Standardizing Differentiation Efficiency in Patient-Specific Stem Cell Lines: From Foundational Challenges to Clinical Translation
This article addresses the critical challenge of variability in differentiation efficiency across patient-specific stem cell lines, a major bottleneck in regenerative medicine and drug development.
Standardizing Differentiation Efficiency in Patient-Specific Stem Cell Lines: From Foundational Challenges to Clinical Translation
Abstract
This article addresses the critical challenge of variability in differentiation efficiency across patient-specific stem cell lines, a major bottleneck in regenerative medicine and drug development. We explore the foundational sources of variability, from genetic and epigenetic heterogeneity to technical protocol inconsistencies. The piece delves into cutting-edge methodological solutions, including non-destructive imaging and machine learning for early prediction, alongside optimization strategies like protocol harmonization and advanced genome editing. Finally, we examine validation frameworks and global regulatory landscapes essential for translating standardized, reproducible stem cell products from the laboratory to the clinic, providing a comprehensive roadmap for researchers and drug development professionals.
Understanding the Bottleneck: Why Differentiation Efficiency Varies in Patient-Specific Lines
The Critical Need for Standardization in Translational Stem Cell Research
FAQs and Troubleshooting Guides
Fundamental Concepts and Standards
Q1: Why is standardization so critical in translational stem cell research?
Standardization is the cornerstone of transforming stem cell research from a promising scientific field into reliable, clinically applicable therapies. Without it, significant variability is introduced from multiple sources, including donor genetic background, culture conditions, reagent inconsistencies, and protocol differences [1]. This variability frustrates attempts to compare results across labs, collaborate effectively, and scale up for translational work. The International Society for Stem Cell Research (ISSCR) and other regulatory bodies emphasize that standards help enable collaborations, support efficient clinical translation, reduce costs, and engender trust among patients [2] [3]. Ultimately, standardization moves the field toward workflows that produce consistent, day-after-day results, which is a prerequisite for developing safe and efficacious cell therapies [4] [1] [5].
Q2: What are the key areas where standards are needed?
The ISSCR highlights numerous areas where standards development would greatly advance stem cell science and its clinical application [2]. Key opportunities include:
- Source Materials: Standards for consent, procurement, manufacturing regulations, and cell potency assays.
- Process Controls: Standards for biobanking, minimally acceptable changes during cell culture, reporting of animal experiments, and trial design.
- Analytical Methods & Data Processing: Standards for characterizing cells and reporting data to ensure reproducibility.
Q3: What is the difference between assessing pluripotency as a "state" versus a "function"?
This is a crucial distinction in cell characterization [6].
- Pluripotency as a State: This involves identifying molecular signatures commonly observed in pluripotent populations, such as the expression of key transcription factors (OCT4, SOX2, NANOG) and cell surface markers (SSEA-4, TRA-1-60) via immunocytochemistry or flow cytometry [6]. While important, these markers in isolation do not necessarily confirm the cell's functional capacity to differentiate.
- Pluripotency as a Function (Developmental Potency): This assesses the actual differentiation capacity of a stem cell population. Assays like the teratoma formation assay (in vivo) or embryoid body formation (in vitro) are used to empirically prove that the cells can generate differentiated progeny from all three developmental germ layers (ectoderm, mesoderm, and endoderm) [6].
Troubleshooting Common Experimental Issues
Q4: My differentiation yields are low and variable. What could be the cause?
Low and variable differentiation efficiency is a common challenge, often stemming from inconsistencies in the starting cell population or differentiation process. Key factors to investigate are:
- Quality of Starting Cells: Ensure your pluripotent stem cells are healthy, free of spontaneous differentiation, and have been properly characterized for pluripotency and genomic integrity [7]. Passaging cells at very high density or when they are over-confluent can reduce their differentiation potential.
- Cell Cluster Size in 3D Differentiation: For protocols involving embryoid body (EB) formation, the size of the cell clusters has a significant impact on differentiation efficiency. EBs that are too large can develop a hypoxic core, leading to cell death and haphazard organization [6] [8]. Using cell cluster sorting or standardized aggregation methods can produce EBs of a defined size, improving reproducibility and yield [8].
- Reagent Consistency: Inconsistencies in growth factors, cytokines, or small molecule inducers between batches can derail a protocol. Using well-validated, GMP-grade reagents where possible helps minimize this variability [1].
Q5: How can I reduce technician-to-technician variability in my stem cell culture and differentiation workflows?
Human handling is a major source of variation. Strategies to mitigate this include:
- Detailed, Validated Protocols: Start with established guidelines from trusted sources like the ISSCR and document every procedural detail, from seeding density and passage number to the exact timing of media changes [1].
- Automation: Implementing automated liquid handling systems for cell passaging, feeding, and differentiation can drastically reduce human error and improve inter-technician consistency [8] [1]. Automated platforms can maintain iPS cells in an undifferentiated state for long periods and ensure highly parallelized processing [8].
- Adoption of Defined Culture Systems: Moving away from poorly defined components like animal feeder layers and serum toward feeder-free, xeno-free, and GMP-grade media and substrates eliminates batch inconsistency associated with biological materials [1].
Q6: I am concerned about genomic instability in my stem cell lines. What are the risks and how can I monitor them?
Stem cells are subject to the acquisition of genetic changes in culture, which can confer a growth advantage and alter the cell's phenotype and behavior [7]. These changes can impact the reproducibility of your results and the safety of any derived therapies.
- Risks: Genetic alterations can affect the differentiation capacity of the stem cells and the functional properties of the cells derived from them.
- Monitoring: Regular genomic characterization is essential. Karyotyping is a standard method to assess chromosome number and integrity [6]. For higher resolution, more sensitive detection methods like genomic sequencing can be employed to identify subtle genetic variants that may not be visible by karyotyping [7].
Analytical and Reporting Standards
Q7: What are the minimal criteria I should report when publishing results with human pluripotent stem cells (hPSCs)?
To ensure reproducibility, published papers should include detailed information on key parameters [7]. The ISSCR Standards provide comprehensive guidance, which includes:
- Basic Characterization: Cell line origin, culture conditions, and mycoplasma status.
- Status of the Undifferentiated State: Evidence of pluripotency, including marker expression and, ideally, a functional assessment of differentiation potential.
- Genomic Characterization: Results of karyotyping or other genetic analysis to confirm genomic integrity.
- Details of Stem Cell-Based Model Systems: For differentiated models, a thorough description of the protocol and characterization of the resulting cells.
- Reporting: Detailed methodology to allow other labs to replicate the work.
Q8: The teratoma assay is considered a gold standard, but what are its limitations?
While the teratoma formation assay is considered a rigorous in vivo method to confirm pluripotency, it has several significant disadvantages [6]:
- Practical Constraints: It is labour-intensive, time-consuming (taking several weeks to months), and expensive due to animal care and maintenance.
- Ethical Considerations: The use of immunocompromised animals raises ethical issues.
- Technical and Analytical Challenges: The assay suffers from protocol variation between laboratories, which impacts tumour differentiation. The analysis is primarily qualitative (morphological identification of tissues) and can be subject to interpretation, with significant inter-tumour heterogeneity. There are also few universally accepted reporting standards for the assay.
Troubleshooting Guide: Common Problems and Solutions
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Differentiation Efficiency | - Poor starting cell quality- Inconsistent EB/organoid size- Unoptimized cytokine/growth factor concentrations- High spontaneous differentiation in PSC culture | - Characterize PSCs for pluripotency before differentiation [7]- Use cell cluster sorting for defined EB size [8]- Perform dose-response experiments for signaling molecules [9]- Improve routine PSC culture; use Rho-associated kinase (ROCK) inhibitor for single-cell survival [10] |
| High Variability Between Replicates/Experiments | - Technician handling differences- Batch-to-batch reagent variability- Inconsistent cell passaging- Fluctuations in incubation conditions (CO₂, temperature) | - Automate key culture and differentiation steps [8] [1]- Source GMP-grade or highly validated reagents [1]- Standardize passaging criteria and methods (e.g., consistent pipetting cycles) [8]- Regularly calibrate incubators and equipment |
| Contamination of Differentiated Cultures with Undifferentiated Cells | - Incomplete differentiation- Lack of selection methods for target cells | - Optimize differentiation protocol timing and factor combinations [10] [9]- Include a passage or freezing step post-differentiation to reduce undifferentiated cells [10]- Use fluorescence-activated cell sorting (FACS) to purify target population |
| Genomic Instabilities in PSC Lines | - Culture-adapted mutations- High passage number- Stress from suboptimal culture conditions | - Regularly karyotype cells and use more sensitive genomic assays [6] [7]- Use low-passage cell banks for experiments- Culture cells in defined, physiologically optimized conditions [1] |
Standardized Experimental Protocols
Protocol 1: Automated Workflow for Clonal iPS Cell Line Establishment and Defined EB Formation
This protocol, adapted from Ma et al. (2022), integrates automation and cell cluster sorting to enhance reproducibility [8].
Key Materials:
- Liquid Handling Unit (LHU): Hamilton STARlet or equivalent.
- Cell Cluster Sorter: Union Biometrica's BioSorter or equivalent.
- iPS Cells: Cultured on MEF feeders or feeder-free.
- Reagents: Collagenase IV, appropriate iPS cell culture media.
Methodology:
- Automated iPS Cell Culture: Maintain iPS cells on the automated platform, with regular feeding and monitoring via integrated microscopy.
- Passaging and Cluster Size Control: Dissociate iPS cell colonies using Collagenase IV. Use the LHU to resuspend the colonies with a predefined number of pipetting cycles (e.g., 5-8 cycles) to break them into uniformly sized clusters.
- Cell Cluster Sorting for Cloning: Analyze and sort the cell clusters using the BioSorter. Individual clusters of 5-10 cells are sorted into individual wells of a 96-well plate to establish clonal iPS cell lines.
- EB Formation of Defined Size: For differentiation, sort larger, defined clusters (e.g., 100-150 µm in diameter) into low-attachment plates to initiate homogeneous EB formation.
- Differentiation: Proceed with directed hematopoietic or other differentiation protocols using these standardized EBs.
Protocol 2: Time-Efficient Differentiation and Cryopreservation of Pancreatic Progenitors
This protocol, based on the work of Lucar et al. (2024), shortens the differentiation timeline and enables banking of intermediate cells [10].
Key Materials:
- iPS Cells: Patient-specific iPS cells.
- Cytokines and Small Molecules: Activin A, CHIR99021, FGF-7, cyclopamine, noggin, all-trans retinoic acid, GLP-1, nicotinamide.
- Media: RPMI 1640, StemMACS iPS-Brew XF.
- Matrix: Matrigel.
Methodology:
- Directed Differentiation:
- Stage I - Definitive Endoderm (4 days): Differentiate iPS cells using Activin A (100 ng/mL) and CHIR99021 (3 µM).
- Stage II - Primitive Gut Tube (3 days): Pattern endoderm with FGF-7 (50 ng/mL).
- Stage III - Pancreatic Progenitors (3 days): Induce pancreatic fate with cyclopamine (0.25 µM), noggin (50 ng/mL), and all-trans retinoic acid (2 µM).
- Cryopreservation of Progenitors: At the end of Stage III, harvest pancreatic progenitor cells. Cryopreserve them in appropriate freezing medium. Upon thawing, the cells can be replated and expanded.
- Final Differentiation and Analysis:
- Stage IV - Pancreatic Exocrine Cells (4-20 days): Differentiate thawed or freshly derived progenitors using FGF-7, GLP-1, and nicotinamide.
- Characterization: Assess efficiency by qPCR (for PDX1, AMY2A/B) and immunofluorescence (for PDX1 and amylase proteins). A reduction in stemness markers like OCT4 and NANOG after passaging or freezing indicates a purer pancreatic cell population [10].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Rationale for Use in Standardized Workflows |
|---|---|---|
| GMP-Grade Media | Provides nutrients and signaling milieu for cell growth/differentiation | Minimizes batch-to-batch variability; supports clinical translation [1] |
| Feeder-Free Matrix | Provides a defined substrate for cell attachment and growth | Eliminates inconsistency and contamination risk from animal feeder cells [1] |
| Validated Antibodies | Detects key pluripotency (OCT4, SOX2) and differentiation (PDX1, Amylase) markers | Critical for accurate characterization; poor antibodies are a major source of irreproducibility [1] |
| Cell Cluster Sorter | Analyzes and sorts cell clusters/EBs by size and fluorescence | Enables production of uniformly sized EBs, critical for reproducible differentiation [8] |
| Liquid Handling Robot | Automates repetitive tasks (media changes, passaging) | Reduces human error and inter-technician variability, enhancing reproducibility [8] [1] |
| ROCK Inhibitor (Y-27632) | Improves survival of single pluripotent stem cells | Increases plating efficiency after passaging or thawing, standardizing initial cell numbers [10] |
Standardized Assessment Workflow
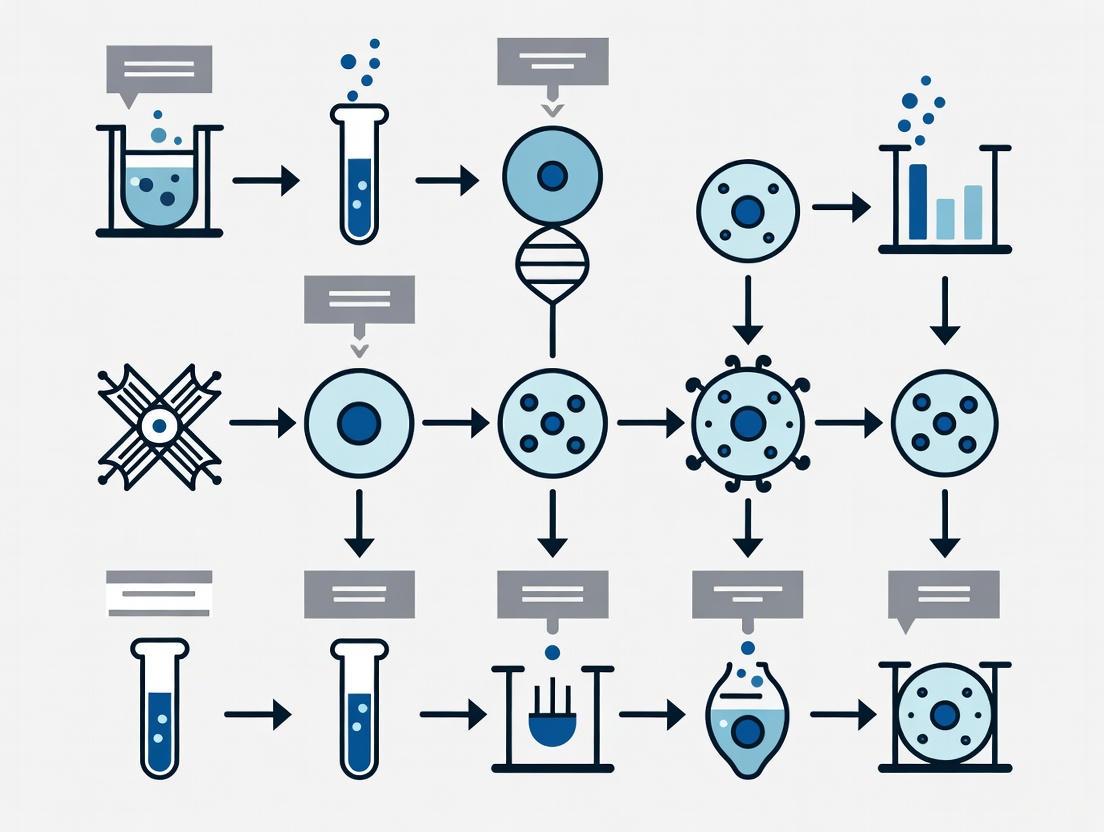
This diagram illustrates a comprehensive, standardized workflow for the characterization of human pluripotent stem cells (hPSCs), integrating assessments of both their "state" and "function" as recommended by the ISSCR [6] [7].
Framework for Standardization
This diagram outlines the multi-level framework necessary for achieving standardization in translational stem cell research, from foundational materials to final application.
What are the primary genetic variations found in iPSCs and how do they originate?
Genetic variations in induced pluripotent stem cells (iPSCs) can originate from multiple sources and manifest as different types of abnormalities. The main types include aneuploidy (abnormal chromosome numbers) and subchromosomal copy number variations (CNVs) [11].
Table 1: Sources and Types of Genetic Variations in iPSCs
| Variation Type | Common Examples | Primary Sources | Frequency/Occurrence |
|---|---|---|---|
| Aneuploidy (Whole chromosome gains/losses) | Trisomy 12 (most common), Trisomy 8, Trisomy X [11] | - Innate instability of in vitro pluripotent state [11]- Prolonged culture (adaptive selection) [11]- Inherited from aneuploid source cells [11] | ~13-33% of hESC/hiPSC cultures [11] |
| Subchromosomal CNVs (Mb-scale deletions/duplications) | Variations around genes like NANOG (Chr. 12), DNMT3B (Chr. 20) [11] | - Reprogramming process (replication stress) [11]- Pre-existing mosaicism in source cells [11]- Prolonged culture [11] | High frequency noted in early-passage iPSCs (deletions often lost through passaging) [11] |
| Single Nucleotide Variations (SNVs) | Point mutations [11] | - Reprogramming-induced mutations [11]- Carried over from source cells [11] | Fewer de novo SNVs detected by sequencing studies [11] |
These variations are significant because they can confer a growth advantage under culture conditions, alter stem cell phenotype and behavior, and impact the reproducibility of downstream differentiation experiments [11] [7].
How does epigenetic variation affect the differentiation capacity of patient-specific iPSC lines?
Epigenetic variation is a strong indicator and determinant of a cell line's ability to differentiate into specific lineages. Donor-specific epigenetic patterns are maintained in iPSCs after reprogramming, creating a "molecular memory" that influences differentiation potential [12] [13].
Key Findings:
- Predictive Epigenetic Marks: Studies integrating molecular signatures with differentiation performance have found that hematopoietic commitment capacity correlates with IGF2 expression levels, which itself depends on signaling-dependent chromatin accessibility. Furthermore, the maturation capacity of derived blood cells is associated with specific patterns of DNA methylation acquired during reprogramming [13].
- Dynamic Relationship with Genetic Variation: The relationship between genetic variation and epigenetic variation is strongest at the iPSC stage. While iPSCs from the same donor cluster closely based on DNA methylation patterns, this donor-dependency decreases after differentiation. Epigenetic variation increases significantly in differentiated cell types, and the donor of origin becomes a less dominant contributor, suggesting cell-type-specific cues override some genetic influences [12].
- Impact on Reproducibility: This inherent epigenetic variation between lines is a major source of heterogeneity in differentiation yields and can affect the purity and functionality of the resulting differentiated cell populations [6] [13].
What are the standard methods for assessing pluripotency and differentiation potential, and what are their limitations?
Confirming pluripotency—the ability to differentiate into all three germ layers—is crucial. Assays are categorized as assessing pluripotency as a "state" (marker expression) or as a "function" (differentiation capacity) [6].
Table 2: Standard Assays for Assessing Pluripotency and Differentiation Potential
| Technique | Key Aspect | Advantages | Disadvantages/Limitations |
|---|---|---|---|
| Immunocytochemistry/Flow Cytometry | Detects protein markers of pluripotency (e.g., Oct4, Sox2, Nanog, SSEA-4, TRA-1-60) [6] | Accessible, provides data on colony homogeneity [6] | Marker expression does not confirm functional differentiation capacity [6] |
| Trilineage Spontaneous Differentiation In Vitro | Formation of embryoid bodies (EBs) containing cells from ectoderm, mesoderm, and endoderm [6] | Inexpensive, accessible, can reveal lineage biases [6] | Produces immature, haphazardly organized tissues; may not reflect full capacity [6] |
| Teratoma Assay In Vivo | Injection of PSCs into immunodeficient mice forms a benign tumour (teratoma) with complex, mature tissues from the three germ layers [6] | Considered the "gold standard"; provides empirical proof of pluripotency and tests for malignancy [6] | Labour-intensive, expensive, ethical concerns, qualitative, protocol variation between labs [6] |
| Modern 3D Cell Culture Technology | Directed differentiation in 3D to form specific tissue rudiments or organoids [6] | Can generate complex structures; avoids animal use; highly customizable [6] | Requires technical skill and optimization; not yet standardized for routine pluripotency assessment [6] |
Troubleshooting Guides: Addressing Experimental Challenges
Issue: Poor or Inefficient Differentiation Across Multiple Patient-Specific iPSC Lines
Potential Causes and Data-Driven Solutions:
Underlying Genetic or Epigenetic Variation
- Cause: Inherent genetic (e.g., CNVs) and epigenetic differences between donor lines can lead to significant variation in differentiation efficiency, a phenomenon called "differential capacity" [13].
- Solution:
- Characterize and Select Lines: Perform integrative molecular analysis to pre-screen lines. Lines with epigenetic features conducive to your target lineage (e.g., specific chromatin accessibility at key genes) should be selected for differentiation experiments [13].
- Use a Positive Control: Always include a well-characterized control PSC line (e.g., H9 or H7 ESC line) in your differentiation experiments to benchmark performance [14].
- Adjust Protocol Parameters: For difficult-to-differentiate iPSC lines, troubleshoot by adjusting cell seeding density or extending the induction time of your differentiation protocol [14].
Inadequate Characterization of Starting Population
- Cause: The pluripotent stem cells (PSCs) used to initiate differentiation are partially differentiated, genetically abnormal, or not maintained in an optimal state, leading to unpredictable results [14] [7].
- Solution:
- Rigorously Characterize hPSCs: Before differentiation, ensure your starting population is fully characterized. This includes confirming morphology, pluripotency marker expression (via flow cytometry/immunocytochemistry), and genomic integrity (e.g., karyotyping) [6] [7].
- Remove Differentiated Cells: Before starting neural induction or other differentiations, carefully remove any differentiated cells observed in the PSC culture [14].
- Monitor Culture Confluency: Prevent routine passaging at high confluency, as this can negatively impact cell health and subsequent differentiation potential [14].
Issue: Low Cell Viability During Differentiation or After Thawing Cryopreserved Cells
Potential Causes and Data-Driven Solutions:
Cryopreservation and Thawing Techniques
- Cause: Incorrect thawing of cryopreserved neural stem cells (NSCs) or other progenitor cells can cause severe osmotic shock and cell death [14].
- Solution:
- Thaw Rapidly and Gently: Do not thaw cells for longer than 2 minutes at 37°C. After thawing, transfer cells to a pre-rinsed tube and add pre-warmed complete medium drop-wise (about one drop per second) while gently swirling the tube. Do not add a large volume of medium at once [14].
- Avoid Centrifugation: For extremely fragile cells like primary neurons, avoid centrifugation upon thawing [14].
- Check Seeding Density: Ensure you are seeding at the recommended density (e.g., >1x10^5 viable cells/cm² for H9-derived NSCs) [14].
Passaging and Apoptosis
- Cause: Passaging PSCs as single cells can induce significant apoptosis, reducing the number of healthy cells available for differentiation.
- Solution:
- Use a ROCK Inhibitor: Include a ROCK inhibitor (e.g., Y-27632) in the culture medium for 18-24 hours after passaging cells. This is critical for improving cell survival after single-cell dissociation [14].
Issue: Failure of Specific Differentiation Protocols (e.g., Neural Induction)
Potential Causes and Data-Driven Solutions:
Suboptimal Initial Conditions
- Cause: The quality of the starting PSCs and the initial seeding conditions are critical for successful neural induction [14].
- Solution:
- Ensure High hPSC Quality: Use a high-quality, fully characterized PSC population and remove any differentiated portions before induction [14].
- Optimize Seeding Confluency: Plate cells at the recommended density. For neural induction, a density of 2–2.5x10^4 cells/cm² is often recommended. Both too low and too high confluency will reduce efficiency [14].
- Plate as Cell Clumps: For some protocols, plating hPSCs as small clumps rather than a single-cell suspension can improve induction efficiency [14].
- Use ROCK Inhibitor at Induction: To prevent extensive cell death at the start of induction, consider overnight treatment with 10 µM ROCK inhibitor Y27632 after splitting hPSCs for the induction protocol [14].
Incorrect Reagent Handling
- Cause: The differentiation medium or critical supplements may have been prepared or stored incorrectly.
- Solution:
- Verify Supplement Usage: For neural differentiation, check that the correct B-27 Supplement is used. It should be a transparent yellow liquid; a green color indicates degradation [14].
- Ensure Reagent Freshness: B-27-supplemented medium is stable for only 2 weeks at 4°C. Thawed B-27 supplement should be stored at 4°C and used within one week, without repeated freeze-thaw cycles [14].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Stem Cell Research and Differentiation
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Significantly improves cell survival after single-cell passaging, thawing, and during the initiation of differentiations [14]. | Use at 10 µM concentration; typically included in medium for 18-24 hours post-disruption [14]. |
| Essential 8 Medium | A feeder-free, defined culture medium for the maintenance of human pluripotent stem cells (PSCs) [14]. | Allows for transition of PSCs from other media systems (e.g., mTeSR) or feeder-dependent cultures [14]. |
| Geltrex / Matrigel / VTN-N | Extracellular matrix proteins used to coat culture vessels, providing a substrate for PSC attachment and growth in feeder-free conditions [14]. | Proper coating is critical for cell health and preventing spontaneous differentiation. |
| B-27 Supplement | A serum-free supplement essential for the survival and growth of post-mitotic neurons and neural differentiation protocols [14]. | Handle with care: stable for 2 weeks at 4°C after preparation; avoid excessive heat and freeze-thaw cycles [14]. |
| StemRNA Clinical Seed iPSCs | Commercially available, clinically compliant iPSC master cell lines. Used as a consistent starting source for deriving differentiated cells for therapy development [15]. | A Drug Master File (DMF) submission to regulators facilitates their use in clinical trial applications [15]. |
| Stemdiff Differentiation Kits | Commercially available, standardized kits for directed differentiation of PSCs into specific lineages (e.g., midbrain organoids, neural precursors) [7]. | Promotes protocol reproducibility and saves optimization time compared to in-house protocol development. |
Experimental Workflows & Molecular Relationships
Workflow for Addressing Differentiation Variability
This diagram outlines a systematic troubleshooting approach when facing inconsistent differentiation results across iPSC lines.
This diagram illustrates the primary origins of genetic and epigenetic variability in iPSCs and how these factors interact to influence differentiation outcomes.
Impact of Donor-Specific Differences on Reproducibility and Experimental Outcomes
FAQs and Troubleshooting Guides
FAQ 1: What are the primary donor-related factors that cause variability in stem cell differentiation outcomes?
Donor-specific differences significantly impact the reproducibility of experimental outcomes in stem cell research. The key factors contributing to this variability include:
- Donor Age: Younger donors often exhibit higher cell proliferation rates and greater regenerative potential. Mesenchymal stem cells (MSCs) from older donors may show reduced viability and differentiation capacity [16] [17].
- Donor Health Status: Underlying conditions such as obesity, diabetes, and systemic inflammation can impair ASC functionality and alter the adipose tissue microenvironment [16].
- Genetic Background: Genetic variations, including single-nucleotide polymorphisms (SNPs) in genes encoding critical receptors, can alter cell expression profiles and functional capacity. This is well-documented in NK cells and solid organ transplantation outcomes [18] [19].
- Sex and Hormonal Influences: Functional differences in cells derived from male and female donors have been observed, potentially due to hormonal influences on cellular environments [16].
- Anatomical Source: The cellular composition, vascularity, and stem cell content of tissue harvested from different body regions can vary, affecting graft viability and integration [16].
FAQ 2: Why do my differentiation results remain inconsistent even when using the same protocol?
Persistent inconsistency, even with standardized protocols, is a common challenge often stemming from these root causes:
- Inherent Donor Variability: The genetic and epigenetic individuality of each donor creates a fundamental baseline variability. Studies on NK cells show marked inter-donor differences in proliferation and receptor expression even under identical culture conditions [19].
- Source Cell Heterogeneity: Using non-clonal induced pluripotent stem cell (iPSC) lines means you are working with a mixed population of cells. A clonal iPSC line, derived from a single reprogrammed cell, provides a genetically uniform population, drastically improving reproducibility [20].
- Protocol Drift and Handling Differences: Subtle differences in reagent batches, operator technique, or cell passaging schedules can introduce variability. The complexity of some differentiation protocols makes them particularly susceptible to this [21].
FAQ 3: How can I improve the reproducibility of my experiments involving donor-derived cells?
Implementing the following strategies can significantly enhance reproducibility:
- Utilize Clonal Cell Lines: For iPSC work, start with clonal lines. The Jackson Laboratory, for instance, offers genetically engineered iPSC lines derived from a characterized clonal parental line (KOLF2.1J), ensuring a uniform genetic baseline [20].
- Adopt Standardized Practices: Follow established guidelines like the ISSCR's "Standards for Human Stem Cell Use in Research" and principles of Good Cell Culture Practice (GCCP) to instill quality in daily cell handling [21].
- Implement Rigorous Quality Control: Perform comprehensive cell characterization (e.g., flow cytometry, karyotyping, RNA sequencing) and establish quality acceptance criteria for every batch of cells used [21] [17].
- Control for Donor Factors: When designing experiments, deliberately account for donor age, sex, and health status. For autologous therapies, strategies like adipose tissue cryopreservation can help mitigate variability related to donor age [16].
- Report Detailed Metadata: Promote transparency by thoroughly documenting donor information, cell handling procedures, and any protocol adjustments [22].
Troubleshooting Common Experimental Issues
Problem: High Variability in MSC Differentiation Outcomes
Potential Causes and Solutions:
| Problem Area | Specific Issue | Recommended Solution |
|---|---|---|
| Donor Selection | Older donor or donor with underlying health condition(s) | Where possible, characterize cells from multiple donors and select those with robust growth kinetics and differentiation potential [17]. |
| Culture Model | Reliance solely on 2D differentiation protocols | Incorporate 3D biomaterial-based culture models (e.g., alginate hydrogels for chondrogenesis), as standard 2D models cannot predict MSC capacity in 3D [23]. |
| Quality Control | Inconsistent cell populations at differentiation start | Implement pre-differentiation checks for viability (e.g., >85% post-thaw), plating efficiency, and surface marker expression [17]. |
Problem: Low Yield or Functionality in Differentiated β-Cells from iPSCs
Potential Causes and Solutions:
| Problem Area | Specific Issue | Recommended Solution |
|---|---|---|
| Starting Material | Use of a non-clonal, heterogeneous iPSC line | Use a clonal, genetically stable iPSC line to ensure a uniform population is directed toward differentiation [20]. |
| Differentiation Protocol | Generation of functionally immature β-cells | Optimize protocol using factors like triiodothyronine (T3), vitamin C (Vc), and adenoviral vectors encoding key transcription factors (Pdx1, Ngn3, MafA) to enhance maturity [24]. |
| Functional Validation | Assays only measure insulin presence | Include glucose-stimulated insulin secretion (GSIS) assays to test functional maturity, as insulin+ cells may not respond properly to glucose [24]. |
Experimental Protocols & Data
Table 1. Documented Impact of Donor Variability Across Cell Types
| Cell Type | Key Variable Measured | Range of Variability | Source/Context |
|---|---|---|---|
| Bone Marrow-MSCs | Post-thaw viability | 42.8% to 84.2% | Clinical doses for ARDS trial [17] |
| Bone Marrow-MSCs | Plating efficiency | 44% to 100% | Clinical doses for ARDS trial [17] |
| Adipose-Derived Stromal Cells (ASCs) | Graft retention rate (clinical) | 10% to 80% within first year | Autologous fat grafting [16] |
| NK Cells | Proliferation & receptor expression | Marked inter-donor differences | Expansion under IL-2 stimulation [19] |
Detailed Protocol: Assessing Donor Variability in MSC Differentiation
This protocol is adapted from studies investigating donor-driven differences in differentiation potential across multiple lineages [23].
Objective: To evaluate and compare the differentiation capacity of MSCs from different human donors using both standard and 3D culture models.
Materials:
- Primary Cells: MSCs from at least 3-6 different human donors.
- Control Cells: A well-characterized MSC line can serve as a reference.
- Chondrogenic Differentiation: Pellet culture system or alginate hydrogels.
- Osteogenic Differentiation: Standard 2D culture or gelatin microribbon (µRB) hydrogels.
- Adipogenic Differentiation: Standard 2D culture or gelatin microribbon (µRB) hydrogels.
- Lineage-Specific Stains: Alcian Blue (chondrogenesis), Alizarin Red (osteogenesis), Oil Red O (adipogenesis).
Methodology:
- Cell Expansion and Seeding:
- Expand MSCs from each donor to the same passage number.
- For each differentiation lineage, seed cells from all donors in parallel at identical densities.
- Tri-lineage Differentiation:
- Chondrogenesis: For each donor, create pellet cultures or encapsulate cells in alginate hydrogels. Culture in chondrogenic induction media for 21-28 days.
- Osteogenesis: Seed cells in 2D or 3D µRB hydrogels. Culture in osteogenic induction media for 14-21 days.
- Adipogenesis: Seed cells in 2D or 3D µRB hydrogels. Culture in adipogenic induction media for 14-21 days.
- Maintain control cultures in base media without induction factors.
- Analysis:
- Quantitative Analysis: Perform quantitative analysis on the stains (e.g., dye elution and spectrophotometry) or measure gene expression (qPCR) for key lineage-specific markers.
- Statistical Comparison: Compare the differentiation outcomes across donors using statistical tests (e.g., ANOVA). Significant inter-donor variability is expected across all three lineages.
Workflow Diagram: Integrating Genetic and Phenotypic Analysis
This diagram outlines an integrated approach to dissect the contributions of genetic and non-genetic factors to donor variability, as applied in NK cell studies [19].
Diagram 1: Integrated analysis workflow for identifying variability drivers.
The Scientist's Toolkit: Research Reagent Solutions
Table 2. Essential Materials and Tools for Managing Donor Variability
| Reagent/Tool | Function/Application | Considerations for Use |
|---|---|---|
| Clonal iPSC Lines (e.g., KOLF2.1J) | Provides a genetically uniform starting population for differentiation and disease modeling, reducing intrinsic noise. | Ensure lines are stable over extended culture (>25 passages) and thoroughly characterized [20]. |
| Deterministic Programming (opti-ox) | Overcomes stochastic differentiation by precisely driving iPSCs to a chosen cell type using transcription factors. | Enables production of highly consistent, defined human cells (e.g., ioCells) with high lot-to-lot uniformity [21]. |
| 3D Biomaterial Scaffolds (e.g., Alginate hydrogels, µRB) | Provides structural support and biochemical cues that more closely mimic the in vivo environment for differentiation. | Significantly influences differentiation outcomes; standard 2D models cannot predict 3D capacity [23]. |
| RosetteSep NK Cell Enrichment Cocktail | Isolation of NK cells directly from donor buffy coats for functional studies. | Used in conjunction with density-gradient centrifugation to study donor variability in immune cell expansion [19]. |
| G-Rex Culture System | A gas-permeable culture platform for scalable in vitro expansion of cells like NK cells. | Enhances nutrient availability and gas exchange, supporting efficient expansion and reducing culture-induced stress [19]. |
The Clinical and Commercial Consequences of Uncontrolled Variability
Troubleshooting Guides and FAQs
This technical support center provides resources for researchers addressing variability in stem cell differentiation. The guides below focus on standardizing differentiation efficiency in patient-specific stem cell lines.
Frequently Asked Questions (FAQs)
1. What are the primary sources of uncontrolled variability in stem cell differentiation protocols? Uncontrolled variability arises from multiple sources, broadly categorized as biological, technical, and procedural. Biological sources include genetic heterogeneity in starting patient cell lines and epigenetic memory from the original somatic cell type, which can create lineage-specific biases [6] [25]. Technical sources encompass inconsistencies in reprogramming efficiency for iPSCs, batch-to-batch variability in critical reagents like growth factors and Matrigel, and suboptimal cell culture conditions (e.g., pH, temperature, CO₂) [6]. Procedural sources involve poorly standardized or complex differentiation protocols and a lack of robust, quantitative potency assays to characterize the starting cell population [6].
2. How can I determine if my differentiation protocol is producing uncontrolled variation? Monitor for these key indicators: high levels of heterogeneity in marker expression within your differentiated cell populations (e.g., mixed cell types when a pure population is expected), significant run-to-run variation in the yield of your target cell type, and poor reproducibility of differentiation outcomes between different technicians or laboratory sites [6]. A well-controlled process should produce consistent, predictable results.
3. My differentiation efficiency is inconsistent between different patient-specific iPSC lines. Is this normal, and how can I address it? Yes, heterogeneity in differentiation capacity between different iPSC lines is a well-documented challenge due to their unique genetic and epigenetic backgrounds [6]. To address this, implement a robust pre-screening process where you characterize the differentiation propensity of new iPSC lines before large-scale experiments. You can also consider developing line-specific "training" protocols that adjust morphogen concentrations or timing based on initial performance. Furthermore, using integrated reporter cell lines to track the expression of key differentiation markers in real-time can help optimize conditions for each specific line [25].
4. What are the clinical and commercial risks of failing to control this variability? Uncontrolled variability poses severe clinical and commercial consequences. Clinically, it can lead to incomplete or incorrect differentiation, raising the risk of tumor formation from residual undifferentiated pluripotent cells or poor therapeutic efficacy of the final cell product [25]. Commercially, variability results in unreliable manufacturing, low batch success rates, and extremely high costs, making therapies economically unviable. It also causes regulatory hurdles, as agencies like the FDA require stringent proof of product consistency, potency, and safety, which is impossible without a controlled process [25].
Troubleshooting Guide: Inconsistent Differentiation Yields
Use this guide to diagnose and resolve common issues leading to variable differentiation outcomes.
| Observed Problem | Potential Root Cause | Recommended Action |
|---|---|---|
| High heterogeneity in final cell population. | Spontaneous differentiation due to suboptimal pluripotency maintenance before differentiation initiation. | Confirm pluripotency marker expression (e.g., Oct4, Nanog) via flow cytometry prior to starting differentiation. Improve passaging technique to maintain healthy, undifferentiated colonies [6]. |
| Significant batch-to-batch variation. | Uncontrolled variability in reagent quality or cell culture conditions. | Implement a rigorous reagent quality control system. Use large, master batches of critical reagents. Strictly monitor and log incubator conditions (temperature, CO₂, humidity). Standardize cell culture handling procedures across all lab personnel [25]. |
| Differentiation fails or is inefficient in a new iPSC line. | Inherent line-to-line variation in differentiation potential. | Do not assume a one-size-fits-all protocol. Perform a small-scale pilot differentiation to "profile" the new line's response. Titrate key morphogens and growth factors to establish a line-specific optimized protocol [6]. |
| Differentiated cells lack mature function. | Protocol may generate immature progenitors but not fully mature, functional cells. | Extend the differentiation timeline. Incorporate maturation factors in the later stages. Consider using advanced 3D culture systems or organoid platforms that better mimic the in vivo microenvironment for terminal maturation [6] [26]. |
Experimental Protocols for Assessing Pluripotency and Differentiation
Standardized characterization of starting stem cell lines is critical for understanding differentiation variability. The table below summarizes key methods for assessing pluripotency as a state (marker expression) and as a function (differentiation capacity) [6].
Table 1: Methods for Assessing Pluripotent State and Function
| Method | Key Aspect | Advantages | Disadvantages |
|---|---|---|---|
| Flow Cytometry | Quantifies expression of multiple pluripotency markers (e.g., Oct4, SSEA-4). | High-throughput, quantitative, accounts for population heterogeneity. | Marker expression does not confirm functional pluripotency [6]. |
| Embryoid Body (EB) Formation | 3D aggregates that spontaneously differentiate into cell types of the three germ layers. | Accessible, inexpensive, indicates broad differentiation capacity. | Structures are immature and disorganized; not a stringent assay [6]. |
| Teratoma Assay | In vivo assay where cells form a benign tumor containing complex, mature tissues from all three germ layers. | Historically the "gold standard"; provides conclusive proof of functional pluripotency. | Labor-intensive, expensive, ethically contentious, primarily qualitative, and protocol variation is high [6]. |
| Modern 3D Organoid Differentiation | Directed differentiation in 3D culture to generate complex, tissue-specific structures. | Mimics organ development; can produce mature, functional cell types; avoids animal use. | Technically challenging to optimize; can be expensive; not yet standardized for all cell types [6] [26]. |
Detailed Protocol: Quantitative Analysis of Differentiation Efficiency via Flow Cytometry
This protocol provides a method to quantitatively assess the purity and efficiency of differentiation toward a specific mesodermal lineage (e.g., cardiomyocytes), a common source of variability.
1. Sample Preparation:
- Differentiate your iPSCs toward the target cell type using your established protocol.
- At the endpoint of differentiation, harvest cells using a gentle cell dissociation reagent to preserve surface markers.
- For intracellular markers (e.g., transcription factors), fix and permeabilize cells using a commercial fixation/permeabilization kit according to the manufacturer's instructions.
2. Staining:
- Prepare antibody master mixes in FACS buffer (e.g., PBS with 1-2% FBS). Include appropriate isotype controls and single-color controls for compensation.
- Resuspend cell pellets in the antibody mix and incubate for 30-60 minutes at 4°C in the dark.
- Wash cells twice with FACS buffer to remove unbound antibody.
3. Data Acquisition and Analysis:
- Resuspend cells in FACS buffer and filter through a cell strainer cap into FACS tubes.
- Acquire data on a flow cytometer, collecting a minimum of 10,000 events per sample.
- Use the unstained and isotype controls to set negative gates. Analyze the percentage of positively stained cells for your target marker (e.g., TNNT2 for cardiomyocytes) to determine differentiation efficiency.
Visualization of Key Concepts
Pluripotency Assay Workflow
This diagram outlines the logical decision process for selecting and implementing assays to confirm pluripotency.
This diagram maps the primary sources of variability in stem cell differentiation experiments and their relationships.
The Scientist's Toolkit: Key Research Reagent Solutions
A critical step in reducing variability is the consistent use of high-quality, well-defined reagents. The table below lists essential materials for stem cell maintenance and differentiation.
Table 2: Essential Reagents for Standardized Stem Cell Research
| Item | Function | Key Considerations for Reducing Variability |
|---|---|---|
| Basal Media (e.g., DMEM/F12, Neurobasal) | Foundation for culture and differentiation media. | Use a single, validated supplier. Pre-mix large batches from a single lot number for long-term projects. |
| Essential Growth Factors (e.g., FGF-2, TGF-β, BMP4) | Direct stem cell fate toward specific lineages. | Source recombinant proteins from reliable vendors. Aliquot upon arrival to avoid freeze-thaw cycles. Perform dose-response titrations for each new lot. |
| Small Molecule Inducers/Inhibitors (e.g., CHIR99021, SB431542) | Chemically define differentiation protocols and improve efficiency. | Verify chemical stability and storage conditions. Prepare concentrated stock solutions in the correct solvent (e.g., DMSO) and use consistent aliquots. |
| Extracellular Matrix (ECM) (e.g., Matrigel, Laminin-521) | Provides physical and chemical cues for cell attachment, survival, and differentiation. | This is a major source of variability. Use a dedicated, large batch for a single project. Thoroughly test dilution factors and polymerization times for consistency. |
| Cell Dissociation Reagents (e.g., EDTA, Accutase) | Used for passaging and harvesting cells. | Standardize concentration, volume, and incubation time to minimize stress and selective pressure on subpopulations. |
| Quality Control Assays (e.g., Mycoplasma tests, Karyotyping G-banding) | Ensures cell culture health and genomic integrity. | Perform tests regularly (e.g., monthly for mycoplasma) and with each new cell line thawed. Document all results. |
Innovative Methods for Monitoring and Controlling Differentiation Outcomes
Frequently Asked Questions (FAQs)
Q1: What is non-destructive monitoring, and why is it critical for stem cell research? Non-destructive monitoring uses imaging and sensing techniques to assess cell status without harming or destroying the samples. This is vital for stem cell research because it allows researchers to monitor the same population of cells throughout a long-term differentiation process, enabling early prediction of efficiency and the selection of high-quality cultures for downstream applications [27] [28].
Q2: My differentiation protocol takes over 80 days. How early can efficiency be predicted? Research on muscle stem cell (MuSC) differentiation from human induced pluripotent stem cells (hiPSCs) has demonstrated that samples with high and low final induction efficiency can be predicted approximately 50 days before the end of the induction period. Specifically, predictions for low-efficiency samples were possible from day 24, and for high-efficiency samples from days 31-34 of an 82-day protocol [27].
Q3: What are the limitations of traditional methods for assessing differentiation? Traditional methods, such as quantitative PCR (qPCR), immunocytochemistry, and flow cytometry, are often:
- Destructive, requiring sample fixation or lysis.
- Time-consuming and require skilled techniques.
- Costly and provide only a single time-point snapshot [27] [6]. While the teratoma assay is a gold standard for assessing pluripotency, it is labor-intensive, time-consuming, expensive, and raises ethical concerns due to its use of animal hosts [6].
Q4: Which machine learning model is best for this task? The "best" model depends on your data and specific goal. Different models have shown success:
- Random Forest was effectively used for classifying differentiation efficiency from phase-contrast image features [27].
- Convolutional Neural Networks (CNNs) are powerful for automatically learning complex features directly from images and have been used for tasks like predicting firmness in agricultural products and analyzing SERS spectra [28] [29].
- Support Vector Machines (SVM) and XGBoost are also commonly applied [29] [30]. It is advisable to test and compare multiple models.
Q5: Our phase-contrast images look similar between efficient and inefficient differentiations. What features can machine learning detect? The human eye may miss subtle, quantitative morphological patterns. Machine learning can analyze features that are not immediately obvious, such as:
- Texture and spatial patterns extracted via Fast Fourier Transform (FFT) [27].
- Complex morphological characteristics learned directly by deep learning models from raw pixels [29].
- Biochemical signatures from the culture medium analyzed via Surface-Enhanced Raman Spectroscopy (SERS) [28].
Troubleshooting Guides
Issue 1: Poor Correlation Between Early Images and Final Differentiation Outcomes
Potential Causes and Solutions:
- Incorrect Timing: The chosen imaging window may not capture the critical decision point in the differentiation pathway.
- Solution: Conduct a correlation study early in your protocol development. Measure key marker expressions (e.g., via qPCR or ICC) at intermediate time points and correlate them with your final efficiency metric to identify the predictive window [27].
- Insufficient Features: The features you are extracting (manually or automatically) may not be discriminatory.
- Solution:
- For traditional ML: Explore different feature extraction methods. The study on hiPSC-MuSC differentiation found that a 100-dimensional, rotation-invariant feature vector generated from the FFT power spectrum was effective [27].
- For deep learning: Use a pre-trained CNN (e.g., ResNet) to leverage its ability to extract rich, hierarchical features automatically [29] [30].
- Solution:
- Model Overfitting: The model performs well on training data but poorly on new data.
- Solution: Increase your dataset size using data augmentation (e.g., rotation, flipping, scaling). Ensure you are using proper validation techniques like k-fold cross-validation and evaluate the model on a completely held-out test set [29].
Issue 2: Inconsistent Model Performance Across Different Cell Lines
Potential Causes and Solutions:
- Cell Line-Specific Bias: The model has learned features specific to the genetic background of the cell lines it was trained on.
- Batch Effects: Variations in culture conditions, media lots, or operator technique can introduce noise.
- Solution: Standardize protocols as much as possible. Document all conditions meticulously. Techniques like batch effect correction algorithms can be applied to the feature data before model training [4].
Issue 3: The "Black Box" Problem – Lack of Interpretability in Predictions
Potential Causes and Solutions:
- Complex Models: Deep learning models, in particular, are often not intrinsically interpretable.
- Solution: Employ Explainable AI (XAI) techniques.
- LIME (Local Interpretable Model-agnostic Explanations): Can highlight which regions of an input image were most influential for a specific prediction [29].
- SHAP (Shapley Additive Explanations): Helps explain the output of any machine learning model [30].
- Using these tools can build trust in the model and provide biological insights by revealing what the model is "seeing" [29].
- Solution: Employ Explainable AI (XAI) techniques.
Experimental Protocol: Early Prediction of hiPSC Differentiation Efficiency
The following methodology is adapted from a published study that successfully predicted muscle stem cell (MuSC) differentiation efficiency [27].
Cell Culture and Differentiation
- Cell Line: Use a reporter hiPSC line (e.g., MYF5-tdTomato) for accurate quantification of final efficiency via flow cytometry.
- Differentiation Protocol: Induce MuSCs from hiPSCs using a directed differentiation protocol. The example protocol involves:
- Days 0-14: Induce dermomyotome cells with a Wnt agonist.
- Days 14-38: Promote myogenic differentiation with growth factors (IGF-1, HGF, bFGF).
- Days 38-82: Mature myotubes in a low-concentration horse serum medium.
- Day 82: Analyze final MuSC induction efficiency (MYF5+ %) by flow cytometry.
Image Acquisition
- Instrument: Standard phase-contrast microscope.
- Schedule: Capture images of cells in multiple wells from the predictive window (days 14-38).
- Dataset: The referenced study used 5,712 images from 34 wells across six independent experiments [27].
Feature Extraction: Fast Fourier Transform (FFT)
This step converts the image into a format that captures its spatial frequency characteristics.
- Procedure:
- Apply FFT to each pre-processed (e.g., cropped, normalized) phase-contrast image.
- Obtain the power spectrum from the FFT output.
- Perform shell integration on the power spectrum to create a 100-dimensional, rotation-invariant feature vector for each image. This vector captures the distribution of spatial frequencies, which correlate with cell morphology.
Machine Learning Classification
- Model: Use a Random Forest classifier.
- Training: Train the model using the feature vectors from days 14-38 as input and the final day-82 efficiency classification (e.g., "High" or "Low") as the target output.
- Validation: Validate model performance using a held-out test set or cross-validation.
Key Quantitative Findings from the Referenced Study
Table 1: Correlation of Mid-Protocol Markers with Final MuSC Efficiency
| Time Point | Marker Type | Marker Name | Correlation with Day 82 Efficiency |
|---|---|---|---|
| Day 38 | Gene Expression (qPCR) | MYH3 | Significant Positive |
| Day 38 | Gene Expression (qPCR) | MYOD1 | Significant Positive |
| Day 38 | Gene Expression (qPCR) | MYOG | Significant Positive |
| Day 38 | Protein (ICC) | MHC-positive area | Significant Positive |
| Days 7 & 14 | Various | T, TBX6, SIX1, DMRT2, PAX3 | No Significant Correlation |
Table 2: Prediction Performance Using FFT and Random Forest
| Prediction For | Effective Prediction Day | Key Outcome |
|---|---|---|
| Low Efficiency Samples | Day 24 | Early identification of failing differentiations |
| High Efficiency Samples | Days 31-34 | Reliable selection of high-yield cultures |
| Overall Workflow | Day 24 & 34 | 43.7% reduction in defective sample rate; 72% increase in good samples |
Essential Research Reagent Solutions
Table 3: Key Materials and Reagents for Implementation
| Item | Function / Explanation | Example / Note |
|---|---|---|
| Reporter hiPSC Line | Enables precise, quantitative measurement of target cell population at the end of differentiation. | e.g., MYF5-tdTomato for muscle stem cells [27]. |
| Directed Differentiation Factors | Drives cells toward the desired lineage in a controlled, step-wise manner. | Wnt agonist, IGF-1, HGF, bFGF (for MuSC protocol) [27]. |
| Quality Control Reagents | Ensures the integrity, function, and safety of cells. Critical for clinical translation. | Karyotyping kits, pathogen tests, pluripotency marker antibodies [31] [4]. |
| SERS-Active Substrate | For SERS-based monitoring; enhances Raman signal from the culture medium for sensitive detection. | Periodical gold gratings on polymer substrates [28]. |
Workflow and Signaling Pathway Diagrams
Experimental Workflow for Early Prediction
hiPSC to Muscle Stem Cell Differentiation Signaling
Machine Learning Model Training Pipeline
Leveraging Prime Editing and CRISPR for Precision Control in hPSCs
Human pluripotent stem cells (hPSCs), including embryonic and induced pluripotent stem cells, represent a cornerstone for regenerative medicine, disease modeling, and drug development due to their capacity for unlimited self-renewal and differentiation into any cell type [32] [33]. The precision manipulation of their genome is crucial for studying gene function, correcting disease-causing mutations, and standardizing differentiation efficiency for patient-specific therapies. While traditional CRISPR-Cas9 systems have enabled targeted gene disruption, their reliance on double-strand breaks (DSBs) leads to undesirable consequences in hPSCs, including p53-mediated apoptosis, chromosomal rearrangements, and low editing efficiency [34] [33]. Prime editing has emerged as a transformative "search-and-replace" technology that directly writes genetic information into target DNA sites without creating DSBs, offering exceptional versatility, specificity, and precision for hPSC engineering [34] [35].
Prime Editing System: Components and Mechanism
Core Components
The prime editing system consists of two primary components:
- Prime Editor (PE) Protein: A fusion of a Cas9 nickase (H840A mutant that cuts only one DNA strand) and an engineered reverse transcriptase (RT) from the Moloney murine leukemia virus [34] [35]. Advanced versions like PEmax feature an optimized architecture for improved nuclear localization and expression in human cells [36].
- Prime Editing Guide RNA (pegRNA): A specially engineered guide RNA that both specifies the target genomic locus and templates the desired edit. Its complex structure includes [35]:
- Spacer Sequence: A ~20-nucleotide region complementary to the target DNA site.
- Scaffold: Binds the Cas9 nickase.
- Reverse Transcription Template (RTT): Encodes the desired genetic alteration (typically 10-25 nucleotides).
- Primer Binding Site (PBS): A ~13-nucleotide sequence that anneals to the nicked DNA strand to initiate reverse transcription.
Mechanism of Action
The following diagram illustrates the multi-step mechanism of prime editing, from target recognition to the completion of the edit.
Step 1: Target Recognition and Strand Nicking: The PE-pegRNA complex binds to the target DNA site via complementary base pairing. The Cas9 nickase domain creates a single-strand cut (nick) in the DNA strand containing the protospacer adjacent motif (PAM) sequence, releasing a 3' DNA end [34] [35].
Step 2: Primer Binding and Reverse Transcription: The liberated 3' DNA end hybridizes with the PBS on the pegRNA. The reverse transcriptase then uses the RTT as a template to synthesize a new DNA strand that contains the desired edit, creating a 3' "edited flap" [34] [35].
Step 3: Edited Flap Incorporation: The newly synthesized 3' edited flap competes with the original 5' non-edited flap. Cellular repair machinery typically favors the 3' flap, ligating the edited strand into the genome. This results in a heteroduplex DNA molecule where one strand carries the new edit and the other retains the original sequence [34] [35].
Step 4: Heteroduplex Resolution (PE2): In the PE2 system, cellular DNA repair or replication processes eventually resolve the heteroduplex, copying the edit to the complementary strand to make the change permanent. However, the mismatch repair (MMR) pathway can sometimes reverse the edit, lowering efficiency [34] [36].
Step 5: Complementary Strand Nicking (PE3/PE3b): In the more advanced PE3 and PE3b systems, a second, standard sgRNA is used to direct the prime editor to nick the non-edited strand. This nick tricks the cell's repair system into using the edited strand as a template, significantly increasing the likelihood that both DNA strands will permanently incorporate the desired change [34] [35].
Optimizing Prime Editing Efficiency in hPSCs
Achieving high editing efficiency in hPSCs is challenging due to their low transfection efficiency and robust DNA repair mechanisms [32]. The following table summarizes key optimization strategies and their quantitative impact on editing efficiency, primarily derived from studies in hPSCs.
Table 1: Optimization Strategies for Prime Editing in hPSCs
| Strategy | Description | Impact on Efficiency | Key Considerations |
|---|---|---|---|
| Inhibit Mismatch Repair (MMR) [36] | Co-express a dominant-negative MLH1 (MLH1dn) to suppress the MMR pathway, which often reverses prime edits. | ~1.4x increase (e.g., from 4.2% to 5.7% for a 2nt deletion at HEK3 site) [36] | Part of the PE4/PE4max and PE5/PE5max systems. Most effective for substitutions and small indels [36]. |
| Inhibit p53 [36] | Co-express a dominant-negative p53 (P53DD) to dampen p53-mediated stress responses activated by editing. | Substantial increase for larger edits (e.g., 30nt deletion: 3.1% to 12.1%; 34nt insertion: 7.9% to 24.3%) [36] | Particularly beneficial for larger edits and in sensitive cell lines. |
| Use Engineered pegRNAs (epegRNAs) [36] | Incorporate stabilizing RNA motifs (e.g., tev or tmp) at the 3' end of the pegRNA to enhance its stability. |
~2x increase (e.g., from 8.4% to ~18-19% when combined with PE4max) [36] | Improves pegRNA half-life, leading to more consistent and robust editing. |
| Employ the PEmax Editor [36] | Use an optimized prime editor with improved nuclear localization and codon usage for human cells. | Synergistic improvement with other strategies (e.g., PE2max + P53DD reached 29.2% in a reporter assay) [36] | Considered a superior backbone for all prime editing experiments. |
| Combine Optimizations [36] | Integrate PEmax, MLH1dn, P53DD, and epegRNA into a single "PE-Plus" system. | ~3x increase over baseline PE4max (e.g., from 8.4% to 24-27%) [36] | Represents the current state-of-the-art for achieving maximal editing efficiency in hPSCs. |
The "PE-Plus" System: A Case Study in Optimization
A comprehensive study systematically compared prime editing configurations in hPSCs and developed a highly efficient "PE-Plus" system. The results demonstrate the additive effect of combining multiple optimizations, as shown in the following workflow diagram.
This integrated approach, combining an optimized editor (PEmax), MMR inhibition (MLH1dn), p53 suppression (P53DD), and stable epegRNAs, resulted in editing efficiencies exceeding 50% in a reporter assay and enabled efficient creation of disease-relevant mutations [36].
Troubleshooting Guide and FAQs
Frequently Asked Questions
Q1: My prime editing efficiency in hPSCs is consistently low. What are the primary factors I should optimize first? A: Low efficiency is common. Prioritize these steps based on the optimization table (Table 1) [36]:
- pegRNA Design: Systematically test pegRNAs with different PBS lengths (typically 10-15 nt) and RTT lengths. Use online design tools (e.g., PE-Designer) and validate multiple designs [32].
- Editor Selection: Switch from PE2 to the PEmax backbone for improved performance [36].
- Cellular Defense Bypass: Co-deliver MMR and p53 inhibitors (MLH1dn and P53DD) to prevent the reversal of edits and reduce stress-induced cell death [36].
Q2: I am observing high background and unintended edits in my edited hPSC pools. How can I improve editing purity? A: Unintended byproducts can arise from several sources:
- pegRNA-independent off-targets: Reassuringly, prime editors (unlike some base editors) do not cause widespread, guide-independent off-target mutations, as confirmed by whole-genome sequencing [33].
- Incorrect flap resolution: To improve purity, use the PE3b system, which employs a nicking sgRNA designed to avoid the edited strand, reducing unwanted indels [34] [35].
- Transfection contamination: Ensure you are working with single-cell clones after editing. When using cleavage selection systems, high background can occur due to plasmid contamination; picking single clones can mitigate this [37].
Q3: What is the best method for delivering prime editing components into hPSCs? A: The delivery method critically impacts efficiency.
- Electroporation of RNP complexes is highly recommended for its high efficiency and transient delivery, which minimizes off-target effects [32]. Deliver the pegRNA as a synthetic nucleic acid alongside mRNA encoding the prime editor protein.
- Plasmid DNA transfection is less efficient in hPSCs due to the need for nuclear entry and transcription [32].
- All-in-one systems stably integrated into a safe-harbor locus (like AAVS1) with inducible expression (e.g., using doxycycline) offer controlled editing and high efficiency, as demonstrated by the iPE-Plus platform [36].
Troubleshooting Table for Common Experimental Issues
Table 2: Troubleshooting Common Prime Editing Problems in hPSCs
| Problem | Possible Cause | Solution |
|---|---|---|
| No editing detected | Poor pegRNA design or activity [32] | Redesign pegRNA with different PBS/RTT. Test multiple targets. Use epegRNAs. |
| Low transfection efficiency [32] | Optimize delivery method (use electroporation). Use a fluorescent reporter to monitor efficiency. | |
| Inefficient nicking or RT activity | Use a more active editor (PEmax) and ensure proper cellular conditions. | |
| Low editing efficiency | MMR reversal of edits [36] | Use PE4/PE5 systems with MLH1dn. |
| p53-mediated stress response [36] | Co-express P53DD during editing. | |
| Unstable pegRNA [36] | Use engineered epegRNAs with stabilizing motifs. | |
| High indel byproducts | Use of basic PE3 system [34] | Switch to the PE3b system, which uses a more specific nicking sgRNA. |
| Overly long transfection/expression | Use transient delivery methods (RNP electroporation) instead of plasmids. | |
| Difficulty isolating edited clones | Low initial efficiency or cell death | Increase starting cell numbers. Optimize post-transfection recovery by using ROCK inhibitor [33]. Use the "PE-Plus" system for higher efficiency. |
Table 3: Key Research Reagent Solutions for Prime Editing in hPSCs
| Reagent / Tool | Function | Example / Note |
|---|---|---|
| Optimized Prime Editors | Core enzyme for editing. | PEmax: An optimized version of PE2 with improved nuclear localization and expression for higher efficiency in human cells [36]. |
| Stable hPSC Lines | Provides controlled, inducible editor expression. | iPE-Plus (AAVS1-integrated): A cell line with the "PE-Plus" system integrated into the AAVS1 safe-harbor locus, allowing for doxycycline-inducible editing [36]. |
| MMR Inhibitor | Blocks the mismatch repair pathway to prevent edit reversal. | MLH1dn: A dominant-negative version of the MLH1 protein, key to the PE4/PE5 systems [36]. |
| p53 Inhibitor | Reduces p53-mediated cellular stress response to editing. | P53DD: A dominant-negative p53 domain that improves editing efficiency, especially for larger edits [36]. |
| Engineered pegRNAs | Increases the stability and half-life of the pegRNA. | epegRNA: pegRNAs with added RNA motifs (e.g., tev or tmp) at the 3' end to protect against degradation [36]. |
| Delivery Method | Method for introducing editing components into cells. | Electroporation of RNP/mRNA: Preferred method for hPSCs due to high efficiency and transient activity. The NEON system is commonly used [33]. |
| Design Software | Computational tools for designing effective pegRNAs. | PE-Designer, pegFinder: Web-based resources to design and optimize pegRNA and nicking sgRNA sequences [32]. |
Standard Experimental Protocol: Prime Editing hPSCs using an All-in-One System
This protocol details the steps for using an inducible, integrated prime editor system (e.g., iPE-Plus) in hPSCs, based on published methodologies [36] [33].
Key Steps:
- Cell Culture Preparation: Maintain iPE-Plus hPSCs in Essential 8 (E8) medium on a suitable matrix (e.g., iMatrix-511). Passage cells using a gentle dissociation reagent like ReLeSR and ensure cells are in a log phase of growth with >90% viability before starting [33].
- Editor Induction: Treat cells with 1 µg/mL doxycycline for 24-48 hours to induce the expression of the prime editor protein [36] [33].
- pegRNA/sgRNA Delivery:
- Prepare a single-cell suspension using Accutase.
- For electroporation, mix 1x10^5 cells with 250-750 ng of pegRNA-encoding plasmid and, for PE3/PE3b systems, 83 ng of nicking sgRNA plasmid.
- Electroporate using a system like the Neon Transfection System (e.g., 1050V, 30ms, 2 pulses) [33].
- Post-Transfection Recovery: Seed the electroporated cells in E8 medium supplemented with a 10 µM ROCK inhibitor (Y-27632) for the first 24 hours to enhance cell survival [33].
- Harvest and Analysis: Culture cells for 3-7 days post-transfection, then harvest for genomic DNA extraction. Analyze editing efficiency via targeted next-generation sequencing (e.g., MiSeq) of PCR-amplified target sites [33].
- Clone Isolation: For clonal isolation, re-seed transfected cells at low density. Pick individual colonies, expand them, and screen by sequencing to identify isogenic clones with the desired edit [36].
Implementing ISSCR Standards for Cell Line Characterization and Banking
Frequently Asked Questions (FAQs)
Q1: What are the most critical first steps for implementing ISSCR standards when acquiring a new cell line?
The most critical first steps involve proper documentation and legal compliance. Before beginning any experiments, researchers must read and understand the Material Transfer Agreement (MTA) or similar agreement, as it captures all donor consent provisions, supplier restrictions, and licensing requirements [38]. Failure to do so could result in violation of donor consent obligations, wasted resources, invalid research, or inability to publish [38]. Additionally, you should establish a Master Cell Bank (MCB) from the earliest possible passage of the established cell line prior to any experimental use or distribution [38]. This MCB should be characterized post-thaw and created as a single homogenous lot by pooling expanded cells prior to cryopreservation to ensure consistency of materials [38].
Q2: How often should I authenticate my cell lines, and what methods are recommended?
Cells for experimental use should be authenticated, with Short Tandem Repeat (STR) analysis recommended as the preferred method [38]. STR analysis has been formally developed into an internationally recognized consensus standard for human cell line authentication and offers advantages including cost efficiency, reproducibility, comparability across platforms, and ability to detect multiple cell sources within a culture [38]. When authenticating cells, a reference sample from the original donor should be used for confirmation of origin where possible [38]. Funding agencies and journals are increasingly requiring evidence of cell line authentication, placing the onus on researchers to properly identify materials used within their laboratory [38].
Q3: What genetic monitoring is required for stem cell cultures according to ISSCR standards?
Cultures should be monitored for culture-acquired genetic changes as these can have irreversible effects on stem cells and their differentiated progeny [39]. The ISSCR recommends a comprehensive genetic monitoring approach:
Table: Recommended Genetic Monitoring Methods
| Method | Detects | Sensitivity for Mosaicism | Key Applications |
|---|---|---|---|
| G-banded Karyotyping | Large chromosomal abnormalities >5Mb (aneuploidies, translocations) | 10-20% of cell population [40] | Baseline monitoring for major chromosomal changes [40] |
| 20q11.21 (BCL2L1) FISH | Specific, common CNVs in hPSCs (0.55-4.6Mb duplications) | 5-10% of cell population [40] | Detecting recurrent hPSC changes missed by karyotyping [40] |
| Higher Resolution Methods | Small CNVs, single nucleotide variants (e.g., in TP53) | Varies by method | When karyotype is normal but cell behavior has changed [39] |
Genetic abnormalities are common in hPSC cultures, with studies indicating 30-35% of cultures analyzed by G-banding harbor a genetic abnormality [40]. Commonly observed abnormalities include gains in chromosomal regions such as 1q, 12p, and 20q11.21, which harbor genes associated with increased proliferation or resistance to apoptosis [40].
Q4: At what timepoints should genetic monitoring be performed?
The ISSCR recommends genetic monitoring at multiple critical stages [39] [40]:
- Before starting experiments: Master and Working Cell Banks should be evaluated to determine their genetic status [39]
- During experiments: Approximately every 10 passages to detect culture-acquired abnormalities early [40]
- After major culture bottlenecks: Events like cloning or genetic modifications increase risk of clonal expansion [40]
- When changes in cell traits are observed: Altered growth or differentiation may indicate genetic changes [39]
- At the end of experiments: To confirm genetic integrity throughout the study period [39]
Cells carrying variants with selective advantage can overtake a culture rapidly, often within 5-10 passages [39]. Not using cells drawn from tested banks beyond passage 10 after thawing significantly decreases risks of genetic drift [39].
Q5: What are the essential elements to report in publications using stem cell lines?
Published reports must include sufficient information to ensure reproducibility [41]:
- Cell line source and derivation details: Include unique cell line identifier, registry number, and specific source [41]
- Complete culture methods: Detailed protocols for maintenance, preservation, passaging, freezing, and thawing [41]
- Passage documentation: Population doublings of cryopreserved MCB or WCB stocks, and number of subsequent passages during experimentation [41]
- Genotyping methodology: Specific methods, timing, and relationship to key experiments [41]
- Pluripotency assessment: Thorough description of assays, reagents, readouts, and quantitation [41]
- Experimental unit definition: Clear explanation of what constitutes n (cell lines, organoids, batches, etc.) [41]
Troubleshooting Guides
Issue: Poor Differentiation Efficiency and High Variability
Problem: Directed differentiation protocols show low reproducibility and robustness, with efficiency varying between hiPSC clones, experimental batches, and even wells in the same plate [27].
Solutions:
Implement early prediction systems: Recent research demonstrates that machine learning analysis of phase contrast images can predict final differentiation efficiency approximately 50 days before the end of induction for long protocols [27]. For muscle stem cell differentiation, samples with high and low induction efficiency could be predicted using images from days 24-34 of an 82-day protocol [27].
Standardize differentiation protocols: Use standardized differentiation kits that contain optimized reagents and succinct protocols to improve yield, minimize time, and provide more reproducible methods compared to "home-brew" protocols that piece together reagents from multiple vendors [42].
Characterize intermediate stages: For MuSC differentiation, significant positive correlations were detected between the expression of skeletal muscle markers (MYH3, MYOD1, MYOG) on day 38 and final efficiency on day 82 [27]. Identify and monitor similar critical checkpoints in your specific differentiation protocol.
Consider 3D culture systems: Implement three-dimensional co-culture systems and microfluidics to control feeding cycles and growth factor gradients, which have been reported to improve differentiation efficiency [43].
Issue: Suspected Cell Line Misidentification or Cross-Contamination
Problem: Uncertain whether cells in culture are the expected line or may have been cross-contaminated.
Solutions:
Perform regular authentication: Implement STR profiling as recommended by ISSCR standards [38]. This is particularly important for cell lines that can be passaged indefinitely, as misidentified lines could corrupt research data on an international basis [38].
Maintain rigorous documentation: Ensure all work is traceable with well-documented routine laboratory protocols [38]. While rigorous documentation by centralized cell banks can reduce potential for misidentification at sourcing, the onus still lies with the end researcher to authenticate materials used within the laboratory [38].
Use reference samples: When authenticating cells, use a reference sample from the original donor for confirmation of origin where available [38]. Where donor material is not available, use a profile obtained from the earliest passage stocks available [38].
Issue: Genetic Drift in Long-Term Culture
Problem: Cells exhibit altered growth characteristics or differentiation potential after extended passaging.
Solutions:
Adhere to monitoring frequency: Perform genetic monitoring every 10 passages and after major culture bottlenecks [40]. Genetic abnormalities are common in hPSC cultures, with up to 30-35% of cultures harboring a genetic abnormality [40].
Use appropriate detection methods: Implement both karyotyping for large-scale changes and FISH for specific common changes like 20q11.21 amplification [40]. The 20q11.21 FISH test can detect duplications ranging from 0.55 Mb to 4.6 Mb that are frequently gained in hPSCs but challenging to detect with standard karyotyping [40].
Establish proper banking practices: Create a two-tier biobanking system with Master Cell Banks and Working Cell Banks [38]. Secure a portion of the characterized MCB off-site, preferably out of region, to guard against loss due to local catastrophic events [38].
Limit experimental passages: Don't use cells drawn from tested banks beyond passage 10 after thawing to significantly decrease risks of genetic drift [39].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents for Stem Cell Characterization and Banking
| Reagent/Service | Function | Application Notes |
|---|---|---|
| STR Analysis Kits | Cell line authentication using internationally recognized standard [38] | Compare profiles to reference sample; protect donor privacy by not making genetic profiles public [38] |
| G-banded Karyotyping Services | Detection of large chromosomal abnormalities >5Mb [40] | Analyzes minimum of 20 metaphase spreads; follows ISCN guidelines; essential for MCB characterization [40] |
| 20q11.21 FISH Assays | Detection of common hPSC CNVs in BCL2L1 region [40] | Analyzes 200+ interphase cells; detects mosaicism as low as 5-10%; identifies changes missed by karyotyping [40] |
| Standardized Differentiation Kits | Optimized, reproducible protocols for specific cell lineages [42] | Provide consistent method for assessing pluripotency; improve workflow efficiency; more reproducible than home-brew protocols [42] |
| Pluripotency Marker Panels | Verification of undifferentiated status [41] | Should be thoroughly described in publications including assay methodology, source of reagents, and readouts [41] |
Experimental Workflows
Cell Line Acquisition and Banking Workflow
Genetic Monitoring Timeline
This technical support content provides researchers with practical guidance for implementing ISSCR standards, addressing common challenges in stem cell banking and characterization, and promoting reproducibility in patient-specific stem cell research.
Frequently Asked Questions (FAQs)
Q1: What are the core differences between organoid and organ-on-a-chip technologies? While both are advanced 3D cell culture models, they differ significantly in their approach and strengths. Organoids are self-organizing 3D structures derived from stem cells that mimic the cellular complexity and architecture of human organs [44] [45]. Organ-on-a-chip systems are microengineered devices that use microfluidics to precisely control the cellular microenvironment, including fluid flow and mechanical stimuli, to mimic organ-level functions [44]. The table below summarizes their key characteristics:
Table 1: Comparison of Organoid and Organ-on-a-Chip Technologies
| Feature | Organoids | Organ-on-a-Chip |
|---|---|---|
| Fundamental Principle | Self-organization from stem cells [45] | Microengineering and precise control of the cellular microenvironment [44] |
| Key Strength | High physiological relevance, cellular heterogeneity, and patient-specific modeling [44] [45] | Precise regulation of biomechanical forces, fluid flow, and multi-tissue integration [44] |
| Typical Cell Source | Pluripotent Stem Cells (PSCs) or Adult Stem Cells (AdSCs) [46] | Often uses pre-differentiated cells or cell lines [44] |
| Microenvironment Control | Limited and often variable | High, with controlled shear stress, strain, and chemical gradients [44] |
| Throughput & Scalability | Moderate, suitable for biobanking and drug screening [47] | Potentially higher for drug discovery, can link multiple organs [44] |
Q2: How can I decide whether to use PSC-derived or AdSC-derived organoids for my research? The choice between Pluripotent Stem Cell (PSC) and Adult Stem Cell (AdSC)-derived organoids depends on your research goal, as they are complementary tools [46]. PSC-derived organoids are ideal for modeling early human organogenesis and developmental diseases, as they can generate complex tissues containing multiple cell lineages (e.g., epithelial, mesenchymal) [46]. In contrast, AdSC-derived organoids are directly generated from adult tissues, exhibit maturity closer to adult organs, typically consist of epithelial cells only, and are better suited for studying adult tissue repair, infectious diseases, and for expanding patient-specific cells for personalized medicine [46].
Q3: What are the most common causes of poor differentiation efficiency in organoid cultures? Poor differentiation efficiency often stems from suboptimal culture conditions. Key factors include:
- Inadequate ECM Signaling: The extracellular matrix (e.g., Matrigel) provides critical biochemical and biophysical cues. Batch-to-batch variability in natural matrices can severely impact reproducibility [48] [47].
- Improper Growth Factor Cocktails: Precise combinations and concentrations of growth factors are essential to guide lineage specification. For example, activating or inhibiting Wnt, TGF-β, and BMP signaling pathways is often required [44] [47].
- Lack of Physiological Cues: Native tissues experience mechanical forces and fluid flow. Static organoid cultures often lack these stimuli, which can limit maturation [44] [48].
Troubleshooting Guides
Problem 1: High Batch-to-Batch Variability in Organoid Cultures
Potential Causes and Solutions:
Table 2: Troubleshooting Organoid Reproducibility
| Observed Issue | Potential Root Cause | Recommended Solution |
|---|---|---|
| Inconsistent organoid size, shape, and cellular composition. | Variability in natural extracellular matrix (ECM) like Matrigel [48] [47]. | Transition to defined synthetic hydrogels (e.g., GelMA) for consistent mechanical and biochemical properties [47]. |
| Unpredictable differentiation outcomes between experiments. | Unstandardized protocols and media components [48]. | Implement a defined, chemically controlled culture medium [49]. Use quality-controlled, aliquoted growth factors to minimize lot variations. |
| Limited reproducibility across different laboratory settings. | Differences in cell source and handling techniques. | Use standardized cell lines from reputable repositories. Establish and meticulously document detailed Standard Operating Procedures (SOPs). |
Problem 2: Failure in Differentiating Stem Cells into Target Lineages
This protocol for differentiating human pluripotent stem cells (hPSCs) into definitive endoderm provides a robust example of a defined system [49]. Failure often relates to incomplete lineage specification.
Step-by-Step Diagnosis:
- Validate Starting Cell Population: Confirm that your hPSCs are healthy, have a high viability (>90%), and are free of mycoplasma contamination before initiating differentiation [49].
- Check Critical Reagents:
- Matrix: Ensure coating matrices like Matrigel or Vitronectin are properly prepared and stored to maintain activity [49].
- Induction Molecules: Verify the activity and concentration of small molecules and growth factors. For example, the GSK3 inhibitor CHIR99021 is critical for efficient definitive endoderm induction in the referenced protocol [49].
- Confirm Differentiation Efficiency: Use immunostaining and flow cytometry to check for the expression of key lineage markers 24-48 hours after induction. For definitive endoderm, this includes transcription factors like SOX17 and FOXA2 [49].
- Troubleshoot Based on Markers:
- Low Expression of SOX17/FOXA2: Suggests inefficient definitive endoderm specification. Re-optimize the concentration and timing of CHIR99021 application [49].
- Presence of Undesired Cell Types: Indicates incomplete inhibition of alternative lineages. Consider adding specific pathway inhibitors (e.g., LDN193189 to suppress BMP signaling) to the base medium [49].
The following workflow diagram illustrates the key steps and quality control checkpoints in a standard differentiation protocol:
Problem 3: Limited Maturation and Functionality in 3D Models
Advanced Solutions to Enhance Physiological Relevance:
- Incorporate Vascularization Cues: Co-culture with endothelial cells and pericytes, or use microfluidic devices to provide perfusion, which improves nutrient delivery and mimics the in vivo vascular environment [48].
- Integrate Mechanical Stimulation: Use bioreactors to apply cyclic mechanical stress (e.g., compression for bone organoids, stretch for lung models) to promote tissue maturation and functional differentiation [48].
- Build Multi-tissue Assembloids: Combine organoids of different lineages (e.g., neural and vascular) to create complex systems that better recapitulate organ-organ interactions and tissue crosstalk [48].
- Adopt Organ-on-a-Chip Principles: Integrate organoids into microfluidic chips to achieve superior control over the microenvironment, including fluid shear stress and paracrine signaling between different tissue types [44].
Research Reagent Solutions
The following table lists essential materials and their functions for establishing and optimizing organoid cultures, based on cited protocols.
Table 3: Key Reagents for Organoid Differentiation and Culture
| Reagent Category | Specific Examples | Function in Culture | Application Example |
|---|---|---|---|
| Extracellular Matrices | Matrigel, Vitronectin, Synthetic Hydrogels (GelMA) | Provides a 3D scaffold that supports cell polarization, proliferation, and self-organization; supplies critical biochemical cues [49] [47]. | Coating culture vessels for hPSC attachment [49]; embedding organoids for 3D growth [47]. |
| Growth Factors & Cytokines | EGF, R-spondin, Noggin, FGF, HGF, Wnt3a | Activates specific signaling pathways to maintain stemness, direct cell fate, and promote differentiation into target lineages [47] [46]. | Noggin and R-spondin are essential for intestinal organoid growth; HGF is critical for liver organoids [47]. |
| Small Molecule Inhibitors/Activators | CHIR99021 (GSK3 inhibitor), Y-27632 (ROCK inhibitor), LDN193189 (BMP inhibitor), A83-01 (TGF-β inhibitor) | Precisely controls key signaling pathways (Wnt, TGF-β/BMP); Y-27632 enhances cell survival after passaging [49] [47]. | CHIR99021 is used to initiate definitive endoderm differentiation from hPSCs [49]. |
| Cell Surface Markers for QC | Anti-SOX17, Anti-FOXA2, Anti-CD184 (CXCR4) | Antibodies used in flow cytometry or immunostaining to validate the identity and purity of differentiated cell populations [49]. | Staining for SOX17 and FOXA2 to confirm definitive endoderm differentiation efficiency [49]. |
Visualizing Key Signaling Pathways in Differentiation
The differentiation of stem cells into specific lineages is guided by the precise manipulation of key signaling pathways. The following diagram summarizes the primary pathways involved and the effect of common modulators used in protocols.
Strategies for Enhancing Protocol Robustness and Reproducibility
Optimizing Culture Conditions and Differentiation Protocols
Troubleshooting Guides
Common hPSC Culture Challenges
This section addresses frequent issues encountered during the maintenance of human pluripotent stem cells (hPSCs), which are foundational for successful differentiation.
Table 1: Troubleshooting Common hPSC Culture Problems
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Excessive Differentiation (>20%) | Old culture medium; overgrown colonies; prolonged time outside incubator; uneven colony size [50]. | Use fresh medium (<2 weeks old); passage when colonies are large and compact but not overgrown; limit plate handling to <15 minutes; remove differentiated areas before passaging; ensure even colony sizing [50]. |
| Poor Cell Attachment After Passaging | Low initial plating density; over-digestion during passaging; sensitive cell line; using incorrect plate for coating matrix [50]. | Plate 2-3x more cell aggregates; reduce incubation time with passaging reagent (e.g., ReLeSR); use non-tissue culture-treated plates for Vitronectin XF [50]. |
| Undesirable Cell Aggregate Size | Incorrect passaging reagent incubation time or manipulation [50]. | For large aggregates (>200µm): Increase incubation time by 1-2 minutes; pipette mixture more [50].For small aggregates (<50µm): Decrease incubation time; minimize post-dissociation manipulation [50]. |
Challenges in Directed Differentiation
Optimizing differentiation protocols is critical for generating high-purity, clinically relevant cell types.
Table 2: Quantitative Analysis of hPSC Epithelial Differentiation Kinetics [51]
| Cell Fate Decision Parameter | Impact on Final Keratinocyte Progenitor Yield | Sensitivity to System Capacity |
|---|---|---|
| Self-renewal rate of progenitor state | High impact; can be a major limiting factor [51]. | Impact varies significantly with the maximum capacity of the culture system [51]. |
| Self-renewal rate of differentiated state | High impact; can be a major limiting factor [51]. | Impact varies significantly with the maximum capacity of the culture system [51]. |
| Differentiation rate between states | Modest impact on final cell yield [51]. | Less sensitive to changes in system scale [51]. |
Frequently Asked Questions (FAQs)
General Optimization Questions
Q1: Why is standardization important in stem cell differentiation, and what tools can help? Standardization is crucial for achieving reproducible and reliable results, especially when comparing different patient-specific cell lines or scaling up processes for drug screening. Using standardized differentiation kits can offer optimized reagents and succinct protocols, ensuring consistent performance, improved workflow efficiency, and easier experimental planning compared to "home-brew" protocols that piece together reagents from multiple vendors [42].
Q2: How does the starting pluripotency state of stem cells affect differentiation? The pluripotency state (or "pre-culture" condition) significantly influences differentiation efficiency and consistency. For example:
- ESLIF medium maintains a naive state, leading to a heterogeneous cell population [52] [53].
- 2i medium promotes a more homogeneous "ground-state" of pluripotency [52] [53]. Research shows that modulating these states, such as using short-term pulses of 2i and ESLIF, can alter the epigenome (e.g., DNA methylation, H3K27me3) and subsequently modulate cell differentiation outcomes, leading to more consistent and complex tissue formation in 3D models like gastruloids [52] [53].
Q3: What is a major source of heterogeneity in embryoid body (EB) differentiation, and how can it be controlled? A major source of heterogeneity is the initial size of the EBs, which affects cell-cell contact and the diffusion of soluble factors [54]. Using size-tunable microfabricated devices, such as concave microwells, to generate uniformly sized EBs from single cells allows for systematic screening of the optimal EB size and growth factor concentration for each specific hPSC line, potentially doubling the differentiation efficiency of target cells like endothelial cells [54].
Technical and Practical Questions
Q4: What are the key ethical guidelines for conducting stem cell research? The International Society for Stem Cell Research (ISSCR) provides comprehensive international guidelines that emphasize rigor, oversight, and transparency. Key principles include [3]:
- Integrity of the Research Enterprise: Ensuring research is trustworthy and subject to independent oversight.
- Primacy of Patient Welfare: Protecting patients and research subjects from undue risk; unproven interventions should not be marketed outside of regulated clinical trials.
- Social Justice: Encouraging fair global distribution of benefits and ensuring clinical trials enroll diverse populations.
Q5: What are the practical steps and timeline for initiating a patient-specific iPSC research project? A typical workflow involves [55]:
- Feasibility Analysis: Conduct a SWOT analysis to ensure the research question is a good fit for iPSC technology.
- iPSC Generation & Validation: Establish and fully characterize multiple iPSC clones from patients and controls (approx. 3-6 months).
- Directed Differentiation: Optimize and execute protocols to differentiate iPSCs into the relevant cell type(s) (approx. 3-6 months).
- Phenotypic Analysis: Use the differentiated cells for disease modeling, mechanism studies, or drug screening (approx. 6-12 months). Consulting or partnering with an experienced iPSC core facility can significantly accelerate this process [55].
Experimental Protocols & Workflows
Workflow for Optimizing a Differentiation Protocol
The following diagram outlines a systematic approach for optimizing a stem cell differentiation protocol, from initial line assessment to final scaled-up application.
Kinetic Model for Differentiation Efficiency
For a more quantitative approach, researchers can fit a kinetic model to time-course data to understand the dynamics of a differentiation process. The model below compartmentalizes the process into distinct cell states and estimates the rate constants (e.g., self-renewal, differentiation, death) for each, helping to pinpoint inefficiencies [51].
The Scientist's Toolkit
Table 3: Essential Reagents and Materials for Optimizing Differentiation
| Category | Item | Function / Rationale |
|---|---|---|
| Culture Media & Supplements | 2i Medium (GSK3b & MEK inhibitors) | Promotes a homogeneous "ground-state" pluripotency, potentially improving differentiation consistency [52] [53]. |
| ESLIF Medium (Serum-based) | Maintains a naive, but more heterogeneous, pluripotency state [52] [53]. | |
| Standardized Differentiation Kits | Provide pre-optimized reagents and protocols for specific lineages, enhancing reproducibility [42]. | |
| Engineering & Analysis Tools | Concave Microwells | Generate uniformly sized embryoid bodies (EBs) from single cells, controlling a key source of heterogeneity [54]. |
| Kinetic Modeling (ODE-based) | A quantitative approach to decouple cell fate decisions (self-renewal, differentiation, death) and identify bottlenecks [51]. | |
| Quality Control | Flow Cytometry Markers (e.g., Nanog, K18, K14) | Enables tracking of distinct cell subpopulations during differentiation for kinetic modeling and protocol assessment [51]. |
Addressing Batch-to-Batch Variability and Scalability Challenges
Troubleshooting Guides
FAQ: Managing Variability in Differentiation Efficiency
1. Why is there significant batch-to-batch variability in my hiPSC differentiations, and how can I address it?
Batch-to-batch variability in hiPSC differentiations arises from multiple sources, including inherent biological fluctuations in pluripotent stem cells, differences in reagent lots, and slight variations in culture conditions. This variability manifests as inconsistent differentiation efficiency across batches [56] [57].
- Root Cause: Biological systems are inherently variable. hiPSC lines can exhibit genetic drift over time, and their differentiation potential can be influenced by minor changes in cell culture microenvironment, passage number, and metabolic state [56].
- Solution: Implement a progenitor cell reseeding and cryopreservation strategy. A 2025 study demonstrated that detaching and reseeding progenitors at specific stages (EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitor stages) can improve cardiomyocyte purity by 10–20% [57]. Furthermore, cryopreserving these intermediate progenitor stages allows for the creation of large, standardized working cell banks. This means you can run a single, large differentiation to generate progenitors, bank them, and then thaw identical vials for future experiments, dramatically reducing batch-to-batch variability [57].
2. How can I improve the scalability of my stem cell manufacturing process while maintaining quality?
Scalability is hindered by manual, labor-intensive processes, donor-dependent variability in starting materials, and the limited expansion capacity of primary cells before they lose potency [58] [59].
- Root Cause: Traditional planar culture systems (e.g., flasks) are not space-efficient for producing clinically relevant cell numbers. Furthermore, primary cells like mesenchymal stromal cells (MSCs) have a finite number of population doublings before entering senescence [60] [59].
- Solution: Transition to automated, closed-system bioreactors [61]. Automation reduces human error and contamination risk while enabling a massive increase in scale. For instance, companies have successfully scaled up to 50-litre xeno-free, batch-fed microcarrier expansion systems for human bone marrow-derived MSCs [59]. Additionally, consider transitioning to induced pluripotent stem cell (iPSC)-derived cells like iMSCs, which offer a more consistent and virtually limitless starting source compared to primary tissue-derived cells, though they require careful characterization to manage their own form of batch variability [60] [15].
3. What tools can I use to objectively assess the quality of stem cell-derived embryo or organoid models before an experiment?
A major challenge is the subjective, researcher-dependent selection of high-quality models, leading to inconsistent experimental outcomes [62].
- Root Cause: Visual assessment of complex 3D structures is qualitative and can vary between users and labs.
- Solution: Employ AI-based deep learning models for quality classification. A 2025 study introduced "StembryoNet," a deep learning model trained on images of hundreds of mouse stem cell-derived embryo models. This model achieved 88% accuracy in classifying models as "normal" or "abnormal" based on morphological features, forecasting developmental trajectories at very early stages [62]. Implementing such image-based AI tools can standardize the selection process.
Experimental Protocols for Standardization
Protocol 1: Progenitor Reseeding for Enhanced Cardiomyocyte Differentiation Purity
This protocol is adapted from iScience (2025) and details a method to improve the consistency and purity of human pluripotent stem cell-derived cardiomyocytes (hPSC-CMs) [57].
- Objective: To increase hPSC-CM differentiation purity by 10–20% (absolute) by reseeding intermediate progenitor cells.
Materials:
- hPSCs (maintained in culture)
- Appropriate differentiation basal medium
- Differentiation induction factors (e.g., CHIR99021, BMP4, etc.)
- Accutase or gentle cell dissociation reagent
- Defined extracellular matrix (e.g., Fibronectin, Vitronectin, Laminin-111)
- Cryopreservation medium
Methodology:
- Mesoderm Induction: Begin standard hPSC-CM differentiation protocol to direct cells toward mesoderm.
- EOMES+ Mesoderm Reseeding: At the EOMES+ mesoderm stage (typically day 1-3), dissociate the cells into a single-cell suspension using Accutase.
- Re-plating: Reseed the cells at a defined density onto dishes coated with a defined ECM (e.g., Fibronectin). Continue the differentiation protocol.
- ISL1+/NKX2-5+ CPC Reseeding: At the cardiac progenitor cell (CPC) stage (typically day 5-7), repeat the dissociation and reseeding process.
- Terminal Differentiation: Continue culture until mature, beating cardiomyocytes are formed.
- (Optional) Cryopreservation: After the reseeding step at either the EOMES+ or ISL1+/NKX2-5+ stage, cells can be cryopreserved. Upon thawing, differentiation can be resumed, yielding CMs with the same improved purity.
Key Outcome Measures: Flow cytometry for cardiac troponin T (cTnT) to assess purity, analysis of contractility and sarcomere structure to ensure functionality is not impaired.
The following workflow diagrams this multi-stage differentiation and quality control process:
Protocol 2: AI-Assisted Quality Control for 3D Stem Cell Models
This protocol is based on Nature Communications (2025) and outlines using deep learning for standardized selection of 3D models [62].
- Objective: To objectively classify stem cell-derived embryo models (ETiX-embryos) as "normal" or "abnormal" using a trained AI model.
Materials:
- Live-imaging platform (e.g., confocal microscope with environmental control)
- Fluorescently labeled stem cells (e.g., ESCs, TSCs)
- Agarose microwells for 3D culture
- Pre-trained deep learning model (e.g., StembryoNet)
Methodology:
- Model Generation: Generate ~100-900 3D ETiX-embryo models by aggregating different stem cell types in agarose microwells.
- Live Imaging: Culture models under the live-imaging platform for ~90 hours, capturing multifocal images at regular intervals.
- Expert Annotation: Have an expert embryologist annotate the dataset, classifying each model at the 90-hour mark based on strict morphological criteria (cylindrical shape, lineage segregation, pro-amniotic cavity formation).
- Model Training/Application: Train a convolutional neural network (e.g., ResNet18-based StembryoNet) on the annotated image dataset. For use, input new time-lapse images of developing models into the trained AI.
- Prediction: The AI model will output a classification ("normal" or "abnormal") with a calculated accuracy, allowing researchers to select only the high-quality models for downstream experiments.
Key Outcome Measures: AI model accuracy, precision, and F1-score in classifying model quality compared to expert annotation.
The logical workflow for implementing this AI-based quality control is as follows:
Data Presentation
Table 1: Quantitative Impact of Standardization Techniques
| Technique | Key Performance Metric | Outcome | Reference |
|---|---|---|---|
| Progenitor Reseeding | Cardiomyocyte Purity | 10-20% absolute improvement | [57] |
| AI Model (StembryoNet) | Classification Accuracy | 88% accuracy in selecting normal embryo models | [62] |
| iPSC-derived MSCs | Anti-inflammatory Effect | Prolonged effect but with batch-to-batch variability | [60] |
| Xeno-Free Medium | Long-term Expansion | Enabled expansion but revealed senescence in primary MSCs by passage 5 | [60] |
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Standardization |
|---|---|
| Defined Extracellular Matrices (e.g., Fibronectin, Vitronectin) | Provides a consistent, xeno-free substrate for cell adhesion and growth, reducing variability compared to biological coatings like Matrigel. Essential for progenitor reseeding protocols [57]. |
| Xeno-Free (XFS) Culture Medium | Eliminates animal-derived components (e.g., FBS), reducing immunogenic risk and improving consistency for clinical translation [60]. |
| Cryopreservation Medium | Allows for the creation of large, standardized banks of intermediate progenitor cells (e.g., EOMES+ mesoderm), enabling on-demand production of differentiated cells from a single, high-quality batch [57]. |
| Microcarriers in Bioreactors | Used in scalable bioreactor systems to dramatically increase the surface area for cell growth, enabling the production of large quantities of cells in a controlled, automated environment [59] [61]. |
Foundational Concepts: Frequently Asked Questions
What is the core value of integrating multi-omics data in stem cell research? Multi-omics integration provides a layered view of biology that no single data type can capture alone. By combining genomics, transcriptomics, proteomics, metabolomics, and epigenomics, researchers can achieve more precise target identification, stronger patient stratification, reduced false positives in biomarker discovery, and improved modeling of complex biological mechanisms like differentiation variability. This integrated approach is essential for understanding the complex factors influencing differentiation efficiency in patient-specific stem cell lines [63] [64].
Why is automation critical in modern stem cell workflows? Automation brings consistency and robustness to stem cell research by replacing human variation with stable, reproducible systems. This is particularly important in differentiation protocols where minor technical variations can significantly impact outcomes. Automated systems range from simple, accessible benchtop units for routine tasks to large, unattended multi-robot workflows for high-throughput screening, all aimed at generating data that can be trusted years later [65].
How can AI and machine learning address variability in differentiation outcomes? AI and ML excel at identifying non-linear patterns across high-dimensional spaces, making them uniquely suited for analyzing multi-omics data to predict differentiation efficiency. For example, models can be trained to link specific molecular signatures with successful differentiation outcomes, enabling researchers to select optimal cell lines early in the process and potentially bypass extensive empirical testing [66] [63] [67].
What are the key bottlenecks in implementing these advanced workflows? Key challenges include data quality and standardization across different omics platforms, interpretability of AI models ("black box" problem), scalability of experimental validation, and integration of disparate data systems. Success depends on both technical solutions and human collaboration between computational and wet-lab researchers [68] [64].
Troubleshooting Guides
Issue 1: High Variability in Differentiation Efficiency Across Cell Lines
Problem: Even when using standardized differentiation protocols, efficiency varies significantly between different patient-specific iPSC lines, leading to inconsistent experimental results and difficulty in comparative studies [69].
Diagnostic Steps:
- Implement early predictive profiling: Before committing to full differentiation protocols, analyze cell culture media at key early stages using multi-analyte profiling technologies such as Luminex assays. This non-invasive method allows you to continue the differentiation process while gathering predictive data [69].
- Identify predictive analytes: Focus on cytokine and growth factor expression profiles that differ between cell lines with robust versus poor differentiation efficiency. Research has identified specific analytes predictive of cardiomyocyte differentiation success [69].
- Cross-validate with molecular characterization: Combine secretory protein data with standard pluripotency assessments (e.g., flow cytometry for OCT4, NANOG) to build a comprehensive predictive model [6] [10].
Solutions:
- Develop line-specific predictive models: Use the analyte profiles from successful differentiations to create reference standards for evaluating new iPSC lines.
- Focus on pathways, not single markers: Analyze the identified predictive analytes in the context of entire signaling pathways involved in your target differentiation, as this provides more robust prediction than single biomarkers [69] [64].
Issue 2: Inefficient and Time-Consuming Differentiation Protocols
Problem: Traditional differentiation protocols for generating specific cell types from iPSCs are often prohibitively long, taking weeks or months, which hinders practical application and high-throughput screening [10].
Diagnostic Steps:
- Conduct stage-specific efficiency analysis: Use qPCR and immunofluorescence to check key markers at each differentiation stage rather than just at the endpoint. This helps identify exactly where protocols fail or become inefficient [10].
- Evaluate cell cycle status: Analyze the cell cycle of undifferentiated and differentiated cells by flow cytometry. A reduction in stemness markers (OCT4, NANOG) after subculturing or cryopreservation often indicates a purer population of differentiated cells [10].
Solutions:
- Protocol optimization through time reduction: Systematically test whether specific stages can be shortened without losing efficiency. Research on pancreatic differentiation successfully reduced protocol time by half while maintaining expression of key differentiation genes [10].
- Implement intermediate cryopreservation: Create banks of intermediate progenitor cells (e.g., pancreatic progenitors) that can be frozen, thawed, and readily differentiated into mature cells, dramatically shortening the timeline for future experiments [10].
Issue 3: Data Fragmentation and Lack of Integration Across Platforms
Problem: Data from omics technologies, high-throughput screening, and clinical annotations remain in separate silos with inconsistent metadata, preventing comprehensive analysis and machine learning applications [65] [64].
Diagnostic Steps:
- Audit data traceability: Determine if your workflow captures sufficient metadata (experimental conditions, processing methods, reagent lots) to ensure data reproducibility and usability for AI training [65].
- Check for batch effects: Analyze data from different experimental batches or platforms for technical artifacts that might obscure biological signals, a common challenge in multi-omics studies [63] [64].
Solutions:
- Implement unified data management platforms: Use systems that connect laboratory information management (LIMS), experimental data, and analysis pipelines to create a seamless data trajectory from bench to analysis [65].
- Prioritize metadata standardization: Establish standardized formats and ontologies before data generation begins, ensuring interoperability across different systems and enabling federated learning approaches [68] [64].
Structured Data for Experimental Planning
Table 1: Methods for Assessing Pluripotency and Differentiation Potential
| Technique | Key Aspects | Advantages | Limitations |
|---|---|---|---|
| Immunocytochemistry/Immunofluorescence | Detects expression of key pluripotency (OCT4, SOX2, NANOG) or differentiation markers (PDX1, Amylase) using antibodies [6] [10]. | Accessible, provides spatial localization within colonies. | Qualitative; marker expression alone does not confirm functional potential [6]. |
| Flow Cytometry | Quantitative analysis of multiple pluripotency or differentiation markers across entire cell populations [6]. | High-throughput, accounts for population heterogeneity. | Does not directly assess functional pluripotency [6]. |
| Teratoma Assay | In vivo test where cells are implanted into immunodeficient mice to form benign tumors containing tissues from three germ layers [6]. | Considered the "gold standard" for providing conclusive proof of pluripotency. | Time-consuming, expensive, ethical concerns, qualitative, and protocol variation between labs [6]. |
| Multi-analyte Profiling (e.g., Luminex) | Measures cytokine/growth factor levels in culture media during early differentiation stages [69]. | Non-invasive, predictive, allows cells to continue differentiation. | Requires prior establishment of predictive analyte profiles for specific cell types [69]. |
| Molecular Analysis (qPCR/RNA-seq) | Quantifies mRNA levels of key lineage-specific genes (e.g., PDX1 for pancreatic progenitors) [10]. | Quantitative, can be performed at multiple stages of differentiation. | Gene expression does not always correlate with protein expression or function [6]. |
Table 2: Key Analytes Predictive of Differentiation Efficiency
This table summarizes the approach for identifying predictive biomarkers, as demonstrated in cardiomyocyte differentiation [69].
| Analysis Method | Stage of Analysis | Key Outcome | Application in Troubleshooting |
|---|---|---|---|
| Luminex Multi-analyte Profiling | Early stages of differentiation; culture media sampling. | Cytokine/growth factor expression profiles differ significantly between cell lines with high vs. low differentiation efficiency. | Serves as an early detection method to screen and select cell lines with high inherent differentiation potential before committing to full protocols. |
| Pathway Analysis | After identifying predictive analytes. | Identification of particular signaling pathways critical for successful differentiation. | Informs mechanistic understanding of failures and guides protocol optimization by focusing on key biological pathways. |
Experimental Protocols
Protocol 1: Non-Invasive Predictive Profiling for Differentiation Potential
Purpose: To assess the likelihood of successful differentiation early in the process without harming the cells, allowing for selective continuation of high-potential lines [69].
Materials:
- Cell culture supernatant from early differentiation stages
- Multi-analyte profiling platform (e.g., Luminex Assays)
- Standard equipment for cell culture
Methods:
- Initiate differentiation of your iPSC lines using your standard protocol (e.g., for cardiomyocytes [69] or pancreatic cells [10]).
- At predetermined early time points (e.g., days 2-4), collect small volumes of cell culture media supernatant.
- Process the samples immediately or store at -80°C for batch analysis.
- Analyze the samples using the multi-analyte platform according to manufacturer's instructions to quantify a panel of cytokines and growth factors.
- Compare the resulting secretory profile of the test line to a pre-established reference profile from lines known to differentiate efficiently.
Interpretation: Cell lines whose secretory profiles closely match the reference profile are considered high-potential candidates for continued differentiation and further experimentation.
Protocol 2: Optimized and Shortened Pancreatic Progenitor Differentiation
Purpose: To efficiently generate patient-specific pancreatic progenitor cells from iPSCs with reduced protocol time and the option for cryopreservation [10].
Materials:
- Human iPS cells
- Matrigel-coated plates
- Stem cell culture medium (e.g., StemMACS iPS-Brew XF)
- Differentiation basal medium: RPMI 1640 with 1% penicillin-streptomycin
- Key differentiation factors: Activin A, CHIR99021, FGF-7, Cyclopamine, Noggin, All-trans Retinoic Acid, GLP-1, Nicotinamide [10]
- TRIzol for RNA extraction, qPCR reagents, antibodies for immunofluorescence (e.g., PDX1)
Methods:
- Stage I - Definitive Endoderm (4 days): Culture iPSCs in RPMI medium supplemented with Activin A (100 ng/mL) and CHIR99021 (3 µM) [10].
- Stage II - Primitive Gut Tube (3 days): Switch to RPMI medium containing FGF-7 (50 ng/mL) [10].
- Stage III - Pancreatic Progenitors (3 days): Culture in RPMI medium with Cyclopamine (0.25 µM), Noggin (50 ng/mL), and All-trans Retinoic Acid (2 µM) [10].
- Validation: Analyze the efficiency of differentiation by qPCR for PDX1 expression and immunofluorescence for PDX1 protein, comparing to undifferentiated iPSCs [10].
- Cryopreservation (Optional): Freeze pancreatic progenitor cells for future use. Upon thawing, they can be expanded or directly differentiated further [10].
Interpretation: Successful differentiation is confirmed by a significant increase in PDX1 mRNA and protein levels in differentiated cells compared to the original iPSCs. A reduction in stemness markers (OCT4, NANOG) after passaging or cryopreservation indicates a purer pancreatic progenitor population [10].
Workflow and Pathway Visualizations
Diagram 1: Predictive Workflow for Efficient Differentiation. This diagram outlines a data-driven strategy that uses multi-omics characterization and AI to predict cell line potential before committing to lengthy differentiation protocols, improving resource allocation.
Diagram 2: Multi-Omics Data Integration for Standardization. This diagram shows how disparate omics data layers are integrated computationally to extract biological insights that drive improvements in experimental outcomes and standardization.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Data-Driven Differentiation Workflows
| Item | Function | Example Application |
|---|---|---|
| Multi-analyte Profiling Kits (e.g., Luminex) | Multiplexed quantification of proteins/cytokines from small volume samples. | Non-invasive prediction of cardiomyocyte differentiation efficiency from culture media [69]. |
| Defined Differentiation Kits | Provide standardized, optimized reagent combinations for specific lineages. | Standardized cardiomyocyte differentiation (e.g., StemXVivo Kit) to reduce protocol variability [69]. |
| Key Growth Factors & Small Molecules | Precisely direct cell fate through specific signaling pathways. | Activin A (definitive endoderm), FGF-7 (gut tube), Retinoic Acid (pancreatic progenitors) [10]. |
| High-Quality Antibodies | Validate pluripotency status and differentiation efficiency via ICC/IF and Flow Cytometry. | Staining for OCT4, NANOG (pluripotency), PDX1 (pancreatic progenitors), Amylase (exocrine cells) [6] [10]. |
| qPCR Reagents & Primers | Quantitatively monitor gene expression dynamics at each differentiation stage. | Tracking mRNA levels of PDX1 and Amylase during pancreatic differentiation [10]. |
| Automated Liquid Handlers | Increase reproducibility and throughput of culture medium changes and differentiation induction. | Enabling robust, large-scale screening of differentiation conditions across multiple cell lines [66] [65]. |
| 3D Cell Culture Systems | Provide a more physiologically relevant microenvironment for differentiation and maturation. | Automated platforms (e.g., MO:BOT) for standardizing organoid culture and improving data quality [65]. |
Automation and Closed-System Bioreactors for Consistent Manufacturing
Technical Support Center
Troubleshooting Guides
Guide 1: Investigating Bacterial Contamination in Bioreactors
Reported Problem: Sudden, unexpected drop in dissolved oxygen (% DO) during a bioreactor run, indicating potential microbial contamination [70].
Investigation Procedure:
Immediate Action and Data Collection:
- Confirm Contamination: Terminate the run and aseptically sample the bioreactor for rapid microbiological testing [70].
- Analyze DO Profile: Use the dissolved oxygen profile to estimate the time of the initial contamination event. The rate of decline in % DO can be used to estimate the growth rate (doubling time) of the contaminating organism [70].
- Estimate Single-Cell Time: By combining the estimated growth rate with a cell count of the contamination, calculate backwards to find when only a single contaminant cell existed in the bioreactor [70].
Identify the Root Cause:
- Review Valve Sterilization: Check temperature profiles of all sample and feed valves used shortly before the estimated contamination time to verify they reached and maintained sterilization temperature [70].
- Correlate with Events: Cross-reference the estimated contamination time with the batch record for events such as sampling, feed additions, or new probe installations [70].
- Identify Contaminant Species: Perform rapid species identification. Gram-positive bacteria and spore formers often originate from sterilization failures, while gram-negative organisms are more likely from water sources [70].
- Inspect Components: Check for micro-cracks in elastomer diaphragms, improperly seated gaskets, or faulty steam traps associated with the suspect events [70].
Corrective and Preventive Actions (CAPA):
- Implement revised sterilization procedures for identified failure points.
- Replace any compromised seals, gaskets, or valves.
- Update standard operating procedures (SOPs) to prevent recurrence [70].
Guide 2: Addressing Inconsistent Stem Cell Product Quality
Reported Problem: Inconsistent results in clinical trials or differentiation experiments, even when using identical cell types and protocols [71].
Investigation Procedure:
Audit Manufacturing Variables:
- Source Material: Verify the consistency of donor tissue and cell isolation techniques [71].
- Culture Media: Review records for any changes or inconsistencies in media formulation, including supplements like Human Serum Albumin (HSA). Even with identical protocols, different commercial media can dramatically alter the biological properties of the final cell product [71].
- Process Control: Ensure all quality control (QC) systems are calibrated and that operators are following standardized protocols [71].
Evaluate Release Criteria:
- Assess whether standard release tests (e.g., surface marker expression) are sufficient to predict the therapeutic functionality of the cells. Current criteria may pass biologically different products as identical [71].
Corrective and Preventive Actions (CAPA):
- Transition to a closed, automated bioreactor system to minimize manual handling and variation [71] [72].
- Implement more predictive release criteria that are linked to the biological function of the cells, rather than just surface markers [71].
- Standardize the manufacturing process, including the use of a single, validated media formulation from start to finish [71].
Frequently Asked Questions (FAQs)
Q1: What are the primary advantages of switching from an open to a closed bioreactor system?
A1: Closed systems offer several critical advantages for clinical manufacturing [72]:
- Reduced Contamination Risk: By minimizing exposure to the room environment, closed systems drastically lower the risk of microbial contamination [72].
- Improved Batch-to-Batch Consistency: Automated, closed processes reduce human error and variability, leading to more reproducible products [72].
- Lower Operational Costs: Closed systems can often operate in a Grade C environment instead of more expensive cleanrooms, and require less labor [72].
- Regulatory Compliance: The inherent contamination control of closed systems aids in meeting stringent regulatory standards for cell and gene therapies [73].
Q2: How can I maintain sterility when integrating supplements into a closed-system bioreactor?
A2: The use of single-use technologies (SUT) is key. Instead of multi-use bottles, use pre-sterilized single-use bags with sterile, weldable tubing and aseptic connectors. This allows materials like media supplements to be added to the bioreactor without breaking the closed loop, enabling a truly aseptic process [73].
Q3: Our differentiation protocols for hiPSCs are long and have low reproducibility. Are there non-destructive methods to predict outcomes earlier?
A3: Yes, emerging techniques combine non-destructive imaging with machine learning. One study successfully predicted the efficiency of muscle stem cell differentiation from hiPSCs approximately 50 days before the protocol endpoint. The method uses phase-contrast images taken between days 14-38, processes them with Fast Fourier Transform (FFT) to extract features, and then employs a random forest classifier to forecast the final differentiation yield. This allows for early selection of high-quality cultures and more efficient protocol optimization [27].
Q4: What is the difference between an integrated and a modular closed automation system?
A4: The choice depends on the needed flexibility and scale.
- Integrated Systems: Are fully automated, all-in-one solutions designed for end-to-end processing of one patient's product at a time. They are easy to use but less flexible [72].
- Modular Systems: consist of separate instruments, each optimized for a single unit operation (e.g., cell isolation, expansion). This offers more versatility and allows mixing of best-in-class equipment from different suppliers, which is advantageous for process development [72].
The table below compares common systems based on a 2023 analysis.
| System Type | Core Technology | Cell Recovery | Input Volume | Key Advantage |
|---|---|---|---|---|
| Modular System | Counterflow Centrifugation | 95% | 30 mL – 20 L | High flexibility for process development [72] |
| Modular System | Electric Centrifugation Motor | 70% | 30 mL – 3 L | Established technology [72] |
| Integrated System | Spinning Membrane Filtration | 70% | 30 mL – 22 L | Streamlined, all-in-one workflow [72] |
The Scientist's Toolkit: Research Reagent Solutions
The table below lists key materials and their functions in standardized stem cell manufacturing, as identified in the search results.
| Item | Function | Application Context |
|---|---|---|
| StemRNA Clinical iPSC Seed Clones | A standardized, GMP-compliant starting material for deriving consistent iPSC lines. A submitted Drug Master File (DMF) aids in regulatory submissions [15]. | Creating reproducible, patient-specific cell lines for therapy [15]. |
| Validated Single-Use Bioreactors (e.g., HyPerforma S.U.B.) | Pre-sterilized, closed-system vessels for cell expansion. They integrate with sterile tubing and connectors to maintain asepsis [73]. | Scalable expansion of stem cells and their derivatives [73]. |
| Sterile, Weldable Tubing & Aseptic Connectors | Tubing that can be fused together and connectors that allow sterile fluid transfer between components without exposing the product to the environment [73]. | Maintaining a closed system during media additions, sampling, or transferring cells between bioreactors [73]. |
| Defined Culture Media Formulations | Chemically defined media that support cell growth and direct differentiation. Consistency in media is critical, as variations can alter the biological properties of the final cell product [71]. | All stages of stem cell culture and directed differentiation [71]. |
| MYF5-tdTomato Reporter iPSC Line | A research tool where a fluorescent protein (tdTomato) is expressed under the control of the MYF5 gene promoter, a marker for muscle stem cells [27]. | Non-destructively monitoring and quantifying the efficiency of muscle stem cell differentiation in real-time [27]. |
Experimental Protocol: Early Prediction of hiPSC Differentiation Efficiency
This protocol summarizes a methodology for non-destructively predicting the final differentiation yield of human induced pluripotent stem cells (hiPSCs) into muscle stem cells (MuSCs) using imaging and machine learning [27].
Objective: To predict MuSC induction efficiency on day 82 from phase-contrast images taken between days 14 and 38.
Materials:
- MYF5-tdTomato reporter hiPSC line [27].
- Materials for MuSC directed differentiation protocol (Wnt agonist, IGF-1, HGF, bFGF, horse serum-based medium) [27].
- Cell culture plates (e.g., 6-well or 24-well plates).
- Phase-contrast microscope with a digital camera.
- Computer with Python/R and libraries for image processing (FFT) and machine learning (Random Forest classifier).
Methodology:
- Cell Culture and Differentiation: Seed the reporter hiPSCs and initiate the directed differentiation protocol toward MuSCs. The protocol involves three main phases: dermomyotome induction (Days 0-14), myogenic induction (Days 14-38), and maturation (Days 38-82) [27].
- Image Acquisition: Between days 14 and 38, acquire phase-contrast images of the cells in multiple culture wells at regular intervals. The cited study captured a total of 5,712 images from 34 wells over six independent experiments [27].
- Feature Extraction: For each acquired image, apply a Fast Fourier Transform (FFT) to obtain its power spectrum. Then, perform shell integration on this spectrum to generate a 100-dimensional, rotation-invariant feature vector. This vector captures the morphological characteristics of the cells in the image [27].
- Model Training and Prediction:
- On day 82, use flow cytometry to measure the final differentiation efficiency (MYF5+ % or CDH13+ %) for each well [27].
- Label each well's image set as "high efficiency" or "low efficiency" based on the flow cytometry results.
- Train a Random Forest classifier using the feature vectors extracted from the images as input and the efficiency labels as the output.
- Validate the model to determine the earliest day (e.g., day 24 or 34) from which images can accurately predict the final outcome [27].
Expected Outcome: The trained machine learning model can identify samples with high and low MuSC induction efficiency approximately 50 days before the protocol endpoint, allowing researchers to prioritize high-yield cultures early in the process [27].
Process Visualization
Diagram 1: ML-integrated differentiation workflow.
Diagram 2: Contamination troubleshooting flowchart.
Benchmarking and Regulatory Pathways for Clinical Translation
For researchers working on standardizing differentiation efficiency in patient-specific stem cell lines, navigating the global regulatory environment is as crucial as optimizing laboratory protocols. The path to clinical translation is paved with stringent and often divergent regulatory requirements across major markets. Understanding the specific frameworks of the U.S. Food and Drug Administration (FDA), the European Union (EU) under its Medical Device Regulation (MDR), and other key agencies is essential for designing compliant and successful research and development strategies. This guide provides a technical support framework to help scientists troubleshoot common regulatory challenges within the context of their thesis work.
Regulatory Agency Comparison: FDA, EU, and PMDA
The following table summarizes the core regulatory characteristics of the FDA and EU MDR, which are the most defined frameworks in the available data. Specific, detailed information on Japan's PMDA (Pharmaceuticals and Medical Devices Agency) was not available in the search results, highlighting a critical area for further investigation.
Table 1: Comparative Overview of Key Regulatory Frameworks
| Aspect | U.S. Food and Drug Administration (FDA) | European Union (EU MDR) | Japan's PMDA |
|---|---|---|---|
| Governing Legislation | Federal Food, Drug, and Cosmetic Act; 21 CFR Regulations [74] | Regulation (EU) 2017/745 (MDR) [74] | Information Not Available |
| Regulatory Philosophy | Risk-based, pragmatic; balances innovation with safety [75] | Prescriptive, precautionary; requires proven compliance [75] | Information Not Available |
| Approval Pathway (for devices) | Centralized review by FDA [74]. Common paths: 510(k) (substantial equivalence), PMA (high risk) [74]. | Decentralized review through Notified Bodies designated by member states [74]. | Information Not Available |
| Clinical Evidence | For 510(k), clinical data may not be required if substantial equivalence can be shown via performance testing [74]. | Clinical evaluation and a Clinical Evaluation Report (CER) are mandatory for all devices, regardless of classification [74]. | Information Not Available |
| Quality Management System (QMS) | 21 CFR 820 (transitioning to QMSR aligned with ISO 13485 by Feb 2026) [74] | ISO 13485:2016 compliance required by law [74] | Information Not Available |
| Timeline (Typical) | 510(k): 6-12 months [74] | CE Marking: 12-18 months [74] | Information Not Available |
| Cost (Typical) | 510(k): $1M-$6M [74] | CE Marking: $500K-$2M [74] | Information Not Available |
Troubleshooting Guides & FAQs
FAQ: Navigating Early-Stage Research and Pre-clinical Development
Q1: Our research uses induced Pluripotent Stem Cell (iPSC)-derived neurons. At what point do our activities require FDA engagement?
A: FDA engagement becomes mandatory when you intend to use the iPSC-derived neurons in human clinical trials or to market them as a therapeutic or diagnostic product. Research and development in a laboratory setting typically do not require FDA submission. However, if your work is preparatory to a clinical trial, you must file an Investigational New Drug (IND) application and receive FDA clearance before beginning human trials [15]. It is a critical distinction that an FDA-authorized trial does not equate to an FDA-approved product; full approval requires a successful Biologics License Application (BLA) [15].
Q2: For the EU MDR, what is the significance of "Person Responsible for Regulatory Compliance (PRRC)" and do we need one for basic research?
A: The PRRC is a mandatory role for manufacturers under EU MDR, requiring a designated individual with expertise in medical device regulations to ensure compliance [74]. If your institution is solely conducting basic research and not placing a finished, CE-marked product on the market, the PRRC requirement likely does not apply. This obligation triggers once you assume the role of a "manufacturer" under the MDR.
Q3: How do regulatory agencies view the use of complex in vitro models like organoids in our pre-clinical data package?
A: Regulatory agencies increasingly recognize the value of human-relevant models. Stem cell- and organoid-based systems are seen as more predictive than traditional 2D cultures or animal models for replicating human-specific pathophysiology, enabling better predictions of therapeutic efficacy and safety [56]. When submitting data, be prepared to provide comprehensive documentation of your protocols, including details on cell line provenance, differentiation efficiency, batch-to-batch variability controls, and validation data to demonstrate the model's reliability and relevance to the disease target [56].
FAQ: Addressing Clinical Evidence and Technical Documentation
Q4: The FDA 510(k) pathway seems efficient, but our stem cell-based product has no true predicate. What are our options?
A: You are correct that the 510(k) pathway relies on demonstrating substantial equivalence to a legally marketed predicate device [74]. If no appropriate predicate exists due to significant technological changes or a novel intended use, the 510(k) path is closed. Your product would likely be classified as Class III and require a Premarket Approval (PMA), which demands rigorous scientific evidence, typically including data from clinical investigations to demonstrate safety and effectiveness [74].
Q5: The EU MDR requires a "Clinical Evaluation Report" for all devices. What does this mean for our novel, patient-specific cell line?
A: This is a key stringent requirement of the EU MDR. A Clinical Evaluation Report (CER) is mandatory for all device classes, and it must be updated throughout the product's lifecycle [74]. For a novel therapy, you cannot rely solely on literature from equivalent devices. You will need to generate and present original clinical data specific to your product to demonstrate safety and performance. This often requires a clinical investigation (trial) within the EU. The principle of equivalence is very strict and difficult to meet for innovative products [74].
Q6: We are experiencing high batch-to-batch variability in our differentiated cell populations. How will this impact our regulatory submissions?
A: High variability is a major red flag for regulators as it challenges the consistency, safety, and efficacy of your final product. You must implement and document a robust control strategy.
- Process Controls: Standardize and tightly control your differentiation protocols, including raw materials (e.g., using clinical-grade iPSC seed clones with a Drug Master File (DMF) [15]).
- Release Criteria: Define and validate critical quality attributes (CQAs) and establish strict acceptance criteria for each batch.
- Risk Management: Document these variability challenges and your mitigation strategies within your risk management file (per ISO 14971). Regulators will expect to see evidence that you can reliably produce a consistent and well-characterized product.
Essential Research Reagent Solutions
Standardizing reagents is fundamental to reducing variability in differentiation protocols. The following table lists key material categories and their functions.
Table 2: Key Research Reagent Solutions for Standardization
| Reagent/Material | Function in Stem Cell Research |
|---|---|
| StemRNA Clinical Seed iPSC Clones | Provides a consistent, GMP-compliant, and well-documented starting cell source. A referenced Drug Master File (DMF) with regulatory agencies can streamline IND filings [15]. |
| Defined Growth Factors & Small Molecules | Directs stem cell fate and differentiation toward specific lineages (e.g., neurons, cardiomyocytes). Using defined, xeno-free, and high-purity lots is critical for protocol consistency and regulatory approval [56]. |
| Characterized & Validated Antibodies | Used for flow cytometry, immunocytochemistry, and other assays to quantify differentiation efficiency and purity by detecting lineage-specific markers. |
| Bioengineered Matrices & Scaffolds | Provides the 3D structural and biochemical support for organoid growth and maturation, mimicking the native tissue microenvironment [56]. |
| Patient-Derived Somatic Cells | The primary source material for generating patient-specific iPSC lines, enabling the creation of disease models and autologous therapies [56]. |
Regulatory Pathway and Oversight Diagrams
Diagram 1: Simplified U.S. FDA Pathway for a Novel Stem Cell-Based Product
The following diagram outlines the key stages a novel product would typically navigate under the FDA's oversight.
Diagram 2: High-Level EU MDR Conformity Assessment for a High-Risk (Class III) Device
This chart illustrates the core process for achieving CE marking under the EU MDR, which involves an external Notified Body.
FAQs: Navigating the Regulatory and Experimental Pathway
Q1: What is the key difference between an FDA-authorized clinical trial and an FDA-approved stem cell product?
An FDA-authorized trial means the agency has permitted a clinical investigation to proceed under an Investigational New Drug (IND) application. This is not product approval. It only allows human trials to begin after a 30-day review period with no FDA objections. In contrast, an FDA-approved product has undergone a rigorous evaluation process and received a Biologics License Application (BLA), confirming it is safe, pure, and potent for its intended use and can be marketed. Referring to a therapy as "FDA-approved" is strictly reserved for products with formal marketing approval [15].
Q2: What are common pitfalls in stem cell differentiation protocols, and how can they be mitigated?
Common pitfalls include high variability in differentiation efficiency between cell lines, immature phenotypes of differentiated cells, and low protocol reproducibility. This is often due to genetic variation in iPSC clones, slight changes in seeding cell numbers, and researcher technique [43] [27]. Mitigation strategies include:
- Thorough Characterization: Use a combination of techniques to assess the identity and functionality of differentiated cells, moving beyond simple marker expression [43].
- Early Quality Prediction: Implement non-destructive, image-based machine learning systems to predict final differentiation efficiency early in the process, allowing for the selection of high-quality cultures long before the protocol is complete [27].
- Protocol Standardization: Meticulously control conditions like seeding numbers and reagent quality to minimize batch-to-batch variation.
Q3: Which FDA-approved stem cell products serve as the most relevant case studies for regenerative medicine?
The FDA's list of approved cellular therapies is selective and provides critical learning opportunities. Key recent approvals include [15] [76]:
- Ryoncil (remestemcel-L): Approved in December 2024, it is the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD). This approval demonstrates the viability of allogeneic, bone marrow-derived MSC therapies for modulating immune responses.
- Omisirge (omidubicel-onlv): Approved in April 2023, this is a nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cell product. It accelerates neutrophil recovery in patients with hematologic malignancies, showcasing the advancement of cord blood-based technologies.
- Lyfgenia (lovotibeglogene autotemcel): Approved in December 2023, this is an autologous cell-based gene therapy for sickle cell disease. It involves genetically modifying a patient's own hematopoietic stem cells, representing the convergence of gene and cell therapy.
Q4: How are novel technologies like AI and machine learning impacting stem cell clinical trials?
AI and ML are being applied to accelerate and improve nearly every stage of stem cell research and therapy development [77] [78] [27]:
- Predicting Differentiation Efficiency: ML models can analyze phase-contrast images of differentiating cells to predict the final yield of target cells weeks in advance, enabling early quality control [27].
- Optimizing Cell Selection and Delivery: AI algorithms can help select the best stem cell lines for individual patients and optimize the route of administration and dosing to enhance therapeutic outcomes [77].
- Accelerating Clinical Trial Design: ML can help with patient recruitment, simulate medical interventions, and analyze complex trial data to identify novel biomarkers and endpoints [78].
Troubleshooting Guides
Guide 1: Addressing Low Differentiation Efficiency and Reproducibility
Problem: The yield of your target differentiated cell type is consistently low or varies significantly between experiments and cell lines.
Solution Steps:
- Implement Early Forecasting: Adopt a non-destructive prediction system. Capture phase-contrast images during the early or mid-phase of differentiation and use a machine learning classifier (e.g., Random Forest) with features extracted via Fast Fourier Transform (FFT) to identify cultures with high potential early on. This allows you to focus resources on the most promising samples [27].
- Verify Pluripotency and Differentiation Potential: Rigorously characterize your starting iPSC population. Do not rely solely on molecular markers of pluripotency (a "state"); confirm developmental potency ("function") using in vitro assays like embryoid body formation [6].
- Recreate Developmental Cues: Ensure your protocol accurately mimics in vivo development. For neural cell types, this involves precise timing and concentration of morphogens like SHH, FGFs, and BMPs to achieve correct anterior/posterior and dorsal/ventral patterning [43].
- Validate Functional Maturity: Assess differentiated cells beyond marker expression. For cholinergic neurons, this includes checking for electrophysiological activity (slow spiking at 4–10 Hz) and the presence of functional proteins like ChAT and vAChT [43].
Guide 2: Preparing for Regulatory Submissions and Clinical Trials
Problem: Navigating the FDA regulatory pathway from preclinical development to clinical trial authorization and eventual approval seems daunting.
Solution Steps:
- Understand the IND Process: Before human trials, submit a detailed IND application to the FDA. This must include animal study data and toxicity profiles, manufacturing information, clinical protocols, and investigator information. The FDA has 30 days to review the application before trials can proceed [79].
- Engage Early with the FDA: Seek FDA assistance during the pre-IND phase and after Phase 2 trials. The agency provides guidance that can help enhance research and design robust Phase 3 studies, even though their suggestions are not mandatory [79].
- Design Pivotal Trials with Clear Endpoints: Phase 3 studies must be designed to demonstrate a clear treatment benefit. Define clinical endpoints (e.g., patient survival, improved function) and surrogate endpoints (e.g., biomarker levels) that are meaningful and measurable. Consider using an independent data monitoring committee (IDMC) to oversee trial integrity [80] [79].
- Leverage Expedited Programs: If your therapy addresses a serious or unmet medical need, explore FDA expedited programs such as Fast Track, Breakthrough Therapy, RMAT (Regenerative Medicine Advanced Therapy), and Priority Review. These can significantly shorten development and review timelines [15] [80].
Data Presentation: Recent Approvals and Clinical Trial Landscape
Table 1: Recently FDA-Approved Stem Cell-Based Therapies (2023-2025)
| Product Name (Approval Year) | Cell Type / Basis | Indication | Key Significance |
|---|---|---|---|
| Ryoncil (2024) [15] | Allogeneic MSCs (bone marrow) | Pediatric steroid-refractory acute Graft-versus-Host Disease (SR-aGVHD) | First FDA-approved MSC therapy; provides an option for a life-threatening condition with limited treatments. |
| Omisirge (2023) [15] | Cord blood-derived hematopoietic progenitor cells | Hematologic malignancies (post-umbilical cord blood transplantation) | Nicotinamide-modified product that accelerates neutrophil recovery, reducing infection risk. |
| Lyfgenia (2023) [15] | Autologous hematopoietic stem cells (gene-modified) | Sickle cell disease (patients with history of vaso-occlusive events) | One-time gene therapy that modifies a patient's own cells to produce anti-sickling hemoglobin. |
Table 2: Select FDA-Authorized Pivotal Stem Cell Clinical Trials (as of 2025)
| Therapy Name | Cell Type / Basis | Indication | Trial Stage / Status |
|---|---|---|---|
| Fertilo [15] | iPSC-derived ovarian support cells (OSCs) | In-vitro oocyte maturation | Phase III (First iPSC-based therapy in U.S. Phase III) |
| OpCT-001 [15] | iPSC-derived therapy | Retinal degeneration (e.g., retinitis pigmentosa) | Phase I/IIa (First iPSC-based therapy for primary photoreceptor diseases) |
| FT819 [15] | iPSC-derived CAR T-cell therapy | Systemic lupus erythematosus (SLE) | Phase I (Granted RMAT designation) |
| MyoPAXon [15] | iPSC-derived muscle progenitor cells | Duchenne Muscular Dystrophy (DMD) | Phase I (ClinicalTrials.gov NCT06692426) |
| Cymerus iMSCs (CYP-001) [15] | iPSC-derived MSCs (iMSCs) | High-Risk Acute Graft-Versus-Host Disease | Clinical Trial (ClinicalTrials.gov NCT05643638) |
Experimental Protocols
This protocol allows for the non-destructive prediction of muscle stem cell (MuSC) differentiation efficiency approximately 50 days before the end of the differentiation process.
1. Cell Culture and Image Acquisition
- Differentiation: Differentiate MYF5-tdTomato reporter hiPSCs toward MuSCs using a directed differentiation protocol.
- Imaging: Between days 14 and 38 of the differentiation process, capture phase-contrast images of the cells in culture wells. A total of 5,712 images from 34 wells were used in the original study.
- Ground Truth: On day 82, analyze the final MuSC induction efficiency using flow cytometry to detect MYF5-tdTomato expression (or an appropriate cell surface marker like CDH13).
2. Feature Extraction using Fast Fourier Transform (FFT)
- Process: Apply FFT to each pre-processed phase-contrast cell image to generate a power spectrum.
- Shell Integration: Perform shell integration on the power spectrum to create a 100-dimensional, rotation-invariant feature vector. This vector captures the global morphological characteristics of the cells in the image.
3. Machine Learning Classification
- Algorithm: Use a Random Forest classifier.
- Training: Train the classifier using the 100-dimensional feature vectors extracted from images taken on specific days (e.g., day 24, 31, or 34) as input, and the corresponding final differentiation efficiency (classified as "high" or "low") as the output.
- Prediction: The trained model can then predict whether a new, unseen sample will have high or low MuSC induction efficiency based on images taken during the early myogenic induction phase.
Diagram 1: Workflow for predicting stem cell differentiation efficiency.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Stem Cell Differentiation and Characterization
| Item | Function / Application | Example in Context |
|---|---|---|
| StemRNA Clinical Seed iPSCs [15] | Standardized, GMP-compliant starting material for generating differentiated cell products. | REPROCELL's iPSC seed clones have an FDA-submitted Drug Master File (DMF), streamlining regulatory submissions for INDs. |
| Morphogens (SHH, FGF8, BMPs, RA) [43] | Direct differentiation by mimicking embryonic developmental signaling pathways. | Used in protocols for cholinergic and dopaminergic neurons to pattern neural tube along dorsal-ventral and anterior-posterior axes. |
| Growth Factors (IGF-1, HGF, bFGF, BDNF, NGF) [43] [27] | Support cell survival, proliferation, and maturation of specific lineages. | IGF-1, HGF, and bFGF are critical for myogenic differentiation of hiPSCs into MuSCs [27]. BDNF and NGF support cholinergic neuron maturation [43]. |
| Reporter Cell Lines [27] | Enable real-time tracking and quantification of specific cell populations without fixation. | MYF5-tdTomato reporter hiPSCs allow for easy flow cytometry analysis of MuSC differentiation efficiency on day 82. |
| Machine Learning Classifier [27] | Non-destructive tool for predicting final differentiation efficiency from early-phase cell images. | A Random Forest model trained on FFT features from phase-contrast images can forecast MuSC yield ~50 days in advance. |
Diagram 2: Methods for assessing stem cell differentiation potential.
Frequently Asked Questions
Q1: What are the primary methods for validating the transcriptomic similarity of stem cell-derived cells to native tissues? The primary method is spatial transcriptomics (ST), which preserves the spatial context of gene expression that is lost in single-cell RNA sequencing. For formalin-fixed paraffin-embedded (FFPE) samples—the standard for clinical archives—imaging-based spatial transcriptomics (iST) platforms are particularly well-suited. These include 10X Xenium, Vizgen MERSCOPE, and Nanostring CosMx. These platforms can recover cell-to-cell interactions, spatially covarying genes, and gene signatures linked to pathology, enabling direct, high-resolution comparison to native tissue [81] [82].
Q2: My stem cell differentiation protocol is long and inefficient. How can I predict the final outcome early on? You can use a non-destructive method combining phase-contrast imaging and machine learning. By capturing cell images during early differentiation and extracting morphological features (e.g., using Fast Fourier Transform), a model can predict final efficiency. One study on muscle stem cell (MuSC) differentiation achieved prediction approximately 50 days before the protocol endpoint, allowing for early selection of high-quality cultures [27].
Q3: What is the "gold standard" for proving a stem cell line's functional differentiation potential? The in vivo teratoma assay has been historically considered the gold standard. It involves implanting pluripotent stem cells into an immunodeficient mouse, leading to benign tumor formation. The conclusive proof of pluripotency is the presence of complex, morphologically recognizable tissues derived from all three embryonic germ layers (ectoderm, mesoderm, and endoderm) within the tumor [6].
Q4: Beyond transcriptomics, how can I validate the functional maturity of my differentiated cells? Functional validation should be tiered. For muscle stem cells, the ultimate validation is the ability to repair damaged muscle in an in vivo model of muscular dystrophy [27]. More broadly, establishing a correlation between early marker expression (e.g., MYH3, MYOD1 proteins for myogenic cells) and the final functional cell output can serve as a robust, predictive functional benchmark [27].
Troubleshooting Guides
Issue 1: Low Concordance with Native Tissue Transcriptomes
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Inappropriate ST platform | Compare your panel to platform-specific gene lists. Check platform sensitivity/specificity data. | Consult recent benchmarking studies. For high transcript counts per gene on FFPE tissue, consider the 10X Xenium platform [81] [83]. |
| Poor RNA integrity in native tissue reference | Perform DV200 assessment on FFPE native tissue samples. Check H&E staining for morphology. | Follow platform-specific sample pre-screening guidelines (e.g., MERSCOPE recommends DV200 > 60%). Use H&E to screen for well-preserved regions [81]. |
| Incorrect cell segmentation | Visually inspect cell boundaries against nuclear (DAPI) and membrane stains. | Utilize platforms that offer improved segmentation capabilities with additional membrane staining, such as Xenium. Manually annotate cells for a ground truth comparison if needed [81] [83]. |
Issue 2: Unpredictable Differentiation Outcomes
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| High variability in starting PSC population | Use flow cytometry to check for pluripotency marker expression (OCT4, SOX2, NANOG). Perform karyotyping. | Ensure a pure, well-characterized starting population by following the ISSCR's minimum reporting standards for stem cell culture [6] [84]. |
| Protocol is overly sensitive to minor technical variations | Correlate early-stage cell morphology (days 14-38) with late-stage differentiation markers (day 82). | Implement an early prediction system using phase-contrast imaging and machine learning to identify cultures with high differentiation potential early in the process [27]. |
| Lack of rigorous in-process quality controls | Perform qRT-PCR for mid-protocol markers (e.g., MYH3, MYOD1 for myogenesis) and correlate with final outcomes. | Establish and validate intermediate biomarker checkpoints. For MuSC differentiation, the expression of skeletal muscle markers on day 38 is a strong predictor of final yield [27]. |
Experimental Protocols & Data
Protocol 1: Benchmarking with Spatial Transcriptomics on FFPE Tissues
This protocol is adapted from comprehensive benchmarking studies [81] [83].
Sample Preparation:
- Obtain serial sections (5-10 µm thick) from the same FFPE block containing your stem cell-derived tissue and a matched native tissue control.
- Use Tissue Microarrays (TMAs) for high-throughput analysis of multiple samples simultaneously.
- Adhere to platform-specific pre-screening requirements (H&E for morphology or DV200 for RNA quality).
Platform Selection and Gene Panel Design:
- Select an iST platform (e.g., Xenium, CosMx, MERSCOPE) based on your needs for sensitivity, gene panel size, and segmentation accuracy. See Table 1 for a comparison.
- Design a custom gene panel or use a pre-defined one that includes key marker genes for your cell type of interest and housekeeping genes.
Data Acquisition and Processing:
- Process TMA sections on each iST platform according to the manufacturer's instructions.
- Perform base-calling and cell segmentation using the vendor's standard pipeline.
Data Analysis and Benchmarking:
- Sensitivity/Specificity: Compare the total transcript counts per gene and the false discovery rates between platforms.
- Concordance: Calculate the gene-wise correlation of transcript counts between the iST data from your stem cell-derived tissue and orthogonal single-cell RNA-seq data from native tissue.
- Cell Typing: Perform spatially resolved cell type identification and cluster analysis. Compare the clusters and their spatial distributions to those in the native tissue control.
Protocol 2: Early Prediction of Differentiation Efficiency
This protocol is adapted from a study on predicting muscle stem cell differentiation [27].
Cell Culture and Imaging:
- Induce differentiation in your hiPSCs according to your directed differentiation protocol.
- Starting at an early, predictive window (e.g., between days 14 and 38 for an 82-day MuSC protocol), acquire phase-contrast images of the cells at regular intervals.
Feature Extraction:
- For each image, apply Fast Fourier Transform (FFT) to obtain its power spectrum.
- Perform shell integration on the power spectrum to generate a 100-dimensional, rotation-invariant feature vector that captures the morphological characteristics of the cells.
Machine Learning Classification:
- Using the final differentiation efficiency (e.g., % of MYF5+ or CDH13+ cells measured by flow cytometry) as the ground truth, label your samples as "high efficiency" or "low efficiency."
- Train a Random Forest classifier using the feature vectors extracted from the early time points to predict the final efficiency label.
Validation and Application:
- Validate the classifier on a held-out test set of images.
- Implement the trained model to screen future differentiation batches early, allowing you to prioritize wells with high predicted efficiency.
The table below summarizes key performance metrics from recent, systematic benchmarking studies of high-throughput spatial transcriptomics platforms, which are crucial for selecting the right tool for validation [81] [83].
Table 1: Benchmarking of High-Throughput Spatial Transcriptomics Platforms
| Platform | Technology Type | Key Strengths | Key Limitations | Notable Application in Validation |
|---|---|---|---|---|
| 10X Xenium (5K) | Imaging-based (iST) | High transcripts per gene; high sensitivity; strong concordance with scRNA-seq [81] [83]. | Targeted gene panel. | Ideal for sensitive detection of marker genes in FFPE tissues. |
| Nanostring CosMx (6K) | Imaging-based (iST) | High total transcript counts; strong concordance with scRNA-seq [81]. | Reported lower correlation with scRNA-seq gene counts in one study [83]. | Suitable for high-plex targeted studies. |
| Vizgen MERSCOPE | Imaging-based (iST) | Direct probe hybridization; amplifies by tiling transcript with many probes [81]. | Lower transcript counts per gene in benchmarked panels [81]. | Useful for applications requiring multiple probes per transcript. |
| Stereo-seq v1.3 | Sequencing-based (sST) | Unbiased whole-transcriptome; very high resolution (0.5 µm) [83]. | Requires fresh-frozen (FF) tissue. | Best for discovery-phase work without a pre-defined gene panel on FF tissue. |
| Visium HD FFPE | Sequencing-based (sST) | Unbiased whole-transcriptome; works on FFPE tissue; 2 µm resolution [83]. | Lower resolution than leading iST platforms. | A strong choice for whole-transcriptome analysis on archived FFPE samples. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Functional and Transcriptomic Validation
| Item | Function in Validation | Example/Note |
|---|---|---|
| FFPE Tissue Microarrays (TMAs) | Enable high-throughput analysis of multiple stem cell lines and native tissue controls on a single slide, reducing batch effects [81]. | Can be custom-made with patient-specific stem cell-derived tissues. |
| MYF5-tdTomato Reporter hiPSC Line | Allows for direct, non-destructive tracking and quantification of muscle stem cell differentiation efficiency via flow cytometry [27]. | A critical tool for establishing ground truth for functional assays. |
| Spatial Transcriptomics Panels | Targeted gene sets for imaging-based ST platforms to quantify cell-type-specific markers and compare to native tissue [81]. | Can be custom-designed or pre-configured (e.g., "multi-tissue" panels). |
| Antibodies for Key Markers | Used for immunocytochemistry (ICC) to validate protein-level expression of critical differentiation markers at intermediate and final stages [27]. | e.g., Anti-MYOD1, Anti-Myosin Heavy Chain (MHC) for myogenesis. |
| CODEX Multiplexed Protein Imaging | Provides high-plex protein expression data from an adjacent tissue section, serving as a robust ground truth for spatial transcriptomics data [83]. | Used in advanced benchmarking to validate transcriptional findings at the protein level. |
Experimental Workflow and Signaling Pathways
Workflow for Stem Cell Validation
This diagram outlines the core experimental workflow for benchmarking stem cell-derived tissues against a native reference.
Predictive Modeling for Differentiation
This diagram illustrates the non-destructive, image-based pipeline for predicting differentiation efficiency long before the protocol is complete.
Conclusion
Standardizing differentiation efficiency in patient-specific stem cell lines is no longer a peripheral concern but a central requirement for advancing credible, reproducible, and clinically impactful science. The integration of foundational understanding, innovative monitoring technologies like machine learning, rigorous optimization strategies, and alignment with evolving regulatory frameworks provides a clear path forward. Future progress hinges on interdisciplinary collaboration to further develop automated, data-driven platforms that can predict and control cell fate with high precision. By systematically addressing these challenges, the field can fully harness the potential of patient-specific stem cells, transforming them from powerful research tools into reliable engines for drug discovery and standardized, off-the-shelf regenerative therapies.
References
- 1. Stem cells in tissue engineering: Why standardization ... [https://www.abcam.com/en-us/stories/articles/stem-cells-in-tissue-engineering]
- 2. 5. Standards in Stem Cell Research [https://www.isscr.org/guidelines/standards-in-stem-cell-research]
- 3. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 4. Promoting the adoption of best practices and standards to ... [https://www.sciencedirect.com/science/article/pii/S2213671125001353]
- 5. An urgent need for standardization of stem cells and stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8560195/]
- 6. Evaluating Strategies to Assess the Differentiation Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762643/]
- 7. ISSCR Standards for Human Stem Cell Use in Research [https://www.stemcell.com/psc-cell-quality/isscr-standards]
- 8. Cell Cluster Sorting in Automated Differentiation of Patient- ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.755983/full]
- 9. Efficient Derivation of Functional Human Airway Epithelium ... [https://www.sciencedirect.com/science/article/pii/S1934590917300723]
- 10. Time-efficient strategies in human iPS cell-derived pancreatic ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04068-6]
- 11. Genetic and epigenetic variations in iPSCs: potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3760008/]
- 12. iPSCs and iPSC-derived cells as a model of human ... [https://www.nature.com/articles/s41467-025-56569-4]
- 13. Epigenetic Variation between Human Induced Pluripotent ... [https://www.sciencedirect.com/science/article/pii/S1934590916301941]
- 14. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 15. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 16. Donor variability in adipose tissue-derived stem cells [https://www.explorationpub.com/Journals/em/Article/1001243]
- 17. Inter- and Intra-donor variability in bone marrow–derived ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924005711]
- 18. The Impact of Donor and Recipient Genetic Variation on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9311456/]
- 19. Donor Variability and Seeding Density Shape NK-Cell ... [https://www.mdpi.com/2073-4409/14/16/1252]
- 20. Why Clonal iPSC Lines? [https://www.jax.org/news-and-insights/jax-blog/2025/june/clonal-ipsc-lines]
- 21. Raising the bar for reproducibility in stem-cell based research [https://www.bit.bio/blog/raising-the-bar-for-reproducibility-in-stem-cell-based-research]
- 22. Reproducibility and transparency: what's going on and how ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11772749/]
- 23. Donor Variability and 3D Culture Models Influence Human ... [https://pubmed.ncbi.nlm.nih.gov/40407303/]
- 24. Differentiation of patient-specific induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305229/]
- 25. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 26. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 27. Early and non-destructive prediction of the differentiation ... [https://www.nature.com/articles/s41598-025-11108-5]
- 28. SERS-CNN approach for non-invasive and non-destructive ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400522014551]
- 29. Explainable AI and mobile imaging for non-destructive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476098/]
- 30. Predictive modelling employing machine learning ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1594728/full]
- 31. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 32. Advances and optimization strategies in prime editing of ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925002562]
- 33. Comprehensive analysis of prime editing outcomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8789035/]
- 34. Prime editing for precise and highly versatile genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10989687/]
- 35. Prime Editing as a Precision Gene Editing Tool [https://www.synthego.com/guide/crispr-methods/prime-editing/]
- 36. Robust and inducible genome editing via an all-in-one ... [https://www.nature.com/articles/s41467-024-55104-1]
- 37. CRISPR-Based Genome Editing Support—Troubleshooting [https://www.thermofisher.com/au/en/home/technical-resources/technical-reference-library/genome-editing-support-center/crispr-based-genome-editing-support/crispr-based-genome-editing-support-troubleshooting.html]
- 38. Section 1: Basic Characterization [https://www.isscr.org/basic-research-standards/basic-characterization]
- 39. Section 3: Genomic Characterization [https://www.isscr.org/basic-research-standards/genomic-characterization]
- 40. Frequently Asked Questions on hPSC Characterization ... [https://www.stemcell.com/hpsc-services-faq.html]
- 41. Section 5: Reporting [https://www.isscr.org/basic-research-standards/reporting]
- 42. Why Use Standardized Kits When Differentiating ... [https://www.rndsystems.com/blog/why-use-standardized-kits-when-differentiating-pluripotent-stem-cells]
- 43. Common pitfalls of stem cell differentiation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5002043/]
- 44. Patient-Specific Organoid and Organ-on-a-Chip: 3D Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8243895/]
- 45. Human organoids: model systems for human biology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7339799/]
- 46. Human organoids in basic research and clinical applications [https://www.nature.com/articles/s41392-022-01024-9]
- 47. Breakthroughs and challenges of organoid models for ... [https://www.nature.com/articles/s41420-025-02505-w]
- 48. Innovative strategies for bone organoid - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362404/]
- 49. Protocol for differentiation of human pluripotent stem cells into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205342/]
- 50. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 51. Improving efficiency of human pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3970199/]
- 52. Stem cell culture conditions affect in vitro differentiation ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0317309]
- 53. Stem cell culture conditions affect in vitro differentiation ... [https://pubmed.ncbi.nlm.nih.gov/40138371/]
- 54. Optimizing human embryonic stem cells differentiation ... [https://pubmed.ncbi.nlm.nih.gov/24780170/]
- 55. A practical guide to induced pluripotent stem cell research ... [https://www.nature.com/articles/labinvest2014104]
- 56. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 57. Enhancing human pluripotent stem cell differentiation to ... [https://www.sciencedirect.com/science/article/pii/S2589004225007138]
- 58. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 59. The resurgence of mesenchymal stem cell therapies [https://www.clinicaltrialsarena.com/sponsored/the-resurgence-of-mesenchymal-stem-cell-therapies/]
- 60. Batch variability and anti-inflammatory effects of iPSC ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1536843/full]
- 61. Automated manufacturing of cell therapies [https://www.sciencedirect.com/science/article/pii/S0168365925001701]
- 62. AI-based approach to dissect the variability of mouse stem ... [https://www.nature.com/articles/s41467-025-56908-5]
- 63. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 64. Making Data Work: How AI and Multi-Omics Integration Are ... [https://ai.northeastern.edu/news/making-data-work]
- 65. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 66. high-throughput technologies and automated workflows to ... [https://www.sciencedirect.com/science/article/pii/S0958166925000643]
- 67. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 68. Data-Driven Biotechnology: How Multi-Omics Analytics Are ... [https://lumagroup.com/data-driven-biotechnology-how-multi-omics-analytics-are-shaping-the-future-of-medicine/]
- 69. Predicting Cell Line Variability in Cardiomyocyte ... [https://www.rndsystems.com/resources/posters/predicting-cell-line-variability-cardiomyocyte-differentiation-efficiency-using]
- 70. Troubleshooting Bacterial Contamination In Bioreactors [https://www.bioprocessonline.com/doc/troubleshooting-bacterial-contamination-in-bioreactors-0001]
- 71. Identifying the REMEDI to problems in stem-cell research [https://www.bioprocessintl.com/upstream-downstream-processing/identifying-the-remedi-to-problems-in-stem-cell-research]
- 72. Closed System Automation for Cell Therapy [https://www.thermofisher.com/blog/behindthebench/closed-system-automation-cell-therapy/]
- 73. Evolving Challenges in Closed-System Biomanufacturing [https://invitria.com/resources/evolving-challenges-in-closed-system-biomanufacturing/]
- 74. EU MDR vs FDA: 2025 US-EU Medical Device Regulatory ... [https://www.complizen.ai/post/eu-mdr-vs-fda-complete-regulatory-comparison-guide-2025]
- 75. FDA vs EU: Regulations compared [https://www.we4cr.com/smart-clinical-trials-fda-vs-eu-2025/]
- 76. Approved Cellular and Gene Therapy Products [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/approved-cellular-and-gene-therapy-products]
- 77. Applications of artificial intelligence in stem cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427078/]
- 78. Machine Learning in Clinical Trials: A Primer with Applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10228463/]
- 79. Step 3: Clinical Research [https://www.fda.gov/patients/drug-development-process/step-3-clinical-research]
- 80. The FDA and Clinical Trials [https://novotech-cro.com/blog/fda-and-clinical-trials]
- 81. Systematic benchmarking of imaging spatial ... [https://www.nature.com/articles/s41467-025-64990-y]
- 82. Systematic benchmarking of imaging spatial ... [https://www.broadinstitute.org/publications/broad1370836]
- 83. Systematic benchmarking of high-throughput subcellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534522/]
- 84. Basic Stem Cell Research Standards [https://www.isscr.org/basic-research-standards]