Overcoming Immune Rejection in Allogeneic Stem Cell Transplantation: From Genetic Engineering to Clinical Applications
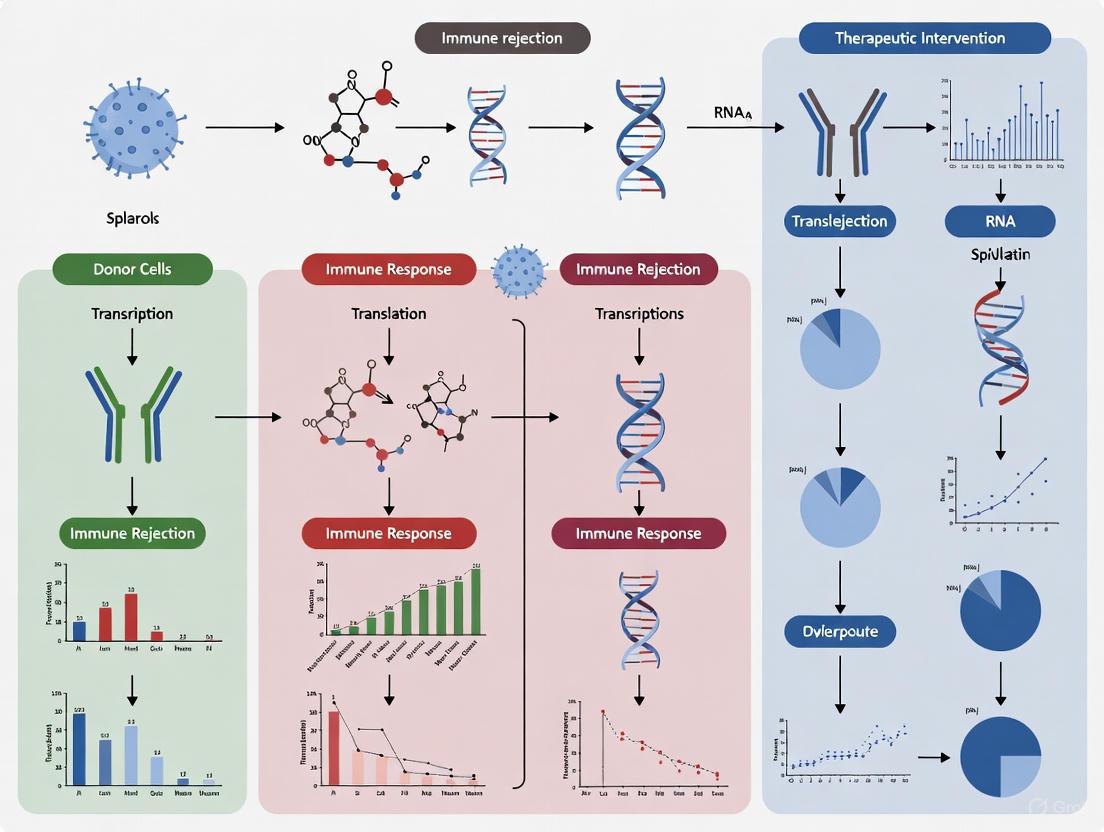
Allogeneic stem cell transplantation holds transformative potential for treating hematologic cancers and genetic disorders, but immune rejection remains a significant barrier to its broad application.
Overcoming Immune Rejection in Allogeneic Stem Cell Transplantation: From Genetic Engineering to Clinical Applications
Abstract
Allogeneic stem cell transplantation holds transformative potential for treating hematologic cancers and genetic disorders, but immune rejection remains a significant barrier to its broad application. This article provides a comprehensive analysis for researchers and drug development professionals, covering the foundational immunology of graft rejection, innovative methodological advances in genetic engineering and conditioning regimens, strategies for troubleshooting innate immunity and optimizing persistence, and a comparative validation of emerging clinical data. By synthesizing the latest preclinical and clinical evidence, this review outlines a path toward universally applicable, off-the-shelf cellular therapies that do not require lifelong immunosuppression.
Decoding the Immune Barriers: Mechanisms of Allograft Rejection
Troubleshooting Guides and FAQs
Frequently Asked Questions
FAQ 1: What are the primary immunological pathways responsible for allograft rejection? Allograft rejection is primarily driven by three pathways of allorecognition [1]:
- Direct Pathway: Donor Antigen-Presenting Cells (APCs) migrate to recipient lymphoid organs and present donor-derived peptide-MHC complexes directly to recipient T cells. This is a dominant pathway in early acute rejection.
- Indirect Pathway: Recipient APCs process and present donor-derived peptides on self-MHC molecules to recipient T cells. This pathway is particularly important for chronic rejection and humoral responses.
- Semi-direct Pathway: Recipient APCs acquire intact donor peptide-MHC complexes from donor cells via extracellular vesicles (e.g., exosomes), allowing a single APC to activate both direct and indirect pathway T cells.
FAQ 2: Why are strategies that induce tolerance in rodent models often ineffective in humans? A key reason is the difference in T-cell memory compartments [2]. Laboratory rodents are typically specific pathogen-free (SPF) and have a T-cell profile similar to human neonates, with a high naïve-to-memory T cell ratio. In contrast, adult humans have a large pool of memory T cells generated through pathogen exposure. These memory T cells, including those generated via heterologous immunity, are more resistant to tolerance induction protocols.
FAQ 3: What are the major immune barriers to 'off-the-shelf' allogeneic cell therapies? The efficacy of allogeneic cell therapies, such as CAR-T or CAR-NK cells, is limited by host versus graft and graft versus host reactions [3] [4]:
- Host T-cell-mediated Rejection: Host CD8+ T cells recognize mismatched HLA class I molecules on the donor cells and eliminate them.
- Host NK-cell-mediated Rejection: Host NK cells attack donor cells that lack "self" HLA class I molecules, a phenomenon known as the "missing-self" response.
- Graft-versus-Host Disease (GvHD): Donor T cells within the therapeutic product recognize alloantigens on host tissues and cause pathology.
- Humoral Rejection: Pre-existing or de novo generated donor-specific antibodies (DSAs) can mediate rejection via antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC).
FAQ 4: How does immune reconstitution after allogeneic hematopoietic stem cell transplantation (HSCT) influence clinical outcomes? The timing and quality of immune cell recovery post-HSCT are critical determinants of patient survival [5] [6]:
- Early Phase (First 100 days): Dominated by innate immunity and homeostatic peripheral expansion of memory T cells. Patients are highly susceptible to viral reactivations (e.g., CMV, EBV) and bacterial/fungal infections due to profound T-cell deficiency.
- Late Phase (Months to Years): Characterized by slow de novo generation of naïve T cells from the thymus and B cells from the bone marrow. Slow B-cell reconstitution and impaired class-switching lead to vulnerability to encapsulated bacteria and delayed humoral immunity.
Troubleshooting Common Experimental Challenges
Challenge 1: Overcoming Host Rejection of Allogeneic Cell Therapies Problem: Adoptively transferred allogeneic T or NK cells are rapidly cleared by the host immune system. Solution: Employ gene editing to modulate the immunogenicity of the donor cells [3] [4].
- Step 1: Knock out the T-cell receptor (TCR) alpha constant (TRAC) locus to prevent GvHD. For a dual approach, simultaneously knock in the CAR gene at this locus.
- Step 2: Knock out Beta-2-microglobulin (B2M) to eliminate surface expression of HLA class I and evade host T-cell recognition.
- Step 3: To prevent the ensuing "missing-self" NK cell attack, co-express a single-chain, non-polymorphic HLA-E variant in the B2M locus. HLA-E engages the inhibitory receptor NKG2A on NK cells, suppressing their activation.
- Step 4: For additional persistence, overexpress CD47 ("don't eat me" signal) to inhibit phagocytosis by host macrophages.
Experimental Workflow for Engineering Allogeneic Cell Therapies
Challenge 2: Poor T-cell Persistence and Function in the Tumor Microenvironment (TME) Problem: Adoptively transferred cells become dysfunctional or exhausted within the immunosuppressive TME. Solution: Engineer cells to resist key suppressive mechanisms [3].
- Step 1: Express a dominant-negative TGF-β receptor II (dnTGFβRII) to block the immunosuppressive TGF-β signal.
- Step 2: Introduce a PD1:CD28 switch receptor. This chimeric receptor converts the inhibitory PD-1 signal from tumor PD-L1 into a co-stimulatory CD28 signal.
- Step 3: Co-express cytokines like IL-15 or membrane-bound IL-12 to promote sustained activation and survival in a cytokine-poor TME.
Challenge 3: Inducing Transplant Tolerance in Pre-clinical Models with High Memory T-cell Load Problem: Tolerance protocols fail in immunologically experienced hosts, limiting translational relevance. Solution: Utilize murine models that better mimic the human immune state and employ regulatory cell therapy [2].
- Step 1: Use "dirty" mice (pet store-derived or wildlings) that have a diverse microbial experience and a T-cell memory compartment similar to adult humans, rather than SPF-housed mice.
- Step 2: Generate and expand donor-specific regulatory T cells (Tregs) in vitro.
- Step 3: Infuse expanded Tregs along with the transplant under reduced immunosuppression. Tregs suppress effector T cell responses and promote a tolerogenic environment.
Quantitative Data on Post-Transplant Immune Reconstitution
The pace of immune recovery is a critical factor in managing post-transplant complications. The table below summarizes normative recovery timelines for key immune cells after allogeneic HSCT, which can serve as a benchmark for evaluating patient progress and identifying delays [5].
Table 1: Timelines for Key Immune Cell Recovery Post-Allogeneic HSCT
| Immune Cell Population | Time to Recovery | Key Functional Implications |
|---|---|---|
| Neutrophils (>0.5 × 10⁹/L) | ~14 days (PBSC), ~21 days (BM), ~30 days (CB) [5] | Protection against bacterial and fungal infections during the aplastic phase. |
| NK Cells | 30–100 days [5] | Early innate defense and anti-leukemic activity. |
| T Cells | ~100 days for initial recovery [5] | Control of viral reactivations (e.g., CMV, EBV); imbalance linked to GvHD and relapse. |
| CD4+ T Cells | Inversion of CD4/CD8 ratio common; numbers of ~200/μL by 3 months [5] | Critical for providing T-cell help; slow recovery correlates with opportunistic infections. |
| CD19+ B Cells | 1–2 years to reach normal numbers [5] | Defective humoral immunity; vulnerability to encapsulated bacteria (e.g., S. pneumoniae). |
| CD19+CD27+ Memory B Cells | Up to 5 years for complete reconstitution [5] | Delayed and restricted antibody repertoire; impaired response to vaccines. |
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Investigating Alloreactivity and Tolerance
| Research Reagent | Primary Function in Experimental Context |
|---|---|
| Alemtuzumab (anti-CD52) | An anti-lymphocyte antibody used for in vivo or in vitro lymphodepletion. Knocking out CD52 in donor cells renders them resistant [4]. |
| Sirolimus (mTOR inhibitor) | Conditions recipient dendritic cells towards a tolerogenic profile, potentially inhibiting alloreactive T-cell survival and promoting tolerance [1]. |
| Anti-thymocyte Globulin (ATG) | Polyclonal T-cell-depleting antibody used in conditioning regimens to reduce host-versus-graft and graft-versus-host reactions [2]. |
| CRISPR-Cas9 System | Gene-editing tool for precise knockout (e.g., TRAC, B2M) or knock-in (e.g., CAR, HLA-E) to create immune-evasive allogeneic cell products [3] [4]. |
| Recombinant IL-2/IL-15 | Cytokines used to expand and maintain T cells and NK cells ex vivo, and to enhance their persistence and function in vivo [3]. |
| TGF-β Inhibitor / dnTGFβRII | Used to block the immunosuppressive effects of TGF-β in the tumor microenvironment, enhancing T-cell cytotoxicity [3]. |
Signaling Pathways in Alloreactive T-cell Activation
The activation of alloreactive T cells requires three distinct signals, which present multiple targets for immunosuppressive and tolerogenic strategies [1].
Diagram: Three-Signal Model of T-Cell Alloreactivity
FAQ: Resolving Key Experimental Challenges
1. In our in vitro cytotoxicity assays, we are not observing consistent NK cell activation against our allogeneic target cells, despite known HLA class I mismatches. What could be the cause?
Inconsistent NK cell activation often stems from an incomplete understanding of the "licensing" or "education" process. NK cell responsiveness is not universal; it is determined by the interaction between the recipient's inhibitory KIRs and their own HLA class I molecules during development. An NK cell that lacks an inhibitory receptor for self-HLA I may be unlicensed and hyporesponsive, even when encountering allogeneic target cells [7] [8].
Troubleshooting Steps:
- Verify KIR-HLA Ligand Status: Genotype both the NK cell donor and the target cell donor for KIR genes and HLA-A, -B, and -C alleles. Focus on the major inhibitory KIR-ligand pairs: KIR2DL1 for HLA-C group 2 (C2), KIR2DL2/3 for HLA-C group 1 (C1), and KIR3DL1 for HLA-Bw4 [7] [8].
- Identify "Missing Self" Conditions: A functional "missing self" scenario exists when the target cell lacks the specific HLA I ligand for an inhibitory KIR expressed on the NK cell. For example, an NK cell expressing KIR2DL1 will be strongly activated by a target cell that is HLA-C2 negative, as the inhibitory signal is absent [7] [8].
- Use Positive Controls: Include a well-characterized target cell line known to be susceptible to NK cell lysis (e.g., K562) to confirm your NK cell effector function is intact.
2. We are investigating chronic rejection in a humanized mouse model of solid organ transplantation. We observe microvascular inflammation but cannot detect donor-specific antibodies (DSAs). What innate immune mechanisms should we explore?
Your observations are consistent with clinical findings where approximately 41% of kidney transplant patients with microvascular inflammation (MVI) do not have detectable DSAs [8]. This antibody-independent MVI is a hallmark of innate allorecognition, primarily driven by NK cells reacting to "missing self" on the graft endothelium [9] [8].
Experimental Investigation Plan:
- Histological Analysis: Perform immunohistochemistry on graft sections using an anti-NKp46 (in mice) or anti-CD56 (in humans) antibody to quantify NK cell infiltration within the microvasculature [8].
- Genetic Analysis: Confirm a mismatch between the donor's HLA I and the recipient's inhibitory KIR repertoire. This creates a "pseudo-missing self" situation where the graft endothelium expresses normal levels of HLA I, but these molecules cannot deliver an inhibitory signal to the recipient's educated NK cells [8].
- Pathway Inhibition: Treat your model with an mTOR inhibitor like rapamycin (sirolimus). Research has shown that the mTORC1 pathway in NK cells is mandatory for this type of endothelial damage, and rapamycin can prevent the development of these lesions [8].
3. Beyond NK cells, what other innate immune cells contribute to allorecognition, and how can we differentiate their roles in rejection?
Myeloid cells, particularly monocytes and macrophages, are now recognized as key players in innate allorecognition through mechanisms distinct from NK cells [10] [11]. They can directly recognize allogeneic non-self via specific receptor-ligand systems, leading to monocyte differentiation into mature dendritic cells and the acquisition of allocytotoxic functions by macrophages [10] [11].
Strategies to Differentiate Roles:
- Target Different Pathways: NK cell "missing self" recognition is primarily mediated by KIR-HLA I interactions. Myeloid allorecognition in mice involves paired immunoglobulin-like receptor type A (PIR-A) recognition of non-self MHC-I and the CD47-SIRPα axis, where polymorphisms in SIRPα trigger monocyte activation [10] [11]. Using blocking antibodies or genetic knockouts for these specific receptors can help isolate their effects.
- Cell Depletion Models: Use clodronate liposomes to deplete phagocytic myeloid cells or anti-asialo GM1 to deplete NK cells in animal models. Comparing rejection outcomes in these conditions can reveal the relative contribution of each cell type [11].
- Analyze Cytokine Profiles: NK cell responses are typically associated with high levels of IFN-γ. Myeloid cell activation, particularly monocyte differentiation into dendritic cells, is characterized by persistent production of IL-12, which drives a Th1 response [11].
Experimental Protocols & Workflows
Protocol 1: In Vitro Model of NK Cell "Missing Self" Activation
This protocol outlines a method to test the functional impact of KIR-HLA ligand mismatches on primary human NK cell activity.
Key Research Reagent Solutions:
| Reagent | Function in the Experiment |
|---|---|
| Ficoll-Paque | Density gradient medium for isolation of peripheral blood mononuclear cells (PBMCs). |
| Human NK Cell Isolation Kit | Negative selection magnetic beads for untouched purification of NK cells. |
| IL-2 | Cytokine used to culture and maintain NK cell viability and activity. |
| K562 Cell Line | HLA class I-negative erythroleukemia cell line; used as a positive control for "missing self" lysis. |
| Lactate Dehydrogenase (LDH) Assay Kit | Measures LDH release from damaged target cells to quantify cytotoxicity. |
Methodology:
- Cell Isolation: Isolate PBMCs from the recipient (NK cell source) using Ficoll-Paque density gradient centrifugation. Subsequently, isolate untouched NK cells from the PBMCs using a negative selection magnetic bead kit [7].
- NK Cell Culture: Culture the purified NK cells in RPMI-1640 medium supplemented with 10% FBS and 500 IU/mL recombinant human IL-2 for 48-72 hours to pre-activate them [7].
- Target Cell Preparation: Culture allogeneic and syngeneic (control) target cells. These can be primary endothelial cells or cell lines with well-defined HLA class I types. Include K562 cells as a positive control.
- Cytotoxicity Assay: Co-culture effector NK cells with target cells at various effector-to-target (E:T) ratios (e.g., 10:1, 5:1, 1:1) in a 96-well plate. Incubate for 4-6 hours.
- Lysis Quantification: Use an LDH release assay according to the manufacturer's instructions. Measure the absorbance and calculate the percentage of specific cytotoxicity [7].
Protocol 2: Assessing Myeloid Allorecognition via the CD47-SIRPα Axis
This protocol uses a mouse model to study how SIRPα polymorphism drives monocyte infiltration and activation.
Workflow:
Methodology Details:
- Step 1: Mouse Strains. Utilize mice with known polymorphisms in the Sirpa gene, such as NOD (non-obese diabetic) and C57BL/6 (B6) strains. NOD SIRPα has a higher binding affinity for CD47 than the B6 variant [11].
- Step 2: Transplantation. Perform transplants (e.g., heart) from a donor of one strain into a RAG-/-γc-/- recipient of another strain. These recipients lack T, B, and NK cells, allowing you to isolate the innate myeloid response [10] [11].
- Steps 3-6: Graft Analysis. Harvest grafts at designated time points. Create a single-cell suspension and stain for monocytes and monocyte-derived dendritic cells (mo-DCs) using antibodies against CD11b, Ly6C, MHC class II (I-A/I-E), and CD80/86. Analyze via flow cytometry. Allogeneic grafts will show a significant and persistent infiltration of mature (MHC-IIhiCD80hi) host-derived mo-DCs compared to syngeneic controls [11].
- Steps 7-8: Mechanism Interrogation. To confirm the role of specific pathways, use congenic mouse strains to map the genetic locus responsible for the alloresponse (often the Sirpa locus) or administer blocking antibodies against CD47 or PIR-A to the recipients to inhibit the allorecognition response [11].
Signaling Pathways in Innate Allorecognition
Diagram 1: NK Cell "Missing Self" Activation Pathway
This diagram details the intracellular signaling events in an NK cell when it encounters a graft endothelial cell lacking self-HLA I.
Title: NK Cell Missing Self Signaling
Key Signaling Molecules:
- Inhibitory KIRs: Contain Immunoreceptor Tyrosine-based Inhibitory Motifs (ITIMs). When engaged by self-HLA I, they recruit phosphatases like SHP-1, which dephosphorylate activation pathway components, suppressing NK cell activity [7].
- Activating Receptors (e.g., NKG2D): Associate with adaptor proteins (DAP10/DAP12) containing Immunoreceptor Tyrosine-based Activation Motifs (ITAMs). Phosphorylated ITAMs recruit kinases like Syk and ZAP70 [7].
- Downstream Pathways (PLC-γ, PI3K, MAPK): These pathways integrate activating signals, leading to calcium flux, cytoskeletal polarization, and the release of perforin/granzyme-containing cytotoxic granules and cytokines like IFN-γ [7].
- mTORC1: This pathway is mandatory for NK cell-mediated endothelial damage in "missing self" responses. Its inhibition by rapamycin can prevent chronic vascular rejection [8].
Diagram 2: Myeloid Allorecognition via SIRPα-CD47
This diagram illustrates how polymorphism in the SIRPα protein on donor cells leads to monocyte activation in the recipient.
Title: Myeloid Allorecognition via SIRPα-CD47
Key Mechanism:
- In a syngeneic setting (donor and recipient have the same SIRPα variant), the bidirectional interaction between CD47 on the graft and SIRPα on the recipient monocyte is balanced. The affinity of binding is equal, resulting in a net inhibitory signal that prevents monocyte activation [11].
- In an allogeneic setting (donor expresses a different SIRPα variant), the affinity of the cross-interaction between donor SIRPα and recipient CD47 is altered. This imbalance upsets the steady-state signaling, leading to a net activating signal that drives monocyte differentiation into mature, IL-12-producing dendritic cells, which can prime naive T cells [11].
Table 1: Clinical Evidence for Antibody-Independent Microvascular Inflammation (MVI) [8]
| Patient Cohort | Prevalence of MVI | Circulating Anti-HLA Donor-Specific Antibodies (DSA) | NK Cell Infiltration in Graft | 5-Year Graft Survival |
|---|---|---|---|---|
| MVI+ / DSA+ (C3d+) | 31% (40/129) | Present & Complement-Activating | Present | Lowest (Worst) |
| MVI+ / DSA+ (C3d-) | 23% (30/129) | Present & Non-Complement-Activating | Present | Intermediate |
| MVI+ / DSA- | 41% (53/129) | Absent | Present | Intermediate |
| MVI- / DSA- (Control) | N/A | Absent | Absent | Highest (Best) |
Table 2: Key Receptor-Ligand Pairs in Innate Allorecognition
| Receptor | Expression | Ligand | Function in Allorecognition | Species |
|---|---|---|---|---|
| Inhibitory KIR (e.g., KIR2DL1) | NK Cells | HLA-C (C2 group) | Inhibits NK cell cytotoxicity upon engagement; absence of ligand ("missing self") triggers activation [7] [8]. | Human |
| PIR-A | Monocytes, Macrophages | MHC Class I | Recognizes non-self MHC-I; engagement triggers monocyte/macrophage activation and memory [10] [11]. | Mouse |
| LILRs (PIR-A orthologs) | Monocytes, Macrophages | HLA Class I | Proposed human equivalent of PIR-A; likely involved in MHC-I allorecognition [11]. | Human |
| SIRPα | Myeloid Cells, Various Non-immune Cells | CD47 | Polymorphic protein; mismatched SIRPα between donor/recipient disrupts balanced signaling, initiating monocyte activation [11]. | Mouse/Human |
In allogeneic stem cell transplantation, the focus has long been on matching Human Leukocyte Antigens (HLA) to minimize immune rejection. However, even with perfect HLA matching, complications like Graft-versus-Host Disease (GVHD), graft rejection, and autoimmune phenomena persist. These events are largely driven by minor histocompatibility antigens (mHAgs) and disruptions in immune tolerance. This technical support center provides troubleshooting guides and experimental protocols to help researchers in the challenging field of transplant immunology overcome these barriers.
FAQs: Core Concepts for Researchers
1. What are minor histocompatibility antigens and why are they significant in transplantation?
Minor histocompatibility antigens (mHAgs) are immunogenic peptides presented by MHC molecules that can elicit T-cell immune responses between transplant recipients and donors who are matched at the HLA loci [12]. They are generated from polymorphic cellular proteins or peptides that differ between donor and recipient due to genetic variations like single nucleotide polymorphisms (SNPs) or insertions/deletions (indels) [12]. In HLA-matched sibling transplants, donor T cells recognize recipient mHAgs, contributing to both graft-versus-leukemia (GVL) effects and graft-versus-host disease (GVHD) [12].
2. What are the primary allorecognition pathways involved in transplant rejection?
The immune system uses three distinct pathways to recognize allografts as foreign [13] [14]:
- Direct Pathway: Recipient T cells directly recognize intact donor MHC molecules on the surface of donor antigen-presenting cells (APCs). This pathway is dominant in early acute rejection.
- Indirect Pathway: Recipient APCs process and present donor MHC molecules as peptides on recipient MHC molecules to recipient T cells. This pathway becomes more important over time and is involved in chronic rejection.
- Semi-direct Pathway: Recipient APCs capture intact donor MHC molecules and present them directly to recipient T cells.
3. How can autoimmune phenomena occur after an allogeneic stem cell transplant?
Autoimmune diseases (ADs) can occur after allogeneic hematopoietic stem cell transplantation (HSCT) due to an imbalance in immune regulation, particularly involving the effect of T-regulatory lymphocytes on autoreactive T-lymphocytes [15]. The transfer of immune cells from the donor can also lead to the transfer of autoimmunity. This immune dysregulation can result in both hematological ADs and non-hematological ADs affecting organs like the thyroid, skin, liver, and nervous system [15]. Autoimmune cytopenias, such as autoimmune neutropenia (AIN), are documented rare complications, with one recent study reporting a cumulative incidence of 14.74% at 2 years post-HSCT in pediatric patients [16].
4. What is the emerging role of non-HLA antibodies in transplant rejection?
Beyond antibodies against HLA and mHAgs, immunity to non-HLA antigenic targets is increasingly recognized. A paradigm-changing example is immunity to the non-HLA angiotensin II type 1 receptor (AT1R) [17]. Antibodies against AT1R have been associated with antibody-mediated rejection and other vascular complications in transplantation. The successful detection and intervention for anti-AT1R antibodies provide a model for understanding the broader pathogenicity of non-HLA antibodies [17].
Troubleshooting Guides: Common Experimental Challenges
Problem 1: Unexpected GVHD in HLA-Matched Animal Models
Observed Issue: Development of clinical or histopathological signs of GVHD in transplanted subjects despite full HLA compatibility.
Potential Root Causes:
- Presence of undiscovered mHAg mismatches.
- Incomplete immune suppression during the peri-transplant period.
- Underlying inflammatory conditions or infections triggering immune activation.
Investigative Steps:
- Confirm Histocompatibility: Re-genotype donor and recipient pairs to verify HLA identity and screen for known genetic disparities.
- Profile mHAgs: Utilize genomic approaches (see Experimental Protocol 1 below) to identify mismatched mHAgs.
- Monitor Immune Reconstitution: Use flow cytometry to track the expansion of alloreactive T-cell populations post-transplant.
- Control for Environment: Ensure sterile housing conditions and screen for common murine pathogens that can incite inflammation.
Solution: Incorporate high-throughput mHAg screening into your donor selection criteria. For established models, consider therapeutic strategies that target alloreactive T cells while preserving regulatory T-cell function.
Problem 2: Detecting Clinically Relevant mHAgs
Observed Issue: Difficulty in linking specific mHAgs to clinical outcomes like GVHD or relapse.
Potential Root Causes:
- Low precursor frequency of T cells for individual mHAgs.
- Lack of specific reagents (e.g., tetramers) for detecting mHAg-specific T cells.
- Heterogeneity in HLA restriction elements among study subjects.
Investigative Steps & Solution: Implement a genome-wide association study (GWAS) approach in well-defined transplant cohorts. The table below summarizes key quantitative findings from such studies.
Table 1: Association between Genetic Mismatching and Clinical Outcomes in HLA-Matched Sibling HCT
| Study Cohort | Number of Sibling Pairs | Key Finding | Statistical Significance |
|---|---|---|---|
| FHCRC Discovery Cohort [12] | 824 HLA-A*02:01-positive pairs | Identification of recipient allele mismatch associations (RAMAs) with GVHD and relapse. | Analyzed via cause-specific hazard ratio (CSHR) |
| FHCRC Discovery Cohort [12] | 929 HLA-A02 supertype-negative pairs | Used as a control to test specificity of HLA-A*02:01-restricted associations. | Associations not replicated in this control group |
| CIBMTR Replication Cohort [12] | 838 HLA-A*02:01-positive pairs | Independent testing of RAMAs discovered in the FHCRC cohort. | Confirmed specific replicated associations |
Problem 3: Post-Transplant Autoimmune Cytopenia
Observed Issue: The patient develops isolated neutropenia, thrombocytopenia, or anemia after engraftment.
Potential Root Causes:
- Autoimmune neutropenia (AIN) or other autoimmune cytopenias (AIC).
- Drug toxicity from immunosuppressive agents.
- Viral reactivation (e.g., CMV, HHV-6).
- Incipient graft failure or disease relapse.
Investigative Steps:
- Confirm Diagnosis: For suspected AIN, obtain at least two consecutive absolute neutrophil counts (ANC) < 0.5 x 10⁹/L and test for anti-granulocyte antibodies via flow cytometry [16].
- Exclude Other Causes: Check donor chimerism to rule out graft failure. Test for viral DNA by PCR and review medication charts.
- Assess Clinical Context: Note that AIC often occurs during immunosuppression tapering and is associated with chronic GVHD [15] [16].
Solution: First-line treatment often involves corticosteroids or rituximab. For steroid-refractory cases, targeted therapies like JAK inhibitors (e.g., ruxolitinib) may be considered [14].
Experimental Protocols for Key Investigations
Protocol 1: Identification of mHAgs via Genomic Sequencing
Objective: To identify minor histocompatibility antigens in HLA-identical donor-recipient pairs.
Workflow: The following diagram illustrates the major steps from sample preparation to statistical analysis.
Materials:
- Pre-transplant blood samples from donor and recipient.
- Genomic DNA extraction kits.
- Genotyping microarray or targeted sequencing platforms (e.g., Illumina MiSeq) [12].
- Bioinformatics pipelines for variant calling (e.g., GATK) and annotation (e.g., Ensembl VEP) [12].
- Computational tools for peptide-HLA binding prediction.
Method:
- Sample Preparation: Extract high-quality genomic DNA from donor and recipient pre-transplant samples [12].
- Genotyping & Imputation: Genotype samples using a high-density SNP array or perform whole-exome/genome sequencing. Use imputation algorithms to fill in missing genotypes [12].
- Variant Annotation: Process variants with the Ensembl Variant Effect Predictor (VEP) to categorize them as "coding" (missense, frameshift, etc.) or "non-coding" [12].
- In Silico Prediction: For coding variants, use algorithms to predict whether the polymorphic peptides they generate will bind to the specific HLA allotypes present in the recipient [12].
- Statistical Analysis: Test for Recipient Allele Mismatch Associations (RAMAs) using Cox regression models, treating death as a competing risk. Compare outcomes between mismatched and non-mismatched pairs [12].
Protocol 2: Detecting Anti-Granulocyte Antibodies for AIN Diagnosis
Objective: To diagnose autoimmune neutropenia (AIN) post-HSCT by detecting anti-granulocyte antibodies.
Materials:
- Patient serum and EDTA blood samples.
- Flow cytometer (e.g., CytoFLEX, Beckman Coulter) [16].
- Antibodies for neutrophil labeling.
- Negative and positive control samples.
Method:
- Sample Collection: Collect patient blood when neutropenia (ANC < 0.5 x 10⁹/L) is observed.
- Direct Test (Detects cell-bound antibodies):
- Isolate neutrophils from the patient's blood.
- Incubate with a fluorescently-labeled anti-human immunoglobulin antibody.
- Analyze by flow cytometry. A positive result is a median fluorescence intensity (MFI) exceeding a validated laboratory cut-off [16].
- Indirect Test (Detects serum antibodies):
- Incubate healthy control neutrophils with the patient's serum.
- Wash and then incubate with a fluorescently-labeled anti-human immunoglobulin antibody.
- Analyze by flow cytometry. A positive result is an MFI at least twice that of a negative control [16].
- Interpretation: A positive result in either test, in the correct clinical context and after excluding other causes, supports a diagnosis of AIN [16].
Key Signaling Pathways in Rejection and Autoimmunity
Understanding these pathways is critical for developing targeted therapies. The diagram below illustrates two key pathways implicated in GVHD.
Pathway 1: JAK-STAT Signaling
- Role in GVHD: This pathway is a critical communication node activated by cytokines. It regulates the development and function of dendritic cells, T cells, and neutrophils, all of which are central to GVHD pathogenesis [14].
- Therapeutic Targeting: Inhibition of JAK signaling with drugs like ruxolitinib has been shown to reduce GVHD severity while potentially preserving graft-versus-leukemia (GVL) activity [14]. The US FDA has approved ruxolitinib for steroid-refractory acute GVHD.
Pathway 2: Notch Signaling
- Role in Rejection: This highly conserved pathway is crucial for innate and adaptive immune cell development and function. It is a key inflammatory pathway in T-cell alloreactivity [14].
- Therapeutic Targeting: Emerging evidence suggests that inhibiting the Notch pathway can prevent allograft rejection and may be beneficial for treating GVHD without interfering with GVL activity [14].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Investigating mHAgs and Autoimmunity
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Genotyping Microarray | Genome-wide SNP profiling | Initial screening for genetic disparities in donor-recipient pairs [12]. |
| GATK Pipeline | Variant calling from sequencing data | Joint genotyping of donor and recipient samples to identify mismatches [12]. |
| Ensembl VEP (Variant Effect Predictor) | Functional annotation of genetic variants | Categorizing variants as coding or non-coding to prioritize mHAg candidates [12]. |
| Peptide-HLA Binding Prediction Algorithms | In silico prediction of mHAg presentation | Predicting which polymorphic peptides will bind to a patient's specific HLA allotypes [12]. |
| Flow Cytometry with Anti-Human Ig | Detection of anti-granulocyte antibodies | Diagnosing Autoimmune Neutropenia (AIN) post-transplant [16]. |
| JAK Inhibitors (e.g., Ruxolitinib) | Inhibition of JAK-STAT signaling | Used in in vivo models or as a therapeutic to investigate pathway role in GVHD [14]. |
FAQ: Understanding IBMIR and Its Impact on Your Research
What is IBMIR and why is it a critical problem in cellular transplantation?
The Instant Blood-Mediated Inflammatory Reaction (IBMIR) is a rapid, innate immune response triggered when transplanted cells or tissues directly contact blood components. It is a major barrier to successful engraftment in intraportal islet transplantation, destroying up to approximately 60% of transplanted islet cells within hours by activating coagulation and complement cascades, inducing platelet activation, recruiting inflammatory cells, and promoting fibrin deposition around the graft [18] [19] [20]. This rapid graft loss severely compromises the initial engraftment and long-term function of transplanted cells.
How does IBMIR differ from other forms of immune rejection?
Unlike T-cell-mediated adaptive immune rejection, which occurs over days to weeks, IBMIR is an innate immune response that begins within minutes to hours of transplantation. Its key distinguishing feature is the simultaneous and powerful activation of both the coagulation system and the complement system, leading to immediate thrombosis and inflammation at the transplant site [18] [20]. This makes it a first-line barrier that must be overcome before addressing chronic rejection.
Which transplant sites are most susceptible to IBMIR?
The intraportal site (transplantation into the liver via the portal vein) is the most clinically established site for islet transplantation and is particularly susceptible to IBMIR [21] [19]. This is due to the direct exposure of islets to the bloodstream immediately upon infusion. Research into alternative sites, such as the subcutaneous space, aims to circumvent IBMIR, but no patient has yet been rendered insulin-free by cellular transplantation in a site other than the liver [21].
Troubleshooting Guide: Investigating and Mitigating IBMIR in Experimental Models
Problem: Poor Early Graft Survival In Vivo
Potential Cause: Uncontrolled IBMIR leading to massive early cell death.
Diagnostic Steps & Solutions:
- Monitor Coagulation Activation: Measure biomarkers like Thrombin-Antithrombin (TAT) complexes and β-thromboglobulin (β-TG). Elevated levels indicate strong coagulation activation and platelet activation, respectively [18].
- Assess Inflammatory Response: Analyze serum for pro-inflammatory cytokines such as TNF-α and examine graft sites for inflammatory cell infiltration (e.g., neutrophils, macrophages) [18] [20].
- Histological Confirmation: Look for significant fibrin deposition and the formation of peri-graft microthrombi [18].
Recommended Interventions:
- Anticoagulant Therapy: Consider using direct thrombin inhibitors like Bivalirudin, which has been shown to more effectively reduce coagulation activation and inflammatory infiltration compared to unfractionated heparin in preclinical models [18].
- Multi-Target Therapy: Explore drugs with combined anti-inflammatory and anti-coagulant properties. For example, Xuebijing (XBJ) injection, a multi-component herbal medicine, has demonstrated efficacy in mitigating IBMIR by suppressing the NF-κB pathway, thereby reducing both thrombosis and inflammation [20].
Problem: Inconsistent IBMIR Readouts In Vitro
Potential Cause: Lack of a robust and standardized assay to model blood-cell interactions.
Solution: Implement a Standardized In Vitro IBMIR Assay. This assay incubates your cell product (e.g., isolated islets) with fresh human blood or plasma to simulate the initial contact [18] [20].
Key Parameters to Quantify:
- Coagulation Activation: Measure TAT complexes and platelet consumption.
- Complement Activation: Measure generation of complement split products like C3a and sC5b-9.
- Cell Activation and Death: Assess leukocyte infiltration and quantify apoptosis/necrosis in the cell product.
This assay provides a controlled system for pre-screening potential IBMIR-inhibiting strategies before moving to complex animal models.
Experimental Protocols: Core Methodologies for IBMIR Research
Detailed Protocol: Evaluating Anticoagulants in a Rodent Intraportal Transplantation Model
The following methodology is adapted from a 2025 study investigating bivalirudin [18].
1. Animal and Diabetes Model:
- Use male Wistar or Sprague Dawley rats (6-8 weeks old).
- Induce diabetes with a single intraperitoneal injection of streptozotocin (70 mg/kg for rats).
- Confirm diabetes by measuring blood glucose levels >300 mg/dL for two consecutive days prior to transplantation [18].
2. Islet Isolation and Preparation:
- Anesthetize donor SD rats and perform an abdominal laparotomy.
- Inject 8 ml of collagenase V (1 mg/ml) into the pancreatic common bile duct to distend the pancreas.
- Remove the enlarged pancreas and digest in a 37°C water bath for 5-6 minutes.
- Purify islets using density gradient centrifugation (e.g., with Histopaque 1077).
- Culture purified islets in RPMI-1640 medium with 10% fetal bovine serum.
- Count islets and determine islet equivalents (IEQ) using dithizone (DTZ) staining [18].
3. Experimental Groups and Dosing: The study design below is critical for a direct comparison of anticoagulants. The following table summarizes the dosing regimen for a rat model [18]:
Table 1: Experimental Groups and Anticoagulant Dosing for Rat Intraportal Islet Transplantation
| Group | Pre-Transplant Bolus (0.5 ml, i.v.) | Continuous Infusion (for 1 hour post-transplant) |
|---|---|---|
| Sham | Physiological Saline | 5 ml/(kg·h) Saline |
| Model (Control) | Physiological Saline | 5 ml/(kg·h) Saline |
| Bivalirudin (BT) | 50 mg/kg Bivalirudin | 70 mg/(kg·h) Bivalirudin |
| Heparin (HT) | 200 U/kg Heparin Sodium | 300 U/(kg·h) Heparin Sodium |
4. Transplantation and Assessment:
- Anesthetize recipient rats and expose the superior mesenteric vein and portal vein.
- Puncture the superior mesenteric vein with a 27G syringe and infuse the islet cells (2000 IEQ per 100g of recipient weight) into the liver.
- Administer treatments via tail vein infusion according to the group design.
- Collect blood via inferior vena cava puncture to assess anticoagulation function (e.g., APTT) and biomarkers (β-TG, TAT, TNF-α).
- Monitor graft function by tracking the time to achieve normoglycemia and the proportion of animals that become normoglycemic [18].
The following tables consolidate quantitative findings from key studies to aid in experimental planning and comparison.
Table 2: Efficacy of Bivalirudin vs. Heparin in Mitigating IBMIR Biomarkers [18]
| Biomarker / Outcome | Model (Saline) | Heparin Treatment (HT) | Bivalirudin Treatment (BT) | Observation |
|---|---|---|---|---|
| Coagulation (TAT complexes) | Baseline (High) | Reduced | Reduced more effectively than HT | BT showed superior anti-thrombotic activity [18] |
| Platelet Activation (β-TG) | Baseline (High) | Reduced | Reduced more effectively than HT | BT more effectively suppressed platelet activation [18] |
| Inflammation (TNF-α) | Baseline (High) | Attenuated | Attenuated, with more pronounced effects | BT demonstrated greater anti-inflammatory activity [18] |
| Graft Normoglycemia | Baseline (Low) | Higher proportion than model | Higher proportion than HT, with shorter time-to-normoglycemia | BT led to superior functional outcomes [18] |
Table 3: Multi-Target Effects of Xuebijing (XBJ) on IBMIR and Islet Function [20]
| Mechanism of Action | Observed Effect | Experimental Model |
|---|---|---|
| Inhibition of NF-κB Pathway | Suppressed pro-inflammatory gene clusters and reduced inflammatory reaction. | Diabetic mouse transplantation model [20] |
| Direct Islet Protection | Protected islet cells against cytokine-induced apoptosis and restored glucose-stimulated insulin secretion. | Cytokine-stimulated mouse islets and β-cells in vitro [20] |
| Improved Transplantation Outcome | Mitigated IBMIR, led to a higher percentage of normoglycemia, and better graft survival. | Intrahepatic islet transplantation in diabetic mice [20] |
Signaling Pathways and Experimental Workflows
IBMIR Mechanism and Therapeutic Blockade
This diagram illustrates the core mechanism of the Instant Blood-Mediated Inflammatory Reaction (IBMIR) and points where therapeutic agents can intervene.
In Vivo IBMIR Investigation Workflow
This diagram outlines a logical workflow for a standard preclinical experiment investigating IBMIR and potential therapeutics.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for IBMIR Research
| Reagent | Function in IBMIR Research | Example Application / Note |
|---|---|---|
| Bivalirudin | Direct thrombin inhibitor; anticoagulant. | Used to mitigate coagulation cascade activation; shown to be more effective than heparin in some models [18]. |
| Heparin Sodium | Indirect thrombin inhibitor (via antithrombin); anticoagulant. | Common clinical anticoagulant; used as a comparative control in IBMIR studies [18]. |
| Xuebijing (XBJ) Injection | Multi-component herbal medicine with anti-inflammatory and anti-coagulant properties. | Suppresses IBMIR via NF-κB pathway inhibition; offers a multi-target approach [20]. |
| Collagenase V | Enzyme for pancreatic digestion. | Critical for isolating islets from the pancreas for transplantation [18]. |
| Histopaque 1077 | Density gradient medium. | Used for purifying isolated islets from exocrine tissue after digestion [18]. |
| Dithizone (DTZ) | Zinc-chelating dye that stains islets red. | Essential for visualizing and counting islet equivalents (IEQ) pre-transplantation [18]. |
| Streptozotocin (STZ) | Chemical agent toxic to pancreatic beta cells. | Used to induce an experimental model of diabetes in rodents [18]. |
Engineering Immune Evasion: Strategies for Hypoimmunogenic Cell Therapies
Genetic Ablation of HLA Class I and II to Thwart T-cell Recognition
Troubleshooting Guide: FAQs on HLA Ablation
FAQ 1: My HLA-ablated cells are being killed by host natural killer (NK) cells after transplantation. How can I prevent this "missing-self" response?
Answer: The "missing-self" response occurs because host NK cells recognize and eliminate cells that lack surface expression of HLA class I molecules, a common outcome of B2M knockout [22] [3]. To overcome this, consider these strategies:
- Express Non-Polymorphic HLA Molecules: Introduce a single-chain HLA-E (SCE) gene or an HLA-E-B2M fusion gene into the B2M locus. HLA-E engages the inhibitory receptor NKG2A on NK cells, providing a "do not eat me" signal that inhibits NK cell-mediated killing [22] [23] [3].
- Use Specific shRNA for HLA-ABC: Employ shRNA (e.g., shRNA #1 from the literature) that selectively knocks down classical HLA-A, -B, and -C molecules without affecting HLA-E expression. This allows retention of HLA-E-mediated inhibition of NK cells while still evading T-cell recognition [23].
FAQ 2: After successful HLA class I ablation, my cellular product still faces rejection. What other immune mechanisms could be responsible?
Answer: Rejection despite HLA class I ablation suggests involvement of other immune components.
- HLA Class II Recognition: Host CD4+ T cells can recognize allogeneic HLA class II molecules. For complete immune evasion, disrupt the class II transactivator (CIITA) gene, which is the master regulator of HLA class II expression [22].
- Macrophage-Mediated Clearance: Host macrophages can phagocytose donor cells. To counter this, overexpress the CD47 protein on your cell product. CD47 binds to SIRPα on macrophages, delivering an inhibitory signal that prevents phagocytosis [3].
- Synapse Formation with Host Immune Cells: Genetic deletion of adhesion ligands CD54 (ICAM-1) and CD58 (LFA-3) can mitigate rejection by host NK cells, as it disrupts the formation of a functional immune synapse necessary for cytotoxicity [24].
FAQ 3: How can I ensure that genetic ablation of HLA does not impair the native therapeutic function of my cell product (e.g., Tregs, CAR cells)?
Answer: It is critical to perform comprehensive functional validation post-editing. Key assessments include:
- Phenotype Stability: Verify the stability of cell-specific surface markers and key transcription factors (e.g., FOXP3 for Tregs) via flow cytometry [22].
- In Vitro Functional Assays: Conduct suppression assays (for Tregs) or cytotoxic killing assays (for CAR cells) to confirm that the engineered cells retain their potent immunosuppressive or anti-tumor activity, comparable to unedited controls [22].
- Epigenetic Stability: For Tregs, assess the methylation status of the Treg-specific demethylation region (TSDR) in the FOXP3 locus. A low methylation state indicates stable FOXP3 expression and Treg lineage commitment [22].
FAQ 4: What is the advantage of using a single-vector system for creating hypo-immunogenic cells?
Answer: A single lentiviral vector that combines a CAR construct, an HLA-knockdown shRNA, and an immune checkpoint protein (e.g., PD-L1 or SCE) enables one-step construction of allogeneic cell products. This strategy simplifies manufacturing, improves efficiency, and ensures that all modifications are present in the final therapeutic product, facilitating clinical translation [23].
The tables below summarize key experimental data from recent studies on HLA engineering, providing a benchmark for expected outcomes.
Table 1: In Vivo Efficacy of HLA-Engineered Human Tregs in a Skin Graft Model [22]
| Treg Treatment Type | Median Graft Survival Time (Days) | Key Genetic Modification |
|---|---|---|
| Autologous Tregs | >100 days (control) | None |
| Allogeneic Tregs (Mismatched) | 24 - 27 days | None |
| HLA-Matched Tregs | >100 days | None |
| HLA-E KI / CIITA KO Tregs | Prolonged, comparable to autologous Tregs | B2M KO, HLA-E fusion knock-in, CIITA KO |
Table 2: Survival of Engineered Cells in Allogeneic Hosts Post-Transplantation [22] [23]
| Host Immune Cell Type | Effect on Unmodified Allogeneic Cells | Proposed Engineering Strategy to Evade Rejection | Outcome of Engineering |
|---|---|---|---|
| Host CD8+ T cells | Swift elimination via HLA mismatch | B2M KO or HLA-ABC-specific shRNA | Significant reduction in T-cell-mediated killing; improved cell persistence |
| Host NK cells | Elimination via "missing-self" recognition | HLA-E overexpression or HLA-E-B2M fusion knock-in | Protection from NK cell lysis; retained inhibition via NKG2A |
| Host Macrophages | Phagocytosis via SIRPα receptor | CD47 overexpression | Reduced phagocytosis; prolonged circulation time |
Experimental Protocols: Key Methodologies
Protocol 1: Multiplex CRISPR-Cas9 Editing for Generation of Hypo-immunogenic Tregs [22]
This protocol describes the generation of HLA class I/II deficient Tregs that incorporate an NK-inhibitory signal.
- Cell Isolation and Activation: Isolate CD4+CD25+ Tregs from human peripheral blood mononuclear cells (PBMCs) of healthy donors using magnetic-activated cell sorting (MACS). Activate the Tregs using anti-CD3/CD28 beads in the presence of IL-2.
- Electroporation with CRISPR RNP: On day 2-3 post-activation, electroporate Tregs with CRISPR-Cas9 ribonucleoprotein (RNP) complexes.
- Target 1: B2M KO and HLA-E Knock-in: Use a single-guide RNA (sgRNA) targeting the B2M gene, co-electroporated with a donor template plasmid containing an HLA-E-B2M fusion gene designed to integrate into the B2M locus via homology-directed repair (HDR).
- Target 2: CIITA KO: Use an sgRNA targeting the CIITA gene. This can be done concurrently or in a second editing step.
- Expansion and Validation: Culture the edited Tregs in expansion medium with IL-2 for 10-14 days.
- Validation of Editing: Use flow cytometry to confirm the loss of HLA class I (using an anti-HLA-ABC antibody) and HLA class II (using an anti-HLA-DR/DP/DQ antibody) surface expression. Verify HLA-E expression using a specific antibody.
- Functional Assay: Perform an in vitro suppression assay to confirm retained Treg function.
Protocol 2: One-Step Lentiviral Engineering of HLA-ABC-Knockdown CAR-NK Cells [23]
This protocol creates allogeneic CAR-NK cells resistant to T and NK cell attack using a single lentiviral vector.
- Lentiviral Vector Design: Construct a lentiviral vector encoding:
- A CAR transgene (e.g., anti-CD19 CAR).
- An shRNA (e.g., shRNA #1) under a U6 promoter for selective knockdown of HLA-A, -B, and -C.
- An immune checkpoint protein (e.g., PD-L1 or a single-chain HLA-E) linked via a P2A or T2A self-cleaving peptide.
- NK Cell Transduction: Isolve NK cells from donor PBMCs or use a cell line. Activate NK cells with IL-2 and IL-15. Transduce the activated NK cells with the lentiviral vector by spinfection.
- Expansion and Selection: Culture transduced NK cells in medium containing IL-2 and IL-15 for 10-14 days to allow expansion and transgene expression. If the vector contains a selection marker (e.g., puromycin resistance), apply selection pressure to enrich for transduced cells. Alternatively, sort cells based on a reporter gene (e.g., GFP).
- Validation:
- Phenotyping: Confirm CAR expression, reduced HLA-ABC expression, and increased PD-L1/SCE expression via flow cytometry.
- Cytotoxicity Assay: Validate anti-tumor function in a standard chromium-51 or luciferase-based killing assay against target tumor cells.
Experimental Workflow Visualization
CRISPR-Cas9 HLA Engineering Workflow
shRNA HLA Knockdown & CAR Engineering
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for HLA Ablation Experiments
| Reagent / Tool | Function in HLA Ablation Research | Example Application |
|---|---|---|
| CRISPR-Cas9 System | Enables precise knockout of HLA-related genes (e.g., B2M, CIITA). | Disruption of B2M to eliminate surface HLA class I expression [22]. |
| Adenine Base Editor (ABE) | Allows precise single nucleotide changes without double-strand breaks; can be used to disrupt gene function. | Silencing of CIITA to ablate HLA class II expression [22]. |
| HLA-E-B2M Fusion Donor Template | A DNA template for HDR; replaces the endogenous B2M gene to express a non-polymorphic HLA-E fusion protein. | Knocked into the B2M locus to inhibit NK cells while avoiding T cell recognition [22]. |
| Lentiviral Vector with shRNA | Delivers genetic material for stable expression of CAR, shRNA, and other transgenes. | One-step generation of CAR-NK cells with shRNA-mediated HLA-ABC knockdown [23]. |
| Anti-HLA-ABC Antibody | Validates successful knockdown or knockout of HLA class I molecules. | Flow cytometry analysis of surface HLA-ABC post-editing [22] [23]. |
| Anti-HLA-DR/DP/DQ Antibody | Validates successful knockdown or knockout of HLA class II molecules. | Flow cytometry analysis of surface HLA class II post-CIITA editing [22]. |
| Recombinant IL-2 | Critical cytokine for the ex vivo expansion and survival of T cells, including Tregs. | Culture and expansion of edited Tregs [22]. |
A major frontier in regenerative medicine and allogeneic stem cell transplantation is overcoming the formidable challenge of immune rejection. The immune system is exceptionally skilled at distinguishing between self and non-self, leading to the rejection of transplanted allogeneic cells through multiple immune mechanisms [25]. These include recognition of highly polymorphic Human Leukocyte Antigens (HLAs), minor histocompatibility antigens (miHA), and newly acquired neoantigens (NA) that can arise during cell culture and differentiation [25].
To address this critical barrier, researchers are developing sophisticated "immune editing" strategies that armor therapeutic cells to evade immune detection. This technical support center focuses on three key immune checkpoint molecules—CD47, HLA-G, and PD-L1—that can be overexpressed to protect allogeneic cells. These strategies aim to create "hypoimmune" or "immune-evasive" cell products that can survive and function in allogeneic recipients without requiring broad immunosuppression, thereby enabling the development of scalable off-the-shelf cell therapies [26] [27].
Key Signaling Pathways and Their Experimental Evidence
Comparative Analysis of Checkpoint Overexpression Strategies
Different immune checkpoint overexpression strategies target distinct components of the immune system. The table below summarizes the function, mechanism, and experimental evidence for CD47, HLA-G, and PD-L1.
Table 1: Comparison of Key Immune Checkpoint Overexpression Strategies
| Checkpoint Molecule | Primary Function | Immune Mechanism Targeted | Key Experimental Evidence |
|---|---|---|---|
| CD47 | "Don't eat me" signal [28] | Innate immunity (macrophages, NK cells) [27] | HIP iPSCs survived 16 weeks in immunocompetent allogeneic rhesus macaques; CD47 protected HLA-deficient cells from NK cell killing [27]. |
| PD-L1 | T-cell inhibitory signal [29] | Adaptive immunity (T cells) [29] | Combined expression with CTLA4-Ig protected hESC-derived teratomas, fibroblasts, and cardiomyocytes from rejection in humanized mice [29]. |
| HLA-G | Tolerogenic HLA signal [27] | Both innate and adaptive immunity (NK cells, T cells) [27] | Engineered expression on K562 cells protected from ILT2+ NK cells but was ineffective against CD94+ NK cells, showing incomplete protection [27]. |
Quantitative Data from Pre-Clinical Models
The efficacy of combining these strategies has been quantified in several rigorous pre-clinical models, demonstrating significant improvements in cell survival.
Table 2: Quantitative Survival Outcomes of Engineered Cells in Pre-Clinical Models
| Cell Type | Engineering Strategy | Model System | Survival Outcome | Reference |
|---|---|---|---|---|
| Human iPSCs | B2M⁻/⁻ CIITA⁻/⁻ CD47⁺ (HIP) | Immunocompetent allogeneic rhesus macaques | Unrestricted survival for 16 weeks [27] | |
| Rhesus macaque primary islets | HIP editing (B2M⁻/⁻ CIITA⁻/⁻ CD47⁺) | Allogeneic rhesus macaque | Survival for 40 weeks without immunosuppression [27] | |
| Human ESC-derived cells | CTLA4-Ig + PD-L1 knock-in | Humanized mice (Hu-mice) | Effective protection of teratomas, fibroblasts, and cardiomyocytes from allogeneic rejection [29] | |
| Human HIP pancreatic islet cells | B2M⁻/⁻ CIITA⁻/⁻ CD47⁺ | Immunocompetent, allogeneic diabetic humanized mice | Survival for 4 weeks and amelioration of diabetes [27] |
Visualizing the Immune Checkpoint Signaling Pathways
The following diagrams illustrate how these overexpressed checkpoint molecules interact with immune cell receptors to suppress rejection.
CD47-SIRPα "Don't Eat Me" Signaling Pathway
Diagram 1: CD47-SIRPα Innate Immune Checkpoint. This diagram shows how donor cell surface CD47 binding to macrophage SIRPα receptors transmits an inhibitory signal that blocks phagocytosis [28] [27].
PD-L1/PD-1 T-Cell Inhibitory Signaling Pathway
Diagram 2: PD-L1/PD-1 Adaptive Immune Checkpoint. This shows how donor cell PD-L1 binding to T-cell PD-1 receptors inhibits T-cell activation and cytotoxic killing, a key adaptive immune evasion pathway [29] [30].
Integrated Hypoimmune Cell Engineering Strategy
Diagram 3: Integrated Hypoimmune Cell Engineering. A combined strategy shows that deleting HLA molecules prevents T-cell recognition via the missing MHC, while simultaneously overexpressing CD47 and/or PD-L1 provides active inhibition of innate and adaptive immunity [25] [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Immune Checkpoint Engineering
| Reagent / Tool | Primary Function | Example Application | Key Considerations |
|---|---|---|---|
| CRISPR-Cas9 System | Gene knockout (e.g., B2M, CIITA) [25] | Creation of HLA class I/II deficient base lines in iPSCs [27] | Enables precise, permanent gene inactivation. Off-target effects must be assessed. |
| Lentiviral Vectors | Stable transgene overexpression (e.g., CD47, PD-L1) [27] | Constitutive expression of immune checkpoint modulators in stem cells and their derivatives. | Ensures transgene is passed to all progeny cells. Requires careful design to avoid insertional mutagenesis. |
| Bispecific Antibodies | Dual targeting of checkpoints (e.g., PD-L1 x CD47) [28] [31] | In vitro and in vivo validation of combined pathway blockade; potential therapeutic agent. | Affinity tuning is critical to minimize on-target, off-tumor toxicity (e.g., RBC binding). |
| Humanized Mouse Models (Hu-mice) | In vivo assessment of human immune rejection [29] [27] | Testing survival and immunogenicity of engineered human cell grafts in a functional human immune system. | Model must be robustly reconstituted with human immune cells for predictive results. |
Detailed Experimental Protocols
Protocol 1: Generating Hypoimmune Pluripotent Stem Cells (HIP)
This protocol outlines the creation of a hypoimmune pluripotent stem cell line via combined gene knockout and overexpression, a foundational methodology in the field [27].
- Design gRNAs and Donor Template: Design CRISPR-Cas9 gRNAs targeting the B2M and CIITA genes to disrupt HLA class I and class II expression, respectively. Simultaneously, design a donor vector for the constitutive overexpression of CD47 (e.g., using a CAG or EF1α promoter).
- Stem Cell Transfection/Transduction: Co-transfect iPSCs with the CRISPR constructs and the CD47 donor vector. This can be achieved via electroporation or nucleofection.
- Single-Cell Cloning and Selection: Plate transfected cells at a very low density to derive single-cell clones. Expand individual clones.
- Genotypic Validation: Screen clones for successful B2M and CIITA knockout using sequencing (e.g., Sanger or NGS). Confirm the site-specific integration and expression of the CD47 transgene via PCR and flow cytometry.
- Phenotypic Validation (Flow Cytometry): Confirm the loss of HLA class I (using a pan-HLA class I antibody) and HLA class II (e.g., HLA-DR) surface expression. Confirm high surface expression of CD47.
- Functional Validation (In Vitro Assay): Co-culture engineered HIP cells with activated human natural killer (NK) cells from an allogeneic donor. Measure cell killing using real-time impedance assays (e.g., xCelligence) or flow cytometry-based cytotoxicity assays. Successful engineering should result in significant protection from NK cell killing.
Protocol 2: In Vivo Teratoma Formation Assay in Humanized Mice
This protocol is used to test the immune evasion capability of engineered stem cells and their differentiated progeny in a model with a functional human immune system [29].
- Prepare Humanized Mouse (Hu-mouse) Recipients: Reconstitute immunodeficient NSG or similar mice with a human immune system. Common methods include co-implantation of human fetal thymus tissue and fetal liver-derived CD34+ hematopoietic stem cells (the BLT model) or injection of human peripheral blood mononuclear cells (PBMC) [29].
- Validate Immune Reconstitution: After 12-16 weeks, bleed the mice and use flow cytometry to confirm robust engraftment of human T cells, B cells, and other immune cell populations.
- Cell Transplantation: Harvest the engineered hPSCs (or their differentiated progeny) into a single-cell suspension. Subcutaneously inject a defined number of cells (e.g., 1-10 million) into the flank of the Hu-mice. The contralateral flank can be injected with wild-type control cells from the same genetic background as an internal control.
- Monitor Graft Survival: Monitor teratoma or graft formation weekly by palpation and caliper measurement. For cells engineered with a luciferase reporter, use bioluminescence imaging (BLI) to quantitatively track viable cell mass over time.
- Endpoint Analysis: After 4-8 weeks, harvest the teratomas/grafts. Compare the size, weight, and viable cell mass (via BLI) of experimental versus control grafts. Perform histological analysis to assess differentiation and immune cell infiltration (e.g., by H&E staining and immunohistochemistry for human CD45+ immune cells).
Troubleshooting Guides and FAQs
FAQ 1: Why is CD47 overexpression favored over HLA-G or PD-L1 alone for protecting HLA-deficient cells from innate immunity?
Answer: Comprehensive in vitro and in vivo studies comparing these strategies have shown that CD47 provides more robust protection. HLA-G only protects from the subset of NK cells expressing its specific receptor (ILT2), and PD-L1 only protects from PD-1+ NK cells, which are a minor population. In contrast, SIRPα, the receptor for CD47, is expressed on almost all macrophages and a majority of activated NK cells. Engineered cells overexpressing CD47 were comprehensively protected from killing by all NK cell subsets, whereas HLA-G and PD-L1 provided only partial protection [27].
FAQ 2: My HIP-edited cells are still being rejected in the Hu-mouse model. What could be the cause?
Answer: Consider these potential issues and troubleshooting steps:
- Incomplete HLA Knockout: Verify at the protein level that HLA class I and II are completely absent from your final differentiated cell product, as their expression can change during differentiation [25].
- Species-Specific CD47-SIRPα Interaction: The CD47-SIRPα interaction is species-specific. If using human cells in a mouse model reconstituted with a mouse immune system, you must use a CD47 transgene matching the recipient species (e.g., macaque CD47 for rhesus models) [27].
- Antibody-Mediated Rejection: While HIP editing removes major targets for donor-specific antibodies, check for pre-existing antibodies against other antigens. Ensure your HIP strategy includes broad disruption of HLA to prevent antibody binding [25].
- Insufficient CD47 Expression Levels: Quantify CD47 surface expression. There may be a threshold required for effective "don't eat me" signaling that your cells have not achieved.
FAQ 3: What are the primary safety concerns associated with overexpressing immune checkpoints like CD47 and PD-L1 in cell therapies?
Answer: The main concern is the potential for the engineered cells to evade immune surveillance in a way that could lead to tumorigenesis. If a pluripotent stem cell contaminates the final therapeutic product, its unchecked growth could form a teratoma that the immune system cannot clear. Furthermore, if the therapeutic cells themselves were to undergo malignant transformation, they might be shielded from anti-tumor immunity. Rigorous testing for residual undifferentiated cells and long-term follow-up in pre-clinical models are essential to quantify this risk [27]. For systemic therapies using bispecific antibodies targeting CD47, a major concern is hematological toxicity, such as anemia and thrombocytopenia, due to CD47's expression on red blood cells and platelets [28] [31]. This is often addressed by engineering lower affinity for CD47.
FAQ 4: Can I use a single immune checkpoint inhibitor, like anti-PD-L1, to protect my allogeneic graft?
Answer: Evidence suggests that single-agent checkpoint inhibition is often insufficient to prevent allograft rejection. Research in humanized mouse models demonstrated that combined expression of CTLA4-Ig and PD-L1 was required to protect hESC-derived cells; neither molecule was sufficient on its own [29]. The immune system has multiple redundant pathways for rejecting foreign cells. A successful strategy likely requires a multi-pronged approach that simultaneously addresses T-cell co-stimulation (e.g., via CTLA4-Ig), T-cell inhibition (e.g., via PD-L1), and innate immune cell clearance (e.g., via CD47) [25] [29].
Troubleshooting Guide: Common Experimental Challenges
This guide addresses specific issues you might encounter while developing universal donor cells through multiplexed gene editing.
Table: Common Problems and Solutions in Gene Editing Experiments
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low editing efficiency [32] | Low transfection efficiency; difficult-to-edit locus. | Optimize transfection protocol; use antibiotic selection or FACS to enrich transfected cells [32]. |
| High off-target effects [32] | crRNA with homology to other genomic regions. | Carefully design crRNA target oligos to avoid off-target homology [32]. |
| No cleavage detected [32] | PAM site unavailable; nucleases cannot access target. | Design a new targeting strategy for a nearby sequence; use TAL effector-based nuclease as an alternative [32]. |
| No PCR product in cleavage detection [32] | Poor PCR primer design; GC-rich region. | Redesign primers (18–22 bp, 45–60% GC content, Tm 52–58°C); add GC Enhancer for GC-rich regions [32]. |
| Smear on cleavage detection gel [32] | Lysate is too concentrated. | Dilute the lysate 2- to 4-fold and repeat the PCR reaction [32]. |
| Immune escape after transplantation [33] | Activation of NK cell "missing-self" response due to absent HLA class I. | Co-express non-classical HLA molecules (e.g., HLA-E, HLA-G) to inhibit NK cell cytotoxicity [33] [34]. |
| Tumor formation from residual undifferentiated cells [33] | Persistence of pluripotent stem cells in the final product. | Implement safety mechanisms (e.g., suicide genes) to enable inactivation or removal of donor cells if needed [33]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary genetic targets for creating hypoimmunogenic pluripotent stem cells? The primary targets are genes within the Major Histocompatibility Complex (MHC). A common and effective strategy is the knockout of Beta-2 microglobulin (B2M), which is essential for the surface expression of all HLA class I molecules, thereby evading CD8+ T cell recognition [33] [25] [34]. To address the subsequent vulnerability to Natural Killer (NK) cell attack, a key strategy is the co-expression of non-classical HLA molecules like HLA-E or HLA-G [33] [34]. Furthermore, eliminating Class II Major Histocompatibility Complex Transactivator (CIITA) prevents the expression of HLA class II molecules, helping to evade CD4+ T cell responses [33] [34].
Q2: Our B2M-knockout cells are being rejected in vivo. What immune cells are likely responsible and how can we prevent this? This rejection is likely mediated by Natural Killer (NK) cells through the "missing-self" response [33] [35]. While B2M knockout removes the ligand for T-cell receptors, it also removes the ligands for inhibitory receptors on NK cells. To overcome this, engineer your cells to express HLA-E or HLA-G. These non-classical HLA molecules bind to inhibitory receptors (e.g., CD94/NKG2A) on NK cells and effectively suppress their cytotoxic activity [33] [34]. A proven method is the targeted knock-in of an HLA-E trimer at the B2M genomic locus, which simultaneously abolishes classical HLA expression and provides NK cell inhibition [34].
Q3: How can I improve the efficiency of my CRISPR/Cas9 editing in stem cells? Several parameters can be optimized:
- Enrich for Transfected Cells: Introduce antibiotic resistance genes alongside your CRISPR constructs and apply selection pressure. Alternatively, use Fluorescence-Activated Cell Sorting (FACS) if a fluorescent marker is co-expressed [32].
- Verify Oligonucleotide Design: For cloning into CRISPR vectors, ensure your single-stranded oligonucleotides contain the correct 5' or 3' nucleotide overhangs required by your specific kit (e.g.,
GTTTTon the 3' end for the top strand in some systems) [32]. - Handle Reagents Properly: Avoid repeated freeze-thaw cycles of annealed oligonucleotides by creating aliquots and storing them at -20°C in an appropriate buffer [32].
Q4: What are the critical quality controls for a newly generated universal donor stem cell line? Beyond standard checks for pluripotency and karyotype, specific quality controls for hypoimmunogenic lines include:
- Genomic Quality Control: Perform rigorous sequencing to screen for and discard clones with undesired on-target or off-target mutations [34].
- Immune Evasion Verification:
- Use flow cytometry to confirm the absence of surface HLA class I and II molecules.
- Demonstrate resistance to allogeneic CD8+ T cell-mediated killing in co-culture assays [33].
- Demonstrate resistance to NK cell-mediated cytotoxicity in co-culture assays, especially if HLA-E/G are expressed [33] [34].
- Functional Differentiation: Confirm that the edited cell line can differentiate normally into your desired therapeutic cell type (e.g., neural, cardiac) [34].
Detailed Experimental Protocols
Protocol 1: Multiplexed KO of B2M and CIITA with HLA-E Knock-in
Objective: To generate a hypoimmunogenic hPSC line lacking T cell recognition (via B2M and CIITA KO) and protected from NK cells (via HLA-E knock-in).
Materials:
- Cell Line: Human ESCs or iPSCs.
- CRISPR System: Cas9 nuclease (mRNA or protein).
- Guide RNAs (gRNAs): Designed for B2M, CIITA, and for a safe harbor locus (e.g., AAVS1) or the B2M locus itself for knock-in.
- Repair Template: Donor vector containing a β2M-HLA-E single-chain trimer fusion gene, flanked by homology arms [33] [34].
- Transfection Reagent: Optimized for your stem cell line (e.g., Lipofectamine 3000).
- Selection Agent: Appropriate antibiotic if the repair template contains a resistance gene.
Methodology:
- Design and Preparation: Design high-efficiency gRNAs for B2M and CIITA. Clone the β2M-HLA-E fusion construct into a donor vector with homology arms.
- Transfection: Co-transfect the stem cells with the Cas9/gRNA ribonucleoprotein (RNP) complexes for B2M, CIITA, and the donor vector.
- Selection and Cloning: Apply antibiotic selection (if applicable) 48-72 hours post-transfection. Manually pick single-cell-derived clones and expand them.
- Genotyping:
- Use PCR and sequencing to confirm biallelic knockout of B2M and CIITA.
- Use junction PCR and sequencing to verify targeted integration of the HLA-E trimer at the intended locus.
- Phenotypic Validation:
- Perform flow cytometry to confirm loss of surface HLA class I (using an antibody like W6/32) and HLA class II.
- Use a specific antibody to confirm surface expression of the HLA-E trimer [34].
- Functional Validation:
- Differentiate the edited clones and conduct in vitro immune cell co-culture assays with allogeneic CD8+ T cells and NK cells to demonstrate evasion of immune rejection [33].
Protocol 2: In Vitro Immune Cell Co-culture Assay
Objective: To quantitatively assess the survival of gene-edited hypoimmunogenic cells when confronted with allogeneic immune cells.
Materials:
- Target Cells: Differentiated progeny of your edited and control (unmodified) stem cells.
- Effector Cells: Peripheral Blood Mononuclear Cells (PBMCs) from an allogeneic donor, or isolated CD8+ T cells and NK cells.
- Assay Plate: 96-well plate.
- Viability Assay: Lactate Dehydrogenase (LDH) release kit, or a flow cytometry-based assay using Annexin V/propidium iodide.
Methodology:
- Seed Target Cells: Plate differentiated target cells and allow them to adhere.
- Co-culture: Add allogeneic PBMCs or isolated immune cells at various effector-to-target (E:T) ratios.
- Incubate: Co-culture for 24-48 hours.
- Measure Cytotoxicity:
- LDH Assay: Measure the LDH enzyme released from the cytosol of damaged cells into the supernatant.
- Flow Cytometry: Harvest and stain cells to distinguish live, apoptotic, and dead target cells.
- Analysis: Calculate the percentage of specific lysis. Successful editing is indicated by significantly reduced lysis in edited cells compared to unmodified controls across all E:T ratios [35].
Key Signaling Pathways and Experimental Workflows
Diagram: Strategies for Generating Universal Donor Cells
Diagram: Immune Recognition and Evasion Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Hypoimmunogenic Cell Generation
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| CRISPR-Cas9 System | Precision genome editing for knocking out genes like B2M and CIITA [25]. | Use high-fidelity Cas9 variants to minimize off-target effects. RNP transfection is often highly efficient. |
| TALENs | Transcription activator-like effector nucleases; an alternative genome editing tool [32]. | Can be used when PAM sites for CRISPR are unavailable [32]. |
| HLA-E Single-Chain Trimer Donor Vector | Repair template for knock-in to confer NK cell resistance [34]. | Ensure the vector includes homology arms for the target locus (e.g., B2M) and a selectable marker. |
| Flow Cytometry Antibodies | Validation of surface protein expression (e.g., anti-HLA-ABC, anti-HLA-DR, anti-HLA-E). | Critical for confirming the knockout of immunogenic HLAs and expression of inhibitory HLAs. |
| In Vitro Immune Assay Kits (e.g., LDH Cytotoxicity) | Quantitative measurement of immune cell-mediated killing of edited cells [35]. | Perform with allogeneic PBMCs or purified immune cells at multiple effector-to-target ratios. |
| PureLink HQ Mini Plasmid Purification Kit | High-quality plasmid DNA preparation for sequencing or transfection [32]. | Using high-quality DNA is crucial for successful sequencing reactions and transfection efficiency. |
Core Concepts: Understanding the New Paradigm
This section answers fundamental questions about the purpose and components of these novel conditioning treatments.
FAQ: What is the primary goal of using non-genotoxic conditioning agents in allogeneic transplantation? The primary goal is to eliminate the need for traditional, DNA-damaging chemotherapy and radiation (genotoxic conditioning) that carries significant risks, including secondary malignancies, infections, and organ toxicity. Non-genotoxic conditioning aims to achieve targeted immunosuppression and create "space" for donor stem cell engraftment through highly specific mechanisms, thereby improving the safety profile of allogeneic stem cell transplantation [36] [37] [26].
FAQ: What are the key biological targets for these novel conditioning agents? The most advanced strategies focus on two key targets:
- CD117 (c-Kit): A receptor tyrosine kinase highly expressed on hematopoietic stem cells (HSCs). Depleting host HSCs with a CD117-targeting antibody-drug conjugate (ADC) creates a niche for donor HSC engraftment without genotoxicity [36] [37].
- TRBV9+ T Cells: A specific T-cell receptor beta variable gene segment identified as a driver in certain autoimmune diseases like ankylosing spondylitis. Targeted depletion of this T-cell subset can eliminate pathologic immune cells without causing broad immunosuppression [38].
FAQ: How does targeted T-cell depletion differ from traditional T-cell depletion? Traditional T-cell depletion is a broad, non-selective removal of all T-cells from a graft (pan-TCD) to prevent Graft-versus-Host Disease (GvHD). While effective at reducing GvHD, it increases risks of graft failure and disease relapse due to the loss of beneficial graft-versus-leukemia effects. In contrast, targeted T-cell depletion aims to remove only specific, disease-causing T-cell clones (e.g., TRBV9+ or PD-1+ alloreactive cells), preserving the broader T-cell repertoire to fight infection and cancer [39] [38] [40].
Troubleshooting Guides
This section provides solutions to common experimental and clinical challenges.
Challenge: Poor Donor Cell Engraftment
Problem: Despite conditioning, donor hematopoietic stem cells fail to engraft or show low-level, transient chimerism.
| Potential Cause | Diagnostic Steps | Recommended Solutions |
|---|---|---|
| Insufficient host HSC clearance | Analyze bone marrow for residual host CD117+ HSCs post-conditioning. | Increase dose of CD117-ADC; combine with transient immunosuppression (e.g., anti-CD4, anti-CD8, anti-CD154 mAbs) [37]. |
| Resistant host immunity | Monitor T-cell chimerism; check for alloreactive T-cells. | Add short-course immunosuppressants (e.g., rapamycin) or target alloreactive T-cells (e.g., anti-PD-1 depletion) [37] [41]. |
| Inadequate cell dose | Quantify the number of donor HSCs infused. | Ensure transplanted cell dose is sufficient (>20 million total bone marrow cells in mouse models) [37]. |
Challenge: Disease Relapse or Autoimmune Symptom Return
Problem: Following initial successful treatment, the underlying malignancy or autoimmune pathology recurs.
| Potential Cause | Diagnostic Steps | Recommended Solutions |
|---|---|---|
| Incomplete depletion of pathologic cells | Use TCR sequencing to track residual or re-emerging pathogenic clones (e.g., TRBV9+ with specific CDR3 motif) [38]. | Implement repeat dosing of the targeted depleting agent (e.g., anti-TRBV9 antibody); consider adjunctive therapy. |
| Loss of tolerance | Monitor for emergence of donor-reactive T cells and loss of chimerism. | Ensure stable mixed chimerism; evaluate need for booster donor lymphocyte infusions under immunosuppression cover. |
Challenge: On-Target, Off-Toxicity
Problem: Adverse effects due to expression of the target antigen on non-target cells.
| Potential Cause | Diagnostic Steps | Recommended Solutions |
|---|---|---|
| CD117 expression on non-HSCs | Monitor for effects on mast cells, melanocytes, or germ cells. | In pre-clinical models, this has been limited to transient liver enzyme elevations [37]. Dose optimization is critical. |
| Cytokine Release Syndrome (CRS) | Monitor for fever, hypotension, and tachycardia following antibody infusion. | Pre-medicate with corticosteroids, antihistamines, and anti-emetics as done in the first human anti-TRBV9 case [38]. |
Experimental Protocols
This section provides detailed methodologies for key experiments cited in the literature.
Objective: To establish durable multi-lineage hematopoietic chimerism and donor-specific tolerance in a fully MHC-mismatched model using CD117-ADC conditioning.
Workflow Diagram:
Key Materials:
- Conditioning Agent: CD117-ADC (e.g., saporin-conjugated anti-CD117 antibody).
- Transient Immunosuppression: Depleting anti-CD8 mAb, non-depleting anti-CD4 mAb, non-depleting anti-CD154 mAb, Rapamycin.
- Model: C57Bl/6 recipients, BALB/c donors (fully MHC-mismatched).
Detailed Procedure:
- Conditioning (Day -6): Administer a single intravenous dose of CD117-ADC to recipient mice.
- Bone Marrow Transplantation (Day 0): Infuse 20 million total bone marrow cells from donor mice via tail vein.
- Transient Immunosuppression:
- Administer one dose each of depleting anti-CD8 mAb, non-depleting anti-CD4 mAb, and non-depleting anti-CD154 mAb on days 0, +2, and +4 relative to BMT.
- Administer rapamycin on days +6 and +30.
- Monitoring: Track donor chimerism in peripheral blood over time using flow cytometry for donor-specific MHC markers across various lineages (T cells, B cells, monocytes, granulocytes).
- Tolerance Assay (Months 5-8): Transplant full-thickness tail skin grafts from both the original bone marrow donor (BALB/c) and a third-party strain (e.g., CBA/Ca). Monitor graft survival long-term without any ongoing immunosuppression.
Expected Outcomes:
- High-level (up to 50%), multi-lineage hematopoietic chimerism lasting >400 days.
- Permanent acceptance of donor-type skin allografts with prompt rejection of third-party grafts.
- No clinical signs of Graft-versus-Host Disease.
Objective: To deplete a specific, disease-driving T-cell population (TRBV9+ T cells) to induce remission in an autoimmune disease model.
Workflow Diagram:
Key Materials:
- Therapeutic Agent: Humanized, cytotoxic anti-TRBV9 monoclonal antibody (e.g., BCD-180).
- Pre-medication: Corticosteroids (e.g., Prednisolone), antihistamine (e.g., Chloropyramine), anti-emetic (e.g., Ondansetron).
Detailed Procedure:
- Patient Selection: Identify patients with active disease (e.g., Ankylosing Spondylitis) and confirm the presence of the pathogenic T-cell population. In the case of AS, this involves HLA-B*27 positivity and confirmation of an expanded TRBV9+ TCRβ CDR3 motif via TCR sequencing.
- Pre-medication: Administer pre-medications approximately 30 minutes before antibody infusion to mitigate infusion-related reactions.
- Treatment Infusion (Day 0): Administer the anti-TRBV9 antibody via slow intravenous infusion. The initial human case used a dose of 60 mg.
- Monitoring:
- Safety: Monitor for infusion reactions (e.g., fever, nausea, hypertension).
- Efficacy: Measure the depletion of TRBV9+ T cells from peripheral blood 10 days post-infusion using TRBV9-specific real-time PCR and high-throughput TCR repertoire sequencing.
- Clinical: Track disease-specific metrics (e.g., BASMI for AS, pain scores).
- Repeat Dosing: Administer subsequent doses based on the re-emergence of symptoms and/or the return of the pathogenic TCRβ CDR3 motif in the blood. The dosing interval may be every 4 months or longer.
Expected Outcomes:
- Profound depletion (>90%) of circulating TRBV9+ T cells within days of infusion.
- Significant clinical improvement within 3 months, potentially allowing cessation of concomitant therapies (e.g., anti-TNF).
- Long-term remission with maintenance dosing.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential reagents and their functions for implementing these novel paradigms.
| Research Reagent | Function & Mechanism | Example Application |
|---|---|---|
| CD117-ADC | Antibody-Drug Conjugate targeting c-Kit on HSCs. Delivers a toxin (e.g., saporin) to selectively ablate host HSCs. | Creating niche for donor HSC engraftment in allogeneic transplantation without genotoxicity [36] [37]. |
| Anti-TRBV9 Antibody | Cytotoxic monoclonal antibody that depletes T cells expressing the TRBV9 gene segment. | Targeted therapy for TRBV9-mediated autoimmune diseases like Ankylosing Spondylitis [38]. |
| Anti-PD-1 Depleting Antibody | Antibody that binds PD-1 and eliminates expressing cells. Targets activated/alloreactive T-cells for depletion. | Reshaping TCR repertoire to induce transplant tolerance or treat autoimmunity [41]. |
| Transient Immunosuppression Cocktail | Combination of non-depleting/depleting antibodies (anti-CD4, anti-CD8, anti-CD154) and mTOR inhibitor (Rapamycin). | Prevents acute rejection of allograft during the peri-transplant period without long-term immunosuppression [37]. |
Navigating Clinical Hurdles: GvHD, Persistence, and Conditioning Toxicity
Allogeneic hematopoietic cell transplantation (allo-HCT) remains the only curative therapy for many aggressive hematological malignancies. However, its success is often limited by graft-versus-host disease (GVHD), a life-threatening complication where donor immunocompetent T cells attack recipient tissues. GVHD occurs in 30-50% of transplant recipients despite standard prophylactic therapies, with approximately half of acute GVHD cases becoming steroid-refractory, creating a critical unmet need for more effective prevention strategies [42]. This technical support document examines two promising approaches for GVHD prevention: T-cell receptor (TCR) ablation and post-transplant cyclophosphamide (PTCy), providing researchers with practical experimental guidance for implementing these methodologies.
Technical FAQs: Mechanism and Application
Q1: What is the fundamental mechanistic difference between TCR ablation and PTCy in preventing GVHD?
A1: While both approaches target alloreactive T cells, they operate through distinct biological mechanisms and temporal applications:
TCR Ablation: This preventive genetic engineering approach involves complete elimination of TCR function in donor T cells before transplantation. Using CRISPR/Cas9 to knockout the TCR α constant (TRAC) locus removes the T cell's ability to recognize any antigen, thereby preventing the initial alloreactive recognition that triggers GVHD [43].
PTCy: This is a pharmacological selective depletion method administered after transplant (typically days +3 and +4). PTCy exploits differential expression of aldehyde dehydrogenase (ALDH), an enzyme that inactivates cyclophosphamide. Hematopoietic stem cells and regulatory T cells (Tregs) with high ALDH activity survive, while alloreactive conventional T cells undergoing rapid division are eliminated by DNA crosslinking [44].
Table 1: Core Mechanism Comparison
| Feature | TCR Ablation | Post-Transplant Cyclophosphamide |
|---|---|---|
| Primary mechanism | Elimination of antigen recognition capability | Selective killing of rapidly dividing alloreactive T cells |
| Timing of intervention | Pre-transplant (ex vivo) | Post-transplant (days +3 and +4) |
| Specificity | Global T cell function ablation | Preferential targeting of activated alloreactive cells |
| Key cellular players | TCR-deficient T cells | ALDH-high stem cells, Tregs, alloreactive T cells |
| Experimental evidence | 80% survival at 90 days in NOG mice [43] | 50 mg/kg on days +3,+4 in haploidentical HCT [44] |
Q2: How can researchers effectively model and assess these interventions preclinically?
A2: The hPBMC-engrafted NOG mouse model has emerged as a gold standard for studying human GVHD mechanisms and interventions:
Model Establishment: Irradiate NOG mice with 200 rads one day prior to intravenous inoculation with donor PBMCs (e.g., 5-10×10^6 cells) [43]. Key endpoints include body weight loss (>20%), survival rate, and clinical GVHD scores over 60-90 days.
TCR Ablation Validation: Confirm TCR knockout efficiency (>95%) via flow cytometry for TCRαβ before transplantation. In vivo, TCR-ablated T cells (via TRAC knockout) should not induce GVHD, with >80% survival at 90 days compared to complete mortality with wild-type T cells [43].
PTCy Modeling: Administer cyclophosphamide 50 mg/kg intraperitoneally on days +3 and +4 post-PBMC transplantation. Monitor for reduced T cell infiltration in target organs (skin, liver, GI tract) and preservation of hematopoietic reconstitution [44].
Q3: What are the critical experimental parameters for PTCy dosing in preclinical models?
A3: Successful PTCy implementation requires careful attention to dosing, timing, and supportive care:
Dosing Regimen: The established clinical dose is 50 mg/kg administered intravenously on days +3 and +4 post-transplantation. This timing coincides with maximal alloreactive T cell activation while sparing quiescent Tregs and hematopoietic stem cells [44].
Toxicity Management: Hydration (e.g., 2-3 mL normal saline per 1 mg cyclophosphamide) and mesna administration (60-100% of cyclophosphamide dose divided into 3-4 doses) are essential to prevent hemorrhagic cystitis. Monitor for cardiotoxicity (acute ECG changes) and hepatotoxicity (serum bilirubin, transaminases) [44].
Pharmacogenetic Considerations: Account for polymorphisms in CYP2B6, CYP2C19, and ALDH genes that significantly impact cyclophosphamide metabolism and toxicity. Consider preemptive genotyping in study designs [44].
Table 2: PTCy Experimental Parameters
| Parameter | Standard Protocol | Key Variations | Troubleshooting Tips |
|---|---|---|---|
| Dose timing | Days +3 and +4 post-transplant | Day +3 only (reduced intensity) | Adjust based on engraftment kinetics |
| Route | Intravenous | Intraperitoneal (preclinical) | Ensure proper hydration support |
| Supportive care | Mesna, forced hydration | Antibiotic prophylaxis | Monitor urine for blood |
| Drug preparation | Fresh preparation in saline | Stability: 24h at room temperature | Discard unused solution |
| Toxicity monitoring | Daily weights, clinical scores | Cardiac echo, liver enzymes | Baseline and weekly labs |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for GVHD Intervention Studies
| Reagent/Cell Type | Specific Function | Experimental Application | Validation Methods |
|---|---|---|---|
| CRISPR/Cas9 TRAC gRNA | Targeted knockout of TCR α constant chain | Generate antigen-insensitive T cells | Flow cytometry (TCRαβ), sequencing |
| NOG (NOD/SCID/IL-2γ-/-) mice | Immunodeficient recipient for human immune cells | Xenogeneic GVHD modeling | PBMC engraftment by flow cytometry |
| Anti-CD3/CD28 beads | Polyclonal T cell activation/expansion | In vitro T cell stimulation | CFSE proliferation assay, cytokine release |
| Cyclophosphamide metabolite standards | HPLC/MS quantification of drug exposure | Pharmacokinetic studies | Calibration curves, internal standards |
| ALDEFLUOR assay kit | Detection of ALDH-bright cell populations | Identify cyclophosphamide-resistant cells | Flow cytometry with DEAB control |
| Anti-human CD127/CD25 antibodies | Regulatory T cell identification | Treg quantification and isolation | FOXP3 intracellular staining |
Experimental Protocols
TCR Ablation Workflow for GVHD Prevention
Principle: Complete elimination of TCR-mediated alloreactivity through genetic engineering while preserving non-alloreactive functions [43].
Step-by-Step Protocol:
T Cell Isolation: Isolate CD3+ T cells from donor PBMCs using magnetic bead separation (purity >95% by flow cytometry).
CRISPR Electroporation: Prepare ribonucleoprotein complexes with Cas9 protein and TRAC-specific gRNA. Electroporate 1×10^6 T cells per condition using manufacturer-optimized settings.
Validation of Knockout: 48-72 hours post-electroporation, assess TCR knockout efficiency by flow cytometry for TCRαβ. Proceed only with preparations showing >90% knockout.
Expansion (Optional): Culture TCR-ablated T cells with IL-7 (10 ng/mL) and IL-15 (5 ng/mL) for 7-14 days to expand cell numbers while maintaining viability.
Functional Assays:
- Mixed Lymphocyte Reaction: Co-culture with allogeneic PBMCs to confirm absence of proliferation.
- Cytokine Release: Stimulate with PMA/ionomycin and measure IFN-γ, IL-2 production (should be significantly reduced).
- Xenogeneic GVHD Model: Transplant 5×10^6 TCR-ablated T cells into irradiated NOG mice alongside 1×10^6 CD34+ hematopoietic stem cells.
PTCy Administration and Monitoring Protocol
Principle: Selective elimination of alloreactive T cells during their peak activation while preserving beneficial immune cells [44].
Step-by-Step Protocol:
Drug Preparation:
- Reconstitute cyclophosphamide in sterile saline to 20 mg/mL final concentration.
- Prepare fresh for each administration and use within 6 hours.
Transplantation and Dosing:
- Perform hematopoietic cell transplantation on day 0.
- Administer first PTCy dose (50 mg/kg) on day +3 via slow IV infusion over 1-2 hours.
- Repeat identical dose on day +4.
Supportive Care:
- Administer mesna at 60-100% of cyclophosphamide dose divided into 3-4 doses.
- Provide forced hydration (2-3 mL normal saline per 1 mg cyclophosphamide).
- Implement antiemetic prophylaxis (ondansetron 0.15 mg/kg pre-infusion).
Toxicity Monitoring:
- Daily: Weights, clinical GVHD scores, fluid balance, urine dipstick for blood.
- Biweekly: Complete blood count, serum creatinine, liver enzymes.
- Weekly: Cardiac function assessment in long-term studies.
Efficacy Assessment:
- Engraftment: Donor chimerism >95% by day +30.
- GVHD Incidence: Clinical scoring of skin, liver, and GI tract.
- Immune Reconstitution: Flow cytometry for T, B, NK cell subsets at days +30, +60, +100.
Troubleshooting Common Experimental Challenges
Problem 1: Incomplete TCR knockout leads to residual GVHD in TCR ablation models.
- Potential Cause: Suboptimal CRISPR efficiency or selection of non-functional gRNA.
- Solution: Validate multiple gRNAs in vitro before proceeding to animal studies. Include a positive control (GFP transfection) to assess delivery efficiency. Implement FACS sorting for TCR-negative populations post-editing to achieve >99% purity [43].
Problem 2: Excessive toxicity or mortality with PTCy in murine models.
- Potential Cause: Inadequate hydration support or incorrect dosing for specific mouse strain.
- Solution: Optimize hydration protocol with subcutaneous fluids (1 mL normal saline) pre- and post-each dose. Consider dose reduction to 30-40 mg/kg for more sensitive strains while monitoring for maintained efficacy [44].
Problem 3: Poor human immune cell engraftment in NOG mouse models.
- Potential Cause: Suboptimal irradiation dose or inadequate cell numbers.
- Solution: Validate irradiation equipment and dose (typically 200-250 rads for NOG mice). Increase PBMC dose to 10×10^6 cells/mouse while monitoring for early GVHD onset. Include engraftment check via flow cytometry for human CD45+ cells at week 2 [43].
Problem 4: Failure to preserve graft-versus-leukemia (GVL) effects while preventing GVHD.
- Potential Cause: Over-suppression of alloreactive responses eliminates beneficial anti-tumor immunity.
- Solution: For TCR ablation approaches, consider retaining or engineering non-alloreactive antitumor specificity (e.g., CAR constructs). For PTCy, optimize timing to preserve tumor-reactive clones [42]. Include tumor challenge models in efficacy studies.
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative therapy for various hematological diseases, but its success is fundamentally challenged by host versus graft reactions, primarily graft-versus-host disease (GVHD). The table below summarizes key clinical outcomes from a recent large-scale meta-analysis, providing a benchmark for evaluating intervention strategies [45].
Table 1: Key Clinical Outcomes of Allo-HSCT
| Outcome Measure | Rate (%) | Details/Subgroups |
|---|---|---|
| Overall Survival (OS) | 94% | Highest with Matched Related Donor (MRD) [45]. |
| Event-Free Survival (EFS) | 86% | Event includes graft rejection, disease relapse, or death [45]. |
| Acute GVHD (aGVHD) | 20% | Lower with non-myeloablative (NMA) conditioning [45]. |
| Chronic GVHD (cGVHD) | 14% | Lower with non-myeloablative (NMA) conditioning and MRD [45]. |
| Graft Failure (GF) | 9% | Lowest with Matched Related Donor (MRD) [45]. |
| Non-Relapse Mortality | 6% | --- |
Core Experimental Protocols
Protocol 1: In Vivo Treg Expansion for GVHD Prohibition
This pre-clinical protocol uses targeted immunotherapy to expand the host's regulatory T cells (Tregs) in vivo before transplant, creating a more tolerant immune environment and reducing reliance on broad immunosuppression [46].
- 1. Primary Objective: To assess the efficacy of pre-transplant Treg expansion in reducing the incidence and severity of acute GVHD without compromising graft-versus-leukemia (GVL) effects.
- 2. Background & Rationale: Tregs are crucial for maintaining immune tolerance. Traditional post-transplant immunosuppression (e.g., calcineurin inhibitors) increases infection risks and may impair GVL. This protocol aims to proactively shape the host's immune system pre-transplant to accept the graft [46].
- 3. Materials & Reagents:
- TL1A-Ig fusion protein: Binds to and stimulates the TNFRSF25 receptor on Tregs.
- Low-dose Interleukin-2 (IL-2): Stimulates the CD25 receptor, promoting Treg survival and proliferation.
- Allogeneic hematopoietic stem cell graft.
- 4. Step-by-Step Methodology:
- Pre-conditioning Therapy: Administer the combination of TL1A-Ig and low-dose IL-2 to the recipient for a defined period (e.g., 5-7 days) before the transplant conditioning regimen begins.
- Conditioning: Initiate standard myeloablative or reduced-intensity conditioning.
- Stem Cell Infusion: Perform the allogeneic HSCT.
- Post-Transplant Monitoring: Monitor for GVHD clinical signs, weight loss, survival, and donor cell engraftment. Analyze Treg populations in key tissues (e.g., colon, liver) and assess the gut microbiome diversity.
- 5. Key Parameters Measured:
- Primary Endpoint: Overall survival and clinical GVHD score.
- Secondary Endpoints: Treg frequency in peripheral blood and target tissues; gut microbiome composition; graft-versus-leukemia (GVL) effect in co-implanted malignancy models.
Protocol 2: Biomarker-Guided Risk Stratification and Preemption
This approach uses validated serum biomarkers to identify patients at high risk for developing severe GVHD before clinical symptoms appear, enabling early intervention [47] [48].
- 1. Primary Objective: To preemptively treat patients at high risk for steroid-refractory GVHD based on biomarker profiles.
- 2. Background & Rationale: The MAGIC algorithm, which combines concentrations of suppression of tumorigenicity 2 (ST2) and regenerating islet-derived protein 3α (REG3α), can predict the onset of severe, treatment-refractory GVHD and non-relapse mortality [48].
- 3. Materials & Reagents:
- ELISA or Multiplex Immunoassay Kits for ST2 and REG3α.
- Patient serum samples collected at specific post-transplant time points (e.g., day 7, 14, 28).
- Therapeutics for preemptive treatment (e.g., Ruxolitinib, a JAK1/2 inhibitor).
- 4. Step-by-Step Methodology:
- Sample Collection: Collect serial serum samples from patients post-allo-HSCT.
- Biomarker Analysis: Measure ST2 and REG3α levels in the serum samples.
- Risk Calculation: Input biomarker concentrations into the MAGIC algorithm to stratify patients as high or standard risk.
- Preemptive Intervention: For patients classified as high-risk, initiate preemptive therapy (e.g., Ruxolitinib) before the full clinical manifestation of severe GVHD.
- Monitoring: Closely monitor clinical GVHD symptoms and biomarker levels for response to preemptive therapy.
- 5. Key Parameters Measured:
- Primary Endpoint: Incidence of severe (Grade III-IV) GVHD.
- Secondary Endpoints: Non-relapse mortality; response rate to preemptive therapy; overall survival.
Troubleshooting Guides & FAQs
FAQ 1: What are the primary strategies to prevent GVHD without completely abolishing the graft-versus-leukemia effect?
Strategies are evolving beyond broad immunosuppression. Promising approaches include:
- Graft Engineering: Using CD34+ selected grafts or alpha-beta T-cell depletion to remove alloreactive T cells while preserving other immune cells [49] [50].
- Pharmacologic Inhibition of Key Pathways: Using post-transplant cyclophosphamide (PTCy) to eliminate alloreactive T-cells, or inhibitors of JAK1/2 (e.g., Ruxolitinib) and ROCK2 (e.g., Belumosudil) which are involved in pro-inflammatory and fibrotic signaling in GVHD [49] [48].
- Cellular Therapy: Infusing donor-derived regulatory T cells (Tregs) to actively suppress immune responses. Recent trials show Treg graft products (e.g., Orca-T) can prevent acute GVHD with less immunosuppression [49].
FAQ 2: Which biomarkers are most clinically useful for predicting and monitoring graft rejection and GVHD?
Biomarkers can be classified by their pathophysiological role [47]:
- Inflammation-Driven: ST2 (a member of the IL-1 receptor family) is a validated marker for predicting treatment-refractory aGVHD and mortality [47] [48]. IL-6 is a key cytokine in the initial "cytokine storm" and is associated with aGVHD diagnosis.
- Tissue Damage-Related: REG3α, a protein secreted by intestinal Paneth cells, is a specific biomarker for gastrointestinal GVHD severity [47] [48]. Elafin is a marker specific to skin damage in aGVHD. The combination of ST2 and REG3α in the MAGIC algorithm is the most clinically utilized panel for predicting steroid resistance and non-relapse mortality [48].
FAQ 3: Our team is exploring non-myeloablative conditioning. What are the key trade-offs?
Non-myeloablative (NMA) conditioning is associated with lower regimen-related toxicity and less tissue damage, which initiates the inflammatory cascade that drives GVHD. This leads to excellent outcomes in terms of reduced GVHD and mortality [45]. The primary trade-off is a potentially higher risk of disease relapse in some advanced malignancies due to less intensive cytoreduction. The choice of regimen must be personalized, balancing the patient's disease status, age, and comorbidities.
FAQ 4: Does the time of day for stem cell infusion influence engraftment or GVHD risk?
Current evidence is conflicting. While circadian rhythms are known to influence immune responses, a recent large retrospective study in patients receiving matched unrelated donor transplants found no significant association between the time of infusion (early vs. late afternoon) and the incidence of aGVHD [51]. The study concluded that logistical factors, rather than circadian timing, can guide scheduling in this setting. This contrasts with earlier studies, suggesting the effect may be dependent on donor type and GVHD prophylaxis regimen [51].
Signaling Pathways & Experimental Workflows
In Vivo Treg Expansion Pathway
The following diagram illustrates the mechanism by which pre-transplant immunotherapy expands regulatory T cells (Tregs) to promote a tolerant environment.
Post-Transplant Rejection Monitoring Workflow
This workflow outlines the key decision points in biomarker-guided monitoring and preemption of graft rejection and GVHD.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating Engraftment and Rejection
| Reagent / Tool | Function / Application | Key Examples / Notes |
|---|---|---|
| Recombinant Cytokines & Proteins | Used for in vivo immune modulation. | TL1A-Ig: Expands Tregs via TNFRSF25 [46]. Low-dose IL-2: Supports Treg survival and function [46]. |
| Pathway Inhibitors | Target specific signaling nodes in GVHD pathogenesis. | JAK1/2 inhibitors (e.g., Ruxolitinib): Suppress inflammatory cytokine signaling [47] [48]. ROCK2 inhibitors (e.g., Belumosudil): Ameliorate cGVHD by reducing fibrosis and shifting balance from Th17 to Tregs [49]. |
| Validated Biomarker Assays | Quantify biomarkers for risk stratification and monitoring. | ST2 & REG3α ELISAs: Core components of the MAGIC algorithm for predicting severe, steroid-refractory GVHD [48]. |
| Treg Expansion & Isolation Kits | For cellular therapy approaches. | Used to generate donor Treg products for adoptive transfer, which can be infused to prevent GVHD [46] [49]. |
| Conditioning Agents | Create marrow space and immunosuppression for engraftment. | Post-Transplant Cyclophosphamide (PTCy): Selectively depletes alloreactive T cells post-infusion, a widely used GVHD prophylaxis [49]. |
Conditioning regimens are a critical, yet double-edged, component of allogeneic stem cell transplantation (allo-SCT). Their purpose is twofold: to create space in the bone marrow for donor stem cells and to suppress the host immune system to prevent graft rejection. However, the intensity required to achieve these goals is directly associated with significant toxicities that can compromise patient outcomes. This technical support guide, framed within the broader thesis of overcoming immune rejection, delves into the specific challenges of conditioning regimen toxicities. It provides researchers and drug developers with targeted FAQs and troubleshooting guides to navigate the delicate balance between achieving sufficient immunosuppression for engraftment and minimizing collateral damage to the patient. The strategies discussed herein are fundamental to improving the safety profile of allo-SCT, thereby expanding its applicability to a broader patient population, including older adults and those with comorbidities [52] [53].
FAQ: Core Concepts for Researchers
Q1: What are the primary immunological goals of a conditioning regimen, and how do they relate to toxicity?
The conditioning regimen must achieve a level of host immune suppression sufficient to prevent graft rejection, a process mediated by residual host T cells, NK cells, and B cells. Insufficient immunosuppression increases rejection risk, necessitating more intensive regimens. However, this intensity is the primary driver of organ toxicities, such as sinusoidal obstruction syndrome (SOS/VOD), mucositis, and prolonged cytopenias. The challenge is that the same cytotoxic agents used for immunosuppression (e.g., alkylators like busulfan) also damage rapidly dividing non-hematopoietic cells, leading to these adverse events. The focus of modern research is to develop agents and protocols that provide more targeted immunosuppression with a reduced off-target toxicity profile [53] [54] [55].
Q2: How do reduced-intensity/reduced-toxicity conditioning (RIC/RTC) regimens differ from myeloablative conditioning (MAC) in their mechanism and toxicity profile?
The distinction lies in the primary mechanism of action and the corresponding safety profile.
- Myeloablative Conditioning (MAC): These regimens utilize high-dose chemotherapy (e.g., busulfan ≥390 mg/m²) and/or radiation to completely eradicate host hematopoiesis and provide potent anti-tumor activity. The trade-off is high rates of non-relapse mortality (NRM) due to organ toxicity, limiting its use to younger, fitter patients [52] [56].
- Reduced-Intensity/Reduced-Toxicity Conditioning (RIC/RTC): RIC regimens rely more heavily on immunosuppression (e.g., with fludarabine) to allow donor engraftment and subsequent Graft-versus-Leukemia (GvL) effect, rather than direct myeloablation for disease control. RTC regimens, often using pharmacokinetic-guided dosing of drugs like intravenous busulfan, are myeloablative but designed with agents that have a more favorable non-hematologic toxicity profile. The core difference is that RIC/RTC regimens prioritize reduced non-relapse mortality, making transplantation feasible for older and less fit patients, though sometimes at the cost of a higher relapse rate in certain high-risk malignancies [52] [53].
Q3: What are the key mechanistic pathways involved in common conditioning regimen toxicities?
Understanding the molecular and cellular pathways is key to developing mitigation strategies.
- Sinusoidal Obstruction Syndrome (SOS/VOD): Conditioning chemotherapy, particularly busulfan and cyclophosphamide, causes damage to the sinusoidal endothelial cells and hepatocytes in the liver. This injury triggers a cascade of events involving inflammation, coagulation, and fibrosis, ultimately leading to sinusoidal obstruction, portal hypertension, and liver failure [55].
- Mucositis: Cytotoxic drugs target the rapidly dividing epithelial cells lining the gastrointestinal tract. This direct DNA damage leads to apoptosis, breakdown of the mucosal barrier, inflammation, and secondary infections. The entire pathophysiological sequence involves multiple steps from initiation to ulceration and healing [55].
- Transplant-Associated Thrombotic Microangiopathy (TA-TMA): Endothelial injury, often from conditioning chemotherapy or calcineurin inhibitors, triggers uncontrolled activation of the complement system and the coagulation cascade. This leads to formation of microthrombi in small vessels, causing thrombocytopenia, microangiopathic hemolytic anemia, and end-organ damage [55].
Troubleshooting Guide: Common Experimental & Clinical Challenges
Problem 1: Graft Rejection in Pre-Clinical Models Despite Conditioning
- Potential Cause: Inadequate lymphodepletion. The conditioning regimen failed to sufficiently deplete host T and NK cells that mediate rejection.
- Investigation & Solution:
- Validate Lymphodepletion: Flow cytometric analysis of peripheral blood, spleen, and bone marrow from control (conditioned, no graft) animals to quantify the extent of T, B, and NK cell clearance.
- Optimize Regimen Intensity: Consider escalating the dose of lymphodepleting agents (e.g., fludarabine, cyclophosphamide) within the tolerated range. Incorporate anti-thymocyte globulin (ATG) or an anti-CD52 antibody (alemtuzumab) for deeper T-cell depletion [53] [54].
- Assess Donor/HLA Disparity: The strength of the alloreactive response is proportional to the degree of HLA mismatch. In highly mismatched models, more intensive conditioning or additional immunosuppression may be necessary [54] [35].
Problem 2: Unacceptable Organ Toxicity (e.g., Hepatotoxicity) in a Novel RTC Protocol
- Potential Cause: The chosen alkylating agent (e.g., busulfan) or its cumulative dose is causing direct tissue damage.
- Investigation & Solution:
- Implement Therapeutic Drug Monitoring (TDM): For drugs like busulfan, use pharmacokinetic-guided dosing to target a specific area-under-the-curve (AUC). This personalizes exposure, maximizing efficacy while minimizing toxicity like SOS/VOD [53].
- Agent Substitution: Replace the toxic agent with one in the same class but with a better safety profile. For example, treosulfan is a structural analog of busulfan with potent immunosuppressive properties and a reportedly more favorable toxicity profile, particularly regarding the liver [53].
- Prophylactic Pharmacotherapy: Introduce proven prophylactic agents. For SOS/VOD, defibrotide has shown prophylactic efficacy. For nausea/vomiting (CINV), a combination of 5-HT3 antagonists, NK1 antagonists, and steroids is standard [55].
Problem 3: Disease Relapse Post-Transplant Using a Novel RIC Regimen
- Potential Cause: The reduced intensity of the regimen provides insufficient direct cytoreduction of the malignancy, and the Graft-versus-Leukemia (GvL) effect is inadequate or delayed.
- Investigation & Solution:
- Evaluate Pre-Transplant Disease Burden: Ensure the novel RIC regimen is tested in a minimal residual disease (MRD) setting, as its efficacy is often dependent on the GvL effect.
- Incorporate Targeted Agents: Add a targeted therapy to the conditioning backbone. For example, in AML with specific mutations, adding a FLT3 inhibitor or BCL-2 inhibitor could enhance cytoreduction without significantly increasing classic chemotherapy toxicities.
- Modulate Regimen Intensity: Consider a "sweet-spot" RTC regimen that uses myeloablative doses of a less toxic drug (e.g., pharmacokinetic-guided busulfan) rather than a purely non-myeloablative approach, thus retaining more direct anti-leukemic activity [52].
Quantitative Data & Regimen Comparison
The following tables summarize key efficacy and safety outcomes from clinical studies of different conditioning platforms, providing a benchmark for evaluating novel regimens.
Table 1: Outcomes of a Fludarabine/i.v. Busulfan-based RTC Platform in AML/MDS [52]
| Parameter | Result (2-Year) | Subgroup Analysis |
|---|---|---|
| Overall Survival | 61.8% | Worse with unfavorable karyotype & disease status >CR1 |
| Progression-Free Survival | 57% | 72.7% (Fav), 60.5% (Int), 45.7% (Unfav) karyotype |
| Relapse Incidence | 29% | 23% (CR1) vs. 39% (>CR1) |
| Non-Relapse Mortality (1-Year) | 11% | - |
| Acute GVHD (Gr 3-4) | 7.9% (by Day 100) | - |
| Chronic GVHD | 21.6% (by 1 Year) | Severe forms: 7.8% |
Table 2: Comparison of Conditioning Regimen Classifications & Properties
| Feature | Myeloablative (MAC) | Reduced-Toxicity (RTC) | Reduced-Intensity (RIC) |
|---|---|---|---|
| Primary Goal | Direct tumor kill & myeloablation | Myeloablation with less toxicity | Immunosuppression for donor engraftment |
| Mechanism | Irreversible cytoreduction | Irreversible cytoreduction | Profound immunosuppression |
| Engraftment Dependency | Mandatory | Mandatory | Mandatory |
| Anti-Tumor Effect | From conditioning chemotherapy | From conditioning chemotherapy | Primarily from Graft-versus-Leukemia |
| Typical Agents | High-dose Busulfan, Cyclophosphamide, TBI | PK-adjusted i.v. Busulfan, Fludarabine, Treosulfan | Fludarabine, Melphalan, Low-dose TBI |
| Non-Hematologic Toxicity | High | Intermediate | Lower |
| Target Patient Population | Young, fit patients | Older patients or those with comorbidities | Elderly, unfit, or with organ dysfunction |
Experimental Protocols for Pre-Clinical Evaluation
Protocol 1: Evaluating Engraftment & Rejection in a Humanized Mouse Model
This protocol is adapted from studies investigating immune rejection of human cell allografts [57].
- Model Generation: Reconstitute immunodeficient mice (e.g., NSG) with a functional human immune system (Hu-mice) via adoptive transfer of human CD34+ hematopoietic stem cells or peripheral blood mononuclear cells (PBMCs).
- Conditioning: Prior to introducing the experimental graft, subject the Hu-mice to a conditioning regimen. A common standard is lymphodepletion with cyclophosphamide (e.g., 100-200 mg/kg) and fludarabine (e.g., 100-150 mg/m² equivalent) administered intraperitoneally over 2-4 days.
- Test Graft Injection: Introduce the allogeneic human cell product (e.g., hESC-derived cardiomyocytes, teratomas) into the conditioned Hu-mice. Include a control group receiving grafts from genetically modified donors engineered for immune evasion (e.g., B2M/CIITA KO to abolish HLA expression).
- Endpoint Analysis:
- Graft Survival: Monitor graft size (if palpable) or use in vivo imaging (e.g., luciferase-expressing grafts) weekly.
- Immunological Analysis: At endpoint, harvest grafts and lymphoid organs. Analyze by flow cytometry for infiltration of human T cells (CD3+, CD8+), NK cells (CD56+), and macrophages. Perform histology (H&E, immunostaining) to assess graft destruction and immune cell infiltration.
- Humoral Response: Measure serum levels of donor-specific antibodies using flow-based crossmatch or ELISA.
Protocol 2: Assessing Hepatotoxicity (SOS/VOD) In Vivo
- Animal Model: Use a susceptible mouse strain (e.g., C57BL/6).
- Conditioning Regimen Administration: Administer the test conditioning regimen (e.g., busulfan 60-120 mg/kg combined with cyclophosphamide 100-200 mg/kg) over several days.
- Monitoring & Endpoints:
- Clinical: Monitor for weight loss, ascites development (increased abdominal girth), and jaundice.
- Biochemical: At sacrifice, collect serum to measure liver enzymes (ALT, AST) and markers of function (bilirubin, albumin).
- Histopathological: Harvest liver tissue, fix in formalin, and section for H&E staining. Key features of SOS/VOD to score include: sinusoidal dilation, erythrocyte extravasation into the space of Disse, hepatocyte necrosis, and occlusion of central venules.
- Prophylaxis/Intervention Arm: Include a group pre-treated with a candidate prophylactic agent like defibrotide (e.g., 60-100 mg/kg i.v.) to assess efficacy in reducing histological and biochemical markers of injury.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Conditioning & Rejection
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Anti-Thymocyte Globulin (ATG) | In vivo T-cell depletion; mimics clinical practice. | Deplete host T cells in pre-clinical models to prevent graft rejection and study its impact on engraftment kinetics and GvHD [53]. |
| Fludarabine | Immunosuppressive nucleoside analog; core component of RIC/RTC. | Create lymphodepleting conditioning regimens in mouse models to enable engraftment of allogeneic or humanized immune systems [52] [53]. |
| Treosulfan | Alkylating agent with myeloablative and immunosuppressive properties. | Investigate as a potentially less hepatotoxic alternative to busulfan in novel RTC protocol development [53]. |
| Anti-CD52 Antibody (Alemtuzumab) | Broadly depletes lymphocytes (T, B, NK); deep immunosuppression. | Use in-vitro to deplete T cells from a graft or in-vivo in models to achieve profound host immunosuppression [53]. |
| Defibrotide | Prophylaxis and treatment of SOS/VOD. | Test as a prophylactic agent in murine models of busulfan-induced hepatotoxicity to assess reduction in SOS/VOD histological scores [55]. |
| Recombinant HLA Tetramers | Detect and isolate antigen-specific T cells. | Identify and quantify host T cells that are alloreactive against donor HLA molecules post-conditioning [54] [35]. |
Signaling Pathways & Experimental Workflows
The diagram below illustrates the core pathways of allorecognition that conditioning regimens must overcome, and the points of intervention for toxicity management.
Diagram 1: Immune Rejection Pathways & Intervention Points. This map illustrates the three principal pathways of allograft rejection (Direct, Indirect, NK cell) triggered by the donor graft. The Conditioning Regimen acts as a primary, broad intervention to blunt these pathways. Specific experimental interventions (e.g., ATG, HLA engineering) can target individual immune effector cells. Parallel strategies for Toxicity Mitigation are crucial to protect host organ function during this process.
Addressing Tumorigenicity and Insertional Mutagenesis in Engineered Products
### Frequently Asked Questions (FAQs)
FAQ 1: What are the primary mechanisms by which engineered cell products, like CAR-T cells, can lead to secondary malignancies?
The development of secondary primary malignancies (SPMs) from engineered cell products is primarily driven by two genotoxic mechanisms:
- Insertional Mutagenesis: This is the main biological mechanism. Viral vectors (lentiviral or gamma-retroviral) used to deliver transgenes like CARs integrate semi-randomly into the host genome. If integration occurs near or within proto-oncogenes or tumor suppressor genes, it can disrupt their regulation and initiate malignant transformation. Gamma-retroviruses are particularly known for integrating near transcription start sites, while lentiviruses favor gene bodies [58].
- Off-Target Effects of Genome Editing: The use of CRISPR/Cas9 and other nucleases for genetic modification introduces risks of off-target double-strand breaks (DSBs). These can lead to chromosomal translocations or the inactivation of critical tumor suppressor genes, further amplifying genomic instability [58].
FAQ 2: How can the risk of insertional mutagenesis be mitigated in allogeneic stem cell therapies?
The most promising strategy is site-directed transgene integration into Genomic Safe Harbors (GSHs). GSHs are loci in the genome validated to support stable, high-level transgene expression without causing oncogenic disruption. They meet stringent criteria: located far from cancer-related genes, resistant to epigenetic silencing, and transcriptionally permissive. Key GSH sites include [58]:
- AAVS1 (19q13.42)
- TRAC (T-cell receptor alpha constant)
- CCR5
- ROSA26
- CLYBL
Targeting these sites using CRISPR/Cas9 or other nucleases eliminates the risks associated with semi-random viral integration.
FAQ 3: Beyond genetic engineering, what host factors influence the risk of tumorigenicity?
Patient-specific factors play a significant role in modulating risk [58]:
- Prior Therapies: Treatments like fludarabine or radiation can induce pre-existing genomic instability.
- Germline Mutations: Inherited mutations in DNA repair pathways (e.g., BRCA genes) increase susceptibility.
- Prolonged Cell Persistence: Long-term persistence of engineered cells, while therapeutically beneficial, increases the window for cumulative genotoxic stress and malignant transformation.
FAQ 4: How does the risk of graft-versus-host disease (GVHD) relate to the strategies for reducing tumorigenicity?
In allogeneic transplants, two main immune reactions can occur. Graft rejection is when the host immune system attacks the donor cells. Conversely, Graft-versus-Host Disease (GVHD) is when donor immune cells attack the recipient's tissues [59] [14]. Strategies to reduce tumorigenicity can intersect with GVHD management. For example, site-directed integration of a CAR transgene into the TRAC locus not only provides a safe harbor but also disrupts the endogenous T-cell receptor (TCR). This reduces the risk of GVHD in allogeneic CAR-T products by minimizing off-target, TCR-driven immune reactions [58].
### Troubleshooting Guides
Problem 1: Suspected Insertional Mutagenesis in Preclinical Models
- Symptoms: Unexplained clonal dominance in culture, emergence of atypical cell morphology, or leukemia/lymphoma in mouse xenograft models.
- Investigation Protocol:
- Integration Site Analysis (ISA):
- Method: Use LAM-PCR or next-generation sequencing-based methods to map the genomic locations of viral vector integrations in the dominant clone [58].
- Analysis: Cross-reference integration sites with databases of known oncogenes (e.g., LMO2) and tumor suppressor genes. Investigate any integrations within a ±100kb window of these genes.
- Oncogene Expression Profiling:
- Method: Perform RNA-Seq or RT-qPCR on the suspect clone to check for dysregulation of genes near the integration site.
- Functional Validation:
- Method: Use CRISPR inhibition (CRISPRi) to silence the dysregulated gene. If this reverses the aggressive phenotype, it strongly supports a role for insertional mutagenesis.
- Integration Site Analysis (ISA):
Problem 2: Low Efficiency in Genomic Safe Harbor (GSH) Targeting
- Symptoms: Low percentage of cells with correct transgene integration after transfection/electroporation.
- Troubleshooting Steps:
- Optimize Nuclease Delivery: Ensure high efficiency of guide RNA and nuclease (e.g., Cas9) delivery. Titrate amounts to maximize cutting efficiency while minimizing toxicity.
- Increase HDR Efficiency: Homology-Directed Repair (HDR) is required for precise integration.
- Strategy: Use the iHDR-3' strategy. Select donor vectors where the 3’ homology arm is extended (e.g., 800-1000 bp) and the 5’ arm is shortened. This asymmetrical design has been shown to significantly boost HDR rates [58].
- Timing: Synchronize donor vector delivery with the cell cycle stage (S/G2 phase) when HDR is active.
- Additives: Supplement with small molecule HDR enhancers like RS-1.
- Validate GSH Locus Accessibility: Check the chromatin state of the target GSH locus (e.g., via ATAC-Seq). If it is closed, consider using epigenetic modifiers to open the chromatin temporarily.
Problem 3: Detecting and Managing Replication-Competent Lentiviruses (RCL)
- Symptoms: Uncontrolled vector spread or mobilization in culture.
- Safety Protocol:
- Prevention: Use third-generation, self-inactivating (SIN) lentiviral vectors with split packaging genes to minimize the chance of recombination.
- Detection Assay:
- Sample: Test the final cell product and vector supernatant.
- Method: Use a functional RCL assay, such as inoculating permissive cells (e.g., HEK293) with the test sample and monitoring for p24 antigen expression over 2-3 weeks.
The tables below summarize key quantitative findings on secondary malignancy risks and the properties of genomic safe harbors.
Table 1: Reported Incidence of Secondary Malignancies Post CAR-T Cell Therapy
| Malignancy Type | Reported Incidence | Median Time to Onset | Key Associated Factors | Source / Study Context |
|---|---|---|---|---|
| All Secondary Malignancies | 3.6% (16/449 patients) | - | Prior therapies, genomic instability | Ghilardi et al. (2024) [58] |
| Solid Tumors | 5-year risk: 15.2% | 26.4 months | Host factors (age, prior genotoxic exposure) | Ghilardi et al. (2024) [58] |
| Hematologic Malignancies | 5-year risk: 2.3% | 9.7 months | Vector type, insertional mutagenesis | Ghilardi et al. (2024) [58] |
| T-cell Lymphoma | Case reports (considered rare) | 3 months | Pre-existing T-cell clones, JAK3 mutations | Ghilardi et al. (2024) [58] |
Table 2: Characteristics of Validated Genomic Safe Harbors (GSHs)
| Genomic Safe Harbor Locus | Cytoband | Key Features and Advantages | Validated Transgene Expression |
|---|---|---|---|
| AAVS1 | 19q13.42 | Well-characterized, permissive chromatin structure, associated with housekeeping genes. | Stable, high-level [58] |
| TRAC | 14q11.2 | Enables concurrent disruption of endogenous TCR, reducing GVHD risk in allogeneic settings. | Uniform, physiological [58] |
| CCR5 | 3p21.31 | Disruption confers HIV resistance; locus is well-tolerated for genetic modifications. | Stable [58] |
| ROSA26 | 3p21.31 (Mouse) | A ubiquitous and strong promoter, widely used in mouse models, with a human homolog. | High-level, ubiquitous [58] |
| CLYBL | 13q32.3 | Gene desert region, minimizes risk of disrupting functional genetic elements. | Stable [58] |
### Experimental Protocols
Protocol 1: Integration Site Analysis (ISA) via Linear Amplification-Mediated PCR (LAM-PCR)
This protocol is used to identify the genomic locations where a viral vector has integrated, which is critical for assessing insertional mutagenesis risk [58].
- Genomic DNA Extraction: Isolate high-molecular-weight genomic DNA from the engineered cell product (≥ 1x10^6 cells). Use a phenol-chloroform extraction method for high purity.
- Digestion: Digest 1-2 µg of gDNA with a frequent-cutting restriction enzyme (e.g., MseI or Tsp509I) to generate fragments suitable for PCR.
- Linker Ligation: Ligate a biotinylated asymmetric linker to the digested DNA fragments.
- Linear PCR (First Amplification): Perform a linear PCR using a biotinylated primer specific to the viral vector's Long Terminal Repeat (LTR). This step linearly amplifies only the fragments containing the vector-genome junction.
- Capture and Purification: Bind the PCR products to streptavidin-coated magnetic beads. Wash away non-specifically bound DNA.
- Second PCR (Exponential Amplification): Perform a nested, exponential PCR using a primer binding to the linker and a nested primer binding to the viral vector. This step adds sequencing adapters.
- Sequencing and Bioinformatic Analysis: Purity the PCR products and subject them to next-generation sequencing. Map the resulting sequences to the human reference genome (e.g., hg38) using specialized software (e.g., INSPIIRED) to identify integration sites.
Protocol 2: Site-Directed CAR Integration into the AAVS1 Safe Harbor Locus
This methodology outlines a non-viral, precise method for CAR integration, minimizing genotoxic risk [58].
- T Cell Activation: Isolate primary human T cells and activate them with anti-CD3/anti-CD28 beads for 24-48 hours.
- Ribonucleoprotein (RNP) Complex Formation: Form complexes by incubating CRISPR/Cas9 protein with a synthetic guide RNA (sgRNA) targeting the AAVS1 locus.
- Donor Template Preparation: Design a single-stranded DNA (ssDNA) or closed-ended linear duplex DNA (CELiD) donor vector containing the CAR expression cassette flanked by ~800bp homology arms matching the sequences around the AAVS1 cut site.
- Co-electroporation: Co-electroporate the RNP complexes and the donor vector into the activated T cells using a nucleofector device. A suggested starting point is 2 µg of RNP and 1 µg of donor DNA per 1x10^6 cells.
- Post-Transfection Culture: Immediately transfer cells to pre-warmed culture medium. Consider adding an HDR enhancer like RS-1 (e.g., 5 µM) for the first 24 hours.
- Validation and Expansion:
- Efficiency Check: 72 hours post-electroporation, analyze a sample of cells by flow cytometry for CAR expression and by genomic PCR to confirm site-specific integration.
- Expansion: Expand the successfully edited T cells for functional assays and further analysis.
### Research Reagent Solutions
Table 3: Essential Reagents for Mitigating Tumorigenicity in Engineered Cells
| Reagent / Tool | Function | Example Product/Catalog Number (if applicable) |
|---|---|---|
| CRISPR/Cas9 System | Creates a targeted double-strand break in the DNA at a specific Genomic Safe Harbor locus to enable precise transgene insertion. | Synthego CRISPR Kit, Alt-R S.p. Cas9 Nuclease |
| GSH-targeting gRNA | Guides the Cas9 nuclease to the specific DNA sequence within a Genomic Safe Harbor (e.g., AAVS1, TRAC). | Custom synthesized from IDT or Synthego. |
| HDR Donor Template | A DNA template containing the transgene (e.g., CAR) flanked by homology arms for precise integration into the cut site via HDR. | ssDNA from IDT; CELiD or AAV6 donor vectors. |
| HDR Enhancers | Small molecules that increase the efficiency of Homology-Directed Repair, improving the rate of correct integration. | RS-1 (Sigma-Aldrich, SML1554) |
| Integration Site Analysis Kit | A specialized kit for mapping the genomic locations of viral vector integrations to assess insertional mutagenesis risk. | LAM-PCR kit (e.g., from Eurofins Genomics) |
| Next-generation Sequencer | For high-throughput sequencing of integration sites and performing off-target analysis after genome editing. | Illumina MiSeq, NovaSeq. |
### Signaling Pathways and Workflow Diagrams
GSH Targeting Mitigates Insertional Mutagenesis
GSH-Targeted CAR-T Cell Workflow
Bench to Bedside: Efficacy and Safety of Allogeneic Platforms in Clinical Trials
The field of adoptive cell therapy has been revolutionized by autologous chimeric antigen receptor (CAR)-T cell treatments, which have demonstrated remarkable efficacy in relapsed/refractory hematological malignancies. However, the autologous approach presents significant logistical challenges, including prolonged manufacturing times (1-3 weeks), variable cell potency, and potential manufacturing failures, particularly in heavily pretreated patients with compromised T-cell fitness [60] [61]. These limitations have accelerated the development of allogeneic "off-the-shelf" cellular therapies derived from healthy donors, which offer the potential for immediate product availability, standardized manufacturing, and reduced costs [62] [60].
Allogeneic CAR-T and CAR-NK cells represent the two most advanced platforms in this emerging paradigm. Both aim to overcome the limitations of autologous products but employ distinct biological mechanisms and face different immunological challenges. This technical analysis examines the comparative efficacy, safety profiles, and persistent immunological barriers associated with these platforms within the broader context of overcoming immune rejection in allogeneic transplantation research. Understanding these dynamics is crucial for researchers and drug development professionals working to optimize next-generation cellular therapies for lymphoid malignancies.
Quantitative Efficacy and Safety Profile Comparison
Table 1: Pooled Efficacy Outcomes from Meta-Analysis of Allogeneic Cell Therapies in R/R LBCL
| Outcome Measure | Allogeneic CAR-T Cells | Allogeneic CAR-NK Cells | Pooled Overall |
|---|---|---|---|
| Best Overall Response Rate (bORR) | 52.5% [95% CI, 41.0-63.9] | 52.5% [95% CI, 41.0-63.9] | 52.5% [95% CI, 41.0-63.9] |
| Best Complete Response Rate (bCRR) | 32.8% [95% CI, 24.2-42.0] | 32.8% [95% CI, 24.2-42.0] | 32.8% [95% CI, 24.2-42.0] |
| Durable Response | Varies by product | 70% 1-year durable remission in largest study | Not reported |
Data compiled from a meta-analysis of 19 studies encompassing 334 patients (155 CAR-NK; 179 CAR-T) [62] and a systematic review of 150 patients [63].
Table 2: Comparative Safety Profiles of Allogeneic Cellular Therapies
| Adverse Event | Allogeneic CAR-T Cells | Allogeneic CAR-NK Cells | Autologous CAR-T Cells (Reference) |
|---|---|---|---|
| Grade 3+ CRS | 0.04% [95% CI 0.00-0.49] | Very rare (no grade 3+ reported) | ~15-20% (varies by product) |
| Grade 3+ ICANS | 0.64% [95% CI 0.01-2.23] | None reported | ~10-15% (varies by product) |
| GvHD Incidence | Only one occurrence across 334 patients | None reported | Not applicable |
| Infections (All Grades) | 25% [95% CI 14-36] | Uncommon | ~20-30% |
| Severe Infections | 7% [95% CI 2-14] | Rare | ~10-15% |
Safety data compiled from meta-analysis of 334 patients [62] and systematic review of 150 patients [63]. CRS=cytokine release syndrome; ICANS=immune effector cell-associated neurotoxicity syndrome; GvHD=graft-versus-host disease.
The quantitative evidence demonstrates that both allogeneic platforms maintain encouraging efficacy while exhibiting remarkably superior safety profiles compared to autologous CAR-T products, particularly regarding severe CRS and ICANS [62]. The absence of significant GvHD across both platforms highlights successful engineering approaches to mitigate this fundamental allogeneic barrier.
Technical Support Center: Troubleshooting Allogeneic Cell Therapy Challenges
Frequently Asked Questions on Immune Rejection Barriers
FAQ 1: What are the primary immune rejection pathways affecting allogeneic cellular therapies?
Allogeneic cells face rejection through multiple immunological pathways:
- Host T-cell-mediated rejection: Occurs when host CD8+ T cells recognize mismatched HLA class I molecules (particularly HLA-A and HLA-B) on donor cells [60] [3]
- NK-cell-mediated "missing-self" response: Activated when donor cells lack expression of host HLA class I molecules that engage inhibitory receptors (KIR, NKG2A) on host NK cells [60] [64]
- Phagocyte-mediated clearance: Macrophages eliminate donor cells through phagocytosis, particularly in reticuloendothelial tissues [3]
- Antibody-mediated rejection: Pre-existing or developing donor-specific antibodies (DSAs) can trigger complement-dependent cytotoxicity and antibody-dependent cellular cytotoxicity [60]
FAQ 2: Why does complete HLA class I ablation create conflicting immune challenges?
Complete elimination of HLA class I expression (e.g., via B2M knockout) effectively prevents T-cell recognition but triggers NK-cell-mediated killing through the "missing-self" response [60] [64]. This creates a fundamental engineering dilemma: solutions that evade one arm of the immune system activate another. Innovative approaches include:
- Expressing single-chain HLA-E (non-polymorphic) to engage NKG2A inhibitory receptors on NK cells [60] [3]
- Selective retention of HLA-C alleles while knocking out HLA-A and HLA-B [60]
- Maintaining full HLA expression while using immunosuppressive regimens [64]
FAQ 3: How can researchers mitigate macrophage-mediated clearance of allogeneic cells?
Macrophage phagocytosis can be reduced through CD47 overexpression. CD47 serves as a "don't eat me" signal by binding to SIRPα on macrophages, inhibiting phagocytosis [3]. However, this strategy requires caution as CD47 is an established immune checkpoint in cancer biology, and its overexpression might interfere with dendritic cell antigen presentation or protect residual tumor cells [3].
Experimental Protocols for Immune Evasion Engineering
Protocol 1: Generation of HLA-Engineered Allogeneic CAR-T Cells with Reduced Immunogenicity
Principle: Disrupt HLA class I and II presentation while providing protection against NK cell-mediated killing [60] [64].
Methodology:
- Isolate T cells from healthy donor leukapheresis product
- Activate T cells using anti-CD3/CD28 beads
- Gene editing workflow:
- Employ CRISPR/Cas9 ribonucleoprotein electroporation to simultaneously target:
- TRAC locus (TCR alpha constant) to prevent GvHD
- B2M locus to eliminate HLA class I surface expression
- CIITA locus to abrogate HLA class II expression
- Incorporate a CAR construct into the TRAC locus via HDR (homology-directed repair)
- Introduce a HLA-E single-chain variant into the B2M locus via HDR
- Employ CRISPR/Cas9 ribonucleoprotein electroporation to simultaneously target:
- Expand edited cells in IL-15 supplemented media for 10-14 days
- Validate editing efficiency via flow cytometry (TCR negativity, HLA expression) and functional assays
Troubleshooting Tip: Low editing efficiency can be improved by optimizing electroporation parameters and using chemically modified sgRNAs with enhanced stability.
Protocol 2: Creating Immune-Evasive iPSC-Derived CAR-NK Cells
Principle: Leverage iPSC platform for multiplex gene editing to generate standardized, scalable allogeneic NK products [3].
Methodology:
- Start with clinical-grade iPSC line with defined HLA haplotype
- Employ sequential CRISPR editing to introduce modifications:
- Knockout B2M to reduce HLA class I expression
- Insert HLA-E gene into B2M locus
- Knockout CD38 to enhance metabolic fitness
- Introduce CAR construct into safe harbor locus (e.g., AAVS1)
- Overexpress membrane-bound IL-15 for enhanced persistence
- Differentiate edited iPSCs to NK cells using a staged protocol:
- Hematopoietic progenitor specification (days 0-10)
- NK progenitor induction (days 10-20)
- NK maturation and expansion (days 20-35)
- Validate phenotype and function through flow cytometry (CD56+, CD16±, NKG2D+), cytotoxicity assays, and cytokine production
Troubleshooting Tip: Poor NK cell differentiation efficiency may require optimization of cytokine combinations (SCF, FLT3L, IL-3, IL-7, IL-15) and stromal co-culture conditions.
Visualizing Immune Recognition Pathways and Engineering Solutions
Figure 1: Immune Recognition Pathways and Engineering Solutions. This diagram illustrates the primary immune rejection mechanisms faced by allogeneic cell therapies and corresponding genetic engineering strategies to overcome them. Red elements represent host immune attacks, while green elements indicate protective genetic modifications.
Figure 2: Allogeneic Cell Therapy Engineering Workflow. This diagram compares the manufacturing and engineering pathways for creating allogeneic CAR-T and CAR-NK cell products, highlighting shared and distinct genetic modification strategies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Allogeneic Cell Therapy Development
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Gene Editing Tools | CRISPR-Cas9 RNPs, TALEN, ZFN | Disruption of immunogenicity genes (TRAC, B2M, CIITA) | CRISPR-Cas9 offers multiplex capability; TALEN may have fewer off-target effects |
| CAR Delivery Systems | Lentiviral vectors, mRNA electroporation, Transposon systems | Stable or transient CAR expression | Lentiviral provides stable integration; mRNA offers transient expression with safety benefits |
| Cell Culture Additives | IL-2, IL-15, IL-21 | T-cell and NK-cell expansion and functional enhancement | IL-15 particularly important for NK cell persistence and function |
| Immunosuppressive Agents | Rapamycin, Tacrolimus, Alemtuzumab | In vitro and in vivo models of immune evasion | Used to test engineered cells with FKBP1A disruption or CD52 knockout |
| Validation Antibodies | Anti-TCRα/β, Anti-HLA-ABC, Anti-CD47, Anti-CD56 | Phenotypic validation of engineered cells | Critical for confirming knockout efficiency and transgene expression |
| In Vivo Models | NSG, NOG, humanized mouse models | Preclinical efficacy and persistence testing | Humanized models essential for evaluating immune rejection |
The evolving landscape of allogeneic cellular immunotherapy demonstrates that both CAR-T and CAR-NK platforms offer viable paths toward "off-the-shelf" cancer treatment. Current evidence indicates that allogeneic CAR-T cells achieve comparable response rates to autologous products with significantly improved safety profiles, while CAR-NK cells present an exceptionally favorable safety advantage with potentially more durable responses in responding patients [62] [63].
The critical challenge remains overcoming the interconnected immune rejection barriers, which requires sophisticated engineering approaches that balance evasion of multiple immune cell types. Future directions include the development of precision-edited iPSC platforms that enable standardized, multiplexed engineering [3] [26], integration of synthetic biology to create dynamic control systems [60] [61], and application of artificial intelligence to optimize HLA matching and editing strategies based on population immunogenetics [3]. As these technologies mature, allogeneic cellular therapies are poised to dramatically expand access to effective immunotherapy while reducing costs and treatment delays, ultimately fulfilling the promise of truly universal cancer treatments.
Transplantation, whether of solid organs or cells, faces a major biological barrier: immune rejection. The recipient's immune system recognizes the transplanted tissue as foreign and mounts a response that can lead to graft damage and failure. While both solid organ and cellular transplants share this challenge, the immune mechanisms involved and their clinical management can differ significantly. Understanding these differences is crucial for developing targeted strategies to overcome immune barriers in allogeneic stem cell transplantation research. This technical support center provides troubleshooting guides and experimental protocols to help researchers navigate these complex immunological landscapes.
Troubleshooting Guides and FAQs
What are the fundamental differences in how the immune system rejects solid organs versus cellular grafts?
Answer: While both involve allorecognition, the primary differences lie in the dominant rejection mechanisms and antigen presentation pathways.
- Solid Organ Transplantation: Rejection is often driven by direct allorecognition, where recipient T cells directly recognize intact donor Major Histocompatibility Complex (MHC) molecules on the surface of donor-derived "passenger" antigen-presenting cells (APCs) within the graft [13] [65]. This pathway elicits a very potent and rapid response. The hallmark of rejection includes T-cell-mediated interstitial inflammation and antibody-mediated injury to the graft's vasculature [66] [65].
- Cellular Transplantation (e.g., Stem Cell-Derived Grafts): These grafts typically lack professional donor APCs. Therefore, rejection is primarily initiated via the indirect allorecognition pathway, where recipient APCs process and present donor antigens (from the transplanted cells) to recipient T cells [67] [25]. The immune response can also be significantly influenced by innate immune cells, particularly if the cells express stress ligands or have altered MHC profiles [25].
My stem cell-derived graft showed initial engraftment but was later rejected. What are potential causes?
Answer: Late rejection after initial engraftment often points to chronic immune activation.
- Minor Histocompatibility Antigens (miHAs): Even with MHC-matched grafts, polymorphisms in other proteins can generate miHAs. These are presented by MHC molecules and can elicit a slow, persistent T-cell response that leads to chronic rejection [25].
- Neoantigens: Genetic changes occurring during in vitro culture or incomplete reprogramming of induced pluripotent stem cells (iPSCs) can create novel proteins (neoantigens) that are recognized as foreign by the host immune system [25].
- Loss of Immunomodulatory Properties: Differentiated cell types derived from stem cells may lose low-level immunomodulatory properties characteristic of pluripotent states, becoming more visible to the immune system over time [25].
How can I experimentally distinguish between T-cell-mediated and innate immune cell-mediated rejection in my transplantation model?
Answer: A combination of in vitro and in vivo assays is required.
- For T-cell mediation:
- In vivo: Use T-cell depletion antibodies (e.g., anti-CD4, anti-CD8) or adoptive transfer experiments. Rejection that is abrogated in T-cell-deficient hosts or by T-cell depletion indicates a T-cell-dependent process.
- In vitro: Perform mixed lymphocyte reactions (MLR) or T-cell proliferation assays using recipient T cells and donor antigens [13].
- For Innate immune mediation (e.g., NK cells):
- Mechanism: NK cells are activated by "missing self," where the absence of donor MHC class I molecules that recipient inhibitory receptors recognize leads to activation [66].
- In vivo: Use NK cell-depleting antibodies. Rejection that persists in T-cell-deficient mice but is blocked by NK cell depletion suggests an NK-mediated pathway [66].
- In vitro: Set up cocultures of purified recipient NK cells with donor-derived target cells (e.g., endothelial cells). Measure NK cell activation markers (e.g., CD69) and target cell cytotoxicity [66].
Table 1: Key Features of Allorecognition Pathways
| Feature | Direct Pathway | Indirect Pathway |
|---|---|---|
| Antigen Presenting Cell (APC) | Donor APC | Recipient APC |
| Antigen Form | Intact donor MHC molecule | Processed donor peptide presented by self-MHC |
| Precursor T-cell Frequency | High (1-10%) | Low (0.01-0.0001%) |
| Dominant Role In | Early/acute rejection | Chronic rejection and late acute rejection |
| Relevance to Transplant Type | Highly relevant for solid organs | Highly relevant for cellular grafts |
What are the best practices for monitoring cytomegalovirus (CMV)-specific cellular immunity in immunosuppressed transplant recipients?
Answer: Monitoring CMV-specific cell-mediated immunity (CMI) is crucial for managing post-transplant viral reactivation risk. Several assays can be employed, each with advantages [68].
- Recommended Assays:
- Enzyme-Linked Immunosorbent Assay (ELISA)-based (e.g., QuantiFERON-CMV): Measures IFN-γ release after stimulating blood with CMV antigens. It has high sensitivity and specificity and is relatively easy to standardize for clinical use [68].
- Activation-Induced Marker (AIM) Assay: Uses flow cytometry to detect T cells that upregulate activation markers (e.g., CD69, CD25) after CMV antigen stimulation. It allows for immunophenotyping of responding T cells (CD4+ vs. CD8+) [68].
- T Cell Proliferation Assay (TCPA): Tracks the division of T cells in response to antigen using dye dilution. It can be less sensitive than other methods [68].
- Proposed Workflow: For routine clinical practice, start with the QuantiFERON-CMV assay due to its practicality. In cases of indeterminate results or for more detailed immune profiling, follow up with the AIM assay [68].
Table 2: Comparison of Assays for CMV-Specific Cellular Immunity
| Assay | Principle | Readout | Advantages | Disadvantages |
|---|---|---|---|---|
| QuantiFERON-CMV | ELISA-based IFN-γ release | Concentration of IFN-γ | High sensitivity & specificity; standardized; short turnaround | Does not differentiate CD4+/CD8+ T cells |
| AIM Assay | Flow cytometry detection of surface activation markers | % of CD4+ or CD8+ T cells expressing markers (e.g., CD69) | Provides immunophenotype; can be highly sensitive | Requires flow cytometry expertise; more complex standardization |
| T Cell Proliferation Assay (TCPA) | Dye dilution to track cell division | % of proliferating (dye-dim) CD3+ T cells | Measures a fundamental functional response | Can be less sensitive; longer culture time (5-7 days) |
Experimental Protocols
Protocol 1: Evaluating NK Cell Alloreactivity via "Missing Self"In Vitro
Background: This protocol tests the hypothesis that recipient NK cells will lyse donor-derived cells that lack expression of MHC class I alleles recognized by the recipient's inhibitory Killer-cell Immunoglobulin-like Receptors (KIRs) [66].
Materials:
- Purified NK cells from recipient (or representative genotype).
- Donor-derived target cells (e.g., endothelial cells, fibroblasts).
- Control target cells expressing the full complement of recipient MHC-I.
- Cell culture medium.
- Cytotoxicity detection kit (e.g., LDH release, calcein-AM).
- Flow cytometry antibodies for KIR and HLA typing.
Method:
- Characterization: Genotype the recipient for inhibitory KIRs and the donor for HLA class I (especially HLA-C groups). Confirm the "missing self" combination in silico [66].
- NK Cell Isolation: Isolate NK cells from recipient peripheral blood using a negative selection kit to maintain cell vitality.
- Coculture: Seed target cells and co-culture with effector NK cells at various effector-to-target (E:T) ratios (e.g., 50:1, 25:1, 10:1) for 4-6 hours.
- Cytotoxicity Measurement: Quantify target cell lysis using a validated method. For LDH release, measure the amount of lactate dehydrogenase enzyme released from damaged target cells.
- Analysis: Calculate specific lysis. A significant increase in lysis of donor cells compared to "self" control cells indicates missing self-induced NK cell activation.
Protocol 2: Assessing T-cell Responses via the Activation-Induced Marker (AIM) Assay
Background: This flow cytometry-based protocol identifies and characterizes antigen-specific T cells by detecting the upregulation of activation markers following stimulation, useful for monitoring responses to viral antigens or alloantigens [68].
Materials:
- Heparinized whole blood or PBMCs from the recipient.
- Peptide pools for the antigen of interest (e.g., CMV pp65, donor HLA-derived peptides).
- Negative control (no antigen).
- Positive control (e.g., PHA, SEB).
- Activation marker antibody cocktail (e.g., anti-CD3, CD4, CD8, CD69, CD25, OX40).
- Cell culture incubator.
- Flow cytometer.
Method:
- Stimulation: Aliquot whole blood or PBMCs into tubes. Stimulate with the antigen peptide pool, negative control, and positive control. Incubate for 18-24 hours at 37°C, 5% CO2 [68].
- Staining: After incubation, stain cells with the surface antibody cocktail for 20 minutes at room temperature in the dark.
- Lysis and Acquisition: Lyse red blood cells (if using whole blood), wash, and resuspend in buffer. Acquire data on a flow cytometer.
- Gating and Analysis: Gate on live, single CD3+ T cells. Further gate on CD4+ and CD8+ populations. A positive response is typically defined as a percentage of T cells expressing activation markers (e.g., CD69) that is at least double (or 20% above, depending on the validated cut-off) the value in the negative control [68].
Visualizing Immune Pathways
The following diagrams illustrate the core immune rejection pathways discussed.
Direct vs Indirect Allorecognition
NK Cell Activation by Missing Self
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Transplant Immune Rejection
| Reagent / Tool | Primary Function | Key Application in Rejection Research |
|---|---|---|
| KIR and HLA Typing Kits | Genotyping of NK cell receptors and their ligands. | Identifying "missing self" pairs predictive of NK cell alloreactivity [66]. |
| T-cell Depletion Antibodies (anti-CD4/CD8) | Selective depletion of T-cell subsets in vivo. | Determining the contribution of T-cell subsets to graft rejection in animal models [13]. |
| NK Cell Depletion Antibodies (anti-NK1.1, anti-asialo GM1) | Selective depletion of NK cells in vivo. | Confirming the role of NK cells in "missing self"-mediated rejection [66]. |
| CMV Peptide Pools (e.g., pp65, IE-1) | Antigens for stimulating virus-specific T cells. | Monitoring CMV-specific cellular immunity in immunosuppressed hosts using AIM or ELISA assays [68]. |
| Recombinant B7-1/B7-2 (CD80/86) and Anti-CD28 | Ligands and antibodies for costimulatory pathways. | Studying the critical "Signal 2" for T-cell activation in mixed lymphocyte reactions [65]. |
| CRISPR/Cas9 Gene Editing Systems | Targeted gene knockout or knock-in. | Generating hypoimmunogenic stem cells by knocking out B2M/MHC Class I or CIITA/MHC Class II [25]. |
| Flow Cytometry Antibodies (for AIM Assay) | Detection of cell surface activation markers. | Phenotyping and quantifying antigen-specific T cells (CD4+/CD8+) via markers like CD69, CD25, OX40 [68]. |
Validating Hypoimmunogenic Stem Cell Derivatives in Large Animal Models
Frequently Asked Questions (FAQs)
Q1: What is the core objective of creating hypoimmunogenic stem cells? The primary goal is to generate "off-the-shelf" universal donor cells that can evade immune rejection in fully immunocompetent, allogeneic recipients. This is achieved by genetically engineering stem cells to eliminate major histocompatibility complex (MHC) molecules and overexpress immunomodulatory factors, thereby avoiding the need for patient-specific cell lines or chronic immunosuppression [69] [70] [27].
Q2: Which large animal models provide the most clinically relevant data for validation? Rhesus macaques are currently the gold standard for preclinical validation. Their immune system is closely related to humans, providing critical insights into immune evasion and long-term cell survival. Recent studies have demonstrated that hypoimmunogenic induced pluripotent stem cells (iPSCs) can survive for 16 weeks in fully immunocompetent, allogeneic rhesus macaques, while similarly engineered primary islets survived for 40 weeks [27].
Q3: What are the primary genetic modifications used to confer hypoimmunogenicity? The most validated strategy involves a triple-modification approach:
- Knockout of B2M: Ablates surface expression of HLA class I molecules, preventing CD8+ T cell recognition [69] [70] [27].
- Knockout of CIITA: Ablates surface expression of HLA class II molecules, preventing CD4+ T cell activation [69] [70] [27].
- Overexpression of CD47: Engages the SIRPα receptor on innate immune cells like macrophages and NK cells, delivering a potent "don't eat me" signal to prevent the "missing-self" response triggered by HLA-I knockout [69] [27].
Q4: How do I address the risk of Natural Killer (NK) cell-mediated rejection? Deleting HLA class I (via B2M KO) can trigger NK cell activation. Strategies to mitigate this include:
- CD47 overexpression: Proven to comprehensively protect HLA-deficient cells from human NK cell killing in vitro and in vivo [27].
- Expression of non-classical HLAs: Engineering cells to express HLA-E or HLA-G, which bind inhibitory receptors on NK cells (NKG2A and ILT2, respectively). This can be achieved via a knock-in strategy, such as inserting an HLA-E/β2M fusion protein at the B2M locus [70] [71].
Q5: What are the key functional assays to validate immune evasion? A multi-faceted approach is essential, combining in vitro and in vivo assays:
- In vitro: Mixed lymphocyte reactions (MLR), ELISpot for IFN-γ, cytotoxicity assays using allogeneic T and NK cells, and FACS analysis for HLA expression [27] [71].
- In vivo: Transplanting engineered cells into immunocompetent, allogeneic large animals (e.g., rhesus macaques) and tracking survival over time using bioluminescence imaging (BLI) and histological analysis for immune cell infiltration [27].
Troubleshooting Guides
Issue 1: Partial Graft Rejection Despite Genetic Modification
Potential Causes and Solutions:
- Cause: Incomplete HLA Knockout.
- Cause: Insufficient CD47 Expression.
- Solution: Ensure high, stable overexpression of CD47. Use a strong constitutive promoter (e.g., EF1α) and verify surface density via flow cytometry. Note that the CD47-SIRPα interaction can be species-specific; use the recipient species' CD47 gene for transplantation studies [27].
- Cause: Rejection by Minor Histocompatibility Antigens (mHAgs).
- Solution: This is a known limitation of the hypoimmunogenic approach. Monitor for chronic, low-grade rejection in long-term studies. No direct genetic solution currently exists, highlighting the need for ongoing immune monitoring [70].
Issue 2: Poor Differentiation or Function of Engineered Cells
Potential Causes and Solutions:
- Cause: Off-Target Effects of Gene Editing.
- Solution: Employ rigorous genomic quality control. Use whole-genome sequencing to screen for off-target mutations and select clonal lines with a clean profile. Differentiate multiple independent clones and compare their function to wild-type controls [70].
- Cause: Impact of HLA Editing on Lineage-Specific Maturation.
Issue 3: Instability of Hypoimmunogenic Phenotype Post-Transplantation
Potential Causes and Solutions:
- Cause: Inflammatory Cytokine-Induced HLA Expression.
- Cause: Loss of Transgene Expression (e.g., CD47).
- Solution: Use site-specific integration (e.g., PiggyBac, CRISPR knock-in) into a safe harbor locus (e.g., AAVS1) rather than random lentiviral integration to promote stable long-term expression [71].
Key Experimental Protocols
Protocol 1: Generating Hypoimmunogenic Pluripotent Stem Cells
This protocol outlines the creation of B2M−/−CIITA−/−CD47+ (HIP) cells [69] [27].
- Knockout of B2M and CIITA:
- Design CRISPR-Cas9 guide RNAs (gRNAs) targeting exon 1 of B2M and key exons of CIITA.
- Co-transfect pluripotent stem cells (iPSCs/ESCs) with Cas9 and gRNA expression vectors.
- Reagent: Use a high-fidelity Cas12iHiFi or similar Cas9 variant to minimize off-target effects [71].
- Selection and Screening:
- At 48-72 hours post-transfection, sort single cells to establish clonal lines.
- Screen clones for loss of HLA-I surface expression using flow cytometry (FITC anti-human HLA-ABC antibody).
- Validate knockout via Sanger sequencing and PCR-based assays (e.g., T7E1) to confirm indels.
- Overexpression of CD47:
- Transduce the B2M−/−CIITA−/− double-knockout cells with a lentiviral vector carrying the CD47 transgene (preferably from the recipient species for large animal studies).
- Use antibiotic selection or FACS to purify populations with high CD47 expression.
- Cell Preparation:
- Engineer rhesus macaque iPSCs to express a reporter gene like firefly luciferase (FLuc) for in vivo tracking.
- Generate HIP cells (B2M−/−CIITA−/−CD47+) and wild-type control cells from the same parental line.
- Animal Transplantation:
- Use fully immunocompetent, MHC-mismatched allogeneic rhesus macaques.
- Administer cells via intramuscular or subcutaneous injection (e.g., 10 million cells per site).
- Long-Term Monitoring:
- Bioluminescence Imaging (BLI): Perform weekly imaging to track cell survival and proliferation quantitatively.
- Immune Monitoring: Collect serial blood samples to assess donor-specific antibodies (DSAs) via flow cross-match and to isolate PBMCs for ELISpot assays against donor antigens.
- Endpoint Analysis: After 16+ weeks, explant grafts for histology. Stain for cell-specific markers (e.g., insulin for islets) and immune cell infiltration (CD3, CD4, CD8, CD68, NK cell markers).
Key Signaling Pathways in Hypoimmunogenic Cell Engineering
The following diagram illustrates the core immune evasion mechanisms engineered into hypoimmunogenic cells.
In Vivo Validation Workflow
The following diagram outlines a standard workflow for validating hypoimmunogenic cells in a large animal model.
Research Reagent Solutions
The table below lists essential reagents and their functions for developing and validating hypoimmunogenic stem cell derivatives.
| Research Reagent | Function / Application | Key Considerations |
|---|---|---|
| CRISPR-Cas9 System | Knocking out immune genes (e.g., B2M, CIITA). |
Use high-fidelity Cas variants (e.g., Cas12iHiFi) to minimize off-target effects [71]. |
| Lentiviral Vectors | Delivering transgenes (e.g., CD47, HLA-E, reporter genes). |
Ensure high titer and test for stable expression in target cells [27]. |
| Anti-HLA-ABC Antibody | Validating HLA-I knockout via flow cytometry. | Clone W6/32 is commonly used to detect all classical HLA-I molecules [71]. |
| Anti-CD47 Antibody | Confirming CD47 overexpression via flow cytometry. | Ensure the antibody is compatible with the species of the transgene [27]. |
| Firefly Luciferase (FLuc) | Non-invasive, longitudinal tracking of cell survival in vivo using BLI. | Critical for quantitative monitoring in large animal studies [27]. |
| IFN-γ ELISpot Kit | Measuring T-cell activation against donor cells in vitro and ex vivo. | A key functional assay to confirm abrogation of alloreactive T-cell responses [27]. |
| Cytotoxicity Assay Kits | Quantifying NK cell and macrophage-mediated killing of target cells. | Use real-time impedance-based assays or standard LDH release assays [27] [71]. |
The table below consolidates critical quantitative findings from recent preclinical studies in large animal models.
| Study Focus | Animal Model | Cell Type | Genetic Modifications | Key Quantitative Outcome | Reference |
|---|---|---|---|---|---|
| Long-term iPSC Survival | Rhesus Macaque | iPSCs | B2M−/− CIITA−/− CD47+ |
16-week survival in immunocompetent allogeneic hosts; wild-type cells were vigorously rejected [27]. | |
| Diabetes Reversal | Humanized Mice / Rhesus Macaque | Pancreatic Islet Cells (from iPSCs) | B2M−/− CIITA−/− CD47+ |
Survived for 4 weeks in diabetic mice, ameliorating diabetes. Primary edited macaque islets survived for 40 weeks in an allogeneic recipient [27]. | |
| NK Cell Protection | In Vitro / Humanized Mice | K562 Cell Line & Derivatives | CD47+ vs. HLA-E+/HLA-G+/PD-L1+ |
Only CD47 overexpression provided comprehensive protection from killing by all IL-2-stimulated human NK cells [27]. | |
| CAR-NK Cell Therapy | In Vitro / Xenograft Mice | ESC-derived CAR-NK Cells | B2M−/− HLA-E+ |
Evaded allogeneic T-cell response and suppressed allogeneic NK-cell response, showing robust anti-tumor activity [71]. |
The development of cell therapies is shaped by the fundamental choice between autologous (patient-specific) and allogeneic (off-the-shelf) approaches, each with distinct economic and logistical implications. The following tables provide a comparative analysis of these models.
Table 1: Economic and Manufacturing Profile Comparison
| Evaluation Criteria | Autologous (Patient-Specific) Therapy | Allogeneic (Off-the-Shelf) Therapy |
|---|---|---|
| Manufacturing Model | Personalized "service-based" production [73] | Standardized, scalable batch production [73] |
| Cost per Dose | Very high (e.g., $300,000–$500,000 for autologous CAR-T) [74] | Potentially lower due to economies of scale [73] |
| Production Timeline | Several weeks [73] | Immediately available from cryopreserved inventory [75] [73] |
| Batch Consistency | High heterogeneity between patient batches [73] | High consistency from a single, well-characterized donor [73] |
| Scalability | Challenging and costly to scale [73] | Highly scalable; one batch treats many patients [73] |
Table 2: Key Immunological and Logistical Challenges
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Primary Immune Risk | Minimal risk of immune rejection [73] | Graft-versus-Host Disease (GvHD) and host-mediated allorejection [75] [59] [73] |
| Need for Immunosuppression | Not required [73] | Required to prevent rejection [73] |
| Cell Source & Quality | Patient's own, potentially compromised cells [74] | Healthy donor-derived, high-quality cells [73] |
| Treatment Readiness | Delay for manufacturing; risk for patients with rapid disease progression [74] [73] | On-demand treatment [73] |
Troubleshooting Guide: FAQs on Allogeneic Therapy Challenges
FAQ: What are the primary causes of immune rejection in allogeneic cell products?
Allogeneic cell products face a dual immune rejection problem:
- Graft-versus-Host Disease (GvHD): This occurs when donor T cells, present in the therapeutic product, attack recipient tissues. This is primarily mediated by the donor T cell receptor (TCR) recognizing the recipient's foreign human leukocyte antigen (HLA) molecules [75] [59] [76].
- Host-versus-Graft (HvG) Rejection (Allorejection): This occurs when the recipient's immune system recognizes the donor cells as foreign and eliminates them. This is also driven by mismatches in HLA markers between the donor and recipient [75] [77].
FAQ: Which genetic engineering strategies can mitigate GvHD and allorejection?
Several gene-editing strategies are being employed to create "immune-evasive" allogeneic cells:
- T Cell Receptor (TCR) Knockout: Disrupting the TCR alpha constant (TRAC) gene in donor T cells using nucleases like TALENs or CRISPR-Cas9 prevents them from recognizing host tissues, thereby eliminating the main mediator of GvHD [75] [74].
- HLA Knockout: Knocking out HLA class I and II molecules on the donor cells makes them "invisible" to the recipient's T cells, reducing host-mediated allorejection [74]. A common target is the Beta-2-microglobulin (B2M) gene, which is essential for HLA class I surface expression [75].
- HLA Camouflage: An alternative to knockout is engineering donor cells to express non-polymorphic HLA molecules like HLA-E or HLA-G, which can inhibit both NK cell and T cell-mediated responses [74].
- Safety Switches: Incorporating "suicide genes" such as RQR8 or inducible Cas9 (iCas9) provides a control mechanism. If toxicity occurs, administering a prodrug can trigger the elimination of the engineered cells [74].
FAQ: How does donor selection and matching impact rejection risk?
The risk of immune rejection is heavily influenced by HLA matching:
- Lower GvHD Risk: Transplants from a genotypically identical sibling or a matched unrelated donor (identical for 10-12 tested HLA antigens) carry a lower risk of GvHD [76].
- Higher GvHD Risk: The use of mismatched or haploidentical (half-matched) donors increases the risk of GvHD and rejection, necessitating more intensive prophylactic strategies [76].
- Umbilical Cord Blood: Cord blood-derived T cells are less mature and have a naturally lower risk of inducing GvHD, though the limited cell number per unit can be a challenge [74].
Experimental Protocols for Overcoming Immune Rejection
Protocol: Generation of TCR-Deficient Allogeneic CAR-T Cells
This protocol outlines the creation of allogeneic CAR-T cells with a reduced potential to cause GvHD.
1. Objective: To manufacture universal allogeneic CAR-T cells by genetically disrupting the endogenous T cell receptor.
2. Materials and Reagents:
- Starting Material: Peripheral blood mononuclear cells (PBMCs) from a healthy donor [74].
- Gene Editing System: CRISPR-Cas9 or TALENs targeting the TRAC locus [74].
- CAR Delivery Vector: A lentiviral or retroviral vector encoding the chimeric antigen receptor [74].
- Cell Culture Media: T cell expansion media supplemented with cytokines (e.g., IL-2).
- Activation Reagents: Anti-CD3/CD28 antibodies or beads.
3. Methodology:
- Step 1: T Cell Activation. Isolate T cells from donor PBMCs and activate them using anti-CD3/CD28 stimulation.
- Step 2: TCR Disruption. Electroporate the activated T cells with CRISPR-Cas9 ribonucleoprotein (RNP) complexes targeting the TRAC gene [74].
- Step 3: CAR Transduction. Transduce the cells with the CAR-encoding lentiviral vector 24-48 hours after activation.
- Step 4: Expansion. Culture the engineered cells in media with IL-2 to expand them to a therapeutic dose.
- Step 5: Validation. Assess the efficiency of TCR knockout via flow cytometry (e.g., loss of CD3ε expression) and confirm CAR expression.
Protocol: CRISPR-Cas9-Mediated B2M Knockout for Immune Evasion
This protocol describes how to knockout the B2M gene to prevent HLA class I-mediated allorejection.
1. Objective: To generate HLA class I-deficient donor cells to evade host T cell recognition.
2. Materials and Reagents:
- Target Cells: Therapeutically relevant cells (e.g., T cells, iPSCs).
- CRISPR Reagents: Synthetic guide RNA (sgRNA) targeting the B2M gene and high-fidelity Cas9 nuclease.
- Delivery Method: Electroporation for primary cells; lipofection or nucleofection for cell lines.
- Analysis Tools: Flow cytometry antibodies for B2M or HLA class I, and genotyping assays.
3. Methodology:
- Step 1: Design and Synthesis. Design and synthesize a highly specific sgRNA targeting an early exon of the B2M gene.
- Step 2: Delivery. Form a complex of Cas9 protein and sgRNA to create an RNP. Deliver the RNP into the target cells via electroporation.
- Step 3: Clonal Selection. For iPSCs, single-cell clone the edited population and expand.
- Step 4: Validation.
- Flow Cytometry: Confirm the loss of B2M/HLA class I surface expression.
- Genotypic Analysis: Use Sanger sequencing or next-generation sequencing (NGS) of the target locus to confirm indels and editing efficiency.
- Step 5: Functional Assay. Co-culture the edited cells with allogeneic peripheral blood lymphocytes (PBLs) to demonstrate reduced T cell activation and cytotoxicity compared to unedited controls.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing Allogeneic Cell Therapies
| Reagent / Solution | Primary Function | Example Application |
|---|---|---|
| CRISPR-Cas9 System | Precise gene knockout (e.g., TRAC, B2M) or knock-in [78] [74] | Creating immune-evasive edits in donor cells. |
| TALENs | Alternative nuclease for gene editing [74] | Disruption of endogenous TCR in UCART19 clinical trials. |
| Lentiviral Vector | Stable integration of transgenes (e.g., CAR) [78] [74] | Engineering cells to express therapeutic receptors. |
| Anti-CD3/CD28 Beads | Polyclonal T cell activation and expansion [74] | Ex vivo stimulation of donor T cells prior to genetic modification. |
| Recombinant IL-2 | T cell growth and survival cytokine [74] | Supporting the expansion and culture of engineered T cells. |
| HLA Typing Kits | Determining HLA allele profiles of donor and recipient [77] | Assessing donor-recipient match and predicting rejection risk. |
Workflow Visualization: Engineering an Off-the-Shelf Cell Product
The diagram below illustrates the key steps in creating an allogeneic, off-the-shelf cell therapy product.
Allogeneic Cell Therapy Engineering Workflow
Conclusion
The field of allogeneic stem cell transplantation is undergoing a paradigm shift, moving from broad immunosuppression toward precise immune evasion through genetic engineering and targeted conditioning. The convergence of strategies—such as creating hypoimmunogenic cells via HLA editing and CD47 overexpression, coupled with non-genotoxic conditioning—paints an optimistic future for off-the-shelf therapeutics. Future research must focus on validating the long-term safety and efficacy of these approaches in larger clinical cohorts, standardizing potency assays for engineered cells, and expanding applications beyond hematology to include solid organ replacement and autoimmune diseases. The ultimate goal is to realize a new class of universally compatible, readily available cellular medicines that can be deployed without the burdens of chronic immunosuppression, thereby democratizing access to curative cell therapies.
References
- 1. Activation and regulation of alloreactive T cell immunity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9968399/]
- 2. Tolerance Induction Strategies in Organ Transplantation [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14958/full]
- 3. Overcoming Immune Barriers in Allogeneic CAR-NK Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292777/]
- 4. Strategies for overcoming bottlenecks in allogeneic CAR-T ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1199145/full]
- 5. Immune Reconstitution after Allogeneic Hematopoietic Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5112259/]
- 6. Immune Reconstitution After Allogeneic Haematopoietic ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2021.786017/full]
- 7. Natural Killer (NK) Cell Alloreactivity in Haploidentical Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293795/]
- 8. Missing self triggers NK cell-mediated chronic vascular ... [https://www.nature.com/articles/s41467-019-13113-5]
- 9. Allorecognition Unveiled: Integrating Recent Breakthroughs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586167/]
- 10. Innate Allorecognition in Transplantation - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11188633/]
- 11. Innate Allorecognition and Memory in Transplantation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.00918/full]
- 12. A Model of Minor Histocompatibility Antigens in Allogeneic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.782152/full]
- 13. Mechanism of cellular rejection in transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2778785/]
- 14. Transplant rejection - GeneGlobe - QIAGEN [https://geneglobe.qiagen.com/us/knowledge/pathways/immunology-inflammation-pathways/transplant-rejection]
- 15. Autoimmune diseases after allogeneic stem cell ... [https://pubmed.ncbi.nlm.nih.gov/35500169/]
- 16. Autoimmune neutropenia: a rare complication of allogeneic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1640546/full]
- 17. The emerging field of non–human leukocyte antigen ... [https://www.sciencedirect.com/science/article/pii/S0085253821005810]
- 18. Effects of bivalirudin on instant blood-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579726/]
- 19. Status of islet transplantation and innovations to ... [https://www.frontiersin.org/journals/transplantation/articles/10.3389/frtra.2024.1485444/full]
- 20. Xuebijing Injection Mitigates Instant Blood‑Mediated ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1671966/full]
- 21. Bioengineered stem cells as an alternative for islet cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4371156/]
- 22. HLA matching or CRISPR editing of HLA class I/II enables ... [https://www.nature.com/articles/s41467-025-64945-3]
- 23. Selective HLA knockdown and PD-L1 expression prevent ... [https://www.nature.com/articles/s41467-025-63863-8]
- 24. Genetic ablation of adhesion ligands mitigates rejection ... [https://www.sciencedirect.com/science/article/pii/S1934590924002194]
- 25. Immune Editing: Overcoming Immune Barriers in Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9643905/]
- 26. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 27. Hypoimmune induced pluripotent stem cells survive long ... [https://www.nature.com/articles/s41587-023-01784-x]
- 28. Blockade of dual immune checkpoint inhibitory signals with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9800731/]
- 29. An effective approach to prevent immune rejection of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4023958/]
- 30. The influence of immune checkpoint blockade on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1491330/full]
- 31. HX009, a novel BsAb dual targeting PD1 x CD47 ... [https://www.nature.com/articles/s41598-023-32547-y]
- 32. CRISPR-Based Genome Editing Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/genome-editing-support-center/crispr-based-genome-editing-support/crispr-based-genome-editing-support-troubleshooting.html]
- 33. Universal cell donor lines: A review of the current research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10679649/]
- 34. Hypoimmunogenic Human iPSCs for Repair and Regeneration in the CNS [https://www.mdpi.com/2073-4409/14/16/1248]
- 35. Immunological considerations and challenges for ... [https://www.nature.com/articles/s42003-021-02237-4]
- 36. Non-genotoxic conditioning facilitates hematopoietic stem cell ... [https://pubmed.ncbi.nlm.nih.gov/34141826/]
- 37. Hematopoietic chimerism and donor-specific skin allograft ... [https://www.nature.com/articles/s41467-018-08202-w]
- 38. Targeted depletion of TRBV9 + T cells as immunotherapy ... [https://www.nature.com/articles/s41591-023-02613-z]
- 39. Overview of T-cell depletion in haploidentical stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3417724/]
- 40. Ex vivo T-cell depletion in allogeneic hematopoietic stem ... [https://www.nature.com/articles/bmt201722]
- 41. Targeted depletion of PD-1-expressing cells induces ... [https://pubmed.ncbi.nlm.nih.gov/38669317/]
- 42. Regulatory T cell approaches for GVHD prevention - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638023/]
- 43. Cell Therapy for Cancer: Preclinical Models to Study T ... [https://www.taconic.com/resources/cell-therapy-cancer-preclinical-models-study-t-cell-mediated-gvhd]
- 44. Post-Transplant Cyclophosphamide for the Prevention of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558021/]
- 45. Efficacy and Safety of Allogeneic Hematopoietic Stem Cell ... [https://www.sciencedirect.com/science/article/pii/S2666636725014472]
- 46. Study demonstrates a safer strategy for allogeneic stem ... [https://www.news-medical.net/news/20251127/Study-demonstrates-a-safer-strategy-for-allogeneic-stem-cell-transplants.aspx]
- 47. Current status, challenges, and integration pathways of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615434/]
- 48. DecodingAcute GVHD: The role of serum biomarkers and ... [https://www.sciencedirect.com/science/article/abs/pii/S0268960X25000748]
- 49. Adult NIH Chronic Graft-Versus-Host Disease Consensus ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725012023]
- 50. EBMT 2025: Exciting Updates and Advancements in ... [https://www.onclive.com/view/ebmt-2025-exciting-updates-and-advancements-in-allohsct]
- 51. Influence of daytime of allogeneic stem cell transplantation ... [https://www.nature.com/articles/s41409-025-02689-w]
- 52. Reduced-toxicity conditioning prior to allogeneic stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4222478/]
- 53. Considerations in Preparative Regimen Selection to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.567423/full]
- 54. The Challenge Of Immune Rejection For Allogeneic Cell ... [https://www.cellandgene.com/doc/the-challenge-of-immune-rejection-for-allogeneic-cell-therapies-0001]
- 55. Prevention and management of acute toxicities from ... [https://chi.scholasticahq.com/article/94952-prevention-and-management-of-acute-toxicities-from-conditioning-regimens-during-hematopoietic-stem-cell-transplantation]
- 56. The Basics of Allogeneic Transplantation: What Fellows ... [https://www.hematology.org/education/trainees/fellows/hematopoiesis/2021/the-basics-of-allogeneic-transplantation]
- 57. An Effective Approach to Prevent Immune Rejection of ... [https://www.sciencedirect.com/science/article/pii/S1934590913005055]
- 58. Preventing secondary primary malignancies (SPMs) in CAR-T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542518/]
- 59. Is There a Risk of Immune Rejection From Stem Cell ... [https://blog.dana-farber.org/insight/2023/04/is-there-a-risk-of-immune-rejection-from-stem-cell-transplants/]
- 60. Strategies for overcoming bottlenecks in allogeneic CAR-T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10405079/]
- 61. CAR-T and CAR-NK as cellular cancer immunotherapy for ... [https://www.nature.com/articles/s41423-024-01207-0]
- 62. Allogeneic CAR-engineered cellular therapy for relapsed ... [https://pubmed.ncbi.nlm.nih.gov/40698082/]
- 63. CAR-NK cells to treat patients with cancer: a systematic ... [https://www.sciencedirect.com/science/article/pii/S1465324925007455]
- 64. Engineering a solution for allogeneic CAR-T rejection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11489523/]
- 65. Immunology of Transplant Rejection: Overview, History, ... [https://emedicine.medscape.com/article/432209-overview]
- 66. Sensitization in Transplantation Assessment of Risk 2025 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331380/]
- 67. Overcoming immunological barriers in regenerative medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC4409427/]
- 68. Comparison of four different assays to evaluate cellular ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1567253/full]
- 69. of induced pluripotent Hypoimmunogenic ... derivatives stem cells [https://pubmed.ncbi.nlm.nih.gov/30778232/]
- 70. Hypoimmunogenic Human iPSCs for Repair and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384217/]
- 71. Frontiers | Hypoimmunogenic CD19 CAR-NK cells from... derived [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1504459/full]
- 72. Hypoimmune stem and islets: hype or a true breakthrough in... cells [https://cmbl.biomedcentral.com/articles/10.1186/s11658-025-00786-8]
- 73. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 74. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 75. Managing allorejection in off-the-shelf CAR-engineered ... [https://www.sciencedirect.com/science/article/pii/S1525001624007627]
- 76. The Toxicities of Allogeneic Transplantation: What Fellows ... [https://www.hematology.org/education/trainees/fellows/hematopoiesis/2022/the-toxicities-of-allogeneic-transplantation]
- 77. Allogeneic Stem Cell Transplant: A Guide for Patients & ... [https://www.mskcc.org/cancer-care/patient-education/allogeneic-stem-cell-transplantation]
- 78. Survival of Transplanted Allogeneic Beta Cells with No ... [https://pubmed.ncbi.nlm.nih.gov/40757665/]