Patient-Specific iPSCs for Neurodegenerative Disease: Modeling, Mechanisms, and Therapeutic Discovery
Patient-specific induced pluripotent stem cells (iPSCs) are revolutionizing the study and treatment of neurodegenerative diseases.
Patient-Specific iPSCs for Neurodegenerative Disease: Modeling, Mechanisms, and Therapeutic Discovery
Abstract
Patient-specific induced pluripotent stem cells (iPSCs) are revolutionizing the study and treatment of neurodegenerative diseases. This article provides a comprehensive resource for researchers and drug development professionals, exploring how iPSC technology enables the creation of genetically accurate in vitro models of conditions like Alzheimer's, Parkinson's, and Amyotrophic Lateral Sclerosis (ALS). It covers foundational reprogramming mechanisms, advanced methodological applications in disease modeling and drug screening, critical troubleshooting for manufacturing and quality control, and rigorous validation against clinical outcomes. By synthesizing recent advances and practical strategies, this guide aims to accelerate the translation of patient-specific iPSC research into validated disease insights and effective therapeutic candidates.
The Foundation of Patient-Specific iPSCs: From Somatic Cell to Disease-Relevant Neuron
Core Principles of Somatic Cell Reprogramming and Pluripotency
The ability to reprogram somatic cells into induced pluripotent stem cells (iPSCs) represents one of the most significant breakthroughs in modern regenerative medicine and disease modeling. Since the initial discovery by Takahashi and Yamanaka, iPSC technology has fundamentally transformed our approach to investigating human development and disease [1]. This technology allows for the generation of patient-specific pluripotent stem cells that can be differentiated into any cell type of the body, providing an unprecedented platform for studying neurodegenerative diseases, drug screening, and developing personalized therapeutic strategies [2] [3]. The core principle of somatic cell reprogramming involves reversing the epigenetic landscape to return differentiated cells to an embryonic-like pluripotent state, thereby erasing their specialized identity and restoring developmental potential [4] [5]. This technical guide examines the molecular mechanisms, methodologies, and applications of somatic cell reprogramming, with particular emphasis on its transformative role in neurodegenerative disease research.
Historical Foundations and Key Discoveries
The conceptual foundation for cellular reprogramming was established through decades of pioneering research that challenged the long-held belief that cell differentiation was an irreversible process. Conrad Waddington's classic "epigenetic landscape" metaphor depicted cell differentiation as a ball rolling downhill toward an increasingly restricted and terminal state [4]. The reversal of this process was first demonstrated by John Gurdon in 1962 through somatic cell nuclear transfer (SCNT) experiments in Xenopus laevis frogs, showing that a nucleus from a terminally differentiated somatic cell could support the development of an entire organism when transplanted into an enucleated egg [1] [5]. This groundbreaking work revealed that the genetic material in specialized cells remains intact and can be reprogrammed to a embryonic state.
The isolation of mouse embryonic stem cells (ESCs) in 1981 by Evans and Kaufman and human ESCs by Thomson in 1998 provided critical reference points for understanding pluripotency [1]. Subsequent cell fusion experiments between ESCs and somatic cells demonstrated that factors within ESCs could reprogram somatic nuclei to pluripotency, suggesting that the process was mediated by specific molecular determinants [1]. The field was revolutionized in 2006 when Takahashi and Yamanaka demonstrated that the forced expression of only four transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as the OSKM or Yamanaka factors)—could reprogram mouse fibroblasts into induced pluripotent stem cells [2] [1]. This discovery was rapidly extended to human cells in 2007 by both Yamanaka's group and Thomson's group, the latter using OCT4, SOX2, NANOG, and LIN28 [2] [1]. These landmark studies earned Gurdon and Yamanaka the 2012 Nobel Prize in Physiology or Medicine and established the fundamental methodology for generating patient-specific pluripotent stem cells without embryonic destruction.
Molecular Mechanisms of Reprogramming
Epigenetic Remodeling and Transcriptional Regulation
The process of somatic cell reprogramming involves profound reorganization of the epigenetic and transcriptional landscape, effectively reversing the Waddington epigenetic landscape to push differentiated cells back up toward a pluripotent state [4] [5]. This complex process occurs through two broad phases: an early, stochastic phase where somatic genes are silenced and early pluripotency-associated genes are activated, followed by a more deterministic late phase where late pluripotency-associated genes are established [1]. The reprogramming factors initiate widespread changes in chromatin structure, DNA methylation patterns, and histone modifications that collectively erase the somatic epigenetic memory and establish a pluripotent state [1].
OCT4 and SOX2 serve as pioneer factors in this process, capable of binding to closed chromatin regions and initiating their opening [4]. These core factors activate endogenous pluripotency networks while repressing somatic-specific genes. KLF4 contributes to this process by regulating downstream targets including NANOG, another critical pluripotency factor [4]. c-MYC plays a distinct role by promoting global chromatin accessibility through histone acetylation and driving proliferation, though it is not absolutely essential for reprogramming [2] [4]. The mesenchymal-to-epithelial transition (MET) represents another critical event during early reprogramming, particularly when starting with fibroblast populations [1].
Table 1: Core Reprogramming Factors and Their Functions
| Factor | Primary Function | Essentiality | Alternative Factors |
|---|---|---|---|
| OCT4 | Pioneer transcription factor; activates pluripotency network | Essential | NR5A2 [2] |
| SOX2 | Pioneer transcription factor; regulates embryonic development | Essential | SOX1, SOX3 [2] |
| KLF4 | Transcriptional regulator; activates NANOG | Non-essential | KLF2, KLF5 [2] |
| c-MYC | Global chromatin modifier; enhances proliferation | Non-essential | L-MYC, N-MYC [2] |
Alternative Reprogramming Factors and Pathways
Subsequent research has identified numerous alternative factors and pathways that can replace or supplement the original Yamanaka factors. The small molecule RepSox can replace SOX2 in reprogramming, while Esrrb and Glis1 can serve as alternatives to c-MYC [2]. Other studies have demonstrated that SALL4, combined with NANOG, Esrrb, and LIN28, can generate high-quality iPSCs [5]. In certain contexts, such as with human neural stem cells, expression of OCT4 alone has proven sufficient to generate iPSCs, highlighting the pivotal role of this factor and the varying requirements across different cell types [2].
Methodologies for Somatic Cell Reprogramming
Delivery Systems for Reprogramming Factors
The initial reprogramming methods relied on integrating viral vectors, particularly retroviruses and lentiviruses, which raised concerns about potential tumorigenesis due to insertional mutagenesis [2]. This limitation has driven the development of non-integrating delivery systems that improve the safety profile of iPSCs for clinical applications. Current delivery methods span multiple technological platforms, each with distinct advantages and limitations for research and therapeutic use.
Table 2: Comparison of Reprogramming Factor Delivery Systems
| Delivery System | Genetic Material | Genomic Integration | Key Applications |
|---|---|---|---|
| Retrovirus/Lentivirus | DNA | Yes | Basic research, proof-of-concept studies [2] |
| Sendai Virus | RNA | No | Clinical-grade iPSC generation [2] |
| Episomal Plasmid | DNA | No | Clinical applications, good manufacturing practice [2] |
| Synthetic mRNA | RNA | No | Clinical applications, high efficiency [2] |
| Recombinant Protein | Protein | No | Basic research, proof-of-concept [2] |
Chemical Reprogramming
A significant advancement in the field has been the development of fully chemical reprogramming approaches that use defined small-molecule combinations to induce pluripotency without genetic manipulation [2] [6]. This method offers a fundamentally different approach with enhanced safety profiles for clinical applications. Chemical reprogramming of human blood cells has been recently achieved with high efficiency, enabling robust generation of human chemically induced pluripotent stem (hCiPS) cells from both cord blood and adult peripheral blood mononuclear cells [6]. Notably, this approach has proven effective even with minimal starting material, generating over 100 hCiPS colonies from a single drop of fingerstick blood [6].
Chemical reprogramming follows a stepwise process with a distinct intermediate cell state that exhibits enhanced chromatin accessibility and activation of early embryonic developmental genes [2]. This transient state shows gene expression signatures analogous to those observed during initial limb regeneration in axolotls, suggesting the activation of conserved regenerative programs [2]. The chemical approach provides a more flexible and standardized platform for reprogramming, as small molecules are easily synthesized, quality-controlled, and administered without the complexities of genetic delivery systems [6].
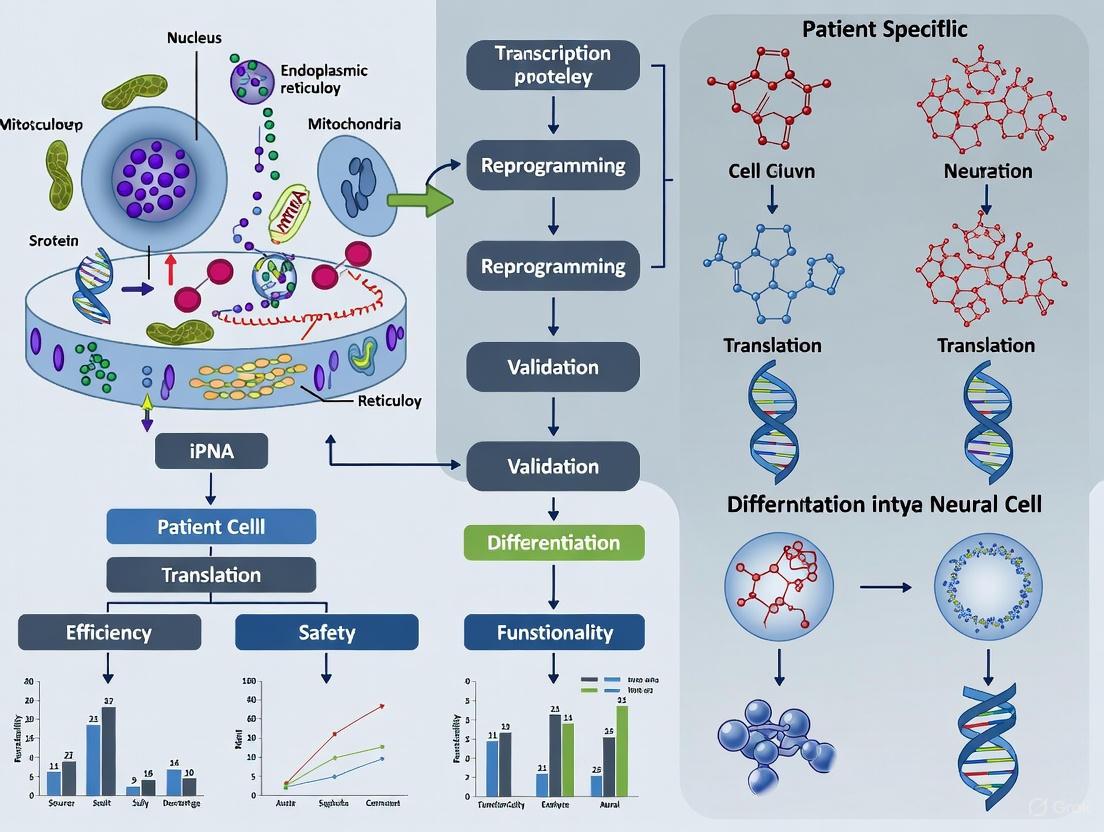
Figure 1: Chemical reprogramming workflow showing the transition from somatic cells to hCiPS cells through a highly plastic intermediate state, driven by small molecule cocktails that trigger epigenetic resetting and regenerative program activation [2] [6].
Enhancing Reprogramming Efficiency
Several strategies have been developed to improve the efficiency and kinetics of somatic cell reprogramming. Inhibition of the p53 tumor suppressor pathway significantly increases reprogramming efficiency, though this approach requires careful consideration due to potential cancer risks [2]. Additional epigenetic modulators, including DNA methyltransferase inhibitors (5-aza-cytidine, RG108), histone deacetylase inhibitors (sodium butyrate, trichostatin A, valproic acid), and the histone methylation regulator neplanocin A, have been shown to enhance reprogramming robustness [2]. The combination of 8-Bromoadenosine 3′,5′-cyclic monophosphate (8-Br-cAMP) with valproic acid increased human fibroblast reprogramming efficiency by up to 6.5-fold [2]. MicroRNAs, particularly the miR-302/367 cluster and miR-372, also significantly improve reprogramming efficiency [2].
Experimental Protocols for iPSC Generation
Fibroblast Reprogramming Using Non-Integrating Methods
For generating clinical-grade iPSCs, non-integrating methods are preferred. The episomal plasmid system provides an effective approach: (1) Culture human dermal fibroblasts in DMEM/F12 medium supplemented with 10% fetal bovine serum; (2) At 60-70% confluency, transfect with episomal plasmids containing OCT4, SOX2, KLF4, L-MYC, LIN28, and p53 shRNA using electroporation; (3) After 48 hours, transfer cells to feeder-free culture conditions with essential 8 medium; (4) Change medium daily and monitor for emergence of embryonic stem cell-like colonies after 14-21 days; (5) Manually pick and expand individual colonies for characterization [2].
Chemical Reprogramming of Human Blood Cells
The chemical reprogramming of blood cells represents a recent advancement: (1) Isolate mononuclear cells from human cord blood or adult peripheral blood; (2) Expand cells in erythroid progenitor cell culture conditions; (3) Treat with a defined cocktail of small molecules targeting key epigenetic barriers and signaling pathways; (4) Transfer cells to adherent culture conditions and continue small molecule treatment; (5) Monitor for emergence of adherent colonies with embryonic stem cell morphology over 25-35 days; (6) Pick and expand hCiPS colonies in chemically defined medium [6]. This method has demonstrated higher efficiency compared to traditional OSKM-based approaches in blood cells and works effectively with both fresh and cryopreserved samples [6].
Characterization of Pluripotent Stem Cells
Validating fully reprogrammed iPSCs requires multiple lines of evidence: (1) Morphological assessment of embryonic stem cell-like colonies with high nucleus-to-cytoplasm ratio; (2) Immunocytochemistry for pluripotency markers including OCT4, SOX2, NANOG, TRA-1-60, and TRA-1-81; (3) RT-PCR analysis for endogenous pluripotency gene expression and silencing of transgenes if applicable; (4) In vitro differentiation through embryoid body formation followed by immunostaining for derivatives of all three germ layers; (5) Karyotype analysis to confirm genomic integrity; (6) Teratoma formation assay in immunodeficient mice to validate differentiation potential in vivo [6] [1].
The Scientist's Toolkit: Essential Reagents for Reprogramming
Table 3: Key Research Reagent Solutions for Somatic Cell Reprogramming
| Reagent Category | Specific Examples | Function in Reprogramming |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC/L-MYC | Core transcription factors inducing pluripotency [2] |
| Epigenetic Modulators | VPA, Sodium Butyrate, Trichostatin A, 5-aza-cytidine | Enhance reprogramming efficiency by modifying chromatin structure [2] |
| Signaling Inhibitors | RepSox (TGF-β inhibitor), DMH1 (BMP inhibitor) | Replace transcription factors and promote MET [2] |
| Metabolic Regulators | 8-Br-cAMP | Enhances reprogramming efficiency through signaling activation [2] |
| Culture Matrices | Matrigel, Vitronectin, Laminin-521 | Provide substrate for pluripotent cell adhesion and expansion [6] |
| Pluripotency Media | Essential 8 Medium, mTeSR1 | Defined, xeno-free media supporting pluripotent state [6] |
| Blood Cell Culture Supplements | Erythropoietin, SCF, IL-3 | Support expansion of blood-derived progenitors for reprogramming [6] |
Applications in Neurodegenerative Disease Research
Disease Modeling and Drug Discovery
iPSC technology has become an invaluable tool for investigating neurodegenerative diseases, particularly amyotrophic lateral sclerosis (ALS), Alzheimer's disease (AD), and frontotemporal dementia (FTD) [2] [7] [8]. Patient-specific iPSCs enable researchers to generate neuronal models that recapitulate disease-specific pathology in vitro. iPSC-derived motor neurons (iPSC-MNs) from ALS patients provide a robust platform to investigate molecular mechanisms underpinning disease pathogenesis and accelerate the discovery of novel therapeutic strategies [2]. Similarly, iPSC models of familial AD with mutations in PSEN1, PSEN2, or APP genes have demonstrated increased production of amyloid-β and altered Aβ42/40 ratios, confirming their utility in modeling disease mechanisms [3].
Several clinical trials based on iPSC research have been initiated for neurodegenerative diseases, including trials of bosutinib, ropinirole, and ezogabine for ALS, and WVE-004 and BII078 for ALS/FTD [7] [8]. iPSC-based screening platforms have identified compounds that target cholesterol metabolism to reduce phospho-Tau accumulation in AD models, revealing promising therapeutic avenues [3]. The integration of artificial intelligence with iPSC-based screening has further enhanced drug discovery efforts for neurodegenerative conditions [7] [8].
Three-Dimensional Models and Organoids
The development of three-dimensional cerebral organoids from patient-specific iPSCs has advanced modeling of neurodegenerative diseases by better recapitulating the complexity of the human brain [3]. For Alzheimer's disease research, cerebral organoids carrying PSEN1 mutations have been successfully established, exhibiting key pathological features including increased Aβ42/40 ratios and reduced synaptic proteins [3]. Similarly, iPSC-derived neurovascular unit models incorporating brain microvascular endothelial cells, astrocytes, and cortical projection neurons have been developed to study cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), revealing impaired barrier function and disorganized tight junctions [3]. These advanced models provide more physiologically relevant systems for investigating disease mechanisms and screening therapeutic candidates.
Figure 2: Application of iPSC technology in neurodegenerative disease research, showing the pathway from patient samples to disease modeling and drug development through two-dimensional neuronal cultures and three-dimensional organoid systems [2] [3].
The core principles of somatic cell reprogramming and pluripotency have established a revolutionary platform for biomedical research and therapeutic development. The molecular mechanisms that govern the reversal of cellular differentiation involve sophisticated reprogramming of the epigenetic landscape, activation of endogenous pluripotency networks, and reorganization of cellular metabolism. Continued refinement of reprogramming methodologies, particularly the development of non-integrating delivery systems and fully chemical approaches, has enhanced the safety and efficiency of iPSC generation. In the context of neurodegenerative diseases, patient-specific iPSCs provide unprecedented opportunities to model pathogenesis, identify novel therapeutic targets, and screen candidate compounds in human neuronal systems. As the field advances, the integration of iPSC technology with emerging techniques in genome editing, three-dimensional organoid culture, and artificial intelligence promises to further accelerate progress toward effective treatments for currently incurable neurological disorders.
The discovery that somatic cells could be reprogrammed into induced pluripotent stem cells (iPSCs) revolutionized biomedical research, creating unprecedented opportunities for disease modeling and regenerative medicine. This breakthrough, achieved by Shinya Yamanaka's team in 2006, demonstrated that the forced expression of four specific transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as OSKM)—could revert adult cells to an embryonic-like pluripotent state [2] [1]. For neurodegenerative disease research, this technology offers a transformative approach: the ability to generate patient-specific neural cells in vitro, including the neurons and glial cells affected in conditions such as amyotrophic lateral sclerosis (ALS), Alzheimer's, and Parkinson's diseases [2]. Patient-derived iPSCs provide a robust platform to recapitulate disease-specific pathology and investigate the molecular mechanisms underpinning these disorders, thereby accelerating the discovery of novel therapeutic strategies [2]. The core of this technology lies in understanding the reprogramming factors—their functions, combinations, and delivery methods—which this review will explore in depth, with a specific focus on applications for neurodegenerative disease research.
Core OSKM Reprogramming Factors
The original OSKM factors were identified through a systematic screening of 24 genes known to be important for maintaining pluripotency in embryonic stem cells [1]. The successful reprogramming of both mouse and human fibroblasts using these factors established a new paradigm in cellular biology, proving that cell fate could be reversed without somatic cell nuclear transfer [1]. Each factor plays a distinct and critical role in the reprogramming process, as detailed below.
Table 1: Core OSKM Reprogramming Factors and Their Functions
| Factor | Full Name | Primary Function in Reprogramming | Key Target Genes |
|---|---|---|---|
| OCT4 | Octamer-binding transcription factor 4 | Master regulator of pluripotency; upregulates embryonic genes and inhibits differentiation genes [4]. | Activates pluripotency genes (e.g., NANOG); essential for stem cell maintenance [4]. |
| SOX2 | SRY (Sex determining region Y)-Box 2 | Partners with OCT4; regulates pluripotency gene expression and inhibits somatic gene programs [4]. | Works with OCT4 to co-activate pluripotency network; critical for early development [4]. |
| KLF4 | Krüppel-like factor 4 | Context-dependent transcriptional activator/suppressor; promotes mesenchymal-to-epithelial transition (MET) [2] [4]. | Regulates NANOG expression; can inhibit p53 to enhance reprogramming efficiency [4] [2]. |
| c-MYC | Cellular Myelocytomatosis | Global chromatin modifier; enhances proliferation and metabolism; increases efficiency but is not essential [4]. | Binds to ~15% of human genes; promotes expression of proliferation-related genes [4]. |
While OCT4 and SOX2 are considered the most essential core factors, KLF4 and c-MYC significantly enhance reprogramming efficiency. However, the use of the oncogene c-MYC poses significant safety risks for clinical applications, including tumorigenesis, which has driven the search for safer alternatives [2].
Alternative Reprogramming Factors and Small Molecules
Subsequent research has revealed that the OSKM combination is not rigid. Many factors can be substituted or supplemented to improve safety, efficiency, and applicability for different somatic cell sources. These alternatives are particularly valuable for generating clinical-grade iPSCs for therapeutic development.
Table 2: Alternative Reprogramming Factors and Small Molecules
| Category | Alternative to | Examples | Mechanism of Action / Rationale | Application Notes |
|---|---|---|---|---|
| Factor Substitutes | c-MYC | L-MYC, N-MYC [2] | Reduced tumorigenic risk compared to c-MYC while maintaining efficiency [2]. | L-MYC is often preferred for its superior safety profile. |
| KLF4 | KLF2, KLF5 [2] | Family members with similar functions can substitute for KLF4. | Most alternatives show lower efficiency than the original factor [2]. | |
| SOX2 | SOX1, SOX3, GLIS1 [2] | SOX family members can replace SOX2; GLIS1 acts as an alternative. | Small molecule RepSox can also replace SOX2 function [2]. | |
| OCT4 | NR5A2 [2] | Can substitute for OCT4 in combination with SOX2 and KLF4. | Demonstrates the flexibility of the core pluripotency network. | |
| Non-OSKM Factors | N/A | NANOG, LIN28 [4] [1] | OCT4, SOX2, NANOG, LIN28 (OSNL) form an alternative combination. | Used by Thomson et al. for human fibroblast reprogramming [4] [1]. |
| Efficiency Enhancers | N/A | miRNAs (e.g., miR-302/367, miR-372), LIN28 [2] | Improve reprogramming to pluripotency; regulate key developmental pathways. | Often used alongside transcription factors. |
| Epigenetic Modulators | N/A | VPA (HDAC inhibitor), Sodium Butyrate, 5-aza-cytidine [2] | Open chromatin structure, facilitating epigenetic remodeling during reprogramming. | Can increase iPSC generation efficiency by up to 6.5-fold when combined (e.g., 8-Br-cAMP + VPA) [2]. |
| Chemical Reprogramming | Genetic Factors | Specific small-molecule cocktails [2] [9] | Fully chemical reprogramming achieved without genetic manipulation, enhancing clinical safety [2]. | Significantly reduces tumorigenicity concerns; a major advance for clinical translation [10]. |
A notable advancement is the finding that the necessity of factors can vary by cell type. For instance, expressing OCT4 alone in human neural stem cells is sufficient to generate iPSCs, highlighting the pivotal role of OCT4 and the influence of the starting cell's epigenetic state [2].
Delivery Systems for Reprogramming Factors
The method used to deliver reprogramming factors is critical, as it impacts efficiency, genomic integrity, and the clinical potential of the resulting iPSCs. The ideal delivery system maximizes reprogramming efficiency while minimizing genomic alterations.
Table 3: Comparison of Reprogramming Factor Delivery Systems
| Vector/Platform | Genetic Material | Genomic Integration? | Key Advantages | Key Disadvantages |
|---|---|---|---|---|
| Retrovirus | RNA | Yes | High efficiency; stable expression. | Integrates into genome; silenced in iPSCs; risk of insertional mutagenesis. |
| Lentivirus | RNA | Yes | Can infect non-dividing cells; high efficiency. | Integrates into genome; risk of insertional mutagenesis. |
| Sendai Virus | RNA | No | High efficiency; does not integrate; viral RNA degrades over time. | Requires effort to clear virus; potential immunogenicity. |
| Adenovirus | DNA | No | Does not integrate; lower immunogenicity than other viruses. | Lower reprogramming efficiency. |
| Episomal Plasmid | DNA | No | Non-viral; does not integrate; simple to use. | Low efficiency; requires repeated transfection. |
| PiggyBac Transposon | DNA | Yes, but reversible | Can be removed after integration; high cargo capacity. | Complex removal process; still involves temporary integration. |
| Synthetic mRNA | RNA | No | Non-viral, non-integrating; high efficiency; controlled dosing. | Can trigger innate immune response; requires multiple transfections. |
| Recombinant Protein | Protein | No | Completely non-genetic; highest safety profile. | Very low efficiency; difficult to produce and deliver. |
The field is increasingly moving toward non-integrating methods, such as Sendai virus, synthetic mRNA, and episomal plasmids, particularly for clinical applications where genomic integrity is paramount [2]. Furthermore, fully chemical reprogramming represents the ultimate safety goal, eliminating the need for genetic material altogether [2] [9].
The Scientist's Toolkit: Key Reagents for iPSC Generation
Table 4: Essential Research Reagents for iPSC Generation
| Reagent Category | Specific Examples | Function in Reprogramming |
|---|---|---|
| Core Transcription Factors | OSKM (OCT4, SOX2, KLF4, c-MYC) factors | Ectopic expression reprograms somatic cells to pluripotency; the foundational components of the process. |
| Delivery Tools | Retroviral/Lentiviral vectors, Sendai virus, mRNA kits | Vehicles for introducing reprogramming factors into target somatic cells. |
| Efficiency Enhancers | Valproic Acid (VPA), Sodium Butyrate, 8-Br-cAMP | Small molecule compounds that increase reprogramming efficiency by modulating epigenetic states and signaling pathways [2]. |
| Cell Culture Media | DMEM/F12, specialized reprogramming media | Provides essential nutrients and a controlled environment to support cell survival and reprogramming. |
| Somatic Cell Sources | Skin fibroblasts, peripheral blood cells | Starting material for reprogramming; chosen for patient-specific applications and accessibility. |
| Characterization Antibodies | Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA4 | Used to confirm the successful establishment of pluripotency in resulting iPSC lines via immunostaining. |
The systematic identification and optimization of reprogramming factors have positioned iPSC technology as a cornerstone of modern biomedical research. The evolution from the canonical OSKM factors to safer, more efficient alternatives, including fully chemical reprogramming, has significantly enhanced the potential of this technology for clinical translation. For neurodegenerative diseases, where access to functional human neurons for study is severely limited, patient-specific iPSCs provide an unparalleled platform. These cells enable researchers to dissect disease mechanisms in relevant cell types, screen for novel therapeutic compounds, and develop autologous cell replacement strategies. As delivery methods become more refined and our understanding of the reprogramming epigenome deepens, the generation of clinical-grade iPSCs will become more standardized. The ongoing refinement of key reprogramming factors continues to push the field closer to its ultimate goal: leveraging a patient's own cells to understand and treat devastating neurodegenerative disorders.
The generation of induced pluripotent stem cells (iPSCs) represents a transformative advancement in regenerative medicine and disease modeling. By reprogramming adult somatic cells back to a pluripotent state, researchers can create patient-specific cell lines for studying disease mechanisms, drug screening, and developing cell-based therapies. The method used to deliver reprogramming factors significantly impacts the genomic integrity, safety profile, and clinical applicability of the resulting iPSCs. This technical guide provides a comprehensive comparison of integrating and non-integrating delivery systems, with particular emphasis on their applications in neurodegenerative disease research.
Core Principles of iPSC Reprogramming
iPSC reprogramming involves the forced expression of specific transcription factors to reverse the developmental clock of somatic cells. The original method utilized four core factors: OCT4, SOX2, KLF4, and c-MYC (collectively known as OSKM) [11]. These factors work in concert to reactivate the endogenous pluripotency network while silencing somatic cell programs. The delivery method for introducing these factors into target cells represents a critical determinant of iPSC quality and safety, particularly for modeling complex neurodegenerative disorders where long-term culture and neuronal differentiation are required.
Integrating Delivery Systems: Methods and Limitations
Integrating delivery systems introduce reprogramming factors into the host cell genome, creating permanent genetic modifications. The primary methods include:
Retroviral Vectors
Retroviruses were used in the pioneering iPSC studies and remain efficient for reprogramming. These vectors require cell division for integration and are typically silenced in fully reprogrammed iPSCs, allowing endogenous pluripotency genes to take over [11]. However, the random nature of integration poses significant risks, including insertional mutagenesis and potential reactivation of transgenes in differentiated cells.
Lentiviral Vectors
Lentiviruses can infect both dividing and non-dividing cells, offering broader applicability than retroviruses. Like retroviral methods, they result in permanent genomic integration. Studies have reported reprogramming efficiencies of approximately 0.27% with lentiviral methods [12]. The major concern with both retroviral and lentiviral systems is the risk of oncogene activation, particularly when using potent factors like c-MYC, which is implicated in approximately 70% of human cancers [11].
Non-Integrating Delivery Systems: Techniques and Applications
Non-integrating methods provide transient expression of reprogramming factors, eliminating the risk of permanent genetic alterations. These approaches are particularly valuable for clinical applications and disease modeling where genomic integrity is paramount.
Sendai Virus (SeV)
Sendai virus is an RNA virus that replicates in the cytoplasm without integrating into the host genome. The CytoTune kit utilizing SeV demonstrates reprogramming efficiencies of approximately 0.077% [12]. A significant advantage is its high reliability, with success rates of 94% in generating multiple iPSC colonies [12]. However, the viral RNA must be actively diluted out through cell passaging, with studies showing 53.8% of lines clear the virus by passages 6-8, and only 21.2% remain positive by passages 9-11 [12].
Episomal Vectors (Epi)
Episomal vectors utilize Epstein-Barr virus-derived sequences that facilitate plasmid replication in dividing cells without genomic integration. These systems achieve reprogramming efficiencies of approximately 0.013% [12]. A concern with this method is the potential persistence of plasmids, with ~39.1% of early-passage iPSC lines retaining EBNA1 DNA, decreasing slowly to 33.3% at passages 9-11 [12]. Fluorescent tagging strategies have been developed to identify plasmid-retaining colonies [12].
mRNA Transfection
The mRNA method involves daily transfections of in vitro-transcribed mRNAs encoding reprogramming factors. This approach achieves the highest reprogramming efficiency at 2.1% but has a lower success rate of 27% due to massive cell death and detachment issues [12]. The method requires chemical measures to limit activation of the innate immune system by foreign nucleic acids. Success rates improve significantly to 73% when combined with microRNA transfections (miRNA + mRNA method) [12].
Additional Non-Integrating Methods
Other non-integrating approaches include adenoviral vectors, plasmid transfection, and protein transduction. Electroporation-based methods (Nucleofector, Neon systems) generally show higher reprogramming efficiency than chemical-based approaches like Lipofectamine 3000 [13]. Protein-induced pluripotent stem cells (piPSCs) generated through direct delivery of recombinant proteins represent perhaps the safest approach, completely avoiding genetic manipulation [14].
Quantitative Comparison of Reprogramming Methods
Table 1: Comprehensive Comparison of iPSC Reprogramming Methods
| Method | Reprogramming Efficiency (%) | Success Rate (%) | Aneuploidy Rate (%) | Hands-on Time (Hours) | Time to Colony Picking (Days) |
|---|---|---|---|---|---|
| mRNA | 2.1 [12] | 27 [12] | 2.3 [12] | ~8 [12] | ~14 [12] |
| miRNA + mRNA | 0.19 [12] | 73 [12] | N/A | N/A | N/A |
| Sendai Virus | 0.077 [12] | 94 [12] | 4.6 [12] | 3.5 [12] | ~26 [12] |
| Episomal | 0.013 [12] | 93 [12] | 11.5 [12] | ~4 [12] | ~20 [12] |
| Lentiviral | 0.27 [12] | 100 [12] | 4.5 [12] | N/A | N/A |
| Retroviral | N/A | N/A | 13.5 [12] | N/A | N/A |
Table 2: Genomic Integrity Assessment Across Reprogramming Methods
| Method | Copy Number Variation Burden | Likely Pathogenic CNVs | Single Nucleotide Variations | Mosaicism |
|---|---|---|---|---|
| Integrating Methods | Maximum CNV sizes 20x higher [15] | Elevated [15] | Increased [15] | More prevalent [15] |
| Non-Integrating Methods | Lower CNV burden [15] | Reduced [15] | Reduced [15] | Less prevalent [15] |
Impact on Genomic Stability and Pluripotency
The choice of reprogramming method significantly impacts the genomic stability of resulting iPSCs. Studies comparing integrating and non-integrating methods have revealed that integrating methods produce significantly larger copy number variations (CNVs) - with maximum sizes up to 20 times higher than non-integrating methods [15]. Additionally, integrating methods show higher numbers of novel CNVs and likely pathogenic CNVs overlapping with databases like ISCA [15].
Regarding pluripotency, all reprogramming methods can generate high-quality iPSCs expressing standard pluripotency markers including TRA160, NANOG, SSEA4, TRA181, OCT4, DNMT3B, SOX2, REX1, LIN28, and UTF1 [12]. However, some studies report differential expression of certain genes (TCERG1L, FAM19A5, MEG3/RIAN) in a subset of iPSC lines regardless of reprogramming method, suggesting additional factors influence complete reprogramming [12].
iPSC Reprogramming Workflow
The following diagram illustrates the general workflow for generating and validating patient-specific iPSCs using non-integrating methods, with particular application to neurodegenerative disease modeling:
Application to Neurodegenerative Disease Research
The generation of patient-specific iPSCs has revolutionized neurodegenerative disease research by enabling the creation of in vitro models that capture patient-specific genetics. Large-scale studies have demonstrated the particular value of non-integrating methods for this application. For instance, in amyotrophic lateral sclerosis (ALS) research, episomal reprogramming has been used to create iPSC libraries from 100 patients with sporadic ALS, enabling population-wide phenotypic screening and drug discovery [16].
These patient-derived models recapitulate key disease aspects including reduced motor neuron survival, accelerated neurite degeneration, and transcriptional dysregulation [16]. Importantly, the use of non-integrating methods ensures that observed phenotypes genuinely reflect the disease pathology rather than artifacts of genomic manipulation. This approach has enabled identification of potential combinatorial therapies (riluzole, memantine, and baricitinib) that rescue motor neuron survival across diverse SALS donors [16].
Similarly, iPSC-based epilepsy models derived from patients with CLCNKB mutations have revealed differentially expressed genes through RNA sequencing, providing insights into disease mechanisms and potential therapeutic targets [17]. The ability to generate genetically accurate models of neurological disorders underscores the critical importance of selecting appropriate reprogramming methods that minimize genomic alterations while maintaining high reprogramming efficiency.
The Scientist's Toolkit: Essential Reagents for iPSC Generation
Table 3: Key Research Reagent Solutions for iPSC Generation and Characterization
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| Reprogramming Kits | CytoTune-iPS Sendai Reprogramming Kit [12], Stemgent mRNA Reprogramming Kit [12] | Commercial systems for efficient non-integrating reprogramming |
| Delivery Systems | Neon Transfection System [13], Nucleofector System [13], Lipofectamine 3000 [13] | Electroporation and chemical-based methods for nucleic acid delivery |
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [11], OCT4, SOX2, NANOG, LIN28 [11] | Core transcription factors to induce pluripotency |
| Culture Media | Knockout Serum Replacement (KSR) Medium [13], Fibroblast Medium [13] | Specialized media formulations for feeder-dependent iPSC culture |
| Pluripotency Markers | TRA160, TRA181, SSEA4, NANOG, OCT4 [12] [13] | Antibodies for immunocytochemical verification of pluripotency |
| Karyotyping Tools | KaryoLite BoBs [13], Affymetrix Cytoscan HD array [15] | Genomic tools for assessing chromosomal integrity and CNVs |
| Differentiation Factors | ChAT, MNX1/HB9, β-tubulin III (Tuj1) [16] | Markers for verifying neural differentiation potential |
Method Selection Framework for Neurodegenerative Disease Applications
The following decision diagram provides a structured approach for selecting the optimal reprogramming method based on research goals and technical constraints:
The selection between integrating and non-integrating reprogramming methods represents a critical decision point in experimental design for neurodegenerative disease research. While integrating methods offer established protocols and good efficiency, non-integrating approaches provide superior genomic integrity essential for clinical translation and accurate disease modeling. For most neurodegenerative disease applications requiring patient-specific iPSCs, Sendai virus and mRNA-based methods offer the optimal balance of efficiency, reliability, and safety. The continued refinement of non-integrating methods, coupled with rigorous genomic quality control, will further enhance our ability to model complex neurological disorders and develop effective therapeutic interventions.
The advent of induced pluripotent stem cells (iPSCs) has revolutionized biomedical research, providing an unprecedented platform for disease modeling, drug screening, and therapeutic development. Within neurodegenerative disease research, patient-specific iPSCs offer the unique capacity to recapitulate disease pathophysiology in vitro, enabling the investigation of molecular mechanisms and personalized therapeutic interventions. The initial step in generating robust neurodegenerative disease models is the selection of an appropriate somatic cell source, a critical decision that directly influences reprogramming efficiency, genomic stability, and the fidelity of subsequent neuronal differentiation. This technical guide provides a comprehensive analysis of somatic cell sources for iPSC-based neurodegenerative disease modeling, detailing methodological considerations, quality control standards, and applications tailored to the requirements of research scientists and drug development professionals.
The choice of somatic cell source significantly impacts the efficiency and quality of resulting iPSC lines, particularly for neurological applications. Key somatic cell types vary in accessibility, reprogramming efficiency, and expansion capability.
Table 1: Characteristics of Somatic Cell Sources for iPSC Generation
| Cell Source | Accessibility | Reprogramming Efficiency | Key Advantages | Limitations for Neurological Modeling |
|---|---|---|---|---|
| Dermal Fibroblasts | Moderate (invasive skin biopsy required) | Variable (0.1%–1%) [18] | High genomic stability; well-established protocols; extensive banking potential [18] | Invasive collection; potential epigenetic memory bias |
| Peripheral Blood Mononuclear Cells (PBMCs) | High (minimally invasive blood draw) | Comparable to fibroblasts [18] | Minimal patient discomfort; renewable source (via blood draws); suitable for longitudinal studies [18] [19] | Lower cell yield per volume; requires specific reprogramming adjustments |
| Urinary Epithelial Cells | Very High (completely non-invasive collection) | Robust [18] | Completely non-invasive; easily repeatable sampling; suitable for pediatric and cognitively impaired patients [18] | Limited initial cell number; potentially higher microbial contamination risk |
| Keratinocytes | Moderate (hair pluck or skin biopsy) | Higher than fibroblasts [18] | Higher reprogramming efficiency than fibroblasts; accessible from minor biopsies [18] | Limited cell yield from plucked hairs; requires specialized culture conditions |
| Dental Pulp Stem Cells | Low (requires dental procedure) | High [18] | Neural crest origin; inherent neurogenic potential; high proliferation rate [18] | Limited availability; requires specialized dental procedures |
| Neural Stem/Progenitor Cells | Very Low (requires specialized tissue access) | High (endogenous expression of pluripotency factors) [19] | Inherent neurological commitment; reduced epigenetic barriers to neural differentiation [19] | Extremely limited accessibility from living donors; ethically complex |
Methodologies for Somatic Cell Reprogramming
Reprogramming Factor Combinations
The foundational reprogramming factors established by Yamanaka and colleagues (OCT4, SOX2, KLF4, c-MYC) remain the benchmark for somatic cell reprogramming. However, subsequent refinements have enhanced safety and efficiency profiles.
Table 2: Reprogramming Factor Combinations and Their Applications
| Factor Combination | Components | Efficiency | Safety Profile | Best Applications |
|---|---|---|---|---|
| OSKM | OCT4, SOX2, KLF4, c-MYC [2] [1] | High | Lower (c-MYC oncogenic potential) [2] | Basic research with robust quality control |
| OSK | OCT4, SOX2, KLF4 (c-MYC omitted) [2] | Moderate | Higher (eliminates c-MYC oncogene) [2] | Preclinical therapeutic development |
| OSNL | OCT4, SOX2, NANOG, LIN28 [2] [1] | Moderate to High | Higher (avoids c-MYC) [2] | Disease modeling and drug screening applications |
| Chemical Reprogramming | Small molecule cocktails (e.g., VPA, CHIR99021, A-83-01) [2] [19] | Lower initially, improving | Highest (non-integrating, transgene-free) [2] | Clinical translation and precision medicine |
Delivery Systems for Reprogramming Factors
The method of introducing reprogramming factors into somatic cells significantly influences genomic integrity and clinical applicability.
Non-integrating methods are strongly preferred for neurodegenerative disease modeling due to the need for genetically stable, clinically relevant models. Sendai virus systems offer an optimal balance of high efficiency and safety, while mRNA-based approaches provide a completely non-viral alternative with comparable safety profiles [18] [19].
Experimental Protocol: iPSC Generation from Peripheral Blood Mononuclear Cells
Materials Required:
- Ficoll-Paque PLUS density gradient medium
- PBMC isolation tubes
- StemSpan H3000 medium with cytokines (SCF, FLT-3 ligand, IL-3, IL-6)
- Sendai virus vectors encoding OSKM factors (CytoTune-iPS 2.0 Sendai Reprogramming Kit)
- mTeSR1 or Essential 8 medium
- Matrigel-coated tissue culture plates
- Rho-associated kinase (ROCK) inhibitor Y-27632
Procedure:
- PBMC Isolation: Collect peripheral blood via venipuncture in heparinized tubes. Isolate PBMCs using density gradient centrifugation with Ficoll-Paque [18].
- Expansion Culture: Resuspend PBMCs in StemSpan H3000 medium supplemented with cytokines. Culture for 5-7 days to expand progenitor populations [18].
- Reprogramming Transduction: On day 0, transduce 1×10^6 PBMCs with Sendai virus vectors at appropriate multiplicities of infection (MOI). Centrifuge plates at 1000×g for 30 minutes to enhance viral contact [19].
- Medium Transition: After 24 hours, replace virus-containing medium with fresh expansion medium. On day 7, transfer transduced cells to Matrigel-coated plates in mTeSR1 medium supplemented with ROCK inhibitor [19].
- Colony Selection: Between days 21-28, identify and manually pick embryonic stem cell-like colonies based on morphology (compact cells with defined borders, high nucleus-to-cytoplasm ratio). Expand selected clones for characterization [18].
Quality Control and Pluripotency Verification
Rigorous quality control is essential to ensure iPSC lines are suitable for neurodegenerative disease modeling. The verification process encompasses molecular characterization and functional assessment.
Key Quality Control Assays:
Pluripotency Marker Verification:
Trilineage Differentiation Potential:
- Embryoid Body Formation: Culture iPSCs in suspension to form embryoid bodies, then plate for spontaneous differentiation [20].
- Germ Layer Marker Analysis: Immunostain differentiated cells for ectoderm (β-III-tubulin), mesoderm (smooth muscle actin), and endoderm (alpha-fetoprotein) markers [20].
- In Vivo Teratoma Assay: Inject iPSCs into immunodeficient mice; analyze resulting teratomas for tissues derived from all three germ layers (requires 2-3 months) [20].
Genomic Integrity Assessment:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for iPSC Generation and Neural Differentiation
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Vectors | CytoTune-iPS Sendai Virus, Episomal plasmids | Delivery of reprogramming factors | Sendai virus preferred for efficiency; episomal for clinical applications [18] [19] |
| Culture Media | mTeSR1, Essential 8, StemFlex | Maintenance of pluripotency | Chemically defined, xeno-free formulations enhance reproducibility [18] |
| Extracellular Matrices | Matrigel, Laminin-521, Vitronectin | Substrate for feeder-free culture | Laminin-521 enhances attachment and survival of neural precursors [18] |
| Neural Induction Media | STEMdiff SMADi Neural Induction, N2/B27 supplements | Direct differentiation to neural lineages | Dual-SMAD inhibition protocol accelerates neural induction [19] |
| Neural Patterning Factors | Retinoic Acid, Sonic Hedgehog, BDNF, GDNF | Regional specification and maturation | Critical for generating disease-relevant neuronal subtypes [2] [21] |
| Gene Editing Tools | CRISPR/Cas9 systems, PiggyBac transposons | Genetic modification for isogenic controls | Essential for correcting mutations or introducing disease variants [20] [19] |
Applications in Neurodegenerative Disease Modeling
Patient-specific iPSCs have enabled significant advances in modeling various neurodegenerative disorders, including Amyotrophic Lateral Sclerosis (ALS), Alzheimer's Disease (AD), and Parkinson's Disease (PD).
Amyotrophic Lateral Sclerosis (ALS) Modeling: iPSCs derived from familial and sporadic ALS patients have been successfully differentiated into motor neurons, recapitulating key disease pathologies including TDP-43 protein aggregation, mitochondrial dysfunction, and neurite degeneration. A recent study utilizing 32 sALS patient-derived iPSC lines identified distinct patient clusters with varying drug responses, leading to the identification of ropinirole hydrochloride as a potential therapeutic candidate [21].
Parkinson's Disease (PD) Modeling: iPSC-derived dopaminergic neurons from PD patients with LRRK2 or SNCA mutations have replicated disease-relevant phenotypes such as α-synuclein accumulation, mitochondrial impairment, and increased susceptibility to oxidative stress. These models have enabled high-throughput screening of compounds that reduce α-synuclein pathology [18] [20].
Alzheimer's Disease (AD) Modeling: iPSC-derived neurons and glial cells from familial AD patients have reproduced hallmark pathological features including β-amyloid deposition, tau hyperphosphorylation, and neuroinflammation. Co-culture systems incorporating microglia have enhanced the modeling of neuroimmune interactions in AD progression [18] [20].
Concluding Recommendations
Selecting the optimal somatic cell source for neurodegenerative disease modeling requires careful consideration of research objectives, patient population, and downstream applications. Peripheral blood mononuclear cells currently represent the optimal balance of accessibility, reprogramming efficiency, and clinical relevance for most neurodegenerative disease modeling applications. For studies requiring maximum neurological relevance, dermal fibroblasts remain valuable for their robust expansion and genomic stability. Emerging sources such as urinary epithelial cells offer particular promise for pediatric neurodegenerative disorders and longitudinal studies requiring repeated sampling.
The integration of advanced gene editing technologies, particularly CRISPR/Cas9, with patient-specific iPSCs enables the generation of isogenic control lines that are fundamental for distinguishing disease-specific phenotypes from background genetic variation. As the field progresses toward increasingly complex 3D model systems including cerebral organoids and assembloids, rigorous quality control of starting somatic cell populations and derived iPSCs becomes increasingly critical for generating physiologically relevant models of neurodegenerative pathogenesis.
Molecular and Epigenetic Remodeling During Neural Fate Acquisition
The process of neural fate acquisition, wherein naive cells are irrevocably committed to a neural lineage, is governed by a precise interplay of extrinsic signaling molecules and intrinsic epigenetic remodeling. This process is fundamental to embryogenesis and is recapitulated in vitro during the differentiation of pluripotent stem cells, including patient-specific induced pluripotent stem cells (iPSCs). The core molecular machinery involves the blockade of Bone Morphogenetic Protein (BMP) signaling, which acts as a master switch to direct cell fate away from epidermal and towards neural lineages. Concurrently, dynamic chromatin modifications, orchestrated by complexes such as the Polycomb Repressor Complex (PRC), silence pluripotency genes and activate neural gene programs. This whitepaper provides a technical guide to the core mechanisms of neural induction, detailing the key signaling pathways, epigenetic regulators, and experimental protocols. Framed within the context of patient-specific iPSC models, this knowledge provides the foundation for advanced in vitro modeling of human neurodevelopment and neurodegenerative diseases, enabling novel drug discovery and therapeutic development.
Core Molecular Mechanisms of Neural Induction
Neural induction is the initial step in embryogenesis where naive cells are converted into committed neural cells [22]. The molecular pathways that govern this binary cell fate decision have been extensively studied and are leveraged in vitro to direct the differentiation of pluripotent stem cells into neural lineages.
The Central Role of BMP Signaling and Its Blockade
The default model of neural induction posits that the blockade of BMP signaling is the pivotal event that drives cells toward a neural fate. In the absence of exogenous inductive signals, mammalian pluripotent stem cells spontaneously differentiate into neural lineages [22]. The presence of BMP signaling promotes differentiation into non-neural ectoderm, characterized by the expression of genes like Id1 [22].
- Key Signaling Molecules: BMP2/4/7 ligands bind to BMP receptors, leading to the phosphorylation of the carboxyl-terminal serine residues of the SMAD1/5/8 proteins. This activated complex then translocates to the nucleus to activate the transcription of genes that promote non-neural fates [22].
- Extracellular Antagonists: Neural inducers such as Noggin, Chordin, and Follistatin are secreted proteins that bind directly to BMP ligands in the extracellular space, preventing them from interacting with their receptors and thus inhibiting the BMP signaling cascade [22].
- Convergence with FGF Signaling: Fibroblast Growth Factor (FGF) signaling also exhibits neural-inducing activity. One mechanism involves FGF promoting the phosphorylation of the intermediate linker domain of SMAD1, which restricts its activity and inhibits the BMP pathway. FGF may also directly induce the expression of neural genes through an independent pathway [22]. The combination of BMP inhibition and FGF signaling is essential for efficient neural induction in amniote embryos and stem cell systems [22].
Table 1: Core Signaling Pathways in Neural Fate Acquisition
| Pathway/Component | Role in Neural Induction | Key Effectors | Outcome of Pathway Activation | Outcome of Pathway Inhibition |
|---|---|---|---|---|
| BMP Signaling | Promotes non-neural (epidermal) fate | BMP2/4/7, BMP Receptors, p-SMAD1/5/8, ID1/ID3 | Differentiation into non-neural ectoderm | Neural fate specification |
| BMP Antagonists | Induces neural fate | Noggin, Chordin, Follistatin | - | Blocks BMP signaling, inducing neural genes |
| FGF Signaling | Supports neural induction | FGF ligands, FGF Receptors | Phosphorylation of SMAD1 linker region; direct neural gene induction | Perturbed neural differentiation |
The "Dual-SMAD Inhibition" Protocol
A widely adopted and efficient method for neural induction from human pluripotent stem cells (hPSCs) is the "dual-SMAD inhibition" protocol [23]. This protocol utilizes small molecule inhibitors to simultaneously suppress both the BMP and TGFβ/Activin/Nodal branches of SMAD signaling.
- BMP Pathway Inhibition: Achieved using molecules like Dorsomorphin or its analogue LDN-193189, which act as BMP receptor kinase inhibitors.
- TGFβ/Activin/Nodal Pathway Inhibition: Achieved using SB431542, an inhibitor of the TGFβ type I receptor ALK5.
- Outcome: The combined inhibition results in highly efficient and rapid conversion of hPSCs into neuroepithelial cells, forming the basis for further differentiation into specific neural subtypes, such as cerebral cortex neural progenitor cells [23].
The following diagram illustrates the core signaling pathway and its experimental inhibition that directs cells toward a neural fate.
Epigenetic Remodeling in Neural Commitment
The shift from a pluripotent to a neural-restricted state requires extensive reprogramming of the epigenetic landscape. This involves the silencing of pluripotency networks and the sequential opening of neural gene loci, a process tightly coupled with extrinsic signaling.
Chromatin Dynamics and Polycomb Complexes
As cells exit pluripotency, chromatin at pluripotent gene loci (e.g., Nanog, Rex) transitions from an open to a condensed, heterochromatic state through DNA methylation and histone modifications [22]. Concurrently, neural gene loci gradually acquire an open chromatin status [22].
- Polycomb Repressor Complexes (PRC): PRC1 and PRC2 are crucial chromatin-modifying complexes that mediate gene silencing through catalysis of specific histone marks.
- Dynamic Subunit Composition: The specificity and function of PRC1 are modulated by the exchange of its subunit components during differentiation. For instance, stem cell-enriched subunits like Cbx7 are replaced by neural progenitor cell (NPC)-enriched subunits like Cbx6, Cbx8, and Pcgf5, which is essential for proper neural differentiation [22].
Integration of Signaling and Epigenetics: The BMP-Phc1 Axis
A direct molecular link exists between the BMP signaling pathway and the epigenetic machinery. Research using mouse embryonic stem (ES) cells has demonstrated that BMP signaling regulates the expression of several PRC component genes, most notably Polyhomeotic Homolog 1 (Phc1) [22] [24].
- BMP Represses Phc1: BMP4 treatment during neural differentiation downregulates the expression of Phc1, a core component of cPRC1 [22].
- Phc1 is Essential for Neural Differentiation: Phc1-knockout (KO) ES cells fail to acquire a neural fate and remain in a pluripotent or primitive non-neural state. Chromatin accessibility analysis (ATAC-seq) revealed that Phc1 is essential for chromatin compaction at pluripotency gene loci during differentiation [22] [24].
- Feedback Loop: Aberrant upregulation of BMP signaling is observed in Phc1 mutant embryos, suggesting a feedback mechanism where the epigenetic regulator Phc1 is required to reinforce and maintain the BMP-inhibited state necessary for neural commitment [22].
The diagram below illustrates the critical role of this epigenetic regulator in neural fate acquisition.
Table 2: Key Epigenetic Regulators in Neural Induction
| Epigenetic Component | Complex/Function | Role in Neural Induction | Consequence of Loss-of-Function |
|---|---|---|---|
| Phc1 | Core component of canonical PRC1 | Essential for silencing pluripotency genes via chromatin compaction; regulated by BMP | Failure to differentiate into neural lineages; cells remain pluripotent [22] [24] |
| Pcgf5 | Component of non-canonical PRC1 | Enriched in NPCs; promotes neural differentiation | Prevents neural differentiation via aberrant SMAD2/TGF-β signaling [22] |
| Cbx7 | PRC1 subunit (Cbx protein) | Enriched in ESCs; maintains pluripotency | - (Subunit exchange during differentiation is crucial) |
| Cbx6/Cbx8 | PRC1 subunits (Cbx proteins) | Enriched in NPCs; promote neural differentiation | Mutants exhibit defective neural development [22] |
| EZH1/EZH2 | Catalytic core of PRC2 | Trimethylates H3K27 (H3K27me3) for gene silencing | Disruption of neural differentiation and patterning |
Experimental Protocols for Neural Differentiation
Standard 2D Cortical Neural Progenitor Differentiation
This protocol is designed for the highly efficient generation of dorsal forebrain neural progenitor cells (NPCs) and neurons from human pluripotent stem cells (hPSCs) [23].
- Core Principle: Dual-SMAD inhibition.
- Base Medium: Chemically defined medium such as GFCDM (growth factor-free chemically defined medium) to allow precise evaluation of exogenous factors [22].
- Key Steps:
- Initiation of Differentiation: hPSCs are dissociated and plated as a monolayer. From day 0, the medium is supplemented with SMAD inhibitors:
- SB431542 (10 µM): A TGFβ receptor inhibitor.
- LDN-193189 (100 nM): A BMP receptor inhibitor.
- Neural Progenitor Expansion: The dual-SMAD inhibitors are maintained for 10-14 days. During this period, cells efficiently differentiate into PAX6+ neuroepithelial cells. The medium can be further supplemented with FGF2 (20 ng/mL) to support progenitor proliferation.
- Patterning and Maturation: To generate specific neuronal subtypes, patterning factors are added. For cortical neurons, SMAD inhibition is continued, and the culture can be transitioned to a medium containing BDNF, GDNF, and ascorbic acid to support neuronal maturation over several weeks. The protocol generates deep-layer neurons followed by upper-layer neurons and astrocytes, recapitulating in vivo corticogenesis [23].
- Initiation of Differentiation: hPSCs are dissociated and plated as a monolayer. From day 0, the medium is supplemented with SMAD inhibitors:
Spinal Motor Neuron Differentiation
This protocol is optimized for generating spinal motor neurons (MNs), which are relevant for diseases like Amyotrophic Lateral Sclerosis (ALS) [16].
- Core Principle: Sequential activation and inhibition of key developmental pathways to pattern the cells toward a caudal spinal cord fate.
- Key Steps:
- Neural Induction: Similar to the cortical protocol, often using dual-SMAD inhibition for the first 1-2 weeks to generate neuroepithelium.
- Caudalization: To specify a spinal cord identity, cells are treated with a Wnt agonist (e.g., CHIR99021) and retinoic acid (RA). This combination promotes a posterior neural fate.
- Ventralization: To generate motor neuron progenitors, the culture is treated with a Sonic Hedgehog (SHH) pathway agonist (e.g., Purmorphamine or SAG). This ventralizes the neural tube to a pMN progenitor domain.
- Maturation: Progenitors are then differentiated into post-mitotic motor neurons expressing markers like HB9 (MNX1) and ChAT in the presence of neurotrophic factors (BDNF, GDNF, CNTF). The entire process from hPSC to mature MNs typically takes 5-7 weeks [16].
Applications in Neurodegenerative Disease Research
Patient-specific iPSCs have revolutionized the modeling of neurodegenerative diseases, providing access to live, human neurons that carry the genetic blueprint of the patient.
Disease Modeling with Patient-Specific iPSCs
iPSC-derived neural models have been generated for all major neurodegenerative disorders, including Parkinson's disease (PD; dopaminergic neurons), Alzheimer's disease (AD; cortical and hippocampal neurons), Amyotrophic Lateral Sclerosis (ALS; motor neurons), and Huntington's disease (HD; striatal neurons) [25] [26]. A key advancement is the ability to model sporadic diseases, which account for over 90% of cases.
- Sporadic ALS Modeling: A landmark study generated an iPSC library from 100 sporadic ALS (SALS) patients. Motor neurons derived from these lines recapitulated key disease pathologies, including reduced survival and accelerated neurite degeneration. The severity of in vitro neurodegeneration correlated with the donor's clinical survival time, validating the model's pathophysiological relevance [16].
- Recapitulating Disease Hallmarks: iPSC-derived neurons from patients with monogenic and sporadic diseases often exhibit disease-specific phenotypes such as protein aggregation (e.g., TDP-43 in ALS), transcriptional dysregulation, and increased susceptibility to cellular stressors [25] [16].
Drug Screening and Therapeutic Discovery
The reproducibility and scalability of iPSC-derived neural models make them ideal for high-throughput drug screening.
- Phenotypic Screening: The SALS motor neuron model was used to screen over 100 drugs that had previously been tested in ALS clinical trials. The model showed a 97% failure rate, accurately reflecting the clinical trial outcomes and validating the model's predictive power [16].
- Identification of Combinatorial Therapies: The same screen identified that a combination of Riluzole (an approved ALS drug), Memantine (an NMDA receptor antagonist), and Baricitinib (a JAK inhibitor) significantly increased the survival of SALS motor neurons, offering a promising new therapeutic avenue [16].
Table 3: Clinical Trial Landscape for Stem Cell Therapies in Neurodegenerative Diseases
| Disease | Total Stem Cell Trials (n=94) | Furthest Clinical Phase | Key Cell Types Used |
|---|---|---|---|
| Alzheimer's Disease (AD) | ~65% of total participants | Phase 2 (Ongoing) | Mesenchymal Stem Cells (MSCs), Neural Stem Cells (NSCs) [26] |
| Parkinson's Disease (PD) | - | Phase 2 (Completed & Ongoing) | iPSCs, ESCs, MSCs [26] |
| Amyotrophic Lateral Sclerosis (ALS) | - | Phase 3 (Completed & Ongoing) | MSCs, NSCs [26] |
| Huntington's Disease (HD) | - | Phase 3 (Ongoing) | MSCs [26] |
Data adapted from a systematic review of 94 clinical trials [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Neural Differentiation and Characterization
| Reagent / Tool | Category | Specific Example(s) | Function in Neural Fate Research |
|---|---|---|---|
| SMAD Inhibitors | Small Molecules | LDN-193189 (BMP inhibitor), SB431542 (TGFβ inhibitor) | Core of "dual-SMAD inhibition"; induces efficient neural induction from PSCs [23] |
| Patterning Molecules | Small Molecules/Growth Factors | CHIR99021 (Wnt agonist), Retinoic Acid, Purmorphamine (SHH agonist) | Specifies regional identity (e.g., caudal spinal cord, ventral motor neurons) [16] |
| Growth Factors | Proteins | FGF2, EGF, BDNF, GDNF | Supports neural progenitor proliferation and neuronal maturation/survival [22] [23] |
| Lineage Reporters | Viral Vectors/Reporter Lines | HB9::GFP, PAX6::tdTomato | Enables live-cell tracking and purification of specific neural populations (e.g., motor neurons) [16] |
| Epigenetic Assays | Kits/Reagents for | ATAC-seq, ChIP-seq (H3K27me3, H2AK119ub) | Profiles chromatin accessibility and histone modifications to map epigenetic remodeling [22] [24] |
Technical Considerations and Variability
A significant challenge in using PSC-derived neural models is the inherent variability in differentiation outcomes.
- Sources of Variation: Analysis of 162 differentiations from 61 hPSC lines revealed that variation occurs primarily along developmental spatial axes (dorsoventral and rostrocaudal) [23]. This variation can be line-independent (stochastic) or line-dependent.
- Endogenous Signaling: Line-dependent variation is largely driven by differences in endogenous signaling pathway activity, most notably Wnt/β-catenin signaling [23].
- Correcting Variability: This bias is not insurmountable. Studies show that modulating the Wnt pathway with exogenous agonists or antagonists during a specific critical window early in differentiation can correct these biases and reduce line-to-line variability, ensuring more consistent and reproducible results [23].
Advanced Methodologies and Applications in Disease Modeling and Drug Discovery
Protocols for Differentiating iPSCs into Key Neural Lineages (Neurons, Microglia, Astrocytes)
The discovery of induced pluripotent stem cells (iPSCs) by Takahashi and Yamanaka in 2006 represented a paradigm shift in biomedical research, enabling the generation of patient-specific pluripotent stem cells from somatic cells [1] [18]. This technology has profound implications for neurodegenerative disease research, as it allows investigators to create patient-specific neural cells that harbor the exact genetic background of individuals with conditions such as Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis (ALS) [27] [2] [28]. Unlike embryonic stem cells, iPSCs are derived from readily accessible adult tissues—including skin fibroblasts, peripheral blood cells, or urinary epithelial cells—circumventing ethical concerns while providing an unlimited source of cells for disease modeling, drug screening, and regenerative approaches [27] [18].
The fundamental principle underlying iPSC technology is cellular reprogramming, typically achieved through the introduction of key transcription factors—most commonly OCT4, SOX2, KLF4, and c-MYC (OSKM)—which collectively reset the epigenetic landscape of somatic cells to a pluripotent state [2] [1] [18]. These iPSCs can subsequently be differentiated into virtually any cell type in the body, including the diverse neural lineages of the central nervous system [1] [29]. For neurodegenerative disease research, the ability to generate human neurons, microglia, and astrocytes from patients with specific genetic vulnerabilities provides an unprecedented opportunity to study disease mechanisms in physiologically relevant human cells, identify novel therapeutic targets, and test candidate drugs in a patient-specific context [29] [28].
Fundamental Principles of iPSC Neural Differentiation
The differentiation of iPSCs into neural lineages recapitulates aspects of embryonic development, guided by the sequential activation and inhibition of key signaling pathways [1] [29]. The process typically begins with the transition from pluripotency to neural progenitor cells (NPCs), which subsequently give rise to the specific neural cell types through the action of regionalizing factors [30].
Table 1: Key Signaling Pathways in Neural Differentiation
| Pathway | Role in Neural Differentiation | Common Modulators |
|---|---|---|
| TGF-β/Activin A | Supports pluripotency; inhibition promotes neural induction | SB431542, A83-01 |
| BMP | Inhibition is required for neural induction | Noggin, DMH1, LDN-193189 |
| WNT/β-catenin | Regulates patterning; precise temporal control required | CHIR99021 (activator), IWR-1 (inhibitor) |
| FGF | Promotes neural proliferation and survival | FGF2 (basic FGF) |
| SHH | Ventralizes neural tissue; critical for specific neuronal subtypes | Purmorphamine, SAG (agonists) |
| RA | Posteriorizes neural tissue; promotes neuronal differentiation | Retinoic acid |
The molecular dynamics of differentiation involve profound epigenetic remodeling and changes to almost every aspect of cell biology, including metabolism, cell signaling, and proteostasis [1]. During the early phase of differentiation, pluripotency genes such as NANOG and OCT4 are silenced, while early neural markers like SOX1 and PAX6 are activated [1] [30]. The late phase involves the activation of lineage-specific genes that define mature neuronal and glial identities, such as MAP2 for neurons, GFAP for astrocytes, and TMEM119 or P2RY12 for microglia [31] [29] [32].
Differentiation Protocols for Specific Neural Lineages
iPSC-Derived Neurons
The generation of cortical neurons from iPSCs can be significantly accelerated through the overexpression of the transcription factor Neurogenin 2 (NGN2), which can produce functional neurons within just 3-4 weeks [31]. This method yields a highly pure population of glutamatergic neurons, providing a robust system for disease modeling and drug screening applications.
Key Protocol Steps:
- iPSC Culture and Maintenance: Maintain iPSCs in feeder-free conditions using defined media such as mTeSR or E8 on matrix-coated plates (e.g., Matrigel, laminin) [18].
- Lentiviral Transduction: Introduce a doxycycline-inducible NGN2 expression system into iPSCs using lentiviral vectors.
- Neural Induction: Upon doxycycline addition, NGN2 expression drives neuronal differentiation. Cells are typically cultured in neural medium supplemented with growth factors (BDNF, NT-3) and small molecules (e.g., dorsomorphin to inhibit BMP signaling) [31].
- Maturation: After 1-2 weeks, cells are replated onto surfaces coated with poly-D-lysine and laminin to promote neurite outgrowth and synaptic formation, with full maturation occurring within 3-4 weeks [31].
For dopaminergic neurons—particularly relevant for Parkinson's disease research—protocols typically employ dual SMAD inhibition combined with ventralization factors. The CORIN sorting strategy has emerged as a milestone for enriching mesencephalic dopaminergic progenitors while eliminating serotonergic neurons and tumorigenic precursors [28].
iPSC-Derived Astrocytes
The directed differentiation of iPSCs into astrocytes employs a developmental approach that passes through a neural progenitor cell (NPC) stage, with protocols typically requiring 60-90 days to generate functional astrocytes [31] [29].
Key Protocol Steps:
- Neural Induction: Use dual SMAD inhibition (SB431542 and LDN-193189) for 10-12 days to convert iPSCs to NPCs.
- NPC Expansion: Expand NPCs in media containing FGF2 to maintain progenitor status.
- Astroglial Specification: Transition cells to astrocyte differentiation medium containing CNTF, BMP4, or LIF to promote glial fate. The transcription factors SOX9 and NFIB can be introduced to accelerate maturation [31].
- Maturation: Maintain cells for 60-90 days to allow for complete maturation, characterized by typical astrocytic morphology and expression of markers including GFAP, S100β, and EAAT1 [29].
Recent advances have significantly shortened this timeline through the use of defined transcription factors, with some protocols generating astrocytes within 20 days post-thaw of pre-differentiated cells [31].
iPSC-Derived Microglia
Microglia differentiation protocols uniquely recapitulate yolk sac hematopoiesis, as microglia originate from primitive macrophages rather than definitive hematopoietic stem cells [29] [32].
Key Protocol Steps:
- Hematopoietic Progenitor Induction: Differentiate iPSCs for 8-10 days in serum-free media with BMP4, VEGF, SCF, and TPO to generate primitive hematopoietic progenitor cells (HPCs) [31] [32].
- Myeloid Specification: Transfer floating HPCs to media containing IL-34, M-CSF, and TGF-β to drive microglial identity.
- Maturation and Expansion: Culture cells for an additional 2-4 weeks to allow for maturation, characterized by expression of microglial markers including TMEM119, P2RY12, and IBA1, and the development of characteristic ramified morphologies [32].
Table 2: Key Markers for Characterizing Neural Lineages
| Cell Type | Pluripotency/ Progenitor Markers | Early Differentiation Markers | Mature Cell Markers | Functional Assays |
|---|---|---|---|---|
| iPSCs | OCT4, NANOG, SOX2, SSEA-4 | - | - | Pluripotency: Teratoma formation, trilineage differentiation |
| Neural Progenitor Cells (NPCs) | SOX2, NESTIN | PAX6, SOX1 | - | Self-renewal, multipotency |
| Neurons | - | βIII-TUBULIN | MAP2, SYN1, VGLUT1 | Electrophysiology (patch clamp), calcium imaging, synaptic activity |
| Astrocytes | - | S100β | GFAP, EAAT1, GLT-1 | Glutamate uptake, calcium signaling, inflammatory response (cytokine release) |
| Microglia | - | CD11b, IBA1 | TMEM119, P2RY12, CX3CR1 | Phagocytosis, chemotaxis, inflammatory response (LPS stimulation) |
Advanced Co-culture Models and Their Applications
The true power of iPSC-derived neural lineages emerges when these cells are combined to create more physiologically relevant systems that capture the complex cell-cell interactions within the brain. A robust triculture system incorporating iPSC-derived neurons, astrocytes, and microglia (iNs, iAs, iMGs) has been developed that enables the study of neuroinflammation and neurodegenerative mechanisms in a controlled human cellular environment [31].
Triculture Protocol Workflow:
- Independent Differentiation: Differentiate iNs, iAs, and iMGs separately using the protocols outlined above.
- Cryopreservation and Quality Control: Cryopreserve each cell type independently, allowing for quality control assessments before triculture assembly.
- Co-culture Assembly: Plate iAs and iMGs onto established iNs at defined ratios (typically 1:1:1) in a optimized triculture medium (TCM).
- Maintenance and Analysis: Maintain co-cultures for 7-20 days before analysis, during which cells develop mature interactions and phenotypes [31].
This triculture system has demonstrated remarkable utility in modeling neurodegenerative disease mechanisms. For example, when microglia are co-cultured with astrocytes and neurons, they exhibit upregulated expression of disease-associated microglia (DAM) genes, including TREM2, APOE, SPP1, and GPNMB—a transcriptional signature observed in Alzheimer's disease brains [31]. Furthermore, when this system incorporates neurons carrying familial Alzheimer's disease (fAD) mutations, the DAM signature is significantly dampened, revealing how disease-specific genetic backgrounds disrupt neuron-glial communication [31].
The Scientist's Toolkit: Essential Research Reagents
Successful differentiation and maintenance of iPSC-derived neural lineages requires carefully selected reagents and culture components. The following table summarizes essential materials and their functions:
Table 3: Essential Research Reagents for iPSC Neural Differentiation
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Reprogram somatic cells to pluripotency | Non-integrating methods (episomal, mRNA, Sendai virus) preferred for clinical applications [2] [33] |
| Small Molecule Inhibitors | SB431542 (TGF-β inhibitor), LDN-193189 (BMP inhibitor), CHIR99021 (GSK-3β inhibitor) | Direct cell fate by modulating signaling pathways | Dual SMAD inhibition critical for efficient neural induction [1] [29] |
| Growth Factors & Cytokines | FGF2, EGF, BDNF, GDNF, IL-34, M-CSF, TGF-β | Support proliferation, survival, and specification | M-CSF and IL-34 essential for microglia differentiation and survival [31] [32] |
| Extracellular Matrices | Matrigel, Laminin-521, Poly-D-lysine | Provide structural support and biochemical cues | Laminin-511/521 supports iPSC expansion and neural differentiation [18] [30] |
| Cell Culture Media | mTeSR, Neural Base Medium, BrainPhys | Provide nutrients and defined environment | BrainPhys optimized for neuronal activity and network formation [31] [18] |
| Cell Sorting Markers | CORIN, PSA-NCAM, CD44 | Isolate specific neural populations | CORIN sorting enriches for dopaminergic progenitors in Parkinson's applications [28] |
Quality Control and Characterization Techniques
Rigorous quality control is essential throughout the differentiation process to ensure the generation of high-quality, lineage-specific cells. Key characterization approaches include:
- Pluripotency Assessment: Confirm the starting iPSC population expresses canonical markers (OCT4, NANOG, SOX2) via immunocytochemistry or flow cytometry, and demonstrate trilineage differentiation potential [18].
- Genomic Stability Monitoring: Regularly screen for chromosomal abnormalities using karyotyping, SNP analysis, or next-generation sequencing, particularly after extended passaging [18] [33].
- Lineage Purity Evaluation: Assess population homogeneity using cell type-specific markers—βIII-TUBULIN/MAP2 for neurons, GFAP for astrocytes, and TMEM119/P2RY12 for microglia [31] [29].
- Functional Validation: Perform physiological assessments including patch-clamp electrophysiology for neuronal activity, glutamate uptake assays for astrocyte function, and phagocytosis assays for microglial function [29].
Emerging technologies are enhancing quality control capabilities. Raman spectroscopy of extracellular vesicles (EVs) in culture supernatants offers a non-invasive method to monitor differentiation status and pluripotency, with lipid-derived Raman signals showing correlation with expression of pluripotency markers like NANOG [30].
Workflow Visualization of Key Protocols
The following diagrams illustrate the core differentiation protocols and advanced co-culture system setup.
Diagram 1: Neural Differentiation Workflow from iPSCs. This diagram illustrates the stepwise differentiation protocols for generating neurons, astrocytes, and microglia from iPSCs, culminating in the assembly of a triculture model.
The protocols for differentiating iPSCs into neurons, microglia, and astrocytes have matured significantly, enabling the creation of increasingly sophisticated human cellular models of neurodegenerative diseases. The ability to generate these key neural lineages from patient-specific iPSCs provides researchers with powerful tools to investigate disease mechanisms in human cells with relevant genetic backgrounds, screen for novel therapeutics, and develop personalized treatment approaches [27] [28].
Current challenges in the field include standardization of protocols across laboratories, reduction of differentiation timelines, and enhancement of functional maturation, particularly for astrocytes and microglia [18] [29]. Future directions are likely to focus on increasing model complexity through the creation of more elaborate multi-culture systems and organoid models that better capture the spatial organization and cellular diversity of the human brain [29] [32]. Additionally, the integration of CRISPR-Cas9 gene editing and AI-guided differentiation protocols will further enhance the precision and reproducibility of these models [33].
As these technologies continue to evolve, iPSC-derived neural lineages will play an increasingly central role in unraveling the pathological mechanisms of neurodegenerative diseases and accelerating the development of effective therapies for conditions that currently lack effective treatment options.
The advent of cerebral organoid technology represents a transformative leap in vitro modeling of human neurodevelopment and disease. These self-organizing three-dimensional structures, derived from human induced pluripotent stem cells (iPSCs), recapitulate defining features of the developing human brain that are inaccessible to conventional models [34]. For researchers focused on neurodegenerative diseases like Alzheimer's and Parkinson's disease, cerebral organoids provide an unprecedented human-relevant platform for probing pathogenesis, identifying genetic risk factors, and performing clinically predictive drug screening [35] [34]. The integration of patient-specific iPSCs enables the creation of models with endogenous expression of mutant genes, offering profound insights into both hereditary and sporadic cases of pathologies while advancing the development of personalized therapeutic approaches [35].
Unlike traditional 2D cultures, cerebral organoids mimic the human brain's developmental process and disease-related phenotypes to a significant extent, including cortical patterning, neural circuit assembly, and the emergence of selective neuronal vulnerability—a hallmark of neurodegenerative conditions [36] [35]. This capability is particularly valuable for studying human-specific developmental processes, such as the expansion of outer radial glia, that are absent in rodent models [34]. However, a major bottleneck persists: extended culture periods (≥6 months) are empirically required to achieve late-stage maturation markers, which severely limits their utility in modeling adult-onset disorders without bioengineering interventions [34].
Fundamental Principles and Protocols for Cerebral Organoid Generation
Core Methodology for Patient-Specific Cerebral Organoids
The creation of a patient-specific iPSCs-based model begins with the collection of biological material from diagnosed patients, typically through skin biopsy or peripheral blood sampling, followed by fibroblast culture establishment [35]. The critical reprogramming phase utilizes transcription factors (Oct-4, Sox2, c-Myc, Klf4) to return differentiated cells to a pluripotent state, employing either integrative methods (lentivirus) or non-integrative approaches (Sendai virus) [35]. Subsequent differentiation involves a meticulously coordinated process of neuronal induction, production of region-specific progenitor cells, and terminal differentiation into the neuronal types most vulnerable in the specific neurodegenerative disease being studied [35].
Protocol selection significantly influences organoid variability and cell-type representation. Systematic analyses have identified that combining multiple protocol approaches—aimed at recapitulating dorsal and ventral forebrain, midbrain, and striatum—can collectively recreate the majority of cell types present in the developing human brain [37]. The NEST-Score computational tool has been developed to evaluate cell-line- and protocol-driven differentiation propensities, providing researchers with quantitative metrics for comparing organoid models to in vivo references [37].
Workflow: From Patient Cells to Cerebral Organoids
The diagram below illustrates the comprehensive workflow for generating patient-specific cerebral organoids.
Advanced Protocol Implementation
Current cerebral organoid protocols can be broadly categorized into guided and unguided approaches. Guided protocols direct hiPSCs toward specific regional identities using media containing neuroectoderm-inducing and mesodermal-inhibiting growth factors [38]. Unguided protocols allow for more spontaneous pattern formation but typically result in higher heterogeneity [38]. For neurodegenerative disease research, guided approaches often provide more reproducible models of specific brain regions affected in conditions like Alzheimer's (cortex) or Parkinson's disease (midbrain) [38].
The emergence of microglial-containing cerebral organoids (MCCOs) addresses a critical limitation of conventional organoids, which lack mesodermal-derived microglia essential for neuroimmune function [38]. Multiple strategies have been developed to generate MCCOs, including endogenous generation through avoidance of mesodermal inhibitors, coculture with hematopoietic or macrophage progenitors, and addition of fully differentiated microglia from various sources [38]. The selection of appropriate protocol depends on the specific research objectives, with each method resulting in organoid microglia with varying degrees of transcriptional, morphological, and functional maturation compared to their in vivo counterparts [38].
Quantitative Profiling of Organoid Protocols and Maturation
Comparative Analysis of Cerebral Organoid Protocols
Systematic evaluation of four established brain organoid protocols across multiple cell lines has revealed significant differences in cellular recapitulation and transcriptional landscapes [37]. The following table summarizes key quantitative findings from comprehensive single-cell RNA sequencing analysis of organoids at day 120 of differentiation.
Table 1: Quantitative Profiling of Brain Organoid Protocols and Cellular Diversity
| Protocol Target | Key Regional Markers | Cell-Type Recapitulation | Protocol Reliability | Recommended Applications |
|---|---|---|---|---|
| Dorsal Forebrain | FOXG1, PAX6, SATB2, TBR1 | High diversity of excitatory neurons, cortical layering | High reproducibility across cell lines | Alzheimer's disease, cortical development |
| Ventral Forebrain | FOXG1, NKX2.1, GABA | Robust GABAergic inhibitory neuron generation | Moderate variability in interneuron subtypes | Epilepsy, neurodevelopmental disorders |
| Midbrain | LMX1A, FOXA2, TH | Functional dopaminergic neurons, tyrosine hydroxylase expression | Consistent dopaminergic differentiation | Parkinson's disease research, drug screening |
| Striatum | CTIP2, DARPP-32, GABA | Medium spiny neuron formation, striatal patterning | Requires validation of striatal identity | Huntington's disease modeling |
Multidimensional Framework for Assessing Organoid Maturity
Evaluating cerebral organoid maturity requires a multimodal approach encompassing structural, functional, and molecular dimensions. The following table outlines the key benchmarks and assessment methodologies for determining organoid maturation status, particularly relevant for modeling late-onset neurodegenerative diseases.
Table 2: Multidimensional Assessment of Brain Organoid Maturity
| Assessment Dimension | Key Markers/Parameters | Analytical Methods | Significance for Neurodegenerative Disease Modeling |
|---|---|---|---|
| Structural Architecture | Cortical lamination (SATB2, TBR1, CTIP2), synaptic markers (SYB2, PSD-95), barrier formation | Immunofluorescence, immunohistochemistry, electron microscopy | Validates tissue organization relevant to disease pathology |
| Cellular Diversity | Neuronal markers (NEUN, βIII-tubulin), astrocyte markers (GFAP, S100β), oligodendrocyte markers (MBP, O4) | Flow cytometry, immunostaining, scRNA-seq | Ensures presence of vulnerable cell types in disease models |
| Functional Maturation | Synchronized network activity, γ-band oscillations, calcium transients, synaptic transmission | Multielectrode arrays, calcium imaging, patch clamp | Confirms physiological relevance for drug testing |
| Molecular & Metabolic Profiling | Transcriptome-wide profiling, mitochondrial function, metabolic activity | scRNA-seq, metabolomics, proteomics | Identifies disease-associated pathways and biomarkers |
Calcium Signaling Dysregulation in Neurodegenerative Disease Models
The calcium hypothesis of neurodegeneration postulates that disturbances in intracellular calcium signaling represent a primary factor triggering neurodegenerative processes [35]. Patient-specific iPSC-based models of major neurodegenerative diseases have consistently demonstrated aberrant calcium signaling, providing compelling evidence for its fundamental role in pathogenesis.
Disease-Specific Calcium Signaling Alterations
Research using patient-specific iPSCs-derived neurons has revealed disease-specific patterns of calcium dysregulation. In Alzheimer's disease models, enhanced endoplasmic reticulum calcium release and upregulated store-operated calcium entry have been consistently observed [35]. Parkinson's disease models demonstrate abnormalities in mitochondrial calcium buffering and voltage-gated calcium channel function, particularly in vulnerable dopaminergic neurons [35]. Huntington's disease models show alterations in glutamate receptor-mediated calcium transients and mitochondrial calcium handling in striatal medium spiny neurons [35]. These findings not only validate the calcium hypothesis of neurodegeneration but also highlight calcium signaling pathways as promising therapeutic targets for multiple neurodegenerative conditions.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful generation and analysis of cerebral organoids requires specialized reagents and tools. The following table compiles essential research solutions for implementing cerebral organoid technology in neurodegenerative disease research.
Table 3: Essential Research Reagent Solutions for Cerebral Organoid Research
| Reagent Category | Specific Examples | Function & Application | Technical Considerations |
|---|---|---|---|
| Reprogramming Factors | Oct-4, Sox2, c-Myc, Klf4 | Fibroblast reprogramming to iPSCs | Non-integrating delivery systems (Sendai virus) preferred for safety |
| Regional Patterning Molecules | SMAD inhibitors, WNT agonists/antagonists, SHH | Direct regional specification (forebrain, midbrain, striatum) | Concentration and timing critical for precise patterning |
| Cell Type-Specific Markers | SATB2, TBR1 (cortical layers), TH (dopaminergic), GABA (inhibitory) | Characterization of cellular diversity and identity | Validate multiple markers for each cell population |
| Microglia Incorporation Reagents | IL-34, CSF-1, TGF-β | Support microglial survival and homeostasis in MCCOs | Essential for modeling neuroimmune aspects of neurodegeneration |
| Functional Assay Tools | Calcium indicators (GCaMP), voltage-sensitive dyes | Assessment of neuronal activity and network formation | Combine with MEAs for comprehensive functional analysis |
| Maturation Promoters | BDNF, NT-3, cAMP analogs | Accelerate functional maturation toward adult phenotypes | Critical for modeling late-onset neurodegenerative diseases |
Current Limitations and Future Perspectives
Despite significant advancements, cerebral organoid technology faces several challenges that must be addressed to enhance its utility for neurodegenerative disease research. Current limitations include the absence of functional vascularization, which restricts nutrient delivery and waste removal in long-term cultures, leading to central necrosis [36] [34]. The incomplete maturation of organoids, which typically arrest at fetal-to-early postnatal stages even after extended culture, limits their applicability for modeling adult-onset disorders like Alzheimer's disease [34]. Additionally, protocol variability and inadequate representation of non-neuronal cell types, particularly microglia and oligodendrocytes, complicate data interpretation and reproducibility [37] [38].
Future developments are focusing on engineering strategies to overcome these limitations. Vascularization approaches include the incorporation of endothelial cells and perfusion using microfluidic systems [34]. Maturation acceleration techniques involve electrical stimulation, biomechanical cues, and optimized culture conditions to promote adult-like phenotypes [34]. The emergence of organoid intelligence initiatives combines cerebral organoids with artificial intelligence to advance understanding of brain function and dysfunction [36]. Standardization efforts, including the development of quantitative assessment tools like the NEST-Score, will enhance reproducibility and enable more reliable disease modeling and drug screening applications [37]. As these technologies mature, cerebral organoids are poised to become indispensable tools for deciphering the pathological mechanisms of neurodegenerative diseases and developing effective therapeutic interventions.
The pursuit of effective therapeutics for amyotrophic lateral sclerosis (ALS) has been persistently hampered by the scarcity of pathophysiologically relevant models, particularly for the sporadic form (SALS) that constitutes approximately 90% of cases [16]. More than 160 drugs shown to slow disease progression in familial ALS (FALS) models have failed to translate into clinically effective treatments, raising critical questions about the pathophysiological relevance of existing models to SALS [16]. This case study examines a groundbreaking approach employing patient-derived induced pluripotent stem cell (iPSC) technologies to conduct large-scale phenotypic screening specifically in SALS motor neurons, framing this methodology within the broader context of patient-specific iPSCs for neurodegenerative disease research.
Experimental Framework and Model Validation
Establishment of a Comprehensive iPSC Library
To capture the clinical, genetic, and biological heterogeneity of the ALS population, researchers generated an iPSC library from 100 patients with sporadic ALS (no family history), 11 suspected monogenic cases, and 25 healthy donors as controls [16]. Fibroblasts isolated from skin biopsy specimens underwent reprogramming with nonintegrating episomal vectors using an automated robotics platform to maximize output and uniformity [16]. All lines underwent rigorous quality control testing, including confirmation of genomic integrity, pluripotency, and trilineage potential.
Table: Donor Cohort Clinical Characteristics
| Characteristic | Distribution | Clinical Significance |
|---|---|---|
| ALS Subtype Classification | 13 lower motor neuron-predominant ALS, 76 classic ALS, 3 upper motor neuron-predominant ALS, 5 suspected PLS | Represents clinical heterogeneity of ALS population |
| Site of Onset | Limb and bulbar regions documented | Reflects natural disease variation |
| Age of Onset | Range representative of typical ALS presentation | Captures age-related disease factors |
| Disease Progression | Measured by ALSFRS-R decline rate | Provides quantitative progression metrics |
| Survival Time | Variable across donor population | Enables correlation with in vitro phenotypes |
Whole-genome DNA sequencing identified pathogenic or likely pathogenic variants or expansions in known ALS genes in only ten ALS donors, confirming the predominantly sporadic nature (98 donors) of the cohort [16]. This genetic characterization ensured accurate classification and provided insights into potential subpopulations within the SALS cohort.
Motor Neuron Differentiation and Phenotyping Pipeline
The research team developed a robust five-stage motor neuron differentiation and phenotyping pipeline adapted from an established spinal motor neuron differentiation protocol [16]. After extensive optimization of maturation and screening conditions, the protocol consistently generated high-purity cultures of mature motor neurons displaying extensive neurite networks.
Table: Cell Culture Composition and Purity Metrics
| Cell Type | Marker | Percentage (Mean ± s.e.m.) | Significance |
|---|---|---|---|
| Motor Neurons | ChAT, MNX1/HB9, Tuj1 | 92.44 ± 1.66% | Definitive motor neuron identity |
| Total Neurons | β-tubulin III (Tuj1) | 97.66 ± 0.99% | Neural lineage purity |
| Astrocytes | GFAP | 0.12 ± 0.01% | Minimal glial contamination |
| Microglia | CD11B | 0.04 ± 0.02% | Minimal microglial presence |
The highly enriched spinal motor neuron cultures (approximately 98% neurons) provided a valuable reductionist system for assessing cell-autonomous effects of ALS without significant confounding influences from other cell types [16]. To quantitatively assess motor neuron health, cultures were monitored daily using live-cell imaging in conjunction with a virally delivered nonintegrating motor neuron-specific reporter (HB9-turbo) [16].
Key Phenotypic Findings in SALS Motor Neurons
Survival Deficits and Neurite Degeneration
The study demonstrated significantly impaired survival and accelerated neurite degeneration in SALS-derived motor neurons compared to those from healthy controls [16]. This recapitulation of key pathological hallmarks of ALS validated the model's relevance for therapeutic screening. Importantly, the severity of neurite degeneration in vitro correlated with donor survival time, establishing a crucial link between the cellular model and clinical outcomes [16].
Transcriptional Profiling Validation
Comprehensive transcriptional profiling identified significant differential expression in SALS motor neurons, generating a disease profile consistent with postmortem spinal cord tissues from ALS patients [16]. This molecular validation confirmed that the iPSC-derived motor neurons recapitulated key aspects of the disease pathophysiology at the transcriptome level, enhancing the model's credibility for mechanistic studies and drug screening.
Large-Scale Drug Screening Platform
Pharmacological Validation of the Model
The researchers implemented the SALS model for systematic drug screening, beginning with reassessment of more than 100 drugs that had previously undergone clinical trials for ALS [16]. Strikingly, less than 5% of these drugs demonstrated efficacy in rescuing motor neuron survival across SALS donors, closely reflecting the clinical trial outcomes for these compounds [16]. This high predictive validity firmly established the utility of the platform for preclinical testing.
Pharmacological testing with the SALS model reproduced the known efficacy of riluzole, the most widely prescribed ALS treatment, which rescued motor neuron survival and reversed both electrophysiological and transcriptomic abnormalities [16]. This further validated the model's responsiveness to known therapeutics.
Combinatorial Therapeutic Discovery
Combinatorial testing of effective drugs identified a promising therapeutic combination of baricitinib, memantine, and riluzole [16]. This triple combination significantly increased the survival of SALS motor neurons, representing the first therapeutic candidates identified and validated across SALS donors to encompass the heterogeneity in drug efficacy within the SALS patient population [16].
Table: Drug Screening Outcomes and Clinical Correlations
| Screening Component | Finding | Clinical Correlation |
|---|---|---|
| Previously Trialed Drugs | 97% failed to mitigate neurodegeneration | Reflects high failure rate in human trials |
| Riluzole Testing | Rescued motor neuron survival | Consistent with known clinical efficacy |
| Effective Single Agents | Baricitinib, memantine, riluzole | Potential individual therapeutic agents |
| Combinatorial Therapy | Significant survival improvement | Addresses patient heterogeneity through multi-target approach |
Research Reagent Solutions Toolkit
Table: Essential Research Reagents and Their Applications
| Reagent/Category | Function | Experimental Application |
|---|---|---|
| Non-integrating Episomal Vectors | Reprogramming without genomic integration | iPSC generation from patient fibroblasts |
| HB9-turbo Reporter | Motor neuron-specific labeling | Live-cell imaging and tracking |
| ChAT, MNX1/HB9, Tuj1 Antibodies | Motor neuron identification | Immunocytochemical validation |
| Live-Cell Imaging Platform | Longitudinal monitoring | Assessment of neurite degeneration and survival |
| Automated Robotics Platform | High-throughput processing | Large-scale iPSC generation and differentiation |
Experimental Workflow and Signaling Pathways
Screening Workflow for SALS Motor Neurons
Therapeutic Mechanisms of Combinatorial Therapy
Discussion and Research Implications
This case study demonstrates that patient-derived iPSC models can successfully recapitulate sporadic disease features, paving the way for a new generation of disease modeling and therapeutic discovery in ALS [16]. The findings have several profound implications for neurodegenerative disease research:
Validation of SALS Modeling Approach
The research provides compelling evidence that SALS can be effectively modeled in patient-derived motor neurons, addressing a critical gap in the field. Previous attempts, including large-scale analyses by consortia such as Answer ALS, had failed to consistently demonstrate survival deficits, TDP-43 pathology, or pharmacological rescue in SALS motor neurons [16]. The success of this approach highlights the importance of rigorous protocol optimization and population-wide screening to capture disease heterogeneity.
Addressing Patient Heterogeneity in Drug Development
By screening across a diverse donor population, the platform accounts for the substantial heterogeneity in SALS, which has likely contributed to the failure of many clinical trials. The identification of a combinatorial therapy effective across SALS donors suggests that multi-target approaches may be necessary to address the complex, multifactorial pathophysiology of sporadic neurodegenerative diseases [16].
Broader Applications for Neurodegenerative Disease Research
The methodologies and insights from this study have significant implications for other neurodegenerative conditions, including Alzheimer's disease and Parkinson's disease, which similarly lack effective treatments and are predominantly sporadic [16] [39]. The demonstration that patient-derived iPSC models can recapitulate key disease phenotypes and predict clinical trial outcomes suggests this approach could transform preclinical testing across neurodegenerative disorders.
This large-scale phenotypic screening platform using iPSC-derived motor neurons from sporadic ALS patients represents a transformative approach for neurodegenerative disease modeling and therapeutic development. By successfully recapitulating disease-specific phenotypes and demonstrating high predictive validity for clinical trial outcomes, the methodology addresses fundamental limitations in the field. The identification of a potential combinatorial therapy effective across a heterogeneous SALS population underscores the power of this patient-specific approach. As the broader scientific community continues to leverage patient-derived iPSC technologies, this case study provides both a methodological framework and a compelling rationale for their expanded application in overcoming the profound challenges of sporadic neurodegenerative disease research.
Integrating CRISPR-Cas9 for Isogenic Controls and Disease Mechanism Elucidation
The convergence of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 technology with human-induced pluripotent stem cells (hiPSCs) represents a transformative approach in biomedical research, particularly for modeling neurodegenerative diseases. This integration enables the precise genetic modification of patient-derived cells, allowing for the creation of isogenic controls that are genetically identical except for a specific pathogenic mutation. Such controls are indispensable for distinguishing disease-causing mutations from background genetic variation, thereby clarifying molecular pathogenesis and accelerating therapeutic development [40]. Within neurodegenerative disease research, where the complexity of the human brain and the inaccessibility of live neuronal tissue present significant challenges, patient-specific iPSCs provide a unique window into disease processes. CRISPR-Cas9 enhances this platform by enabling the precise introduction or correction of mutations in genes such as APP, PSEN1, PSEN2, and APOE, which are critically involved in Alzheimer's disease (AD) pathology [40]. This technical guide details the methodologies for creating and validating these essential research tools and their application in elucidating disease mechanisms.
Technical Foundation: CRISPR-Cas9 and iPSC Integration
The Role of Isogenic Controls in Disease Research
In disease modeling, an isogenic control is a cell line derived from a patient-specific iPSC line where the disease-causing mutation has been reverted to the wild-type sequence (or a wild-type line where the mutation has been introduced). The key utility of this pair is that they share an identical genetic background; any phenotypic differences observed between them can therefore be confidently attributed to the specific genetic modification, rather than to the natural genetic variation between different individuals [41] [42]. This is particularly crucial for studying complex neurodegenerative diseases with multifactorial etiology. The generation of a genetically corrected iPSC line, such as the BIHi261-A-1 line correcting the POMC:W84X mutation for monogenic obesity modeling, demonstrates the principle of using a patient-derived line as the starting material for creating a perfectly matched control [41].
CRISPR-Cas9 Mechanism and Workflow
The CRISPR-Cas9 system functions as a programmable gene-editing tool. The core components are the Cas9 nuclease, which cuts DNA, and a single-guide RNA (sgRNA), which directs Cas9 to a specific DNA sequence. The sgRNA binds to a complementary ~20-nucleotide target sequence adjacent to a Protospacer Adjacent Motif (PAM), typically 5'-NGG-3' for the commonly used Streptococcus pyogenes Cas9. Upon binding, Cas9 creates a double-strand break (DSB) approximately 3 base pairs upstream of the PAM site [40] [43].
The cell then repairs this DSB primarily through one of two pathways:
- Non-Homologous End Joining (NHEJ): An error-prone repair process that often results in small insertions or deletions (indels). This is typically used for gene knockout studies.
- Homology-Directed Repair (HDR): A precise repair pathway that uses a DNA template, such as a single-stranded oligodeoxynucleotide (ssODN) or a donor plasmid, to introduce specific nucleotide changes. This is the mechanism for generating precise point mutations or corrections [43] [44].
The following diagram illustrates the integrated workflow for generating isogenic iPSC lines using CRISPR-Cas9, from sgRNA design to final clone validation.
Experimental Protocols for Isogenic Line Generation
Detailed Methodology: CRISPR-Cas9 Mediated Gene Correction
The following protocol outlines the key steps for correcting a pathogenic mutation in a patient-derived iPSC line, based on established methods [41] [42].
1. sgRNA and Donor Template Design:
- sgRNA Selection: Design sgRNAs to target a genomic site as close as possible to the mutation (within 10 bp or less is ideal). Use online tools (e.g., CRISPOR, ChopChop) to minimize predicted off-target effects. The sgRNA target sequence should be unique in the genome and have a high-quality score.
- HDR Donor Template: Design a single-stranded oligodeoxynucleotide (ssODN) donor template (~100-200 nucleotides) containing the desired corrective sequence. Flank the correction with homologous arms (at least 40-50 nucleotides on each side) that are identical to the genomic sequence. Incorporate silent mutations (synonymous SNPs) within the protospacer sequence of the donor to prevent re-cleavage by Cas9 after successful HDR.
2. iPSC Culture and Transfection:
- Cell Culture: Maintain patient-derived iPSCs (e.g., line BIHi261-A) in feeder-free conditions using essential media like mTeSR or StemFlex on a suitable substrate (e.g., Matrigel, Geltrex). Ensure cells are in a state of optimal growth and >90% viability before transfection.
- RNP Transfection: For high efficiency and reduced off-target effects, use a ribonucleoprotein (RNP) complex. Complex purified Cas9 protein with the synthesized sgRNA in vitro and deliver it along with the ssODN donor template into iPSCs using an efficient method such as electroporation (e.g., Neon Transfection System). Electroporation parameters for HCT116 cells, for instance, are 1130 V, 30 ms, 2 pulses [43].
3. Single-Cell Cloning and Expansion:
- After transfection, culture cells for 48-72 hours to allow for editing and recovery.
- Dissociate the cells into a single-cell suspension and seed them at a very low density in a plate containing conditioned media supplemented with a ROCK inhibitor (e.g., Y-27632) to enhance single-cell survival.
- Manually pick individual, undifferentiated colonies after 10-14 days and expand them in 96-well plates for genomic DNA extraction and screening.
4. Genotypic Screening and Validation:
- Primary Screening: Extract genomic DNA from expanded clones. Perform PCR amplification of the targeted genomic region. Initial screening can be done using a mismatch detection assay (e.g., T7E1 or Surveyor nuclease) or by PCR-RFLP if the edit creates or destroys a restriction site. However, these methods are not quantitative and can miss some edits [43] [44].
- Sequencing Confirmation: Sanger sequence the PCR products from candidate clones. Use computational tools like Inference of CRISPR Edits (ICE) or Tracking of Indels by Decomposition (TIDE) to deconvolute the sequencing chromatograms and quantify editing efficiency. For definitive confirmation, especially of heterozygous edits, subclone the PCR product and sequence multiple clones, or perform targeted Next-Generation Sequencing (NGS) [44].
- Comprehensive Characterization: As performed for the BIHi261-A-1 line, validated clones must undergo rigorous quality control [41] [42]:
- Karyotyping: Ensure genomic integrity (e.g., G-band analysis).
- Pluripotency Validation: Confirm expression of key markers (e.g., OCT4, NANOG, SOX2) via immunocytochemistry or flow cytometry.
- Trilineage Differentiation: Demonstrate the ability to differentiate into endoderm, mesoderm, and ectoderm lineages in vitro.
- Off-Target Analysis: PCR-amplify and sequence the top in silico-predicted off-target sites to ensure no unintended edits occurred.
Quantitative Analysis of CRISPR Editing Efficiency
A critical step in the protocol is the accurate assessment of editing outcomes. Several methods are available, each with distinct advantages and limitations, as summarized in the table below.
Table 1: Comparison of Methods for Analyzing CRISPR-Cas9 Editing Efficiency
| Method | Principle | Key Advantages | Key Limitations | Best Use Case |
|---|---|---|---|---|
| T7 Endonuclease 1 (T7E1) [44] | Cleaves mismatched DNA in heteroduplexes. | Low cost, quick, requires basic lab equipment. | Not quantitative; cannot detect homozygous edits or large indels reliably. | Initial, low-cost screening during protocol optimization. |
| Restriction Fragment Length Polymorphism (RFLP) [44] | Relies on loss or gain of a restriction enzyme site. | Inexpensive and straightforward if edit alters a restriction site. | Only applicable if a restriction site is created or destroyed. | Screening for specific HDR events that change a restriction site. |
| Tracking of Indels by Decomposition (TIDE) [44] | Decomposes Sanger sequencing data to quantify indels. | Cost-effective (uses Sanger data), provides indel sequence information. | Limited ability to detect large insertions/deletions and complex edits. | Rapid quantification of editing efficiency for simple indel spectra. |
| Inference of CRISPR Edits (ICE) [44] | Analyzes Sanger sequencing data to model editing outcomes. | High accuracy comparable to NGS; detects a wide range of edits including large indels. | Requires data upload to a web-based platform (Synthego). | Standard for most labs needing detailed, cost-effective analysis. |
| Next-Generation Sequencing (NGS) [43] [44] | Deep, targeted sequencing of the amplified genomic region. | Gold standard; highly sensitive and comprehensive; detects all mutation types. | Expensive, time-consuming, requires bioinformatics expertise. | Definitive validation and detailed analysis of editing spectrum. |
| qEva-CRISPR [43] | Quantitative, multiplex ligation-based probe amplification. | Detects all mutation types; suitable for difficult genomic regions; multiplex capable. | Requires specific probe design and optimization. | Quantitative, parallel analysis of multiple targets or off-targets. |
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of these protocols relies on a suite of specialized reagents and tools. The following table outlines essential materials and their functions.
Table 2: Essential Research Reagents for CRISPR-iPSC Work
| Reagent / Tool Category | Specific Examples | Function / Application |
|---|---|---|
| CRISPR-Cas9 System | pSpCas9(BB)-2A-GFP (PX458) plasmid [43]; purified Cas9 protein for RNP; synthetic sgRNA. | Provides the core gene-editing machinery. Plasmid-based expression or RNP delivery. |
| HDR Donor Template | Single-stranded oligodeoxynucleotide (ssODN); donor plasmid with homology arms. | Serves as the repair template for precise gene correction or mutation knock-in. |
| iPSC Culture Media | mTeSR Plus, StemFlex Media | Maintains hiPSCs in a pluripotent, undifferentiated state. |
| Cell Dissociation Reagent | Accutase, ReLeSR | Gentle enzymatic dissociation of iPSCs into single cells for cloning or transfection. |
| Transfection Reagent/System | Lipofectamine LTX [43]; Neon Transfection System [43] | Efficient delivery of CRISPR components (RNP, plasmid) into hard-to-transfect iPSCs. |
| Cell Survival Enhancer | ROCK inhibitor (Y-27632) | Critical for enhancing survival of iPSCs after single-cell dissociation and cloning. |
| Genotyping & Analysis | PCR kits; T7E1 enzyme [44]; ICE or TIDE software [44]; NGS services. | For amplifying the target locus, screening clones, and quantifying editing efficiency. |
| Pluripotency Markers | Antibodies against OCT4, SOX2, NANOG, SSEA-4 | Confirmation of pluripotent state in the generated isogenic line via immunostaining/flow cytometry. |
Elucidating Disease Mechanisms in Neurodegeneration
The primary application of CRISPR-engineered, patient-specific iPSCs is the dissection of disease mechanisms. By comparing the isogenic pair—one with the disease mutation and the corrected control—researchers can pinpoint the specific molecular and cellular consequences of the mutation.
Key Pathogenic Pathways Investigated:
- Amyloid-β Processing: In Alzheimer's disease, isogenic iPSCs with mutations in APP, PSEN1, or PSEN2 have been used to demonstrate increased production of the pathogenic Aβ1-42 isoform and an altered Aβ42/Aβ40 ratio, directly linking these mutations to a key pathological feature [40].
- Tau Hyperphosphorylation: The relationship between Aβ accumulation and Tau pathology can be studied. CRISPR-Cas9 has been used to create models that recapitulate the abnormal phosphorylation of Tau and its aggregation into neurofibrillary tangles [40] [45].
- Neuroinflammation: The role of microglia, the brain's resident immune cells, can be explored using iPSC-derived microglia from isogenic lines. This allows for the study of how specific mutations exacerbate inflammatory responses, such as chronic glial activation, which contributes to neuronal loss [40].
- Oxidative Stress: The connection between Aβ and oxidative stress is a vicious cycle in AD. Aβ peptides can inhibit mitochondrial function and promote the accumulation of reactive oxygen species (ROS), leading to neuronal damage. Isogenic models allow researchers to test if correcting a mutation reduces ROS and improves mitochondrial health [40].
The following diagram maps the logical flow of how an isogenic iPSC model is used to elucidate such disease mechanisms, from hypothesis to therapeutic insight.
The strategic integration of CRISPR-Cas9 genome editing with iPSC technology has bridged a critical gap in neurodegenerative disease research. By providing perfectly matched isogenic controls, this powerful combination allows for the unambiguous attribution of cellular phenotypes to specific genetic lesions, thereby enabling a more precise elucidation of disease mechanisms. The detailed experimental protocols for generating and validating these lines, supported by quantitative analysis methods and a defined toolkit of reagents, provide a robust framework for researchers. As these methodologies continue to evolve, particularly with improvements in HDR efficiency and delivery systems, their application will be instrumental in deconvoluting the complex pathophysiology of disorders like Alzheimer's and Parkinson's disease, ultimately paving the way for the development of targeted, effective therapies.
High-Throughput Drug Screening and Toxicity Testing Using iPSC-Derived Cells
The integration of induced pluripotent stem cell (iPSC)-derived models into high-throughput screening (HTS) platforms represents a paradigm shift in preclinical drug development and toxicity assessment. For neurodegenerative disease research, patient-specific iPSCs provide a physiologically relevant human context that bridges the critical translational gap between traditional animal models and human clinical trials. These platforms enable population-wide phenotypic screening, the identification of patient-specific therapeutic responses, and robust safety pharmacology profiling. This technical guide details the experimental methodologies, key applications, and essential reagents that underpin the use of iPSC-derived cells in industrial-scale drug discovery, with a specific focus on addressing the unique challenges of developing treatments for conditions such as amyotrophic lateral sclerosis (ALS), Alzheimer's disease, and Parkinson's disease.
Scientific Foundations of iPSC-Based Screening Platforms
The discovery that somatic cells could be reprogrammed into pluripotent stem cells fundamentally expanded the toolbox for disease modeling. For drug discovery, iPSCs offer three distinct advantages over immortalized cell lines or animal models: patient specificity, human relevance, and scalability [46].
- Patient Specificity: iPSCs retain the complete genetic background of the donor, including all disease-associated mutations and polymorphisms. This allows for the creation of in vitro models that capture the complex, multifactorial etiology of sporadic neurodegenerative diseases, which constitute the majority of cases [16] [47].
- Human Relevance: Differentiated iPSC-derived neurons, cardiomyocytes, and hepatocytes recapitulate key functional aspects of native human tissue, such as synaptic activity, contractility, and metabolic capacity. This results in more physiologically accurate data on drug efficacy and mechanism of action [46].
- Scalability: Once a robust differentiation protocol is established, iPSC lines can be expanded indefinitely, enabling the generation of the large, consistent cell quantities required for high-throughput compound screening [48] [46].
The FDA Modernization Act 2.0, which permits the use of human-relevant cell-based assays in lieu of animal testing for certain drug applications, has provided significant regulatory momentum for the adoption of these platforms [47].
High-Throughput Screening for Neurodegenerative Disease
ALS Case Study: Large-Scale Phenotypic Screening
A landmark study demonstrated the power of this approach by establishing an iPSC library from 100 patients with sporadic ALS (SALS) and conducting population-wide phenotypic screening [16]. The experimental workflow and key outcomes are summarized below and in the accompanying diagram.
Experimental Protocol:
- iPSC Library Generation: Dermal fibroblasts from 100 SALS donors and 25 healthy controls were reprogrammed using non-integrating episomal vectors on an automated robotics platform to ensure uniformity [16].
- Motor Neuron Differentiation: A optimized five-stage protocol was used to differentiate iPSCs into highly enriched (>92%) cultures of spinal motor neurons expressing ChAT, MNX1/HB9, and Tuj1 [16].
- Longitudinal Live-Cell Imaging: A motor neuron-specific reporter (HB9-turboGFP) was used to track neuronal health over time. Key phenotypic endpoints included:
- Compound Screening: The platform was used to test over 100 drugs that had previously entered ALS clinical trials. Compounds were applied to the SALS motor neuron cultures, and their ability to rescue the neurodegeneration phenotype was assessed [16].
Figure 1: High-Throughput Screening Workflow for ALS. This diagram outlines the key stages of a large-scale phenotypic screening campaign using a patient-derived iPSC library, from cell line generation to therapeutic candidate identification [16].
Key Quantitative Findings from ALS Drug Screening:
| Screening Parameter | Result | Implication |
|---|---|---|
| Clinical Trial Drug Re-evaluation | 97% (over 100/103) failed to mitigate neurodegeneration | High predictive validity of the SALS model for clinical trial outcomes [16] |
| Effective Single Agents | <5% of tested drugs rescued motor neuron survival | Reflects the high failure rate of ALS clinical trials and highlights recalcitrant targets [16] |
| Combinatorial Therapy Efficacy | Baricitinib + Memantine + Riluzole significantly increased SALS motor neuron survival | First therapeutic combination validated across a heterogeneous SALS donor population [16] |
| Phenotype-Donor Correlation | Accelerated neurite degeneration correlated with donor survival | Confirms clinical relevance of the in vitro phenotype for disease progression [16] |
Protocol for Neurotoxicity Screening
Beyond efficacy screening, iPSC-derived neural cultures are critical for assessing compound neurotoxicity. A standardized protocol for a multi-parametric neurotoxicity screen is as follows [49]:
- Cell Culture Models: Utilize a panel of iPSC-derived neural models, including neural progenitor cells (NPCs), 2D mature neuronal co-cultures (with astrocytes and microglia), and 3D cerebral organoids.
- Plate Formatting: Plate cells in 384-well plates optimized for high-content imaging.
- Compound Treatment: Treat cultures with test compounds across a range of clinically relevant concentrations. Include acute (minutes to hours) and chronic (days) exposure periods.
- Endpoint Multiplexing: Simultaneously assess multiple toxicity endpoints:
- Cell Viability: Using nuclear dyes to identify dead/dying cells.
- Cell Proliferation: Using Click-iT EdU assays (for NPCs).
- Calcium Activity: Using fluorescent calcium dyes to image spontaneous calcium transients and synchronization.
- Synaptic Integrity: Immunostaining for pre- and post-synaptic markers (e.g., PSD-95, Synapsin) followed by automated puncta counting.
- Image Acquisition and Analysis: Perform high-speed imaging on a Kinetic Image Cytometer (e.g., Vala KIC IC200). Analyze images with single-cell resolution software (e.g., CyteSeer) to extract quantitative data for each endpoint [49].
Toxicity Testing and the CiPA Initiative
A major application of iPSC-derived cells is in toxicity testing, most notably in cardiotoxicity screening under the Comprehensive in vitro Proarrhythmia Assay (CiPA) initiative. CiPA aims to move beyond traditional hERG channel testing to a more holistic assessment of proarrhythmic risk using human iPSC-derived cardiomyocytes (hiPSC-CMs) [50] [46].
Experimental Protocol for CiPA-Compliant Cardiotoxicity Testing [50]:
- Cell Source: Use a qualified hiPSC-CM line (e.g., YBLiCardio, iCell Cardiomyocytes).
- Platform: Employ a high-throughput extracellular field potential (EFP) measurement system, such as the CardioExcyte 96, which functions similarly to a microelectrode array.
- Compound Testing: Test 28 or more drugs, each at a minimum of four concentrations. The drug panel should include high, intermediate, and low-risk compounds defined by the CiPA consortium.
- Data Analysis: Record and analyze extracellular signals to determine dynamic changes in beat patterns. The key parameter is QT prolongation, assessed by measuring the interval between the sodium spike (depolarization) and the peak of the T-wave (repolarization).
- Risk Classification: Classify drug risk based on the degree of QT prolongation and other waveform perturbations compared to established controls. For example, drugs like droperidol and domperidone show significant QT prolongation (>170%) and are correctly identified as high-risk [50].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of an iPSC-based screening platform relies on a suite of specialized reagents and tools. The following table details key components.
| Tool/Reagent | Function | Example Products/Providers |
|---|---|---|
| iPSC-Derived Cells | Biologically relevant human cells for screening assays. | iCell Cardiomyocytes/Neurons (FUJIFILM CDI), ReproCardio Cardiomyocytes (REPROCELL), ioCells (bit.bio), Axol Human iPSC-Derived Neural Cells (Axol Bioscience) [48] [51] |
| Reprogramming & Differentiation Kits | Consistent, scalable production of specific cell types from iPSCs. | MyCell Kits (FUJIFILM CDI), opti-ox powered differentiation (bit.bio), Standardized Hepatic Differentiation (Takara Bio) [48] [51] |
| Specialized Culture Media | Supports the growth, maintenance, and functional maturity of differentiated cells. | Cell-type specific media (e.g., for neurons, cardiomyocytes) from various suppliers like Axol Bioscience and Thermo Fisher Scientific [51] |
| High-Content Imaging Reporters | Enables longitudinal tracking of cell health and function. | HB9-turboGFP motor neuron reporter [16], Fluorescent calcium dyes (e.g., for Ca²⁺ transient imaging) [49] |
| Automated Imaging & Analysis Systems | High-throughput data acquisition and quantitative analysis of complex phenotypes. | CardioExcyte 96 System (Nanion Technologies), Kinetic Image Cytometer (KIC IC200, Vala Science), CyteSeer Image Analysis Software [50] [49] |
The deployment of patient-specific iPSC-derived models in high-throughput screening and toxicity testing has irrevocably altered the landscape of drug discovery for neurodegenerative diseases. By providing a human-pathophysiological context with endogenous gene expression, these platforms offer unparalleled predictive power, as evidenced by their ability to recapitulate the high failure rate of ALS clinical trials and identify novel combinatorial therapies. The ongoing standardization of protocols, commercialization of high-quality reagents, and integration of these models into regulatory frameworks like the CiPA initiative promise to further enhance their reliability and throughput. As these technologies mature, they will undoubtedly accelerate the development of safer and more effective, patient-tailored therapeutics for some of the most challenging neurodegenerative disorders.
Overcoming Technical Hurdles: Quality Control, Scalability, and Standardization
Addressing Batch-to-Batch Variability and Genetic Instability
The promise of induced pluripotent stem cells (iPSCs) in modeling neurodegenerative diseases and advancing drug discovery is immense, yet significant challenges in reproducibility threaten progress. Batch-to-batch variability and genetic instability introduce confounding experimental variables that can obscure disease-specific phenotypes and compromise translational research [52]. Within patient-specific iPSC models for neurodegenerative disease research, these challenges become particularly critical, as subtle disease manifestations may be masked by technical artifacts. This technical guide examines the sources of this variability and provides evidence-based strategies to enhance experimental reproducibility, ensuring that iPSC-derived models reliably contribute to our understanding of disease mechanisms and therapeutic development.
The fundamental sources of variation in iPSC models are multifaceted. Genetic background differences between individual donors account for 5-46% of variation in iPSC phenotypic traits, surpassing other non-genetic factors [52]. Additionally, the reprogramming process itself, culture conditions, and differentiation protocols each introduce their own layers of variability that accumulate throughout the experimental workflow [52]. For neurodegenerative disease research using patient-specific iPSCs, controlling these variables is essential for distinguishing true disease pathology from technical artifacts.
Genetic Instability in iPSC Cultures
iPSCs possess a remarkable capacity for self-renewal, but this proliferative potential comes with inherent genomic vulnerabilities. During extended culture, iPSCs frequently acquire non-random genomic abnormalities that may provide selective growth advantages [53]. These mutations can alter differentiation potency, cellular heterogeneity, and transcriptional profiles, fundamentally compromising the reliability of disease models [52]. Some acquired abnormalities mirror changes observed in human cancers, raising concerns about their suitability for clinical applications [53].
The mechanisms driving genetic instability include:
- Oxidative stress from suboptimal culture conditions
- Replication stress during rapid cell division
- Selection pressures favoring mutations that enhance survival or proliferation
- Incomplete reprogramming leading to epigenetic aberrations
These genetic changes can manifest as karyotypic abnormalities, copy number variations, or point mutations that may go undetected without rigorous quality control measures.
Batch-to-Batch Technical Variability
Technical variability arises throughout the multi-step process of iPSC generation, maintenance, and differentiation. Small variations at each stage accumulate, generating significantly different outcomes in the resulting cellular models [52]. Key sources include:
- Reprogramming method efficiency: Lentiviral, episomal, and mRNA methods exhibit different integration patterns and reprogramming efficiencies
- Culture conditions: Differences in media composition, passaging techniques, and substrate coatings
- Differentiation protocol consistency: Variations in reagent batches, timing, and cell handling
- Cellular heterogeneity: Presence of multiple cell types and diversity in maturation states within differentiated populations
This technical variability is particularly problematic for neurodegenerative disease modeling, where the fetal-like maturity of iPSC-derived neurons may already limit phenotype manifestation [52]. When combined with batch effects, the ability to detect subtle disease-associated cellular phenotypes becomes significantly compromised.
Table 1: Major Sources of Variability in iPSC Models
| Variability Source | Impact on Research | Detection Methods |
|---|---|---|
| Genetic Drift | Altered differentiation potential, transcriptional profiles, and cellular function | Karyotyping, digital PCR, array CGH [54] |
| Donor Genetic Background | 5-46% of variation in iPSC phenotypes [52] | Genotyping, STR analysis [54] |
| Reprogramming Method | Differential epigenetic memory, integration artifacts | Epigenomic profiling, vector presence detection |
| Differentiation Efficiency | Variable cell type proportions and maturity states | Flow cytometry, immunocytochemistry, functional assays |
| Culture Conditions | Changes in proliferation, metabolism, and pluripotency | Morphological assessment, pluripotency marker analysis [55] |
Quality Control Frameworks
Comprehensive Quality Control Testing
Implementing a robust, ongoing quality control program is essential for identifying and addressing sources of variability. A strategic QC protocol should include both initial characterization and periodic reassessment throughout the research timeline.
Genetic Integrity Assessment
- Karyotyping: G-banding remains the gold standard for detecting chromosomal abnormalities, but should be supplemented with more sensitive methods [54]
- Digital PCR and array CGH: Provide higher resolution detection of subchromosomal copy number variations and smaller genetic alterations [54]
- Whole genome sequencing: Offers the most comprehensive assessment of genetic integrity but at higher cost and computational requirements
Pluripotency Verification
- Pluripotency marker expression: Confirm expression of hallmark genes including Nanog, Oct3/4, SSEA-4, TRA-1-60, and TRA-1-81 via immunofluorescence staining or flow cytometry [54]
- Functional pluripotency assessment: Evaluate trilineage differentiation potential through directed differentiation into ectoderm, mesoderm, and endoderm lineages [54] [53]
Identity and Sterility Testing
- Short tandem repeat (STR) analysis: Authenticate cell lines and confirm identity matches original donor material [54]
- Mycoplasma testing: Essential for detecting these common, destructive contaminants that alter gene expression and induce karyotypic abnormalities [54]
- Sterility testing: Ensure absence of bacterial and fungal contaminants through direct inoculation or membrane filtration methods [54]
Table 2: Essential Quality Control Measures for iPSCs
| QC Category | Specific Test | Frequency | Acceptance Criteria |
|---|---|---|---|
| Genetic Integrity | G-band karyotyping | Every 10 passages | Normal male/female karyotype |
| Digital PCR/array CGH | Every 20 passages | No detectable CNVs | |
| Pluripotency | Flow cytometry for surface markers | Every 5 passages | >90% positive for pluripotency markers |
| Trilineage differentiation | For new lines/quarterly | Robust differentiation to all three germ layers | |
| Identity | STR profiling | For new lines/annually | Match to donor tissue |
| Sterility | Mycoplasma testing | Monthly | Negative results |
| Bacterial/fungal culture | With each freeze | No contamination detected |
Morphological Quality Assessment
Daily morphological assessment provides a rapid, non-invasive method for monitoring iPSC culture quality. Undifferentiated hiPSCs exhibit characteristic morphology including prominent nucleoli, high nucleus:cytoplasm ratio, and formation of compact colonies with well-defined edges [55]. Quantitative image analysis algorithms can now reproducibly classify iPSC quality based on biological features that experts visually assess, providing objective quality metrics [55].
Key morphological indicators of differentiation or poor quality include:
- Appearance of cracks in intercellular spaces
- Loss of colony definition and increased cell spacing
- Dark, flat cellular appearance indicating differentiation
- Decreased nucleoli prominence and visibility
Automated systems using machine learning can now classify iPSC quality with accuracy equivalent to expert visual inspection, standardizing this assessment across laboratories [55].
Strategies for Standardization
Protocol Optimization and Standardization
Standardized, rigorously optimized protocols are fundamental for minimizing technical variability in iPSC generation and differentiation. The NGN2-driven iPSC-to-neuron conversion protocol exemplifies how defined methods can produce consistent excitatory neurons maintainable for at least 150 days [56]. Critical optimization steps include:
Determining Optimal Reagent Concentrations
- Doxycycline concentration: Testing revealed 3 μg/mL provides optimal induction efficiency with low toxicity in NGN2 induction [56]
- Small molecule selection: Noggin performed better in neuronal induction and morphology than the more economical alternative LDN-193189 [56]
- Anti-proliferative agents: Including compounds like AraC (Cytarabine), mitomycin-C (MMC) at 0.25 μM, or fluorouracil (5-FU) at 60 μM inhibits formation of clumps in long-term cultures [56]
Engineering Consistency Through Cell Line Design
- Utilizing clonal, targeted-engineered iPSC lines with inducible NGN2 transgenes engineered into safe-harbor sites (such as AAVS1) eliminates batch-to-batch variabilities associated with lentiviral introduction [56]
- Implementing defined reagents and elimination of co-culture requirements (such as with astrocytes) reduces complexity and variability in downstream analyses [56]
Bulk Culture Strategies to Minimize Clonal Variation
Clonal variations present significant challenges in iPSC research, particularly when using transcription factor overexpression for differentiation. Innovative bulk culture approaches can mitigate these concerns while maintaining high differentiation efficiency:
Puromycin Selection for Bulk MYOD1-iPSCs
- Puromycin selection of bulk MYOD1-hiPSCs results in 82.2% HA+ and 80.0% MyoD1+ cells, compared to only 47.3% HA+ and 46.5% MyoD1+ cells with G418 selection [57]
- Bulk cultures established with puromycin selection exhibited differentiation properties representing the average of clonally established lines, minimizing clonal variation effects [57]
- This approach enables efficient skeletal muscle differentiation without time-consuming clonal selection, facilitating larger-scale disease modeling studies [57]
Standardized Culture Practices
- Consistent passaging techniques: Aggregation-based passaging enables long-term expansion while maintaining normal karyotype [53]
- pH stability maintenance: Careful monitoring and maintenance of optimal culture medium pH prevents acidification-induced stress [53]
- Antibiotic-free culture: Continuous antibiotic use alters gene expression profiles and should be avoided in routine culture [54]
Experimental Design and Data Analysis
Robust Experimental Design Principles
Appropriate experimental design is crucial for accounting for residual variability that cannot be eliminated through protocol standardization:
Implementing Control Strategies
- Isogenic controls: Engineered lines derived from the same individual that differ only at specific disease-relevant loci provide the most matched controls [52]
- Multiple clone analysis: Assessing several independent clones from the same reprogramming experiment controls for reprogramming and clonal variation artifacts
- Longitudinal batch controls: Including standardized control lines across experimental batches enables normalization across time
Population-Based Approaches
- Utilizing multiple patient-derived lines representing genetic diversity of the disease population
- Incorporating sufficient sample sizes to account for individual genetic background effects
- Balancing experimental batches with representative samples from each experimental group
Analytical Approaches for Addressing Variability
Advanced analytical methods can identify and account for technical variability in downstream data analysis:
Statistical Methods for Variability Correction
- Principal component analysis: Identifies major sources of variation in high-dimensional data, enabling detection of batch effects [52]
- Removal of unwanted variation (RUV): Normalization method that identifies and removes technical sources of variation within omics readouts [52]
- Probabilistic estimation of expression residuals (PEER): Identifies hidden factors that explain expression variability, including technical artifacts [52]
Reference-Based Standardization
- Rosetta lines: Including standardized iPSC lines common across experiments and laboratories enables cross-study comparison and normalization [52]
- Inter-laboratory calibration: Using shared reference materials to standardize protocols and assessments across research sites
Signaling Pathways and Molecular Mechanisms
The molecular processes governing iPSC behavior and differentiation provide targets for enhancing reproducibility through precise pathway modulation. The following diagram illustrates key signaling pathways manipulated in directed differentiation protocols, such as for cardiomyocyte generation, highlighting opportunities for standardization:
Cardiac Differentiation Signaling Pathway
Similar pathway precision is exemplified in neuronal differentiation protocols. In optimized NGN2 protocols, incorporation of DD factors during neural induction achieves more homogeneous and targeted neuron types [56]. Additionally, including Notch inhibitors like DAPT in both induction and replating media produces the most consistent, clump-free cultures [56]. These targeted interventions demonstrate how understanding and precisely controlling key developmental pathways enhances reproducibility.
Research Reagent Solutions
Consistent, high-quality reagents are fundamental for reducing technical variability in iPSC research. The following table details essential materials and their functions in establishing reproducible experimental systems:
Table 3: Essential Research Reagents for Standardized iPSC Work
| Reagent Category | Specific Examples | Function in Protocol | Variability Reduction Role |
|---|---|---|---|
| Inducible Transcription Factors | Dox-inducible NGN2 [56]; Dox-inducible MYOD1 [57] | Drives differentiation toward specific lineages | Enables precise temporal control; reduces line-to-line variation |
| Small Molecule Inhibitors/Activators | CHIR99021 (GSK-3β inhibitor) [58]; LDN-193189 (BMP inhibitor); DAPT (Notch inhibitor) [56] | Modulates key signaling pathways | Defined, consistent activity compared to protein factors |
| Selection Agents | Puromycin [57]; G418 [57] | Enriches for successfully transduced cells | Puromycin provides more uniform transgene expression in bulk cultures |
| Extracellular Matrix Components | Matrigel; recombinant laminin-521 | Provides substrate for cell attachment and growth | Defined matrices reduce batch variability |
| Cryopreservation Media | Commercial formulated media; DMSO-based solutions | Enables long-term storage and banking | Protects cell viability and recovery consistency |
Addressing batch-to-batch variability and genetic instability in patient-specific iPSC models requires a comprehensive, multifaceted approach. Through rigorous quality control, protocol standardization, strategic experimental design, and advanced analytical methods, researchers can significantly enhance the reproducibility of iPSC-based neurodegenerative disease models. As the field progresses toward clinical applications and high-throughput drug screening, these standardization efforts become increasingly critical for generating reliable, translatable findings. The strategies outlined in this technical guide provide a framework for maximizing the tremendous potential of iPSC technology while minimizing the confounding effects of technical variability.
Strategies for Scalable, Automated Manufacturing of Clinical-Grade iPSCs
The development of patient-specific induced pluripotent stem cells (iPSCs) has revolutionized the approach to neurodegenerative disease research and therapeutic development. These cells provide a unique platform for modeling conditions such as Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis in a patient-specific context [27]. However, the translation of iPSC technology from research tools to clinically applicable therapies faces significant manufacturing challenges. Approval of iPSCs for manufacturing cell therapies to support clinical trials is now becoming realized after more than 20 years of research, yet manufacturing these therapies at the scale required for patient treatment and clinical trial enabling activities remains a substantial challenge [59].
The inherent variability of neurodegenerative diseases necessitates patient-specific models, creating an urgent need for scalable manufacturing solutions that can produce standardized, clinical-grade iPSCs while maintaining their critical quality attributes. This technical guide examines the current state of automated iPSC manufacturing platforms, process optimization strategies, and quality control frameworks essential for advancing iPSC-based applications in neurodegenerative disease research. By addressing the bottlenecks in scalability, standardization, and cost-effectiveness, researchers can accelerate the development of meaningful personalized therapies for devastating neurological conditions that currently lack effective treatments [26] [60].
Current Challenges in iPSC Manufacturing for Neurodegenerative Disease Applications
Manufacturing Complexities and Scalability Limitations
The manufacturing of clinical-grade iPSCs for neurodegenerative disease research presents multiple interconnected challenges that impact both research validity and potential clinical translation. A primary constraint lies in the high variability of starting materials, where donor-specific differences produce cells with varying metabolic profiles and differentiation capabilities [61]. This variability complicates the establishment of standardized processes and consistent differentiation into neural lineages necessary for disease modeling. Current manufacturing processes often struggle to normalize these inherent biological differences, leading to inconsistencies in downstream applications [61].
The legacy manufacturing processes commonly employed remain complex, resource-intensive, and difficult to scale, creating bottlenecks that inflate costs and limit accessibility [61]. These processes are frequently labor-intensive, requiring specialized expertise and expensive raw materials, which collectively increase manufacturing costs and reduce reproducibility. Additionally, the risk of tumorigenicity presents a significant barrier to clinical adoption. This risk arises from multiple factors including the reprogramming process itself, the use of specific viral vectors, and the potential presence of residual undifferentiated iPSCs in the final product that could proliferate uncontrollably [62].
For neurodegenerative disease applications specifically, additional challenges emerge in differentiation efficiency toward specific neural phenotypes and the long-term stability of these cultures during extended studies that model progressive disorders. The high cost of production remains particularly prohibitive for academic research settings, where funding limitations can restrict access to iPSC technologies despite their scientific value for understanding disease mechanisms [63].
Analytical and Regulatory Hurdles
A critical challenge in iPSC manufacturing lies in understanding how manufacturing conditions affect therapeutic efficacy—particularly how expansion protocols and culture conditions impact cell persistence, functionality, and genomic stability [61]. The inability to fully characterize these relationships creates uncertainties in process validation and quality control. Furthermore, the lack of universal quality standards complicates commercialization and international collaboration, as researchers must navigate variable regulatory frameworks across regions [63].
The complex logistics of patient-specific supply chains introduce additional challenges for autologous approaches, including cold-chain maintenance, strict time constraints, and the critical need for end-to-end traceability and chain-of-identity [61]. For neurodegenerative disease research, where patient-derived iPSCs are particularly valuable for modeling genetic forms of disorders, these logistical challenges can significantly impact project timelines and consistency.
Table 1: Key Challenges in Scalable iPSC Manufacturing for Neurodegenerative Disease Research
| Challenge Category | Specific Limitations | Impact on Neurodegenerative Disease Research |
|---|---|---|
| Process Scalability | High variability of donor cells; Inability to normalize biological differences; Complex, resource-intensive legacy processes | Limited production capacity for large-scale drug screening; Inconsistent neural differentiation outcomes |
| Safety Concerns | Risk of tumorigenicity from reprogramming process; Residual undifferentiated iPSCs; Vector-related mutagenesis | Barriers to clinical translation; Safety concerns for transplant studies |
| Economic Factors | High production costs; Labor-intensive processes; Expensive raw materials | Limited access for academic researchers; Restricted scale of disease modeling projects |
| Quality Control | Lack of universal standards; Variable regulatory frameworks; Difficulties in characterizing manufacturing impacts | Challenges comparing results across studies; Uncertain validation pathways for clinical applications |
| Technical Limitations | Differentiation efficiency toward specific neural subtypes; Long-term culture stability; Genetic instability during reprogramming | Incomplete disease modeling; Limited study duration for progressive disorders |
Automated Platforms and Bioreactor Systems for Scalable Expansion
Advanced Automation Systems
Automation represents a transformative approach to addressing the scalability and standardization challenges in iPSC manufacturing. The implementation of automated systems provides multiple significant advantages, including reduced contamination risk by minimizing human intervention, decreased operational costs through reduced labor requirements, and improved process consistency by eliminating operator-dependent variability [64]. For neurodegenerative disease research, where reproducibility across patient-specific lines is essential for valid comparisons, this consistency is particularly valuable.
Current automated platforms for iPSC manufacturing employ modular design approaches that allow flexibility in processing steps while maintaining closed-system environments [64]. These systems typically integrate multiple processing modules for critical operations such as cell passaging, medium exchange, and quality monitoring, creating a continuous manufacturing workflow. The emerging trend toward patient-adjacent, regionalized manufacturing models incorporates advanced end-to-end digital logistics to maintain chain-of-identity while improving accessibility [61]. For academic research settings, where large-scale production may be unnecessary, scaled-down automated systems offer the same standardization benefits at appropriate throughput levels.
The integration of process analytical technologies (PAT) within automated platforms enables real-time monitoring of critical quality attributes, allowing for dynamic process adjustments and improved control over cell状态. These technologies are particularly important for neural differentiation processes, where specific morphological changes and marker expression patterns can serve as indicators of differentiation efficiency and lineage specification [59].
Bioreactor Technologies
Bioreactor systems have emerged as essential tools for scaling iPSC production from laboratory to industrial scale. These systems overcome the limitations of traditional 2D culture by enabling three-dimensional cell culture environments that more closely mimic physiological conditions and support higher cell densities. The suspended aggregate or microcarrier-based cultures in bioreactors facilitate efficient mass transfer of nutrients, gases, and signaling molecules, which is crucial for maintaining uniform cell growth and differentiation [59].
Modern bioreactor platforms for iPSC expansion and neural differentiation incorporate advanced monitoring and control systems that continuously track parameters such as dissolved oxygen, pH, metabolite concentrations, and biomass. This detailed process information supports the implementation of quality by design (QbD) approaches by identifying critical process parameters that influence critical quality attributes [59]. For neural differentiation protocols, which often require precise temporal control of signaling pathways, this level of process control is invaluable.
The transition from planar culture to bioreactor-based expansion can achieve significant scale-up factors, with some systems capable of producing clinically relevant cell numbers in single batches. This scalability is essential for generating sufficient quantities of neural progenitor cells or specific neuronal subtypes for high-throughput drug screening campaigns targeting neurodegenerative diseases. Additionally, the use of bioreactors supports better documentation and process validation through comprehensive data logging, addressing important regulatory requirements for potential clinical applications [59].
Automated iPSC Manufacturing Workflow: This diagram illustrates the integrated process from reprogramming to neural differentiation within an automated bioreactor system, highlighting continuous monitoring and quality control checkpoints.
Process Optimization and Quality by Design (QbD) Framework
Quality by Design Implementation
The application of Quality by Design (QbD) principles is essential for developing robust, scalable iPSC manufacturing processes that consistently yield high-quality cells appropriate for neurodegenerative disease research. A QbD approach begins with establishing a Quality Target Product Profile (QTPP) that defines the critical quality attributes (CQAs) necessary for the intended research application [59]. For iPSCs destined for neurodegenerative disease modeling, these CQAs might include specific pluripotency marker expression, genomic stability, differentiation efficiency toward neural lineages, and electrophysiological functionality in derived neurons.
The implementation of QbD relies on systematically identifying the relationship between critical process parameters (CPPs) and CQAs through structured experimentation. This approach enables researchers to establish a design space within which process parameters can be varied while still ensuring product quality. For neural differentiation processes, which often require precise temporal control of multiple signaling pathways, understanding these relationships is particularly important for achieving consistent results across different cell lines [59]. The use of design of experiment (DOE) methodologies allows for efficient exploration of complex parameter interactions while minimizing experimental runs, accelerating process optimization [59].
Process Analytical Technology Integration
Process Analytical Technology (PAT) forms the monitoring framework within the QbD system, providing real-time or near-real-time assessment of critical process parameters and quality attributes. Advanced PAT systems for iPSC manufacturing may include in-line sensors for continuous monitoring of biochemical parameters (pH, dissolved oxygen, metabolites), on-line sampling systems for automated cell counting and viability assessment, and at-line tools for more complex analyses such as flow cytometry or PCR [59] [64].
The integration of multivariate data analysis with PAT systems enables the detection of subtle process deviations that might impact final product quality, allowing for proactive process adjustments. For neural differentiation processes, which are particularly sensitive to environmental fluctuations, this level of process control can significantly improve reproducibility. The application of machine learning algorithms to PAT data can further enhance process understanding by identifying complex patterns that may not be apparent through conventional analysis [63].
Table 2: Critical Process Parameters and Quality Attributes for iPSC Manufacturing
| Process Stage | Critical Process Parameters | Critical Quality Attributes | Analytical Methods |
|---|---|---|---|
| Reprogramming | Reprogramming method; Vector type; Starting cell type; Culture conditions | Reprogramming efficiency; Genomic stability; Pluripotency marker expression; Off-target integration | Flow cytometry; Karyotyping; Pluripotency tests; PCR |
| Expansion | Seeding density; Passaging method; Medium composition; Feeding schedule | Doubling time; Morphology; Pluripotency maintenance; Karyotype stability; Metabolic profile | Microscopy; Metabolite analysis; Flow cytometry; Genetic analysis |
| Neural Differentiation | Differentiation protocol; Signaling molecules; Matrix composition; Oxygen tension | Neural marker expression; Neuronal subtype specification; Electrophysiological function; Synapse formation | Immunocytochemistry; RNA sequencing; Patch clamping; Calcium imaging |
| Harvest & Preservation | Detachment method; Formulation solution; Cooling rate; Storage temperature | Post-thaw viability; Recovery rate; Function retention; Phenotype stability | Viability assays; Functional tests; Marker expression analysis |
Analytical Technologies and Quality Control Measures
Comprehensive Characterization Methods
Rigorous quality control is essential for ensuring that manufactured iPSCs exhibit consistent characteristics appropriate for neurodegenerative disease research. A comprehensive characterization strategy should assess multiple quality dimensions including identity, purity, potency, and safety. Standard identity tests for iPSCs typically include analysis of pluripotency marker expression (OCT4, NANOG, SOX2, TRA-1-60) through flow cytometry or immunocytochemistry, as well as assessment of differentiation potential through embryoid body formation or directed differentiation toward all three germ layers [59].
For iPSCs intended specifically for neurodegenerative disease applications, additional neural differentiation efficiency assessments are crucial. These typically involve quantification of neural progenitor markers (SOX1, SOX2, PAX6) and neuronal markers (TUJ1, MAP2) following standardized differentiation protocols. More advanced functional assessments might include electrophysiological measurements using patch clamping or multi-electrode arrays to verify the functionality of derived neurons, particularly for disease modeling applications where neuronal activity is relevant [26] [60].
Genomic stability represents a particularly important safety consideration, given the association between prolonged culture and karyotypic abnormalities. Regular karyotype analysis using G-banding or higher-resolution methods such as array comparative genomic hybridization can detect chromosomal abnormalities that might impact research validity or safety. Additionally, whole-genome sequencing provides comprehensive assessment of genetic integrity, including point mutations that might arise during reprogramming or culture [62].
Release Criteria and Specifications
Establishing well-defined release criteria is essential for ensuring consistent quality across manufactured iPSC lines. These criteria should be tailored to the specific research application, with more stringent requirements for cells intended for therapeutic development compared to basic research use. Typical release criteria for clinical-grade iPSCs include minimum viability thresholds (typically >80-90% post-thaw), pluripotency marker expression (>80-90% positive for key markers), sterility (absence of microbial contamination), and mycoplasma testing [59].
For neurodegenerative disease applications, additional criteria might include specifications for neural differentiation efficiency, such as minimum percentages of TUJ1-positive cells following standardized differentiation protocols. Banks of iPSCs intended for distribution across multiple research sites should undergo even more comprehensive characterization, including whole-genome sequencing to establish a reference genetic profile and epigenetic analysis to confirm complete reprogramming [63].
The documentation supporting quality control should include detailed method descriptions, raw data, and certificate of analysis for each cell batch. This transparency enables researchers to appropriately interpret results generated using these cells and facilitates comparison across studies. Furthermore, establishing a system for tracking quality trends over time can help identify gradual process drift and support continuous improvement initiatives [59].
The Scientist's Toolkit: Essential Reagents and Technologies
Table 3: Key Research Reagent Solutions for iPSC Manufacturing and Neural Differentiation
| Reagent Category | Specific Examples | Function in iPSC Workflow | Considerations for Neurodegenerative Disease Applications |
|---|---|---|---|
| Reprogramming Systems | Sendai virus vectors; Episomal plasmids; mRNA reagents; Small molecule cocktails | Reprogram somatic cells to pluripotent state; Define efficiency and safety profile | Non-integrating methods preferred; Consider genetic stability; Efficiency impacts number of clones needed |
| Culture Media | Essential 8 Medium; mTeSR Plus; StemFit | Maintain pluripotency; Support expansion; Define culture environment | Xeno-free formulations for clinical applications; Consistent performance across lines; Support genetic stability |
| Neural Differentiation Kits | Commercial neural induction media; Patterning factors; Small molecule inhibitors | Direct differentiation toward neural lineages; Regional specification; Maturation | Efficiency for specific neuronal subtypes; Batch-to-batch consistency; Relevance to disease modeling |
| Extracellular Matrices | Geltrex; Laminin-521; Vitronectin; Synthetic polymers | Provide structural support; Influence signaling; Affect cell behavior | Impact on neural differentiation; Defined composition preferred; Scalability for manufacturing |
| Quality Control Assays | Pluripotency flow cytometry kits; Genetic analysis tools; Mitochondrial function assays | Characterize cell state; Ensure safety; Monitor functionality | Sensitivity for detecting abnormalities; Correlation with in vivo behavior; Validation for specific neural subtypes |
The development of scalable, automated manufacturing processes for clinical-grade iPSCs requires an integrated approach that addresses both technical and regulatory challenges. Implementation of quality by design principles from the earliest stages of process development establishes a scientific foundation for understanding the relationship between process parameters and product quality. The strategic incorporation of automation and bioreactor technologies addresses scalability constraints while improving process consistency and reducing contamination risks. Furthermore, the application of advanced analytical technologies ensures comprehensive characterization of critical quality attributes relevant to neurodegenerative disease research.
For the field of neurodegenerative disease research, these advances in scalable manufacturing are particularly significant. The ability to efficiently generate standardized, high-quality iPSCs from multiple patients enables larger-scale disease modeling studies that can capture the heterogeneity of these complex disorders. Additionally, the improved consistency and scalability support the development of more robust drug screening platforms that can identify potential therapeutics with greater reliability. As these manufacturing technologies continue to evolve, they will accelerate the translation of iPSC-based research into meaningful advances in understanding and treating devastating neurodegenerative conditions.
The translation of induced pluripotent stem cells (iPSCs) from research tools to clinically relevant models for neurodegenerative diseases hinges on the rigorous assessment of critical quality attributes (CQAs). For patient-specific iPSCs destined to model complex disorders such as Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis (ALS), three CQAs are paramount: potency, purity, and tumorigenicity [65] [33]. Establishing robust, standardized assays for these attributes is not merely a regulatory formality but a fundamental scientific requirement to ensure that experimental outcomes accurately reflect disease biology rather than artifacts of cellular reprogramming or differentiation [18]. The inherent variability of iPSC lines, compounded by the genetic diversity of neurodegenerative diseases, necessitates a comprehensive quality framework to generate physiologically relevant neurons, glia, and cerebral organoids for mechanistic studies and drug discovery [66] [16].
The challenge is particularly acute in the context of sporadic neurodegenerative diseases, which account for the majority of cases. Recent large-scale studies utilizing iPSC-derived motor neurons from sporadic ALS patients have demonstrated that only with stringent quality control can these models successfully recapitulate key pathological hallmarks like reduced neuronal survival and accelerated neurite degeneration [16]. This article provides a technical guide for researchers and drug development professionals, detailing the definitive assays and methodologies required to characterize iPSC lines for potency, purity, and tumorigenicity, thereby underpinning the validity and reproducibility of patient-specific neurodegenerative disease research.
Defining and Assessing Potency
In the context of patient-specific iPSCs for neurodegenerative disease research, potency is defined as the qualitative and quantitative capacity of a cell population to generate a defined, terminally differentiated output, such as functional neurons or glial cells, with specific morphological and functional characteristics. It is the benchmark that confirms the iPSCs' differential potential and the functional relevance of the derived cells [18] [65].
Key Markers for Potency Assessment
A multi-tiered analytical approach is required to thoroughly assess the potency of iPSCs and their neuronal derivatives. The table below summarizes the core markers and their significance in potency evaluation.
Table 1: Key Assays and Markers for Evaluating iPSC Potency in Neurodegenerative Research
| Assessment Tier | Target | Specific Markers/Assays | Significance in Neurodegenerative Models |
|---|---|---|---|
| Pluripotency | Endogenous Transcription Factors | OCT4, SOX2, NANOG [18] [66] | Verifies successful reprogramming and baseline quality of the master iPSC line. |
| Trilineage Potential | Germ Layer Formation | In vitro differentiation to ectoderm (e.g., PAX6), mesoderm (e.g., Brachyury), endoderm (e.g., SOX17) [18] | Confirms fundamental pluripotency, a prerequisite for efficient neural induction. |
| Neural Differentiation | Neural Progenitors & Neurons | SOX1, NESTIN (Neural Progenitors); β-III-Tubulin (Tuj1), MAP2 (Mature Neurons) [16] | Ensures robust and specific commitment to the neural lineage. |
| Subtype Specification | Disease-Relevant Neurons | Tyrosine Hydroxylase (Dopaminergic, for PD); HB9 (MNX1), ChAT (Motor Neurons, for ALS) [16] [28] | Critical for modeling specific diseases; confirms generation of therapeutically relevant cell types. |
| Functional Maturity | Electrophysiology | Patch-clamp recording of action potentials and postsynaptic currents [16] | Validates that neurons are not merely present but are functionally active, enabling physiological studies. |
Experimental Protocol: Directed Motor Neuron Differentiation
The following protocol, adapted from a large-scale ALS study, details the differentiation of iPSCs into spinal motor neurons, a key model for ALS [16]. This process typically spans 5 stages over several weeks.
Key Materials:
- Base Medium: DMEM/F-12, Neurobasal, or similar defined medium.
- Small Molecules: CHIR99021 (GSK-3β inhibitor), Retinoic Acid (RA), Smoothened Agonist (SAG) or Purmorphamine (SHH pathway agonists) [16].
- Growth Factors: BDNF, GDNF, CNTF.
- Coating Substrate: Poly-ornithine/laminin.
Procedure:
- Induction of Neural Precursors: Culture iPSCs to ~70% confluence. Begin differentiation by switching to a neural induction medium supplemented with dual SMAD signaling pathway inhibitors (e.g., LDN-193189 for BMP, SB431542 for TGF-β) for 10-14 days to direct cells toward a neural fate.
- Patterning to Spinal Motor Neuron Fate: Replace the medium with a patterning medium containing 1µM Retinoic Acid (RA) to confer caudal (spinal) identity and 1µM Smoothened Agonist (SAG) to ventralize the cells and induce a motor neuron progenitor phenotype. Maintain for another 7-10 days.
- Terminal Differentiation: Dissociate the patterned progenitors and plate them on a poly-ornithine/laminin-coated substrate in a terminal differentiation medium containing brain-derived neurotrophic factor (BDNF), glial cell line-derived neurotrophic factor (GDNF), and ciliary neurotrophic factor (CNTF) to support motor neuron survival and maturation for 2-4 weeks.
- Quality Control: Validate the resulting culture by immunocytochemistry. A high-quality differentiation should yield >90% of cells expressing the motor neuron marker HB9 (MNX1) and the pan-neuronal marker β-III-tubulin (Tuj1), with minimal contamination by GFAP+ astrocytes or CD11B+ microglia [16].
Figure 1: Motor Neuron Differentiation Workflow. A standardized 5-stage protocol for generating mature motor neurons from iPSCs, crucial for modeling ALS [16].
Establishing and Validating Purity
Purity in a patient-specific iPSC product encompasses both the homogeneity of the target cell population and the absence of contaminants. These contaminants can include undifferentiated iPSCs, which pose a tumorigenic risk; off-target cell types that may confunctional experimental readouts; and non-cellular impurities like endotoxins or residuals from the manufacturing process [18] [65]. In neurodegenerative disease modeling, even small populations of undifferentiated iPSCs or aberrant glial cells can significantly alter neuronal survival, synaptic activity, and drug response data.
Analytical Methods for Purity Assessment
A combination of techniques is required to achieve a comprehensive purity profile.
Table 2: Comprehensive Purity Assays for iPSC-Derived Neural Cultures
| Contaminant | Detection Method | Specific Marker/Target | Acceptance Criterion |
|---|---|---|---|
| Undifferentiated iPSCs | Flow Cytometry | Surface markers: TRA-1-60, SSEA4 [18] | < 1% positive cells |
| Off-Target Neural Cells | Immunocytochemistry | GFAP (Astrocytes); CD11B/IBA1 (Microglia) [16] | Context-dependent; often <5% non-target neural cells |
| Mesenchymal Cells | PCR or Flow Cytometry | CD44, CD73, CD105 [18] | Not detected |
| Genetic Abnormalities | Karyotyping / SNP Array | Chromosomal aberrations [18] [65] | Normal, stable karyotype |
| Microbiological Contaminants | Mycoplasma Testing | PCR-based assay | Not detected |
| Process Residuals | ELISA/LAL | Beta-glucans, endotoxins [65] | Below specified limit |
Experimental Protocol: Flow Cytometry for Residual Pluripotent Cells
This protocol details the quantification of residual undifferentiated iPSCs in a differentiated neuronal culture using flow cytometry, a highly sensitive and quantitative method.
Key Materials:
- Antibodies: Conjugated antibodies against TRA-1-60 and SSEA4.
- Buffer: Flow cytometry staining buffer (e.g., PBS with 1% BSA).
- Cells: A single-cell suspension of the differentiated culture. Include an unstained control and a sample of pure, undifferentiated iPSCs as a positive control.
- Equipment: Flow cytometer.
Procedure:
- Cell Harvesting: Gently dissociate the differentiated neuronal culture to create a single-cell suspension. Avoid over-digestion, which can damage surface epitopes.
- Staining: Aliquot approximately 1x10^6 cells per sample. Resuspend the cell pellet in 100µL of flow buffer containing the pre-titrated, conjugated anti-TRA-1-60 and anti-SSEA4 antibodies. Incubate for 30-60 minutes on ice or at 4°C in the dark.
- Washing and Resuspension: Wash the cells twice with 2mL of flow buffer to remove unbound antibody. Resuspend the final pellet in 300-500µL of flow buffer containing a viability dye (e.g., DAPI or 7-AAD) to exclude dead cells from the analysis.
- Data Acquisition and Analysis: Acquire data on a flow cytometer. First, gate on single, live cells based on forward/side scatter and viability dye exclusion. Then, analyze the gated population for dual positivity for TRA-1-60 and SSEA4. The percentage of double-positive cells in the differentiated culture should be below the pre-defined acceptance criterion (e.g., <1%) [18].
Tumorigenicity Testing and Risk Mitigation
Tumorigenicity is the most significant safety concern associated with iPSC-based therapies and models. The risk stems primarily from two sources: the inadvertent transplantation of residual undifferentiated iPSCs, which can form teratomas, and the genomic instability acquired during reprogramming or prolonged culture, which could lead to malignant transformation [65] [33]. While the immediate risk in in vitro research is lower than in clinical transplantation, undetected overgrowth of aberrant cells can compromise the integrity of long-term disease modeling experiments.
Comprehensive Tumorigenicity Testing Strategies
A robust tumorigenicity safety profile is built on multiple, orthogonal assays.
Table 3: Tumorigenicity Assays for iPSC-Derived Products
| Assay Category | Specific Assay | Readout | Risk Assessed |
|---|---|---|---|
| In Vitro Pluripotency | Flow Cytometry (TRA-1-60/SSEA4) | Quantification of residual pluripotent cells [18] | Teratoma formation from undifferentiated cells |
| In Vivo Tumorigenicity | Soft Agar Colony Formation | Anchorage-independent growth [65] | Malignant transformation potential |
| In Vivo Tumorigenicity (Gold Standard) | Teratoma Assay (Immunodeficient Mice) | Histology of teratomas with three germ layers [65] [33] | Functional pluripotency and tumorigenic potential |
| Genomic Stability | Karyotyping (G-banding) | Gross chromosomal abnormalities [18] [65] | Genomic instability leading to transformation |
| Oncogene Expression | PCR or RNA-Seq | Expression of reprogramming factors (e.g., c-MYC) [66] | Reactivation of integrated transgenes |
Experimental Protocol:In VitroSoft Agar Colony Formation Assay
The soft agar assay is a critical in vitro method for assessing anchorage-independent growth, a hallmark of cellular transformation. It serves as a scalable and ethically favorable alternative to initial animal studies for screening multiple cell lines.
Key Materials:
- Base Agar: Noble Agar or Agarose.
- Culture Medium: Appropriate medium for the cell type being tested (e.g., neuronal maintenance medium).
- Cells: Test iPSC-derived neural progenitors, positive control (e.g., HeLa cells), and negative control (e.g., primary human fibroblasts).
- Equipment: 6-well plates, water bath.
Procedure:
- Prepare Base Agar Layer: Create a 1.2% agar solution in water and autoclave. Mix this with 2x concentration of culture medium to create a 0.6% agar solution. Quickly add 1.5 mL of this mixture to each well of a 6-well plate to form the base layer and allow it to solidify at room temperature.
- Prepare Cell Layer: Trypsinize and count the test cells. Create a 0.3% agar solution in 1x culture medium. Suspend the cells in this solution at a density of 10,000-20,000 cells per mL. Carefully layer 1.5 mL of this cell-agar suspension over the solidified base layer.
- Culture and Feed: Allow the top layer to solidify. Incubate the plates at 37°C with 5% CO2 for 3-4 weeks. Every 5-7 days, add a fresh 0.5 mL of liquid culture medium on top of the agar to nourish the cells.
- Stain and Score: After the incubation period, add 0.5 mL of 0.005% Crystal Violet solution to each well for 1 hour. Examine the plates under a microscope. Count the number of colonies larger than 50µm in diameter. A significant number of colonies in the test sample compared to the negative control indicates transformation potential [65].
Figure 2: Tumorigenicity Testing Strategy. A multi-tiered approach to de-risk iPSC lines, progressing from in vitro to in vivo assays.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues critical reagents and their functions for establishing CQA assays in an iPSC laboratory focused on neurodegenerative disease modeling.
Table 4: Research Reagent Solutions for CQA Assays
| Reagent / Kit | Function | Application in CQA Testing |
|---|---|---|
| Anti-TRA-1-60 & SSEA4 Antibodies | Detection of pluripotency-associated surface antigens | Purity (residual iPSCs), Tumorigenicity [18] |
| Lineage-Specific Antibodies (e.g., Tuj1, MAP2, GFAP, HB9) | Immunophenotyping of differentiated cells | Potency (differentiation efficiency), Purity (off-target cells) [16] |
| G-banding Karyotyping Kit | Analysis of chromosomal structure and number | Tumorigenicity (genomic stability) [18] [65] |
| Mycoplasma Detection Kit (PCR-based) | Detection of mycoplasma contamination | Purity (microbiological contaminants) |
| Sendai Virus Reprogramming Kit | Non-integrating method for iPSC generation | Tumorigenicity (avoids insertional mutagenesis) [66] [65] |
| CRISPR/Cas9 Gene Editing System | Precision genetic correction in patient iPSCs | Potency (creation of isogenic controls) [65] [33] |
| Defined Neural Induction Media (e.g., with SMAD inhibitors) | Directing iPSC differentiation to neural lineage | Potency (standardized protocol) [16] |
The systematic implementation of potency, purity, and tumorigenicity assays forms the bedrock of reliable and reproducible science using patient-specific iPSCs for neurodegenerative disease research. As the field advances towards more complex models like cerebral organoids and embarks on high-throughput drug screening campaigns, the rigor of quality control will directly determine the translational value of the findings [8] [16]. The integration of advanced technologies such as CRISPR-Cas9 for genetic correction and AI-guided image analysis for phenotypic screening further empowers researchers to deconvolute disease mechanisms with unprecedented precision [65] [33]. By adhering to a stringent framework for defining these critical quality attributes, the scientific community can fully harness the potential of iPSC technology to unravel the complexities of the human brain and develop desperately needed therapeutics for debilitating neurodegenerative diseases.
Managing Raw Material and Supply Chain Inconsistencies
In the pioneering field of patient-specific induced pluripotent stem cell (iPSC) research for neurodegenerative diseases, consistency is not merely a logistical goal—it is a fundamental scientific necessity. The reprogramming of somatic cells into a pluripotent state creates a powerful platform for modeling conditions like Alzheimer's disease (AD), Parkinson's disease (PD), and Amyotrophic Lateral Sclerosis (ALS) [8] [67]. However, the complex differentiation processes involved are exquisitely sensitive to even minor perturbations in raw material quality and supply chain reliability.
Supply chain variability represents the difference between actual and planned lead times and performance, creating what practitioners term "anti-flows" that disrupt the essential movement of materials [68] [69]. For researchers working with iPSCs, this variability manifests as inconsistent culture media components, variable matrix coatings, and unreliable availability of critical reagents—all of which can compromise experimental validity and translational potential. The challenges of standardizing iPSC manufacturing are substantial, as the differentiation process is influenced by multiple cell-line and process-related variables that hinder standardization and consistency [70]. Consequently, managing these inconsistencies becomes paramount for advancing robust, reproducible neurodegenerative disease research.
Understanding and Categorizing Supply Chain Variability
Fundamental Types of Variability
In the context of iPSC research, supply chain variability can be systematically categorized into four distinct types, each with specific impacts on research outcomes [68]:
- Demand Variability: Fluctuations in the requirement for specific reagents, differentiation kits, or culture components due to changing research priorities or unexpected experimental needs.
- Supply Variability: Inconsistencies in the quality, composition, or delivery of raw materials from vendors, including lot-to-lot variations in growth factors, small molecules, and extracellular matrices.
- Operational Variability: Process inconsistencies within the laboratory environment, including technician techniques, equipment performance, and environmental conditions.
- Managerial Variability: Decisions, policies, and strategic changes that introduce disruption, including funding cycles, vendor selection changes, and inventory management practices.
Consequences of Variability in iPSC Research
The impacts of supply chain variability extend throughout the iPSC research pipeline, creating significant scientific and operational challenges [71]:
Table 1: Impacts of Supply Chain Variability on iPSC Research
| Impact Category | Research Consequences | Long-Term Implications |
|---|---|---|
| Differentiation Inconsistency | Variable purity and maturity of neuronal populations; poor reproducibility of disease phenotypes [72] | Compromised disease modeling; unreliable drug screening results |
| Experimental Noise | Increased inter-batch and inter-line variability obscures genuine pathological mechanisms [67] | Reduced statistical power; need for larger sample sizes |
| Process Inefficiency | Increased time and resource expenditure on quality control and protocol re-optimization [70] | Slowed research progress; increased costs |
| Translational Risk | Inability to standardize processes for clinical application [73] | Barriers to transitioning from basic research to clinical trials |
Strategic Framework for Managing Variability in iPSC Research
Demand Signal Management
Capturing the true demand signal is the foundation of variability reduction. For iPSC laboratories, this involves:
- Consumption-Based Planning: Aligning reagent procurement with actual experimental consumption patterns rather than forecasted usage alone. This requires implementing inventory tracking systems specifically designed for research environments [68].
- Aggregate Forecasting: Forecasting needs at the most aggregate level possible—for example, projecting requirements for "neural differentiation media components" rather than individual small molecules—then disaggregating based on actual experimental schedules [68].
Strategic Buffer Implementation
While eliminating all variability is impossible, strategic buffers can mitigate its impact:
- Safety Inventory: Maintaining minimum stock levels of critical reagents with known lead time variability, particularly for essential components like basal media, growth factors, and extracellular matrices [69].
- Capacity Buffering: Implementing flexible capacity solutions such as cross-trained personnel, modular equipment arrangements, and shared resource facilities to absorb fluctuations in experimental workloads [69].
Process Standardization and Rhythm
Establishing rhythmic, standardized processes provides stability against variability:
- Protocol Harmonization: Developing and adhering to standardized operating procedures (SOPs) for all critical processes, particularly iPSC culture maintenance, passaging, and differentiation protocols [73].
- Temporal Anchoring: Implementing regular, rhythmic schedules for core activities such as media preparation, quality control testing, and cell culture maintenance to create predictable workflow patterns [68].
Essential Quality Control Systems for iPSC Manufacturing
iPSC Characterization and Quality Metrics
Robust quality control systems are essential for identifying and controlling variability in iPSC lines. The following characterization should be routinely performed [20] [73]:
Table 2: Essential Quality Control Metrics for iPSC Research
| Quality Attribute | Assessment Method | Acceptance Criteria | Frequency |
|---|---|---|---|
| Pluripotency | Immunostaining for markers (SSEA-4, TRA-1-80); Trilineage differentiation potential [20] | >90% expression of markers; spontaneous differentiation to three germ layers | Each major passage |
| Cell Morphology | Microscopic evaluation of colony structure, edges, and nucleus:cytoplasm ratio [73] | Compact colonies with clear edges; prominent nucleoli | Daily |
| Proliferation Capacity | Doubling time calculation; cell counting and viability assessment [73] | Doubling time ~16-20 hours; >85% viability | Each passage |
| Genomic Stability | Karyotype analysis; Whole genome sequencing [20] | Normal karyotype; absence of major translocations | Every 10 passages |
| Lineage-Specific Differentiation | Expression of markers (e.g., β-III-tubulin for neurons) [20] [72] | Protocol-specific marker expression | Each differentiation |
Critical Process Controls
Implementing statistical process control for key iPSC manufacturing parameters enables early detection of variability:
- Control Charts for Critical Quality Attributes: Establishing control charts with upper and lower limits for metrics like doubling time, viability, and differentiation efficiency to distinguish common-cause from special-cause variation [69].
- Differentiation Efficiency Monitoring: Regularly quantifying the efficiency of differentiation protocols toward target neural lineages using flow cytometry or immunocytochemistry for lineage-specific markers [72].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details critical reagents and materials for iPSC-based neurodegenerative disease research, with special attention to variability management considerations:
Table 3: Essential Research Reagents for iPSC-Based Neurodegenerative Disease Modeling
| Reagent Category | Specific Examples | Function in iPSC Research | Variability Considerations |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) [20] | Reprogram somatic cells to pluripotent state | Use non-integrating methods (episomal DNA, mRNA) to reduce genomic variability [20] |
| Culture Matrices | Vitronectin, Synthemax II-SC, Laminin-521 [73] | Support iPSC attachment and proliferation | Standardize on xeno-free, defined matrices to reduce batch variability [73] |
| Culture Media | Essential 8 Medium, mTeSR [73] | Maintain pluripotency and support expansion | Use fully defined, albumin-free formulations to minimize lot-to-lot variability [73] |
| Neural Induction Agents | LDN193189, SB431542, DMH-1, Noggin [72] | Dual SMAD inhibition for neural induction | Pre-qualify small molecule inhibitors for consistent activity across lots |
| Patterning Factors | Retinoic Acid, SHH, SAG, CHIR99021 [72] | Direct regional specification (caudal, ventral) | Establish quality control checks for biological activity of recombinant proteins |
| Neuronal Maturation Supplements | BDNF, GDNF, NT-3, cAMP, Ascorbic Acid [72] | Enhance neuronal survival, maturation, and connectivity | Use GMP-grade growth factors when possible for highest consistency |
| Gene Editing Tools | CRISPR/Cas9 systems, gRNA [20] | Generate isogenic controls; introduce disease mutations | Validate editing efficiency and off-target effects for each gRNA lot |
Experimental Workflows for Managing Variability
cGMP-Compliant iPSC Culture Protocol
Implementing current Good Manufacturing Practice (cGMP) principles provides a structured approach to reducing variability in iPSC culture [73]:
cGMP iPSC Culture Workflow
Protocol for Differentiation to Disease-Relevant Neurons
Differentiation of iPSCs to specific neuronal subtypes for disease modeling requires precise control of timing and reagent quality:
Neuronal Differentiation Workflow
Case Studies: Variability Management in Neurodegenerative Disease Research
Clinical Trial Translation Successes
Several clinical trials for neurodegenerative diseases have emerged from iPSC research, demonstrating effective management of supply chain inconsistencies:
- ALS Clinical Trials: Candidate drugs including bosutinib, ropinirole, and ezogabine have advanced to clinical trials for ALS based on iPSC-based screening platforms [8].
- Gene-Targeted Therapies: WVE-004 and BII078 have entered clinical trials for ALS/FTD (amyotrophic lateral sclerosis/frontotemporal dementia), highlighting the translation of iPSC-based discoveries to human therapies [8].
- Parkinson's Disease Trial: The first clinical trial using iPSC-derived dopaminergic neurons for Parkinson's disease was announced by Kyoto University in 2018, demonstrating the clinical application of consistently manufactured iPSC-derived cells [73].
Technical Approaches to Variability Reduction
Advanced technical strategies have been developed specifically to address variability in iPSC-based disease modeling:
- Isogenic Controls: Using CRISPR/Cas9 gene editing to correct or introduce disease-causing mutations in patient-derived iPSCs, creating genetically matched controls that reduce background variability [67] [3].
- Standardized Differentiation Protocols: Implementing small molecule-based differentiation protocols that reduce batch variability associated with recombinant proteins [72].
- 3D Culture Systems: Employing cerebral organoids and 3D culture systems that better recapitulate tissue architecture and demonstrate improved reproducibility for disease modeling [67] [3].
Managing raw material and supply chain inconsistencies is not merely an operational concern but a fundamental scientific requirement in patient-specific iPSC research for neurodegenerative diseases. The strategies outlined in this technical guide—from systematic variability categorization to implementation of cGMP-compliant processes and quality control systems—provide a framework for enhancing research reproducibility and translational potential.
As the field advances toward more complex models including 3D organoids, assembloids, and microfluidic systems [72] [3], the importance of supply chain resilience will only increase. By adopting the principles of demand-driven planning, strategic buffering, and rigorous quality management, research institutions can build the foundation necessary to translate iPSC-based discoveries into meaningful therapies for neurodegenerative diseases.
Optimizing Neuronal Maturation and Functional Characterization
The utilization of induced pluripotent stem cells (iPSCs) in neurodegenerative disease research represents a paradigm shift toward patient-specific disease modeling and therapeutic development. A core challenge in this field is the consistent generation of functionally mature and characterized neurons that accurately recapitulate the phenotypic hallmarks of neurological conditions. This technical guide details optimized protocols for the maturation and functional characterization of iPSC-derived neurons, framed within the context of advancing personalized medicine for disorders such as amyotrophic lateral sclerosis (ALS), Parkinson's disease (PD), and epilepsy [28]. The methodologies outlined herein are designed to provide researchers with a robust framework for producing high-fidelity in vitro models suitable for mechanistic studies and preclinical drug screening.
iPSC Differentiation and Cortical Neuron Maturation
A defined, xeno-free protocol for differentiating iPSCs into cortical neurons is critical for producing a consistent and physiologically relevant population. The following workflow outlines a multi-stage process that yields a highly pure culture of functionally mature cortical neurons, free from glial cell influence [74].
Figure 1. Cortical Neuron Differentiation Workflow
Detailed Experimental Protocol
Initial Differentiation (DIF1, Days 1-5): Induce early neural lineages by treating iPSCs with the SMAD signaling inhibitors LDN193189 (100 nM) and SB431542 (10 µM) in neural induction medium. This dual inhibition promotes efficient neural commitment [74].
Neural Patterning (DIF2, Days 6-10): Specify telencephalic fate by adding the Wnt/β-catenin antagonist DKK-1 (100 ng/mL) alongside the BMP inhibitor DMH-1 (500 nM). This combination guides cells toward a rhombomeric neuroepithelia identity [74].
Cortical Specification (DIF3, Days 11-20): Withdraw DKK-1 and introduce the SHH inhibitor cyclopamine (1 µM) to promote dorsal cortical fate and enhance generation of cortical glutamate neurons [74].
Neuronal Maturation (Days 21-40): Culture the specified neural progenitors in maturation medium containing Brain-Derived Neurotrophic Factor (BDNF, 20 ng/mL), Glial Cell-Derived Neurotrophic Factor (GDNF, 20 ng/mL), cAMP (1 µM), ascorbic acid (200 µM), and laminin (1 µg/mL) to support survival, neurite outgrowth, and functional maturation [74].
Quality Control and Characterization
Immunocytochemistry analysis at day 40 should reveal a culture comprising >95% neurons (β-III tubulin+) with cortical identity (ctip2+), and minimal glial contamination (GFAP+ <1%) [74]. Longitudinal tracking demonstrates a critical transition around day 21-40, where cultures shift from simultaneously expressing excitatory (VGlut1) and inhibitory (GABA) markers to a purely excitatory phenotype (VGlut1+ only) by day 40 [74].
Functional Characterization of Mature Neurons
Comprehensive functional assessment is essential to validate the electrophysiological maturity and network integrity of iPSC-derived neurons. The following methodologies provide a multi-modal approach to functional characterization.
Electrophysiological Analysis
Patch Clamp Electrophysiology: Verify the presence of voltage-gated sodium and potassium channels capable of generating action potentials in response to depolarizing current injections. Mature neurons (day 40+) should exhibit repetitive firing patterns and spontaneous postsynaptic currents, indicating functional synaptic integration [74].
Multi-Electrode Array (MEA) Recording: Monitor network-level activity by plating neurons on MEA chips. Record spontaneous spiking activity and network bursting behavior over multiple weeks. Key parameters include mean firing rate, burst frequency, and synchrony index. Functionally mature cortical networks (day 40+) demonstrate the ability to undergo long-term potentiation (LTP) following high-frequency electrical stimulation, a hallmark of synaptic plasticity [74].
Figure 2. Functional Characterization Framework
Synaptic and Molecular Characterization
Immunocytochemistry for Synaptic Markers: Confirm the presence of mature synaptic structures by staining for pre-synaptic (synaptophysin) and post-synaptic markers (GluR1 for AMPA receptors, NMDAR1, and PICK1). Co-localization of pre- and post-synaptic proteins demonstrates the formation of functional synaptic connections [74].
Calcium Imaging: Measure intracellular calcium transients using fluorescent indicators (e.g., Fluo-4 AM) to monitor neuronal activity and network synchronization. Pharmacological validation with glutamate receptor agonists and antagonists can confirm the functional integrity of excitatory signaling pathways.
Table 1: Key Markers for Neuronal Maturation and Characterization
| Marker Category | Specific Marker | Expression in Mature Neurons | Assessment Method |
|---|---|---|---|
| Neuronal Identity | β-III tubulin | >95% of cells | Immunocytochemistry [74] |
| Cortical Identity | ctip2 (layer V) | >90% of neurons | Immunocytochemistry/Flow Cytometry [74] |
| Excitatory Phenotype | VGlut1 | Exclusive expression by day 40 | Immunocytochemistry [74] |
| Inhibitory Phenotype | GABA | Absent by day 40 | Immunocytochemistry [74] |
| Pre-synaptic | Synaptophysin | Punctate staining along processes | Immunocytochemistry [74] |
| Post-synaptic | PICK1, GluR1, NMDAR1 | Co-localized with synaptophysin | Immunocytochemistry [74] |
| Glial Contamination | GFAP | <1% of cells | Immunocytochemistry/Flow Cytometry [74] |
Application to Disease Modeling and Drug Screening
Optimized maturation protocols enable the development of phenotypically robust models for neurodegenerative diseases. These models are particularly valuable for studying sporadic cases, which constitute the majority of patients.
ALS Disease Modeling
A large-scale study utilizing iPSCs from 100 sporadic ALS (SALS) patients demonstrated that optimized motor neuron differentiation protocols can recapitulate key disease pathologies, including reduced motor neuron survival and accelerated neurite degeneration [16]. The motor neuron health was monitored using longitudinal live-cell imaging with a motor neuron-specific reporter (HB9-turbo), revealing a correlation between in vitro degeneration and donor survival time [16].
This model demonstrated high pharmacological predictivity when screening drugs previously tested in ALS clinical trials, with 97% failing to mitigate neurodegeneration—reflecting actual clinical trial outcomes [16]. Combinatorial drug testing identified a promising therapeutic combination of baricitinib, memantine, and riluzole for SALS [16].
Epilepsy Modeling and Compound Screening
Functionally mature cortical neurons (day 40) provide a robust platform for modeling hyperexcitability disorders such as epilepsy. Treatment with the GABAA receptor antagonist bicuculline induces epileptiform activity, which can be quantified by MEA through increased synchronous bursting [74]. This model can be used for preclinical drug screening, as demonstrated by the successful suppression of epileptiform activity with the anti-epileptic drug valproic acid [74].
Table 2: Quantitative Outcomes from iPSC-Based Disease Modeling Studies
| Disease Model | Cell Type | Key Phenotype | Pharmacological Validation | Source |
|---|---|---|---|---|
| Sporadic ALS | Spinal Motor Neurons | Reduced survival & accelerated neurite degeneration | Riluzole efficacy confirmed; <5% of trial drugs effective | [16] |
| Epilepsy | Cortical Neurons | Bicuculline-induced hyperexcitability & bursting | Valproic acid suppressed epileptiform activity | [74] |
| Parkinson's | Dopaminergic Neurons | NA (Therapeutic cell replacement) | NA (Clinical trials ongoing) | [28] |
| Age-related Macular Degeneration | Retinal Pigment Epithelium | NA (Therapeutic cell replacement) | NA (Clinical trials ongoing) | [28] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for iPSC Neuronal Differentiation and Characterization
| Reagent/Category | Specific Examples | Function in Protocol | Application Notes |
|---|---|---|---|
| Small Molecule Inhibitors | LDN193189, SB431542, DMH-1, Cyclopamine | Direct differentiation toward neural and cortical fates | Critical for defined, xeno-free protocols [74] |
| Trophic Factors | BDNF, GDNF | Support neuronal survival, maturation, and neurite outgrowth | Used during final maturation stage [74] |
| Maturation Supplements | cAMP, Ascorbic Acid, Laminin | Enhance neuronal health, synaptic function, and adherence | Promotes functional maturity [74] |
| Neuronal Markers | β-III tubulin, ctip2, MAP2 | Identify neuronal identity and cortical layer specification | Quality control via ICC/flow cytometry [74] |
| Synaptic Markers | Synaptophysin, GluR1, NMDAR1, PICK1 | Validate synapse formation and maturation | Co-localization indicates functional synapses [74] |
| Functional Assay Tools | Multi-electrode arrays, Patch clamp equipment | Characterize electrophysiological properties and network activity | Essential for functional validation [74] |
| Cell Type-Specific Reporters | HB9-turbo (for motor neurons) | Enable live-cell tracking of specific neuronal populations | Crucial for longitudinal health studies [16] |
The protocols and characterization methods detailed in this guide provide a comprehensive framework for generating functionally mature iPSC-derived neurons that closely mimic their in vivo counterparts. The emphasis on defined, xeno-free conditions ensures reproducibility and clinical relevance, while multi-modal functional assessment guarantees robust phenotypic readouts. These advanced in vitro models are already accelerating drug discovery, as evidenced by their successful application in large-scale screening for ALS and epilepsy research. By implementing these optimized maturation and characterization strategies, researchers can enhance the translational potential of iPSC-based models, ultimately advancing the development of patient-specific therapeutics for neurodegenerative diseases.
Validating iPSC Models: Correlating In Vitro Phenotypes with Clinical Reality
The advent of patient-specific induced pluripotent stem cell (iPSC) technology has revolutionized neurodegenerative disease research by providing a human-relevant, genetically accurate platform for investigating pathogenesis and therapeutic interventions. This technical guide outlines established methodologies for recapitulating three fundamental hallmarks of neurodegenerative diseases—protein aggregation, neuronal death, and transcriptomic alterations—within in vitro iPSC models. Focusing on conditions such as Alzheimer's disease (AD), Parkinson's disease (PD), and Amyotrophic Lateral Sclerosis (ALS), we detail the experimental frameworks that enable researchers to model disease progression, identify underlying mechanisms, and perform high-throughput compound screening. The integration of these approaches allows for a comprehensive analysis of disease pathology, from molecular triggers to phenotypic outcomes, thereby accelerating the development of targeted therapies.
Recapitulating Protein Aggregation
Core Mechanisms and Pathological Proteins
Protein aggregation is a defining pathological feature of major neurodegenerative diseases, characterized by the accumulation of misfolded proteins that assemble into insoluble fibrils with prion-like propagation properties [75] [76]. The process typically begins with the formation of soluble, oligomeric intermediates that are now regarded as primary drivers of neurotoxicity due to their exposed hydrophobic regions and high reactivity [76]. These oligomers can subsequently undergo a structural transition into stable, β-sheet-rich amyloid fibrils that accumulate intracellularly or extracellularly [75] [76]. The major pathogenic proteins include amyloid-β (Aβ) and tau in Alzheimer's disease, α-synuclein (α-Syn) in Parkinson's disease, and TAR DNA-binding protein 43 (TDP-43) in amyotrophic lateral sclerosis and frontotemporal lobar degeneration [75].
Table 1: Major Pathogenic Proteins in Neurodegenerative Diseases
| Disease | Primary Aggregating Proteins | Cellular Location of Aggregates | Key Aggregation Promoters |
|---|---|---|---|
| Alzheimer's Disease (AD) | Amyloid-β (Aβ), Tau | Extracellular (Plaques), Intracellular (NFTs) | BACE1/γ-secretase mutations, AEP activation, APP mutations [75] |
| Parkinson's Disease (PD) | α-synuclein (α-Syn) | Intracellular (Lewy bodies) | Gene mutations (SNCA), oxidative stress, impaired clearance [76] |
| Amyotrophic Lateral Sclerosis (ALS) | TDP-43, SOD1 | Intracellular (Cytoplasmic inclusions) | Gene mutations, oxidative stress, prion-like propagation [76] |
| Huntington's Disease (HD) | Huntingtin (with polyQ expansion) | Intracellular (Nuclear & cytoplasmic inclusions) | CAG repeat expansions in HTT gene [75] |
Experimental Modeling in iPSC Systems
iPSC Differentiation and Seeding Protocols: To model protein aggregation, researchers first differentiate patient-derived iPSCs into relevant neuronal subtypes (e.g., cortical neurons for AD, dopaminergic neurons for PD, motor neurons for ALS) using established patterning factors [77] [16]. A common approach involves exposing these cultures to pre-formed fibrils generated from recombinant pathogenic proteins to initiate the aggregation process. This seeding method accelerates the formation of protein aggregates that exhibit prion-like propagation between cells [75] [76]. The internalization of these seeds by recipient cells triggers the templated misfolding of endogenous, natively folded proteins, leading to the amplification and spreading of pathological aggregates [76].
Detection and Quantification Methods:
- Immunocytochemistry: Utilize conformation-specific antibodies (e.g., OC for amyloid fibrils) and phospho-specific antibodies (e.g., anti-pTau) to detect and localize aggregates [75] [76].
- FRET-Based Biosensors: Implement biosensors that undergo fluorescence resonance energy transfer upon protein misfolding to monitor aggregation dynamics in live cells [76].
- Filter Trap Assay: Use cellulose acetate membranes to separate and quantify insoluble aggregates from soluble protein fractions [76].
- Superresolution Microscopy: Apply STORM or PALM techniques to visualize the structural organization of protein aggregates at nanoscale resolution [76].
Diagram 1: Protein Aggregation Pathway. The diagram illustrates the progression from native proteins to toxic oligomers and mature fibrils, highlighting the prion-like propagation that enables disease progression.
Modeling Neuronal Death
Cell Death Mechanisms in Neurodegeneration
Neurodegenerative diseases involve multiple regulated cell death pathways that are activated in response to protein aggregation and other cellular stresses. The execution of these pathways leads to the irreversible loss of neuronal populations, which correlates with clinical disease progression [78] [79] [80]. Different death programs can be activated simultaneously or sequentially, contributing to the complex pathophysiology of these disorders.
Table 2: Neuronal Death Mechanisms in Neurodegenerative Diseases
| Cell Death Type | Key Regulators | Primary Triggers in Neurodegeneration | Detection Methods |
|---|---|---|---|
| Apoptosis | Caspases, Bcl-2 family, JAK-STAT pathway | Aβ oligomers, oxidative stress, neuroinflammation [80] | Caspase-3/7 activity, TUNEL staining, Annexin V staining |
| Ferroptosis | GPX4, Nrf2, iron homeostasis | Glial activation, abnormal iron homeostasis, lipid peroxidation [78] [80] | C11-BODIPY⁵⁸¹/⁵⁹¹ lipid peroxidation sensor, iron assays |
| Necroptosis | RIPK1/RIPK3/MLKL pathway, TNF-α | Neuroinflammation, cytokine signaling [80] | p-MLKL immunohistochemistry, necrostatin-1 inhibition |
| Pyroptosis | NLRP3 inflammasome, gasdermin D | Aβ and tau pathology, microglial activation [80] | LDH release, caspase-1 activity, IL-1β measurement |
| Autophagy | AMPK/mTOR/ULK1 pathway | Protein aggregate burden, mitochondrial dysfunction [80] | LC3-I/II conversion, p62 degradation, autophagosome imaging |
Quantitative Assessment of Neuronal Viability
Longitudinal Live-Cell Imaging: Implement automated microscopy systems to track neuronal survival in real-time using motor neuron-specific reporters (e.g., HB9::GFP) [16]. This approach enables the quantification of both somal degeneration and neurite fragmentation, providing dynamic readouts of disease progression. In a large-scale iPSC study involving 100 sporadic ALS patients, researchers demonstrated significantly reduced survival of SALS motor neurons compared to controls, establishing a key pathological hallmark [16].
High-Content Analysis of Death Pathways:
- Multiplexed Caspase Activity Assays: Use fluorescently-labeled inhibitors of caspases (FLICA) combined with cell permeability markers to distinguish apoptotic cells.
- Mitochondrial Function Assessment: Employ TMRE or JC-1 dyes to measure mitochondrial membrane potential, combined with MitoSOX Red for mitochondrial superoxide detection.
- Metabolic Activity Assays: Apply resazurin-based viability assays or ATP quantification kits as complementary measures of cellular health.
- High-Throughput Screening: In the aforementioned large-scale ALS study, researchers developed a robust phenotypic screening pipeline that identified only 3 out of 100+ tested drugs (riluzole, memantine, and baricitinib) that effectively rescued motor neuron survival across SALS donors [16].
Diagram 2: Neuronal Death Signaling Network. This diagram illustrates how protein aggregates trigger multiple parallel cell death pathways through neuroinflammation, mitochondrial dysfunction, and oxidative stress, culminating in neuronal loss.
Capturing Transcriptomic Signatures
Dynamic Transcriptomic Alterations in Disease
Transcriptomic profiling enables the identification of gene expression patterns that reflect underlying disease mechanisms, often before overt pathological changes occur. In Alzheimer's Disease Spectrum (ADS), dynamic functional connectivity (dFC) changes emerge early and progress through distinct stages from subjective cognitive decline to mild cognitive impairment and frank dementia [81]. Single-cell RNA sequencing of iPSC-derived neuronal cultures can capture cell-type-specific transcriptomic vulnerabilities that drive disease pathogenesis.
Key Transcriptomic Pathways in Neurodegeneration:
- Neuroinflammatory Signaling: Upregulation of NF-κB pathway components, cytokine and chemokine receptors, and complement system genes [80].
- Metabolic Dysregulation: Alterations in glycolytic enzymes, mitochondrial electron transport chain components, and glutamate catabolism pathways [81] [82].
- Proteostatic Failure: Downregulation of ubiquitin-proteasome system components, molecular chaperones, and autophagy-related genes [76].
- Synaptic Dysfunction: Changes in genes encoding synaptic vesicle proteins, neurotransmitter receptors, and neuronal cytoskeletal elements [81].
Analytical Frameworks for Transcriptomic Data
Leading Eigenvector Dynamics Analysis (LEiDA): This data-driven method captures time-resolved whole-brain dynamic functional connectivity by identifying transient brain states and calculating their occupancy rates, dwell times, and transition probabilities [81]. Applying this approach to ADS reveals how brain network stability and transition patterns change with disease severity, with later stages showing pronounced alterations in dwell time and occurrence rates of specific states that correlate with cognitive decline [81].
Pathway-Based Similarity Scoring: A novel computational framework integrates multi-database enrichment analysis to quantify functional convergence across diseases [83]. This approach has identified over 1,000 disease combinations that share molecular pathways despite divergent clinical presentations, revealing fundamental biological mechanisms that transcend traditional disease classification systems [83].
Table 3: Transcriptomic Analysis Methods in Neurodegenerative Disease Research
| Methodology | Key Applications | Resolution | Data Outputs |
|---|---|---|---|
| Bulk RNA-Seq | Pathway analysis, biomarker identification | Tissue/ population | Differential expression, enriched pathways |
| Single-Cell RNA-Seq | Cell-type-specific vulnerability, heterogeneity | Single-cell | Cell clusters, rare cell populations, trajectory inference |
| Spatial Transcriptomics | Topographic gene expression, microenvironment | Cellular/ subcellular | Spatial localization, cell-cell interactions |
| Dynamic Functional Connectivity | Brain network states, stage-dependent changes | Systems level | State occupancy, transition probabilities, dwell times [81] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for iPSC-Based Neurodegenerative Disease Modeling
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [77] | Somatic cell reprogramming to pluripotency | Use non-integrating episomal vectors for clinical relevance |
| Neural Differentiation | Retinoic acid, Sonic hedgehog, BDNF, GDNF | Pattern and mature specific neuronal subtypes | Optimize concentrations for regional specification |
| Cell Type Markers | ChAT, MNX1/HB9, Tuj1 (neurons), GFAP (astrocytes) [16] | Identify and quantify cellular populations | Use combinatorial markers for purity assessment |
| Pathological Protein Antibodies | Anti-Aβ (6E10, 4G8), anti-pTau (AT8), anti-pα-syn | Detect and quantify protein aggregates | Validate for specific oligomeric vs. fibrillar forms |
| Viability Reporters | HB9-turboGFP [16], Caspase-3/7 sensors | Longitudinal tracking of neuronal health | Use constitutive and inducible promoters |
| Pathway Modulators | Riluzole, memantine, baricitinib [16] | Pharmacological rescue experiments | Test combinations for enhanced efficacy |
Integrated Experimental Workflow
Diagram 3: Integrated iPSC Experimental Workflow. This workflow illustrates the comprehensive approach from iPSC generation through multi-parametric phenotyping to therapeutic screening.
The integrated experimental framework presented here enables the systematic recapitulation of neurodegenerative disease hallmarks using patient-specific iPSC models. By simultaneously monitoring protein aggregation, neuronal death pathways, and transcriptomic alterations, researchers can establish causal relationships between molecular triggers and phenotypic outcomes. The standardization of these protocols across research laboratories will enhance the reproducibility of findings and accelerate the development of effective therapies for these devastating disorders.
Benchmarking Against Animal Models and Post-Mortem Human Tissues
The study of neurodegenerative diseases presents a formidable challenge to global health, with the prevalence of conditions like Alzheimer's disease (AD) predicted to more than double in the next 30 years, affecting nearly 15 million Americans and costing over $1 billion by 2050 [84]. Traditional approaches to understanding disease mechanisms and developing therapeutics have relied heavily on animal models and post-mortem human tissues, yet these models have significant limitations in recapitulating the complexity of human neurodegenerative diseases [84] [85]. Despite providing crucial insights into disease mechanisms, the translation of findings from these traditional models into effective clinical therapies has been mostly unsuccessful [84] [85]. In fact, over 90% of drugs for neurodegenerative diseases fail during human clinical trials despite promising pre-clinical results [86].
The emergence of patient-specific induced pluripotent stem cell (iPSC) technology has created a paradigm shift in neurodegenerative disease modeling [1] [35]. By enabling the generation of disease-relevant human cell types while maintaining the complete genetic background of individual patients, iPSC-based models offer an unprecedented opportunity to bridge the translational gap between pre-clinical research and clinical applications [35] [87]. This technical guide provides a comprehensive benchmarking analysis of iPSC-based models against traditional animal models and post-mortem human tissues, with specific focus on their application in neurodegenerative disease research and drug development.
Limitations of Conventional Modeling Approaches
Animal Models in Neurodegenerative Research
Animal models, including rodents [85], Drosophila melanogaster [84], and non-human primates [87], have been instrumental in advancing our understanding of basic neurodegenerative mechanisms. These models offer several advantages, including the ability to study complex behaviors, intact nervous system circuitry, and the effects of aging and drugs in a whole-organism context [84]. The fruit fly Drosophila melanogaster, for instance, has positioned itself as a prominent model organism due to its cost effectiveness, short developmental time, and minimal genetic redundancy [84].
However, significant limitations constrain the translational relevance of animal models:
- Inadequate recapitulation of human disease complexity: Most animal models fail to recapitulate the complexity of an intact human nervous system and fully capture human disease phenotypes [84] [85].
- Species-specific differences: Fundamental differences in gene regulation, brain circuitry complexity, and cortical expansion between animals and humans limit translational potential [87]. Despite conservation of brain disorder-related genes across species, their precise function and relevance often vary [87].
- Ethical considerations: Increasing ethical concerns and regulatory restrictions surrounding animal research present additional challenges [86].
- High development costs: Developing and maintaining animal models involves substantial financial investment and time commitments [86].
Post-Mortem Human Tissues
Post-mortem human brain tissues have provided invaluable insights into the neuropathological hallmarks of neurodegenerative diseases. These tissues allow direct examination of human-specific disease pathology, including protein aggregation, neuronal loss, and glial responses at end-stage disease.
Nevertheless, critical limitations include:
- Static snapshot limitation: Post-mortem tissues provide only a single time point from the end-stage disease, offering no insight into disease initiation or progression dynamics [35].
- Technical artifacts: Variables such as post-mortem interval, agonal state, and tissue processing methods can introduce confounding technical artifacts.
- Limited availability and accessibility: Procurement of high-quality, well-characterized human brain tissues remains challenging, particularly for rare neurodegenerative conditions.
- Genetic and clinical heterogeneity: Difficulty in matching tissues with comprehensive clinical and genetic data limits mechanistic insights.
The Emergence of Patient-Specific iPSC Technology
Historical Development and Technical Foundations
The development of iPSC technology represents a watershed moment in biomedical research. The seminal work by Takahashi and Yamanaka in 2006 demonstrated that somatic cells could be reprogrammed to a pluripotent state through forced expression of defined transcription factors (Oct4, Sox2, Klf4, and c-Myc, known collectively as OSKM or Yamanaka factors) [1]. This discovery built upon foundational research including somatic cell nuclear transfer (SCNT) experiments by John Gurdon in 1962, which first demonstrated that differentiated somatic cells retain the genetic information needed to generate entire organisms [1].
The molecular mechanisms of somatic cell reprogramming involve profound epigenetic remodeling, wherein somatic cell signatures are erased and pluripotency networks are activated [1]. Reprogramming occurs in two principal phases: an early stochastic phase where somatic genes are silenced and early pluripotency-associated genes are activated, followed by a more deterministic late phase where late pluripotency-associated genes are activated [1].
Table 1: Evolution of Cellular Reprogramming Technologies
| Year | Development | Key Researchers/Institutions | Significance |
|---|---|---|---|
| 1962 | Somatic Cell Nuclear Transfer (SCNT) | John Gurdon | Demonstrated reversibility of cellular differentiation |
| 1981 | Mouse Embryonic Stem Cells (ESCs) | Evans, Kaufman, Martin | Established pluripotent stem cell reference |
| 1998 | Human Embryonic Stem Cells (ESCs) | James Thomson | Enabled human pluripotent stem cell research |
| 2006 | Mouse iPSCs | Takahashi and Yamanaka | First reprogramming with defined factors |
| 2007 | Human iPSCs | Yamanaka and Thomson | Enabled human-specific disease modeling |
| 2008 | Small Molecule-Enhanced Reprogramming | Multiple groups | Improved efficiency and safety |
| 2013 | Fully Chemical Reprogramming | Deng group | Virus-free reprogramming method |
Methodological Workflow for iPSC-Based Disease Modeling
The standard workflow for establishing patient-specific iPSC models of neurodegenerative diseases involves multiple critical stages [35]:
- Patient Recruitment and Biological Material Collection: Patients with specific neurodegenerative diseases are recruited through neurological centers, with informed consent obtained. Biological material (typically skin biopsy or peripheral blood samples) is collected.
- Somatic Cell Culture Establishment: Fibroblast cultures are established from skin biopsies, or peripheral blood mononuclear cells (PBMCs) are isolated from blood samples.
- Reprogramming to Pluripotency: Somatic cells are reprogrammed using integrative (lentivirus, retrovirus) or non-integrative (Sendai virus, episomal vectors, mRNA) methods to deliver reprogramming factors.
- iPSC Characterization and Validation: Pluripotency is confirmed through assessment of marker expression, differentiation potential, and genetic stability.
- Directed Differentiation to Relevant Neural Lineages: Using established protocols, iPSCs are differentiated into disease-relevant cell types (e.g., cortical neurons, motor neurons, dopaminergic neurons).
- Disease Phenotyping and Experimental Analysis: Resulting neural cells are analyzed for disease-specific phenotypes using molecular, cellular, functional, and omics approaches.
Diagram 1: Workflow for Establishing Patient-Specific iPSC Models of Neurodegenerative Diseases. This diagram illustrates the sequential process from patient sample collection to neuronal differentiation and phenotypic analysis.
Comparative Benchmarking of Modeling Platforms
Quantitative Comparison of Key Parameters
Table 2: Comprehensive Benchmarking of Neurodegenerative Disease Modeling Platforms
| Parameter | Animal Models | Post-Mortem Tissues | iPSC-Based Models |
|---|---|---|---|
| Human Genetic Background | Limited (species differences) | Yes (but static) | Yes (patient-specific) |
| Dynamic Disease Progression | Yes (longitudinal studies possible) | No (end-stage only) | Yes (in vitro maturation) |
| Access to Vulnerable Cell Populations | Indirect (requires tissue dissection) | Direct but fixed | Direct and dynamic |
| Temporal Resolution | High (throughout lifespan) | Single time point | Medium (weeks to months) |
| Throughput for Drug Screening | Low to medium | Not applicable | High (96/384-well formats) |
| Complex Circuitry/Network Analysis | High (intact brain) | Limited (fixed tissue) | Emerging (organoids, assembloids) |
| Genetic Manipulation Efficiency | Medium to high (transgenics) | Not applicable | High (CRISPR/Cas9) |
| Recapitulation of Human Pathology | Variable (often incomplete) | High (but static) | High for cellular phenotypes |
| Model Development Timeline | Months to years | N/A | 3-6 months |
| Cost Considerations | High | Medium | Medium to high |
Functional and Phenotypic Benchmarking
Disease Modeling Fidelity
iPSC-based models demonstrate superior performance in recapitulating key aspects of human neurodegenerative diseases compared to animal models. For example, in Alzheimer's disease, iPSC-derived neurons from patients recapitulate pathological features including increased Aβ production, elevated phosphorylated tau, and endosomal abnormalities [35]. Similarly, in Parkinson's disease, iPSC-derived dopaminergic neurons from patients show key pathological features such as α-synuclein accumulation, mitochondrial dysfunction, and increased susceptibility to oxidative stress [35].
The calcium hypothesis of neurodegeneration posits that disturbances in intracellular calcium signaling represent a central triggering factor for neurodegenerative processes [35]. iPSC-based models have provided compelling evidence supporting this hypothesis across multiple neurodegenerative conditions:
- Alzheimer's disease: iPSC-derived neurons exhibit enhanced endoplasmic reticulum calcium storage and increased store-operated calcium entry, potentially contributing to synaptic dysfunction and neurodegeneration [35].
- Parkinson's disease: iPSC-derived dopaminergic neurons with mutations in LRRC2 show increased expression of L-type voltage-gated calcium channels, resulting in elevated cytosolic calcium concentrations and increased susceptibility to excitotoxicity [35].
- Huntington's disease: iPSC-derived medium spiny neurons demonstrate abnormalities in store-operated calcium entry accompanied by decreased ER storage capacity, potentially contributing to their selective vulnerability [35].
Predictive Validity for Drug Discovery
The predictive validity of disease models—their ability to accurately forecast clinical efficacy—represents perhaps the most significant advantage of iPSC-based platforms. Traditional animal models have demonstrated poor predictive validity for neurodegenerative diseases, with a 95% failure rate for AD drugs in clinical trials despite promising pre-clinical results in animal models [86].
iPSC-based platforms are increasingly being used for drug discovery and toxicity screening, with several notable successes:
- Clinical trial candidates: iPSC-based screening has identified several clinical trial candidates, including bosutinib, ropinirole, and ezogabine for ALS, and WVE-004 and BII078 for ALS/FTD [8].
- High-throughput screening: iPSC-derived neuronal models enable high-throughput screening of chemical libraries in human-relevant systems, improving the likelihood of clinical success [86] [35].
- Toxicity assessment: iPSC-derived neural cells provide human-relevant platforms for assessing compound toxicity, potentially reducing late-stage drug failures [1].
Advanced Methodological Protocols for iPSC-Based Modeling
Directed Differentiation to Disease-Relevant Neural Lineages
The value of iPSC-based models depends critically on the efficient and reproducible differentiation of pluripotent cells into disease-relevant neural populations. Established protocols for generating specific neuronal subtypes include:
Motor Neuron Differentiation Protocol [88]:
- Neural Induction: Treat iPSCs with CHIR99021 (3 μM), DMH-1 (2 μM), and SB431542 (2 μM) for 6 days to generate neuroepithelial progenitors (NEPs).
- Motor Neuron Progenitor Induction: Differentiate NEPs in the presence of CHIR99021 (1 μM), DMH-1 (2 μM), SB431542 (2 μM), retinoic acid (0.1 μM), and Purmorphamine (0.5 μM) for 6 days.
- Neurosphere Formation: Culture motor neuron progenitors as neurospheres with retinoic acid (0.5 μM) and Purmorphamine (0.1 μM) for 5 days.
- Terminal Differentiation: Plate dissociated neurospheres and mature in medium containing retinoic acid (0.5 μM), Purmorphamine (0.1 μM), and Compound E (0.1 μM).
Neural Progenitor and Cortical Neuron Differentiation [87]:
- Dual-SMAD Inhibition: Use Noggin or DMH-1 (BMP inhibition) combined with SB431542 (TGF-β inhibition) to efficiently direct neural induction.
- Regional Patterning: Apply specific morphogens (e.g., SHH for ventral patterning, FGF8 for frontal cortex) to generate region-specific neural progenitors.
- Terminal Differentiation: Withdraw mitogens and promote neuronal maturation through neurotrophic factors (BDNF, GDNF, NT-3) and cAMP activators.
3D Organoid and Assembloid Models
While 2D cultures provide valuable reductionist models, the development of 3D cerebral organoids represents a significant advancement for modeling the complex cellular interactions and tissue architecture of the human brain [89] [1]. Sophisticated protocols now enable the generation of region-specific organoids (cortical, striatal, midbrain) that can be combined to form "assembloids" modeling circuit-level interactions [89].
Cortical Organoid Protocol [89] [1]:
- Embryoid Body Formation: Aggregate iPSCs in low-attachment plates with neural induction medium.
- Neuroectoderm Specification: Maintain aggregates in Matrigel droplets with neural induction factors.
- Unpatterned Organoid Culture: Transfer to spinning bioreactors with differentiation medium containing BDNF, GDNF, and cAMP.
- Long-term Maturation: Culture for extended periods (months) to promote neuronal maturation, synaptic development, and network activity.
Genetic Engineering and Isogenic Controls
A critical consideration in iPSC-based disease modeling is addressing the genetic heterogeneity between individuals. To control for background genetic variation, researchers establish isogenic control lines through precise genetic correction of disease-associated mutations in patient-derived iPSCs [35]. CRISPR/Cas9 technology enables efficient generation of these matched control lines, ensuring that observed phenotypic differences can be confidently attributed to the specific mutation of interest rather than unrelated genetic variation [35].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for iPSC-Based Neurodegenerative Disease Modeling
| Reagent Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Reprogramming Factors | OSKM (OCT4, SOX2, KLF4, c-MYC), OSK (without c-MYC), OSNL (OCT4, SOX2, NANOG, LIN28) | Somatic cell reprogramming to pluripotency | Non-integrating methods (Sendai virus, mRNA) preferred for clinical applications |
| Small Molecule Enhancers | Valproic acid, 5-azacytidine, CHIR99021, sodium butyrate | Improve reprogramming efficiency, replace transcription factors | Enable fully chemical reprogramming approaches |
| Neural Induction Agents | Noggin, DMH-1, SB431542, LDN-193189, dorsomorphin | Direct differentiation toward neural lineages | Dual-SMAD inhibition dramatically improves efficiency |
| Regional Patterning Factors | Retinoic acid (posterior), SHH (ventral), FGF8 (anterior), BMPs (dorsal) | Specify regional identity of neural progenitors | Concentration-dependent effects require careful optimization |
| Neuronal Maturation Factors | BDNF, GDNF, NT-3, NGF, cAMP, ascorbic acid | Promote terminal neuronal differentiation, synaptic maturation | Extended maturation periods (≥60 days) often required |
| Gene Editing Tools | CRISPR/Cas9, TALENs, zinc finger nucleases | Genetic correction for isogenic controls, introduce disease mutations | Off-target effects must be carefully assessed |
| Characterization Antibodies | OCT4, NANOG (pluripotency), SOX1, PAX6 (neural progenitors), Tuj1, MAP2 (neurons) | Validate pluripotency and differentiation efficiency | Species compatibility critical for immunocytochemistry |
Calcium Signaling Pathway Analysis in Neurodegenerative Disease Models
The investigation of calcium signaling abnormalities represents a prime example of how iPSC-based models can reveal disease-specific phenotypes with therapeutic relevance. The diagram below illustrates key calcium signaling pathways that can be studied using iPSC-derived neurons:
Diagram 2: Calcium Signaling Pathways in Neuronal Function and Dysfunction. This diagram illustrates key calcium regulatory mechanisms that are frequently disrupted in neurodegenerative diseases, including voltage-gated calcium channels, receptor-operated channels, store-operated calcium entry, and endoplasmic reticulum calcium storage and release.
Integration with Cutting-Edge Technologies and Future Perspectives
Complementary Technological Advancements
The utility of iPSC-based models is greatly enhanced through integration with other advanced technologies:
- Artificial Intelligence and Machine Learning: AI algorithms can analyze complex multidimensional data from iPSC-based screens, identifying subtle phenotypic patterns and predicting compound efficacy [8] [90].
- Microfluidic and Organ-on-a-Chip Platforms: These systems enable precise control of microenvironmental conditions and creation of complex tissue-tissue interfaces [86] [90].
- High-Content Imaging and Analysis: Automated imaging systems allow quantitative analysis of neuronal morphology, protein aggregation, and organelle dynamics in high-throughput formats [35].
- Multi-Omics Integration: Combining transcriptomic, proteomic, metabolomic, and epigenomic data from iPSC-derived neurons provides comprehensive insights into disease mechanisms [1] [35].
- Xenografting Approaches: Transplantation of human iPSC-derived neural cells into animal models creates human/animal chimeras that combine the advantages of in vivo modeling with human-specific biology [89].
Clinical Translation and Commercial Landscape
The iPSC-based platforms market is experiencing significant growth, projected to generate substantial revenue increases in the coming years [90]. Key commercial trends include:
- Drug Discovery & Toxicology Screening: This application segment holds a dominant 42% market share, reflecting widespread adoption in pharmaceutical development [90].
- Personalized Medicine: The fastest-growing application segment, enabled by patient-specific iPSC models that facilitate tailored therapeutic approaches [90].
- Neural Progenitors & Neurons: Among cell types, neural progenitors and neurons represent the fastest-growing segment, driven by increasing focus on neurological disorders [90].
- Regional Markets: North America currently leads with 46% market share, but Asia-Pacific is expected to demonstrate the fastest growth, supported by government initiatives and regenerative medicine emphasis [90].
The benchmarking analysis presented in this technical guide demonstrates that patient-specific iPSC models offer significant advantages over traditional animal models and post-mortem human tissues for neurodegenerative disease research. While each modeling approach has distinctive strengths and limitations, iPSC-based platforms provide unprecedented access to live, functional human neurons with disease-relevant genetic backgrounds. The capacity to observe dynamic disease processes, perform high-throughput drug screening, and establish isogenic controls positions iPSC technology as an indispensable component of the modern neurodegenerative disease research toolkit.
As the field continues to advance through integration with AI, organ-on-a-chip systems, and multi-omics technologies, iPSC-based models are poised to dramatically accelerate the development of effective therapies for neurodegenerative conditions. By enabling researchers to move beyond the limitations of species-specific differences and static pathological snapshots, these human cellular models offer a powerful path toward understanding and ultimately treating devastating neurodegenerative diseases.
The Power of Population-Scale iPSC Libraries to Capture Disease Heterogeneity
Induced pluripotent stem cells (iPSCs), generated by reprogramming somatic cells through the introduction of transcription factors like Oct4, Sox2, Klf4, and c-Myc, have revolutionized biomedical research by providing patient-specific cellular models [18]. Population-scale iPSC libraries represent the next evolutionary step, comprising collections of iPSC lines derived from hundreds of genetically diverse donors, including both healthy individuals and patients with various diseases [91] [16]. These libraries directly address the critical challenge of disease heterogeneity—the natural variation in disease presentation, progression, and treatment response observed across patient populations—by enabling researchers to study how genetic background influences disease mechanisms and therapeutic outcomes [16].
The fundamental value of these resources lies in their ability to model human genetic diversity in vitro. By capturing a wide spectrum of human genetic variation, population-scale iPSC libraries facilitate the identification of molecular networks underlying disease susceptibility and progression, moving beyond single-gene models to address complex polygenic disorders [91]. For neurodegenerative diseases, which exhibit substantial heterogeneity in clinical presentation and pathological mechanisms, these libraries provide an unprecedented platform for mechanistic studies that account for genetic variability while controlling environmental factors [16].
The Construction and Characterization of iPSC Libraries
Library Generation and Quality Control
Establishing a population-scale iPSC library begins with the careful selection of donor cohorts that represent the genetic and clinical diversity of the target population. Donor somatic cells can be obtained from various sources, including dermal fibroblasts (via skin biopsy), peripheral blood mononuclear cells (via blood draw), or urinary epithelial cells (completely non-invasive) [18]. The reprogramming process typically employs non-integrating methods such as episomal vectors or Sendai virus to minimize genomic alterations while restoring pluripotency [18] [16].
Following reprogramming, rigorous quality control is essential to ensure line fidelity and functionality. This includes:
- Verification of pluripotency markers (OCT4, NANOG, SOX2) via PCR, immunocytochemistry, or flow cytometry
- Demonstration of trilineage differentiation potential into ectoderm, mesoderm, and endoderm derivatives
- Assessment of genomic integrity through karyotyping and whole-genome sequencing
- Evaluation of line-specific identity through genotyping [18] [16]
Large-scale initiatives like the Human Induced Pluripotent Stem Cell Initiative (HipSci) have established standardized protocols for generating and characterizing iPSC libraries, with some collections featuring hundreds to thousands of lines [91] [92].
Capturing Population Diversity
The power of population-scale libraries stems from their deliberate inclusion of donors representing the spectrum of human genetic variation. The HipSci project, for instance, established iPSC lines from over 500 healthy donors and patients, creating a resource that captures common genetic variants present in the broader population [91] [92]. Similarly, disease-specific libraries, such as the sporadic ALS (SALS) library comprising 100 patient-derived lines, intentionally encompass the clinical heterogeneity of the disease, including variations in age of onset, site of onset, and progression rate [16].
Table 1: Exemplary Population-Scale iPSC Libraries
| Library Name/Focus | Number of Lines | Key Characteristics | Primary Applications |
|---|---|---|---|
| HipSci General Population [91] [92] | 215+ | Healthy donors and multiple disease states; extensive multi-omics characterization | Mapping dynamic eQTLs during differentiation; studying differentiation biases |
| Sporadic ALS Library [16] | 100 SALS patients + 25 controls | Clinically heterogeneous donors; comprehensive clinical data | Modeling sporadic neurodegeneration; large-scale drug screening |
| CiRA Haplobank [93] | 27 HLA-homozygous lines | Matches ~40% of Japanese population immunologically | Allogeneic therapeutic development |
Technical Approaches for Large-Scale iPSC Studies
Multiplexed Experimental Designs
A key innovation enabling population-scale iPSC research is multiplexing—pooling multiple iPSC lines together during differentiation and subsequent analyses to minimize batch effects and improve throughput [91] [92]. In this approach, lines are combined at the pluripotent stage, differentiated together, and then assigned to their line of origin through genetic demultiplexing using tools like demuxlet, which leverages natural genetic variation as cellular barcodes [91]. This method significantly enhances experimental reproducibility while controlling for technical variability that often plagues individual differentiations.
The multiplexing approach was successfully implemented in a study differentiating 215 iPSC lines toward midbrain dopaminergic neurons, where cells from 7-24 lines were pooled in each differentiation experiment [91]. This design allowed researchers to profile over 1 million cells across three differentiation time points while effectively controlling for batch effects, enabling robust identification of cell-intrinsic differences between lines [91].
Single-Cell Multi-Omic Technologies
Advanced single-cell technologies provide unprecedented resolution for characterizing cell types, states, and molecular networks within heterogeneous populations of differentiated cells. Single-cell RNA sequencing (scRNA-seq) has been particularly transformative, enabling researchers to:
- Map differentiation trajectories at single-cell resolution
- Identify novel cell subpopulations and transitional states
- Characterize cell-type-specific genetic effects on gene expression [91] [94] [92]
In one of the largest scRNA-seq studies of iPSCs, researchers profiled 18,787 individual cells, identifying four distinct subpopulations within supposedly homogeneous pluripotent cultures, including a core pluripotent population (48.3%), proliferative cells (47.8%), and subpopulations primed for differentiation (2.8% and 1.1%) [94]. This resolution is crucial for understanding how pre-existing heterogeneity in pluripotent states influences differentiation outcomes.
Complementing transcriptomic approaches, proteomic profiling via tandem mass tag mass spectrometry (TMT-MS) has been applied to population-scale iPSC libraries, revealing that approximately 30% of genetic variants affecting protein abundance do not manifest at the RNA level [95]. This highlights the importance of multi-layer molecular characterization for comprehensively understanding genetic effects.
Table 2: Core Analytical Methods for Population-Scale iPSC Studies
| Method Category | Specific Technologies | Key Applications | Considerations |
|---|---|---|---|
| Cell Pooling & Demultiplexing | demuxlet, genotype-based assignment [91] | Batch effect control; high-throughput differentiation | Requires pre-existing genotype data; optimization of pool size |
| Single-Cell Profiling | scRNA-seq (Smart-Seq2, 10X) [91] [92] | Lineage reconstruction; cell type identification; eQTL mapping | Cost at scale; computational analysis challenges |
| Proteomic Characterization | Tandem Mass Tag Mass Spectrometry [95] | pQTL mapping; post-transcriptional regulation | Lower throughput than transcriptomics; limited proteome coverage |
| High-Content Screening | Automated live-cell imaging [16] | Longitudinal phenotypic assessment; drug screening | Requires specialized instrumentation; data storage challenges |
Application in Neurodegenerative Disease Research
Modeling Sporadic Neurodegenerative Diseases
Population-scale iPSC libraries have proven particularly valuable for studying sporadic neurodegenerative diseases, which account for the majority of cases and involve complex interactions between multiple genetic risk factors and environmental influences [16]. Traditional models based on monogenic familial forms have limited translational relevance for these sporadic cases, as evidenced by the failure of more than 160 drugs that showed efficacy in familial ALS models but failed in clinical trials encompassing predominantly sporadic patients [16].
The application of population-scale iPSC libraries to sporadic amyotrophic lateral sclerosis (SALS) has demonstrated that patient-derived motor neurons recapitulate key disease phenotypes, including reduced survival, accelerated neurite degeneration, and transcriptional dysregulation [16]. Critically, the heterogeneity in phenotypic severity across lines from different donors mirrored the clinical heterogeneity observed in patients, with the rate of neurite degeneration in vitro correlating with donor survival time [16]. This suggests that these models capture biologically relevant aspects of disease heterogeneity.
Identifying Molecular Determinants of Disease Susceptibility
By combining iPSC-based models with genetic data, researchers can identify molecular markers that predict disease susceptibility or progression. In a study of midbrain dopaminergic neuron differentiation from 215 iPSC lines, researchers observed substantial variation in the differentiation efficiency of individual lines—the proportion of neurons produced by each line—which was highly reproducible across different experiments and even across different differentiation protocols (R = 0.75) [91]. This differentiation bias was predictable by molecular markers expressed in pluripotent cells, suggesting the existence of cell-intrinsic factors that predispose certain genetic backgrounds to more efficient neuronal differentiation [91].
Similarly, studies of endoderm differentiation from 125 iPSC lines identified molecular markers predictive of differentiation efficiency, enabling researchers to prospectively identify lines with poor differentiation potential [92]. These findings have important implications for both disease modeling and therapeutic development, as they suggest that inherent biological properties of a patient's cells may influence both disease susceptibility and response to regenerative therapies.
Experimental Workflows and Methodologies
Large-Scale Differentiation and Phenotyping
The following diagram illustrates a representative workflow for population-scale iPSC differentiation and phenotyping, as implemented in a large-scale study of sporadic ALS:
Diagram 1: Population-scale iPSC differentiation and phenotyping workflow
Detailed Methodologies for Key Experiments
Motor Neuron Differentiation and Phenotypic Screening for ALS Modeling
For large-scale modeling of ALS, researchers developed a robust five-stage protocol adapted from established spinal motor neuron differentiation methods [16]. Critical optimization steps included:
- Culture conditions: Extensive testing of maturation and screening conditions to discriminate between healthy control and diseased motor neurons
- Purity assessment: Implementation of highly stringent quantification criteria, resulting in cultures with 92.44 ± 1.66% motor neurons (co-expressing ChAT, MNX1/HB9, and Tuj1)
- Longitudinal live-cell imaging: Daily monitoring using automated microscopy with a motor neuron-specific reporter (HB9-turbo) to assess survival and neurite degeneration
- Pharmacological validation: Confirmation of model relevance through demonstration of riluzole efficacy, consistent with its clinical effects [16]
This optimized protocol enabled researchers to detect significant survival deficits in SALS motor neurons compared to controls—a key pathological hallmark that had proven elusive in previous smaller-scale studies [16].
Single-Cell RNA Sequencing and eQTL Mapping
Comprehensive molecular profiling of differentiating iPSCs involves:
- Cell collection: Sampling at multiple time points (e.g., days 0, 11, 30, and 52 for dopaminergic differentiation) to capture dynamic processes [91]
- Library preparation: Using either full-length Smart-Seq2 protocols for deep sequencing or droplet-based methods for higher throughput [92]
- Cell type annotation: Combining literature-curated marker genes with computational alignment to existing single-cell atlases [91]
- Expression Quantitative Trait Loci (eQTL) mapping: Testing for associations between genetic variants and gene expression using linear mixed models that account for batch effects and population structure [91] [92]
In one study profiling endoderm differentiation across 125 iPSC lines, this approach identified 1,833 eGenes in iPSCs, with over 30% of eQTLs being specific to a single differentiation stage [92]. This dynamic regulation highlights the importance of studying genetic effects across developmental contexts rather than only in mature cell types.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents for Population-Scale iPSC Studies
| Reagent Category | Specific Examples | Function & Application | Technical Considerations |
|---|---|---|---|
| Reprogramming Systems | Episomal vectors; Sendai virus (CytoTune); mRNA systems [18] [16] | Footprint-free reprogramming of somatic cells; clinical compatibility | Efficiency varies by cell source; require optimization |
| Culture Media | mTeSR1; E8 medium [18] | Chemically defined maintenance of pluripotency; xeno-free applications | Lot-to-lot variability; cost at scale |
| Extracellular Matrices | Matrigel; recombinant laminin [18] | Feeder-free culture substrate; enhanced reproducibility | Complexity of Matrigel composition; laminin specificity |
| Neural Differentiation Kits | Commercial dopaminergic or motor neuron kits [16] | Standardized differentiation; protocol harmonization across labs | May require optimization for specific lines |
| Demultiplexing Tools | demuxlet [91] | Genetic assignment of pooled cells to line of origin | Requires pre-existing genotype data |
| Cell Type-Specific Reporters | HB9::GFP; other fluorescent constructs [16] | Live monitoring of specific cell populations; sorting | Potential perturbation of native biology |
| Viability Assays | Longitudinal live-cell imaging dyes [16] | High-content screening of cellular phenotypes | Compatibility with long-term culture |
Data Analysis and Computational Approaches
Genetic Demultiplexing and Batch Effect Correction
The analysis of pooled single-cell data begins with sample demultiplexing to assign cells to their original donor lines. The tool demuxlet uses natural genetic variation as cellular barcodes, leveraging pre-existing genotype data to probabilistically assign each cell to a specific donor [91]. Following demultiplexing, batch effect correction is critical, as even pooled differentiations may exhibit technical variability. Tools like Harmony effectively integrate data across multiple experiments, removing technical artifacts while preserving biological heterogeneity [91].
QTL Mapping Across Cellular Contexts
Mapping quantitative trait loci (QTLs) in population-scale iPSC studies involves several key considerations:
- Cell state stratification: Rather than analyzing cells solely by experimental time point, researchers first assign cells to specific differentiation stages or cell types based on transcriptional profiles, then perform QTL mapping within each population [92]. This approach increases power by analyzing more homogeneous cell states.
- Dynamic QTL analysis: Using sliding-window approaches along differentiation pseudotime to identify genetic effects that change during development [92].
- Multi-level QTL integration: Combining eQTL (expression), pQTL (protein), and sQTL (splicing) data to comprehensively characterize genetic effects across molecular layers [95].
These approaches have revealed that a substantial fraction of genetic effects on molecular phenotypes are context-specific, appearing only in certain cell types or developmental stages [91] [92] [95].
Future Directions and Clinical Translation
Population-scale iPSC libraries are increasingly being applied to drug discovery and development, particularly for heterogeneous neurodegenerative diseases. In one large-scale screen using 100 SALS lines, researchers found that 97% of drugs previously tested in ALS clinical trials failed to mitigate neurodegeneration in this more representative model, accurately reflecting clinical trial outcomes [16]. However, combinatorial testing identified baricitinib, memantine, and riluzole as a promising therapeutic combination that rescued motor neuron survival across the heterogeneous SALS donor population [16].
The integration of artificial intelligence with population-scale iPSC data represents another promising direction, enabling the identification of complex patterns in high-dimensional molecular and phenotypic data [8]. These approaches may help decode the relationship between genetic variation, molecular networks, and cellular phenotypes, ultimately improving patient stratification and treatment selection.
As the field advances, population-scale iPSC libraries are also facilitating the development of allogeneic cell therapies through the creation of haplobanks—collections of HLA-homozygous lines that can immunologically match large segments of the population [93]. The CiRA Foundation in Japan, for instance, has generated 27 clinical-grade iPSC lines from just seven donors that match approximately 40% of the Japanese population, demonstrating the potential of this approach to enable off-the-shelf regenerative therapies [93].
The continued expansion and characterization of population-scale iPSC libraries, coupled with advances in differentiation protocols, single-cell technologies, and computational methods, promises to further enhance our ability to understand and address heterogeneity in neurodegenerative diseases, ultimately enabling more effective, personalized therapeutic interventions.
The high failure rate of therapeutics in neurodegenerative disease clinical trials underscores a critical translational gap between preclinical models and human pathophysiology. Induced pluripotent stem cell (iPSC) technology has emerged as a transformative platform for addressing this challenge, enabling the development of human-specific disease models that more accurately recapitulate disease mechanisms. Pharmacological validation—the process of using clinical trial outcomes to assess and refine the predictive accuracy of these preclinical models—represents a crucial methodology for strengthening the drug development pipeline. Within the context of patient-specific iPSC models, pharmacological validation establishes a feedback loop where clinical results inform model refinement, thereby enhancing the predictive power of subsequent preclinical studies [86] [96].
The discovery of iPSCs in 2006 by Takahashi and Yamanaka, who reprogrammed somatic cells using the transcription factors Oct4, Sox2, Klf4, and c-Myc (OSKM), created unprecedented opportunities for neurodegenerative disease modeling [1]. Unlike animal models that may lack human-specific disease phenotypes, iPSC-derived neuronal and glial cells preserve the patient's complete genetic background, including risk variants associated with complex disorders like Alzheimer's disease (AD) and Parkinson's disease (PD) [97] [96]. This technological advance enables researchers to move beyond traditional drug screening in non-human systems to human-based platforms where disease mechanisms and therapeutic responses can be studied in clinically relevant cellular environments.
Table 1: Global Distribution of Ongoing iPSC Clinical Trials (Therapeutic vs. Nontherapeutic)
| Country/Region | Therapeutic Trials | Nontherapeutic Trials | Primary Applications |
|---|---|---|---|
| Japan | Leading in therapeutic applications | Limited | Cell replacement therapies |
| United States | Developing | Highest number (33.3%) | Disease modeling (75.8%) |
| France | Limited | Substantial (20.6%) | Drug screening (12.9%) |
| Multiple Countries (Germany, UK, etc.) | Varying | Moderate (6.3% each) | Cell bank development (8.1%) |
Source: Adapted from current trends in clinical trials involving iPSCs [98]
Foundations of Pharmacological Validation
Conceptual Framework
Pharmacological validation operates on the principle that a preclinical model's response to therapeutic interventions should predict corresponding human clinical outcomes. For iPSC-based models of neurodegenerative diseases, this validation process occurs across multiple dimensions. The face validity of a model examines how accurately it recapitulates the key pathological features of the human disease, such as amyloid-β accumulation in Alzheimer's or α-synuclein aggregation in Parkinson's. Construct validity assesses how well the model incorporates the known etiological mechanisms of the disease, while predictive validity specifically evaluates the model's ability to correctly identify therapeutics that will succeed or fail in human trials [96].
The validation process follows a structured approach: (1) establishing baseline disease phenotypes in patient-derived iPSC models, (2) administering compounds with known clinical efficacy profiles, (3) quantifying functional and molecular responses, and (4) correlating these responses with clinical trial outcomes. This methodology creates a quantitative framework for assessing a model's predictive accuracy before its deployment in screening novel therapeutic candidates. For neurodegenerative diseases, this is particularly crucial given the lengthy and costly nature of clinical trials and the urgent need for effective treatments [86] [97].
Clinical Trial Data as a Validation Benchmark
Clinical trial outcomes provide the essential benchmark for pharmacological validation, offering standardized metrics of therapeutic efficacy and safety in human populations. For iPSC model validation, several types of clinical data prove most informative: primary endpoints that directly measure clinical improvement (e.g., cognitive scores), secondary endpoints that capture functional or biomarker changes, adverse event profiles, and pharmacokinetic/pharmacodynamic data [99]. These datasets enable researchers to determine whether compound effects observed in iPSC models correspond meaningfully to human responses.
Regulatory standards for clinical data quality, outlined in guidelines such as ICH-GCP and FDA 21 CFR Part 11, emphasize the importance of data accuracy, completeness, and consistency [100]. These same principles extend to the pharmacological validation process, where rigorous documentation of experimental conditions, standardized operating procedures, and quality control measures ensure the reliability of validation outcomes. Modern clinical data management increasingly employs Electronic Data Capture (EDC) systems with real-time validation checks, targeted Source Data Validation (tSDV) for critical data points, and batch validation techniques for large datasets—methodologies that can be adapted to the validation of iPSC-based screening platforms [100].
iPSC-Based Disease Modeling for Drug Screening
Development of Patient-Specific Neural Models
The generation of functionally relevant neural cells from iPSCs requires precisely orchestrated differentiation protocols that mimic developmental cues. For pharmacological validation in neurodegenerative disease research, the most valuable models include iPSC-derived midbrain dopaminergic neurons for Parkinson's disease, cortical and hippocampal neurons for Alzheimer's disease, and supporting glial populations such as astrocytes and microglia that contribute significantly to disease pathogenesis [101] [96]. These differentiation protocols typically involve sequential exposure to morphogens including SHH (sonic hedgehog) and FGF8 (fibroblast growth factor 8) for dopaminergic neurons, or dual SMAD inhibition followed by neuronal patterning factors for cortical populations.
Recent advances have enabled the creation of more complex 3D organoid systems that better recapitulate the cellular diversity and structural organization of the human brain. Cerebral organoids can exhibit features such as cortical layering, regional specification, and even primitive connectivity, offering enhanced platforms for modeling network-level dysfunction in neurodegenerative diseases [97]. For pharmacological validation, these 3D systems may provide significant advantages over 2D cultures by capturing cell-cell interactions and tissue-level drug distribution effects that more closely resemble the in vivo environment. The incorporation of multiple brain cell types (neurons, astrocytes, microglia) into these models enables researchers to evaluate compound effects on neuroinflammation, trophic support, and other glia-mediated mechanisms increasingly recognized as crucial to neurodegenerative processes [97] [96].
Capturing Disease-Relevant Phenotypes
A critical step in pharmacological validation is demonstrating that iPSC-based models exhibit disease-specific phenotypes that can be modulated by therapeutic interventions. In Alzheimer's disease models, these phenotypes include amyloid-β pathology (altered Aβ42/Aβ40 ratios), tau hyperphosphorylation, endosomal dysfunction, oxidative stress, and synaptic deficits [96]. Parkinson's disease models may display α-synuclein accumulation, mitochondrial dysfunction, lysosomal impairment, and increased susceptibility to oxidative stress [101]. The measured response of these phenotypes to reference compounds with established clinical profiles forms the basis for assessing a model's predictive validity.
Table 2: Key Disease Phenotypes in iPSC-Derived Neurodegenerative Models
| Disease | Cellular Phenotypes | Molecular Markers | Functional Assays |
|---|---|---|---|
| Alzheimer's Disease | Aβ plaque formation, neurite dystrophy | Increased Aβ42/Aβ40 ratio, p-tau | Synaptic activity (MEA), calcium imaging |
| Parkinson's Disease | Lewy body-like inclusions, neuronal death | α-synuclein aggregation, DJ-1 mutation | Dopamine release, mitochondrial stress |
| Diabetic Neuropathy | Axonal degeneration, myelin defects | Advanced glycation end products | Nerve conduction velocity, apoptosis assays |
Source: Adapted from iPSC applications in neurodegenerative disorders [86] [96]
Methodological Framework for Pharmacological Validation
Experimental Workflow for Validation Studies
The pharmacological validation process follows a structured workflow that integrates iPSC technology, clinical data, and computational analysis. The first stage involves iPSC generation and characterization from patients with specific neurodegenerative diseases and appropriate healthy controls. Somatic cells (typically fibroblasts or peripheral blood mononuclear cells) are reprogrammed using non-integrating methods such as Sendai virus or episomal vectors to minimize genomic alterations, with rigorous quality control including pluripotency marker expression, karyotyping, and genetic integrity verification [1].
Following differentiation into relevant neural cell types, the next stage establishes baseline disease phenotypes through multi-omics profiling, functional analyses, and morphological assessment. The critical validation phase then involves compound testing with reference therapeutics that have unequivocal clinical trial outcomes—both successful and failed compounds—across a range of concentrations. High-content screening approaches capture multidimensional readouts including transcriptomic changes, protein-level modifications, cellular imaging, and functional metrics. The resulting data undergoes correlation analysis with clinical outcomes to quantify predictive accuracy, followed by model refinement to improve alignment with human responses [97] [96].
Quantitative Framework for Predictive Accuracy
A robust quantitative framework is essential for objective assessment of a model's predictive validity. Key metrics include sensitivity (true positive rate in identifying clinically effective compounds), specificity (true negative rate in identifying clinical failures), and overall accuracy (proportion of correct predictions). These metrics can be calculated using the following relationships:
- Sensitivity = True Positives / (True Positives + False Negatives)
- Specificity = True Negatives / (True Negatives + False Positives)
- Accuracy = (True Positives + True Negatives) / Total Compounds Tested
The receiver operating characteristic (ROC) curve and corresponding area under the curve (AUC) provide comprehensive assessments of predictive performance across different classification thresholds. For example, a recent machine learning approach to predicting neurodegenerative disease progression in type 2 diabetes patients achieved an AUC of 0.83 using the AdaBoost model, demonstrating the potential for quantitative predictive modeling in complex diseases [102]. Similar analytical frameworks can be applied to pharmacological validation of iPSC models, with the goal of achieving AUC values that exceed 0.8, indicating strong predictive power.
Beyond binary classification, effect size correlation analyses quantify how well the magnitude of response in the iPSC model predicts the clinical effect size. This is particularly valuable for dose-response predictions and for understanding translational relationships between cellular phenotypes and clinical outcomes. Advanced computational approaches, including machine learning algorithms and ensemble transfer learning methods similar to those used in Alzheimer's disease prediction from MRI data, can further enhance predictive accuracy by integrating multiple parameters and identifying complex nonlinear relationships [103].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for iPSC-Based Pharmacological Validation
| Category | Specific Reagents/Solutions | Function in Validation | Example Applications |
|---|---|---|---|
| Reprogramming Tools | Sendai viral vectors, episomal plasmids | Non-integrating iPSC generation | Patient-specific line creation |
| Neural Differentiation Kits | Commercial dopaminergic neuron kits | Standardized neural differentiation | Parkinson's disease modeling |
| Phenotypic Assays | Amyloid-β ELISA kits, calcium imaging dyes | Quantitative phenotype measurement | Alzheimer's therapeutic screening |
| Reference Compounds | Donepezil, L-DOPA, clinical failures | Establishing response benchmarks | Model validation controls |
| Cell Culture Platforms | 3D organoid matrices, microfluidic devices | Complex tissue modeling | Neuroinflammation studies |
Source: Compiled from multiple sources on iPSC methodologies [86] [97] [101]
Signaling Pathways and Experimental Workflows
Case Studies in Pharmacological Validation
Alzheimer's Disease Models and Anti-Amyloid Therapeutics
iPSC-derived models of Alzheimer's disease have been pharmacologically validated using clinical trial data from anti-amyloid therapies. Models incorporating presenilin mutations associated with familial AD consistently demonstrate elevated Aβ42/Aβ40 ratios, which can be normalized by γ-secretase inhibitors and modulators [96]. However, the clinical failure of multiple γ-secretase inhibitors due to toxicity and lack of efficacy has prompted refinement of these models to include additional endpoints beyond amyloid processing. More comprehensive models now incorporate tau pathology, axonal transport deficits, endosomal dysfunction, and neuroinflammatory responses to better predict clinical outcomes [96].
The recent conditional approval of anti-amyloid immunotherapies provides additional validation data for iPSC models. Models that successfully predicted the differential efficacy of these therapies demonstrated not only reduction of amyloid pathology but also effects on microglial activation and synaptic protection. These case studies highlight the importance of incorporating multiple cell types, particularly microglia and astrocytes, into pharmacological validation paradigms, as their responses to immunotherapies significantly influence clinical outcomes [97] [96].
Parkinson's Disease and Dopaminergic Cell Therapy
Parkinson's disease represents a compelling case study in pharmacological validation, particularly for cell replacement therapies. iPSC-derived dopaminergic neurons have been extensively characterized in preclinical models and are now advancing to clinical trials [101]. The validation process for these cells incorporates functional endpoints such as dopamine release, electrophysiological activity, integration into host circuitry, and long-term survival without tumor formation. Clinical outcomes from early trials provide critical data for refining differentiation protocols and potency assays.
For small molecule therapeutics, iPSC-based Parkinson's models have been validated using drugs with well-established clinical profiles such as L-DOPA and dopamine agonists. These models successfully recapitulate expected responses while also identifying potential mechanisms underlying treatment complications such as L-DOPA-induced dyskinesias. The ability to model both therapeutic benefits and adverse effects enhances the predictive validity of these systems for evaluating novel compounds [86] [101].
Future Directions and Implementation Challenges
Advancing Model Complexity and Standardization
Future improvements in pharmacological validation will require increasingly complex iPSC-based models that better capture the multicellular environment of the human brain. The development of assembloids—fused organoids containing multiple brain regions—enables modeling of circuit-level dysfunction in neurodegenerative diseases. Similarly, the incorporation of blood-brain barrier models allows for more accurate prediction of CNS penetrance and distribution. As these complex models evolve, pharmacological validation must adapt to address their additional layers of complexity while maintaining reproducibility and scalability for drug screening [97].
Standardization remains a significant challenge in iPSC-based pharmacological validation. Sources of variability include genetic background differences, epigenetic memory from source cells, differentiation efficiency, and batch effects. Addressing these requires implementation of robust quality control measures, standardized operating procedures, and reference standards for assay performance. Computational approaches for batch effect correction and data normalization can further enhance reproducibility and predictive accuracy [98] [1].
Integration with Emerging Technologies
The integration of iPSC-based models with emerging technologies represents a promising direction for enhancing pharmacological validation. Machine learning algorithms can identify complex patterns in multidimensional response data that predict clinical outcomes, as demonstrated by recent approaches predicting neurodegenerative disease incidence in diabetic patients with AUC values exceeding 0.8 [102]. High-content imaging combined with computer vision approaches enables quantification of subtle morphological changes that may serve as early predictors of therapeutic efficacy.
Genome editing technologies, particularly CRISPR-Cas9 systems, facilitate the introduction of specific disease-associated mutations into control iPSC lines, enabling precise dissection of genotype-phenotype relationships and their modulation by therapeutic interventions. Similarly, reporter lines with labeled disease-relevant proteins (e.g., tau, α-synuclein) enable real-time tracking of pathological processes in response to compound treatment. These technological advances, when coupled with rigorous pharmacological validation against clinical trial data, promise to significantly improve the predictive accuracy of iPSC-based neurodegenerative disease models [1] [96].
Pharmacological validation using clinical trial outcomes provides an essential framework for establishing the predictive accuracy of patient-specific iPSC models in neurodegenerative disease research. As the technology evolves toward more complex multicellular systems and integrates with advanced computational approaches, these validated models offer unprecedented opportunities to de-risk drug development and identify more effective therapeutics for devastating conditions like Alzheimer's and Parkinson's diseases. The ongoing refinement of validation methodologies will further strengthen the translational bridge between iPSC-based screening platforms and clinical success, ultimately accelerating the delivery of effective treatments to patients.
Identifying and Modeling Epigenetic Drivers of Sporadic Neurodegeneration
Sporadic neurodegenerative diseases (NDDs), which constitute the vast majority of cases for conditions like Alzheimer's disease (AD) and Parkinson's disease (PD), arise from a complex interplay between genetic risk factors and environmental exposures. Epigenetic mechanisms serve as the critical interface decoding these interactions, orchestrating long-term changes in gene expression without altering the DNA sequence. The integration of patient-specific induced pluripotent stem cells (iPSCs) provides a revolutionary platform for modeling this sporadic pathogenesis. This whitepaper offers a technical guide for researchers and drug development professionals, detailing the methodologies for using iPSC-derived neural models to identify and characterize aberrant epigenetic marks—including DNA methylation, histone modifications, and non-coding RNAs—in sporadic NDDs. It further outlines experimental protocols for quantifying these changes, modeling their functional consequences, and exploiting them for high-throughput drug screening, thereby paving the way for personalized epigenetic therapies.
Neurodegenerative diseases are a pressing global health concern, with sporadic cases representing 90-95% of all instances of AD, PD, and amyotrophic lateral sclerosis (ALS) [104] [25]. Unlike familial forms, sporadic NDDs lack a clear Mendelian inheritance pattern and are believed to result from sustained neuronal dysfunction due to aging, superimposed by complex interactions between polygenic risk factors and environmental influences such as toxins, pesticides, and air pollutants [104]. The epigenome is particularly vulnerable to these environmental influences, with changes in gene expression persisting over many years and influencing functional processes and mechanisms [104].
Epigenetics refers to heritable yet reversible modifications to gene expression that occur without altering the underlying DNA sequence. The three primary epigenetic mechanisms are:
- DNA methylation: The addition of a methyl group to cytosine residues, typically leading to gene silencing.
- Histone modifications: Post-translational changes, such as acetylation and methylation, that alter chromatin structure and gene accessibility.
- Non-coding RNAs: RNA molecules that regulate gene expression post-transcriptionally.
In healthy neurons, these mechanisms ensure precise expression of genes necessary for synaptic activity, plasticity, and cellular homeostasis [104]. However, disruptions to these processes—epigenetic dysregulation—are increasingly linked to NDD pathogenesis, contributing to neuronal dysfunction and degeneration by repressing neuroprotective genes and activating deleterious pathways [104]. The reversible nature of these epigenetic alterations presents a promising therapeutic window for countering neurodegenerative processes.
iPSCs as a Platform for Epigenetic Research
The inaccessibility of living human neurons has long been a major challenge in neurodegeneration research. Patient-specific iPSCs overcome this barrier by providing a limitless source of disease-relevant neural cell types with the patient's complete genetic background [25] [1].
Generation of Patient-Specific iPSCs
iPSCs are generated by reprogramming adult somatic cells (e.g., dermal fibroblasts or blood cells) back to a pluripotent state. This process involves the reintroduction of specific transcription factors, most commonly the Yamanaka factors (OSKM: Oct4, Sox2, Klf4, and Myc) [1]. The reprogramming process itself entails profound remodeling of the chromatin structure and the epigenome, erasing somatic cell signatures and re-establishing a pluripotent state [1].
Key Advantages for Modeling Sporadic NDDs
- Patient-specificity: iPSC-derived neurons and glia retain the individual's unique genetic and epigenetic predispositions, allowing for the study of sporadic cases in a human context [1] [105].
- Disease-relevant cell types: Protocols exist for differentiating iPSCs into various neural cell types affected in NDDs, including dopaminergic neurons for PD, cortical neurons for AD, and motor neurons for ALS [25].
- Modeling environmental influence: The inherent epigenetic memory of iPSCs and the ability to expose differentiated cells to environmental toxins (e.g., pesticides, heavy metals) allow for the modeling of gene-environment interactions implicated in sporadic NDDs [104] [25].
Technical Guide: Profiling Epigenetic Modifications in iPSC-Derived Models
A robust, multi-optic approach is required to comprehensively profile the epigenetic landscape of iPSC-derived neural models.
Workflow for Epigenomic Analysis
The following workflow outlines the key steps from sample preparation to data integration, applicable to both bulk and single-cell analyses.
Core Methodologies and Protocols
Profiling DNA Methylation
DNA methylation is a key regulatory mechanism in the brain, with roles in memory consolidation and synaptic plasticity [104]. Aberrant patterns are observed in both AD and PD.
- Recommended Technique: Whole-genome bisulfite sequencing (WGBS). This is the gold standard for unbiased, base-resolution detection of 5-methylcytosine (5mC) across the entire genome.
- Alternative for large cohorts: Infinium HumanMethylation BeadArray. This array-based technology provides a cost-effective solution for profiling methylation at pre-defined CpG sites and is suitable for studies with many samples [106].
- Protocol Summary:
- DNA Extraction: Use a phenol-chloroform or column-based method to extract high-quality, high-molecular-weight DNA from iPSC-derived neurons.
- Bisulfite Conversion: Treat DNA with sodium bisulfite, which deaminates unmethylated cytosines to uracils, while methylated cytosines remain unchanged.
- Library Preparation & Sequencing: Prepare sequencing libraries from the converted DNA and sequence on a high-throughput platform (e.g., Illumina).
- Bioinformatic Analysis: Align sequences to a bisulfite-converted reference genome. Calculate methylation levels as the proportion of reads reporting a cytosine (vs. thymine) at each CpG site. Differentially methylated regions (DMRs) can be identified using tools like
methylKitorDSS.
Mapping Histone Modifications
Histone modifications, such as acetylation and methylation, regulate chromatin accessibility. Decreased histone acetylation, for instance, is associated with the silencing of neuroprotective genes [104].
- Recommended Technique: Chromatin Immunoprecipitation followed by sequencing (ChIP-seq). This method allows for genome-wide mapping of histone marks or transcription factor binding sites.
- Protocol Summary:
- Cross-linking & Fragmentation: Cross-link proteins to DNA in living cells using formaldehyde. Lyse cells and fragment chromatin by sonication to ~200-500 bp.
- Immunoprecipitation: Incubate chromatin with a specific antibody against the histone mark of interest (e.g., H3K27ac for active enhancers, H3K4me3 for active promoters). Capture the antibody-chromatin complex.
- Library Preparation & Sequencing: Reverse cross-links, purify DNA, and prepare sequencing libraries.
- Bioinformatic Analysis: Align sequences to the reference genome. Call peaks (enriched regions) using tools like
MACS2. Integrate with RNA-seq data to correlate histone marks with gene expression changes.
Assessing Chromatin Accessibility
- Recommended Technique: Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq). This technique identifies open, accessible chromatin regions by using a hyperactive Tn5 transposase to insert sequencing adapters.
- Protocol Summary: The key advantage is its simplicity and low cell number requirement, making it suitable for iPSC-derived cultures.
- Nuclei Isolation: Isolate nuclei from iPSC-derived neurons.
- Tagmentation: Incubate nuclei with the Tn5 transposase, which simultaneously fragments accessible DNA and adds adapter sequences.
- Library Preparation & Sequencing: Purify the tagged DNA and amplify by PCR to create the sequencing library.
- Bioinformatic Analysis: Align sequences and call peaks to identify regions of significant openness. Tools like
MACS2are also used for ATAC-seq peak calling.
Data Analysis Workflow
The generic workflow for quantitative omics data analysis involves several critical steps to ensure robust and interpretable results [106].
- Quality Control (QC1): Assess raw data quality. For sequencing, use
FastQC; for arrays, use packages likearrayQualityMetrics. - Data Type-Specific Processing: For sequencing, trim adapters and align reads to a reference genome. For arrays, perform background correction.
- Data Summarization: Summarize data to features of interest (e.g., reads per gene for RNA-seq, methylation beta-values per CpG site).
- Normalization: Remove technical variation between samples to make them comparable. Methods like
DESeq2for RNA-seq orBMIQfor methylation arrays are commonly used. - Quality Control (QC2): Post-normalization QC to identify outliers or batch effects, often using Principal Component Analysis (PCA).
- Hypothesis Testing: Identify statistically significant features (e.g., differentially expressed genes, DMRs) using moderated statistical tests (e.g., in
limmaorDESeq2packages). - Multiple Testing Correction: Correct P-values for the thousands of tests performed using False Discovery Rate (FDR) methods (e.g., Benjamini-Hochberg).
The Scientist's Toolkit: Research Reagent Solutions
The table below details essential reagents and tools for conducting epigenetic research using iPSC models of neurodegeneration.
Table 1: Key Research Reagents and Resources for iPSC-based Epigenetic Studies
| Item/Category | Function/Application | Examples & Notes |
|---|---|---|
| Reprogramming Kits | Generation of iPSCs from patient somatic cells. | Non-integrating episomal vectors or Sendai virus kits (e.g., CytoTune-iPS) to minimize genomic alteration. |
| Neural Differentiation Kits | Directed differentiation of iPSCs into specific neural lineages. | Commercially available kits for dopaminergic neurons (PD model), cortical neurons (AD model), or motor neurons (ALS model). |
| Reference iPSC Lines | Genetically stable control lines to minimize experimental variability. | KOLF2.1J (JAX) [27] or other widely characterized control lines. |
| HDAC Inhibitors | Small molecule tools to reverse histone deacetylation, a common epigenetic aberration in NDDs. | Sodium butyrate, Trichostatin A, Vorinostat (SAHA). Used for proof-of-concept therapeutic experiments [104]. |
| DNMT Inhibitors | Small molecules to reverse hypermethylation and reactivate silenced genes. | 5-Azacytidine, Decitabine. Useful for probing the functional role of specific methylation events [104]. |
| Antibodies for ChIP-seq | Immunoprecipitation of specific histone modifications for genome-wide mapping. | Validated antibodies for H3K27ac (active enhancers), H3K4me3 (active promoters), H3K9me3 (heterochromatin). |
| Bisulfite Conversion Kits | Critical sample preparation step for DNA methylation analysis. | Kits from Zymo Research or Qiagen that ensure high and efficient conversion rates for WGBS or arrays. |
| Toxins for Modeling | Induce epigenetic dysregulation and sporadic disease phenotypes in iPSC-derived cultures. | Dieldrin (pesticide linked to PD risk [104]), heavy metals (e.g., lead, mercury), or air pollutant components. |
Quantitative Data from Epigenetic Studies in Neurodegeneration
Epigenetic profiling studies consistently reveal quantifiable alterations in iPSC-derived models and post-mortem brains of NDD patients.
Table 2: Summary of Key Epigenetic Alterations in Neurodegenerative Diseases
| Disease | Epigenetic Change | Genomic Locus / Gene | Quantitative Change & Functional Outcome | Model System |
|---|---|---|---|---|
| Alzheimer's Disease (AD) | DNA Hypermethylation | SORBS3 | ~20-30% increased methylation in cortical neurons, associated with synaptic deficits [104]. | Post-mortem brain / iPSC-derived neurons. |
| Alzheimer's Disease (AD) | Histone Hypoacetylation | BDNF | Global reduction of H3K9ac and H4K12ac; linked to impaired learning and memory [104]. | Animal models / Cell culture. |
| Parkinson's Disease (PD) | DNA Hypermethylation | SNCA | Increased methylation in intron 1, potentially repressing alpha-synuclein overexpression, though findings are complex [104]. | Post-mortem substantia nigra / Toxin models. |
| Parkinson's Disease (PD) | Dysregulated microRNA | Multiple | e.g., miR-34b/c is downregulated, leading to mitochondrial dysfunction and oxidative stress [104]. | iPSC-derived dopaminergic neurons / PD patient biofluids. |
| Huntington's Disease (HD) | Histone H3 Hypoacetylation | BDNF | Specific loss of H3K9/K14 acetylation at the BDNF promoter, reducing its transcription and contributing to striatal vulnerability [25]. | HD mouse models / Patient-derived cells. |
Therapeutic Applications and Drug Discovery
The reversible nature of epigenetic marks and the predictive power of iPSC models open two primary therapeutic avenues.
Epigenetic Modulators as Therapeutics
Histone deacetylase (HDAC) inhibitors and DNA methyltransferase (DNMT) inhibitors have shown promise in preclinical models.
- Mechanism: HDAC inhibitors increase histone acetylation, promoting a more open chromatin state and reactivating silenced neuroprotective genes. DNMT inhibitors reverse hypermethylation to achieve a similar outcome [104].
- Evidence: In toxin-induced models of NDDs, these inhibitors have demonstrated restoration of normal gene expression, improvement of neuronal function, and reduction in pathological markers [104]. Encouragingly, HDAC inhibitors have shown improvements in cognition and memory in clinical trials for Alzheimer's disease [104].
iPSC-based Drug Screening Platforms
Patient-specific iPSC-derived neurons are being used for high-throughput screening of compound libraries.
- Process: iPSCs from sporadic AD or PD patients are differentiated into relevant neural cell types. These are cultured in high-density plates and exposed to thousands of small molecules. Readouts can include epigenetic markers (e.g., H3 acetylation via immunofluorescence), cell survival, and disease-related phenotypes (e.g., amyloid-beta or phosphorylated tau levels) [8] [1].
- Outcomes: This approach has already led to the identification of candidate drugs and their progression into clinical trials. For example, iPSC-based screening has contributed to trials of bosutinib, ropinirole, and ezogabine for ALS [8] [7]. The integration of artificial intelligence (AI) is further enhancing the analysis of the complex, high-dimensional data generated from these screens [8].
The convergence of epigenetics and iPSC technology provides an unprecedented, patient-specific framework for deconstructing the multifaceted pathology of sporadic neurodegenerative diseases. By employing the detailed methodologies for epigenetic profiling and functional validation outlined in this guide, researchers can systematically identify disease-driving epigenetic alterations, elucidate their functional consequences, and validate them as therapeutic targets. The future of neurodegeneration research lies in leveraging these human-relevant models to develop personalized epigenetic therapies that can halt or reverse the devastating progression of diseases like Alzheimer's and Parkinson's.
Conclusion
Patient-specific iPSCs have unequivocally matured into a powerful, clinically predictive platform for neurodegenerative disease research. By providing a genetically faithful, human-relevant system, they bridge critical gaps left by traditional animal models. Success hinges on robust methodological execution, from standardized differentiation and sophisticated 3D modeling to stringent quality control. The demonstrated ability of these models to recapitulate patient-specific disease phenotypes and accurately reflect clinical drug responses, as seen in large-scale ALS studies, underscores their transformative potential. Future progress will be driven by the integration of advanced gene editing, multi-omics profiling, and machine learning to fully decode disease mechanisms. Ultimately, the strategic application of patient-specific iPSC technology promises to de-risk drug development, usher in an era of personalized neurology, and deliver much-needed effective therapies for these devastating disorders.
References
- 1. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 2. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 3. Advances in induced pluripotent stem cell-based in vitro ... [https://www.pfmjournal.org/journal/view.php?number=169]
- 4. Current advances and future prospects of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1546423/full]
- 5. Cell reprogramming: methods, mechanisms and applications [https://cellregeneration.springeropen.com/articles/10.1186/s13619-025-00229-x]
- 6. Chemical reprogramming of human blood cells to ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925002607]
- 7. Drug discovery research with the iPSC models of ... [https://pubmed.ncbi.nlm.nih.gov/41213329/]
- 8. Drug discovery research with the iPSC models of ... [https://www.sciencedirect.com/science/article/pii/S0168010225001683]
- 9. Chemically induced reprogramming to reverse cellular aging [https://www.aging-us.com/article/204896/text]
- 10. Contrast Checker [https://webaim.org/resources/contrastchecker/]
- 11. Induced Pluripotent Stem Cells: Problems and Advantages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3347549/]
- 12. A comparison of non-integrating reprogramming methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC4329913/]
- 13. A Comparative View on Easy to Deploy non-Integrating ... [https://link.springer.com/article/10.1007/s12015-015-9619-3]
- 14. Advantages & Disadvantages of Induced Pluripotent Stem ... [https://bioinformant.com/induced-pluripotent-stem-cell-ipsc-market/]
- 15. Effects of Integrating and Non-Integrating Reprogramming ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0131128]
- 16. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 17. Development of patient-specific iPSC-based epilepsy ... [https://pubmed.ncbi.nlm.nih.gov/40600194/]
- 18. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 19. Current Development of iPSC-Based Modeling in ... [https://www.mdpi.com/1422-0067/26/8/3774]
- 20. iPSC for modeling neurodegenerative disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7770414/]
- 21. Modeling ALS with Patient-Derived iPSCs [https://www.mdpi.com/2076-3425/15/2/134]
- 22. of Acquisition by combination of BMP blockade and... neural fate [https://pmc.ncbi.nlm.nih.gov/articles/PMC10522999/]
- 23. Variable Outcomes in Neural Differentiation of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7296348/]
- 24. Acquisition of neural fate by combination of BMP blockade ... [https://www.sciencedirect.com/science/article/pii/S2589004223019648]
- 25. Epigenetic Research of Neurodegenerative Disorders Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4677257/]
- 26. Stem Cell Clinical Trials and Promise of Engineered Exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409071/]
- 27. Reprogramming biology: iPSCs and the future of predictive ... [https://www.jax.org/news-and-insights/2025/november/reprogramming-biology-ipscs-and-the-future-of-predictive-research]
- 28. Transforming Neurodegenerative Disease Research With ... [https://www.cellandgene.com/doc/transforming-neurodegenerative-disease-research-with-ipscs-a-path-to-innovation-and-therapeutic-breakthroughs-0001]
- 29. Human iPSC-derived glia models for the study of ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02919-2]
- 30. Evaluation of induced pluripotent stem cell differentiation ... [https://www.sciencedirect.com/science/article/abs/pii/S1389172324002792]
- 31. Astrocyte induction of disease-associated microglia is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12282607/]
- 32. Human pluripotent stem cell (hPSC)-derived microglia for ... [https://www.sciencedirect.com/science/article/pii/S2667242124000290]
- 33. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 34. Navigating Brain Organoid Maturation: From Benchmarking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383812/]
- 35. Patient-Specific iPSCs-Based Models of Neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8776084/]
- 36. Emerging brain organoids: 3D models to decipher, identify ... [https://www.sciencedirect.com/science/article/pii/S2452199X25000258]
- 37. Quantitative profiling of human brain organoid cell diversity ... [https://www.sciencedirect.com/science/article/pii/S2211124725009398]
- 38. Building Immunocompetent Cerebral Organoids From a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436987/]
- 39. Review article Neurodegenerative disorders: Mechanisms ... [https://www.sciencedirect.com/science/article/pii/S1568163724001752]
- 40. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291668/]
- 41. Generation of an isogenic iPSC line via CRISPR correction ... [https://pubmed.ncbi.nlm.nih.gov/40752254/]
- 42. Generation of an isogenic iPSC line via CRISPR correction ... [https://www.sciencedirect.com/science/article/pii/S1873506125001369]
- 43. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 44. How to Pick the Best CRISPR Data Analysis Method for ... [https://www.synthego.com/guide/how-to-use-crispr/analysis-methods/]
- 45. CRISPR-Cas9: bridging the gap between aging ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1681891/full]
- 46. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 47. Editorial: Studying rare diseases using induced pluripotent ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/full]
- 48. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 49. 072 An iPSC-derived neurotoxicity screening platform ... [https://www.sciencedirect.com/science/article/pii/S1056871925000851]
- 50. A new frontier in toxicity testing by evaluating drug-induced ... [https://pubmed.ncbi.nlm.nih.gov/40482844/]
- 51. How Human iPSCs are Revolutionizing Drug Discovery in ... [https://bioinformant.com/ipsc-drug-discovery/]
- 52. Addressing variability in iPSC-derived models of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6994963/]
- 53. Assess and Maintain Human Pluripotent Stem Cell Quality [https://www.stemcell.com/psc-cell-quality]
- 54. Quality Control: What is really in your hiPSC culture? [https://www.reprocell.com/blog/key-quality-controls-of-human-induced-pluripotent-stem-cells]
- 55. Method for evaluation of human induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5668125/]
- 56. Fully defined NGN2 neuron protocol reveals diverse signatures of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11440061/]
- 57. Simple and efficient differentiation of human iPSCs into ... [https://www.nature.com/articles/s41598-023-34445-9]
- 58. Patient and Disease–Specific Induced Pluripotent Stem Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6934989/]
- 59. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 60. Stem cells therapy in neurodegenerative and ... [https://www.sciencedirect.com/science/article/pii/S1043661825003858]
- 61. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 62. Induced Pluripotent Stem Cell (iPSC) Therapy Market Size, ... [https://www.precedenceresearch.com/induced-pluripotent-stem-cell-therapy-market]
- 63. Induced Pluripotent Stem Cells Market Report 2025–2033 [https://syg.ma/@renubresearch/induced-pluripotent-stem-cells-market-report-2025-2033-cell-type-country?comments=all]
- 64. Automated manufacturing of cell therapies [https://www.sciencedirect.com/science/article/pii/S0168365925001701]
- 65. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 66. Current Development of iPSC-Based Modeling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027653/]
- 67. Opportunities and challenges for the use of induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6367134/]
- 68. 5 Effective Solutions to Reduce Supply Chain Variability [https://demanddriventech.com/blog/reduce-supply-chain-variability]
- 69. Variability in supply chains adds to uncertainty [https://www.learnaboutlogistics.com/variability-in-supply-chains-adds-to-uncertainty/]
- 70. Mastering Consistency and Quality in iPSC-Derived Cell ... [https://www.ncardia.com/webinar-registration-mastering-consistency-and-quality-in-ipsc-derived-cell-manufacturing]
- 71. Supply Chain Variability: what it is, why it's bad & ... [https://www.linkedin.com/pulse/supply-chain-variability-what-why-its-bad-how-can-minimised-eagle-xmq5e]
- 72. Advances and challenges in modeling inherited peripheral ... [https://www.nature.com/articles/s12276-024-01250-x]
- 73. Human‐Induced Pluripotent Stem Cell Culture Methods Under ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7507179/]
- 74. A functional hiPSC-cortical neuron differentiation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8758945/]
- 75. Protein aggregation in neurodegenerative diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574514/]
- 76. Current Understanding of Protein Aggregation in ... [https://www.mdpi.com/1422-0067/26/21/10568]
- 77. Advances in Induced Pluripotent Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/41179113/]
- 78. Editorial: Cell death mechanisms in neurodegenerative ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1694173/full]
- 79. Editorial: Cell death mechanisms in neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547129/]
- 80. Unravelling neuronal death mechanisms: The role of ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725002296]
- 81. Dynamic functional connectivity and transcriptomic ... [https://pubmed.ncbi.nlm.nih.gov/41239516/]
- 82. Spatial transcriptomics of progression gene signature and ... [https://www.sciencedirect.com/science/article/pii/S2473952925001934]
- 83. Discovery of Disease Relationships via Transcriptomic ... [https://arxiv.org/html/2508.04742v1]
- 84. Animal Models of Neurodegenerative Disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9063566/]
- 85. Prospects of Directly Reprogrammed Adult Human ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.546484/full]
- 86. iPSCs in Neurodegenerative Disorders: A Unique Platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9500601/]
- 87. Transition from Animal-Based to Human Induced ... [https://www.mdpi.com/2073-4409/12/4/538]
- 88. Quantitative comparison of the mRNA content of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7876496/]
- 89. Benchmarking in vitro, in vivo, ex vivo, and xenografting ... [https://www.sciencedirect.com/science/article/pii/S2213671124001462]
- 90. iPSC-based Platforms Market 2025 Report and Trends [https://www.towardshealthcare.com/insights/ipsc-based-platforms-market-sizing]
- 91. Population-scale single-cell RNA-seq profiling across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7610897/]
- 92. Single-cell RNA-sequencing of differentiating iPS ... [https://www.nature.com/articles/s41467-020-14457-z]
- 93. Induced pluripotent stem cells: The advantages, ... [https://www.clinicaltrialsarena.com/sponsored/induced-pluripotent-stem-cells-the-advantages-challenges-and-advances/]
- 94. Single-cell RNA-seq of human induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6028138/]
- 95. Population-scale proteome variation in human induced ... [https://elifesciences.org/articles/57390]
- 96. Modeling Alzheimer's disease with iPSC-derived brain cells [https://www.nature.com/articles/s41380-019-0468-3]
- 97. Induced pluripotent stem cells in disease modelling and drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584039/]
- 98. Review of the Current Trends in Clinical Trials Involving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8445612/]
- 99. Introduction - Assuring Data Quality and Validity in Clinical ... [https://www.ncbi.nlm.nih.gov/books/NBK224582/]
- 100. Data Validation in Clinical Data Management [https://www.quanticate.com/blog/data-validation-in-clinical-data-management]
- 101. iPSC-based cell replacement therapy: from basic research ... [https://www.sciencedirect.com/science/article/pii/S1465324925000532]
- 102. Machine Learning–Based Prediction of Neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11487204/]
- 103. An integrated predictive model for Alzheimer's disease ... [https://www.nature.com/articles/s41598-025-13478-2]
- 104. Reversing Epigenetic Dysregulation in Neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12112518/]
- 105. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 106. Quantitative transcriptomic and epigenomic data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10997052/]