Optimizing Cryopreservation and Thawing for Personalized Stem Cell Products: A Guide for Maximizing Viability and Therapeutic Potential
This article provides a comprehensive guide for researchers and drug development professionals on optimizing cryopreservation and thawing processes for personalized stem cell therapies.
Optimizing Cryopreservation and Thawing for Personalized Stem Cell Products: A Guide for Maximizing Viability and Therapeutic Potential
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on optimizing cryopreservation and thawing processes for personalized stem cell therapies. Covering foundational principles, current methodological applications, and advanced troubleshooting, it synthesizes the latest research and survey data to address key challenges in post-thaw cell recovery, viability, and functional integrity. By presenting evidence-based strategies and comparative analyses of different processing methods, this resource aims to support the development of robust, standardized protocols that ensure the consistent quality and efficacy of stem cell-based therapeutics, from research to clinical application.
The Science of Stem Cell Cryopreservation: Preserving Cellular Potential
Frequently Asked Questions (FAQs)
1. What is the fundamental principle behind cryopreservation? Cryopreservation works by cooling biological materials to extremely low temperatures (typically between -80°C and -196°C) to dramatically reduce all biochemical and metabolic activity, effectively placing cells in a state of suspended animation. This process halts biological decay and preserves cell viability and functionality for future use [1] [2].
2. Why is the cooling rate so critical, and what is the ideal rate? The cooling rate is vital because cooling too quickly leads to lethal intracellular ice crystal formation, while cooling too slowly causes excessive cell dehydration and solute imbalance. A controlled rate of approximately -1°C per minute is ideal for freezing many cell types, as it allows water to safely exit the cell before freezing [2] [3].
3. What are cryoprotective agents (CPAs) and how do they work? CPAs are chemicals that protect biological materials from freezing damage. They function primarily by preventing the formation of damaging ice crystals inside cells. Common examples include Dimethyl Sulfoxide (DMSO) and glycerol. They are categorized as:
- Intracellular CPAs: Small molecules that penetrate the cell membrane (e.g., DMSO, glycerol).
- Extracellular CPAs: Large molecules that do not penetrate the cell (e.g., sucrose, dextrose) [1] [3].
4. What is the difference between controlled-rate freezing and passive freezing? The choice between these methods involves a trade-off between control and simplicity, which is crucial for process development in personalized medicine.
Table: Comparison of Freezing Methods
| Feature | Controlled-Rate Freezing | Passive Freezing |
|---|---|---|
| Process Control | High control over critical cooling parameters [4] | Low control; relies on passive heat transfer [4] |
| Consistency | High, ideal for reproducible manufacturing [4] | Lower, potential vial-to-vial variability [4] |
| Cost & Complexity | High; requires specialized equipment and expertise [4] | Low-cost and simple operation [4] |
| Best Application | Late-stage clinical & commercial products; sensitive cells [4] | Early R&D and early-stage clinical development [4] |
5. What are the key challenges in cryopreserving cells for therapy? Major challenges include:
- Scaling: The "ability to process at a large scale" was identified as the biggest hurdle by 22% of industry survey respondents [4].
- Cryoprotectant Toxicity: Reducing the concentration of potentially toxic agents like DMSO in final therapeutic formulations [5].
- Post-Thaw Viability: Ensuring high cell recovery, viability, and maintained functionality after thawing [4] [3].
Troubleshooting Guides
Poor Post-Thaw Viability
Problem: Cells show low viability or poor recovery after thawing.
Possible Causes and Solutions:
Cause 1: Poor Pre-Freeze Cell Health
Cause 2: Suboptimal Freezing Rate
Cause 3: Inadequate Thawing Technique
Cause 4: Incorrect Cell Concentration
- Solution: Freeze cells at an optimal concentration. A very high concentration can lead to clumping, while a very low concentration can result in low viability. A typical range is 1x10^3 to 1x10^6 cells/mL; determine the ideal concentration for your specific cell type [2].
Low Efficiency in iPSC Colony Formation Post-Thaw
Problem: Thawed induced Pluripotent Stem Cells (iPSCs) fail to form colonies or show poor attachment.
Specific Troubleshooting Steps:
- Check Cell Condition Pre-Freeze: Feed iPSCs daily before cryopreservation and freeze them 2-4 days after passaging. Ensure cell clumps are properly dissolved to allow cryoprotectant penetration [3].
- Validate Cryopreservation Protocol: Handle cells gently during harvesting (centrifuge at 200-300 x g for 2 minutes) and use fresh freezing media. The recommended freezing density for iPSCs is typically 1-2 x 10^6 cells/mL [3].
- Optimize Thawing and Seeding: After rapid thawing, transfer the cell suspension drop-by-drop into 10 volumes of warm medium to gently dilute the cryoprotectant. Seed cells at a high density (e.g., 2x10^5 - 1x10^6 viable cells per well of a 6-well plate) onto Matrigel-coated plates [3].
Contamination and Genetic Instability
Problem: Cultures show contamination or exhibit genetic drift over time.
Preventative Best Practices:
- Aseptic Technique: Use proper sterile techniques and wipe all containers with 70% ethanol or isopropanol before opening [2].
- Rigorous Testing: Test cells for mycoplasma and other microbial contamination before freezing [2].
- Detailed Record Keeping: Maintain accurate records of passage numbers, lot numbers for all reagents, and freezing protocols. This ensures traceability and helps identify the source of any problems [6].
- Proper Long-Term Storage: For long-term storage, use liquid nitrogen tanks in the vapor phase (-135°C to -196°C). Storage at -80°C is acceptable for less than a month but leads to declining viability over time [2] [7].
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Reagents for Cryopreservation Workflows
| Item | Function & Application | Example Use Case |
|---|---|---|
| DMSO | An intracellular cryoprotectant that penetrates the cell to prevent ice crystal formation. | Standard cryopreservation of many cell lines at a final concentration of ~10% [1] [3]. |
| Serum-Free Freezing Media | A chemically-defined, ready-to-use solution providing a safe, protective environment; often GMP-manufactured. | Critical for cell and gene therapy products (e.g., CryoStor CS10) [2]. |
| Specialized Cell Media | Formulated for specific, sensitive cell types to maximize post-thaw recovery and functionality. | mFreSR for human ES/iPS cells; STEMdiff media for cardiomyocytes [2]. |
| Controlled-Rate Freezer | Equipment that precisely controls the cooling rate, typically at -1°C/min, for optimal viability. | Essential for freezing cell therapy products like CAR-T cells or iPSCs [4] [7]. |
| Cryogenic Vials | Single-use, sterile vials designed for ultra-low temperature storage. | Use internally-threaded vials to minimize contamination risk during storage [2] [3]. |
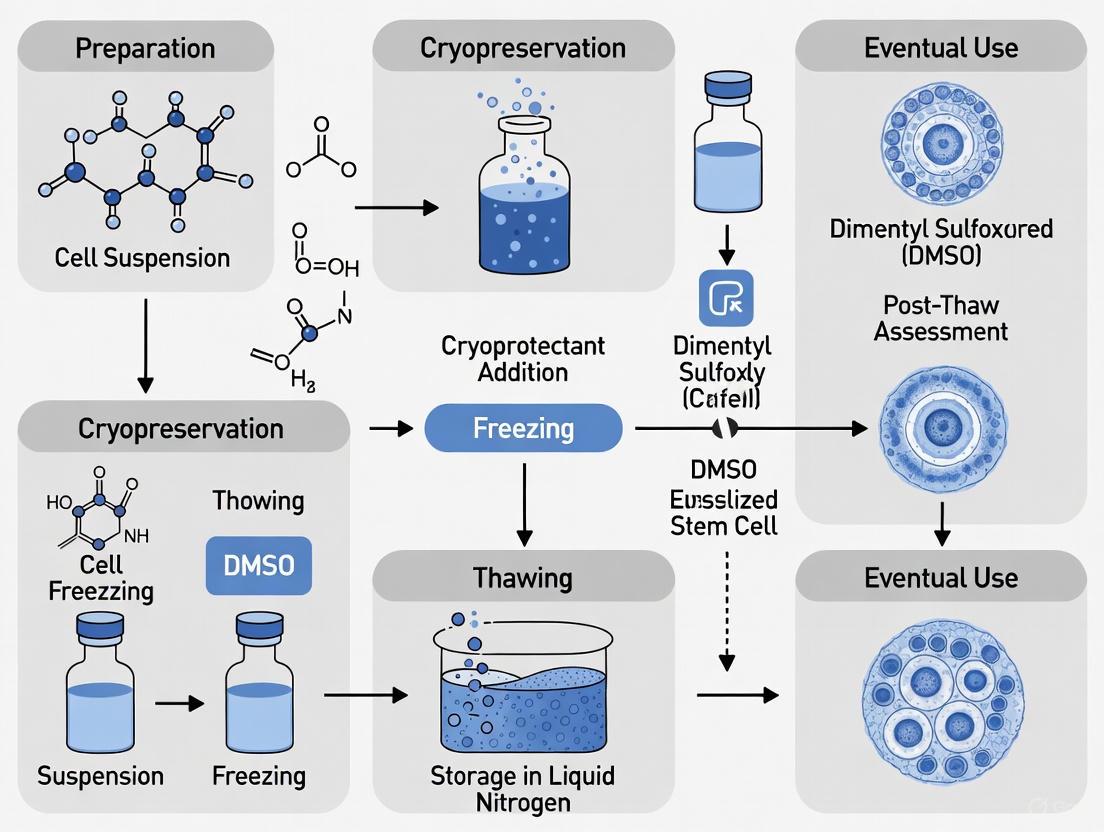
Experimental Workflow and Protocol
The following diagram illustrates the core cryopreservation workflow, highlighting the critical parameters at each stage that ensure biochemical activity is successfully halted while maintaining cell viability.
Detailed Step-by-Step Protocol for Freezing Cells
Harvesting:
- Culture cells to their maximum growth phase, typically >80% confluency and in the log phase of growth [2] [6].
- Detach cells using standard methods (e.g., trypsin) and collect them in a centrifuge tube.
- Centrifuge to pellet the cells (e.g., 200-300 x g for iPSCs). Carefully remove the supernatant [2] [3].
Preparation of Freezing Medium:
- Resuspend the cell pellet in an appropriate, cold freezing medium.
- For many standard cell types, a medium containing 10% DMSO in FBS is used. For sensitive or therapeutic cells, use a specialized, commercially available, serum-free medium like CryoStor CS10 [2] [3].
- Keep the mixture cold to minimize CPA toxicity.
Aliquoting and Cooling:
- Quickly aliquot the cell suspension into labeled cryogenic vials.
- Place the vials immediately into a controlled-rate freezing container (e.g., CoolCell) and transfer it to a -80°C freezer. Alternatively, use a programmable controlled-rate freezer [2] [3].
- Leave the vials in the -80°C freezer for a minimum of 2-4 hours, or preferably overnight.
Long-Term Storage:
Troubleshooting Guides
Low Post-Thaw Viability
Problem: Cell viability is unacceptably low immediately after thawing.
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Intracellular Ice Crystal Formation [8] [9] | Check cooling rate documentation; review freeze curves if available. [4] | Implement controlled-rate freezing at -1°C/min to -3°C/min. [9] Validate the freezing profile for your specific cell type. [4] |
| Osmotic Stress & Cryoprotectant Toxicity [4] [8] | Audit cryoprotectant composition (DMSO concentration, additives) and equilibration time. [10] | Optimize DMSO concentration (test between 5-10%); [10] use serum-free, chemically defined cryomedium; [11] ensure gradual addition and removal of cryoprotectant. |
| Suboptimal Thawing Process [4] [9] | Observe thawing technique; check water bath temperature consistency. | Adopt a rapid thawing protocol (e.g., 37°C water bath until just ice-free). [9] Standardize the thawing process across all staff. [4] |
| Extended Storage Duration [12] | Review inventory records for storage time. | Note that viability can decline ~1.02% per 100 days at -80°C. [12] Prioritize use of older batches and ensure storage at ≤ -150°C or in liquid nitrogen vapor phase for long-term stability. [10] [9] |
Poor Functional Integrity Post-Thaw
Problem: Cells are viable but show impaired therapeutic function (e.g., differentiation, immunomodulation).
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Cryo-Induced Apoptosis [13] | Perform a Live/Apoptosis-Negative (LAN) assay post-thaw, not just viability staining. [13] | Include caspase inhibitors in recovery media; allow a 24-hour recovery period post-thaw before functional assays. [8] |
| Inadequate Post-Thaw Processing [13] | Analyze recovery and purity metrics for different isolation methods (e.g., Wash-only vs. Bead depletion). | Select a post-thaw processing method that aligns with the functional goal (e.g., bead depletion for high purity and long-term function). [13] |
| Damage to Critical Cell Subpopulations | Use flow cytometry to characterize immune subset recovery (e.g., T-cells, CD14+ cells) before and after culture. [13] | Modify the cryopreservation formula; avoid methods that aggressively deplete critical subsets like CD14+ cells if they are required for function. [13] |
| Inconsistent Freezing Profiles [4] | Analyze freeze curves for deviations; correlate with post-thaw functional data. | Move away from "default" controlled-rate freezer (CRF) profiles. [4] Develop and validate an optimized freezing protocol for your specific cell product (e.g., T-cells, iPSCs). [4] |
Frequently Asked Questions (FAQs)
Q1: What is the most reliable method for assessing post-thaw viability, and why is there sometimes a discrepancy between viability and actual function?
A1: The choice of viability assay significantly impacts results. The acridine orange (AO) staining method has been shown to demonstrate greater sensitivity to delayed cellular damage compared to some other methods like 7-AAD [12]. Viability and function can decouple because cryopreservation can induce early-stage apoptosis, where cells still exclude dyes but are destined for cell death and are functionally compromised [13]. For a more predictive assessment, incorporate a Live/Apoptosis-Negative (LAN) assay or a functional assay like a Colony-Forming Unit (CFU) test alongside simple viability staining [13].
Q2: Our lab uses uncontrolled-rate freezing in a -80°C freezer. Is this sufficient for clinically-oriented research?
A2: Evidence suggests that long-term storage at -80°C can maintain sufficient CD34+ hematopoietic stem cell viability for successful engraftment, albeit with a gradual, time-dependent decline in viability (~1.02% per 100 days) [12]. However, the field is moving towards controlled-rate freezing (CRF), with 87% of survey respondents in the cell and gene therapy industry using CRF for its superior control over critical process parameters [4]. CRF reduces variability, improves consistency, and is strongly recommended for late-stage clinical development and commercialization [4].
Q3: We observe good cell recovery after thawing, but the cells perform poorly in subsequent experiments. What could be happening?
A3: This is a classic sign of compromised functional integrity. Key factors include:
- Post-Thaw Processing: The method used to process cells after thawing involves critical trade-offs. A simple "wash-only" method may yield high cell numbers but low purity, while bead-based depletion can provide high purity and better preserve long-term function [13].
- Cryoprotectant Toxicity: Extended exposure to DMSO post-thaw is toxic [4] [8]. Ensure rapid and gentle dilution and removal of cryoprotectant immediately upon thawing.
- Lack of Recovery Time: Thawed cells are under metabolic stress. Allowing an overnight recovery period in culture before using them in assays can significantly improve functional outcomes [8].
Q4: What are the key considerations for scaling up our cryopreservation process from research to clinical-grade manufacturing?
A4: Scaling is identified as a major hurdle [4]. Key considerations include:
- Process Consistency: When cryopreserving an entire manufacturing batch, the time between the start and end of freezing can introduce variability. Staggering sub-batches adds risk of process irreproducibility [4].
- Quality Control: Move beyond post-thaw analytics alone. Incorporate process data, such as freeze curves, as part of manufacturing controls to identify deviations in Controlled-Rate Freezer (CRF) performance [4].
- Automation & Innovation: To enhance scalability and consistency, the industry is integrating automation, AI-driven predictive modeling for freezing protocols, and novel technologies like ice-free vitrification and nanoparticle-based cryoprotectants [11] [8].
Table 1: Impact of Storage Conditions on Cell Viability
| Cell Type | Storage Condition | Storage Duration | Post-Thaw Viability | Key Finding | Source |
|---|---|---|---|---|---|
| CD34+ HSC Products | -80°C (uncontrolled-rate) | Median 868 days | 94.8% (median) | Viability decline of ~1.02% per 100 days; sufficient for engraftment. | [12] |
| Cord Blood Mononuclear Cells (CBMCs) | Not Specified (Likely ≤ -150°C) | N/A | Varies by method | Post-thaw processing method critically impacts recovery & function, not just viability. | [13] |
| Mesenchymal Stem Cells (MSCs) | Liquid Nitrogen (with CS-SC-D1 medium) | N/A | >90% | Clinical-grade, GMP cryomedium can consistently maintain high viability. | [14] |
Table 2: Comparison of Post-Thaw Processing Methods for Cord Blood
| Processing Method | Purity (Depletion Efficiency) | CBMC Yield/Recovery | Impact on Functional Fitness | [13] |
|---|---|---|---|---|
| Wash-Only | Lowest | Highest | Retains all cell types, but may include debris. | [13] |
| Density Gradient | Moderate | Moderate | Standardized separation of mononuclear cells. | [13] |
| Bead Depletion (CD15/CD235a) | Highest | Lower | Best preserved cell viability over 5 days in culture. | [13] |
| EasySep PBMC Isolation Kit | High | Lower | Highest initial viable cells (Day 0); significantly depletes CD14+ cells, reducing T-cell proliferation. | [13] |
Experimental Protocol: Evaluating Post-Thaw Recovery & Function
This protocol outlines a comprehensive method to assess not only viability but also the functional integrity of thawed stem cell products, based on current research practices [13].
Objective: To systematically evaluate the impact of different post-thaw processing methods on cell recovery, viability, and functional fitness.
Materials:
- Cryopreserved cell product (e.g., Cord Blood Unit, PBSCs)
- Water bath or automated warmer (37°C)
- Pre-warmed complete culture medium
- Centrifuge
- Materials for post-thaw processing (e.g., wash buffers, density gradient media, depletion beads/kits)
- Flow cytometer with appropriate antibodies for viability (e.g., 7-AAD) and immunophenotyping
- Cell culture incubator (37°C, 5% CO₂)
- Reagents for functional assays (e.g., CFU assay kit, apoptosis/LAN assay kit, T-cell stimulation cocktail)
Procedure:
- Thawing: Rapidly thaw the cryovial/cryobag in a 37°C water bath until only a small ice crystal remains. Immediately proceed to the next step [9].
- Dilution & Primary Wash: Gently transfer the thawed contents to a tube containing a pre-warmed volume of culture medium (e.g., 10x volume). Mix gently. Centrifuge at a moderate speed (e.g., 300-400 x g) for 5-10 minutes. Carefully decant the supernatant [8].
- Post-Thaw Processing (Split into Groups): Resuspend the cell pellet and divide into aliquots for different processing methods as per your experimental design:
- Group A (Wash-Only): Resuspend in medium, centrifuge, and resuspend for counting.
- Group B (Density Gradient): Isolate mononuclear cells using a standard Ficoll or similar density gradient centrifugation protocol.
- Group C (Bead Depletion): Follow manufacturer's instructions for immunomagnetic bead-based depletion of unwanted cells (e.g., CD15/CD235a).
- Group D (PBMC Isolation Kit): Process cells using a direct isolation kit per manufacturer's guide.
- Day 0 Analysis:
- Cell Count & Viability: Perform a cell count and viability assessment for all groups using your preferred method (e.g., trypan blue, AO/Propidium Iodide, or flow cytometry with 7-AAD) [12].
- Immunophenotyping: Use flow cytometry to analyze the composition of immune cell subsets in each group (e.g., CD3+ T-cells, CD14+ monocytes, CD34+ HSCs) [13].
- Apoptosis Assay: Perform a Live/Apoptosis-Negative (LAN) assay on a portion of the cells from each group to quantify early apoptotic events [13].
- Functional Assessment (Culture):
- Culture a defined number of viable cells from each group under standard conditions for 5 days. Optionally, add T-cell activation stimuli to assess proliferation capacity.
- Day 5 Analysis:
- Re-assess cell count and viability.
- Perform a T-cell proliferation assay (e.g., CFSE dilution).
- Repeat the LAN assay to evaluate the stability of the culture.
- For HSCs, perform a Colony-Forming Unit (CFU) assay to assess clonogenic potential.
Workflow and Decision Diagrams
Diagram 1: Post-Thaw Viability Assessment Workflow
Diagram Title: Comprehensive Viability and Function Assessment Pathway
Diagram 2: Post-Thaw Processing Method Decision Tree
Diagram Title: Post-Thaw Processing Method Selection Guide
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Cryopreservation Optimization
| Item | Function & Rationale | Example / Specification |
|---|---|---|
| Controlled-Rate Freezer (CRF) | Provides precise control over cooling rate, a critical process parameter (CPP) that minimizes intracellular ice formation and osmotic stress, ensuring batch-to-batch consistency. [4] | Industry standard for clinical-grade manufacturing; preferred over passive freezing. [4] |
| DMSO-based Cryomedium | The most common permeating cryoprotectant. Disrupts hydrogen bonding to prevent ice crystal formation and stabilizes cell membranes. [8] | Concentrations typically 5-15%; often combined with cell culture media, albumin, or other supplements. [10] |
| Serum-Free / Chemically Defined Media | Redishes variability and safety risks associated with animal serum. Supports regulatory compliance for clinical applications. [11] | Commercially available GMP-grade formulations (e.g., CS-SC-D1 for MSCs). [14] |
| Programmable Water Bath / Thawing Device | Ensures rapid, consistent, and controlled thawing at ~37°C, which is critical for high viability. Reduces contamination risk vs. traditional water baths. [4] [9] | Provides the recommended warming rate of ~45°C/min for many cell types. [4] |
| Immunomagnetic Bead Kits | For post-thaw cell processing to achieve high purity of specific cell populations (e.g., CD15/CD235a depletion from CBMCs), which can enhance functional outcomes. [13] | Kits like EasySep; selection depends on target cell population and required purity. [13] |
Impact of Cryopreservation on Critical Quality Attributes (CQAs)
Cryopreservation is an indispensable process in the development of personalized stem cell products, enabling vital pause points between manufacturing and final administration. However, this process introduces significant stresses that can directly compromise the Critical Quality Attributes (CQAs) essential for therapeutic efficacy and safety. CQAs are defined biological, chemical, or physical properties that must be controlled within appropriate limits to ensure product quality. For cell-based therapies, these typically include cell viability, identity, potency, and purity [4] [15].
The journey from a controlled-rate freezer to the patient involves multiple risks. During freezing and thawing, cells are subjected to physical and chemical stresses that can lead to osmotic damage, intracellular ice crystal formation, and prolonged exposure to cytotoxic cryoprotectants like dimethyl sulfoxide (DMSO) [4] [16] [15]. These insults can diminish cell viability and recovery, alter cell surface markers, and impair critical biological functions. Furthermore, the industry faces a major challenge in scaling cryopreservation processes without introducing variability that affects CQAs [4]. This technical support center provides targeted guidance to troubleshoot these challenges, ensuring that your cryopreserved stem cell products consistently meet the stringent CQA standards required for clinical application.
Troubleshooting Guides
FAQ 1: How does the choice between controlled-rate freezing and passive freezing impact my stem cell product's CQAs?
Answer: The freezing method directly influences the consistency of your process and the viability of your final product. Controlled-rate freezing (CRF) provides precise manipulation of cooling parameters, which is critical for managing ice crystal formation and minimizing osmotic stress—key factors affecting cell viability and potency [4] [2]. In contrast, passive freezing in a -80°C isopropanol chamber offers a low-cost, simple alternative but sacrifices control over critical process parameters, leading to greater variability in post-thaw CQAs [4] [2].
Industry surveys reveal that 87% of cell therapy developers use controlled-rate freezing, with its adoption being nearly universal for late-stage and commercial products [4]. The table below summarizes the core trade-offs:
Table: Impact of Freezing Method on Process and Product CQAs
| Feature | Controlled-Rate Freezing (CRF) | Passive Freezing |
|---|---|---|
| Control over Cooling Rate | Precise control (e.g., -1°C/min) [2] | Uncontrolled, variable rate |
| Impact on Viability | Maximized by avoiding intracellular ice [2] | Often lower and more variable |
| Process Consistency | High, suitable for cGMP and late-stage clinical products [4] | Low, common in early research [4] |
| Infrastructure Cost | High (specialized equipment, LN2) [4] | Low (freezing container, -80°C freezer) [4] |
| Scale-Up Bottleneck | Can be a bottleneck for large batches [4] | Simple to scale in terms of vial numbers [4] |
Recommendation: For programs advancing toward clinical trials, adopting controlled-rate freezing early is a best practice. Switching from passive to controlled-rate freezing later requires complex and costly process comparability studies [4].
FAQ 2: My post-thaw viability is low. What are the primary causes, and how can I address them?
Answer: Low post-thaw viability is a common symptom of cryo-injury, which manifests as three primary types of damage: osmotic damage, mechanical damage from ice crystals, and oxidative damage from reactive oxygen species (ROS) [15]. The root cause often lies in suboptimal protocols for freezing or, just as critically, thawing.
The diagram below illustrates the interconnected mechanisms of cryo-injury that lead to reduced viability and impaired CQAs.
Troubleshooting Steps:
- Audit Your Thawing Rate: A rapid thaw is non-negotiable. Quickly thaw cells by gently swirling the vial in a 37°C water bath until only a small ice crystal remains, then immediately dilute out the cryoprotectant. Slow thawing dramatically increases exposure to cytotoxic DMSO and allows damaging ice recrystallization [17] [2] [18].
- Verify Your Freezing Profile: For controlled-rate freezers, do not assume the "default" profile is optimal. While 60% of users employ default profiles, challenging cell types like iPSC-derived cardiomyocytes or neural progenitors often require optimized cooling rates to minimize chilling injury and intracellular ice formation [4].
- Investigate Cryoprotectant Toxicity: If you are required to use DMSO-free or low-DMSO media, be aware that standard slow-freeze protocols may perform poorly. This often necessitates dedicated process development to optimize freezing profiles for alternative cryoprotectant formulations [16].
- Implement Process Analytical Technology (PAT): Use freeze curve data from your controlled-rate freezer as a process control. Deviations from a qualified "golden batch" profile can predict low viability before you even run post-thaw analytics, allowing you to investigate the freezing system's performance [4].
FAQ 3: The CQAs of my thawed cells are inconsistent across vials from the same batch. How can I improve uniformity?
Answer: Inconsistency in CQAs, such as variable viability or potency, between vials of the same batch points to issues in process robustness and a lack of well-qualified equipment.
Key Investigation Areas and Solutions:
- Qualify Your Controlled-Rate Freezer (CRF): A leading cause of variability is an unqualified freezing process. Nearly 30% of labs rely solely on vendor qualification, which may not represent your specific use case [4].
- Action: Perform a full temperature mapping study of your CRF chamber. This should evaluate a range of conditions, including full vs. empty loads, different vial locations, and various container types and fill volumes. This ensures all vials experience the same thermal environment [4].
- Standardize the Thawing Process: Manual thawing in a water bath is a significant source of variability. It introduces contamination risk and relies on operator technique to judge the endpoint [4].
- Control Pre-Freeze Cell State: Inconsistency can originate from the starting material.
- Action: Ensure cells are harvested during their maximum growth phase (log phase) with >80% confluency and are free of microbial contamination [2]. Standardize the cell concentration and volume per vial to ensure uniform heat transfer during freezing and thawing.
The Scientist's Toolkit: Essential Reagents and Materials
Optimizing your cryopreservation workflow requires high-quality, purpose-built reagents and materials. The table below details key solutions for protecting CQAs.
Table: Essential Research Reagent Solutions for Cryopreservation
| Item | Function & Rationale | Key Considerations |
|---|---|---|
| Defined Cryomedium (e.g., CryoStor) | A ready-to-use, serum-free freezing medium containing DMSO. Provides a safe, defined, and protective environment, minimizing lot-to-lot variability and contamination risks associated with homemade FBS-containing media [2]. | Essential for GMP compliance. Using a defined medium is critical for ensuring consistent production and quality control [2]. |
| DMSO-Free Formulations | Cryopreservation media using alternatives like trehalose, sucrose, or polyampholytes. Mitigates the cytotoxicity and patient side effects associated with DMSO, which is crucial for therapies administered via novel routes (e.g., intracerebral, intraocular) [16] [15]. | Often requires optimization of freezing profiles, as they may not perform well with standard -1°C/min protocols [16]. |
| Liquid Nitrogen Storage Systems | Long-term storage of cryopreserved cells at -135°C to -196°C. Dramatically reduces biological and chemical activity, ensuring long-term stability of CQAs. Short-term storage at -80°C leads to progressive viability loss [2] [19]. | Use internal-threaded cryogenic vials to prevent contamination. Ensure systems have temperature monitoring and backup for security [2]. |
| Controlled-Rate Freezer (CRF) | Equipment that precisely controls cooling rate (typically -1°C/min). Allows definition of critical process parameters to control ice nucleation and minimize intracellular ice formation, directly impacting viability and potency CQAs [4] [2]. | Requires user qualification for specific container types and load configurations. Vendor factory testing is often insufficient for cGMP use [4]. |
| Automated Thawing Device (e.g., ThawSTAR) | Provides consistent, rapid thawing at a defined rate. Eliminates variability and contamination risk from manual water bath thawing, ensuring high and consistent cell recovery [4] [18]. | Ensures bedside and GMP-thawing reproducibility, a frequent failure point in the cold chain [4]. |
Advanced Protocol: Qualification of a Controlled-Rate Freezer for CQA Consistency
Objective: To qualify a new or existing controlled-rate freezer (CRF) to ensure it provides a uniform and reproducible thermal environment for cryopreserving stem cell products, thereby minimizing inter-vial CQA variability.
Background: Relying solely on vendor certification is insufficient for a cGMP environment. This protocol establishes performance limits for your specific process conditions (vial type, fill volume, cell type) [4].
Materials:
- Controlled-rate freezer
- Validated temperature logging system (e.g., thermocouples)
- Empty cryovials of the primary container type used
- Freezing medium (e.g., CryoStor CS10)
- CRF racking system
Methodology:
- Define Operational Ranges: Determine the minimum, typical, and maximum loads (e.g., 10 vials, 50 vials, 100 vials) and configurations that will be used in production.
- Instrument Vials: Fill cryovials with freezing medium at the standard volume (e.g., 1 mL). Place temperature probes in vials located at strategic, challenged locations within the CRF chamber (e.g., top-center, bottom-corner, near the LN2 inlet). A typical mapping strategy involves a 3D grid of locations [4].
- Execute Freezing Runs: Run the standard freezing profile (e.g., -1°C/min to -80°C) for each load condition defined in Step 1. Record the temperature from every probe at frequent intervals (e.g., every 10 seconds).
- Analyze Data: For each run, analyze the data to determine:
- Temperature Uniformity: The maximum temperature difference between any two vials at any point during the run should be within a pre-defined acceptance criterion (e.g., ±3°C).
- Cooling Rate Consistency: The actual cooling rate for each vial through the critical phase (e.g., +4°C to -40°C) should match the set point within a defined range (e.g., ±0.5°C/min).
- Establish Alert and Action Limits: Based on the data, set limits for routine monitoring. If a production run shows a freeze curve that deviates beyond these limits, it can be flagged for investigation before post-thaw analytics are even available [4].
This qualification protocol directly supports the quality of your stem cell product by ensuring the process-related data from the CRF is a reliable indicator of consistent manufacturing, thereby safeguarding your CQAs.
Regulatory Landscape for Cellular Starting Materials (US, EU, and APAC perspectives)
Frequently Asked Questions (FAQs)
1. How do different regions classify the cryopreservation of cellular starting materials, and what are the regulatory consequences? The classification of cryopreservation—whether as a "minimal manipulation" or "substantial manipulation"—dictates the level of regulatory control. This classification varies by region, impacting whether Good Manufacturing Practice (GMP) standards are required.
- United States (US): Under 21 CFR 1271, cryopreservation is typically considered a minimal manipulation unless it alters relevant biological characteristics. Minimal manipulation activities are subject to less stringent regulations compared to more than minimally manipulated products [20].
- European Union (EU): The ATMP Regulation (1394/2007) and the Tissue and Cells Directive (2004/23/EC) provide the framework. Similar to the US, cryopreservation itself (freezing, cryopreservation) is generally not considered a substantial manipulation. Substantial manipulations include activities like cell expansion or genetic modification, which would classify the product as an Advanced Therapy Medicinal Product (ATMP) [21] [20].
- Asia-Pacific (APAC): Perspectives vary:
- Japan: The Good Gene, Cellular, and Tissue-based Products Manufacturing Practice (GCTP) applies. The health authority determines the impact on product quality and safety based on scientific data [20].
- Australia: Follows the Australian Code of GMP for Human Blood and Blood Components, Human Tissues and Human Cellular Therapy Products, which generally considers cryopreservation as minimal manipulation [20].
- South Korea: Governed by the Act on the Safety of and Support for Advanced Regenerative Medicine and Advanced Biological Products (ARMAB), with a perspective similar to the US and EU [20].
2. What are the key regulatory trends for Advanced Therapy Medicinal Products (ATMPs) in 2024-2025? Regulatory bodies are continuously adapting to the rapid growth of cell and gene therapies. Key recent trends include:
- US FDA Policy Shift: The FDA has eliminated the Risk Evaluation and Mitigation Strategies (REMS) for all approved BCMA- and CD19-directed autologous CAR-T cell immunotherapies. This removes requirements for special hospital certification and on-site, immediate access to tocilizumab, simplifying treatment administration [22].
- UK MHRA Innovation: New UK regulations for Modular Manufacture and Point of Care came into effect in July 2025. This allows manufacturing steps for personalized therapies like CAR-T to be performed in hospitals or local clinics, reducing patient wait times [22].
- EMA Regulatory Support: The EMA is running a pilot program to provide dedicated regulatory support, including fee reductions, to academia and non-profit organizations developing ATMPs for unmet clinical needs [23].
- Security and Data Concerns: The US FDA has announced a review of clinical trials that involve sending American citizens' cells to "hostile countries" for genetic engineering and re-infusion, highlighting growing concerns over genetic data security and patient consent [24].
3. What are the major challenges in scaling up cryopreservation processes for commercial cell therapies? Scaling cryopreservation is identified as a major hurdle for the cell and gene therapy industry [4]. Key challenges include:
- Batch Processing: The majority of respondents (75%) in an ISCT survey cryopreserve all units from an entire manufacturing batch together. This can create a bottleneck and increase the time variance between the start and end of freezing for a single batch [4].
- Process Consistency: Dividing a batch into sub-batches for sequential cryopreservation introduces a risk of freezing process variability between the sub-batches, potentially impacting product consistency [4].
- Infrastructure and Cost: Scaling requires significant investment in controlled-rate freezers, liquid nitrogen infrastructure, and specialized personnel [4].
4. Why is there a industry push towards DMSO-free cryopreservation media? While DMSO is the traditional cryoprotectant, its cytotoxicity is a significant concern, especially for sensitive cell types. DMSO-free cryosolutions offer several advantages [25]:
- Reduced Toxicity: Eliminates the risk of DMSO-induced cell damage and potential adverse effects in patients.
- Simplified Workflow: Often reduces or eliminates the need for post-thaw washing steps, saving time and improving efficiency, which is critical in high-throughput and automated settings [25].
- Improved Reproducibility: Defined, serum-free formulations reduce lot-to-lot variability compared to lab-made media containing fetal bovine serum (FBS) [2]. Challenges to adoption include higher cost, limited accessibility, and ongoing regulatory evaluations for broader clinical use [25].
Troubleshooting Guides
Problem: Poor Post-Thaw Cell Viability and Recovery
Potential Causes and Solutions
| Potential Cause | Diagnostic Checks | Corrective Action |
|---|---|---|
| Suboptimal Cooling Rate | Review controlled-rate freezer (CRF) validation records and freeze curve data [4]. | - Use a controlled cooling rate of -1°C/min [2].- Validate CRF performance across different container types and load configurations [4]. |
| Improper Thawing Technique | Confirm thawing method and rate. | Thaw cells rapidly (e.g., in a 37°C water bath) to minimize ice recrystallization damage and DMSO exposure [4] [2]. |
| Cryoprotectant Agent (CPA) Toxicity | Check CPA concentration and post-thaw washing protocol. | - Consider switching to a DMSO-free, serum-free commercial medium (e.g., CryoStor, Bambanker DMSO-Free) [25] [2].- If using DMSO, ensure concentration is optimized for your cell type (typically 5-10%) [10]. |
| Inconsistent CRF Performance | Analyze freeze curves for deviations from the set profile [4]. | - Qualify CRFs using a range of masses and container types, not just a vendor's default profile [4].- Establish alert limits for freeze curves as part of process monitoring [4]. |
Experimental Protocol: Optimizing a Cryopreservation Protocol for a New Stem Cell Line
This protocol provides a methodology to systematically develop a cryopreservation process, addressing common failure points.
Cell Harvest:
- Harvest cells during their maximum growth phase (log phase) at >80% confluency [2].
- Perform a cell count and viability assay to establish a baseline.
CPA and Media Formulation Testing:
- Prepare multiple cryomedias: Test a traditional DMSO-based medium (e.g., 10% DMSO in culture medium with FBS) against commercially available, defined alternatives (e.g., CryoStor CS10, Bambanker DMSO-Free) [2] [25].
- Resuspend cell pellets in the different cryomedias at a target concentration (e.g., 1x10^6 cells/mL).
Cooling Rate Optimization:
- Aliquot cell suspensions into cryovials.
- Freeze using different methods:
- Controlled-rate freezer: Use a standard profile (e.g., -1°C/min).
- Passive freezing containers: Place vials in a Mr. Frosty or CoolCell and store at -80°C [2].
Storage and Thawing:
- After freezing, transfer vials to long-term storage in the vapor phase of liquid nitrogen (<-135°C).
- Thaw rapidly by immersing vials in a 37°C water bath with gentle agitation until only a small ice crystal remains [2].
Post-Thaw Analysis:
- Immediately upon thawing, assess:
- Viability: Using trypan blue exclusion or flow cytometry.
- Recovery: Calculate the percentage of viable cells recovered relative to the pre-freeze count.
- Functionality: Perform a cell-type specific functional assay (e.g., differentiation potential, proliferation assay).
- Immediately upon thawing, assess:
Problem: Regulatory Compliance During Tech Transfer and Scale-Up
Potential Causes and Solutions
| Potential Cause | Diagnostic Checks | Corrective Action |
|---|---|---|
| Lack of Process Understanding | Review process development data and CRF qualification reports [4]. | - Quality CRFs for the specific container types and load configurations used in production, not just vendor defaults [4].- Use freeze curves as part of process monitoring, not just post-thaw analytics for release [4]. |
| Inadequate Quality Control (QC) | Audit QC data and batch records for completeness. | - Implement post-thaw quality assessment (e.g., viability, sterility) for every batch [10].- Ensure robust record-keeping for full traceability [2]. |
| Open vs. Closed Processing | Evaluate the cleanroom classification and environmental monitoring data. | - Implement closed system processing (e.g., sterile tubing welders) for formulation and cryopreservation to reduce contamination risk [20].- A validated closed system may allow processing in a controlled, non-classified space, reducing costs [20]. |
Experimental Protocol: Qualifying a Controlled-Rate Freezer (CRF) for cGMP Compliance
This protocol outlines key steps to qualify a CRF, addressing a major industry challenge where nearly 30% of users rely solely on vendor qualification [4].
Define User Requirements Specification (URS): Document the intended use, including common container types (vials, cryobags), fill volumes, and cell product types.
Installation Qualification (IQ): Verify the CRF is installed correctly according to manufacturer specifications.
Operational Qualification (OQ): Verify that the CRF operates within specified parameters across its defined range.
- Temperature Mapping: Perform full and empty chamber mapping across a grid of locations to identify hot/cold spots [4].
- Use thermocouples to monitor temperature uniformity.
Performance Qualification (PQ): Demonstrate the CRF performs reliably under actual production conditions.
- Simulate Production Loads: Use cryocontainers filled with a placebo solution that mimics the thermal mass of your cell product.
- Freeze Curve Mapping: Run standard and worst-case freezing profiles and monitor the freeze curves at different locations within the load [4].
- Mixed Load Testing: If applicable, test configurations with different container types frozen together to establish performance limits [4].
Documentation: Compile a qualification report summarizing all data, establishing alert and action limits for freeze curves, and defining the approved operational ranges.
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key reagents and equipment for cryopreservation workflows, incorporating best practices for regulatory compliance.
| Item | Function & Regulatory Consideration | Example Products / Notes |
|---|---|---|
| Cryopreservation Media | Protects cells from ice crystal damage during freeze-thaw. Using cGMP-manufactured, defined, serum-free media is recommended for regulated applications to ensure consistency and safety [2]. | DMSO-based: CryoStor [2]DMSO-free: Bambanker DMSO-Free [25]Specialized: mFreSR (for ES/iPS cells) [2] |
| Controlled-Rate Freezer (CRF) | Provides a consistent, controlled cooling rate (typically -1°C/min), which is critical for process control and reproducibility in cGMP [4] [10]. | Must be qualified for intended use with specific container types and load configurations [4]. |
| Cryogenic Storage Vials/Bags | Primary container for long-term storage. Internal-threaded vials are preferred to prevent contamination [2]. Cryobags are common for larger volumes like PBSCs [10]. | Corning Cryogenic Vials; Various cryobag sizes (50mL - 500mL) [2] [10]. |
| Passive Freezing Containers | Provides an approximate cooling rate of -1°C/min in a standard -80°C freezer, offering a lower-cost alternative to CRFs for R&D or early-stage work [2]. | Nalgene Mr. Frosty (isopropanol-based), Corning CoolCell (isopropanol-free). |
| Liquid Nitrogen Storage | For long-term storage at <-135°C. Essential for maintaining cell viability over extended periods [2]. | Storage in the vapor phase is standard practice. |
| Closed System Equipment | Enables aseptic processing without relying on a classified cleanroom, reducing contamination risk and facility costs. Critical for minimal manipulation processes [20]. | Sterile tubing welders, closed-system cell processors. |
From Principle to Practice: Current Protocols and Industry Standards
Frequently Asked Questions (FAQs)
1. What is the current industry adoption rate for controlled-rate freezing? A 2025 survey by the ISCT Cold Chain Management & Logistics Working Group indicates high adoption, with 87% of respondents reporting the use of controlled-rate freezing for cell-based products. The remaining 13% using passive freezing have products predominantly in early clinical stages (up to phase II) [4].
2. When is controlled-rate freezing strongly preferred over passive freezing? Controlled-rate freezing is the preferred method for late-stage clinical and commercial products due to superior control over critical process parameters [4]. It is particularly crucial for sensitive cell types like iPSCs, CAR-T cells, engineered cells, and differentiated cells (hepatocytes, cardiomyocytes) that often require optimized, non-default freezing profiles [4].
3. Are there any cell types where passive freezing is sufficient? Yes. A 2025 clinical study found that for hematopoietic progenitor cells (HPCs), passive freezing outcomes were comparable to controlled-rate freezing regarding CD34+ cell viability and engraftment, suggesting it is an acceptable alternative for this cell type [26].
4. What are the primary technical challenges associated with controlled-rate freezers? Key challenges include a lack of consensus on qualification methods (with nearly 30% of users relying on vendor qualification) and underutilization of freeze curves in the release process, as many facilities still rely solely on post-thaw analytics [4].
5. Why is scaling cryopreservation a major industry hurdle? In the same 2025 survey, 22% of respondents identified the "Ability to process at a large scale" as the single biggest hurdle. Most respondents (75%) cryopreserve all units from an entire manufacturing batch together, which can create variance and present scaling challenges [4].
Troubleshooting Guides
Issue 1: Poor Post-Thaw Viability of iPSCs
Problem: Low cell survival and extended recovery time (beyond 4-7 days) after thawing induced pluripotent stem cells (iPSCs).
Solution:
- Freezing Protocol: Ensure a slow, controlled cooling rate.
- Thawing Protocol: Thaw cells rapidly.
- Pre-freezing Cell Status: Harvest cells during their maximum growth phase (log phase) and at >80% confluency for best results [2].
- Prevent Osmotic Shock: During thawing, carefully dilute out the cryoprotectant to prevent sudden osmotic stress that can further damage cells [27].
Issue 2: Inconsistent Performance Across a Controlled-Rate Freezer (CRF) Batch
Problem: Variable post-thaw results from vials frozen in the same CRF run.
Solution:
- Comprehensive Freezer Qualification:
- Do not rely solely on vendor factory testing. Perform qualification based on your specific use case [4].
- The qualification protocol should include a range of masses, container configurations, and temperature profiles [4].
- Perform temperature mapping across a grid of locations and freeze curve mapping for different container types to identify hot or cold spots [4].
- Utilize Freeze Curves for Process Control:
- Implement monitoring of freeze curves for every run. Establish action or alert limits to identify deviations in CRF performance before they lead to critical failures [4].
Issue 3: Choosing Between Controlled-Rate and Passive Freezing for a New Product
Problem: Deciding on a cryopreservation strategy early in process development.
Solution:
- Weigh the pros and cons based on your product's needs and development stage. The table below summarizes key considerations [4]:
| Factor | Controlled-Rate Freezing | Passive Freezing |
|---|---|---|
| Process Control | High control over critical parameters (e.g., cooling rate) [4]. | Lack of control over critical process parameters [4]. |
| Product Consistency | Effective tool for controlling quality and consistency [4]. | Advanced technology may be needed to mitigate freezing damage [4]. |
| Cost & Infrastructure | High cost (instrument, liquid nitrogen, staffing) [4]. | Low-cost, low-consumable infrastructure [4]. |
| Operational Complexity | Specialized expertise required [4]. | Simple, one-step operation; low technical barrier [4]. |
| Scaling | Can be a bottleneck for batch scale-up [4]. | Ease of scaling [4]. |
| Best Application | Late-stage clinical and commercial products; sensitive cell types [4]. | Early R&D and early clinical stages (up to phase II); robust cell types [4]. |
- Consider the impact of process changes: Adopting controlled-rate freezing early on can avoid the significant effort of making a major manufacturing change later and establishing product comparability [4].
Adoption Rates and Resource Allocation
The following table consolidates key quantitative findings from recent industry surveys and research [4]:
| Metric | Finding | Context / Implication |
|---|---|---|
| Adoption of Controlled-Rate Freezing | 87% | High prevalence in cell and gene therapy industry [4]. |
| Use of Default Freezer Profiles | 60% | Remaining 40% require optimized profiles for sensitive cells [4]. |
| Resources Dedicated to Cryopreservation/Post-Thaw Analytics | 33% | This area faces the most challenges and attracts the most R&D effort [4]. |
| Biggest Hurdle: Large-Scale Processing | 22% | Identified as the single largest challenge to overcome [4]. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Application Note |
|---|---|---|
| CryoStor CS10 | A ready-to-use, serum-free cryopreservation medium containing 10% DMSO. | Provides a safe, protective environment; suitable for a wide variety of cell types and recommended for GMP workflows [2] [29]. |
| mFreSR | A defined, serum-free freezing medium. | Optimized for cryopreserving human embryonic and induced pluripotent stem cells (ES and iPS cells) [2]. |
| Dimethyl Sulfoxide (DMSO) | A permeating cryoprotectant agent (CPA). | Prevents ice crystal formation by penetrating cells; standard concentration is 5-10% [27] [16]. |
| Rho Kinase (ROCK) Inhibitor (Y-27632) | A small molecule that improves cell survival after thawing. | Often added to culture medium post-thaw to enhance attachment and survival of sensitive cells like iPSCs [29]. |
| Ficoll 70 | A non-permeating polymer. | Can be added to freezing solution to enable potential long-term storage of iPSCs at -80°C [27]. |
Experimental Protocol for Controlled-Rate Freezing
This is a generalized detailed protocol for cryopreserving cells using a controlled-rate freezer, compiled from industry standards [2].
Cell Harvesting:
- Harvest cells during the logarithmic growth phase at >80% confluency.
- Centrifuge the cell suspension and carefully remove the supernatant.
Resuspension in Freezing Medium:
- Resuspend the cell pellet in an appropriate, pre-cooled cryopreservation medium (e.g., CryoStor CS10) at a specific concentration. Typical concentrations range from 1x10^3 to 1x10^6 cells/mL.
- Note: It is good practice to test freezing at multiple concentrations to determine the optimum for your cell type.
Aliquoting:
- Aliquot the cell suspension into cryogenic vials. Using internal-threaded vials is preferable to prevent contamination.
Controlled-Rate Freezing:
Long-Term Storage:
Cryopreservation Strategy Decision Workflow
Cell Freezing Experimental Workflow
DMSO Concentration Guide and Safety Profile
Table 1: Clinical DMSO Concentration Guidelines for Cell Therapy Products
| Cell Type | Common DMSO Concentration | Key Comparative Findings | Reported Post-Thaw Viability | Primary Safety Concerns |
|---|---|---|---|---|
| Hematopoietic Stem Cells (HSCs) [31] | 10% (Standard) | Higher infusional toxicity | -- | Nausea, vomiting, cardiac events [31] |
| Hematopoietic Stem Cells (HSCs) [31] | 5% (Reduced) | Improved CD34+ cell viability, reduced side effects | -- | Significantly reduced adverse effects [31] |
| Mesenchymal Stromal Cells (MSCs) [32] [33] | ~10% (Standard) | Doses 2.5-30x lower than 1 g/kg deemed acceptable [32] [33] | -- | Isolated infusion-related reactions with premedication [32] [33] |
| hiPSC-Derived Cardiomyocytes [34] | 10% (Conventional) | Lower performance vs. DMSO-free cocktails | 69.4% ± 6.4% | Functional alterations, epigenetic effects [34] |
DMSO-Free Cryoprotectant Formulations
Table 2: Experimentally Validated DMSO-Free Formulations
| Cell Type | DMSO-Free Formulation | Post-Thaw Viability/Recovery | Key Advantages |
|---|---|---|---|
| hiPSC-Derived Cardiomyocytes [34] | Cocktail of Trehalose, Glycerol, Isoleucine | >90% recovery [34] | Preserved function, avoids DMSO toxicity & epigenetic effects [34] |
| Mesenchymal Stromal Cells (MSCs) [32] | 30 mM Sucrose + 5% Glycerol + 7.5 mM Isoleucine | 83% Viability, 93% Recovery [32] | Serum-free, defined composition [32] |
| Adipose Tissue MSCs [32] | 3% Trehalose + 5% Dextran 40 + 4% Polyethylene Glycol | ~95% Viability, ~95% Recovery [32] | High efficiency, non-penetrating CPAs [32] |
| Embryonic Stem Cell-Derived MSCs [32] | 150 mM Sucrose + 300 mM Ethylene Glycol + 30 mM Alanine + 0.5 mM Taurine + 0.02% Ectoine | 96% Viability, 103% Recovery [32] | Complex cocktail mimicking intracellular environment [32] |
Experimental Protocols
Differentiation and Purification:
- Culture hiPSCs to 80-90% confluency.
- Initiate cardiac differentiation using 6.5 µM CHIR99021 in RPMI/B-27 minus insulin medium for 48 hours.
- On Day 2, replace medium with RPMI minus supplemented with 5 µM IWP2.
- On Day 8, switch to RPMI/B-27 maintenance medium.
- Between Days 10-14, purify cardiomyocytes using glucose-free DMEM with 4 mM sodium L-lactate.
Freezing Process:
- Harvest cardiomyocytes on Days 14-16 using 0.25% Trypsin-EDTA.
- Resuspend in recovery medium (RPMI/B-27 with 20% FBS and 5 µM ROCK inhibitor Y-27632) for 30 minutes.
- Prepare the optimized DMSO-free cryoprotectant solution.
- Mix the cell suspension with the cryoprotectant.
- Use a controlled-rate freezer with the following parameters:
- Store cryovials at -80 °C or in liquid nitrogen.
Tissue Processing and Crypt Isolation:
- Collect human colorectal tissue samples under sterile conditions and IRB approval.
- Transfer samples in cold Advanced DMEM/F12 medium supplemented with antibiotics.
- For short-term delays (≤6-10 hours), wash tissues with antibiotic solution and store at 4°C.
- For longer delays, cryopreserve tissue pieces in freezing medium (e.g., 10% FBS, 10% DMSO in 50% L-WRN conditioned medium).
- Isolate crypts from the processed tissue through mechanical and enzymatic dissociation.
Organoid Culture and Cryopreservation:
- Embed isolated crypts in Matrigel droplets.
- Culture with specialized medium containing growth factors (EGF, Noggin, R-spondin).
- For cryopreservation, harvest organoids and resuspend in an appropriate freezing medium (e.g., 10% DMSO in FBS or a commercial serum-free alternative).
- Freeze at a controlled rate of -1 °C/min or using a -80 °C freezer overnight before transferring to liquid nitrogen for long-term storage.
Troubleshooting Common Cryopreservation Issues
FAQ 1: How can I reduce DMSO-related toxicity in cell therapy products?
- Strategy A: Reduce DMSO Concentration. For autologous HSC transplants, reducing DMSO from 10% to 5% in the freezing medium improves post-thaw CD34+ cell viability and significantly reduces adverse effects in patients, such as nausea and vomiting, without negatively impacting engraftment [31].
- Strategy B: Implement Post-Thaw Washing. Remove the cryoprotectant after thawing by centrifuging the cell product and resuspending it in a compatible solution like normal saline or plasma. Note that this can lead to cell loss and requires careful handling [31].
- Strategy C: Use DMSO-Free Formulations. For research applications, adopt validated DMSO-free media. These formulations use combinations of sugars, sugar alcohols, and amino acids to protect cells, eliminating DMSO-related toxicity concerns entirely [25] [34].
FAQ 2: What are the critical parameters for optimizing controlled-rate freezing? The cooling rate and nucleation temperature are crucial. For example, in hiPSC-derived cardiomyocytes, a rapid cooling rate of 5 °C/min and a low nucleation temperature of -8 °C were found to be optimal, achieving post-thaw recoveries over 90% with a DMSO-free formulation [34]. The optimal parameters are cell-type specific and must be determined experimentally.
FAQ 3: Why is post-thaw cell viability low even with high viability pre-freeze? This can be due to several factors:
- Suboptimal Cooling Rate: An incorrect cooling rate causes lethal intracellular ice formation or excessive osmotic stress [34].
- Improper Thawing Technique: Rapid thawing at 37°C is standard, but uneven thawing or failure to promptly dilute cryoprotectants can damage cells [35].
- Cryoprotectant Toxicity: DMSO exposure time and temperature post-thaw are critical; prolonged exposure at room temperature is toxic [34] [35].
- Cell-Type Specific Sensitivity: Some primary cells and stem cells are inherently more sensitive to cryopreservation stresses and may require tailored formulations [25] [34].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Cryopreservation Research
| Reagent / Solution | Function | Example Use Cases |
|---|---|---|
| DMSO (Dimethyl Sulfoxide) [32] [31] | Penetrating cryoprotectant; prevents intracellular ice formation. | Standard cryopreservation of HSCs, MSCs, and many cell lines. |
| Trehalose [32] [34] | Non-penetrating cryoprotectant; stabilizes cell membranes and proteins. | Key component in many DMSO-free formulations for MSCs and hiPSC-CMs [32] [34]. |
| Glycerol [32] [34] | Penetrating cryoprotectant; less toxic alternative to DMSO for some cell types. | Used in DMSO-free cocktails for MSCs and hiPSC-CMs [32]. |
| ROCK Inhibitor (Y-27632) [29] | Enhances cell survival by inhibiting apoptosis following dissociation and freezing. | Added to recovery medium post-thaw for hiPSCs and sensitive primary cells [29]. |
| CryoStor CS10 [29] | A proprietary, serum-free, GMP-compliant cryopreservation solution containing 10% DMSO. | Used in clinical-grade cell therapy products and research for improved, standardized recovery [29]. |
| Bambanker DMSO-Free [25] | A commercial, serum-free, DMSO-free cryopreservation medium. | Provides a ready-to-use, defined solution for sensitive cells like stem cells and primary cells [25]. |
Visualizing Cryopreservation Workflows and Strategies
DMSO-Free Formulation Development
Post-Thaw Cell Processing Decision Guide
For researchers and drug development professionals working with personalized stem cell products, the post-thaw phase is a critical determinant of experimental success and therapeutic efficacy. The period immediately following the removal of cells from cryostorage represents a vulnerable window where processing decisions directly impact cell fitness, function, and suitability for downstream applications. This technical support center addresses the key challenges in post-thaw processing, providing evidence-based troubleshooting guidance to navigate the inherent trade-offs between cell purity, recovery yield, and functional integrity. The following sections offer detailed protocols, comparative data, and strategic frameworks to optimize your post-thaw workflows within the broader context of advancing cryopreservation research for stem cell-based therapies.
FAQs: Navigating Post-Thaw Processing Decisions
What is the fundamental trade-off between purity and recovery in post-thaw processing?
There is an inherent inverse relationship between the purity of your target cell population and the total number of cells you recover post-thaw. Methods designed to achieve high purity, such as bead-based depletion or specialized isolation kits, typically involve more processing steps that can mechanically stress cells or require longer handling times, leading to greater overall cell loss. Conversely, simpler methods like wash-only protocols maximize total cell recovery but retain more unwanted cell populations and debris, which can interfere with downstream applications [13] [36].
How does the choice of post-thaw method impact long-term cell function?
The processing method selected immediately after thawing can significantly influence cell fitness days later. For instance, in cord blood mononuclear cells (CBMCs), the EasySep Direct Human PBMC Isolation Kit yielded the highest percentage of viable cells on Day 0. However, when cells were cultured for five days, the Beads (CD15/CD235 depletion) method demonstrated superior preservation of viability under stimulation [13] [37]. Some methods that enhance initial purity may inadvertently remove critical supportive cells; the PBMC Isolation Kit's depletion of CD14+ cells was correlated with reduced T-cell proliferation, highlighting a functional trade-off [36].
My post-thaw viability is good, but the cells fail to expand in culture. What could be wrong?
Good viability immediately post-thaw, as measured by assays like trypan blue exclusion, primarily indicates membrane integrity. Failure to expand suggests underlying functional deficits not captured by basic viability tests. Potential causes include:
- Cryo-induced Apoptosis: Cryopreservation can trigger programmed cell death. Consider implementing an apoptosis assay, such as the Live, Apoptosis-Negative (LAN) assay, validated for post-thaw cells [13].
- Metabolic or Mitochondrial Damage: The freezing process can damage mitochondria. Assessing metabolic activity (e.g., with a colony-forming unit assay) or mitochondrial membrane potential can provide a deeper functional readout [13] [38].
- Improper Pre-freeze Handling: The cell growth phase before freezing is critical. Cells should be harvested during their maximum growth phase (log phase) and at high confluency (>80%) to ensure robust recovery [39] [2].
Are there alternatives to chemical cryoprotectants like DMSO to improve post-thaw fitness?
Yes, research is actively exploring DMSO-free solutions and physical methods to mitigate cryodamage. Photobiomodulation (PBM), the application of specific light wavelengths, has shown promise as a non-chemical, post-thaw intervention. One study found that irradiating thawed human stem cells with 950 nm near-infrared light at 30 Hz and a 30% duty cycle reduced apoptosis and reactive oxygen species (ROS), while increasing mitochondrial membrane potential and ATP generation [38]. Furthermore, DMSO-free cryoprotectant cocktails using naturally occurring osmolytes (e.g., trehalose, glycerol, isoleucine) have been developed for hiPSC-derived cardiomyocytes, achieving post-thaw recoveries over 90% [34].
Troubleshooting Guides
Problem: Low Cell Yield After Post-Thaw Processing
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Excessive processing | Compare cell counts after thawing and after each processing step. | Simplify the protocol. If high purity is not immediately required, use a wash-only method and perform isolation after a short period in culture [13]. |
| Osmotic shock during DMSO removal | Check protocol for direct dilution. Observe cell morphology for swelling or lysis. | Use a sequential dilution method. Gently add warm culture medium dropwise to the cell suspension while gently mixing to gradually reduce DMSO concentration [39]. |
| Overly aggressive centrifugation | Review speed and duration of spin. | Optimize centrifugation force and time. Use the lowest possible g-force and shortest time adequate for pelleting the specific cell type (e.g., 160g for 18 min for PBSCs) [40]. |
| Incorrect cell concentration | Count cells before cryopreservation. | Aim for a general range of 1x10^3 to 1x10^6 cells/mL in the cryovial. Test multiple concentrations to find the optimum for your cell type [2]. |
Problem: Poor Functional Outcomes Despite High Viability
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Loss of critical accessory cells | Use flow cytometry to characterize immune subset composition pre-freeze and post-processing. | Switch to a gentler or more specific purification method. If using a kit that depletes CD14+ monocytes, be aware this may impair T-cell function [36]. |
| Residual cryoprotectant toxicity | Note the DMSO concentration during culture. | Ensure thorough but gentle washing post-thaw. For sensitive applications, consider DMSO-free cryopreservation formulations [34]. |
| Mitochondrial dysfunction | Perform a metabolic activity assay (e.g., MTT) or measure ROS and ATP levels [38]. | Incorporate a recovery period with antioxidants or consider non-invasive PBM to boost mitochondrial function post-thaw [38]. |
| Cryo-induced senescence | Check for enlarged, flat morphology and low proliferation rates. | Ensure cells are frozen in the log growth phase and use early-passage cells for critical applications [39]. |
Experimental Protocols & Data
Comparative Analysis of Post-Thaw Processing Methods for CBMCs
The following table summarizes quantitative outcomes from a systematic study comparing four post-thaw processing methods for cord blood mononuclear cells, illustrating the key trade-offs [13] [36].
| Processing Method | CBMC Recovery Yield | Purity (Depletion of Non-Target Cells) | Day 0 Viability (LAN Cells) | Day 5 Viability After Stimulation |
|---|---|---|---|---|
| Wash-Only | Highest | Lowest | Moderate | Moderate |
| Density Gradient | Moderate | Moderate | Moderate | Moderate |
| CD15/CD235 Bead Depletion | Low | Highest | Moderate | Best Preserved |
| EasySep PBMC Isolation Kit | Low | Highest | Highest | Low (Reduced T-cell prolif.) |
Detailed Protocol: Post-Thaw Processing via Density Gradient
This protocol is adapted for processing volume-reduced cord blood units after thawing [36].
Materials:
- Thawed CBU sample
- DPBS (Dulbecco's Phosphate Buffered Saline), without calcium and magnesium
- Ficoll-Paque PLUS or similar density gradient medium
- Good Manufacturing Practice (GMP)-grade Dextran
- Centrifuge with swing-bucket rotor
- Sterile serological pipettes
- Processing tube (e.g., 50 mL conical tube)
Method:
- Dilution: Gently dilute the thawed CBU sample with an equal volume of DPBS supplemented with 1% GMP-grade Dextran. Mix gently by inversion.
- Layer: Carefully layer the diluted cell suspension over the Ficoll-Paque medium in a 2:1 ratio (e.g., 30 mL diluted cells over 15 mL Ficoll) without disrupting the interface.
- Centrifugation: Centrifuge at 800g for 20-30 minutes at room temperature, with the brake turned off. This is critical for a clean separation.
- Harvest MNCs: After centrifugation, carefully aspirate the upper plasma/platelet layer. Using a sterile pipette, transfer the mononuclear cell layer (the cloudy interface between the plasma and Ficoll) to a new sterile tube.
- Wash: Resuspend the harvested cells in a large volume (e.g., 3-4 times the volume collected) of DPBS. Centrifuge at 300g for 10 minutes to wash the cells.
- Final Resuspension: Aspirate the supernatant and resuspend the cell pellet in an appropriate culture medium or buffer for counting and subsequent use.
Workflow Diagram: Post-Thaw Processing Decision Pathway
The following diagram outlines a logical workflow for selecting an appropriate post-thaw processing strategy based on your primary experimental objective.
The Scientist's Toolkit: Essential Reagents & Materials
| Item | Function & Application | Key Considerations |
|---|---|---|
| Dextran (GMP-grade) | Sedimentation agent used in dilution buffers for density gradient separation to improve cell recovery [36]. | Using GMP-grade reagents enhances protocol standardization and is critical for therapeutic applications. |
| EasySep Direct Human PBMC Isolation Kit | Immunomagnetic negative selection kit for high-purity isolation of PBMCs post-thaw [13] [37]. | Excellent for Day 0 viability but may deplete critical CD14+ cells, impacting long-term T-cell function. |
| CD15/CD235 Depletion Beads | Immunomagnetic beads for specifically removing granulocytes and red blood cells from thawed samples [13]. | Superior for preserving long-term cell viability and function over 5 days in culture. |
| Ficoll-Paque PLUS | Density gradient medium for isolating mononuclear cells based on buoyant density [36]. | A standard, well-established method. Ensure the brake is turned off during centrifugation for optimal separation. |
| CryoStor CS10 | A commercially available, serum-free, GMP-manufactured cryopreservation medium containing 10% DMSO [2]. | Provides a defined, protective environment, reducing lot-to-lot variability compared to lab-made FBS/DMSO mixtures. |
| Photobiomodulation Device | Applies specific near-infrared light (e.g., 950nm) to reduce ROS and apoptosis, and boost mitochondrial function post-thaw [38]. | A novel, non-chemical intervention. Parameters like frequency (30Hz) and duty cycle (30%) are critical for efficacy. |
| DMSO-Free CPA Cocktails | Mixtures of osmolytes (e.g., Trehalose, Glycerol, Isoleucine) to replace DMSO, avoiding its toxicity and epigenetic effects [34]. | Can achieve >90% recovery for sensitive cells like hiPSC-CMs. Requires optimization of composition and cooling rates. |
Best Practices for Ultra-Low Temperature Storage and Cold Chain Management
Troubleshooting Guides
Problem: Low Post-Thaw Cell Viability
Issue: Stem cells show poor recovery and viability after thawing, characterized by low attachment rates and failure to form colonies.
Investigation & Resolution:
- Audit Your Freezing Protocol: Ensure cells were frozen at a controlled rate of approximately -1°C/minute, which is critical for most cell types, including iPSCs [2] [27]. Verify the use of a proper freezing container (e.g., isopropanol-based Mr. Frosty or alcohol-free CoolCell) placed in a -80°C freezer before transfer to long-term storage [2] [3].
- Check Cell Health and Confluency Pre-Freeze: Cells must be harvested during their maximum growth phase (log phase) at >80% confluency and confirmed to be free of microbial contamination (e.g., mycoplasma) before freezing [2] [3].
- Review Cryoprotectant Agent (CPA): The standard is 5-10% DMSO [15]. To reduce DMSO cytotoxicity, consider using commercially available, serum-free, defined freezing media (e.g., CryoStor CS10, mFreSR) or supplementing your medium with non-permeable CPAs like sucrose or trehalose [2] [15].
- Validate Thawing Technique: Thaw cells rapidly by placing cryovials in a 37°C water bath until only a small ice crystal remains [2] [3]. Immediately after thawing, dilute the cell suspension drop-wise into pre-warmed culture medium to minimize osmotic shock and gently pellet the cells to remove the CPA-containing supernatant [3].
Problem: Temperature Excursions During Storage or Transport
Issue: Data loggers or monitoring systems record temperatures rising above the acceptable range for your stored or shipped products.
Investigation & Resolution:
- Confirm Storage Equipment Performance: For ultra-low (-80°C) or cryogenic (≤ -135°C) storage, qualify equipment with regular validation and temperature mapping. Ensure redundant power systems (e.g., backup generators) and continuous monitoring with real-time alerts are in place [41] [42].
- Inspect Storage Vials: Use internally-threaded cryogenic vials to minimize the risk of contamination, especially when stored in liquid nitrogen [2] [3].
- Audit Shipping and Handling Procedures:
- Packaging: Use validated thermal shipping systems. For long journeys or ultra-cold temperatures, select packaging with sufficient dry ice or active cooling containers to maintain temperature for the entire duration, including potential delays [41].
- Monitoring: Equip all shipments with real-time temperature loggers and GPS trackers. Establish clear contingency plans for interventions if alerts are triggered [41] [43].
- Training: Ensure all personnel are trained in the safe handling of dry ice and proper procedures for moving materials [41].
Problem: iPSCs Fail to Form Colonies Post-Thaw
Issue: Specific to induced pluripotent stem cells (iPSCs); cells attach but do not proliferate or form characteristic colonies.
Investigation & Resolution:
- Optimize Freezing and Thawing as Cell Aggregates: iPSCs are particularly vulnerable. Freezing and thawing them as small, defined aggregates (clumps) rather than single cells can improve recovery by preserving cell-cell contacts [27].
- Prevent Osmotic Shock During Thawing: The rapid dilution of CPAs post-thaw is a critical step for sensitive iPSCs. Slowly and gently diluting the thawed cell suspension drop-wise into a larger volume of warm medium is essential [27].
- Ensure Proper Seeding Density: Plate thawed iPSCs at a high density (e.g., 2x10^5 - 1x10^6 viable cells per well of a 6-well plate) on a Matrigel-coated surface to support attachment and colony formation [3].
- Assess Pre-Freeze Culture Health: Feed iPSC cultures daily before cryopreservation and freeze during the 2-4 day window after passaging. Avoid using overgrown or unhealthy cultures [3].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental principle behind "slow freeze, rapid thaw"? The principle balances two main causes of cell damage. Slow freezing (at about -1°C/min) allows water to gradually exit the cell, minimizing the formation of lethal intracellular ice crystals that mechanically damage membranes and organelles [27] [15]. Rapid thawing (in a 37°C water bath) quickly passes through the dangerous temperature zone where ice recrystallization can occur, reducing exposure to concentrated solutes and cytotoxic cryoprotectants like DMSO [2] [15] [3].
Q2: How can I reduce or replace DMSO in my freezing media for clinical applications? Strategies include:
- Combination with other CPAs: Supplementing a lower concentration of DMSO (e.g., 5%) with non-permeable agents like sucrose, trehalose, or hydroxyethyl starch can provide synergistic protection, allowing for DMSO reduction [15].
- Using defined, commercial media: Several GMP-manufactured, serum-free, and xeno-free freezing media (e.g., CryoStor series) are optimized to be effective while mitigating DMSO-related toxicity [2].
- Novel CPA exploration: Polymers like polyvinylpyrrolidone (PVP) and methylcellulose have shown promise as partial or complete replacements for DMSO in some stem cell types [3].
Q3: What are the critical temperature thresholds for long-term storage of stem cells? For true long-term storage, temperatures at or below the glass transition temperature (Tg') of the system (around -123°C for DMSO) are required, where all molecular motion and damaging biochemical reactions cease [27]. Storage in the vapor phase of liquid nitrogen (typically -135°C to -180°C) or in ultra-low -150°C mechanical freezers is recommended [27] [3]. Storage at -80°C is acceptable only for short periods (e.g., <1 month) as cell viability will decline over time [2].
Q4: What are the key parameters to monitor for cold chain compliance? A robust cold chain monitoring system should track and document:
- Temperature continuously, with setpoints and alarms for excursions.
- Location via GPS for shipments.
- Chain of custody, including all hand-off points.
- Equipment performance (e.g., freezer/fridge metrics, backup power status) [44] [41] [43].
Q5: What are the main types of cryodamage and how do they manifest?
- Osmotic Damage: Caused by water leaving the cell during freezing, leading to harmful solute concentration and cell shrinkage [15].
- Mechanical Damage: Resulting from the physical shearing of cell membranes and organelles by intracellular and extracellular ice crystals [27] [15].
- Oxidative Damage: Caused by the generation of reactive oxygen species (ROS) during the freezing/thawing process, leading to oxidation of lipids, proteins, and DNA [15].
Experimental Protocols & Data
Standardized Freezing and Thawing Protocol for Cell Aggregates
This protocol is adapted for freezing stem cells, particularly iPSCs, as small aggregates to enhance post-thaw recovery [2] [27] [3].
Materials:
- Healthy, log-phase cells (~80-90% confluent)
- Appropriate cell culture medium
- Cryopreservation medium (e.g., with 10% DMSO or commercial alternative)
- Cryogenic vials
- Controlled-rate freezing container (e.g., CoolCell) or programmable freezer
- -80°C freezer
- Long-term storage unit (liquid nitrogen vapor phase or -150°C freezer)
- 37°C water bath
- Centrifuge
Methodology:
Freezing:
- Harvest: Gently dissociate cells to form small clumps of ~10-20 cells (aggregates), avoiding a single-cell suspension. Use minimal enzyme exposure.
- Centrifuge: Pellet cells at 200-300 x g for 2-5 minutes. Carefully remove supernatant.
- Resuspend: Gently resuspend the cell pellet in cold cryopreservation medium at a recommended density (e.g., 1-2 x 10^6 cells/mL). Keep the tube on ice.
- Aliquot: Dispense 1 mL of cell suspension into each cryogenic vial. Place vials immediately into the pre-cooled (4°C) freezing container.
- Freeze: Place the freezing container in a -80°C freezer for a minimum of 4 hours (or overnight) to achieve a cooling rate of ~-1°C/min.
- Store: Quickly transfer the vials to their designated long-term storage location in the vapor phase of liquid nitrogen or a -150°C freezer. Record the location.
Thawing:
- Retrieve: Quickly retrieve the vial from long-term storage, keeping it cool.
- Thaw: Immerse the vial immediately in a 37°C water bath with gentle agitation until only a small ice crystal remains (approx. 1-2 minutes). Do not submerge the vial cap.
- Decontaminate: Wipe the vial exterior with 70% ethanol and transfer to a sterile biosafety cabinet.
- Dilute: Gently transfer the thawed suspension drop-wise into a 15mL tube containing 10mL of pre-warmed complete culture medium. This slow dilution is critical to prevent osmotic shock.
- Wash: Centrifuge the cell suspension at 200 x g for 2-5 minutes. Carefully aspirate the supernatant containing the cryoprotectant.
- Reseed: Gently resuspend the cell pellet in fresh, pre-warmed culture medium and plate at a high density onto a suitably coated culture vessel.
Temperature and Logistics Specifications for Cold Chain Management
Table 1: Key Temperature Ranges and Their Applications in the Biopharma Cold Chain [41] [43] [45]
| Temperature Range | Typical Products | Key Handling & Equipment |
|---|---|---|
| 2–8 °C (Refrigerated) | Many vaccines (e.g., MMR), insulin, biologics | Medical-grade refrigerators, gel packs, temperature data loggers |
| -18 to -25 °C (Frozen) | Some pharmaceuticals, seafood, meat | Standard frozen logistics |
| -40 to -80 °C (Ultralow) | mRNA vaccines, certain biologics, gene therapies | Ultra-low freezers, dry ice for shipping, validated packaging |
| Cryogenic (< -150 °C) | Stem cells (iPSCs, MSCs), CAR-T therapies, cell banks | Liquid nitrogen (vapor phase storage), cryogenic tanks, dry ice shippers |
Table 2: Critical Monitoring Parameters for Cold Chain Integrity [44] [41] [43]
| Parameter | Purpose | Best Practice Tools |
|---|---|---|
| Temperature | Ensure product stability and prevent degradation | Real-time IoT sensors with cloud alerts, calibrated data loggers |
| Location | Track shipment progress and prevent loss/theft | GPS tracking integrated with monitoring platform |
| Chain of Custody | Document every hand-off for regulatory compliance | Digital systems (e.g., blockchain, centralized databases) |
| Equipment Health | Prevent failures in storage units | Predictive maintenance with AI, backup power systems |
Workflow and System Diagrams
Stem Cell Cryopreservation Workflow
Three-Zone Model of Cryogenic Freezing
The Scientist's Toolkit
Table 3: Essential Reagents and Materials for Cryopreservation Workflows [2] [15] [3]
| Item | Function & Rationale |
|---|---|
| Intracellular CPAs (e.g., DMSO) | Penetrate the cell membrane, lower the freezing point, and reduce ice crystal formation. The most common permeable CPA. |
| Extracellular CPAs (e.g., Sucrose, Trehalose) | Do not enter the cell; they stabilize the cell membrane and create a hypertonic environment that promotes gentle dehydration before freezing. |
| Defined, Serum-Free Freezing Media | Commercially available, GMP-manufactured media (e.g., CryoStor, mFreSR) provide a consistent, xeno-free environment, reducing lot-to-lot variability and regulatory concerns for clinical applications. |
| Controlled-Rate Freezing Containers | Insulated containers (e.g., CoolCell, Mr. Frosty) ensure a consistent, reproducible cooling rate of ~-1°C/min when placed in a -80°C freezer, making controlled-rate freezing accessible without a programmable freezer. |
| Internally-Threaded Cryogenic Vials | Designed to minimize the risk of contamination during filling or when stored in liquid nitrogen, as the thread is not exposed to the storage environment. |
| Real-Time Temperature Data Loggers | IoT-enabled sensors provide continuous monitoring and instant alerts for temperature excursions during storage and transport, enabling proactive intervention. |
Overcoming Critical Hurdles: Scaling, Viability, and Consistency
Addressing Scalability as a Major Industry Bottleneck
Frequently Asked Questions (FAQs)
Q1: What are the key factors for successfully cryopreserving induced pluripotent stem cells (iPSCs) to ensure high colony formation post-thaw?
The success of iPSC cryopreservation hinges on four critical areas [3]:
- Good Cell Condition: iPSCs should be fed daily before cryopreservation and frozen when they are in the log phase of growth (typically 2-4 days after passaging). Avoid freezing overgrown cultures. Ensure cell clumps are properly dissolved before freezing to allow cryoprotectants to penetrate effectively [3].
- Correct Use of Cryoprotective Agent: Use fresh freezing media. A final concentration of 10% DMSO is common, often supplemented with other components like FBS or Ficoll. Many commercial, serum-free formulations are also available [3].
- A Controlled Freezing Rate: The ideal cooling rate is -1°C per minute. This can be achieved using a programmable freezing unit or a passive cooling device like a Corning CoolCell placed in a -80°C freezer [3].
- Proper Storage: For long-term storage, cells should be kept in the vapor phase of liquid nitrogen (between -140°C and -180°C) to maintain viability and prevent the risk of vial explosion [3].
Upon thawing, seed cells at a high density (between 2x10^5 - 1x10^6 viable cells per well of a 6-well plate) on a Matrigel-coated plate. Properly thawed cells should attach within 30 minutes and reach 70-80% confluence within 24-48 hours [3].
Q2: Our lab is experiencing variable post-thaw cell viability. What are the main checkpoints to investigate?
Low and variable post-thaw viability can be frustrating. We recommend systematically checking these four major points [3]:
- Pre-freeze Cell Health & Density: Freeze only healthy, log-phase cells at the recommended density (e.g., 1-2 x 10^6 cells/mL). High cell density can lead to nutrient and cryoprotectant insufficiency. Minimize the time cells are exposed to dissociation reagents and cryoprotectants at room temperature during harvesting [3].
- Controlled Freezing Rate: Ensure you are using a reliable method to achieve the -1°C/minute cooling rate, such as a validated freezing container or controlled-rate freezer [3] [2].
- Proper Storage and Handling: Avoid transient warming events when transferring vials to long-term storage. Store cells at or below -135°C (preferably in liquid nitrogen vapor) and minimize how often the storage unit is opened [2].
- Rapid Thawing and Gentle CPA Removal: Thaw cells quickly in a 37°C water bath, but dilute the cryoprotectant-containing medium drop-by-drop into a large volume of warm culture medium to prevent osmotic shock [3] [2].
Q3: Are there alternatives to DMSO for cell therapy applications, and what are their pros and cons?
Yes, alternatives are being actively researched, particularly for cell therapies where DMSO toxicity is a concern. Cryoprotectants are generally classified as penetrating (intracellular) or non-penetrating (extracellular) [3].
The table below summarizes common cryoprotectants and their applications:
| Cryoprotectant | Type | Examples & Applications |
|---|---|---|
| Penetrating (Intracellular) | Small molecules that enter the cell. | DMSO: The most common CPA; effective but has known cytotoxicity and can influence cell differentiation [3] [46].Glycerol, Ethylene Glycol: Alternative penetrating agents [3].Cell Banker Series: Commercial formulations [3]. |
| Non-Penetrating (Extracellular) | Large molecules that remain outside the cell. | Sucrose, Dextrose: Act as osmotic buffers [3].Polyvinylpyrrolidone (PVP): Shown to work as well as DMSO for some adult stem cells when used with human serum [3].Methylcellulose: Can be used alone or with reduced DMSO concentrations (as low as 2%) [3]. |
Q4: Is it acceptable to re-freeze cells that have been previously thawed?
No, this is not recommended. Cryopreservation is a traumatic process for cells. Refreezing previously thawed cells typically results in very low viability, as the cumulative stress from multiple freeze-thaw cycles is too great for most cells to survive [3]. It is best practice to plan experiments to use all thawed cells or to culture them fresh and then freeze down new, healthy vials for future use.
Q5: How can we scale our cryopreservation protocols while maintaining consistency and cell quality?
Scalability requires standardization and optimization. Key strategies include:
- Standardize Freezing Media: Move from homemade, serum-containing formulations to defined, commercial, serum-free freezing media (e.g., CryoStor or mFreSR). This reduces batch-to-batch variability and eliminates undefined components, which is critical for clinical applications [2].
- Automate Processes: Where possible, use automated systems for cell counting, vial filling, and sealing to reduce human error and increase throughput.
- Validate Cooling Rates: Ensure your freezing method (whether using controlled-rate freezers or passive coolers like CoolCell or Mr. Frosty) is validated and provides a consistent -1°C/minute cooling rate for the number of vials you are processing simultaneously [3] [2].
- Implement Robust Tracking: Use a laboratory information management system (LIMS) or detailed inventory logs to track vial location, passage number, and freeze date to ensure you are always using the highest quality stock [2].
Troubleshooting Guides
Poor Post-Thaw Viability
Use the following workflow to diagnose and resolve common issues leading to poor cell recovery after thawing.
Low iPSC Colony Formation Post-Thaw
When thawed iPSCs fail to form characteristic colonies, the issue often lies in the pre-freeze handling or the thawing protocol [3].
Problem: Low Cell Survival or Attachment
- Potential Cause 1: Cells were overgrown or unhealthy before freezing.
- Solution: Ensure cells are fed daily and frozen at 2-4 days post-passage, during maximal growth. Avoid freezing confluent, differentiated cultures [3].
- Potential Cause 2: Cell clumps were too large during freezing, preventing cryoprotectant penetration.
- Solution: Gently dissociate cells into small clumps before freezing. Centrifuge at 200-300 x g for 2 minutes and resuspend gently [3].
- Potential Cause 3: Seeding density after thaw was too low.
- Solution: Seed cells at a high density (2x10^5 - 1x10^6 viable cells per well of a 6-well plate) to encourage colony formation and recovery [3].
Problem: Spontaneous Differentiation
- Potential Cause: Inadequate or poor-quality extracellular matrix coating.
- Solution: Use a fresh, properly aliquoted, and high-quality matrix like Corning Matrigel for coating plates to provide the necessary signals for self-renewal [3].
Research Reagent Solutions
For scalable and reproducible cryopreservation, selecting the right reagents is crucial. The table below lists key materials and their functions.
| Product Category | Specific Examples | Function & Application |
|---|---|---|
| Serum-Free Freezing Media | CryoStor CS10 [2], mFreSR (for ES/iPS cells) [2], STEMdiff Cardiomyocyte Freezing Medium [2] | Defined, xeno-free formulations that provide a protective environment during freezing/thawing. Critical for clinical applications and reducing variability [2]. |
| Cryoprotectants | Dimethyl Sulfoxide (DMSO), Glycerol, Polyvinylpyrrolidone (PVP) [3] | Penetrating (DMSO, Glycerol) or non-penetrating (PVP) agents that protect cells from ice crystal damage. PVP is explored as a DMSO alternative [3]. |
| Passive Freezing Containers | Corning CoolCell [3] [2], Nalgene Mr. Frosty [2] | Insulated containers designed to achieve an approximate -1°C/minute cooling rate when placed in a -80°C freezer, providing a low-cost alternative to controlled-rate freezers [3] [2]. |
| Cryogenic Storage Vials | Corning Cryogenic Vials [2] | Single-use, sterile vials designed for low-temperature storage. Internal-threaded designs can help minimize contamination risks [3] [2]. |
Optimized Cryopreservation Workflow for Scalability
The following diagram outlines a standardized workflow for scaling up the cryopreservation of stem cell products, integrating best practices for viability and consistency.
Optimizing Thawing Protocols to Minimize Osmotic Stress and DMSO Toxicity
Troubleshooting Guide: Common Thawing Challenges and Solutions
1. Problem: Low Post-Thaw Cell Viability
- Potential Causes:
- Recommended Solutions:
- Ensure rapid thawing by placing cryovials directly from storage into a 37°C water bath with gentle swirling until only a small ice crystal remains [17].
- Dilute DMSO immediately after thawing by adding pre-warmed growth medium dropwise to the cell suspension [27].
- Consider using controlled-rate freezing equipment or isopropanol-based freezing containers to ensure optimal cooling rate of approximately -1°C/min [3] [27].
2. Problem: Osmotic Shock During Thawing
- Potential Causes:
- Recommended Solutions:
- Employ gradual dilution methods by adding wash medium slowly to the thawed cell suspension [27].
- Use osmotically balanced wash solutions containing non-penetrating cryoprotectants like sucrose to stabilize cell membranes during CPA removal [49].
- Perform dilution and washing steps at appropriate temperatures (typically 20-25°C) to minimize temperature-induced stress [48].
3. Problem: Functional Impairment Despite Good Viability
- Potential Causes:
- Recommended Solutions:
- Implement DMSO-free cryopreservation using alternative CPAs like polyampholytes, sugars, or macromolecules [47] [49].
- Reduce DMSO concentration through hydrogel microencapsulation, enabling effective cryopreservation with as low as 2.5% DMSO [50].
- Assess functional recovery through differentiation assays and potency tests rather than relying solely on viability metrics [50] [49].
4. Problem: Inconsistent Recovery Between Batches
- Potential Causes:
- Recommended Solutions:
Quantitative Data on DMSO Toxicity and Cryoprotection
Table 1: DMSO Toxicity Across Temperature and Concentration Ranges
| DMSO Concentration | Exposure Temperature | Exposure Time | Effect on Cell Viability | Reference |
|---|---|---|---|---|
| 12% (v/v) | 0°C to 37°C | 10 minutes | No negative effect on viability | [48] |
| 40% (v/v) | Room Temperature | 10 minutes | Immediate loss of functional viability | [48] |
| 10% (v/v) | 37°C | Standard thaw | Cytotoxic effects observed | [50] [49] |
| 2.5% (v/v) with microencapsulation | 37°C | Standard thaw | Maintained >70% viability (clinical threshold) | [50] |
Table 2: Alternative Cryoprotectants and Their Efficacy
| Cryoprotectant | Cell Type | Post-Thaw Viability | Advantages | Reference |
|---|---|---|---|---|
| Polyvinyl alcohol (PVA) | Mesenchymal stem cells | Increased from 71.2% to 95.4% | Synthetic polymer, ice recrystallization inhibition | [47] |
| Carboxylated poly-L-lysine (COOH-PLL) | Rat MSCs | Significantly higher than 10% DMSO | Does not cause inappropriate differentiation | [47] |
| PEG−PA (5000−500) block copolymer | Stem cells | Acceptable survival, proliferation and multilineage differentiation | Excellent cryoprotectant properties | [49] |
| Osmolyte-based solutions (sucrose, glycerol, creatine, isoleucine, mannitol) | Mesenchymal stromal cells | Comparable to DMSO | Retained differentiation capacity, modulated epigenome | [49] |
Experimental Protocols for Thawing Optimization
Protocol 1: Standardized Thawing Procedure for DMSO-Cryopreserved Cells
Materials Required:
- Cryovial containing frozen cells
- Complete growth medium pre-warmed to 37°C
- Water bath or bead bath calibrated to 37°C
- Centrifuge tubes
- 70% ethanol for decontamination
- Tissue culture flasks or plates [17]
Methodology:
- Remove cryovial from liquid nitrogen storage, ensuring proper personal protective equipment.
- Immediately place vial in 37°C water bath with gentle swirling until only a tiny ice crystal remains (typically <1 minute).
- Transfer to biological safety cabinet and decontaminate vial exterior with 70% ethanol.
- Transfer thawed cell suspension to centrifuge tube containing 10 volumes of pre-warmed growth medium, adding dropwise with gentle agitation.
- Centrifuge at 200 × g for 5-10 minutes (adjust based on cell type).
- Aspirate supernatant carefully without disturbing cell pellet.
- Resuspend cells gently in fresh growth medium and transfer to culture vessel.
- Plate at high density to optimize recovery [17] [27].
Protocol 2: DMSO Removal and Wash Procedure for Clinical Applications
Rationale: Complete DMSO removal is essential for clinical applications to prevent patient side effects including neurotoxicity, cardiac arrhythmia, and hepatic dysfunction [48] [49].
Materials:
- Thawed cell product
- Wash solution (e.g., glucose-supplemented DMEM)
- Refractometer for DMSO concentration measurement [48]
Methodology:
- Perform three sequential washes using wash solution at a cell product to wash ratio of 1:2.
- Between washes, centrifuge at appropriate g-force for cell type (typically 200-300 × g).
- After final wash, measure supernatant DMSO concentration using refractometry to confirm reduction to <1%.
- Resuspend cells in final formulation buffer or infusion medium [48].
Visual Workflow: Optimized Thawing Process
Frequently Asked Questions (FAQs)
Q: What is the scientific basis for rapid thawing versus slow thawing? A: Rapid thawing in a 37°C water bath is critical to minimize the time spent in dangerous temperature zones where ice recrystallization and devitrification can occur. During warming, samples pass through temperatures between -123°C and -47°C where extracellular and intracellular glass transitions occur, potentially causing stressful events that reduce viability. Rapid warming minimizes the duration of this exposure [27].
Q: Why is gradual dilution necessary when removing DMSO after thawing? A: Gradual dilution prevents osmotic shock by allowing equilibration of intracellular and extracellular solute concentrations. When cells are exposed to high DMSO concentrations intracellularly and suddenly placed in DMSO-free medium, water rapidly enters cells to equilibrate the osmotic difference, potentially causing membrane damage and cell lysis. Dropwise dilution maintains osmotic balance throughout the process [27] [49].
Q: Can DMSO be completely eliminated from cryopreservation protocols? A: Yes, emerging research demonstrates successful DMSO-free cryopreservation using alternative strategies including:
- Polyampholyte-based cryoprotectants that adsorb to cell membranes [49]
- Sugar-based solutions (trehalose, sucrose) with electroporation for intracellular delivery [49]
- Combination approaches using ethylene glycol, sucrose, and other biocompatible compounds [49]
- Hydrogel microencapsulation that enables reduced DMSO requirements (as low as 2.5%) [50]
Q: How does cell encapsulation technology reduce DMSO toxicity? A: Hydrogel microcapsules, particularly alginate-based systems, create a protective three-dimensional environment that shields cells from direct ice crystal damage. This physical protection enables effective cryopreservation with significantly reduced DMSO concentrations (as low as 2.5% versus conventional 10%) while maintaining viability above the 70% clinical threshold [50].
Q: What are the critical parameters for successful thawing of stem cell products? A: Four critical parameters must be controlled:
- Thawing rate: Rapid warming to minimize time in dangerous temperature zones [27]
- Dilution technique: Slow, controlled dilution to prevent osmotic shock [27]
- Temperature management: Maintenance of appropriate temperatures during DMSO removal [48]
- Cell handling: Gentle processing to avoid mechanical damage to vulnerable post-thaw cells [17]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Thawing Optimization Research
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cryoprotectant Solvents | DMSO, glycerol, ethylene glycol | Penetrating cryoprotectants that reduce ice formation | DMSO concentration and temperature-dependent toxicity must be managed [48] [49] |
| Non-Penetrating CPAs | Sucrose, trehalose, dextrose, hydroxyethyl starch | Extracellular protection, osmotic stabilization | Effective in combination approaches for DMSO reduction [3] [49] |
| Polymer-Based CPAs | Polyvinyl alcohol (PVA), carboxylated poly-L-lysine, polyampholytes | Ice recrystallization inhibition, membrane stabilization | Emerging class with potential for DMSO-free cryopreservation [47] [49] |
| Hydrogel Materials | Alginate, collagen, synthetic polymers | 3D microenvironments for cell protection during freezing | Enable significant DMSO reduction; compatible with clinical applications [50] |
| Commercial DMSO-Free Media | StemCell Keep, CryoSOfree, XT-Thrive | Formulated alternatives to DMSO-containing media | Require validation for specific cell types; limited independent studies [49] |
In the field of personalized stem cell research, the integrity of your biological products is paramount. Contamination during cryopreservation and thawing can compromise months of painstaking research, leading to unreliable data, lost time, and depleted resources. The choice between open and closed processing systems represents a critical decision point in safeguarding your valuable samples. Open systems, while sometimes offering technical simplicity, inherently expose your products to the environment. In contrast, closed systems are designed to provide a sealed, protected environment throughout processing and storage. This technical support center is designed to help you navigate these risks through practical troubleshooting guides and FAQs, framed within the broader context of optimizing cryopreservation for personalized medicine applications.
FAQs: Understanding Contamination Risks and System Selection
Q1: What fundamentally defines an open versus a closed processing system in biopharmaceutical manufacturing?
In biopharmaceutical production, the terms "open" and "closed" describe the extent to which a process is isolated from its external environment.
- Closed System: A process that is entirely shielded from outside exposure by design or through validated sanitization methods. It is effectively sealed during production, preventing contamination from airborne particles, microbes, or other environmental factors. These systems can often operate in a Controlled Non-Classified (CNC) space.
- Open System: A process that involves any level of exposure to the surrounding environment, typically during component transfer or manual additions. This exposure increases contamination risk and necessitates operation within a rigorously controlled cleanroom setting [51].
Q2: What are the specific contamination risks associated with liquid nitrogen in cryostorage?
Liquid nitrogen itself is not sterile and poses two primary contamination risks:
- Direct Contamination: Pathogens or environmental contaminants present in the liquid nitrogen can directly infect stored samples.
- Cross-Contamination: Viruses or other contaminants from one patient's sample can be transmitted to another via the liquid nitrogen medium [52] [53].
This is a significant concern for germplasm and cell therapies stored in "open" systems where the storage container directly contacts the liquid nitrogen. The COVID-19 pandemic further highlighted the need to mitigate viral contamination risks in cryostorage [53].
Q3: How does the choice between open and closed systems impact operational efficiency and regulatory compliance?
The choice between systems involves a trade-off between initial investment, operational costs, and compliance burden, as summarized in the table below.
Table: Operational and Compliance Comparison of Open vs. Closed Systems
| Aspect | Open System | Closed System |
|---|---|---|
| Initial Investment | Lower | Higher |
| Operational Costs | Higher (labor, cleaning, downtime) | Lower long-term savings |
| Cleaning Protocol | Rigorous manual cleaning, high downtime | Automated Clean-In-Place (CIP) technology |
| Regulatory Burden | Higher scrutiny, meticulous documentation | Designed to meet/exceed standards, simpler compliance |
| Environmental Control | Requires high-classification cleanroom | Can operate in Controlled Non-Classified (CNC) space [54] [51] |
Q4: For sensitive induced pluripotent stem cells (iPSCs), what are the critical factors for successful recovery post-thaw?
Successful recovery of iPSCs depends on a meticulously optimized protocol:
- Freezing Protocol: Use a controlled-rate freezer, cooling at approximately -1°C to -3°C/min to balance the risks of intracellular ice formation and cell dehydration [27].
- Cell State: Freeze cells when they are healthy and in the late logarithmic phase of growth [27].
- Thawing Technique: Thaw rapidly (e.g., in a 37°C water bath) to minimize damage, but prevent osmotic shock by diluting the cryoprotectant agent (e.g., DMSO) drop-wise with pre-warmed medium [55] [27].
- Contamination Prevention: Confirm the absence of microbial contamination (e.g., Mycoplasma) before freezing. Simple measures like wearing face masks can prevent the transfer of contaminants from the experimenter [27].
Troubleshooting Guides
Guide 1: Poor Post-Thaw Cell Viability and Recovery
Problem: Low cell survival rates and poor attachment after thawing cryopreserved stem cells.
Investigation and Resolution: Table: Troubleshooting Poor Post-Thaw Cell Recovery
| Possible Cause | Investigation Steps | Recommended Solutions |
|---|---|---|
| Suboptimal Freezing Rate | Review controlled-rate freezer protocol and cooling curve data. | For iPSCs, use a controlled freezing rate of -1°C to -3°C/min. Avoid passive freezing methods for sensitive cells [27]. |
| Improper Thawing Technique | Audit thawing procedure in the lab. | Thaw cells rapidly in a 37°C water bath or warming device. Immediately transfer to pre-warmed medium to dilute cryoprotectant [9]. |
| Osmotic Shock During Thawing | Observe cell lysis immediately after thawing. | After thawing, add pre-warmed medium to the cell suspension drop-wise (approximately one drop per second) while gently swirling the tube to gradually reduce DMSO concentration [55] [27]. |
| Incorrect Cell State at Freezing | Check culture logs for confluency and passage number at time of freezing. | Freeze cells when they are healthy and in the late logarithmic growth phase. Do not use over-confluent or unhealthy cultures [27]. |
| Cryoprotectant Agent (CPA) Toxicity | Verify the type and concentration of CPA used. | Use the appropriate CPA (e.g., DMSO for many mammalian cells) at the correct concentration. For sensitive iPSCs, include a ROCK inhibitor in the recovery medium to enhance survival [9] [55]. |
Guide 2: Suspected Contamination in Cryopreserved Samples
Problem: Microbial contamination (e.g., bacteria, fungi, or Mycoplasma) is detected in samples after thawing.
Investigation and Resolution: Table: Troubleshooting Contamination in Cryopreserved Samples
| Possible Cause | Investigation Steps | Recommended Solutions |
|---|---|---|
| Open System Contamination | Determine if the freezing, storage, or thawing steps were performed in an open manner. | Transition to closed vitrification devices and closed storage systems that eliminate direct contact with non-sterile liquid nitrogen [52]. |
| Non-Sterile Liquid Nitrogen | Assume liquid nitrogen is not sterile. | For open systems, use sterile liquid nitrogen. However, the most robust solution is to move to a closed system that provides a physical barrier [52] [53]. |
| Cross-Contamination in Storage | Check for improper sealing of cryovials or storage in an open tank. | Ensure all samples are properly sealed. Store samples in the vapor phase of liquid nitrogen instead of the liquid phase to minimize the risk of cross-contamination through fluid transfer [52] [27]. |
| Operator-Induced Contamination | Review aseptic technique during sample preparation. | Implement stricter aseptic techniques. Wear face masks to prevent oral microbiomes (e.g., Mycoplasma orale) from contaminating samples during handling [27]. |
Experimental Protocols for Risk Mitigation
Protocol 1: Controlled-Rate Freezing of iPSCs Using a Closed Device
Aim: To cryopreserve induced pluripotent stem cell aggregates while maximizing viability and minimizing contamination risk.
Materials:
- Healthy, late-log phase iPSC culture
- Appropriate cryoprotectant medium (e.g., containing 10% DMSO)
- Closed system freezing device (e.g., Cryotip)
- 37°C water bath or warming device
- 15 mL centrifuge tube
- 10 mL of pre-warmed, complete culture medium
Method:
- Preparation: Harvest iPSCs as cell aggregates of consistent size using a gentle method like EDTA passaging.
- Loading: Resuspend the cell aggregates in cryoprotectant medium. Quickly load the mixture into the closed freezing device, ensuring no air bubbles are trapped.
- Freezing: Place the device in a controlled-rate freezer. Initiate a freeze program with a cooling rate of -1°C per minute until the temperature reaches at least -80°C [27].
- Storage: Immediately transfer the frozen device to a long-term storage unit (liquid nitrogen vapor phase or -150°C freezer).
Protocol 2: Rapid Thawing and Osmotic Shock Prevention for Sensitive Cells
Aim: To rapidly thaw cryopreserved cells while preventing the dual damages of ice crystal formation and osmotic shock.
Materials:
- Cryovial of frozen cells
- 70% ethanol for decontamination
- 37°C water bath or controlled-thawing device
- 15 mL conical tube
- 10 mL of pre-warmed complete growth medium
Method:
- Rapid Thaw: Remove the cryovial from storage and immediately place it in a 37°C water bath. Gently agitate until only a small ice crystal remains (usually about 2 minutes). Do not thaw completely at 37°C [55].
- Decontamination: Wipe the outside of the vial thoroughly with 70% ethanol.
- Gentle Dilution: Transfer the thawed cell suspension directly into a 15 mL tube containing 10 mL of pre-warmed medium. To prevent osmotic shock, add the medium drop-wise to the cell suspension initially (about 1 drop per second) while gently swirling the tube [55] [27].
- Seeding: Centrifuge the cell suspension at a gentle speed, aspirate the supernatant, and resuspend the cell pellet in fresh, pre-warmed culture medium. Seed the cells at the recommended density in a coated culture vessel.
System Selection and Contamination Control Workflow
The following diagram outlines a logical decision-making workflow for selecting and validating a cryopreservation system based on contamination risk control.
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagent Solutions for Cryopreservation
| Item | Function | Application Notes |
|---|---|---|
| Closed Vitrification Device (e.g., Cryotop) | Allows ultra-rapid cooling with minimal volumes in a sealed system, preventing direct contact with liquid nitrogen [52]. | Critical for high-contamination-risk applications like clinical-grade cell banking. |
| Dimethyl Sulfoxide (DMSO) | A permeable cryoprotectant that penetrates cells, disrupts ice crystal formation, and reduces freezing damage [27]. | Standard concentration is 10%. Can be cytotoxic; requires rapid removal post-thaw. |
| ROCK Inhibitor (Y-27632) | Improves survival of single pluripotent stem cells by inhibiting apoptosis following dissociation and thawing [55]. | Add to culture medium for 24 hours after thawing to enhance cell attachment and recovery. |
| Controlled-Rate Freezer (CRF) | Provides precise control over cooling rate, which is critical for balancing ice formation and dehydration damage [4] [27]. | Superior to passive freezing for sensitive cells like iPSCs, CAR-T cells, and differentiated progeny. |
| Liquid Nitrogen Vapor Phase Storage | Provides temperatures below -150°C for stable long-term storage while minimizing the risk of cross-contamination via liquid medium [53] [27]. | Preferred over liquid phase storage for biobanking where sample integrity is paramount. |
Troubleshooting Guides
Freeze Curve Analysis and Interpretation
Problem: Sample probe curve does not follow the theoretical curve.
- Potential Cause 1: Inappropriate freezing parameters for the cell type or cryoprotectant.
- Solution: Develop optimized, cell-specific freezing curves. The flexibility of programmable freezers allows theoretical curves to be "tailored to specific media extenders; specific cryoprotectant molecules or content" [56]. Consult published literature for your specific primary cell type and adjust the cooling rate accordingly.
- Preventive Action: Always validate new freezing protocols by comparing the sample probe curve to the theoretical curve and performing post-thaw viability and functionality assays [57].
- Potential Cause 2: Malfunctioning equipment or incorrect probe placement.
- Solution: Verify calibration of the programmable freezer and ensure the sample probe is inserted correctly into a representative sample vial. The "sample probe curve answers specific questions as to how the sample reacted during the cycle" [56], so its accuracy is paramount.
- Preventive Action: Perform regular maintenance and calibration of the controlled-rate freezer as per the manufacturer's schedule.
Problem: Poor post-thaw cell viability and recovery.
- Potential Cause 1: Suboptimal freezing curve, particularly during the phase transition stage.
- Solution: Analyze the sample probe curve to ensure it clearly shows the four main freezing stages: liquid cooling, liquid to crystalline, cooling to crystal state, and stable stage [56]. A poorly managed "liquid to crystalline" phase (latent heat of fusion release) can cause excessive ice crystal formation and cell damage.
- Preventive Action: The sample curve should be closely monitored in real-time to "confirm that the theoretical freezing curve can provide the essential environment to ensure premium sample quality" [56].
- Potential Cause 2: Inconsistent or incorrect thawing technique.
- Solution: Follow a standardized, rapid-thaw protocol. Thaw cells quickly in a 37°C water bath by "gently swirling the vial until a small amount of ice remains," which should take about 1-2 minutes [18]. Do not vortex the cells. Using an automated thawing system can ensure consistency and sterility [18].
- Preventive Action: Always pre-warm culture medium and have all materials ready before removing cells from storage to minimize processing time [17].
Data and Documentation
Problem: Incomplete data for quality control of the freezing process.
- Potential Cause: Relying on a single temperature curve.
- Solution: Ensure your programmable freezer and standard operating procedures capture all three critical curves: the theoretical curve, the chamber probe curve, and the sample probe curve [56]. Together, they "form a complete power team that can provide the necessary data documenting the freezing of valuable samples" [56].
- Preventive Action: Use a freezer that generates a standard report displaying these curves for quality control checks of the freezing event [56].
Frequently Asked Questions (FAQs)
Q1: Why is it critical to monitor the sample probe curve in addition to the chamber temperature? The chamber probe monitors the air temperature in the freezer, which is important for the entire inventory. The sample probe curve, however, shows precisely how the sample itself reacts to the changing temperatures, revealing the four main freezing stages and confirming that the sample is following the intended theoretical path for optimal survival [56].
Q2: What are the key stages I should look for in a sample freeze curve? When monitoring the sample probe curve, you want your sample to achieve the four main freezing stages [56]:
- Liquid Cooling: The sample temperature decreases.
- Liquid to Crystalline: The phase change where water freezes and latent heat is released (often seen as a plateau or spike in the curve).
- Cooling to Crystal State: The temperature of the now-frozen sample decreases further.
- Stable Stage: The final, stable storage temperature is reached.
Q3: My frozen primary cells have low viability post-thaw. Should I adjust the freezing curve or the thawing process? Both processes are critical and interconnected. First, verify your thawing technique is optimal by ensuring it is quick and gentle, using pre-warmed media, and that you are not subjecting the cells to a second freeze-thaw cycle, which "typically results in high cell death" [57]. If thawing is confirmed to be correct, then analyze your sample freeze curves for deviations from the theoretical path, particularly during the phase change, as this indicates a need to optimize the freezing parameters [56].
Q4: Can I use the same theoretical freezing curve for different types of primary cells? While base curves can be a starting point, "curves may have to be tailored to specific media extenders; specific cryoprotectant molecules or content" [56]. The flexibility of programmable freezers allows you to adapt curves to specific sample needs, goal temperatures, or cooling rates. It is essential to validate the freeze curve and post-thaw recovery for each primary cell type and cryopreservation medium formulation.
Key Freezing Stages and Parameters
The following table outlines the critical stages of the freezing process that must be monitored via the sample probe curve to ensure quality.
| Freezing Stage | Description | Key Parameter to Monitor | Data Source |
|---|---|---|---|
| Liquid Cooling | Initial cooling of the sample in its liquid state. | Consistent, controlled cooling rate. | [56] |
| Liquid to Crystalline | Phase change where water freezes, releasing latent heat. | Characteristic temperature plateau or exothermic peak. | [56] |
| Cooling to Crystal State | Further cooling of the now-frozen sample. | Resumption of a controlled cooling rate. | [56] |
| Stable Stage | Final cooling to the storage temperature. | Achievement and maintenance of target storage temperature (e.g., -135°C or colder). | [57] [56] |
Post-Thaw Cell Analysis and Acceptance Criteria
After thawing, cells should be evaluated against key metrics. The following table summarizes critical quality control checks.
| Analysis Metric | Method | Typical Acceptance Criteria | Data Source |
|---|---|---|---|
| Cell Count & Viability | Hemocytometer with Trypan Blue exclusion. | Viability should be specified on the CoA. Cell loss of up to 30% can be expected during wash steps. | [57] [18] |
| Purity | Flow cytometry or other characterization assays. | Guaranteed on the Certificate of Analysis (CoA) provided with cells. | [57] |
| Functionality | Cell-specific assays (e.g., CFU assays, immunological assessments). | Dependent on downstream application; should be established and validated by the researcher. | [57] |
Experimental Protocols
Detailed Methodology: Thawing Cryopreserved Primary Cells
Principle: Quickly melt frozen cells while minimizing the toxic effects of cryoprotectants like DMSO, and remove them via washing to recover viable, functional cells for downstream applications [18] [17].
Materials:
- Cryovial of frozen primary cells
- Pre-warmed complete growth medium (e.g., RPMI 1640 with 10% FBS, IMDM with 10% FBS) [18]
- Water bath or bead bath at 37°C
- 70% ethanol or isopropanol
- Serological pipettes (2 mL, 25 mL)
- 50 mL conical tubes
- DNase I Solution (1 mg/mL) - if clumping is observed
- Hemocytometer and Trypan Blue for counting
Procedure:
- Setup: Pre-warm medium in a 37°C water bath. Prepare the biosafety cabinet with all materials [18].
- Thawing:
- Remove the cryovial from liquid nitrogen storage and immediately place it in a 37°C water bath. Submerge only the lower part of the vial.
- Gently swirl the vial until only a small ice crystal remains (approximately 1-2 minutes). Do not vortex [18] [17].
- Wipe the outside of the vial with 70% ethanol and transfer it to the biosafety cabinet [17].
- Washing and Counting:
- Gently transfer the thawed cell suspension to a 50 mL conical tube using a pipette.
- Rinse the cryovial with 1 mL of pre-warmed medium and add it dropwise to the cells while gently swirling the tube.
- Slowly add 15-20 mL of pre-warmed medium dropwise, while gently swirling the tube to dilute the cryoprotectant [18].
- Centrifuge at 300 x g for 10 minutes at room temperature [18].
- Critical Step: Immediately after thawing, before washing, remove a 20 µL aliquot of cells for counting to determine the total number of cells provided and track cell loss during washing [18].
- Carefully decant the supernatant without disturbing the cell pellet. Gently resuspend the pellet by flicking the tube.
- If cells are clumping, add 100 µg/mL DNase I Solution and incubate at room temperature for 15 minutes. Do not do this if cells will be used for DNA/RNA extraction [18].
- Add another 15-20 mL of medium and centrifuge again at 300 x g for 10 minutes.
- Decant the supernatant and resuspend the cell pellet in the appropriate medium for your downstream application.
Notes:
- Thaw only one vial at a time to prevent prolonged exposure of cells to DMSO at higher temperatures [18].
- Always work quickly and use aseptic technique throughout the procedure.
- Plate thawed cells at a high density to optimize recovery [17].
Process Visualization
Freeze Curve Quality Control Workflow
Primary Cell Thawing and Analysis Protocol
The Scientist's Toolkit
Research Reagent Solutions
| Essential Material | Function in Cryopreservation/Thawing |
|---|---|
| Programmable Freezer | Enables controlled-rate cooling and generates critical data (theoretical, chamber, and sample curves) for quality monitoring [56]. |
| Cryopreservation Medium | Typically contains a base medium, serum (e.g., FBS), and a cryoprotectant (e.g., DMSO) to protect cells during freezing [17]. |
| Thawing Medium | Pre-warmed medium (e.g., IMDM, RPMI 1640 with 10% FBS) used to dilute and wash cells post-thaw, removing cryoprotectants [18]. |
| DNase I Solution | Added post-thaw to dissociate cell clumps caused by DNA release from damaged cells, improving cell recovery [18]. |
| Automated Thawing System | Provides consistent, sterile thawing to minimize variability and contamination risk [18]. |
| Hemocytometer & Trypan Blue | Essential tools for performing cell counts and assessing viability immediately after thawing [18]. |
Ensuring Product Quality: Analytical Methods and Comparative Outcomes
Troubleshooting Post-Thaw Quality Issues
Why is there delayed engraftment despite adequate post-thaw viable CD34+ cell counts?
Post-thaw viable CD34+ cell counts, while important, do not guarantee the functional activity of your stem cell product. A 2016 investigation was initiated at Great Ormond Street Hospital after 8 patients experienced delayed engraftment despite adequate post-thaw viable CD34+ counts. The root cause analysis identified the freezing process itself as a contributing factor.
Experimental Evidence: In a key experiment, a single PBSC product was divided and cryopreserved in parallel using:
- A control-rate freezer (CRF) at GOSH.
- A passive freezing method (-80°C freezer) at GOSH.
- The same passive freezing method at another laboratory.
While post-thaw viable CD34+ counts were equivalent and adequate across all three methods, functional assessment told a different story. The Granulocyte-Monocyte Colony-Forming Unit (CFU-GM) assay showed robust colonies from both passively frozen products, but no colonies grew from the product frozen using the CRF, despite the equipment operating within the manufacturer's specifications [58] [59].
Key Implication: This finding is critical for all transplant programs. It demonstrates that routine quality assurance must extend beyond simple viability and cell counts to include potency or functional assays like CFU formation to ensure the graft will perform as expected [58].
What is the typical recovery of viable CD34+ cells after thawing, and what factors affect it?
Recovery of viable CD34+ cells after thawing is generally high, but can be influenced by several factors, including the patient's underlying disease and the type of mobilization therapy used.
Typical Recovery Rates: A study of 79 autologous stem cell products found a median recovery of viable CD34+ cells after thawing to be over 90% [60]. The table below summarizes the recovery rates observed in different patient populations.
Table 1: Viable CD34+ Cell Recovery in Autologous Products by Disease Type [60]
| Disease | Median Post-Thaw Recovery of Viable CD34+ Cells |
|---|---|
| Non-Hodgkin's Lymphoma (NHL) | 90% |
| Multiple Myeloma | 83% |
| Acute Leukemia | 92.3% |
| Non-hematological Malignancies | 94.5% |
| Bone Marrow (All) | 90% |
Factors Affecting Viable CD34+ Cell Loss: A 2023 study in NHL patients identified two key factors:
- Mobilization Capacity: A higher yield of CD34+ cells at the first apheresis was linked with a greater percentage loss of viable cells after cryopreservation [61].
- G-CSF Type: The use of Filgrastim (FIL) for mobilization was associated with significantly higher viable CD34+ cell loss compared to Pegfilgrastim (PEG) or Lipegfilgrastim (LIPEG). The median loss was 37% with FIL versus 15% with PEG and 13% with LIPEG in one patient group [61].
How do different cell subpopulations within a leukapheresis product withstand cryopreservation?
Not all cells survive the freeze-thaw process equally. Different leukocyte subpopulations show variable recovery, which is crucial if the product is intended for therapies beyond simple stem cell rescue.
Variable Recovery of Cell Subtypes: A prospective study analyzing autologous and allogeneic leukapheresis products found that CD34+ hematopoietic stem cells and CD14+ monocytes are particularly susceptible to cryopreservation damage, showing the lowest post-thaw recovery. In contrast, certain lymphocyte populations, such as CD3+/CD8+ T-cells in autologous products and CD19+ B-cells in allogeneic products, demonstrate higher recovery rates [62].
Table 2: Median Post-Thaw Recovery of Different Cell Subpopulations [62]
| Cell Population | Autologous Product Recovery | Allogeneic Product Recovery |
|---|---|---|
| CD34+ Cells | 73.7% | 68.1% |
| CD14+ Monocytes | Low (specific value not provided) | Low (specific value not provided) |
| CD3+ T Cells | 85.4% | 80.6% |
| CD3+/CD4+ T Cells | 83.9% | 79.4% |
| CD3+/CD8+ T Cells | 89.3% | 80.7% |
| CD19+ B Cells | 85.2% | 90.7% |
| CD16+/CD56+ NK Cells | 82.6% | 83.3% |
Factors Influencing Recovery:
- In autologous products, a higher platelet concentration and longer storage time before freezing weakly correlated with lower recovery of some T-cell subsets [62].
- In allogeneic products, a high percentage of granulocytes in the fresh product had a strong negative correlation with the recovery of T-cell populations (CD3+, CD3+/CD4+, CD3+/CD8+) [62].
Experimental Protocols & Best Practices
Protocol: Thawing and Pre-culture of Cryopreserved CD34+ HSPCs for Downstream Applications
This protocol is essential for ensuring high cell viability and recovery after thawing, particularly before sensitive applications like gene editing [63].
Workflow Overview:
Materials:
- Cryopreserved CD34+ HSPCs
- Pre-warmed complete StemSpan SFEM II medium (supplemented with CD34+ Expansion Supplement and 1µM UM729)
- Pre-warmed wash medium (e.g., basal StemSpan SFEM II or IMDM + 2% FBS)
- 37°C water bath
- Centrifuge
Procedure:
- Rapid Thawing: Gently shake the cryovial in a 37°C water bath. Remove it immediately once only a small frozen pellet remains. Work quickly in the subsequent steps [63].
- Decontaminate and Dilute: Wipe the vial with 70% ethanol or isopropanol. Slowly add pre-warmed wash medium to the vial at a 1:1 (v/v) ratio [63].
- Transfer and Wash: Gently mix and transfer the cell suspension to a conical tube containing 10 mL of pre-warmed wash medium. Rinse the pipette tip and cryovial with more wash medium at least three times to maximize cell recovery [63].
- Centrifuge: Centrifuge at 250 x g for 10 minutes with a low brake setting, at room temperature [63].
- Resuspend and Count: Aspirate the supernatant and resuspend the cell pellet in 1 mL of pre-warmed complete StemSpan SFEM II medium. Perform a viable cell count [63].
- Pre-culture: Adjust the cell density to 1 x 10^5 cells/mL with complete medium. Transfer to an appropriate culture plate and incubate in a humidified incubator at 37°C and 5% CO2 [63].
- Culture Duration Note: For standard applications, a 24-hour pre-culture is used. To better retain the primitive hematopoietic stem cell population (CD34+CD45RA-CD90+), reduce the pre-culture period to 4 hours [63].
Protocol: Validating Sterility Testing for Cellular Therapy Products
Ensuring the sterility of a cell product is a fundamental GMP requirement. This protocol outlines a validated method based on European Pharmacopoeia guidelines [64] [65].
Materials:
- Automated microbial detection system (e.g., BacT/Alert)
- Culture media bottles (Aerobic FA Plus and Anaerobic FN Plus)
- Thioglycollate broth (FTM) and Soybean Casein broth (TSB)
Procedure (Direct Inoculation Method):
- Sample Collection: Under a sterile laminar flow cabinet, collect a sample representing ≥1% of the final cell product volume (typically 0.5–4 mL) [65].
- Sample Preparation: Dilute the sample in 10 mL of autologous or compatible plasma used for cryopreservation [65].
- Inoculation: Inoculate the diluted sample into a set of two culture bottles: one for aerobic and one for anaerobic microorganisms [65].
- Incubation and Monitoring: Incubate the cultures in the automated system for 14 days. The system continuously monitors for microbial growth. Extending the culture beyond the 7-day minimum increases the chance of detecting low levels of slow-growing microorganisms [65].
- Validation with Positive Controls: For method validation, positive controls should be performed. All cultures in Fastidious Anaerobic Broth (FTM) should show growth after 3 days. For Tryptic Soy Broth (TSB) cultures, B. subtilis should be positive after 3 days and Mycetes after 5 days, with a detection limit of 1-10 colonies [64].
Best Practices for Thawing Cryopreserved Cells
The thawing process is critical for maximizing cell survival. Adhering to standardized protocols minimizes variability and maximizes recovery [8].
- Rapid Thawing: Use a 37°C water bath and remove the vial the moment it is thawed. Do not allow cells to sit at elevated temperatures for extended periods [8] [63].
- Gentle Handling: Avoid harsh pipetting, mixing, or vortexing, as these can damage delicate cells that have just undergone the stress of freezing and thawing [8].
- DMSO Removal: Dilute and wash cells gradually to reduce the toxicity of the cryoprotectant DMSO. A sudden osmotic shock can be detrimental [8].
- Recovery Period: Allow cells a rest period post-thaw (e.g., overnight incubation) before using them in downstream applications or assays [8].
FAQ on Critical Quality Assessment Topics
Is routine sterility testing necessary, and what is the clinical impact of a contaminated product?
Yes, routine sterility testing is a mandatory part of Good Manufacturing Practice (GMP) and JACIE standards for both minimally and extensively manipulated cell products [64] [65].
Clinical Impact: Data from a 10-year analysis showed that infusing contaminated hematopoietic stem cell (HSC) products did not result in any documented adverse impact on hematologic engraftment or directly linked infections in patients. In this study, 22 patients received contaminated HSCs, and while 5 had positive hemocultures post-infusion, none could be linked to the graft contamination. This is likely due to optimized antibiotic prophylaxis in patients [65].
Contamination Rates:
- Apheresis Products: 1.3% (22 out of 1643 products) [65].
- Bone Marrow Harvests: 17.8% (14 out of 73 harvests), highlighting the higher risk associated with bone marrow collection [65].
Best Practice Recommendation: The act of routine testing and feedback to collection centers itself improves clinical practices, leading to a observed decrease in contamination rates over time [65].
Does a low number of infused viable CD34+ cells impact long-term patient survival?
For NHL patients undergoing autologous stem cell transplantation, a low infused dose of viable CD34+ cells (< 2.0 x 10^6/kg) may delay hematologic recovery, but it does not appear to negatively impact long-term survival outcomes [61].
Key Evidence: A 2023 post-hoc study found that while patients receiving a lower dose of cells (Group A: < 2.0 x 10^6/kg) had slower engraftment than those receiving a higher dose (Group B: ≥ 2 x 10^6/kg), the low cell dose did not affect Progression-Free Survival (PFS) or Overall Survival (OS) [61]. This suggests that other factors beyond the sheer number of CD34+ cells are critical for long-term success.
What are the advanced concepts in cryopreservation-induced cell damage?
Beyond immediate ice crystal damage, scientists now recognize a complex stress response triggered by the freeze-thaw process.
Cryopreservation-Induced Delayed-Onset Cell Death (CIDOCD): This phenomenon describes apoptotic and necrotic cell death that occurs hours or days after thawing. It is driven by the activation of biochemical pathways, including apoptotic caspase activation, oxidative stress, and unfolded protein response [66].
Novel Research Approaches: The field is shifting from a focus solely on ice control (chemo-osmometric) to an integrated approach that includes molecular modulation of these cell death pathways. For example, applying Rho-associated protein kinase inhibitors post-thaw has been shown to increase the yield of cryopreserved T-cells by reducing the expression of the Fas death receptor [66].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Cryopreservation and Quality Assessment
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectant; disrupts ice crystal formation, lowers freezing point, and stabilizes cell membranes [66] [8]. | Standard component (5-10%) in cryopreservation media for HPCs [66]. |
| Hydroxyethyl Starch (HES) | Non-permeating extracellular cryoprotectant; increases solution viscosity and reduces osmotic shock [66]. | Often used in combination with DMSO in cryopreservation protocols. |
| StemSpan SFEM II Medium | A serum-free, cytokine-rich medium designed for the expansion of hematopoietic stem and progenitor cells [63]. | Used for thawing, washing, and pre-culturing CD34+ HSPCs before functional assays or gene editing [63]. |
| CD34+ Expansion Supplement | A defined supplement containing cytokines (e.g., SCF, TPO, FLT-3 Ligand) to support the survival and growth of CD34+ cells [63]. | Added to StemSpan SFEM II to create a complete culture medium for CD34+ HSPCs [63]. |
| 7-Aminoactinomycin D (7-AAD) | A fluorescent dye that binds to DNA but is excluded by viable cells. It identifies cells in late apoptosis and necrosis [62]. | Used in flow cytometry to determine the viability of specific cell populations, such as CD34+ cells and lymphocyte subsets, in fresh and thawed products [62]. |
| BacT/Alert Culture Media Bottles | Automated culture bottles for detecting aerobic and anaerobic microorganisms through colorimetric or sensor-based detection [65]. | Used for 14-day sterility testing of cellular therapy products in compliance with Pharmacopoeia guidelines [65]. |
Quality Assurance Decision Pathway
The following diagram synthesizes key information from the search results into a recommended pathway for comprehensive quality assurance of a cryopreserved stem cell product.
Comparative Analysis of Pre-Cryopreservation Processing Strategies
Troubleshooting Guide: Common Pre-Cryopreservation Issues
Poor Post-Thaw Viability
- Problem: Low cell survival rates after thawing.
- Potential Cause: Inconsistent or suboptimal cooling rates during freezing. [3] [9]
- Solution: Use a controlled-rate freezing device. Avoid homemade insulated boxes, which do not provide uniform cooling. [3] The ideal cooling rate for many cells is -1°C per minute. [3] [2]
- Potential Cause: Cells were not in optimal health or growth phase before freezing. [9] [27]
- Solution: Harvest cells for cryopreservation when they are healthy and in the late logarithmic phase of growth. [9] [2] For iPSCs, ensure they are fed daily and frozen 2-4 days after passaging, avoiding overgrowth. [3]
Low iPSC Colony Formation Post-Thaw
- Problem: Induced Pluripotent Stem Cells (iPSCs) fail to form colonies after thawing. [3]
- Potential Cause: Cryoprotectant cannot penetrate large cell clumps, leading to only peripheral cell survival. [3]
- Solution: Gently dissociate cell clumps before freezing to ensure cryoprotectant penetrates the entire aggregate. [3]
- Potential Cause: Incorrect cell density or handling during centrifugation. [3]
- Solution: Use a cell density of 1-2 x 10^6 cells/mL for cryopreservation. Centrifuge cells gently at 200-300 x g for 2 minutes and avoid overly vigorous pipetting. [3]
Osmotic Shock During Thawing
- Problem: Cells are damaged by rapid changes in solute concentration during the thawing process. [27]
- Potential Cause: Cryoprotectant is not removed properly after thawing. [3] [9]
- Solution: After rapid thawing, dilute the cell suspension dropwise into pre-warmed culture medium. This gentle dilution slowly reduces the concentration of cryoprotectant like DMSO, minimizing osmotic stress. [3] [17]
Frequently Asked Questions (FAQs)
Q1: What are the key differences between freezing cells as single cells versus as aggregates? Freezing cells as aggregates (clumps) or single cells presents distinct advantages and disadvantages for post-thaw recovery. [27]
- Aggregates (Clumps):
- Single Cells:
- Advantages: Enables better quality control through accurate cell counting and viability measurement, leading to more consistent recovery from vial to vial. [27]
- Disadvantages: Cells may require more time after thawing to re-form aggregates and may need Rho-associated kinase (ROCK) inhibitor to improve survival. [27]
Q2: How can I reduce or replace DMSO in my cryopreservation media for sensitive applications like cell therapy? DMSO can exhibit cytotoxicity, prompting research into alternatives. [3]
- Partial Replacement: Research indicates that 1% methylcellulose can produce comparable results when combined with DMSO concentrations as low as 2%. [3]
- Full Replacement: Polyvinylpyrrolidone (PVP) has been investigated as an alternative. One study observed that recovery of adipose tissue-derived stem cells cryopreserved in 10% PVP with human serum was similar to cells frozen with DMSO and animal serum. [3]
- Commercial Formulations: Use commercially available, defined, serum-free freezing media (e.g., CryoStor, Synth-a-Freeze) which are optimized for performance and regulatory compliance. [2] [67]
Q3: What are the best practices for the long-term storage of cell therapy products?
- Storage Temperature: For optimal long-term stability, store cryopreserved cells at or below -135°C, typically in the vapor phase of liquid nitrogen (between -140°C and -180°C). [3] [2] Storage at -80°C is acceptable for short periods (<1 month) but is not recommended for long-term storage as cell viability will decline over time. [2]
- Container Integrity: Use internally-threaded cryogenic vials to help prevent contamination during storage in liquid nitrogen. [2]
- Storage Monitoring: Continuously monitor liquid nitrogen levels in storage tanks, as the temperature of the vapor phase is dependent on the volume of liquid nitrogen. [27]
Table 1: Key Quantitative Parameters for Cell Cryopreservation
| Parameter | Typical Range / Value | Key Considerations | Supporting References |
|---|---|---|---|
| Cooling Rate | -1°C / minute | A rate between -0.3°C/min and -3°C/min is optimal for many cell types, including stem cells. Controlled-rate freezing or specialized containers (e.g., CoolCell) are required. [3] [2] [27] | [3] [2] [27] |
| Cell Concentration | 1x10^5 - 1x10^6 cells/mL | Too high a density can cause clumping and nutrient/CPA insufficiency; too low a density can lead to poor viability. Optimization for specific cell types is recommended. [2] | [3] [2] |
| DMSO Concentration | 5% - 10% | 10% is common, but lower concentrations (e.g., 2%) with supplements like methylcellulose are feasible. High concentrations can cause chromosomal instability. [3] [9] | [3] [9] |
| Post-Thaw Seeding Density | Varies by cell type | Plate thawed cells at a high density to optimize recovery. For iPSCs in a 6-well plate, seed between 2x10^5 - 1x10^6 viable cells. [3] | [3] [17] |
Table 2: Comparison of Cryopreservation Methods for Different Cell Types
| Cell Type | Recommended Cryoprotectant | Recommended Freezing Method | Special Notes |
|---|---|---|---|
| iPSCs (as aggregates) | 10% DMSO in culture medium, potentially with Ficoll or other supplements. [3] [27] | Slow freezing at -1°C/min in a controlled-rate freezer or freezing container. [3] [27] | Ensure cells are healthy and dissociated into small clumps. Post-thaw, colony formation may take 4-7 days. [3] [27] |
| Hepatocytes | 10% DMSO, potentially supplemented with oligosaccharides. [3] | Slow freezing at a controlled rate. | 10% DMSO is the most common minimum concentration. Commercial formulations like STEM-CELLBANKER can provide higher viability. [3] |
| Peripheral Blood Mononuclear Cells (PBMCs) | CryoStor CS10 or lab-made formulation with DMSO and serum. [2] | Slow freezing at a controlled rate. | Standardized protocols are available for reproducible results. [2] |
| Mesenchymal Stromal/Stem Cells (MSCs) | Defined, serum-free commercial media (e.g., MesenCult-ACF Freezing Medium) or DMSO-based formulations. [2] | Slow freezing at a controlled rate. | Using defined, xeno-free media is critical for therapeutic applications. [2] |
Experimental Protocols for Key Processes
Protocol 1: Standard Slow-Freezing Cryopreservation
This protocol is a general guideline for freezing many adherent and suspension cell types using a controlled cooling device. [2]
- Harvesting: Harvest cells according to standard procedures. For adherent cells, use a gentle dissociation reagent. Ensure cells are healthy and in the log phase of growth. [2]
- Centrifugation: Centrifuge the cell suspension to pellet the cells. Carefully decant the supernatant. [2]
- Resuspension: Resuspend the cell pellet in an appropriate, chilled freezing medium (e.g., CryoStor CS10 or culture medium with 10% DMSO) at a concentration of 1x10^5 - 1x10^6 cells/mL. [2] [67] Keep the suspension cold.
- Aliquoting: Aliquot the cell suspension into cryogenic vials. [2]
- Freezing:
- Option A (Controlled-Rate Freezer): Place vials in the freezer and program a freeze rate of -1°C per minute until at least -40°C to -80°C, after which the cooling rate can be increased. [67]
- Option B (Freezing Container): Place vials into an isopropanol-free freezing container (e.g., Corning CoolCell) and immediately transfer the container to a -80°C freezer for 18-24 hours. [2]
- Long-Term Storage: After freezing, promptly transfer the vials to a long-term storage location, such as the vapor phase of a liquid nitrogen tank. [2]
Protocol 2: Thawing and Recovering Cryopreserved Cells
Rapid thawing and gentle handling are critical for success. [17]
- Preparation: Pre-warm complete growth medium in a 37°C water bath. [17]
- Rapid Thawing: Remove the cryovial from storage and immediately place it in a 37°C water bath. Gently swirl the vial until only a small ice crystal remains (usually <1 minute). [17]
- Decontamination: Wipe the outside of the vial with 70% ethanol and transfer it to a laminar flow hood. [17]
- Dilution: Gently transfer the thawed cell suspension, drop by drop, into a centrifuge tube containing pre-warmed medium. This slow dilution minimizes osmotic shock. [3] [17]
- Centrifugation: Centrifuge the cell suspension at a low speed (e.g., 200 x g for 5-10 minutes) to pellet the cells and remove the cryoprotectant-containing supernatant. [17]
- Plating: Resuspend the cell pellet in fresh, pre-warmed culture medium and transfer to a culture vessel. Plate cells at a high density to support recovery. [17]
Workflow Visualization: Pre-Cryopreservation Processing
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for Cryopreservation Workflows
| Item | Function | Examples & Notes |
|---|---|---|
| Defined Cryopreservation Media | Provides a protective, serum-free environment for cells during freezing, storage, and thawing. Reduces lot-to-lot variability and safety concerns associated with serum. [2] | CryoStor [2] [68]: A cGMP-manufactured, serum-free platform. Synth-a-Freeze [67]: A defined, protein-free medium for various stem cells. |
| Cell-Type Specific Media | Optimized formulations designed for the specific needs of sensitive cell types, improving post-thaw recovery and functionality. [2] | mFreSR: For human ES/iPS cells. [2] MesenCult-ACF Freezing Medium: For Mesenchymal Stromal Cells (MSCs). [2] |
| Cryoprotective Agents (CPAs) | Penetrating (intracellular) or non-penetrating (extracellular) agents that reduce ice crystal formation and protect cells from cryo-injury. [3] [9] | Intracellular: DMSO, Glycerol. [3] Extracellular: Sucrose, Dextrose, Methylcellulose, PVP. [3] |
| Controlled-Rate Freezing Devices | Ensures a consistent, optimal cooling rate (e.g., -1°C/min), which is critical for high cell viability and process reproducibility. [3] [2] [68] | Programmable Freezing Units: Gold standard for control. [3] Passive Cooling Devices: e.g., Corning CoolCell, Nalgene Mr. Frosty. [3] [2] |
| Cryogenic Storage Vials | Sterile containers designed for low-temperature storage. Choice of thread type can impact contamination risk and automation compatibility. [3] [2] | Internal Thread: May reduce contamination risk. [3] External Thread: May be preferred for automation. [3] |
Within research on optimizing the cryopreservation and thawing of personalized stem cell products, functional fitness assays are indispensable for quantifying the true therapeutic potential of these cells. While basic viability stains can indicate immediate membrane integrity post-thaw, they often overestimate cell health. Assays that measure the ability to form Colony-Forming Units (CFU) and assess metabolic activity provide a deeper, more functional readout of cell survival, proliferative capacity, and biological fitness. This guide addresses common challenges and provides troubleshooting support for researchers employing these critical assays in the development of advanced cell therapies.
Troubleshooting Common Assay Challenges
Colony-Forming Unit (CFU) Assays
CFU assays evaluate a single cell's capacity to proliferate and form a large colony, directly testing its long-term clonogenic potential and reproductive health [69].
Q1: Our CFU assays show low plating efficiency and high variability after seeding cryopreserved cells. What are the key factors we should investigate?
- A: Low and variable plating efficiency often stems from issues in the pre-assay handling and thawing process. Key areas to investigate include:
- Thawing Technique: Rapid thawing in a 37°C water bath is critical to minimize ice crystal damage [17] [18]. Diluting the cryoprotectant (e.g., DMSO) dropwise with pre-warmed medium immediately after thawing is essential to prevent toxicity [18] [35].
- Cell Handling: Post-thaw, cells are particularly fragile. Avoid vortexing or high-speed centrifugation, as these practices can further reduce viability and clonogenic potential [17] [35]. Gently resuspend cells and use low centrifugal forces (e.g., 200-300 × g) for washing [18].
- Plating Density: Plate thawed cells at a high density as recommended by the supplier to optimize recovery. Over-diluted samples can lead to poor colony formation [17].
- Culture Medium: Use the complete growth medium recommended for your specific cell type. An imbalance in serum concentration (e.g., reducing from 10% to 5% FBS) can significantly lower colony yield [69].
- A: Low and variable plating efficiency often stems from issues in the pre-assay handling and thawing process. Key areas to investigate include:
Q2: How can we accurately distinguish a true colony from a simple cell cluster during counting?
- A: A true colony is biologically defined as a cluster of 50 or more cells, originating from a single progenitor cell, which reflects approximately 5-6 cell divisions [69]. To ensure accurate counting:
- Use Staining and Thresholds: After a suitable incubation period (typically 1-3 weeks), fix and stain cells with dyes like crystal violet or Giemsa. Establish a size threshold in your imaging or analysis software to count only clusters meeting the 50-cell minimum.
- Understand the Purpose: This threshold distinguishes cells with sustained proliferative capacity from those that have merely survived or undergone a few divisions before succumbing to reproductive cell death [69].
- A: A true colony is biologically defined as a cluster of 50 or more cells, originating from a single progenitor cell, which reflects approximately 5-6 cell divisions [69]. To ensure accurate counting:
Q3: What are the common sources of contamination in long-term CFU assays and how can we prevent them?
- A: Maintaining sterility over the assay's duration is paramount.
- Aseptic Technique: Always work in a Class II biosafety cabinet using sterile lab coats, gloves, and minimal movement [69].
- Reagents and Equipment: Use sterile, filtered media and supplements. Include antibiotics like penicillin and streptomycin in the culture media, though be aware that long-term use may slightly reduce colony yield in sensitive lines [69].
- Incubator Management: Maintain a clean CO₂ incubator with humidity levels between 95-98%. Using a water pan containing copper sulfate can help deter microbial growth [69].
- A: Maintaining sterility over the assay's duration is paramount.
Metabolic Activity Assays
These assays, which often measure fluorescence or absorbance as proxies for cellular health, can be influenced by numerous factors beyond just the number of living cells.
Q1: Why might metabolic activity data from a quick assay not correlate with the results from a longer-term CFU assay?
- A: This discrepancy is common and highlights the fundamental difference between what these assays measure.
- Short-term vs. Long-term: Metabolic assays measure immediate biochemical activity (e.g., enzyme activity or membrane potential) but cannot distinguish between cells that are truly clonogenic and those that are alive but have lost the ability to proliferate long-term (reproductive cell death) [69]. CFU assays directly measure this long-term proliferative capacity.
- Overestimation by Metabolic Assays: Studies show that short-term viability assays often overestimate cell survival compared to CFU assays, making CFU a more reliable gold standard for evaluating the impact of treatments like cryopreservation on reproductive health [69].
- A: This discrepancy is common and highlights the fundamental difference between what these assays measure.
Q2: After thawing cryopreserved PBMCs, we get acceptable viability with trypan blue, but our flow cytometry data is inconsistent. What could be wrong?
- A: Trypan blue and similar vitality dyes only assess cell membrane integrity at the moment of thaw and can miss underlying damage.
- Cell Fitness vs. Viability: Research indicates that a combined measurement of metabolic activity and early apoptosis markers is a better indicator of "cell fitness" than membrane integrity alone [70].
- Establish Fitness Thresholds: Data suggests that for reliable biomarker assays, cryopreserved cells should be >60-70% live and apoptosis-negative. Below this threshold, assay results may be determined by cell fitness rather than the inherent biology of the cells [70]. Letting cells rest overnight post-thaw can allow early apoptotic cells to become detectable, providing a more accurate health assessment [70].
- A: Trypan blue and similar vitality dyes only assess cell membrane integrity at the moment of thaw and can miss underlying damage.
Q3: How does the culture vessel affect the outcome of metabolic growth curves?
- A: The choice of vessel can significantly impact the results. A study comparing growth in 96-well plates, culture flasks, and culture tubes found that fitness conclusions for the same engineered E. coli mutants changed depending on the vessel used [71]. This was attributed to differences in environmental conditions, such as oxygenation and pH, which can affect microbial physiology and distort fitness measurements. It is crucial to use a vessel that replicates the experimental evolution environment as closely as possible [71].
Essential Protocols & Data Tables
Standardized Protocol: Thawing Cryopreserved Cells for Functional Assays
This protocol is critical for maximizing cell recovery and fitness prior to assay setup [17] [18].
- Preparation: Pre-warm complete growth medium in a 37°C water bath. Prepare a centrifuge tube with a suitable volume (e.g., 10 mL) of this medium.
- Rapid Thaw: Retrieve the cryovial from liquid nitrogen storage and immediately place it in a 37°C water bath. Gently swirl the vial until only a small ice crystal remains (approximately 1-2 minutes).
- Decontaminate and Transfer: Wipe the vial with 70% ethanol and transfer to a biosafety cabinet. Slowly transfer the thawed cell suspension dropwise into the prepared tube of pre-warmed medium to dilute the cryoprotectant.
- Wash: Centrifuge the cell suspension at 200-300 × g for 5-10 minutes.
- Resuspend and Count: Carefully decant the supernatant and gently resuspend the cell pellet in fresh, pre-warmed medium. Perform a cell count and viability assessment.
- Proceed to Assay: Plate cells directly into the functional assay (CFU or metabolic activity) at the recommended density. For some cell types, a short recovery period in culture may be beneficial.
Experimental Workflow Diagram
The following diagram outlines the logical workflow from cell thawing to functional fitness analysis, integrating key decision points for troubleshooting.
The table below summarizes key quantitative findings from recent studies on the impact of cryopreservation on functional outcomes, particularly in a clinical stem cell transplant context.
Table 1: Impact of Graft Cryopreservation on Functional Engraftment Outcomes
| Functional Outcome | Fresh Graft Performance | Cryopreserved Graft Performance | Significance & Notes |
|---|---|---|---|
| Platelet Engraftment Time | 15 days (median) [72] | 18 days (median) [72] | Significant delay (P<0.01) [72] |
| Neutrophil Engraftment Time | 13 days (median) [72] | 14 days (median) [72] | Significant delay (P<0.01) [72] |
| Primary Graft Failure | Lower odds [73] | Higher odds (OR: 0.58 for composite failure) [73] | Associated with significantly lower odds of failure for fresh grafts [73] |
| Cell Fitness Threshold | Not Applicable | >60-70% Live/Apoptosis-Negative [70] | Minimum for reliable immunological assay results [70] |
| Overall Survival (1-Year) | Favored fresh grafts in some analyses [73] | Comparable in some studies [72] | Associations can vary by statistical model and study [73] [72] |
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Functional Fitness Assays
| Reagent / Material | Function in Assay | Key Considerations |
|---|---|---|
| Complete Growth Medium | Supports cell viability and continuous proliferation. | Must be balanced for specific cell type. Serum concentration (e.g., 10% FBS) is critical for colony formation [69]. |
| Semi-Solid Media (e.g., Methylcellulose) | Prevents cell movement in CFU assays, ensuring each colony arises from a single cell. | Essential for non-adherent/hematopoietic cells. Can be supplemented with cytokines (Epo, GM-CSF) [69]. |
| Trypsin/EDTA | Creates viable single-cell suspensions from adherent cultures for accurate plating. | Concentration and incubation time must be optimized to avoid damaging cell surface proteins [69]. |
| Fixatives & Stains (e.g., Crystal Violet) | Preserves and visualizes colonies for counting. | Crystal violet offers clear boundaries for automated counting; Giemsa provides morphological detail [69]. |
| Viability/Fitness Dyes | Assesses cell health post-thaw. | Trypan blue checks membrane integrity. Advanced kits measuring metabolism + apoptosis (e.g., CC-450/Apopxin) better predict assay success [70]. |
| Cryoprotectant (DMSO) | Protects cells during freezing. | Must be diluted effectively post-thaw. Exposure to room temperature after thawing is toxic [18] [35]. |
FAQs on Core Concepts
Q: Why is the CFU assay considered a "gold standard" in stem cell research?
- A: The CFU assay directly measures a cell's long-term, functional capacity to proliferate and self-renew, which is the defining biological function of a stem cell. Unlike metabolic assays that provide a snapshot of general health, CFU proves clonogenic potential, making it a more stringent test for therapeutic quality [69].
Q: For personalized cell products, should we always use fresh cells over cryopreserved ones for assays?
- A: While fresh grafts are associated with better outcomes in some clinical studies (e.g., lower graft failure rates) [73], cryopreservation is logistically essential for off-the-shelf and banked therapies. The goal of optimization research is not to eliminate cryopreservation but to refine the process so that the functional fitness of thawed cells closely mirrors that of fresh cells. The UK multicenter study showed that despite delays in engraftment, cryopreserved grafts can still achieve similar overall survival, highlighting the potential of the approach [72].
Q: What is the single most critical step to ensure success in these functional assays post-thaw?
- A: While the entire process is a chain, the most critical phase is the immediate post-thaw handling. This includes the rapidity of thawing, the gentle yet swift dilution of cryoprotectant, and the use of low-stress centrifugation and resuspension techniques. Errors introduced at this stage cause damage that no downstream assay can overcome [17] [18] [35].
Cryopreservation is a critical unit operation in the manufacturing of advanced therapeutic medicinal products (ATMPs), including Chimeric Antigen Receptor T-cell (CAR-T) and Hematopoietic Stem Cell (HSC) therapies. This process enables long-term storage and logistical flexibility by halting cellular metabolism at ultra-low temperatures (typically -135°C to -196°C) [28] [2]. However, the freezing and thawing procedures can induce various forms of cellular damage that may compromise the quality, potency, and ultimately, the therapeutic efficacy of these living drugs [28] [15]. Understanding and mitigating these challenges is essential for advancing personalized stem cell products from research to clinical application.
Key Challenges and Impact on Therapeutic Efficacy
Fundamental Cryodamage Mechanisms
Cryopreservation inflicts damage through three primary mechanisms, each with distinct consequences for therapeutic cell products:
- Osmotic Damage: During slow freezing, extracellular ice formation increases solute concentration in the unfrozen fraction, creating a hypertonic environment that drives osmotically forced water efflux from cells. This dehydration can cause irreversible damage to cellular structures and functions [15].
- Mechanical Damage: Rapid cooling prevents sufficient water from leaving the cell, leading to intracellular ice formation. This ice can puncture membranes and damage organelles, compromising cell viability [15] [74].
- Oxidative Damage: The cryopreservation process generates reactive oxygen species (ROS), which can oxidize lipids, proteins, and nucleic acids, leading to impaired cell function and apoptosis post-thaw [15].
Functional Consequences for CAR-T and HSC Products
The physical damage from cryopreservation translates into specific functional deficits that directly impact therapeutic performance:
- Reduced Cell Viability and Recovery: Ice crystal formation and osmotic stress directly kill cells, resulting in lower viable cell counts upon thawing. This reduces the effective therapeutic dose [74].
- Impaired Engraftment and Persistence: For HSCs and CAR-T cells, long-term engraftment in vivo is crucial for sustained therapeutic effect. Cryodamage can impair homing, adhesion, and proliferation capacities, diminishing persistence [28] [75].
- Loss of "Stemness" and Differentiation Potential: Particularly critical for HSCs, cryopreservation can disrupt epigenetic regulation and cell-extracellular matrix interactions, reducing the ability to self-renew and differentiate into mature blood lineages [74].
- Altered Immunophenotype and Function: Cryopreservation stress can change the surface marker expression and functional characteristics of therapeutic cells. For CAR-T cells, this may shift the population toward more differentiated, short-lived effector phenotypes rather than the desired long-persisting memory subsets (e.g., TSCM, TCM), compromising long-term efficacy [76] [77].
- Metabolic Reprogramming: CD28-based CAR-T cells undergoing cryopreservation stress may experience PI3K-AKT pathway activation leading to glycolytic metabolic reprogramming. This promotes differentiation into short-lived effector cells at the expense of long-persisting memory T cells, reducing in vivo durability [77].
Table 1: Functional Deficits in Cryopreserved Cell Therapies and Their Clinical Impact
| Functional Deficit | Affected Cell Type | Impact on Therapeutic Efficacy |
|---|---|---|
| Reduced Viability | CAR-T, HSC, MSC | Lower effective dose; potential treatment failure |
| Impaired Engraftment/Persistence | HSC, CAR-T | Shortened duration of effect; disease relapse |
| Loss of Stemness | HSC | Poor long-term reconstitution; cytopenias |
| Phenotype Shift | CAR-T | Reduced memory subsets; shorter persistence |
| Metabolic Alteration | CAR-T | Enhanced differentiation; exhaustion |
| Immunomodulatory Loss | MSC | Reduced therapeutic potency in inflammatory environments |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: What are the primary factors influencing post-thaw recovery and viability of CAR-T cells?
A: Multiple factors contribute to post-thaw recovery:
- Cell Source and Phenotype: CAR-T products derived from cord blood, which contains a higher proportion of naïve and TSCM cells, often show better recovery and persistence than those from heavily pre-treated peripheral blood [76].
- Freezing Rate: A controlled rate of -1°C/minute is critical to minimize ice crystal formation [2] [3].
- Cryoprotectant Formulation: DMSO concentration (typically 5-10%) must balance protection and toxicity. Combining DMSO with non-permeable agents like trehalose or sucrose can allow for concentration reduction [15].
- Pre-freeze Cell State: Cells should be harvested during log-phase growth at >80% confluency and be free from microbial contamination [2].
Q2: How does cryopreservation specifically contribute to prolonged cytopenias after CAR-T therapy?
A: Cytopenias post-CAR-T are biphasic and multifactorial [75]. Cryopreservation exacerbates this by:
- Damaging HSCs in the graft, impairing their ability to reconstitute hematopoiesis.
- Inducing inflammatory responses (e.g., elevated IL-6, CRP, ferritin) that promote hematopoietic stem cell exhaustion in the bone marrow niche [75].
- The CAR-HEMATOTOX score, which incorporates baseline blood counts and inflammatory markers, can help predict patients at high risk for prolonged cytopenias [75].
Q3: What are the key differences in cryopreservation requirements between autologous and allogeneic cell therapy products?
A:
- Autologous products (e.g., patient-specific CAR-T) face challenges related to patient health status—cells from heavily pre-treated patients may be more cryosensitive. The entire chain from apheresis to infusion must be meticulously planned, and cryopreservation provides essential scheduling flexibility [78].
- Allogeneic "off-the-shelf" products (e.g., cord blood CAR-T/NK, HSCs) require large-scale banking. Here, cryopreservation is a core manufacturing step, not just a logistical convenience. Consistency across batches and donor units is paramount, requiring extremely standardized protocols [76] [78].
Q4: Our lab observes variable recovery of MSCs after thawing. Which parameters should we prioritize to improve consistency?
A: For Mesenchymal Stromal/Stem Cells (MSCs), focus on:
- Freezing Density: Optimize within 5×10^5 to 1×10^6 cells/mL [74].
- Post-Thaw Revival: Use specialized media and provide essential growth factors to help MSCs recover functionality [74].
- Quality Assessment: Go beyond viability. Routinely check differentiation potential (adipo-, osteo-, chondrogenesis), immunomodulatory function (e.g., T-cell suppression assays), and surface marker expression (CD90, CD105, CD73 positive; CD34, CD45 negative) post-thaw [74].
Step-by-Step Experimental Protocol: Assessing Post-Thaw CAR-T Cell Potency
This protocol provides a framework for evaluating the critical quality attributes of CAR-T cells after cryopreservation.
Objective: To determine the functional competence of cryopreserved CAR-T cells through a multi-parameter assessment of viability, phenotype, and cytotoxic activity.
Materials:
- Cryopreserved CAR-T cell vial
- 37°C water bath or automated thawing device (e.g., ThawSTAR)
- Pre-warmed complete culture medium (e.g., RPMI-1640 + 10% FBS)
- Centrifuge
- Flow cytometer with appropriate antibodies
- Target cells expressing the cognate antigen
- Incubator (37°C, 5% CO2)
- Cytotoxicity detection kit (e.g., LDH release, real-time cell analysis)
Procedure:
Rapid Thawing:
Cryoprotectant Removal & Washing:
- Gently transfer the cell suspension to a tube containing 10 volumes of pre-warmed medium. Add the medium drop-wise to minimize osmotic shock.
- Centrifuge at 200-300 x g for 5 minutes. Carefully aspirate the supernatant containing the DMSO.
- Resuspend the cell pellet in fresh, pre-warmed complete medium [2] [3].
Viability and Cell Counting:
- Mix a cell sample with Trypan Blue or use an automated cell counter. Calculate total and viable cell concentration.
- For a more detailed analysis of apoptosis/necrosis, perform Annexin V/Propidium Iodide staining and analyze by flow cytometry [74].
Immunophenotyping by Flow Cytometry:
- Aliquot 5×10^5 - 1×10^6 cells into a flow tube.
- Stain with fluorescently labeled antibodies to identify key T cell subsets. A critical panel includes:
- Analyze on a flow cytometer. A high-quality product should retain a significant proportion of naïve/TSCM and TCM phenotypes.
In Vitro Cytotoxicity Assay:
- Co-culture thawed CAR-T cells with fluorescently labeled target cells at various Effector:Target (E:T) ratios (e.g., 40:1, 20:1, 10:1, 5:1) in a 96-well plate.
- Include controls (target cells alone, effector cells alone).
- After 12-48 hours, measure specific lysis using a real-time cell analyzer or by quantifying LDH release in the supernatant.
- Calculate % Specific Cytotoxicity = (Experimental LDH - Effector Spontaneous LDH - Target Spontaneous LDH) / (Target Maximum LDH - Target Spontaneous LDH) * 100.
Cytokine Secretion Profile:
Interpretation: Compare the post-thaw viability, phenotype distribution, and cytotoxic potency to pre-freeze samples or established release criteria. A successful cryopreservation process should maintain >70% viability, preserve memory subsets, and exhibit potent, antigen-specific killing.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Cryopreservation Optimization
| Reagent/Material | Function/Purpose | Key Considerations |
|---|---|---|
| DMSO (Dimethyl Sulfoxide) | Penetrating cryoprotectant; reduces ice crystal formation. | Cytotoxic at high concentrations/ prolonged exposure; standard use at 5-10%; requires gradual removal post-thaw [15] [3]. |
| Trehalose/Sucrose | Non-penetrating cryoprotectants; provide extracellular stabilization and reduce osmotic stress. | Allows for reduction of DMSO concentration; improves post-thaw recovery of HSCs and others [15]. |
| cGMP-manufactured, Xeno-Free Freezing Media (e.g., CryoStor) | Ready-to-use, serum-free cryopreservation medium. | Ensures consistency, eliminates lot-to-lot variability and risk from animal sera; critical for clinical applications [2] [74]. |
| Controlled-Rate Freezer (or passive devices like CoolCell) | Ensures optimal cooling rate of -1°C/minute. | Vital for reproducible viability; passive containers are a cost-effective alternative to programmable freezers [2] [3]. |
| Internal-Thread Cryogenic Vials | Secure containment for frozen cells. | Reduces risk of contamination during filling and storage in liquid nitrogen [2] [3]. |
| Annexin V / PI Apoptosis Detection Kit | Distinguishes viable, early apoptotic, and necrotic cells post-thaw. | Provides a more accurate assessment of cell health than viability dyes alone [74]. |
| Cell-Specific Phenotyping Antibody Panels | Characterizes differentiation/activation state (e.g., CD45RA/RO, CCR7, CD62L for T cells). | Essential for correlating post-thaw phenotype with in vivo persistence potential [76]. |
Visualizing Critical Relationships and Workflows
Cryopreservation Impact on CAR-T Cell Fate
This diagram illustrates how cryopreservation stress can influence CAR-T cell differentiation and metabolic state, ultimately affecting therapeutic persistence.
Post-Thaw Quality Assessment Workflow
This flowchart outlines the key experiments for a comprehensive functional assessment of therapeutic cells after thawing.
Conclusion
Optimizing cryopreservation and thawing is not a one-size-fits-all endeavor but a critical, application-specific process that directly influences the therapeutic potential of personalized stem cell products. Success hinges on understanding the fundamental trade-offs between cell recovery, purity, and long-term functional fitness. The integration of controlled-rate freezing, optimized cryoprotectant formulations, and rigorous post-thaw analytics forms the foundation of a robust protocol. As the stem cell market continues its rapid growth, future efforts must focus on standardizing methods, embracing closed-system technologies for scalability and safety, and deepening the understanding of how cryopreservation impacts critical quality attributes. By adopting these evidence-based strategies, researchers and developers can enhance product consistency, ensure regulatory compliance, and ultimately accelerate the delivery of reliable and effective stem cell therapies to patients.
References
- 1. Cryopreservation of biological materials: applications and ... [https://link.springer.com/article/10.1007/s11626-025-01027-0]
- 2. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 3. Cryopreservation of Cells: Dos and Don'ts [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/the-dos-and-donts-of-cryopreservation.html]
- 4. Cryopreservation - Key Survey Findings from the ISCT ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/05/28/cryopreservation-key-survey-findings-from-the-isct]
- 5. How To Overcome The Challenges In Cryopreservation? [https://www.kosheeka.com/overcome-the-challenges-in-cryopreservation/]
- 6. Poor Cell Growth Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/poor-cell-growth?srsltid=AfmBOormM8StRiEusLyXR-m-5frPp_jsPRzjZzc8KQ4ogLda9zYt4Xqa]
- 7. Best Practices for Ultra-Low Temperature Storage [https://custombiogenics.com/cryopreservation-best-practices-for-ultra-low-temperature-storage/]
- 8. Cryopreservation in Cell and Gene Therapy [https://cgt.global/cryopreservation-in-cell-and-gene-therapy-ensuring-high-viability-cells-for-research-manufacturing/]
- 9. Why Aren't My Cells Surviving Cell Thawing? [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/why-arent-my-cells-surviving-cell-thawing.html]
- 10. Current practices in peripheral blood stem cell processing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283502/]
- 11. Cell Cryopreservation Market Size and Forecast – 2025-2032 [https://www.coherentmarketinsights.com/market-insight/cell-cryopreservation-market-1698]
- 12. Viable and Functional: Long-Term -80 °C Cryopreservation ... [https://pubmed.ncbi.nlm.nih.gov/41096113/]
- 13. Impact of pre- and post-thaw processing on recovery ... [https://pubmed.ncbi.nlm.nih.gov/41026081/]
- 14. Powering China's Stem Cell Therapy Revolution in 2025 [http://www.cellstore-global.com/news/cellstore-stem-cell-cryopreservation-medium-powering-chinas-stem-cell-therapy-revolution-in-2025.html]
- 15. Principles and Protocols For Post-Cryopreservation Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9113563/]
- 16. Optimizing cryopreservation strategies for scalable cell therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659802/]
- 17. Thawing Cells | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/thawing-cells.html]
- 18. How to Thaw Frozen Primary Cells [https://www.stemcell.com/how-to-thaw-frozen-primary-cells.html]
- 19. Cryopreservation Systems | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/lab-equipment/cold-storage/cryopreservation-systems-accessories.html]
- 20. Practice of Cryopreservation of Cellular Starting Materials from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446400/]
- 21. Regulation of stem cell use in the EU [https://www.hoganlovells.com/en/publications/regulation-of-stem-cell-use-in-the-eu]
- 22. Regulatory Round-up - July 2025 - Cell and Gene Therapy [https://ct.catapult.org.uk/news/regulatory-round-up-july-2025]
- 23. Advanced therapy medicinal products: Overview [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview]
- 24. FDA Halts New Clinical Trials That Export Americans' Cells ... [https://www.fda.gov/news-events/press-announcements/fda-halts-new-clinical-trials-export-americans-cells-foreign-labs-hostile-countries-genetic]
- 25. Freezing cells for success: DMSO-free redefining the future ... [https://www.news-medical.net/news/20251125/Freezing-cells-for-success-DMSO-free-redefining-the-future-of-cryopreservation.aspx]
- 26. Passive freezing is equivalent to controlled-rate ... [https://pubmed.ncbi.nlm.nih.gov/40323255/]
- 27. Improving Cell Recovery: Freezing and Thawing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8909336/]
- 28. Impact of Cryopreservation and Freeze-Thawing on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9045030/]
- 29. 3D culture and cryopreservation/thawing strategy of human ... [https://www.sciencedirect.com/science/article/abs/pii/S2214552425000951]
- 30. The Importance of Controlling the Rate of Freezing [https://www.thermofisher.com/blog/life-in-the-lab/the-importance-of-controlling-the-rate-of-freezing/]
- 31. Impact of lower concentrations of dimethyl sulfoxide on ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924000537]
- 32. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362920/]
- 33. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell therapy... [https://pubmed.ncbi.nlm.nih.gov/40826088/]
- 34. -free cryopreservation of hiPSC-derived cardiomyocytes: low... DMSO [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04384-5]
- 35. Thawing cells – process, difficulties & recommendations [https://www.susupport.com/blogs/knowledge/thawing-cells-process-difficulties-recommendations]
- 36. Impact of pre- and post-thaw processing on recovery ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008400]
- 37. Optimizing Cord Blood for Best Therapeutic Outcomes [https://www.linkedin.com/posts/cytotherapy_%F0%9D%97%99%F0%9D%97%BF%F0%9D%97%BC%F0%9D%97%BA-%F0%9D%97%A7%F0%9D%97%B5%F0%9D%97%AE%F0%9D%98%84-%F0%9D%98%81%F0%9D%97%BC-%F0%9D%97%A7%F0%9D%97%B5%F0%9D%97%B2%F0%9D%97%BF%F0%9D%97%AE%F0%9D%97%BD%F0%9D%98%86-%F0%9D%97%A2-activity-7376006550546608128-saEB]
- 38. Photobiomodulation as an antioxidant substitute in post - thawing ... [https://www.nature.com/articles/s41598-021-96841-3?error=cookies_not_supported&code=45d8a329-4009-47c8-b8e2-bced18f7b394]
- 39. Improving Cell Recovery: Freezing and Thawing ... [https://www.mdpi.com/2073-4409/11/5/799]
- 40. Collection, cryopreservation and thawing of stem cells for ... [https://www.htct.com.br/pt-collection-cryopreservation-thawing-stem-cells-articulo-S2531137922000025]
- 41. Ultra Cold Chain Logistics: Definition, Trends & Optimization ... [https://www.tempcontrolpack.com/knowledge/ultra-cold-chain-logistics-definition-trends-optimization-tips-for-2025/]
- 42. ISBER Releases Position Statement for Management and ... [https://www.isber.org/news/547382/ISBER-Releases-Position-Statement-for-Management-and-Use-of-Ultra-Low-Temperature-Freezers.htm]
- 43. Best Practices for Cold Chain Vaccine Storage | solution [https://www.phchd.com/apac/biomedical/service-downloads/evolving-science-for-the-future/cold-chain-vaccine-storage]
- 44. The EasyLog Guide to Cold Chain Compliance in 2025 [https://lascarelectronics.com/cold-chain-compliance-in-2025/]
- 45. Cold Chain Management : A Comprehensive Guide [https://pharmasource.global/content/guides/category-guide/cold-chain-management-a-comprehensive-guide/]
- 46. From Freezer to Failure? The Hidden Risks ... [https://cellbox-solutions.com/cellbox-blog/from-freezer-to-failure-the-hidden-risks-of-cryopreservation-in-cell-therapy]
- 47. the critical step to utilize stem cell products [https://pmc.ncbi.nlm.nih.gov/articles/PMC10393932/]
- 48. Dimethyl sulfoxide for cryopreservation of alginate ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224022000396]
- 49. Strategies in developing dimethyl sulfoxide (DMSO)-free ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1030965/full]
- 50. Hydrogel microcapsulation technology reduces the DMSO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639263/]
- 51. Open vs. Closed Processing in Biopharmaceuticals [https://www.cpduk.co.uk/news/open-vs-closed-processing-in-biopharmaceuticals-a-guide-to-effective-contamination-control]
- 52. Cryopreservation in ART and concerns with contamination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5892987/]
- 53. mitigating the viral contamination risk to reproductive cells ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648320305186]
- 54. Food Safety Insights: Comparing Open and Closed Systems [https://nhkmachineryparts.com/food-safety-insights-comparing-open-and-closed-systems/]
- 55. Culture Support— Stem Cell Troubleshooting [https://www.thermofisher.com/br/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 56. Data in Motion: Freezing Curves in the Digitcool [https://www.imv-technologies.us/academy/data-in-motion-freezing-curves-in-the-digitcool]
- 57. Frequently Asked Questions on Primary Cells [https://www.stemcell.com/primary-cells-faq.html]
- 58. Post- thaw of viability peripheral blood cryopreserved ... stem cells [https://pubmed.ncbi.nlm.nih.gov/27291859/]
- 59. (PDF) Post- thaw of viability peripheral blood cryopreserved ... stem [https://www.academia.edu/52769771/Post_thaw_viability_of_cryopreserved_peripheral_blood_stem_cells_PBSC_does_not_guarantee_functional_activity_important_implications_for_quality_assurance_of_stem_cell_transplant_programmes]
- 60. Recovery of viable CD34+ cells from cryopreserved ... [https://pubmed.ncbi.nlm.nih.gov/15937512/]
- 61. Loss of CD34+ Cells and Effect of the Number of Viable ... [https://www.sciencedirect.com/science/article/pii/S2152265023002562]
- 62. Variable recovery of cryopreserved hematopoietic stem ... [https://www.sciencedirect.com/science/article/abs/pii/S1473050223001477]
- 63. How to Perform Gene Editing of Human CD34+ HSPCs ... [https://www.stemcell.com/gene-editing-human-cd34-hematopoietic-stem-and-progenitor-cells-with-the-cellpore-transfection-system.html]
- 64. A practical approach for the validation of sterility, endotoxin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2753319/]
- 65. Utility of routine evaluation of sterility of cellular therapy ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324917307727]
- 66. Pros and Cons of Cryopreserving Allogeneic Stem Cell ... [https://www.mdpi.com/2073-4409/13/6/552]
- 67. Synth-a-Freeze™ Cryopreservation Medium - FAQs [https://www.thermofisher.com/order/catalog/product/A1254201/faqs]
- 68. Overcoming Cryopreservation Challenges [https://www.biolifesolutions.com/resource-center/insights-blog/overcoming-cryopreservation-challenges/]
- 69. Colony formation assay: A tool to study cell survival [https://www.abcam.com/en-us/knowledge-center/cell-biology/colony-formation-assay]
- 70. Improving Reliability of Immunological Assays by Defining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447670/]
- 71. Case Studies in the Assessment of Microbial Fitness [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276084/]
- 72. Hematopoietic Stem Cell (HSC) Graft Cryopreservation ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725011145]
- 73. Comparison of Fresh Versus Frozen Allogenic Peripheral ... [https://pubmed.ncbi.nlm.nih.gov/40998263/]
- 74. Dealing with Cryopreservation Challenges in ... [https://www.atlantisbioscience.com/blog/dealing-with-cryopreservation-challenges-in-mesenchymal-stem-cell-culture/?srsltid=AfmBOorIk1_FOVDXHP9mM1wvO7r91RtNMizBnCZLDrnMnFGYECQqR1Rw]
- 75. Chimeric Antigen Receptor T-Cell Therapy and ... [https://www.mdpi.com/2073-4409/12/4/531]
- 76. New player in CAR-T manufacture field: comparison of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1561174/full]
- 77. Advances in CAR optimization strategies based on CD28 [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1548772/full]
- 78. Fresh or frozen? Navigating the cryopreservation dilemma ... [https://www.europeanpharmaceuticalreview.com/article/229851/fresh-or-frozen-navigating-the-cryopreservation-dilemma-for-cgt/]
- 79. Current Advances and Challenges in CAR-T Therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212355/]