Safeguarding iPSC Integrity: Strategies to Prevent Genomic Instability in Long-Term Culture
This article provides a comprehensive guide for researchers and drug development professionals on managing genomic instability in induced pluripotent stem cells (iPSCs) during extended culture.
Safeguarding iPSC Integrity: Strategies to Prevent Genomic Instability in Long-Term Culture
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on managing genomic instability in induced pluripotent stem cells (iPSCs) during extended culture. It explores the fundamental causes and consequences of karyotypic abnormalities, details practical methodologies for routine monitoring and stable culture maintenance, offers troubleshooting and optimization strategies to minimize variability, and establishes validation frameworks for ensuring iPSC quality. By synthesizing recent advances, this resource aims to enhance the reliability of iPSC models for disease research, drug discovery, and clinical applications.
Understanding Genomic Instability: The Silent Challenge in iPSC Culture
Induced pluripotent stem cells (iPSCs) hold transformative potential for disease modeling, drug discovery, and regenerative medicine. However, their clinical application is significantly challenged by genomic instability, which can arise during reprogramming, long-term culture, and differentiation processes. This technical support center provides a comprehensive guide to identifying, troubleshooting, and preventing the genetic alterations that compromise iPSC quality and safety, framed within a broader thesis on maintaining genomic integrity in long-term iPSC culture research.
FAQs: Understanding Genomic Instability in iPSCs
1. What types of genomic instability are most commonly observed in iPSC cultures? iPSC cultures frequently acquire both numerical and structural chromosomal abnormalities. Common findings include trisomy of chromosomes 12, 17, 20, and 8, and gains of chromosomal regions 1q and 20q11.21 [1] [2]. Structural alterations such as acentric fragments, chromosomal fusions, double minutes, radial figures, ring chromosomes, and inversions are also regularly detected [3]. The frequency of karyotype abnormalities in iPSC lines has been reported to be approximately 21-23%, with some studies observing rates as high as 80% in prolonged passaging [2].
2. At what stage does genomic instability typically arise? Genetic variations can originate from multiple stages:
- Pre-existing variations in parental somatic cells that are clonally expanded during reprogramming [1].
- Reprogramming-induced mutations that occur during the reprogramming process itself [1].
- Passage-induced mutations that accumulate during prolonged in vitro culture [1]. Studies note that abnormal clones can emerge or be selected over time, generating altered lineages, with aberrations becoming more common in later passages [3].
3. Does the reprogramming method influence genomic instability? Yes, the choice of reprogramming method significantly impacts genomic instability. Recent research comparing Sendai virus (SV) and episomal vector (Epi) methods found that all SV-iPS cell lines exhibited copy number alterations (CNAs) during reprogramming, while only 40% of Epi-iPS cells showed such alterations. Additionally, single-nucleotide variations (SNVs) were observed exclusively in SV-derived cells during passaging and differentiation [4].
4. How does long-term culture affect genomic stability? Prolonged passaging selectively enriches for clones with growth advantages, often through specific chromosomal gains. The percentage of abnormal samples increases with passage number. One study analyzing passages P6 to P34 found that while abnormal clones can emerge early, they become increasingly prevalent in later passages [3]. Another study noted that the frequency of clonal aberrations in lines from healthy donors increased from 2 out of 10 to 4 out of 10 when re-karyotyped at later passages [2].
5. Can genomic instability be transmitted during differentiation? Yes, genomic alterations can persist or newly arise during differentiation into downstream lineages. Studies have identified copy number alterations (CNAs) and single-nucleotide variations (SNVs) during the differentiation of iPSCs into induced mesenchymal stromal/stem cells (iMS cells) [4]. Additionally, genomic abnormalities may appear as a result of in vitro differentiation protocols, highlighting the importance of monitoring both pluripotent cells and their differentiated progeny [5].
Troubleshooting Guides
Problem 1: Excessive Differentiation in Cultures
Potential Causes and Solutions:
- Cause: Overgrown colonies or suboptimal culture conditions.
- Solution: Ensure cultures are passaged when majority of colonies are large and compact with dense centers. Remove differentiated areas prior to passaging [6].
- Cause: Old or degraded culture medium.
- Solution: Use complete cell culture medium less than 2 weeks old when stored at 2-8°C [6].
- Cause: Prolonged exposure to non-incubator conditions.
- Solution: Minimize time culture plates remain outside the incubator to less than 15 minutes [6].
- Cause: Inappropriate colony density.
- Solution: Decrease colony density by plating fewer cell aggregates during passaging [6].
Problem 2: Declining Cell Viability After Passaging
Potential Causes and Solutions:
- Cause: Over-confluent cultures at time of passaging.
- Solution: Passage cells at 40-85% confluency for optimal health. Avoid routine passaging at high confluencies [7].
- Cause: Inadequate protection during single-cell passaging.
- Solution: Include ROCK inhibitor (e.g., RevitaCell Supplement) during passaging, especially for sensitive lines or when cultures are overly confluent [7].
- Cause: Excessive manipulation of cell aggregates.
- Solution: Minimize pipetting and manipulation of cell aggregates after dissociation to maintain proper cluster size [6].
Problem 3: Low Cell Attachment After Plating
Potential Causes and Solutions:
- Cause: Insufficient initial cell density.
- Solution: Plate 2-3 times higher number of cell aggregates initially and maintain more densely confluent culture [6].
- Cause: Prolonged suspension of cell aggregates.
- Solution: Work quickly after treatment with passaging reagents to minimize time aggregates spend in suspension [6].
- Cause: Incorrect plate coating or handling.
- Solution: Ensure non-tissue culture-treated plates are used when coating with Vitronectin XF; use tissue culture-treated plates when coating with Corning Matrigel [6].
Problem 4: Suspected Genetic Instability in Established Lines
Potential Causes and Solutions:
- Cause: Accumulation of mutations during prolonged culture.
- Solution: Implement regular genomic monitoring at key passages (e.g., P10, P20, P30) using G-banding karyotyping and higher-resolution methods [3] [1].
- Cause: Selective pressure favoring abnormal clones.
- Solution: Maintain lower passage stock banks and avoid extended culture beyond 30-40 passages when possible [3] [2].
- Cause: Reprogramming method-related instability.
- Solution: Consider episomal vector methods if Sendai virus-derived lines show persistent instability [4].
Quantitative Data on Genomic Instability
Table 1: Frequency and Types of Chromosomal Aberrations in iPSC Cultures
| Aberration Type | Specific Alterations | Frequency/Notes | Reference |
|---|---|---|---|
| Overall Karyotype Abnormalities | Any clonal aberration | 21-23% of cell lines (increasing to 80% with prolonged passaging) | [2] |
| Common Trisomies | Trisomy 12, 17, 20, 8 | Most recurrent aneuploidies | [1] [2] |
| CNV Hotspots | 20q11.21 amplification | Most recurrent CNV; contains DNMT3B, ID1, BCL2L1 genes | [1] |
| Structural Rearrangements | 1q duplications, translocations | Most frequently affected region in structural changes | [2] |
| Method-Specific Instability | Sendai virus vs. episomal | 100% of SV-iPS vs. 40% of Epi-iPS showed CNAs during reprogramming | [4] |
Table 2: Detection Methods for Genomic Instability
| Method | Resolution | Key Applications | Advantages/Limitations |
|---|---|---|---|
| G-banding Karyotyping | ~5-10 Mb | Detection of numerical and large structural abnormalities | Low cost, detects low-level mosaicism (>5%); cannot detect small alterations [3] [1] |
| Array-based Technologies (aCGH, SNP array) | ~kb level | Genome-wide CNV detection | Higher resolution than karyotyping; cannot detect balanced translocations [1] [5] |
| Next-Generation Sequencing (WGS, WES) | Single nucleotide | Comprehensive SNV and CNV detection | Highest resolution, detects low-frequency variants; higher cost and computational requirements [1] [4] |
| M-FISH | Chromosomal arm level | Detection of complex structural rearrangements | Visualizes multiple chromosomes simultaneously; lower resolution than arrays [5] |
Experimental Protocols for Monitoring Genomic Instability
Materials:
- KaryoMAX Colcemid (Life Technologies)
- Hypotonic solution (0.075 M KCl with HEPES)
- Fixative (methanol-acetic acid 3:1)
- Trypsin and Giemsa stain
- Microscope with image capture capability (e.g., Leica DM Microscope)
Method:
- Harvest chromosomes when cultures reach 60-80% confluence.
- Incubate with 0.1 µg/ml Colcemid for one hour at 37°C.
- Trypsinize cells and add to 6 ml of hypotonic solution.
- Fix cells with methanol-acetic acid solution (3:1).
- Prepare slides by dropping cell suspension onto pre-warmed slides.
- Perform G-banding using trypsin and Giemsa staining.
- Analyze at least 20 metaphases per sample.
- For clonal definition: same structural aberration or chromosome gain must be present in ≥2 metaphases; chromosome loss must be detected in ≥3 cells.
Background: Residual reprogramming vectors can contribute to genomic instability.
Method:
- After 10+ passages, perform RT-PCR to confirm absence of Klf4 vector.
- If only c-Myc and KOS vectors remain, incubate iPSCs at 38-39°C for 5 days.
- Confirm clearance with subsequent RT-PCR testing.
- Note: Only perform temperature shift with sensitive lines and after appropriate validation.
Research Reagent Solutions
Table 3: Essential Research Reagents for Genomic Stability Maintenance
| Reagent Category | Specific Products | Function/Application | References |
|---|---|---|---|
| Reprogramming Systems | CytoTune-iPS Sendai Reprogramming Kit; Episomal vectors | Non-integrating reprogramming; Episomal methods show lower instability | [3] [4] [7] |
| Culture Media | mTeSR Plus, Essential 8 Medium | Feeder-free culture maintenance | [6] [7] |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent, EDTA | Enzymatic and non-enzymatic passaging | [6] [7] |
| Genomic Stability Enhancers | ROCK inhibitor (Y-27632), RevitaCell Supplement | Improves cell survival after passaging, reduces selective pressure | [7] |
| Extracellular Matrices | Vitronectin XF, Geltrex, Matrigel | Defined substrates for feeder-free culture | [6] [7] |
Maintaining genomic stability in iPSCs requires a multifaceted approach encompassing careful reprogramming method selection, controlled culture conditions, regular monitoring, and appropriate troubleshooting. By implementing the guidelines and protocols outlined in this technical support center, researchers can significantly improve the genetic quality of their iPSC lines, enabling more reliable research outcomes and advancing the path toward safe clinical applications. Regular genomic surveillance using the described methodologies should be integrated as a standard practice in any iPSC research program focused on long-term culture maintenance.
For researchers working with induced pluripotent stem cells (iPSCs), genomic instability presents a critical challenge that can compromise experimental results and therapeutic applications. Karyotypic changes—including aneuploidies, copy number variations (CNVs), and structural chromosomal aberrations—can arise from two primary stressors: the reprogramming process itself and prolonged in vitro passaging [8] [1]. Understanding these drivers is essential for developing robust protocols that maintain genetic integrity throughout your experiments.
This technical support guide provides targeted troubleshooting advice and FAQs to help you identify, prevent, and manage karyotypic instability in your iPSC research. The strategies outlined below are framed within a comprehensive approach to preserving genomic stability in long-term iPSC cultures.
Frequently Asked Questions (FAQs)
Q1: What are the most common karyotypic abnormalities observed in iPSC cultures, and how frequently do they occur?
The following table summarizes the frequency and types of genetic variations commonly detected in iPSC cultures:
Table 1: Common Genetic Variations in iPSC Cultures
| Variation Type | Specific Examples | Reported Frequency | Potential Functional Impact |
|---|---|---|---|
| Aneuploidy | Trisomy 12, Trisomy 8, Trisomy X [8] [1] | ~13-33% of hESC/hiPSC lines [8] | Confers growth advantage; alters pluripotency gene dosage (e.g., NANOG on Chr12) [8] |
| Subchromosomal CNVs | Amplification of 20q11.21 [8] [1] | Frequently recurrent [1] | Enriches genes associated with pluripotency and anti-apoptosis (e.g., DNMT3B, BCL2L1) [1] |
| Single Nucleotide Variants (SNVs) | Point mutations in protein-coding regions [1] | ~10 mutations per line (WGS/WES data) [1] | Can introduce aberrant or immunogenic proteins [9] |
| Chromosomal Aberrations | Translocations, inversions, breaks [10] | 6.12% of new iPS clones (in one study) [10] | May compromise differentiation potential or lead to tumorigenesis [10] |
Q2: Does the choice of reprogramming method influence genomic instability?
Yes, the reprogramming method is a significant factor. Studies comparing Sendai virus (SV) and episomal vector (Epi) methods have found clear differences:
- Sendai Virus (SV): A higher frequency of copy number alterations (CNAs) was observed during the reprogramming phase in all SV-iPS cell lines. Furthermore, single-nucleotide variations (SNVs) were detected exclusively in SV-derived cells during subsequent passaging and differentiation [4].
- Episomal Vectors (Epi): Only 40% of Epi-iPS cell lines showed CNAs during reprogramming, and no SNVs were detected in Epi-derived lines during passaging and differentiation [4]. Gene expression analysis also revealed upregulation of chromosomal instability-related genes in late-passage SV-iPSCs, further indicating increased genomic instability with this method [4].
Q3: How does extended cell passaging contribute to genomic instability?
Prolonged culturing introduces or selects for genetic alterations that facilitate cell propagation, a process known as culture adaptation [8]. The frequency of recurrent aneuploidy generally increases with continuous passaging, as subpopulations with growth-advantageous mutations (like Trisomy 12) expand [8]. Furthermore, long-term culture can lead to the accumulation of genetic mutations due to errors in DNA replication and oxidative stress [9]. One study also demonstrated that even long-term cryopreservation (e.g., 10 years) can lead to genomic instability, causing variability in chromosome number and random chromosomal rearrangements upon thawing and subsequent culturing [11].
Q4: What are the practical consequences of these karyotypic changes for my research?
Karyotypic instability can directly impact your experimental outcomes and the safety of potential therapies.
- Altered Cell Behavior: Genetic changes can affect differentiation potential, proliferation rates, and cellular function [12] [10].
- Immunogenicity: Mutations can lead to the production of altered or new proteins that may be recognized as foreign by the immune system, triggering rejection even in autologous transplantation settings [9].
- Tumorigenic Risk: The presence of mutations in tumor suppressor genes (e.g., TP53) or amplification of oncogenic regions raises serious safety concerns for clinical applications [1] [4] [13].
Troubleshooting Guides
Issue 1: High Incidence of Karyotypic Abnormalities in Newly Generated iPSC Clones
Potential Cause: Reprogramming-induced replication stress and oxidative damage.
Solution: Mitigate the stress encountered by cells during reprogramming.
- Experimental Protocol: Limiting Replication Stress
- Nucleoside Supplementation: Add a nucleoside supplement to the culture medium during the reprogramming process. This provides the raw materials for DNA synthesis and has been shown to reduce the load of DNA damage and genomic rearrangements in resulting iPSCs [14].
- Antioxidant Treatment: Include the antioxidant N-Acetyl-Cysteine (NAC) in the culture medium for the first few days of reprogramming. This has been proven to effectively reduce the occurrence of chromosomal aberrations at this critical early stage [10].
- Modulate Reprogramming Factors: Be cautious with the dosage and combination of reprogramming factors. High expression of factors like cMYC can exacerbate replication stress. Using a cocktail that excludes cMYC or using small molecules to enhance reprogramming efficiency can be beneficial [14] [9].
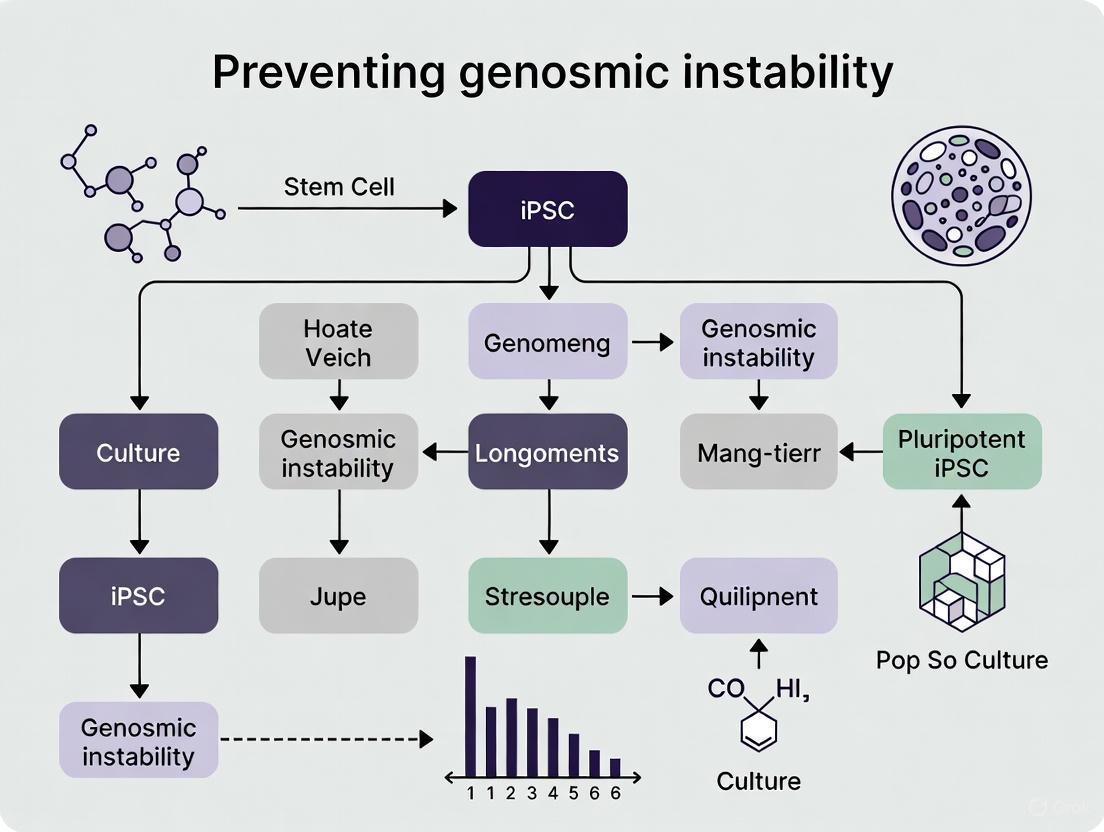
The diagram below illustrates how reprogramming factors induce replication stress and two effective strategies to mitigate it.
Issue 2: Emergence of Genomic Instability During Long-Term Culture and Differentiation
Potential Cause: Culture adaptation and selective pressure.
Solution: Implement rigorous monitoring and optimized culture conditions.
- Experimental Protocol: Routine Genomic Surveillance
- Regular Karyotyping: Perform G-banded karyotyping every 10-15 passages to screen for gross chromosomal abnormalities and aneuploidy [1]. This is a basic but essential requirement.
- High-Resolution CNV Detection: Use higher-resolution technologies like SNP arrays or array Comparative Genomic Hybridization (aCGH) to detect subchromosomal CNVs, particularly in regions like 20q11.21 [8] [1].
- Sequencing-Based Screening: For the most comprehensive assessment, employ whole-genome sequencing (WGS) or whole-exome sequencing (WES) to identify single nucleotide variants (SNVs) and low-frequency pre-existing variations that might be captured during cloning [1].
- Limit Passages: As a general practice, establish a master cell bank and working cell bank system. Use cells within a strictly defined passage range (e.g., below passage 20-30) for key experiments and differentiation protocols to minimize the impact of culture-accumulated variations [8] [11].
Issue 3: Genomic Instability in Differentiated Cell Products (e.g., iMS Cells)
Potential Cause: Mutations carried over from the parent iPSC line or acquired during differentiation.
Solution: Ensure the genetic integrity of the starting material and the differentiation process.
- Experimental Protocol: Ensuring Genomic Stability of Final Products
- Source Cell Validation: Only begin differentiation with iPSC lines that have recently been confirmed as karyotypically normal and genetically stable via the surveillance methods described above.
- Clonal Selection: Select specific, well-characterized iPSC clones for differentiation rather than using a mixed population, which may contain subclones with heterogeneous genetic aberrations [4].
- Monitor Differentiation: Perform genetic analysis on the final differentiated cell product (e.g., iMS cells) to confirm the absence of major de novo abnormalities, especially if the cells are intended for therapeutic use [4].
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Managing Genomic Instability
| Reagent / Tool | Function | Application Context |
|---|---|---|
| N-Acetyl-Cysteine (NAC) [10] | Antioxidant that reduces oxidative stress and chromosomal breaks. | Added to medium during the first few days of reprogramming. |
| Nucleoside Supplement [14] | Provides substrates (dNTPs) for DNA synthesis, alleviating replication stress. | Added to medium during the reprogramming process. |
| CHK1 Expression Vector [14] | Genetically increases levels of the checkpoint kinase 1, which stabilizes replication forks. | Used to generate cells with enhanced ability to cope with replication stress. |
| Non-Integrating Reprogramming Vectors (e.g., Episomal, mRNA) [4] [9] | Deliver reprogramming factors without integrating into the host genome, reducing mutation risk. | Preferred method for generating clinical-grade iPSCs. |
| Giemsa (G) Banding Kit [1] | Standard cytogenetic method for detecting numerical and large structural chromosomal changes. | Routine karyotyping of iPSC cultures. |
| SNP/Array CGH Platform [1] [12] | High-resolution detection of copy number variations (CNVs) across the genome. | Identifying subchromosomal gains/losses. |
| Next-Generation Sequencer | Enables whole genome/exome sequencing to detect SNVs and low-frequency variants. | Comprehensive genomic profiling of master cell banks and final products. |
Frequently Asked Questions (FAQs)
FAQ 1: What types of genomic abnormalities are most commonly found in iPSCs, and how do they originate? Genomic instability in iPSCs manifests in several forms, which can originate from different stages of cell handling. The table below summarizes the primary types and their origins.
Table 1: Common Genomic Abnormalities in iPSCs
| Abnormality Type | Description | Primary Origins |
|---|---|---|
| Chromosomal Aberrations | Gains or losses of entire chromosomes (aneuploidy). Recurrent examples include trisomy of chromosomes 12, 8, 17, and X [15] [1]. | Acquired during long-term culture; can provide a selective growth advantage [15] [1]. |
| Copy Number Variations (CNVs) | Deletions or duplications of DNA sections, ranging from kilobases to megabases. A recurrent hotspot is amplification of 20q11.21 [15] [1]. | Pre-existing as low-frequency variants in the parental somatic cell population that are fixed during reprogramming, or acquired de novo during reprogramming [15] [1]. |
| Single Nucleotide Variants (SNVs) | Single point mutations in the protein-coding regions. iPSC lines can contain an average of 6-12 such mutations [15] [1]. | A combination of pre-existing mutations in parental somatic cells and mutations acquired during the reprogramming process itself [15] [1]. |
| Uniparental Disomy (UPD) | Inheritance of two copies of a chromosome from one parent and none from the other, leading to loss of heterozygosity [15]. | Can occur during the reprogramming process, sometimes as a compensatory mechanism to correct a chromosomal aberration [15]. |
FAQ 2: Can you provide a specific example of how a somatic mutation directly derails a differentiation protocol? Yes. A large-scale study differentiating 238 iPSC lines into dopaminergic neurons found that loss-of-function mutations in the BCOR gene were strongly associated with differentiation failure [16]. BCOR is a key developmental gene. Lines with deleterious BCOR mutations produced significantly fewer dopaminergic neurons and exhibited a larger proliferation rate in culture, indicating that the mutation disrupted the normal developmental pathway and inhibited successful neurogenesis [16]. This is a clear example where a single mutation can compromise an entire disease-modeling experiment.
FAQ 3: What are the best methods to detect these abnormalities in my iPSC lines? Detection methods vary in resolution and what they can find. A combination of techniques is often necessary for comprehensive quality control.
Table 2: Genomic Instability Detection Methods
| Technique | What It Detects | Resolution/Limitations |
|---|---|---|
| G-banding Karyotyping | Numerical abnormalities (aneuploidy) and large structural chromosomal changes [1]. | Low resolution; cannot detect small CNVs or SNVs [15]. |
| SNP Array / CGH Array | Copy Number Variations (CNVs) and Loss of Heterozygosity (LOH), which can indicate UPD [15] [1]. | Kilobase resolution. Cannot detect balanced translocations or single nucleotide variants [15] [1]. |
| Whole Exome/Genome Sequencing (WES/WGS) | Single Nucleotide Variants (SNVs) and small insertions/deletions across the entire exome or genome [1]. | Single-nucleotide resolution. Essential for a complete picture of genomic integrity [1]. |
FAQ 4: How can I adjust my culture practices to minimize the acquisition of genomic abnormalities? Proper culture techniques are crucial for maintaining genomic integrity. The table below outlines common problems and their solutions based on established protocols.
Table 3: Troubleshooting Guide for iPSC Culture to Maintain Genomic Integrity
| Problem | Potential Impact on Genomic Integrity | Recommended Solution |
|---|---|---|
| Excessive Differentiation in Cultures | Differentiated cells may overgrow and outcompete pluripotent cells, potentially selecting for aberrant clones. | Remove differentiated areas before passaging. Do not allow cultures to overgrow. Plate evenly sized aggregates and optimize passage timing [6]. |
| Prolonged Culture & Over-confluence | Increases selective pressure for mutations that confer growth advantage (e.g., trisomy 12, 20q11.21 amplification) [15] [1]. | Avoid excessive passaging. Use low-density freezing stocks to minimize long-term culture. Passage cultures when colonies are large and dense but before multi-layering [6] [17]. |
| Low Cell Survival After Passaging | Can selectively pressure the survival of a small number of potentially abnormal cells that are more resistant to stress. | Use a Rho-associated kinase (ROCK) inhibitor to improve survival. Plate a higher density of cell aggregates and work quickly with passaging reagents [6] [17]. |
| Switching to Feeder-Free Conditions | Adaptation stress can induce apoptosis and differentiation, potentially allowing minor abnormal populations to expand. | Proceed carefully. Test different matrices (e.g., Geltrex, Matrigel, Laminin-521) and media (e.g., mTeSR Plus, StemFlex) to find the optimal condition for your line to minimize stress [17]. |
Essential Research Reagent Solutions
The following reagents are critical for the successful culture, quality control, and adaptation of iPSC lines.
Table 4: Key Reagents for iPSC Culture and Genomic Integrity Monitoring
| Reagent / Material | Function / Application | Example |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Improves cell survival after passaging and thawing by inhibiting apoptosis, helping to maintain a representative cell population [17]. | Stemgent; available from various suppliers. |
| Gentle Cell Dissociation Reagent | A non-enzymatic reagent for passaging cells in aggregates, minimizing DNA damage and stress compared to traditional trypsinization [6] [17]. | STEMCELL Technologies. |
| Defined Matrices for Feeder-Free Culture | Provide a consistent, xeno-free substrate for iPSC attachment and growth, reducing variability and contamination risk. | Geltrex (Thermo Fisher), Matrigel (Corning), Laminin-521 (Thermo Fisher) [17]. |
| High-Quality Culture Media | Specially formulated media support pluripotency and healthy growth under feeder-free conditions. | mTeSR Plus, StemFlex (STEMCELL Technologies) [6] [17]. |
| SNP Microarray Kits | For high-resolution detection of CNVs and LOH (UPD) as part of routine genomic quality control [15] [18]. | Affymetrix, Illumina. |
| Whole Exome Sequencing Services | For comprehensive detection of single nucleotide variants and small indels in the coding regions of the genome [1] [16]. | Various commercial and core facility providers. |
Experimental Protocols for Monitoring Genomic Integrity
Protocol 1: Routine Karyotyping and SNP Analysis for iPSC Lines Objective: To screen for gross chromosomal abnormalities and sub-chromosomal CNVs. Methodology:
- Cell Preparation: Harvest a confluent well of a 6-well plate of iPSCs during an active log-phase growth period.
- Karyotyping: Submit cells to a cytogenetics core facility for G-banding analysis. A minimum of 20 metaphase spreads are typically analyzed to confirm a normal karyotype [1].
- SNP Genotyping: Extract high-quality genomic DNA from iPSCs. Use a commercial SNP array platform according to the manufacturer's instructions. This will identify CNVs and regions of LOH that are invisible to karyotyping [15] [18]. Frequency: This analysis should be performed when establishing a new master cell bank and periodically (e.g., every 10-15 passages) on working cell banks, especially if cells are maintained in long-term culture.
Protocol 2: Assessing Differentiation Capacity via Directed Differentiation Objective: To functionally validate that an iPSC line has not acquired mutations that impair its ability to differentiate into a specific lineage. Methodology (Example: Dopaminergic Neurons):
- Base Protocol: Follow an established, robust protocol for the differentiation of iPSCs into dopaminergic neurons [16].
- Single-Cell RNA Sequencing (scRNA-seq): At key time points during differentiation (e.g., day 11, 30, and 52), harvest cells and perform scRNA-seq.
- Data Analysis: Use computational clustering to identify the different cell types present in the culture. Quantify the proportion of cells that have successfully reached the desired dopaminergic neuron fate.
- Correlation with Genomics: Compare the differentiation efficiency (percentage of target cells) across multiple lines. Lines that consistently fail to differentiate, like those with BCOR mutations, should be subjected to whole-exome sequencing to identify potential causative mutations [16]. Application: This functional test is critical for ensuring that iPSC-based disease models will yield relevant and reproducible results.
Visualizing the Origins and Impacts of Genomic Instability
The following diagram illustrates the pathways through which genomic abnormalities arise and how they ultimately compromise research outcomes.
FAQ: Understanding Karyotypic Abnormalities in iPSC Cultures
What are the most common karyotypic abnormalities found in human iPSC lines?
The most frequently observed karyotypic abnormalities in human iPSC lines are recurrent gains of entire chromosomes or specific chromosomal regions. These changes confer a selective growth advantage under standard culture conditions. The table below summarizes the most common recurrent abnormalities.
Table 1: Recurrent Karyotypic Abnormalities in Human iPSCs
| Abnormality Type | Specific Chromosomal Region | Reported Frequency |
|---|---|---|
| Whole Chromosome Gain | Trisomy 20 | 8.6% of all tests, 38.5% of unique aberrant lines [19] |
| Whole Chromosome Gain | Trisomy 8 | 2.9% of all tests, 15.4% of unique aberrant lines [19] |
| Partial Chromosome Gain | Gain of 1q arm | 7.2% of all tests, 30.8% of unique aberrant lines [19] |
| Partial Chromosome Gain | Gain of 20q | A recurrent CNV hotspot [1] |
| Partial Chromosome Gain | Gain of 12p | Associated with prolonged culture [1] |
| Whole Chromosome Loss | Loss of Chromosome 18 | A well-recognized recurrent loss [19] |
| Whole Chromosome Loss | Loss of Chromosome 10 | A well-recognized recurrent loss [19] |
Why do these specific abnormalities keep appearing?
These recurrent aberrations are not random. They undergo selection in vitro because the genetic changes they confer improve the cells' ability to survive and proliferate in the artificial culture environment, a process known as culture adaptation [19]. For example:
- Trisomy 12 is recurrent because chromosome 12 contains pluripotency-associated genes like NANOG and other cell cycle-related genes, which boost proliferation and reprogramming efficiency [1].
- Gain of 20q11.21 is a common CNV hotspot enriched with genes that support pluripotency and inhibit apoptosis (such as BCL2L1), favoring survival after single-cell passaging [19] [1].
- Gain of the 1q arm has been associated with feeder-free and high-density cell culture protocols [19].
How does the reprogramming process itself contribute to genomic instability?
The cellular stress of reprogramming, coupled with the unique physiology of pluripotent cells, creates a perfect storm for genomic instability. Key factors include [19] [14]:
- Reprogramming-Induced Replication Stress: The forced expression of reprogramming factors (like OSKM) can induce replication stress, leading to DNA breakage, similar to the phenomenon of oncogene-induced replication stress in cancer [14].
- Low Mitotic Fidelity & Relaxed Checkpoint Control: Pluripotent stem cells have relaxed cell cycle checkpoints, which can allow errors to propagate [19].
- Basal Levels of Replication Stress: iPSCs inherently have high basal levels of replication stress, predisposing them to damage at fragile sites in the DNA [19].
The following diagram illustrates the primary mechanisms and outcomes of genomic instability in iPSCs.
Troubleshooting Guide: Preventing and Managing Genomic Instability
How can I reduce the occurrence of genomic instability during reprogramming?
Evidence suggests that mitigating replication stress during the reprogramming process can significantly reduce DNA damage and resultant genomic rearrangements [14].
Table 2: Strategies to Limit Reprogramming-Induced Instability
| Strategy | Method | Effect |
|---|---|---|
| Nucleoside Supplementation | Adding nucleosides to the culture medium during reprogramming. | Increases nucleotide pool, reduces replication stress, DNA damage, and de novo CNVs [14]. |
| Checkpoint Kinase 1 (CHK1) Overexpression | Genetically increasing levels of the CHK1 kinase. | Limits replication stress and increases reprogramming efficiency [14]. |
| Choosing a Low-Stress Reprogramming Method | Using non-integrating methods (e.g., Sendai virus, episomal vectors). | Minimizes risk of insertional mutagenesis and associated DNA damage [19] [20]. |
What is the recommended schedule for karyotypic monitoring of my iPSC cultures?
Regular monitoring is a cornerstone of quality control. The following workflow provides a robust strategy for maintaining genetic integrity.
Which techniques should I use to detect different types of genetic variations?
No single method captures all genomic aberrations. A combination of techniques is recommended for comprehensive quality control [15] [1].
Table 3: Genomic Integrity Assessment Toolkit
| Technique | Primary Use | Detects | Limitations |
|---|---|---|---|
| G-Banding Karyotyping | Initial screening for large-scale abnormalities. | Aneuploidy, translocations, large deletions/duplications (>5-10 Mb). | Limited resolution; cannot detect small CNVs or SNVs [1] [21]. |
| SNP Array / CGH Array | Higher-resolution screening for sub-chromosomal changes. | Copy Number Variations (CNVs) at kilobase resolution. | Cannot detect balanced translocations or low-level mosaicism reliably [15] [1]. |
| Whole Genome/Exome Sequencing | Most comprehensive analysis of the genome. | Single Nucleotide Variants (SNVs), small insertions/deletions, and CNVs. | Higher cost and complex data analysis; may not detect low-frequency mosaicism [1]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagents for Genetic Stability Workflows
| Reagent / Material | Function in iPSC Culture & Quality Control |
|---|---|
| Nucleoside Supplement | Chemical means to reduce replication stress during reprogramming and culture, limiting DNA damage and CNVs [14]. |
| Versene (EDTA Solution) | A non-enzymatic, gentle method for dissociating iPSCs, improving cell survival and reducing stress during passaging [20]. |
| Matrigel / Geltrex / Laminin-521 | Defined extracellular matrix coatings for feeder-free culture, supporting cell attachment and expansion while reducing variability [20]. |
| Essential 8 (E8) Medium | A chemically defined, xeno-free medium that provides a simpler and more controlled environment for hiPSC propagation [20]. |
| Giemsa Stain | The standard dye used in G-banding karyotyping to produce a distinct banding pattern for chromosome identification [21]. |
Genomic instability is a critical factor that can compromise the validity of disease models and the reproducibility of preclinical data. In the context of long-term cell culture, particularly with sensitive models like induced pluripotent stem cells (iPSCs), accumulated genetic alterations can lead to inconsistent differentiation, functional deficiencies, and unreliable experimental results. This guide provides troubleshooting and best practices for researchers to identify, monitor, and prevent genomic instability in their experiments.
Troubleshooting Common Genomic Instability Issues
FAQ 1: My iPSC culture shows inconsistent differentiation into the target cell type. Could genomic instability be the cause?
Yes, this is a common consequence of genomic instability. Alterations in the expression of genes that maintain pluripotency and control differentiation pathways can directly impair an iPSC line's ability to differentiate reliably into specific cell types [22]. This inconsistency undermines the reliability of downstream assay data.
- Diagnosis Steps:
- Karyotype Analysis: Perform G-banding to check for large-scale chromosomal abnormalities (e.g., trisomy 12 or 20) that are known to provide a growth advantage and alter differentiation potential [1].
- Functional Assay: Differentiate the suspect iPSC line in parallel with a low-passage, well-characterized control line. Compare the efficiency and purity of the resulting differentiated cells using cell-type-specific markers.
- Solution: Implement a routine genetic integrity check. If abnormalities are found, thaw an earlier, validated stock of the cell line with a known stable differentiation profile.
FAQ 2: After several passages, my cell line's growth rate and functional characteristics have changed. What should I do?
Genetic alterations acquired during prolonged culture (passage-induced mutations) can affect proliferation rates, viability, and functional characteristics [1] [22]. This is a typical sign of genomic instability and has been documented even in widely used lines like Jurkat cells, leading to marked variations in immunophenotype and cytokine production between laboratories [23].
- Diagnosis Steps:
- Monitor Proliferation: Keep detailed records of population doubling times and confluency at each passage. A significant increase in growth rate can indicate the expansion of a clone with a selective advantage, such as a gain of chromosome 12p or the 20q11.21 region [1].
- Genetic Screening: Use a high-resolution method like SNP array or whole-genome sequencing to identify copy number variations (CNVs) and single nucleotide variants (SNVs) that may have arisen during culture [1] [23].
- Solution: Establish a strict cell culture policy: avoid culturing cells for excessive passages, create large master banks of low-passage stocks, and routinely authenticate and characterize cell lines to prevent the dominance of genetically variant subpopulations.
FAQ 3: My experimental results are not reproducible between different stocks of the same cell line. How can I troubleshoot this?
Substantial genomic heterogeneity both between and within cell lines is a major source of irreproducibility. Genomic instability leads to a heterogeneous population of cells with different functional characteristics, growth rates, and differentiation potentials [22] [23].
- Diagnosis Steps:
- Cell Line Authentication: Use Short Tandem Repeat (STR) profiling to confirm the identity of your cell lines and rule out cross-contamination [23].
- Multi-Omic Comparison: For critical cell lines, compare the genomic (karyotype, CNVs), transcriptomic (RNA-seq), and functional (e.g., cytokine production, surface marker expression) profiles of the different stocks [23].
- Solution: Standardize cell culture protocols across laboratories. Replace old, high-passage cell stocks with newly authenticated, low-passage stocks from a reliable source. Clearly document the passage number and culture history for all experiments.
FAQ 4: How can I determine if a detected genetic variation in my iPSCs poses a safety risk for clinical applications?
It remains challenging to distinguish between innocuous genomic aberrations and those that may cause adverse effects like malignant transformation [1] [18]. However, certain mutations are considered higher risk.
- Diagnosis Steps:
- Focus on Hotspots: Prioritize the screening for mutations in known cancer-driver genes and recurrent CNV hotspots like 20q11.21, which contains anti-apoptosis and pluripotency-associated genes like BCL2L1 [1].
- Functional Validation: Conduct in vitro tumorigenicity assays (e.g., soft agar colony formation) and in vivo teratoma formation assays to assess the malignant potential of iPSC-derived cells.
- Solution: Employ high-resolution monitoring (e.g., SNP genotyping) throughout the preparation of cells for transplant [18]. Regulatory agencies typically require comprehensive genetic analysis, including karyotyping and higher-resolution methods like array genomic hybridization (AGH), to identify microdeletions before clinical use [22].
Detailed Experimental Protocols for Monitoring Genomic Instability
Protocol 1: Comprehensive Genetic Integrity Workflow for iPSCs
This workflow combines multiple techniques to detect different types of genomic instability at various scales.
Table 1: Methods for Detecting Genomic Instability in Cell Cultures
| Method | Detects | Resolution | Best For | Limitations |
|---|---|---|---|---|
| Karyotyping (G-banding) [1] | Numerical & large structural chromosomal changes (aneuploidy, translocations) | ~5-10 Mb | Routine quality control, gold standard for regulatory submissions [22] | Low resolution; cannot detect small CNVs or SNVs |
| Array Genomic Hybridization (AGH) [22] | Copy Number Variations (CNVs) | Kilobase level | Identifying microdeletions and recurrent CNV hotspots (e.g., 20q11.21) [1] | Cannot detect balanced translocations or low-frequency mosaicism [1] |
| Whole Genome Sequencing (WGS) [1] | Single Nucleotide Variants (SNVs), CNVs, structural variants | Single nucleotide | Most comprehensive profiling; identifying low-frequency variants and mutations of unknown origin [1] | Higher cost and complex data analysis |
Workflow Diagram: Genetic Integrity Monitoring Pathway
Protocol 2: Assessing Functional Consequences of Instability
Genomic instability must be linked to phenotypic outcomes. This protocol assesses the functional impact on a model T-cell line (Jurkat), but the principles are applicable to other cell types.
Method:
- Cell Stimulation: Stimulate cells from different laboratory stocks or passages in parallel. For Jurkat cells, use CD3/CD28 Dynabeads or PMA/Ionomycin [23].
- Phenotypic Analysis by Flow Cytometry: At 24 hours post-stimulation, analyze the cells for activation markers (e.g., CD69, CD25) to detect immunophenotype variations [23].
- Cytokine Production Profiling: Collect supernatant at 6-24 hours post-stimulation. Use a multiplex cytokine bead array (e.g., for IL-2, IFN-γ) to quantify functional output [23].
- Correlation with Genomic Data: Integrate functional data with genomic data (e.g., from WES or CMA) to link specific mutations or karyotypic changes to the observed phenotypic variations [23].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Genomic Instability Research
| Item | Function | Example Product(s) | Specific Use Case |
|---|---|---|---|
| Karyotyping Kit | Detects chromosomal aberrations via G-banding | Giemsa Stain | Routine cytogenetic analysis required by regulatory agencies for cell therapy applications [22]. |
| CGH/SNP Array | High-resolution detection of CNVs | Agilent GenetiSure Cyto CGH + SNP array [23] | Identifying recurrent CNV hotspots in iPSCs (e.g., 20q11.21) and confirming karyotype results [1] [23]. |
| Mycoplasma Detection Kit | Detects mycoplasma contamination | MycoAlert Mycoplasma Detection Kit [23] | Essential quality control step, as mycoplasma infection can induce chromosomal abnormalities and alter gene expression, confounding results [23]. |
| T-cell Activation Reagents | Functional assessment of immune cells | Human T-activator CD3/CD28 Dynabeads, PMA/Ionomycin [23] | Testing the functional impact of genomic instability in T-cell models like Jurkat cells by measuring activation and cytokine production [23]. |
| Multiplex Cytokine Assay | Quantifies multiple cytokines simultaneously | Multiplex cytokine bead array (e.g., for IL-2, IFN-γ) [23] | Profiling functional changes in cell secretome due to accumulated mutations, linking genotype to phenotype [23]. |
Workflow Diagram: From Instability to Functional Deficit
Practical Monitoring: Essential Tools for Detecting Genomic Drift
In long-term induced pluripotent stem cell (iPSC) culture research, maintaining genomic integrity is not optional—it is foundational. iPSCs possess an inherent propensity for genomic instability, with studies revealing that a genetically abnormal clone can overtake a culture in less than five passages [24]. This technical support guide provides a comprehensive framework for establishing a routine karyotyping schedule, a critical component in preventing genomic instability and ensuring the validity of your research and the safety of future therapeutic applications.
Frequently Asked Questions (FAQs)
1. Why is routine karyotyping non-negotiable in iPSC research? Karyotyping is a primary quality control measure because chromosomal abnormalities frequently arise during reprogramming, gene editing, and maintenance cultivation [24]. These aberrations can compromise differentiation efficiency, alter cellular function, and pose significant safety risks in cell replacement therapies [24]. Routine monitoring is the only way to catch these changes early.
2. What is the recommended baseline schedule for karyotyping my iPSC lines? A proactive schedule is essential for catching genomic drift before it compromises your cell lines. The following table summarizes the key timepoints:
| Cell Culture Stage | Recommended Action | Rationale & Supporting Data |
|---|---|---|
| Newly Established Line | Perform initial karyotyping at early passage (Passage 7-10) [20]. | Establishes a genomic baseline for the line post-reprogramming. |
| During Routine Maintenance | Karyotype every 10-15 passages during propagation [20]. | Monitors for instability acquired during long-term culture. |
| Pre-Differentiation | Validate karyotype before initiating major differentiation protocols [4]. | Ensures genomic integrity of the starting material for downstream experiments. |
| Post-Gene Editing | Karyotype after selection and expansion of edited clones [24]. | Confirms that the editing process has not introduced chromosomal aberrations. |
| After Cell Line Recovery | Karyotype after re-expansion from cryopreserved stocks [20]. | Verifies stability after the freeze-thaw cycle. |
3. What are the most common chromosomal abnormalities I should look for in iPSCs? Research has identified a consistent bias in the genetic changes acquired in human pluripotent stem cells (hPSCs). The most frequent anomalies involve [24] [15]:
- Trisomy of chromosome 12, 17, or X.
- Amplification of specific regions like chromosome 1, 12p, 17q, or 20q11.21.
4. My karyotype results are normal. Are my cells genetically pristine? Not necessarily. A normal karyotype is crucial but does not guarantee full genomic integrity. Traditional G-banding karyotyping has a resolution of 5-10 Mb, meaning smaller abnormalities can be missed [24]. It also cannot detect copy-neutral loss of heterozygosity (CN-LOH) or single point mutations [24] [15]. A comprehensive quality control panel should include additional assays like SNP arrays or sequencing.
Troubleshooting Guide: Interpreting Karyotyping Results
Problem: A suspected chromosomal abnormality is reported. Solution:
- Verify the Nomenclature: Ensure you understand the International System for Human Cytogenetic Nomenclature (ISCN). Common symbols include [25] [26]:
- del: Deletion
- t: Translocation
- inv: Inversion
- + / -: Gain or loss of a chromosome
- i: Isochromosome
- mar: Marker chromosome
- dn: De novo (not inherited from parents)
- Correlate with Biology: Determine if the abnormality is a known, culture-adapted mutation (e.g., gain of 20q11.21) that provides a growth advantage [24].
- Action: Discard the affected iPSC clone. The identified abnormality is likely to confer a selective advantage and may impact your research outcomes [20].
Problem: Subclonal abnormalities or mosaic cells are detected. Solution:
- Understand the Limitation: Karyotyping has a limited ability to identify sub-clonal populations; its sensitivity depends on the proportion of the abnormal cells and the number of metaphases analyzed [24].
- Action: If a minor sideline is detected, it is a strong indicator of emerging genomic instability. The culture should be considered compromised and regenerated from an earlier, fully characterized stock.
Problem: The karyotype is normal, but the cell line shows poor differentiation performance. Solution:
- Investigate Further: A normal karyotype rules out large chromosomal aberrations, but not smaller genetic lesions.
- Employ Higher-Resolution Techniques: Use SNP array analysis to detect copy number variations (CNVs) and copy-neutral loss of heterozygosity (CN-LOH) as small as 350 kb [24]. Consider whole-exome sequencing to identify single point mutations that can accumulate in iPSCs [15].
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and kits are essential for establishing and monitoring iPSC genomic integrity.
| Reagent / Kit | Primary Function | Application in Genomic Health Checks |
|---|---|---|
| Colcemid | Inhibits spindle fiber formation, arresting cells in metaphase. | Used in the preparation of samples for G-banding karyotype analysis to obtain analyzable metaphase spreads [24]. |
| QIAamp DNA Blood Mini Kit | Extracts high-quality genomic DNA from cell samples. | Prepares DNA for high-resolution analysis techniques like SNP arrays or next-generation sequencing (NGS) [24]. |
| Illumina Global Screening Array | A single-nucleotide polymorphism (SNP) genotyping platform. | Used for molecular karyotyping to sensitively detect CNVs and CN-LOH with high resolution [24]. |
| STEMdiff Mesenchymal Progenitor Kit | Differentiates iPSCs into mesenchymal stromal/stem cells (iMS cells). | Used in studies to trace genomic instability from the iPSC stage through differentiation, a key quality control step [4]. |
Experimental Workflow for Comprehensive Genomic Screening
The diagram below illustrates a multi-tiered experimental workflow for monitoring genomic integrity in iPSCs, integrating both routine checks and higher-resolution follow-up analyses.
Figure 1: A tiered workflow for genomic health checks in iPSC cultures, from routine karyotyping to advanced molecular analysis.
Leveraging Targeted qPCR Assays for Rapid, Cost-Effective Screening of Common Abnormalities
The utility of induced pluripotent stem cells (iPSCs) in research and regenerative medicine is often compromised by genomic instability that arises during reprogramming and long-term culture. This instability can manifest as copy number variations (CNVs), single nucleotide variants (SNVs), and chromosomal aberrations, which collectively impact the reliability and safety of iPSC-based models and therapies [1]. Targeted qPCR assays offer a rapid and cost-effective solution for routine monitoring of the most common karyotypic abnormalities, serving as a critical quality control checkpoint to ensure genomic integrity in iPSC cultures [27].
Frequently Asked Questions (FAQs)
1. Why is genomic instability a particular concern in long-term iPSC culture? Genomic instability in iPSCs originates from multiple sources: pre-existing variations in parental somatic cells, reprogramming-induced mutations, and passage-induced mutations acquired during prolonged culture [1]. Certain abnormalities, such as gains on chromosome 12 or 20q11.21, confer a selective growth advantage, allowing affected cells to overtake the culture over time and leading to reduced differentiation capacity and increased neoplastic risk [1] [27].
2. How does targeted qPCR compare to other methods like karyotyping or aCGH for abnormality screening? While traditional karyotyping and array-based methods like aCGH provide broad genomic coverage, they are often lower in resolution, more time-consuming, and costlier. Targeted qPCR is specifically designed for high-throughput, rapid screening of known common abnormality hotspots. It offers a practical solution for frequent monitoring, allowing researchers to identify problematic cultures early before committing resources to extensive differentiations [27].
3. My iPSC line shows a common abnormality. Should I immediately discard it? The decision depends on the specific abnormality and your research application. Gains in regions like 20q11.21 are well-documented to impair differentiation potential and increase tumorigenicity [1] [27]. For most therapeutic or rigorous preclinical studies, discarding the line is the safest course. For basic research, you might proceed with extreme caution and clear documentation, but be aware that results may be irreproducible or misleading.
4. Can the reprogramming method influence the genomic instability of the resulting iPSCs? Yes. Reprogramming methods that utilize integrating vectors or specific oncogenes (e.g., c-MYC) can contribute to genomic instability [28]. Non-integrating methods, such as episomal vectors or Sendai virus, are generally preferred for generating clinical-grade iPSCs as they lower the risk of insertional mutagenesis and viral immunogenicity [28].
Troubleshooting Guides
Problem 1: Inconsistent Differentiation Outcomes
- Symptoms: High variability in differentiation efficiency and purity between passages or batches of the same iPSC line. Presence of non-target cell types or abnormal cellular morphology [27].
- Potential Cause: The accumulation of genomic abnormalities in the iPSC master cell bank or during culture expansion. Common abnormalities like trisomy 12 or 20q11.21 amplification can directly alter differentiation capacity [27].
- Solutions:
- Implement Routine Screening: Integrate a targeted qPCR assay for common karyotypic abnormalities as a mandatory quality control check before initiating any differentiation experiment.
- Monitor Culture Passages: Assess genomic stability at key passages (e.g., every 10 passages) to track the emergence of abnormalities over time.
- Establish Clear Thresholds: Define acceptable cut-off values for chromosomal copy number (e.g., 1.5 to 2.5 for autosomes) based on your assay validation data. Discard lines that fall outside this range [27].
Problem 2: Amplification in No Template Control (NTC)
- Symptoms: The NTC well, which contains all qPCR reagents except the nucleic acid template, shows amplification and a Ct value [29] [30].
- Potential Causes:
- Contamination: Aerosol contamination from amplified PCR products or concentrated positive control templates in the lab environment [29].
- Primer-Dimer Formation: The forward and reverse primers anneal to each other and are amplified, typically resulting in a low efficiency reaction and a melt curve peak at a lower temperature than the specific product [30].
- Solutions:
- Prevent Contamination: Use separate physical areas for reagent preparation, sample handling, and post-amplification analysis. Clean workspaces and pipettes with 10% bleach or 70% ethanol [29].
- Use a Uracil-DNA Glycosylase (UDG) System: Employ a master mix containing dUTP and UDG. This enzyme will degrade any contaminating amplicons from previous PCRs before the new reaction begins [29].
- Optimize Primer Design: Re-design primers to avoid self-complementarity and check for dimer formation using oligonucleotide analysis tools. Increase the annealing temperature during the qPCR cycle to discourage non-specific binding [31] [30].
- Physical Separation: Place NTC wells away from high-concentration sample wells on the qPCR plate to prevent splashing or aerosol cross-contamination [30].
Problem 3: Poor qPCR Assay Efficiency or Non-Specific Amplification
- Symptoms: A standard curve with an efficiency below 90% or above 110%, or a melt curve with multiple peaks indicating non-specific products [30].
- Potential Causes: Suboptimal primer/probe design, incorrect annealing temperature, or contaminated reagents [31] [29].
- Solutions:
- Verify Oligo Design: Ensure primers and probes meet optimal design criteria (see Table 2). Use tools like IDT's OligoAnalyzer to check for secondary structures and dimer formation [31].
- Perform BLAST Analysis: Confirm that your primer sequences are unique to the intended target to avoid amplifying non-specific genomic regions [31].
- Optimize Annealing Temperature: Perform a temperature gradient experiment to determine the ideal annealing temperature for your specific assay [31].
- Use High-Purity Reagents: Source oligonucleotides from manufacturers that take steps to prevent bacterial DNA contamination during synthesis and purification [29].
Common Karyotypic Abnormalities in iPSCs
The following table summarizes the most frequent genomic abnormalities identified in human iPSCs, which are ideal targets for a focused qPCR screening panel [1] [27].
Table 1: Common Genomic Abnormalities in Human iPSCs
| Chromosomal Abnormality | Functional Consequence | Impact on Differentiation |
|---|---|---|
| Trisomy 12 | Contains pluripotency genes (e.g., NANOG); confers selective growth advantage [1]. | Recurrent aneuploidy; alters pluripotency network. |
| Amplification of 20q11.21 | Harbors anti-apoptosis (BCL2L1) and pluripotency-associated genes (DNMT3B, ID1) [1]. | Well-documented to reduce differentiation capacity and purity [27]. |
| Trisomy 8 | Another recurrent aneuploidy observed in both iPSCs and ESCs [1]. | Can alter differentiation propensity and culture stability. |
| Trisomy X (in female lines) | A common sex chromosome aneuploidy [1]. | Effect on differentiation requires further study. |
Experimental Protocol: Targeted qPCR Screening for Common iPSC Abnormalities
This protocol provides a detailed methodology for using a bulk qPCR assay to screen for common karyotypic abnormalities in human iPSCs, based on the approach validated in scientific studies [27].
Sample Preparation and DNA Extraction
- Cell Lysis: Harvest a minimum of 1x10^6 iPSCs. Extract high-quality, high-molecular-weight genomic DNA using a silica column-based kit to minimize inhibitor carryover.
- DNA Quantification: Precisely quantify the DNA using a fluorometer. Normalize all samples to the same concentration (e.g., 10 ng/µL) in nuclease-free water.
Primer and Probe Design
- Target Selection: Design assays to target the nine most common karyotypic abnormalities in human iPSCs (e.g., chromosomes 1, 8, 12, 17, 20, and X) [27].
- Reference Genes: Include at least two reference assays targeting genomically stable regions on different chromosomes (e.g., chromosome 14).
- Design Parameters:
- Amplicon Length: 70–150 bp.
- Tm: Primers: 60–64°C; Probes: 5–10°C higher than primers.
- GC Content: 35–65% for both primers and probes.
- Specificity: Ensure primers span an exon-exon junction if targeting an RNA sequence for reverse-transcribed samples, and run a BLAST analysis for specificity [31].
qPCR Setup and Run
- Reaction Mix: Prepare a master mix for each sample containing:
- 1X double-quenched probe master mix (e.g., TaqMan).
- Primers and probe for the target abnormality.
- Primers and probe for the reference gene.
- 50 ng of normalized genomic DNA.
- Controls:
- No Template Control (NTC): Contains all reaction components except DNA.
- Positive Control: Genomic DNA from a cell line with a known, validated abnormality.
- Negative Control: Genomic DNA from a confirmed karyotypically normal cell line.
- Cycling Conditions:
- UDG incubation (if using): 50°C for 2 minutes.
- Polymerase activation: 95°C for 20 seconds.
- 40 cycles of: Denature at 95°C for 3 seconds, Anneal/Extend at 60°C for 30 seconds.
Data Analysis
- Copy Number Calculation: Use the ΔΔCt method. Normalize the Ct of the target assay to the reference assay in the test sample and a diploid control sample.
- Copy Number = 2 × 2^(–ΔΔCt)
- Interpretation:
- Normal: Copy number between 1.5 and 2.5 for autosomes (or 0.7-1.3 for chromosome X in male lines).
- Abnormal: Copy number ≤ 1.5 or ≥ 2.5 (for autosomes) indicates a potential deletion or amplification, respectively [27].
The workflow for this screening process is outlined below.
Best Practices for qPCR Assay Design and Validation
Adhering to established design principles is crucial for developing a robust and reliable targeted qPCR assay.
Table 2: qPCR Primer and Probe Design Guidelines [31]
| Parameter | Recommended Guideline | Rationale |
|---|---|---|
| Primer Length | 18–30 bases | Balances specificity and binding efficiency. |
| Primer Tm | 60–64°C (ideal: 62°C); pair within 2°C | Ensures simultaneous and efficient binding of both primers. |
| Probe Tm | 5–10°C higher than primers | Ensures probe is bound before primer extension. |
| GC Content | 35–65% (ideal: 50%) | Provides sequence complexity while avoiding stable secondary structures. |
| Amplicon Length | 70–150 bp | Ideal for efficient amplification under standard cycling conditions. |
| Specificity Check | BLAST analysis; avoid poly-G sequences | Confirms uniqueness to the target and prevents G-quadruplex formation. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Targeted Genomic Screening
| Item | Function | Consideration |
|---|---|---|
| High-Fidelity DNA Polymerase | Amplifies target sequences with low error rates. | Essential for accurate quantification in pre-amplification steps, if used. |
| Double-Quenched Probes | Provides specific signal detection during qPCR. | Lowers background fluorescence, increasing signal-to-noise ratio compared to single-quenched probes [31]. |
| dUTP/UDG Master Mix | Prevents carryover contamination from previous PCR products. | UDG enzymatically degrades uracil-containing amplicons before PCR begins [29]. |
| Commercial gDNA Extraction Kits | Isolates high-purity, inhibitor-free genomic DNA. | Silica-column based kits are preferred for removing PCR inhibitors. |
| Predesigned Assay Panels | Targets the most common iPSC abnormalities. | Available from vendors like STEMCELL Technologies; saves development time [27]. |
| Nucleoside Supplements | Reduces replication stress during reprogramming/culture. | Adding nucleosides to culture media can decrease DNA damage and CNV load in resulting iPSCs [14]. |
The diagram below illustrates how replication stress from reprogramming can lead to genomic instability and how targeted screening and mitigation strategies form a complete quality control cycle.
Foundational Principles and Applications in iPSC Research
What are the fundamental principles distinguishing SNP microarray and aCGH?
SNP microarray and aCGH are powerful genomic profiling technologies, but they operate on different principles and are suited for detecting distinct types of genomic aberrations.
Array Comparative Genomic Hybridization (aCGH) is primarily designed to detect copy number variations (CNVs), which are gains or losses of genomic DNA. Its principle is based on a competitive hybridization between a test DNA and a reference DNA, each labeled with different fluorescent dyes (typically Cyanine 3 for test and Cyanine 5 for reference). The mixture is applied to a microarray chip containing thousands of known DNA probes. The resulting color at each probe spot reveals the copy number: a green-to-red ratio indicates equal copy number, a shift towards red suggests a loss in the test sample, and a shift towards green indicates a gain [32].
Single Nucleotide Polymorphism (SNP) Microarray is designed to detect single nucleotide polymorphisms and can also infer copy number. Its principle is based on hybridizing a single sample's DNA to a chip containing probes for known SNP loci. By measuring the hybridization signal intensity and, crucially, the allelic composition (the "B allele frequency"), it can determine both the copy number at each locus and the genotype (e.g., AA, AB, BB). This dual measurement allows SNP microarrays to detect not only CNVs but also copy-neutral loss of heterozygosity (LOH), a change in the genome where both copies of a gene are from one parent, without a change in copy number [33] [34].
Table 1: Core Differences Between aCGH and SNP Microarray
| Feature | aCGH | SNP Microarray |
|---|---|---|
| Primary Principle | Competitive, two-color hybridization | Single-sample hybridization with intensity and allelic ratio measurement |
| Detects CNVs | Yes | Yes |
| Detects SNPs & Genotypes | No | Yes |
| Detects Copy-Neutral LOH | No | Yes |
| Key Outputs | Log R ratio (intensity) | Log R ratio (intensity) & B Allele Frequency |
Why are these techniques critical for monitoring genomic instability in iPSC cultures?
Genomic instability is a major concern in induced pluripotent stem cell (iPSC) research, potentially compromising their use in disease modeling and regenerative medicine. SNP microarrays and aCGH are essential for identifying the following types of genetic alterations that arise during reprogramming and long-term culture [1] [22]:
- Copy Number Variations (CNVs): These are recurrently observed in iPSCs. A common hotspot is an amplification of 20q11.21, a region containing genes associated with pluripotency and anti-apoptosis (e.g., DNMT3B, BCL2L1), which can provide a selective growth advantage [1].
- Chromosomal Aberrations: Aneuploidy, particularly gains of chromosomes 12, 8, and X, is frequently reported in both iPSCs and ESCs, likely conferring a proliferative advantage [1].
- Copy-Neutral Loss of Heterozygosity (LOH): This can unmask recessive mutations and is implicated in tumorigenesis. SNP arrays are uniquely capable of detecting this abnormality, which aCGH cannot [33] [34].
These aberrations originate from multiple sources: pre-existing mutations in parental somatic cells that are clonally expanded during reprogramming; reprogramming-induced mutations caused by replication stress from the forced expression of factors like OCT4 and c-MYC; and passage-induced mutations accumulated during prolonged culture [1] [14] [22]. Routine screening with these technologies is therefore paramount for quality control in iPSC banking and for ensuring the safety of future cell therapies.
Troubleshooting Guides
Our aCGH data shows high background noise and poor signal-to-noise ratio. What steps can we take?
Poor data quality in aCGH often stems from suboptimal sample preparation or hybridization conditions. Follow this checklist to resolve these issues [32]:
Table 2: Troubleshooting aCGH Quality Control Metrics
| QC Metric | Target Value | Problem | Potential Causes & Solutions |
|---|---|---|---|
| Background Noise | < 25 | High Background | Cause: Contaminated DNA, inefficient washing, or incorrect hybridization stringency.Solution: Re-purify DNA using columns or ethanol precipitation. Ensure wash buffers are fresh and follow washing protocols strictly. Verify hybridization temperature and buffer composition. |
| Signal Intensity | > 200 | Low Signal | Cause: Inefficient fluorescent labeling or degraded DNA.Solution: Check DNA integrity via gel electrophoresis. Ensure the labeling reaction is performed at the correct temperature and for the full recommended duration. Do not shorten the primer extension step. |
| Signal-to-Noise Ratio | > 30 | Low Ratio | Cause: Combination of high background and low signal.Solution: Address both issues above. Also, verify the amount of Cot-1 DNA in the hybridization mix, as it blocks non-specific binding of repetitive sequences. |
| Derivative Log Ratio (DLR) | < 0.2 | High DLR | Cause: Poor DNA quality and/or inefficient labeling efficiency. A high DLR indicates high noise, reducing the ability to call CNVs accurately.Solution: Start with high-quality, high-molecular-weight DNA (A260/280 > 1.8; A260/230 ~2.0-2.2). Re-check the labeling reaction efficiency using a NanoDrop before hybridizing to the expensive chip. |
Our SNP microarray results show unusual clustering or a high failure rate. How can we improve this?
Unusual clustering in SNP genotyping can arise from several technical and biological factors [35].
Problem: Trailing or Multiple Clusters
- Cause 1 (Technical): Variation in gDNA quality or concentration across samples. This is a common cause of "trailing" where data points smear between clusters.
- Solution: Accurately quantify all DNA samples and use a standardized, high-quality isolation method to ensure consistent purity and integrity. Avoid degraded DNA [35].
- Cause 2 (Biological): A hidden SNP under the probe or primer binding site.
- Solution: Query the dbSNP database for other known polymorphisms near your target SNP. If found, redesign the assay to avoid this region by masking the position as an "N" in the design tool [35].
- Cause 3 (Biological): The genomic region being assayed is within a copy number variation.
- Solution: Evaluate the sample with a dedicated TaqMan Copy Number Assay to confirm if the region is amplified or deleted, which would explain the abnormal genotype clustering [35].
Problem: No Amplification or High Failure Rate
- Cause: Inaccurate DNA quantitation, degraded DNA, or the presence of PCR inhibitors in the sample.
- Solution: Re-quantify DNA using a fluorescence-based method for higher accuracy. Check DNA integrity on a gel. If inhibitors are suspected, clean up the DNA sample with a purification column [35].
How can we mitigate replication stress during iPSC reprogramming to reduce genomic instability?
A key driver of genomic instability during iPSC generation is replication stress, triggered by the expression of reprogramming factors. Proactively reducing this stress leads to iPSC lines with fewer genetic alterations [14].
- Chemical Mitigation: Supplement the reprogramming medium with nucleosides. This provides the raw materials for DNA synthesis, alleviating the nucleotide depletion that contributes to replication stress. Studies show this treatment reduces the load of DNA damage (γH2AX foci) and lowers the number of de novo CNVs in the resulting iPSC lines without increasing reprogramming efficiency [14].
- Genetic Mitigation: Increasing the levels of the checkpoint kinase CHK1, a key regulator of the replication stress response, has been shown to reduce reprogramming-induced DNA damage. While this is often done genetically, it underscores the importance of the CHK1 pathway in maintaining genomic integrity during reprogramming [14].
Detailed Methodologies
What is a standardized workflow for performing SNP microarray analysis?
The general workflow for SNP microarray is robust and can be broken down into several key stages [33]:
- Chip Fabrication: Predesigned oligonucleotide probes, specific to the target SNP loci, are synthesized and arranged in a high-density pattern on a solid glass carrier. Technologies like Affymetrix's GeneChip allow for in-situ oligonucleotide synthesis with extreme density [33].
- Sample Preparation: High-quality, high-molecular-weight genomic DNA is isolated from the sample (e.g., iPSCs). The concentration and purity (A260/280 > 1.8) are critically important. The DNA is then fluorescently labeled [33].
- Hybridization: The labeled DNA is denatured and applied to the SNP microarray chip under controlled conditions of temperature, salt concentration, and time to allow for specific hybridization between the sample DNA and the complementary probes on the array [33].
- Washing and Scanning: After hybridization, the chip is washed stringently to remove any non-specifically bound DNA. It is then scanned with a high-resolution fluorescence scanner to detect the signal at each probe [33].
- Data Analysis: Specialized software analyzes the scanned image, extracting raw signal data. This data is processed to generate the two key values for each SNP: the Log R Ratio (normalized intensity for copy number) and the B Allele Frequency (allelic ratio for genotype). These are plotted along the genome for visualization and detection of aberrations [33] [34].
What is the detailed protocol for aCGH in profiling iPSC lines?
For reliable aCGH results, meticulous attention to protocol details is required [32]:
- Step 1: DNA Quality Control. Isolate genomic DNA from your iPSC line and a reference control. Assess purity by spectrophotometry (A260/280 ~1.8; A260/230 ~2.0-2.2) and check integrity by gel electrophoresis (should be a high molecular weight band). Store DNA at 4°C to avoid freeze-thaw cycle-induced breaks.
- Step 2: Fluorescent Labeling. Label 1 µg of test and reference DNA with different cyanine dyes (e.g., Cy3 and Cy5) using a validated labeling kit (e.g., Enzo's CYTAG series). The reaction, based on random priming and primer extension, must be performed at the correct temperature and for the full duration to ensure efficient dye incorporation.
- Step 3: Probe Purification and Quality Check. Purify the labeled DNA to remove unincorporated nucleotides, using silica columns or ethanol precipitation. Check the labeling efficiency with a NanoDrop: for a 4x180k array, aim for a DNA yield >5.0 µg, with specific activity of at least ~60 pmol/µg for Cy3 and ~40 pmol/µg for Cy5.
- Step 4: Hybridization. Mix the labeled test and reference DNA with Cot-1 DNA (to block repetitive sequences) and hybridization buffer. Denature the mixture and apply it to the aCGH microarray. Incubate in a hybridization chamber at the recommended temperature and duration (typically ~24-40 hours).
- Step 5: Washing, Scanning, and Analysis. After hybridization, wash the array according to the manufacturer's protocol to remove non-specific binding. Scan the slide with a dual-laser scanner and extract the log2 ratio of test/reference signal for each probe using the appropriate software. Aberrations are called when the log2 ratio significantly deviates from zero.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Genomic Analysis
| Reagent / Kit | Function | Application Notes |
|---|---|---|
| CYTAG TotalCGH Labeling Kit | Fluorescent labeling of DNA for aCGH. | Allows for SNP arrays in addition to standard CGH, providing flexibility [32]. |
| CYTAG SuperCGH Labeling Kit | Fluorescent labeling for limited DNA input. | Designed for samples with as little as 50 ng of starting DNA, crucial for rare iPSC clones [32]. |
| Infinium Whole-Genome Genotyping BeadChip | High-density SNP genotyping platform. | Available in various densities (e.g., 109K, 317K SNPs); enables simultaneous measurement of intensity and allelic ratios [34]. |
| Nucleoside Supplement | Chemical mitigation of replication stress. | Adding to reprogramming media reduces DNA damage and CNVs in resulting iPSCs [14]. |
| PCR & Gel Clean-up Kit | Purification of labeled DNA probes. | Typically included in labeling kits to remove unincorporated dyes and nucleotides post-labeling [32]. |
| Cot-1 DNA | Blocking of repetitive genomic sequences. | Added in excess to the hybridization mix to prevent non-specific binding and reduce background "wave effects" [32]. |
Integrating Genomic Stability Assessment into Standard iPSC Culture Workflows
FAQs on Genomic Instability in iPSC Cultures
What types of genomic abnormalities are most common in iPSCs?
The most frequent genomic abnormalities in iPSCs are copy number variations (CNVs) and single nucleotide variants (SNVs) [36]. CNVs are deletions or amplifications of DNA sections that often confer a selective advantage for proliferation and survival, while SNVs can disrupt differentiation capacities and increase the risk of malignant transformation [36]. Specific recurrent abnormalities include:
- Trisomy of chromosome 12, 17, or X [15]
- Amplification of 20q11.21, a region containing pluripotency and anti-apoptosis genes [1]
- Uniparental disomy (UPD), where both copies of a chromosome come from a single parent [15]
When should I test my iPSC cultures for genomic instability?
Regular monitoring at key process stages is essential for maintaining genomic integrity [36]:
| Testing Stage | Purpose | Recommended Methods |
|---|---|---|
| Acquisition of a new line | Establish baseline genomic stability | G-banding + digital PCR or NGS [36] |
| After reprogramming/gene editing | Screen for procedure-induced aberrations | Digital PCR for clone screening [36] |
| During cell amplification & maintenance | Monitor for culture-acquired defects | Digital PCR every 5-10 passages [36] |
| Pre-banking characterization | Ensure quality before preservation | NGS or G-banding + digital PCR [36] |
| During differentiation | Check stability until full differentiation | Digital PCR at media change points [36] |
| End of process | Final validation before publication/therapy | NGS or G-banding + digital PCR [36] |
How does the reprogramming process contribute to genomic instability?
Reprogramming induces replication stress (RS) similar to oncogene-induced DNA damage [14]. Expression of reprogramming factors (especially OSKM) causes:
- Increased DNA damage marked by elevated γH2AX levels [14]
- Reduced replication fork speed [14]
- Generation of copy number variations enriched at fragile sites [14]
This replication stress originates from multiple sources: pre-existing variations in parental somatic cells, reprogramming-induced mutations occurring during the process, and passage-induced mutations arising during prolonged culture [1].
What culture practices can minimize genomic instability?
- Limit replication stress during reprogramming by adding nucleoside supplements [14]
- Avoid overgrowth and passage when colonies are large but not overly dense [6]
- Minimize time out of incubator (under 15 minutes at a time) [6]
- Use quality-controlled reagents with fresh culture medium (less than 2 weeks old when stored at 2-8°C) [6]
- Ensure even cell aggregate sizing during passaging to prevent selective pressure [6]
Troubleshooting Guides
Problem 1: Excessive Differentiation (>20%) in Cultures
Potential Causes and Solutions [6]:
| Cause | Solution | Prevention Tip |
|---|---|---|
| Old or compromised culture medium | Use fresh complete medium (<2 weeks old at 2-8°C) | Label medium with preparation date |
| Overgrown colonies | Passage when colonies are large and compact with dense centers | Establish consistent passaging schedule |
| Prolonged exposure outside incubator | Limit plate removal to <15 minutes at a time | Plan all procedures before removing cells |
| Uneven cell aggregate sizing | Ensure evenly sized aggregates during passaging | Standardize dissociation protocol |
Additional Steps:
- Remove differentiated areas manually before passaging [6]
- Decrease colony density by plating fewer aggregates [6]
- For ReLeSR users: reduce incubation time if your cell line is particularly sensitive [6]
Problem 2: Low Cell Attachment After Passaging
Solutions [6]:
- Plate 2-3 times more cell aggregates initially and maintain more confluent cultures
- Work quickly after treatment with passaging reagents to minimize suspension time
- Reduce incubation time with passaging reagents for sensitive cell lines
- Avoid excessive pipetting; instead increase incubation time by 1-2 minutes for dense colonies
- Verify appropriate plate type: non-tissue culture-treated for Vitronectin XF; tissue culture-treated for Corning Matrigel [6]
Problem 3: Managing Replication Stress During Reprogramming
Experimental Protocol to Reduce Genomic Instability [14]:
Nucleoside Supplementation Method:
- Preparation: Create nucleoside stock solution containing adenosine, guanosine, cytidine, and uridine at 10 mM each in DMEM
- Supplementation: Add nucleoside mix to reprogramming medium at 10-50 μM final concentration
- Timing: Maintain nucleoside supplementation throughout the reprogramming process
- Validation: Monitor γH2AX levels to confirm reduction in DNA damage
Expected Outcomes:
- Reduced replication stress and DNA damage markers [14]
- Lower incidence of copy number variations in resulting iPSC lines [14]
- Decreased multi-telomeric signals indicating reduced chromosomal fragility [14]
The Scientist's Toolkit: Essential Reagents for Genomic Stability
| Reagent/Category | Function | Examples & Notes |
|---|---|---|
| Quality Control Tools | Detect genomic abnormalities | Digital PCR (targeted CNVs), NGS (SNVs/indels), Karyotyping (large structural changes) [36] |
| Nucleoside Supplements | Reduce replication stress during reprogramming | Adenosine, guanosine, cytidine, uridine mix [14] |
| Advanced Culture Media | Support robust expansion and maintenance | HiDef B8 Growth Medium: precisely balanced nutrients, growth factors, cytokines [37] |
| Cell Recovery Supplements | Enhance viability during passaging and thawing | Ready-CEPT: improves cell recovery post-thawing [37] |
| Passaging Reagents | Gentle dissociation for maintenance | ReLeSR, Gentle Cell Dissociation Reagent [6] |
| Checkpoint Kinase Modulators | Limit replication stress | CHK1 enhancement reduces reprogramming-induced DNA damage [14] |
Comprehensive Genomic Stability Testing Workflow
Detailed Experimental Protocol: Nucleoside Supplementation for Stable Reprogramming
Background: Reprogramming factors induce replication stress similar to oncogene activation, leading to DNA damage and genomic rearrangements [14]. Nucleoside supplementation addresses nucleotide pool imbalances during this high-stress period.
Step-by-Step Procedure:
Preparation of Nucleoside Stock Solution:
- Dissolve solid nucleosides (adenosine, guanosine, cytidine, uridine) in DMEM to create individual 10 mM stock solutions
- Sterilize by passing through 0.22μm filter
- Combine equal volumes to create a 10 mM mixed nucleoside stock
- Aliquot and store at -20°C for up to 6 months
Reprogramming with Supplementation:
- Add mixed nucleoside stock to reprogramming medium to achieve 10-50 μM final concentration
- Include nucleosides throughout the entire reprogramming process (typically 14-21 days)
- Refresh nucleoside-containing medium daily during critical reprogramming phases
Validation and Quality Control:
- Monitor γH2AX levels by immunofluorescence to confirm reduction in DNA damage
- Assess replication fork speed by DNA combing analysis if available
- Perform CNV analysis on resulting iPSC lines by aCGH or digital PCR
Expected Results:
- 40-60% reduction in γH2AX foci during reprogramming [14]
- Significant decrease in multi-telomeric signals (indicator of chromosomal fragility) [14]
- 30-50% reduction in de novo CNVs in supplemented iPSC lines [14]
Troubleshooting Notes:
- If nucleoside supplementation shows no effect, verify stock solution concentration and activity
- Excessive nucleoside concentrations may be toxic; perform dose-response testing for new cell types
- Combine with CHK1 enhancement for synergistic reduction of replication stress [14]
Frequently Asked Questions (FAQs)
Q1: What constitutes a CNV that requires action in a research iPSC line? A CNV likely requires investigative action if it is: (1) de novo (not present in the parental somatic cell line); (2) large in size (often >1-5 Mb, though this threshold can vary); (3) located in a genomic region harboring tumor suppressor genes or oncogenes (e.g., deletions affecting PTEN or amplifications of MYC); and/or (4) demonstrates increasing prevalence or allele frequency over successive passages in culture, suggesting a selective growth advantage [38] [15] [39]. The joint ACMG/ClinGen recommendations provide a quantitative, evidence-based framework for classifying CNVs into five tiers (Pathogenic, Likely Pathogenic, Variant of Uncertain Significance (VUS), Likely Benign, Benign) to guide this decision [38].
Q2: My NGS-based CNV detection shows high noise. How can I distinguish true positive CNVs from artifacts? High noise can stem from several sources. To mitigate this:
- Verify Input DNA Quality: Ensure your input DNA is not degraded and is free of contaminants (e.g., phenol, salts) by checking 260/230 and 260/280 ratios [40].
- Cross-validate with an Orthogonal Method: Use a different technology platform to confirm the call. A true positive CNV should be consistently detected by, for example, both NGS read-depth analysis and digital PCR or array CGH [41] [42].
- Check for GC Bias and Library Complexity: Over-amplification during library prep can exacerbate coverage noise in GC-rich or poor regions. Ensure your library has high complexity and avoid excessive PCR cycles [40].
- Utilize Healthy Control Samples: Process control samples (e.g., well-characterized, genomically stable iPSC lines) in parallel. CNVs not found in these controls are more likely to be genuine calls in your test samples [39].
Q3: During long-term iPSC culture, how do I differentiate between a random genetic drift and a true clonal expansion of a CNV? Monitoring the variant allele frequency (VAF) or prevalence of the CNV across passages and across multiple subclones is key.
- Random Genetic Drift: The VAF of the CNV will fluctuate stochastically around a mean value and will not consistently increase over time [43].
- Clonal Expansion: The VAF of the CNV will show a consistent, directional increase over successive passages. If you perform single-cell cloning, the CNV will be present in a growing proportion of the daughter clones, indicating it confers a selective advantage [15] [43]. Intracellular selection can shape the mutational landscape during culture expansion, often selecting against putatively actionable mutations [43].
Q4: What are the critical quality control checkpoints for CNV analysis in iPSCs? A robust QC pipeline includes:
- Parental Line Characterization: Establish a baseline CNV profile for the somatic cell source used for reprogramming [15].
- Post-Reprogramming CNV Screening: Perform a comprehensive CNV analysis on early passage master cell banks of the iPSC clone [15].
- Routine Monitoring at Regular Passage Intervals: Incorporate CNV screening (e.g., every 10-20 passages) during long-term culture to detect newly acquired variants [15] [43].
- Pre-Differentiation Check: Screen the iPSC batch immediately before initiating differentiation experiments, as genomic alterations can impact differentiation efficiency and the functionality of the resulting cells [15].
Troubleshooting Guides
Problem 1: Low Yield or Quality in NGS-based CNV Library Preparation
Symptoms:
- Low final library concentration.
- Broad or multi-peaked fragment size distribution on the BioAnalyzer/Fragment Analyzer.
- High percentage of adapter-dimers (sharp peak ~70-90 bp).
| Root Cause | Corrective Action |
|---|---|
| Degraded or contaminated DNA input | Re-purify input DNA; check absorbance ratios (260/280 ~1.8, 260/230 >1.8); use fluorometric quantification (Qubit) over UV absorbance [40]. |
| Inefficient fragmentation/ligation | Optimize fragmentation time/enzyme concentration; titrate adapter-to-insert molar ratio; ensure fresh ligase buffer [40]. |
| Overly aggressive purification | Optimize bead-to-sample ratio during clean-up steps to avoid discarding desired fragments; avoid over-drying beads [40]. |
| Over-amplification (PCR bias) | Reduce the number of PCR cycles during library amplification; use a high-fidelity polymerase [40]. |
Problem 2: Inconsistent CNV Calls Across Different Analysis Platforms
Symptoms:
- A CNV is called by one algorithm or platform (e.g., from NGS data) but not confirmed by another (e.g., array CGH or digital PCR).
- Poor confidence scores for called CNVs.
| Root Cause | Corrective Action |
|---|---|
| Differences in platform resolution and probe/target coverage | Use a platform with CNV-focused design (e.g., arrays with probes targeting known CNV regions) for validation. For NGS, ensure sufficient sequencing depth (>30x for WGS) and use multiple complementary detection methods (read-depth, paired-end, split-read) [41] [42]. |
| Low sample quality or quantity | Re-check DNA quality and concentration. For single-cell CNV analysis, be aware that Whole Genome Amplification (WGA) artifacts are a major confounder; use WGA methods with robust quality metrics [39] [41]. |
| Inappropriate reference or control | Use matched, high-quality control samples processed identically to the test samples. Ensure the reference genome and algorithm parameters are appropriate for your data type [41]. |
Problem 3: Suspected CNV-Driven Genomic Instability in iPSC Culture
Symptoms:
- Observed rapid change in cell growth rate or morphology.
- Previous CNV screening identified a VUS or likely pathogenic CNV.
- Differentiation efficiency suddenly drops without explanation.
Diagnostic and Mitigation Workflow:
Action Thresholds and Classification Framework
The following table summarizes key quantitative and qualitative criteria to help establish action thresholds for CNVs in iPSCs, synthesizing consensus recommendations [38] and research findings [15] [39] [42].
Table 1: CNV Classification and Action Thresholds for iPSC Research
| CNV Category | Typical Size Range | Key Characteristics & Gene Content | Recommended Action for iPSC Research |
|---|---|---|---|
| Pathogenic / Likely Pathogenic | Often >1 Mb; can be smaller if key gene is affected. | - Overlaps well-established, dosage-sensitive microdeletion/duplication syndromes.- Contains a gene with a known triplosensitivity or haploinsufficiency score.- Recurrent in disease databases (e.g., DECIPHER, ClinGen).- De novo origin relative to parental line. | IMMEDIATE ACTION. Discard the cell line or bank it with clear warnings. Do not use for therapy or publication as a "normal" control. |
| Variant of Uncertain Significance (VUS) | Variable. | - Inherited from parental line but phenotype association is unclear.- Contains genes of unknown dosage-sensitivity.- Absent or at very low frequency in population databases (e.g., DGV).- No clear link to current phenotype. | INVESTIGATE & MONITOR. Bank the line but conduct further studies (e.g., segregation in family/donor, functional assays). Monitor VAF over passages. If VAF increases significantly, consider discarding. |
| Likely Benign / Benign | Variable. | - High frequency in healthy population databases (DGV).- Inherited from phenotypically normal parent.- Does not contain protein-coding genes or known regulatory elements. | NO ACTION REQUIRED. Can be used for research. Still document in cell line metadata. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for CNV Analysis in iPSC Research
| Item | Function in CNV Workflow | Example Notes & Considerations |
|---|---|---|
| High-Quality DNA Extraction Kits (e.g., QIAamp DNA Mini, DNeasy Blood & Tissue) | Obtain pure, high-molecular-weight DNA for accurate analysis. | Ensure kits are validated for cultured cells. Check for RNAse A treatment to prevent RNA contamination affecting quantification [40]. |
| Fluorometric Quantitation Kits (e.g., Qubit dsDNA HS/BR Assay, PicoGreen) | Accurately measure double-stranded DNA concentration. | Critical: More accurate than UV spectrophotometry (NanoDrop) for NGS library prep, as it ignores RNA, salts, and free nucleotides [40]. |
| NGS Library Prep Kits with Robust WGA | For single-cell or low-input CNV analysis. Essential for analyzing heterogeneity within an iPSC population. | For single-cell CNVs, use kits with proven low amplification bias (e.g., SeqPlex Enhanced) [39]. Always include WBC controls from healthy donors [39]. |
| CNV-Focused Microarray Kits (e.g., Affymetrix CytoScan, Illumina Infinium Cytosnp-850k) | Genome-wide CNV detection with high resolution and standardized analysis. | Often used as a first-tier clinical test. Provides a robust, cost-effective method for routine screening of iPSC banks [38] [41] [42]. |
| Digital PCR (dPCR) Assays (e.g., Bio-Rad QX200, Thermo Fisher QuantStudio) | Absolute quantification of copy number for a specific locus. Used for orthogonal validation. | Excellent for confirming suspected CNVs in specific genes (e.g., PTEN loss, AR amplification). Requires pre-existing knowledge of the target [39] [44]. |
| CopyCaller Software / CNV Analysis Algorithms | Specialized software for analyzing qPCR or dPCR data to determine copy number. | Ensure data is exported from the instrument in the correct format (Well, Sample, Target, CT). Use multiple reference assays for confidence [44]. |
Experimental Protocol: Routine Monitoring of CNVs in Long-Term iPSC Culture
Objective: To periodically screen iPSC lines for acquired copy number variations during extended in vitro culture.
Materials:
- iPSC cultures at designated passages (e.g., p10, p20, p30, etc.).
- DNA extraction kit.
- Qubit fluorometer and associated reagents.
- Selected CNV detection platform (e.g., NGS library prep kit or SNP microarray).
Methodology:
- Sample Collection: Harvest at least 1x10^6 iPSCs at each target passage. Ensure high viability (>90%) to minimize DNA degradation from apoptotic cells.
- Genomic DNA Extraction: Extract genomic DNA according to the manufacturer's protocol. Include a DNase-free step if possible. Elute in a low-EDTA TE buffer or nuclease-free water.
- DNA Quantification and Quality Control:
- Quantify DNA using a fluorometric method (Qubit).
- Check purity by measuring A260/A280 and A260/A230 ratios. Acceptable ranges are ~1.8-2.0 for both.
- Run a small aliquot on an agarose gel or Fragment Analyzer to confirm high molecular weight and lack of degradation.
- CNV Profiling:
- For NGS: Proceed with library preparation using a minimum of 100 ng input DNA. Avoid over-amplification during the PCR step. Sequence to an appropriate depth (e.g., 30-50x for whole genome sequencing).
- For Microarray: Process the sample according to the array kit's instructions (e.g., fragmentation, labeling, hybridization, washing, and scanning).
- Data Analysis:
- NGS Data: Process raw sequencing reads through a bioinformatics pipeline that includes read alignment to a reference genome (e.g., GRCh38) and CNV calling using read-depth-based algorithms (e.g., from packages like CNVkit or Control-FREEC). Use matched normal (parental or early passage) DNA as a control if possible [41].
- Microarray Data: Analyze the intensity data using the manufacturer's software and genotype-calling algorithm (e.g., Affymetrix Power Tools, Illumina GenomeStudio) to generate log R ratio (LRR) and B allele frequency (BAF) values for segmentation and CNV calling.
- Interpretation and Reporting:
- Annotate all called CNVs with genomic coordinates, size, type (gain/loss), and genes involved.
- Filter against database of common benign variants (e.g., DGV).
- Classify each variant using the ACMG/ClinGen framework (See Table 1) [38].
- Compare the profile to previous passages to identify newly emerging or expanding CNVs.
- Document all findings in a cell line-specific genomic stability report.
Proactive Culture Management: Minimizing Instability at the Bench
In long-term induced pluripotent stem cell (iPSC) culture, maintaining genomic integrity is a cornerstone for ensuring the validity of research data and the safety of subsequent clinical applications. The culture environment itself is a critical determinant of genetic stability. Using chemically defined media and matrices moves the field away from variable, ill-defined components and toward a standardized system that minimizes selective pressures and stress-induced DNA damage. This technical support center provides targeted guidance to help researchers optimize these conditions to safeguard their cell lines.
FAQs: Media, Matrices, and Genomic Stability
FAQ 1: How do chemically defined media help prevent genomic instability in iPSCs? Chemically defined media provide a consistent and reproducible culture environment free of unknown biological components like serum. This consistency reduces cellular stress and unintended differentiation, which are key drivers of genomic instability. By eliminating variability, these media prevent selective pressures that can favor the outgrowth of subpopulations with genetic aberrations, such as copy number variations (CNVs) in regions like 20q11.21, which are associated with growth advantage and are frequently observed in iPSCs [28] [1].
FAQ 2: What is the role of the culture matrix in maintaining stable iPSCs? The extracellular matrix (ECM) provides essential signals for cell survival, proliferation, and pluripotency. A defined matrix ensures these signals are consistent and free from contaminants. An inappropriate or variable matrix can cause poor attachment and detachment-induced stress (anoikis), compromising cell health and potentially leading to DNA damage responses. Using a qualified, defined matrix is crucial for robust and stable cultures [45] [46].
FAQ 3: Why is basic Fibroblast Growth Factor (bFGF) critical, and how should its concentration be optimized? bFGF is a key cytokine that supports iPSC self-renewal and pluripotency by activating signaling pathways that suppress spontaneous differentiation [47]. Suboptimal bFGF levels can lead to differentiation or cell stress, increasing the risk of genomic instability. Research using response surface methodology has demonstrated that optimizing bFGF concentration is vital for maximizing pluripotency marker expression. For example, one study identified 111 ng/mL for optimal expansion and 130 ng/mL for maintaining pluripotency, highlighting the need for fine-tuning rather than using a one-size-fits-all approach [47].
FAQ 4: How does cell seeding density impact genetic quality? Incorrect seeding density creates a suboptimal microenvironment. Too low a density can lead to poor cell-cell contact and increased stress, while excessive density can accelerate nutrient depletion and waste accumulation. Both scenarios can induce stress and increase the risk of mutations. Studies have shown that optimizing seeding density, such as 70,000 cells/cm², works synergistically with correct bFGF levels to maintain pluripotency and support healthy, stable growth [47].
FAQ 5: At what passage should I be most concerned about genomic instability? Genetic abnormalities can accumulate over time. A study on mesenchymal stem cells (a relevant model for long-term culture risks) found a statistically significant increase in DNA damage from passage 5 onwards, with a notable rise in micronucleus formation (indicative of chromosomal loss or breakage) from passage 7 [48]. While the exact passage number may vary for iPSCs, this underscores the importance of monitoring genetic integrity in mid- to late-passage cells and establishing a low-passage master cell bank [48] [1].
Troubleshooting Guides
Problem 1: Excessive Spontaneous Differentiation in Cultures
- Potential Cause: Inconsistent media components (e.g., old growth factors, improperly stored media) or suboptimal concentration of key factors like bFGF.
- Solutions:
- Ensure complete culture medium is less than two weeks old [6].
- Systematically optimize the concentration of bFGF for your specific cell line [47].
- Manually remove differentiated areas from colonies before passaging.
- Avoid letting colonies overgrow; passage when they are large and compact [6].
- Decrease colony density during passaging to reduce competition for nutrients and signaling molecules [6].
Problem 2: Poor Cell Attachment After Passaging
- Potential Cause: Inadequate or inactive matrix coating, or environmental stress on the cells.
- Solutions:
- Verify that the correct cultureware is being used (e.g., non-tissue culture-treated for some defined matrices) [6].
- Confirm the matrix preparation procedure and expiration date.
- Check for incubator temperature and CO₂ fluctuations [45].
- Plate a higher number of cell aggregates initially to improve survival and attachment [6].
- Work quickly after cells are treated with passaging reagents to minimize suspension time [6].
Problem 3: Low Proliferation Rate
- Potential Cause: Suboptimal concentration of growth factors or poor cell culture conditions.
- Solutions:
- Optimize the concentration of bFGF in the culture medium, as it directly supports proliferation [47].
- Ensure the culture is passaged at the recommended density to maintain paracrine signaling.
- Check the quality of all media components and the activity of the matrix.
Key Experimental Data and Protocols
Table 1: Optimized Culture Conditions for hiPSCs Using Response Surface Methodology [47] This table summarizes key findings from a systematic optimization of hiPSC culture conditions, highlighting the interaction between bFGF concentration and cell seeding density.
| Parameter | Goal | Optimized Value | Key Outcome |
|---|---|---|---|
| bFGF Concentration | Cell Expansion | 111 ng/mL | Maximized cell proliferation |
| bFGF Concentration | Maintain Pluripotency | 130 ng/mL | Enhanced expression of pluripotency markers |
| Seeding Density | Maintain Pluripotency | 70,000 cells/cm² | Optimal density for pluripotency when combined with 130 ng/mL bFGF |
Table 2: Onset of Genomic Instability in Long-Term Culture of Stem Cells [48] Data from a study on Adipose-Derived Mesenchymal Stromal Cells (ADSC) illustrates the progression of genomic damage with increasing passages, a critical consideration for iPSC culture.
| Passage Number | DNA Damage (Comet Assay) | Chromosomal Alterations (Micronucleus Test) |
|---|---|---|
| Passage 1 & 3 | Baseline level | Baseline level |
| Passage 5 | Statistically significant increase | Not statistically significant |
| Passage 7 | Increased level | Statistically significant increase |
| Passage 9 & 11 | Further increased level | Further increased level |
Detailed Protocol: Systematic Optimization of bFGF and Seeding Density [47]
Objective: To empirically determine the optimal concentration of bFGF and cell seeding density for maintaining hiPSC pluripotency and proliferation.
Methodology:
- Experimental Design: Utilize a two-factor, three-level Central Composite Design (CCD) within the Response Surface Methodology (RSM) framework. The two factors are bFGF concentration and seeding density.
- Factor Levels: Assign low, medium, and high levels to each factor (e.g., for density: 30,000, 50,000, and 70,000 cells/cm²).
- Cell Culture: Culture the hiPSC line (e.g., UMN PCBC16iPS) on a feeder layer of mitomycin C-treated mouse embryonic fibroblasts (MEFs) in a specialized medium.
- Response Measurement:
- Cell Proliferation/Viability: Assess using the MTT assay on cells cultured for 24 hours under the nine different conditions generated by the DoE software.
- Pluripotency: Evaluate key pluripotency gene expression (e.g., OCT4, SOX2) via quantitative RT-PCR and flow cytometric analysis of markers (e.g., SSEA-4) after 48 hours and 7 days in culture under selected conditions.
- Validation: Culture hiPSCs in the predicted optimal condition (e.g., bFGF 130 ng/mL and 70,000 cells/cm²) and a control group for seven days. Analyze pluripotency markers, apoptosis, and colony morphology to validate the model's predictions.
Signaling Pathways and Workflows
Figure 1. How defined components promote genomic stability. Chemically defined media and matrices provide a consistent foundation, while optimized bFGF activates FGF signaling. This sustains pluripotency and suppresses stress, preventing genomic instability [47] [28] [46].
Figure 2. A workflow for optimizing culture conditions. This diagram outlines the step-by-step process for using Response Surface Methodology (RSM) to empirically derive optimal culture conditions, leading to a robust and defined protocol [47].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Defined iPSC Culture Systems
| Reagent / Material | Function in Maintaining Genomic Stability |
|---|---|
| Chemically Defined Media (e.g., mTeSR Plus, StemFlex, Essential 8) | Provides a consistent, xeno-free nutrient base to minimize cellular stress and unintended selective pressures. Supports self-renewal and pluripotency [6] [49] [46]. |
| Defined Matrices (e.g., Vitronectin XF, Geltrex) | Provides a consistent, non-variable substrate for cell attachment, signaling, and survival, reducing stress from poor attachment [6] [49]. |
| Recombinant Human bFGF | The key growth factor for maintaining pluripotency and preventing spontaneous differentiation. Concentration must be optimized for each cell line and culture condition [47]. |
| Small Molecule Inhibitors (e.g., ROCK inhibitor) | Improves cell survival after passaging and freezing by reducing apoptosis (anoikis), thereby minimizing stress-induced genetic damage during routine culture manipulations [46]. |
| Quality Control Kits (Mycoplasma PCR, Pluripotency Scorecards) | Essential for routine monitoring. Ensures cultures are free of contamination and confirms pluripotency, preventing the use of compromised or differentiated cells in experiments [6] [49]. |
Frequently Asked Questions (FAQs)
Q1: How does extended passaging actually lead to more genomic changes in my iPSC culture? Prolonged passaging introduces genomic stress primarily through replication stress, a type of DNA damage that occurs at stalled replication forks during cell division [14]. The cumulative number of cell divisions increases the probability of errors. Furthermore, specific genomic regions are more vulnerable; CNVs that arise are frequently enriched in fragile sites and areas harboring genes associated with growth and survival, which can then be selectively favored in the culture, allowing cells with these advantages to outcompete others [50] [14].
Q2: I've found a CNV in my culture. Did it come from the donor cell, the reprogramming process, or the passaging? Determining the origin of a CNV is crucial for troubleshooting. The variations can stem from three main sources, which are outlined in the following workflow. The presence of identical CNVs in multiple, independently derived iPSC clones from the same donor strongly suggests a pre-existing variation in the original somatic cell population [50]. In contrast, CNVs that are unique to a single clone and are detected in later passages but not in the early-passage cells are likely passage-induced mutations acquired during culture expansion [50] [1].
Q3: What are the most common genomic changes I should look out for in long-term cultures? Recurrent genomic alterations provide a signature of the selective pressures in iPSC culture. You should be particularly vigilant for copy number variations (CNVs) on specific chromosomes. Data from large-scale studies have identified consistent hotspots [1] [51].
Table 1: Common Recurrent Genomic Alterations in iPSC Cultures
| Genomic Alteration Type | Recurrent Genomic Loci | Key Genes in the Region | Potential Functional Consequence |
|---|---|---|---|
| Copy Number Variation (CNV) | Amplification of 20q11.21 [1] [51] | BCL2L1 (anti-apoptosis), ID1, DNMT3B [1] | Enhanced survival, resistance to cell death, improved self-renewal. |
| Copy Number Variation (CNV) | Amplification of 12p [1] | NANOG (pluripotency) [1] | Enhanced self-renewal and reprogramming efficiency. |
| Aneuploidy | Gains of entire chromosome 12, 8, or X [1] | Multiple cell cycle and pluripotency genes [1] | Provides a proliferative advantage. |
Q4: Can I modify my passaging technique to reduce replication stress and genomic instability? Yes. A key strategy is to limit replication stress by ensuring an adequate supply of nucleotides during DNA replication. Supplementing your culture medium with a nucleoside mix has been demonstrated to reduce the load of DNA damage and lower the number of de novo CNVs in resulting iPSC lines [14]. The experimental protocol for this is detailed in the section "Experimental Protocol: Reducing Replication Stress with Nucleoside Supplementation".
Q5: How frequently should I karyotype my cells or perform other genetic quality control checks? There is no one-size-fits-all answer, but a common and critical practice is to establish a genetic baseline and monitor at key points [1] [22]. You should perform a genetic quality control check:
- Before starting a new project: Analyze your starting iPSC line.
- After major manipulations: Check cells after thawing, following clonal selection, or after genetic engineering.
- At regular intervals during long-term culture: For example, every 10 passages, or according to your lab's established SOP.
- Before any final application: Always analyze the specific cell population immediately before using them for terminal differentiation, a key experiment, or (especially) clinical application [1] [22].
A combination of karyotyping (to detect large chromosomal changes) and a higher-resolution method like aCGH or SNP array (to detect CNVs) is recommended for a comprehensive assessment [1] [22].
Troubleshooting Guides
Problem: Sudden Increase in Proliferation Rate
Potential Cause: Acquisition of a growth-advantage mutation. Investigation & Solution:
- Confirm the Phenotype: Perform a growth curve analysis to quantitatively confirm the increased proliferation.
- Genetic Analysis: Immediately subject the culture to genetic analysis (e.g., karyotyping and aCGH/SNP array). Pay close attention to the recurrent regions listed in Table 1, particularly 20q11.21 and 12p [1] [51].
- Decision Point:
- If a known high-risk alteration (e.g., 20q11.21 amplification) is detected, it is safest to discard the culture and go back to an earlier, genetically validated stock.
- If the alteration is unknown or the cell line is irreplaceable, you must consider the risk for your specific application. For in vivo transplantation or clinical use, discard the line. For in vitro research, you may proceed with extreme caution, clearly documenting the genetic status and interpreting all data in this context.
Problem: Inconsistent or Failed Differentiation
Potential Cause: Accumulation of genetic alterations that affect pluripotency or differentiation pathways. Investigation & Solution:
- Control Check: Ensure your differentiation protocol is working correctly with a control iPSC line.
- Genetic Quality Control: Perform genetic analysis on the problematic line. Alterations in key developmental genes or imbalances in pluripotency networks (e.g., via NANOG) can block or skew differentiation [1] [22].
- Characterize Pluripotency State: Analyze the expression of core pluripotency markers (OCT4, SOX2, NANOG) to ensure they are normal before initiating differentiation.
- Solution: If genetic defects are found, thaw a low-passage, validated bank of the same line. Re-initiate the differentiation and compare results.
Problem: High Level of Cell Death Post-Passaging
Potential Cause: Elevated genomic instability leading to mitotic catastrophe or apoptosis. Investigation & Solution:
- Check Passaging Technique: First, rule out technical issues like over-trypsinization or inaccurate cell counting.
- Assess DNA Damage: Perform an immunofluorescence stain for γH2AX, a marker of DNA double-strand breaks and replication stress. A high level of γH2AX foci indicates significant genomic stress [14].
- Mitigate Replication Stress: Consider adapting your protocol to reduce replication stress. This can be achieved by using a CHK1-overexpressing iPSC line (if genetically feasible) or, more practically, by adding nucleoside supplements to the culture medium during expansion [14].
Experimental Protocols from Key Studies
Detailed Methodology: Monitoring CNV Dynamics Across Passages
This protocol is adapted from studies that tracked the emergence of genomic instability over time [50] [1].
Objective: To identify the timing and origin of de novo CNVs in an iPSC line.
Materials:
- iPSC culture at various passages (e.g., P5, P10, P15, P20).
- DNA extraction kit.
- DNA from parental somatic cells (if available).
- Array Comparative Genomic Hybridization (aCGH) platform or materials for Whole Genome Sequencing (WGS).
Procedure:
- Sample Collection: Harvest cells and extract high-quality genomic DNA at each predetermined passage.
- Genomic Analysis: Hybridize the DNA to an aCGH array or prepare libraries for WGS. Always include the parental somatic cell DNA (or the earliest passage iPSC DNA) as a reference.
- Data Analysis:
- Identify all CNVs present at each passage.
- Classify each CNV based on its first appearance:
- Pre-existing: Present in the parental cells or all passages.
- Reprogramming-induced/Early passage: Appears in the first analyzed passage of the iPSCs.
- Passage-induced: Appears for the first time in a later passage (e.g., P15) and was absent in earlier passages (e.g., P5 and P10).
Interpretation: This longitudinal design allows you to pinpoint when specific CNVs arose, providing direct evidence for the impact of passaging on genomic integrity [50].
Experimental Protocol: Reducing Replication Stress with Nucleoside Supplementation
This protocol is based on the work of Ruiz et al. (2015), which demonstrated that nucleoside supplementation during reprogramming and culture reduces genomic instability [14].
Objective: To reduce the load of replication stress-associated DNA damage and CNV formation in iPSCs.
Materials:
- Standard iPSC culture medium.
- Nucleoside solution for mammalian cells (e.g., 100x solution, typically containing adenosine, guanosine, cytidine, uridine).
Procedure:
- Prepare Supplemented Medium: Add nucleosides to your standard iPSC culture medium at a final concentration of 20-50 µM for each nucleoside [14].
- Culture Cells: Maintain the iPSCs in the nucleoside-supplemented medium. The medium should be replaced with fresh supplemented medium every 24-48 hours.
- Validate Reduction in Stress:
- To confirm the effect, you can perform immunofluorescence for γH2AX and compare foci counts between supplemented and non-supplemented cultures.
- For a long-term readout, perform aCGH on cells cultured for multiple passages with and without nucleosides and compare the number of de novo CNVs [14].
The Scientist's Toolkit: Essential Reagents for Monitoring and Mitigating Genomic Stress
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Example Use in Troubleshooting |
|---|---|---|
| Giemsa Stain (G-banding) | Cytogenetic test to detect numerical chromosome abnormalities (aneuploidy) and large structural variations [1]. | Routine karyotyping to ensure chromosomal integrity at a resolution of ~5-10 Mb [22]. |
| aCGH or SNP Array | High-resolution (kb-scale) genome-wide detection of copy number variations (CNVs) [1]. | Identifying microdeletions/amplifications at known hotspots like 20q11.21 [50] [51]. |
| Anti-γH2AX Antibody | Marker for DNA double-strand breaks and replication stress via immunofluorescence [14]. | Quantifying replication stress levels in different culture conditions or after chemical interventions. |
| Nucleoside Supplement | Provides nucleotide precursors to mitigate replication stress by supporting DNA synthesis [14]. | Added to culture medium to reduce DNA damage and CNV formation, as per the protocol above. |
| dPGA-coated Cultureware | A cytocompatible substrate that improves cell adhesion and reduces aggregation in long-term neuronal cultures [52]. | Used for long-term differentiation experiments (e.g., with motor neurons) to prevent aggregate-related stress and cell death. |
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What are the most significant sources of non-genetic variability in iPSC differentiation? Statistical analysis of motor neuron differentiations has shown that operator-induced variability and induction set variations are the predominant non-genetic factors, outweighing the contribution from cell line genetics. One study found that "Operator," followed by "Induction Set" explained large amounts of variation within quality control metrics, while "Cell Line" was a significant but lesser explanatory factor with R² values <12% in most cases [53].
Q2: How can laboratories reduce operator-induced variability in iPSC workflows? Implementing automated cell culture systems can significantly reduce this variability by performing normally manual actions (pipetting, picking cells under a microscope) and key iPSC workflows under standardized culture conditions. Automation also allows passive collection of imaging and workflow data, providing insights into biological processes [54]. AI-powered automated systems can execute intricate, multi-step protocols without deviation, managing complex workflows with exacting precision [55].
Q3: What specific quality control metrics are most affected by induction set variability? Analysis of motor neuron differentiation revealed that culture purity markers and cell proliferation metrics show high sensitivity to induction set variations. Specifically, coefficients of variance exceeded 30% for most quantifiable factors, with over half of these metrics exceeding 40%, far beyond acceptable levels for an industrial environment (ideally <20%) [53].
Q3: Does genomic instability in iPSCs interact with operator and induction set effects? Yes, research shows that iPSC genomic instability, as assessed by targeted assays for common karyotypic abnormalities, significantly affects differentiation efficiency and purity. Cultures derived from genomically stable iPSCs exhibited reduced variance and improved marker expression profiles, suggesting that routine genomic assessment enhances reliability of iPSC-derived models [53].
Q4: What practical steps can be taken to standardize induction sets across experiments? Using defined protocols with precise timing and reagent specifications is crucial. Studies recommend implementing rigorous quality control benchmarks at each differentiation stage and using the same reagent batches across induction sets when possible. Statistical modeling has shown that controlling for induction set factors can explain over 50% of variance in certain quality metrics [53].
Troubleshooting Guides
Problem: Excessive differentiation (>20%) in iPSC cultures
- Potential Solutions:
- Ensure complete cell culture medium is less than 2 weeks old [6]
- Remove areas of differentiation prior to passaging [6]
- Avoid having culture plates out of the incubator for more than 15 minutes [6]
- Ensure cell aggregates generated after passaging are evenly sized [6]
- Passage cultures when majority of colonies are large, compact, and have dense centers [6]
Problem: High variability in differentiation outcomes between operators
- Potential Solutions:
- Implement automated pick-passaging systems that use robotics and algorithm-directed cell selection [54]
- Establish standardized training protocols for all technical staff
- Use integrated automation systems that combine liquid handling, incubation, and imaging [55]
- Implement blind coding of samples to reduce operator bias
Problem: Inconsistent results between induction sets
- Potential Solutions:
- Conduct routine genomic assessment of iPSCs using targeted assays for common karyotypic abnormalities [53]
- Use predefined quality control metrics at each differentiation stage [53]
- Maintain detailed records of all experimental conditions, including reagent lot numbers and environmental factors
- Implement statistical process control to identify and correct drift in differentiation protocols
Problem: Low cell attachment after plating
- Potential Solutions:
- Plate a higher number of cell aggregates initially (e.g., 2-3 times higher) and maintain a more densely confluent culture [6]
- Work quickly after cells are treated with passaging reagents to minimize duration cell aggregates are in suspension [6]
- Reduce incubation time with passaging reagents, particularly if cells are passaged prior to cell multi-layering within the colony [6]
- Ensure proper plate coating based on tissue culture treatment requirements [6]
Table 1: Sources of Variability in iPSC-Derived Motor Neuron Differentiation [53]
| QC Metric | Coefficient of Variance (%) | R² - Cell Line (%) | R² - Induction Set (%) | R² - Operator (%) |
|---|---|---|---|---|
| NPC:D3 Ratio | 59.5 | - | - | 67.1 |
| D3:D10 Ratio | 67.0 | 31.5 | - | 31.4 |
| D10 Neurite Area | 53.7 | 7.1 | - | - |
| PAX6+OLIG2+ (%) | 46.3 | 1.5 | 51.1 | - |
| SMI32+MAP2+ (D3) | 46.5 | 9.7 | 42.5 | - |
| SMI32+MAP2+ (D10) | 36.8 | 6.3 | 57.2 | - |
| ISL1+MAP2+ (D3) | 36.8 | 11.2 | 45.4 | 39.6 |
Table 2: Impact of Genomic Stability on Differentiation Variability [53]
| QC Metric | Coefficient of Variance - All Sets (%) | Coefficient of Variance - No Abnormalities (%) | Improvement with Stable Karyotype |
|---|---|---|---|
| NPC:D3 Ratio | 32.14 | 35.61 | Increased variance |
| D3:D10 Ratio | 49.16 | 36.44 | 25.9% reduction |
| PAX6+OLIG2+ (%) | 46.3 | Not reported | Significantly greater purity |
| SMI32+MAP2+ (D3) | 46.5 | Not reported | Significantly greater purity |
Experimental Protocols
Purpose: To address inherent cell-line variability and enable efficient cleaning up of cultures through robotic selection.
Procedure:
- Culture iPSCs under standard conditions until 70-80% confluent
- Using automated platform, identify and map 'good' and 'bad' quality culture regions within the same iPSC population
- Employ algorithm-directed robotic picking to selectively passage cells from designated regions
- For 'good' regions: Select compact colonies with defined edges and high nucleus-to-cytoplasm ratio
- For 'bad' regions: Identify areas showing spontaneous differentiation, irregular colony morphology, or excessive vacuolization
- Expand selected populations separately for downstream differentiation assays
- Collect continuous imaging and workflow data throughout the process
Applications: This methodology was validated across three different iPSC cell lines for expansion and differentiation into cardiomyocytes, demonstrating that potential for random differentiation was largely dependent on the selected picking regions.
Purpose: To evaluate iPSC karyotypic abnormalities and their impact on differentiation variability.
Procedure:
- Extract RNA from iPSC cultures at passage 15-25
- Perform bulk RT-qPCR using primers targeting the nine most common karyotypic abnormalities in human iPSCs
- Analyze chromosomal copy numbers with thresholds:
- Autosomes: <1.5 or >2.5 considered abnormal
- Chromosome X (male donors): <0.7 or >1.3 considered abnormal
- Confirm chromosomal deletions using one-way ANOVAs comparing chromosomal copy number across all loci with post hoc Tukey test p-value adjustment
- Correlate genomic stability findings with differentiation efficiency metrics
Quality Control: Cultures derived from genomically stable iPSCs should exhibit reduced variance and improved differentiation marker expression profiles.
Experimental Workflow Diagrams
Automated vs Manual iPSC Culture Workflow
Major Variability Sources in iPSC Differentiation
Research Reagent Solutions
Table 3: Essential Materials for Mitigating Non-Genetic Variability
| Reagent/Platform | Function | Application in Variability Control |
|---|---|---|
| Automated Cell Culture Systems (e.g., CellXpress.ai) | AI-powered robotic culture maintenance | Reduces operator-induced variability through standardized protocols and continuous monitoring [55] |
| Selective Pick-Passaging Platform (e.g., Celligent) | Algorithm-directed cell selection | Addresses inherent cell-line variability by precise selection of optimal culture regions [54] |
| Genomic Stability Assay Kits | Detection of karyotypic abnormalities | Identifies iPSC lines with chromosomal abnormalities that contribute to differentiation variance [53] |
| Defined Culture Media (e.g., mTeSR Plus) | Maintenance of pluripotency | Ensures consistent nutrient composition and reduces batch-to-batch variability [6] |
| Non-enzymatic Passaging Reagents (e.g., ReLeSR) | Gentle cell dissociation | Maintains consistent aggregate size and viability during passaging [6] |
| Quality Control Antibody Panels | Assessment of differentiation markers | Enables standardized quantification of culture purity and differentiation efficiency [53] |
Maintaining genomic integrity is a fundamental challenge in long-term induced pluripotent stem cell (iPSC) culture. As iPSCs transition from research tools to clinical therapeutics, establishing robust procedures to document and standardize handling is paramount for preventing genomic instability. This technical support center provides targeted guidance to help researchers identify, control, and troubleshoot the critical process parameters (CPPs) that are essential for maintaining the genetic and epigenetic stability of iPSC cultures over extended periods.
FAQs: Addressing Genomic Instability in iPSC Culture
1. What are the most common genetic abnormalities acquired in long-term iPSC culture? Human iPSCs exhibit a propensity for genomic instability during extended in vitro culture. The most frequently observed abnormalities include:
- Aneuploidies: Recurrent trisomies of chromosomes 12, 17, or X [15].
- Copy Number Variations (CNVs): DNA sequence deletions or amplifications, often affecting common fragile sites or sub-telomeric regions [15].
- Single Point Mutations: Protein-coding mutations that can arise during reprogramming or culture expansion [15].
- Uniparental Disomy (UPD): Inheritance of two chromosomal copies from one parent, which can lead to loss of heterozygosity [15].
2. How does the reprogramming method impact genomic integrity? The choice of reprogramming method significantly influences the mutational load in resulting iPSC lines. Non-integrating methods, such as episomal vectors or synthetic mRNA, are preferred as they avoid insertional mutagenesis [15] [56]. Furthermore, the starting cell type is important due to somatic mosaicism, where pre-existing mutations in the source population can be selectively amplified during reprogramming [15].
3. Which culture parameters are most critical for preventing genetic instability?
- Cell Density Management: Seeding cells at optimal density is critical; high density can lead to over-confluence and increased genomic stress, while low density can induce senescence [56].
- Culture Medium Formulation: Using a chemically defined, xeno-free medium like Essential 8 reduces batch-to-batch variability and provides a consistent environment that supports genomic stability [57].
- Passaging Techniques: Consistent, gentle dissociation methods and the use of ROCK inhibitor (Y-27632) help maintain cell viability and prevent stress-induced mutations [58] [57].
- Culture System: Adaptation to suspension culture in bioreactors requires careful optimization of factors like shear stress and aggregate size to minimize selective pressures that favor aberrant cells [58].
Troubleshooting Guides
Problem: Increased Spontaneous Differentiation in Culture
Potential Causes and Solutions:
- Cause: Over-confluence during culture.
- Solution: Standardize sub-culture timing to maintain exponential growth. Adherent iPSCs should typically be passaged every 4-5 days [57].
- Cause: Inconsistent extracellular matrix coating.
- Solution: Implement strict quality control for coating reagents like vitronectin or Synthemax II-SC. Use consistent coating procedures and validate with test cultures [57].
- Cause: Suboptimal medium composition or preparation.
- Solution: Use only fresh, properly prepared cGMP-grade E8 medium. Document preparation dates and pre-warm only the amount needed for immediate use [57].
Problem: Detection of Karyotypic Abnormalities
Potential Causes and Solutions:
- Cause: Extended culture duration leading to selection of advantageous mutations.
- Solution: Establish a cell banking strategy with early passage master and working cell banks. Limit the number of passages for experimental use [59].
- Cause: Selective pressure from suboptimal culture conditions.
- Solution: Document and standardize all critical process parameters including oxygen levels, pH fluctuation, and feeding schedules to minimize selective pressures [60].
- Cause: Inadequate monitoring of genetic integrity.
- Solution: Implement a routine genomic quality control schedule as detailed in the experimental protocols section below.
Experimental Protocols for Monitoring Genomic Stability
Regular Karyotyping and Genetic Analysis
Methodology:
- Perform G-banding karyotype analysis at a minimum of every 10 passages and before creating master cell banks [15].
- Conduct higher resolution analyses such as SNP genotyping or comparative genomic hybridization (CGH) array to detect copy number variations that may be missed by standard karyotyping [15].
- For comprehensive mutation screening, implement whole exome or whole genome sequencing on a regular basis, particularly for lines intended for therapeutic applications [15] [59].
Documentation and Tracking System
Establish a standardized documentation system that records:
- Passage number and population doubling times
- Cell morphology assessments with representative images
- Regular pluripotency marker validation (Oct4, Sox2, Nanog) by flow cytometry
- Differentiation potential assays
- All observed irregularities and corrective actions taken
This documentation should be maintained in a searchable format to identify correlations between handling procedures and genomic stability outcomes.
Research Reagent Solutions for Genomic Stability
Table: Essential Reagents for Maintaining Genomic Integrity in iPSC Culture
| Reagent/Category | Specific Examples | Function & Importance for Genomic Stability |
|---|---|---|
| Culture Medium | Essential 8 Medium (cGMP-grade) | Chemically defined, xeno-free formulation that eliminates lot-to-lot variability and provides consistent growth factors supporting stable expansion [57]. |
| Extracellular Matrix | Vitronectin, Synthemax II-SC | Defined, synthetic substrates that replace variable animal-derived matrices (e.g., Matrigel), reducing selective pressures that can favor genetically abnormal cells [57]. |
| Passaging Reagents | TrypLE, Accutase, ROCK inhibitor (Y-27632) | Gentle, enzyme-based dissociation combined with apoptosis inhibition minimizes cellular stress and DNA damage during sub-culture [58] [57]. |
| Cell Banking Medium | CryoStor CS10 | Serum-free, defined cryopreservation medium that enhances post-thaw viability, reducing the need for extensive post-recovery expansion and associated replicative stress [57]. |
| Quality Control Assays | G-banding kits, SNP arrays, Flow cytometry panels | Regular assessment tools to monitor karyotypic status, pluripotency marker expression, and detect early signs of genetic drift or differentiation [15] [59]. |
Process Optimization and Workflow Diagrams
iPSC Culture Process Flow
Genomic Instability Risk Factors
Preventing genomic instability in long-term iPSC culture requires meticulous documentation and standardization of handling procedures. By implementing the troubleshooting guides, experimental protocols, and reagent solutions outlined above, researchers can systematically control the critical process parameters that influence genetic integrity. Consistent application of these practices, combined with regular genomic monitoring, forms the foundation for producing reliable, clinically relevant iPSC lines suitable for both research and therapeutic applications.
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common morphological signs that my iPSC cultures are becoming genetically unstable?
Excessive and spontaneous differentiation within your colonies is a primary morphological red flag. While some differentiation is normal, levels exceeding 20% indicate culture stress and can be associated with underlying genomic instability [6]. Other key signs include changes in colony morphology, such as loss of defined, compact colony edges, and the appearance of heterogeneous cell sizes and shapes within a colony [61]. Also, watch for changes in growth dynamics, such as a significant increase or decrease in proliferation rates, which can be a sign of emerging aneuploidy [62].
FAQ 2: I see differentiated cells in my culture. How can I tell if it's a normal level or a sign of instability?
A normal, manageable level of differentiation is typically sporadic and confined to the edges of colonies. You can often control it by physically removing the differentiated areas before passaging and ensuring your culture conditions are optimal [6]. However, if differentiation is rapid, widespread throughout the colony center, and recurs aggressively after passaging, it is a strong indicator of systemic instability. This suggests the cells may have acquired genetic or epigenetic changes that disrupt the maintenance of pluripotency [61].
FAQ 3: What specific chromosomal aberrations should I be most concerned about in iPSC cultures?
Certain recurrent chromosomal abnormalities are frequently observed in unstable iPSC cultures. Trisomy 12 is one of the most common, as it contains genes like NANOG and GDF3 that confer a selective growth advantage to pluripotent cells [1] [62]. Another frequent aberration is the amplification of the 20q11.21 region, which harbors anti-apoptosis and pluripotency-related genes such as BCL2L1 [1]. Monitoring for these specific changes is crucial, as they are hallmarks of culture adaptation.
FAQ 4: Can I prevent genomic instability, or can I only monitor for it?
While vigilant monitoring is essential, proactive strategies can significantly reduce the onset of instability. Two key approaches are:
- Limiting Replication Stress: Supplementing culture media with nucleosides during reprogramming and routine passaging has been shown to reduce replication stress, DNA damage, and the load of copy number variations (CNVs) [14].
- Choosing the Right Reprogramming Method: Studies show that using non-integrating episomal vectors instead of Sendai virus vectors can result in fewer copy number alterations (CNAs) and single nucleotide variations (SNVs) in the resulting iPSCs [4].
Troubleshooting Guides
Problem 1: Excessive Spontaneous Differentiation (>20%)
| Potential Cause | Recommended Action | Preventive Strategy |
|---|---|---|
| Suboptimal culture medium | Ensure complete medium is fresh (e.g., less than 2 weeks old when stored at 2-8°C) [6]. | Use defined, high-quality media formulations designed for robust iPSC maintenance [61]. |
| Overgrown colonies | Passage cultures when colonies are large and compact but before they become overly dense and start differentiating in the center [6]. | Maintain a consistent passaging schedule and do not allow cultures to become over-confluent. |
| Improper passaging | Ensure cell aggregates after passaging are evenly sized. Reduce incubation time with passaging reagents if the cell line is particularly sensitive [6]. | Standardize passaging techniques to minimize mechanical and enzymatic stress. |
| Low colony density | If differentiation persists after passaging, it may be due to plating too few cell aggregates. Plate 2-3 times more aggregates to maintain a denser, more supportive culture [6]. | Optimize and document the ideal seeding density for each specific iPSC line. |
Problem 2: Changes in Colony Morphology and Growth Rate
| Observation | Potential Genetic Cause | Investigation & Action |
|---|---|---|
| Rapid dominance of a fast-growing cell population | Aneuploidy (e.g., Trisomy 12): Provides a growth advantage [1] [62]. | Karyotype Analysis: Perform regular G-banding analysis to check for gross chromosomal abnormalities.Doubling Time Monitoring: Track cell counts at each passage; a significant change can indicate an emerging aneuploid population [62]. |
| Heterogeneous colony appearance, inconsistent growth | Accumulation of Structural Variants or Point Mutations: These can disrupt genes involved in cell cycle and pluripotency [1] [62]. | High-Resolution Genotyping: Use techniques like optical mapping or next-generation sequencing to identify structural variants and single nucleotide variants (SNVs) not visible by karyotyping [62]. |
Quantitative Data on Genomic Instability in iPSCs
The table below summarizes types of genetic variations and their frequencies as reported in the literature.
| Genetic Variation Type | Key Chromosomal Hotspots | Frequency / Load | Detection Method |
|---|---|---|---|
| Chromosomal Aberration | Trisomy 12, Trisomy 8, Trisomy X [1] | Found in 12.5% of iPSC cultures; Trisomy 12 represents ~32% of aberrations [1] [62] | G-banding, Karyotype Analysis [1] |
| Copy Number Variation (CNV) | Amplification of 20q11.21 [1] | Higher numbers in early-passage iPSCs; selected against during culture [1] [63] | Array CGH, SNP array [1] |
| Single Nucleotide Variant (SNV) | No highly recurrent hotspots reported [1] | Average of ~6 protein-coding mutations per line [1] [63] | Whole Genome Sequencing (WGS), Whole Exome Sequencing (WES) [1] |
| Structural Variants (SVs) | Found across the genome [62] | Hundreds identified per line, many disrupting protein-coding sequences [62] | Optical Mapping, Long-Read Sequencing [62] |
Experimental Protocols for Assessing Instability
Protocol 1: Detecting DNA Damage via γH2AX Immunocytochemistry
This protocol is used to measure replication stress, a key source of DNA damage during reprogramming and culture [14].
- Cell Culture and Preparation: Plate iPSCs on Matrigel-coated coverslips in a 12-well plate. Culture until they reach ~70% confluence.
- Fixation: Aspirate media and wash cells with PBS. Fix cells with 4% formaldehyde in PBS for 15 minutes at room temperature.
- Permeabilization and Blocking: Permeabilize cells with 0.1% Triton X-100 in PBS for 30 minutes. Block non-specific binding with 4% Bovine Serum Albumin (BSA) for 2 hours.
- Primary Antibody Incubation: Incubate cells with a primary antibody against phospho-Histone H2A.X (Ser139) (e.g., clone JBW301) at a 1:500 dilution overnight at 4°C [4].
- Secondary Antibody Incubation: Wash and incubate with an appropriate Alexa Fluor-conjugated secondary antibody (e.g., 1:200 dilution) for 2 hours at room temperature in the dark.
- Counterstaining and Imaging: Stain nuclei with DAPI. Mount coverslips and image using a fluorescence or confocal microscope. The number of γH2AX foci per nucleus is a quantitative measure of DNA damage [14].
Protocol 2: Assessing Genomic Instability Across Workflow Phases
This systematic approach helps pinpoint when instability is introduced during iPS cell generation and differentiation [4].
- Experimental Design: Generate iPSCs from a somatic source (e.g., fibroblasts) using different methods (e.g., Sendai virus vs. episomal vectors). Differentiate them into a target cell type (e.g., mesenchymal stem cells).
- Sample Collection: Collect samples at key phases:
- Parental somatic cells
- Early-passage iPSCs
- Late-passage iPSCs
- Differentiated cells
- Passaged differentiated cells
- Genomic Analysis: Subject all samples to a battery of tests:
- Karyotyping (G-banding): For gross chromosomal abnormalities [1].
- Chromosomal Microarray: To detect copy number alterations (CNAs) and copy number variations (CNVs) [4].
- Next-Generation Sequencing (NGS): Whole genome or exome sequencing to identify single nucleotide variations (SNVs) and small insertions/deletions [4].
- Data Integration: Map the specific CNAs and SNVs to the phase in which they first appeared (reprogramming, differentiation, or passaging).
Key Signaling Pathways in Instability and Detection
The diagram below illustrates the PI3K-Akt signaling pathway, which is implicated in early-warning signals of cellular stress and is a known hotspot in genomic instability studies.
Diagram Title: PI3K-Akt Signaling Pathway in Early-Warning Detection
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Tool | Function | Example Use-Case |
|---|---|---|
| HiDef B8 Growth Medium | A chemically defined medium for robust expansion and maintenance of iPSCs. Helps minimize spontaneous differentiation and preserve pluripotency [61]. | Routine culture to maintain high-quality, undifferentiated iPSCs under standardized conditions. |
| Ready-CEPT Supplement | A supplement designed to improve cell viability and recovery during critical steps like passaging and thawing [61]. | Used when dissociating iPSCs to single cells or after cryopreservation to enhance survival and reduce stress-induced instability. |
| Nucleoside Supplement | Provides raw materials for DNA synthesis, reducing replication stress during reprogramming and cell division [14]. | Added to the culture medium during the reprogramming of somatic cells into iPSCs to lower the load of DNA damage and CNVs. |
| CHEK1 (CHK1) Gene | A checkpoint kinase gene that limits replication stress. Overexpression reduces reprogramming-induced DNA damage [14]. | A genetic strategy to create more genomically stable iPSC lines by mitigating replication stress. |
| Non-Integrating Episomal Vectors | A reprogramming method that avoids viral integration into the host genome, reducing the risk of insertional mutagenesis [4] [63]. | Generating clinical-grade iPSC lines with a lower initial burden of genetic alterations compared to viral methods. |
Ensuring Model Fidelity: Quality Control and Functional Validation
Frequently Asked Questions (FAQs)
Q1: What are the most critical quality control checks for a new human induced pluripotent stem cell (hiPSC) line? A comprehensive QC program for a new hiPSC line should include checks for sterility, pluripotency, and genetic integrity. Key tests are summarized in the table below. [64]
Table 1: Essential Quality Control Tests for a New hiPSC Line
| Test Category | Specific Test | Key Metrics & Purpose |
|---|---|---|
| Sterility & Safety | Mycoplasma Testing | Ensure culture is free of this common, invisible contaminant that alters gene expression. [64] |
| Bacterial/Fungal Sterility | Confirm absence of microbial contamination, typically assessed by direct inoculation or membrane filtration. [64] | |
| Human Viral Pathogen Testing | Verify cells are free of hazardous viruses like HIV or HCV. [64] | |
| Identity & Pluripotency | Pluripotency Marker Assessment | Confirm expression of hallmark genes (e.g., Nanog, Oct3/4, SSEA-4, TRA-1-60, TRA-1-81) via flow cytometry or immunofluorescence. [64] |
| Trilineage Differentiation Potential | Functionally validate pluripotency by demonstrating ability to differentiate into ectoderm, mesoderm, and endoderm. [64] | |
| Genetic Integrity | Karyotyping (G-banding) | Identify gross chromosomal abnormalities (e.g., aneuploidy, translocations). This is the gold standard. [1] [64] |
| Copy Number Variation (CNV) Analysis | Detect smaller duplications or deletions across the genome using array CGH or SNP arrays. [1] |
Q2: My iPSC culture has become contaminated with mycoplasma. What should I do? Mycoplasma contamination is a serious issue as it cannot be detected by routine microscopy and can alter gene expression and induce karyotype abnormalities. A lab typically enters a decontamination protocol upon confirmation of an infestation. While some investigators may attempt to salvage rare cells through antibiotic treatment, strict adherence to aseptic technique and regular testing of cultures are the best preventive measures. [64] [65]
Q3: Why is genomic instability a major concern in iPSCs, and what are its main types? Genomic instability in iPSCs raises serious safety concerns for clinical applications, primarily due to the risk of tumorigenicity. [1] The main types of genetic variations found in iPSCs include:
- Chromosomal Aberrations: Numerical changes (e.g., trisomy 12, 8, or X) or large structural changes. Trisomy 12 is recurrent and may confer a selective growth advantage. [1]
- Copy Number Variations (CNVs): Duplications or deletions of DNA segments. A common hotspot is amplification of 20q11.21, which contains genes associated with pluripotency and anti-apoptosis. [1]
- Single Nucleotide Variants (SNVs): Point mutations in the protein-coding regions. [1]
Q4: How can I reduce the risk of introducing genomic instability during the reprogramming process? Reprogramming itself induces replication stress, a key driver of DNA damage and genomic instability. You can mitigate this by:
- Genetic Strategy: Increasing levels of the checkpoint kinase 1 (CHK1) has been shown to reduce replication stress and increase reprogramming efficiency. [14]
- Chemical Strategy: Supplementing the culture medium with nucleosides during reprogramming reduces the load of DNA damage and genomic rearrangements in the resulting iPSCs. [14]
Q5: For GMP-compliant release of an hiPSC intermediate drug product, what are the validated criteria for key QC assays? For GMP release, assays must be rigorously validated. One study established the following criteria: [66]
- Residual Episomal Vectors (REVs): A minimum input of 20,000 cells (120 ng genomic DNA) is required for accurate determination. Screening is recommended between passages 8 and 10, as testing too early may lead to unnecessary rejection of lines. [66]
- Undifferentiated State Markers: The cutoff was set to expression of at least three individual markers on at least 75% of the cells. When using multi-color flow cytometry, a "fluorescence minus one" control is advised. [66]
- Directed Differentiation Potential: The detection limit was set to two of three positive lineage-specific markers for each of the three germ layers. [66]
Troubleshooting Guides
Problem: Suspected Genetic Instability in Long-Term hiPSC Culture
Potential Causes and Solutions:
Cause: Accumulation of mutations during prolonged cell passaging.
Cause: Selective overgrowth of a subclone with a competitive advantage (e.g., trisomy 12).
- Solution: Carefully monitor culture morphology. If a rapidly dividing subclone is suspected, isolate individual clones and re-characterize them. Regularly authenticate your cell line using Short Tandem Repeat (STR) analysis to confirm identity and check for cross-contamination. [64]
Cause: Inadequate culture conditions leading to replication stress.
- Solution: Ensure media and supplements are consistent and of high quality. Batch-to-batch variation in media can introduce inconsistencies that affect cell growth and genomic stability. [65]
Problem: Low Reprogramming Efficiency and Poor-Quality iPSC Colonies
Potential Causes and Solutions:
Cause: High levels of reprogramming-induced replication stress and DNA damage.
- Solution: As outlined in FAQ #4, consider supplementing your reprogramming medium with nucleosides to alleviate replication stress and reduce DNA damage, leading to clones with fewer genomic rearrangements. [14]
Cause: Use of an inefficient or mutagenic reprogramming method.
Workflow: Comprehensive QC Pipeline for Genomic Stability
The following diagram outlines a logical workflow for monitoring genomic stability from reprogramming through to long-term culture.
Mechanism: Replication Stress in iPSC Reprogramming
This diagram illustrates the mechanism of reprogramming-induced replication stress and two strategies to mitigate it, as discovered in the cited research. [14]
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for iPSC QC and Genomic Stability
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Nucleoside Supplements | Reduces replication stress and DNA damage during the reprogramming process, leading to iPSCs with fewer copy number variations (CNVs). [14] | A chemically defined supplement that can be added to the reprogramming medium without the need for genetic modification. |
| CHK1 Expression Vector | Genetically increasing levels of the CHK1 kinase protects against reprogramming-induced replication stress and can increase reprogramming efficiency. [14] | Involves genetic modification of the starting cells, which may not be suitable for all therapeutic applications. |
| Non-Integrating Reprogramming Vectors | Generating iPSCs using methods like Sendai virus or episomal vectors avoids the risk of insertional mutagenesis from integrating viruses. [1] [67] | Essential for creating clinical-grade iPSC lines. Requires confirmation of clearance from the final iPSC product. |
| Validated Flow Cytometry Panels | Quantitative assessment of pluripotency surface markers (e.g., SSEA-4, TRA-1-60) for identity testing and release criteria. [66] [64] | Must include appropriate controls like "fluorescence minus one" (FMO) to ensure accurate gating and interpretation. [66] |
| G-Banding Staining Kits | Enables classical karyotype analysis to detect gross chromosomal abnormalities, a standard release test for cell banks. [1] [64] | Consider supplementing with higher-resolution methods like array CGH or SNP arrays for a more comprehensive view of genomic integrity. [1] |
The Critical Link Between Genomic Stability and iPSC Differentiation Efficacy
Induced pluripotent stem cells (iPSCs) hold transformative potential for disease modeling, drug discovery, and regenerative medicine. However, a significant challenge in their reliable application is genomic instability, which can arise from pre-existing mutations in somatic cells, the reprogramming process itself, or prolonged culture [22]. This instability directly impacts the differentiation capacity of iPSCs, particularly for sensitive lineages like motor neurons.
Research demonstrates that genomic instability in iPSCs is not merely a quality control concern but a critical determinant of differentiation outcomes. A 2025 study examining iPSC-derived motor neurons found that cultures originating from genomically stable iPSCs exhibited reduced variance and significantly improved motor neuron marker expression profiles compared to those with detectable abnormalities [53]. The statistical analysis revealed that differentiations from cell lines with no detectable abnormalities commonly displayed decreased coefficient of variance values for key quality control metrics, making them less variable and more reliable for research and therapeutic development [53].
The consequences of genomic instability extend beyond motor neuron differentiation, affecting multiple lineages by:
- Altering expression of genes governing pluripotency and differentiation
- Selecting for genetic variants that provide a growth advantage in culture but impair specialized function
- Creating heterogeneous cell populations with different functional characteristics and differentiation potential [22]
Table 1: Quantitative Impact of Genomic Stability on Motor Neuron Differentiation Metrics
| QC Metric | Coefficient of Variance - All Sets | Coefficient of Variance - No Detectable Abnormalities | Impact of Stability |
|---|---|---|---|
| NPC: D3 | 32.14% | 35.61% | Slightly more variable |
| D3:D10 | 49.16% | 36.44% | Significantly less variable |
| PAX6 + OLIG2 (NPC) | 46.3% | Not specified | Significantly greater purity |
| SMI32 + MAP2 (D10) | 36.8% | Not specified | Significantly greater purity |
Troubleshooting Guides & FAQs
Common Issues and Solutions in iPSC Differentiation
Q1: Why does my motor neuron differentiation show high variability in purity and efficiency between experiments?
A: High variability often stems from non-genetic factors overshadowing even genetic contributions. Statistical modeling indicates that operator technique and induction set variations explain large amounts of variation (R² values >50% for some metrics), while cell line genetics generally accounts for less than 12% of variability [53].
Solution:
- Implement standardized operating procedures with detailed documentation
- Provide comprehensive training for all technical staff
- Control reagent batches by using large, aliquoted lots for related experiments
- Regularly assess genomic stability using karyotyping or targeted assays
Q2: How can I improve the maturity and functional purity of my iPSC-derived motor neurons?
A: Immature motor neurons lacking functional characteristics typically result from suboptimal differentiation protocols or genomically unstable starter populations.
Solution:
- Employ small molecule-guided differentiation using optimized combinations like CHIR99021 (WNT agonist), SB431542 (activin-nodal inhibitor), DMH1 (BMP inhibitor), retinoic acid, and purmorphamine (SHH agonist) to achieve >95% pure motor neuron progenitors [68]
- Utilize Notch inhibitors to promote functional maturation after initial specification
- Validate genomic stability before initiating differentiations, as abnormalities significantly impact terminal differentiation efficiency [53]
Q3: What are the signs that my iPSC line has acquired problematic genetic abnormalities?
A: Indicators include:
- Sudden changes in growth characteristics or morphology
- Decreased differentiation efficiency despite previously established protocols
- Increased heterogeneity in differentiation outcomes
- Altered expression of pluripotency markers [69] [22]
Genomic Stability-Specific FAQ
Q4: How frequently should I perform genomic stability assessment on my iPSC cultures?
A: Regular monitoring is essential. Current research supports:
- Comprehensive karyotyping at master cell bank creation and every 10-15 passages during routine culture
- Targeted assays for common abnormalities (e.g., RT-qPCR for common karyotypic abnormalities) more frequently, especially before critical differentiations [53]
- Array Genomic Hybridization (AGH) for detecting microdeletions missed by standard karyotyping [22]
Q5: Which chromosomal abnormalities most significantly impact motor neuron differentiation capacity?
A: While any significant abnormality can be problematic, targeted RT-qPCR assays focusing on the nine most common karyotypic abnormalities in human iPSCs have shown significant correlation with reduced differentiation efficiency [53]. Cells with chromosomal copy numbers <1.5 or >2.5 (<0.7 or >1.3 for chromosome X in male lines) are considered "abnormal" and show impaired performance.
Q6: Can I "rescue" an iPSC line with detected genomic abnormalities?
A: Generally, no. Most abnormalities provide selective growth advantages and will expand in culture. The recommended approach is to:
- Return to an earlier, validated bank confirmed to be genomically normal
- Establish new lines if no stable bank exists
- Implement more rigorous monitoring to detect issues earlier in future cultures [69] [22]
Experimental Protocols for Validation
Protocol 1: Assessing Genomic Stability Using Targeted RT-qPCR Assay
Purpose: To routinely monitor common karyotypic abnormalities in iPSCs without full karyotyping.
Materials:
- iPSCs at 70-85% confluence
- RNA extraction kit
- RT-qPCR system with primers for the nine most common karyotypic abnormalities in human iPSCs
- Normalization primers for reference chromosomes
Method:
- Culture cells under standardized conditions until 70-85% confluence
- Extract total RNA following manufacturer's protocol
- Perform reverse transcription to generate cDNA
- Run qPCR with target and reference primers
- Analyze using ΔΔCt method to determine relative copy number
- Interpret results: chromosomal copy numbers <1.5 or >2.5 (<0.7 or >1.3 for chromosome X in male donors) indicate abnormalities [53]
Validation: Compare with karyotyping results to establish correlation for your specific cell lines and culture conditions.
Protocol 2: High-Purity Motor Neuron Differentiation with Quality Control Assessment
Purpose: Generate highly pure, functionally mature motor neurons from iPSCs with integrated quality control checkpoints.
Materials:
- Genomically stable iPSCs
- Essential 8 or similar defined medium
- Small molecules: CHIR99021, SB431542, DMH1, retinoic acid, purmorphamine
- Notch inhibitor for maturation (e.g., DAPT)
- Immunocytochemistry antibodies: OLIG2, NKX2.2, ISL1, MAP2, SMI32, PAX6
Method:
- Neural Induction & Caudalization (Days 1-6): Treat iPSCs with CHIR99021 (3µM) + SB431542 (2µM) + DMH1 (2µM) to generate caudal neuroepithelial progenitors [68]
- Ventralization & MNP Specification (Days 7-12): Switch to CHIR99021 (1µM) + SB431542 (2µM) + DMH1 (2µM) + retinoic acid (0.1µM) + purmorphamine (0.5µM) to specify OLIG2+ motor neuron progenitors (MNPs)
- Quality Checkpoint (Day 12): Assess MNP purity by immunostaining for OLIG2+/NKX2.2- population (>95% target)
- MNP Expansion (Optional): Passage MNPs maintaining same small molecule combination for controlled expansion
- Terminal Differentiation & Maturation (Days 13-28): Withdraw mitogens, add Notch inhibitor to promote maturation to ISL1+/MAP2+/SMI32+ motor neurons
Quality Control Metrics:
- Culture Purity: PAX6+OLIG2+ (>80%), ISL1+MAP2+ (quantified)
- Neuronal Health: D10 neurite area (>40,000 µm²)
- Cell Proliferation: NPC:D3 ratio (<3), D3:D10 ratio (<1) [53]
Signaling Pathways and Experimental Workflows
Diagram 1: Motor Neuron Differentiation Workflow with Quality Control Checkpoints. This diagram illustrates the staged differentiation process from pluripotent stem cells to mature motor neurons, highlighting critical quality control checkpoints and the negative impact of genomic instability.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagents for Genomic Stability and Motor Neuron Differentiation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor, WNT pathway activator | Promotes neural induction, caudalization; concentration critical (1-3µM) [68] |
| SB431542 | TGF-β/Activin-Nodal inhibitor | Enhances neural induction; blocks dorsalizing signals (2µM) [68] |
| DMH1 | BMP signaling inhibitor | Promotes ventralization; suppresses dorsal fate (2µM) [68] |
| Purmorphamine | Smoothened agonist, SHH pathway activator | Specifies motor neuron progenitors; concentration affects OLIG2/NKX2.2 balance (0.5-1µM) [68] |
| Retinoic Acid | Morphogen, caudalizing factor | Patterns anterior-posterior axis; combined with SHH for motor neuron induction (0.1µM) [68] |
| Karyotyping Services | Chromosomal analysis | Detects balanced translocations, copy number variations; gold standard for genomic integrity [22] |
| Array Genomic Hybridization (AGH) | High-resolution genomic analysis | Identifies microdeletions missed by karyotyping; complementary to traditional methods [22] |
| Targeted RT-qPCR Panel | Common abnormality screening | Routine monitoring of frequent karyotypic abnormalities; faster than full karyotyping [53] |
Diagram 2: Signaling Pathway Integration for Motor Neuron Specification. This diagram illustrates how coordinated signaling pathways direct cells toward motor neuron fate while suppressing alternative lineages, highlighting the importance of balanced pathway activation.
Quantitative Data Synthesis
Table 3: Sources of Variability in Motor Neuron Differentiation (Statistical Analysis)
| Source of Variability | Explanatory Power (R²) | Statistical Significance | Practical Implications |
|---|---|---|---|
| Operator | High (>50% for some metrics) | p < 0.05 | Standardized training essential; major impact on reproducibility [53] |
| Induction Set | Moderate to High | p < 0.05 | Reagent batches, environmental conditions significantly influence outcomes [53] |
| Cell Line Genetics | Low (<12% for most metrics) | p < 0.05 | Less impactful than handling factors; enables focus on controllable variables [53] |
| Genomic Stability Status | Significant for purity metrics | p < 0.05 | Stable cells show significantly greater purity at neural precursor and terminal differentiation stages [53] |
The consistent theme across recent research is that genomic stability provides the foundation for reliable differentiation, but optimal outcomes require integration of stable cell lines with standardized protocols and experienced technique. By implementing the systematic approaches outlined in this technical support guide—regular genomic assessment, standardized differentiation protocols, and comprehensive quality control—researchers can significantly enhance the reliability and reproducibility of their motor neuron differentiations and other lineage specification efforts.
Technical Support Center
Troubleshooting Guides
Problem 1: High and Variable Differentiation Rates in iPSC Cultures During Assay Setup
- Potential Cause: Spontaneous differentiation due to suboptimal culture conditions or overgrowth.
- Solution: Ensure cultures are passaged when colonies are large and compact but before they overgrow. Actively remove any areas of differentiation prior to passaging. Avoid keeping culture plates out of the incubator for extended periods and ensure cell aggregates are evenly sized during passaging [6]. Decrease colony density by plating fewer cell aggregates [6].
Problem 2: Poor Cell Survival and Low Attachment After Passaging for Assay Plating
- Potential Cause: Excessive single-cell dissociation or enzymatic over-exposure during passaging.
- Solution: Reduce incubation time with passaging reagents if your cell line is particularly sensitive [6]. For low attachment, initially plate 2–3 times the number of cell aggregates and ensure the use of correctly coated plates (e.g., use non-tissue culture-treated plates for Vitronectin XF) [6]. Use of a ROCK inhibitor (e.g., in RevitaCell Supplement) can significantly improve cell survival post-passaging and post-thaw [70] [71].
Problem 3: Inconsistent Data and High Well-to-Well Variability in Screening Readouts
- Potential Cause: Underlying genomic instability and genetic heterogeneity in the iPSC lines.
- Solution: Regularly monitor the genomic integrity of your master and working cell banks. Implement strategies to limit the acquisition of mutations during cell line generation and culture, such as nucleoside supplementation [14]. Use defined culture systems like HiDef B8 Growth Medium to minimize variability and spontaneous differentiation [71].
Problem 4: Confirmation of Genomic Instability in Poor-Performing Lines
- Potential Cause: Accumulation of copy number variations (CNVs) or single nucleotide variants (SNVs) during reprogramming or long-term culture.
- Solution: Perform regular genetic characterization. Techniques include:
Frequently Asked Questions (FAQs)
Q1: Why should I be concerned about genomic instability in iPSCs for drug screening? Genomic instability can lead to the accumulation of genetic variations, such as copy number variations (CNVs) and single nucleotide variants (SNVs) [1]. In drug screening, this means your cell populations are not genetically uniform. Unstable lines can exhibit altered differentiation potential, inconsistent responses to compounds, and general unpredictability, which severely compromises the reliability and reproducibility of your assay data [1] [14].
Q2: What are the main origins of genetic variations in my iPSC lines? Variations have at least three key origins:
- Pre-existing in Parental Cells: Low-frequency somatic variants in the original somatic cell population that are clonally expanded during reprogramming [1].
- Reprogramming-Induced: Mutations caused by replication stress during the reprogramming process itself [1] [14].
- Passage-Induced: Mutations that arise during prolonged in vitro culture [1].
Q3: How can I practically reduce genomic instability when generating new iPSC lines? A key strategy is to limit replication stress during reprogramming. Supplementing the culture medium with nucleosides has been shown to reduce the load of DNA damage and genomic rearrangements in resulting iPSCs [14]. This provides a simple, chemical means to generate genomically more stable lines.
Q4: What are the critical quality control checkpoints I should implement for my screening lines?
- Regularly Monitor Genomic Integrity: Schedule periodic checks using methods like karyotyping or SNP arrays for your actively cultured lines [1].
- Assess Pluripotency and Differentiation Potential: Confirm that your lines maintain their ability to differentiate into the relevant cell types for your assay.
- Check for Mycoplasma: Conduct routine mycoplasma testing to prevent contamination that can affect cell health and data [71].
- Document Culture History: Keep detailed records of passage numbers and culture conditions, as genomic instability can increase over time [1].
The performance of stable versus unstable iPSC lines can be quantified through various metrics. The tables below summarize key comparative data relevant to drug screening assays.
Table 1: Impact of Genomic Instability on iPSC Culture and Assay Readiness
| Performance Metric | Stable iPSC Line | Unstable iPSC Line | Impact on Drug Screening |
|---|---|---|---|
| Growth Rate Consistency | High, reproducible doubling times | Variable and unpredictable | Affects plating uniformity and timing for assay setup. |
| Spontaneous Differentiation | Low and consistent (<20%) [6] | High and variable | Creates heterogeneous cell populations, confounding results. |
| Clonal Survival Post-Passaging | High, with predictable attachment | Low and inconsistent | Leads to variable cell density across assay plates. |
| Karyotypic Abnormalities | Normal and stable | Frequent anomalies (e.g., Trisomy 12, 20q11.21 gain) [1] | Alters fundamental cell biology and drug response pathways. |
Table 2: Molecular Markers of Instability and Their Detection
| Marker Type | Detection Method | Stable iPSC Line | Unstable iPSC Line | Assay Relevance |
|---|---|---|---|---|
| DNA Damage Foci (γH2AX) | Immunofluorescence [72] [14] | Low number of foci per cell (<10) [72] | High number of foci per cell (>10) or pan-nuclear staining [72] | Indicates ongoing replication stress and DNA damage, affecting cell health. |
| Copy Number Variations (CNVs) | SNP array, aCGH, WGS [1] [14] | Few to no de novo CNVs | High number of de novo CNVs, often in fragile sites [1] [14] | Major source of genetic heterogeneity and functional variability. |
| Multi-Telomeric Signals (MTS) | Metaphase spread analysis [14] | Low number per metaphase | High number per metaphase [14] | Indicator of replication stress-induced chromosomal fragility. |
Experimental Protocols
Protocol 1: Reducing Reprogramming-Induced Genomic Instability via Nucleoside Supplementation
This protocol is adapted from Ruiz et al., 2015, and outlines a method to generate iPSC lines with reduced genomic instability [14].
- Reprogramming Initiation: Begin reprogramming of somatic cells (e.g., human dermal fibroblasts) using your method of choice (e.g., Sendai virus, episomal vectors).
- Supplementation: Upon initiation, supplement the reprogramming medium with a nucleoside solution.
- Final Concentration: Use a 1X final concentration of a commercially available nucleoside supplement (e.g, 100 μM dA, 100 μM dG, 100 μM dC, 100 μM dT/U).
- Continuous Exposure: Maintain the cells in the nucleoside-supplemented medium throughout the entire reprogramming process until iPSC colonies are picked and established.
- Validation: The resulting iPSC lines should be characterized for reduced markers of genomic instability, such as lower γH2AX foci counts, fewer multi-telomeric signals, and a reduced burden of de novo CNVs compared to lines generated without supplementation [14].
Protocol 2: Immunofluorescence Detection of γH2AX Foci as a Marker of DNA Damage
This protocol is used to quantify DNA double-strand breaks, a key indicator of genomic stress, in your iPSC cultures [72].
- Cell Seeding: Plate iPSCs on coated glass coverslips in a multi-well plate and culture until they reach ~60-70% confluency.
- Fixation: Aspirate the medium and wash cells with PBS. Fix cells with 4% paraformaldehyde in PBS for 15 minutes at room temperature.
- Permeabilization and Blocking: Wash with PBS and permeabilize with 0.5% Triton X-100 in PBS for 10 minutes. Block non-specific binding with 5% bovine serum albumin (BSA) in PBS for 1 hour.
- Primary Antibody Incubation: Incubate with anti-γH2AX (phospho-S139) primary antibody diluted in blocking buffer overnight at 4°C.
- Secondary Antibody Incubation: Wash and incubate with an appropriate fluorescently conjugated secondary antibody for 1 hour at room temperature in the dark.
- Counterstaining and Mounting: Wash and counterstain nuclei with DAPI (or Hoechst) for 5 minutes. Mount the coverslips onto glass slides using a mounting medium.
- Imaging and Analysis: Image cells using a fluorescence microscope. Score the number of distinct γH2AX foci per nucleus in a blinded manner. A high number of foci (>10 per nucleus) indicates significant DNA damage [72].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their functions for maintaining stable iPSC cultures and investigating genomic instability.
Table 3: Research Reagent Solutions for iPSC Genomic Stability
| Reagent / Tool | Function in Research | Example Product(s) |
|---|---|---|
| Chemically Defined Medium | Provides a consistent, xeno-free environment to support pluripotency and minimize spontaneous differentiation and variability. | mTeSR Plus, Essential 8 Medium, HiDef B8 Growth Medium [6] [70] [71] |
| ROCK Inhibitor | Improves survival of single iPSCs after passaging and cryopreservation by reducing apoptosis. | Y-27632, RevitaCell Supplement [70] [71] |
| Nucleoside Supplement | Reduces replication stress during reprogramming and culture, leading to fewer DNA damage events and CNVs. | Not specified in search results, but various commercial mixes are available. |
| Passaging Reagents | Enables gentle, non-enzymatic dissociation of iPSCs into ideal-sized aggregates for maintenance and expansion. | ReLeSR, Gentle Cell Dissociation Reagent [6] |
| Cell Recovery Supplement | Enhances viability and recovery of iPSCs after thawing cryopreserved vials. | Ready-CEPT [71] |
| γH2AX Antibody | A key immunofluorescence reagent for detecting and quantifying DNA double-strand breaks, a marker of genomic instability. | Various validated suppliers [72] [14] |
Experimental Workflow and Pathways
This workflow diagram outlines the key steps for analyzing and ensuring the quality of iPSC lines used in drug screening.
The diagram below illustrates the link between the source of instability and its functional consequences in a screening assay.
Troubleshooting Guides
Frequently Asked Questions on Genomic Stability in iPSC Cultures
What are the most common genetic variations found in iPSCs and how do they affect my experiments? iPSCs frequently acquire chromosomal aberrations and copy number variations (CNVs) during reprogramming and long-term culture. The most recurrent chromosomal aberration is trisomy 12, which contains pluripotency-associated genes and may confer a selective growth advantage [1]. The most common CNV hotspot is an amplification of 20q11.21, a region enriched with genes associated with pluripotency and anti-apoptosis [1]. These variations can significantly increase variance in differentiation experiments, as altered gene dosage may skew cells toward or away from specific lineages, compromising experimental reproducibility and outcome consistency.
How does genomic instability directly increase variance in my experimental data? Genomic instability introduces subpopulations of cells with different genetic backgrounds within your culture. During differentiation or functional assays, these subpopulations may respond differently to the same cues. For example:
- Differentiation Efficiency: A CNV affecting a key developmental gene can cause clones to have vastly different differentiation efficiencies into a target cell type (e.g., cardiomyocytes or neurons).
- Gene Expression Profiles: Bulk RNA-seq results can show high variability due to the presence of multiple genomic subtypes in your sample.
- Drug Response: Instability in genes related to drug metabolism or targets can lead to inconsistent results in pharmacological screens [1] [59].
Quantitatively, studies have shown that human iPSC lines can contain an average of approximately 10 protein-coding single nucleotide variants (SNVs) per line, in addition to CNVs and chromosomal changes [1].
I am observing inconsistent differentiation results between different passages of the same iPSC line. Could genomic instability be the cause? Yes, this is a classic sign. As iPSCs are passaged, new genetic variations can arise or pre-existing minor variants can clonally expand due to selective pressure [1]. Laurent et al. (2011) observed that deletions of tumor-suppressor genes are frequent in early-passage iPSCs, but duplications of oncogenic genes increase during cell passages [1]. This evolving genetic landscape means that differentiation cues may interact with a changing genome over time, directly increasing the passage-to-passage variance in your experimental outcomes.
What practical steps can I take to minimize replication stress during reprogramming? Reprogramming factor expression induces replication stress, a major source of DNA damage and genomic instability [14]. You can mitigate this:
- Chemically: Supplement the reprogramming medium with nucleosides. This has been shown to reduce the load of DNA damage (γH2AX levels) and lower the number of de novo CNVs in the resulting iPSC lines [14].
- Genetically: If modifying your reprogramming system is feasible, increasing the levels of the checkpoint kinase 1 (CHK1) can reduce replication stress and improve genomic stability [14].
My iPSC cultures are showing high rates of spontaneous differentiation. Is this linked to genetic instability? While often a culture condition issue, spontaneous differentiation can be a consequence of genomic instability. Aneuploidies or CNVs can alter the expression of pluripotency genes, making cells more prone to exit the pluripotent state. Furthermore, differentiated cells in culture can overgrow if they acquire a proliferative advantage due to mutations, creating a vicious cycle that increases the perceived "variance" in pluripotency marker expression across experiments [6].
Quantitative Impact of Instability and Interventions
The table below summarizes key quantitative findings from research on how specific interventions can reduce genomic instability and its associated variance.
| Intervention / Observation | Measured Outcome | Quantitative Impact | Effect on Experimental Variance |
|---|---|---|---|
| Nucleoside Supplementation (during reprogramming) | Reduction in de novo Copy Number Variants (CNVs) [14] | Lowered the average number of de novo CNVs in human iPSC lines [14] | Reduces variance in differentiation efficiency and functional assays between clones. |
| Nucleoside Supplementation (during reprogramming) | Reduction in DNA Damage (γH2AX foci) and chromosomal fragility (Multi-telomeric signals) [14] | Reduced γH2AX and significantly lower number of MTS/metaphase [14] | Leads to more consistent cell populations and reduces karyotypic variability. |
| CHK1 Overexpression (in MEFs) | Reduction in Reprogramming-Induced DNA Damage (γH2AX levels) [14] | Increased reprogramming efficiency (Chk1TG/TG > Chk1TG/+ > wt) [14] | Generates a more stable starting population, reducing inter-clonal variance. |
| Presence of Common CNVs (e.g., 20q11.21 amp) | Altered gene dosage of pluripotency/anti-apoptosis genes (BCL2L1, ID1, DNMT3B) [1] | Confers selective growth advantage; frequently observed in iPSCs and ESCs [1] | Major source of batch-to-batch variance; can dominate phenotype. |
Essential Protocols for Maintaining Genomic Stability
Protocol 1: Reducing Replication Stress During Reprogramming with Nucleoside Supplementation
This protocol is adapted from Ruiz et al., Nature Communications, 2015 [14].
- Preparation of Nucleoside Stock: Prepare a 1000X nucleoside stock solution containing 10 mM each of adenosine, guanosine, cytidine, and uridine in sterile DMSO.
- Reprogramming Initiation: Begin your standard reprogramming protocol (e.g., using OSKM transcription factors) in human fibroblasts.
- Supplementation: Add the nucleoside stock solution directly to the reprogramming medium to achieve a 1X working concentration immediately after viral transduction/induction.
- Continuous Exposure: Maintain the nucleoside supplementation throughout the entire reprogramming process, refreshing the medium every day.
- iPSC Colony Picking: Pick emerging iPSC colonies as per standard procedure. The nucleoside supplementation can be discontinued once stable clonal lines are established and expanded.
Expected Outcome: iPSC lines generated with this protocol have been shown to possess a lower load of DNA damage and fewer de novo genomic rearrangements, providing a more stable foundation for downstream experiments [14].
Protocol 2: Routine Genomic Monitoring of Cultured iPSCs
Implementing a schedule for genetic characterization is critical for identifying instability that could increase experimental variance.
- Short-Term Check (Every 5-10 passages):
- Method: Giemsa (G)-banding karyotyping.
- Purpose: To detect gross chromosomal abnormalities (e.g., trisomy 12, trisomy 8). This is a low-cost, readily applicable method for monitoring numerical and large structural changes [1].
- In-Depth Analysis (For key cell lines pre-critical experiments):
- Method: SNP array or Array Comparative Genomic Hybridization (aCGH).
- Purpose: To identify copy number variations (CNVs) at a higher resolution (kilobase level). This is effective for detecting recurrent CNVs like the amplification of 20q11.21 [1].
- High-Resolution Screening (For comprehensive characterization):
- Method: Whole Genome Sequencing (WGS).
- Purpose: To identify single nucleotide variants (SNVs) and all classes of structural variations across the entire genome at single-base resolution. This is the most thorough method for quantifying the overall mutational load [1].
Signaling Pathways and Experimental Workflows
The following diagram illustrates the relationship between reprogramming, replication stress, genomic instability, and the interventions that can break this cycle to reduce experimental variance.
The Scientist's Toolkit: Key Research Reagent Solutions
This table lists essential reagents mentioned in the search results for maintaining genomic integrity and managing iPSC culture health.
| Reagent / Material | Function / Purpose | Key Consideration for Genomic Stability |
|---|---|---|
| Nucleosides (Adenosine, Guanosine, Cytidine, Uridine) | Reduces replication stress during reprogramming by providing nucleotide precursors [14]. | Critical for minimizing the introduction of de novo CNVs during the initial derivation of iPSC lines. |
| Rho-associated kinase (ROCK) inhibitor (Y-27632) | Improves cell survival after passaging and cryopreservation by inhibiting apoptosis [73] [17] [74]. | Promotes clonal recovery without selective pressure, helping to maintain a genetically heterogeneous and representative culture. |
| Gentle Cell Dissociation Reagent (e.g., EDTA, Dispase) | Promotes detachment of iPSC colonies as clumps with minimal enzymatic activity [6] [74]. | Gentle handling preserves cell viability and reduces stress, which can be a source of genomic instability. |
| bFGF (Basic Fibroblast Growth Factor) | Key growth factor for maintaining pluripotency in culture media [17] [74]. | Use animal component-free, high-quality bFGF for consistent signaling; instability or variability can induce stress and differentiation. |
| CHK1 Expression Vector | Genetic tool to increase levels of the checkpoint kinase 1 [14]. | A genetic strategy to directly combat replication stress during reprogramming, improving efficiency and genomic fidelity. |
| Mycoplasma Detection Kit | Regular testing for mycoplasma contamination [74]. | Chronic mycoplasma infection can cause pervasive genetic and metabolic stress, profoundly impacting genomic stability and data variance. |
In the field of induced pluripotent stem cell (iPSC) research, genomic instability presents a significant challenge, particularly during long-term culture. Genetic variations can accumulate through the reprogramming process, during extended passaging, and throughout differentiation protocols, potentially compromising experimental reproducibility and therapeutic safety [1]. This technical support center provides a comprehensive framework for utilizing reference iPSC lines as critical tools for quality assurance, enabling researchers to monitor, benchmark, and maintain genomic integrity in their studies.
The Critical Role of Reference iPSC Lines in Quality Control
Reference iPSC lines serve as standardized benchmarks across laboratories and experiments, providing a constant against which experimental variables can be measured. Well-characterized reference lines like KOLF2.1J and those in the Allen Cell Collection offer thoroughly documented genetic backgrounds, stable pluripotency, and known differentiation capabilities [75] [76]. By regularly comparing in-house iPSC cultures to these reference standards, researchers can:
- Detect culture-induced anomalies through comparative genomic analysis
- Validate experimental protocols including differentiation efficiency and genome editing outcomes
- Establish inter-laboratory reproducibility for collaborative projects
- Monitor long-term genomic stability across multiple passages
The KOLF2.1J line exemplifies an effective reference standard, demonstrating robust growth, stable pluripotency across passages, absence of high-risk neurodegenerative alleles, and efficient differentiation into relevant cell types, particularly neural lineages [77]. Its selection criteria provide a framework for evaluating other potential reference lines for specific research applications.
Troubleshooting Genomic Instability in iPSC Cultures
Problem: Excessive Spontaneous Differentiation in Cultures
- Potential Causes and Solutions:
- Check media age and quality: Ensure complete cell culture media has been stored properly and is less than two weeks old [6].
- Optimize passaging timing: Passage cultures when colonies are large and compact with dense centers, before overgrowth occurs [6].
- Manage colony density: Decrease colony density by plating fewer cell aggregates during passaging to prevent nutrient competition [6].
- Remove differentiated areas: Physically remove differentiated regions prior to passaging to maintain pluripotent populations [6].
- Limit external exposure: Avoid having culture plates out of the incubator for more than 15 minutes at a time [6].
Problem: Declining Pluripotency Marker Expression
- Verification Protocol:
- Confirm pluripotency markers: Assess expression of hallmark genes (Nanog, OCT4, SSEA-4, TRA-1-60, TRA-1-81) via immunofluorescence staining or flow cytometry [64].
- Perform functional validation: Conduct trilineage differentiation assays to confirm developmental potential into ectoderm, mesoderm, and endoderm derivatives [64] [78].
- Check culture conditions: Ensure appropriate extracellular matrices and media formulations with quality growth factors are being used [78].
Problem: Detection of Genetic Aberrations
- Monitoring and Intervention Strategy:
- Regular karyotyping: Perform G-banding analysis every 10-15 passages to detect chromosomal abnormalities, with particular attention to chromosomes 12, 17, 20, and X, which are common hotspots for iPSC abnormalities [1] [64].
- Implement higher-resolution methods: Supplement G-banding with array CGH or digital PCR to identify copy number variations (CNVs) that may be missed by conventional karyotyping [1] [64].
- Utilize NGS technologies: For comprehensive variant detection, employ whole genome or whole exome sequencing to identify single nucleotide variants (SNVs) and small indels at single-base resolution [1].
- Compare to reference lines: Sequence reference lines in parallel to distinguish culture-specific mutations from background variants [75].
Essential Quality Control Methodologies
Genomic Stability Assessment Workflow
The following diagram illustrates a comprehensive workflow for maintaining and assessing genomic stability in iPSC cultures using reference lines:
Performance Benchmarking Against Reference Lines
Regular comparison of experimental iPSC lines with reference standards provides critical quality metrics. The following table summarizes key parameters for assessment:
| Quality Parameter | Assessment Method | Frequency | Acceptance Criteria | Reference Standard Data |
|---|---|---|---|---|
| Pluripotency | Flow cytometry for TRA-1-60, NANOG | Every 5 passages | >90% positive cells [75] | KOLF2.1J: >90% positive [75] |
| Karyotype | G-banding analysis | Every 10-15 passages | Normal euploidy (46, XY/XX) | Allen Cell Collection: Normal karyotype [76] |
| CNV Burden | Array CGH or digital PCR | Every 20 passages | No recurrent CNVs at 12p, 20q11.21 | WTC-11 line: CNV profile documented [76] |
| SNV Load | Whole exome sequencing | At banking and critical milestones | <10 novel protein-coding mutations | KOLF2.1J: WGS variants documented [75] |
| Differentiation Potential | Trilineage differentiation assay | After reprogramming and at banking | Robust differentiation to all germ layers | KOLF2.1J: Excellent neuronal differentiation [77] |
| Growth Rate | Cell counting and confluence assays | Continuous monitoring | Stable population doubling time | Reference line-specific proliferation data [75] |
Frequently Asked Questions (FAQs)
Q: How often should I compare my iPSC cultures to reference lines? A: Regular benchmarking should occur at minimum during initial culture establishment, before and after critical manipulations (such as genome editing), at banking milestones, and every 10-15 passages during long-term culture [1] [64]. More frequent comparison is recommended when establishing new protocols or noticing phenotypic changes.
Q: What are the key genetic hotspots to monitor in iPSCs? A: Current evidence identifies several recurrent instability regions: trisomy of chromosome 12 (containing pluripotency genes), amplifications of chromosomes 8 and X, and copy number variations at 20q11.21 (containing anti-apoptotic genes) [1]. TP53 mutations are also frequently observed and should be specifically monitored [4].
Q: How can I distinguish pre-existing mutations from culture-acquired variants? A: This requires sequencing of the parental somatic cells and the derived iPSC line. Ultra-deep sequencing of parental cells can identify low-frequency pre-existing variants that may become fixed during reprogramming. Comparison with reference line data helps identify technical artifacts [1].
Q: What reference lines are available for specific disease modeling applications? A: The Allen Cell Collection provides extensively characterized base lines, while specialized collections like the iNDI initiative offer lines optimized for neurodegenerative disease research [76] [77]. KOLF2.1J has demonstrated particular utility for neural differentiation and neurodegenerative disease modeling [77].
Q: How does the choice of reprogramming method impact genomic stability? A: Studies indicate that Sendai virus reprogramming may result in a higher frequency of copy number alterations and single nucleotide variations compared to episomal vector methods [4]. Non-integrating methods generally produce more genomically stable lines suitable as reference standards [79] [77].
Research Reagent Solutions for Quality Assurance
The following table outlines essential reagents and their functions in maintaining genomic stability and quality control:
| Reagent Category | Specific Examples | Function in Quality Assurance |
|---|---|---|
| Culture Media | mTeSR Plus, Essential 8 Medium | Defined formulations that support pluripotency while minimizing spontaneous differentiation [6] [73] |
| Extracellular Matrices | Matrigel, Geltrex, Laminin, Vitronectin XF | Provide consistent substrate for attachment and growth, reducing selective pressures that can cause genomic instability [73] [78] |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent, EDTA | Gentle dissociation methods that minimize cellular stress and DNA damage [6] [78] |
| ROCK Inhibitors | Y-27632, RevitaCell Supplement | Improve cell survival after passaging and freezing, reducing selective pressures that favor abnormal clones [73] [78] |
| Growth Factors | Animal component-free bFGF, TGF-β1 | High-quality recombinant proteins that maintain pluripotency without introducing contaminants [78] |
| Genomic Analysis Kits | G-banding kits, SNP arrays, WGS library prep | Enable regular monitoring of genomic integrity and comparison with reference standards [1] [64] |
Implementing a robust quality assurance program centered on well-characterized reference iPSC lines is essential for producing reliable, reproducible research outcomes. By establishing regular benchmarking practices, utilizing comprehensive genomic stability assessments, and maintaining detailed documentation, researchers can significantly enhance the validity of their findings while advancing our understanding of genomic instability mechanisms in pluripotent stem cells.
Conclusion
Preventing genomic instability is not merely a technical challenge but a fundamental prerequisite for generating reliable, reproducible iPSC models. A proactive, integrated approach—combining routine genomic monitoring with optimized culture practices and rigorous validation—significantly enhances differentiation purity, reduces experimental variance, and strengthens the translational potential of iPSC-based research. Future efforts must focus on developing more sensitive, accessible monitoring tools and establishing universally accepted stability criteria. As the field advances toward clinical applications, mastering the long-term genomic stability of iPSCs will be paramount for realizing the full promise of regenerative medicine and personalized drug discovery.
References
- 1. Genomic Instability of iPSCs: Challenges Towards Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5346115/]
- 2. Chromosomal Aberrations in Induced Pluripotent Stem Cells [https://www.mdpi.com/1422-0067/26/16/7728]
- 3. Chromosomal aberrations after induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8425414/]
- 4. Tracing genomic instability in induced mesenchymal ... [https://www.nature.com/articles/s12276-025-01439-8]
- 5. Comprehensive characterization of genomic instability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5121198/]
- 6. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 7. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/ca/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 8. Genetic and epigenetic variations in iPSCs: potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3760008/]
- 9. How To Overcome Immune Rejection In iPSC-based Gene ... [https://www.cellandgene.com/doc/how-to-overcome-immune-rejection-in-ipsc-based-gene-therapy-0001]
- 10. Chromosomal aberration arises during somatic ... - Cell Division [https://celldiv.biomedcentral.com/articles/10.1186/s13008-020-00068-z]
- 11. Long-Term Cryopreservation May Cause Genomic ... [https://www.mdpi.com/1422-0067/25/3/1467]
- 12. Jurkat T-cell lines exhibit marked genomic instability affecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12214745/]
- 13. Exploring the promising potential of induced pluripotent ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01873-0]
- 14. Limiting replication stress during somatic cell ... [https://www.nature.com/articles/ncomms9036]
- 15. Genomic integrity of human induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC6828592/]
- 16. Somatic mutations alter the differentiation outcomes of ... [https://www.sciencedirect.com/science/article/pii/S2666979X2300040X]
- 17. Tips and tricks for successfully culturing and adapting human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8640166/]
- 18. Minireviews Genomic Instability in Pluripotent Stem Cells [https://www.sciencedirect.com/science/article/pii/S0021925820440992]
- 19. Chromosomal Aberrations in Induced Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387029/]
- 20. A Protocol for Culture and Characterization of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10506163/]
- 21. Karyotype Analysis for iPSC [https://www.creative-biolabs.com/stem-cell-therapy/karyotype-analysis-for-ipsc.htm]
- 22. Genetic instability of iPSCs: Why does it matter? [https://www.cellgs.com/blog/genetic-instability-of-ipscs-why-does-it-matter.html]
- 23. Jurkat T-cell lines exhibit marked genomic instability ... [https://www.nature.com/articles/s41598-025-95903-0]
- 24. Chromosomal quality control in hPSCs: A practical guide to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259632/]
- 25. Cytogenetics Basics - Wisconsin State Laboratory of Hygiene [https://www.slh.wisc.edu/clinical/cytogenetics/education/basics/]
- 26. Help File - ISCN Symbols and Abbreviated Terms [https://www.coriell.org/0/Sections/Support/Global/iscn_help.aspx?PgId=263]
- 27. Examining iPSC derived motor neuron variability and ... [https://www.nature.com/articles/s41598-025-23378-0]
- 28. The Challenges to Advancing Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 29. Controlling for contamination in qPCR testing - LGC [https://blog.biosearchtech.com/how-to-control-for-contamination-in-qpcr-testing]
- 30. qPCR Troubleshooting Guide [https://azurebiosystems.com/qpcr-resources/troubleshooting/]
- 31. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 32. Tips for Successful aCGH [https://www.enzo.com/note/tips-for-successful-acgh/]
- 33. The Principles and Workflow of SNP Microarray [https://www.cd-genomics.com/the-principles-and-workflow-of-snp-microarray.html]
- 34. High-resolution genomic profiling of chromosomal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1557768/]
- 35. SNP Genotyping Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/snp-genotyping-support/snp-genotyping-support-troubleshooting.html]
- 36. Stem Genomics publishes latest genomic stability QC for ... [https://www.stemgenomics.com/blog/genomic-stability-workflow-for-pluripotent-stem-cells-psc-introducing-practical-guidelines-for-regular-in-process-testing-of-psc-lines/]
- 37. iPSC Maintenance Challenges and How to Overcome Them [https://definedbioscience.com/blogs/news/ipsc-maintenance-challenges-and-how-to-overcome-them?srsltid=AfmBOoqmGonqQ3Gi9ZRFnw0tR2YuUQNJm4cPzRaIzqHFOp7Py6OYHo_F]
- 38. Technical standards for the interpretation and reporting of... [https://pubmed.ncbi.nlm.nih.gov/31690835/]
- 39. Chromosomal Instability Estimation Based on Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5112954/]
- 40. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 41. Current analysis platforms and methods for detecting copy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3544484/]
- 42. Clinical interpretation of copy in the human genome number variants [https://link.springer.com/article/10.1007/s13353-017-0407-4]
- 43. iPSC culture expansion selects against putatively ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8514965/]
- 44. Copy Number Variation (CNV) Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/copy-number-variation-support/copy-number-variation-support-troubleshooting.html]
- 45. Poor Adherent Cell Attachment Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/poor-adherent-cell-attachment-troubleshooting?srsltid=AfmBOoqRilPvzfHRn2OMXmlIU22bGgHvvnR9fRNdDhOxZ7MjL7SqkCb-]
- 46. iPSC Maintenance Challenges and How to Overcome Them [https://definedbioscience.com/blogs/news/ipsc-maintenance-challenges-and-how-to-overcome-them?srsltid=AfmBOoq89i2v7X-G4h-AjC59YM_5aZHCXDsHd4CzudNshFyIMX29K_CA]
- 47. Systematic optimization of culture media for maintenance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11226774/]
- 48. Genomic instability in long-term culture of human adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10361644/]
- 49. Pluripotent Stem Cell (PSC) Protocols [https://www.thermofisher.com/us/en/home/references/protocols/cell-culture/stem-cell-protocols/ipsc-protocols.html]
- 50. Passage Number is a Major Contributor to Genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4165691/]
- 51. Genomic integrity of human induced pluripotent stem cells ... [https://www.sciencedirect.com/science/article/pii/S1873506120301057]
- 52. Optimization of Long-Term Human iPSC-Derived Spinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8784909/]
- 53. Examining iPSC derived motor neuron variability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612198/]
- 54. Automating iPSC Manufacturing: Overcoming inherent and ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925006759]
- 55. Automated Cell Culture [https://www.moleculardevices.com/applications/automated-cell-culture]
- 56. A Highly Optimized Protocol for Reprogramming Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4312798/]
- 57. Human‐Induced Pluripotent Stem Cell Culture Methods Under ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7507179/]
- 58. Identifying and optimizing critical process parameters for large ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03973-0]
- 59. The consequences of recurrent genetic and epigenetic ... [https://www.sciencedirect.com/science/article/pii/S1934590922004532]
- 60. Developing iPSC Therapies: Why Your CMC Strategy ... [https://www.exmoorpharma.com/blog/ipsc-cmc-strategy-development/]
- 61. iPSC Maintenance Challenges and How to Overcome Them [https://definedbioscience.com/blogs/news/ipsc-maintenance-challenges-and-how-to-overcome-them?srsltid=AfmBOoo-5SZdb5Ao6h3Qdr9z6IJirMkuzD-SoVfD2kSvCYqzGSwl14JH]
- 62. Dynamic Features of Chromosomal Instability during Culture of Induced Pluripotent Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9318709/]
- 63. iPSCs: Unstable Origins? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3129555/]
- 64. Quality Control: What is really in your hiPSC culture? [https://www.reprocell.com/blog/key-quality-controls-of-human-induced-pluripotent-stem-cells]
- 65. Troubleshoot cell growth | PHCbi [https://www.phchd.com/apac/biomedical/service-downloads/evolving-science-for-the-future/troubleshoot-cell-growth]
- 66. Validating human induced pluripotent stem cell-specific ... [https://www.sciencedirect.com/science/article/pii/S1465324924006108]
- 67. What are the disadvantages of pluripotent stem cells? [https://int.livhospital.com/disadvantages-of-pluripotent-stem-cells/]
- 68. Generation and expansion of highly pure motor neuron ... [https://www.nature.com/articles/ncomms7626]
- 69. Long-term single-cell passaging of human iPSC fully ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7586033/]
- 70. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/ar/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 71. iPSC Maintenance Challenges and How to Overcome Them [https://definedbioscience.com/blogs/news/ipsc-maintenance-challenges-and-how-to-overcome-them?srsltid=AfmBOoqEWieEy5f27ODT2lcWX6B-ty5hNJx0Jg9wIq3QVlUrJjYojffK]
- 72. Tools used to assay genomic instability in cancers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8891418/]
- 73. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 74. Tips and tricks for iPSC culture [https://www.ptglab.com/news/blog/tips-and-tricks-for-ipsc-culture/?srsltid=AfmBOoq5qPYQMVPlm1tYGEl9YQBvq-M7ToEP91D5Cv8QZOqow-9koJ4o]
- 75. A reference human induced pluripotent stem cell line for large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9782786/]
- 76. FAQ [https://www.coriell.org/1/AllenCellCollection/FAQ]
- 77. Defining a Reference iPSC Line [https://www.jax.org/news-and-insights/jax-blog/2025/august/universal-reference-ipsc-line]
- 78. Tips and tricks for iPSC culture [https://www.ptglab.com/news/blog/tips-and-tricks-for-ipsc-culture/?srsltid=AfmBOoqrm_Cs8rHsdojVSU9adenGmIXlpbleilO4878i_olJmeKKINoE]
- 79. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]