Revolutionizing ALS Research: iPSC-Derived Motor Neurons as Predictive Models for Drug Discovery
This article provides a comprehensive overview of the transformative role of induced pluripotent stem cell (iPSC)-derived motor neurons in modeling Amyotrophic Lateral Sclerosis (ALS).
Revolutionizing ALS Research: iPSC-Derived Motor Neurons as Predictive Models for Drug Discovery
Abstract
This article provides a comprehensive overview of the transformative role of induced pluripotent stem cell (iPSC)-derived motor neurons in modeling Amyotrophic Lateral Sclerosis (ALS). It covers the foundational biology of reprogramming patient cells to create clinically relevant in vitro models, details the latest protocols for efficient differentiation and high-throughput screening, and addresses key challenges in model validation and optimization. Highlighting successful translations from phenotypic screens to clinical trials, we evaluate how these human cell models are overcoming the limitations of traditional animal studies to de-risk drug development and enable personalized therapeutic strategies for both familial and sporadic ALS.
From Patient to Dish: Building a Human-Relevant Foundation for ALS Disease Modeling
The quest to understand and treat Amyotrophic Lateral Sclerosis (ALS) has been persistently challenged by the inadequacy of existing animal and cellular models, particularly for the sporadic form (SALS) which constitutes approximately 90% of all cases [1] [2]. The development of induced pluripotent stem cell (iPSC) technology has revolutionized this landscape by enabling the generation of patient-specific motor neurons (MNs) that retain the complete genetic background of donors, offering an unprecedented platform for disease modeling and therapeutic discovery [1] [2]. This application note details the critical methodologies and experimental frameworks essential for leveraging iPSC-derived motor neurons to faithfully recapitulate both sporadic and familial ALS (FALS) pathophysiology, underscoring their indispensable role in modern ALS research and drug development.
Establishing a Phenotypically Validated iPSC Library for ALS
The foundational step in robust ALS modeling is the creation of a comprehensively characterized iPSC library that captures the clinical and genetic heterogeneity of the patient population.
Library Generation and Quality Control
A seminal study established a library from 100 sporadic ALS (SALS) patients, 11 suspected monogenic cases, and 25 healthy controls [1]. Fibroblasts isolated from donor skin biopsies were reprogrammed using non-integrating episomal vectors on an automated robotics platform to maximize output uniformity and minimize technical variability. All lines underwent rigorous quality control (QC), including:
- Confirmation of genomic integrity
- Verification of pluripotency
- Demonstration of trilineage differentiation potential [1]
Clinical annotation of donors encompassed ALS subtype classification (e.g., lower motor neuron-predominant, classic ALS, upper motor neuron-predominant), site of onset, age of onset, disease progression rate (ALSFRS-R decline), and survival time, ensuring the library reflected the broad clinical spectrum of ALS [1]. Whole-genome sequencing identified pathogenic variants in known ALS genes in a subset of donors, enabling stratification of familial and sporadic cases [1].
Quantitative Phenotyping of ALS-Specific Pathology
Implementing a robust motor neuron differentiation and phenotyping pipeline is crucial for modeling neurodegeneration. A five-stage spinal motor neuron differentiation protocol adapted from established methods has demonstrated exceptional efficacy, generating cultures with:
- 92.44 ± 1.66% motor neurons (co-expressing ChAT, MNX1/HB9, and Tuj1)
- 97.66 ± 0.99% Tuj1+ neurons
- Minimal contamination from astrocytes (0.12 ± 0.01% GFAP+ cells) and microglia (0.04 ± 0.02% CD11B+ cells) [1]
Longitudinal live-cell imaging with motor neuron-specific reporters (HB9-turbo) enabled quantitative assessment of key disease phenotypes, including significantly reduced motor neuron survival and accelerated neurite degeneration in SALS lines compared to controls—a critical pathological hallmark historically difficult to recapitulate in vitro [1]. Importantly, the severity of in vitro neurite degeneration correlated with donor survival time, establishing face validity for the model [1].
Table 1: Key Quality Control Metrics for iPSC-Derived Motor Neuron Cultures
| Parameter | Measurement | Assessment Method |
|---|---|---|
| Motor Neuron Purity | 92.44% ± 1.66% | ICC: Co-expression of ChAT, MNX1/HB9, Tuj1 |
| Total Neuronal Population | 97.66% ± 0.99% | ICC: Tuj1+ cells |
| Astrocyte Contamination | 0.12% ± 0.01% | ICC: GFAP+ cells |
| Microglia Contamination | 0.04% ± 0.02% | ICC: CD11B+ cells |
Protocol: Motor Neuron Differentiation and Phenotypic Screening
The following protocol details the optimized methodology for generating high-purity motor neurons and conducting phenotypic screening for ALS disease modeling and drug discovery.
Motor Neuron Differentiation Protocol
Adapted from: Hall et al. (as cited in [3]) and Bye et al. [1]
Stage 1: Neural Induction (Days 1-7)
- Base Medium: DMEM/F-12 with N2 supplement
- Small Molecules:
- Culture Format: Pluripotent iPSCs are dissociated and plated as a single-cell suspension in the presence of ROCK inhibitor (Y-27632, 10 µM) [4].
- Key QC Checkpoint (Day 7): >90% of cells should express neural precursor markers PAX6 and SOX1 [5].
Stage 2: Motor Neuron Progenitor Patterning (Days 8-14)
- Base Medium: Neurobasal medium with B27 supplement
- Small Molecules:
- Dorsomorphin (1 µM)
- Retinoic Acid (0.1 µM)
- Smoothed Agonist (SAG, 1 µM) or Purmorphamine (1 µM)
- Key QC Checkpoint (Day 14): High co-expression of neural precursor (SOX1, N-Cadherin, Nestin) and motor neuron progenitor (OLIG2) markers. Emergence of ISL1 expression [5].
Stage 3: Motor Neuron Maturation (Days 15-28)
- Base Medium: Neurobasal medium with B27 supplement, BDNF (10 ng/mL), GDNF (10 ng/mL), CNTF (10 ng/mL)
- Small Molecules:
- Substrate: Cultures are plated on Laminin-coated surfaces (1-2 µg/cm²) [4].
- Key QC Checkpoint (Day 28): >90% of cells express mature motor neuron markers HB9 and Neurofilament (NF). Cultures can be cryopreserved for future use [5].
Phenotypic Screening and Live-Cell Imaging
Critical Parameters for Modeling ALS Neurodegeneration [1]
- Longitudinal Health Monitoring: Utilize a motor neuron-specific reporter (e.g., HB9-driven fluorescent protein) for selective tracking.
- Image Acquisition: Acquire high-content images daily for at least 14-21 days during the maturation stage.
- Key Outcome Measures:
- Motor Neuron Survival: Quantify the number of fluorescently-labeled motor neurons over time.
- Neurite Degeneration: Measure neurite network integrity, including total neurite length/area and number of branches per neuron.
- Data Validation: Correlate in vitro degeneration kinetics (e.g., rate of neurite loss) with clinical data from the cell donor, such as survival time, to establish clinical relevance [1].
Addressing Variability in iPSC-Derived Motor Neuron Models
A significant challenge in utilizing iPSC-derived models is technical variability. A systematic analysis of 15 differentiation sets across 8 cell lines identified that non-genetic factors—specifically the "Induction Set" (batch effects) and "Operator"—were the predominant sources of variability, outweighing the contribution from "Cell Line" genetics [3].
Table 2: Sources of Variability in Motor Neuron Differentiation QC Metrics
| QC Metric | Coefficient of Variance (%) | Variation Explained by Cell Line (R²) | Variation Explained by Induction Set (R²) | Variation Explained by Operator (R²) |
|---|---|---|---|---|
| NPC:D3 Cell Ratio | 59.5 | - | - | 67.1% |
| D3:D10 Cell Ratio | 67.0 | 31.5% | - | 31.4% |
| D10 Neurite Area | 53.7 | 7.1% | - | - |
| PAX6+OLIG2+ (NPC) | 46.3 | 1.5% | 51.1% | - |
| SMI32+MAP2+ (D10) | 36.8 | 6.3% | 57.2% | - |
Mitigation Strategy: Genomic Stability Monitoring Differentiations from iPSCs with no detectable karyotypic abnormalities (assessed via targeted RT-qPCR for common abnormalities) showed:
- Reduced coefficient of variance for key QC metrics
- Significantly higher purities at neural precursor and mature motor neuron stages [3] Recommendation: Implement routine genomic assessment of iPSCs as a standard QC procedure to enhance model reliability and reproducibility [3].
Advanced Functional and Multi-Cellular Models
Functional Characterization of Hyperexcitability
A key ALS pathological trait is neuronal hyperexcitability. Functional screening of iPSC-derived MNs from unaffected donors and donors with ALS-linked mutations (C9orf72, SOD1, TDP43) using Multi-Electrode Array (MEA) and spontaneous neuronal activity (SNA) analysis revealed:
- Unaffected Donors: Highly synchronized firing, higher mean burst duration, lower burst rate.
- ALS Donors (C9orf72, TDP43): Hyperexcitable phenotype, less synchronized firing, increased burst rate [6]. These reproducible functional phenotypes provide a physiologically relevant platform for testing therapeutics aimed at modulating neuronal excitability [6].
Rapid Neuromuscular Junction (NMJ) Model
To model the "dying-back" axonopathy in ALS, a rapid 12-day human NMJ model using cryopreserved iPSC-derived MNs and skeletal muscle cells (SKMs) was developed [5]. Protocol Summary:
- Days 1-5: Thaw and mature cryopreserved skeletal myoblasts into SKMs.
- Day 5: Thaw and seed ready-to-use MN spheres onto the myotube layer.
- Days 5-12: Co-culture to facilitate NMJ formation. Key Outcomes: Within 12 days, the model demonstrates:
- Colocalization of NF/SV2 (neuronal), TTN (muscle), and AChR clusters at NMJ endplate-like sites
- Spontaneous and inducible myotube contractions
- ALS-specific cytopathies, including altered AChR properties and impaired contractions, dominantly initiated by SOD1 mutant MNs [5].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for iPSC-Derived Motor Neuron Differentiation and Screening
| Reagent / Material | Function / Application | Example Catalog Number/Supplier [4] |
|---|---|---|
| Dorsomorphin | BMP inhibitor for neural induction | Sigma-Aldrich |
| Purmorphamine / SAG | Hedgehog pathway agonists for motor neuron patterning | Sigma-Aldrich |
| Retinoic Acid (RA) | Rostrocaudal patterning, specifies spinal identity | Various |
| Compound E (γ-Secretase Inhibitor) | Accelerates neuronal maturation | Sigma-Aldrich |
| Laminin | Extracellular matrix for neuronal plating | Sigma-Aldrich (Laminin from EHS) |
| ROCK Inhibitor (Y-27632) | Enhances survival of dissociated cells | Sigma-Aldrich |
| Cytosine β-D-arabinofuranoside | Anti-mitotic; eliminates proliferating non-neuronal cells | Sigma-Aldrich |
| Anti-ChAT Antibody | Immunocytochemistry for motor neuron identity | Chemicon (Sigma-Aldrich) |
| HB9-turbo Reporter | Live-cell imaging of motor neuron health | N/A |
The imperative for human iPSC-derived models in ALS research is unequivocal. The protocols and application notes detailed herein provide a roadmap for generating phenotypically robust and reproducible models of both sporadic and familial ALS that recapitulate critical disease hallmarks, including motor neuron degeneration, transcriptomic dysregulation, hyperexcitability, and NMJ pathology. By adhering to rigorous quality control, mitigating sources of variability, and implementing functional and physiological screening assays, these human models are poised to dramatically accelerate the identification and validation of novel therapeutic strategies for this devastating disease.
The discovery of induced pluripotent stem cells (iPSCs) represents a paradigm shift in regenerative medicine and disease modeling. This technology enables the reprogramming of adult somatic cells back to an embryonic-like pluripotent state through the forced expression of specific transcription factors. The groundbreaking work by Shinya Yamanaka and colleagues in 2006 demonstrated that introducing four key transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as the OSKM factors)—could reprogram mouse fibroblasts into pluripotent stem cells [7]. This achievement, which earned Yamanaka the Nobel Prize in Physiology or Medicine in 2012, provided an ethically acceptable alternative to embryonic stem cells and opened new avenues for personalized medicine [8].
In the context of amyotrophic lateral sclerosis (ALS) research, iPSC technology has become an indispensable tool. iPSCs can be generated from ALS patients with both familial and sporadic forms of the disease and differentiated into motor neurons, the specific cell type affected in ALS [9] [2]. This approach has enabled researchers to create in vitro models that recapitulate key aspects of the disease, providing unprecedented opportunities to study disease mechanisms and screen potential therapeutics in human cells [1]. The ability to model sporadic ALS (which constitutes 85-90% of cases) is particularly valuable, as these cases lack known monogenic causes and have been challenging to model in animals [9] [2].
Somatic Cell Reprogramming Fundamentals
Core Reprogramming Factors
The reprogramming process involves epigenetic remodeling that reverses the developmental clock of somatic cells, restoring them to a pluripotent state. While the original OSKM factors remain foundational, research has identified numerous alternatives and optimizations that enhance safety and efficiency [7]:
- OCT4 Substitutes: NR5A2 can replace OCT4 in combination with SOX2 and KLF4.
- SOX2 Substitutes: SOX1 and SOX3 can substitute for SOX2, and the small molecule RepSox can also fulfill this role.
- KLF4 Substitutes: KLF2 and KLF5 can replace KLF4 in the reprogramming process.
- c-MYC Substitutes: Due to its oncogenic potential, c-MYC can be replaced with L-MYC, N-MYC, SALL4, Esrrb, or Glis1 to reduce tumorigenic risk.
The table below summarizes the core reprogramming factors and their functions:
Table 1: Core Reprogramming Factors and Their Functions
| Factor | Full Name | Primary Function in Reprogramming | Safe Substitutes |
|---|---|---|---|
| OCT4 | Octamer-binding transcription factor 4 | Establishes and maintains pluripotency; regulates self-renewal | NR5A2 |
| SOX2 | SRY-box transcription factor 2 | Maintains pluripotent state; collaborates with OCT4 | SOX1, SOX3, RepSox (small molecule) |
| KLF4 | Krüppel-like factor 4 | Promotes mesenchymal-to-epithelial transition; cell cycle regulation | KLF2, KLF5 |
| c-MYC | Cellular myelocytomatosis oncogene | Enhances proliferation; promotes chromatin remodeling (often omitted for safety) | L-MYC, N-MYC, SALL4, Esrrb, Glis1 |
The initial step in iPSC generation is the isolation of somatic cells from a donor. The choice of cell source significantly influences reprogramming efficiency, quality of resulting iPSCs, and subsequent applications [8]:
- Dermal Fibroblasts: Historically the first cell type used for iPSC generation, obtained via skin biopsy. They offer high genomic stability and can be readily expanded and banked, despite the moderately invasive collection procedure [8].
- Peripheral Blood Mononuclear Cells (PBMCs): Isolated from blood samples, these cells provide a less invasive collection alternative with comparable reprogramming efficiency to fibroblasts. They are increasingly favored in translational studies [8].
- Urinary Epithelial Cells: Represent a completely non-invasive, reproducible source with robust reprogramming capacity, enabling generation of multiple iPSC lines from the same donor [8].
- Keratinocytes: Derived from hair follicles, these cells offer higher reprogramming efficiency compared to fibroblasts, though the yield of starting material is typically lower [8].
Delivery Systems for Reprogramming Factors
Multiple delivery methods have been developed to introduce reprogramming factors into somatic cells, each with distinct advantages and limitations concerning efficiency, genomic integration, and safety profiles [8] [7].
Table 2: Comparison of Reprogramming Factor Delivery Systems
| Delivery System | Genomic Integration | Efficiency | Safety Profile | Primary Applications |
|---|---|---|---|---|
| Retrovirus/Lentivirus | Yes (Random integration) | High | Lower (Risk of insertional mutagenesis) | Basic research |
| Sendai Virus | No (Viral RNA persists transiently) | High | High (Non-integrating, diluted upon passaging) | Basic and translational research |
| Episomal Vectors | No (Replicated extra-chromosomally) | Moderate | High (Non-integrating) | Clinical applications, large-scale studies [1] |
| Synthetic mRNA | No | Moderate to High | High (Non-integrating, transient expression) | Clinical applications |
| Recombinant Protein | No | Low | High (Non-integrating) | Basic research, safety-focused applications |
For ALS modeling, non-integrating methods like episomal vectors are particularly valuable for generating clinical-grade iPSCs, as demonstrated in large-scale studies involving 100 sporadic ALS patients [1].
Detailed Experimental Protocols
Protocol: iPSC Generation from Dermal Fibroblasts
This protocol outlines the generation of iPSCs from human dermal fibroblasts using non-integrating episomal vectors, adapted from methodologies used in recent large-scale ALS studies [1].
Materials and Reagents:
- Human dermal fibroblasts from ALS patient or control
- Fibroblast culture medium: DMEM supplemented with 10% FBS, 1% GlutaMAX, 1% non-essential amino acids
- Reprogramming vectors: Episomal plasmids containing OCT4, SOX2, KLF4, L-MYC, LIN28, and shRNA for p53
- Transfection reagent: Appropriate for episomal vectors (e.g., Lipofectamine)
- iPSC culture medium: mTeSR1 or Essential 8 Medium
- Extracellular matrix: Matrigel or recombinant laminin-521
- ROCK inhibitor (Y-27632)
Procedure:
- Cell Preparation: Culture human dermal fibroblasts in fibroblast medium until 70-80% confluent. Passage cells at least twice after thawing before reprogramming.
- Transfection: Transfect fibroblasts with episomal reprogramming vectors using the appropriate transfection reagent according to manufacturer's protocol.
- Media Transition: 3-5 days post-transfection, transition cells to iPSC culture medium supplemented with ROCK inhibitor.
- Colony Monitoring: Monitor cultures daily for emergence of iPSC colonies with distinct embryonic stem cell-like morphology (tightly packed cells with defined borders, high nucleus-to-cytoplasm ratio).
- Colony Picking: Between days 21-28, manually pick individual iPSC colonies and transfer to 24-well plates coated with extracellular matrix.
- Expansion and Banking: Expand clonal lines and cryopreserve stocks at early passages (P2-P5).
Quality Control:
- Confirm pluripotency marker expression (OCT4, NANOG, SOX2, TRA-1-60) via immunocytochemistry or flow cytometry.
- Verify trilineage differentiation potential (ectoderm, mesoderm, endoderm) in vitro.
- Perform karyotype analysis to ensure genomic integrity.
- Confirm absence of episomal vectors after passage 10-12 using PCR.
Protocol: Motor Neuron Differentiation from iPSCs
This protocol describes efficient differentiation of iPSCs into spinal motor neurons, optimized for ALS disease modeling and drug screening applications [1] [10].
Materials and Reagents:
- Established iPSC lines
- Neural induction medium: DMEM/F12 and Neurobasal medium (1:1) supplemented with N2, B27, and appropriate small molecules
- Motor neuron patterning factors: Retinoic acid (RA), Smoothened Agonist (SAG) or Purmorphamine
- Motor neuron maturation medium: Neurobasal medium with BDNF, GDNF, CNTF, and ascorbic acid
- Motor neuron markers for characterization: Antibodies against HB9 (MNX1), ISL1, ChAT, and β-tubulin III (Tuj1)
Procedure:
- Neural Induction: Dissociate iPSCs to single cells and culture in neural induction medium with dual SMAD inhibition (using SB431542 and LDN-193189) for 7-10 days.
- Motor Neuron Patterning: Between days 3-7, add retinoic acid (0.1 µM) and Smoothened Agonist (SAG, 1 µM) to pattern cells toward caudal spinal motor neuron identity.
- Maturation: From day 10 onward, transition cells to motor neuron maturation medium to support terminal differentiation and neurite outgrowth.
- Purification: Optional purification using fluorescence-activated cell sorting (FACS) with motor neuron-specific surface markers.
- Characterization: Validate motor neuron identity by immunostaining for HB9, ISL1, and ChAT. Assess functional properties via electrophysiology where possible.
Timeline and Efficiency:
- Using optimized protocols, functional motor neurons can be obtained within 28-32 days [11].
- Advanced protocols combining small molecules with transcription factors can achieve approximately 80% induction efficiency within just two weeks [10].
- Typical yields include >90% HB9+/Tuj1+ cells, indicating high-purity motor neuron cultures suitable for disease modeling [1].
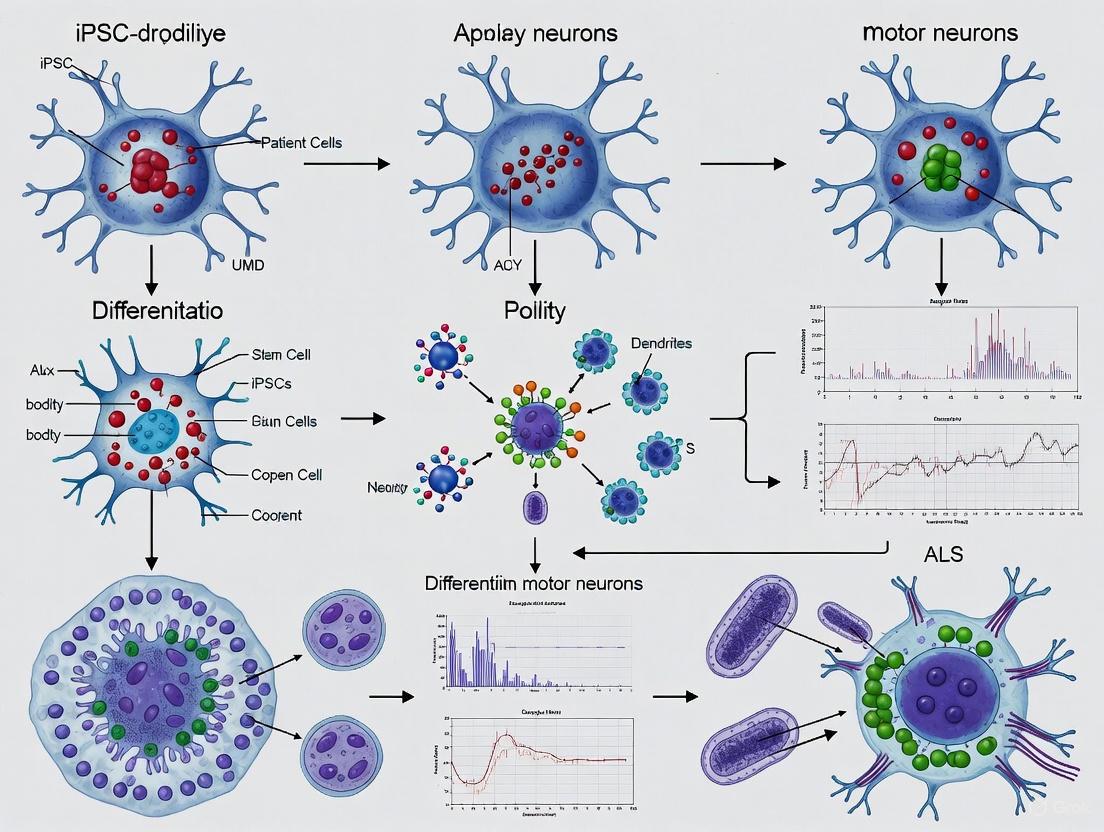
Diagram 1: Workflow for Generating Motor Neurons from Somatic Cells via iPSC Reprogramming and Differentiation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for iPSC Generation and Motor Neuron Differentiation
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, L-MYC | Induce pluripotency in somatic cells | L-MYC preferred over c-MYC for reduced tumorigenic risk [7] |
| Reprogramming Enhancers | Valproic acid (VPA), Sodium butyrate, 8-Br-cAMP | Improve reprogramming efficiency | 8-Br-cAMP with VPA can increase efficiency by 6.5-fold [7] |
| Culture Media | mTeSR1, Essential 8 Medium | Maintain pluripotency and self-renewal | Chemically defined, feeder-free systems enhance standardization [8] |
| Neural Induction Agents | SB431542, LDN-193189, Noggin | Inhibit SMAD signaling to direct neural fate | Dual SMAD inhibition dramatically improves neural induction efficiency |
| Motor Neuron Patterning Factors | Retinoic acid (RA), Purmorphamine, SAG | Pattern neural progenitors to caudal spinal motor neuron fate | RA provides anterior-posterior patterning; SHH agonists provide dorsal-ventral patterning |
| Motor Neuron Maturation Factors | BDNF, GDNF, CNTF, Ascorbic acid | Support motor neuron survival, maturation, and neurite outgrowth | Critical for generating electrophysiologically active motor neurons [1] |
| Extracellular Matrices | Matrigel, Laminin-521, Vitronectin | Provide structural support and signaling cues for cell attachment | Recombinant matrices (e.g., laminin-521) enhance reproducibility for clinical applications |
| Cell Characterization Markers | Antibodies against OCT4, NANOG, HB9, ISL1, ChAT, Tuj1 | Identify and validate cell identity at each stage | Essential for quality control and protocol validation |
Applications in ALS Research
iPSC-derived motor neurons have become a cornerstone in ALS research, particularly for modeling sporadic forms of the disease that lack known genetic causes and have been challenging to study with traditional animal models [9]. These patient-specific cellular models recapitulate key pathological features of ALS, including reduced motor neuron survival, accelerated neurite degeneration, and transcriptional dysregulation [1].
In large-scale drug screening initiatives, iPSC-derived motor neurons from sporadic ALS patients have validated known therapeutics such as riluzole and identified novel potential treatment combinations. A recent study screening over 100 drugs that had previously undergone ALS clinical trials found that less than 5% showed efficacy in rescuing motor neuron survival across diverse patient donors, reflecting the high failure rate of clinical trials [1]. Combinatorial testing identified baricitinib, memantine, and riluzole as a promising therapeutic combination for sporadic ALS [1].
The technology also enables personalized medicine approaches, as demonstrated by studies showing variable drug responses among motor neurons derived from different sporadic ALS patients [9] [2]. For instance, the drug ropinirole hydrochloride showed protective effects in motor neurons derived from some but not all sporadic ALS patients, highlighting the pathological heterogeneity of the disease and the potential for patient stratification in clinical trials [9] [2].
Diagram 2: Application Pipeline of iPSC-Derived Motor Neurons in ALS Research and Drug Discovery.
Reprogramming somatic cells into pluripotent stem cells represents a transformative technology that has fundamentally advanced our approach to studying human diseases, particularly complex neurodegenerative disorders like ALS. The protocols and methodologies outlined in this document provide a foundation for generating high-quality iPSCs and differentiating them into the motor neurons specifically affected in ALS. As the field continues to evolve, further refinements in reprogramming efficiency, differentiation protocols, and three-dimensional modeling will enhance the physiological relevance of these systems. The integration of iPSC technology with advanced genomic editing and multi-omics approaches holds particular promise for unraveling the complex pathophysiology of sporadic ALS and developing effective, personalized therapeutic strategies for this devastating disease.
Key Pathogenic Hallmarks Modeled in iPSC-Derived Motor Neurons
Induced pluripotent stem cell (iPSC)-derived motor neurons have revolutionized the study of amyotrophic lateral sclerosis (ALS), providing a critical human model for a disease that is predominantly sporadic (sALS) and notoriously difficult to model [1]. These patient-derived cells capture key pathological features of ALS while encompassing the genetic and clinical heterogeneity of the patient population. This application note details the primary pathogenic hallmarks recapitulated in iPSC-derived motor neurons and provides standardized protocols for their investigation, enabling robust disease modeling and drug screening for researchers and therapeutic developers.
iPSC-derived motor neurons from ALS patients consistently demonstrate specific, quantifiable pathological features. The table below summarizes the key hallmarks and their experimental readouts.
Table 1: Key Pathogenic Hallmarks in iPSC-Derived ALS Motor Neurons
| Pathogenic Hallmark | Experimental Readout | Quantitative Findings | Technical Assay |
|---|---|---|---|
| Reduced Neuronal Survival [1] | Motor neuron count over time | Significantly reduced survival in SALS MNs vs. controls [1] | Longitudinal live-cell imaging, viability staining |
| Accelerated Neurite Degeneration [1] | Neurite length & complexity | Correlates with donor survival time [1] | High-content image analysis (e.g., MAP2/Tuj1 staining) |
| Transcriptional Dysregulation [1] [12] | RNA-sequencing profile | ~1/3 of gene changes in postmortem sALS MNs captured in iPSC-MNs [12] | Bulk or single-cell RNA-sequencing |
| TDP-43 Pathology [12] | Splicing dysregulation | Downregulation of TDP-43 splicing targets in relevant genotypes [12] | RT-qPCR of known TDP-43 targets |
| Hyperexcitability [13] | Electrophysiological activity | Increased firing activity in sALS MNs [13] | Whole-cell patch clamp, multielectrode array (MEA) |
| Pharmacological Response [1] | Rescue of survival/degeneration | Riluzole rescues survival; 97% of failed clinical trial drugs ineffective [1] High-throughput drug screening |
Detailed Experimental Protocols
Protocol 1: Efficient Monolayer Differentiation of Cervical Spinal Motor Neurons
This protocol enables rapid, high-yield generation of functional motor neurons suitable for disease modeling and electrophysiological detection of hyperexcitability phenotypes within 28 days [13].
Table 2: Key Reagents for Motor Neuron Differentiation
| Reagent | Function | Signaling Pathway Role |
|---|---|---|
| CHIR99021 [13] | GSK-3β inhibitor | Activates WNT signaling for caudalization |
| SB431542 [13] | TGF-β inhibitor | Dual SMAD inhibition for neural induction |
| DMH1 [13] | BMP inhibitor | Dual SMAD inhibition for neural induction |
| Retinoic Acid (RA) [13] | Morphogen | Rostrocaudal patterning (spinal identity) |
| Purmorphamine [13] | Smoothened agonist | Activates SHH signaling for ventralization |
| Compound E [13] | γ-secretase inhibitor | Inhibits Notch signaling to accelerate MN maturation |
Day 0-6: Induction of Caudalized Ventral Neural Stem Cells (NSCs)
- Plate and maintain human iPSCs at 80-90% confluency in essential basal medium.
- Treat with 3 μM CHIR99021 (WNT activator), 2 μM SB431542 (TGF-β inhibitor), and 2 μM DMH1 (BMP inhibitor) for 6 days.
- Quality Control: Confirm NSC identity by immunocytochemistry for NESTIN (96.6% ± 2.7%), PAX6 (91.9% ± 4.3%), and SOX2 (97.8% ± 2.1%). Verify caudalization by high expression of HOXB4 and HOXC5 via RT-qPCR [13].
Day 6-12: Specification of Motor Neuron Progenitors (MNPs)
- Continue culture with 1 μM CHIR99021, 2 μM SB431542, 2 μM DMH1, and add 0.1 μM Retinoic Acid (RA) and 0.5 μM Purmorphamine (SHH agonist) for 6 days.
- Quality Control: On day 12, assess for OLIG2+ (81.5% ± 6.9%, up to 91.4%) and NKX6.1+ (94.3% ± 0.7%) MNPs via immunocytochemistry. Minimal NKX2.2+ interneuron progenitors (2.8% ± 1.5%) should be present [13].
Day 12-18: Maturation to Post-Mitotic Motor Neurons
- Replace medium with maturation medium containing 0.5 μM RA, 0.1 μM Purmorphamine, and 0.1 μM Compound E (γ-secretase/Notch inhibitor) to promote cell cycle exit and terminal differentiation.
- Quality Control: By day 18, cultures should contain 88%-97% CHAT+ spinal motor neurons. Assess functional maturity from day 28 using whole-cell patch clamp or MEA to detect hyperexcitability, a key ALS phenotype [13].
Protocol 2: Phenotypic Screening for Neurodegeneration
This protocol outlines a method for longitudinal tracking of motor neuron health and survival to quantify key ALS pathologies, including neurite degeneration and cell death [1].
- Reporter System: Implement a motor neuron-specific reporter, such as an HB9::turboGFP construct, to enable precise identification and tracking.
- Longitudinal Live-Cell Imaging: Plate differentiated motor neurons and transfer to an automated live-cell imaging system. Acquire high-resolution images of defined fields every 24 hours for a minimum of 14 days.
- Image Analysis:
- Survival: Quantify the number of GFP-positive motor neurons in each field over time. Normalize data to day 0 to generate survival curves.
- Neurite Integrity: Use automated neurite tracing algorithms to measure total neurite length per neuron and analyze complexity. A significant reduction in SALS MNs compared to controls indicates accelerated degeneration [1].
- Pharmacological Validation: Include the approved drug riluzole as a positive control. A valid model should show a significant rescue of motor neuron survival with riluzole treatment [1].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for iPSC-Derived Motor Neuron ALS Modeling
| Reagent/Category | Specific Examples | Critical Function in Workflow |
|---|---|---|
| Small Molecule Inducers [13] | CHIR99021, SB431542, DMH1, RA, Purmorphamine, Compound E | Guides developmental patterning from pluripotency to mature MNs. |
| Cell Culture Medium | Essential basal medium (DMEM/F12 + Neurobasal), N2/B27 Supplements | Supports neural differentiation and long-term MN health. |
| Characterization Antibodies | Anti-Tuj1 (neurons), Anti-ChAT (MNs), Anti-HB9/MNX1 (MNs), Anti-ISL1 (MNs), Anti-SMI-32 (mature MNs) [1] [14] | Confirms MN identity, purity (≥88% ChAT+), and maturity. |
| Critical Assay Kits | Live-cell imaging dyes, RNA extraction kits, scRNA-seq library prep kits | Enables phenotyping (survival, degeneration) and transcriptomics. |
| Pharmacological Agents | Riluzole, Baricitinib, Memantine [1] | Positive controls and candidate therapeutics for screening. |
Signaling Pathways in Motor Neuron Differentiation
The stepwise differentiation of iPSCs into spinal motor neurons is governed by key developmental signaling pathways, which are precisely manipulated using small molecules.
iPSC-derived motor neurons provide a physiologically relevant and scalable platform for modeling sporadic and familial ALS. By recapitulating core pathogenic hallmarks such as reduced survival, neurite degeneration, transcriptional dysregulation, and hyperexcitability, these models offer an unparalleled tool for deconstructing disease mechanisms. The standardized protocols and reagents detailed herein provide a framework for generating robust, reproducible data, thereby accelerating the path from in vitro modeling to therapeutic discovery for ALS.
The study of amyotrophic lateral sclerosis (ALS) has been revolutionized by the ability to model genetic mutations in patient-derived induced pluripotent stem cell (iPSC) motor neurons. This approach has provided unprecedented insights into the pathophysiological mechanisms driving this fatal neurodegenerative disease. Approximately 90% of ALS cases are sporadic (SALS), while 10% are familial (FALS), with mutations in C9orf72, SOD1, TARDBP, and FUS accounting for a significant proportion of familial cases [1] [15]. The development of large-scale iPSC libraries from patients with sporadic ALS has enabled population-wide phenotypic screening and drug discovery, validating these models as physiologically relevant systems for preclinical testing [1]. This Application Note details experimental protocols for modeling these key ALS-associated mutations, providing researchers with standardized methodologies for investigating disease mechanisms and screening therapeutic candidates.
Molecular Mechanisms of ALS-Linked Genes
ALS-linked genes converge on several core pathological pathways despite their diverse molecular functions. The table below summarizes the primary mechanisms associated with each major ALS gene.
Table 1: Key Pathogenic Mechanisms of Major ALS-Linked Genes
| Gene | Primary Function | Main Pathogenic Mechanisms | Key Pathological Hallmarks |
|---|---|---|---|
| C9orf72 | DENN protein involved in GDP/GTP exchange, endocytosis, autophagy regulation [16] | • Haploinsufficiency: Reduced C9orf72 transcripts [16]• RNA Toxicity: G4C2 RNA foci sequester RNA-binding proteins [16] [17]• DPR Toxicity: RAN translation produces toxic dipeptide repeats (poly-GA, -GP, -GR, -PR, -PA) [16] [17] | • TDP-43 cytoplasmic inclusions• RNA foci in nuclei [16]• p62+/Ubiquitin+/TDP43- cytoplasmic inclusions containing DPRs [16] |
| SOD1 | Antioxidant enzyme detoxifying superoxide radicals [18] | • Gain of Function: Misfolding and aggregation of mutant protein [15] [18]• Mitochondrial Dysfunction: Toxic aggregates in mitochondria [18] | • SOD1-positive inclusions in mitochondria [18]• Mitochondrial swelling, oxidative stress [18] |
| TARDBP | RNA-binding protein involved in multiple aspects of RNA metabolism | • Loss of Function: Disrupted RNA processing [19]• TDP-43 Proteinopathy: Cytoplasmic mislocalization and aggregation [20] | • Cytoplasmic TDP-43 inclusions [19]• Nuclear clearance of TDP-43 |
| FUS | RNA-binding protein involved in multiple aspects of RNA metabolism, essential paraspeckle component [21] | • Nuclear Loss of Function: Disrupted paraspeckle integrity and RNA processing [21]• Cytoplasmic Gain of Function: Formation of stress granules and inclusions [21] | • FUS-positive cytoplasmic inclusions [21]• Dysfunctional paraspeckles, excess free NEAT1 [21] |
Signaling Pathway Diagram
The following diagram illustrates the complex molecular interactions and pathways implicated in ALS pathogenesis across the four major genes:
Figure 1: Molecular Pathways in ALS Pathogenesis. The diagram illustrates how mutations in C9orf72, SOD1, TARDBP, and FUS converge on common pathological pathways leading to motor neuron degeneration. Each gene triggers distinct initial mechanisms (yellow nodes) that evolve into pathological processes (red nodes) before ultimately driving shared degenerative outcomes (green nodes) and clinical symptoms (blue node).
Experimental Protocols for iPSC-Derived Motor Neuron Models
iPSC Library Generation and Motor Neuron Differentiation
Protocol 1: Large-Scale iPSC Library Generation from ALS Donors
- Objective: Generate a curated iPSC library capturing clinical, genetic, and biological heterogeneity of the ALS patient population [1].
- Starting Material: Fibroblasts isolated from skin biopsy specimens from 100 sporadic ALS patients, 11 suspected monogenic cases, and 25 healthy donors [1].
- Reprogramming Method: Non-integrating episomal vectors using an automated robotics platform to maximize output and uniformity [1].
- Quality Control:
- Confirm genomic integrity, pluripotency, and trilineage potential
- Perform whole-genome DNA sequencing to establish ancestry and identify pathogenic variants
- Confirm presence of expansions (e.g., C9ORF72) in both donor blood and iPSC lines [1]
- Clinical Data Collection: Classify ALS subtypes, site of onset, onset age, disease progression (ALSFRS-R), and survival time [1].
Protocol 2: Motor Neuron Differentiation and Maturation
- Base Protocol: Adapted five-stage protocol from established spinal motor neuron differentiation methods [1] [19].
- Key Modifications:
- Purity Assessment:
Phenotypic Screening and Functional Assessment
Protocol 3: Longitudinal Live-Cell Imaging of Motor Neuron Health
- Imaging System: Live-cell imaging with virally delivered non-integrating motor neuron-specific reporter (HB9-turbo) for tracking neuronal health [1].
- Key Readouts:
- Motor neuron survival over time
- Neurite degeneration and retraction
- Correlation of in vitro degeneration with donor survival [1]
- Experimental Timeline:
- Daily monitoring beginning at week 3-4 post-plating
- Continue through week 10 to capture progressive degeneration [19]
Protocol 4: Electrophysiological Characterization
- Technique: Whole-cell patch-clamp recordings from the largest neurons visualized via IR-DIC microscopy [19].
- Recording Parameters:
- Passive membrane properties: capacitance (Cm), input resistance (RN), resting membrane potential (RMP)
- Active properties: action potential generation, voltage-activated Na+ and K+ currents
- Synaptic activity: spontaneous postsynaptic currents [19]
- Temporal Analysis: Recordings from 2 to 10 weeks post-plating to track functional progression [19].
- Cell Identification: Post-hoc SMI-32 labelling of neurons filled with Alexa Fluor dye during recordings (78% recovery rate of SMI-32 positive cells) [19].
Protocol 5: Molecular Pathology Assessment
- RNA Foci Detection:
- TDP-43 Localization:
- Method: Immunocytochemistry with anti-TDP-43 antibodies
- Assessment: Nuclear clearance and cytoplasmic aggregation [19]
- Paraspeckle Integrity (for FUS mutations):
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for ALS iPSC Modeling
| Category | Specific Product/Kit | Application | Key Features |
|---|---|---|---|
| Reprogramming | Non-integrating episomal vectors | iPSC generation | Avoids insertional mutagenesis, suitable for clinical applications [1] |
| Motor Neuron Differentiation | Modified spinal motor neuron protocol [1] [19] | Generate mature motor neurons | Five-stage protocol producing high-purity cultures (92.44% motor neurons) [1] |
| Cell Line Validation | Whole-genome DNA sequencing | Genetic characterization | Identifies pathogenic variants and repeat expansions [1] |
| Live-Cell Imaging | HB9-turbo reporter | Motor neuron-specific labeling | Non-integrating, enables tracking of motor neuron health [1] |
| Electrophysiology | Whole-cell patch-clamp setup | Functional assessment | Measures passive/active membrane properties, synaptic activity [19] |
| RNA FISH | Stellaris Quasar 570-labelled NEAT1 probes [21] | RNA foci detection | Visualizes sense and antisense RNA foci in nuclei |
| Protein Interaction | Duolink In Situ Orange Starter Kit Mouse/Rabbit [21] | Proximity ligation assay | Detects protein-protein interactions (e.g., FUS-NONO) in paraspeckles |
| CRISPR/Cas9 Editing | Alt-R CRISPR/Cas9 system (IDT) [20] | Isogenic line generation | Creates mutation-corrected controls or introduces specific mutations |
Data Analysis and Interpretation
Quantitative Assessment of ALS Phenotypes
Table 3: Key Phenotypic Metrics in ALS iPSC-Motor Neuron Models
| Phenotypic Category | Specific Assay | Control Values | ALS Mutant Phenotype | Technical Notes |
|---|---|---|---|---|
| Cell Survival | Longitudinal live-cell imaging with MN reporter | Stable survival over 10 weeks | Significant reduction in survival across SALS donors [1] | Use automated counting for objectivity |
| Neurite Integrity | Neurite length quantification | Extensive, stable neurite networks | Accelerated neurite degeneration correlating with donor survival [1] | Correlate with clinical donor data |
| Electrophysiology | Whole-cell patch clamp | Normal development of Na+/K+ currents, action potentials | Initial hyperexcitability followed by progressive loss of activity [19] | Track temporal progression weekly |
| Ionic Currents | Voltage-clamp recordings | Stable Na+ and K+ current density | Progressive decrease in voltage-activated Na+ and K+ currents [19] | precedes viability changes |
| RNA Pathology | RNA-FISH for C9orf72 | No RNA foci | Nuclear RNA foci in neurons and glia [16] | Count foci per nucleus |
| Protein Aggregation | Immunocytochemistry for TDP-43 | Nuclear TDP-43 localization | Cytoplasmic TDP-43 inclusions, nuclear clearance [19] | Quantify mislocalization percentage |
Pharmacological Validation
The ALS iPSC-motor neuron model has been validated through comprehensive pharmacological testing:
- Clinical Trial Correlation: Screening of drugs previously tested in ALS clinical trials revealed that 97% failed to mitigate neurodegeneration in the SALS model, reflecting clinical trial outcomes [1].
- Riluzole Validation: The model reproduced the efficacy of riluzole, rescuing motor neuron survival and reversing electrophysiological and transcriptomic abnormalities [1].
- Combinatorial Therapy Identification: Combinatorial testing identified baricitinib, memantine, and riluzole as a promising therapeutic combination for SALS [1].
- Novel Compound Screening: Ropinirole hydrochloride was identified through phenotypic screening and shown to reduce neuronal cell death, ROS production, and neuronal hyperexcitation in TARDBP-mutant motor neurons [20].
Modeling ALS-linked mutations in C9orf72, SOD1, TARDBP, and FUS using iPSC-derived motor neurons provides a physiologically relevant system for investigating disease mechanisms and screening therapeutic candidates. The protocols outlined in this Application Note enable researchers to recapitulate key aspects of ALS pathology, including reduced motor neuron survival, accelerated neurite degeneration, electrophysiological dysfunction, and molecular pathologies characteristic of each genetic subtype. The ability to conduct population-wide studies using iPSC libraries from sporadic ALS patients captures the clinical and biological heterogeneity of the disease, enhancing the translational relevance of findings. These standardized methodologies support the discovery and validation of potential therapeutics, as demonstrated by the identification of promising drug combinations and novel compounds that rescue ALS phenotypes in patient-derived models.
The Promise of Large-Scale iPSC Libraries for Population-Wide Studies
The advent of large-scale induced pluripotent stem cell (iPSC) libraries represents a transformative approach for modeling human diseases, enabling unprecedented population-wide studies that capture the extensive genetic and clinical heterogeneity inherent in patient populations. For amyotrophic lateral sclerosis (ALS), where 90% of cases are sporadic with unknown etiology, this technology offers particular promise where traditional models have fallen short [1]. The development of iPSC repositories from hundreds of ALS patients provides the research community with biologically relevant human models that recapitulate key disease pathologies in a dish, paving the way for more effective therapeutic discovery and personalized medicine approaches [1] [22].
These extensive iPSC collections facilitate the generation of specialized cells, particularly motor neurons, which are the primary cells affected in ALS. By deriving these cells from a diverse array of patients, researchers can now conduct population-wide phenotypic screening, identify subtype-specific pathologies, and perform large-scale drug testing across the full spectrum of disease presentation [1]. This resource marks a quantum leap over existing models, providing ready-to-investigate motor neurons in just 7-10 days compared to the approximately 45 days typically required to generate motor neurons from iPSCs, offering efficiency that is crucial for fast-tracking the development of effective ALS treatments [22].
Large-Scale iPSC Libraries for ALS Research
Recent initiatives have established unprecedented iPSC resources for ALS research, enabling population-wide studies that capture clinical and biological diversity. The table below summarizes two major large-scale iPSC libraries currently advancing ALS research.
Table 1: Major Large-Scale iPSC Libraries for ALS Research
| Initiative | Library Size | Key Characteristics | Major Findings |
|---|---|---|---|
| SALS iPSC Library [1] | 100 sporadic ALS (SALS) patients, 25 healthy controls | Captured clinical heterogeneity; rigorous QC including genomic integrity, pluripotency, and trilineage potential | Recapitulated reduced motor neuron survival and accelerated neurite degeneration; identified combinatorial therapy (baricitinib, memantine, riluzole) |
| Answer ALS [23] [22] | ~1,000 ALS patients and controls | Comprehensive multi-omics data (clinical, genetic, transcriptomic, proteomic); open-access resource | Revealed sex and cell composition as major variability sources; higher Islet1+ cells in male ALS-derived cultures; no clear transcriptomic separation between ALS and controls |
These repositories have revealed critical insights into disease modeling requirements. The SALS library demonstrated that patient-derived motor neurons can recapitulate key disease pathologies including reduced survival and neurite degeneration that correlated with donor survival [1]. Notably, this study achieved what previous efforts had struggled with - demonstrating consistent survival deficits in SALS motor neurons compared to controls, a fundamental pathological hallmark of ALS [1].
The Answer ALS project, while not finding clear transcriptomic separation between ALS and controls, identified significant confounding variables that must be controlled in experimental design, particularly sex differences and cell composition effects [23]. Their analysis revealed that male ALS samples generated significantly higher percentages of ISL1+ motor neurons (17.0% ± 0.4% vs 14.1% ± 0.8% in controls) and motor neuron progenitor markers, suggesting intrinsic biological differences that may influence disease susceptibility or progression [23].
Experimental Protocols for iPSC-Derived Motor Neurons
Motor Neuron Differentiation and Maturation
Several optimized protocols have been developed for efficient differentiation of iPSCs into functional motor neurons. The most effective protocols share common elements but differ in their specific approaches to neural induction, patterning, and maturation.
Table 2: Comparison of Motor Neuron Differentiation Protocols
| Protocol Aspect | SALS Library Protocol [1] | Rapid Monolayer Protocol [13] | Answer ALS Protocol [23] |
|---|---|---|---|
| Duration | Not specified | 18 days to enriched CHAT+ cervical spinal MNs (88%-97%); 28 days to functional maturity | 32-day standardized protocol |
| Efficiency | 92.44% ± 1.66% motor neurons (ChAT+, MNX1/HB9+, Tuj1+) | 73%-91% OLIG2+ pMNs; 88%-97% CHAT+ cervical spinal MNs | 17.0% ± 0.4% ISL1+ cells in ALS vs 14.1% ± 0.8% in controls |
| Key Signaling Modulators | Not fully detailed | Dual SMAD inhibition (SB431542, DMH1) + WNT activation (CHIR99021); RA + SHH agonist (purmorphamine); Notch inhibition (Compound E) | Based on dual SMAD inhibition and ventral patterning |
| Unique Features | Highly enriched spinal motor neuron cultures with minimal non-neuronal cells (0.12% GFAP+, 0.04% CD11B+) | Notch inhibition accelerates maturation; enables detection of hyperexcitability in sALS MNs | Includes batch technical controls and batch differentiation controls for quality assurance |
The rapid monolayer protocol developed by Shen et al. represents a significant advancement in efficiency [13]. This approach generates nearly pure neural stem cells in 6 days through combined dual SMAD inhibition (using SB431542 and DMH1) and WNT activation (using CHIR99021), followed by robust motor neuron progenitors (73%-91% OLIG2+) in 12 days with additional RA and purmorphamine treatment [13]. A critical innovation is the application of Compound E, a γ-secretase inhibitor that blocks Notch signaling, effectively promoting the conversion of motor neuron progenitors into spinal motor neurons and accelerating functional maturation [13].
The SALS library protocol emphasizes purity and reductionist modeling, generating cultures containing 92.44% ± 1.66% motor neurons with minimal contamination from astrocytes (0.12% ± 0.01% GFAP+ cells) or microglia (0.04% ± 0.02% CD11B+ cells) [1]. This high purity enables clearer assessment of cell-autonomous effects in ALS pathology.
Diagram 1: Signaling Pathway for Rapid Motor Neuron Differentiation. This workflow illustrates the key stages and signaling modulators in an efficient monolayer protocol for generating functional spinal motor neurons from human iPSCs.
Phenotypic Screening and Quality Assessment
Robust phenotypic screening pipelines are essential for characterizing ALS-specific pathologies in iPSC-derived motor neurons. The SALS library implementation employed longitudinal live-cell imaging with a motor neuron-specific reporter (HB9-turbo) to quantitatively assess neurodegeneration parameters including cell survival and neurite degeneration [1]. This approach demonstrated that neurite degeneration correlated with donor survival, providing critical validation of the model's pathological relevance.
Functional characterization of neuronal activity represents another key phenotypic assessment. Multi-electrode array (MEA) analysis and calcium imaging have revealed hyperexcitability as a consistent phenotype in ALS iPSC-derived motor neurons [6] [13]. ALS motor neurons display less synchronized firing and increased burst rates compared to unaffected controls, reflecting expected ALS clinical pathology [6]. These functional assays are now being incorporated into quality control processes to ensure batch-to-batch consistency in iPSC-derived motor neuron differentiations [6].
Rigorous quality control throughout iPSC generation and differentiation is paramount. Standard QC measures include sterility testing, mycoplasma testing, viability assessment, stem cell marker FACS analysis, and alkaline phosphatase staining [24]. Additional optional QC steps include karyotyping, embryoid body formation assays, pluritest arrays, and testing for persistence of reprogramming vectors [24]. The inclusion of batch technical controls and batch differentiation controls, as implemented in the Answer ALS protocol, helps monitor technical variability and differentiation consistency across experiments [23].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for iPSC-derived Motor Neuron Studies
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [25] | Reprogram somatic cells to pluripotent state; non-integrating delivery methods preferred for clinical applications |
| Neural Induction Agents | SB431542 (TGF-β inhibitor), DMH1 (BMP inhibitor), CHIR99021 (WNT activator) [13] | Dual SMAD inhibition + WNT activation for efficient neural induction and caudalization |
| Patterning Molecules | Retinoic Acid (RA), Purmorphamine (SHH agonist) [13] | Specify rostrocaudal and dorsoventral patterning to generate spinal motor neurons |
| Maturation Enhancers | Compound E (γ-secretase/Notch inhibitor) [13] | Accelerate motor neuron maturation and functional development |
| Motor Neuron Markers | CHAT, MNX1/HB9, ISL1, Tuj1 [1] [23] | Identify and quantify motor neuron populations; assess differentiation efficiency |
| Functional Assay Reagents | Multi-electrode arrays, Calcium indicators, IncuCyte Neuroburst Orange [6] [13] | Assess electrophysiological properties, neuronal activity, and network synchronization |
Applications in Disease Modeling and Drug Discovery
Modeling Sporadic ALS Pathology
The development of large-scale iPSC libraries has enabled crucial advances in modeling sporadic ALS, which constitutes approximately 90% of all cases and has been particularly challenging to model using traditional approaches. The SALS library demonstrated that motor neurons derived from sporadic ALS patients recapitulate key disease features including reduced survival, accelerated neurite degeneration, and transcriptional dysregulation [1]. Importantly, the neurite degeneration phenotype correlated with donor survival, providing a clinically relevant readout for therapeutic screening [1].
These models also successfully recapitulate functional abnormalities observed in ALS patients. Multiple studies have identified hyperexcitability as a consistent phenotype in iPSC-derived motor neurons from both familial and sporadic ALS patients [6] [13]. This hyperexcitability manifests as less synchronized firing and increased burst rates in ALS-derived motor neurons compared to unaffected controls, reflecting similar observations in human patients [6]. The rapid monolayer protocol developed by Shen et al. enables detection of these electrophysiological phenotypes within 28 days, significantly accelerating the timeline for functional studies [13].
Drug Screening and Therapeutic Discovery
Large-scale iPSC libraries provide powerful platforms for high-throughput drug screening that more accurately predicts clinical outcomes. Screening of the SALS library with drugs previously tested in ALS clinical trials revealed that 97% failed to mitigate neurodegeneration, reflecting trial outcomes and validating the model's predictive value [1]. This high concordance between in vitro results and clinical trial outcomes demonstrates the potential of iPSC-based screening to de-risk drug development pipelines.
Combinatorial testing in the SALS library identified baricitinib, memantine, and riluzole as a promising therapeutic combination for sporadic ALS [1]. The combination significantly increased survival of SALS motor neurons across multiple donors, representing the first therapeutic candidates validated across SALS donors to encompass heterogeneity in drug efficacy within the patient population [1]. This approach highlights the advantage of large-scale libraries for identifying treatments effective across diverse genetic backgrounds.
Several clinical trials have been initiated based on iPSC research findings, including trials of bosutinib, ropinirole, and ezogabine for ALS, and WVE-004 and BII078 for ALS/FTD [26]. The integration of artificial intelligence into screening platforms is further enhancing drug discovery efforts, enabling more sophisticated analysis of complex screening datasets [26].
Future Directions and Clinical Translation
The field of iPSC-based disease modeling is rapidly evolving toward clinical applications. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct pluripotent stem cell-derived products targeting indications in ophthalmology, neurology, and oncology [27]. Over 1,200 patients have been dosed with more than 10¹¹ cells, with no significant class-wide safety concerns reported to date [27].
In February 2025, the FDA granted IND clearance for Fertilo, the first iPSC-based therapy to enter a U.S. Phase III trial [27]. For neurological applications, several iPSC-based therapies targeting Parkinson's disease, spinal cord injury, and ALS received FDA IND clearance in June 2025 [27]. These off-the-shelf products are designed to address neurodegenerative conditions with scalable, allogeneic cell sources, marking significant progress toward clinical translation.
Key challenges that remain include ensuring genomic stability during reprogramming and differentiation, managing immune responses to allogeneic cells, achieving reliable scale-up under GMP conditions, and demonstrating long-term engraftment and functional integration of transplanted cells [25]. Emerging technologies such as CRISPR/Cas9 gene editing and AI-guided differentiation are helping to address these challenges by enhancing iPSC quality and enabling more precise differentiation protocols [25].
The creation of HLA-matched iPSC banks represents another promising direction for facilitating clinical translation. These banks aim to provide HLA-homozygous lines that can match a significant proportion of the population with reduced immune rejection risk, making off-the-shelf iPSC therapies more feasible [25]. As these resources expand and differentiation protocols continue to improve, large-scale iPSC libraries will likely play an increasingly central role in both disease modeling and therapeutic development for ALS and other complex disorders.
Advanced Protocols and High-Throughput Applications in iPSC-Based ALS Screening
The generation of human induced pluripotent stem cell (iPSC)-derived motor neurons (MNs) represents a cornerstone of modern in vitro modeling for Amyotrophic Lateral Sclerosis (ALS). These models provide a pathophysiologically relevant system to study disease mechanisms and conduct drug screening [1]. A major challenge, however, has been the efficient, rapid, and subtype-specific differentiation of iPSCs into functional MNs that accurately recapitulate the selective vulnerability observed in patients [28]. This application note details optimized protocols that leverage small molecules and transcription factors to overcome these limitations, providing researchers with robust methodologies for ALS research and drug development.
Small Molecule-Based Differentiation Strategies
Small molecules that modulate key developmental signaling pathways can be used to direct iPSCs through a precise sequence of neural induction, patterning, and maturation stages. These defined compounds offer advantages in terms of cost, reproducibility, and scalability compared to recombinant protein-based methods.
Protocol: Efficient Induction of Spinal Motor Neurons
The following protocol, adapted from large-scale screening studies, outlines a highly efficient method for generating enriched cultures of spinal MNs from human iPSCs [1].
Key Reagents:
- Dorsomorphin: An inhibitor of BMP signaling, used for neural induction.
- SB431542: An inhibitor of TGF-β signaling, used in conjunction with Dorsomorphin for dual SMAD inhibition to enhance neural conversion.
- Retinoic Acid (RA): A caudalizing factor that confers a spinal cord identity to the developing neural progenitor cells.
- Purmorphamine (Pur.): A small molecule agonist of the Sonic Hedgehog (SHH) pathway, which ventralizes the neural tube to specify motor neuron progenitors.
- BDNF, GDNF, CNTF: Neurotrophic factors critical for MN survival and maturation.
Detailed Methodology:
- Neural Induction: Culture human iPSCs to ~70% confluence. Initiate differentiation by replacing the maintenance medium with a neural induction medium containing Dorsomorphin (1 µM) and SB431542 (10 µM) for 10-12 days.
- Motor Neuron Patterning: Passage the resulting neural progenitor cells (NPCs) and pattern them toward an MN fate by adding RA (0.1-1 µM) and Purmorphamine (0.125-0.5 µM) for an additional 10-14 days. The specific concentrations can be optimized to bias toward different MN subtypes (see Section 2.2).
- Terminal Differentiation: Switch the medium to a terminal differentiation medium lacking mitogens but containing BDNF (10 ng/mL), GDNF (10 ng/mL), and CNTF (10 ng/mL). Maintain cultures under these conditions for at least 14 days to allow for the expression of mature MN markers and the development of electrophysiological properties.
- Quality Control: Validate MN identity and purity via immunocytochemistry for markers such as ISL1, HB9 (MNX1), and ChAT. This protocol typically yields MN cultures with >90% purity [1].
Subtype Specification: Generating Phrenic-like Motor Neurons
Respiratory failure from phrenic MN (phMN) degeneration is a primary cause of death in ALS. A specialized protocol has been developed to enrich for phrenic-like MNs, which exhibit distinct vulnerability [28].
Key Optimization: Standard protocols using 0.1 µM RA and 0.5 µM Pur. ("generic condition") primarily yield limb-innervating MNs. To specify phrenic-like MNs, a "dorsal-most" progenitor identity must be induced.
- Optimized Condition: Treat NPCs with a higher concentration of RA (1 µM) and a lower concentration of Purmorphamine (0.125 µM). This
RAHIGH/Pur.LOWcondition enriches for OLIG2+/PAX6HIGH/TLELOW dorsal MN progenitors with cervical identity, as evidenced by a 3-fold increase in HOXA5+ progenitors compared to the generic condition [28]. - Further Enrichment: Following patterning, fluorescence-activated cell sorting (FACS) can be used to isolate MN progenitors based on surface expression of IGDCC3, yielding cultures where ~25% of MNs express the phMN marker SCIP, a significant enrichment over generic protocols [28].
Table 1: Quantitative Outcomes of Small Molecule-Based Differentiation Protocols
| Protocol Objective | Key Signaling Molecules | Patterning Duration | Resulting MN Population | Efficiency / Purity | Key Markers |
|---|---|---|---|---|---|
| General Spinal MNs [1] | RA (0.1 µM), Pur. (0.5 µM) | ~24 days | Mixed spinal MNs (LMC, MMC) | >90% MN purity (ISL1+/HB9+) | HB9, ISL1, ChAT |
| Phrenic-like MNs [28] | RA (1 µM), Pur. (0.125 µM) | ~30 days | Phrenic-like MNs (enriched) | ~25% of MNs are SCIP+ | SCIP, HOXA5, FOXP1- |
Figure 1: Signaling pathway for phrenic-like MN specification. A dorsalized progenitor identity is induced by low SHH and high RA signaling, leading to HOXA5 expression and phrenic-like MN fate.
Combined Transcription Factor and Small Molecule Strategies
For maximum speed and efficiency, the direct transduction of key transcription factors can be combined with small molecule patterning. This approach bypasses some of the slower morphogen-driven patterning steps.
Protocol: Rapid Induction of Lower Motor Neurons
A recently published protocol demonstrates a highly efficient method for generating spinal lower motor neurons (LMNs) in just two weeks by combining transcription factors with a small molecule-based approach [10].
Key Reagents:
- Transcription Factors: A combination of critical MN fate-determining factors, typically including NGN2, ISL1, and LHX3, is delivered via lentiviral or sendai viral vectors.
- Small Molecules: The protocol utilizes a background of small molecules (likely including RA and a SHH agonist) to create a permissive environment for MN differentiation.
Detailed Methodology:
- Pre-patterning: Culture iPSCs and begin neural induction using a dual-SMAD inhibition protocol for approximately 5-7 days to generate neural progenitors.
- Transduction: Transduce the neural progenitors with viral vectors expressing the transcription factor cocktail.
- Maturation: After transduction, continue culturing the cells in a maturation medium containing neurotrophic factors.
- Outcome: This combined approach achieves around 80% induction efficiency of LMNs within two weeks, significantly faster than small-molecule only protocols [10]. The resulting cells express characteristic MN markers and are suitable for single-cell analysis and high-content screening.
Experimental Workflow for ALS Modeling and Screening
A complete, optimized workflow from iPSC to drug screening integrates the differentiation strategies above with robust phenotyping.
Figure 2: Integrated experimental workflow for ALS modeling. iPSCs are differentiated into MNs via small molecules or combined methods, followed by phenotypic validation and high-content drug screening.
Phenotypic Validation and Screening Readouts
Following differentiation, MNs must be rigorously validated for disease-relevant phenotypes.
- Longitudinal Live-Cell Imaging: A key method involves daily imaging of MN cultures using a motor neuron-specific reporter (e.g., HB9::GFP) to track survival and neurite integrity over time. This approach has demonstrated reduced survival and accelerated neurite degeneration in sporadic ALS (SALS) MNs compared to controls, correlating with donor survival [1].
- Electrophysiology: Multi-electrode array (MEA) recordings or patch-clamp can validate the functional activity of MNs. C9orf72-mutated phrenic-like MNs, for instance, show progressive loss of electrophysiological activity [28].
- High-Content Analysis: Combining live-cell imaging with machine learning-based single-cell analysis allows for the quantification of morphology and viability on a large scale, enabling robust drug screening [10].
Table 2: Key Reagent Solutions for iPSC-derived Motor Neuron Differentiation and Screening
| Reagent Category | Specific Example | Function in Protocol |
|---|---|---|
| Small Molecules | Retinoic Acid (RA) | Confers spinal cord (caudal) identity during patterning. |
| Purmorphamine | Activates SHH pathway to ventralize neural progenitors toward MN fate. | |
| Dorsomorphin / SB431542 | Dual-SMAD inhibition for efficient neural induction from iPSCs. | |
| Transcription Factors | NGN2, ISL1, LHX3 | Cocktail for direct reprogramming of progenitors to MN fate; enhances speed and efficiency. |
| Cell Surface Markers | IGDCC3 | Used for FACS enrichment of phrenic motor neuron progenitors. |
| Culture Additives | BDNF, GDNF, CNTF | Neurotrophic factors supporting MN survival and maturation post-differentiation. |
| Reporter Systems | HB9::turboGFP | Enables live-cell tracking and isolation of MNs for screening and analysis. |
Application in ALS Drug Discovery
These optimized differentiation strategies enable biologically relevant disease modeling and screening. A large-scale study using a SALS iPSC model derived from 100 patients demonstrated that over 97% of drugs previously tested in ALS clinical trials failed to mitigate neurodegeneration in vitro, accurately reflecting clinical trial outcomes [1]. Furthermore, combinatorial drug testing identified baricitinib, memantine, and riluzole as a promising therapeutic combination for SALS, highlighting the utility of these models for discovering new treatment strategies [1].
Achieving High-Purity Motor Neuron Cultures for Cell-Autonomous Studies
The development of robust, high-purity human induced pluripotent stem cell-derived motor neuron (iPSC-MN) models represents a critical advancement for studying amyotrophic lateral sclerosis (ALS) pathogenesis and therapeutic development. The predominant sporadic form of ALS (SALS), accounting for 90-95% of cases, has been particularly challenging to model due to its complex etiology and high clinical heterogeneity [1] [29]. Traditional models relying on familial ALS (FALS) mutations often fail to recapitulate the sporadic disease state, with over 160 drugs effective in FALS models failing clinical trials in broader ALS populations [1]. High-purity motor neuron cultures enable researchers to isolate cell-autonomous disease mechanisms from non-cell autonomous contributions, providing a controlled system for investigating intrinsic motor neuron vulnerability in ALS. Recent large-scale studies have demonstrated that iPSC-derived motor neurons from sporadic ALS patients can recapitulate key disease features including reduced survival, accelerated neurite degeneration, transcriptional dysregulation, and pharmacological responses to established treatments like riluzole [1]. The reproducibility and translational relevance of these models depend critically on achieving consistent, high-purity motor neuron differentiations that minimize confounding variables and enhance detection of disease-relevant phenotypes.
Established Differentiation Protocols and Methodologies
Rapid Monolayer Protocol for Cervical Spinal Motor Neurons
A novel, highly efficient protocol for generating cervical spinal motor neurons from human iPSCs has been developed, producing functionally mature sMNs within 28 days [13]. This method employs a streamlined, monolayer-adherent culture system that eliminates the need for embryoid body formation or complex purification steps, making it particularly suitable for standardized, high-throughput applications.
Key Protocol Steps:
- Days 0-6 (Neural Induction): Treat iPSCs with 2 μM SB431542 (TGF-β inhibitor), 2 μM DMH1 (BMP inhibitor), and 3 μM CHIR99021 (WNT activator) in monolayer culture to generate caudalized and ventralized neural stem cells (NSCs). This combination yields highly pure NSCs (96.6% ± 2.7% NESTIN+, 91.9% ± 4.3% PAX6+, 97.8% ± 2.1% SOX2+) while suppressing pluripotency markers (OCT4-) [13].
- Days 6-12 (Motor Neuron Progenitor Specification): Continue culture with the above inhibitors while adding 0.1 μM retinoic acid (RA) and 0.5 μM purmorphamine (SHH agonist) to pattern NSCs toward motor neuron progenitors. This stage generates 81.5% ± 6.9% OLIG2+ MNPs (up to 91.4% ± 1.4%) and 94.3% ± 0.7% NKX6.1+ ventral progenitors [13].
- Days 12-18 (Motor Neuron Differentiation): Transition cells to maturation medium with 0.1 μM Compound E (γ-secretase inhibitor) to inhibit Notch signaling and promote cell cycle exit and terminal differentiation. This critical step accelerates maturation, yielding 88%-97% CHAT+ cervical spinal MNs by day 18 [13].
- Days 18-28 (Functional Maturation): Maintain cultures in maturation medium to enable functional development, with extensive network activity and electrophysiological properties detectable by day 28 [13].
Large-Scale Screening-Optimized Protocol
For population-wide studies and drug screening applications, an alternative five-stage protocol has been optimized for consistency across multiple cell lines [1]. This approach emphasizes reproducibility and scalability while maintaining high purity, achieving cultures with 92.44% ± 1.66% of cells defined as motor neurons (co-expressing ChAT, MNX1/HB9, and Tuj1), with minimal contamination from astrocytes (0.12% ± 0.01% GFAP+) and microglia (0.04% ± 0.02% CD11B+) [1]. The protocol employs rigorous quality control measures and longitudinal live-cell imaging to track motor neuron health and degeneration kinetics, enabling correlation with donor clinical data.
Diagram Title: Motor Neuron Differentiation Workflow
Quality Control and Validation Metrics
Quantitative Purity Assessment
Rigorous quality control is essential for validating culture purity and ensuring experimental reproducibility. The following table summarizes key quality control metrics from recent studies achieving high-purity motor neuron cultures:
Table 1: Quality Control Metrics for High-Purity Motor Neuron Cultures
| QC Metric | Assessment Method | Target Value | Reported Performance | Study |
|---|---|---|---|---|
| Motor Neuron Purity | Co-expression of ChAT, MNX1/HB9, Tuj1 | >90% | 92.44% ± 1.66% | [1] |
| Neuronal Population | Tuj1+ staining | >95% | 97.66% ± 0.99% | [1] |
| Motor Neuron Progenitors | OLIG2+ expression | >80% | 81.5% ± 6.9% (up to 91.4%) | [13] |
| Cervical Spinal MNs | CHAT+ expression | >85% | 88%-97% | [13] |
| Astrocyte Contamination | GFAP+ staining | <0.5% | 0.12% ± 0.01% | [1] |
| Microglia Contamination | CD11B+ staining | <0.1% | 0.04% ± 0.02% | [1] |
| Neural Stem Cells | PAX6+OLIG2+ co-expression | >80% | >80% | [3] |
Functional Validation
Beyond marker expression, functional validation is crucial for confirming motor neuron identity and maturity:
- Electrophysiological Properties: Whole-cell patch clamp recording should demonstrate characteristic action potentials and voltage-gated ion channel activity [30] [13]. Mature cultures show spontaneous network activity and appropriate responses to depolarizing stimuli.
- Calcium Imaging: Functional networks should exhibit synchronized calcium oscillations, indicating established synaptic connections and network maturity [13].
- Molecular Profiling: Transcriptomic analysis should confirm expression of mature motor neuron markers and appropriate HOX gene patterns corresponding to cervical identity when relevant [13]. Single-cell RNA sequencing can provide detailed characterization of population homogeneity.
Managing Differentiation Variability
Even with optimized protocols, significant variability can arise from technical and biological factors. A comprehensive analysis of differentiation outcomes across 15 differentiation sets and 8 cell lines identified that non-genetic factors—particularly induction set and operator—were the predominant sources of variability, outweighing the contribution from cell line genetics [3]. Key findings included:
- Operator influence accounted for the majority of variance in multiple quality metrics, highlighting the need for standardized training and procedures [3].
- Induction set variations (environmental conditions, reagent lots) significantly impacted culture morphology and clustering [3].
- iPSC genomic instability emerged as a critical factor, with cultures derived from genomically stable iPSCs exhibiting reduced variance and improved marker expression profiles [3].
Advanced Culture Systems for Long-Term Maintenance
Maintaining high-purity motor neuron cultures beyond initial differentiation presents unique challenges, including cell aggregation, detachment, and declining viability. Recent advancements address these limitations:
- Dendritic Polyglycerol Amine (dPGA) Substrates: Culture surfaces coated with dPGA significantly improve long-term adherence and reduce cluster formation compared to conventional Matrigel coatings [31]. This cytocompatible substrate enhances neurite outgrowth, network stability, and suitability for single-cell applications like RNA sequencing.
- Indirect Coculture Systems: Physically separating motor neurons from supportive astrocytes using culture inserts provides trophic support while maintaining neuronal purity [32]. This system enables extended culture duration (≥3 weeks) without compromising purity, facilitating the study of age-related phenotypes in mature neurons.
Table 2: Research Reagent Solutions for High-Purity Motor Neuron Cultures
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Small Molecule Inducers | SB431542 (TGF-β inhibitor), DMH1 (BMP inhibitor), CHIR99021 (WNT activator) | Neural induction and patterning | Triple combination caudalizes and ventralizes NSCs [13] |
| Patterning Molecules | Retinoic acid (RA), Purmorphamine (SHH agonist) | Motor neuron specification | Establishes cervical identity and pMN domain [13] |
| Maturation Enhancers | Compound E (γ-secretase inhibitor) | Accelerates terminal differentiation | Inhibits Notch signaling to promote cell cycle exit [13] |
| Advanced Substrates | Dendritic Polyglycerol Amine (dPGA) | Improves long-term adhesion | Reduces clustering and enhances neurite outgrowth [31] |
| Trophic Factors | BDNF, GDNF, IGF-1, NT-3 | Supports neuronal survival and maturation | Critical for long-term culture maintenance [31] |
Applications in ALS Disease Modeling and Therapeutic Development
Modeling Sporadic ALS Pathogenesis
The availability of high-purity motor neuron cultures has enabled unprecedented insights into sporadic ALS mechanisms. A landmark study utilizing a 100-patient SALS iPSC library demonstrated that patient-derived motor neurons recapitulate key disease features including reduced survival, accelerated neurite degeneration correlating with donor survival, and transcriptional dysregulation [1]. Importantly, this model system exhibited pharmacological rescue by riluzole, validating its pathophysiological relevance.
Drug Screening and Therapeutic Discovery
High-purity cultures provide a robust platform for therapeutic screening and development:
- Target Validation: Well-characterized cultures enable rigorous testing of candidate therapies in a controlled, cell-autonomous context. Screening of drugs previously tested in ALS clinical trials revealed that 97% failed to mitigate neurodegeneration in the SALS model, reflecting clinical trial outcomes and validating the model's predictive value [1].
- Combinatorial Therapy Development: The reduced noise and enhanced consistency of high-purity systems facilitates identification of synergistic drug combinations. Recent work identified baricitinib, memantine, and riluzole as a promising therapeutic combination for SALS using such approaches [1].
- Personalized Medicine Applications: Population-wide screening across donor-specific lines helps account for heterogeneity in drug response, supporting the development of tailored therapeutic strategies [1].
Diagram Title: Signaling Pathways in MN Differentiation
The development of reliable methods for generating high-purity human iPSC-derived motor neuron cultures represents a transformative advancement for ALS research, particularly for the study of sporadic disease. By implementing optimized differentiation protocols, rigorous quality control measures, and advanced culture systems, researchers can now establish highly reproducible, physiologically relevant models that faithfully recapitulate disease-specific phenotypes. These tools have already demonstrated significant value in elucidating cell-autonomous disease mechanisms, validating therapeutic targets, and identifying novel treatment combinations. As the field continues to evolve, further refinements in standardization, maturation, and integration with non-cell autonomous components will enhance the predictive validity of these systems and accelerate the development of effective therapies for this devastating disorder.
Functional phenotyping of human induced pluripotent stem cell (hiPSC)-derived motor neurons (MNs) is crucial for modeling the pathobiology of amyotrophic lateral sclerosis (ALS) and conducting preclinical drug discovery. These assays capture key neurodegenerative processes, including neuronal hyperexcitability, neurite degeneration, and loss of neuronal survival, which are hallmark features of ALS. The development of robust, quantitative protocols for these phenotypic measures has enabled more accurate in vitro modeling of both familial and sporadic ALS, paving the way for more reliable drug screening and mechanistic studies. This application note provides detailed methodologies and data analysis frameworks for implementing these critical functional assays in ALS research.
Key Phenotypic Assays in ALS Research
Advanced functional phenotyping in hiPSC-derived MNs encompasses multiple assays that quantify distinct aspects of neurodegeneration. The table below summarizes the primary phenotypic measures, their biological significance, and common assessment methodologies.
Table 1: Core Functional Phenotyping Assays for iPSC-Derived Motor Neurons
| Phenotypic Measure | Biological Significance in ALS | Common Assessment Methods |
|---|---|---|
| Neuronal Survival | Models motor neuron death, a definitive pathological hallmark; correlates with donor survival [1]. | Longitudinal live-cell imaging, cell viability assays, caspase activation detection [1] [33]. |
| Neurite Degeneration | Early-stage event preceding neuronal death; quantifies fragmentation of axons and dendrites [34] [35]. | Degeneration Index (DI) analysis, neurite length quantification, fragmentation scoring [34] [35]. |
| Hyperexcitability | Altered electrophysiological function; manifests as increased firing frequency or reduced activation threshold [36]. | Patch-clamp electrophysiology, Ca²⁺ imaging, multi-electrode arrays (MEAs) [36]. |
Quantitative Data from Phenotypic Screening
Large-scale phenotypic screening of iPSC-derived motor neurons from sporadic ALS (SALS) patients generates quantitative data essential for validating disease models and evaluating therapeutic efficacy. The following table consolidates key findings from a recent large-scale study.
Table 2: Key Quantitative Findings from a Large-Scale iPSC Screening Study in SALS [1]
| Parameter | Finding in SALS vs. Control | Implications for Disease Modeling |
|---|---|---|
| Motor Neuron Survival | Significantly reduced survival in SALS motor neurons. | Recapitulates core pathological hallmark of ALS; validates model face validity [1]. |
| Neurite Degeneration | Accelerated neurite degeneration that correlated with donor survival. | Provides a continuous, quantifiable metric of disease progression; links in vitro and clinical outcomes [1]. |
| Pharmacological Rescue | Riluzole rescued survival and electrophysiological/transcriptomic deficits. | Confirms clinical efficacy and validates model for drug screening [1]. |
| Clinical Trial Drug Re-screening | 97% of previously tested drugs failed to mitigate neurodegeneration. | Mirrors clinical trial failures, highlighting model predictive validity [1]. |
| Combinatorial Therapy | Baricitinib, memantine, and riluzole combination significantly increased survival. | Identifies a promising therapeutic strategy validated across a heterogeneous SALS population [1]. |
Detailed Experimental Protocols
Protocol: Automated Quantification of Neurite Degeneration
The Degeneration Index (DI) is a quantitative measure of neurite fragmentation. This protocol describes an enhanced, automated method using an ImageJ macro (ANDI) for improved accuracy and efficiency [34] [35].
Key Reagents and Materials
- Cell Culture: Human iPSC-derived motor neurons (e.g., 30+ days differentiated).
- Fixation: 4% Paraformaldehyde (PFA) in PBS.
- Staining: Primary antibodies (e.g., anti-β-tubulin III/Tuj1), fluorescent secondary antibodies.
- Imaging: High-content fluorescence microscope.
- Software: Fiji/ImageJ with ANDI Macro.
Step-by-Step Procedure
- Culture and Differentiation: Generate high-purity spinal motor neurons from hiPSCs using a validated 5-stage protocol involving sequential patterning with small molecules [1]. Culture neurons on appropriate substrates (e.g., poly-L-ornithine/laminin).
- Fixation and Staining: At the desired time point (e.g., day 30-60 of differentiation), fix cells with 4% PFA for 15-20 minutes at room temperature. Permeabilize with 0.1% Triton X-100, block with serum, and immunostain for a neuronal cytoskeletal marker (e.g., β-tubulin III/Tuj1) to visualize the entire neurite network.
- Image Acquisition: Acquire high-resolution fluorescent images (10x or 20x objective) of multiple random fields per well, ensuring even illumination and avoiding signal saturation.
- Automated DI Analysis with ANDI Macro:
- Open the image stack in ImageJ/Fiji.
- Run the ANDI Macro, which automatically:
- Removes cell bodies from the micrographs to isolate neurites.
- Applies filters to remove image artifacts and non-neurite materials.
- Optimizes image contrast and thresholds to detect neurite fragments.
- Uses the "Analyze Particles" tool to calculate the total area of neurite fragments.
- The macro outputs the Degeneration Index (DI), calculated as: DI = (Area of Fragments) / (Total Neurite Area + Area of Fragments). A DI of 0 represents a healthy, intact network, while a DI approaching 1 indicates widespread fragmentation [34] [35].
Protocol: Longitudinal Live-Cell Imaging for Survival and Health
This protocol uses live-cell imaging to simultaneously track motor neuron survival and neurite health over time, providing kinetic data on degeneration.
Key Reagents and Materials
- Reporter Line: hiPSC-derived MNs transduced with a non-integrating, motor neuron-specific fluorescent reporter (e.g., HB9::GFP/TurboGFP) [1].
- Culture Vessels: 96 or 384-well imaging-optimized microplates.
- Equipment: Automated live-cell imaging system with environmental control (37°C, 5% CO₂).
Step-by-Step Procedure
- Cell Plating and Validation: Plate the reporter-expressing motor neurons at an optimized density in Matrigel-coated 384-well plates. Confirm that >90% of fluorescent cells co-express MN markers like HB9 and ChAT to ensure population purity [1].
- Experimental Setup: After allowing cells to adhere, add compounds or vehicles to the wells. Include controls (e.g., healthy control MNs, SALS MNs).
- Image Acquisition and Analysis:
- Program the live-cell imager to capture images of each well at regular intervals (e.g., every 4-24 hours) over the course of the experiment (e.g., 14-28 days).
- Survival Quantification: Use automated image analysis software to count the number of GFP-positive motor neuron cell bodies in each well at each time point. Normalize data to the initial cell count to generate survival curves.
- Neurite Health Analysis: From the same images, analyze the neurite network. This can be done by measuring total neurite length per image or by calculating a DI from the live images, though this is typically done more accurately post-fixation.
Protocol: Electrophysiological Profiling for Hyperexcitability
Assessing the electrophysiological properties of MNs reveals hyperexcitability, an early dysfunction in ALS.
Key Reagents and Materials
- Cells: Mature hiPSC-derived MNs (day 50+).
- Solution: Artificial Cerebrospinal Fluid (aCSF) for recording.
- Equipment: Patch-clamp rig or Multi-Electrode Array (MEA) system.
Step-by-Step Procedure (Whole-Cell Patch-Clamp)
- Cell Preparation: Plate MNs at low density for patch-clamp or higher density for MEA on appropriate substrates.
- Recording: For whole-cell patch-clamp configuration:
- Target healthy-looking neurons.
- Establish a giga-ohm seal and break into the whole-cell mode.
- Record intrinsic properties in current-clamp mode. Key parameters include:
- Resting Membrane Potential: Often depolarized in ALS models.
- Input Resistance: Can be altered.
- Action Potential Threshold: Often reduced, indicating hyperexcitability.
- Firing Frequency: In response to a series of current injections, ALS MNs often fire at a higher frequency compared to controls [36].
- Alternative Method - MEA: Plate MNs on MEA chips to record network-level activity simultaneously from multiple electrodes. Parameters like mean firing rate and burst frequency can indicate network hyperexcitability.
Signaling Pathways and Experimental Workflow
The following diagram illustrates the logical workflow for conducting a comprehensive functional phenotyping screen, from iPSC differentiation to data analysis.
The Scientist's Toolkit: Key Research Reagents
Successful implementation of these phenotyping assays relies on a standardized set of high-quality reagents. The table below lists essential materials and their functions.
Table 3: Essential Research Reagents for Functional Phenotyping of hiPSC-Derived MNs
| Reagent / Material | Function / Application | Specific Example(s) |
|---|---|---|
| Small Molecule Inducers | Directs hiPSC differentiation toward spinal motor neuron fate. | Retinoic Acid (RA), Purmorphamine (SHH agonist) [1] [37] [38]. |
| Culture Substrates | Provides adhesive surface for neuron attachment and neurite outgrowth. | Poly-L-Ornithine (PLO), Laminin [34] [37]. |
| Neurotrophic Factors | Supports motor neuron survival and maturation in vitro. | BDNF, GDNF, CNTF, IGF-1 [37]. |
| Cell Type Markers (Antibodies) | Identifies and validates motor neuron identity and purity. | Anti-HB9, Anti-ISLET1, Anti-ChAT, Anti-Tuj1 (β-tubulin III) [1] [37]. |
| Fluorescent Reporters | Enables live-cell tracking of motor neurons for survival assays. | HB9::turboGFP, HB9::RFP [1]. |
| Pharmacological Agents | Tool compounds for assay validation and mechanism study. | Riluzole (rescue), Memantine, Baricitinib (combinatorial therapy) [1]. |
High-Content and Live-Cell Imaging for Longitudinal Analysis
The integration of high-content screening (HCS) and live-cell imaging technologies has revolutionized longitudinal analysis in neurodegenerative disease research, particularly for amyotrophic lateral sclerosis (ALS) modeling using induced pluripotent stem cell-derived motor neurons (iPSC-MNs). These approaches enable researchers to capture dynamic disease-related phenotypes and cellular events over extended periods, providing unprecedented insights into disease mechanisms and therapeutic interventions [1] [39]. For ALS research, where patient-specific iPSCs can capture the complex and sporadic nature of the disease, these technologies offer a pathophysiologically relevant human model system with endogenous gene expression and regulation [1] [40]. This application note details established protocols and analytical frameworks for implementing these technologies in iPSC-MN ALS modeling, supporting drug discovery and disease mechanism investigation.
Key Research Reagent Solutions
The table below outlines essential reagents and tools for establishing robust high-content and live-cell imaging workflows for iPSC-derived motor neurons.
Table 1: Essential Research Reagents and Tools for iPSC-MN Imaging
| Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Line Development | iPSCs from sporadic and familial ALS patients [1] [23]; Non-integrating episomal vectors for reprogramming [1] | Establishes genetically relevant disease models; Enables generation of patient-specific lines without genomic integration |
| Cell Type Markers | Choline acetyltransferase (ChAT), MNX1/HB9, β-tubulin III (Tuj1) for motor neurons [1]; SMI-32/neurofilament heavy chain [23]; ISL1 for motor neuron quantification [23]; S100B for astrocyte-like cells [23] | Identifies and validates cell populations; Assesses culture purity and composition |
| Viability & Staining | HCS LIVE/DEAD Green Kit [41]; HCS Mitochondrial Health Kit [41]; CellROX reagents for oxidative stress [41]; HCS NuclearMask stains [41] | Measures cell death/apoptosis; Evaluates mitochondrial function; Quantifies oxidative stress; Labels cellular structures |
| Reporters & Biosensors | HB9-turbo fluorescent reporter for motor neuron-specific labeling [1]; Genetically encoded fluorescent biosensors for cell cycle, DNA damage, apoptosis [42] | Enables live-cell tracking of specific cell types; Monitors dynamic cellular processes longitudinally |
High-Content Screening Protocol for iPSC-MN Phenotyping
This protocol details a standardized methodology for conducting high-content screening of iPSC-derived motor neurons to quantify disease-relevant phenotypes, adapted from established large-scale studies [1] [23].
Motor Neuron Differentiation and Plating
- iPSC Culture and Differentiation: Maintain iPSC lines from healthy controls and ALS patients (both sporadic and familial). Differentiate iPSCs into spinal motor neurons using a standardized 32-day protocol based on dual SMAD inhibition and ventral patterning [23]. An optimized five-stage protocol can generate highly pure cultures (>92%) of mature motor neurons with extensive neurite networks [1].
- Experimental Plating: Plate differentiated motor neurons in 96-well or 384-well imaging-optimized microplates with #1.5 glass bottoms to ensure optimal image quality. Plate cells at a density achieving 60-80% confluency at time of imaging to minimize density-related artifacts while allowing sufficient cells for analysis [42] [43]. Include appropriate controls in each plate (healthy control lines, batch differentiation controls, and technical replicates).
Staining and Fixation
- Fixation and Permeabilization: Fix cells with 4% paraformaldehyde for 15 minutes at room temperature, then permeabilize with 0.1% Triton X-100 for 10 minutes.
- Immunofluorescence Staining: Incubate with primary antibodies against motor neuron markers (ISL1, Tuj1, SMI-32) and other cell type markers (S100B for astrocyte-like cells) for 2 hours at room temperature or overnight at 4°C [23]. Follow with appropriate fluorescently-labeled secondary antibodies for 1 hour at room temperature protected from light.
- Nuclear Counterstaining: Include Hoechst 33342 or DAPI (1 µg/mL for 10 minutes) to label all nuclei for segmentation and cell counting [41].
Image Acquisition and Analysis
- Image Acquisition: Acquire images using a high-content screening system (e.g., PerkinElmer Opera LX, Thermo Scientific ArrayScan XTI) with a 20x or 40x objective. Capture multiple fields of view (≥50 per well) to ensure statistical power [1] [43]. Maintain consistent exposure times across plates and experimental runs.
- Image Analysis Workflow:
- Cell Segmentation: Use nuclear staining to identify individual cells and define regions of interest.
- Neurite Outgrowth Analysis: Quantify neurite length, branching, and complexity using dedicated neurite tracing algorithms.
- Cell Type Classification: Identify motor neurons based on co-expression of specific markers (e.g., ISL1+).
- Phenotypic Quantification: Measure survival (number of ISL1+ cells), neurite degeneration, and inclusion body formation.
Table 2: Key Quantitative Readouts from iPSC-MN High-Content Screening
| Parameter | Measurement Method | Representative Finding in ALS Models |
|---|---|---|
| Motor Neuron Survival | Percentage of ISL1+ cells relative to total nuclei [23] | Significantly reduced survival in SALS motor neurons versus controls [1] |
| Neurite Degeneration | Total neurite length per cell, number of branches [1] | Accelerated neurite degeneration correlating with donor survival [1] |
| Cell Composition | Percentage of S100B+ cells, Tuj1+ neurons [23] | S100B+ astrocyte-like cells present from day 18 of differentiation [23] |
| Culture Purity | Percentage of ChAT+, MNX1/HB9+, Tuj1+ cells [1] | High-purity cultures (92.44 ± 1.66%) achievable with optimized protocols [1] |
Figure 1: High-content screening workflow for iPSC-derived motor neurons
Longitudinal Live-Cell Imaging Protocol
This protocol describes the setup for long-term live-cell imaging of iPSC-derived motor neurons to track dynamic disease processes, incorporating best practices for maintaining cell health during extended imaging sessions [42].
Microscope and Environmental Control Setup
- Microscope Configuration: Utilize an automated inverted microscope (widefield epifluorescence or spinning-disc confocal) equipped with motorized stage, digital camera, and environmental chamber. Phase contrast or differential interference contrast (DIC) is ideal for label-free imaging, while fluorescent capabilities enable tracking of expressed reporters or biosensors [42] [39].
- Environmental Chamber Setup:
- Configure the stage-top environmental chamber to maintain 37°C, 5% CO₂, and ~80% humidity.
- Pre-equilibrate the chamber for 30-60 minutes before introducing cells using a "dummy" dish with water to stabilize temperature.
- Use pre-mixed, certified 5% CO₂/balance air gas with appropriate flow rates as per manufacturer directions [42].
- Ensure no tension on connection cords to prevent motion artifacts during time-lapse acquisition.
Sample Preparation and Time-Lapse Acquisition
- Cell Preparation: Plate iPSC-derived motor neurons in specialized live-cell imaging vessels with #1.5 glass bottoms. For fluorescent biosensor expression, use BacMam gene delivery or stable expression of biosensors for cell cycle progression, apoptosis, or mitochondrial health [41] [42].
- Image Acquisition Parameters:
- Set appropriate sampling intervals based on the biological process: 5-15 minutes for cell motility and process extension, 30-60 minutes for survival tracking, and 2-6 hours for proliferation assessment.
- Use the lowest practical light intensity and shortest exposures to minimize phototoxicity while maintaining sufficient signal-to-noise ratio.
- For multi-position experiments, ensure adequate time for stage movement and focus maintenance between positions.
Data Analysis and Cell Tracking
- Cell Recognition and Tracking: Implement instance segmentation algorithms to identify and track individual cells across time points. Either brightfield microscopy or fluorescent markers can be used for this purpose [39].
- Multi-Modal Readouts: Extract both single-timepoint (cell morphology, intensity, texture) and multiple-timepoint metrics (migration speed, genealogy, lineage information) from the tracking data [39].
- Validation: Manually review a subset of tracks to ensure algorithm accuracy, particularly for challenging scenarios like cell division or death.
Figure 2: Longitudinal live-cell imaging workflow for dynamic process analysis
Application in ALS Research: Key Findings and Data Presentation
The implementation of these imaging technologies has yielded significant insights into ALS disease mechanisms and therapeutic discovery, as demonstrated by several landmark studies.
Modeling Sporadic ALS and Drug Screening
Large-scale phenotypic screening of iPSC-derived motor neurons from 100 sporadic ALS (SALS) patients has demonstrated the ability to recapitulate key disease features, including reduced survival, accelerated neurite degeneration correlating with donor survival, and transcriptional dysregulation [1]. This model system has proven valuable for therapeutic discovery:
- Pharmacological testing reproduced the efficacy of riluzole, rescuing motor neuron survival and reversing electrophysiological and transcriptomic abnormalities [1].
- Screening of drugs previously tested in ALS clinical trials revealed that 97% failed to mitigate neurodegeneration, reflecting clinical trial outcomes and validating the SALS model [1].
- Combinatorial testing identified baricitinib, memantine, and riluzole as a promising therapeutic combination for SALS [1].
Addressing Variability in Large-Scale Studies
Recent large-scale differentiation efforts have highlighted important considerations for experimental design:
- Sex Differences: Motor neuron cultures from male ALS patients showed significantly higher percentages of ISL1+ cells (17.0% ± 0.4%) compared to controls (14.1% ± 0.8%) and female ALS samples, indicating sex-specific differences in differentiation efficiency or motor neuron vulnerability [23].
- Cell Composition: Unsupervised principal component analysis of gene expression data revealed high correlations with the percentage of S100B+ cells, emphasizing the need to account for varying cell type composition in differentiated cultures [23].
- Transcriptomic Signatures: Sex drove a strong transcriptomic signature that could completely separate males and females, associated with a large number of differentially expressed autosomal and sex-linked genes [23].
Table 3: Key Considerations for Large-Scale iPSC-MN Studies Based on Experimental Findings
| Factor | Impact on Data | Recommendation |
|---|---|---|
| Sex of Cell Donor | Significantly affects ISL1+ motor neuron percentage and transcriptomic profiles [23] | Balance experimental groups by sex; Include as covariate in analyses |
| Cell Culture Composition | Variable percentages of S100B+ astrocyte-like cells and other non-neuronal cells affect transcriptomics [23] | Quantify and account for cell composition in analyses; Consider purification strategies |
| Reprogramming Method | T cell vs. non-T cell reprogramming leads to specific gene expression patterns in motor neuron cultures [23] | Document and account for reprogramming method; Standardize where possible |
| Differentiation Batch | Technical variability across differentiations affects multiple readouts [23] | Include batch differentiation controls; Randomize samples across batches |
These imaging approaches provide powerful tools for addressing the complexity of ALS, enabling researchers to capture disease-relevant phenotypes in patient-specific models and paving the way for more effective therapeutic development.
Amyotrophic lateral sclerosis (ALS) presents a formidable challenge in neurodegenerative disease research, with approximately 90% of cases classified as sporadic (SALS) with unknown etiology and highly heterogeneous clinical presentation [1]. The failure of over 160 drugs tested in clinical trials for ALS over the past three decades can be partially attributed to the reliance on animal or cell models expressing gene mutations linked to rare familial forms of ALS (FALS), often with non-physiological levels of expression and regulation [1]. The development of induced pluripotent stem cell (iPSC) technologies has created unprecedented opportunities to model sporadic disease from across the patient population, providing human pathophysiological models with endogenous gene expression and regulation [1] [26]. This Application Note details experimental protocols and case studies demonstrating how iPSC-derived motor neuron models are advancing ALS therapeutic development from screening to clinical trials, with specific focus on ropinirole, ezogabine, and combinatorial therapies identified through this approach.
Case Study 1: Ropinirole - From Phenotypic Screening to Clinical Validation
Experimental Protocol for iPSC Screening
Motor Neuron Differentiation Protocol: The identification of ropinirole as a candidate ALS therapeutic employed a standardized motor neuron differentiation protocol [44]. Human iPSCs from sporadic ALS patients and healthy controls were differentiated into spinal motor neurons using a five-stage process with small molecules. Briefly, neural induction was achieved using dual SMAD signaling inhibition (LDN-193189 and SB431542) for 10 days, followed by caudalization with retinoic acid (0.1 µM) and ventralization using the sonic hedgehog agonist purmorphamine (1 µM) for 10-14 days. Motor neuron precursors were selected using CD171 (L1CAM) magnetic-activated cell sorting before final maturation for 21-28 days [44].
Phenotypic Screening Method: Differentiated motor neurons were plated in 384-well plates at 10,000 cells per well and treated with ropinirole hydrochloride across a concentration range (0.1-100 µM) for 48-72 hours. Key phenotypic endpoints included:
- Neurite Degeneration: Quantified via high-content imaging of β-tubulin III-stained neurons using Harmony software.
- Cell Survival: Measured using CellTiter-Glo luminescent cell viability assay.
- Oxidative Stress: Assessed via CellROX Green reagent staining.
- Mitochondrial Function: Evaluated using MitoStress kit on Seahorse Analyzer.
- Dopamine D2 Receptor Expression: Confirmed via immunocytochemistry and qPCR [45] [44].
Key Findings and Translational Data
Table 1: Key Experimental Findings for Ropinirole in ALS Models
| Parameter | In Vitro Effect | Clinical Trial Outcome | Proposed Mechanism |
|---|---|---|---|
| Motor Neuron Survival | Increased survival by 25-40% in SALS iPSC-MNs [44] | 27.9 weeks additional progression-free survival in open-label extension [45] | Dopamine D2 receptor agonism modulating SREBP2-cholesterol pathway [45] |
| Neurite Degeneration | Significant reduction vs. untreated controls [44] | Not directly measured | Independent of antioxidant activity or mitochondrial rescue [44] |
| Disease Progression | N/A | Significant suppression of ALSFRS-R decline in open-label extension [45] | Regulation of cholesterol homeostasis and reduction of lipid peroxides [45] |
| Clinical Trial Design | N/A | 24-week double-blind, 24-week open-label extension; 20 participants [45] | Lipid peroxide as potential surrogate biomarker [45] |
Signaling Pathway
Figure 1: Proposed signaling pathway for ropinirole's neuroprotective effects in ALS models, involving dopamine D2 receptor-mediated modulation of cholesterol synthesis and reduction of toxic lipid peroxides [45] [44].
Case Study 2: Ezogabine (Retigabine) - Targeting Neuronal Hyperexcitability
Experimental Protocol for Hyperexcitability Assessment
Motor Neuron Differentiation: Cortical and spinal motor neurons were differentiated from both familial (SOD1, C9orf72) and sporadic ALS patient-derived iPSCs using a modified protocol with small molecules for neural induction (dual SMAD inhibition), caudalization (retinoic acid), and patterning (purmorphamine) over 28-35 days [46] [47]. Motor neuron identity was confirmed by immunostaining for ISL1, HB9, and ChAT, with cultures containing >90% motor neurons.
Electrophysiological Assessment: Functional characterization of motor neuron hyperexcitability was performed using multiple complementary approaches:
- Whole-Cell Patch Clamp Recording: Cells were analyzed at 30-35 days post-differentiation. Spontaneous action potentials were recorded in current-clamp mode, and potassium currents were measured in voltage-clamp mode with and without ezogabine (1-20 µM) [46].
- Multi-Electrode Array (MEA): Network-level activity was recorded using Maestro MEA systems. Parameters included mean firing rate, burst duration, and synchrony index before and after drug application [6] [47].
- Calcium Imaging: Cells were loaded with Fluo-4 AM dye, and calcium transients were recorded to assess synchronous network activity [47].
Clinical Translation Metrics: The phase 2 randomized clinical trial (NCT02450552) assessed cortical and spinal motor neuron excitability in 65 ALS participants using:
- Transcranial Magnetic Stimulation (TMS): Measuring short-interval intracortical inhibition (SICI) and resting motor threshold (RMT).
- Threshold Tracking Nerve Conduction Studies (TTNCS): Quantifying strength-duration time constant (SDTC) [46].
Key Findings and Pharmacodynamic Effects
Table 2: Ezogabine Effects on Neuronal Hyperexcitability in ALS Models and Patients
| Excitability Parameter | In Vitro Effect | Clinical Trial Result | Dose Dependency |
|---|---|---|---|
| Cortical Inhibition (SICI) | Not directly measured | Increased by 53% with 900 mg/d (P=.009) [46] | Dose-dependent; 600 mg/d not significant [46] |
| Resting Motor Threshold | Not directly measured | Increased with 600 mg/d (P=.04) [46] | Inverse dose relationship [46] |
| Spinal Excitability (SDTC) | Reduced in SOD1 & C9orf72 MNs [46] | Decreased with 900 mg/d (P<.001) [46] | Dose-dependent [46] |
| KCNQ Channel Activity | Increased potassium currents [46] | Inferred from excitability measures [46] | Dose-dependent [46] |
| Network Hyperexcitability | Reduced burst firing and synchronicity in MEA [6] | Not directly measured | Concentration-dependent [6] |
Mechanism of Action Pathway
Figure 2: Ezogabine mechanism of action involving direct opening of KCNQ potassium channels, leading to membrane hyperpolarization and reduced neuronal hyperexcitability, subsequently decreasing ER stress and improving motor neuron survival [46].
Case Study 3: Combinatorial Therapies - Addressing Multifactorial Pathogenesis
Experimental Protocol for Combination Screening
Large-Scale Screening Approach: A comprehensive combinatorial drug screening was performed using an iPSC library derived from 100 sporadic ALS patients and 25 healthy controls [1]. Motor neurons were differentiated using a rigorously optimized five-stage protocol capable of discriminating between healthy control and diseased motor neurons, achieving cultures with >92% purity (confirmed by ChAT, MNX1/HB9, and Tuj1 co-expression) [1].
Screening Methodology:
- Longitudinal Live-Cell Imaging: Motor neuron cultures were monitored daily using live-cell imaging with a virally delivered nonintegrating motor neuron-specific reporter (HB9-turbo) to track survival and neurite degeneration over 28 days.
- High-Content Analysis: Automated imaging and analysis quantified neurite length, branching complexity, and cell survival.
- Compound Libraries: Testing included more than 100 drugs previously tested in ALS clinical trials, with combinatorial testing of effective agents.
- Transcriptomic Analysis: RNA sequencing was performed to assess pathway-level responses to combination therapies [1].
PrimeC Combination Protocol: Separate investigations examined the PrimeC combination (ciprofloxacin and celecoxib) using:
- Survival Assays: ALS iPSC-derived motor neurons treated with individual compounds vs. combination.
- Drug Concentration Profiling: Measurements in brain tissue and serum of C57BL mice treated with single compounds versus combination [48].
Key Findings for Combinatorial Approaches
Table 3: Combinatorial Therapies in ALS iPSC Models
| Therapeutic Combination | Experimental Findings | Proposed Synergistic Mechanisms | Validation Level |
|---|---|---|---|
| Baricitinib + Memantine + Riluzole | Significant increase in SALS motor neuron survival across heterogeneous donor population [1] | Multi-target: JAK/STAT inhibition (baricitinib), NMDA receptor antagonism (memantine), glutamatergic modulation (riluzole) [1] | In vitro validation across 100 SALS iPSC lines; patent filed [1] [49] |
| PrimeC (Ciprofloxacin + Celecoxib) | Enhanced survival vs. individual compounds; increased ciprofloxacin brain penetration [48] | Dual-pathway: COX-2 inhibition (celecoxib) and RNA regulation (ciprofloxacin) with improved pharmacokinetics [48] | In vitro human iPSC-MNs and in vivo rodent pharmacokinetics [48] |
| Clinical Trial Drugs | 97% failed to mitigate neurodegeneration in SALS models, reflecting clinical trial outcomes [1] | N/A | Large-scale validation against historical clinical trial data [1] |
Experimental Workflow for iPSC-based Drug Discovery
Figure 3: Integrated workflow for iPSC-based ALS drug discovery, from patient cell reprogramming through motor neuron differentiation, phenotypic screening, and clinical translation [1] [26].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagent Solutions for iPSC-based ALS Research
| Reagent/Platform | Function | Application Example |
|---|---|---|
| Human iPSC Lines | Disease modeling foundation | Sporadic ALS donor libraries (n=100) for population-wide screening [1] |
| Motor Neuron Differentiation Kits | Generate target cells | Accelerated protocols producing CHAT+ cervical spinal MNs (88%-97% purity) [47] |
| HB9-turbo Reporter | Motor neuron-specific labeling | Longitudinal tracking of survival and neurite degeneration [1] |
| Multi-Electrode Array (MEA) | Network-level functional assessment | Detecting hyperexcitability phenotypes in ALS motor neurons [6] [47] |
| IncuCyte S3 System | Live-cell imaging and analysis | Quantifying spontaneous neuronal activity and synchronicity [6] |
| CD171 (L1CAM) Magnetic Sorting | Motor neuron purification | Isolation of spinal motor neuron precursors for high-purity cultures [44] |
The case studies presented herein demonstrate the transformative potential of iPSC-derived motor neuron models in advancing ALS therapeutic development from screening to clinical application. Ropinirole exemplifies successful translation from phenotypic screening to clinical trial validation, while ezogabine highlights the utility of iPSC models for targeting specific pathological mechanisms like neuronal hyperexcitability with clinically measurable pharmacodynamic effects. Combinatorial approaches address the multifactorial pathogenesis of ALS, with promising in vitro results across heterogeneous patient populations. These application notes provide validated protocols and analytical frameworks that researchers can implement to advance their own ALS drug discovery programs using human iPSC-based models that faithfully recapitulate sporadic disease features.
Navigating Challenges: Strategies for Enhancing Reproducibility and Maturation in iPSC-ALS Models
The use of induced pluripotent stem cell (iPSC)-derived motor neurons (MNs) represents a transformative approach for modeling amyotrophic lateral sclerosis (ALS) and advancing therapeutic discovery. However, the significant variability inherent in iPSC generation and differentiation poses a substantial challenge to experimental reproducibility and reliability. This variability stems from multiple sources, including donor genetic background, reprogramming methodologies, and differentiation protocol efficiency. Addressing these factors is crucial for establishing robust, standardized models that accurately recapitulate ALS pathology, particularly for the predominantly sporadic forms of the disease. This Application Note details the primary sources of variability in iPSC-derived MN studies and provides standardized protocols and analytical frameworks to enhance reproducibility in ALS research.
Understanding the relative contribution of different factors to experimental variability is essential for designing robust studies. The table below summarizes quantitative findings on key sources of variance in iPSC-derived motor neuron models.
Table 1: Quantitative Summary of Variability Sources in iPSC-Derived Motor Neuron Models
| Source of Variability | Quantitative Impact | Experimental Evidence |
|---|---|---|
| Genetic Background | Explains 2-30% of variance in differentiation outcomes [50]; 5-46% of variation in iPSC phenotypic traits [51]. | Significant inter-individual differences in gene expression, eQTLs, and DNA methylation observed across lines from different donors [51]. |
| Non-Genic Factors (Induction Set) | Largest contributor, explaining up to 70% of variance in culture purity metrics [50]. | Differentiation attempts ("induction sets") significantly associated with morphological outcomes and cluster formation (p < 0.05) [50]. |
| Operator Effect | Second largest contributor after induction set [50]. | Linear modeling identified operator as a significant factor (p < 0.05), independent of years of experience [50]. |
| Sex of Donor | Significant source of variation in large-scale differentiations [11]. | Male ALS cultures showed increased MN numbers and enrichment of stress-related pathways [11]. |
| Genomic Instability | Cultures from abnormal karyotype lines show high variance and morphological defects [50]. | qPCR-identified chromosomal abnormalities (<1.5 or >2.5 copy number) linked to failed differentiations and dense cellular clusters [50]. |
Experimental Protocols for Variability Mitigation
Protocol: Large-Scale iPSC Library Generation and Quality Control
Background: Generating a well-characterized iPSC library is foundational for capturing the heterogeneity of ALS and controlling for genetic variability. This protocol is adapted from a large-scale study that established an iPSC library from 100 sporadic ALS (SALS) patients and 25 healthy controls [1].
Procedure:
- Somatic Cell Source: Obtain skin biopsy specimens from clinically assessed ALS donors and healthy controls. Fibroblasts are isolated as the primary somatic cell source.
- Reprogramming: Use non-integrating episomal vectors for reprogramming to minimize genomic alterations.
- Automation: Employ an automated robotics platform to maximize output uniformity and reduce operator-induced variability during reprogramming and subsequent culture [1].
- Rigorous Quality Control: Implement a multi-tiered QC pipeline:
- Genomic Integrity: Confirm via whole-genome DNA sequencing. Identify any pathogenic variants or expansions in known ALS genes (e.g., C9ORF72) [1].
- Pluripotency Verification: Confirm expression of standard pluripotency markers.
- Trilineage Differentiation Potential: Demonstrate the capacity to differentiate into all three germ layers.
Troubleshooting Note: Regular monitoring for karyotypic abnormalities is critical. Utilize a targeted RT-qPCR assay for the nine most common karyotypic abnormalities in human iPSCs. Lines with chromosomal copy numbers < 1.5 or > 2.5 (or < 0.7 / > 1.3 for chromosome X in male lines) should be considered "abnormal" and excluded from differentiations, as they significantly increase variance and failure rates [50].
Protocol: Standardized Motor Neuron Differentiation and Phenotyping
Background: A consistent, high-purity MN differentiation protocol is vital for reproducible disease modeling. This protocol yields mature MNs suitable for longitudinal health assessment and drug screening [1].
Procedure:
- Differentiation Method: Adapt a five-stage, small molecule-based spinal motor neuron differentiation protocol [1]. This method was selected after optimization for its ability to discriminate between healthy control and diseased motor neurons.
- Maturation and Culture Purity: Culture cells under optimized maturation conditions. The protocol should consistently generate cultures with >90% MNs, defined by co-expression of ChAT, MNX1/HB9, and β-tubulin III (Tuj1), and minimal contamination from astrocytes (<0.2%) and microglia (<0.1%) [1].
- Phenotypic Screening: Implement a longitudinal live-cell imaging pipeline to assess MN health over time.
- Reporter System: Use a virally delivered, non-integrating, MN-specific reporter (e.g., HB9-turboGFP) to accurately identify and track MNs [1].
- Key Metrics: Quantify fundamental hallmarks of ALS pathology, including:
- Motor neuron survival and death rates.
- Accelerated neurite degeneration (which should correlate with donor survival data) [1].
Figure 1: Experimental workflow for the generation and phenotyping of iPSC-derived motor neurons, highlighting key steps for quality control and standardized output.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Resources for iPSC-Derived Motor Neuron Studies
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| Non-integrating Episomal Vectors | Reprogramming somatic cells to iPSCs | Avoids genomic integration, improves genomic safety [1]. |
| HB9-turboGFP Reporter | Motor neuron-specific live-cell identification | Enables accurate tracking of MN health and morphology in longitudinal studies [1]. |
| Anti-MNX1/HB9 Antibody | Immunocytochemistry for MN identification | Critical for validating differentiation efficiency and culture purity. |
| Anti-ChAT Antibody | Immunocytochemistry for MN identification | Confirms cholinergic phenotype of differentiated MNs. |
| Anti-β-tubulin III (Tuj1) Antibody | Pan-neuronal marker | Used in conjunction with MN-specific markers to assess neuronal purity. |
| Karyotyping RT-qPCR Assay | Genomic stability monitoring | Targets 9 most common karyotypic abnormalities; essential for routine QC [50]. |
| "Rosetta" iPSC Lines | Inter-laboratory standardization | Commonly used reference lines to normalize data and remove technical variation between labs [50]. |
Analysis and Data Interpretation
Effective management of variability extends beyond the bench to data analysis. The following strategies are recommended:
- Account for Genetic Background: For studies involving multiple cell lines, incorporate "genetic background" as a covariate in statistical models. The use of "Rosetta" or reference lines can help normalize data across different genetic backgrounds and laboratories [51] [50].
- Statistical Modeling of Variance: Employ linear modeling to quantify the variance (e.g., via R² values) attributable to key factors such as induction set, operator, and cell line. This helps identify the most significant sources of noise in a specific experimental setup [50].
- Address Sex as a Biological Variable: Given that donor sex is a significant source of variation in large-scale MN differentiations, studies should be designed to account for and analyze potential sex-specific effects [11].
Figure 2: A hierarchical breakdown of the primary factors contributing to variability in iPSC-derived motor neuron models, highlighting their relative impact.
The successful implementation of iPSC-derived motor neuron models for ALS research hinges on a systematic and vigilant approach to managing variability. Key strategies include the establishment of well-curated, genomically stable iPSC libraries; the use of standardized, highly efficient differentiation protocols with rigorous quality control; and the application of statistical methods that account for both genetic and non-genetic sources of variance. By adopting the protocols and analytical frameworks outlined in this Application Note, researchers can significantly enhance the reliability and reproducibility of their models, thereby accelerating the discovery of effective therapies for ALS.
The use of human induced pluripotent stem cell-derived motor neurons (iPSC-MNs) has emerged as a transformative approach for modeling amyotrophic lateral sclerosis (ALS) and conducting drug discovery. However, a significant challenge persists: the inherent immaturity of these cells relative to their adult human counterparts. Most differentiation protocols yield motor neurons with fetal-like characteristics, limiting their ability to fully recapitulate late-onset disease pathophysiology [2] [52]. This application note details the critical hurdles in achieving adult-like maturation of iPSC-MNs and provides validated protocols and tools to advance ALS research toward more physiologically relevant models.
The maturation hurdle is multifaceted, encompassing electrophysiological, metabolic, structural, and transcriptional domains. Electrophysiologically, immature iPSC-MNs often exhibit depolarized resting membrane potentials, slower action potential upstroke velocities, and spontaneous activity, contrasting with the stable electrophysiological profile of adult motor neurons [53] [54]. Transcriptional analyses reveal that in vivo mouse motor neurons undergo pervasive gene expression changes until the third postnatal week, after which their transcriptional profile stabilizes into an adult state [52]. A critical finding is that stem cell-derived motor neurons recapitulate only approximately 40% of this intrinsic maturation program in vitro, indicating a substantial deficiency in capturing the complete adult phenotype [52]. Overcoming these limitations is paramount for establishing iPSC-MNs as reliable platforms for ALS disease modeling and therapeutic screening.
Quantitative Assessment of Maturation Status
Evaluating the success of maturation protocols requires benchmarking against defined metrics. The tables below summarize key phenotypic differences between fetal-state and adult-like motor neurons and catalog the essential markers for assessing maturation status.
Table 1: Comparative Characteristics of Fetal-state vs. Adult-like Motor Neurons
| Parameter | Fetal-State iPSC-MNs | Adult-like Motor Neurons | Citation |
|---|---|---|---|
| Resting Membrane Potential | -44 mV to -49 mV (depolarized) | Progressively more hyperpolarized (towards -65 mV) | [53] [55] |
| Action Potential Upstroke Velocity | ~4.2 V/s | Increases to ~11 V/s | [55] |
| Repetitive Firing Capability | Often single spike; limited trains | Sustained, high-frequency trains | [53] |
| Input Resistance | Higher | Decreases with maturation | [53] |
| Metabolic Profile | Glycolysis-dependent | Increased oxidative phosphorylation | [55] [56] |
| Sarcomeric Organization | Random orientation | Highly organized, aligned myofibrils | [55] |
Table 2: Key Markers for Evaluating Motor Neuron Maturation
| Marker Category | Key Markers | Function & Significance in Maturation |
|---|---|---|
| Structural & Identity | TUJ1 (β-tubulin III), HB9 (MNX1), ChAT | Confirms neuronal and motor neuron identity; high purity (>90%) is achievable. |
| Electrophysiological | Kir2.1 (for IK1 current), Voltage-gated Na+ channels | Kir2.1 expression is crucial for stable resting potential; its absence is a key sign of immaturity. |
| Synaptic & Connectivity | Connexin 43 (Cx43), RYR2 | Mature localization to membrane and colocalization with sarcomeres indicates advanced development. |
| Transcriptional Regulators | ISL1, LHX3, NFI factors, Hormone receptors | ISL1/LHX3 dominate early specification; NFI/activity-dependent factors emerge later. |
Experimental Protocols for Enhanced Maturation
This section outlines specific methodologies to generate and characterize mature iPSC-MNs suitable for ALS research.
Protocol A: Rapid High-Efficiency Motor Neuron Induction
This protocol, adapted from recent work, enables swift production of lower motor neurons with high purity [10].
- Initial Seeding: Plate human iPSCs on a suitable extracellular matrix (e.g., Matrigel) in essential 8 medium.
- Neural Induction: At approximately 70% confluence, switch to a neural induction medium containing dual-SMAD inhibition (e.g., LDN-193189 and SB431542) for 5-7 days.
- Motor Neuron Patterning: Add caudalizing (e.g., retinoic acid) and ventralizing (e.g., purmorphamine or SAG) factors to the medium for another 7-10 days to specify spinal motor neuron fate.
- Transcription Factor Transduction: To boost efficiency and speed, transduce cells with lentiviral vectors expressing motor neuron-specific transcription factors (e.g., NGN2, ISL1, LHX3). This step can be combined with small molecules.
- Maturation: Following a 2-week induction period, dissociate and plate the resulting motor neuron progenitors on a poly-ornithine/laminin substrate. Maintain cells in a maturation medium containing neurotrophic factors (BDNF, GDNF, CNTF) for up to 4 weeks, refreshing the medium every 2-3 days.
- Quality Control: Validate cultures via immunocytochemistry for HB9 and TUJ1. This protocol achieves around 80% induction efficiency within two weeks [10].
Protocol B: A Multi-Modal Maturation Strategy
Inspired by advances in cardiomyocyte maturation, this protocol applies combinatorial cues to drive adult-like phenotypes [55].
- Metabolic Maturation: After initial differentiation, transition cells to a maturation medium (MM) enriched with lipids (fatty acids), a high concentration of calcium, and hormones (e.g., T3/T4 thyroid hormone) to shift metabolism from glycolysis to oxidative phosphorylation.
- Structural Patterning: Plate cells on nanopatterned (NP) culture surfaces. These surfaces are coated with parallel microgrooves to guide cytoskeletal and sarcomeric alignment, promoting anisotropic tissue structure.
- Electrostimulation: After cells adhere, apply chronic electrical field stimulation (ES) using a commercial system (e.g., C-Pace EP). A regimen of 2 Hz mimics physiological activity levels and promotes electrophysiological maturation.
- Functional Analysis: After 2-4 weeks of combined treatment, assess maturity via patch clamp electrophysiology and multi-electrode array (MEA) recordings.
Diagram: A sequential combinatorial maturation workflow. Integrating metabolic, structural, and activity-dependent cues drives iPSC-MNs toward an adult-like state.
Key Assays for Phenotypic Validation in ALS Models
For ALS disease modeling, functional phenotyping is critical. The following assays are essential for validating both maturation and disease-relevant phenotypes.
Longitudinal Live-Cell Imaging for Neurodegeneration:
- Purpose: To quantitatively assess motor neuron survival and neurite degeneration, a key pathological hallmark of ALS [1].
- Method: Transfer MN cultures to imaging-ready plates. Use a motor neuron-specific reporter (e.g., Hb9::GFP). Acquire brightfield and fluorescence images every 4-6 hours for 7-14 days using an automated live-cell imaging system.
- Analysis: Utilize machine learning-based single-cell tracking software to analyze soma counts, neurite length, and branching complexity over time. In SALS models, accelerated neurite degeneration correlates with donor survival [1].
Functional Screening with Multi-Electrode Array (MEA):
- Purpose: To detect disease-associated hyperexcitability and network dysfunction non-invasively [6].
- Method: Plate matured iPSC-MNs on MEA plates. Record spontaneous electrical activity after cultures stabilize (typically 10-20 days post-thaw).
- Analysis: Compare parameters like mean firing rate, burst duration, number of network bursts, and synchrony index between control and ALS lines. ALS donor cells typically show a reproducible loss of synchronous firing and different degrees of hyperexcitability [6].
Patch Clamp Electrophysiology:
- Purpose: To perform a detailed investigation of intrinsic electrical properties.
- Method: Perform whole-cell patch clamp on single iPSC-MNs. Key measurements include resting membrane potential (RMP), action potential (AP) threshold, AP amplitude, and maximum upstroke velocity (Vmax). Also, test for the ability to fire repetitively in response to sustained depolarization and for the presence of spike frequency adaptation (SFA) [53].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for iPSC-MN Maturation and Screening
| Reagent / Material | Function | Example Application |
|---|---|---|
| Nanopatterned Culture Surfaces | Provides topological cues to guide cell alignment and sarcomere organization, improving structural maturity. | Used in Protocol B to enhance cytoskeletal alignment and sarcomere structure [55]. |
| Electrostimulation Systems (e.g., C-Pace) | Applies chronic electrical pacing to mimic in vivo activity, driving electrophysiological and metabolic maturation. | Key component of Protocol B; shown to be a primary driver of mitochondrial development [55]. |
| Metabolic Maturation Medium | A lipid/Fatty Acid-enriched medium with high calcium and hormones; shifts cell metabolism from glycolysis to oxidative phosphorylation. | Base medium in Protocol B; promotes metabolic maturation and adult-like electrophysiology [55]. |
| Hb9::GFP Reporter System | Allows for specific identification and live imaging of motor neurons, facilitating purity analysis and single-cell tracking. | Used in live-cell imaging assays to track motor neuron survival and health over time [1] [53]. |
| Multi-Electrode Array (MEA) Systems | Non-invasively records network-level electrophysiological activity (firing, bursting, synchrony) from cultures. | Essential for functional QC and detecting ALS-related hyperexcitability phenotypes [6]. |
| IncuCyte Neuroburst Reagent | Lentiviral reagent for imaging spontaneous neuronal firing (calcium flux) in live cells over time. | Alternative to MEA for quantifying synchronicity and burst rate in ALS donor cells [6]. |
Signaling Pathways and Molecular Regulation of Maturation
The transition from a fetal to an adult state is governed by a hardwired transcriptional program and modulated by extrinsic signals. Understanding this network is key to rationally engineering maturation protocols.
Diagram: Molecular and behavioral regulation of motor neuron maturation. The hardwired core program is recapitulated in vitro, while the context-dependent program requires in vivo-like cues.
The molecular roadmap of maturation involves a profound shift in transcriptional regulators. In vivo, nascent motor neurons are defined by selector transcription factors like ISL1 and LHX3 [52]. As maturation progresses, the regulatory landscape changes, with motifs for NFI factors, activity-dependent factors (e.g., AP-1), and hormone receptors becoming enriched in maturation-specific enhancers [52]. This explains why extrinsic cues like electrostimulation (activating AP-1) and hormonal supplementation are critical in vitro. A seminal finding is that stem cell-derived motor neurons successfully execute the hardwired, cell-autonomous part of the maturation program (approximately 40%), but fail to activate the extensive context-dependent program that relies on the systemic environment of a living organism [52]. This underscores the necessity of providing complex external cues, as outlined in the protocols above.
Overcoming the maturation hurdle is no longer an insurmountable challenge. By implementing the detailed protocols and validation assays described herein—particularly combinatorial approaches that integrate metabolic, structural, and activity-dependent cues—researchers can robustly generate iPSC-derived motor neurons with more adult-like properties. These advanced models are proving their value, as demonstrated by their ability to mirror clinical trial failures and identify novel therapeutic combinations for sporadic ALS [1]. The continued refinement of these maturation strategies is essential for unlocking the full potential of iPSC technology in ALS disease modeling, mechanistic studies, and the development of effective, patient-specific therapies.
Batch-to-Batch Consistency and Quality Control in Manufacturing
In the field of amyotrophic lateral sclerosis (ALS) research, the transition towards human-induced pluripotent stem cell (iPSC)-derived motor neurons marks a significant advancement for disease modeling and drug discovery. A core challenge in utilizing these models for robust preclinical screening is ensuring batch-to-batch consistency during the manufacturing and differentiation of these cells. The inherent biological variability of patient-derived cells, combined with the complexity of multi-stage differentiation protocols, introduces substantial variability that can obscure disease-relevant phenotypes and compromise drug screening outcomes. Therefore, implementing a rigorous, multi-parametric Quality Control (QC) framework is not merely a procedural step but a foundational requirement for generating reliable and reproducible data. This document outlines detailed application notes and protocols for establishing QC processes to ensure the consistency of iPSC-derived motor neurons, specifically within the context of ALS research.
Establishing a QC Framework for iPSC-Derived Motor Neurons
A comprehensive QC strategy for iPSC-derived motor neurons must extend beyond traditional identity and purity checks to include functional assessment, ensuring that the cells not only look the part but also behave in a manner consistent with motor neuron biology and ALS pathology.
Determining Quality Standards and Critical Quality Attributes (CQAs)
The first step is to define the Critical Quality Attributes (CQAs) that characterize a high-fidelity motor neuron culture. These attributes should be objectively measurable and align with the intended use of the cells in disease modeling.
Key CQAs for ALS Motor Neuron Models:
- Morphology: Presence of extensive neurite networks and large cell bundles.
- Purity and Identity: High percentage of cells expressing motor neuron-specific markers.
- Functional Competence: Exhibiting spontaneous and synchronous electrophysiological activity.
- Disease Phenotype Recapitulation: For ALS lines, displaying expected pathological hallmarks such as hyperexcitability and reduced synchrony.
Selection of QC Methods
A combination of QC methods, adapted from established manufacturing principles, should be employed [57]. A prevention-based approach, akin to Quality Assurance (QA) and Statistical Process Control (SPC), is ideal for standardizing the differentiation process itself [58] [59]. This is complemented by inspection-based methods, akin to Quality Control (QC), which verify the quality of the final cell product [58] [60].
Table 1: Quality Control Methods and Their Application in Cell Manufacturing
| QC Method | Core Principle | Application in iPSC-Derived Motor Neuron Manufacturing |
|---|---|---|
| Total Quality Management (TQM) | Organization-wide culture of quality and continuous improvement [59] [60]. | Empowering all personnel involved in the differentiation process to identify and address sources of variability. |
| Statistical Process Control (SPC) | Data-driven monitoring and control of process variation [59] [60]. | Tracking key differentiation metrics (e.g., cell count, viability) over time to identify and correct process drift. |
| 100% Inspection Method | Thorough examination of all units against standards [60]. | High-content imaging and analysis of every batch for morphological and molecular markers. |
| Lean Manufacturing | Eliminating waste and optimizing processes [59] [60]. | Streamlining the differentiation protocol to reduce unnecessary steps and improve reproducibility. |
Detailed QC Experimental Protocols for iPSC-Derived Motor Neurons
The following protocols provide a multi-parametric approach to batch quality assessment.
Protocol 1: Morphological Characterization via Brightfield Imaging
1.1 Objective: To visually assess the health, neurite outgrowth, and structural network formation of motor neuron cultures, identifying any gross morphological deviations between batches.
1.2 Materials:
- Differentiated motor neuron cultures (e.g., at Day 10 in vitro (DIV10))
- Phase-contrast or brightfield microscope with a digital camera
- Image analysis software (e.g., Sartorius IncuCyte, ImageJ)
1.3 Methodology:
- Plate cells on imaging-compatible plates according to your differentiation protocol.
- On the designated day (e.g., DIV10), capture at least 5-10 non-overlapping, representative brightfield images per well using a 10x or 20x objective.
- Maintain consistent lighting and exposure settings across all batches.
1.4 Data Analysis:
- Qualitatively assess images for expected neuronal morphology, including the presence of large cell bundles, thick cabling (neurites) between bundles, and the absence of excessive cellular debris [6].
- As shown in studies, control lines should display "uniform cultures with large cell bundles and thick cabling," while ALS lines (e.g., C9orf72) may show "smaller irregular cell-body clusters... with thinner cabling" [6].
- Quantitative analysis can be performed using software to measure parameters like neurite length and branching points.
Protocol 2: Molecular Identity and Purity via Immunocytochemistry (ICC)
2.1 Objective: To quantitatively determine the proportion of cells that have successfully differentiated into motor neurons and to characterize the cellular composition of the culture.
2.2 Materials:
- Differentiated motor neuron cultures fixed with 4% paraformaldehyde
- Permeabilization and blocking buffer
- Primary antibodies: Anti-TUJ1 (neuron-specific class III β-tubulin), Anti-ISL1 (motor neuron marker), Anti-S100B (astrocyte-like cell marker)
- Fluorescently-labeled secondary antibodies
- Nuclear stain (e.g., DAPI)
- High-content imager or fluorescent microscope
2.3 Methodology:
- Fix, permeabilize, and block cells according to standard ICC protocols.
- Incubate with primary antibodies overnight at 4°C, followed by appropriate secondary antibodies.
- Image multiple fields per well to ensure statistical power.
2.4 Data Analysis:
- Quantify the percentage of DAPI-positive cells that are positive for TUJ1 (general neurons) and ISL1 (motor neurons). High-quality differentiations should yield >90% TUJ1+ and >90% ISL1+ of the neuronal population [1].
- Quantify the percentage of S100B+ cells to monitor the presence of astrocyte-like cells, which can be a source of variability [23].
- Document batch-to-batch variability in the percentage of ISL1+ cells, which has been shown to be a significant variable, particularly influenced by donor sex in ALS lines [23].
Table 2: Key Markers for QC of iPSC-Derived Motor Neurons
| Marker | Cell Type | Expected Result (QC Pass) | Significance in ALS Models |
|---|---|---|---|
| TUJ1 (TUBB3) | Neurons | >90% of cells [1] | Confirms successful neuronal differentiation. |
| ISL1 / HB9 (MNX1) | Spinal Motor Neurons | >90% of TUJ1+ cells [1] | Verifies correct ventral spinal identity. |
| S100B | Astrocyte-like cells | Low percentage (e.g., <5%) [23] | A high percentage is a confounder for cell-autonomous studies. |
| GFAP | Astrocytes | Very low/absent [1] | Confirms minimal astrocyte contamination. |
Protocol 3: Functional Characterization via Electrophysiology and Activity Assays
3.1 Objective: To validate that the motor neurons are not only morphologically and molecularly correct but also functionally mature and capable of firing action potentials, a key requirement for modeling ALS hyperexcitability.
3.2 Materials:
- Differentiated motor neuron cultures plated on MEA plates or suitable dishes for calcium imaging
- Multi-Electrode Array (MEA) system (e.g., Axion Biosystems Maestro Pro) or fluorescent imaging platform (e.g., Sartorius IncuCyte S3)
- IncuCyte Neuroburst Orange lentiviral reagent or other calcium-sensitive dyes
3.3 Methodology:
- For MEA: Plate cells directly on MEA plates and record electrical activity at multiple time points (e.g., DIV30-DIV40). Record for at least 10 minutes per well.
- For Spontaneous Neuronal Activity (SNA) imaging: Transduce cells with IncuCyte Neuroburst Orange reagent and record activity using the IncuCyte live-cell analysis system.
3.4 Data Analysis:
- Key Metrics: Mean firing rate, number of bursts, burst duration, synchrony index, and spike amplitude [6].
- QC Pass Criteria: Control motor neurons should demonstrate synchronized firing, characterized by a higher mean burst duration and lower burst rate [6].
- ALS Phenotype Check: ALS motor neurons should display a reproducible functional phenotype, such as "less synchronized firing and different degrees of hyperexcitability" [6], including an increased burst rate.
Table 3: Quantitative Functional Parameters for Motor Neuron QC
| Functional Parameter | Unaffected / Control Motor Neurons | ALS Motor Neurons (e.g., C9orf72, TDP43) |
|---|---|---|
| Mean Firing Rate | Consistent, moderate rate | Often increased (hyperexcitability) [6] |
| Burst Rate | Lower | Increased [6] |
| Synchrony Index | Higher, synchronized firing | Reproducible loss of synchronous firing [6] |
| Burst Duration | Longer bursts | Shorter, more frequent bursts |
The Scientist's Toolkit: Research Reagent Solutions
A list of essential materials and their functions for the QC of iPSC-derived motor neurons is provided below.
Table 4: Essential Research Reagents for Motor Neuron QC
| Item Name | Function in QC Process | Example Application |
|---|---|---|
| Anti-TUJ1 Antibody | Labels neuronal microtubules to confirm neuronal identity and purity. | Immunocytochemistry to quantify % neurons. |
| Anti-ISL1 Antibody | Labels spinal motor neuron nuclei to confirm specific subtype differentiation. | Immunocytochemistry to quantify % motor neurons. |
| Anti-S100B Antibody | Labels astrocyte-like cells to monitor culture composition and variability. | Identifying a key source of transcriptional variance [23]. |
| IncuCyte Neuroburst Orange | Lentiviral reagent for non-invasive, live-cell imaging of spontaneous neuronal firing. | Measuring synchronicity and burst rate in live cultures [6]. |
| Multi-Electrode Array (MEA) Plate | Provides a substrate for recording extracellular electrical activity from neuronal networks. | Directly measuring firing parameters and network synchrony. |
| HB9::GFP Reporter | Motor neuron-specific live-cell reporter for isolating or monitoring motor neurons. | Longitudinal tracking of motor neuron health and survival [1]. |
Data Analysis and Batch Acceptance Criteria
Collecting data is only the first step; establishing clear, data-driven acceptance criteria is essential for releasing consistent batches.
- Data Collection and SPC: Implement a system for collecting all QC data (morphological, molecular, functional) in a centralized database. Use control charts to monitor each CQA over time, setting upper and lower control limits to visually identify when the differentiation process is going out of specification [59].
- Root Cause Analysis: When a batch fails QC, employ techniques like the "5 Whys" to determine the underlying cause, whether it's a reagent lot change, technician error, or equipment malfunction [57].
- Batch Acceptance/Rejection: A batch should be accepted only when it meets all pre-defined criteria across all assays. For example, a batch might be rejected if the ISL1+ percentage falls outside the control limits, even if the morphology appears normal, as this molecular composition significantly impacts transcriptomic data [23].
Workflow and Pathway Diagrams
The following diagrams summarize the overall QC workflow and the logical relationship between QC findings and their interpretation.
QC Workflow for Motor Neuron Batches
Interpreting QC Findings in ALS Research
Amyotrophic lateral sclerosis (ALS) is no longer considered purely a motor neuron disorder but rather a complex multisystem disease where non-neuronal cells play crucial roles in disease pathogenesis and progression. The non-cell-autonomous hypothesis posits that the degeneration of motor neurons in ALS results from dysfunctional interactions between multiple cell types within the motor neuron microenvironment. While motor neurons derived from induced pluripotent stem cells (iPSCs) provide valuable insights into cell-autonomous mechanisms, they fail to fully recapitulate the complex cellular interactions that occur in vivo. The development of co-culture systems incorporating glial cells and other non-neuronal elements has revealed that these cells actively contribute to motor neuron vulnerability and degeneration through multiple pathways, including neuroinflammation, excitotoxicity, and impaired trophic support [61] [2].
Evidence from both sporadic and familial ALS models demonstrates that non-neuronal cells undergo significant pathological changes that actively influence disease progression. Microglia, the resident immune cells of the central nervous system (CNS), exhibit dual roles in ALS pathogenesis, shifting from a neuroprotective phenotype in early disease stages to a neurotoxic phenotype as disease progresses [61]. Similarly, astrocytes show impaired glutamate clearance capabilities and release toxic factors that contribute to motor neuron degeneration. Oligodendrocytes, which provide critical metabolic support to axons, also display dysfunction in ALS models, with abnormalities observed even prior to symptom onset in rodent models [61]. The integration of these non-neuronal cells into ALS models is therefore essential for accurate disease modeling and therapeutic screening.
Quantitative Analysis of Non-Neuronal Cell Contributions
Table 1: Immune and Glial Cell Alterations in ALS Pathogenesis
| Cell Type | Pathogenic Changes | Protective Functions | Key Mediators |
|---|---|---|---|
| Microglia | M1 phenotype: Increased ROS, Cox-2, pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) [61] | M2 phenotype: Anti-inflammatory factors (IL-4, IL-10), growth factors [61] | TLRs, HMGB1, NLRP3 inflammasome [61] |
| Astrocytes | Loss of EAAT2, glutamate excitotoxicity, release of toxic factors [61] | Glutamate uptake, growth factor secretion (BDNF, GDNF) [61] | FGF-1, S100β, inflammatory markers [61] |
| Oligodendrocytes | Myelin abnormalities, NG2+ cell deficiency, impaired metabolic support [61] | Axonal integrity maintenance, energy substrate provision | Mutant SOD1, TDP-43, FUS aggregates [61] |
| Peripheral Immune Cells | Infiltration of macrophages, T cell dysregulation, autoantibodies [61] | Regulatory T cells, anti-inflammatory cytokines | CD4+ T cells, CD8+ T cells, autoantibodies [61] |
Table 2: Efficacy of ALS Therapies in iPSC-Derived Co-culture Models
| Therapeutic Intervention | Molecular Target | Reported Efficacy in Models | Effect on Motor Neuron Survival |
|---|---|---|---|
| Riluzole | Glutamate signaling | Rescue of survival and transcriptomic abnormalities [1] | Significant improvement across SALS donors [1] |
| Memantine | NMDA receptors | Reduction of excitotoxicity | Effective in combination therapy [1] |
| Baricitinib | JAK-STAT pathway | Modulation of neuroinflammation | Effective in combination therapy [1] |
| Ropinirole (ROPI) | D2 dopamine receptors | Protection against oxidative stress [2] | Effective in 9/22 sALS models; not in SOD1 models [2] |
Experimental Protocols for ALS Co-culture Systems
Protocol 1: Generation of iPSC-Derived Motor Neurons
Principle: This protocol outlines the differentiation of human iPSCs into highly enriched spinal motor neuron cultures using a modified five-stage methodology adapted from established motor neuron differentiation protocols [1].
Materials:
- Human iPSCs from ALS patients and healthy controls
- Matrigel-coated culture plates
- Neural induction medium
- Motor neuron differentiation supplements (retinoic acid, sonic hedgehog agonist)
- Motor neuron maturation medium
- Immunocytochemistry reagents
Procedure:
- Maintenance of iPSCs: Culture human iPSCs on Matrigel-coated plates in essential 8 medium until 70-80% confluent.
- Neural Induction: Dissociate iPSCs and transfer to low-attachment plates in neural induction medium to form embryoid bodies for 5 days.
- Patterning: Transfer embryoid bodies to poly-ornithine/laminin-coated plates and pattern toward caudal neural fate using 1µM retinoic acid and 1µM purmorphamine (Shh agonist) for 7 days.
- Motor Neuron Progenitor Expansion: Dissociate patterned neural progenitors and plate at 50,000 cells/cm² in motor neuron proliferation medium containing brain-derived neurotrophic factor (BDNF), glial cell-derived neurotrophic factor (GDNF), and insulin-like growth factor 1 (IGF-1).
- Terminal Differentiation: After 7 days, switch to motor neuron maturation medium containing cAMP and continue culture for additional 14-21 days.
- Quality Control: Validate motor neuron identity by immunocytochemistry for HB9 (92.44 ± 1.66% purity), ChAT, and Tuj1 [1].
Validation: Cultures should contain >92% motor neurons (HB9+/ChAT+), with minimal contamination by astrocytes (<0.12% GFAP+) and microglia (<0.04% CD11B+) [1].
Protocol 2: Establishment of Motor Neuron-Glia Co-culture Systems
Principle: This protocol describes the integration of iPSC-derived microglia and astrocytes with motor neurons to model non-cell-autonomous pathology in ALS.
Materials:
- iPSC-derived motor neurons (from Protocol 1)
- iPSC-derived microglia precursors
- iPSC-derived astrocyte precursors
- Co-culture medium
- Transwell inserts (for non-contact co-culture)
Procedure:
- Generation of Glial Cells: Differentiate iPSCs into microglia and astrocytes using established protocols [2].
- Direct Co-culture System:
- Plate motor neurons at desired density and allow to adhere for 24 hours
- Add microglia and astrocytes at defined ratios (recommended starting ratio: 60:20:20 motor neurons:astrocytes:microglia)
- Maintain in co-culture medium with half-medium changes every 48 hours
- Indirect Co-culture System:
- Plate motor neurons in main chamber of transwell system
- Plate glial cells in transwell inserts with permeable membrane (0.4µm pores)
- Culture for desired duration to study paracrine effects
- Conditioned Media Studies:
- Collect conditioned media from ALS and control glial cultures
- Apply to motor neurons to assess soluble factor-mediated effects
- Phenotypic Assessment: Monitor motor neuron survival, neurite degeneration, and inflammatory markers over 2-4 weeks.
Technical Notes: The use of isogenic lines (all cell types derived from same patient iPSCs) controls for genetic background effects. For studies of specific cell contributions, consider using iPSCs from different genotypes in cross-over experiments.
Signaling Pathways in Non-Cell-Autonomous Pathology
Cellular Signaling in ALS Non-Cell-Autonomous Pathology
The diagram illustrates the key signaling pathways through which non-neuronal cells contribute to motor neuron pathology in ALS. Microglia activation occurs through pattern recognition receptors (TLRs, RAGE) that respond to damage-associated molecular patterns (DAMPs) such as HMGB1 and pathogen-associated molecular patterns (PAMPs), as well as direct activation by mutant proteins including SOD1 and TDP-43 [61]. Activated microglia polarize toward either M1 (pro-inflammatory) or M2 (anti-inflammatory) phenotypes. M1 microglia release pro-inflammatory cytokines (IL-1β, IL-6, TNF-α), reactive oxygen species (ROS), and Cox-2, which collectively contribute to motor neuron damage. In contrast, M2 microglia secrete anti-inflammatory factors (IL-4, IL-10) and growth factors that support neuronal survival pathways [61].
Simultaneously, astrocyte activation leads to pathological changes including downregulation of excitatory amino acid transporter 2 (EAAT2), resulting in impaired glutamate clearance and subsequent excitotoxicity. Activated astrocytes also release toxic factors that directly damage motor neurons. These parallel pathways from microglia and astrocytes converge to cause motor neuron damage, while protective pathways from M2 microglia promote neuronal survival. The balance between these pathogenic and protective signals determines the overall trajectory of motor neuron degeneration in ALS.
Experimental Workflow for Co-culture Studies
Workflow for ALS Co-culture Model Development
The experimental workflow begins with iPSC generation from patient somatic cells (typically fibroblasts or peripheral blood mononuclear cells) using non-integrating episomal vectors to ensure genomic integrity [1]. Following rigorous quality control assessment of pluripotency and genomic stability, iPSCs undergo parallel differentiation into motor neurons and glial cells (astrocytes and microglia) using optimized protocols that generate highly pure populations. Motor neuron cultures should achieve >92% purity (HB9+/ChAT+), while glial cultures are characterized using cell-specific markers [1] [2].
The established cell populations are then combined in co-culture systems at defined ratios, with common configurations including direct contact co-cultures and transwell-based indirect co-culture systems that allow separation of cell types while permitting soluble factor exchange. Following quality assessment of the established co-cultures, the system proceeds to phenotypic screening where key disease-relevant phenotypes are quantified, including motor neuron survival, neurite degeneration, inflammatory marker expression, and electrophysiological properties [1]. The validated model then advances to therapeutic testing of candidate compounds, with promising hits undergoing further validation through transcriptomic and proteomic analyses. This comprehensive workflow enables the assessment of both cell-autonomous and non-cell-autonomous disease mechanisms and provides a platform for evaluating potential therapeutics that target glial-mediated pathogenic pathways.
Research Reagent Solutions
Table 3: Essential Research Reagents for ALS Co-culture Studies
| Reagent Category | Specific Examples | Function/Application | Key References |
|---|---|---|---|
| iPSC Reprogramming | Non-integrating episomal vectors, Sendai virus vectors | Generation of integration-free iPSCs from patient somatic cells | [1] |
| Motor Neuron Differentiation | Retinoic acid, Purmorphamine (Shh agonist), BDNF, GDNF, IGF-1 | Pattern neural progenitors to caudal fate and promote motor neuron specification | [1] |
| Glial Differentiation | IL-34, M-CSF, GM-CSF (microglia); CNTF, BMPs (astrocytes) | Direct differentiation of iPSCs to microglia and astrocyte lineages | [2] |
| Cell Type Markers | Anti-HB9, Anti-ChAT (motor neurons); Anti-Iba1, Anti-GFAP (glia) | Validation of cellular identity and purity in cultures | [1] |
| Cytokine/Analyte Detection | ELISA kits for IL-1β, IL-6, TNF-α; Neurofilament light chain assays | Quantification of inflammatory mediators and neuronal damage markers | [61] |
| Live-Cell Imaging Reporters | HB9-turbo fluorescent protein constructs, Calcium indicators | Longitudinal monitoring of motor neuron health and function | [1] |
Applications in Drug Discovery and Therapeutic Screening
The implementation of co-culture systems for ALS modeling has significant implications for drug discovery and development. Traditional monoculture systems have demonstrated poor predictive value for clinical outcomes, with over 97% of drugs showing efficacy in familial ALS models failing in clinical trials [1]. Co-culture systems that incorporate non-cell-autonomous mechanisms offer improved pathological relevance and potentially better predictive validity.
Recent studies utilizing patient-derived co-culture systems have identified promising therapeutic combinations that target multiple aspects of ALS pathology. The combination of riluzole, memantine, and baricitinib has demonstrated significant improvements in motor neuron survival across sporadic ALS donors, representing one of the first therapeutic strategies validated across heterogeneous SALS patient populations [1]. This combinatorial approach targets both neuronal excitotoxicity (riluzole, memantine) and neuroinflammation (baricitinib), addressing multiple pathological mechanisms simultaneously.
Similarly, high-throughput screening using iPSC-derived motor neurons from 32 SALS patients identified ropinirole hydrochloride as a promising candidate that protected against mitochondrial dysfunction and oxidative stress in a subset of SALS models [2]. Importantly, the response to ropinirole was heterogeneous across SALS donors, with protection observed in approximately 40% of patient-derived lines. This finding highlights the value of patient-specific models for identifying subgroups that may respond to specific therapeutic approaches and supports the movement toward personalized medicine strategies for ALS.
The integration of co-culture systems with advanced screening technologies, including automated live-cell imaging and multi-omics approaches, provides a powerful platform for evaluating drug efficacy across the spectrum of ALS heterogeneity. These systems enable not only the assessment of motor neuron survival but also the evaluation of effects on glial cell function, neuroinflammation, and other non-cell-autonomous processes, offering a more comprehensive evaluation of therapeutic candidates before advancement to clinical trials.
Leveraging 3D Cultures and Organoids for Enhanced Physiological Complexity
The study of Amyotrophic Lateral Sclerosis (ALS) has been fundamentally transformed by induced pluripotent stem cell (iPSC) technology, which enables the generation of patient-specific motor neurons for disease modeling. However, traditional two-dimensional (2D) monocultures lack the physiological complexity to fully recapitulate the in vivo environment. The emergence of three-dimensional (3D) cultures and organoids represents a paradigm shift, offering enhanced physiological relevance through improved cell-to-cell interactions, maturation, and spatial organization. These advanced models are particularly crucial for ALS, a condition where multiple cell types contribute to motor neuron degeneration and where sporadic cases (comprising 85-90% of all ALS) have been exceptionally difficult to model [2] [62]. This protocol outlines standardized methods for generating and characterizing 3D motor neuron models that more accurately mimic the pathological landscape of ALS, thereby providing more translational platforms for therapeutic discovery.
Quantitative Validation of 3D Models in ALS Research
The transition to 3D modeling is supported by empirical data demonstrating their advantages over conventional 2D systems for ALS research. The table below summarizes key comparative findings:
Table 1: Quantitative Advantages of 3D Models in ALS Research
| Parameter | 2D Monoculture Findings | 3D Model Findings | Implication for ALS Research |
|---|---|---|---|
| Motor Neuron Survival | Limited survival deficits demonstrated in SALS models [1] | Enhanced maturation and long-term culture (>28 days) support phenotype development [63] | Enables study of later-stage disease mechanisms |
| Cellular Complexity | Primarily motor neurons (92.44% purity reported) [1] | Presence of interneurons and oligodendrocyte progenitors [63] | Captures non-cell-autonomous disease mechanisms |
| Functional Activity | Technical challenges due to random cell clustering [63] | Demonstrated action potentials and burst patterns via MEA [63] | Facilitates electrophysiological screening of compounds |
| Transcriptomic Fidelity | Variable correlation with post-mortem human spinal cord [1] | Improved maturation trajectories reflecting primary tissue [64] | Enhances molecular relevance of disease modeling |
Protocol 1: Generation of Motor Neuron Spheroids
Background and Principles
Motor neuron spheroids represent a scaffold-free 3D model system that bridges the gap between simple 2D cultures and complex organoids. These structures self-assemble from motor neuron progenitor cells (MNPCs), forming organized clusters that enhance maturation and facilitate long-term culture—a critical requirement for modeling chronic neurodegenerative processes in ALS [63]. Compared to matrix-dependent organoids, spheroids offer advantages of reduced technical variability, minimal necrosis due to smaller size, and cost-effectiveness for higher-throughput applications [63].
Materials and Equipment
Table 2: Essential Reagents and Equipment for Spheroid Generation
| Category | Specific Item | Function/Application |
|---|---|---|
| Starting Cells | iPSC-derived Motor Neuron Progenitor Cells (MNPCs) [63] | Foundation for spheroid formation and differentiation |
| Culture Vessels | Low-attachment U-bottom plates [63] | Promotes spontaneous cell aggregation and spheroid formation |
| Culture Medium | Motor neuron differentiation medium [63] | Supports maturation and maintenance of motor neurons |
| Analysis Tools | Tissue-clearing reagents (e.g., CUBIC) [63] | Enables 3D imaging and immunostaining of whole spheroids |
| Functional Assay | Microelectrode Array (MEA) system [63] | Records electrophysiological activity and network function |
Step-by-Step Procedure
- MNPC Preparation: Generate MNPCs from validated iPSC lines using established monolayer differentiation protocols [63]. Ensure MNPCs are at 70-80% confluence and in optimal health prior to spheroid formation.
- Cell Dissociation: Gently dissociate MNPC cultures using Accutase or similar enzymatic solution to create a single-cell suspension. Avoid vigorous pipetting to maintain cell viability.
- Cell Seeding for Spheroid Formation: Resuspend cells in motor neuron differentiation medium and seed into low-attachment U-bottom plates at a density of 5,000-10,000 cells per well [63]. Centrifuge plates at 100 x g for 2 minutes to encourage aggregate formation at the bottom of wells.
- Spheroid Maintenance: Culture spheroids at 37°C with 5% CO2. Perform 50% medium changes every 2-3 days, carefully removing spent medium without disturbing the settled spheroids.
- Long-Term Culture: Maintain spheroids for up to 28 days or longer, with periodic monitoring of size and morphology. Spheroids typically reach a stable size of 200-500 μm in diameter within 7-10 days [63].
- Quality Control: Regularly inspect spheroids under a bright-field microscope. Discard any cultures showing signs of disintegration or excessive size variation.
Technical Notes and Troubleshooting
- Optimizing Size: If spheroids are too large (>500 μm), which can lead to necrotic cores, reduce the initial seeding density.
- Preventing Clumping: If multiple spheroids form and fuse in a single well, increase the volume of medium or use plates with ultra-low attachment coating.
- Handling Precision: Always use wide-bore pipette tips when transferring spheroids to prevent structural damage and cell loss.
Protocol 2: Characterization of 3D Motor Neuron Models
Morphological Analysis
- Size and Shape Profiling: Acquire bright-field images of spheroids using an inverted microscope. Use image analysis software (e.g., ImageJ) to measure cross-sectional area, diameter, and circularity. Establish baseline parameters for quality control.
- Tissue Clearing and 3D Immunostaining:
- Fix spheroids with 4% paraformaldehyde for 30 minutes at room temperature.
- Permeabilize with 0.5% Triton X-100 for 1 hour.
- Apply primary antibodies (e.g., anti-HB9, anti-ISL1, anti-Tuj1, anti-ChAT) diluted in PBS with 1% BSA and 0.1% Tween-20 for 48 hours at 4°C with gentle agitation [63].
- Wash thoroughly and apply secondary antibodies for 24-48 hours at 4°C.
- Implement tissue-clearing using CUBIC or similar protocol to reduce light scattering [63].
- Image using confocal or light-sheet microscopy to visualize internal structure and protein localization in three dimensions.
Gene Expression Analysis
- RNA Extraction: Collect 10-15 spheroids per condition and extract total RNA using a commercial kit with a homogenization step to ensure complete lysis.
- qPCR Profiling: Perform quantitative PCR using primers for motor neuron markers (HB9, ISL1, ChAT), pan-neuronal markers (Tuj1), and glial markers (GFAP, OLIG2) to comprehensively characterize cellular composition [63].
Functional Characterization with Microelectrode Arrays (MEA)
- Spheroid Transfer: Carefully transfer individual mature spheroids (day 28+) to MEA chips coated with a thin layer of laminin or Matrigel to enhance attachment.
- Acclimation: Allow spheroids to adhere for 24-48 hours in culture medium before recording.
- Recording Parameters: Set up recordings in a temperature-controlled (37°C) environment with 5% CO2. Record spontaneous activity for at least 10 minutes per sample at a sampling rate of 10-50 kHz.
- Data Analysis: Analyze recordings for key parameters including mean firing rate, burst frequency, network synchronization, and interspike intervals to assess functional maturity and network integrity [63].
Integrating 3D Models into ALS Drug Discovery Pipelines
The application of 3D models in screening paradigms requires adaptation of traditional approaches. The workflow below outlines this integrated process:
Implementing Phenotypic Screening in 3D
Large-scale drug screening using 3D ALS models has demonstrated superior predictive validity. A recent study screening over 100 drugs previously tested in ALS clinical trials found that 97% failed to mitigate neurodegeneration in patient-derived 3D models, accurately reflecting clinical trial outcomes [1]. This high concordance underscores the value of 3D systems for de-risking drug development.
For screening campaigns:
- Standardize spheroid size and age at treatment initiation to minimize variability.
- Implement automated imaging systems for high-content analysis of motor neuron survival and neurite integrity.
- Include isogenic controls (CRISPR-corrected lines from the same patient) when available to confirm on-target effects [63].
- Assess combinatorial therapies, as 3D models have identified promising synergistic drug combinations (e.g., baricitinib, memantine, and riluzole) that may address the multifactorial pathology of ALS [1].
The adoption of 3D cultures and organoids represents a critical evolution in ALS modeling, providing unprecedented physiological complexity for investigating disease mechanisms and evaluating therapeutic candidates. The protocols outlined here for generating and characterizing motor neuron spheroids offer researchers a robust framework to implement these advanced models, bridging the translational gap between traditional in vitro systems and clinical reality. As these technologies continue to mature, their integration with multi-omics approaches and microfluidic systems will further enhance their predictive power, accelerating the development of effective treatments for this devastating disease.
Benchmarking Success: Validating Phenotypes and Comparative Analysis with Animal Models and Human Tissue
Within the field of amyotrophic lateral sclerosis (ALS) research, establishing the face validity of in vitro models—how well they recapitulate observable clinical features of the disease—is a critical first step toward ensuring their translational relevance. For models based on induced pluripotent stem cell (iPSC)-derived motor neurons (MNs), the most compelling evidence of face validity is a direct correlation between in vitro phenotypic measurements and the original donor's clinical outcomes [1]. This protocol details the methods for establishing such correlations, a process central to validating iPSC-based models for sporadic ALS (SALS), which constitutes 85-90% of all cases and lacks known monogenic causes [2]. The following sections provide a comprehensive guide for generating a clinically annotated iPSC library, conducting longitudinal phenotypic screening of patient-derived MNs, and performing statistical analyses to link cellular phenotypes with donor disease progression and survival.
Key Research Reagent Solutions
The following reagents and tools are essential for implementing the protocols described in this application note.
Table 1: Essential Research Reagents and Materials
| Item | Function/Description | Application in Protocol |
|---|---|---|
| Human iPSC Library | A curated collection of iPSC lines from 100+ SALS patients and healthy controls; requires rigorous quality control for genomic integrity and pluripotency [1]. | Serves as the foundational patient-specific material for motor neuron differentiation. |
| Non-integrating Episomal Vectors | Used for reprogramming somatic cells (e.g., skin fibroblasts) to iPSCs, minimizing genomic alterations [1]. | Generation of footprint-free iPSC lines from donor biopsies. |
| Motor Neuron Differentiation Kit | A standardized set of factors for the efficient differentiation of iPSCs into spinal motor neurons. | Production of high-purity, mature motor neuron cultures. |
| HB9-turboGFP Reporter | A virally delivered, motor neuron-specific reporter that labels live MNs for tracking [1]. | Enables longitudinal live-cell imaging of motor neuron health and survival. |
| Longitudinal Live-Cell Imaging System | An automated microscopy system for continuous, non-invasive monitoring of cell cultures. | Quantification of motor neuron survival and neurite degeneration over time. |
| Multi-Electrode Array (MEA) Platform | A system for recording extracellular electrical activity from neuronal networks [6]. | Functional assessment of motor neuron hyperexcitability and network synchronicity. |
Protocol: Establishing Face Validity in SALS iPSC-Derived Motor Neurons
Stage 1: Generation of a Clinically Annotated iPSC Library
- Donor Recruitment and Clinical Annotation: Recruit a cohort of patients with Sporadic ALS (SALS) and age-matched healthy controls. For each donor, collect comprehensive clinical data, which must include:
- Site of disease onset (bulbar or limb)
- Age at onset
- Disease progression rate (e.g., decline in ALSFRS-R score per month)
- Survival time from symptom onset [1]
- Cell Reprogramming: Isolate fibroblasts from skin punch biopsies of consented donors. Reproblem the fibroblasts into induced pluripotent stem cells (iPSCs) using non-integrating episomal vectors to ensure a footprint-free reprogramming process [1].
- Quality Control (QC): Subject all established iPSC lines to rigorous QC. This includes:
- Pluripotency Validation: Confirm expression of key pluripotency markers.
- Trilineage Differentiation Potential: Verify the ability to differentiate into all three germ layers.
- Genomic Integrity: Perform karyotyping and whole-genome sequencing to identify any pathogenic variants and confirm the absence of familial ALS mutations, thereby classifying lines as SALS [1].
Stage 2: Motor Neuron Differentiation & Phenotypic Screening
Motor Neuron Differentiation: Differentiate iPSCs into spinal motor neurons using a standardized, five-stage protocol optimized for high yield and maturity [1]. The workflow for the entire screening process is summarized in the diagram below.
Diagram Title: Workflow for Validating iPSC Models
Phenotypic Screening via Live-Cell Imaging:
- Culture Preparation: Plate mature motor neurons and transduce with an HB9-turboGFP reporter to specifically label motor neurons.
- Image Acquisition: Use an automated live-cell imaging system to capture high-resolution images of the cultures daily for a period of 2-4 weeks.
- Quantitative Analysis: Analyze the acquired images using stringent quantification criteria to extract key parameters of neurodegeneration:
- Motor Neuron Survival: The number of GFP-positive MNs over time.
- Neurite Degeneration: The total neurite length per field or the number of fragmented neurites [1].
- Functional Characterization (Optional): To complement survival data, perform functional assays such as Multi-Electrode Array (MEA) analysis to measure network-level hyperexcitability, a known pathological trait in ALS [6].
Stage 3: Data Integration and Statistical Correlation
Data Compilation: Compile all quantitative in vitro data and corresponding donor clinical data into a structured table for analysis.
Table 2: Correlation between In Vitro Phenotypes and Donor Clinical Outcomes
iPSC Line (Donor ID) In Vitro MN Survival (Day 14) In Vitro Neurite Degeneration Rate Donor Age at Onset Donor Disease Progression Rate (ALSFRS-R decline/month) Donor Survival (Months) Ctrl-1 95% Low N/A N/A N/A SALS-021 45% High 58 -1.2 38 SALS-078 65% Medium 42 -0.8 52 SALS-101 30% Very High 67 -1.5 24 SALS-045 75% Low 48 -0.5 68 Statistical Analysis: Perform statistical correlation analyses (e.g., Pearson or Spearman correlation) to test for significant relationships between in vitro phenotypes and clinical outcomes. Key analyses include:
- Correlating the rate of in vitro neurite degeneration with donor survival time.
- Correlating the final motor neuron survival percentage with the donor's disease progression rate [1].
- Interpretation: A statistically significant inverse correlation between, for example, in vitro motor neuron survival and donor disease progression rate provides strong evidence for the face validity of the model. This indicates that the accelerated degeneration observed in the dish mirrors the aggressive disease course experienced by the patient.
Discussion
The protocol outlined above provides a robust framework for demonstrating that iPSC-derived motor neurons from SALS patients are not merely cellular artifacts but models with strong face validity. The key strength of this approach is its ability to directly link a quantifiable cellular phenotype—accelerated motor neuron death and neurite degeneration—to the ultimate clinical outcome of the individual from whom the cells were derived [1]. This correlation is the cornerstone for using these models in downstream applications, including elucidation of disease mechanisms and high-throughput drug screening.
Successful implementation of this protocol, as demonstrated in a large-scale study, shows that less than 5% of drugs that failed in clinical trials showed efficacy in this SALS model, highlighting its predictive validity [1]. Furthermore, the model's ability to identify a potential combinatorial therapy (riluzole, memantine, and baricitinib) underscores its utility in discovering new treatment strategies for a heterogeneous patient population. By ensuring that in vitro models faithfully reflect the clinical reality of ALS, researchers can significantly de-risk the drug discovery pipeline and accelerate the development of effective therapies.
Transcriptomic Benchmarking Against Post-Mortem Human Spinal Cord Tissue
Induced pluripotent stem cell-derived motor neurons (iPSC-MNs) have emerged as a transformative model for studying amyotrophic lateral sclerosis (ALS), offering access to living human motor neurons that are otherwise impossible to sample in patients [1]. However, a critical question remains: how faithfully do these in vitro models recapitulate the molecular pathology of the human disease in vivo? Transcriptomic benchmarking against post-mortem human spinal cord tissue provides an essential validation framework, ensuring that iPSC-MNs capture biologically relevant disease mechanisms for meaningful therapeutic development [65]. This protocol details comprehensive methodologies for comparing transcriptional profiles between iPSC-MN models and post-mortem ALS tissue, enabling researchers to quantify the physiological relevance of their cellular models.
Background and Significance
ALS is characterized by progressive motor neuron degeneration, with TDP-43 proteinopathy observed in 97% of cases [66]. While iPSC-MNs can model both familial and sporadic ALS, their validation requires demonstration that they recapitulate key transcriptional networks observed in patient tissues. Large-scale integrated analyses have revealed that iPSC-MNs from familial ALS patients capture approximately one-third of the transcriptional dysregulation observed in laser-captured motor neurons from sporadic ALS post-mortem spinal cords [65]. This conservation of disease signatures across in vitro and in vivo contexts provides a strong foundation for using iPSC-MNs to study ALS mechanisms and screen therapeutics.
Recent studies analyzing 429 iPSC-MNs from 15 datasets alongside 271 post-mortem spinal cord samples have identified robust upregulation of p53 signaling and DNA damage response pathways in ALS across both systems [66]. These conserved pathways represent core disease mechanisms that can be targeted therapeutically and serve as benchmarks for model validation.
Experimental Design and Workflows
Study Design Considerations
Cohort Sizing and Powering: For iPSC-MN studies, include a minimum of 20-30 donor lines per group (ALS vs. control) to account for biological variability [1]. For post-mortem validation, leverage publicly available datasets from consortia like Answer ALS [67] and the New York Genome Center ALS Consortium [68] [69], which provide substantial statistical power through meta-analysis approaches.
Batch Effect Mitigation: Technical variability between iPSC-MN differentiations and sequencing batches represents a major confounding factor. Implement balanced experimental designs that distribute samples from different experimental groups across differentiation batches and sequencing runs [66]. Include reference RNA samples or external controls to monitor technical variability.
Temporal Matching: iPSC-MNs typically represent early disease stages, while post-mortem tissue represents end-stage pathology. Compare iPSC-MNs at multiple maturation timepoints (e.g., 30-42 days in vitro) to identify when disease signatures emerge [66].
Integrated Analysis Workflow
The diagram below illustrates the core computational workflow for transcriptomic benchmarking:
Key Methodological Protocols
iPSC-MN Differentiation and Transcriptomic Profiling
Motor Neuron Differentiation Protocol:
- Base Protocol: Adapt a five-stage spinal motor neuron differentiation protocol from established methods [1]
- Induction: Use dual-SMAD inhibition with LDN193189 (100nM) and SB431542 (10μM) for neural induction days 0-5
- Patterning: Add retinoic acid (100nM) and purmorphamine (1μM) days 5-12 for caudal and motor neuron patterning
- Maturation: Culture for 30-42 days in neurotrophic factors (BDNF, GDNF, CNTF at 10ng/mL each) [66]
- Quality Control: Verify >90% purity by immunostaining for HB9/MNX1, ChAT, and TUJ1 [1]
RNA Sequencing:
- Library Preparation: Use poly-A selection for mRNA enrichment; avoid Ribo-Zero protocols which create batch effects [66]
- Sequencing Depth: Target 30-50 million reads per sample with 150bp paired-end sequencing
- Replication: Include at least 3 technical replicates per donor line
Post-Mortem Tissue Processing and Analysis
Tissue Selection and Quality Control:
- Regions: Prioritize lumbar and cervical spinal cord regions showing maximal motor neuron vulnerability [69]
- Quality Metrics: Require RNA Integrity Number (RIN) >7.0 for optimal transcriptome preservation [68]
- Covariate Adjustment: Account for post-mortem interval, age, sex, and RIN in statistical models [69]
Cell Type Deconvolution:
- Method Selection: For spatial transcriptomics, use CARD, Cell2location, or Tangram which show superior performance in benchmarking studies [70]
- Reference Atlas: Build scRNA-seq reference from matched tissue using 10-15 major CNS cell types
- Validation: Verify deconvolution accuracy with known cell-type marker genes [68]
Computational Analysis Pipeline
Differential Expression Analysis:
- Software: Use DESeq2 or limma-voom with robust normalization methods
- Covariates: Include dataset batch, sex, and relevant technical factors in design matrix [66]
- Thresholds: Apply false discovery rate (FDR) <0.05 with minimum log2 fold change of 0.5
Pathway and Network Analysis:
- Functional Enrichment: Implement over-representation analysis with hypergeometric testing using Gene Ontology, Reactome, and KEGG databases
- Pathway Activity: Infer signaling pathway changes using PROGENy [66]
- Transcription Factor Activity: Calculate regulon activity using DoRothEA database [66]
Cross-Platform Integration:
- Batch Correction: Apply ComBat or Harmony algorithms to remove technical variability while preserving biological signals
- Conserved Signature Identification: Use rank-based methods (Robust Rank Aggregation) to identify consistently dysregulated genes across platforms
Key Analytical Findings and Data Tables
Conserved Transcriptomic Signatures in ALS
Table 1: Core Transcriptional Pathways Conserved Between iPSC-MNs and Post-Mortem ALS Tissue
| Pathway/Domain | Direction in ALS | iPSC-MN Evidence | Post-Mortem Evidence | Key Genes |
|---|---|---|---|---|
| p53 Signaling | Upregulated | PROGENy NES +13.0 [66] | Significant enrichment [66] | CDKN1A, SESN1, RRM2B |
| DNA Damage Response | Upregulated | 43 DEGs FDR<0.05 [66] | 213 DEGs identified [68] | RNASEL, TNFRSF10B |
| Immune/Inflammatory | Upregulated | 1,504 DEGs [1] | 144 increased DEGs [68] | MHC class II genes |
| Synaptic Function | Downregulated | 3,700 DEGs [65] | 69 decreased DEGs [68] | STMN2, UNC13A |
| RNA Metabolism | Dysregulated | TDP-43 pathology genotypes [65] | RNA metabolism biodomain [69] | TARDBP, TAF15 |
| Myelination | Downregulated | Oligodendrocyte genes [66] | Oligodendrocyte decreased DEGs [68] | MBP, PLP1 |
Cellular Deconvolution Performance Metrics
Table 2: Performance Benchmarking of Cellular Deconvolution Methods for Spatial Transcriptomics
| Method | Computational Approach | Recommended Use Case | Accuracy (JSD) | Robustness | Usability |
|---|---|---|---|---|---|
| CARD | Probabilistic | High-resolution spatial mapping | High | High | Medium |
| Cell2location | Probabilistic | Large tissue sections | High | High | Medium |
| Tangram | Deep learning | Cellular spatial organization | High | Medium | High |
| DestVI | Probabilistic | Small spot numbers | High | Low | Medium |
| SpatialDWLS | NMF-based | Simulated data | Medium | Low | High |
| RCTD | Probabilistic | General purpose | Medium | Medium | High |
| STdeconvolve | Reference-free | Unknown cell types | Medium | Medium | High |
Experimental Parameters for Transcriptomic Studies
Table 3: Optimal Experimental Parameters for Transcriptomic Benchmarking Studies
| Parameter | iPSC-MN Profiling | Post-Mortem Tissue Profiling | Integrated Analysis |
|---|---|---|---|
| Minimum Sample Size | 20-30 donors/group [1] | 45 controls, 151 ALS [69] | 429 iPSC-MNs, 271 post-mortem [66] |
| Sequencing Depth | 30-50M reads/sample | 20-40M reads/sample | Matched depth recommended |
| Key Quality Metrics | >90% MN purity [1] | RIN >7.0 [68] | Batch effect correction |
| Primary Analysis Tools | DESeq2, limma | DESeq2, linear mixed models | Harmony, ComBat |
| Validation Approach | Post-mortem overlap [65] | Cell type proportion [68] | Correlation analysis |
Signaling Pathways in ALS Transcriptomics
The diagram below illustrates the core signaling pathways identified through transcriptomic benchmarking:
The Scientist's Toolkit: Essential Research Reagents and Computational Tools
Table 4: Essential Research Resources for Transcriptomic Benchmarking
| Category | Specific Tool/Reagent | Application/Purpose | Key Features |
|---|---|---|---|
| iPSC Differentiation | LDN193189, SB431542 | Dual-SMAD inhibition | Neural induction |
| Retinoic acid, Purmorphamine | Motor neuron patterning | Caudal/ventral specification | |
| BDNF, GDNF, CNTF | Motor neuron maturation | Survival and functional maturation | |
| Transcriptomic Profiling | Poly-A selection mRNA | Library preparation | mRNA enrichment |
| RIN metrics | RNA quality assessment | Sample quality control | |
| DESeq2, limma | Differential expression | Statistical analysis | |
| Cellular Deconvolution | CARD | Spatial deconvolution | High accuracy for spatial mapping |
| Cell2location | Large tissue sections | Scalable for big datasets | |
| Scaden | Bulk tissue deconvolution | Accurate proportion estimation | |
| Pathway Analysis | PROGENy | Pathway activity inference | Context-specific pathway scores |
| DoRothEA | TF activity assessment | Regulon-based analysis | |
| WGCNA | Co-expression networks | Module-trait relationships | |
| Advanced Modeling | SuStaIn | Subtype and stage inference | Temporal dynamics from cross-sectional data [69] |
| Harmony, ComBat | Batch integration | Multi-dataset integration |
Applications and Validation Case Studies
Drug Screening Validation
Large-scale drug screening in iPSC-MNs from 100 sporadic ALS patients demonstrated the critical importance of transcriptomic benchmarking for therapeutic development. Only 3% of drugs that showed efficacy in traditional familial ALS models rescued motor neuron survival in sporadic ALS iPSC-MNs, closely reflecting clinical trial failure rates [1]. This highlights how transcriptomic benchmarking against sporadic human pathology can filter out compounds that work in artificial systems but lack relevance to human disease.
Molecular Subtyping Applications
The Subtype and Stage Inference (SuStaIn) algorithm applied to post-mortem spinal cord transcriptomes identified two molecular ALS subtypes with distinct temporal trajectories [69]:
- Immune/Apoptosis/Proteostasis Subtype (54% of cases): Characterized by early immune/apoptotic/proteostatic dysregulation, worse prognosis, and higher microglia proportions
- Synapse/RNA-Metabolism Subtype (26% of cases): Shows early synaptic/RNA-processing deficits, lower male prevalence, and prominent neuron loss
These subtypes demonstrate how transcriptomic benchmarking can unravel disease heterogeneity and inform personalized therapeutic approaches.
Technical Validation Framework
Implement a multi-level validation framework to ensure benchmarking reliability:
- Technical Reproducibility: Assess consistency across replicate samples and processing batches
- Biological Consistency: Verify that directionality of gene expression changes aligns across platforms
- Functional Relevance: Correlate transcriptional changes with functional readouts (neuronal survival, electrophysiology)
- Clinical Correlation: Relate transcriptional signatures to patient clinical outcomes where possible
Troubleshooting and Technical Considerations
Low Concordance Between Models:
- If iPSC-MNs show poor transcriptional overlap with post-mortem tissue, verify maturation status; extended maturation (42+ days) may be necessary for late-onset disease signatures to emerge [66]
- Check for batch effects and implement more aggressive batch correction methods
- Consider cell type purity; contamination with non-motor neurons can dilute disease signals
Spatial Transcriptomics Challenges:
- For low-resolution spatial technologies (like 10X Visium), apply advanced deconvolution methods (CARD, Cell2location) to infer cellular composition [70]
- Address spot swapping effects in Visium data using SpotClean, particularly for manual tissue placement protocols [71]
Post-Mortem Tissue Quality:
- Account for RNA degradation using RIN values as covariates in statistical models
- Address cellular composition changes due to end-stage pathology rather than primary disease mechanisms
By implementing these comprehensive transcriptomic benchmarking protocols, researchers can rigorously validate their iPSC-MN models against human post-mortem tissue, ensuring that therapeutic development builds upon molecularly faithful representations of human ALS pathology.
Within the broader thesis on utilizing induced pluripotent stem cell (iPSC)-derived motor neurons for Amyotrophic Lateral Sclerosis (ALS) modeling, a critical validation step is demonstrating that these in vitro systems accurately recapitulate known drug responses. The successful recapitulation of riluzole efficacy—the first FDA-approved ALS drug—provides a crucial benchmark for confirming the pathophysiological relevance of iPSC-based models. This application note details protocols and quantitative data for using riluzole response as a key pharmacological validation metric in patient-derived motor neurons, enabling researchers to qualify their models for subsequent drug discovery applications.
The pressing need for such validated models is underscored by the high failure rate of ALS clinical trials; a recent large-scale screening revealed that 97% of drugs previously tested in ALS clinical trials failed to mitigate neurodegeneration in iPSC-derived motor neuron models, accurately reflecting disappointing trial outcomes [1]. This emphasizes the critical importance of establishing physiologically relevant screening platforms that can bridge the translational gap between preclinical studies and human clinical efficacy.
Experimental Workflow for Pharmacological Validation
The diagram below illustrates the integrated workflow for establishing and validating an iPSC-derived motor neuron model for pharmacological screening, with emphasis on recapitulating known drug responses.
Quantitative Validation of Disease Phenotypes and Drug Response
Key Phenotypic Hallmarks in SALS Motor Neurons
Table 1: Phenotypic characterization of sporadic ALS (SALS) iPSC-derived motor neurons demonstrating relevant disease hallmarks for pharmacological validation.
| Parameter | Control Motor Neurons | SALS Motor Neurons | Significance | Measurement Technique |
|---|---|---|---|---|
| Neuronal Survival | Normalized to 100% | Significantly reduced [1] | p < 0.001 | Longitudinal live-cell imaging |
| Neurite Degeneration | Minimal degeneration | Accelerated, correlates with donor survival [1] | p < 0.01 | Automated neurite tracing |
| Electrophysiological Properties | Repetitive firing capacity | Limited firing capacity, depolarized RMP [72] | p < 0.05 | Whole-cell patch clamp |
| Transcriptional Profile | Healthy control profile | Consistent with post-mortem ALS tissue [1] | FDR < 0.05 | RNA sequencing |
Recapitulation of Riluzole Efficacy
Table 2: Quantitative assessment of riluzole efficacy in SALS iPSC-derived motor neurons, confirming known clinical drug response.
| Assay Readout | SALS Baseline (Vehicle) | SALS + Riluzole | % Rescue/Improvement | Clinical Correlation |
|---|---|---|---|---|
| Motor Neuron Survival | Significantly reduced | Significant rescue [1] | Not specified | Extends lifespan by 2-3 months [73] |
| Neurite Degeneration | Accelerated | Significant reduction in degeneration [1] | Not specified | Functional preservation in patients |
| Repetitive Firing | Impaired | Partial restoration of firing patterns [74] | Not specified | Modulates neuronal hyperexcitability |
| Transcriptional Dysregulation | ALS disease signature | Partial reversal towards healthy state [1] | Not specified | Unknown |
Detailed Experimental Protocols
Motor Neuron Differentiation and Maturation
Protocol: High-Purity Motor Neuron Differentiation
This protocol adapts established spinal motor neuron differentiation methods [1] with optimizations for enhanced maturation and screening robustness.
Culture Conditions:
Quality Control Assessment:
- Purity Analysis: At day 30-35 of differentiation, fix cells and immunostain for motor neuron markers. A rigorously optimized protocol should yield cultures with:
Functional Phenotyping and Drug Screening
Protocol: Longitudinal Assessment of Motor Neuron Health
Live-Cell Imaging and Survival Analysis:
- Monitor cultures daily using automated live-cell imaging systems.
- Implement a motor neuron-specific reporter (e.g., HB9-turbo) for unambiguous identification [1].
- Quantify survival and neurite morphology using highly stringent criteria and automated image analysis pipelines.
Electrophysiological Characterization:
- Perform whole-cell patch clamp recordings from day 10-15 in vitro (DIV) [72].
- Solutions:
- Extracellular: 125 mM NaCl, 3 mM KCl, 1.2 mM CaCl₂, 1 mM MgSO₄, 25 mM NaHCO₃, 1.25 mM NaH₂PO₄, 10 mM glucose, 3 mM myo-inositol, 3 mM Na-pyruvate, and 0.5 mM L-ascorbic acid (pH 7.4) [72].
- Pipette: 120 mM K-gluconate, 20 mM KCl, 2 mM MgCl₂, 2 mM Na-ATP, 0.25 mM Na-GTP, and 10 mM HEPES (pH 7.4) [72].
- Assess passive membrane properties, action potential kinetics, and repetitive firing in response to 500-ms depolarizing current pulses.
Protocol: Pharmacological Testing with Riluzole
Drug Preparation:
- Prepare a 10 mM riluzole stock solution in DMSO. Aliquot and store at -20°C.
- Dilute stock directly into culture medium to final testing concentrations (typically 1-10 µM) [74]. Include vehicle control (DMSO ≤ 0.1%).
Treatment Paradigm:
- Initiate drug treatment upon establishment of mature motor neuron cultures (e.g., DIV 20-25).
- Maintain treatment for a duration sufficient to observe disease phenotype modulation (e.g., 2-4 weeks), with medium and drug replenishment every 2-3 days.
Endpoint Analysis:
- Assess key parameters as listed in Table 1 and Table 2.
- A validated model should demonstrate significant rescue of survival deficits and neurite degeneration by riluzole, mirroring its modest but reproducible clinical benefit.
Mechanism of Action Analysis
The diagram below illustrates the primary molecular targets of riluzole in motor neurons, which contribute to its neuroprotective effects in ALS models.
Riluzole exerts its neuroprotective effects through multiple mechanisms that are quantifiable in iPSC-derived motor neurons:
Ion Channel Modulation: At clinically relevant concentrations (low micromolar), riluzole primarily inhibits the persistent sodium current (IC₅₀ ~0.3-1 µM), which stabilizes neuronal firing and reduces excitotoxicity [74]. At higher concentrations, it also inhibits fast Na⁺ currents and voltage-gated Ca²⁺ channels [74].
Synaptic Effects: Riluzole inhibits neurotransmitter release and potentiates glutamate transport, reducing excitotoxic signaling at synapses [74].
Integrated Functional Outcomes: These molecular actions converge to decrease repetitive firing without blocking single action potentials, ultimately promoting motor neuron survival [74]. This mechanistic profile should be reflected in the electrophysiological and survival readouts from the validation protocols.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents and resources for establishing and validating iPSC-derived motor neuron models for ALS research.
| Resource Category | Specific Example / Source | Application / Function |
|---|---|---|
| iPSC Biobanks | Target ALS Data Portal (postmortem tissue, stem cells) [75] | Access to well-characterized patient-derived biological materials |
| Keio University (32 sALS iPSC lines) [2] | Pre-established sALS model systems | |
| Differentiation Kits | Applied StemCell Inc. Motor Neuron Starter Kit [72] | Ready-to-use, pre-differentiated motor neurons |
| Critical Antibodies | Anti-MNX1/HB9 (Sigma #ABN174) [72] | Motor neuron identity confirmation |
| Anti-Tuj1 (R&D Systems #MAB1195) [72] | Pan-neuronal marker | |
| Anti-CHAT (R&D Systems #AF3447) [72] | Cholinergic neuron marker | |
| Pharmacological Agents | Riluzole (Tocris, Sigma) [1] | Reference compound for model validation |
| TTX, Calcium Channel Blockers (e.g., ω-Conotoxin GVIA) [72] | Electrophysiological characterization | |
| Data Resources | PRO-ACT Database (Pooled Resource Open-Access ALS Clinical Trials) [73] | Clinical trial data for comparative analysis |
| Target ALS Data Portal (multi-omic data) [75] | Access to transcriptomic, genetic, and clinical data |
The pharmacological validation of iPSC-derived motor neuron models using established drugs like riluzole provides an essential benchmark for qualifying these systems for preclinical ALS research. The protocols and quantitative frameworks outlined herein enable researchers to rigorously confirm that their in vitro models recapitulate key pathological features of ALS and demonstrate appropriate responsiveness to therapeutic intervention. This validation step is critical for building confidence in subsequent drug screening efforts aimed at identifying novel therapeutic combinations and candidates for this devastating neurodegenerative disease.
The high failure rate of amyotrophic lateral sclerosis (ALS) clinical trials presents a major challenge in drug development. Over 120 Phase II and III trials conducted in the decade to 2019 yielded minimal success, with only riluzole achieving widespread licensing and modest survival benefit [76]. This translational gap highlights the critical need for preclinical models that better predict human therapeutic responses.
Induced pluripotent stem cell (iPSC)-derived motor neurons (iPSC-MNs) have emerged as a promising platform for modeling sporadic and familial ALS. These patient-derived cells maintain the genetic background of donors and recapitulate key disease pathologies, offering a human-relevant system for preclinical screening [2] [77]. This application note examines how iPSC-based screening platforms are increasingly mirroring clinical trial outcomes, providing researchers with validated tools to prioritize therapeutic candidates before human studies.
Validating Predictive Capacity: Comparative Performance Data
Recent large-scale studies have quantitatively demonstrated that iPSC-MN drug screening platforms can accurately reflect clinical trial success and failure rates, providing a crucial validation of their predictive value.
Table 1: Comparison of Clinical Trial Outcomes vs. iPSC Screening Predictions
| Therapeutic Category | Clinical Trial Outcome | iPSC Screening Result | Concordance |
|---|---|---|---|
| Drugs previously tested in ALS clinical trials (n>100) | >97% failure rate | 97% failed to mitigate neurodegeneration | High concordance [1] |
| Riluzole (approved medication) | Modest survival benefit (2-3 months) | Consistently rescued motor neuron survival | High concordance [1] |
| Ropinirole hydrochloride (ROPI) | Phase 1/2a trial showed slowed ALSFRS-R decline | Protected MNs in 9/22 sALS and FUS/TDP-43 models | High concordance [2] |
| Edaravone/AMX0035 | Limited efficacy, restricted approval/market removal | Not reported | N/A [1] |
The striking concordance between iPSC predictions and clinical outcomes extends beyond single compounds. A landmark study screening over 100 drugs that had previously entered ALS clinical trials found that less than 5% demonstrated efficacy in rescuing motor neuron survival in sporadic ALS (sALS) models – closely reflecting the approximately 3% success rate in human trials [1]. This high predictive validity was further demonstrated by the consistent detection of riluzole's neuroprotective effects across multiple iPSC-MN models [1].
Table 2: iPSC Screening Platform Technical Validation Metrics
| Performance Parameter | Specification | Experimental Support |
|---|---|---|
| Motor Neuron Purity | 92.44 ± 1.66% (co-expressing ChAT, MNX1/HB9, Tuj1) | Highly enriched cultures [1] |
| Culture Composition | 97.66 ± 0.99% Tuj1+ neurons; 0.12% astrocytes; 0.04% microglia | Reductionist system for cell-autonomous effects [1] |
| Donor Cohort Size | 100 sALS patients, 11 monogenic cases, 25 healthy controls | Population-wide heterogeneity representation [1] |
| Clinical Correlation | Accelerated neurite degeneration correlated with donor survival | Pathophysiological relevance [1] |
| Differentiation Protocol | 32-day standardized motor neuron differentiation | Reproducible across multiple laboratories [11] |
Experimental Protocols for Predictive Screening
Large-Scale iPSC-MN Differentiation and Phenotyping Protocol
This standardized protocol enables population-wide phenotypic screening capable of discriminating between healthy control and diseased motor neurons.
Materials and Reagents
- Human iPSCs from ALS patients and matched controls
- Matrigel or Geltrex-coated culture plates
- Neural induction medium (DMEM/F12, NEAA, N2 supplement)
- Motor neuron patterning molecules (retinoic acid, purmorphamine/SAG)
- Motor neuron maturation medium (BDNF, GDNF, CNTF)
- HB9-turbo fluorescent reporter for motor neuron identification
- Live-cell imaging compatible culture plates
Procedure
- iPSC Culture and Quality Control: Maintain iPSCs in feeder-free conditions on coated plates. Confirm genomic integrity, pluripotency markers (OCT3/4, SOX2, NANOG), and trilineage differentiation potential for all lines [1].
- Neural Induction (Days 1-7): Transfer iPSCs to neural induction medium containing dual SMAD inhibitors (dorsomorphin, SB431542) to promote neural progenitor formation.
- Motor Neuron Patterning (Days 8-18): Add retinoic acid (0.1µM) and purmorphamine (0.5µM) to specify spinal motor neuron identity through caudalization and ventralization.
- Motor Neuron Maturation (Days 19-32): Replace with maturation medium containing neurotrophic factors (BDNF, GDNF, CNTF at 10ng/mL each) to promote terminal differentiation and functional maturation.
- Phenotypic Validation: Verify motor neuron identity by immunocytochemistry for ChAT, MNX1/HB9, and Tuj1. Cultures should achieve >92% purity with minimal glial contamination (<0.2% combined astrocytes and microglia) [1].
- Longitudinal Live-Cell Imaging: Monitor motor neuron health daily using automated imaging systems. Track survival, neurite degeneration, and soma size changes over 14-21 days.
Technical Notes
- Maintain consistent culture conditions across all lines; patient sex and cell culture composition represent significant sources of variability that must be controlled [11].
- Implement stringent quantification criteria; define motor neurons as cells co-expressing ChAT, MNX1/HB9, and Tuj1 with appropriate morphology.
- For high-content screening, use motor neuron-specific reporters (e.g., HB9-turbo) to enable automated tracking while excluding non-neuronal cells from analysis.
Compound Screening and Combination Therapy Protocol
This protocol outlines the systematic approach for evaluating single agents and combination therapies in validated iPSC-MN models.
Materials and Reagents
- Test compounds prepared in DMSO or appropriate vehicle
- Positive control (riluzole, 10µM)
- Vehicle control (DMSO, <0.1% final concentration)
- Cell viability assay reagents (LDH, MTT, or ATP-based)
- Immunocytochemistry supplies for cleaved caspase-3, TDP-43 pathology
- RNA extraction kit for transcriptomic analysis
Procedure
- Platform Establishment: Plate differentiated iPSC-MNs at day 32 onto 96-well or 384-well plates optimized for high-content imaging.
- Compound Administration: Add test compounds across a concentration range (typically 100nM-100µM) in triplicate wells. Include vehicle and positive controls on every plate.
- Chronic Exposure: Maintain compounds in culture for 14 days with medium changes every 48-72 hours to ensure consistent exposure.
- Endpoint Assessment:
- Viability Metrics: Quantify cell survival using automated imaging and nuclear staining.
- Neurite Integrity: Analyze neurite length and branching using neurite tracing algorithms.
- Functional Assessment: Measure electrophysiological activity using multi-electrode arrays where available.
- Pathological Markers: Fix parallel wells for TDP-43 localization and aggregation analysis.
- Combination Screening: For effective single agents, test combinations using matrix dosing designs. The baricitinib, memantine, and riluzole combination demonstrated synergistic effects in SALS models [1].
- Data Analysis: Normalize results to vehicle controls and compare across donor cohorts. Apply statistical models that account for donor-to-donor variability.
Validation Criteria
- Effective compounds should demonstrate rescue across multiple sALS donors, not just individual lines.
- Efficacy should be reproducible across minimum two independent differentiations.
- Compounds should show dose-dependent effects on primary endpoints (survival, neurite integrity).
Signaling Pathways in ALS Pathogenesis and Therapeutic Intervention
The complexity of ALS pathogenesis involves multiple interconnected cellular processes that can be modeled in iPSC-MN systems. The most promising therapeutic combinations target several of these pathways simultaneously.
Figure 1: ALS Pathogenic Pathways and Therapeutic Intervention Targets. The diagram illustrates key pathological processes in ALS and evidence-based therapeutic interventions that target these mechanisms. The validated three-drug combination (baricitinib, memantine, riluzole) simultaneously addresses multiple disease pathways, potentially explaining its enhanced efficacy in iPSC-MN models [1].
Advanced Workflow for Predictive iPSC-based Screening
Implementing a robust, standardized workflow is essential for generating clinically predictive data from iPSC-based ALS models.
Figure 2: Comprehensive Workflow for Predictive iPSC-based ALS Drug Screening. The standardized protocol encompasses patient-derived cell line generation through validated phenotypic screening, with quality control checkpoints at each stage to ensure reproducibility and clinical relevance [1] [11].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for iPSC-based ALS Modeling
| Tool Category | Specific Product/Platform | Application in ALS Research |
|---|---|---|
| iPSC Lines | Answer ALS iPSC collection (1,000+ lines) [11] | Large-scale disease modeling incorporating population heterogeneity |
| Differentiation Kits | Commercial motor neuron differentiation kits | Standardized generation of iPSC-MNs with reduced protocol variability |
| Characterization Antibodies | Anti-ChAT, MNX1/HB9, Tuj1, TDP-43 | Motor neuron identification and pathological assessment |
| Cell Programming | opti-ox enabled ioCells [78] | Deterministic programming for highly consistent neuronal populations |
| Screening Platforms | Longitudinal live-cell imaging systems | Continuous monitoring of motor neuron health and compound effects |
| Functional Assays | Multi-electrode arrays (MEAs) | Electrophysiological assessment of motor neuron function |
| Data Integration | Answer ALS Data Portal [11] | Multi-omics data integration and collaborative analysis |
Discussion and Future Directions
The demonstrated concordance between iPSC-MN screening outcomes and clinical trial results represents a significant advancement in preclinical ALS modeling. The 97% concordance in predicting clinical failures underscores the potential of these platforms to de-risk drug development by identifying likely ineffective compounds before human trials [1]. Furthermore, the identification of effective combination therapies (baricitinib, memantine, and riluzole) through iPSC screening highlights the platform's utility not only for weeding out failures but also for discovering novel therapeutic approaches [1].
Several key factors enhance the predictive validity of modern iPSC platforms:
- Population-Relevant Cohort Sizes: Moving beyond minimal sample sizes to incorporate 100+ sALS patients captures the biological heterogeneity of the disease [1].
- Standardized Phenotyping: Automated, longitudinal assessment of multiple disease-relevant parameters (survival, neurite integrity, pathology) reduces bias and increases reproducibility [1].
- Clinical Correlation: Establishing relationships between in vitro phenotypes and donor clinical outcomes (e.g., neurite degeneration correlating with survival) strengthens pathophysiological relevance [1].
Future developments will likely focus on increasing model complexity through microfluidics, organoid systems, and incorporation of non-cell autonomous contributors (astrocytes, microglia) to better capture the multicellular pathophysiology of ALS [2] [77]. Additionally, initiatives like Project Mosaic aim to industrialize sALS models and establish them as a new preclinical standard, potentially accelerating the development of effective precision medicines for this devastating disease [79].
The landscape of preclinical testing for neurodegenerative diseases, particularly Amyotrophic Lateral Sclerosis (ALS), is undergoing a fundamental transformation. Traditional reliance on animal models has faced significant challenges due to species-specific differences in biology and their limited ability to recapitulate sporadic disease forms, which constitute approximately 90% of ALS cases [1] [2]. The emergence of induced pluripotent stem cell (iPSC) technology offers an unprecedented opportunity to create human-derived disease models that capture patient-specific pathophysiology. However, the future lies not in replacing animal models entirely, but in strategically integrating iPSC-derived data with traditional in vivo approaches to create more predictive preclinical pipelines. This paradigm shift enables researchers to leverage the human relevance of iPSC systems while maintaining the systemic context provided by animal studies, ultimately accelerating the development of effective therapies for ALS.
The critical need for this integrated approach is underscored by the historical failure rate of ALS clinical trials. More than 160 drugs demonstrated efficacy in familial ALS (fALS) models, primarily in rodents, yet over 97% failed to provide clinical benefit in human trials, reflecting a profound translational gap [1]. This discrepancy highlights the limitations of models that do not fully capture the complexity of human sporadic ALS (sALS). iPSC-derived motor neurons from ALS patients provide a human-based system that recapitulates key disease features, including reduced neuronal survival, accelerated neurite degeneration, TDP-43 proteinopathy, and transcriptional dysregulation patterns consistent with postmortem patient tissues [1] [80]. The integration of these human-specific insights with animal data creates a more comprehensive foundation for therapeutic development.
Current Landscape of ALS Modeling Approaches
Limitations of Traditional Animal Models
Traditional animal models, including genetically modified rodents, zebrafish, and fruit flies, have provided valuable insights into ALS mechanisms, particularly for familial forms linked to specific gene mutations such as SOD1, C9orf72, and FUS [2]. These systems enable the study of disease progression in a whole-organism context, including complex physiological interactions between the nervous system and other tissues. However, these models fundamentally lack the complete genetic background of human patients and cannot replicate the complex, multifactorial etiology of sporadic ALS [2]. Additionally, species-specific differences in lifespan, metabolism, and neural architecture limit their predictive value for human therapeutic responses. The failure of numerous compounds that showed efficacy in animal models to translate to human clinical benefit emphasizes these limitations and underscores the need for complementary human-relevant models [1].
Advancements in iPSC-Derived Motor Neuron Models
The development of iPSC technology has enabled the generation of patient-specific motor neurons that retain the complete genetic profile of the donor, including polygenic risk factors and epigenetic modifications relevant to sporadic disease [1]. Recent large-scale initiatives have established extensive iPSC resources, such as the Answer ALS repository comprising iPSCs from nearly 1,000 patients with associated clinical and multi-omics data [81]. These resources provide unparalleled opportunities for disease modeling and drug screening across a population that reflects the heterogeneity of human ALS.
Technological advances in differentiation protocols have significantly improved the efficiency and physiological relevance of iPSC-derived motor neurons. Recent studies describe optimized protocols that generate high-purity cultures (92.44% ± 1.66% motor neurons) with extensive neurite networks within 18-28 days, compared to traditional methods requiring 45 days or more [1] [47]. These protocols incorporate small molecules for notch inhibition to accelerate maturation, resulting in functionally active neurons that exhibit disease-relevant phenotypes such as hyperexcitability and TDP-43 mislocalization [47] [80]. The enhanced efficiency and reproducibility of these methods make them suitable for large-scale screening applications while providing physiologically relevant models of human disease.
Table 1: Comparison of ALS Model Systems
| Feature | Animal Models | iPSC-Derived Motor Neurons | Integrated Approach |
|---|---|---|---|
| Genetic Relevance | Limited to introduced mutations; lacks human genetic background | Complete human genetic background including polygenic risk factors | Combines human genetics with systemic validation |
| Sporadic ALS Modeling | Poorly recapitulated; primarily models familial forms | Recapitulates key features of sporadic disease (90% of cases) | Enables validation of sporadic mechanisms in whole organism context |
| Throughput | Low to moderate; time-intensive for disease progression | High; suitable for large-scale screening [1] | Sequential screening: high-throughput iPSC followed by targeted animal studies |
| Systemic Complexity | Whole-organism physiology including immune interactions | Reduced system; primarily cell-autonomous effects with some co-culture options | Human cellular insights guide focused systemic investigations |
| Pharmacological Predictive Value | Limited translation for sporadic ALS; 97% clinical trial failure rate [1] | Recapitulates known drug effects (e.g., riluzole); identifies patient-specific responses [1] | Improved prediction through human mechanism validation in physiological context |
| Temporal Resolution | Months for disease progression | Weeks for phenotype emergence [47] [80] | Rapid human cellular insights followed by longitudinal whole-organism studies |
Experimental Protocols for iPSC-Derived Motor Neuron Generation and Phenotyping
Motor Neuron Differentiation Protocol
The following protocol, adapted from recent large-scale studies, details an optimized method for generating spinal motor neurons from human iPSCs with high efficiency and reproducibility [1] [47]:
Stage 1: Neural Induction (Days 1-6)
- Culture iPSCs in monolayer on Matrigel-coated plates in neural induction medium containing DMEM/F12, N2 supplement, non-essential amino acids, and dual SMAD signaling inhibitors (LDN-193289 100nM and SB431542 10μM).
- Change medium daily for 6 days until neural rosette structures appear.
- Quality Control: Verify presence of PAX6+ neural progenitor cells via immunostaining (>85% purity expected).
Stage 2: Motor Neuron Progenitor Specification (Days 7-12)
- Replace medium with motor neuron induction medium: Neurobasal medium, B27 supplement, retinoic acid (0.1μM), and smoothened agonist (SAG 1μM).
- Culture for 5 days with medium change every other day.
- Quality Control: Assess OLIG2+ motor neuron progenitors via flow cytometry (73%-91% purity expected) [47].
Stage 3: Motor Neuron Maturation (Days 13-18)
- Switch to motor neuron maturation medium: Neurobasal, B27, BDNF (10ng/mL), GDNF (10ng/mL), CNTF (10ng/mL), and ascorbic acid (0.2μM).
- Culture for 6 days with medium change every other day.
- Quality Control: Verify CHAT+ and HB9+ motor neurons via immunocytochemistry (88%-97% purity expected) [47].
Stage 4: Functional Maturation (Days 19-28)
- Maintain cultures in maturation medium with the addition of cAMP (1μM) to enhance synaptic development.
- Change medium every other day for 10 days.
- Quality Control: Assess electrophysiological activity via patch-clamp recording or calcium imaging; cultures should exhibit spontaneous electrical activity and calcium transients [47].
This optimized protocol reduces the typical differentiation timeline from 45 days to approximately 28 days while achieving high purity (92.44% ± 1.66% motor neurons) and functional maturity suitable for disease modeling and drug screening applications [1].
Phenotypic Screening and Validation Assays
Comprehensive phenotypic characterization is essential for validating disease-relevant features in iPSC-derived motor neurons. The following assays provide quantitative assessment of ALS-associated pathologies:
Neurite Degeneration and Survival Analysis
- Plate differentiated motor neurons in 96-well imaging plates at day 28 of differentiation.
- Perform live-cell imaging over 7-14 days using motor neuron-specific reporters (e.g., HB9::GFP).
- Quantify neurite length and branching using automated image analysis (e.g., NeuronJ or commercial platforms).
- Assess cell survival via nuclear staining (Hoechst) and membrane integrity markers.
- Validation: SALS motor neurons typically exhibit 25-40% reduced survival and significant neurite fragmentation compared to controls by day 14 [1].
Electrophysiological Profiling
- Perform whole-cell patch-clamp recordings at day 28-35 of differentiation.
- Measure resting membrane potential, action potential generation, and synaptic activity.
- Validation: SALS motor neurons demonstrate hyperexcitability with increased firing frequency and depolarized resting membrane potentials [47].
TDP-43 Pathology Assessment
- Fix cultures at multiple time points (e.g., day 32, 46, 60) for immunofluorescence analysis.
- Stain for TDP-43 localization (nuclear vs. cytoplasmic) and quantify using high-content imaging.
- Assess TDP-43 function via qRT-PCR panel of known targets (ELAVL3, STMN2, UNC13A, etc.) [80].
- Validation: Nuclear depletion of TDP-43 and mis-splicing of target genes emerges in a time-dependent manner, with significant pathology apparent by day 46-60 [80].
Multi-Omic Integration
- Perform RNA sequencing to identify transcriptional dysregulation patterns.
- Integrate with proteomic and epigenetic data where available.
- Compare signatures to postmortem ALS patient tissues for validation.
- Validation: Transcriptional profiles of SALS motor neurons should correlate with postmortem spinal cord signatures [1] [82].
Diagram 1: iPSC Motor Neuron Differentiation and Screening Workflow
Strategic Integration Framework for Preclinical Testing
Complementary Data Integration Strategy
The integration of iPSC and animal model data requires a systematic framework that leverages the unique strengths of each approach while mitigating their individual limitations. The following strategy provides a structured pathway for comprehensive preclinical assessment:
Phase 1: iPSC-Based Mechanistic Screening
- Utilize patient-derived motor neurons for high-content screening to identify disease mechanisms and therapeutic targets across genetically diverse populations.
- Implement large-scale drug screening (100+ compounds) to identify candidate therapeutics with efficacy across sALS models.
- Recent example: A screen of 100 SALS iPSC lines identified baricitinib, memantine, and riluzole as a promising combinatorial therapy [1].
- Output: Prioritized therapeutic targets and compounds with demonstrated efficacy in human neuronal contexts.
Phase 2: Animal Model Validation
- Test prioritized compounds in animal models to assess pharmacokinetics, blood-brain barrier penetration, and systemic effects.
- Evaluate therapeutic effects on complex physiological processes including neuromuscular junction function, respiratory capacity, and motor coordination.
- Output: Validation of human-derived insights in whole-organism context with assessment of systemic parameters.
Phase 3: Patient Stratification Biomarker Development
- Use iPSC-derived molecular signatures (transcriptomic, proteomic) to identify patient subgroups with distinct therapeutic responses.
- Develop biomarkers for clinical trial enrichment based on in vitro response patterns.
- Recent example: Molecular profiling of 180 iPSC lines revealed variable TDP-43 dysfunction signatures, enabling patient stratification [80].
- Output: Biomarker-stratified clinical trial designs with higher predictive success rates.
Phase 4: Clinical Correlation and Model Refinement
- Compare preclinical predictions with clinical outcomes to continuously refine both iPSC and animal models.
- Incorporate postmortem validation to confirm that in vitro phenotypes recapitulate human neuropathology.
- Output: Iteratively improved preclinical models with enhanced predictive validity.
Table 2: Successful iPSC-Based Therapeutic Discovery in ALS
| Study Focus | iPSC Model Scale | Key Findings | Validation Approach | Reference |
|---|---|---|---|---|
| Large-scale drug screening | 100 sALS patients | Identified baricitinib, memantine, and riluzole as effective combination; 97% of clinical trial drugs failed in sALS model | Pharmacological rescue of survival and electrophysiological deficits; transcriptomic reversal | [1] |
| ROP1 efficacy screening | 32 sALS patients + controls | Identified ropinirole as protective in 9/22 sALS models; mechanism via mitochondrial protection and reduced TDP-43 aggregation | Phase 1/2a clinical trial showing slowed ALSFRS-R decline and reduced CSF neurofilament | [2] |
| TDP-43 dysfunction mapping | 180 individuals (controls and ALS) | Time-dependent TDP-43 loss of function signatures; nuclear pore injury as therapeutic target | Postmortem tissue correlation; nuclear pore repair reversed TDP-43 pathology | [80] |
| Multi-omic pathway analysis | C9orf72 ALS patients | Identified novel dysregulated pathways conserved across differentiation protocols | Drosophila model validation; postmortem spinal cord confirmation | [82] |
Signaling Pathways in ALS Pathogenesis and Therapeutic Targeting
The integration of iPSC and animal models has elucidated key signaling pathways involved in ALS pathogenesis, revealing both cell-autonomous and non-cell-autonomous mechanisms. The following diagram illustrates the principal pathways and corresponding therapeutic intervention points:
Diagram 2: ALS Signaling Pathways and Therapeutic Intervention Points
Table 3: Key Research Reagent Solutions for iPSC-Based ALS Modeling
| Reagent/Category | Specific Examples | Function/Application | Validation Notes |
|---|---|---|---|
| iPSC Lines | Answer ALS repository (1,000+ lines) [81]; Keio University collection (32 sALS) [2] | Population-wide disease modeling; genotype-phenotype correlation | Extensive multi-omic characterization; clinical data integration |
| Differentiation Kits | Commercial motor neuron differentiation kits; Modified protocol small molecules [47] | Efficient, reproducible motor neuron generation | Yield: >90% purity; 28-day protocol; functional maturity |
| Cell Type Markers | HB9, ChAT, ISLET1 (motor neurons); S100β (astrocytes); CD11B (microglia) [1] | Cell identity confirmation; culture purity assessment | Multiplex immunocytochemistry; flow cytometry validation |
| Pathology Assays | TDP-43 immunofluorescence; STMN2, UNC13A qPCR panels [80] | Assessment of ALS-associated cellular pathology | Time-dependent emergence (day 46-60); correlates with postmortem tissue |
| Live-Cell Imaging Reporters | HB9::GFP; Tuj1::RFP; Caspase-3 activation reporters [1] | Longitudinal survival and neurite dynamics | Automated quantification; 7-14 day imaging protocols |
| Electrophysiology Tools | Multi-electrode arrays; Patch-clamp systems [47] | Functional assessment of neuronal activity | Hyperexcitability phenotype in sALS models |
| Multi-Omic Platforms | RNA sequencing; ATAC-seq; Proteomic profiling [82] | Comprehensive molecular profiling | Integration with clinical data; pathway analysis |
The integration of iPSC-derived motor neuron models with traditional animal data represents a transformative approach to preclinical testing for ALS. This synergistic framework leverages the human relevance and scalability of iPSC systems while maintaining the physiological context provided by animal models. The emergence of large-scale iPSC resources, such as the Answer ALS repository with nearly 1,000 patient lines, combined with optimized differentiation protocols that recapitulate key disease phenotypes, has established a robust foundation for this integrated paradigm [1] [81]. The future of preclinical testing will increasingly focus on leveraging these complementary approaches to de-risk therapeutic development, enhance clinical trial design through patient stratification, and ultimately accelerate the delivery of effective treatments for this devastating disease.
Looking forward, several key advancements will further strengthen this integrated approach. First, the development of more complex in vitro systems, including 3D organoids and microfluidic-based co-culture models that incorporate non-neuronal cells, will enhance the physiological relevance of iPSC-based assays [2]. Second, the application of artificial intelligence and machine learning to multi-omic datasets from both iPSC and animal models will enable the identification of conserved molecular networks and predictive biomarkers [26]. Finally, the standardization of protocols and validation metrics across laboratories will facilitate data integration and comparison, creating a more collaborative and efficient preclinical research ecosystem. Through the continued refinement and strategic integration of these complementary model systems, the field is poised to significantly advance our understanding of ALS mechanisms and accelerate the development of effective therapies.
Conclusion
iPSC-derived motor neuron models have fundamentally shifted the paradigm for ALS research, providing an unprecedented platform to study disease mechanisms in a patient-specific context. The successful identification of clinical candidates like ropinirole and the validation of combinatorial therapies demonstrate the tangible translational impact of this technology. Future progress hinges on standardizing protocols to reduce variability, advancing maturation to model late-onset disease, and integrating complex multi-cell type systems to fully capture disease pathophysiology. As these models continue to mature, they promise to de-risk drug development, enable patient stratification, and accelerate the delivery of effective therapies for this devastating disease.
References
- 1. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 2. Modeling ALS with Patient-Derived iPSCs: Recent Advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852857/]
- 3. Examining iPSC derived motor neuron variability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612198/]
- 4. Cross-Comparison of Human iPSC Motor Neuron Models ... [https://www.merckmillipore.com/GW/en/tech-docs/paper/1536511]
- 5. Rapid iPSC-derived neuromuscular junction model ... [https://www.nature.com/articles/s41420-025-02302-5]
- 6. Advancing ALS drug discovery with iPSC-derived motor ... [https://www.news-medical.net/health/Advancing-ALS-drug-discovery-with-iPSC-derived-motor-neuron-models.aspx]
- 7. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 8. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 9. Modeling ALS with Patient-Derived iPSCs [https://www.mdpi.com/2076-3425/15/2/134]
- 10. Swift induction of human spinal lower motor neurons and ... [https://www.sciencedirect.com/science/article/pii/S2213671124003217]
- 11. Large-scale differentiation of iPSC-derived motor neurons ... [https://www.sciencedirect.com/science/article/pii/S089662732300034X]
- 12. iPSC motor neurons, but not other derived cell types ... [https://www.sciencedirect.com/science/article/pii/S2211124723010574]
- 13. A novel protocol to derive cervical motor neurons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10545486/]
- 14. Quantitative comparison of the mRNA content of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7876496/]
- 15. SOD1 mutations associated with amyotrophic lateral ... [https://www.nature.com/articles/s41598-021-03891-8]
- 16. Modeling the C9ORF72 repeat expansion mutation using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8029270/]
- 17. Modeling C9orf72-Related Frontotemporal Dementia and ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2021.770937/full]
- 18. The Role of Superoxide Dismutase 1 in Amyotrophic Lateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9857031/]
- 19. Human iPSC-derived motoneurons harbouring TARDBP or ... [https://www.nature.com/articles/ncomms6999]
- 20. Mutant iPSC‐Derived Motor Neurons [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361731/]
- 21. ALS-linked FUS mutations confer loss and gain of function in ... [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-019-0658-x]
- 22. Largest ALS patient-based iPSC repository opens new ... [https://www.news-medical.net/news/20241115/Largest-ALS-patient-based-iPSC-repository-opens-new-frontiers-in-research.aspx]
- 23. Large-scale differentiation of iPSC-derived motor neurons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10557526/]
- 24. iPSC Quality Control - Sampled [https://sampled.com/services/cellular-services/ipsc-services/ipsc-quality-control/]
- 25. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 26. Drug discovery research with the iPSC models of ... [https://www.sciencedirect.com/science/article/pii/S0168010225001683]
- 27. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 28. Generation of human iPSC-derived phrenic-like motor ... [https://www.nature.com/articles/s42003-024-05925-z]
- 29. ALS Disease Statistics: Insights from Latest Research [https://www.targetals.org/2025/01/30/als-statistics/]
- 30. All-Optical Electrophysiology for High-Throughput ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/29779896/]
- 31. Optimization of Long-Term Human iPSC-Derived Spinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8784909/]
- 32. Assembling a Coculture System to Prepare Highly Pure ... [https://www.eneuro.org/content/11/7/ENEURO.0165-24.2024]
- 33. Modeling Cell-Autonomous Motor Neuron Phenotypes in ALS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7002167/]
- 34. Quantification of Neurite Degeneration with Enhanced ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8938979/]
- 35. Quantification of Neurite Degeneration with Enhanced ... [https://www.eneuro.org/content/9/2/ENEURO.0327-21.2022.abstract]
- 36. Neuronal hyperexcitability in Alzheimer's disease [https://www.nature.com/articles/s41398-022-02024-7]
- 37. and Culture of Enriched Phrenic-Like Derivation From... Motor Neurons [https://bio-protocol.org/en/bpdetail?id=5363&type=0]
- 38. and Culture of Enriched Phrenic-Like Derivation From... Motor Neurons [https://pubmed.ncbi.nlm.nih.gov/40655414/]
- 39. Label-free live cell recognition and tracking for biological ... [https://www.nature.com/articles/s44303-024-00046-y]
- 40. Modeling ALS and FTD with iPSC-derived Neurons - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4833714/]
- 41. High-Content Analysis (Quantitative Imaging) Information [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/cell-imaging-information/high-content-analysis-information.html]
- 42. Time-lapse Microscopy and Longitudinal Tracking of Single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4942147/]
- 43. High-content screening image dataset and quantitative image ... [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-019-4844-5]
- 44. Ropinirole, a New ALS Drug Candidate Developed Using ... [https://www.sciencedirect.com/science/article/pii/S0165614719302743]
- 45. Phase 1/2a clinical trial in ALS with ropinirole, a drug ... [https://pubmed.ncbi.nlm.nih.gov/37267913/]
- 46. Effect of Ezogabine on Cortical and Spinal Motor Excitability... Neuron [https://pmc.ncbi.nlm.nih.gov/articles/PMC7684515/]
- 47. Article A novel protocol to derive cervical motor neurons ... [https://www.sciencedirect.com/science/article/pii/S2213671123002667]
- 48. Elucidating the Synergistic Effect of the PrimeC ... [https://pubmed.ncbi.nlm.nih.gov/40283960/]
- 49. Large-scale drug screening in iPSC-derived motor neurons ... [https://pubmed.ncbi.nlm.nih.gov/41286450/]
- 50. Examining iPSC derived motor neuron variability and ... [https://www.nature.com/articles/s41598-025-23378-0]
- 51. Addressing variability in iPSC-derived models of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6994963/]
- 52. Transcriptional dynamics of murine motor neuron ... [https://www.nature.com/articles/s41467-022-33022-4]
- 53. Maturation of Spinal Motor Neurons Derived from Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3388990/]
- 54. 050 Electrophysiological maturation of human induced ... [https://www.sciencedirect.com/science/article/pii/S1056871925000632]
- 55. Comprehensive promotion of iPSC-CM maturation by ... [https://www.nature.com/articles/s41467-025-58044-6]
- 56. Adult human heart extracellular matrix improves human iPSC ... [https://pubmed.ncbi.nlm.nih.gov/39862185/]
- 57. How to Establish Quality Control Processes in Manufacturing [https://www.fastfieldforms.com/blog/how-to-establish-quality-control-processes-in-manufacturing.html]
- 58. Quality Control in Manufacturing | Basics and Best Practices [https://www.machinemetrics.com/blog/quality-control-in-manufacturing]
- 59. Quality Control in Manufacturing: Overview and Best ... [https://www.6sigma.us/manufacturing/quality-control-in-manufacturing/]
- 60. What Are 5 Different Quality Control Methods [https://www.employbridge.com/blog/career-path/what-are-5-different-quality-control-methods]
- 61. Non‐neuronal Cells in ALS: Role of Glial, Immune cells and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8029111/]
- 62. Induced Pluripotent Stem Cells and Their Applications ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10047679/]
- 63. An Optimized Workflow to Generate and Characterize iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9954647/]
- 64. An integrated transcriptomic cell atlas of human neural ... [https://www.nature.com/articles/s41586-024-08172-8]
- 65. iPSC motor neurons, but not other derived cell types ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10622181/]
- 66. Integrated transcriptome landscape of ALS identifies ... [https://www.nature.com/articles/s41467-023-37630-6]
- 67. Large-scale differentiation of iPSC-derived motor neurons ... [https://pubmed.ncbi.nlm.nih.gov/40441139/]
- 68. Meta-Analysis of Gene Expression in Bulk-Processed Post ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12286074/]
- 69. Unraveling temporal dynamics of the post-mortem ... [https://www.medrxiv.org/content/10.1101/2025.06.10.25329061v1.full-text]
- 70. A comprehensive benchmarking with practical guidelines ... [https://www.nature.com/articles/s41467-023-37168-7]
- 71. Benchmarking spatial transcriptomics technologies with the ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03543-4]
- 72. Electrophysiological characterization of sourced human iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11938304/]
- 73. What can a Clinical Trial Database Reveal About ALS? [https://pmc.ncbi.nlm.nih.gov/articles/PMC4404433/]
- 74. A Review of the Neural Mechanisms of Action and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6493865/]
- 75. Target ALS Launches New Data Portal for ALS Research [https://www.targetals.org/2024/03/28/target-als-launches-groundbreaking-data-portal-with-dnastack-and-verily-to-fuel-breakthroughs-in-als-research/]
- 76. Drug repurposing in amyotrophic lateral sclerosis (ALS) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11974926/]
- 77. Motor neuron-derived induced pluripotent stem cells as a ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.962881/full]
- 78. Cell-based drug discovery: Why human iPSC-derived ... [https://www.bit.bio/blog/cell-based-drug-discovery-with-human-ipsc-models]
- 79. iXCells Biotechnologies Selected to Perform the First Pilot ... [https://projectmosaic.org/2025/08/26/ixcells-biotechnologies-selected-to-perform-the-first-pilot-in-patient-led-als-precision-medicine-effort/]
- 80. Sporadic ALS induced pluripotent stem cell derived neurons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318032/]
- 81. Answer ALS Releases World's Largest ALS Patient-Based ... [https://www.answerals.org/answer-als-releases-worlds-largest-als-patient-based-ipsc-and-bio-data-repository/]
- 82. An integrated multi-omic analysis of iPSC-derived motor ... [https://www.sciencedirect.com/science/article/pii/S2589004221011895]