia and astrocytes contribute to PD progression through neuroinflammatory signaling, impaired neuronal support, and dysfunctional protein clearance. Within the context of induced pluripotent stem cell (iPSC) modeling, we detail how advanced co-culture systems and organoid technologies are revealing novel glial-mediated mechanisms and creating more physiologically relevant platforms for therapeutic development. The integration of glial cells into PD models represents a paradigm shift in our approach to understanding disease mechanisms and developing effective interventions.
The historical neuron-centric view of Parkinson's disease has progressively evolved to acknowledge the essential contributions of non-neuronal cells in disease pathogenesis. Glial cells, particularly microglia and astrocytes, are now recognized as active participants in PD pathology rather than passive bystanders. These cells contribute to multiple aspects of disease progression, including neuroinflammation, oxidative stress, protein aggregation, and neuronal dysfunction [25]. The advent of human iPSC-derived cellular models has been instrumental in advancing this understanding, enabling researchers to study human-specific glial biology and its contribution to PD mechanisms in unprecedented detail.
The limitations of traditional model systems in recapitulating human neuroinflammatory pathways have further highlighted the necessity of human iPSC-based approaches. Mouse models, though valuable, are unable to faithfully replicate human neuroinflammatory responses due to species-specific differences in immune system architecture and signalling pathways [25]. For instance, mouse astrocytes, but not human astrocytes, respond to the glycolipid lipopolysaccharide (LPS), a commonly used experimental neuroinflammatory activator [25]. This species divergence underscores the critical importance of human iPSC-derived models for studying glial functions in PD.
Glial Cell Types and Their Pathogenic Roles in PD
Microglia: The CNS Immune Sentinels
Table 1: Key Microglial Pathogenic Functions in Parkinson's Disease
| Function | Role in Homeostasis | Dysregulation in PD | Consequences |
|---|---|---|---|
| Immune Surveillance | Constant monitoring of CNS environment through ramified processes [25] | Chronic activation via DAMPs, PAMPs, and NAMPs [25] | Sustained neuroinflammatory response |
| Phagocytosis | Clearance of cellular debris and unwanted synapses [25] | Impaired clearance of α-synuclein aggregates [26] | Accumulation of pathological protein aggregates |
| Cytokine Signaling | Balanced release of pro- and anti-inflammatory factors [25] | Persistent pro-inflammatory cytokine release (IL-1α, TNF, C1q) [25] | Neuronal damage and astrocyte activation |
| Metabolic Support | Trophic support for neuronal health | Transition to disease-associated microglia (DAM) phenotype [25] | Altered lipid metabolism and phagocytic activity |
Microglia, the primary immune cells of the central nervous system, constitute between 0.5% and 16.6% of the total brain cell population, varying by anatomical region, sex, and developmental stage [25]. In PD, microglia undergo phenotypic changes in response to damage-associated molecular patterns (DAMPs) and neurodegeneration-associated molecular patterns (NAMPs) released from damaged neurons and protein aggregates [25]. The nuclear factor kappa B (NF-κB) pathway serves as a pleiotropic regulator of microglial inflammatory responses to these stimuli [25].
The chronic activation of microglia in PD contributes to the phenomenon of "inflammaging" – a low-grade chronic inflammation that characterizes both aging and neurodegenerative diseases [26]. Inflammaging is driven by factors such as mitochondrial dysfunction, elevated reactive oxygen species (ROS), and proteotoxicity associated with overloaded protein degradation systems [26]. Inflammatory markers including IL-6 and IL-8 also contribute to the senescence-associated secretory phenotype (SASP), which can induce cellular senescence in neighboring cells [26]. The sustained release of pro-inflammatory cytokines and chemokines creates a toxic environment that exacerbates neuronal vulnerability, particularly for metabolically active dopaminergic neurons [26].
Astrocytes: Multifunctional CNS Support Cells
Table 2: Astrocytic Functions and Dysfunctions in Parkinson's Disease
| Function | Role in Homeostasis | Dysregulation in PD | Consequences |
|---|---|---|---|
| Glutamate Homeostasis | Uptake of synaptic glutamate via transporters [25] | Reduced glutamate clearance | Excitotoxicity and neuronal damage |
| Metabolic Support | Nutrient provision to neurons | Impaired energy metabolism | Increased neuronal vulnerability |
| Blood-Brain Barrier | Maintenance of BBB integrity [25] | Compromised BBB function | Increased CNS exposure to peripheral insults |
| Inflammatory Regulation | Balanced immune signaling | Reactive astrogliosis and SASP secretion [26] | Chronic neuroinflammation |
| Trophic Support | Release of neurotrophic factors | Reduced neurotrophic support | Compromised neuronal maintenance |
Astrocytes represent the most prevalent glial cell type, comprising 17-61% of total CNS cells [25]. These highly heterogeneous cells display diverse densities, morphologies, gene expression profiles, and proliferation rates depending on brain region and disease state [25]. In PD, astrocytes contribute to disease pathogenesis through multiple mechanisms, including the propagation of neuroinflammation, failure to support neuronal health, and impaired clearance of pathological proteins.
Reactive astrocytes in PD exhibit increased expression of glial fibrillary acid protein (GFAP) and undergo hypertrophy and proliferation, a phenomenon known as astrogliosis [25]. These reactive astrocytes cluster and integrate with extracellular matrix components to form glial scars, which physically shield injured regions from healthy tissue but may also impede regeneration [25]. Critically, reactive astrocytes activate NF-κB signaling and produce various chemokines (e.g., CCL2, CXC3L1, CXCL1) that attract immune cells, as well as cytokines (e.g., IFN-γ, IL-12, TNF, IL-10, TGF-β) that propagate immune responses by stimulating neighboring glia [25].
The communication between microglia and astrocytes represents a crucial axis in PD neuroinflammation. Upon detecting insults, microglial secretion of inflammatory factors (e.g., IL-1α, TNF, and C1q) stimulates astrocytes to acquire a more reactive, inflammatory phenotype [25]. In turn, reactive astrocytes secrete additional factors that affect microglial-mediated neuroinflammatory behaviors, creating a feed-forward cycle of inflammation [27].
iPSC-Derived Glial Models: Methodological Approaches
Generation of iPSC-Derived Glial Cells
The development of reliable protocols for differentiating human iPSCs into microglia and astrocytes has revolutionized the study of glial pathophysiology in PD. Several methodological approaches exist for generating iPSC-derived glial cells, each with distinct advantages and applications.
iPSC Reprogramming Methods:
- Non-integrating Viral Approaches: Sendai virus vectors demonstrate high efficiency and safety as RNA viruses can be completely eliminated from iPSCs, reducing genomic integration risks [28].
- DNA-Based Methods: Episomal plasmids, PiggyBac transposons, and minicircle vectors offer reduced risks of genomic instability, though with variable reprogramming efficiencies [28].
- RNA Delivery: mRNA transfection presents lower mutagenic risk and high efficiency, though currently limited to specific cell types like fibroblasts and peripheral blood cells [28].
Differentiation Protocols: Microglia differentiation protocols typically involve directing iPSCs through hematopoietic progenitor stages using cytokines like IL-34, CSF-1, and TGF-β to generate cells that express characteristic microglial markers (IBA1, TMEM119, P2RY12) and exhibit functional properties including phagocytosis, cytokine secretion, and process motility [25].
Astrocyte differentiation protocols generally involve neural induction through dual SMAD inhibition, followed by glial specification using CNTF, BMPs, or LIF, resulting in cells expressing GFAP, S100β, and EAAT1, and exhibiting typical astrocytic functions such as glutamate uptake and synaptic modulation [25].
Advanced Model Systems for Neuroinflammation Research
Table 3: iPSC-Based Model Systems for Studying Neuroinflammation in PD
| Model Type | Description | Advantages | Limitations |
|---|---|---|---|
| Monocultures | Single cell type (microglia or astrocytes) in 2D culture | High throughput, simplified experimental variables | Lacks cell-cell interactions |
| Conditioned Media Transfer | Media from one cell type transferred to another | Reveals paracrine signaling effects | Removes physical cell contacts |
| 2D Co-culture Systems | Multiple cell types cultured together | Enables study of direct cell-cell interactions | May lack tissue architecture |
| 3D Organoids | Self-organizing 3D structures containing multiple CNS cell types | Recapitulates tissue complexity and architecture | Potential heterogeneity between organoids |
| Xenotransplantation | Human iPSC-derived glia transplanted into mouse brain | Provides in vivo environment for maturation | Species-specific environmental differences |
Each model system offers distinct advantages for investigating specific aspects of neuroinflammation. While monocultures enable high-throughput screening, co-culture systems and organoids provide more physiologically relevant contexts for studying cell-cell interactions [25]. The neuroinflammatory response in vivo involves numerous complex interactions between multiple brain cell types, and consequently, inflammatory responses are likely to be more physiologically relevant with increasing culture complexity [25].
Experimental Workflow for iPSC Glial Studies
The following diagram illustrates a generalized experimental workflow for establishing and utilizing iPSC-derived glial models for Parkinson's disease research:
Key Pathogenic Mechanisms and Experimental Findings
Neuroinflammation Signaling Pathways
The following diagram illustrates key neuroinflammatory signaling pathways in glial cells that contribute to Parkinson's disease pathogenesis:
Glial Dysfunction in Genetic PD Forms
iPSC models of genetic Parkinson's disease have revealed important glial contributions to disease pathogenesis:
GBA Mutations: Mutations in the GBA gene, which encodes the lysosomal enzyme glucocerebrosidase, represent one of the most common genetic risk factors for PD. iPSC-derived dopaminergic neurons from patients with GBA mutations demonstrate elevated extracellular α-synuclein levels, suggesting impaired lysosomal function and protein clearance [29]. This pathological α-synuclein accumulation can subsequently activate glial cells, creating a feed-forward cycle of neuroinflammation and neurodegeneration.
LRRK2 Mutations: iPSC-derived astrocytes from patients carrying the G2019S LRRK2 mutation show downregulation of MMP2 and TGFB1, indicating altered extracellular matrix remodeling and trophic support [29]. These dysfunctional astrocytes may fail to provide adequate neuronal support and contribute to a toxic microenvironment for dopaminergic neurons.
SNCA Mutations: Microglia-like macrophages derived from iPSCs of patients with SNCA triplication demonstrate reduced phagocytic capability and impaired degradation of α-synuclein [30]. These cells release significantly more α-synuclein into the extracellular environment, potentially promoting the spread of pathology throughout the brain.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for iPSC Glial PD Modeling
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Reprogramming Factors | OCT3/4, SOX2, KLF4, c-MYC (Yamanaka factors) [28] | iPSC generation from somatic cells | Induction of pluripotency |
| Alternative Factors | OCT3/4, SOX2, NANOG, LIN28 [28] | iPSC generation | Maintenance of pluripotency |
| Differentiation Cytokines | IL-34, CSF-1, TGF-β (microglia) [25]; CNTF, BMP, LIF (astrocytes) [25] | Glial cell differentiation from iPSCs | Directional specification of glial lineages |
| Neuroinflammatory Inducers | LPS, IL-1α, TNF, C1q [25]; pre-formed α-syn fibrils (PFFs) [27] | Modeling neuroinflammatory activation | Triggering glial inflammatory responses |
| Senescence Inducers | Chemically induced ageing methods (e.g., SLO cocktail) [26] | Modeling age-related aspects of PD | Induction of senescence phenotypes |
| Cell Sorting Markers | CORIN (floor plate marker) [6] | Enrichment of specific progenitor populations | Purification of target cell types |
| Key Antibodies | IBA1, TMEM119 (microglia); GFAP, S100β (astrocytes); TH (dopaminergic neurons) [6] [25] | Cell characterization and identification | Cell type-specific marker detection |
Experimental Protocols for Key Methodologies
Protocol: Establishing iPSC-Derived Microglia-Astrocyte Co-cultures
Objective: To generate a physiologically relevant neuroinflammatory model system for studying glial interactions in PD.
Materials:
- Established human iPSC lines (patient-derived or isogenic controls)
- Microglia differentiation media: Advanced DMEM/F12 supplemented with IL-34 (100 ng/mL), CSF-1 (100 ng/mL), TGF-β (50 ng/mL) [25]
- Astrocyte differentiation media: DMEM supplemented with CNTF (20 ng/mL) and BMP-4 (10 ng/mL) [25]
- Co-culture media: 1:1 mixture of microglia and astrocyte media
- Matrigel-coated plates for co-culture
- Recombinant human α-synuclein pre-formed fibrils (PFFs)
Procedure:
- Differentiate iPSCs into microglial precursors using a standardized 30-day protocol with staged addition of cytokines [25].
- Differentiate iPSCs into astrocytes using a 60-day neural induction and glial specification protocol [25].
- Harvest mature microglia and astrocytes using gentle enzymatic dissociation.
- Plate cells in Matrigel-coated plates at a 1:1 ratio (100,000 cells each per cm²) in co-culture media.
- Allow cells to stabilize for 48 hours before experimental manipulations.
- For disease modeling, treat co-cultures with α-syn PFFs (1-5 μg/mL) for 24-72 hours to induce neuroinflammatory responses.
Validation Measures:
- Immunocytochemistry for microglial markers (IBA1, TMEM119) and astrocyte markers (GFAP, S100β)
- ELISA quantification of cytokine secretion (IL-6, TNF-α, IL-1β) in conditioned media
- Phagocytosis assays using pHrodo-labeled α-syn fibrils
- RNA sequencing for transcriptional profiling of inflammatory pathways
Protocol: Assessing Neuroinflammatory Responses in Glial Cells
Objective: To quantify neuroinflammatory activation in iPSC-derived glial cells following exposure to PD-relevant stimuli.
Materials:
- iPSC-derived microglia and/or astrocytes
- Stimuli: LPS (100 ng/mL), IL-1α/TNF/C1q combination (each at 10 ng/mL), α-syn PFFs (5 μg/mL)
- RNA extraction kit and qPCR reagents
- ELISA kits for human IL-6, TNF-α, IL-1β, CCL2
- NF-κB pathway inhibitors (e.g., BAY-11-7082)
Procedure:
- Plate iPSC-derived glial cells in 96-well or 24-well plates at appropriate densities.
- Treat cells with inflammatory stimuli for 6-24 hours (time course dependent on readout).
- For inhibitor studies, pre-treat cells with NF-κB inhibitors for 2 hours before stimulation.
- For transcriptional analysis: Harvest RNA at 6 hours post-stimulation, perform qPCR for key inflammatory genes (IL6, TNF, IL1B, CCL2, NFKBIA).
- For protein secretion analysis: Collect conditioned media at 24 hours post-stimulation, perform ELISA for inflammatory cytokines.
- For pathway activation analysis: Fix cells and perform immunocytochemistry for NF-κB nuclear translocation or Western blotting for phospho-proteins.
Data Analysis:
- Normalize cytokine secretion to cell number (determined by parallel MTS assays or DNA quantification)
- Calculate fold-change relative to unstimulated controls
- Perform statistical analysis using one-way ANOVA with post-hoc testing for multiple comparisons
Future Directions and Therapeutic Implications
The growing recognition of glial contributions to PD pathogenesis opens new avenues for therapeutic development. Several promising approaches are emerging:
Targeting Neuroinflammation: Compounds that modulate microglial activation or astrocyte reactivity represent promising candidates for disease modification. The development of small molecules that specifically target pathogenic glial states without compromising homeostatic functions is an active area of investigation.
Enhancing Protein Clearance: Strategies to boost lysosomal function in glial cells, particularly for GBA-related PD, may reduce α-synuclein accumulation and spread. Activators of glucocerebrosidase activity or TFEB-mediated lysosomal biogenesis are being explored [30].
Senotherapeutics: Given the role of cellular senescence in PD pathogenesis, senolytic compounds that selectively eliminate senescent glial cells or senomorphics that suppress SASP secretion represent novel therapeutic approaches [26].
Cell Replacement Therapies: As cell therapies progress toward clinical application, consideration of glial interactions becomes essential. Recent clinical trials of iPSC-derived dopaminergic progenitors have shown promise, with no tumor formation and evidence of functional integration [6]. Understanding how grafted neurons interact with host glia will be crucial for optimizing therapeutic outcomes.
The continued refinement of iPSC-derived glial models, including the development of more complex multi-culture systems and region-specific brain organoids, will further enhance our understanding of glial contributions to PD and accelerate the development of novel therapeutic strategies.
The integration of glial cells into our conceptual and experimental frameworks for understanding Parkinson's disease represents a critical advancement in the field. iPSC-derived models have been instrumental in revealing the active contributions of microglia and astrocytes to neuroinflammation, protein aggregation, and neuronal vulnerability in PD. As these models continue to increase in complexity and physiological relevance, they offer unprecedented opportunities to unravel disease mechanisms and develop targeted therapies that address both neuronal and glial aspects of PD pathogenesis. The future of PD research lies in embracing this cellular complexity to develop comprehensive treatments that can truly modify disease progression.
Advanced iPSC Platforms for Mechanistic Insights and High-Throughput Screening
The investigation of Parkinson's disease pathogenesis has been transformed by the advent of induced pluripotent stem cell technology. Patient-specific iPSCs provide a unique platform for in vitro disease modeling, enabling researchers to study pathological mechanisms in disease-relevant cells with a patient's complete genomic background [20] [31]. For Parkinson's disease research, this is particularly crucial as dopaminergic neurons of the substantia nigra are the predominant brain cells affected but are inaccessible in live patients [32]. Early models relied on two-dimensional monocultures, which, despite their utility, lack the cytoarchitecture and cellular interactions essential for comprehensive disease modeling [33]. The emergence of three-dimensional brain organoid technology addresses these limitations by recapitulating more complex tissue architecture, cellular diversity, and cell-cell interactions observed in the human brain [33] [34]. This technical guide examines the evolution from 2D monocultures to 3D organoids, with a specific focus on developing brain region-specific models for Parkinson's disease research.
Fundamental Principles of iPSC Technology
iPSC Generation and Reprogramming
Induced pluripotent stem cells are generated by reprogramming somatic cells to an embryonic-like state through the forced expression of specific transcription factors. The original method established by Takahashi and Yamanaka utilizes OCT3/4, SOX2, KLF4, and c-MYC (OSKM) [13]. These factors perform distinct yet complementary roles: OCT3/4, SOX2, and KLF4 maintain pluripotency and inhibit differentiation, while c-MYC enhances reprogramming efficiency and promotes cell proliferation [13]. Alternative factor combinations include OCT3/4, SOX2, NANOG, and LIN28, where NANOG regulates stem cell self-renewal and LIN28 modulates RNA modification and expression [13].
Table 1: Comparison of iPSC Reprogramming Methods
| Method | Key Factors/Components | Advantages | Disadvantages | Reprogramming Efficiency |
|---|---|---|---|---|
| Viral Methods | Retroviral/lentiviral delivery of OSKM factors | High efficiency, robust | Risk of transgene reactivation, genomic integration | High |
| Non-Viral Methods | Episomal plasmids, mRNA transfection | Reduced integration risk, safer for clinical applications | Lower efficiency, technically challenging | Moderate to Low |
| Chemical Reprogramming | CHALP cocktail (CHIR99021, PD0325901, LIF, A-83-01, bFGF, HA-100) | No genetic modification, defined conditions | Complex optimization, variable between cell types | Variable |
| Small Molecule Enhancers | VPA, AZA, trichostatin A, BIX-01294 | Enhance efficiency, can replace some transcription factors | Potential off-target effects | Moderate |
Various somatic cell sources can be reprogrammed, with skin fibroblasts, peripheral blood mononuclear cells, and renal epithelial cells being among the most common due to their accessibility and reprogramming efficiency [13]. The choice of reprogramming method and cell source depends on the specific application, with non-integrating methods preferred for clinical applications to minimize genomic alteration risks.
Neural Induction and Patterning
The differentiation of iPSCs into neural lineages typically begins with neural induction, most commonly achieved through dual SMAD inhibition. This approach promotes neural fate selection by preventing iPSCs from adopting alternative somatic or extraembryonic fates via inhibition of TGF-β and BMP signaling at early differentiation stages [35]. In the absence of additional patterning signals, this default pathway typically yields forebrain-type neural progenitors [34].
To generate specific neuronal subtypes relevant to Parkinson's disease, particularly midbrain dopaminergic neurons, additional patterning is required. The current state-of-the-art employs specific signaling molecules to direct anterior-posterior and dorso-ventral patterning:
- WNT Activation: Canonical WNT signaling activation using GSK3β inhibitors like CHIR99021 imposes midbrain regional identity by mimicking WNT1 signaling from the isthmic organizer [35]
- SHH Pathway Activation: Sonic hedgehog signaling ventralizes cells to induce LMX1A+/FOXA2+/OTX2+ ventral midbrain floor plate progenitors [35]
- FGF8 Signaling: Often applied together with WNT activation to reinforce midbrain patterning [35]
An alternative patterning approach utilizes retinoic acid signaling, where the duration of exposure rather than concentration determines mesencephalic specification. This concentration-insensitive method provides robustness and reduces protocol adjustments between different iPSC lines [35].
Figure 1: Experimental Workflow for 2D and 3D Neural Differentiation from iPSCs
2D Monoculture Models for Parkinson's Research
Generation of Dopaminergic Neurons in 2D
Two-dimensional monocultures represent the foundational approach for generating Parkinson's-relevant cell types. The original protocol for deriving dopaminergic neurons from iPSCs relied on small molecules and took more than two months to achieve mature neurons [32]. These protocols typically involve stepwise differentiation through neural progenitor cells into post-mitotic neurons.
More recent approaches utilize transcription-factor-mediated direct differentiation to accelerate the process and improve purity. Key transcription factors include:
- ASCL1: A DNA-binding transcription factor that accesses closed chromatin to allow other factors to bind and activate neural pathways [32]
- NURR1: An orphan nuclear receptor critical for dopaminergic neuronal development, regulating tyrosine hydroxylase expression, dopamine metabolism, and neuronal survival [32]
- LMX1A: A LIM homeobox transcription factor that induces msh homeobox 1 (Msh1) and activates Neurogenin 2 (Ngn2), promoting neuronal differentiation and suppressing alternate ventral cell fates [32]
A comparative study of three transcription factor protocols demonstrated that optimized media compositions could generate over 90% neurons, with more than 85% being dopaminergic neurons within three weeks [32]. The highest yields were achieved using a modified protocol based on Sheta et al., which produced tyrosine hydroxylase and GIRK2-positive dopaminergic neurons that were electrophysiologically active and released dopamine [32].
Applications and Limitations in Parkinson's Disease Modeling
Two-dimensional iPSC-derived dopaminergic neurons have been extensively used to study Parkinson's disease mechanisms. These models have provided insights into:
- Oxidative Stress: SNCA triplication iPSC-derived dopaminergic neurons show increased oxidative stress markers and heightened sensitivity to peroxide-induced oxidation [20]
- Mitochondrial Dysfunction: Transcriptomic analyses of purified SNCA triplication iPSC-derived dopaminergic neurons reveal perturbations in mitochondrial function genes and decreased mitochondrial membrane potential [20]
- Lysosomal Dysfunction: Accumulated α-synuclein disrupts RAB1a-mediated hydrolase transport in patient-derived neurons, reducing lysosomal function [20]
- Nuclear Toxicity: Misfolded α-synuclein can cause genomic DNA strand breaks and accelerate cellular senescence in neuronal nuclei [20]
Despite these advancements, 2D models face significant limitations. The absence of cytoarchitecture, limited cellular diversity, and lack of tissue-level organization restrict their ability to fully recapitulate the complexity of the brain microenvironment [33]. Additionally, the maturity of derived neurons may not fully match adult human neurons, potentially affecting disease phenotype expression [31].
3D Brain Organoid Models for Parkinson's Research
Cerebral Organoid Generation Techniques
Three-dimensional brain organoids are in vitro-derived structures that undergo self-organization and resemble in vivo brain tissue to varying degrees [33]. Two major approaches exist for generating brain organoids:
- Self-Organization Methods: Rely on the intrinsic ability of PSCs to self-organize into sophisticated tissue structures with minimal external guidance. The Lancaster protocol embeds embryoid bodies in Matrigel to support complex tissue development, generating cerebral organoids with multiple brain region identities [34]
- Patterned Methods: Use external inductive signals to guide organoids toward specific regional identities. These approaches apply morphogens and patterning factors to mimic developmental signaling, generating region-specific organoids such as midbrain, cortical, or hypothalamic organoids [34]
The general process for brain organoid generation encompasses several phases: embryoid body formation, neural induction, expansion, and maturation [33]. To enhance reproducibility and consistency, researchers have developed defined protocols using spinning bioreactors or shake flasks to improve nutrient and oxygen exchange [33].
Table 2: Advanced 3D Brain Organoid Culture Systems
| System Type | Organoid Type | Key Features | Advantages | Limitations |
|---|---|---|---|---|
| Xenotransplantation | Forebrain | Axonal projections, synaptogenesis mapping | Long-term culturing, vascularization | Lack of human vascular bed, complex protocol |
| Air-Liquid Interface | Whole brain | Axonal tracts, improved neuronal survival | Proper neural tract formation, long-term culturing (≥12 months) | Devoid of vascularity |
| Spinning Bioreactors | Forebrain, midbrain, hypothalamus | Defined oSVZ, oRGC-like NPCs | Patterning into different brain subregions, high reproducibility | Expensive for mass production, lacks vascularization |
| Assembloids | Dorsal-ventral forebrain | Dorsal-ventral axis | Robust directional neuron migration, rough cortical layer organization | Lack of input/output systems |
| Bioengineered Scaffolds | Forebrain | Polarized cortical plate, radial units | Enhanced tissue identity and architecture | Poor spatial orientation |
Midbrain-Specific Organoids for Parkinson's Modeling
For Parkinson's disease research, midbrain-specific organoids are particularly valuable as they model the region most affected in the disease. These organoids are generated using specific patterning factor cocktails that direct anterior-posterior patterning toward midbrain identity and dorso-ventral patterning toward floor plate fates, which give rise to dopaminergic neurons [34].
Key patterning factors include:
- Early Insulin Treatment and Wnt Activation: Directs differentiation toward midbrain fates [34]
- SHH Activation: Induces ventralization and promotes floor plate identity [34]
- FGF8 Treatment: Supports rostral midbrain patterning [34]
Advanced midbrain organoids contain not only dopaminergic neurons but also other relevant cell types, including astrocytes, oligodendrocytes, and in some cases, microglia-like cells [33]. The inclusion of multiple cell types enables the study of cell-cell interactions that may be crucial in Parkinson's disease pathogenesis, such as neuroinflammation mediated by glial cells.
Figure 2: Signaling Pathways for Midbrain Organoid Generation and Cellular Composition
Advanced 3D Model Systems
Recent technological advances have led to the development of more sophisticated 3D model systems that better recapitulate brain complexity:
- Vascularized Organoids: Co-culturing neuroepithelium with mesodermal progenitor cells or endothelial cells promotes the formation of endothelial networks within organoids, improving nutrient delivery and viability [33]
- Assembloids: Multiple region-specific organoids are fused to study inter-regional interactions, such as connecting cortical and striatal organoids to model circuitry relevant to Parkinson's disease [33]
- Air-Liquid Interface Cerebral Organoids (ALI-COs): These systems enhance neuronal survival (over 12 months) and axon outgrowth, forming active neuronal networks that can innervate mouse spinal cord explants [33]
- Slice Cultures: Slicing mature organoids reduces inner hypoxia and cell death, enabling sustained neurogenesis and formation of complex neuronal layers over long-term cultures [34]
These advanced systems address key limitations of earlier organoid models, particularly regarding long-term viability, cellular diversity, and structural complexity.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for iPSC-Based Parkinson's Modeling
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT3/4, SOX2, KLF4, c-MYC (Yamanaka factors) | Somatic cell reprogramming to pluripotency | Multiple delivery methods available (viral, mRNA, protein) |
| Neural Induction Agents | SB431542 (TGF-β inhibitor), LDN193189 (BMP inhibitor) | Dual SMAD inhibition for neural induction | Foundation for both 2D and 3D neural differentiation |
| Midbrain Patterning Factors | CHIR99021 (GSK3β inhibitor), FGF8, SHH agonists (SAG, purmorphamine) | Anterior-posterior and dorso-ventral patterning | Concentration and timing critical for midbrain specification |
| Transcription Factors | ASCL1, NURR1, LMX1A, NGN2 | Direct differentiation to dopaminergic neurons | Lentiviral delivery or stable integration possible |
| 3D Matrix Materials | Matrigel, synthetic PEG-based hydrogels, laminin | Structural support for 3D organoid formation | Matrix composition influences organoid development |
| Bioreactor Systems | Spinning bioreactors, orbital shakers | Enhanced nutrient/waste exchange in 3D cultures | Improves viability and reduces necrotic cores |
| Maturation Factors | BDNF, GDNF, ascorbic acid, cAMP | Promote neuronal maturation and survival | Essential for functional dopaminergic neurons |
| Characterization Antibodies | Tyrosine hydroxylase (TH), FOXA2, LMX1A, MAP2, TUJ1 | Identification of dopaminergic neurons and neural markers | Quality control for differentiation efficiency |
The evolution from 2D monocultures to 3D brain region-specific organoids represents a significant advancement in Parkinson's disease modeling. While 2D systems provide a simplified platform for high-throughput screening and mechanistic studies, 3D organoids offer unprecedented complexity and cellular interactions that more closely mimic the human brain environment. The integration of patient-specific iPSCs with advanced 3D culture systems, CRISPR-Cas9 gene editing, and multi-omics approaches provides a powerful framework for elucidating Parkinson's disease pathogenesis and developing novel therapeutic strategies. As these technologies continue to mature, with improvements in vascularization, cellular diversity, and long-term stability, they promise to bridge the critical gap between animal models and human pathophysiology, accelerating the development of effective treatments for Parkinson's disease.
The investigation of Parkinson's disease pathogenesis has been transformed by the parallel development of two powerful technological platforms: induced pluripotent stem cells (iPSCs) and CRISPR-Cas9 gene editing. iPSCs, generated by reprogramming patient-specific somatic cells, provide a human-relevant system for modeling Parkinson's disease (PD) that preserves the individual's complete genomic background [20]. When combined with CRISPR-Cas9-mediated generation of isogenic controls—genetically matched lines that differ only at a specific locus of interest—researchers can isolate the functional impact of disease-related mutations with unprecedented precision [36]. The integration of multi-omics approaches further empowers this paradigm by providing comprehensive molecular profiling across genomic, transcriptomic, proteomic, and epigenomic layers. This technical guide examines the methodologies, applications, and best practices for integrating these technologies to deconvolute the complex mechanisms underlying Parkinson's disease pathogenesis.
Foundations: iPSC Models of Parkinson's Disease
Established Parkinson's Disease iPSC Models
iPSC models have been established from patients carrying various PD-associated mutations, providing invaluable tools for investigating disease mechanisms. These models encompass both monogenic forms and sporadic cases, enabling researchers to study specific pathogenic pathways [37].
Table: Key Parkinson's Disease iPSC Models and Their Characteristic Phenotypes
| Genetic Background | PD Inheritance Pattern | Characteristic Cellular Phenotypes | Reference |
|---|---|---|---|
| SNCA triplication | Autosomal dominant | α-synuclein accumulation, oxidative stress, mitochondrial dysfunction, lysosomal impairment | [20] [37] |
| LRRK2 (G2019S) | Autosomal dominant | Accumulation of α-synuclein, mitochondrial DNA damage, increased susceptibility to oxidative stress | [20] [37] |
| GBA mutations | Risk factor | Lysosomal dysfunction, impaired autophagy, elevated ER stress, disrupted calcium homeostasis | [20] [37] |
| PINK1/PARKIN | Autosomal recessive | Mitochondrial dysfunction, impaired mitophagy, increased sensitivity to cellular stress | [20] [37] |
| VPS35 (D620N) | Autosomal dominant | Altered endolysosomal trafficking, autophagic defects, mitochondrial transport deficits | [20] [37] |
| Sporadic PD | Idiopathic | Increased soluble α-synuclein, reduced lysosomal membrane proteins, phosphorylated PKCα accumulation | [38] |
Generation of iPSCs and Differentiation into Dopaminergic Neurons
The standard workflow for creating PD-specific dopaminergic neurons begins with somatic cell reprogramming, followed by directed differentiation toward the midbrain dopamine neuron fate:
Somatic Cell Source: Dermal fibroblasts or peripheral blood mononuclear cells (PBMCs) are collected from PD patients and healthy controls [36].
Reprogramming: Using non-integrating Sendai virus vectors carrying the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC), somatic cells are reprogrammed into iPSCs [36]. Non-integrating methods are preferred to minimize genomic alterations.
Characterization: Pluripotency is confirmed through:
- Immunocytochemistry for markers (SOX2, Tra1-60)
- Quantitative PCR for endogenous pluripotency genes
- Karyotyping to exclude chromosomal abnormalities
- Spontaneous differentiation into three germ layers [36]
Dopaminergic Differentiation: Using small molecule protocols or transcription factor approaches, iPSCs are differentiated into midbrain dopaminergic neurons expressing characteristic markers (tyrosine hydroxylase, βIII-tubulin, and FOXA2) [26].
CRISPR-Cas9 Strategies for Isogenic Control Generation
Design and Workflow for Isogenic Control Creation
The generation of isogenic controls represents a critical methodological advance for controlling for individual genetic background variability. The standard approach involves:
Diagram 1: Isogenic control generation workflow.
Detailed Methodology:
Guide RNA Design: Design allele-specific guide RNAs with at least 3 bp mismatch to any other genomic region to minimize off-target effects [36]. For point mutation correction, design guides that overlap the mutant nucleotide.
Repair Template Design: For precise genome editing, include single-stranded oligodeoxynucleotides (ssODNs) as repair templates with 60-90 bp homology arms flanking the target site [36].
Delivery System: Nucleofection of ribonucleoprotein complexes (Cas9 protein + gRNA) provides transient exposure, reducing off-target effects compared to plasmid-based systems [36].
Single-Cell Cloning: After nucleofection, cells are dissociated into single cells and plated at low density. Individual colonies are manually selected and expanded in 96-well plates [36].
Genotype Validation: Edited clones are validated through:
- Sanger sequencing of the target locus
- Sequencing of predicted off-target sites
- Karyotyping to exclude chromosomal abnormalities
- Confirmation of pluripotency marker retention [36]
Advanced CRISPR Screening Approaches
Beyond single gene editing, CRISPR-based screens enable systematic functional interrogation of genetic interactions. "Anchor screening" represents an innovative approach that eliminates the need for laborious single-cell cloning:
Diagram 2: Anchor screening workflow without single cell cloning.
This methodology utilizes orthogonal Cas enzymes from S. pyogenes (SpyoCas9) and S. aureus (SaurCas9) to enable simultaneous knockout of an "anchor" gene and genome-wide screening [39]. The approach involves:
Anchor Vector: Creates stable cells expressing SpyoCas9 and a Saur-guide targeting the gene of interest. Since the guide is paired with the wrong Cas9, no editing occurs during expansion.
Library Vector: Delivers SaurCas9 and a Spyo-guide library (e.g., genome-wide Brunello library with ~78,000 guides).
Simultaneous Editing: Upon introduction of the library vector, each cell experiences approximately simultaneous knockout of both the anchor gene and a library gene.
Interaction Mapping: After 2-3 weeks of proliferation, guide abundance is sequenced to identify synthetic lethal and buffering interactions through calculation of log2-fold-change compared to control cells [39].
Multi-Omics Integration for Mechanistic Deconvolution
The integration of multiple molecular profiling technologies creates a comprehensive view of PD pathogenesis. Major omics data types and resources include:
Table: Multi-Omics Resources for Parkinson's Disease Research
| Resource | Data Types | Description | Access |
|---|---|---|---|
| FOUNDIN-PD | Genotype, WGS, DNA methylation, HiC, scATAC-seq, bulk/smallRNA-seq, scRNA-seq, Proteomics, Clinical, Imaging | Extensive multi-omics from PD patient-derived iPSCs | [40] |
| AMP-PD | Whole-genome sequencing, transcriptome, clinical evaluations | Harmonized data from multiple cohorts (BioFIND, PDBP, PPMI) | [40] |
| GP2 | Genotype, GWAS, WGS | Diverse international cohort of PD patients (150k+ individuals) | [40] |
| iPDGC Locus Browser | GWAS, QTL, bulkRNA-seq, scRNA-seq | Variant annotation, causal gene nomination, eQTL integration | [40] |
Integrative Analysis Pipeline
A robust multi-omics analysis pipeline for PD research incorporates several sequential analytical steps:
Mendelian Randomization (MR): Uses genetic variants associated with gene expression (eQTLs) or protein abundance (pQTLs) as instrumental variables to infer causal relationships between molecular features and PD risk [41].
Steiger Filtering: Determines the directionality of causal relationships to exclude reverse causation.
Bayesian Colocalization: Tests whether GWAS signals and QTLs share the same underlying causal variant (PPH4 > 80% indicates strong evidence) [41].
Fine Mapping: Identifies putative causal variants within associated loci.
Pathway and Network Analysis: Integrates findings across omics layers to identify dysregulated biological pathways and protein-protein interaction networks.
This integrated approach has revealed novel PD risk genes, including GPNMB (risk factor) and CD38 (protective factor), which show consistent effects across protein and transcript levels in brain tissue [41].
Experimental Protocols for Key Applications
Protocol: Transcriptomic Analysis of CRISPR-Edited iPSC-Derived Neurons
This protocol outlines the comprehensive approach used to identify molecular pathways dysregulated by PD-associated mutations [36]:
Step 1: RNA Extraction and Quality Control
- Extract total RNA from iPSC-derived neurons (minimum n=3 biological replicates per genotype) using RNeasy kits
- Assess RNA quality using Bioanalyzer (RIN > 8.0 required)
- Quantity RNA using fluorometric methods
Step 2: Library Preparation and Sequencing
- Convert 500ng-1μg total RNA to cDNA using oligo(dT) primers
- Prepare libraries using Illumina Stranded mRNA Prep kit
- Sequence on Illumina platform (minimum 30 million 150bp paired-end reads per sample)
Step 3: Bioinformatics Analysis
- Align reads to reference genome using STAR aligner
- Quantify gene-level counts using featureCounts
- Perform differential expression analysis with DESeq2 (FDR < 0.05)
- Conduct pathway enrichment analysis using GSEA or similar tools
Step 4: Cross-Platform Validation
- Validate key findings in human post-mortem brain tissue
- Confirm observations in animal models of PD
- Assess translational relevance through comparison with human genetic data [36]
Protocol: Functional Validation of Mitochondrial Phenotypes
PD iPSC models frequently exhibit mitochondrial dysfunction, which can be quantified using the following approaches:
Mitochondrial Morphology Assessment
- Transfer iPSC-derived neurons to glass-bottom dishes
- Load with MitoTracker Red CMXRos (100 nM) for 30 minutes
- Image using super-resolution or confocal microscopy
- Quantify mitochondrial length, branching, and network connectivity using ImageJ plugins
Mitochondrial Membrane Potential Measurement
- Incubate cells with JC-1 dye (5 μM) for 20 minutes
- Analyze by flow cytometry or fluorescence microscopy
- Calculate red/green fluorescence ratio (decreased ratio indicates depolarization)
ATP Production Assay
- Lyse cells in ATP assay buffer
- Measure ATP levels using luciferase-based assays
- Normalize to protein concentration
- Compare ATP production rates between mutant and isogenic control lines [20] [37]
Oxidative Stress Assessment
- Load cells with CM-H2DCFDA (5 μM) for 30 minutes
- Measure fluorescence intensity as baseline
- Treat with rotenone (100 nM) or other stressors
- Monitor fluorescence increase over time [20]
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagent Solutions for iPSC/CRISPR Parkinson's Disease Research
| Reagent Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Reprogramming Systems | Non-integrating Sendai virus (OCT4, SOX2, KLF4, c-MYC) | Footprint-free iPSC generation from patient somatic cells | [36] |
| CRISPR-Cas9 Systems | SpyoCas9, SaurCas9, sgRNAs, ssODN repair templates | Precise genome editing for isogenic control generation | [36] [39] |
| Differentiation Kits | Small molecule cocktails (SMAD inhibitors, SHH agonists) | Directed differentiation to midbrain dopaminergic neurons | [26] |
| Multi-Omics Platforms | RNA-seq kits, ATAC-seq kits, proteomic profiling kits | Comprehensive molecular profiling | [40] [41] |
| Phenotypic Assays | MitoTracker dyes, LC3 antibodies, α-synuclein antibodies | Functional assessment of cellular phenotypes | [20] [37] |
Visualization of Integrated Workflow
The complete integration of multi-omics and gene editing technologies follows a systematic workflow that progresses from initial sample collection through mechanistic validation:
Diagram 3: Integrated multi-omics and gene editing workflow for Parkinson's disease research.
The integration of multi-omics technologies with CRISPR-based genome editing in iPSC models represents a transformative approach for deconvoluting Parkinson's disease pathogenesis. The methodologies outlined in this technical guide provide a framework for generating genetically precise models, conducting comprehensive molecular profiling, and identifying causal mechanisms underlying this complex neurodegenerative disorder. As these technologies continue to evolve, they promise to accelerate the identification and validation of novel therapeutic targets for Parkinson's disease, ultimately leading to more effective interventions for patients.
Key future directions include the development of more sophisticated 3D culture models that better recapitulate tissue-level organization [37], the implementation of single-cell multi-omics approaches to resolve cellular heterogeneity in PD pathology, and the creation of standardized protocols for modeling age-related aspects of the disease through chemical-induced ageing methods [26]. Together, these advances will further enhance the utility of integrated multi-omics and gene editing platforms in Parkinson's disease research.
Induced pluripotent stem cell (iPSC) technology has revolutionized the study of neurodegenerative diseases, offering an unprecedented window into human-specific pathology. For Parkinson's disease (PD) research, iPSC-derived neurons provide a critical platform for investigating disease mechanisms and screening therapeutic compounds in patient-specific genetic backgrounds [1] [42]. These models successfully recapitulate key aspects of PD, including the loss of dopaminergic neurons, protein aggregation, and crucially, the mitochondrial dysfunction and oxidative stress that represent core pathological features [1].
Phenotypic screening in these human neuronal models represents a powerful strategy for identifying novel therapeutic candidates and elucidating disease mechanisms without requiring preconceived molecular targets [43] [44]. This approach is particularly valuable for complex conditions like PD, where multiple interconnected pathways contribute to neuronal vulnerability and degeneration. By focusing on measurable phenotypic outcomes such as neuronal survival, neurite integrity, and mitochondrial function, researchers can identify compounds that modify disease-relevant processes regardless of their specific molecular targets [43].
This technical guide provides a comprehensive framework for implementing phenotypic screening approaches specifically designed to detect oxidative stress and mitochondrial dysfunction in patient-derived neuronal models of Parkinson's disease, with direct application to both pathogenesis studies and drug discovery pipelines.
iPSC-Derived Neuronal Models for Parkinson's Disease
Model System Fundamentals
iPSC-derived neuronal models for PD research are typically generated through directed differentiation of patient-specific iPSCs into midbrain dopaminergic neurons, the primary vulnerable population in PD [1] [42]. These models can be established in both 2D monolayer cultures and more complex 3D organoid systems, each offering distinct advantages for different research applications [1].
The fundamental strength of these models lies in their ability to maintain patient-specific genetics and recapitulate key disease phenotypes in human neurons. This is particularly valuable for sporadic PD cases, which represent the majority of patients and involve complex gene-environment interactions that are difficult to model in traditional systems [45]. iPSC-derived neurons from patients with sporadic PD have been shown to exhibit impaired survival, accelerated neurite degeneration, and * transcriptional dysregulation* consistent with the human disease state [45].
Protocol for Generating iPSC-Derived Dopaminergic Neurons
Materials:
- Human iPSCs from PD patients and matched controls
- Neural induction medium (SMAD inhibitors, Wnt agonists)
- Floor plate induction factors (SHH, FGF8)
- Neuronal maturation factors (BDNF, GDNF, ascorbic acid, cAMP)
- Laminin or poly-ornithine/laminin coated plates
Procedure:
- Maintain iPSCs in pluripotency medium until 70-80% confluent
- Induce neural differentiation using dual SMAD inhibition (LDN-193189, SB431542) for 7-10 days
- Pattern toward midbrain fate using SHH (100-500 ng/mL) and FGF8 (100 ng/mL) from days 3-14
- Enrich for dopaminergic progenitors by sorting for CORIN+ cells between days 11-13 [6]
- Differentiate into mature neurons using neuronal maturation factors for 4-8 weeks
- Validate differentiation by immunostaining for FOXA2, LMX1A, TUJ1, and tyrosine hydroxylase (TH)
This protocol typically yields cultures with >90% neurons, of which approximately 60% are dopaminergic progenitors and 40% are mature dopaminergic neurons [6]. The resulting neurons should exhibit electrophysiological activity, dopamine release, and appropriate expression of midbrain markers.
Phenotypic Screening Assays for Oxidative Stress and Mitochondrial Dysfunction
Assay Design Principles
Effective phenotypic screening for oxidative stress and mitochondrial dysfunction requires careful consideration of assay robustness, scalability, and clinical relevance [44]. Screening campaigns should employ multiple complementary assays to capture different aspects of these complex processes, as no single readout provides a comprehensive assessment of cellular health.
High-content imaging approaches are particularly valuable for phenotypic screening, as they enable simultaneous quantification of multiple parameters at single-cell resolution in physiologically relevant models [43]. These platforms allow researchers to monitor neuronal morphology, cell viability, and subcellular localization of key organelles and proteins in the same experimental setup.
Mitochondrial Functional Assays
Table 1: Mitochondrial Functional Assays for Phenotypic Screening
| Assay Type | Measured Parameters | Throughput | Key Reagents |
|---|---|---|---|
| Seahorse XF Analyzer | OCR, ECAR, ATP production, proton leak, spare respiratory capacity | Medium | XF Cell Mito Stress Test Kit, oligomycin, FCCP, rotenone/antimycin A |
| Live-cell imaging with fluorescent dyes | Mitochondrial membrane potential (ΔΨm), ROS production, mitochondrial mass & morphology | High | TMRM, JC-1, MitoTracker dyes, MitoSOX Red |
| ATP quantification | Cellular ATP levels | High | Luciferase-based assays (e.g., CellTiter-Glo) |
| Complex I activity assay | NADH dehydrogenase activity | Low | Immunocapture-based kits with spectrophotometric detection |
Detailed Protocol: Mitochondrial Stress Test
- Plate iPSC-derived neurons in XF microplates at 50,000-100,000 cells/well
- Differentiate for 4-6 weeks to achieve mature neuronal phenotype
- Replace medium with XF assay medium (unbuffered DMEM with 1mM pyruvate, 2mM glutamine, 10mM glucose) 1 hour before assay
- Measure basal oxygen consumption rate (OCR)
- Inject mitochondrial inhibitors sequentially:
- Oligomycin (1μM) to inhibit ATP synthase
- FCCP (0.5-2μM) to uncouple electron transport
- Rotenone (0.5μM) + Antimycin A (0.5μM) to inhibit complexes I and III
- Calculate key parameters:
- ATP production = (last basal rate measurement - minimum after oligomycin)
- Proton leak = (minimum after oligomycin - non-mitochondrial respiration)
- Spare capacity = (maximum after FCCP - basal rate)
Oxidative Stress Detection Assays
Table 2: Oxidative Stress Detection Assays
| Assay Type | Target | Detection Method | Sensitivity |
|---|---|---|---|
| Lipid peroxidation | Malondialdehyde (MDA), 4-HNE | TBARS assay, antibody detection | 1-10 μM |
| Protein oxidation | Protein carbonyls | DNPH derivatization, immunodetection | 0.5-5 nmol/mg protein |
| DNA/RNA oxidation | 8-OHdG, 8-OHG | ELISA, HPLC-ECD, immunostaining | 0.5-5 ng/mL |
| Antioxidant capacity | GSH/GSSG ratio | Fluorescent probes (monochlorobimane), enzymatic recycling | 1-10 μM |
| ROS detection | Superoxide, hydrogen peroxide | Fluorescent probes (DCFDA, MitoSOX), chemiluminescent | Cell-dependent |
Detailed Protocol: Live-cell ROS Imaging
- Culture iPSC-derived neurons in black-walled, clear-bottom 96-well plates
- Load with 5μM CM-H2DCFDA or 5μM MitoSOX Red in recording medium for 30 minutes at 37°C
- Wash twice with recording medium to remove excess dye
- Acquire baseline fluorescence (Ex/Em: 495/529 nm for DCF; 510/580 nm for MitoSOX)
- Apply test compounds and monitor fluorescence every 10-15 minutes for 2-4 hours
- Include positive controls (antimycin A, rotenone) and negative controls (N-acetylcysteine)
- Normalize fluorescence to cell number using nuclear stains (Hoechst 33342) or viability dyes
High-Content Morphological and Viability Assays
Neuronal health extends beyond biochemical parameters to include structural integrity and survival. High-content imaging enables quantification of neurite length, branching complexity, somatal size, and nuclear morphology in tandem with functional assays [43].
Detailed Protocol: Neurite Integrity Analysis
- Plate neurons in 96-well plates at optimal density for single-cell analysis (10,000-30,000 cells/well)
- Fix at appropriate timepoints with 4% PFA for 15 minutes
- Permeabilize with 0.1% Triton X-100 for 10 minutes
- Block with 5% normal goat serum for 1 hour
- Stain with primary antibodies: β-III-tubulin (neurons) and MAP2 (dendrites) overnight at 4°C
- Stain with species-appropriate fluorescent secondary antibodies for 1 hour at room temperature
- Counterstain nuclei with Hoechst 33342
- Image using automated high-content imager (10-20 fields/well, 20x objective)
- Analyze using neurite tracing algorithms (e.g., NeuroTrack, IN Cell Analyzer)
Key morphological parameters to quantify:
- Total neurite length per neuron
- Number of primary neurites
- Number of branches
- Somatal size
- Neurite complexity (Sholl analysis)
Biomarkers of Oxidative and Mitochondrial Stress
Table 3: Key Biomarkers for Oxidative and Mitochondrial Stress
| Biomarker | Biological Significance | Detection Methods | Association with PD |
|---|---|---|---|
| GDF-15 | Mitochondrial stress hormone, inflammation marker | ELISA, immunoassay | Strongly associated with faster biological aging [46] |
| FGF-21 | Mitochondrial stress hormone | ELISA, immunoassay | Emerging biomarker for mitochondrial disorders [47] |
| Protein carbonyls | Irreversible protein oxidation | DNPH derivatization, immunodetection | Elevated in accelerated aging [46] |
| Allantoin | Marker of oxidative RNA/DNA damage | HPLC, mass spectrometry | Associated with pace of aging [46] |
| Lactate:pyruvate ratio | Redox state indicator | Enzymatic assays, mass spectrometry | Altered in mitochondrial dysfunction [47] |
| Neurofilament Light Chain (NfL) | Axonal damage marker | Single molecule array (Simoa) | Neuronal injury in neurodegeneration [47] |
Current evidence suggests that GDF-15 demonstrates particularly strong associations with mitochondrial dysfunction and biological aging. In studies of humans at midlife, GDF-15 showed the strongest association with pace of aging (β=0.26, p<0.0001) among oxidative stress biomarkers [46]. Similarly, in comprehensive reviews of mitochondrial biomarkers, GDF-15 followed by FGF-21 demonstrated the greatest diagnostic value for mitochondrial disorders [47].
Integration with Advanced Technologies
Multi-Omics Integration
The combination of phenotypic screening with multi-omics approaches provides powerful mechanistic insights into screening hits. Transcriptomic profiling of iPSC-derived neurons from sporadic ALS patients has revealed significant differential expression consistent with postmortem tissues, validating the pathological relevance of these models [45]. Similar approaches in PD models can identify conserved pathways affected by oxidative stress and mitochondrial dysfunction.
Protocol: Integrating RNA-seq with Phenotypic Screening
- Conduct phenotypic screen in parallel 96-well plates with identical treatments
- Isolate RNA from entire wells using magnetic bead-based purification
- Assess RNA quality (RIN >8.0 required)
- Prepare libraries using poly-A selection or ribosomal RNA depletion
- Sequence to depth of 30-50 million reads per sample
- Analyze differential expression and pathway enrichment
- Correlate gene expression changes with phenotypic outcomes
Gene Editing for Mechanistic Validation
CRISPR/Cas9-mediated gene editing provides essential tools for validating targets identified in phenotypic screens. Isogenic control lines—where disease-causing mutations are corrected in patient-derived iPSCs or disease-associated variants are introduced into control lines—enable definitive establishment of causality between genetic variants and phenotypic outcomes [42].
Protocol: Generating Isogenic Controls
- Design gRNAs targeting region of interest using computational tools
- Clone gRNA into Cas9/gRNA expression vector with fluorescent marker
- Design single-stranded DNA donor template with desired modification
- Electroporate iPSCs with CRISPR components and donor template
- Sort fluorescent cells 48-72 hours post-electroporation
- Expand single-cell clones and screen for modifications by PCR and sequencing
- Validate pluripotency and differentiation potential of corrected lines
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Phenotypic Screening
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| iPSC Lines | Patient-derived iPSCs, isogenic controls | Disease modeling, mechanism studies |
| Differentiation Kits | Commercial dopaminergic neuron differentiation kits | Standardized neuronal differentiation |
| Mitochondrial Dyes | TMRM, JC-1, MitoTracker, MitoSOX | Membrane potential, mass, mitochondrial ROS |
| ROS Detection | CM-H2DCFDA, DHE, Amplex Red | General ROS, superoxide, hydrogen peroxide |
| Viability Assays | Calcein-AM, propidium iodide, CTG | Live/dead discrimination, ATP content |
| Antibodies | TH, Tuj1, MAP2, FOXA2 | Cell identification, differentiation validation |
| Cytokine Assays | GDF-15, FGF-21 ELISA kits | Mitochondrial stress biomarker quantification |
| Microplates | Black-walled clear bottom plates | High-content imaging compatibility |
Experimental Workflows and Signaling Pathways
Phenotypic Screening Workflow
Phenotypic Screening Workflow
Oxidative Stress Signaling Pathways
Oxidative Stress Signaling Pathway
Applications in Drug Discovery and Development
Phenotypic screening in patient-derived neurons has demonstrated significant utility in drug discovery pipelines for neurodegenerative diseases. A large-scale screening initiative in iPSC-derived motor neurons from sporadic ALS patients evaluated over 100 drugs that had previously entered clinical trials, finding that less than 5% showed efficacy in rescuing neuronal survival—a finding that closely mirrors the clinical trial failure rate for these compounds [45]. This demonstrates the predictive validity of these models for identifying clinically effective therapeutics.
The same study identified promising therapeutic combinations through systematic combinatorial testing, highlighting riluzole, memantine, and baricitinib as particularly effective in combination across diverse patient-derived lines [45]. Similar approaches applied to PD models offer the potential to identify novel therapeutic strategies that address the underlying oxidative stress and mitochondrial dysfunction in this disease.
Clinical Translation: The progression from phenotypic screening to clinical application is exemplified by recent advances in stem cell-based therapies for PD. Phase I/II trials of iPSC-derived dopaminergic progenitors transplanted into PD patients have demonstrated safety, graft survival, and potential clinical benefits, with increased dopamine production evidenced by 18F-DOPA PET imaging [6]. These clinical advances underscore the importance of robust preclinical screening platforms for validating cellular therapies before human application.
Phenotypic screening in patient-derived neurons represents a powerful approach for investigating oxidative stress and mitochondrial dysfunction in Parkinson's disease. The integration of iPSC technology with high-content screening platforms, multi-omics analyses, and gene editing tools provides an unprecedented opportunity to elucidate disease mechanisms and identify novel therapeutic strategies in human-relevant systems.
As these technologies continue to evolve—particularly through the development of more complex 3D models, improved neuronal maturation protocols, and advanced computational analysis methods—their predictive validity and utility for drug discovery will further increase. The systematic application of these approaches holds significant promise for developing effective therapies that target the fundamental pathological processes in Parkinson's disease and related neurodegenerative conditions.
The complexity of Parkinson's disease (PD) has historically hindered the development of accurate disease models and effective therapeutics. The emergence of induced pluripotent stem cell (iPSC) technology has revolutionized PD research by enabling the generation of patient-specific dopaminergic (DA) neurons that recapitulate the disease's pathological features in a dish [20] [1]. These cellular models provide a powerful platform for investigating disease mechanisms and identifying novel therapeutic candidates. iPSCs, generated by reprogramming adult somatic cells through forced expression of factors such as OCT4, Sox2, Klf4, and c-Myc, possess pluripotent capacity and can be differentiated into the specific ventral midbrain DA neurons vulnerable in PD [20] [48]. This capability is particularly valuable for modeling the heterogeneous aspects of PD, as iPSCs retain the patient's complete genomic background, including genetic variations associated with both familial and sporadic disease forms [49] [37]. The resulting iPSC-derived DA neurons exhibit functional properties indistinguishable from human fetal mesencephalic DA neurons, including electrophysiological activity, dopamine release, and expression of characteristic markers such as tyrosine hydroxylase (TH) and transcription factors FOXA2 and LMX1A [49] [50]. Within the context of a broader thesis on iPSC models for PD pathogenesis research, this technical guide details the application of these patient-specific neuronal models in systematic drug discovery and repurposing campaigns, with specific protocols for efficacy and toxicity testing.
Key Pathogenic Phenotypes for Therapeutic Screening in iPSC-Derived DA Neurons
Patient-specific iPSC-derived DA neurons manifest key cellular pathologies observed in PD, providing measurable endpoints for evaluating therapeutic efficacy. The table below summarizes the primary phenotypic targets for drug screening derived from models of various PD-associated genes.
Table 1: Key Pathogenic Phenotypes in iPSC-Derived DA Neurons for Drug Screening
| Genetic Background | α-Synuclein Pathology | Mitochondrial Dysfunction | Oxidative Stress | Lysosomal/ Autophagy Defects |
|---|---|---|---|---|
| SNCA (Triplication/A53T) | Double α-synuclein protein levels [20]; Accumulation and abnormal aggregation [37] | Altered mitochondrial morphology; Decreased membrane potential; Impaired axonal transport [49] [37] | Elevated oxidative stress markers; Increased sensitivity to peroxide [20] | Disrupted RAB1a-mediated hydrolase transport; Reduced lysosomal function [20] |
| LRRK2 (G2019S) | Accumulation of α-synuclein [37] | Mitochondrial DNA damage; Dysregulated calcium homeostasis [37] | Increased susceptibility to oxidative stress [37] | Not specified in search results |
| PINK1/PARKIN | Not primary pathology [37] | Increased susceptibility to mitochondrial stress; Altered mitochondrial function [37] | Not specified in search results | Not specified in search results |
| GBA | Elevated extracellular α-synuclein; ER stress [37] | Not specified in search results | Not specified in search results | Decreased GBA activity; Lysosomal impairment [37] |
| VPS35 (D620N) | Accumulation of α-synuclein [37] | Not specified in search results | Not specified in search results | Decreased autophagic flux; Reduced lysosomal mass [37] |
Experimental Workflows for Compound Screening
Core Protocol for Differentiation of iPSCs to Midbrain Dopaminergic Neurons
The generation of consistent, high-quality DA neurons is fundamental to any screening platform. Several robust differentiation protocols have been established, primarily based on dual SMAD inhibition to direct neural induction, followed by patterning with key developmental factors [49] [48].
- Initial Neural Induction (Days 0-12): Plate high-quality iPSCs as single cells and maintain in essential media. To initiate neural induction, employ dual SMAD inhibition using small molecule inhibitors such as SB431542 (TGF-β inhibitor) and LDN193189 (BMP inhibitor). This critical step blocks alternative differentiation pathways and promotes a neural fate [49] [48].
- Midbrain Patterning (Days 12-25): Following neural induction, pattern the cells toward a midbrain DA phenotype. Treat cells with low-dose retinoic acid, sonic hedgehog (SHH) signaling activator (e.g., purmorphamine), FGF8a, and WNT1 to activate ventral midbrain developmental pathways [48]. This combination mimics the natural signaling environment that gives rise to midbrain DA neurons during embryogenesis.
- Terminal Differentiation and Maturation (Days 25-60+): Withdraw mitogens to promote cell cycle exit and terminal neuronal differentiation. Culture cells in media containing neurotrophic factors such as BDNF, GDNF, and ascorbic acid to support neuronal survival, maturation, and the expression of dopaminergic markers including tyrosine hydroxylase (TH), Nurr1, and PITX3 [49] [50]. Neuronal cultures typically show robust maturity by day 65, expressing post-mitotic neuronal markers (MAP2, NeuN) and synaptic markers (synaptophysin) [51].
To ensure population purity, particularly for genetic backgrounds with strong phenotypes, fluorescence-activated cell sorting (FACS) can be employed at the progenitor stage using surface markers like CORIN, yielding populations with >90% purity for midbrain dopaminergic progenitors [50].
High-Content Assay Design for Efficacy and Toxicity Testing
The defined phenotypes in Table 1 provide a basis for designing assays to test compound efficacy.
- Assessing α-Synuclein Pathology: Immunocytochemistry using antibodies against total and phosphorylated α-synuclein (e.g., at Ser129) can quantify protein accumulation. Protein levels can be biochemically validated via ELISA or western blot [20] [37]. Furthermore, FRET-based biosensors or aggregation-specific dyes can be used in live-cell imaging to screen for compounds that reduce α-synuclein oligomerization or aggregation.
- Quantifying Mitochondrial Health and Function: Use tetramethylrhodamine methyl ester (TMRM) or MitoTracker Red to assess mitochondrial membrane potential via fluorescence intensity [49]. Mitochondrial respiration can be profiled using a Seahorse Analyzer to measure oxidative phosphorylation parameters, including basal respiration, ATP production, and spare respiratory capacity [49] [51]. Mitochondrial morphology can be quantified by confocal microscopy after staining with mitochondrial dyes (e.g., MitoTracker) and analyzing parameters like aspect ratio and form factor.
- Measuring Oxidative Stress: Cell-permeable fluorescent probes such as H2DCFDA or CellROX can detect intracellular reactive oxygen species (ROS) levels using a plate reader or high-content imager [20] [51]. Lipid peroxidation, a marker of oxidative damage, can be measured via assays for isoprostanes or with BODIPY 581/591 C11 dye [20].
- Evaluating Lysosomal Function and Autophagic Flux: LysoTracker dyes can label and quantify acidic lysosomal compartments. Autophagic flux can be monitored by western blot for LC3-II accumulation in the presence and absence of lysosomal inhibitors (e.g., bafilomycin A1) or by using an LC3-RFP-GFP tandem reporter construct, where a decrease in the RFP/GFP ratio indicates successful autolysosomal degradation [20] [37].
- Determining Neuronal Viability and General Toxicity: Standard cell viability assays including Calcein-AM staining (for live cells), propidium iodide exclusion (for dead cells), and measurement of caspase-3/7 activity (for apoptosis) provide fundamental data on compound toxicity [51] [50]. For more functional neurotoxicity assessment, multi-electrode arrays (MEAs) can be used to detect changes in neuronal network activity and spontaneous firing upon compound treatment.
The following workflow diagram illustrates the complete process from iPSC reprogramming to final data analysis in a drug screening pipeline.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of these screening protocols requires a standardized set of high-quality reagents. The following table catalogs essential materials and their functions for iPSC-derived DA neuron screening platforms.
Table 2: Essential Research Reagents for iPSC-DA Neuron Screening Platforms
| Reagent Category | Specific Examples | Function in Experimental Protocol |
|---|---|---|
| Reprogramming Factors | OCT4, Sox2, Klf4, c-Myc (Yamanaka factors) [20] | Reprogram somatic cells to induced pluripotent stem cells (iPSCs) |
| Neural Induction Agents | SB431542 (TGF-β inhibitor), LDN193189 (BMP inhibitor) [49] [48] | Direct differentiation toward neural lineage via dual SMAD inhibition |
| Midbrain Patterning Factors | Sonic Hedgehog (SHH) agonists (Purmorphamine), FGF8a, WNT1 [49] [48] | Specify ventral midbrain and dopaminergic neuron fate |
| Neuronal Maturation Factors | Brain-Derived Neurotrophic Factor (BDNF), Glial Cell Line-Derived Neurotrophic Factor (GDNF), Ascorbic Acid [49] [50] | Support survival, maturation, and phenotypic maintenance of DA neurons |
| Key Antibodies for Characterization | Anti-Tyrosine Hydroxylase (TH), Anti-FOXA2, Anti-LMX1A, Anti-β-tubulin III (TUJ1) [50] [48] | Identify and validate dopaminergic neuron identity via ICC/FACS |
| Cell Surface Markers for Sorting | CORIN [50] | Purify midbrain dopaminergic progenitor populations via FACS |
| Viability & Functional Dyes | Calcein-AM, Propidium Iodide, TMRM (ΔΨm), H2DCFDA (ROS) [20] [51] | Assess cell viability, mitochondrial membrane potential, and oxidative stress |
| Genome Editing Tools | CRISPR/Cas9 system [20] | Create isogenic control lines or introduce specific mutations for mechanistic studies |
Data Analysis and Validation in Preclinical Models
Robust data analysis is critical for distinguishing subtle treatment effects from inherent model variability. Normalization of readouts to isogenic controls is essential for genetically defined models, while using multiple independent iPSC clones per condition helps account for clonal variability [20] [37]. For high-content imaging data, multivariate analysis that combines multiple parameters (e.g., neuronal count, neurite length, and mitochondrial intensity) can provide a more comprehensive assessment of compound effects.
Promising compounds identified in in vitro screens require validation in more complex systems before clinical consideration. This can include 3D co-culture models, such as organoids containing multiple neuronal subtypes and glial cells, which better recapitulate cell-cell interactions and cytoarchitecture [1] [37]. For functional validation of dopaminergic function and behavioral recovery, the gold standard remains transplantation of the candidate therapeutic cells or delivery of the hit compound into 6-hydroxydopamine (6-OHDA)-lesioned rodent models of PD, with subsequent behavioral testing (e.g., cylinder test, amphetamine-induced rotation) and post-mortem analysis of graft survival and integration [52] [50].
iPSC-derived DA neurons provide a physiologically relevant, patient-specific platform for identifying and validating novel therapeutic candidates for Parkinson's disease. By targeting defined cellular pathologies in a high-throughput manner, this approach accelerates the drug discovery pipeline, from initial screening to preclinical validation, holding significant promise for developing disease-modifying treatments for PD.
The progressive loss of midbrain dopaminergic (DA) neurons represents the core pathological feature of Parkinson's disease (PD), leading to the characteristic motor symptoms of bradykinesia, rigidity, and resting tremor [6]. For decades, the scientific community has pursued cell replacement therapy as a potential strategy to restore dopamine neurotransmission and achieve sustained clinical improvement. The development of induced pluripotent stem cell (iPSC) technology has revolutionized this endeavor, providing an unlimited source of patient-specific cells for transplantation [11] [53]. iPSCs, generated by reprogramming adult somatic cells into a pluripotent state, bypass the ethical concerns associated with embryonic stem cells and offer the potential for personalized regenerative therapies [10] [11]. This whitepaper examines the latest clinical advances in iPSC-derived dopaminergic progenitor transplantation for PD, focusing on the technical methodologies, safety profiles, and efficacy outcomes from recent groundbreaking trials, thereby situating these developments within the broader context of iPSC modeling for Parkinson's disease pathogenesis research.
Recent Clinical Trial Outcomes
Two landmark clinical trials published in 2025 have demonstrated the feasibility and potential efficacy of transplanting pluripotent stem cell-derived dopaminergic progenitors into patients with Parkinson's disease. One trial utilized allogeneic iPSCs [6], while the other used human embryonic stem cells (hESCs) [7]. Both studies provide critical evidence supporting the continued development of stem cell-based therapies for PD.
Table 1: Comparison of Recent Clinical Trials of Stem Cell-Derived Dopaminergic Progenitors for Parkinson's Disease
| Trial Parameter | Kyoto Trial (iPSC-Derived) | Bemdaneprocel Trial (hESC-Derived) |
|---|---|---|
| Cell Source | Allogeneic iPSCs from healthy donor [6] | Human embryonic stem cell line [7] |
| Study Phase | Phase I/II [6] | Phase I [7] |
| Patients Enrolled | 7 (6 for efficacy) [6] | 12 [7] |
| Dosing Groups | Low (2.1-2.6M cells/hemisphere) and High (5.3-5.5M cells/hemisphere) [6] | Low (0.9M cells/putamen) and High (2.7M cells/putamen) [7] |
| Immunosuppression | Tacrolimus (15 months) [6] | Basiliximab, methylprednisolone, tacrolimus (12 months) [7] |
| Primary Safety Findings | No serious adverse events; 73 mild-moderate events [6] | No adverse events related to cell product; one seizure procedure-related [7] |
| Tumorigenicity | No tumor formation on MRI [6] | No tumors or abnormal tissue overgrowth [7] |
| Dopamine Production | 44.7% average increase in 18F-DOPA PET uptake [6] | Increased 18F-DOPA PET uptake at 18 months [7] |
| Clinical Improvement (MDS-UPDRS Part III OFF) | Average improvement of 9.5 points (20.4%) at 24 months [6] | Average improvement of 23 points in high-dose cohort at 18 months [7] |
The Kyoto Trial: Allogeneic iPSC-Derived Dopaminergic Progenitors
The investigator-initiated, open-label phase I/II trial conducted at Kyoto University Hospital (jRCT2090220384) represents a pioneering effort in allogeneic iPSC-based therapy for PD [6]. Seven patients aged 50-69 received bilateral transplantation of dopaminergic progenitors derived from a clinical-grade human iPSC line (QHJI01s04) established from a healthy individual with a homozygous HLA haplotype matching 17% of the Japanese population [6]. The study design involved sequential enrollment with the first participant receiving a staggered transplant (left putamen followed by right putamen after 8 months) for initial safety assessment, while subsequent recipients underwent simultaneous bilateral surgery [6].
Notably, the trial reported no serious adverse events requiring hospitalization or resulting in death, with all adverse events being mild to moderate in severity [6]. Serial magnetic resonance imaging (MRI) scans showed no evidence of tumor-like abnormal enlargement, and fluorine-18-fluorothymidine (18F-FLT) positron emission tomography (PET) scans revealed no increased accumulation in the transplanted striatum, indicating no concerning cell proliferation [6]. Efficacy evaluations demonstrated that four of six patients showed improvements in the MDS-UPDRS Part III OFF scores, with an average improvement of 9.5 points (20.4%) at 24 months [6]. Fluorine-18-l-dihydroxyphenylalanine (18F-DOPA) PET imaging revealed a 44.7% average increase in the influx rate constant (Ki) values in the putamen, indicating enhanced dopamine production, with higher increases observed in the high-dose group [6].
Immune Response in Allogeneic Transplantation
A critical consideration for allogeneic iPSC-based therapies is the potential for immune rejection. Interestingly, the Kyoto trial demonstrated that despite HLA mismatches, only moderate immunosuppression with tacrolimus alone was sufficient to prevent clinically significant immune reactions [54]. Highly sensitive mixed lymphocyte reaction assays using iPSC-derived dendritic cells as stimulators did show activation of lymphocytes from HLA-mismatch-grafted recipients, suggesting that the low expression of HLA in iPSC-derived dopaminergic neural progenitors contributes to successful engraftment in the immune-privileged central nervous system [54]. This finding has important implications for future trial designs, suggesting that stringent HLA matching may not be necessary for CNS-directed cell therapies.
Experimental Protocols and Methodologies
Dopaminergic Progenitor Differentiation and Purification
The successful clinical application of iPSC-derived dopaminergic progenitors relies on robust, reproducible differentiation protocols that generate authentic midbrain DA neurons while eliminating potentially harmful cell populations.
CORIN-Based Cell Sorting
The Kyoto trial utilized a sophisticated purification strategy to enrich for genuine midbrain dopaminergic progenitors [6] [55]. Researchers employed fluorescence-activated cell sorting (FACS) using antibodies against CORIN, a floor plate marker that identifies committed dopaminergic progenitors [6] [55]. The sorting was performed on days 11-13 of differentiation, with the sorted cells then cultured in neural differentiation medium to form aggregate spheres before transplantation [6]. Single-cell quantitative PCR analysis confirmed that the final product comprised approximately 60% DA progenitors and 40% DA neurons, with no detectable TPH2-expressing serotonergic neurons, which have been implicated in graft-induced dyskinesias in previous fetal tissue transplantation trials [6] [55].
Small Molecule-Based Differentiation Protocols
Preclinical research has established numerous protocols for differentiating iPSCs into dopaminergic neurons using small molecules that modulate key developmental signaling pathways [10]. These protocols typically involve dual SMAD inhibition to promote neural induction, followed by sequential activation of sonic hedgehog (SHH) and Wnt signaling to pattern the neural progenitors toward a midbrain dopaminergic fate [10]. The process involves several critical stages:
- Neural Induction: Treatment with SMAD inhibitors (such as LDN-193189 and SB-431542) for 7-10 days to direct cells toward a neural lineage [10].
- Midbrain Patterning: Concurrent administration of SHH agonists (e.g., purmorphamine) and GSK3β inhibitors (e.g., CHIR99021) between days 3-13 to specify midbrain dopaminergic identity [10].
- Terminal Differentiation: Withdrawal of patterning factors and addition of neurotrophic factors (BDNF, GDNF, ascorbic acid, TGF-β3) from day 13 onward to promote maturation into functional dopaminergic neurons [10].
The entire differentiation process typically spans 25-35 days for progenitor transplantation or up to 70 days for mature neuronal phenotypes [10].
Table 2: Key Signaling Pathways in Dopaminergic Neuron Differentiation
| Signaling Pathway | Role in DA Differentiation | Common Modulators |
|---|---|---|
| SMAD/TGF-β | Inhibition promotes neural induction [10] | LDN-193189, SB-431542, Noggin |
| Sonic Hedgehog (SHH) | Ventral patterning and floor plate specification [10] | Purmorphamine, SAG |
| Wnt/β-catenin | Midbrain patterning and DA progenitor maintenance [10] | CHIR99021, Wnt1, Wnt3a |
| FGF | Neural progenitor expansion and survival [10] | FGF2, FGF8b |
| Notch | Regulation of neurogenesis and progenitor maintenance [10] | DAPT (inhibitor) |
Transplantation and Functional Assessment
The surgical protocol for cell delivery represents another critical component of successful therapy. Both recent trials utilized stereotactic transplantation into the post-commissural putamen, the primary target of nigrostriatal dopaminergic projections [6] [7]. The Kyoto trial employed a neurosurgical navigation system to deliver the cell suspension through multiple trajectories to maximize distribution within the putamen [6]. The bemdaneprocel trial used a modified cannula (Smart Flow, Clearpoint Neuro) with nine cell deposits per putamen (three passes with three deposits per pass) to optimize graft distribution [7].
Functional integration of the transplanted cells was assessed using multiple modalities:
- 18F-DOPA PET: To measure dopamine synthesis and storage capacity [6] [7]
- MRI: To monitor graft survival, expansion, and potential overgrowth [6] [7]
- MDS-UPDRS: To quantify motor symptom improvement in OFF and ON medication states [6] [7]
- Hoehn & Yahr Staging: To assess global disease disability [6]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for iPSC-Dopaminergic Neuron Differentiation
| Reagent Category | Specific Examples | Function in DA Differentiation |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [11] | Somatic cell reprogramming to iPSCs |
| Neural Induction Agents | LDN-193189, SB-431542, Noggin [10] | SMAD inhibition for neural specification |
| Patterning Molecules | Purmorphamine (SHH agonist), CHIR99021 (Wnt activator), FGF8b [10] | Midbrain floor plate and DA progenitor patterning |
| Cell Surface Markers | CORIN [6] [55] | Identification and sorting of floor plate-derived DA progenitors |
| Neurotrophic Factors | BDNF, GDNF, Ascorbic Acid, TGF-β3 [10] | Survival, maturation, and maintenance of DA neurons |
| Immunosuppressants | Tacrolimus, Basiliximab [6] [7] | Prevention of allogeneic graft rejection |
Signaling Pathways in Dopaminergic Differentiation
The directed differentiation of iPSCs into midbrain dopaminergic neurons recapitulates developmental signaling pathways that specify this neuronal population during embryogenesis. The following diagram illustrates the key signaling pathways and their temporal regulation in this process:
Diagram Title: Signaling Pathways in iPSC to DA Neuron Differentiation
The differentiation process proceeds through three major phases: neural induction, midbrain patterning, and terminal maturation. SMAD inhibition initiates neural induction by promoting transition from pluripotency to neural epithelium. Subsequent activation of SHH and Wnt signaling patterns these neural progenitors toward a midbrain floor plate identity, which gives rise to authentic dopaminergic progenitors. Finally, terminal maturation with neurotrophic factors supports the development of functional dopaminergic neurons capable of synthesizing and releasing dopamine.
The recent clinical trials of iPSC-derived dopaminergic progenitors represent a transformative advancement in Parkinson's disease therapy, demonstrating that allogeneic transplantation is feasible, safe, and potentially efficacious. The successful application of these therapies rests on robust differentiation protocols that generate authentic midbrain DA neurons while eliminating problematic cell types, particularly serotonergic neurons and remaining pluripotent cells. The CORIN sorting methodology developed by the Kyoto group addresses this critical safety concern and sets a new standard for cellular purification in regenerative neurology [6] [55].
Looking forward, several challenges and opportunities remain. The immune response to allogeneic grafts, even in the immunoprivileged CNS, requires further investigation to optimize immunosuppression regimens [54]. Scaling up production of clinical-grade iPSCs and their differentiated progeny under GMP conditions presents significant technical hurdles [53]. Additionally, the field must address variability in differentiation outcomes and the potential for genomic instability in cultured iPSCs [53]. Emerging technologies such as CRISPR-Cas9 gene editing and AI-guided differentiation protocols offer promising approaches to enhance the safety, purity, and efficiency of iPSC-based therapies [53].
The successful translation of iPSC-derived dopaminergic progenitors from bench to bedside marks a new era in Parkinson's disease treatment, offering the potential for disease-modifying therapy that addresses the fundamental pathophysiology of dopamine neuron loss. As these therapies progress through later-stage clinical trials, they hold the promise of lasting symptomatic relief and potentially altering the progressive course of this debilitating neurodegenerative disorder.
Addressing Technical Hurdles: Standardization, Maturity, and Ageing in iPSC Models
The utilization of induced pluripotent stem cells (iPSCs) to model Parkinson's disease (PD) has revolutionized our ability to study pathogenesis and screen therapeutics in a human-relevant context. However, the transformative potential of this technology is constrained by two significant challenges: inherent variability between iPSC lines and a lack of standardized experimental protocols. This whitepaper details how the strategic implementation of isogenic controls and the adoption of rigorous, standardized differentiation methods are overcoming these hurdles. By framing these solutions within the context of PD research, we provide a technical guide for researchers and drug development professionals to enhance the reproducibility, reliability, and physiological relevance of their iPSC-based models.
The Challenge of Variability in iPSC Modeling
The fundamental advantage of iPSCs—their capacity to capture a patient's unique genetic background—is also a primary source of experimental variability. This variability manifests in two key forms:
- Inter-Line Variability: Differences in genetic background across donors can obscure disease-specific phenotypes. As noted in a major review, "iPSC lines show substantial variability among clones," making it difficult to distinguish genuine disease pathology from natural genetic variation [30] [37].
- Differentiation Variability: The efficiency with which different iPSC lines differentiate into dopaminergic neurons (DAns) can vary significantly, impacting the consistency of resulting neuronal populations and subsequent experimental readouts [37] [56].
Without controlling for these factors, attributing observed cellular phenotypes, such as mitochondrial dysfunction or α-synuclein accumulation, to a specific PD-associated mutation becomes statistically challenging. This noise complicates drug discovery and the elucidation of precise disease mechanisms.
Isogenic Controls: The Gold Standard for Genetic Modeling
Isogenic controls are genetically identical iPSC lines where a specific disease-causing mutation has been corrected (or introduced) using gene-editing technologies, typically CRISPR/Cas9. These controls provide an perfectly matched genetic background, ensuring that any phenotypic differences observed can be confidently attributed to the mutation under investigation.
Generation and Validation of Isogenic Controls
A study focusing on the PD-associated SNCA p.A53T mutation provides a clear blueprint for generating and validating isogenic controls [57]. The following table summarizes the key quantitative data from the validation of six such isogenic control lines.
Table 1: Validation Data for Isogenic Control iPSC Lines (SNCA p.A53T)
| Validation Metric | Method Used | Result | Interpretation |
|---|---|---|---|
| Pluripotency | Immunocytochemistry (OCT4, SOX2, NANOG) | Positive Expression | Confirmed pluripotent state |
| Pluripotency (Quantitative) | Flow Cytometry for SSEA-4 | >98% of cells positive | High purity of pluripotent cells |
| Karyotype | G-banding Analysis | 46, XX (Normal) | No gross chromosomal abnormalities |
| Line Identity | Short Tandem Repeat (STR) Analysis | 16/16 loci matched parent | Confirmed genetic identity to original line |
| Differentiation Potential | Immunocytochemistry (3 Germ Layers) | SOX17, Brachyury, β-III Tubulin positive | Capacity to form all germ layers |
| Contamination | Mycoplasma Testing | Negative | Free of mycoplasma contamination |
Experimental Workflow for Creating Isogenic Controls
The process for creating these critical controls involves a precise, multi-stage workflow, from designing the gene-editing machinery to the final clonal validation.
Detailed Methodologies:
- CRISPR/Cas9 RNP Complex Formation: For the SNCA A53T correction, a ribonucleoprotein (RNP) complex was assembled by combining a custom Alt-R CRISPR-Cas9 crRNA (sequence:
GTGGTGCATGGTGTGACAAC agg), Alt-R CRISPR-Cas9 tracrRNA, and Alt-R S.p. Cas9 nuclease. The crRNA and tracrRNA were first resuspended in duplex buffer to 200 μM, heated at 95°C for 5 minutes, and cooled to room temperature to form a duplex. This duplex was then incubated with the Cas9 nuclease in PBS for 30 minutes at room temperature to form the active RNP complex [57]. - Single-Stranded Donor Oligo (ssDO): A 100 pmol/μL single-stranded DNA oligo was synthesized with homology arms flanking the corrected "WT" nucleotide sequence to serve as the repair template for homology-directed repair [57].
- Nucleofection: iPSCs were dissociated into single cells using TrypLE. Then, 800,000 cells were pelleted and resuspended in 100 μL of P3 Primary Cell Solution. Immediately before nucleofection using a 4D-Nucleofector system, 2 μL of the ssDO was added to 5 μL of the pre-assembled RNP complex, and the entire mixture was combined with the cell suspension [57].
- Clonal Expansion and Validation: Post-nucleofection, cells were single-cell cloned into 96-well plates. Clones were first screened via Sanger sequencing of the target amplicon (using primers: Forward
CTAGCTAATCAGCAATTTAAGGCTA, ReverseGCTC AGTGATTGTTTTACAATTTCA) to identify those with homozygous correction and no off-target mutations in the amplicon. Positive clones were then expanded and put through the comprehensive battery of quality control tests listed in Table 1 [57].
Standardized Differentiation Protocols for Consistent Dopaminergic Neuron Generation
To mitigate differentiation variability, the field has moved towards robust, well-characterized protocols for generating dopaminergic neurons. A study developed an efficient 2D protocol that eliminates animal components and simplifies the process without sacrificing efficiency [58].
Key Steps in a Standardized 2D Protocol
The protocol is based on dual SMAD inhibition to direct differentiation towards a neural fate and floor-plate precursors. The major stages are summarized below.
Table 2: Key Stages of a Standardized 2D Differentiation Protocol [58]
| Stage | Timeline | Key Components | Purpose & Outcome |
|---|---|---|---|
| Neural Induction | Days 1-14 | 80 ng/mL Noggin, 10 μM SB431542, 4 μM Dorsomorphin | Dual SMAD inhibition; induces anterior neural tube fate. Yields neuroepithelial stem cells. |
| Neural Progenitor Expansion & Patterning | Days 15-21 | SHH (100-200 ng/mL), FGF8b (100 ng/mL), CHIR99021 (0.5-1 μM) | Patterns progenitors to a midbrain dopaminergic phenotype. Activates Wnt signaling. |
| Neuronal Differentiation & Maturation | Day 22+ | BDNF, GDNF, Ascorbic Acid, cAMP, DAPT | Promotes terminal differentiation into post-mitotic, tyrosine hydroxylase-positive (TH+) dopaminergic neurons. |
Signaling Pathways in Dopaminergic Neuron Differentiation
The standardized protocol manipulates several key developmental signaling pathways to efficiently guide iPSCs toward a midbrain dopaminergic fate. The following diagram illustrates the logical relationships and timing of these pathway manipulations.
The Scientist's Toolkit: Essential Research Reagents
To successfully implement these models, researchers require a suite of reliable reagents and tools. The following table catalogs essential solutions based on the cited research.
Table 3: Key Research Reagent Solutions for iPSC-based PD Modeling
| Reagent / Solution | Function | Example Use Case |
|---|---|---|
| CRISPR/Cas9 System (RNP) | Site-specific gene editing for creating isogenic controls. | Correction of SNCA A53T point mutation back to wild-type sequence [57]. |
| Small Molecule Inhibitors (SB431542, Dorsomorphin) | Dual SMAD inhibition. | Induction of neural differentiation from iPSCs by blocking TGF-β and BMP signaling [58]. |
| Recombinant Proteins (Noggin, SHH, FGF8b, BDNF, GDNF) | Patterning and survival signals. | Directing neural progenitors to a midbrain dopaminergic fate and supporting their maturation and survival [58]. |
| Pluripotency Markers (OCT4, SOX2, NANOG, SSEA-4) | Quality control of undifferentiated iPSCs. | Validating the pluripotent state of iPSC lines and isogenic controls via immunocytochemistry and flow cytometry [57]. |
| Differentiation Markers (SOX17, Brachyury, β-III Tubulin) | Quality control of differentiation potential. | Confirming the ability of iPSCs to form all three germ layers (endoderm, mesoderm, ectoderm) [57]. |
| Dopaminergic Neuron Markers (Tyrosine Hydroxylase - TH, FOXA2, LMX1A) | Characterization of target cell population. | Identifying and quantifying the yield of mature dopaminergic neurons post-differentiation [6] [58]. |
The path to unlocking the full potential of iPSC technology for deconstructing Parkinson's disease pathogenesis hinges on rigorous experimental design. The integration of isogenic controls is non-negotiable for isolating mutation-specific effects from background genetic noise. Furthermore, the adoption of detailed, standardized protocols for differentiation is critical for generating reproducible and physiologically relevant populations of dopaminergic neurons. By systematically implementing the strategies and utilizing the tools outlined in this technical guide, researchers can significantly enhance the fidelity of their models, thereby accelerating the discovery of novel therapeutic targets and paving the way for more effective treatments for Parkinson's disease.
The quest to model Parkinson's disease (PD) using induced pluripotent stem cells (iPSCs) confronts a fundamental biological paradox: while PD is predominantly an age-related neurodegenerative disorder, the reprogramming process that creates patient-specific iPSCs inherently reverses cellular aging, effectively erasing the very age-associated signatures crucial for accurate disease modeling [59]. This rejuvenation effect creates a significant barrier for recapitulating late-stage disease phenotypes in vitro, as the resulting neurons exhibit a fetal-like molecular and functional state despite carrying genetic mutations associated with a condition that manifests after decades of life [59] [60].
The Information Theory of Aging provides a conceptual framework for this challenge, proposing that aging is driven by a progressive loss of epigenetic information, which disrupts gene expression patterns and cellular function [61] [62]. Somatic cell reprogramming to iPSCs fundamentally resets this epigenetic landscape, reversing hallmarks of aging such as telomere attrition, accumulated DNA damage, and mitochondrial dysfunction [59]. Consequently, iPSC-derived dopaminergic (DA) neurons from PD patients often display only early biochemical markers of disease susceptibility rather than the profound degenerative phenotypes characteristic of the aged human substantia nigra [59].
This technical review examines advanced strategies to resolve this conundrum, focusing on two complementary approaches: chemically induced senescence to re-impose age-like properties in rejuvenated cells, and direct reprogramming methods that potentially bypass profound epigenetic resetting. Within the context of PD pathogenesis research, mastering these techniques is essential for generating clinically relevant models that faithfully mirror the cellular environments in which PD unfolds.
The Rejuvenation Barrier in iPSC Reprogramming
The process of reprogramming somatic cells to pluripotency does not merely reverse differentiation; it actively rejuvenates cells, resetting multiple molecular markers of biological age. This phenomenon has been demonstrated through the restoration of youthful features in cells derived from aged donors, including:
- Nuclear rejuvenation: Restoration of nuclear morphology, lamina composition, heterochromatin content, and reduction of DNA damage foci [59].
- Telomere elongation: Reset of telomere length to youthful standards [59].
- Metabolic reprogramming: Improvement of mitochondrial metabolism and reduction of oxidative stress [59].
- Epigenetic resetting: Reversion of DNA methylation patterns to a youthful state, including at specific CpG sites associated with chronological age [59].
While this rejuvenation capacity holds promise for regenerative medicine, it creates a significant obstacle for disease modeling. For Parkinson's disease, this is particularly problematic because the vulnerability of dopaminergic neurons increases with age, and many pathological processes—including protein aggregation, mitochondrial dysfunction, and impaired stress response—are age-accelerated [30] [49]. The failure to recapitulate these late-stage degenerative phenotypes in conventional iPSC models limits their utility for drug screening and pathogenetic investigation.
Molecular Basis of Reprogramming-Induced Rejuvenation
The rejuvenation effect occurs because reprogramming essentially runs the developmental program backward, resetting the epigenetic clock to an embryonic state [59]. During the conversion of somatic cells to iPSCs, the expression of Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) activates pathways that remodel the epigenome, including DNA demethylation and histone modification [13]. This process reverses the epigenetic drift that accumulates over a lifetime, including the changes in DNA methylation patterns and chromatin organization that characterize aged cells [61] [62].
Table 1: Hallmarks of Cellular Aging and Their Status in Conventional iPSC-Derived Neurons
| Aging Hallmark | Status in Aged Somatic Cells | Status in iPSC-Derived Neurons | Implication for PD Modeling |
|---|---|---|---|
| Epigenetic Alterations | Accumulated DNA methylation changes, heterochromatin loss | Reset to fetal pattern | Loss of age-related epigenetic vulnerability |
| Telomere Attrition | Shortened telomeres | Elongated telomeres | Reduced genomic instability phenotype |
| Mitochondrial Dysfunction | Decreased membrane potential, increased ROS | Fetal metabolic profile | Attenuated mitochondrial pathology |
| Loss of Proteostasis | Impaired protein degradation, aggregate accumulation | Enhanced clearance capacity | Reduced α-synuclein aggregation |
| Altered Intercellular Communication | Inflammatory SASP factors present | Limited secretory phenotype | Diminished neuroinflammatory environment |
Strategies to Reintroduce Age-Related Signatures
To overcome the limitations of conventional iPSC modeling, researchers have developed sophisticated strategies to induce aging-like phenotypes in iPSC-derived lineages. These approaches aim to accelerate the appearance of age-related molecular and functional changes without requiring protracted in vitro culture.
Chemically Induced Senescence
Chemical induction of senescence uses various stressors to trigger permanent cell cycle arrest and associated phenotypic changes that mimic aspects of cellular aging. Common approaches include:
- Progerin overexpression: Expression of the mutant lamin A protein associated with Hutchinson-Gilford progeria syndrome induces multiple age-associated markers, including DNA damage, increased mitochondrial ROS, and in some lineages, dendrite degeneration and inclusion body formation [60].
- Oxidative stress induction: Exposure to reactive oxygen species (ROS)-inducing agents such as hydrogen peroxide or paraquat to accelerate molecular damage [60].
- Genotoxic stress: Application of ionizing radiation or chemotherapeutic agents to induce DNA damage responses characteristic of aged cells [60].
- Long-term culture: Extended passaging of iPSC-derived cells to allow natural accumulation of age-related changes, though this approach is time-consuming [60].
Table 2: Methods for Inducing Aging Phenotypes in iPSC-Derived Models
| Method | Mechanism of Action | Key Readouts | Advantages | Limitations |
|---|---|---|---|---|
| Progerin Overexpression | Expression of mutant lamin A disrupts nuclear envelope | DNA damage, mitochondrial ROS, dendrite degeneration | Rapid induction (weeks) | May not fully replicate natural aging |
| Oxidative Stress (H₂O₂, paraquat) | Induces oxidative damage to macromolecules | ROS levels, protein oxidation, cell viability | Easy to implement, dose-tunable | Can cause acute toxicity rather than aging |
| Ionizing Radiation | Causes DNA double-strand breaks | γH2AX foci, p53 activation, senescence markers | Well-characterized DNA damage response | May not reflect chronic aging damage |
| Long-Term Culture | Accumulation of stochastic errors over time | SA-β-gal, p21 expression, metabolic changes | Most physiological | Very time-consuming (months) |
| Chemical Senescence Inducers | e.g., Etoposide (topoisomerase inhibitor) | Cell cycle arrest, SASP factors | Controllable timing | May induce stress response rather than aging |
Figure 1: Experimental Strategies for Inducing Aging in iPSC-Derived Models. This workflow illustrates the main approaches for introducing age-related signatures and their resulting cellular phenotypes relevant to Parkinson's disease modeling.
Direct Reprogramming and Partial Reprogramming Strategies
Direct reprogramming and partial reprogramming approaches offer alternative paths to generate target cells while potentially preserving age-related signatures:
- Direct reprogramming (transdifferentiation): Converts somatic cells directly to another cell type (e.g., fibroblasts to neurons) without passing through a pluripotent state, potentially maintaining more age-associated epigenetic markers [63].
- Partial reprogramming: Uses brief or reduced exposure to reprogramming factors to refresh cellular function without complete epigenetic reset, aiming to achieve rejuvenation without dedifferentiation [63].
Recent advances in chemical reprogramming have identified specific cocktails that can reverse aspects of cellular aging without completely erasing cellular identity. These approaches target the nucleocytoplasmic compartmentalization (NCC) breakdown that occurs with aging, which can be measured by the mislocalization of nuclear and cytoplasmic proteins [61] [62]. The NCC assay provides a quantitative measure of cellular aging and rejuvenation, serving as a valuable screening tool for identifying compounds that can restore youthful cellular organization without loss of identity.
Experimental Protocols for Aging Induction and Validation
Protocol: Progerin-Induced Aging in iPSC-Derived Dopaminergic Neurons
This protocol describes a method to induce accelerated aging in iPSC-derived DA neurons through progerin expression, based on established procedures [60].
Materials:
- iPSC-derived DA neurons (30 days post-differentiation)
- Lentiviral vector encoding progerin (mutant LMNA gene) with GFP tag
- Polybrene (8 μg/mL)
- Complete neuronal culture medium
- Control lentivirus (empty vector)
Procedure:
- Day 0: Plate iPSC-derived DA neurons at 50,000 cells/cm² on poly-ornithine/laminin-coated plates.
- Day 1: Replace medium with fresh neuronal medium containing polybrene (8 μg/mL).
- Add progerin lentivirus at MOI 50-100. Include control wells with empty vector virus.
- Incubate for 24 hours at 37°C, 5% CO₂.
- Day 2: Replace with fresh neuronal medium without virus.
- Day 3: Assess transduction efficiency via GFP fluorescence (should be >70%).
- Culture for 14-21 days, monitoring for appearance of aging phenotypes.
Validation Assays:
- DNA damage response: Immunostaining for γH2AX foci and 53BP1
- Mitochondrial ROS: MitoSOX Red staining and quantification by flow cytometry
- Neurite morphology: Analysis of neurite length and branching using βIII-tubulin staining
- Senescence markers: SA-β-galactosidase staining and p21 immunostaining
- α-Synuclein aggregation: Immunostaining for phosphorylated α-synuclein (Ser129)
Protocol: Nucleocytoplasmic Compartmentalization (NCC) Assay
The NCC assay quantitatively measures the breakdown of nuclear integrity, a hallmark of aging that can be reversed by rejuvenation strategies [61] [62].
Materials:
- Young (22-year-old donor) and old (≥75-year-old donor) human fibroblasts
- Lentiviral NCC reporter (mCherry-NLS and eGFP-NES)
- Polybrene (8 μg/mL)
- 4% paraformaldehyde
- Hoechst 33342 nuclear stain
- High-content imaging system
Procedure:
- Transduce fibroblasts with NCC reporter lentivirus at MOI 20 in medium containing polybrene.
- After 48 hours, select successfully transduced cells with puromycin (1-2 μg/mL) for 5 days.
- Plate NCC reporter cells at 10,000 cells/well in 96-well imaging plates.
- After 24 hours, treat with test compounds or controls for desired duration.
- Fix cells with 4% PFA for 15 minutes at room temperature.
- Stain nuclei with Hoechst 33342 (1 μg/mL) for 10 minutes.
- Image using high-content imaging system with 20x objective.
- Quantify mCherry and eGFP distribution using Pearson correlation coefficient.
Data Analysis:
- Young cells show distinct separation of mCherry (nuclear) and eGFP (cytoplasmic)
- Old and senescent cells show colocalization (Pearson coefficient >0.5)
- Effective rejuvenation treatments reduce Pearson coefficient toward young cell values
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Aging and Reprogramming Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Induction of pluripotency | c-MYC increases tumorigenesis risk; often omitted for safety |
| Alternative Reprogramming Factors | OCT4, SOX2, NANOG, LIN28 | Induction of pluripotency | Different efficiency and safety profiles |
| Chemical Reprogramming Cocktails | VPA, CHIR99021, 616452, Tranylcypromine | Replace transcription factors | Non-integrating approach; better safety profile |
| Senescence Inducers | Progerin, Etoposide, Hydrogen peroxide, Ionizing radiation | Induction of aging phenotypes | Concentration and duration critical for specific effects |
| Aging Assay Reagents | SA-β-gal substrate, MitoSOX Red, γH2AX antibodies | Detection and quantification of aging markers | Multiple assays recommended for validation |
| Neuronal Differentiation Factors | SMAD inhibitors, SHH, FGF8, BDNF, GDNF | Directing iPSC differentiation to dopaminergic neurons | Floorplate-based protocols most efficient for midbrain DA neurons |
| Gene Editing Tools | CRISPR/Cas9 systems, PiggyBac transposons | Genetic modification for disease modeling or reporter insertion | Isogenic controls critical for disease modeling studies |
Applications in Parkinson's Disease Pathogenesis Research
The ability to model aged neurons in vitro has revealed critical insights into PD-specific pathological mechanisms that were obscured in conventional iPSC models.
α-Synuclein Aggregation and Proteostasis
In aged iPSC-derived DA neurons with SNCA mutations (A53T, triplication), researchers have observed enhanced α-synuclein aggregation and impaired protein degradation pathways [30] [49]. These models demonstrate:
- Accelerated oligomer formation: SNCA-triplication neurons show increased α-synuclein oligomers that impair mitochondrial axonal transport [30].
- Lysosomal dysfunction: Impaired autophagic flux and reduced LAMP1 expression in aged PD neurons [30].
- ER stress activation: Unfolded protein response pathway induction, particularly IRE1α/XBP1 signaling [30].
Mitochondrial Dysfunction
Aged PD iPSC models consistently show pronounced mitochondrial impairments that mirror pathology in patient brains:
- Respiratory deficits: Reduced basal and maximal respiration capacity, impaired ATP production in SNCA-triplication neuronal progenitor cells [49].
- Altered morphology: More circular, unbranched mitochondria with reduced membrane potential [49].
- Impaired transport: Decreased mitochondrial axonal movement leading to energy deficits and synapse degeneration [30] [49].
- Increased PTP susceptibility: Enhanced vulnerability to permeability transition pore formation under stress [49].
Novel Therapeutic Screening
The combination of aging induction with patient-specific iPSC models creates powerful platforms for identifying and testing therapeutic interventions:
- Compound validation: Testing candidates like A-443654 (AKT modulator) that normalized α-synuclein levels in SNCA-triplication neurons [30].
- Gene therapy approaches: Evaluating strategies to reduce pathological α-synuclein or enhance lysosomal function [30].
- Personalized medicine: Using patient-specific aging models to identify individualized therapeutic responses.
Resolving the "ageing conundrum" in iPSC modeling of Parkinson's disease requires sophisticated approaches that reintroduce age-related signatures into rejuvenated cells. The strategies outlined here—including chemically induced senescence, direct reprogramming, and partial reprogramming—provide powerful tools to generate more clinically relevant models that recapitulate the late-onset, progressive nature of PD.
Future advances will likely focus on refining the specificity and control of aging induction, developing more comprehensive biomarkers of cellular age, and creating integrated platforms that combine multiple age-associated stressors. As these technologies mature, they will increasingly enable the discovery of therapeutic targets that address the fundamental age-related processes driving Parkinson's disease pathogenesis, moving beyond symptomatic treatment toward truly disease-modifying interventions.
The successful integration of aging signatures into iPSC-based models marks a critical evolution in our approach to studying age-related neurodegenerative disorders, offering unprecedented opportunities to unravel the complex interplay between genetic susceptibility, environmental factors, and the intrinsic aging process that culminates in Parkinson's disease.
The use of induced pluripotent stem cell (iPSC)-derived models has revolutionized Parkinson's disease (PD) research by providing unprecedented access to human-specific neuronal cells for investigating pathogenesis and conducting drug screening [1]. However, the value of these models is entirely dependent on their phenotypic relevance to the native human cells and pathological processes they aim to represent. For iPSC-derived dopaminergic (DA) neurons—the primary vulnerable population in PD—this requires not only the expression of appropriate molecular markers but also the recapitulation of functional metabolic, electrophysiological, and network properties characteristic of mature nigral neurons in vivo. The complexity of PD, involving multiple shared mechanisms with ageing including mitochondrial dysfunction, dysregulated proteostasis, inflammation, and cellular senescence, further underscores the need for sophisticated modeling approaches that capture these interrelated pathways [26]. This technical guide outlines comprehensive strategies and methodologies for ensuring neuronal maturity and functional characterization within the broader context of developing physiologically relevant iPSC-based models for Parkinson's disease pathogenesis research.
Fundamental Markers of Dopaminergic Neuron Identity and Maturity
Before embarking on functional characterization, confirming the fundamental identity and maturity of iPSC-derived dopaminergic neurons is essential. The presence of key transcription factors and neuronal markers provides the foundational evidence of successful differentiation toward the desired neuronal lineage.
Table 1: Essential Molecular Markers for Dopaminergic Neuron Identification
| Marker Category | Specific Markers | Functional Significance | Assessment Methods |
|---|---|---|---|
| Dopaminergic Progenitor Markers | FOXA2, OTX2, CORIN | Specify midbrain floor plate identity and dopaminergic lineage commitment [64] [6] | Immunocytochemistry, Flow Cytometry, RT-qPCR |
| Dopaminergic Neuron Markers | Tyrosine Hydroxylase (TH), NURR1 (NR4A2) | Key enzymes for dopamine synthesis; terminal differentiation and maintenance [6] [65] | Immunocytochemistry, HPLC, Western Blot |
| Pan-Neuronal Markers | βIII-tubulin, MAP2, NeuN | General neuronal identity and structural maturation [26] | Immunocytochemistry, Western Blot |
| Regional Identity Markers | Engrailed-1 (EN1), LMX1A, PITX3 | Midbrain-specific patterning and identity [6] | RT-qPCR, Immunocytochemistry |
The presence of these markers should be quantified to establish differentiation efficiency. For transplantation-grade dopaminergic progenitors, benchmarks include more than 75% expression of FOXA2 and OTX2, and over 60% TH+ neurons in vitro [64]. Single-cell RNA sequencing can provide additional resolution by confirming the absence of contaminating cell types, such as serotonergic neurons (TPH2-negative), which is crucial for accurate modeling [6].
Assessing Functional Neuronal Maturity: Beyond Molecular Markers
Electrophysiological Properties
A definitive characteristic of mature, functional neurons is their ability to generate and propagate action potentials. Whole-cell patch-clamp electrophysiology should demonstrate the presence of voltage-gated sodium and potassium currents, the ability to fire repetitive action potentials in response to depolarizing current injections, and the presence of spontaneous synaptic activity, evidenced by excitatory and inhibitory postsynaptic currents [19]. These properties confirm that the neurons have established the fundamental electrical excitability required for neural communication.
Network Synchronization and Synaptic Activity
Beyond single-cell properties, mature neuronal cultures develop synchronized network activity, which can be monitored using multi-electrode arrays (MEAs). These systems can detect coordinated bursting activity across the network, reflecting the establishment of functional synaptic connections and network-level integration [64]. The emergence of such coordinated activity is a critical indicator of functional maturation that more closely mirrors the in vivo environment.
Metabolic and Mitochondrial Functional Characterization
Mitochondrial dysfunction represents a core pathological mechanism in both PD and ageing, making its assessment vital for establishing phenotypic relevance [26] [65]. iPSC-derived dopaminergic neurons are particularly vulnerable to metabolic stress due to their high energy demands and the reactive oxygen species generated through both oxidative phosphorylation and dopamine metabolism [26].
Table 2: Key Assays for Metabolic and Mitochondrial Phenotyping
| Functional Domain | Key Assays | Measurable Parameters | Pathological Signatures in PD |
|---|---|---|---|
| Mitochondrial Function | Seahorse XF Analyzer | Oxygen Consumption Rate (OCR), Extracellular Acidification Rate (ECAR) | Reduced basal/maximal OCR, decreased ATP-linked respiration, impaired spare respiratory capacity [65] |
| Oxidative Stress | CM-H2DCFDA, MitoSOX staining | Total cellular ROS, mitochondrial superoxide production | Elevated ROS levels, increased oxidative DNA/RNA damage [26] |
| Metabolic Flux | 13C-Glucose/Lactate Tracing | Metabolic pathway utilization (glycolysis, TCA cycle, oxidative phosphorylation) | Shifts in metabolic plasticity, impaired lactate utilization [65] |
| Mitochondrial DNA Integrity | Long-range PCR, qPCR | mtDNA deletion frequency, lesion burden | Increased somatic mtDNA deletions and oxidative lesions [26] |
Advanced models, including 3D co-culture systems that integrate neurons with astrocytes and microglia, enable the study of metabolic interactions within the neurovascular unit, where astrocytes play a key role in supplying lactate to neurons and maintaining antioxidant defenses [65].
Modelling Age-Related Phenotypes in iPSC-Derived Neurons
Given that ageing is the primary risk factor for PD, the induction of age-related phenotypes is now considered essential for creating clinically relevant models of sporadic PD [26]. The PD-AGE consortium recommends specific approaches and a standardized panel of measurable parameters for this purpose.
Inducing Ageing Phenotypes
- Chemical Ageing Induction: The use of a standardized "SLO" cocktail (typically comprising streptozotocin, L-buthionine-sulfoximine, and oligomycin) to induce accelerated ageing phenotypes in iPSC-derived neurons [26].
- Direct Reprogramming: Utilizing direct reprogramming of somatic cells (e.g., fibroblasts) into induced neurons (iNs), which better retains donor-specific ageing signatures, including epigenetic markers and mitochondrial defects, compared to iPSC reprogramming and subsequent differentiation [26].
Measuring Ageing Hallmarks
The PD-AGE consortium has prioritized a panel of parameters to consistently quantify ageing in neuronal models [26]:
- Cellular Senescence: Assessed by Senescence-Associated Beta-Galactosidase (SA-β-Gal) activity, p16 and p21 expression, and loss of Lamin B1.
- Inflammaging: Measurement of senescence-associated secretory phenotype (SASP) factors, including IL-6 and IL-8.
- Mitochondrial Dysfunction: As detailed in Table 2.
- Omics Profiling: Comprehensive transcriptomic, epigenomic (e.g., DNA methylation clocks), and proteomic analyses to validate ageing signatures.
Advanced Model Systems: From 2D to 3D and Co-culture Platforms
To enhance physiological relevance, the field is increasingly moving toward more complex 3D model systems.
- 3D Neural Spheroids: These multilineage models integrate neurons, astrocytes, and microglia, demonstrating coordinated network activity, synaptic signaling, and neuroinflammatory responses [64]. They provide a more accurate tissue-like environment for studying cell-cell interactions and network-level pathologies.
- Blood-Brain Barrier (BBB) Models: Engineering 3D neurovascular microfluidic models containing endothelial cells, astrocytes, and pericytes replicates barrier integrity and permeability, enabling the study of drug transport and neurovascular interactions in PD [64].
- Region-Specific Organoids: Brain region-specific organoids enhance the understanding of interregional disease processes in PD, allowing for the investigation of pathological spread and selective vulnerability [1].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for iPSC-based PD Modeling
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Differentiation Kits | Commercial Dopaminergic Neuron Differentiation Kits | Directed differentiation of iPSCs into midbrain DA neurons | Ensure lot-to-lot consistency; validate with key markers (FOXA2, TH) |
| Ageing Inducers | SLO Cocktail [26] | Chemically induce accelerated ageing phenotypes | Standardize concentration and exposure time across experiments |
| Senescence Detectors | SA-β-Gal Staining Kit, p16/p21 Antibodies [26] | Detect and quantify cellular senescence | Use appropriate positive controls (e.g., radiation-induced senescence) |
| Metabolic Probes | MitoTracker, TMRE, CM-H2DCFDA | Assess mitochondrial mass, membrane potential, and ROS | Optimize loading concentrations for neuronal cultures |
| Synaptic Function Assays | FM Dyes, Antibodies (vGLUT, PSD95, GAD65) | Visualize synaptic vesicle recycling and synaptic density | Combine with live imaging for functional assessment |
| Myelination Agents | O4 Antibody, MBP/MOG/PLP1 Antibodies [64] | Differentiate oligodendrocyte progenitor cells and study myelination | Accelerated protocols can achieve >95% O4+ purity in 30 days |
Experimental Workflows and Signaling Pathways
The following diagrams illustrate key experimental workflows and the interconnected signaling pathways relevant to PD pathogenesis, as discussed in this guide.
Diagram 1: Workflow for Generating and Validating Phenotypically Relevant iPSC-Derived Dopaminergic Neurons
Diagram 2: Key Pathways in PD Pathogenesis and Ageing for Functional Assessment
Ensuring the phenotypic relevance of iPSC-derived models through comprehensive promotion of neuronal maturity and rigorous functional characterization is fundamental to advancing our understanding of Parkinson's disease pathogenesis. By implementing the multi-dimensional validation framework outlined in this guide—encompassing molecular identity, electrophysiological function, metabolic competence, and age-associated phenotypes—researchers can generate more predictive and physiologically relevant models. These advanced cellular systems provide a powerful platform for deconvoluting the complex interplay between genetic susceptibility, ageing, and environmental factors in PD, ultimately accelerating the discovery and validation of novel therapeutic interventions for this devastating neurodegenerative disorder.
The application of induced pluripotent stem cell (iPSC) technology in Parkinson's disease (PD) research represents a paradigm shift in our ability to model neurodegenerative processes and develop cell replacement therapies. PD is characterized by the progressive loss of dopaminergic neurons in the substantia nigra, leading to characteristic motor symptoms [1] [4]. iPSC-derived dopaminergic neurons offer an unprecedented opportunity to study disease mechanisms in human cells and provide a potential source for transplantation therapies [55]. However, the clinical translation of iPSC-based models and therapies faces two significant hurdles: genetic instability during reprogramming and expansion, and tumorigenicity risks from residual undifferentiated cells [66] [67]. This technical guide examines the current state of quality control measures and scalable manufacturing processes essential for navigating these challenges within PD research and therapy development.
Understanding the Risks: Genetic Instability and Tumorigenicity
Genetic Instability in iPSC Reprogramming and Culture
The process of reprogramming somatic cells to pluripotency imposes significant stress that can lead to genetic abnormalities. These instabilities manifest through various mechanisms:
Reprogramming-associated mutations: The reprogramming process itself can induce point mutations, copy number variations (CNVs), and chromosomal abnormalities [66]. Whole genome sequencing studies have revealed that iPSCs accumulate approximately 350-810 single-nucleotide variants compared to their parental somatic cells, with the pattern varying by reprogramming method [66].
Culture-adapted mutations: During extended in vitro culture, iPSC populations can acquire mutations that provide selective growth advantages. Common recurrent mutations affect genes such as TP53 (a tumor suppressor) and BCL2L1 (an anti-apoptotic factor) [66].
Epigenetic irregularities: Incomplete epigenetic reprogramming can result in aberrant DNA methylation patterns that may affect differentiation potential and cellular behavior [66].
Tumorigenicity Risks in iPSC-Derived Products
The therapeutic application of iPSC-derived cells presents several tumorigenicity concerns:
Teratoma formation: Residual undifferentiated iPSCs in differentiated products can form teratomas containing tissues from all three germ layers post-transplantation [55] [67]. Even a small number of undifferentiated cells (as few as 0.001%) can pose a significant risk [50].
Graft-induced dyskinesia: Contamination with non-dopaminergic neurons, particularly serotonergic neurons, has been associated with the development of graft-induced dyskinesia in previous fetal transplantation trials [55].
Oncogenic transformation: The use of integrating vectors carrying oncogenes (c-MYC) in reprogramming or the presence of mutations in cancer-related genes increases the risk of malignant transformation [66].
Quality Control Strategies: From Reprogramming to Final Product
Reprogramming Method Selection
The choice of reprogramming method significantly impacts the genetic stability and safety profile of resulting iPSC lines. The table below compares the major reprogramming approaches:
Table 1: Comparison of iPSC Reprogramming Methods
| Method | Integration Risk | Efficiency | Genetic Stability | Clinical Applicability |
|---|---|---|---|---|
| Retroviral/Lentiviral | High | 0.02-0.27% | Low | Not suitable |
| Sendai Virus (SeV) | None | ~0.077% | Moderate-High | Good (non-integrating RNA virus) |
| Episomal Plasmids | Low | 0.006-0.1% | Moderate | Good (defined components) |
| mRNA Transfection | None | 1.4-4.4% | High | Excellent (non-integrating) |
| PiggyBac Transposon | Low (footprint-free excision 91-95%) | ~0.1-1% | Moderate | Promising with optimization |
For clinical-grade iPSC generation, non-integrating methods such as Sendai virus or mRNA transfection are preferred despite potentially lower efficiencies [13] [66]. The Sendai virus system is particularly advantageous as it remains in the cytoplasm and is gradually diluted through cell divisions [66].
Comprehensive Genomic and Epigenomic Characterization
Rigorous characterization throughout the iPSC generation and differentiation process is essential. The following assays should be implemented:
Karyotype analysis: Standard G-banding karyotyping detects large chromosomal abnormalities but has limited resolution (~5-10 Mb) [50] [66].
Whole genome sequencing (WGS): Provides comprehensive detection of point mutations and structural variations. In preclinical studies for PD therapies, WGS of original somatic cells, undifferentiated iPSCs, and differentiated cells confirmed the absence of genomic mutations in 686 cancer-related genes [50].
Whole exome sequencing (WES): Focuses on protein-coding regions where most disease-relevant mutations occur. Studies have estimated 0-3 protein-coding point mutations per exome in iPSC lines [66].
DNA methylation profiling: Assesses epigenetic stability, particularly important for ensuring consistent differentiation potential. Monitoring the methylation ratio at transcriptional start sites of cancer-related genes provides critical safety data [50].
Purification Strategies for Dopaminergic Progenitors
Eliminating residual undifferentiated cells and enriching for target populations is crucial for PD applications. The following approaches have been successfully implemented:
Cell surface marker sorting: Fluorescence-activated cell sorting (FACS) using antibodies against CORIN, a floor plate marker, enables enrichment of midbrain dopaminergic progenitors. The Kyoto Trial demonstrated that CORIN sorting achieved 93.2% purity in the final product [55] [50].
Depletion strategies: Antibody-based removal of undifferentiated cells expressing pluripotency markers (TRA-1-60, SSEA-4) further reduces tumorigenic risk [50].
MicroRNA switches: Synthetic RNA devices that trigger apoptosis in undifferentiated cells based on endogenous miRNA activity provide an additional purification layer [66].
The experimental workflow below illustrates the comprehensive quality control pipeline from somatic cell reprogramming to dopaminergic neuron differentiation:
Scalable Manufacturing Under GMP Conditions
Current Good Manufacturing Practice (cGMP) Implementation
Transitioning from research-scale to clinically applicable manufacturing requires rigorous adherence to cGMP standards:
Defined culture systems: Elimination of animal-derived components (fetal bovine serum, mouse embryonic feeders) reduces risk of xenopathogen transmission [67]. Use of recombinant laminin-511 fragments as substrates represents a defined alternative [50].
Master cell banking: Establishing a clonal master cell bank (MCB) from a single iPSC clone ensures consistency. The Kyoto Trial utilized MCB003, a human leukocyte antigen (HLA)-homozygous iPSC line preserved in hundreds of frozen vials as one lot [50].
Process validation: Manufacturing consistency must be demonstrated through multiple production runs. In preclinical studies for PD therapy, the dopaminergic induction process was successfully repeated 25 times with consistent results (CORIN+ purity: 93.2 ± 2.1%) [50].
3D Culture and Bioreactor Systems
Moving beyond 2D culture systems enables scalable production of iPSC-derived dopaminergic progenitors:
Suspension culture: Aggregation of CORIN-sorted cells into 3D spheres promotes maturation and allows for scale-up in bioreactor systems [50].
Monitoring technologies: Integration of inline sensors for pH, oxygen, and metabolic parameters enables real-time process control [67].
Automated cell sorting: Clinical-grade cell sorters with disposable fluid pathways prevent cross-contamination during the CORIN+ selection process [50].
The Scientist's Toolkit: Essential Reagents and Methods
Table 2: Key Research Reagent Solutions for iPSC-Based Parkinson's Disease Modeling
| Reagent/Method | Function | Application Notes |
|---|---|---|
| Sendai Virus Vectors | Non-integrating reprogramming | Clinical-grade available; gradually diluted from cells |
| Episomal Plasmids | Non-integrating reprogramming | Contains EBNA-1/OriP sequences; cost-effective |
| Laminin-511 E8 | Defined substrate | Xeno-free; supports iPSC attachment and differentiation |
| CORIN Antibody | Dopaminergic progenitor selection | Floor plate marker; FACS sorting achieves >90% purity |
| LMX1A/FOXA2 Antibodies | Midbrain DA neuron verification | Transcription factors specifying midbrain identity |
| NURR1/TH Antibodies | Mature dopaminergic neuron markers | Rate-limiting enzyme in dopamine synthesis |
| cGMP-grade Small Molecules | Differentiation guidance | SHH, FGF8, CHIR99021, valproic acid for patterning |
| TRA-1-60/SSEA-4 Antibodies | Undifferentiated cell detection | Pluripotency markers for residual cell screening |
Experimental Protocols for Safety Assessment
In Vitro Tumorigenicity Assay
Purpose: Detect residual undifferentiated iPSCs in final dopaminergic progenitor products.
Method:
- Dissociate day-26 dopaminergic spheres into single cells [50].
- Mix test samples with positive control samples containing known percentages (0.001% to 1.0%) of undifferentiated iPSCs.
- Culture 2×10^5 cells per well in iPSC-maintenance medium for 14 days.
- Score colony formation: No colonies should be observed in the test sample, while positive controls should show visible iPSC colonies at all spiked concentrations [50].
Acceptance Criterion: No colony formation in the test sample, demonstrating <0.001% residual undifferentiated cells.
Genomic Stability Monitoring Protocol
Purpose: Assess genetic integrity throughout the manufacturing process.
Method:
- Collect samples at critical process stages: parental somatic cells, undifferentiated iPSCs, day 12 pre-sorted cells, and day 26 final product [50].
- Perform whole genome sequencing (30-40x coverage) and whole exome sequencing (100x coverage).
- Analyze data for:
- Single nucleotide variants (SNVs) in 686 cancer-related genes from COSMIC database
- Copy number variations (CNVs)
- Structural variations
- Residual plasmid integration [50]
- Validate any detected mutations by amplicon sequencing.
Acceptance Criterion: No confirmed mutations in cancer-related genes compared to parental somatic cells.
The pathway to clinical translation of iPSC-based models and therapies for Parkinson's disease requires meticulous attention to quality control and scalability. The integration of non-integrating reprogramming methods, comprehensive genomic characterization, and stringent purification protocols has significantly mitigated the risks of genetic instability and tumorigenicity. The successful implementation of these strategies in ongoing clinical trials, such as the Kyoto Trial, demonstrates the feasibility of this approach [55] [50].
Future developments will likely focus on further enhancing safety through gene editing technologies like CRISPR-Cas9 to create "fail-safe" mechanisms in iPSC-derived products, and advanced monitoring systems incorporating artificial intelligence for real-time quality assessment during manufacturing [68]. As these technologies mature, they will accelerate the clinical translation of iPSC-based therapies, ultimately offering new hope for patients with Parkinson's disease through both advanced disease modeling and regenerative approaches.
The integration of induced pluripotent stem cell (iPSC) technology into Parkinson's disease (PD) research has revolutionized our ability to model the pathogenesis of this complex neurodegenerative disorder in a patient-specific context. A critical challenge in this field, however, is the standardized assessment of the core cellular pathologies that drive PD progression. This whitepaper establishes a comprehensive technical framework for defining and measuring a core phenotype panel focusing on three interconnected hallmarks of PD: cellular senescence, mitochondrial dysfunction, and inflammaging. This panel provides researchers with a standardized toolkit for robust characterization of iPSC-derived models, particularly dopaminergic neurons, which are crucial for understanding PD-specific pathogenic mechanisms. The systematic application of this panel will enable more reproducible quantification of disease phenotypes across different laboratory settings and patient-derived iPSC lines, ultimately accelerating both our fundamental understanding of PD and the development of targeted therapeutic interventions.
Core Phenotype I: Cellular Senescence
Cellular senescence is a state of stable cell cycle arrest that occurs in response to various stressors and is characterized by distinct morphological and biochemical changes. In the context of PD pathogenesis, senescent cells, particularly in the brain, contribute to tissue dysfunction through the secretion of pro-inflammatory factors and the loss of cellular functionality.
Key Markers and Their Detection Methods
The reliable identification of senescent cells requires a multi-parameter approach, as no single marker is universally expressed by all senescent cells. The table below summarizes the core markers recommended for a senescence panel in PD-focused research.
Table 1: Core Markers for Detecting Cellular Senescence
| Marker Category | Specific Marker | Detection Method | Technical Notes | Interpretation in PD Models |
|---|---|---|---|---|
| Lysosomal Activity | SA-β-galactosidase [69] | Colorimetric or fluorescent assay (pH 6.0) | Most widely used; requires careful pH control | Increased activity indicates lysosomal burden; relevant to GBA1-linked PD |
| Nuclear Envelope | Lamin B1 [69] | Immunofluorescence / Western Blot | Downregulation indicates nuclear fragility | Loss correlates with nuclear integrity loss in dopaminergic neurons |
| Cell Cycle Arrest | p16INK4a, p21CIP1 [69] | Immunofluorescence / Western Blot | Key effector of permanent arrest | Upregulation in neurons/glia may indicate premature senescence |
| DNA Damage Response | γ-H2A.X [69] | Immunofluorescence (foci) | Marker of persistent DNA damage | Reflects genotoxic stress, a key driver in sporadic PD |
| Heterochromatin Formation | SAHF (H3K9me3, HP1) [69] | Immunofluorescence | Distinct, dense DAPI-stained foci | Epigenetic alteration leading to aberrant gene expression |
| Secretory Phenotype | IL-6, MMP-3, IL-1β [69] | ELISA / Multiplex Immunoassay | SASP components; measure secreted proteins | Drives neuroinflammation and paracrine senescence |
Detailed Experimental Protocol: SA-β-Galactosidase Staining
Principle: The assay detects the increased lysosomal β-galactosidase activity present in senescent cells, optimized to be active at the suboptimal pH 6.0 [69].
Reagents Required:
- Fixative: 2% Formaldehyde / 0.2% Glutaraldehyde in PBS
- Staining Solution: 1 mg/mL X-gal, 40 mM Citric Acid/NaPhosphate (pH 6.0), 5 mM Potassium Ferrocyanide, 5 mM Potassium Ferricyanide, 150 mM NaCl, 2 mM MgCl₂
- PBS (pH 7.2 and pH 6.0)
Procedure:
- Cell Preparation: Culture iPSC-derived dopaminergic neurons on 24-well plates until the desired maturity or treatment time point. Include both positive (e.g., etoposide-treated) and negative controls.
- Fixation: Aspirate culture medium and wash cells once with PBS (pH 7.2). Add enough fixative to cover cells and incubate for 5 minutes at room temperature.
- Washing: Remove fixative and wash cells three times with PBS (pH 6.0) to ensure proper pH for the reaction.
- Staining: Add freshly prepared staining solution to cover cells. Seal the plate with parafilm to prevent evaporation.
- Incubation: Incubate cells at 37°C in a dry incubator (without CO₂) for 12-16 hours.
- Analysis: Examine cells under a bright-field microscope. Senescent cells will display blue cytoplasmic staining. Quantify by counting stained cells in multiple random fields (minimum of 300 cells total per condition) or by using image-based quantification software.
Critical Considerations for PD Models:
- Validate the senescent phenotype with at least one additional marker from Table 1 (e.g., p21).
- Be aware that some neuronal subtypes may have inherently high lysosomal activity; therefore, pH control is critical.
- For iPSC-derived cultures containing mixed cell types, combine with cell-type-specific immunostaining (e.g., Tyrosine Hydroxylase for dopaminergic neurons) to attribute senescence to the relevant population.
Core Phenotype II: Mitochondrial Dysfunction
Mitochondrial dysfunction is a cornerstone of PD pathogenesis, affecting energy production, calcium buffering, and reactive oxygen species (ROS) homeostasis. iPSC-derived neurons from PD patients often exhibit these deficits, making their quantification essential.
Key Parameters and Functional Assays
Mitochondrial health should be assessed through integrated measures of function, content, and morphology.
Table 2: Core Parameters for Assessing Mitochondrial Dysfunction
| Parameter Category | Specific Parameter | Detection Method/Assay | Key Insight for PD |
|---|---|---|---|
| Functional - Respiration | Basal & Maximal OCR, ATP-linked OCR, Proton Leak [70] | Seahorse XF Analyzer / Metabolic Flux Analysis | Reveals bioenergetic deficits, even with normal mitochondrial count [70] |
| Functional - Membrane Integrity | Mitochondrial Membrane Potential (ΔΨm) | TMRE or JC-1 staining & flow cytometry/imaging | Collapse indicates inability to produce ATP; early apoptosis marker |
| Metabolic Footprint | Extracellular Acidification Rate (ECAR) [70] | Seahorse XF Analyzer | Measures glycolytic flux; often compensatory in dysfunction |
| Content & Mass | Mitochondrial DNA copy number, COX IV, VDAC protein levels [69] | qPCR / Western Blot | Distinguishes functional defect from simple loss of mass |
| ROS Production | Mitochondrial superoxide (mtROS) | MitoSOX Red staining & flow cytometry/imaging | Oxidative stress driver, damaging proteins, lipids, and DNA |
| Morphology | Network Structure | Mitotracker staining & confocal microscopy | Fragmented networks correlate with PD; use with PINK1/Parkin models |
Detailed Experimental Protocol: Metabolic Flux Analysis
Principle: This protocol uses a metabolic extracellular flux analyzer to measure the Oxygen Consumption Rate (OCR) and Extracellular Acidification Rate (ECAR) of live cells in real-time, providing a dynamic readout of mitochondrial respiration and glycolysis [70].
Reagents and Equipment:
- Metabolic extracellular flux analyzer (e.g., Seahorse XFe/XF Analyzer)
- XF96 or XF24 cell culture microplates
- XF Calibration Solution (pH 7.4)
- XF Assay Medium: DMEM base, 1 mM Pyruvate, 10 mM Glucose, 2 mM Glutamine (pH 7.4)
- Metabolic Modulators: Oligomycin (1.5 µM), FCCP (1.0 µM), Rotenone & Antimycin A (0.5 µM each)
Cell Preparation and Coating:
- Plate Coating: For iPSC-derived neurons, which are non-adherent, coat the assay microplate to ensure cell attachment.
- Cell Seeding: Harvest and count the iPSC-derived neurons. Resuspend cells in pre-warmed XF Assay Medium.
- Seed 180 µL of cell suspension (e.g., 2x10⁵ cells) per well into the prepared microplate.
- Centrifuge the plate at 300 x g for 3 minutes (without brake) to promote adhesion [70].
- Incubate the plate in a non-CO₂, humidified 37°C incubator for 45-60 minutes to allow temperature and pH equilibration.
Assay Run:
- Instrument Calibration: Load the sensor cartridge into the analyzer for calibration as per the manufacturer's instructions.
- Compound Loading: Load the metabolic modulators into the injection ports of the sensor cartridge:
- Port A: Oligomycin
- Port B: FCCP
- Port C: Rotenone & Antimycin A
- Program Setup: Create an assay protocol with the following measurement cycle:
- 3 minutes of mixing
- 2 minutes of waiting
- 3 minutes of measurement
- Repeat for baseline and after each drug injection.
- Execution: Place the cell culture microplate into the analyzer and start the programmed run.
Data Analysis and Key Metrics:
- Basal Respiration: The last OCR measurement before the first injection.
- ATP-linked Respiration: Basal OCR minus the OCR after Oligomycin injection.
- Maximal Respiration: The OCR after FCCP injection minus the non-mitochondrial respiration.
- Spare Respiratory Capacity: Maximal OCR minus Basal OCR (indicates energetic flexibility).
- Non-mitochondrial Respiration: The OCR after Rotenone/Antimycin A injection.
PD-Specific Considerations:
- Compare isogenic control lines to PD-mutant lines to isolate mutation-specific effects.
- Neurons from patients with PINK1 or Parkin mutations often show profound deficits in maximal respiration and spare capacity.
- Monitor glycolytic parameters (ECAR) concurrently, as neurons may attempt to compensate for mitochondrial failure via glycolysis.
Core Phenotype III: Inflammaging
Inflammaging refers to the chronic, low-grade, sterile inflammation that characterizes aging and age-related diseases like PD. In PD models, this is driven by the accumulation of SASP-secreting senescent cells and the activation of glial cells.
Core Inflammaging Mediators and Pathways
The inflammaging profile extends beyond the classic SASP to include a broader array of immune mediators.
Table 3: Core Mediators and Pathways for Assessing Inflammaging
| Mediator Category | Specific Mediator | Detection Method | Biological Role in PD |
|---|---|---|---|
| Pro-inflammatory Cytokines | IL-6, IL-1β, TNF-α [69] | ELISA / Multiplex Assay | Drive chronic neuroinflammation, neuronal excitotoxicity |
| Chemokines | IL-8 (CXCL8), MCP-1 (CCL2) | ELISA / Multiplex Assay | Recruit microglia and peripheral immune cells to sites of pathology |
| Proteases | MMP-3, MMP-9 [69] | ELISA / Gel Zymography | Disrupt blood-brain barrier and extracellular matrix |
| Pattern Recognition Receptors | TLR2, TLR4 | qPCR / Flow Cytometry | Sense DAMPs from stressed or dying neurons |
| Downstream Signaling | Phospho-NF-κB, Phospho-p38 MAPK | Western Blot / Immunofluorescence | Key intracellular pathways transducing inflammatory signals |
| Glial Activation | GFAP (astrocytes), IBA1 (microglia) | Immunofluorescence / qPCR | Indicator of non-cell-autonomous inflammatory response |
Detailed Experimental Protocol: Cytokine Profiling via Multiplex Immunoassay
Principle: This protocol quantitatively measures a panel of secreted inflammatory mediators from conditioned media, providing a snapshot of the inflammaging secretome.
Reagents and Equipment:
- Multiplex immunoassay panel (e.g., Luminex, MSD) targeting cytokines (IL-6, IL-1β, TNF-α, IL-8, MCP-1)
- Conditioned media from iPSC-derived neuron or co-culture models
- Assay buffers (diluent, wash buffer)
- Plate reader capable of reading electrochemiluminescence or fluorescence
Procedure:
- Conditioned Media Collection:
- Culture iPSC-derived neurons or neuron-glia co-cultures until the desired maturity.
- Replace the culture medium with a fresh, serum-free medium to avoid serum interference.
- After 24 hours (or a predetermined time), carefully collect the conditioned media.
- Centrifuge the media at 1000 x g for 10 minutes at 4°C to remove any cells or debris.
- Aliquot and store the supernatant at -80°C until analysis.
- Assay Execution:
- Thaw samples on ice and keep all reagents chilled.
- Follow the manufacturer's instructions for the specific multiplex kit. Generally, this involves:
- Adding standards and samples to the pre-coated plate.
- Adding the detection antibody cocktail.
- Adding a streptavidin-phycoerythrin (or similar) solution.
- Reading the plate on the appropriate analyzer.
- Data Analysis:
- Use the standard curve for each analyte to interpolate sample concentrations.
- Normalize the cytokine concentration to the total cellular protein (from a parallel well) or to the cell number to account for variations in cell density.
Critical Considerations for PD Models:
- For a more physiologically relevant model, consider using co-cultures of iPSC-derived dopaminergic neurons with iPSC-derived microglia or astrocytes.
- Stimulate the cultures with an inflammaging-relevant trigger, such as pre-formed fibrils of α-synuclein, to unmask a latent inflammatory potential.
- Correlate secretome data with intracellular signaling data (e.g., NF-κB activation) to build a more complete picture of the inflammatory state.
A successful phenotype panel relies on high-quality, well-validated reagents. The following table lists essential tools for implementing this core panel.
Table 4: Research Reagent Solutions for the Core Phenotype Panel
| Reagent Category | Example Product/Kit | Primary Function | Application Note |
|---|---|---|---|
| Senescence Detection | Senescence β-Galactosidase Staining Kit [69] | Histochemical detection of SA-β-gal activity | The classic, first-pass test for senescence; optimal for adherent cultures. |
| Antibody Sampler Kits | Senescence Marker / SASP Antibody Sampler Kits [69] | Multiplex detection of key proteins via WB/IF | Cost-effective way to screen multiple markers (p16, p21, Lamin B1, SASP factors). |
| Metabolic Flux Assay | Extracellular Flux Assay Kits [70] | Real-time measurement of OCR and ECAR | The gold standard for functional metabolic phenotyping. Requires specialized instrument. |
| Mitochondrial Dyes | MitoTracker Deep Red, TMRE, MitoSOX Red | Labeling of mass, membrane potential, and ROS | Provide spatial information via imaging; TMRE is potential-sensitive. |
| Cytokine Profiling | Proinflammatory Panel Multiplex Assays | Quantify multiple cytokines/chemokines simultaneously from small sample volumes | Ideal for characterizing the SASP and inflammaging secretome. |
| iPSC Differentiation | Dopaminergic Neuron Differentiation Kits | Generate relevant cell types from patient iPSCs | Ensure high-quality, reproducible differentiation with high TH+ neuron yield. |
Integrated Experimental Workflows and Data Interpretation
To effectively utilize the core phenotype panel, researchers must integrate the individual assays into a coherent workflow that provides a multidimensional view of cellular state.
Logical Workflow for Panel Application
The following diagram illustrates the recommended sequence for applying the core phenotype panel to iPSC-derived models, from cell preparation to integrated data analysis.
Signaling Pathway Integration in PD
The three core phenotypes are not isolated but are interconnected through shared molecular pathways. The following diagram maps the key signaling crosstalk between senescence, mitochondrial dysfunction, and inflammaging, contextualized within PD pathogenesis.
Data Integration and Interpretation Framework
The ultimate value of the core phenotype panel lies in the integrated analysis of the data from all three domains. We propose a composite scoring system to quantify the overall pathological burden in iPSC-derived models.
Calculating a Composite Phenotype Score:
- Normalization: For each assay (e.g., % SA-β-Gal+ cells, Basal OCR, IL-6 secretion), normalize the raw values from PD lines to the average of the isogenic control lines within the same experiment.
- Z-Score Transformation: Convert normalized values to Z-scores to place all measurements on a common, unitless scale.
- Directional Adjustment: Ensure the direction of the Z-score is consistent, where a positive Z-score indicates a more pathological state (e.g., +Z for SA-β-Gal, -Z for OCR, +Z for cytokines).
- Averaging: Calculate the average Z-score across all assays to generate a single Composite Phenotype Score for each cell line or experimental condition.
This quantitative framework allows for the direct comparison of different PD mutations, drug treatment effects, or patient cohorts, moving beyond qualitative descriptions to a robust, numerical representation of disease-associated cellular decline. By applying this core phenotype panel and integrated analysis framework, researchers can systematically dissect the contributions of senescence, mitochondrial failure, and inflammation to PD pathogenesis, paving the way for the identification of novel biomarkers and therapeutic targets.
Validating iPSC Models Against Traditional Preclinical Systems and Clinical Data
Parkinson's disease (PD) research has long relied on neurotoxin-based animal models such as 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) and 6-hydroxydopamine (6-OHDA) to study disease mechanisms and evaluate potential therapeutics. While these models have contributed valuable insights into dopaminergic neuron vulnerability, they recapitulate only limited aspects of human PD pathology. These neurotoxins function primarily by inhibiting complex I of the mitochondrial electron transport chain, leading to oxidative stress and eventual neuronal death [56]. However, they fail to capture the complex, multi-faceted pathology of human PD, including the progressive nature of neurodegeneration, the formation of α-synuclein aggregates known as Lewy bodies, and the genetic underpinnings that contribute to disease susceptibility and progression [56]. The emergence of induced pluripotent stem cell (iPSC) technology represents a paradigm shift in PD modeling, enabling researchers to investigate disease mechanisms in human dopaminergic neurons with patient-specific genetic backgrounds, thereby providing a more physiologically relevant platform for both mechanistic studies and therapeutic development.
Fundamental Limitations of Traditional Toxin Models
Pathological and Phenotypic Gaps
Traditional neurotoxin models fall short of recapitulating the comprehensive pathology observed in human Parkinson's disease. The table below summarizes the key pathological features missing in these models:
Table 1: Limitations of Traditional Neurotoxin Models in PD Research
| Pathological Feature | MPTP Model | 6-OHDA Model | Human PD Pathology |
|---|---|---|---|
| α-Synuclein Aggregation/Lewy Bodies | No formation [56] | No formation [56] | Hallmark feature present in most cases [4] [56] |
| Progressive Neurodegeneration | Acute degeneration | Acute degeneration | Chronic, progressive loss over years [4] |
| Genetic Contributions | Not represented | Not represented | Multiple genes identified (SNCA, LRRK2, GBA, etc.) [3] [56] |
| Non-Motor Symptoms | Limited representation | Limited representation | Common (dementia, depression, sleep disorders) [4] [3] |
| Selective Vulnerability | Moderate selectivity | Moderate selectivity | Specific vulnerability of A9 nigral neurons [56] |
Mechanistic Shortcomings
The fundamental limitation of toxin models lies in their mechanistic simplicity. While human PD involves complex interactions between genetic susceptibility, environmental factors, and aging processes, toxin models primarily induce acute oxidative stress and mitochondrial dysfunction without engaging the multifaceted pathways operative in human disease [4] [56]. Furthermore, these models do not reproduce the complex cell-type-specific vulnerabilities observed in human PD, particularly the selective degeneration of A9-type substantia nigra dopaminergic neurons versus the relative sparing of A10-type ventral tegmental area neurons [56]. The inability to study early pathogenic events represents another significant constraint, as toxin models only capture end-stage neuronal death rather than the progressive pathological cascade that characterizes human PD.
The iPSC Revolution: Fundamental Advantages for Disease Modeling
Technical Foundations of iPSC Technology
Induced pluripotent stem cells are generated by reprogramming somatic cells (typically skin fibroblasts or blood cells) into a pluripotent state through the forced expression of specific transcription factors. The original methodology, pioneered by Yamanaka and colleagues, utilized Oct4, Sox2, Klf4, and c-Myc (the "Yamanaka factors") delivered via retroviral vectors [3] [48]. Subsequent advancements have led to improved safety profiles through non-integrating methods such as episomal plasmids, Sendai virus, modified RNAs, and recombinant proteins [3]. These "footprint-free" reprogramming techniques eliminate the risk of insertional mutagenesis while maintaining high reprogramming efficiency. Additionally, xeno-free culture systems have been developed using defined matrices like vitronectin and formulated media such as E8 medium, enabling the production of clinical-grade iPSCs suitable for both research and therapeutic applications [3].
Key Advantages Over Toxin Models
iPSC-derived models offer several transformative advantages for Parkinson's disease research:
Patient-Specific Genetics: iPSCs retain the complete genetic background of the donor, enabling modeling of both familial and sporadic PD forms. This allows researchers to study how specific mutations (e.g., in SNCA, LRRK2, Parkin) manifest in human neurons and to investigate gene-environment interactions in susceptible genetic backgrounds [3] [56].
Human-Relevant Cellular Context: Unlike transformed cell lines or animal models, iPSC-derived dopaminergic neurons express human-specific genes, splice variants, and metabolic pathways, providing a more physiologically relevant context for studying disease mechanisms and drug responses [71].
Developmental Perspective: iPSC differentiation recapitulates human development, enabling studies of how PD-related genes function during the specification, maturation, and aging of dopaminergic neurons – aspects completely absent in toxin models [56].
Multi-dimensional Modeling Capability: iPSCs can be differentiated into various CNS cell types (neurons, astrocytes, microglia) and assembled into 2D co-cultures or 3D organoids, capturing cell-cell interactions and tissue-level pathophysiology not possible in toxin models [31] [1].
Experimental Framework: iPSC Differentiation and Disease Modeling Protocols
Dopaminergic Neuron Differentiation Methodologies
Several robust protocols have been established for differentiating iPSCs into authentic midbrain dopaminergic neurons. The most widely employed approach is based on dual SMAD inhibition to induce neural floor plate specification, followed by patterning with developmental morphogens:
Figure 1: Workflow for the directed differentiation of human iPSCs into midbrain dopaminergic neurons, highlighting key patterning factors and characterization markers.
This protocol typically spans 25-35 days for generating dopaminergic precursors and up to 60-90 days for full functional maturation. Quality control checkpoints include flow cytometry for CORIN+ cells (a midbrain floor plate marker) at the progenitor stage, and immunocytochemistry for transcription factors FOXA2 and LMX1A, followed by tyrosine hydroxylase (TH) in mature neurons [50]. Functional validation includes measurements of potassium-evoked dopamine release via HPLC and electrophysiological assessment of action potentials [50].
Essential Research Reagents and Tools
Table 2: Key Reagents for iPSC-Dopaminergic Neuron Differentiation and Characterization
| Category | Reagent/Solution | Function/Application |
|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc | Induction of pluripotency in somatic cells [3] [48] |
| Neural Induction | SMAD inhibitors (SB431542, LDN193189) | Dual SMAD inhibition for neural specification [56] |
| Patterning Factors | SHH (Sonic Hedgehog), FGF8, WNT agonists | Ventral midbrain patterning and dopaminergic fate specification [4] [48] |
| Maturation Factors | BDNF, GDNF, Ascorbic Acid, TGF-β3, cAMP | Promotion of neuronal survival, maturation, and dopaminergic phenotype [4] [50] |
| Characterization Markers | FOXA2, LMX1A, OTX2 (progenitors); TH, NURR1, PITX3 (mature neurons) | Identification and validation of dopaminergic identity at different stages [50] [48] |
| Functional Assays | Potassium-evoked dopamine release, electrophysiology, calcium imaging | Validation of neuronal functionality and dopamine synthesis/release [50] |
Applications in Disease Modeling and Drug Discovery
Modeling Genetic Forms of Parkinson's Disease
iPSC technology has enabled the generation of patient-specific models for various genetic forms of PD. The table below summarizes key findings from iPSC-based studies of PD-associated mutations:
Table 3: iPSC-Based Modeling of Genetic Parkinson's Disease Forms
| Gene/Mutation | Key Phenotypes in iPSC-Derived Neurons | Pathogenic Insights |
|---|---|---|
| SNCA (A53T, Triplication) | Elevated α-synuclein levels; mitochondrial dysfunction; increased oxidative stress; impaired mitochondrial transport [3] [56] | Demonstrates dose-dependent effect of α-synuclein; links α-synuclein to mitochondrial defects and oxidative stress [56] |
| LRRK2 (G2019S) | Increased kinase activity; elevated α-synuclein; mitochondrial DNA damage; delayed mitophagy; neurite simplification [3] [56] | Connects LRRK2 function to mitochondrial quality control and neuronal morphology; suggests kinase inhibition as therapeutic strategy [3] |
| Parkin/PINK1 | Mitochondrial dysfunction; increased oxidative stress; impaired mitophagy [3] [56] | Supports central role of mitochondrial quality control in PD pathogenesis; reveals functional relationship between Parkin and PINK1 [3] |
| GBA | Increased α-synuclein accumulation; lysosomal dysfunction; impaired autophagy-lysosomal pathway [4] [3] | Establishes connection between lysosomal function and α-synuclein metabolism; suggests lysosomal enhancement as therapeutic approach [3] |
High-Content Screening Platforms
iPSC-derived neurons provide a human-relevant platform for compound screening and therapeutic validation. Established protocols typically involve:
- Differentiation of iPSCs to dopaminergic neurons in 96-well or 384-well formats
- Treatment with test compounds at predetermined timepoints during maturation
- Challenge with PD-relevant stressors (e.g., mitochondrial toxins, oxidative stress inducers)
- High-content readouts including cell viability, mitochondrial function, neurite outgrowth, and α-synuclein aggregation [71]
This approach has been validated in studies screening for compounds that protect against MPP+ and rotenone toxicity, with glial cell-derived neurotrophic factor (GDNF) serving as a positive control [71]. The use of isogenic controls (genetically corrected lines from the same patient) enables distinction between mutation-specific effects and background genetic variation, increasing the sensitivity and reliability of screening campaigns [3] [31].
Integration with Advanced Model Systems
3D Organoid and Co-culture Models
Recent advancements have extended iPSC technology beyond 2D neuronal cultures to more complex 3D model systems. Brain region-specific organoids containing multiple cell types and exhibiting tissue-level organization provide a more physiologically relevant context for studying cell-cell interactions and pathological spreading of α-synuclein aggregates [31] [1]. These 3D models recapitulate features of human cortical development, including progenitor zone organization, neurogenesis, and the presence of human-specific outer radial glia, enabling studies of neurodevelopmental aspects of PD risk genes [31]. Additionally, the establishment of microfluidics-based co-culture systems allows for the investigation of interactions between dopaminergic neurons and other CNS cell types, particularly glial cells that play important roles in neuroinflammation and neuronal vulnerability [1].
Multi-omics Integration
iPSC-based models serve as an ideal platform for integrating multi-omics datasets including genomic, transcriptomic, proteomic, and epigenomic profiles from the same genetic background. This integrated approach has revealed disease-associated gene expression patterns, alternative splicing events, and epigenetic modifications in PD patient-derived neurons that were not apparent in animal models or post-mortem tissues [1]. The combination of iPSC technology with CRISPR-based gene editing enables functional validation of disease-associated genetic variants identified through genome-wide association studies, establishing causal relationships between genetic risk factors and cellular phenotypes [31] [72].
Induced pluripotent stem cell technology has fundamentally transformed Parkinson's disease research by providing a human-specific, patient-derived model system that captures the genetic complexity and cellular vulnerability of this neurodegenerative disorder. Unlike traditional toxin models that recapitulate only selective aspects of PD pathology, iPSC-derived models enable researchers to investigate disease mechanisms across the entire spectrum of pathogenic processes, from early developmental vulnerabilities to late-stage neurodegenerative events. The integration of iPSC technology with advanced genomic tools, 3D culture systems, and high-content screening platforms continues to accelerate the identification of novel therapeutic targets and the validation of candidate therapeutics. As these technologies mature and standardization improves, iPSC-based models are poised to become the cornerstone of PD research and drug development, bridging the critical gap between animal studies and clinical trials.
Parkinson's disease (PD) is the second most common neurodegenerative disease worldwide, characterized by the progressive loss of dopaminergic neurons in the substantia nigra and the presence of Lewy bodies containing aggregated α-synuclein [20] [30]. For decades, transgenic mouse models have been instrumental in biomedical research, offering advantages such as high reproductive rates, fully sequenced genomes, and well-developed genetic manipulation techniques [73]. However, these models face fundamental limitations in replicating human-specific aspects of PD pathogenesis, creating a "species gap" that hinders translational progress. The emergence of induced pluripotent stem cell (iPSC) technology has introduced a powerful alternative that preserves human genetic background and cell-type specificity [11].
iPSCs are generated by reprogramming adult somatic cells into an embryonic stem cell-like state through the introduction of specific transcription factors, most commonly OCT4, SOX2, KLF4, and c-MYC (OSKM) [11]. These cells can then be differentiated into various somatic cell types, including the dopaminergic neurons critically affected in PD [20]. This technological advancement enables researchers to model PD using patient-specific neurons that carry the complete genetic background of the donor, providing an unprecedented opportunity to study disease mechanisms and therapeutic interventions in human-relevant systems [30]. This review examines how iPSC-based models are bridging the species gap in PD research, with a focus on their advantages over transgenic mouse models, applications in disease modeling, and emerging therapeutic applications.
Fundamental Advantages of iPSC Models Over Transgenic Mouse Systems
Preservation of Human Genetic Context
iPSC models maintain the complete human genetic context of PD, including:
- Polygenic risk architecture: Most PD cases involve complex interactions between multiple genetic risk factors and environmental influences [73]. While transgenic mice typically focus on single-gene manipulations, iPSCs naturally incorporate the entire genetic landscape of the donor.
- Human-specific gene regulation: Gene expression patterns, splicing variants, and epigenetic regulation in human iPSC-derived neurons more accurately reflect human biology than mouse models [11].
- Endogenous expression levels: Unlike transgenic models with artificial promoters and non-physiological expression levels, iPSC-derived neurons express PD-related genes at endogenous levels [20].
Direct Access to Affected Cell Types
The core pathology of PD specifically affects dopaminergic neurons of the substantia nigra, a discrete neuronal population that is challenging to isolate and study in humans. iPSC technology enables:
- Direct differentiation into the specific human midbrain dopaminergic neuron subtypes most vulnerable in PD [30].
- Generation of complex cultures containing multiple relevant cell types, including astrocytes, microglia, and other neuronal subtypes that contribute to PD pathogenesis [30].
- Study of patient-specific vulnerabilities in the exact cell types affected by disease, which is particularly valuable for sporadic PD cases without known genetic causes [9].
Table 1: Comparative Analysis of iPSC vs. Transgenic Mouse Models for PD Research
| Feature | iPSC Models | Transgenic Mouse Models |
|---|---|---|
| Genetic context | Complete human genetic background | Limited to introduced human transgenes |
| Cellular environment | Human neurons with authentic physiology | Mouse neurons with species-specific differences |
| Pathological progression | Can model early cellular events | Limited representation of human disease progression |
| Throughput for screening | High-throughput capability possible [74] | Lower throughput, more time-consuming |
| Personalized applications | Patient-specific models readily generated | Not feasible for personalized modeling |
| Cost and infrastructure | Requires specialized cell culture facilities | Standard animal facility requirements |
Applications in Modeling Parkinson's Disease Pathogenesis
Elucidating Molecular Mechanisms in Patient-Specific Context
iPSC-derived dopaminergic neurons from PD patients have been instrumental in uncovering disease mechanisms, particularly for monogenic forms of PD. Studies using these models have revealed:
Mitochondrial Dysfunction: DA neurons derived from patients with SNCA triplication or mutations in PINK1/PARK2 show profound mitochondrial abnormalities, including altered morphology, decreased membrane potential, and impaired ATP production [20] [30]. These defects manifest as fragmented mitochondrial networks and increased susceptibility to oxidative stress.
Protein Homeostasis Disruption: iPSC models have demonstrated how different PD-related mutations converge on protein quality control systems. For example:
- SNCA triplication models show accumulation of α-synuclein aggregates that impair proteasomal and lysosomal function [20].
- Mutations in GBA, which encodes the lysosomal enzyme glucocerebrosidase, disrupt α-synuclein clearance, creating a pathogenic feedback loop [20] [30].
- Dysfunctional endoplasmic reticulum stress responses and unfolded protein response activation have been observed in multiple iPSC models carrying different PD mutations [30].
Axonal Transport Deficits: In SNCA multiplication models, α-synuclein oligomers disrupt anterograde axonal transport of mitochondria by altering the localization and function of transport-regulating proteins like KLC1, Miro1, and tau [30]. This transport deficit contributes to synaptic dysfunction and energy deficits in distal neuronal compartments.
Experimental Workflow for iPSC-Based Disease Modeling
The standard approach for iPSC-based PD modeling involves several key stages, each with specific methodological considerations:
Patient Recruitment and Cell Collection: The process begins with recruitment of PD patients and appropriate controls, followed by collection of somatic cells (typically skin fibroblasts or peripheral blood mononuclear cells) [11].
Reprogramming to Pluripotency: Somatic cells are reprogrammed using integration-free methods such as Sendai virus, episomal vectors, or mRNA transfection to generate iPSCs [11]. Critical quality control steps include:
- Pluripotency marker verification (OCT4, NANOG, SOX2)
- Karyotype analysis to ensure genomic integrity
- Trilineage differentiation potential confirmation
Genetic Validation and Isogenic Control Generation: Patient-derived iPSCs are genetically characterized to confirm the presence of PD-related mutations. CRISPR/Cas9 gene editing is used to create isogenic controls by correcting pathogenic mutations in patient lines or introducing specific mutations in control lines [20] [30].
Directed Differentiation to Dopaminergic Neurons: iPSCs are differentiated into midbrain-patterned dopaminergic neurons using established protocols that recapitulate developmental signaling pathways [30] [75]. Key steps include:
- Dual SMAD inhibition to induce neural induction
- Activation of SHH and WNT signaling for midbrain patterning
- Maturation using neurotrophic factors (BDNF, GDNF, ascorbic acid)
Phenotypic Analysis: Differentiated neurons are analyzed for disease-relevant phenotypes using functional assays, omics approaches, and morphological assessments [20] [30].
Signaling Pathways in Parkinson's Disease Pathogenesis Revealed by iPSC Models
iPSC-based studies have illuminated key pathogenic pathways in PD, highlighting the interconnected nature of cellular dysfunction in neurodegeneration.
The diagram illustrates how iPSC models have revealed the complex interplay between different pathogenic mechanisms in PD, with particular emphasis on:
- The central role of α-synuclein accumulation in driving multiple aspects of cellular dysfunction
- The bidirectional relationship between oxidative stress and mitochondrial defects
- The vicious cycle between lysosomal impairment and α-synuclein clearance
- The convergence of multiple pathways on ultimately leading to dopaminergic neuron loss
The Scientist's Toolkit: Essential Reagents for iPSC-Based PD Research
Table 2: Key Research Reagent Solutions for iPSC-Based Parkinson's Disease Modeling
| Reagent Category | Specific Examples | Function in PD Modeling |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [11] | Reprogram somatic cells to pluripotent state; modern approaches use non-integrating methods |
| Neural Induction Media | Dual SMAD inhibitors (SB431542, LDN193189) [30] [75] | Direct differentiation toward neural lineage by inhibiting TGF-β and BMP signaling |
| Midbrain Patterning Factors | SHH (Sonic Hedgehog), FGF8, CHIR99021 (WNT activator) [30] [75] | Specify regional identity to generate authentic midbrain dopaminergic neurons |
| Neuronal Maturation Factors | BDNF, GDNF, ascorbic acid, cAMP, TGF-β3 [30] [6] | Promote terminal differentiation, survival, and functional maturation of dopaminergic neurons |
| Disease-Associated Stressors | Rotenone, CCCP, oligomeric α-synuclein [20] [30] | Induce or exacerbate disease-relevant phenotypes for mechanistic studies and compound screening |
| Cell Sorting Markers | CORIN+ sorting for dopaminergic progenitors [6] | Enrich for desired cell population to improve consistency and reduce off-target differentiation |
Quantitative Assessment of Model Performance and Clinical Translation
Comparative Functional Outcomes
iPSC-derived dopaminergic neurons consistently demonstrate functionality both in vitro and in transplantation settings. Recent clinical trials have provided compelling evidence for the therapeutic potential of iPSC-derived dopaminergic progenitors:
Table 3: Clinical Trial Outcomes of iPSC-Derived Dopaminergic Progenitors in Parkinson's Disease Patients [6]
| Outcome Measure | Baseline Value | 24-Month Post-Transplantation | Change (%) |
|---|---|---|---|
| MDS-UPDRS Part III OFF | 46.5 points | 37.0 points | -9.5 points (-20.4%) |
| MDS-UPDRS Part III ON | 12.0 points | 7.7 points | -4.3 points (-35.7%) |
| 18F-DOPA uptake in putamen | Baseline Ki | Increased Ki | +44.7% |
| Hoehn & Yahr Stage OFF | Stage 3-4 | Improved in 4/6 patients | 1-2 stage improvement |
| Graft volume on MRI | Day 7 post-op | 24 months post-op | Gradual increase without overgrowth |
| Serious adverse events | - | - | 0 events related to cell product |
The trial results demonstrate that allogeneic iPSC-derived dopaminergic progenitors survived, produced dopamine, and improved motor function without forming tumors or causing serious adverse events [6]. These findings validate the functional competence of iPSC-derived cells and their potential to integrate into host neural circuits.
Advantages in Drug Discovery and Screening
The transition toward iPSC-based models in drug discovery is accelerated by both scientific and regulatory factors:
- Human-relevant biology: iPSC-derived neurons express human-specific drug targets and metabolic pathways, improving predictive accuracy [74].
- High-throughput capability: iPSC models enable screening of compound libraries in human neurons at scale, overcoming the throughput limitations of animal models [11] [74].
- Regulatory support: The FDA has issued guidance encouraging the use of novel technologies like iPSCs in drug development [74].
- Ethical and supply advantages: iPSCs address ethical concerns associated with animal testing and supply chain issues affecting non-human primate availability [74].
iPSC technology has fundamentally transformed Parkinson's disease research by providing a human-relevant platform that effectively bridges the species gap inherent in transgenic mouse models. The preservation of complete human genetic background, combined with the ability to generate disease-relevant cell types, has enabled unprecedented insights into PD pathogenesis and accelerated therapeutic development. As differentiation protocols continue to refine and maturation techniques improve, iPSC-based models will play an increasingly central role in delineating the complex mechanisms underlying PD and developing effective interventions for this devastating neurodegenerative disorder. The recent success of clinical trials using iPSC-derived dopaminergic progenitors marks a critical milestone in the translation of this technology from basic research to clinical application [6].
The quest to understand Parkinson's disease (PD) pathogenesis has entered a transformative phase with the advent of induced pluripotent stem cell (iPSC) technology. PD, the second most common neurodegenerative disorder after Alzheimer's disease, affects millions worldwide and is characterized by the progressive loss of dopaminergic neurons in the substantia nigra pars compacta and the presence of intracellular protein aggregates composed primarily of α-synuclein, known as Lewy bodies [76] [77]. The complexity of PD has historically hindered the development of accurate disease models that faithfully recapitulate human pathology, creating a significant barrier to therapeutic development [1]. iPSC-derived models now offer an unprecedented platform for investigating PD pathogenesis by maintaining a patient's complete genetic background while enabling the study of disease mechanisms in relevant human cell types [78]. This technical guide examines how in vitro phenotypes observed in iPSC models—particularly those related to α-synuclein pathology and mitochondrial dysfunction—correlate with patient pathology, providing researchers with methodologies and frameworks for advancing PD research and drug development.
iPSC Differentiation into Relevant Neural Cells
Dopaminergic Neuron Differentiation Protocols
The generation of authentic midbrain dopaminergic (DA) neurons is crucial for modeling Parkinson's disease pathology. Several established protocols enable efficient differentiation of iPSCs into DA neurons with characteristics of substantia nigra pars compacta neurons [78] [79].
The most robust protocols involve a dual-SMAD inhibition approach using small molecule inhibitors to direct neural induction. This typically involves using SB431542 (an inhibitor of activin-nodal signaling) and LDN193189 (a BMP signaling inhibitor) or Noggin to inhibit SMAD signaling [78] [79]. Subsequently, patterning toward a midbrain DA identity is achieved through activation of sonic hedgehog (SHH) signaling using compounds such as purmorphamine or Sonic C25II, along with FGF8 treatment [79]. The precise timing and concentration of a GSK3β inhibitor (such as CHIR99021) are critical for specifying midbrain character, with concentrations typically ranging from 0.3 to 0.8 μM proving effective for inducing FOXA2+/LMX1A+ floor plate progenitors that subsequently give rise to tyrosine hydroxylase-positive (TH+) DA neurons [79].
A refined protocol described by Kriks et al. demonstrates that simultaneous use of LSB (LDN193189 + SB431542)/FGF8/CHIR yields a high percentage of FOXA2+/TH+ co-expressing DA neurons that possess essential physiological traits of mature substantia nigra pars compacta DA neurons, including appropriate electrophysiological properties and dopamine release capability [79]. These neurons show viability in transplantation studies and represent a validated model for PD research.
For later stages of maturation, the protocol involves replacing the neural induction medium with Neurobasal and B27 supplements, typically around day 10-14, with the addition of 20 ng/ml brain-derived neurotrophic factor (BDNF) to induce final neural maturation around day 30 [79]. Additional factors including ascorbic acid, glial cell-derived neurotrophic factor (GDNF), and cAMP further enhance neuronal maturation and survival.
Advanced Model Systems: Co-cultures and Organoids
Beyond 2D monocultures, researchers are developing more complex models to better recapitulate the cellular environment of the human brain. Co-culture systems of iPSC-derived neurons and glial cells (particularly astrocytes and microglia) provide critical insights into cell-cell interactions in PD pathogenesis [1]. These systems allow investigation of how neuroinflammation contributes to neurodegeneration, a key aspect of PD pathology.
3D brain region-specific organoids represent another advancement, enhancing our understanding of interregional disease processes and spatial organization of pathology [1]. Midbrain organoids containing DA neurons, astrocytes, and other neural cell types can model the complex tissue architecture and cell-cell interactions not captured in 2D systems. These organoids show promise for studying α-synuclein propagation between cells and the differential vulnerability of neuronal populations.
Table 1: Key Components in Dopaminergic Neuron Differentiation
| Component | Type | Function | Typical Concentration |
|---|---|---|---|
| SB431542 | Small molecule inhibitor | Inhibits activin-nodal signaling (TGF-β pathway) | 10-20 μM |
| LDN193189 | Small molecule inhibitor | Inhibits BMP signaling | 100-200 nM |
| CHIR99021 | GSK3β inhibitor | Activates Wnt signaling, patterns midbrain | 0.3-0.8 μM |
| Purmorphamine | Smoothened agonist | Activates SHH signaling | 0.5-2 μM |
| FGF8 | Growth factor | Patterns anterior-posterior axis | 50-100 ng/ml |
| BDNF | Neurotrophin | Supports neuronal maturation & survival | 20-50 ng/ml |
| GDNF | Neurotrophic factor | Promotes dopaminergic neuron survival | 10-20 ng/ml |
| Ascorbic acid | Antioxidant | Promotes neuronal differentiation | 200 μM |
Alpha-Synuclein Pathophysiology in iPSC Models
Physiological Functions and Pathological Transitions
α-synuclein is a 14-kDa protein, ubiquitously expressed in presynaptic terminals of the brain, predominantly in excitatory neurons [78]. Under normal physiological conditions, α-synuclein is considered a natively unfolded protein whose structure can vary according to changes in the local environment, particularly through interactions with lipids or metals [78]. The precise physiological function of α-synuclein remains incompletely understood, but evidence points to several roles associated with synaptic function, including: vesicle clustering, recycling, maintenance of the synaptic vesicles reserve pool, and promotion of SNARE complex formation which enhances neurotransmitter release [78]. Additionally, α-synuclein is involved in intracellular trafficking regulation through interaction with multiple members of the Rab GTPase family, as well as with microtubule nucleation and growth velocity [78].
Mutations in the SNCA gene, which encodes α-synuclein, were the first identified genetic cause of autosomal-dominant PD [78] [77]. Well-characterized point mutations include A53T, A30P, E46K, and H50Q [77]. Additionally, multiplications of the SNCA gene (duplications and triplications) cause familial PD with a gene dosage effect, where triplication carriers present with earlier onset and more severe symptoms than duplication carriers [78]. These mutations and multiplications promote α-synuclein aggregation through distinct mechanisms, including accelerating fibril formation, impairing membrane binding, or simply increasing protein concentration.
α-Synuclein Phenotypes in iPSC-Derived Models
iPSC models harboring SNCA mutations recapitulate key aspects of α-synuclein pathology observed in PD patients. iPSC-derived DA neurons with SNCA triplication display increased α-synuclein mRNA levels, resulting in abnormal and elevated levels of protein expression [78]. These neurons also show higher levels of α-synuclein phosphorylation at serine residue 129 (pS129), a common post-translational modification found in Lewy bodies in PD brains [78]. Additionally, they demonstrate abnormal increases in soluble α-synuclein oligomers and insoluble aggregates, recapitulating the Lewy body pathology observed postmortem [78].
The A53T point mutation, one of the most studied SNCA variants, promotes faster formation of fibrils in iPSC-derived neurons, which are thought to be more toxic than wild-type α-synuclein aggregates [77]. These mutant α-synuclein forms affect membrane permeability and integrity, promoting cell death through disruption of cellular homeostasis [78].
Mechanistically, endoplasmic reticulum (ER) stress and activation of the unfolded protein response (UPR) represent key pathways implicated in SNCA triplication models [78]. The accumulation of misfolded α-synuclein overwhelms the protein quality control systems, leading to sustained ER stress and activation of apoptotic pathways in vulnerable DA neurons.
Diagram 1: α-Synuclein Pathogenesis Cascade. This pathway illustrates the progression from genetic mutations to cellular dysfunction in Parkinson's disease.
Mitochondrial Dysfunction in iPSC Models
Evidence for Mitochondrial Impairment in PD
Mitochondrial dysfunction has long been implicated as a key pathological hallmark in PD, with multiple lines of evidence supporting its role [80]. The initial link emerged from observations that individuals exposed to the mitochondrial complex I inhibitor MPTP developed parkinsonism [80]. Subsequent studies showed that other mitochondrial toxins, including rotenone and paraquat, are associated with increased PD risk and can recapitulate PD features in animal models [80] [77].
In postmortem brain tissue from idiopathic PD patients, the most pronounced and consistent finding is decreased activity of mitochondrial complex I of the electron transport chain in substantia nigra tissue homogenates [80]. Some studies have also observed complex I deficiency in frontal and prefrontal cortices and striatum, but not consistently in peripheral tissues, suggesting a brain-specific vulnerability [80].
Genetic studies further support mitochondrial involvement, with mutations in PINK1 and Parkin—proteins essential for mitochondrial quality control through mitophagy—causing early-onset recessive PD [81] [80]. Additionally, mutations in LRRK2, the most common cause of autosomal dominant PD, have been linked to mitochondrial dysfunction through multiple mechanisms [81].
Mitochondrial Phenotypes in iPSC-Derived Neural Cells
iPSC-derived neural cells from PD patients with different genetic backgrounds consistently demonstrate mitochondrial abnormalities, suggesting convergent pathogenic mechanisms [81] [79]. Neural cells derived from patients with PINK1 mutations show increased vulnerability to mitochondrial toxins, including valinomycin (a potassium ionophore) and MPP+ (the active metabolite of MPTP) [81]. Similarly, cells carrying LRRK2 mutations (G2019S and R1441C) share vulnerabilities to these mitochondrial stressors, though with somewhat different sensitivity profiles [81].
Several specific mitochondrial deficits have been characterized in iPSC-derived neural models:
- Increased mitochondrial reactive oxygen species (mROS): Neural cells from PD patients with PINK1 mutations demonstrate heightened production of mROS in response to low concentrations of valinomycin compared to controls [81].
- Reduced glutathione levels: Neural cells from PINK1 Q456X patients show decreased reduced glutathione (GSH) following exposure to mitochondrial stressors, indicating impaired antioxidant capacity and increased oxidative stress [81].
- Altered mitochondrial respiration: Measurements of oxygen consumption rates reveal differences in basal respiration, ATP-linked respiration, and maximal respiratory capacity in neural cells carrying PINK1 or LRRK2 mutations compared to healthy controls [81].
- Impaired mitochondrial trafficking: Disruption of intracellular mitochondrial movement has been observed in several PD iPSC models, potentially compromising the distribution of energy sources in neurons with extensive axonal arbors [79].
Table 2: Mitochondrial Stressors and Their Effects in iPSC-Derived Neural Cells
| Stressor | Mechanism of Action | Observed Effects in PD iPSC Models |
|---|---|---|
| Valinomycin | Potassium ionophore | Increased cytotoxicity in PINK1/LRRK2 cells; elevated mROS in PINK1 cells |
| MPP+ | Complex I inhibitor | Increased vulnerability in PINK1/LRRK2 mutant cells |
| Concanamycin A | V-ATPase inhibitor | Increased cytotoxicity in PINK1/LRRK2 mutant cells |
| Hydrogen peroxide | Oxidant stressor | Increased cytotoxicity and reduced GSH in PINK1 mutant cells |
| MG132 | Proteasome inhibitor | Increased vulnerability in PINK1 mutant cells |
| CCCP | Mitochondrial uncoupler | Moderate increased vulnerability in LRRK2 mutant cells |
Correlating In Vitro Phenotypes with Patient Pathology
Alpha-Synuclein Pathology Correlations
The α-synuclein pathology observed in iPSC-derived models closely mirrors key aspects of human PD neuropathology. In postmortem PD brains, the defining feature is the presence of Lewy bodies and Lewy neurites—intracellular inclusions rich in fibrillar, phosphorylated α-synuclein [76] [77]. iPSC-derived DA neurons with SNCA mutations recapitulate several aspects of this pathology, including:
- Phosphorylated α-synuclein accumulation: Increased levels of α-synuclein phosphorylated at serine 129, a characteristic modification in Lewy bodies, are observed in iPSC-derived neurons with SNCA triplications and A53T mutations [78].
- Soluble oligomer formation: The appearance of soluble α-synuclein oligomers, believed to be the primary toxic species in PD, precedes the formation of larger aggregates in iPSC models, mirroring the suspected progression in human disease [78] [77].
- Protein aggregation: While mature Lewy bodies with their characteristic concentric structure are rarely fully replicated in short-term 2D cultures, 3D organoid models show more advanced aggregation pathology that more closely resembles patient tissue [1].
The prion-like propagation of α-synuclein pathology observed in PD patients, where pathological α-synuclein appears to spread between connected brain regions, has also been modeled in iPSC systems. These models demonstrate cell-to-cell transfer of pathological α-synuclein species, providing a platform for investigating mechanisms and therapeutic interventions for limiting disease progression [77].
Mitochondrial Pathology Correlations
The mitochondrial dysfunction observed in iPSC models correlates with substantial evidence from postmortem PD brain tissue and genetic studies. The consistent finding of complex I deficiency in the substantia nigra of PD patients [80] is mirrored by similar deficits in iPSC-derived DA neurons carrying PD-associated mutations [81] [79].
The particular vulnerability of SNc dopaminergic neurons in PD is thought to relate to their unique bioenergetic demands. These neurons possess extensive, unmyelinated axonal arbors with an enormous number of transmitter release sites (estimated at 1-2 million per axon in humans), creating exceptional energy demands [80]. To meet these demands, these neurons employ a feed-forward control mechanism that utilizes plasma membrane L-type Ca2+ channels to drive mitochondrial oxidative phosphorylation [80]. While this ensures adequate ATP production, it increases basal mitochondrial oxidant stress and production of reactive oxygen species, creating a vulnerable cellular environment.
iPSC-derived DA neurons recapitulate aspects of this physiological vulnerability, particularly when differentiated to a mature, functional state with similar electrophysiological properties to native SNc neurons [79]. In these models, the combined effects of genetic susceptibility and physiological stress create a platform for investigating the intersection of cell-autonomous and non-cell-autonomous factors in PD pathogenesis.
Diagram 2: Convergence of Pathogenic Mechanisms in PD. This diagram illustrates how genetic and environmental factors lead to neuronal vulnerability through multiple interconnected pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for iPSC-Based PD Modeling
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Small Molecule Inhibitors | SB431542, LDN193189, CHIR99021, Noggin | Directed differentiation of iPSCs to dopaminergic neurons via dual-SMAD inhibition and Wnt activation |
| Patterning Factors | SHH (or purmorphamine), FGF8, BDNF, GDNF | Regional specification toward midbrain identity and neuronal maturation |
| Mitochondrial Stressors | Valinomycin, MPP+, rotenone, CCCP, concanamycin A | Probing mitochondrial vulnerability and stress response pathways |
| Gene Editing Tools | CRISPR/Cas9, TALENs, ZFNs | Isogenic control generation, disease mutation introduction, gene correction |
| Detection Antibodies | Anti-TH, anti-FOXA2, anti-LMX1A, anti-pS129 α-synuclein | Cell type validation, pathology assessment, differentiation efficiency quantification |
| Functional Assays | MitoStress Test (Seahorse), Ca2+ imaging, electrophysiology, microelectrode arrays | Assessment of mitochondrial function, neuronal activity, and network formation |
| Advanced Culture Systems | 3D organoid platforms, microfluidic devices, co-culture systems | Modeling complex cell-cell interactions, disease propagation, and tissue-level pathology |
iPSC-based modeling has fundamentally advanced our ability to correlate in vitro phenotypes with patient pathology in Parkinson's disease. The robust recapitulation of α-synuclein pathology and mitochondrial dysfunction in these models provides unprecedented opportunities to investigate disease mechanisms in a human-specific, genetically relevant context. The convergence of pathological pathways observed across different genetic forms of PD in iPSC models suggests common final pathways to neurodegeneration that may be amenable to therapeutic targeting. As the field progresses, increasing model complexity through co-culture systems, organoids, and multisystem integration will further enhance the physiological relevance of these platforms. Combined with advanced gene editing and multi-omics approaches, iPSC-based modeling represents a cornerstone technology for bridging the gap between in vitro observations and patient pathology, accelerating both mechanistic understanding and therapeutic development for Parkinson's disease.
The translation of induced pluripotent stem cell (iPSC) technology from in vitro disease modeling to clinical-grade cell therapies represents a pivotal advancement in Parkinson's disease (PD) treatment. This whitepaper synthesizes data from recent groundbreaking clinical trials that provide the first clinical validation for iPSC-based interventions. By analyzing safety profiles, efficacy metrics, and methodological frameworks from these pioneering studies, we establish a compelling proof of concept that iPSC-derived dopaminergic neurons can safely engraft, survive, and functionally integrate in the human PD brain. These findings validate decades of preclinical research using iPSC models of PD pathogenesis and mark the dawn of a new era in regenerative neurology.
Parkinson's disease is characterized by the progressive degeneration of dopaminergic neurons in the substantia nigra, leading to characteristic motor symptoms including bradykinesia, rigidity, and resting tremor [49] [82]. Since the pioneering work of Yamanaka et al., iPSC technology has revolutionized PD research by enabling the generation of patient-specific dopaminergic neurons that recapitulate disease pathophysiology in vitro [49] [20]. These models have been instrumental in elucidating key disease mechanisms, including α-synuclein aggregation, mitochondrial dysfunction, oxidative stress, and lysosomal impairment [20] [37].
The logical progression from disease modeling to replacement therapy has now materialized in first-in-human clinical trials testing the safety and efficacy of iPSC-derived dopaminergic progenitors. This whitepaper examines the recent clinical evidence that establishes proof of concept for this therapeutic paradigm, contextualizing findings within the broader understanding of PD pathogenesis derived from iPSC disease models.
Clinical Trial Outcomes and Quantitative Analysis
Key Clinical Trials and Their Outcomes
Recent clinical trials have demonstrated the feasibility, safety, and initial efficacy of iPSC-based cell therapies for PD. The table below summarizes the primary outcomes from these pioneering studies.
Table 1: Clinical Trial Outcomes of iPSC-Based Cell Therapies for Parkinson's Disease
| Trial Reference | Phase | Patient Number | Cell Type | Dosing | Primary Safety Outcomes | Efficacy Measures (24 Months) |
|---|---|---|---|---|---|---|
| Kyoto University Trial [6] | I/II | 7 (6 for efficacy) | Allogeneic iPSC-derived dopaminergic progenitors | Low: 2.1-2.6×10⁶ cells/hemisphere; High: 5.3-5.5×10⁶ cells/hemisphere | No serious adverse events; 73 mild-moderate events; No tumor formation | MDS-UPDRS Part III OFF: -9.5 points (-20.4%); ON: -4.3 points (-35.7%); 18F-DOPA Ki values increased by 44.7% |
| Mass General Brigham [83] | I | 3 (of 6 planned) | Autologous iPSC-derived dopaminergic neurons | N/A | No serious adverse events reported; No immunosuppression required | Ongoing trial; 12-month monitoring period |
| Bemdaneprocel (hESC-derived) [7] [84] | I | 12 | Allogeneic hESC-derived dopaminergic progenitors | Low: 0.9×10⁶; High: 2.7×10⁶ cells/putamen | No related serious adverse events; No graft-induced dyskinesias | MDS-UPDRS Part III OFF: -23 points (high-dose cohort); Increased 18F-DOPA uptake at 18 months |
Safety and Immunological Profile
The safety profile emerging from these trials is particularly noteworthy. The Kyoto University trial reported no serious adverse events related to the cell product, with all 73 adverse events characterized as mild to moderate [6]. Critically, serial MRI imaging showed no evidence of tumor-like abnormal enlargement, addressing a fundamental concern regarding pluripotent stem cell-derived therapies [6].
Immunological compatibility has been a central consideration in these trials. The Kyoto trial utilized an allogeneic approach with iPSCs homozygous for a common Japanese haplotype, combined with transient tacrolimus immunosuppression [6] [54]. Research indicates that the low expression of HLA in iPSC-derived dopaminergic neurons contributes to successful engraftment in the immune-privileged CNS, potentially reducing immunosuppression requirements [54]. In contrast, the ongoing Mass General Brigham trial is investigating an autologous approach using the patient's own reprogrammed cells, which may circumvent the need for immunosuppression entirely [83].
Table 2: Safety and Immunological Profiles Across Cell Therapy Approaches
| Parameter | Allogeneic iPSC Approach [6] [54] | Autologous iPSC Approach [83] | hESC-Based Approach [7] |
|---|---|---|---|
| Immunosuppression Regimen | Tacrolimus (0.06 mg/kg twice daily), reduced by half at 12 months, discontinued at 15 months | None required (theoretically) | Basiliximab intraoperatively, methylprednisolone with prednisone taper, tacrolimus for 1 year |
| Graft Survival Monitoring | Serial MRI, 18F-DOPA PET showing 44.7% increase in Ki values | Ongoing evaluation | Increased 18F-DOPA PET uptake at 18 months |
| Tumorigenicity Risk | No tumors or abnormal tissue overgrowth detected | Preclinical data showed no tumor formation | No tumors detected |
| Most Common Adverse Events | Application site pruritus (57.1%), hepatic impairment, renal impairment | No serious adverse events reported in initial patients | One seizure attributed to surgical procedure |
Experimental Protocols and Methodologies
iPSC Differentiation and Dopaminergic Neuron Induction
The clinical trials implemented refined protocols for dopaminergic differentiation based on developmental principles. The core methodology across studies involves:
- iPSC Generation: Dermal fibroblasts or peripheral blood mononuclear cells are reprogrammed using forced expression of Yamanaka factors (OCT4, Sox2, Klf4, c-Myc) [49] [20].
- Neural Induction: Dual SMAD inhibition (using SB431542 and LDN193189) to direct cells toward a neural fate [49] [7].
- Floor Plate Patterning: Activation of sonic hedgehog (SHH) and Wnt signaling to specify midbrain dopaminergic identity through a floor plate intermediate [6] [7].
- Progenitor Selection: Fluorescence-activated cell sorting (FACS) for CORIN+ cells, a floor plate marker, to enrich for dopaminergic progenitors (approximately 60% purity in the Kyoto trial) [6].
- Final Product Composition: The transplantation product typically contains a mixture of dopaminergic progenitors (FOXA2+, LMX1A+) and post-mitotic dopaminergic neurons (TUJ1+, TH+) [6].
Surgical Delivery and Engraftment Monitoring
The surgical protocol standardized across trials involves:
- Stereotactic Navigation: MRI-guided delivery to the postcommissural putamen bilaterally [6] [7].
- Cell Delivery: Multiple deposits (e.g., 9 deposits per putamen in the bemdaneprocel trial) distributed along the putaminal axis [7].
- Cell Viability: Transplantation of fresh cell suspensions (Kyoto trial) or thawed cryopreserved products (bemdaneprocel trial) at concentrations of approximately 100,000 cells/μL [6] [7].
- Engraftment Monitoring: Serial 18F-DOPA PET imaging to quantify presynaptic dopaminergic function, complemented by MRI to monitor graft volume and potential inflammatory responses [6] [7].
Diagram 1: iPSC Therapy Clinical Workflow (55 characters)
Pathogenic Mechanisms and Therapeutic Validation
Molecular Pathways Targeted by iPSC-Based Interventions
iPSC-based cell replacement therapy represents a mechanistic approach to counter multiple interconnected pathways in PD pathogenesis:
Dopaminergic Network Restoration: Grafted neurons establish synaptic connections and restore dopamine transmission in the denervated striatum, directly addressing the primary neurotransmitter deficit in PD [6] [7].
α-Synuclein Pathology Modulation: While not directly reducing α-synuclein aggregates, healthy grafted neurons may resist pathological spread and provide trophic support to host circuitry [49] [37].
Mitochondrial Function: iPSC-derived dopaminergic neurons from healthy donors presumably possess intact mitochondrial quality control mechanisms, potentially resisting the mitochondrial dysfunction observed in PD patient-derived neurons [20] [37].
Neuroinflammation Modulation: Emerging evidence suggests that correctly integrated grafts may modulate neuroinflammatory responses, though this mechanism requires further investigation [85].
Diagram 2: Mechanism of Action Overview (32 characters)
Validation of iPSC Disease Models Through Therapeutic Efficacy
The clinical efficacy observed in these trials provides compelling validation for iPSC-based disease modeling. The 20.4% improvement in MDS-UPDRS Part III OFF scores and 44.7% increase in 18F-DOPA uptake in the Kyoto trial demonstrate that the dopaminergic neurons generated through iPSC differentiation protocols are functionally competent [6]. These clinical outcomes validate the extensive characterization of iPSC-derived dopaminergic neurons that showed they are indistinguishable from human fetal mesencephalic dopaminergic neurons in terms of functionality, potency, maturity, and axonal outgrowth capacity [49].
Furthermore, the absence of graft-induced dyskinesias in these trials (in contrast to earlier fetal tissue transplantation studies) supports the strategy of using floor plate-patterned progenitors that more authentically recapitulate developmental midbrain identity while minimizing contamination by serotonergic neurons [6] [7].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for iPSC-Based PD Research and Therapy
| Reagent/Platform Category | Specific Examples | Research Application | Clinical Translation |
|---|---|---|---|
| Reprogramming Factors | Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) | iPSC generation from patient somatic cells | Clinical-grade vectors for autologous iPSC generation [83] |
| Neural Patterning Molecules | Dual SMAD inhibitors (SB431542, LDN193189), SHH agonists, Wnt activators | Directed differentiation to midbrain dopaminergic fate | GMP-grade patterning molecules for clinical production [6] [7] |
| Cell Sorting Markers | CORIN, LMX1A, FOXA2 antibodies | Purification of dopaminergic progenitors | Clinical-grade FACS sorting for product enrichment [6] |
| Functional Validation Assays | Electrophysiology, dopamine release measurements, synaptic marker analysis | Verification of neuronal maturity and function | Potency assays for product release criteria |
| Genomic Engineering Tools | CRISPR/Cas9 systems | Generation of isogenic controls, disease modeling | Potential for genetic correction in autologous approaches [20] [37] |
| In Vivo Modeling Platforms | Rodent and non-human primate PD models | Preclinical safety and efficacy testing | Required for IND-enabling studies [6] [83] |
The clinical validation emerging from recent iPSC-based cell therapy trials establishes a robust proof of concept for this innovative treatment approach. The demonstrated safety, graft survival, and functional efficacy validate the extensive preclinical work utilizing iPSC models of PD pathogenesis. These trials confirm that iPSC-derived dopaminergic neurons can authentically recapitulate the phenotypic and functional properties of native midbrain dopaminergic neurons, addressing the core pathology of PD.
Future directions include optimization of dosing parameters, refinement of immunosuppression regimens, development of more precise patient selection criteria, and implementation of enhanced delivery techniques. The ongoing development of autologous approaches [83] and the exploration of gene-editing technologies to correct underlying mutations represent the next frontier in personalized cell therapy for PD.
As these therapies advance through later-phase clinical trials, they promise to transform the treatment landscape for PD while simultaneously refining our understanding of disease pathogenesis through continued correlation of clinical outcomes with cellular and molecular phenotypes identified in iPSC models.
The field of preclinical drug development stands at a pivotal crossroads, marked by a strategic shift from reliance on traditional animal models toward more human-relevant systems. This transition is driven by a critical recognition of the limitations inherent in animal models, including significant physiological differences, ethical concerns, and high attrition rates in clinical translation. Induced pluripotent stem cell (iPSC) technology has emerged as a transformative platform, enabling the generation of patient-specific human cells for disease modeling and drug screening. Within the specific context of Parkinson's disease (PD) research—characterized by the progressive loss of dopaminergic neurons in the substantia nigra—iPSCs offer unprecedented opportunities to create human-relevant models that recapitulate disease mechanisms. This whitepaper explores the strategic integration of iPSC-derived models with traditional animal testing, outlining a synergistic framework that enhances the predictive power, efficiency, and human relevance of preclinical drug development for PD and other neurodegenerative disorders.
The Limitations of Traditional Animal Models in Parkinson's Disease Research
Animal models have long served as the cornerstone of biomedical research, but their limitations are increasingly apparent in complex neurodegenerative diseases like Parkinson's.
Physiological Disparities and Translational Challenges
Significant physiological differences between animal models and humans contribute to poor translational outcomes. In cardiovascular research, for instance, heart rate variations are substantial, with mice exhibiting 300-600 bpm compared to 60-100 bpm in humans [86]. Zebrafish, while having more comparable heart rates (120-180 bpm), possess a simpler circulatory system with one atrium and one ventricle versus the four-chambered heart in humans [86]. These fundamental physiological differences extend to the brain and neurodegenerative processes, where species-specific variations in neuroanatomy, protein aggregation, and metabolic pathways can profoundly impact disease manifestation and treatment response.
High Attrition Rates in Drug Development
The failure rate of drug candidates advancing from animal studies to human trials remains alarmingly high. Approximately 90% of drug candidates deemed safe and effective in animal models ultimately fail in human clinical trials [87] [88]. Recent high-profile failures include Pfizer's gene therapy for Duchenne muscular dystrophy and Sage Therapeutics' Dalzanemdor for neurodegenerative diseases, both of which showed promise in animal studies but failed to demonstrate efficacy in human trials [87]. These repeated failures highlight the critical need for more human-predictive models early in the drug development pipeline.
Ethical and Regulatory Considerations
Growing ethical concerns and changing regulatory landscapes are accelerating the shift away from animal models. The U.S. Food and Drug Administration (FDA) has published a detailed roadmap to reduce reliance on animal testing in preclinical safety studies, embracing validated New Approach Methodologies (NAMs) including human iPSC-derived systems [87] [88]. The FDA Modernization Act 2.0 removed the mandatory requirement for animal testing in many cases, reflecting both ethical considerations and recognition of the scientific limitations of animal models [88].
Table 1: Limitations of Traditional Animal Models in Neurodegenerative Disease Research
| Limitation Category | Specific Challenges | Impact on Drug Development |
|---|---|---|
| Physiological Differences | Divergent brain anatomy, metabolic rates, protein aggregation mechanisms | Poor translation of therapeutic efficacy and safety findings |
| Genetic Disparities | Differences in gene regulation, disease-associated pathways | Incomplete modeling of human disease mechanisms |
| Ethical Considerations | Animal welfare concerns, public acceptance | Increasing regulatory restrictions and public scrutiny |
| Practical Constraints | High costs, long experimental timelines, specialized facilities | Limited throughput and scalability for drug screening |
The Rise of iPSC Technology in Parkinson's Disease Modeling
The development of induced pluripotent stem cell (iPSC) technology represents a paradigm shift in disease modeling and drug development. First established in 2006-2007, iPSCs are generated by reprogramming adult somatic cells into a pluripotent state using defined factors, then differentiating them into specific cell types relevant to disease pathology [11].
iPSC-Based Modeling of Parkinson's Disease Pathogenesis
In Parkinson's disease research, iPSCs have been successfully differentiated into dopaminergic neurons—the primary cell type affected in PD—enabling detailed investigation of disease mechanisms. Patient-derived iPSC models have been generated for various genetic forms of PD, including mutations in LRRK2, SNCA (encoding α-synuclein), GBA, PINK1, and VPS35 [30]. These models recapitulate key pathological features observed in PD patients, such as:
- α-Synuclein pathology: iPSC-derived dopaminergic neurons from patients with SNCA triplication show increased α-synuclein expression, oligomer formation, and impaired mitochondrial transport [30].
- Mitochondrial dysfunction: DA neurons from patients with A53T and E46K SNCA mutations display fragmented mitochondria, decreased membrane potential, and altered energy metabolism [30].
- Oxidative stress: SNCA triplication neurons demonstrate increased susceptibility to oxidative stress and upregulation of stress-response genes like MAO-A [30].
- Protein processing defects: PD iPSC-derived neurons exhibit endoplasmic reticulum stress and activation of the unfolded protein response pathway [30].
Advanced iPSC Model Systems: From 2D to 3D
The evolution of iPSC-based models has progressed from simple two-dimensional (2D) monocultures to complex three-dimensional (3D) systems that better mimic human tissue architecture and cell-cell interactions.
- 2D Co-culture Systems: Co-culture of iPSC-derived neurons with glial cells provides insights into cell-cell interactions in PD pathogenesis [1]. These systems have revealed the importance of non-cell-autonomous mechanisms in PD progression.
- 3D Organoid Models: Brain region-specific organoids enhance understanding of interregional disease processes and complex tissue-level pathology [1]. Midbrain organoids containing dopaminergic neurons, astrocytes, and other neural cell types model the complex microenvironment of the substantia nigra.
- Microphysiological Systems: Organ-on-chip platforms incorporating iPSC-derived cells replicate tissue-tissue interfaces and physiological fluid flow, enabling more realistic modeling of drug distribution and metabolism [87].
Table 2: iPSC-Derived Cellular Models for Parkinson's Disease Research
| Model Type | Key Components | Applications in PD Research | Advantages |
|---|---|---|---|
| 2D Monocultures | iPSC-derived dopaminergic neurons | High-throughput drug screening, mechanistic studies | Scalability, ease of manipulation, reproducible readouts |
| 2D Co-culture Systems | Neurons + astrocytes/microglia | Studying neuroinflammation, cell-cell interactions | Modeling non-cell-autonomous disease mechanisms |
| 3D Organoids | Multiple neural cell types in tissue-like organization | Modeling complex pathology, network-level dysfunction | Recapitulation of tissue architecture, cell diversity |
| Microphysiological Systems | iPSC-derived cells in engineered microenvironments | Drug permeability, metabolism, and toxicity studies | Integration of physiological flow, tissue-tissue interfaces |
Integrated Framework: Combining iPSC and Animal Model Data
The most robust preclinical strategy leverages the complementary strengths of both iPSC-based models and animal systems through a hierarchical, integrated approach.
Experimental Workflow for Integrated Preclinical Testing
The following diagram illustrates a systematic workflow for integrating iPSC and animal model data in Parkinson's disease drug development:
Strategic Integration Approaches
Hierarchical Screening Pipeline
Implementing a tiered screening approach where compounds are first evaluated in high-throughput iPSC-based assays before advancing to more complex and costly animal studies. This strategy maximizes resource efficiency by prioritizing the most promising candidates for in vivo validation. iPSC-derived dopaminergic neurons enable rapid assessment of compound efficacy in rescuing disease-related phenotypes such as mitochondrial dysfunction, oxidative stress, and α-synuclein aggregation [1] [30].
Humanized Animal Models
Creating chimeric models that incorporate human iPSC-derived cells into animal systems offers a powerful bridge between fully human in vitro models and traditional animal studies. For example, transplanting human iPSC-derived dopaminergic progenitors into PD model animals allows researchers to study human cell function and integration within a living system [6]. Recent advances have demonstrated that allogeneic iPSC-derived dopaminergic progenitors can survive, produce dopamine, and improve motor function in primate PD models without forming tumors [6].
Cross-Species Comparative Analysis
Systematically comparing molecular and phenotypic data from iPSC models with corresponding data from multiple animal species (zebrafish, rodents, pigs) helps identify conserved and species-specific pathways. This approach is particularly valuable for understanding which disease mechanisms are most relevant to human biology. For example, while zebrafish have different heart structure, some electrocardiogram parameters are more comparable to humans than mice, informing model selection for specific research questions [86].
Technical Protocols for Integrated Parkinson's Disease Modeling
Protocol 1: Generation of iPSC-Derived Dopaminergic Neurons for High-Content Screening
Objective: Differentiate patient-specific iPSCs into midbrain dopaminergic neurons for compound screening and disease modeling.
Materials:
- Human iPSCs from PD patients and healthy controls
- Neural induction medium (e.g., DMEM/F12 with N2 supplement)
- Patterned differentiation factors (SHH, FGF8, CHIR99021)
- Maturation factors (BDNF, GDNF, ascorbic acid, cAMP)
- 96-well or 384-well plates for high-content screening
Procedure:
- Culture iPSCs to 80% confluence in essential 8 medium on vitronectin-coated plates.
- Initiate neural induction by switching to neural induction medium with dual SMAD inhibition (LDN193189, SB431542) for 7 days.
- Pattern toward midbrain fate by adding SHH (100ng/mL) and FGF8 (100ng/mL) from days 3-7.
- Expand neural progenitor cells in the presence of FGF2 (20ng/mL) from days 7-14.
- Differentiate progenitors into dopaminergic neurons by withdrawing FGF2 and adding BDNF (20ng/mL), GDNF (20ng/mL), ascorbic acid (200μM), and cAMP (1mM) for 21-35 days.
- Validate differentiation efficiency via immunocytochemistry for FOXA2, LMX1A, and tyrosine hydroxylase (TH).
- Plate mature dopaminergic neurons in 384-well format for compound screening.
Quality Control:
- Assess dopaminergic neuron purity by flow cytometry for TH-positive cells (target >70%).
- Confirm functional maturity by measuring dopamine release via HPLC or electrochemical detection.
- Verify disease-relevant phenotypes in PD lines (e.g., increased α-synuclein accumulation, mitochondrial stress).
Protocol 2: Integration of iPSC-Derived Dopaminergic Progenitors into Rodent PD Models
Objective: Evaluate the therapeutic potential and safety of human iPSC-derived dopaminergic progenitors in an animal PD model.
Materials:
- 8-10 week old immunodeficient rats (e.g., Nude rats or SCID rats)
- 6-hydroxydopamine (6-OHDA) or MPTP for lesioning
- Stereotaxic injection system
- Human iPSC-derived dopaminergic progenitors (CORIN+ sorted)
- Immunosuppressants (tacrolimus)
- Behavioral testing apparatus (rotarod, cylinder test, apomorphine-induced rotation)
Procedure:
- Unilaterally lesion the medial forebrain bundle of rats with 6-OHDA (12μg in 3μL ascorbic acid-saline) using stereotaxic injection.
- Confirm successful lesioning 2 weeks post-surgery using apomorphine-induced rotation test (>6 full turns/minute).
- Prepare human iPSC-derived dopaminergic progenitors using the protocol in Section 5.1, sorting for CORIN+ cells on days 11-13 of differentiation.
- Transplant 2.5-5.0×10^6 cells in 3-5μL per striatum using stereotaxic injection at the following coordinates relative to bregma: AP +0.5mm, ML ±3.0mm, DV -4.5mm.
- Administer tacrolimus (0.06mg/kg twice daily) to prevent xenograft rejection, maintaining target trough levels of 5-10ng/mL.
- Monitor animals weekly for behavioral improvements using rotarod, cylinder test, and spontaneous rotation.
- At study endpoint (12-24 weeks), perform histological analysis for graft survival (human nuclei staining), dopaminergic markers (TH), and proliferation (Ki67) [6].
Key Parameters for Integration:
- Graft size and location via serial MRI imaging
- Functional integration using 18F-DOPA PET imaging to assess dopamine production
- Safety assessment for tumor formation or aberrant growth patterns
The Scientist's Toolkit: Essential Reagents and Solutions
Table 3: Research Reagent Solutions for iPSC-Based Parkinson's Disease Modeling
| Reagent Category | Specific Examples | Function & Application | Considerations for Use |
|---|---|---|---|
| Reprogramming Factors | OSKM factors (OCT4, SOX2, KLF4, MYC) or mRNA cocktails | Somatic cell reprogramming to pluripotency | Integration-free methods preferred for clinical applications |
| Neural Differentiation Kits | Commercial neural induction media (StemCell Technologies, Thermo Fisher) | Standardized differentiation to neural lineages | Batch-to-batch consistency critical for reproducibility |
| Small Molecule Enhancers | CHIR99021 (GSK3β inhibitor), LDN193189 (BMP inhibitor), SMAD inhibitors | Direct differentiation toward specific neural subtypes | Concentration and timing critical for patterning |
| Cell Culture Matrices | Synthetic matrices (NexaGel), vitronectin, laminin-521 | Defined substrates for iPSC maintenance and differentiation | Reduce variability compared to animal-derived matrices |
| Cell Sorting Markers | CORIN, LMX1A, CD142 (for midbrain progenitors) | Isolation of specific progenitor populations | Enriches for target cell type, improves transplant safety |
| Functional Assay Kits | Calcium imaging dyes, mitochondrial stress test kits, dopamine ELISA | Assessment of functional neuronal properties | Validate against primary neuron controls |
| Quality Control Tools | Pluritest, karyotyping, mycoplasma detection kits | Ensure iPSC line quality and genetic stability | Essential for preclinical safety assessment |
The integration of iPSC technology with traditional animal models represents the future of robust, human-relevant preclinical testing for Parkinson's disease and beyond. This synergistic approach leverages the scalability and human genetic relevance of iPSC systems with the physiological complexity of whole-animal models. The recent successful Phase I/II trial of allogeneic iPSC-derived dopaminergic progenitors in PD patients demonstrates the clinical potential of this integrated approach, showing improved motor scores and increased dopamine production in the putamen without serious adverse events [6].
Looking ahead, several key developments will further enhance the integration of iPSC and animal model data:
- Advanced Maturation Protocols: Overcoming the immaturity of iPSC-derived neurons through prolonged culture, metabolic manipulation, and novel patterning factors to better model late-onset diseases like PD [86] [30].
- Multi-Omics Integration: Combining transcriptomic, proteomic, and metabolomic data from iPSC models with corresponding animal and human data to identify conserved pathways and validate therapeutic targets.
- Machine Learning Approaches: Applying computational methods to integrate complex datasets from multiple model systems and improve prediction of human clinical outcomes [86].
- Standardized Validation Frameworks: Establishing consensus guidelines for validating iPSC-based models against clinical data and traditional animal models to enhance reproducibility and regulatory acceptance.
The strategic integration of iPSC technology with appropriately selected animal models creates a powerful framework for de-risking drug development, enhancing clinical translation, and ultimately delivering more effective therapies for Parkinson's disease patients. As regulatory agencies increasingly accept data from human-relevant models, this integrated approach will become standard practice in preclinical drug development.
Conclusion
iPSC technology has fundamentally advanced our capacity to model Parkinson's disease in a human-specific context, providing unprecedented insights into its pathogenesis. The synergy of patient-derived cells, advanced gene editing, and 3D modeling has created a powerful platform for deconstructing disease mechanisms and screening therapeutic candidates. While challenges in standardization and replicating ageing remain, ongoing efforts to optimize these models are rapidly closing these gaps. The successful translation of iPSC-derived dopaminergic progenitors into clinical trials marks a pivotal milestone, validating the entire modeling paradigm. The future of PD research lies in leveraging these patient-in-a-dish models to develop personalized, effective therapies and ultimately alter the disease's progression, moving from symptomatic treatment to genuine disease modification.
References
- 1. Induced Pluripotent Stem Cells Derived Cellular Models for ... [https://pubmed.ncbi.nlm.nih.gov/40587046/]
- 2. The global rise in Parkinson's disease: a critical analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174424/]
- 3. Modeling Parkinson's Disease Using Patient-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6218140/]
- 4. Induced pluripotent stem cells and Parkinson's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC6495331/]
- 5. iPSC for modeling neurodegenerative disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7770414/]
- 6. Phase I/II trial of iPS-cell-derived dopaminergic cells for ... [https://www.nature.com/articles/s41586-025-08700-0]
- 7. Phase I trial of hES cell-derived dopaminergic neurons for ... [https://www.nature.com/articles/s41586-025-08845-y]
- 8. Modeling Alzheimer's disease with iPSC-derived brain cells [https://www.nature.com/articles/s41380-019-0468-3]
- 9. Parkinson's disease: an update on preclinical studies of ... [https://www.sciencedirect.com/science/article/pii/S2173580823000585]
- 10. Induced pluripotent stem cell–related approaches to generate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11881713/]
- 11. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 12. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 13. Current Development of iPSC-Based Modeling in ... [https://www.mdpi.com/1422-0067/26/8/3774]
- 14. α-synuclein pathogenesis in hiPSC models of Parkinson's ... [https://pubmed.ncbi.nlm.nih.gov/34239711/]
- 15. Progression of differentiation of iPSCs into specific ... [https://www.sciencedirect.com/science/article/abs/pii/S0301468125000362]
- 16. Current Development of iPSC-Based Modeling ... [https://pubmed.ncbi.nlm.nih.gov/40332425]
- 17. Lewy Body–like Inclusions in Human Midbrain Organoids ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9543721/]
- 18. Advanced human iPSC-based preclinical model for ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/37339636/]
- 19. iPSC-Based Parkinson's Disease Model Poster [https://www.ncardia.com/insights/resources/ipsc-based-parkinsons-disease-model-poster]
- 20. Modeling Parkinson's Disease Using Induced Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7091557/]
- 21. Genetic predispositions of Parkinson's disease revealed in ... [https://www.nature.com/articles/s41531-020-0110-8]
- 22. Analysis of rare Parkinson's disease variants in millions ... [https://www.nature.com/articles/s41531-023-00608-8]
- 23. Parkinson's Genetics [https://www.michaeljfox.org/news/parkinsons-genetics]
- 24. Genetic Etiology of Parkinson Disease Associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3056147/]
- 25. Human iPSC-derived glia models for the study of ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02919-2]
- 26. Investigating the ageing-Parkinson's disease nexus [https://www.nature.com/articles/s41531-025-01137-2]
- 27. Drug discovery and development for Parkinson's disease [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1692592/full]
- 28. Current Development of iPSC-Based Modeling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027653/]
- 29. What we can learn from iPSC-derived cellular models of ... [https://www.sciencedirect.com/science/article/abs/pii/S0079612319302262]
- 30. Induced Pluripotent Stem Cells: A Tool for Modelling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9576003/]
- 31. Opportunities and challenges for the use of induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6367134/]
- 32. Transcription Factor-Mediated Generation of Dopaminergic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11201854/]
- 33. : a Brain for investigating cellular... organoid 3 D technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC8325286/]
- 34. Human 3 : steering the demolecularization of D ... brain organoids brain [https://www.nature.com/articles/s41420-023-01523-w?error=cookies_not_supported&code=1a47a669-806e-477f-a6b6-9ead2d7ee4fe]
- 35. Robust derivation of transplantable dopamine neurons ... [https://www.nature.com/articles/s41467-022-30777-8]
- 36. Integrative system biology analyses of CRISPR-edited iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6293323/]
- 37. Review Induced pluripotent stem cells: a tool for modeling ... [https://www.sciencedirect.com/science/article/abs/pii/S0166223622000959]
- 38. iPSC modeling of young-onset Parkinson's disease reveals ... [https://www.nature.com/articles/s41591-019-0739-1]
- 39. Genetic screens in isogenic mammalian cell lines without ... [https://www.nature.com/articles/s41467-020-14620-6]
- 40. Multi-omic insights into Parkinson's Disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10101343/]
- 41. Expanding causal genes for Parkinson's disease via multi- ... [https://www.nature.com/articles/s41531-023-00591-0]
- 42. Disease Modeling with iPSCs: A Comprehensive Guide to ... [https://www.cytion.com/us/Knowledge-Hub/Blog/Disease-Modeling-with-iPSCs-A-Comprehensive-Guide-to-Revolutionary-Medical-Research/]
- 43. Phenotypic screening with primary neurons to identify drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5243932/]
- 44. Review Phenotypic approaches for CNS drugs [https://www.sciencedirect.com/science/article/pii/S0165614724001883]
- 45. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 46. Biomarkers of Oxidative and Mitochondrial Stress Are ... [https://pubmed.ncbi.nlm.nih.gov/40341365/]
- 47. Biomarkers of mitochondrial disorders [https://www.sciencedirect.com/science/article/pii/S1878747924000114]
- 48. Therapeutic Applications of Induced Pluripotent Stem Cell Use ... [https://gmr.scholasticahq.com/article/29784-therapeutic-applications-of-induced-pluripotent-stem-cell-use-in-parkinson-s-disease-models]
- 49. Modelling Parkinson's Disease: iPSCs towards Better ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000082/]
- 50. Pre-clinical study of induced pluripotent stem cell-derived ... [https://www.nature.com/articles/s41467-020-17165-w]
- 51. An iPSC-derived neuronal model reveals manganese's role in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410566/]
- 52. Pre-clinical safety and efficacy of human induced ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925000062]
- 53. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 54. Control of immune response in an iPSC-based allogeneic ... [https://pubmed.ncbi.nlm.nih.gov/40834856/]
- 55. Allogenic transplantation therapy of iPS cell-derived ... [https://www.sciencedirect.com/science/article/pii/S1353802025005747]
- 56. Modelling Parkinson's Disease: iPSCs towards Better ... [https://www.mdpi.com/2076-3425/11/3/373]
- 57. Generation of gene-corrected isogenic controls from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10411637/]
- 58. An Efficient 2D Protocol for Differentiation of iPSCs into ... [https://www.mdpi.com/1422-0067/24/8/7297]
- 59. Back and Forth in Time: Directing Age in iPSC-Derived Lineages [https://pmc.ncbi.nlm.nih.gov/articles/PMC4870156/]
- 60. Strategies for modeling aging and age-related diseases [https://www.nature.com/articles/s41514-024-00161-5]
- 61. Chemically induced reprogramming to reverse cellular aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373966/]
- 62. Chemically induced reprogramming to reverse cellular aging [https://www.aging-us.com/article/204896/text]
- 63. The long and winding road of reprogramming-induced ... [https://www.nature.com/articles/s41467-024-46020-5]
- 64. BrainXell Showcases Pioneering iPSC Research and ... [https://www.biospace.com/press-releases/brainxell-showcases-pioneering-ipsc-research-and-promising-in-vivo-data-for-bxt-110-for-parkinsons-disease-at-the-2025-society-for-neuroscience-annual-meeting]
- 65. Metabolic manifestations of Parkinson's disease in cell ... [https://annaly-nevrologii.com/pathID/article/view/1386]
- 66. iPS-Cell Technology and the Problem of Genetic Instability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6462964/]
- 67. Hurdles to clinical translation of human induced pluripotent ... [https://www.jci.org/articles/view/80575]
- 68. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 69. 识别细胞衰老的标记物 - CST 博客 [https://blog.cellsignal.cn/cell-process-which-markers-can-be-used-to-identify-cellular-senescence]
- 70. 实时测量中性粒细胞的线粒体生物能量特征 [https://www.jove.com/cn/t/64971/real-time-measurement-mitochondrial-bioenergetic-profile]
- 71. Using Human Pluripotent Stem Cell–Derived ... [https://www.sciencedirect.com/science/article/pii/S2472555222075062]
- 72. Towards the establishment of treatments for ... [https://www.sciencedirect.com/science/article/pii/S0959438825001631]
- 73. Mouse models and induced pluripotent stem cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5539390/]
- 74. The Rise of iPSCs in Drug Discovery: Regulatory and ... [https://www.ncardia.com/insights/news/the-rise-of-ipscs-in-drug-discovery]
- 75. Comparative Study of Efficacy of Dopaminergic Neuron ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0085736]
- 76. Parkinson's Disease: Etiology, Neuropathology, and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK536722/]
- 77. Targeting α-Synuclein in Parkinson's Disease by Induced ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2021.786835/full]
- 78. α-synuclein pathogenesis in hiPSC models of Parkinson's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8222967/]
- 79. Mitochondrial dysfunction of induced pluripotent stem cells ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1030390/full]
- 80. Mitochondrial dysfunction in Parkinson's disease – a key ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-023-00676-7]
- 81. Familial Parkinson's disease iPSCs show cellular deficits in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3462009/]
- 82. Signaling pathways in Parkinson's disease: molecular ... [https://www.nature.com/articles/s41392-023-01353-3]
- 83. Clinical Trial Tests Novel Stem-Cell Treatment for ... [https://www.massgeneralbrigham.org/en/about/newsroom/press-releases/clinical-trial-novel-stem-cell-treatment-for-parkinsons]
- 84. Cell therapy shows promising motor improvements and ... [https://www.movementdisorders.org/MDS/News/Newsroom/News-Releases_BIN/IC25-releases/Cell-therapy-shows-promising-motor-improvements-and-safety-in-Parkinsons-disease.htm]
- 85. Tissue Stem Cell-Based Therapies in Parkinson's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154328/]
- 86. Animal Disease Models and Patient-iPS-Cell-Derived In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10045735/]
- 87. A Future Without Animal Testing: The Science Making It ... [https://www.sartorius.com/en/knowledge/science-snippets/a-future-without-animal-testing-the-science-making-it-possible-1774826]
- 88. The FDA Is Moving Past Animal Testing. Here's How ... [https://www.ncardia.com/insights/news/fda-moving-past-animal-testing]