Optimizing Post-Thaw Stem Cell Viability: A 2025 Guide for Enhanced Recovery in Research & Therapy
This article provides a comprehensive guide for researchers and drug development professionals on the critical factors influencing stem cell viability and recovery after cryopreservation.
Optimizing Post-Thaw Stem Cell Viability: A 2025 Guide for Enhanced Recovery in Research & Therapy
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical factors influencing stem cell viability and recovery after cryopreservation. Covering foundational principles, advanced methodological protocols, and systematic troubleshooting, it synthesizes current best practices for optimizing post-thaw outcomes. The content explores the balance between intracellular ice formation and cell dehydration, details controlled-rate freezing and thawing techniques, and validates strategies through industry survey data and comparative analytics. The goal is to equip scientists with actionable knowledge to improve cell fitness, ensure experimental reproducibility, and enhance the efficacy of cell-based therapies.
The Science of Cell Survival: Understanding Cryopreservation Fundamentals
Fundamental Mechanisms and FAQs
FAQ: What are the primary competing risks of cellular damage during cryopreservation? The two principal competing risks are intracellular ice formation (IIF) and excessive cell dehydration. During freezing, ice forms outside the cell first. This increases the solute concentration in the remaining liquid, creating an osmotic pressure difference that draws water out of the cell—a process known as dehydration. A slow cooling rate allows time for this water to exit, preventing deadly intracellular ice. However, if the cooling is too slow, excessive dehydration occurs, leading to a harmful increase in intracellular solute concentration and cell shrinkage. Conversely, if cooling is too fast, water does not have time to exit and freezes inside the cell, forming intracellular ice crystals that can disrupt organelles and the cell membrane, which is almost always fatal [1] [2] [3].
FAQ: How does the ice nucleation temperature influence cell survival? Controlling the temperature at which ice nucleates extracellularly (Tnuc) is critical. Research on Jurkat T-cells shows that a higher Tnuc, closer to the solution's equilibrium freezing point (e.g., -6°C), is beneficial. This promotes more extensive intracellular dehydration during the freezing process, which in turn leads to less intracellular ice formation and results in higher post-thaw cell membrane integrity and viability, compared to a lower Tnuc (e.g., -10°C) or uncontrolled nucleation [1].
FAQ: What role does the warming rate play? The warming rate is crucial, particularly in preventing damage from recrystallization. During slow warming, small intracellular ice crystals can melt and refreeze into larger, more damaging crystals. A rapid warming rate is therefore preferred to minimize the time spent in temperature zones where this recrystallization occurs, thereby reducing damage to the cell membrane [2] [3]. Computational models suggest that for some cell types, adding a high-power pulse at the start of warming can further mitigate recrystallization effects [3].
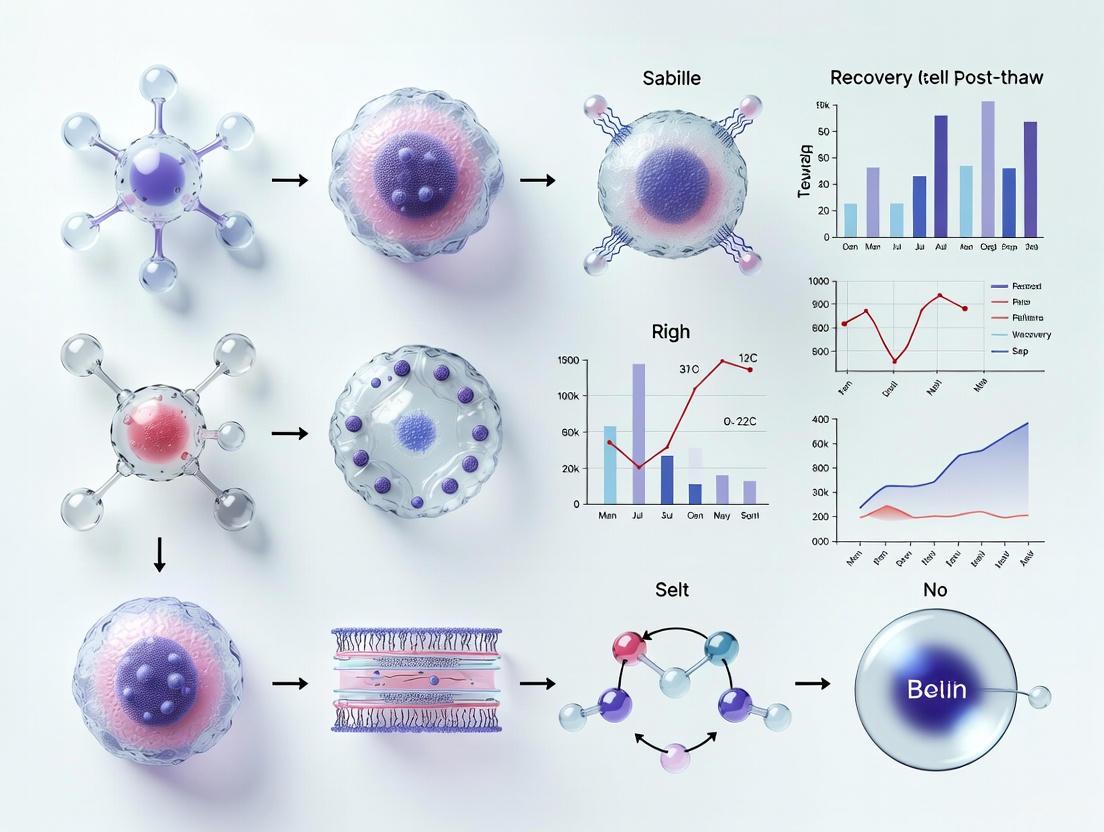
The following diagram illustrates the core principles and competing risks during the freeze-thaw cycle:
Quantitative Parameters and Data
Table 1: Impact of Controlled Ice Nucleation on T-Cell (Jurkat) Outcomes [1]
| Nucleation Temperature | Intracellular Dehydration | Intracellular Ice Formation | Post-Thaw Viability |
|---|---|---|---|
| -6°C (Controlled) | High | Low | High |
| -10°C (Controlled) | Moderate | Moderate | Moderate |
| Uncontrolled (Spontaneous) | Low | High | Low |
Table 2: Recommended Cooling Rates for Different Cell Types [2] [3]
| Cell Type | Optimal Cooling Rate | Key Consideration |
|---|---|---|
| Mouse Oocytes | 0.5 - 1.0 °C/min | Modeled to minimize intracellular ice volume and solute damage [3]. |
| Many Mammalian Cells | ~1 °C/min | A standard slow rate to balance dehydration and IIF [2]. |
| T-Cells (Jurkat) | ~1 °C/min (Starting) | Often part of a multi-step protocol [1]. |
Table 3: Comparison of Post-Thaw Processing Methods for Cord Blood Mononuclear Cells [4] [5]
| Processing Method | Purity | CBMC Yield | Key Functional Outcome |
|---|---|---|---|
| Wash-Only | Low | High | Highest cell yield, but lowest purity due to contaminants. |
| Density Gradient | Moderate | Moderate | Standard method for purity and recovery. |
| Beads (CD15/CD235 depletion) | High | Moderate | Best preserved cell viability over 5 days of stimulation. |
| EasySep PBMC Isolation Kit | High | Moderate | Highest initial viability (LAN cells); significantly depletes CD14+ cells. |
Troubleshooting Common Experimental Issues
FAQ: Our post-thaw stem cell viability is low, but we use a standard protocol. What could be wrong? Beyond the cooling rate, several factors can degrade recovery. First, examine your graft composition. For hematopoietic stem cells, extreme concentrations of platelets (both very low and very high) in the product have been correlated with reduced post-thaw CD34+ cell recovery [6]. Second, evaluate your post-thaw processing. The choice of method involves a trade-off: a simple "wash-only" step gives the highest yield but lower purity, while bead-based depletion or specific isolation kits offer higher purity and can better preserve long-term T-cell function, which is critical for cell therapy applications [4] [5]. Third, ensure your storage conditions are stable. Physical disturbances during storage (e.g., "pick-and-place" of vials) can induce recrystallization. It is recommended to store below -160°C and limit handling time to under 90 seconds to mitigate this risk [3].
FAQ: How can we reduce the cytotoxic effects of Cryoprotective Agents (CPAs) like DMSO? This is a major research focus. Promising strategies include:
- Controlled Ice Nucleation: Using a defined nucleation temperature can improve post-thaw recovery, potentially allowing for a reduction in the required CPA concentration for some cell types [1].
- Novel CPA Formulations: Research into nature-inspired antifreeze peptides (AFpeps) is ongoing. These compounds are biocompatible, can inhibit ice growth, and some variants possess additional cell-penetrating, antioxidant, or antimicrobial properties, offering a multi-functional alternative to conventional CPAs [7].
- Optimized CPA Loading/Unloading: Following precise, multi-step protocols for adding and removing CPAs can minimize osmotic shock and toxicity [2].
The workflow below outlines a systematic approach to diagnosing and resolving low post-thaw viability:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Cryopreservation Research
| Reagent / Tool | Function | Example & Notes |
|---|---|---|
| Permeating CPAs | Penetrate cells, reduce IIF by replacing water, and mitigate solute effects. | DMSO (most common, but has toxicity concerns); Glycerol [8] [7]. |
| Non-Permeating CPAs | Remain outside cells, providing osmotic balance and extracellular protection. | Sucrose, Trehalose, HES (Hydroxyethyl starch) [4] [7]. |
| Antifreeze Peptides (AFpeps) | Novel, bio-inspired CPAs that inhibit ice growth, reduce freezing point, and offer low toxicity. | Synthetic or insect-derived AFpeps form round crystals and are broad-spectrum; marine/plant AFpeps form sharp crystals, potentially useful for cryosurgery [7]. |
| Bead-based Depletion Kits | For post-thaw processing to remove specific contaminants (e.g., RBCs, granulocytes) and improve purity. | CD15/CD235 depletion beads; shown to best preserve long-term T-cell viability in cord blood [4] [5]. |
| Controlled Rate Freezers | Precisely control cooling rates to systematically navigate the dehydration-IIF balance. | Enables protocols with steps (e.g., hold for nucleation) and is commercially relevant for cell therapy [1]. |
| Plasma-Lyte A | A balanced salt solution used as a base for formulating cryomedicine. | Used in commercially relevant cryoformulations for T-cells [1]. |
Fundamental Mechanisms of DMSO Action
What is the primary cryoprotective mechanism of Dimethyl Sulfoxide (DMSO)?
DMSO provides cryoprotection through a combination of colligative properties and specific molecular interactions. As a penetrating cryoprotectant, DMSO enters cells and reduces the freezing point of intracellular solutions, thereby minimizing intracellular ice formation which is typically lethal to cells. Recent molecular dynamics simulations using updated AMBER force fields reveal that at low concentrations (1.5-10 vol%), DMSO's protective action arises mainly from modulation of water and ice behavior rather than direct perturbation of lipid bilayers. DMSO slows ice crystal growth by approximately a factor of five and gets excluded from the ice lattice, accumulating at ice-membrane interfaces to form protective, ice-free layers [9].
How does DMSO interact with cell membranes at the molecular level?
DMSO exhibits a complex relationship with lipid membranes. Contrary to some earlier simulation studies that exaggerated DMSO-membrane interactions, recent research indicates that low concentrations of DMSO (1.5-10 vol%) cause negligible changes to membrane thickness, area per lipid, hydration, or acyl-chain order. DMSO shows mild enrichment at the hydrophobic-hydrophilic interface of membranes, particularly near carbonyl and glycerol groups, but most molecules remain in the solvent phase. This represents an improvement in understanding over earlier models and aligns better with experimental evidence [9].
Osmotic Stress During Cryopreservation
Osmotic stress occurs throughout the cryopreservation workflow from multiple sources:
- Freezing phase: As extracellular water freezes, solute concentration in the unfrozen fraction increases, creating hypertonic conditions that draw water out of cells, potentially causing excessive dehydration.
- CPA addition: Introduction of cryoprotectants like DMSO creates a strong osmotic gradient, causing rapid water efflux and cell shrinkage if not properly controlled.
- Thawing phase: As temperatures rise, melting ice creates hypotonic extracellular conditions, driving water influx and cell swelling.
- CPA removal: Dilution or removal of cryoprotectants post-thaw can cause massive water influx and potential membrane rupture if not performed gradually with proper osmotic buffers.
How does osmotic stress manifest in cellular damage?
Osmotic stress during cryopreservation causes both immediate and delayed cellular damage:
- Membrane tension from rapid volume changes can exceed elastic limits, causing rupture
- Activation of mechanosensitive ion channels disrupting electrochemical gradients
- Cytoskeletal disorganization and disruption of organelle positioning
- Generation of reactive oxygen species (ROS) leading to oxidative damage
- DNA damage and cell cycle arrest, as documented in human bone mesenchymal stem cells [10]
Table 1: Documented Cellular Damage from DMSO Cryopreservation
| Damage Type | Affected Cellular Component | Functional Consequences | Reference |
|---|---|---|---|
| Apoptosis | Membrane integrity & caspase activation | 10-15% immediate post-thaw cell death | [10] |
| Genetic Damage | DNA integrity | 3.8x increase in DNA damage/repair markers | [10] |
| Cell Cycle Disruption | Cell cycle checkpoints | G0/G1 phase arrest | [10] |
| Oxidative Stress | Redox homeostasis | Significantly increased ROS levels | [10] |
| Functional Impairment | Differentiation capacity | Reduced adipogenic & osteogenic potential | [10] |
Troubleshooting Common CPA Challenges
How can researchers mitigate DMSO toxicity while maintaining cryoprotective efficacy?
Strategies to balance efficacy and toxicity include:
- Concentration reduction: Hydrogel microencapsulation enables effective cryopreservation of mesenchymal stem cells with as low as 2.5% DMSO while sustaining viability above the 70% clinical threshold [11].
- Combination approaches: Using DMSO with non-toxic additives like trehalose, ectoine, or betaine allows reduction of DMSO concentration while maintaining protection [12].
- Controlled-rate freezing: Precision freezing protocols improve outcomes at lower DMSO concentrations by optimizing cooling kinetics [13].
- Post-thaw processing: Effective DMSO removal methods including washing, density gradient separation, or bead-based depletion improve post-thaw recovery [5].
What are the key considerations for optimizing freezing and thawing rates?
Optimal thermal protocols must balance competing damage mechanisms:
- Slow cooling rates (<1°C/min) minimize intracellular ice formation but increase exposure to solute effects and osmotic stress
- Rapid cooling rates (>50°C/min) minimize solution effects but risk lethal intracellular ice
- Thawing rates significantly impact recovery; rapid thawing (45°C/min or higher) typically provides best outcomes by minimizing devitrification and recrystallization [13]
- Container-specific optimization is essential as vial, bag, and straw configurations have distinct thermal transfer properties
Table 2: Quantitative Effects of DMSO Concentration on Stem Cell Viability
| DMSO Concentration (vol%) | Post-thaw Viability | Key Observations | Reference |
|---|---|---|---|
| 0% | Below clinical threshold | Insufficient cryoprotection | [11] |
| 1.0% | Below 70% | Below clinical minimum requirement | [11] |
| 1.5-3% | Viable | Threshold where cryoprotective effects diminish | [9] [11] |
| 2.5% | ~70% | Minimum clinical threshold with microencapsulation | [11] |
| 5% | Variable | Intermediate efficacy | [11] |
| 10% | High viability | Significant toxicity concerns: DNA damage, ROS, functional impairment | [11] [10] |
Experimental Protocols for DMSO Optimization
Protocol: Evaluating DMSO Concentration Effects with Hydrogel Microencapsulation
This protocol enables systematic testing of low-dose DMSO cryopreservation for sensitive cell types [11]:
Cell Preparation:
- Culture human umbilical cord mesenchymal stem cells (hUC-MSCs) to 80-90% confluence in complete DMEM/F12 medium with 10% FBS
- Harvest using standard trypsinization and centrifugation
Hydrogel Microencapsulation:
- Prepare core solution: 0.68g mannitol + 0.15g hydroxypropyl methylcellulose in sterile water
- Prepare shell solution: 0.46g mannitol + 0.2g sodium alginate in sterile water
- Resuspend cell pellet in core solution at appropriate density
- Use high-voltage electrostatic coaxial spraying device with:
- Core solution flow rate: 25 μL/min
- Shell solution flow rate: 75 μL/min
- Voltage: 6 kV
- Collect microcapsules in calcium chloride solution for crosslinking
DMSO Exposure and Cryopreservation:
- Prepare cryomedium with DMSO concentrations: 0%, 1.0%, 2.5%, 5.0%, 10.0% (v/v)
- Exchange culture medium with respective cryomedium
- Implement controlled-rate freezing: 1°C/min to -80°C
- Transfer to liquid nitrogen for long-term storage
Post-thaw Analysis:
- Rapid thaw in 37°C water bath
- Assess viability via flow cytometry with Annexin V/PI staining
- Evaluate phenotype retention (CD markers)
- Test differentiation potential (osteogenic/adipogenic induction)
- Measure stemness gene expression (Nanog, Oct4, Sox2)
Protocol: Assessing DNA Damage and Functional Integrity Post-Cryopreservation
Comprehensive safety assessment for therapeutic cell applications [10]:
Cell Culture and Cryopreservation:
- Culture human bone mesenchymal stem cells (hBMSCs) in α-MEM with 10% FBS
- Use passages 3-6 for experiments
- Cryopreserve in standard medium with 10% DMSO using slow cooling
- Store in liquid nitrogen vapor phase
Viability and Apoptosis Assessment:
- Perform AO/PI staining immediately post-thaw
- Calculate viability: (live cells/total cells) × 100%
- Assess apoptosis using Annexin V-FITC/PI flow cytometry
- Include fresh cells as control
DNA Damage Evaluation:
- Culture post-thaw cells for 48 hours
- Fix and stain for γH2AX foci (DNA damage marker)
- Quantify foci per nucleus compared to fresh controls
- Calculate DNA damage ratio: (foci in frozen-thawed)/(foci in fresh)
Cell Cycle Analysis:
- Culture post-thaw cells for 24 hours
- Fix and stain with propidium iodide
- Analyze DNA content by flow cytometry
- Compare cell cycle distribution with fresh controls
Functional Capacity Tests:
- Induce osteogenic and adipogenic differentiation
- Analyze lineage-specific gene expression (Runx2, PPARγ)
- Evaluate migration capacity via transwell assays
- Stain F-actin to assess cytoskeletal organization
Emerging Alternatives and Advanced Solutions
What DMSO-free strategies show promise for stem cell cryopreservation?
Several innovative approaches are advancing toward clinical application:
- Hydrogel microencapsulation: Alginate-based hydrogels provide physical protection and enable radical DMSO reduction to 2.5% while maintaining viability above clinical thresholds and preserving differentiation potential [11].
- Deep Eutectic Solvents (DES): Choline chloride-glycerol mixtures show promising cryoprotection with minimal toxicity, achieving platelet recovery of 88.2% in DMSO-free protocols [14].
- DNA frameworks: Nanoscale DNA structures functionalized with cholesterol provide membrane-targeted cryoprotection, inhibit ice growth, and undergo biodegradation post-thaw to avoid toxicity concerns [15].
- Intracellular trehalose delivery: Using electroporation, nanoparticles, or extended incubation to load non-penetrating sugars provides cryoprotection without chemical toxicity [12].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for DMSO and Osmotic Stress Research
| Reagent/Category | Specific Examples | Research Application | Mechanistic Role |
|---|---|---|---|
| Penetrating CPAs | DMSO, Glycerol, Ethylene Glycol | Standard cryopreservation protocols | Colligative freezing point depression, intracellular penetration |
| Non-penetrating CPAs | Sucrose, Trehalose, Raffinose | Osmotic buffering, vitrification | Extracellular stabilization, glass formation |
| Osmolytes | Ectoine, Hydroxyectoine, Betaine | Osmotic stress protection | Membrane and protein stabilization |
| Hydrogel Materials | Sodium Alginate, Calcium Chloride | Microencapsulation protocols | Physical barrier, 3D microenvironment |
| Membrane Modulators | Cholesterol-DNA Frameworks | Advanced nanomaterial approaches | Membrane stabilization, ice growth inhibition |
| Deep Eutectic Solvents | Choline Chloride-Glycerol | DMSO-free cryopreservation | Hydrogen-bond networks, membrane protection |
| Viability Indicators | AO/PI, Annexin V-FITC, LDH assays | Post-thaw quality assessment | Membrane integrity, apoptosis detection |
| Damage Markers | γH2AX, CD62P, CD63, ROS probes | Cellular stress and damage quantification | DNA damage, activation, oxidative stress |
Frequently Asked Questions
What is the minimum effective DMSO concentration for stem cell cryopreservation?
The minimum effective DMSO concentration depends on cell type and preservation strategy. For mesenchymal stem cells, 2.5% DMSO combined with hydrogel microencapsulation can maintain viability above the 70% clinical threshold [11]. However, concentrations below 2% typically show diminished cryoprotective effects, marking a critical threshold [9]. The optimal concentration balances sufficient ice inhibition with acceptable toxicity levels for your specific application.
How does DMSO cause DNA damage in cryopreserved cells?
DMSO-induced DNA damage occurs through both direct and indirect mechanisms. Research on human bone mesenchymal stem cells reveals approximately 3.8-fold increase in DNA damage/repair markers post-thaw, with DMSO contributing to:
- Reactive oxygen species (ROS) generation causing oxidative DNA lesions
- Cell cycle disruption leading to G0/G1 arrest and impaired DNA repair
- Direct interactions with nucleic acids and associated proteins
- Activation of apoptotic pathways that involve DNA fragmentation [10]
What are the advantages of controlled-rate freezing versus passive freezing?
Controlled-rate freezing provides significant advantages for reproducibility and cell quality:
- Parameter control: Precisely manage cooling rate before/after nucleation, nucleation temperature, and final sample temperature
- Process documentation: Automated recording of critical process parameters
- Consistency: Minimize batch-to-batch variability in post-thaw recovery
- Optimization capability: Systematically test freezing profiles for sensitive cell types
- Regulatory compliance: Better alignment with GMP requirements for therapeutic applications [13]
Industry surveys indicate 87% of respondents use controlled-rate freezing for cell-based products, with particularly high adoption in late-stage clinical development [13].
Technical Support & Troubleshooting Center
This technical support center is designed to assist researchers in navigating the specific vulnerabilities of induced pluripotent stem cells (iPSCs), with a focus on improving post-thaw recovery and viability. The following guides and FAQs address common experimental challenges, providing practical solutions grounded in current research.
Frequently Asked Questions (FAQs)
Q1: Why are iPSCs particularly vulnerable to cryopreservation compared to other cell types? iPSCs possess a unique biological sensitivity to environmental and handling conditions, making them especially vulnerable to losses in viability and function during freezing and thawing. They are more susceptible to cryopreservation-induced stresses like intracellular ice formation, osmotic shock, and dehydration than many conventional cell types [16] [17]. Their large surface area-to-volume ratio also contributes to this sensitivity [17].
Q2: My post-thaw iPSC viability is low. What are the first parameters I should check? First, verify your freezing rate. A controlled rate of -1°C to -3°C per minute is often optimal for iPSCs; deviations can drastically reduce survival [17]. Next, check the concentration of DMSO in your cryoprotectant; consider testing formulations with lower DMSO (e.g., 5%) supplemented with ice recrystallization inhibitors (IRIs) to mitigate toxicity [18]. Finally, ensure you are using high-quality, GMP-grade reagents to avoid introducing variability [16].
Q3: How can I reduce the risk of contamination during the post-thaw QC sampling process? To maintain aseptic conditions, minimize direct product contact by using container closure strategies and sampling through sterile connectors. Process engineering solutions, such as integrated sampling ports in cryo-containers or automated thaw-and-transfer systems, can further reduce manual handling and standardize sampling across sites [16].
Q4: What is a risk-based approach to post-thaw quality control (QC)? A risk-based QC panel focuses on minimal, essential criteria to verify product integrity without excessive manipulation. This typically includes cell count, viability, and critical quality markers associated with potency or pluripotency. Working with regulatory agencies to align on a scientifically justified panel balances robust verification with the need to protect the final drug product from contamination or loss [16].
Q5: When should I consider automating my thawing and downstream processes? Automation becomes critical when seeking enhanced batch consistency, process closure, and contamination control. While manual methods offer flexibility for early-phase research, automated systems standardize critical steps like thawing rates and wash protocols, locking in consistent post-thaw recovery. A hybrid strategy, automating high-risk steps like fill-finish first, can be a practical approach for many developers [16].
Troubleshooting Guides
Problem: Poor Post-Thaw Cell Recovery and Viability
Potential Causes and Solutions:
Suboptimal Freezing Rate
- Cause: Uncontrolled or incorrect cooling rates lead to destructive intracellular ice crystal formation or excessive cell dehydration [17].
- Solution: Use a controlled-rate freezer. Research indicates that a cooling rate within -0.3°C to -1.8°C/min is optimal for many pluripotent stem cells. A rate of -1°C/min is frequently used successfully for iPSCs [17].
Cryoprotectant-Associated Toxicity
- Cause: High concentrations of DMSO (e.g., 10%) are cytotoxic and can damage cells [18] [17].
- Solution: Explore alternative cryoprotectant formulations. Recent studies show that solutions containing 15 mM ice recrystallization inhibitors (IRIs) in 5% DMSO can be an efficient cryoprotective solution, reducing DMSO-associated toxicities while maintaining post-thaw recovery, viability, and pluripotency [18].
Improper Handling During Thawing
- Cause: Osmotic shock during the removal of cryoprotectants [17].
- Solution: During thawing, add pre-warmed complete medium to the cell suspension drop-wise (approximately one drop per second) while gently swirling the tube. This gradual dilution prevents rapid osmotic changes that can damage fragile cells [19].
Problem: Excessive Differentiation in Cultures After Thawing
Potential Causes and Solutions:
Poor Initial Culture Health
Over-manipulation Post-Thaw
Incorrect Seeding Density
Data & Protocol Summaries
Table 1: Comparison of Cryoprotectant Solutions for iPSCs
| Solution Formulation | Post-Thaw Viability | Pluripotency Maintenance | Key Advantages | Key Disadvantages |
|---|---|---|---|---|
| 10% DMSO (Standard Solution) | Variable, can be suboptimal [18] | Maintained, but with risk of toxicity | Widely used, simple formulation | High DMSO toxicity, batch-to-batch variability [16] |
| 5% DMSO + 15 mM IRIs (Advanced Formulation) | High [18] | Maintained, with reduced transcriptomic changes [18] | Reduces DMSO toxicity, improves consistency, robust transcriptomic profile [18] | Requires sourcing of specialized IRIs |
| CryoStor CS10 (Commercial Solution) | High (used as a benchmark in studies [18]) | Maintained | Commercially available, GMP-manufactured | Proprietary formulation, cost |
Table 2: Post-Thaw Recovery Timeline Under Optimized vs. Non-optimized Conditions
| Parameter | Optimized Protocol | Non-Optimized Protocol |
|---|---|---|
| Time to Ready for Experiments | 4-7 days after thawing and seeding [17] | Up to 2-3 weeks [17] |
| Key Influencing Factors | Controlled freezing rate, advanced cryoprotectants, proper handling to prevent osmotic shock [18] [17] | Uncontrolled freezing, high DMSO toxicity, osmotic shock during thawing [17] |
| Experimental Complications | Minimal, predictable timeline [17] | Significant delays, unpredictable cell behavior, resource waste [17] |
Experimental Protocol: Assessing Post-Thaw Cell Quality
A comprehensive assessment of post-thaw iPSCs goes beyond simple viability. The following methodology outlines key steps for evaluating recovery and function.
1. Thawing and Plating:
- Quickly thaw cryovials in a 37°C water bath until only a small ice crystal remains [17].
- Transfer the contents to a tube and slowly add pre-warmed complete medium drop-wise to dilute the cryoprotectant [19].
- Centrifuge the cell suspension to pellet the cells, resuspend in fresh culture medium, and plate onto Matrigel-coated plates.
2. Viability and Recovery Assessment:
- Timepoint: 24 hours post-thaw.
- Method: Perform a cell count using an automated cell counter (e.g., Countess II) with Trypan Blue exclusion to assess immediate post-thaw viability [21].
3. Pluripotency and Phenotype Verification:
- Timepoint: 3-5 days post-thaw, upon reaching confluency.
- Method: Immunocytochemistry (ICC) or flow cytometry for key markers.
- Neurons (if differentiated): Antibodies against NeuN and βIII-tubulin (Tuj1) [21].
- Astrocytes (if differentiated): Antibodies against GFAP and CD44 [21].
- Microglia (if differentiated): Antibodies against IBA1 and P2RY12 [21].
- Undifferentiated iPSCs: Staining for pluripotency markers like OCT4, SOX2, and NANOG is recommended to confirm maintenance of pluripotent state.
- Success Criterion: Differentiation efficiency or pluripotency marker expression should exceed 95% with no evidence of a contaminating proliferative population (assessed with Ki67 staining) [21].
The Scientist's Toolkit: Essential Research Reagents
| Item | Function | Example & Notes |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Improves single-cell survival by inhibiting apoptosis; used during passaging and post-thaw plating [21] [19]. | Add to medium at 10 µM for 24 hours after thawing [19]. |
| Ice Recrystallization Inhibitors (IRIs) | Small molecules that inhibit the growth of ice crystals during thawing, reducing cell damage and enabling lower DMSO concentrations [18]. | e.g., carbohydrate-based IRIs; used at 15 mM in 5% DMSO [18]. |
| GMP-Grade Matrigel/VTN-N | Defined extracellular matrix substrate for feeder-free culture, providing a consistent surface for cell attachment and growth [19]. | Essential for scalable and compliant manufacturing; ensures consistency [16] [19]. |
| mTeSR or Essential 8 Medium | Chemically defined, xeno-free culture media optimized for the maintenance and growth of pluripotent stem cells [21] [19]. | Supports robust cell growth; Essential 8 allows transition from other media systems [19]. |
| Annexin V Apoptosis Assay | Sensitive assay to detect early-stage apoptosis (phosphatidylserine exposure), which can reveal subtle cell stress not detected by Trypan Blue [16]. | Useful for uncovering delayed apoptosis or loss of functionality 24-72 hours post-thaw [16]. |
Experimental Workflow Visualization
The following diagram illustrates the critical stages of the iPSC thawing and recovery process, highlighting key vulnerabilities and intervention points.
The three-zone freezing model represents a sophisticated approach to cryopreservation that moves beyond constant cooling rates. This model is particularly crucial for sensitive cell types like human induced pluripotent stem cells (hiPSCs), where optimal post-thaw viability is essential for research and clinical applications. The model is founded on the "two-factor theory" of cryoinjury, which posits that cells are primarily damaged by two competing factors: intracellular ice formation and cell dehydration [22]. The three-zone framework strategically balances these competing risks by applying specific cooling rates at different temperature ranges to maximize cell survival [23] [22].
For hiPSCs, which are more vulnerable to intracellular ice formation than many other cell types, strict control of the cooling rate is particularly critical [23]. Research by Hayashi et al. suggests that a constant cooling rate does not yield the best cell survival outcomes. Instead, their model-based assessment of 16,206 temperature profiles demonstrated that a specific sequence of cooling rates applied across three distinct temperature zones produces superior results [22]. This approach forms the foundation of modern, optimized cryopreservation protocols for regenerative medicine applications.
Detailed Zone Specifications and Protocols
The Three Zones: Mechanisms and Parameters
The three-zone freezing model divides the cryopreservation process into distinct phases, each addressing specific physicochemical challenges. The table below summarizes the key characteristics of each zone:
Table 1: Specifications of the Three-Zone Freezing Model
| Zone Name | Temperature Range | Cooling Rate | Primary Cellular Process | Main Risk to Mitigate |
|---|---|---|---|---|
| Dehydration Zone | From initial temperature to below freezing | Fast cooling | Extracellular ice formation, cellular dehydration | Excessive dehydration and solute effects |
| Nucleation Zone (Intracellular Ice Formation Zone) | Critical temperature range where intracellular ice forms | Slow cooling | Intracellular ice nucleation | Intracellular ice crystal formation |
| Further Cooling Zone | From nucleation completion to final storage temperature | Fast cooling | Stabilization of frozen state | Re-crystallization and mechanical damage |
Experimental Protocol for Three-Zone Freezing
Materials Required:
- STEM-CELLBANKER GMP grade or similar cryopreservation solution [22]
- Programmable freezing system or appropriate cryocontainers
- Cryogenic vials
- hiPSCs in logarithmic growth phase [23]
Methodology:
- Cell Preparation: Harvest hiPSCs during the logarithmic growth phase to ensure optimal recovery post-thaw [23]. Prepare cell suspension in appropriate cryopreservation solution containing cryoprotectants such as DMSO.
Dehydration Zone Protocol:
- Transfer cryovials containing cell suspension to the freezing apparatus.
- Apply rapid cooling from initial temperature to below freezing point.
- This rapid initial cooling minimizes prolonged cellular dehydration.
Nucleation Zone Protocol:
Further Cooling Zone Protocol:
- Once through the nucleation danger zone, increase cooling rate again.
- Rapidly cool cells to the final storage temperature (typically -80°C or below).
- Transfer to long-term storage in liquid nitrogen vapor phase or -150°C freezers [23].
Storage Considerations:
- Maintain storage below -123°C (extracellular glass transition temperature of DMSO) to prevent stressful thermal events [23].
- Avoid temperature fluctuations during storage to prevent ice crystal growth.
Troubleshooting Common Issues
Frequently Asked Questions
Table 2: Troubleshooting Common Cryopreservation Problems
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Poor post-thaw viability | Suboptimal cooling rate through nucleation zone; improper pre-freeze culture conditions | Test different cooling rates in nucleation zone between -0.3 to -1.8°C/min; ensure cells are in logarithmic growth phase before freezing [23] | Standardize pre-freeze culture protocols; validate cooling rates for specific cell line |
| High intracellular ice formation | Cooling too rapidly through nucleation zone; inappropriate cryoprotectant concentration | Slow cooling rate through nucleation zone; verify cryoprotectant concentration and permeability [23] [22] | Implement controlled-rate freezing equipment; optimize cryoprotectant addition/removal steps |
| Excessive cell dehydration | Cooling too slowly through dehydration zone; overexposure to hypertonic cryoprotectant | Increase cooling rate in dehydration zone; reduce incubation time in cryoprotectant before freezing [22] | Optimize timing of cryoprotectant addition; implement fast-slow-fast cooling pattern |
| Variable recovery between vials | Inconsistent temperature profiles during freezing; improper storage conditions | Validate temperature uniformity in freezing system; ensure consistent fill volume in cryovials [23] | Use controlled-rate freezing equipment; monitor storage temperature stability |
Q1: Why is the logarithmic growth phase important before freezing hiPSCs?
Cells in the logarithmic growth phase are physiologically more uniform and robust, exhibiting better recovery post-thaw compared to cells from stationary or decline phases. This ensures higher viability and more consistent experimental results [23].
Q2: How can I determine the optimal cooling rate for my specific cell type in the nucleation zone?
The optimal cooling rate is cell type-specific. For hiPSCs, research indicates that rates between -0.3 and -1.8 °C/min are generally effective [23]. However, systematic experimentation with different rates while monitoring post-thaw viability is recommended for specific cell lines. Computational modeling approaches can also help predict optimal parameters [22].
Q3: What is the impact of cryoprotectant choice on the three-zone model?
Cryoprotectants like DMSO reduce ice crystal formation by penetrating cells and altering ice formation dynamics. The hypertonic nature of cryoprotectant solutions (approximately 1.4 osm/L for 10% DMSO) causes initial cellular dehydration, which interacts with the dehydration zone processes. Different cryoprotectants may require adjustments to zone cooling rates [23].
Q4: How long should the acclimation period be after thawing, and why is it important?
Research on mesenchymal stem cells demonstrates that a 24-hour acclimation period post-thaw allows cells to regain functional potency. Immediately after thawing (freshly thawed cells), various aspects of cell characteristics and function are deleteriously affected by cryopreservation. The acclimation period 'reactivates' thawed cells, enabling recovery of diminished stem-cell function [24].
Research Reagent Solutions
Table 3: Essential Materials for Three-Zone Freezing Experiments
| Reagent/Equipment | Function | Example Products | Application Notes |
|---|---|---|---|
| Controlled-Rate Freezer | Implements precise temperature profiles across the three zones | Programmable freezing systems; FZ-2000 direct-contact freezer [22] | Essential for consistent application of three-zone protocol |
| Cryopreservation Media | Provides cryoprotection and osmotic balance | STEM-CELLBANKER GMP grade [22] [25] | Contains DMSO and other cryoprotectants; specific formulations may enhance recovery |
| Cryogenic Vials | Contain cell suspension during freezing and storage | Standard 2.0 mL cryovials [26] | Consistent vial material and fill volumes improve temperature uniformity |
| Temperature Monitoring System | Validates temperature profiles during freezing | T-type thermocouples [26] | Critical for protocol validation and troubleshooting |
| DMSO (Dimethyl Sulfoxide) | Penetrating cryoprotectant agent | Various GMP-grade sources | Reduces ice crystal formation; typically used at 10% concentration [23] |
| Post-Thaw Recovery Media | Supports cell recovery after thawing | Media supplemented with Y-27632 (10 μM) [22] | Enhances survival of sensitive stem cells during critical post-thaw period |
Visualizing the Three-Zone Model
The following diagram illustrates the temperature profile and cellular processes in the three-zone freezing model:
Figure 1: Three-Zone Freezing Model Workflow. This diagram illustrates the sequential temperature zones and primary cellular processes during controlled-rate cryopreservation.
Advanced Applications and Computational Modeling
The three-zone model has evolved beyond empirical optimization to incorporate sophisticated computational approaches. Recent research has demonstrated the effectiveness of Computational Fluid Dynamics (CFD) models for designing continuous freezing processes for hiPSCs [27] [26]. These models combine single-cell freezing mechanisms with system-level heat transfer calculations to predict cell survival rates under various process parameters [27].
For advanced applications such as the cryopreservation of 3D structures like cell sheets or microcardiac spheroids, the three-zone principle requires adaptation. Research shows that freezing 100-200 μm diameter microcardiac spheroids using optimized protocols can maintain approximately 80% viability after 6 months of cryopreservation in liquid nitrogen [28]. The integrity of cell-cell contacts in these 3D structures contributes significantly to their cryoresistance.
The following diagram illustrates the experimental workflow for implementing and validating the three-zone freezing model:
Figure 2: Experimental Workflow for Three-Zone Freezing Protocol. This diagram shows the implementation process from cell preparation to post-thaw analysis, including computational modeling feedback for protocol optimization.
These computational approaches enable researchers to scale up freezing processes significantly. One study demonstrated that properly designed continuous freezing processes could be scaled to up to 170-fold compared to currently used equipment for hiPSC freezing while maintaining average cell survival rates above 0.90 [26]. This scalability is essential for the clinical translation and commercialization of stem cell-based therapies.
The three-zone freezing model represents a significant advancement in cryopreservation science, moving beyond empirical approaches to a mechanistic, computationally-enhanced framework. By understanding and optimizing the processes in each zone, researchers can significantly improve post-thaw recovery of valuable cell resources, accelerating progress in regenerative medicine and drug development.
Frequently Asked Questions
Q1: Why is the logarithmic growth phase so critical for cryopreserving stem cells? Freezing cells during the log phase ensures they are at their most robust state of metabolic activity and proliferation. Cells in this phase are healthiest and most resilient, which allows them to better withstand the significant stresses of the freezing and thawing process. This leads to higher post-thaw viability and faster recovery of a stable, proliferative culture, typically within 4–7 days. In contrast, freezing cells from the stationary or death phases can result in poor recovery and extended culture times of up to 2–3 weeks [23] [29].
Q2: What are the consequences of cryopreserving a contaminated cell culture? Cryopreservation does not eliminate contamination; it preserves it. Upon thawing, microbial contaminants will proliferate, competing with your cells for nutrients and secreting toxic metabolites. This compromises cell health, viability, and experimental results, and risks spreading the contamination to other cell lines in your laboratory. Microbial contamination can also increase cell death, leading to a higher burden of cellular debris in the cryopreserved vial, which can further impair the recovery of healthy cells [23] [30] [29].
Q3: How can I visually identify the logarithmic growth phase in my adherent stem cell cultures? For adherent cultures, the log phase is characterized by active cell division, high confluency (typically between 70% to 90%), and healthy, undifferentiated morphology. Cells should be actively proliferating but not yet fully confluent. You should observe a rapid drop in media pH (yellowing of phenol red) due to high metabolic activity, requiring frequent medium changes. A drop in pH of more than 0.1–0.2 units often indicates a high cell concentration and active growth [31].
Q4: Does pre-freeze processing, like switching from aggregates to single cells, affect recovery? Yes, the passaging method significantly impacts post-thaw recovery. The choice involves a trade-off:
- Freezing as Aggregates: This method preserves cell-cell contacts, which can support survival. Recovery can be faster as cells are already in their natural clustered state. However, variable aggregate size can lead to inconsistent penetration of cryoprotectant, causing vial-to-vial variability in viability [23].
- Freezing as Single Cells: This allows for precise cell counting and more consistent seeding densities, leading to more standardized recovery. The downside is that single cells may be more vulnerable to cryo-damage and require more time to re-form aggregates after thawing [23]. The optimal method depends on your specific cell line and experimental requirements.
Troubleshooting Guides
Problem: Low Post-Thaw Viability and Slow Proliferation
Potential Causes and Solutions:
Cause 1: Cells were frozen from a non-logarithmic growth phase.
Cause 2: Undetected microbial contamination (e.g., Mycoplasma) compromising cell health pre-freeze.
- Solution: Integrate routine mycoplasma testing into your workflow before freezing. Use PCR-based detection kits. Always wear a face mask during freezing procedures to prevent oral microbial transfer (e.g., Mycoplasma orale) into cryovials [23].
Cause 3: Suboptimal freezing rate causing ice crystal formation.
- Solution: Use a controlled-rate freezer or an isopropanol freezing chamber (e.g., "Mr. Frosty") placed in a -80°C freezer to ensure a consistent cooling rate of approximately -1°C per minute. This slow freezing is vital for preventing lethal intracellular ice formation in sensitive stem cells [23] [32] [29].
The logic for investigating poor post-thaw recovery, focusing on the pre-freeze cell state, can be summarized as follows:
Problem: Inconsistent Recovery Between Frozen Vials
Potential Causes and Solutions:
Cause 1: Inconsistent cell passaging and aggregation before freezing.
Cause 2: Fluctuations in incubator temperature, CO2, or humidity affecting pre-freeze cell health.
- Solution: Regularly calibrate and monitor incubator conditions. Ensure temperature is stable at 37°C and CO2 is appropriate for your medium's bicarbonate buffer (typically 5%) [31].
Table 1: Impact of Cell Growth Phase on Post-Thaw Recovery
| Growth Phase | Key Characteristics | Impact on Post-Thaw Recovery | Recommended Action |
|---|---|---|---|
| Lag Phase | Cells are adapting, not dividing; metabolic preparation [33]. | Slow and poor recovery; cells are not at peak resilience. | Do not freeze. Wait for exponential growth. |
| Log (Exponential) Phase | Active cell division; high metabolic activity; rapid nutrient consumption [33] [31]. | Optimal recovery; high viability; rapid proliferation post-thaw (4-7 days) [23] [29]. | Ideal for freezing. Harvest at 70-90% confluency. |
| Stationary Phase | Growth plateaus due to contact inhibition or nutrient depletion; stress responses may begin [33] [31]. | Suboptimal recovery; reduced viability; potential for increased differentiation or apoptosis. | Avoid freezing. Subculture to re-establish log phase growth. |
| Death Phase | Widespread cell death and lysis; accumulation of debris [33]. | Very poor recovery and viability; culture is often unrecoverable. | Do not freeze. Discard and thaw a new vial. |
Table 2: Consequences and Detection of Common Contaminations
| Contamination Type | Pre-freeze Indicators | Impact on Cryopreservation & Post-Thaw Recovery |
|---|---|---|
| Mycoplasma | Often subtle; possible granularity in cytoplasm, slight changes in growth rate [23] [34]. | Compromised cell health leads to low viability. Contamination persists post-thaw, invalidating experiments and risking cross-contamination [23]. |
| Bacterial | Turbid medium; rapid pH shift to yellow (acidic); possible visible films or spots [29] [35]. | High cell death; toxicity from bacterial wastes; likely complete culture loss upon thawing. |
| Fungal | Fuzzy, filamentous, or spherical particles in medium; resistant to common antibiotics [34]. | Overgrowth post-thaw, consuming nutrients and secreting toxins, leading to culture loss. |
Experimental Protocols
Protocol 1: Standardized Cryopreservation of Stem Cells in Logarithmic Growth Phase
Objective: To freeze high-quality stem cell stocks with maximum post-thaw viability by ensuring cells are harvested during the logarithmic growth phase.
Materials:
- Log-phase stem cell culture (>90% viability, 70-90% confluent) [29]
- Pre-warmed complete growth medium
- Cryoprotective agent (e.g., DMSO-based solution like CryoStor CS10 or mFreSR) [29]
- Sterile cryogenic vials
- Controlled-rate freezing apparatus (e.g., isopropanol chamber like "Mr. Frosty" or programmable freezer)
Method:
- Confirm Log Phase: Visually inspect cultures under a microscope. Cells should be sub-confluent (70-90%), displaying healthy, undifferentiated morphology, and the medium should be rapidly acidifying (if using phenol red) [31].
- Harvest Cells: Detach adherent cells gently using a suitable dissociation reagent. For cells frozen as aggregates, use a method that yields clumps of uniform size [23].
- Prepare Cell Suspension: Centrifuge the cell suspension, aspirate the supernatant, and resuspend the cell pellet in an appropriate amount of cold freezing medium to achieve a final concentration of ~1x10^6 cells/mL (adjust based on cell type) [32] [29] [35].
- Aliquot: Dispense the cell suspension into cryovials. Gently mix the suspension frequently to maintain homogeneity [32].
- Controlled-Rate Freezing: Place cryovials in a pre-cooled isopropanol freezing chamber and immediately transfer to a -80°C freezer for 24 hours. This achieves a cooling rate of approximately -1°C/min, which is critical for cell survival [23] [32] [29].
- Long-Term Storage: After 24 hours, quickly transfer the vials to a liquid nitrogen tank for long-term storage in the vapor phase (-135°C to -196°C) [23] [29].
Protocol 2: Pre-freeze Contamination Screening Workflow
Objective: To routinely screen stem cell cultures for microbial contamination prior to cryopreservation.
Materials:
- Conditioned medium from the stem cell culture to be frozen
- Mycoplasma detection kit (PCR-based)
- Bacterial/fungal culture media (e.g., blood agar plates)
- Microscope
Method:
- Visual Inspection: Examine the culture medium for unexplained turbidity or a sudden, drastic color change. Check the cells for any unusual morphology or debris under a microscope [35].
- Mycoplasma Testing: Collect conditioned medium and perform a PCR-based mycoplasma test according to the manufacturer's instructions. This is the most reliable method for detecting this common and invisible contaminant [23] [34].
- Microbial Culture (Optional but Recommended): Inoculate a small sample of conditioned medium into sterile broth or onto agar plates. Incubate separately at 37°C and at room temperature for several days and observe for microbial growth [34].
- Decision Point: Only proceed with cryopreservation if all contamination tests return negative results. If contamination is detected, the culture must be discarded, and the lab space and equipment decontaminated [29].
The workflow for ensuring a contamination-free, log-phase culture ready for cryopreservation is outlined below:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Pre-freeze Quality Control
| Reagent / Material | Function | Example Products |
|---|---|---|
| Defined Cryomedium | Provides a protective, consistent environment during freezing; contains cryoprotectants like DMSO to prevent ice crystal formation. | CryoStor [29], Synth-a-Freeze [32] |
| Controlled-Rate Freezer | Ensures a consistent, optimal cooling rate (approx. -1°C/min) to minimize cryo-damage from ice crystals. | "Mr. Frosty" [32], Corning CoolCell [29], programmable freezers |
| Mycoplasma Detection Kit | Essential for detecting this common, invisible cell culture contaminant that compromises pre-freeze cell health. | PCR-based detection kits [23] [34] |
| Cell Dissociation Reagents | For gentle and effective harvesting of adherent cells, either as single cells or uniform aggregates. | Trypsin-EDTA, TrypLE Express [32] |
| Serum-Free Media | Provides a defined, consistent culture environment free of unknown variables present in serum, supporting robust log-phase growth. | mTeSR [29] |
From Protocol to Practice: Advanced Freezing, Thawing, and Processing Techniques
Technical Troubleshooting Guides
Troubleshooting Poor Post-Thaw Cell Viability
Problem: Low cell viability recovery after thawing cryopreserved samples.
Possible Causes and Solutions:
Cause: Suboptimal freezing rate
- For Controlled-Rate Freezers (CRF): Validate and adjust the cooling profile. Different cell types require specific cooling rates; for example, human iPSCs often recover best at rates between -1°C/min and -3°C/min [23].
- For Passive Freezing: Ensure consistent conditions in the -80°C mechanical freezer. Use insulating devices like isopropanol (IPA) containers or styrofoam to help achieve a cooling rate of approximately 1-2°C/min, which is critical for HPCs [36].
Cause: Inadequate cryoprotectant handling
Cause: Osmotic shock during thawing
- Thaw cells rapidly in a 37°C water bath to minimize exposure to toxic cryoprotectant concentrations and avoid osmotic stress. Use controlled-thawing devices to improve reproducibility and minimize contamination risks associated with conventional water baths [13].
Troubleshooting Inconsistent Results Between Batches
Problem: Significant variation in post-thaw viability between different freezing runs.
Possible Causes and Solutions:
Cause: Improper CRF qualification
- Conduct comprehensive freezer qualification that includes temperature mapping across a grid of locations, using different container types, and testing mixed load configurations. Do not rely solely on vendor Factory Acceptance Testing, as it may not represent your specific use case [13].
Cause: Variable sample characteristics
- Freeze cells during the logarithmic growth phase for improved recovery [23].
- For iPSCs, consider the passaging method; freezing as cell aggregates (clumps) can support cell survival but may lead to variability in cryoprotectant penetration, while single-cell freezing allows for better quantification but may require more recovery time [23].
Cause: Lack of process monitoring
- Implement freeze curves as part of process monitoring and manufacturing controls. Establish action or alert limits for curves to identify changes in CRF performance before critical failure occurs [13].
Frequently Asked Questions (FAQs)
Q1: When should I choose controlled-rate freezing over passive freezing for my cell therapy product?
The choice depends on your development stage, cell type, and resources. Survey data indicates that 87% of cell therapy professionals use CRF in their current practice, while passive freezing is predominantly used (86%) for products in early clinical development (up to phase II) [13]. Adopting CRF early can avoid the challenging process of making a significant manufacturing change later. However, for certain cell types like Hematopoietic Progenitor Cells (HPCs), recent evidence suggests passive freezing can be an acceptable alternative, showing comparable engraftment outcomes [36] [38].
Q2: Is the default profile on my controlled-rate freezer sufficient, or do I need to optimize it?
Industry surveys show that 60% of users rely on default CRF profiles, which work for a wide variety of products [13]. However, optimized profiles are often necessary for sensitive or specialized cells, including iPSCs, hepatocytes, cardiomyocytes, and certain immune cells like macrophages and B cells. The need for optimization should be determined case-by-case, considering cell type, cryoprotectant formulation, primary container, and critical quality attributes [13].
Q3: Can I store my cells long-term at -80°C, or do I need liquid nitrogen storage?
For true long-term storage (years), temperatures below -130°C are required where all molecular processes cease [23]. However, recent research demonstrates that hematopoietic stem cells can maintain sufficient viability for durable engraftment even after long-term storage at -80°C (median 868 days in one study) despite a gradual, time-dependent decline in viability of approximately 1.02% per 100 days [39]. For other cell types like Dental Pulp-derived Stem Cells (DPSCs), viability, proliferative capacity, and stemness can be maintained for up to 13 years with proper cryopreservation before storage [40].
Q4: What are the most critical factors for successful thawing of cryopreserved cells?
Successful thawing requires:
- Rapid warming: Established good practice includes a warming rate of 45°C/min, though optimal rates may vary by cell type [13].
- Prevention of osmotic shock: Rapid dilution to minimize DMSO exposure is critical [23].
- Use of controlled-thawing devices: These provide more reproducible results and lower contamination risk compared to conventional water baths [13].
- Proper training of bedside staff: Particularly important for clinical applications where thawing is often poorly regulated [13].
Comparative Data Analysis
Table 1: Direct Comparison of Controlled-Rate vs. Passive Freezing Methods
| Parameter | Controlled-Rate Freezing (CRF) | Passive Freezing (PF) |
|---|---|---|
| Control over process parameters | High - Precise control over cooling rates, nucleation temperature, and final sample temperature [13] | Low - Uncontrolled nucleation and inconsistent cooling rates [36] |
| Initial equipment cost | High - Substantial investment required [41] | Low - Utilizes standard -80°C mechanical freezers [41] |
| Operational complexity | High - Requires specialized expertise for use and optimization [13] | Low - Simple, one-step operation with low technical barrier [13] |
| Batch scalability | Can be a bottleneck for large-scale batch processing [13] | Easier scaling due to simplicity [13] |
| Documentation & compliance | Built-in data logging for traceability and regulatory compliance [41] | Limited monitoring and documentation capabilities [36] |
| Typical cell viability outcomes | Higher TNC viability reported for HPCs (74.2% ± 9.9%) [36] | Slightly lower TNC viability for HPCs (68.4% ± 9.4%) but comparable CD34+ viability [36] |
| Clinical engraftment results | Similar neutrophil (12.4 ± 5.0 days) and platelet engraftment (21.5 ± 9.1 days) for HPCs [36] | Similar neutrophil (15.0 ± 7.7 days) and platelet engraftment (22.3 ± 22.8 days) for HPCs [36] |
Table 2: Research Reagent Solutions for Cryopreservation
| Reagent/Material | Function | Example Applications & Concentrations |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating cryoprotectant that prevents intracellular ice crystal formation [23] | 5-15% concentration in various media; 10% DMSO has osmolarity of ~1.4 osm/L [37] [23] |
| Human Serum Albumin | Protein stabilizer that reduces cryoinjury and membrane damage [37] | Commonly used at 9% concentration in combination with DMSO for HPC cryopreservation [36] |
| Ficoll 70 | Non-penetrating polymer enabling long-term storage at -80°C [23] | Added to freezing solution for iPSC preservation at -80°C for at least one year [23] |
| Cryobags | Primary containers for cryopreservation with integral tubing [37] | Volumes from 50-500 mL; most centers use 2-4 bags per collection [37] |
| Isopropanol (IPA) containers | Passive freezing devices providing approximately -1°C/min cooling rate [41] | Placed in -80°C mechanical freezer for uncontrolled-rate freezing of various cell types [41] |
Experimental Protocols
Protocol 1: Qualification of Controlled-Rate Freezers
Purpose: To ensure CRF performance meets specific use case requirements and regulatory standards.
Methodology:
- Temperature Mapping: Perform full versus empty chamber mapping across a three-dimensional grid of locations to identify hot/cold spots [13].
- Freeze Curve Mapping: Test different container types (vials, bags) in various locations within the chamber [13].
- Mixed Load Validation: Evaluate performance with different sample masses and configurations to define operational limits [13].
- Profile Verification: Confirm that actual temperature profiles match programmed parameters for both default and customized freezing protocols.
Reference Standards: Consult the ISPE Good Practice Guide: Controlled Temperature Chambers 2nd Edition, 2021, for comprehensive guidance [13].
Protocol 2: Viability Assessment Post-Thaw
Purpose: To accurately determine cell recovery and functionality after cryopreservation.
Methodology:
- Viability Staining:
- Functional Assays:
- Senescence Evaluation:
Experimental Workflow and Decision Pathways
Diagram 1: Decision Pathway for Cryopreservation Method Selection. This workflow guides researchers in selecting the appropriate freezing method based on clinical development stage, cell type, and available resources.
Diagram 2: Comprehensive Cryopreservation Experimental Workflow. This diagram outlines the complete experimental protocol from cell preparation through post-thaw assessment, highlighting critical steps for both freezing methods.
Technical Troubleshooting Guide
FAQ: Addressing Common Cryopreservation Challenges
Q: My post-thaw iPSC viability is consistently low. What is the most critical factor I should check?
A: The cooling rate is a primary suspect. Evidence confirms that human iPSCs are particularly vulnerable to intracellular ice formation and require a slow, controlled freezing rate. While a cooling rate of -1°C/min is a frequently used and effective standard for iPSCs, optimal recovery has been demonstrated within the -1°C/min to -3°C/min range [17]. You should verify that your controlled-rate freezer is correctly calibrated and programmed for this specific rate. Furthermore, ensure you are using a cryoprotectant such as DMSO, which penetrates cells to prevent ice crystal formation [42] [17].
Q: I am cryopreserving multiple cell types. Can I use the same cooling rate for all of them?
A: No, a "one-size-fits-all" approach is not optimal. Different cell types have unique biological characteristics, such as membrane permeability and volume, which demand specific cooling rates [43]. For instance, algorithm-driven optimization found that the ideal cooling rate for Jurkat lymphocytes was 10°C/min, while for mesenchymal stem cells (MSCs) it was 1°C/min [44]. Using an incorrect rate can lead to cell death from either intracellular ice formation (if too fast) or excessive dehydration and "solution effects" (if too slow) [45] [17]. The table below summarizes optimal rates for various cell types.
Q: What does the "two-factor hypothesis of cryo-injury" mean for my protocol?
A: This hypothesis explains the inverted 'U'-shaped cell survival curve seen when testing different cooling rates [45]. Injury occurs for two distinct reasons:
- At cooling rates SLOWER than the optimum: Damage is caused by "solution effects," where prolonged exposure to hyperosmotic solute concentrations in the unfrozen extracellular fluid leads to toxic levels of electrolytes and cellular dehydration [45].
- At cooling rates FASTER than the optimum: Damage is caused by lethal intracellular ice formation, as water does not have sufficient time to leave the cell before freezing [45].
Your goal is to find the cooling rate that best balances these two opposing dangers, which is cell-type-specific [45] [44].
Optimized Cooling Rates for Different Cell Types
The following table synthesizes evidence-based cooling rates for a variety of cells, demonstrating that protocol optimization must be cell-type-specific.
Table 1: Evidence-Based Optimal Cooling Rates for Different Cell Types
| Cell Type | Optimal Cooling Rate | Key Evidence and Notes |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | -1°C/min to -3°C/min | A rate of -1°C/min is frequently used. Testing shows better recovery at -1 to -3°C/min compared to -10°C/min [17]. |
| Mesenchymal Stem Cells (MSCs) | 1°C/min | Identified as optimal via a differential evolution algorithm, using a specific non-DMSO cryoprotectant solution [44]. |
| Jurkat Lymphocytes | 10°C/min | Algorithm-driven optimization determined this faster rate was ideal for this cell line [44]. |
| Lizard Sperm (V. panoptes) | 73°C/min | An intermediate rate was optimal, providing the first direct evidence for the two-factor hypothesis in reptile sperm [45]. |
| Human Oocytes | -0.3°C/min to -30°C, then -50°C/min to -150°C | A multi-step cooling protocol is required due to high susceptibility to ice crystal damage [17]. |
| General Mammalian Cells | 1-3°C/min | A standard range when using cryoprotective agents like DMSO or glycerol [42]. |
The Science of Cryo-Injury: The Two-Factor Hypothesis
The following diagram illustrates the fundamental principle of cryo-injury that underpins the need for cell-type-specific cooling rates. Finding the peak of the curve is the objective of protocol optimization.
Experimental Protocol: Algorithm-Driven Optimization of Cryopreservation Protocols
For researchers looking to move beyond published protocols and systematically optimize conditions for a novel cell type, the following methodology, adapted from [44], provides a powerful, high-throughput framework.
Objective: To simultaneously optimize cryopreservation solution composition and cooling rate for a specific cell type using a Differential Evolution (DE) algorithm, minimizing experimental effort while maximizing post-thaw recovery.
Materials:
- Cell culture of the target cell type.
- Candidate cryoprotectant agents (e.g., trehalose, glycerol, ethylene glycol, sucrose, taurine, ectoine).
- Controlled-rate freezer capable of precise cooling rates (e.g., 0.5°C/min to 10°C/min).
- Multi-well plates for high-throughput testing.
- Viability assay reagents (e.g., flow cytometry with viability dyes).
Methodology:
- Define Parameter Space: Establish discrete concentration levels (e.g., 0-300 mM for solutes) and a range of cooling rates (e.g., 0.5, 1, 3, 5, 10°C/min) to be tested.
- Initialize Algorithm: The DE algorithm randomly generates an initial population of "vectors," where each vector represents a unique combination of solute concentrations and a cooling rate.
- High-Throughput Freezing: Cells are combined with the solution specified by each vector and frozen in a 96-well plate at the designated cooling rate.
- Assess Cell Recovery: Post-thaw live cell recovery is measured for each condition.
- Algorithm Iteration: The experimental recovery data is fed back into the DE algorithm. The algorithm uses this information to mutate and recombine the best-performing vectors to generate a new, "evolved" set of test conditions for the next experimental round.
- Convergence and Validation: Steps 3-5 are repeated. The process converges when new generations no longer produce significant improvements in recovery. The best-performing solution and cooling rate are then validated in a larger-scale vial freezing experiment.
Key Research Reagent Solutions: Table 2: Key Reagents for Advanced Cryopreservation Optimization
| Reagent / Tool | Function / Explanation |
|---|---|
| Differential Evolution (DE) Algorithm | A stochastic search algorithm that efficiently navigates a multi-parameter space (solute concentrations, cooling rate) to find the global optimum for cell recovery [44]. |
| Non-DMSO Cryoprotectants (e.g., Trehalose, Ectoine) | Used to create less toxic, defined freezing solutions. Trehalose is a disaccharide that helps maintain structural integrity, while ectoine is an osmolyte that protects against stress [42] [44]. |
| Controlled-Rate Freezer | Essential for applying precise, reproducible cooling rates critical for protocol optimization and validation [42] [17]. |
| High-Throughput Viability Screening | Using 96-well plates and automated analysis allows for the simultaneous testing of dozens of conditions, making complex optimization feasible [44]. |
Scientific Background and Rationale
Why is a specialized thawing protocol necessary? Dimethyl sulfoxide (DMSO) is the most common cryoprotectant used for cryopreservation of hematopoietic stem cells (HSCs) and mesenchymal stromal cells (MSCs) due to its high efficiency and ability to rapidly penetrate cell membranes [46] [47]. However, when cryopreserved cells are thawed for autologous or allogeneic transplantation, the accompanying DMSO can induce significant adverse effects in patients, including nausea, vomiting, chills, tachycardia, dyspnea, and in rare cases, more severe cardiopulmonary or neurological reactions [46] [47]. Furthermore, the thawing process itself poses a risk of osmotic shock to the cells, which can compromise cell viability, recovery, and ultimately, the efficacy of the transplant [48].
The dual challenge of minimizing DMSO-associated toxicity for the patient and osmotic stress for the cells during the phase transition necessitates a robust and carefully balanced post-thaw protocol. The goal is to ensure high cell recovery and viability while reducing the infusion of toxic agents into the patient [49] [48].
Step-by-Step Thawing and DMSO Reduction Protocol
This protocol is designed for a 100 mL cryobag of peripheral blood stem cells (PBSCs) and is based on established methods used in clinical settings [46]. The process should be performed in a Grade A laminar flow cabinet with a Class B background.
Table 1: Key Reagents and Equipment
| Item | Function/Description |
|---|---|
| Water Bath | For thawing cells, must be calibrated to maintain 37°C. |
| Washing Solution | Normosol-R, Plasma-Lyte 148, or 0.9% NaCl supplemented with agents like hydroxychyl starch (HES) or human serum albumin (HSA) [46]. |
| Anticoagulant | Acid Citrate Dextrose Solution (ACD-A) to prevent clot formation during processing [46]. |
| Centrifuge | Capable of cooling to 4°C and running at 400 g. |
| Cryoprotectant | Dimethyl Sulfoxide (DMSO), typically used at a final concentration of 10% (v/v) for freezing [46] [48]. |
Step 1: Thawing
- Remove the cryobag from liquid nitrogen storage.
- Immediately place the sealed bag in a 37°C water bath.
- Gently agitate the bag until the contents are completely thawed (approximately 5 minutes). Avoid overwarming.
Step 2: Dilution and Washing
- Transfer the entire volume of the thawed cell suspension (mean 98 mL) to a larger, sterile washing bag.
- Gradually add 258 mL of washing solution (e.g., HES) and 42 mL of ACD-A anticoagulant solution to the bag. Gradual dilution is critical to reduce the extracellular DMSO concentration slowly and minimize osmotic shock.
- Mix the suspension gently but thoroughly.
Step 3: Centrifugation
- Centrifuge the bag for 20 minutes at 400 g and 4°C.
- After centrifugation, approximately 300 mL of the supernatant, which contains the majority of the DMSO, is carefully removed without disturbing the cell pellet.
Step 4: Product Formulation and Infusion
- The resulting cell pellet is resuspended in an appropriate infusion solution.
- The final product is labeled and transferred to the clinical department at 2–8°C.
- The product should be administered to the patient within two hours after thawing [46].
Figure 1: DMSO Reduction Workflow. This diagram outlines the key steps for the post-thaw washing process.
Quantitative Data on Cell Recovery
The DMSO reduction process has variable effects on different cell populations. The table below summarizes median recovery rates from a clinical study [46].
Table 2: Cell Recovery Post DMSO Reduction
| Cell Type / Function | Median Recovery (%) | Key Interpretation |
|---|---|---|
| Viable Nucleated Cells (NC) | 120.85% | High recovery; possible explanation is the removal of non-viable cells and debris during washing, effectively concentrating the viable cells. |
| Viable Mononuclear Cells (MNC) | 104.53% | Good recovery, indicating the process is gentle enough to preserve this population. |
| Viable CD34+ Cells | 51.49% | Significant decrease. This highlights a potential risk of losing crucial progenitor cells during processing. |
| Colony-Forming Unit (CFU-GM) Capacity | 93.37% | No significant decrease, suggesting the function of the remaining progenitors is well-preserved. |
Alternative Strategy: Using Lower DMSO Concentrations
An alternative to post-thaw washing is to reduce the DMSO concentration in the freezing media itself. A 2024 systematic review and meta-analysis provides compelling evidence for this approach [48].
Table 3: 5% vs. 10% DMSO Cryopreservation
| Parameter | 5% DMSO Performance vs. 10% DMSO |
|---|---|
| CD34+ Cell Viability | Greater post-thaw viability [48]. |
| Patient Side Effects | Lower rates of adverse events [48]. |
| Engraftment Rates | Minimal impact on neutrophil and platelet engraftment rates [48]. |
Troubleshooting and Frequently Asked Questions (FAQs)
FAQ 1: What are the primary indications for performing DMSO reduction? This procedure is typically reserved for patients at high risk for adverse reactions. Key indications include [46]:
- Impaired Renal Function: Patients with severe renal impairment, such as those with renal failure caused by secondary amyloidosis in multiple myeloma.
- Cardiac Involvement: Patients with primary or secondary amyloidosis of the heart.
- History of Severe Reaction: Patients who have previously experienced a severe adverse reaction to a DMSO-containing stem cell infusion.
FAQ 2: We observed a significant loss of CD34+ cells after washing. What could be the cause? A substantial loss of viable CD34+ cells (median ~50% in some studies) is a known risk of the washing process [46]. This can be due to:
- Physical Cell Loss: Cells are lost during the supernatant removal step.
- Osmotic Stress: Inadequate control of osmotic pressure during dilution and centrifugation can damage sensitive progenitor cells.
- Cell Clumping: Aggregation of cells can lead to inconsistent pellets and loss during processing. Solution: To minimize the risk of prolonged engraftment, ensure the initial collected cell dose is sufficient to tolerate the expected loss. This process should be applied judiciously.
FAQ 3: Is there a safe DMSO dose limit for patient infusion? Yes. The widely accepted safety limit is a daily DMSO dose not exceeding 1 gram per kilogram of patient body weight [46] [47]. For MSC therapies, the delivered DMSO doses are often 2.5–30 times lower than this threshold [47].
FAQ 4: What are the pros and cons of DMSO reduction vs. using lower DMSO concentrations from the start?
Figure 2: Strategy Comparison for DMSO Management. Weighing two primary methods to mitigate DMSO-related issues.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for the Protocol
| Reagent / Solution | Function in Protocol |
|---|---|
| DMSO (cGMP Grade) | Penetrating cryoprotectant that prevents ice crystal formation during freezing [46] [48]. |
| Hydroxyethyl Starch (HES) | Extracellular cryoprotectant and volume expander; used in washing solutions to help maintain osmotic balance [46]. |
| Human Serum Albumin (HSA) | Protein supplement added to washing or freezing media; helps stabilize cell membranes and reduces mechanical stress [46]. |
| ACD-A Anticoagulant | Citrate-based solution; prevents activation of the coagulation cascade during the washing process [46]. |
| Normosol-R / Plasma-Lyte 148 | Balanced electrolyte solutions used as the base for washing cells; physiocompatible and help maintain cell viability post-thaw [46]. |
Frequently Asked Questions (FAQs)
Q1: What are the key trade-offs when choosing a post-thaw processing method for Cord Blood Mononuclear Cells (CBMCs)? The choice involves balancing cell recovery, purity, and functional fitness, and the optimal method depends on your specific downstream application [4]. The Wash-Only method provides the highest cell yield but results in the lowest purity due to contaminants like red blood cells and granulocytes [4]. Density Gradient and Bead-based methods (e.g., CD15/CD235 depletion) offer higher purity [4]. Functional outcomes also vary; for instance, the EasySep Direct Human PBMC Isolation Kit significantly depletes CD14+ cells, which can correlate with reduced T-cell proliferation, while the Beads method best preserves cell viability over several days in culture [4] [5].
Q2: Does isolating mononuclear cells before cryopreservation improve post-thaw outcomes for cord blood units? No, current research indicates that pre-cryopreservation mononuclear cell isolation does not improve post-thaw CBMC recovery or function compared to the standard practice of using volume-reduced units [4] [5]. Therefore, focusing on optimizing the post-thaw processing method is more impactful for enhancing cell fitness.
Q3: How does granulocyte contamination in a PBMC sample affect downstream experiments? Granulocyte contamination can negatively impact the integrity and function of other immune cells in your sample. Studies have shown a correlation between granulocyte contamination and a significant decline in T-cell proliferation following stimulation. It can also lead to loss of cell number, reduced cell integrity, and increased variability in assays involving Regulatory T cells [50].
Q4: What are the best practices for thawing cryopreserved cells to maximize viability? The thawing process is critical and stressful for cells. Key practices include [51] [52]:
- Thaw Quickly: Remove the vial from liquid nitrogen and immediately place it in a 37°C water bath, gently swirling until only a small ice crystal remains [51].
- Dilute Slowly: Transfer the thawed cells dropwise into a tube containing pre-warmed complete growth medium to gradually reduce the concentration of the cryoprotectant (e.g., DMSO) [51].
- Use Controlled Thawing Devices: For GMP workflows or bedside administration, using a controlled thawing device is recommended over conventional water baths to minimize contamination risk and ensure a consistent, rapid warming rate [13].
- Plate at High Density: Plate the thawed cells at a high density to optimize recovery [51].
Troubleshooting Guides
Poor Cell Recovery Post-Thaw
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Low cell yield after processing | Excessive cell loss during washing steps | Centrifuge at appropriate, gentle speeds (e.g., 200 × g for 5-10 min); avoid harsh handling [51]. |
| High level of cell death before or during freezing | Ensure consistent, controlled-rate freezing; use fresh, high-quality cryopreservation reagents; avoid prolonged storage at non-optimal temperatures [52] [13]. | |
| High granulocyte contamination (leading to DNA release and cell clumping) | For Leukopaks or old blood samples, consider using a density gradient or CD15/CD16 MicroBeads to deplete granulocytes, acknowledging this may reduce total recovery [50]. |
Low Cell Viability or Function After Thawing
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Low viability immediately post-thaw | Improper thawing technique (slow thawing, prolonged DMSO exposure) | Thaw cells quickly in a 37°C water bath and dilute slowly in pre-warmed medium. Work efficiently to minimize DMSO contact time [50] [51]. |
| Old or improperly stored freezing media | Prepare fresh cryopreservation media; note that glycerol, if used, can convert to toxic acrolein if stored in light [51]. | |
| Reduced T-cell proliferation after culture | High granulocyte contamination | Deplete granulocytes using bead-based methods (e.g., CD15 depletion) to improve T-cell function [50]. |
| Significant loss of CD14+ monocytes (e.g., from certain bead kits) | If antigen presentation is required for your assay, select a processing method that preserves monocytes, such as Wash-Only or Density Gradient [4]. | |
| Cells not rested post-thaw | Culture thawed PBMCs at high density for several hours (e.g., overnight) before stimulation to restore immunogenicity [52]. |
The following table summarizes key performance metrics for different post-thaw processing methods, as reported in a study on cord blood mononuclear cells [4] [5].
Table 1: Comparison of Post-Thaw CBMC Processing Methods
| Processing Method | CBMC Yield | Purity (Depletion of Contaminants) | Viability on Day 0 | Viability Preservation (After 5 Days) | Impact on T-cell Proliferation |
|---|---|---|---|---|---|
| Wash-Only | Highest | Lowest | Moderate | Not Specified | Maintained |
| Density Gradient | Moderate | Moderate | Moderate | Not Specified | Maintained |
| Beads (CD15/CD235 depletion) | Moderate | Highest | Moderate | Best Preserved | Maintained |
| EasySep Direct PBMC Isolation Kit | Low | Highest | Highest (LAN cells) | Moderate | Reduced (due to CD14+ depletion) |
Experimental Protocols
Protocol 1: Comparing Post-Thaw Processing Methods
This protocol is adapted from a study evaluating wash-only, density gradient, and bead-based isolation methods for cord blood mononuclear cells (CBMCs) [4] [5].
- Starting Material: Use cryopreserved, volume-reduced cord blood units (CBUs).
- Thawing: Rapidly thaw CBUs in a 37°C water bath.
- Processing Methods:
- Wash-Only: Dilute the thawed product in a buffer and centrifuge. Resuspend the pellet for analysis.
- Density Gradient: Layer the diluted thawed product onto a density gradient medium (e.g., Ficoll-Paque). Centrifuge and carefully collect the mononuclear cell layer at the interface.
- Bead-Based Isolation: Use commercial kits (e.g., for CD15/CD235 depletion or the EasySep Direct Human PBMC Isolation Kit) according to the manufacturer's instructions, typically involving antibody incubation and magnetic separation.
- Assessment:
- Day 0: Assess immune subset recovery and the percentage of Live, Apoptosis-Negative (LAN) cells using flow cytometry.
- Day 5: After culture with stimulation, assess T-cell proliferation and perform additional viability/apoptosis assays.
Protocol 2: General Thawing and Culture of PBMCs
This protocol outlines a general best-practice procedure for thawing and handling cryopreserved PBMCs [51] [52].
- Materials: Pre-warmed complete growth medium (37°C), centrifuge tubes, 70% ethanol, water bath or bead bath at 37°C.
- Thawing:
- Retrieve the cryovial from liquid nitrogen. Caution: Vials stored in liquid phase present an explosion risk.
- Immediately place the vial in a 37°C water bath and gently swirl until only a small ice crystal remains.
- Wipe the vial with 70% ethanol and transfer the contents to a centrifuge tube.
- Slowly add pre-warmed medium dropwise to dilute the cells.
- Washing:
- Centrifuge the cell suspension at approximately 200 × g for 5-10 minutes.
- Carefully decant the supernatant without disturbing the cell pellet.
- Gently resuspend the cells in fresh, pre-warmed complete medium.
- Culture: Plate the cells at a high density in an appropriate culture vessel. For functional assays, it is often recommended to "rest" the cells by culturing them for several hours or overnight before stimulation [52].
Workflow Diagram
The diagram below illustrates the logical decision-making process for selecting a post-thaw processing method based on the primary goal of the downstream application.
The Scientist's Toolkit: Essential Research Reagents & Materials
The table below lists key materials and reagents used in post-thaw processing and viability research, along with their primary functions [4] [5] [50].
Table 2: Key Reagents and Materials for Post-Thaw Processing
| Item | Function & Application |
|---|---|
| Density Gradient Medium (e.g., Ficoll-Paque) | Separates mononuclear cells from other blood components (e.g., granulocytes, red blood cells) based on density during centrifugation [50]. |
| Bead-Based Isolation Kits (e.g., for CD15/CD235 depletion) | Immunomagnetic beads for high-purity negative selection and depletion of specific contaminating cell populations [4]. |
| EasySep Direct Human PBMC Isolation Kit | A commercial kit designed for the direct isolation of PBMCs from whole blood or thawed cord blood, resulting in high purity and initial viability [4] [5]. |
| Cryopreservation Medium (with DMSO) | A cryoprotectant solution (often 10% DMSO in FCS) that reduces intracellular ice crystal formation and osmotic stress during freezing and thawing [52]. |
| Dimethyl Sulfoxide (DMSO) | A common cryoprotective agent (CPA). Its concentration and the time cells are exposed to it pre-freeze and post-thaw are critical for viability [50] [52]. |
| Complete Growth Medium | A culture medium containing serum and supplements, pre-warmed and used to dilute thawed cells, providing nutrients and helping to remove DMSO [51]. |
| Controlled-Rate Freezer (CRF) | Equipment that controls the cooling rate (e.g., -1°C/min) during cryopreservation, which is crucial for maximizing cell viability and process consistency [13]. |
The Role of Automated Thawing Systems in Ensuring Consistency and Sterility
Within stem cell research and therapy development, post-thaw cell viability and functionality are critical determinants of experimental success and therapeutic efficacy. Automated thawing systems have emerged as a pivotal technology, directly addressing the core challenges of variability and contamination inherent in manual, water-bath-based methods. By providing a standardized, sterile thawing process, these systems significantly improve the consistency and quality of cell recovery, directly supporting the overarching research goal of enhancing stem cell viability post-thaw. This technical resource center provides detailed guidance on leveraging this technology to overcome common experimental hurdles.
Performance Comparison: Automated vs. Manual Thawing
The following table summarizes quantitative data from controlled experiments comparing automated and manual thawing methods for different cell types, demonstrating the direct impact on post-thaw recovery.
Table 1: Comparison of Cell Recovery and Viability Post-Thaw
| Cell Type | Thawing Method | Live Cell Recovery (Mean) | Cell Viability (Mean) | Source / Context |
|---|---|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Automated (ThawSTAR CFT2) | 2.78 x 107 cells | 92.8% | [53] |
| Manual (Water Bath) | 2.96 x 107 cells | 93.9% | [53] | |
| Monocytes | Automated (ThawSTAR CFT2) | 2.05 x 107 cells | 95.0% | [53] |
| Manual (Water Bath) | 1.89 x 107 cells | 94.6% | [53] | |
| Human Pluripotent Stem Cells (hPSCs) | Automated (ThawSTAR CFT2) | 9.05 x 105 cells | 83.04% | [53] |
| Manual (Water Bath) | 9.35 x 105 cells | 82.93% | [53] | |
| Clinical-Grade MSCs (Industry Standard) | N/A (Post-Thaw Benchmark) | N/A | 95% - 98% | [54] |
Standardized Operational Protocol
Adhering to a precise workflow is fundamental for success. The following diagram and protocol outline the optimized steps for thawing cryopreserved cells using an automated system.
Detailed Methodology:
- Preparation: Warm an appropriate cell culture medium (e.g., IMDM with 10% FBS or other recommended medium) in a 37°C water bath. Ensure all other materials, such as serological pipettes and 50 mL conical tubes, are ready within the biosafety cabinet [55].
- Vial Retrieval and Transport: Minimize the frozen vial's exposure to room temperature. If not thawing immediately, place the vial on dry ice or use a specialized portable transporter (e.g., ThawSTAR CFT2 Transporter) during movement from storage to the workstation [55] [53].
- Decontamination: Wipe the outside of the cryovial thoroughly with 70% ethanol or isopropanol before introducing it into the biosafety cabinet [55].
- Automated Thawing: Inside the biosafety cabinet, place the frozen vial directly into the automated thawing system and initiate the thaw cycle. The system will complete the process in approximately 2.5 minutes and alert you when finished [53].
- Immediate Dilution and Washing: Once thawed, use a pipette to transfer the cell suspension to a 50 mL conical tube. Rinse the original vial with 1 mL of warm medium and add it dropwise to the cells while gently swirling the tube. Then, add 15-20 mL of warm medium dropwise, continuing to gently swirl the tube to dilute the cryoprotectant (e.g., DMSO) gradually and prevent osmotic shock [55] [23].
- Centrifugation and Resuspension: Centrifuge the cell suspension at 300 x g for 10 minutes at room temperature. Carefully remove the supernatant without disturbing the cell pellet. Resuspend the cells in fresh, pre-warmed culture medium for counting and downstream applications [55].
- Viability Assessment: It is critical to perform a viable cell count immediately after thawing (before washing) and again after resuspension to confirm cell yield and track any loss during the wash process. Use Trypan Blue staining and a hemocytometer or an automated cell counter. Cell loss of up to 30% can be expected during washing [55].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Cell Thawing Experiments
| Item | Function / Application | Example / Note |
|---|---|---|
| Automated Thawing System | Provides a standardized, sterile thawing profile to maximize consistency and cell viability. | ThawSTAR CFT2 System [53] |
| Cell Culture Medium | Provides nutrients and environment for cell recovery and growth post-thaw. | Iscove's Modified Dulbecco's Medium (IMDM), RPMI 1640, often supplemented with Fetal Bovine Serum (FBS) [55] |
| Cryoprotectant | Protects cells from ice crystal formation during freezing and thawing. | Dimethyl sulfoxide (DMSO); newer DMSO-free, glucose-based alternatives are available [56] [54] |
| DNase I Solution | Reduces cell clumping post-thaw by digesting free DNA released from damaged cells. | Add 100 µg/mL to cell suspension if clumping is observed. Do not use if cells are for DNA/RNA extraction [55] |
| Trypan Blue | Dye exclusion test to assess cell viability; non-viable cells with compromised membranes take up the blue dye. | Use with a hemocytometer or automated cell counter for quantification [55] |
| ROCK Inhibitor | Enhances survival of single pluripotent stem cells by inhibiting apoptosis; can be used in recovery media post-thaw. | Y-27632; often used in hPSC and iPSC culture after thawing [19] |
Troubleshooting and FAQs
Q1: My post-thaw cell viability is consistently low, even when using the automated system. What could be the cause? Low viability can stem from factors preceding the thawing process itself. Investigate these areas:
- Pre-thaw Cell Health: Ensure cells were frozen during the logarithmic growth phase and were not over-confluent, as this impacts their ability to withstand cryopreservation stresses [23].
- Freezing Protocol: The cooling rate during initial cryopreservation is critical. An unoptimized, non-controlled rate freezing step can cause irreparable damage from intracellular ice crystals, which no thawing method can rectify [23].
- Storage Conditions: Transient warming events during storage above key glass transition temperatures (e.g., -123°C for extracellular DMSO vitrification) can be highly detrimental to cell viability over time. Ensure stable storage in the vapor phase of liquid nitrogen or sub -150°C freezers [23].
- Post-thaw Handling: After dilution, cells are fragile. Harsh pipetting or vortexing can significantly reduce viability. Always use gentle swirling and avoid creating shear forces [56].
Q2: I am observing microbial contamination in my cultures shortly after thawing. How can an automated system help prevent this? Automated systems directly address a primary contamination vector: the water bath. By thawing cells directly within the biosafety cabinet, they eliminate the risk of contaminated water contacting vial seals and being drawn into the vial upon opening. This closed, sterile process is a major advantage over water baths, which are known reservoirs for microbes [53] [57].
Q3: The automated system provides high viability, but my cell recovery (yield) is lower than expected. What steps should I take? Focus on the steps immediately following the thaw cycle:
- Prevent Clumping: If cells are starting to clump after resuspension, add DNase I Solution (e.g., 100 µg per mL of cell suspension) and incubate at room temperature for 15 minutes before proceeding with a second wash. This digests DNA from dead cells that can trap live cells in aggregates [55].
- Optimize Washing: Ensure you are rinsing the original cryovial with medium to recover all cells. During dilution, add the medium dropwise while gently swirling the tube to ensure gradual mixing and prevent osmotic shock, which can kill cells [55] [23].
- Gentle Centrifugation: Verify that the centrifugation speed and time are appropriate for your cell type. Excessive g-force or duration can damage the freshly thawed cells.
Q4: For sensitive cells like iPSCs, what specific post-thaw practices are recommended? iPSCs are particularly vulnerable post-thaw. In addition to using an automated thawer, consider these practices:
- Use of ROCK Inhibitor: Supplement the recovery medium with a ROCK inhibitor (e.g., Y-27632) for the first 24 hours after thawing. This significantly improves cell attachment and survival by reducing apoptosis [19].
- Optimal Seeding Density: Seed cells at a higher, recommended density to support cell-cell contact and survival signaling. Refer to cell-specific protocols for guidance [23] [58].
- Allow Recovery Time: Understand that iPSCs may require a recovery period of 4-7 days before they are ready for passaging or differentiation experiments. Do not passage cells too soon after thawing [23].
Solving the Puzzle: A Systematic Troubleshooting Guide for Poor Recovery
Insufficient cell recovery post-thaw is a critical bottleneck in stem cell research and therapy, directly impacting experimental consistency, therapeutic efficacy, and commercial viability. This process exposes cells to multiple stressors, including hypothermic shock, osmotic injury, and intracellular ice crystal formation, which can collectively trigger apoptotic and necrotic pathways [59]. A systematic approach to diagnosing the root cause is therefore essential for improving post-thaw viability, phenotype retention, and functional potency. This guide provides a structured, stepwise troubleshooting methodology to help researchers identify and resolve the most common factors leading to poor cell recovery.
Key Questions for Initial Diagnosis
Begin your investigation by answering these foundational questions. The answers will quickly guide you toward the most likely root cause categories.
- What is the specific viability metric? Is the issue low immediate post-thaw viability (e.g., Trypan Blue exclusion) or a later manifestation like poor attachment or reduced proliferation after several days in culture?
- When was the recovery issue first observed? Is it a new problem with a previously reliable protocol, or an issue with a newly established cell line or cryopreservation method?
- Which cell type is affected? Are you working with mesenchymal stromal cells (MSCs), hematopoietic progenitors, or iPSC-derived cells like cardiomyocytes? Different cell types have distinct sensitivities.
- What is your current cryopreservation solution? Does it contain DMSO at what concentration? Is it a standard in-house formulation (e.g., PlasmaLyte/Albumin/DMSO) or a commercial, intracellular-like solution (e.g., CryoStor)?
Troubleshooting Guide: Root Causes and Solutions
The following table outlines the primary categories of failure, their symptoms, and the recommended corrective actions.
| Root Cause Category | Specific Symptoms | Recommended Corrective Actions |
|---|---|---|
| Suboptimal Cryopreservation Solution [59] [60] | Consistently low viability across multiple cell lines and operators; high levels of apoptosis post-thaw (Annexin V+). | Transition to an intracellular-like, protein-free formulation (e.g., CryoStor CS10). Test solutions with lower DMSO concentrations (e.g., 5% vs. 10%). For clinical applications, consider DMSO-free cocktails of osmolytes [61]. |
| Inefficient Freezing Parameters [61] | Low recovery specific to a new cell type; variable results between experiments. | For hiPSC-CMs, a rapid cooling rate (e.g., 5°C/min) and lower nucleation temperature (-8°C) may be optimal. Systematically test cooling rates (1°C/min to 10°C/min) to find the ideal for your cell type. |
| Damaging Thawing & Post-Thaw Handling [59] [60] | Good initial viability that plummets after washing or plating; poor cell attachment and spreading. | Ensure a rapid thaw in a 37°C water bath. Dilute the cryoprotectant (DMSO) gradually post-thaw; for MSCs, a 1:2 dilution of a high-concentration cryopreserved product can improve viability. Minimize the DMSO exposure time before washing. |
| Inappropriate Cell State or Concentration [60] | Low recovery yield and poor growth even with acceptable initial viability. | Avoid cryopreserving cells at too high or too low densities. For MSCs, concentrations between 3-9 million cells/mL have been tested successfully. Ensure cells are in a healthy, logarithmic growth phase pre-freeze. |
Experimental Protocols for Systematic Diagnosis
Protocol 1: Comparative Viability and Recovery Assay
This protocol is designed to systematically evaluate the impact of different cryopreservation solutions on your specific cell type.
- Cell Preparation: Culture your cells (e.g., MSCs) under standard conditions to 80-90% confluency. Harvest and create a single-cell suspension. Determine the total nucleated cell count and viability (should be >95% pre-freeze).
- Experimental Arm Setup: Divide the cell suspension into aliquots to be cryopreserved in different solutions:
- Test Solution A: Commercial intracellular-like solution (e.g., CryoStor CS10).
- Test Solution B: Standard in-house formulation (e.g., PlasmaLyte-A with 5% HA and 10% DMSO).
- Test Solution C: A solution with a lower DMSO concentration (e.g., 5%).
- Cryopreservation: Cryopreserve the aliquots at a controlled cell concentration (e.g., 3-6 million cells/mL) using a controlled-rate freezer. Store in the vapor phase of liquid nitrogen for at least one week.
- Thawing and Analysis: Rapidly thaw vials in a 37°C water bath. Dilute the thawed product gradually with a suitable buffer (e.g., PlasmaLyte with 1% HSA). Assess the following:
- Total Nucleated Cell (TNC) Recovery: Using an automated cell counter.
- Viability: Using Trypan Blue exclusion and/or Annexin V/Propidium Iodide flow cytometry to distinguish between live, early apoptotic, and necrotic cells.
- Functional Potency: Perform colony-forming unit (CFU) assays for progenitors or immunomodulation assays for MSCs.
Protocol 2: Post-Thaw Time-Course Viability
This protocol assesses the stability of your recovered cells over time, simulating the window between thaw and infusion or plating.
Methodology [60]:
- Thaw a vial of your cryopreserved cells using your standard procedure.
- After the initial dilution/wash, resuspend the cells in a holding medium (e.g., PlasmaLyte with 5% Human Albumin) and maintain them at room temperature.
- Take samples at time points: 0-hours (immediately post-thaw), 2-hours, 4-hours, and 6-hours.
- At each time point, measure cell count and viability (Trypan Blue). A sharp decline over time indicates sensitivity to post-thaw handling or the inability to recover from cryo-injury.
Quantitative Data for Informed Decision-Making
The following table summarizes key findings from recent studies, providing benchmarks for evaluating your own recovery outcomes.
| Cryopreservation Solution | Cell Type | Key Viability/Recovery Metrics | Reference |
|---|---|---|---|
| CryoStor CS10 (5% DMSO) | Peripheral Blood Stem Cells | 1.8x increase in viable CD34+ cells; 1.5x increase in CFU-GM vs. standard FHCRC formulation. | [59] |
| CryoStor CS5 (5% DMSO) | Mesenchymal Stromal Cells | Decreasing trend in viability and recovery over 6 hours post-thaw. 10-fold less proliferative capacity after 6-day culture vs. other solutions. | [60] |
| PHD10 (10% DMSO) | Mesenchymal Stromal Cells | Comparable viability and recovery to NutriFreez up to 6 hours post-thaw. Similar post-thaw immunomodulatory potency. | [60] |
| Optimized DMSO-Free CPA | hiPSC-Derived Cardiomyocytes | Post-thaw recoveries >90%, significantly higher than 10% DMSO (69.4 ± 6.4%). Preserved calcium transient function and cardiac markers. | [61] |
Visual Workflow: Diagnostic Pathway
The following diagram illustrates the logical, step-by-step process for diagnosing the cause of low cell recovery.
The Scientist's Toolkit: Essential Research Reagents
This table details key reagents and their critical functions in optimizing cell recovery, as featured in the cited research.
| Research Reagent | Function in Cryopreservation & Recovery |
|---|---|
| CryoStor (CS5, CS10) [59] | A defined, intracellular-like cryopreservation solution that reduces ice crystal formation and cold-induced apoptosis, improving post-thaw viability and function. |
| Dimethyl Sulfoxide (DMSO) [60] | A permeating cryoprotectant that prevents intracellular ice formation. High concentrations (e.g., 10%) can be toxic and are linked to adverse patient events. |
| Human Serum Albumin (HSA) [60] | A protein source commonly added to in-house cryopreservation formulations to provide colloidal support and mitigate some damaging effects of freezing. |
| Annexin V / Propidium Iodide (PI) [60] | Fluorescent stains used in flow cytometry to distinguish between viable (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells. |
| Trehalose [61] | A non-permeating sugar used in DMSO-free CPA cocktails. It stabilizes cell membranes and proteins in a dehydrated state during freezing. |
| ROCK Inhibitor (Y27632) [61] | Significantly improves the survival and attachment of single-cell suspensions (especially stem cells) after thawing by inhibiting apoptosis. |
FAQs on Cell Recovery
Q1: My post-thaw viability is >90% by Trypan Blue, but the cells fail to attach and proliferate. What could be wrong? This is a classic sign that your viability assay is only detecting membrane integrity, while the cells have undergone significant cryo-injury. The root cause is often related to apoptosis induction [59]. Trypan Blue cannot detect early apoptosis. Implement an Annexin V/PI flow cytometry assay to get a more accurate picture of cell health. Furthermore, this can indicate a problem with the cryopreservation solution or freezing parameters, which may preserve membrane integrity but not cellular function. Switching to an intracellular-like solution or optimizing cooling rates may be necessary [59] [61].
Q2: Is reducing the DMSO concentration in my cryopreservation solution always beneficial? Not necessarily. While reducing DMSO from 10% to 5% can mitigate its toxic side effects [62], it can also lead to reduced cryoprotection and lower recovery if not compensated for. Studies show that MSCs cryopreserved in a 5% DMSO solution (CryoStor CS5) showed a decreasing trend in viability and a significant reduction in proliferative capacity post-thaw compared to 10% DMSO formulations [60]. The optimal approach is to either carefully validate the lower concentration for your specific cell type or transition to a DMSO-free CPA cocktail that has been explicitly optimized for it [61].
Q3: How long can I hold my cells in the cryopreservation solution after thawing before they need to be used or washed? The post-thaw "holding time" is critical. Research indicates that cell viability begins to decline after thawing, especially if the DMSO is not diluted. One study on MSCs showed that viability starts to drop measurably over a 6-hour window post-thaw when held in the cryopreservation solution [60]. To maximize recovery, it is recommended to dilute and wash the cells as soon as possible after the thawing process is complete, following a standardized and gentle dilution protocol [59].
Optimizing Cell Seeding Density and Aggregate Size for Enhanced Post-Thaw Attachment
Key Quantitative Data for Post-Thaw Seeding
The table below summarizes evidence-based recommendations for cell seeding after thawing, crucial for ensuring high viability and successful attachment in subsequent experiments.
| Cell Type / System | Recommended Seeding Density | Key Finding / Rationale | Source |
|---|---|---|---|
| hiPSCs (for neuroectodermal differentiation) | 1.23 × 10⁵ cells/cm² | This high density was used in spatial heterogeneity studies; improper seeding led to lower differentiation yield. [63] | |
| hiPSCs (General 2D Monolayer) | Information Missing | Plating thawed cells at a high density optimizes recovery. [51] | |
| General Cell Culture | 1x10³ - 1x10⁶ cells/mL (general range for cryovials) | A very high concentration can lead to undesirable cell clumping, while a very low concentration could lead to low cell viability. [29] | |
| 3D hPSC Aggregates (for freezing) | Information Missing | Using a 70-micron reversible strainer instead of a 37-micron one maintains slightly larger clumps, which improves post-thaw viability. [64] |
Troubleshooting FAQs
1. After thawing, my cells show poor attachment and survival. Could the seeding density be the issue?
Yes, this is a common problem. Seeding at a density that is too low can result in poor viability, as cells may require cell-to-cell contact for survival signals. [23] [29] Conversely, seeding at a very high density can cause excessive clumping, which leads to necrotic centers in aggregates and inefficient nutrient/waste exchange. [29] Solution: For hiPSCs, ensure you are plating at a high density as recommended. [51] Furthermore, the uniformity of the initial cell distribution (spatial heterogeneity) after seeding is critical. High heterogeneity, caused by errors like prolonged cell suspension time or tilting the culture vessel during seeding, is directly correlated with reduced yield in downstream differentiation. [63]
2. I am transitioning my hiPSCs from 2D to 3D suspension culture. How does this affect freezing and thawing?
The format in which cells are frozen (as single cells or as aggregates) significantly impacts recovery strategy. [23] Freezing and thawing hiPSCs as cell aggregates (clumps) is often advantageous because existing cell-cell contacts support survival and lead to faster post-thaw recovery compared to single cells, which need time to re-form aggregates. [23] Solution: For 3D cultures, a proven method is to cryopreserve cells as clumps generated from 3D cultures using a medium like CryoStor CS10. Using a 70-micron reversible strainer during preparation helps maintain optimally-sized aggregates, which has been shown to improve post-thaw viability. [64]
3. What are the best practices for handling the cryoprotectant DMSO during thawing to minimize cell stress?
DMSO is essential but toxic at higher temperatures. The key is rapid thawing to minimize its exposure to cells in a concentrated state. [56] Solution: Thaw cells quickly in a 37°C water bath until only a small ice crystal remains, then immediately and gently dilute the cell suspension dropwise into a larger volume of pre-warmed culture medium. This gradual dilution reduces osmotic shock. Subsequent centrifugation and removal of the DMSO-containing supernatant is recommended. [55] [51] Allowing cells a recovery period post-thaw before any downstream applications is also beneficial. [56]
Detailed Experimental Protocols
Protocol for Thawing and Seeding Frozen Primary Cells or hiPSCs
This standard protocol is designed to maximize cell viability and attachment after thawing. [55] [51]
Materials:
- Cryovial of frozen cells
- Pre-warmed complete growth medium (e.g., TeSR-E8 for hiPSCs [65])
- Water bath or automated thawing device (e.g., ThawSTAR) at 37°C
- 70% ethanol
- Centrifuge tubes
- DNase I Solution (optional, for clumping)
- Culture vessel coated with appropriate matrix (e.g., Matrigel for hiPSCs [65])
Method:
- Preparation: Warm complete growth medium in a 37°C water bath. Prepare the culture vessel.
- Thawing: Remove the cryovial from liquid nitrogen and thaw it quickly by gently swirling in a 37°C water bath for approximately 1-2 minutes. Remove the vial when a small amount of ice remains. Do not vortex. [55]
- Decontamination: Wipe the outside of the vial with 70% ethanol and move to a biosafety cabinet. [55]
- Dilution: Transfer the thawed cell suspension to a centrifuge tube using a pipette. Rinse the vial with 1 mL of medium and add it to the tube. Then, gently add a larger volume (e.g., 15-20 mL) of pre-warmed medium dropwise while swirling the tube to dilute the DMSO gradually. [55]
- Washing: Centrifuge the cell suspension at approximately 200-300 x g for 5-10 minutes at room temperature. [55] [51]
- Resuspension: Carefully decant the supernatant and gently resuspend the cell pellet in a fresh, small volume of medium.
- Seeding: Plate the cell suspension at the recommended high density into the prepared culture vessel.
- Post-Seeding Care: If cells show signs of clumping, add DNase I Solution (100 µg/mL) and incubate at room temperature for 15 minutes before proceeding. [55] Allow cells to adhere for 24-48 hours before the first medium change.
Protocol for Freezing hiPSCs as 3D Aggregates for Optimal Post-Thaw Recovery
This method leverages the benefits of aggregate freezing for improved survival. [23] [64]
Materials:
- Healthy, log-phase hiPSC culture (>80% confluency) [29]
- Accutase or Gentle Cell Dissociation Reagent (GCDR) [65] [64]
- Cryopreservation medium (e.g., CryoStor CS10 [64] or mFreSR [29])
- 70-micron reversible strainer [64]
- Cryogenic vials
- Controlled-rate freezing container (e.g., CoolCell [29])
Method:
- Harvesting: Dissociate the hiPSC culture to form cell aggregates of appropriate size. For 3D cultures, this may involve using a strainer to size the aggregates.
- Preparation: Centrifuge the cell aggregates and carefully remove the supernatant.
- Resuspension: Resuspend the cell pellet in cold cryopreservation medium. Using a specialized medium like CryoStor CS10, potentially supplemented with a Rho kinase inhibitor (Y-27632), can significantly enhance post-thaw viability. [65]
- Aliquoting: Aliquot the cell suspension into cryovials.
- Freezing: Place the cryovials in a controlled-rate freezing container and transfer them to a -80°C freezer for overnight freezing. This ensures an optimal cooling rate of approximately -1°C/minute. [29]
- Storage: The next day, transfer the vials to long-term storage in liquid nitrogen or a -150°C freezer. [29]
Experimental Workflow and Optimization Logic
The following diagram illustrates the critical steps and decision points for optimizing post-thaw cell attachment.
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and materials referenced in the protocols and studies, which are essential for optimizing post-thaw recovery.
| Reagent / Material | Function / Application | Example Product Names / Components |
|---|---|---|
| Cryopreservation Medium | Protects cells during freezing and thawing by preventing ice crystal formation. | CryoStor CS10 [29] [64], mFreSR [29] |
| Rho Kinase (ROCK) Inhibitor | Improves post-thaw cell survival and attachment, particularly for sensitive stem cells. | Y-27632 [65] |
| Defined Culture Medium | Provides nutrients and signals for cell growth and maintenance post-thaw. | TeSR-E8 [65], mTeSR 3D [64] |
| Hydrogel Matrix | Provides a 3D scaffold for cell growth that mimics the natural extracellular matrix. | Matrigel [65], VitroGel Hydrogel Matrix [65] |
| Enzymatic Dissociation Reagent | Gently breaks down cell-cell and cell-matrix adhesions for passaging or creating aggregates. | Accutase [65], Gentle Cell Dissociation Reagent (GCDR) [64] |
| Reversible Strainer | Used to size cell aggregates to a uniform, optimal diameter before freezing. | 70-micron reversible strainer [64] |
Frequently Asked Questions (FAQs)
Q1: Why do my cells clump together after thawing? Cell clumping post-thaw typically occurs due to the release of genomic DNA from dying or damaged cells. When cells undergo cryodamage during the freeze-thaw process, their membranes become compromised, releasing "sticky" DNA strands that act as a physical glue, trapping neighboring cells together. This is particularly common in samples subjected to repeated freeze/thaw cycles or enzymatic tissue dissociation [66] [67]. Clumping can also be exacerbated by high cell density, over-digestion with enzymes like trypsin, and various environmental stresses that accelerate cell death rates [68] [67].
Q2: How does DNase I work to reduce cell clumping? DNase I is an endonuclease enzyme that specifically cleaves DNA into small fragments. When added to a clumped cell suspension, it targets and degrades the extracellular DNA released from dead cells that is responsible for forming the viscous, sticky network that holds cells together. By fragmenting this DNA, DNase I disrupts the physical bridges between cells, allowing them to separate into a single-cell suspension without harming the living cells' genetic material [66] [67].
Q3: What is the recommended working concentration and incubation time for DNase I? For reducing cell clumping, the recommended final concentration of DNase I is 100 µg per mL of cell suspension. The treated sample should be incubated at room temperature for 15 minutes to allow for complete DNA degradation [66]. This protocol is effective for thawed primary cells and frozen peripheral blood mononuclear cells (PBMCs) [55] [69].
Q4: Are there any downstream applications where DNase I should not be used? Yes, DNase I should be avoided if you plan to perform downstream DNA extraction from the cells. However, RNase-free DNase I may be used if performing downstream RNA extraction. For applications sensitive to DNase, such as hematopoietic colony assays, cells should be washed once in the appropriate assay buffer (without DNase) before continuing [66] [69].
Q5: What are some alternative strategies to prevent cell clumping besides using DNase I? Several strategies can help minimize clumping:
- Optimize Cell Density: Maintain optimal cell density during culture and avoid letting cells reach 100% confluency before passaging. Subculture at approximately 80% confluence [68].
- Gentle Handling: Use wide-bore pipettes, minimize physical agitation, and avoid excessive pipetting or vortexing. Centrifuge at lower speeds (200-300 x g) for shorter durations (3-5 minutes) [68].
- Proper Dissociation: Avoid over-trypsinization during passaging, which can damage cell membranes and increase stickiness. Consider using gentler enzymes or adding EDTA to block cell surface adhesion molecules [68].
- Use of Chelators: Ethylenediaminetetraacetic acid (EDTA) can dissolve calcium bonds that contribute to cell adhesion [67].
- Trituration: Gentle, repetitive pipetting can help break up weak bonds between cells [67].
Troubleshooting Guides
Problem: Poor Cell Recovery After Thawing Due to Clumping
Possible Causes and Solutions:
Cause: Excessive Cell Death During Freeze-Thaw
- Solution: Optimize your cryopreservation protocol. Ensure cells are frozen in logarithmic growth phase at 70-80% confluency [70]. Use a controlled-rate freezer or an isopropanol freezing container to achieve a slow cooling rate of approximately -1°C/min, which is critical for preventing lethal intracellular ice crystal formation [23] [70]. Thaw cells rapidly in a 37°C water bath and immediately dilute in pre-warmed medium containing serum or protein [55] [71].
Cause: DNA-Mediated Clumping
- Solution: Implement a DNase I treatment step during the thawing process. After the initial wash, if cells appear clumpy, add DNase I solution to a final concentration of 100 µg/mL and incubate for 15 minutes at room temperature before proceeding with a second wash [55].
Cause: Suboptimal Post-Thaw Handling
- Solution: Always include protein in your thawing solution. Reconstituting cryopreserved cells in protein-free vehicles can result in significant cell loss (up to 50%). Using simple isotonic saline with 2% human serum albumin (HSA) can prevent thawing- and dilution-induced cell loss, ensuring >90% viability [71]. Avoid diluting cells to very low concentrations (<10^5/mL) in protein-free solutions, as this causes instant cell loss [71].
Problem: Clumping During Routine Cell Culture
Possible Causes and Solutions:
Cause: High Cell Density and Over-confluence
- Solution: Subculture cells before they reach over-confluence. For mesenchymal stem cells (MSCs), for example, low seeding densities (e.g., 5,000-6,000 cells/cm²) can reduce cell-to-cell contact and minimize clumping. Do not let cells grow to 100% confluency before subculturing [68].
Cause: Over-digestion with Enzymes
- Solution: Standardize enzymatic passaging. Avoid over-trypsinization, which damages cells and makes them stickier. Use chelating agents like EDTA or gentler enzymes such as TrypLE for dissociation [68].
Cause: Mechanical Stress
- Solution: Handle cultures gently. Use wide-bore pipettes for passaging and avoid creating excessive shear forces. Ensure centrifuges are calibrated and use appropriate g-force (200-300 x g) and time (3-10 minutes) for pelleting cells [68].
Experimental Protocols
Detailed Protocol: Using DNase I to Reduce Clumping in Thawed Cells
This protocol is adapted from established methods for thawing frozen primary cells and preparing single-cell suspensions [66] [55].
Materials Required:
- DNase I Solution (1 mg/mL)
- Culture medium or buffer free of EDTA (e.g., HBSS, PBS)
- Fetal bovine serum (FBS) or Human Serum Albumin (HSA)
- 50 mL conical tubes
- Cell strainer (37-70 µm)
- PBS containing 2% FBS
Procedure:
- Thaw Cells: Quickly thaw cell vials in a 37°C water bath until only a small ice crystal remains. Gently swirl the vial; do not vortex [55].
- Transfer and Dilute: Transfer the thawed cell suspension to a sterile 50 mL conical tube. Optional: Add 0.25 to 0.5 mL of DNase I solution directly to the tube prior to transferring the cells [66]. Slowly add 10-15 mL of pre-warmed medium or buffer containing 10% FBS dropwise, while gently swirling the tube [55].
- Wash Cells: Centrifuge the tube at 300 x g for 10 minutes at room temperature. Carefully discard the supernatant without disturbing the cell pellet [66] [55].
- Assess Clumping: Gently tap the tube to resuspend the pellet. If cells appear clumpy, proceed to DNase I treatment.
- DNase I Treatment: Calculate the volume of DNase I Solution needed to achieve a final concentration of 100 µg/mL. Add the DNase I dropwise to the cell suspension while gently swirling the tube. Incubate at room temperature for 15 minutes [66].
- Wash Again: Add 25 mL of culture medium or buffer containing 2% FBS to wash the cells. Centrifuge at 300 x g for 10 minutes. Discard the supernatant and gently resuspend the pellet [66].
- Final Filtration (if needed): If clumping persists, pass the sample through a 37-70 µm cell strainer into a fresh conical tube. Rinse the sample tube with buffer and pass through the strainer [66].
- The single-cell suspension is now ready for cell counting and downstream applications.
Table 1: Comparison of Cryoprotectant Solutions on Post-Thaw Recovery of Hematopoietic Stem Cells (HSC) from Cord Blood [72]
| Cryoprotectant Formulation | Nucleated Cell (NC) Recovery | Viable CD34+ Recovery | Colony-Forming Unit (CFU) Numbers |
|---|---|---|---|
| 10% DMSO in Dextran-40 | Baseline | Baseline | Baseline |
| 10% DMSO in CryoStor | Significantly Improved (P < 0.001) | Significantly Improved (P < 0.001) | Significantly Improved (P < 0.001) |
| 5% DMSO in CryoStor | Significantly Improved (P < 0.001) | Similar to Dextran Control | Significantly Improved (P < 0.001) |
Table 2: Impact of Reconstitution Solution on Post-Thaw Recovery and Stability of Mesenchymal Stromal Cells (MSCs) [71]
| Reconstitution Solution | Cell Loss After Thawing | Viability After 1h Storage | Stability Observation |
|---|---|---|---|
| Protein-Free Solutions (e.g., PBS) | Up to 50% | <80% | Poor stability (>40% cell loss) |
| Isotonic Saline | No observed cell loss | >90% | Stable for at least 4 hours |
| Culture Medium | >40% cell loss | <80% | Poor stability |
| Saline with 2% HSA | Prevented cell loss | >90% | High yield and stability maintained |
Workflow and Mechanism Diagrams
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Managing Cell Clumping and Improving Post-Thaw Recovery
| Reagent / Material | Function / Purpose | Example Application Notes |
|---|---|---|
| DNase I Solution (1 mg/mL) | Degrades extracellular DNA to break up cell clumps. | Use at 100 µg/mL final concentration for 15 min at RT. Do not use for downstream DNA extraction [66]. |
| Cryoprotectants (DMSO) | Penetrates cells to prevent ice crystal formation during freezing. | Standard concentration is 10%. New formulations like CryoStor allow reduced DMSO (5%) with improved recovery [23] [72]. |
| Protein Supplement (FBS/HSA) | Prevents cell loss during thawing and reconstitution; improves viability. | Essential in thawing solution. 2% HSA in saline is an effective, clinically compatible option [71]. |
| EDTA | Chelating agent that binds calcium ions; reduces cell adhesion. | Can be added to dissociation buffers to block cell surface adhesion molecules and minimize clumping [68] [67]. |
| Cell Strainers (37-70 µm) | Physically separate remaining cell clumps from single cells. | Use after DNase treatment if clumping persists. Rinse tube with medium to recover cells [66]. |
| Controlled-Rate Freezer | Provides optimal, reproducible cooling rate (~-1°C/min) for cryopreservation. | Critical for preventing intracellular ice crystals in sensitive cells like iPSCs [23] [70]. |
Frequently Asked Questions (FAQs)
1. Why is storing cells below -123°C so critical for their survival? Storing cells below -123°C is essential because this temperature represents the extracellular glass transition point for common cryoprotectants like Dimethyl Sulfoxide (DMSO). Below this temperature, the extracellular medium undergoes a phase change into a stable, glass-like state that halts all molecular activity. Storing cells above this transition point, even in the -80°C freezer, subjects them to stressful conditions where damaging chemical reactions and the formation of intracellular ice crystals can still occur, leading to mechanical damage to cell membranes and reduced post-thaw viability [17].
2. What are the practical consequences of storing my cell products at -80°C instead of in vapor-phase nitrogen? While short-term storage (less than one month) at -80°C may be acceptable for some cell types, it is not suitable for long-term preservation. Cells stored at -80°C will inevitably degrade over time [29]. In contrast, a 2025 study on hematopoietic stem cells (HSCs) demonstrated that even with a moderate, time-dependent decline in viability (approximately 1.02% per 100 days), products stored long-term at -80°C can still maintain viability sufficient for durable engraftment, highlighting that the impact is both cell type- and process-dependent [39].
3. My post-thaw cell recovery is low, but the storage temperature seems correct. What else should I investigate? Low cell recovery can stem from multiple factors in the pre- and post-thaw workflow. Key areas to investigate include:
- Pre-thaw Processing: The method used to isolate cells before freezing can impact recovery. For cord blood mononuclear cells (CBMCs), pre-cryopreservation isolation did not improve post-thaw recovery or function compared to standard volume-reduced units [5] [4].
- Post-thaw Processing Method: The technique used to process cells after thawing involves significant trade-offs. For example, a "Wash-only" method may retain the highest cell yield but the lowest purity, while methods using specialized kits or bead depletion can achieve high purity but may affect the recovery of specific immune cell subsets, such as CD14+ cells, which can in turn impact T cell proliferation [5] [4].
- Graft Composition: For hematopoietic stem cells, extreme platelet concentrations (either very low or very high) in the graft have been correlated with reduced post-thaw CD34+ cell recovery [6].
Troubleshooting Guides
Problem: Poor Viability and Functionality After Thawing
Potential Cause: Inconsistent or suboptimal storage temperature, allowing cellular stress.
Solutions:
- Verify Storage Equipment: Ensure liquid nitrogen tanks are consistently monitored and maintained. The vapor phase should reliably stay below -150°C. Note that the temperature can vary based on the distance from the liquid nitrogen level [17].
- Avoid Transient Warming Events: Minimize the time that storage freezers or tanks are open. Frequent opening can cause temperature fluctuations above the critical glass transition point, accelerating cell degradation [29].
- Audit Your Inventory: Maintain a log of vial locations to reduce searching time within the storage tank.
Potential Cause: The post-thaw processing method is not suitable for your downstream application.
Solutions:
- Application-Specific Method Selection:
- If your goal is maximum cell yield and you can tolerate lower purity, a simple "Wash-only" method may be appropriate [5] [4].
- If your goal is high purity for specific cell subsets, consider bead-based depletion or specialized isolation kits [5] [4].
- If long-term viability in culture is critical, the "Beads" method was shown to best preserve viability over five days of stimulation [5] [4].
Problem: Low Cell Yield Post-Thaw
Potential Cause: The freezing protocol itself was not optimized, leading to intracellular ice crystal formation or excessive dehydration.
Solutions:
- Use Controlled-Rate Freezing: Always use a controlled-rate freezer or an isopropanol-based freezing container (e.g., "Mr. Frosty") placed in a -80°C freezer to ensure a consistent cooling rate of approximately -1°C/minute, which is ideal for many cell types [17] [29].
- Freeze During Log Phase: Harvest and freeze cells when they are in their maximum growth phase (log phase) and at greater than 80% confluency to ensure health and robustness [29].
- Optimize Cell Concentration: Freeze cells at a concentration that avoids clumping and supports good recovery, typically within 1x10^3 to 1x10^6 cells/mL. Testing multiple concentrations is recommended [29].
Experimental Protocols for Validation
Protocol: Assessing the Impact of Post-Thaw Processing on CBMC Fitness
This protocol is adapted from Coutu-Godbout et al. (2025) to evaluate different methods for recovering cells after thawing [5] [4].
1. Materials
- Cryopreserved, volume-reduced Cord Blood Units (CBUs)
- Cell culture medium
- Ficoll-Paque PLUS or equivalent density gradient medium
- EasySep Direct Human PBMC Isolation Kit (or similar)
- Depletion beads (e.g., for CD15/CD235)
- Flow cytometry antibodies for immune subsets (e.g., CD14, CD3)
2. Methods
- Thawing: Rapidly thaw CBUs in a 37°C water bath.
- Post-Thaw Processing: Immediately process the thawed sample using four parallel methods:
- Wash-Only: Dilute and centrifuge to remove cryoprotectant.
- Density Gradient: Isolate mononuclear cells using standard Ficoll separation.
- Bead Depletion: Use magnetic beads to deplete unwanted lineages (e.g., CD15/CD235).
- Isolation Kit: Process cells using a direct PBMC isolation kit.
- Analysis:
- Day 0: Assess immune subset recovery and percentage of Live, Apoptosis-Negative (LAN) cells via flow cytometry.
- Day 5: After culture with stimulation, assess T-cell proliferation and re-evaluate cell viability via apoptosis assay.
3. Expected Outcomes A well-executed experiment will reveal clear trade-offs, allowing you to select the optimal processing method for your specific application, such as maximizing yield versus preserving long-term function [5] [4].
Viability Assessment Methods
| Method | Principle | Key Advantage | Consideration |
|---|---|---|---|
| Acridine Orange (AO) / Propidium Iodide (PI) | Viable cells with intact membranes fluoresce green; dead cells with compromised membranes fluoresce red. | Rapid, non-toxic; shows enhanced sensitivity to delayed cellular degradation post-thaw [39]. | Requires fluorescence microscopy. |
| Flow Cytometry with 7-AAD | 7-AAD is a fluorescent dye that penetrates cells with compromised membranes and is excluded by viable cells. | Quantitative, allows for multiplexing with cell surface marker staining. | May be less sensitive than AO for detecting delayed damage in some HSC products [39]. |
| Live, Apoptosis-Negative (LAN) Assay | Uses flow cytometry to distinguish live, early apoptotic, and late apoptotic/necrotic cells. | Provides a more nuanced view of cell health beyond simple membrane integrity. | More complex staining protocol [5] [4]. |
Signaling Pathways and Workflows
Stem Cell Storage Integrity Workflow
The Scientist's Toolkit
Research Reagent Solutions
| Reagent / Kit | Function | Application Note |
|---|---|---|
| CryoStor CS10 | A ready-to-use, serum-free cryopreservation medium containing 10% DMSO. | Provides a defined, protective environment for cells during freezing and thawing; recommended for use in regulated fields [29]. |
| EasySep Direct Human PBMC Isolation Kit | Immunomagnetic kit for isolating peripheral blood mononuclear cells directly from whole blood. | Post-thaw processing with this kit achieved high depletion of unwanted cells and the highest percentage of viable cells on Day 0, though it may reduce CD14+ cells [5] [4]. |
| MesenCult-ACF Freezing Medium | Animal component-free freezing medium formulated for mesenchymal stromal cells (MSCs). | Supports GMP-compliant workflows for MSC therapy development, helping to maintain viability and sterility after thawing [73] [29]. |
| CD15/CD235 Depletion Beads | Magnetic beads for negatively selecting and removing granulocytes and red blood cells. | The "Beads" method best preserved cord blood cell viability over five days of culture post-thaw [5] [4]. |
Technical Support Center
Troubleshooting Guide: FAQs on Large-Batch Cryopreservation
This guide addresses common challenges researchers face when scaling up cryopreservation processes for stem cell therapies and other advanced treatments, with a focus on improving post-thaw viability and recovery.
FAQ 1: Our post-thaw viability is consistently low when processing large batches. What are the key process parameters we should investigate?
Low post-thaw viability at scale often stems from inconsistent cooling rates or inadequate cryoprotectant formulation. To address this:
- Audit Your Controlled-Rate Freezer (CRF) Performance: Merely using a CRF is insufficient. System qualification should include temperature mapping across a grid of locations and freeze curve mapping for different container types and load configurations, not just a vendor's factory acceptance test [13].
- Analyze Freeze Curves as a Process Control: Incorporate freeze curve analysis into your process monitoring. Establishing action or alert limits for these curves can identify deviations in CRF performance before they lead to critical failures, explaining why some batches fail post-thaw analytics [13].
- Review Cooling Rates for Sensitive Cells: While a standard cooling rate of -1°C/min is common, it may not be optimal for all cell types. Evidence suggests that certain sensitive cells, like some T-cells and iPSC-derived lineages (e.g., cardiomyocytes, hepatocytes), require optimized, non-default freezing profiles [13] [74].
FAQ 2: How can we standardize the thawing process across multiple clinical sites to reduce variability?
Non-standardized thawing is a major source of variability and cell damage. To ensure consistency:
- Transition to Controlled-Thawing Devices: Replace conventional water baths, which are a source of contamination risk and rely on manual operation, with automated thawing systems [13] [75]. These devices provide control over warming rates and improve process robustness [13].
- Establish a Defined Warming Rate: The established good practice for thawing includes a warming rate of 45°C/min, though the optimal rate may vary based on the cell type and its corresponding cooling rate [13].
- Implement a Reproducible Thawing Program: Develop a consistent thawing protocol that can be executed reproducibly at any clinical site. Automated thawing systems are preferred to limit site-to-site variability [75].
FAQ 3: We are developing an "off-the-shelf" allogeneic therapy. How can we eliminate the logistically complex post-thaw wash step?
The post-thaw wash to remove cytotoxic DMSO is a significant bottleneck. Solutions include:
- Develop DMSO-Free Cryopreservation Media: There is a critical need to explore Me₂SO-free cryopreservation methods for novel administration routes (e.g., intracerebral, epicardial) where DMSO is not tolerated [74].
- Optimize Freezing Profiles for New Media: DMSO-free methods often yield suboptimal viability with standard slow-freeze protocols. Enhancing their performance requires dedicated optimization of freezing profiles [74].
- Consider Advanced CPA Formulations: Investigate cryoprotectant agents (CPAs) beyond DMSO. Alternatives include intracellular agents like glycerol and ethylene glycol, or extracellular agents like sucrose, dextrose, and methylcellulose, which can be used alone or in combination with reduced DMSO levels [76].
FAQ 4: What are the best practices for filling and aliquoting large batches to ensure homogeneity and viability?
The fill-and-aliquot step is critical for batch consistency.
- Maintain Solution Agitation: Use commercially available fluid transfer systems and maintain solution agitation throughout the aliquot process to ensure homogeneity and avoid issues like sinking cells or coagulation [75].
- Select the Right Primary Containers: Choose containers that meet performance, quality, and regulatory requirements. Review them for integrity, extractable and leachable profiles, and scalability for downstream processes [75].
- Incorporate a "Seeding" Step: During controlled-rate freezing, introduce an ice-nucleation step ("seeding") to reduce the risk of supercooling, which improves sample consistency and process reproducibility [75].
FAQ 5: Our post-thaw quality control (QC) sampling risks contamination and product loss. How can we mitigate this?
Minimizing risk during QC sampling is essential.
- Use Closed-System Sampling: Employ container closure strategies and sample through sterile connectors to maintain aseptic conditions. Integrated sampling ports in cryo-containers can reduce manual handling [16].
- Adopt a Risk-Based QC Panel: Work with regulatory agencies to define minimal, scientifically justified post-thaw release criteria. Balance the need for robust product verification with the imperative to protect the final drug product from contamination during manipulation [16].
- Plan for Scalable QC Assays: Choose QC assays that are practical, reproducible, and transferable across multiple clinical sites. Highly specialized assays can become logistical bottlenecks [16].
Quantitative Data for Large-Batch Cryopreservation
The following tables summarize key quantitative data relevant to scaling up cryopreservation processes, helping to inform protocol development and expectation management.
Table 1: Industry Survey Data on Scaling Challenges & Practices
| Survey Topic | Key Finding | Implication for Scaling |
|---|---|---|
| Biggest Hurdle | 22% of respondents identified "Ability to process at a large scale" as the single biggest hurdle [13]. | Scaling production capacity is a primary bottleneck for the cell and gene therapy industry. |
| Batch Processing | 75% of respondents cryopreserve all units from an entire manufacturing batch together [13]. | Manufacturing scale is often small, but cryopreserving sub-batches introduces reproducibility risks. |
| Freezing Method | 87% of survey participants use controlled-rate freezing; its adoption is high for late-stage and commercial products [13]. | Controlled-rate freezing is seen as critical for controlling quality and consistency at scale. |
| Default Freezer Profiles | 60% of users rely on the CRF's default freezing profile [13]. | Default profiles may be insufficient for sensitive or specialized cell types, requiring optimization. |
Table 2: Post-Thaw Viability & Storage Duration Data
| Cell Type | Storage Condition | Key Viability Finding | Reference |
|---|---|---|---|
| Hematopoietic Stem Cells (HSCs) | -80°C (uncontrolled-rate), median 868 days | Median post-thaw viability remained high at 94.8%, despite a moderate decline of ~1.02% per 100 days [39]. | [39] |
| Human induced Pluripotent Stem Cells (hiPSCs) in 3D culture | -80°C with optimized cryomedium | Achieved a cell survival rate exceeding 85% after thawing [65]. | [65] |
| General Cell Lines | Liquid Nitrogen (-196°C) | Theoretical storage duration is unlimited; cells can be recovered after decades without significant viability loss [76]. | [76] |
Essential Research Reagent Solutions
The following reagents and materials are critical for developing robust and scalable cryopreservation protocols.
Table 3: Key Reagents and Materials for Scalable Cryopreservation
| Reagent / Material | Function / Application | Considerations for Scaling |
|---|---|---|
| Cryoprotective Agents (CPAs) | Protect cells from ice crystal formation and osmotic stress during freeze-thaw [76]. | DMSO is standard, but cytotoxicity drives need for DMSO-free or alternative formulations [74]. |
| Controlled-Rate Freezer (CRF) | Provides precise control over cooling rate, a critical process parameter [13]. | System qualification must reflect actual use cases (container types, load configurations) [13]. |
| Controlled-Thawing Device | Provides rapid, standardized warming to maximize cell recovery and minimize contamination [13] [75]. | Replaces variable water baths; essential for multi-site clinical trials [77]. |
| Specialized Cryopreservation Media (e.g., CryoStor CS10) | A ready-to-use, GMP-compliant solution designed to improve post-thaw viability and function [65] [75]. | Redves formulation burden; often contains non-penetrating CPAs and energy substrates. |
| Rho Kinase (ROCK) Inhibitor (e.g., Y-27632) | Improves survival of human pluripotent stem cells (hPSCs) after thawing by inhibiting apoptosis [65]. | Crucial for improving the post-thaw recovery of sensitive iPSCs and their derivatives [65]. |
| Primary Containers (Cryovials, Bags) | Hold the cell product during freezing and storage. | Must be qualified for integrity, extractables/leachables, and scalability [75]. |
Experimental Protocols for Scaling
Protocol 1: Qualification of a Controlled-Rate Freezer for a Mixed Load
This protocol ensures your CRF performs adequately with the specific containers and cell types you use.
- Define Boundary Conditions: Identify the range of masses, container types (vials, bags), and configurations (full, partial load) used in your process [13].
- Execute Temperature Mapping: Place thermocouples across a grid of locations within the CRF chamber, including the center, corners, and near the cooling source [13].
- Perform Freeze Curve Mapping: Run standard freeze cycles using the identified boundary conditions. Record and analyze freeze curves for each container type and location to identify hot/cold spots and ensure uniform cooling [13].
- Establish Alert and Action Limits: Based on the data, set limits for critical freeze curve parameters (e.g., supercooling point, cooling rate after nucleation) to trigger maintenance or process intervention [13].
Protocol 2: Optimizing a DMSO-Free Cryopreservation Formulation
This protocol outlines a systematic approach to developing a safer, non-DMSO dependent process.
- Base Formulation Selection: Select a base DMSO-free cryomedium, which may include combinations of penetrating CPAs (e.g., glycerol, ethylene glycol) and non-penetrating CPAs (e.g., sucrose, trehalose) [74] [76].
- Cooling Rate Optimization: Systematically test a range of cooling rates (e.g., from -0.5°C/min to -2.5°C/min) with your selected formulation. DMSO-free methods often perform poorly with the standard -1°C/min rate and require optimization [74].
- Post-Thaw Functional Assessment: Beyond simple viability (e.g., trypan blue), assess cell function post-thaw using assays for metabolic activity, phenotype (flow cytometry), pluripotency markers (for stem cells), or specific secretory functions [16].
- Stress Testing: Subject the optimized protocol to simulated transport and freeze-thaw condition challenges to evaluate robustness [16].
Workflow and Process Diagrams
The following diagrams illustrate key workflows for large-batch processing.
Large-Batch Cryopreservation Workflow
Standardized Thawing and Post-Thaw Workflow
Benchmarking Success: Validation Metrics, Industry Standards, and Functional Assays
Frequently Asked Questions (FAQs)
What are the most critical metrics for assessing cell health after thawing?
Three key metrics are essential for a comprehensive assessment:
- Viability: The percentage of live cells in the population immediately after thawing.
- Recovery: The proportion of the total number of viable cells recovered post-thaw compared to the pre-freeze count.
- Live, Apoptosis-Negative (LAN) Cells: This combined metric identifies cells that are not only viable but also functionally healthy and not undergoing programmed cell death, which is a crucial indicator for downstream success [4] [5].
Why is my post-thaw cell viability good, but the cells fail to expand in culture?
High initial viability can sometimes be misleading, as it may not detect early apoptotic cells. Cells can be viable but stressed from the cryopreservation process, leading them to enter apoptosis hours or days later. This is why measuring Live, Apoptosis-Negative (LAN) cells is critical. A method like the LAN assay can more accurately predict long-term culture success by identifying these healthy cells [4]. Furthermore, the choice of post-thaw processing method can significantly impact long-term fitness, with some methods better preserving the ability of cells to proliferate over several days [4].
What is the best method for isolating mononuclear cells from thawed cord blood?
The "best" method involves a trade-off and should be selected based on your downstream application. The table below summarizes findings from a systematic comparison of four post-thaw processing methods for cord blood units [4] [5]:
| Processing Method | Key Characteristic | Impact on Viability/Recovery | Best Suited For |
|---|---|---|---|
| Wash-Only | Minimal processing; retains contaminants. | Highest total cell yield, but lowest purity. | Applications where maximum cell number is critical and contaminants are less concerning. |
| Density Gradient | Standard separation based on cell density. | Moderate yield and purity. | General purpose use when a balance of yield and purity is acceptable. |
| CD15/CD235 Depletion (Beads) | Negative selection to remove granulocytes & RBCs. | High purity; best preserved viability over 5 days in culture. | Applications requiring long-term culture and high purity, such as extended in vitro studies. |
| EasySep PBMC Isolation Kit | Negative selection kit. | Highest percentage of viable (LAN) cells on Day 0; significantly depletes CD14+ cells. | Applications where immediate high viability is key, or where antigen-presenting cell depletion is desired. |
How does the pre-cryopreservation processing method affect post-thaw outcomes?
A study found that performing mononuclear cell isolation prior to cryopreservation did not improve post-thaw recovery or function compared to the standard practice of freezing volume-reduced cord blood units [4] [5]. This suggests that optimizing post-thaw processing methods is a more effective strategy for enhancing cell fitness for therapy.
Should I use flow cytometry or fluorescence microscopy for viability assessment?
While both are valid, flow cytometry (FCM) offers several advantages for precise, quantitative analysis:
- Superior Precision: FCM provides high-throughput, single-cell analysis and is particularly more precise under conditions of high cytotoxic stress [78].
- Detailed Apoptosis/Necrosis Distinction: Multiparametric FCM staining can classify viable, early apoptotic, and late apoptotic/necrotic populations, giving a more detailed picture of cell health [78] [79].
- Objective Quantification: FCM analyses thousands of cells automatically, reducing sampling bias and operator subjectivity, which can be a limitation of manual fluorescence microscopy [78].
Troubleshooting Guides
Poor Cell Recovery Post-Thaw
| Problem | Potential Cause | Solution |
|---|---|---|
| Low viability and yield | Intracellular ice formation during freezing. | Optimize the cooling rate. For many stem cells, a controlled rate of ~-1°C/min is effective. Use controlled-rate freezers instead of passive freezing devices [13] [17]. |
| Osmotic shock during thawing or dilution. | Thaw cells rapidly, but dilute the cryoprotectant (e.g., DMSO) slowly using a drop-wise addition of pre-warmed culture medium [17]. | |
| Cryoprotectant toxicity. | Consider using advanced cryopreservation formulations. Studies show that supplementing DMSO with macromolecular cryoprotectants like polyampholytes can double post-thaw recovery by reducing intracellular ice formation [80]. | |
| Good initial viability, poor long-term growth | High levels of early apoptosis not detected by simple viability stains. | Implement an apoptosis-specific assay like the Live, Apoptosis-Negative (LAN) assay or use Annexin V/PI staining to detect early apoptotic cells [4] [79]. |
| Contaminating cells and debris affecting growth. | Re-evaluate your post-thaw processing. Switch from a "Wash-Only" method to a beads-based or kit-based isolation method for higher purity, which improves the culture environment [4]. |
High Levels of Apoptosis in Post-Thaw Cultures
| Problem | Potential Cause | Solution |
|---|---|---|
| High early apoptosis (Annexin V+/PI-) | Cryopreservation-induced activation of apoptotic pathways. | Ensure cells are frozen in the logarithmic growth phase, not from an over-confluent or stressed culture [17]. |
| Suboptimal cryopreservation formula. | Test cryopreservation media supplemented with macromolecular cryoprotectants. Research demonstrates these can reduce apoptosis post-thaw, leading to healthier cells [80]. | |
| High late apoptosis/necrosis (Annexin V+/PI+) | Damage from intracellular ice crystals or severe osmotic stress. | Verify that your frozen cells are stored below the glass transition temperature (e.g., in liquid nitrogen vapor phase) to prevent destructive ice recrystallization [17]. |
| Overly aggressive thawing or processing. | Use a controlled-thawing device or a 37°C water bath with gentle agitation to ensure a consistent and rapid thaw. Avoid leaving cells in diluted DMSO for extended periods before centrifugation [13]. |
Experimental Protocols
Protocol: Combined Viability, Apoptosis, and Protein Expression Analysis by Flow Cytometry
This protocol, adapted from a published method, allows for the simultaneous assessment of viability, apoptosis, and surface marker expression in defined subpopulations [79].
Key Steps:
- Harvest and Stain: Collect cells, wash with PBS, and resuspend in Annexin V Binding Buffer.
- Antibody Incubation: Incubate cells with a fluorochrome-conjugated antibody against your protein of interest (e.g., anti-CD44-APC) for 20-30 minutes on ice in the dark.
- Viability/Apoptosis Staining: Add Annexin V-FITC and Propidium Iodide (PI) to the cell suspension. Incubate for 15 minutes at room temperature in the dark.
- Acquisition: Analyze the cells immediately on a flow cytometer equipped with 488 nm (for FITC/PI) and 630-640 nm (for APC) lasers.
Gating Strategy:
- Use FSC-A vs. SSC-A to gate on the main cell population.
- On a dot plot of Annexin V-FITC vs. PI, identify four distinct populations:
- Viable: Annexin V-/PI-
- Early Apoptotic: Annexin V+/PI-
- Late Apoptotic/Necrotic: Annexin V+/PI+
- Necrotic/Debris: Annexin V-/PI+ (if present)
- Finally, analyze the fluorescence of your protein of interest (e.g., APC channel) within each of these gated populations to track expression changes from viable to apoptotic cells.
Workflow Diagram: Post-Thaw Cell Analysis
The diagram below illustrates the logical workflow for a comprehensive post-thaw cell analysis, integrating multiple metrics.
Protocol: Applying the Live, Apoptosis-Negative (LAN) Assay to Post-Thaw Cells
This protocol is based on a study that successfully adapted the LAN assay, previously used for fresh cells, to evaluate thawed cord blood mononuclear cells [4] [5].
Methodology:
- Thaw and Process: Thaw your cell product and isolate mononuclear cells using your chosen method (e.g., Beads, Density Gradient).
- Stain for Viability and Apoptosis: Follow a staining procedure similar to the flow cytometry protocol above, using a viability dye (like PI or a live/dead fixable dye) in combination with an early apoptosis marker (like Annexin V or a caspase activity probe). The specific fluorescent markers should be compatible with your flow cytometer.
- Flow Cytometry Analysis: Acquire data on the flow cytometer.
- Gating for LAN: The "Live, Apoptosis-Negative" population is defined as the subset of cells that are negative for both the viability dye (live) and the early apoptosis marker (not undergoing apoptosis) [4]. This population represents the most robust and functionally fit cells in your sample.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function/Explanation | Reference |
|---|---|---|
| Annexin V & Propidium Iodide (PI) | A classic dual-stain combination to distinguish viable (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells by flow cytometry. | [79] |
| Macromolecular Cryoprotectants (e.g., Polyampholytes) | Advanced additives used alongside DMSO. They function as extracellular cryoprotectants, demonstrated to reduce intracellular ice formation and osmotic shock, thereby improving post-thaw recovery and reducing apoptosis. | [80] |
| CD15/CD235 Depletion Beads | A negative selection method for post-thaw cord blood processing. It effectively removes granulocytes and red blood cells, achieving high purity and preserving T-cell function and long-term viability. | [4] [5] |
| EasySep Direct Human PBMC Isolation Kit | A negative selection kit for isolating PBMCs. It results in a high percentage of viable (LAN) cells immediately post-thaw but may deplete specific populations like CD14+ monocytes, which can impact T-cell proliferation assays. | [4] [5] |
| Controlled-Rate Freezer (CRF) | Equipment that provides precise control over the cooling rate during freezing. This is crucial for balancing cell dehydration and intracellular ice formation, a key determinant of post-thaw viability. | [13] [17] |
| GMP-compliant, Animal Component-Free Media | Culture media formulations designed for clinical applications. They eliminate risks associated with animal-derived components (e.g., immunogenicity, batch variability) and are essential for translating therapies to the clinic. | [81] |
This technical support center resource is developed within the broader research context of a thesis focused on improving stem cell viability post-thaw recovery. For researchers and drug development professionals, cryopreservation represents both a critical enabling technology and a significant bottleneck in the advancement of cell and gene therapies. The following troubleshooting guides and FAQs synthesize the most current industry findings from the International Society for Cell & Gene Therapy (ISCT), highlighting both established consensus and critical knowledge gaps that require further investigation. This resource aims to provide practical, evidence-based guidance to address common experimental challenges while framing them within the larger scientific context of improving post-thaw cell recovery and functionality.
Current Industry Landscape: Survey Data and Identified Gaps
Recent survey data from the ISCT Cold Chain Management and Logistics Working Group reveals several key trends and challenges in current cryopreservation practices. The table below summarizes the most critical quantitative findings:
Table 1: Key Survey Findings on Cryopreservation Practices from ISCT [13]
| Survey Category | Finding | Percentage of Respondents | Implications |
|---|---|---|---|
| Freezing Method Adoption | Use Controlled-Rate Freezing (CRF) | 87% | High adoption of controlled methods, especially for late-stage products |
| Use Passive Freezing | 13% | Primarily products in early clinical stages (up to Phase II) | |
| CRF Profile Usage | Use default CRF profiles | 60% | Majority use standard settings across clinical stages |
| Use optimized CRF profiles | 40% | Particularly for challenging cell types (iPSCs, CAR-T, etc.) | |
| Qualification Practices | Rely on vendors for system qualification | ~30% | Potential gaps in understanding specific use cases |
| Resource Allocation | Dedicate most resources to freezing process & cryomedium | 33% | Indicates area of highest technical challenge |
| Scale-up Challenges | Identify "ability to process at large scale" as biggest hurdle | 22% | Scaling recognized as major industry bottleneck |
Troubleshooting Guides & FAQs
FAQ 1: What are the most critical gaps in cryopreservation standardization identified by ISCT?
The ISCT survey highlights two significant standardization gaps that impact manufacturing consistency and regulatory compliance [13]:
Lack of Consensus on Controlled-Rate Freezer Qualification: Currently, there is little industry agreement on how to properly qualify controlled-rate freezers or whether different container form factors should be frozen together. Nearly 30% of respondents rely solely on vendors for system qualification, which often does not represent final use cases. Proper qualification should include a range of mass, container configurations, and temperature profiles specific to the user's intended application [13].
Underutilization of Freeze Curve Data: A large number of respondents indicated that freeze curves are not used for product release, relying instead on post-thaw analytics alone. However, freeze curves provide valuable information about ongoing CRF system performance and can identify why samples did not perform as expected in post-thaw analytics. Establishing action or alert limits for curves can help users intervene before critical failures occur [13].
FAQ 2: How can I improve post-thaw viability for sensitive cell types like iPSCs or CAR-T cells?
Improving viability for challenging cell types requires addressing multiple critical factors in the cryopreservation workflow:
Implement Controlled Cooling Rates: Human iPSCs are particularly vulnerable to intracellular ice formation. Evidence suggests that a freezing rate between -1°C/min and -3°C/min is optimal for iPSC survival, compared to faster rates of -10°C/min which show poorer recovery [23] [17]. The optimal cooling rate may follow a "fast-slow-fast" pattern through different temperature zones: fast in the dehydration zone, slow in the nucleation zone, and fast again in the further cooling zone [23] [17].
Optimize Cell Processing Method: For iPSCs, the choice between freezing as cell aggregates versus single cells involves important trade-offs. Cell aggregates maintain cell-cell contacts that support survival and typically recover faster post-thaw. Single cells enable better quality control and more consistent vial-to-vial recovery but require more time to re-form aggregates after thawing [23] [17].
Ensure Proper DMSO Handling: Use fresh cryoprotectant solutions prepared on the day of experimentation. For iPSC cryopreservation, gently resuspend cell clumps to ensure cryoprotectant penetration, and centrifuge at 200-300 × g for 2 minutes when harvesting [82].
The following workflow diagram illustrates the optimal cryopreservation process for challenging cell types:
FAQ 3: What are the best practices for qualifying controlled-rate freezing systems?
Proper qualification of controlled-rate freezers should extend beyond vendor specifications to ensure they meet your specific use cases [13]:
Comprehensive Temperature Mapping: Conduct full versus empty chamber mapping, temperature mapping across a grid of locations, freeze curve mapping across different container types, and mixed load freeze curve mapping.
Process-Relevant Parameters: Include a range of mass, container configurations, and temperature profiles that reflect your actual manufacturing conditions rather than relying solely on vendor qualification profiles.
Ongoing Monitoring: Implement freeze curve monitoring as part of routine manufacturing controls, establishing action and alert limits to identify performance changes before they impact product quality.
FAQ 4: What post-thaw processing methods optimize recovery for cord blood mononuclear cells?
A 2025 study systematically evaluated different post-thaw processing methods for cord blood mononuclear cells (CBMCs), revealing significant trade-offs between recovery, purity, and functional outcomes [5] [4]. The table below compares the performance characteristics of four different processing methods:
Table 2: Comparison of Post-Thaw Processing Methods for Cord Blood Mononuclear Cells [5] [4]
| Processing Method | CBMC Yield | Purity | Viability on Day 0 | Viability After 5 Days | Best For Applications Requiring |
|---|---|---|---|---|---|
| Wash-Only | Highest | Lowest | Moderate | Moderate | Maximum cell yield over purity |
| Density Gradient | Moderate | Moderate | Moderate | Moderate | Balanced recovery & purity |
| Beads (CD15/CD235 depletion) | Moderate | Highest | Moderate | Best | Long-term culture & stimulation |
| PBMC Isolation Kit | Moderate | High | Best | Moderate | Immediate viability & function |
The study also found that pre-cryopreservation mononuclear cell isolation did not improve post-thaw CBMC recovery or function compared to standard volume-reduced units, suggesting that optimization efforts should focus on post-thaw processing rather than additional pre-freeze manipulation [5] [4].
FAQ 5: How does the choice between controlled-rate and passive freezing impact cell quality?
The selection between controlled-rate freezing (CRF) and passive freezing involves significant trade-offs that should be considered based on your product's stage of development and target product profile [13]:
Table 3: Controlled-Rate vs. Passive Freezing Method Comparison [13]
| Parameter | Controlled-Rate Freezing | Passive Freezing |
|---|---|---|
| Process Control | High control over critical process parameters (cooling rate, nucleation temperature) | Limited control over critical parameters |
| Impact on CQAs | Can control impacted Critical Quality Attributes (e.g., cytokine release) | Advanced pre-freeze or thawing technology may be needed to mitigate damage |
| Infrastructure Cost | High (equipment, liquid nitrogen, staffing) | Low-cost, low-consumable infrastructure |
| Operational Complexity | Specialized expertise required | Simple, one-step operation with low technical barrier |
| Scalability | Potential bottleneck for batch scale-up | Easier scaling |
| Regulatory Position | Preferred for late-stage and commercial products | Mainly used in early clinical development (up to Phase II) |
Adopting controlled-rate freezing early in clinical development can avoid the challenging effort of making significant manufacturing changes later, but requires substantial resource investment in infrastructure, operating costs, and process development expertise [13].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagents and Materials for Cryopreservation Workflows [29] [82] [55]
| Product Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Cryopreservation Media | CryoStor CS10, BloodStor | Serum- and animal component-free, cGMP-manufactured for regulated applications |
| Cell-Type Specific Media | mFreSR (hES/iPS cells), MesenCult-ACF (MSCs), STEMdiff (cardiomyocytes) | Chemically-defined formulations optimized for specific cell types |
| Controlled-Rate Freezing Containers | Corning CoolCell, Nalgene Mr. Frosty | Achieve approximately -1°C/minute cooling rate in standard -80°C freezers |
| Cryogenic Storage Vials | Corning Cryogenic Vials | Internal-threaded designs minimize contamination risk during filling/storage |
| Automated Thawing Systems | ThawSTAR CFT2 | Ensure consistent thawing performance and maintain sample sterility |
| Ancillary Reagents | DNase I Solution | Reduce cell clumping in post-thaw processing (not for DNA/RNA extraction) |
Advanced Technical Guide: Three-Zone Cooling Optimization
Emerging research suggests that a constant cooling rate may not be optimal for all cell types. Advanced protocols for sensitive cells like iPSCs may implement variable cooling rates through three critical temperature zones [23] [17]:
This approach applies fast cooling in the dehydration zone to minimize prolonged exposure to cryoprotectant toxicity, slow cooling in the nucleation zone to prevent intracellular ice formation, and fast cooling in the final zone to minimize dehydration effects [23] [17].
The cryopreservation landscape for advanced therapies is characterized by rapid technological advancement alongside significant standardization challenges. While consensus exists on the preference for controlled-rate freezing in late-stage development, critical gaps remain in qualification methodologies, process monitoring, and scaling capabilities. By addressing these challenges through systematic optimization of both freezing and thawing processes, researchers can significantly improve post-thaw cell recovery and functionality. The troubleshooting guides and FAQs presented here provide a framework for navigating these complex technical decisions while contributing to the broader research goal of enhancing stem cell viability after cryopreservation.
Proliferation Assays: FAQs and Troubleshooting
Q1: What are the primary non-radioactive methods for quantifying T-cell proliferation, and how do they compare?
Several robust methods have replaced traditional radioactive assays. The table below summarizes the key characteristics of three common techniques.
| Assay Method | Principle of Detection | Optimal Readout Time | Key Advantages | Reported Optimal Concentration/Conditions |
|---|---|---|---|---|
| CFSE Dye Dilution [83] | Fluorescent dye diluted in daughter cells with each division. | 6 days post-stimulation [83] | Tracks multiple rounds of division; allows for downstream cell sorting. | 2.5 μM CFSE, cell density of 1 × 10^6 cells/mL [83] |
| Ki-67 Intracellular Staining [83] | Detection of a nuclear protein expressed in all active cell cycle phases (G1, S, G2, M). | 69-96 hours post-stimulation [83] | No pre-labeling required; flexible processing window. | Antibody titration required; stable expression window of 69-96 hours [83] |
| EdU (Click-iT) Incorporation [84] | Click chemistry detection of a thymidine analog incorporated into new DNA. | Pulse-dependent (e.g., 2-24 hours) | Faster than BrdU; no DNA denaturation required. | Requires optimization of EdU concentration and pulse time [84] |
Q2: I am observing no signal or very low signal in my Click-iT EdU proliferation assay. What could be wrong?
Low signal in an EdU assay can be attributed to several factors related to the "click" reaction or analog incorporation [84]:
- Inadequate Fixation/Permeabilization: Cells must be adequately fixed and permeabilized to allow the click reaction reagents access to the nucleus.
- Copper Chelation: The presence of metal chelators (e.g., EDTA, EGTA, citrate) in any buffer prior to the click reaction can bind copper, which is essential for the catalysis. Perform extra wash steps to remove chelators.
- Inactive Reagents: The click reaction mixture must be used immediately after preparation. The additive buffer must be colorless; a yellow color indicates it is no longer active.
- Low EdU Incorporation: The cells may not be proliferating, or the EdU concentration or incubation time may be insufficient. Ensure cells are healthy and at an appropriate density.
Q3: My CFSE assay shows poor proliferation. Is this a true biological effect or an artifact of my cells' condition?
Especially in a post-thaw context, the cell condition is critical. Artificially low proliferation can result from:
- Reduced Cell Viability: Always check post-thaw viability before assay setup. Cryopreservation-induced apoptosis can reduce the responsive cell pool [4].
- Inappropriate Stimulation: Verify the activity and concentration of your T-cell activator (e.g., anti-CD3/CD28 antibodies, PHA). Use a positive control from a healthy donor if possible.
- Impact of Post-Thaw Processing: The method used to process cells after thawing can significantly impact function. For example, one study found that using a specific PBMC Isolation Kit post-thaw significantly depleted CD14+ monocytes, which correlated with reduced T-cell proliferation, likely due to loss of antigen-presenting cells [4] [5].
Metabolic Activity Assays: FAQs and Troubleshooting
Q4: What functional metabolic assays can I use to profile the fitness of my recovered T-cells?
Metabolic reprogramming is a hallmark of T-cell activation and function. The table below outlines key assays to profile different aspects of T-cell metabolism.
| Metabolic Parameter | Assay Method | Principle of Detection | Key Insights Provided |
|---|---|---|---|
| Glycolytic Activity | L-Lactate Assay [85] | Fluorescent measurement of lactate concentration in the culture medium. | Indicates glycolytic flux; high lactate production is associated with effector T-cell differentiation. |
| Glycolytic Capacity | Hexokinase Activity Assay [85] | Fluorometric measurement of the activity of hexokinase, the first enzyme in glycolysis. | Reflects the cell's commitment to glucose metabolism; increased activity is associated with activation and some cancers. |
| Cytotoxicity / Membrane Integrity | LDH Cytotoxicity Assay [85] | Measures lactate dehydrogenase (LDH) released from damaged cells into the culture medium. | Useful for assessing cytotoxicity of CAR-T cells or for monitoring cryo-induced damage during thaw recovery. |
| Global Metabolic Phenotype | Spectral Flow Cytometry [86] | Integrates analysis of metabolic protein expression (e.g., GLUT1), functional probes, and metabolite uptake. | Enables single-cell metabolic profiling of antigen-specific T cells across activation states. |
| Real-Time Metabolic Flux | Hyperpolarized 13C-NMR [87] | Tracks the conversion of 13C-labeled substrates (e.g., glucose) to products (e.g., lactate) in real-time. | Reveals dynamic metabolic plasticity; e.g., a shift from oxidative phosphorylation to glycolysis during early CAR-T expansion [87]. |
Q5: The background signal in my LDH cytotoxicity assay is too high. How can I reduce it?
High background in LDH assays is often due to interference from the serum present in the growth medium [85]. To mitigate this:
- Use culture medium with minimal serum (e.g., 1-2%) during the assay period.
- Always include a medium-only control (without cells) and subtract its signal from your experimental values to account for background LDH activity in the serum itself.
Q6: When measuring intracellular metabolites, how can I ensure my measurements are accurate and not artifacts of the sampling process?
Accurate metabolite measurement is challenging due to their fast turnover. Key pitfalls and practices include [88]:
- Rapid Quenching: Metabolism must be stopped instantly. Slow methods like cell pelleting or cold PBS washing can perturb metabolite levels. Fast filtration or direct addition of cold, acidic acetonitrile:methanol:water is recommended.
- Effective Extraction: Use an organic solvent extraction method that provides quantitative yields. Incomplete extraction or artifactual production of metabolites from higher-energy species during extraction can occur.
- Absolute Quantitation: For concentration comparisons, use internal isotopic standards or external calibration curves to account for different ionization efficiencies of metabolites in MS-based assays.
The Scientist's Toolkit: Essential Reagents for Functional Assays
The following table lists key reagents and their functions for setting up the discussed assays.
| Reagent / Kit | Primary Function | Key Consideration for Post-Thaw T-Cells |
|---|---|---|
| CFSE (Carboxyfluorescein succinimidyl ester) | Fluorescent cell staining dye for tracking cell division by flow cytometry [83]. | Optimize concentration for post-thaw cells; 2.5 μM is a validated starting point [83]. |
| Anti-Ki-67 Antibody | Intracellular staining marker for cells in active phases of the cell cycle [83]. | Does not require pre-labeling, ideal for assaying thawed cells directly. Expression stable from 69-96h [83]. |
| Click-iT EdU Kit | Chemical detection of a thymidine analog incorporated into DNA during synthesis [84]. | Avoid metal chelators in buffers. Ensure cells are fixed and permeabilized properly for reagent access [84]. |
| LDH Cytotoxicity Assay Kit | Measures lactate dehydrogenase release as a marker of cell membrane damage and death [85]. | Use low-serum medium during assay to reduce background. Differentiate between thaw-induced death and experimental cytotoxicity [85]. |
| EasySep Human T Cell Isolation Kit | Negative selection for isolating untouched T cells from PBMCs [87]. | Post-thaw cell isolation method impacts function. Beads and isolation kits offer high purity but may affect subset recovery [4]. |
| CD3/CD28 Dynabeads | Artificial antigen-presenting system for polyclonal T-cell activation and expansion [87]. | Standardized method to stimulate T-cells for proliferation and metabolic assays post-recovery. |
Experimental Workflow and Troubleshooting Pathways
Diagram 1: Post-Thaw T-Cell Functional Validation Workflow
Diagram 2: Proliferation Assay Troubleshooting Guide
FAQs: Core Concepts and Trade-offs
Q1: What is the fundamental "purity vs. yield" trade-off in post-thaw cell processing?
A1: The purity vs. yield trade-off describes the inverse relationship where efforts to increase the proportion of desired cells in a final sample (purity) often lead to a loss in the total number of those desired cells recovered (yield), and vice versa. This occurs because highly selective separation methods, which remove unwanted cell types to achieve high purity, can also inadvertently discard some target cells or subject them to stress, reducing overall yield. Researchers must balance this based on their downstream application: high purity is critical for precise analytical assays, while high yield is often prioritized for cell therapies and expansion cultures [89].
Q2: What are the primary causes of cell loss and contamination that impact post-thaw purity and yield?
A2: Post-thaw cell loss and contamination stem from several sources:
- Cryoinjury: The freezing and thawing process itself inflicts damage, primarily through three mechanisms:
- Osmotic Damage: Extracellular ice formation causes water to osmotically leave the cell, leading to harmful dehydration and solute imbalance [30] [90].
- Mechanical Damage: Intracellular ice crystal formation physically ruptures cell membranes and organelles [30].
- Oxidative Damage: The process generates reactive oxygen species (ROS), which oxidize lipids, proteins, and nucleic acids [30].
- Cryoprotectant Toxicity: While Dimethyl sulfoxide (DMSO) is the most common cryoprotectant, it can cause cytotoxicity and, upon infusion in patients, adverse reactions like abdominal cramps or cardiac arrhythmias [30]. High concentrations exacerbate this risk.
- Suboptimal Cell Quality: Starting with cells that are not in their maximum growth phase (log phase) or are overly confluent before freezing can significantly reduce post-thaw viability and recovery [23] [29].
Q3: How does the initial cell passaging method (single cells vs. aggregates) influence post-thaw recovery?
A3: The choice between passaging and freezing cells as single cells or aggregates (clumps) has a direct impact on the recovery profile [23]:
- Cell Aggregates (Clumps):
- Advantages: Cell-cell contacts support survival, and recovery is typically faster as cells do not need to reform connections.
- Disadvantages: Variable aggregate size can lead to inconsistent cryoprotectant penetration, causing variability in viability. This can impact the consistency of purity and yield from vial to vial.
- Single Cells:
- Advantages: Allow for accurate cell counting and viability measurement, leading to more consistent and quantifiable recovery.
- Disadvantages: Cells require more time to recover and re-establish contacts after thawing, which can delay experiments.
Troubleshooting Guides
Problem: Low Post-Thaw Cell Yield
Potential Causes and Solutions:
- Cause 1: Inadequate Cryoprotection
- Solution: Optimize cryoprotectant agent (CPA) composition. Consider using a combination of permeable (e.g., DMSO) and non-permeable (e.g., sucrose, trehalose) CPAs. Non-permeable CPAs help reduce the required concentration of toxic permeable CPAs like DMSO, mitigating osmotic shock and improving yield [30] [91].
- Cause 2: Suboptimal Freezing Rate
- Solution: Implement controlled-rate freezing. A cooling rate of approximately -1°C/minute is optimal for many cell types, including stem cells. This can be achieved using a programmable freezer or an isopropanol-based freezing container placed in a -80°C freezer. This controlled rate minimizes lethal intracellular ice formation by allowing water to exit the cell gradually [23] [29].
- Cause 3: Low Starting Cell Viability or Health
- Solution: Ensure cells are harvested during their logarithmic growth phase (typically >80% confluency) and are free from microbial contamination (e.g., mycoplasma) before initiating cryopreservation [29].
Problem: Low Post-Thaw Cell Purity
Potential Causes and Solutions:
- Cause 1: Selective Loss of Target Cells
- Solution: Re-evaluate the post-thaw cell separation method. If using immunomagnetic selection, check for antibody over-labeling or under-labeling, which can cause non-specific binding or reduced recovery of target cells, respectively. The use of Fc receptor blocking agents can minimize non-specific antibody binding, improving purity [89].
- Cause 2: High Apoptosis/Necrosis in Target Population
- Solution: Incorporate apoptosis inhibitors in the post-thaw wash and recovery media. Additionally, the use of defined, serum-free freezing media can provide a more consistent environment than homemade FBS-containing media, reducing lot-to-lot variability and unintended selective pressures that can harm specific cell populations [30] [29].
- Cause 3: Excessive Cell Clumping
- Solution: Optimize the cell concentration during freezing. A very high cell concentration can promote clumping. Freeze cells at a concentration that balances high yield with the prevention of aggregation, typically within 1x10^3 to 1x10^6 cells/mL [29]. After thawing, use gentle yet effective dissociation techniques to disperse clumps without damaging cells.
The following tables consolidate key quantitative findings from recent research on post-thaw processing.
Table 1: Impact of Freezing Protocol on Enteric Neural Stem Cell Neurospheres [92]
| Freezing Protocol | Description | Post-Thaw Survival | RNA Expression Impact | Protein Expression Impact |
|---|---|---|---|---|
| M1 | Slow freezing (FCS + 10% DMSO) | High | Low (least affected) | Unchanged |
| M2 | Slow freezing | High | Low (least affected) | Altered |
| M3 | Slow freezing | High | Affected | Altered |
| M4 | Flash-freezing (Vitrification) | Low | Affected | Altered |
Table 2: Performance of Xenogeneic-Free Cryopreservation Solutions [91]
| Solution Name | Type | Key Composition | Post-Thaw Viability | Key Findings |
|---|---|---|---|---|
| Ti5 | Tissue-specific | Low-DMSO, pathogen-inactivated hPL (ihPL) | Maintained | Preserved matrix integrity & biomechanical properties of bioengineered tissues. |
| CeA | Cell-specific | Undisclosed ihPL-based | >80% (BM-MSCs, FBs, NSCs) | Preserved immunomodulatory properties of MSCs; promoted good recovery. |
Table 3: Effect of Long-Term Cryopreservation on Stromal Vascular Fraction (SVF) Cells [93]
| Cryopreservation Duration | Cell Viability & Stemness | Wound-Healing Potential (In Vivo) |
|---|---|---|
| Short-Term (2 months) | High | High (Superior) |
| Long-Term (12-13 years) | Significantly Reduced | Retained, but Inferior to Short-Term |
Experimental Protocols
Methodology:
- Harvesting: Culture-induced pluripotent stem cells (iPSCs) to an appropriate confluence. Passage cells as aggregates (clumps) using non-enzymatic methods (e.g., EDTA) to preserve cell-cell contacts.
- Freezing Medium Preparation: Resuspend cell aggregates in a suitable freezing medium. A common base is a culture medium supplemented with 10% DMSO. For improved performance, consider a defined, commercial serum-free freezing medium.
- Cooling: Aliquot the cell suspension into cryovials. Place vials in an isopropanol freezing container or a controlled-rate freezer. Cool at a rate of -1°C/min to -80°C.
- Storage: After 24 hours, transfer vials to long-term storage in liquid nitrogen vapor phase (<-135°C) to prevent warming above the critical glass transition temperature [23].
Methodology:
- Thawing: Rapidly thaw cryovials in a 37°C water bath until only a small ice crystal remains.
- Cell Washing: Gently transfer the cell suspension to a pre-warmed culture medium. Centrifuge to remove the cryoprotectant-containing supernatant.
- Cell Counting and Viability Assessment:
- Resuspend the cell pellet.
- Mix with a viability dye (e.g., Trypan Blue or 7-AAD).
- Use an automated cell counter or hemocytometer to count live (unstained) and dead (stained) cells.
- Calculate Viability: (Number of live cells / Total number of cells) x 100.
- Purity Assessment via Flow Cytometry:
- Label the washed cells with fluorescent antibodies against specific cell surface markers (e.g., CD45, CD34 for hematopoietic stem cells).
- Analyze using a flow cytometer.
- Calculate Purity: (Number of labeled target cells / Total number of live cells) x 100 [89].
- Yield and Recovery Calculation:
- Calculate Total Yield: Total number of live target cells recovered post-thaw.
- Calculate Recovery: (Number of target cells in the final isolate / Number of target cells in the starting sample) x 100 [89].
Signaling Pathways and Workflows
Diagram Title: Post-Thaw Processing Decision Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Post-Thaw Processing
| Item | Function & Rationale |
|---|---|
| Defined, Serum-Free Freezing Media (e.g., CryoStor) | Provides a consistent, xeno-free environment with optimized cryoprotectants to maximize post-thaw viability and reduce variability compared to lab-made FBS/DMSO mixtures [29]. |
| Controlled-Rate Freezing Container (e.g., Mr. Frosty) | Ensures an approximate cooling rate of -1°C/min when placed in a -80°C freezer, which is critical for preventing intracellular ice formation in many cell types [29]. |
| Non-Permeable Cryoprotectants (e.g., Sucrose, Trehalose) | Added to freezing media to act as osmotic buffers, allowing for a reduction in the concentration of toxic permeable CPAs like DMSO, thereby mitigating osmotic shock and cytotoxicity [30]. |
| Viability Dyes (e.g., Trypan Blue, 7-AAD) | Used to distinguish live from dead cells based on membrane integrity during cell counting, enabling accurate calculation of post-thaw viability and yield [89]. |
| Fc Receptor Blocking Reagent | Critical for immunomagnetic or FACS-based cell separation. Prevents non-specific antibody binding, thereby improving the purity of the isolated target cell population [89]. |
| Pathogen-Inactivated Human Platelet Lysate (ihPL) | A xeno-free supplement that can replace FBS in both culture and cryopreservation media, enhancing safety for clinical-grade cell therapy products [91]. |
Leveraging Freeze Curve Data as a Process Control and Release Criterion
Frequently Asked Questions (FAQs)
Q1: Why should we use freeze curve data as a release criterion when our post-thaw cell viability is already acceptable?
A1: Relying solely on post-thaw analytics provides a snapshot of the final outcome but lacks insight into the process. Freeze curve data acts as a real-time process control tool. It can identify subtle deviations in controlled-rate freezer (CRF) performance that may not immediately impact viability but could affect other Critical Quality Attributes (CQAs) like cell functionality or long-term health. Furthermore, if a batch shows poor post-thaw recovery, analyzing its freeze curve can help you pinpoint whether the cause was related to the freezing process itself, enabling faster and more accurate root-cause analysis [13].
Q2: Our lab uses default freezing profiles on our controlled-rate freezer. Is this sufficient for rigorous process control?
A2: Default profiles are a good starting point and are used by about 60% of the industry for many cell types [13]. However, they are not one-size-fits-all solutions. Sensitive or engineered cell types, such as iPSC-derived cardiomyocytes, photoreceptors, or certain CAR-T cells, often require optimized freezing profiles [13]. To determine if your default profile is sufficient, you should compare the freeze curves across multiple runs. Significant variation or deviations from the expected curve shape indicate a need for process optimization and profile customization.
Q3: What are the critical parameters to look for in a freeze curve for stem cell products?
A3: For stem cells like iPSCs, which are vulnerable to intracellular ice formation, the following phases are critical [23]:
- The Cooling Rate before Nucleation: This affects chilling injury and cryoprotectant agent (CPA) toxicity.
- The Temperature of Ice Nucleation: This is critical for managing osmotic stress and preventing intracellular ice formation.
- The Cooling Rate after Nucleation: This influences cell dehydration and intracellular ice formation. Research suggests that a constant cooling rate may not be optimal. A profile with a fast-slow-fast pattern in different temperature zones can lead to better iPSC survival [23].
Q4: We see variation in freeze curves between vials in the same run. Is this normal?
A4: Some variation is normal, but consistent or large variations can signal a problem with your system qualification. A proper CRF qualification should account for different load configurations. Nearly 30% of labs rely solely on vendor qualifications, which may not represent your specific use case [13]. To ensure uniformity, your qualification protocol should include temperature and freeze curve mapping across a grid of locations within the CRF chamber, using different container types and load masses that reflect your actual operations [13].
Q5: How can freeze curve data help with scaling up our cryopreservation process?
A5: Scaling is a major industry hurdle [13]. As you move from freezing a few vials to an entire manufacturing batch, the thermal mass and configuration within the CRF change. Freeze curve data is essential for establishing process consistency and reproducibility during scale-up. By comparing freeze curves from small-scale validation runs to those from full-scale production batches, you can ensure the freezing kinetics remain within defined parameters, thereby protecting the critical quality attributes of your therapy during scaling [13].
Troubleshooting Guides
Problem 1: Poor Post-Thaw Viability Despite Acceptable Freeze Curve Shape
| Possible Cause | Investigation Steps | Recommended Solution |
|---|---|---|
| Suboptimal Thawing Process | Review thawing method. Non-controlled thawing can cause osmotic stress and ice crystal damage [23]. | Implement a controlled-thawing device and standardize the thawing rate. Evidence points to the relevance of specific warming rates (e.g., ~45°C/min) for cell recovery [13]. |
| Improper Cell Handling Pre-Freeze | Check the confluency and health of cultures before freezing. | Ensure cells are harvested during their maximum growth phase (log phase) and are over 80% confluent for best freezing results [29]. |
| Osmotic Shock During Thawing | Review the protocol for diluting the cryoprotectant post-thaw. | Slowly dilute the thawed cell suspension with fresh culture medium to gradually reduce the concentration of DMSO and prevent osmotic shock [23]. |
Problem 2: High Variability in Freeze Curves Between Runs
| Possible Cause | Investigation Steps | Recommended Solution |
|---|---|---|
| Inconsistent CRF Load Configuration | Document the mass, vial type, and arrangement for each run. | Develop and adhere to a Standard Operating Procedure (SOP) that defines a standardized load configuration for your process [13]. |
| Inadequate CRF Qualification | Review the CRF qualification and mapping records. | Perform an extended qualification that includes "mixed load freeze curve mapping" to understand the limits of your freezer's performance with different sample types [13]. |
| Hardformance Degradation | Check the CRF maintenance logs and monitor for increasing deviations. | Implement a preventive maintenance schedule and use freeze curve monitoring with established alert limits to identify performance drift before critical failure [13]. |
Problem 3: Freeze Curve Shows Unexpected "Spikes" or "Dips"
| Possible Cause | Investigation Steps | Recommended Solution |
|---|---|---|
| Supercooling and Spontaneous Nucleation | Check if the curve shows a sudden, sharp temperature increase at a specific point. | Implement a "seeding" step in your freezing profile. This involves briefly holding the temperature at a point just below the freezing point and manually or automatically inducing ice nucleation to ensure a consistent process [94]. |
| Faulty Temperature Probe or Sensor | Calibrate all temperature probes. Run an empty chamber test to identify sensor malfunction. | Regularly calibrate sensors according to the manufacturer's schedule and during system qualification [13]. |
Data and Evidence Table: Key Findings on Freezing Parameters and Cell Recovery
The table below synthesizes quantitative data and findings from recent research on cryopreservation parameters impacting post-thaw recovery.
| Cell Type | Optimal Cooling Rate | Key Finding | Reference |
|---|---|---|---|
| Human iPSCs | -1 °C/min | A rate of -1 °C/min is frequently used and provides good recovery. Rates of -10 °C/min lead to poorer outcomes. [23] | |
| Human iPSCs | Variable (Fast-Slow-Fast) | A model suggests optimal survival is not achieved by a constant rate, but by a fast cooling in the dehydration zone, slow cooling in the nucleation zone, and fast cooling in the further cooling zone. [23] | |
| Human Oocytes | -0.3 °C/min to -30°C, then -50 °C/min to -150°C | A two-step cooling protocol is optimal for these large, ice-susceptible cells. [23] | |
| HSCs (at -80°C) | Uncontrolled (passive) | Post-thaw viability shows a time-dependent decline of ~1.02% per 100 days, but can remain high enough for engraftment after long-term storage. [39] | |
| Various (CAR-T, iPSC-differentiated) | Default vs. Optimized | 60% of surveyed professionals use default CRF profiles, but optimized profiles are often needed for challenging cells like iPSC-derived cells, CAR-Ts, and hepatocytes. [13] |
Experimental Protocol: Qualifying Your Controlled-Rate Freezer and Profile
This protocol provides a methodology for generating the freeze curve data necessary for robust process control.
Objective: To qualify the performance of a Controlled-Rate Freezer (CRF) for a specific cell type and load configuration by establishing a characterized freeze profile and defining acceptable parameter limits.
Materials (Research Reagent Solutions)
| Item | Function |
|---|---|
| Cryoprotectant Media (e.g., CryoStor CS10) | A ready-to-use, serum-free freezing medium that provides a defined and protective environment for cells during freezing. [29] |
| Validated Temperature Probes | For accurate, real-time monitoring of temperature within sample vials during the freeze cycle. |
| Data Logging System | To record time-temperature data from the probes for generating and analyzing freeze curves. |
| Cell-specific Culture Media | For suspending cells or as a base for in-house cryomedium. |
| Cryogenic Vials | For containing the cell suspension during freezing. |
Methodology:
- Experimental Setup: Fill cryogenic vials with a cell-free cryopreservation medium or a placebo solution that matches the thermal properties of your product. Place validated temperature probes in the center of representative vials located in different areas of the CRF chamber (e.g., center, corners, top, bottom).
- Profile Execution: Program the CRF with the freezing profile you wish to qualify (e.g., the manufacturer's default profile or an optimized profile). Initiate the freeze cycle while simultaneously recording data from all temperature probes.
- Data Collection: Record the temperature from all probes at frequent intervals (e.g., every 5-10 seconds) throughout the entire freeze cycle, from the start until the final transfer temperature is reached.
- Curve Analysis: Plot the temperature against time for each probe to generate a set of freeze curves. Analyze the curves for key events:
- Initial Cooling Phase: Confirm the rate matches the setpoint.
- Phase Change Plateau: Identify the supercooling point and the subsequent release of latent heat.
- Post-Crystallization Cooling: Confirm the rate and linearity of the curve down to the end temperature.
- Establish Ranges: Calculate the average curve and determine the upper and lower control limits (alert and action limits) for the entire profile based on the variability observed across multiple runs (e.g., 3-5 runs).
Diagram: Freeze Curve Analysis Workflow
Conceptual Diagram: Integrating Freeze Curves into a Quality Framework
This diagram illustrates how freeze curve monitoring integrates into a broader quality control system for cell therapy manufacturing, directly supporting the thesis of improving post-thaw recovery.
Conclusion
Optimizing stem cell viability post-thaw is a multifaceted challenge that hinges on a deep understanding of cryobiology, the meticulous application of tailored protocols, and rigorous validation. Success is not defined by a single parameter but by the integration of controlled freezing rates, gentle thawing processes, and functional post-thaw assessments. The industry is moving towards greater control and standardization, as evidenced by the widespread adoption of controlled-rate freezing and controlled thawing devices. Future progress will be driven by overcoming scaling hurdles, developing advanced cryoprotectant formulations, and integrating process analytics like freeze curve monitoring into routine quality control. By adopting these evidence-based strategies, researchers can significantly enhance cell recovery, ensuring that high-quality stem cells are available to power the next generation of biomedical research and clinical therapies.
References
- 1. Impact of controlled ice nucleation on intracellular ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517324009281]
- 2. Advanced technologies for the preservation of mammalian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8765766/]
- 3. Modeling and typical cases analyze at the cell-scale of ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224025000161]
- 4. Impact of pre- and post-thaw processing on recovery ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008400]
- 5. Impact of pre- and post-thaw processing on recovery ... [https://pubmed.ncbi.nlm.nih.gov/41026081/]
- 6. Post-thaw CD34+ cell recovery likely degraded under ... [https://www.nature.com/articles/s41409-024-02409-w]
- 7. Expanding the cryoprotectant toolbox in biomedicine by ... [https://www.sciencedirect.com/science/article/abs/pii/S073497502500031X]
- 8. Cryopreservation of biological materials: applications and ... [https://link.springer.com/article/10.1007/s11626-025-01027-0]
- 9. Reassessing DMSO–lipid interactions: Improved AMBER ... [https://www.sciencedirect.com/science/article/abs/pii/S0005273625000756]
- 10. Cryopreservation with DMSO affects the DNA integrity ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224024000026]
- 11. Hydrogel microcapsulation technology reduces the DMSO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639263/]
- 12. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362920/]
- 13. Cryopreservation - Key Survey Findings from the ISCT ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/05/28/cryopreservation-key-survey-findings-from-the-isct]
- 14. Innovations in Platelet Cryopreservation: Evaluation of DMSO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563202/]
- 15. Membrane-targeted DNA frameworks with biodegradability ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925003130]
- 16. Strategies for Optimizing iPSC Cryopreservation Storage ... [https://www.cellandgene.com/doc/strategies-for-optimizing-ipsc-cryopreservation-storage-and-post-thaw-quality-0001]
- 17. Improving Cell Recovery: Freezing and Thawing ... [https://www.mdpi.com/2073-4409/11/5/799]
- 18. Ice recrystallization inhibitors enable efficient ... [https://www.sciencedirect.com/science/article/pii/S1873506124002812]
- 19. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 20. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 21. Protocol for generating a human iPSC-derived tri-culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590421/]
- 22. Model-based assessment of temperature profiles in slow ... [https://www.sciencedirect.com/science/article/abs/pii/S0098135420307225]
- 23. Improving Cell Recovery: Freezing and Thawing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8909336/]
- 24. Cryopreserved mesenchymal stem cells regain functional ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-019-2038-5]
- 25. Freezing of cell sheets using a 3D freezer produces ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8579153/]
- 26. Computational fluid dynamics model-based design of ... [https://www.sciencedirect.com/science/article/pii/S0263876224004295]
- 27. A CFD-model-based approach to continuous freezing ... [https://www.sciencedirect.com/science/article/abs/pii/B9780443152740500111]
- 28. Effect and application of cryopreserved three‐dimensional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8800481/]
- 29. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 30. Principles and Protocols For Post-Cryopreservation Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9113563/]
- 31. Seeding, Subculturing, and Maintaining Cells [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/maintaining-cultured-cells.html]
- 32. Cell Freezing Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 33. What are the Stages of the Bacterial Growth Curve? [https://www.scientificbio.com/blog/what-are-the-stages-of-the-bacterial-growth-curve/]
- 34. Cell Culture FAQs [https://lifescience.invitro.com.au/l/cell-culture-faqs]
- 35. Cell culture and maintenance protocol [https://www.abcam.com/en-us/technical-resources/protocols/cell-culture-and-maintenance-protocol]
- 36. Passive freezing is equivalent to controlled-rate ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925006796]
- 37. Current practices in peripheral blood stem cell processing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283502/]
- 38. Passive freezing is equivalent to controlled-rate ... [https://pubmed.ncbi.nlm.nih.gov/40323255/]
- 39. Viable and Functional: Long-Term −80 °C Cryopreservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525932/]
- 40. Viability of dental pulp derived stem cells after long-term ... [https://www.sciencedirect.com/science/article/pii/S0099239925005977]
- 41. Freeze Down Methods featuring Controlled Rate Freezers [https://strexcell.com/blog/freeze-down-methods-for-cryopreservation/]
- 42. Effects of storage media, supplements and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8474714/]
- 43. “One Size Fits All” Approach May Not Be Optimal When ... [https://www.thermofisher.com/blog/biobanking/one-size-fits-all-approach-may-not-be-optimal-when-selecting-a-cryopreservation-protocol/]
- 44. Algorithm-driven optimization of cryopreservation protocols ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5769925/]
- 45. Optimal cooling rates for sperm cryopreservation in a ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224021001474]
- 46. Post-thaw dimethyl sulfoxide reduction in autologous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398813/]
- 47. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06807-6]
- 48. Impact of lower concentrations of dimethyl sulfoxide on ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924000537]
- 49. The role of depletion of dimethyl sulfoxide before autografting [https://pubmed.ncbi.nlm.nih.gov/14750079/]
- 50. Optimizing PBMC Viability and Recovery: Updated Best ... [https://cgt.global/pbmc-viability-and-recovery/]
- 51. Thawing Cells | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/thawing-cells.html]
- 52. Technical pitfalls when collecting, cryopreserving, thawing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11133553/]
- 53. ThawSTAR® CFT2 Automated Thawing System [https://www.stemcell.com/products/thawstar-cft2-automated-thawing-system.html]
- 54. How to Recognize a High-Quality Stem Provider in Cell : A Physicia 2025 [https://bioregenwellness.com/blogs/news/how-to-recognize-a-high-quality-stem-cell-provider-in-2025-a-physician-s]
- 55. How to Thaw Frozen Primary Cells [https://www.stemcell.com/how-to-thaw-frozen-primary-cells.html]
- 56. Cryopreservation in Cell and Gene Therapy | CGT Global [https://cgt.global/cryopreservation-in-cell-and-gene-therapy-ensuring-high-viability-cells-for-research-manufacturing/]
- 57. Thawing cells – process, difficulties & recommendations [https://www.susupport.com/blogs/knowledge/thawing-cells-process-difficulties-recommendations]
- 58. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 59. Improved Post-Thaw Recovery of Peripheral Blood Stem/Progenitor Cells Using a Novel Intracellular-like Cryopreservation Solution - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3021966/]
- 60. Frontiers | Key quality parameter comparison of mesenchymal stem cell product cryopreserved in different cryopreservation solutions for clinical applications [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1412811/full]
- 61. DMSO-free cryopreservation of hiPSC-derived cardiomyocytes: low temperature characterization and protocol development | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04384-5]
- 62. What Not to Do After Stem Cell Treatment [https://stemcellmia.com/what-not-to-do-after-stem-cell-treatment/]
- 63. Spatial heterogeneity analysis of seeding of human ... [https://www.sciencedirect.com/science/article/pii/S2352320424001846]
- 64. Scaling Up and Differentiating hPSCs in 3D Suspension ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/03/12/scaling-up-and-differentiating-hpscs-in-3d-suspens]
- 65. 3D culture and cryopreservation/thawing strategy of human ... [https://www.sciencedirect.com/science/article/abs/pii/S2214552425000951]
- 66. How to Reduce Cell Clumping in Single Cell Suspensions [https://www.stemcell.com/how-to-reduce-cell-clumping-in-single-cell-suspensions-with-dnase.html]
- 67. How to Reduce Cell Clumping in Cell Cultures [https://www.akadeum.com/blog/cell-clumping/?srsltid=AfmBOorhhtX4eBVcdiFrYb8f1Zra_rouMV0L7QRfzGOZV5smQLRCzrIe]
- 68. Strategies to Mitigate Cell Clumping in Mesenchymal Stem ... [https://www.atlantisbioscience.com/blog/overcoming-a-sticky-situation-strategies-to-mitigate-cell-clumping-in-mesenchymal-stem-cell-cultures/?srsltid=AfmBOooVBSDcUVDwEyX2p1UWgBr6_9T2VjHDr-igAiGxonPDMQ7nhPHp]
- 69. EasySep™ Cell Isolation Starting Guide: Tips & Tricks [https://www.stemcell.com/easysep-cell-isolation-starting-guide-tips-and-tricks.html]
- 70. Freezing Cells and Thawing Cells to Maintain Viability [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/top-tips-for-freezing-and-thawing-cells-to-maintain-viability.html]
- 71. Reconstitution and post-thaw storage of cryopreserved ... [https://www.sciencedirect.com/science/article/pii/S2352320423000275]
- 72. Novel cryoprotectant significantly improves the post-thaw ... [https://www.stemcell.com/novel-cryoprotectant-significantly-improves-the-post-thaw-recovery-and-quality-of-hsc-from-cb.html]
- 73. Optimizing mesenchymal stem cell therapy: from isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054297/]
- 74. Optimizing cryopreservation strategies for scalable cell therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659802/]
- 75. Overcoming Cryopreservation Challenges [https://www.biolifesolutions.com/resource-center/insights-blog/overcoming-cryopreservation-challenges/]
- 76. Cell Cryopreservation: Common Protocols, Thawing Tips ... [https://www.genfollower.com/cell-cryopreservation-thawing-guide/]
- 77. Cell Thawing Device 2025 Trends and Forecasts 2033 [https://www.archivemarketresearch.com/reports/cell-thawing-device-772191]
- 78. Evaluating cell viability assessment techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492793/]
- 79. Flow cytometry-based quantitative analysis of cellular ... [https://www.sciencedirect.com/science/article/pii/S2405844024096968]
- 80. Cryopreservation and post-thaw differentiation of monocytes ... [https://pubs.rsc.org/it-it/content/articlehtml/2025/lp/d5lp00131e]
- 81. Optimizing mesenchymal stem cell therapy: from isolation to ... [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-025-00539-7]
- 82. Cryopreservation of Cells: Dos and Don'ts [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/the-dos-and-donts-of-cryopreservation.html]
- 83. Standardization of CFSE and Ki-67 based lymphocyte ... [https://www.medrxiv.org/content/10.1101/2025.08.12.25333468v1.full-text]
- 84. Click-iT™ EdU Microplate Assay - FAQs [https://www.thermofisher.com/store/v3/products/faqs/C10214]
- 85. How Do You Assess Your Cell's Health and Metabolic ... [https://sciencellonline.com/en/how-do-you-assess-your-cells-health-and-metabolic-activity?srsltid=AfmBOopzTw5cTJkgf1BZvp4tz192bbpEUPckHIUx27c2fEcfnN-MD1R4]
- 86. Metabolic profiling of antigen-specific CD8+ T cells by ... [https://pubmed.ncbi.nlm.nih.gov/41015027/]
- 87. Mapping real-time metabolic kinetics of expanded CAR T ... [https://www.nature.com/articles/s41598-025-24712-2]
- 88. Metabolite Measurement: Pitfalls to Avoid and Practices to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5734093/]
- 89. Evaluating the Performance of Cell Separation Methods [https://www.stemcell.com/cell-separation/parameters]
- 90. Cryopreservation and its clinical applications [https://www.sciencedirect.com/science/article/pii/S221342201630155X]
- 91. Bioengineered tissue and cell therapy products are efficiently ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03300-z]
- 92. Impact of cryopreservation on viability, gene expression ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1196472/full]
- 93. Investigation of the stemness and wound-healing potential ... [https://www.sciencedirect.com/science/article/pii/S2352320425000306]
- 94. Optimization of freezing and thawing protocols for human ... [https://www.sciencedirect.com/science/article/pii/S0011224025000513]