Mycoplasma Contamination in Stem Cell Culture: Prevention, Detection, and Control Strategies for Researchers
This article provides a comprehensive guide for researchers and drug development professionals on addressing mycoplasma contamination in stem cell cultures.
Mycoplasma Contamination in Stem Cell Culture: Prevention, Detection, and Control Strategies for Researchers
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on addressing mycoplasma contamination in stem cell cultures. Covering the foundational biology and risks of these stealth contaminants, it details advanced detection methodologies like qPCR and next-generation sequencing. The content offers practical troubleshooting protocols for decontamination and outlines rigorous, phase-appropriate validation strategies to meet global pharmacopeia standards (USP, Ph. Eur., JP), ensuring data integrity, product safety, and regulatory compliance in both research and clinical applications.
The Stealth Contaminant: Understanding Mycoplasma Biology and Risks in Stem Cell Research
What Are Mycoplasmas? Defining the Cell Wall-Lacking Prokaryotes
Mycoplasmas represent a unique genus of bacteria that are a significant concern in cell culture laboratories worldwide. As prokaryotes that naturally lack a cell wall, they are resistant to many common antibiotics and can persistently contaminate cultures, leading to altered experimental outcomes and irreproducible data. This technical support center provides essential guides and FAQs to help researchers, particularly those in stem cell research, prevent, detect, and address mycoplasma contamination.
Frequently Asked Questions (FAQs)
What are mycoplasmas and why are they a problem in cell culture? Mycoplasmas are the smallest self-replicating bacteria, belonging to the class Mollicutes (meaning "soft skin") [1]. Their defining characteristic is the absence of a rigid cell wall [2] [3]. This makes them naturally resistant to beta-lactam antibiotics, such as penicillin, which target cell wall synthesis [2]. In cell culture, they are a major problem because they are difficult to detect visually, can significantly alter the physiology and metabolism of host cells, and are highly contagious, risking the contamination of entire laboratory cell stocks [4] [5].
How can I tell if my cell culture is contaminated with mycoplasma? Visual identification is nearly impossible as mycoplasma contamination does not cause media turbidity [6]. However, chronic signs may include subtle changes in cell growth rate, morphology, or overall cell health [4]. Definitive identification requires specific tests. The table below summarizes the common detection methods.
Table: Common Mycoplasma Detection Methods
| Method | Principle | Duration | Key Advantage | Key Limitation |
|---|---|---|---|---|
| PCR-Based Assays | Amplifies specific mycoplasma DNA sequences [7] [3] | Hours to 1 day | Rapid, highly sensitive, can detect multiple species [5] | Does not distinguish between viable and non-viable organisms |
| DNA Staining (e.g., DAPI, Hoechst) | Stains extranuclear DNA in the cytoplasm of infected indicator cells [5] [6] | 1-2 days | Visually demonstrates contamination on cells | Requires experience to interpret, may have false positives |
| Microbiological Culture | Grows mycoplasma on agar plates; forms "fried-egg" colonies [1] [5] | Up to 4 weeks | The "gold standard" for viability confirmation [5] | Very slow, some species are difficult to culture |
| Enzymatic Assays | Detects specific mycoplasma enzymes (e.g., arginine deiminase) [5] | 1-2 days | Can be adapted for high-throughput | May be less sensitive than PCR or staining |
What are the most common sources of mycoplasma contamination in the lab? The primary sources are other contaminated cell cultures introduced into the laboratory, followed by laboratory personnel. Human-borne species like M. orale and M. fermentans can be introduced via poor aseptic technique [5]. While less common today, contaminated reagents like fetal bovine serum (source of M. arginini and A. laidlawii) or trypsin (source of M. hyorhinis) are also potential sources [5].
Table: Common Mycoplasma Species in Cell Culture and Their Sources
| Mycoplasma Species | Primary Source | Frequency in Cell Culture |
|---|---|---|
| Mycoplasma orale | Human oropharyngeal tract [5] | Very High |
| Mycoplasma fermentans | Human oropharyngeal tract [5] | High |
| Mycoplasma hyorhinis | Swine (via trypsin) [5] | Common |
| Mycoplasma arginini | Bovine serum [5] | Common |
| Acholeplasma laidlawii | Bovine serum [5] | Common |
My culture is contaminated. Can I eradicate mycoplasma, or must I discard the cells? Eradication is possible but should only be attempted for unique, irreplaceable cell lines due to the high risk of treatment failure and laboratory spread [5]. Standard practice is to discard contaminated cultures immediately [5]. If treatment is necessary, antibiotics like Plasmocin are added to the culture media for 1-2 weeks [4]. Following treatment, cells must be cultured antibiotic-free for 1-2 weeks and then rigorously re-tested to confirm eradication [4].
Troubleshooting Guides
Guide 1: Preventing Mycoplasma Contamination
Prevention is the most effective and economical strategy for managing mycoplasma.
- Adhere to Strict Aseptic Technique: Always wear proper personal protective equipment (PPE) and use a biosafety cabinet correctly. Spray all items with 70% ethanol before introducing them into the cabinet, and avoid cluttering the work surface [4] [6].
- Implement a Quarantine System: All new cell lines arriving in the lab should be cultured in a separate incubator until they test negative for mycoplasma [4].
- Establish a Routine Testing Schedule: Test all active cell cultures for mycoplasma on a regular basis (e.g., monthly) and with every new cell stock frozen down [4] [5].
- Avoid Routine Use of Antibiotics: Using antibiotics in standard culture media can mask low-level contamination, allowing it to spread undetected and promoting the development of resistant strains [6].
- Maintain a Clean Incubator: Adhere to a strict schedule for cleaning and disinfecting incubators and water baths, as these are common cross-contamination points [4].
Guide 2: Detecting Mycoplasma Contamination
When contamination is suspected or as part of routine screening, follow this workflow for reliable detection.
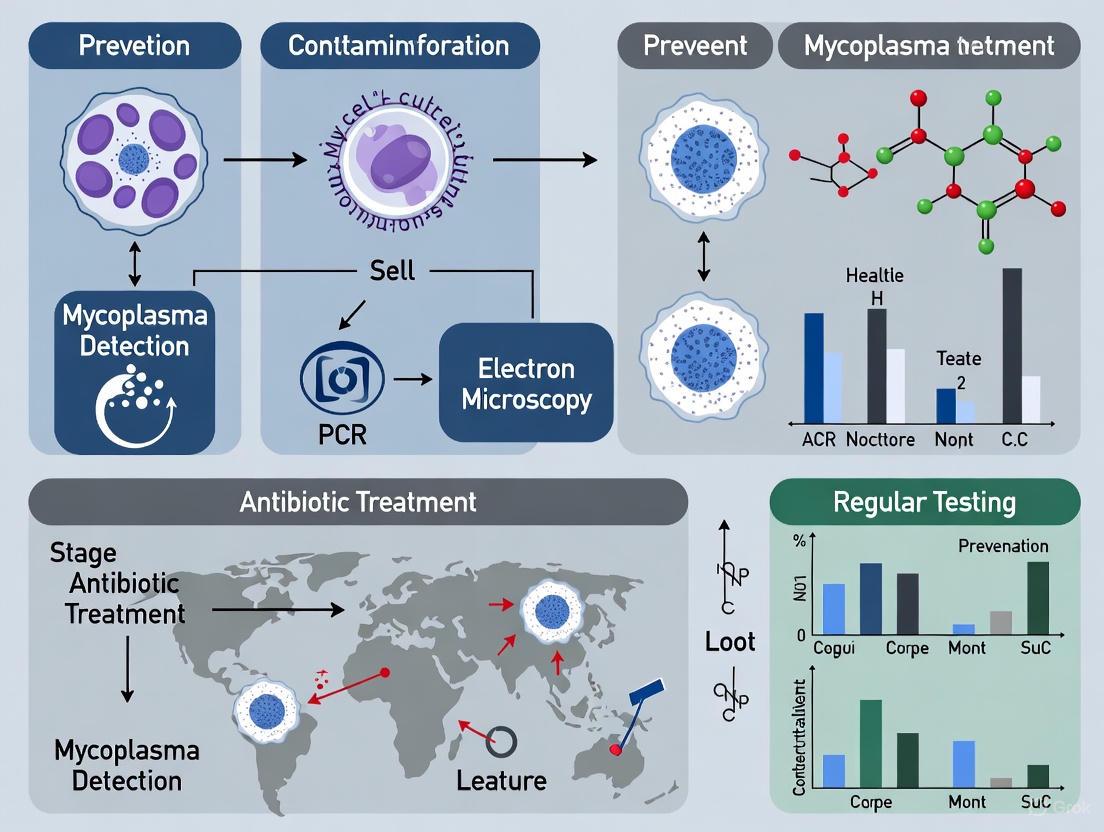
Diagram Title: Mycoplasma Detection Workflow
Experimental Protocol: DNA Staining for Mycoplasma Detection
This is a widely used, indirect method to visualize mycoplasma DNA adherent to host cells.
- Prepare Indicator Cells: Seed a sterile coverslip in a culture dish with an appropriate indicator cell line, such as Vero cells, and grow to 50-60% confluency.
- Inoculate with Test Sample: Add the sample to be tested (e.g., cell culture supernatant) to the indicator cells. Include a positive control (known mycoplasma-contaminated supernatant) and a negative control (known mycoplasma-free medium). Incubate for 3-5 days.
- Fix Cells: Aspirate the medium and wash the cells gently with phosphate-buffered saline (PBS). Fix the cells with a fresh mixture of acetic acid and methanol (1:3 ratio) for 10-15 minutes.
- Stain DNA: Prepare a DNA-binding fluorescent stain solution, such as Hoechst 33258 or DAPI, according to the manufacturer's instructions. Apply the stain to the fixed cells and incubate in the dark for 15-30 minutes.
- Mount and Visualize: Wash the coverslip with PBS to remove excess stain. Mount the coverslip on a microscope slide with a mounting medium. Examine the cells using a fluorescence microscope with the appropriate filter set.
- Interpret Results:
Guide 3: Eradicating Mycoplasma Contamination
This high-risk procedure should be performed in a dedicated quarantine space.
Experimental Protocol: Antibiotic Elimination of Mycoplasma
- Quarantine: Immediately move the contaminated culture to a separate, designated incubator and biosafety cabinet.
- Select an Antibiotic: Choose a proven anti-mycoplasma antibiotic, such as Plasmocin. Standard antibiotics like penicillin-streptomycin are ineffective [4].
- Treat Cells: Add the antibiotic to the culture medium at the recommended concentration (e.g., 25 μg/mL for Plasmocin). Culture the cells with the antibiotic for the prescribed duration, typically 1-2 weeks, with regular medium changes to maintain antibiotic activity [4].
- Passage without Antibiotics: After the treatment period, passage the cells into antibiotic-free medium and culture for a further 1-2 weeks. This "cure period" is crucial to ensure the bacteria are eliminated and not just suppressed.
- Validate Eradication: Test the cured cells for mycoplasma using at least two different methods (e.g., PCR and DNA staining) after the antibiotic-free period. If the tests are negative, the treatment was successful. If positive, consider a second, longer treatment cycle or discard the cells [4].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Mycoplasma Management
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Plasmocin | A specialized antibiotic mixture used to treat mycoplasma-contaminated cell lines [4]. | Ineffective against all species; resistance can develop; treatment can stress cells. |
| Hoechst 33258 / DAPI Stains | Fluorescent DNA dyes used in indirect detection methods to visualize mycoplasma DNA on indicator cells [6]. | Requires fluorescence microscopy and experience to interpret; can produce false positives. |
| Mycoplasma PCR Detection Kit | A commercially available kit for the highly sensitive and rapid detection of mycoplasma-specific DNA sequences [7]. | Does not confirm cell viability; can detect non-viable organism fragments. |
| 0.1 μm Pore Filter | Used for sterilizing solutions and media to physically remove mycoplasma [5] [6]. | Essential for filtering reagents; standard 0.22 μm filters are not sufficient. |
| Mycoplasma Experience Stock | A confirmed positive control culture used for validating detection assays and training personnel. | Must be handled with extreme caution in a quarantined area to prevent laboratory spread. |
Mycoplasma contamination represents one of the most significant yet stealthy challenges in cell culture laboratories. These bacteria, which lack a cell wall, are the smallest self-replicating organisms and can profoundly affect cell physiology and experimental outcomes without causing the obvious turbidity associated with common bacterial contaminants. For researchers in stem cell biology and drug development, where reproducibility and data accuracy are paramount, understanding and preventing mycoplasma contamination is not just good practice—it's essential for scientific integrity.
Prevalence and Resistance Patterns: The Quantitative Data
Mycoplasma contamination is widespread, affecting a substantial proportion of cell cultures globally. The tables below summarize key epidemiological and resistance data.
Table 1: Global Prevalence of Mycoplasma pneumoniae (MP) Infections and Resistance
| Location/Context | Prevalence/Resistance Rate | Key Findings | Source |
|---|---|---|---|
| Global Cell Cultures | 15-35% of continuous cultures [8] | Contamination rates can reach 65-80% in extreme cases; 8 species account for ~95% of contaminations. | |
| Southern Italy (Post-COVID) | 7.5% macrolide-resistant MP (MRMP) [9] | MRMP peaks at 12.6% in preadolescents (10-14 years); A2063G mutation predominates (96%). | |
| United States | <10% macrolide-resistant MP overall [10] | Higher resistance proportions (>20%) observed in the South and East, and within clusters. | |
| Europe | ~5% average macrolide-resistant MP [10] | Italy has a notably higher resistance rate, around 20%. | |
| Eastern China (Genital Mycoplasmas) | 43.74% infection rate in suspected cases [11] | High resistance to fluoroquinolones; Ureaplasma spp. most prevalent. |
Table 2: Impact of Mycoplasma Contamination on Cell Biology and Research
| Impact Area | Specific Consequences | Experimental Implications |
|---|---|---|
| Cell Physiology | Chromosomal aberrations; disruption of nucleic acid synthesis; changes in membrane antigenicity [8]. | Compromised genetic studies; unreliable cell surface marker analysis. |
| Cell Growth & Metabolism | Inhibition of cell proliferation and metabolism; competition for essential nutrients (e.g., arginine) [5] [12]. | Altered growth curves; inconsistent cell counts; erroneous metabolic assays. |
| Gene Expression & Epigenetics | Dysregulation of hundreds of host genes; alteration of chromatin accessibility (affects ATAC-seq) [12]. | Misleading transcriptomics and epigenomics data; incorrect conclusions about treatment effects. |
| Virus Production & Transfection | Affects virus production; decreased transfection rates [8]. | Failed or inconsistent production of viral vectors; poor genetic manipulation efficiency. |
Detection and Diagnosis: Methodologies and Protocols
Routine testing is the cornerstone of mycoplasma contamination control. The following are established detection methods used in laboratories.
DNA Fluorescence Staining Method
This indirect method is a standard for many labs.
- Principle: Uses fluorescent dyes like Hoechst 33258 that bind to the A-T rich regions of DNA. In contaminated cultures, fluorescent spots appear in the cytoplasm around the host cell nuclei, which is the mycoplasma DNA [8] [13].
- Protocol: Culture cells on a sterile cover slip for 48-72 hours. Fix the cells with Carnoy's fixative (acetic acid:methanol, 1:3) and stain with Hoechst dye for 30 minutes. Examine under a fluorescence microscope [8].
- Advantages & Limitations: Relatively rapid (a few hours) but requires an indicator cell line and can sometimes yield false positives from apoptotic bodies or cellular debris.
PCR-Based Detection
PCR is one of the most sensitive, specific, and rapid methods.
- Principle: Universal PCR primers target the conserved 16S rRNA gene in the mycoplasma genome, allowing for the detection of over 60 species [8] [13].
- Protocol:
- Sample Preparation: Incubate cell culture supernatant at 95°C for 5 minutes to inactivate nucleases [12].
- Amplification: Use specific primers (e.g., F: GGGAGCAAACAGGATTAGTATCCCT; R: TGCACCATCTGTCACTCTGTTAACCTC) in a touchdown PCR protocol to increase sensitivity [12] [8].
- Analysis: Run the PCR product on a 1.5% agarose gel. A positive result is indicated by a band of the expected size (e.g., ~500 bp) [12].
- Advantages & Limitations: Extremely sensitive and can provide results within 3-4 hours. However, it requires specialized equipment and can detect non-viable organisms.
Frequently Asked Questions (FAQs) for Researchers
Q1: Our lab routinely uses penicillin/streptomycin in all cell cultures. Are we protected from mycoplasma contamination? No. Mycoplasmas lack a cell wall, rendering penicillin completely ineffective. While streptomycin may inhibit some strains, mycoplasmas are generally resistant to the antibiotic mixtures commonly used in cell culture [8] [14]. Reliance on antibiotics can mask low-level bacterial contamination and provide a false sense of security, allowing mycoplasma to spread undetected.
Q2: We are setting up a new stem cell culture lab. What are the most critical steps to prevent mycoplasma contamination? For a new stem cell lab, the following are crucial [12] [8] [14]:
- Source Cells Wisely: Only acquire cell lines from reputable sources that provide certification of being mycoplasma-free.
- Quarantine: Isolate and test all new cell lines in a designated incubator before introducing them to your main culture space.
- Aseptic Technique: Mandate strict use of personal protective equipment (PPE), minimize talking in the hood, and avoid working with multiple cell lines simultaneously.
- Routine Screening: Implement a policy of routine mycoplasma testing for all active cultures every 2 weeks to 3 months.
Q3: I suspect my precious, irreplaceable stem cell line is contaminated. Can it be saved? While the most recommended action is to discard contaminated cultures to prevent spread, eradication is sometimes attempted for unique or invaluable lines. Treatments can include specific antibiotics (e.g., plasmocin), fluoroquinolones, or macrolides, but success is not guaranteed [5]. Any "cured" cell line must be rigorously re-tested and its behavior closely monitored, as the eradication process and original contamination can alter its characteristics [5] [12].
Q4: How does mycoplasma contamination specifically impact high-throughput sequencing data in stem cell research? Mycoplasma contamination has severe effects on sequencing data:
- RNA-seq: Can dysregulate host gene expression profiles, leading to false interpretations of differential gene expression [12].
- ATAC-seq: Mycoplasma DNA, being prokaryotic, is highly accessible and will be preferentially tagmented by the Tn5 transposase. This can overwhelmingly dominate your sequencing library, drastically reducing the mapping rate to the host genome and invalidating the experiment [12].
- Genomic DNA-seq: Contaminating mycoplasma DNA can lead to misassembly and false alignment during analysis [12].
Troubleshooting Guide: Common Experimental Issues
Table 3: Troubleshooting Common Problems Linked to Mycoplasma Contamination
| Problem | Potential Signs of Contamination | Recommended Actions |
|---|---|---|
| Poor Cell Growth | Cells require frequent medium changes; reduced proliferation rate despite high confluence [13]. | Test for mycoplasma; check nutrient competition; review culture conditions. |
| Unexplained Changes in Cell Morphology | Increased granularity; unhealthy appearance without clear cause. | Perform DNA staining or PCR; check for contaminants affecting physiology. |
| Inconsistent Experimental Results | High variability in assays between passages; failure to replicate previous data. | Initiate systematic mycoplasma screening; authenticate cell lines. |
| Low Transfection/Virus Production Efficiency | Consistently low yields or efficiency despite protocol optimization. | Test for mycoplasma; known to disrupt transfection and viral production [8]. |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Mycoplasma Prevention, Detection, and Eradication
| Reagent/Kit | Function | Specific Use Case |
|---|---|---|
| Hoechst 33258 Stain | DNA-binding fluorescent dye for indirect detection. | Staining fixed cells on coverslips to visualize extranuclear mycoplasma DNA via fluorescence microscopy [8]. |
| Mycoplasma Detection PCR Kits | Contains primers targeting 16S rRNA for sensitive molecular identification. | Routine screening of cell culture supernatants; fast results (3-4 hours) with high specificity [12] [8]. |
| Mycoplasma Growth Supplement | Enriches broth and agar media for growing fastidious mycoplasma. | Used for the direct culture method, which is considered the gold standard for detection [8]. |
| Antibiotic/Eradication Reagents (e.g., Plasmocin) | Formulations specifically targeting mycoplasma metabolism. | Attempting to rescue unique, contaminated cell lines; not recommended for general use [5]. |
| Zell Shield | A cocktail of antibiotics, antifungals, and antimycoplasmal agents. | Added to media to protect against a broad spectrum of contaminants, though not a substitute for good technique [12]. |
Best Practices for Prevention
Preventing mycoplasma contamination is far more effective than dealing with its consequences. Key strategies include [12] [8] [14]:
- Strict Aseptic Technique: Always wear PPE, use a certified laminar flow hood, and disinfect all surfaces and equipment.
- Quarantine New Cell Lines: Isolate and test all new arrivals before integrating them with your main cell stock.
- Avoid Antibiotic Overreliance: Do not use antibiotics as a crutch; they can mask contamination.
- Maintain Good Record Keeping: Track cell lineages, test results, and contamination incidents.
- Routine Screening: Test all active cultures every few weeks and always before freezing or publishing.
In stem cell culture, even minor microbiological contamination can compromise research integrity and pose serious risks for clinical applications. Mycoplasma contamination, a particularly prevalent and stealthy threat, underscores the critical importance of understanding contamination pathways. This guide details common contamination sources and provides actionable protocols to safeguard your stem cell research.
1. What are the most common sources of mycoplasma contamination in a stem cell lab?
Mycoplasma contamination primarily originates from five key sources, each requiring specific control measures [15]:
- Laboratory Personnel: Technicians are a major source of human-origin mycoplasma species (e.g., M. orale, M. fermentans), often introduced via poor aseptic technique [5].
- Contaminated Culture Reagents: While less common with reputable suppliers, raw materials like fetal bovine serum (a source of M. arginini and A. laidlawii) and trypsin (a source of M. hyorhinis) can be vectors [5].
- Contaminated Cell Lines: The introduction of new, untested cell lines from other labs is currently a major route of contamination spread [5].
- Nonsterile Laboratory Equipment: Pipettes, water baths, and other equipment can harbor contaminants if not properly sterilized [15].
- Environmental Contamination: Mycoplasma can persist in the cell culture room, incubator, or biosafety cabinet, leading to cross-contamination across multiple cell lines [15].
2. How does contamination from personnel actually spread?
Mycoplasma spreads readily via aerosols and surface contact. A model demonstrated that after trypsinizing an infected culture in a laminar flow hood, live mycoplasma were found on the technician, the hemocytometer, pipettor, and the hood surface. Contamination persisted on the hood surface for up to six days, and a clean culture processed in the same hood weeks later became infected. This shows how a single contaminated culture can rapidly compromise an entire laboratory's work [5].
3. What is the documented rate of contamination in stem cell cultures?
Microbiological control programs in stem cell banks provide clear data on contamination rates. One study analyzing 32 stem cell and feeder cell lines over 158 passages found that 12% of passages were contaminated. The breakdown of contaminants is shown in the table below [16]:
Table 1: Contamination Profile in Stem Cell Cultures
| Contaminant Type | Number of Contaminated Passages | Percentage of Total Contaminants |
|---|---|---|
| Gram-Positive Cocci | 10 | 53% |
| Mycoplasma species | 7 | 37% |
| Gram-Negative Rods | 3 | 16% |
| Gram-Positive Rods | 2 | 11% |
| Note: Three passages had co-contamination with two microorganisms. |
4. Why is mycoplasma considered a more serious problem than bacterial contamination?
Mycoplasma is particularly problematic due to its subtle nature. Unlike bacteria, which often cause turbidity in the medium, mycoplasma does not typically kill the host cells or change the medium's appearance. It lacks a cell wall, making it resistant to common antibiotics like penicillin and allowing it to pass through standard 0.22µm filters. With a size of only 0.1-0.3 µm, it is impossible to detect with a regular microscope. Mycoplasma infection can chronically alter cell metabolism, growth, and gene expression, leading to unreliable and erroneous experimental results without any obvious signs of trouble [17] [5].
5. What are the best methods for detecting mycoplasma contamination?
Several methods are available, with varying levels of expertise and time required. The following table summarizes the common detection methodologies [15] [5]:
Table 2: Mycoplasma Detection Methods
| Method | Principle | Notes |
|---|---|---|
| Culture-Based | Direct growth of mycoplasma on agar. | Considered the "gold standard" but can take weeks for results [15]. |
| DNA Staining (e.g., DAPI, Hoechst) | Fluorescent dyes bind to mycoplasma DNA attached to indicator cells, visible under a fluorescence microscope. | A common indirect method; requires an indicator cell line [17] [5]. |
| PCR and qPCR | Amplification of mycoplasma-specific DNA sequences. | Highly sensitive and fast; allows for specific identification of mycoplasma species [15]. |
| Enzymatic or Chemiluminescent Assays | Detection of an enzyme activity specific to mycoplasma. | Provides a robust and specific detection method [15]. |
The following workflow diagram outlines the strategic process for monitoring and responding to potential contamination:
Experimental Protocols for Prevention and Detection
Protocol 1: Routine Mycoplasma Detection via DNA Staining
This protocol uses fluorescent dyes to detect mycoplasma DNA adherent to host cells, a widely used and effective method [17].
Principle: DNA-binding dyes like DAPI or Hoechst stain both mammalian and mycoplasma DNA. Because mycoplasmas adhere to the cell surface and in the pericellular space, they appear as a characteristic particulate or filamentous staining pattern on the background of the larger host cell nuclei.
Materials:
- Indicator cells (e.g., Vero cells or the cells being tested) grown on a cover slip or in a chamber slide.
- DAPI (4',6-diamidino-2-phenylindole) or Hoechst stain solution.
- Phosphate-Buffered Saline (PBS), pH 7.4.
- Fixative solution (e.g., 3:1 Methanol:Acetic Acid or 4% Paraformaldehyde).
- Fluorescence microscope with appropriate filter sets.
Methodology:
- Cell Preparation: Grow indicator cells to about 50-70% confluency on a sterile cover slip placed in a culture dish. Alternatively, test the cells in question directly.
- Fixation: Aspirate the culture medium and wash the cells gently with PBS. Add the fixative solution and incubate for 15-30 minutes at room temperature.
- Staining: Aspirate the fixative, wash twice with PBS, and add the DAPI or Hoechst stain solution (diluted according to manufacturer's instructions). Incubate for 15-30 minutes in the dark.
- Washing and Mounting: Aspirate the stain and wash the cells thoroughly three times with PBS to remove unbound dye. If using a cover slip, mount it on a glass slide with a mounting medium.
- Microscopy: Observe the cells under a fluorescence microscope. A positive mycoplasma contamination is indicated by the presence of small, bright, particulate or filamentous staining in the intercellular spaces, in addition to the larger, well-defined nuclei of the host cells.
Protocol 2: Decontamination of Irreplaceable Cell Cultures
This protocol provides a stepwise procedure for attempting to salvage a valuable, contaminated cell line using antibiotics, noting that this is a last resort and carries risks of inducing resistance or cellular changes [18].
Principle: High doses of specific anti-mycoplasma antibiotics are applied to infected cultures for a limited time to eradicate the contaminant, followed by a rigorous validation period to confirm eradication.
Materials:
- Contaminated cell culture.
- Appropriate mycoplasma elimination reagent (e.g., antibiotic-based or non-antibiotic like membrane-active peptides) [15].
- Antibiotic-free culture medium.
- Multi-well culture plates or small flasks.
Methodology:
- Toxicity Test: Dissociate, count, and dilute the contaminated cells in antibiotic-free medium. Dispense the cell suspension into a multi-well plate. Add the elimination reagent to the wells in a range of concentrations. Observe the cells daily for signs of toxicity (e.g., sloughing, vacuolation, decreased confluency) over several days to determine the maximum non-toxic concentration [18].
- Treatment Phase: Culture the cells for 2-3 passages using the elimination reagent at a concentration one- to two-fold lower than the determined toxic level.
- Post-Treatment Validation: Culture the cells for one passage in antibiotic-free media. Then, culture the cells in antibiotic-free medium for 4-6 additional passages. At the end of this period, test the cells again for mycoplasma using a sensitive method (e.g., PCR) to confirm the contamination has been eliminated [18].
The Scientist's Toolkit: Key Reagent Solutions
The following reagents are essential for the effective prevention, detection, and elimination of mycoplasma in stem cell cultures.
Table 3: Essential Reagents for Mycoplasma Management
| Reagent / Kit | Function | Application Notes |
|---|---|---|
| Mycoplasma Elimination Reagents | To treat and eradicate mycoplasma from contaminated cultures. | Includes DNA synthesis inhibitors (e.g., fluoroquinolones), protein synthesis inhibitors (e.g., macrolides), and non-antibiotic membrane disruptors. Alternating or combining agents is advised to prevent resistance [15]. |
| PCR or qPCR Detection Kit | Sensitive and specific molecular detection of mycoplasma DNA. | Ideal for routine screening; provides rapid results. Kits often include primers for common mycoplasma species [15]. |
| DNA Fluorescent Stains (DAPI/Hoechst) | Histochemical staining for microscopic visualization of mycoplasma. | A standard indirect method; requires indicator cells and fluorescence microscopy. Can yield false positives from cellular debris [17] [15]. |
| Mycoplasma Culture Kits | Gold-standard method based on microbial growth. | Used for definitive confirmation. Requires a long incubation time (several weeks) but is highly reliable [15]. |
| Validated Mycoplasma-Free FBS | Critical culture supplement certified to be free of mycoplasma and other viruses. | Sourcing from reputable suppliers who provide certification is a fundamental preventive measure [5] [19]. |
Effective control of contamination in stem cell research requires a proactive, multi-layered strategy. This involves rigorous environmental monitoring, strict adherence to aseptic technique, careful sourcing and quarantine of new cell lines and reagents, and implementing a routine, reliable testing schedule for mycoplasma. By understanding the common sources and integrating these troubleshooting guides and protocols into your daily practice, you can significantly mitigate risk and protect the integrity of your research and potential clinical products.
Mycoplasma contamination represents one of the most significant yet frequently overlooked challenges in stem cell research. Unlike bacterial or fungal contaminants that produce obvious turbidity or pH changes, mycoplasma contamination is covert, potentially lingering for extended periods without noticeable cell damage [5]. This hidden nature makes it particularly dangerous, as contaminated cultures can produce published data that are irreproducible, wasting valuable research resources and time [20].
The particular vulnerability of stem cell cultures to mycoplasma contamination necessitates specialized vigilance. Stem cells, with their unique metabolic profiles and pluripotent capabilities, respond differently to mycoplasma infection compared to traditional cell lines. The contamination can alter their differentiation potential, compromise their genetic integrity, and ultimately invalidate experimental results [20] [21]. This guide provides comprehensive troubleshooting resources to help researchers identify, address, and prevent mycoplasma contamination within the critical context of stem cell research.
Frequently Asked Questions (FAQs)
Q1: What are the specific effects of mycoplasma contamination on stem cell metabolism and gene expression?
Mycoplasma contamination systematically compromises fundamental cellular functions in stem cells through multiple mechanisms:
- Nutrient Competition: Mycoplasmas compete with stem cells for essential nutrients in the culture medium, particularly amino acids and nucleic acid precursors, leading to hindered cell growth and proliferation [20].
- Metabolic Interference: Mycoplasmas expose stem cells to unwanted metabolites and alter levels of protein, RNA, and DNA synthesis [20]. This metabolic stress can manifest as slowed proliferation and premature cell death [22].
- Gene Expression Alterations: Contamination induces significant changes in gene expression patterns and cell signaling pathways, potentially affecting stem cell differentiation and pluripotency markers [20].
- Genomic Impact: Mycoplasma infection can cause mutations and chromosomal changes, directly threatening genomic integrity [20]. Research has shown that transcription processes themselves can be sources of DNA damage, including double-strand breaks, which mycoplasma contamination may exacerbate [23].
Q2: Why is mycoplasma contamination particularly problematic for stem cell research and drug development?
Mycoplasma contamination poses unique threats to stem cell research and therapeutic development:
- Compromised Cellular Identity: Contamination alters gene expression, cell signaling, and morphology, potentially changing a stem cell's fundamental identity and differentiation capacity [20]. This is particularly critical for stem cells used in regenerative medicine.
- Irreproducible Results: Experiments conducted with contaminated cells often cannot be replicated with clean cells, and vice versa, leading to false interpretations and invalid conclusions [20].
- Therapeutic Safety Risks: For stem cell-based therapies, mycoplasma contamination presents direct patient safety concerns through altered cellular function and potential product contamination [24] [5].
- Regulatory Challenges: In GMP manufacturing, contamination can lead to batch failures, costly production delays, and regulatory scrutiny [24].
Q3: What are the most reliable methods for detecting mycoplasma contamination in stem cell cultures?
Detection methods vary in sensitivity, time requirements, and regulatory acceptance. The table below summarizes the primary detection approaches:
Table 1: Mycoplasma Detection Methods Comparison
| Method | Principle | Time Required | Sensitivity | Suitable for Stem Cells |
|---|---|---|---|---|
| Direct Agar Culture | Growth on specialized agar plates | 3-5 weeks | High (Gold Standard) | Yes, for definitive confirmation [20] |
| PCR-Based Tests | DNA amplification of mycoplasma-specific sequences | Hours to 1 day | High | Yes, for rapid screening [25] [20] |
| Fluorescence Staining | DNA-binding dyes (e.g., Hoechst) visualize mycoplasma DNA | 1-2 days | Moderate | Yes, with proper controls [22] |
| Enzyme Immunoassays | Detection of mycoplasma-specific enzymes | Several hours | Moderate | Yes, for high-throughput screening [22] |
| Indicator Cell Culture | Culture on Vero cells with DAPI staining | 1-2 weeks | High | Yes, but time-consuming [5] |
For stem cell research, a combination of PCR-based screening for regular monitoring and agar culture for definitive confirmation provides optimal security [20] [26].
Q4: Our lab follows aseptic techniques, yet we still experience mycoplasma contamination. What are we missing?
Even with proper aseptic technique, several overlooked factors can introduce mycoplasma:
- Cross-Contamination in Shared Spaces: Working with multiple cell lines simultaneously in the same biosafety cabinet significantly increases contamination risk [25] [26]. Implement a "one cell line at a time" policy in the hood.
- Inadequate Incubator Maintenance: Water baths and incubator water pans are common contamination reservoirs—clean these regularly and use antimicrobial solutions like Aquaguard [20].
- Improper Hood Management: Storing equipment or materials in the biosafety cabinet can disrupt laminar airflow, compromising sterility [25].
- Antibiotic Misuse: Routine antibiotic use in stem cell culture can mask low-level contamination and promote antibiotic resistance [25] [26]. Reserve antibiotics for specific, justified applications.
- Human Carriers: An estimated 80.6% of laboratory technicians are mycoplasma carriers [20]. Proper personal protective equipment, including lab coats dedicated to mammalian cell culture and gloves, is essential.
Troubleshooting Guides
Mycoplasma Contamination: Detection Workflow
The following diagram outlines a systematic approach to detecting mycoplasma contamination in stem cell cultures:
Systematic Prevention Strategy
Implementing a robust prevention strategy requires addressing multiple potential contamination sources simultaneously:
Quantitative Impact of Mycoplasma Contamination
The table below summarizes the documented effects of mycoplasma contamination on cellular systems:
Table 2: Documented Effects of Mycoplasma Contamination on Cellular Systems
| Affected System | Specific Effects | Experimental Consequences |
|---|---|---|
| Cell Metabolism | Competition for nucleic acid precursors and amino acids [20] | Altered metabolic profiling, reduced ATP production |
| Gene Expression | Changes in expression of up to 5-10% of mammalian genes [20] | False conclusions in transcriptome studies |
| Genomic Integrity | Chromosomal aberrations and mutations [20]; interference with DNA damage repair pathways [23] | Compromised genetic stability in stem cell lines |
| Proliferation Rate | Reduction in growth rate by 30-50% [22] | Extended experiment timelines, skewed population dynamics |
| Cell Physiology | Membrane damage, organelle dysfunction [20] | Abnormal response to differentiation signals |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Mycoplasma Prevention and Detection in Stem Cell Research
| Reagent/Category | Specific Examples | Function in Mycoplasma Management |
|---|---|---|
| Detection Kits | EZ-PCR Mycoplasma Detection Kit [25]; Sartorius MycoSEQ PCR kits [26] | Regular screening and confirmation of contamination |
| Disinfectants | Pharmacidal Spray [20]; 70% ethanol; bleach solutions | Surface decontamination of work areas and equipment |
| Water Pan Additives | Aquaguard Solutions 1 & 2 [20] | Prevention of microbial growth in incubator water reservoirs |
| Antibiotics for Eradication | Fluoroquinolones; Macrolides; Tetracyclines [20] [26] | Elimination of mycoplasma from irreplaceable cell lines |
| Cell Culture Media Components | Quality-controlled FBS; Antibiotic-free media [5] | Reducing introduction and masking of contaminants |
| Personal Protective Equipment | Dedicated lab coats; sterile gloves; masks [25] | Prevention of human-derived contamination |
Vigilance against mycoplasma contamination is not merely a technical consideration but a fundamental ethical responsibility in stem cell research. The hidden toll on cell metabolism, gene expression, and genomic integrity can compromise years of research and potentially endanger future therapeutic applications. By implementing the systematic detection, prevention, and troubleshooting strategies outlined in this guide, researchers can protect their valuable stem cell lines, ensure the validity of their findings, and contribute to the advancement of reproducible, high-quality science.
Technical Support Center
Frequently Asked Questions (FAQs)
What are the most critical ISSCR recommendations for preventing cell culture contamination? The ISSCR emphasizes that researchers must demonstrate and document that cell lines are free of microbial contamination [27]. Key recommendations include handling stem cell cultures aseptically, ideally without antibiotics to avoid hidden contaminations, and conducting daily microscopic observation of cultures to monitor for signs of infection such as cell death, turbidity, and color changes in culture media [27]. Robust microbiological testing of Master Cell Banks (MCBs) is strongly advised.
My cell culture shows no visible contamination but has a reduced growth rate. Could it be mycoplasma? Yes. Unlike other contaminants, mycoplasma contamination does not typically cause turbidity and is too small to be seen with regular microscopy [5] [28]. A reduced rate of cell proliferation is one of the first visible signs, as mycoplasmas compete with your cells for nutrients [28]. Other indications can include cell aggregation, morphological changes, and a sudden drop in transfection efficiency [28]. Specific testing is required for confirmation.
Are we obligated to test for mycoplasma even if our cells look healthy? Absolutely. The ISSCR recommends regular mycoplasma testing as part of good cell culture practice [29]. Mycoplasma contamination can persist without noticeable cell damage but can alter almost every aspect of cell physiology, leading to unreliable and erroneous results [5] [30]. Establishing a routine testing protocol (e.g., via PCR) for all cultures is essential for research integrity [29].
According to ISSCR, what should we do with a contaminated cell line? The ISSCR's general recommendation is that contaminated cell lines should be discarded, barring exceptional circumstances [27]. While methods to eliminate mycoplasma contamination exist and can be considered for unique, irreplaceable cultures, the safest and most standard practice to protect your other cell lines and the validity of your research is to dispose of the contaminated culture properly [5] [27].
What are the ethical implications of using contaminated cells in research? Using contaminated cells violates the core ethical principles of research integrity and transparency upheld by the ISSCR [31]. Data generated from contaminated cells is not trustworthy, as mycoplasma can profoundly alter cell physiology and metabolism [5]. This can lead to the publication of false and irreproducible results, wasting scientific resources and potentially misleading future research and clinical efforts, which is a breach of ethical scientific practice [31] [21].
Troubleshooting Guides
Guide 1: Preventing Mycoplasma Contamination
Mycoplasma contamination is a serious problem in cell culture. The following diagram outlines the primary sources and pathways of contamination, which are critical to understand for effective prevention.
Workflow Overview: The diagram illustrates that contamination primarily originates from laboratory personnel, contaminated reagents, cross-contamination from infected cultures, and non-sterile supplies [5]. These sources introduce species like M. orale and M. arginini. The recommended prevention measures form a multi-layered defense to block these pathways [5] [29].
Detailed Prevention Protocols:
- Aseptic Technique: Maintain strict procedures and disinfect all surfaces with 70% ethanol/isopropanol. Avoid actions that can introduce contamination, such as talking or coughing near cultures [29].
- Quarantine New Cultures: Place all new cell sources in quarantine and perform quality control, including mycoplasma testing, before integrating them into your main laboratory workflow [29].
- Careful Reagent Handling: Use high-quality, well-screened reagents. Filter raw animal-derived sera and media with 0.1µm pore size filters, especially if sterility is dubious, as 0.2µm filters may not be sufficient under high pressure [5].
- Environmental Control: Keep the laboratory and laminar flow hoods clean and uncluttered. Regularly clean incubators and water baths [29].
- Antibiotic-Free Culture: Periodically culture cells for 2-3 weeks without antibiotics to reveal any hidden, low-level contaminations that antibiotics might be masking [29].
Guide 2: Detecting Mycoplasma Contamination
When contamination is suspected, a systematic approach to detection is required. The following workflow guides you through the process from observation to confirmation.
Workflow Overview: The detection process begins with observing subtle culture signs and proceeds to specific testing, as visual confirmation under a standard microscope is impossible [28]. A positive result typically leads to discarding the culture, with decontamination being a last resort for valuable lines [27].
Detailed Detection Methodologies: The ISSCR recommends robust testing and notes that different methods can be used [27]. The table below summarizes common techniques.
| Method | Principle | Duration | Key Advantage | Key Limitation |
|---|---|---|---|---|
| PCR [30] | Amplifies mycoplasma-specific DNA sequences | ~1 day | High sensitivity, rapid, easy to establish in lab [30] [27] | Does not distinguish between viable and dead organisms |
| Microbiological Culture [30] | Grows mycoplasma on agar or in broth | 3-4 weeks | The "gold standard" for direct detection [30] | Very slow, requires specific culture conditions |
| DNA Fluorochrome Staining [30] [28] | Stains DNA on indicator cells; mycoplasma appear as fluorescent foci | 1-2 days | Detects a broad range of species visually | Requires fluorescence microscope, may have lower sensitivity |
Table: Comparison of major mycoplasma detection methods. It is recommended that two techniques be used, selected from a PCR-based method, indirect staining, and agar/broth culture [30].
The Scientist's Toolkit
| Reagent / Material | Function in Prevention/Detection |
|---|---|
| 0.1µm Pore Filter | Sterilizing media and reagents; more effective at removing mycoplasma than standard 0.2µm filters [5]. |
| PCR Mycoplasma Test Kit | A rapid and sensitive method for routine screening of cell cultures for mycoplasma DNA [30] [29]. |
| DNA Staining Kit (e.g., Hoechst) | A fluorescent dye used in indirect staining methods to detect mycoplasma DNA on indicator cells [30]. |
| Mycoplasma Culture Media | Specialized agar and broth for the cultivation and direct detection of mycoplasma contaminants [30]. |
| 70% Ethanol/Isopropanol | A standard disinfectant for sterilizing surfaces, laminar flow hoods, and equipment to maintain an aseptic environment [29]. |
| Antibiotic-Free Medium | Used for routine culture to prevent the masking of low-level bacterial or mycoplasma contaminations [27] [29]. |
Navigating ISSCR Guidelines and Ethics
The ISSCR Guidelines stress that the primary mission of biomedical research is to alleviate human suffering, and this collective effort depends on public trust and rigorous ethical standards [31]. Contamination control is not just a technical issue but an ethical imperative directly tied to the core principles of:
- Integrity of the Research Enterprise: Ensuring that information obtained from research is trustworthy and reliable [31]. Data from contaminated cells is not, rendering subsequent experiments worthless [30].
- Transparency: Researchers are expected to share data and methods and communicate the state of the art, including uncertainties [31]. This includes being transparent about the quality control measures, like mycoplasma testing, applied to cell lines.
- Social Justice: Wasting resources on flawed research due to contamination diverts funds and effort from addressing unmet medical needs [31].
Furthermore, the ISSCR's clinical translation guidelines mandate that stem cell-based interventions must be processed with scrupulous oversight to ensure integrity, function, and safety before patient use [32]. Using a contaminated cell line in the development of a therapy introduces an unacceptable risk of pathogen transmission and invalidates preclinical safety data, constituting a serious breach of patient welfare [31] [32]. Adherence to these guidelines is fundamental to conducting scientifically sound and ethically responsible stem cell research.
Detection and Defense: Implementing Robust Mycoplasma Screening and Aseptic Protocols
Mycoplasma contamination represents a pervasive and serious threat to the integrity of stem cell research and the safety of resulting cellular therapies. These cell-wall-less bacteria can profoundly alter cell physiology and metabolism without causing visible turbidity in culture media, often going undetected for extended periods [5]. For stem cell lines, which are frequently cultured over long durations and exchanged between laboratories, the risk is particularly acute [14]. Compendial culture methods outlined in United States Pharmacopeia (USP) <63>, European Pharmacopoeia (Ph. Eur.) 2.6.7, and Japanese Pharmacopeia (JP) remain the regulatory gold standard for mycoplasma testing, providing the most comprehensive detection system despite the emergence of faster molecular alternatives [33] [34]. This guide details the implementation, troubleshooting, and contextual application of these mandated methods within a stem cell research environment.
Understanding the Compendial Framework: USP <63> and Ph. Eur. 2.6.7
What are the core principles of the compendial culture method?
The compendial culture method is a dual-phase enrichment and detection system designed to support the growth of a wide spectrum of fastidious Mollicutes. Its core principle is to provide both liquid and solid culture media that are exceptionally enriched with nutrients and growth factors to accommodate mycoplasmas' auxotrophic nature [33]. The method requires a substantial sample volume (typically ~15 mL) and an extended incubation period of 28 days to allow slow-growing contaminants to reach detectable levels [33] [34]. This prolonged incubation is necessary because mycoplasmas lack many biosynthetic pathways and are therefore fastidious, requiring complex media and extended incubation times [33].
Which mycoplasma species are targeted by these standards?
The pharmacopeias specify a panel of reference organisms that must be detected for a method to be considered valid. These organisms were selected based on their relevance as cell culture contaminants, their origin (human, bovine, or swine), and their clinical significance. The table below summarizes key indicator organisms.
Table 1: Key Mycoplasma Reference Strains in Compendial Testing
| Organism | Relevance in Pharmacopeia | Reported as Cell Culture Contaminant | Typical Source |
|---|---|---|---|
| Acholeplasma laidlawii | USP <63>, Ph. Eur. 2.6.7, JP XVIII [33] | Yes [33] [5] | Fetal Bovine Serum [5] |
| Mycoplasma fermentans | USP <63>, Ph. Eur. 2.6.7 [33] | Yes [33] | Laboratory Personnel [5] |
| Mycoplasma orale | USP <63>, Ph. Eur. 2.6.7, JP XVIII [33] | Yes [33] [5] | Laboratory Personnel (Human Oropharyngeal) [5] |
| Mycoplasma pneumoniae | USP <63>, Ph. Eur. 2.6.7, JP XVIII [33] | No [33] | Vaccines/Cell Banks for Human Use [33] |
| Mycoplasma hyorhinis | USP <63>, Ph. Eur. 2.6.7, JP XVIII [33] | Yes [33] [5] | Trypsin Solutions of Porcine Origin [5] |
It is important to note that some species, like Spiroplasma citri (or a genetically similar substitute), are also included to account for contaminants that may originate from insect or plant material used during production processes [33].
The Experimental Protocol: A Step-by-Step Workflow
The following diagram and protocol outline the standard compendial culture method as per USP <63> and Ph. Eur. 2.6.7.
Figure 1: Workflow of the compendial mycoplasma testing method as per USP <63> and Ph. Eur. 2.6.7, combining both broth/agar culture and indicator cell culture methods.
Detailed Methodology
- Sample Preparation: Aseptically collect at least 15 mL of the test cell culture supernatant [33]. The sample should be taken from a culture that has not received antibiotics for at least a week to avoid suppressing low-level contamination.
- Broth Inoculation and Incubation: Inoculate the sample into specialized, enriched broth media (e.g., Hayflick's broth or SP4 medium). The choice of medium may need to be optimized for certain fastidious species [33].
- Agar Subculture and Examination: On days 3, 7, and 14 of incubation, subculture a portion of the broth onto solid agar plates [33] [35].
- Wrap plates in parafilm to prevent drying and incubate under the same conditions as the broth [33].
- Periodically examine the agar plates under a dissection microscope (at up to 20x magnification) for the appearance of characteristic "fried egg" colonies, which result from central growth into the agar and superficial surface growth [34].
- Indicator Cell Culture Method (Parallel Test): As not all mycoplasma strains grow in artificial media, a parallel test is run. Inoculate a sample of the test material onto indicator cells (typically Vero cells) and culture for 3-5 days [34] [35]. The cells are then fixed and stained with a DNA-binding fluorochrome like Hoechst 33258 or DAPI. Under a fluorescence microscope, a mycoplasma-positive sample will show fluorescent staining not just in the cell nuclei, but also as a particulate or filamentous pattern on the cell surface due to the adhered mycoplasmas [34] [35].
A final negative result is only reported after a full 28-day incubation with no growth observed on agar plates and a negative indicator cell culture result [34] [35].
Troubleshooting Common Issues in Compendial Testing
What are the major limitations, and how can we address them?
The primary challenge of the compendial method is its 28-day duration, which is incompatible with biological products that have a short shelf-life, such as many cell therapy products (e.g., 48-72 hours) [33]. Furthermore, the method is technically demanding, labor-intensive, and requires a large sample volume [34] [36]. The following table outlines common problems and solutions.
Table 2: Troubleshooting Guide for Compendial Culture Methods
| Problem | Potential Cause | Solution & Prevention |
|---|---|---|
| No growth of positive control strains. | Improper media preparation, incorrect incubation conditions (temperature, CO₂), or excessive passaging of reference strains. | Use freshly prepared, validated media batches. Verify incubator settings. Keep reference strain passages below 15 from the original stock as per USP <63> [33]. |
| Contaminated test articles (other bacteria/fungi). | Non-sterile sample or technique. Overgrowth of contaminants can mask mycoplasma growth. | Ensure aseptic sampling technique. For non-sterile products, consider filtration or specific inactivating agents as described in the pharmacopeia. |
| Inconsistent results between tests. | Low-level or intermittent contamination, sample not representative, or technique variability. | Increase sample volume as per guidelines. Test cultures that are in the log phase of growth and have not been recently treated with antibiotics. Standardize protocols and analyst training. |
| Method is too slow for product release. | Inherent 28-day incubation period. | For short-shelf-life products, implement a validated, rapid molecular method (e.g., PCR) for product release, while using the compendial method for parallel validation and environmental monitoring [33] [34]. |
Comparison with Alternative Detection Methods
While the culture method is the gold standard, several other techniques are used, especially in time-sensitive R&D settings. The European and Japanese pharmacopeias accept validated molecular methods with a limit of detection of ≤10 CFU/mL as an alternative to culture [33]. The table below compares the primary methods.
Table 3: Comparison of Mycoplasma Detection Methods
| Method | Principle | Approx. Time | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Compendial Culture [33] [34] | Growth in enriched broth/agar. | 28 days | Regarded as the gold standard; can detect viable organisms; high sensitivity when fully executed. | Very long turnaround time; labor-intensive; cannot detect non-cultivable species without indicator cell method. |
| DNA Staining [35] [28] | Staining with fluorescent DNA dyes (e.g., Hoechst). | 1-2 days | Rapid and relatively simple. | Low sensitivity; requires high level of contamination (~10⁶ CFU/mL); subjective interpretation; requires indicator cells. |
| PCR-Based Methods [33] [34] [35] | Amplification of conserved 16S rRNA gene sequences. | 2-5 hours | Very fast, highly sensitive, can detect a broad spectrum of species. Ideal for screening and short-shelf-life products [33]. | May detect non-viable DNA; requires rigorous validation to avoid false positives/negatives; considered an alternative method in the US [33]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) [36] | Detection of specific mycoplasma antigens. | 4-6 hours | Easy to perform, reproducible, and easily interpreted [36]. | Lower specificity and sensitivity compared to PCR and culture methods. |
The Scientist's Toolkit: Essential Reagents for Compendial Testing
Table 4: Key Research Reagent Solutions for Compendial Culture Methods
| Reagent/Item | Function | Example & Notes |
|---|---|---|
| Enriched Broth Media | Supports the growth and metabolism of fastidious mycoplasma in liquid culture. | Hayflick's broth, SP4 broth [33]. The choice depends on the target species; SP4 is often used for more fastidious strains. |
| Enriched Solid Agar | Allows for the formation of characteristic mycoplasma colonies for visual identification. | Hayflick's agar, SP4 agar [33]. Must be sealed to prevent drying during long incubation. |
| Indicator Cell Line | Host cells for the detection of mycoplasma that do not grow in artificial culture media. | Vero cells (a mammalian cell line) [34]. |
| DNA Fluorochrome Stain | Binds to DNA, allowing visualization of mycoplasma adhered to indicator cells under fluorescence microscopy. | Hoechst 33258 or DAPI [34] [35]. |
| Reference Strains | Positive controls to validate that the media and methods are functioning correctly. | ATCC strains (e.g., M. pneumoniae ATCC 15531, A. laidlawii ATCC 23206) [33]. |
Frequently Asked Questions (FAQs)
Q1: Our stem cell therapies have a shelf-life of 48 hours. Is a 28-day test relevant?
This is a critical industry challenge. While the 28-day test is the regulatory ideal, it is impractical for product release. The current strategy is to use a rigorously validated, rapid method (like a validated PCR assay) for product release, while the compendial method is used for qualifying the manufacturing process, testing master cell banks, and ongoing system suitability [33]. The European Pharmacopoeia is currently being revised to better reflect this practice and the state of current technology [37].
Q2: Why is the sample volume requirement so large (~15 mL)?
The large volume is necessary to ensure a representative sample and to detect a low-level contamination. Mycoplasma contamination can be present at very low concentrations, and a large sample volume increases the probability of capturing the organism for detection, especially given the potential for uneven distribution in the culture [33].
Q3: Can we rely solely on PCR for our stem cell research?
For definitive product release in regulated environments, a validated PCR method may be acceptable as an alternative, but it requires extensive comparative validation against the compendial method to demonstrate equivalence as per USP <1223> [33]. For basic research, PCR is an excellent, highly sensitive tool for routine screening. However, it is crucial to remember that PCR detects DNA, not necessarily viability. A positive PCR result could be from dead organisms, while a culture-based method confirms the presence of viable, replicating mycoplasma.
Q4: What are the best practices for preventing mycoplasma contamination in a stem cell lab?
Prevention is paramount. Key tips include [14]:
- Routine Screening: Test all cells regularly, including all new cell lines entering the lab.
- Aseptic Technique: Use proper sterile technique, work with one cell line at a time, and keep all containers covered.
- Lab Hygiene: Sterilize work surfaces and equipment meticulously and regularly clean water baths and incubators.
- Antibiotic Responsibility: Avoid the routine use of antibiotics, as they can mask low-level bacterial contamination and are ineffective against mycoplasma, potentially leading to persistent, hidden infections [14].
- Good Record Keeping: Maintain thorough records of cell sources, test results, and contamination incidents for traceability.
Troubleshooting Guide: Common qPCR Issues in Mycoplasma Testing
This guide addresses specific qPCR issues you might encounter when testing for mycoplasma contamination in stem cell cultures, providing targeted solutions to ensure assay reliability.
Table 1: Common qPCR Abnormalities and Corrective Actions
| Problem Observed | Possible Causes | Recommended Solutions |
|---|---|---|
| Amplification in No Template Control (NTC) | Contamination from sample splashing, reagent contamination, or primer-dimer formation [38] [39]. | Clean work area and pipettes with 10% bleach or 70% ethanol; prepare fresh primer dilutions; spatially separate NTC wells on the plate; include a melt curve to detect primer-dimer [38] [39]. |
| Ct Values Too Early | Genomic DNA contamination in RNA samples, highly expressed transcript, or sample evaporation increasing concentration [38] [39]. | DNase treat samples prior to reverse transcription; ensure primers span an exon-exon junction; dilute template to an ideal Ct range [38] [39]. |
| Poor Replicate Reproducibility | Pipetting error, insufficient mixing of reaction solutions, or low copy number of the target [38] [40] [39]. | Calibrate pipettes; mix all solutions thoroughly; perform technical replicates; use positive-displacement pipettes and filtered tips [40] [39]. |
| Abnormal Melt Curve (Multiple Peaks) | Primer-dimer formation (if Tm <80°C) or non-specific amplification/gDNA contamination (if Tm >80°C) [40]. | Optimize primers and increase annealing temperature; Blast-check primer specificity; use a no-reverse-transcriptase control (NAC) to check for gDNA [40] [41]. |
| Low Amplification Efficiency (Slope > -3.1 or < -3.6) | Presence of PCR inhibitors, inaccurate dilutions for standard curve, or suboptimal primer design [38] [39] [41]. | Dilute template to reduce inhibitors; prepare standard curve fresh and accurately; redesign primers using specialized software [38] [41]. |
| No Amplification | Failed reverse transcription, reaction inhibitors, or incorrect instrument settings [42] [39]. | Check RNA quality and cDNA synthesis; verify correct dye and well selection in instrument software; run a positive control [42] [39]. |
| High Background Noise or Jagged Curves | Probe degradation, bubbles in the reaction well, or unstable fluorescence due to system inhibitors [40] [39]. | Ensure sufficient probe concentration; centrifuge plates to remove bubbles; improve template purity; calibrate the instrument [40] [39]. |
Frequently Asked Questions (FAQs)
Q1: My No Template Control (NTC) is showing amplification. What does this mean and how can I resolve it? Amplification in your NTC indicates contamination of your reaction reagents or primer-dimer formation. This is a critical issue for mycoplasma testing as it can lead to false positives. To resolve it, decontaminate your work surface and pipettes with 10% bleach or 70% ethanol [39]. Prepare fresh primer and probe dilutions, and ensure you are using nuclease-free water [38]. When setting up your plate, position the NTC wells away from any sample wells to prevent splashing or aerosol contamination [38]. Finally, run a dissociation curve; a peak at a lower melting temperature (Tm) than your target amplicon typically indicates primer-dimer [40].
Q2: How can I prevent genomic DNA from causing false positives in my mycoplasma qPCR assay? Genomic DNA (gDNA) contamination is a common pitfall. The most effective strategy is to use primers that are designed to span an exon-exon junction, which will not efficiently amplify gDNA [38] [41]. Furthermore, you should always treat your RNA samples with DNase I prior to the reverse transcription step [38]. It is also crucial to include a mandatory "No Amplification Control" (NAC) or "No Reverse Transcriptase Control" (-RT control) in every experiment. This control contains all reaction components except the reverse transcriptase. Amplification in this control signals the presence of contaminating DNA [41].
Q3: My amplification curves for mycoplasma standards are inconsistent, with poor reproducibility between replicates. What should I check? Poor replicate reproducibility is often related to pipetting technique and reaction homogeneity. First, check the calibration of your micropipettes, as small volumetric errors can significantly impact qPCR results [38] [43]. Ensure all reaction components are mixed thoroughly but gently before plate loading [39]. For low-concentration targets, which can exhibit stochastic amplification, it is advisable to increase the number of technical replicates [40]. Using an automated liquid handler can dramatically improve precision and consistency by eliminating manual pipetting error [43].
Q4: My qPCR assay has low efficiency. How does this affect mycoplasma quantification, and how can I improve it? A qPCR reaction with low efficiency (slope > -3.1) will not double the product each cycle, leading to an underestimation of the target quantity and inaccurate quantification of mycoplasma load [41]. To improve efficiency, first verify the purity of your template, as PCR inhibitors from the cell culture medium can be carried over [38] [39]. Check your primer design for specificity and secondary structures, and consider optimizing their concentration [39] [41]. Finally, ensure that your standard curve is prepared from fresh, serial dilutions, as stored samples can evaporate and alter concentrations [38].
Experimental Workflow: qPCR for Mycoplasma Detection
The following diagram illustrates the core workflow for detecting mycoplasma in stem cell cultures using qPCR, from sample preparation to data interpretation.
Research Reagent Solutions for Mycoplasma qPCR
Table 2: Essential Reagents for qPCR-Based Mycoplasma Detection
| Item | Function in the Experiment | Key Considerations |
|---|---|---|
| SYBR Green qPCR Master Mix | Fluorescent dye that binds double-stranded DNA, enabling real-time detection of amplified mycoplasma DNA [40]. | Check for compatibility with your qPCR instrument and the inclusion of a reference dye like ROX for well-to-well normalization [40] [41]. |
| Mycoplasma-Specific Primers | Oligonucleotides designed to anneal to a conserved, specific region of the mycoplasma genome [41]. | Specificity is critical. Validate primers with BLAST; design to generate a short amplicon (100-150 bp) for high efficiency [40] [39]. |
| No Template Control (NTC) | Critical control containing nuclease-free water instead of template to detect reagent or environmental contamination [39] [41]. | Must be included in every run. Any amplification in the NTC invalidates the experiment and necessitates decontamination [38]. |
| Positive Amplification Control (PAC) | A sample with known, low-level mycoplasma DNA to verify the assay is functioning with the expected sensitivity [39]. | Confirms that the entire qPCR system (reagents, thermal cycling, detection) is working correctly. |
| DNase I | Enzyme that degrades contaminating genomic DNA from host stem cells during RNA preparation [38]. | Essential for preventing false positives. Use prior to the reverse transcription step if detecting RNA, or as part of the DNA extraction for DNA-based tests. |
| Automated Liquid Handler | Precision instrument for dispensing small-volume reagents to minimize pipetting error and improve reproducibility [43]. | Highly recommended for high-throughput testing. Reduces human error and cross-contamination risk [43]. |
For researchers, scientists, and drug development professionals working with stem cells, the threat of contamination represents a significant risk to data integrity, experimental reproducibility, and patient safety in regenerative medicine. Mycoplasma contamination, in particular, is a pervasive and stealthy threat that can alter cell metabolism and gene expression without visible signs, potentially compromising years of research. This technical support center provides a comprehensive framework of aseptic techniques, troubleshooting guides, and frequently asked questions designed to fortify your laboratory's defense against contamination, with a specific focus on safeguarding precious stem cell cultures.
#1 Foundational Principles of Aseptic Technique
Aseptic technique is a set of procedures designed to create a barrier between microorganisms in the environment and your sterile cell culture. It is fundamentally different from sterilization, though the two concepts are complementary. Sterilization is a process that destroys or eliminates all forms of microbial life, creating an absolute state of being free from microorganisms. Aseptic technique, conversely, refers to the practices and procedures performed under controlled conditions to prevent contamination from microorganisms, thereby maintaining that sterile state [44] [45].
The core elements of aseptic technique are:
- A Sterile Work Area: Typically a biosafety cabinet (BSC) or laminar flow hood.
- Good Personal Hygiene: Including proper use of personal protective equipment (PPE).
- Sterile Reagents and Media: Ensuring all solutions and media are sterilized and properly handled.
- Sterile Handling: Manipulating cultures without introducing contaminants [44].
#2 The Scientist's Toolkit: Essential Materials and Reagents
The following table details key reagents and materials essential for maintaining sterile stem cell cultures and addressing contamination issues.
| Item Name | Function/Application | Key Considerations |
|---|---|---|
| 70% Ethanol | Surface disinfection for biosafety cabinets, gloves, and reagent bottles [44] [45]. | Effective concentration for microbial kill; allows for sufficient contact time. |
| ROCK Inhibitor (Y-27632) | Improves survival of human pluripotent stem cells (hPSCs) after passaging or thawing [46] [47]. | Use at recommended concentrations; typically included for 18-24 hours post-dissociation. |
| Gentle Cell Dissociation Reagent | Passages hPSCs into small, evenly-sized aggregates ideal for subsequent growth [47]. | Incubation time is cell line-dependent; avoid over-pipetting to prevent overly small clumps. |
| Mycoplasma Elimination Reagents (e.g., Mynox) | Rescues contaminated cultures by selectively disrupting mycoplasma membranes [48]. | Treatment can affect eukaryotic cells; goal is to rescue a subset of healthy cells for culture restart. |
| Validated Extracellular Matrices (e.g., Geltrex, Vitronectin) | Provides a defined, feeder-free substrate for hPSC attachment and growth [46] [47]. | Ensure correct plate coating (TC-treated vs. non-TC treated) per manufacturer's instructions. |
| B-27 Supplement | Serum-free supplement used in neural differentiation and other culture media [46]. | Check expiration; prepare fresh medium frequently; avoid repeated thawing/freezing of supplement. |
#3 Troubleshooting Common Stem Cell Culture Issues
This section addresses specific problems encountered during human pluripotent stem cell (hPSC) culture.
Problem: Excessive Differentiation (>20%) in hPSC Cultures
- Ensure Medium Freshness: Use complete cell culture medium that is less than two weeks old when stored at 2-8°C [47].
- Remove Differentiated Areas: Manually scrape or pick off differentiated regions from colonies prior to passaging [47].
- Optimize Handling Time: Minimize the time culture plates are outside the incubator to less than 15 minutes at a time [47].
- Control Colony Density: Passage cultures when colonies are large and compact but before they overgrow. Plate fewer cell aggregates during passaging to decrease density [47].
- Check Passaging Parameters: For sensitive cell lines, reduce incubation time with passaging reagents like ReLeSR [47].
Problem: Low Cell Attachment After Passaging or Thawing
- Increase Seeding Density: Plate 2 to 3 times the normal number of cell aggregates initially to maintain a denser culture [47].
- Work Quickly: Minimize the time cell aggregates are in suspension after treatment with passaging reagents [47].
- Optimize Aggregate Size: Do not over-pipette to break up clumps. If aggregates are too large, slightly increase incubation time with the dissociation reagent by 1-2 minutes [47].
- Verify Coating and Plates: Use non-tissue culture-treated plates with Vitronectin XF and tissue culture-treated plates with Matrigel [47].
Problem: Suspected Microbial Contamination
The flowchart below outlines the logical decision-making process for identifying and addressing a contaminated culture.
Problem: Cell Aggregate Size After Passaging is Not Ideal
- If Aggregates Are Too Large (>200 µm): Gently pipette the mixture up and down (without creating single cells) and consider increasing incubation time with the passaging reagent by 1-2 minutes [47].
- If Aggregates Are Too Small (<50 µm): Minimize manipulation and pipetting of aggregates after dissociation and decrease the incubation time with the passaging reagent by 1-2 minutes [47].
#4 Aseptic Technique Checklist and Best Practices
A disciplined, zero-tolerance approach is the best defense against contamination. Adhere to the following protocols to maintain a sterile environment [44] [49].
Personal Hygiene and Preparation
- Wash Hands: Thoroughly with antiseptic soap and warm water before and after handling cultures [44] [50].
- Wear Appropriate PPE: Always wear a clean lab coat, sterile gloves, and safety glasses. Tie back long hair [44] [45] [49].
- Dedicated Lab Coats: Use separate lab coats for the cell culture room and other laboratory areas [49].
Workspace Management
- Biosafety Cabinet (BSC) Setup: Turn on the BSC for at least 15 minutes prior to use. Wipe all interior surfaces with 70% ethanol before and after work. Keep the work surface uncluttered [44] [45].
- Create a Sterile Field: Work in an area free from drafts, doors, and through traffic. When using a Bunsen burner (not inside a BSC), work within the sterile updraft of the flame [44] [50].
- Organize Materials Strategically: Arrange all necessary items in the BSC before starting. Place plates to your left, bottles/flasks in the center, and the Bunsen burner (if used) to your right [50].
Sterile Handling Procedures
- Disinfect Everything: Wipe gloved hands, the outside of all bottles, flasks, and equipment with 70% ethanol before introducing them to the work area [44] [45].
- Flame Bottle Necks: Briefly pass the necks of glass bottles and flasks through a Bunsen burner flame to create an upward convection current that prevents airborne contaminants from entering [50] [45].
- Cap Management: When setting a cap down, place it with the opening facing down on the sterile work surface. Never leave sterile containers uncovered [44].
- Pipetting Precautions: Use sterile pipettes and a pipettor for all liquids. Use each pipette only once to avoid cross-contamination. Never let the pipette tip touch anything non-sterile [44].
- Work Efficiently: Perform experiments as rapidly as possible to minimize exposure of sterile materials to the open environment [44].
#5 Mycoplasma Focus: Prevention, Detection, and Elimination
Mycoplasma contamination is a critical concern, as these bacteria are invisible under routine microscopy and are primarily spread from one culture to another by laboratory personnel [26].
Prevention and Detection Strategies
- Regular Testing: Implement a routine testing schedule using PCR-based methods, fluorescence staining, or culture on agar plates. PCR offers the fastest results [24] [26].
- Avoid Prophylactic Antibiotics: Do not use antibiotics in routine culture maintenance, as this can mask low-level contamination and lead to antibiotic resistance [26].
- Work on One Cell Line at a Time: This golden rule minimizes the risk of cross-contamination between cultures [26].
- Use Dedicated Media: Have separate media bottles for each cell line [26].
Mycoplasma Elimination Workflow
For irreplaceable, contaminated cell lines, a dedicated decontamination protocol can be attempted. The workflow below outlines the key steps for this rescue process.
#6 Frequently Asked Questions (FAQs)
Q1: What is the most critical step of aseptic technique for cell culture? While all steps are important, the most critical element is the consistent and correct use of the biosafety cabinet, coupled with the meticulous disinfection of all surfaces and materials with 70% ethanol before starting work. This establishes the foundational sterile field for all subsequent manipulations [45].
Q2: My culture medium is cloudy. What does this mean? Cloudy or turbid media is a classic sign of bacterial contamination. You may also see a rapid shift in pH (color change in phenol red) or, under a microscope, tiny floating particles. Immediately quarantine and dispose of the contaminated culture following biosafety guidelines [24] [45].
Q3: Is it necessary to flame the neck of bottles during aseptic procedures? Yes, when working at an open bench with a Bunsen burner, flaming the neck of a sterile bottle or flask is a crucial step. The heat creates an upward convection current of sterile air, which prevents airborne microorganisms from falling into the container while it is open [45].
Q4: How can I prevent cross-contamination between my cell lines? Always work on one cell line at a time in the biosafety cabinet. Use dedicated media and reagents for each cell line whenever possible, and always change pipette tips between handling different cultures. Proper labeling and spatial separation of materials in the BSC are also essential [24] [26].
Q5: Why is mycoplasma contamination so problematic? Mycoplasmas are problematic because they are very small and lack a cell wall, making them invisible under standard light microscopy and resistant to some common antibiotics. They do not cause visible turbidity in the medium but can subtly alter cell metabolism, growth, and gene expression, leading to unreliable and irreproducible experimental data [24] [26] [48].
Q6: My pluripotent stem cells are not attaching well after passaging. What should I check? First, ensure you are using the correct extracellular matrix and the right type of culture plate. Second, optimize your passaging technique to generate cell aggregates of an ideal size (not too large or small). Third, consider plating at a higher density and using a ROCK inhibitor to improve cell survival and attachment post-dissociation [46] [47].
Contamination poses a significant risk to stem cell research and therapy development. Mycoplasma species, in particular, represent a prevalent and challenging form of microbial contamination in cell cultures. Traditional detection methods like PCR and culture-based techniques present limitations, including cross-reactivity issues and lengthy turnaround times. This technical support center guide explores the application of Next-Generation Sequencing (NGS) and broad-spectrum assays for advanced monitoring and troubleshooting of contamination in stem cell research.
NGS Performance and Advantages
Comparative Diagnostic Performance
Next-Generation Sequencing demonstrates superior performance characteristics compared to Conventional Microbiological Tests (CMT), offering a powerful tool for contamination monitoring.
Table 1: Comparison of NGS and Conventional Microbiological Test (CMT) Performance [51]
| Parameter | NGS (Peripheral Blood) | Conventional Microbiological Test (CMT) |
|---|---|---|
| Sensitivity | 91.2% | 41.2% |
| Time to Identify Monomicrobial Infections | Significantly less (P=0.0185) | Slower |
| Time to Identify Polymicrobial Infections | Significantly less (P=0.0027) | Slower |
| Effect of Immunosuppressant Use | Not affected | Can be affected |
Advantages Over Traditional Methods
- Broad-Range Detection: Unlike PCR, NGS does not require prior knowledge of the contaminant's genetic sequence, enabling detection of both known and unknown adventitious agents, including viruses, bacteria, fungi, and Mycoplasma species [52].
- Overcoming PCR Cross-Reactivity: In complex samples, universal PCR primers can cross-react with non-target species. For example, in veterinary vaccines, Mycoplasma universal primers show near-complete complementarity with Erysipelothrix rhusiopathiae, leading to non-specific amplification and false positives. NGS bioinformatics pipelines can effectively filter these non-specific reads [53] [54].
- Superior Sensitivity: NGS-based methods can demonstrate up to a 100-fold improvement in detection limits for certain Mycoplasma species compared to conventional PCR [53] [54].
Experimental Protocols for Mycoplasma Detection Using NGS
Sample Preparation and DNA Extraction
- Sample Collection: Suspect cell culture supernatant or other test materials are collected.
- Spike-In Controls (Optional): For validation or sensitivity assessment, specific Mycoplasma species (e.g., M. fermentans, M. orale, M. hyorhinis, M. synoviae) and Acholeplasma laidlawii can be spiked into the sample [53] [54].
- DNA Extraction: Use an automated magnetic bead-based nucleic acid extraction platform or manual kits. Elute DNA in a suitable buffer [53] [54]. A combination of DNA and RNA sequencing is recommended for comprehensive viral detection [52].
Library Preparation and Sequencing
- Library Construction: Following DNA extraction, construct sequencing libraries. This involves fragmentation, end-repair, adapter ligation, and amplification.
- Quality Control: Check the library's size distribution and concentration using an instrument like a BioAnalyzer to ensure a lack of adapter dimers (sharp peaks at ~70-90 bp) which can indicate preparation failure [55].
- Sequencing: Sequence the libraries on an NGS platform, such as the MGISEQ-2000 [51].
Bioinformatics Analysis
Two primary approaches can be employed:
- Reference-Mapping Method (Recommended): This method uses a two-step alignment process to filter non-specific reads and accurately reconstruct Mycoplasma-derived contigs, demonstrating superior sensitivity and specificity [53] [54].
- 16S rRNA-based Metabarcoding: This approach uses tools like DADA2 and Qiime2 for taxonomic profiling and can provide quantitative resolution but is more prone to non-specific hits [53] [54].
Diagram: NGS Workflow for Mycoplasma Detection
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Why should I use NGS for Mycoplasma detection when PCR is faster and cheaper? NGS is invaluable when broad-range, unbiased detection is needed. PCR can fail due to cross-reactivity with other bacteria in the sample or if the specific Mycoplasma species is not targeted by the primers. NGS overcomes these limitations by detecting all nucleic acids present without prior assumption [53] [52] [54].
Q2: My cell culture is contaminated, and traditional methods have failed to identify the culprit. What is the fastest way to get an answer using NGS? In time-critical contamination events, the NGS testing process can be accelerated by adapting the sample preparation, reducing sequencing runtimes, and using streamlined bioinformatics pipelines. High contaminant concentrations often allow for these adjustments without compromising result reliability [52].
Q3: What are the most common reasons for NGS library preparation failure? Common issues include:
- Poor Input Quality: Degraded DNA/RNA or contaminants (phenol, salts) inhibit enzymes [55].
- Fragmentation/Ligation Errors: Over- or under-shearing, improper adapter-to-insert ratios leading to adapter dimers [55].
- Amplification Problems: Too many PCR cycles cause duplicates and bias [55].
- Purification Errors: Incorrect bead-based cleanup ratios lead to sample loss or adapter dimer carryover [55].
Troubleshooting Common NGS Problems
Table 2: NGS Library Preparation Troubleshooting Guide [55]
| Problem Category | Typical Failure Signals | Common Root Causes | Corrective Actions |
|---|---|---|---|
| Sample Input / Quality | Low starting yield; smear in electropherogram | Degraded DNA/RNA; sample contaminants (phenol, salts) | Re-purify input sample; use fluorometric quantification (Qubit) over UV; ensure purity ratios (260/280 ~1.8) |
| Fragmentation & Ligation | Unexpected fragment size; sharp peak at ~70-90 bp (adapter dimers) | Over-/under-shearing; improper adapter-to-insert ratio; poor ligase performance | Optimize fragmentation parameters; titrate adapter ratios; ensure fresh ligase/buffer |
| Amplification / PCR | Overamplification artifacts; high duplicate rate; bias | Too many PCR cycles; enzyme inhibitors; primer exhaustion | Reduce PCR cycles; use hot-start polymerases; additives like BSA to reduce inhibition |
| Purification & Cleanup | Incomplete removal of small fragments; sample loss | Wrong bead:sample ratio; over-dried beads; inadequate washing | Precisely follow bead cleanup protocols; avoid over-drying beads; use fresh wash buffers |
Case Study: NGS for Contaminant Identification in a Bioreactor
Background: A bulk harvest from a bioreactor culturing hamster cells for recombinant protein production showed a cytopathic effect (CPE) in Vero cells during routine in-vitro adventitious agent testing [52].
Initial Investigation: The positive result triggered an out-of-specification (OOS) investigation. Traditional follow-up methods like qPCR and transmission electron microscopy (TEM) were considered but deemed less suitable due to the potential for unknown contaminants and limited specificity [52].
NGS Analysis: The sample underwent both DNA and RNA sequencing. Initial runs were complicated by background retroviral sequences also found in negative controls. The process was optimized with an additional step to denature dsRNA to ssRNA, which significantly improved the dataset [52].
Result: The optimized NGS analysis identified the contaminant as Ephemerovirus (EHDV), a reovirus that infects cattle, with nearly complete coverage of all ten genome segments. Follow-up PCR confirmed high titers (~8 log10 gc/mL). The source was likely bovine components used in the cell culture media [52].
Conclusion: NGS was crucial for rapidly identifying an unexpected viral contaminant that traditional methods might have missed, allowing for targeted corrective actions and safeguarding the production process.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for NGS-Based Contamination Detection
| Item | Function / Application | Examples / Notes |
|---|---|---|
| Magnetic Bead-Based Nucleic Acid Kits | Automated extraction of DNA and RNA from complex samples. | TANBead Nucleic Acid Extraction Kit; essential for purifying nucleic acids while removing enzyme inhibitors [53]. |
| NGS Library Prep Kits | Preparation of sequencing libraries from extracted nucleic acids. | Kits for fragmentation, adapter ligation, and index PCR. Quality control is critical to check for adapter dimers [55]. |
| Positive Control Organisms | Validation of the NGS detection assay for Mycoplasma and other contaminants. | Five species including A. laidlawii, M. fermentans, M. orale, M. hyorhinis, and M. synoviae [53] [54]. |
| Bioinformatics Tools | Analysis of NGS data to identify contaminants. | Reference-Mapping: BWA, Bowtie2. Metabarcoding: DADA2, Qiime2 (for 16S rRNA analysis) [53] [54]. |
| Pathogen Database | Reference for classifying sequenced reads. | PMDB (Pathogens Metagenomics Database) from NCBI; should contain genomes of bacteria, fungi, viruses, and parasites [51]. |
Quality by Design (QbD) is a systematic, risk-based approach to pharmaceutical development that begins with predefined objectives and emphasizes product and process understanding and control. According to ICH Q8 guidelines, QbD focuses on building quality into the product throughout development and manufacturing, rather than relying solely on end-product testing [56] [57]. For stem cell cultures and biological products, this approach is particularly crucial for preventing microbiological contamination that can compromise product safety and efficacy.
Applying QbD principles to microbiological control involves identifying Critical Quality Attributes (CQAs) related to contamination prevention, understanding the impact of process parameters on these CQAs, and implementing a control strategy to minimize risks. This technical support center provides troubleshooting guidance and best practices for researchers implementing QbD principles to prevent microbiological contamination, with particular emphasis on mycoplasma prevention in stem cell culture systems.
QbD Framework for Microbiological Control
Core QbD Elements for Contamination Prevention
Table 1: Essential QbD Elements for Microbiological Control
| QbD Element | Description | Application to Microbiological Control |
|---|---|---|
| Quality Target Product Profile (QTPP) | Prospective summary of quality characteristics | Defines sterility requirements, microbial limit specifications for final product |
| Critical Quality Attributes (CQAs) | Physical, chemical, biological, or microbiological properties that must be controlled | Sterility, endotoxin levels, bioburden, absence of specific pathogens (e.g., mycoplasma) |
| Critical Process Parameters (CPPs) | Process parameters whose variability impacts CQAs | Holding times, sterilization parameters, environmental conditions, filtration parameters |
| Critical Material Attributes (CMAs) | Physical, chemical, biological properties of input materials | Bioburden of raw materials, quality of feeder cells, sterility of reagents |
| Control Strategy | Planned set of controls derived from product and process understanding | Environmental monitoring, in-process testing, validated sterilization processes, aseptic techniques |
Establishing the Quality Target Product Profile
The QTPP for stem cell products should clearly define microbiological quality targets based on intended clinical use. Key considerations include:
- Intended use and route of administration: Determines stringency of sterility requirements
- Dosage form and delivery system: Influences vulnerability to contamination
- Container closure system: Impacts ability to maintain sterility
- Drug product quality criteria: Explicit sterility, purity, and stability requirements [56]
For stem cell therapies, the QTPP should specify:
- Sterility assurance level (e.g., ≤1 × 10⁻⁶ for injectables)
- Endotoxin limits
- Absence of specific pathogens (especially mycoplasma)
- Microbial limits for non-sterile intermediates
Troubleshooting Guides: Common Microbiological Contamination Issues
Mycoplasma Contamination
Q: Our stem cell cultures repeatedly test positive for mycoplasma despite using aseptic techniques. What could be the source and how can we address it?
A: Mycoplasma contamination is particularly challenging due to its small size (0.2-0.8 µm) and lack of cell wall. Studies indicate approximately 4% of cell cultures show mycoplasma contamination [16].
Table 2: Mycoplasma Contamination Sources and Solutions
| Source | Detection Methods | Prevention Strategies |
|---|---|---|
| Primary starting materials | PCR, culture methods (PPLO agar/fluid), DNA staining | Quarantine and test new cell lines, use certified mycoplasma-free reagents |
| Laboratory personnel | Regular environmental monitoring | Training in aseptic techniques, proper gowning procedures |
| Contaminated reagents | Direct inoculation methods | Use of gamma-irradiated sera, filter sterilization of additives |
| Cross-contamination | Routine testing of all cell lines | Physical separation of cell lines, dedicated media for each cell line |
Experimental Protocol for Mycoplasma Detection:
- Sample Collection: Collect supernatant from test cultures after 72-96 hours of growth without antibiotics
- Culture Method:
- Inoculate 0.1 mL into PPLO broth and onto PPLO agar plates
- Incubate aerobically and anaerobically at 36±1°C for 14-28 days
- Examine plates weekly for characteristic "fried egg" colonies
- DNA Fluorochrome Method:
- Fix cells on glass slides
- Stain with DNA-binding fluorochrome (e.g., Hoechst 33258)
- Examine under fluorescence microscopy for cytoplasmic DNA
- PCR Method:
Bacterial and Fungal Contamination
Q: We're experiencing sporadic bacterial contamination in our stem cell cultures. How can we identify the root cause?
A: Bacterial contamination affects approximately 12% of cell culture passages, with gram-positive cocci being the most common contaminants [16].
Troubleshooting Workflow:
Root Cause Analysis:
- Sporadic contamination: Typically indicates technique failures - review aseptic technique, gowning procedures, biosafety cabinet maintenance
- Systematic contamination: Suggests issues with materials or equipment - test media, supplements, trypsin, water baths, incubators
- Specific microorganisms: Can indicate source (e.g., gram-positive cocci often from skin flora; gram-negative rods from water sources)
Environmental Monitoring Failures
Q: Our environmental monitoring program keeps detecting contaminants, but we can't identify the source. What approach should we take?
A: Implement a systematic environmental monitoring program with data trending:
Comprehensive Environmental Monitoring Protocol:
- Air Monitoring: Settle plates, active air samplers, particle counters
- Surface Monitoring: Contact plates, swabs of critical surfaces
- Personnel Monitoring: Finger plates, gown contact plates
- Water System Monitoring: Regular bioburden and endotoxin testing
Data Analysis Approach:
- Trend data by location, time, and personnel
- Investigate deviations from established baselines
- Correlate environmental findings with product contamination events
- Implement geographic mapping of contamination hotspots
Frequently Asked Questions
Donor Screening and Testing
Q: What testing is essential for donors of biological materials used in stem cell cultures?
A: Comprehensive donor screening should include:
Table 3: Essential Donor Screening Tests
| Test Category | Specific Tests | Rationale |
|---|---|---|
| Mandatory Viral Screening | HIV-1/2 antibody, HBsAg, HCV antibody, Treponemal-specific antibody (syphilis) | Prevents transmission of serious blood-borne pathogens [19] |
| Additional Testing for Cell-Associated Viruses | HTLV-I/II, CMV antibody | Important for leucocyte-rich cells and tissues [19] |
| Nucleic Acid Testing (NAT) | HIV RNA, HCV RNA, HBV DNA | Reduces window period of viral infections [19] |
| Emerging Pathogens | Based on epidemiology and risk assessment | Addresses regional concerns and outbreak situations |
Experimental Protocol for Donor Testing:
- Collect blood samples at time of donation
- Perform serological testing using FDA-approved/CE-marked tests
- Implement NAT testing in pools or individual samples based on sensitivity requirements
- Maintain samples for additional testing if needed
- Document all results in traceable format [19] [58]
Process Control and Validation
Q: How can we apply QbD principles to our aseptic processing operations?
A: Implement a risk-based approach focusing on Critical Process Parameters (CPPs):
Key CPPs for Aseptic Processing:
- Filtration parameters: Filter type, pore size, pressure, volume, integrity testing
- Environmental conditions: Particle counts, viable monitoring, pressure differentials
- Process timing: Maximum holding times for solutions and intermediates
- Personnel factors: Training, gowning qualification, intervention patterns
Control Strategy Elements:
- Real-time monitoring of CPPs
- Automated data collection and trend analysis
- Clear action limits for process intervention
- Regular review of process capability indices
Material and Reagent Control
Q: What controls should we implement for biological reagents like fetal bovine serum and feeder cells?
A: Biological materials represent significant contamination risks and require rigorous control:
Feeder Cell Quality Control Protocol:
- Source Qualification:
- Obtain from reputable banks with complete testing documentation
- Verify mycoplasma, virus, and sterility testing
- Incoming Testing:
- Sterility testing per European Pharmacopoeia methods
- Mycoplasma testing by culture and PCR methods
- Species identity confirmation
- Process Controls:
- Irradiation validation for growth arrest
- Storage conditions validation
- Expiry dating based on stability studies
Serum and Reagent Controls:
- Use gamma-irradiated serum when possible
- Implement in-house sterility testing for critical reagents
- Establish inventory rotation to prevent extended storage
- Qualify secondary suppliers for critical materials [19] [16]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Microbiological Control in Stem Cell Research
| Reagent/Category | Function | Quality Considerations |
|---|---|---|
| Culture Media | Cell growth and maintenance | Endotoxin testing, sterility assurance, composition consistency |
| Fetal Bovine Serum | Provides growth factors and hormones | Gamma-irradiated, mycoplasma-free, virus-screened, traceable origin |
| Trypsin/ Dissociation Reagents | Cell passaging | Sterility, absence of mycoplasma, performance qualification |
| Antibiotics | Contamination control (limited use) | Qualified for stem cell culture, concentration optimization |
| Water | Reagent preparation | Pyrogen-free, controlled bioburden, resistivity monitoring |
| Sterility Testing Media | Microbial detection | Trypticase soy agar/fluid, thioglycollate media, quality-controlled |
| Mycoplasma Detection Kits | Mycoplasma screening | Validated sensitivity/specificity, internal controls included |
| PCR Reagents | Viral and mycoplasma detection | Quality-controlled, minimal contamination risk |
Visualizing the QbD Approach to Microbiological Control
Advanced Contamination Control Strategies
Implementing Process Analytical Technology (PAT)
PAT tools can provide real-time monitoring of critical process parameters:
- Air particle monitoring: Continuous monitoring during aseptic operations
- Rapid microbiological methods: Reduce detection time for contaminants
- Total organic carbon monitoring: For water system control
- Bio-fluorescent particle counting: Real-time viable particle monitoring
Quality Risk Management
Apply formal risk assessment methodologies to prioritize contamination control efforts:
- Risk Identification: Brainstorm potential contamination sources
- Risk Analysis: Evaluate severity, probability, and detectability
- Risk Evaluation: Compare against risk acceptance criteria
- Risk Control: Implement mitigation strategies
- Risk Review: Periodic reassessment based on data
Continual Improvement Programs
Establish systems for ongoing quality enhancement:
- Trend analysis: Statistical review of contamination events
- Investigation CAPA: Robust corrective and preventive actions
- Change management: Controlled implementation of improvements
- Knowledge management: Capture and transfer lessons learned
By implementing this comprehensive QbD approach to microbiological control, researchers can build quality into their processes, reduce contamination risks, and develop more robust and reliable stem cell culture systems.
Crisis Management and Proactive Prevention: Decontamination and Corrective Action
Frequently Asked Questions (FAQs)
What are the first signs that my stem cell culture might be contaminated? While some contaminants like bacteria cause visible turbidity or pH changes (media color change), mycoplasma and viruses are often covert. Signs can include subtle changes like a persistent decrease in cell growth rate, abnormal cell morphology, unexplained cellular death, or inconsistent experimental results [5] [24]. Mycoplasma specifically can alter cellular metabolism and gene expression without causing media cloudiness [4] [24].
My culture is suspected of mycoplasma contamination. What is the first thing I should do? Immediately quarantine the suspected culture. Move it to a separate incubator, if possible, and use dedicated equipment (pipettes, media) to prevent cross-contamination to other cell lines. Decontaminate the work area and inform other lab members [4] [59].
What is the most reliable method to confirm a mycoplasma infection? No single method is perfect, but a combination is often used for confirmation. The traditional 'gold standard' is culturing the supernatant on specialized agar plates/broth to observe mycoplasma colony growth. However, this is slow. Currently, PCR-based detection is widely used for its speed, high sensitivity, and reliability [5] [59].
Can I salvage a stem cell line that is contaminated with mycoplasma? Yes, but it is a time-consuming process and risks are involved. The common approach is treatment with specific antibiotics like Plasmocin or BM Cyclin for several weeks. Crucially, after treatment, cells must be cultured without antibiotics for 1-2 weeks and then re-tested to confirm eradication. For irreplaceable cell lines, this may be worthwhile, but for others, discarding the culture is often the safest choice to protect the rest of your lab's work [4] [59].
How can I prevent viral contamination in stem cell cultures derived from human donors? The primary risk is from the source material. Ideally, donors should be pre-screened for major viral pathogens. If this is not possible, the cell lines themselves should be tested at the earliest possible timepoint. Minimum screening should include tests for HIV-1/2, Hepatitis B, and Hepatitis C. All human materials should be handled using BSL2 containment standards [60] [27].
Troubleshooting Guide: Step-by-Step Diagnostic Workflows
Suspected Microbial Contamination (Bacteria, Yeast, Fungi)
This type of contamination is often visually detectable.
- Step 1: Visual and Microscopic Inspection. Check for macroscopic signs like media cloudiness or a sudden, sharp drop in pH (yellowing of phenol-red containing media). Under a standard light microscope, look for rapid movement of bacteria or fungal hyphae at a higher magnification [27] [24].
- Step 2: Confirm with Sterility Testing. Use microbial culture media to reveal hidden contaminants. The European Pharmacopoeia Method 2.6.1 for sterility is a robust standard. Alternatively, incubate a sample of the culture in antibiotic-free, glucose-rich media for 14 days and monitor for signs of growth [27].
- Step 3: Action. If contamination is confirmed, the standard protocol is to discard the culture via autoclaving, decontaminate all surfaces and equipment, and retrain personnel on aseptic technique [27] [24].
Suspected Mycoplasma Contamination
Mycoplasma is invisible under a standard light microscope and requires specific detection methods. The following workflow outlines the diagnostic process.
Detailed Experimental Protocols for Mycoplasma Detection
1. PCR-Based Detection
- Principle: Amplifies specific 16S rRNA genes unique to common mycoplasma species.
- Protocol: a. Sample Collection: Collect supernatant from a test cell culture that has not been passaged or had its media changed for at least 2-3 days to allow potential contaminants to accumulate [59]. b. DNA Extraction: Isolate total DNA from the sample using a standard kit. c. PCR Amplification: Perform PCR using universal or species-specific primers for mycoplasma. Common targets include sequences from M. orale, M. arginini, M. hyorhinis, and A. laidlawii [5] [59]. d. Analysis: Run the PCR product on an agarose gel. A positive band indicates contamination.
- Advantages: Quick (results in hours), highly sensitive, and cost-effective [59].
2. Agar Culture Method (Gold Standard)
- Principle: Directly culture mycoplasmas on nutrient-rich agar plates.
- Protocol: a. Inoculation: Spread 100-200 µL of cell culture supernatant onto specialized mycoplasma agar plates. b. Incubation: Incubate plates anaerobically at 37°C for up to 3 weeks. c. Observation: Periodically check for the appearance of characteristic "fried-egg" colonies, which can be seen with a microscope or sometimes by naked eye [5] [59].
- Advantages: Can detect a wide range of species and provides a viable isolate.
- Disadvantages: Very slow, requiring up to 3 weeks for a definitive result [59].
3. Fluorescent DNA Staining (e.g., Hoechst 33258 or DAPI)
- Principle: A DNA-binding dye stains all DNA, including mycoplasma DNA that adheres to the surface of infected cells.
- Protocol: a. Prepare Indicator Cells: Grow an uncontaminated indicator cell line (e.g., Vero cells) on a coverslip. b. Inoculate: Inoculate these cells with the supernatant from the suspect culture and incubate for several days. c. Stain: Fix the cells and stain with Hoechst 33258 or DAPI. d. Visualize: Examine under a fluorescence microscope. Mycoplasma DNA will appear as tiny, bright specks or filaments in the cytoplasm and around the nuclei of the infected indicator cells [5] [59].
- Advantages: Visually demonstrates the presence of mycoplasma on cells.
- Disadvantages: Requires expertise in interpretation and a fluorescence microscope [59].
Quantitative Data on Mycoplasma Contamination
Table 1: Mycoplasma Species and Their Common Sources in Cell Culture
| Mycoplasma Species | Primary Source | Estimated Frequency in Contaminations |
|---|---|---|
| M. orale | Human oropharyngeal tract (lab personnel) | Very High (>50% of infections) [5] |
| M. fermentans | Human | High [5] |
| M. hyorhinis | Swine (trypsin) | ~5-35% of contaminations [5] |
| M. arginini | Bovine (serum) | ~5-35% of contaminations [5] |
| Acholeplasma laidlawii | Bovine (serum) | ~5-35% of contaminations [5] |
Table 2: Comparison of Major Mycoplasma Detection Methods
| Method | Time to Result | Sensitivity | Key Advantage | Key Disadvantage |
|---|---|---|---|---|
| Agar Culture | Up to 3 weeks | High (10² - 10³ CFU/mL) [5] | Gold standard, detects viable organism | Very slow, requires specific culture conditions |
| PCR | Several hours | Very High (10¹ - 10² genome copies) [5] | Fast, highly sensitive, specific | Does not distinguish between viable and dead cells |
| Fluorescent Staining | 1-3 days | Moderate | Visually shows spatial distribution of infection | Requires fluorescence microscope, subjective interpretation |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Contamination Prevention and Diagnosis
| Reagent / Material | Function | Key Consideration |
|---|---|---|
| Mycoplasma Removal Agents (e.g., Plasmocin) | Antibiotic treatment to eliminate mycoplasma from contaminated cultures [59]. | Use only for valuable, irreplaceable cell lines. Requires follow-up testing after antibiotic-free culture [4]. |
| PCR Mycoplasma Detection Kit | Contains primers and controls for sensitive DNA-based detection of a broad range of mycoplasma species [5] [59]. | Preferred for routine, rapid screening. Choose kits with universal primers for maximum coverage. |
| Fluorescent DNA Stains (e.g., Hoechst 33258) | Used in indirect staining methods to visualize mycoplasma DNA on the surface of infected indicator cells [5] [59]. | Excellent for visual confirmation but requires a fluorescence microscope and some expertise. |
| Validated Fetal Bovine Serum (FBS) | Nutrient-rich supplement for cell culture media. A historical source of bovine-derived mycoplasma [5]. | Always source from reputable suppliers who provide certification of testing for mycoplasma and viruses [5] [24]. |
| 0.1 µm Pore Filters | Sterile filtration of media and sensitive solutions (e.g., trypsin) to remove microbial contaminants [5] [59]. | More effective than standard 0.2 µm filters at removing small, flexible mycoplasma. |
To Treat or Discard? Evaluating Decontamination Options like Mynox
Mycoplasma contamination represents a significant challenge in stem cell research, capable of altering cellular characteristics, compromising experimental data, and jeopardizing long-term studies. This technical support center provides stem cell researchers and drug development professionals with evidence-based troubleshooting guides and FAQs for managing mycoplasma contamination, with a specific focus on evaluating the use of decontamination reagents like Mynox.
Quick Decision Guide: To Treat or Discard
The flowchart below outlines the critical decision-making process for managing mycoplasma-contaminated stem cell cultures.
Troubleshooting Mynox Treatment in Stem Cell Cultures
Mynox and its advanced formulation Mynox Gold represent biophysical decontamination approaches that utilize surfactin to compromise mycoplasma membrane integrity. Mynox Gold combines this mechanism with the antibiotic ciprofloxacin, virtually eliminating resistance development [61]. The treatment protocol involves an initial treatment to eliminate most mycoplasmas followed by several maintenance treatments to destroy remaining contaminants [61].
Frequently Encountered Issues & Solutions
Problem: Mycoplasma remains detectable after Mynox treatment.
Root Cause & Solution:
- Extracellular DNA Interference: Mynox lyses mycoplasmas but leaves DNA in supernatant. Wait 4 passages after treatment before retesting to allow DNases to hydrolyze free DNA [62].
- Excessive FCS Concentration: FCS cholesterol binds Mynox, reducing efficacy. Ensure FCS concentration does not exceed 5% during treatment [62].
- High Cell Density or Clumping: Lower cell concentration and extend incubation time. Prepare single-cell suspensions through extended trypsination [62].
- Extremely High Initial Titer: Perform second treatment after 2-day cell recovery period [62].
Problem: Cytotoxic effects observed during treatment.
Root Cause & Solution:
- Improper Mixture Preparation: Most cytotoxicity cases result from incorrect Mynox concentrations. Immediately stop treatment via medium change if toxicity appears [62].
- Cell Line Sensitivity: For sensitive stem cell lines, reduce treatment time (30 minutes for adherent cells, 15 minutes for suspension cells) [62].
Problem: Ineffective elimination from virus stocks.
Root Cause & Solution:
- Cellular Debris Interference: Centrifuge supernatant at 1,000 rpm for 5 minutes, discard pellet, then treat clear supernatant [62].
Treatment Parameters for Stem Cell Cultures
The table below summarizes critical parameters for successful Mynox implementation in stem cell research.
| Parameter | Optimal Condition | Considerations for Stem Cells |
|---|---|---|
| Cell Confluence | 40-60% confluence [62] | Ensures effective single-cell preparation |
| FCS Concentration | Maximum 5% [62] | Critical for treatment efficacy |
| Treatment Duration | Varies by sensitivity [62] | Monitor closely for toxicity signs |
| Validation Timing | After 4 passages [62] | Use PCR-based detection methods |
| Concurrent Antibiotics | Penicillin/Streptomycin acceptable [62] | Avoid routine antibiotic use in stem cell culture [27] |
Essential Research Reagent Solutions
The following reagents and equipment are essential for effective mycoplasma prevention, detection, and elimination in stem cell research.
| Reagent/Equipment | Primary Function | Application Notes |
|---|---|---|
| Mynox Gold [61] | Mycoplasma elimination | Combination surfactin/ciprofloxacin; low resistance risk |
| Mycoplasma Off [62] [63] | Surface decontamination | Effective against enveloped/non-enveloped viruses & spores |
| VenorGeM PCR Kit [61] | Mycoplasma detection | Gold-standard validation post-treatment |
| CO₂ Incubator with Copper Inlay [64] [62] | Contamination prevention | Do not polish copper surfaces; oxide layer is bacteriostatic |
| WaterShield [62] | Incubator water pan protection | Maintains antibiotic action for 4 weeks; non-cytotoxic |
| Cell Locker Systems [64] | Cross-contamination prevention | Essential for multi-user stem cell facilities |
Prevention: The Cornerstone of Stem Cell Culture Integrity
Strategic Antibiotic Use
The International Society for Stem Cell Research recommends stem cell cultures be handled "in the absence of antibiotics which can affect the biochemistry of cultured cells" [27]. While Mynox provides a solution for established contamination, preventive strategies are paramount:
- Routine Monitoring: Implement quarterly mycoplasma testing using PCR-based methods [65] [27]
- Aseptic Technique: Maintain strict handling procedures and controlled access to cell culture areas [24]
- Environmental Control: Utilize HEPA-filtered biosafety cabinets and validated incubator sterilization cycles [64]
- Cell Bank Validation: Regularly test frozen stem cell stocks to prevent latent contamination issues [24]
The decision to treat or discard mycoplasma-contaminated stem cells requires careful consideration of scientific value, resource availability, and contamination scope. While Mynox products provide effective decontamination options for irreplaceable cell lines, successful implementation depends on strict adherence to protocols and comprehensive validation. In stem cell research, where genetic stability and phenotypic consistency are paramount, robust prevention strategies combined with routine monitoring remain the most reliable approach to safeguarding culture integrity and ensuring reproducible research outcomes.
FAQs on Mycoplasma Contamination
1. What are the common sources of mycoplasma contamination in a stem cell culture laboratory? Mycoplasma contamination typically originates from three main sources:
- Laboratory Personnel: Technicians are a primary source. Speaking, coughing, or sneezing can generate aerosols containing species like M. orale, M. fermentans, and M. hominis [13] [5].
- Contaminated Reagents: Animal-derived products, particularly fetal bovine serum (FBS) and trypsin, can introduce species such as M. arginini, Acholeplasma laidlawii, and M. hyorhinis [5] [66].
- Cross-Contamination: The handling of multiple cell lines, especially with shared equipment like pipettes, can spread mycoplasma from an infected culture to clean ones. A single contaminated culture can lead to widespread infection in a lab space within weeks [13] [5].
2. Why is mycoplasma contamination particularly problematic for stem cell research and therapy? Mycoplasma contamination poses a severe threat to stem cell applications for several reasons:
- Metabolic Competition: Mycoplasmas compete with host cells for essential nutrients in the culture medium, impairing stem cell growth, viability, and function [13] [67].
- Altered Cell Physiology: They can cause chromosomal aberrations, alter gene expression patterns, and disrupt cell signaling pathways, which compromises the genomic integrity and differentiation potential crucial for stem cells [13] [5] [66].
- Product Safety: For clinical applications, mycoplasma contamination in a stem cell product can transmit infection to the recipient and lead to the complete loss of a therapeutic batch, emphasizing the need for rigorous testing as outlined in tissue bank guidelines [19] [66].
3. What are the most effective methods for detecting mycoplasma contamination? The table below summarizes the key detection methods, highlighting their principles and suitability for a stem cell lab.
| Method | Principle | Duration | Key Advantage | Consideration for Stem Cell Labs |
|---|---|---|---|---|
| Culture Method [13] [5] | Isolates and grows mycoplasma on agar. | Several weeks | Gold standard, highly specific. | Slow; not ideal for rapid screening. |
| DNA Fluorescence Staining [13] [5] | Fluorescent dye (e.g., Hoechst) binds to mycoplasma DNA. | 1-2 days | Visually identifies infection location. | Requires indicator cells; subjective interpretation. |
| PCR [13] [68] [66] | Amplifies conserved mycoplasma DNA sequences. | Hours to a day | High sensitivity, speed, and specificity. | Can detect non-viable organisms; risk of false positives. |
| Enzyme-Linked Immunosorbent Assay (ELISA) [13] | Detects specific mycoplasma antigens. | Several hours | Can process many samples at once. | Lower specificity compared to other methods. |
4. We suspect a mycoplasma contamination. What is the immediate containment procedure? Upon suspicion of contamination, take these immediate steps to contain it:
- Isolate: Immediately move the suspected culture from the incubator and cell culture hood to a designated quarantine area [18].
- Decontaminate: Thoroughly clean the incubator, laminar flow hood, and all work surfaces with a sporicidal laboratory disinfectant. Live mycoplasma can persist on surfaces for days [5] [69].
- Verify: Use a reliable detection method (e.g., PCR or fluorescence staining) to confirm the presence and species of mycoplasma [13] [67].
- Discard: The safest and most recommended practice is to autoclave the contaminated culture and all reagents it contacted [5] [69].
5. Can a valuable, irreplaceable mycoplasma-contaminated stem cell line be saved? Yes, salvage is possible but challenging and should only be attempted for irreplaceable lines. The primary method is antibiotic treatment [69] [67].
- Procedure:
- Determine Toxicity: Dissociate the cells and culture them in a multi-well plate with a range of antibiotic concentrations (e.g., Plasmocin) to find a non-toxic dose [18] [67].
- Treat: Culture the cells for several passages (e.g., 2-3) using the antibiotic at a concentration one- to two-fold lower than the toxic level.
- Validate: Culture the cells in antibiotic-free medium for 4-6 passages and re-test thoroughly to ensure complete eradication [18].
- Caution: Treatment may not fully eradicate the infection, can induce selective pressure, and the recovered cell line may have altered characteristics. Always bank treated cells and use untreated, clean cells as a control where possible [69] [67].
Experimental Protocols for Detection
Protocol 1: Detection by DNA Fluorescence Staining
This protocol uses Hoechst 33258, a dye that binds the A-T rich regions of mycoplasma DNA [13] [5].
Key Reagents:
- Hoechst 33258 stain solution
- Fresh Carnoy's fixative (methanol:glacial acetic acid, 3:1)
- Indicator cells (e.g., Vero cells)
Method:
- Prepare Indicator Cells: Grow sterile indicator cells on a coverslip in a multi-well plate until 50-60% confluent.
- Inoculate with Test Sample: Add 1-2 mL of the supernatant from the suspect cell culture to the indicator cells. Include positive and negative controls.
- Incubate: Incubate for 3-5 days to allow mycoplasma to adhere and grow.
- Fix: Aspirate the medium, rinse with PBS, and fix the cells with Carnoy's fixative for 10 minutes.
- Stain: Aspirate the fixative, add Hoechst 33258 solution, and incubate for 30 minutes in the dark.
- Analyze: Rinse with water, mount the coverslip, and observe under a fluorescence microscope. Mycoplasma will appear as bright, punctate, extra-nuclear staining (small, fluorescent dots in the cytoplasm and around the cell periphery).
Protocol 2: Detection by PCR
PCR is a sensitive and rapid method for detecting mycoplasma DNA [13] [68].
Key Reagents:
- Mycoplasma-specific primers (targeting 16S rRNA genes)
- DNA polymerase master mix
- DNA extraction kit
- Nuclease-free water
Method:
- Sample Collection: Collect 1-2 mL of supernatant from a test cell culture that has been grown for at least 72 hours without antibiotics.
- DNA Extraction: Extract total nucleic acids from the sample using a commercial DNA extraction kit, following the manufacturer's instructions.
- PCR Setup: Prepare the PCR reaction mix containing master mix, specific forward and reverse primers, and the extracted DNA template.
- Amplification: Run the PCR using a validated thermal cycling program (e.g., initial denaturation at 95°C for 5 min; 35 cycles of 95°C for 30s, 55°C for 30s, 72°C for 1 min; final extension at 72°C for 5 min).
- Analysis: Separate the PCR products by gel electrophoresis. The presence of a band at the expected size (e.g., ~500 bp, depending on the primer set) indicates mycoplasma contamination.
The Scientist's Toolkit: Key Reagent Solutions
| Reagent / Kit | Function | Application Note |
|---|---|---|
| Plasmocin [67] | Antibiotic mixture for eradication of mycoplasma. | Used as a therapeutic treatment for contaminated irreplaceable cell lines; typically used for 2-3 passages. |
| Hoechst 33258 [13] [5] | DNA-binding fluorescent dye for staining. | Used in the DNA fluorescence staining method to visualize mycoplasma DNA under a fluorescence microscope. |
| Mycoplasma PCR Kit [66] [67] | Contains primers and controls for DNA amplification. | Enables highly sensitive and specific detection of mycoplasma DNA in a few hours; ideal for routine screening. |
| Normocin [67] | Broad-spectrum antibiotic for prevention of bacterial, fungal, and mycoplasma contamination. | Can be added to cell culture media as a prophylactic measure, though routine use of antibiotics is generally discouraged. |
Root Cause Analysis Workflow and Detection Selection
The following diagram illustrates a systematic workflow for investigating a suspected contamination event, from initial observation to final corrective actions.
Mycoplasma Detection Method Selection Logic
When multiple detection methods are available, use the following logic to select the most appropriate one based on your experimental constraints and needs.
In the context of stem cell research, the Corrective and Preventive Action (CAPA) system is a fundamental quality management process designed to address deviations and prevent their recurrence. For researchers working with valuable cell lines, a robust CAPA system is not merely a regulatory formality but a critical tool for safeguarding research integrity. It ensures that issues like mycoplasma contamination are systematically investigated, rectified, and prevented from compromising future experiments or therapeutic applications [70] [71].
The purpose of CAPA is to collect and analyze information, identify and investigate product and quality problems, and take appropriate and effective action to prevent their recurrence [70]. This is especially vital in stem cell culture, where contamination events can lead to the loss of irreplaceable samples, invalidate months of research, and potentially endanger patients if those cells are destined for clinical use.
CAPA Fundamentals: A Structured Workflow
A typical CAPA process follows a logical, closed-loop sequence. The workflow below outlines the key stages from problem identification to resolution and verification.
The CAPA Form: A Core Documentation Tool
The CAPA form is the primary tool for documenting this process. It serves as a living record from initiation to closure, ensuring all necessary steps are completed and auditable [72]. A well-structured CAPA form should include, at a minimum, the following elements [72]:
- Problem Description: A clear, concise statement of the issue.
- Immediate Actions Taken: Containment measures to stabilize the situation.
- Root Cause Analysis (RCA): Documentation of the investigation into the underlying cause.
- Corrective and Preventive Actions: Steps to fix the current problem and prevent recurrence.
- Timelines and Responsibilities: Defined deadlines and assigned personnel.
- Effectiveness Checks: Evidence that the actions resolved the problem and did not introduce new risks.
- Sign-offs and Approvals: Formal review and closure.
Frequently Asked Questions (FAQs) on CAPA
Q1: What is the key difference between a corrective and a preventive action?
Corrective Action addresses an existing, identified problem or nonconformity. For example, if a batch of cell culture media is found to be contaminated with mycoplasma, the corrective action involves investigating that specific event, disposing of the contaminated media, and decontaminating the work area.
Preventive Action, however, addresses a potential problem that has not yet occurred. It is proactive. Analyzing data from various sources might reveal an unfavorable trend, such as a gradual increase in ambient humidity in the cleanroom during summer months, which could increase the risk of fungal contamination. A preventive action would be taken to install or service dehumidifiers before any actual contamination occurs [71].
Q2: How do I perform an effective Root Cause Analysis (RCA) for a complex issue like recurring contamination?
Effective RCA requires a systematic approach and a team with the right knowledge to minimize bias [70]. Two common and effective techniques are:
- The 5 Whys Technique: Repeatedly ask "Why?" to peel back the layers of a problem. For example: Why is the cell culture contaminated? → Because the biosafety cabinet was contaminated. Why was the cabinet contaminated? → Because the regular weekly cleaning was not performed. Why was it not performed? → Because the staff member responsible was on leave, and no backup was assigned. This reveals a systemic flaw in personnel scheduling, not just a simple human error.
- The Fishbone (Ishikawa) Diagram: This method helps visually categorize all potential causes of a problem (e.g., People, Process, Equipment, Materials, Environment, Measurement) to ensure a comprehensive investigation [72]. This is particularly useful for complex issues with multiple contributing factors.
Q3: Our lab often struggles with setting realistic timelines for CAPA. What is a good practice?
CAPA procedures often fail due to unreasonable timeframes and deadlines [70]. To avoid this:
- Break down the CAPA plan into distinct phases (e.g., Investigation, Action Plan Development, Implementation, Effectiveness Check).
- Assign estimated completion times for each milestone, consulting with the personnel responsible for the tasks.
- Utilize project management tools or simple timeline software to track progress and identify potential delays early [72].
Troubleshooting Guide: Common Scenarios in Stem Cell Labs
Scenario 1: Suspected Mycoplasma Contamination in a Stem Cell Line
| Step | Action | Documentation / Output |
|---|---|---|
| 1. Identification | Routine PCR test returns a positive result for mycoplasma. | Quality Record / Lab Notebook entry. |
| 2. Immediate Action | Quarantine the affected culture and all cultures handled in the same biosafety cabinet. Notify the Principal Investigator. | CAPA Form: "Immediate Actions" section. |
| 3. Investigation (RCA) | Use the 5 Whys. Review recent procedures: was aseptic technique breached? Were new reagents introduced? Was the biosafety cabinet recently serviced? | CAPA Form: "Root Cause Analysis" section. Conclusion: e.g., "Mycoplasma-positive cell line introduced into the lab without prior screening." |
| 4. Corrective Action | Safely dispose of the contaminated culture. Decontaminate the work area and equipment used. | CAPA Form: "Corrective Actions" section. |
| 5. Preventive Action | Update lab SOP: Mandatory mycoplasma screening for all new incoming cell lines. Implement quarterly training on aseptic technique. | CAPA Form: "Preventive Actions" section. |
| 6. Effectiveness Check | Audit incoming cell logs for the next 3 months to verify 100% compliance with pre-screening policy. Re-test other cell lines from the same cabinet. | CAPA Form: "Effectiveness Verification" report. |
Background: Mycoplasmas are small bacteria that lack a cell wall and can pass through sterilizing filters. They can persist in culture without causing turbidity, making them a frequent and cryptic contaminant [73] [21]. They alter cell function and metabolism, compromising research data [18].
Scenario 2: Unexplained Drop in Stem Cell Viability Post-Thawing
| Step | Action | Documentation / Output |
|---|---|---|
| 1. Identification | Consistent, significant reduction in post-thaw viability noted for a specific stem cell line over multiple cycles. | Trend analysis data from cell bank records. |
| 2. Immediate Action | Flag the specific cell bank batch for further investigation. Use an alternative batch if available. | Non-Conformance Report. |
| 3. Investigation (RCA) | Form a team. Use a Fishbone diagram. Investigate: People (training on thawing protocol), Method (changes to freezing/thawing SOP), Machine (calibration of water bath, freezer temperature logs), Material (quality of cryopreservation medium, DMSO age), Measurement (viability assay method). | CAPA Form: "Root Cause Analysis" with investigation notes. Conclusion: e.g., "Uncalibrated water bath led to deviant thawing temperature." |
| 4. Corrective Action | Re-calibrate the water bath. Discard the compromised cell batch. | CAPA Form: "Corrective Actions" section. |
| 5. Preventive Action | Implement a monthly calibration schedule for the water bath. Update the freezing/thawing SOP to include a mandatory temperature check before use. | CAPA Form: "Preventive Actions" section. |
| 6. Effectiveness Check | Monitor post-thaw viability for the next 5 batches thawed using the calibrated equipment. | CAPA Form: "Effectiveness Verification" showing a return to normal viability levels. |
The Scientist's Toolkit: Key Reagents for Contamination Control
The following table details essential reagents and tools used in the prevention, detection, and management of contamination in stem cell culture.
| Reagent / Tool | Function | Application Note |
|---|---|---|
| Mycoplasma Detection Kit (PCR-based) | Highly sensitive and specific detection of mycoplasma DNA in cell culture supernatants [74]. | Use for routine, mandatory screening of all cell lines and culture lots every 2-4 weeks. |
| Mycoplasma Removal Treatment | Reagent for decontaminating infected cultures; not a substitute for good practice [74]. | Consider for irreplaceable, contaminated cell lines. Always re-culture from a treated stock. |
| ROCK Inhibitor (Y-27632) | A small molecule that enhances survival of human pluripotent stem cells (hPSCs) after passaging and thawing by inhibiting apoptosis [75]. | Add to culture medium for 24-48 hours after thawing or single-cell passaging to improve viability and cloning efficiency. |
| Surface Decontaminants | Reagents (e.g., sporicidal disinfectants) for disinfecting biosafety cabinets and work surfaces [74]. | Use a validated two-step process: clean with a detergent to remove residue, then apply an effective disinfectant. Rotate disinfectants periodically. |
| Antibiotics/Antimycotics | Suppress microbial growth. Note: Should not be used routinely as they can mask low-level contamination, like mycoplasma, and promote resistant strains [18]. | Reserve for short-term applications only (e.g., during primary culture establishment). Maintain antibiotic-free cultures as a standard practice. |
Signaling Pathways in Stem Cell Culture and Contamination Stress
Mycoplasma contamination can directly interfere with critical signaling pathways essential for stem cell self-renewal and differentiation. Understanding these pathways helps in diagnosing culture health and selecting appropriate culture additives to maintain robust stem cells.
Key Pathways and Additives:
- JAK-STAT Pathway: Activated by cytokines like Leukemia Inhibitory Factor (LIF), this pathway is crucial for maintaining the pluripotent state of mouse embryonic stem cells [75].
- MAPK/ERK and PI3K/AKT Pathways: These are key signaling routes activated by growth factors like Fibroblast Growth Factor (FGF-2) and Insulin-like Growth Factor (IGF), promoting stem cell survival and proliferation [75].
- TGF-β/SMAD Pathway: This pathway has dual roles. In human pluripotent stem cells, it helps maintain self-renewal in concert with FGF; however, it also is a potent driver of differentiation into various lineages [75]. The small molecule inhibitor SB431542 is used to block this pathway to direct differentiation.
- Impact of Contamination: Mycoplasma infection can dysregulate these precise signaling environments by causing nutrient depletion and triggering a cellular stress response, leading to aberrant differentiation, cell death, and unreliable experimental results [18].
Mycoplasma contamination represents one of the most significant yet stealthy challenges in cell culture laboratories worldwide. With an estimated 15-35% of cell lines contaminated globally, these microorganisms pose a persistent threat to research integrity, biopharmaceutical production, and experimental reproducibility [5] [76] [77]. Unlike bacterial or fungal contaminants that cause obvious turbidity, mycoplasma contamination typically progresses unnoticed, without visible signs or cell death, yet it extensively alters cellular physiology and metabolism [5] [78]. For researchers working with stem cells or developing cell-derived biopharmaceuticals, implementing rigorous routine monitoring and reagent quality control is not merely best practice—it is essential for generating reliable, reproducible data and ensuring product safety.
FAQs: Understanding Mycoplasma Contamination
Q: What are mycoplasmas and why are they particularly problematic for cell culture?
Mycoplasmas are a distinct group of bacteria classified under the class Mollicutes, characterized by their complete lack of a cell wall and exceptionally small size (0.15-0.3 μm) [5] [76]. These features make them difficult to detect visually and allow them to pass through many filtration systems (0.2 μm filters) commonly used for sterilizing cell culture media [5]. Their small genome drastically reduces their biosynthetic capabilities, causing them to heavily rely on nutrients from their host cell culture, which they deplete while producing waste products [76].
The main sources of mycoplasma contamination include:
- Laboratory personnel: Human oral flora is a significant source, with species like M. orale, M. fermentans, and M. hominis accounting for more than half of all mycoplasma infections in cell cultures [5].
- Contaminated cell cultures: Introduction of already-infected cell lines is a major route for spreading mycoplasma to uncontaminated cultures [5] [78].
- Reagents and media: Animal-derived products, particularly fetal bovine serum (source of M. arginini and A. laidlawii) and porcine trypsin (source of M. hyorhinis) can introduce contamination [5] [79].
- Laboratory environment: Mycoplasma can spread via aerosols, contaminated equipment, and liquid nitrogen storage [5] [78].
Q: What effects can mycoplasma contamination have on my cell cultures and experimental results?
Mycoplasma contamination can extensively impact nearly all aspects of cell physiology [5] [76]:
- Induction of chromosomal abnormalities and disruption of DNA/RNA synthesis
- Alterations in cell metabolism, growth rates, and viability
- Changes in membrane composition and antigenicity
- Inhibition of cell proliferation due to nutrient competition
- Modification of gene expression profiles
- Interference with differentiation processes, particularly critical in stem cell research
- Altered response to chemical compounds and therapeutic agents, potentially leading to erroneous conclusions in drug screening
Mycoplasma Detection Methods: A Comparative Analysis
Various methods are available for detecting mycoplasma contamination, each with distinct advantages, limitations, and appropriate applications. The table below summarizes the key characteristics of the most commonly used techniques:
| Method | Sensitivity | Time Required | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Direct Culture | High | ~28 days | Considered "gold standard"; detects viable cells indicating active infection [76] | Laborious; time-consuming; not all strains grow well in culture [76] [78] |
| PCR-based Methods | High | 1-2 days | Rapid; highly sensitive and specific; detects broad range of species including non-culturable strains [76] [78] | Cannot distinguish between viable and non-viable cells; requires optimization to prevent false results [76] |
| DNA Staining (Hoechst/DAPI) | Moderate | 1-2 days | Rapid; cost-effective; easy to perform [76] | Not specific to mycoplasma; requires expert interpretation; lower sensitivity for low-level contamination [76] [78] |
| Enzymatic/Bioluminescence Assays | Moderate | ~1 hour | Very rapid; simple procedure; inexpensive [77] [78] | May not detect all species; limited to detecting contamination above a certain threshold [78] |
| ELISA/Immunostaining | Moderate | 1-2 days | Can identify specific species; relatively fast [78] | Limited range of detectable species; subjective interpretation [78] |
Troubleshooting Guide: Common Cell Culture Issues and Solutions
Problem: Excessive differentiation (>20%) in human pluripotent stem cell cultures
Potential Solutions [47]:
- Ensure complete cell culture medium is fresh (less than 2 weeks old when stored at 2-8°C)
- Remove areas of differentiation prior to passaging
- Limit time culture plates remain outside the incubator (no more than 15 minutes at a time)
- Ensure cell aggregates generated during passaging are evenly sized
- Passage cultures when colonies are large, compact, and dense in the centers
- Decrease colony density by plating fewer cell aggregates during passaging
- Reduce incubation time with dissociation reagents if your cell line is particularly sensitive
Problem: Poor cell attachment after passaging
Potential Solutions [46] [47]:
- Plate a higher number of cell aggregates initially (2-3 times higher) to maintain more densely confluent cultures
- Work quickly after cells are treated with passaging reagents to minimize time aggregates spend in suspension
- Reduce incubation time with passaging reagents, particularly if cells are passaged prior to multi-layering within colonies
- Avoid excessive pipetting to break up cell aggregates; instead increase incubation time with passaging reagent by 1-2 minutes
- Ensure proper coating matrix is used (e.g., non-tissue culture-treated plates for Vitronectin XF; tissue culture-treated for Matrigel)
Problem: Failed neural induction from pluripotent stem cells
Potential Solutions [46]:
- Remove differentiated and partially differentiated hPSCs before neural induction
- Optimize plating density for induction (recommended: 2-2.5 × 10⁴ cells/cm²)
- Plate cell clumps rather than single cell suspensions for induction
- Consider overnight treatment with 10 μM ROCK inhibitor Y27632 at the time of hPSC splitting to prevent extensive cell death
- Verify the quality and proper storage of essential supplements like B-27:
- Check expiration date
- Ensure supplemented medium is fresh (stable for only 2 weeks at 4°C)
- Avoid excessive heat exposure
- Note proper appearance (should be transparent yellow liquid; green indicates deterioration)
Problem: Suspected mycoplasma contamination
Potential Solutions [5] [77] [79]:
- Implement routine testing of all cell lines at least monthly, and whenever thawed from cryovial stocks
- Test cell lines immediately prior to critical experiments, such as high-throughput screening
- Destroy contaminated cell lines immediately whenever possible
- For irreplaceable contaminated lines, consider treatment with anti-mycoplasma antibiotics (e.g., plasmocin) with strict quarantine protocols
- Re-source contaminated cell lines from reputable cell banks when possible
- Review and enhance aseptic techniques throughout the laboratory
Experimental Protocols for Mycoplasma Detection
Protocol 1: PCR-Based Mycoplasma Detection
Principle: This method amplifies specific DNA sequences unique to mycoplasma species, particularly targeting the conserved 16S rRNA region [76].
Materials:
- Universal Mycoplasma Detection Kit (commercial kits are available)
- PCR thermal cycler
- DNA extraction reagents (phenol-chloroform or column-based)
- Agarose gel electrophoresis equipment
- Positive and negative control templates
Procedure:
- Sample Collection: Collect supernatant from test cell cultures after 3-5 days of growth without antibiotic treatment.
- DNA Extraction: Purify DNA using phenol-chloroform extraction or commercial column kits to ensure sample quality and prevent PCR inhibition.
- PCR Setup: Prepare reaction mixtures according to kit instructions, including:
- Universal primers specific to the 16S rRNA gene
- dNTPs
- Taq polymerase
- Buffer with magnesium
- Template DNA (test samples, positive control, negative control)
- Amplification: Run PCR with optimized cycling conditions, typically including:
- Initial denaturation: 94°C for 2-5 minutes
- 35-40 cycles of: Denaturation (94°C, 30 sec), Annealing (55-65°C, 30 sec), Extension (72°C, 45-60 sec)
- Final extension: 72°C for 5-10 minutes
- Analysis: Separate PCR products by agarose gel electrophoresis. Mycoplasma contamination is indicated by distinct bands ranging from 434 to 468 base pairs, depending on species [76].
Validation: Include appropriate controls in each run: positive control (known mycoplasma DNA), negative control (nuclease-free water), and internal control to detect PCR inhibition.
Protocol 2: Mycoplasma Detection by Cultural Methods
Principle: This gold standard method detects viable mycoplasma cells through growth on selective agar and broth media [76] [78].
Materials:
- Selective mycoplasma broth medium
- Mycoplasma agar plates
- Anaerobic incubation system
- Sterile pipettes and culture tubes
Procedure:
- Inoculation: Aseptically inoculate 0.1 mL of test cell culture supernatant into selective mycoplasma broth medium.
- Broth Incubation: Incubate broth cultures at 36±1°C under anaerobic conditions for 14 days.
- Subculture: On days 3, 7, and 14 post-inoculation, subculture 0.1 mL from broth onto solid mycoplasma agar plates.
- Agar Incubation: Incubate agar plates anaerobically at 36±1°C for 14 additional days.
- Observation: Examine agar plates periodically for characteristic mycoplasma colony formation using microscopic examination (20-100× magnification). Typical "fried-egg" colonies indicate positive contamination.
Interpretation: The sample is considered positive if colonies form on agar at any subculture point. The entire process requires 28 days for definitive negative results [76].
Essential Research Reagent Solutions
The following table details key reagents and materials essential for maintaining mycoplasma-free cell cultures and conducting proper quality control:
| Reagent/Material | Function | Quality Control Considerations |
|---|---|---|
| Fetal Bovine Serum | Nutrient supplement for cell culture media | Screen for mycoplasma and bovine viral diarrhea virus (BVDV); request Certificate of Analysis; consider batch testing [79] |
| Cell Culture Media | Supports cell growth and maintenance | Filter-sterilized through 0.1μm filters for better mycoplasma removal; test for sterility and performance [5] |
| PCR Detection Kits | Molecular detection of mycoplasma contamination | Validate sensitivity and specificity; ensure inclusion of positive and negative controls [76] [80] |
| Mycoplasma Treatment Agents | Elimination of contamination from valuable cultures | Use only for irreplaceable cell lines; follow with rigorous re-testing; maintain treated cultures in quarantine [77] |
| Antibiotics | Prevention of bacterial contamination | Avoid continuous use to prevent masking low-level contamination and developing resistant strains [79] |
Quality Control Implementation Framework
Establishing a Routine Monitoring Program
Implementing a systematic quality control program is essential for maintaining culture health. The following workflow outlines key decision points in mycoplasma testing and response:
Contamination Response Protocol
When mycoplasma contamination is detected, a systematic response is critical to prevent laboratory-wide spread:
Maintaining mycoplasma-free cell cultures requires diligent implementation of comprehensive quality control measures. By establishing routine monitoring protocols, validating critical reagents, training personnel in proper aseptic technique, and responding systematically to contamination events, research laboratories can protect valuable cell lines, ensure experimental reproducibility, and generate reliable scientific data. In stem cell research and biopharmaceutical development, where cellular integrity directly impacts scientific conclusions and product safety, this vigilance is not merely optional—it is fundamental to scientific integrity and advancement.
Ensuring Compliance: Validating Methods and Comparing International Standards
The following table summarizes the key methodological differences for the compendial mycoplasma tests as outlined in the United States Pharmacopeia (USP), European Pharmacopoeia (Ph. Eur.), and Japanese Pharmacopoeia (JP).
| Testing Parameter | USP <63> | Ph. Eur. 2.6.7 | Harmonization Status & JP |
|---|---|---|---|
| Core Reference | USP Chapter <63> Mycoplasma Tests [81] | Ph. Eur. Chapter 2.6.7 Mycoplasmas [81] | JP methods are harmonized; many general microbiology chapters are aligned across the three pharmacopeias [82]. |
| Nutritive Properties (Solid Media) | Count must be within a 0.5-log unit range of the inoculate (e.g., 32-316 CFU for a 100 CFU inoculum) [81]. | Growth must not differ by a factor greater than 5 from the inoculate (e.g., 20-500 CFU for a 100 CFU inoculum) [81]. | Not specified in available search results, but general harmonization efforts are ongoing [82] [83]. |
| Inhibitory Substances (Solid Media) | Plates with test article must be within a 0.5-log unit range of plates without it [81]. | Plates with product must have no fewer than 1/5 the colonies of plates without it [81]. | Not specified in available search results. |
| Incubation Temperature | 36 ± 1 °C [81] | 35–38 °C [81] | Not specified in available search results. |
| Incubation Atmosphere | Microaerophilic (nitrogen with 5-10% CO₂) [81] | Microaerophilic (hydrogen with <0.5% O₂ and/or nitrogen with 5-10% CO₂) [81] | Not specified in available search results. |
| Positive Controls | At least two species: one dextrose fermenter and one arginine hydrolyzer [81]. | At least one species from a list of six [81]. | Not specified in available search results. |
| Alternative/Nucleic Acid Testing | Alternative methods may be used if validated and comparable to culture methods; specifics are not detailed [81]. | Includes foundational requirements for validation and use of nucleic acid-based tests (e.g., PCR) [81]. | The JP is part of the Pharmacopeial Discussion Group (PDG) working on harmonization, including alternative methods [82]. |
Frequently Asked Questions (FAQs) for Researchers
Q1: Our stem cell culture is critical and cannot be held for 28 days. Are faster mycoplasma testing methods accepted by the pharmacopeias?
Yes, rapid Nucleic Acid Testing (NAT) methods are increasingly accepted. While the traditional culture-based method takes 28 days, rapid techniques like PCR can deliver results in hours to a few days [84] [85].
- Regulatory Status: Ph. Eur. 2.6.7 explicitly includes foundations for validating and using nucleic acid-based tests [81]. USP <63> also allows for validated alternative methods that are comparable to the culture assay [81]. The JP, as part of the international harmonization efforts, also recognizes this trend [82].
- Available Technologies: Real-time quantitative PCR (qPCR) assays, such as the MycoSEQ, can provide results within 3-5 days and meet regulatory guidelines [85]. Even faster cartridge-based systems like BioFire can generate results in 24 hours to 3 days by targeting RNA, which helps indicate viable contamination [85].
Q2: We suspect our fetal bovine serum (FBS) is a contamination source. What is the most effective way to sterilize it?
Mycoplasma contamination from raw materials like FBS is a known risk [5]. Filtration is the primary method for sterilization.
- Filtration Pore Size: Use 0.1 µm-rated membrane filters instead of the more common 0.2 µm filters. The small size and plasticity of mycoplasma allow some species to penetrate 0.2 µm filters [5] [84].
- Process Validation: Be aware that 0.1 µm filtration is not an absolute guarantee of removal. Filter performance can vary by mycoplasma species and process parameters (e.g., differential pressure). It is critical to validate the filtration process for your specific application [84].
- Heat Inactivation: While heat (e.g., 30 minutes at 45°C or 10 minutes at 60°C) can inactivate mycoplasmas, it may also denature heat-sensitive components in the serum, altering its growth-promoting properties [84].
Q3: Our valuable master stem cell bank is contaminated with mycoplasma. Is discarding it the only option?
No, several elimination strategies exist, but they carry risks and should be used as a last resort for irreplaceable cultures.
- Antibiotic Treatment: Using antibiotics like Plasmocin is a common and relatively simple approach. However, it carries risks of generating antibiotic-resistant mycoplasma or causing cytotoxicity in your cells [86] [87].
- In Vivo Passage in Mice: This sophisticated technique involves injecting contaminated cells into the peritoneal cavity of immunodeficient mice. The mouse immune system clears the contamination, and clean cells can be recovered from the ascites. A study demonstrated success in eliminating M. hyorhinis from human hepatocytes in 14 days using this method, with confirmation that cell function was not significantly altered [86]. This method requires specialized animal facilities and rigorous checks to ensure no cross-contamination with mouse cells occurs [86].
Q4: Why are there differences between the pharmacopeias, and what is being done to harmonize them?
The USP, Ph. Eur., and JP are independent organizations with different histories and structures. Harmonization is a ongoing, collaborative process to align standards and reduce the burden on manufacturers who operate globally [82].
- The Pharmacopeial Discussion Group (PDG): Since 1989, the USP, Ph. Eur., JP, and now the Indian Pharmacopoeia have been working through the PDG to harmonize excipient monographs and general chapters [82] [83].
- Progress: Key general microbiology chapters, such as the sterility test (<71>), microbial enumeration test (<61>), and test for specified microorganisms (<62>), are already harmonized between the three major pharmacopeias [82].
- Recent Initiatives: The Ph. Eur. and JP have recently launched a bilateral prospective harmonization project specifically for active substance and medicinal product monographs, building upon their long-standing collaboration [83].
Essential Research Reagent Solutions
The following table lists key reagents and their applications for mycoplasma testing and contamination control in stem cell research.
| Reagent / Material | Primary Function | Application in Mycoplasma Management |
|---|---|---|
| Hayflick Medium (Broth & Agar) | Culture medium specifically formulated for the growth of mycoplasmas [84]. | Used as the primary medium in the compendial 28-day direct culture method for detecting viable mycoplasma [84]. |
| Hoechst 33258 Stain | A fluorescent dye that binds to DNA [84]. | Used in the indicator cell culture method (indirect test). Stained cells are examined under a fluorescence microscope to detect extranuclear mycoplasma DNA [84]. |
| PCR/Q-PCR Kits (e.g., MycoSEQ) | Kits containing primers and probes for the amplification of mycoplasma-specific DNA sequences [84] [85]. | Used for rapid and sensitive detection of mycoplasma contamination via nucleic acid testing, significantly reducing time-to-result compared to culture [85]. |
| Plasmocin | A combination of antibiotics targeting mycoplasmas [87]. | Used as a curative treatment to eliminate mycoplasma contamination from precious, irreplaceable cell lines or viral supernatants [87]. |
| Specific Positive Control Strains (e.g., M. pneumoniae, A. laidlawii) | Viable mycoplasma organisms used as controls [81] [85]. | Essential for validating the nutritive properties of each batch of media and for serving as a positive control in every assay to ensure the test is functioning correctly [81]. |
Experimental Workflow for Mycoplasma Testing and Management
The diagram below outlines a comprehensive workflow for preventing, detecting, and managing mycoplasma contamination in a stem cell research laboratory, integrating both compendial and rapid methods.
Frequently Asked Questions (FAQs)
Q1: What are the key differences between Limit of Blank (LOB), Limit of Detection (LOD), and Limit of Quantitation (LOQ)?
A: These three parameters form a crucial hierarchy for understanding an assay's detection capabilities:
- Limit of Blank (LOB): The highest apparent analyte concentration expected to be found when replicates of a sample containing no analyte are tested. It represents the background noise of your assay system [88].
- Limit of Detection (LOD): The lowest analyte concentration likely to be reliably distinguished from the LOB and at which detection is feasible. According to CLSI EP17 guidelines, a sample at the LOD should be distinguishable from the LOB 95% of the time [88].
- Limit of Quantitation (LOQ): The lowest concentration at which the analyte can not only be reliably detected but at which some predefined goals for precision and bias are met. The LOQ must be equal to or greater than the LOD [88].
Q2: Why is mycoplasma detection particularly challenging in cell culture, and what are the consequences of contamination?
A: Mycoplasma contamination is problematic because:
- Difficult Detection: Infection is persistent and difficult to detect without specialized testing. Contamination doesn't produce turbidity or visible cytopathic effects in cultures, even at high concentrations (10⁵–10⁸ organisms/mL) [36] [89].
- Altered Cell Behavior: Mycoplasma contamination can change many cell reactions, including altering cell growth rate, inducing morphological changes or cell transformation, and mimicking virus infection [36].
- Data Compromise: Experimental data derived from contaminated cell lines is likely to be invalid due to significant but unseen influences on cellular processes [36].
- Product Safety: For biological products, contamination can lead to unsafe final products [89].
Q3: What are the best practices for determining analytical sensitivity/LOD in molecular assays?
A: For robust LOD determination:
- Replicate Testing: Perform 20 measurements at, above, and below the likely analytical sensitivity [90].
- Include Extraction Controls: Assays using nucleic acid extraction must include controls to detect errors in the extraction process [90].
- Use Appropriate Controls: Employ whole bacteria or viruses as control material for nucleic acid isolation, preparation, or process [90].
- Matrix Considerations: Account for potential environmental inhibitors, loss of organisms, or impurities when testing clinical or environmental samples [91].
Q4: How do I address uneven colony counts in triplicate CFU assays?
A: Uneven colony distribution in Colony-Forming Unit (CFU) assays typically stems from improper mixing. After adding cells to MethoCult medium, vortex for at least 4 seconds for equal distribution. Also ensure that [92]:
- Thawed MethoCult medium is thoroughly mixed before dispensing into tubes
- Cell volumes added to MethoCult do not exceed a 1:10 ratio to avoid viscosity issues
- Tubes containing cells and MethoCult medium are thoroughly mixed before plating
Troubleshooting Guides
Problem: High variability in LOD determination studies
Potential Causes and Solutions:
| Cause | Solution | Validation Approach |
|---|---|---|
| Insufficient replicates | Increase replicates to 20-60 per dilution as recommended by guidelines [91] [90] | Use statistical analysis to determine 95% positivity cut-off [89] |
| Improper dilution series | Prepare serial dilutions around target concentration determined through range-finding studies [91] | Ensure linear response across the range with correlation coefficient R² ≥ 0.99 [93] |
| Matrix effects | Spike samples into relevant matrices (PBS, broth, serum, cell culture supernatant) [89] | Demonstrate specificity with maximal unspiked matrix concentration below LLOQ [93] |
| Inhibition issues | Include exogenous RNA/DNA controls to verify absence of inhibition in extraction [89] | Recovery rates should be between 85%-105% for accuracy [93] |
Problem: Mycoplasma detection assay lacks sensitivity
Troubleshooting Steps:
- Verify Nucleic Acid Extraction: Use column purification systems with guanidine thiocyanate buffer for efficient lysis and DNase treatment to remove contaminating DNA [89].
- Optimize Target Selection: For RT-PCR methods, target 16S rRNA which is typically present in more copies per cell than corresponding DNA, thus increasing assay sensitivity [89].
- Validate with Appropriate Controls: Use authenticated reference standards that are titered or quantitated, such as ATCC strains with pre-established concentrations [91] [89].
- Assay Design: Employ multiple primer-probe sets targeting different phylogenetic groups within Mollicutes to ensure broad detection range [89].
Problem: CFU assays showing dehydration or irregular colony growth
Troubleshooting Guide:
| Symptom | Possible Cause | Solution |
|---|---|---|
| Speckled or cracked culture appearance | Low humidity in incubator | Maintain high humidity (≥95%) using water dishes [92] |
| Colonies floating or smearing | Runny methylcellulose medium | Ensure MethoCult is thoroughly mixed; avoid exceeding 1:10 cell suspension dilution [92] |
| Uneven colony distribution | Improper vortexing after cell addition | Vortex cell-MethoCult mixture for at least 4 seconds before plating [92] |
| Grainy background | Excessive RBCs in sample | Deplete red blood cells before assay setup [92] |
| No colonies detected | Complete culture dehydration | Verify water dishes are maintained throughout culture period; check incubator humidity controls [92] |
Experimental Protocols and Validation Data
Protocol: Validation of Mycoplasma Detection Assay Using RT-PCR
Materials and Methods based on [89]:
Primer-Design: Test three primer-probe sets in three reaction mixes based on phylogenetic relationships within Mollicutes class:
- Master mix "Orale" (MMO): For group including M. hominis, M. orale, M. arginini, M. fermentans, M. hyorhinis
- Master mix "Pneumoniae" (MMP): For group including M. pneumoniae, M. gallisepticum
- Master mix "Laidlawii" (MML): For Acholeplasma species
Reference Strains: Use well-characterized Mycoplasma and Acholeplasma organisms titered by CFU determination:
- M. arginini (ATCC #23243), M. fermentans (ATCC #19989)
- M. hyorhinis (ATCC #17981), M. orale (ATCC #23714)
- M. pneumoniae (ATCC #15531), A. laidlawii (ATCC #23206)
RNA Extraction: Use column purification system with:
- Initial lysis with denaturing buffer containing guanidine thiocyanate
- On-column DNase treatment to remove contaminating DNA
- Low-speed centrifugation for debris removal from cell lysates
RT-PCR Amplification:
- Perform two-step RT-PCR
- Use sequence detection system with fluorescent signal analysis
- Express results as CT (threshold cycle) values
- Perform all PCR reactions in triplicate
Protocol: Determination of Limit of Detection (LOD)
Step-by-Step Procedure based on [91] [90]:
- Sample Quantification: Use authenticated samples with pre-established concentration or quantify control samples.
- Dilution Series Preparation: Create serial dilutions around appropriate concentration determined through range-finding study.
- Replicate Testing: Test each dilution in at least 20-60 replicates.
- Statistical Analysis: Determine the minimum concentration that can be reliably distinguished from absence of sample with 95% confidence.
Table: LOD Validation Data Template
| Dilution Factor | Target Concentration | Positive/Total Replicates | % Positive | Meets LOD Criteria? |
|---|---|---|---|---|
| 1:10 | 1000 copies/mL | 20/20 | 100% | No (above LOD) |
| 1:50 | 200 copies/mL | 20/20 | 100% | No (above LOD) |
| 1:100 | 100 copies/mL | 19/20 | 95% | Yes (at LOD) |
| 1:200 | 50 copies/mL | 10/20 | 50% | No (below LOD) |
| 1:500 | 20 copies/mL | 2/20 | 10% | No (below LOD) |
Validation Parameters for Potency Assays in Cell Therapy
Table: Validation Parameters for VEGF Potency Assay in CD34+ Cell Therapy [93]
| Parameter | Acceptance Criteria | Experimental Results | Method |
|---|---|---|---|
| Linearity | R² ≥ 0.95 | R² = 0.9972 | 8 concentrations (20-2800 pg/mL) |
| Range | 20-2800 pg/mL | Covered 80% of low limit to 120% of high limit | Spiked StemFeed medium |
| Repeatability Precision | CV ≤ 10% | CV ≤ 10% | Multiple replicates per concentration |
| Intermediate Precision | CV ≤ 20% | CV ≤ 20% | Different days, different operators |
| Accuracy | Recovery 85-105% | 85-105% recovery for each concentration | Spiked vs measured comparison |
| Specificity | Unspiked < LLOQ (20 pg/mL) | Max 2 pg/mL in unspiked medium | StemFeed medium without VEGF |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Assay Validation in Stem Cell Research
| Item | Function | Example Products/Sources |
|---|---|---|
| Authenticated Reference Standards | Provide accurately quantified materials for LOD determination | ATCC Genuine Cultures, ATCC Genuine Nucleics [91] |
| Methylcellulose-based Media | Support colony growth in CFU assays | MethoCult H4034 Optimum for human hematopoietic progenitors [92] |
| Quantitative Immunoassay Systems | Automated potency assay quantification | ELLA system with VEGF cartridge for automated immunoassay [93] |
| Mycoplasma Detection Primers | Broad-range detection of contamination | Custom primer-probe sets for MMO, MMP, MML master mixes [89] |
| Nucleic Acid Purification Kits | RNA extraction with DNase treatment | Column purification systems with guanidine thiocyanate buffer [89] |
| Viability Stains | Cell viability assessment | Trypan blue, 7AAD, AO/PI (note: trypan blue typically gives higher viability vs nuclear dyes) [92] |
| Low Adherence Cultureware | Prevent cell adhesion in CFU assays | Specialized plates for methylcellulose cultures [92] |
| Molecular Controls | Quality control for molecular assays | ACCURUN molecular controls, AccuSeries linearity panels [90] |
In the field of stem cell research, maintaining contamination-free cultures is not merely a best practice but a fundamental prerequisite for data integrity and reproducibility. Mycoplasma contamination, in particular, represents a pervasive threat due to its cryptic nature, altering cellular functions and compromising experimental outcomes without causing turbidity in media [24]. This performance review evaluates leading commercial mycoplasma detection kits, providing a critical resource for researchers, scientists, and drug development professionals dedicated to safeguarding their stem cell lines. Our analysis is framed within a broader thesis on contamination prevention, focusing on providing actionable data and troubleshooting guidance to empower your quality control processes.
Comparative Analysis of Leading Kits
To facilitate an informed selection, we have summarized the key performance metrics and specifications of several prominent mycoplasma detection kits in the table below. This comparison focuses on attributes critical for sensitive stem cell applications.
Table 1: Performance Comparison of Commercial Mycoplasma Detection Kits
| Company / Kit Name | Technology | Detection Sensitivity | Time to Result | Key Features | Price (USD, unless noted) |
|---|---|---|---|---|---|
| SouthernBiotech Mycoplasma Detection Kit [94] | PCR | 2-5 femtograms of DNA | < 3 hours | Detects over 95% of common cell culture contaminants; includes an internal control to prevent false negatives. | $217.00 (50 reactions) |
| Minerva Biolabs VenorGeM Classic [95] | PCR | Information Missing | Information Missing | Designed for routine screening of cell cultures, supernatants, and media. | €159.90 |
| Minerva Biolabs VenorGeM qEP [95] | Quantitative PCR (qPCR) | Information Missing | Information Missing | Designed for rapid and quantitative results. | €362.30 |
| abcam Mycoplasma PCR Detection Kit (ab289834) [96] | PCR | 200+ species | < 2 hours | No DNA extraction required; includes a ready-to-use primer mix. | Information Missing |
| General Market Pricing (PCR Kits) [97] | PCR | Information Missing | Information Missing | General market price range for PCR-based detection kits. | $300 – $1,200 per kit |
Vendor Selection Guidance
Different research and production environments have varying requirements for throughput, regulatory compliance, and budget. The following breakdown aligns vendor strengths with specific use cases:
- Regulated Environments (Biopharma Manufacturing): For highly regulated environments like biopharmaceutical manufacturing, vendors like Lonza, Charles River, and BioMerieux offer validated, compliant solutions with extensive documentation required for regulatory filings [98].
- High-Throughput & Automated Screening: Large-scale testing facilities requiring scalable, high-throughput solutions should explore Hyclone or MilliporeSigma for their robust, adaptable offerings [98]. The market is also seeing a trend toward fully automated platforms to minimize human error and increase throughput [97].
- Research Labs & Cost-Effectiveness: Academic research labs or startups with limited budgets might prefer cost-effective options from vendors like VWR International or Biotool, which provide reliable performance at lower price points [98]. Hain Lifescience is also noted for its ease of use and affordability [99].
Essential Reagent Toolkit for Mycoplasma Detection
Implementing a robust detection protocol requires more than just a kit. The following table details key reagents and materials essential for successful mycoplasma testing in your stem cell lab.
Table 2: Research Reagent Solutions for Mycoplasma Detection
| Reagent / Material | Function | Example & Key Characteristics |
|---|---|---|
| PCR Master Mix | Amplifies target DNA sequences for detection. | ExpressTaq 2X PCR MasterMix [96] - Pre-mixed for convenience and reliability. |
| Species-Specific Primers | Binds to conserved genomic regions of Mycoplasma for specific amplification. | Mycoplasma PCR Primer Mix [96] - Designed for broad detection of over 200 species. |
| Positive Control | Validates that the PCR amplification process is working correctly. | Purified Mycoplasma DNA (e.g., M. orale) [94] - Provides a known positive result for comparison. |
| Internal Control | Rules out false negatives caused by PCR inhibitors in the sample. | Non-mycpolasma DNA supplied in the kit [94] - Confirms the reaction environment is optimal. |
| Nuclease-Free Water | Used to reconstitute reagents without degrading sensitive nucleotides. | Provided in kits to ensure stability and reaction integrity [96]. |
| Electrophoresis Reagents | Visualizes amplified PCR products. | Agarose gel, DNA ladder, and staining dye - Confirms the presence and size of the amplification product. |
FAQs and Troubleshooting Guide
Q1: Our stem cell cultures show no visible signs of contamination, but our experimental results are inconsistent. Could mycoplasma be the cause? Yes. Mycoplasma contamination does not typically cause cloudiness in media and is invisible under standard light microscopy [24]. Instead, it leads to subtle but critical alterations in cell function, including changes in gene expression, metabolism, and proliferation rates [24] [100]. These effects can severely compromise data reproducibility. The National Center for Advancing Translational Sciences (NCATS) found an initial contamination rate of over 10% in incoming cell lines, underscoring the need for routine testing [100].
Q2: What is the recommended frequency for testing our master stem cell banks for mycoplasma? A multi-tiered testing approach is recommended. Master Cell Banks and Working Cell Banks must be tested before use and prior to cryopreservation. For ongoing cultures, testing should be performed every 1-2 weeks, or at a minimum, when a new culture is initiated from a frozen stock and before publishing results or using cells in a critical experiment [24] [100]. Most scientific publishers now require proof of mycoplasma testing for manuscript submission [95].
Q3: We got a positive mycoplasma result. What are the immediate steps we should take?
- Quarantine: Immediately move the contaminated culture to a separate, designated incubator to prevent aerosol spread.
- Dispose: Autoclave the contaminated culture and all associated media and consumables that came into contact with it.
- Decontaminate: Thoroughly clean and decontaminate the work area, incubator, and any shared equipment used for the culture.
- Investigate: Test all other cell lines that were handled concurrently. Review and reinforce aseptic techniques with all lab personnel [24].
Q4: Our PCR assay shows a weak or ambiguous band. How should we interpret this? A weak band is indicative of a positive result, potentially from a low-level infection. First, verify the result by running the PCR products on an agarose gel alongside the provided positive control; a band in the expected size range (e.g., ~370-550 bp for the abcam kit) confirms contamination [96]. Ensure you have used the internal control to rule out PCR inhibition, which can cause false negatives [94]. If the result remains ambiguous, repeat the test with a fresh sample of supernatant or consider using a more sensitive qPCR assay.
Q5: How does the choice between conventional PCR and qPCR impact our detection capability?
- Conventional PCR: Is rapid, cost-effective, and suitable for routine screening. It provides a qualitative (yes/no) result through gel electrophoresis [94] [95].
- qPCR (Quantitative PCR): Offers greater sensitivity and speed, and provides quantitative data on the level of contamination. It does not require gel electrophoresis, reducing hands-on time and contamination risk. It is ideal for high-throughput settings and for monitoring the effectiveness of eradication efforts [97] [95].
Experimental Workflow for PCR-Based Mycoplasma Detection
The following diagram illustrates the generalized workflow for detecting mycoplasma contamination in a stem cell culture using a standard PCR-based kit. This protocol is adapted from common procedures described in commercial kits [94] [96].
Diagram 1: Mycoplasma PCR Detection Workflow
Detailed Protocol: PCR-Based Detection
Objective: To detect the presence of mycoplasma DNA in a sample of stem cell culture supernatant.
Materials:
- Mycoplasma Detection Kit (e.g., from SouthernBiotech [94] or abcam [96])
- Cell culture supernatant sample (avoid excessive cell carryover)
- Nuclease-free water
- Thermal cycler
- Agarose gel electrophoresis equipment
Methodology:
- Sample Collection: Aseptically collect approximately 100 µL of supernatant from a test culture that has been grown for at least 3 days without antibiotic treatment [94].
- Reaction Setup:
- Thaw all kit components on ice and briefly centrifuge.
- Prepare a PCR premix solution according to the kit instructions. This typically includes PCR buffer, nucleotides, Taq polymerase, and the specific primer mix designed to amplify a conserved 16S rRNA region of the mycoplasma genome [94] [96].
- Aliquot the premix into PCR tubes.
- Add a small volume (e.g., 1-5 µL) of the supernatant sample directly to the premix. No prior DNA extraction is needed for some kits [96]. Include a positive control (supplied mycoplasma DNA) and a no-template control (nuclease-free water) in each run.
- PCR Amplification: Place the tubes in a thermal cycler and run the amplification program. A typical program might include:
- Initial Denaturation: 95°C for 2 minutes.
- 35-40 Cycles of:
- Denaturation: 95°C for 30 seconds.
- Annealing: 55-60°C for 30 seconds.
- Extension: 72°C for 1 minute.
- Final Extension: 72°C for 5 minutes.
- Result Analysis: Analyze the PCR products using agarose gel electrophoresis.
The mycoplasma detection landscape is evolving rapidly. Key trends include the increased adoption of qPCR and automated, high-throughput platforms to enhance efficiency and reduce human error [98] [97]. Furthermore, Artificial Intelligence (AI) is beginning to shape the field, with companies like Eurofins Scientific and Cytena GmbH integrating AI-driven tools for data analysis and cell line quality control to improve detection accuracy and reduce false negatives [97]. Regulatory landscapes are also tightening globally, particularly with the implementation of the European Union's In Vitro Diagnostic Regulation (IVDR), pushing vendors to provide more robustly validated and compliant solutions [97].
For stem cell researchers, the imperative for routine, reliable mycoplasma detection is clear. The selection of a detection kit should be guided by the specific application—whether for rigorous, compliant manufacturing or for fundamental academic research. By integrating the comparative data, troubleshooting guides, and standardized protocols provided in this review, laboratories can establish a formidable defense against mycoplasma contamination. This proactive approach is indispensable for ensuring the authenticity of cellular models, the reproducibility of scientific data, and the ultimate safety of any cell-based therapies derived from stem cell research.
In stem cell research and therapy development, phase-appropriate testing is a risk-based framework for designing validation strategies that evolve from initial research through to commercial product release. This approach ensures that the level of control and testing is commensurate with the stage of development, the specific risks of the product, and its intended clinical use. For stem cell-based products, which are inherently variable and susceptible to contaminants like mycoplasma, a rigorous, phase-appropriate quality control system is not just a regulatory requirement but a critical component of scientific integrity and patient safety [32] [101]. This guide provides troubleshooting and FAQs for professionals navigating this complex landscape, with a special focus on mycoplasma prevention.
FAQs and Troubleshooting Guides
Fundamental Concepts and Strategies
Q1: What does "phase-appropriate" mean in the context of stem cell testing? A phase-appropriate approach tailors the stringency of quality control and the extent of validation to the specific stage of product development.
- Early R&D: Focus is on proof-of-concept and basic characterization. Testing may use research-grade reagents and focus on identity and pluripotency markers [101].
- Preclinical Development: As a product moves toward clinical trials, testing must become more rigorous. This includes implementing early Good Manufacturing Practice (GMP) principles and conducting extensive safety testing, such as sterility and mycoplasma screening [32] [19].
- Clinical Trials & Commercial Release: At this stage, full GMP compliance is required. The testing panel is most extensive, requiring validated methods for potency, purity, identity, and safety, including comprehensive adventitious agent testing [32] [19].
Q2: Why is mycoplasma a particularly serious contaminant in stem cell cultures? Mycoplasma contamination is a major concern because:
- It is difficult to detect visually as it does not cause turbidity in the media and lacks a cell wall, making it resistant to common antibiotics like penicillin [5].
- It can extensively alter cell physiology and metabolism, leading to unreliable experimental data and potentially dangerous clinical products [5].
- Contamination can persist undetected for extended periods while compromising the quality of your cells and all downstream experiments or products [5].
Q3: What are the primary sources of mycoplasma contamination in a cell culture lab? The most common sources are:
- Laboratory Personnel: Human-derived species like M. orale and M. fermentans are frequently introduced via poor aseptic technique [5].
- Contaminated Cell Lines: The single biggest source is receiving already-infected cultures from other labs or suppliers [5].
- Contaminated Reagents: While less common with reputable suppliers, animal-derived products like fetal bovine serum (source of M. arginini and A. laidlawii) and trypsin (source of M. hyorhinis) can be a source [5].
Testing and Validation Protocols
Q4: What are the key quality control checkpoints for a stem cell line? Integrated quality control should be performed at key stages [101]:
- Cell Banking: Test master and working cell banks for identity, viability, sterility, and mycoplasma.
- Pluripotency Verification: Confirm expression of markers like SSEA-4, TRA-1-60, and Oct4.
- Culture Purity: Routinely monitor for the absence of spontaneously differentiated cells.
- Batch-to-Batch Consistency: Ensure consistency across different production runs using standardized reagents and assays.
Q5: What methods are used to detect mycoplasma, and what are their pros and cons? The following table summarizes common detection methods:
| Method | Principle | Pros | Cons | Phase Applicability |
|---|---|---|---|---|
| PCR-based Kits [101] | DNA amplification of mycoplasma-specific sequences | - Rapid (hours)- High sensitivity- Easy to perform | - May detect non-viable organisms- Requires specific equipment | All phases (R&D to Commercial) |
| Indicator Cell Culture (DNA Stain) [5] | Staining DNA in indicator cells; mycoplasma appear as fluorescent specks on the cell surface. | - Can detect very low levels of infection- Visual confirmation | - Longer turnaround (1-3 weeks)- Subject to interpretation | Preclinical & Clinical |
| Microbiological Culture [5] | Growth of mycoplasma on agar plates. | - "Gold standard"- Confirms viability | - Very slow (up to 4 weeks)- Some strains do not grow | Commercial Release (for regulatory filing) |
Q6: Our lab is transitioning a research-stage iPSC line toward clinical application. What is the most critical shift in testing philosophy? The most critical shift is from a reactive to a proactive and documented quality system. In research, problems are often fixed as they arise. For clinical applications, you must:
- Establish a Quality Management System (QMS) with strict documentation of all procedures (SOPs).
- Implement rigorous environmental monitoring of your cleanrooms and equipment [19].
- Move from research-grade to GMP-grade reagents and qualify your critical raw materials [32].
- Formalize your mycoplasma testing strategy, making it a routine and documented release test for cell banks [19].
Troubleshooting Common Scenarios
Scenario 1: You get a positive mycoplasma test result.
- Immediate Action: Isolate the contaminated culture immediately. Do not open it inside your main tissue culture hood.
- Containment: Treat all media, reagents, and equipment that came into contact with the culture as contaminated. Quarantine and test all other cultures that were handled in the same hood or incubator.
- Decontamination: Perform a thorough decontamination of the laminar flow hood, incubators, and any shared equipment.
- Long-term Decision: The safest and most recommended course of action is to discard the contaminated culture. While eradication methods exist (e.g., antibiotics), they are not always reliable, can induce cellular stress, and may mask the problem without fully resolving it [5].
Scenario 2: Your stem cell line shows inconsistent differentiation results between batches.
- Troubleshooting Steps:
- Check Pluripotency: Verify that your starting population has a consistent and high level of pluripotency markers before differentiation begins [101].
- Audit Reagents: Check the lot numbers and certificates of analysis for all growth factors and differentiation media components. Small variations can have major effects.
- Monitor Karyotype: Extended culture can lead to genomic and epigenetic instabilities that alter differentiation potential [32].
- Test for Contamination: Rule out low-level, non-visible microbial contamination, including mycoplasma, which can profoundly affect cell metabolism and behavior [5].
Phase-Appropriate Testing Workflow
The following diagram illustrates the evolution of testing strategies from basic research to commercial release, highlighting the increasing rigor and scope of quality control.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and materials essential for maintaining quality control and preventing contamination in stem cell culture.
| Item | Function/Application | Key Considerations |
|---|---|---|
| Pluripotency Antibodies (e.g., Anti-SSEA-4, TRA-1-60) [101] | Verification of undifferentiated stem cell status via flow cytometry or immunocytochemistry. | Use validated, specific monoclonal antibodies to ensure batch-to-batch consistency and reliable results. |
| Mycoplasma Detection Kit (PCR-based) [101] | Rapid and sensitive screening for mycoplasma contamination in cell culture supernatants. | Choose a kit with high sensitivity and broad species coverage. Perform tests regularly (e.g., monthly). |
| GMP-Grade Growth Factors & Media [32] | Used in the manufacture of cells for clinical trials to ensure product quality and safety. | Sourced with full traceability and certificates of analysis. Essential for clinical-stage manufacturing. |
| Good Manufacturing Practice (GMP) [32] | A quality assurance system to ensure products are consistently produced and controlled according to quality standards. | Required for clinical applications. Involves strict control of processes, materials, documentation, and facility design. |
Experimental Protocol: Routine Mycoplasma Screening by PCR
This is a generalized protocol based on common best practices and commercially available kits [101].
1. Sample Collection:
- Collect at least 0.5 mL of cell culture supernatant from a test culture that has been incubated for at least 3 days without antibiotic treatment. Include a known positive control (e.g., purposefully contaminated culture) and a negative control (fresh culture medium).
2. Sample Preparation (if required by kit):
- Some kits allow direct use of supernatant without DNA purification. If purification is needed, follow the manufacturer's instructions.
3. PCR Setup:
- On ice, prepare the PCR master mix according to the kit's instructions. This typically includes Taq polymerase, dNTPs, reaction buffer, and primers specific for the conserved 16S rRNA region of mycoplasma.
- Aliquot the master mix into PCR tubes and add the template DNA (your sample and controls).
- Briefly centrifuge the tubes to collect the contents.
4. PCR Amplification:
- Place the tubes in a thermal cycler and run the programmed protocol. A typical program might be:
- Initial Denaturation: 95°C for 2 minutes
- 35-40 Cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing: 55-60°C for 30 seconds
- Extension: 72°C for 1 minute
- Final Extension: 72°C for 5 minutes
5. Analysis of Results:
- Prepare a 1.5-2% agarose gel with an appropriate DNA stain.
- Load the PCR products and a DNA ladder into the gel.
- Run the gel at a constant voltage until bands are sufficiently separated.
- Visualize the gel under UV light.
- Interpretation: A distinct band at the expected size (e.g., ~500 bp) in the test sample indicates mycoplasma contamination. The positive control should show a band, and the negative control should not. Any contaminated cultures should be discarded immediately.
Technical Support Center
Troubleshooting Guides
This guide assists researchers in diagnosing and resolving common issues encountered when adapting their mycoplasma testing protocols to comply with the revised European Pharmacopoeia (EP) Chapter 2.6.7, effective April 2026.
Problem 1: Inconsistent Limit of Detection (LOD) in NAT Validation
- Problem Description: During the validation of a Nucleic Acid Amplification Technique (NAT) method, the achieved Limit of Detection (LOD) is inconsistent and fails to meet the new requirement of ≤ 10 CFU/mL or < 100 genomic copies (GC)/mL [102] [103].
- Potential Cause 1: The reference standards used for spiking the product matrix have a high Genomic Copy to Colony Forming Unit (GC/CFU) ratio. A ratio greater than 10 can artificially inflate the GC count, making it difficult to accurately correlate with the required CFU sensitivity [104].
- Solution: Use ready-to-use, CFU-calibrated mycoplasma reference standards with a confirmed low GC/CFU ratio (optimally between 1 and 9) [104]. These standards are prepared from mycoplasma cells in the exponential growth phase, ensuring one CFU corresponds to one or two GCs, enabling an accurate and objective comparison between NAT and culture methods [104].
- Potential Cause 2: Inhibitory substances present in the specific product matrix (e.g., your cell culture medium or biopharmaceutical product) are interfering with the PCR amplification [102].
- Solution: The revised chapter mandates method validation in the user’s own product matrix [102]. Always include an internal control within the NAT assay to rule out inhibition. Spike the candidate matrix with a low number of mycoplasma cells (e.g., 10 CFU) or genomic copies (e.g., 100 GC) to confirm the assay can detect mycoplasma in the presence of that specific material [102] [104].
Problem 2: Failure to Detect Non-Cultivable Mycoplasma Species
- Problem Description: A cell culture batch tests negative for mycoplasma using a culture method but shows cellular physiological defects consistent with contamination.
- Potential Cause: The culture method may fail to detect "non-cultivable" mycoplasma species, which can still adversely affect cell physiology and metabolism [105] [5].
- Solution: The revised EP Chapter 2.6.7 specifies a testing strategy based on risk assessment. For critical products like stem cell lines, it is recommended to use both the culture method and a NAT method conjointly to ensure detection of both cultivable and non-cultivable species [105]. NAT methods are now recognized as fully equivalent for this purpose [103].
Problem 3: Cross-Contamination of Cell Cultures
- Problem Description: Unexplained mycoplasma contamination appears in previously clean cell lines.
- Potential Cause: Mycoplasma contamination spreads easily via aerosols, contaminated equipment, or personnel handling multiple cell lines without adequate aseptic technique. Studies show live mycoplasma can be recovered from laminar flow hood surfaces days after working with an infected culture [5].
- Solution:
- Quarantine: All new cell lines received from external labs should be quarantined and tested for mycoplasma before incorporation into your main culture facility [5] [100].
- Aseptic Technique: Implement strict aseptic techniques, including the use of personal protective equipment and regular disinfection of work surfaces and equipment [5].
- Discard Policy: Wherever possible, immediately destroy contaminated cell lines to prevent the spread to other cultures [100]. For irreplaceable, contaminated stem cell lines, seek validated elimination protocols.
Frequently Asked Questions (FAQs)
Q1: What is the most significant change in the revised EP Chapter 2.6.7? The most significant update is the formal recognition of Nucleic Acid Amplification Techniques (NAT) as fully equivalent to traditional culture-based methods for mycoplasma testing in a regulatory context. This is coupled with a clear, harmonized sensitivity requirement: a detection limit of ≤ 10 CFU/mL or < 100 genomic copies/mL [102] [103].
Q2: Our lab currently uses a validated NAT method. What must we do to comply with the new chapter? You must re-validate your NAT method according to the new guidelines. Key steps include:
- Matrix-Specific Validation: Demonstrate your method achieves the required LOD in your specific product matrix (e.g., your stem cell culture supernatant) to check for inhibitory substances [102].
- Control Requirements: Ensure your test includes an internal control (to detect inhibition) and an external positive control with a defined GC or CFU content close to the LOD [102].
- Reference Standards: Use appropriate reference standards with a GC/CFU ratio of less than 10 for validation [104].
Q3: Why is the GC/CFU ratio for reference standards so important, and what is the new requirement? The GC/CFU ratio ensures an accurate comparison between NAT methods (which detect genomic copies) and culture methods (which detect colony-forming units). A high ratio would make a NAT method appear more sensitive than it actually is. The revised chapter sets an acceptance criterion of a GC/CFU ratio of less than 10 for reference preparations, unless otherwise justified [102] [104]. Commercially available standards with a ratio of 1-9 are ideal [104].
Q4: What are the consequences of mycoplasma contamination in stem cell research? Mycoplasma contamination can extensively compromise stem cell physiology and metabolism, leading to unreliable and irreproducible experimental data [5]. Effects include alterations in cell growth, gene expression, and metabolism, which are particularly critical in translational research and therapy development [5] [100].
Q5: When do the new regulations come into force? The revised EP Chapter 2.6.7 was published in Ph. Eur. Issue 12.2 (October 2025) and will enter into force on 1 April 2026 [105] [102].
The following table summarizes the core quantitative requirements for NAT methods as per the updated regulatory framework.
| Parameter | Old Requirement | New Requirement (EP 2.6.7, 12.2) | Significance |
|---|---|---|---|
| Detection Limit | Not formally defined for NAT. | ≤ 10 CFU/mL or < 100 GC/mL [102] [103]. | Establishes a clear, harmonized benchmark for sensitivity, aligning with USP and JP [102]. |
| GC/CFU Ratio | No specific requirement. | < 10, unless otherwise justified [102] [104]. | Ensures objective comparability between NAT and culture method results during validation [104]. |
| Testing Strategy | Method not specified. | Use of both culture and NAT methods conjointly is recommended unless a risk assessment justifies otherwise [105]. | Ensures detection of both cultivable and non-cultivable mycoplasma species [105]. |
Experimental Protocol: Validating a NAT Method for Compliance
This protocol outlines the key methodology for validating a NAT-based mycoplasma detection test to meet the revised EP Chapter 2.6.7.
1. Principle To demonstrate that a Nucleic Acid Amplification Technique (NAT) achieves a detection limit of ≤ 10 CFU/mL for mycoplasma in a specific product matrix by using calibrated reference standards and appropriate controls.
2. Materials
- Test NAT kit (e.g., qPCR-based, compliant with EP 2.6.7)
- Mycoplasma reference standards (e.g., M. orale, M. fermentans, A. laidlawii) with a defined, low GC/CFU ratio (<10) [104]
- Product matrix (e.g., your stem cell culture supernatant)
- Sterile, mycoplasma-free diluent
- qPCR instrument and consumables
3. Procedure Step 1: Preparation of Spiked Samples
- Thaw the mycoplasma reference standard according to the manufacturer's instructions.
- Prepare a dilution series of the standard in both a sterile diluent and your target product matrix. The dilution series should bracket the target LOD of 10 CFU / 100 GC.
- Include a negative control (un-spiked matrix) for each matrix type.
Step 2: Nucleic Acid Amplification
- Extract nucleic acids from each spiked and control sample.
- Run the NAT assay (e.g., qPCR) following the manufacturer's protocol. Ensure the test includes an internal control to monitor for inhibition in each reaction [102].
Step 3: Data Analysis and LOD Determination
- Analyze the amplification data to determine the proportion of positive replicates at each spiking level.
- The LOD is the lowest concentration at which 95% of the tested replicates are positive. This value must be ≤ 10 CFU/mL or < 100 GC/mL in your product matrix to be compliant [102].
Experimental Workflow for Mycoplasma Testing
The diagram below outlines the decision-making workflow for mycoplasma testing according to the revised chapter's risk-based approach.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents required for implementing compliant mycoplasma testing.
| Item | Function | Key Specification for Compliance |
|---|---|---|
| NAT Test Kit (e.g., Venor Mycoplasma qPCR) | Provides a ready-to-use solution for the rapid and reliable detection of mycoplasma DNA/RNA [103]. | Detection limit of < 100 GC/mL and ≤ 10 CFU/mL; detects >130 mollicute species; includes internal and positive controls [102] [103]. |
| Mycoplasma Reference Standards (e.g., Mycosafe Standards, 100GC Standards) | Used for method validation, as positive controls, and for comparability studies [104]. | CFU-calibrated with a defined GC/CFU ratio of less than 10; covers all pharmacopoeial reference strains [102] [104]. |
| Cell Culture Media & Sera | Growth medium for cell cultures. | Sourced from reputable manufacturers that provide certification of being mycoplasma-free [5]. |
| 0.1µm Pore Size Filters | For sterilizing solutions that might contain mycoplasma, such as raw animal-derived sera. | More effective at removing small, pliable mycoplasma than standard 0.2µm filters [5]. |
Conclusion
Effective management of mycoplasma contamination is a non-negotiable pillar of credible stem cell research and safe clinical translation. A multi-layered defense strategy—combining rigorous aseptic practice, routine monitoring with sensitive molecular assays, and a clear decontamination protocol—is essential. The evolving regulatory landscape, including the 2025 Ph. Eur. revisions, emphasizes a risk-based, scientifically robust approach. Future success hinges on the widespread adoption of these integrated control strategies, ensuring the integrity of scientific data and the safety of transformative cell therapies for patients.
References
- 1. Mycoplasmas - Medical Microbiology - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK7637/]
- 2. Mycoplasma [https://en.wikipedia.org/wiki/Mycoplasma]
- 3. Mycoplasma Infection Types: Causes & Prevention [https://my.clevelandclinic.org/health/diseases/23545-mycoplasma]
- 4. Mycoplasma Contamination: Prevention, Testing & Treatment [https://blog.cellsignal.com/mycoplasma-contamination]
- 5. Prevention and Detection of Mycoplasma Contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584481/]
- 6. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOooaS2InYrH_GbiqwHCunq7wbwUbn6v_i1uLMCRJ8CGfAHnOSgn0]
- 7. Mycoplasma Pneumonia - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430780/]
- 8. Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 9. Prevalence of Macrolide-Resistant Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602751/]
- 10. Mycoplasma pneumoniae Infection Surveillance and Trends [https://www.cdc.gov/mycoplasma/php/surveillance/index.html]
- 11. 6-year trends of Ureaplasma spp. and Mycoplasma ... [https://pubmed.ncbi.nlm.nih.gov/41174608/]
- 12. Prevention, Diagnosis and Eradication of Mycoplasma ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668599/]
- 13. How to Deal with Mycoplasma Contamination in Cell Culture [https://www.creative-biogene.com/blog/how-to-deal-with-mycoplasma-contamination-in-cell-culture]
- 14. 10 Tips for Preventing Mycoplasma Contamination [https://www.regmednet.com/10-tips-for-preventing-mycoplasma-contamination/]
- 15. FAQs on Mycoplasma Elimination - Yeasen [https://www.yeasenbio.com/blogs/cell/faqs-on-mycoplasma-elimination]
- 16. Microbiological contamination in stem cell cultures [https://www.sciencedirect.com/science/article/abs/pii/S1065699507000807]
- 17. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOoqJBrrPZ_aNcQjNnEBuMB2_J3tI2Kz1dE7oegn5Np6n3dOsMI9x]
- 18. Cell Culture Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 19. Microbiological control in stem cell banks - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7080164/]
- 20. Cell Culture Basics - Mycoplasma 101 – A practical guide ... [https://cellculturedish.com/cell-culture-basics-mycoplasma-101-a-practical-guide-to-prevention-detection-and-elimination-of-mycoplasma-contamination/]
- 21. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 22. Troubleshooting Cell Culture Contamination [https://www.creative-bioarray.com/support/troubleshooting-cell-culture-contamination-a-comprehensive-guide.htm]
- 23. Transcription-associated events affecting genomic integrity [https://pmc.ncbi.nlm.nih.gov/articles/PMC5577466/]
- 24. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 25. 10 tips for preventing mycoplasma contamination [https://captivatebio.com/tips-for-preventing-mycoplasma-contamination/]
- 26. On the frontline of the fight against cell culture contamination [https://www.nature.com/articles/d42473-019-00306-1]
- 27. Appendix 3: Cell Culture Hygiene Practices [https://www.isscr.org/basic-research-standards/appendix-3]
- 28. Mycoplasma contamination of cell cultures | Lonza [https://bioscience.lonza.com/lonza_bs/CH/en/mycoplasma-contamination-in-cell-culture]
- 29. Prevention of Contaminations in Cell Culture [https://ibidi.com/content/436-prevention-of-contaminations]
- 30. Detection of Mycoplasma in cell cultures [https://www.nature.com/articles/nprot.2010.43]
- 31. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 32. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 33. Comparison of Five Commercial Molecular Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9945500/]
- 34. Mycoplasma Detection in Cell Cultures [https://www.rapidmicrobiology.com/test-method/rapid-detection-of-mycoplasmas]
- 35. How to Detect a Mycoplasma Contamination? [https://news.minerva-biolabs.com/informative-articles/2024/05]
- 36. Mycoplasma detection in cell cultures: a comparison of four ... [https://pubmed.ncbi.nlm.nih.gov/11204859/]
- 37. Revision of Chapter 2.6.7 of the European Pharmacopoeia ... [https://www.gmp-compliance.org/gmp-news/revision-of-chapter-2-6-7-of-the-european-pharmacopoeia-published-for-comment]
- 38. qPCR Troubleshooting Guide [https://azurebiosystems.com/qpcr-resources/troubleshooting/]
- 39. Troubleshooting qPCR: Interpreting Amplification Curves [https://blog.biosearchtech.com/thebiosearchtechblog/bid/63622/qpcr-troubleshooting]
- 40. What to do when the qPCR results are weird? - Yeasen [https://www.yeasenbio.com/blogs/molecular-biology/what-to-do-when-the-qpcr-results-are-weird]
- 41. Top Ten Most Common Real-Time qRT-PCR Pitfalls [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rtpcr-analysis/general-articles/ten-most-common-real-time-qrt-pcr-pitfalls.html]
- 42. Real-Time PCR Basics Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/real-time-pcr-basics-support/real-time-pcr-basics-support-troubleshooting.html]
- 43. qPCR Troubleshooting: How to Ensure Successful ... [https://dispendix.com/blog/qpcr-troubleshooting]
- 44. Aseptic Laboratory Techniques and Safety in Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 45. Mastering Aseptic Technique: The Foundation of ... [https://www.labmanager.com/mastering-aseptic-technique-the-foundation-of-successful-cell-culture-34208]
- 46. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 47. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 48. How to Eliminate a Mycoplasma Contamination? [https://news.minerva-biolabs.com/informative-articles/2025/08]
- 49. Zero Tolerance: A Perfectionist's Guide to Aseptic Technique [https://bitesizebio.com/9263/zero-tolerance-a-perfectionists-guide-to-aseptic-technique/]
- 50. Aseptic Laboratory Techniques: Plating Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846335/]
- 51. Application of Next-Generation Sequencing in Infections After ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9239075/]
- 52. NGS testing for identification of contamination events [https://services.virusure.com/next-generation-sequencing/ngs-testing-for-adventitious-agent-detection/ngs-testing-for-identification-of-contamination-events/]
- 53. Application of next-generation sequencing for detecting ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1657098/full]
- 54. Application of next-generation sequencing for detecting ... [https://pubmed.ncbi.nlm.nih.gov/41142556/]
- 55. How to Troubleshoot Preparation Sequencing ( Errors ) NGS Guide [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 56. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 57. Quality by Design for Pharmaceutical Microbiology [https://www.americanpharmaceuticalreview.com/Featured-Articles/114489-Quality-by-Design-for-Pharmaceutical-Microbiology/]
- 58. Donor selection, donor testing and pathogen reduction [https://professionaleducation.blood.ca/en/transfusion/clinical-guide/donor-selection-donor-testing-and-pathogen-reduction]
- 59. Mycoplasma Contamination: Where Does It Come From ... [https://blog.addgene.org/mycoplasma-contamination-where-does-it-come-from-and-how-to-prevent-it]
- 60. Diagnostic approaches for viruses and prions in stem cell banks [https://pmc.ncbi.nlm.nih.gov/articles/PMC7118799/]
- 61. Mynox® Gold - Minerva Biolabs GmbH [https://minerva-biolabs.com/en/mycoplasma-elimination/mynox-gold]
- 62. Minerva Biolabs GmbH - FAQ [https://minerva-biolabs.com/en/faq]
- 63. Mycoplasma Elimination [https://minerva-biolabs.com/en/mycoplasma-elimination]
- 64. Mastering tomorrow's cell culture challenges - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/mastering-tomorrows-cell-culture-challenges/]
- 65. Stem Cell Research [https://www.mpbio.com/us/stem-cell-research?srsltid=AfmBOoruuDxNXUs-UfzDSNwjgA3b3-k6qkdjYcblj4DzUyhDHmYIPUIy]
- 66. Considerations for risk and control of mycoplasma in ... [https://www.sciencedirect.com/science/article/abs/pii/S2211339818300224]
- 67. Mycoplasma Contamination of Cell Culture | Review [https://www.invivogen.com/review-mycoplasma]
- 68. Resurgence of Mycoplasma pneumoniae Infections in the ... [https://pubmed.ncbi.nlm.nih.gov/41220194/]
- 69. Cell Culture Contamination, Containment, and Correction [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/cell-contamination-containment-and-correction-good-cell-culture-practices-in-3d.html]
- 70. Corrective and Preventive Action (CAPA): The Definitive ... [https://www.thefdagroup.com/blog/definitive-guide-to-capa]
- 71. Corrective and Preventive Actions (CAPA) [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/corrective-and-preventive-actions-capa]
- 72. CAPA (Corrective and Preventive Action) Form [https://simplerqms.com/capa-form/]
- 73. Mycoplasma Contamination Why It ... [https://hardydiagnostics.com/media/wysiwyg/MICRObits/Pharma/2025/06-June/microbits-pharma-june-2025-newsletter.html]
- 74. Contamination Control Compass Edition #07/2025 [https://news.minerva-biolabs.com/newsletter/2025/07/]
- 75. How to Boost Your Stem Cell Culture for Cell Therapy with ... [https://www.enzo.com/note/how-to-boost-your-stem-cell-culture-for-cell-therapy-with-cell-culture-additives/]
- 76. Mycoplasma quality control of cell substrates and ... [https://www.atcc.org/resources/white-papers/mycoplasma-quality-control-of-cell-substrates-and-biopharmaceuticals]
- 77. Keeping it clean: the cell culture quality control experience at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8506661/]
- 78. Why Test for Mycoplasma in My Cell Culture? [https://www.goldbio.com/blogs/articles/testing-for-mycoplasma?srsltid=AfmBOoonj1fORAIQd8r9pRj0AM8F06Y5oN39NzEijOOa6GJtrBR_m1VX]
- 79. Quality Control Considerations in Cell Culture [https://www.merckmillipore.com/CI/fr/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/quality-control-considerations]
- 80. Mycoplasma Testing for Quality Control | ATCC [https://www.atcc.org/microbe-products/applications/quality-control/mycoplasma-testing]
- 81. USP <63> Mycoplasma Tests: A New Regulation for Mycoplasma Testing | BioPharm International [https://www.biopharminternational.com/view/usp-mycoplasma-tests-new-regulation-mycoplasma-testing]
- 82. Alternatives and rapid Microbiological methods & Pharmacopeias world [https://www.a3p.org/en/alternatives-rapid-microbiological-methods-pharmacopeias-world/]
- 83. JP and Ph. Eur. launch a bilateral prospective harmonisation ... [https://www.edqm.eu/en/-/jp-and-ph.-eur.-launch-a-bilateral-prospective-harmonisation-project-for-active-substance-and-medicinal-product-monographs]
- 84. The Reoccurrence of Mycoplasma Contamination [https://www.bioprocessintl.com/filtration/the-reoccurrence-of-mycoplasma-contamination-prevention-strategies]
- 85. Mycoplasma Testing - Eurofins Scientific [https://www.eurofins.com/biopharma-services/product-testing/services/biopharma-product-testing-services/microbiology/mycoplasma-testing/]
- 86. Elimination of Mycoplasma Contamination from Infected ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2017.00440/full]
- 87. Mycoplasma removal: simple curative methods for viral ... [https://pubmed.ncbi.nlm.nih.gov/23117065/]
- 88. Approaches to Assay Characterization and Validation: Part 1 [https://www.quanterix.com/approaches-to-assay-characterization-and-validation-part-1-limit-of-detection-and-lower-limit-of-quantitation/]
- 89. Assay Validation for Rapid Detection of Mycoplasma ... [https://www.bioprocessintl.com/assays/assay-validation-for-rapid-detection-of-mycoplasma-contamination]
- 90. Molecular Diagnostics - Part 5: Analytical Sensitivity and ... [https://blog.seracare.com/molecular-serology-blog/verification-part5]
- 91. Infectious disease assay development determining the limit ... [https://www.atcc.org/resources/white-papers/infectious-disease-assay-development-determining-the-limit-of-detection]
- 92. Frequently Asked Questions on Performing the CFU Assay [https://www.stemcell.com/frequently-asked-questions-cfu-assay.html]
- 93. Validation of a potency assay for CD34 + cell based therapy [https://www.nature.com/articles/s41598-025-14828-w]
- 94. Mycoplasma Detection Kit [https://www.southernbiotech.com/mycoplasma-detection-kit-13100-01]
- 95. Mycoplasma Detection Kits [https://minerva-biolabs.com/en/mycoplasma-detection-kits]
- 96. Mycoplasma PCR Detection Kit (ab289834) [https://www.abcam.com/en-us/products/assay-kits/mycoplasma-pcr-detection-kit-ab289834]
- 97. Mycoplasma Testing Market Size & Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/global-mycoplasma-testing-market]
- 98. Evaluation Criteria for Mycoplasma Detection Kits [https://www.linkedin.com/pulse/top-mycoplasma-detection-kit-companies-how-compare-739de/]
- 99. Top Mycoplasma Test Kit Companies & How to Compare ... [https://www.linkedin.com/pulse/top-mycoplasma-test-kit-companies-how-compare-wy2cf/]
- 100. Keeping It Clean: The Cell Culture Quality Control ... [https://www.sciencedirect.com/science/article/pii/S2472555222065649]
- 101. Quality Control of Stem Cells [https://www.amsbio.com/research-areas/stem-cell/stem-cells-quality-control]
- 102. New EP 2.6.7 Revision: Compliant Mycoplasma Testing [https://www.rapidmicrobiology.com/news/ep-2-6-7-revision-compliant-mycoplasma-testing-for-biopharma-and-atmps]
- 103. Contamination Control Compass Edition #10/2025 [https://news.minerva-biolabs.com/newsletter/2025/10/]
- 104. CFU-Calibrated, Low-GC/CFU Mycoplasma Standards ... [https://www.rapidmicrobiology.com/news/the-advantages-of-ready-to-use-calibrated-mycoplasma-strains-for-microbial-qc]
- 105. EPC adopts mycoplasmas general chapter and monographs ... [https://www.edqm.eu/en/-/epc-adopts-mycoplasmas-general-chapter-and-monographs-updated-to-incorporate-latest-analytical-developments]