Modeling Tau Hyperphosphorylation in Human iPSC-Derived Neurons: From Mechanisms to Therapeutic Discovery
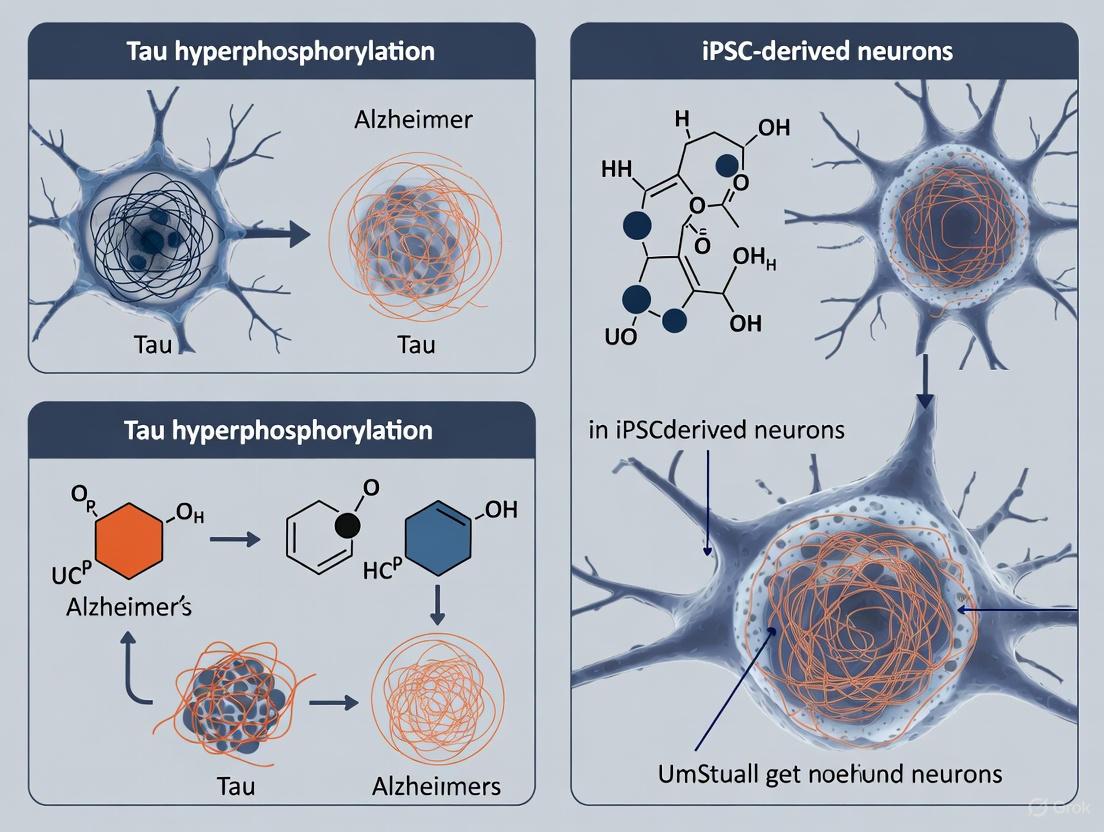
This article synthesizes current research on modeling tau hyperphosphorylation using human induced pluripotent stem cell (iPSC)-derived neurons, a system that recapitulates key aspects of Alzheimer's disease and related tauopathies.
Modeling Tau Hyperphosphorylation in Human iPSC-Derived Neurons: From Mechanisms to Therapeutic Discovery
Abstract
This article synthesizes current research on modeling tau hyperphosphorylation using human induced pluripotent stem cell (iPSC)-derived neurons, a system that recapitulates key aspects of Alzheimer's disease and related tauopathies. We explore the foundational role of stress-induced kinases like SGK1 in driving pathological tau phosphorylation and subsequent microtubule destabilization. The content details advanced methodological approaches, including 3D culture and high-throughput screening assays, for consistent phenotype generation. Furthermore, we address common challenges in model optimization and compare the pathophysiological relevance of iPSC-derived models against other experimental systems. Finally, we evaluate how these human neuronal models are validating novel therapeutic strategies, including small molecule inhibitors and immunotherapies, providing a robust platform for translational drug development.
Unraveling the Molecular Drivers of Tau Hyperphosphorylation in Human Neurons
SGK1 as a Central Stress-Induced Kinase in Alzheimer's Patient-Derived Neurons
Alzheimer's disease (AD) is a progressive neurodegenerative disorder and the most common cause of dementia, characterized by the pathological accumulation of hyperphosphorylated tau protein and amyloid-beta (Aβ) plaques. While numerous kinases have been implicated in tau pathology, recent evidence has identified serum and glucocorticoid-regulated kinase 1 (SGK1) as a central stress-induced kinase that is significantly elevated in AD and contributes critically to disease pathogenesis. This technical guide examines the role of SGK1 in Alzheimer's disease, with particular focus on mechanisms elucidated through human induced pluripotent stem cell (iPSC)-derived neuronal models that recapitulate both familial and sporadic AD pathology.
The development of iPSC-derived cortical neurons expressing adult isoforms of tau has enabled unprecedented investigation of human tauopathy mechanisms in patient-specific models [1]. These models have revealed that SGK1 elevation represents a key point of convergence in AD pathophysiology, connecting cellular stress responses to microtubule destabilization through coordinated effects on tau phosphorylation and tubulin acetylation. This whitepaper provides a comprehensive technical resource for researchers investigating SGK1 signaling in AD models, detailing experimental findings, methodological approaches, and practical research tools for therapeutic development.
SGK1 Structure, Regulation, and Expression in Alzheimer's Disease
SGK1 Molecular Characteristics and Activation Mechanism
SGK1 is a serine/threonine protein kinase belonging to the AGC family (protein kinases A, G, and C) [2]. The SGK1 gene is localized on chromosome 6q23, with a total length of 2.4 kb encoding a protein with a relative molecular mass of 49 KD [3]. SGK1 is structurally composed of an N-terminal domain, an intermediate catalytic domain, and a C-terminal hydrophobic motif [3] [2].
SGK1 activation requires phosphorylation at two critical sites: Thr256 in the activation loop of the catalytic domain by phosphoinositide-dependent kinase 1 (PDK1), and Ser422 in the C-terminal hydrophobic motif by mammalian target of rapamycin complex 2 (mTORC2) [3] [2]. This phosphorylation cascade is initiated by extracellular stimuli through the phosphoinositide 3-kinase (PI3K) signaling pathway. The resulting activated SGK1 phosphorylates numerous target proteins, including those directly implicated in AD pathogenesis such as tau, GSK-3β, and histone deacetylase 6 (HDAC6) [1] [2].
Table 1: SGK1 Structural Domains and Functional Characteristics
| Domain | Location | Function | Phosphorylation Sites |
|---|---|---|---|
| N-terminal | Amino-terminus | Protein localization and regulation | None |
| Catalytic domain | Intermediate region | Serine/threonine kinase activity | Thr256 (phosphorylated by PDK1) |
| C-terminal hydrophobic motif | Carboxy-terminus | Regulation of kinase activity | Ser422 (phosphorylated by mTORC2) |
SGK1 Elevation in Alzheimer's Disease Pathology
Multiple lines of evidence demonstrate significant SGK1 elevation in Alzheimer's disease. Transcriptomic analysis of the prefrontal cortex in P301S human tau transgenic mice identified Sgk1 as one of the most significantly upregulated genes [1]. This finding has been validated in human postmortem AD brain tissue, which shows significantly higher levels of SGK1 mRNA [1]. Single-cell RNA sequencing of AD human frontal cortex and neuron-specific RNAseq data from P301S mice further confirm SGK1 upregulation [1].
Recent research using iPSC-derived cortical neurons from AD patients has provided direct evidence of SGK1 elevation in disease-relevant human cells. Immunostaining and Western blot analysis revealed significantly increased SGK1 protein levels in AD-derived cortical neurons compared to controls [1]. This elevation was observed as early as day 25 of neuronal differentiation, coinciding with increased tau phosphorylation [1]. SGK1 mRNA levels were also significantly elevated in RT-qPCR measurements, confirming upregulation at the transcriptional level [1].
Figure 1: SGK1 Activation Pathway in Alzheimer's Disease. Multiple stress signals converge to increase SGK1 transcription and activation through PI3K/mTORC2/PDK1 signaling, leading to tau phosphorylation and microtubule destabilization.
SGK1-Mediated Tau Phosphorylation and Microtubule Destabilization
Tau Hyperphosphorylation in AD Patient-Derived Neurons
Cortical neurons differentiated from iPSCs of AD patients demonstrate marked increase of phosphorylated tau (pTau) compared to controls from normal subjects [1]. Immunostaining with AT8 antibody (recognizing phosphorylation at S202/T205) and S214 phospho-specific antibody showed significant increases in tau phosphorylation, while total tau levels remained consistent across AD and control lines [1]. Western blot analysis confirmed these findings, demonstrating that tau hyperphosphorylation is a consistent feature of AD patient-derived neurons in this model system.
The functional consequence of tau hyperphosphorylation is decreased ability to stabilize microtubules, which are essential for maintaining neuronal structure and function [1]. Research has demonstrated that hyperphosphorylated tau shows reduced binding to microtubules and increased propensity to form aggregates, ultimately leading to the neurofibrillary tangles that represent a hallmark of AD pathology [1].
SGK1 Direct Regulation of Tau Phosphorylation
Multiple experimental approaches have established a direct relationship between SGK1 activity and tau phosphorylation in AD models. Pharmacological inhibition of SGK1 using specific inhibitors GSK650394 (100 nM) or EMD638683 (6 µM) for 72 hours resulted in marked reduction of tau phosphorylation at both S202/T205 and S214 sites in AD-derived cortical neurons [1]. The reduction was more pronounced in AD neurons than in controls, which had lower basal pTau levels.
Genetic manipulation of SGK1 expression further confirmed its role in tau phosphorylation. SGK1 overexpression in control neurons significantly increased tau phosphorylation at S202/T205 and S214, while SGK1 knockdown using shRNA significantly decreased phosphorylation at these sites in AD neurons [1]. Control experiments using lentiviruses expressing scrambled shRNA or the reverse tetracycline transactivator M2rtTA confirmed the specificity of these effects.
Table 2: Quantitative Changes in AD Patient-Derived Cortical Neurons Compared to Controls
| Parameter | Change in AD Neurons | Experimental Method | Citation |
|---|---|---|---|
| Tau phosphorylation (S202/T205) | Significant increase | Immunostaining, Western blot | [1] |
| Tau phosphorylation (S214) | Significant increase | Immunostaining, Western blot | [1] |
| SGK1 protein levels | Significant increase | Western blot, immunostaining | [1] |
| SGK1 mRNA levels | Significant increase | RT-qPCR | [1] |
| Acetylated tubulin | Significant decrease | Immunostaining, Western blot | [1] |
| Microtubule stability | Significant decrease | Free/polymerized tubulin assay | [1] |
| HDAC6 expression | Significant increase | Western blot | [1] |
Microtubule Destabilization Through HDAC6 Regulation
Beyond direct tau phosphorylation, SGK1 contributes to microtubule destabilization through regulation of HDAC6, a tubulin deacetylase [1]. AD-derived cortical neurons show significantly increased HDAC6 expression alongside decreased acetylated tubulin, a marker of stable microtubules [1]. Fractionation experiments measuring free tubulin (cytoplasmic) versus polymerized tubulin (microtubules) confirmed significantly higher free tubulin and lower polymerized tubulin in AD neurons, indicating reduced microtubule stability [1].
SGK1 manipulation directly affected these parameters. SGK1 inhibition or knockdown significantly reduced HDAC6 levels and increased acetylated tubulin in AD neurons, while SGK1 overexpression in control neurons decreased acetylated tubulin [1]. This demonstrates that SGK1 elevation in AD promotes microtubule destabilization through both tau hyperphosphorylation and HDAC6-mediated tubulin deacetylation.
Experimental Models and Methodologies
iPSC-Derived Cortical Neuron Model of Alzheimer's Disease
A critical advancement in modeling Alzheimer's disease has been the development of methods to differentiate human iPSCs into cortical neurons expressing all six major splicing isoforms of tau found in adult human brains [1]. Previous iPSC-derived neuronal models were limited to producing only the fetal 0N3R tau isoform, even after extended differentiation periods [1]. The newer method installs dorsal forebrain fate on neuralizing embryoid bodies, generating neurons with more complete tau isoform expression that better recapitulates adult human brain physiology [1].
For AD modeling, iPSCs from both normal subjects and AD patients are differentiated into cortical neurons. In published studies, all iPSC lines were generated using footprint-free plasmid methods by the California Institute for Regenerative Medicine [1]. Neurons are typically analyzed at day 40 of differentiation, though increased SGK1 expression and pTau levels can be detected as early as day 25 [1]. These models have been successfully applied to both familial and sporadic AD, with neurons from both conditions showing increased phosphorylation of TAU protein at multiple sites and elevated levels of extracellular Aβ1-40 and Aβ1-42 compared to controls [4].
Figure 2: Experimental Workflow for iPSC-Derived Cortical Neuron AD Models. Patient somatic cells are reprogrammed to iPSCs, which are differentiated into cortical neurons expressing adult tau isoforms for disease modeling and therapeutic testing.
SGK1 Manipulation Protocols
Pharmacological Inhibition
SGK1 Inhibitor Treatment: Two well-characterized SGK1 inhibitors have been successfully used in AD neuronal models:
- GSK650394: Applied at 100 nM concentration for 72 hours [1]
- EMD638683: Applied at 6 µM concentration for 72 hours [1]
Treatment validation includes Western blot analysis of pSGK1, which recognizes activated SGK1, confirming inhibition of SGK1 phosphorylation in both AD and control neurons [1]. These treatments significantly reduce tau phosphorylation and HDAC6 levels while increasing acetylated tubulin in AD neurons.
Genetic Manipulation
SGK1 Overexpression: Lentiviral vectors with doxycycline-inducible SGK1 expression systems are used to overexpress SGK1 in control neurons. This approach significantly increases tau phosphorylation at S202/T205 and S214 in control neurons, though it does not further increase the already elevated levels in AD neurons [1].
SGK1 Knockdown: Lentiviral vectors expressing SGK1 shRNA are used to knock down SGK1 expression in AD neurons. This significantly decreases the high endogenous SGK1 level in AD neurons and reduces tau phosphorylation at key sites [1]. Control neurons with low endogenous SGK1 show minimal response to SGK1 shRNA.
Appropriate controls include lentiviruses expressing the reverse tetracycline transactivator M2rtTA or scrambled shRNA, which have no significant effect on SGK1 expression or tau phosphorylation [1].
Analytical Methods for Phenotypic Characterization
Immunostaining: Cells are costained for markers such as MAP2 (neuronal marker), DAPI (nuclear marker), and target proteins including SGK1, phosphorylated tau (using AT8 or S214 phospho-specific antibodies), and acetylated tubulin [1]. Quantification of fluorescence intensity provides comparative data between AD and control neurons.
Western Blotting: Total cell lysates are analyzed for protein levels of SGK1, phosphorylated tau, total tau, HDAC6, and acetylated tubulin [1]. Phospho-specific antibodies against SGK1 (pThr256 and pSer422) confirm SGK1 activation status.
Microtubule Stability Assay: Cells are lysed at 37°C to preserve microtubules, followed by fractionation into supernatant (containing free tubulin) and pellet (containing polymerized tubulin/microtubules) fractions [1]. Western blotting of both fractions quantifies free versus polymerized tubulin ratios.
RT-qPCR: mRNA levels of SGK1 and other targets are quantified to assess transcriptional regulation [1].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SGK1 in Alzheimer's Models
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| SGK1 Inhibitors | GSK650394 (100 nM), EMD638683 (6 µM) | Pharmacological inhibition of SGK1 kinase activity | Treat for 72 hours; validate with pSGK1 Western blot |
| Genetic Manipulation Tools | Lentiviral SGK1 shRNA, Doxycycline-inducible SGK1 overexpression vectors | Knockdown or overexpression of SGK1 | Use scrambled shRNA and empty vectors as controls |
| Cell Line Models | iPSC-derived cortical neurons from AD patients and controls | Disease modeling | Ensure expression of adult tau isoforms; validate at day 25-40 |
| Tau Phosphorylation Antibodies | AT8 (S202/T205), S214 phospho-specific antibodies | Detection of tau hyperphosphorylation | Use alongside total tau antibodies for normalization |
| Microtubule Stability Assay Reagents | Acetylated tubulin antibodies, tubulin fractionation kits | Assessment of microtubule stability | Lysate cells at 37°C to preserve microtubule structure |
| SGK1 Activity Assays | Phospho-SGK1 (Thr256/Ser422) antibodies, kinase activity assays | Measurement of SGK1 activation | mTORC2 and PDK1 activity can affect SGK1 phosphorylation |
SGK1 in the Broader Context of Alzheimer's Disease Mechanisms
Connections to Type 2 Diabetes and Metabolic Dysregulation
Epidemiological studies have established type 2 diabetes mellitus (T2DM) as a significant risk factor for AD, with diabetics showing a 2.5-fold increased risk for cognitive dysfunction [5]. Research has revealed that SGK1 provides a molecular link between these conditions. High-fat diet (HFD) administration in mouse models causes upregulation and activation of SGK1 in the hippocampus, leading to tau pathology through phosphorylation of tau at Ser214 and activation of GSK-3β, forming an SGK1-GSK-3β-tau complex [5].
Notably, SGK1 is activated under conditions of elevated glucocorticoids and hyperglycemia associated with HFD, but not in fatty acid-mediated insulin resistance [5]. This suggests that SGK1 mediates tau pathology specifically in response to metabolic and hormonal disturbances common in T2DM. Elevated expression of SGK1 in mouse hippocampus leads to neurodegeneration and impairments in learning and memory, mirroring aspects of AD pathophysiology [5].
Dual Role of SGK1 in Neurological Diseases
The role of SGK1 in neurological diseases appears complex and context-dependent. Beyond its detrimental role in promoting tau pathology in AD, SGK1 has demonstrated neuroprotective functions in certain contexts. SGK1 can inhibit amyloidogenic processing of APP by downregulating the stability of the γ-secretase component nicastrin and by phosphorylating the brain-enriched articulin FE65 at Ser610, which attenuates FE65 binding to APP [3].
SGK1 also plays important roles in hippocampal synaptic plasticity, spatial learning, and memory formation [3]. SGK1 enhances memory by upregulating the hydrochloride receptor GluR6, thereby enhancing neuronal excitability [3]. This dual nature of SGK1 - both contributing to AD pathology and supporting normal cognitive function - presents challenges for therapeutic targeting that must carefully preserve physiological functions while inhibiting pathological ones.
SGK1 has emerged as a central stress-induced kinase in Alzheimer's disease pathophysiology, with compelling evidence from iPSC-derived neuronal models demonstrating its critical role in tau hyperphosphorylation and microtubule destabilization. The coordinated increases in SGK1, phosphorylated tau, and HDAC6, along with decreased acetylated tubulin and microtubule stability in AD neurons, offer attractive targets for therapeutic development.
Future research should focus on elucidating the upstream regulators that trigger SGK1 elevation in sporadic AD, developing more specific SGK1 inhibitors with optimal blood-brain barrier penetration, and exploring the timing of SGK1 inhibition for maximal therapeutic benefit. The established protocols for iPSC-derived cortical neuron differentiation and SGK1 manipulation provide valuable tools for these investigations, enabling patient-specific modeling of AD mechanisms and high-throughput screening of potential therapeutics.
As our understanding of SGK1's multifaceted roles in AD continues to expand, targeting this kinase represents a promising avenue for developing much-needed disease-modifying treatments for Alzheimer's disease.
In Alzheimer's disease (AD) research, a critical pathological cascade connects the hyperphosphorylation of tau protein to the destabilization of the microtubule network, ultimately compromising neuronal structure and function. This whitepaper delineates the molecular pathway wherein elevated phosphorylated tau (p-tau) leads to microtubule instability through the coordinated action of key enzymes, particularly Histone Deacetylase 6 (HDAC6). Recent investigations using induced pluripotent stem cell (iPSC)-derived cortical neurons from AD patients have provided human-relevant experimental validation of this cascade, revealing significantly elevated expression of both p-tau and the stress-induced kinase SGK1, accompanied by markedly reduced levels of acetylated tubulin, a key marker of microtubule stability [1]. The diagram below illustrates the core signaling pathway and experimental workflow used to validate it in iPSC-derived models.
Core Mechanistic Pathway: From p-Tau to Cytoskeletal Collapse
The pathway from tau hyperphosphorylation to microtubule destabilization involves a precisely coordinated series of molecular events that compromise neuronal integrity.
Tau Hyperphosphorylation and Microtubule Dissociation
In its physiological state, tau protein promotes microtubule assembly and stabilizes microtubule structure, with its binding affinity regulated by phosphorylation levels [6]. Normal brain tau contains only 2-3 moles of phosphate per mole of protein, but in AD, this stoichiometry increases dramatically, reducing tau's ability to bind and stabilize microtubules [6] [7]. Hyperphosphorylated tau exhibits impaired microtubule binding and actually sequesters normal tau, MAP1, and MAP2, further disrupting microtubule integrity [6]. This pathological transformation represents the initial step in the cascade toward cytoskeletal collapse.
SGK1 as a Key Regulatory Kinase
Serum and Glucocorticoid-regulated Kinase-1 (SGK1) has emerged as a critical upstream regulator in this pathway. RNA sequencing of AD patient brains and P301S tau transgenic mice identified SGK1 as one of the top-ranking upregulated genes [1]. In iPSC-derived cortical neurons from AD patients, SGK1 mRNA and protein levels were significantly elevated compared to controls [1]. As an immediate early gene induced by various cellular stresses, SGK1 directly phosphorylates tau and creates a feedforward loop that amplifies the pathological cascade [1].
HDAC6-Mediated Tubulin Deacetylation
Histone Deacetylase 6 (HDAC6) serves as the crucial link between tau pathology and microtubule destabilization. This cytoplasmic deacetylase targets α-tubulin, removing acetyl groups from lysine 40 and thereby destabilizing microtubule structure [1] [8] [9]. AD-derived cortical neurons demonstrate significantly elevated HDAC6 expression alongside markedly reduced acetylated tubulin levels [1]. HDAC6 also interacts directly with tau through its microtubule-binding domain, potentially facilitating the localized disruption of microtubule integrity [9]. Beyond its deacetylase function, HDAC6's ubiquitin-binding domain (ZnF UBP) participates in aggresome formation and protein quality control, positioning it as a multifunctional regulator in AD pathogenesis [10] [11].
Table 1: Quantitative Changes in Key Pathway Components in AD Patient-Derived Cortical Neurons
| Analyte | Change in AD Neurons | Measurement Method | Functional Consequence |
|---|---|---|---|
| pTau (S202/T205) | Significant increase | Immunostaining (AT8 antibody), Western blot | Reduced microtubule binding, aggregation propensity |
| pTau (S214) | Significant increase | Immunostaining, Western blot | Impaired tau function, pathological conformation |
| SGK1 mRNA | Significant increase | RT-qPCR | Enhanced tau phosphorylation capacity |
| SGK1 Protein | Significant increase | Immunostaining, Western blot | Increased kinase activity in pathway |
| HDAC6 Protein | Significant increase | Immunostaining, Western blot | Enhanced tubulin deacetylation |
| Acetylated Tubulin | Significant decrease | Immunostaining, Western blot | Microtubule destabilization |
| Polymerized Tubulin | Significant decrease | Fractionation assay, Western blot | Loss of structural microtubule network |
Experimental Validation in Human iPSC-Derived Neurons
The development of advanced differentiation protocols for generating cortical neurons expressing adult-like tau isoforms has enabled robust modeling of AD pathology in a human neuronal context.
iPSC-Derived Cortical Neuron Model
A critical advancement in modeling tauopathy has been the development of methods to generate cortical neurons expressing all six major splicing isoforms of tau, including the 4R Tau isoform found in adult human brains [1]. Earlier models predominantly produced only the fetal 0N3R splicing isoform, limiting their pathological relevance. Using a dorsal forebrain fate induction protocol, researchers have established iPSC-derived cortical neurons from both normal subjects and AD patients that recapitulate key aspects of adult tau biology and pathology [1]. This model system demonstrates increased Tau phosphorylation and SGK1 elevation as early as day 25 of differentiation, providing a robust platform for mechanistic and therapeutic investigations [1].
Functional Consequences on Microtubule Stability
Direct assessment of microtubule stability in AD-derived neurons reveals profound cytoskeletal alterations. Measurements of acetylated tubulin (a marker of stable microtubules) show significantly decreased levels in AD-derived cortical neurons compared to controls [1]. Furthermore, fractionation assays separating free tubulin from polymerized tubulin (microtubules) demonstrate significantly higher free tubulin and lower polymerized tubulin in AD neurons, confirming substantial microtubule network disruption [1]. These structural changes likely underlie the compromised cellular functions that ultimately impair cognition in AD patients.
Table 2: Experimental Assessment of Microtubule Stability in AD Patient-Derived Neurons
| Experimental Method | Specific Target | Key Finding in AD Neurons | Technical Details |
|---|---|---|---|
| Immunostaining | Acetylated tubulin (AcTub) | Significant decrease | Costaining with MAP2 and DAPI; fluorescence quantification |
| Western Blot | Acetylated tubulin (AcTub) | Significant reduction | Total cell lysates; normalized to total protein |
| Cellular Fractionation | Free vs. polymerized tubulin | Increased free tubulin; decreased polymerized tubulin | Lysis at 37°C to preserve microtubules; supernatant (free) vs. pellet (polymerized) |
| Immunostaining | Tau phosphorylation (S202/T205, S214) | Significant increase | AT8 and S214 phospho-specific antibodies; costaining with MAP2 |
| SGK1 Inhibition | pSGK1 (activated SGK1) | Marked reduction with inhibitors | Treatment with GSK650394 (100 nM) or EMD638683 (6 µM) for 72h |
Interventional Studies: Validating Therapeutic Targets
Intervention experiments in iPSC-derived neuronal models provide compelling evidence for the causal relationships within this pathway and highlight potential therapeutic strategies.
SGK1 Inhibition and Knockdown
Targeted manipulation of SGK1 expression and activity demonstrates its pivotal role in driving tau pathology. Treatment of AD-derived cortical neurons with SGK1 inhibitors (GSK650394 or EMD638683) for 72 hours produces a marked reduction in Tau phosphorylation at both S202/T205 and S214 sites [1]. Similarly, shRNA-mediated SGK1 knockdown significantly decreases tau phosphorylation in AD neurons, while having minimal effect on control neurons with low basal p-tau levels [1]. Conversely, SGK1 overexpression in normal neurons increases tau phosphorylation, confirming SGK1's sufficiency to drive this pathological modification [1]. These interventions establish SGK1 as a genuine regulator rather than correlative factor in the pathway.
HDAC6 Manipulation and Microtubule Rescue
HDAC6 modulation directly impacts microtubule stability downstream of tau phosphorylation. SGK1 inhibition or knockdown in AD neurons significantly reduces HDAC6 levels while increasing acetylated tubulin, indicating that SGK1 operates upstream of HDAC6 expression [1]. Direct HDAC6 inhibition through genetic or pharmacological methods suppresses neuritic tau bead formation and increases acetylated α-tubulin levels, promoting microtubule stability [12] [8]. In AD mouse models, HDAC6 inhibition improves axonal transport rates, decreases tau phosphorylation, and ameliorates cognitive deficits, further validating this nodal point in the pathway [8].
The following diagram illustrates the key experimental approaches and their outcomes in validating this pathological cascade.
The Scientist's Toolkit: Essential Research Reagents and Protocols
This section details critical experimental resources and methodologies for investigating the p-tau to microtubule destabilization cascade.
Table 3: Essential Research Reagents for Investigating the p-Tau/HDAC6/Microtubule Pathway
| Reagent Category | Specific Examples | Key Applications | Experimental Notes |
|---|---|---|---|
| Cell Models | iPSC-derived cortical neurons from AD patients and controls [1] | Disease modeling, therapeutic screening | Must produce adult 4R tau isoforms; multiple donor lines recommended |
| SGK1 Inhibitors | GSK650394 (100 nM) [1], EMD638683 (6 µM) [1] | Target validation, pathway interrogation | 72-hour treatment effective in reducing p-tau in AD neurons |
| HDAC6 Inhibitors | Tubastatin A [8], ACY-738 [8], ACY-1215 [8] | Microtubule stabilization studies | Varying selectivity profiles; assess brain bioavailability for in vivo studies |
| Tau Phosphorylation Antibodies | AT8 (S202/T205) [1], S214 phospho-specific [1], PHF-1 (S396/S404) [9] | Phospho-tau quantification, pathology assessment | Multiple epitopes recommended for comprehensive assessment |
| Microtubule Stability Reagents | Acetylated tubulin antibodies [1], tubulin fractionation kits | Microtubule integrity assessment | Combine immunostaining with biochemical fractionation |
| HDAC6 Modulators | HDAC6 shRNA [1], HDAC6 expression constructs [9] | Genetic manipulation studies | BUZ domain mutants help dissect deacetylase-independent functions |
| Vectors | Doxycycline-inducible lentivirus for SGK1 expression/kd [1] | Controlled gene expression | Tight regulation essential for manipulating this stress-responsive kinase |
Key Experimental Protocols
iPSC-Derived Cortical Neuron Differentiation
The protocol involves installing dorsal forebrain fate on neuralizing embryoid bodies to generate cortical neurons expressing all six major tau isoforms, overcoming previous limitations in producing adult-specific 4R tau [1]. Neurons are typically analyzed at day 40 of differentiation, with pathological manifestations (elevated p-tau and SGK1) detectable as early as day 25 [1]. This method produces MAP2+ neurons from day 18 onward, enabling sufficient material for Western blotting and other analyses by day 25 [1].
Microtubule Stability Assessment
The microtubule stability assay involves two complementary approaches: (1) Immunostaining and Western blotting for acetylated tubulin, a specific marker of stable microtubules [1]; and (2) Biochemical fractionation of free versus polymerized tubulin through cell lysis at 37°C to preserve microtubule integrity, followed by separate quantification of supernatant (free tubulin) and pellet (polymerized tubulin) fractions [1]. This combined approach provides both spatial distribution and quantitative assessment of microtubule stability.
SGK1 Pathway Intervention
For pharmacological inhibition, treat iPSC-derived cortical neurons with SGK1 inhibitors GSK650394 (100 nM) or EMD638683 (6 µM) for 72 hours, with confirmation of pathway inhibition via pSGK1 Western blotting [1]. For genetic manipulation, use doxycycline-inducible lentivirus for either SGK1 overexpression or shRNA-mediated knockdown, with M2rtTA or scrambled shRNA as appropriate transduction controls [1].
The pathway linking p-tau elevation to microtubule destabilization through HDAC6 represents a core pathological cascade in Alzheimer's disease, with robust validation in human iPSC-derived neuronal models. The experimental evidence demonstrates that cellular stress-induced SGK1 elevation drives both tau hyperphosphorylation and increased HDAC6 expression, culminating in microtubule network disruption through tubulin deacetylation [1]. The consistent observation that SGK1 inhibition or knockdown reduces tau phosphorylation, decreases HDAC6, and increases acetylated tubulin in AD neurons confirms the mechanistic relationship between these pathway components [1].
Future research should leverage increasingly sophisticated human neuronal models to identify additional pathway components and validate therapeutic targets. The development of more selective HDAC6 inhibitors with improved blood-brain barrier penetration represents a promising therapeutic approach [8] [11]. Similarly, SGK1-specific inhibitors may offer complementary benefits by targeting the upstream driver of this cascade. The integration of structural biology, medicinal chemistry, and human cellular models will be essential for translating these mechanistic insights into effective disease-modifying therapies for Alzheimer's disease and related tauopathies.
In neurodegenerative diseases known as tauopathies, including Alzheimer's disease (AD) and frontotemporal lobar degeneration (FTLD), the microtubule-associated protein tau undergoes a pathological transformation from a soluble, natively unfolded protein into a spectrum of toxic assemblies [13] [14]. For decades, research focused on end-stage neurofibrillary tangles (NFTs) as the primary toxic entity. However, a paradigm shift has occurred with growing evidence that soluble tau species, particularly tau oligomers and soluble tau assemblies (STAs), are more closely associated with synaptic dysfunction, neuronal death, and the spread of pathology throughout the brain [13] [14]. Characterizing this heterogeneous mixture of pathological tau is crucial for understanding disease mechanisms and developing effective therapeutic strategies for tauopathies.
This shift in focus is particularly relevant in human cellular models, such as induced pluripotent stem cell (iPSC)-derived neurons. In these systems, which recapitulate human physiology, the study of early tau pathology provides a critical window into the initial molecular events of neurodegeneration [15] [16]. Framed within the context of a broader thesis on tau hyperphosphorylation in iPSC-derived neurons, this review details the molecular characteristics, detection methodologies, and pathogenic significance of the various pathological tau species, with an emphasis on the soluble oligomeric forms that are now considered primary drivers of toxicity.
Tau Isoforms and Post-Translational Modifications: The Genesis of Pathology
Tau Isoform Diversity
The MAPT gene, located on chromosome 17q21, undergoes alternative splicing of exons 2, 3, and 10 to generate six major tau isoforms in the adult human central nervous system [17] [14]. These isoforms differ by the presence of either 0, 1, or 2 N-terminal inserts (0N, 1N, 2N) and the inclusion of either three or four microtubule-binding repeats (3R or 4R) [18] [13]. In a healthy adult brain, the ratio of 3R to 4R tau is approximately 1:1. An imbalance in this ratio is a hallmark of specific tauopathies; for example, Pick's disease is characterized by accumulated 3R tau, while progressive supranuclear palsy (PSP) and corticobasal degeneration (CBD) feature 4R tau aggregates [13].
Post-Translational Modifications and Hyperphosphorylation
Physiological tau is a phosphoprotein, but under pathological conditions, it becomes abnormally hyperphosphorylated. The 2N4R tau isoform contains 85 potential phosphorylation sites for serine (S), threonine (T), and tyrosine (Y) residues [14]. In Alzheimer's disease brain tissue, approximately 45 different phosphorylation sites have been identified [14]. This hyperphosphorylation is driven by an imbalance between kinase and phosphatase activity. Key kinases implicated include proline-directed protein kinases (PDPKs) like GSK-3β and CDK5, non-PDPKs such as MARKs and PKA, and tyrosine kinases including Fyn [13] [14]. The resulting hyperphosphorylation reduces tau's affinity for microtubules and promotes its aggregation [17] [19].
Beyond phosphorylation, tau undergoes other post-translational modifications (PTMs) that influence its aggregation propensity. These include acetylation, which can impair tau degradation and promote accumulation; truncation by enzymes like caspase-3, which generates aggregation-prone fragments; and glycosylation, ubiquitination, and SUMOylation [17] [13] [19]. These PTMs collectively contribute to the misfolding and assembly of tau into toxic species. The table below summarizes the key features of different tau species.
Table 1: Characteristics of Different Tau Species in Tauopathies
| Tau Species | Key Features | Putative Role in Toxicity | Detection Methods |
|---|---|---|---|
| Tau Oligomers | Soluble, low molecular weight aggregates; altered conformation; phosphorylated and often truncated [13] [14]. | Synaptic dysfunction, mitochondrial impairment, seeding of further aggregation [13]. | Size-exclusion chromatography, native-PAGE, conformation-specific antibodies [13]. |
| Soluble Tau Assemblies (STAs) | Heterogeneous mixture of soluble aggregates, potentially including oligomers and small filaments [20]. | Disruption of synaptic vesicle release, receptor trafficking, and axonal transport [17] [19]. | Sarkosyl extraction, ultracentrifugation, high-content imaging assays [20]. |
| Paired Helical Filaments (PHFs) | Insoluble, filamentous structures with characteristic twisted morphology; major component of NFTs [13]. | Historically considered the toxic entity, but correlation with cognitive decline is weaker than for soluble species [14]. | Electron microscopy, Thioflavin-S staining, sarkosyl-insoluble fractionation [13]. |
| Neurofibrillary Tangles (NFTs) | Insoluble, intracellular inclusions of hyperphosphorylated tau; end-stage aggregates [17] [13]. | May represent a protective sequestration of toxic soluble tau; presence does not directly correlate with neuronal loss [14]. | Immunohistochemistry (e.g., AT8, PHF1), Gallyas-Braak silver staining [13]. |
Mechanisms of Toxicity and Propagation
The toxicity of pathological tau species is not merely a consequence of protein aggregation but arises from specific gains of toxic function. Tau oligomers and STAs are potent disruptors of synaptic integrity. They can reduce the mobility and release of presynaptic vesicles, decrease glutamatergic receptors at the postsynaptic density, impair dendritic spine maturation, and disrupt mitochondrial transport and function at synapses [17]. Furthermore, pathological tau can disturb autophagy, leading to the accumulation of vesicles and dysfunctional organelles [17].
A critical feature of tau pathology is its progressive spread through the brain in a prion-like manner. This propagation follows a stereotypical pattern, originating in the locus coeruleus and transentorhinal cortex before spreading to the limbic system and neocortex [21]. Misfolded tau is thought to be released from affected neurons, possibly in extracellular vesicles or as free protein, and then internalized by connected neurons, where it acts as a seed to template the misfolding and aggregation of endogenous, native tau [19]. This process of seeding and propagation is an active area of research and a key therapeutic target.
Table 2: Experimental Models for Studying Pathological Tau Species
| Model System | Key Features & Applications | Limitations | Relevance to Tau Species Study |
|---|---|---|---|
| iPSC-Derived Neurons (Patient-Derived) | Recapitulate patient genetics; human physiological context; ideal for studying early pathogenic events [15] [16]. | Neurons often exhibit fetal-like tau isoform expression; long culture times may be needed for pathology [16] [22]. | Excellent for studying initial tau oligomerization, phosphorylation, and early STAs in a human neuronal context [15]. |
| iPSC-Derived Neurons (Genetically Engineered) | TET-on tau overexpression enables rapid aggregation and cell death within two weeks; suitable for high-throughput screening [15]. | Overexpression may not reflect physiological levels; potential for artifactual aggregation [15]. | Rapid model for inducing and studying tau aggregation-dependent neuronal death and evaluating tau-targeting compounds [15]. |
| Primary Neuronal Seeding Models | Neurons expressing wild-type human tau are seeded with pathological tau from AD brain; high pathophysiological relevance [20]. | Requires access to well-characterized human brain-derived tau seeds. | Robust model for studying cell-to-cell propagation of tau pathology and the effects of endogenous tau aggregation [20]. |
| 3D Cerebral Organoids | Multiple cell types and rudimentary brain architecture; can develop amyloid and tau pathology over time [16]. | Resource-intensive; variable morphology; gene expression resembles fetal brain [16]. | Allows study of tau pathology in a more complex, multi-cellular environment. |
Detection and Methodologies for Tau Species Characterization
Accurately detecting and quantifying specific tau species is technically challenging due to their heterogeneous and dynamic nature. The following section outlines key experimental protocols and methodologies.
Biochemical Fractionation
A foundational technique for separating tau species based on solubility is sequential extraction. The protocol typically begins with a high-salt buffer to extract soluble tau. This is followed by a sarkosyl (detergent) extraction, which separates soluble proteins from insoluble aggregates. The sarkosyl-insoluble pellet, which contains filamentous tau like PHFs and NFTs, can then be analyzed by western blot or mass spectrometry [20] [13]. To isolate soluble oligomers, techniques such as size-exclusion chromatography (SEC) or sucrose density gradient centrifugation are employed [14].
Establishing a Rapid Tau Aggregation Model in iPSC-Derived Neurons
A 2025 study established a robust model for inducing tau aggregation in iPSC-derived neurons within a short timeframe [15].
- Cell Line Generation: An iPSC line was engineered to express Ngn2 and miR-9/9*-124 for rapid neuronal differentiation. A TET-on inducible system was incorporated to allow controlled overexpression of wild-type or mutant tau (e.g., P301S) upon doxycycline addition [15].
- Neuronal Differentiation: The engineered iPSCs are differentiated into excitatory neurons using a neuronal induction medium containing doxycycline to initiate tau expression. After 5 days, neurons are re-plated for experiments [15].
- Tau Overexpression & Aggregation: Neurons are transduced with lentivirus carrying the tau transgene. Tau overexpression leads to aggregation and neuronal cell death within two weeks, a process that can be quantified using high-content imaging and immunofluorescence [15].
- Compound Screening: This model's rapid phenotype makes it suitable for testing tau-targeting compounds. Known tau-targeting drugs have demonstrated neuroprotective effects in this system, validating its use for drug discovery [15].
Immunoassays and Conformation-Specific Antibodies
Antibodies are indispensable tools for detecting specific tau epitopes and conformations. Phospho-specific antibodies (e.g., AT8 for pS202/pT205) are widely used to detect hyperphosphorylated tau. A key advancement is the development of conformation-specific antibodies that recognize unique structural epitopes presented by oligomeric tau but not monomers or filaments [20]. Ultrasensitive immunoassays, particularly Single Molecular Array (Simoa) technology, have enabled the quantification of specific tau fragments (e.g., pTau217) from plasma and cerebrospinal fluid, providing critical biomarkers for diagnosis and monitoring [21].
The following diagram illustrates the core workflow for establishing and utilizing a neuronal model of tau pathology.
The Therapeutic Landscape: Targeting Pathological Tau
The recognition of tau oligomers and STAs as key toxic entities has reshaped therapeutic development. Currently, there are no approved disease-modifying therapies that directly target tau pathology, underscoring the urgent need for effective treatments [18]. The therapeutic pipeline is diverse, with 170 drugs in development as of early 2025 [18]. These strategies can be broadly categorized as follows:
- Immunotherapies: Monoclonal antibodies (comprising 20% of the pipeline) and vaccines (11%) are designed to target extracellular tau seeds for clearance or to neutralize intracellular toxic species. The challenge lies in designing antibodies that selectively bind pathogenic tau without depleting functional tau [18] [19].
- Small Molecule Inhibitors: This category (44% of the pipeline) includes kinase inhibitors (targeting GSK-3β, etc.), tau aggregation inhibitors, and microtubule stabilizers (e.g., Epothilone D). Their goal is to prevent the initial steps of tau misfolding and aggregation [18] [19].
- Gene-Targeting Approaches: Antisense oligonucleotides (ASOs) and siRNA are being developed to reduce the overall production of tau protein, a strategy that has shown promise in preclinical models [18].
The following diagram maps the core pathogenic pathways of tau and the corresponding therapeutic strategies being investigated to block them.
Advancing research into pathological tau requires a well-characterized set of reagents and cellular models. The table below details key resources for building experimental workflows in this field.
Table 3: Essential Research Reagents and Resources for Tau Pathology Studies
| Reagent/Resource | Type | Key Function/Application | Examples & Notes |
|---|---|---|---|
| iPSC & NPC Collections | Cell Lines | Provide physiologically relevant human neuronal models with patient-specific or engineered mutations [22]. | Tau Consortium collection (140 samples), includes MAPT mutations (P301L, R406W) and isogenic controls [22]. |
| Conformation-Specific Antibodies | Antibody | Detect oligomeric or misfolded tau species without binding monomers or filaments [20]. | MC1 (conformational epitope); T22, TOMA (oligomers). Critical for specific quantification [20] [14]. |
| Phospho-Specific Tau Antibodies | Antibody | Detect and quantify tau hyperphosphorylation at specific pathological epitopes. | AT8 (pS202/pT205), PHF1 (pS396/pS404). Standard for assessing tau pathology [13] [14]. |
| Polyclonal Antibody to Proline-Rich Region | Antibody | Capture a broader range of tau fragments in plasma/serum for biomarker development [21]. | Sheep P.pAb (targets tau 113-251). Used in Simoa assays to distinguish AD from controls [21]. |
| Tau Seeds (AD Brain-Derived) | Biochemical Reagent | Induce aggregation of endogenous tau in neuronal models, studying seeding and propagation [20]. | Sarkosyl-insoluble tau extracts from confirmed AD brains. Essential for pathophysiologically relevant models [20]. |
| Ngn2-Transduced iPSC Lines | Engineered Cell Line | Enable rapid, synchronous differentiation into excitatory neurons for high-throughput studies [15] [22]. | Available in Tau Consortium resource. Ideal for uniform neuronal differentiation and drug screening [22]. |
The characterization of pathological tau species, from oligomers to STAs, represents a frontier in understanding and ultimately treating tauopathies. The move beyond NFTs to focus on these soluble, pre-fibrillar aggregates has been catalyzed by evidence of their primary role in synaptic toxicity and disease propagation. The integration of advanced human cellular models, particularly iPSC-derived neurons, with sensitive biochemical and imaging techniques provides an unprecedented opportunity to dissect the earliest molecular events in tau pathogenesis. As the therapeutic landscape evolves, the successful translation of these insights into effective treatments will depend on our continued ability to accurately identify, quantify, and target the most relevant toxic tau species driving neurodegeneration.
Within the context of tauopathy research using induced pluripotent stem cell (iPSC)-derived neurons, understanding the downstream cellular consequences is paramount for developing targeted therapies. This technical guide examines the critical pathophysiological events in neurodegenerative disease: mitochondrial dysfunction and the activation of specific neuronal death pathways. The accumulation of hyperphosphorylated tau (pTau) not only disrupts microtubular stability but also initiates a cascade of subcellular failures, ultimately leading to neuronal loss. Research using human iPSC-derived neuronal models has become indispensable for elucidating these mechanisms in a human-specific context, providing a platform for drug discovery that bridges the gap between animal models and clinical trials [15]. This review synthesizes current findings on how tau pathology compromises mitochondrial biology and activates regulated cell death, focusing on data generated from patient-specific iPSC models.
Data from iPSC-derived neuronal models and other experimental systems consistently reveal a pattern of bioenergetic failure and oxidative damage in tauopathies and related neurodegenerative diseases. The tables below summarize key quantitative findings.
Table 1: Mitochondrial Functional Parameters in Aged and Diseased iPSC-Derived Neuronal Models
| Cell Model | ATP Level | Mitochondrial Membrane Potential | ROS Production | Oxidative Phosphorylation (OCR) | Glycolysis (ECAR) | Citation |
|---|---|---|---|---|---|---|
| Aged iPSCsNs | Decreased (Trend) | Decreased (Trend) | Increased (Significant for mtROS) | Not Reported | No shift to glycolysis | [23] |
| Aged iNs | Decreased | Decreased | Increased | Decreased | Increased | [23] |
| PARK2 iPSCsNs | Impaired (Inferred) | Impaired (Inferred) | Increased | Not Reported | Not Reported | [24] |
| MERRF iPSCsNs | Impaired (Inferred) | Not Reported | Increased | Impaired | Not Reported | [25] |
Table 2: Neuronal Death Pathway Activation in Tauopathy Models
| Experimental Model | Cell Death Pathway | Key Molecular Markers | Observed Effect | Citation |
|---|---|---|---|---|
| HT22 Neuronal Cells | Necroptosis | RIPK1/RIPK3/MLKL necrosome formation | pTau induces necroptosis | [26] |
| iPSC-Derived Neurons | Tau Aggregation-Driven Death | Tau oligomers/filaments | Overexpression-induced death in 2 weeks | [15] |
| PC12 Cells | Apoptosis & Cell Cycle Reactivation | Caspase-3, Cyclin B1, Cyclin D1 | OA-induced tau hyperphosphorylation | [27] |
| Primary Neurons | Apoptosis | Early tau hyperphosphorylation, later cleavage | PI3K inhibition | [28] |
Mitochondrial Dysfunction: A Core Consequence of Tauopathy
Bioenergetic Deficit and Oxidative Stress
In-depth studies using iPSC-derived neurons (iPSCsNs) and directly converted neurons (iNs) from aged donors have provided a quantitative profile of tauopathy-associated mitochondrial failure. Key impairments include a significant decrease in cellular ATP levels and a reduction in the mitochondrial membrane potential (MMP), which is the fundamental driving force for ATP synthesis [23]. This is coupled with a measurable impairment in mitochondrial respiration, evidenced by decreased oxygen consumption rates (OCR) across basal respiration, ATP-linked respiration, and maximal respiratory capacity [23]. Concurrently, these models exhibit a substantial increase in reactive oxygen species (ROS), including mitochondrial superoxide anions, leading to elevated oxidative stress [23]. This phenomenon is also observed in iPSC-derived models of other neurodegenerative conditions, such as PARK2 Parkinson's disease, where patient neurons showed increased oxidative stress and abnormal mitochondrial morphology [24].
Morphological and Metabolic Shifts
Beyond functional metrics, the mitochondrial network itself undergoes structural deterioration. In aged neuronal models, the normally tubular and interconnected mitochondrial network becomes fragmented, exhibiting a more circular and shorter morphology, as quantified by decreases in parameters like Form Factor and Aspect Ratio [23]. This fragmentation is associated with an upregulation of gene expression for both mitochondrial fission (e.g., FIS1) and fusion (e.g., MFN1, MFN2, OPA1) proteins, suggesting a dynamic but ultimately pathological remodeling of the network [23]. Furthermore, a critical metabolic shift appears to be model-dependent; while aged directly converted neurons (iNs) show a compensatory shift towards glycolysis, aged iPSCsNs do not, indicating potential differences in how these models handle bioenergetic stress [23].
Tau-Induced Neuronal Death Pathways
Necroptosis: A Regulated Form of Necrotic Death
Beyond apoptosis, hyperphosphorylated tau has been shown to directly activate necroptosis, a programmed form of inflammatory cell death. Research demonstrates that pTau promotes the formation of the RIPK1/RIPK3/MLKL necrosome complex [26]. This process is critical for neuronal loss in Alzheimer's disease models. Importantly, the same study found that this RIPK1/RIPK3/MLKL axis is also essential for pTau-mediated activation of the NF-κB signaling pathway, driving a cell-autonomous cytokine and chemokine storm that exacerbates neuroinflammation. Blocking necroptosis with the RIPK1 inhibitor Nec-1s ameliorated behavioral deficits and neuroinflammation in a TauP301S mouse model, highlighting the therapeutic potential of targeting this pathway [26].
Aberrant Cell Cycle Reactivation and Apoptosis
Post-mitotic neurons can be driven into an abortive cell cycle by tau pathology, culminating in apoptosis. In a PC12 cell model of okadaic acid-induced tau hyperphosphorylation, this was evidenced by the upregulated expression of Cyclin B1 and Cyclin D1 [27]. This reactivation is a direct precursor to neuronal apoptosis, marked by the activation of caspase-3 [27]. The relationship between tau phosphorylation and apoptosis is complex and stage-dependent; in primary cerebellar granule neurons, a transient hyperphosphorylation of tau occurs at an early stage of apoptosis, which is followed by subsequent dephosphorylation and proteolytic cleavage of the protein as cell death progresses [28].
Experimental Protocols for Key Assays
Protocol: Generating and Utilizing iPSC-Derived Neuronal Models
The use of human iPSC-derived neurons is critical for modeling human-specific aspects of tau toxicity [15]. The following workflow outlines a standard protocol for generating a neuronal model for studying tau aggregation and toxicity.
Title: iPSC-derived Neuron Tau Toxicity Model Workflow
Procedure:
- iPSC Generation and Culture: Generate and maintain iPSCs from patient fibroblasts or peripheral blood mononuclear cells (PBMCs) using a feeder-free system, such as culture on Geltrex-coated plates with StemFlex medium [25]. For the first 24 hours after passaging, supplement the medium with a 10 µM ROCK inhibitor (Y-27632) to enhance cell survival.
- Neuronal Differentiation: Differentiate iPSCs into cortical glutamatergic neurons. One established protocol involves generating stable iPSC lines that inducibly express neurogenin-2 (Ngn2) and microRNAs (miR-9/9*-124) upon doxycycline (DOX) treatment. Culture cells in Neuronal Induction Medium (e.g., Neurobasal Plus with B27 Plus, CultureOne, GlutaMAX, L-ascorbic acid, dbcAMP, Y-27632, DAPT, and DOX) for 5 days on plates pre-coated with Poly-L-ornithine and iMatrix-511 [15].
- Inducing Tau Pathology:
- Overexpression Model: Transduce the neurons with lentiviral particles carrying wild-type or mutant (e.g., P301S) human tau (1N4R isoform) under a TET-on promoter system. Induce expression with doxycycline (e.g., 2 µg/mL) to drive tau aggregation and cell death within a two-week timeframe [15].
- Pharmacological Model: Treat neurons with a reagent like okadaic acid (OA, 30-70 nM for 24 hours), a potent phosphatase inhibitor, to induce rapid tau hyperphosphorylation [27].
- Intervention Studies: Apply therapeutic compounds (e.g., DOR agonists, necroptosis inhibitors) to the culture medium to assess their ability to rescue mitochondrial function or prevent cell death.
Protocol: Assessing Mitochondrial Function via Seahorse XF Analyzer
The Seahorse XF Analyzer provides real-time, live-cell measurement of mitochondrial function by monitoring the Oxygen Consumption Rate (OCR) and Extracellular Acidification Rate (ECAR).
Procedure:
- Cell Seeding: Seed iPSC-derived neurons at a density of 3.0 x 10^4 to 5.0 x 10^4 cells per well in a XF96 cell culture microplate that has been pre-coated with the appropriate substrate (e.g., Poly-L-ornithine/iMatrix-511) [23].
- Assay Medium Preparation: One day before the assay, replace the growth medium with unbuffered XF Assay Medium (e.g., XF Base Medium supplemented with 1 mM pyruvate, 2 mM glutamine, and 10 mM glucose). Incubate the cells overnight in a non-CO2 incubator.
- Mitochondrial Stress Test:
- Basal Measurements: Record basal OCR.
- Oligomycin Injection: Inject oligomycin (1.5 µM final concentration) to inhibit ATP synthase. The resulting drop in OCR represents ATP-linked respiration.
- FCCP Injection: Inject the uncoupler FCCP (1.0 µM final concentration) to collapse the proton gradient and induce maximum electron transport chain activity. The rise in OCR indicates maximal respiratory capacity.
- Rotenone/Antimycin A Injection: Inject a mix of rotenone and antimycin A (0.5 µM final concentration each) to completely shut down mitochondrial respiration. The remaining OCR is non-mitochondrial respiration.
- Data Calculation: Calculate key bioenergetic parameters from the OCR profile: Basal Respiration, ATP Production, Maximal Respiration, and Spare Respiratory Capacity [23].
Protocol: Evaluating Neuronal Death Pathways
Necroptosis and Apoptosis Analysis via Western Blotting and Flow Cytometry:
- Protein Extraction and Western Blot: Lyse cells in RIPA buffer with protease and phosphatase inhibitors. Resolve proteins by SDS-PAGE, transfer to PVDF membranes, and probe with specific antibodies [26] [27].
- Flow Cytometry for Cell Death: To quantify death pathways, use probes such as:
- Propidium Iodide (PI) / Annexin V staining to distinguish apoptotic from necrotic/necroptotic populations.
- Antibodies against activated MLKL to specifically detect necroptotic cells [26].
Signaling Pathways in Tau-Mediated Neurodegeneration
The diagram below synthesizes the core signaling pathways that connect hyperphosphorylated tau to mitochondrial dysfunction and neuronal death, as identified in the cited research.
Title: Signaling in Tau-Mediated Neurodegeneration
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating Tauopathy Mechanisms
| Reagent / Tool | Function / Target | Application in Research |
|---|---|---|
| AT8 Antibody | Detects tau phosphorylated at Ser202/Thr205 | Immunostaining, Western blot to confirm pTau pathology [29]. |
| Necrostatin-1 (Nec-1s) | RIPK1 inhibitor (specific for necroptosis) | To interrogate the role of necroptosis in pTau-mediated neuronal death [26]. |
| UFP-512 | δ-opioid receptor (DOR) agonist | To probe DOR-mediated neuroprotection against tau hyperphosphorylation via CDK5/AMPK [27]. |
| Okadaic Acid (OA) | Potent PP2A phosphatase inhibitor | To induce rapid and robust tau hyperphosphorylation in neuronal cell cultures [27]. |
| Seahorse XF Cell Mito Stress Test Kit | Measures mitochondrial bioenergetics (OCR) | To profile mitochondrial function (basal respiration, ATP production, spare capacity) [23]. |
| Lentiviral TET-on Tau Vectors | Doxycycline-inducible tau expression | To create iPSC-neuron models with controlled tau (wild-type or mutant) overexpression [15]. |
| CDK5 siRNA/Drug Inhibitors | Targets Cyclin-dependent kinase 5 | To investigate the role of CDK5 in driving tau hyperphosphorylation and subsequent pathology [27]. |
| MitoSOX Red | Mitochondrial superoxide indicator | Flow cytometry or fluorescence microscopy to measure mitochondrial oxidative stress [23]. |
Advanced Protocols for Robust Tau Pathology Modeling in iPSC Neurons
The microtubule-associated protein tau plays a central role in neurodegenerative tauopathies, including Alzheimer's disease (AD) and Frontotemporal Dementia (FTD). A significant challenge in modeling these diseases has been recapitulating the precise balance of tau isoforms found in the adult human brain, particularly the six isoforms generated through alternative splicing that differ by the inclusion of 0, 1, or 2 N-terminal inserts and the presence of either 3 or 4 microtubule-binding repeats (3R or 4R tau). This technical guide examines recent advances in generating human neuronal models that faithfully express adult-like 4R tau isoforms, a critical requirement for accurate disease modeling and therapeutic screening. Framed within the broader context of tau hyperphosphorylation research, we detail methodologies, quantitative outcomes, and essential reagents for overcoming this persistent experimental hurdle.
Tau pathology is a defining characteristic of multiple neurodegenerative disorders, and there is strong genetic and experimental evidence supporting a central role for tau dysfunction in neuronal death [16]. The development of tau pathology can precede symptom onset by several years, making understanding the earliest molecular events in tauopathy a research priority [16]. A major limitation in this research has been the availability of experimental models that recapitulate key features of human disease, particularly the precise expression profile of tau isoforms.
In the adult human brain, the equal ratio between 3R and 4R tau isoforms is maintained for normal function, and dysregulation of this ratio causes tauopathy [31]. However, certain aspects of tau biology, notably its alternative splicing, are species-specific, and common experimental models often fail to replicate patterns observed in the adult human central nervous system [16]. This technical gap has hindered our understanding of disease mechanisms and the development of effective therapies. The emergence of induced pluripotent stem cell (iPSC) technology and direct neuronal reprogramming methods has provided new opportunities to generate human neurons that capture the precise genetic makeup of donors, offering a powerful tool for studying disease mechanisms [16]. This whitepaper consolidates the most effective strategies for generating authentic 4R tau expression in human neuronal models, providing a technical roadmap for researchers and drug development professionals.
Tau Isoform Fundamentals and Pathological Significance
Tau is a microtubule-binding protein expressed in neurons, and the equal ratios between 4-repeat (4R) and 3-repeat (3R) isoforms are critically maintained in normal adult brain function [31]. The six major tau isoforms result from alternative splicing of exons 2, 3, and 10 of the MAPT gene. The inclusion or exclusion of exon 10 determines whether the isoform contains 4 microtubule-binding repeats (4R tau) or 3 repeats (3R tau). This distinction is functionally and pathologically significant, as 4R and 3R tau exhibit differences in their microtubule-binding properties and propensity for aggregation.
Dysregulation of the 3R:4R tau ratio is a well-established mechanism in several tauopathies. For example, mutations in the MAPT gene that alter splicing, such as the IVS10+16 splice site mutation, cause increased 4R tau expression and lead to familial tauopathy [31]. The H1 haplotype of the MAPT locus is associated with increased susceptibility to several sporadic tauopathies, including progressive supranuclear palsy (PSP) and corticobasal degeneration (CBD) [16]. Beyond genetic tauopathies, abnormal tau accumulation is a hallmark of Alzheimer's disease, where hyperphosphorylated tau forms neurofibrillary tangles that correlate with disease progression and neuronal cell death [32] [4].
Table 1: Tau Isoforms in Human Brain and Model Systems
| Model System | 3R:4R Tau Ratio | Developmental Regulation | Pathological Relevance |
|---|---|---|---|
| Fetal Human Brain | ~90:10 (Higher 3R) | Yes | Developmental regulation |
| Adult Human Brain | ~50:50 (Balanced) | Stable | Normal function |
| Standard iPSC-Neurons | Variable, often fetal-like | Limited | Limited disease relevance |
| miR Neurons [31] | Equivalent to adult brain | Yes | Recapitulates familial mutation effects |
| Optimized iPSC-Cortical Neurons [33] | Adult-like, all 6 isoforms | Developmentally regulated | Accelerated timeline |
Methodological Approaches for Recapitulating Adult Tau Isoforms
Direct Neuronal Reprogramming with microRNAs
One promising approach for generating neurons with adult-like tau expression is microRNA-induced neuronal reprogramming (miR neurons). This method involves the direct conversion of adult fibroblasts into neurons, bypassing the pluripotent state and potentially preserving age-related characteristics.
Detailed Protocol:
- Starting Material: Obtain human dermal fibroblasts from adult donors (including tauopathy patients with IVS10+16 or other MAPT mutations for disease modeling).
- Reprogramming: Transduce fibroblasts with lentiviral vectors expressing microRNAs (miR-9/9*-124) known to promote neuronal fate.
- Culture Conditions: Maintain cells in neuronal induction medium supplemented with growth factors (BDNF, CNTF, GDNF).
- Maturation: Culture for 8-12 weeks to allow for full neuronal maturation and establishment of adult tau isoform profiles.
- Validation: Perform transcript and protein analyses to confirm expression of all six tau isoforms with the 3R:4R ratio equivalent to human adult brains.
Key Outcomes: This method has demonstrated successful recapitulation of endogenous 4R tau expression and the formation of insoluble tau with seeding activity when using fibroblasts from familial tauopathy patients with 3R:4R ratio-altering mutations [31]. The increased 4R tau expression in patient-derived miR neurons provides evidence that this system can capture disease-relevant molecular changes.
Optimized iPSC-Derived Cortical Neuron Differentiation
An alternative approach involves developing refined differentiation protocols for iPSC-derived cortical neurons that promote the expression of all six adult tau isoforms.
Detailed Protocol:
- Neural Induction: Differentiate hiPSCs through embryoid body (EB) formation with combined inhibition of WNT (using XAV939), SHH (using cyclopamine), and SMAD signaling pathways.
- Dorsal Forebrain Specification: The specific combination and timing of morphogen inhibition generate neuroepithelial cells expressing appropriate dorsal forebrain markers while suppressing ventral, midbrain, and hindbrain genes.
- Neuronal Differentiation: Further differentiate in neurogenic and neurotrophic factors to produce MAP2+ neurons by approximately day 18.
- Maturation: Continue culture for extended periods (up to 80 days) to allow developmental expression of all six tau isoforms in a regulated manner.
- Characterization: Verify cortical layer markers, synapse formation, and synaptic physiology to confirm neuronal maturity.
Key Outcomes: This chemically defined differentiation method produces a key hallmark of mature human cortical neurons by expressing the six main splicing isoforms of tau, modeling the situation in human brains on an accelerated timeline [33]. The neurons express markers of all cortical layers and exhibit synapse formation and synaptic physiology, indicating functional maturity.
Three-Dimensional Culture Systems
Both directly reprogrammed neurons and iPSC-derived neurons can be adapted to 3D culture formats to better mimic the brain microenvironment and enhance tau pathology development.
Detailed Protocol:
- Matrix Embedding: Embed neurons in a 3D support matrix such as Matrigel to provide scaffolding and reduce shearing stress.
- Long-term Culture: Maintain cultures for extended periods (up to 90 days or more) to allow accumulation of pathological tau species.
- Assay Integration: Combine with detection methods like AlphaLISA technology for high-throughput-compatible tau aggregate detection.
Key Outcomes: 3D neuronal cultures accelerate the accumulation of insoluble Aβ monomers and oligomers together with sarkosyl-insoluble, hyperphosphorylated, filamentous tau [16]. This format has been downscaled to 384-well plate formats, creating a robust and scalable tau aggregation model compatible with high-throughput screening [34].
Signaling Pathways Regulating Tau Isoform Expression
The following diagram illustrates the key signaling pathways involved in directing iPSCs toward cortical neurons with adult tau isoform expression:
Diagram Title: Signaling Pathway to Cortical Neurons with Adult Tau
Research Reagent Solutions for Tau Isoform Studies
Table 2: Essential Research Reagents for Tau Isoform Modeling
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Small Molecule Inhibitors | XAV939 (WNT inhibitor), Cyclopamine (SHH inhibitor) | Dorsal forebrain patterning | iPSC differentiation to cortical neurons [33] |
| Reprogramming Factors | miR-9/9*-124 | Direct neuronal reprogramming | Generation of miR neurons from fibroblasts [31] |
| Growth Factors | BDNF, CNTF, GDNF | Neuronal maturation and survival | Maintenance of human neurons in long-term culture [31] |
| 3D Scaffolding Matrices | Matrigel | 3D culture environment | Enhanced tau pathology development [16] [34] |
| Tau Detection Assays | AlphaLISA technology | High-throughput tau aggregate detection | Screening platforms for tau-targeting therapeutics [34] |
| Cell Lines | Familial tauopathy patient iPSCs (e.g., IVS10+16 MAPT mutation) | Disease modeling | Studying 4R tau increase and insoluble tau formation [31] |
Relationship Between 4R Tau Expression and Tau Hyperphosphorylation
The successful recapitulation of adult-like 4R tau expression in human neuronal models has enabled more accurate study of its relationship with tau hyperphosphorylation, a key pathological event in tauopathies. Neurons derived from both familial and sporadic AD iPSCs show increased phosphorylation of tau protein at multiple sites, including S396, S404, T181, and S235 [4] [35]. Active glycogen synthase kinase 3β (GSK3B), a physiological kinase of tau, is increased in AD-derived neurons, providing a potential mechanism for hyperphosphorylation [4].
Notably, the expression of adult 4R tau isoforms appears to create a permissive environment for pathological changes. In optimized models, increased 4R tau expression leads to the formation of insoluble, seed-competent tau species that recapitulate key features of human tauopathy [31]. This pathological tau shows characteristics similar to those found in human AD brains, including fragmentation and detergent-insolubility [35]. The relationship between 4R tau expression and hyperphosphorylation underscores the importance of accurate isoform representation for meaningful disease modeling.
The following experimental workflow demonstrates how these elements integrate in a comprehensive tau pathology study:
Diagram Title: Experimental Workflow for Tau Pathology Modeling
Quantitative Assessment of Tau Pathology in Advanced Models
Table 3: Quantitative Measures of Tau Pathology in Human Neuronal Models
| Pathological Feature | Assessment Method | Key Findings | Experimental System |
|---|---|---|---|
| Tau Hyperphosphorylation | Phospho-specific antibodies (S396/404, T181, S235) | Increased at multiple sites in fAD and sAD neurons | iPSC-derived neurons [4] [35] |
| Tau Insolubility | Sarkosyl extraction and Western blot | Seed-competent, insoluble tau in patient-derived neurons | miR neurons with MAPT mutations [31] |
| Neuronal Death | Cell viability assays, caspase activation | Tau aggregation-dependent death within 2 weeks with overexpression | iPSC-derived neuronal model [32] |
| Axonal Degeneration | Immunofluorescence (MAP2, Tau) | Axon fragmentation and dendrite retraction | Aβ42 oligomer-treated neurons [35] |
| Synaptic Alterations | Synaptic marker staining (PSD95, Synapsin) | Significant synapse loss with tau pathology | Automated iPSC neuron platform [35] |
The generation of human neuronal models that faithfully recapitulate adult-like 4R tau expression represents a significant advancement in tauopathy research. Through optimized differentiation protocols, direct reprogramming approaches, and advanced 3D culture systems, researchers can now overcome the historical hurdle of modeling adult tau isoform regulation. These technical improvements have enabled more accurate study of tau hyperphosphorylation mechanisms and the development of screening platforms for tau-targeting therapeutics.
The ability to capture the endogenous regulation of tau isoforms, including the balanced 3R:4R ratio of the adult brain and its dysregulation in disease, provides a critical platform for elucidating pathogenic processes [31]. As these models continue to evolve—incorporating multiple cell types, enhancing maturity, and improving throughput—they offer promising avenues for identifying and validating novel therapeutic strategies for Alzheimer's disease and other tauopathies. The integration of these advanced cellular models with automated culturing platforms and high-content screening technologies will further accelerate the translation of basic research findings into clinical applications.
Implementing 3D Culture and Scaffolding to Enhance Pathological Phenotypes
The study of tau hyperphosphorylation in Alzheimer's disease (AD) and related tauopathies has been historically challenged by the limitations of conventional two-dimensional (2D) neuronal cultures. These traditional systems fail to recapitulate the complex three-dimensional microenvironment of the human brain, often resulting in pathological phenotypes that lack key disease characteristics observed in patients. The advent of three-dimensional (3D) cell culture models using induced pluripotent stem cell (iPSC)-derived neurons represents a transformative approach for neurodegenerative disease modeling [36] [37]. These advanced systems provide a more physiologically relevant context that better mimics the architectural and cellular complexity of native brain tissue, enabling researchers to study disease mechanisms with unprecedented accuracy.
For researchers focusing on tau pathology, 3D cultures offer particular advantages for observing the progression of tau hyperphosphorylation and aggregation. The restricted diffusion of secreted factors in 3D environments allows for the accumulation of pathological proteins, including amyloid-β (Aβ) and hyperphosphorylated tau, facilitating the formation of neurofibrillary tangle-like structures that are hallmarks of AD [36] [38]. This technical guide provides comprehensive methodologies for implementing 3D culture systems and scaffolding techniques specifically designed to enhance pathological tau phenotypes in iPSC-derived neuronal models, enabling more robust mechanistic studies and drug discovery applications.
Theoretical Foundation: 3D Systems for Enhanced Neuropathology
Comparative Advantages of 3D Culture Systems
Three-dimensional culture systems provide critical advantages over conventional 2D systems for modeling tau pathology in neurodegenerative diseases. The enhanced pathological relevance stems from several key factors:
Accumulation of Pathological Proteins: Unlike 2D systems where culture medium changes regularly remove secreted factors, 3D environments restrict diffusion and enable accumulation of Aβ species and tau proteins, creating localized concentrations that drive aggregation [38]. This is particularly crucial for tau pathology, as the hyperphosphorylated forms require sufficient concentration and time to form the oligomeric species and filamentous aggregates that characterize disease states.
Cell-Cell and Cell-ECM Interactions: 3D cultures preserve the intricate network of interactions between neurons, astrocytes, oligodendrocytes, and microglia that significantly influence tau phosphorylation states [37]. These interactions, combined with more physiological cell-ECM engagement, create signaling environments that better mimic the in vivo conditions under which tau pathology develops.
Spatial Organization and Biochemical Gradients: The three-dimensional architecture allows for establishing biochemical gradients and polarized cellular structures that influence tau localization and function within neuronal processes [36]. This spatial organization is essential for recapitulating the compartment-specific vulnerability to tau pathology observed in human brain tissue.
Scaffolding Materials and Their Properties
The choice of scaffolding material fundamentally influences the development of pathological phenotypes in 3D cultures. The table below summarizes key biomaterials used in neurodegenerative disease modeling:
Table 1: Scaffolding Biomaterials for 3D Neuronal Culture Systems
| Material Type | Examples | Key Properties | Impact on Tau Pathology |
|---|---|---|---|
| Natural Hydrogels | Matrigel, Collagen, Laminin | Bioactive ligands, tunable stiffness, high permeability | Enhances neuronal differentiation and network formation; promotes endogenous Aβ and tau accumulation [34] [37] |
| Synthetic Hydrogels | PEG-based, PA hydrogels | Defined mechanical properties, controllable degradation | Allows systematic study of stiffness effects on tau phosphorylation; minimal bioactive interference [37] |
| Hybrid Systems | Peptide-functionalized PEG | Combined bioactivity and control | Enables investigation of specific ECM component effects on tau pathology |
| Scaffold-Free | Spheroids, Organoids | Self-organizing, complex cell interactions | Recapitulates Aβ and tau pathology without exogenous factors [36] |
Experimental Implementation
iPSC-Derived Neuronal Culture in 3D Format
Protocol 1: Establishment of 3D Human iPSC-Derived Cortical Neurons for Tau Aggregation Studies
This protocol adapts a scalable, high-throughput-compatible assay to detect tau aggregates using iPSC-derived cortical neurons maintained in a 3D culture format [34]:
iPSC Neural Differentiation:
- Differentiate human iPSCs into cortical neuronal progenitors using dual SMAD inhibition protocol (LDN-193189 100nM, SB431542 10μM) for 10-12 days [36].
- Confirm neural commitment via immunocytochemistry for Nestin (neural progenitor marker) and PAX6 (cortical progenitor marker).
3D Culture Seeding:
- Prepare ice-cold Matrigel solution (8-10 mg/mL concentration) in DMEM/F-12 medium.
- Mix neuronal progenitors with Matrigel at density of 1×10^7 cells/mL.
- Plate 30μL droplets (3×10^5 cells) into center of 384-well plates pre-warmed to 37°C.
- Incubate plates for 30 minutes at 37°C to allow gel polymerization.
- Carefully add 50μL of neuronal maintenance medium (Neurobasal medium with B-27, BDNF 20ng/mL, GDNF 10ng/mL, cAMP 1mM).
Long-term Maintenance:
- Replace 50% of medium twice weekly for up to 90 days.
- For tau pathology enhancement, avoid agitation and limit medium exchange frequency after day 30 to promote protein accumulation [34].
Protocol 2: Hydrogel-Based 3D Culture of iPSC-Derived Neurons Carrying AD Mutations
This method utilizes a hydrogel-based 3D model with iPSCs carrying the A246E mutation in the PSEN1 gene that produces Aβ oligomers and enhances tau pathology [36]:
iPSC Generation from AD Patients:
- Obtain human fibroblasts from AD patients harboring PSEN1 mutations (e.g., A246E mutation, Coriell Cat# AG07768).
- Reprogram using lentiviral vectors containing Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) [36].
- Validate pluripotency through expression of Nanog, OCT4, SOX2, TRA-1-60, and SSEA4.
3D Neural Differentiation in Hydrogel:
- Encapsulate iPSCs in defined neural induction hydrogel (e.g., PEG-based matrix with RGD adhesion peptides).
- Culture in neural induction medium (N2B27 supplements, dual SMAD inhibitors) for 14 days.
- Switch to neuronal maturation medium for additional 4-6 weeks.
Pathological Phenotype Validation:
- Confirm Aβ oligomer production via Western Blot from day 14 onward.
- Assess tau hyperphosphorylation at multiple time points (days 30, 60, 90) using phospho-tau specific antibodies (AT8, PHF-1).
Tau Aggregation Assessment in 3D Cultures
Protocol 3: High-Throughput Tau Aggregation Detection Using AlphaLISA
This protocol enables quantitative detection of tau aggregates in 3D cultures in a high-throughput-compatible format [34]:
Sample Preparation from 3D Cultures:
- Aspirate culture medium from 384-well 3D cultures.
- Add 20μL of lysis buffer (50mM Tris-HCl pH7.4, 150mM NaCl, 1% NP-40, protease and phosphatase inhibitors).
- Incubate with orbital shaking (300rpm) for 30 minutes at 4°C.
- Transfer lysates to microplate for analysis.
AlphaLISA Detection:
- Use anti-tau capture antibody (e.g., Tau5) conjugated to AlphaLISA acceptor beads.
- Employ anti-phospho-tau detection antibody (e.g., AT8 for pS202/pT205) conjugated to biotin.
- Add streptavidin-coated donor beads to form detection complex.
- Quantify tau aggregates using AlphaLISA signal measured at 615nm.
- Normalize values to total protein content.
Table 2: Temporal Development of Pathological Markers in 3D AD Models
| Time Point | Aβ Pathology | Tau Pathology | Key Molecular Events |
|---|---|---|---|
| Day 14 | Aβ oligomers detectable by WB [36] | Phospho-tau barely detectable | Initial amyloid precursor protein processing |
| Day 30 | Aβ deposits immunostaining positive | Elevated p-tau levels by AlphaLISA [34] | Early hyperphosphorylation begins |
| Day 60 | Significant Aβ aggregation | Robust tau hyperphosphorylation | NFT-like phosphorylation patterns emerge |
| Day 90 | Mature Aβ plaques | Filamentous tau aggregates | Neurofibrillary tangle-like structures |
Research Reagent Solutions
Table 3: Essential Research Reagents for 3D Tau Pathology Models
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Factors | Lentiviral OSKM factors (OCT4, SOX2, KLF4, c-MYC) [36] | Generation of patient-specific iPSCs from somatic cells |
| Neural Induction | Dual SMAD inhibitors (LDN-193189, SB431542) [36] | Efficient differentiation toward neural lineage |
| 3D Scaffolding | Matrigel, PEG-based hydrogels, laminin-containing matrices [34] [37] | Provides 3D structural support and biochemical cues |
| Tau Detection | AlphaLISA detection system, AT8, PHF-1 antibodies [34] | Quantification and detection of tau aggregates and phospho-epitopes |
| Cell Type Markers | Nestin (progenitors), MAP2 (neurons), GFAP (astrocytes) [36] | Characterization of cellular composition in 3D cultures |
Signaling Pathways in Tau Hyperphosphorylation
The following diagram illustrates key signaling pathways involved in tau hyperphosphorylation within 3D neuronal cultures:
Signaling Pathways in Tau Hyperphosphorylation
Experimental Workflow
The following diagram outlines the comprehensive workflow for establishing 3D cultures to enhance tau pathology:
3D Culture Workflow for Tau Pathology
The implementation of 3D culture systems and advanced scaffolding technologies represents a significant advancement in modeling tau hyperphosphorylation using iPSC-derived neurons. These systems successfully address critical limitations of traditional 2D cultures by providing a more physiologically relevant microenvironment that enables the accumulation and aggregation of pathological proteins, enhanced cell-cell interactions, and superior spatial organization. The methodologies outlined in this technical guide—from the establishment of hydrogel-based 3D cultures to the high-throughput quantification of tau aggregates—provide researchers with robust tools to study disease mechanisms and screen potential therapeutic compounds. As the field continues to evolve, these 3D model systems will play an increasingly vital role in bridging the gap between conventional in vitro models and clinical reality, ultimately accelerating the development of effective treatments for Alzheimer's disease and related tauopathies.
Designing High-Throughput Screening (HTS) Assays for Tau Aggregation Modulators
The pathological aggregation of tau protein into neurofibrillary tangles (NFTs) is a defining neuropathological hallmark of Alzheimer's disease (AD) and related tauopathies, directly correlating with cognitive decline and neuronal loss [39] [4]. Under normal physiological conditions, tau is an intrinsically disordered, soluble protein; its transition to a pathogenic, aggregation-prone state is driven by complex molecular events including hyperphosphorylation, acetylation, and conformational changes [39]. Research using induced pluripotent stem cell (iPSC)-derived neurons from patients with both familial and sporadic AD has demonstrated that these neurons recapitulate key disease phenotypes, including tau hyperphosphorylation at multiple serine and threonine residues and increased sensitivity to oxidative stress [4] [32]. This establishes iPSC-derived neuronal models as a physiologically relevant platform for investigating tau pathobiology. The development of high-throughput screening (HTS) assays capable of identifying modulators of tau aggregation within such biologically complex systems is therefore a critical endeavor for therapeutic discovery, offering the potential to halt or reverse disease progression in tauopathies [39] [32].
Core HTS Technologies for Monitoring Tau Aggregation
Conventional in vitro tau aggregation assays often rely on recombinant protein and artificial inducers like heparin, lacking the cellular context necessary for modeling the full complexity of tau pathology [39] [40]. Cell-based models, particularly those utilizing mammalian cells like HEK293 and human iPSC-derived neurons, offer a more physiologically relevant environment as they support disease-relevant post-translational modifications (PTMs) of tau and allow for simultaneous assessment of compound cytotoxicity and cell penetration [39] [4]. Several fluorescence-based technologies have been engineered to monitor intracellular tau aggregation in living cells.
Bimolecular Fluorescence Complementation (BiFC) and Split GFP Systems: These are "turn-on" sensors where fluorescence is reconstituted only upon tau-tau interaction and aggregation. Tau proteins are fused to complementary, non-fluorescent fragments of a fluorescent protein (e.g., Venus or GFP). When tau aggregates, the fragments are brought into proximity, allowing the fluorescent protein to reassemble and emit a signal with minimal background under basal conditions [39] [32]. This system is particularly useful for detecting early aggregation events.
Fluorescence Resonance Energy Transfer (FRET): In FRET-based assays, tau is tagged with both a donor fluorophore (e.g., CFP) and an acceptor fluorophore (e.g., YFP). Upon close proximity during aggregation, energy is transferred from the donor to the acceptor, resulting in a detectable emission shift. While valuable, FRET can have limitations in sensitivity and dynamic range, and the large fluorophore tags may potentially interfere with protein dynamics [39].
Flow Cytometry-Compatible Assays: The integration of cell-based aggregation sensors (like split GFP) with flow cytometry enables rapid, quantitative analysis of thousands of cells per second. This combination is ideal for HTS, as it allows for the processing of large compound libraries while providing multiparametric data on both fluorescence intensity (aggregation level) and cell viability [39].
Table 1: Comparison of Core HTS Assay Technologies for Tau Aggregation
| Technology | Principle | Advantages | Disadvantages/Limitations |
|---|---|---|---|
| Split GFP/Venus (BiFC) | "Turn-on" fluorescence via fragment complementation upon aggregation [39]. | Low background; detects early aggregates; suitable for live-cell imaging and flow cytometry. | Fluorescence is irreversible after complementation. |
| FRET | Energy transfer between two fluorophores tagged on tau proteins in close proximity [39]. | Can monitor dynamic interactions. | Lower sensitivity; large tags may interfere; requires specialized equipment. |
| Flow Cytometry | Quantitative analysis of fluorescence per cell in suspension [39]. | Very high-throughput; multiparametric (aggregation & viability). | Requires cells in suspension; equipment cost. |
| iPSC-Derived Neurons | Patient-specific human neurons that model disease pathology [4] [32]. | High physiological relevance; contains human genetic background. | Lower throughput; higher cost; more variable. |
Experimental Design and Protocols
A High-Throughput Cell-Based Assay Using Split GFP and Flow Cytometry
A robust HTS assay has been developed using suspension-adapted HEK293 cells co-transfected with tau proteins (0N4R isoform) fused to complementary split GFP fragments [39]. This system demonstrates key advantages for screening.
Key Experimental Workflow:
- Cell Line Engineering: Suspenion-adapted HEK293 cells are co-transfected with plasmids encoding tau-0N4R fused to GFP1-10 and tau-0N4R fused to GFP11.
- Cell Culture and Seeding: Cells are maintained in suspension culture and seeded into multi-well plates (e.g., 384-well format) containing the compound library.
- Incubation and Induction: The cells are incubated with compounds for a defined period (e.g., 24-48 hours). Notably, this specific system demonstrates tau aggregation without requiring external aggregation inducers, which is attributed to enhanced protein expression in suspension-adapted cells [39].
- Flow Cytometry Analysis: Cells are analyzed using a flow cytometer. The fluorescence signal from reconstituted GFP is quantified as a measure of tau aggregation. Simultaneously, a viability dye (e.g., propidium iodide) can be added to gate out dead cells and assess compound cytotoxicity [39].
- Data Analysis: Fluorescence intensity data is processed to calculate the Z'-factor, a statistical parameter for assessing assay quality and robustness for HTS. A Z'-factor > 0.5 is generally indicative of an excellent assay. Dose-response curves are generated for hit compounds to determine IC₅₀ values [39].
The following diagram illustrates the core principle of the split GFP Tau aggregation assay and the subsequent HTS workflow:
Validation in iPSC-Derived Neuronal Models
While overexpression systems are valuable for primary HTS, validation of hit compounds in more physiologically relevant models is essential. iPSC-derived neurons from AD patients provide a powerful secondary assay platform.
Protocol for iPSC-Derived Neuron Validation:
- iPSC Generation and Differentiation: Generate iPSCs from healthy controls, patients with familial AD (e.g., PSEN1 mutations), and patients with sporadic AD. Differentiate these iPSCs into mature cortical neurons using established protocols [4].
- Compound Treatment: Treat the mature iPSC-derived neurons with hit compounds identified from the primary HTS.
- Phenotype Assessment:
- Tau Phosphorylation: Analyze lysates by Western blot to measure tau hyperphosphorylation at specific epitopes (e.g., using antibodies against p-tau Thr181, Ser202, Ser396) [4].
- Neuronal Cell Death: Quantify cell death using assays like TUNEL staining or Caspase-3 activation to confirm the neuroprotective effects of aggregation inhibitors [32].
- Other Pathological Markers: Measure extracellular Aβ₁–₄₀ and Aβ₁–₄₂ levels by ELISA and assess the activity of kinases like GSK3β, which is known to phosphorylate tau [4].
Table 2: Key Parameters for Validating Modulators in iPSC-Derived Neurons
| Validation Parameter | Experimental Method | Significance in Disease Modeling |
|---|---|---|
| TAU Hyperphosphorylation | Western Blot with phospho-specific tau antibodies [4]. | Core pathological event driving aggregation; confirmed in both fAD and sAD iPSC-neurons [4]. |
| Neuronal Cell Death TUNEL, Caspase-3/7 assay, LDH release [32]. | Functional readout of neuroprotection; tau aggregation induces death in human neurons [32]. | |
| Aβ1-42 / Aβ1-40 Ratio | ELISA [4]. | Indicator of amyloidogenic processing; typically increased in fAD neurons [4]. |
| GSK3β Activity | Western Blot for active (phospho-) GSK3β [4]. | A key physiological kinase for tau; found upregulated in AD iPSC-neurons [4]. |
| Oxidative Stress Sensitivity Viability after H₂O₂ or amyloid oligomer exposure [4]. | Models environmental stress interactions; fAD/sAD neurons show elevated sensitivity [4]. |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for HTS Assay Development
| Reagent / Material | Function in Assay | Specific Examples / Notes |
|---|---|---|
| Suspension-Adapted HEK293 Cells | A scalable cellular host for high-throughput transfection and flow cytometry [39]. | Chosen for high protein expression, enabling aggregation without external inducers [39]. |
| Split GFP-Tau Plasmids | Engineered DNA constructs for expressing tau fused to non-fluorescent GFP fragments [39]. | Tau-0N4R isoform fused to GFP1-10 and GFP11; acts as a "turn-on" sensor for aggregation [39]. |
| Known Inhibitor for Validation | A reference compound for assay validation and as a positive control [39]. | A urea-based tau aggregation inhibitor shown to cause dose-dependent fluorescence reduction [39]. |
| Flow Cytometer with HTS Capability | Instrument for rapid, quantitative analysis of fluorescence and viability in single cells [39]. | Essential for processing 384-well plates; allows multiplexed readouts. |
| iPSC-Derived Cortical Neurons | A physiologically relevant human model for secondary validation of hit compounds [4] [32]. | Can be derived from fAD or sAD patients; recapitulate hyperphosphorylation and Aβ pathology [4]. |
| Phospho-Specific Tau Antibodies | Detect and quantify disease-relevant hyperphosphorylation of tau in validation assays [4]. | Target sites like pThr181, pSer202, pSer396 for Western Blot [4]. |
| Congo Red / Anionic Surfactants | Aggregation agonists used in some models to induce or accelerate tau fibril formation [39] [40]. | Useful in mechanistic studies but not required in the described split GFP HEK293 system [39]. |
Assay Validation and Hit Qualification
A critical step in HTS is validating that the assay robustly identifies true modulators of the biological pathway. For the split GFP tau aggregation assay, this is achieved by treating cells with a known urea-based tau aggregation inhibitor, which produces a dose-dependent reduction in fluorescence signal, confirming the assay's ability to detect inhibition [39]. The statistical parameter Z'-factor should be calculated to confirm the assay's robustness and suitability for HTS; a value greater than 0.5 is considered excellent.
Hit qualification from the primary screen must involve counter-screens to rule out false positives. This includes:
- Cytotoxicity Assessment: Ensuring reduced fluorescence is not due to compound-induced cell death, which is facilitated by the multiplexed nature of flow cytometry [39].
- Mechanistic Studies: Investigating whether hit compounds directly interact with tau to prevent aggregation (true inhibitors) or indirectly modulate the pathway by affecting kinases/phosphatases. This can be assessed in in vitro aggregation assays with recombinant tau [40].
- Secondary Validation: Confirming efficacy in iPSC-derived neuronal models, as described in Section 3.2, to ensure activity in a more disease-relevant human system [4] [32].
Rapid Tau Aggregation Models for Efficient Therapeutic Candidate Screening
In the quest to develop disease-modifying therapies for Alzheimer's disease (AD) and related tauopathies, the hyperphosphorylation and subsequent aggregation of the microtubule-associated protein tau represents a critical therapeutic target. The progression of cognitive decline in these diseases correlates more closely with the burden of tau pathology than with other pathological hallmarks [19]. A significant challenge in therapeutic development has been the translation of promising preclinical findings to clinical benefit, underscoring the urgent need for robust, physiologically relevant, and efficient models of tau aggregation for candidate screening [20]. This whitepaper provides an in-depth technical guide to contemporary rapid tau aggregation models, with a specific focus on their application in human iPSC-derived neuronal systems, which recapitulate key features of sporadic AD-related tauopathies, including tau hyperphosphorylation.
The Central Role of Tau Hyperphosphorylation in Pathogenesis
In its physiological state, tau is a neuron-enriched microtubule-associated protein that stabilizes axonal microtubules, thereby supporting neuronal morphology, integrity, and intracellular transport [19] [41]. The protein is encoded by the MAPT gene, and alternative splicing of exons 2, 3, and 10 generates six major isoforms in the adult human central nervous system, which differ in their microtubule-binding affinity and aggregation propensity [19] [18].
Under pathological conditions, a shift in post-translational modification homeostasis—particularly a kinase/phosphatase imbalance—drives the hyperphosphorylation of tau. This hyperphosphorylation severely impairs tau's normal function, reducing its microtubule-binding capacity and promoting its mislocalization from axons to the somatodendritic compartments [19] [1]. The somatodendritic accumulation of hyperphosphorylated tau is a key step in its transition into a pathogenic species. Specific kinases, such as Serum and Glucocorticoid-regulated Kinase 1 (SGK1), are significantly upregulated in AD patient-derived iPSC cortical neurons and post-mortem brain tissue, and have been mechanistically linked to increased tau phosphorylation on pathologically relevant epitopes like S202/T205 (detected by AT8 antibody) and S214 [1]. This hyperphosphorylation disrupts synaptic integrity, dendritic spine morphology, mitochondrial function, and ultimately leads to cognitive deterioration [19] [1]. Crucially, hyperphosphorylation enhances tau's propensity to self-assemble, through key aggregation-prone motifs (e.g., VQIVYK and VQIINK), into soluble oligomers and insoluble fibrils that accumulate as neurofibrillary tangles [41] [42]. Furthermore, pathological tau exhibits prion-like properties, whereby misfolded aggregates can be released from cells and taken up by neighboring neurons, seeding the aggregation of native tau and propagating pathology through connected brain circuits [41] [43].
Table 1: Key Phosphorylation Sites in Pathological Tau and Their Detection
| Phosphorylation Site | Significance / Associated Antibody | Detection Method |
|---|---|---|
| S202/T205 | Early pathological event; AT8 antibody epitope | Immunostaining, Western Blot [1] |
| S214 | Increased in AD neurons; linked to pathology | Immunostaining, Western Blot [1] |
| pTau217 | Strongly correlates with tau seeding activity; potential diagnostic biomarker | Western Blot, Mass Spectrometry [43] |
| pTau396 | AD-specific phospho-species; correlates with seeding activity | Western Blot, Mass Spectrometry [43] |
| pTau262 | AD-specific phospho-species; correlates with seeding activity | Mass Spectrometry [43] |
| pTau231 | AD-specific phospho-species; correlates with seeding activity | Mass Spectrometry [43] |
Advanced Tau Aggregation Models for High-Throughput Screening
Traditional models often failed to capture the gradual, concentration-dependent accumulation of insoluble tau aggregates observed in human disease. The following next-generation models have been developed to overcome these limitations, offering superior pathophysiological relevance and compatibility with high-content screening.
Primary Neuronal Seeding and Propagation Model
This model utilizes primary neurons expressing wild-type human tau at physiological levels. The key to its rapid and robust aggregation is the seeding with sub-nanomolar concentrations of pathological tau derived from human AD brain tissue. This seeding event initiates the templated misfolding and aggregation of endogenous tau in the neurons [20].
Key Advantages:
- High Pathophysiological Relevance: Employs native neuronal context and authentic AD tau seeds.
- Quantitative Readouts: Tau aggregation is quantitatively measured using automated high-content imaging algorithms, making it suitable for screening.
- Functional Correlates: The resulting aggregates lead to impaired mitochondrial function, reflecting a downstream pathological consequence [20].
Optogenetic Tau (optoTAU) Aggregation Model
The optoTAU system is an inducible model that provides superior light-specific control over tau aggregation. It is based on a fusion protein of full-length (2N4R) tau and a small, engineered photoreceptor called Vivid (VVD). Upon exposure to light, VVD undergoes rapid homodimerization, forcing the tau component to cluster and initiate the aggregation process [44].
Key Advantages:
- Temporal and Concentration-Dependent Control: Aggregation can be induced with precise timing and exhibits gradual, concentration-dependent formation of insoluble aggregates, mirroring the disease process.
- Irreversibility: Once initiated by light, optoTAU aggregates persist and are irreversible after light cessation, modeling the persistent nature of tau pathology in disease.
- Live-Cell Visualization of Solubility Transition: When combined with the AggTag method, this model allows for the direct visualization of the transition from soluble oligomers to insoluble aggregates in live cells.
iPSC-Derived Cortical Neuron Model for Tau Hyperphosphorylation
This model leverages human induced pluripotent stem cells (iPSCs) differentiated into cortical neurons that express all six major adult isoforms of tau, overcoming a significant limitation of earlier stem cell models. Neurons derived from AD patients inherently exhibit elevated levels of phosphorylated tau (pTau) and increased expression of stress-induced kinase SGK1, providing a native pathological environment for studying tau hyperphosphorylation [1].
Key Advantages:
- Human Genetic Background: Captures the patient-specific genetic context of AD.
- Endogenous Hyperphosphorylation: Recapitulates the kinase/phosphatase imbalances and elevated pTau levels found in AD brain.
- Isoform Complexity: Expresses the full repertoire of adult human tau isoforms, which is critical for modeling isoform-specific pathophysiology [1].
Detailed Experimental Protocols
Protocol: Primary Neuronal Tau Seeding Assay
This protocol describes the establishment of a robust, physiologically relevant neuronal tau aggregation model suitable for screening modulators of tau aggregation [20].
- Cell Culture: Maintain primary neuronal cultures (e.g., from E18 rat cortex or human iPSC-derived neurons) expressing wild-type human tau under a physiological promoter.
- Tau Seed Preparation: Isate Sarkosyl-insoluble tau from confirmed AD post-mortem brain tissue. Alternatively, use sonicated recombinant tau pre-formed fibrils (PFFs). The critical step is to use a sub-nanomolar final concentration of seeds to initiate the process without causing overt toxicity [20].
- Seeding Transduction: At days in vitro (DIV) 7-10, add the prepared tau seeds to the neuronal culture medium. Lipofection reagents can be used to enhance the uptake of seeds by neurons.
- Incubation and Aggregation: Allow the aggregation process to proceed for 14-21 days, with regular medium changes absent of new seeds.
- Fixation and Staining: At the endpoint, fix cells and immunostain for pathological tau conformations (e.g., using MC1 or AT8 antibodies) and a neuronal marker (e.g., MAP2).
- High-Content Imaging and Analysis: Use an automated high-content imaging system to capture images. Quantify tau aggregation by measuring the number, size, and intensity of pTau-positive puncta per neuron using integrated analysis algorithms [20].
Protocol: Live-Cell Visualization with OptoTAU and AggFluor Probes
This protocol enables the direct, real-time observation of tau solubility changes and aggregation kinetics in live cells [44].
- Cell Line Engineering: Generate a stable, inducible cell line (HEK293 or human neurons) expressing the optoTAU-Halo fusion construct. The HaloTag allows for covalent labeling with fluorescent probes.
- Protein Expression Induction: Induce optoTAU-Halo expression with a low dose of doxycycline to achieve near-physiological protein levels, which is crucial for concentration-dependent aggregation.
- AggFluor Probe Labeling: Label the cells with two distinct viscosity-sensitive AggFluor probes:
- P1h: Fluoresces in lower viscosity environments, reporting on soluble oligomers (Ex/Em: 450/520 nm).
- P18h: Fluoresces in high viscosity environments, reporting on insoluble aggregates (Ex/Em: 540/640 nm) [44].
- Light Induction and Live-Cell Imaging: Expose the cells to blue light to initiate VVD dimerization and tau aggregation. Immediately commence longitudinal time-lapse imaging using a confocal microscope equipped with an environmental chamber to maintain cell viability.
- Data Analysis: Quantify the fluorescence intensity of P1h (soluble oligomers) and P18h (insoluble aggregates) over time. The kinetic curve will typically show a rapid rise in P1h signal, followed by a progressive increase in P18h signal, visually capturing the transition in tau solubility [44].
Diagram 1: Experimental workflow for the optoTAU live-cell aggregation assay.
Protocol: Assessing Tau Seeding Activity via RT-QuIC
The Real-Time Quaking-Induced Conversion (RT-QuIC) assay is a highly sensitive, plate-based method to quantify the seeding activity of pathological tau from brain homogenates or biofluids [43].
- Sample Preparation: Prepare brain homogenates or biofluids from AD and control cases. Serially dilute samples in a clear-bottom, low-binding plate.
- Reaction Mixture: Add a reaction mixture containing recombinant tau fragment (e.g., τ306/K19CFh mixture) as a substrate, Thioflavin T (ThT) dye, and reaction buffer.
- Cyclic Incubation: Seal the plate and place it in a fluorescent plate reader pre-heated to 37°C or 42°C. Subject the plate to cycles of shaking and rest (e.g., 1 min shake, 1 min rest).
- Fluorescence Monitoring: Measure ThT fluorescence (excitation ~450 nm, emission ~480 nm) every 15-45 minutes. The ThT fluorescence increases upon binding to the growing β-sheet-rich amyloid fibrils.
- Data Analysis: Determine the lag time (time to reach a fluorescence threshold) and the maximum fluorescence amplitude for each sample. The lag time is inversely proportional to the concentration of seeding-competent tau in the original sample [43].
Table 2: Quantitative Comparison of Advanced Tau Aggregation Models
| Model | Key Readout | Assay Duration | Throughput Potential | Key Advantage |
|---|---|---|---|---|
| Primary Neuronal Seeding [20] | pTau-positive aggregates per neuron (High-content imaging) | 2-3 weeks | Medium | Uses authentic AD seeds; native neuronal context |
| optoTAU with AggFluor [44] | Fluorescence kinetics of soluble (P1h) and insoluble (P18h) species | 24-72 hours | High | Live-cell, real-time kinetics of solubility transition |
| iPSC-Derived Cortical Neurons [1] | Endogenous pTau levels (Western Blot/ICC); Microtubule stability | 4-6 weeks (differentiation) | Low-Medium | Patient-specific genetics; endogenous hyperphosphorylation |
| Biochemical RT-QuIC [43] | ThT fluorescence (Lag time, Amplitude) | 24-48 hours | Very High | Ultra-sensitive detection of seeding activity from tissue/biofluid |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Tau Aggregation Studies
| Reagent / Tool | Function / Target | Example Use-Case |
|---|---|---|
| optoTAU Construct [44] | Light-inducible tau aggregation protein | Controlled, rapid induction of tau aggregation in live cells. |
| AggFluor Probes (P1h, P18h) [44] | Viscosity-sensitive fluorophores for HaloTag | Live-cell distinction between soluble oligomers and insoluble aggregates. |
| Phospho-Specific Tau Antibodies (e.g., AT8, anti-pTau217) [1] [43] | Detect specific tau phosphorylation epitopes | Quantifying hyperphosphorylation in models (ICC, WB); immunodepletion. |
| SGK1 Inhibitors (e.g., GSK650394, EMD638683) [1] | Inhibit kinase responsible for tau phosphorylation | Validating role of specific kinases in hyperphosphorylation; potential therapeutic. |
| τ306/K19CFh Tau Fragment [43] | Optimal substrate for RT-QuIC assays | Sensitive in vitro amplification and detection of pathological tau seeds. |
| iPSC-Derived Cortical Neurons [1] | Human neurons expressing adult tau isoforms | Studying tau hyperphosphorylation and pathology in a human genetic context. |
The development of rapid, physiologically relevant tau aggregation models marks a significant advancement in the preclinical screening of therapeutic candidates for Alzheimer's disease and other tauopathies. The integration of human iPSC-derived neurons, which model the endogenous hyperphosphorylation of tau, with sophisticated tools like optogenetic aggregation and sensitive seeding assays, provides a powerful, multi-faceted platform. These models enable researchers to not only identify compounds that inhibit the formation of tau aggregates but also to dissect the underlying molecular mechanisms, such as the role of specific kinases like SGK1. By employing these advanced tools and protocols, the drug discovery pipeline can be populated with more promising candidates, increasing the likelihood of clinical success for desperately needed tau-targeted therapies.
Solving Key Challenges in iPSC-based Tauopathy Modeling
Addressing Variability in Sporadic AD Lines and Phenotype Penetrance
The study of sporadic Alzheimer's disease (sAD) using induced pluripotent stem cell (iPSC)-derived neurons represents a transformative approach for modeling this complex neurodegenerative disorder. However, a significant challenge persists: the inherent variability in phenotypic penetrance and expression across different iPSC lines. This variability often obscures robust disease-related phenotypes, particularly in tau hyperphosphorylation, which is a critical pathological hallmark of AD [34]. The successful identification of disease-modifying therapies hinges on overcoming this challenge through standardized, sensitive, and biologically relevant experimental paradigms.
In sAD, intracellular neurofibrillary tangles composed of hyperphosphorylated tau protein correlate strongly with cognitive decline and neuronal loss [45] [43]. While iPSC technology allows for the generation of human neurons carrying the genetic background of sAD patients, the unpredictable expressivity of tau pathology in two-dimensional cultures often necessitates large sample sizes and complex study designs to achieve statistical power. This technical guide outlines strategic experimental approaches to mitigate variability and enhance the detection of tau hyperphosphorylation in sAD iPSC-derived models, thereby providing a robust platform for mechanistic studies and drug discovery.
Core Strategies to Minimize Variability and Enhance Phenotypes
To address the central issue of phenotypic variability, researchers should integrate the following core strategies into their experimental design. These approaches aim to standardize culture conditions, employ sensitive detection methods, and incorporate external stressors to reveal latent pathological tendencies.
Implementation of Three-Dimensional Culture Systems
Transitioning from traditional two-dimensional (2D) monocultures to three-dimensional (3D) culture systems can significantly enhance the phenotypic relevance and stability of iPSC-derived models.
- Rationale: 3D cultures, utilizing scaffolds like Matrigel, introduce physical protection against cell detachment and reduce shearing stress, better recapitulating the in vivo microenvironment and promoting the accumulation of disease-relevant protein aggregates [34].
- Protocol Outline:
- Differentiate iPSCs into cortical neurons using established protocols.
- Downscale cell culture conditions to a 384-well plate format for high-throughput compatibility.
- Embed cells in a Matrigel matrix to create a protective 3D scaffold.
- Maintain cultures over extended periods (e.g., 3-6 months) to allow for the spontaneous development of tau pathology, including hyperphosphorylation and aggregation [34].
Application of Pro-Apoptotic Stress to Unmask Latent Vulnerability
Sporadic AD iPSC-derived neurons may harbor a latent vulnerability to stress that is not apparent under basal conditions. Applying a controlled, sub-lethal stressor can unmask this vulnerability and reveal differences between sAD and control lines.
- Rationale: Neurons carrying pathogenic mutations, such as those in MAPT, show a time-dependent accumulation of toxic tau species and increased vulnerability to pro-apoptotic stress. This principle can be applied to sAD lines to precipitate a tau hyperphosphorylation phenotype [46].
- Protocol Outline:
- Culture sAD and age-matched control iPSC-derived neurons for extended periods (e.g., 1-3 months post-differentiation).
- Treat cultures with a pro-apoptotic stimulus (e.g., a low-dose caspase activator or other cellular stressor).
- Quantify subsequent markers of pathology, including caspase activation, tau cleavage, and tau hyperphosphorylation, using immunofluorescence or Western blotting [46].
- Assess the neuroprotective effects of candidate therapeutic compounds, such as caspase inhibitors, in this paradigm.
Utilization of Sensitive Assays for Tau Aggregation
The direct detection of tau aggregates, which are downstream of hyperphosphorylation, provides a robust and quantifiable endpoint.
- AlphaLISA Assay for Tau Aggregates: This bead-based proximity assay is highly suitable for high-throughput screening and can detect tau aggregates in a sensitive, quantitative manner within complex 3D culture lysates, providing a scalable readout for phenotypic severity [34].
Detailed Experimental Protocols
Protocol 1: Scalable Tau Aggregation Assay in 3D Culture
This protocol is adapted from a study that developed a high-throughput-compatible assay to detect tau aggregates [34].
Key Materials:
- Commercially available iPSC lines (e.g., from healthy controls and sAD patients).
- 384-well cell culture plates.
- Matrigel matrix.
- Neuronal differentiation media.
- Lysis buffer (e.g., RIPA buffer with protease and phosphatase inhibitors).
- AlphaLISA assay kit for tau detection.
Methodology:
- iPSC Maintenance and Neural Induction: Maintain iPSCs in a pluripotent state and then differentiate them into cortical neurons using a standardized protocol.
- 3D Seeding in 384-Well Plates:
- Mix the neuronal cell suspension with cold Matrigel on ice.
- Seed the cell-Matrigel suspension into 384-well plates.
- Centrifuge plates briefly to ensure even distribution and incubate at 37°C to polymerize the gel.
- Long-Term Culture and Maintenance: Culture the 3D neural constructs for up to 6 months, with half-media changes performed bi-weekly.
- Cell Lysis and Sample Preparation:
- At designated time points, lyse cells in the wells using an appropriate lysis buffer.
- Homogenize the lysate and clarify by centrifugation.
- AlphaLISA Detection:
- Transfer clarified lysates to a white 384-well optiplate.
- Add AlphaLISA anti-tau acceptor and donor beads according to the manufacturer's instructions.
- Incubate the plate in the dark and read the signal using an AlphaLISA-compatible reader.
Protocol 2: Assessing Caspase-Mediated Tau Cleavage and Phosphorylation
This protocol leverages the finding that caspase-6 cleaved tau is a prevalent feature in tauopathies and can be pharmacologically modulated [46].
Key Materials:
- iPSC-derived neurons from sAD patients and controls.
- Monoclonal antibodies targeting caspase-6 cleavage sites (e.g., mAbD402 for cleavage at D402).
- Phospho-tau antibodies (e.g., AT8 for p-S202/p-T205).
- Pro-apoptotic stimulus (e.g., Staurosporine).
- Pan-caspase or caspase-6 specific inhibitor (e.g., Z-VEID-FMK).
Methodology:
- Long-Term Culture of Neurons: Differentiate and maintain iPSC-derived cortical neurons for 1-3 months to allow for maturation and latent pathology development.
- Stress Induction and Pharmacological Intervention:
- Pre-treat a subset of cultures with a caspase inhibitor (e.g., 20 µM) for 24 hours.
- Expose cultures to a pro-apoptotic stressor for a defined period (e.g., 6-24 hours).
- Immunocytochemical and Biochemical Analysis:
- Fix cells for immunostaining or prepare lysates for Western blotting.
- Probe for cleaved tau (using mAbD402 or similar), phospho-tau (e.g., AT8), and total tau.
- Assess apoptotic markers like active caspase-6 or cleaved PARP.
- Quantification and Analysis: Quantify the fluorescence intensity or band density to determine the extent of tau cleavage and phosphorylation, normalized to total tau and control conditions.
Quantitative Data and Key Reagents
The following tables summarize expected experimental outcomes and essential research reagents based on current literature.
Table 1: Representative Quantitative Data from Tau Pathology Assays
| Assay Type | Measurement | Control Neurons | sAD Neurons | Intervention (e.g., Caspase Inhib.) | Source |
|---|---|---|---|---|---|
| Tau RT-QuIC | Seeding Activity (Lag Time, h) | ~42.9 ± 3.8 | ~11.4 ± 3.5* | Not Reported | [43] |
| Tau RT-QuIC | Seeding Activity (Fluorescence, a.u.) | ~1.05e3 ± 0.42e3 | ~12.93e3 ± 3.83e3* | Not Reported | [43] |
| Western Blot | pTau217 / pTau396 levels | Baseline | Significantly higher in ITG vs. STG/CER* | Not Reported | [43] |
| Cell Death Assay | Viability after stress | High | Reduced in V337M MAPT neurons* | Rescued to near control levels | [46] |
| AlphaLISA | Tau Aggregation (Signal) | Low | High in 3D culture over time* | Reduced by aggregation inhibitors | [34] |
*Indicates a statistically significant difference compared to control.
Table 2: Research Reagent Solutions for Tau Hyperphosphorylation Studies
| Reagent / Tool | Type | Specific Function / Target | Key Application in Experimental Protocol |
|---|---|---|---|
| Anti-pTau (AT8) | Monoclonal Antibody | Phospho-Tau (Ser202, Thr205) | Immunostaining, Western blot to detect hyperphosphorylation [47]. |
| Anti-Cleaved Tau (mAbD402) | Neoepitope Monoclonal Antibody | Caspase-6 cleaved tau (at Asp402) | Detects caspase-mediated tau truncation, an early pathological event [46]. |
| 3D Culture Matrix (Matrigel) | Scaffolding Biomaterial | Provides a protective 3D microenvironment | Enhances tau aggregation and promotes long-term neuronal survival in culture [34]. |
| Caspase-6 Inhibitor (e.g., Z-VEID-FMK) | Pharmacological Inhibitor | Potent and selective caspase-6 inhibition | Used to probe the role of caspase-6 in tau cleavage and neuronal death [46]. |
| τ306/K19CFh tau fragment | Recombinant Protein | Substrate for RT-QuIC assay | Used to measure tau-seeding activity in brain or cell lysates [43]. |
| GSK-3β Inhibitor (e.g., CHIR99021) | Pharmacological Inhibitor | Key tau kinase | Used to investigate the role of GSK-3β in driving tau hyperphosphorylation [48]. |
Signaling Pathways and Experimental Workflows
Key Signaling Pathways in Tau Hyperphosphorylation
The following diagram illustrates the core signaling pathways involving major tau kinases and phosphatases, and their perturbation in Alzheimer's disease, leading to tau hyperphosphorylation and aggregation.
Key Pathways in Tau Hyperphosphorylation and Aggregation
Integrated Experimental Workflow for sAD iPSC Studies
This workflow diagram outlines a comprehensive experimental strategy for modeling sporadic Alzheimer's disease using iPSC-derived neurons, from line generation to phenotypic analysis and therapeutic testing.
Integrated Workflow for sAD iPSC Modeling
Optimizing Neuronal Maturation to Overcome Fetal-like Tau Signatures
The use of human induced pluripotent stem cell (iPSC)-derived neurons has revolutionized the modeling of tauopathies, including Alzheimer's disease and frontotemporal dementia. However, a significant challenge persists: these neurons often retain fetal-like characteristics, including an immature tau isoform profile and heightened susceptibility to hyperphosphorylation, which limits their utility in modeling age-related neurodegenerative diseases [49]. The slow maturation timeline of human neurons, which can extend over months to reach adult-like function, presents a major bottleneck for disease modeling and drug discovery [49]. This whitepaper details the core mechanisms underlying this developmental limitation and provides evidence-based, technical strategies to accelerate neuronal maturation to overcome fetal-like tau signatures, thereby creating more physiologically relevant models for tauopathy research.
The Problem of Fetal-like Tau in iPSC-Derived Neuronal Models
Tau Isoform Regulation During Development
Under physiological conditions, the expression of tau isoforms is tightly regulated through development. The fetal human brain predominantly expresses the 3R tau isoform, which contains three microtubule-binding repeats [50]. In the healthy adult brain, alternative splicing of the MAPT gene yields six primary isoforms, resulting in an approximately equal ratio of 3R and 4R tau isoforms [50] [51]. This balance is critical for maintaining neuronal health and microtubule function, and its disruption is a hallmark of multiple tauopathies.
- 3R Tau Predominance in Immature Neurons: iPSC-derived neurons typically recapitulate the fetal tau signature, with a 3R-dominated profile that fails to mirror the 3R:4R balance of the adult human brain [50].
- Consequences for Disease Modeling: This immature tau environment affects fundamental neuronal properties, including microtubule stability, axonal transport, and synaptic function, thereby compromising the pathological relevance of these models for studying adult neurodegenerative diseases [52].
Tau Hyperphosphorylation in Immature Neuronal Environments
The fetal-like environment of standard iPSC-derived neuronal cultures creates conditions ripe for aberrant tau hyperphosphorylation, a key pathological event in tauopathies.
- Developmental Phosphorylation Patterns: Certain tau phosphorylation sites are more prevalent during development, and these same epitopes are often hyperphosphorylated in pathological conditions [51].
- Cellular Stress Drivers: Immature neuronal cultures exhibit heightened susceptibility to cellular stressors, including mitochondrial dysfunction, oxidative stress, and neuroinflammation, all of which can activate kinases directly involved in tau phosphorylation [53] [51].
Table 1: Key Challenges of Fetal-like Tau Signatures in iPSC Models
| Challenge | Impact on Disease Modeling | Consequence for Drug Screening |
|---|---|---|
| 3R Tau Predominance | Does not recapitulate the 3R:4R balance of adult human brain or specific tauopathies | Reduced predictive power for therapies targeting 4R tau or isoform balance |
| Immature Phosphorylation Patterns | May confuse developmental and pathological tau phosphorylation events | Risk of identifying compounds that target developmental rather than disease-specific pathways |
| Underdeveloped Neuronal Networks | Limited synaptic connectivity and network activity affects tau spreading and pathology | Functional rescue of immature networks may not translate to mature, diseased brains |
| Incomplete Cytoskeletal Maturation | Altered microtubule dynamics and axonal transport, key pathways in tau pathology | Missed opportunities to identify compounds stabilizing the axonal cytoskeleton |
Strategic Approaches to Accelerate Neuronal Maturation
Small-Molecule Cocktails for Transcriptional and Epigenetic Reprogramming
A groundbreaking approach to accelerate maturation involves the use of small-molecule cocktails that target epigenetic and transcriptional regulators of neuronal development. A combination of four compounds, collectively termed GENtoniK, has demonstrated remarkable efficacy in driving maturation across multiple neuronal lineages [49].
- GSK2879552: An inhibitor of lysine-specific demethylase 1 (LSD1/KDM1A) that promotes epigenetic changes conducive to neuronal maturation.
- EPZ-5676: A disruptor of telomerase-like 1 (DOT1L) histone methyltransferase inhibitor that facilitates transcriptional changes associated with maturity.
- N-methyl-d-aspartate (NMDA): Activates NMDA-type glutamate receptors to stimulate calcium-dependent transcription.
- Bay K 8644: An L-type calcium channel (LTCC) agonist that works synergistically with NMDA to enhance calcium signaling and activity-dependent gene expression.
This combination has been shown to trigger comprehensive maturation, including enhanced synaptic density, electrophysiological function, and adult-like transcriptomic profiles in cortical neurons, spinal motoneurons, and cortical organoids [49].
Targeting Mitochondrial Dysfunction to Rescue Tau Pathology
Recent evidence highlights mitochondrial dysfunction as both a consequence and driver of pathological tau accumulation, creating a vicious cycle in developing neurons. Targeting this pathway presents a promising strategy to break this cycle and promote maturation.
In cortical organoids harboring the FTD-linked MAPT IVS10+16 mutation, researchers observed significant mitochondrial abnormalities, including reduced mitochondrial content and impaired function, concomitant with tau hyperphosphorylation and aggregation [53]. Treatment with bezafibrate (5 μM), an agonist of the mitochondrial biogenesis master regulator PGC1α, from day 70 to 100 of organoid differentiation:
- Restored mitochondrial parameters
- Enhanced neuronal integrity and synaptic maturation
- Reduced tau hyperphosphorylation
- Restored network functionality [53]
This approach demonstrates that targeting fundamental cellular energetics can indirectly promote tau physiology by creating a more metabolically mature environment.
Advanced Culture Systems to Support Maturation
The choice of culture platform significantly influences neuronal maturation outcomes. Moving beyond traditional two-dimensional cultures to more sophisticated systems can provide the necessary physical and signaling context for proper development.
- Three-Dimensional Cortical Organoids: These systems better recapitulate the cellular diversity and tissue architecture of the human brain, providing a more physiological environment for maturation [53].
- Matrigel-Embedded 3D Cultures: Embedding neurons in Matrigel provides physical protection against shearing stress and creates a more in vivo-like environment that supports mature tau pathology development, making it suitable for high-throughput screening applications [34].
- Extended Culture Duration: Despite acceleration strategies, extended culture periods (≥90 days) remain necessary for the emergence of mature tau signatures, including isoform stabilization and adult-like phosphorylation patterns.
Table 2: Quantitative Comparison of Neuronal Maturation Strategies
| Strategy | Experimental System | Key Readouts | Efficacy | Timeline |
|---|---|---|---|---|
| GENtoniK Cocktail [49] | hPSC-derived cortical neurons (2D) | Synaptic density, Electrophysiology, Transcriptomics | Significant acceleration across all parameters | Days 7-14 treatment, analysis at day 21 |
| Bezafibrate Treatment [53] | MAPT-mutant cortical organoids (3D) | Mitochondrial content, Synaptic markers, Tau phosphorylation | Rescue of mutant phenotypes | Day 70-100 treatment |
| Matrigel 3D Culture [34] | iPSC-derived cortical neurons (3D) | Tau aggregation, Neuronal viability | Enhanced tau aggregation vs. 2D cultures | 4-6 weeks |
| Extended Maturation | Various neuronal subtypes | 3R:4R tau ratio, Adult isoform expression | Gradual improvement | ≥90 days |
Experimental Protocols for Key Assays
High-Content Screening for Neuronal Maturity
A multi-parametric high-content screening (HCS) assay enables quantitative assessment of neuronal maturation status. This protocol was validated in hPSC-derived cortical neurons and can be adapted for various neuronal subtypes [49].
Procedure:
- Differentiation: Generate nearly pure populations of hPSC-derived, deep-layer cortical neurons using established protocols.
- Compound Treatment: Apply maturation compounds (e.g., GENtoniK cocktail) from days 7-14 of differentiation.
- Withdrawal Period: Culture in compound-free medium for an additional 7 days (days 14-21) to identify hits that trigger long-lasting maturation.
- Immunostaining: Fix cells and stain for:
- Microtubule-associated protein 2 (MAP2) for dendritic tracing
- DAPI for nuclear morphology
- Immediate early gene products (FOS and EGR1) after 2 hours of KCl stimulation
- Image Acquisition and Analysis:
- Use automated tracing of MAP2 staining to quantify total neurite length and branching
- Measure nuclear size and roundness from DAPI staining
- Quantify the fraction of KCl-induced FOS+ and EGR1+ cells
Validation:
- Compare parameters to primary embryonic rat cortical neurons, which quickly develop mature-like functionality
- Benchmark against extended cultures of hPSC-derived neurons (50+ days)
Functional Assessment of Tau Physiology in 3D Organoids
This protocol details the generation and analysis of cortical organoids containing a frontotemporal dementia-associated MAPT mutation to study tau pathology and therapeutic intervention [53].
Cortical Organoid Generation:
- Initial Aggregation: Use AggreWell800 plates (800 μm microwells) to form uniformly sized spheroids from dissociated iPSCs (approximately 2×10^6 cells per well).
- Neural Induction (Days 1-8): Culture in neural induction medium (NIM) supplemented with heparin, SB 431542, DORSO, and XAV 939.
- Neural Differentiation (Day 8+): Transfer spheroids to ultra-low attachment dishes with neural differentiation medium (NDM) on an orbital shaker (40-60 RPM).
- Maturation Enhancement: At approximately day 30, replace FGF2 and heparin with BDNF, GDNF, and ascorbic acid. From day 50, use Neurobasal A-based NDM with only BDNF.
Therapeutic Intervention:
- Treatment Window: Administer bezafibrate (5 μM) or other compounds from day 70 to day 100.
- Functional Assessment: Perform calcium imaging to assess network functionality.
- Molecular Analysis:
- Immunofluorescence for synaptic markers (PSD95, synapsin), mitochondrial markers, and phosphorylated tau
- Nanostring gene expression analysis for neuronal development and synaptic maturation genes
- Assessment of 3R:4R tau ratio via RT-PCR or isoform-specific antibodies
Signaling Pathways and Molecular Mechanisms
The following diagrams illustrate the key molecular pathways targeted by maturation strategies, detailing how they converge to overcome fetal-like tau signatures.
Mitochondrial-Tau Feedback Loop in Neuronal Maturation
GENtoniK Cocktail Mechanism of Action
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Tau Maturation Studies
| Reagent/Category | Specific Examples | Function/Application | Key References |
|---|---|---|---|
| Maturation Cocktails | GENtoniK (GSK2879552, EPZ-5676, NMDA, Bay K 8644) | Accelerates morphological, transcriptional, and functional neuronal maturation | [49] |
| Mitochondrial Therapeutics | Bezafibrate (5 μM) | Activates PGC1α to rescue mitochondrial content and function in tau mutant neurons | [53] |
| 3D Culture Matrices | Matrigel, AggreWell800 plates | Provides structural support for complex neuronal network formation and mature tau pathology | [53] [34] |
| Tau Pathology Detection | AlphaLISA assays, phospho-tau antibodies (e.g., AT8, AT100) | High-throughput compatible detection of tau aggregates and phosphorylation | [34] |
| Neuronal Differentiation Kits | Commercial motor neuron/cortical neuron differentiation kits | Standardized, reproducible generation of specific neuronal subtypes | [54] [55] |
| Functional Assessment Tools | Calcium imaging dyes, multi-electrode arrays | Measurement of network activity and synaptic function in mature neurons | [53] [49] |
Overcoming the fetal-like tau signatures in iPSC-derived neuronal models requires a multi-faceted approach that addresses both the intrinsic maturation clock and the extracellular environment. The strategies outlined here—including small-molecule acceleration of epigenetic and transcriptional programs, targeted rescue of mitochondrial dysfunction, and implementation of advanced 3D culture systems—provide a roadmap for generating more physiologically relevant models of tauopathy. As these optimized maturation protocols become more widely adopted, they will enhance our understanding of tau pathogenesis and improve the predictive validity of preclinical drug screening, ultimately accelerating the development of effective therapies for Alzheimer's disease and related tauopathies.
Strategies for Inducing Aggregation and Toxicity Within Practical Timeframes
In the study of tauopathies, such as Alzheimer's disease (AD), a significant challenge is replicating the slow, progressive neuropathology of the human condition within experimentally practical timeframes. Research utilizing induced pluripotent stem cell (iPSC)-derived neurons has been transformative, providing a human-relevant platform for disease modeling and drug discovery. However, the spontaneous development of tau hyperphosphorylation and aggregation in these cultures can take many months, mirroring the protracted timeline of human disease and hindering rapid research progress. This guide details established and emerging strategies to accelerate the induction of tau aggregation and associated neurotoxicity in iPSC-derived neuronal models, thereby creating more efficient and scalable systems for pathomechanistic investigation and therapeutic screening. These approaches are integral to a broader thesis on modeling tau hyperphosphorylation, enabling the controlled study of this critical process within accessible experimental windows.
Core Strategies for Accelerated Tau Pathology
Several key methodologies have been developed to induce tau hyperphosphorylation, aggregation, and subsequent neuronal death in iPSC-derived models. The most prominent strategies are summarized in the table below and discussed in detail in the subsequent sections.
Table 1: Core Strategies for Inducing Tau Aggregation and Toxicity
| Strategy | Core Principle | Key Agents/ Methods | Typical Timeframe | Key Readouts |
|---|---|---|---|---|
| Exogenous Tau Seeding | Introduce pre-formed tau aggregates ("seeds") to act as templates for endogenous tau misfolding in a prion-like manner [56] [57] [58] | Brain lysates from tauopathy models (e.g., rTg4510 mice); synthetic tau fibrils [56] | Days to a few weeks [56] | Tau biosensor aggregation (FRET/CFP-YFP); neuronal death; emergence of distinct tau strains [56] |
| Genetic Manipulation | Introduce genetic mutations known to cause tauopathy, enhancing intrinsic tau aggregation propensity [59] [60] | Overexpression of wild-type or mutant (e.g., P301L) tau; use of iPSCs with fAD (PSEN1) or FTD-associated MAPT mutations [56] [59] | Varies (weeks); can be combined with seeding for further acceleration [56] [60] | Increased Aβ and p-tau levels; elevated Aβ42/40 ratio (in fAD); caspase activation [59] [60] |
| Manipulation of Cellular Environment | Perturb cellular pathways to disrupt tau homeostasis and promote hyperphosphorylation [59] [58] | GSK3β activation; oxidative stress inducers (e.g., H₂O₂); proteasome inhibitors [59] | Hours to days [59] | Site-specific tau hyperphosphorylation; increased sensitivity to oligomers/oxidative stress [59] |
Exogenous Tau Seeding
The prion-like hypothesis of tau propagation posits that misfolded tau can template the misfolding of native tau in recipient cells, leading to the spread of pathology [56] [57]. This principle is leveraged by exposing iPSC-derived neurons to exogenous tau "seeds" to rapidly induce aggregation.
Detailed Protocol: Induction using Brain Lysates
- Seed Preparation: Homogenize whole brains from 12-month-old rTg4510 mice (which overexpress human tau with the P301L mutation) or control littermates in ice-cold PBS with protease inhibitors. Use 5 mL of PBS per gram of brain tissue [56].
- Clarification: Centrifuge the homogenate at 3000 × g for 10 minutes at 4°C. Collect the supernatant, resuspend the pellet in 500 µL of PBS with protease inhibitor, and sonicate on ice [56].
- Final Clearance: Centrifuge the sonicated suspension again at 3000 × g for 10 minutes. The resulting supernatant is used as the seed material [56].
- Neuronal Transduction and Treatment: Use iPSC-derived neurons stably expressing a TauRD (Tau Repeat Domain) biosensor (e.g., lentivirally delivered TauRD-CFP-2A-TauRD-YFP). Treat these neurons with the prepared brain lysate seeds [56].
- Live Imaging and Quantification: Continuously monitor the neurons for over one week using live-cell imaging. Aggregation is indicated by the emergence of CFP/YFP puncta, and subsequent cell death is tracked at single-cell resolution [56].
Genetic Manipulation
Introducing disease-associated genetic backgrounds into iPSC models predisposes neurons to develop pathology more rapidly.
- Familial AD Mutations: iPSC neurons carrying mutations in genes like PSEN1 (e.g., L435F) provide a predisposed background. These neurons exhibit accelerated tau seeding kinetics and increased phosphorylated tau levels, likely due to altered Aβ profiles that promote tau pathology [56] [59].
- Direct Tau Manipulation: Overexpression of full-length tau, or the aggregation-prone repeat domain (TauRD) containing mutations like P301L, can directly drive aggregation and has been shown to be sufficient to induce cell death in iPSC-derived neurons [60].
Manipulation of the Cellular Environment
Cellular stressors can trigger key kinases and disrupt proteostasis, pushing neurons toward a pathological state.
Detailed Protocol: GSK3β Activation and Oxidative Stress
- Culture Preparation: Differentiate control and patient-derived iPSCs into mature cortical neurons [59].
- Pharmacological Induction:
- GSK3β Activation: The activity of GSK3B, a key tau kinase, is found to be elevated in both fAD- and sAD-derived neurons. To mimic this, treatments like specific GSK3β activators or lithium chloride (which can have complex, concentration-dependent effects on pathways) can be applied [59].
- Oxidative Stress: Treat neurons with sub-toxic concentrations of hydrogen peroxide (H₂O₂) or amyloid oligomers to probe the increased sensitivity of AD neurons. For example, apply 50-100 µM H₂O₂ for 24 hours [59].
- Analysis: Assess outcomes via Western blot for site-specific tau hyperphosphorylation (e.g., Thr231, Ser396) and cell viability assays to confirm elevated vulnerability [59].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of the above strategies requires a suite of specialized reagents and tools.
Table 2: Essential Research Reagents for Tau Aggregation Studies
| Reagent / Tool | Function and Utility | Example Usage |
|---|---|---|
| TauRD Biosensor | A construct (e.g., TauRD-CFP-2A-TauRD-YFP) that only fluoresces upon seeded aggregation, enabling real-time visualization of tau misfolding [56]. | Live-cell imaging to track aggregation kinetics and correlate with neuronal death at a single-cell level [56]. |
| rTg4510 Mouse Brain Lysate | A source of potent, pre-formed tau seeds with the P301L mutation, used to initiate prion-like propagation in human neuronal cultures [56]. | Serves as a positive control and highly effective seed material in exogenous seeding protocols [56]. |
| PSEN1 Mutant iPSCs | iPSC lines with familial AD mutations (e.g., L435F) that provide a genetically predisposed background with accelerated tau seeding and altered Aβ profiles [56] [59]. | Used to model patient-specific susceptibilities and investigate interactions between Aβ and tau pathology [56]. |
| GSK3β Modulators | Pharmacological agents to manipulate the activity of GSK3B, a primary kinase responsible for tau hyperphosphorylation [59]. | Used to directly probe the relationship between kinase activity, tau phosphorylation, and neuronal health [59]. |
Visualization of Experimental Workflow and Pathways
The following diagrams illustrate the core experimental workflow for exogenous seeding and the key signaling pathways involved in tau hyperphosphorylation and toxicity.
Exogenous Tau Seeding Workflow
Key Pathways in Tau Hyperphosphorylation & Toxicity
The convergence of exogenous seeding, genetic predisposition, and environmental stressor strategies provides a robust and flexible toolkit for researchers to model tau-induced aggregation and neurotoxicity within experimentally feasible timeframes. The integration of biosensors, patient-derived iPSCs, and longitudinal single-cell analysis allows for an unprecedented, granular view of the molecular events leading from initial tau misfolding to neuronal death. These accelerated models are indispensable for validating the pathophysiological role of specific tau strains, elucidating the mechanisms of toxicity, and, most critically, serving as high-throughput platforms for the screening of novel therapeutic agents designed to halt the progression of tauopathies.
In the study of neurodegenerative diseases, particularly those involving tau protein pathology such as Alzheimer's disease (AD) and frontotemporal dementia (FTD), the development of robust, quantifiable endpoints has revolutionized our ability to model disease mechanisms and screen therapeutic candidates. Research using induced pluripotent stem cell (iPSC)-derived neurons has been instrumental in recapitulating human tau pathology, including the hyperphosphorylation and aggregation that characterize tauopathies [4]. Studies have demonstrated that neurons derived from both familial and sporadic AD patients show increased phosphorylation of TAU protein at multiple sites, providing a physiologically relevant system for investigating disease mechanisms and therapeutic interventions [4].
Within this context, the selection of appropriate detection technologies becomes paramount for generating reliable, reproducible data. FRET (Förster Resonance Energy Transfer)-based biosensors, AlphaLISA (Amplified Luminescent Proximity Homogeneous Assay), and traditional immunoassays each offer distinct advantages and limitations for quantifying tau pathology endpoints. This technical guide provides an in-depth comparison of these platforms, with specific application to monitoring tau hyperphosphorylation, aggregation, and seeding activity in iPSC-derived neuronal models, enabling researchers to make informed decisions when designing experiments for basic research or drug discovery campaigns.
Technology Platform Comparison
The quantitative assessment of tau pathology requires sensitive, specific, and reproducible detection methods. The table below provides a systematic comparison of the major assay platforms used in tau research.
Table 1: Comparative Analysis of Tau Detection Technologies
| Parameter | FRET-Based Biosensors | AlphaLISA | Traditional Immunoassays (ELISA) |
|---|---|---|---|
| Detection Principle | Energy transfer between fluorophores upon tau aggregation | Singlet oxygen transfer between donor and acceptor beads | Enzyme-linked colorimetric or chemiluminescent detection |
| Sample Throughput | Moderate | High | Moderate to Low |
| Sensitivity | High (detection limit ~3 pg for optimized assays) [61] | High (femtomolar range) | Moderate to High (picogram range) |
| Dynamic Range | ~3-4 logs | ~4-5 logs | ~2-3 logs |
| Assay Format | Homogeneous (no-wash) | Homogeneous (no-wash) | Heterogeneous (multiple wash steps) |
| Multiplexing Capability | Limited | Possible with spectral discrimination | Limited |
| Primary Application | Tau seeding and aggregation [61] [62] | Total tau, phospho-tau, and aggregate quantification [63] [64] | Total tau and phospho-tau quantification [4] |
| Sample Volume | Not specified | 5-30 µL [63] [64] | Typically 50-100 µL |
| Key Advantage | Measures functionally relevant seeding activity | Homogeneous, no-wash format suitable for HTS | Well-established, widely validated |
FRET-Based Tau Biosensors
Principle and Applications
FRET-based biosensors have become indispensable tools for detecting tau seeding activity, a process fundamental to the prion-like propagation of tau pathology in Alzheimer's disease and related tauopathies [61] [62]. These cellular assays typically utilize HEK293T cells stably expressing the tau repeat domain (RD) with aggregation-prone mutations (e.g., P301S) fused to donor and acceptor fluorophores. When seed-competent tau from patient-derived samples is introduced, it templates the aggregation of the tau RD probes, bringing the fluorophores into close proximity and generating a FRET signal quantifiable by flow cytometry or fluorescence microscopy [61].
The relevance of these biosensors is particularly evident in disease modeling, where they have demonstrated that tau seeding propensity correlates with disease severity and rate of clinical progression [62]. Furthermore, their application extends to human biofluids, offering potential for diagnostic development, though sensitivity limitations with CSF require additional optimization [62].
Experimental Protocol for Tau Seeding Assay
Day 1: Cell Seeding and Treatment
- Seed HEK293T tau biosensor cells (e.g., clone 18 with pseudoacetylated (EAAAK)3 linker) in white, opaque-bottom 384-well plates at 3,000-5,000 cells/well in complete medium [61].
- Incubate plates for 12-24 hours at 37°C, 5% CO₂ to allow cell attachment.
Day 2: Sample Transduction
- Prepare tau seeds from iPSC-derived neuron conditioned medium or cell lysates. For human brain samples, homogenize in PBS with protease inhibitors and clarify by centrifugation [61] [62].
- Mix samples with lipofectamine (e.g., 0.1-0.2 mg/mL final concentration) to enhance transduction efficiency [61] [62].
- Add sample-lipofectamine complexes to biosensor cells (typically 5-10% of total well volume).
- Incubate plates for 24-72 hours at 37°C, 5% CO₂.
Day 3: Analysis and Data Acquisition
- For flow cytometry: Harvest cells using trypsinization, fix with 4% paraformaldehyde, and analyze using a flow cytometer with 405 nm excitation and 450/50 nm (CFP) and 535/25 nm (YFP) emission filters [61].
- For plate reading: Measure FRET directly from plates using a compatible plate reader.
- Calculate FRET efficiency as the ratio of acceptor emission to donor emission after background subtraction.
Graphviz diagram illustrating the FRET-based tau seeding detection principle:
Recent Optimizations and Enhancements
Recent structural insights into tau aggregates have guided the rational design of improved FRET probes. Key optimizations include:
- Linker Design: Replacement of flexible linkers with rigid (EAAAK)3 linkers increases FRET efficiency by maintaining closer proximity between fluorophores during aggregation [61].
- Pseudoacetylation: Mutation of lysine residues 311, 317, and 321 to glutamine to mimic acetylation increases sensitivity approximately threefold for detecting Alzheimer's-derived tau seeds [61].
- Codon Optimization: Implementing codon-optimized sequences prevents recombination during genomic integration and improves expression stability [61].
- Advanced Fluorophores: Utilization of mTurquoise2 and mNeonGreen fluorophore pairs enhances energy transfer efficiency and photostability compared to original CFP/YFP pairs [61].
These optimizations have yielded biosensors with significantly improved sensitivity, such as HEK293T clone 18, which demonstrates a lower detection limit of 3 pg of tau seed protein - more than 10 times more sensitive than previous generations [61].
AlphaLISA Technology
Principle and Assay Formats
AlphaLISA is a homogeneous, no-wash immunoassay platform that utilizes bead-based energy transfer for highly sensitive protein detection. The technology employs donor beads containing a photosensitizer that converts ambient oxygen to excited singlet oxygen upon illumination at 680nm. When acceptor beads are within proximity (≤200nm), the singlet oxygen triggers a chemiluminescent emission at 615nm [63] [65] [66]. This proximity-dependent signal generation eliminates the need for separation steps, making it ideal for high-throughput applications.
For tau research, specialized AlphaLISA kits are available for different analytical endpoints:
- Total Tau Detection: Quantifies overall tau expression levels using two antibodies recognizing different epitopes [63].
- Tau Aggregate Detection: Specifically measures pathological tau aggregates using an antibody that recognizes an exposed epitope on aggregated tau [64].
- Phospho-Tau Detection: Can be configured with phospho-specific antibodies to quantify hyperphosphorylation at specific epitopes.
Experimental Protocol for Tau Aggregate Detection
Sample Preparation
- Culture iPSC-derived neurons in appropriate differentiation media for 4-8 weeks to achieve mature neuronal phenotypes [4].
- Treat neurons with experimental compounds or vehicle control for desired duration.
- Lyse cells using recommended lysis buffer (e.g., 1X SureFire Lysis Buffer) with protease and phosphatase inhibitors.
- Clarify lysates by centrifugation at 10,000 × g for 10 minutes at 4°C.
- Adjust protein concentration to 0.1-1 mg/mL for optimal detection within the assay's dynamic range.
AlphaLISA Procedure (Two-Plate Protocol)
- Transfer 10-30 µL of clarified lysate to a 384-well white OptiPlate [64].
- Add 5 µL of Acceptor Mix (anti-tau aggregate antibody conjugated to acceptor beads) to each well.
- Incubate for 1 hour at room temperature protected from light.
- Add 5 µL of Donor Mix (streptavidin-coated donor beads) to each well.
- Incubate for 1 hour at room temperature protected from light.
- Read plate using an Alpha-compatible plate reader (e.g., EnVision, PerkinElmer) with standard AlphaLISA settings.
Data Analysis
- Generate a standard curve using recombinant tau aggregate protein serially diluted in the same matrix as samples [64].
- Normalize sample signals to the standard curve to determine tau aggregate concentration.
- Express data as fold-change relative to control or absolute concentration when appropriate.
Graphviz diagram illustrating the AlphaLISA detection workflow:
Advantages for Tau Hyperphosphorylation Studies
AlphaLISA technology offers several distinct advantages for monitoring tau pathology in iPSC-derived neuronal models:
- Compatibility with Complex Matrices: The platform performs robustly in cell lysates, serum, and culture media, making it ideal for analyzing iPSC-derived neuron conditioned media or lysates without extensive sample cleanup [65].
- Sensitivity in Physiological Contexts: The technology can detect tau hyperphosphorylation and aggregation in patient-derived neuronal models, as demonstrated in studies where fAD and sAD iPSC-derived neurons showed increased phosphorylation at multiple tau sites [4].
- High-Throughput Capability: The homogeneous, no-wash format enables screening of thousands of compounds in 384- or 1536-well formats, with automation compatibility for drug discovery campaigns [65] [64].
- Flexibility in Sample Volume: While standard protocols use 5µL sample volume, increasing to 20µL can enhance analytical sensitivity for low-abundance targets [65].
Experimental Design for iPSC-Derived Neuron Models
Modeling Tau Hyperphosphorylation in Human Neurons
iPSC-derived neurons provide a physiologically relevant platform for studying tau pathology, as they recapitulate key aspects of human neuronal biology and disease mechanisms. When designing experiments to investigate tau hyperphosphorylation, several critical factors must be considered:
Neuronal Maturation and Characterization
- Differentiate iPSCs to cortical neurons using established protocols, ensuring adequate maturation (typically 4-8 weeks) [4].
- Confirm neuronal identity using markers such as MAP2, βIII-tubulin, and synapsin.
- Verify expression of all six human tau isoforms and establish baseline 3R:4R tau ratio, as isoform imbalance represents an early etiological event in tauopathies [30].
Disease Modeling Approaches
- Familial AD Models: Utilize iPSCs carrying PSEN1, APP, or MAPT mutations associated with autosomal dominant AD [4].
- Sporadic AD Models: Employ iPSCs from patients with late-onset AD or introduce genetic risk factors (e.g., APOE ε4) via gene editing [4].
- Pharmacological Induction: Treat control neurons with compounds such as okadaic acid or oxidative stress inducers to trigger tau hyperphosphorylation.
Multi-Parametric Assessment of Tau Pathology
A comprehensive evaluation of tau pathology in iPSC-derived neurons should incorporate multiple assay platforms to capture different aspects of the disease process:
Table 2: Integrated Experimental Approach for Tau Pathology Assessment
| Pathological Process | Primary Detection Method | Secondary Validation | Key Readouts |
|---|---|---|---|
| Tau Hyperphosphorylation | AlphaLISA phospho-tau assays [63] | Western blotting [4] | Site-specific phosphorylation (e.g., pT181, pS396) |
| Tau Aggregation | AlphaLISA tau aggregate assay [64] | Immunocytochemistry | Oligomeric and fibrillar tau species |
| Seeding Activity | FRET-based biosensor assay [61] [62] | Sarkosyl insolubility [61] | Tau seeding potency and efficacy |
| Neuronal Health | Viability assays (e.g., ATP content) | Synaptic markers | Synaptic density, neurite degeneration |
| Functional Consequences | Electrophysiology (MEA) | Axonal transport assays | Network activity, cargo trafficking |
This multi-parametric approach enables researchers to establish correlations between molecular tau pathology and functional neuronal deficits, providing a more complete understanding of disease mechanisms.
Research Reagent Solutions
The following table outlines essential materials and reagents for implementing the described assay technologies in tau hyperphosphorylation research.
Table 3: Essential Research Reagents for Tau Pathology Studies
| Reagent Category | Specific Examples | Application and Function |
|---|---|---|
| Cell Models | iPSC-derived cortical neurons [4] | Physiologically relevant human model for tau pathology |
| FRET biosensor cell lines (HEK293T clone 18) [61] | Sensitive detection of tau seeding activity | |
| Detection Kits | AlphaLISA SureFire Ultra Human Total Tau Kit [63] | Quantification of total tau expression levels |
| AlphaLISA SureFire Ultra Human Tau Aggregate Kit [64] | Specific detection of pathological tau aggregates | |
| Antibodies | Anti-phospho-tau antibodies (site-specific) [4] | Detection of tau hyperphosphorylation at specific epitopes |
| Anti-tau aggregate conformation-specific antibodies | Selective recognition of pathological tau conformers | |
| Reference Materials | Recombinant tau proteins (monomeric, pre-formed fibrils) | Assay standards and controls |
| Recombinant human tau aggregate protein [64] | Standard curve generation for aggregate quantification | |
| Specialized Reagents | Liposomes/Lipofectamine [61] [62] | Enhance tau seed transduction in biosensor assays |
| Proteasome inhibitors (e.g., MG132) | Stabilize tau aggregates by inhibiting degradation | |
| Lysis buffers with protease/phosphatase inhibitors | Preserve tau phosphorylation states during extraction |
The integration of FRET, AlphaLISA, and complementary immunoassays provides a powerful toolkit for defining robust, quantifiable endpoints in tau pathology research. FRET-based biosensors excel at detecting the biologically relevant seeding activity of tau, with recent optimizations significantly enhancing sensitivity and disease relevance [61]. AlphaLISA technology offers superior throughput and flexibility for screening applications, particularly for quantifying tau hyperphosphorylation and aggregation in complex samples like iPSC-derived neuron lysates [63] [64]. When implemented in physiologically relevant iPSC-derived neuronal models, these technologies enable comprehensive assessment of tau pathology from molecular mechanisms to functional consequences, accelerating both basic research and therapeutic development for Alzheimer's disease and other tauopathies.
Benchmarking iPSC Models Against Human Neuropathology and Therapeutics
Cross-Validation with Post-Mortem Brain Tissue and Biofluid Biomarkers
The study of tau hyperphosphorylation, a pivotal process in neurodegenerative tauopathies including Alzheimer's disease (AD), has been revolutionized by human induced pluripotent stem cell (iPSC) technology. iPSC-derived neurons provide a patient-specific, human-relevant platform for modeling disease mechanisms and screening therapeutic candidates [67] [15]. However, the translational validity of findings from these in vitro models must be established through rigorous cross-validation against the gold standards of neurodegenerative disease research: post-mortem human brain tissue and clinically validated biofluid biomarkers [68] [69]. This whitepaper provides a technical guide for researchers and drug development professionals on the methodologies and frameworks for this essential multi-modal validation, contextualized within the broader thesis of understanding tau hyperphosphorylation in human models.
Tau Proteoform Landscapes in Human Brain Tissue
Post-mortem brain studies from neuropathologically confirmed cases provide the definitive molecular signatures of tauopathies, against which iPSC models must be calibrated. A recent high-resolution mass spectrometry (MS) study characterized tau in soluble and insoluble brain fractions from multiple tauopathies, revealing distinct proteoform profiles [68].
Table 1: Tau Peptide Abundance in Sarkosyl-Insoluble Brain Fractions Across Tauopathies
| Tau Peptide / Measure | Alzheimer's Disease (AD) | Progressive Supranuclear Palsy (PSP) | Corticobasal Degeneration (CBD) | Pick's Disease (PiD) |
|---|---|---|---|---|
| MTBR-containing peptides | 12-72x increase vs. controls | Moderate increase | Moderate increase | Moderate increase |
| Predominant Tau Isoform | Mixed 3R/4R | 4R | 4R | 3R |
| Phosphorylated peptides (general) | Pronounced increase | Modest increase | Modest increase | Modest increase |
| Doubly/Triply phosphorylated peptides | Significant increase (soluble & insoluble) | Not significant (soluble) | Not significant (soluble) | Not significant (soluble) |
Key Findings from Brain Tissue Analysis:
- AD is characterized by a massive accumulation of microtubule-binding region (MTBR) peptides in insoluble aggregates, far exceeding levels in primary tauopathies [68].
- Isoform-specific signatures differentiate primary tauopathies: 3R predominance in PiD and 4R in PSP and CBD, while AD shows a mixed 3R/4R profile [68].
- Complex phosphorylation patterns, particularly doubly and triply phosphorylated peptides, are a pronounced feature of AD even in soluble brain fractions, suggesting they may represent early pathological changes [68].
Table 2: Clinically Validated Fluid Biomarkers for Tau Pathology
| Biomarker | Biological Matrix | Primary Pathological Association | Performance & Context of Use |
|---|---|---|---|
| eMTBR-tau243 | Plasma | Insoluble tau tangles | Strong correlation with tau-PET (β=0.72, R²=0.56) and cognitive performance (β=0.60, R²=0.40); specifically elevated in symptomatic AD stages [70] |
| P-tau217 | Plasma / CSF | Amyloid-β plaques | Highly sensitive to cerebral Aβ load; emerges early in pre-clinical AD around Aβ plaques; reduced by anti-Aβ immunotherapy [70] [71] |
| P-tau181 | CSF | AD-type tau pathology | Established CSF biomarker for AD; increased in AD but not in primary tauopathies like PSP/CBD [72] [68] |
| T-tau | CSF | Neuronal injury / neurodegeneration | Marker of acute neuronal injury; not specific to AD [72] |
Experimental Workflows for Cross-Validation
Protocol for Tau Profiling in Post-Mortem Brain Tissue
The following workflow, adapted from [68], details the steps for comprehensive tau characterization against which iPSC-derived findings can be validated.
Methodology Details:
- Tissue Homogenization: Flash-frozen brain tissue (e.g., frontal cortex Brodmann area 9) is homogenized in Tris-buffered saline (TBS) containing protease and phosphatase inhibitors [68].
- Sequential Extraction: The homogenate is centrifuged at 100,000 × g to generate a TBS-soluble fraction (S1), containing soluble tau and small oligomers. The pellet is subsequently extracted with sarkosyl detergent to isolate the sarkosyl-insoluble fraction (P3), enriched for pathological tau aggregates [68].
- Immunoprecipitation and MS: Tau is immunoprecipitated from both fractions using specific antibodies, followed by tryptic digestion and LC-MS/MS analysis. This allows for absolute quantification of specific tau peptides, mapping of phosphorylation sites, and determination of 3R/4R isoform ratios [68].
Protocol for Validating iPSC-Derived Neuronal Models
iPSC-based disease models can be engineered to recapitulate key aspects of tau pathology. The following workflow, integrating methodologies from [15], provides a framework for generating and validating these models.
Key Methodological Considerations for iPSC Models:
- Rapid Tau Aggregation Model: A recently developed system utilizes lentiviral delivery of wild-type tau (1N4R isoform) under a TET-on inducible promoter in iPSC-derived neurons. This system induces tau aggregation and tau-dependent cell death within two weeks, enabling rapid drug screening [15].
- CRISPR-Cas9 Engineering: Isogenic controls are critical. Correcting or introducing mutations (e.g., in MAPT) creates genetically matched pairs that isolate the effects of specific variants on tau pathology [67].
- Differentiation Protocol: Efficient generation of high-purity (>90%), functionally mature neurons is achieved through inducible expression of neurogenic transcription factors like Ngn2 combined with microRNAs such as miR-9/9*-124 [15].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Tau Pathology and Biomarker Research
| Reagent / Tool | Function & Utility | Specific Examples / Assays |
|---|---|---|
| Anti-Tau Antibodies | Immunoprecipitation, immunoassay, and immunohistochemistry for specific tau epitopes and phospho-sites | Antibodies for p-tau181, p-tau217, p-tau205, p-tau231, MTBR-tau243; AT8 (p-S202/p-T205) for immunohistochemistry [70] [71] [68] |
| Tau PET Ligands | In vivo quantification and spatial mapping of tau aggregates in brain | First- and second-generation ligands (e.g., Flortaucipir); second-gen shows improved off-target binding profiles [72] |
| MS-Based Assays | Precise quantification of specific tau proteoforms and modifications in biofluids and tissue | LC-MS/MS for eMTBR-tau243 in plasma; multiplex assays for phosphorylated and non-phosphorylated tau peptides in brain extracts [70] [68] |
| CRISPR-Cas9 Systems | Genetic engineering of iPSCs for disease modeling and creation of isogenic controls | Correction of disease-associated mutations (e.g., SNCA A53T, LRRK2); introduction of reporter tags [67] |
| iPSC Reprogramming Systems | Generation of patient-specific pluripotent cells | Non-integrating methods: Sendai virus, episomal plasmids, mRNA reprogramming [67] [69] |
| Neuronal Differentiation Kits | Directed differentiation of iPSCs into relevant neuronal subtypes | Inducible transcription factor systems (e.g., Ngn2) for cortical or motor neurons [15] [54] |
Integration with Broader Tau Hyperphosphorylation Research
The cross-validation framework solidifies the role of iPSC-derived neurons in the broader landscape of tau research. Key integrative insights include:
- Biomarker Specificity: Fluid biomarkers reflect different aspects of pathology. P-tau217 increases early in response to Aβ plaques, while eMTBR-tau243 is a specific marker for insoluble tau tangle load that correlates with cognitive impairment [70] [71]. iPSC models can be used to elucidate the cellular mechanisms that generate these distinct biomarker species.
- Interspecies Differences: Human iPSC-derived neurons address a critical limitation of animal models, as the susceptibility to toxic tau aggregates differs between human and mouse neuronal cells [15]. Validation against human post-mortem tissue confirms the human-relevance of pathogenic mechanisms discovered in iPSC models.
- Drug Discovery Platform: Validated iPSC models enable high-throughput screening. The demonstration that tau overexpression induces aggregation and cell death within two weeks provides a rapid platform for evaluating tau-targeting compounds [15]. Furthermore, the ability of these models to correctly identify clinically effective drugs (e.g., riluzole in an ALS iPSC model) reinforces their predictive validity [54].
Cross-validation with post-mortem brain tissue and biofluid biomarkers is not merely a supplementary step but a fundamental requirement for establishing the scientific and translational relevance of iPSC-based models of tau hyperphosphorylation. The integrated workflows, quantitative benchmarks, and toolkit presented herein provide a roadmap for researchers to ensure that their in vitro findings accurately reflect human disease biology. As tau-targeting therapies move into clinical trials, rigorously validated iPSC models will be indispensable for identifying novel targets, screening for effective compounds, and ultimately personalizing therapeutic strategies for tauopathies.
Comparing iPSC Neuron Vulnerability to Mouse and Immortalized Cell Models
The study of tau hyperphosphorylation, a critical pathological event in Alzheimer's disease (AD) and frontotemporal dementia (FTD), has long relied on animal models and immortalized cell lines. While these systems have contributed valuable insights, they possess inherent limitations in fully recapitulating human-specific disease processes. The emergence of induced pluripotent stem cell (iPSC)-derived neuronal models represents a transformative approach for investigating tau pathology in human cells with patient-specific genetic backgrounds. iPSCs are generated by reprogramming somatic cells using transcription factors (OCT4, SOX2, KLF4, and MYC) to a pluripotent state, enabling their differentiation into virtually any cell type, including various neuronal subtypes and glial cells [73] [74]. This technical guide examines the comparative vulnerability of iPSC-derived neurons against traditional mouse models and immortalized cell lines, focusing on their application in tau hyperphosphorylation research. We evaluate these models through multiple parameters including physiological relevance, genetic fidelity, phenotypic recapitulation, and experimental utility, providing researchers with a framework for selecting appropriate model systems for neurodegenerative disease research and drug development.
Model System Comparisons: Technical Specifications and Applications
Fundamental Model Characteristics and Limitations
Table 1: Core Characteristics of Neuronal Model Systems
| Parameter | iPSC-Derived Neurons | Immortalized Cell Lines | Mouse Models |
|---|---|---|---|
| Species Origin | Human | Human (e.g., SH-SY5Y) or rodent | Mouse |
| Genetic Background | Patient-specific genomic retention [73] | Oncogenic transformation; cancer-derived [75] | Human transgene expression or mouse mutagenesis |
| Cellular Proliferation | Differentiated post-mitotic neurons [75] | Continuous proliferation [75] | In vivo development |
| Tau Isoform Expression | Endogenous human tau isoforms [76] | Variable, often fetal or abnormal patterns | Mostly 4R-tau (mouse), potentially chimeric human/mouse tau |
| Key Advantages | • Patient-specific mutations• Human genomic context• Differentiate into relevant subtypes [73] | • Low cost, high scalability• Homogeneous populations• Simplified experimental protocols [75] | • Intact neural circuitry• Behavioral correlates• Systemic physiology |
| Major Limitations | • Fetal-like maturity• Protocol variability• Time-intensive differentiation [73] [59] | • Proliferation signaling alters responses• Lack cellular diversity• Non-physiological metabolism [75] | • Species differences in tau sequence/expression• Incomplete phenotype recapitulation [73] |
Quantitative Performance in Tau Pathology Modeling
Table 2: Model Performance in Recapitulating Tau Hyperphosphorylation Phenotypes
| Experimental Readout | iPSC-Derived Neurons | Immortalized Cell Lines | Mouse Models |
|---|---|---|---|
| TAU Hyperphosphorylation | Elevated p-tau sites (Thr231, Ser202/Thr205) in fAD/sAD neurons [59] | Can be induced but may not reflect physiological regulation | Often requires aggressive mutant tau transgenes |
| Amyloid-β Pathology | Increased Aβ1-40, Aβ1-42; altered Aβ42/40 ratio in fAD [59] | Limited APP processing fidelity; constitutive cleavage differences [75] | Extensive amyloid plaque pathology in specific models |
| Neuronal Vulnerability | Mutation-specific death (e.g., V337M MAPT) [77]; caspase-3/6 activation [77] | Generally high resistance to stressors; proliferation can confound death assays [75] | Age-dependent neuronal loss in some models; often minimal |
| GSK3B Activation | Significantly increased in AD neurons [59] | Can be chemically induced but may not reflect disease context | Variable depending on model and age |
| Neuroinflammation | Microglia/astrocyte activation in co-cultures; cytokine release [78] [79] | Limited innate immune responses; lack glial interactions [75] | Robust neuroinflammatory response but species-specific signatures |
| Therapeutic Predictive Value | High for human biomarker response (e.g., p-tau reduction) [73] | Poor clinical translation record for neuroprotective drugs [73] | Mixed; successful for amyloid-targeting but failures for tau/nuroprotection |
Experimental Paradigms for Investigating Tau Hyperphosphorylation in iPSC Neurons
Protocol 1: Establishing 2D Monocultures of Cortical Neurons from iPSCs
Principle: Guided differentiation of iPSCs into cortical glutamatergic neurons using dual-SMAD inhibition and appropriate patterning factors, generating a homogeneous population for tau pathology studies [73] [59].
Procedure:
- Neural Induction: Culture iPSCs to 70-80% confluence in essential 8 medium. Initiate differentiation by switching to neural induction medium containing DMEM/F-12, N2 supplement, MEM-NEAA, and heparin. Add small molecule inhibitors for dual-SMAD inhibition: SB431542 (10 µM, TGF-β inhibitor) and LDN193189 (100 nM, BMP inhibitor) for 10-14 days [73].
- Neural Progenitor Expansion: Mechanically dissect neural rosettes and plate on poly-ornithine/laminin-coated surfaces in neural progenitor medium (DMEM/F-12, N2 supplement, B27 supplement, FGF2 [20 ng/mL]). Passage every 7-10 days for expansion [80].
- Cortical Neuron Differentiation: Upon neural progenitor confluence, switch to neuronal differentiation medium (Neurobasal, B27 supplement, BDNF [20 ng/mL], GDNF [10 ng/mL], cAMP [1 mM], ascorbic acid [200 µM]). Culture for 6-12 weeks with half-medium changes every 3-4 days, monitoring neuronal maturity via MAP2 expression and synaptic markers [59].
- Validation: At day 60-80, assess cortical identity by immunocytochemistry for CTIP2, TBR1, and SATB2. Confirm glutamatergic phenotype by VGLUT1 expression and electrophysiological activity (patch clamp) [59].
Protocol 2: Generating 3D Cerebral Organoids for Tau Spreading Studies
Principle: Create complex three-dimensional models containing multiple neuronal subtypes and glial cells to investigate tau propagation and cell-type-specific vulnerability in a tissue-like context [78].
Procedure:
- Embryoid Body Formation: Detach iPSC colonies using EDTA and transfer to low-attachment 96-well plates in embryoid body medium (DMEM/F-12, 20% KnockOut Serum Replacement, MEM-NEAA, β-mercaptoethanol) to form uniform aggregates [78].
- Neural Induction: At day 5, transfer embryoid bodies to neural induction medium (DMEM/F-12, N2 supplement, MEM-NEAA, heparin) for 5 days without agitation.
- 3D Maturation: Embed organoids in Matrigel droplets at day 10 and transfer to differentiation medium (DMEM/F-12, Neurobasal, N2 supplement, B27 without vitamin A, insulin, ascorbic acid). Culture with constant rotation for 100+ days to achieve advanced maturity with cortical layer formation [78].
- Tau PFF Challenge: At day 100, introduce sonicated tau pre-formed fibrils (PFFs) at 10 µg/mL or 100 µg/mL concentrations. Refresh medium containing PFFs every 5 days for 10-15 days total exposure [78].
- Outcome Measures: Process organoids for cryosectioning and immunostaining for pTau181, pTau217, AT8 (Ser202/Thr205), and GFAP. Analyze tau pathology spread from surface to deep layers and correlate with astrocyte activation [78].
Protocol 3: CRISPR-Cas9 Engineering of Isogenic iPSC Lines
Principle: Generate genetically matched control lines through precise genome editing to isolate the pathogenic contribution of specific MAPT mutations, controlling for background genetic variability [80].
Procedure:
- gRNA Design: Design and validate guide RNAs targeting sequences flanking the V337M MAPT mutation or to introduce specific mutations into the endogenous MAPT locus.
- Electroporation: Deliver ribonucleoprotein complexes (Cas9 protein, gRNA) and single-stranded DNA donor template (for base editing) to iPSCs using nucleofection technology.
- Clonal Selection: Single-cell sort edited iPSCs after 48 hours and expand individual clones for 2-3 weeks. Screen clones by PCR and Sanger sequencing to identify precise edits.
- Isogenic Validation: Confirm pluripotency (OCT4, NANOG expression) and normal karyotype in edited clones. Differentiate alongside the original patient line to confirm mutation-specific phenotypes while controlling for genetic background [80].
Signaling Pathways in Tau Hyperphosphorylation Using iPSC-Derived Neurons
Molecular Mechanisms of Tau Pathology
Investigations using iPSC-derived neurons have elucidated key signaling pathways driving tau hyperphosphorylation in human neurons. A central pathway involves amyloid-β-mediated activation of glycogen synthase kinase 3 beta (GSK3B), which phosphorylates tau at multiple pathological epitopes [59]. iPSC studies have demonstrated that neurons from both familial and sporadic AD patients show significantly increased levels of active GSK3B, providing a direct link to tau hyperphosphorylation observed in these models [59]. The vulnerability of specific neuronal subtypes appears linked to their intrinsic expression of tau isoforms, with recent evidence indicating that the 1N4R tau isoform confers particular sensitivity to amyloid-β oligomer-induced toxicity in human neurons [76].
Complementing these findings, caspase activation represents another critical pathway in tau pathogenesis. In iPSC-derived neurons carrying the FTD-associated V337M MAPT mutation, researchers have documented a time-dependent accumulation of tau cleaved by caspase-6 at D13 and D402 residues, creating aggregation-prone tau species that precede neuronal death [77]. This caspase activation creates a feed-forward loop where cleaved tau promotes further misfolding and phosphorylation. The integration of these pathways—amyloid-driven kinase activation, isoform-specific vulnerability, and caspase-mediated proteolysis—provides a more comprehensive understanding of tau pathogenesis derived specifically from human cellular models.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for iPSC-Based Tau Pathology Studies
| Reagent/Catalog Number | Application | Experimental Function |
|---|---|---|
| Tau Pre-formed Fibrils (TAU-H5113/TAU-H5116) [78] | Tau seeding and propagation | Induce tau aggregation and spreading in human neurons; model prion-like tau pathology |
| iPSC-Derived Cerebral Organoids (CIPO-BWL002K) [78] | 3D disease modeling | Provide complex tissue-like environment with multiple neuronal subtypes and glial cells |
| Cerebral Organoid Differentiation Kit (RIPO-BWM001K) [78] | 3D model generation | Direct iPSC differentiation into patterned cerebral organoids with cortical layers |
| SB431542 [73] | Neural induction | TGF-β inhibitor for efficient neural conversion via dual-SMAD inhibition |
| CHIR99021 [73] | Neural patterning | GSK3β inhibitor for dorsal forebrain patterning; WNT pathway modulation |
| Dorsomorphin [73] | Neural induction | BMP pathway inhibitor for efficient neural conversion via dual-SMAD inhibition |
| Purmorphamine [73] | Neuronal subtyping | Smoothened agonist for SHH pathway activation; ventral neuron patterning |
| Caspase Inhibitors (Z-VAD) [77] | Pathway modulation | Pan-caspase inhibitor to rescue tau mutation-associated neuronal death |
| Phospho-Tau Antibodies (AT8, pTau181, pTau217) [59] [78] | Pathology readout | Detect and quantify disease-relevant tau phosphorylation epitopes |
| Neoepitope Tau Antibodies (mAbD402, mAbD13) [77] | Cleavage detection | Specifically recognize caspase-cleaved tau fragments not present in full-length tau |
Discussion and Future Perspectives in Tauopathy Modeling
The comprehensive comparison of model systems reveals distinct advantages of iPSC-derived neurons for studying tau hyperphosphorylation mechanisms and therapeutic interventions. The demonstrated capacity of these human cellular models to recapitulate disease-relevant phenotypes including tau phosphorylation, caspase activation, isoform-specific vulnerability, and neuroinflammation provides unprecedented opportunities for both basic research and drug development [59] [78] [77]. The consistency of findings across multiple laboratories using different patient-derived lines strengthens the validation of iPSC technology for disease modeling.
Future directions in the field will likely focus on enhancing model complexity through the incorporation of multiple brain cell types in defined ratios, the development of accelerated neuronal aging protocols, and the implementation of high-content screening platforms for drug discovery. The integration of 3D model systems with advanced functional readouts including multi-electrode arrays and calcium imaging will further strengthen the physiological relevance of these models. Additionally, the generation of comprehensive iPSC libraries from patients with diverse tauopathies provides a resource for identifying subtype-specific mechanisms and therapeutics [80]. As these technologies mature, iPSC-derived neuronal models are positioned to significantly advance our understanding of tau-driven neurodegeneration and bridge the translational gap between preclinical discovery and clinical therapeutic development for Alzheimer's disease, frontotemporal dementia, and related tauopathies.
Alzheimer's disease (AD) is a progressive neurodegenerative disorder whose pathogenesis is strongly linked to the abnormal accumulation of the microtubule-associated protein tau. In healthy neurons, tau promotes microtubule assembly and stability, which are essential for maintaining axonal structure and facilitating intracellular transport [19] [81]. However, under pathological conditions, tau undergoes hyperphosphorylation, detaching from microtubules and aggregating into neurofibrillary tangles (NFTs) [15] [81]. This hyperphosphorylation is driven by dysregulation of various kinase and phosphatase activities. The presence of hyperphosphorylated tau (pTau) correlates more closely with cognitive decline in AD than other pathological hallmarks, making it a prime therapeutic target [1] [19]. The study of tau pathology has been revolutionized by human induced pluripotent stem cell (iPSC) technology, which enables the generation of patient-derived neurons that recapitulate key aspects of AD, including the adult isoforms of tau and disease-relevant phosphorylation patterns [1]. This whitepaper evaluates two promising therapeutic strategies for attenuating tau pathology: SGK1 inhibitors and tau-targeting antibodies, with a focus on their efficacy in human iPSC-derived neuronal models.
SGK1 Inhibitors: Mechanism and Therapeutic Potential
The Role of SGK1 in Tau Pathology
Serum and Glucocorticoid-regulated Kinase 1 (SGK1) is a stress-responsive kinase that has emerged as a significant regulator of tau phosphorylation and microtubule stability in Alzheimer's disease. Research using cortical neurons differentiated from iPSCs of AD patients has demonstrated a marked increase in both SGK1 expression and tau phosphorylation compared to neurons from healthy controls [1]. This elevated SGK1 expression is observed at the mRNA and protein levels and is accompanied by significantly increased levels of phosphorylated Tau (pTau) at specific epitopes, including S202/T205 (recognized by the AT8 antibody) and S214 [1]. Beyond its direct role in phosphorylating tau, SGK1 also influences microtubule dynamics by regulating the expression of Histone Deacetylase 6 (HDAC6), an enzyme that deacetylates tubulin. Increased HDAC6 activity leads to reduced levels of acetylated tubulin (AcTub), a marker of stable microtubules, thereby contributing to microtubule destabilization—a key consequence of tau dysfunction in AD [1].
Efficacy of SGK1 Inhibition in iPSC-Derived Neurons
Intervention studies in human iPSC-derived cortical models have provided compelling evidence for SGK1 as a therapeutic target. Both pharmacological inhibition and shRNA-mediated knockdown of SGK1 effectively reduce tau phosphorylation and restore microtubule stability in AD patient-derived neurons.
Table 1: SGK1 Inhibitors and Their Effects in iPSC-Derived Neuronal Models
| Intervention Method | Specific Agent/Approach | Observed Effects in AD Neurons | Citation |
|---|---|---|---|
| Pharmacological Inhibition | GSK650394 (100 nM) | Decreased pSGK1, reduced Tau phosphorylation (AT8, S214), increased acetylated tubulin | [1] |
| Pharmacological Inhibition | EMD638683 (6 µM) | Decreased pSGK1, reduced Tau phosphorylation (AT8, S214) | [1] |
| Genetic Knockdown | SGK1 shRNA (lentivirus) | Reduced Tau phosphorylation, decreased HDAC6, increased acetylated tubulin | [1] |
| SGK1 Overexpression | SGK1 (lentivirus) in control neurons | Increased Tau phosphorylation, increased HDAC6, decreased acetylated tubulin | [1] |
The efficacy of SGK1 inhibition extends beyond tau biochemistry. In animal models of Parkinson's disease, SGK1 inhibition in glial cells has been shown to correct pro-inflammatory properties, protect dopamine neurons from degeneration, and ameliorate behavioral deficits, suggesting a broader neuroprotective role that could be relevant across neurodegenerative conditions [82].
Tau-Targeting Antibodies: Mechanism and Therapeutic Potential
Immunotherapeutic Approaches to Tau Pathology
Tau-targeting antibodies represent a passive immunotherapeutic strategy designed to recognize and neutralize pathological forms of tau. The theoretical basis for this approach hinges on the "prion-like" propagation of tau pathology, wherein misfolded tau spreads between neurons, seeding further aggregation in a stereotypical pattern through the brain [81]. Antibodies can target extracellular tau to prevent its cell-to-cell transmission or, in some cases, enter neurons to engage intracellular tau aggregates [19]. The specificity of these antibodies for particular pathological tau conformations or phosphorylation states is crucial for minimizing off-target effects and ensuring engagement of the most toxic species.
MK-2214: A Case Study in Tau-Targeting Antibodies
MK-2214, an anti-tau monoclonal antibody developed by Merck, exemplifies this therapeutic class. This antibody specifically recognizes tau phosphorylated at serine 413 (pSer413), an epitope found in pathological tau from AD brains but not in tau from healthy brain tissue [83]. This selectivity for disease-associated tau is a critical feature intended to enhance therapeutic safety. Preclinical data demonstrates that MK-2214 binds with picomolar affinity to aggregated tau in AD patient samples and can deplete tau seeding activity from brain extracts [83]. Furthermore, the antibody has been engineered with a specific mutation to extend its half-life, potentially allowing for less frequent dosing in clinical settings [83].
Table 2: Profile of Tau-Targeting Antibody MK-2214
| Characteristic | Description | Citation |
|---|---|---|
| Target Epitope | Phosphorylated Serine 413 (pSer413) | [83] |
| Binding Affinity | Picomolar to aggregated tau in AD brain and CSF samples | [83] |
| Mechanistic Actions | Binds extracellular pSer413 tau; depletes tau seeding activity; blocks development of tau pathology in iPSC-derived neurons | [83] |
| Engineering Feature | Mutated for extended half-life | [83] |
| Clinical Status | Phase 2 trial initiated July 2025 (NCT07033494) | [83] |
Experimental Protocols for Evaluating Therapeutics in iPSC-Derived Neurons
Protocol 1: Differentiating Cortical Neurons from Human iPSCs
The ability to generate consistent and physiologically relevant human neurons is foundational to screening and validating tau-directed therapies.
- iPSC Line Selection: Use footprint-free human iPSC lines from both healthy donors and AD patients. Ensure lines are karyotypically normal and express standard pluripotency markers.
- Neural Induction via Embryoid Bodies: Adapt a method that installs dorsal forebrain fate to generate cortical neurons expressing all six major adult tau isoforms [1]. This overcomes a historical limitation of many iPSC-neuron protocols that produce only fetal tau isoforms.
- Neuronal Differentiation and Maturation: Plate neuralized cells on appropriate substrates (e.g., poly-L-ornithine/laminin). Maintain cultures in neuronal maintenance medium, typically containing Neurobasal medium, B27 supplement, BDNF, and other factors. Neurons are typically ready for experimentation by Day 25-40 post-differentiation, as evidenced by MAP2 staining and the presence of mature tau isoforms [1].
- Validation: Confirm neuronal identity (MAP2+), purity, and tau isoform expression via immunocytochemistry and Western blotting. Verify elevated pTau and SGK1 in AD lines compared to controls [1].
Protocol 2: Assessing Therapeutic Efficacy of SGK1 Inhibitors
This protocol details the treatment and analysis of iPSC-derived neurons to evaluate SGK1-targeted compounds.
- Compound Preparation: Prepare stock solutions of SGK1 inhibitors (e.g., GSK650394, EMD638683) in DMSO. Create working dilutions in neuronal maintenance medium, ensuring the final DMSO concentration is low (e.g., <0.1%) to avoid cytotoxicity.
- Neuronal Treatment: Treat mature (Day 40) control and AD iPSC-derived cortical neurons with the inhibitor or vehicle control for 72 hours. Include a positive control, such as neurons transduced with SGK1 shRNA lentivirus [1].
- Cell Lysis and Analysis:
- Western Blotting: Lyse cells in RIPA buffer with protease and phosphatase inhibitors. Resolve proteins via SDS-PAGE and probe with the following antibodies:
- Primary Antibodies: anti-pSGK1, anti-total SGK1, anti-pTau (AT8, pS214), anti-total tau, anti-HDAC6, anti-acetylated tubulin, anti-β-actin (loading control).
- Secondary Antibodies: HRP-conjugated anti-mouse/rabbit IgG.
- Immunocytochemistry: Fix neurons in 4% PFA, permeabilize with Triton X-100, and block with BSA. Incubate with primary antibodies (e.g., AT8, MAP2) followed by fluorophore-conjugated secondary antibodies and DAPI. Image using a high-content imaging system or confocal microscope [1].
- Western Blotting: Lyse cells in RIPA buffer with protease and phosphatase inhibitors. Resolve proteins via SDS-PAGE and probe with the following antibodies:
- Functional Assay - Microtubule Stability: To directly assess microtubule polymerization, lyse cells at 37°C to preserve microtubules. Centrifuge to separate supernatant (free tubulin) from pellet (polymerized tubulin/microtubules). Analyze both fractions by Western blotting for tubulin [1].
Protocol 3: Evaluating Tau Antibodies in Seeding and Uptake Assays
This protocol is used to test the ability of antibodies like MK-2214 to inhibit tau propagation and engage their targets.
- Tau Seeding Assay:
- Utilize biosensor cell lines (e.g., HEK293T) engineered to express tau fusion proteins (e.g., tau repeat domain fused to CFP/YFP) that fluoresce upon tau aggregation [81].
- Pre-incubate brain homogenates from AD patients or tauopathy mouse models with the therapeutic antibody or an isotype control for 1-2 hours.
- Add the mixture to the biosensor cells. After a set period (e.g., 48-72 hours), quantify fluorescence as a measure of tau seeding activity inhibited by the antibody [83].
- Antibody Uptake and Target Engagement in Neurons:
- Treat control or AD iPSC-derived neurons with the tau antibody (e.g., MK-2214).
- After treatment, fix and stain neurons for the antibody itself (using a secondary antibody against human IgG) and for intracellular markers like total tau or pTau.
- Use high-content imaging analysis to quantify the co-localization of the therapeutic antibody with intracellular tau aggregates, indicating successful internalization and target engagement [83].
Signaling Pathways and Experimental Workflows
SGK1 Signaling in Tau Phosphorylation and Microtubule Destabilization
The following diagram illustrates the central role of SGK1 in driving tau pathology and how its inhibition exerts a therapeutic effect.
Workflow for High-Content Screening of Tau-Lowering Compounds
This diagram outlines a streamlined process for using iPSC-derived neurons to screen for compounds that reduce tau levels, a method applicable to evaluating both small molecules and antibodies.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and tools used in the featured experiments for studying tau pathology and evaluating therapeutics in iPSC-derived neuronal models.
Table 3: Research Reagent Solutions for Tauopathy Studies in iPSC-Derived Neurons
| Reagent/Tool | Specific Example(s) | Function and Application | Citation |
|---|---|---|---|
| iPSC-derived Cortical Neurons | AD patient-derived lines; Isogenic Ngn2-iPSCs (AAVS1-integrated) | Provides physiologically relevant human neuronal model expressing adult tau isoforms for disease modeling and HTS. | [1] [84] |
| Phospho-Specific Tau Antibodies | AT8 (pS202/pT205); pS214; pT231; pS262; pS413 | Detect and quantify specific pathological tau phosphorylation events via Western blot (WB) and immunocytochemistry (ICC). | [1] [83] [27] |
| SGK1 Inhibitors | GSK650394 (100 nM); EMD638683 (6 µM) | Small molecule inhibitors used to pharmacologically validate SGK1 as a target and assess its role in tau phosphorylation. | [1] |
| Microtubule Stability Markers | Anti-acetylated tubulin antibody | Detects levels of acetylated tubulin (AcTub), a marker for stable microtubules, by WB and ICC. | [1] |
| Lentiviral Vectors | SGK1 overexpression; SGK1 shRNA; M2rtTA (control) | Enables genetic manipulation (knockdown/overexpression) of targets in neurons to confirm pharmacological findings. | [1] |
| Tau Seeding Assay | Biosensor cell lines (e.g., HEK293T with tau RD-CFP/YFP) | Measures the prion-like seeding activity of tau aggregates from patient samples, used to evaluate antibody efficacy. | [83] [81] |
| HDAC6 Antibody | Anti-HDAC6 | Measures expression of HDAC6, a tubulin deacetylase linked to SGK1 signaling and microtubule instability. | [1] |
The development of effective tau-directed therapies is a critical frontier in the fight against Alzheimer's disease and related tauopathies. Human iPSC-derived neuronal models have become indispensable tools in this endeavor, providing a physiologically relevant platform for target validation and drug screening. The evidence gathered from these models strongly supports the therapeutic potential of both SGK1 inhibitors and conformation-specific tau antibodies like MK-2214. SGK1 inhibitors address the upstream kinase dysregulation that drives tau hyperphosphorylation and microtubule destabilization, offering a multi-faceted approach to preserving neuronal function. Conversely, tau-targeting antibodies aim to directly neutralize and clear the pathological tau species responsible for disease propagation. The ongoing clinical evaluation of MK-2214 and the robust preclinical data for SGK1 inhibitors highlight a dynamic and promising landscape. Future work will likely focus on combination therapies, improved biomarker development for patient stratification, and further refinement of human cellular models to fully capture the complexity of tau-driven neurodegeneration.
The study of Non-Demented Individuals with Alzheimer's Neuropathology (NDAN) represents a crucial frontier in Alzheimer's disease (AD) research. These unique individuals maintain cognitive function despite possessing the hallmark neuropathological features of AD—amyloid plaques and neurofibrillary tangles. Understanding the molecular mechanisms underlying this resilience provides unprecedented opportunities for developing novel therapeutic strategies that mimic natural neuroprotective pathways. Within the broader context of tau hyperphosphorylation research in iPSC-derived neurons, NDAN models offer a powerful platform to investigate endogenous protective mechanisms against tau-driven neurodegeneration.
The pathological progression of AD is characterized by the accumulation of amyloid-β (Aβ) peptides and hyperphosphorylated tau protein, which aggregates into neurofibrillary tangles (NFTs). While these features are consistently observed in post-mortem brains of AD patients, a subset of individuals exhibits significant AD pathology without corresponding cognitive decline. Investigating these resilient individuals through human iPSC-derived neuronal models enables researchers to probe the molecular basis of this protection in a controlled, physiologically relevant system. This approach allows for direct comparison between vulnerable AD neurons and resilient NDAN neurons, identifying key differences in tau processing, phosphorylation patterns, and cellular stress responses.
Methodological Approaches for Modeling NDAN
iPSC-Derived Neuronal Models
The foundation of NDAN research relies on establishing robust human cellular models that recapitulate key aspects of the condition. Induced pluripotent stem cell (iPSC) technology enables generation of patient-specific neurons that capture the complete genetic background of NDAN individuals. The standard protocol involves:
- iPSC Generation: Dermal fibroblasts or peripheral blood mononuclear cells are obtained from genetically characterized NDAN donors, sporadic AD patients, and healthy controls. These somatic cells are reprogrammed using non-integrating Sendai virus vectors expressing the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) to establish pluripotent stem cell lines.
- Neuronal Differentiation: iPSCs are differentiated into mature cortical neurons using dual-SMAD inhibition protocols, typically requiring 60-90 days for full maturation. This process generates functionally active, glutamatergic neurons that express appropriate cortical layer markers and exhibit spontaneous electrical activity.
- Characterization: Resulting neurons are validated through immunocytochemistry for neuronal markers (β-III-tubulin, MAP2), synaptic proteins (synapsin, PSD95), and electrophysiological assessments to confirm functional maturity.
Three-Dimensional Culture Systems
While traditional 2D neuronal cultures have provided valuable insights, 3D model systems better recapitulate the complexity of the human brain microenvironment. Cerebral organoids and Matrigel-embedded cultures enable the study of tau pathology in a more physiological context:
- Cerebral Organoids: iPSCs are guided through embryonic brain development patterns using specialized culture conditions, generating self-organizing structures containing multiple neuronal subtypes and rudimentary layered architecture. These organoids develop spontaneous tau pathology when derived from fAD or sAD patients, with hyperphosphorylated tau appearing after approximately 90 days in culture [16].
- Matrigel-Embedded 3D Cultures: Cortical neurons are embedded in Matrigel matrix, providing scaffolding that reduces shearing stress and promotes enhanced neuronal network formation. This system accelerates the accumulation of insoluble Aβ and hyperphosphorylated tau, making it particularly suitable for modeling later-stage AD pathology [34].
Tau Aggregation Assays
Quantifying tau aggregation is essential for evaluating pathological progression and treatment responses. High-throughput-compatible assays have been developed specifically for iPSC-derived neuronal models:
- AlphaLISA Technology: This bead-based proximity assay detects tau aggregates in a 384-well plate format, enabling high-throughput screening. The assay demonstrates excellent reproducibility across users and different iPSC lines, representing a highly translational tool for identifying tau-modifying compounds [34].
- Seeding-Based Models: To accelerate tau aggregation, neurons can be transduced with tau harboring the pro-aggregating P301L mutation and seeded with preformed aggregates consisting of the tau-microtubule binding repeat domain. This approach triggers robust tau aggregation and hyperphosphorylation within 2 weeks without affecting general cell health, enabling rapid screening of therapeutic interventions [85].
Table 1: Key Methodological Approaches for NDAN Modeling
| Method | Key Features | Applications in NDAN Research | References |
|---|---|---|---|
| iPSC-derived 2D neuronal cultures | Patient-specific, mature cortical neurons, 60-90 day differentiation | Comparison of tau phosphorylation between NDAN, AD, and control neurons | [4] [86] |
| Cerebral organoids | Self-organizing 3D structures, multiple neuronal subtypes | Study of spontaneous tau pathology development in tissue-like context | [16] |
| Matrigel-embedded 3D cultures | Enhanced neuronal networking, reduced shearing stress | Accelerated accumulation of insoluble, hyperphosphorylated tau | [34] |
| AlphaLISA tau detection | High-throughput compatible, 384-well format | Quantification of tau aggregates for therapeutic screening | [34] |
| Seeding models | Rapid aggregation (2 weeks), P301L tau mutation | Evaluation of tau propagation and compound efficacy | [85] |
Key Findings in Tau Hyperphosphorylation
Comparative Phenotypes in Familial and Sporadic AD
Research using iPSC-derived neurons has revealed important similarities and differences in tau pathology between genetic and sporadic AD forms:
- TAU Hyperphosphorylation: Neurons derived from both familial AD (fAD, caused by PSEN1 mutations) and sporadic AD (sAD) patients show increased phosphorylation of TAU protein at all investigated phosphorylation sites compared to control neurons. This hyperphosphorylation impairs microtubule-binding capacity and leads to microtubule destabilization, disrupting critical neuronal functions including axonal transport [4] [86].
- Amyloid-β Profiles: Both fAD and sAD neurons exhibit higher levels of extracellular amyloid-β 1-40 (Aβ1-40) and amyloid-β 1-42 (Aβ1-42) compared to controls. However, the significantly increased Aβ1-42/Aβ1-40 ratio, a pathological hallmark of fAD, is observed only in fAD samples, suggesting distinct mechanisms of amyloid processing in different AD forms [4].
- GSK3B Activation: Neurons derived from AD iPSCs show increased levels of active glycogen synthase kinase 3 β (GSK3B), a physiological kinase of TAU. GSK3B phosphorylates serine and threonine residues in TAU and its activity corresponds with increased Aβ expression and Aβ-mediated neuronal death [4] [86].
- Oxidative Stress Sensitivity: Both fAD- and sAD-derived neurons display elevated sensitivity to oxidative stress induced by amyloid oligomers or peroxide, indicating shared vulnerability pathways despite potentially different disease origins [4].
Signaling Pathways in Tau Pathology
The molecular mechanisms driving tau hyperphosphorylation involve complex signaling networks that represent potential therapeutic targets:
Diagram 1: Tau Hyperphosphorylation Signaling Pathways. This diagram illustrates the key molecular pathways leading to tau hyperphosphorylation in Alzheimer's disease, highlighting potential points for therapeutic intervention.
Blood Biomarkers of Disease Progression
Recent advances in blood-based biomarkers provide minimally invasive tools for tracking disease progression:
- Phosphorylated Tau Isoforms: Elevated levels of p-tau181 and p-tau217 show strong associations with faster progression from MCI to all-cause and AD dementia, with p-tau217 demonstrating particularly robust predictive value [87].
- Neurofilament Light Chain (NfL): Increased NfL levels, indicating axonal damage, show the strongest associations with progression from MCI to dementia among all biomarkers tested [87].
- Glial Fibrillary Acidic Protein (GFAP): Elevated GFAP, reflecting astrocytic activation, is associated with faster progression from MCI to dementia and reduced likelihood of reversion from MCI to normal cognition [87].
- Amyloid-β42/40 Ratio: Lower Aβ42/40 ratios in blood are associated with faster progression from MCI to all-cause and AD dementia, correlating with brain amyloid deposition [87].
Table 2: Key Blood Biomarkers in Alzheimer's Disease Progression
| Biomarker | Biological Significance | Association with Cognitive Decline | Performance in Prediction | |
|---|---|---|---|---|
| p-tau217 | Tau phosphorylation at residue 217 | Faster progression from MCI to dementia | Strongest predictor for AD dementia (HR 2.11) | [87] |
| Neurofilament Light (NfL) | Axonal damage marker | Faster progression from MCI to dementia | Strongest association with all-cause dementia (HR 1.84) | [87] |
| GFAP | Astrocytic activation | Faster progression, reduced MCI reversion | Significant for both all-cause and AD dementia | [87] |
| Aβ42/40 ratio | Amyloid plaque formation | Faster progression from MCI to dementia | Moderate predictive value | [87] |
| p-tau181 | Tau phosphorylation at residue 181 | Faster progression from MCI to dementia | Strong predictor, especially in younger participants | [87] |
Research Reagent Solutions
Successful modeling of NDAN requires carefully selected reagents and tools optimized for iPSC and neuronal applications:
Table 3: Essential Research Reagents for NDAN Modeling
| Reagent/Category | Specific Examples | Function in NDAN Research | Application Notes | |
|---|---|---|---|---|
| iPSC Lines | NDAN-derived, sAD-derived, fAD-derived (PSEN1 mutations), isogenic controls | Provide patient-specific disease models with complete genetic backgrounds | Essential for comparative studies of resilience mechanisms | [4] [86] |
| Neuronal Differentiation Kits | Commercial cortical neuron differentiation kits | Generate consistent populations of mature, functional cortical neurons | Standardized protocols enhance reproducibility across laboratories | [16] [85] |
| TAU Aggregation Detection | AlphaLISA tau aggregation assays | Quantify soluble tau aggregates in high-throughput format | Compatible with 384-well plates, works across multiple iPSC lines | [34] |
| 3D Culture Systems | Matrigel, specialized scaffolding biomaterials | Create tissue-like environments for neuronal culture | Accelerates pathological protein accumulation, enhances physiological relevance | [34] |
| Phospho-TAU Antibodies | Anti-p-tau (multiple epitopes: T181, S396, S404) | Detect and quantify tau hyperphosphorylation at specific residues | Essential for evaluating tau pathology progression | [4] [16] |
| GSK3B Activity Assays | Phospho-GSK3B antibodies, kinase activity kits | Monitor activation state of key tau kinase | Connates amyloid and tau pathologies | [4] [86] |
Experimental Workflows
A standardized approach to NDAN modeling ensures consistent, reproducible results across studies:
Diagram 2: NDAN Modeling Experimental Workflow. This diagram outlines the key stages in establishing, characterizing, and utilizing iPSC-based models of cognitive resilience in NDAN.
Data Presentation and Analysis
Effective data presentation ensures clear communication of complex experimental results:
Quantitative Analysis of Tau Pathology
Standardized metrics enable direct comparison between NDAN, AD, and control models:
- Phospho-TAU ELISA Quantification: Electrochemiluminescence assays provide precise measurement of tau phosphorylation at specific epitopes (e.g., T181, S396, S404). Neurons from both fAD and sAD patients typically show 2.5 to 4-fold increases in phospho-tau levels compared to controls across multiple phosphorylation sites [4].
- Amyloid-β Secretion Profiles: Multiplex ELISAs quantifying Aβ1-40 and Aβ1-42 in conditioned media reveal distinct secretion patterns. While both fAD and sAD neurons show elevated absolute levels of both peptides, only fAD neurons exhibit the characteristically elevated Aβ42/40 ratio associated with enhanced aggregation propensity [4] [86].
- GSK3B Activity Measurements: Kinase activity assays demonstrate 1.5 to 2-fold increases in active GSK3B in AD-derived neurons compared to controls, establishing a direct link between kinase activation and tau hyperphosphorylation [4].
High-Content Imaging Analysis
Automated microscopy and image analysis provide single-cell resolution of pathological features:
- Neuronal Viability Assays: Cell health assessments using multiplexed viability markers (calcein-AM for live cells, ethidium homodimer for dead cells) reveal that both fAD and sAD neurons show 30-50% reduced survival under oxidative stress conditions compared to control neurons, indicating shared vulnerability pathways [4].
- Tau Localization Analysis: Subcellular fractionation and immunostaining demonstrate mislocalization of hyperphosphorylated tau from axonal to somatodendritic compartments in AD neurons, with 60-70% of AD neurons showing abnormal somatic tau accumulation compared to 10-15% in control cultures [16].
The development of robust iPSC-derived neuronal models of NDAN represents a transformative approach to understanding cognitive resilience in the face of significant Alzheimer's pathology. By leveraging advanced 3D culture systems, high-throughput tau aggregation assays, and comprehensive biomarker profiling, researchers can now systematically investigate the molecular mechanisms that protect against tau-mediated neurodegeneration. These models not only provide insights into fundamental disease processes but also serve as powerful platforms for identifying and validating novel therapeutic strategies aimed at promoting resilience rather than merely preventing pathology. As these technologies continue to evolve, they hold exceptional promise for delivering much-needed interventions for Alzheimer's disease and related tauopathies.
Conclusion
Human iPSC-derived neuronal models have matured into indispensable tools for deconstructing the mechanism of tau hyperphosphorylation and accelerating therapeutic discovery. They have firmly established the role of kinases like SGK1 in human neuronal contexts and revealed downstream consequences on microtubule stability. The development of robust, scalable, and physiologically relevant assays now enables the systematic evaluation of diverse therapeutic strategies, from kinase inhibitors and aggregation blockers to immunotherapies. Future research must focus on integrating these models with complex systems, such as glial co-cultures and organoids, to capture the full spectrum of tau-driven neurodegeneration. The convergence of iPSC technology with emerging biomarker data and cryo-EM structural insights promises to unlock a new era of precision medicine for Alzheimer's disease and primary tauopathies, ultimately guiding the selection of the right patients for the right tau-targeted therapies.
References
- 1. Elevated SGK1 increases Tau phosphorylation and ... [https://www.nature.com/articles/s41380-025-03225-4]
- 2. Serum and glucocorticoid-regulated kinase 1 - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9706101/]
- 3. The role of SGK1 in neurologic diseases: A friend or foe? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11683284/]
- 4. Neurons derived from sporadic Alzheimer's disease iPSCs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5709977/]
- 5. High-fat diet–induced activation of SGK1 promotes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8411983/]
- 6. Mechanisms of tau-induced neurodegeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2872491/]
- 7. Does modulation of tau hyperphosphorylation represent a ... [https://www.nature.com/articles/s41380-023-02113-z]
- 8. HDAC6 Modulates Signaling Pathways Relevant to ... [https://www.mdpi.com/1422-0067/20/7/1605]
- 9. Histone deacetylase 6 interacts with the microtubule ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2574575/]
- 10. Histone deacetylase-6 modulates Tau function in ... [https://www.sciencedirect.com/science/article/pii/S0167488922000660]
- 11. Advancing histone deacetylase 6 (HDAC6) as a promising ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2025.1662691/full]
- 12. The Deacetylase HDAC6 Mediates Endogenous Neuritic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578720/]
- 13. Tau in neurodegenerative diseases: molecular mechanisms ... [https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-024-00429-6]
- 14. Frontiers | The Importance of Tau Phosphorylation for ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2013.00083/full]
- 15. Tau aggregation induces cell death in iPSC-derived neurons [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018045/]
- 16. Modeling tau pathology in human stem cell derived neurons [https://pmc.ncbi.nlm.nih.gov/articles/PMC8029337/]
- 17. Role of Tau Protein in Neurodegenerative Diseases and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11206543/]
- 18. Revisiting the therapeutic landscape of tauopathies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12135284/]
- 19. Tau-Targeted Therapeutic Strategies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523266/]
- 20. Development of a robust, physiologically relevant neuronal ... [https://www.sciencedirect.com/science/article/pii/S002192582502705X]
- 21. Quantification of plasma tau species containing the proline- ... [https://www.nature.com/articles/s41598-025-25864-x]
- 22. Introducing: iPSC Collection from Tauopathy Patients [https://www.alzforum.org/news/research-news/introducing-ipsc-collection-tauopathy-patients]
- 23. Tracing mitochondrial marks of neuronal aging in iPSCs- ... [https://www.nature.com/articles/s42003-025-08152-2]
- 24. associated with increased oxidative stress... Mitochondrial dysfunction [https://pubmed.ncbi.nlm.nih.gov/23039195/]
- 25. impairment and synaptic Mitochondrial are associated... dysfunction [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-023-00966-8]
- 26. Hyperphosphorylated tau mediates neuronal death by ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-022-02567-y]
- 27. A new pathway for neuroprotection against tau ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1587219/full]
- 28. Modifications of tau protein during neuronal cell death [https://pubmed.ncbi.nlm.nih.gov/12214023/]
- 29. Neurogenesis and cell cycle-reactivated neuronal death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2239302/]
- 30. In vivo hyperphosphorylation of tau is associated with ... [https://www.nature.com/articles/s41593-024-01829-7]
- 31. Recapitulation of endogenous 4R tau expression and ... [https://www.sciencedirect.com/science/article/pii/S1934590922002004]
- 32. Tau aggregation induces cell death in iPSC-derived neurons [https://www.sciencedirect.com/science/article/pii/S2589958925000027]
- 33. Generation of human induced pluripotent stem cell-derived ... [https://pubmed.ncbi.nlm.nih.gov/40267294/]
- 34. Development of a Scalable, High-Throughput-Compatible ... [https://www.sciencedirect.com/science/article/pii/S2472555222071350]
- 35. Improved modeling of human AD with an automated ... [https://www.nature.com/articles/s41467-021-25344-6]
- 36. A Three-Dimensional Alzheimer's Disease Cell Culture Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7325960/]
- 37. Advances in current in vitro models on neurodegenerative ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1260397/full]
- 38. 2D versus 3D human induced pluripotent stem cell- ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-018-0258-4]
- 39. A high-throughput drug screening assay for anti-tau ... [https://www.nature.com/articles/s41598-025-21680-5]
- 40. Modulation and detection of tau aggregation with small- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3725300/]
- 41. Mechanisms of secretion and spreading of pathological tau ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7190606/]
- 42. The Rational Discovery of a Tau Aggregation Inhibitor - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7021323/]
- 43. Regional variations in seeding activity, phosphorylation ... [https://www.nature.com/articles/s44328-025-00056-9]
- 44. Live-cell visualization of tau aggregation in human neurons [https://www.nature.com/articles/s42003-024-06840-z]
- 45. Alzheimer's disease - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7201870/]
- 46. iPSC-induced neurons with the V337M MAPT mutation are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11866097/]
- 47. Amyloid, tau, and astrocyte pathology in autosomal ... [https://www.nature.com/articles/s41380-020-0817-2]
- 48. An Unbiased Approach to Identifying Tau Kinases That ... [https://www.sciencedirect.com/science/article/pii/S0021925820453554]
- 49. Combined small-molecule treatment accelerates ... [https://www.nature.com/articles/s41587-023-02031-z]
- 50. Prion-Like Propagation Mechanisms in Tauopathies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7692808/]
- 51. Cellular and molecular mechanisms of pathological tau ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00842-z]
- 52. Revisiting the grammar of Tau aggregation and pathology ... [https://pubs.rsc.org/en/content/articlehtml/2022/cs/d1cs00127b]
- 53. Bezafibrate treatment rescues neurodevelopmental and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351496/]
- 54. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 55. SfN 2025 - A Human iPSC-Derived Motor Neuron Platform [https://www.sygnaturediscovery.com/publications/posters/a-human-ipsc-derived-motor-neuron-platform-applications-for-drug-discovery-and-als-research/]
- 56. Continuous Monitoring of Tau -Induced Neurotoxicity in Patient- Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8143197/]
- 57. Protein aggregation in neurodegenerative diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574514/]
- 58. Current Understanding of Protein Aggregation in ... [https://www.mdpi.com/1422-0067/26/21/10568]
- 59. from sporadic Alzheimer’s disease Neurons reveal... derived iPSCs [https://alzres.biomedcentral.com/articles/10.1186/s13195-017-0317-z]
- 60. (PDF) Tau induces cell death in aggregation - iPSC derived neurons [https://www.academia.edu/144222710/Tau_aggregation_induces_cell_death_in_iPSC_derived_neurons]
- 61. Specific detection of tau seeding activity in Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10408046/]
- 62. Quantitative Methods for the Detection of Tau Seeding ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.654176/full]
- 63. AlphaLISA SureFire Ultra Human Total Tau Detection Kit, ... [https://www.revvity.com/product/alpha-sf-ultra-tau-total-500-alsu-ttau-a500]
- 64. AlphaLISA SureFire Ultra Human Tau Aggregate Detection ... [https://www.revvity.com/product/alpha-sf-ultra-tau-aggregate-hv-alsu-atau-a-hv]
- 65. AlphaLISA Immunoassay Kits [https://www.revvity.com/ask/alphalisa-immunoassay-kits]
- 66. Development of a Cell-Based AlphaLISA Assay for High- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10157846/]
- 67. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 68. Tau protein profiling in tauopathies: a human brain study [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-024-00741-9]
- 69. Translational Prospects and Challenges in Human Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5187530/]
- 70. Plasma MTBR-tau243 biomarker identifies tau tangle ... [https://www.nature.com/articles/s41591-025-03617-7]
- 71. Biomarker-related phospho-tau217 appears in synapses ... [https://www.sciencedirect.com/science/article/pii/S221112472500974X]
- 72. Biomarkers for tau pathology - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584358/]
- 73. Modeling neurological diseases using iPSC-derived neural cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6029980/]
- 74. Human Induced Pluripotent Stem Cell Models of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.766773/full]
- 75. Immortalized neuronal lines versus human induced ... [https://www.sciencedirect.com/science/article/abs/pii/S2468748024000195]
- 76. The tau isoform 1N4R confers vulnerability of MAPT knockout human... [https://pubmed.ncbi.nlm.nih.gov/40019008/]
- 77. -induced iPSC with the V337M MAPT... | Research Square neurons [https://www.researchsquare.com/article/rs-300172/v2]
- 78. Exploring tau PFF and cerebral organoid co-culture [https://www.news-medical.net/whitepaper/20250922/Tau-PFF-and-cerebral-organoid-co-culture-in-the-fight-against-neurodegenerative-diseases.aspx]
- 79. Human iPSC-derived glia models for the study of ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02919-2]
- 80. A Comprehensive Resource for Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S2213671119303352]
- 81. Tau tangles and the evolving landscape of Alzheimer's ... [https://www.abcam.com/en-us/stories/articles/tau-tangles-and-alzheimers-research]
- 82. SGK1 inhibition in glia ameliorates pathologies and ... [https://link.springer.com/article/10.15252/emmm.202013076]
- 83. MK-2214 [https://www.alzforum.org/therapeutics/mk-2214]
- 84. Scalable Production of iPSC-Derived Human Neurons to ... [https://www.sciencedirect.com/science/article/pii/S2213671117303764]
- 85. Using human iPSC-derived neurons to model TAU ... [https://www.stemcell.com/using-human-ipsc-derived-neurons-to-model-tau-aggregation.html]
- 86. Neurons derived from sporadic Alzheimer's disease iPSCs ... [https://pubmed.ncbi.nlm.nih.gov/29191219/]
- 87. Blood biomarkers of Alzheimer's disease and progression ... [https://www.nature.com/articles/s41467-025-66728-2]