Precision Immunomodulation: Decoding Patient-Specific Stem Cell Mechanisms for Clinical Translation
This article synthesizes current research on the intricate mechanisms by which stem cells, particularly mesenchymal stem cells (MSCs), modulate the immune system in a patient-specific manner.
Precision Immunomodulation: Decoding Patient-Specific Stem Cell Mechanisms for Clinical Translation
Abstract
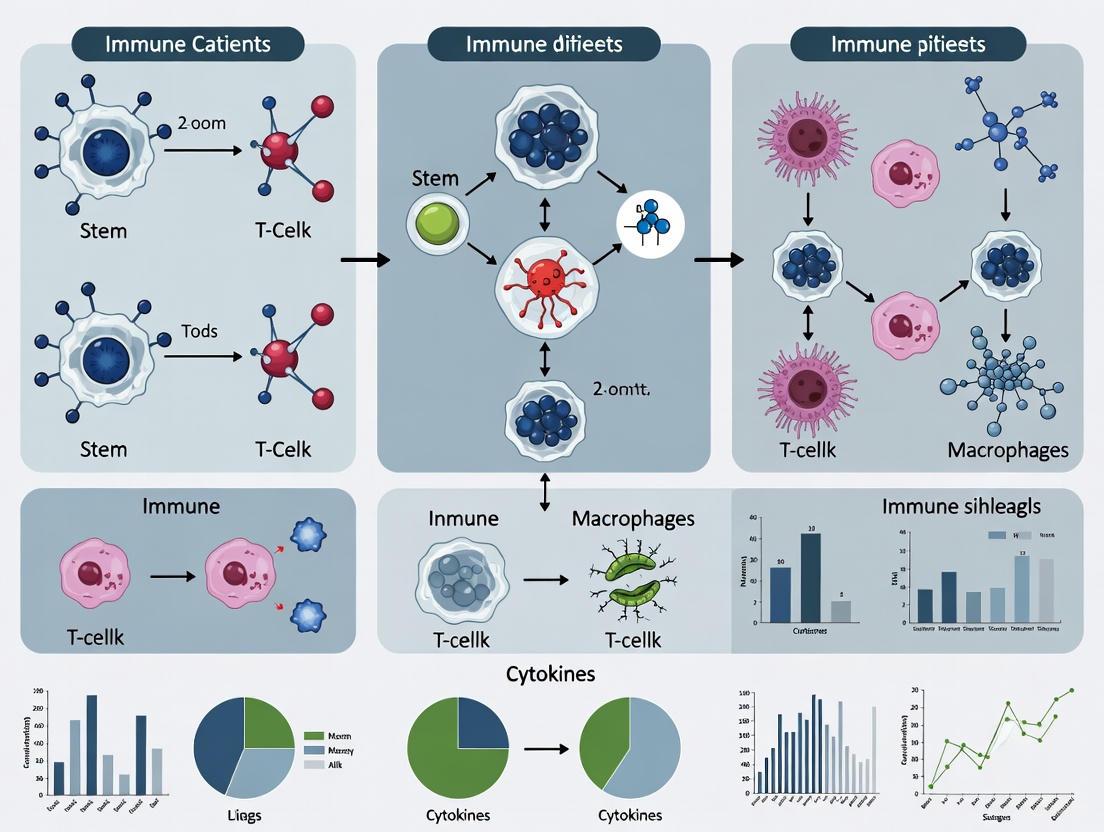
This article synthesizes current research on the intricate mechanisms by which stem cells, particularly mesenchymal stem cells (MSCs), modulate the immune system in a patient-specific manner. It explores the foundational biology of stem cell-immune interactions, advanced methodologies for profiling heterogeneous cell populations, strategies to overcome clinical challenges like immune rejection, and the validation of these approaches through contemporary clinical trials and regulatory milestones. Aimed at researchers and drug development professionals, this review provides a comprehensive framework for developing personalized regenerative therapies by addressing the critical sources of inter-patient variability that impact therapeutic efficacy and safety.
Core Mechanisms: How Stem Cells Intrinsically Modulate the Immune Landscape
The immunomodulatory prowess of mesenchymal stem cells (MSCs) is not merely a function of direct cellular contact but is predominantly mediated through a sophisticated paracrine apparatus. This system comprises soluble factors and exosomal cargo, which collaboratively recalibrate the immune landscape in pathological conditions. The core mediators—Transforming Growth Factor-Beta (TGF-β), Prostaglandin E2 (PGE2), Indoleamine 2,3-Dioxygenase (IDO), and an array of regulatory microRNAs (miRNAs)—orchestrate a shift from pro-inflammatory to anti-inflammatory and tolerogenic immune states. This whitepaper delineates the mechanistic roles, signaling pathways, and experimental methodologies for investigating these key players, providing a technical framework for researchers and drug development professionals engaged in developing patient-specific stem cell-based immunomodulatory strategies.
MSCs exert their therapeutic effects primarily through paracrine activity, secreting a multitude of bioactive molecules that modulate innate and adaptive immune responses [1] [2]. The immunomodulatory functions of MSCs are not constitutive but are potently enhanced by a process of "licensing" or "priming," where exposure to an inflammatory microenvironment, particularly cytokines like interferon-gamma (IFN-γ), triggers the upregulation of key immunosuppressive factors [3] [4]. Among these, TGF-β, PGE2, and IDO form a triad of critical soluble mediators, while MSC-derived exosomes serve as vital nanocarriers for regulatory miRNAs and proteins, enabling targeted intercellular communication and amplification of immunosuppressive signals [5] [6] [2]. This cell-free approach, utilizing exosomes, mitigates risks associated with whole-cell transplantation, such as lung entrapment and immune rejection, presenting a promising therapeutic avenue [3] [4].
In-Depth Analysis of Key Soluble Mediators
Transforming Growth Factor-Beta (TGF-β)
Mechanism of Action: TGF-β is a pivotal cytokine secreted by MSCs that plays a central role in immune regulation and the induction of tolerance. Its primary mechanism involves the TGF-β/Smad signaling pathway. TGF-β binds to its receptor TGF-βRII, which then recruits and phosphorylates TGF-βRI, forming a heterotetrameric complex. This activation triggers the phosphorylation of receptor-regulated Smads (R-Smads), specifically Smad2 and Smad3. The phosphorylated Smad2/3 forms a complex with the common mediator Smad4, which translocates to the nucleus to regulate the transcription of target genes involved in immune suppression and tissue repair [1] [7]. A key function of this pathway in immunomodulation is the induction and expansion of regulatory T cells (Tregs), which are critical for maintaining immune homeostasis and suppressing aberrant immune responses [1] [6].
Experimental Evidence: Preclinical studies demonstrate that TGF-β secretion by MSCs is instrumental in restoring the Treg/Th2 balance in allergic rhinitis models and contributes to immune regulation in Crohn's disease [1] [7]. Furthermore, the licensing of MSCs with TGF-β1 enhances their immunomodulatory potency, leading to improved outcomes in experimental models [4].
Diagram 1: The TGF-β/Smad Signaling Pathway. This pathway illustrates the key steps from ligand binding to gene regulation, culminating in the induction of regulatory T cells.
Prostaglandin E2 (PGE2)
Mechanism of Action: PGE2 is a lipid-soluble mediator synthesized by MSCs in response to inflammatory cues. It exerts broad immunomodulatory effects by suppressing the proliferation and function of several immune cells, including T lymphocytes, natural killer (NK) cells, and antigen-presenting cells like dendritic cells (DCs) [1] [5]. A crucial mechanism is its role in inhibiting the differentiation and priming of naive T cells into pro-inflammatory T helper 1 (Th1) and Th17 subsets, while simultaneously promoting the expansion of anti-inflammatory Tregs [1] [6]. PGE2 also acts synergistically with other mediators, such as IDO, to amplify the overall immunosuppressive microenvironment [5].
Experimental Evidence: Studies have shown that the co-culture of induced pluripotent stem cell-derived MSCs (iPSC-MSCs) with T cells from allergic rhinitis patients inhibits T cell proliferation through a mechanism involving cell-to-cell contact and PGE2 expression [1]. Furthermore, PGE2 is identified as a key soluble factor in MSC-conditioned media responsible for suppressing T cell receptor signaling [1].
Indoleamine 2,3-Dioxygenase (IDO)
Mechanism of Action: IDO is a heme-containing enzyme whose expression in MSCs is strongly induced by inflammatory cytokines, particularly IFN-γ [5] [4]. It catalyzes the first and rate-limiting step in the kynurenine pathway of tryptophan degradation. Immunosuppression is achieved through a dual mechanism:
- Tryptophan Depletion: Rapid depletion of the essential amino acid tryptophan in the local microenvironment starves proliferating T cells, leading to their cell cycle arrest in the G0/G1 phase and inhibition of clonal expansion [5] [6].
- Production of Kynurenines: The catabolic products of tryptophan degradation, known as kynurenines, are themselves biologically active and can induce apoptosis in activated T cells and contribute to the generation of Tregs [3].
Experimental Evidence: The critical role of IDO is highlighted in studies where MSC-derived exosomes licensed with IFN-γ increased levels of immunosuppressive IDO in co-cultures with peripheral blood mononuclear cells (PBMCs), correlating with reduced pro-inflammatory cytokines and improved outcomes in experimental autoimmune encephalomyelitis (EAE) models [3]. IDO is consistently listed among the most important soluble factors for MSC-mediated immunomodulation [5] [2].
Table 1: Key Soluble Mediators in MSC Immunomodulation
| Mediator | Chemical Nature | Primary Induction Signal | Key Immunomodulatory Mechanisms | Target Immune Cells |
|---|---|---|---|---|
| TGF-β | Cytokine | Inflammatory Microenvironment | Activates Smad pathway; induces Treg differentiation; suppresses T effector cells [1] [7]. | T cells, B cells, Macrophages, Dendritic Cells |
| PGE2 | Lipid Mediator (Prostaglandin) | Inflammatory Cytokines (e.g., IFN-γ) | Inhibits T cell, NK cell, and DC function; promotes Treg expansion; acts synergistically with IDO [1] [5]. | T cells, NK cells, Dendritic Cells |
| IDO | Enzyme | IFN-γ | Depletes local tryptophan; generates immunosuppressive kynurenines; induces T cell cycle arrest and apoptosis [5] [3]. | T cells |
The Role of MSC-Derived Exosomes and Regulatory miRNAs
Exosomes as Paracrine Effectors
MSC-derived exosomes are nano-sized extracellular vesicles (30-150 nm) that function as key paracrine effectors [2]. They are encapsulated by a lipid bilayer and carry a diverse cargo of proteins, lipids, mRNAs, and non-coding RNAs (including miRNAs) that reflect the biological state of their parent MSCs [8] [2]. Because of their nanoscale, they can easily bypass biological barriers, and as a cell-free product, they avoid the risks of immune rejection and tumor formation associated with whole-cell transplants [7] [3]. Their therapeutic potential can be enhanced by licensing the parent MSCs with cytokines like IFN-γ and TGF-β1, which enriches the exosomes with anti-inflammatory molecules [3] [4].
Key Regulatory miRNAs in Exosomal Cargo
Exosomal miRNAs are among the most significant cargoes responsible for mediating the immunomodulatory effects of MSCs. They function by being delivered to recipient immune cells and post-transcriptionally regulating the expression of target genes.
Table 2: Key Regulatory miRNAs in MSC-Derived Exosomes
| miRNA | Reported Function in Immunomodulation | Proposed Target/Pathway | Experimental Context |
|---|---|---|---|
| miR-146a-5p | Inhibits eosinophil activation and IgE production; downregulation promotes MSC senescence via TRAF6/NF-κB [1] [6]. | TRAF6, NF-κB signaling pathway | Allergic Rhinitis, Systemic Lupus Erythematosus (SLE) [1] [6] |
| miR-23a-3p | Promotes CD4+ T cell differentiation toward a regulatory phenotype (Treg) [6]. | TGF-β receptor 2 (post-transcriptional regulation) | In vitro T cell culture [6] |
| miR-223 | Can modulate inflammation by activating IL-32 cascade or regulating CX3CR1+ macrophage differentiation [7]. | IL-32, CX3CR1 | Inflammatory Bowel Disease (IBD) [7] |
| miR-21 | Highly enriched in exosomes during active IBD; modulates intestinal barrier and immune cell function [7]. | Not Specified in Search Results | Inflammatory Bowel Disease (IBD) [7] |
The following diagram summarizes the biogenesis of MSC-derived exosomes and their mechanism of action on a recipient immune cell.
Diagram 2: MSC-Derived Exosome Biogenesis and Mechanism. This workflow outlines the formation of exosomes from MSCs and their subsequent action on target immune cells to elicit an immunomodulatory response.
Experimental Protocols and Methodologies
Protocol for Licensing MSCs and Isoling Exosomes
This protocol is synthesized from recent research on enhancing the immunomodulatory potency of MSCs and their derived exosomes [3] [4].
Part A: Licensing of Human Bone Marrow-MSCs
- Cell Culture: Culture human bone marrow-MSCs in standard growth medium (e.g., α-MEM supplemented with 10% FBS and 1% penicillin/streptomycin) until passage 3-4.
- Cytokine Licensing: At ~90% confluency, wash cells twice with PBS and replace the medium with a serum-free or xeno-free licensing medium.
- Stimulation: Supplement the licensing medium with a combination of IFN-γ (50 ng/mL) and TGF-β1 (50 ng/mL).
- Incubation: Incubate the cells for 48-72 hours at 37°C with 5% CO₂.
- Collection: After the incubation period, collect the conditioned medium for exosome isolation. The licensed MSCs can also be harvested for direct cell therapy applications or molecular analysis.
Part B: Isolation of Exosomes from Conditioned Medium
- Pre-clearing: Centrifuge the conditioned medium at 2,000 × g for 20 minutes to remove dead cells and debris. Follow with a centrifugation at 10,000 × g for 30 minutes to remove larger vesicles and apoptotic bodies.
- Ultracentrifugation: Ultracentrifuge the supernatant at 100,000 × g for 70-120 minutes at 4°C to pellet the exosomes.
- Washing: Resuspend the pellet in a large volume of PBS and perform a second ultracentrifugation under the same conditions to wash the exosomes.
- Resuspension: Finally, resuspend the purified exosome pellet in a small volume of PBS or storage buffer.
- Characterization: Characterize the isolated exosomes using Nanoparticle Tracking Analysis (NTA) for size and concentration, Transmission Electron Microscopy (TEM) for morphology, and Western Blotting for exosomal markers (e.g., CD63, CD81, TSG101).
In Vitro Assay for Evaluating Immunomodulatory Efficacy
T Cell Proliferation Suppression Assay [3] [4]:
- PBMC Isolation: Isolate PBMCs from human peripheral blood using density gradient centrifugation (e.g., Ficoll-Paque).
- T Cell Activation: Activate the PBMCs using a mitogen like phytohemagglutinin (PHA) or anti-CD3/CD28 antibodies.
- Co-culture: Co-culture the activated PBMCs with varying concentrations of licensed MSC-derived exosomes (e.g., 10-100 μg/mL) for 3-5 days.
- Proliferation Measurement: Quantify T cell proliferation using methods such as:
- CFSE Dilution: Flow cytometry-based tracking of carboxyfluorescein succinimidyl ester (CFSE) dye dilution in dividing cells.
- ³H-Thymidine Incorporation: Measure the incorporation of radioactive thymidine into the DNA of proliferating cells.
- Flow Cytometry Analysis: Analyze the cells by flow cytometry to assess the induction of Tregs (CD4+CD25+FOXP3+). Advanced data analysis techniques like t-SNE can be employed for deep immune profiling [4].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Investigating MSC Mediators
| Reagent / Tool | Specific Example | Primary Function in Research |
|---|---|---|
| Licensing Cytokines | Recombinant Human IFN-γ, Recombinant Human TGF-β1 | To pre-condition MSCs to enhance the production of target mediators (IDO, PGE2, TGF-β) and enrich exosomal cargo [3] [4]. |
| Exosome Isolation Kits | Ultracentrifugation-based kits; Size-exclusion chromatography (SEC) kits; Precipitation kits | To isolate and purify exosomes from MSC-conditioned medium for functional studies and cargo analysis [2]. |
| Characterization Antibodies | Anti-CD63, Anti-CD81, Anti-TSG101 (for exosomes); Anti-CD73, CD90, CD105 (for MSCs) | To confirm the identity and purity of isolated exosomes and MSCs via Flow Cytometry or Western Blot [3] [4]. |
| Enzyme Activity Assays | IDO Activity Assay (e.g., via Tryptophan/Kynurenine measurement by HPLC) | To functionally quantify the activity of key immunomodulatory enzymes like IDO in MSC cultures or supernatants [3]. |
| Pathway Inhibitors | SB-431542 (TGF-βRI inhibitor); NS-398 (COX-2/PGE2 inhibitor); 1-MT (IDO inhibitor) | To mechanistically dissect the contribution of specific pathways (TGF-β, PGE2, IDO) in MSC-mediated immunomodulation [1]. |
| miRNA Analysis Tools | miRNA microarrays; Next-generation sequencing (NGS); qRT-PCR assays; miRNA mimics/inhibitors | To profile exosomal miRNA content and perform functional validation of candidate miRNAs (e.g., miR-146a, miR-23a) [6] [2]. |
The strategic manipulation of soluble mediators like TGF-β, PGE2, and IDO, along with the harnessed delivery power of exosomal miRNAs, represents the forefront of precision immunomodulation. The experimental frameworks and tools detailed in this whitepaper provide a roadmap for deconstructing the complex mechanisms of MSC function and translating these insights into reproducible, cell-free therapeutic products. Future research must prioritize the standardization of exosome production, rigorous functional characterization of cargo, and the development of targeted delivery systems to fully realize the potential of these biological nanotherapeutics in patient-specific treatment paradigms.
Within the broader thesis exploring mechanisms of stem cell immune modulation, direct cell-cell contact represents a fundamental paradigm. While the immunomodulatory capabilities of mesenchymal stem cells (MSCs) are exerted through both paracrine activity and direct cellular interactions, this guide focuses specifically on the latter mechanism [9]. MSCs participate in both innate and adaptive immunity through physical interactions with immune cells, including T cells, natural killer (NK) cells, and antigen-presenting cells (APCs) such as dendritic cells and macrophages [9]. These interactions are not merely adjuncts to soluble factor-mediated suppression but are essential for initiating and enhancing immunomodulatory effects, particularly in the context of treating inflammatory and autoimmune diseases [10]. The direct contact between MSCs and immune cells facilitates critical signaling events that regulate immune activation, tolerance, and homeostasis, making this mechanism a pivotal component of MSC-based therapeutic strategies for individual patient research and drug development.
Molecular Mechanisms of Direct Cellular Interactions
Interactions with T Lymphocytes
MSCs employ multiple surface molecules to modulate T-cell function through direct contact. These interactions primarily inhibit T-cell proliferation and alter cytokine profiles to promote an anti-inflammatory state.
Table 1: Key Molecular Interactions Between MSCs and T Cells
| MSC Surface Molecule | Immune Cell Receptor | Signaling Pathway | Functional Outcome |
|---|---|---|---|
| Programmed Death-Ligand 1 (PD-L1) [10] | Programmed Cell Death Protein 1 (PD-1) on T cells [10] | Recruitment of SHP-1/SHP-2 phosphatases; inhibition of TCR-mediated ZAP70/PKCθ phosphorylation; suppression of PI3K/AKT and MAPK/ERK pathways [10] | Suppression of T-cell activation; cell cycle arrest in G0/G1 phase [10] |
| Programmed Death-Ligand 2 (PD-L2) [10] | Cytotoxic T-Lymphocyte-Associated Protein 4 (CTLA-4) on T cells [10] | Competition with CD28 for binding to B7 molecules (CD80/CD86) on APCs [10] | Reduction of co-stimulatory signals required for T-cell activation [10] |
| Galectin-1 [9] | Not specified on T cells [9] | Not fully elucidated [9] | Inhibition of CD4+ and CD8+ T-cell proliferation [9] |
| Inducible Co-Stimulatory Ligand (ICOSL) [10] | Inducible Co-Stimulator (ICOS) on Tregs [10] | Activation of regulatory T cells (Tregs) [10] | Inhibition of Th2 cell activity [10] |
| Adhesion Molecules (ICAM-1, VCAM-1) [9] | Leukocyte integrins [9] | Facilitation of strong immunological synapse [9] | Critical for T-cell activation and recruitment; enables subsequent immunosuppression [9] |
| Notch1 [9] | Notch receptor on CD4+ T-cells [9] | Notch1/FOXP3 pathway activation [9] | Increase in CD4+CD25+FOXP3+ regulatory T-cell percentage [9] |
The functional consequences of these interactions are profound. Human placenta-derived MSCs (PMSCs) expressing high levels of PD-L1 and PD-L2 inhibit T-cell proliferation by arresting the cell cycle in the G0/G1 phase [9] [10]. Furthermore, the knockdown of Galectin-1 in MSCs results in a loss of immunomodulatory properties and restores the proliferation of CD4+ and CD8+ T-cells, underscoring its critical role [9]. MSCs also activate the Notch1/FOXP3 pathway in CD4+ T-cells, increasing the population of regulatory T-cells (Tregs), which are essential for maintaining immune tolerance [9].
Interactions with Natural Killer (NK) Cells
The crosstalk between MSCs and NK cells involves direct contact that modulates the cytotoxic activity of NK cells. Co-culture studies of MSCs with different NK cell lines (KHYG-1 and NK-92) have demonstrated that MSCs can either suppress or induce granule polarization, indicating a complex and potentially context-dependent relationship [9]. This differential crosstalk suggests that MSCs can fine-tune NK cell responses, potentially preventing unwanted tissue damage while maintaining anti-viral and anti-tumor immunity. The precise molecular mechanisms governing this interaction remain an active area of investigation, but it is clear that direct cell-cell contact is a significant component.
Interactions with Antigen-Presenting Cells (APCs)
MSCs directly influence the function of key APCs, including monocytes, macrophages, and dendritic cells. A pivotal mechanism involves the phagocytosis of MSCs by monocytes. Tracking studies reveal that infused umbilical cord MSCs (UC-MSCs) briefly reside in the lungs and are rapidly phagocytosed by monocytes, which subsequently migrate to other body sites [9]. This phagocytosis induces phenotypical and functional changes in monocytes, which in turn modulate cells of the adaptive immune system, thereby distributing the immunomodulatory effect of MSCs systemically [9].
Furthermore, MSCs directly interact with macrophages through cell contact. It has been shown that MSCs increase production of Tumor Necrosis Factor-Stimulated Gene 6 (TSG-6) through intercellular contact with pro-inflammatory M1 macrophages [10]. This TSG-6-dependent mechanism promotes the transformation of pro-inflammatory M1 macrophages into anti-inflammatory M2 macrophages, alleviating excessive inflammation [10]. Adipose-derived MSCs (A-MSCs) are also known to switch activated M1-like inflammatory macrophages to an M2-like phenotype, an effect mediated in part by prostaglandin E2 (PGE2), which requires close cellular proximity for optimal effect [9].
Diagram 1: MSC interactions with Antigen-Presenting Cells (APCs). MSCs are phagocytosed by monocytes, which then modulate adaptive immunity. Direct contact also drives M1 to M2 macrophage conversion.
Experimental Models and Methodologies
Key Experimental Protocols
To study these direct cell-cell contact mechanisms, researchers employ specific co-culture systems and animal models.
Transwell Co-Culture System: This is a fundamental tool for distinguishing contact-dependent from soluble factor-mediated effects. In this setup, MSCs and immune cells (e.g., T cells) are cultured in separate chambers separated by a semi-permeable membrane that allows for the free diffusion of soluble factors but prevents physical cell contact. A study demonstrated that when T cells were co-cultured with bone marrow-derived MSCs (BM-MSCs) in a Transwell system or with BM-MSC conditioned medium, the inhibitory activity on T cells was eliminated, providing direct evidence that BM-MSC-mediated inhibition of T cells requires cell-to-cell contact [10].
In Vivo Mouse Models: These models are crucial for validating contact-dependent mechanisms in a physiologically relevant context. For instance, in a syngeneic orthotopic mouse model of ovarian cancer, compact bone-derived MSCs (CB-MSCs) exhibited anti-tumor effects in combination with a fusion protein (VIC-008), which was associated with the activation of CD4+ and CD8+ T-cells and inhibition of Tregs in the tumor microenvironment [9]. Furthermore, in fetal abortion models, MSCs have been shown to enhance the suppressive regulation of T-cells and macrophages [9]. The critical role of contact-mediated priming is supported by experiments where MSCs primed by activated T cells derived from IFN-γ −/− mice exhibited a dramatically reduced ability to suppress T cell proliferation [9].
Table 2: Summary of Key Experimental Findings on Direct Cell-Cell Contact
| Experimental Model | MSC Source | Immune Cell Target | Key Finding |
|---|---|---|---|
| Transwell Co-culture [10] | Bone Marrow (BM-MSC) | T cells | T-cell inhibition was eliminated without direct contact, proving its necessity. |
| In vivo mouse model (Ovarian Cancer) [9] | Compact Bone (CB-MSC) | CD4+/CD8+ T-cells, Tregs | Activated CD4+/CD8+ T-cells and inhibited Tregs in the tumor microenvironment. |
| In vitro Co-culture [9] | Not Specified | T cells from IFN-γ −/− mouse | Priming by IFN-γ-producing T-cells via contact is critical for immunosuppression. |
| In vivo tracking study [9] | Umbilical Cord (UC-MSC) | Monocytes | Phagocytosis of UC-MSCs by monocytes induced phenotypical/functional changes. |
| In vitro Co-culture [10] | Induced Pluripotent Stem Cell (iPSC-MSC) | Tregs, Th2 cells | ICOSL-ICOS interaction activated Tregs and inhibited Th2 cells. |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying MSC-Immune Cell Interactions
| Reagent / Tool | Function / Target | Application in Research |
|---|---|---|
| Transwell System | Physically separates cells while allowing soluble factor exchange. | To definitively distinguish contact-dependent effects from paracrine effects [10]. |
| Recombinant Cytokines (e.g., IFN-γ) | Prime MSCs to enhance immunosuppressive molecule expression. | To mimic inflammatory microenvironment and study MSC licensing [9]. |
| Neutralizing/Antibodies (e.g., anti-PD-L1, anti-Galectin-1) | Block specific surface protein interactions. | To functionally validate the role of a specific ligand-receptor pair (e.g., PD-1/PD-L1) [9] [10]. |
| Small Interfering RNA (siRNA) | Knock down specific gene expression in MSCs (e.g., Galectin-1). | To confirm the necessity of a specific MSC molecule for immunomodulation [9]. |
| Flow Cytometry Antibodies | Detect surface markers (CD73, CD90, CD105, CD45, CD34, HLA-DR) and immune cell markers (CD4, CD8, CD25, FOXP3). | To characterize MSC purity and analyze immune cell populations and activation status [9] [11] [10]. |
| CFSE (Carboxyfluorescein succinimidyl ester) | Fluorescent cell staining dye that dilutes with each cell division. | To quantitatively measure the proliferation inhibition of immune cells (e.g., T-cells) by MSCs [9]. |
Integrated Signaling in MSC-Mediated Immunomodulation
The following diagram synthesizes the primary direct cell-cell contact mechanisms MSCs use to modulate the activity of T cells, NK cells, and Antigen-Presenting Cells.
Diagram 2: Integrated view of MSC immunomodulation via direct contact with T cells, NK cells, and APCs, showing key receptor-ligand pairs and functional outcomes.
Direct cell-cell contact is a non-redundant mechanism underpinning the immunomodulatory power of MSCs. The interactions, mediated by a sophisticated array of surface molecules, enable precise control over T-cell activation and proliferation, NK cell cytotoxicity, and APC phenotype and function. A comprehensive understanding of these contact-dependent pathways, as outlined in this guide, provides researchers and drug development professionals with the foundational knowledge and experimental framework necessary to advance MSC-based therapies from foundational research to targeted clinical applications for individual patients.
The C-X-C chemokine receptor type 4 (CXCR4) and its primary ligand, stromal cell-derived factor-1 (SDF-1, also known as CXCL12), constitute a fundamental biological axis critical for stem cell trafficking in physiological and pathological states. This receptor-ligand pair operates as a central regulatory system, guiding the mobilization and homing of stem cells to sites of tissue injury, inflammation, and damage [12] [13]. The SDF-1/CXCR4 axis is exploited by various cell types, including hematopoietic stem cells (HSCs), mesenchymal stem cells (MSCs), and endothelial progenitor cells (EPCs), facilitating their recruitment from reservoirs such as the bone marrow into the peripheral circulation and subsequent navigation to compromised tissues [12]. Upon tissue injury, damaged cells release endogenous molecules known as Damage-Associated Molecular Patterns (DAMPs), which trigger a localized increase in SDF-1 expression [12] [13]. Stem cells expressing CXCR4 on their surface detect this SDF-1 gradient and undergo a multistep homing process—tethering, activation, arrest, transmigration, and migration—culminating in their extravasation and recruitment to the inflamed microenvironment [14]. The axis not only directs cellular migration but also contributes directly to tissue preservation by activating pro-survival signaling pathways in CXCR4-expressing parenchymal cells [13]. This orchestrated response positions the SDF-1/CXCR4 axis as a cornerstone mechanism in the body's innate repair system and a compelling target for therapeutic intervention in regenerative medicine.
Molecular Mechanisms of Homing
Initiation: Injury Detection and DAMP Release
The homing process begins with tissue injury, which prompts the release of intracellular molecules collectively known as Damage-Associated Molecular Patterns (DAMPs) [12]. These molecules, which include ATP, high-mobility group box 1 (HMGB1), heat shock proteins (HSPs), and reactive oxygen species (ROS), function as distress signals upon their release into the extracellular space [12]. DAMps are recognized by Pattern Recognition Receptors (PRRs), such as Toll-like receptors (TLRs) and the receptor for advanced glycation end-products (RAGE), on resident immune and stromal cells [12]. This recognition activates pivotal intracellular signaling cascades, most notably the NF-κB pathway, leading to the transcriptional upregulation and secretion of pro-inflammatory cytokines and chemokines, chief among them being SDF-1 [12]. The upregulation of SDF-1 at the injury site establishes a soluble chemical gradient, creating the primary directional cue for CXCR4-expressing stem cells.
The Multi-Step Homing Process
Systemically administered or endogenously mobilized stem cells must execute a precise, multi-step sequence to exit the circulation and reach the injured tissue. This process, analogous to leukocyte trafficking, is outlined below and illustrated in Figure 1 [14].
- Step 1: Tethering and Rolling. The initial weak adhesion of stem cells to the activated endothelium near the injury site is facilitated by selectins. Mesenchymal stromal cells (MSCs) utilize surface molecules like CD44 to interact with endothelial P-selectin, causing the cells to slow down and roll along the vascular wall [14].
- Step 2: Activation. Chemokines presented on the endothelial surface, particularly SDF-1, engage their G protein-coupled receptors (e.g., CXCR4) on the rolling stem cell. This binding triggers intracellular signaling that activates integrins, inducing a conformational change that increases their affinity for endothelial ligands [14].
- Step 3: Arrest. Activated integrins, such as VLA-4 (α4β1 integrin) on MSCs, mediate firm adhesion to endothelial counter-ligands like VCAM-1 [14]. This step halts the stem cell, preparing it for transmigration.
- Step 4: Transmigration (Diapedesis). The adhered stem cell traverses the endothelial barrier, a process that may involve paracellular (between endothelial junctions) or transcellular (through the endothelial cell body) routes. This step often requires the action of matrix-remodeling enzymes like matrix metalloproteinases (MMPs) [14].
- Step 5: Migration. Once in the extravascular space, the stem cell continues to migrate through the interstitial matrix, guided by the established SDF-1 concentration gradient, until it reaches the specific niche of tissue injury [12] [14].
Figure 1: The multi-step homing process of stem cells to injured tissue.
Downstream Intracellular Signaling
The binding of SDF-1 to CXCR4 activates several downstream signaling pathways that are essential for cytoskeletal reorganization, directional migration, and cell survival. The two most characterized pathways are the PI3K/Akt and MAPK/ERK pathways [15]. As detailed in Figure 2, SDF-1 binding induces a conformational change in the G-protein-coupled receptor CXCR4, leading to the activation of phosphoinositide 3-kinase (PI3K). PI3K then phosphorylates Akt, a central kinase that regulates multiple processes, including actin polymerization and cell survival. Concurrently, the MAPK/ERK pathway is activated, influencing cell proliferation and differentiation. The critical role of the PI3K/Akt pathway is demonstrated by studies where its inhibition with LY294002 significantly impairs SDF-1-directed MSC migration in vitro and homing in vivo [15].
Figure 2: Key intracellular signaling pathways activated by the SDF-1/CXCR4 axis.
Quantitative Data in Stem Cell Homing and Modulation
The function of the SDF-1/CXCR4 axis has been quantified across various experimental models, providing insights into its efficacy and modulation. The table below summarizes key quantitative findings from recent research.
Table 1: Quantitative Findings on the SDF-1/CXCR4 Axis in Disease Models
| Disease Model | Key Parameter Measured | Experimental Findings | Citation |
|---|---|---|---|
| Chemotherapy-induced Premature Ovarian Insufficiency (POI) in Rats | SDF-1 levels in ovaries | Significantly increased in POI rats compared to controls | [15] |
| Homing of hAD-MSCs to ovaries | Blocking with AMD3100 significantly reduced the number of homing cells | [15] | |
| DSS-Induced Colitis in Mice | Immune cell modulation in vitro | SDF-1-pretreated ERCs increased anti-inflammatory IL-4, IL-10 and decreased pro-inflammatory IL-6, TNF-α | [16] |
| Postoperative Colon Cancer Patients | Serum CXCR4 levels | 0.163 ± 0.012 pg/mL in patients vs. 0.376 ± 0.025 pg/mL in controls (p=0.001) | [17] |
| Serum SDF-1 levels | 0.376 ± 0.025 pg/mL in patients vs. 0.699 ± 0.110 pg/mL in controls (p=0.001) | [17] | |
| Myocardial Infarction | Homing efficiency of systemically infused MSCs | Only ~1% of administered MSCs reach the ischemic tissue | [18] |
The impact of CXCR4 expression levels on cellular migration has been directly demonstrated through in vitro transwell migration assays. Furthermore, experimental modulation of the axis via receptor antagonists or genetic approaches yields predictable and quantifiable changes in homing efficiency, as summarized below.
Table 2: Impact of CXCR4 Modulation on Stem Cell Migration and Homing
| Method of Modulation | Effect on CXCR4/SDF-1 Axis | Outcome on Cell Behavior | Citation |
|---|---|---|---|
| SDF-1 Pre-treatment (50 ng/ml, 72 hrs) | Increased CXCR4 expression on Endometrial Regenerative Cells (ERCs) | Enhanced migration towards SDF-1 gradient; improved immunomodulation in colitis | [16] |
| AMD3100 (CXCR4 antagonist) | Blocks SDF-1 from binding to CXCR4 receptor | Significantly reduced homing of hAD-MSCs to injured ovaries in rats | [15] |
| Cell Surface Engineering (DMPE-PEG-CXCR4) | Incorporates recombinant CXCR4 protein onto MSC membrane within 10 minutes | Confirmed improved migration of MSCs toward an SDF-1 gradient in vitro | [18] |
| PI3K Inhibition (LY294002) | Inhibits downstream PI3K/Akt signaling pathway | Significantly inhibited SDF-1-induced migration of hAD-MSCs in vitro | [15] |
Experimental Protocols for Investigating the Axis
Protocol 1: In Vitro Transwell Migration Assay
The Transwell migration assay is a foundational method for quantifying the chemotactic response of stem cells to an SDF-1 gradient.
- Apparatus Setup: Use a Transwell plate, which consists of an upper chamber and a lower well separated by a porous membrane (typically 8.0 μm pore size for MSCs).
- Gradient Establishment: Prepare a solution of recombinant human SDF-1α (e.g., from ProSpec-Tany TechnoGene) in serum-free medium. Add this chemokine solution to the lower well of the chamber. Serum-free medium alone serves as a negative control.
- Cell Preparation: Harvest the stem cells (e.g., MSCs, ERCs, or hAD-MSCs) and resuspend them in serum-free medium. If testing the role of CXCR4, pre-treat a cell aliquot with an antagonist like AMD3100 (e.g., 1 μg/ml for 30 minutes) [16] [15].
- Assay Execution: Seed the cell suspension into the upper chamber of the Transwell insert. Incubate the plate for a predetermined period (e.g., 6-24 hours) at 37°C in a 5% CO₂ incubator to allow for cell migration.
- Quantification: After incubation, carefully remove the non-migratory cells from the upper surface of the membrane using a cotton swab. Fix the cells that have migrated to the lower surface with 4% paraformaldehyde and stain them with a crystal violet solution. Count the number of migrated cells in multiple random fields under a light microscope or use a spectrophotometer for dissolved stain quantification [15] [18].
Figure 3: Workflow for the Transwell Migration Assay.
Protocol 2: In Vivo Homing Analysis in a Disease Model
This protocol evaluates the homing efficiency of systemically transplanted stem cells to a target organ in an animal model of disease, such as chemotherapy-induced POI or colitis.
- Disease Model Induction:
- Cell Labeling and Preparation: Label stem cells (e.g., hAD-MSCs or ERCs) with a fluorescent marker such as PKH26 or CM-Dil according to the manufacturer's protocol. For experimental groups, pre-treat cells with SDF-1 (50 ng/ml for 72 hours) to upregulate CXCR4, or with AMD3100 (e.g., 5 mg/kg per test for 30 minutes) to block the receptor [16] [15].
- Cell Administration: Systemically transplant the labeled cells (e.g., 1×10⁶ cells/mouse) via tail vein injection at specified time points post-injury (e.g., days 2, 5, and 8 in the colitis model) [16].
- Tissue Collection and Analysis: Sacrifice the animals at a predetermined endpoint post-transplantation. Harvest the target organs (e.g., ovaries, colon) and process them for cryosectioning or flow cytometry.
- Homing Quantification:
- Fluorescence Microscopy: Identify and count the PKH26-labeled cells in multiple sections of the target tissue using a fluorescence microscope. The number of labeled cells per field or per mm² provides a measure of homing efficiency [15].
- Flow Cytometry: For tissues that can be dissociated into single-cell suspensions, use flow cytometry to quantify the percentage of fluorescently labeled cells within the total cell population [16].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating the SDF-1/CXCR4 Axis
| Reagent / Tool | Category | Primary Function in Research | Example Source / Citation |
|---|---|---|---|
| Recombinant SDF-1α | Chemokine | Creates a chemotactic gradient in in vitro migration assays and for pre-treating cells to upregulate CXCR4. | ProSpec-Tany TechnoGene [16] [15] |
| AMD3100 (Plerixafor) | Small Molecule Antagonist | Selectively blocks SDF-1 from binding to CXCR4; used to validate the specific role of the axis in vitro and in vivo. | Sigma-Aldrich [16] [15] |
| Anti-CXCR4 Antibody | Antibody | Detects and quantifies CXCR4 receptor expression on stem cells via flow cytometry or immunofluorescence. | BioLegend (e.g., anti-CD184-PE) [16] |
| DMPE-PEG-CXCR4 | Chemical Tool | Rapidly engineers cell surface by incorporating recombinant CXCR4 protein onto MSC membranes to enhance homing potential. | Nanocs, Inc. (for DMPE-PEG) [18] |
| LY294002 | Small Molecule Inhibitor | Inhibits the PI3K/Akt signaling pathway downstream of CXCR4; used to dissect mechanism of migration. | Multiple commercial suppliers [15] |
| PKH26 / CM-Dil | Fluorescent Cell Linker | Labels cell membranes for tracking and quantification of transplanted stem cells in host tissues. | Multiple commercial suppliers [16] [15] |
Therapeutic Implications and Clinical Translation
The profound role of the SDF-1/CXCR4 axis in stem cell homing has paved the way for numerous therapeutic strategies aimed at enhancing regenerative medicine. These approaches can be broadly categorized into cell-based strategies and pharmacological/biological strategies.
Cell-Based Strategies: A significant challenge in MSC therapy is the downregulation of CXCR4 during ex vivo expansion, leading to poor homing efficiency [18]. To counter this, researchers have developed methods to enhance CXCR4 expression on therapeutic cells. These include:
- Genetic Modification: Transducing MSCs with viral vectors to overexpress CXCR4, which has been shown to increase homing to target tissues like bone marrow and infarcted myocardium [14].
- Cell Priming: Pre-treating MSCs with cytokines or under hypoxic conditions to upregulate endogenous CXCR4 expression [18]. For instance, SDF-1 pretreatment of Endometrial Regenerative Cells (ERCs) enhanced their immunomodulatory capacity in a murine colitis model [16].
- Cell Surface Engineering: A rapid, non-genetic approach that involves chemically conjugating recombinant CXCR4 protein onto the surface of MSCs using lipid-PEG tethers. This method can significantly improve migration toward an SDF-1 gradient within minutes, offering a clinically viable strategy for acute conditions like myocardial infarction [18].
Pharmacological/Biological Strategies: An alternative to manipulating the cells is to modulate the axis within the patient. This can be achieved by:
- Direct SDF-1 Delivery: Administering recombinant SDF-1 protein to injured tissues to create a sustained or amplified homing signal for endogenous CXCR4-positive stem cells. This strategy is the basis of an ongoing clinical trial for chronic heart failure (NCT01082094) [13].
- Modulating SDF-1 Expression: Using gene therapy to induce local SDF-1 expression in damaged organs, thereby creating a "regenerative niche" [13].
- Complement System Modulation: Evidence suggests that cleavage fragments of the third complement component (C3), which are released during tissue injury, can modulate the responsiveness of CXCR4+ stem cells to SDF-1, forming an optimal gradient for homing [19].
The therapeutic application of this axis extends beyond regenerative medicine. In oncology, the SDF-1/CXCR4 axis is co-opted by cancer cells to promote metastasis, angiogenesis, and the creation of an immunosuppressive tumor microenvironment [17]. Consequently, CXCR4 antagonists are being investigated not only to impair stem cell homing but also as a potential anti-metastatic therapy. The dual role of this axis in regeneration and disease underscores its biological potency and the need for context-specific therapeutic interventions.
The Hedgehog (Hh), Wnt, Notch, and TGF-β signaling pathways represent evolutionarily conserved communication systems that orchestrate fundamental biological processes during embryonic development and maintain tissue homeostasis in adult organisms [20] [21]. In post-natal life, these pathways operate at low activity levels, playing restricted but crucial roles in stem cell maintenance and tissue repair [20]. When these pathways become unbalanced, impaired cross-talk contributes significantly to disease development, particularly in cancer, where more than one of these pathways are frequently active simultaneously [20]. Understanding the molecular interlinking networks between these pathways provides a rational basis for combined anticancer drug development and offers critical insights into stem cell biology and immunomodulation [20] [22].
The biological and pathogenic importance of these signaling pathways emphasizes the need to tightly control their activity, both physiologically and therapeutically. Evidence of extensive cross-talk between Hh and other signaling pathways is reported in many tumor types, and this complexity is mirrored in the regulation of stem cell immune privilege and immunomodulatory functions [20] [22]. The integration of several signaling pathways is a key step able to determine more aggressive behavior of tumor cells and their resistance to pharmacological approaches, while in stem cells, this integration supports their quiescence, regenerative capacity, and immune suppressive properties [20] [22]. This whitepaper explores the intricate protein-protein interaction networks between key components of these signaling pathways and examines how their integration ultimately affects cellular behavior in the context of stem cell research and therapeutic development.
Core Pathway Mechanics and Molecular Components
Hedgehog Signaling Pathway
First discovered in Drosophila, the Hedgehog signaling pathway is an evolutionarily conserved system that functions as a critical morphogenesis driver for embryonic and post-natal development [20]. It regulates diverse cellular processes, including cell proliferation, tissue differentiation, and repair of normal tissues, and is also implicated in the regulation and survival of both normal and malignant stem cells [20].
Canonical Hedgehog pathway activation is characterized by the interaction of Hh ligands—Sonic (SHh), Indian (IHh), and Desert (DHh)—with the Patched1 (Ptch1) receptor, which resides in the primary cilium, a key organelle consisting of microtubules emanating from the cell surface where SHh signaling takes place [20]. In the absence of Hh ligand, Ptch localizes to the base of the primary cilium and catalytically represses the activity of Smoothened (SMO), a member of G-protein-coupled receptor-like proteins, by inhibiting its translocation into the primary cilium [20]. Hh ligand binding causes internalization of the ligand/receptor complex from the cell surface towards lysosomes for degradation and promotes accumulation of SMO at the cell surface [20].
Once activated, SMO becomes hyperphosphorylated by casein kinase 1 (CK1) and G-protein-coupled receptor kinase 2 (GRK2), resulting in release of its inhibition and movement from the base into the tip of the primary cilium [20]. This activation triggers a cascade of intracellular processes that involve a dynamic association between Gli transcription factors (the final effectors of Hh signaling) and Suppressor of Fused (SuFu), a negative regulator of Hedgehog signaling [20]. Hh ligand binding sustains the release of Gli from SuFu, allowing Gli to move into the nucleus and activate Hh target genes, including Gli1 itself, creating a feedback loop that serves as a readout of Hh activity [20].
Table 1: Key Components of the Hedgehog Signaling Pathway
| Component | Type | Function in Pathway |
|---|---|---|
| SHh, IHh, DHh | Ligands | Bind to Ptch1 receptor to initiate signaling |
| Ptch1 | Receptor | Catalytically represses SMO in absence of ligand |
| SMO | Transducer | Seven-transmembrane protein that activates downstream signaling |
| SuFu | Negative Regulator | Binds Gli proteins to regulate activity, processing, localization |
| Gli1, Gli2, Gli3 | Transcription Factors | Final effectors that regulate expression of Hh target genes |
| Primary Cilium | Cellular Structure | Platform for Hh signal transduction |
Wnt Signaling Pathway
The Wnt signaling pathway is a highly conserved regulator of diverse cellular processes that governs embryonic development, cell proliferation, differentiation, migration, and tissue homeostasis [21]. The pathway is categorized into canonical and non-canonical branches based on β-catenin's involvement in transcriptional activation [21]. The canonical Wnt pathway is characterized by β-catenin's nuclear translocation and subsequent activation of target genes through T-cell factor/lymphoid enhancer factor (TCF/LEF) transcription factors, primarily driving cell proliferation [21]. Conversely, the non-canonical Wnt pathway functions independently of the β-catenin-TCF/LEF axis, modulating cell polarity and migration, and establishes a complex, interdependent network with the canonical pathway [21].
In the absence of Wnt ligands, β-catenin is phosphorylated by a multiprotein destruction complex comprising Axin, adenomatous polyposis coli (APC), glycogen synthase kinase 3β (GSK3β), casein kinase 1α (CK1α), protein phosphatase 2A (PP2A), and β-transducin repeat-containing E3 ubiquitin-protein ligase (β-TrCP) [21]. This phosphorylation marks β-catenin for ubiquitination, targeting it for proteasomal degradation [21]. When Wnt proteins are present, they bind to the N-terminal cysteine-rich domain of Frizzled (Fzd) family receptors, disrupting the formation of the destruction complex by recruiting cytosolic disheveled (Dvl) proteins, thus initiating Wnt signaling [21].
The non-canonical Wnt signaling pathway, also known as the non-canonical Wnt-Fzd signaling pathway, comprises two major intracellular signaling cascades: the Wnt/planar cell polarity (PCP) pathway and the Wnt/calcium (Ca²⁺) pathway [21]. Unlike the canonical pathway, these function independently of β-catenin and are essential for regulating cell polarity, Ca²⁺ signaling, and other cellular processes [21].
Table 2: Wnt Signaling Pathway Classification and Components
| Pathway Type | Key Ligands | Core Components | Primary Functions |
|---|---|---|---|
| Canonical (β-catenin-dependent) | Wnt1, Wnt3, Wnt3a, Wnt8a, Wnt8b | Fzd, LRP5/6, Dvl, β-catenin, TCF/LEF | Regulation of cell proliferation, target gene expression |
| Non-canonical PCP Pathway | Wnt5a, Wnt7, Wnt11 | Fzd, Dvl, Rho/Rac GTPases, JNK | Control of cell polarity, migration, tissue organization |
| Non-canonical Calcium Pathway | Wnt1, Wnt5a, Wnt11 | Fzd, Dvl, PLC, intracellular Ca²⁺ | Regulation of cell adhesion, migration, early development |
Notch and TGF-β Signaling Pathways
The Notch signaling pathway operates through direct cell-to-cell communication, where transmembrane ligands on one cell activate transmembrane receptors on adjacent cells. This pathway plays crucial roles in cell fate determination, differentiation, and stem cell maintenance. While the search results provide limited specific details about Notch signaling mechanics, they consistently highlight its significant cross-talk with Hh, Wnt, and TGF-β pathways in both developmental and pathological contexts [20].
The TGF-β signaling pathway is a critical regulator of cell proliferation, differentiation, migration, and apoptosis. TGF-β binds to its receptor TGF-βRII, which then recruits and phosphorylates TGF-βRI, forming a heterotetrameric complex [10]. This activation triggers the phosphorylation of R-Smads (receptor-regulated Smads), specifically Smad2 and Smad3 [10]. Phosphorylated Smad2/3 forms a complex with the common mediator Smad4, which translocates to the nucleus to regulate the transcription of target genes involved in immune suppression, such as FOXP3, the master regulator of regulatory T cells (Tregs) [10]. This pathway is particularly important in the context of mesenchymal stem cell (MSC) immunomodulation, as TGF-β is a pivotal cytokine secreted by MSCs that plays a central role in immune regulation and tissue repair [10].
Pathway Cross-Talk: Molecular Integration Points
Hh and Wnt Pathway Interconnections
The cross-talk between Hh and Wnt pathways represents a fundamental interaction that collaboratively regulates growth factor expression during embryonic development, influencing cell differentiation and tissue morphology [21]. Research indicates that Hh signaling can potentiate Wnt pathway activity, while Wnt signaling, in turn, modulates Hh effectors—a dynamic interplay essential in tissue regeneration and cancer progression [21]. These two pathways share several common regulatory components and mechanisms that facilitate their integration at multiple molecular levels.
One significant connection point involves the primary cilium, which serves as a signaling hub for both pathways [20]. The primary cilium provides a physical platform where components of both pathways can interact and influence each other's activity. Additionally, several kinases and ubiquitin ligases, including GSK3β and β-TrCP, participate in both Hh and Wnt signaling, creating nodes of functional convergence [20] [21]. These shared components allow for coordinated regulation of both pathways in response to cellular cues and environmental signals.
The integration between Hh and Wnt pathways has particular significance in stem cell biology and cancer. In stem cells, this cross-talk helps maintain the balance between self-renewal and differentiation, while in cancer cells, simultaneous activation of both pathways contributes to more aggressive tumor phenotypes and therapy resistance [20] [21]. Understanding these interactions provides insights for developing combination therapies that simultaneously target multiple pathways in cancer treatment.
Integration with Notch and TGF-β Pathways
The communication between Hh and Notch pathways is reported in many tumor types, with evidence of physical interactions between key components and transcriptional coordination [20]. Similarly, TGF-β signaling intersects with Hh, Wnt, and Notch pathways through multiple mechanisms, including shared transcriptional targets and synergistic regulation of developmental processes [20] [10]. In the context of mesenchymal stem cells, TGF-β secretion plays a central role in immune regulation by restoring Treg/Th2 balance through the TGF-β/Smad pathway [10].
Notch signaling engages in cross-talk with other pathways through various mechanisms, including direct protein-protein interactions between pathway components and coordination of transcriptional responses [20]. This integration allows cells to process multiple environmental signals in a coordinated manner, resulting in appropriate cellular responses during development and tissue homeostasis. When dysregulated, these interconnected networks contribute to pathological processes, including cancer progression and immune dysregulation.
In MSCs, the immunomodulatory functions are mediated through the integrated activity of multiple signaling pathways, including TGF-β, which binds to its receptor TGF-βRII, recruits and phosphorylates TGF-βRI, and triggers phosphorylation of R-Smads (Smad2 and Smad3) [10]. The phosphorylated Smad2/3 then forms a complex with Smad4 that translocates to the nucleus to regulate transcription of target genes involved in immune suppression, such as FOXP3, the master regulator of Tregs [10]. This molecular pathway is essential for MSCs' ability to modulate immune responses and maintain tissue homeostasis.
Cross-Talk in Stem Cell Immunomodulation
The cross-talk between Hh, Wnt, Notch, and TGF-β pathways takes on particular significance in the context of stem cell immunomodulation [22]. MSCs, also identified as immunomodulatory stem cells (IMSCs), demonstrate pronounced and diverse immune modulation capabilities [22]. These cells not only evade cytotoxic immune action but also actively attract immune cells and can activate or reprogram them depending on the molecular context [22]. The immunomodulatory capabilities are more pronounced in IMSCs than in other differentiated cells, highlighting the importance of these pathway interactions in stem cell function [22].
MSCs have been shown to express a range of immunosuppressing molecules, including PGE2, TGF-β, HLA-G5, IL-10, HGF, galectins, CD73, CD39, PD-L1, and HLA-G1 [22]. The activation of MSCs and subsequent induction of the regenerative program results in suppression of the inflammatory program [22]. This immunomodulatory function is closely linked to the quiescent state of stem cells and relates to regeneration and inflammation regulation [22]. The integration of multiple signaling pathways allows MSCs to fine-tune their immunomodulatory activities in response to local environmental cues.
The functional significance of IMSCs is of particular evolutionary importance with respect to the stem and immune systems [22]. The existing mutual integration of stem and immune systems highlights the evolutionary significance of this integration, as it provides an additional mechanism for maintaining tissue homeostasis and responding to injury or infection [22]. This integrated system represents a sophisticated regulatory network that balances the regenerative capacity of stem cells with the protective functions of the immune system.
Experimental Approaches for Studying Pathway Cross-Talk
Methodologies for Analyzing Pathway Interactions
Studying the complex cross-talk between signaling pathways requires sophisticated experimental approaches that can capture dynamic interactions and functional outcomes. Several key methodologies have been developed to elucidate these intricate networks, each with specific applications and limitations. Below is a comprehensive table of experimental protocols for investigating pathway cross-talk.
Table 3: Experimental Methods for Analyzing Signaling Pathway Cross-Talk
| Method Category | Specific Techniques | Key Applications | Technical Considerations |
|---|---|---|---|
| Genetic Manipulation | CRISPR/Cas9 knockout, RNA interference, Dominant-negative constructs | Identify essential pathway components, test functional requirements | Off-target effects, compensation mechanisms |
| Protein Interaction Analysis | Co-immunoprecipitation, Proximity ligation assays, Yeast two-hybrid | Detect physical interactions between pathway components | May not reflect functional consequences in living cells |
| Imaging Approaches | Immunofluorescence, Live-cell imaging, FRET-based biosensors | Visualize pathway component localization and dynamics in real-time | Technical limitations in resolution and multiplexing capacity |
| Transcriptional Reporting | Luciferase reporter assays, GFP reporters, Chromatin immunoprecipitation | Measure pathway activity and target gene regulation | May not capture all relevant regulatory contexts |
| Proteomic & Genomic Analysis | Phosphoproteomics, RNA-seq, ATAC-seq | Comprehensive profiling of pathway activities and outputs | Complex data analysis, integration challenges |
Detailed Experimental Protocols
Co-culture Systems for MSC-Immune Cell Interactions: To study how MSCs modulate immune responses through signaling pathways, researchers employ co-culture systems where MSCs are cultured with immune cells such as T lymphocytes [10]. When T cells were co-cultured with bone marrow-derived MSCs (BM-MSCs) in Transwell systems or with BM-MSC conditioned medium, the inhibitory activity of T cells was eliminated, suggesting that inhibition of T cells by BM-MSCs requires MSC-T cell contact [10]. This protocol involves: (1) Isolating and expanding MSCs from relevant tissues (adipose, bone marrow, umbilical cord); (2) Culturing MSCs to 70-80% confluence; (3) Isolating peripheral blood mononuclear cells (PBMCs) or specific immune cell populations; (4) Setting up direct contact co-culture or Transwell systems; (5) Measuring outcomes including T cell proliferation, cytokine secretion, and differentiation markers.
Pathway Activity Reporter Assays: Luciferase-based reporter systems are widely used to monitor the activity of specific signaling pathways in living cells. For Wnt pathway analysis, constructs containing TCF/LEF binding sites driving luciferase expression are transfected into target cells. For Hh pathway analysis, Gli-responsive elements are used similarly. Protocol steps include: (1) Cloning consensus binding sequences for transcription factors (Gli for Hh, TCF/LEF for Wnt) into luciferase reporter vectors; (2) Transfecting reporter constructs into target cells; (3) Treating cells with pathway-specific agonists or inhibitors; (4) Measuring luciferase activity after specified time points; (5) Normalizing results to control reporters for transfection efficiency.
Advanced Imaging of Primary Cilium Signaling: Given the importance of the primary cilium in Hh and other signaling pathways, advanced imaging techniques have been developed to visualize pathway components in this specialized organelle. The protocol involves: (1) Culturing cells on glass coverslips; (2) Serum starvation to promote ciliogenesis; (3) Immunostaining for ciliary markers (acetylated tubulin) and pathway components (SMO, Gli); (4) High-resolution confocal or STORM microscopy; (5) Quantitative analysis of protein localization and co-localization within the cilium.
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for Studying Pathway Cross-Talk
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Pathway Modulators | SAG (SMO agonist), Cyclopamine (SMO antagonist), CHIR99021 (GSK-3 inhibitor), DAPT (γ-secretase/Notch inhibitor) | Pathway activation/inhibition studies | Selective modulation of specific pathway components |
| Antibodies for Detection | Anti-Gli1, Anti-β-catenin, Anti-Smad2/3, Anti-active β-catenin, Anti-acetylated tubulin | Protein localization, Western blot, immunofluorescence | Detection and visualization of pathway components |
| Reporter Systems | TCF/LEF-luciferase, Gli-luciferase, CBF1-luciferase reporters | Pathway activity quantification | Measurement of transcriptional activity downstream of pathways |
| Cell Lines | C3H10T1/2, HEK293, MSC lines, Primary MSCs from various tissues | In vitro pathway analysis | Model systems for studying pathway mechanics and cross-talk |
| Cytokines & Ligands | Recombinant SHh, Wnt3a, TGF-β, Dll4 (Notch ligand) | Pathway stimulation | Activation of specific signaling pathways |
Visualization of Pathway Cross-Talk
To facilitate understanding of the complex interactions between these signaling pathways, we have created comprehensive diagrams using Graphviz DOT language. These diagrams adhere to the specified color palette and contrast requirements, ensuring optimal readability and visual clarity.
Hedgehog Signaling Pathway Diagram
Wnt Signaling Pathway Diagram
Pathway Cross-Talk Integration Diagram
Implications for Therapeutic Development and Future Directions
The intricate cross-talk between Hh, Wnt, Notch, and TGF-β signaling pathways has profound implications for therapeutic development, particularly in the areas of cancer treatment and regenerative medicine [20] [21]. The simultaneous activation of multiple pathways in various tumors suggests that targeting a single pathway may be insufficient for effective treatment, providing a rational basis for combined anticancer drug development [20]. Understanding these molecular interlinking networks will enable the design of more effective therapeutic strategies that address the complexity of signaling pathway interactions in disease states.
In the context of stem cell biology and immunomodulation, the integration of these signaling pathways supports the quiescence, regenerative capacity, and immune suppressive properties of mesenchymal stem cells [22]. This has significant implications for developing MSC-based therapies for inflammatory and autoimmune conditions, including allergic rhinitis, where MSCs have shown promise in restoring immune balance through multipronged strategies that include TGF-β secretion to restore Treg/Th2 balance, PGE2 and IDO to suppress DC-mediated Th2 priming, and exosomal miRNAs that directly inhibit eosinophil activation and IgE production [10]. The immunomodulatory capabilities of MSCs are more pronounced than in other differentiated cells, highlighting the therapeutic potential of targeting these pathway interactions [22].
Future research directions should focus on elucidating the precise molecular mechanisms of pathway cross-talk in specific cellular contexts and developing more sophisticated models to capture the dynamics of these interactions. Additionally, standardized protocols for studying and targeting these pathways in therapeutic contexts will be essential for translating our understanding of pathway cross-talk into effective treatments for cancer, inflammatory diseases, and regenerative medicine applications.
The therapeutic paradigm for stem cell applications is shifting from a cell-based to a cell-free approach, centered on the stem cell secretome. Defined as the complete repertoire of bioactive molecules secreted by cells, the secretome is a complex mixture of soluble factors and extracellular vesicles (EVs) that orchestrates immunomodulation, tissue repair, and regeneration [23]. This whitepaper delineates the secretome's composition, its context-dependent biological effects, and the experimental frameworks for its study. We emphasize that the immunomodulatory potency of the secretome is not a fixed property but is dynamically regulated by factors such as the cellular source, microenvironmental cues, and downstream processing methods, with profound implications for developing patient-specific cell-free therapies [24] [23] [25].
The mesenchymal stem cell secretome has emerged as a primary mediator of the therapeutic effects once attributed solely to the cells themselves. This shift is supported by evidence demonstrating that the paracrine factors secreted by MSCs are largely responsible for modulating the immune environment and promoting repair processes [23] [11]. The secretome comprises two major fractions: (1) the soluble component, including growth factors, cytokines, and chemokines; and (2) the vesicular component, primarily extracellular vesicles such as exosomes and microvesicles, which carry a cargo of proteins, lipids, and nucleic acids [23]. The composition of this mixture is highly dynamic and can be engineered through preconditioning, making it a versatile tool for regenerative medicine and immunomodulation [23].
Composition and Functional Annotation of the Secretome
The secretome's functional capacity is determined by its molecular composition, which varies based on the tissue source and the state of the parent cells.
2.1 Core Components. A systematic analysis of the secretome from bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs) reveals a substantial overlap in their functional protein annotations. Common biological processes include regulation of inflammatory response, extracellular matrix organization, and angiogenesis [26]. Key molecular functions involve cytokine activity and growth factor receptor binding. Notably, proteins commonly secreted by both sources interact with multiple druggable targets for bone diseases and are associated with critical KEGG pathways such as the PI3K-Akt signaling pathway and Rap1 signaling pathway [26].
2.2 Source-Dependent Variations. While a core set of functions is conserved, the specific tissue origin introduces functional biases. For instance, the secretome from adipose-derived stem cells (ADSCs) is enriched with a broader range of angiogenic factors, while that from Wharton's Jelly MSCs (WJ-MSCs) demonstrates superior capabilities in promoting neurogenesis and angiogenesis compared to BM-MSCs [23]. Furthermore, a comparative study showed that the secretome of placental MSCs enhanced the migration of endothelial progenitor cells, whereas the BMSC-secretome had a more pronounced effect on the cells' invasion and vessel-forming capacity [23]. These distinctions are critical for selecting the appropriate cell source for targeted therapeutic applications.
Table 1: Quantitative Immunomodulatory Effects of Secretome Fractions
| Secretome Fraction / Parameter | Experimental System | Key Immunomodulatory Effect | Reference |
|---|---|---|---|
| Soluble Factors (< 5 kDa) | PBMCs + THP-1 dual reporter cells | Dose-dependent inhibition of NF-κB and IRF pathways; effect partially mediated by PGE2 | [24] |
| Concentrated Secretome (> 100 kDa) | PBMCs + PHA/IL-2 | Inhibition of T-cell proliferation in a dose-dependent manner | [24] |
| Clarified Secretome | PBMCs + THP-1 dual reporter cells | Strong anti-inflammatory activity; inhibition of innate immune pathways | [24] |
| CCM (50% concentration) | CD3+ T-cells from aGVHD patients | Maximal inhibition of T-cell proliferation at 48h collection time, enhanced by hypoxia preconditioning | [25] |
| WJ-MSCs Hypoxia CCM | CD3+ T-cell co-culture | Superior suppression of proliferation & reduction of CD4+ T-cell activation vs. BM-MSCs | [25] |
Context-Dependent Immunomodulatory Effects
The immunomodulatory actions of the MSC secretome are highly plastic and can be directed by specific experimental and pathological contexts.
3.1 Size-Dependent Mechanisms. Research reveals a functional dichotomy within the secretome based on molecular size. The inhibition of innate immune pathways, specifically the NF-κB and IRF axes, is primarily mediated by soluble factors smaller than 5 kDa, an effect partially dependent on Prostaglandin E2 (PGE2) [24]. In contrast, the suppression of adaptive T-cell proliferation is a function of the concentrated secretome containing larger components, irrespective of the molecular weight cutoff used during filtration [24]. This indicates that the secretome modulates innate and adaptive immunity through distinct molecular actors and pathways.
3.2 Engineering the Secretome through Preconditioning. The secretory profile of MSCs is not static but can be potently modulated by the cellular microenvironment, a process known as preconditioning.
- Hypoxic Preconditioning: Culture under low oxygen tension (e.g., 1% O₂) is a widely used strategy to enhance the therapeutic potential of the secretome. It promotes the secretion of numerous pro-survival and pro-angiogenic factors, such as VEGF, b-FGF, HGF, and IL-6 [23] [25]. A dose-response study in an acute Graft-versus-Host-Disease model confirmed that hypoxia-preconditioned CCM, particularly from WJ-MSCs, demonstrated superior efficacy in suppressing T-cell proliferation and reducing CD4+ T-cell activation compared to CCM from naive MSCs [25].
- Inflammatory Priming: Exposing MSCs to inflammatory mediators like TNF-α, IFN-γ, or IL-1β triggers the cells to produce a respondent set of immunomodulatory molecules. This includes cytokines, chemokines, and factors that contribute to anti-inflammatory, antifibrotic, and neuroprotective effects [23]. This priming is essential for licensing MSCs to exert their full immunosuppressive capacity.
Diagram 1: Secretome modulation and immunomodulatory mechanisms.
Experimental Protocols for Secretome Analysis
Robust and reproducible methodologies are crucial for the isolation, characterization, and functional validation of the secretome.
4.1 Secretome Preparation and Concentration. The standard workflow begins with culturing MSCs to 70-80% confluency in serum-containing medium. To eliminate contaminating serum proteins, cells are thoroughly washed and subsequently cultured in a serum-free medium for a defined period (12-48 hours) [23]. This step often doubles as the preconditioning phase. The resulting Conditioned Medium is collected and clarified by centrifugation to remove cells and debris. For downstream analysis and concentration, methods such as tangential flow filtration with specific molecular weight cutoffs or ultrafiltration are employed [24] [23].
4.2 Functional Potency Assays. Assessing the immunomodulatory capacity of secretome preparations requires robust bioassays.
- Innate Immunity Potency Assay: This involves treating human peripheral blood mononuclear cells with an immunostimulant and then exposing a reporter cell line to the supernatant. Activation of key pathways like NF-κB and IRF is measured in the reporter cells, allowing for the quantification of anti-inflammatory activity [24].
- T-cell Proliferation Assay: Isolated CD3+ T-cells are activated with mitogens and co-cultured with different concentrations of the secretome preparation. Proliferation is quantified using dye dilution assays and flow cytometry, providing a direct measure of the secretome's effect on adaptive immunity [24] [25].
Diagram 2: Experimental workflow for secretome preparation.
4.3 The Scientist's Toolkit: Essential Research Reagents. Table 2: Key Reagents for Secretome Research
| Reagent / Tool | Specific Example | Function in Experimentation |
|---|---|---|
| Reporter Cell Line | THP-1 dual cells (Invivogen) | Quantifies activation of NF-κB and IRF pathways in innate immunomodulation assays [24]. |
| Cell Isolation Kits | CD3+ T-cell isolation kits | Isulates pure populations of primary T-cells from PBMCs for proliferation and activation studies [25]. |
| EV Phenotyping Kit | MACSPlex Exosome Kit (Miltenyi) | Characterizes the surface protein profile of extracellular vesicles via flow cytometry [24]. |
| Cytokine/Chemokine Array | Prostaglandin E2 ELISA Kit (Cayman) | Quantifies specific soluble factors (e.g., PGE2, kynurenine) in the secretome [24]. |
| Tangential Flow Filtration | TFF systems with 5-100 kDa membranes | Concentrates and fractionates the secretome based on molecular weight for mechanistic studies [24]. |
The MSC secretome represents a sophisticated, multifactorial signaling system that mediates tissue repair and immunomodulation. Its effects are not monolithic but are determined by a complex interplay of its cellular origin, molecular composition, and the specific biological context. The move toward cell-free therapies necessitates a deep understanding of how to standardize production, engineer the secretome through preconditioning, and rigorously validate its potency. Future research focused on deciphering the contributions of specific vesicular and soluble components will be key to unlocking the full potential of the secretome for personalized regenerative medicine.
Advanced Profiling and Engineering: Tools to Decode and Harness Patient-Specific Responses
Single-cell RNA sequencing (scRNA-seq) has revolutionized our ability to dissect cellular heterogeneity within stem cell populations, moving beyond bulk tissue analysis to reveal previously obscured subpopulations with distinct functional properties. This technical advancement is particularly transformative for understanding the immunomodulatory capabilities of mesenchymal stem/stromal cells (MSCs), which exhibit remarkable functional diversity that standard characterization methods often miss. The therapeutic potential of MSCs lies fundamentally in their immunomodulatory characteristics, trophic capabilities, and high in vitro self-renewal ability [9]. However, this potential is constrained by substantial cell-to-cell heterogeneity in gene expression that remains poorly characterized, especially in vivo in humans [27].
The integration of scRNA-seq technologies allows researchers to deconvolute this heterogeneity at unprecedented resolution, identifying distinct subpopulations corresponding to specific differentiation trajectories (osteogenic, chondrogenic, adipogenic) and immunomodulatory phenotypes [27]. This capability is critically important for advancing personalized medicine approaches, as it enables the identification of patient-specific subpopulations that may predict therapeutic responses. For drug development professionals, these technological advances offer new pathways for developing targeted therapies that leverage specific immunomodulatory stem cell subpopulations, potentially increasing treatment efficacy while reducing off-target effects.
Technical Foundations of scRNA-seq
Core Experimental Workflow
The standard scRNA-seq workflow incorporates multiple critical stages from sample preparation to data generation. Typical workflows begin with single-cell dissociation, where biological tissue samples are digested to create a single-cell suspension. Cells are then isolated using plate-based techniques or droplet-based methods, with each approach having implications for doublet rates and cell viability. During library construction, intracellular mRNA is captured, reverse-transcribed to cDNA, and amplified with cellular barcodes that enable multiplexing. Unique Molecular Identifiers (UMIs) are incorporated in many protocols to distinguish between amplified copies of the same mRNA molecule and reads from separate mRNA molecules [28].
Following sequencing, raw data processing pipelines such as Cell Ranger perform read quality control, demultiplexing, genome alignment, and quantification to produce count matrices of dimension number of barcodes × number of transcripts [28]. It is crucial to distinguish that the term "barcode" does not automatically equate to "cell," as barcodes may tag multiple cells (doublets) or no cells (empty droplets), necessitating rigorous quality control procedures before biological interpretation [28].
Essential Bioinformatics Tools and Pipelines
The analysis of scRNA-seq data requires specialized computational tools that continue to evolve rapidly. By 2025, the bioinformatics landscape features several mature platforms that address distinct aspects of the analytical pipeline. Scanpy dominates large-scale scRNA-seq analysis, especially for datasets exceeding millions of cells, with architecture optimized for memory use and scalable workflows [29]. Seurat remains the R standard for versatility and integration, featuring robust data integration across batches, tissues, and modalities including spatial transcriptomics and multiome data [29]. For preprocessing of 10x Genomics data, Cell Ranger remains the gold standard for transforming raw FASTQ files into gene-barcode count matrices [29].
Advanced analytical needs are addressed by specialized tools. scvi-tools brings deep generative modeling into the mainstream using variational autoencoders (VAEs) to model noise and latent structure, providing superior batch correction and imputation [29]. CellBender employs deep learning to clean ambient RNA contamination in droplet-based technologies, significantly improving downstream clustering [29]. For trajectory inference, Monocle 3 advances pseudotime analysis using graph-based abstraction to model lineage branching, while Velocyto introduces RNA velocity to infer cellular dynamics by quantifying spliced and unspliced transcripts [29].
Table 1: Essential Bioinformatics Tools for scRNA-seq Analysis
| Tool | Primary Function | Key Features | Language |
|---|---|---|---|
| Scanpy | Large-scale analysis | Scalable workflows, memory optimization, integrates with scverse ecosystem | Python |
| Seurat | Data integration & analysis | Multi-modal support, spatial transcriptomics, label transfer | R |
| Cell Ranger | Preprocessing | Processes raw FASTQ to count matrices, supports multiome data | Pipeline |
| scvi-tools | Deep generative modeling | Probabilistic modeling, superior batch correction, transfer learning | Python |
| Monocle 3 | Trajectory inference | Graph-based lineage modeling, UMAP integration | R |
| CellBender | Ambient RNA removal | Deep probabilistic modeling, denoised matrices | Python |
| Velocyto | RNA velocity | Predicts future cell states, dynamics visualization | Pipeline |
Deconvoluting Stem Cell Heterogeneity with scRNA-seq
Identifying Distinct Subpopulations and Lineage Trajectories
scRNA-seq has enabled systematic in vivo dissection of human bone marrow-derived mesenchymal stem cells (BM-MSCs), revealing their cellular heterogeneity and roles in maintaining bone homeostasis. A landmark study analyzing CD271+ BM-derived mononuclear cells from human subjects successfully identified LEPRhiCD45low BM-MSCs and further codified them into distinct subpopulations corresponding to osteogenic, chondrogenic, and adipogenic differentiation trajectories, along with terminal-stage quiescent cells [27]. Biological functional annotations revealed that osteoblast precursors induce angiogenesis coupled with osteogenesis, while chondrocyte precursors demonstrated potential to differentiate into myocytes [27].
This study also discovered novel cluster of differentiation (CD) markers that were either highly expressed (CD167b, CD91, CD130, CD118) or absent (CD74, CD217, CD148, CD68) in BM-MSCs, representing potential new markers for human BM-MSC purification [27]. The ability to identify these distinct subpopulations and their characteristic markers at single-cell resolution provides critical insights for regenerative medicine applications where specific differentiation pathways are desired.
Experimental Protocol for scRNA-seq of Stem Cell Populations
A standardized protocol for scRNA-seq analysis of stem cell populations incorporates multiple critical steps with specific quality control checkpoints:
Sample Preparation and Single-Cell Suspension: Generate single-cell suspension through tissue dissociation appropriate for the stem cell source (bone marrow, adipose tissue, umbilical cord). Filter through flow cytometry strainers (30-40μm) to remove aggregates [28].
Cell Viability Assessment: Assess viability using trypan blue exclusion or fluorescent viability dyes. Maintain viability >90% to minimize technical artifacts [28].
Library Preparation: Use droplet-based (10x Genomics) or plate-based (Smart-seq2) systems depending on required sequencing depth and budget. Incorporate UMIs to account for amplification biases [28].
Sequencing: Aim for 50,000-100,000 reads per cell depending on experimental goals. Higher depth may be required for detecting low-abundance transcripts of interest [28].
Quality Control and Filtering: Perform rigorous quality control using Scater, Scran, or Seurat based on three key covariates [28]:
- Number of counts per barcode (count depth)
- Number of genes per barcode
- Fraction of counts from mitochondrial genes per barcode
Thresholds must be set carefully to exclude dying cells (low counts/genes, high mitochondrial content) and doublets (unexpectedly high counts/genes) while preserving biological heterogeneity [28].
Downstream Analysis: Apply appropriate tools for normalization, feature selection, dimensionality reduction, clustering, and trajectory inference based on experimental questions [28].
Identifying Immunomodulatory Subpopulations
Multimodal Approaches to Discover Immunomodulatory Subsets
The identification of immunomodulatory subpopulations within heterogenous stem cell populations requires sophisticated analytical approaches. A 2025 study integrated scRNA-seq with bulk proteomics to characterize subpopulations of adipose stromal vascular fraction (SVF) and stem/stromal cells that resemble cytokine-licensed, cultured ASCs [30]. Using the Scissor algorithm to integrate proteomics data with uncultured SVF scRNA-seq data, researchers identified distinct ASC subpopulations with differing immunomodulatory phenotypes [30].
Interactome analysis revealed that Scissor-positive ASCs function as stress adaptive immune regulators primarily through IL6 and broad SEMA4 interactions with higher Visfatin signaling, while Scissor-negative ASCs showed strong signatures of ECM remodeling through FN1 and immunosuppression through THY1 and MIF signaling [30]. This multimodal, integrative approach enabled identification of previously unrecognized ASC subpopulations with distinct immunomodulatory phenotypes that can potentially be selected from uncultured SVF populations, offering new avenues for therapeutic development [30].
Network-Based Methods for Phenotype Association
Advanced computational methods have been developed specifically to identify cell subpopulations associated with disease phenotypes from scRNA-seq data. PACSI (Phenotype-Associated Cell Subpopulation Identification) represents a novel network-based approach that utilizes topological properties of biological networks to introduce a proximity-based measure quantifying correlation between individual cells and disease phenotypes of interest [31]. Unlike methods that assess associations with predefined cell clusters, PACSI can identify phenotype-associated cells even when distributed across diverse clusters, addressing a critical limitation in heterogeneous stem cell populations [31].
The method constructs gene signatures for each cell and bulk sample, then computes network-based proximity using protein-protein interaction networks. Application to head and neck squamous cell carcinoma data successfully identified malignant cells associated with tumor phenotype, with subsequent regulatory network analysis revealing JUND, JUNB, and FOSB as top regulators in these cells [31]. This approach has broad utility for identifying stem cell subpopulations with enhanced immunomodulatory capacity associated with positive therapeutic outcomes.
Differential State Analysis for Multi-Condition Studies
As scRNA-seq datasets increasingly incorporate multiple samples and conditions, differential state (DS) analysis has emerged as a critical framework for identifying subpopulation-specific responses. The muscat R package provides robust tools for multi-condition analysis, enabling researchers to detect state transitions across experimental conditions within specific subpopulations [32]. This approach is particularly valuable for identifying immunomodulatory subpopulations that respond differently to inflammatory stimuli or patient-specific factors.
muscat implements both cell-level mixed models and aggregation-based pseudobulk methods, with comprehensive simulations demonstrating that pseudobulk approaches generally provide superior performance for sample-level inferences [32]. The framework can detect diverse differential expression patterns including changes in mean expression (DE), proportion of expression states (DP), differential modality (DM), or both (DB), offering comprehensive characterization of subpopulation-specific state changes [32].
Signaling Pathways in Stem Cell Immunomodulation
Molecular Mechanisms of Immunomodulation
MSCs exert their immunomodulatory effects through multiple interconnected mechanisms involving both cell-to-cell contacts and paracrine activity. They participate in both innate and adaptive immunity, interacting with T cells, B cells, natural killer (NK) cells, macrophages, monocytes, dendritic cells (DCs) and neutrophils [9]. The immunomodulatory functions of MSCs are mainly communicated via MSC-secreted cytokines; however, more recent evidence shows that apoptotic and metabolically inactivated MSCs also possess immunomodulatory potential, with regulatory T-cells and monocytes playing a key role [9].
Through cell-to-cell contact, MSCs inhibit naive and memory T-cell responses by upregulating intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), critical for T-cell activation and leukocyte recruitment to inflammation sites [9]. MSCs co-cultured with CD4+ T-cells activate the Notch1/forkhead box P3(FOXP3) pathway and increase the percentage of CD4+CD25 FOXP3+ cells [9]. Additionally, programmed-death ligand 1 (PD-L1) and PD-L2 expression on MSCs can inhibit T-cell proliferation by arresting the cell cycle [9].
Through paracrine activity, MSCs secrete a diverse repertoire of multifaceted cytokines, growth factors, and chemokines including transforming growth factor-β1 (TGF-β1), prostaglandin E2 (PGE2), indoleamine-pyrrole 2,3-dioxygenase (IDO), hepatocyte growth factor (HGF), and nitric oxide [9]. These factors are found encapsulated in cell-secreted extracellular vesicles (EVs) including exosomes, microvesicles (MVs), and apoptotic bodies, which display immunoregulatory functions similar to the parent MSCs [9].
Diagram 1: MSC Immunomodulation Pathways. This diagram illustrates the key mechanisms through which mesenchymal stem cells exert immunomodulatory effects, including both cell-cell contact and paracrine signaling pathways.
TGF-β/Smad Signaling Pathway
The TGF-β/Smad pathway represents a central mechanism through which MSCs regulate immune responses. TGF-β secreted by MSCs binds to TGF-βRII, which then recruits and phosphorylates TGF-βRI, forming a heterotetrameric complex [10]. This activation triggers phosphorylation of R-Smads (Smad2 and Smad3), which then form a complex with the common mediator Smad4 that translocates to the nucleus to regulate transcription of target genes including FOXP3, the master regulator of Tregs [10]. Through this pathway, MSCs enhance Treg differentiation and activity, crucial for restoring immune balance in conditions like allergic rhinitis where Th2 dominance drives pathology [10].
Analytical Framework for scRNA-seq Data
Comprehensive Analytical Workflow
A robust analytical workflow for scRNA-seq data incorporates multiple sequential steps with current best-practice recommendations at each stage. The process begins with pre-processing including quality control, normalization, data correction, feature selection, and dimensionality reduction [28]. Downstream analysis then proceeds to cell-level and gene-level investigations including clustering, differential expression, and trajectory inference [28].
Table 2: Key Analytical Steps in scRNA-seq Processing
| Analytical Step | Purpose | Best-Practice Methods |
|---|---|---|
| Quality Control | Filter low-quality cells | Thresholding based on counts, genes, mitochondrial percentage |
| Normalization | Remove technical variability | SCTransform, Scran, LogNormalize |
| Integration | Correct batch effects | Harmony, Seurat CCA, scVI |
| Feature Selection | Identify highly variable genes | Variance-stabilizing transformation |
| Dimensionality Reduction | Visualize and compress data | PCA, UMAP, t-SNE |
| Clustering | Identify cell subpopulations | Louvain, Leiden, hierarchical clustering |
| Differential Expression | Find marker genes | Wilcoxon rank-sum test, MAST, DESeq2 |
| Trajectory Inference | Model cell differentiation | Monocle 3, Slingshot, PAGA |
Research Reagent Solutions
Essential research reagents and platforms form the foundation of reliable scRNA-seq experiments in stem cell research:
Table 3: Essential Research Reagents and Platforms
| Reagent/Platform | Function | Application Notes |
|---|---|---|
| 10x Genomics Chromium | Single-cell partitioning | High-throughput droplet-based system; optimized for cell suspensions |
| Smart-seq2 | Full-length scRNA-seq | Plate-based; superior transcript coverage for biomarker discovery |
| Cell Ranger | Data processing pipeline | Converts FASTQ to count matrices; essential for 10x Genomics data |
| UMIs (Unique Molecular Identifiers) | Molecular counting | Distinguishes biological duplicates from technical amplification artifacts |
| Viability Dyes | Cell quality assessment | Critical for ensuring high-quality input material (e.g., DAPI, propidium iodide) |
| CD271 Antibodies | BM-MSC isolation | Magnetic or fluorescent sorting for primary human BM-MSC purification |
| Liberase TL | Tissue dissociation | Enzymatic blend for gentle tissue dissociation preserving cell surface markers |
Clinical Implications and Therapeutic Applications
Translation to Personalized Medicine Approaches
The identification of immunomodulatory subpopulations through scRNA-seq has profound implications for developing personalized stem cell therapies. Different tissue sources of MSCs exhibit varying immunomodulatory potencies, with adipose-derived MSCs (A-MSCs) demonstrating more potent immunomodulatory effects than bone marrow-derived MSCs (BM-MSCs), while umbilical cord-derived MSCs (UC-MSCs) show minimal risk of initiating an allogeneic immune response in vivo [9]. Understanding these source-specific differences at single-cell resolution enables more precise matching of MSC sources to specific clinical applications.
In allergic rhinitis, for example, preclinical studies demonstrate that MSCs from adipose, bone marrow, umbilical cord, and tonsils reduce symptoms and serum IgE levels by restoring Th1/Th2 immune equilibrium and enhancing Treg activity [10]. Emerging approaches using MSC-derived exosomes and hydrogel-encapsulated formulations further improve targeting and safety [10]. The ability to identify particularly potent immunomodulatory subpopulations within these heterogeneous cell products represents a crucial advancement toward more consistent and effective therapies.
Analytical Framework for Patient-Specific Responses
The muscat package provides a robust framework for detecting subpopulation-specific state transitions from multi-sample multi-condition single-cell transcriptomics data [32]. This approach enables researchers to make sample-level inferences that account for both sample-to-sample and cell-to-cell variability, moving beyond simple cross-condition comparisons to identify patient-specific responses. Application of this method to mouse cortex cells successfully uncovered subpopulation-specific responses to lipopolysaccharide treatment, demonstrating its utility for identifying nuanced immunomodulatory responses [32].
For drug development professionals, this analytical capability enables more precise assessment of how specific patient characteristics or disease states might influence therapeutic responses at the cellular level. This is particularly valuable for clinical trials of MSC-based therapies, where understanding responder versus non-responder mechanisms at single-cell resolution could identify biomarkers for patient stratification and personalized treatment approaches.
Single-cell RNA sequencing has fundamentally transformed our ability to deconvolute stem cell heterogeneity and identify novel immunomodulatory subpopulations with high precision. The integration of advanced computational methods like PACSI and muscat with multimodal data integration approaches provides unprecedented insights into the cellular mechanisms underlying stem cell immunomodulation. As these technologies continue to evolve, they offer a pathway toward truly personalized stem cell therapies where specific immunomodulatory subpopulations can be matched to individual patient needs and disease states. For researchers and drug development professionals, these advances represent critical tools for developing more effective, targeted regenerative medicine approaches with enhanced therapeutic consistency and predictable clinical outcomes.
The convergence of artificial intelligence (AI) with immunology is heralding a new era in precision medicine, particularly in the development of small-molecule immunomodulators. These therapies are designed to precisely control the immune system, drawing inspiration from the body's own sophisticated mechanisms for maintaining immune balance. Among the most powerful natural modulators are mesenchymal stem/stromal cells (MSCs), which possess a remarkable ability to suppress excessive immune responses and resolve inflammation through multiple contact-dependent and soluble mechanisms [9] [33]. The therapeutic goal is to mimic these refined natural processes with orally available, tunable small molecules.
Small-molecule immunomodulators present a compelling alternative to biologic-based therapies, such as monoclonal antibodies. Their advantages include oral bioavailability, greater tissue penetration, lower production costs, and the ability to target intracellular pathways that are inaccessible to larger biologics [34] [35]. This is particularly critical for treating complex diseases and reaching therapeutic targets protected by biological barriers, such as the blood-brain barrier in glioblastoma [35].
AI and machine learning (ML) are now transforming the discovery of these precise therapeutics. By decoding the complex immunomodulatory mechanisms of MSCs—such as their secretion of factors like PGE2, IDO, and TGF-β, and their influence on T-cells and macrophages—researchers can identify novel molecular targets and engineer compounds that replicate these effects with high specificity [9] [10]. AI accelerates this process from target identification to lead optimization, harnessing multi-omics data to usher in a new generation of targeted immunomodulatory drugs [34] [36].
Foundations of MSC Immunomodulation as a Therapeutic Blueprint
The therapeutic effects of MSCs are not primarily due to their differentiation capacity but rather their potent paracrine activity and direct cell-to-cell communication with various immune cells. These innate mechanisms provide a biological blueprint for designing small-molecule therapies aimed at achieving immune tolerance.
Key Immunomodulatory Mechanisms of MSCs
MSCs exert their effects through two primary modes of action, which are well-documented in both in vitro and in vivo models:
Cell-to-Cell Contact: MSCs express surface molecules such as PD-L1, PD-L2, and ICAM-1 that engage with receptors on immune cells. For instance, the interaction between PD-L1 on MSCs and PD-1 on T cells leads to the dephosphorylation of key signaling molecules like ZAP70, ultimately suppressing T-cell activation and arresting the cell cycle in the G0/G1 phase [9] [10]. This direct contact is also crucial for MSC-mediated polarization of pro-inflammatory M1 macrophages towards an anti-inflammatory M2 phenotype, an effect dependent on factors like TSG-6 [10].
Paracrine Activity via Soluble Factors: MSCs secrete a wide array of immunomodulatory factors, including TGF-β, PGE2, IDO, HGF, and IL-10 [9] [10]. The TGF-β/Smad signaling pathway is particularly important. Upon TGF-β secretion, it binds to its receptor (TGF-βRII/RI), leading to the phosphorylation of Smad2/3. This complex then translocates to the nucleus to promote the expression of FOXP3, the master regulator of regulatory T-cells (Tregs), thereby enhancing immune suppression [10]. Similarly, IDO catalyzes tryptophan metabolism in the local microenvironment, which can inhibit T-effector cells and promote Treg differentiation [9] [34].
Table 1: Key Soluble Factors in MSC-Mediated Immunomodulation and Their Primary Actions
| Soluble Factor | Primary Immunomodulatory Action |
|---|---|
| TGF-β (Transforming Growth Factor-β) | Promotes differentiation and function of Tregs via the Smad pathway; inhibits T-cell activation [10]. |
| IDO (Indoleamine 2,3-dioxygenase) | Depletes local tryptophan, suppressing T-cell proliferation and promoting Treg induction [9] [34]. |
| PGE2 (Prostaglandin E2) | Suppresses dendritic cell maturation and drives macrophage switch from M1 to M2 phenotype [9] [10]. |
| HGF (Hepatocyte Growth Factor) | Inhibits T-cell receptor signaling, contributing to the suppression of T-cell activation [10]. |
MSC Influence on Key Immune Cells
The functional outcome of these mechanisms is a coordinated regulation of both innate and adaptive immunity:
- T-Lymphocytes: MSCs inhibit the proliferation and function of pro-inflammatory Th17 cells and promote the expansion and activation of anti-inflammatory Tregs [9] [10]. This restoration of the Th17/Treg balance is a cornerstone of their therapeutic effect in autoimmune and inflammatory conditions.
- B-Lymphocytes: MSCs can inhibit B-cell proliferation and antibody production, partly by activating p38 MAPK pathways and arresting the B-cell cycle in the G0/G1 phase [9].
- Macrophages: As mentioned, MSCs are potent inducers of M2 macrophage polarization, which is associated with tissue repair and resolution of inflammation [9] [35].
- Dendritic Cells (DCs): MSC-soluble factors like PGE2 can suppress the maturation of DCs, reducing their capacity to activate naive T-cells and initiate an inflammatory response [10].
The following diagram synthesizes the core immunomodulatory pathways and cell interactions initiated by MSCs, which serve as a foundational model for therapeutic targeting.
Diagram 1: Core immunomodulatory pathways of MSCs, highlighting key contact-dependent and paracrine mechanisms that can be targeted by small molecules.
AI and Machine Learning in the Drug Discovery Pipeline
The traditional drug discovery pipeline is notoriously lengthy, expensive, and prone to failure. AI and ML are now being integrated at every stage to increase efficiency, reduce costs, and improve the predictive power of research outcomes [34] [37]. This is particularly impactful for the complex field of immunomodulation, where AI can help navigate the vast chemical and biological space to find optimal small-molecule candidates.
Core AI Techniques and Their Applications
AI in drug discovery encompasses a range of techniques, each suited to specific tasks.
Table 2: Key AI/ML Techniques and Their Applications in Drug Discovery
| AI Technique | Category | Primary Application in Immunomodulator Discovery |
|---|---|---|
| Random Forests, SVMs | Supervised Learning | Quantitative Structure-Activity Relationship (QSAR) modeling, toxicity prediction, and virtual screening of compound libraries [34] [37]. |
| Variational Autoencoders (VAEs) | Deep Learning / Generative Models | De novo molecular design by learning a compressed latent representation of chemical space to generate novel, drug-like structures [34]. |
| Generative Adversarial Networks (GANs) | Deep Learning / Generative Models | Generating novel molecular structures with optimized properties through a competitive process between a generator and discriminator network [34]. |
| Reinforcement Learning (RL) | Machine Learning | Iterative optimization of generated molecules for desired properties like binding affinity, solubility, and synthetic accessibility [34]. |
| Convolutional Neural Networks (CNNs) | Deep Learning | Processing image-based molecular representations (e.g., 2D/3D structures) for property prediction and activity classification [38]. |
AI-Driven Workflow for Immunomodulator Discovery
The application of AI follows a structured workflow, from initial data preparation to final lead compound identification.
Diagram 2: An AI-driven drug discovery workflow, showing the pipeline from data input to lead candidate output using various molecular representation methods.
Step 1: Data Sourcing and Curation The process begins with aggregating large-scale datasets from public and proprietary sources. Key databases include:
- ChEMBL: A manually curated database of bioactive molecules with drug-like properties [38].
- PubChem: A comprehensive public database of chemical substances and their biological activities [38].
- ZINC: A curated collection of commercially available compounds for virtual screening [38].
Step 2: Molecular Representation To be processed by AI models, molecules must be converted into a machine-readable format. Common approaches include:
- SMILES (Simplified Molecular Input Line Entry System): A string-based notation that can be processed using Natural Language Processing (NLP) techniques [38].
- Molecular Graphs: Representing atoms as nodes and bonds as edges, analyzed using Graph Neural Networks (GNNs) [38].
- Image-Based Representation: Converting molecular structures into 2D or 3D images, which can then be analyzed using Convolutional Neural Networks (CNNs) [38]. This method can intuitively capture structural features and relationships.
Step 3: Model Training and Validation AI models are trained on the represented data to predict key properties, such as:
- Binding affinity to specific immunomodulatory targets (e.g., PD-L1, IDO1).
- ADMET properties (Absorption, Distribution, Metabolism, Excretion, and Toxicity), crucial for predicting in vivo efficacy and safety [34] [37].
- Synthetic accessibility.
Step 4: De Novo Molecular Generation and Virtual Screening Generative AI models, such as VAEs and GANs, can create entirely new molecular structures from scratch (de novo design) that are optimized for the desired immunomodulatory profile and drug-like properties [34]. These generated libraries, along with existing virtual compound libraries, are then rapidly screened in silico (virtual high-throughput screening) to prioritize the most promising candidates for synthesis and laboratory testing.
Experimental Protocols for Validating AI-Designed Immunomodulators
Once AI models have proposed candidate small molecules, rigorous experimental validation is essential. The following protocols outline key methodologies for confirming the biological activity and mechanism of action of these candidates, with a focus on replicating MSC-like effects.
Protocol 1:In VitroT-Cell Suppression Assay
This assay directly tests the candidate molecule's ability to mimic MSC-mediated suppression of T-cell proliferation [9] [10].
- T-Cell Isolation and Labeling: Isolate human peripheral blood mononuclear cells (PBMCs) from healthy donors using density gradient centrifugation (e.g., Ficoll-Paque). Further isolate CD4+ or CD8+ T-cells using magnetic-activated cell sorting (MACS) or fluorescence-activated cell sorting (FACS). Label the T-cells with a cell proliferation dye, such as CFSE (Carboxyfluorescein succinimidyl ester).
- T-Cell Activation: Activate the labeled T-cells using plate-bound anti-CD3 and soluble anti-CD28 antibodies to simulate antigen exposure.
- Compound Treatment: Co-culture the activated T-cells with a range of concentrations of the AI-designed small-molecule candidate. Include appropriate controls: non-activated T-cells (negative control), activated T-cells with a DMSO vehicle (positive control), and activated T-cells with a reference immunosuppressant (e.g., Cyclosporin A).
- Flow Cytometry Analysis: After 72-96 hours of culture, harvest the cells and analyze them by flow cytometry. The dilution of the CFSE dye in daughter cells is a direct measure of proliferation. The percentage of suppression is calculated by comparing the proliferation in treated wells to the vehicle-controlled wells.
- Cytokine Profiling: Collect culture supernatants and analyze them using a multiplex ELISA or Luminex assay to quantify the levels of key cytokines (e.g., IFN-γ, IL-17, IL-10, TGF-β), providing insight into the immunomodulatory phenotype induced by the compound.
Protocol 2: Macrophage Polarization Assay
This protocol assesses the candidate's capacity to drive a shift from a pro-inflammatory (M1) to an anti-inflammatory (M2) macrophage phenotype, a key MSC-like function [9] [35].
- Macrophage Differentiation: Isolate human monocytes from PBMCs via CD14+ MACS selection. Differentiate them into M0 macrophages by culturing with Macrophage Colony-Stimulating Factor (M-CSF) for 5-7 days.
- M1 Polarization and Compound Treatment: Polarize the M0 macrophages into an M1 state by adding IFN-γ and LPS. Concurrently, treat the cultures with the AI-designed small molecule. Include controls for M0, M1 (vehicle-treated), and M2 (induced by IL-4/IL-13) phenotypes.
- Flow Cytometry for Surface Markers: After 48 hours, detach the macrophages and stain for surface markers characteristic of M1 (e.g., CD80, CD86) and M2 (e.g., CD206, CD163) phenotypes. Analyze using flow cytometry.
- Gene Expression Analysis: Extract total RNA from the macrophages and perform quantitative RT-PCR (qRT-PCR) to measure the expression of M1-associated genes (e.g., TNF-α, IL-6, IL-12) and M2-associated genes (e.g., ARG1, MRC1, IL-10).
Success in this interdisciplinary field relies on a suite of specialized reagents, datasets, and computational tools.
Table 3: Essential Research Reagents and Resources for Developing Small-Molecule Immunomodulators
| Resource Category | Specific Example(s) | Key Function in R&D |
|---|---|---|
| Public Chemical/Bioactivity Databases | ChEMBL [38], PubChem [38], ZINC [38] | Provide large-scale, annotated data on chemical structures and biological activities for training and validating AI models. |
| Cell-Based Assay Reagents | Anti-CD3/CD28 antibodies, CFSE, M-CSF, IFN-γ, IL-4/IL-13 | Enable functional in vitro validation of immunomodulatory activity (e.g., T-cell suppression, macrophage polarization). |
| AI/Modeling Software & Tools | RDKit [38], Graph Neural Networks (GNNs), CNN-based image processors | Facilitate molecular representation, property prediction, and de novo molecular design. |
| Key In Vivo Disease Models | Experimental Autoimmune Encephalomyelitis (EAE), Glioma models, Allergic Rhinitis models [10] [35] | Provide preclinical in vivo systems for testing the efficacy and safety of lead compounds in a complex immune environment. |
The integration of AI and machine learning with a deep understanding of stem cell immunobiology is poised to revolutionize the development of small-molecule immunomodulators. By systematically decoding and mimicking the sophisticated mechanisms of MSCs, researchers can design precise therapeutics that target specific immune pathways with unprecedented accuracy. The AI-driven pipeline—from target identification and de novo molecular generation to predictive ADMET profiling—dramatically accelerates the transition from concept to viable therapeutic candidate.
Future progress will be fueled by the integration of ever more complex multi-omics data and the development of more sophisticated AI models, such as "digital twins" for simulating individual patient responses [34]. Furthermore, the exploration of novel molecular representation methods, including image-based learning using CNNs, offers a powerful and intuitive approach to capturing critical structural information [38]. As these technologies mature and are validated through robust experimental protocols, they will unlock a new frontier of personalized, effective, and safe immunomodulatory therapies for a wide spectrum of inflammatory, autoimmune, and oncological diseases.
The field of regenerative medicine is increasingly focused on harnessing the power of stem cells, particularly their immunomodulatory properties, for therapeutic applications. Mesenchymal stem cells (MSCs) have emerged as a promising candidate due to their low immunogenicity and ability to modulate immune responses through cell-to-cell contact and secretion of soluble factors [10]. A key mechanism involves the expression of immune checkpoint ligands like PD-L1, which interacts with PD-1 on T cells to suppress their activation and proliferation, thereby promoting an immunotolerant environment [10]. However, the inherent immunomodulatory capacity of stem cells can be insufficient to overcome host immune responses in allogeneic transplantation settings. This limitation has spurred the development of advanced genetic engineering strategies designed to enhance the immune-evasive and immunosuppressive properties of therapeutic stem cells. By systematically editing Human Leukocyte Antigen (HLA) genes to reduce immunogenicity and overexpressing checkpoint ligands to actively suppress immune responses, researchers aim to create universally compatible "off-the-shelf" stem cell products that can survive, engraft, and function effectively in a broad patient population, thereby making cell therapies more accessible, scalable, and effective [39].
The primary goal of HLA gene editing is to create hypoimmunogenic cells that can evade detection and rejection by the host's immune system. This is crucial for developing universal cell therapies that do not require patient-specific matching. The immune system recognizes and attacks foreign cells primarily through alloreactive T cells and natural killer (NK) cells, which identify targets via surface HLA molecules. HLA Class I molecules (encoded by genes HLA-A, -B, and -C) are expressed on nearly all nucleated cells and present peptides to CD8+ cytotoxic T cells. HLA Class II molecules (encoded by genes like HLA-DR, -DQ, -DP) are typically expressed on professional antigen-presenting cells and present antigens to CD4+ helper T cells. The high polymorphism of HLA genes across individuals is the main driver of transplant rejection [39].
Two predominant engineering strategies have emerged to address this challenge. The first involves the complete or partial knockout of HLA genes to prevent the expression of polymorphic proteins recognizable by the host T cells. The second, more sophisticated strategy involves replacing polymorphic HLA molecules with non-polymorphic variants that provide inhibitory signals to immune cells.
Knockout of HLA Class I and II
The most direct approach to prevent T-cell-mediated recognition is to disrupt the genes necessary for HLA expression. CRISPR-Cas9-mediated knockout of Beta-2-microglobulin (B2M), a essential subunit for HLA class I surface expression, effectively eliminates HLA class I presentation. This prevents CD8+ T cell recognition [39]. However, cells lacking HLA class I become targets for NK cell-mediated lysis via the "missing-self" response. To address this, researchers have simultaneously knocked out Class II Major Histocompatibility Complex Transactivator (CIITA), the master regulator of HLA class II expression, thereby also eliminating CD4+ T cell recognition [39]. While B2M and CIITA knockout cells are shielded from T cells, they remain vulnerable to NK cells.
Expression of Non-Polymorphic HLA Variants
To protect HLA-silenced cells from NK cell attack, a leading strategy involves introducing a non-polymorphic HLA molecule. A key innovation is the knock-in of an HLA-E-B2M fusion gene into the endogenous B2M locus [39]. HLA-E is a non-polymorphic molecule that engages the inhibitory receptor NKG2A on NK cells and a subset of T cells, transmitting a potent "do not kill" signal. This gene fusion strategy effectively replaces diverse HLA class I molecules with a single, uniform inhibitory ligand, conferring resistance to both T and NK cells [39]. Engineered cells displaying this phenotype—HLA class I/II negative but HLA-E positive—demonstrate significantly prolonged survival in vivo in immunocompetent hosts.
A related, highly precise approach known as "anchor-position editing" focuses on modulating the peptide-presenting function of HLA molecules rather than eliminating them. This technique, which involves editing a single amino acid in the invariant region of the HLA molecule (e.g., position 82), substantially reduces its ability to bind and present specific disease-driving self-peptides (such as citrullinated peptides in rheumatoid arthritis) to T cells. This method selectively "quiets" the autoimmune response without completely abolishing HLA expression, thereby minimizing the risk of global immune suppression [40].
Table 1: Key Genetic Targets for HLA Engineering
| Target Gene | Molecule Type | Engineering Strategy | Immune Cell Affected | Functional Outcome |
|---|---|---|---|---|
| B2M | HLA Class I subunit | CRISPR Knockout / Knock-in | CD8+ T Cells / NK Cells | Eliminates HLA Class I; Triggers "missing-self" NK cell activation unless combined with HLA-E. |
| CIITA | Transcriptional Regulator | CRISPR Knockout / Base Editing | CD4+ T Cells | Eliminates HLA Class II expression. |
| HLA-E | Non-polymorphic HLA | B2M-HLA-E fusion gene knock-in | NKG2A+ NK & T Cells | Provides inhibitory signal, protects from NK cell lysis. |
| HLA-DRA/DRB1 | HLA Class II | Anchor-position editing (e.g., N82L) | CD4+ T Cells | Reduces binding of specific arthritogenic peptides, modulating T cell response without global suppression [40]. |
While HLA editing reduces the immunogenicity of therapeutic cells, overexpression of immune checkpoint ligands (ICLs) actively suppresses the local immune response, fostering a tolerogenic microenvironment. This strategy is particularly relevant for stem cells used in treating inflammatory or autoimmune diseases. The most prominent target for this approach is the Programmed Death-Ligand 1 (PD-L1; CD274).
PD-L1 expressed on the surface of stem cells binds to its receptor PD-1 on activated T cells. This interaction recruits phosphatases SHP-1 and SHP-2, which dephosphorylate key signaling molecules in the T cell receptor (TCR) cascade (e.g., ZAP70, PKCθ). This leads to the suppression of downstream pathways like PI3K/AKT and MAPK/ERK, resulting in cell cycle arrest at the G0/G1 phase, inhibition of T cell proliferation, and reduction in cytokine production [10]. In the context of allergic rhinitis, for example, MSCs expressing PD-L1 can correct the Th1/Th2 imbalance and promote the proliferation of regulatory T cells (Tregs), thereby alleviating allergic inflammation [10].
The expression of PD-L1 can be intrinsic or induced by extrinsic factors within the tissue microenvironment. Interferon-gamma (IFN-γ) is one of the most potent inducers of PD-L1 expression, acting through the JAK/STAT signaling pathway and direct binding of Interferon Regulatory Factor 1 (IRF1) to the PD-L1 promoter [41]. Other inflammatory mediators, including TNF-α, IL-6, and IL-27, can also upregulate PD-L1 through pathways such as NF-κB and STAT3 [41]. From an engineering perspective, understanding these regulatory mechanisms is key. Strategies can involve constructing expression cassettes for PD-L1 under the control of a constitutive promoter or, more sophisticatedly, using synthetic biology to place the PD-L1 gene under the control of a promoter responsive to inflammatory signals like IFN-γ, creating a self-regulating feedback loop that amplifies immunosuppression precisely when and where it is needed.
Detailed Experimental Protocols
This section provides a technical breakdown of key methodologies for creating and validating hypoimmunogenic stem cells, from genome editing to functional assays.
Protocol 1: Multiplex CRISPR-Cas9 Editing of HLA Genes in Human Tregs
This protocol, adapted from a recent Nature Communications study, details the generation of hypoimmunogenic human regulatory T cells (Tregs) capable of evading both T and NK cell responses [39].
1. Isolation and Activation of Human Tregs:
- Isolate CD4+CD25+CD127- Tregs from healthy donor leukapheresis products using clinical-grade magnetic bead separation.
- Activate cells using anti-CD3/anti-CD28 antibodies in X-VIVO 15 serum-free medium supplemented with 500 IU/mL recombinant human IL-2 and 10 ng/mL recombinant human TGF-β.
2. Electroporation and RNP Delivery:
- On day 2 post-activation, harvest and wash Tregs. Prepare a CRISPR ribonucleoprotein (RNP) complex by combining:
- For B2M knockout: A mix of synthetic crRNAs targeting exon 2 of the B2M gene and tracrRNA, complexed with recombinant Cas9 protein.
- For CIITA knockout: A mix of crRNAs targeting the CIITA gene, complexed with Cas9.
- Electroporate the RNP complexes into Tregs using a Neon Transfection System (e.g., 1600V, 10ms, 3 pulses).
- Include a non-targeting RNP as a negative control.
3. Knock-in of HLA-E-B2M Fusion Gene:
- Co-electroporate the RNP complex with a single-stranded DNA (ssDNA) donor template for homology-directed repair (HDR).
- The ssDNA donor template should contain: the HLA-E cDNA sequence, a short linker (e.g., GSG), the B2M exon 2 sequence (to maintain the open reading frame), and homologous arms matching the sequences flanking the Cas9 cut site in the B2M gene.
4. Post-Editing Culture and Expansion:
- Immediately after electroporation, transfer cells to pre-warmed culture medium with IL-2.
- Expand cells for 10-14 days, feeding with fresh medium and IL-2 every 2-3 days.
5. Validation of Editing Efficiency:
- Flow Cytometry: Confirm loss of HLA class I (using an anti-HLA-A,B,C antibody) and HLA class II (anti-HLA-DR/DP/DQ) surface expression. Confirm surface expression of HLA-E using a specific antibody.
- Genomic Analysis: Use T7 Endonuclease I assay or Sanger sequencing of the target loci to confirm insertion/deletion mutations. Verify precise knock-in via PCR and sequencing across the integration junction.
Protocol 2: In Vivo Assessment of Engineered Cell Survival and Function
This protocol describes a humanized mouse model to test the persistence and immunosuppressive capability of engineered cells [39].
1. Human Skin-Xenograft Transplant Model:
- Utilize immunodeficient NSG mice.
- Implant a 4-mm punch of human skin onto the dorsal flank.
- On the day of transplant, intravenously inject a cohort of mice with either:
- Unmodified allogeneic Tregs (control)
- HLA-matched Tregs (control)
- HLA-engineered Tregs (B2M/CIITA KO + HLA-E KI)
- PBS vehicle (control)
2. Graft Monitoring and Endpoint Analysis:
- Monitor grafts daily for signs of rejection, defined as >80% graft shrinkage, desiccation, or eschar formation.
- At defined endpoints (e.g., day 100 or upon rejection), harvest grafts for analysis.
- Histology: Process graft tissue for H&E staining to assess lymphocytic infiltration and graft integrity.
- Spatial Transcriptomics: Use platforms like 10x Genomics Visium to profile gene expression directly on tissue sections, identifying enriched immunoregulatory and tissue-repair pathways in grafts protected by engineered Tregs.
3. In Vivo Cytolytic Assay:
- To directly quantify cell survival, label engineered Tregs with CFSE and host PBMCs with a cell proliferation dye (e.g., CellTrace Violet).
- Co-inject the labeled cells intraperitoneally into immunodeficient mice reconstituted with human immune cells.
- After 7 days, perform peritoneal lavage and analyze recovered cells by flow cytometry.
- Calculate the recovery ratio of engineered Tregs to host cells. A higher recovery rate indicates successful evasion of host immune killing.
Table 2: Key Reagents for HLA Engineering and Validation
| Research Reagent / Tool | Function / Application | Example / Specification |
|---|---|---|
| CRISPR-Cas9 RNP Complex | Precise genomic DNA cleavage at target loci. | Recombinant Cas9 protein, synthetic crRNA & tracrRNA. |
| ssDNA HDR Donor Template | Template for inserting new genetic sequences via homology-directed repair. | ~200 nt single-stranded DNA with homology arms and HLA-E-B2M fusion payload. |
| Electroporation System | Efficient delivery of macromolecules (RNP, DNA) into cells. | Neon Transfection System (Thermo Fisher). |
| Anti-HLA Antibodies | Validation of surface protein expression by flow cytometry. | Anti-HLA-A,B,C (Clone W6/32), Anti-HLA-DR/DP/DQ, Anti-HLA-E (Clone 3D12). |
| T7 Endonuclease I Assay | Detection of insertion/deletion mutations at the target site. | Surveyor Mutation Detection Kit (IDT). |
| Humanized Mouse Model | In vivo functional testing of engineered cells in a context with a human immune system. | NSG mouse engrafted with human skin and PBMCs. |
Critical Data and Findings
The efficacy of the described genetic engineering strategies is supported by robust preclinical data. The following table synthesizes key quantitative findings from recent studies.
Table 3: Summary of Preclinical Efficacy Data for Engineered Cell Therapies
| Cell Type | Genetic Modification | Experimental Model | Key Quantitative Outcome | Source |
|---|---|---|---|---|
| Human Tregs | Allogeneic (unmodified) | Human skin-xenograft model | Median graft survival: 24-27 days (partially mismatched) | [39] |
| Human Tregs | HLA-matched | Human skin-xenograft model | Median graft survival: >100 days | [39] |
| Human Tregs | B2M KO & CIITA KO (HLA-E KI) | Human skin-xenograft model | Median graft survival: >100 days (comparable to autologous Tregs) | [39] |
| Human Tregs | B2M KO & CIITA KO (HLA-E KI) | In vitro suppression assay | Retained potent, dose-dependent suppression of allogeneic T cell proliferation (comparable to autologous Tregs) | [39] |
| HLA Gene Editing | Anchor-position editing (N82L) | In vitro peptide binding assay | Substantially reduced binding of citrullinated arthritogenic peptides and collagen [40] | [40] |
Visualization of Signaling Pathways and Workflows
The following diagrams illustrate the core engineering workflow and the molecular mechanism of an overexpressed checkpoint ligand.
HLA Engineering Workflow for Hypoimmunogenic Cells
PD-L1 Checkpoint Signaling Mechanism
The synergistic combination of HLA gene editing and checkpoint ligand overexpression represents a paradigm shift in the development of stem cell-based therapeutics. By first reducing the inherent immunogenicity of cells through strategic manipulation of the HLA complex and then actively suppressing residual immune responses via ligands like PD-L1, researchers can create powerful, universally compatible "off-the-shelf" products. These engineered cells, as demonstrated in preclinical models, are capable of prolonged survival and potent regulatory function in immunocompetent allogeneic hosts. As the field progresses, the focus will shift towards optimizing the safety and specificity of these genetic modifications, standardizing manufacturing protocols, and translating these transformative therapies into clinical trials for a wide range of autoimmune, inflammatory, and degenerative diseases. The ultimate goal is to realize the full potential of regenerative medicine by making effective cell therapies accessible to a broad patient population.
The success of regenerative medicine strategies, particularly those involving stem cell therapies, is profoundly influenced by the host immune response to the implanted biomaterial scaffold. Rather than acting as a passive delivery vehicle, the biomaterial itself actively instructs the local immune microenvironment, a process that can either potentiate or undermine therapeutic outcomes [42] [43]. The polarization of CD4+ T helper (Th) cells, specifically the balance between pro-regenerative Th2 and pro-inflammatory Th17 subsets, serves as a critical nexus in this process, determining the trajectory toward functional integration or chronic inflammation and fibrosis [42] [10]. This technical guide examines the mechanisms by which biomaterial scaffolds modulate this pivotal decision, framing the discussion within the broader objective of harnessing stem cell immunomodulation for personalized patient outcomes. A deep understanding of these interactions is paramount for researchers and drug development professionals aiming to engineer next-generation scaffolds that predictably steer the immune system toward a pro-regenerative phenotype.
Core Principles of Biomaterial-Driven Immune Polarization
The implantation of a biomaterial initiates a well-orchestrated sequence of immune cell recruitment and activation, beginning with the innate immune response. The ultimate polarization of the adaptive immune system, particularly T cells, is directly influenced by the biomaterial's physicochemical properties and the phenotype of innate immune cells it first encounters [42] [43].
- Innate Immune Instruction: Neutrophils and macrophages are the first responders. Their activation state in response to the biomaterial sets the stage for subsequent T cell polarization. Macrophages, in particular, are crucial intermediaries; their functional phenotype dictates the cytokine milieu that directs naive T cell differentiation [42] [44].
- The Th2/Th17 Balance: A pro-regenerative environment is typically associated with a Th2-skewed response, characterized by the production of cytokines like IL-4, IL-5, and IL-13, which promote tissue repair, alternative macrophage activation (M2), and antibody production. In contrast, a Th17-dominant response, defined by IL-17A and IL-17F secretion, drives neutrophilic inflammation, autoimmunity, and fibrosis, ultimately hindering regeneration [42] [10].
- Biomaterial as an Instructive Platform: Biomaterial properties—including chemistry, topography, stiffness, and degradation profile—can be engineered to deliver specific cues to immune cells. By presenting the right signals, the scaffold can promote tolerogenic dendritic cells and M2 macrophages, which in turn favor the expansion of Th2 and regulatory T cells (Tregs) over Th1 and Th17 subsets [43] [45].
Quantitative Analysis of Biomaterial Properties on Immune Cell Fate
The intrinsic properties of a biomaterial significantly impact the ensuing immune response. The following table summarizes key findings from in vivo and in vitro studies investigating how different biomaterials influence innate immune cell activation and subsequent T cell polarization.
Table 1: Impact of Biomaterial Bulk Chemistry on Immune Cell Recruitment and Polarization
| Biomaterial | Neutrophil Response | Macrophage-Induced T Cell Polarization | Overall Inflammatory Profile |
|---|---|---|---|
| Polyetheretherketone (PEEK) | High recruitment; elevated NE, MPO, and NETs production [42] | Increased Th1/Th17; decreased Th2/Treg [42] | Robust inflammation; high risk of fibrous encapsulation [42] |
| 316L Stainless Steel (SS) | High recruitment; elevated NE, MPO, and NETs production [42] | Increased Th1/Th17; decreased Th2/Treg [42] | Robust inflammation; high risk of fibrous encapsulation [42] |
| Titanium Alloy (TiAlV) | Lower neutrophil activation vs. PEEK/SS [42] | Increased Th1/Th17; decreased Th2/Treg (less than PEEK/SS) [42] | Moderate inflammation [42] |
| Pure Titanium (Ti) | Lowest recruitment and activation [42] | Most favorable balance; less Th1/Th17 drive [42] | Least inflammatory; supports osseointegration [42] |
Beyond bulk chemistry, other physicochemical parameters are critical levers for immune engineering. Surface topography and wettability have been shown to directly affect macrophage polarization, with specific micro- and nano-scale patterns promoting an anti-inflammatory M2 phenotype [42]. Furthermore, the mechanical stiffness of a scaffold is a potent determinant of cell fate; materials with stiffnesses mimicking the target tissue are more likely to support a regenerative outcome by reducing the activation of pro-inflammatory pathways in resident cells [45].
Table 2: Engineering Biomaterial Properties for a Pro-Regenerative Immune Response
| Biomaterial Property | Pro-Inflammatory Signal (Promoting Th17) | Pro-Regenerative Signal (Promoting Th2/Treg) | Key Immune Mechanisms |
|---|---|---|---|
| Surface Chemistry | High wettability alone on certain chemistries [42] | Titanium oxide layer [42] | Modulates protein adsorption, DAMP release, and macrophage cytokine secretion [42] [43] |
| Topography/Roughness | Smooth surfaces on Ti (increases MPO, NE, NETs) [42] | Rough, hydrophilic surfaces on Ti [42] | Directs macrophage polarization toward M2; reduces neutrophil hyperactivation [42] |
| Stiffness | Mismatch with native tissue (e.g., high modulus metals) [42] | Matching native tissue (e.g., PEEK's bone-like modulus) [42] | Activates mechanosensing pathways; influences fibroblast and MSC differentiation [42] [45] |
| Degradation Profile | Fast, acidic degradation (e.g., some polyesters) [43] | Slow, controlled degradation with neutral byproducts [43] | Degradation products can act as DAMPs; chronic release sustains inflammation [43] |
Experimental Protocols for Evaluating Biomaterial-Immune Interactions
To systematically evaluate the immunomodulatory capacity of novel biomaterials, standardized in vitro and in vivo protocols are essential. The following sections detail key methodologies for assessing immune cell recruitment and T cell polarization.
In Vitro Macrophage:T Cell Co-culture Assay
This protocol is designed to test how a biomaterial-primed macrophage influences the polarization of naive T cells, a critical step in the adaptive immune response [42].
- Step 1: Macrophage Culture and Priming on Biomaterials. Isolate and differentiate primary human or mouse monocyte-derived macrophages. Seed macrophages onto the test biomaterial surfaces (e.g., 15mm disks) or tissue culture plastic (TCP) controls. Culture for 24-48 hours in standard medium to allow for biomaterial-dependent priming [42].
- Step 2: T Cell Isolation and Co-culture. Isolate naive CD4+ T cells from peripheral blood or spleen using a magnetic-activated cell sorting (MACS) kit. Activate the T cells with plate-bound anti-CD3 and soluble anti-CD28 antibodies. Establish a Transwell co-culture system, with the primed macrophages in the lower chamber and the activated T cells in the upper insert, or use a direct contact system depending on the hypothesis [42] [10].
- Step 3: Phenotypic Analysis. After 72-96 hours of co-culture, analyze T cell polarization by flow cytometry. Key surface markers include: CD4 (T helper), CXCR5 (T follicular helper), CCR6 (Th17), and CD25/FoxP3 (Treg). Intracellular cytokine staining for IFN-γ (Th1), IL-4 (Th2), and IL-17A (Th17) provides functional validation [42]. Collect supernatant for multiplex cytokine analysis (e.g., IL-4, IL-5, IL-13, IL-17A, IFN-γ) to quantify the secretory profile.
In Vivo Murine Femoral Implant Model
This model allows for the assessment of the local and systemic immune response to an implanted biomaterial in a relevant physiological environment [42].
- Step 1: Implant Preparation and Sterilization. Machine test and control materials (e.g., Ti, PEEK, SS) into 1mm diameter rods. Sterilize all implants thoroughly using gamma irradiation or ethylene oxide to prevent confounding immune responses from endotoxin contamination [42] [43].
- Step 2: Surgical Implantation. Anesthetize 12-week-old male C57BL/6 mice using an approved protocol. Make a lateral incision to expose the distal femur. Drill a bicortical defect and surgically implant the material rod into the medullary canal. Close the wound with sutures or staples [42].
- Step 3: Tissue Harvest and Analysis. At predetermined endpoints (e.g., 7, 14, 28 days post-implantation), euthanize the animals and explant the femurs with the surrounding tissue.
- Flow Cytometry: Create a single-cell suspension from the bone marrow and surrounding tissue. Analyze for immune cell infiltration using antibodies against: Ly6G (neutrophils), F4/80 (macrophages), CD206 (M2 macrophage), CD4 (T helper), and CD8 (cytotoxic T). Intracellular staining defines Th subsets [42].
- Histology: Fix and section the explanted tissue. Use Hematoxylin and Eosin (H&E) to assess general morphology and cellularity. Masson's Trichrome or Picrosirius Red staining to evaluate collagen deposition and fibrous encapsulation [42] [43]. Immunohistochemistry for specific cytokines (e.g., IL-17, IL-4) can localize protein expression.
The following diagram illustrates the logical workflow and key analysis endpoints for these protocols.
Signaling Pathways in Biomaterial-Mediated T Cell Polarization
The differentiation of naive CD4+ T cells into specific effector subsets is governed by distinct signaling pathways, which can be modulated by cytokines released from biomaterial-instructed antigen-presenting cells (APCs). The following diagram maps the key signaling cascades that drive Th2 and Th17 commitment.
Biomaterial scaffolds that promote the release of IL-4 from basophils or other innate cells will engage the JAK/STAT6 pathway in T cells, leading to the upregulation of the master transcription factor GATA3. GATA3 drives the genetic program for Th2 differentiation, resulting in the production of IL-4, IL-5, and IL-13 [10] [44]. In contrast, materials that induce a strong inflammatory response in macrophages and dendritic cells, characterized by the secretion of IL-6, TGF-β, and IL-23, will activate the JAK/STAT3 pathway in T cells. This, in turn, upregulates the transcription factor RORγt, which is essential for Th17 lineage commitment and the production of IL-17 and IL-22 [42] [10]. The specific cytokine milieu presented by the biomaterial-conditioned innate immune cells is therefore the decisive factor in T cell fate.
The Scientist's Toolkit: Research Reagent Solutions
To effectively investigate biomaterial-immune interactions, a standardized set of research tools and reagents is required. The following table catalogues essential items for characterizing the immune response and probing underlying mechanisms.
Table 3: Essential Research Reagents for Investigating Biomaterial-Driven Immune Polarization
| Reagent / Tool Category | Specific Examples | Primary Function in Experimental Workflow |
|---|---|---|
| Model Biomaterials | Ti, TiAlV, 316L Stainless Steel, PEEK, PLGA, Agarose [42] [43] | Serve as positive/negative controls for immune activation; baseline for testing novel materials. |
| Immune Cell Isolation Kits | MACS or FACS kits for CD4+ T cells, monocytes, neutrophils [42] | Isulate pure populations of primary immune cells for in vitro co-culture studies. |
| Cell Culture Supplements | Recombinant cytokines: IL-4, IL-6, TGF-β, IL-23; Polarizing antibodies: anti-IFN-γ, anti-IL-4 [42] [10] | Directly polarize T cells or macrophages in vitro to establish control conditions. |
| Flow Cytometry Antibodies | Surface: CD4, CD25, CCR6, CXCR3. Intracellular: FoxP3, RORγt, GATA3, T-bet, IFN-γ, IL-4, IL-17A [42] [10] | Identify and quantify distinct immune cell populations and their activation states. |
| Cytokine Detection Assays | ELISA or Luminex kits for IFN-γ, IL-4, IL-5, IL-13, IL-17A, IL-10, TGF-β [42] [10] | Quantify soluble mediators in culture supernatant or serum to define immune phenotype. |
| Histology Stains | H&E, Masson's Trichrome, Picrosirius Red, Immunofluorescence (IF) for cytokines [42] [43] | Visualize tissue integration, fibrosis, and cellular localization in explanted scaffolds. |
| Small Molecule Inhibitors | STAT3 inhibitors (e.g., Stattic), STAT6 inhibitors, RORγt inverse agonists [10] | Mechanistic studies to block specific signaling pathways and confirm their role. |
The paradigm in regenerative medicine is shifting from viewing the biomaterial scaffold as a passive structural component to recognizing it as an active, instructive platform for immune system modulation. The deliberate engineering of biomaterials to promote a Th2/Treg-weighted response over a Th17-driven reaction represents a powerful strategy to enhance the efficacy of stem cell therapies and improve regenerative outcomes. This approach requires a multidisciplinary effort, integrating principles from materials science, immunology, and molecular biology. By employing the quantitative analyses, experimental protocols, and reagent tools outlined in this guide, researchers and drug developers can systematically design and validate next-generation delivery scaffolds that harness the body's own immune mechanisms to create a pro-regenerative environment, ultimately paving the way for more predictable and successful patient-specific therapies.
The advent of advanced cell-based therapies, including various forms of stem cell transplantation and chimeric antigen receptor (CAR)-T cell therapy, has revolutionized treatment for numerous malignant, autoimmune, and degenerative diseases. However, significant challenges remain, including risks of relapse, severe toxicities such as cytokine release syndrome (CRS), and unpredictable treatment responses [46] [47]. A critical factor determining clinical outcomes is the dynamic interplay between administered therapeutic cells and the patient's immune system. To decipher this complex relationship, researchers are increasingly turning to high-dimensional single-cell technologies—specifically, high-parameter flow cytometry and mass cytometry (CyTOF)—for deep immunophenotyping. These technologies enable comprehensive monitoring of immune reconstitution, therapeutic cell persistence, and functional status, providing invaluable insights into mechanisms of action, treatment efficacy, and toxicity [47] [48] [49]. This technical guide outlines standardized methodologies and analytical frameworks for implementing these powerful immune monitoring tools in the context of stem cell therapies, framed within a broader thesis on understanding patient-specific mechanisms of immune modulation.
Technology Comparison: High-Parameter Flow Cytometry versus Mass Cytometry
Selecting the appropriate high-parameter technology depends on experimental needs, sample availability, and analytical requirements. The table below provides a systematic comparison of spectral flow cytometry and mass cytometry (CyTOF) for deep immunophenotyping applications.
Table 1: Technical Comparison of Spectral Flow Cytometry and Mass Cytometry (CyTOF)
| Feature | Spectral Flow Cytometry | Mass Cytometry (CyTOF) |
|---|---|---|
| Core Principle | Measurement of full emission spectra from fluorochrome-labeled antibodies using multiple lasers and calibrated spectral libraries [50]. | Measurement of metal isotope-tagged antibodies via time-of-flight mass spectrometry [48]. |
| Parameter Capacity | Up to 40+ markers simultaneously with current instruments [50]. | 50+ markers simultaneously, limited primarily by panel design and metal availability [48]. |
| Throughput Speed | High (≥10,000 cells/second) [48]. | Low (300-500 cells/second) [48]. |
| Cell Loss | Minimal with standard protocols. | Significant during acquisition and staining; protocols often require enrichment steps for rare populations [48]. |
| Key Advantage | High-speed analysis of complex samples, ability to use well-established fluorochromes. | Minimal signal overlap, extreme multiplexing capacity, stable metal tags enabling sample barcoding and batch analysis [48]. |
| Primary Limitation | Complex spectral unmixing requires reference controls and specialized software [50]. | Slow acquisition speed, requires cell fixation, no native side-scatter equivalent, destructive to samples [48]. |
| Ideal Use Case | Longitudinal monitoring requiring high cell throughput, functional assays (e.g., intracellular cytokine staining) [47]. | Maximal phenotypic depth from limited samples, deep immune profiling discovery studies, high-plex fixed sample analysis [48] [49]. |
Experimental Protocols for Immune Monitoring
Standardized protocols are essential for generating reproducible and reliable data in immune monitoring studies. The following sections detail methodologies for sample preparation, staining, and data acquisition for both flow and mass cytometry.
Sample Preparation and Staining for High-Parameter Flow Cytometry
The following protocol is adapted from a standardized 13-colour/15-parameter flow cytometry assay for monitoring CAR-T cell patients [47].
- Blood Sample Collection: Collect peripheral blood in EDTA or heparin tubes. Note: The choice of anticoagulant may depend on subsequent staining steps (e.g., heparinized blood is recommended for intracellular staining involving stimulation).
- Absolute Leukocyte Counting and Viability Assessment:
- Add 100 µL of EDTA-anticoagulated whole blood to a ready-to-use dry antibody tube containing anti-CD45-FITC and a viability dye (e.g., 7-AAD).
- Add reference beads for absolute counting.
- Mix for 6-8 seconds and incubate for 15 minutes at room temperature (RT) in the dark.
- Lyse red blood cells by adding 2 mL of lysing solution (e.g., VersaLyse), mix, and incubate for 10 minutes at RT in the dark.
- Acquire on a flow cytometer. The absolute count of CD45+ leukocytes is used to estimate cellular concentrations in subsequent staining panels [47].
- Surface Marker Staining:
- Use pre-formulated dry antibody panels (e.g., DURA Innovations format) to minimize technical variability. These can be supplemented with additional liquid "drop-in" antibodies for customization.
- Add the custom antibody mix to a test tube.
- Add 100 µL of EDTA-anticoagulated whole blood, mix, and incubate for 15 minutes at RT in the dark.
- Lyse red blood cells with 2 mL of lysing solution, incubate for 10 minutes, then centrifuge at 200 g for 5 minutes.
- Discard the supernatant, wash the cell pellet with 3 mL of phosphate-buffered saline (PBS), and centrifuge again.
- Discard the supernatant and resuspend the cells in 0.5 mL of PBS containing 0.1% formaldehyde for acquisition [47].
- Intracellular Staining (for cytokines, transcription factors, etc.):
- Start with 50 µL of heparinized blood. Stimulate cells if detecting cytokines (e.g., using PMA and Ionomycin with Brefeldin A for 3-4 hours at 37°C). Use an unstimulated control.
- Fix and permeabilize cells using a commercial buffer system (e.g., FoxP3 / Transcription Factor Staining Buffer Set).
- Add the fixed and permeabilized sample to a tube containing a pre-configured intracellular antibody panel.
- Incubate for 30 minutes at RT in the dark.
- Wash with permeabilization buffer, centrifuge, and resuspend in an appropriate stabilization buffer before acquisition [47].
Mass Cytometry (CyTOF) Staining and Barcoding Protocol
This protocol is based on longitudinal immune profiling of multiple sclerosis patients after autologous hematopoietic stem cell transplantation (AHSCT) [49].
- PBMC Isolation and Cryopreservation:
- Isolate Peripheral Blood Mononuclear Cells (PBMCs) from heparinized blood using density gradient centrifugation (e.g., Ficoll-Paque PLUS).
- Cryopreserve PBMCs in fetal bovine serum (FBS) supplemented with 10% DMSO and store in liquid nitrogen until use.
- Cell Thawing and Recovery:
- Thaw cryopreserved PBMCs rapidly at 37°C.
- Wash cells and incubate in Benzonase-supplemented culture media for 2 hours at 37°C and 5% CO₂ to allow for recovery.
- Sample Barcoding:
- To minimize staining variability and inter-sample acquisition bias, barcode individual samples using a live-cell barcoding kit (e.g., Cell-ID 20-Plex Pd Barcoding Kit).
- Label live cells from different samples (e.g., different time points or patients) with unique combinations of palladium isotopes.
- After barcoding, pool all samples into a single tube.
- Surface Antigen Staining:
- Wash the pooled, barcoded cells.
- Resuspend the cell pellet in a master mix of metal-tagged antibodies targeting surface markers. Incubate for 30-60 minutes at RT.
- Wash cells to remove unbound antibodies.
- Intracellular Staining:
- Fix and permeabilize the stained cells using a commercial buffer system.
- Incubate cells with metal-tagged antibodies against intracellular targets (e.g., CTLA-4, Ki-67) for 45 minutes.
- DNA Staining and Acquisition:
- Stain cellular DNA with an intercalator-Iridium solution to facilitate cell identification.
- Acquire data on a mass cytometer (e.g., Helios CyTOF). Use normalization beads during acquisition to correct for instrument sensitivity fluctuations over time [49].
Figure 1: CyTOF Experimental Workflow. The workflow outlines the key steps from patient sample collection to data acquisition, highlighting the sample barcoding and pooling steps that reduce technical variability.
Analytical Workflows for High-Dimensional Cytometry Data
The complex, high-dimensional data generated by these technologies require specialized computational tools and workflows for unbiased analysis.
Preprocessing and Quality Control
- Data Cleaning: Remove technical artifacts, doublets, and dead cells. In CyTOF, use DNA and viability staining (e.g., cisplatin) to exclude debris and dead cells [48] [50].
- Data Transformation: Apply arcsinh (inverse hyperbolic sine) transformation to normalize the skewed distribution of cytometry data and stabilize variance across markers.
- Batch Effect Correction: When integrating data from multiple batches or time points, use algorithms to remove technical variation while preserving biological signals [50].
Dimensionality Reduction and Clustering
- Dimensionality Reduction: Use algorithms like t-Distributed Stochastic Neighbor Embedding (t-SNE) or Uniform Manifold Approximation and Projection (UMAP) to project high-dimensional data into 2D or 3D maps for visualization, allowing for the identification of cellular clusters [51] [50].
- Automated Clustering: Apply clustering algorithms such as FlowSOM or PhenoGraph to group cells into phenotypically distinct populations in an unbiased manner, without manual gating. This is essential for discovering novel or rare cell subsets [50].
Mapping and Interpretation
- Phenotyping: Manually or automatically annotate the resulting cell clusters based on the expression of known marker combinations. Statistical comparison of cluster abundances between patient groups (e.g., responders vs. non-responders) can identify biologically relevant populations [51] [49].
Figure 2: High-Dimensional Data Analysis Pipeline. The core steps for analyzing high-parameter cytometry data, from raw files to biological insight.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of these complex assays relies on a suite of specialized reagents and tools. The following table catalogs key solutions used in the field.
Table 2: Essential Research Reagent Solutions for Deep Immunophenotyping
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| Pre-configured Dry Antibody Panels (e.g., DURA Innovations) | Pre-formulated, dry antibody layers in ready-to-use tubes minimize pipetting errors and inter-operator variability, enhancing standardization [47]. | Standardized 13+ color T cell and NK cell phenotyping in CAR-T clinical trials [47]. |
| Cell Barcoding Kits (e.g., Cell-ID 20-Plex Pd Barcoding) | Allows pooling of multiple samples for simultaneous staining and acquisition, reducing technical variability and reagent costs [48] [49]. | Longitudinal tracking of patient PBMCs from multiple time points in a single CyTOF run [49]. |
| Maxpar Direct Immune Profiling Assay | A fixed, pre-optimized panel for CyTOF providing a broad immune overview, which can be customized with additional markers [52]. | Rapid, standardized immune profiling in clinical studies, such as MSC therapy for COVID-19 pneumonia [52]. |
| Viability Stains (e.g., Cisplatin for CyTOF, Zombie dyes for flow) | Distinguishes live from dead cells during analysis, which is critical for data quality, especially when using cryopreserved samples [48] [50]. | Exclusion of dead cells in PBMC samples to prevent non-specific antibody binding and false positives. |
| Metal-Labeled Antibodies | Antibodies conjugated to stable metal isotopes (e.g., Lanthanides) are the primary detection reagents for CyTOF [48]. | Custom panel design for simultaneous detection of 30+ cell surface and intracellular proteins. |
| Data Analysis Software (e.g., FlowJo, Cytobank) | Platforms offering both traditional manual gating and integrated machine learning tools (clustering, UMAP, t-SNE) for high-dimensional data exploration [51]. | Unbiased identification of novel T cell subsets associated with treatment response in AHSCT patients [49]. |
Application in Stem Cell Therapy Monitoring
The application of these technologies in clinical studies has yielded critical insights into the immune mechanisms underlying treatment success and failure.
- Monitoring CAR-T Cell Therapies: Standardized high-parameter flow cytometry enables longitudinal tracking of CAR-T cell persistence and activation status (e.g., CD69, PD-1), differentiation, and cytotoxic potential (e.g., perforin, granzyme B). Concurrently, it assesses the depletion of target cells (e.g., CD19+ B cells) and the systemic immune response, providing data to correlate with toxicities like CRS [47].
- Unraveling Mechanisms of AHSCT: CyTOF-based deep immunophenotyping has revealed that the efficacy of AHSCT in multiple sclerosis is associated with a profound reconfiguration of the immune system. Key findings include a preferential recovery of naïve B cells with prolonged depletion of memory B cells and plasmablasts, a shift in CD4+ T cells from central memory to effector memory phenotypes, and a selective loss of polyfunctional Th1/Th17 cells. These changes collectively contribute to the "immune reset" observed in successfully treated patients [49].
- Evaluating Mesenchymal Stem Cell (MSC) Therapies: Mass cytometry was used to profile immune changes in patients with COVID-19 pneumonia treated with MSCs. The analysis revealed that clinical improvement was linked to the disappearance of overactivated cytokine-secreting immune cells and an expansion of regulatory dendritic cell subsets, providing a mechanistic explanation for how MSCs may mitigate cytokine storm [52].
High-parameter flow cytometry and mass cytometry are indispensable tools for deconstructing the complex immunological consequences of stem cell therapies. By providing a high-resolution, systems-level view of the immune landscape, these technologies move beyond simple correlative analyses to reveal patient-specific mechanisms of immune modulation, persistence, and toxicity. The continued standardization of experimental protocols, coupled with advanced computational analytics, is paving the way for these methods to transition from research tools to routine clinical monitoring assays. This will ultimately enhance our ability to predict patient outcomes, optimize therapeutic protocols, and develop novel interventions with improved efficacy and safety profiles.
Navigating Clinical Hurdles: Strategies to Mitigate Rejection and Enhance Efficacy
The success of advanced therapies, including stem cell transplantation and regenerative medicine, is critically dependent on overcoming the formidable barriers posed by the recipient's innate immune system. Two of the most significant components of this response are natural killer (NK) cell-mediated "missing-self" recognition and complement activation. NK cells, large granular lymphocytes of the innate immune system, rapidly identify and eliminate target cells that lack or downregulate major histocompatibility complex (MHC) class I molecules—a phenomenon termed "missing-self" recognition [53]. Simultaneously, the complement system can initiate a cascade of events leading to opsonization and direct lysis of foreign or transplanted cells. Within the context of stem cell-based therapies, understanding and mitigating these immune responses is paramount for achieving therapeutic efficacy and long-term persistence of administered cells. This technical guide examines the molecular mechanisms underlying these immune hurdles and details experimental approaches for their investigation and modulation, providing researchers with the frameworks needed to advance the clinical application of stem cell therapies.
Molecular Mechanisms of NK Cell Activation and "Missing-Self" Recognition
Fundamental NK Cell Biology
Natural killer cells are innate lymphocytes that play central roles in immune surveillance, tissue homeostasis, and the regulation of adaptive immunity [54]. Their defining feature is the ability to mediate rapid cytotoxicity against stressed target cells without prior sensitization, utilizing effector mechanisms including perforin and granzyme release, death receptor signaling, and cytokine production [55]. Unlike T cells, NK cells do not express CD3, B-cell receptors, or T-cell receptors, instead relying on an intricate balance of germline-encoded activating and inhibitory receptors to discriminate between healthy and aberrant cells [53].
The cytotoxic machinery of NK cells is contained within cytoplasmic vesicles filled with perforin and various granzymes. Upon target recognition, these granules polarize toward the immunological synapse—the interface between the NK cell and its target—where their contents are released. Perform creates pores in the target cell membrane, allowing granzymes to enter and initiate apoptosis through caspase activation [55]. Additionally, NK cells can eliminate targets via Fas/FasL and TRAIL pathways, which trigger apoptotic signaling cascades [56].
The "Missing-Self" Recognition Paradigm
The "missing-self" hypothesis, first advanced in 1986, explains how NK cells identify cells with downregulated or absent MHC class I molecules, a common evasion strategy employed by malignant and virally infected cells [55] [53]. Under steady-state conditions, inhibitory receptors on NK cells—including killer-cell immunoglobulin-like receptors (KIRs), CD94/NKG2A, and ILT2—engage with self-MHC class I molecules on potential target cells, transmitting dominant negative signals that prevent NK cell activation [57] [56].
When target cells lack sufficient MHC class I expression, these inhibitory signals are absent, tipping the balance toward activation and triggering NK cell-mediated cytotoxicity. This mechanism is particularly relevant in transplantation settings, where donor cells may not express the recipient's specific MHC class I haplotypes, rendering them vulnerable to NK cell attack [57]. The clinical significance of this phenomenon was highlighted in a translational study of kidney transplant recipients, where "missing-self" identified through donor and recipient genotyping was an independent predictor of worse allograft survival in patients with complement-independent chronic antibody-mediated rejection [57].
Table 1: Key NK Cell Receptors and Their Ligands
| Receptor | Type | Ligand | Function | Signaling Pathway |
|---|---|---|---|---|
| KIRs | Inhibitory/Activating | HLA class I | Inhibition via ITIM domains; limited activation via ITAM adapters | DAP12/FcεRγ for activating KIRs |
| NKG2A | Inhibitory | HLA-E | Inhibition through ITIM domains | Recruits SHP-1/SHP-2 phosphatases |
| NKG2D | Activating | MICA/B, ULBP | Stress surveillance; potent activation | DAP10/PI3K pathway |
| DNAM-1 | Activating | PVR, Nectin-2 | Adhesion and co-activation | ??? |
| CD16 (FcγRIIIA) | Activating | IgG Fc | Mediates ADCC | ITAM via DAP12/FcεRγ |
| NKp46 | Activating | Viral hemagglutinins? | Natural cytotoxicity; viral recognition | ITAM via CD3ζ/FcεRγ |
Complement Activation Pathways
The complement system represents another critical innate immune barrier, comprising over 30 plasma and membrane-bound proteins that orchestrate a proteolytic cascade leading to opsonization, inflammation, and direct membrane attack. Three pathways—classical, lectin, and alternative—converge on C3 convertase formation, ultimately generating the membrane attack complex (MAC) that creates pores in target cell membranes. In transplantation and cellular therapy contexts, complement activation occurs primarily through the classical pathway initiated by antibody binding to donor antigens, though the alternative and lectin pathways may also contribute [57].
The significance of complement activation is particularly evident in antibody-mediated rejection (AMR), where donor-specific antibodies (DSAs) bind to graft endothelium and activate complement, accelerating rejection. However, complement activation is not mandatory for rejection, as demonstrated in experimental models where complement-independent pathways still mediate significant injury [57].
Strategic Approaches to Mitigate NK Cell and Complement Responses
Genetic Engineering of Therapeutic Cells
Genetic modification of donor cells represents a powerful strategy to circumvent innate immune recognition. For evasion of NK cell activity, several approaches show promise:
- Forced expression of non-classical MHC molecules: Introduction of HLA-E or HLA-G can engage inhibitory receptors NKG2A and KIR2DL4, respectively, transmitting inhibitory signals to NK cells even in the absence of classical MHC class I [56].
- Modification of activating ligand expression: Downregulation of stress-induced ligands for NKG2D and other activating receptors reduces "stress-surveillance" mediated NK cell activation.
- Expression of complement regulatory proteins: Introduction of human complement regulators (hCD46, hCD55, hCD59) protects donor cells from complement-mediated lysis [56]. This approach has demonstrated success in pig-to-non-human primate xenotransplantation models, where expression of these regulators alongside knockout of major xenocarbohydrate antigens prevented hyperacute and acute vascular rejection [56].
The efficacy of these genetic strategies is evidenced in advanced xenotransplantation models, where pigs engineered with multiple genetic modifications (including αGal knockout combined with human complement regulator and thrombomodulin expression) supported life-supporting xenograft function for up to 195 days in non-human primates [56].
Stem Cell-Mediated Immunomodulation
Mesenchymal stem cells (MSCs) possess potent immunomodulatory properties that can be harnessed to mitigate innate immune responses. MSCs modulate immune function through both direct cell-cell contact and paracrine secretion of bioactive molecules including growth factors, cytokines, and extracellular vesicles [11]. They interact with various immune cells—including T cells, B cells, dendritic cells, and NK cells—to suppress excessive inflammation and promote tolerance [11].
The molecular mechanisms underlying MSC-mediated immunomodulation include:
- Secretion of soluble mediators: TGF-β, PGE2, IDO, and other factors suppress immune cell activation and proliferation [58].
- Metabolic disruption: IDO-mediated tryptophan depletion creates a local immunosuppressive microenvironment.
- Exosome-mediated signaling: Regulatory miRNAs such as miR-21 and miR-146a packaged within MSC-derived exosomes modulate recipient immune responses [58].
MSCs also exhibit homing capabilities, migrating to inflamed sites in a CXCR4/SDF-1 axis-dependent manner, where they can exert localized immunomodulatory effects and directly participate in tissue repair [58]. These properties have been leveraged in clinical applications such as graft-versus-host disease (GVHD), where the recently FDA-approved MSC product Ryoncil (remestemcel-L) demonstrated efficacy for pediatric steroid-refractory acute GVHD [59].
Table 2: Clinical Trials of Stem Cell Therapies in Autoimmune Conditions (2006-2025)
| Disease Focus | Number of Trials | Primary Cell Type | Key Therapeutic Mechanisms |
|---|---|---|---|
| Crohn's Disease | 85 | Mesenchymal Stem Cells (MSCs) | Immune modulation, tissue repair via growth factors |
| Systemic Lupus Erythematosus | 36 | Hematopoietic Stem Cells (HSCs), MSCs | Re-establishment of immune tolerance, suppression of autoreactive cells |
| Scleroderma | 32 | HSCs, MSCs | Immune reset, tissue repair |
| Rheumatoid Arthritis | Not specified | MSCs | Modulation of T and B cell responses, anti-inflammatory signaling |
| Inflammatory Bowel Disease | Not specified | MSCs | Regulation of Th cell responses, intestinal barrier repair |
Biomaterial and Surface Engineering Approaches
Emerging biomaterial-based strategies offer promising alternatives to genetic modification for customizing cellular therapeutics. Surface engineering techniques enable the direct modification of cell membranes with immunomodulatory molecules without genetic manipulation. Key approaches include:
- Covalent conjugation: Immobilization of proteins or ligands directly onto surface residues.
- Metabolic glycoengineering: Incorporation of modified sugars that can be selectively functionalized.
- Bio-orthogonal click chemistry: Highly specific coupling reactions for attaching complex molecules.
- Hydrophobic insertion: Spontaneous integration of lipid-modified compounds into the cell membrane [60].
These techniques have been applied to NK cells themselves to enhance their therapeutic efficacy in cancer immunotherapy, demonstrating the potential for similar approaches to modify therapeutic cells for enhanced evasion of immune responses. Biomaterial-assisted surface engineering supports programmable cell-cell interactions while maintaining native cellular functions, offering practical advantages in flexibility, reversibility, and manufacturing scalability [60].
Experimental Protocols for Assessing Immune Evasion
In Vitro Assessment of NK Cell Responses
Robust in vitro assays are essential for evaluating the success of immune evasion strategies. The following protocols represent key methodologies for assessing NK cell responses:
CD107a Degranulation Assay
- Principle: Surface exposure of CD107a (LAMP-1) indicates fusion of cytotoxic granules with the plasma membrane during degranulation.
- Procedure:
- Co-culture effector NK cells with target cells at appropriate effector-to-target ratios (typically 10:1 to 1:1).
- Add anti-CD107a antibody at the beginning of the assay to label degranulating cells.
- Include protein transport inhibitor (e.g., monensin) to prevent internalization of surface CD107a.
- Incubate for 3-6 hours at 37°C, 5% CO₂.
- Harvest cells and perform surface staining for NK cell markers (CD56, CD3) and intracellular staining for cytokines if desired.
- Analyze by flow cytometry; CD107a expression on CD3⁻CD56⁺ cells indicates NK cell degranulation.
Cytotoxicity Release Assay
- Principle: Measures membrane damage in target cells by quantifying release of incorporated labels.
- Procedure:
- Label target cells with ⁵¹Chromium or BATDA for 1-2 hours.
- Wash excess label and co-culture with effector NK cells at various ratios in round-bottom plates.
- Centrifuge briefly to initiate cell contact and incubate for 4 hours at 37°C.
- Collect supernatant and quantify released radioactivity (⁵¹Cr) or fluorescence (BATDA).
- Calculate specific lysis as: (Experimental release - Spontaneous release) / (Maximum release - Spontaneous release) × 100.
Adhesion and Transendothelial Migration (TEM) Assay
- Principle: Evaluates NK cell recruitment and interaction with endothelial barriers.
- Procedure:
- Culture endothelial cells to confluence on Transwell inserts with porous membranes.
- Add NK cells to the upper chamber with chemoattractant in the lower chamber.
- Incubate 2-4 hours to allow migration.
- Collect cells from the lower chamber and quantify by flow cytometry.
- For advanced assessment, use 3D microfluidic systems that better mimic physiological flow conditions [56].
Assessment of Complement Activation
C3d Binding Assay
- Principle: Detects complement activation via deposition of C3d fragment on target cells.
- Procedure:
- Incubate target cells with human serum containing complement sources.
- Wash unbound components and stain with anti-C3d antibody.
- Analyze by flow cytometry or fluorescence microscopy.
- Quantify mean fluorescence intensity as a measure of complement activation.
Membrane Attack Complex (MAC) Deposition Assay
- Principle: Measures terminal complement pathway activation through detection of C5b-9 complexes.
- Procedure:
- After serum incubation, fix cells and permeabilize if necessary.
- Stain with anti-C5b-9 antibody and appropriate secondary reagent.
- Quantify deposition by flow cytometry or confocal microscopy.
Visualization of Signaling Pathways and Experimental Workflows
NK Cell Activation Signaling Pathway
Diagram 1: NK cell activation signaling pathway, showing the balance between inhibitory and activating signals that determines NK cell responses. The inhibitory pathway (red) predominates when MHC class I is present, while the activating pathway (green) triggers cytotoxicity when stress ligands are encountered, particularly in the context of reduced MHC class I expression.
Experimental Workflow for Immune Evasion Testing
Diagram 2: Experimental workflow for comprehensive evaluation of immune evasion strategies, showing the sequential process from therapeutic cell preparation through in vitro testing to in vivo validation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Investigating NK Cell and Complement Responses
| Reagent/Category | Specific Examples | Research Application | Experimental Notes |
|---|---|---|---|
| NK Cell Isolation Kits | CD3⁻ CD56⁺ selection; CD3⁻ CD19⁻ depletion | Purification of NK cells from PBMC | Magnetic bead-based systems (e.g., CliniMACS) enable clinical-grade isolation |
| Feeder Cell Lines | K562-mbIL-21; K562-mbIL-15 | Ex vivo NK cell expansion | Membrane-bound cytokines enhance expansion and persistence |
| Flow Cytometry Antibodies | CD56, CD3, CD107a, IFN-γ, NKG2D, KIRs | Phenotyping and functional assessment | Multi-panel designs enable comprehensive subset analysis |
| Complement Reagents | Normal human serum; C3d, C5b-9 antibodies | Complement activation assays | Serum batch variability requires careful standardization |
| Cytokines | IL-2, IL-15, IL-21 | NK cell activation and expansion | IL-15 preferred over IL-2 for selective NK expansion without Treg stimulation |
| Genetic Engineering Tools | CRISPR/Cas9; Lentiviral vectors | Modification of therapeutic cells | Enable knockout of xenoantigens and insertion of protective transgenes |
| Biomaterial Systems | Hyaluronic acid scaffolds; functionalized nanoparticles | 3D expansion and surface engineering | Macroporous architecture supports NK cell clustering and proliferation |
Overcoming the innate immune hurdles posed by NK cell "missing-self" recognition and complement activation represents a critical frontier in advancing stem cell-based therapies and transplantation medicine. The strategic integration of genetic engineering, stem cell-mediated immunomodulation, and emerging biomaterial approaches provides a multifaceted toolkit for researchers developing next-generation cellular therapeutics. The experimental frameworks and technical protocols outlined in this guide offer systematic approaches for evaluating and validating immune evasion strategies, with particular relevance to the advancing field of stem cell immune modulation. As these technologies mature, the continued refinement of personalized approaches—tailored to individual patient immune profiles and specific therapeutic applications—will be essential for maximizing clinical efficacy while maintaining safety. The convergence of these disciplines holds significant promise for transforming outcomes in transplantation, regenerative medicine, and autoimmune disease treatment.
The success of solid organ and cellular transplants, including those involving stem cells, is fundamentally limited by the recipient's adaptive immune response, a process known as allorecognition. Allorecognition occurs when the recipient's immune system identifies genetically encoded polymorphisms between donor and recipient tissues, triggering rejection responses. In vertebrates, T lymphocytes play a central role in this process through their recognition of polymorphic proteins, primarily major histocompatibility complex (MHC) molecules [61]. What makes transplantation immunologically unique is that T cells can recognize alloantigen through at least three distinct pathways: direct, indirect, and semi-direct allorecognition [62] [63] [61]. The conventional view that acute rejection is mediated primarily by the direct pathway while chronic rejection is driven by the indirect pathway represents an oversimplification of a highly complex process [62]. Recent breakthroughs have revealed significant roles for innate immune components and novel mechanisms of antigen transfer that challenge traditional paradigms [63].
For researchers developing stem cell-based therapies, understanding these pathways is particularly crucial. Stem cells, including mesenchymal stem cells (MSCs), possess immunomodulatory properties that can be harnessed to mitigate allorecognition [22] [10]. However, stem cell transplants themselves face immune rejection challenges, necessitating sophisticated strategies to address allorecognition. This technical guide comprehensively examines the molecular mechanisms underlying each allorecognition pathway and outlines evidence-based strategies to modulate these pathways, with particular emphasis on their application in stem cell research and therapy development.
Molecular Mechanisms of Allorecognition Pathways
Direct Allorecognition Pathway
The direct pathway involves recipient T cells recognizing intact MHC molecules displayed on the surface of donor antigen-presenting cells (APCs) [62] [61]. This pathway is remarkably potent, with 1-10% of a recipient's T cell repertoire capable of recognizing a single MHC alloantigen—a frequency 100 to 10,000 times higher than conventional antigen-specific responses [62] [63] [61]. Two non-mutually exclusive models explain this high precursor frequency:
Multiple Binary Complex Model: This model posits that T cell receptors (TCRs) recognize specific combinations of donor MHC molecules and their bound peptides. Each allogeneic MHC molecule can present numerous different peptides, creating diverse pMHC complexes recognizable by different T cell clones [62] [63]. Crystallographic analyses support this model, showing similar TCR-pMHC interaction orientations in alloresponses and conventional responses [62].
High Determinant Density Model: This alternative model suggests TCRs directly recognize polymorphic regions of allogeneic MHC molecules largely independently of the bound peptide. According to this model, every MHC molecule on a donor APC appears foreign, creating an exceptionally high density of recognizable determinants compared to host APCs presenting conventional antigens [62] [63] [61].
The direct pathway was traditionally considered short-lived, primarily mediating acute rejection, as it depends on donor passenger leukocytes that diminish within weeks post-transplantation [62]. However, recent evidence suggests this pathway may persist longer through mechanisms involving extracellular vesicles [62].
Indirect Allorecognition Pathway
The indirect pathway involves recipient T cells recognizing processed allopeptides presented by self-MHC molecules on recipient APCs [62] [61]. This pathway mirrors conventional T cell responses to foreign antigens and is now recognized as a major driver of chronic allograft rejection [62]. Unlike the broad polyclonal response characteristic of direct recognition, indirect alloresponses typically begin as oligoclonal reactions focused on a limited number of immunodominant epitopes [61]. However, epitope spreading can occur over time, where responses expand to include formerly cryptic determinants, potentially underpinning chronic rejection [62] [61].
The indirect pathway can persist indefinitely post-transplantation because it relies on recipient APCs that continuously acquire and present donor antigens shed from the graft [62]. This pathway is particularly important for responses against minor histocompatibility antigens—polymorphic housekeeping proteins that can elicit potent immune responses even in MHC-matched transplants [61].
Semi-Direct Allorecognition Pathway
The semi-direct pathway represents a hybrid mechanism where recipient APCs acquire intact MHC-allopeptide complexes from donor cells and present them to recipient T cells [62] [63] [61]. This pathway blurs the traditional distinction between direct and indirect recognition and may explain certain clinical observations not adequately addressed by the classical model, such as late T-cell mediated rejection episodes occurring long after donor passenger leukocytes have disappeared [63].
Mechanisms for antigen transfer in the semi-direct pathway include:
- Trogocytosis: Cell-to-cell contact resulting in membrane exchange [61]
- Extracellular Vesicles: Exosomes and other vesicles carrying intact MHC molecules [62] [61]
- Nanotubes: Membrane channels connecting cells and enabling molecular transfer [61]
Notably, the semi-direct pathway enables a single APC to present both intact donor MHC molecules and processed donor peptides, potentially facilitating collaborative interactions between CD4+ and CD8+ T cells within a "three-cell cluster" [63]. This pathway may sustain direct allorecognition beyond the initial post-transplant period by dissociating direct-pathway T cell activation from the presence of donor APCs [62].
Table 1: Characteristics of T Cell Allorecognition Pathways
| Feature | Direct Pathway | Indirect Pathway | Semi-Direct Pathway |
|---|---|---|---|
| Antigen Form | Intact allogeneic MHC molecules | Processed allopeptides presented by self-MHC | Intact allogeneic MHC molecules on recipient APCs |
| Presenting Cell | Donor antigen-presenting cells | Recipient antigen-presenting cells | Recipient antigen-presenting cells |
| Precursor Frequency | Very high (1-10% of T cells) [62] [61] | Low (conventional frequency) | Same clones as direct pathway |
| Time Course | Short-lived (weeks), but may persist via extracellular vesicles [62] | Long-lasting (months to years) [62] | Potentially persistent |
| Role in Rejection | Acute cellular rejection [62] | Chronic rejection [62] | Acute and chronic rejection [63] |
| Therapeutic Targeting | Deplete donor passenger leukocytes; costimulation blockade | Promote tolerance to immunodominant epitopes | Inhibit extracellular vesicle transfer |
Experimental Analysis of Allorecognition Pathways
Research Reagent Solutions
Table 2: Essential Research Reagents for Allorecognition Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| T Cell Analysis | TCR transgenic mice with defined allospecificity [62] | Tracking alloreactive T cell responses |
| CFSE, cell proliferation dyes | Monitoring T cell division and expansion | |
| Antigen Presentation | MHC tetramers with defined peptides [62] | Detecting alloantigen-specific T cells |
| Antibodies to MHC class I/II | Blocking allorecognition pathways | |
| Cell Tracking | Fluorescent proteins (GFP, RFP) [64] | Visualizing cell interactions and movement |
| Cytokine/Chemokine Analysis | Multiplex cytokine arrays | Profiling immune responses to alloantigens |
| Neutralizing antibodies to cytokines | Defining functional roles of specific mediators |
Key Methodologies for Pathway Analysis
Mixed Lymphocyte Reaction (MLR): This in vitro assay measures T cell proliferation in response to allogeneic stimulator cells, primarily assessing direct allorecognition [61]. The high frequency of directly alloreactive T cells enables robust proliferation without prior sensitization. MLR can be adapted to study indirect allorecognition by using synthetic allopeptides or donor cell lysates presented by recipient APCs.
Adoptive T Cell Transfer Models: TCR transgenic T cells with defined allospecificity are transferred into transplant recipients to track the activation, expansion, and differentiation of alloreactive T cells in vivo [62]. This approach allows precise dissection of which allorecognition pathways are operational at different times post-transplantation.
Transcriptomic Analysis: RNA sequencing of alloresponses reveals pathway-specific gene expression patterns. Studies in model systems have identified temporal changes in gene expression during allorecognition, with distinct signatures emerging during the establishment of multicellularity and segregation of incompatible allotypes [64].
Intravital Microscopy: This technique enables real-time visualization of cell-cell interactions during allorecognition. Research in model systems has demonstrated that cells with incompatible allotypes exhibit impaired coordinated movement and polarization compared to compatible cells [64].
Strategic Interventions for Allorecognition Pathways
Targeting Direct Allorecognition
Donor Leukocyte Depletion: Reducing passenger leukocytes in donor grafts can diminish direct allorecognition. However, complete elimination is challenging, and some donor APCs may persist or be reintroduced through semi-direct mechanisms [62].
Costimulation Blockade: Agents that block CD28-B7 or CD40-CD154 interactions can inhibit T cell activation via the direct pathway. Belatacept, a CTLA4-Ig fusion protein, represents a clinical success in this category.
T Cell Depletion Strategies: Polyclonal or monoclonal antibodies targeting T cell surface molecules can reduce the overall alloreactive T cell pool. However, these approaches lack specificity and increase infection risks.
Modulating Indirect Allorecognition
Tolerance Induction to Immunodominant Epitopes: Administration of immunodominant allopeptides via tolerogenic routes (oral, subcutaneous) can promote regulatory T cell responses and reduce indirect alloreactivity [62].
Treg-Based Therapies: Regulatory T cells with indirect allospecificity show particular promise for controlling chronic rejection driven by the indirect pathway [62]. These cells can be expanded ex vivo or induced in vivo through appropriate antigen presentation.
B Cell Targeting: Since indirect allorecognition provides help for alloantibody production, B cell depletion or inhibition may complement T cell-directed therapies [63].
Emerging Approaches for Semi-Direct Allorecognition
Extracellular Vesicle Modulation: Strategies to inhibit the transfer of extracellular vesicles or modify their cargo could potentially limit semi-direct allorecognition [62] [61]. However, such approaches must carefully preserve beneficial vesicle functions.
APC-Targeted Therapies: Since recipient APCs mediate semi-direct presentation, agents that modulate APC function may impact this pathway. This includes drugs that affect antigen uptake, processing, or presentation.
Stem Cell-Based Immunomodulation of Allorecognition
Mesenchymal stem cells (MSCs) and other immunomodulatory stem cells (IMSCs) represent promising therapeutic tools for addressing allorejection due to their multifaceted immunosuppressive capabilities [22] [10]. These cells employ multiple mechanisms to suppress alloresponses:
Cell Contact-Dependent Mechanisms
MSCs express surface molecules that directly inhibit T cell activation through contact-dependent mechanisms:
- PD-L1/PD-L2 Interactions: MSCs express programmed death-ligand 1 and 2, which engage PD-1 on T cells, inhibiting TCR-mediated signaling by recruiting SHP-1 and SHP-2 phosphatases that dephosphorylate ZAP70 and PKCθ, ultimately blocking T cell cycle progression at G0/G1 phase [10].
- Other Co-inhibitory Signals: MSCs also express additional surface molecules that deliver inhibitory signals to T cells, including members of the B7 family and adhesion molecules [10].
Soluble Factor-Mediated Immunomodulation
MSCs secrete numerous immunosuppressive factors that modulate alloresponses:
- TGF-β: This pivotal cytokine secreted by MSCs activates the TGF-β/Smad pathway, promoting the differentiation and function of regulatory T cells [10]. TGF-β binds to TGF-βRII, recruiting and phosphorylating TGF-βRI, which then phosphorylates Smad2/3. The resulting complex with Smad4 translocates to the nucleus to regulate transcription of genes including FOXP3, the master regulator of Tregs [10].
- PGE2 and IDO: Prostaglandin E2 and indoleamine 2,3-dioxygenase suppress dendritic cell maturation and Th2 priming, particularly relevant in allergic inflammation but also applicable to alloresponses [10].
- Additional Factors: MSCs also produce IL-10, HGF, TSG-6, and other mediators that collectively create an immunosuppressive microenvironment [10].
MSC Integration with Allorecognition Pathways
The immunomodulatory properties of MSCs can potentially target all three allorecognition pathways:
- MSCs can directly inhibit T cell activation regardless of the allorecognition pathway involved [10].
- MSC-derived extracellular vesicles may deliver immunosuppressive cargo while potentially avoiding the transfer of allogeneic MHC molecules [22].
- MSCs can promote the generation of allopeptide-specific Tregs that specifically suppress indirect alloresponses [62] [10].
However, challenges remain in clinical translation, including heterogeneous protocols, unresolved long-term risks, and the need for standardized production methods [10]. Future efforts should prioritize combination strategies that simultaneously target multiple allorecognition pathways.
Visualization of Allorecognition Pathways and Therapeutic Strategies
Allorecognition Pathways and Intervention Strategies
The complex interplay between direct, indirect, and semi-direct allorecognition pathways presents both challenges and opportunities for researchers and clinicians working in transplantation and stem cell therapy. While each pathway has distinct characteristics, they operate concurrently and can influence each other in shaping the overall alloimmune response. The semi-direct pathway, in particular, bridges the classical direct and indirect pathways and may sustain alloresponses beyond the initial post-transplant period.
Future directions in addressing adaptive immune rejection should include:
- Personalized Approaches: Mapping individual immunodominance patterns to tailor tolerance induction strategies [62]
- Combination Therapies: Simultaneously targeting multiple allorecognition pathways while preserving protective immunity
- Stem Cell Engineering: Enhancing the immunomodulatory properties of therapeutic stem cells through genetic modification or preconditioning [22] [10]
- Novel Delivery Systems: Utilizing exosomes and hydrogel-encapsulated formulations to improve the targeting and safety of immunomodulatory agents [10]
As our understanding of allorecognition mechanisms continues to evolve, particularly with insights from stem cell biology, we move closer to the ultimate goal of achieving transplant tolerance without the need for lifelong immunosuppression.
The therapeutic application of stem cells, particularly mesenchymal stromal cells (MSCs), represents a transformative approach in regenerative medicine and immunomodulation. However, the efficacy of these treatments is profoundly influenced by patient-specific variables that create a complex biological context for cellular interventions. Understanding how age, underlying disease, microbiome composition, and prior antigen exposure interact with administered stem cells is critical for advancing personalized therapeutic strategies. This technical guide examines the mechanisms through which these patient-specific factors modulate stem cell function and immune responses, providing researchers and drug development professionals with a comprehensive framework for optimizing clinical outcomes.
The inherent plasticity and immunomodulatory capacity of MSCs make them particularly sensitive to recipient environment. These multipotent stromal cells reside in perivascular niches and can differentiate into multiple lineages, but their primary therapeutic value lies in their paracrine secretion and immune regulatory functions [65] [66]. MSCs act as "sensors and switchers" of the immune system, responding to inflammatory cues by secreting factors that can either promote or suppress immune activity depending on the context [67]. This dynamic responsiveness, while therapeutically advantageous, also renders MSC efficacy vulnerable to patient-specific variables that shape the host microenvironment.
Impact of Chronological Age and Immunosenescence
Molecular Hallmarks of Aging in Stem Cells and Immune Function
Aging introduces multidimensional changes in both administered stem cells and the host immune system. Cellular aging is characterized by telomere shortening, genomic instability, and cellular senescence, marked by persistent DNA damage foci, increased senescence-associated β-galactosidase activity, elevated p16INK4A and p21CIP1 expression, and secretion of senescence-associated secretory phenotype (SASP) components including IL-6, IL-8, TNF-α, and CCL2 [68]. These changes create a hostile microenvironment for both endogenous and administered stem cells.
Immunosenescence affects both innate and adaptive immunity. In innate immune cells, aging macrophages show reduced phagocytic capacity with increased pro-inflammatory cytokine expression, neutrophils exhibit elevated intracellular calcium and reduced ROS production, and dendritic cells demonstrate impaired antigen presentation despite elevated pro-inflammatory cytokine secretion [68]. The adaptive immune system experiences more profound alterations, with reduced T and B cell receptor diversity, diminished naïve lymphocyte populations, accumulated memory cells, and impaired antigen clearance capacity [68].
Table 1: Age-Associated Changes in Immune Cell Function and Implications for Stem Cell Therapy
| Immune Cell Type | Age-Related Functional Changes | Impact on Stem Cell Therapy |
|---|---|---|
| Macrophages | Reduced phagocytosis, increased IL-6/TNF-α secretion, decreased antioxidant capacity | Creates pro-inflammatory microenvironment that may polarize MSCs toward anti-inflammatory phenotype prematurely |
| Neutrophils | Reduced chemotaxis and bactericidal capacity, increased pro-inflammatory activity | May exacerbate initial inflammatory response to cell administration |
| Dendritic Cells | Impaired antigen presentation, reduced migration, increased inflammatory cytokines | Alters T-cell priming and may affect adaptive immune response to administered cells |
| T Cells | Decreased naïve T cell population, increased memory T cells, reduced receptor diversity | Limits de novo immune responses, may affect long-term therapeutic persistence |
| B Cells | Reduced immunoglobulin diversity, increased autoreactive B cells, altered BCR repertoire | May increase risk of autoimmunity or reduce functional antibody responses |
Experimental Protocols for Assessing Age-Related Impacts
Protocol 1: Evaluation of MSC Senescence in Aged Microenvironments
- Culture Conditions: Plate early-passage MSCs (P3-P5) at 5,000 cells/cm² in serum-free media supplemented with 10% human serum from young (25-35 years) and aged (65-75 years) donors
- Senescence Assessment: After 72 hours, assess SA-β-gal activity using commercial senescence detection kits, quantify p16INK4A and p21 expression via qRT-PCR, and analyze SASP factors (IL-6, IL-8, MCP-1) via ELISA
- Functional Assays: Perform trilineage differentiation potential assessment using standard osteogenic, adipogenic, and chondrogenic induction media with quantification of differentiation markers
Protocol 2: Analysis of Immune Cell-MSC Interactions in Aging
- Co-culture System: Establish transwell co-cultures with peripheral blood mononuclear cells (PBMCs) from young and aged donors in the upper chamber and MSCs in the lower chamber
- Immune Activation: Stimulate with anti-CD3/CD28 antibodies or phytohemagglutinin for 72 hours
- Readouts: Quantify T-cell proliferation via CFSE dilution, analyze Treg differentiation (CD4+CD25+FoxP3+) by flow cytometry, and measure key immunomodulatory factors (IDO, PGE2, TGF-β) in supernatant
Microbiome Influence on Stem Cell Function
Gut-Bone Marrow Axis and Microbial Metabolites
The gut microbiome exerts profound effects on stem cell function through microbial metabolites, immune modulation, and epigenetic regulation. Dysbiosis, or compositional changes in gut microbiota, is linked to stem cell aging through metabolic alterations, aberrant immune activation, and epigenetic instability [69]. Short-chain fatty acids (SCFAs) including acetate, butyrate, and propionate—produced by bacterial fermentation of dietary fiber—directly impact stem cell function through multiple mechanisms.
Butyrate impedes colonic epithelial stem and progenitor proliferation through FOXO3 stress signaling pathway activation, while propionate inhibits differentiation capacity of human chorion-derived MSCs [69]. SCFAs regulate stem cell function by binding to G-protein coupling receptors, suppressing insulin signaling, and causing mitochondrial electron transport chain dysfunction, leading to NAD+/NADH ratio imbalance and dysregulation of SIRT1/PGC1α pathway [69]. The resulting mitochondrial damage and ROS accumulation drive erroneous differentiation and depletion of stem cell pools.
Microbial metabolites also induce epigenetic modifications in stem cells. Butyrate enhances repressive histone mark H3K27me3 through polycomb repressive complex 2, facilitating metabolic shifts away from glycolysis and increasing susceptibility to ROS [69]. Additionally, microbiota-derived uracil activates G-protein-coupled receptors on intestinal cells, triggering ROS release that stimulates p38 and JNK signaling pathways to promote intestinal stem cell proliferation [69].
Table 2: Microbial Metabolites and Their Impact on Stem Cell Function
| Metabolite | Microbial Source | Impact on Stem Cells | Molecular Mechanisms |
|---|---|---|---|
| Short-chain Fatty Acids (Butyrate, Propionate, Acetate) | Bacteroides, Firmicutes | Inhibits proliferation and differentiation, alters metabolism | GPCR signaling, insulin signaling suppression, mitochondrial dysfunction, HDAC inhibition |
| Endogenous Ethanol | Proteobacteria (E. coli, Enterobacteriaceae) | Depletes hippocampal stem/progenitor cells, increases gut permeability | Disrupts epithelial tight junctions, direct cytotoxicity |
| Uracil | Various commensals | Promotes intestinal stem cell proliferation | GPCR activation, ROS production, p38/JNK pathway activation |
| Bacterially Derived ROS | Commensal microbiota | Janus-faced: appropriate levels support differentiation, excess causes aberrant differentiation | p38 and Foxhead box protein signaling, oxidative stress responses |
Experimental Protocols for Microbiome-Stem Cell Investigations
Protocol 3: Assessing Microbiome Influence on MSC Function
- Animal Model: Utilize germ-free versus conventionalized mice, or employ antibiotic cocktail treatment (1g/L ampicillin, 0.5g/L vancomycin, 1g/L neomycin, 1g/L metronidazole) for 4 weeks to deplete microbiota
- SCFA Administration: Supplement drinking water with physiological SCFA mixture (100mM acetate, 50mM propionate, 50mM butyrate) for 8 weeks
- MSC Analysis: Isolate bone marrow MSCs and assess differentiation potential, immunomodulatory capacity, and transcriptomic changes via RNA sequencing
Protocol 4: Human Microbiome-MSC Interaction Studies
- Cohort Design: Recruit patients with characterized microbiome profiles (16S rRNA sequencing of stool samples) undergoing MSC therapy
- Sample Processing: Correlate microbial diversity indices with MSC potency markers in vitro
- Functional Assays: Treat MSCs with patient-derived serum and quantify immunomodulatory factor secretion (IDO, PGE2, TGF-β) in response to IFN-γ stimulation
Underlying Disease and Prior Antigen Exposure
Disease-Specific Microenvironments and Immune Memory
The host disease state creates distinct microenvironments that significantly influence MSC behavior. In autoimmune conditions like multiple sclerosis, dysregulated immune responses and chronic inflammation alter the tissue landscape that administered stem cells encounter [70]. The success of autologous hematopoietic stem cell transplantation in MS is influenced by the pre-treatment immune state and associated microbiome configuration, particularly oral microbiota diversity and composition [70].
Prior antigen exposure shapes the adaptive immune repertoire, creating immunological memory that can recognize allogeneic MSC antigens. While MSCs are considered immunoprivileged due to low MHC class II expression, they do express MHC class I molecules and can elicit immune responses in pre-sensitized hosts [66]. The history of infections, vaccinations, and previous cell therapies contributes to the antigen experience of the immune system, potentially affecting the persistence and function of administered stem cells.
Experimental Protocols for Disease Context Assessment
Protocol 5: Modeling Disease-Specific Microenvironments
- Conditioned Media Preparation: Generate disease-specific conditioned media from patient-derived PBMCs or tissue biopsies cultured for 48 hours
- MSC Priming: Incubate MSCs with 30% disease-conditioned media for 72 hours prior to functional assays
- Potency Analysis: Quantify changes in MSC immunophenotype (CD73, CD90, CD105, HLA-DR), secretome profile (multiplex cytokine array), and transcriptome (RNA-seq)
Protocol 6: Assessing Impact of Prior Antigen Exposure
- ELISpot Assay: Perform IFN-γ ELISpot using patient PBMCs co-cultured with allogeneic MSCs to detect pre-existing cellular immunity
- Antibody Detection: Screen patient serum for anti-HLA antibodies against donor MSC HLA profile using Luminex-based single antigen bead assay
- Functional Correlation: Correlize pre-treatment immune reactivity with post-administration MSC persistence via PCR-based tracking of donor DNA in patient blood
Technical Approaches and Research Reagent Solutions
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Patient-Specific Variables in Stem Cell Therapy
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Senescence Detection | SA-β-gal staining kits, p16INK4A antibodies, SASP cytokine panels | Quantifying cellular aging in donor MSCs and host tissues | Combine multiple markers for definitive senescence identification |
| Immunophenotyping Panels | CD73, CD90, CD105, CD45, CD34, HLA-DR, CD14, CD19 | MSC characterization per ISCT criteria | Include viability dye to exclude dead cells from analysis |
| Microbiome Profiling | 16S rRNA V3-V4 primers, INVITEK DNA extraction kits, DNAGenotek collection kits | Assessing gut and oral microbiota composition | Standardize collection time and method to reduce variability |
| Immunomodulation Assays | IDO functional assays, PGE2 ELISA, iNOS detection, Treg differentiation panels | Evaluating MSC immune function | Use standardized IFN-γ concentrations for activation (typically 10-50ng/mL) |
| SCFA Analysis | GC-MS SCFA standards, β-hydroxybutyrate assay kits | Quantifying microbial metabolites | Stabilize samples immediately after collection as SCFAs are volatile |
| Cell Tracking | CFSE cell proliferation kit, luciferase-expressing MSCs, PCR-based human Alu repeats | Monitoring MSC persistence in vivo | For clinical studies, PCR-based methods are most feasible |
Pathway Visualization: MSC-Immune Cell Interactions in Variable Patient Contexts
The following diagram illustrates the key molecular pathways through which MSCs interact with immune cells, and how patient-specific variables modulate these interactions:
Diagram 1: MSC-Immune Interactions Modulated by Patient Context. This diagram illustrates how patient-specific variables (age, microbiome, underlying disease, and prior antigen exposure) influence the molecular interactions between MSCs and immune cells, ultimately affecting therapeutic outcomes.
Experimental Workflow for Comprehensive Patient Profiling
The following diagram outlines a systematic approach for evaluating patient-specific variables in stem cell therapy research:
Diagram 2: Comprehensive Workflow for Patient-Specific Variable Assessment. This experimental approach systematically integrates patient profiling with MSC characterization to predict and optimize therapeutic outcomes.
The integration of patient-specific variables into stem cell therapy development is essential for advancing personalized regenerative medicine. Age, microbiome composition, underlying disease states, and prior antigen exposure collectively create a unique biological context that significantly influences MSC function and therapeutic efficacy. By employing comprehensive profiling approaches and mechanistic studies, researchers can identify critical determinants of treatment response and develop strategies to mitigate negative influences.
Future directions should focus on developing standardized potency assays that incorporate patient-specific factors, creating predictive algorithms for treatment response, and engineering next-generation MSCs that are resistant to hostile microenvironmental factors. Additionally, combinatorial approaches that modulate the patient environment through microbiome interventions or immunomodulatory preconditioning may enhance MSC therapy outcomes. As our understanding of these complex interactions deepens, the field will progress toward truly personalized stem cell therapies optimized for individual patient contexts.
Stem cell therapy stands at the forefront of regenerative medicine, offering promising solutions for repairing tissues and treating degenerative diseases and cancer. The therapeutic efficacy of stem cells is critically dependent on their capacity for survival, controlled differentiation, and safe integration without tumorigenic complications. This whitepaper delves into the strategic use of small molecules to precisely modulate stem cell behavior by targeting key signaling pathways. Framed within the context of personalized stem cell immune modulation research, we provide an in-depth analysis of pharmacological enhancement mechanisms, complete with structured quantitative data, detailed experimental protocols, and essential research toolkits. The integration of these pharmacological strategies is pivotal for advancing safer, more effective, and personalized stem cell-based therapies, ultimately revolutionizing regenerative and onco-medicine.
The behavior of stem cells, including their self-renewal, differentiation, and migration, is collectively regulated by a complex network of essential signaling pathways such as Hedgehog (Hh), Wnt, Hippo, TGF-β, FGF, BMP, and Notch [71]. These pathways offer multiple pharmacological entry points to fine-tune stem cell behavior for therapeutic purposes. Pharmacological interventions have emerged as powerful tools to overcome the significant challenges limiting the clinical success of stem cell therapies, namely poor cell survival, uncontrolled differentiation, immune rejection, and the risk of tumorigenesis associated with pluripotent stem cells like ESCs and iPSCs [71].
Small molecules, in particular, present a compelling strategy for enhancing stem cell therapy. They can enhance the survival, proliferation, and functionality of stem cells, ensuring their successful integration and performance in damaged tissues [71]. A key advantage is their ability to direct stem cell differentiation into specific lineages needed for tissue regeneration, such as cardiac or neural cells [71]. Furthermore, they can stimulate a patient's endogenous stem cells to participate in tissue repair, reducing the need for external transplantation [71]. From a manufacturing and clinical perspective, small-molecule drugs often possess superior pharmacokinetic properties, lower costs, and better patient compliance compared to biologic drugs, making them highly attractive for clinical translation [72].
Key Signaling Pathways as Pharmacological Targets
Understanding the key signaling pathways that govern stem cell fate is fundamental to developing targeted pharmacological enhancements. The following sections detail the primary pathways and the small molecules used to modulate them.
Table 1: Key Stem Cell Signaling Pathways and Their Roles
| Pathway | Primary Role in Stem Cells | Key Components | Outcome of Modulation |
|---|---|---|---|
| TGF-β | Tissue homeostasis, immune response, growth inhibition of early progenitors | TGF-β (1-3), Activins, SMAD1/5/8, SMAD2/3, TAB/TAK [71] | Modulates immunomodulation, inhibits proliferation of multipotent progenitors [71] |
| Wnt | Tissue homeostasis, self-renewal, differentiation | β-catenin, GSK-3β | Supports stem cell self-renewal and differentiation; key regulator of stem cell function [71] |
| Hedgehog (Hh) | Embryonic development, limb and bone formation | Patched, Smoothened, GLI transcription factors | Regulates epithelial-mesenchymal interactions during development [71] |
| Notch | Cell fate decisions, proliferation | Notch receptors (1-4), DLL/Jagged ligands | Strategic target for preventing tumor recurrence by targeting cancer stem cells (CSCs) [71] |
| FGF | Embryonic development, angiogenesis, wound healing | FGF receptors, RAS/MAPK, PI3K/AKT | Regulates cell proliferation and survival [71] |
| BMP | Bone and cartilage formation, cell differentiation | BMPs (1-20), SMAD1/5/8 | Promotes differentiation into osteogenic and other mesodermal lineages [71] |
The complex crosstalk between these pathways means that modulation of one can influence others, allowing for multi-faceted pharmacological strategies to fine-tune stem cell behavior [71].
Figure 1: Pharmacological Targeting of Stem Cell Signaling Pathways. Small molecules modulate core pathways to direct therapeutic outcomes.
Quantitative Analysis of Small Molecule Efficacy
The efficacy of pharmacological enhancement is demonstrated through quantitative metrics from preclinical and clinical studies. The tables below summarize key data on small molecule performance in enhancing stem cell therapy and their application in targeted cancer therapy, which is relevant for suppressing tumorigenesis in stem cell-based treatments.
Table 2: Efficacy of Small Molecules in Stem Cell Enhancement
| Small Molecule / Class | Target Pathway | Experimental Model | Key Efficacy Metrics | Outcome |
|---|---|---|---|---|
| ALK Inhibitors (e.g., Crizotinib, Alectinib) | ALK, c-Met, ROS1 [72] | ALK-positive NSCLC [72] | PFS vs. chemotherapy; CNS metastasis prevention [72] | Overcomes crizotinib resistance (L1196M, G1269A); superior BBB permeability [72] |
| Immunomodulators | TGF-β, PGE2, IDO pathways [73] | MSC therapy in Autoimmune Diseases (Clinical Trials) [73] | Promotion of Treg expansion; Suppression of Th1/Th17 [73] | Mediates immune tolerance and homeostasis via paracrine effects [73] |
| Tyrosine Kinase Inhibitors (TKIs) | Various Kinases (ROS, TRK) [72] | Solid Tumors (Clinical) [72] | Tumor response rate in TRK fusion solid tumors [72] | Approved for clinical use (e.g., Entrectinib) [72] |
| Differentiation Inducers | Notch, Wnt, BMP [71] | In vitro stem cell cultures [71] | Lineage-specific differentiation efficiency (%) [71] | Directs differentiation into cardiac, neural, osteogenic, etc. lineages [71] |
Table 3: Small Molecules in Targeted Cancer Therapy (Relevant to Suppressing Tumorigenesis)
| Small Molecule Category | Number of Approved Drugs (US FDA & China NMPA) | Example Targets | Key Challenges |
|---|---|---|---|
| Kinase Inhibitors | 89 (as of Dec 2020) [72] | ALK, ROS1, TRK, c-Met [72] | Low response rate, drug resistance [72] |
| Epigenetic Modifiers | Included in the 89 approved drugs [72] | HDACs, DNMTs | Cumulative toxicity, managing immune-related effects |
| DNA Damage Repair Enzymes | Included in the 89 approved drugs [72] | PARP | Off-target effects, patient selection |
| Proteasome Inhibitors | Included in the 89 approved drugs [72] | 20S Proteasome | Resistance mechanisms |
Experimental Protocols for Pharmacological Enhancement
To ensure reproducibility and translational validity, detailed methodologies for key experiments are crucial. The following protocols outline standardized procedures for evaluating the core aspects of pharmacological enhancement.
Protocol for Assessing Small Molecule-Mediated Differentiation
This protocol evaluates the capacity of small molecules to direct stem cell differentiation into specific lineages.
- Cell Culture: Maintain human iPSCs or MSCs in appropriate culture conditions. For MSCs, use standard media (e.g., α-MEM supplemented with 10% FBS and 1% penicillin/streptomycin) and confirm adherence to plastic and expression of surface markers (CD73, CD90, CD105 ≥95%; lack of CD34, CD45, CD14, CD19, HLA-DR ≤2%) as per International Society for Cellular Therapy (ISCT) guidelines [11].
- Differentiation Induction: Upon reaching 80% confluency, passage cells and seed them into differentiation plates. Replace the standard growth medium with specific differentiation induction media supplemented with the small molecule(s) of interest.
- Osteogenic Differentiation: Culture MSCs in medium containing dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate, with or without a BMP pathway activator [11]. Confirm differentiation by Alizarin Red S staining for calcium deposits after 21 days.
- Chondrogenic Differentiation: Pellet MSCs and culture in a defined medium with TGF-β3 and other relevant small molecules. Confirm differentiation by Alcian Blue staining for sulfated proteoglycans.
- Neural Differentiation: For iPSCs, use a staged protocol involving dual SMAD inhibition (e.g., using small molecule inhibitors of TGF-β and BMP pathways) to induce neural precursors.
- Flow Cytometric Analysis: Harvest differentiated cells and stain with fluorescently labeled antibodies against lineage-specific markers (e.g., Runx2 for osteoblasts, SOX9 for chondrocytes, β-III-tubulin for neurons). Analyze using a high-parameter flow cytometer.
- High-Dimensional Data Analysis: Export single-cell data and analyze using algorithms like PhenoGraph or viSNE to visualize and quantify heterogeneous differentiation outcomes and identify novel subpopulations [74]. The R package
cytofastcan be used for downstream quantification and visualization of specific cell clusters [75].
Protocol for Evaluating Cell Survival and Anti-Tumorigenic Effects
This protocol assesses the impact of small molecules on promoting stem cell survival and suppressing undesired proliferation.
- In Vitro Survival/Proliferation Assay: Seed stem cells at a low density in 96-well plates. Treat with a range of concentrations of the pro-survival small molecule (e.g., an FGF pathway activator). After 24-72 hours, measure cell viability using assays like MTT or CellTiter-Glo.
- Apoptosis Assay: To model stress conditions, expose stem cells to serum-free medium or inflammatory cytokines (e.g., TNF-α). Co-treat with the test small molecule. After 24 hours, stain cells with Annexin V and Propidium Iodide (PI) and analyze by flow cytometry to quantify early and late apoptotic cells.
- Soft Agar Colony Formation Assay: This is a gold-standard assay for detecting anchorage-independent growth, a hallmark of tumorigenicity. Plate iPSCs or ESCs transfected with a luciferase reporter in a soft agar layer with or without the anti-tumorigenic small molecule (e.g., a Wnt or Notch pathway inhibitor). Allow colonies to form for 2-4 weeks.
- Quantification and Imaging: Stain colonies with iodonitrotetrazolium chloride (INT) or measure luciferase activity. Image the plates and use automated colony counting software to quantify the number and size of colonies. A significant reduction in colony formation in treated groups indicates suppression of tumorigenic potential.
Figure 2: Experimental Workflow for Pharmacological Enhancement. A sequential pipeline from cell culture to high-dimensional data analysis.
Protocol for Mass Cytometry (CyTOF) Analysis of Immune Modulation
This protocol is essential for profiling the immune modulatory effects of stem cells in a patient-specific context, as framed by the thesis.
- Sample Preparation: Co-culture pharmacologically enhanced MSCs with peripheral blood mononuclear cells (PBMCs) from a donor. Include conditions that activate the PBMCs (e.g., with anti-CD3/CD28 beads). After 48-72 hours, harvest all cells.
- Antibody Staining: Stain the cell mixture with a metal-tagged antibody panel targeting immune cell markers (CD3, CD4, CD8, CD25, CD127, CD19, CD14, CD56, etc.) and functional markers (Ki-67, cleaved caspase-3, cytokines). Include a viability marker (cisplatin) and an intercalator (Iridium) for DNA content [74].
- Data Acquisition on Helios Mass Cytometer: Resuspend stained cells in water containing normalization beads and run on the CyTOF. The instrument measures the abundance of metal isotopes per single cell [74].
- Data Preprocessing: Normalize the data using software like the Nolan lab's Normalizer. Use FlowJo to gate for single, viable cells before exporting the data for downstream analysis [74].
- High-Dimensional Analysis: Import the fcs files into an analysis platform (e.g., Cytobank or R).
- Dimensionality Reduction: Run the viSNE algorithm to visualize the high-dimensional data in two dimensions, revealing the landscape of all immune cells [74].
- Clustering: Use the PhenoGraph algorithm to objectively identify distinct clusters of immune cells (e.g., T cell subsets, B cells, monocytes) without researcher bias [74].
- Differential Abundance/Expression: Compare the abundance of PhenoGraph clusters and the median marker expression between experimental conditions (e.g., MSC-treated vs. untreated PBMCs) to identify statistically significant changes in immune cell populations and their functional states induced by the pharmacologically enhanced MSCs [74].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Reagents for Pharmacological Stem Cell Research
| Item | Function / Application |
|---|---|
| Defined Culture Media (e.g., mTeSR1 for iPSCs, α-MEM for MSCs) | Provides a standardized, reproducible base for culturing stem cells and executing differentiation protocols. |
| Small Molecule Libraries (e.g., Selleckchem, Tocris) | Collections of bioactive compounds for high-throughput screening to discover novel inducers of differentiation, survival, or anti-tumorigenic agents. |
| Recombinant Human Proteins (e.g., TGF-β3, BMP-4, FGF-2) | Positive controls for activating specific signaling pathways in differentiation and proliferation assays. |
| Flow Cytometry Antibodies (e.g., CD73, CD90, CD105, CD34, CD45, HLA-DR) | Essential for characterizing stem cell populations according to ISCT criteria and assessing lineage-specific differentiation [11]. |
| Mass Cytometry (CyTOF) Antibody Panel | Metal-tagged antibodies for deep immunophenotyping of >30 parameters simultaneously to analyze complex cellular interactions and immune modulation [74]. |
| Viability & Apoptosis Kits (e.g., Annexin V/PI, MTT, CellTiter-Glo) | Quantifying cell survival, proliferation, and death in response to pharmacological treatment. |
R Packages (cytofast, cytofkit) |
For comprehensive downstream analysis, visualization, and quantification of high-dimensional cytometry data [75] [74]. |
Therapy-induced senescence (TIS), a stable cell cycle arrest triggered by cytotoxic stress, represents a double-edged sword in oncology. While it halts tumor proliferation, it can also drive persistent tissue dysfunction, particularly fibrosis, through the senescence-associated secretory phenotype (SASP). This in-depth technical guide explores the central role of TIS in propagating fibrotic pathways and details how stem cell immune modulation, especially by mesenchymal stem cells (MSCs), presents a promising therapeutic avenue. Framed within a broader thesis on personalized patient research, this review synthesizes current mechanistic understanding, provides standardized experimental protocols, and outlines a toolkit for developing novel senotherapies aimed at mitigating treatment-related chronic damage.
Therapy-induced senescence (TIS) is a critical cellular response to anti-cancer treatments such as radiotherapy and chemotherapy, characterized by an irreversible proliferation arrest. Initially intended as a tumor-suppressive mechanism, TIS can have detrimental long-term consequences. A primary mediator of this damage is the senescence-associated secretory phenotype (SASP), a robust pro-inflammatory and pro-fibrotic secretome that alters the tissue microenvironment [76]. In the context of cancer treatment, over 50% of patients receive radiotherapy, alone or in combination, making TIS a widespread concern [77].
Radiation-induced tissue fibrosis (RIF) is a classic example of TIS-driven pathology. It is characterized by the abnormal activation of myofibroblasts and excessive accumulation of extracellular matrix (ECM), leading to irreversible tissue damage and organ dysfunction [77]. This fibrotic process, which can manifest in lungs, skin, liver, and kidneys, is propelled by chronic inflammation, oxidative stress, and metabolic reprogramming stemming from senescent cells. The interplay between TIS and the immune system is complex; while immune cells initially clear senescent cells, persistent TIS can lead to immune dysregulation and a pro-fibrotic communication network. Understanding this crosstalk is paramount for developing interventions that preserve the benefits of cancer therapy while preventing the debilitating sequelae of fibrosis.
Molecular Mechanisms Linking Senescence and Fibrosis
Core Senescence Pathways
The establishment of TIS is governed by two principal tumor suppressor pathways: p53/p21CIP1 and p16INK4a/RB. These pathways respond to diverse stressors, including ionizing radiation, which causes significant DNA damage, particularly telomere dysfunction [76]. This damage triggers a persistent DNA damage response (DDR), which is a hallmark of stable senescence enforcement [76].
- p53/p21CIP1 Pathway: DNA double-strand breaks activate kinases like ATM, leading to p53 stabilization. p53 then transactivates the cyclin-dependent kinase inhibitor p21CIP1, which promotes cell cycle arrest [76].
- p16INK4a/RB Pathway: The CDK inhibitor p16INK4a accumulates in senescent cells, inhibiting CDK4/6 and preventing the phosphorylation of the retinoblastoma (RB) protein. Hypophosphorylated RB actively represses E2F target genes, enforcing a permanent G1 cell cycle arrest [76].
Oncogenic stress and persistent DDR signaling amplify these pathways, ensuring the maintenance of the senescent state. While this arrest is crucial for preventing the proliferation of damaged cells, it sets the stage for the deleterious effects of the SASP.
The Senescence-Associated Secretory Phenotype (SASP)
The SASP is a key mediator through which senescent cells impact their environment and drive fibrosis. It comprises a diverse array of secreted factors, including:
- Pro-inflammatory Cytokines: IL-6, IL-1β, IL-8
- Growth Factors: TGF-β, connective tissue growth factor (CTGF)
- Matrix Remodeling Enzymes: Matrix metalloproteinases (MMPs) and their inhibitors (TIMPs)
The release of these factors, particularly TGF-β, creates a pro-fibrotic signaling milieu that promotes the activation and persistence of myofibroblasts, the primary effector cells in fibrosis [77]. Myofibroblasts are characterized by their secretion of α-smooth muscle actin (α-SMA) and collagens (types I, III, IV), leading to excessive ECM deposition and tissue stiffening [77]. The cGAS/STING pathway, activated by cytosolic DNA, is a crucial intracellular regulator of the SASP and a potential therapeutic target [77].
Table 1: Key SASP Factors and Their Pro-Fibrotic Roles
| SASP Factor Category | Key Examples | Pro-Fibrotic Function |
|---|---|---|
| Growth Factors | TGF-β, CTGF | Directly activates fibroblast-to-myofibroblast differentiation; stimulates collagen production [77]. |
| Interleukins | IL-6, IL-1β, IL-8 | Drives chronic inflammation; recruits immune cells; synergizes with TGF-β [77] [76]. |
| Matrix Enzymes & Inhibitors | MMP-2, MMP-9, TIMP-1 | Remodels ECM; altered MMP/TIMP balance favors matrix accumulation [77]. |
| Chemokines | CXCL1, CXCL8 | Recruits neutrophils and macrophages to sustain inflammatory response. |
Figure 1: Signaling Pathway from Therapy-Induced Stress to Fibrosis. Therapy (e.g., IR) causes DNA damage, activating the DDR and leading to senescence via p53/p21 and p16/RB. Senescent cells secrete SASP factors (TGF-β, IL-6, MMPs), which activate myofibroblasts and drive fibrosis.
Immune System Communication in Senescence and Fibrosis
The immune system plays a paradoxical role in the lifecycle of senescent cells, acting as both a scavenger and a propagator of damage. Effective immune surveillance is crucial for the timely clearance of senescent cells; however, TIS and the SASP can disrupt this delicate balance.
Immune Cell Recruitment and Dysregulation
The SASP acts as a powerful chemoattractant for innate and adaptive immune cells. Key interactions include:
- Macrophages: SASP factors like CCL2 recruit monocytes to the tissue. While M1 macrophages may initially attempt to clear senescent cells, the microenvironment can polarize them toward an M2 phenotype, which is pro-fibrotic and supports tissue repair in a dysregulated manner [77] [11].
- T Lymphocytes: The SASP can suppress cytotoxic T-cell activity while promoting the expansion of T-helper cells that favor fibrosis, such as Th2 and Th17 cells. This impairs the immune system's ability to eliminate senescent cells effectively [11].
- Natural Killer (NK) Cells: These are primary effector cells for senescent cell clearance. However, senescent cells can upregulate ligands like HLA-E that inhibit NK cell activity, allowing them to evade immune destruction [76].
The failure to clear senescent cells leads to their accumulation, resulting in a chronic, low-grade inflammatory state that perpetuates myofibroblast activity and ECM deposition.
Immunomodulatory Role of Mesenchymal Stem Cells
Mesenchymal stem cells (MSCs) have emerged as potent modulators of the immune response in fibrotic microenvironments. Their therapeutic potential is largely attributed to their paracrine activity and direct cell-cell interactions, which can be harnessed to counteract the deleterious effects of TIS [22] [11].
MSCs are defined by their adherence to plastic, specific surface marker expression (CD73, CD90, CD105), and capacity for trilineage differentiation [11]. They can be derived from bone marrow (BM-MSCs), adipose tissue (AD-MSCs), umbilical cord (UC-MSCs), and other sources. In the context of senescence and fibrosis, MSCs exert their effects through:
- SASP Modulation: MSCs release a diverse array of immunoregulatory molecules, including PGE2, TGF-β, HLA-G5, IL-10, HGF, and galectins [22] [11]. These factors can directly suppress the pro-inflammatory components of the SASP.
- Immune Cell Reprogramming: MSCs interact with various immune cells, promoting the transition of macrophages from a pro-inflammatory M1 to an anti-inflammatory M2 phenotype, suppressing T-cell proliferation, and modulating dendritic cell maturation [22] [11].
- Trophic Support and Tissue Repair: By secreting growth factors and extracellular vesicles, MSCs promote tissue repair, angiogenesis, and cell survival, thereby opposing the tissue-destructive effects of fibrosis [11].
The low numbers and quiescent state of endogenous MSCs are evolutionarily conserved traits that may prevent excessive immunosuppression, highlighting the need for carefully timed therapeutic administration [22].
Table 2: MSC-Derived Immunomodulatory Molecules and Their Functions
| Molecule Category | Key Examples | Mechanism of Action in Senescence/Fibrosis |
|---|---|---|
| Soluble Immunosuppressors | PGE2, IL-10, TGF-β, HLA-G5 | Suppresses T-cell activation and pro-inflammatory cytokine production; polarizes macrophages to M2 anti-inflammatory state [22] [11]. |
| Trophic Growth Factors | HGF, VEGF, FGF | Promotes tissue repair, angiogenesis, and survival of parenchymal cells; counteracts cell death from senescence-related stress [11]. |
| Metabolizing Enzymes | CD73, CD39 | Catalyzes production of immunosuppressive adenosine from extracellular ATP, dampening local inflammation [22] [11]. |
| Checkpoint Ligands | PD-L1, PD-L2 | Binds to PD-1 on T cells to inhibit their effector function and reduce immune-mediated tissue damage [22]. |
Experimental Approaches for Investigating TIS and Fibrosis
In Vitro Model of Radiation-Induced Senescence and Fibrosis
Purpose: To establish a reproducible cellular model to study TIS mechanisms, SASP composition, and the efficacy of senotherapeutic agents.
Materials:
- Cell Lines: Primary human fibroblasts (e.g., IMR-90, WI-38) or cell lines relevant to the tissue of interest (e.g., pulmonary, dermal).
- Culture Reagents: Dulbecco's Modified Eagle Medium (DMEM), fetal bovine serum (FBS), penicillin-streptomycin, trypsin-EDTA.
- Irradiation Source: X-ray or Gamma-ray irradiator.
- Staining Reagents: PBS, formaldehyde, Triton X-100, SA-β-Gal staining kit, antibodies for immunofluorescence (p21, γH2AX, α-SMA).
Protocol:
- Cell Culture: Maintain fibroblasts in complete DMEM supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C and 5% CO₂.
- Senescence Induction: At 70-80% confluence, irradiate cells with a single dose of 10 Gy (Gray). Include a sham-irradiated control (0 Gy) handled identically but without irradiation.
- Post-Irradiation Culture: Replace the medium and culture the cells for 5-10 days to allow for full senescence establishment. Refresh medium every 2-3 days.
- Senescence Validation (5-10 days post-irradiation):
- Senescence-Associated β-Galactosidase (SA-β-Gal) Staining: Fix cells and incubate with X-Gal solution at pH 6.0 overnight. Senescent cells will stain blue.
- Immunofluorescence for DDR and Cycle Arrest: Stain for markers like γH2AX (DNA damage) and p21 (CDK inhibitor).
- SASP Analysis: Collect conditioned medium and analyze SASP factors (e.g., IL-6, IL-8, TGF-β) via ELISA or multiplex immunoassay.
- Fibrosis Readouts: Co-culture senescent fibroblasts with naive fibroblasts or analyze treated cultures for upregulation of fibrotic markers (α-SMA, Collagen I) via immunofluorescence or qPCR.
Figure 2: In Vitro Workflow for TIS Model. Fibroblasts are cultured, irradiated, and incubated to establish senescence. Validation is done via SA-β-Gal and IF, followed by SASP and fibrosis analysis.
Protocol for Testing MSC-Mediated Senescence Alleviation
Purpose: To evaluate the efficacy of MSCs or their derivatives in mitigating TIS and its pro-fibrotic consequences.
Materials:
- MSCs: Human bone marrow-derived or umbilical cord-derived MSCs (confirm CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR- by flow cytometry).
- Transwell Co-culture System: Permeable supports (e.g., 0.4 µm pore) for indirect co-culture.
- MSC-Conditioned Medium (MSC-CM): Serum-free medium conditioned by MSCs for 48 hours, centrifuged, and filtered.
- Senescence/Fibrosis Assay Kits: As in Section 4.1.
Protocol:
- Establish Senescence: Generate senescent fibroblasts as described in Section 4.1.
- Therapeutic Intervention:
- Conditioned Medium Transfer: Replace medium on senescent fibroblasts with MSC-CM.
- Direct Co-culture: Seed MSCs directly onto the senescent fibroblast culture.
- Transwell Co-culture: Seed MSCs in the insert above the senescent fibroblasts.
- Co-culture Duration: Maintain co-cultures for 48-72 hours.
- Outcome Assessment:
- Senescence Clearance: Quantify the percentage of SA-β-Gal positive cells pre- and post-treatment.
- SASP Modulation: Analyze conditioned media for changes in IL-6, IL-8, and TGF-β levels.
- Fibrotic Marker Expression: Assess α-SMA and Collagen I levels in fibroblasts via qPCR or immunofluorescence.
- Apoptosis Assay: Perform TUNEL staining or Caspase-3 activity assay to determine if MSCs induce apoptosis in senescent cells.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Senescence, Fibrosis, and MSC Therapy
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Senescence Inducers | Ionizing Radiation (X-ray, γ-ray), Chemotherapeutics (Doxorubicin, Etoposide) | Induce stable cellular senescence in vitro and in vivo for modeling TIS [77] [76]. |
| Senescence Detection | SA-β-Gal Staining Kit, Antibodies vs p21, p16, γH2AX | Histochemical and immunological identification and validation of senescent cells in culture or tissue sections [76]. |
| SASP Analysis | ELISA Kits (IL-6, IL-8, TGF-β), Multiplex Cytokine Array | Quantify the levels of key pro-inflammatory and pro-fibrotic factors secreted by senescent cells [77] [76]. |
| Fibrosis Markers | Antibodies vs α-SMA, Collagen I, Fibronectin; Sirius Red Stain | Detect and quantify the activation of myofibroblasts and deposition of extracellular matrix [77]. |
| MSC Characterization | Antibodies vs CD73, CD90, CD105, CD34, CD45, HLA-DR | Validate MSC identity and purity via flow cytometry according to ISCT standards [11]. |
| Senolytic Compounds | ABT-263 (Navitoclax), ABT-737, Dasatinib + Quercetin (D+Q) | Selectively induce apoptosis in senescent cells; used as positive controls in therapeutic experiments [76]. |
The intricate interplay between therapy-induced senescence, fibrosis, and immune communication presents a significant challenge in oncology, but also a profound therapeutic opportunity. Targeting senescent cells and their pro-fibrotic SASP represents a paradigm shift in managing the long-term side effects of cancer treatment. The immunomodulatory prowess of MSCs, mediated through paracrine signaling and direct cellular crosstalk, offers a multifaceted strategy to disrupt this damaging cycle. Future research must focus on personalizing these approaches, potentially by deriving patient-specific MSCs to fine-tune immune modulation. Furthermore, combining senolytics (to clear senescent cells) with MSC-based therapies (to modulate the immune response and promote repair) presents a highly promising combinatorial strategy. As our understanding of the molecular mechanisms deepens, so too will our ability to combat TIS-driven fibrosis, ultimately improving the quality of life for cancer survivors.
From Bench to Bedside: Clinical Trial Insights and Evolving Regulatory Frameworks
Autoimmune diseases represent a significant challenge in modern medicine, occurring when the immune system targets the body's own tissues, leading to inflammation and tissue damage [78]. Among these conditions, systemic lupus erythematosus (SLE), Crohn's disease, and systemic sclerosis (scleroderma) affect millions globally and pose considerable challenges in treatment efficacy, safety, and long-term disease control [78]. This whitepaper provides a comprehensive analysis of global clinical trials for these diseases, focusing on emerging therapeutic strategies, efficacy and safety trends, and their alignment with novel paradigms in stem cell immune modulation.
The treatment landscape is rapidly evolving from broad immunosuppression toward targeted immunomodulation that addresses underlying disease mechanisms [78]. This analysis synthesizes findings from recent clinical trials to identify consistent trends and novel approaches that offer the potential for long-term disease remission and possibly cures.
Methodology: Clinical Trial Analysis Framework
Literature Search and Selection Criteria
This analysis employed a systematic approach to identify relevant clinical trials and research studies. A targeted literature search was conducted using PubMed/MEDLINE, ClinicalTrials.gov, and proceedings of major international rheumatology congresses (EULAR, ACR) up to October 2025 [79]. Search terms included combinations of: "systemic lupus erythematosus," "Crohn's disease," "systemic sclerosis," "scleroderma," "clinical trials," "efficacy," "safety," "emerging therapies," and "stem cell therapy."
Priority was given to phase II–III clinical trials, recent international guidelines, and ongoing trials investigating novel therapeutic targets. Foundational or landmark studies published prior to this timeframe were included where they remain essential to guiding current clinical practice. Additional references were identified through citation chaining and based on expert consensus in autoimmune disease clinical care and research.
Data Extraction and Analysis
For each included study, data were extracted using a standardized template capturing: primary endpoints, secondary outcomes, safety parameters, study duration, patient population, and key efficacy metrics. Quantitative data were synthesized into structured tables for cross-trial comparison, while qualitative findings were analyzed thematically to identify emerging trends and consensus positions.
Efficacy and Safety Trends Across Autoimmune Diseases
Systemic Lupus Erythematosus (SLE)
Table 1: Clinical Trial Outcomes for Systemic Lupus Erythematosus (SLE) Therapies
| Therapy | Mechanism | Trial Phase | Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|
| Upadacitinib + Elsubrutinib [80] | JAK inhibitor + BTK inhibitor | Phase 2 (104 weeks) | SRI-4: 85.4%; BICLA: 78.0%; LLDAS: 78.0% | Consistent with known profiles, no new safety signals |
| Deucravacitinib [81] | TYK2 inhibitor | Phase 2 (up to 4 years) | Sustained SRI-4, BICLA, LLDAS, and CLASI-50 responses | Consistent safety profile, no new safety signals |
| CD19 CAR-T Cells [78] | B-cell depletion via CAR-T therapy | Early Phase | Durable drug-free remission, normalized complement levels, decreased anti-dsDNA titers | Mild, short-lived cytokine release syndrome |
| Ianalumab [82] | B-cell targeting | Phase 3 | Significant reduction in disease activity in two large trials (NEPTUNUS-1, NEPTUNUS-2) | Not specified in detail |
Recent findings in SLE have revealed how severely this disease can affect the heart, with a nationwide case-control study showing that people with SLE face a much higher risk of cardiovascular disease and heart tissue damage than the general population [82]. These results emphasize the importance of regular heart health monitoring for anyone living with lupus.
Novel therapeutic approaches for SLE include JAK/BTK inhibition, TYK2 inhibition, and CAR-T cell therapy. The 104-week long-term extension study of upadacitinib alone or combined with elsubrutinib demonstrated maintained or increased efficacy responses from weeks 48 to 104, with SRI-4 responses of 82.1%, 85.4%, and 61.3% for upadacitinib, upadacitinib/elsubrutinib, and placebo-switched groups respectively [80]. Similarly, deucravacitinib maintained a consistent safety profile and durable efficacy with up to four years of drug exposure, with no new safety signals despite complex background therapies [81].
The most revolutionary approach comes from CD19-directed CAR T-cell therapy, which demonstrated remarkable results in patients with refractory SLE, with all patients entering durable drug-free remission, normalized complement levels, decreased anti-dsDNA titers, and no further disease flares during follow-up [78].
Crohn's Disease
Table 2: Clinical Trial Outcomes for Crohn's Disease Therapies
| Therapy | Mechanism | Trial Phase | Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|
| Upadacitinib (15 mg) [83] | JAK inhibitor | Phase 3 (104 weeks) | Clinical remission: 78.3%-82.9%; Endoscopic response: 59.6%-67.1% | 283.1 events/100 PYs |
| Upadacitinib (30 mg) [83] | JAK inhibitor | Phase 3 (104 weeks) | Clinical remission: 84.7%-76.6%; Endoscopic response: 71.2%-69.6% | 273.4 events/100 PYs |
The U-ENDURE long-term extension study evaluated the efficacy and safety of upadacitinib in patients with moderate to severe Crohn's disease over two years of total maintenance treatment [83]. From long-term extension week 0 to week 48, as-observed efficacy rates for clinical remission and endoscopic response remained stable, demonstrating sustained therapeutic effects.
The safety profile of the cumulative maintenance population observed through the long-term extension week 48 was consistent with previous trials in the upadacitinib Crohn's disease program [83]. Treatment-emergent adverse event rates were 283.1 and 273.4 events per 100 patient-years for upadacitinib 15 mg and 30 mg, respectively. The most common adverse events of special interest (≥5.0 events/100 patient-years) were hepatic disorder, lymphopenia, creatine phosphokinase elevation, herpes zoster, and anemia.
Systemic Sclerosis (Scleroderma)
Table 3: Clinical Trial Outcomes for Systemic Sclerosis Therapies
| Therapy | Mechanism | Trial Phase | Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|
| Rapcabtagene autoleucel [84] [79] | CD19-targeted CAR-T therapy | Phase 1/2 | 100% probability of improvement per ACR-CRISS; mRSS decreased by 31%; FVC increased by 195 mL | Cytokine release syndrome risk |
| Belimumab [79] [85] | BAFF inhibition | Phase 2b | Targets B-cell survival, reducing autoantibody production | Not fully characterized |
| Anifrolumab [79] [85] | Type I interferon receptor blockade | Phase 2b | Previously approved for SLE, now explored in SSc | Not fully characterized |
| BMS-986278 [84] [85] | LPA1 receptor antagonist | Phase 2 | For progressive pulmonary fibrosis in SSc | Not fully characterized |
Systemic sclerosis is characterized by vasculopathy, immune dysregulation, and progressive fibrosis, leading to significant morbidity and mortality [79]. Recent studies evaluating CAR-T19 therapy in diffuse cutaneous systemic sclerosis have yielded promising results, with patients demonstrating a 100% probability of improvement based on the ACR-CRISS score at 6 months post-treatment, suggesting complete resolution of active disease [79].
Median modified Rodnan skin scores decreased by 31% within the first 100 days, indicating rapid and substantial reduction in skin fibrosis [79]. High-resolution CT scans revealed a 4% decrease in disease extent, with improvements in ground-glass opacities, while forced vital capacity increased by a median of 195 mL, a notable improvement given the typically progressive nature of SSc-associated interstitial lung disease.
Multiple clinical trials are currently investigating novel therapies for systemic sclerosis, including belimumab, anifrolumab, and BMS-986278 for progressive pulmonary fibrosis [85]. These emerging therapies reflect a shift toward personalized and biomarker-driven approaches that offer the potential to alter disease trajectory and support early, targeted intervention.
Stem Cell Immune Modulation: Mechanisms and Therapeutic Applications
Mesenchymal Stem Cells as Biological Drugs
Stem cells are increasingly recognized as "living drugs" due to their dynamic and adaptive therapeutic properties [86]. Unlike conventional medicines derived from chemical or biological compounds, living drugs such as stem cells are derived from living tissues and are administered as viable, functional cells. The effects of conventional medicine are often temporary, whereas living drugs can integrate into damaged tissues and organs, exerting longer-lasting effects [86].
Mesenchymal stem cells possess two defining characteristics: self-renewal (the ability to divide and produce identical copies) and differentiation (the ability to differentiate into specialized cell types) [86]. These characteristics make them promising candidates for repairing and regenerating damaged tissues and organs. Their functional properties, however, can vary significantly depending on tissue source, donor age, health status, and production protocols [86].
Immunomodulatory Mechanisms of Stem Cells
Diagram 1: Stem Cell Immunomodulatory Mechanisms in Autoimmunity
MSCs counteract autoimmune pathophysiology through multipronged strategies [10]. The immunomodulatory mechanisms can be divided into two primary categories:
Immunoregulatory Mechanisms of Intercellular Contact
When MSCs are kept in close contact with activated immune cells, they enhance their immunosuppressive effects [10]. MSCs express integrins, intercellular adhesion molecules, vascular cell adhesion molecule, CD72, and CD58 on their surface, enabling them to bind to T lymphocytes with high affinity [10]. Studies have shown that when T cells were co-cultured with bone marrow-derived MSCs in Transwell systems or with conditioned medium, the inhibitory activity of T cells was eliminated, suggesting that inhibition of T cells by MSCs requires direct MSC-T cell contact [10].
Specific mechanisms include:
- Human placenta-derived MSCs bind to co-inhibitory receptors on T cell surfaces through high expression of PDL1 and PDL2, inhibiting T cell proliferation and cytokine production by blocking the cell cycle in the G0/G1 phase [10].
- Induced pluripotent stem cell-derived MSCs and bone marrow MSCs inhibit proliferation of CD3 T cells isolated from peripheral blood mononuclear cells of allergic rhinitis patients through cell-to-cell contact and PGE2 expression [10].
- MSCs increase TNF-stimulated gene 6 production through intercellular contact with pro-inflammatory M1 macrophages, promoting transformation into anti-inflammatory M2 macrophages in a TSG-6-dependent manner to alleviate excessive inflammation [10].
Mechanisms of Immunomodulation by Soluble Factors
MSCs can treat autoimmune conditions by modulating pro-inflammatory and anti-inflammatory cytokines, ameliorating the severity of acute injury and fibrosis, restoring epithelial barrier integrity, and modulating networks of interactions between various immune cells [10]. Soluble factors associated with MSC treatment include TGF-β, IL-10, PGE2, IDO, hepatocyte growth factor, NO, TSG-6, IL-6, leukemia inhibitory factor, HLA-G5, and IL1RA [10].
Key pathways include:
- TGF-β/Smad pathway: TGF-β binds to its receptor TGF-βRII, recruiting and phosphorylating TGF-βRI to form a heterotetrameric complex, triggering phosphorylation of R-Smads (Smad2 and Smad3) which translocate to the nucleus to regulate transcription of target genes like FOXP3, the master regulator of Tregs [10].
- Soluble factors secreted by MSCs can restore Th1/Th2 cell balance by modulating T cell-mediated immune responses. MSC-conditioned media contain significantly increased concentrations of TGF-β1, PGE2, and hepatocyte growth factor, which have been implicated in suppressing T cell activation through inhibition of T cell receptor signaling [10].
Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation stands as the prototypical success of cell therapy in autoimmune diseases [86]. Its effectiveness rests on the remarkable ability of donor-derived stem cells to engraft, self-renew, and reconstitute the immune and hematopoietic systems after intensive conditioning [86]. For multiple sclerosis patients who fail to respond to conventional therapy, hematopoietic stem cell transplantation can reboot the immune system, halting disease progression or even reversing some neurological damage [86].
Recent data from experienced centers using optimized conditioning regimens indicate improved safety profiles and lower transplant-related mortality for systemic sclerosis patients [79]. While early trials reported considerable treatment-related risks, hematopoietic stem cell transplantation remains an important option for selected patients with rapidly progressive systemic sclerosis at risk of organ failure [79].
Experimental Protocols and Research Methodologies
CAR-T Cell Therapy Protocol for Autoimmune Diseases
Diagram 2: CAR-T Cell Therapy Workflow for Autoimmunity
The development of CAR-T cell therapy for autoimmune diseases follows a standardized protocol with specific modifications for autoimmunity:
Leukapheresis and T-cell Collection: Patients undergo leukapheresis to collect peripheral blood mononuclear cells, from which T-cells are isolated and enriched [78].
T-cell Activation and Genetic Modification: Isolated T-cells are activated using anti-CD3/CD28 antibodies and genetically modified to express chimeric antigen receptors targeting B-cell markers such as CD19 or BCMA [78].
CAR Transgene Insertion: The CAR transgene is typically inserted using lentiviral or retroviral vectors, though non-viral methods like transposon systems are also being investigated [78].
Ex Vivo Expansion: Genetically modified T-cells are expanded in culture using cytokines such as IL-2 and IL-7 to achieve sufficient cell numbers for therapeutic efficacy [78].
Lymphodepleting Chemotherapy: Before CAR-T cell infusion, patients receive lymphodepleting chemotherapy (typically fludarabine and cyclophosphamide) to enhance engraftment and persistence of the modified cells [78].
CAR-T Cell Infusion: The expanded CAR-T cells are infused back into the patient, where they expand further and mediate their therapeutic effects [78].
Monitoring and Management: Patients are closely monitored for efficacy endpoints and adverse events, particularly cytokine release syndrome, with appropriate management protocols implemented [78].
JAK Inhibitor Clinical Trial Methodology
Clinical trials for JAK inhibitors such as upadacitinib follow rigorous methodology to evaluate efficacy and safety:
Study Design: Randomized, double-blind, placebo-controlled trials with long-term extension phases, such as the SLEek study (NCT03978520) and its long-term extension (NCT04451772) for SLE, or the U-ENDURE study (NCT03345823) for Crohn's disease [80] [83].
Patient Population: Adults with moderately to severely active disease, often with specific criteria such as SLEDAI-2K score ≥6 and clinical manifestations for SLE, or Crohn's Disease Activity Index scores for Crohn's disease [80].
Primary Endpoints: Typically composite measures such as SRI-4 (SLE Responder Index-4) for lupus or clinical remission per stool frequency/abdominal pain score for Crohn's disease [80] [83].
Secondary Endpoints: Include BICLA (British Isles Lupus Assessment Group-based Combined Lupus Assessment), LLDAS (Lupus Low Disease Activity State), glucocorticoid dose reduction, flare rates, and patient-reported outcomes [80].
Safety Assessments: Comprehensive evaluation of adverse events, laboratory parameters, vital signs, and electrocardiograms throughout the study period [80] [83].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Autoimmunity Investigations
| Reagent/Category | Specific Examples | Research Function | Application Context |
|---|---|---|---|
| Immune Cell Markers | CD19, CD3, CD4, CD8, CD20, CD38 | Identification and isolation of specific immune cell populations | Flow cytometry, immunohistochemistry, cell sorting |
| Cytokine Detection | IL-6, IL-10, TGF-β, IFN-α, IFN-γ | Quantification of inflammatory and regulatory mediators | ELISA, multiplex immunoassays, intracellular staining |
| Signaling Pathway Inhibitors | JAK inhibitors (upadacitinib), BTK inhibitors (elsubrutinib), TYK2 inhibitors (deucravacitinib) | Targeted disruption of specific immune signaling pathways | Mechanism of action studies, combination therapy approaches |
| CAR-T Components | Lentiviral vectors, anti-CD19 scFv, CD3ζ, 4-1BB | Genetic modification of T cells for adoptive cell therapy | CAR-T development, optimization, and manufacturing |
| Stem Cell Media & Supplements | Mesenchymal stem cell media, FBS alternatives, differentiation kits | Maintenance and directed differentiation of stem cell populations | MSC expansion, characterization, and therapeutic preparation |
| Autoantibody Assays | Anti-dsDNA, ANA, Scl-70, rheumatoid factor | Detection and quantification of disease-specific autoantibodies | Patient stratification, disease monitoring, biomarker discovery |
Comparative Analysis of Therapeutic Mechanisms
Diagram 3: Therapeutic Targeting in Autoimmune Signaling
The therapeutic approaches analyzed demonstrate distinct but complementary mechanisms of action:
Targeted Small Molecule Therapies
Small molecule inhibitors such as JAK inhibitors (upadacitinib), BTK inhibitors (elsubrutinib), and TYK2 inhibitors (deucravacitinib) target intracellular signaling pathways critical for immune cell activation and cytokine production [80] [81]. These orally administered agents provide convenient dosing but require careful safety monitoring due to potential effects on multiple cell types and physiological processes.
The efficacy of these approaches across multiple autoimmune conditions suggests shared pathogenic pathways, particularly in cytokine signaling and B-cell/T-cell activation. The maintenance of efficacy over extended periods (up to 104 weeks in some trials) supports their role as long-term management strategies [80] [83].
Cellular Therapies: CAR-T and Stem Cells
Cellular therapies represent a paradigm shift in autoimmune disease treatment, offering the potential for durable remissions and possibly cures. CD19-directed CAR T-cell therapy achieves profound B-cell depletion, potentially "resetting" immune tolerance and allowing reconstitution with naïve, non-autoreactive B-cells [78]. This approach has demonstrated remarkable efficacy in refractory SLE, with patients maintaining drug-free remission even after B-cell recovery [78].
Mesenchymal stem cells function as multimodal biological drugs that sense environmental cues and adapt their therapeutic effects accordingly [86]. Their mechanisms include differentiation into specific cell types, paracrine signaling, immunomodulation, homing to injury sites, tissue integration, and anti-apoptotic and anti-fibrotic actions [86]. Unlike pharmacologic agents with specific molecular targets, MSCs employ multiple coordinated strategies to restore immune homeostasis.
The analysis of global clinical trials for Crohn's disease, SLE, and scleroderma reveals several consistent trends in autoimmune disease treatment. There is a clear movement away from broad immunosuppression toward targeted immunomodulation that addresses specific disease mechanisms while preserving protective immunity. Additionally, the success of cellular therapies, particularly CAR-T cells and stem cells, demonstrates the potential for durable remissions and possibly cures in conditions previously managed only with lifelong immunosuppression.
Future research directions should focus on several key areas:
- Optimization of patient selection through biomarker development to match specific therapies to individual disease mechanisms
- Combination approaches that leverage complementary mechanisms of action while minimizing toxicity
- Development of next-generation cellular therapies with improved safety profiles and manufacturing scalability
- Long-term follow-up to understand the durability of responses and late-emerging effects of novel therapies
The convergence of targeted small molecules, cellular therapies, and stem cell approaches represents a transformative period in autoimmune disease treatment. These advances align with the broader thesis of stem cell immune modulation, demonstrating how harnessing and directing fundamental biological processes can achieve therapeutic outcomes not possible with conventional pharmacotherapy alone. As these technologies continue to evolve, they offer the promise of truly personalized medicine for patients with autoimmune diseases.
The period from 2023 to 2025 has marked significant regulatory milestones in stem cell therapy, with the U.S. Food and Drug Administration (FDA) approving several innovative products that demonstrate the expanding therapeutic potential of cellular technologies. This whitepaper provides a comparative analysis of three groundbreaking therapies—Omisirge (omidubicel-onlv), Lyfgenia (lovotibeglogene autotemcel), and Ryoncil (remestemcel-L)—approved during this timeframe. Each product represents a distinct technological approach: Omisirge is a nicotinamide-modified ex vivo expanded cord blood-derived graft for hematopoietic reconstitution; Lyfgenia is an autologous hematopoietic stem cell-based gene therapy for sickle cell disease; and Ryoncil is the first allogeneic bone marrow-derived mesenchymal stromal cell therapy for steroid-refractory acute graft-versus-host disease. Beyond their distinct clinical applications, these therapies collectively highlight the critical role of immune modulation in achieving therapeutic efficacy, from creating permissive environments for engraftment to actively suppressing pathological immune responses. This analysis examines their mechanisms of action, clinical profiles, and contributions to the evolving understanding of stem cell-mediated immune regulation in therapeutic contexts.
Product Profiles and Clinical Indications
Omisirge (omidubicel-onlv)
Omisirge, approved on April 17, 2023, is a first-in-class, nicotinamide-modified ex vivo expanded umbilical cord blood-derived cellular therapy developed by Gamida Cell Ltd. It is indicated for patients 12 years and older with hematologic malignancies who are planned for umbilical cord blood transplantation following myeloablative conditioning [87]. This patient-specific allogeneic product consists of two fractions derived from a single cord blood unit: a cultured fraction containing nicotinamide-modified hematopoietic stem and progenitor cells (HSPCs) and a non-cultured T-cell containing fraction [87]. The primary therapeutic goals are to accelerate hematopoietic recovery and reduce infection risk post-transplantation.
Lyfgenia (lovotibeglogene autotemcel or Lovo-cel)
Lyfgenia, approved on December 8, 2023, is an autologous cell-based gene therapy developed by bluebird bio for patients aged 12 years and older with sickle cell disease and a history of vaso-occlusive events (VOEs) [88]. This one-time treatment involves genetically modifying the patient's own hematopoietic stem cells to produce HbAT87Q, a gene-therapy derived hemoglobin with anti-sickling properties designed to reduce sickling of red blood cells and improve blood flow [89]. The therapy represents a significant advancement in addressing the underlying pathophysiology of sickle cell disease through genetic modification.
Ryoncil (remestemcel-L)
Ryoncil, approved on December 18, 2024, developed by Mesoblast, represents a landmark as the first FDA-approved allogeneic, off-the-shelf, bone marrow-derived mesenchymal stromal cell (MSC) therapy [90]. It is indicated for the treatment of pediatric patients aged 2 months and older with steroid-refractory acute graft-versus-host disease (SR-aGVHD), a life-threatening complication following allogeneic hematopoietic stem cell transplantation with historically limited treatment options and high mortality rates [90]. Unlike the other products, Ryoncil's mechanism centers on immunomodulation rather than reconstitution or genetic correction.
Comparative Analysis of Key Characteristics
Table 1: Comparative Product Profiles
| Characteristic | Omisirge | Lyfgenia | Ryoncil |
|---|---|---|---|
| Brand Name | Omisirge | Lyfgenia | Ryoncil |
| Generic Name | omidubicel-onlv | lovotibeglogene autotemcel (lovo-cel) | remestemcel-L |
| Manufacturer | Gamida Cell Ltd. | bluebird bio, Inc. | Mesoblast, Inc. |
| FDA Approval Date | April 17, 2023 [87] | December 8, 2023 [59] | December 18, 2024 [90] |
| Therapeutic Category | Cord blood-derived hematopoietic progenitor cells | Cell-based gene therapy | Allogeneic mesenchymal stromal cells |
| Cell Source | Allogeneic umbilical cord blood | Autologous hematopoietic stem cells | Allogeneic bone marrow |
| Key Technology | Nicotinamide modification & ex vivo expansion | Gene addition (lentiviral vector) | Native immunomodulatory cells |
| Administration | Single intravenous infusion | Single intravenous infusion | Multiple intravenous infusions (twice weekly for 4 weeks) [90] |
Table 2: Clinical Efficacy and Safety Profiles
| Parameter | Omisirge | Lyfgenia | Ryoncil |
|---|---|---|---|
| Primary Indication | Hematologic malignancies requiring cord blood transplant | Sickle cell disease with history of VOEs | Pediatric steroid-refractory acute GVHD |
| Key Efficacy Outcomes | Median time to neutrophil engraftment: 12 days (vs. 22 days control); Lower infection incidence (37% vs. 57%) [87] | 88% (28/32) achieved complete resolution of VOEs between 6-18 months post-infusion [89] | Clinical trials demonstrated response in life-threatening condition with limited options [90] |
| Mechanism of Action | Hematopoietic reconstitution | Production of anti-sickling hemoglobin (HbAT87Q) | Immunomodulation via MSC-secreted factors |
| Common Adverse Reactions | Infections, febrile neutropenia | Stomatitis, thrombocytopenia, neutropenia [59] | Viral/bacterial infections, pyrexia, respiratory failure [90] |
| Unique Safety Considerations | Graft failure, graft-versus-host disease | Hematologic malignancies required monitoring [89] | Hypersensitivity reactions, ectopic tissue formation potential [90] |
Mechanisms of Action and Immune Modulation
Omisirge: Enhanced Hematopoietic Reconstitution
Omisirge functions through hematopoietic reconstitution with an enhanced profile. The nicotinamide modification technology expands functional hematopoietic stem and progenitor cells while inhibiting differentiation, resulting in a graft with improved engraftment capacity [87]. This leads to more rapid neutrophil recovery (12 days versus 22 days with standard cord blood transplantation), directly reducing the window of vulnerability to life-threatening infections [91]. The accelerated reconstitution represents an indirect immunomodulatory effect by rapidly restoring innate immune defenses in immunocompromised patients.
Lyfgenia: Genetic Correction of Erythrocytes
Lyfgenia employs a gene addition approach using a lentiviral vector to introduce functional genetic material into autologous CD34+ hematopoietic stem cells, enabling them to produce HbAT87Q [89]. This anti-sickling hemoglobin substitutes for defective hemoglobin S, reducing polymerization under deoxygenating conditions and subsequent erythrocyte sickling. The resolution of vaso-occlusive events (achieved in 88% of patients) demonstrates how genetic correction at the hematopoietic stem cell level can systemically alleviate inflammatory cascades and tissue damage driven by sickle cell pathophysiology.
Ryoncil: Multimodal Immunomodulation
Ryoncil exemplifies direct therapeutic immunomodulation through multiple synchronized mechanisms. As a mesenchymal stromal cell therapy, it counteracts the excessive immune activation in SR-aGVHD through:
- Soluble factor secretion: Production of TGF-β, PGE2, IDO, HLA-G5, and other immunoregulatory molecules that suppress T-cell activation and proliferation [10]
- Cell contact-dependent suppression: Expression of PD-L1/PD-L2 that interacts with PD-1 on T cells, inhibiting TCR-mediated activation and cell cycle progression [10]
- Immune cell reprogramming: Facilitation of macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes [10]
- Treg enhancement: Promotion of regulatory T cell activity through Notch1 and NF-κB signaling pathways, restoring immune balance [10]
These coordinated actions position MSCs as central regulators in the immune network, making them particularly effective for inflammatory conditions like SR-aGVHD where immune dysregulation is paramount.
Experimental Protocols and Clinical Trial Designs
Omisirge Phase III Clinical Trial (NCT02730299)
The regulatory approval of Omisirge was based on a Phase III randomized study of 125 patients with hematologic malignancies comparing omidubicel (n=62) to standard umbilical cord blood transplantation (n=63) [87]. The trial implemented a myeloablative conditioning regimen followed by transplantation of either the investigational or control product. Primary endpoints included time to neutrophil engraftment and incidence of bacterial and fungal infections. The experimental protocol demonstrated statistically significant improvements in both endpoints, with the omidubicel group showing faster neutrophil recovery (median 12 days vs. 22 days) and reduced infection risk (37% vs. 57%) through day 100 post-transplant [87].
Lyfgenia Phase I/2 Study (Study 1-C)
Lyfgenia's approval was supported by a single-arm, 24-month, open-label, multicenter Phase 1/2 study and long-term follow-up data [89]. The study enrolled 32 patients with sickle cell disease and a history of at least 4 vaso-occlusive events in the 24 months prior to consent. The experimental protocol involved: (1) hematopoietic stem cell collection via apheresis following mobilization with granulocyte colony-stimulating factor; (2) ex vivo genetic modification using a lentiviral vector to introduce the anti-sickling hemoglobin gene; (3) myeloablative conditioning with busulfan; and (4) reinfusion of the genetically modified autologous cells [89]. The primary efficacy endpoint was complete resolution of VOEs between 6 and 18 months post-infusion, which was achieved in 88% of evaluable patients.
Ryoncil Clinical Program (MSB-GVHD001)
Ryoncil's approval was based on Study MSB-GVHD001, which evaluated 54 pediatric patients with SR-aGVHD [90]. The dosing protocol consisted of intravenous administration at 2 × 10⁶ MSCs/kg twice weekly for four consecutive weeks (total of eight infusions). Patients with partial or mixed response at Day 28 received additional weekly infusions for four weeks. The median number of doses administered was 10 (range 1-16) over a median of 43 days [90]. The primary outcomes included Day 28 overall response and survival, with safety assessed through 100 days post-treatment. This intensive dosing regimen reflects the need for sustained immunomodulation to counteract the aggressive immune activation in SR-aGVHD.
Signaling Pathways and Mechanistic Diagrams
Ryoncil Immunomodulatory Pathways
Diagram 1: Ryoncil multimodal immunomodulation network. MSC immunosuppression integrates cell contact-dependent pathways (PD-L1/PD-L2 interactions) with soluble factor secretion (TGF-β, PGE2, IDO), collectively inhibiting T-cell activation while promoting Treg expansion and macrophage polarization.
Hematopoietic Stem Cell Therapeutic Applications
Diagram 2: Therapeutic applications of hematopoietic stem cells. Omisirge utilizes allogeneic cord blood with nicotinamide modification to enhance engraftment, while Lyfgenia employs autologous genetic modification to confer anti-sickling properties, demonstrating divergent applications of HSC platforms.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Stem Cell Therapy Development
| Reagent/Category | Function in Research | Example Applications |
|---|---|---|
| Nicotinamide | Small molecule expansion agent; inhibits differentiation and enhances stem cell function [87] | Ex vivo expansion of hematopoietic stem cells (Omisirge platform) |
| Lentiviral Vectors | Gene delivery system for stable integration of therapeutic transgenes [89] | Genetic modification of autologous HSCs (Lyfgenia platform) |
| Mesenchymal Stromal Cells | Primary immunomodulatory cells with soluble factor secretion and cell contact-dependent suppression capabilities [10] | Allogeneic cell therapy for inflammatory conditions (Ryoncil platform) |
| CD34 Microbeads | Immunomagnetic selection of hematopoietic stem/progenitor cells | Isolation of target cell population for genetic manipulation or expansion |
| Myeloablative Agents (Busulfan) | Conditioning regimen to create niche space for engrafted cells | Pre-transplant preparation in both oncologic and genetic applications |
| Cryopreservation Media | Maintain cell viability and function during frozen storage | Preservation of cellular products between manufacturing and administration |
| Cytokine Cocktails | Promote specific cell differentiation, expansion, or maintenance | Culture systems for stem cell propagation and genetic modification |
The approval of Omisirge, Lyfgenia, and Ryoncil between 2023-2025 represents a maturation of the stem cell therapy field, showcasing three distinct paradigms: enhanced hematopoietic reconstitution, genetic correction, and active immunomodulation. Each product addresses fundamentally different disease mechanisms yet collectively highlights the central role of immune regulation in therapeutic success. For researchers and drug development professionals, these products offer valuable insights into platform technologies with expanding applications.
Future directions will likely include: (1) platform extension of these validated technologies to additional indications; (2) next-generation improvements in cell manufacturing, potency, and persistence; (3) combination approaches leveraging complementary mechanisms; and (4) predictive biomarkers for patient stratification. The continued elucidation of stem cell immune modulatory mechanisms will further refine these therapeutic platforms and inspire novel approaches for managing complex immune and inflammatory conditions.
The field of regenerative medicine has been transformed by the discovery of induced pluripotent stem cells (iPSCs), which possess the unique dual properties of unlimited self-renewal and differentiation potential into all cell types of the body [92]. This breakthrough has enabled the development of a new generation of cell therapies designed to overcome the limitations of traditional patient- or donor-sourced treatments. iPSC-derived therapies represent a paradigm shift in cellular medicine, offering the potential for well-defined, uniform cell products that can be manufactured at scale, stored in inventory for off-the-shelf availability, and administered in combination with other therapies [92]. The therapeutic landscape for iPSC-derived products has expanded rapidly, with clinical trials now spanning oncology, ophthalmology, neurology, and autoimmune diseases [59]. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products, with over 1,200 patients dosed and more than 10¹¹ cells administered without significant class-wide safety concerns [59].
The clinical translation of iPSC technologies has been accelerated by advances in precision gene editing, particularly CRISPR/Cas9 systems, which enable precise genetic modifications to enhance therapeutic efficacy and safety profiles [93] [94]. These technologies allow researchers to create clonal master iPSC lines that serve as a consistent starting cell source for manufacturing engineered cell products [92]. This comprehensive review examines three prominent iPSC-derived therapeutic approaches—FT819 CAR-T cells, OpCT-001 photoreceptor cells, and iPSC-derived mesenchymal stromal cells (iMSCs)—evaluating their mechanisms of action, clinical progress, and potential to address unmet medical needs across diverse disease areas.
The clinical landscape for iPSC-derived therapies has consolidated around several key therapeutic areas where localized delivery, immune privilege, or clear mechanistic pathways offer strategic advantages. Ophthalmology and central nervous system (CNS) disorders represent leading targets, followed by oncology applications and autoimmune conditions [59]. This consolidation reflects both biological considerations and practical clinical development factors, including delivery feasibility and endpoint measurement.
Table 1: Global Pluripotent Stem Cell Clinical Trial Landscape (2020-2025)
| Therapeutic Area | Number of Trials | Notable Candidates | Development Stage |
|---|---|---|---|
| Ophthalmology | 35+ | OpCT-001, Eyecyte-RPE | Phase I/II to Phase III |
| Neurology | 30+ | Dopaminergic progenitors for Parkinson's | Phase I to Phase II |
| Oncology | 25+ | FT536, CAR-T/NK therapies | Phase I to Phase I/II |
| Autoimmune | 10+ | FT819, iMSCs for GVHD | Phase I to Phase II |
Recent regulatory milestones underscore the accelerating clinical translation of iPSC platforms. In February 2025, the FDA granted IND clearance for Fertilo, the first iPSC-based therapy to enter U.S. Phase III trials for supporting ex vivo oocyte maturation [59]. Similarly, multiple iPSC-derived neural progenitor cell therapies for Parkinson's disease, spinal cord injury, and ALS received FDA IND clearance in June 2025 [59]. The RMAT (Regenerative Medicine Advanced Therapy) designation has further facilitated development pathways, as seen with FT819 for systemic lupus erythematosus in April 2025 [92] [59].
Table 2: Recent FDA Regulatory Milestones for iPSC-Derived Therapies (2023-2025)
| Therapy | Indication | Regulatory Status | Date | Developer |
|---|---|---|---|---|
| Fertilo | In vitro oocyte maturation | FDA IND clearance for Phase III | February 2025 | Gameto |
| FT819 | Systemic lupus erythematosus | RMAT designation | April 2025 | Fate Therapeutics |
| Neural progenitors | Parkinson's disease, SCI, ALS | FDA IND clearance | June 2025 | Multiple |
| OpCT-001 | Retinal degeneration | FDA IND clearance for Phase I/IIa | September 2024 | BlueRock Therapeutics |
The safety profile of iPSC-based clinical trials to date has been encouraging, with no class-wide safety concerns observed across more than 1,200 dosed patients [59]. However, specific considerations remain regarding administration route, disease context, and long-term surveillance, particularly for therapies with proliferative potential or those targeting immunocompromised populations.
FT819: Off-the-Shelf CAR T-Cell Therapy for Autoimmune Disease
Mechanism of Action and Engineering Strategy
FT819 represents a groundbreaking approach in autoimmune therapy as the first off-the-shelf, iPSC-derived CAR T-cell product candidate targeting CD19-positive B cells [92]. This therapy is engineered from a clonal master iPSC line that incorporates multiple synthetic controls of cell function, including a novel CD19-targeted 1XX CAR construct integrated into the T-cell receptor alpha constant (TRAC) locus to eliminate endogenous TCR expression and prevent graft-versus-host disease [92]. The manufacturing approach enables the production of uniform, dose-controlled CAR T-cell products that can be administered immediately upon diagnosis, eliminating the treatment delays associated with autologous CAR T-cell therapies.
The therapeutic mechanism of FT819 in autoimmune conditions involves rapid depletion of CD19+ B cells, which are central to the pathogenesis of diseases like systemic lupus erythematosus (SLE) [92]. Following B-cell depletion, FT819 facilitates immune remodeling toward a naïve and less pathogenic B-cell repertoire, essentially resetting the immune system. This remodeling is evidenced by the emergence of naïve B cells beyond baseline levels upon return of the B-cell compartment, correlating with reduction in disease burden [92]. The dual mechanism of direct B-cell depletion followed by immune reconstitution distinguishes FT819 from conventional B-cell targeting therapies.
Clinical Trial Design and Outcomes
Fate Therapeutics is currently conducting a multi-center, Phase 1 clinical trial of FT819 for patients with moderate-to-severe SLE, including lupus nephritis and extrarenal lupus (NCT06308978) [92]. The study is evaluating the safety, pharmacokinetics, and activity of a single dose of FT819 administered with either a less-intensive conditioning regimen (fludarabine-free conditioning with cyclophosphamide alone or bendamustine alone) or a conditioning-free regimen for patients on standard-of-care maintenance therapy [92].
As of the data cut-off date of October 26, 2025, clinical results have demonstrated promising efficacy across multiple patient cohorts. In patients with active refractory lupus nephritis treated with the less-intensive conditioning regimen, two patients at dose level 1 (360 million cells) showed significant reductions of 16 and 12 points, respectively, in SLEDAI-2K from baseline, with Urine Protein-to-Creatinine ratio reduction to <0.5 mg/mg at 6 months [92]. One patient discontinued steroids and achieved DORIS (Definition of Remission in SLE) and complete renal response at 6 months, maintaining steroid-free DORIS and CRR at 15-month follow-up [92].
The safety profile observed in over 60 patients treated with FT819 across autoimmune disease and oncology has been favorable, with low incidence of low-grade cytokine release syndrome (CRS), no events of immune effector cell-associated neurotoxicity (ICANS), and no graft-versus-host disease [92]. Specifically, in the 8 safety-evaluable SLE patients with at least one month follow-up, no dose-limiting toxicities were observed, and all patients were discharged following short-duration hospitalization, supporting the potential for outpatient administration and same-day discharge [92].
Experimental Protocols and Methodologies
The clinical trial employs comprehensive assessment protocols to evaluate both efficacy and safety endpoints. Key methodological approaches include:
- Disease Activity Assessment: SLE Disease Activity Index (SLEDAI-2K) scores and Physician's Global Assessment (PGA) are measured at baseline and regular intervals post-treatment [92].
- Renal Function Monitoring: For lupus nephritis patients, Urine Protein-to-Creatinine ratio (UPCr) is tracked with complete renal response defined as UPCr reduction to <0.5 mg/mg [92].
- Remission Criteria: Definition of Remission in SLE (DORIS) criteria are applied, incorporating clinical and serological measures [92].
- B-cell Monitoring: Flow cytometry and immunological assays track CD19+ B-cell depletion and repertoire reconstitution [92].
- Safety Monitoring: Standardized grading for cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), and other adverse events using established criteria [92].
Conditioning regimens are tailored to patient subgroups, with the less-intensive regimen (Regimen A) utilizing cyclophosphamide alone or bendamustine alone, while the conditioning-free approach (Regimen B) allows FT819 administration as an add-on to existing maintenance therapies like mycophenolate mofetil [92].
OpCT-001: iPSC-Derived Therapy for Retinal Degeneration
Therapeutic Approach and Biological Rationale
OpCT-001 represents a pioneering iPSC-derived therapy targeting retinal degeneration, including retinitis pigmentosa and cone-rod dystrophy [59]. The therapy involves the transplantation of photoreceptor progenitor cells derived from clinical-grade human induced pluripotent stem cells. The eye presents an ideal target for iPSC-based therapies due to its relative immune privilege, facilitating local administration that minimizes systemic exposure and potential immune rejection [59]. This immunological advantage, combined with precise delivery methods and established functional endpoints for visual assessment, has positioned ophthalmology as a leading area in pluripotent stem cell clinical trials.
The therapeutic strategy behind OpCT-001 centers on replacing lost photoreceptor cells and potentially preserving remaining retinal architecture through trophic support. In degenerative retinal conditions, the progressive loss of photoreceptors—the light-sensing cells of the retina—leads to irreversible vision impairment. By introducing functional progenitor cells capable of maturing into photoreceptors, OpCT-001 aims to restore visual function at the cellular level. The therapy builds upon previous advances in retinal pigment epithelium (RPE) transplantation, with products like Eyecyte-RPE having received IND approval in India in 2024 for geographic atrophy associated with AMD [59].
Clinical Development Status and Protocol Design
In September 2024, OpCT-001 received FDA clearance of its IND application to enter a Phase I/IIa clinical trial to assess safety and visual restoration in patients with photoreceptor diseases [59]. This milestone marks OpCT-001 as the first iPSC-based cell therapy to be clinically tested for treating primary photoreceptor diseases, representing a significant advancement beyond RPE-focused approaches.
The Phase I/IIa trial is designed to evaluate:
- Primary Safety Endpoints: Incidence and severity of adverse events, including ocular inflammation, increased intraocular pressure, tumor formation, and retinal detachment [59].
- Efficacy Measures: Visual acuity testing, visual field assessments, retinal imaging (OCT), and electrophysiological studies (ERG) to evaluate functional integration [59].
- Dose Escalation: Sequential cohort enrollment with increasing cell doses to establish the therapeutic window [59].
- Immunosuppression Regimen: Typically involves local and systemic corticosteroids to manage post-transplantation inflammation, though the immune privilege of the eye may permit lower immunosuppression burdens compared to other sites [59].
The immune compatibility of allogeneic iPSC-derived products in the retinal space is enhanced by the ocular immune environment, which exhibits altered antigen presentation capabilities and contains immunosuppressive factors that promote tolerance [95].
iPSC-Derived Mesenchymal Stromal Cells (iMSCs)
Advantages Over Primary MSCs and Manufacturing Considerations
iPSC-derived mesenchymal stromal cells (iMSCs) represent an innovative approach to overcoming the limitations of primary MSCs, including donor-dependent variability, limited expansion capacity, and senescence-associated functional decline [59]. By differentiating iPSCs into MSCs, researchers can generate highly consistent, scalable cell populations with enhanced proliferative capacity while maintaining the immunomodulatory and tissue-reparative properties that make MSCs therapeutically valuable [93].
The manufacturing process for iMSCs begins with established clonal master iPSC lines, which undergo directed differentiation toward mesodermal lineages using specific cytokine cocktails and culture conditions [93]. This approach enables the production of standardized, well-characterized cell banks that meet regulatory requirements for off-the-shelf therapies. The resulting iMSCs express typical MSC surface markers (CD73, CD90, CD105) while lacking hematopoietic markers (CD34, CD45, CD14/CD11b, CD79α/CD19, HLA-DR), consistent with International Society for Cellular Therapy (ISCT) criteria [96] [97].
Genetic Engineering to Enhance Therapeutic Potential
CRISPR/Cas9 technology has emerged as a powerful tool for enhancing iMSC functionality and overcoming immunological barriers [93]. Key engineering strategies include:
- Immune Evasion: Knockout of beta-2 microglobulin (β2M) to abrogate HLA class I surface expression, reducing recognition by alloreactive CD8+ T-cells [93].
- Enhanced Immunomodulation: Augmentation of anti-inflammatory mediators like interleukin (IL)-10 and TNF-alpha stimulated gene/protein 6 (TSG-6) to amplify suppressive effects on immune responses [93].
- Targeted Delivery: Engineering iMSCs to express homing receptors or therapeutic transgenes for site-specific activity in conditions like rheumatoid arthritis or solid tumors [93].
These genetic modifications enable the creation of "immune stealth" iMSCs designed for allogeneic use without matching requirements, potentially broadening patient access and enabling off-the-shelf availability [93].
Clinical Applications and Trial Status
iMSCs are gaining momentum in regenerative medicine trials targeting conditions such as osteoarthritis, tissue repair, and immune-mediated disorders [59]. An ongoing FDA-approved clinical trial in the U.S. is evaluating Cymerus iMSCs (CYP-001) for the treatment of High-Risk Acute Graft-Versus-Host Disease (HR-aGvHD) in combination with corticosteroids (NCT05643638) [59]. This trial builds on the recent FDA approval of Ryoncil (remestemcel-L), a primary MSC therapy for pediatric steroid-refractory acute GVHD, demonstrating the clinical validation of the MSC platform for immune modulation [59] [97].
The therapeutic effects of iMSCs are mediated primarily through paracrine signaling rather than direct differentiation and engraftment [97]. iMSCs secrete a diverse array of bioactive molecules, including growth factors, cytokines, and extracellular vesicles, that modulate local cellular environments, promote tissue repair, stimulate angiogenesis, and exert anti-inflammatory effects [97]. This mechanism aligns with the understanding that MSCs function as "trophic mediators" that coordinate repair processes through communication with resident cells [97].
Immune Modulation Mechanisms of iPSC-Derived Therapies
Hypoimmunogenic Engineering Strategies
A central challenge in allogeneic cell therapy is preventing immune rejection without requiring intensive immunosuppression. iPSC-derived products address this through multiple hypoimmunogenic engineering approaches designed to evade host immune recognition [95]. These strategies include:
- HLA Silencing: Targeted disruption of beta-2 microglobulin or HLA genes to reduce surface expression of major histocompatibility complex class I molecules, minimizing CD8+ T-cell recognition [93] [95].
- Immunomodulatory Molecule Expression: Engineering cells to overexpress immunosuppressive factors like PD-L1, CD47, CD200, indoleamine 2,3-dioxygenase (IDO), and heme oxygenase-1 (HO-1) that inhibit T-cell proliferation, NK cell activation, and macrophage phagocytosis [95].
- HLA Matching Banks: Establishing banks of HLA-haplotyped iPSC lines to enable matching for common population haplotypes, reducing immunogenicity through compatibility rather than genetic modification [94].
Research on GStemHep cells (iPSC-derived hepatic progenitors) demonstrates the potential of these approaches, showing complete loss of HLA-I expression while maintaining high expression of immunoregulatory molecules like IDO and HO-1 [95]. These cells exhibited low immunogenic activity on T cells and a suppressive effect on proliferation partially mediated by IDO [95].
Metabolic and Signaling Pathway Modulation
iPSC-derived therapies additionally modulate immune responses through metabolic reprogramming and signaling pathway interactions. Key mechanisms include:
- Tryptophan Metabolism: IDO-mediated tryptophan catabolism depletes this essential amino acid from the local microenvironment, suppressing T-cell activation and proliferation [95].
- Heme Degradation: HO-1 expression breaks down heme into biliverdin, carbon monoxide, and free iron, exerting anti-inflammatory, antioxidant, and cytoprotective effects [95].
- Checkpoint Molecule Expression: Surface expression of PD-L1 engages PD-1 on activated T cells, delivering inhibitory signals that limit effector functions [95].
- Cytokine Secretion: Production of anti-inflammatory cytokines (IL-10, TGF-β) and growth factors that shift immune responses toward tolerance and tissue repair [97].
These multifaceted immunomodulatory capacities enable iPSC-derived therapies to persist in allogeneic environments while actively suppressing detrimental immune responses that drive disease pathology.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for iPSC-Derived Therapy Development
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | iPSC generation | Reprogramming somatic cells to pluripotent state |
| CRISPR/Cas9 Systems | SpCas9, gRNA constructs, HDR templates | Genetic engineering | Targeted gene knockout (β2M, CIITA) or knock-in (therapeutic transgenes) |
| Cell Culture Matrices | iMatrix-511, Vitronectin, Laminin | iPSC maintenance | Support pluripotent cell growth and differentiation |
| Differentiation Factors | CHIR99021 (GSK3β inhibitor), HGF, BMPs, FGFs | Directed differentiation | Guide lineage-specific differentiation (mesodermal, ectodermal) |
| Phenotypic Characterization | CD73, CD90, CD105 antibodies; Flow cytometry | Cell product validation | Confirm surface marker expression per ISCT criteria |
| Immunomodulatory Reagents | IFN-γ, TNF-α, IL-1β | In vitro potency assays | Activate immunomodulatory pathways; assess therapeutic potential |
The development of clinical-grade iPSC lines requires stringent quality control and documentation. In July 2025, REPROCELL submitted a Type II Drug Master File (DMF) for its StemRNA Clinical iPSC Seed Clones, providing comprehensive regulatory documentation including donor screening, GMP-compliant manufacturing, quality control, and raw material sourcing [59]. This resource enables researchers to reference established iPSC platforms in their IND filings, streamlining regulatory submissions for Phase I-III trials.
Advanced research tools also include single-cell RNA sequencing for characterizing differentiation heterogeneity, automated colony morphology classification systems using AI/machine learning, and functional potency assays that measure immunomodulatory capacity through T-cell suppression or cytokine secretion profiles [94]. These tools collectively enable the rigorous characterization required for clinical translation of iPSC-derived therapies.
The clinical landscape for iPSC-derived therapies has progressed substantially, with multiple products now in advanced clinical trials and demonstrating promising safety and efficacy profiles. FT819, OpCT-001, and iMSCs represent diverse applications of iPSC technology across autoimmune, ophthalmologic, and regenerative indications, collectively highlighting the transformative potential of this platform. The ongoing clinical evaluation of these therapies will provide critical insights into manufacturing scalability, long-term safety, and real-world efficacy across different disease contexts.
Future development will likely focus on enhancing product consistency through improved differentiation protocols, advancing hypoimmunogenic engineering strategies to enable universal donor approaches, and developing combination therapies that integrate iPSC-derived cells with other treatment modalities. The continued refinement of CRISPR-based engineering approaches will further enable precise customization of therapeutic attributes, potentially leading to next-generation products with enhanced potency, specificity, and safety profiles [93] [94]. As the field matures, addressing challenges related to manufacturing standardization, regulatory alignment, and reimbursement models will be essential for realizing the full potential of iPSC-derived therapies to transform treatment paradigms across medicine.
The clinical success of stem cell therapies, particularly those utilizing mesenchymal stromal cells (MSCs), hinges on effectively managing immunogenic responses. While MSCs possess inherent immunomodulatory properties, their transplantation can still provoke immune reactions that compromise therapeutic efficacy and safety [11] [22]. The primary mechanism of action of MSCs is now understood to be predominantly paracrine signaling, whereby they secrete bioactive molecules—cytokines, growth factors, and extracellular vesicles—that modulate the local immune environment and promote tissue repair [97]. This immunomodulatory function is tightly regulated by key signaling pathways, including Hedgehog, TGF-β, Wnt, Hippo, FGF, BMP, and Notch [71]. Assessing the immunogenicity of these advanced therapies presents unique challenges, as it requires evaluating not only protein-specific immune responses but also cellular integration, persistence, and functional modulation. This guide examines the predictive value of preclinical models for evaluating immunogenicity, framing the discussion within the context of stem cell immune modulation mechanisms and their implications for patient-specific responses.
Stem Cell Immune Modulation: Mechanisms and Assessment Challenges
Key Immunomodulatory Mechanisms of MSCs
The therapeutic potential of mesenchymal stromal cells extends beyond differentiation capacity to encompass complex immune regulatory functions. MSCs achieve immunomodulation through several interconnected mechanisms:
- Soluble Factor Secretion: MSCs constitutively express an array of immunosuppressive molecules including PGE2, TGF-β, HLA-G5, IL-10, HGF, galectins, CD73, CD39, PD-L1, and HLA-G1 [22]. These factors collectively suppress T-cell proliferation, modulate dendritic cell maturation, and promote regulatory immune cell phenotypes.
- Metabolic Reprogramming: The quiescent metabolic state of stem cells enables survival in damaged tissues while contributing to their immune-privileged status [22]. This metabolic profile may protect against infection hijacking while facilitating regeneration in inflammatory environments.
- Paracrine Signaling: MSC-derived extracellular vesicles facilitate intercellular communication by transferring proteins, lipids, and nucleic acids that regulate immune responses and tissue repair processes [97].
- Direct Cell-Cell Contact: MSCs modulate immune cells through direct interactions involving surface proteins that influence immune cell activation and function [11].
Challenges in Predicting Clinical Immunogenicity
Despite understanding these mechanisms, predicting individual patient responses remains challenging due to several factors:
- Patient-Specific Variables: Genetic background, disease status, age, and concomitant medications significantly influence immunogenic responses to stem cell therapies [98].
- Product Heterogeneity: MSC properties vary considerably based on tissue source (bone marrow, adipose, umbilical cord), donor characteristics, manufacturing processes, and culture expansion methods [97].
- Dynamic Immune Interactions: The immunomodulatory effects of MSCs are not static but depend on the local inflammatory milieu, creating context-dependent responses that are difficult to model predictively [11] [22].
Current Preclinical Immunogenicity Assessment Models
In Vitro Model Systems
Table 1: In Vitro Assays for Immunogenicity Assessment
| Assay Type | Key Components | Measured Endpoints | Utility in Stem Cell Therapy |
|---|---|---|---|
| T-cell Activation Assays | PBMCs, antigen-presenting cells, MSC cocultures | T-cell proliferation, cytokine secretion, activation markers | Measures allogeneic T-cell responses to MSC antigens [98] |
| Dendritic Cell (DC) Assays | Monocyte-derived DCs, MSC-derived factors | DC maturation markers, cytokine secretion, phagocytic activity | Evaluates innate immune activation by MSC products [98] |
| MHC-Associated Peptide Proteomics (MAPPs) | Antigen-presenting cells, mass spectrometry | HLA-bound peptide identification and quantification | Identifies immunogenic MSC-derived peptides [98] |
| Cell-Based Potency Assays | Reporter cell lines, primary human cells | Expression of immunomodulatory factors, suppression of immune cell activation | Quantifies MSC functional potency and batch consistency [99] |
In Vivo Model Systems
Table 2: In Vivo Models for Immunogenicity Assessment
| Model System | Key Features | Measured Endpoints | Limitations |
|---|---|---|---|
| Humanized Mouse Models | Immunodeficient mice engrafted with human immune cells | Human-specific immune responses, cell persistence, functional assessment | Incomplete recapitulation of human immune system; high cost and technical complexity [100] |
| Syngeneic/Allogeneic Animal Models | Immunocompetent animals with MSC transplantation | Anti-drug antibody formation, cell clearance, efficacy reduction | Species-specific immune differences limit human translatability [100] |
| Disease-Specific Models | Animals with condition mimicking human disease (e.g., arthritis, GvHD) | Integrated assessment of immunogenicity and therapeutic effect | Disease pathology may alter immune responses unpredictably [96] |
Establishing Correlation Between In Vitro and In Vivo Assays
Experimental Approaches for Correlation Studies
Establishing robust correlations between preclinical assays and clinical outcomes requires systematic approaches:
- Sample Destabilization Studies: Intentional stress (thermal, photo) applied to create samples with varying potencies enables parallel testing of in vitro and in vivo responses [99]. For mRNA vaccines, thermal stress-induced mRNA integrity loss correlated directly with reduced in vitro protein expression and in vivo antibody induction [99].
- Parallel Method Comparison: Comparing multiple assay formats (binding antibodies, neutralizing antibodies, cell-based assays) against gold standard in vivo responses helps identify the most predictive in vitro endpoints [99].
- Multi-laboratory Validation: Reproducibility across different laboratories and operators strengthens confidence in predictive models and facilitates technology transfer [101].
Quantitative Systems Pharmacology (QSP) Approaches
QSP modeling integrates knowledge of biological mechanisms with physiological and drug-specific parameters to predict immunogenicity dynamics and their impact on pharmacokinetics [98]. The Immunogenicity Simulator (IG Simulator) represents one such platform that mechanistically models humoral immune responses to non-self therapeutic proteins [98]. These models incorporate:
- Drug-specific parameters: Clearance rates, biodistribution, and MHC-II binding affinity
- Patient factors: HLA haplotypes, immune status, and genetic background
- System biology: Immune cell dynamics, antigen presentation, and T-cell help
For 13 monoclonal antibodies and fusion proteins, this approach accurately predicted ADA impact on drug concentration in 10 cases, demonstrating the potential of computational approaches to supplement traditional models [98].
Detailed Experimental Protocols
In Vitro T-cell Activation Assay Protocol
Purpose: To measure the potential of MSC preparations to stimulate allogeneic T-cell responses, a key indicator of immunogenic potential.
Materials:
- Research Reagent Solutions:
- Ficoll-Paque PLUS: Density gradient medium for PBMC isolation from human blood
- RPMI-1640 complete medium: Culture medium supplemented with 10% heat-inactivated human AB serum, 2 mM L-glutamine, 100 U/mL penicillin, 100 μg/mL streptomycin
- CFSE dye: Cell proliferation tracking dye (carboxyfluorescein succinimidyl ester)
- Anti-CD3/CD28 beads: Positive control T-cell activator
- Flow cytometry antibodies: Anti-CD3, CD4, CD8, CD25, CD69, and viability dye
Procedure:
- PBMC Isolation: Isolate PBMCs from healthy donor buffy coats using Ficoll-Paque density gradient centrifugation (400 × g, 30 min).
- T-cell Labeling: Resuspend PBMCs at 10×10^6 cells/mL in PBS, add CFSE to final concentration of 1 μM, incubate 10 min at 37°C, quench with 5 volumes of ice-cold complete medium.
- Coculture Setup: Plate irradiated (30 Gy) MSCs in 96-well U-bottom plates at 1×10^4 cells/well. Add CFSE-labeled PBMCs at 1×10^5 cells/well (1:10 ratio). Include wells with anti-CD3/CD28 beads (positive control) and PBMCs alone (negative control).
- Culture Conditions: Incubate plates for 5 days at 37°C, 5% CO₂.
- Flow Cytometry Analysis: Harvest cells, stain with surface antibodies and viability dye, acquire data on flow cytometer. Analyze CFSE dilution in CD3+CD4+ and CD3+CD8+ populations to determine proliferation.
Data Analysis: Calculate stimulation index (SI) as (percentage of proliferating T-cells in coculture)/(percentage of proliferating T-cells in negative control). SI > 2 considered positive response.
In Vitro-In Vivo Correlation Study Protocol
Purpose: To establish correlation between in vitro potency measurements and in vivo immunogenicity for stem cell-based products.
Materials:
- Research Reagent Solutions:
- HepG2 cells: Human hepatoma cell line with high transfection efficiency for mRNA-based therapies
- Lipid nanoparticles (LNPs): Delivery vehicle for mRNA vaccines
- RSVpreF-specific antibodies: Capture and detection antibodies for protein quantification
- ELISA reagents: Substrate, wash buffer, stop solution
Procedure:
- Sample Preparation: Generate MSC samples with varying potencies through controlled stress conditions (thermal stress at 25°C, 30°C, 37°C for 0-14 days).
- In Vitro Potency Assessment:
- For mRNA-based therapies: Transfect HepG2 cells with mRNA-LNP formulations, quantify antigen expression after 24h using immunofluorescence or ELISA [99].
- For cell therapies: Measure immunosuppressive capacity via T-cell inhibition assays as described in section 5.1.
- In Vivo Immunogenicity Testing:
- Administer stressed MSC samples to animal models (mice, rats, or humanized mice) via clinically relevant route.
- Collect serum samples at predetermined intervals (days 7, 14, 28, 42).
- Measure antigen-specific antibody titers using ELISA.
- For functional assessment, perform neutralization assays if applicable.
- Correlation Analysis:
- Plot in vitro potency values (EC50) against in vivo antibody titers or neutralization potency (ED50).
- Calculate correlation coefficient (R²) using linear regression analysis.
Signaling Pathways in Stem Cell Immune Modulation
Stem cell immunogenicity and immune modulatory functions are regulated by complex signaling pathways that represent potential targets for pharmacological intervention to control immune responses [71].
Figure 1: Key Signaling Pathways Regulating Stem Cell Immune Modulation. These pathways represent pharmacological targets for enhancing therapeutic efficacy and managing immunogenicity [71].
Industry Practices and Regulatory Landscape
Current Industry Approaches
A recent survey of 19 pharmaceutical companies revealed current immunogenicity risk assessment practices:
- 89.5% of companies perform immunogenicity risk assessments (IRAs) as part of drug development strategy [101]
- 70.6% follow a defined internal process and/or document template for IRA [101]
- 76.5% initiate IRA during preclinical discovery stage [101]
- Multi-disciplinary teams typically include Bioanalytical, Clinical Pharmacology, CMC, and Preclinical experts [101]
Table 3: Computational Tools for Immunogenicity Risk Assessment
| Tool Category | Specific Tools/Methods | Application | Limitations |
|---|---|---|---|
| In Silico T-cell Epitope Prediction | NetMHCIIpan, MHC-associated peptide proteomics (MAPPs) | Identification of potential T-cell epitopes in protein sequences | Variable predictive value; may overestimate risk [98] |
| B-cell Epitope Prediction | Sequence-based algorithms, structural modeling | Prediction of potential B-cell epitopes and ADA development | Less established than T-cell epitope prediction [98] |
| Quantitative Systems Pharmacology (QSP) | Immunogenicity Simulator (IG Simulator) | Prediction of ADA incidence and impact on pharmacokinetics | Requires extensive compound-specific input parameters [98] |
Regulatory Considerations and New Approach Methodologies (NAMs)
Regulatory landscapes are evolving toward reduced animal testing, with the FDA Modernization Act 2.0 (2022) removing mandatory animal testing requirements for new drug applications [100]. This shift accelerates adoption of New Approach Methodologies (NAMs):
- Organ-on-a-chip systems: Microphysiological models that better recapitulate human tissue environments
- Human-based in vitro systems: 3D organoids and complex coculture systems incorporating human immune components
- In silico modeling: AI and machine learning approaches to predict immunogenicity risk based on compound properties
These approaches are particularly relevant for stem cell therapies, where species differences in immune responses often limit the predictive value of traditional animal models [100].
The predictive value of preclinical immunogenicity assays for stem cell therapies continues to improve with advances in human-relevant model systems and computational approaches. Key considerations for enhancing predictability include:
- Model Selection: Prioritizing human-based systems (humanized mice, in vitro human immune models) over conventional animal models to better capture human immune responses
- Multi-parameter Assessment: Combining T-cell activation assays, epitope mapping, and functional immunomodulation assays rather than relying on single endpoints
- QSP Integration: Incorporating mechanistic modeling to interpret complex immune responses and their clinical implications
- Standardization: Developing standardized protocols and acceptance criteria for immunogenicity assessment of cell-based products
As the field advances, the integration of patient-specific factors—including HLA haplotypes, disease state, and concomitant medications—will be essential for developing truly predictive models that account for individual variation in immune responses to stem cell therapies. The ongoing transition from animal-based to human-based systems promises more accurate immunogenicity prediction, potentially improving the success rate of stem cell therapies in late-stage clinical development.
In the rapidly advancing field of stem cell research, regulatory designations from the U.S. Food and Drug Administration (FDA) serve as critical validation milestones that accelerate the translation of promising therapies from bench to bedside. For researchers and drug development professionals focusing on stem cell immune modulation, understanding the strategic importance of the Regenerative Medicine Advanced Therapy (RMAT) and Fast Track designations is essential for navigating the complex regulatory pathway. These designations not only provide development advantages but also signal that a therapeutic approach has demonstrated sufficient potential to address serious conditions with unmet medical needs.
The development of stem cell therapies for immune-related disorders represents a paradigm shift in treating conditions ranging from autoimmune diseases to graft-versus-host disease (GVHD). As of 2025, global clinical trials have expanded significantly, with over 244 trials registered for autoimmune conditions alone, including Crohn's disease, systemic lupus erythematosus (SLE), and scleroderma [73]. Within this vibrant research landscape, regulatory designations provide a structured framework for prioritizing the most promising therapeutic candidates while maintaining rigorous safety and efficacy standards.
Understanding FDA Expedited Development Programs
The FDA has established several expedited programs to accelerate the development and review of drugs and biologics for serious conditions. These programs include Fast Track (FT), Breakthrough Therapy (BTD), Regenerative Medicine Advanced Therapy (RMAT), and Accelerated Approval pathways [102]. While these designations share the common goal of facilitating faster availability of therapies to patients, they differ significantly in their qualifying criteria, evidence requirements, and specific benefits.
For stem cell researchers, these designations represent more than just regulatory shortcuts; they provide a structured development pathway with enhanced FDA interaction, potentially de-risking the complex journey from preclinical discovery to market authorization. The strategic pursuit of these designations requires careful planning regarding timing, data collection, and evidentiary standards.
Comparative Analysis of RMAT and Fast Track
Table 1: Comparison of RMAT and Fast Track Designations
| Feature | RMAT Designation | Fast Track Designation |
|---|---|---|
| Qualifying Criteria | Drug must be a regenerative medicine therapy intended to treat, modify, reverse, or cure a serious condition; preliminary clinical evidence must show potential to address unmet medical needs [103] | Drug intended to treat a serious condition; non-clinical or clinical data must demonstrate potential to address unmet medical need [102] |
| Data Requirements | Preliminary clinical evidence [103] | Preliminary non-clinical, mechanistic, or clinical data [102] |
| Designation-specific Benefits | Early interactions to discuss surrogate endpoints; eligibility for accelerated approval and priority review [102] | More frequent meetings and written communication; eligibility for rolling review and accelerated approval [102] |
| Success Rate (CBER) ~50% grant success rate (2023-2024) [104] | 70.3% historical grant success rate [104] | |
| Popularity | Most requested high-order designation for CBER [104] | Most applied-for and granted FDA expedited designation [104] |
The choice between pursuing RMAT versus Fast Track designation depends on multiple factors, including the nature of the stem cell product, the stage of clinical development, and the strength of the available evidence. According to regulatory trend analyses, CGT developers have increasingly favored RMAT designation due to its lower qualifying bar compared to Breakthrough Therapy Designation and its tailored applicability to regenerative medicine products [104]. As noted by CBER Director Peter Marks, "the standard is a little bit lower to receive this designation—one simply has to show that you have possible clinical benefit, not that you are better than existing standard of care" [104].
The RMAT Designation: Deep Dive
Eligibility and Qualification Criteria
The RMAT designation, created under the 21st Century Cures Act (Section 3033), has specific eligibility requirements that stem cell therapies must meet. A drug is eligible for RMAT designation if it qualifies as a regenerative medicine therapy, which includes cell therapies, therapeutic tissue engineering products, human cell and tissue products, or any combination products using such therapies or products [103]. The therapy must be intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and preliminary clinical evidence must indicate the potential to address unmet medical needs for such disease or condition [103].
Based on the FDA's interpretation of the statute, certain human gene therapies and xenogeneic cell products may also meet the definition of a regenerative medicine therapy [103]. This broad interpretation has significant implications for stem cell researchers working on genetically modified or engineered stem cell products aimed at modulating immune responses in individual patients.
Application Process and Timeline
Sponsors must submit requests for RMAT designation either concurrently with an Investigational New Drug (IND) application or as an amendment to an existing IND [103]. The submission must include specific language in the cover letter clearly identifying the RMAT designation request. The FDA's Office of Tissues and Advanced Therapies (OTAT) will notify the sponsor of their decision within 60 calendar days of receipt of the designation request [103].
Table 2: RMAT Designation Request Requirements
| Submission Context | Cover Letter Requirement |
|---|---|
| With IND Amendment | Must specify "REQUEST FOR REGENERATIVE MEDICINE ADVANCED THERAPY DESIGNATION" in bold, uppercase letters [103] |
| With Initial IND | Must specify both "INITIAL INVESTIGATIONAL NEW DRUG SUBMISSION" and "REQUEST FOR REGENERATIVE MEDICINE ADVANCED THERAPY DESIGNATION" in bold, uppercase letters [103] |
| Submission Address | FDA Center for Biologics Evaluation and Research, Office of Tissues and Advanced Therapies, Document Control Center [103] |
Benefits and Strategic Advantages
RMAT designation offers sponsors several tangible benefits that can significantly accelerate stem cell therapy development programs. These include early interactions with the FDA to discuss potential surrogate or intermediate endpoints, eligibility for priority review, and eligibility for accelerated approval [102]. Additionally, RMAT-designated products gain access to rolling review of the Biologics License Application (BLA), more frequent FDA meetings, and written communication throughout the development process [102].
The strategic value of RMAT designation extends beyond these formal benefits. As noted by Parexel experts, "some sponsors view an RMAT designation request as a way to gain earlier insight than would be possible with a BTD request as to whether the company and the FDA are seeing eye-to-eye on the potential for the product to fulfill unmet needs" [104]. This early alignment opportunity is particularly valuable for stem cell therapies targeting immune modulation, where the mechanisms of action may be complex and multifactorial.
Fast Track Designation: Comprehensive Analysis
Qualification Requirements
Fast Track designation is available for drugs intended to treat serious conditions that demonstrate the potential to address unmet medical needs [102]. Unlike RMAT, which requires preliminary clinical evidence, Fast Track designation can be granted based on preclinical data, mechanistic data, or clinical data that shows the product's potential [102]. This lower evidence threshold makes Fast Track an attractive option for stem cell therapies in earlier stages of development.
The flexibility in evidentiary standards for Fast Track designation is particularly advantageous for novel stem cell approaches where early clinical data may be limited but strong scientific rationale exists. For stem cell therapies targeting immune modulation, mechanistic data demonstrating effects on relevant signaling pathways or immune cell populations may support a Fast Track designation request.
Benefits and Strategic Implementation
Fast Track designation provides several development advantages, including more frequent meetings with the FDA, more frequent written communication, eligibility for rolling review of the BLA, and potential eligibility for accelerated approval and priority review if supported by clinical data at the time of application [102]. Despite perceptions that it offers fewer regulatory advantages than higher-order designations, Fast Track designation remains popular, with request numbers hitting consecutive records in recent years [104].
The strategic value of Fast Track designation for stem cell therapies was highlighted by the market response to Candel's FT designation in February 2024, which triggered a 25% stock surge [104]. This demonstrates that despite being considered a "lower-level" designation, Fast Track still commands significant attention and validation from both regulatory agencies and the investment community.
Integration with Stem Cell Immune Modulation Research
Current Landscape of Stem Cell Therapies for Immune Disorders
Stem cell therapies, particularly those utilizing mesenchymal stem cells (MSCs), have demonstrated significant potential for modulating immune responses in various disease contexts. MSCs possess potent immunomodulatory and regenerative properties that enable them to regulate immune tolerance and maintain immune homeostasis through multiple mechanisms [73]. These include secreting soluble factors such as TGF-β, PGE2, and IDO, releasing exosomes enriched with regulatory miRNAs, and directly interacting with immune cells through cell-to-cell contact [73].
The therapeutic application of MSCs for immune disorders is supported by their ability to migrate to sites of inflammation in a CXCR4/SDF-1 axis-dependent manner and differentiate into functional stromal cells within the local microenvironment [73]. These properties make MSC-based therapies particularly attractive for conditions characterized by dysregulated immune responses, such as autoimmune diseases, graft-versus-host disease, and inflammatory disorders.
Diagram 1: Stem Cell Immune Modulation Signaling Pathways. This diagram illustrates the key molecular mechanisms through which stem cells, particularly MSCs, modulate immune responses. These mechanisms represent potential targets for engineered stem cell therapies and provide mechanistic rationale for regulatory designation requests.
Recent Clinical Advances and Regulatory Successes
The clinical translation of stem cell therapies for immune modulation has achieved significant milestones in recent years, with several products receiving regulatory approval or advanced designations. Notable examples include:
Ryoncil (remestemcel-L): Received FDA approval in December 2024 as the first MSC therapy for pediatric steroid-refractory acute graft versus host disease (SR-aGVHD) [59]. This approval represents a landmark achievement for MSC-based immune modulation, demonstrating the viability of allogeneic bone marrow-derived MSCs for modulating immune responses in life-threatening conditions.
FT819: An off-the-shelf, iPSC-derived CAR T-cell therapy for active moderate to severe systemic lupus erythematosus (SLE) that received FDA RMAT designation in April 2025 [59]. This designation highlights the regulatory validation of iPSC-derived approaches for autoimmune conditions.
Omisirge (omidubicel-onlv): Approved in April 2023 for patients with hematologic malignancies undergoing cord blood transplantation [59]. While primarily a hematopoietic progenitor cell product, its approval demonstrates the regulatory pathway for cell-based therapies with immunomodulatory properties.
These regulatory successes reflect the growing maturity of the stem cell field and provide valuable precedents for researchers developing novel stem cell therapies for immune modulation.
Experimental Design and Methodological Considerations
Essential Research Reagents and Tools
Table 3: Key Research Reagent Solutions for Stem Cell Immune Modulation Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Stem Cell Sources | Bone marrow-derived MSCs, Umbilical cord-derived MSCs, iPSC-derived MSCs, Hematopoietic stem cells [105] [106] [11] | Provide cellular material for therapeutic development and mechanism studies |
| Characterization Markers | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) [11] | Standardized phenotyping according to ISCT criteria |
| Differentiation Media | Osteogenic, chondrogenic, and adipogenic induction cocktails [11] | Validation of multilineage differentiation potential |
| Immune Cell Assays | Mixed lymphocyte reactions, T cell suppression assays, macrophage polarization assays [73] | Functional assessment of immunomodulatory properties |
| Signaling Pathway Modulators | TGF-β inhibitors, Wnt agonists/antagonists, Notch inhibitors [71] | Mechanistic studies of immunomodulatory pathways |
| Analytical Tools | Flow cytometry, single-cell RNA sequencing, cytokine arrays [105] | Comprehensive profiling of cellular responses |
Methodological Framework for Regulatory Designation
Securing RMAT or Fast Track designation requires a strategic approach to experimental design and evidence generation. The following methodological framework provides a structured pathway for researchers:
1. Preclinical Proof-of-Concept Development
- Establish robust in vitro models of immune modulation using primary human immune cells
- Demonstrate dose-dependent effects on relevant immune cell populations (T cells, B cells, macrophages, dendritic cells)
- Validate mechanisms through pathway-specific inhibition studies [71]
- Conduct in vivo studies in clinically relevant disease models with appropriate immune profiling
2. Clinical Evidence Generation for RMAT
- Design early-phase clinical trials with biologically relevant endpoints
- Incorporate biomarker assessments that reflect mechanism of action
- Collect preliminary evidence of clinical activity in targeted patient population
- Implement robust monitoring for safety signals, particularly tumorigenicity and immunogenicity [105]
3. Regulatory Strategy Implementation
- Request informal feedback on potential Breakthrough Therapy designation (for context on agency expectations) [104]
- Prepare comprehensive designation request with emphasis on unmet need and preliminary evidence
- Align clinical development plan with potential accelerated approval pathways
- Plan for post-marketing requirements to confirm clinical benefit
Diagram 2: Regulatory Designation Strategy Workflow. This diagram outlines a systematic approach for integrating regulatory strategy into stem cell therapy development, from preclinical studies through early clinical evaluation and regulatory engagement.
The strategic pursuit of RMAT and Fast Track designations represents a critical component of modern stem cell therapy development, particularly for approaches targeting immune modulation. These designations provide not only regulatory benefits but also external validation of a therapy's potential to address serious unmet medical needs. For researchers and drug development professionals, understanding the nuances of these programs enables more efficient navigation of the complex pathway from discovery to clinical application.
The evolving landscape of stem cell immune modulation research, coupled with increasingly sophisticated regulatory frameworks, offers unprecedented opportunities to advance transformative therapies for patients with limited treatment options. By strategically integrating regulatory considerations into research planning and experimental design, scientists can accelerate the development of promising stem cell approaches while maintaining the rigorous evidence standards required for regulatory approval.
As the field continues to mature, with an increasing number of stem cell therapies achieving regulatory milestones, these designations will play an increasingly important role in prioritizing development resources and facilitating the delivery of innovative treatments to patients in need. The successful integration of robust science with strategic regulatory planning will ultimately determine how quickly the field can realize the full potential of stem cell immune modulation.
Conclusion
The successful clinical translation of stem cell therapies hinges on a nuanced understanding of their patient-specific immunomodulatory mechanisms. A multidisciplinary approach that integrates deep immunological profiling, advanced engineering, and precision medicine is paramount. Future directions must focus on defining robust predictive biomarkers, standardizing potency assays that reflect immune function, and developing next-generation 'off-the-shelf' universal donor cells. By systematically addressing the sources of inter-patient variability—from cellular heterogeneity and immune history to the tissue-specific microenvironment—researchers can unlock the full potential of stem cells to deliver safe, effective, and personalized regenerative medicines for a broad spectrum of debilitating conditions.
References
- 1. The Immunomodulatory mechanism and research progress of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12008879/]
- 2. Current Knowledge and Future Perspectives on ... [https://www.mdpi.com/1422-0067/21/3/727]
- 3. Stem Cell-Derived Exosomes as Nanotherapeutics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6880946/]
- 4. In-vitro immunomodulatory efficacy of extracellular vesicles ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04476-2]
- 5. The Unique Immunomodulatory Properties of MSC-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8055852/]
- 6. Immunomodulatory Effect of MSCs and MSCs-Derived ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.714832/full]
- 7. Therapeutic potential and mechanistic insights into adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12659562/]
- 8. The role of mesenchymal stem cell-derived exosomes in ... [https://www.sciencedirect.com/org/science/article/pii/S0327954523000865]
- 9. Mesenchymal Stem Cell Immunomodulation: Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7751844/]
- 10. The Immunomodulatory mechanism and research progress of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04333-2]
- 11. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 12. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 13. SDF-1:CXCR4 Axis Is Fundamental for Tissue Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2966775/]
- 14. Mesenchymal Stromal Cell Homing: Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6529790/]
- 15. Important role of the SDF-1/CXCR4 axis in the homing of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02759-6]
- 16. SDF-1/CXCR4 axis enhances the immunomodulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6615145/]
- 17. Estimate the relationship between CXCR4-SDF-1 axis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11731802/]
- 18. Cell surface engineering to enhance mesenchymal stem ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961214003305]
- 19. Review Article Modulation of the SDF-1–CXCR4 axis by ... [https://www.sciencedirect.com/science/article/pii/S0301472X06002360]
- 20. Wnt, Notch, and TGF-β Pathways Impinge on Hedgehog ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2019.00711/full]
- 21. Wnt signaling pathways in biology and disease [https://www.nature.com/articles/s41392-025-02142-w]
- 22. Immune modulatory stem cells represent a significant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11911480/]
- 23. Emergence of the Stem Cell Secretome in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7666064/]
- 24. Size-dependent immunomodulation by MSC secretome [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512777/]
- 25. Dose-response immunomodulatory effects of ... [https://www.sciencedirect.com/science/article/pii/S2352320425001981]
- 26. A systematic review of mesenchymal stem cell secretome [https://www.sciencedirect.com/science/article/abs/pii/S8756328224002588]
- 27. Single-cell RNA sequencing deconvolutes the in vivo ... [https://pubmed.ncbi.nlm.nih.gov/34803492/]
- 28. Current best practices in single‐cell RNA‐seq analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC6582955/]
- 29. Top 10 Bioinformatics Tools for scRNA-seq in 2025 [https://neovarsity.org/blogs/top-bioinformatics-tools-for-scrna-seq]
- 30. Identifying Immunomodulatory Subpopulations of Adipose ... [https://pubmed.ncbi.nlm.nih.gov/40366552/]
- 31. Identification of cell subpopulations associated with disease ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-023-01658-3]
- 32. muscat detects subpopulation-specific state transitions ... [https://www.nature.com/articles/s41467-020-19894-4]
- 33. Immunomodulatory properties of mesenchymal stem cells ... [https://www.nature.com/articles/s41423-023-00998-y]
- 34. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 35. Small Molecule Immunomodulators as Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814352/]
- 36. Unlocking the future of drug discovery through advances in AI [https://www.astrazeneca.com/content/astraz/what-science-can-do/topics/data-science-ai/unlocking-future-drug-discovery-through-AI-advances.html]
- 37. Machine Learning in Drug Discovery: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8356896/]
- 38. Image-based molecular representation learning for drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11200195/]
- 39. HLA matching or CRISPR editing of HLA class I/II enables ... [https://www.nature.com/articles/s41467-025-64945-3]
- 40. RheumaGen Presents HLA Gene-Editing Preclinical Data ... [https://www.rheumagen.com/news-events/rheumagen-presents-hla-gene-editing-preclinical-data-for-nearly-universal-autoimmune-disease-target-at-acr-convergence-2025-oral-session/]
- 41. Perspectives on immune checkpoint ligands: expression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8411045/]
- 42. Immune Cell Response to Orthopedic and Craniofacial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10269274/]
- 43. Biomaterial adjuvant effect is attenuated by anti- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2988402/]
- 44. Regenerative potential of immune cells after traumatic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1610119/full]
- 45. Modulating the immune system towards a functional ... [https://www.sciencedirect.com/science/article/pii/S0169409X24001649]
- 46. Immune Monitoring after Cell Therapy and Hematopoietic ... [https://www.sciencedirect.com/science/article/pii/S1465324925006905]
- 47. Advanced Flow Cytometry Assays for Immune Monitoring of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8127837/]
- 48. CyTOF as a suitable tool for stratification and monitoring of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220477/]
- 49. insights into immune reconstitution and disease modulation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1601223/full]
- 50. How to Prepare Spectral Flow Cytometry Datasets for High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8640183/]
- 51. Advanced flow cytometry data analysis ... [https://www.flowjo.com/advanced_analysis.html]
- 52. Fluidigm CyTOF Technology Used to Evaluate Stem Cell ... [https://investors.standardbio.com/news-releases/news-release-details/fluidigm-cytof-technology-used-evaluate-stem-cell-therapy]
- 53. Strategies to Enhance NK Cell Function for the Treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6343663/]
- 54. Natural killer cell immunotherapies beyond cancer [https://www.sciencedirect.com/science/article/pii/S3050538025000420]
- 55. Comprehensive snapshots of natural killer cells functions ... [https://www.nature.com/articles/s41392-024-02005-w]
- 56. Cytotoxic Responses Mediated by NK Cells and Cytotoxic T ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.13867/full]
- 57. Missing Self-Induced Activation of NK Cells Combines with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8054908/]
- 58. Global clinical trials on stem cell therapy for autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328461/]
- 59. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 60. Natural killer cell membrane manipulation for augmented ... [https://www.sciencedirect.com/science/article/pii/S2590006425005356]
- 61. Allorecognition by T Lymphocytes and Allograft Rejection [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2016.00582/full]
- 62. T cell Allorecognition Pathways in Solid Organ Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6230624/]
- 63. Allorecognition Unveiled: Integrating Recent Breakthroughs ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2024.13523/full]
- 64. Allorecognition, via TgrB1 and TgrC1, mediates the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4631765/]
- 65. Patient-Specific Age: The Other Side of the Coin in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4667069/]
- 66. Mesenchymal stromal cell therapies: immunomodulatory ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01855-9]
- 67. Immune modulation by mesenchymal stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6985662/]
- 68. a qualitative review of their potential and challenges | Stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04360-z]
- 69. The role of the microbiome in stem cell ageing [https://pmc.ncbi.nlm.nih.gov/articles/PMC6653314/]
- 70. Understanding the microbiome in autologous ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1590601/full]
- 71. Pharmacological modulation of stem cells signaling pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210473/]
- 72. Small molecules in targeted cancer therapy [https://www.nature.com/articles/s41392-021-00572-w]
- 73. Global clinical trials on stem cell therapy for autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 74. A Beginner's Guide To Analyzing and Visualizing Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5765874/]
- 75. Cytofast: A workflow for visual and quantitative analysis of ... [https://www.sciencedirect.com/science/article/pii/S200103701830059X]
- 76. Cellular senescence in ageing: from mechanisms to therapeutic ... [https://www.nature.com/articles/s41580-020-00314-w?error=cookies_not_supported]
- 77. Tissue fibrosis by radiotherapy: current understanding of the... induced [https://pmc.ncbi.nlm.nih.gov/articles/PMC10563272/]
- 78. Innovations in immunotherapy for autoimmune diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 79. New horizons in systemic sclerosis treatment: advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12215137/]
- 80. results through 104 weeks in a long-term extension study [https://pubmed.ncbi.nlm.nih.gov/40829888/]
- 81. Corporate news details [https://news.bms.com/news/details/2025/Bristol-Myers-Squibb-Presents-Two-Late-Breaking-Presentations-Demonstrating-Sotyktu-deucravacitinib-Efficacy-in-Psoriatic-Arthritis-and-Systemic-Lupus-Erythematosus/default.aspx]
- 82. Breakthrough Autoimmune Findings at ACR 2025 [https://www.autoimmuneinstitute.org/research_updates/breakthrough-autoimmune-findings-at-acr-2025/]
- 83. Efficacy and safety of upadacitinib maintenance therapy in ... [https://pubmed.ncbi.nlm.nih.gov/40704669/]
- 84. UCSF Diffuse Scleroderma Clinical Trials for 2025 [https://clinicaltrials.ucsf.edu/diffuse-scleroderma]
- 85. UCLA Diffuse Scleroderma Clinical Trials — Los Angeles [https://ucla.clinicaltrials.researcherprofiles.org/diffuse-scleroderma]
- 86. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 87. First FDA Approved Ex Vivo Expanded Cord Blood Graft for ... [https://www.cbcspecialtyservices.org/blog/omisirge-first-fda-approved-ex-vivo-expanded-cord-blood-graft-for-stem-cell-transplantation]
- 88. LYFGENIA™ (lovotibeglogene autotemcel) | An FDA ... [https://www.lyfgenia.com/]
- 89. LYFGENIA™ (lovotibeglogene autotemcel) Gene Therapy ... [https://www.lyfgeniahcp.com/]
- 90. Ryoncil.com: SR-aGVHD Treatment | Pediatric Patients [https://www.ryoncil.com/]
- 91. Gamida Cell's Omisirge Administered to First Patient in ... [https://www.cgtlive.com/view/gamida-cell-omisirge-administered-first-patient-commercial-setting]
- 92. Fate Therapeutics Presents New Clinical Data at ACR ... [https://ir.fatetherapeutics.com/news-releases/news-release-details/fate-therapeutics-presents-new-clinical-data-acr-convergence]
- 93. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04723-6]
- 94. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 95. Human pluripotent stem cell-derived hepatic progenitors ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1507317/full]
- 96. Advances in cell therapy for orthopedic diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1567640/full]
- 97. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 98. a novel model-informed metric to assess immunogenicity risk [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1677925/full]
- 99. Establishing correlation between in vitro potency and in ... [https://www.nature.com/articles/s41541-025-01181-2]
- 100. How new approach methodologies are reshaping drug ... [https://www.mckinsey.com/industries/life-sciences/our-insights/the-synthesis/how-new-approach-methodologies-are-reshaping-drug-discovery]
- 101. IQ Survey Results on Current Industry Practices—Part 1 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087687/]
- 102. Expedited programs [https://bgtcplaybook.document360.io/docs/expedited-programs-1]
- 103. Regenerative Medicine Advanced Therapy Designation [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/regenerative-medicine-advanced-therapy-designation]
- 104. Parexel Introduces FDA Expedited Designation Trends for ... [https://www.parexel.com/insights/new-medicines-novel-insights/accelerating-development-cell-gene-therapies/effective-regulatory-strategies/parexel-introduces-fda-expedited-designation-trends-for-advanced-therapies]
- 105. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 106. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]