Overcoming Immune Rejection in Stem Cell Therapies: From Foundational Mechanisms to Clinical Applications
This article provides a comprehensive analysis of the immunological barriers and evolving immunosuppression strategies in stem cell-based therapies.
Overcoming Immune Rejection in Stem Cell Therapies: From Foundational Mechanisms to Clinical Applications
Abstract
This article provides a comprehensive analysis of the immunological barriers and evolving immunosuppression strategies in stem cell-based therapies. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational science on innate and adaptive immune drivers of graft rejection with cutting-edge methodological advances in genetic engineering and cell-based tolerance induction. The content explores troubleshooting for safety and optimization challenges, validates approaches through recent clinical trial data and comparative efficacy analyses, and outlines a translational roadmap for enhancing the survival and functional integration of regenerative cellular products.
The Immune Battlefield: Foundational Mechanisms of Stem Cell Graft Rejection
FAQ: Troubleshooting Common Experimental Challenges
FAQ 1: In our mouse model of stem cell transplantation, we observe unexpected graft loss even with MHC-matched donors. What innate immune mechanisms could be responsible?
Unexpected graft loss in MHC-matched scenarios can often be attributed to innate immune triggers outside classical adaptive recognition pathways. Key players include:
- NK Cell "Missing-Self" Recognition: NK cells can become activated if the graft lacks host inhibitory MHC class I molecules, a scenario possible even with some MHC matching. This is mediated through killer immunoglobulin-like receptors (KIRs) in humans and Ly49 receptors in mice. Educated NK cells, which have undergone maturation in the presence of self-MHC, are particularly responsive to this missing self, leading to graft injury through direct cytotoxicity and IFN-γ secretion [1].
- Complement System Activation: The complement cascade can be activated by ischemia-reperfusion injury (IRI) inherent to the transplantation process. DAMPs released from stressed or dying graft cells can trigger the lectin pathway, while natural antibodies may activate the classical pathway, even in the absence of high-titer donor-specific antibodies [2] [3]. The anaphylatoxins C3a and C5a generated during this process recruit and activate innate immune cells, exacerbating inflammation.
- Antibody-Dependent Cellular Cytotoxicity (ADCC): The presence of low-level, pre-existing antibodies, potentially against non-HLA antigens, can bind to the graft. NK cells, via their FcγRIIIA (CD16) receptor, then recognize these antibody-coated cells and mediate ADCC, contributing to graft damage [1].
Troubleshooting Guide:
- Experimental Check: Analyze your graft for the expression of ligands for NK cell activating receptors (e.g., MICA/B, ULBPs). Their upregulation under cellular stress can trigger NK cells independently of MHC.
- Model Validation: Confirm the specific MHC matching in your model. Use NK cell-depleting antibodies (e.g., anti-NK1.1, anti-asialo GM1) or complement inhibitors (e.g., C3aR/C5aR antagonists, soluble CR1) to test the functional role of these pathways.
- Readout Expansion: Beyond graft survival, include histology for NK cell infiltration (e.g., NKp46 staining) and complement deposition (e.g., C4d, C3d staining) to identify the involved mechanism.
FAQ 2: Our data on NK cells in graft rejection seem contradictory, with some studies showing a pro-tolerogenic role. How can we explain this duality?
NK cell function in transplantation is highly plastic and context-dependent, which explains apparent contradictions. Their role is dictated by a balance of signals and specific interactions.
- Checkpoint 1: Interaction with Donor Antigen-Presenting Cells (APCs): A pivotal "checkpoint" is the early interaction between host NK cells and donor dendritic cells (DCs). If donor DCs are perceived as "missing self," NK cells can eliminate them via perforin-mediated killing. This reduces direct allorecognition by T-cells and can divert the immune response toward indirect presentation, which in some contexts promotes tolerance [4] [5].
- Checkpoint 2: Interaction with Host APCs: Conversely, NK cells can also license host DCs, enhancing their maturation and ability to prime alloreactive T-cells, thereby promoting rejection [4].
- Checkpoint 3: Direct Interaction with T-cells: NK cells can directly enhance T-cell responses via cytokine production (e.g., IFN-γ) or, alternatively, suppress them through direct killing of activated T-cells or secretion of immunoregulatory cytokines like IL-10 [4].
Troubleshooting Guide:
- Timing is Critical: The net effect of NK cells can depend on the timing of their activation. Analyze their phenotype and function at different post-transplant periods (e.g., early vs. late).
- Microenvironment Matters: The cytokine milieu (e.g., levels of IL-15, IL-12, IL-18, TGF-β) can skew NK cell function. Profile the local cytokine environment in your graft.
- Define the Subset: Do not treat NK cells as a uniform population. Characterize the subsets involved (e.g., CD56bright vs. CD56dim in humans; CD27+ vs. CD11b+ in mice) as they have divergent functions.
FAQ 3: What are the primary experimental methods to differentiate between complement-mediated and NK cell-mediated damage in vivo?
Disentangling these pathways requires a combination of genetic, pharmacological, and analytical tools.
- Table 1: Key Experimental Approaches for Differentiating Innate Immune Pathways
Target Pathway Experimental Method Key Reagents / Models Readouts & Measurements NK Cell Activity Cell Depletion Anti-NK1.1 (mice), anti-asialo GM1 (mice/rats) Graft survival, histology for cytotoxicity, IFN-γ ELISpot Functional Blockade Anti-NKG2D, anti-CD16 (FcγRIII), anti-KIR antibodies Cytokine production, donor cell lysis in co-culture assays Genetic Models β2-microglobulin deficient grafts (lacks MHC I, "missing-self") Graft rejection kinetics, NK cell infiltration by flow cytometry Complement Activity Inhibitors C1-inhibitor, C3aR/C5aR antagonists, Cobra Venom Factor (CVF) Graft function, C3/C5a levels by ELISA, C4d deposition by IHC Genetic Models C3 knockout mice, Factor B knockout (blocks alternative pathway) Serum creatine (kidney), transaminases (liver), histology Integrated Analysis Multiplex Imaging Immunofluorescence (IF) for NKp46+ cells & C4d+ areas Spatial relationship between NK cells and complement deposition Transcriptomics RNA-seq of graft tissue Gene expression signatures for NK cell and complement pathways
Troubleshooting Guide:
- Specificity of Depletion/Inhibition: Always confirm the efficacy and specificity of your depletion/inhibition strategy. For example, ensure that anti-NK1.1 does not deplete NKT cells in your model.
- Combination Studies: To test for synergistic or additive effects, perform experiments combining NK cell depletion with complement inhibition.
- Functional Assays: Move beyond descriptive data. Use in vivo cytotoxicity assays to measure NK cell function and measure complement activation products (C3a, C5a, SC5b-9) in serum or graft tissue to confirm pathway engagement.
Experimental Protocols for Key Assays
Protocol 1: Assessing NK Cell Cytotoxicity Against Donor Cells via In Vivo Rejection Assay
This protocol measures the ability of host NK cells to eliminate "missing self" target cells in vivo [1].
- Target Cell Preparation: Isolate splenocytes from a donor mouse strain that is MHC class I-deficient (e.g., β2m-/-) or has a specific MHC mismatch with the recipient. Label these cells with a high concentration of CFSE (e.g., 5 µM, CFSEhigh).
- Control Cell Preparation: Isolate splenocytes from a syngeneic host-type mouse. Label these cells with a low concentration of CFSE (e.g., 0.5 µM, CFSElow).
- Cell Injection: Mix the two populations at a 1:1 ratio and inject intravenously into the recipient mouse that has been transplanted or is undergoing a transplant experiment.
- NK Cell Depletion Control: In a parallel group of recipients, deplete NK cells using an appropriate antibody (e.g., anti-NK1.1) prior to target cell injection.
- Analysis: After 16-20 hours, harvest the recipient's spleen and analyze by flow cytometry. The ratio of CFSEhigh (donor) to CFSElow (host) cells is calculated. Specific rejection is indicated by a reduced donor-to-host ratio in the control group compared to the NK-depleted group.
Key Reagent Solutions:
- CFSE (Carboxyfluorescein succinimidyl ester): A cell-permanent fluorescent dye for tracking cell division and fate.
- Anti-NK1.1 Antibody (PK136): For specific depletion of NK cells in C57BL/6 mice.
- β2-microglobulin deficient mice: A model to provide "missing self" target cells.
Protocol 2: Measuring Complement Activation in Graft Tissue by C4d Immunohistochemistry
C4d deposition is a stable marker of classical and lectin pathway activation and is a key diagnostic feature in antibody-mediated rejection [2] [1].
- Tissue Fixation and Sectioning: Fix graft tissue in formalin and embed in paraffin. Section at 4-5 µm thickness.
- Deparaffinization and Antigen Retrieval: Deparaffinize sections in xylene and rehydrate through a graded ethanol series. Perform heat-induced epitope retrieval using a citrate-based or EDTA-based buffer (pH 6.0 or 9.0) appropriate for your anti-C4d antibody.
- Blocking and Staining:
- Block endogenous peroxidase activity with 3% H₂O₂.
- Block non-specific binding with 10% normal serum from the species of your secondary antibody.
- Incubate with primary anti-C4d antibody (monoclonal or polyclonal) at the manufacturer's recommended dilution overnight at 4°C.
- Incubate with a biotinylated secondary antibody followed by an avidin-biotin-enzyme complex (ABC).
- Detection and Counterstaining:
- Develop the signal with 3,3'-Diaminobenzidine (DAB) substrate, which produces a brown precipitate.
- Counterstain with hematoxylin to visualize nuclei.
- Scoring: Analyze staining under a light microscope. C4d deposition is typically scored as positive when there is linear, diffuse staining along capillary endothelial cells. Scoring can be semi-quantitative (e.g., 0 to 3+) or based on the percentage of positive capillaries.
Key Reagent Solutions:
- Anti-C4d Antibody: Specific antibody for detecting the C4d fragment.
- ABC Kit (Avidin-Biotin Complex): A high-sensitivity detection system for immunohistochemistry.
- DAB Substrate Kit: A chromogen for producing a visible, insoluble reaction product.
Signaling Pathways and Experimental Workflows
Diagram 1: NK Cell Activation in Graft Recognition
Diagram 2: Complement Activation in Transplantation
Diagram 3: Experimental Workflow for Differentiating Innate Immune Damage
The Scientist's Toolkit: Key Research Reagents
- Table 2: Essential Research Reagents for Investigating Innate Immunity in Transplantation
Reagent / Model Category Primary Function in Experiments Anti-NK1.1 (PK136) Antibody Biological Tool Depletes NK cells in vivo in C57BL/6 mice to test their functional role. Anti-Asialo GM1 Antiserum Biological Tool Depletes NK cells and some T-cell subsets in vivo in various rodent models. Cobra Venom Factor (CVF) Biological Tool A potent and transient decomplementing agent that depletes C3, used to study the role of complement. C3a Receptor Antagonist (SB 290157) Pharmacological Inhibitor Specifically blocks the C3a-C3aR signaling axis, mitigating anaphylatoxin-mediated inflammation. β2-microglobulin KO Mice Genetic Model Provides grafts or cells that lack MHC class I, creating a "missing-self" scenario for NK cell studies. C3 Knockout Mice Genetic Model Allows for the study of transplantation in the absence of the central complement component C3. Recombinant Human IL-15 Cytokine Used to expand and activate NK cells in vitro and in vivo. Anti-C4d Antibody Analytical Reagent Critical for detecting classical/lectin pathway complement activation in graft tissue via IHC. Anti-NKG2D Blocking Antibody Biological Tool Inhibits a major NK cell activating receptor, used to test its contribution to rejection. Factor B Knockout Mice Genetic Model Specifically blocks the alternative pathway of complement activation.
Troubleshooting Guides & FAQs
FAQ: T-Cell Allorecognition Pathways
Q1: In our mixed lymphocyte reaction (MLR) assay, we observe unexpectedly high T-cell proliferation even with matched HLA-DR. Which allorecognition pathway is likely responsible and how can we confirm this?
A1: The semi-direct allorecognition pathway is the most probable cause. Donor antigen-presenting cells (APCs) can transfer intact Major Histocompatibility Complex (MHC) molecules to recipient APCs via trogocytosis or exosomes, enabling recipient T-cells to see donor MHC peptides presented by self-MHC. To confirm:
- Perform an MLR using purified CD4+ T-cells as responders and recipient-derived, donor peptide-pulsed dendritic cells as stimulators.
- Use flow cytometry to detect the presence of donor MHC molecules on recipient APCs using specific antibodies.
- Employ transwell assays to physically separate cell populations and quantify cross-talk.
Q2: Our immunosuppressive drug effectively inhibits the direct pathway but graft rejection still occurs. What experimental approach can identify if the indirect pathway is active?
A2: This indicates a likely failure to control the indirect pathway. To investigate:
- ELISPOT Assay: Measure the frequency of recipient T-cells producing IFN-γ in response to donor-derived MHC peptides.
- Tetramer Staining: Use MHC class II tetramers loaded with donor-derived MHC peptides to identify and quantify T-cell clones specific for these indirectly presented antigens.
- Adoptive Transfer: Transfer T-cells from rejected hosts into naïve, matched hosts challenged with the same donor peptides to demonstrate pathogenicity.
Q3: We are developing a CAR-Treg therapy to suppress alloreactivity. Which allorecognition pathway should the CAR target for broad-spectrum efficacy?
A3: Targeting the semi-direct pathway may offer the broadest suppression. A CAR that recognizes a conserved region of donor MHC class I or II would allow Tregs to inhibit T-cell activation regardless of the presenting APC (donor for direct, recipient for indirect/semi-direct). This requires a CAR construct with a scFv domain specific for a non-polymorphic region of the MHC molecule.
Troubleshooting: B-Cell and Antibody Responses
Q4: In our stem cell transplant model, we detect high-titer donor-specific antibodies (DSAs) but cannot identify the immunizing source. How can we determine if T-cell help is coming from the direct or indirect pathway?
A4: This is a classic problem in chronic rejection. Use a two-pronged approach:
- Indirect Pathway Help: Isolate CD4+ T-cells from the recipient and test their proliferation and cytokine production (e.g., IL-21) in response to recipient APCs pulsed with donor MHC peptides.
- Direct/Semi-Direct Help: Co-culture recipient B-cells with donor-derived B-cells or recipient APCs that have acquired donor MHC (semi-direct) and measure B-cell activation and differentiation using CD86/CD69 upregulation.
Q5: Our protocol for detecting memory B-cells specific to donor HLA is yielding inconsistent results. What is a reliable method?
A5: Use an optimized Antigen-Specific Memory B-Cell ELISpot.
- Issue: Inconsistency often stems from suboptimal antigen coating or inadequate B-cell stimulation.
- Solution:
- Coat ELISpot plates with purified, recombinant donor HLA monomers (not multimers) to ensure correct conformation.
- Use a polyclonal stimulation cocktail (e.g., CpG + R848) for 4-6 days to differentiate memory B-cells into antibody-secreting cells (ASCs) in vitro before plating.
- Include positive controls (anti-Ig) and negative controls (irrelevant protein) in every assay.
Table 1: Frequency of Alloreactive T-Cells in Naïve Repertoire
| Allorecognition Pathway | Frequency of Precursor T-Cells | Primary MHC Restriction | Key Readout Assay |
|---|---|---|---|
| Direct | 1-10% of total T-cell pool | Donor MHC | Primary MLR, CFSE dilution |
| Indirect | 0.01-0.1% of total T-cell pool | Recipient MHC | Peptide-specific ELISpot, Tetramer staining |
| Semi-Direct | Not fully quantified (estimated <1%) | Recipient MHC | Flow cytometry for donor MHC on recipient APCs |
Table 2: Efficacy of Immunosuppressive Agents on Allorecognition Pathways
| Drug/Target | Direct Pathway Inhibition | Indirect Pathway Inhibition | Semi-Direct Pathway Inhibition | Effect on DSA Production |
|---|---|---|---|---|
| Calcineurin Inhibitors (Cyclosporin, Tacrolimus) | Strong | Moderate | Moderate | Moderate |
| mTOR Inhibitors (Sirolimus) | Moderate | Strong | Strong (blocks exosome function) | Strong |
| Anti-CD25 (Basiliximab) | Strong (early) | Weak | Weak | Weak |
| Co-stimulation Blockade (Belatacept) | Strong | Strong | Strong | Strong |
Experimental Protocols
Protocol 1: Distinguishing Direct vs. Indirect Allorecognition In Vitro
Title: MLR Co-culture Assay for Pathway Analysis
- Cell Isolation:
- Isolate CD4+ T-cells (responders) from recipient spleen or PBMCs using magnetic-activated cell sorting (MACS).
- Isolate APCs (stimulators) from donor (for direct pathway) and recipient (for indirect pathway) spleen. Irradiate (30 Gy) or treat with Mitomycin C to prevent proliferation.
- Antigen Pulsing (Indirect Pathway):
- Incubate recipient APCs with a panel of synthetic 15-mer peptides spanning the polymorphic regions of donor MHC class I and II (10 µg/mL) for 4-6 hours.
- Co-culture:
- Set up co-cultures in a 96-well U-bottom plate:
- Direct: Recipient T-cells + Donor APCs
- Indirect: Recipient T-cells + Recipient APCs (donor peptide-pulsed)
- Control: Recipient T-cells + Recipient APCs (unpulsed)
- Use a 1:1 responder:stimulator ratio (e.g., 1x10^5 cells each) in complete RPMI-1640 medium.
- Set up co-cultures in a 96-well U-bottom plate:
- Readout (Day 5-7):
- Proliferation: Add ³H-thymidine for the final 16-18 hours and measure incorporation.
- Cytokines: Collect supernatant for IFN-γ and IL-17 measurement by ELISA.
- Flow Cytometry: Use CFSE dilution to track proliferation divisions.
Protocol 2: Detection of Donor-Specific Antibodies (DSAs)
Title: Flow Cytometric Crossmatch (FCXM) for DSA Detection
- Target Cell Preparation:
- Isolate lymphocytes from donor spleen or use donor-derived cell lines expressing the relevant HLA.
- Wash cells twice with PBS + 1% BSA (FACS buffer). Adjust concentration to 5x10^6 cells/mL.
- Serum Incubation:
- Incubate 50 µL of donor cells with 50 µL of test recipient serum (heat-inactivated at 56°C for 30 mins) for 30 minutes at room temperature, protected from light.
- Detection:
- Wash cells twice with FACS buffer to remove unbound antibody.
- Resuspend cell pellet in 100 µL of FACS buffer containing a fluorochrome-conjugated anti-human IgG antibody (e.g., F(ab')₂ fragment to avoid Fc receptor binding). Incubate for 30 minutes on ice in the dark.
- Analysis:
- Wash cells twice and resuspend in fixation buffer.
- Acquire data on a flow cytometer. Gate on lymphocytes and analyze the median fluorescence intensity (MFI) of the fluorochrome channel. A positive shift in MFI compared to a negative control serum indicates the presence of DSAs.
Pathway & Workflow Visualizations
Title: T-Cell Allorecognition Pathways
Title: B-Cell Alloantibody Production Workflow
The Scientist's Toolkit
Table 3: Key Research Reagents for Alloimmunity Studies
| Research Reagent | Function & Application in the Field |
|---|---|
| Recombinant HLA Monomers/Tetramers | Used to identify and isolate T-cells specific for donor MHC or its peptides via flow cytometry. Critical for quantifying indirect pathway T-cells. |
| CFSE / Cell Proliferation Dyes | A fluorescent dye that dilutes with each cell division. Essential for tracking and quantifying T-cell and B-cell proliferation in MLR and other co-culture assays. |
| CpG ODN + R848 (Resiquimod) | Toll-like receptor agonists (TLR9 and TLR7/8) used in combination to polyclonally activate and differentiate human memory B-cells into ASCs for ELISpot assays. |
| Anti-CD40 Agonistic Antibody | Mimics T-cell help (CD40L) for B-cell activation, isotype switching, and germinal center formation in in vitro B-cell culture systems. |
| Transwell Inserts | Permeable supports for cell culture plates that allow physical separation of cell populations while permitting soluble factor exchange. Used to dissect cell-contact dependent vs. independent effects. |
| MHC-Specific Antibodies (One-HLA) | Antibodies that recognize a single allele of HLA. Used in flow cytometry and FCXM to confirm HLA expression and detect donor MHC on recipient APCs in the semi-direct pathway. |
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: What are the core mechanisms by which an HLA mismatch leads to transplant rejection? An HLA mismatch triggers rejection through two primary immunological pathways:
- Direct Allorecognition: Recipient T cells directly recognize intact mismatched HLA molecules on the surface of donor antigen-presenting cells (APCs). This pathway is dominant in the early post-transplant period [6].
- Indirect Allorecognition: Recipient CD4+ T cells recognize peptides derived from donor HLA molecules that are presented by the recipient's own APCs. This pathway is operational throughout the life of the graft and is a potent inducer of allograft rejection via antibody-mediated and CD8+ T cell–mediated rejection [6].
FAQ 2: How does pre-sensitization occur, and why is it a major barrier to transplantation? Pre-sensitization refers to the pre-existence of anti-HLA antibodies in a transplant candidate's blood. Sensitizing events include [6]:
- Previous blood transfusions
- Pregnancies
- Previous organ transplants These pre-formed anti-HLA antibodies represent a significant immunological barrier because high-titer donor-specific HLA antibodies (DSA) can cause hyperacute antibody-mediated rejection (AMR), leading to rapid graft loss. Lower titer antibodies can also cause rejection via NK cell activation or endothelial cell proliferation [6].
FAQ 3: What is the difference between antigen-level and molecular-level HLA matching?
- Antigen-Level Matching: The conventional approach, which counts mismatches for HLA-A, -B, and -DR antigens. A "0-antigen mismatch" means no mismatch is detected for these loci at the antigen level [6] [7].
- Molecular-Level Matching (Eplet Matching): A more granular method that assesses mismatches at the level of small configurations of polymorphic amino acids called eplets, which are the actual targets for antibodies. An HLA antigen-mismatched graft could theoretically be matched at the eplet level, potentially reducing immunogenicity [8].
FAQ 4: My patient is highly sensitized with high PRA. What strategies can increase transplant opportunities?
- Advanced Histocompatibility Testing: Use single-antigen bead (SAB) assays to precisely define antibody specificities and identify "unacceptable" HLA antigens [6].
- Eplet-Based Matching: Use the HLAMatchmaker algorithm to assess donor-recipient compatibility at the epitope level, which can help identify acceptable donors among those who might appear mismatched at the antigen level [9] [8].
- Desensitization Protocols: Therapeutic options to reduce antibody levels prior to transplantation [6].
- Paired Donation Programs: Increase the pool of potential donors [7].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or Ambiguous HLA Typing Results
- Potential Cause: Use of low-resolution typing methods that cannot distinguish between closely related alleles.
- Solution: Implement next-generation sequencing (NGS) technologies, such as single-molecule real-time (SMRT) sequencing or Oxford Nanopore (ONT) sequencing. These third-generation systems analyze long-read sequences spanning entire intronic-exonic regions of HLA genes, effectively resolving ambiguity and phasing issues [10].
- Protocol: High-Resolution HLA Typing via NGS
- DNA Extraction: Obtain high-quality, high-molecular-weight genomic DNA.
- Target Amplification: Use locus-specific primers to amplify HLA genes of interest (e.g., HLA-A, -B, -C, -DRB1, -DQB1, -DPB1).
- Library Preparation: Fragment amplicons and attach sequencing adapters.
- Sequencing: Run on a long-read sequencer (e.g., PacBio Sequel or Nanopore MinION).
- Data Analysis: Use specialized software (e.g., HLA Twin or specific NGS HLA typing suites) to align sequences and assign alleles based on the IMGT/HLA database.
Challenge 2: Differentiating Clinically Relevant Donor-Specific Antibodies (DSA) from Benign Signals
- Potential Cause: False positivity in single-antigen bead (SAB) assays, which are highly sensitive but can be prone to non-specific binding.
- Solution: Employ a multi-method verification approach. Do not rely on SAB results alone [6] [8].
- Protocol: Verification of Clinically Relevant HLA Antibodies
- Initial Screening: Use a solid-phase SAB assay to identify potential DSA.
- Cross-Correlation: Correlate SAB results with clinical history (e.g., known sensitizing events).
- Functional Assays: For antibodies detected by SAB, perform a complement-dependent cytotoxicity (CDC) assay to confirm their ability to activate complement and cause cell lysis, which is a marker of clinical relevance [6].
- Antibody Verification (Research Setting): Use advanced techniques like site-directed mutagenesis of HLA molecules or cryogenic electron microscopy (cryo-EM) to visualize the epitope-paratope interaction and confirm which specific amino acid residues are crucial for antibody binding [8].
Challenge 3: Investigating Antibody-Mediated Rejection (AMR) in a Patient with No Detectable DSA
- Potential Cause: Antibodies targeting non-HLA antigens or HLA epitopes not represented on standard SAB panels.
- Solution: Explore non-HLA pathways. Recent research highlights the role of innate immune mismatches, such as in the SIRPa-CD47 pathway [11].
- Protocol: Assessing Non-HLA SIRPa Mismatch
- Genotyping: Determine the SIRPa haplotypes (A or B) of both the donor and recipient using DNA from stored samples.
- Mismatch Directionality Analysis: Note that the immunogenic risk is particularly high when a recipient with SIRPa haplotype A receives an organ from a donor with SIRPa haplotype B [11].
- Functional Analysis (Research): In mouse models, blocking the SIRPa-CD47 interaction can prevent monocyte activation and subsequent chronic damage, providing mechanistic insight [11].
Data Presentation: HLA System in Transplantation
Table 1: Key HLA Loci and Their Characteristics in Transplantation [6] [10] [9]
| Locus Category | Loci | Polymorphism (Approx. Alleles) | Expression | Primary Role in Immune Response |
|---|---|---|---|---|
| Class I | HLA-A, HLA-B, HLA-C | >7,500 known alleles | All nucleated cells | Present endogenous peptides to CD8+ cytotoxic T cells |
| Class II | HLA-DR, HLA-DQ, HLA-DP | High polymorphism | Antigen-presenting cells (B cells, macrophages, dendritic cells) | Present exogenous peptides to CD4+ helper T cells |
Table 2: Impact of HLA-A, -B, -DR Mismatch on Kidney Transplant Outcomes [7]
| Number of Mismatches (A, B, DR) | Incidence of Rejection (%) | 5-Year Graft Survival (%) | Key Contextual Factors |
|---|---|---|---|
| 0-2 | 4.4% | ~100% | Data from highly sensitized patients (PRA >80%) |
| 3-4 | 11.4% | ~81% | Data from highly sensitized patients (PRA >80%) |
| 5-6 | 31.3% | ~74% | Data from highly sensitized patients (PRA >80%) |
Experimental Protocols & Methodologies
Protocol 1: HLA Antibody Screening and Characterization Using Single-Antigen Bead (SAB) Assay
Purpose: To detect and identify specific anti-HLA antibodies in a patient's serum to assess pre-sensitization risk. Workflow:
- Serum Preparation: Collect and heat-inactivate patient serum.
- Incubation: Mix serum with SAB panel. Each bead is coated with a single, purified HLA antigen.
- Detection: Add fluorescently labelled anti-human IgG antibody.
- Analysis: Run the bead mixture through a flow cytometry-based analyzer (e.g., Luminex). The mean fluorescence intensity (MFI) indicates the strength of antibody binding to each specific HLA antigen.
- Interpretation: Correlate reactive beads with the patient's HLA typing and potential donor HLA types to identify unacceptable antigens and potential DSA [6] [9].
Protocol 2: Eplet Mismatch Load Analysis Using HLAMatchmaker
Purpose: To provide a granular assessment of donor-recipient HLA compatibility beyond the antigen level, predicting the risk of de novo DSA development. Workflow:
- High-Resolution Typing: Obtain high-resolution (allele-level) HLA typing for both donor and recipient.
- Data Input: Enter the allele-level HLA types for both pairs into the HLAMatchmaker software.
- Analysis: The algorithm compares the amino acid sequences of the donor and recipient HLA molecules and counts the number of mismatched eplets—small, antibody-accessible configurations of polymorphic amino acids.
- Risk Stratification: A higher eplet mismatch load is associated with an increased risk of de novo DSA formation, rejection, and graft loss [8]. The analysis can inform on the immunogenic potential of a specific donor-recipient pair.
Visualization: Signaling Pathways and Workflows
Diagram 1: T Cell Allorecognition Pathways
Diagram 2: HLA Typing Technology Evolution
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Transplant Immunology Research
| Reagent / Material | Primary Function | Key Application in HLA/Rejection Research |
|---|---|---|
| Single-Antigen Bead (SAB) Kits | Multiplex detection of anti-HLA antibodies | Pre-transplant risk assessment; identification of DSA post-transplant [6] |
| Recombinant HLA Monoclonal Antibodies (mAbs) | Define specific HLA epitopes | Antibody verification; crucial for validating the immunogenicity of specific eplets [8] |
| Site-Directed Mutagenesis Kits | Introduce specific point mutations in HLA genes | Determine the exact amino acid residues critical for antibody binding (epitope mapping) [8] |
| Anti-Thymocyte Globulin (ATG) | T-cell depleting induction therapy | Suppresses T-cell mediated rejection, particularly important in the context of HLA mismatch [6] |
| CRISPR-Cas9 Systems | Gene editing in cell lines | Create knock-out or specific HLA-variant cell lines to study functional interactions (e.g., with KIRs) [8] |
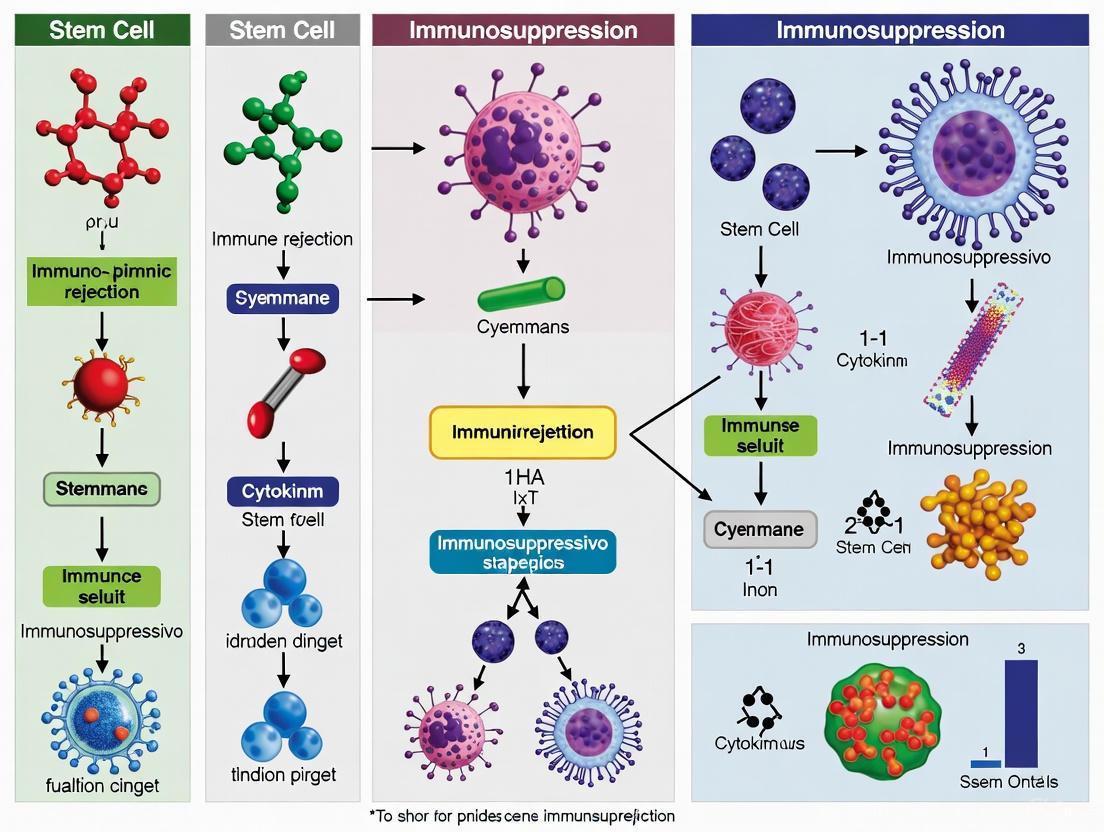
The immunogenic potential of stem cells is a critical parameter determining their survival and efficacy upon transplantation. Different stem cell types exhibit distinct immunological properties due to variations in their expression of major histocompatibility complex (MHC) molecules and immunomodulatory factors. Understanding these profiles is essential for selecting appropriate cell types for specific therapeutic applications and for designing effective immunosuppression strategies.
Table 1: Immunogenicity and Immunomodulatory Properties of Major Stem Cell Types
| Stem Cell Type | Key MHC Expression Features | Immunogenic Potential | Immunomodulatory Properties | Primary Immune Evasion Mechanisms |
|---|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Low/absent MHC-I; negative for MHC-II [12]. | Low in undifferentiated state; potential increase upon differentiation [12] [13]. | Capable of immunosuppression via arginase I, preventing dendritic cell maturation, and up-regulating regulatory T cells [12]. | Low MHC profile reduces T-cell activation; soluble factors that suppress immune responses [12]. |
| Induced Pluripotent Stem Cells (iPSCs) | Low/absent MHC-I; negative for MHC-II; limited upregulation with IFN-γ [12]. | Conflicting in vivo reports; generally low in vitro [12]. | Potent immunomodulatory effects; can suppress T-cell proliferation more effectively than MSCs in some assays [12]. | Low antigen-presenting function; active suppression of responder immune cell proliferation [12] [14]. |
| Mesenchymal Stromal Cells (MSCs) | High MHC-I; low/negative MHC-II (can be upregulated by IFN-γ) [12]. | Low in autologous use; rejection reported in allogeneic settings [12]. | Significant; inhibit T-cell proliferation, alter dendritic cell maturation, induce regulatory lymphocytes [12]. | Dynamic immunophenotype; secretion of soluble immunosuppressive factors; lack of co-stimulatory molecules [12]. |
| iPSC-Derived Neural Stem/Progenitor Cells (NS/PCs) | Low HLA-DR (MHC-II) and co-stimulatory molecules, even with cytokine stimulation [14]. | Low, even in allogeneic HLA-mismatched settings [14]. | Suppressive effects on peripheral blood mononuclear cell (PBMC) proliferation [14]. | Low antigen-presenting function and active immunosuppression [14]. |
Essential Experimental Protocols for Immunogenicity Assessment
In Vitro Immunogenicity Assay (Modified Mixed Leukocyte Reaction - MLR)
The Mixed Leukocyte Reaction is a cornerstone assay for evaluating the immunogenic potential of stem cells by measuring T-cell proliferation in response to foreign antigens [12] [14].
Protocol Steps:
- Cell Preparation:
- Responder Leukocytes: Isolate peripheral blood mononuclear cells (PBMCs) or splenocytes from a donor. These represent the host's immune system [12] [14].
- Stimulator Cells: Use the stem cell population under investigation (e.g., iPSCs, MSCs, or differentiated progeny). These should be irradiated or treated with mitomycin-C to prevent their proliferation while retaining antigen-presenting capability [12].
- Controls: Include positive controls (MHC-mismatched leukocytes) and negative controls (MHC-matched leukocytes or self-leukocytes) [12].
Co-culture Setup:
- Culture responder and stimulator cells together in a culture plate for 5-7 days. A typical ratio is 1:1 (responder:stimulator), but dose-dependence should be tested (e.g., 1:1, 1:0.3, 1:0.1) [12] [14].
- Culture conditions: Use RPMI 1640 medium supplemented with 10% human serum, L-glutamine, and penicillin/streptomycin at 37°C in 5% CO₂ [12].
Proliferation Measurement:
- Assess T-cell proliferation after the culture period. Common methods include:
- ³H-thymidine incorporation: Add ³H-thymidine to the culture for the last 6-18 hours. Measure incorporated radioactivity using a beta-counter [12].
- CFSE dilution: Label responder cells with Carboxyfluorescein succinimidyl ester (CFSE) prior to co-culture. Flow cytometry analysis of CFSE dilution in daughter cells indicates proliferation.
- Assess T-cell proliferation after the culture period. Common methods include:
Data Analysis:
- Compare the proliferation of responder cells when stimulated with test stem cells versus control stimulators.
- Significant proliferation in test groups compared to negative controls indicates immunogenicity.
- For immunomodulatory assessment, the suppression of proliferation in a standard MLR by the addition of stem cells is measured [12].
Diagram 1: Experimental workflow for a Mixed Leukocyte Reaction (MLR) assay to assess stem cell immunogenicity.
Flow Cytometry Analysis of MHC and Co-stimulatory Molecules
Quantifying the expression of immune-related surface markers is fundamental for profiling stem cells.
Protocol Steps:
- Cell Harvest: Gently dissociate stem cells into a single-cell suspension.
- Staining: Aliquot cells and incubate with fluorochrome-conjugated antibodies against target molecules (e.g., HLA-ABC (MHC-I), HLA-DR (MHC-II), CD80, CD86, CD40). Include isotype-matched control antibodies.
- Analysis: Analyze stained cells using a flow cytometer. The expression levels of MHC and co-stimulatory molecules are determined by the fluorescence intensity compared to the isotype control.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Stem Cell Immunogenicity Research
| Reagent / Material | Function in Immunogenicity Research | Example Application |
|---|---|---|
| Doxycycline-inducible Lentiviral Vectors | Delivery of reprogramming factors (e.g., OSKM) for iPSC generation [12]. | Creating isogenic iPSC lines for controlled differentiation and immunogenicity testing. |
| Interferon-gamma (IFN-γ) | Proinflammatory cytokine used to mimic an inflammatory environment and test immune plasticity [12] [14]. | Upregulating MHC expression on stimulator cells in MLR assays or pre-treating stem cells. |
| ROCK Inhibitor (Y-27632) | Improves survival of dissociated human pluripotent stem cells (hPSCs) [15]. | Used during passaging or thawing of iPSCs/ESCs for MLR to maintain cell viability. |
| RevitaCell Supplement | A cocktail supplement containing a ROCK inhibitor, antioxidants, and other components to enhance cell recovery [15]. | Improving survival of single-cell clones after genetic modification of stem cells. |
| mTeSR Plus / Essential 8 Medium | Defined, feeder-free cell culture media for maintaining hPSCs in an undifferentiated state [15]. | Culturing iPSCs and ESCs to ensure a consistent, high-quality cell source for experiments. |
| Geltrex / Vitronectin (VTN-N) | Defined, xeno-free extracellular matrices for feeder-free culture of hPSCs [15]. | Coating cultureware for the adherent growth of iPSCs and ESCs under defined conditions. |
| Carboxyfluorescein succinimidyl ester (CFSE) | Fluorescent cell dye for tracking cell division by flow cytometry [12]. | Labeling responder leukocytes in MLR to track and quantify T-cell proliferation. |
Troubleshooting Guides & FAQs
FAQ 1: Our iPSC lines show high variability in immunogenicity between different clones. How can we standardize our assessments? Answer: Clone-to-clone variation is a recognized challenge. To standardize assessments:
- Thorough Screening: Implement rigorous screening for genetic stability and karyotype abnormalities before immunogenicity testing [12].
- Isogenic Controls: Where possible, use isogenic controls (e.g., iPSCs derived from the same genetic background) to minimize genetic variability.
- Differentiation Status: Confirm the purity and maturity of your differentiated cell populations, as undifferentiated cells contaminating a culture can have different immune properties [15] [16].
- Internal Controls: Always include reference cell lines (e.g., a well-characterized MSC line) as an internal control across your MLR experiments to calibrate assay sensitivity [12].
FAQ 2: We are observing poor survival of our iPSCs in suspension during MLR setup, leading to inconclusive results. What can we do? Answer: Pluripotent stem cells are particularly sensitive to dissociation-induced apoptosis.
- Use ROCK Inhibitor: Include a ROCK inhibitor (e.g., Y-27632) at 10 µM in the culture medium during cell passaging, plating, and for the first 24 hours of the MLR assay to significantly improve cell survival [15] [16].
- Avoid Over-Dissociation: When preparing stimulator cells, avoid creating a single-cell suspension. Small, uniform cell aggregates survive better than single cells [16].
- Irradiation: Ensure proper irradiation of stimulator cells to prevent overgrowth, but optimize the dose to avoid excessive cellular stress.
FAQ 3: For regenerative neurology applications, is HLA-matching necessary for iPSC-derived neural stem/progenitor cells (NS/PCs)? Answer: Current in vitro evidence suggests that HLA-matching may be less critical for certain neural cells. Studies show that iPSC-derived NS/PCs have low expression of HLA-DR and co-stimulatory molecules even under inflammatory stimulation. Furthermore, they exhibit active immunosuppressive properties [14]. Modified MLR assays demonstrate similarly low allogeneic immune responses in both HLA-matched and mismatched settings for these cells [14]. However, these are in vitro findings, and their confirmation in clinical settings is crucial.
Troubleshooting Guide: Excessive Differentiation in Stem Cell Cultures Pre-Experiment
- Problem: Differentiated cells in your pluripotent stem cell culture can confound immunogenicity results.
- Solutions:
- Quality Control Media: Ensure culture medium (e.g., mTeSR Plus) is fresh and has been stored correctly at 2-8°C for less than two weeks [16].
- Manual Removal: Prior to passaging, manually remove areas of spontaneous differentiation under a microscope [16].
- Optimize Passaging: Passage cells when colonies are large and compact but before they overgrow and differentiate in the center. Ensure cell aggregates after passaging are evenly sized [15] [16].
- Limit Handling Time: Avoid having culture plates outside the incubator for extended periods (>15 minutes) [16].
Clinical Perspectives and Immunosuppression Strategies
Translating stem cell therapies from the lab to the clinic requires bridging in vitro findings with in vivo application. The choice of stem cell type and its inherent immunogenicity directly influences the immunosuppression regimen required.
Table 3: Clinical Immunosuppression Approaches in Stem Cell Trials
| Therapy / Cell Type | Common Immunosuppression Regimen | Clinical Context & Evidence |
|---|---|---|
| hESC-Derived Retinal Pigment Epithelial (RPE) Cells | Systemic: Tacrolimus + Mycophenolate Mofetil (MMF), sometimes with corticosteroids. Local: Intravitreal fluocinolone acetonide implant [17]. | Used in trials for macular degeneration. No clear signs of immune rejection reported with these regimens. Adverse events include infections and GI symptoms [17]. |
| Allogeneic Stem Cell Transplants (Neural, Retinal) | Varies by trial; often a combination of Tacrolimus (targeting serum concentration), MMF, and steroids, tapered over months [17]. | Regimen aims to prevent acute rejection while allowing long-term graft survival. Some studies report long-term graft survival even after immunosuppression cessation [17]. |
| Future/Trial Strategies: T-regulatory cell (Treg) Therapy | Infusion of ex vivo expanded alloantigen-specific Tregs [18]. | Aims to induce immune tolerance, potentially eliminating need for chronic drug therapy. Early trials in organ transplantation and GVHD show safety and feasibility of this approach [18]. |
Diagram 2: The three-signal model of T-cell activation, a key pathway targeted by immunosuppressive strategies. Signal 1 (antigen recognition), Signal 2 (co-stimulation), and Signal 3 (cytokine differentiation) are all potential points for therapeutic intervention [19].
Armoring the Graft: Methodological Strategies for Immune Evasion and Tolerance
Pharmacologic immunosuppression is a critical component in clinical trials involving stem cell and gene therapies. It mitigates host immune rejection, promoting the survival and viability of transplanted cells. The strategies and regimens vary significantly depending on the target tissue, cell type, and the specific immune challenges posed by allogeneic or xenograft transplants. This technical resource summarizes key regimens and experimental protocols from recent clinical trials and preclinical studies, providing a structured reference for researchers developing therapies for neural, retinal, and other specialized cell types.
The table below summarizes immunosuppression regimens from key clinical trials in neural and retinal cell therapies, providing a comparison of drugs, durations, and applications [20].
| Therapy / Indication | Immunosuppression Regimen | Duration | Key Findings / Rationale | Clinical Trial Context |
|---|---|---|---|---|
| Retinal Cell Transplants [20] [21] | Systemic: Tacrolimus, Mycophenolate Mofetil (MMF).Local: Corticosteroids (e.g., peri-ocular). | Short-term (tapering over weeks to months). | Grafted cells remained viable months to years after cessation. Local steroids manage intraocular inflammation. | Phase 1/2 trials for inherited retinal diseases (e.g., Retinitis Pigmentosa). |
| Spinal Cord Injury & ALS [20] | Multi-drug regimen: Tacrolimus, MMF, tapering corticosteroids. | Short-term course. | Detected immune responses in treated patients were rare. Regimen deemed efficacious for promoting graft survival. | Phase 1/2 trials for stem cell-derived neural precursor transplantation. |
| AAV Gene Therapy (Duchenne Muscular Dystrophy) [22] [23] | Standard: Systemic corticosteroids.Enhanced (under investigation): Addition of Sirolimus (pre- and post-infusion). | Corticosteroids: Before and after infusion.Sirolimus: 14 days prior to 12 weeks post-infusion. | Enhanced regimen aims to mitigate the risk of acute liver injury (ALI) and acute liver failure (ALF) associated with AAV vectors. | Phase 1b trial (ENDEAVOR Cohort 8) for non-ambulant patients. |
| Huntington's Disease Gene Therapy [24] | Optimized immunosuppression regimen (details not fully public). | Specific duration not disclosed; linked to one-time neurosurgical administration. | Protocol includes a dedicated cohort to investigate an optimized regimen for AAV-based therapy delivered directly to the brain. | Phase I/II clinical trial of AMT-130 (first gene therapy in HD). |
| Stem Cell Transplant (Fanconi Anemia) [25] | Non-Chemo Conditioning: Anti-CD117 antibody (Briquilimab) + immune-suppressing medications. | Antibody administered 12 days pre-transplant. | Replaced toxic busulfan chemotherapy/radiation. Achieved near 100% donor chimerism without graft rejection. | Phase 1 clinical trial for a genetic disease, enabling transplant from haploidentical donors. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the rationale behind using a multi-drug immunosuppression regimen in most cell therapy trials? Using a combination of drugs that target different pathways of the immune system allows for synergistic effects, enabling lower doses of each drug and potentially reducing individual drug-related toxicities. A common combination is Tacrolimus (a calcineurin inhibitor that suppresses T-cell activation) with Mycophenolate Mofetil (an antiproliferative agent that inhibits lymphocyte proliferation) [20]. This approach comprehensively targets both T-cell activation and expansion.
Q2: How long is immunosuppression typically maintained in retinal cell therapy trials? A short-term course is commonly employed. Evidence suggests that a tapering regimen over weeks to months can be efficacious, with some studies showing grafted cells remaining viable for months to years after immunosuppression has been stopped [20]. The "immune-privileged" status of the eye may contribute to this phenomenon, though local immunosuppression with steroids is also frequently used to control inflammation at the site [20] [21].
Q3: What are the key immune cell populations targeted by standard immunosuppressive drugs, and how are they monitored? The primary targets are T-lymphocytes. Tacrolimus inhibits calcineurin, blocking IL-2 production and T-cell activation. Mycophenolate Mofetil inhibits inosine monophosphate dehydrogenase, impairing lymphocyte proliferation. Sirolimus inhibits mTOR, disrupting T-cell activation and proliferation. Monitoring is critical and often involves [21]:
- Immunophenotyping: Using flow cytometry to track lymphocyte populations (e.g., T-helper, T-cytotoxic cells) in peripheral blood.
- Drug Level Monitoring: Using LC-MS to ensure therapeutic levels of drugs like tacrolimus are maintained.
- Cytokine Assays: Measuring pro-inflammatory cytokines to assess the overall immune state.
Q4: Our pre-clinical data shows graft rejection despite immunosuppression. What strategies can we investigate to induce immune tolerance? Beyond general immunosuppression, several advanced strategies are emerging:
- Engineered Immune Tolerance: Co-transplanting therapeutic cells with regulatory T-cells (Tregs) engineered to protect them. For example, beta cells engineered to express EGFRt can be protected by CAR-Tregs designed to recognize this tag, creating a "lock-and-key" system for local immune tolerance [26].
- Gene-Edited "Immune-Evasive" Cells: Using gene editing tools like CRISPR-Cas9 to modify allogeneic cells, for example, by knocking out Major Histocompatibility Complex (MHC) molecules to avoid T-cell recognition [27] [28].
- Novel Conditioning Regimens: Replacing toxic chemotherapies with targeted antibodies. Using an anti-CD117 antibody (e.g., Briquilimab) to clear host hematopoietic stem cells creates space for the donor graft without genotoxic side effects, which is particularly beneficial for fragile patients [25].
Q5: What are the primary safety concerns linked to prolonged immunosuppression in clinical trials? The main concerns are [20] [22]:
- Increased susceptibility to infections (including serious respiratory infections).
- Potential for organ toxicity (e.g., acute liver injury, nephrotoxicity from calcineurin inhibitors).
- Specific drug-related risks (e.g., sirolimus requires monitoring for metabolic issues and myelosuppression). Notably, in recent neural and retinal trials, side effects directly related to immunosuppression were reported to be uncommon [20].
Experimental Protocols
Protocol: In Vitro Assessment of Immunosuppressant Toxicity on hESC-Derived Retinal Organoids (ROs)
This protocol is used to evaluate the direct effects of immunosuppressive drugs on the viability and function of candidate cell products before transplantation [21].
1. Materials
- hESC-derived Retinal Organoids (ROs) at relevant stages of differentiation.
- Immunosuppressant drugs: Tacrolimus (TAC), Mycophenolic Acid (MPA; the active metabolite of MMF).
- Culture medium suitable for ROs.
- qPCR system with primers for key retinal identity and differentiation markers (e.g., CRX, NRL, OPSIN).
- Functional and Structural Fluorescence Lifetime Imaging Microscopy (FLIM) setup.
- Cell viability assay kit (e.g., MTT, CellTiter-Glo).
2. Methodology
- Step 1: RO Exposure. Expose ROs to therapeutic concentrations of TAC, MPA, or a combination for 1-4 weeks. Refresh drugs and medium regularly.
- Step 2: Gene Expression Analysis (qPCR). Harvest ROs after exposure. Extract RNA, synthesize cDNA, and perform qPCR for retinal identity and photoreceptor-specific genes. Compare to untreated control ROs.
- Step 3: Metabolic Function Analysis (FLIM). Use FLIM to assess the metabolic activity of live ROs. The autofluorescence of metabolic co-enzymes (e.g., NAD(P)H) provides a readout of cellular metabolic states, which should remain unchanged if the drugs are non-toxic.
- Step 4: Structural and Viability Assessment. Perform immunohistochemistry on fixed ROs for standard retinal cell markers and synaptic proteins. Perform a cell viability assay to quantify potential cytotoxicity.
3. Expected Outcomes & Analysis A successful result shows no significant negative effects on RO gene expression, metabolic function, or structural integrity compared to controls. This data supports the tolerability of the proposed immunosuppression regimen for the retinal cells in a clinical setting [21].
Protocol: In Vivo Evaluation of Immunosuppression in an Immunocompetent Retinal Degeneration (RD) Model
This protocol outlines the steps to test the efficacy of a systemic immunosuppression regimen in preventing the rejection of a xenograft in a pre-clinical RD model [21].
1. Materials
- Animals: Immunocompetent retinal degenerate rats (e.g., SD-foxn1 Tg(S334ter)3Lav strain).
- Transplant: hESC-derived Retinal Organoid sheets.
- Drugs: Tacrolimus (TAC) pellets for sustained release, Mycophenolate Mofetil (MMF) in chow.
- Analytical Tools: LC-MS for drug level monitoring, flow cytometer for immunophenotyping, ELISA kits for cytokines, Optical Coherence Tomography (OCT) for in vivo imaging, Optokinetic Test (OKT) for visual function.
2. Methodology
- Step 1: Determine Minimum Effective Dosing. Administer TAC and MMF at varying doses to healthy immunocompetent rats. Use serial blood collection and LC-MS to establish pharmacokinetics. Use flow cytometry immunophenotyping to link drug levels to the degree of lymphocyte suppression, thereby defining the minimum effective dosing range.
- Step 2: Transplantation and Immunosuppression. Perform subretinal transplantation of RO sheets into RD rats. Implant TAC pellets and provide MMF-medicated chow to the treatment group starting at the time of surgery.
- Step 3: Post-Operative Monitoring.
- Drug Efficacy: Regularly collect blood for LC-MS (drug levels) and flow cytometry (T-cell, B-cell counts).
- Graft Survival: Use in vivo OCT imaging at defined intervals to monitor the presence and structure of the transplant.
- Visual Function: Assess visual acuity using OKT and electrophysiological recordings.
- Immune Activation: Measure serum cytokine levels (e.g., IFN-γ, TNF-α) post-surgery.
- Step 4: Endpoint Analysis. At study endpoint, perform immunohistochemistry on retinal sections to evaluate immune cell infiltration (e.g., with microglia/macrophage markers like IBA1) and assess donor photoreceptor integration into the host retina.
3. Expected Outcomes & Analysis Effective immunosuppression will result in significantly reduced immune cell infiltration into the graft, improved long-term graft survival, and significant visual improvement in OKT compared to non-immunosuppressed controls. This model helps characterize the critical immune populations involved in rejection and validates the efficacy of the chosen drug regimen [21].
Signaling Pathways and Experimental Workflows
T-cell Activation and Immunosuppression Pathways
This diagram illustrates the mechanism of action of key immunosuppressant drugs on the T-cell activation pathway.
Pre-clinical In Vivo Immunosuppression Efficacy Workflow
This diagram outlines the logical workflow for evaluating an immunosuppression regimen in an immunocompetent animal model of retinal degeneration.
The Scientist's Toolkit: Research Reagent Solutions
The table below details key reagents and their functions for implementing the experimental protocols discussed [25] [21] [26].
| Research Reagent / Tool | Function / Application | Experimental Context |
|---|---|---|
| Anti-CD117 Antibody (Briquilimab) | Targets and depletes host hematopoietic stem cells via the CD117 (c-Kit) receptor. | Replaces toxic chemotherapy/radiation in conditioning regimens for stem cell transplantation [25]. |
| Tacrolimus (FK-506) | Calcineruin inhibitor; blocks T-cell activation by suppressing IL-2 transcription. | Core component of systemic immunosuppression regimens in neural and retinal cell therapy trials [20] [21]. |
| Mycophenolate Mofetil (MMF) | Inhibitor of inosine monophosphate dehydrogenase (IMPDH); blocks lymphocyte proliferation. | Used in combination with Tacrolimus for multi-pathway immunosuppression [20] [21]. |
| Sirolimus (Rapamycin) | mTOR inhibitor; suppresses T-cell activation and proliferation. | Investigated in enhanced regimens for AAV gene therapy to mitigate liver toxicity [22] [23]. |
| Alpha/Beta T-Cell Depletion Kit | Immunomagnetic selection to remove αβ T-cells from a donor graft. | Reduces the risk of Graft-versus-Host Disease (GvHD) in haploidentical transplants, expanding donor pools [25]. |
| Engineered CAR-Treg Cells | Regulatory T-cells engineered with a Chimeric Antigen Receptor (CAR) to target a specific tag (e.g., EGFRt) on co-transplanted cells. | Creates localized immune tolerance, protecting therapeutic cells from rejection without broad immunosuppression [26]. |
| hESC-Derived Retinal Organoids | 3D in vitro model containing laminated retinal layers and photoreceptors. | Used for pre-clinical safety testing of immunosuppressants and as a source for transplantation studies [21]. |
Technical Support Center
Troubleshooting Guides & FAQs
FAQ: General Concepts
Q1: Why target both CTLA4-Ig and PD-L1 for creating immune-privileged stem cells?
- A: These molecules target complementary pathways in T-cell activation. CTLA4-Ig acts early, blocking the CD28-B7 costimulatory signal required for naive T-cell activation. PD-L1 acts later, delivering an inhibitory signal to already-activated T-cells via PD-1, promoting tolerance and exhaustion. Combining them provides a multi-layered defense against immune rejection.
Q2: What is the primary advantage of a "knock-in" strategy over viral transduction?
- A: A knock-in strategy, using CRISPR/Cas9 for example, allows for targeted integration of the transgenes into a defined, active genomic "safe harbor" locus (e.g., AAVS1). This ensures consistent, stable, and physiological expression of CTLA4-Ig and PD-L1, avoiding the risks of insertional mutagenesis and transgene silencing associated with random viral integration.
Troubleshooting Guide: Molecular Cloning & Vector Design
Q1: Our donor vector for CRISPR/Cas9 knock-in is yielding very low homologous recombination (HR) efficiency. What could be the issue?
- A: Low HR efficiency is common. Please check the following:
- Homology Arm Length: Ensure arms are sufficiently long (typically 800-1000 bp each).
- Donor Vector Concentration: Titrate the donor plasmid concentration; too high can be toxic, too low reduces HR events.
- sgRNA Efficiency: Validate that your sgRNA has high cutting efficiency using a T7E1 assay or next-generation sequencing.
- Cell Health: Use low-passage, healthy stem cells. Pre-treating cells with a small molecule like Alt-R HDR Enhancer can boost HR rates.
- A: Low HR efficiency is common. Please check the following:
Q2: We are concerned about off-target effects of CRISPR/Cas9. How can we mitigate this?
- A: Employ the following strategies:
- Use a high-fidelity Cas9 variant (e.g., SpCas9-HF1, eSpCas9).
- Design and validate multiple sgRNAs with high on-target scores using tools like CRISPRscan or ChopChop.
- Perform a computational prediction of off-target sites and sequence the top candidate loci in your final cell lines to confirm specificity.
- A: Employ the following strategies:
Troubleshooting Guide: Cell Culture & Selection
Q1: After transfection and selection, we see no surviving colonies. What steps should we take?
- A: This indicates potential cytotoxicity.
- Check Transfection Efficiency: Use a fluorescent reporter plasmid to determine your baseline transfection efficiency. If low, optimize your delivery method (electroporation parameters, lipofection reagent).
- Titrate Selection Antibiotic: Perform a kill curve assay on wild-type cells to determine the minimal effective concentration and optimal timing for antibiotic application post-transfection.
- Confirm Cas9 Activity: High levels of Cas9-induced double-strand breaks can be toxic. Consider using a lower concentration of Cas9 plasmid/RNP.
- A: This indicates potential cytotoxicity.
Q2: Our cloned stem cell colonies show heterogeneous transgene expression. How do we address this?
- A: Heterogeneity suggests variable integration or silencing.
- Single-Cell Cloning: Isolate single cells from a mixed population and expand them into clonal lines.
- Genomic Validation: Perform PCR and Southern blotting on clonal lines to confirm precise, mono-allelic or bi-allelic integration.
- Expression Analysis: Use flow cytometry (for surface PD-L1) and ELISA (for secreted CTLA4-Ig) to quantify expression levels across different clones and select high expressors.
- A: Heterogeneity suggests variable integration or silencing.
Experimental Protocols
Protocol 1: CRISPR/Cas9-Mediated Knock-in into the AAVS1 Safe Harbor Locus
- sgRNA Design: Design an sgRNA targeting the human AAVS1 locus (PPP1R12C gene).
- Donor Vector Construction: Clone your expression cassettes (a constitutive promoter driving PD-L1 and a separate cassette for CTLA4-Ig, linked by a P2A self-cleaving peptide if desired) into a donor plasmid flanked by AAVS1-specific left and right homology arms (~800 bp each). Include a puromycin resistance gene flanked by loxP sites for selection and subsequent removal.
- Stem Cell Transfection: Co-transfect human pluripotent stem cells (hPSCs) with the donor vector and a plasmid encoding Cas9 and the AAVS1 sgRNA using a high-efficiency method like nucleofection.
- Selection and Expansion: 48 hours post-transfection, apply puromycin (e.g., 0.5-1.0 µg/mL) for 7-10 days. Manually pick and expand resistant colonies.
- Cre-Recombinase Excision: Transfer the puromycin-resistant clones with a Cre-recombinase plasmid to excise the selection cassette, leaving behind a single loxP site.
- Validation: Confirm correct integration via genomic PCR, Southern blot, and Sanger sequencing of the junction sites.
Protocol 2: In Vitro T-Cell Suppression Assay (Mixed Lymphocyte Reaction - MLR)
- Prepare Effector Cells: Isolate peripheral blood mononuclear cells (PBMCs) from a mismatched donor and label with CFSE.
- Prepare Target Cells: Differentiate your engineered and wild-type hPSCs into the desired cell type (e.g., cardiomyocytes, beta-cells). Irradiate them to prevent proliferation.
- Co-culture: Co-culture CFSE-labeled PBMCs (effectors) with the irradiated, differentiated cells (targets) at various ratios (e.g., 10:1, 5:1, 1:1) in a 96-well U-bottom plate for 5-7 days.
- Analysis: Harvest cells and analyze T-cell proliferation by flow cytometry, measuring CFSE dilution in the CD3+ T-cell population. Include wells with PBMCs alone (negative control) and PBMCs stimulated with anti-CD3/CD28 beads (positive control).
Data Presentation
Table 1: Comparison of Key Immune Evasion Transgenes
| Transgene | Mechanism of Action | Expression Format | Key Interacting Partner |
|---|---|---|---|
| CTLA4-Ig | Soluble decoy receptor that blocks CD28 costimulation by binding CD80/CD86 on Antigen Presenting Cells (APCs). | Secreted | CD80 (B7-1), CD86 (B7-2) |
| PD-L1 | Membrane-bound ligand that engages PD-1 on activated T-cells, delivering an inhibitory signal. | Surface Membrane | PD-1 (Programmed Death-1) |
Table 2: Expected Outcomes from In Vitro T-Cell Suppression Assay
| Cell Type | Co-culture with Allogeneic PBMCs | Expected CFSE Proliferation Profile | Interpretation |
|---|---|---|---|
| Wild-Type Differentiated Cells | Yes | High % of CFSE-low proliferating T-cells | Strong immune rejection |
| CTLA4-Ig+PD-L1 Knock-in Differentiated Cells | Yes | Low % of CFSE-low proliferating T-cells; high % of CFSE-high non-proliferating T-cells | Significant immune evasion |
| Positive Control (anti-CD3/CD28) | N/A | Very high % of CFSE-low proliferating T-cells | Maximum T-cell activation |
| Negative Control (PBMCs only) | N/A | Very high % of CFSE-high non-proliferating T-cells | Baseline, no stimulation |
Diagrams
Diagram 1: T-cell Inhibition Pathways
Diagram 2: CRISPR Knock-in Workflow
The Scientist's Toolkit
| Research Reagent | Function & Application |
|---|---|
| AAVS1 Safe Harbor Targeting Kit | Pre-validated sgRNA and homology arm templates for reliable, safe integration. |
| High-Fidelity Cas9 Nuclease | Reduces off-target editing while maintaining high on-target activity. |
| Alt-R HDR Enhancer | Small molecule that improves Homology-Directed Repair (HDR) efficiency. |
| Recombinant Human CTLA4-Ig Protein | Positive control for functional assays (e.g., ELISA, T-cell suppression). |
| Anti-PD-L1 Antibody (for flow cytometry) | Validates surface expression of the knocked-in PD-L1 transgene. |
| LIVE/DEAD Fixable Viability Dyes | Distinguishes live from dead cells in flow cytometry-based co-culture assays. |
| CFSE Cell Division Tracker | Fluorescent dye to monitor T-cell proliferation in suppression assays. |
FAQs and Troubleshooting Guide
This section addresses common technical challenges in the development and analysis of CHAR-Tregs and CAR-MSCs, providing evidence-based solutions.
Q1: My engineered CAR Tregs are losing their FoxP3 expression and suppressive function in long-term culture. What could be the cause and how can I prevent this?
A: Loss of FoxP3 expression and subsequent instability in CAR Tregs is a documented challenge. This can be caused by several factors:
- Cytokine Environment: Exposure to inflammatory cytokines like IL-6 can promote conversion to pro-inflammatory Th17-like cells [29].
- Costimulatory Domain Selection: The choice of intracellular signaling domains significantly impacts stability. CARs containing a CD28 domain have demonstrated superior stability and function in GvHD models compared to those with 4-1BB, which may exhibit decreased lineage stability [29].
- Mitigation Strategy: To enhance stability, consider transient exposure to mTOR inhibitors (e.g., rapamycin) and Vitamin C, which have been shown to improve the in vivo function and stability of 4-1BB-based CAR Tregs [29].
Q2: What are the primary mechanisms through which CAR-MSCs mediate immunosuppression in the tumor microenvironment?
A: CAR-MSCs leverage both their engineered specificity and innate immunomodulatory capacities. Key mechanisms include:
- Precision Targeting: The CAR directs MSC homing to specific antigen-expressing cells within the tumor microenvironment (TME) [30].
- Secreted Factors: They can be engineered to secrete high levels of immunoregulatory factors like TRAIL (TNF-related apoptosis-inducing ligand) to induce apoptosis in target cells, or produce bispecific antibodies to engage immune effector cells [30].
- Immune Cell Modulation: CAR-MSCs can promote the induction of regulatory T cells (Tregs), thereby amplifying local immunosuppression [30].
- Bystander Suppression: Through their secretome, they can suppress immune responses in a non-antigen-specific manner within the local microenvironment [31].
Q3: How can I effectively monitor the persistence and in vivo functionality of administered CAR Tregs or CAR-MSCs?
A: A multi-parameter approach is recommended for accurate assessment.
- Phenotypic Tracking: For CAR Tregs, monitor canonical markers (CD4, CD25, FoxP3) alongside the CAR transgene to confirm stable identity [29].
- Functional Assays: Utilize multiplex immunoassays (e.g., Luminex technology) to quantify the profile of secreted cytokines in serum or tissue culture supernatant. This allows you to detect increases in suppressive cytokines like IL-10 and TGF-β, indicative of functional activity [32].
- Imaging and Biodistribution: For pre-clinical models, in vivo imaging can track cell homing, while PCR-based methods on explanted tissues can quantify cellular persistence [33].
Q4: What strategies can be employed to generate "off-the-shelf" hypoimmunogenic cell therapies to avoid host immune rejection?
A: Creating universal donor cells involves engineering to evade both T-cell and NK-cell surveillance. Key gene edits include:
- Abrogating T-cell Recognition: Knock out Beta-2 microglobulin (B2M) to prevent surface expression of HLA class I molecules [33].
- Evading NK-cell Mediated Lysis: To counter the "missing self" response from NK cells due to low HLA, overexpress CD47 (a "don't eat me" signal) and non-classical HLA molecules like HLA-G or HLA-E, which inhibit NK cell activity [33].
- Expressing Local Immunosuppressants: Engineer cells to overexpress surface immunomodulators like PD-L1 (Programmed Death-Ligand 1), which engages PD-1 on activated T cells to induce tolerance [33].
Key Experimental Protocols and Data
Protocol: In Vitro Suppression Assay for CAR Tregs
This protocol is used to quantify the antigen-specific suppressive function of engineered CAR Tregs.
- Prepare Responder T Cells (Tresps): Isolate CD4+ CD25- T cells from human PBMCs and label them with a cell division tracker like CFSE.
- Stimulate Tresps: Co-culture the labeled Tresps with anti-CD3/CD28 activation beads or antigen-presenting cells (APCs).
- Set Up Co-culture: Add your engineered CAR Tregs to the stimulated Tresps at various ratios (e.g., 1:1, 1:2, 1:4 Treg:Tresp). Include controls with no Tregs (maximal proliferation) and no stimulation (background).
- Provide Antigen Specificity: Ensure the co-culture contains the target antigen recognized by the CAR (e.g., a peptide or expressed on APCs) to activate the CAR Tregs specifically.
- Incubate and Analyze: After 3-5 days, analyze Tresp proliferation by flow cytometry via CFSE dilution. The suppressive capacity is calculated as the percentage reduction in proliferation compared to the maximal proliferation control [29].
Protocol: Assessing CAR-MSC Mediated Treg Induction
This protocol evaluates the ability of CAR-MSCs to promote the differentiation of regulatory T cells.
- Co-culture Setup: Isolate naive CD4+ T cells from human PBMCs. Co-culture them with your CAR-MSCs (or control MSCs) in the presence of the target antigen and T-cell activation stimuli (e.g., soluble anti-CD3/CD28).
- Polarizing Conditions: Include TGF-β in the medium to favor Treg differentiation.
- Analysis by Flow Cytometry: After 5-7 days, harvest the T cells and stain for Treg markers, primarily CD4, CD25, and the transcription factor FoxP3.
- Functional Validation: To confirm functionality, the induced Tregs can be isolated and tested in a standard in vitro suppression assay as described above [30].
The tables below consolidate key quantitative findings from the literature on CAR Tregs and CAR-MSCs.
Table 1: Comparison of CAR Treg Costimulatory Domains and Functional Outcomes
| CAR Generation | Costimulatory Domain(s) | Model System | Key Functional Outcome | Reference |
|---|---|---|---|---|
| Second Generation | CD28 | Human, GvHD | Significant prevention of GvHD; enhanced suppressive efficacy. | [29] |
| Second Generation | 4-1BB | Human, GvHD | Prevention of GvHD, but with decreased lineage stability. | [29] |
| Second Generation | CD28 | Human, Skin Allograft | Suppressed HLA-mismatched immune responses; preserved human skin grafts for 100 days. | [29] |
| Second Generation | CD28 | Murine, Islet Allograft | Prolonged survival of pancreatic islet allografts. | [29] |
Table 2: Documented Clinical and Preclinical Efficacy of MSCs and CAR-MSCs
| Cell Type | Disease / Model | Key Efficacy Metric | Outcome / Mechanism | Reference |
|---|---|---|---|---|
| Third-party MSCs | Steroid-resistant aGVHD (Clinical trial, n=47) | Treatment Response Rate | 75.0% response in MSC group vs. 42.1% in control. | [31] |
| Third-party MSCs | Haploidentical HSCT (Clinical, n=50) | Hematopoietic Reconstitution | Rapid, stable engraftment; median neutrophil (12d) and platelet (15d) recovery. | [31] |
| CAR-MSCs | Glioblastoma, Ewing's Sarcoma (Preclinical) | Tumor Suppression | Mediated via TRAIL secretion and induction of local Tregs. | [30] |
| MSC + IL-37b gene | DSS-induced Colitis (Murine) | Therapeutic Efficacy | Gene-modified MSCs alleviated colitis by inducing regulatory T cells. | [34] |
Signaling Pathway and Workflow Visualizations
CAR Treg Signaling and Stability Pathway
This diagram illustrates the intracellular signaling within a CAR Treg and the factors influencing its stability.
Title: CAR Treg Signaling and Stability Regulation
CAR-MSC Immunomodulation Mechanism
This diagram outlines the multi-modal mechanisms by which CAR-MSCs exert targeted immunosuppression.
Title: CAR-MSC Mechanisms of Targeted Immunomodulation
Workflow for Generating Hypoimmunogenic "Off-the-Shelf" Cells
This flowchart details the genetic engineering steps required to create universal donor cells resistant to immune rejection.
Title: Engineering Workflow for Hypoimmunogenic Cells
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and tools essential for research and development in engineered cell-based immunomodulation.
Table 3: Essential Reagents for CHAR-Treg and CAR-MSC Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Luminex Multiplex Immunoassays | Simultaneously quantify up to 50 soluble analytes (e.g., cytokines, chemokines) from a single small sample volume [32]. | Profiling suppressive cytokine secretion (IL-10, TGF-β) by CAR Tregs or CAR-MSCs in culture supernatant. |
| Lentiviral / Retroviral Vectors | Efficient and stable gene delivery for the expression of CAR constructs or gene-editing tools in primary immune cells and stem cells [29]. | Engineering CAR Tregs with antigen-specific receptors or creating hypoimmunogenic MSCs via gene overexpression. |
| CRISPR-Cas9 System | Precision gene-editing technology for targeted knock-out (e.g., B2M) or knock-in (e.g., CAR into TCR locus) [29]. | Generating universal donor cells by disrupting HLA genes or creating stable, potent CAR Tregs. |
| Anti-human CD4, CD25, FoxP3 Antibodies | Flow cytometry antibodies for the identification, isolation, and purity check of Treg populations by surface and intracellular staining [29]. | Characterizing the phenotype of engineered CAR Tregs before and after in vitro or in vivo experiments. |
| Recombinant Immunomodulatory Proteins (e.g., IL-10, TGF-β) | Recombinant cytokines used to polarize T cells towards a regulatory phenotype or to test the functionality of engineered cells in suppression assays [29]. | Differentiating naive T cells into iTregs for subsequent CAR engineering or as positive controls in functional assays. |
| Treg Isolation Kits (e.g., CD4+CD25+) | Magnetic or fluorescence-activated cell sorting (FACS) kits for the high-purity isolation of Tregs from PBMCs as a starting population for engineering [29]. | Obtaining a pure population of primary human Tregs for CAR transduction to ensure a well-defined cellular product. |
Frequently Asked Questions (FAQs)
Mixed Chimerism and Tolerance Induction
Q1: What is the fundamental difference between graft acceptance and true transplant tolerance? Graft acceptance is often a transient state of immune nonresponsiveness, commonly achieved by immunosuppression and can be reversible. In contrast, true transplant tolerance is an active immunological process of mutual education between two immune systems to accept donor antigenic makeups, requiring either modulation of central selection or institution of indefinite peripheral suppression. It is characterized by specific unresponsiveness to donor alloantigens without ongoing immunosuppressive treatment [35].
Q2: Why is mixed chimerism preferred over complete chimerism for tolerance induction in solid organ transplantation? Mixed chimerism (coexistence of donor and host immune cells) induces true immune tolerance through central and peripheral mechanisms, with minimal risk of graft-versus-host disease (GVHD). Complete chimerism (full replacement of recipient hematopoiesis with donor cells), typically requiring myeloablative conditioning, carries significant risks including GVHD, infections, and is considered overly toxic for organ transplant recipients without underlying malignancy [36] [37].
Q3: Is stable, long-term mixed chimerism always necessary for sustained organ graft tolerance? No. Studies in large animal models and some clinical cases demonstrate that transient mixed chimerism can be sufficient for long-term graft acceptance. In MHC-mismatched transplantation in non-human primates, loss of detectable chimerism after several weeks did not preclude maintained renal allograft function without immunosuppression, suggesting that a limited period of chimerism may adequately "reset" the immune system [36].
HLA Matching and Stem Cell Banking
Q4: What are the current standardized HLA matching recommendations for different donor types? The Blood and Marrow Transplant Clinical Trials Network (BMT CTN) has established evidence-based guidelines for donor HLA assessment [38]:
Table: Standardized HLA Matching Recommendations for Allogeneic Transplantation
| Donor Type | Minimum HLA Matching Requirement | Key Loci Assessed |
|---|---|---|
| Matched Sibling | 6/6 match | HLA-A, -B (intermediate/high resolution), -DRB1 (high resolution) |
| 1 Antigen Mismatched Related | 7/8 match | HLA-A, -B, -C (intermediate/high resolution), -DRB1 (high resolution) |
| Haploidentical Related | ≥4/8 match | HLA-A, -B, -C (intermediate/high resolution), -DRB1 (high resolution) |
| Adult Unrelated Donor | 8/8 match preferred | HLA-A, -B, -C, -DRB1 (all high resolution) |
| Umbilical Cord Blood | ≥4/6 match | HLA-A, -B (intermediate resolution), -DRB1 (high resolution) |
Q5: What are the critical quality control checkpoints when establishing a stem cell bank for clinical applications? The International Society for Stem Cell Research (ISSCR) recommends a two-tiered banking system with rigorous characterization [39]:
Table: Characterization Testing for Stem Cell Banks
| Characteristic | Master Cell Bank | Working Cell Bank |
|---|---|---|
| Post-thaw viability | ||
| Authentication (donor match) | ||
| Sterility (mycoplasma, adventitious agents) | ||
| Genomic stability | ||
| Gene/marker expression (undifferentiated status) | ||
| Functional pluripotency |
Technical and Translational Challenges
Q6: Why have tolerance strategies successful in murine models been difficult to translate to humans? Key challenges include the compartment of memory T cells in humans generated through lifelong pathogen exposure, which are largely absent in specific pathogen-free laboratory mice. These memory T cells, including those generated via heterologous immunity, confer significant resistance to tolerance induction. Additionally, the lack of universally validated biomarkers of tolerance precludes safe, personalized withdrawal of immunosuppression in clinical practice [37].
Q7: What role do regulatory T cells (Tregs) play in maintaining mixed chimerism and graft tolerance? Tregs are critical for sustaining mixed chimerism and preventing graft rejection through multiple mechanisms: suppressing alloreactive effector T cells, promoting functional inactivation of reactive T cells (anergy), and facilitating peripheral tolerance. In mixed chimerism models, Tregs are necessary for sustained chimerism and exhibit allo-antigen specific regulation [40] [18].
Troubleshooting Guides
Problem 1: Failure to Establish Stable Mixed Chimerism
Potential Causes and Solutions:
Insufficient conditioning: Residual host immunity may reject donor hematopoietic cells.
Inadequate donor cell dose: Low hematopoietic stem cell numbers may not engraft effectively.
- Solution: Ensure minimum CD34+ cell dose of 2-5×10^6/kg recipient weight. For cord blood, aim for total nucleated cell dose ≥3×10^7/kg [38].
Immunological barriers: Pre-existing donor-specific antibodies or host NK cell activity.
- Solution: Screen for donor-specific antibodies pre-transplant. Consider incorporating CD117 antibody-based conditioning to enhance engraftment, as demonstrated in recent diabetes models [41].
Problem 2: Rejection of Stem Cell-Derived Tissues Despite HLA Matching
Potential Causes and Solutions:
Indirect allorecognition: Recipient antigen-presenting cells process and present donor peptides.
Innate immune activation: NK cell-mediated killing due to "missing self" recognition.
- Solution: Engineer stem cells to express NK inhibitory ligands (HLA-E, CD47) or consider pharmacological mitigation of instant blood-mediated inflammatory reaction (IBMIR) [42].
Autoimmune recurrence: Particularly relevant in type 1 diabetes models where autoimmunity targets newly transplanted islets.
Problem 3: Instability of Stem Cell Bank Quality
Potential Causes and Solutions:
Genetic drift during prolonged culture:
- Solution: Establish early-passage Master Cell Banks. Limit working cell bank passages (recommend thawing fresh vials every 10-20 passages). Implement regular karyotyping and genomic stability assessment [39].
Inconsistent differentiation capacity:
- Solution: Perform rigorous pluripotency validation (teratoma formation, pluripotency marker expression) on master cell bank. Monitor differentiation efficiency as quality indicator for working cell banks [39].
Experimental Protocols
Protocol 1: Induction of Mixed Chimerism for Islet Transplantation Tolerance (Murine Model)
Based on Stanford University approach for curing autoimmune diabetes in mice [41]
Pre-conditioning Regimen (initiated day -4):
- Administer CD117 antibody (to target c-Kit on hematopoietic stem cells)
- Add an immunomodulatory drug for autoimmune protection (e.g., drug used for autoimmune diseases)
- Apply low-dose radiation (0.5-1.0 Gy) to create niche space
Cell Transplantation (day 0):
- Harvest donor bone marrow: Flush femurs and tibias from donor mice, isolate mononuclear cells
- Prepare pancreatic islets: Collagenase digestion and density gradient purification
- Combine transplants: Infuse 1-2×10^7 bone marrow cells with 500-1000 islet equivalents via intraportal or kidney subcapsular route
Post-transplantation Monitoring:
- Track chimerism: Monthly flow cytometry of peripheral blood for donor vs. host HLA markers
- Assess graft function: Blood glucose measurements, glucose tolerance tests
- Evaluate tolerance: In vitro T cell response assays to donor vs. third-party antigens
Protocol 2: Two-Tiered Stem Cell Banking According to ISSCR Standards
Master Cell Bank (MCB) Establishment:
- Cell expansion: Expand cells from earliest possible passage in culture conditions free of animal components
- Cell pooling: Pool cells from multiple vessels to ensure homogeneity
- Cryopreservation: Aliquot into 10-15 vials using controlled-rate freezing, store in vapor phase liquid nitrogen
- Quality control: Thaw one representative vial for comprehensive characterization:
- Sterility testing (bacteria, fungi, mycoplasma)
- Viability assessment (post-thaw recovery >70%)
- Identity confirmation (STR profiling, HLA typing)
- Pluripotency verification (flow cytometry for markers, teratoma assay)
- Genomic stability (karyotyping, SNP microarray)
Working Cell Bank (WCB) Generation:
- Thaw MCB vial: Expand cells for limited passages (recommended <10 passages from MCB)
- Repeat pooling: Ensure homogeneous population
- Large-scale cryopreservation: Create 50-100 vials based on projected needs
- Reduced QC testing: Assess post-thaw viability, sterility, and identity confirmation only
Visualization: Mixed Chimerism Induction Workflow
Diagram Title: Mixed Chimerism-Mediated Tolerance Induction Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Tolerance Induction Research
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Conditioning Agents | CD117 (c-Kit) antibodies, low-dose radiation, anti-thymocyte globulin (ATG) | Create niche space for donor cell engraftment with reduced toxicity |
| Cell Isolation | CD34+ selection kits, Pan T cell isolation kits, HLA typing antibodies | Purify hematopoietic stem cells, deplete alloreactive T cells |
| Tolerance Modulation | Treg expansion kits, IL-2 pathway modulators, costimulation blockers (abatacept) | Expand regulatory populations, block T cell activation pathways |
| Monitoring Tools | HLA typing panels, chimerism quantification standards, donor-specific antibody assays | Track engraftment, detect rejection biomarkers |
| Stem Cell Banking | Defined culture media, cryopreservation solutions, mycoplasma detection kits | Maintain pluripotency, ensure bank sterility and genetic stability |
Key Experimental Considerations
Critical Parameters for Success:
Timing of tolerance induction: For solid organ transplantation, establishing chimerism before or simultaneously with organ transplant yields superior outcomes compared to post-transplant induction [36].
HLA matching level: While perfect matching is ideal, strategic selection of permissible mismatches (particularly at HLA-DP and HLA-DQ loci) can expand donor pools without significantly increasing rejection risk [38].
Autoimmune considerations: In autoimmune settings like type 1 diabetes, tolerance strategies must address both alloreactivity and autoreactivity, requiring more comprehensive immune resetting [41] [40].
Biomarker monitoring: Implement regular assessment of chimerism levels, Treg frequencies, and donor-specific antibodies as early indicators of protocol success or failure.
The field continues to evolve with emerging strategies including engineered Tregs, genetic modification of stem cells to reduce immunogenicity, and increasingly sophisticated non-myeloablative conditioning regimens bringing the goal of routine transplantation tolerance closer to clinical reality [42] [18] [37].
Navigating Clinical Hurdles: Troubleshooting Safety, Efficacy, and Practical Challenges
Technical Support Center: Troubleshooting Teratoma Risk
Frequently Asked Questions (FAQs)
What is the minimum number of undifferentiated cells required to form a teratoma? Evidence from transplantation studies in immunodeficient mice indicates that as few as 245 undifferentiated human embryonic stem cells (hESCs) are sufficient to form a teratoma [43]. Another study confirmed that the injection of only a few hundred human pluripotent cells can result in teratoma formation in immunocompromised mice [44].
Which immune cells are most critical for preventing teratoma formation in an immune-competent host? Natural Killer (NK) cells play a critical role. Research using humanized mouse models showed that the presence of NK cells alone was sufficient to prevent teratoma formation from autologous human induced pluripotent stem cells (hiPSCs). Conversely, teratomas formed in mice reconstituted with autologous peripheral blood mononuclear cells (PBMCs) that had been depleted of NK cells [44].
Can established teratomas be targeted and eliminated by the immune system? Yes, but the effectiveness depends on the immune cell type and donor matching. Studies show that established teratomas are not efficiently targeted by NK cells. However, they can be effectively rejected by allogeneic T cells, though not by autologous T cells [44].
Are there targeted therapies to eliminate residual undifferentiated cells? Yes, monoclonal antibodies (mAbs) offer a promising strategy. The chimerised monoclonal antibody ch2448, which targets Annexin A2 (an oncofetal antigen), has been shown to kill human embryonic stem cells (hESCs) in vivo. It acts via Antibody-Dependent Cell-mediated Cytotoxicity (ADCC) and as an Antibody-Drug Conjugate (ADC), thereby preventing or delaying teratoma formation [43].
Troubleshooting Guides
Problem: Teratoma formation after transplantation of differentiated cell products.
- Potential Cause: The final cell product contains residual undifferentiated pluripotent stem cells (PSCs) that escaped purification.
- Solutions:
- Implement a cell purification step: Use fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) with antibodies specific to undifferentiated cells (e.g., TRA-1-60, SSEA-4, or mAb 2448) to remove them from the population [43].
- Pre-treatment with small molecules: Incubate cells with small molecule inhibitors, cardiac glycosides, or ceramide analogues that are selectively toxic to undifferentiated PSCs prior to transplantation [43].
- Employ a safety switch: Use a monoclonal antibody like ch2448 as a post-transplant surveillance tool to eliminate any residual undifferentiated cells that may cause teratomas in vivo [43].
Problem: Inconsistent results in teratoma formation assays using humanized mouse models.
- Potential Cause: The specific human immune cell populations engrafted in the mouse model are insufficient or lack functionality.
- Solutions:
- Verify immune cell reconstitution: Use flow cytometry to routinely monitor the levels and functionality of key human immune cells (e.g., CD45+ leukocytes, CD3+ T cells, CD56+ NK cells) in the peripheral blood of humanized mice [44].
- Select the appropriate model: Be aware that different humanized mouse models have varying immune capabilities. For example, Hu-BLT mice, which develop competent T cells but may lack functional NK cells, might not prevent teratoma initiation, whereas models reconstituted with PBMCs (containing NK cells) can [44].
- Confirm cell characterization: Always validate the pluripotency of your stem cell line (via markers like OCT4, SOX2, SSEA-4, TRA-1-60) and its lack of differentiation before injection to ensure consistent tumorigenic potential [44].
Experimental Protocols for Key Assays
Protocol 1: In Vivo Assessment of Teratoma Risk in Humanized Mice
- Objective: To evaluate the capacity of the human immune system to prevent teratoma formation by hiPSCs.
- Materials: NOD/SCID/IL2Rγnull (NSG) mice, hiPSCs, human fetal tissues (for Hu-BLT) or human PBMCs (for Hu-AT) [44].
- Methods:
- Generate Humanized Mice:
- Hu-BLT Model: Irradiate NSG mice (2 Gy) and implant with human fetal thymus tissue under the renal capsule. Intravenously inject autologous CD34+ hematopoietic stem cells (e.g., 1 × 10^7 cells) isolated from fetal liver [44].
- Hu-AT Model: Intravenously inject adult NSG mice with freshly isolated human PBMCs (e.g., 1 × 10^7 cells). For NK cell studies, inject with purified NK cells (e.g., 5–15 × 10^5 cells) or NK-depleted PBMCs [44].
- Monitor Engraftment: Track human immune cell (e.g., CD45+, CD3+, CD19+) reconstitution in peripheral blood via flow cytometry for up to 13 weeks [44].
- Teratoma Assay: Harvest hiPSCs into small clumps. Resuspend ~1 × 10^6 cells in a PBS/Geltrex mixture (e.g., 50%) and inject under the renal capsule or subcutaneously into humanized mice [44].
- Analysis: Monitor mice for teratoma formation over several weeks. Excise and analyze suspected tumors histologically for the presence of tissues from all three germ layers [44].
- Generate Humanized Mice:
Protocol 2: Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC) Assay Against hPSCs
- Objective: To test the efficacy of a monoclonal antibody (e.g., ch2448) in directing immune cells to kill undifferentiated hPSCs.
- Materials: hPSCs, effector cells (e.g., human PBMCs or NK cells), target mAb, ADCC Reporter Bioassay kit [43].
- Methods:
- Prepare Cells: Harvest hPSCs using a gentle dissociation reagent to maintain cell clumps. Wash cells with PBS [43].
- Coculture: Add hPSCs to a 96-well plate. Co-culture hPSCs with effector cells at a specific ratio (e.g., 1:2) in the presence of the target mAb [43].
- Measure Cytotoxicity: Use a bioassay (e.g., Promega ADCC Reporter Bioassay) to quantify the cytotoxicity, which is based on the activation of a signaling pathway in the effector cells upon successful antigen-antibody engagement [43].
- Analysis: Measure luminescence or fluorescence to determine the level of ADCC activity.
Table 1: Critical Thresholds in Teratoma Research
| Parameter | Quantitative Value | Experimental Context | Source |
|---|---|---|---|
| Minimum Teratoma-Forming Cell Number | ~245 hESCs | Sufficient to form teratomas in SCID mice | [43] |
| NK Cell Prevention | Prevents teratoma formation | Hu-AT mice reconstituted with purified NK cells (5-15 x 10^5) | [44] |
| mAb 2448 Binding Capacity | 8.3 × 10^7 molecules/hESC | Maximum binding capacity (q~m~) to HES-3 cells | [43] |
Table 2: Immune Cell Roles in Teratoma Prevention and Elimination
| Immune Cell Type | Role in Teratoma Initiation | Role Against Established Teratomas |
|---|---|---|
| Natural Killer (NK) Cells | Prevents formation in autologous setting. Critical for initial surveillance. | Not effective at targeting established teratomas. |
| Autologous T Cells | Limited data on prevention. | Not effective at rejecting established teratomas. |
| Allogeneic T Cells | Limited data on prevention. | Effective at rejecting established teratomas. |
Research Reagent Solutions
Table 3: Essential Reagents for Teratoma Mitigation Research
| Reagent | Function / Target | Specific Example |
|---|---|---|
| Anti-Annexin A2 mAb | Binds to Annexin A2 on PSCs; enables ADCC/ADC killing. | ch2448 (chimerised, human IgG1) [43] |
| NK Cell Isolation Kit | Isulates human NK cells for functional studies in vivo or in vitro. | NK-cell enrichment negative selection kit (e.g., STEMCELL #19055) [44] |
| Pluripotency Marker Antibodies | Identifies and removes residual undifferentiated cells via FACS/MACS. | Anti-SSEA-4, Anti-TRA-1-60, Anti-OCT4, Anti-SOX2 [44] |
| ADCC Reporter Bioassay | Measures the potency of mAbs to elicit NK cell-mediated killing. | Promega ADCC Reporter Bioassay [43] |
| Humanized Mouse Model | Provides an in vivo platform to study human immune responses to PSCs. | NOD/SCID/IL2Rγnull (NSG) mice, Hu-BLT, Hu-AT [44] |
Signaling Pathways and Experimental Workflows
Immune-Mediated Teratoma Prevention and Rejection Pathways
Experimental Workflow for Teratoma Risk Mitigation
FAQs: Modern Immunosuppression Strategies in Research
Q1: What are the primary strategies to minimize the toxicity of broad-spectrum immunosuppressants in cell therapy? A1: Researchers are developing several key strategies to reduce reliance on broad-spectrum immunosuppressants like calcineurin inhibitors (e.g., tacrolimus, cyclosporine). These include:
- Targeted Cellular Therapies: Engineering regulatory T-cells (Tregs) with chimeric antigen receptors (CHARs) to specifically suppress only the immune cells responsible for rejection, thereby avoiding global immunosuppression [45].
- Hypoimmunogenic Stem Cells: Using CRISPR/Cas9 gene editing to create stem cells that evade immune detection by downregulating Major Histocompatibility Complex (MHC) molecules and overexpressing immunomodulatory proteins like PD-L1 and CD47 [46].
- Calcineurin Inhibitor (CNI)-Sparing Regimens: Implementing maintenance immunosuppression protocols that use alternative drug classes (e.g., co-stimulation blockers, mTOR inhibitors) to reduce long-term CNI exposure and its associated toxicities [47].
Q2: How do engineered hypoimmunogenic stem cells function to reduce the need for drugs? A2: Hypoimmunogenic pluripotent stem cells (hPSCs) are bioengineered to create "universal donor" cell lines. They function through a dual mechanism [46]:
- Reducing Immunogenicity: CRISPR/Cas9 is used to ablate MHC class I and II molecules, the primary signals that trigger T-cell-mediated immune recognition and rejection.
- Enhancing Immune Evasion: These cells are engineered to overexpress immunomodulatory molecules such as HLA-G, PD-L1, and CD47. These proteins send "do not attack" signals to various immune cells, including T cells and macrophages, thereby promoting tolerance and reducing the need for pharmacologic immunosuppression.
Q3: What are common side effects of traditional immunosuppressants that new strategies aim to avoid? A3: Traditional regimens, often based on calcineurin inhibitors, corticosteroids, and anti-proliferative agents, are associated with a significant side effect profile that impacts patient quality of life and long-term health [48]. New strategies aim to mitigate these, which include:
- Nephrotoxicity and Hypertension: Common with tacrolimus and cyclosporine.
- Metabolic Disorders: Such as high blood sugar and elevated cholesterol/triglycerides.
- Increased Infection Risk: Due to broad suppression of the entire immune system.
- Other Specific Toxicities: Neurotoxicity (tremors, headaches), gastrointestinal issues (diarrhea), bone thinning, and increased cancer risk [48].
Q4: What is the role of extracellular vesicles (EVs) as an alternative to whole cell therapy? A4: Research indicates that extracellular vesicles (EVs) derived from mesenchymal stem cells (MSCs) offer a promising cell-free alternative. A 2025 study demonstrated that xenogeneic (human-to-mouse) EVs triggered a less vigorous humoral (antibody) response compared to whole MSCs, while still providing immunosuppressive effects. This suggests EVs may be less immunogenic and could circumvent some rejection risks associated with whole-cell transplants, potentially reducing the immunosuppressive load required [49].
Troubleshooting Guide: Common Experimental Challenges
Table: Troubleshooting Common Immunosuppression Experiments
| Challenge | Potential Cause | Solution |
|---|---|---|
| Poor Graft Survival Despite Immunosuppression | Inadequate immune evasion; strong host-vs-graft response. | Consider using hypoimmunogenic PSCs with multiple edits (e.g., MHC knockout + PD-L1 overexpression) [46]. |
| Significant Side Effects in Animal Models | High doses or narrow therapeutic index of conventional drugs (e.g., CNIs). | Transition to a CNI-sparing regimen (e.g., using belatacept or mTOR inhibitors) or test targeted therapies like CHAR-Tregs to lower drug exposure [47] [45]. |
| Inconsistent Efficacy of Engineered Cells | Low persistence or unstable phenotype of cellular product. | Optimize the engineering protocol and include a "suicide gene" system in the design for safety. Use precise gene editing tools (CRISPR/Cas9) to ensure stable genetic modifications [46]. |
| Unexpected Immune Activation | Recognition of non-MHC antigens or immunogenic components in the cell product. | Analyze the immune response in detail (e.g., T-cell assays, antibody production). Purity the cell product or use EVs, which show lower immunogenicity than their parent MSCs [49]. |
Research Reagent Solutions
Table: Essential Reagents for Advanced Immunosuppression Research
| Reagent / Tool | Function in Research | Example Use Case |
|---|---|---|
| CRISPR/Cas9 System | Precision gene editing to create immune-evasive cell lines. | Knocking out B2M (for MHC-I ablation) in pluripotent stem cells to generate universal donor cells [46]. |
| CHAR (Chimeric HLA Antibody Receptor) | Engineered receptor for targeted immunosuppression. | Creating CHAR-Tregs that specifically recognize and suppress B-cells producing anti-HLA antibodies, preventing transplant rejection [45]. |
| Immunomodulatory Proteins (e.g., HLA-G, PD-L1) | Overexpression to induce immune tolerance. | Genetically engineering stem cells to overexpress PD-L1, which engages the PD-1 receptor on T-cells to inhibit their activation [46]. |
| Mycophenolate Mofetil | Anti-proliferative immunosuppressant; inhibits lymphocyte division. | Used in combination drug regimens to prevent rejection in pre-clinical transplant models [50] [48]. |
| Belatacept | CNI-sparing agent; blocks T-cell co-stimulation. | A key drug in clinical trials for CNI-sparing regimens to protect kidney function post-transplant [47] [48]. |
Quantitative Data on Immunosuppressive Strategies
Table: Comparing Immunosuppression Strategies and Outcomes
| Strategy / Component | Key Mechanism | Potential to Reduce Side Effects | Key Risks / Challenges |
|---|---|---|---|
| Calcineurin Inhibitors (Tacrolimus) | Inhibits T-cell activation | Low (High side effect profile) | Nephrotoxicity, neurotoxicity, diabetes [48] |
| CHAR-Tregs | Suppresses specific antibody-producing B-cells | High (Targeted action) | Complex manufacturing, cell persistence [45] |
| Hypoimmunogenic PSCs | Evades immune detection via MHC knockout | High (Potentially drug-free) | Tumorigenicity, genetic instability [46] |
| Extracellular Vesicles (EVs) | Cell-free immunomodulation | Moderate (Less immunogenic than cells) | Standardization of production and dosing [49] |
| CNI-Sparing Regimens | Replaces toxic CNIs with safer drugs | High (Reduces direct CNI toxicity) | Requires careful patient selection and monitoring [47] |
Detailed Experimental Protocols
Protocol 1: Generating Hypoimmunogenic Pluripotent Stem Cells using CRISPR/Cas9
This protocol outlines the creation of PSCs that evade immune rejection, a foundational strategy for reducing overall immunosuppression [46].
Key Steps:
- Guide RNA Design: Design sgRNAs targeting genes for immune-related molecules, specifically B2M (for MHC Class I knockout) and CIITA (for MHC Class II knockout).
- CRISPR/Cas9 Transfection: Transfect pluripotent stem cells (iPSCs or ESCs) with the Cas9 enzyme and designed sgRNAs using a high-efficiency method like electroporation.
- Clonal Selection: Single-cell sort the transfected cells and allow them to expand into clonal colonies.
- Genotypic Validation: Screen clones for successful gene edits using genomic PCR and sequencing to confirm frameshift mutations or deletions in the target genes.
- Phenotypic Validation:
- Use flow cytometry to confirm the loss of MHC Class I (using an anti-HLA-A,B,C antibody) and MHC Class II surface expression.
- Perform an in vitro mixed lymphocyte reaction (MLR) co-culture to demonstrate reduced T-cell activation compared to unedited PSCs.
- Functional Characterization: Differentiate the validated hypoimmunogenic clones into the desired cell type (e.g., cardiomyocytes, beta cells) to ensure the edits do not impair differentiation capacity.
Protocol 2: Evaluating Efficacy of CHAR-Tregs in Suppressing Alloantibody Response
This protocol tests the functionality of engineered, targeted Tregs, a promising targeted cellular therapy [45].
Key Steps:
- CHAR-Treg Engineering:
- Isolate naive T-cells from a human donor.
- Transduce with a lentiviral vector encoding a chimeric receptor (CHAR) specific for a defined HLA alloantigen (e.g., HLA-A2).
- Differentiate the transduced T-cells into a stable regulatory T-cell (Treg) phenotype.
- Target Cell Preparation: Isolate B-cells from a "pre-sensitized" patient (e.g., one with high levels of anti-HLA-A2 antibodies).
- Co-culture Assay: Co-culture the CHAR-Tregs with the target B-cells at various effector-to-target ratios.
- Outcome Measurement:
- After several days, collect culture supernatants.
- Quantify the concentration of anti-HLA-A2 antibodies using a specific ELISA.
- A significant reduction in antibody titer in wells with CHAR-Tregs compared to controls indicates successful suppression.
- Flow Cytometry Analysis: Analyze co-cultured cells to assess markers of B-cell apoptosis and Treg activation.
Signaling Pathways and Experimental Workflows
For researchers and drug development professionals working in stem cell therapy, achieving high rates of cell delivery, engraftment, and functional integration remains a significant translational challenge. Low cell retention and engraftment after delivery is a key factor limiting the successful application of cell therapy, irrespective of the cell type or delivery method used [51]. This technical support center provides evidence-based troubleshooting guidance to help you optimize your experimental protocols, overcome common hurdles in stem cell viability, homing, and integration, and advance your research on immunosuppression strategies.
Quantitative Data on Cell Delivery and Engraftment
Understanding typical engraftment efficiencies and the factors that influence them is crucial for experimental design and interpretation of results. The data below summarize key quantitative findings from the literature.
Table 1: Documented Cell Engraftment Efficiencies and Fates
| Cell Type / Model | Delivery Route | Engraftment Efficiency / Cell Fate | Key Findings |
|---|---|---|---|
| Bone marrow-derived stem cells (Human, post-heart attack) [52] | Intracoronary artery | 1-2% in heart region | Majority of cells trapped in liver and spleen |
| Bone marrow-derived stem cells (Human, post-heart attack) [52] | Intravenous (IV) | Not detectable in heart region | Vast majority sequestered in liver and spleen |
| Mesenchymal Stem Cells (MSCs) [53] | Intra-arterial | Higher than IV | Avoids "first-pass" lung accumulation |
| MSCs (Systemic infusion) [52] | Intravenous (IV) | Low numbers at target site | Most cells found in liver, spleen, and lungs |
| Hematopoietic Stem Cells (HSCs) [52] | Intravenous (IV) | Rapid & Efficient to bone marrow | Cross endothelium into marrow within hours |
Table 2: Methods for Assessing Cell Engraftment: Strengths and Limitations [51]
| Method Category | Specific Techniques | Key Strengths | Major Limitations |
|---|---|---|---|
| Histological | Immunofluorescence, Reporter genes (eGFP, RFP), Quantum dots | Widely available; provides data on cell location, viability, and fate | Requires animal sacrifice; longitudinal tracking impossible; prone to artifacts (e.g., autofluorescence, phagocytosis of labels) |
| Genetic/Species-Specific | FISH (for Y-chromosome, human-specific ALU sequences), qPCR | Does not require pre-labeling; stable genomic targets | Labor-intensive; requires specific models (xeno/sex-mismatch); limited quantitation potential |
| In Vivo Imaging | Bioluminescence, Magnetic Resonance Imaging (MRI), Radionuclide imaging (PET, SPECT) | Enables longitudinal, non-invasive tracking in the same subject | Limited penetration (optical methods); radionuclide half-life; cost and complexity of equipment |
Experimental Protocols for Key Investigations
Protocol 1: Assessing Engraftment via Histology and Immunofluorescence
This protocol is adapted from methods used to track cardiosphere-derived cells (CDCs) in immunodeficient mouse hearts [51].
- Cell Labeling: Transduce your therapeutic stem cells (e.g., MSCs) with a lentiviral vector encoding a reporter gene such as eGFP to ensure stable, long-term expression. Use untransduced cells as a negative control.
- Transplantation: Administer cells into your animal model (e.g., intramyocardial injection for cardiac studies). Include a sham-injected control group.
- Tissue Harvest and Sectioning: At predetermined endpoints, euthanize animals and perfuse with PBS. Excise the target organ and fix in 4% paraformaldehyde. Embed in OCT compound and section into 5-10 µm thick slices.
- Immunostaining: Block sections with serum from the secondary antibody host. Incubate with primary antibodies against:
- The reporter (e.g., anti-GFP).
- Lineage-specific markers (e.g., Troponin I for cardiomyocytes, CD31 for endothelium).
- A nuclear stain (e.g., DAPI).
- Imaging and Analysis: Image using a confocal microscope to avoid superimposition artifacts. Quantify engrafted cells (e.g., GFP+ cells per mm² of tissue) across multiple, systematically random sections to avoid sampling bias.
Protocol 2: Optimizing MSC Homing via Genetic Modification of the SDF-1/CXCR4 Axis
This protocol outlines a strategy to enhance homing by overexpressing a key homing receptor [54].
- Genetic Modification: Transduce MSCs with a lentiviral vector carrying the CXCR4 gene. Use MSCs transduced with an empty vector as a control.
- In Vitro Validation:
- Confirm CXCR4 overexpression using flow cytometry.
- Perform a Transwell migration assay to verify enhanced chemotaxis of modified MSCs toward an SDF-1α gradient compared to controls.
- In Vivo Homing Assay:
- Induce a focal injury in your animal model (e.g., myocardial infarction, skin wound).
- Systemically administer (IV) a known number of CXCR4-overexpressing MSCs and control MSCs. Cells can be pre-labeled with a fluorescent dye or luciferase for tracking.
- Assessment:
- Longitudinal: Use in vivo bioluminescence imaging at 24, 48, and 72 hours post-injection to quantify signal intensity at the injury site.
- Endpoint: Harvest tissues at 72 hours and quantify cell presence using histology (as in Protocol 1) or quantitative PCR for a human-specific gene (in xenotransplantation models).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Stem Cell Engraftment and Homing Research
| Reagent / Material | Primary Function | Example Application |
|---|---|---|
| Lentiviral Vectors | Stable gene delivery for reporter genes (eGFP, luciferase) or homing genes (CXCR4) | Creating stably modified cell lines for long-term tracking or functional enhancement [51] |
| ROCK Inhibitor (Y-27632) | Improves cell viability and survival after passaging, thawing, and single-cell dissociation | Critical for maintaining high cell health and number during preparation for transplantation [15] |
| Matrigel / Geltrex | Basement membrane matrix providing a scaffold for cell growth and differentiation | Used for coating plates during in vitro differentiation protocols and 3D culture systems [15] |
| B-27 Supplement | Serum-free supplement optimized for the survival and growth of neuronal cells | Essential component in media for neural stem cell culture and differentiation [15] |
| Recombinant Human Vitronectin (VTN-N) | Defined, xenogeneic-free substrate for feeder-free pluripotent stem cell culture | Maintaining undifferentiated hPSCs before directed differentiation into target lineages [15] |
| SDF-1α (CXCL12) | Key chemokine ligand for the CXCR4 receptor | Used in in vitro Transwell assays to test and validate the migratory capacity of stem cells [54] |
Frequently Asked Questions (FAQs)
Q1: Our systemically delivered MSCs are not reaching the target tissue in significant numbers. What are the primary reasons for this?
The inefficient homing of non-hematopoietic cells like MSCs is a well-documented bottleneck [52]. The primary reasons include:
- Physical Trapping: After IV infusion, a significant proportion of cells get trapped in filter organs, primarily the lungs (due to size restriction), and subsequently in the liver and spleen [53] [52].
- Lack of Specific Homing Signals: The molecular "homing" process is a multi-step cascade involving tethering, activation, arrest, and transmigration. MSCs may lack sufficient levels of the required adhesion molecules (e.g., specific selectin ligands) or chemokine receptors (e.g., CXCR4) to efficiently navigate this process toward your specific target site [54].
- Inflammatory Environment: The hostile, pro-inflammatory microenvironment of the target tissue (e.g., with high levels of reactive oxygen species) can lead to significant apoptosis of the delivered cells before they can engraft.
Q2: What are the most reliable methods to quantify cell engraftment, and how do I choose?
The choice of method depends on your experimental question, resources, and need for longitudinal data.
- For initial, endpoint validation: Histology with genetic reporters (e.g., eGFP) or FISH for species-specific sequences provides spatial context and can confirm cell location and identity. However, they are semi-quantitative and require animal sacrifice [51].
- For longitudinal tracking in the same subject: In vivo imaging (e.g., bioluminescence) is ideal. It allows you to monitor the kinetics of cell arrival and persistence over days or weeks, providing powerful temporal data. The limitation is that it gives a whole-organ signal and does not show single-cell distribution [53] [51].
- For high sensitivity and quantification in tissues: Quantitative PCR (qPCR) for a species-specific or genetically introduced sequence is highly sensitive and quantitative but requires tissue homogenization, losing all spatial information [53].
A robust strategy often combines a longitudinal method (like bioluminescence) with an endpoint, spatial method (like histology) for confirmation.
Q3: We are deriving beta-cells from hPSCs for diabetes research. What strategies can we use to protect them from immune rejection without long-term immunosuppression?
This is a critical area of investigation. Strategies to evade immune rejection include:
- Encapsulation: Using semi-permeable biomaterials (e.g., alginate microspheres) to encase the stem cell-derived islets. This physically blocks immune cells and antibodies from contacting the graft while allowing for the diffusion of oxygen, nutrients, and secreted insulin [55].
- Genetic Manipulation: Genetically engineering the hPSCs to reduce their immunogenicity before differentiation. This can involve knocking out Classical HLA class I and II genes to prevent T-cell recognition, or overexpressing immunomodulatory molecules like PD-L1 [55].
- Inducing Immune Tolerance: Differentiating hPSCs into regulatory T cells (Tregs) or other tolerogenic immune cells that can be co-administered with the graft to promote local immune tolerance [56].
Q4: Our stem cell cultures show high rates of spontaneous differentiation before we can use them for experiments. How can we reduce this?
Excessive differentiation (>20%) in human pluripotent stem cell (hPSC) cultures is a common issue. Key troubleshooting steps include [16]:
- Check Media Quality: Ensure your complete culture medium is fresh (less than 2 weeks old when stored at 2-8°C).
- Manage Passaging: Remove differentiated areas manually before passaging. Ensure cell aggregates after passaging are evenly sized and do not allow colonies to overgrow.
- Minimize Stress: Avoid having culture plates out of the incubator for extended periods (>15 minutes). Optimize passaging reagent incubation times for your specific cell line.
- Optimize Density: Plate an appropriate number of cell aggregates to maintain optimal density, as both under- and over-confluency can promote differentiation.
Visualizing Key Concepts
Diagram: The Multistep MSC Homing Cascade
This diagram illustrates the sequential molecular events that mesenchymal stromal cells (MSCs) must undergo to exit circulation and home to a site of injury, a process critical for their therapeutic efficacy [54].
Diagram: Experimental Workflow for Engraftment Optimization
This workflow outlines a integrated experimental approach to test a homing-enhancement strategy and rigorously assess its impact on cell engraftment.
Technical Support Center
Troubleshooting Guide: Stem Cell Therapy Manufacturing
This guide addresses common operational challenges in the manufacturing of stem cell therapies, providing step-by-step solutions to ensure product quality and compliance.
Table 1: Troubleshooting Common Manufacturing Challenges
| Challenge | Root Cause | Solution | Preventive Action |
|---|---|---|---|
| High process variability | Non-standardized protocols; inconsistent raw materials [57] | Implement automated, closed-system bioreactors; establish raw material qualification program [58] | Create a centralized database of standardized work instructions (SOPs) accessible across all shifts [59] |
| Supply chain disruption | Reliance on single-source suppliers; trade policy uncertainty [58] | Use Agentic AI systems to identify and qualify alternative suppliers; diversify supplier base [58] | Develop a digital supply chain control tower for real-time visibility and risk monitoring [58] [60] |
| Skilled labor shortage | Retiring workforce; complex new technologies [60] [59] | Implement a "build, buy, borrow" workforce framework; use augmented reality for guided training [58] | Partner with local educational institutions for creative recruiting and create internal upskilling programs [60] |
| Data security risks | Disconnected systems; unsecured data storage [59] | Migrate to cloud-based platforms with automated security updates and AI-driven threat detection [60] | Conduct regular employee training on cybersecurity threats like phishing and implement strict access controls [60] |
| Scale-up failures | Process drift during expansion; artificial bottlenecks [59] | Use digital twins for process simulation before physical scale-up; implement real-time capacity monitoring [58] | Base scaling strategies on real-time production data and ensure process repeatability across sites [60] [59] |
Frequently Asked Questions (FAQs)
GMP Compliance & Regulatory Challenges
Q1: What are the most critical GMP considerations for stem cell therapies to prevent immune rejection?
The most critical GMP considerations are identity, purity, and potency [61]. For therapies aimed at mitigating immune rejection, this means:
- Identity & Purity: Ensuring the final product contains a well-characterized cell population with minimal undifferentiated cells or contaminants that could trigger an immune response [57] [61]. The presence of residual undifferentiated cells (e.g., in hESC or hiPSC products) is a key risk factor [57].
- Potency: Demonstring the biological function of your therapy, such as the immunosuppressive capacity of engineered Tregs [45] or MSCs [62]. CGMP requires robust operating procedures and reliable testing laboratories to build quality into every step, as testing alone on a small sample of a batch is not adequate to ensure quality [61].
Q2: How can we efficiently manage evolving global regulations for our cell-based product?
- Establish a Regulatory Intelligence Team: Proactively track updates from the FDA, EMA, and other relevant agencies. Utilize a Compliance Management System (CMS) to centralize documentation [63].
- Engage Early with Regulators: Seek guidance through pre-IND meetings. The FDA provides resources on its website and through public conferences to help companies understand expectations [61].
- Leverage Referenced Systems: For iPSC-based products, using established starting materials, such as those described in a submitted Drug Master File (DMF), can streamline regulatory submissions by referencing existing quality and manufacturing data [62].
Q3: Our internal documentation is inconsistent, creating audit risks. How can we fix this?
- Digitize Processes: Replace paper records with electronic batch records (EBR) and document control systems to enforce standardization and prevent errors [63].
- Standardize Templates: Create and use uniform templates for all documentation, aligned with standards like ISO 9001, across all sites and shifts [63] [59].
- Conduct Regular Internal Audits: Perform frequent self-inspections to identify and correct documentation gaps before a regulatory audit [63].
Tumorigenicity Assessment
Q4: What are the key factors influencing tumorigenicity risk for a cell-based therapy?
Tumorigenicity risk is multifactorial. Key considerations include [57] [64]:
- Cell Type: Stem cell-based therapies (hESCs, hiPSCs) carry a higher inherent risk due to the potential for residual undifferentiated cells with high proliferative capacity [57] [64].
- Phenotype & Differentiation Status: The characteristics and maturity of the cells in the final product are critical.
- Manufacturing Process: Factors like ex vivo culture conditions, processing methods, and the duration of culture can influence risk [57].
- Delivery Method: The injection site and route of administration (e.g., local vs. systemic) are important factors in the overall risk assessment [57].
Q5: Is there a globally harmonized guideline for tumorigenicity testing of cell-based therapies?
No. Currently, there is no unified global regulatory consensus or technical implementation guide for tumorigenicity evaluation [57] [64]. Requirements and practices vary across different regulatory agencies. Manufacturers must design their non-clinical safety evaluation strategy based on the specific characteristics of their product and the regulatory expectations of each target region [57] [64].
Q6: What strategies can be used to mitigate tumorigenicity risk in iPSC-derived therapies?
- Purity Optimization: Improve differentiation protocols to rigorously minimize the number of residual undifferentiated pluripotent cells in the final product [57].
- Cell Engineering: Introduce "safety switches" (e.g., suicide genes) that allow for the selective elimination of the transplanted cells if uncontrolled growth is detected.
- Comprehensive Testing: Employ a combination of in vitro (e.g., soft agar colony formation) and in vivo (e.g., transplantation into immunodeficient mice) assays to assess tumor-forming potential, tailored to the product's specific risk profile [57] [64].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents for Stem Cell Therapy Development
| Item | Function | Application Example |
|---|---|---|
| Clinical-Grade iPSC Seed Stock | A standardized, well-characterized starting cell source for deriving therapeutic cell types. Ensures consistency and scalability [62]. | REPROCELL StemRNA Clinical iPSC Seed Clones, which have a submitted DMF for regulatory streamlining [62]. |
| Cell Sorting Reagents (e.g., Antibodies, Beads) | Isulates specific cell populations (e.g., CD54+ muscle progenitors, dopaminergic neural progenitors) to ensure product purity and minimize tumorigenic risk from heterogeneous cultures [62]. | Isolation of allogeneic muscle progenitor cells (MyoPAXon) or autologous dopaminergic progenitors for clinical trials [62]. |
| Gene Editing Systems (e.g., CRISPR) | Genetically modifies cells to enhance function, introduce safety switches, or create receptors. | Engineering Chimeric Anti-HLA Antibody Receptors (CHAR) into Tregs to suppress alloantigen-specific B-cells [45]. |
| GMP-Grade Culture Media & Cytokines | Supports the expansion and specific differentiation of stem cells into target lineages under defined, xeno-free conditions. Critical for CGMP compliance [61]. | Manufacturing of allogeneic, off-the-shelf NK cell therapies (e.g., FT536) from a master hiPSC line [62]. |
| Tumorigenicity Assay Kits | Evaluates the potential of a cell product to form tumors in non-clinical studies. | Using in vitro and in vivo methods for safety assessment of iPSC-derived products, as part of a risk-based strategy [57] [64]. |
Experimental Protocols & Workflows
Detailed Methodology: Tumorigenicity Assessment of iPSC-Derived Progenitor Cells
Objective: To evaluate the tumorigenic potential of a candidate iPSC-derived neural progenitor cell (NPC) product in an in vivo model.
Materials:
- Test Article: iPSC-derived NPCs (final formulated product).
- Control Articles: Parental iPSCs (positive control), Human fibroblasts (negative control), Vehicle (formulation buffer).
- Animals: Immunodeficient mice (e.g., NOD-scid gamma), 8-10 weeks old, n=10 per group.
- Reagents: Matrigel, anesthesia, tissue fixative (e.g., 10% Neutral Buffered Formalin).
Procedure:
- Cell Preparation: Harvest and resuspend test and control cells in an appropriate medium, mixed 1:1 with Matrigel on ice to a final concentration of 1x10^7 cells per 100 µL injection.
- Animal Dosing: Anesthetize mice. Using a sterile syringe, administer a subcutaneous injection of 100 µL of the cell-Matrigel suspension into the right flank of each mouse. Assign animals to groups as per the experimental design.
- In-Life Observations:
- Clinical Observations: Perform daily checks for mortality and moribundity.
- Palpation: Twice per week, palpate the injection site to detect the presence, size, and progression of any masses.
- Tumor Measurement: Using digital calipers, measure any palpable mass twice weekly. Record the length (L) and width (W). Calculate the tumor volume using the formula: Volume = (L x W²) / 2.
- Body Weight: Measure and record the body weight of all animals twice weekly.
- Study Termination: The study terminates at 6 months post-injection, or earlier if a mass reaches a predefined ethical volume (e.g., 1500 mm³) or if animals show signs of distress.
- Necropsy and Histopathology:
- Euthanize all animals humanely.
- Perform a gross necropsy. Excise the injection site, including any mass and surrounding tissue.
- Fix tissues in 10% NBF for 48 hours, process, and embed in paraffin.
- Section tissues and stain with Hematoxylin and Eosin (H&E).
- A board-certified pathologist should examine the slides for evidence of tumor formation, classifying any lesions.
Data Analysis: Compare the incidence, latency, and histology of any masses in the test article group against the positive and negative controls.
Detailed Methodology: In Vitro Suppression Assay for CHAR-Tregs
Objective: To validate the suppressive function of novel Chimeric anti-HLA Antibody Receptor Tregs (CHAR-Tregs) on alloantigen-specific B cells from pre-sensitized patients.
Materials:
- Effector Cells: Engineered CHAR-Tregs.
- Target Cells: Peripheral Blood Mononuclear Cells (PBMCs) isolated from pre-sensitized patients (e.g., high anti-HLA-A2 antibody titer) [45].
- Control Cells: Unmodified Tregs, CHAR-Tregs co-cultured with HLA-A2-negative PBMCs.
- Reagents: Cell culture medium (RPMI-1640 + 10% FBS), Ficoll-Paque PLUS, CFSE Cell Division Tracker, Anti-human CD19 MicroBeads, ELISpot kit for IgG, Flow Cytometry antibodies (CD3, CD4, CD25, CD127, CD19).
Procedure:
- Cell Isolation:
- Isolate PBMCs from patient blood using density gradient centrifugation with Ficoll-Paque.
- Isolate B cells from PBMCs using anti-CD19 MicroBeads.
- Label target B cells with CFSE according to manufacturer's protocol to track proliferation.
- Co-culture Setup:
- Plate CFSE-labeled B cells (1x10^5 cells/well) in a 96-well U-bottom plate.
- Add CHAR-Tregs at different ratios (e.g., 1:1, 2:1, 4:1 Treg:B cell).
- Include appropriate controls: B cells alone (max proliferation), B cells with unmodified Tregs.
- Stimulate the culture with anti-CD3/CD28 T cell activator and IL-2.
- Incubate for 5-7 days at 37°C, 5% CO₂.
- Analysis:
- Flow Cytometry: Harvest cells. Analyze CFSE dilution on CD19+ B cells to quantify suppression of proliferation.
- ELISpot: On day 5, transfer a portion of cells to an anti-IgG coated ELISpot plate. Develop after 24 hours to count the number of antibody-secreting cells (ASCs). The key metric is a reduction in spots in CHAR-Treg co-cultures [45].
- Flow Cytometry for Phenotype: Stain cells with antibodies for Treg markers (CD4, CD25, CD127) to confirm Treg stability post-culture.
Data Analysis: Calculate the percentage suppression of B cell proliferation and antibody secretion compared to the B-cell-only control.
Bench to Bedside: Validating Strategies Through Clinical Data and Comparative Analysis
Troubleshooting Guide: Navigating Immunosuppression in Stem Cell Clinical Trials
This guide addresses common challenges researchers face when designing experiments to evaluate immunosuppression regimens for stem cell-based therapies.
| Problem | Possible Cause | Recommended Action |
|---|---|---|
| Poor graft survival despite standard immunosuppression. | Inadequate regimen potency; high degree of HLA mismatch; activation of innate immune pathways (e.g., NK cells, complement) [42]. | Consider a combination regimen (e.g., Tacrolimus + MMF) [17]. Pre-screen for HLA matching where feasible and evaluate innate immune activation in vitro [42]. |
| High rate of infectious adverse events. | Systemic immunosuppression causing broad suppression of adaptive immunity [17]. | Evaluate the use of local/targeted immunosuppression (e.g., intravitreal implants) to minimize systemic exposure [17]. Monitor drug levels (e.g., Tacrolimus) to maintain within target therapeutic window [17]. |
| Uncertainty in determining the duration of immunosuppression. | Lack of consensus on the risk of late-onset rejection versus long-term drug toxicity [17]. | Taper drugs sequentially based on their roles; MMF may be used for a longer period than corticosteroids [17]. Monitor for operational tolerance after cessation [17]. |
| Differentiated stem cell product shows unexpected immunogenicity. | Residual immature cells expressing embryonic antigens; inflammatory cytokine-induced upregulation of HLA molecules on grafted cells [42]. | Implement rigorous purification of the differentiated cell product. Conduct in vitro co-culture assays with immune cells to profile immunogenicity before in vivo use [42]. |
Frequently Asked Questions (FAQs) on Immunosuppression Protocols
Q1: What are the most common immunosuppressive regimens used in recent stem cell clinical trials for neural and retinal applications? Systematic review data indicates that a combination of tacrolimus and mycophenolate mofetil (MMF) is the most frequently used systemic regimen [17]. This is often supplemented with corticosteroids (e.g., prednisone) for induction [17]. For localized applications, such as in the eye, local delivery via an intravitreal fluocinolone acetonide implant has been successfully used to minimize systemic side effects [17].
Q2: How do short-term and long-term immunosuppression outcomes compare in supporting graft survival? Evidence from clinical trials, particularly in retinal diseases, shows that defined courses of immunosuppression can support long-term graft survival even after cessation. The regimens are often designed for the short to medium term. For instance, in hESC-derived retinal pigment epithelial (RPE) cell trials, immunosuppression with tacrolimus and MMF was maintained for periods ranging from a few months to over a year. Notably, graft survival and visual acuity improvements were sustained for years after the immunosuppression was stopped, suggesting the induction of a stable, tolerant state in these immunoprivileged sites [17].
Q3: What is the efficacy and safety profile of Tacrolimus compared to other immunosuppressants? A recent 2025 systematic review and meta-analysis for autoimmune conditions provides comparative efficacy and safety data, which can inform stem cell trial design [65]. Key findings are summarized in the table below.
Table 1: Comparative Efficacy and Safety of Tacrolimus vs. Other Immunosuppressants (Meta-Analysis Data) [65]
| Comparison | Complete Remission (CR) Rate | Infection Rate | Key Safety Findings |
|---|---|---|---|
| Tacrolimus vs. Cyclophosphamide (CYC) | Superior (OR=1.83, 95% CI: 1.33-2.51) | No significant difference | |
| Tacrolimus vs. Mycophenolate Mofetil (MMF) | No significant difference (OR=0.93, 95% CI: 0.58-1.47) | Lower with Tacrolimus (OR=0.48, 95% CI: 0.31-0.75) | |
| Tacrolimus vs. Azathioprine (AZA) | No significant difference (OR=0.95, 95% CI: 0.49-1.84) | No significant difference | Lower leukopenia than AZA (OR=0.13, 95% CI: 0.04-0.43) |
Q4: What are the primary immune rejection pathways that immunosuppression must overcome in allogeneic stem cell therapies? Rejection is a coordinated effort by innate and adaptive immunity. The key pathways are visualized in the diagram below.
Q5: What experimental workflows are used to assess the immunogenicity of a cellular therapy and the efficacy of an immunosuppressive regimen? A combination of in vitro and in vivo models is essential for a comprehensive assessment. The typical workflow progresses from simple screening to complex systemic models, as outlined below [42].
Detailed Experimental Protocol: Evaluating Immunosuppression in a Preclinical Model
The following protocol is synthesized from methodologies described in the search results [42] [17].
Aim: To assess the efficacy and safety of a short-term versus long-term Tacrolimus/MMF regimen in supporting the survival of allogeneic stem cell-derived grafts in a humanized mouse model.
Materials Required:
- Research Model: Immunodeficient NSG mice engrafted with a human immune system (e.g., PBMC- or CD34+-humanized).
- Test Article: Allogeneic stem cell-derived product (e.g., RPE cells, neural precursors).
- Immunosuppressants: Tacrolimus (for subcutaneous injection or oral gavage), Mycophenolate Mofetil (for oral gavage).
- Key Reagents: Flow cytometry antibodies (for human immune cell phenotyping: CD3, CD4, CD8, CD56, CD19), ELISA kits (for measuring human cytokines: IFN-γ, TNF-α, IL-2), equipment for functional graft assessment (e.g., ophthalmology tools for retinal grafts, behavioral assays for neural grafts).
Methodology:
- Cell Transplantation: Administer the allogeneic stem cell-derived product to the humanized mice at the target site (e.g., subretinal space for RPE cells, intraspinal for neural cells).
- Group Randomization: Randomize mice into the following groups:
- Group 1 (Short-term): Receive Tacrolimus (e.g., target serum level 3-5 ng/mL) and MMF (e.g., 100 mg/kg/day) for 45 days post-transplant.
- Group 2 (Long-term): Receive the same Tacrolimus/MMF regimen for 120 days.
- Group 3 (Control): Receive vehicle only (no immunosuppression).
- Monitoring and Analysis:
- Graft Survival: Assess weekly using in vivo imaging (if applicable) and terminal histology at defined endpoints (e.g., days 45, 120, and 180) for the presence and integrity of grafted cells.
- Immune Monitoring: Collect blood and spleen samples at regular intervals. Use flow cytometry to track changes in human T, B, and NK cell populations. Measure serum levels of pro-inflammatory cytokines by ELISA.
- Graft Function: Perform functional tests relevant to the cell type (e.g., electroretinography for retinal grafts, motor function scoring for spinal cord grafts).
- Safety & Toxicity: Monitor mouse body weight, behavior, and overall health. Perform blood counts and chemistry to assess drug-related hematological or organ toxicity.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Stem Cell Immunosuppression
| Reagent / Material | Function in Experimental Design |
|---|---|
| Humanized Mouse Models | In vivo platform for studying human-specific immune responses to allogeneic grafts and for testing immunosuppression efficacy [42]. |
| Flow Cytometry Panels | To quantitatively analyze host immune cell infiltration (T, B, NK cells) and activation status in the graft site and peripheral lymphoid organs [66] [42]. |
| Tacrolimus & MMF | The current standard-of-care combination immunosuppressants for many clinical trials; used as a positive control benchmark for new regimens [17]. |
| Cytokine ELISA/Kits | To measure the levels of key inflammatory (e.g., IFN-γ, TNF-α) and suppressive (e.g., IL-10, TGF-β) cytokines in serum or tissue homogenates, indicating the immune state [66] [42]. |
| HLA Typing Kits | To characterize the HLA profile of donor cells and recipient models, enabling the study of the impact of HLA matching/mismatching on rejection [42] [27]. |
| Immunofluorescence Staining Reagents | For histological visualization of graft survival, immune cell infiltration (e.g., CD3+ T cells), and complement deposition within the grafted tissue [42] [17]. |
FAQ: Safety of Immunomodulators in Research
What does head-to-head evidence reveal about the safety profiles of JAK inhibitors versus TNF antagonists?
A large-scale systematic review and meta-analysis provides direct, comparative safety data. The analysis included 42 studies and data from 813,881 patients with immune-mediated inflammatory diseases (IMIDs) such as rheumatoid arthritis, inflammatory bowel disease, and psoriasis. The table below summarizes the key findings for critical adverse events, showing incidence rates (IR) per 100 person-years and pooled hazard ratios (HR) for JAK inhibitors compared to TNF antagonists [67] [68].
| Safety Outcome | JAK Inhibitors IR (95% CI) | TNF Antagonists IR (95% CI) | Pooled Hazard Ratio (95% CI) |
|---|---|---|---|
| Serious Infections | 3.79 (2.85 - 5.05) | 3.03 (2.32 - 3.95) | 1.05 (0.97 - 1.13) |
| Malignant Neoplasms | 1.00 (0.77 - 1.31) | 0.94 (0.72 - 1.22) | 1.02 (0.90 - 1.16) |
| Major Adverse Cardiovascular Events (MACE) | 0.72 (0.56 - 0.92) | 0.66 (0.49 - 0.89) | 0.91 (0.80 - 1.04) |
| Venous Thromboembolism (VTE) | 0.57 (0.40 - 0.82) | 0.52 (0.37 - 0.73) | 1.26 (1.03 - 1.54) |
Interpretation for Researchers: This data suggests that for a broad IMID population, the risks of serious infections, cancer, and MACE are not significantly different between the two drug classes. However, there is a statistically significant 26% increased risk of Venous Thromboembolism (VTE) associated with JAK inhibitor use compared to TNF antagonists. This finding is critical for risk-benefit assessments, especially for patients with additional VTE risk factors [67] [68].
How do these findings relate to the context of stem cell transplantation research?
While the meta-analysis above focused on IMIDs, immunosuppression is equally critical in regenerative medicine. The host immune response is a major barrier to the successful engraftment of transplanted cells [69] [42]. For example, in preclinical models, a combined regimen of tacrolimus and sirolimus significantly prolonged the survival of transplanted human embryonic stem cells (hESCs) for up to 28 days [69]. Clinical trials for stem cell-derived retinal pigment epithelial (RPE) cells commonly use a combination of tacrolimus and mycophenolate mofetil (MMF), sometimes with corticosteroids, to prevent rejection [17]. Understanding the safety profiles of these and other immunomodulators, like JAK inhibitors and TNF antagonists, is essential for designing safe and effective transplantation protocols.
What are the clinical implications of these safety findings?
The evidence indicates that the strict regulatory guidance requiring JAK inhibitors to be used only after TNF antagonist failure may need reconsideration for a broader IMID population. The absolute risks for serious events were low, and the study did not find meaningful differences in the risks of serious infections, cancer, or MACE [68]. This supports a case-by-case clinical decision-making process that balances effectiveness, patient comorbidities, and these nuanced safety profiles. For instance, a JAK inhibitor might be a suitable first-line option for a patient without VTE risk factors, while a TNF antagonist could be preferred for another.
Troubleshooting Guide: Common Scenarios in Immunomodulator Research
Scenario: Managing Confounding in Comparative Safety Studies
Challenge: Observational studies comparing drug safety are susceptible to confounding by indication, where the reason for prescribing a drug is also associated with the outcome.
Solution:
- Protocol Design: Prioritize study designs that minimize confounding, such as new-user active comparator designs.
- Statistical Analysis: In your analysis plan, pre-specify methods to adjust for key confounders. The meta-analysis by Solitano et al. adjusted for variables including age, sex, comorbidities, and concomitant medication use [67] [68].
- Sensitivity Analysis: Conduct sensitivity analyses to test the robustness of your findings. This can include using different statistical models or excluding studies with a high risk of bias.
Scenario: Translating Safety Evidence from IMIDs to Transplant Models
Challenge: Safety data from IMIDs may not directly translate to stem cell transplantation models due to different disease mechanisms and concomitant treatments (e.g., chemotherapy).
Solution:
- Preclinical Modeling: Conduct dedicated safety studies in your specific animal model of transplantation. Monitor for the same adverse events (e.g., infections, VTE) identified in human studies.
- Combination Regimens: Carefully evaluate the safety of immunomodulators when used in combination with other transplant-related drugs, as synergistic toxicities may occur.
- Endpoint Selection: Include relevant safety biomarkers and histological analyses as endpoints in your efficacy studies to build a preliminary safety profile for your specific cellular therapy context.
The Scientist's Toolkit: Key Reagents for Investigating Immunosuppression
| Research Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Tacrolimus | Calcineurin inhibitor; suppresses T-cell activation. | Used in combination with sirolimus to prolong survival of hESC transplants in murine models [69]. |
| Mycophenolate Mofetil (MMF) | Inhibits inosine monophosphate dehydrogenase, suppressing lymphocyte proliferation. | Common component of systemic immunosuppression in clinical trials for hESC-derived retinal pigment epithelial (RPE) cells [17]. |
| Sirolimus (Rapamycin) | mTOR inhibitor; suppresses T-cell and B-cell activation. | Combined with tacrolimus to enhance hESC survival in immunocompetent mice [69]. |
| B2M-Knockout Stem Cells | CRISPR/Cas9-edited cells lacking β-2-microglobulin, which eliminates surface HLA class I expression. | Used to create "hypoimmunogenic" stem cells that evade CD8+ T-cell recognition [70]. |
| PD-L1 Expressing Cells | Cells engineered to overexpress programmed death-ligand 1 (PD-L1), an immune checkpoint protein. | Overexpression on human islet-like cells restricts T-cell activation and delays rejection in diabetic mouse models [42]. |
| Bioluminescent Reporter Genes (e.g., fLuc) | Enables longitudinal, non-invasive tracking of cell survival in vivo via bioluminescent imaging (BLI). | Used to longitudinally monitor the rejection of transplanted hESCs in immunocompetent vs. immunodeficient mice [69]. |
Experimental Workflow for Evaluating an Immunomodulator in a Stem Cell Transplant Model
The following diagram outlines a core methodology for testing the efficacy of an immunomodulator in a preclinical stem cell transplantation setting, based on established approaches [69] [42].
JAK-STAT and TNF Signaling Pathway in Immune Rejection
Understanding the molecular targets of these immunomodulators is key. JAK inhibitors block cytokine signaling, while TNF antagonists target a specific inflammatory cytokine. This diagram illustrates the core signaling pathways relevant to their function in the context of transplant rejection.
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary advantages of using CAR-MSCs over CAR-T cells in solid tumor therapy?
CAR-MSCs combine the precise targeting of CAR technology with the innate biological properties of mesenchymal stem cells (MSCs). Unlike CAR-T cells, which primarily exert cytotoxic effects, CAR-MSCs can modulate the tumor microenvironment (TME) through immunomodulatory functions and tissue-repair capabilities. Preclinical studies demonstrate that CAR-MSCs are effective against glioblastoma, Ewing sarcoma, acute myeloid leukemia, and lung cancer. Their mechanisms of action include secretion of TNF-related apoptosis-inducing ligand (TRAIL), production of bispecific antibodies, and induction of regulatory T cells (Tregs). This provides a dual therapeutic modality targeting both cancer cells and the immunosuppressive TME [71].
FAQ 2: Our CAR-Treg therapy needs to target the central nervous system. What administration route and preclinical evidence should we consider?
For neuroinflammatory diseases like multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS), intrathecal administration (directly into the cerebrospinal fluid) is a promising route. A clinical study with intrathecally delivered polyclonal Tregs (PTG-007) in relapsing-remitting MS patients showed no increase in existing brain lesions and almost no new lesions, a result superior to intravenous administration. A preclinical development program for a CAR-Treg candidate for these diseases, involving studies in humanized mouse models, is underway, with data expected by March 2025. This supports intrathecal delivery as a viable strategy for engineered Treg therapies targeting neuroinflammatory conditions [72].
FAQ 3: What are the major immunological barriers facing allogeneic cell therapies, and how can we test for them?
The host immune response is a critical barrier. The innate immune system, particularly Natural Killer (NK) cells, can target and kill therapy cells that lack or have mismatched self-HLA class I molecules. The adaptive immune system, specifically host T cells, can reject the transplant by recognizing foreign donor antigens via direct, indirect, or semi-direct pathways of allorecognition. Experimental platforms to study this include:
- In vitro assays: Co-culture of your cell product with human peripheral blood mononuclear cells (PBMCs) or specific immune cell populations (e.g., NK cells, T cells) to measure activation, cytokine release, and cytotoxicity.
- In vivo models: Humanized mouse models engrafted with a human immune system are essential for assessing the survival, integration, and immunogenicity of your cellular therapy in a more physiologically relevant context [42].
FAQ 4: Which generation of CAR design is most suitable for initial CAR-MSC development?
Second-generation CARs are a validated starting point. They incorporate a single costimulatory domain (e.g., CD28 or 4-1BB) alongside the CD3ζ activation domain, which significantly improves persistence and functionality compared to first-generation designs. Most FDA-approved CAR-T cell therapies use this design, making it a well-characterized and reliable platform for initial CAR-MSC development. Later-generation CARs (e.g., fourth-generation TRUCKs) can be explored to add functionalities like inducible cytokine secretion once a foundational platform is established [71].
Troubleshooting Guides
Problem: Poor In Vivo Persistence of CAR-MSCs
- Potential Cause 1: Cell Senescence. MSCs can undergo senescence during in vitro expansion, limiting their therapeutic longevity.
- Solution: Isolate and use senescence-resistant MSC clones. Implement metabolic engineering strategies to enhance cell fitness [71].
- Potential Cause 2: Host Immune Rejection. Allogeneic MSCs may be recognized and eliminated by the recipient's immune system.
Problem: Inconsistent CAR Expression in Final MSC Product
- Potential Cause: Heterogeneous MSC Tissue Sourcing and Inefficient Transfection. MSCs derived from different donors or tissues (bone marrow, adipose, umbilical cord) may have varying transfection efficiencies.
- Solution: Standardize the MSC source and manufacturing workflow. Utilize high-efficiency transfection systems like electroporation. Implement rigorous quality control (QC) checks for CAR expression and functionality during production [71].
Problem: Insufficient Trafficking or Efficacy in Solid Tumors
- Potential Cause: The Immunosuppressive Tumor Microenvironment (TME). The TME can inhibit the function and homing of therapeutic cells.
- Solution: Engineer fourth-generation CAR-MSCs (TRUCKs) to secrete immunomodulatory cytokines (e.g., IL-12) or chemokines (e.g., CCL19) upon CAR activation. This can help remodel the TME, enhance immune cell recruitment, and improve the therapy's own survival and function [71].
Data Presentation
Table 1: Preclinical Applications of CAR-MSCs in Oncology
| Target Disease | Proposed Mechanism of Action | Key Findings/Status | Research Support |
|---|---|---|---|
| Glioblastoma | TRAIL secretion, tumor homing, induction of apoptosis | Preclinical studies show targeted antitumor activity. | [71] |
| Ewing Sarcoma | Bispecific antibody production, TME modulation | Demonstrated effectiveness in preclinical models. | [71] |
| Acute Myeloid Leukemia | Precise targeting of tumor-associated antigens (TAAs) | Effective against hematological malignancy in preclinical studies. | [71] |
| Lung Cancer | Immunomodulation, targeted cytotoxicity | Preclinical evidence of efficacy. | [71] |
| Graft-versus-Host Disease (GvHD) | Treg induction, immunomodulation | Shows application in immune-related disorders. | [71] |
Table 2: Evolution of CAR Signaling Domains
| CAR Generation | Costimulatory Domains | Key Features | Considerations for Development | |
|---|---|---|---|---|
| First Generation | None (only CD3ζ) | Basic cytotoxic signal; requires exogenous IL-2. | Limited persistence and efficacy; largely superseded. | [71] |
| Second Generation | CD28 or 4-1BB | One costimulatory domain enhances persistence, proliferation, and cytotoxicity. | Well-established, reliable platform; 4-1BB domain associated with longer persistence. | [71] |
| Third Generation | CD28 and 4-1BB (or two others) | Dual costimulatory signals for enhanced activation. | Can lead to excessive signaling, exhaustion, or increased toxicity; results are variable. | [71] |
| Fourth Generation (TRUCK) | CD28 or 4-1BB | Inducible secretion of transgenic proteins (e.g., IL-12, IL-15) to modulate the TME. | Ideal for solid tumors; can recruit and activate secondary immune effectors. | [71] |
Experimental Protocols
Protocol 1: In Vitro Cytotoxicity Assay for CAR-MSCs Objective: To quantify the specific killing of target cells by CAR-MSCs.
- Label Target Cells: Culture tumor cell lines expressing the target antigen (positive control) and those that do not (negative control). Label both with a fluorescent dye, such as calcein AM.
- Co-culture: Seed the labeled target cells in a multi-well plate. Add CAR-MSCs or unmodified MSCs (control) at various effector-to-target (E:T) ratios (e.g., 1:1, 5:1, 10:1).
- Incubate: Incubate the co-culture for a predetermined period (e.g., 6-24 hours).
- Measure Cytotoxicity: Collect supernatant from each well and measure the fluorescence released from lysed target cells using a fluorometer. Calculate specific lysis using the formula:
(Experimental Release – Spontaneous Release) / (Maximum Release – Spontaneous Release) * 100[71].
Protocol 2: Assessing Allorecognition Pathways In Vitro Objective: To determine how a cellular therapy activates alloreactive T cells.
- Generate Monocyte-Derived Dendritic Cells (moDCs): Differentiate CD14+ monocytes from human PBMCs into immature DCs using GM-CSF and IL-4.
- Co-culture Setup:
- Direct Pathway: Co-culture irradiated (non-proliferative) cellular therapy directly with allogeneic PBMCs.
- Indirect Pathway: Co-culture the cellular therapy with allogeneic moDCs for antigen uptake and processing, then co-culture these primed moDCs with autologous T cells.
- Readout: After 5-7 days, measure T-cell proliferation (e.g., via CFSE dilution) and activation (e.g., via IFN-γ ELISpot or cytokine flow cytometry) [42].
Diagram: CAR-MSC Construction and Mechanism
CAR-MSC recognizes tumor antigens and modulates the tumor microenvironment.
Diagram: Cell Therapy Manufacturing and Validation Workflow
Engineered cell therapy manufacturing and validation workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Engineered Cell Therapy Development
| Reagent/Material | Function/Purpose | Application Example |
|---|---|---|
| Non-viral Transfection System | High-efficiency delivery of CAR constructs into cells (e.g., MSCs) with potentially lower immunogenicity than viral methods. | Electroporation for engineering CAR-MSCs [71]. |
| Humanized Mouse Models | In vivo testing of cell therapy survival, integration, and immunogenicity in the context of a human immune system. | Preclinical safety and efficacy studies for CAR-Tregs in neuroinflammation [72] [42]. |
| Recombinant Human Cytokines | Direct T-cell or Treg differentiation, expansion, and culture maintenance (e.g., IL-2). | Critical for the in vitro expansion and stability of CAR-Treg products [72]. |
| Flow Cytometry Antibodies | Characterization of cell product phenotype (e.g., MSC markers: CD73, CD90, CD105) and quantification of CAR expression. | Essential for quality control during manufacturing to ensure product identity and purity [71]. |
| HLA Typing Kits | Assessing the degree of HLA matching between donor cells and recipient, which is a major factor in allorecognition. | Used in studies to correlate HLA mismatch with the strength of the immune response to the cell therapy [42]. |
This technical support guide provides researchers and scientists with a foundational overview of key metrics and methodologies in stem cell transplantation research. The content focuses on assessing critical outcomes—graft survival, patient morbidity, and infection rates—across different immunosuppressive and conditioning regimens, framed within the context of stem cell immune rejection and immunosuppression strategies. The following sections offer troubleshooting guides, frequently asked questions, and essential tools to support the design and interpretation of related experiments.
▎Key Outcome Metrics at a Glance
The tables below summarize core quantitative data on graft survival, infection rates, and Graft-versus-Host Disease (GVHD) to serve as a quick reference for benchmarking experimental outcomes.
Table 1: Graft Survival and Failure Rates
| Regimen or Donor Type | Graft Survival / Failure Rate | Context and Notes |
|---|---|---|
| HLA-Matched Unrelated Donor (MUD) | Graft Failure Rate: 3.8% [73] | Recent large cohort study (2006-2012); disease status at transplant was a significant risk factor [73]. |
| Haploidentical with PTCy | Graft Failure with DSA >10,000 MFI: Significantly Increased [74] | High levels of Donor-Specific Antibody (DSA) are a major risk factor for graft failure, necessitating donor avoidance or desensitization [74]. |
| Combined Kidney & HSC Transplant | Successful Immunosuppression Withdrawal: >80% (24/29 patients) [75] | Protocol for HLA-identical donors using total lymphoid irradiation and anti-thymocyte globulin (ATG) [75]. |
Table 2: Infection and Morbidity Rates Post-Allo-HCT
| Complication | Rate | Context and Notes |
|---|---|---|
| Any Infection (within 2 years post-HCT) | Nearly Universal [76] | Occurrence of infections following allogeneic hematopoietic cell transplant (HCT) is nearly universal. |
| Life-Threatening Infections (with aGVHD) | Hazard Ratio: 1.97 (95% CI 1.33-2.90) [76] | Acute GVHD significantly increases the risk of severe and fatal infections [76]. |
| Fatal Infections (with aGVHD) | Hazard Ratio: 2.8 (95% CI 1.10-7.08) [76] | The increased immunosuppression used to treat GVHD heightens infection-related mortality [76]. |
| Hospital Readmission (within 100 days post-HCT) | 54.9% of patients [77] | In a study of patients with grades II-IV acute GVHD, over half required readmission; 22.3% had ≥2 readmissions [77]. |
| 1-Year Non-Relapse Mortality (with aGVHD) | 25.5% [77] | Mortality not due to relapse of the underlying disease [77]. |
Table 3: Graft-versus-Host Disease (GVHD) Outcomes
| Metric | Rate | Context and Notes |
|---|---|---|
| Acute GVHD (Grades II-IV) Progression | 40% of patients [77] | Patients experienced an increase in disease severity or developed new organ involvement after diagnosis [77]. |
| Steroid Dependence (inability to taper below 10 mg/day) | 44.4% of patients [77] | A significant proportion of patients with acute GVHD could not reduce their corticosteroid dose [77]. |
| Steroid-Refractory Acute GVHD | 23.8% of patients [77] | Defined as requiring ≥1 additional systemic GVHD therapy after corticosteroids [77]. |
| Overall Mortality (with aGVHD) | 52.8% during follow-up [77] | Median follow-up of 524 days from acute GVHD diagnosis [77]. |
Frequently Asked Questions (FAQs) and Troubleshooting
Graft Failure and Rejection
Q: What are the primary risk factors for graft failure in modern transplantation regimens?
- A: Key risk factors include:
- Donor-Specific Antibodies (DSA): The presence of high levels of DSA (>10,000 MFI, particularly if C1q positive) is a major risk factor for graft failure, especially in haploidentical transplantation with post-transplant cyclophosphamide (PTCy) [74]. Always screen for DSA during donor selection.
- Disease Status: In a large study of unrelated donor transplants, the disease status before graft was a significant risk factor for graft failure [73]. Patients with active or advanced disease are at higher risk.
- Tolerance Induction: In protocols aiming for immune tolerance, the loss of donor hematopoietic chimerism is often followed by solid organ graft rejection [75]. Monitoring chimerism is critical.
Q: How can we mitigate the risk of antibody-mediated rejection?
- A: Employ a structured strategy:
- Donor Selection: Avoid donors for whom the recipient has pre-formed DSA with MFI > 5000 [74].
- Desensitization: For patients with high DSA levels, desensitization protocols (e.g., using rituximab, IVIG, plasma exchange) can be attempted to reduce DSA to a safer level (<5000 MFI) prior to transplant [74].
- Crossmatch: The goal of desensitization is to achieve a negative flow cytometric crossmatch [74].
Infection and Morbidity
Q: Why are infection rates so high after allogeneic HCT, and how can they be predicted?
- A: Infections are nearly universal due to several factors [76]:
- Conditioning Regimen Toxicity: Causes breakdown of mechanical barriers like the skin and GI tract lining [76].
- Delayed Immune Reconstitution: The immune system rebuilds slowly post-transplant, leaving the patient vulnerable [78].
- Immunosuppression: Pharmacologic immunosuppression used to prevent or treat GVHD further increases infection risk [76] [78].
- Predictive Factor: A history of frequent bacterial infections in the year before transplant is a strong predictor of post-transplant bacterial infections [76].
Q: What is the relationship between GVHD and infection?
- A: This is a complex, bidirectional relationship. GVHD itself causes immune dysregulation, impairing the ability to fight infections. Furthermore, the intensified immunosuppressive therapy required to treat GVHD (e.g., high-dose corticosteroids) further increases the risk of severe and fatal infections [76]. Patients with acute GVHD experience approximately 60% more infections than those without [76].
Graft-versus-Host Disease (GVHD)
Q: What are the clinical outcomes for patients who develop steroid-refractory acute GVHD?
- A: Outcomes are poor, highlighting a significant unmet need. In a large study, 23.8% of acute GVHD patients were steroid-refractory [77]. These patients often require multiple subsequent lines of therapy (e.g., sirolimus, extracorporeal photopheresis, monoclonal antibodies), and this population experiences high mortality, with a 1-year overall mortality rate of 35.2% from the date of acute GVHD diagnosis [77].
Q: In the context of novel regimens, how does donor selection influence GVHD risk?
- A: With modern prophylaxis like PTCy, the influence of HLA matching on GVHD is evolving.
- Haploidentical with PTCy: The degree of HLA mismatch may have less impact on survival. Some evidence suggests mismatches at HLA-DRB1 or non-permissive HLA-DPB1 may be associated with improved outcomes, potentially through a enhanced graft-versus-leukemia effect [74].
- Unrelated Donor with PTCy: HLA class I matching may still be preferred, as class I mismatches have been associated with inferior survival in this setting [74].
- Donor Age: Younger donors are generally associated with improved survival outcomes regardless of HLA matching [74].
Experimental Protocols and Methodologies
Protocol: Establishing Mixed Chimerism for Tolerance Induction
This protocol is used to create a state of donor-specific immune tolerance, potentially eliminating the need for lifelong immunosuppression [75].
- Objective: To achieve stable mixed hematopoietic chimerism, enabling donor-specific immune tolerance without graft rejection.
- Key Applications: Solid organ transplantation combined with hematopoietic stem cell (HSC) infusion; research into immune reconstitution and tolerance.
- Materials: See "Research Reagent Solutions" below.
Detailed Workflow:
- Non-Myeloablative Conditioning: The recipient undergoes a reduced-intensity conditioning regimen to create "space" in the bone marrow without complete myeloablation. Example regimens include total lymphoid irradiation or low-dose total body irradiation combined with fludarabine and cyclophosphamide [75].
- HSC and Solid Organ Graft: The patient receives an infusion of donor-derived hematopoietic stem cells, followed by transplantation of the solid organ (e.g., kidney) from the same donor.
- Post-Transplant Cyclophosphamide (PTCy): On days +3 and +4 post-transplant, high-dose cyclophosphamide is administered. This selectively eliminates alloreactive, proliferating T cells that cause graft rejection and GVHD, while sparing regulatory T cells and non-dividing HSCs [75] [74].
- Concurrent Immunosuppression: Tacrolimus or mycophenolate mofetil is typically started after PTCy to provide further prophylaxis against GVHD.
- Monitoring: Peripheral blood chimerism is quantified regularly using flow cytometry or PCR-based methods. The goal is to maintain a stable percentage of donor-derived hematopoietic cells. Operational tolerance is assessed by the ability to wean off all immunosuppression without graft rejection [75].
The following diagram illustrates the logical workflow and key mechanisms of this protocol.
Protocol: Quantifying Infection Burden in Preclinical HCT Models
This methodology provides a framework for systematically analyzing infection rates and severity in the context of different transplant regimens.
- Objective: To categorize and quantify infectious complications in a translational transplant model to compare the infectious toxicity of different regimens.
- Key Applications: Preclinical testing of novel immunosuppressive drugs or conditioning regimens; studying the impact of GVHD on immune competence.
- Materials: Animal HCT model, pathogen banks (e.g., CMV, Aspergillus), diagnostic tools (PCR, culture, histopathology).
- Detailed Workflow:
- Categorization by Timing: Record infections based on post-transplant phases (e.g., pre-engraftment, post-engraftment, late phase).
- Categorization by Causative Organism: Classify infections as bacterial, viral, or fungal. Sub-categorize by specific pathogens (e.g., CMV, adenovirus, invasive aspergillosis).
- Assign Severity Grade: Use a standardized grading system like the BMT CTN severity scale. For example:
- Grade 2: Moderate infection requiring therapeutic intervention.
- Grade 3: Life-threatening infection requiring intravenous treatment or intensive care.
- Grade 4: Fatal infection [76].
- Statistical Analysis: Correlate infection frequency and severity with other variables such as the presence and grade of GVHD, the level of immune reconstitution (e.g., T-cell counts), and the specific transplant regimen being tested [76].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Transplantation Immunology Research
| Reagent / Material | Primary Function in Research | Key Considerations |
|---|---|---|
| Anti-Thymocyte Globulin (ATG) | In vivo T-cell depletion; part of conditioning regimens to prevent graft rejection and GVHD [75]. | Varies by source (rabbit, horse); impacts depletion efficacy and side-effect profile. |
| Post-Transplant Cyclophosphamide (PTCy) | Selective elimination of alloreactive T cells post-transplant; a cornerstone of modern GVHD prophylaxis in haploidentical and MUD transplants [75] [74]. | Timing is critical (typically days +3, +4). Key for promoting tolerance in mixed chimerism models. |
| Calcineurin Inhibitors (Tacrolimus, Cyclosporine A) | Foundation of GVHD prophylaxis; inhibits T-cell activation [77]. | Nephrotoxic and neurotoxic; drug level monitoring is essential. Often used in combination with other agents. |
| Sirolimus (mTOR inhibitor) | Alternative immunosuppressant for GVHD prophylaxis or treatment; used in steroid-refractory cases [77]. | Has antiproliferative effects and may exhibit less nephrotoxicity than calcineurin inhibitors. |
| Donor-Specific Antibody (DSA) Assays | Detect pre-formed HLA antibodies in recipient against donor HLA; critical for assessing risk of antibody-mediated rejection [74]. | Luminex-based single antigen bead assay is standard. MFI >5000-10,000 or positive C1q assay indicates high risk [74]. |
Analytical Pathways in Transplantation Immunology
The diagram below maps the logical decision points and key biological relationships in transplantation immunology, from initial donor selection to major clinical outcomes.
Conclusion
The convergence of genetic engineering, cell-based immunomodulation, and refined pharmacologic strategies is decisively shifting the paradigm from broad immunosuppression toward targeted, graft-specific immune protection. The integration of mechanisms like CTLA4-Ig/PD-L1 co-expression and the deployment of engineered suppressor cells such as CHAR-Tregs represent a promising path to induce durable tolerance. Future progress hinges on establishing standardized safety and tumorigenicity assessments, advancing the development of 'off-the-shelf' universal donor cells, and executing robust long-term clinical studies. For researchers and drug developers, the priority must be on creating integrated platforms that combine these multidisciplinary strategies to ensure the clinical safety, efficacy, and scalability of stem cell therapies, ultimately unlocking their full regenerative potential.
References
- 1. NK Cells: Not Just Followers But Also Initiators of Chronic ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2024.13318/full]
- 2. The Role of Complement in Organ Transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6788431/]
- 3. Activation of immune signals during organ transplantation [https://www.nature.com/articles/s41392-023-01377-9]
- 4. NK Cells: Elusive Participants in Transplantation Immunity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2967580/]
- 5. Direct and indirect allograft recognition: pathways dictating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4701596/]
- 6. Immunological considerations—HLA matching and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9226257/]
- 7. HLA Mismatching Strategies for Solid Organ Transplantation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2016.00575/full]
- 8. The Progress and Challenges of Implementing HLA Molecular ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14716/full]
- 9. HLA and non-HLA polymorphisms in renal transplantation [https://smw.ch/index.php/smw/article/download/1576/2037?inline=1]
- 10. Advancements in HLA Typing Techniques and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11175610/]
- 11. Innate Immune 'Mismatch' Could Transform Kidney Transplant ... [https://news.feinberg.northwestern.edu/2025/08/13/innate-immune-mismatch-could-transform-kidney-transplant-outcomes/]
- 12. Induced pluripotent stem cells have similar immunogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4352342/]
- 13. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 14. Evaluation of the immunogenicity of human iPS cell- ... [https://www.sciencedirect.com/science/article/pii/S1873506117300077]
- 15. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 16. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 17. Immunosuppression in stem cell clinical trials of neural and ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0304073]
- 18. Immune Tolerance and Stem Cell Transplantation: A CIRM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4275016/]
- 19. Assay format diversity in pre-clinical immunogenicity risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8726688/]
- 20. Immunosuppression in stem cell clinical trials of neural and ... [https://pubmed.ncbi.nlm.nih.gov/38968328/]
- 21. Effect of immunosuppression on hESC-derived retina ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04271-z]
- 22. Press Release - Investor Relations | Sarepta Therapeutics, Inc. [https://investorrelations.sarepta.com/news-releases/news-release-details/sarepta-announces-approval-begin-endeavor-cohort-8-evaluate]
- 23. Sarepta gets FDA's go-ahead to study immunosuppressive ... [https://www.fiercepharma.com/pharma/sarepta-gets-fdas-go-ahead-add-new-immunosuppressive-regimen-elevidys-study-key-population]
- 24. Phase I/II Clinical Trial of AMT-130 | Programs & Pipeline [https://www.uniqure.com/programs-pipeline/phase-1-2-clinical-trial-of-amt-130]
- 25. Stem cell transplant without toxic preparation successfully ... [https://med.stanford.edu/news/all-news/2025/07/stem-cell-transplant.html]
- 26. A combination strategy for stem cell graft rejection [https://www.regmednet.com/a-combination-strategy-for-stem-cell-graft-rejection/]
- 27. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 28. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 29. CAR-T Regulatory (CAR-Treg) Cells: Engineering and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8869296/]
- 30. CAR-MSCs在细胞免疫治疗中的最新研究 [https://www.cyagen.cn/frontier-express/FE001940]
- 31. Research status and application prospect of mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7342131/]
- 32. Luminex 分析,多重免疫分析 [https://www.bio-techne.com/cn/reagents/luminex-assays]
- 33. Hypoimmune stem cells and islets: hype or a true ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492583/]
- 34. 用AI辅助撰写国自然申请书,效率提高不止10倍:实操演示 [http://www.360doc.com/content/25/0203/19/44325450_1145848254.shtml]
- 35. Mechanisms of Tolerance Induction by Hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5442770/]
- 36. Chimerism and immunological tolerance in solid organ ... [https://link.springer.com/article/10.1007/s00281-025-01052-x]
- 37. Tolerance Induction Strategies in Organ Transplantation [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14958/full]
- 38. Recommendations for Donor HLA Assessment and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4272893/]
- 39. Human Pluripotent Stem Cell Banking [https://www.stemcell.com/psc-cell-quality/cell-banking]
- 40. Tregs and Mixed Chimerism as Approaches for Tolerance ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.612737/full]
- 41. Stanford's new cell therapy cures type 1 diabetes in mice [https://www.sciencedaily.com/releases/2025/11/251126095018.htm]
- 42. Immunological considerations and challenges for ... [https://www.nature.com/articles/s42003-021-02237-4]
- 43. In vivo surveillance and elimination of teratoma‐forming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6790577/]
- 44. Natural Killer Cells Prevent the Formation of Teratomas ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.02580/full]
- 45. Teaching the immune system a new trick could one day ... [https://web.musc.edu/about/news-center/2025/08/15/tackling-organ-rejection]
- 46. Hypoimmunogenic pluripotent stem cells: A game-changer ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925011245]
- 47. Advances in Post-Kidney Transplant Immunosuppression ... [https://primeinc.org/live/advances-post-kidney-transplant-immunosuppression-applying-latest-cni-sparing]
- 48. Immunosuppression: Watching For and Managing Side ... [https://connect.mayoclinic.org/blog/transplant/newsfeed-post/immunosuppression-watching-for-and-managing-side-effects/]
- 49. Immune rejection of human mesenchymal stem cells ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079651/]
- 50. Immunosuppressants: Definition, Uses & Side Effects [https://my.clevelandclinic.org/health/treatments/10418-immunosuppressants]
- 51. Assessment and Optimization of Cell Engraftment after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826722/]
- 52. The “Myth” of Homing: Why Do Cells Need A Delivery ... [https://likarda.com/resources/bio-blog/homing/the-myth-of-homing-why-do-cells-need-a-delivery-system/]
- 53. MSCs: Delivery Routes and Engraftment, Cell-Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755386/]
- 54. Mesenchymal Stromal Cell Homing: Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6529790/]
- 55. Evasion in Immune -Based Diabetes Therapy—Current... Stem Cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853723/]
- 56. Frontiers | Global clinical trials on stem therapy for autoimmune... cell [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 57. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 58. 2026 Manufacturing Industry Outlook | Deloitte Insights [https://www.deloitte.com/us/en/insights/industry/manufacturing-industrial-products/manufacturing-industry-outlook.html]
- 59. Top 15 Manufacturing Challenges in 2025 & How to Solve ... [https://www.orcalean.com/article/15-manufacturing-challenges-in-2025]
- 60. 18 Challenges the Manufacturing Industry Faces in 2025 [https://www.netsuite.com/portal/resource/articles/erp/manufacturing-industry-challenges.shtml]
- 61. Facts About the Current Good Manufacturing Practice ... [https://www.fda.gov/drugs/pharmaceutical-quality-resources/facts-about-current-good-manufacturing-practice-cgmp]
- 62. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 63. Compliance in Manufacturing: The Ultimate Guide 2025 [https://springsapps.com/knowledge/compliance-in-manufacturing-the-ultimate-guide-2025]
- 64. Global regulatory considerations and practices for ... [https://pubmed.ncbi.nlm.nih.gov/39743127/]
- 65. Efficacy of tacrolimus and other immunosuppressants in ... [https://pubmed.ncbi.nlm.nih.gov/40599615/]
- 66. Analysis of short-term clinical efficacy and immune function ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1667205/full]
- 67. Comparative Safety of JAK Inhibitors vs TNF Antagonists in ... [https://pubmed.ncbi.nlm.nih.gov/40928778/]
- 68. Comparative Safety of JAK Inhibitors vs TNF Antagonists in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423869/]
- 69. Immunosuppressive therapy mitigates immunological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2529073/]
- 70. Immune Editing: Overcoming Immune Barriers in Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9643905/]
- 71. Recent advances in CAR-MSCs: the new engine of cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557984/]
- 72. PolTREG starts preclinical CAR-Treg development for ... [https://poltreg.com/poltreg-starts-preclinical-car-treg-development-for-neuroinflammatoryautoimmune-diseases/]
- 73. Risk factors and outcome of graft failure after HLA matched ... [https://pubmed.ncbi.nlm.nih.gov/26855158/]
- 74. HLA and Non-HLA Factors for Donor Selection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11674641/]
- 75. Tolerance Induction Strategies in Organ Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539449/]
- 76. Infectious Risk Following Allogeneic Hematopoietic Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5551893/]
- 77. a multicenter chart review | Bone Marrow Transplantation [https://www.nature.com/articles/s41409-022-01764-w]
- 78. Selection of Autologous or Allogeneic Transplantation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK12844/]