Optimizing Stem Cell Differentiation Efficiency: Foundational Principles, Advanced Methods, and AI-Driven Solutions
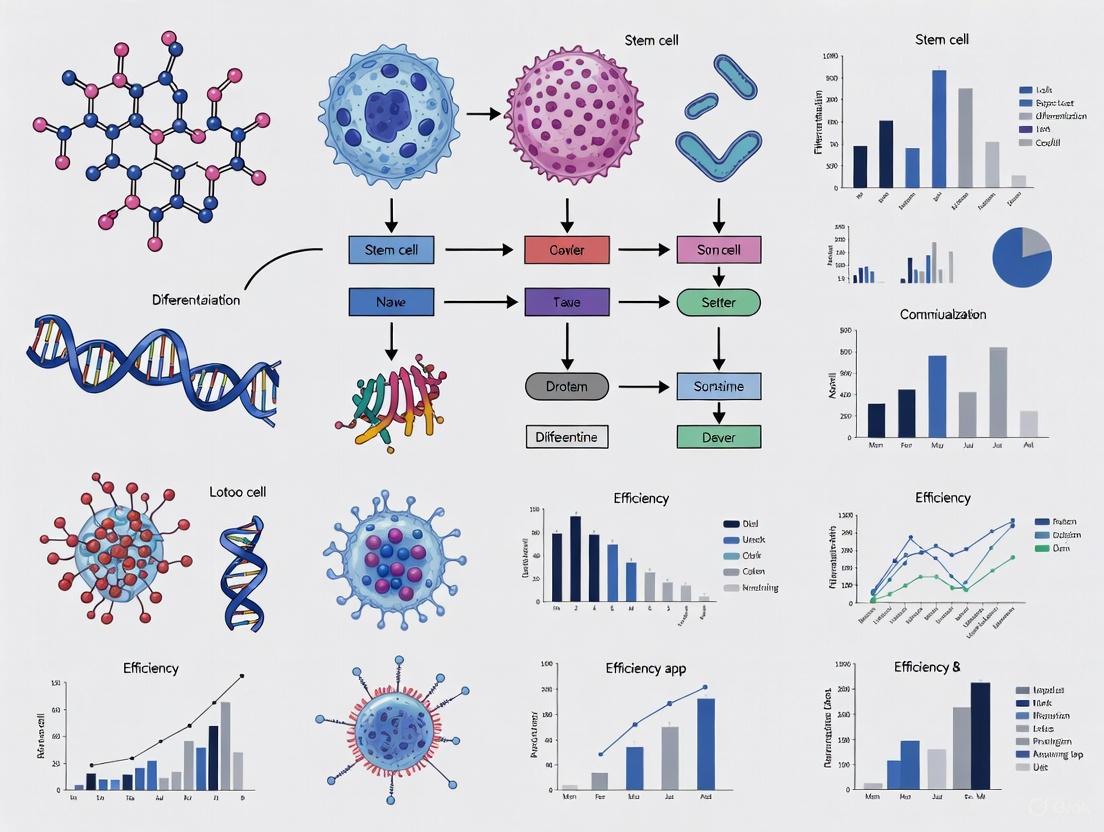
This article provides a comprehensive guide for researchers and drug development professionals on optimizing stem cell differentiation efficiency, a critical bottleneck in regenerative medicine and disease modeling.
Optimizing Stem Cell Differentiation Efficiency: Foundational Principles, Advanced Methods, and AI-Driven Solutions
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on optimizing stem cell differentiation efficiency, a critical bottleneck in regenerative medicine and disease modeling. It explores the foundational biological principles governing cell fate, details established and emerging differentiation protocols for key cell lineages like hepatic, hematopoietic, and neural cells, and addresses major challenges such as protocol reproducibility and long differentiation timelines. Crucially, it highlights innovative troubleshooting strategies, including the integration of artificial intelligence and machine learning for non-destructive quality prediction and protocol optimization. The scope also covers rigorous validation techniques and comparative analyses of differentiation methods to ensure the generation of high-quality, clinically relevant cell populations.
Understanding the Blueprint: Core Principles of Stem Cell Fate and Differentiation
Frequently Asked Questions (FAQs)
Q1: My stem cell differentiation yields highly heterogeneous cultures. Is this a sign of a failed protocol? Not necessarily. Heterogeneity is an inherent property of stem cell populations and can emerge from high-dimensional gene-regulatory networks [1]. Rather than indicating failure, this may reflect a diverse differentiation landscape. To assess your protocol, use single-cell RNA sequencing to characterize the distribution of cell states and confirm the presence of your target progenitors [2].
Q2: How can I improve the low transduction efficiency in my liver progenitor cell models? Your choice of delivery method is critical. Research shows that using recombinant adeno-associated viral (rAAV) vectors, particularly serotype 2/2 at a high multiplicity of infection (MOI of 100,000), can achieve transduction efficiencies over 90% in liver progenitor cells. For non-viral methods, electroporation can achieve moderate efficiency (around 54%) [3]. Optimize your viral titer or electroporation parameters specific to your cell line.
Q3: Can physical cues alone direct stem cell fate decisions? Yes. Surface topography is a powerful cue. Hierarchical micro-nano topographies can maintain mesenchymal stem cell (MSC) viability while significantly enhancing osteogenic differentiation, even without biochemical inducers. These physical features modulate focal adhesions, triggering downstream signaling that influences cell morphology, migration, and lineage commitment [4].
Q4: My primary hepatocytes dedifferentiate rapidly in 2D culture. What are more robust models for liver disease research? This is a common challenge. Consider moving to 3D organoid cultures derived from induced pluripotent stem cells (iPSCs). These models better maintain functional properties and cellular characteristics of liver tissue. We recommend using optimized directed differentiation protocols to generate bipotent liver progenitor cells (LPCs) that can self-renew and differentiate into both hepatocyte- and cholangiocyte-like cells [3].
Troubleshooting Guides
Issue 1: Poor Differentiation Efficiency into Target Lineage
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Inconsistent Signaling Molecule Concentration | Review protocol logs; check reagent preparation and storage. | Standardize concentrations of small molecules/growth factors (e.g., CHIR99021, Activin A, BMP4) to reduce need for line-specific optimization [3]. |
| Inaccurate Developmental Timing | Perform single-cell RNA-seq at multiple time points to map trajectory [2]. | Strictly adhere to timed media changes; use a detailed differentiation workflow chart for reference. |
| Unsuitable Extracellular Matrix | Immunofluorescence for pluripotency markers (OCT-4, NANOG) post-seeding. | Use Matrigel-coated plates for hiPSC maintenance and differentiation initiation [3] [2]. |
Issue 2: High Bacterial Contamination in Implant Co-culture Studies
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Non-sterile Implant Surface | Standard microbiological culture tests. | Use polymers (PDMS, PMMA) with integrated mechano-bactericidal nanotopographies like Moth-Eye nanocones to physically kill bacteria [4]. |
| Ineffective Antibiotic Prophylaxis | Check for antibiotic resistance in contaminants. | Combine hierarchical micro-nano topographies with a short, targeted course of antibiotics [4]. |
Issue 3: Low Transduction Efficiency in Progenitor Cells
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Suboptimal Transgene Delivery Method | Titrate viral vectors; test electroporation parameters on a small scale. | For high efficiency (>90%), use rAAV serotype 2/2. For non-viral delivery, use optimized electroporation protocols (~54% efficiency) [3]. |
| Incorrect Cell State/Health | Check viability and marker expression (e.g., FOXA2 for LPCs) pre-transduction. | Transduce during the progenitor cell stage; ensure >80% confluent monolayer at induction [3]. |
Experimental Protocols & Data
Optimized Directed Differentiation of hiPSCs to Liver Progenitor Cells (LPCs)
This protocol is optimized for rapid, cost-effective, and straightforward generation of LPCs with high marker expression efficiency [3].
Key Materials:
- Cell Line: Human induced pluripotent stem cells (hiPSCs)
- Basal Medium: RPMI 1640, 1% B-27 supplement (without Vitamin A), 1% Glutamax, 1% sodium pyruvate [3].
- Small Molecules/Growth Factors: CHIR99021, Activin A, FGFβ, FGF10, SB431542, Retinoic acid, BMP4 [3].
- Coating Material: Matrigel-coated plates [3].
Methodology:
- Maintenance: Culture hiPSCs on Matrigel-coated plates in mTeSR1 medium [2].
- Initiation (Day -1): Harvest hiPSCs and seed at high density (100,000 cells per cm²) in mTeSR1 with ROCK inhibitor [3].
- Definitive Endoderm (Day 0-3):
- Days 0-1: Switch to basal medium supplemented with 100 ng/mL Activin A and 3 µM CHIR99021.
- Days 1-3: Change to basal medium with 100 ng/mL Activin A and 10 ng/mL FGFβ. Change media daily [3].
- Anteroposterior Foregut (Day 3-5): Change to basal medium supplemented with 50 ng/mL FGF10, 10 µM SB431542, and 10 µM retinoic acid. Change media daily [3].
- Liver Progenitor Cells (Day 5+): Culture in basal medium with 50 ng/mL FGF10 and 10 µM BMP4 to obtain LPCs [3].
Table 1: Comparison of transgene delivery methods in Liver Progenitor Cells.
| Delivery Method | Specific Type | Key Parameter (MOI) | Average Efficiency | Key Application |
|---|---|---|---|---|
| Viral (rAAV) | Serotype 2/2 | 100,000 | 93.6% | High-efficiency gene delivery for therapy [3] |
| Non-Viral | Electroporation | N/A | 54.3% | Gene delivery avoiding viral vectors [3] |
Signaling Pathway Perturbation in Mesendoderm Differentiation
This methodology uses single-cell RNA sequencing to study the role of specific signaling pathways during differentiation [2].
Methodology:
- Differentiate hiPSCs towards mesendoderm for 2 days (as in the protocol above).
- On day 2, apply signaling perturbations by adding small molecules or recombinant proteins (e.g., targeting WNT, BMP4, VEGF pathways) to the culture medium.
- Remove the perturbation agents on day 5.
- Collect cells for scRNA-seq at baseline (day 2), progenitor (day 5), and committed stages (day 9) to analyze the effects [2].
Table 2: Key research reagents for stem cell differentiation and manipulation.
| Reagent / Solution | Category | Function in Research |
|---|---|---|
| CHIR99021 | Small Molecule | GSK-3 inhibitor; activates WNT signaling to initiate differentiation [3] [2] |
| Activin A | Growth Factor | Promotes differentiation into definitive endoderm lineage [3] |
| BMP4 | Growth Factor | Signals for hepatic specification from foregut [3] |
| ROCK Inhibitor | Small Molecule | Improves survival of dissociated single hiPSCs during passaging [3] |
| rAAV Vectors | Viral Delivery | High-efficiency tool for introducing transgenes into progenitor cells [3] |
| Matrigel | Extracellular Matrix | Provides a basement membrane matrix for cell attachment and polarization [3] [2] |
| SB431542 | Small Molecule | TGF-β inhibitor; used in foregut patterning [3] |
Signaling Pathways and Workflows
Stem Cell Differentiation State Space
hiPSC to Liver Progenitor Workflow
Signaling Perturbation Experimental Design
Stem cell differentiation is a tightly regulated process orchestrated by key signaling pathways. Among these, the Wnt, BMP (Bone Morphogenetic Protein), and FGF (Fibroblast Growth Factor) pathways play particularly critical and interconnected roles in determining cell fate. In the context of stem cell differentiation efficiency optimization, precise control of these pathways is paramount. These pathways do not function in isolation; they engage in complex crosstalk that can either promote or constrain differentiation toward specific lineages, influencing the overall success and reproducibility of experimental protocols [5] [6]. This technical support center provides troubleshooting guides and FAQs to help researchers navigate the challenges associated with manipulating these pathways for robust stem cell differentiation.
Pathway Diagrams and Crosstalk
The following diagrams illustrate the core components and transduction mechanisms of the Wnt, BMP, and FGF signaling pathways, which are frequently manipulated in differentiation protocols.
Canonical Wnt/β-catenin Signaling Pathway
Wnt signaling is categorized into canonical (β-catenin-dependent) and non-canonical (β-catenin-independent) pathways [7]. The canonical pathway, crucial for lineage specification, is activated when Wnt ligands bind to Frizzled receptors and LRP5/6 co-receptors. This disrupts the β-catenin destruction complex, preventing β-catenin degradation and allowing its nuclear translocation to activate target genes via TCF/LEF transcription factors [7] [8]. In stem cell differentiation, this pathway must be temporally controlled, often initially activated to induce mesoderm, then inhibited to promote cardiac specification [8].
BMP Signaling Pathway
BMP signaling is initiated when BMP ligands form a complex with type I and type II serine/threonine kinase receptors, leading to the phosphorylation of R-SMADs (1/5/8) [5] [9]. These then complex with SMAD4 and translocate to the nucleus to regulate gene expression alongside lineage-specific transcription factors like NKX2.5 and Hand1 [5]. The pathway is finely tuned by extracellular antagonists (e.g., Noggin, Chordin) and inhibitory SMADs (6/7) [5] [9]. BMP signaling promotes differentiation by antagonizing pluripotency and is essential for mesoderm and cardiac lineage commitment [5] [10].
FGF Signaling Pathway
FGF signaling begins with FGF ligands binding to FGFRs (Fibroblast Growth Factor Receptors), a process facilitated by heparan sulfate proteoglycans [5] [11]. Receptor activation triggers intracellular signaling through several downstream cascades, including RAS-MAPK, PI3K-AKT, PLCγ, and STAT pathways [5] [11] [12]. These effectors regulate fundamental processes like proliferation, survival, and differentiation. The role of FGF signaling is highly context-dependent, exhibiting biphasic effects where early activation promotes cardiac mesoderm formation, but continued signaling can inhibit further cardiomyocyte differentiation [5].
Troubleshooting Common Experimental Issues
FAQ: Addressing Low Differentiation Efficiency
Q1: My stem cells are not efficiently differentiating into the target lineage (e.g., cardiomyocytes). What could be wrong?
A: Low differentiation efficiency often stems from improper temporal control of signaling pathways. Consider these factors:
- Check Wnt Pathway Timing: For cardiac differentiation, the initial activation of Wnt signaling via CHIR99021 is crucial for mesoderm induction. However, premature or delayed inhibition can drastically reduce efficiency. Adhere strictly to the optimal window for adding Wnt inhibitors like IWP-2 [8].
- Optimize BMP Concentration: BMP signaling levels are dose-sensitive. Low concentrations may favor intermediate mesoderm, while higher concentrations promote lateral plate mesoderm and cardiomyocyte differentiation [13]. Titrate BMP4 concentrations (e.g., 4-100 ng/mL) to find the optimal level for your target lineage [13].
- Account for Pathway Crosstalk: Be aware that activating one pathway can cross-activate others. For instance, BMP signaling can cross-activate FGF, Nodal, and Wnt pathways, which may divert cells from the intended totipotent or differentiation state [6]. Using specific inhibitors for these cross-activated pathways might be necessary to enhance target population proportions.
Q2: I observe high variability between differentiation experiments. How can I improve reproducibility?
A: Variability often arises from inconsistent cell culture practices and reagent handling.
- Standardize Cell Confluency: Initiate differentiation at a consistent and recommended cell confluency (e.g., 70-90%). High confluency can lead to spontaneous differentiation, while low density can result in poor survival and differentiation [8].
- Quality Control of Critical Reagents: Test the activity of small molecules like CHIR99021 and recombinant proteins like BMP4 in a pilot assay. Use the same batch of Matrigel and growth factor-reduced media for a series of experiments to minimize lot-to-lot variability [13] [8].
- Monitor Pluripotency State: The starting state of pluripotent stem cells (naïve vs. primed) significantly impacts differentiation competency. Use standardized conditions and validated markers (e.g., Oct4, Sox2, Nanog) to ensure a consistent starting population [11].
Q3: My differentiated cultures are contaminated with off-target cell types. How can I enhance purity?
A: Purity issues suggest incomplete lineage specification or the presence of signaling factors promoting alternative fates.
- Fine-tune Wnt Inhibition: The choice and combination of Wnt inhibitors (e.g., IWP-2 + IWR-1-endo vs. IWP-2 + XAV939) can influence the balance between cardiomyocytes and other mesodermal derivatives like smooth muscle cells [8].
- Apply Selective Pressure: Use metabolic selection (e.g., lactate purification) or antibiotic resistance genes driven by cardiac-specific promoters (e.g., α-MHC) to enrich for the target cardiomyocyte population.
- Re-evaluate BMP and FGF Signaling: BMP levels must be precisely controlled, as incorrect concentrations can promote alternative mesodermal lineages instead of cardiac [13]. Similarly, the duration of FGF signaling should be limited, as its prolonged activity can inhibit terminal cardiomyocyte differentiation [5].
Quantitative Data for Protocol Optimization
Table 1: Key signaling pathway modulators used in stem cell differentiation protocols.
| Pathway | Modulator | Common Concentrations | Function in Differentiation | Key Considerations |
|---|---|---|---|---|
| Wnt | CHIR99021 (Agonist) | 3-6 µM [13] [8] | Induces mesoderm progenitor formation (e.g., TBXT+/MIXL1+ cells) [13]. | Concentration and exposure time are critical; excess can inhibit cardiac specification. |
| IWP-2/IWR-1 (Inhibitor) | 3-5 µM [8] | Inhibits Wnt production/response to promote cardiac specification from mesoderm. | Often used after initial Wnt activation; choice of inhibitor can affect maturation [8]. | |
| BMP | BMP4 | 4-100 ng/mL [13] | Promotes mesoderm and cardiac lineage commitment; concentration dictates lineage specificity [13]. | Low concentrations may favor IM; higher concentrations favor LPM and CMs [13]. |
| Noggin (Inhibitor) | Varies | Extracellular antagonist that binds BMP ligands, preventing receptor activation. | Can be used to block endogenous BMP signaling that may cause heterogeneity. | |
| FGF | FGF2 (bFGF) | Varies (e.g., 100 ng/mL [13]) | Supports pluripotency in hPSCs; roles in differentiation are context and stage-dependent. | Required for maintaining primed pluripotency; its role in differentiation is complex [11]. |
Comparison of Differentiation Protocol Schedules
Table 2: Impact of temporal control on differentiation outcomes based on optimized protocols.
| Differentiation Schedule | Key Steps | Reported Outcome | Maturation State of Derived Cells |
|---|---|---|---|
| "2 + 2" Schedule [8] | 2 days CHIR99021 → 2 days IWP-2 + IWR-1-endo. | High efficiency (>80% TNNT2+ CMs) [8]. | Improved structural and metabolic maturation compared to some other schedules [8]. |
| "1 + 2 + 2" Schedule [8] | 1 day CHIR -> 2 days medium -> 2 days IWP-2 + XAV939. | High efficiency (>80% TNNT2+ CMs) [8]. | Altered gene expression profiles related to maturation; may yield less mature CMs [8]. |
| IM Differentiation Protocol [13] | 2 days CHIR99021 → 2 days CHIR99021 + BMP4. | Generation of OSR1+/GATA3+/PAX2+ intermediate mesoderm (IM) cells [13]. | Used for generating precursors for urogenital system organoids. |
Research Reagent Solutions
Essential Materials for Pathway Manipulation
Table 3: Essential reagents for studying Wnt, BMP, and FGF signaling in differentiation.
| Reagent Category | Specific Examples | Function/Brief Explanation |
|---|---|---|
| Small Molecule Agonists | CHIR99021 (GSK3β inhibitor) [13] [8] | Activates canonical Wnt signaling by stabilizing β-catenin, used for mesoderm induction. |
| Small Molecule Inhibitors | IWP-2, IWR-1-endo, XAV939 (Wnt inhibitors) [8] | Blocks Wnt ligand secretion or response, crucial for cardiac specification after mesoderm induction. |
| Recombinant Growth Factors | BMP4, BMP2, BMP7, BMP9 (Osteogenic) [5] [13] [14] | Activates BMP signaling to promote mesodermal and osteogenic differentiation. Concentration is critical for lineage direction. |
| FGF2 (bFGF), FGF4, FGF10 [5] [11] | Activates FGF signaling. Roles vary from maintaining pluripotency to promoting specific differentiation stages. | |
| Extracellular Antagonists | Noggin, Chordin [5] | Binds to BMP ligands in the extracellular space, preventing them from activating receptors. |
| Cell Culture Supplements | Heparin [13] | Used with FGFs to stabilize ligand-receptor interaction and enhance FGF signaling efficiency. |
Advanced Technical Guide: Optimizing a Cardiac Differentiation Protocol
The following workflow summarizes an optimized protocol for generating cardiomyocytes, highlighting the critical control points for the key signaling pathways.
Experimental Workflow for Cardiac Differentiation
Detailed Methodology:
Starting Cell Preparation: Culture human pluripotent stem cells (hPSCs) in defined conditions (e.g., mTeSR or E8 medium) on Matrigel-coated plates. Passage cells at 70-90% confluency, as this is critical for achieving reproducible differentiation [8]. Accurately count cells and ensure >90% viability.
Mesoderm Induction (Day 0): Initiate differentiation by adding CHIR99021 (3-6 µM) in a chemically defined medium like CDM3 [8]. This activation of Wnt signaling is essential for directing cells toward a mesodermal fate (inducing TBXT+/MIXL1+ mesoderm progenitors) [13] [8]. The optimal concentration may vary between cell lines and should be determined empirically.
Cardiac Specification (Day 2-4): After precisely 48 hours, replace the medium containing CHIR99021 with fresh medium containing a combination of Wnt inhibitors, such as IWP-2 and IWR-1-endo (5 µM each) [8]. This inhibition of Wnt signaling is the key step that drives the specified mesoderm to commit to the cardiac lineage. The "2 + 2" schedule (2 days agonist, 2 days inhibitor) has been shown to yield high-purity cardiomyocyte cultures with improved maturation traits [8].
Culture and Maturation (Day 4+): After 48 hours of Wnt inhibition, transition to a basal medium (e.g., CDM3 or RPMI supplemented with B27) without small molecules, refreshing the medium every 2-3 days [8]. Spontaneously contracting areas typically appear between days 8-10.
Analysis and Validation (Day 10+): Assess differentiation efficiency by analyzing the percentage of cells expressing cardiac troponin T (TNNT2) via flow cytometry or immunocytochemistry [8]. Evaluate functional maturity through calcium transient imaging, metabolic assays (shift from glycolysis to fatty acid oxidation), and analysis of sarcomeric structure (e.g., via α-actinin staining) [8].
Frequently Asked Questions
Q1: What are the core transcription factors (TFs) in pluripotency, and how do they interact? A core network of transcription factors, including OCT4, SOX2, and NANOG, stabilizes the pluripotent state in stem cells through a positive feedback loop. These TFs activate their own expression and each other's, creating a robust network that maintains stem cell identity [15] [16]. This network represses the expression of differentiation-promoting genes. The stability of this state is influenced by the intrinsic half-life of its components, such as NANOG, which helps the network filter out short-lived stochastic fluctuations in gene expression and only respond to sustained differentiation signals [16].
Q2: How can a single transcription factor induce differentiation? Lineage-specific transcription factors can drive differentiation by competing with and destabilizing the core pluripotency network. A key mechanism is transcription factor competition [16]. For example, during neural differentiation, the pro-neural factor BRN2 (an OCT4 homolog) competes with OCT4 for binding to SOX2 [16]. Successful competition disrupts the OCT4-SOX2-NANOG pluripotency complex, leading to its destabilization and initiating a neural differentiation program [16]. Similar competition mechanisms govern other lineage choices, such as endoderm differentiation [16].
Q3: What is the role of epigenetics beyond transcription factors in directing cell fate? While TFs initiate gene expression changes, epigenetic mechanisms provide a crucial layer of regulation that stabilizes cell fate decisions by modifying chromatin structure without altering the DNA sequence itself [17]. These modifications create heritable patterns of gene expression and include:
- DNA Methylation: The addition of methyl groups to DNA, typically repressing transcription of genes, including tumor suppressor genes in cancer [17].
- Histone Modifications: A variety of chemical modifications (e.g., acetylation, methylation, phosphorylation) to histone proteins that can either activate or repress gene transcription depending on the specific modification and genomic context [17].
- Non-coding RNAs: RNA molecules that regulate gene expression post-transcriptionally and are implicated in diverse cellular processes [17]. These epigenetic marks are dynamically regulated by "writer," "eraser," and "reader" enzymes, and their widespread dysregulation is highly correlated with malignant phenotypes and therapy resistance in cancer [17].
Q4: How can I identify the right transcription factors to differentiate stem cells into a specific target cell type? High-throughput, unbiased screening of transcription factor libraries is a powerful method for this. A state-of-the-art approach involves:
- Creating a Library: Generate a comprehensive, barcoded library of human TF open reading frames (ORFs) or splice isoforms [18] [19].
- Pooled Transfection: Transfect this library into human induced pluripotent stem cells (iPSCs) in a pooled format.
- Single-Cell RNA Sequencing: Use scRNA-seq to profile the gene expression of the transfected cells and simultaneously detect which TF(s) each cell received via barcode sequencing [18].
- Data Analysis: Computational analysis identifies TFs or TF combinations that drive the expression profile closest to your target cell type [18] [19]. This method has been successfully used to identify TF combinations for generating microglia and many other cell types [18] [19].
Q5: Why does my transcription factor-driven differentiation protocol yield heterogeneous or incomplete cell types? This common challenge arises from several factors:
- Insufficient TF Combination: A single TF may be insufficient. Many cell types require a specific combination of TFs to fully suppress the original cell identity and activate the complete new genetic program [18]. For example, generating microglia-like cells required a combination of six TFs (SPI1, CEBPA, FLI1, MEF2C, CEBPB, and IRF8) [18].
- Incomplete Maturation: The induced cells may lack the necessary epigenetic landscape or proper cellular microenvironment (niche) signals to reach full maturity [20]. The new cell state must be stabilized through epigenetic remodeling [15] [17].
- Off-Target Effects: Exogenous expression of TFs can have unintended binding and activation effects, leading to a mixture of cell fates [20]. Using inducible systems and optimizing the timing of TF expression can help improve synchrony.
Troubleshooting Guides
Issue 1: Low Efficiency in Transcription Factor-Driven Differentiation
| Potential Cause | Investigation Method | Recommended Solution |
|---|---|---|
| Insufficient TF delivery/expression | Quantify vector copy number per cell via qPCR (as in [18]); Check exogenous TF expression via barcode-amplification from cDNA [18]. | Optimize DNA dose during transfection to ensure single-digit copy number of multiple TFs per cell [18]. |
| Suboptimal TF combination | Perform iterative TF screening; use scRNA-seq to rank TFs by their ability to drive target gene expression [18]. | Employ a polycistronic vector to ensure co-expression and co-delivery of multiple TFs. Test different gene orders in the cassette, as this affects expression levels [18]. |
| Incorrect culture conditions | Analyze expression of maturity markers (electrophysiology for neurons, phagocytosis for microglia). | Review literature for target-cell specific soluble factors (e.g., TGF-β for tissue-resident memory T cells [21]). Co-culture with supportive cell types may be necessary. |
Issue 2: Poor Reproducibility Across Different Stem Cell Lines
| Potential Cause | Investigation Method | Recommended Solution |
|---|---|---|
| Variable epigenetic background | Perform multi-omics profiling (e.g., scATAC-seq) to compare chromatin accessibility between cell lines [21]. | Pre-screen iPSC lines for differentiation competence. Consider using an intermediate progenitor cell bank (e.g., neuronal progenitors) as a more uniform starting population [22]. |
| Heterogeneous transgene integration | Use FACS to select a population with homogeneously integrated inducible TF cassettes [22]. | Utilize site-specific integration systems (e.g., PiggyBac transposase [18]) instead of random integration to minimize position effects. |
| Inconsistent cell state at start | Monitor key pluripotency markers (e.g., NANOG) before induction. | Standardize passaging and maintenance protocols rigorously. Ensure cells are in a consistent, healthy pluripotent state at the initiation of differentiation. |
Key Experimental Data and Protocols
Table 1: Transcription Factor Screening Data for Directed Differentiation
| Target Cell Type | Key Identified Transcription Factors (TFs) | Number of TFs Screened | Protocol Duration | Key Functional Validation | Source |
|---|---|---|---|---|---|
| Microglia-like cells (TFiMGL) | SPI1, CEBPA, FLI1, MEF2C, CEBPB, IRF8 | 40 (initial screen) | 4 days | Phagocytosis, cytokine response, transcriptional similarity to primary microglia [18] | [18] |
| Various Cell Types | 290 TFs (e.g., for neural progenitors, trophoblasts) | 3,548 (all human TF isoforms) | Varies by target | Matching to reference cell type expression profiles from single-cell RNA-seq atlas [19] | [19] |
| Neurons (iGluNeurons) | Neurogenin-2 (NGN2) | N/A (Literature-based) | N/A | Single-cell and network electrophysiological recordings [22] | [22] |
Table 2: Major Epigenetic Modifications and Their Roles in Cell State Regulation
| Epigenetic Modification | Key Enzymes (Examples) | Primary Function | Role in Cell State/Cancer |
|---|---|---|---|
| DNA Methylation | DNA methyltransferases (Writers), TET proteins (Erasers) | Transcriptional repression of genes, including tumor suppressors; genome stability [17]. | Widespread dysregulation (hypermethylation of promoters); contributor to therapy resistance [17]. |
| Histone Acetylation | HATs (Writers), HDACs (Erasers) | Generally associated with open, active chromatin and gene activation [17]. | Aberrantly activated oncogenes or repressed differentiation programs; target of epigenetic drugs [17]. |
| Histone Methylation | KMTs (Writers), KDMs (Erasers) | Can be activating or repressing depending on the modified residue (e.g., H3K4me3 active, H3K27me3 repressive) [17]. | Altered in tumors; can maintain cells in a stem-like, undifferentiated state [17]. |
| N6-methyladenosine (m6A) RNA Modification | METTL3/14 (Writers), FTO/ALKBH5 (Erasers) | Regulates mRNA stability, translation efficiency, and splicing [17]. | Affects tumor proliferation, invasion, metastasis, and immune evasion [17]. |
This protocol enables the identification of optimal TF combinations for differentiating iPSCs into a target cell type.
Key Reagents:
- Cell Line: Human iPSCs (e.g., PGP1).
- TF Library: A custom barcoded library of 40 TF clones in a doxycycline-inducible PiggyBac vector (pBAN2).
- Transfection Reagent: PiggyBac Transposase.
- Culture Media: Standard iPSC media and differentiation media.
Workflow:
- Clone & Barcode: Clone each TF from the selected library into the pBAN2 vector. Incorporate a unique 20-nucleotide barcode between the stop codon and poly-A sequence of each TF for tracking.
- Transfect & Integrate: Co-transfect the TF library and PiggyBac transposase into iPSCs at a 4:1 mass ratio. Determine the optimal DNA dose (e.g., 5 µg) to achieve a single-digit copy number of multiple TFs per cell.
- Select & Induce: Select for successfully transfected cells using puromycin. Induce TF expression by adding doxycycline (Dox) to the culture medium for 4 days to initiate differentiation.
- Sort & Sequence: Use Fluorescent Activated Cell Sorting (FACS) to sort differentiated cells (e.g., TRA-1-60 negative). Perform single-cell RNA sequencing (scRNA-seq) on the sorted population.
- Analyze & Rank: From the scRNA-seq data, quantify exogenous TF expression via barcode amplicon sequencing. Correlate TF presence with the expression of target cell-type-specific genes (e.g., ITGAM, P2RY12 for microglia). Rank TFs based on their ability to induce the desired gene signature.
- Iterate & Validate: For complex lineages, a second round of screening with the top TFs from the first round may be necessary. Validate the final TF combination by testing its ability to generate cells with the correct molecular and functional properties of the target cell.
Figure 1: Core Gene Regulatory Network Logic. The pluripotency network (OCT4, SOX2, NANOG) maintains the stem cell state via mutual activation. A sustained differentiation signal induces a lineage-specific TF, which competes with and disrupts the pluripotency network, allowing activation of a new differentiation gene program [15] [16].
Figure 2: Iterative Transcription Factor Screening Workflow. This high-throughput screening method involves multiple rounds of transfection, induction, and single-cell analysis to efficiently identify optimal TF combinations for generating specific cell types from iPSCs [18].
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Tool | Function in Experiment | Key Features & Considerations |
|---|---|---|
| Barcoded TF ORF Library [18] [19] | Comprehensive screening of transcription factor effects. | Contains thousands of human TF isoforms; each TF has a unique nucleotide barcode for tracking in pooled screens; often in inducible vectors. |
| Inducible Expression System (e.g., Dox-inducible) [18] | Precise temporal control over TF expression. | Allows separation of transfection/integration from differentiation induction; enables testing of duration thresholds for TF activity [16]. |
| Polycistronic Vector (2A peptide-linked) [18] | Co-expression of multiple TFs from a single transcript. | Ensures delivery of all required TFs to a cell; gene order matters for expression levels and must be optimized. |
| PiggyBac Transposon System [18] | High-efficiency genomic integration of large DNA cargo. | Provides stable, long-term expression; preferred over random plasmid integration for higher consistency. |
| Single-Cell Multi-Omics (scRNA-seq + scATAC-seq) [21] | Simultaneous profiling of gene expression and chromatin accessibility. | Reveals enhancer-driven gene regulatory networks and the epigenetic state of differentiating cells. |
| Dominant-Negative REST (DN:REST) [23] | Tool to block activity of the transcriptional repressor REST. | Used to dissect the role of REST-mediated repression in maintaining stem cell states or blocking differentiation. |
Within stem cell research and regenerative medicine, a central challenge persists: the inherent limitations of native biological systems. Primary cells, isolated directly from living tissue, are the gold standard for physiological relevance but suffer from finite lifespans and a strong tendency to dedifferentiate—lose their specialized characteristics—in culture. This instability drives the need for robust, standardized models that can reliably generate high-quality, functional cells for disease modeling, drug screening, and therapeutic development. This technical support center is framed within the broader thesis of optimizing stem cell differentiation efficiency, providing actionable solutions to common pitfalls.
Frequently Asked Questions (FAQs)
1. What is the main advantage of using primary cells over cell lines? Primary cells are isolated directly from tissues (e.g., blood, bone marrow, skin) and are therefore more representative of the in vivo physiological state of that tissue compared to immortalized cell lines. Data generated from primary cells has increased physiological relevance, making them an ideal model for investigative research [24] [25].
2. Why do my primary cells keep dedifferentiating or losing their phenotype in culture? Dedifferentiation is a common challenge. Primary cells have a finite lifespan and a limited number of population doublings before they enter senescence. This process can be accelerated by:
- Over-confluence: Culturing cells beyond 100% confluence can trigger differentiation and slow proliferation [25].
- Sub-optimal culture medium: The lack of tissue-specific cytokines and growth factors fails to maintain the specialized phenotype [25].
- Extended culture time: Primary cells should not be maintained for extended periods; for example, plateable cryopreserved hepatocytes are generally not recommended for culture beyond five days [26].
3. My stem cell differentiation efficiency is low and variable. What are the common causes? Low and variable differentiation efficiency is a widely recognized hurdle. Key causes include:
- Inconsistent Starting Material: The genetic and epigenetic state of human pluripotent stem cell (hPSC) clones can vary, impacting their differentiation potential [27] [28].
- Protocol Variability: Slight changes in seeding cell number, growth factor composition, or timing can lead to marked differences in the resulting cultures [29].
- Insufficient Characterization: Many protocols fail to fully characterize the intermediate progenitor cells, leading to heterogeneous final populations [29] [27].
- Incorrect Primitive Streak Patterning: For mesoderm and endoderm differentiation, the specific subtype of primitive streak induced (anterior, mid, posterior) dictates the downstream cell types that can be formed. Using broad markers like BRACHYURY is insufficient to ensure the correct intermediate has been generated [27].
4. How can I improve the reproducibility of my differentiation protocols?
- Use 3D Embryoid Body (EB)-based Systems: EB formation can improve differentiation efficiency for many cell lineages and allows for early prediction of differentiation potential by analyzing gene expression markers like SALL3 [30].
- Ensure High-Quality hPSCs: Before neural induction, remove any differentiated or partially differentiated hPSCs. Cell counting is also recommended to ensure optimal seeding density, as too low or too high confluency will reduce induction efficiency [31].
- Employ Early Prediction Tools: Emerging technologies using phase-contrast imaging and machine learning can predict the final differentiation efficiency of induced muscle stem cells (MuSCs) as early as 50 days before the end of the induction period, allowing for early sample selection [28].
5. What are the key considerations for choosing between 2D and 3D culture systems? Both systems have distinct advantages. While 2D culture is simpler, 3D embryoid body (EB)-based suspension culture systems often demonstrate higher stable differentiation efficiency and are better suited for generating complex organoids that mimic human organs [30]. The choice depends on the target cell type and the research application.
Table 1: Common Primary Cell Culture Challenges and Solutions
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low post-thaw viability | Improper thawing technique, rough handling | Thaw cells rapidly (<2 mins at 37°C). Use wide-bore pipette tips and mix slowly [26]. |
| Poor cell attachment | Coating matrix dried, suboptimal substratum | Shorten time between coating and cell seeding. Use appropriate extracellular matrix (e.g., Matrigel, Collagen I) [26] [25]. |
| Excessive differentiation in hPSC cultures | Old culture medium, overgrown colonies | Use fresh medium (<2 weeks old). Remove differentiated areas before passaging. Do not allow colonies to overgrow [31]. |
| Heterogeneous differentiation outcomes | Inconsistent cell aggregate size during passaging | Ensure cell aggregates are evenly sized. Avoid generating a single-cell suspension for protocols requiring clump passaging [31]. |
Troubleshooting Guides
Problem: Inefficient Neural Differentiation from Human Pluripotent Stem Cells (hPSCs)
Possible Causes and Recommendations:
- Cause: Low-quality starting hPSCs.
- Recommendation: Regularly characterize hPSCs for pluripotency markers and genomic integrity. Remove any differentiated regions from the culture before initiating differentiation [31].
- Cause: Incorrect seeding density for induction.
- Recommendation: Perform cell counting before plating. The recommended plating density for neural induction is often in the range of 2–2.5 x 10^4 cells/cm². Plating cells as small clumps, not as a single-cell suspension, can also improve efficiency [26].
- Cause: Sub-optimal or expired differentiation supplements.
- Recommendation: Check the expiration date of all supplements. For example, B-27 Supplement, once thawed, should be stored at 4°C and used within one week. Prepared medium supplemented with B-27 is stable for only two weeks at 4°C [26].
Problem: Low Attachment Efficiency in Primary Cells
Possible Causes and Recommendations:
- Cause: Improper thawing technique.
- Cause: Inadequate or dried-out extracellular matrix coating.
- Recommendation: Ensure the culture vessel is coated with the appropriate attachment factor (e.g., Collagen, Matrigel, Vitronectin). Do not let the coating solution dry out. Work with a few wells at a time to prevent drying during the coating process [26].
- Cause: Seeding density is too low.
- Recommendation: Check the lot-specific specification sheet for the recommended seeding density. Observe cells under a microscope after seeding to ensure appropriate density [26].
Table 2: Key Research Reagent Solutions for Stem Cell Differentiation
| Reagent / Tool | Function | Example in Context |
|---|---|---|
| Growth Factors (e.g., FGF, BMP, SHH) | Mimic developmental signaling to direct lineage specification. | SHH and FGF8 are used for ventral patterning in dopaminergic neuron differentiation [29]. |
| Small Molecule Agonists/Antagonists | Precisely control key signaling pathways (Wnt, TGF-β). | A Wnt agonist is used at high concentration to induce dermomyotome cells from hiPSCs [28]. |
| EB-Based 3D Culture Systems | Improve differentiation efficiency and stability for various lineages. | Used for robust differentiation into neural, hepatic, and cardiac cells [30]. |
| Defined Culture Media & Supplements | Provide tailored nutrients and factors for specific cell types. | B-27 Supplement is critical for neuronal cell culture and health; its quality must be assured [26]. |
| Lineage Reporter Systems | Enable real-time tracking of differentiation efficiency. | MYF5-tdTomato reporter hiPSCs allow for flow cytometry analysis of muscle stem cell induction efficiency [28]. |
Detailed Methodology: Early Prediction of Muscle Stem Cell (MuSC) Differentiation Efficiency
This protocol, based on a 2025 study, outlines a non-destructive method to predict the final differentiation efficiency of hiPSC-derived MuSCs approximately 50 days in advance [28].
1. Cell Line and Differentiation:
- Use MYF5-tdTomato reporter hiPSCs.
- Induce MuSC differentiation using a directed protocol:
- Days 0-14: Treat with a high concentration of a Wnt agonist to generate dermomyotome cells.
- Days 14-38: Treat with growth factors (IGF-1, HGF, bFGF) to promote myogenic differentiation (myogenic induction phase).
- Days 38-82: Switch to a muscle culture medium with low-concentration horse serum for maturation.
2. Image Acquisition and Feature Extraction:
- Between days 14 and 38, capture phase-contrast images of the cells in culture.
- Apply Fast Fourier Transform (FFT) to each image to obtain a power spectrum.
- Perform shell integration on the power spectrum to generate a 100-dimensional, rotation-invariant feature vector that captures cell morphology characteristics.
3. Machine Learning and Classification:
- Use a random forest classifier trained on the feature vectors from days 14-38.
- The model predicts the final MYF5+ percentage (measured by flow cytometry on day 82).
- Key Finding: Samples with high and low induction efficiency can be predicted from images taken on day 34 and day 24, respectively.
Signaling Pathways in Directed Differentiation
The following diagram illustrates the critical initial stages of germ layer differentiation from hPSCs, highlighting the importance of precise primitive streak patterning.
Diagram 1: Pathway to Germ Layer Formation. Successful differentiation requires inducing the correct primitive streak subtype, as each has restricted lineage potential [27].
Table 3: Correlation Between Early Markers and Final Differentiation Efficiency in MuSC Induction [28]
| Day of Induction | Marker Analyzed | Marker Type | Correlation with Final MYF5+ % (Day 82) |
|---|---|---|---|
| Day 7 | T (Brachyury) | Gene Expression (qRT-PCR) | Not Significant |
| Day 14 | PAX3 | Gene Expression (qRT-PCR) | Not Significant |
| Day 38 | MYH3 | Gene Expression (qRT-PCR) | Significant Positive |
| Day 38 | MYOD1 | Gene Expression (qRT-PCR) | Significant Positive |
| Day 38 | Myosin Heavy Chain (MHC) | Protein (Immunocytochemistry) | Significant Positive |
```
This technical support content underscores that overcoming the challenges of primary cell dedifferentiation and variable differentiation requires a multi-faceted approach. By integrating robust, standardized protocols, rigorous quality control of starting materials, and the adoption of advanced predictive technologies, researchers can generate more reliable and physiologically relevant models to advance the field of regenerative medicine.
From Theory to Practice: Protocols for Differentiating Hepatic, Hematopoietic, and Mesenchymal Lineages
Directed Differentiation of iPSCs into Liver Progenitor Cells and Organoids
This technical support center is designed within the context of ongoing research to optimize the efficiency and reproducibility of stem cell differentiation. It addresses frequent experimental challenges encountered when differentiating induced Pluripotent Stem Cells (iPSCs) into liver progenitor cells (LPCs) and subsequent 3D hepatic organoids. The following FAQs, troubleshooting guides, and summarized data are compiled to assist researchers, scientists, and drug development professionals in standardizing protocols and achieving robust, high-quality results for downstream applications in disease modeling, drug screening, and toxicology studies.
Frequently Asked Questions (FAQs) & Troubleshooting
Protocol Efficiency and Differentiation Success
Q1: What is a typical differentiation efficiency for obtaining definitive endoderm (DE) and hepatocyte-like cells (HLCs) from iPSCs?
Achieving high differentiation efficiency is a primary goal in optimization research. Performance can vary based on the specific protocol and cell line used. The table below summarizes key efficiency metrics from established methods.
Table 1: Typical Differentiation Efficiencies for Key Stages
| Differentiation Stage | Typical Efficiency | Measurement Method | Citation |
|---|---|---|---|
| Definitive Endoderm (DE) | Up to 97% | Sox17-positive cells (Immunofluorescence) [32] | |
| Liver Progenitor Cells (LPCs) | High-level expression achieved | Expression of specific LPC markers [3] | |
| Hepatocyte-like Cells (HLCs) | Up to 94% | HNF4α-positive cells (Immunofluorescence) [32] | |
| Transduction of LPCs | 93.6% | eGFP expression using rAAV serotype 2/2 [3] | |
| Transfection of LPCs | 54.3% | eGFP expression using electroporation [3] |
Q2: My differentiation efficiency is low. What are the most critical steps to optimize?
Low efficiency often stems from inconsistencies in early stages. The most critical steps include:
- Accurate Cell Counting: The initial seeding density of iPSCs is paramount. Inaccurate counts can severely impact yield. It is recommended to use a hemocytometer/Bürker chamber for validation, especially when setting up an automated cell counter [32].
- Strict Protocol Adherence: Small deviations, such as delayed medium changes, can significantly affect the functionality of the final hepatocytes. Adhere strictly to the timing and formulation of media changes [32].
- Cell Line Variability: Different iPSC lines have inherent variations in differentiation potential. One study found that a self-reprogrammed hiPSC line had a higher differentiation tendency than a commercially sourced line [33]. Protocol optimization for each specific cell line may be necessary.
Q3: Can the definitive endoderm (DE) or hepatocyte-like cells (HLCs) be expanded or cryopreserved for later use?
- Definitive Endoderm (DE): Yes, DE cells can be dissociated, cryopreserved using a provided protocol, and later reseeded for differentiation [32]. Some protocols also support the expansion of DE/foregut endoderm cells [32].
- Hepatocyte-like Cells (HLCs): Differentiated hepatocytes are generally terminally differentiated and cannot be expanded [32]. While custom protocols for dissociation and cryopreservation of HLCs exist as customized solutions [32], it is noted that differentiated hepatic organoid cultures cannot be passaged or cryopreserved [34].
Organoid Culture and 3D Modeling
Q4: What seeding density is recommended for forming hepatic organoids, and why is high density often used?
Seeding at higher densities is recommended for two primary reasons:
- Improved Formation Probability: Not every single cell or fragment will develop into an organoid; higher densities increase the chances of successful establishment.
- Paracrine Signaling: Liver organoids benefit from "neighboring cells," as paracrine signaling between them supports growth and health [34]. A common recommendation for differentiation experiments is to seed approximately ~2000 fragments between 30 - 100 µm in size [34]. It is crucial to avoid overseeding, as this can negatively affect culture quality and viability.
Q5: How long can hepatic organoids be maintained in culture, and what is a typical passage number?
Human hepatic organoid expansion cultures can be maintained long-term. One established protocol maintains cultures up to passage 14 - 15 with the potential for indefinite culture [34]. The ability to culture long-term is a key advantage for generating a sustainable cell model.
Q6: My organoids show high heterogeneity in size. Is this normal, and how can it be controlled?
Heterogeneity in organoid size is normal, especially if the fragments generated during passaging are not uniform [34]. To standardize size:
- Generate Uniform Fragments: Aim for fragments between 30 - 100 µm during passaging.
- Use Strainers: Employ reversible strainers to generate more uniformly sized fragment suspensions [34].
- Control Final Size: Actively maintain organoids under 500 µm in diameter. Larger organoids risk core cell death due to limited oxygen and nutrient diffusion in the absence of a vascular system [35].
Characterization and Functional Validation
Q7: What key hepatic functions should I validate in my differentiated HLCs or organoids?
To confirm successful differentiation and maturation, researchers should assess a panel of classic hepatic functions. The table below lists key functions and common assessment methods.
Table 2: Key Hepatic Functions for Model Validation
| Hepatic Function | Description | Common Assessment Method |
|---|---|---|
| Albumin Secretion | Major plasma protein synthesized by hepatocytes | ELISA on culture supernatant [34] |
| CYP450 Enzyme Activity | Critical for drug metabolism (e.g., CYP3A4, CYP1A2) | P450-Glo Assay or LC/MS [34] [32] |
| Urea Synthesis | Key metabolic function of hepatocytes | Colorimetric assay [34] |
| Bile Acid Production | Indicator of hepatocyte metabolic function | Total bile acid assay [34] |
| LDL Uptake | Functional receptor-mediated endocytosis | Fluorescent LDL uptake assay [32] |
Q8: Do hepatic organoids contain non-parenchymal cells (e.g., stellate, Kupffer cells)?
Most standard protocols for deriving hepatic organoids from iPSCs focus on the parenchymal lineage (hepatocytes and cholangiocytes). One FAQ explicitly states, "We have not looked for the presence of non-parenchymal cells in human hepatic organoids" [34]. However, one optimized protocol reported the establishment of a 2D culture comprising stellate-like cells alongside the organoid cultures, suggesting that with specific protocol modifications, certain non-parenchymal cell types can be obtained [3].
Essential Experimental Protocols & Workflows
Optimized Differentiation Workflow
The following diagram outlines a generalized and optimized workflow for the directed differentiation of iPSCs into liver progenitor cells and subsequent 2D or 3D cultures, integrating steps from multiple sources [3] [36] [32].
Key Signaling Pathways for Directed Differentiation
The directed differentiation of iPSCs into liver cell fates is achieved by sequentially modulating key signaling pathways to mimic embryonic liver development. The following diagram summarizes the critical factors and their roles.
The Scientist's Toolkit: Research Reagent Solutions
A successful differentiation experiment relies on a suite of high-quality reagents. The following table details essential materials and their functions as cited in the literature.
Table 3: Essential Reagents for iPSC to Hepatic Differentiation
| Reagent Category | Specific Examples | Function in Protocol |
|---|---|---|
| Basal Media | RPMI 1640, Advanced DMEM | Serves as the base for differentiation media formulations [3]. |
| Critical Growth Factors & Cytokines | Activin A, BMP4, FGF10, FGFβ, HGF, KGF, OSM | Key signaling molecules that direct each stage of differentiation from definitive endoderm to hepatocyte maturation [3] [33]. |
| Small Molecules & Pathway Modulators | CHIR99021 (WNT agonist), SB431542 (TGF-β inhibitor), Retinoic Acid | Precisely controls developmental signaling pathways to steer cell fate [3]. |
| 3D Culture Matrix | Matrigel, synthetic hydrogels, recombinant protein gels | Provides a scaffold for 3D organoid formation, mimicking the native extracellular matrix [3] [35]. |
| Specialized Organoid Media | HepatiCult Organoid Growth & Differentiation Media | Commercially available, optimized media systems for robust expansion and maturation of hepatic organoids [34] [3]. |
| Cell Dissociation Reagents | TrypLE, Versen solution | Enzymatic or non-enzymatic solutions for passaging organoids and dissociating cells during protocol steps [34] [3]. |
Frequently Asked Questions (FAQs)
1. Why is stromal cell seeding density critical in co-culture systems? The initial seeding density of stromal cells directly influences the efficiency of stem cell differentiation. An optimal density creates the correct cellular microenvironment and signaling gradients needed to direct differentiation, while suboptimal densities can lead to reduced efficiency or incorrect cell fate specification [37] [38]. For example, in OP9-hESC co-cultures for hematopoietic differentiation, a precise density of 10.4 × 10⁴ cells/cm² achieved high efficiency five days faster than traditional overgrown cultures [37].
2. What are common signs of suboptimal co-culture conditions? Common indicators include low expression of target differentiation markers (e.g., CD34 for hematopoietic cells), delayed appearance of differentiated cell populations, and inconsistent results across experimental replicates [37] [28]. For instance, prolonged differentiation timelines (14-18 days) with variable CD34+ cell yields can signal inefficient OP9 stromal preparation [37].
3. How can I non-destructively monitor differentiation efficiency early in the process? Phase-contrast imaging combined with machine learning algorithms can predict final differentiation efficiency long before traditional marker analysis. One system using Fast Fourier Transform (FFT)-based feature extraction from images successfully predicted muscle stem cell differentiation efficiency approximately 50 days before the end of the induction period [28].
4. What are the key differences between research-grade and GMP-grade stromal cells? The isolation process and quality control criteria are often similar, but GMP-grade cells require manufacturing in B-grade clean rooms, more comprehensive documentation, and additional testing for chromosomal stability [39]. Both types should be negative for hematopoietic markers (CD45, CD34, CD14) and positive for typical mesenchymal markers (CD105, CD73, CD90) [39].
Troubleshooting Guides
Problem: Low Hematopoietic Differentiation Efficiency in OP9 Co-culture Systems
Symptoms: Reduced CD34+ cell yield, prolonged differentiation time (exceeding 14 days), inconsistent results between batches [37].
Solution: Optimize OP9 stromal cell preparation method and density.
- Step 1: Replace the traditional 4-day overgrowth protocol with a 24-hour pre-culture of OP9 cells at optimal density [37].
- Step 2: Plate OP9 cells at (10.4 \times 10^4) cells/cm² in a 6-well plate format [37].
- Step 3: Co-culture with hESCs after exactly 24 hours of OP9 cell attachment.
- Step 4: Evaluate CD34+ cell appearance by flow cytometry on day 8-10, expecting peak efficiency 2 days earlier than traditional methods [37].
Prevention: Use low-passage OP9 cells (passages 3-15) and maintain consistent culture conditions. Pre-test different OP9 cell batches for differentiation-supporting capability [37].
Problem: Variable Efficiency in Long-Term Differentiation Protocols
Symptoms: High well-to-well variability in final differentiation outcomes, inefficient use of resources due to long protocol durations (up to 80+ days) [28].
Solution: Implement early prediction systems to identify high-efficiency cultures.
- Step 1: Capture phase-contrast images during the early differentiation phase (days 14-38 for an 82-day protocol) [28].
- Step 2: Apply Fast Fourier Transform (FFT) feature extraction to generate rotation-invariant feature vectors from images [28].
- Step 3: Use machine learning classification (e.g., Random Forest) to predict high and low-efficiency samples [28].
- Step 4: Focus resources on cultures predicted to have high differentiation efficiency, discarding low-performing samples early.
Validation: Correlation between early image-based predictions and late-stage marker expression (e.g., MYF5+% or CDH13+% for MuSCs) should be established for each protocol [28].
Problem: Poor Factor Diffusion in Filter-Based Co-culture Systems
Symptoms: Inadequate paracrine signaling between cell types, reduced co-culture effect, inconsistent results across the culture area [40].
Solution: Ensure proper filter preparation and adequate culture volumes.
- Step 1: Degas filters thoroughly before use to remove air trapped in pores [40].
- Step 2: Pre-treat filters by washing with pure water, followed by 100% ethanol for 1 minute, then PBS before assembling the co-culture plate [40].
- Step 3: Use sufficient culture medium volume to ensure complete contact with the filter surface [40].
- Step 4: For extracellular vesicle studies, note that proteins and vesicles may adhere to filters, requiring optimization of recovery methods [40].
Table 1: Optimized Seeding Densities for Various Co-culture Applications
| Cell Type/System | Optimal Seeding Density | Culture Format | Key Efficiency Metrics | Reference |
|---|---|---|---|---|
| OP9 stromal cells (for hESC hematopoietic differentiation) | (10.4 \times 10^4) cells/cm² (total (1.0 \times 10^6) cells/well) | 6-well plate | CD34+ cells appeared 2 days earlier; Same efficiency achieved 5 days faster | [37] |
| Adipose-derived Stem Cells (ASCs for epithelial differentiation) | (5.0 \times 10^6) cells/cm² | Composite scaffold | Highest expression of epithelial markers; Supported further air-liquid interface culture | [38] |
| Primary Endometrial Stromal Cells (for tissue modeling) | Tissue explants method-dependent | 6-cm culture dish | Successful outgrowth in 2-3 days; 75-80% confluency for passaging | [41] |
Table 2: Comparison of Stromal Cell Preparation Methods
| Parameter | Traditional Overgrowth Method | Optimized Density Method | Advantage of Optimization | |
|---|---|---|---|---|
| Preparation Time | 4 days | 24 hours | Reduces total process time by 3 days | [37] |
| Cell State at Co-culture | Overgrown, confluent | Log-phase growth | Better recapitulates physiological stromal signaling | [37] |
| Differentiation Timeline | 14-18 days | 9-13 days | Achieves peak CD34+ population 2 days earlier | [37] [42] |
| Reproducibility | Variable between batches | Higher consistency | Standardized density reduces experimental variability | [37] [28] |
Detailed Experimental Protocols
Protocol 1: Optimized OP9 Stromal Cell Preparation for Hematopoietic Differentiation
Materials:
- OP9 mouse stromal cell line (passages 3-15 recommended)
- α-MEM medium supplemented with 15% FBS
- 0.1% gelatin-coated 6-well plates
- hPSC medium (mTeSR1 or equivalent)
- Differentiation medium: α-MEM with 10% FBS and 100 μmol/L monothioglycerol (MTG)
Method:
- Thawing and Maintenance: Culture OP9 cells on gelatin-coated plates in α-MEM/15% FBS until 70-80% confluent. Use 0.25% trypsin for passaging (1 minute at 37°C) [37].
- Experimental Seeding: Harvest OP9 cells and seed at exactly (10.4 \times 10^4) cells/cm² in 6-well plates [37].
- Pre-culture Incubation: Incubate OP9 cells for 24 hours at 37°C, 5% CO₂ [37].
- hESC Preparation: Harvest hESCs using 2 mg/ml dispase, maintaining cells in small clumps. Plate at (0.7-1.0 \times 10^6) cells per well onto OP9 monolayer [37].
- Co-culture Maintenance: Culture in differentiation medium with complete medium change on day 1 and half-medium changes on days 4, 6, 8, and 10 [37].
- Efficiency Assessment: Harvest co-culture cells by 20-minute trypsinization on days 8, 10, and 12. Analyze CD34+ population by flow cytometry using PE-Cy5.5 anti-human CD34 and APC-human TRA-1-85 antibodies [37].
Protocol 2: Early Efficiency Prediction via Imaging and Machine Learning
Materials:
- Phase-contrast microscope with digital camera
- MYF5-tdTomato reporter hiPSCs (for MuSC differentiation)
- Computational resources for image analysis
- Python/R with machine learning libraries (e.g., scikit-learn)
Method:
- Image Acquisition: Capture phase-contrast images during early differentiation phase (days 14-38 for an 82-day protocol) [28].
- Feature Extraction: Process images using Fast Fourier Transform (FFT) to generate power spectra. Apply shell integration to create 100-dimensional, rotation-invariant feature vectors [28].
- Model Training: Label images based on final differentiation efficiency (e.g., MYF5+% on day 82). Train a Random Forest classifier using feature vectors from multiple independent experiments [28].
- Prediction Application: Use the trained model to classify new cultures based on early images. For MuSC differentiation, images from days 24-34 were most predictive [28].
- Decision Making: Prioritize cultures predicted to have high efficiency for further experimentation and resource allocation.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Reagent/Cell Line | Function in Co-culture Systems | Application Notes |
|---|---|---|
| OP9 Mouse Stromal Cells | Supports hematopoietic differentiation from hPSCs; provides critical microenvironmental signals | Use passages 3-15; pre-test differentiation support capability; culture on gelatin-coated surfaces [37] |
| Fibrin Sealant (Tisseel) | Bioengineered scaffold for 3D co-culture; enhances cell attachment and tissue ingrowth | Composed of fibrinogen, thrombin, factor XIII, CaCl₂, and aprotinin; forms gel when combined; FDA-approved [38] |
| Mesenchymal Stem Cells (MSCs) | Multipotent stromal cells with immunomodulatory properties; can differentiate into multiple lineages | Source matters (bone marrow, umbilical cord, adipose); characterized by CD105+, CD73+, CD90+ and lack of hematopoietic markers [39] |
| Defined Xeno-Free Media | Clinically relevant culture conditions without animal components; reduces variability | Essential for GMP-compliant processes; supports MSC expansion and differentiation without FBS [39] |
| Air-Liquid Interface (ALI) Systems | Promotes epithelial differentiation and maturation; mimics physiological tissue interfaces | Requires specialized culture inserts; enables study of polarization and specialized cell functions [38] |
Workflow and Signaling Diagrams
Co-culture Optimization Workflow
Stromal Cell Signaling in Co-culture Systems
Selecting the appropriate cell culture model is a critical strategic decision in stem cell differentiation efficiency optimization research. While two-dimensional (2D) cultures have been the laboratory standard for decades, three-dimensional (3D) cultures are emerging as a powerful tool for their ability to better mimic the in vivo microenvironment. This technical support center guide provides researchers, scientists, and drug development professionals with a practical framework for choosing between these models, troubleshooting common experimental issues, and implementing protocols that enhance the reliability and predictive power of their work in stem cell research.
Model Comparison: 2D vs. 3D at a Glance
The choice between 2D and 3D culture models involves balancing practical considerations with physiological relevance. The following table summarizes their core characteristics based on current literature [43] [44].
Table 1: Fundamental Characteristics of 2D and 3D Cell Culture Models
| Feature | 2D Cell Culture | 3D Cell Culture |
|---|---|---|
| Growth Pattern | Monolayer on a flat plastic surface [44] | Cells grow in all directions, forming structures like spheroids and organoids [43] |
| In Vivo Imitation | Does not mimic the natural 3D structure of tissues [44] | Better mimics the natural morphology and architecture of tissues and organs [43] [44] |
| Cell Interactions | Limited cell-cell and cell-ECM interactions; no in vivo-like microenvironment [44] | Proper cell-cell and cell-ECM interactions; creates environmental "niches" [43] [44] |
| Cell Morphology & Polarity | Altered morphology; loss of native phenotype and polarity [44] | Preserved native morphology, diverse phenotype, and polarity [43] [44] |
| Gradients (Oxygen, Nutrients) | Unlimited access to oxygen, nutrients, and signaling molecules [44] | Variable access, creating natural gradients (e.g., hypoxic cores) as found in vivo [43] [44] |
| Gene Expression & Biochemistry | Changes in gene expression, splicing, and biochemistry compared to in vivo [44] | Gene expression, splicing, and biochemistry more closely resemble in vivo conditions [43] [44] |
| Cost & Infrastructure | Simple, low-cost maintenance; well-established protocols [43] [45] | More expensive, time-consuming; fewer commercially available standardized tests [44] |
| Throughput & Ease of Use | High performance, reproducibility; easy to culture and interpret; compatible with High-Throughput Screening (HTS) [43] [44] | Often more cumbersome; can be difficult to interpret and maintain; throughput is improving with new technologies [44] [45] |
Table 2: Strategic Application of Culture Models in Stem Cell Research
| Research Objective | Recommended Model | Rationale |
|---|---|---|
| High-Throughput Drug Screening (Early Stage) | 2D | Allows for quick, inexpensive screening of thousands of compounds due to simplicity and compatibility with HTS formats [43]. |
| Basic Genetic Manipulations (e.g., CRISPR) | 2D | Well-established, straightforward protocols for genetic modifications in a controlled environment [43]. |
| Stem Cell Differentiation & Protocol Optimization | 3D | Provides a more physiologically relevant context for differentiation, leading to more mature and accurate cell phenotypes [43] [28]. |
| Disease Modeling (e.g., Cancer, Neurodegenerative) | 3D | Captures complex tissue architecture and cell interactions crucial for understanding disease mechanisms [43] [46]. |
| Personalized Therapy Testing | 3D (Patient-Derived Organoids) | Enables the creation of patient-specific models for predicting individual treatment responses [43]. |
| Toxicology & Safety Pharmacology | 3D | Offers more accurate prediction of drug toxicity and metabolism due to better preservation of tissue-specific functions [43]. |
Troubleshooting Guides
Issue 1: Poor Differentiation Efficiency in 3D Cultures
Problem: The differentiation of human induced pluripotent stem cells (hiPSCs) into target cells (e.g., muscle stem cells) is inefficient and highly variable, leading to unreliable results and wasted resources.
Investigation & Solution:
- Monitor Early Differentiation Markers: Biological analyses suggest that the efficiency of muscle stem cell (MuSC) differentiation on day 82 can be predicted by assessing the expression of skeletal muscle markers (like MYH3, MYOD1, and MYOG) around day 38 [28]. Implement non-destructive quality checks during early induction phases.
- Implement Early Prediction Systems: Adopt machine learning-based prediction systems that use phase-contrast imaging and feature analysis (e.g., Fast Fourier transform) during the early stages of differentiation (e.g., days 14-38). This non-destructive method can forecast final induction efficiency approximately 50 days before the end of the protocol, allowing for early intervention or termination of poorly differentiating samples [28].
- Verify Pluripotency Status: Ensure that the starting hiPSCs have a high, homogeneous expression of established undifferentiated stem cell markers. Using a cost-effective flow cytometry protocol to verify pluripotency before initiating differentiation can help reduce line-to-line variability [47].
Issue 2: Choosing Between 2D and 3D for a Specific Project
Problem: A researcher is unsure whether to use a 2D or 3D culture system for a new project, balancing the need for physiological relevance with practical constraints like budget, time, and throughput.
Investigation & Solution:
- Define the Primary Research Question:
- Is the goal high-speed screening of many compounds? → Choose 2D for its speed, low cost, and compatibility with HTS [43] [45].
- Is the goal to understand a complex biological process where tissue architecture and cell-ECM interactions are critical? → Choose 3D for its physiological relevance [43] [46].
- Adopt a Tiered Workflow: Many advanced labs use a hybrid approach. Start with 2D to rapidly screen and eliminate a large number of candidates. Then, validate the shortlisted candidates in more physiologically relevant 3D models (e.g., spheroids, organoids) for better predictive power [43].
- Consider the Endpoint Analysis: If the required readout (e.g., high-resolution microscopy, protein isolation) is not yet fully optimized for 3D models, a 2D system might be more practical. However, technologies for 3D analysis are rapidly improving [45].
Issue 3: Challenges with 3D Culture Analysis and Throughput
Problem: 3D cultures are perceived as cumbersome, difficult to analyze with standard equipment, and low-throughput, making them unsuitable for large-scale screening projects.
Investigation & Solution:
- Address Throughput with Advanced Plates: Use modern microfluidic 3D culture plates, such as the OrganoPlate, which are based on standard 384-well plate formats. These are specifically designed to provide the high throughput needed for large-scale drug screening and research [45].
- Simplify Microscopy and Assays: Select 3D systems that are engineered to allow for easy microscopy, assays, and readouts. The architecture of these systems is designed to overcome the challenges of light penetration and focus in thicker 3D structures [45].
- Leverage AI-Driven Image Analysis: Implement artificial intelligence (AI) tools for the analysis of 3D cultures. AI can enable predictive analytics and non-destructive assessment of complex parameters like differentiation efficiency from simple phase-contrast images, reducing the reliance on complex, low-throughput assays [28] [46].
Experimental Protocols
Protocol 1: Early, Non-Destructive Prediction of hiPSC Differentiation Efficiency
This protocol is adapted from Saware et al. and demonstrates how to predict the final differentiation efficiency of human induced pluripotent stem cells (hiPSCs) into muscle stem cells (MuSCs) long before the protocol is complete, using imaging and machine learning [28].
Application: Optimizing and screening long-term hiPSC differentiation protocols non-destructively.
Workflow Diagram:
Key Research Reagent Solutions:
Table 3: Essential Reagents and Materials for the Prediction Protocol
| Item | Function/Description | Example/Note |
|---|---|---|
| MYF5-tdTomato Reporter hiPSC Line | Allows for quantification of final MuSC induction efficiency via flow cytometry by expressing a fluorescent protein under a muscle-specific promoter [28]. | Custom-generated cell line. |
| Phase Contrast Microscope | For non-destructive, daily imaging of cell cultures during the differentiation induction period [28]. | Standard equipment. |
| Directed Differentiation Media | Specific combinations of growth factors and small molecules to direct hiPSCs toward the muscle lineage. | Includes Wnt agonist, IGF-1, HGF, and bFGF [28]. |
| Flow Cytometer | For final analysis of differentiation efficiency on day 82 by measuring the percentage of MYF5-tdTomato positive cells [28]. | e.g., FACSCalibur. |
| Machine Learning Software | For analyzing extracted image features (FFT data) and building a predictive classification model [28]. | Random Forest classifier used in the study. |
Protocol 2: Flow Cytometry Analysis of Pluripotency Markers in hiPSCs
This protocol, based on Saware et al., outlines a cost-effective method to verify the pluripotent status of hiPSCs before beginning differentiation experiments, which is crucial for ensuring consistent and high-quality starting material [47].
Application: Defining the pluripotency status of hiPSC cultures by evaluating the expression of surface and intracellular undifferentiated stem cell markers.
Workflow Diagram:
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between 2D and 3D cell culture? The fundamental difference lies in the growth environment. In 2D culture, cells grow as a monolayer attached to a flat plastic surface (e.g., flask, Petri dish). In 3D culture, cells are allowed to grow in three dimensions, expanding in all directions to form tissue-like structures such as spheroids, organoids, or cells embedded within an extracellular matrix (ECM) scaffold. This 3D architecture more closely mimics the natural tissue environment [43] [44].
Q2: My 2D culture results are inconsistent when transitioning to a new cell line. Could the culture model be the issue? Yes. While 2D cultures are simple, they are known for altering cell morphology, polarity, and gene expression. Different cell lines can respond uniquely to the artificial 2D environment, leading to variability. Furthermore, the lack of a natural 3D microenvironment in 2D culture means that critical cell-ECM and complex cell-cell interactions are absent, which can significantly impact differentiation capacity and other cellular functions. For sensitive work like stem cell differentiation, moving to a 3D system might provide more consistent and physiologically relevant results across different cell lines [44].
Q3: Are there any scenarios where 2D culture is still the preferred or recommended method? Absolutely. 2D culture is not obsolete. It remains the preferred method for:
- High-throughput screening (HTS) applications where thousands of compounds need to be tested quickly and cost-effectively [43].
- Basic cytotoxicity assays and initial genetic manipulations (e.g., CRISPR knockouts) due to its simplicity and well-standardized protocols [43].
- Projects with significant budget or time constraints, or when a vast amount of comparative historical data from 2D models exists [45].
Q4: What are the main practical challenges when starting with 3D cell cultures, and how can I overcome them? The main challenges include:
- Cost and Infrastructure: 3D cultures are generally more expensive and may require specialized materials (e.g., ECM hydrogels, specialized plates) [44].
- Protocol Standardization: Protocols can be less standardized and more time-consuming than for 2D [44].
- Analysis Complexity: Analyzing 3D structures can be difficult with standard microscopy and biochemical assays [45].
- Solution: Begin with well-established 3D protocols for your cell type. Invest in technologies designed for 3D throughput and analysis (e.g., microfluidic plates). Leverage AI and advanced imaging techniques to simplify data extraction from complex 3D models [46] [45].
Q5: How is AI being integrated with 3D cell culture models to advance drug discovery? AI is playing a transformative role by:
- Enabling Predictive Analytics: Machine learning models can analyze data from 3D cultures (e.g., imaging, gene expression) to predict outcomes like drug efficacy or toxicity with high accuracy [46].
- Automating Image Analysis: AI can non-destructively assess complex parameters in 3D cultures, such as predicting future differentiation efficiency from simple phase-contrast images, which is a major bottleneck in protocol optimization [28].
- Facilitating Personalized Medicine: AI can help analyze data from patient-derived 3D organoids to identify personalized therapeutic regimens [43] [46].
Troubleshooting Guide: Common Issues & Solutions
Problem 1: Low Differentiation Efficiency and High Variability
| Problem Cause | Recommended Solution | Key Reagents & Concentrations |
|---|---|---|
| Inconsistent starting cell quality [47] [48] | Verify pluripotency status of hiPSCs prior to differentiation using flow cytometry for established undifferentiated stem cell markers (e.g., OCT4, SOX2). [47] | Flow cytometry antibodies panel for pluripotency markers. [47] |
| Suboptimal cell seeding density [48] | Accurately count cells and plate at protocol-specific density. For neural induction, a density of 2–2.5 x 10⁴ cells/cm² is often recommended. [48] | ROCK inhibitor (Y27632, 10 µM) to improve cell survival after passaging. [48] [49] |
| Spontaneous differentiation in culture [31] [50] | Remove differentiated areas from hPSC cultures before induction. Maintain cultures by passaging when colonies are large and compact, avoiding overgrowth. [31] | N/A |
| Inherent line-to-line variability [47] [50] | Include a control hPSC line (e.g., H9 or H7) as a positive control in differentiation experiments. Adjust cell density or extend induction time for difficult lines. [48] | N/A |
Problem 2: Inconsistent Cell Aggregate Size During Passaging
| Problem Cause | Recommended Solution | Key Reagents & Concentrations |
|---|---|---|
| Aggregates too large [31] | Increase incubation time with dissociation reagent by 1-2 minutes. Increase pipetting to break up aggregates. [31] | Gentle Cell Dissociation Reagent; Non-enzymatic passaging reagents (e.g., ReLeSR). [31] |
| Aggregates too small [31] | Minimize manipulation of aggregates after dissociation. Decrease incubation time with passaging reagent by 1-2 minutes. [31] | Non-enzymatic passaging reagents (e.g., ReLeSR). [31] |
Problem 3: Slow or Incomplete Maturation of Differentiated Cells
| Problem Cause | Recommended Solution | Key Reagents & Concentrations |
|---|---|---|
| Protracted intrinsic maturation timing [51] | Employ small-molecule cocktails to accelerate maturation. A combination called "GENtoniK" has been shown to enhance maturation in neurons and other lineages. [51] | GENtoniK Cocktail [51]: GSK2879552 (LSD1 inhibitor), EPZ-5676 (DOT1L inhibitor), NMDA (receptor agonist), Bay K 8644 (LTCC agonist). |
| Incorrect medium preparation [48] | Use fresh supplementation and check reagent expiration. For example, B-27-supplemented medium is stable for only 2 weeks at 4°C. Avoid multiple freeze-thaw cycles. [48] | B-27 Supplement. [48] |
Frequently Asked Questions (FAQs)
Q1: How can I non-destructively monitor differentiation efficiency early in a long protocol? Early prediction is possible by combining phase-contrast imaging with machine learning. One study successfully predicted muscle stem cell (MuSC) differentiation efficiency on day 82 using images taken as early as day 24-38. Features were extracted from images using Fast Fourier Transform (FFT) and classified with a random forest model. [28] This non-destructive method allows for early quality assessment and protocol adjustment.
Q2: Are there general strategies to boost maturation across multiple cell lineages? Yes, targeting chromatin remodeling and calcium signaling is a promising strategy. A high-content screen identified that inhibiting lysine-specific demethylase 1 (LSD1/KDM1A) and disruptor of telomerase-like 1 (DOT1L), while activating calcium-dependent transcription via LTCC agonists, can collectively accelerate maturation in hPSC-derived neurons, cortical organoids, and even non-neural lineages like melanocytes. [51]
Q3: What are the critical steps for transitioning from feeder-dependent to feeder-free culture systems? When adapting cells to a feeder-free system, passage the cells either manually or with EDTA into the new system. Using a ROCK inhibitor (e.g., Y27632) at the first passage can significantly improve cell survival and attachment. Ensure you are using the correct culture vessel (tissue culture-treated or non-treated) as specified by the coating matrix protocol. [48] [50]
Q4: How can I improve the survival of fragile differentiated cells, such as neurons, after thawing? For fragile cells like primary neurons or NSCs, fast thawing is critical. Do not thaw cells for longer than 2 minutes at 37°C. After thawing, transfer cells to a tube and add pre-warmed complete medium drop-wise while swirling to prevent osmotic shock. Do not centrifuge the cells immediately upon thawing, as they are extremely fragile. [48]
The Scientist's Toolkit: Research Reagent Solutions
| Reagent Category | Specific Example | Function in Differentiation & Standardization |
|---|---|---|
| Small Molecule Inhibitors | CHIR99021 (GSK-3β inhibitor) [49] | Activates Wnt signaling; commonly used for definitive endoderm and mesoderm induction. [49] |
| Small Molecule Inhibitors | LDN193189 (BMP inhibitor) [49] | Inhibits BMP signaling to promote neural ectoderm formation. [49] |
| Small Molecule Inhibitors | GSK2879552 (LSD1 inhibitor) [51] | Promotes neuronal maturation by modulating histone methylation. [51] |
| Small Molecule Inhibitors | EPZ-5676 (DOT1L inhibitor) [51] | Works synergistically with LSD1 inhibitors to drive a mature transcriptional state. [51] |
| Signaling Agonists | Bay K 8644 (LTCC Agonist) [51] | Activates L-type calcium channels to stimulate calcium-dependent transcription for maturation. [51] |
| Signaling Agonists | N-methyl-D-aspartate (NMDA) [51] | Activates NMDA receptors to work with LTCC agonists in promoting neuronal maturity. [51] |
| Rho-Kinase (ROCK) Inhibitor | Y-27632 2HCI [49] | Enhances single-cell survival after passaging and thawing, improving reproducibility of seeding. [48] [49] |
| Extracellular Matrix (ECM) | Matrigel, Vitronectin, Synthemax [49] [50] | Provides a defined substrate for cell attachment and growth in feeder-free systems, signaling cues that influence cell fate. [49] [50] |
| Culture Medium Supplements | B-27 Supplement [48] | A serum-free supplement essential for the long-term health and function of neurons and other differentiated cells. [48] |
Featured Experimental Protocol: Accelerated Neuronal Maturation
This protocol utilizes a small-molecule cocktail (GENtoniK) to accelerate the maturation of hPSC-derived cortical neurons, standardizing the timeline to achieve adult-like function [51].
Key Materials:
- Cell Type: hPSC-derived cortical neurons (e.g., deep-layer TBR1+ cells) [51].
- Small Molecules: GSK2879552 (LSD1 inhibitor), EPZ-5676 (DOT1L inhibitor), Bay K 8644 (LTCC agonist), N-methyl-D-aspartate (NMDA) [51].
- Key Media: Appropriate cortical neuron maturation medium [51].
Procedure:
- Differentiate and Plate Neurons: Differentiate hPSCs into cortical neurons according to your established protocol. Plate the resulting post-mitotic neurons for the maturation assay.
- Compound Treatment (Day 7-14): On day 7 after plating, replace the medium with fresh medium containing the GENtoniK cocktail.
- The cocktail consists of GSK2879552, EPZ-5676, Bay K 8644, and NMDA [51].
- Treat the cells for 7 days, with medium changes as needed.
- Compound Withdrawal (Day 14-21): On day 14, remove the compound-containing medium. Wash the cells and culture them in compound-free medium for an additional 7 days. This step identifies compounds that trigger a long-lasting maturation "memory" [51].
- Functional Assessment (Day 21+): On day 21 or later, assess maturation parameters. This multi-phenotypic assessment is crucial [51]:
- Morphology: Immunostain for MAP2 and use automated tracing to quantify total neurite length and branching [51].
- Nuclear Changes: Use DAPI staining to measure nuclear size and roundness [51].
- Function: Measure the nuclear expression of immediate-early genes (IEGs) FOS and EGR-1 after a 2-hour KCl stimulation to assess synaptic activity and excitability. Calculate the specific depolarization-induced signal by subtracting the baseline signal [51].
The workflow for this protocol is summarized in the diagram below:
Quality Control Workflow for Standardized Differentiation
Implementing a standardized quality control workflow is essential for maintaining reproducibility across experiments and cell lines. The following diagram outlines a recommended process from cell line selection to final validation.
Overcoming Roadblocks: AI, Predictive Modeling, and Protocol Refinement
Frequently Asked Questions (FAQs)
1. Why does the differentiation efficiency of my hiPSCs vary so much between experiments? Variability in directed differentiation protocols for human induced pluripotent stem cells (hiPSCs) is a well-known challenge. The efficiency can be influenced by the genetic and epigenetic state of individual hiPSC clones, experimental batches, and even slight changes in seeding cell number or researcher skill [28]. This is because hiPSCs are acutely sensitive to their microenvironment, including nutrient availability, gas exchange, and pH [52].
2. At what stage can I predict the final differentiation outcome for a long protocol? For long-term differentiation protocols, such as an 82-day induction of muscle stem cells (MuSCs), research indicates that the final induction efficiency can be predicted at a very early stage. Biological analyses have shown that the expression of key skeletal muscle markers on day 38 is significantly correlated with the final MuSC efficiency on day 82. By using phase-contrast imaging and machine learning, samples with high and low induction efficiency can be classified approximately 50 days before the end of induction [28].
3. What are the best methods for non-destructive, real-time quality control during differentiation? Artificial intelligence (AI)-driven approaches are transforming quality control. Combining simple phase-contrast imaging with machine learning allows for continuous, non-invasive tracking of morphological changes that are predictive of future differentiation states [28] [52]. For instance, convolutional neural networks (CNNs) can analyze high-resolution images to dynamically track critical quality attributes like cell morphology and predict differentiation outcomes with high accuracy [52].
4. How can I improve the reproducibility of my co-differentiation protocols? Engineering a controlled co-differentiation process for generating multiple cell types simultaneously is complex. A robust strategy involves dividing the process into stages (e.g., progenitor induction and trilineage differentiation) and using statistical design of experiments (DoE) for stage-specific optimization. This approach allows for the development of multi-response models that delineate differentiation ratios within a defined parameter space, significantly enhancing process controllability and reproducibility [53].
5. What critical quality attributes (CQAs) should I monitor in my stem cell cultures? Key CQAs that directly influence cell fate and function include [52]:
- Cell morphology and viability: Primary indicators of stem cell quality.
- Differentiation potential and lineage fidelity: The ability to commit to target lineages.
- Genetic and molecular stability: Crucial for safety and reproducibility.
- Environmental conditions: Including pH, oxygen, and nutrient levels.
- Contamination risk: One of the most costly risks in manufacturing.
Troubleshooting Guides
Issue 1: High Well-to-Well Variability in the Same Experimental Batch
Potential Causes:
- Slight variations in seeding cell number or bias of seeded cells in the culture dish [28].
- Inconsistent aggregate size and cell distribution in 3D suspension cultures [54].
- Minor fluctuations in the microenvironment of individual wells.
Solutions:
- Standardize Seeding: Use automated liquid handlers for precise cell counting and dispensing to ensure consistent seeding density across all wells [53].
- Implement In-Process Monitoring: Employ non-destructive imaging and AI-based analysis to classify samples early. For example, one study used Fast Fourier Transform (FFT)-based feature extraction from phase-contrast images and a random forest classifier to identify wells with high and low potential at early time points [28].
- Monitor Aggregate Morphology: In 3D cultures, consistently monitor aggregate size and morphology, as "pockmarking" can be an indicator of quality [54].
Issue 2: Low Differentiation Efficiency Across Multiple hiPSC Clones
Potential Causes:
- Inherent variability in the genetic and epigenetic state of different hiPSC clones [28] [55].
- Suboptimal concentration of critical differentiation factors, such as growth factors or small molecules, for a specific cell line.
- Inefficient induction of progenitor cells in the initial differentiation stage.
Solutions:
- Clone Selection: If possible, pre-screen and select hiPSC clones that demonstrate robust differentiation toward your target lineage.
- Protocol Optimization using DoE: Systematically optimize factor concentrations using statistical design of experiments rather than one-factor-at-a-time approaches. For example, one study used sequential DoE to optimize activin A and CHIR-99021 concentrations to achieve ~95% induction efficiency of cardiogenic mesoderm cells with minimal batch-to-batch variability [53].
- Validate Progenitor Induction: Carefully quality-control the initial stages of differentiation. For cardiac co-differentiation, this meant ensuring high efficiency in generating KDR+/PDGFR-α+ cardiogenic mesoderm cells, as this stage critically influences the entire process [53].
Issue 3: Poor Reproducibility Between Technicians
Potential Causes:
- Differences in technical skill, particularly for manual processes like media changes, passaging, and aggregate handling in 3D cultures [28] [54].
- Lack of detailed, step-by-step documentation for critical protocol steps.
Solutions:
- Automation: Utilize automated platforms for media changes, feeding, and passaging to reduce human error [55] [52].
- Structured Training: Ensure all technicians are trained against a standardized protocol. Utilize available on-demand courses for complex techniques like 3D suspension culture [54].
- Detailed Documentation: Create protocols that specify exact parameters for common techniques. For example, when dissociating 3D aggregates, note that it "typically requires a longer incubation time with the dissociation reagent" compared to 2D cultures [54].
Issue 4: Inconsistent Results When Scaling Up from 2D to 3D Culture
Potential Causes:
- Failure to properly adapt a protocol designed for 2D adherent culture to 3D suspension conditions.
- Formation of necrotic cores in 3D aggregates due to suboptimal size or agitation.
- Differences in cell-cell interactions and exposure to nutrients/growth factors in 3D.
Solutions:
- Follow a Structured Workflow: A recommended workflow for transitioning to 3D includes [54]:
- Confirm high-quality hPSCs in 3D culture over multiple passages.
- First, validate the differentiation protocol works robustly in 2D.
- Master reproducible 3D hPSC culture techniques (aggregate formation, passaging) before differentiating.
- Optimize differentiation at a small scale (e.g., 6-well plates on an orbital shaker).
- Scale up gradually to larger bioreactor vessels.
- Optimize Agitation and Density: Monitor and optimize agitation rates in bioreactors to maintain consistent aggregate size and prevent necrosis. Implement sampling strategies to track differentiation progress and make data-driven adjustments [54].
- Use Specialized Media: Employ media specifically formulated for 3D fed-batch workflows to ensure efficient nutrient use and consistent expansion [54].
The following table summarizes quantitative data from recent studies on predicting and improving differentiation efficiency.
Table 1: Machine Learning for Early Prediction of Differentiation Outcomes
| Cell Type | Total Protocol Duration | Early Prediction Timepoint | Prediction Method | Key Performance Metric |
|---|---|---|---|---|
| Muscle Stem Cells (MuSCs) [28] | 82 days | Day 24 (for low efficiency)Day 31/34 (for high efficiency) | Phase-contrast imaging + FFT feature extraction + Random Forest | Accurate classification ~50 days before protocol end |
| Mouse Stem Cell-derived Embryo Models (ETiX-embryos) [56] | 90 hours | 65-90 hours post-seeding | Live imaging + Deep Learning (StembryoNet - ResNet18) | 88% accuracy in classifying normal vs. abnormal development |
Table 2: Strategies for Protocol Optimization and Control
| Strategy | Application | Key Outcome | Reference |
|---|---|---|---|
| Statistical Design of Experiments (DoE) | Cardiac trilineage (CMs, ECs, MCs) co-differentiation from iPSCs | Achieved high process controllability with a close match between actual and predicted differentiation ratios. | [53] |
| Sequential DoE for Factor Optimization | Cardiogenic mesoderm induction from iPSCs | Achieved ~95% induction efficiency of KDR+/PDGFR-α+ cells with minimal batch-to-batch variability. | [53] |
| AI-driven Quality Monitoring | General stem cell biomanufacturing | Enables real-time tracking of CQAs like morphology, predicts culture trajectories, and allows for proactive process interventions. | [52] |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Stem Cell Differentiation and Quality Control
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| TeSR-AOF 3D / mTeSR 3D Media | Animal-origin free and standard media for fed-batch expansion of hPSCs in 3D suspension culture. | Scalable production of hPSCs and their derivatives for therapeutic applications [54]. |
| STEMdiff Differentiation Kits | Specialized, optimized media kits for directed differentiation of hPSCs into specific lineages. | Provides a validated starting point for 2D differentiation before adapting to 3D systems [54]. |
| Recombinant Adeno-associated Virus (rAAV) | Highly efficient viral vector for transgene delivery into stem cell derivatives. | Transduction of liver progenitor cells, achieving up to 93.6% efficiency for genetic manipulation studies [3]. |
| Critical Quality Attribute (CQA) Tracking with AI | Non-destructive, real-time monitoring of cell morphology, predicting differentiation potential, and detecting anomalies. | Using CNN-based image analysis to predict iPSC colony formation with >90% accuracy [52]. |
Experimental Workflow & Signaling Pathways
The following diagram illustrates a generalized, robust workflow for developing and monitoring a stem cell differentiation protocol, integrating best practices from the cited research.
Robust Stem Cell Differentiation Workflow
For complex processes like cardiac co-differentiation, multiple signaling pathways are carefully manipulated. The diagram below outlines the key stages and factors involved in one such optimized protocol.
Controlled Cardiac Co-Differentiation Pathway
Technical Support Center
This guide provides troubleshooting and methodological support for researchers employing phase-contrast imaging and machine learning to non-destructively predict stem cell differentiation efficiency. The content is framed within the context of optimizing hiPSC differentiation protocols for regenerative medicine, specifically focusing on muscle stem cells (MuSCs) [28] [57] [58].
Frequently Asked Questions (FAQs)
Q1: What is the core principle behind predicting differentiation efficiency from phase-contrast images? The core principle is that morphological changes in cells during early differentiation stages (e.g., days 14-38) contain predictive information about the final differentiation outcome (e.g., on day 82). These subtle, visually indiscernible morphological patterns can be captured computationally using feature extraction methods like the Fast Fourier Transform (FFT) and analyzed by machine learning classifiers [28] [58].
Q2: Why use FFT for feature extraction from my cell images? FFT converts image data from the spatial domain to the frequency domain, generating a power spectrum. This spectrum captures repetitive patterns and textural information in the cell culture. Performing shell integration on this spectrum creates a rotation-invariant feature vector, ensuring the analysis is not affected by the orientation of cellular structures [28].
Q3: My model's predictions are inaccurate. What could be wrong? Inaccurate predictions can stem from several issues:
- Insufficient Data: The model may not have seen enough examples to learn robust patterns. One referenced study used 5,712 images from 34 wells [28] [58].
- Incorrect Feature Extraction: Verify the parameters of your FFT and shell integration process.
- Poor Image Quality: Blurry or inconsistently lit images will hinder feature extraction. Ensure standardized imaging protocols.
- Suboptimal Model Parameters: The machine learning classifier (e.g., Random Forest) may need hyperparameter tuning [28].
Q4: How do I determine the optimal time point for image acquisition and prediction? This requires empirical validation. Biological validation (e.g., qRT-PCR, ICC) should first identify a phase where marker expression (e.g., MYH3, MYOD1 on day 38) correlates with final efficiency (e.g., MYF5+% on day 82). Subsequently, images from this phase should be tested for predictive power. For MuSC differentiation, days 24 (for low-efficiency) and days 31/34 (for high-efficiency) were found to be effective [28].
Q5: What are common artifacts in phase-contrast imaging, and how can I mitigate them? In Talbot-Lau phase-contrast imaging, artifacts like Moiré patterns can arise from grating misalignments or phase step fluctuations. Using software toolkits like XPCIpy, which includes algorithms for correcting these instabilities, can help mitigate such reconstruction artifacts [59].
Troubleshooting Guides
Problem: Low Classification Accuracy in Predicting Differentiation Efficiency
Possible Causes and Solutions:
Cause 1: Inadequate Training Data
- Solution: Increase the number of biological replicates. Aim for a large dataset of images across multiple time points and independent differentiation batches to improve model generalizability [28].
Cause 2: Non-informative Feature Vectors
- Solution: Re-examine the FFT feature extraction pipeline. Confirm that the generated feature vectors show discernible patterns when visualized (e.g., via PCA) for samples with known high and low efficiency. Consider experimenting with the number of shells used in integration [28].
Cause 3: Class Imbalance
- Solution: If your dataset has many more "high-efficiency" samples than "low-efficiency" ones, the model may become biased. Employ strategies such as oversampling the minority class, undersampling the majority class, or using algorithmic approaches that adjust for class weight [28].
Problem: Poor Generalization to New Data Batches
Possible Causes and Solutions:
- Cause: Batch Effects from Cell Culture or Imaging Conditions
- Solution: Implement strict standardization protocols for cell culture, seeding density, and image acquisition (light intensity, exposure time). Techniques like data augmentation (e.g., rotation, flipping) on training images can also make models more robust to minor variations [28].
Experimental Protocol: Predicting MuSC Differentiation Efficiency
This protocol details the methodology for non-destructively predicting muscle stem cell (MuSC) differentiation efficiency from human induced pluripotent stem cells (hiPSCs) [28] [57] [58].
1. Cell Culture and Differentiation
- Cell Line: Use a reporter hiPSC line (e.g., MYF5-tdTomato) for validation [28].
- Differentiation Protocol: Employ a directed differentiation protocol toward MuSCs. The process typically involves:
- Induction of dermomyotome cells using a Wnt agonist (Days 0-14).
- Myogenic induction using growth factors (IGF-1, HGF, bFGF) (Days 14-38).
- Maturation in muscle culture medium to obtain MuSCs (Days ~38-82) [28].
2. Image Acquisition
- Microscopy: Use a phase-contrast microscope.
- Timing: Capture images of cell cultures between days 14 and 38 of differentiation.
- Standardization: Image multiple wells and fields of view under consistent lighting and magnification. The referenced study collected 5,712 images from 34 wells [28] [58].
3. Ground Truth Validation
- Flow Cytometry: On the final day of differentiation (e.g., day 82), analyze cells using flow cytometry to quantify the percentage of MYF5-positive cells (MYF5+%), which serves as the ground truth for differentiation efficiency [28].
- Biological Correlation: Validate that intermediate markers (e.g., MHC, MYOD1 protein expression on day 38) correlate with the final MYF5+% [28].
4. Computational Analysis
- Feature Extraction with FFT:
- Apply FFT to each pre-processed phase-contrast image to obtain its 2D power spectrum.
- Perform shell integration (radial averaging) on the power spectrum to create a 1D, rotation-invariant feature vector (e.g., 100-dimensional) [28].
- Machine Learning Classification:
- Data Labeling: Label each image's feature vector based on its final MYF5+% outcome (e.g., "High" or "Low" efficiency).
- Model Training: Train a classifier, such as a Random Forest, using the labeled feature vectors.
- Prediction: Use the trained model to predict the differentiation efficiency of new, unseen samples based on their phase-contrast images [28].
The workflow for this experimental protocol is summarized in the following diagram:
Key Experimental Data and Performance
The following table summarizes quantitative data from a referenced study on predicting MuSC differentiation efficiency [28].
Table 1: Prediction Performance for MuSC Differentiation
| Prediction Target | Optimal Prediction Day | Key Outcome Metric | Result |
|---|---|---|---|
| Low Induction Efficiency | Day 24 | Effective identification of low-efficiency samples | ~50 days before induction end [28] |
| High Induction Efficiency | Day 31 or 34 | Effective identification of high-efficiency samples | ~50 days before induction end [28] |
| Overall Workflow Impact | Days 24 & 34 | Reduction in defective sample rate | 43.7% reduction [28] |
| Overall Workflow Impact | Days 24 & 34 | Increase in good samples | 72% increase [28] |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for the Featured Experiment
| Item | Function / Explanation | Example / Note |
|---|---|---|
| hiPSC Line | The starting cell material with pluripotent potential. | MYF5-tdTomato reporter line for validation [28]. |
| Wnt Agonist | Directs initial differentiation toward mesodermal lineages. | Used at high concentration for dermomyotome induction (Days 0-14) [28]. |
| Growth Factors | Promotes myogenic specification and proliferation. | Insulin-like growth factor 1 (IGF-1), Hepatocyte growth factor (HGF), basic Fibroblast growth factor (bFGF) [28]. |
| Antibodies for Validation | Used to confirm protein expression for ground truth. | Antibodies against MYH3 (Myosin Heavy Chain), MYOD1 for ICC; Flow cytometry antibodies for MYF5 or CDH13 [28]. |
| Phase-Contrast Microscope | For non-destructive, label-free imaging of cell morphology. | Essential for collecting the primary image data [28] [58]. |
| FFT Software Library | To perform the Fast Fourier Transform on acquired images. | Available in many programming languages (e.g., Python via NumPy/SciPy) [28]. |
| Machine Learning Library | To implement the classification algorithm. | Scikit-learn for Python (includes Random Forest) [28]. |
The logical relationship between the computational steps in the prediction pipeline is shown below:
AI-Driven Optimization of Reprogramming and Differentiation Parameters
Technical Support Center
Troubleshooting Guides & FAQs
This section addresses common challenges researchers face when integrating Artificial Intelligence (AI) and Machine Learning (ML) into stem cell reprogramming and differentiation workflows. The guidance is framed within the context of optimizing differentiation efficiency for research and therapeutic applications.
FAQ 1: Our AI model for predicting iPSC colony formation performs well on training data but generalizes poorly to new cell lines. What could be wrong?
- Potential Cause: The model is likely overfitting to the specific morphological features or imaging conditions of your original training dataset. This is a common issue given the inherent biological variability in stem cell lines.
- Solution:
- Data Augmentation: Artificially expand your dataset by applying transformations (e.g., rotations, contrast adjustments, slight distortions) to your training images to improve model robustness [60].
- Incorporate Multi-Omics Data: Relying solely on imaging data may be insufficient. Integrate other data types, such as gene expression or epigenetic markers, to create a more comprehensive digital phenotype of the cell lines. Adopting community standards for cell line registration, as recommended by the ISSCR, can facilitate this by creating unambiguous links between a cell line's physical entity and its digital data [61].
- Explore Federated Learning: Consider using federated learning approaches, which allow you to train models across multiple institutions without sharing raw data, thereby accessing more diverse datasets and improving generalizability [52].
FAQ 2: How can we achieve real-time, non-invasive quality control during stem cell differentiation?
- Potential Cause: Traditional quality control methods, such as flow cytometry or immunostaining, are destructive, endpoint assays that provide only a snapshot in time and disrupt the culture process [52].
- Solution:
- Implement AI-Driven Live-Cell Imaging: Use convolutional neural networks (CNNs) to analyze time-lapse bright-field or phase-contrast microscopy images. These models can be trained to track critical quality attributes (CQAs) like cell morphology, confluency, and even early signs of differentiation in real-time, without labels [52] [60].
- Sensor Integration: Combine imaging with real-time sensor data (e.g., pH, dissolved oxygen). Predictive models can analyze these high-frequency data streams to forecast deviations in culture conditions hours in advance, allowing for preemptive corrections [52].
FAQ 3: Our differentiation protocols yield inconsistent results. Can AI help optimize them systematically?
- Potential Cause: Manual optimization of differentiation protocols, which involves manipulating numerous variables (growth factors, cell density, nutrient levels), is inherently trial-and-error and prone to variability [62].
- Solution:
- Leverage Reinforcement Learning (RL): Implement RL algorithms that iteratively adjust culture parameters (e.g., growth factor concentrations, timing of additions) based on feedback from the culture's outcome. This allows the system to autonomously explore a vast parameter space and discover highly effective, reproducible differentiation protocols [62].
- Predictive Modeling for Lineage Commitment: Use support vector machines (SVMs) or other classifiers trained on time-series imaging and gene expression data to forecast differentiation outcomes. One study achieved over 90% sensitivity in distinguishing endocrine lineage commitment stages, enabling early intervention [52].
FAQ 4: We are concerned about the "black box" nature of AI models. How can we trust their predictions for critical research decisions?
- Potential Cause: Complex AI models like deep neural networks can lack interpretability, making it difficult to understand the biological rationale behind their predictions, which undermines trust and hampers biological discovery [63].
- Solution:
- Prioritize Interpretable Models: When possible, use models that provide insight into feature importance, such as random forests, which can indicate which parameters (e.g., a specific morphological feature or gene) were most influential in a prediction [64].
- Model Validation and Human Oversight: Always correlate AI predictions with established biological assays. Maintain human oversight to ensure that the model's outputs are biologically plausible. The goal is a partnership where AI handles data-intensive pattern recognition, and researchers provide domain expertise and validation [62].
Experimental Protocols & Methodologies
This section provides detailed methodologies for key experiments cited in AI-driven stem cell research.
Protocol 1: AI-Driven Real-Time Morphological Analysis for Quality Monitoring
- Objective: To non-invasively track stem cell morphology, proliferation, and predict pluripotency or early differentiation in real-time using convolutional neural networks (CNNs) [52] [60].
- Materials:
- Phase-contrast or bright-field microscope with time-lapse imaging capabilities.
- Computational environment (e.g., Python with TensorFlow/PyTorch).
- Labeled dataset of stem cell images (annotated for colony formation, differentiation stage, etc.).
- Methodology:
- Data Acquisition: Capture high-resolution time-lapse images of stem cell cultures at regular intervals (e.g., every 30 minutes) throughout the reprogramming or differentiation process.
- Model Training: Train a CNN (e.g., ResNet, U-Net) on a curated dataset where images are labeled with specific outcomes (e.g., "successful iPSC colony," "differentiated neuron"). The model learns to associate morphological features with these states.
- Deployment and Inference: Integrate the trained model into the live imaging system. The model analyzes new images as they are acquired and provides predictions on cell state.
- Validation: Correlate the AI's predictions with endpoint assays, such as immunostaining for pluripotency markers (OCT4, SOX2) or lineage-specific markers, to confirm accuracy [52] [60].
Protocol 2: Reinforcement Learning for Differentiation Protocol Optimization
- Objective: To use a Reinforcement Learning (RL) algorithm to autonomously discover optimal differentiation protocols by dynamically adjusting culture conditions [52] [62].
- Materials:
- Automated bioreactor or cell culture system with parameter control (e.g., for media perfusion, additive dosing).
- In-line sensors for monitoring CQAs (e.g., dissolved oxygen, pH sensors, automated microscope).
- RL software platform.
- Methodology:
- Define Environment and Agent: The environment is the stem cell culture system. The agent is the RL algorithm.
- Set State, Action, and Reward:
- State (s): A vector of current culture conditions (e.g., metabolite levels, cell morphology data from imaging, time point).
- Action (a): The adjustments the agent can make (e.g., "increase growth factor A by 10%," "change media now").
- Reward (R): A numerical score based on desired outcomes. For example, a high reward is given for high expression of a target cell marker detected later in the process.
- Training Loop: The agent explores the environment by taking actions, receiving rewards, and learning a policy that maximizes cumulative reward over time. For instance, Komarova et al. used an RL algorithm to adjust gas composition, which improved the expansion efficiency of stem cell cultures by 15% [52].
- Protocol Validation: The optimized protocol discovered by the RL agent must be rigorously validated in independent experiments against standard protocols.
Data Presentation
Table 1: Mapping Critical Quality Attributes (CQAs) to AI Monitoring Strategies
| Critical Quality Attribute (CQA) | Traditional Challenge | AI-Based Monitoring Strategy | Key Algorithms & Techniques |
|---|---|---|---|
| Cell Morphology & Viability | Manual microscopy is subjective, labor-intensive, and offers limited temporal resolution [52]. | CNN-based analysis of high-resolution time-lapse imaging for continuous, non-invasive tracking [52]. | Convolutional Neural Networks (CNNs), Generative Adversarial Networks (GANs) for synthetic data [52]. |
| Differentiation Potential & Lineage Fidelity | Endpoint assays (e.g., flow cytometry) fail to provide real-time insights during critical transitions [52]. | Trajectory-based modeling using time-series data to forecast differentiation outcomes [52]. | Support Vector Machines (SVM), Regression Models, Multitask Learning [52] [64]. |
| Environmental Conditions | Offline sampling or simple threshold-based control cannot predict subtle, future anomalies [52]. | Predictive modeling of sensor data (pH, O₂) for dynamic control [52]. | Reinforcement Learning (RL), Predictive Modeling from IoT sensor data [52]. |
| Genetic Stability | Low-throughput techniques like karyotyping offer limited scope [52]. | Multi-omics data fusion (genomics, transcriptomics) to model instability patterns [52]. | Deep Learning, Attention-Based Models [52]. |
| Contamination Risks | Relies on visual inspection or delayed microbial assays [52]. | Anomaly detection in real-time sensor data and microscopy images [52]. | Random Forest Classifiers, CNNs [52] [64]. |
Table 2: Essential Research Reagent Solutions for AI-Integrated Workflows
| Item | Function in AI-Driven Workflows |
|---|---|
| High-Resolution Live-Cell Imaging System | Generates the primary morphological data (videos and images) required for training and deploying CNN models for non-invasive quality control [52] [60]. |
| In-line Bioreactor Sensors (pH, DO, metabolites) | Provides continuous, high-frequency data on culture environment. This data is the input for predictive models that forecast culture trajectories and enable real-time feedback control [52]. |
| Multi-Omics Assay Kits (e.g., RNA-seq) | Generate genomic, transcriptomic, and epigenomic data used to build digital phenotypes of cell lines. This data is fused with imaging data in deep learning models to predict genetic stability and differentiation potential [52] [63]. |
| Validated Pluripotency & Lineage Marker Panels | Provides the "ground truth" data for training supervised machine learning models. The AI learns to correlate real-time imaging features with these definitive endpoint molecular markers [52] [60]. |
Workflow & Pathway Visualizations
AI-Driven Stem Cell Analysis Workflow
AI for iPSC Reprogramming and Differentiation
The strategic selection of a gene delivery vector is a critical determinant of success in stem cell differentiation efficiency optimization research. Vectors function as microscopic delivery trucks, transporting genetic material (transgenes) into the nucleus of target cells to instruct new functions or correct defects [65]. The choice between viral and non-viral methods hinges on a matrix of experimental needs, including required duration of transgene expression, size of the genetic cargo, target cell type, and sensitivity to immunogenic responses [66] [67].
For researchers engineering stem cell-derived models, this decision directly impacts the efficiency of generating genetically defined tissues. The two primary vector categories are:
- Viral Vectors: Engineered from viruses, leveraging their natural ability to efficiently enter cells. They are the current delivery vehicle in most FDA-approved gene therapies [65] [67].
- Non-Viral Vectors: Rely on physical or chemical methods to deliver genetic material, offering safer and more scalable alternatives that are rapidly advancing [65] [68].
The following sections provide a detailed technical guide, structured as FAQs and troubleshooting guides, to assist in selecting and optimizing these systems for your stem cell differentiation protocols.
Frequently Asked Questions (FAQs)
Q1: Which delivery method offers the highest transduction efficiency for hard-to-transduce stem cells? Viral vectors, particularly Lentivirus (LV) and Adeno-Associated Virus (AAV), generally provide the highest transduction efficiency. A recent 2025 study on liver progenitor cell models achieved a 93.6% transduction efficiency using the rAAV2/2 serotype [3]. Lentiviral vectors are also highly efficient for transducing a broad range of dividing and non-dividing cells and are a backbone for ex vivo cell therapy [66] [67]. For non-viral methods, electroporation can achieve moderate efficiency (e.g., 54.3% plasmid delivery in the same liver progenitor study [3]), but this can vary significantly by cell type. Lipid Nanoparticles (LNPs) are highly efficient for mRNA delivery but face challenges with endosomal escape, a rate-limiting step where often less than 2-3% of the LNP payload successfully reaches the cytoplasm [66].
Q2: I need persistent transgene expression in a stem cell-derived organoid model. What is my best option? The need for persistent expression narrows your choice to vectors that enable stable genetic maintenance.
- For in vivo delivery to non-dividing cells: AAV vectors are the gold standard. They predominantly exist as long-lasting episomes within the cell's nucleus, providing durable expression without integrating into the host genome [66].
- For ex vivo engineering of stem cells and their differentiated progeny: Lentiviral vectors are ideal. Their key advantage is the ability to integrate into the host genome, ensuring the transgene is passed on to all daughter cells, which is essential for long-term studies in dividing cell populations [66] [67] [69].
- Non-viral methods like electroporation of plasmids typically result in transient expression. While transposon systems (e.g., PiggyBac) can facilitate stable integration, they are less common and come with their own risks of insertional mutagenesis [69].
Q3: What are the primary safety concerns associated with viral and non-viral vectors? Each vector class carries distinct safety profiles:
- Viral Vector Concerns:
- Immunogenicity: Pre-existing neutralizing antibodies (NAbs) to AAV can exclude 30-60% of patients from treatment and prevent re-dosing. Adenoviruses are highly immunogenic [66] [68].
- Insertional Mutagenesis: Primarily a concern for retroviral and lentiviral vectors, where random integration could disrupt a tumor suppressor gene or activate an oncogene. Third-generation self-inactivating (SIN) vectors have significantly mitigated this risk [66] [70].
- Cargo Capacity Limitations: AAV's strict ~4.7 kb limit can be a major constraint for large genes or complex editing machinery [66].
- Non-Viral Vector Concerns:
- Cytotoxicity: Certain cationic lipids and polymers can be cytotoxic, impacting cell viability [71] [72].
- Lower Efficiency: While safer, they often fall short of the high transduction efficiency achieved by viral vectors, particularly in challenging primary cells [68].
- Material-Specific Toxicity: Impurities in lipid or polymer raw materials can alter stability and induce unwanted immune responses [66].
Q4: My genetic cargo is large (>8 kb). Can I still use viral vectors? This is a significant challenge for viral vectors. AAV's ~4.7 kb capacity is often insufficient. While Lentivirus can accommodate up to ~10 kb, production efficiency can drop with larger cargo [66] [68]. For large cargos, non-viral vectors are superior. Lipid Nanoparticles (LNPs) offer flexible and high cargo capacity, making them suitable for delivering large CRISPR-based editing machinery or multiple genes simultaneously [66] [72]. Physical methods like electroporation also have minimal size constraints for plasmid DNA [69].
Vector Selection and Comparison Tables
Quantitative Comparison of Major Delivery Systems
Table 1: Technical Specifications of Key Delivery Vectors
| Feature | AAV (Viral) | Lentivirus (Viral) | LNP (Non-Viral) | Electroporation (Non-Viral) |
|---|---|---|---|---|
| Primary Use Case | In vivo gene replacement (CNS, Eye, Liver) [66] | Ex vivo cell therapy (CAR-T, HSCs) [66] | Gene editing (CRISPR/mRNA), Vaccines [66] | Ex vivo delivery to immune cells, stem cells [71] |
| Cargo Capacity | ~4.7 kb (Strict) [66] | ~10 kb (Moderate) [66] | Flexible / High [66] | Flexible (plasmid size) |
| Genetic Persistence | Episomal (Long-term) [66] | Integrated (Permanent) [66] | Transient [66] | Transient or Stable (with integrase systems) [69] |
| Typical Efficiency | Very High (e.g., >90% [3]) | Very High [69] | Variable; High for mRNA [66] | Moderate to High (e.g., 30-70% [3] [69]) |
| Immunogenicity | High (Pre-existing NAbs, no re-dosing) [66] | Low (Mostly used ex vivo) [66] | Low (Re-dosable) [66] | Low (Physical method) |
| Key Advantage | Well-trodden regulatory path, durable in vivo expression [66] | Stable expression in dividing cells, large cargo [66] | Scalable manufacturing, re-dosability, large cargo [66] | Viral-free, applicable to a wide range of nucleic acids [71] |
| Key Bottleneck | Empty/Full capsid separation, pre-existing immunity [66] | Viral stability & titer, insertional mutagenesis risk [66] | Endosomal escape, "Liver Trap" for biodistribution [66] | Low cell viability, optimization required [71] |
Decision Workflow for Vector Selection
The following diagram outlines a logical workflow for selecting the most appropriate transgene delivery method based on key experimental parameters:
Troubleshooting Guides
Low Transduction/Efficiency
Problem: Low levels of transgene delivery or expression in your stem cell culture.
Possible Causes and Solutions:
- Cause 1: Suboptimal Vector Dose or Cell Health.
- Solution: Perform a Multiplicity of Infection (MOI) gradient test to determine the optimal viral particle-to-cell ratio. Ensure cells are healthy and actively dividing at the time of transduction, as cell state profoundly impacts efficiency [69].
- Cause 2: Low Transfection Efficiency in Non-Viral Methods.
- Cause 3 (Viral): Inefficient Viral Entry.
- Solution: Utilize tissue-specific viral serotypes (e.g., AAV2/2 for liver progenitors [3]) or pseudotyped lentiviral envelopes (e.g., VSV-G) that enhance tropism for your target cell. Add enhancers like polybrene to viral media.
- Cause 4 (Non-Viral): Poor Endosomal Escape.
High Cytotoxicity
Problem: Significant cell death following the delivery procedure.
Possible Causes and Solutions:
- Cause 1: Excessive Viral Load.
- Solution: High MOIs can trigger immune responses and cellular toxicity. Titrate the virus to find the lowest effective dose [66].
- Cause 2: Electroporation-Induced Stress.
- Solution: Electroporation can be harsh. Use a square-wave protocol if available, as it can be gentler than exponential decay. Optimize pulse parameters and ensure cells are recovered in enriched media supplemented with Rho-kinase inhibitors (Y-27632) to prevent anoikis [69].
- Cause 3: Impurities or Cytotoxic Formulations.
Inconsistent or Transient Expression
Problem: Transgene expression is mosaic across the cell population or fades over time.
Possible Causes and Solutions:
- Cause 1: Epigenetic Silencing of the Transgene.
- Solution: This is common with viral vectors using certain promoters. Use promoters less prone to silencing (e.g., EF1α, PGK) instead of CMV. Consider vectors with chromatin insulators [69].
- Cause 2: Targeting Non-Stem Cells in Organoid Cultures.
- Solution: In organoids, only modified stem cells will propagate the transgene long-term. Use stem-cell specific promoters (e.g., an Ascl2 reporter) and perform transduction/transfection on dissociated single cells to maximize stem cell access, followed by selection to enrich for successfully modified clones [69].
- Cause 3: Use of Transient Non-Viral Delivery.
- Solution: If persistent expression is needed, switch to a viral vector or use a non-viral integrating system like the PiggyBac transposon delivered via electroporation [69].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Transgene Delivery Experiments
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Rho-kinase Inhibitor (Y-27632) | Inhibits anoikis (cell death due to detachment); dramatically improves viability of single stem cells after dissociation and electroporation [69]. | Critical for any single-cell cloning or transfection workflow with sensitive epithelial or stem cells. |
| Ionizable Cationic Lipids | Key component of LNPs; enables complexation with nucleic acids and facilitates endosomal escape through a charge shift at acidic pH [66] [73]. | The specific pKa of the lipid is a major determinant of in vivo targeting beyond the liver. |
| Stem Cell-Specific Promoters | Drives transgene expression specifically in stem cells (e.g., EF1α, PGK, synthetic STAR element); prevents silencing and ensures expression is maintained in proliferating compartments [69]. | Essential for achieving homogeneous, long-term expression in organoid cultures. |
| Polybrene | A cationic polymer that reduces electrostatic repulsion between viral particles and the cell membrane, thereby enhancing viral transduction efficiency [69]. | Can be cytotoxic; requires dose optimization. |
| Accutase | A gentle enzyme blend for dissociating cells into single suspensions; preserves cell surface receptors and improves viability compared to trypsin [69]. | Ideal for creating single-cell suspensions for electroporation or viral transduction. |
| Matrigel / ECM | A basement membrane extract providing a 3D environment that supports stem cell survival, self-organization, and differentiation into organoids [3] [69]. | Lot-to-lot variability can significantly impact experimental reproducibility. |
| Selection Antibiotics | Allows for the enrichment of stably transduced cells (e.g., Puromycin, Blasticidin, Zeocin). Often co-expressed with the transgene via P2A or IRES sequences [69]. | Killing curve must be established for each new cell type to determine the minimal effective concentration. |
Experimental Protocol: Transducing Stem Cell-Derived Liver Progenitor Cells
This protocol, adapted from a 2025 study, details an optimized method for achieving high-efficiency transduction of liver progenitor cells (LPCs) derived from human induced pluripotent stem cells (hiPSCs), a relevant model for optimizing stem cell differentiation [3].
Objective: To deliver a transgene (e.g., eGFP reporter) to LPCs using recombinant Adeno-Associated Virus (rAAV) and assess transduction efficiency.
Materials:
- Differentiated 2D culture of hiPSC-derived LPCs.
- rAAV vector of choice (e.g., serotype 2/2), carrying eGFP.
- Control: Plasmid DNA for electroporation comparison.
- Matrigel-coated culture plates.
- Appropriate growth medium (e.g., RPMI 1640 with B-27 supplement, FGF10, BMP4 [3]).
- Flow cytometry buffer and access to a flow cytometer.
Method:
- Cell Preparation: Culture LPCs in a 12-well plate pre-coated with Matrigel until they reach 70-80% confluence.
- Viral Transduction:
- Prepare dilutions of the rAAV stock in the growth medium to achieve the desired Multiplicity of Infection (MOI). The referenced study used an MOI of 100,000 for rAAV2/2 [3].
- Remove the existing medium from the LPCs and add the virus-containing medium.
- Incubate the cells for 24-48 hours. Consider including polybrene at an optimized concentration to enhance transduction.
- Expression Analysis: After 48-72 hours, analyze the cells for transgene expression.
- Quantitative Analysis: Harvest the cells using Accutase and analyze the percentage of eGFP-positive cells using flow cytometry. The referenced protocol achieved 93.6% efficiency with rAAV2/2 [3].
- Qualitative Analysis: Fix the cells and perform immunofluorescence staining for eGFP and key LPC markers (e.g., HNF4α, AFP) to confirm cell identity and transgene co-expression.
Troubleshooting Notes:
- Low Efficiency: Confirm the LPCs express the primary receptor for the AAV serotype used. Titrate the MOI and test different AAV serotypes (e.g., AAV-DJ, AAVrh10) for optimal tropism.
- High Cell Death: Reduce the viral load. Ensure cells are healthy prior to transduction and that the media is fresh.
- As a comparative control, the same study achieved 54.3% plasmid delivery efficiency using electroporation, highlighting the efficiency difference between methods for this cell type [3].
Ensuring Fidelity: Metrics, Models, and Comparative Analysis of Differentiation Outcomes
Within stem cell differentiation efficiency optimization research, robust analytical techniques are paramount. Confirming successful differentiation into target cells is critical for applications in basic research, drug discovery, and regenerative medicine. This technical support center provides essential guidance on using flow cytometry and immunostaining (including immunocytochemistry (ICC) and immunohistochemistry (IHC)) to characterize stem cell populations, troubleshoot common experimental issues, and validate differentiation protocols.
FAQ: Core Techniques
Q1: What is the fundamental difference between flow cytometry and immunostaining?
The primary difference lies in the format of the sample and the type of data generated.
- Flow Cytometry is a laser-based technique that analyzes a suspension of single cells. It is quantitative and provides high-throughput, multi-parameter data on marker expression across thousands of cells in a population [74] [75].
- Immunostaining (ICC/IHC) is a microscopy-based technique used to visualize antigen location within cells on a culture plate (ICC) or within tissue sections (IHC). It provides qualitative or semi-quantitative data on the spatial distribution of markers within a sample [75].
Q2: When should I use flow cytometry versus immunostaining to assess differentiation?
Your choice depends on the research question.
- Use Flow Cytometry when you need quantitative data on the percentage of cells expressing specific markers, to assess population homogeneity, or to sort sub-populations for downstream applications [74] [76]. It is ideal for routine, quantitative assessment of differentiation efficiency.
- Use Immunostaining when you need to confirm co-localization of markers within the same cell, observe cellular or tissue morphology, or analyze complex structures like 3D organoids [28] [3]. IHC is essential for analyzing teratomas, a traditional in vivo assay for pluripotency [77].
Q3: Can these techniques be used together?
Absolutely. They are highly complementary. For instance, immunostaining can first identify promising markers and spatial patterns in a sample, which can then be quantified at a population level using flow cytometry [78]. A 1998 study on colorectal cancer found that flow cytometry was superior for detecting low-abundance antigens, while the techniques complemented each other for comprehensive analysis [78].
Troubleshooting Guides
Common Issues in Flow Cytometry
| Problem Area | Specific Problem | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Sample Preparation | High cell death/clumping; Low event rate | Over-digestion during dissociation; Mechanical stress; Improper filtering | Optimize enzymatic dissociation cocktail and time for your cell type [78]; Use gentle pipetting; Filter cells through a fine mesh (e.g., 40-70µm) before analysis. |
| Staining | High background/noise; No signal | Antibody concentration too high/low; Inadequate permeabilization; Fluorophore degradation | Perform a titration experiment for each antibody; Validate permeabilization buffer for intracellular targets (e.g., transcription factors); Protect fluorophores from light. |
| Data Analysis | High variability between replicates; Inconsistent gating | Uncontrolled cell seeding density; Gating strategy subjectivity | Standardize initial cell seeding numbers [28]; Establish and document a consistent gating strategy using appropriate negative controls (e.g., FMO, isotype). |
| Differentiation-Specific | Low expression of target differentiation marker | Differentiation protocol did not work; Marker not specific for the cell type | Include a positive control (e.g., a well-differentiated cell line); Validate markers for your specific protocol and cell type, as some recommended markers can be non-specific [79]. |
Common Issues in Immunostaining (ICC/IHC)
| Problem Area | Specific Problem | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Staining | High background fluorescence; Non-specific staining | Antibody cross-reactivity; Inadequate blocking; Over-fixation | Optimize antibody dilution; Use a blocking buffer (e.g., with serum, BSA) for 1 hour; Titrate fixation time and concentration. |
| Signal | Weak or no signal | Under-fixation; Low antibody concentration; Epitope masked | Ensure fresh fixative is used; Increase primary antibody concentration and/or incubation time; Include an antigen retrieval step. |
| Microscopy & Analysis | Poor morphology; Inconsistent quantification | Photobleaching; Non-standardized imaging settings | Use an anti-fade mounting medium; Capture all images for an experiment using identical microscope settings (exposure, gain); Use automated image analysis software for objectivity. |
| Differentiation-Specific | Failure to detect mature tissue structures in teratomas | Assay protocol variation; Insufficient differentiation time | Standardize implantation site (e.g., subcutaneous vs. kidney capsule) and cell number [77]; Allow adequate time (often 8-12 weeks) for complex tissue formation [77]. |
Optimized Markers for Stem Cell Characterization
Selecting the correct markers is critical. A 2024 study reassessed marker genes using long-read sequencing and found that many traditionally recommended markers show overlapping expression or lack specificity for directed differentiation protocols [79]. The tables below summarize validated markers for different states.
Table 1: Key Markers for Pluripotency and Germ Layers
| Cell State | Marker | Type | Key Function / Specificity | Notes |
|---|---|---|---|---|
| Pluripotency | NANOG | Transcription Factor | Core pluripotency network regulator [79] | Validated as a unique marker for pluripotency state [79]. |
| OCT-4 (POU5F1) | Transcription Factor | Core pluripotency network regulator [3] | Standard marker; high levels in undifferentiated cells. | |
| SSEA-4 | Cell Surface Glycolipid | Pluripotency-associated surface antigen [79] | Useful for live-cell sorting and flow cytometry. | |
| Ectoderm | PAX6 | Transcription Factor | Eye, brain, and neural tube development [79] | Validated as a unique marker for ectoderm [79]. |
| HES5 | Transcription Factor | Notch signaling effector; neural progenitor cells [79] | Validated as a unique marker for ectoderm [79]. | |
| Mesoderm | APLNR (APJ) | G-Protein Coupled Receptor | Early mesoderm and cardiovascular development [79] | Validated as a unique marker for mesoderm [79]. |
| HAND1 | Transcription Factor | Cardiogenesis and trophoblast differentiation [79] | Validated as a unique marker for mesoderm [79]. | |
| T/Brachyury | Transcription Factor | Early mesoderm formation [79] | Classic marker, but expression is transient. | |
| Endoderm | CER1 | Secreted Factor | Anterior primitive streak and endoderm specification [79] | Validated as a unique marker for endoderm [79]. |
| GATA6 | Transcription Factor | Definitive endoderm and hepatic specification [79] | Validated as a unique marker for endoderm [79]. | |
| SOX17 | Transcription Factor | Definitive endoderm formation [79] | Standard marker for definitive endoderm. |
Table 2: Markers for Specific Differentiated Cell Lineages
| Cell Lineage | Marker | Type | Key Function / Specificity |
|---|---|---|---|
| Cardiomyocytes | TNNT2 / cTNT | Structural Protein | Cardiac Troponin T; contractile apparatus [76] |
| MLC2v | Structural Protein | Myosin Light Chain 2, ventricular isoform [76] | |
| Liver Progenitors | FOXA2 | Transcription Factor | Definitive endoderm and hepatic progenitor fate [3] |
| Myogenic Lineage | MYOD1 | Transcription Factor | Master regulator of myogenic differentiation [28] |
| Myosin Heavy Chain (MHC) | Structural Protein | Contractile protein of muscle cells [28] |
Experimental Workflows
Workflow 1: Assessing Differentiation Efficiency
The following diagram outlines a generalized workflow for assessing stem cell differentiation using key techniques.
Workflow 2: Marker Validation for Quality Control
This diagram illustrates a modern, qPCR-based workflow for enhanced quality control of stem cell populations, as identified in recent research [79].
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and materials essential for experiments involving stem cell differentiation and characterization.
| Item | Function / Application | Example in Context |
|---|---|---|
| Small Molecules & Growth Factors | Direct cell fate by activating or inhibiting specific signaling pathways during differentiation. | CHIR99021 (Wnt agonist for mesendoderm induction [3]), Activin A (for definitive endoderm specification [3]), Retinoic Acid (for patterning, e.g., foregut [3]). |
| Extracellular Matrix (ECM) | Provides a physiological substrate for cell attachment, growth, and organization, crucial for 2D and 3D culture. | Matrigel (used for coating plates for hiPSC culture and as a scaffold for 3D organoid formation [3]). |
| Validated Antibody Panels | Detect specific protein markers for pluripotency and differentiation via flow cytometry and immunostaining. | Antibodies against NANOG (pluripotency), PAX6 (ectoderm), SOX17 (endoderm), TNNT2 (cardiomyocytes) [3] [79] [76]. |
| Reporter Cell Lines | Enable real-time, non-destructive monitoring of specific cell populations based on marker expression. | MYF5-tdTomato reporter hiPSCs used to track muscle stem cell differentiation and sort populations [28]. |
| qPCR Assays | Quantitative, sensitive measurement of gene expression for validated marker genes. | Used in standardized quality control pipelines like hiPSCore to assess pluripotency and germ layer marker expression [79]. |
Mastering flow cytometry and immunostaining is fundamental to optimizing stem cell differentiation protocols. By selecting validated, specific markers, following standardized protocols, and understanding how to troubleshoot common pitfalls, researchers can generate reliable, reproducible, and quantitative data on differentiation efficiency. The integration of modern techniques, like machine learning-based scoring of qPCR data [79] and non-destructive image-based prediction models [28], represents the future of robust stem cell quality control, accelerating progress in regenerative medicine and drug development.
FAQs on Core Functional Assays
Q1: What are the key functional assays for evaluating hematopoietic stem and progenitor cells (HSPCs), and how do they compare? Two primary assays for evaluating HSPC functionality are the in vitro colony-forming unit (CFU) assay and the in vivo mouse engraftment study [80]. The CFU assay is a clonal assay that measures the growth and frequency of functionally viable HSPCs and their ability to differentiate into mature cells of specific lineages found in normal peripheral blood [80]. While the in vivo engraftment study is considered the gold standard for assessing long-term engraftment potential, the CFU assay is a quantitative in vitro assay that correlates strongly with engraftment potential in patients and is recommended for evaluating the quality and potency of HSPCs in cell therapy products [80].
Q2: Why is the CFU assay recommended for potency assessment of cell therapy products by regulatory bodies? The U.S. Food and Drug Administration (FDA) recommends that potency assays for cell therapy products demonstrate product activity, have a quantitative readout, and indicate product stability and consistency [80]. The CFU assay meets these requirements as it demonstrates the functional activity of HSPCs (their ability to proliferate and differentiate), provides quantitative data on colony numbers and types, and can be used to monitor product quality over time [80]. Viability alone is not accepted as a sole measure of efficacy, making the functional data from CFU assays crucial [80].
Q3: How do HSPCs from different sources compare in CFU assay performance? The three main sources of primary CD34+ HSPCs are cord blood (CB), bone marrow (BM), and mobilized peripheral blood (mPB) [80]. Their performance varies significantly. Research shows that CB engraftment can be 5- to 10-fold higher per CD34+ input cell compared to BM [80]. Furthermore, CD34+ cells derived from pluripotent stem cell (PSC) cultures, such as induced pluripotent stem cells (iPSCs), are not functionally identical to those from adult sources. The total CFU frequency and lineage progenitor frequency are often lower for PSC-derived CD34+ cells, and not all lineages may be represented [80].
Q4: My MethoCult cultures are drying out or appear runny. What could be the cause? Dehydration is commonly caused by improper culture setup, specifically not using water dishes in the incubator or low humidity [81]. Dehydrated cultures appear speckled or cracked and may have a grainy gradient from one edge [81]. Runny media and floating or smearing colonies can result from several issues: inadequately mixed MethoCult before dispensing, adding overly large volumes of cells or components that dilute the medium's viscosity, or insufficient mixing of cells with the medium before plating [81]. Maintaining high humidity (≥95%) and following precise preparation protocols is essential.
Q5: Why are my CFU assay triplicate counts uneven, and how can I improve reproducibility? Uneven colony counts in replicates are most frequently due to incorrect vortexing of the cell-MethoCult mixture [81]. After adding cells to the MethoCult medium, it is critical to vortex the mixture for at least four seconds to ensure equal cell distribution before dispensing it into culture dishes [81]. Consistent and thorough mixing is key to achieving reproducible results.
Troubleshooting Guides
Troubleshooting Common CFU Assay Problems
Table 1: Common Issues and Solutions in the CFU Assay
| Problem | Potential Causes | Solutions |
|---|---|---|
| Runny medium / streaming colonies [81] | - Medium not thoroughly mixed post-thaw- Excessive volume of added cells/components- Tubes not mixed well before plating | - Mix thawed medium vigorously before use- Ensure cell suspension is concentrated (10X) to minimize added volume- Vortex cell-medium mix thoroughly |
| Culture dehydration [81] | - Low incubator humidity- No water dishes used | - Maintain ≥95% humidity- Always place open water dishes in incubator |
| Uneven colony distribution [81] | - Inadequate vortexing of cell-medium mixture | - Vortex for at least 4 seconds after adding cells- Ensure homogeneous mixture before plating |
| Yellow/violet medium after thawing [81] | - pH shift during transport/storage | - The medium is typically still usable. Performance is unaffected if stored correctly and used before expiry. pH will adjust in incubator with 5% CO₂ [81]. |
| Low or no colony growth | - Overplating or underplating cells- Incorrect cell concentration- Non-viable cells | - Plate a range of 2-3 cell concentrations to find the linear range [81]- Use a recommended viability stain (e.g., 7AAD) to assess cell health [81] |
| Excessive background, grainy appearance [81] | - High presence of red blood cells (RBCs) in sample | - Deplete RBCs from the cell sample before assay setup [81] |
Quantitative Data for Assay Design
Table 2: Key Quantitative Parameters for Functional Assays
| Parameter | Typical Range / Value | Application Note |
|---|---|---|
| CFU Assay Plating [81] | Plate 2-3 cell concentrations within a recommended range | Prevents overplating (causes nutrient depletion, counting errors >100 colonies/dish) or underplating (statistically inaccurate data) [81]. |
| Human HSPC Engraftment Success [80] | >500 neutrophils/μL & >50,000 platelets/μL blood | Defined as transfusion-independent engraftment in humans post-transplant [80]. |
| VCA Preservation Window [82] | 4-6 hours | Viability window for Vascularized Composite Allografts using static cold storage [82]. |
| iPSC to Endothelial Cell Efficiency [83] | >99% CD31+ CD144+ cells in 5 days | Achieved with optimized, inducible ETV2 overexpression protocol without cell sorting [83]. |
Essential Experimental Protocols
Protocol: Standard CFU Assay Setup
Principle: This protocol enables the quantification of functionally viable hematopoietic stem and progenitor cells (HSPCs) based on their ability to form clonal colonies in a semi-solid medium [80].
Materials:
- MethoCult Medium: A semi-solid methylcellulose-based medium supplemented with cytokines and supplements (e.g., MethoCult H4034 Optimum for human cells) [81].
- Cells: Bone marrow (BM), cord blood (CB), peripheral blood mononuclear cells (PB MNCs), or purified CD34+ cells [81].
- Culture Dishes: 35 mm low-adherence petri dishes [81].
- Dispensers: 3 mL or 6 mL syringes with 16-gauge blunt-end needles [81].
- Other: CO₂ incubator (maintained at ≥95% humidity), inverted microscope.
Procedure:
- Thaw and Prepare MethoCult:
- Thaw the frozen MethoCult medium bottle overnight at 2-8°C or for 1-2 hours at room temperature. Do not thaw at 37°C as this can cause lumps [81].
- Once thawed, mix the bottle vigorously for 1-2 minutes to ensure a homogeneous solution [81].
- Dispense the required volume (e.g., 3 mL for duplicates, 4 mL for triplicates) into tubes using a syringe with a blunt-end needle. Avoid serological pipettes for inaccurate dispensing [81].
Prepare Cell Suspension:
Mix Cells and Medium:
Plate Cultures:
Culture and Incubate:
Score and Identify Colonies:
- After the incubation period, count and classify colonies based on their distinct morphology using an inverted microscope [81] [80].
- BFU-E (Burst-Forming Unit-Erythroid): Large, diffuse colonies composed of small, red-colored erythroblasts [80].
- CFU-GM (Colony-Forming Unit-Granulocyte/Macrophage): Colonies of larger, clear and shiny granulocytes and/or macrophages [80].
- CFU-GEMM (Colony-Forming Unit-Granulocyte, Erythrocyte, Monocyte, Megakaryocyte): Large colonies containing a mixture of myeloid and erythroid cells [80].
Protocol: Antibody Validation for Flow Cytometry
Principle: To confirm the specificity and performance of an antibody for flow cytometry in a specific experimental setup, ensuring accurate and reproducible data [84].
Materials:
- Antibody of interest.
- Validated positive and negative control cell lines or samples.
- Flow cytometry buffer, viability dye.
- (Optional) siRNA/shRNA for knockdown, CRISPR/Cas9 for knockout, or expression plasmids for overexpression.
Procedure:
- Knockout/Knockdown Validation:
- Use CRISPR/Cas9 to create a full knockout of the target gene or RNAi (siRNA/shRNA) for transient knockdown in a relevant cell line [84] [85].
- Confirm the loss of target protein expression via Western blot or RT-qPCR [84].
- Stain the knockout/knockdown cells and the wild-type control cells with the antibody. A specific antibody will show a significant reduction or loss of signal in the modified cells compared to the control [84].
Orthogonal Correlation:
- Use cell lines or mixed cell populations (e.g., PBMCs) with known, varying expression levels of the target protein, as determined by independent methods like RNA sequencing or proteomics [85].
- Correlate the flow cytometry staining intensity from your antibody with the expected expression levels from the orthogonal data. The antibody staining should reflect the known expression differences [85].
Overexpression Validation:
- Transiently transfect a cell line (preferably one with no endogenous target expression) with an expression plasmid for the target protein, often fused to a tag like GFP [85].
- The antibody should show strong staining in transfected cells compared to non-transfected controls. This is useful for confirmation but does not validate performance at endogenous expression levels [85].
Use of Validated Resources:
- Consult databases from organizations like the Human Cell Differentiation Molecules (HCDM), which run HLDA workshops to characterize and validate antibodies against CD markers [85]. Using antibody clones approved in these workshops can save time and resources.
Signaling Pathways and Experimental Workflows
CFU Assay Experimental Workflow
Antibody Validation Strategy for Flow Cytometry
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Functional Validation
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| MethoCult Media [81] [80] | Semi-solid medium for CFU assays. Supports clonal growth and differentiation of HSPCs. | Choose formulation optimized for species and cell source (e.g., H4034 Optimum for human BM, CB, PB MNCs). Contains pre-qualified serum and cytokines [81]. |
| Low-Adherence Culture Dishes [81] | Prevents cell attachment for proper colony formation in semi-solid media. | Essential because adherent cells (e.g., fibroblasts) can inhibit colony growth and obscure visualization [81]. |
| Blunt-End Needles & Syringes [81] | Accurate dispensing of viscous methylcellulose media. | Serological pipettes are not recommended due to inaccurate volume dispensing and medium adherence to pipette walls [81]. |
| Validated Flow Cytometry Antibodies [84] [85] | Identification and characterization of cell surface and intracellular markers. | Requires application-specific validation (e.g., via knockout, knockdown, orthogonal correlation) to ensure specificity and reproducibility [84]. |
| Inducible Transcription Factor Systems [83] | Overexpression of master regulators (e.g., ETV2, SOX17) to efficiently drive differentiation. | Enables rapid, high-yield differentiation of PSCs to target cells (e.g., >99% pure endothelial cells in 5 days) [83]. |
| Machine Perfusion Systems [82] | Ex vivo preservation of tissues and organs for transplantation research. | Mitigates ischemic damage compared to static cold storage, prolonging viability and enabling better assessment of graft quality [82]. |
This technical support center resource is designed to assist researchers and drug development professionals in optimizing transduction methods for stem cell differentiation efficiency. The following guides and data address common experimental challenges, providing troubleshooting advice and detailed protocols to enhance the reproducibility and safety of your work. The information is framed within the broader context of stem cell research, emphasizing the critical role of efficient and safe gene delivery in developing advanced therapeutic applications.
The choice of transduction method significantly impacts experimental outcomes and therapeutic safety. The tables below summarize key quantitative data for comparing efficiency and safety profiles.
Table 1: Comparative Transduction Efficiency and Processing Data
| Method/Platform | Transduction Efficiency | Process Time | Vector Consumption | Key Application Notes |
|---|---|---|---|---|
| Transduction Boosting Device (TransB) | ~0.5 to 0.7-fold increase vs. 24-well plate [86] | 1-fold decrease vs. conventional methods [86] | 3-fold reduction vs. conventional methods [86] | Scalable, automated, closed-system for T cells [86] |
| Lumbar Puncture (LP) - AAV9 | Effective CNS transduction, even with pre-existing anti-AAV9 antibodies [87] | N/A | Enables lower doses vs. intravenous [87] | Targets CNS; circumvents pre-existing immunity [87] |
| Intracerebroventricular (ICV) - AAV9 | Robust GFP expression in hippocampus and fimbria [88] | N/A | N/A | Effective for direct CNS targeting [88] |
| Intra-arterial (IA) - AAV9 | Moderate transduction in CNS and peripheral tissues [88] | N/A | N/A | Balanced CNS and peripheral distribution [88] |
| Intravenous (IV) - AAV9 | Limited CNS penetration; robust expression in liver and lungs [88] | N/A | N/A | Widespread peripheral distribution [88] |
Table 2: Key Safety and Profiling Endpoints
| Assessment Category | Specific Endpoints & Findings | Relevant Method |
|---|---|---|
| Immunogenicity & Humoral Response | Anti-AAV9 pre-existing antibodies; humoral response to viral capsid and transgene [87] | AAV9 via Lumbar Puncture [87] |
| Clinical Pathology | Differences in liver enzyme activities [87] | AAV9 via Lumbar Puncture [87] |
| Histopathology | Tissue changes observed [87] | AAV9 via Lumbar Puncture [87] |
| Biomarker Analysis | Altered levels of 276 neural injury, organ damage, and inflammatory protein markers in serum and CSF [87] | AAV9 via Lumbar Puncture [87] |
| Tumorigenicity Risk | Risk of malignant transformation; analyzed via in vitro methods and in vivo models in immunocompromised animals [89] | Pluripotent Stem Cell Therapies [89] |
| Biodistribution | Tracking via quantitative PCR and imaging (PET, MRI) [89] | General for Cell Therapies [89] |
Experimental Protocols for Key Transduction Methods
Protocol: T Cell Transduction Using the TransB Device
This protocol details the use of the novel TransB platform for efficient lentiviral transduction of human T cells [86].
Key Materials:
- Donor PBMCs: Source of primary T cells.
- Lentiviral Vector: e.g., Lenti-CMV-GFP-Puro.
- TransB Device: An automated, closed-system platform with a hollow fiber.
- Cell Culture Medium: RPMI-1640 supplemented with 10% FBS and 2 mM L-glutamine.
- T Cell Activator: ImmunoCult Human CD3/CD28/CD2 T Cell Activator.
- Recombinant Human IL-2
Procedure:
- T Cell Preparation and Activation: Thaw and culture donor PBMCs in complete medium. Activate cells using CD3/CD28/CD2 T Cell Activator (25 µl/ml) and IL-2 (50 IU/ml) for 3 days prior to transduction [86].
- Prepare Cell-Virus Mixture: On the day of transduction (Day 0), premix the activated PBMCs with the lentiviral vector at the desired Multiplicity of Infection (MOI), defined as virus volume-to-cell volume ratio [86].
- Load the TransB Device: Introduce the cell-virus mixture (e.g., 200 µl) into the intracapillary (IC) space of the hollow fiber in the TransB device [86].
- Transduction Incubation: Place the loaded device in a 37°C, 5% CO₂ incubator. During the incubation, the device's pump system continuously perfuses IL-2-supplemented complete culture medium through the extracapillary (EC) space at a low flow rate (e.g., 0.1 mL/min). This step can be significantly shorter than static incubation [86].
- Harvest Cells: After transduction (e.g., Day 1), harvest cells by flushing both the IC and EC spaces of the hollow fiber with complete culture medium [86].
- Post-Transduction Culture: Centrifuge the harvested medium, resuspend the cell pellet, and seed the cells into a culture plate (e.g., at 1 × 10⁶ cells/mL). Culture for an additional 3-4 days before analysis [86].
- Analysis: On Day 4, assess transduction efficiency (e.g., via GFP expression by flow cytometry), cell count, viability, and phenotype (e.g., CD3 staining) [86].
Protocol: Assessing AAV9 Transduction in Non-Human Primates via Lumbar Puncture
This methodology outlines the delivery of AAV9 vectors into the cerebrospinal fluid (CSF) of cynomolgus macaques to evaluate CNS transduction efficiency and safety, particularly in the context of pre-existing immunity [87].
Key Materials:
- AAV9 Vector: e.g., AAV9-GFP.
- Experimental Model: Juvenile cynomolgus macaques, with and without pre-existing serum anti-AAV9 antibodies.
- Delivery System: Equipment for lumbar puncture (LP).
- Assay Kits: For clinical pathology (e.g., liver enzymes) and proteomic analysis.
- Tissue Fixation and Staining Reagents: For histopathology.
Procedure:
- Vector Administration: Administer the AAV9-GFP vector via lumbar puncture at a defined dose (e.g., 5.0 × 10¹³ vg/mL) to juvenile cynomolgus macaques. Include groups with and without pre-existing anti-AAV9 antibodies [87].
- Observation Period: Monitor animals for a defined study duration (e.g., 28 days) [87].
- Tissue Collection and Analysis: At the endpoint, survey CNS and peripheral tissues for:
- Safety and Immune Response Profiling:
- Histopathology: Perform macroscopic and microscopic examination of tissues [87].
- Clinical Pathology: Analyze blood for parameters like liver enzyme activities [87].
- Humoral Immune Response: Measure antibody responses against the viral capsid and the transgene product [87].
- Proteomic Analysis: Analyze serum and CSF samples using multiplex assays for biomarkers of neural injury, organ damage, and inflammation [87].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Transduction Experiments
| Reagent/Material | Function in Experiment | Example Use Case |
|---|---|---|
| Lentiviral Vectors (e.g., Lenti-CMV-GFP) | Stable gene delivery and expression in dividing and non-dividing cells. | Genetic modification of T cells for CAR-T therapy manufacturing [86]. |
| Adeno-Associated Virus 9 (AAV9) | In vivo gene delivery with broad tropism, particularly for CNS targets. | Preclinical gene therapy studies targeting the central nervous system via ICV, IA, or IV injection [87] [88]. |
| T Cell Activator (CD3/CD28/CD2) | Polyclonal activation and expansion of T cells ex vivo. | Essential pre-step to activate T cells prior to transduction, improving transduction efficiency and cell growth [86]. |
| Recombinant Human IL-2 | T cell growth factor that promotes proliferation and survival. | Added to culture medium during and after T cell activation and transduction [86]. |
| Hollow Fiber (TransB Device) | Provides high surface-area-to-volume ratio to enhance cell-virus interactions. | Core component of the TransB platform, creating an optimized microenvironment for efficient viral transduction [86]. |
| Proteomic Biomarker Panels | Multiplexed measurement of protein markers for safety assessment. | Profiling neural injury, organ damage, and inflammatory responses in serum and CSF in preclinical studies [87]. |
Troubleshooting Guides and FAQs
FAQ 1: Our primary T cell transduction efficiency is consistently low with static culture methods. What are the main limitations of these methods, and what strategies can improve efficiency?
Answer: Conventional static incubation in cultureware often suffers from inefficient cell-virus interactions, leading to suboptimal transduction efficiency, particularly for hard-to-transduce cells like primary T cells. These methods also involve manual, open-system manipulations, increasing process variability and contamination risk [86].
Troubleshooting Steps:
- Consider Advanced Platforms: Evaluate scalable systems like the TransB device, which is designed to enhance cell-virus proximity and has demonstrated a 0.5 to 0.7-fold increase in transduction efficiency with a 3-fold reduction in vector consumption compared to 24-well plates [86].
- Optimize Activation: Ensure T cells are properly activated before transduction. Use a combination of CD3/CD28/CD2 activators and IL-2, and confirm cell viability and blast formation pre-transduction [86].
- Evaluate Alternative Methods: If new platforms are not accessible, consider optimizing spinoculation parameters (centrifugation speed and time) to enhance vector entry, though this method may have scalability limits [86].
FAQ 2: For in vivo studies, how does the route of administration for AAV vectors impact transduction efficiency and safety in the central nervous system (CNS)?
Answer: The administration route critically determines the biodistribution, transduction profile, and potential toxicity of AAV vectors [88].
Troubleshooting Guide:
- Goal: Robust & Widespread CNS Targeting
- Recommended Route: Intracerebroventricular (ICV) delivery.
- Rationale: ICV administration results in robust transgene expression in key brain regions like the hippocampus and fimbria [88].
- Goal: Balanced CNS & Peripheral Expression
- Recommended Route: Intra-arterial (IA) delivery.
- Rationale: IA delivery facilitates moderate transduction in both CNS and peripheral tissues [88].
- Goal: Minimizing CNS Exposure
- Recommended Route: Intravenous (IV) delivery.
- Rationale: IV administration leads to widespread peripheral organ transduction (e.g., liver, lungs) with limited CNS penetration [88].
- Safety Note: Lumbar puncture delivery of AAV9 can achieve CNS transduction while circumventing pre-existing immunity, but it is associated with differential safety endpoints, including changes in liver enzymes and histopathology, which must be monitored [87].
FAQ 3: What are the critical safety issues we must assess when translating stem cell-based therapies involving transduced cells, particularly for clinical trials?
Answer: Rigorous biosafety assessment is mandatory for clinical translation. Key risks include tumorigenicity, immunogenicity, and off-target biodistribution [89] [90].
Critical Safety Checklist:
- Tumorigenicity/Oncogenicity: Analyze the risk of malignant transformation using a combination of in vitro assays and in vivo models in immunocompromised animals. This is especially critical for therapies derived from pluripotent stem cells [89].
- Immunogenicity: Assess the potential for immune responses against the cellular product. This includes evaluating T-cell and NK-cell responses, cytokine release, and, for allogeneic therapies, ensuring appropriate HLA typing [89].
- Biodistribution: Track the movement, persistence, and fate of cells post-administration over time. This is typically done using quantitative PCR (for vector genomes or cellular DNA) and imaging techniques like PET or MRI [89].
- Cell Product Quality: Ensure final product sterility, identity, potency, viability, and genetic stability. Manufacturing must adhere to quality-by-design principles and evolving regulatory guidelines for cellular products [89] [90].
Workflow and Safety Assessment Visualizations
The following diagrams illustrate the comparative analysis workflow for transduction methods and the logical pathway for safety assessment.
Comparative Analysis Workflow
Safety Assessment Logic Pathway
This technical support center provides troubleshooting guides and FAQs to help researchers overcome common challenges in benchmarking the maturity of stem cell-derived cells against their native counterparts.
A critical step in optimizing stem cell differentiation protocols is rigorously assessing how closely the resulting cells resemble their in vivo counterparts. This process, known as benchmarking, ensures that the cells are functionally and molecularly mature enough for use in downstream applications like disease modeling, drug screening, or regenerative medicine. Effective benchmarking relies on a multi-omics approach, integrating data from transcriptomics, genomics, and functional assays to build a comprehensive maturity profile [91] [92] [93].
A common bottleneck, especially in complex models like brain organoids, is that extended culture periods are often needed to achieve late-stage maturation markers. Furthermore, prolonged culture can exacerbate issues like metabolic stress and central necrosis, leading to asynchronous tissue maturation where electrophysiologically active layers may coexist with degenerating cores [91]. The guides below are designed to help you navigate these challenges.
Troubleshooting Common Benchmarking Challenges
FAQ 1: My stem cell-derived cells express key marker genes, but their global transcriptomic profile still doesn't closely match native cells. What could be wrong?
This is a frequent challenge where targeted validation and global profiling yield different results. The issue often lies in the immaturity of fundamental cellular processes.
- Potential Cause: The cells may be focusing energy on differentiation pathways while downregulating essential "housekeeping" genes responsible for basic cellular homeostasis. This is a documented phenomenon in ageing brains, where genes involved in translation, metabolism, and intracellular transport are commonly downregulated across cell types [92].
- Solution:
- Expand Your Gene Panel: Move beyond a handful of lineage-specific markers. Incorporate a broader transcriptomic analysis using single-cell RNA sequencing (scRNA-seq) to assess the entire cellular population [93].
- Analyze Housekeeping Functions: Use your transcriptomic data to check the expression levels of genes involved in core cellular functions like ribosome formation, metabolism, and transport. Widespread downregulation in these pathways is a strong indicator of immaturity [92].
- Leverage Benchmarking Studies: Consult recent benchmarking studies that evaluate computational methods for clustering transcriptomic data. Algorithms like scDCC, scAIDE, and FlowSOM have been shown to perform well across different omics data types and can help in robustly identifying cell types and states based on your transcriptomic data [94].
FAQ 2: How can I non-destructively predict the final differentiation efficiency early in my long-term protocol?
Waiting for the end of a multi-month differentiation protocol to assess efficiency is time-consuming and resource-intensive. Non-destructive prediction methods can drastically optimize this process.
- Potential Cause: The morphological and molecular cues predictive of final efficiency are present at early stages but are not being captured or quantified [28].
- Solution: Implement a machine learning-based imaging system.
- Image Acquisition: Capture phase-contrast images of cells during the early or mid-phase of differentiation (e.g., days 14-38 in an 82-day protocol) [28].
- Feature Extraction: Use computational methods like the Fast Fourier Transform (FFT) to convert images into a rotation-invariant, quantitative feature vector that captures cell morphology characteristics [28].
- Classification: Train a machine learning classifier (e.g., a Random Forest model) on these extracted features to predict samples that will ultimately have high or low differentiation efficiency. This allows for early intervention or selection of the best cultures weeks before the protocol ends [28].
FAQ 3: My brain organoids show mixed maturity profiles—some markers are present, but others are absent. How can I standardize their assessment?
Brain organoids are notorious for developing asynchronously, with mature superficial layers often surrounding a necrotic core [91].
- Potential Cause: Microenvironmental limitations, particularly inadequate nutrient and oxygen diffusion into the organoid's core, create metabolic stress that impedes uniform maturation [91].
- Solution: Adopt a multidimensional assessment framework and consider bioengineering interventions.
- Standardize Multi-Modal Metrics: Do not rely on a single metric. Systematically evaluate your organoids across multiple dimensions as outlined in the table below [91]:
- Improve the Culture System: To overcome microenvironmental limitations, explore advanced culture methods such as bioreactors, vascularized co-cultures, or microfluidic devices to enhance nutrient delivery and waste removal, promoting more uniform growth and maturation [91].
Table 1: Multidimensional Framework for Assessing Brain Organoid Maturity
| Assessment Dimension | Key Benchmarks | Common Techniques |
|---|---|---|
| Structural Architecture | Cortical lamination (e.g., SATB2, TBR1), synaptic proteins (e.g., PSD-95, SYB2), barrier formation (e.g., glia limitans) [91] | Immunofluorescence (IF), Immunohistochemistry (IHC), Electron Microscopy (EM) [91] |
| Cellular Diversity | Presence of neurons (NEUN, MAP2), astrocytes (GFAP, S100β), and oligodendrocytes (MBP, O4) [91] | IF, IHC, Fluorescence-Activated Cell Sorting (FACS) [91] |
| Functional Maturation | Synchronized neuronal network activity, action potentials, calcium transients [91] | Multielectrode Arrays (MEA), Calcium Imaging, Patch Clamp [91] |
| Molecular Profiling | Transcriptomic signatures of mature neuronal and glial subtypes, postnatal transcriptional programs [91] | Single-cell RNA sequencing (scRNA-seq) [91] [93] |
Experimental Protocols for Key Benchmarking Experiments
Protocol: Transcriptomic Benchmarking Using Single-Cell RNA Sequencing
This protocol outlines a standard workflow for comparing your stem cell-derived cells to a native reference dataset using scRNA-seq [95] [93].
- Sample Preparation: Generate your stem cell-derived cells and secure a reference dataset of native cells (e.g., from a public repository or processed in parallel).
- Single-Cell Library Preparation: Use a platform like the 10x Genomics Chromium to create barcoded scRNA-seq libraries.
- Sequencing and Quality Control (QC): Sequence the libraries and perform rigorous QC. Filter out low-quality cells, high mitochondrial read counts, and doublets.
- Data Integration and Clustering: Use a tool like Seurat to normalize the data, identify highly variable genes, and scale the dataset. Integrate your stem cell-derived data with the native reference dataset to correct for technical batch effects [95]. Perform linear dimensionality reduction (PCA) and cluster the cells using graph-based methods (e.g., Louvain, Leiden) [94].
- Differential Expression and Interpretation: Identify differentially expressed genes (DEGs) between your clusters and the native reference clusters. Perform gene ontology (GO) enrichment analysis on the DEGs to identify which biological processes are dysregulated [95].
Protocol: Early Prediction of Differentiation Efficiency via Imaging and ML
This protocol is adapted from a study on predicting muscle stem cell (MuSC) differentiation [28].
- Hypothesis and Timing: Based on preliminary data (e.g., qPCR or ICC), identify an early time window where marker expression correlates with final efficiency. For example, in an 82-day MuSC protocol, days 14-38 were predictive [28].
- Image Acquisition: In multiple independent differentiation experiments, capture high-quality phase-contrast images of cells within the predictive time window.
- Feature Extraction with FFT: For each image, apply a 2D Fast Fourier Transform (FFT) to obtain its power spectrum. Perform shell integration on the power spectrum to generate a 100-dimensional, rotation-invariant feature vector that describes the image's morphological properties [28].
- Model Training and Prediction: Label your samples based on their final, experimentally confirmed differentiation efficiency (e.g., "High" vs. "Low"). Use these labels and the extracted feature vectors to train a Random Forest classifier. Validate the model's accuracy on a held-out test set of images [28].
Research Reagent Solutions
Table 2: Essential Materials for Benchmarking Experiments
| Item | Function / Explanation | Example(s) |
|---|---|---|
| scRNA-seq Platform | High-resolution profiling of transcriptional states in individual cells to assess heterogeneity and identity. | 10x Genomics Chromium [93] |
| Spatial Transcriptomics | Preserves the spatial context of RNA expression within a tissue section, crucial for assessing structural organization. | MERFISH [92] |
| Flow Cytometry Antibodies | Quantifies protein expression of key undifferentiated stem cell or lineage-specific markers at the population level. | Antibodies against NANOG, SSEA4 [47] |
| Clustering Algorithms | Computational tools to identify distinct cell populations from scRNA-seq data. | scDCC, scAIDE, FlowSOM [94] |
| Data Integration Tools | Software packages for analyzing and integrating single-cell data, especially for comparing to reference datasets. | Seurat [95] |
| Machine Learning Libraries | For building predictive models from imaging or other high-dimensional data (e.g., in Python or R). | Scikit-learn (for Random Forest) [28] |
Visualization of Workflows
Experimental and Computational Benchmarking Pipeline
This diagram illustrates the integrated workflow for benchmarking stem cell-derived models, combining wet-lab experiments with computational analysis.
Transcriptomic Data Analysis Pipeline
This diagram details the key steps and decisions in the computational analysis of scRNA-seq data for benchmarking.
Conclusion
Optimizing stem cell differentiation efficiency is a multifaceted endeavor that hinges on a deep understanding of developmental biology, the application of robust and standardized protocols, and the strategic adoption of advanced technologies like AI and machine learning. The integration of non-destructive, image-based prediction models can dramatically accelerate protocol development and quality control, addressing the critical challenge of long differentiation timelines. Moving forward, the field must focus on enhancing the functional maturity of differentiated cells, improving the scalability of production for clinical applications, and establishing universally accepted benchmarking standards. By converging foundational knowledge with cutting-edge computational tools, researchers can unlock the full potential of stem cells for transformative advances in regenerative medicine, precise disease modeling, and drug discovery.
References
- 1. Systems biology of stem cells: three useful perspectives to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3130416/]
- 2. A pluripotent stem cell atlas of multilineage differentiation [https://www.nature.com/articles/s41597-025-05549-w]
- 3. The Optimization of a Protocol for the Directed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189164/]
- 4. Hierarchical micro-nano topographies to control Bacteria ... [https://www.nature.com/articles/s41598-025-08415-2]
- 5. Signaling Pathways Governing Cardiomyocyte Differentiation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11202427/]
- 6. Cross-activation of FGF, NODAL, and WNT pathways ... [https://www.sciencedirect.com/science/article/pii/S2211124723004497]
- 7. Wnt signaling pathways in biology and disease [https://www.nature.com/articles/s41392-025-02142-w]
- 8. Temporal Control of the WNT Signaling Pathway During ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.714008/full]
- 9. The roles and regulatory mechanisms of TGF-β and BMP ... [https://www.nature.com/articles/s41422-023-00918-9]
- 10. Review BMP signaling and stem cell regulation [https://www.sciencedirect.com/science/article/pii/S0012160605003015]
- 11. FGF Signaling Pathway: A Key Regulator of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7040165/]
- 12. Roles of FGF signaling in stem cell self-renewal ... [https://www.aging-us.com/article/100369/text]
- 13. Optimizing Nodal, Wnt and BMP signaling pathways for robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11182123/]
- 14. BMP signaling in mesenchymal stem cell differentiation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4725591/]
- 15. interconnected regulators of stem cell differentiation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11210451/]
- 16. Transcription factor competition allows embryonic stem cells to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4576702/]
- 17. Targeting epigenetic regulators as a promising avenue to ... [https://www.nature.com/articles/s41392-025-02266-z]
- 18. Iterative transcription factor screening enables rapid ... [https://www.nature.com/articles/s41467-025-59596-3]
- 19. A transcription factor atlas of directed differentiation [https://www.sciencedirect.com/science/article/pii/S0092867422014702]
- 20. Transcription Factor-Based Differentiation of Pluripotent ... [https://www.mdpi.com/2227-9059/13/11/2783]
- 21. Enhancer-driven gene regulatory networks reveal ... [https://www.sciencedirect.com/science/article/abs/pii/S1074761325001931]
- 22. Optimization of Transcription Factor-Driven Neuronal ... [https://pubmed.ncbi.nlm.nih.gov/39888571/]
- 23. REST Regulates Distinct Transcriptional Networks in ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.0060256]
- 24. Frequently Asked Questions on Primary Cells [https://www.stemcell.com/primary-cells-faq.html]
- 25. Primary Cell Culture Guide [https://www.atcc.org/resources/culture-guides/primary-cell-culture-guide]
- 26. Primary Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/primary-cell-culture-support/primary-cell-culture-support-troubleshooting.html]
- 27. A critical look: challenges in differentiating human pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7397816/]
- 28. Early and non-destructive prediction of the differentiation ... [https://www.nature.com/articles/s41598-025-11108-5]
- 29. Common pitfalls of stem cell differentiation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5002043/]
- 30. Practical choice for robust and efficient differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7477655/]
- 31. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 32. Cellartis iPS Cell to Hepatocyte Differentiation System FAQs [https://www.takarabio.com/learning-centers/stem-cell-research/stem-cell-faqs/cellartis-ips-cell-to-hepatocyte-differentiation-system-faqs?srsltid=AfmBOopZioUDay_yyDZEk6Vg4_Yy5ULxtQWH8mbdNKmDQ6sWQ4sR10dx]
- 33. Optimization of differentiation methods from various human ... [https://www.ahbps.org/journal/view.html?doi=10.14701/ahbps.2023S1.OP-6-5]
- 34. FAQs on Human Hepatic Organoid Cultures [https://www.stemcell.com/human-liver-organoid-faqs.html]
- 35. Organoid Experiments: 40 FAQs You Need to Know - Yeasen [https://www.yeasenbio.com/pt/blogs/organoid/organoid-experiments-40-faqs-you-need-to-know]
- 36. Using iPSCs to optimize human hepatic organoid ... [https://www.news-medical.net/health/How-to-optimize-human-hepatic-organoid-development-using-iPSCs.aspx]
- 37. Optimization of seeding density of OP9 cells to improve ... [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-024-00503-x]
- 38. Optimization of seeding cell density for differentiation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0301468125000374]
- 39. FAQ - Clinical MSCs [https://www.reprocell.com/clinical-stem-cell-services/faq-mscs]
- 40. Troubleshooting | Horizontal co-culture plate [https://i-coculture.com/troubleshooting/]
- 41. Two Methods for Establishing Primary Human Endometrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4207099/]
- 42. Optimization of seeding density of OP9 cells to improve ... [https://pubmed.ncbi.nlm.nih.gov/38523262/]
- 43. 3D vs 2D Cell Culture: Which Model Suits Your Lab in 2025? [https://www.pharmanow.live/knowledge-hub/research/3d-vs-2d-cell-culture-comparison]
- 44. 2D and 3D cell cultures – a comparison of different types of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6040128/]
- 45. 2D Versus 3D Cell Cultures: Advantages and Disadvantages [https://www.mimetas.com/en/blogs/315/2d-versus-3d-cell-cultures-advantages-and-disadvantages.html]
- 46. Leveraging 3D cell culture and AI technologies for next- ... [https://www.sciencedirect.com/science/article/pii/S3050562325000418]
- 47. Optimized, Efficient Measurement of the Expression ... [https://pubmed.ncbi.nlm.nih.gov/40028708/]
- 48. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 49. Protocol for differentiation of human pluripotent stem cells into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205342/]
- 50. Stem Cell Culture Guide [https://www.atcc.org/resources/culture-guides/stem-cell-culture-guide]
- 51. Combined small-molecule treatment accelerates ... [https://www.nature.com/articles/s41587-023-02031-z]
- 52. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 53. Engineering a controlled cardiac multilineage co ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04408-0]
- 54. Scaling Up and Differentiating hPSCs in 3D Suspension ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/03/12/scaling-up-and-differentiating-hpscs-in-3d-suspens]
- 55. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 56. AI-based approach to dissect the variability of mouse stem ... [https://www.nature.com/articles/s41467-025-56908-5]
- 57. Streamlining Differentiation with Non - Destructive AI-Based Imaging ... [https://www.cira.kyoto-u.ac.jp/e/pressrelease/news/250724-100000.html]
- 58. Early and non - destructive of the differentiation prediction ... efficiency [https://pubmed.ncbi.nlm.nih.gov/40702033/]
- 59. XPCIpy: A Python toolkit for X-ray phase-contrast imaging [https://opg.optica.org/oe/abstract.cfm?uri=oe-33-22-45949]
- 60. Smarter stem cells: how AI is supercharging iPSC technology [https://link.springer.com/article/10.1007/s00441-025-03999-7]
- 61. Guidelines for managing and using the digital phenotypes ... [https://www.sciencedirect.com/science/article/pii/S2213671124002479]
- 62. Harnessing AI and Machine Learning to Revolutionize Stem ... [https://www.openaccessjournals.com/articles/harnessing-ai-and-machine-learning-to-revolutionize-stem-cell-culture-and-differentiation-18355.html]
- 63. Artificial Intelligence Driven Innovation [https://www.mdpi.com/2306-5354/12/12/1302]
- 64. The Applications of Machine Learning in the Management ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11816169/]
- 65. Viral and Non-viral Vectors | Lentiviral, Adenoviral & AAV [https://www.thegenehome.com/how-does-gene-therapy-work/vectors]
- 66. Viral vs. Non-Viral Gene Delivery: A Critical Choice for ... [https://www.drugdiscoverynews.com/viral-vs-non-viral-gene-delivery-a-critical-choice-for-gene-therapy-developers-16819]
- 67. Viral and non-viral vectors in gene therapy: current state and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271757/]
- 68. Gene delivery systems explained. "Viral vs. Non ... [https://www.lqventures.com/gene-delivery-systems-explained-viral-vs-non-viral-vectors-debate/]
- 69. Strategies for genetic manipulation of adult stem cell- ... [https://www.nature.com/articles/s12276-021-00609-8]
- 70. Retroviral Vector Technology for Gene Therapy [https://www.sciencedirect.com/science/article/pii/S002228362500539X]
- 71. Delivery Approaches for Therapeutic Genome Editing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7597956/]
- 72. The Delivery Dilemma Looking Beyond Viral Vectors for ... [https://www.bioprocessintl.com/gene-therapies/the-delivery-dilemma-looking-beyond-viral-vectors-for-gene-therapy]
- 73. Hurdles to healing: Overcoming cellular barriers for viral ... [https://www.sciencedirect.com/science/article/pii/S0378517325003060]
- 74. Cytometry in Stem Cell Research and Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4293101/]
- 75. What are the differences between flow cytometry and ... [https://www.aatbio.com/resources/faq-frequently-asked-questions/what-are-the-differences-between-flow-cytometry-and-immunohistochemistry]
- 76. High efficiency differentiation of human pluripotent stem ... [https://pure.johnshopkins.edu/en/publications/high-efficiency-differentiation-of-human-pluripotent-stem-cells-t]
- 77. Evaluating Strategies to Assess the Differentiation Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762643/]
- 78. A comparison of flow cytometry and immunohistochemistry ... [https://pubmed.ncbi.nlm.nih.gov/9674894/]
- 79. Reassessment of marker genes in human induced ... [https://www.nature.com/articles/s41467-024-52922-1]
- 80. Six considerations when evaluating functionality of ... [https://www.regmednet.com/six-considerations-when-evaluating-functionality-of-hematopoietic-stem-and-progenitor-cells-in-cell-therapy-products/]
- 81. Frequently Asked Questions on Performing the CFU Assay [https://www.stemcell.com/frequently-asked-questions-cfu-assay.html]
- 82. Methods of ex vivo analysis of tissue status in vascularized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10492401/]
- 83. ETV2 Overexpression Promotes Efficient Differentiation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152468/]
- 84. Validation of Antibodies for Flow Cytometry [https://fluorofinder.com/antibody-validation/]
- 85. Antibody Validation for Flow Cytometry [https://blog.addgene.org/antibody-validation-for-flow-cytometry]
- 86. a novel transduction device for efficient and scalable gene ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06836-1]
- 87. Comparative assessment of the transduction efficiency and ... [https://pubmed.ncbi.nlm.nih.gov/39717225/]
- 88. Evaluation of AAV transduction efficiency via multiple ... [https://www.sciencedirect.com/science/article/pii/S0306452225002283]
- 89. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 90. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 91. Navigating Brain Organoid Maturation: From Benchmarking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383812/]
- 92. Single-cell transcriptomic and genomic changes in the ... [https://www.nature.com/articles/s41586-025-09435-8]
- 93. Advancements in single-cell RNA sequencing and spatial ... [https://www.frontierspartnerships.org/journals/acta-biochimica-polonica/articles/10.3389/abp.2025.13922/full]
- 94. Comparative benchmarking of single-cell clustering ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03719-y]
- 95. A practical guide for single-cell transcriptome data analysis ... [https://www.sciencedirect.com/science/article/pii/S0168010225000653]