Overcoming Stem Cell Scalability Manufacturing Challenges: A 2025 Roadmap for Researchers and Developers
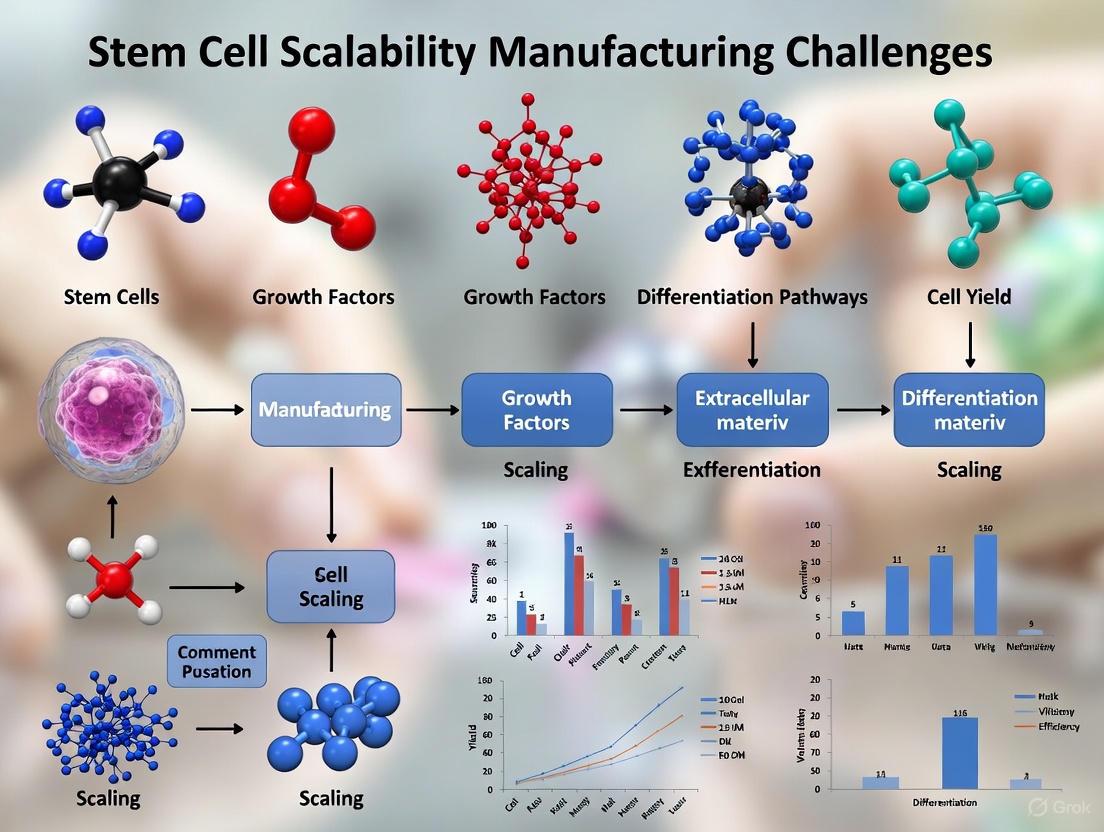
This article provides a comprehensive analysis of the critical challenges and innovative solutions in scaling up stem cell manufacturing for clinical and commercial applications.
Overcoming Stem Cell Scalability Manufacturing Challenges: A 2025 Roadmap for Researchers and Developers
Abstract
This article provides a comprehensive analysis of the critical challenges and innovative solutions in scaling up stem cell manufacturing for clinical and commercial applications. It explores the foundational biological and economic hurdles, details emerging methodologies in bioreactor technology and process automation, outlines strategies for troubleshooting quality control and regulatory compliance, and examines validation frameworks for commercial translation. Aimed at researchers, scientists, and drug development professionals, this review synthesizes current industry perspectives and technological advancements to guide the development of robust, scalable, and cost-effective manufacturing processes for stem cell-based therapies.
The Core Hurdles: Understanding the Biological and Economic Barriers to Scalable Stem Cell Production
The field of stem cell therapy stands at a pivotal crossroads, with remarkable clinical potential tempered by profound manufacturing challenges. As cell therapies advance through clinical trials toward commercialization, prohibitive production costs and complex manufacturing processes threaten to limit patient access and scalability. The global stem cell therapy market, projected to grow at a robust CAGR of 25.26% to reach approximately USD 4,777.4 million by 2034, faces a critical bottleneck: translating laboratory success into economically viable, large-scale production [1].
This manufacturing crisis manifests differently across the two primary therapeutic paradigms. Autologous therapies, which utilize a patient's own cells, offer personalized treatment but face scalability limitations due to their patient-specific nature. Allogeneic therapies, derived from donor cells, promise "off-the-shelf" availability but require massive scaling and sophisticated engineering to avoid immune rejection. Both pathways confront substantial hurdles in achieving the stringent quality standards, regulatory compliance, and economic sustainability necessary for widespread clinical adoption [2] [3].
Understanding the distinct cost drivers for each approach is essential for advancing the field. This technical support center provides researchers and drug development professionals with targeted troubleshooting guidance and analytical frameworks to navigate the complex economic landscape of stem cell therapy manufacturing.
Quantitative Analysis of Cost Drivers
The production costs for stem cell therapies are influenced by multiple interconnected factors that vary significantly between autologous and allogeneic approaches. The table below summarizes the primary cost components and their relative impact on each therapy type.
Table 1: Key Cost Drivers in Stem Cell Therapy Manufacturing
| Cost Component | Impact on Autologous Therapies | Impact on Allogeneic Therapies |
|---|---|---|
| Starting Material Acquisition | Variable patient-specific collection; multiple small batches | Standardized donor screening; large-volume procurement |
| Manufacturing Process | Labor-intensive, small-scale parallel processes | Capital-intensive bioreactor systems; scale-up optimization |
| Quality Control & Testing | Repeated batch-release testing for each patient | Extensive donor cell banking characterization; batch testing |
| Personnel & Expertise | Highly trained technicians for multiple parallel processes | Specialized engineers for bioreactor operation and process control |
| Facility & Equipment | Cleanroom space for multiple simultaneous batches | Large-scale bioreactors and downstream processing equipment |
| Regulatory Compliance | Complex tracking of patient-specific chain of identity | Rigorous characterization of master cell banks; safety studies |
The fundamental economic challenge lies in the inherent tension between personalized medicine and industrial scalability. Autologous therapies typically cost patients between $15,000 and $30,000 for expanded cell products, with higher prices for complex conditions [4]. These costs reflect the labor-intensive nature of manufacturing individual batches, each requiring separate quality validation, sterility testing, and release procedures.
For allogeneic therapies, while the "off-the-shelf" model promises better economics at scale, it requires substantial upfront investment in process development, donor screening, and the establishment of master cell banks that can cost millions of dollars before a single dose is produced [2] [5]. The emerging integration of automation and artificial intelligence offers promising pathways to reduce these costs by enhancing process consistency, predicting optimal culture parameters, and minimizing human intervention [2] [5].
Troubleshooting Guide: Manufacturing Cost Challenges
Frequently Asked Questions on Cost and Scalability
Table 2: Manufacturing Cost and Scalability FAQ
| Question | Expert Insight & Recommendations |
|---|---|
| Why does stem cell manufacturing remain so expensive despite technological advances? | High costs persist due to complex processes requiring specialized equipment, strict environmental controls, extensive quality control testing, and highly trained personnel. Manual, labor-intensive workflows further limit scalability and increase variability [2] [5]. |
| What are the key economic differences between autologous and allogeneic manufacturing? | Autologous therapies involve multiple small batches with repeated quality control, leading to high per-dose costs. Allogeneic requires massive upfront investment in donor screening and process development but offers lower marginal costs through large-scale production [2]. |
| How can automation address current cost challenges? | Automated systems and closed processing reduce manual intervention, minimize contamination risks, enhance process consistency, and enable higher throughput. This is particularly valuable for autologous therapies requiring multiple parallel processes [2] [5]. |
| What role does quality control play in overall costs? | QC can account for 20-30% of total costs. Each batch requires sterility, purity, potency, identity, and viability testing. For autologous therapies, this repeated per-patient testing creates significant economic burden without economies of scale [2] [3]. |
Troubleshooting High Production Costs
Problem: Inconsistent cell yields leading to batch failures and costly manufacturing losses.
Solution: Implement advanced process analytical technologies (PAT) and real-time monitoring systems to detect early deviations. Utilize design of experiment (DOE) approaches to identify critical process parameters and establish proven acceptable ranges for key culture conditions [3].
Prevention Strategy: Develop standardized protocols with clearly defined critical quality attributes (CQAs) and process parameters. Establish robust cell banking systems with comprehensive characterization to ensure starting material consistency [6] [7].
Problem: High labor costs associated with manual processing in cleanroom environments.
Solution: Transition to automated, closed-system bioreactor platforms that reduce manual manipulation and minimize contamination risk. Implement semi-automated systems for routine media exchanges and monitoring tasks [3] [5].
Prevention Strategy: Conduct thorough process mapping to identify automation opportunities. Invest in staff training for automated system operation and maintenance to maximize equipment utilization and efficiency [6].
Problem: Excessive quality control costs from repeated testing regimens.
Solution: Implement quality-by-design (QbD) principles to build quality into the process rather than testing it in the final product. Utilize in-line and at-line monitoring to reduce reliance on end-product testing [3].
Prevention Strategy: Develop platform approaches for similar product types to standardized testing regimens. Work with regulators to establish risk-based testing strategies that maintain safety while reducing redundant analyses [3].
Process Optimization and Workflow Diagrams
Scalable Manufacturing Workflow
The diagram below illustrates a streamlined workflow for scaling up stem cell manufacturing, integrating cost-saving technologies and approaches for both autologous and allogeneic production.
Scalable Manufacturing Pathways for Autologous and Allogeneic Therapies
Process Optimization Decision Framework
Researchers must navigate critical decision points when designing scalable, cost-effective manufacturing processes. The following framework outlines key considerations for process development.
Process Optimization Decision Framework for Cost-Effective Manufacturing
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful scale-up requires carefully selected reagents and materials that maintain cell quality while supporting manufacturing objectives. The table below outlines key solutions for stem cell manufacturing workflows.
Table 3: Essential Research Reagent Solutions for Stem Cell Manufacturing
| Reagent Category | Key Function | Scale-Up Considerations |
|---|---|---|
| Chemically Defined Media | Supports consistent cell growth and maintenance without variable components | Enables standardized manufacturing; fed-batch formulations reduce media consumption in large-scale cultures [6] |
| 3D Culture Matrices | Provides structural support for cell growth in suspension systems | Facilitates transition to bioreactor systems; critical for high-density 3D culture applications [8] [6] |
| Cell Dissociation Reagents | Enables gentle cell passaging and harvesting with high viability | Optimized formulations maintain cell functionality during scale-up; automation-compatible for high-throughput systems [9] [10] |
| Cryopreservation Solutions | Maintains cell viability and functionality during long-term storage | Critical for cell banking; specialized formulations enhance recovery post-thaw, reducing cell loss costs [7] |
| Quality Control Assays | Monitors critical quality attributes throughout manufacturing | Platform approaches reduce testing costs; in-process assays enable real-time decision making [3] [7] |
The journey toward economically sustainable stem cell manufacturing requires coordinated advances across multiple fronts. Strategic integration of automation platforms, artificial intelligence for process optimization, and quality-by-design principles represents the most promising pathway to reduce costs while maintaining product quality and safety [2] [5].
For autologous therapies, the development of standardized, closed automated systems that can process multiple patient-specific batches in parallel is essential for improving efficiency. For allogeneic approaches, advancing high-density bioreactor technologies and optimizing cryopreservation methods will enable the true "off-the-shelf" potential of these therapies [3] [6].
The future of stem cell manufacturing will likely see convergence between these approaches, with hybrid models emerging that leverage the economic advantages of allogeneic platforms while maintaining the personalized benefits of autologous approaches. Through continued innovation in process development, analytical methods, and regulatory science, the field can overcome current cost barriers and fulfill the promise of regenerative medicine for broader patient populations.
Technical Support Center
This technical support center provides targeted guidance for researchers addressing the critical challenge of biological variability in stem cell manufacturing. The following troubleshooting guides, FAQs, and structured protocols are designed to help you mitigate the impact of donor and starting material inconsistency on your process robustness and final product quality.
Troubleshooting Guides
Troubleshooting Excessive Differentiation in hPSC Cultures
Problem: Excessive differentiation (>20%) in human pluripotent stem cell (hPSC) cultures.
| Potential Cause | Recommended Action | Rationale & Additional Context |
|---|---|---|
| Old or degraded culture medium | Ensure complete medium kept at 2-8°C is less than 2 weeks old [9]. | Culture medium stability is critical for consistent performance. |
| Over-manipulation of cultures | Avoid having the culture plate out of the incubator for more than 15 minutes at a time [9]. | Environmental fluctuations stress cells and can induce differentiation. |
| Suboptimal colony size and density | Passage cultures when colonies are large and compact; avoid overgrowth. Decrease colony density by plating fewer cell aggregates [9]. | Over-confluence is a common trigger for spontaneous differentiation. |
| Inconsistent cell aggregate size | Ensure cell aggregates generated after passaging are evenly sized [9]. | Uniform aggregate size ensures consistent growth and differentiation signals. |
| Oversensitivity to passaging reagents | Reduce incubation time with passaging reagents (e.g., ReLeSR) [9]. | Cell lines can exhibit variable sensitivity to enzymatic or chemical dissociation. |
Troubleshooting Low Cell Recovery and Viability Post-Cryopreservation
Problem: Low cell recovery or viability after thawing starting material or final product.
| Potential Cause | Recommended Action | Rationale & Additional Context |
|---|---|---|
| Suboptimal thawing technique | Thaw cells quickly (≤2 mins at 37°C). Do not thaw cells directly in medium; instead, transfer to a tube first, then add pre-warmed medium drop-wise while swirling [10]. | Rapid, controlled dilution minimizes osmotic shock, which is critical for fragile primary and stem cells. |
| Incorrect cryopreservation medium | Use specialized, serum-free cryopreservation media (e.g., CryoStor CS10) instead of standard DMSO-containing media [11]. | Formulated cryomedia provide superior protection and enhance post-thaw recovery and function. |
| Insufficient or excessive cell concentration | Count cell viability with trypan blue after thawing. Seed at recommended density (e.g., >1x10^5 viable cells/cm² for H9-derived NSCs) [10]. | Seeding at improper densities impedes recovery and expansion. |
| Transient warming events during storage | Monitor and control storage conditions; minimize cumulative impact of transient warming events [12]. | Temperature fluctuations during storage degrade product quality even in nominally frozen conditions. |
| Incorrect analysis | Characterize cells post-thaw, accounting for cells lost to lysis [12]. | Standard viability assays may not capture full functional competence. |
Frequently Asked Questions (FAQs)
Donor and Starting Material
Q1: Why does my manufacturing success rate vary significantly between different donor samples?
The donor is the primary driver of variability in cell manufacturing processes. The mononuclear cell product will always be a direct reflection of the cell populations circulating in the donor at the time of collection [12]. Key factors include:
- Clinical Indication: Patients with different diseases have vastly different starting blood counts (e.g., chronic lymphocytic leukemia vs. lymphoma) [12].
- Prior Treatment: Years of cytotoxic chemotherapy can lead to a T-cell population that is suboptimal for expansion [12].
- Donor Demographics: Age, genetics, and health status contribute to inherent biological variability [12].
Q2: What are the risks of developing therapies using only healthy donor material?
Relying solely on healthy donor material introduces substantial risks for clinical translation [13]:
- Faulty Preclinical Data: Healthy cells may not accurately reflect disease-specific mechanisms, leading to inaccurate predictions of therapeutic efficacy and safety [13].
- Manufacturing Failures: Processes optimized for robust healthy cells might prove ineffective or damaging for more fragile diseased cells, leading to low yields and high variability [13].
- Clinical Failure: Therapies showing promise in healthy models may fail in patients, as diseased cells can respond differently, leading to unforeseen adverse events [13].
Q3: How can I extend the shelf-life and stability of my starting material to gain manufacturing flexibility?
While fresh material is ideal, its quality declines immediately post-collection. Two primary methods can extend stability [11]:
- Hypothermic Storage: Using specialized storage media (e.g., HypoThermosol) at 2-8°C can maintain viable cell recovery and function for up to 48 hours post-collection [11].
- Cryopreservation: Freezing starting material (e.g., in CryoStor CS10) is the best method for long-term stability (beyond 96 hours) and enables simplified, "level-loaded" manufacturing scheduling rather than on-demand processing [11].
Process and Manufacturing
Q4: My process performs well at a small scale but becomes variable and inefficient when scaled up. What could be wrong?
Scaling a process that was not optimized for robustness early in development often leads to substandard reproducibility. Variability can occur at multiple levels [14]:
- Raw Materials: Media and reagent variations can cause differences in titer and critical quality attributes (CQAs) [14].
- Equipment Transition: Cell behavior can change when moving from 2D flasks to 3D bioreactors, affecting transfection efficacy and cell quality [14].
- Process Parameters: Critical process parameters (CPPs) that were easy to control in small-scale equipment may be harder to manage consistently at larger scales [14].
Q5: How can I make my bioprocess more robust against inherent biological variability?
Implementing a systematic approach is key to improving robustness [15]:
- Adopt QbD Principles: Use Quality-by-Design (QbD) and Design of Experiments (DoE) to identify and control critical process parameters [15] [14].
- Leverage Advanced Monitoring: Integrate advanced sensors and AI-driven models to dynamically track CQAs and predict culture trajectories, allowing for proactive interventions [16].
- Standardize and Automate: Use standardized automated methods to overcome inter- and intra-observer variation in assays and cell culture handling [12].
Protocol: Evaluating Preservation Methods for Leukapheresis Starting Material
This protocol, based on collaborative studies, outlines how to compare hypothermic storage versus cryopreservation for extending the shelf-life of donor-derived leukapheresis products [11].
1. Objective: To assess the impact of different preservation methods and storage durations on the viability, recovery, and function of leukapheresis starting material.
2. Materials:
- Donor leukapheresis product
- HypoThermosol storage medium
- CryoStor CS10 cryopreservation medium
- Controlled-rate freezer
- Liquid nitrogen storage vapor
- Cell culture reagents for functional assays (e.g., for CD14+ cell function)
- Flow cytometry equipment and antibodies (e.g., for CD14, CD3, CD45RA, CCR7)
3. Methodology:
- Collection & Splitting: Following leukapheresis collection, process the product and split it into multiple, identical aliquots.
- Preservation Conditions:
- Condition A (Hypothermic): Mix leukapheresis product with HypoThermosol at a 1:1 ratio. Hold at 2-8°C [11].
- Condition B (Cryopreserved): Mix leukapheresis product with CryoStor CS10 at a 1:1 ratio. Freeze using a controlled-rate freezer and store in liquid nitrogen vapor [11].
- Condition C (Unmanipulated Control): Hold a portion of the leukapheresis product at 2-8°C without any additive [11].
- Time-Point Analysis: At predetermined time points (e.g., 0, 24, 48, 96, 120 hours), thaw cryopreserved samples and analyze all conditions in parallel.
- Key Assessments:
- Viable Cell Recovery: Use trypan blue exclusion and cell counting.
- Cell-Specific Recovery & Viability: Use flow cytometry to analyze specific cell populations (e.g., WBC, CD14+ monocytes, CD3+ T cells).
- Cell Function: Perform functional assays relevant to the cell type (e.g., monocyte function assays).
- Phenotypic Markers: Analyze markers of cell state, such as T cell naivety (CD45RA+/CCR7+) [11].
4. Data Analysis: Compare the recovery, viability, and function across the different preservation conditions and over time to determine the optimal storage method for your specific downstream manufacturing process.
The table below summarizes typical outcomes from the protocol above, illustrating the trade-offs between different preservation strategies [11].
| Preservation Method & Condition | Storage Temp | Viable WBC Recovery (at 48-96h) | Key Functional/Phenotypic Notes | Ideal Use Case |
|---|---|---|---|---|
| Unmanipulated Leukapheresis | 2-8°C | Dramatic decrease after 48 hours | T cell naivety ~50-60% at 96h | Manufacturing within 48h of collection |
| Hypothermic (HypoThermosol) | 2-8°C | 78-94% (similar to cryo at 24h) | CD14+ cell function maintained | Short-term stability (up to 48-72h); maintains function |
| Cryopreserved (CryoStor CS10) | ≤-135°C | Stable over 120h | T cell naivety reduced to ~30% | Long-term storage; geo-graphical separation; scheduling flexibility |
Experimental Workflow for Evaluating Starting Material Preservation
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and their functions for managing variability in stem cell and cell therapy processes.
| Item | Function & Application | Key Consideration |
|---|---|---|
| Specialized Cryopreservation Media (e.g., CryoStor) | Serum-free, formulated media designed to minimize freezing-induced cell damage and improve post-thaw recovery and function [11]. | Superior to homemade DMSO/serum mixes; provides consistent, xeno-free composition for clinical applications. |
| Hypothermic Storage Media (e.g., HypoThermosol) | An optimized solution for the short-term (2-8°C) storage and shipment of cells, designed to slow metabolism and support viability better than saline or plasma [11]. | Extends the viable shelf-life of starting materials, providing a buffer for logistical delays. |
| Rock Inhibitor (Y-27632) | A small molecule that significantly improves the survival of human pluripotent stem cells (hPSCs) after single-cell passaging and thawing from cryopreservation [10]. | Critical for preventing anoikis; use at time of passaging or post-thaw for challenging cell lines. |
| Defined, Feeder-Free Culture Systems (e.g., mTeSR, Essential 8) | Chemically defined, xeno-free media and matrix combinations that support the robust growth of hPSCs without feeder cells, reducing variability [9] [10]. | Essential for standardizing the culture environment and minimizing introduction of undefined components. |
| GMP-Grade Cell Separation Reagents | Reagents (e.g., for Ficoll density gradient, CD3+ selection) that are manufactured under Good Manufacturing Practice for clinical-grade cell processing [12]. | Availability of GMP-grade reagents for cell enrichment is currently limited but crucial for clinical translation. |
Logical Flow for Managing Donor Variability
Troubleshooting Guide: 3D Suspension Culture
This guide addresses common challenges researchers face when transitioning from 2D planar cultures to 3D suspension systems for scaling stem cell production.
Problem 1: Poor Cell Viability and Growth in 3D Suspension
- Symptoms: Slow or no cell growth, excessive cell debris, low viability post-passaging.
- Potential Causes and Solutions:
- Cause: Inoculation density is too low. Suspension cells are density-dependent and state is better at high density [17].
- Solution: Ensure routine inoculation density is maintained at 3-5×10⁵ cells/mL. When cells are in poor condition, passage via replenishment or half-medium exchange to avoid centrifugation cell loss [17].
- Cause: Excessive shear stress from agitation damaging delicate cells [18] [19].
- Solution: Optimize agitation speed and impeller design; use gentle rocking platforms for shear-sensitive cells. Supplement media with surfactants like Pluronic F-68 to protect cells [18] [19].
- Cause: Cells are undergoing an adaptation phase after transition from 2D [20].
- Solution: Monitor key metrics. In mTeSR 3D, some cell lines show lower expansion for 1-2 passages but should fully adapt by passage three. Use TeSR-AOF 3D medium which may not require an adaptation phase [20].
Problem 2: Excessive Cell Aggregation or Clumping
- Symptoms: Cells form large, irregular clumps instead of well-defined aggregates; necrotic centers may develop in large clumps.
- Potential Causes and Solutions:
- Cause: Normal characteristic for some cell lines (e.g., NK92, JURKAT grow in clusters) [17].
- Solution: For cells that naturally grow in clusters, avoid frequent blowing of aggregates. When density increases and state improves, cells may disperse naturally [17].
- Cause: Suboptimal culture conditions or serum quality [17].
- Solution: Rest cultures (less operation/observation). For low cell density clumping, add serum (5%). If all cells clump unexpectedly, consider testing different serum brands [17].
- Cause: Aggregation leads to necrotic core formation due to diffusion limitations [21] [20].
- Solution: Control aggregate size by optimizing passaging techniques and agitation rates. For hPSCs, target aggregate size of 50-200 μm [9] [20].
Problem 3: Unintended Differentiation in hPSC 3D Cultures
- Symptoms: Loss of pluripotency markers, spontaneous differentiation despite using growth media.
- Potential Causes and Solutions:
- Cause: Suboptimal aggregate size or culture conditions [22] [9].
- Solution: Ensure cell aggregates generated after passaging are evenly sized. Remove differentiated areas prior to passaging. Do not allow cultures to overgrow [9].
- Cause: Mechanical forces in bioreactors causing epigenetic changes [22].
- Solution: Use specialized bioreactors like PBS-MINI designed for shear-sensitive hPSCs. Monitor pluripotency markers (OCT4, TRA-1-60) every 5 passages [22] [20].
- Cause: Old or suboptimal culture medium [9].
- Solution: Use fresh complete cell culture medium (less than 2 weeks old when stored at 2-8°C). Avoid having culture vessels out of incubator for more than 15 minutes [9].
Problem 4: Challenges in Monitoring and Characterization
- Symptoms: Difficulty assessing cell density, viability, and differentiation status in 3D aggregates.
- Potential Causes and Solutions:
- Cause: Traditional sampling techniques ineffective in 3D systems [22].
- Solution: For counting clumpy suspensions, use automated counters like NucleoCounter NC-250 with lysis protocols to obtain total and viable cell counts. Alternatively, use clump counting with consistent clump sizes [20].
- Cause: Limited visualization and microscopy in 3D structures [23].
- Solution: Implement regular sampling with dissociation for flow cytometry analysis. Use systems designed for easy microscopy like OrganoPlates [23] [20].
Frequently Asked Questions (FAQs)
Q1: What are the key advantages of 3D suspension culture over 2D for large-scale production?
A: 3D suspension culture offers several critical advantages for scale-up:
- Enhanced Scalability: Enables large-scale production in bioreactors, overcoming surface area limitations of 2D systems [20].
- Efficiency: Fed-batch workflows minimize labor and media costs while preventing aggregate loss [20].
- Matrix Elimination: Reduces reliance on expensive extracellular matrices required for 2D cultures [20].
- Homogeneity: Provides more homogeneous cell population compared to adherent cultures [18].
- Physiological Relevance: Better mimics in vivo conditions with enhanced cell-cell interactions and tissue-like structures [21] [23].
Q2: How long does adaptation take when transitioning hPSCs from 2D to 3D suspension culture?
A: Adaptation time depends on cell line, medium, and culture conditions:
- With TeSR-AOF 3D medium, little to no adaptation phase may be needed [20].
- In mTeSR 3D, some cell lines experience lower expansion during first 1-2 passages but typically fully adapt by passage 3 [20].
- Monitor key quality attributes including aggregate morphology, viability, and expansion at each passage to gauge adaptation success [20].
Q3: Can we cryopreserve and recover hPSCs directly in 3D suspension culture?
A: Yes, cryopreserved hPSCs can be thawed directly into 3D suspension culture, bypassing 2D expansion [20]. For optimal recovery:
- Freeze clumps generated from 3D hPSC cultures using CryoStor CS10 [20].
- Use a 70-micron reversible strainer instead of 37-micron to maintain slightly larger clumps, improving post-thaw viability [20].
Q4: How do we prevent necrotic core formation in 3D aggregates?
A: Necrotic cores form due to diffusion limitations in large aggregates. Prevention strategies include:
- Controlling aggregate size through optimal passaging and agitation [20].
- Ensuring adequate oxygen and nutrient exchange through proper bioreactor design and mixing [18].
- Monitoring aggregate morphology and adjusting culture parameters when "pockmarking" appears [20].
Q5: What bioreactors are most effective for sensitive hPSCs in 3D suspension?
A: hPSCs are highly shear-sensitive. The most reproducible results have been observed with:
- Nalgene Storage Bottles (15-60 mL scale) [20].
- PBS-MINI Bioreactors (100-500 mL scale) [20].
- For cultures larger than 500 mL, further optimization is ongoing [20].
Quantitative Data Comparison: 2D vs 3D Culture Systems
Table 1: Performance Metrics for Scalable Culture Systems
| Parameter | Traditional 2D | 3D Suspension (Microcarrier) | 3D Spheroid/Aggregate |
|---|---|---|---|
| Max Scale Achievable | Limited by surface area (multilayer stacks, roller bottles) [22] | High (bioreactors with microcarriers) [22] | High (suspension bioreactors) [20] |
| Relative Cell Yield per Volume | Low (surface area-limited) [22] | High (increased volumetric density) [22] | High (3D structure enables density) [20] |
| Labor Intensity | High (multiple vessels, manual handling) [22] | Moderate (automation possible) [18] | Low (fed-batch workflows) [20] |
| Media Consumption | Higher per cell [23] | Optimized [18] | Efficient (fed-batch approach) [20] |
| Physiological Relevance | Low (monolayer, unnatural polarization) [21] [23] | Moderate (3D environment) [21] | High (tissue-like structures) [23] [24] |
| Shear Stress Sensitivity | Low (static culture) [19] | High (agitation required) [18] [19] | Moderate (aggregates more resilient) [20] |
| Typical hPSC Expansion (Daily Fold) | Variable [20] | 1.4-2.0 [20] | 1.4-2.0 [20] |
Table 2: Troubleshooting 3D Culture Parameters
| Problem | Critical Parameters to Monitor | Optimal Range/Target |
|---|---|---|
| Poor Cell Growth | Inoculation density [17] | 3-5×10⁵ cells/mL [17] |
| Excessive Aggregation | Aggregate size [9] | 50-200 μm for hPSCs [9] |
| Unintended Differentiation | Pluripotency markers [20] | OCT4, TRA-1-60 (regular monitoring) [20] |
| Necrotic Core Formation | Aggregate size & morphology [20] | Uniform aggregates, avoid oversized clusters [20] |
| Low Post-Thaw Viability | Cryopreservation clump size [20] | Use 70-micron strainer for larger clumps [20] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for 3D Suspension Culture
| Reagent/Product | Function | Application Notes |
|---|---|---|
| TeSR-AOF 3D Medium | Animal-origin free media for fed-batch 3D culture [20] | Provides most consistent expansion across passages; enhanced viral safety [20] |
| mTeSR 3D Medium | First media enabling fed-batch workflows [20] | Saves time and media with daily feeds; no medium exchanges on non-passaging days [20] |
| Gentle Cell Dissociation Reagent (GCDR) | Non-enzymatic dissociation for aggregate breakdown [20] | For single-cell passaging: longer incubation (10-15 min at 37°C) with trituration [20] |
| CryoStor CS10 | Cryopreservation medium for 3D cultures [20] | Preserves viability when freezing clumps from 3D hPSC cultures [20] |
| Extracellular Matrices (ECMs) | Hydrogels providing 3D scaffolding [23] | Collagen, laminin, fibrin; provides microenvironment for morphogenesis [24] |
| Microcarriers | Beads providing growth substrate in suspension [19] | Enables adherent cells to grow in suspension bioreactors [19] |
| Anti-Clumping Agents | Supplements to reduce cell aggregation [18] | Pluronic F-68 protects against shear stress [18] |
Experimental Protocols
Protocol 1: Transitioning hPSC Differentiation from 2D to 3D Suspension Culture
Purpose: Adapt existing 2D differentiation protocols to 3D suspension systems for scalable production.
Workflow Overview:
Step-by-Step Methodology:
Confirm High-Quality hPSCs Before Differentiation
- Expand hPSCs in TeSR-AOF 3D for at least two passages
- Assess key quality metrics: aggregate morphology, marker expression (OCT4, TRA-1-60), and genetic stability [20]
Validate the Standard 2D Differentiation Protocol
- Use existing STEMdiff kits or established protocols
- Confirm differentiation efficiency in 2D culture first - if it doesn't work in 2D, it likely won't work in 3D [20]
Develop Reproducible 3D hPSC Culture Techniques
- Master aggregate formation, media change techniques, and passaging before differentiation
- Utilize resources like 3D hPSC On-Demand Courses and technical manuals [20]
Optimize Differentiation at Small Scale
- Begin with 6-well plates on an orbital shaker
- Optimize key parameters: media change strategy, differentiation timing, and seeding density [20]
Scale Up in Bioreactors
- Progress to Nalgene Storage Bottles (15-60 mL) then PBS-MINI Bioreactors (100-500 mL)
- Monitor differentiation efficiency through marker expression and yield
- Optimize agitation rates and media exchange protocols [20]
Protocol 2: Assessing Pluripotency in 3D hPSC Aggregates
Purpose: Regularly monitor stem cell quality and prevent spontaneous differentiation during 3D culture.
Key Assessment Metrics:
Monitoring Framework:
- At Each Passage: Assess expansion and viability. Expected daily fold expansion ranges from 1.4 to 2 - deviations may indicate suboptimal conditions [20].
- Daily Monitoring: Evaluate aggregate morphology. "Pockmarking" often correlates with undifferentiated hPSC marker expression [20].
- Every 5 Passages: Dissociate aggregates for flow cytometry analysis of undifferentiated hPSC markers (OCT4, TRA-1-60) [20].
- Every 5-10 Passages: Assess genetic stability and functional pluripotency using trilineage differentiation kits [20].
Technical Diagrams
3D Culture System Decision Framework
This technical support resource provides stem cell researchers and bioproduction professionals with practical guidance for overcoming the scalability bottleneck through implementation of 3D suspension culture systems. The contained troubleshooting guides, FAQs, and protocols address the most common challenges encountered when transitioning from 2D to 3D systems for large-scale manufacturing applications.
Troubleshooting Guides
This section addresses common challenges in scaling up stem cell manufacturing and provides evidence-based corrective actions to protect critical quality attributes (CQAs).
Guide 1: Troubleshooting Loss of Cell Potency During Bioreactor Scale-Up
Problem: A significant drop in cell differentiation potential and therapeutic functionality is observed when transitioning from 2D flask cultures to 3D bioreactor systems.
| Observation | Potential Root Cause | Corrective Action |
|---|---|---|
| Reduced differentiation to osteoblasts, adipocytes, and chondroblasts [25] | Suboptimal dissolved oxygen (DO) levels [25] | Implement DO control strategies and establish a proven acceptable range for your cell line. |
| Decreased expression of key immunophenotype markers (CD105, CD73, CD90) [25] | Inadequate nutrient supply or waste product accumulation [25] | Monitor key metabolites (e.g., glucose, lactate) and establish feeding schedules or perfusion rates. |
| High cell viability but low in vivo efficacy | Inconsistent microcarrier colonization in agitated systems | Optimize inoculation strategy and agitation parameters to minimize shear stress while ensuring uniform cell distribution. |
| Increased batch-to-batch variability | Uncontrolled physiochemical properties (e.g., pH shifts) [25] | Tighten process controls on pH and temperature; define acceptable operating ranges for all critical process parameters (CPPs). |
Guide 2: Addressing Product Variability and Contamination Risks
Problem: Inconsistent cell product quality and safety between manufacturing batches, including failed safety tests.
| Observation | Potential Root Cause | Corrective Action |
|---|---|---|
| Positive sterility test (bacterial, fungal, mycoplasma) [26] | Compromised aseptic processing during manual operations [26] | Implement closed-system processing and automated bioreactors where possible; validate aseptic techniques with media fills [26]. |
| Detection of endotoxin [26] | Contaminated raw materials or reagents | Source GMP-grade reagents and establish rigorous quality control testing for all incoming materials [26]. |
| Karyotype abnormalities after successive cultures [26] | Genetic instability due to prolonged expansion [26] | Establish a maximum in vitro cell age limit; perform regular karyotype and genetic stability testing [26]. |
| Failed tumorigenicity assays (e.g., positive in soft agar) [26] | Presence of residual undifferentiated cells or transformed cells [26] | Improve purification processes; employ more sensitive tumorigenicity assays like digital soft agar or cell proliferation characterization tests [26]. |
Frequently Asked Questions (FAQs)
Q1: What are the minimal quality attributes that must be tested for a mesenchymal stem cell (MSC) product before release? According to the International Society for Cell & Gene Therapy (ISCT), the minimal criteria include plastic adherence, positive expression of CD105, CD73, and CD90, lack of expression of hematopoietic markers (CD45, CD34, etc.), and the ability to differentiate into osteoblasts, adipocytes, and chondroblasts in vitro [25]. Cell count and viability are also ubiquitously measured as they define the product dosage [25].
Q2: How can we ensure our scaled-up manufacturing process is compliant with regulatory standards? A Quality-by-Design (QbD) approach is recommended [25]. Begin by defining a Quality Target Product Profile (QTPP). Use this to identify your product's CQAs. Then, systematically evaluate your production process to define the Critical Process Parameters (CPPs) that control these CQAs. This risk-based framework, detailed in ICH Q8, is recognized by regulators like the EMA and FDA [25].
Q3: What are the major challenges when translating a research-scale process to GMP-compliant manufacturing? Key challenges include ensuring a reliable supply of GMP-grade raw materials, managing donor-to-donor variability, developing scalable cell expansion protocols that maintain phenotype, and adapting facilities to meet GMP requirements for contamination control. A critical step is process validation to ensure consistent product quality, safety, and efficacy [26].
Q4: What advanced technologies can help overcome scaling challenges for Advanced Therapy Medicinal Products (ATMPs)? Novel technologies such as automated closed-system bioreactors, organoids for more accurate disease modeling, and artificial intelligence (AI) for improved process monitoring and data management are being explored to enhance the consistency, scalability, and precision of ATMP production [26].
| CQA Category | Specific Attribute | Standard Analytical Method | Typical Target / Acceptance Criterion |
|---|---|---|---|
| Dosage & Viability | Total Cell Number | Automated cell counter / Hemocytometer | Defined by dose; >70-90% viability (product-specific) |
| Cell Viability | Trypan blue exclusion / Flow cytometry | ||
| Identity / Potency | Immunophenotype (Positive) | Flow Cytometry | ≥ 95% positive for CD105, CD73, CD90 |
| Immunophenotype (Negative) | Flow Cytometry | ≤ 2% positive for CD45, CD34, etc. | |
| Differentiation Potential | In vitro trilineage differentiation (Staining, qPCR) | Demonstrated differentiation into fat, bone, and cartilage | |
| Product Quality | Genetic Stability | Karyotype analysis / SNP array | No major abnormalities detected |
| Sterility | Sterility test (e.g., BacT/ALERT) | No growth of aerobic/anaerobic bacteria, fungi | |
| Endotoxin | LAL test | Below specified limit (e.g., <5.0 EU/kg/hr) |
| Critical Process Parameter (CPP) | Related Unit Operation | Impact on Critical Quality Attributes (CQAs) |
|---|---|---|
| Dissolved Oxygen (DO) | Bioreactor Cultivation | Affects cell growth, metabolism, differentiation potential, and overall potency [25]. |
| pH Level | Bioreactor Cultivation | Impacts cell health, viability, and growth rate; shifts can indicate metabolic changes [25]. |
| Agitation Speed | Bioreactor Cultivation | Influences cell attachment to microcarriers, nutrient distribution, and shear stress (which can damage cells). |
| Nutrient & Metabolite Levels | Media Formulation & Feeding | Glucose, glutamine, lactate levels directly affect volumetric productivity, cell growth, and viability [25]. |
| Cell Source & Donor | Cell Isolation | A primary source of biological variability impacting growth rate, potency, and functionality [25]. |
Experimental Protocols
Protocol 1: In Vitro Trilineage Differentiation Potency Assay for MSCs
Objective: To confirm the differentiation capacity of manufactured MSCs into adipocytes (fat), osteoblasts (bone), and chondroblasts (cartilage) as a key potency assay [25].
Materials:
- Cells: Human MSCs at passage number P3-P5.
- Media: Commercial, standardized differentiation kits for adipogenesis, osteogenesis, and chondrogenesis are recommended.
- Staining Reagents:
- Adipogenesis: Oil Red O stain for lipid droplets.
- Osteogenesis: Alizarin Red S stain for calcium deposits.
- Chondrogenesis: Alcian Blue stain for sulfated proteoglycans.
- Equipment: 6-well and 24-well tissue culture plates, centrifuge, CO₂ incubator, microscope.
Methodology:
- Cell Seeding:
- Adipogenic/Osteogenic Differentiation: Seed MSCs at a defined density (e.g., 2.1x10⁴ cells/cm²) in 6-well plates in standard growth media. Allow cells to reach 100% confluence. Change to differentiation media 24 hours post-confluence.
- Chondrogenic Differentiation: Pellet 2.5x10⁵ MSCs in a 15mL conical tube. Culture the pellet in chondrogenic differentiation media.
- Differentiation:
- Maintain cultures for 14-21 days, changing the differentiation media every 2-3 days.
- Include control groups cultured in standard growth media for each lineage.
- Staining and Analysis:
- At endpoint, wash cells/pellets with PBS and fix with 4% paraformaldehyde.
- Perform lineage-specific staining:
- Adipocytes: Stain with Oil Red O and counterstain with Hematoxylin. Red lipid vacuoles confirm differentiation.
- Osteoblasts: Stain with Alizarin Red S. Red-orange mineralized matrix confirms differentiation.
- Chondrocytes: Embed pellets in paraffin, section, and stain with Alcian Blue. Blue-stained extracellular matrix confirms differentiation.
- Documentation: Image stained cultures under a brightfield microscope. A successful assay shows clear positive staining in differentiation groups compared to controls.
Protocol 2: Monitoring Process Parameters in a Stirred-Tank Bioreactor
Objective: To monitor and control key process parameters during MSC expansion in a bioreactor to ensure consistent product quality.
Materials:
- Bioreactor System: Stirred-tank bioreactor with control unit.
- Sensors: Pre-calibrated pH and dissolved oxygen (DO) probes.
- Media: Serum-free or xeno-free cell culture media.
- Cells & Carriers: Human MSCs and compatible microcarriers.
- Analytical Tools: Bioanalyzer or blood gas analyzer for metabolite testing.
Methodology:
- Bioreactor Setup & Calibration: Assemble the bioreactor vessel and sterilize (e.g., by autoclaving). Calibrate the pH and DO probes according to the manufacturer's instructions.
- Parameter Setpoints: Define and set the acceptable ranges for CPPs based on prior development data. Common setpoints include:
- pH: Typically 7.2 - 7.4
- Dissolved Oxygen (DO): Often 20-50% air saturation
- Temperature: 37°C
- Agitation Speed: Speed must be sufficient to keep microcarriers in suspension without causing excessive shear stress (e.g., 50-100 rpm).
- Process Monitoring:
- Real-time: The control system should log pH, DO, and temperature data continuously.
- Off-line Sampling: Take daily samples to count cells and assess viability (e.g., with trypan blue). Measure metabolite concentrations (glucose, lactate, glutamine) to understand nutrient consumption and waste accumulation.
- Process Control: Use the controller to automatically adjust gas flow rates (O₂, N₂, CO₂) to maintain pH and DO within their set ranges. Adjust feeding strategies based on metabolite data.
Workflow and Pathway Diagrams
Diagram Title: QbD Framework for Process Development
Diagram Title: MSC Manufacturing Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material / Reagent | Function in MSC Manufacturing |
|---|---|
| GMP-grade Culture Media | Provides nutrients and growth factors for cell expansion. Using standardized, GMP-grade media reduces batch-to-batch variability and supports regulatory compliance [26]. |
| Microcarriers | Provides a high-surface-area scaffold for adherent MSCs to grow on in 3D bioreactor systems, enabling scalable expansion. |
| Characterized Cell Banks | A well-characterized Master Cell Bank (MCB) ensures a consistent and reliable starting material, reducing variability caused by the cell source [25]. |
| Flow Cytometry Antibody Panels | Kits containing fluorescently-labeled antibodies against positive (CD105, CD73, CD90) and negative (CD45, CD34) markers to confirm MSC immunophenotype identity [25]. |
| Trilineage Differentiation Kits | Standardized, off-the-shelf kits containing optimized media and reagents for performing adipogenic, osteogenic, and chondrogenic differentiation assays to assess cell potency [25]. |
| Closed-System Bioprocess Containers | Single-use bags and tubing sets for fluid transfer and cell culture that minimize the risk of contamination during manufacturing, supporting aseptic processing [26]. |
Technical Support Center: Cold Chain Management for Advanced Therapies
Frequently Asked Questions (FAQs)
Q1: What are the most critical points for temperature monitoring in a stem cell product's journey? The most critical points are during cross-docking, last-mile delivery, and loading/unloading, where products are most vulnerable to temperature excursions [27]. Real-time monitoring with IoT sensors at these stages allows for immediate corrective action.
Q2: Our facility faces frequent power outages. How can we ensure the integrity of cryogenically stored cell therapies? Implement redundant systems and contingency protocols [27]. This includes backup power generators (e.g., UPS systems) and backup transport plans. For long-term storage in off-grid areas, investing in liquid nitrogen dry shippers that can maintain temperatures below -150°C for extended periods without external power is recommended [28].
Q3: What is the primary regulatory challenge when scaling out a manufacturing process to a new location? The most critical challenge is demonstrating product comparability after the manufacturing process change [26]. Regulatory authorities like the FDA and EMA require a risk-based comparability assessment, extended analytical characterization, and staged testing to ensure that the change does not impact the product's critical quality attributes (CQAs), safety, or efficacy.
Q4: How can we improve supply chain resilience for critical single-source reagents? For reagents facing shortages, such as Hespan in cord blood processing, a dual strategy is effective [29]. Short-term, establish "good-neighbor" agreements with other facilities to share available lots. Long-term, qualify alternative international vendors or supplement approved procedures to include a method that does not use the scarce reagent, though this requires a demonstration of product comparability.
Q5: What logistical model can help extend the reach of cell and gene therapies to remote clinics? The hub and spoke model is a promising framework [30]. In this model, a central, well-resourced facility (the hub) handles complex manufacturing and storage, while smaller, local health facilities (spokes) manage patient identification, cell collection, and final product administration. This model is scalable, efficient, and adaptable to different regional needs.
Troubleshooting Guides
Guide 1: Addressing Temperature Excursions During Transport
Problem: A temperature tracker alert indicates a cryogenic shipment of CAR-T cells has experienced a temperature rise above the -150°C threshold for 15 minutes.
Immediate Actions:
- Isolate the Shipment: Upon receipt, do not mix the affected shipment with other inventory. Move it to a designated quarantine area in the cryogenic storage unit [27].
- Document Everything: Record the IoT sensor data, including the exact duration and magnitude of the temperature deviation. Note the external conditions and any potential causes noted by the logistics provider [27].
- Assess Product Impact: Consult pre-defined stability data for the product. The quality control unit must review the deviation against validated stability parameters to determine if the product's critical quality attributes (CQAs) are likely compromised [26].
Corrective and Preventive Actions (CAPA):
- Investigate Root Cause: Was the excursion due to equipment failure (e.g., liquid nitrogen tank issue), prolonged handling during transfer, or a transport delay?
- Review Packaging: Evaluate the integrity of the dry shipper and the remaining liquid nitrogen volume. Consider using advanced thermal packaging with phase-change materials for better thermal buffering [27].
- Optimize Routing: Use AI-driven route planning to minimize transit times and avoid routes prone to delays [27].
Guide 2: Managing Supply Disruption of a Critical Processing Reagent
Problem: The sole supplier of a GMP-grade reagent essential for your cell culture process announces a discontinuation or allocation.
Immediate Actions:
- Inventory Assessment: Quantify your current stock of the reagent and calculate the "runway" based on your production forecast.
- Communicate with Stakeholders: Inform clinical teams and management of the potential risk to production timelines.
Mitigation Strategies:
- Short-Term: Contact the supplier to secure any remaining lots. Inquire about "good-neighbor" commitments where other institutions might share small quantities to bridge the gap [29].
- Long-Term:
- Supplier Qualification: Begin the process of qualifying an alternative reagent from a different vendor. This requires extensive testing to demonstrate comparability [29].
- Process Adaptation: If no direct alternative exists, investigate if the manufacturing process can be modified to eliminate the need for the reagent. This is a significant undertaking requiring regulatory approval [29].
Guide 3: Implementing a Hub and Spoke Model for a Regional Trial
Problem: A clinical trial for a new stem cell therapy needs to enroll patients from widespread, underserved regions.
Implementation Steps:
- Define Roles: Establish a central Hub (e.g., a university hospital) for complex manufacturing, long-term cryostorage, and centralized quality control. Identify several local Spokes (e.g., community clinics) for patient identification, cell collection (apheresis/biopsy), and final product infusion [30].
- Standardize Protocols: Develop and validate standardized protocols for cell collection, interim storage, and transport from the spoke to the hub. This ensures the starting material's quality is consistent regardless of the collection site [30].
- Establish Robust Logistics: Set up a reliable, monitored transport network for moving patient cells from the spoke to the hub and the finished product back to the spoke. This includes trained couriers and real-time tracking [30] [28].
Key Experimental Data and Protocols
Table 1: Cold Chain Temperature Requirements for Different Biologicals
| Product Category | Temperature Range | Primary Storage Equipment | Key Challenge |
|---|---|---|---|
| Pluripotent Stem Cells | Cryogenic (< -150°C) | Liquid Nitrogen Dewars | Risk of tumorigenesis; genetic instability during thaw [26] [28] |
| CAR-T Cell Therapies | Cryogenic or Refrigerated (2-8°C) | Liquid Nitrogen Dewars or Pharmaceutical Refrigerators | Extremely short shelf-life if refrigerated (hours/days) [28] |
| Vaccines (Standard) | Refrigerated (2-8°C) | Pharmaceutical Refrigerators | Temperature control during last-mile delivery [31] |
| Cord Blood Units | Cryogenic (< -150°C) | Liquid Nitrogen Dewars | Maintaining temperature during transport in non-disposable tanks [29] [28] |
Table 2: Research Reagent Solutions for Cell Therapy Manufacturing
| Reagent / Material | Function in Experiment | Critical Consideration |
|---|---|---|
| Hespan (HES) | Sedimentation agent for red blood cell agglutination in cord blood processing [29] | Facing industry-wide shortages; requires qualification of alternatives [29] |
| GMP-grade Cytokines | Direct cell differentiation and expansion in culture [26] | High cost; supply chain vulnerability; requires strict vendor qualification [26] |
| Cell Dissociation Agents | Detach adherent cells (e.g., stem cells) from culture surfaces [26] | Can affect cell viability and surface markers; requires validation for each cell type [26] |
| Cryopreservation Media | Protect cells during freeze-thaw cycles using DMSO and serum/serum-free alternatives [28] | DMSO can have toxic effects; formulation is critical for post-thaw viability and function [28] |
Standard Operating Procedure: Validation of a Cold Chain Shipping Container
Objective: To validate that a selected shipping container can maintain the required internal temperature range for a specified duration under simulated summer and winter conditions.
Materials:
- Shipping container (e.g., insulated shipper)
- Qualified temperature data loggers (IoT sensors preferred)
- Environmental chamber or validated cold/hot room
- Thermal mass simulant (e.g., water or gel packs)
Methodology:
- Protocol Design: Define the test parameters, including required temperature range (e.g., -175°C to -125°C), duration (e.g., 72 hours), and ambient test conditions (e.g., +40°C for summer, -20°C for winter).
- Sensor Placement: Place pre-calibrated temperature data loggers at predetermined critical locations within the empty container (e.g., geometric center, near the walls, top, and bottom).
- Thermal Load: Fill the container with a thermal mass that simulates the product load.
- Pre-conditioning: Pre-condition the container and thermal mass to the required initial transport temperature.
- Stability Testing: Place the loaded and sealed container into the pre-set environmental chamber. Start data loggers and monitor for the predefined duration.
- Data Analysis: At the end of the test period, retrieve the data and analyze it to confirm that all internal monitoring points remained within the specified temperature range for the entire duration.
Workflow Visualizations
Hub and Spoke Logistics Workflow
Temperature Excursion Response Protocol
Scalable Solutions: Implementing Advanced Bioreactor Systems and Automated Platforms
Troubleshooting Guides
Aggregation and Scalability
Problem: Excessive Aggregate Size or Inhomogeneous Aggregate Formation
- Potential Cause: Inoculation density too high or stirring speed too low.
- Solution: Optimize initial seeding density and increase agitation rate to improve hydrodynamic control. For hPSCs, single cell-based inoculation helps establish a well-controlled starting point [32].
Problem: Poor Scalability from Multi-well to Bioreactor
- Potential Cause: Differences in physical conditions (shear stress, mixing efficiency) between static and dynamic culture systems.
- Solution: Implement a scaled-up approach: first validate in rotated Erlenmeyer flasks before moving to stirred tank bioreactors. Process parameters like aggregate formation during expansion can dominate subsequent differentiation efficiency [32].
Differentiation Efficiency
Problem: Low Differentiation Efficiency in 3D vs. 2D
- Potential Cause: Cell density, aggregate size, or nutrient gradients within 3D aggregates differing from 2D monolayers.
- Solution: Systematically screen critical differentiation factors in small-scale suspension culture. For cardiac differentiation of hPSCs, performance is highly sensitive to the concentration of small molecules like CHIR99021 [32].
Problem: High Batch-to-Batch Variability
- Potential Cause: Uncontrolled process parameters and lack of real-time monitoring.
- Solution: Utilize bioreactors with integrated sensors for pH, dissolved oxygen, and metabolites. Implement controlled feeding strategies (e.g., batch or cyclic perfusion) for more consistent outcomes [33] [32].
Contamination Control
Problem: Recurring Bioreactor Contamination
- Potential Cause: Compromised sterility from inoculum, faulty seals, or inadequate sterilization.
- Solution:
- Check the inoculum: Ensure the seed train is contamination-free using plating and staining methods [34].
- Inspect bioreactor components: Regularly check and replace O-rings, valve seals, and tubing. Replace O-rings after 10-20 sterilization cycles [34].
- Validate sterilization: Use autoclave test strips or phials to confirm correct sterilization temperature and time [34].
Problem: "Hidden" Mycoplasma or Viral Contamination
- Potential Cause: Contaminants not visible via light microscopy, leading to poor cell growth.
- Solution: Use specialized test kits, PCR, or conduct regular checks for poor cell culture performance as an early indicator [34].
Frequently Asked Questions (FAQs)
Why transition from 2D flasks to 3D suspension bioreactors for PSC work? 2D cell culture is limited by surface area, manual operations, and difficulty in monitoring, making it unsuitable for large-scale production [35]. Transitioning to 3D suspension culture in bioreactors enables scalable expansion and differentiation, provides a controlled environment, and allows for the mass production of cells required for therapeutic and industrial applications [32].
What are the key process parameters to control in a stirred-tank bioreactor? Critical parameters include inoculation density, stirring speed (to control aggregate size and minimize shear stress), dissolved oxygen, pH, temperature, and feeding strategies [32]. For differentiation, the pattern of aggregate formation during the expansion phase can be a dominant factor [32].
Can I directly transfer my existing 2D differentiation protocol to a 3D bioreactor? Protocols often cannot be transferred directly and require re-optimization for 3D suspension culture. Key factors like small molecule concentrations and timing may need adjustment. It is recommended to first establish the protocol in static suspension (e.g., multi-well plates), then scale up to dynamic systems like Erlenmeyer flasks before final implementation in a stirred bioreactor [32].
How does bioreactor culture impact the quality and phenotype of the differentiated cells? Bioreactor culture conditions can influence the final cell product. For example, research has shown that culture platforms can affect the expression of key developmental signals like BMP agonists/antagonists, thereby influencing cell fate. Furthermore, stress-related markers like metallothionein may be expressed differently in bioreactor-expanded cells [32].
What are the advantages of perfusion systems? Perfusion systems allow for continuous media exchange, which helps maintain nutrient levels, remove waste products, and support higher cell densities over extended periods. This is particularly useful for sensitive cells and for processes like differentiating and maturing cells over long timeframes [33].
Experimental Protocols & Data
This protocol combines hPSC expansion as matrix-independent aggregates with cardiomyogenic differentiation using chemical Wnt pathway modulators.
Workflow Overview
1. hPSC Expansion as Aggregates
- Inoculation: Inoculate single cell-dissociated hPSCs (e.g., HES3 NKX2-5eGFP/w line) into mTeSR1 medium.
- Culture Vessel: Use stirred tank bioreactors.
- Aggregate Control: Control aggregate formation and growth by adjusting inoculation density and stirring speed.
- Feeding Strategy: Apply controlled feeding strategies such as batch or cyclic perfusion.
- Pluripotency Check: Confirm maintenance of pluripotency (e.g., >98% TRA-1-60 positive cells) before initiating differentiation.
2. Cardiomyogenic Differentiation
- Day 0: Replace mTeSR1 with differentiation medium. Add GSK3 inhibitor CHIR99021 to activate Wnt signaling. Optimal concentration is critical (e.g., 7.5 μM determined from screening).
- Day 3: Add Wnt production inhibitor IWP2 for 48 hours to inhibit Wnt pathway and specify cardiac lineage.
- Day 10 onwards: Harvest and analyze cardiomyocytes.
Quantitative Outcomes from Scaled-Up Process [32]
| Process Parameter | Multi-well Plate | Erlenmeyer Flask | 100 mL Stirred-Tank Bioreactor |
|---|---|---|---|
| Average Aggregate Size | 214 ± 65 μm | 389.4 ± 13.8 μm | Controlled by stirring |
| Optimal CHIR99021 Concentration | 7.5 μM | 7.5 μM | 7.5 μM |
| Cardiomyocyte Purity (NKX2.5-GFP+ or cTNT+) | ~52% - 60% | ~55% - >60% | Up to 85% |
| Total CM Yield per Run | Not specified | Not specified | ~40 million cells |
| Key Finding | Protocol established | Protocol transferable to dynamic culture | Production scale-up achievable; expansion pattern dictates differentiation |
The differentiation protocol relies on precise temporal modulation of the Wnt/β-catenin signaling pathway.
Research Reagent Solutions
Essential materials and reagents for implementing the described scalable PSC expansion and differentiation protocol.
| Reagent/Material | Function/Description | Example/Reference |
|---|---|---|
| mTeSR1 Medium | Defined, serum-free medium for maintenance of hPSC pluripotency in suspension culture. | [32] |
| CHIR99021 | A GSK-3 inhibitor that activates Wnt/β-catenin signaling, used for mesoderm induction at differentiation initiation. | [32] |
| IWP2 or IWR1 | Small molecule inhibitors of Wnt production/response, used after initial activation to specify cardiac lineage. | [32] |
| Bombyx mori Silk | Natural protein fiber used to fabricate porous 3D scaffolds for advanced 3D cell culture models. | [36] |
| 3D Bioreactor System | Controlled system (e.g., stirred-tank) for scalable suspension culture, allowing parameter monitoring and control. | [33] [32] |
| Nanofiber Microcarriers | Advanced microcarriers for 3D cell culture enabling high cell densities and scalability in bioreactors. | [37] |
Core Concepts: Hydrodynamic Principles in Bioreactor Design
The Critical Link Between Hydrodynamics and Cell Culture Outcomes
In stirred suspension bioreactors, the hydrodynamic environment—governed by fluid flow patterns, shear stress, and energy dissipation—directly impacts the success of stem cell cultures. For pluripotent stem cells (PSCs) grown as aggregates, this environment dictates critical quality attributes including cell viability, proliferation rates, pluripotency maintenance, and differentiation potential [38] [39]. The hydrodynamic parameters directly influence aggregate characteristics; higher shear stress and turbulent energy dissipation rates result in smaller aggregate sizes, while lower levels permit the formation of larger aggregates [40]. Controlling these parameters is essential, as excessively large aggregates (typically >300-500 μm) develop necrotic cores due to diffusion limitations of oxygen and nutrients, while overly small aggregates may exhibit reduced expansion and differentiation efficiency [40] [41].
Vertical-Wheel Technology: A Paradigm Shift in Impeller Design
The Vertical-Wheel (VW) bioreactor system incorporates an innovative impeller design that operates within a distinctive U-shaped vessel. Unlike traditional horizontal-blade impellers that create uneven hydrodynamic environments with "hot zones" of high turbulence near the impeller tips, the Vertical-Wheel generates a uniquely homogeneous distribution of hydrodynamic forces throughout the culture volume [40] [42]. The VW impeller combines radial and axial flow components, ensuring particles circulate throughout the entire bioreactor rather than becoming trapped in high-shear or low-shear zones [43]. This homogeneous environment translates to a much tighter distribution of PSC aggregate sizes, promoting consistent spherical morphology and similar diameters across the population [40] [42].
Table 1: Key Hydrodynamic Differences Between Bioreactor Impeller Types
| Hydrodynamic Characteristic | Traditional Horizontal-Blade Impeller | Vertical-Wheel Impeller |
|---|---|---|
| Flow Pattern | Predominantly axial flow | Combined radial and axial flow |
| Shear Stress Distribution | Wide variation with high-shear zones at impeller tips | Narrow, homogeneous distribution |
| Energy Dissipation Rate (EDR) Distribution | Broad range throughout vessel | Narrow distribution |
| Aggregate Size Control | Wide, heterogeneous size distribution | Tight, consistent size distribution |
| Scalability | Variable hydrodynamic environment across scales | Maintains consistent environment across scales |
Technical Support: Troubleshooting Guides and FAQs
FAQ 1: How does the Vertical-Wheel impeller achieve more uniform aggregate size distribution compared to traditional impellers?
Answer: The Vertical-Wheel impeller achieves uniform aggregate size distribution through its unique capacity to create a homogeneous hydrodynamic environment. Computational Fluid Dynamics (CFD) analysis reveals that traditional horizontal-blade impellers generate significantly uneven hydrodynamic conditions, with the highest levels of shear stress and turbulent energy dissipation rates near the rapidly spinning impeller tips, creating decreasing gradients as distance from the impeller increases [40]. This wide variation results in a broad distribution of aggregate sizes. In contrast, the Vertical-Wheel impeller, in conjunction with its U-shaped vessel, provides a consistently low shear stress profile across all impeller surfaces and maintains a narrow distribution of energy dissipation rates throughout the entire vessel [40] [42]. The fluid mixing pattern ensures all aggregates experience similar hydrodynamic conditions, resulting in a much tighter size distribution [40].
FAQ 2: What specific hydrodynamic parameters should we monitor when scaling up a PSC process from PBS-MINI to larger Vertical-Wheel bioreactors?
Answer: When scaling up PSC processes in Vertical-Wheel bioreactors, the key parameters to maintain constant are the volume-average energy dissipation rate (EDR) and maximum shear stress. Research demonstrates that keeping the volume-average EDR constant during scale-up enables maintenance of consistent aggregate sizes between different bioreactor scales [39]. CFD modeling provides precise calculations of these parameters across scales. For example, one scaling approach using Vertical-Wheel bioreactors maintained consistent hiPSC growth kinetics and aggregate sizes from 0.1L to 3L scales by applying scale-up correlations based on volume-average hydrodynamic variables [38] [43]. This method is more reliable than traditional scale-up parameters like impeller tip speed or Reynolds number, which may not adequately maintain aggregate size consistency [39].
FAQ 3: Our hiPSC aggregates are becoming too large (>400μm), leading to necrotic centers. What adjustments can we make in a Vertical-Wheel bioreactor to control aggregate size?
Answer: To reduce average aggregate size in Vertical-Wheel bioreactors, systematically increase the agitation rate within the validated operating range. Multiple studies have confirmed an inverse correlation between agitation rate and average aggregate size in Vertical-Wheel systems [40] [41]. For example:
- In PBS MINI 0.1 bioreactors (60-100mL working volume), increasing agitation from 30 rpm to higher rates (e.g., 40-60 rpm) significantly reduces average aggregate diameter [41].
- One study demonstrated that adjusting agitation rates enabled precise control of hiPSC aggregate diameters, with averages reaching 346±11 μm under optimized conditions [41].
The homogeneous hydrodynamic environment of the Vertical-Wheel ensures that increasing agitation rate uniformly reduces aggregate sizes throughout the vessel without creating a wide size distribution [40]. Additionally, consider supplementing culture media with dextran sulfate, which has been shown to reduce aggregation and increase maximum cell density by up to 106% in Vertical-Wheel bioreactors [41].
FAQ 4: We are experiencing low cell viability after inoculation in our Vertical-Wheel bioreactor. What might be causing this, and how can we optimize our inoculation protocol?
Answer: Low cell viability post-inoculation often results from suboptimal inoculation methods or hydrodynamic conditions. Implement these evidence-based solutions:
Adopt single-cell inoculation protocols: Research has established successful single-cell inoculation methods for hiPSCs in Vertical-Wheel bioreactors, achieving over 30-fold expansion in 6 days without sacrificing cell quality [38]. This approach eliminates heterogeneity associated with clump seeding.
Optimize agitation rate during early culture: Begin with lower agitation rates (e.g., 30 rpm in PBS MINI systems) to promote initial aggregate formation, then gradually increase to operational rates for complete suspension [41] [38].
Ensure proper bioreactor filling: Maintain a working volume sufficient to cover the vertical wheel (e.g., 60mL in PBS MINI 0.1) to ensure the optimized hydrodynamic profile [41].
Validate seed train quality: Cells harvested from 2D culture should be in exponential growth phase, as cells entering plateau phase may exhibit extended lag phases and varied growth kinetics in 3D culture [43].
Diagram 1: Hydrodynamic Environment Troubleshooting Guide for Common Bioreactor Challenges
Experimental Protocols & Methodologies
Protocol: hiPSC Expansion as Aggregates in PBS MINI 0.1 Bioreactor
This protocol adapts established methodologies for the expansion of human induced pluripotent stem cells as floating aggregates in Vertical-Wheel bioreactors [41] [38].
Materials:
- PBS MINI 0.1 MAG bioreactor system (PBS Biotech)
- mTeSR1 or mTeSR3D culture medium
- Dextran sulfate (optional, for enhanced yield)
- hiPSC line (e.g., TCLab, Gibco, or 4YA)
- Tris(2,2-bipyridyl) ruthenium chloride hexahydrate (for oxygen measurements)
Method:
- Bioreactor Preparation: Ensure the U-shaped vessel is properly positioned with minimal working volume of 60mL to cover the vertical wheel and ensure optimized hydrodynamic profile.
Inoculation: Use single-cell inoculation protocol established for Vertical-Wheel systems [38]:
- Harvest hiPSCs as single cells using appropriate enzymatic dissociation
- Inoculate at optimized density (protocols demonstrate success with standard densities)
- Begin with agitation rate of 30 rpm to promote initial aggregate formation
Culture Conditions:
- Maintain temperature at 37°C
- Set initial agitation rate to 30 rpm, increasing incrementally as needed to control aggregate size
- For fed-batch cultures, add concentrated medium without replacing vessel contents
- For repeated batch cultures, replace 80% of medium daily from day 2 onwards
Aggregate Monitoring:
- Monitor aggregate size daily using microscopy
- Maintain aggregate diameters between 200-400 μm through agitation adjustment
- Sample for metabolic analysis (glucose consumption, lactate production)
Harvesting: Utilize in-vessel dissociation protocol [38]:
- Apply proteolytic enzymes within the agitated bioreactor
- Control agitation exposure time to achieve single-cell harvest
- Achieve >95% recovery efficiency
Expected Outcomes:
- Maximum cell density: (2.3 ± 0.2) × 10⁶ cells∙mL⁻¹ after 5 days with mTeSR1 + dextran sulfate [41]
- Average aggregate diameter: 346 ± 11 μm under optimized conditions [41]
- Maintenance of pluripotency markers and normal karyotype [41] [38]
Protocol: Computational Fluid Dynamics Analysis for Bioreactor Optimization
CFD modeling enables detailed characterization of hydrodynamic environments without extensive empirical testing [44] [38] [39].
Software Requirements:
- OpenFOAM-8 (open source) or ANSYS Fluent (commercial)
- CAD software (e.g., AutoCAD) for geometry creation
- Meshing software (e.g., ICEM ANSYS)
Methodology:
- Geometry Creation: Develop virtual model of bioreactor vessel and impeller using CAD software.
Mesh Generation: Discretize geometry using tetrahedral elements with appropriate refinement levels.
Boundary Conditions:
- Apply wall boundary conditions to vessel wall and impeller (no-slip condition)
- Set liquid surface with free surface boundary condition (frictionless wall)
- Implement impeller rotation using moving reference frame
Solver Setup:
- Use LES-WALE turbulence modeling or k-epsilon model
- Employ SIMPLE algorithm for pressure-velocity coupling
- Set fluid properties for water at 37°C (density: 0.993 g/cm³, dynamic viscosity: 7.01 × 10⁻⁴ kg/(m·s))
Simulation Parameters:
- Run models for agitation rates between 20-100 rpm
- Ensure Courant-Friedrich-Lewy number remains below 1
- Collect volume-average values for velocity, shear stress, and energy dissipation rate
Validation: Compare simulated mass transfer coefficients with experimental spectroscopy-based oxygen measurements [44].
Table 2: Key Research Reagent Solutions for Vertical-Wheel Bioreactor Studies
| Reagent/Equipment | Function/Application | Example Usage in Protocol |
|---|---|---|
| mTeSR1/mTeSR3D Medium | Feeder-free, serum-free culture medium for hiPSCs | Expansion of hiPSCs as aggregates in VWBR [41] |
| Dextran Sulfate | Polysulfated compound reduces aggregation, increases yield | 97-106% increase in maximum cell number [41] |
| Tris(2,2-bipyridyl) ruthenium chloride | Dissolved oxygen indicator for spectroscopy | Measurement of oxygen transport coefficients [44] |
| hESC-qualified Matrigel | Feeder-free substrate for static culture expansion | Coating T-flasks for pre-bioreactor expansion [38] |
| OpenFOAM-8/ANSYS Fluent | CFD simulation software | Hydrodynamic characterization of bioreactors [44] [38] |
| Proteolytic Enzymes (Trypsin/Accutase) | Cell dissociation for harvesting | In-vessel aggregate dissociation protocol [38] |
Advanced Applications & Scaling Strategies
Scale-Up Correlations for Vertical-Wheel Bioreactors
Successful scale-up of stem cell processes requires systematic approaches to maintain consistent hydrodynamic environments across different bioreactor volumes. For Vertical-Wheel systems, CFD modeling enables development of precise scale-up correlations [43] [39]. Research demonstrates that maintaining constant volume-average energy dissipation rate (EDR) during scale-up most effectively preserves aggregate sizes and biological outcomes [39]. The stepwise approach includes:
Process Optimization at Small Scale: Optimize agitation rate for desired aggregate size and cell growth in PBS-MINI (0.1L) systems.
CFD Modeling: Develop computational models of target production scales (e.g., PBS-3, PBS-15, PBS-80).
Agitation Rate Calculation: Calculate agitation rates for larger scales that maintain constant volume-average EDR values.
Experimental Validation: Conduct limited verification runs to confirm predicted outcomes.
This approach has successfully enabled scale-up from 0.1L to 3L scales while maintaining consistent hiPSC growth kinetics, with potential for expansion to 80L production scales [40] [43].
Integration with Stem Cell Manufacturing Workflows
Vertical-Wheel bioreactor technology addresses critical bottlenecks in stem cell manufacturing, particularly for allogeneic therapies requiring large cell quantities. The technology supports:
- Serial passaging: Studies demonstrate consistent 32-fold expansion of iPSCs during 6-8 day culture periods per passage, achieving cumulative expansion greater than one million-fold in 28 days [40].
- Differentiation processes: Successful differentiation of iPSC aggregates into neural cells, beta cells, cardiomyocytes, and organoids within Vertical-Wheel bioreactors [40].
- cGMP compliance: Single-use systems compatible with current Good Manufacturing Practice requirements for clinical manufacturing [41].
Diagram 2: Scale-Up Methodology Using Computational Fluid Dynamics and Hydrodynamic Correlations
Through systematic implementation of these principles and protocols, researchers can effectively master the hydrodynamic environment in bioreactors, enabling robust control of shear stress and aggregate size distribution for successful stem cell manufacturing.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between a Critical Quality Attribute (CQA) and a Critical Process Parameter (CPP) in stem cell manufacturing?
A1: A Critical Quality Attribute (CQA) is a physical, chemical, biological, or microbiological property or characteristic of the final stem cell product that must be within an appropriate limit, range, or distribution to ensure the desired product quality, safety, and efficacy. Examples include cell identity, potency, viability, and purity [45]. A Critical Process Parameter (CPP) is a process variable whose variability has a direct and significant impact on a CQA. Therefore, it must be closely monitored or controlled to ensure the process produces the desired quality. In stem cell bioprocessing, an example of a CPP is the agitation rate in a bioreactor, which directly impacts the critical quality attribute of cell aggregate size [40].
Q2: Why is a one-factor-at-a-time (OFAT) experimental approach insufficient for a QbD-based process characterization?
A2: OFAT studies, where only one parameter is changed at a time, are inefficient and cannot detect interactions between process parameters. In a complex biological process like stem cell expansion, parameters often interact. For instance, the effect of temperature might depend on the dissolved oxygen level. A multivariate Design of Experiments (DoE) approach varies all relevant parameters simultaneously, which allows for the efficient identification of these critical interactions and the establishment of a robust design space [46] [47].
Q3: How can we control stem cell aggregate size in a suspension bioreactor, and why is this critical?
A3: Cell aggregate size is a critical intermediate attribute because it directly impacts nutrient diffusion, cell viability, and differentiation efficiency [40]. The primary method to control aggregate size is by adjusting the bioreactor's agitation rate. The hydrodynamic environment (shear stress and turbulent energy dissipation rate) created by the impeller is inversely correlated with aggregate size [40]. A homogeneous hydrodynamic environment, such as that provided by a Vertical-Wheel bioreactor, results in a tighter distribution of aggregate sizes, leading to more consistent cell expansion and differentiation outcomes [40].
Q4: What are the common stages in a staged DoE approach for process characterization?
A4: A typical staged approach includes [47]:
- Screening Designs (e.g., fractional factorial): To identify which of many potential parameters have a significant impact on CQAs.
- Refining Designs (e.g., full factorial): To quantify the main effects and interactions of the shortlisted parameters.
- Optimization Designs (e.g., central composite, Box-Behnken): To model nonlinear relationships and identify the optimal set points within the design space.
Q5: What are the major scalability challenges when moving from 2D culture to 3D bioreactors for stem cells?
A5: Transitioning from 2D planar vessels to 3D suspension bioreactors introduces several challenges, including [40] [14]:
- Inconsistent Cell Quality: Cell behavior (expansion, differentiation) can change significantly.
- Process Control: Parameters like agitation, pH, and dissolved oxygen are more complex to control at larger scales.
- Aggregate Formation: Ensuring the formation of uniformly sized cell aggregates is difficult with traditional impellers that create heterogeneous mixing environments.
- Reproducibility: Highly manual 2D processes are variable and do not translate well to automated, larger-scale manufacturing.
Troubleshooting Guides
Issue 1: High Variability in Final Cell Yield and Quality
Problem: Inconsistent performance and quality of stem cell batches, leading to failures in meeting specifications.
| Possible Cause | Diagnostic Steps | Corrective and Preventive Actions |
|---|---|---|
| Uncontrolled Cell Aggregate Size [40] | Measure aggregate diameter distribution daily using microscopy or an automated analyzer. | Implement a bioreactor technology that provides a homogeneous hydrodynamic environment (e.g., Vertical-Wheel). Establish a controlled agitation rate protocol to maintain optimal aggregate size. |
| Unidentified CPPs [45] [47] | Conduct a risk assessment (e.g., FMEA) to identify potential parameters. Perform a screening DoE to verify their impact. | Use a systematic QbD approach to define the QTPP and CQAs first. Use DoE to scientifically link CPPs to CQAs and establish a validated design space. |
| Raw Material Variability [45] [14] | Test multiple lots of critical raw materials (e.g., growth factors, media). Include raw material attributes as factors in DoE studies. | Strengthen supplier qualification and set tight acceptance criteria for Critical Material Attributes (CMAs). Use QbD principles to understand the impact of material variability. |
Issue 2: Failure in DoE – Inability to Identify Significant Factors
Problem: After running a designed experiment, the analysis shows no statistically significant factors, or the results are unreliable.
| Possible Cause | Diagnostic Steps | Corrective and Preventive Actions |
|---|---|---|
| Poor Measurement System [46] [47] | Perform a Gage R&R (Repeatability & Reproducibility) study on analytical methods. | Ensure measurement system error is <20% and has sufficient distinct categories. Improve assay precision before conducting DoE. |
| Insufficient Range for Parameters [46] | Review the selected ranges for each factor against the process capability. | In screening studies, set parameter ranges wide enough (e.g., 3-4x the desired operating range) to detect an effect. |
| High Uncontrolled Noise [46] | Analyze the variation between replicate runs at the same conditions. | Use DoE principles of blocking (to account for known noise like different operators or material lots) and randomization (to account for unknown noise over time). Include replicate and center points in the design. |
Issue 3: Inefficient Differentiation into Target Cell Type
Problem: Stem cells do not reliably differentiate into the desired functional cells, or the resulting population is heterogeneous.
| Possible Cause | Diagnostic Steps | Corrective and Preventive Actions |
|---|---|---|
| Suboptimal Aggregate Size [40] | Correlate final differentiation efficiency with initial and median aggregate size during differentiation induction. | Determine the optimal aggregate size for your specific differentiation protocol. For example, one study showed 450 µm was ideal for cardiogenesis, while 150–300 µm was better for endothelial cells [40]. Control size via agitation rate. |
| Poor Control of Process Parameters | Monitor and log key differentiation parameters (e.g., dissolved oxygen, metabolite levels) in real-time if possible. | Implement Process Analytical Technology (PAT) for better control. Use a DoE-optimized differentiation protocol to define the precise combination and timing of growth factors and other cues [48]. |
Key Experimental Protocols
Protocol 1: A Staged DoE for Bioreactor Process Characterization
This protocol outlines a systematic approach to defining the design space for a stem cell expansion process in a bioreactor [47].
1. Objective: To identify the CPPs and establish a design space for agitation rate and dissolved oxygen (DO) that maximizes cell yield and viability while maintaining pluripotency.
2. Screening DoE (Fractional Factorial)
- Factors: Agitation rate, DO, pH, feeding schedule.
- Levels: Two levels (low and high) for each factor.
- Responses (CQAs): Fold expansion, % viability, % pluripotency marker expression.
- Execution: This design allows for the testing of multiple factors in a minimal number of runs to screen out non-significant factors.
3. Refining DoE (Full Factorial)
- Factors: Agitation rate, DO (the significant factors from the screening study).
- Levels: Two levels, plus center points (to estimate curvature and pure error).
- Execution: This design quantifies the main effects and the interaction between agitation and DO on the CQAs.
4. Optimization DoE (Central Composite)
- Factors: Agitation rate, DO.
- Levels: At least five levels (to model a quadratic response surface).
- Execution: This design allows for the identification of the optimal set point and the shape of the response surface, formally defining the design space.
Protocol 2: Determining Optimal Cell Aggregate Size
Objective: To empirically determine the optimal aggregate size for efficient cell expansion or differentiation [40].
Methodology:
- Inoculation: Seed pluripotent stem cells as single cells into a bioreactor system with a homogeneous mixing environment (e.g., Vertical-Wheel).
- Agitation Setting: Set up multiple bioreactors or sequential experiments with different, controlled agitation rates (e.g., low, medium, high).
- Monitoring: Culture cells for the duration of the expansion or differentiation process. Sample daily to measure:
- Aggregate Size: Using microscopy and image analysis to determine the mean and distribution of diameters.
- Viability and Metabolites: Use off-line analyzers.
- Cell Count: To calculate fold expansion.
- Endpoint Analysis: At the end of the process, analyze the final CQAs:
- For expansion: Fold increase, viability, and pluripotency markers.
- For differentiation: Efficiency via flow cytometry for specific lineage markers and functional assays.
- Correlation: Correlate the average aggregate size during the culture with the final CQAs to identify the optimal size range.
Workflow and Relationship Diagrams
QbD and DoE Workflow
Staged DoE Approach
Research Reagent Solutions
The following table details key materials and technologies used in scalable stem cell manufacturing processes developed under QbD principles.
| Item | Function in Process | Key Consideration |
|---|---|---|
| Vertical-Wheel Bioreactor [40] | Provides a homogeneous hydrodynamic environment for consistent cell aggregate formation and growth. | Ensures uniform shear stress and energy dissipation, leading to tight control over aggregate size distribution. |
| Microcarriers [48] | Provides a surface for adherent stem cells to attach and grow in suspension bioreactors, enabling high-volume expansion. | Material composition, size, and density are Critical Material Attributes (CMAs) that must be optimized. |
| Xeno-Free/Sera-Free Media [14] | Provides nutrients and growth factors for cell culture without animal-derived components, enhancing safety and consistency. | Reduces lot-to-lot variability and eliminates the risk of xenogenic immunogenic responses. Critical for CMC regulatory filings. |
| Lentiviral Vectors [14] | Used as a tool for genetic modification of cells (e.g., for induced pluripotency or CAR-T engineering). | Their production and purification are themselves a complex bioprocess that can be optimized using QbD and DoE. |
| Single-Use Bioreactors [14] | Disposable culture vessels that eliminate cross-contamination and reduce cleaning validation requirements. | Enables flexible, multi-product manufacturing facilities and is a cornerstone of modern bioprocessing. |
The transition of cell therapies from research laboratories to clinical-scale manufacturing presents significant scalability challenges. A primary hurdle is the traditional reliance on manual, open-process steps, which are susceptible to human error, contamination, and high labor costs, ultimately limiting production consistency and volume. Automation and closed systems represent a transformative approach to overcoming these barriers. By integrating robotic systems and minimizing human intervention, this strategy enhances process robustness, ensures product quality, and improves the economic viability of advanced therapies [49] [50]. This technical support center provides targeted guidance to help researchers and manufacturing professionals troubleshoot and optimize their use of these critical technologies.
Frequently Asked Questions (FAQs)
What are the primary benefits of automating cell therapy manufacturing?
Automation in cell therapy manufacturing delivers several critical advantages that address fundamental production challenges:
- Reduced Contamination Risk: Closing the manufacturing workflow and automating steps that were traditionally manual drastically lowers the number of touchpoints where microbial contamination can be introduced [49].
- Enhanced Process Consistency: Automated systems perform repetitive tasks with high precision, minimizing human error and donor-to-donor variation. This leads to more consistent cell products, which is vital for meeting release specifications [49] [50].
- Lower Operational Costs: While initial investment can be significant, automation reduces long-term labor costs and the high expenses associated with manual processing and manufacturing failures [50].
- Increased Production Speed: Automation can significantly accelerate specific process steps. For example, one study showed an automated bead removal process reduced time from two hours to 29 minutes, a 76% improvement [49].
What are "closed systems" and how do they relate to automation?
A closed system is a manufacturing environment where the cell product is never exposed to the open room environment, typically through the use of sterile connectors, tubing sets, and single-use bioprocess containers [49]. Automation involves using robotic systems and software to control the process steps with minimal human intervention.
These concepts are deeply interconnected. A workflow must first be "closed" to effectively and safely introduce automation. Automation then enhances the reliability and efficiency of the closed process. Together, they form the backbone of a scalable, robust manufacturing platform [49].
Our facility is considering automation. What is the difference between a rigid and a modular approach?
Choosing between these two engineering philosophies is a critical strategic decision.
- Rigid (All-in-One) Approach: This system is a walled-off, single solution with fixed protocols for each manufacturing step. It aims to create speed and scale through standardization.
- Modular (Flexible) Approach: This system focuses on delivering flexibility at individual steps within the workflow. It allows therapy developers to use specific protocols and instrumentation best suited for a particular therapy and allows for in-process adjustments to cater to donor variation [49].
For a rapidly evolving field where processes are still being optimized, a modular approach often better supports a wider range of cell therapy manufacturers by providing the adaptability needed to advance therapies without being locked into a single, rigid process [49].
Which critical steps in the cell therapy workflow can be automated?
Many traditionally manual steps in the cell therapy workflow are now addressable with automation. Key examples include:
- Cell Isolation: Technologies exist that create automated environments for cell isolation, consistently delivering high efficiency and purity [49].
- Genetic Manipulation: Steps involving transduction or transfection can be carried out in a closed fashion [49].
- Cell Expansion: The introduction of automated bioreactors has been a major advancement, eliminating error-prone manual interventions required when using flasks and bags [49].
- Media Exchange and Formulation: Automated liquid handlers can perform these tasks with high reproducibility.
- In-process Monitoring and Sampling: Auto-sampling and in-line analytics are key enabling technologies for automated quality control [49].
What are common points of failure in automated robotic systems used in biomanufacturing?
While industrial robots are robust, the surrounding system components can experience issues. Common problems include:
- Component Wear: Cables, even high-flex versions, can fail over time due to repeated movement [51].
- End-Effector (Gripper) Issues: Suction cups can split in pneumatic systems, and grippers can lose holding force, leading to dropped parts [51].
- Sensor Malfunction: Part-presence sensors can become dirty or misaligned, preventing the system from receiving correct signals to proceed [51].
- Software and Programming Errors: These can cause the robot arm to attempt unattainable positions or behave erratically [51].
- Maintenance Neglect: Irregular servicing of components like joints and motors can lead to grease breakdown, causing abnormal motion, noise, and overheating [52].
Troubleshooting Guides
Guide 1: Addressing Intermittent System Stoppages
| Symptoms | The system stops unexpectedly without a clear, persistent fault code. Stoppages may be brief and resolve after a reset. |
|---|---|
| Potential Causes | Intermittent electrical noise; faulty sensors or wiring; software glitches; safety mechanism triggers. |
Step-by-Step Diagnostic Protocol:
- Review System Logs: Check the robot's pendant and control software for any stored fault history or alarm codes, even if the system is currently running [51].
- Inspect Safety Circuits: Verify that all safety gates, light curtains, and emergency stops are fully engaged and functioning correctly. A loose safety switch is a common culprit [51].
- Check Sensor Operation: Inspect part-presence sensors and other critical sensors for dirt, misalignment, or damage. Confirm their operational status via the PLC diagnostic interface [51].
- Examine Electrical Components: Look for loose connections, damaged cables in high-flex areas, and blown fuses [51].
- Assess Electrical Noise: If the cell is near heavy equipment like welders, electrical noise spikes can cause seemingly random faults. Ensure all shielding and grounding is proper [51].
- Perform a Controlled Restart: Sometimes, a full system power cycle is needed to clear registers and reset flags causing the intermittent issue [51].
Guide 2: Troubleshooting Poor Cell Recovery or Viability After an Automated Process
| Symptoms | Post-process cell counts are low, or cell viability is significantly reduced compared to pre-process values or manual process controls. |
|---|---|
| Potential Causes | Excessive shear stress from pump speeds; inaccurate timing in reagent addition; improper temperature control; contamination. |
Step-by-Step Diagnostic Protocol:
- Verify Consumables and Reagents:
- Confirm that the correct single-use sterile fluid path (e.g., tubing set, kit) is installed.
- Check that all reagents (media, buffers, enzymes) are within their expiration dates and have been stored correctly.
- Audit Process Parameters:
- Review the automated method's setpoints. Pay close attention to centrifugation speeds, perfusion rates in bioreactors, and wait times during activation or transduction steps. Compare them to validated manual protocols.
- Ensure that parameters like temperature on heated stages and CO₂ levels in integrated incubators are calibrated and maintained throughout the run.
- Inspect for Mechanical Stress:
- Examine the fluid path for sharp kinks or crimps in tubing that could damage cells.
- Check that peristaltic pump heads are correctly adjusted—over-tightening can cause high shear and cell lysis.
- Assess Aseptic Integrity:
- Check the integrity of all sterile welds and tube connections for potential leaks that could break the closed system and introduce contamination [49].
- Take samples for sterility and mycoplasma testing if contamination is suspected.
Guide 3: Resolving Abnormal Robot Motion or Performance
| Symptoms | The robot arm moves jerkily, drifts from the programmed path, makes unusual grinding/whining noises, or exhibits reduced accuracy. |
|---|---|
| Potential Causes | Mechanical wear in joints; lubrication issues (wrong grease, over/under-greasing); encoder or motor failure; controller issues [52]. |
Step-by-Step Diagnostic Protocol:
- Power Down and Lock Out: Always begin by shutting down the robot and following lockout/tagout procedures for safety [52].
- Visual Inspection:
- Check Motion Behavior: If the model allows, move the robot manually and feel for stiffness, drag, or resistance in specific axes. Jerky or uneven motion often points to lubrication problems [52].
- Take a Grease Sample: If possible, extract a small amount of grease from the affected joint. Check its color, consistency (gritty or watery), and smell. A burnt smell typically indicates excessive heat exposure [52].
- Corrective Actions:
Quantitative Data on Automation Benefits
The following table summarizes specific performance improvements achieved through automation, as documented in recent studies.
Table 1: Documented Efficiency Gains from Automation in Cell Therapy Manufacturing
| Process Step | Manual Process Duration | Automated Process Duration | Efficiency Improvement | Key Outcome |
|---|---|---|---|---|
| Cell Isolation (from 1L volume) | 3 - 4 hours (average) | 70 - 100 minutes | ~60-70% reduction | Processed ≥10 billion target cells with >86% efficiency and 96% purity [49] |
| Bead Removal (Debeading) | 2 hours | 29 minutes | 76% reduction | Achieved without impacting cell recovery rates [49] |
| Cell Purity (in a pre-clinical workflow) | < 40% purity | > 95% purity | > 137% relative increase | Automation consistently delivered high purity levels where manual methods struggled [49] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials and Reagents for Automated Cell Therapy Manufacturing
| Item | Function in Automated Workflow | Key Considerations |
|---|---|---|
| Ancillary Materials (AMs) [53] | Components and reagents used during manufacture but not intended for the final product (e.g., cell isolation reagents, culture media). | Must be carefully qualified. Sourcing under a robust Quality Management System (QMS) reduces the manufacturer's qualification burden. "GMP-grade" is preferable but not always mandatory for early trials [53]. |
| cGMP-Grade iPSCs/MSCs [54] [7] | A consistent, well-characterized, and qualified starting cell source for allogeneic therapies. | Master Cell Banks manufactured under current Good Manufacturing Practices (cGMP) provide a reliable, scalable, and regulatory-compliant foundation for production [54] [7]. |
| Xeno-Free Culture Media [54] [55] | A cell culture medium free of animal-derived components (e.g., no Fetal Bovine Serum). | Eliminates risks associated with xenogeneic serum, such as adverse immune reactions and batch-to-batch variability, enhancing product safety and consistency [54] [55]. |
| Single-Use Bioprocess Containers & Kits | Pre-sterilized, closed-system fluid path assemblies (bags, tubing) designed for automated bioreactors and processing systems. | Maintains a closed, sterile environment, eliminates cleaning validation, and allows for rapid product changeover, which is ideal for multi-product facilities [49]. |
Automated Cell Therapy Manufacturing Workflow
The diagram below illustrates a simplified, integrated workflow for the automated manufacturing of cell therapies, highlighting the closed and interconnected nature of the process.
FAQ: Troubleshooting Common PAT Implementation Issues
Q1: Our real-time metabolite readings are inconsistent with offline sample analysis. What could be causing this discrepancy? Discrepancies between real-time and offline measurements often stem from calibration drift, sensor fouling, or improper sensor placement. First, verify calibration against standard reference materials and ensure sensors are properly maintained. Second, confirm that the sensor is located in a representative region of the bioreactor to avoid dead zones or gradient effects. Third, review the sampling frequency; real-time sensors capture dynamic changes that static offline samples might miss [56] [57].
Q2: We are observing high variability in cell differentiation outcomes despite tight control of basic parameters like pH and temperature. What other factors should we investigate? Basic environmental parameters are only part of the picture. You should investigate dissolved CO₂ (dCO₂) levels and metabolic waste product accumulation. dCO₂ can become toxic beyond specific thresholds and significantly impact cell metabolism and product quality attributes [56]. Furthermore, implement monitoring of Critical Quality Attributes (CQAs) like cell morphology and differentiation markers using AI-driven image analysis to detect subtle phenotypic changes that precede off-target differentiation [16].
Q3: Our PAT system generates large amounts of data. How can we effectively use this for process improvement without being overwhelmed? Leverage data analytics and machine learning for pattern recognition. Use multivariate data analysis to identify correlations between Critical Process Parameters (CPPs) and CQAs. AI models, such as convolutional neural networks (CNNs), can analyze high-resolution imaging and sensor data to dynamically track CQAs and forecast culture trajectories, providing actionable insights for process control [16].
Q4: When scaling up a process from a small-scale bioreactor, which PAT tools are most critical for maintaining process comparability? Prioritize PAT tools that monitor parameters with known scale-dependence. Real-time off-gas analysis (e.g., using mass spectrometry) for calculating oxygen uptake and carbon evolution rates is essential for understanding metabolic shifts [57]. Additionally, inline refractive index or metabolite probes can help track culture composition and metabolic activity dynamics that often change with scale [58].
Troubleshooting Guide: PAT in Stem Cell Bioprocesses
Table 1: Common PAT Challenges and Resolution Strategies
| Problem | Potential Root Cause | Recommended Action | Verification Method |
|---|---|---|---|
| Unpredictable drop in cell viability | Accumulation of toxic metabolites (e.g., lactate, ammonia) or suboptimal dCO₂ levels [56]. | Implement real-time metabolite and dCO₂ monitoring. Use data to create feedback control for media perfusion or base addition [16]. | Trend viability and metabolite data pre- and post-intervention. |
| High batch-to-batch variability in differentiation efficiency | Uncontrolled subtle fluctuations in the cellular microenvironment leading to lineage drift [16]. | Integrate AI-driven morphology analysis to track differentiation in real-time. Use predictive models to adjust process parameters preemptively [16]. | Compare real-time AI classification with endpoint immunostaining or flow cytometry. |
| Sensor fouling leading to data drift | Protein adhesion or cell attachment to sensor surfaces. | Establish a preventive maintenance and cleaning-in-place (CIP) schedule. Consider using sensor designs with self-cleaning mechanisms or fouling-resistant materials. | Regular calibration checks against offline reference measurements [57]. |
| Failure to detect early-stage contamination | Traditional methods are too slow and not real-time. | Implement anomaly detection algorithms on multi-sensor data (e.g., pH, O₂, metabolite consumption rates) to flag deviations indicative of contamination [16]. | Confirm with rapid microbiological methods (e.g., PCR-based tests). |
Experimental Protocol: Implementing a Refractometry-Based PAT System for Monitoring Metabolic Activity
Objective: To deploy a novel refractometry-based PAT system for real-time, non-invasive monitoring of cellular metabolic activity during stem cell culture, enabling the development of an optimized process control strategy.
Background: Refractometry-based PAT relies on advanced refractive index (RI) profiling to identify changes in cell culture composition associated with cellular metabolism in real-time [58].
Table 2: Required Reagents and Equipment
| Item | Function/Application |
|---|---|
| Bioreactor System | Provides the controlled environment for cell culture. Must have ports for PAT probe integration. |
| Refractometry-based PAT System (e.g., Ranger system) | In-line probe for continuous monitoring of refractive index profiles as a surrogate for culture composition and metabolic activity [58]. |
| HEK293T cells or relevant stem cell line | Model system for process development (e.g., lentiviral vector production or stem cell expansion). |
| Cell Culture Media | Formulated media specific to the cell line. |
| pH Probe & Controller | For monitoring and controlling bioreactor pH. |
| Off-gas Analyzer (Mass Spectrometer) | For measuring oxygen and carbon dioxide in the exhaust gas to calculate metabolic rates [57]. |
| Data Acquisition Software | To collect, synchronize, and visualize data from all PAT tools (e.g., 21 CFR Part 11 compliant software). |
Methodology:
- System Setup and Calibration:
- Install and calibrate the refractometry PAT probe, pH probe, and off-gas analyzer according to manufacturer specifications [57].
- Integrate all analyzers with the data acquisition system to enable synchronized, real-time data collection.
- Inoculation and Process Operation:
- Inoculate the bioreactor with the stem cell line at the standard seeding density.
- Initiate the culture process, allowing the PAT system to begin continuous data logging.
- Data Correlation and Model Building:
- Collect data on the refractive index profile, standard process parameters (pH, dO₂, temperature), and off-gas analysis throughout the culture run.
- Correlate the refractive index data with metabolic activity. For example, a study found a correlation between bioreactor pH and metabolic activity revealed by the RI profile [58].
- Use this correlation to build a process understanding. In the referenced case, this understanding was used to create a pH operating strategy that increased metabolic activity by 1.8-fold [58].
- Process Optimization and Control:
- Use the insights gained to design a new control strategy. This could involve using the RI signal as a trigger for media feeds or parameter adjustments.
- Validate the new strategy by running comparative batches against the unoptimized process and assessing impact on both metabolic activity and critical quality attributes (e.g., viral vector titer or differentiation markers).
The workflow for this experimental protocol is outlined below.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for PAT-Enabled Stem Cell Bioprocessing
| Category / Item | Specific Example / Technology | Function in PAT Context |
|---|---|---|
| Inline Sensors | Dissolved CO₂ probe [56] | Monitors dCO₂ in real-time to prevent toxicity and optimize cell metabolism. |
| Refractometry-based system (Ranger) [58] | Tracks metabolic activity via refractive index changes in culture media. | |
| Off-gas Analyzers | Process Mass Spectrometer (e.g., Thermo Scientific Prima PRO) [57] | Provides fast, precise multi-component analysis of bioreactor off-gases (O₂, CO₂) for metabolic quotient calculation. |
| AI & Image Analysis | Convolutional Neural Networks (CNNs) [16] | Analyzes high-resolution images for real-time tracking of CQAs like cell morphology, confluence, and differentiation. |
| Software & Control | 21 CFR Part 11 compliant software (e.g., GasWorks) [57] | Manages data from multiple PAT tools, ensures data integrity, and facilitates process control. |
| Bioreactor Systems | Single-use bioreactors with integrated sensor ports [14] | Provides flexible, scalable platform for integrating various PAT tools in a closed system. |
PAT Data Integration and Control Logic
The power of PAT is fully realized when multiple data streams are integrated into a cohesive control system. The following diagram illustrates the logical relationship and feedback loop between data acquisition, analysis, and process control.
Navigating Production Pitfalls: Strategies for Quality Control, Safety, and Regulatory Compliance
For researchers and drug development professionals working to scale pluripotent stem cell (PSC) manufacturing, ensuring product safety is a critical hurdle. The very properties that make human induced pluripotent stem cells (iPSCs) and embryonic stem cells (hESCs) so therapeutically promising—their capacity for self-renewal and differentiation—also present significant safety challenges. The risks of tumorigenicity and genomic instability are not just laboratory concerns but fundamental barriers to clinical translation and commercial viability [59] [60]. This technical support center article provides targeted strategies to identify, assess, and mitigate these risks within scalable manufacturing workflows.
FAQs on Tumorigenicity and Genomic Instability
FAQ 1: What are the primary tumorigenicity risks associated with PSC-derived therapies?
There are two major tumorigenicity concerns for PSC-based products. First, residual undifferentiated PSCs in the final product may form teratomas—typically benign germ cell tumors—upon transplantation [60]. Second, genomically unstable cells with acquired mutations may lead to malignant transformation [60] [26]. The source cells, phenotype, differentiation status, proliferative capacity, ex vivo culture conditions, processing methods, and route of administration all influence the overall tumorigenic risk profile [59].
FAQ 2: Which chromosomes are most vulnerable to instability in PSC cultures, and why does this matter?
Table 1: Recurrent Genomic Abnormalities in Human Pluripotent Stem Cells
| Chromosomal Region | Frequency | Key Genes Involved | Functional Consequence |
|---|---|---|---|
| Chr 20q11.21 | Very Common | BCL2L1 (Bcl-xL) | Enhanced cell survival, anti-apoptosis [60] |
| Chr 12p | Common | NANOG, GDF3 | Enhanced self-renewal, pluripotency [61] |
| Chr 1 | Common | Multiple | Associated with growth advantage [61] |
| Chr 17 | Common | TP53 | Loss of tumor suppressor function [61] |
| Chr 8 | Observed | MYC | Increased proliferation [61] |
| Chr X | Observed | Multiple | Altered gene dosage effects [61] |
These abnormalities are of high concern because they are repeatedly selected for during culture, provide a growth advantage, and are also found in human cancers, raising significant safety concerns for clinical applications [60] [61].
FAQ 3: How do manufacturing processes influence genomic instability?
Scalable manufacturing processes can exert significant selective pressure on PSC cultures. Single-cell passaging, a common method in large-scale bioreactors, is associated with higher rates of cytogenetic changes compared to cluster-based passaging [61]. Karyotypically abnormal PSCs often bypass the growth bottlenecks (e.g., post-plating cell death) that restrict normal cells, allowing them to outcompete genetically normal populations over successive passages [61]. Furthermore, the reprogramming method itself can impact stability; Sendai virus (SV)-reprogrammed iPSCs have been shown to acquire a higher frequency of copy number alterations (CNAs) and single-nucleotide variations (SNVs) compared to those generated with episomal (Epi) vectors [62].
FAQ 4: What are the critical quality control checkpoints in a scalable PSC manufacturing workflow?
A rigorous, multi-stage quality control system is essential. The diagram below illustrates a comprehensive safety assessment strategy integrated into the manufacturing pipeline.
Troubleshooting Common Experimental Challenges
Problem: Detecting Low-Level Mosaicism in PSC Cultures
- Challenge: Standard G-banding karyotyping has a detection limit of ~5-20% mosaicism, meaning a culture deemed "normal" could harbor a significant population of abnormal cells [61].
- Solution: Implement more sensitive methods such as SNP genotyping or digital droplet PCR (ddPCR). These can detect subchromosomal copy number variations (CNVs) and mosaicism at levels below 5% [60] [61]. For critical checkpoints like MCB testing, use high-resolution methods.
Problem: High Spontaneous Differentiation Rates Compromising Final Product Purity
- Challenge: Excessive differentiation (>20%) in cultures increases heterogeneity and the risk of residual undifferentiated cells in the final product [9].
- Solution:
- Ensure culture medium is fresh (less than 2 weeks old when stored at 2-8°C) [9].
- Manually remove differentiated areas from colonies before passaging [9].
- Minimize time that culture plates are outside the incubator to less than 15 minutes [9].
- Optimize passaging to ensure cell aggregates are evenly sized and prevent overgrowth [9].
Problem: Inconsistent Results in Tumorigenicity Assays
- Challenge: Traditional in vitro assays like the soft agar colony formation assay have limited sensitivity for detecting rare transformed cells in a therapeutic product [26].
- Solution:
- For PSC-derived products, use the in vivo teratoma formation assay in immunocompromised mice to detect residual undifferentiated PSCs [26].
- For somatic cell-based therapies, employ more sensitive in vitro methods like digital soft agar assays or detailed cell proliferation characterization tests [26].
- Always include appropriate controls and validate the assay sensitivity for your specific cell product.
The Scientist's Toolkit: Essential Reagents and Assays
Table 2: Key Research Reagent Solutions for Safety Assessment
| Tool Category | Specific Examples | Function in Safety Assessment |
|---|---|---|
| Culture Media | mTeSR Plus, mTeSR1, TeSR media [9] [62] | Defined, feeder-free culture systems for maintaining genomic stability and reducing variability. |
| Differentiation Kits | STEMdiff Mesenchymal Progenitor kit [62], STEMdiff media systems [7] | Standardized protocols for generating differentiated lineages, reducing batch-to-batch variability. |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent [9] | Gentle, enzyme-free passaging to maintain cell cluster size and minimize stress-induced genomic damage. |
| Characterization Antibodies | Oct3/4, Nanog, Tra-1-60, SSEA-4 [62] | Immunocytochemistry for confirming pluripotency and monitoring undifferentiated cell populations. |
| Genomic Analysis | Karyotyping, SNP Microarray, Whole Exome Sequencing [7] [62] | Detecting chromosomal abnormalities, copy number variations (CNVs), and single-nucleotide variations (SNVs). |
Experimental Protocols for Safety Assessment
Protocol 1: Longitudinal Genomic Stability Monitoring During Scale-Up
This protocol tracks the acquisition of genomic variants from the master cell bank through expansion and differentiation.
- Step 1: Cell Sampling. Collect cell samples at defined stages: Master Cell Bank (MCB), Working Cell Bank (WCB), post-bioreactor expansion, and final differentiated cell product [62] [61].
- Step 2: DNA Extraction. Use a commercial kit to extract high-quality, high-molecular-weight genomic DNA from each sample.
- Step 3: High-Resolution Genotyping. Perform SNP (Single Nucleotide Polymorphism) genotyping or Whole Exome Sequencing (WES) on all samples. This allows for the detection of copy number alterations (CNAs) and single-nucleotide variations (SNVs) with high sensitivity [62].
- Step 4: Data Analysis. Align sequencing data to a reference genome. Use bioinformatics tools to call CNAs and SNVs. Focus on recurrently altered regions in PSCs (see Table 1) and mutations in key tumor suppressor genes like TP53 [62] [61].
- Step 5: Correlation with Culture Conditions. Correlate the appearance of specific genomic variants with manufacturing parameters (e.g., passage method, time in culture, bioreactor conditions) to identify and mitigate pressure points [61].
The workflow below visualizes this multi-stage monitoring process.
Protocol 2: In Vitro Tumorigenicity Assay for Final Product Release
This assay provides a sensitive method to detect rare transformed cells in the final product before patient administration.
- Step 1: Cell Preparation. Prepare the final PSC-derived drug product and a positive control (e.g., a known cancerous cell line).
- Step 2: Digital Soft Agar Assay. Instead of a conventional soft agar assay, use a digital format. Seed a high number of cells (e.g., 1x10^6 to 5x10^6) in a semi-solid matrix like soft agar in a 96-well format. This increases the probability of detecting a rare colony-forming cell [26].
- Step 3: Incubation and Monitoring. Inculture the assay for 3-4 weeks, monitoring weekly for colony formation.
- Step 4: Analysis and Quantification. Use automated imaging and analysis software to count the number and size of colonies formed. Compare the colony-forming frequency of the drug product against the positive control and a negative control (normal somatic cells).
- Step 5: Interpretation. A statistically significant increase in colony formation compared to the negative control may indicate the presence of transformed cells, requiring further investigation and potential batch rejection [26].
Troubleshooting Guides
Troubleshooting Contamination Control in Aseptic Processing
| Problem | Possible Causes | Recommended Solutions | Preventive Measures |
|---|---|---|---|
| Microbial Contamination in Final Product | - Failure in sterile filtration- Inadequate environmental controls- Compromised operator aseptic technique- Faulty sterilized component transfer | - Perform pre-use post-sterilization integrity testing (PUPSIT) of filters [63]- Review environmental monitoring data (viable & non-viable particulates) [26]- Retrain personnel on aseptic techniques in ISO 5 environments [26] | - Implement closed-system technologies like isolators or single-use systems [64]- Use Rapid Transfer Ports (RTPs) for material transfer [64] |
| High Particulate Matter in Vials | - Shedding from personnel or equipment- Improper component preparation (vials, stoppers)- Inadequate cleaning of filling line | - Enhance gowning procedures- Validate depyrogenation tunnel cycles for vials [63]- Implement more robust line clearance and cleaning procedures | - Utilize automated visual inspection systems to detect particulates [63]- Use pre-sterilized, ready-to-use components [14] |
| Loss of Product Sterility during Lyophilization | - Loss of container closure integrity during the cycle- Non-sterile conditions during loading/unloading | - Validate container closure integrity for the lyophilization cycle [63]- Implement closed system transfer from filler to lyophilizer | - Use lyophilizers with integrated CIP/SIP (Clean-in-Place/Sterilize-in-Place) [63] |
Troubleshooting Closed System Implementation
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Cell Aggregates in Bioreactor Vary in Size | - Non-homogeneous hydrodynamic environment in bioreactor [40]- Agitation rate not optimized for cell type and process step | - Transition to bioreactors with a more homogeneous hydrodynamic environment (e.g., Vertical-Wheel) [40]- Establish a DOE to correlate agitation rate with optimal aggregate size [40] |
| Inconsistent Cell Yield & Quality at Scale | - Process parameters not scalable from R&D to production- High shear stress in traditional impeller bioreactors damages cells [40] | - Adopt scalable single-use bioreactor systems that maintain consistent hydrodynamic properties from 0.1L to 50L+ scales [40] [14]- Use computational fluid dynamics (CFD) to model and predict shear stress at larger scales [40] |
| System Integrity Failure During Sampling/Fluid Transfer | - Improper connection/disconnection of tubing sets- Failure of single-use connector seals | - Standardize and validate aseptic connection/disconnection procedures (e.g., via welders or diaphragm connectors) [64]- Implement 100% integrity testing of single-use components post-manufacture |
Frequently Asked Questions (FAQs)
Q1: What exactly defines a "closed system" in regulatory terms, and how does it change my monitoring responsibilities?
A1: According to industry guidance, a closed system is designed to prevent microbial ingress by physically separating the product from the environment. It must be sterilized in place (SIP) or closed prior to use, maintain integrity under all operating conditions, and allow for aseptic fluid transfers and connections [64]. For a validated closed system, extensive internal environmental monitoring (e.g., air and surface sampling) is not required, as the primary control is the system's physical barrier. Monitoring focus shifts to ensuring the system remains closed and its integrity is maintained throughout the process [64].
Q2: For our pluripotent stem cell (PSC) process, we see variable differentiation outcomes at larger scales. Could this be related to our bioreactor's hydrodynamic environment?
A2: Yes, absolutely. Hydrodynamic environment is a critical process parameter (CPP) for suspension culture of PSCs. Traditional horizontal-blade impellers create uneven shear stress, leading to a wide variation in cell aggregate sizes [40]. Since nutrient and differentiation factor diffusion is highly dependent on aggregate size, this heterogeneity directly causes inconsistent differentiation. The solution is to use a bioreactor that provides a homogeneous hydrodynamic environment, enabling tight control over aggregate size distribution simply by adjusting the agitation rate [40].
Q3: We have a terminally sterilized product. Why should we consider aseptic processing instead?
A3: Regulatory agencies mandate that terminal sterilization (e.g., autoclaving) is the preferred method when the product can withstand it [63]. Aseptic processing is reserved for products that are heat-labile, such as most biologics, vaccines, monoclonal antibodies, and live cell therapies [63]. The fragility of these advanced therapy medicinal products (ATMPs) means the heat from terminal sterilization would destroy their efficacy, making aseptic processing the only viable option.
Q4: What are the biggest gaps in our current aseptic process that could lead to a contamination event?
A4: The most significant risks typically are:
- Personnel: Operators are the primary source of contamination. Gaps in gowning, technique, and movement in the cleanroom pose a constant risk [26] [63].
- Manual Interventions: Any open manipulation, such as aseptic assembly or sampling, introduces risk [26].
- Material Transfer: The process of introducing sterilized components, equipment, and raw materials into the critical zone is a vulnerable point [64]. The overarching strategy to close these gaps is to remove the operator from the direct processing environment through automation, robotics, and the implementation of fully closed systems like isolators and single-use disposable fluid paths [64].
Experimental Protocols & Workflows
Protocol: Validating a Closed Aseptic Processing System
Objective: To demonstrate that a closed aseptic processing system maintains sterility throughout a simulated production campaign.
Materials:
- Closed system (e.g., single-use bioreactor assembly with sterilizing filters, connected tubing, and transfer ports)
- Sterile growth medium (e.g., Tryptic Soy Broth)
- Incubator
- Integrity test equipment for filters
Methodology:
- Assemble & Sterilize: Assemble the closed system according to the manufacturer's instructions and subject it to a validated sterilization process (e.g., gamma irradiation for single-use systems, steam-in-place for fixed systems).
- Integrity Test: Perform and document integrity tests on all sterilizing filters post-sterilization and prior to use (PUPSIT) [63].
- Media Fill Simulation: Aseptically introduce sterile growth media into the system. Process the media through the entire system, simulating all normal unit operations (mixing, holding, transfers) and the maximum number of intended connections and disconnections [64].
- Incubation: Incubate the media-filled units at controlled temperatures (e.g., 20-25°C and 30-35°C) for 14 days.
- Observation & Analysis: Visually inspect units for microbial growth (turbidity) at intervals (e.g., days 3, 7, and 14). The acceptance criteria are zero growth from all units processed in the closed system.
Workflow: Scaling Up Pluripotent Stem Cell Expansion
The following workflow diagrams a scalable process for PSC expansion, from cell bank to production-scale bioreactor, integrating contamination control and critical quality monitoring.
Diagram Title: Scalable PSC Expansion Workflow
Key Steps:
- Seed Train: Initiate culture from a characterized cryovial into a small-scale (e.g., 0.1L) Vertical-Wheel (VW) bioreactor to promote uniform aggregate formation [40].
- In-Process Analytics: Monitor critical quality attributes (CQAs) like aggregate size distribution, viability, and pluripotency markers. Adjust agitation rate to control aggregate size [40].
- Scale-Up: Serially passage and expand cells into progressively larger VW bioreactors. The consistent hydrodynamic environment across scales ensures process comparability [40].
- Production & Harvest: Expand to production scale (e.g., 50L). At harvest, perform full quality control, including tests for karyotype and pluripotency, to ensure the final cell product is suitable for differentiation into the target therapeutic cell [40].
The Scientist's Toolkit: Essential Reagents & Technologies
| Item | Function in Aseptic Stem Cell Manufacturing |
|---|---|
| Single-Use Bioreactor (SUB) | A closed, pre-sterilized culture vessel that eliminates cleaning and sterilization validation, drastically reducing contamination risk during cell expansion [14]. |
| Vertical-Wheel Bioreactor | A specific SUB design that creates a homogeneous hydrodynamic environment, enabling precise control over stem cell aggregate size and improving yield and quality consistency [40]. |
| Rapid Transfer Port (RTP) | A standardized docking system that allows the aseptic transfer of materials in and out of closed systems (e.g., isolators, bioreactors) without breaking containment [64]. |
| Sterilizing Grade Filter | A membrane filter (0.22 µm) used to remove microorganisms from gases and liquid media; integrity testing pre- and post-use is critical for validation [63]. |
| Peristaltic Pump | A pump type preferred for biologics filling and transfer in closed systems; it prevents foaming and splashing and operates without contaminating the fluid path [63]. |
| Xeno-Free/Sera-Free Media | Chemically defined cell culture media that eliminates the use of animal-derived components (e.g., FBS), reducing the risk of introducing adventitious agents and improving product consistency [26]. |
For researchers and drug development professionals working with Advanced Therapy Medicinal Products (ATMPs), demonstrating process consistency after scale-up is a critical regulatory hurdle. The inherent biological variability of stem cells, combined with the complexities of moving from laboratory-scale to clinically relevant batch sizes, poses a significant risk to product quality and therapeutic efficacy [26]. A successful scale-up or scale-out strategy requires a robust framework of standardized assays and protocols to prove that the critical quality attributes (CQAs) of your cell therapy product remain unchanged despite modifications in the manufacturing process [14] [65]. This technical support center provides a foundational guide to navigating these challenges, ensuring your scaled process delivers a consistent, safe, and potent product.
Core Concepts: Comparability and Quality Attributes
Before troubleshooting, it is essential to understand the key framework regulators expect you to follow: the Comparability Assessment.
- Process Changes Requiring Assessment: Any change in scale, equipment, or manufacturing site (scale-out) for an autologous or allogeneic cell therapy product necessitates a formal comparability exercise [65].
- The Goal of Comparability: To demonstrate with a high degree of confidence that the manufacturing process change does not adversely impact the product's CQAs, and thus, its safety and efficacy profile [14].
- Critical Quality Attributes (CQAs): These are the physical, chemical, biological, and functional properties of your cell product that must be maintained within an appropriate limit, range, or distribution to ensure the desired product quality. Common CQAs for stem cell products include:
- Identity (Cell surface markers, genotype)
- Potency (Therapeutic mechanism of action)
- Purity (Freedom from contaminants)
- Viability
- Safety (e.g., free from replication-competent viruses, endotoxin)
The following diagram illustrates the strategic workflow for planning and executing a successful comparability study following a process change.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: What are the most common mistakes during assay scale-up and how can we avoid them?
Moving from a research-grade assay to a validated, scalable one is a frequent pain point. Common pitfalls and their solutions are outlined below.
| Common Mistake | Consequence | Expert Solution |
|---|---|---|
| Neglecting Regulatory Planning | Costly re-development and re-validation to meet FDA/EMA standards later [66]. | Adopt a "Quality by Design" (QbD) approach early. Use an ISO 13485 phase-gated development process from the start if a diagnostic product is the long-term goal [66] [14]. |
| Poorly Defined Workflow | Incompatibility with automated systems or cartridge-based formats, leading to failure upon technology transfer [66]. | Fully define the final product workflow early. Visualize how the assay will be used (e.g., cartridge, plate) and understand all physical (time, temperature) and chemical boundaries [66]. |
| Ignoring Component Stability | Short shelf-life, product failure during transport or storage, and batch-to-batch variability [66]. | Conduct small-scale accelerated stability studies during development. Evaluate lyophilization vs. air-drying for critical reagents like enzymes to extend shelf life [66]. |
| Weak Supply Chain Strategy | Manufacturing delays and batch failures due to inconsistent reagent quality or availability [66] [14]. | Audit and engage with reputable suppliers early. Ensure they have robust inventory management, can support scale-up, and provide high-quality, GMP-grade raw materials [66]. |
FAQ 2: Our cell therapy product's potency seems to drop after scaling up in a bioreactor. How can we investigate this?
A drop in potency is a critical failure that directly impacts efficacy. Your investigation should be systematic, focusing on how the new process environment affects cell biology.
Step 1: Re-assay the Scaled-Up Product with a Robust Potency Assay.
- Protocol: Ensure your potency assay is quantitative, reproducible, and relevant to the biological mechanism of action (MoA). It should not just be a marker expression check but a functional assay [26]. Re-test multiple batches of the scaled-up product against pre-defined acceptance criteria and historical lab-scale data.
- Troubleshooting: If the assay itself shows high variability, it cannot accurately detect a process-induced change. Re-optimize or develop a more robust potency assay first [67].
Step 2: Profile Critical Process Parameters (CPPs) in the New Bioreactor System.
- Protocol: Cell behavior is highly sensitive to its environment. Use Design of Experiment (DoE) approaches to profile CPPs in your new bioreactor, such as dissolved oxygen (DO), pH, shear stress, and feeding schedules [14]. Compare these parameters directly to your well-controlled small-scale system (e.g., T-flasks, small-volume bioreactors).
- Troubleshooting: A common issue is inadequate control of CPPs at larger scales. Sub-optimal DO or high shear stress can induce differentiation, senescence, or alter secretome profiles, directly reducing potency [14].
Step 3: Conduct Deep Cellular Characterization.
- Protocol: Go beyond standard CQAs. Perform transcriptomic (RNA-seq) and proteomic analyses to compare cells from the old and new processes. This can identify unintended differentiation, stress response pathways, or shifts in metabolic states that a standard potency assay might miss [26].
- Troubleshooting: If characterization reveals a shift to an undesired cell state, you must re-optimize the bioreactor process conditions (from Step 2) to maintain the correct phenotypic and functional identity.
FAQ 3: We are planning to scale out our autologous therapy to a second manufacturing site. What is needed to demonstrate comparability?
"Scale-out" to multiple sites presents a profound comparability challenge, particularly for autologous therapies where the starting material (patient cells) is inherently variable [65].
- The Core Challenge: Under a single market authorization, establishing and maintaining comparability between multiple sites can become an "unsurmountable burden beyond two or three sites" due to process and analytical variability [65].
- Key Strategy: Process Validation and Standardization.
- Protocol: Before technology transfer, the process must be locked and fully validated at the primary site. This means it must be highly robust and minimally variable. Then, execute a pre-defined comparability protocol at the new site using the same, standardized:
- Equipment and Consumables (e.g., same bioreactor model, same media source)
- Standard Operating Procedures (SOPs) for every unit operation
- Analytical Methods and Assays (transferred and qualified at the new site)
- Training Programs for personnel [65]
- Data Requirement: Generate data from multiple batches (e.g., 3-5) produced at the new site and compare them directly to the historical data from the primary site, focusing on all CQAs.
- Protocol: Before technology transfer, the process must be locked and fully validated at the primary site. This means it must be highly robust and minimally variable. Then, execute a pre-defined comparability protocol at the new site using the same, standardized:
The following workflow details the critical phases of assay development and validation, which form the bedrock of any successful comparability assessment.
The Scientist's Toolkit: Essential Reagents and Materials
A successful, scalable process depends on consistent, high-quality starting materials. The table below lists key reagents and their critical functions in stem cell manufacturing and analytics.
| Item | Function in Manufacturing & Analytics | Key Considerations for Scalability |
|---|---|---|
| cGMP-grade Cell Culture Media | Provides nutrients and signaling molecules for cell growth and maintenance. | Secure a reliable, GMP-compliant supply chain. Move from research-grade to cGMP-grade to ensure consistency and regulatory compliance [14]. |
| Micro/Mini Bioreactor Systems (e.g., Ambr) | Enables high-throughput process optimization and DoE studies with minimal cell resource. | Critical for scaling up suspension cells (e.g., T-cells) or adherent cells on microcarriers (e.g., MSCs). Data from these systems are directly scalable to larger single-use bioreactors [14]. |
| Cell Dissociation Reagents | Passages adherent stem cells and harvests the final cell product. | Enzyme lot-to-lot variability can significantly impact cell yield, viability, and phenotype. Qualify multiple lots early and implement rigorous in-process testing [14]. |
| Flow Cytometry Antibodies | Characterizes cell identity, purity, and critical markers for CQA assessment. | Validation of antibody clones for specific cell types is crucial. Plan for multi-lot testing to ensure consistent performance in your standardized assays [66]. |
| qPCR/PCR Reagents | Tests for identity, genetic stability, and detection of contaminants (e.g., mycoplasma). | Use GMP-grade, lyophilized master mixes to improve stability, simplify workflow, and reduce inter-operator variability in a scaled-out model [66]. |
Within the broader research on stem cell scalability manufacturing challenges, securing a robust supply chain for GMP-grade reagents is not merely a logistical concern—it is a fundamental prerequisite for success. The inherent variability of biological raw materials, combined with complex global supply chains and stringent regulatory requirements, creates a significant bottleneck for the transition from laboratory-scale research to commercial-scale production [14]. In stem cell manufacturing, raw material variability can directly impact Critical Quality Attributes (CQAs), such as cell potency, differentiation efficiency, and genomic stability, ultimately compromising product safety and efficacy [48] [14]. This technical support center provides targeted guidance to help researchers, scientists, and drug development professionals identify, troubleshoot, and mitigate these risks, ensuring that the foundation of their manufacturing process is as reliable as the science behind it.
FAQs: Addressing Common Supply Chain Challenges
Q1: What are the primary risks associated with raw material variability in stem cell processes? Raw material variability introduces significant risks at both process and product levels. Key impacts include:
- Process Performance: Variability in growth factors, cytokines, or serum alternatives can lead to inconsistent cell expansion rates, differentiation yields, and harvest viability [14]. This lack of reproducibility can halt production and requires extensive re-validation.
- Product Quality: Inconsistent raw materials can alter Critical Quality Attributes (CQAs), such as cell surface marker expression, secretome profiles, and genomic stability, potentially affecting the therapeutic function of the final cell product [48].
- Regulatory Compliance: Failure to demonstrate control over raw material quality and its impact on the manufacturing process is a major source of Chemistry, Manufacturing, and Controls (CMC) issues, which can result in clinical holds by regulatory agencies like the FDA [14].
Q2: How can we qualify a new supplier for a critical GMP-grade reagent? A robust supplier qualification process is essential. Key steps include:
- Documentation Review: Obtain and review the supplier's Quality Management System (QMS) certificates, Drug Master Files (DMF), and comprehensive Certificates of Analysis (CoA) for the specific material [68] [14].
- Audit: Conduct an on-site or remote GMP audit of the supplier's facilities. This verifies their adherence to quality standards, data integrity practices, and control over their own supply chain [69] [68].
- Testing and Evaluation: Perform identity, purity, and functionality testing on multiple lots of the material. This should include small-scale "bench-top" models of your critical process steps to assess performance impact [14].
- Quality Agreements: Establish a formal Quality Agreement that clearly defines roles, responsibilities, specifications, and communication protocols for handling deviations and changes [69].
Q3: Our cell expansion is inconsistent between lots. How do we determine if raw materials are the cause? Follow this systematic troubleshooting workflow to isolate the variable:
Experimental Protocol: Split-Batch Testing for Raw Material Investigation
- Objective: To conclusively determine if a specific raw material lot is causing inconsistent cell expansion.
- Materials: Two different lots of the suspected reagent (e.g., basal medium, growth factor), a stable working cell bank, and all other standardized reagents.
- Method:
- Design: Inoculate cells from the same vial of the Working Cell Bank (WCB) into two parallel bioreactors or culture vessels [48].
- Variable: Use the two different lots of the suspected raw material. Keep all other process parameters (seeding density, temperature, pH, other media components) identical.
- Monitoring: Monitor and record Viable Cell Density (VCD), viability, metabolite consumption/production (e.g., glucose, lactate), and pH daily.
- Endpoint Analysis: At harvest, compare key CQAs, such as cell potency markers and differentiation potential (if applicable).
- Data Analysis: Statistical comparison (e.g., t-test) of growth kinetics and CQAs between the two groups. A significant and reproducible difference confirms the raw material as the root cause.
Q4: What strategies can mitigate supply chain disruptions for single-use consumables? To build resilience against disruptions, consider a multi-pronged approach:
- Supplier Diversification: Qualify secondary or tertiary suppliers for critical single-use items like bioreactor bags, filters, and tubing sets to avoid single-point failures [69].
- Inventory Management: Maintain a strategic buffer stock of high-criticality consumables, calculated based on lead times and production forecasts [69].
- Supply Chain Visibility: Implement digital tracking tools (e.g., RFID, IoT sensors) to gain real-time visibility into inventory levels and shipment status, enabling proactive response to potential delays [69].
- Reshoring/Nearshoring: Evaluate sourcing consumables from geographically closer suppliers to reduce logistics complexity and exposure to international trade volatility [70] [69].
Q5: What are the key regulatory considerations for managing raw material variability under GMP? Regulatory compliance requires a proactive, science-based approach to raw material control.
- Traceability: Maintain full traceability of all raw materials from receipt to the final product batch. This is critical for investigations and recalls [71] [68].
- Specifications and Testing: Establish strict acceptance criteria for all raw materials, based on understanding their Critical Process Parameter (CPP) impact. Perform identity and purity testing on every GMP lot [68].
- Change Management: Implement a rigorous change control process. Any change proposed by a supplier must be assessed for its potential impact on your process and product, and may require re-qualification [68].
- Data Integrity: Ensure all data related to raw material qualification, testing, and inventory is recorded and maintained in compliance with ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, and Accurate) [68].
Troubleshooting Guide: From Symptom to Solution
This guide helps diagnose and address common problems linked to raw material variability.
| Observed Symptom | Potential Raw Material Cause | Immediate Action | Long-Term Corrective Action |
|---|---|---|---|
| Reduced cell expansion yield [14] | - Low potency of growth factors.- Sub-optimal basal medium formulation. | - Check CoA and expiry dates.- Switch to a qualified backup lot. | - Enhance functionality testing for new lots.- Strengthen supplier qualification. |
| Unusual cell differentiation [48] | - High variability in differentiation-inducing small molecules or cytokines.- Inconsistent attachment matrix (e.g., laminin). | - Characterize differentiation markers to confirm defect.- Test with a reference material. | - Implement more sensitive identity/purity assays (e.g., HPLC).- Source xeno-free, defined matrices. |
| Increased cell clumping or aggregation | - Variability in enzyme activity (e.g., passaging enzymes).- Changes in surface treatment of microcarriers. | - Visually inspect culture and adjust agitation if possible.- Test enzymatic activity. | - Adopt a Vertical-Wheel bioreactor for more homogeneous aggregate control [40].- Strictly qualify microcarrier surface properties. |
| Batch failure due to contamination | - Microbial contamination in raw material.- Compromised sterility of single-use systems. | - Quarantine and test the suspected material lot.- Review sterilization validation data from supplier. | - Enforce supplier sterilization quality agreements.- Audit supplier's aseptic processing controls. |
The Scientist's Toolkit: Essential Reagents & Solutions
This table details key materials and their roles in establishing a robust stem cell manufacturing process.
| Tool / Material | Function in Stem Cell Manufacturing | Key Considerations for Supply Chain Security |
|---|---|---|
| Chemically Defined Media [14] | Provides essential nutrients in a consistent, xeno-free formulation, supporting scalable expansion. | - Primary Risk: Serum-free adaptation and component variability.- Strategy: Secure long-term supply agreements with manufacturers who provide full traceability and change notification. |
| Microcarriers [48] | Provides a surface for adherent stem cells to grow in 3D bioreactors, dramatically increasing surface area for scale-up. | - Primary Risk: Lot-to-lot variability in surface charge, coating, and size.- Strategy: Qualify multiple microcarrier types and suppliers. Perform split-batch qualification for each new lot. |
| Cell Separation Reagents [e.g., citation:6] | Used to purify specific stem cell populations (e.g., using magnetic-activated cell sorting) based on surface markers. | - Primary Risk: Antibody specificity and efficiency vary, affecting purity and yield.- Strategy: Use GMP-grade, conjugated antibodies. Establish internal purification performance standards for qualifying new reagent lots. |
| Vertical-Wheel Bioreactors [40] | Provides a homogeneous hydrodynamic environment for suspension culture, enabling uniform cell aggregate size and improved reproducibility during scale-up. | - Primary Risk: Single-use equipment supply chain bottlenecks.- Strategy: Diversify suppliers for single-use bioreactor vessels and integrate with digital twins to simulate and manage inventory [69]. |
| Intensified Design of Experiments (iDoE) [72] | A modeling approach that uses intra-experimental parameter shifts to maximize process understanding with fewer experiments, accelerating characterization of raw material impacts. | - Primary Risk: High experimental burden for process characterization.- Strategy: Use iDoE and hybrid modeling to efficiently define the acceptable range for raw material attributes, reducing future testing burden [72] [73]. |
Proactive Strategy: Building a Resilient Raw Material Control Strategy
A proactive, holistic approach is required to secure the supply chain. The following workflow outlines the key components of a robust control strategy, from initial risk assessment to continuous monitoring.
Moving from a reactive to a proactive stance involves:
- Risk-Based Classification: Use Quality by Design (QbD) principles to identify Critical Material Attributes (CMAs) that significantly impact your process [14]. Not all materials require the same level of control.
- Leverage Advanced Modeling: Employ hybrid modeling and intensified Design of Experiments (iDoE) to efficiently characterize the design space for raw materials. This defines acceptable ranges for variability, reducing the need for extensive re-testing with every new lot [72] [73].
- Embrace Digital Tools: Implement digital twins to simulate supply chain disruptions and blockchain technology for enhanced traceability, providing a transparent and auditable record from raw material origin to final product [69] [68].
By integrating these strategies, your organization can build a resilient supply chain that not only mitigates the risks of raw material variability but also becomes a strategic asset in the scalable and compliant manufacturing of stem cell therapies.
Frequently Asked Questions (FAQs) on CMC Strategy
1. How do CMC requirements differ between early-phase and late-phase clinical trials for ATMPs? Regulatory expectations for CMC are phase-appropriate and evolve throughout development. For early-phase trials, the focus is on ensuring patient safety through controlled manufacturing and basic characterization. As you advance to late-phase trials, requirements intensify, demanding a more robust process with rigorous validation, extensive characterization, and comprehensive comparability data to support marketing applications. Immature quality systems in early phases can jeopardize the use of that clinical data in a future marketing authorization application [74].
2. What is the most critical CMC challenge when scaling up a pluripotent stem cell (PSC)-based therapy? The most critical challenge is demonstrating product comparability after any manufacturing process change [26]. Regulatory authorities require a risk-based comparability assessment to prove that changes in scale or process do not adversely impact the product's critical quality attributes (CQAs), safety, or efficacy [26]. This often involves extensive analytical characterization and staged testing.
3. How do FDA and EMA perspectives on GMP compliance for investigational ATMPs differ? A key difference lies in the timing of verified GMP compliance. The EMA requires adherence to GMP guidelines, verified through mandatory self-inspections, as a prerequisite for clinical trials [74]. The FDA operates on a phase-appropriate approach, relying on sponsor attestation early in development, with full GMP compliance verified via a pre-license inspection only upon submission of a Biologics License Application (BLA) [74].
4. What CMC strategies can help manage the high cost of ATMP manufacturing? Prioritizing strategies that drive efficiency is crucial. This includes adopting process automation and closed systems to reduce labor and contamination risks [75], implementing advanced analytics for real-time quality monitoring [75], and simplifying process steps wherever possible [75]. Focusing on a scalable, sustainable, and repeatable "vein-to-vein" process from the outset is essential for long-term viability [75].
5. What are the key CMC considerations for using an allogeneic (donor-derived) cell source? For allogeneic therapies, a primary CMC focus is on controlling the starting material. This involves rigorous donor eligibility determination, including screening and testing for infectious diseases [74]. There is a lack of global harmonization on specific donor testing requirements, which can complicate development. Furthermore, processes must be designed to manage the inherent variability between different donors to ensure a consistent final product [75].
Troubleshooting Guides for Common CMC Challenges
Issue 1: Inconsistent Product Potency During Process Scale-Up
Problem: As you transition from small-scale R&D to large-scale GMP manufacturing, the critical quality attributes (CQAs) of your cell therapy product, particularly its potency, show significant batch-to-batch variation.
Solution Approach:
- Implement a Quality by Design (QbD) Framework: Systematically identify the relationship between your process parameters and the product's CQAs. Use Design of Experiments (DOE) to understand the impact of interacting variables [3].
- Enhance In-Process Monitoring: Integrate Process Analytical Technologies (PAT) to monitor critical process parameters (CPPs) in real-time, allowing for better control over the process [3].
- Adopt Scalable Technologies Early: Move away from planar culture systems to closed-system bioreactors that offer better control over the cellular microenvironment (e.g., pH, dissolved oxygen, nutrients) during expansion and differentiation [3] [26].
- Develop a Robust Potency Assay: The potency assay should be biologically relevant, measuring the product's mechanism of action. It must be quantitative, validated, and capable of demonstrating stability and comparability [76].
Table: Key Reagent Solutions for Scalable PSC Manufacturing
| Research Reagent / Material | Function in Manufacturing | Key Consideration for GMP |
|---|---|---|
| Closed-System Bioreactors | Enables scalable, 3D cell expansion under controlled conditions; improves process consistency. | Ensure the system is qualified for GMP use and allows for aseptic processing [3]. |
| GMP-Grade Culture Media | Supports cell growth, expansion, and maintains cell phenotype. | Requires strict vendor qualification and supply chain security to prevent shortages [26]. |
| GMP-Grade Growth Factors/Cytokines | Directs stem cell differentiation towards a specific lineage. | Focus on sourcing materials with high purity, potency, and traceable origin to ensure batch-to-batch consistency [26]. |
| Cell Separation Materials | Isolates or purifies the target therapeutic cell population. | Moving away from research-grade antibodies to GMP-compliant isolation methods (e.g., non-antibody based) is often necessary for clinical production. |
Issue 2: Navigating Regulatory Pathways for a Global Development Program
Problem: Your ATMP is intended for patients in both the US and EU, but you are encountering divergent CMC requirements from the FDA and EMA, leading to delays and increased costs.
Solution Approach:
- Engage Early with Both Agencies: Seek regulatory advice (e.g., FDA INTERACT, EMA ITF briefing) to understand specific CMC expectations for your product [77] [74].
- Leverage Recent Guidances: Familiarize yourself with new FDA draft guidances on innovative trial designs, post-approval data collection, and expedited programs (RMAT) that offer regulatory flexibility [78].
- Understand Key Divergence Points: Be prepared to address specific areas of difference, such as:
- Design a Global CMC Strategy: From the beginning, design your manufacturing process and control strategy to meet the most stringent requirements from either region, facilitating a smoother global application.
Table: Comparison of Key CMC-Related Regulatory Elements for ATMPs (FDA vs. EMA)
| Regulatory Element | U.S. FDA (CBER) | European EMA (CAT) |
|---|---|---|
| Primary Legislation | FD&C Act, PHSA, 21 CFR [77] | Regulation (EC) No 1394/2007 [77] |
| Expedited Pathway | Regenerative Medicine Advanced Therapy (RMAT) [77] [78] | Priority Medicines (PRIME) [77] |
| CMC Guidances | Multiple product-specific guidances (e.g., CAR-T, Genome Editing) [76] | Multidisciplinary guideline for investigational ATMPs [79] [74] |
| Donor Eligibility | Prescriptive requirements; restrictions on pooling [74] | Must comply with EU and member state laws; general guidance on risks [74] |
| GMP Verification for Trials | Phase-appropriate attestation; verified at pre-BLA inspection [74] | Mandatory self-inspections and compliance for clinical trial authorization [74] |
Issue 3: Designing a Control Strategy for a Complex, Differentiated Cell Product
Problem: Your PSC-derived therapy is a complex mixture of multiple cell types, making it difficult to define and control the critical quality attributes that predict clinical efficacy and safety.
Solution Approach:
- Define a Comprehensive Panel of CQAs: Go beyond basic identity and purity. CQAs should include:
- Identity: Specific markers of the target cell population and absence of residual undifferentiated PSCs.
- Purity & Viability: Percentage of target cells, cell viability, and presence of unwanted cell types.
- Potency: A quantitative measure of the biological activity linked to the mechanism of action (e.g., secretion of a therapeutic factor, electrophysiological function).
- Safety: Tests for sterility, mycoplasma, endotoxin, and adventitious viruses [26].
- Employ Orthogonal Analytical Methods: Use multiple, independent methods to characterize the same attribute. For example, characterize the cell population using flow cytometry, qPCR, and functional assays to build a complete picture of the product.
- Implement Real-Time Release Testing (RTRT): Where possible, develop non-destructive, rapid methods (e.g., inline PAT) that can be used to release a product batch based on data collected during manufacturing, rather than relying solely on lengthy end-product tests.
- Plan for Long-Term Stability: Design stability studies that account for the product's storage, transport, and administration conditions (e.g., cryopreserved in liquid nitrogen vapor phase) [75].
CMC Workflow for PSC Therapies
ATMP CMC Strategy Pillars
From Bench to Bedside: Validating Scalable Processes and Assessing Commercial Viability
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental purpose of a scale-down model in bioprocess development?
Scale-down models are small-scale laboratory systems designed to mimic the heterogeneous environment found in large-scale commercial bioreactors. Their primary purpose is to study the impact of gradients in parameters like substrate concentration, dissolved oxygen (DO), and pH on cell physiology and process performance, which is difficult and expensive to investigate directly at production scale. These models allow researchers to understand and mitigate scale-up risks, thereby reducing development time and increasing the precision and reliability of bioprocess scale-up [80] [81].
FAQ 2: What are the most common gradients encountered in large-scale bioreactors, and why are they problematic?
In large-scale bioreactors, inadequate mixing leads to the formation of distinct microenvironments or gradients. The most common and studied gradients are:
- Substrate Concentration: Occurs near the feed port, creating zones of excess and starvation [80].
- Dissolved Oxygen (DO): Oxygen-depleted zones can form, leading to periodic oxygen limitation for cells [80].
- pH and Dissolved CO₂: Gradients can develop due to inadequate mixing of acid/base additions or CO₂ accumulation [80] [82]. These gradients expose cells to fluctuating conditions, which can alter their metabolism, cause phenotypic population heterogeneity, and lead to reduced productivity, increased byproduct formation, and decreased biomass yield [80].
FAQ 3: What are the key configuration types for scale-down bioreactors?
Scale-down bioreactors typically fall into three main configurations, each with its own approach to mimicking large-scale conditions [80]:
- Single Stirred-Tank Bioreactors (STRs) with Special Feeding Regime: A single, well-mixed vessel where gradients are created by controlling the feeding strategy, such as pulsing a concentrated substrate to simulate a feed zone.
- Multi-Compartment Bioreactors: These systems physically separate different environments. A common setup links a well-mixed, aerated "bulk" zone with a smaller, stagnant "recirculation" zone that becomes oxygen-limited and substrate-rich.
- Combinations of Bioreactors: This involves connecting two or more independent bioreactors, each maintained at different setpoints (e.g., one with high and one with low substrate concentration) through which cells are continuously circulated.
FAQ 4: How do I select the most appropriate scale-down configuration for my process?
The choice of configuration depends on the specific large-scale challenge being studied and the organism used.
- For studying substrate gradients and overflow metabolism in microbial systems like E. coli, a two-compartment system or a linked bioreactor setup is highly effective as it directly simulates the circulation between feed and starvation zones [80].
- For mammalian cell cultures, which are more sensitive to shear, a single stirred-tank reactor with a controlled feeding strategy to create subtle nutrient gradients is often preferable.
- For high-throughput screening of process parameters or clone selection, miniaturized or microfluidic bioreactor systems are emerging as powerful tools [80] [83].
FAQ 5: What are the critical parameters to match when qualifying a scale-down model?
A qualified scale-down model should replicate the key environmental stresses cells experience at large scale. Critical parameters include [80] [82]:
- Mixing Time: The time required to achieve homogeneity should be proportional to the large-scale tank.
- Circulation Time: The average time for a cell to circulate through the entire bioreactor volume.
- Power Input per Unit Volume (P/V): This influences mixing and shear forces.
- Oxygen Mass Transfer Coefficient (kLa): This should be matched to ensure similar oxygen availability.
- Impeller Tip Speed: This can be related to shear stress.
Troubleshooting Guides
Poor Correlation Between Scale-Down Model and Large-Scale Performance
| Symptom | Potential Cause | Recommended Action |
|---|---|---|
| Metabolic byproducts (e.g., lactate) are elevated in the large-scale run but not in the scale-down model. | The scale-down model is not accurately replicating the duration or severity of nutrient/oxygen gradients experienced by cells at large scale [80]. | Re-evaluate and adjust the model's mixing time, circulation time, or compartment volume ratios using computational fluid dynamics (CFD) or tracer studies to better match large-scale hydrodynamics [80]. |
| Cell growth and viability are significantly lower in the scale-down model compared to historical large-scale data. | The shear stress in the scale-down model (e.g., from higher agitation) is too high, damaging cells [82]. | Review the scale-up criterion used. If using constant P/V, consider the impact on tip speed. Adjust agitation and aeration to maintain kLa while reducing shear, potentially by using different impeller types [82]. |
| Product quality attributes (e.g., glycosylation patterns) differ between scales. | The scale-down model is not capturing pH or CO₂ gradients that can affect cellular metabolism and post-translational modifications [82]. | Incorporate dynamic pH control strategies or model CO₂ accumulation. Ensure that the acid/base addition points and mixing are representative of large-scale conditions. |
Challenges in Stem Cell-Specific Scale-Down Models
| Symptom | Potential Cause | Recommended Action |
|---|---|---|
| Increased cellular heterogeneity and off-target cell populations in the final product. | The gradients in the bioreactor create divergent microenvironments that push sub-populations of cells toward different differentiation fates [84]. | Implement strategies to reduce heterogeneity, such as adding small molecule inhibitors (e.g., aphidicolin) to control cell proliferation and promote uniform maturation, as demonstrated in hiPSC-derived islet differentiation [84]. |
| Significant cell loss during differentiation in a scaled-down suspension bioreactor. | The process involves manual steps for cell aggregation/disaggregation, or the hydrodynamic environment causes excessive cluster breakup or fusion [84]. | Transition to a single-vessel, single-batch process within a suspension bioreactor (e.g., a Vertical Wheel bioreactor) to eliminate disruptive transfer and aggregation steps [84]. Optimize agitation speed to control cluster size. |
| Inconsistent differentiation yields across different scales and bioreactor platforms. | The bioreactor's physical parameters (mixing, mass transfer) are not adequately controlled or matched between the development scale and the scale-down model. | Use a scale-down model to systematically map the impact of critical process parameters (CPPs) like agitation and feeding strategies on critical quality attributes (CQAs). Establish a robust design space for the process [81]. |
Quantitative Data for Scale-Down Modeling
Table 1: Characteristic Times and Their Impact on Gradients
| Parameter | Formula / Description | Typical Range (Lab vs. Production Scale) | Impact on Process |
|---|---|---|---|
| Mixing Time (tₘ) | Time to achieve 95% homogeneity after tracer addition [80]. | Lab: < 5-10 s [80]. Production: 10s to 100s of seconds [80]. | If tₘ > cellular response time, gradients form. |
| Circulation Time (t꜀) | Average time for a fluid element to return to a reference point. | Increases with scale; can be several minutes in large cell culture reactors [82]. | Determines frequency of cell exposure to different zones. |
| Cell Reaction Time (τ꜀) | τ꜀ = c꜀ / (q꜀ × cⱼ) ; c꜀=substrate concentration, q꜀=specific consumption rate, cⱼ=cell concentration [80]. | Varies with metabolism; can be in the magnitude of seconds on the transcriptome level [80]. | If τ꜀ ≤ tₘ, cells react to local gradients, leading to heterogeneity. |
Table 2: Common Scale-Down Criteria and Their Consequences
| Scale-Up Criterion Held Constant | Impact on Other Parameters During Scale-Up | Typical Application |
|---|---|---|
| Power per Unit Volume (P/V) | Results in lower impeller speed but higher tip speed and longer mixing time [82] [85]. | Common for microbial fermentations where oxygen transfer is critical. |
| Impeller Tip Speed | Reduces P/V and kLa, while increasing mixing time [82]. | Used for shear-sensitive cells, like mammalian and stem cells. |
| Oxygen Mass Transfer Coefficient (kLa) | Maintains similar oxygen availability; may require adjustments to agitation and aeration. | Applied when dissolved oxygen is a limiting factor for growth. |
| Mixing Time | Results in a very large (often infeasible) increase in P/V [82]. | Not typically used as a primary criterion due to impractical power needs. |
Experimental Protocol: Developing a Two-Compartment Scale-Down Model
Objective: To establish a two-compartment scale-down model for studying the impact of substrate gradients on a microbial process (e.g., using E. coli or S. cerevisiae).
Principle: This model separates the large-scale environment into two distinct zones: a well-mixed, aerated section representing the bulk of the reactor, and a smaller, stagnant, substrate-rich zone that simulates the area near the feed point. Cells are circulated between these zones to mimic their large-scale experience [80].
Materials:
- Stirred-Tank Bioreactor (STR): Represents the well-mixed, aerated bulk zone (e.g., 1-2 L working volume).
- Plug-Flow Reactor (PFR) or Stirred Tank without Baffles: Represents the stagnant, feed zone. A simple glass column or a small, unbaffled vessel can be used.
- Peristaltic Pumps (Two): For continuous circulation between the STR and PFR.
- Control System: For pH, DO, and temperature in the STR.
- Feed Reservoir: Containing concentrated substrate.
Methodology:
- System Setup and Sterilization: Connect the STR and PFR in a closed loop via the peristaltic pumps. Sterilize the entire assembly in place or autoclave individual components aseptically.
- Inoculation and Baseline Operation: Inoculate the STR. Begin operation in batch mode with both recirculation pumps off. Maintain standard environmental conditions (pH, DO, temperature) in the STR.
- Initiation of Fed-Batch and Gradient Simulation: Once the batch phase is complete, initiate the fed-batch phase by:
- Starting the recirculation pumps to establish a defined circulation time between the STR and PFR.
- Continuously feeding a concentrated substrate solution directly into the inlet of the PFR.
- Optional: Sparge the PFR with nitrogen to create an oxygen-limiting environment, simulating conditions that can occur near a feed point in a large fermenter.
- Process Monitoring: Sample from both the STR and PFR outlets periodically to measure:
- Cell density (OD₆₀₀) and viability
- Substrate (e.g., glucose) and metabolite (e.g., acetate) concentrations
- Dissolved oxygen levels
- Analysis: Compare the performance (e.g., biomass yield, product titer, byproduct formation) and physiology (e.g., transcriptomics) of cells cultivated in the two-compartment model against both a homogeneous lab-scale control and historical large-scale data.
The following workflow diagram outlines the key stages in developing and qualifying a scale-down model.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Scale-Down Modeling
| Item | Function in Scale-Down Modeling | Example & Notes |
|---|---|---|
| High-Throughput Mini Bioreactors | Enable parallel experimentation with multiple parameters or clones using minimal resources, accelerating process characterization [83] [86]. | Systems like the ambr250 (250 mL volume) provide automated control of pH, DO, and temperature in a single-use format, serving as qualified scale-down models [83]. |
| Computational Fluid Dynamics (CFD) Software | Provides insights into fluid dynamics and gradient formation in large-scale bioreactors, guiding the design of scale-down models [80]. | Used to simulate flow patterns, shear stress, and concentration fields, helping to define parameters like mixing and circulation times for the scale-down system. |
| Single-Use Bioreactors | Offer flexibility and reduce cross-contamination risk during process development and model testing. | Many suppliers provide families of single-use bioreactors with geometrically similar designs from 10 L to 2000 L, facilitating more consistent scale-down/up studies [82]. |
| Aphidicolin | A cell growth inhibitor used in stem cell differentiation processes to reduce proliferation of off-target cells and enhance uniform maturation of the target cell population [84]. | Used in the differentiation of human iPSCs into islets within bioreactors to mitigate cellular heterogeneity [84]. |
| Vertical Wheel Bioreactors | Provide uniform mixing with low shear stress, suitable for the expansion and differentiation of shear-sensitive cells, including stem cells and organoids [84]. | PBS Vertical-Wheel Bioreactors have been used for single-vessel, 3D differentiation of human iPSCs into functional islet cells, enabling scale-up from 0.1 L to 0.5 L [84]. |
The following diagram illustrates the key parameters and their logical relationships that must be characterized when designing a scale-down experiment.
The transition from research-scale to commercial-scale production of induced pluripotent stem cells (iPSCs) represents a critical challenge in regenerative medicine and drug development. While traditional 2D planar culture systems have supported early-stage research and clinical trials, they are inadequate and cost-prohibitive for producing the trillions of high-quality cells required for late-stage clinical trials and commercial manufacturing [40]. This case study examines the technical achievements and solutions enabling trillion-fold expansion of iPSCs in bioreactor systems while rigorously maintaining pluripotency and genetic stability.
Advanced bioreactor technologies, particularly those employing innovative impeller designs like the Vertical-Wheel system, have demonstrated potential to overcome traditional manufacturing bottlenecks. These systems provide a homogeneous hydrodynamic environment that ensures uniform cell aggregate sizes—a critical factor for efficient nutrient diffusion and consistent cell quality during expansion and differentiation processes [40]. Independent biological studies have confirmed the ability to achieve a cumulative cell expansion of greater than one million-fold in just 28 days through serial passaging in progressively larger bioreactors, projecting that commercial-scale production of over one trillion high-quality iPSCs is feasible in a 50L working volume bioreactor [40].
Key Technical Parameters for Scalable Expansion
Table 1: Critical Process Parameters and Their Impact on iPSC Expansion in Bioreactors
| Parameter | Optimal Range | Impact on Expansion & Pluripotency | Scale-Up Consideration |
|---|---|---|---|
| Aggregate Size | 130-450μm (process-dependent) [40] | Prevents necrotic cores; maximizes expansion & differentiation efficiency [40] | Size distribution narrows with homogeneous mixing [40] |
| Agitation Rate | Process-dependent (e.g., 40-60 RPM) [87] | Controls average aggregate size; higher rates yield smaller aggregates [40] | Homogeneous environment maintained at larger scales [40] |
| Shear Stress | Low, uniform levels [40] | High stress causes DNA breaks, cell death, karyotypic instability [87] | Vertical-Wheel design maintains low, uniform stress across scales [40] |
| Media Additives | Heparin, PEG, PVA [87] | Reduces aggregate fusion; controls size; protects against shear [87] | Defined, xeno-free formulations essential for cGMP [87] |
| Expansion Rate | 32-fold per passage (6-8 days) [40] | Achieving trillion cells requires maintained doubling time of 1-1.4 days [40] [87] | Serial passaging from 0.1L to 80L demonstrated [40] |
Research Reagent Solutions for Scalable iPSC Culture
Table 2: Essential Media Components and Their Functions in Bioreactor Culture
| Reagent | Function | Concentration Range | Mechanism of Action |
|---|---|---|---|
| Heparin Sodium Salt (HS) | Aggregate stability control [87] | 0.1-1 μg/mL [87] | Prevents unwanted cell adhesion and aggregate fusion [87] |
| Polyethylene Glycol (PEG) | Shear protection & fusion control [87] | 0.1-1% [87] | Reduces surface tension; limits aggregate agglomeration [87] |
| Poly (Vinyl Alcohol) (PVA) | Matrix enhancement [87] | 0.1-1 mg/mL [87] | Enhances extracellular matrix and cell membrane interactions [87] |
| Pluronic F-68 | Shear protection [87] | 0.1-1% [87] | Protects cells from hydrodynamic shear stress in bioreactor [87] |
| L-Tryptophan | Growth enhancement [88] | Fortified concentration | Essential amino acid that promotes proliferation in defined media [88] |
| FGF-2 & TGF-β1 | Pluripotency maintenance [87] | Essential 8 formulation | Critical growth factors for maintaining self-renewal and pluripotency [87] |
| Y-27632 (ROCK inhibitor) | Survival post-passaging [87] | 10μM [87] | Enhances cell survival after dissociation and single-cell seeding [87] |
Experimental Protocol: Media Optimization for Aggregate Stability and Expansion
Background
Maintaining uniform aggregate size and minimizing fusion events are critical challenges in suspension bioreactor cultures. The following protocol employs a Design of Experiments (DoE) approach to systematically optimize media additives for controlling aggregate stability while maintaining pluripotency during iPSC expansion [87].
Materials
- Base medium: Essential 8 (E8) formulation [87]
- Additives: Heparin sodium salt (HS), polyethylene glycol (PEG), poly (vinyl alcohol) (PVA), Pluronic F68, dextran sulfate (DS) [87]
- Bioreactor: PBS Vertical-Wheel bioreactors (100ml working volume) [87]
- Cell line: Human iPSCs [87]
Method
DoE Design Generation
- Use MODDE software or equivalent to generate a D-optimal interaction design [87]
- Include 5 factors (HS, PEG, PVA, Pluronic F68, DS) across predetermined concentration ranges [87]
- Create 16 reaction conditions plus 3 center point replicates [87]
- Include one control condition with E8 base medium only [87]
Cell Culture Preparation
Process Monitoring and Sampling
- Sample 3ml daily for cell counting and aggregate size analysis [87]
- Dissociate samples with Accutase for 10 minutes for accurate cell counting [87]
- Image aggregates daily (minimum 30 aggregates per condition) using brightfield microscopy [87]
- Analyze aggregate size distribution using ImageJ software [87]
Assessment Criteria
Expected Results
- Optimal expansion: Combination of PVA and PEG with E8 base reduces doubling time by 40% compared to E8 alone [87]
- Optimal pluripotency: Addition of 1% PEG to E8 medium enhances maintenance of pluripotency markers [87]
- Optimal aggregate stability: Interaction of Heparin and PEG limits aggregation while supporting expansion [87]
- Validated performance: Consistent doubling time of 1-1.4 days with >90% expression of OCT4 and SOX2 across cell lines [87]
Experimental Workflow Visualization
Troubleshooting Guide for Scalable iPSC Expansion
FAQ 1: How can I control aggregate size and prevent formation of necrotic cores in bioreactor culture?
Problem: Heterogeneous aggregate sizes with large aggregates (>500μm) showing central necrosis and reduced viability [40].
Solutions:
- Optimize agitation rate: Systematically test agitation rates between 40-60 RPM. Higher agitation rates generate smaller aggregates due to increased turbulent energy dissipation rates [40].
- Implement media additives: Use heparin (0.1-1μg/mL) and PEG (0.1-1%) to reduce aggregate fusion. The interaction of these components limits uncontrolled agglomeration [87].
- Strategic agitation adjustment: Begin with low agitation after seeding to promote initial spheroid formation, then increase to operational rates to prevent unwanted fusion [40].
- Monitor size distribution: Daily imaging and analysis of aggregate sizes using brightfield microscopy and ImageJ software. Target size range of 130-450μm depending on specific cell line and process requirements [40] [87].
FAQ 2: What strategies maintain pluripotency during serial passaging in suspension culture?
Problem: Gradual loss of pluripotency markers (OCT4, SOX2) during repeated bioreactor passaging.
Solutions:
- Media optimization: Include 1% PEG in E8 medium, which has been shown to enhance maintenance of pluripotency markers [87].
- Quality control checkpoints: Assess pluripotency at each passage via flow cytometry for OCT4 and SOX2 (target >90% positive cells) [87].
- ROCK inhibitor application: Use 10μM Y-27632 during passaging to enhance cell survival after dissociation [87].
- Comprehensive characterization: Perform regular teratoma assays to confirm differentiation potential into all three germ layers, in addition to molecular marker analysis [89].
FAQ 3: How can I overcome low cell viability and recovery during bioreactor harvest?
Problem: Poor cell recovery (<70%) and viability after harvest from large-scale bioreactors.
Solutions:
- Implement low-shear processing: Use tubular bowl centrifugation systems specifically designed for sensitive cell types. This approach can achieve 90% cell recovery and 95% aggregate viability [90].
- Optimize harvest timing: Harvest cells during exponential growth phase before nutrient depletion or waste product accumulation affects viability [40].
- Closed-system processing: Employ automated, closed processing technologies to minimize contamination risk and maintain consistent processing conditions [90].
- Avoid over-dissociation: When passaging as clumps, minimize mechanical disruption to maintain small, uniform aggregates rather than single cells [87].
FAQ 4: How do I address excessive differentiation (>20%) in bioreactor cultures?
Problem: High levels of spontaneous differentiation compromising product quality.
Solutions:
- Monitor culture confluence: Passage cultures when colonies are large and compact but before overgrowth occurs. Over-confluent cultures promote differentiation [9].
- Ensure medium freshness: Use complete cell culture medium less than 2 weeks old to guarantee growth factor activity [9].
- Maintain optimal environment: Limit time outside incubator to less than 15 minutes during handling to minimize environmental stress [9].
- Remove differentiated areas: Physically remove or selectively dissociate differentiated regions prior to passaging [9].
- Adjust seeding density: Decrease colony density by plating fewer cell aggregates if differentiation persists [9].
Advanced Technical Considerations
Computational Fluid Dynamics in Bioreactor Design
The homogeneous hydrodynamic environment created by Vertical-Wheel bioreactors has been modeled using computational fluid dynamics (CFD) analysis up to 80L scale and beyond. These models demonstrate consistently low shear stress levels on all impeller surfaces and a narrow distribution of turbulent energy dissipation rates throughout the U-shaped vessel [40]. This engineering approach enables prediction of mixing properties and hydrodynamic environment at manufacturing scales based on process development done at small scale, significantly de-risking the scale-up process [40].
Aggregate Size Optimization for Differentiation
Different target cell types require specific aggregate size ranges for optimal differentiation efficiency:
- Cardiomyocyte differentiation: ~450μm average diameter [40]
- Neural differentiation: 139±26μm average diameter [40]
- Endoderm induction: 130±40μm average diameter [40]
- Endothelial cell differentiation: 150-300μm diameter range [40]
This process-dependent optimization necessitates careful control of aggregate sizes throughout expansion and differentiation processes.
The implementation of advanced bioreactor systems with defined culture parameters enables unprecedented scale-up of iPSC manufacturing. Through the systematic optimization of critical process parameters—including agitation rate, media composition, and aggregate size control—researchers can achieve trillion-fold expansion of high-quality iPSCs suitable for clinical applications [40]. The reproducible generation of over one trillion cells from a single vial of cryopreserved iPSCs represents a transformative capability for the field of regenerative medicine, potentially enabling treatment of vast patient populations with standardized, high-quality cell products [40].
The integration of computational modeling, systematic DoE approaches, and robust quality control measures provides a roadmap for transitioning from laboratory-scale research to commercial-scale manufacturing of iPSC-based therapies. As these technologies continue to mature, they will play a pivotal role in realizing the full clinical potential of induced pluripotent stem cells.
Troubleshooting Guide: Manufacturing Strategy Selection
1. How do I choose between centralized and decentralized manufacturing for a new therapy? Selecting a model depends on a balanced assessment of therapy-specific, economic, and operational factors. No single model is superior for all scenarios; the choice is a strategic trade-off [91].
- Check: Is the target patient population geographically concentrated or dispersed? Solution: A centralized model is often more cost-effective for serving concentrated, high-demand populations [92] [91].
- Check: What is the disease aggressiveness and required vein-to-vein time? Solution: For highly aggressive diseases with rapid progression, a Point-of-Care (POC) model with shorter turnaround is preferable [93] [91].
- Check: Is the therapy autologous (patient-specific) or allogeneic (off-the-shelf)? Solution: Centralized models can manage the complex logistics of autologous products, but POC can mitigate shipping risks for these same products [93] [91].
- Check: What is the level of process standardization and technological readiness? Solution: Centralized models better handle complex, multi-step processes. POC requires robust, closed, and automated systems to ensure consistency across sites [93] [91].
2. Our manufacturing costs are too high. Could a decentralized model reduce them? Not necessarily. While POC can reduce cold chain shipping costs, it often introduces higher operational overhead.
- Check: Analyze your current Cost of Goods Sold (COGS) breakdown. Solution: If labor constitutes a large portion (40-50%), automation in a centralized facility can reduce costs more effectively than deploying multiple smaller POC units [91].
- Check: Is your facility utilization rate low? Solution: Centralized models benefit from high resource utilization. POC units can have low individual utilization, increasing the cost per dose [92].
- Check: Are you using legacy, manual manufacturing processes? Solution: Transitioning to automated, closed systems in a centralized model can drive down costs more predictably than building a POC network [75].
3. We are experiencing long vein-to-vein times, causing patient attrition. Long turnaround times are a key limitation of centralized models for autologous therapies [93].
- Check: Map your current vein-to-vein process to identify bottlenecks. Solution: If the delay is primarily in logistics and shipping, a regional or POC model can drastically cut this time [93] [92].
- Check: Is the apheresis-to-manufacturing start interface efficient? Solution: POC manufacturing eliminates the need to ship the patient's cells to a distant facility, shaving days or weeks off the timeline [93].
- Check: Is the manufacturing process itself too long? Solution: Investigate adopting newer, faster manufacturing platforms (e.g., CliniMACS Prodigy, Lonza Cocoon) that can reduce production from 2-4 weeks to 8-14 days, regardless of location [93].
4. How can we ensure consistent product quality across multiple POC sites? Lack of standardization is a primary challenge for decentralized manufacturing [75] [91].
- Check: Are your manufacturing protocols and quality control assays fully harmonized? Solution: Implement identical, validated, automated manufacturing platforms and standardized QC assays at every POC site [91].
- Check: Is there a robust training program for local technicians? Solution: Develop comprehensive and recurring training programs to ensure consistent operational expertise across all sites [93] [91].
- Check: Do you have a centralized data monitoring system? Solution: Use a digital platform for real-time monitoring of process parameters and quality data from all decentralized units to quickly identify and correct deviations [91].
Frequently Asked Questions (FAQs)
Q1: What are the key performance indicators (KPIs) for comparing these models? When evaluating manufacturing strategies, key KPIs include cost per dose, fulfillment time (vein-to-vein time), service level (ability to meet demand), and resource utilization [92]. These metrics help quantify the trade-offs between cost, speed, and efficiency.
Q2: What manufacturing technologies are enabling decentralized production? Automated, closed-system platforms are critical for POC production. Technologies like the CliniMACS Prodigy and Lonza Cocoon integrate T-cell isolation, activation, transduction, and expansion within a single-use kit, minimizing manual intervention and allowing operation in less stringent cleanroom environments [93]. Microfluidic devices are also emerging as a promising technology for streamlining cell separation, purification, and formulation [48].
Q3: Is there a hybrid approach between fully centralized and POC models? Yes, a regional hub model is a common hybrid strategy. This approach uses centralized facilities that are geographically closer to patient populations than a single global facility, offering a compromise that improves vein-to-vein time over a fully centralized model while being more cost-effective than a fully decentralized one [92] [91].
Q4: How do regulatory challenges differ between the models? Centralized manufacturing has a well-established regulatory pathway with quality control consolidated in one location. Decentralized manufacturing is more complex, as it requires harmonizing quality control, validation, and reporting across multiple manufacturing sites, which can be challenging under different national regulatory frameworks [91].
Data Comparison: Centralized vs. Point-of-Care Manufacturing
Table 1: Quantitative Comparison of Manufacturing Models (Based on Simulation Studies)
| Key Performance Indicator (KPI) | Centralized Manufacturing | Point-of-Care (POC) Manufacturing |
|---|---|---|
| Production Cost per Dose | Lower at current demand levels (few thousand/year) [92] | Higher due to operational overhead of multiple sites [92] [91] |
| Vein-to-Vein Time | Longer (3-5 weeks including logistics) [93] | Shorter (as little as 8-12 days with fresh cells) [93] |
| Facility Resource Utilization | High, leading to better economies of scale [92] | Can be low per unit, requiring optimal network capacity planning [92] |
| Cold Chain Logistics Cost | Higher (two-way shipping of apheresis and final product) [93] | Significantly lower or eliminated [93] [91] |
| Labor Cost as % of COGS | High (40-50%) but can be optimized centrally [91] | Proportionally high, with added cost of governance across sites [91] |
Table 2: Qualitative Comparison of Manufacturing Models
| Factor | Centralized Manufacturing | Point-of-Care (POC) Manufacturing |
|---|---|---|
| Quality Control & Consistency | Easier to maintain standardized processes and batch consistency in one location [91]. | Challenging; requires stringent harmonization of protocols and assays across all sites to ensure consistency [75] [91]. |
| Regulatory Path | Well-established and familiar to regulators [91]. | More complex; requires regulatory alignment for multi-site production and quality reporting [91]. |
| Scalability for Global Demand | High for concentrated demand; requires robust global logistics [92]. | Potentially high for distributed demand, but scaling requires replicating full manufacturing units [92]. |
| Best-Suited Therapy Profile | Allogeneic (off-the-shelf) products; autologous products for less aggressive diseases [91]. | Autologous products for aggressive diseases with rapid progression; therapies requiring high personalization [93] [91]. |
Experimental Protocol: Simulating Supply Chain Strategies
This protocol outlines a methodology for comparing manufacturing supply chain strategies using computational simulation, as referenced in the literature [92].
Objective: To evaluate and compare the performance of centralized and point-of-care (POC) autologous cell therapy supply chains based on cost, fulfillment time, and resource utilization.
Methodology: Agent-Based Simulation
1. System Definition and Data Acquisition:
- Agents: Define key actors in the supply chain (e.g., patients, manufacturing facilities, testing labs, logistics providers).
- Environment: Set the geographical landscape (e.g., USA, EU) and treatment center locations.
- Input Parameters:
- Demand: Patient arrival rate (e.g., Poisson distribution with a defined lambda).
- Process Times: Apheresis duration, manufacturing time (e.g., 2-4 weeks for centralized, 8-14 days for POC), quality control (QC) testing time, logistics transit times.
- Costs: Manufacturing fixed and variable costs, labor costs, shipping costs, QC testing costs.
- Capacities: Manufacturing slot availability per facility, resource constraints (e.g., bioreactors, staff).
2. Model Implementation:
- Develop or use a pre-validated agent-based simulation framework (e.g., AnyLogic, MATLAB Simulink).
- Program agent behaviors and interaction rules (e.g., a patient agent enters the system, is assigned a manufacturing slot, their cell sample is shipped, etc.).
- Model the two scenarios:
- Centralized: All manufacturing occurs at a single, large-scale facility.
- POC: Manufacturing occurs at multiple, smaller facilities co-located with treatment centers.
3. Simulation Execution and Data Collection:
- Run the simulation for a predefined period (e.g., 1-2 years) with multiple replications to account for stochastic variability.
- Collect output data for Key Performance Indicators (KPIs):
- Cost: Average total cost per dose.
- Fulfillment Time: Average vein-to-vein time (from apheresis to product infusion).
- Service Level: Percentage of patients treated without unacceptable delay.
- Utilization: Average utilization of manufacturing resources.
4. Data Analysis and Scenario Comparison:
- Perform statistical analysis (e.g., t-tests) on the output KPIs to determine significant differences between the centralized and POC models.
- Conduct sensitivity analysis on key input parameters (e.g., demand level, shipping time, production success rate) to identify the most influential factors.
Decision Workflow for Manufacturing Strategy
The following diagram illustrates the key decision factors and logical flow for selecting an appropriate manufacturing strategy.
The Scientist's Toolkit: Research Reagent & Platform Solutions
Table 3: Key Technologies and Materials for Advanced Therapy Manufacturing
| Item | Function / Application in Manufacturing | Example Use Case |
|---|---|---|
| CliniMACS Prodigy | An integrated, automated closed-system for cell processing, culture, and formulation [93]. | Used in decentralized trials for the production of CAR-T cells, reducing hands-on time and maintaining consistency [93]. |
| Lentiviral Vector | A viral vector commonly used for the genetic modification of T-cells to express a Chimeric Antigen Receptor (CAR) [93]. | Critical raw material for CAR-T manufacturing; can be produced centrally or locally (impacting POC feasibility) [93]. |
| CD3/CD28 Activator | Antibody-coated beads or soluble factors used to activate T-cells ex vivo, a critical step before transduction [93]. | A standard reagent in the T-cell activation step of most CAR-T manufacturing protocols [93]. |
| Microfluidic Devices | Platforms for manipulating small fluid volumes in microchannels for cell separation, purification, and analysis [48]. | Potential use in downstream processing (DSP) to purify a uniform population of stem cells with high precision and low cost [48]. |
| Mesenchymal Stem Cells (MSCs) | A type of adult stem cell with multipotent differentiation potential, used in regenerative medicine [94] [48]. | Served as a starting material for allogeneic cell therapies and as a subject for scaling up production processes [48]. |
The field of regenerative medicine holds immense promise for treating a wide range of chronic and degenerative diseases, from heart disease and Parkinson's to cancer and autoimmune conditions [95]. However, a significant barrier persists in translating promising research into widely accessible treatments: the high cost of manufacturing these complex living therapies [96]. For cell and gene therapies, particularly autologous treatments tailored to individual patients, production costs are substantially higher than for traditional pharmaceuticals or biologics because each product requires a dedicated, individualized workflow [96]. These cost challenges directly impact therapy affordability and patient access, creating an urgent need for innovative manufacturing solutions.
Automation and scalable technologies represent the most promising pathway to overcoming these economic hurdles. This technical support article, framed within a broader thesis on stem cell scalability manufacturing challenges, provides researchers, scientists, and drug development professionals with a practical framework for quantifying the impact of these technologies on Cost of Goods (CoGS). By integrating troubleshooting guidance, experimental protocols, and quantitative analysis, this resource aims to support the industry-wide transition from manual, small-scale laboratory procedures to robust, scalable, and cost-effective industrial manufacturing [97].
Economic Impact: Quantifying the Value of Automation
Comparative Cost Analysis: Automated vs. Manual Manufacturing
A fundamental understanding of cost structures is essential for evaluating manufacturing approaches. The transition from manual to automated processes significantly alters both fixed and variable cost components, ultimately driving down CoGS and enhancing therapy accessibility.
Table 1: Cost-Benefit Analysis of Automated vs. Manual Cell Manufacturing
| Cost & Efficiency Factor | Manual Flask-Based Method | Automated Bioreactor System |
|---|---|---|
| Manufacturing Cost per Dose | Higher due to intensive labor | Significantly lower [98] |
| Labor Time & Effort | Substantially higher | Reduced requirements [98] |
| Production Consistency | Operator-dependent variability | High consistency and reproducibility [97] |
| Contamination Risk | Higher in open systems | Reduced via closed systems [50] |
| Scalability Potential | Limited by physical space and labor | Highly scalable [99] |
| Facility Footprint | Larger cleanroom space needed | Reduced footprint [95] |
Market Growth and Technology Adoption Projections
The economic advantage of automation is reflected in robust market growth projections across the manufacturing landscape. Multiple analyses confirm rapid expansion driven by efficiency gains and scalability improvements.
Table 2: Market Growth Projections for Stem Cell and Automated Therapy Manufacturing
| Market Segment | 2024/2025 Market Size | 2034 Projected Market Size | CAGR | Key Growth Drivers |
|---|---|---|---|---|
| Stem Cell Manufacturing Market | $14.18B (2024) [100] | $41.45B [100] | 11.32% [100] | Rising chronic disease prevalence, regenerative medicine adoption [100] |
| Automated & Closed Cell Therapy Market | $1.86B (2025) [97] | $11.20B [97] | 22.19% [97] | Need for consistency, contamination reduction, scalability requirements [97] |
| U.S. Automated Cell Therapy Market | $610M (2025) [97] | $3,920M [97] | 23.11% [97] | Strong healthcare infrastructure, regulatory frameworks, biotech investment [97] |
Technical Support Center: Troubleshooting Automated Manufacturing
Frequently Asked Questions (FAQs) on Automation Implementation
Q1: What are the most critical steps in cell therapy manufacturing to target for initial automation? Certain process steps offer greater returns on automation investment than others. Washing and expansion operations are considered "low-hanging fruit" for automation across the industry, providing immediate benefits in consistency and efficiency [99]. These foundational automations allow organizations to focus resources on developing more specialized solutions for product-specific steps like transfection or differentiation [99]. Standardizing these common steps first creates a platform approach that can support multiple therapy pipelines.
Q2: How can we mitigate contamination risks during scale-up? Implementing closed processing systems is critical for minimizing contamination risks during scaling operations [99]. Automated technologies that reduce manual manipulations directly decrease contamination vectors [99]. Furthermore, integrating at-line or online analytics enables real-time quality monitoring without breaking the closed system, maintaining sterility while ensuring process control [99]. The transition from open to closed systems represents a fundamental shift in contamination control strategy.
Q3: Our organization struggles with process variability in raw materials. How can automation help? Automation introduces superior process control capabilities that can compensate for raw material variability [99]. By maintaining precise environmental parameters (pH, temperature, oxygen levels) throughout culture processes, automated systems reduce performance fluctuations associated with material inconsistencies [101]. Additionally, automated systems generate comprehensive data logs that can help identify correlations between raw material attributes and process outcomes, enabling more sophisticated quality-by-design approaches.
Q4: What data integration challenges should we anticipate when implementing automated systems? Many available automation platforms lack adequate data integration capabilities, requiring companies to develop custom solutions [99]. Prior to implementation, thoroughly vet supplier capabilities for data export, system interoperability, and compatibility with existing manufacturing execution systems (MES) or laboratory information management systems (LIMS). Incomplete data integration can limit the ability to demonstrate process robustness to regulators and hinder process optimization efforts.
Q5: How do we justify the significant capital investment required for automated systems? Beyond the direct labor reduction captured in traditional ROI calculations, consider the comprehensive value proposition including: reduced batch failure rates through enhanced consistency [97], decreased quality control costs via built-in process analytical technologies (PAT), lower facility costs through reduced cleanroom footprint requirements [95], and accelerated tech transfer through standardized, validated processes. Additionally, factor in the strategic value of increased scalability to meet clinical and commercial demand [99].
Essential Research Reagent Solutions for Automated Manufacturing
Table 3: Key Research Reagent Solutions for Automated Stem Cell Manufacturing
| Reagent/Material | Function in Automated Manufacturing | Automation-Specific Considerations |
|---|---|---|
| GMP-Grade Human Platelet Lysate | Serum replacement for MSC expansion [98] | Consistency critical for automated bioreactor systems; must demonstrate batch-to-batch reproducibility |
| Specialized Culture Media | Supports cell growth and maintenance | Formulation optimized for 3D culture systems; enhanced nutrient composition for high-density bioreactor cultures [101] |
| Dissociation Reagents | Cell harvesting from microcarriers or 3D cultures | Gentle enzymatic action preserving cell viability and functionality; compatibility with closed-system fluidic paths |
| Cryopreservation Media | Long-term storage of final cell product | Formulated for automated fill-finish systems; compatible with high-throughput vialing and labeling equipment |
| Cell Separation Reagents | Isolation of target cell populations from source material | Compatibility with automated separation systems; gentle on cells to maintain viability and potency [97] |
Experimental Protocols for CoGS Reduction Analysis
Protocol: Comparative Cost Analysis of Manual vs. Automated Expansion
Objective: Quantify the economic impact of automating the cell expansion process using a standardized methodology suitable for technology assessment and business case development.
Materials and Equipment:
- Manual control arm: Multilayer flasks (e.g., Cell Stack, HyperStack) [98]
- Automated test arm: Hollow-fiber bioreactor system (e.g., Quantum, Terumo BCT) or comparable automated platform [98]
- Cell line: Bone marrow-derived mesenchymal stem cells (BM-MSCs) [98]
- Culture media: αMEM supplemented with 5% human platelet lysate [98]
- Laboratory equipment: Centrifuge, cell counter, flow cytometer for quality assessment
- Data collection: Labor tracking system, material consumption logs, equipment utilization tracker
Methodology:
- Process Mapping: Document all unit operations for both manual and automated processes, including:
- Cell seeding, feeding, monitoring, harvesting, and quality assessment
- Material preparation, equipment setup, and cleanup
- [98]
Resource Tracking:
- Record labor time (operator hours, technical support) for each process step
- Document material consumption (media, reagents, disposables)
- Track equipment utilization (capital depreciation, maintenance)
- [98]
Quality Assessment:
- Evaluate cell phenotype (CD73, CD90, CD105 expression) via flow cytometry
- Assess functionality (adipogenic and osteogenic differentiation capacity)
- Measure cytokine and growth factor secretion profiles
- [98]
Cost Calculation:
- Compute total cost per dose for both methods
- Factor in labor, materials, quality control, and equipment costs
- Perform sensitivity analysis on key cost drivers
- [98]
Expected Outcome: The automated bioreactor system demonstrates significantly lower manufacturing costs with equivalent or superior cell quality, providing quantitative support for automation investment [98].
Protocol: Scalability Assessment of Automated Bioprocessing Systems
Objective: Evaluate the scalability of an automated bioprocessing system from research and development scale to commercial production, identifying potential scale-up bottlenecks and cost implications.
Materials and Equipment:
- Automated bioreactor system (e.g., stirred-tank, hollow-fiber, or fixed-bed bioreactor)
- Cell line: Human mesenchymal stem cells (hMSCs) or induced pluripotent stem cells (iPSCs)
- Scale-down models: Microbioreactors or ambr systems for high-throughput parameter screening
- Analytics: Metabolite analyzers, cell counters, flow cytometers, ELISA kits for potency markers
Methodology:
- Process Parameter Translation:
- Identify critical process parameters (CPPs) at small scale (e.g., 0.1-1L)
- Systematically scale up to pilot (1-10L) and commercial (10-100L) scales
- Monitor impact on critical quality attributes (CQAs) at each scale
Economic Modeling:
- Document material utilization efficiency at each scale
- Track labor requirements relative to output volume
- Calculate facility utilization and footprint requirements
- Model CoGS projections across scales based on empirical data
Quality Comparability:
- Assess cell identity, purity, viability, and potency across scales
- Document any scale-dependent changes in cell characteristics
- Establish acceptance criteria for quality consistency
Expected Outcome: A comprehensive scalability assessment providing both technical and economic data to inform process scale-up decisions and capital investment planning.
Automation Impact on Therapy Affordability
Implementation Roadmap and Future Directions
Strategic Implementation Framework
Successfully integrating automation technologies requires a phased, strategic approach that aligns with organizational capabilities and therapeutic development timelines. The following framework provides guidance for structured implementation:
Phase 1: Technology Assessment & Business Case Development
- Conduct thorough process mapping to identify automation priorities
- Perform comparative cost analysis using Protocol 4.1
- Evaluate vendor capabilities, focusing on data integration and support services
- Develop comprehensive business case with ROI calculations
Phase 2: Pilot Implementation & Staff Training
- Install core automation platforms for highest-impact unit operations
- Implement remote training and simulation tools to build operator competency [102]
- Establish standardized operating procedures (SOPs) and change control processes
- Conduct limited runs to demonstrate technical feasibility
Phase 3: Scale-Up & Digital Integration
- Expand automation to additional process steps
- Implement data integration with LIMS/MES systems
- Develop process analytical technology (PAT) capabilities for real-time monitoring
- Establish maintenance and calibration programs
Phase 4: Continuous Improvement & Optimization
- Leverage accumulated data for process optimization
- Implement advanced control strategies
- Explore AI integration for predictive maintenance and process control [100]
- Share best practices across organization
Emerging Technologies and Future Trends
The automation landscape continues to evolve with several emerging technologies poised to further impact CoGS and scalability:
Artificial Intelligence and Machine Learning: AI is revolutionizing cell manufacturing by optimizing culture conditions, predicting optimal cell growth parameters, and enabling real-time quality assessment [100]. These technologies reduce batch failure rates through advanced analytics and predictive modeling, directly impacting CoGS through improved success rates and reduced material waste [97].
Allogeneic ("Off-the-Shelf") Therapy Platforms: The transition from autologous to allogeneic therapies represents a fundamental shift in manufacturing paradigm [99]. Allogeneic approaches enable true mass production of cell therapies, dramatically reducing per-dose costs through economies of scale and eliminating the logistical challenges of patient-specific manufacturing [99].
Decentralized Manufacturing Models: Emerging approaches aim to distribute manufacturing capacity to point-of-care locations, potentially reducing logistics costs and expanding patient access [102]. The ARPA-H NEBULA project exemplifies this trend, focusing on developing modular biomanufacturing approaches that enable healthcare facilities to generate cell-based therapies on demand [95].
Automation Implementation Roadmap
The integration of automation and scalable technologies represents a transformative opportunity to address the critical challenge of therapy affordability in regenerative medicine. Through systematic implementation of the technologies, protocols, and frameworks outlined in this article, researchers and manufacturing professionals can directly quantify and realize significant CoGS reductions while maintaining or enhancing product quality. The quantitative data presented demonstrates that automation drives economic value through multiple mechanisms: reducing labor requirements, improving process consistency, minimizing contamination-related losses, and enabling scalable production models.
As the field continues to evolve, emerging technologies—particularly artificial intelligence, allogeneic platforms, and decentralized manufacturing approaches—promise to further accelerate progress toward affordable, accessible cell therapies. By adopting a strategic, data-driven approach to automation implementation, the regenerative medicine field can overcome the manufacturing challenges that currently limit patient access to these transformative treatments. The protocols and troubleshooting guidance provided here offer a practical foundation for organizations embarking on this critical journey toward scalable, cost-effective manufacturing.
Stem Cell Manufacturing Market and Key Player Innovations
The global stem cell manufacturing market is experiencing robust growth, driven by rising demand for regenerative medicine and cell-based therapies for chronic diseases. The market's expansion is supported by significant investments in research and development, favorable regulatory changes, and technological advancements in manufacturing processes [103] [5].
Quantitative Market Outlook
The table below summarizes the projected growth of the global stem cell manufacturing market from 2024 to 2034:
| Market Metric | 2024 Value | 2025 Value | 2034 Projection | CAGR (2025-2034) |
|---|---|---|---|---|
| Global Market Size | USD 14.22 billion [103] | USD 15.79 - 16.42 billion [100] [5] | USD 41.45 - 43.18 billion [103] [100] [5] | 11.32% - 11.35% [103] [100] |
Table 1: Global Stem Cell Manufacturing Market Size and Projections
Regional Market Landscape
North America dominated the market in 2024, attributed to its advanced healthcare infrastructure, presence of leading academic institutions, and significant biotechnology investments [103] [100]. However, the Asia-Pacific region is projected to be the fastest-growing market during the forecast period, fueled by increasing investments in biotechnology, government support for stem cell research, and a growing focus on advanced medical treatments in countries like China, Japan, and South Korea [103] [100] [5].
Market Segmentation Analysis
| Segment | Dominant Sub-Segment (2024) | Fastest-Growing Sub-Segment (2025-2034) |
|---|---|---|
| By Product | Consumables (culture media, reagents, growth factors) [103] [100] [5] | Instruments (bioreactors, cell sorters) [103] [100] [5] |
| By Application | Clinical Applications (therapeutic use) [103] [100] [5] | Research Applications [103] [100] [5] |
| By End-User | Pharmaceutical & Biotechnology Companies [103] [100] [5] | Academic Institutes, Research Laboratories & CROs [103] [100] [5] |
Table 2: Stem Cell Manufacturing Market Segmentation
Key Player Innovations and Strategic Developments
Leading companies and research organizations are driving innovation through strategic investments, partnerships, and technological breakthroughs to overcome manufacturing challenges and scale production.
Recent Strategic Initiatives
- STEMCELL Technologies Canada Inc. received a USD 49.9 million investment from Canada's Strategic Innovation Fund in March 2025 to establish large-scale production of essential inputs for research and manufacturing, creating 460 jobs and 900 student co-ops [103].
- Bayer AG opened a new USD 250 million cell therapy production plant in Berkeley, California, in October 2023 to supply cell therapies globally and support the clinical development and potential commercial launch of bemdaneprocel for Parkinson's disease [103].
- Aspen Neuroscience, Inc. announced plans in January 2025 to automate production of its Parkinson's cell therapy, ANPD001, and entered a collaboration with Mytos to advance automated production of dopaminergic neuronal precursor cells [5].
- Fujifilm Corporation allocated USD 200 million in December 2023 to two subsidiaries, Fujifilm Diosynth Biotechnologies and Fujifilm Cellular Dynamics, to expand cell therapy and induced pluripotent stem cell (iPSC) production capacity [100].
Biotech Companies Advancing Clinical Pipelines
- Mesoblast is advancing its Phase III clinical trial for rexlemestrocel-L, an allogeneic cellular therapy for chronic low back pain, which utilizes mesenchymal precursor cells to reduce inflammation and promote tissue healing [94].
- Capricor Therapeutics received FDA Priority Review for its Biologics License Application for CAP-1002, a cell-based therapy for Duchenne muscular dystrophy-associated cardiomyopathy, with a target action date of August 31, 2025. Clinical trials showed a 52% reduction in disease progression over three years [94].
Technical Support Center: Troubleshooting Scalability and Manufacturing Challenges
Frequently Asked Questions (FAQs)
Q1: What are the primary scalability challenges in transitioning from lab-scale to large-scale stem cell manufacturing?
Scaling up poses multiple challenges, including maintaining product comparability after process changes, which requires rigorous risk-based assessments and analytical characterization [26]. There is a shortage of specialized professionals, and manufacturing costs remain high due to labor-intensive processes and expensive raw materials [75]. Furthermore, donor cell variability leads to unpredictable drug product performance, complicating the establishment of a robust, repeatable vein-to-vein process, especially for autologous therapies [75].
Q2: How can we control the high operational costs associated with stem cell manufacturing?
Cost control strategies include adopting automation and closed-system bioreactors to reduce labor inputs and contamination risks [75] [5]. Investing in process optimization and advanced analytics enables better process control and shorter production workflows [75]. Furthermore, a strategic shift towards allogeneic "off-the-shelf" therapies can offer greater scalability and cost-efficiency compared to autologous treatments [75] [104].
Q3: What are the critical safety concerns, particularly regarding tumorigenesis, and how are they addressed?
A major safety concern is the potential for stem cells to undergo neoplastic transformation. For pluripotent stem cell (PSC)-derived products, the in vivo teratoma formation assay is used to validate pluripotency and detect residual undifferentiated PSCs [26]. For somatic cell-based therapies, tumorigenicity is assessed using in vivo studies in immunocompromised models. To improve detection sensitivity, digital soft agar assays or cell proliferation characterization tests are now recommended over conventional methods [26].
Q4: What key design considerations are crucial for a GMP-compliant large-scale stem cell facility?
Facility design must prioritize closed processing systems over open processes to minimize contamination risk and reduce the need for higher-grade cleanrooms [104]. A comprehensive risk assessment is essential upfront, focusing on whether the facility will be single-product, multiproduct, or a CMO, as this dictates segregation and campaigning strategies [104]. The design must also integrate workflows for material, personnel, waste, and equipment flow, and ensure compliance with relevant GMP regulations such as 21 CFR Part 1271 in the US and EudraLex Volume 4 in Europe [104].
Troubleshooting Common Experimental and Manufacturing Issues
| Challenge | Potential Root Cause | Solution & Best Practice |
|---|---|---|
| High Contamination Rates | Open processing steps; inadequate aseptic technique. | Implement closed processing systems (e.g., single-use tubing assemblies); perform media fill simulations to validate aseptic processes [26] [104]. |
| Variable Cell Product Quality/Potency | Donor-to-donor variability; inconsistent culture conditions. | Use standardized cell characterization assays; employ automated platforms with real-time monitoring for consistent culture parameters [75] [26]. |
| Low Cell Yield in Expansion | Senescence due to high number of population doublings; suboptimal plating density. | Limit population doublings (e.g., <20); use low plating densities (1,000-4,000 cells/cm²) and consider adding defined growth factors like FGF2 [105]. |
| Genetic Instability | Successive long-term culture. | Perform regular karyotype analysis and select genetically stable cell lines for master cell banks [26]. |
| Failure in Product Comparability | Process changes during scale-up. | Conduct tiered, risk-based comparability studies per FDA/EMA guidance, focusing on Critical Quality Attributes (CQAs) [26]. |
Table 3: Troubleshooting Guide for Common Stem Cell Manufacturing Challenges
The Scientist's Toolkit: Essential Reagents and Materials
| Item | Function in Manufacturing |
|---|---|
| Defined Culture Media | Supports stem cell growth and maintenance under xeno-free conditions; ensures reproducibility and safety [105]. |
| GMP-grade Growth Factors (e.g., FGF2) | Promotes cell proliferation and helps maintain stemness; use of defined concentrations improves process consistency [105]. |
| Cell Dissociation Reagents | Enables gentle harvesting of adherent cells (e.g., MSCs, iPSCs) for sub-culturing and bioreactor inoculation while maintaining viability [105]. |
| Single-Use Bioreactors | Provides a closed, scalable environment for the expansion of adherent or suspension cells, enhancing productivity and reducing contamination risk [104]. |
| Quality Control (QC) Assay Kits | Used for in-process testing and release criteria, including sterility, mycoplasma, potency, and identity assays [26] [105]. |
Table 4: Key Research Reagent Solutions for Stem Cell Manufacturing
Visualized Processes and Workflows
Stem Cell Manufacturing Facility Workflow
Tumorigenicity Risk Assessment Pathway
Conclusion
Scaling stem cell manufacturing is a multifaceted challenge demanding integrated solutions across biology, engineering, and regulation. The path forward hinges on the widespread adoption of scalable bioreactor platforms, comprehensive automation, and rigorous application of QbD principles. Success will be measured by the ability to transition from bespoke, laboratory-scale processes to robust, standardized, and cost-effective industrial operations. Future progress will be driven by advancements in AI-driven process optimization, enhanced safety profiling for tumorigenicity, and greater regulatory harmonization. By systematically addressing these scalability challenges, the field can unlock the full potential of stem cell therapies, enabling broad patient access and cementing their role as transformative medicines for a range of debilitating diseases.
References
- 1. Stem Cell Therapy Market Attains USD 4777.4 Mn Driving at [https://www.globenewswire.com/news-release/2025/09/08/3146196/0/en/Stem-Cell-Therapy-Market-Attains-USD-4-777-4-Mn-Driving-at-25-26-CAGR-by-2034.html]
- 2. Cell Therapy Manufacturing Market Size to Hit USD 18.89 ... [https://www.precedenceresearch.com/cell-therapy-manufacturing-market]
- 3. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 4. Stem Cell Therapy Cost (2025 Update) [https://www.dvcstem.com/post/stem-cell-therapy-cost-2020]
- 5. Stem Cell Manufacturing Market Size 2024 To 2034 [https://www.novaoneadvisor.com/report/stem-cell-manufacturing-market]
- 6. Tips to Optimize Your hPSC Scale-Up Workflows [https://www.isctglobal.org/telegrafthub/blogs/lauren-reville/2023/10/12/tips-to-optimize-your-hpsc-scale-up-workflows]
- 7. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 8. Navigating stem cell culture: insights, techniques, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586186/]
- 9. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 10. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 11. Managing starting material stability to maximize ... [https://www.insights.bio/immuno-oncology-insights/journal/article/209/managing-starting-material-stability-to-maximize-manufacturing-flexibility-and-downstream-efficiency]
- 12. Addressing Variability in Donor Tissues and Cells - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK544028/]
- 13. OrganaBio: Risks of Healthy Donor Material in Cell Therapy [https://www.organabio.com/the-hidden-risks-of-over-reliance-on-healthy-donor-material/?srsltid=AfmBOoqNuok6anUbsJmrbHNA3fVf7zsXeFVTip5dj9j7BxFqsdABTrB3]
- 14. Addressing Performance, Scalability, and Regulatory ... [https://www.biopharminternational.com/view/addressing-performance-scalability-and-regulatory-challenges-to-accelerate-cell-therapy-manufacturing]
- 15. Analyzing and understanding the robustness of bioprocesses [https://www.sciencedirect.com/science/article/abs/pii/S0167779923000641]
- 16. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 17. How to Troubleshoot Suspension Cell Culture Problems [https://www.procellsystem.com/resources/cell-culture-academy/how-to-troubleshoot-suspension-cell-culture-problems-62]
- 18. Suspension Cell Culture: Methods, Benefits & Applications [https://lifesciences.danaher.com/us/en/library/suspension-cell-culture.html]
- 19. The Pros and Cons of Adherent Versus Suspension Cell ... [https://www.biopharminternational.com/view/the-pros-and-cons-of-adherent-versus-suspension-cell-culture]
- 20. Scaling Up and Differentiating hPSCs in 3D Suspension ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/03/12/scaling-up-and-differentiating-hpscs-in-3d-suspens]
- 21. Current Advances in 3D Dynamic Cell Culture Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9778081/]
- 22. 2D vs 3D cell culture: What's best for scalable ... [https://greenelephantbiotech.com/blog/2d-vs-3d-cell-culture-what-s-best-for-scalable-biopharmaceutical-production/]
- 23. 2D Versus 3D Cell Cultures: Advantages and Disadvantages [https://www.mimetas.com/en/blogs/315/2d-versus-3d-cell-cultures-advantages-and-disadvantages.html]
- 24. 3D Cell Culture - A Rapidly Emerging Technique for Drug ... [https://www.ddw-online.com/3d-cell-culture-a-rapidly-emerging-technique-for-drug-discovery-973-201704/]
- 25. Identification of critical process parameters and quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408662/]
- 26. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 27. Cold Chain Logistics: Challenges, Solutions & Best ... [https://www.hopstack.io/blog/cold-chain-logistics-challenges-solutions-best-practices]
- 28. Challenges of cell & gene therapy supply chains [https://www.n-side.com/en/insights/the-challenges-of-a-cell-gene-therapy-supply-chain/]
- 29. Mitigation of supply chain challenges in cell therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11386209/]
- 30. A practical approach for adoption of a hub and spoke ... [https://www.nature.com/articles/s41434-023-00425-x]
- 31. Cold chain equipment management - technical resources [https://www.technet-21.org/en/topics/supply-chain-and-logistics/cold-chain-equipment-management-technical-resources]
- 32. Controlling Expansion and Cardiomyogenic Differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4264033/]
- 33. Trends in Bioprocessing for 2025 | Innovative Insights [https://www.tecnic.eu/trends-in-bioprocessing-for-2025/]
- 34. How to troubleshoot bioreactor contamination [https://infors-ht.com/en/blog/how-to-troubleshoot-bioreactor-contamination]
- 35. The future of cell therapy: scaling production for global reach [https://www.drugtargetreview.com/article/156266/the-future-of-cell-therapy-scaling-production-for-global-reach/]
- 36. Setup and utilization of a 3D in vitro bioreactor system for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12065549/]
- 37. CPHI Frankfurt 2025: Unlocking the Potential of 3D Cell ... [https://www.thepharmanavigator.com/news/cphi-frankfurt-2025-unlocking-the-potential-of-3d-cell-cultures-in-vaccine-production-with-novel-nanofiber-platform]
- 38. Overcoming bioprocess bottlenecks in the large-scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7805206/]
- 39. Scale-up of embryonic stem cell aggregate stirred ... [https://www.sciencedirect.com/science/article/abs/pii/S1369703X18300561]
- 40. Challenges and Solutions for Commercial Scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7355837/]
- 41. Strategies for the expansion of human induced pluripotent ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-019-0204-1]
- 42. Innovative Vertical-Wheel Impeller Technology [https://www.pbsbiotech.com/technology]
- 43. Vertical-wheel bioreactors: a promising panacea for iPSC ... [https://www.regmednet.com/pbs_sccgt_vertical-wheel-bioreactors-a-promising-panacea-for-ipsc-scale-up/]
- 44. Characterization of the Aeration and Hydrodynamics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405225/]
- 45. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 46. Practical Considerations for DoE Implementation in Quality ... [https://www.bioprocessintl.com/information-technology/practical-considerations-for-doe-implementation-in-quality-by-design]
- 47. Determining Criticality—Process Parameters and Quality ... [https://www.biopharminternational.com/view/determining-criticality-process-parameters-and-quality-attributes-part-ii-design-experiments-and-dat]
- 48. Scaling up stem cell production: harnessing the potential of ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975023001787]
- 49. Addressing Cell Therapy Challenges Through a Modular ... [https://www.biopharminternational.com/view/addressing-cell-therapy-challenges-through-a-modular-closed-and-automated-manufacturing-system]
- 50. Automated manufacturing of cell therapies [https://www.sciencedirect.com/science/article/pii/S0168365925001701]
- 51. Troubleshooting Common Robot Problems [https://www.acieta.com/blog/robot-troubleshooting/]
- 52. How to Troubleshoot Common Issues Related to Robot Grease [https://content.fanucworld.com/how-to-troubleshoot-common-robot-grease-issues/]
- 53. Regulatory Support [https://www.stemcell.com/regulatory-support]
- 54. FAQ - Clinical MSCs [https://www.reprocell.com/clinical-stem-cell-services/faq-mscs]
- 55. Manufacturing Cell and Gene Therapies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10961620/]
- 56. The Importance of Real-Time CO2 Monitoring in Cell Culture [https://www.bioprocessintl.com/sponsored-content/the-importance-of-real-time-co2-monitoring-in-cell-culture]
- 57. Process Analytical Technology | PAT Testing [https://www.thermofisher.com/sr/en/home/industrial/pharma-biopharma/manufacturing-control-pharma-biopharma/process-analytical-technology.html.html?erpType=Global_E1]
- 58. Implementing Process Analytical Technology into Cell and ... [https://oxfordglobal.com/nextgen-biomed/resources/implementing-process-analytical-technology-into-cell-and-gene-therapy-manufacturing]
- 59. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 60. Genomic Instability in Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3931019/]
- 61. PSC Genomic Integrity and Stability | Cell Quality [https://www.stemcell.com/psc-cell-quality/genomic-integrity]
- 62. Tracing genomic instability in induced mesenchymal ... [https://www.nature.com/articles/s12276-025-01439-8]
- 63. The current state of aseptic processing & fill-finish manufacturing [https://www.crbgroup.com/insights/pharmaceuticals/aseptic-processing]
- 64. Straight Talk on Closed Aseptic Systems [https://www.biopharminternational.com/view/straight-talk-closed-aseptic-systems]
- 65. Manufacturing models permitting roll out/scale out of ... [https://www.sciencedirect.com/science/article/pii/S1465324914005453]
- 66. Scaling Up Assays: 4 tips to help avoid the most common ... [https://blog.biosearchtech.com/mastering-assay-scale-up-4-tips]
- 67. Assay Guidance Manual - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK53196/]
- 68. Top GMP Guidelines and Best Practices for 2025 [https://jafconsulting.com/top-gmp-guidelines-and-best-practices-for-2025/]
- 69. 2025 Supply Chain Challenges for the Life Sciences Industry [https://medmarc.com/life-sciences-news-and-resources/publications/2025-supply-chain-challenges-for-the-life-sciences-industry]
- 70. 2026 Chemical Industry Outlook [https://www.deloitte.com/us/en/insights/industry/chemicals-and-specialty-materials/chemical-industry-outlook.html]
- 71. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 72. Model Transferability and Reduced Experimental Burden ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8733703/]
- 73. Accelerating bioprocess development by analysis of all ... [https://www.sciencedirect.com/science/article/pii/S0264410X1930917X]
- 74. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect [https://www.cellandgene.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 75. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 76. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 77. Navigating the ATMP Regulatory Landscape ... [https://www.evotec.com/sciencepool/navigating-the-atmp-regulatory-landscape]
- 78. Cell & gene therapy clinical trials, development promoted ... [https://www.hoganlovells.com/en/publications/cell-gene-therapy-clinical-trials-development-promoted-in-three-new-fda-guidance-documents]
- 79. Guideline on quality, non-clinical and clinical requirements for ... [https://www.ema.europa.eu/en/guideline-quality-non-clinical-clinical-requirements-investigational-advanced-therapy-medicinal-products-clinical-trials-scientific-guideline]
- 80. Scale-down bioreactors—comparative analysis of configurations [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460589/]
- 81. Uncovering the potential of ultra scale-down tools to ... [https://insights.bio/immuno-oncology-insights/journal/article/470/uncovering-the-potential-of-ultra-scale-down-tools-to-enable-cost-effective-quality-by-design]
- 82. Exploring Principles of Bioreactor Scale-Up [https://www.bioprocessintl.com/bioreactors/lessons-in-bioreactor-scale-up-part-1-mdash-exploring-introductory-principles]
- 83. Scale-Down Models to Support Process Characterization [https://bioprocessingjournal.com/scale-down-models-to-support-process-characterization/]
- 84. Scale up manufacturing approach for production of human ... [https://www.nature.com/articles/s41536-025-00409-y]
- 85. Bioprocessing Scale Up [https://www.eppendorf.com/us-en/lab-academy/applied-industries/bioprocessing/introduction-to-bioprocessing/bioprocessing-scale-up/]
- 86. How Predictive Modeling Can Benefit Bioreactor ... [https://www.biopharminternational.com/view/how-predictive-modeling-can-benefit-bioreactor-performance]
- 87. Addressing bioreactor hiPSC aggregate stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11218057/]
- 88. Protocol for enhanced proliferation of human pluripotent ... [https://www.sciencedirect.com/science/article/pii/S2666166722002210]
- 89. Defining synthetic surfaces for human pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4230363/]
- 90. Overcoming Scale-Up Challenges in iPSC Production [https://www.pbsbiotech.com/carr-biosystems-use-case-overcoming-scale-up-challenges-in-ipsc-production]
- 91. The Cell and Gene Therapy Dilemma Centralized Vs ... [https://www.cellandgene.com/doc/the-cell-and-gene-therapy-dilemma-centralized-vs-decentralized-manufacturing-0001]
- 92. A simulation-based comparison of centralized and point-of- ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324923010381]
- 93. Promises and challenges of a decentralized CAR T-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11235344/]
- 94. The 2025 Surge in Stem-Cell Research and Development [https://vasro.de/en/stem-cell-research-resurgence-2025/]
- 95. ARPA-H announces project to scale methods for making ... [https://arpa-h.gov/news-and-events/arpa-h-announces-project-scale-methods-making-more-affordable-personalized-cell]
- 96. Automation and Standardization Will Cut Cell and Gene ... [https://regmedfoundation.org/2024/09/04/automation-and-standardization-will-cut-cell-and-gene-therapy-production-costs/]
- 97. automated and closed cell therapy market size [https://www.biospace.com/press-releases/automated-and-closed-cell-therapy-market-size-worth-usd-11-20-bn-by-2034]
- 98. Characterization and cost-benefit analysis of automated ... [https://pubmed.ncbi.nlm.nih.gov/30203447/]
- 99. Driving Down COGS Leveraging Automation Technologies ... [https://www.cellandgene.com/doc/driving-down-cogs-leveraging-automation-technologies-and-mitigating-risk-0001]
- 100. Stem Cell Manufacturing Market Size to Surpass USD ... [https://www.precedenceresearch.com/stem-cell-manufacturing-market]
- 101. Stem Cell Manufacturing Market Growth Rate, Industry ... [https://www.datamintelligence.com/research-report/stem-cell-manufacturing-market]
- 102. Addressing the Challenges of Cell Therapy Manufacturing [https://www.scaleready.com/addressing-the-challenges-of-cell-therapy-manufacturing/]
- 103. Stem Cell Manufacturing Market Surges 11.35% CAGR ... [https://www.towardshealthcare.com/insights/stem-cell-manufacturing-market-sizing]
- 104. Design Considerations for Large-Scale Stem Cell ... [https://ispe.org/pharmaceutical-engineering/november-december-2023/design-considerations-large-scale-stem-cell]
- 105. Production of mesenchymal stromal/stem cells according to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3707032/]