Stem Cell Potency Assays: From Foundational Concepts to In Vitro and In Vivo Applications in Drug Development
This article provides a comprehensive overview of stem cell potency assays, essential tools for quantifying the biological activity and therapeutic potential of cell-based products.
Stem Cell Potency Assays: From Foundational Concepts to In Vitro and In Vivo Applications in Drug Development
Abstract
This article provides a comprehensive overview of stem cell potency assays, essential tools for quantifying the biological activity and therapeutic potential of cell-based products. Aimed at researchers, scientists, and drug development professionals, it covers the foundational principles of stem cell potency, explores a spectrum of in vitro and in vivo methodological approaches, and addresses critical challenges in assay troubleshooting and optimization. Furthermore, the article delves into the rigorous process of assay validation and the strategic use of assay matrices to meet regulatory standards, serving as a practical guide for the development and implementation of robust potency assays in both research and clinical settings.
Defining Potency: The Cornerstone of Stem Cell Biology and Therapeutic Potential
Cell potency is a fundamental concept in stem cell biology, defining a cell's ability to differentiate into other cell types [1]. This hierarchical classification system ranges from totipotent cells, which possess the greatest differentiation potential, to unipotent cells, which have the most restricted developmental capacity [1] [2]. Understanding this potency spectrum is crucial for advancing stem cell research, disease modeling, and regenerative medicine applications [3] [4].
The potency of stem cells is traditionally demonstrated through a combination of functional assays and molecular marker evaluation [4] [5]. These assessments are vital for quality control in research and clinical applications, particularly as the global stem cell assay market expands—projected to grow from USD 3.15 billion in 2025 to USD 13.5 billion by 2034 [6]. This growth reflects the increasing importance of standardized potency measurements in translating stem cell technologies into therapeutic applications.
The Potency Hierarchy Spectrum
Defining the Hierarchy Levels
The traditional developmental paradigm follows a hierarchical progression from the most potent to the least potent cell states [4] [5]. This journey begins with totipotent cells and progresses through pluripotent, multipotent, and finally unipotent states, with both self-renewal capacity and differentiation potential diminishing at each stage [4] [5].
Table: Stem Cell Potency Hierarchy Classification
| Potency Level | Developmental Potential | Representative Cell Types | Key Characteristics |
|---|---|---|---|
| Totipotent | Can generate all embryonic and extra-embryonic tissues (including placenta) [3] [1] | Zygote, early blastomeres (up to 4-cell stage in some species) [3] [7] | Can form a complete, viable organism [1]; highest potency level [2] |
| Pluripotent | Can differentiate into all three embryonic germ layers (ectoderm, mesoderm, endoderm) but NOT extra-embryonic tissues [3] [4] | Embryonic Stem Cells (ESCs), Induced Pluripotent Stem Cells (iPSCs) [3] [4] | Found in inner cell mass of blastocyst [3]; can form teratomas containing tissues from all three germ layers [1] |
| Multipotent | Can differentiate into multiple cell types within a specific tissue or organ lineage [4] [2] | Hematopoietic Stem Cells (all blood cell types) [4], Mesenchymal Stem Cells (bone, cartilage, fat) [3] | Limited to particular tissue/organ system [2]; adult tissue-specific [8] |
| Oligopotent | Can differentiate into only a few cell types within a specific lineage [8] | Lymphoid or Myeloid progenitor cells [8] | More restricted than multipotent cells [8] |
| Unipotent | Can produce only one cell type [4] [5] | Epidermal stem cells, muscle satellite cells [5] | Most restricted potency; capable of self-renewal to maintain tissue [4] |
Molecular Regulation of Potency States
The transitions between potency states are governed by sophisticated molecular mechanisms involving transcription factors, epigenetic modifications, and signaling pathways [3] [7]. Core transcription factors including OCT4, SOX2, and NANOG play essential roles in maintaining pluripotency in both ESCs and iPSCs [3] [4]. The molecular profile of totipotent cells differs significantly, expressing unique markers such as Zscan4 and Eomes alongside a more open chromatin structure with fewer repressive histone modifications [3].
The diagram below illustrates the key molecular features and transcriptional networks that define totipotent and pluripotent stem cell states:
Experimental Assessment of Cell Potency
Functional Potency Assays
Functional assays remain the gold standard for definitively establishing stem cell potency [4] [5]. These assays test the functional capacity of stem cells in both in vitro and in vivo environments, providing crucial validation of their developmental potential [1].
Table: Functional Assays for Assessing Stem Cell Potency
| Assay Type | Experimental Approach | Interpretation & Significance | Key Applications |
|---|---|---|---|
| Teratoma Formation Assay [1] | Injection of test cells into immunodeficient mice (e.g., kidney capsule, testis, muscle) [1] | Formation of benign tumor containing differentiated tissues from all three germ layers confirms pluripotency [1] | Gold standard for pluripotency verification; quality check for ESCs and iPSCs [1] |
| Embryoid Body (EB) Formation [9] | Suspension culture to form 3D aggregates; spontaneous differentiation via hanging drop method [9] | Differentiation into derivatives of three germ layers confirmed by immunostaining for specific markers [9] | In vitro assessment of pluripotency; study of early differentiation events [9] |
| Chimera Formation [7] | Injection of test cells into host blastocyst; assessment of contribution to developing embryo [7] | Ability to incorporate into embryonic tissues and contribute to different lineages indicates pluripotent state [7] | Assessment of developmental potential; generation of genetically modified animal models [7] |
| In Vitro Differentiation [3] | Directed differentiation using specific growth factors, small molecules, and signaling cues [3] | Efficient generation of specific cell types (e.g., cardiomyocytes, neurons) demonstrates differentiation capacity [3] [9] | Disease modeling; drug screening; regenerative medicine applications [3] |
| Tetraploid Complementation [7] | Injection of test cells into tetraploid embryo; most stringent test of developmental potential [7] | Generation of entire organism from test cells confirms naive pluripotency in mouse ESCs [7] | Ultimate validation of naive pluripotent state (primarily in murine systems) [7] |
Standards in Stem Cell Assay Development
The International Society for Stem Cell Research (ISSCR) emphasizes the importance of developing standardized protocols for stem cell research, including potency assays [10]. Standardization enables comparison of trial outcomes across laboratories and facilitates reproduction of treatments reported in published studies [10]. Key areas for standards development include source materials, process controls, analytical methods, and data processing [10].
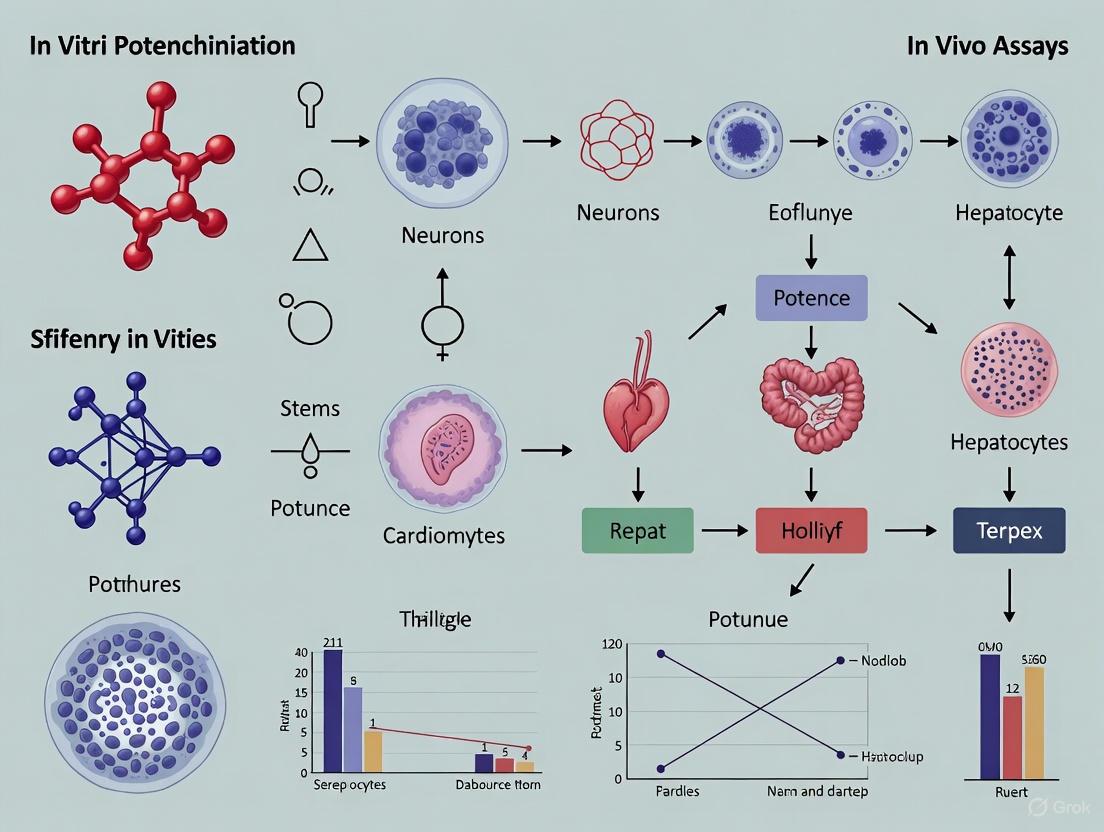
The experimental workflow below outlines a typical approach for generating and validating pluripotent stem cells and their differentiated derivatives:
Research Reagent Solutions for Potency Assessment
Table: Essential Research Reagents for Stem Cell Potency Studies
| Reagent Category | Specific Examples | Research Application | Function in Potency Assessment |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) [1] | Generation of iPSCs from somatic cells [1] | Induction of pluripotent state from differentiated cells [1] |
| Pluripotency Markers | Antibodies against OCT4, NANOG, SSEA-4, TRA-1-60 [9] [1] | Immunofluorescence staining, flow cytometry [9] | Identification and validation of pluripotent stem cells [9] |
| Differentiation Media Components | Activin A, bFGF, BMP4, DKK-1, VEGF [9] | Directed differentiation of pluripotent stem cells [9] | Lineage-specific differentiation; demonstration of developmental potential [9] |
| Cell Culture Supplements | LIF (Leukemia Inhibitory Factor) [7], MEK/GSK3 inhibitors (2i/L system) [7] | Maintenance of pluripotent stem cells in culture [7] | Support self-renewal and maintain undifferentiated state [7] |
| Germ Layer Markers | Alpha-fetoprotein (endoderm), Nestin (ectoderm), SMA (mesoderm) [9] | Characterization of differentiated cells [9] | Verification of trilineage differentiation potential [9] |
Signaling Pathways and Pluripotency States
Pluripotent stem cells exist in multiple states—naïve, formative, and primed—that represent developmental transitions from pre-implantation to post-implantation epiblast stages [7]. These states are stabilized in vitro through specific signaling pathway manipulations [7].
Naïve pluripotency is characterized by an unfettered developmental capacity to differentiate into all somatic and germline lineages [7]. Mouse ESCs cultured in "2i/L" conditions (MEK inhibition + GSK3 inhibition + LIF) represent the benchmark for naïve pluripotency [7]. These cells can generate all adult lineages in chimeras and whole mice through tetraploid complementation [7].
Primed pluripotency represents a more developmentally advanced state similar to the post-implantation epiblast [1]. These cells have undergone X-chromosome inactivation and exhibit limited ability to contribute to blastocyst chimeras [1]. Signaling pathways including FGF, TGF-β, and WNT regulate the transition between these pluripotency states [7].
The diagram below illustrates the signaling pathways that regulate the transition between different pluripotency states:
Clinical Implications and Therapeutic Applications
The therapeutic potential of stem cells is directly influenced by their position in the potency hierarchy [2]. Multipotent stem cells currently form the backbone of clinical applications, with hematopoietic stem cell transplantation representing the most established therapy [8]. These cells present lower risks of teratoma formation and immune rejection, making them suitable for current clinical use, though their limited differentiation potential restricts applications to specific tissue types [2].
Pluripotent stem cells offer broader therapeutic possibilities but require more sophisticated control mechanisms [2]. iPSC technology enables generation of patient-specific pluripotent cells for personalized regenerative medicine [1]. These cells hold promise for treating conditions including Parkinson's disease, macular degeneration, and diabetes, though most applications remain in clinical trial phases [2]. Research using human urine-derived epithelial cells reprogrammed into iPSCs and differentiated into functional cardiomyocytes demonstrates the potential of minimally invasive approaches for generating patient-specific cells for regenerative medicine [9].
The choice between potency levels for therapeutic interventions depends on multiple patient-specific factors including age, disease severity, immune status, and treatment timeline [2]. As stem cell technologies advance, potency assessment remains crucial for ensuring both safety and efficacy in clinical applications [10].
The Critical Link Between Mechanism of Action (MoA) and Potency Assay Design
For cell therapy products (CTPs), potency is defined as the specific attribute that enables a product to achieve its intended mechanism of action (MoA) [11]. The potency test is the quantitative measurement of this attribute [11] [12]. Regulatory agencies, including the U.S. Food and Drug Administration (FDA), require that every CTP demonstrates potency through assays that are biologically relevant and ideally based on the product's MoA [13] [14]. This requirement presents a significant challenge for developers, as many approved CTPs have incompletely understood MoAs, making the design of truly mechanism-based potency assays difficult [11] [12].
The relationship between these core concepts can be visualized as a process flow from biological mechanism to clinical outcome.
This framework illustrates that while a potency test (a laboratory measurement) and an efficacy endpoint test (a clinical measurement) are distinct, their alignment strengthens the validity of the potency assay [11] [12]. The following analysis compares potency assay strategies across approved and experimental CTPs, providing researchers with a data-driven guide for assay design.
Comparative Analysis of Potency Assays in Approved Therapies
An analysis of the 31 U.S. FDA-approved CTPs (2010-2024) reveals the current landscape of potency testing. A total of 104 potency tests have been used for these products, with an average of 3.4 potency tests per product (standard deviation 2.0) [15]. The measurements can be categorized as follows:
Table 1: Categorization of 71 Non-Redacted Potency Tests for 31 FDA-Approved CTPs
| Assay Category | Number of Tests | Percentage | Example CTPs |
|---|---|---|---|
| Viability and Count | 37 | 52% | Hemacord, Allocord, Laviv |
| Expression (Gene/Protein) | 19 | 27% | Kymriah, Yescarta, Tecartus |
| Bioassays | 7 | 7% | Kymriah (IFN-γ release) |
| Genetic Modification | 6 | 9% | Zynteglo, Skysona |
| Histology | 2 | 3% | Gintuit, Rethymic |
| Redacted/Uncategorized | 33 | 32% | Abecma, Breyanzi, Aucatzyl |
Data sourced from Simon et al. (2025) analysis of FDA regulatory documents [15]
The data shows a heavy reliance on "Viability and Count" and "Expression" assays, which are often used together [15]. While these are reproducible, they may act as surrogates for more complex biological functions. True bioassays, which measure functional biological responses, are less commonly reported, though redactions in public documents mean as many as 77% of CTPs could potentially employ them [15].
Case Studies: MoA Clarity and Potency Assay Correlation
Table 2: MoA and Potency Assay Relationship in Select Approved CTPs
| Product (Year) | Indication | Reported MoA | Potency Test(s) | MoA-Potency Link |
|---|---|---|---|---|
| Provenge (2011) | Prostate Cancer | "Precise mechanism of action is unknown" [11] | CD54+ cell count & increased CD54 expression after culture [15] [11] | Assay measures an immune activation marker; link to clinical effect is indirect. |
| Kymriah (2017) | B-cell Leukemia | CD19 recognition leads to T-cell activation, expansion, and target cell elimination [11] | IFN-γ release upon CD19+ cell stimulation [15] [11] | Measures a key activation response; FDA noted difficulty correlating results with clinical efficacy [11] [12]. |
| Gintuit (2012) | Gingival Defects | "MOA... has not been identified" [11] | Histology (tissue morphology) [15] [11] | Assay measures structural integrity, not a known biological activity. |
| MACI (2016) | Knee Cartilage Defects | "A mechanism of action has not been established" [11] | Cell number, PCR for aggrecan gene expression [15] [11] | Measures a marker of chondrocyte phenotype (aggrecan), but link to cartilage repair is unverified. |
| Amtagvi (2024) | Melanoma | "The specific mechanism of action... is unknown." [11] | Dose (total viable cells) and multiple redacted tests [11] | Cell number is a surrogate; functional assays are undisclosed. |
A critical example of the correlation challenge comes from Kymriah. The FDA's briefing document showed that while interferon-gamma (IFN-γ) production (the potency test) was higher, on average, in patients who achieved remission, there was significant overlap between responders and non-responders. The agency concluded it was "difficult to correlate IFN-γ production in vitro with... efficacy" [11] [12]. This highlights that even for a successful product, a single-parameter potency assay may be an imperfect predictor of clinical outcome.
MoA-Based Assay Design: A Checklist and Workflow for Developers
Grounding potency assay design in a hypothesized MoA is essential for regulatory acceptance and clinical relevance [13]. The following checklist provides a strategic guide for developers and quality teams.
Checklist for Mechanism-Informed Potency Testing [13]
- Start with MoA: Clearly define the intended biological function of the cell product and identify the key pathways involved in its therapeutic effect. Use preclinical models to support the proposed MoA.
- Select Assays That Reflect Function: Choose assays directly linked to the MoA, not just surrogate markers. For complex MoAs, use multiparameter or functional readouts. strive to correlate in vitro results with clinical outcomes.
- Validate and Justify: Confirm the assay is sensitive enough to detect changes in product quality that could impact function. Provide a strong scientific rationale for the chosen method and document performance characteristics (accuracy, precision, linearity, etc.).
- Review and Reassess: Revalidate potency tests after any significant manufacturing change. Continuously monitor assay performance during routine production and use the data for product comparability assessments.
- Embrace Innovation Thoughtfully: Integrate advanced tools like omics, systems biology, or high-content imaging if they provide a deeper understanding of the MoA. Ensure any new method remains interpretable, reproducible, and aligned with regulatory expectations.
The process of developing and validating a mechanism-based potency assay follows a structured workflow, as demonstrated in the following case study.
Experimental Protocol: A Model VEGF Potency Assay for CD34+ Cell Therapy
A 2025 study by Shrotti et al. provides a exemplary model for developing and validating a mechanism-based potency assay for an advanced therapy medicinal product (ATMP) [16]. The product, ProtheraCytes, consists of expanded autologous CD34+ cells for cardiac repair. Its proposed MoA is the revascularization of damaged myocardial tissue via the secretion of pro-angiogenic factors like Vascular Endothelial Growth Factor (VEGF) [16].
Detailed Methodology
- Cell Source: CD34+ cells isolated from acute myocardial infarction (AMI) patients or healthy donors.
- Culture Conditions: Cells are expanded for 9 days in a defined medium (StemFeed).
- Sample Collection: Cell culture supernatant is collected at the end of the expansion process.
- VEGF Quantification: The concentration of VEGF in the supernatant is quantified using an automated immunoassay platform (ELLA system, Bio-Techne).
- Principle: The ELLA system uses a microfluidic cartridge with a sandwich-type quantitative ELISA. Fluorescence (RFU) is proportional to VEGF concentration, calculated against a factory-calibrated standard curve.
- Key Optimization: The team transitioned from a traditional manual ELISA (which showed high variability, with CVs >15%) to the automated ELLA system, which reduced CVs to below 7.5% and improved reproducibility [16].
Validation Data and Results
The VEGF potency assay was validated according to ICH Q2(R2) guidelines, with the following performance characteristics [16]:
Table 3: Validation Parameters for the VEGF Potency Assay
| Validation Parameter | Result | Acceptance Criteria |
|---|---|---|
| Linearity (Range) | 20 pg/mL - 2800 pg/mL | R² = 0.9972 |
| Repeatability Precision | Coefficient of Variation (CV) ≤ 10% | Met |
| Intermediate Precision | CV ≤ 20% | Met |
| Accuracy (Mean Recovery) | 85% - 105% | Met |
| Specificity | VEGF in blank medium < LLOQ (2 pg/mL) | Met (LLOQ = 20 pg/mL) |
| Robustness | Demonstrated under varied conditions | Met |
The assay was successfully used to release 38 clinical batches. VEGF concentrations in patient samples were high (mean 650 ± 303.0 pg/mL) and significantly greater than in culture medium alone (2.8 ± 0.2 pg/mL), confirming the biological attribute was being measured [16].
The Scientist's Toolkit: Essential Reagents for a VEGF Potency Assay
Table 4: Key Research Reagent Solutions for a VEGF Potency Assay
| Reagent / Material | Function in the Assay | Example from Protocol |
|---|---|---|
| CD34+ Cells | The active biological product whose critical quality attribute (VEGF secretion) is being measured. | Expanded autologous CD34+ cells from AMI patients [16]. |
| Defined Cell Culture Medium | Supports cell expansion and secretion without interfering with the downstream detection assay. | StemFeed medium [16]. |
| Automated Immunoassay System | Provides a reproducible, low-handling platform for quantitative protein analysis, reducing operator variability. | ELLA system (Bio-Techne) with microfluidic cartridges [16]. |
| VEGF-Specific Immunoassay Cartridge | Contains immobilized antibodies specific for VEGF-A, enabling sandwich ELISA-based quantification. | Simple Plex Cartridge Kit for VEGF-A (Bio-Techne) [16]. |
| Recombinant VEGF Protein | Serves as a positive control and for generating standard curves to ensure assay accuracy and linearity. | Used for spiking experiments and validation [16]. |
Emerging Trends and Multi-Omics in Potency Assessment
For complex CTPs like CAR T-cells, the field is moving beyond single-parameter assays (e.g., IFN-γ release) toward a multi-parametric approach that better captures the product's functional complexity [17] [13]. Next-generation potency testing leverages advances in multi-omics to deconstruct the MoA into measurable critical quality attributes (CQAs).
Table 5: Emerging Multi-Omics Approaches for CAR T-Cell Potency Profiling
| Omics Layer | Measurable Attributes | Insights for Potency |
|---|---|---|
| Genomics | Vector Copy Number (VCN), Integration Sites, TCR Repertoire | Assesses genetic integrity, safety (risk of insertional mutagenesis), and clonal diversity [17]. |
| Epigenomics | DNA methylation, Chromatin Accessibility | Defines T-cell differentiation states (e.g., memory vs. exhausted) which are critical for in vivo persistence and efficacy [17]. |
| Transcriptomics | Bulk and Single-cell RNA Sequencing | Identifies gene expression signatures of T-cell activation, exhaustion, and metabolic fitness [17]. |
| Proteomics | Surface Marker Expression, Intracellular Signaling Proteins | Quantifies proteins critical for cytotoxicity (e.g., granzymes) and defines T-cell subsets [17]. |
| Metabolomics | Glycolytic Activity, Mitochondrial Fitness | Evaluates metabolic pathways that fuel T-cell expansion and long-term function [17]. |
The integration of artificial intelligence (AI) and machine learning (ML) is also beginning to transform potency assay development. AI can analyze complex multi-omics datasets to identify novel biomarkers of potency and predict the in vivo performance of cell products, thereby creating more predictive and mechanism-relevant assays [18].
The critical link between MoA and potency assay design is the foundational principle for successful CTP development. While current regulatory approvals show a mix of direct functional assays and indirect surrogate tests, the clear trend is toward multiparameter, mechanism-informed potency assessments. The validation of the VEGF assay for ProtheraCytes demonstrates that a robust, quantitative, and MoA-based potency test is achievable when the product's biological function is well-defined [16]. As the field evolves, leveraging advanced omics technologies and data analytics will enable developers to create more predictive potency assays that not only meet regulatory requirements but also ensure that every batch of a cellular therapy possesses the biological activity needed to deliver a consistent clinical benefit to patients.
Potency assays represent a fundamental pillar in the development and quality control of Advanced Therapy Medicinal Products (ATMPs). These sophisticated biological assays serve as essential tools to guarantee that cell-based therapies consistently deliver their intended biological effect, making them non-negotiable for regulatory approval and clinical success. For somatic cells expanded in vitro, with or without genetic modification, potency testing provides the critical link between product characterization and clinical efficacy, ensuring that each batch meets stringent quality standards before patient administration [19].
The development of robust potency assays presents significant challenges due to the inherent variability of biological starting materials and the complex, often multifactorial, mechanisms of action (MOA) involved in ATMP function. These assays must quantitatively measure the relevant biological attributes that directly correlate with the product's therapeutic performance in vivo. According to regulatory reviews, nearly 50% of ATMP applications encounter potency-related issues during assessment, often resulting in significant clinical delays [20]. As noted by former FDA CBER Director Peter Marks, "Potency-related problems have been among the most common reasons for delayed approvals in the field" [20].
The Unavoidable Necessity: Regulatory and Clinical Imperatives
The Consequences of Inadequate Potency Testing
The absence of robust, validated potency assays can derail ATMP development programs with profound implications for both patients and developers. For patients facing aggressive diseases, delays in ATMP availability are not merely inconveniences—they can be dangerous. Clinical data suggests that 20-25% of patients may lose performance status each month without effective therapy, potentially disqualifying them from receiving advanced treatments like CAR-T cell therapy [20].
The cumulative impact of such delays is staggering. In a high-yield allogeneic CAR-T scenario where one batch may treat 100 patients, a one-month potency-related delay equals 3,000 patient-days without therapy—more than eight years of cumulative lost treatment time across the waiting population [20]. For developers, each month of delay for a high-value therapy can cost $5–$15 million in lost revenue, excluding added costs of prolonged manufacturing holds and supply chain disruptions [20].
Regulatory Framework and Requirements
Global regulatory agencies, including the FDA and EMA, mandate potency testing as an indispensable component of ATMP batch release. According to Regulation (EC) n. 1394/2007 and subsequent EU Directives, and FDA regulations for Cellular and Gene Therapy Products (CGTs), ATMPs must be produced according to Good Manufacturing Practice (GMP) in authorized laboratories, with potency assays representing a fundamental aspect of quality control [19] [21]. These regulations aim to guarantee both safety and efficacy of cell products for patients, with potency testing providing the quantitative measure of biological activity essential for consistent dosing and therapeutic effect.
Comparative Analysis of Potency Assay Strategies Across ATMP Categories
ATMP Classification and Corresponding Potency Approaches
Table 1: Potency Assay Strategies for Major ATMP Categories
| ATMP Category | Primary Mechanism of Action | Common Potency Assay Methods | Surrogate Markers | Regulatory Status |
|---|---|---|---|---|
| CAR-modified T/NK cells | MHC-unrestricted cytotoxicity against specific targets | Direct cytotoxicity (dye release, flow cytometry), cytokine secretion (IFNγ, TNFα) | CAR quantification by flow cytometry or qPCR, degranulation markers (CD107a) | Multiple FDA/EMA approvals [19] |
| Antigen-specific T-cell lines | MHC-restricted cytotoxicity against viral or tumor targets | Cytotoxicity against peptide-primed APCs or autologous tumor cells, Elispot | Tetramer staining, Th1 cytokine secretion | Clinical trial phase [19] |
| Mesenchymal Stromal Cells (MSCs) | Paracrine signaling, immunomodulation, tissue repair | Secreted factor quantification (VEGF, IDO, TSG-6), T-cell suppression assays | Surface marker profiling (CD73+, CD90+, CD105+) | Marketing approval for some indications [19] |
| CD34+ hematopoietic cells | Angiogenesis, tissue revascularization | VEGF secretion via automated ELISA, colony-forming unit assays | CD34+ cell quantification, viability assays | Phase I/IIb clinical trials (NCT02669810) [16] |
| mRNA vaccines | Intracellular antigen expression, immune activation | Cell-based antigen expression, capillary gel electrophoresis for mRNA integrity | LNP size distribution (80-120 nm optimal), mRNA encapsulation efficiency | Multiple approvals (COVID-19) [22] |
Quantitative Comparison of Potency Assay Performance
Table 2: Performance Metrics of Validated Potency Assays Across ATMP Types
| Assay Type | Precision (%CV) | Linear Range | Accuracy (% Recovery) | Turnaround Time | Key Validation Parameters |
|---|---|---|---|---|---|
| VEGF ELISA (CD34+ cells) | ≤10% (repeatability), ≤20% (intermediate precision) | 20-2800 pg/mL (R²=0.9972) | 85-105% | Hours (vs. days for animal models) | Specificity, linearity, accuracy, precision, robustness [16] |
| CAR quantification | Varies by method | Correlation with cytotoxicity (R value not specified) | Not specified | Minutes to hours | Correlation with functional potency [19] |
| In vivo immunogenicity | 34-125% (high variability) | Dependent on model | Not applicable | Weeks to months | Immune response correlation with protection [23] |
| Cell-based antigen expression (mRNA vaccines) | <10% (in vitro) vs. high variability (in vivo) | Correlation with intact mRNA % | Not specified | Days | Correlation with in vivo neutralizing antibody response [22] |
Experimental Protocols: Methodologies for Robust Potency Assessment
VEGF Potency Assay for CD34+ Cell-Based Therapy
Background: ProtheraCytes (expanded autologous CD34+ cells) promote cardiac regeneration through secretion of vascular endothelium growth factor (VEGF), making VEGF quantification an ideal potency assay [16].
Protocol Details:
- Platform: Automated ELISA system (ELLA) with microfluidic cartridge design
- Sample Preparation: Cell culture supernatants collected after 9 days of CD34+ cell expansion
- Assay Principle: Sandwich-type quantitative ELISA using specific antibodies against VEGF-A
- Detection Method: Fluorometer measures relative fluorescence units (RFU) proportional to antibody/antigen complexes
- Validation Parameters: Specificity, linearity (working range 20-2800 pg/mL), accuracy (85-105% recovery), precision (repeatability CV ≤10%, intermediate precision CV ≤20%), robustness [16]
Experimental Data: Analysis of 38 clinical batches demonstrated VEGF concentrations ranging from 185.6 pg/mL to 1032.4 pg/mL in AMI patient samples, with no significant difference compared to healthy donor samples (mean 516.2 ± 208.1 pg/mL) [16]. The assay showed significantly reduced variability compared to traditional ELISA methods, with CVs below 15% versus traditional method CVs as high as 30.1%.
CAR-Modified Cell Potency Assessment
Background: For CAR-modified CIK (cytokine-induced killer) cells, quantifying cytotoxic potential is essential for potency assessment [19].
Protocol Details:
- Cytotoxicity Assay: Co-culture with target cells (e.g., CD19+ B-ALL cell lines for anti-CD19 CAR)
- Duration: 4 hours for dye release assays, 4-24 hours for flow cytometry-based assays
- Effector:Target Ratios: Variable (40:1 to 1:1)
- Readout Methods:
- Dye release (calcein, 51chromium, LDH)
- Flow cytometry with dead/live cell dyes
- Surrogate markers: CD107a degranulation, granzyme B production, inflammatory cytokine secretion (IFNγ, TNFα, IL2)
- Correlation Analysis: Percentage of CAR-positive cells by flow cytometry correlated with cytotoxicity against standard target cell lines [19]
Experimental Data: In validation studies for CAR-CIK clinical trials (NCT03389035 and NCT05252403), the percentage of CAR-CD19 positive cells demonstrated significant correlation with cytotoxicity in vitro, supporting its use as a rapid surrogate potency assay for GMP release [19].
mRNA Vaccine Potency Correlation Protocol
Background: Establishing correlation between in vitro and in vivo potency is particularly challenging for mRNA vaccines, which require intracellular translation before antigen expression [22].
Protocol Details:
- Sample Preparation: mRNA-LNP samples with varying relative potencies created by gradual structural destabilization under thermal stress
- In Vitro Testing: Antigen expression in transfected cells (HepG2 cell line selected after evaluation of six mammalian cell lines)
- Detection Method: Quantitative imaging using fluorescently labeled protein-specific capture and detection antibodies
- In Vivo Testing: Antigen-specific antibody induction and immune response in vaccinated animals
- Parallel Analysis: Intact mRNA percentage measurement by capillary gel electrophoresis (CGE) and particle size distribution by dynamic light scattering (DLS) [22]
Experimental Data: Studies demonstrated that loss of intact mRNA as a function of time at elevated temperatures was accompanied by loss of in vitro potency. Furthermore, pseudovirus neutralizing potency (ED50) correlated with statistical significance with in vitro relative potency (EC50), supporting the predictive value of the in vitro assay [22].
Visualizing Potency Assay Development and Implementation
ATMP Potency Assay Workflow
In Vitro - In Vivo Correlation Strategy
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Solutions for ATMP Potency Assays
| Reagent/Solution | Function in Potency Testing | Example Applications | Technical Considerations |
|---|---|---|---|
| VEGF ELISA Kits | Quantification of pro-angiogenic secreted factor | CD34+ cell potency (cardiac regeneration) | Automated platforms (ELLA) reduce variability vs. traditional ELISA [16] |
| Fluorochrome-conjugated Antibodies | Detection of surface markers (CAR, TCR) and intracellular cytokines | Flow cytometry-based CAR quantification, CD107a degranulation | Correlation with functional potency must be established [19] |
| Cytotoxicity Detection Reagents | Measurement of target cell killing (dye release, LDH) | CAR-T/NK cell potency assessment | Variable effector:target ratios and timing require standardization [19] |
| Cell Culture Media for Expansion | Maintenance of cell viability and function during testing | All cell-based ATMPs | Composition affects secreted factors and functional properties |
| Reference Standards | Calibration and relative potency calculation | All quantitative potency assays | Essential for assay validation and inter-batch comparison [23] |
| mRNA Integrity Assay Kits | Measurement of intact mRNA percentage | mRNA vaccine potency | Capillary gel electrophoresis correlates with protein expression [22] |
The development of robust, validated potency assays is not merely a regulatory requirement but a fundamental component of responsible ATMP development. As demonstrated across multiple ATMP categories, successful potency strategies share common elements: direct linkage to mechanism of action, rigorous validation under GMP conditions, demonstration of correlation between in vitro measurements and biological function, and implementation of quantitative, reproducible analytical methods.
The scientific evidence overwhelmingly supports early integration of potency assay development into ATMP programs, with proactive engagement with regulatory agencies to align on expectations. This strategic approach not only mitigates the risk of clinical delays but, more importantly, ensures that transformative therapies reach patients with consistent quality and predictable therapeutic effect. In the rapidly evolving field of advanced therapies, potency assays remain the non-negotiable cornerstone that bridges innovative science with reliable medicine.
The core transcriptional regulatory circuitry comprising OCT4, SOX2, and NANOG constitutes the fundamental molecular machinery governing pluripotency in mammalian stem cells. These transcription factors function as master regulators that maintain embryonic stem cells (ESCs) in a undifferentiated state, enable lineage specification during development, and facilitate the reprogramming of somatic cells into induced pluripotent stem cells (iPSCs). In the context of stem cell potency assays—critical quality control measures for cell therapy products—these three factors serve as essential markers for evaluating pluripotent character and differentiation potential. Their expression levels and functional interactions provide crucial insights into stem cell quality, functionality, and therapeutic potential, making them indispensable tools for both in vitro research and in vivo applications in regenerative medicine.
This guide provides a comprehensive comparison of OCT4, SOX2, and NANOG by synthesizing current scientific understanding of their distinct and overlapping functions, expression patterns, regulatory mechanisms, and experimental approaches for their detection and quantification. For researchers and drug development professionals, mastering the nuances of these pluripotency markers is paramount for developing robust potency assays that can reliably predict the biological performance of stem cell-based therapeutics.
Molecular Characteristics and Expression Profiles
Comparative Analysis of Key Attributes
Table 1: Fundamental characteristics of core pluripotency transcription factors
| Feature | OCT4 | SOX2 | NANOG |
|---|---|---|---|
| Gene Symbol | POU5F1 | SOX2 | NANOG |
| Protein Family | POU (Pit-Oct-Unc) domain | SRY-related HMG-box | Homeodomain |
| Human Chromosomal Location | Chromosome 6 | Chromosome 3 | Chromosome 12 |
| Protein Isoforms | OCT4A, OCT4B (OCT4A maintains pluripotency) | Single major isoform | Multiple splice variants |
| Expression in Early Embryo | Inner Cell Mass (ICM) of blastocyst | Inner Cell Mass (ICM) of blastocyst | Inner Cell Mass (ICM) of blastocyst |
| Expression in Adult Tissues | Primordial germ cells | Adult stem cell niches (brain, testes, stomach, cervix) | Generally silenced except in certain malignancies |
| Essential for Embryonic Development | Lethal at implantation [24] | Lethal; failure to form pluripotent epiblast [25] | Lethal due to failed epiblast formation |
| Regulation of Expression | Dose-dependent; precise levels critical [26] | Stringent level requirements; dynamic equilibrium with partners [25] | Threshold-dependent; maintains pluripotency network |
Expression Patterns During Development and in Adult Tissues
The expression dynamics of these pluripotency factors throughout development follow distinct yet overlapping patterns. OCT4 is initially present as maternal mRNA and protein in oocytes and zygotes, with zygotic transcription activating at the 4- to 8-cell stage in mice. It remains highly expressed in all blastomeres until the morula stage, becomes restricted to the inner cell mass (ICM) in blastocysts, and after implantation, is progressively down-regulated during gastrulation, eventually becoming confined to primordial germ cells [24] [26]. In adults, OCT4 expression is largely restricted to germ cells, though it may be re-activated in certain pathological contexts such as cancer.
SOX2 expression initiates at the morula stage, becomes localized to the ICM of the blastocyst and epiblast, and persists in the central nervous system after gastrulation [25] [27]. Unlike OCT4, SOX2 maintains expression in multiple adult stem cell compartments, including the brain, stomach, cervix, anus, testes, lens, and various glands [28]. These SOX2-expressing adult stem cells continuously self-renew and generate mature cell types within their respective tissues, contributing to tissue regeneration and homeostasis [28].
NANOG expression follows a similar pattern to OCT4 during early development, with high expression in the ICM and down-regulation upon differentiation. However, in adults, NANOG is typically silenced in somatic tissues, with its expression being predominantly associated with pluripotent states and maligned transformations rather than normal tissue homeostasis [29].
Functional Roles and Regulatory Networks
Core Pluripotency Regulatory Circuitry
The three transcription factors form an interconnected autoregulatory loop that maintains the pluripotent state. They co-occupy their own promoters and those of each other, creating a robust network that reinforces pluripotency while suppressing differentiation genes [24] [25] [26]. This core transcriptional circuitry activates genes involved in self-renewal (including themselves) while simultaneously repressing developmental genes that would otherwise promote differentiation [24] [25]. The partnership between OCT4 and SOX2 is particularly critical, as these proteins physically interact through their HMG and POU domains, respectively, forming a complex that binds to composite DNA elements and regulates target gene expression [25] [26].
Figure 1: Core pluripotency regulatory network. OCT4, SOX2, and NANOG form an interconnected autoregulatory loop that activates self-renewal genes while repressing differentiation genes, maintaining the pluripotent state.
Context-Dependent Functions and Lineage Specification
Beyond maintaining pluripotency, these factors play critical roles in lineage specification through dose-dependent effects and partnership switching. OCT4 exhibits a remarkable "rheostat" behavior where its expression level determines ESC fate: reduced expression promotes trophoblast differentiation, moderate levels maintain pluripotency, and elevated levels drive differentiation toward primitive endoderm and mesoderm [24] [26]. This dosage sensitivity extends to its partnership capabilities—at standard levels, OCT4 complexes with SOX2 to maintain pluripotency, but increased expression enables partnership with SOX17, forming a complex that binds to different DNA motifs and activates endodermal and mesendodermal differentiation genes [24].
SOX2 demonstrates dual functionality in both maintaining pluripotency and directing neural differentiation. While it sustains OCT4 expression to preserve the pluripotent state, it also functions as a critical factor for neural commitment and maintains multipotential neural stem cells derived from ESCs, embryos, or adult sources [25] [27]. This context-dependent functionality makes SOX2 a persistent marker along the neural lineage pathway, from pluripotent cells to specialized neural progenitors.
NANOG functions as a key stabilizer of the pluripotent state, with its name deriving from the Celtic mythological figure "Tír na nÓg," representing the mythical land of eternal youth. Its expression is associated with ground-state pluripotency, and it reinforces the network by positively regulating its own expression along with OCT4 and SOX2. In pathological contexts, NANOG upregulation is strongly associated with advanced cancer stages and poor prognosis, where it promotes stemness, self-renewal, metastasis, invasiveness, and chemoresistance in various malignancies through signaling pathways including JAK/STAT and Wnt/β-catenin [29].
Experimental Analysis and Detection Methodologies
Detection Techniques and Assay Platforms
Table 2: Experimental approaches for detecting and quantifying pluripotency markers
| Methodology | Target | Application Context | Key Considerations |
|---|---|---|---|
| Reverse Transcription PCR (RT-PCR) | mRNA expression | Semi-quantitative detection in cell lines and tissues [30] | Requires specific primers for isoforms (e.g., OCT4A vs. OCT4B) |
| Immunocytohistochemistry | Protein localization and expression | Subcellular localization in cultured cells [30] | Distinguishes nuclear vs. cytoplasmic localization; antibody specificity critical |
| Immunofluorescent Staining | Protein expression with spatial context | Characterization of stem cell colonies and heterogeneous cultures [30] | Enables visualization of nuclear localization patterns |
| Western Blotting | Protein expression and modification | Detection of protein isoforms and post-translational modifications | Can differentiate between OCT4 isoforms based on molecular weight |
| Flow Cytometry | Protein expression at single-cell level | Quantification of marker expression in heterogeneous cell populations | Enables isolation of subpopulations based on pluripotency marker expression |
| Single-Cell RNA Sequencing | Transcriptomic profiling | Resolution of cellular heterogeneity in stem cell cultures | Identifies distinct cell states based on coordinated marker expression |
Detailed Experimental Protocol: Combined RT-PCR and Immunofluorescence
For comprehensive characterization of pluripotency markers in cultured cells, researchers often employ a combined molecular and cytological approach. The following protocol has been successfully applied to human breast cancer cell lines but can be adapted for various stem cell populations [30]:
Cell Culture and Preparation: Culture cells under standard conditions appropriate for the cell type. For the cited study, MCF7, T-47D, and MDA-MB-231 human breast cancer cell lines were maintained in Dulbecco's Modified Eagle's Medium (DMEM)/F12 medium supplemented with 10% fetal bovine serum at 37°C in a humidified atmosphere of 5% CO₂ [30].
RNA Extraction and Reverse Transcription: Harvest cells in the log phase of growth. Extract total RNA using an RNeasy Mini kit or similar. Perform reverse transcription using a SuperScript First-Strand Synthesis kit with oligo(dT) primers to generate cDNA.
Semi-Quantitative PCR Amplification:
- Prepare PCR reactions using Hotstar Taq DNA polymerase or similar high-fidelity enzyme.
- Use the following cycling parameters: 35 cycles of 94°C for 30 sec, 55°C for 30 sec, and 72°C for 1 min.
- Employ primer sequences specific for each pluripotency marker:
- OCT3/4A: Forward 5'-TGGAGAAGGAGAAGCTGGAGCAAAA-3', Reverse 5'-GGCAGAGGTCGTTTGGCTGAATAGACC-3'
- NANOG: Forward 5'-TCCTCCTCTTCCTCTATACTAAC-3', Reverse 5'-CCCACAATCACAGGCATAG-3'
- SOX-2: Forward 5'-GGGAAATGGAGGGGTGCAAAAGAGG-3', Reverse 5'-TTGCGTGAGTGTGGATGGGATTGGTG-3'
- Include β-actin or GAPDH as housekeeping controls for normalization.
- Separate PCR products on 1.2% agarose gels stained with ethidium bromide and visualize under UV illumination.
Immunofluorescent Staining:
- Fix cells in BD Cytofix/Cytoperm solution or similar fixative for 20 min at 4°C.
- Block nonspecific binding with donkey serum in BD Perm/Wash Buffer for 20 min.
- Incubate with primary antibodies overnight at 4°C:
- Goat anti-Oct3/4 antibody (e.g., sc-8628; Santa Cruz Biotechnology)
- Mouse anti-Sox-2 antibody (e.g., MAB-4343; 1:100; Millipore)
- For Nanog staining, use FITC-conjugated anti-human Nanog antibody (e.g., eBioscience)
- For non-conjugated primaries, incubate with appropriate fluorescent secondary antibodies (e.g., Rhodamine red conjugated donkey anti-goat antibody, 1:200) for 1 hr at room temperature.
- Include negative controls with primary antibodies replaced by PBS.
- Visualize using fluorescence microscopy and capture digital images.
Data Analysis: For RT-PCR, quantify band intensities using densitometry software and normalize to housekeeping genes. For immunofluorescence, document the subcellular localization patterns (nuclear vs. cytoplasmic) and relative expression levels across cell lines.
Figure 2: Experimental workflow for combined RT-PCR and immunofluorescence analysis of pluripotency markers. This integrated approach provides both molecular quantification and subcellular localization data.
Application in Potency Assays for Cell Therapy Products
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents for pluripotency marker analysis
| Reagent Category | Specific Examples | Application Function |
|---|---|---|
| Cell Culture Media | DMEM/F12 supplemented with fetal bovine serum | Maintenance of stem cell cultures and cancer cell lines for experimentation [30] |
| RNA Isolation Kits | RNeasy Mini kit (Qiagen) | High-quality total RNA extraction for gene expression analysis [30] |
| Reverse Transcription Kits | SuperScript First-Strand Synthesis kit (Invitrogen) | cDNA synthesis from RNA templates for PCR amplification [30] |
| PCR Enzymes | Hotstar Taq DNA polymerase (Qiagen) | High-fidelity amplification of target sequences with minimal background [30] |
| Primary Antibodies | Goat anti-Oct3/4 (Santa Cruz), Mouse anti-Sox-2 (Millipore) | Specific detection of target proteins in immunofluorescence and other applications [30] |
| Secondary Antibodies | Rhodamine red conjugated donkey anti-goat antibody | Fluorescent detection of primary antibodies with high sensitivity and specificity [30] |
| Fixation Solutions | BD Cytofix/Cytoperm solution (BD Biosciences) | Cell structure preservation and permeabilization for intracellular staining [30] |
| Blocking Reagents | Donkey serum in BD Perm/Wash Buffer | Reduction of non-specific antibody binding in immunofluorescence [30] |
Regulatory Considerations for Potency Testing
The development of robust potency assays is essential for regulatory approval of cell therapy products (CTPs). A comprehensive analysis of potency tests used for the 31 United States Food and Drug Administration-approved CTPs reveals that products typically employ multiple complementary approaches, with an average of 3.4 potency tests per product [31]. These assays are categorized into five main bins: "Viability and count" (52%), "Expression" (27%), "Bioassays" (7%), "Genetic modification" (9%), and "Histology" (3%) [31].
Within this regulatory framework, assessment of pluripotency markers falls primarily under "Expression" testing, which has been employed by 20 of the 31 approved CTPs (65%) [31]. The most common combination involves "Viability and count" together with "Expression" tests, implemented for 16 CTPs (52%) [31]. For advanced therapy medicinal products, including those based on pluripotent stem cells, the expression of OCT4, SOX2, and NANOG often serves as a critical quality attribute that must be carefully monitored throughout product development and manufacturing.
The emerging field of multi-omics approaches—including genomics, epigenomics, transcriptomics, proteomics, and metabolomics—provides unprecedented resolution for characterizing pluripotency markers in CTPs [17]. These advanced profiling techniques enable comprehensive assessment of the molecular features that underlie product potency, including the expression and functional status of core pluripotency factors. As the cell therapy field advances toward more complex products, potency assays will increasingly need to capture the dynamic regulation of these key markers and their downstream effects on cellular identity and function.
OCT4, SOX2, and NANOG represent the core transcriptional machinery governing pluripotency, with each factor playing distinct yet interconnected roles in maintaining stem cell identity. OCT4 serves as the central rheostat, with its precise expression levels determining cell fate decisions between self-renewal and lineage specification. SOX2 functions as both a pluripotency sustainer and a neural lineage specifier, maintaining flexibility across developmental contexts. NANOG stabilizes the pluripotent ground state and reinforces the core regulatory network through positive feedback mechanisms.
For researchers and therapy developers, these markers provide indispensable tools for characterizing stem cell populations, evaluating differentiation status, and ensuring product quality. Their expression patterns and functional interactions offer critical insights into the biological potency of stem cell-based therapeutics, forming the foundation of robust assays that can predict clinical performance. As the field advances toward more sophisticated cell therapies, understanding the nuanced relationships between these pluripotency factors will remain essential for harnessing the full potential of stem cells in regenerative medicine and drug development.
A Practical Guide to In Vitro and In Vivo Potency Assay Techniques
This guide provides an objective comparison of core functional assays used to characterize cell products, with a specific focus on their application in stem cell potency evaluation for preclinical and clinical research.
Stem cell potency—the functional capacity of a cell product to elicit a specific biological effect—is a critical quality attribute that must be quantified for clinical translation. [32] While in vivo studies are the ultimate test of function, in vitro assays provide essential, reproducible metrics for lot-to-lot consistency and correlation with clinical outcomes. [32] Three cornerstone in vitro functional assays form the basis of this evaluation: colony-forming unit (CFU) assays, which measure clonogenic potential and proliferative capacity; cytotoxicity assays, which assess the ability to kill target cells (for immunotherapies) or, more broadly, a cell product's toxicological profile; and cytokine secretion profiling, which quantifies the secretion of immunomodulatory and trophic factors that mediate a cell's therapeutic mechanism of action. [32] The integration of data from these assays provides a multi-faceted view of cell product quality and functional potency, which is increasingly important for regulatory approval. [33] [32]
Experimental Protocols for Key Assays
Cytokine Secretion Profiling
Cytokine profiling is crucial for understanding the in vivo functionality and safety of cell therapies, particularly for predicting and managing adverse events like cytokine release syndrome (CRS). [33] Standardization of cytokine measurement platforms, however, remains a challenge in the field. [33]
One-Step Flow Cytometry-Based Multiplex Cytokine Assay [34] This protocol details a simplified method for simultaneously quantifying 12 cytokines, reducing both operation time and cold-chain dependency for reagents.
- Principle: Uses capture-antibody-modified fluorescent microspheres and phycoerythrin (PE)-labeled detection antibodies in a single reaction step. [34]
- Key Reagents:
- Capture Microspheres: Carboxylated fluorescently encoded microspheres conjugated to cytokine-specific capture antibodies via EDC/sulfo-NHS chemistry. [34]
- Detection Antibodies: Phycoerythrin (PE) conjugated to detection antibodies via SMCC crosslinking. [34]
- Lyophilization Buffer: PBS with BSA, mannitol, and trehalose to stabilize reagents for storage without refrigeration. [34]
- Procedure:
- Preparation: Combine capture microspheres and PE-labeled detection antibodies in lyophilization buffer, aliquot, and freeze-dry to form reagent beads. [34]
- Assay Execution: Add 100 µL of sample or standard to a well containing a lyophilized reagent bead. [34]
- Incubation: Incubate with shaking at room temperature for 1.5 hours. [34]
- Wash and Analyze: Wash to remove unbound components, add reading buffer, and analyze using a flow cytometer (e.g., Beckman Coulter DxFlex). [34]
- Data Analysis: Use machine learning models (e.g., logistic regression, random forest) on cytokine data, along with other clinical parameters, to build predictive models for disease severity or viral load. [34]
High-Throughput Homogeneous Time-Resolved Fluorescence (HTRF) Assay [35] This protocol is designed for high-throughput screening of environmental chemicals using human induced pluripotent stem cell-derived microglia (hiMG).
- Principle: A homogenous, plate-based immunoassay that uses fluorescence resonance energy transfer (FRET) between donor and acceptor molecules to quantify cytokines like IL-6 and TNF-α. [35]
- Key Reagents:
- Procedure:
- Cell Seeding and Stimulation: Seed hiMG cells in a 1536-well plate format and stimulate with LPS (e.g., EC50 ~50 ng/mL for IL-6). [35]
- Detection: Add HTRF detection reagents directly to the culture well. [35]
- Incubation and Reading: Incubate and read the time-resolved fluorescence on a compatible plate reader. [35]
- Data Analysis: Calculate the fold-change in cytokine secretion over the vehicle control group. A significant increase (e.g., 3.71-fold for IL-6) indicates a robust inflammatory response. [35]
The following diagram illustrates the core workflow of a multiplex cytokine detection assay:
Cytotoxicity Testing
Cytotoxicity testing evaluates cell viability and death mechanisms, which is vital for toxicology screening and for assessing the effector function of immune cell therapies. [36] [37] A multimodal approach is recommended to capture the complex nature of cell death. [36]
Multimodal Cytotoxicity Assessment in 3D Microtissues [36] This protocol uses a linear mixed-effects regression model to integrate data from multiple assays, providing a more comprehensive evaluation of cytotoxicity.
- Principle: Different assays with distinct mechanisms of action (e.g., metabolic activity, membrane integrity, apoptosis) are used in parallel to capture multifaceted cellular injuries. [36]
- Key Assays and Reagents:
- ATP Assay (CellTiter-Glo 3D): Measures metabolic activity via ATP content. Used for metabolic inhibitors like 2-Deoxy-D-glucose (2DG) and oligomycin A. [36]
- Live/Dead Viability/Cytotoxicity Assay: Uses calcein-AM (live) and ethidium homodimer-1 (dead) stains to assess plasma membrane integrity. Used for membrane disruptors like Triton X-100 and melittin. [36]
- Caspase-Glo 3/7 Assay: Measures caspase-3/7 activity as a marker of apoptosis. Used for DNA-damaging agents like cisplatin and melphalan. [36]
- Click-iT EdU Proliferation Assay: Measures DNA synthesis to assess proliferative capacity. Used for anti-mitotic agents like paclitaxel. [36]
- Procedure:
- Dose-Response Curves: Treat 3D microtissues (e.g., HepG2 spheroids, primary neurospheroids) with a compound and measure response using the relevant "gold-standard" assay. [36]
- Model Fitting: Fit data to a nonlinear mixed-effects (NLME) model to derive lethal concentration (LC) values (e.g., LC25, LC50, LC75). [36]
- Multimodal Testing: Test all assay-treatment combinations at the derived LC values. [36]
- Data Integration: Analyze the full dataset using a linear mixed-effects (LME) model to capture inter-assay sensitivity and off-target effects. [36]
- Data Analysis: The slope from the LME model indicates assay-treatment sensitivity. A slope of -1.0 indicates the viability captured by an assay decreases proportionally to the increase in LC value. [36]
Standardized In Vitro Cytotoxicity Testing per ISO 10993-5 [38] This is a standardized method for assessing the cytotoxicity of medical device materials, such as biodegradable magnesium alloys.
- Principle: Evaluates the effect of material extracts on cell viability, morphology, and proliferation. [38]
- Key Reagents:
- Procedure:
- Cell Culture: Culture L-929 cells in a monolayer at 37°C with 5% CO2. [38]
- Exposure: Expose cells to the material extract (e.g., 100%, 50%, 25% concentrations) for a defined period. [38]
- Viability Assessment: After incubation, assess cell morphology microscopically and quantify cell viability using the MTT assay. [38]
- Data Analysis: Calculate cell viability as a percentage of the negative control. A cell viability of 71.51% with an undiluted extract, improving with dilution, is indicative of a non-cytotoxic material. [38]
On-Chip 3D Potency Assay for Cell Therapies
This advanced protocol uses a microfluidic 3D culture system to create a clinically predictive potency assay for cell therapies, specifically for bone marrow aspirate concentrate (BMAC) used in a phase 3 trial for osteoarthritis. [32]
- Principle: A 3D microphysiological system with media perfusion better emulates the in vivo environment, leading to a secretory profile that is more predictive of clinical outcomes compared to 2D culture. [32]
- Key Reagents:
- Microfluidic Device: PDMS device with a cell-laden hydrogel chamber. [32]
- Hydrogel: 4-arm maleimide-functionalized poly(ethylene-glycol) (PEG-4MAL) hydrogel presenting RGD peptide and cross-linked with protease-degradable peptide. [32]
- Culture Media: Supplemented with a simulated synovial fluid (simSF) mimic to replicate the joint environment. [32]
- Multiplex Immunoassay: To quantify 24 immunomodulatory and trophic proteins (e.g., cytokines, chemokines, MMPs). [32]
- Procedure:
- Cell Encapsulation: Thaw BMAC samples and encapsulate in the PEG-4MAL hydrogel within the microfluidic device. [32]
- Perfusion Culture: Perfuse the device with media (with or without simSF) at 1.0 µL/min for 24 hours. [32]
- Secretome Analysis: Collect perfusate and analyze secreted analyte levels using a multiplex immunoassay. [32]
- Model Building: Use secreted analyte data in a linear regression model to predict patient-matched clinical outcomes (e.g., pain scores). [32]
- Data Analysis: The 3D on-chip system demonstrated elevated levels of immunomodulatory and trophic proteins and improved cross-validation accuracy for predicting clinical pain scores compared to the 2D assay. [32]
Comparative Performance Data
Cytokine Detection Platforms
Table 1: Comparison of cytokine detection platforms used in clinical trials and research. [33]
| Platform | Method | Sample Volume | Proteins Measured | Dynamic Range | Advantages | Limitations |
|---|---|---|---|---|---|---|
| ELISA | Antibody-based immunofluorescence | ~50–100 µL | 1 at a time | 1–2 logs | Sensitive, rapid, high-throughput | Sample preparation, false positives, time-intensive |
| Luminex / MSD | Bead-based multiplexing (Fluorescence/Electrochemiluminescence) | ~25 µL | 4 to 48+ | 3–4 log+ | Multiplexing, linear range | Specialized instrumentation required |
| Proximity Extension Assay (e.g., Olink) | Combined antibody and PCR | 1 µL | >3,000 | 5 log+ | High-plex, sensitive, low sample volume | Output is relative value; validated for serum/plasma |
| One-Step Flow Cytometry | Bead-based with single-step incubation | 100 µL | 12-plex (as reported) | Similar to conventional | Reduced hands-on time, reagents lyophilizable | Requires flow cytometer |
Cytotoxicity Assay Performance
Table 2: Performance of different cytotoxicity assays in detecting various mechanisms of cell death. [36]
| Assay | Mechanism of Action Measured | Example Treatments | Key Performance Metric (Lethal Concentration 50 - LC50) |
|---|---|---|---|
| ATP Assay (CellTiter-Glo 3D) | Metabolic Activity | 2DG, Oligomycin A | Derived from dose-response curve using NLME model |
| Live/Dead Viability/Cytotoxicity | Membrane Integrity | Triton X-100, Melittin | Derived from dose-response curve using NLME model |
| Caspase-Glo 3/7 | Apoptosis | Cisplatin, Melphalan | Derived from dose-response curve using NLME model |
| Click-iT EdU | Proliferation | Paclitaxel | Derived from dose-response curve using NLME model |
2D vs. 3D Potency Assay Predictive Power
Table 3: Comparison of 2D culture and on-chip 3D potency assay for predicting clinical outcomes. [32]
| Assay Characteristic | 2D Culture Assay | On-Chip 3D Potency Assay |
|---|---|---|
| Structural Cues | Planar, rigid surface | 3D hydrogel matrix with RGD peptides |
| Biophysical Environment | Static culture | Perfused system (interstitial flow) |
| Secretory Profile | Lower levels of immunomodulatory/trophic proteins | Elevated levels of secreted proteins |
| Correlation with Clinical Outcomes | Lower correlative power with patient pain scores | Higher correlative power and improved prediction accuracy |
| Predictive Validity | Limited | Improved, enabling better clinical decision-making |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key reagents and materials for in vitro functional assays.
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| Functionalized Microspheres | Capture and detect multiple analytes in multiplex assays | Carboxylated fluorescently encoded microspheres for cytokine detection [34] |
| PEG-4MAL Hydrogel | Synthetic ECM for 3D cell encapsulation in microfluidic devices | Creates a defined 3D microenvironment for BMAC potency testing [32] |
| Simulated Synovial Fluid (simSF) | Biorelevant culture medium mimicking the in vivo joint environment | Used in on-chip 3D assays to test BMAC samples for OA [32] |
| CellTiter-Glo 3D | Luminescent assay to quantify ATP as a measure of metabolically active cells in 3D cultures | Used for cytotoxicity testing of 3D microtissues [36] |
| Click-iT EdU | Fluorescent assay to measure DNA synthesis and cell proliferation | Used to assess anti-mitotic toxicity (e.g., paclitaxel) [36] |
| Caspase-Glo 3/7 | Luminescent assay to measure caspase activity as a marker of apoptosis | Used to assess cytotoxicity of DNA-damaging agents [36] |
| Lyophilization Stabilizers | Preserve assay reagents for storage and shipping without cold chain | Trehalose and mannitol in PBS/BSA buffer [34] |
Integrated Workflow for Potency Assessment
The following diagram summarizes a data-driven workflow for developing a predictive potency assay, integrating multiple in vitro functional data points with clinical outcomes:
The comparative data presented in this guide underscores a critical evolution in in vitro functional assay design: moving from single-endpoint, 2D formats toward integrated, multimodal, and physiologically relevant 3D systems. [36] [32] [37] The performance of an assay is no longer judged solely on its reproducibility, but increasingly on its predictive validity—its ability to correlate with in vivo efficacy and clinical outcomes. [32] For researchers developing stem cell therapies, this means that combining data from CFU, cytotoxicity, and cytokine secretion profiles within advanced assay systems like organ-on-chip platforms provides the most robust and regulatorily compelling potency data. [32] This integrated approach is essential for de-risking clinical translation and ensuring that cell therapies are characterized by their clinically relevant biological functions.
Stem cell potency, defined as the ability to self-renew and differentiate into specialized cell types, is a foundational property that must be rigorously confirmed for successful downstream applications in research, drug discovery, and regenerative medicine [39]. The accurate assessment of differentiation capacity is particularly crucial when considering the therapeutic potential of human pluripotent stem cells (hPSCs), including both embryonic and induced pluripotent stem cells, as variability in differentiation capacity between cell lines can significantly impact experimental outcomes and clinical safety [39] [40]. Within this context, two principal assays have emerged for evaluating pluripotency: the in vivo teratoma assay and in vitro directed differentiation approaches.
The teratoma assay has historically been regarded as the "gold standard" for assessing developmental potency, providing empirical proof of a cell population's ability to form derivatives of all three embryonic germ layers [39] [41]. In contrast, directed differentiation assays leverage defined culture conditions to steer pluripotent cells toward specific lineages in vitro. This guide provides a comprehensive comparative analysis of these two methodologies, examining their technical execution, applications, advantages, and limitations to inform researchers and drug development professionals in selecting appropriate assessment strategies for their specific needs.
The Teratoma Assay: An In Vivo Gold Standard
Fundamental Principles and Historical Context
The teratoma assay is an in vivo test that assesses pluripotency through the formation of benign tumors containing differentiated tissues from the three primary germ layers—ectoderm, mesoderm, and endoderm—following transplantation of putative pluripotent stem cells into immunocompromised mice [39] [41] [42]. This method has its roots in 1950s tumor research and gained prominence as a functional validation tool during the emergence of human stem cell research [42]. The assay operates on the principle that only truly pluripotent cells can generate the complex, organized tissue structures characteristic of teratomas when placed in an in vivo environment, even if that environment is non-physiological [42].
The teratoma assay serves a dual purpose in stem cell characterization. First, it confirms developmental pluripotency through the histological identification of mature, morphologically recognizable tissues derived from all three germ layers [39]. Second, it provides valuable safety information by detecting malignant elements within the formed tumors; the presence of undifferentiated cells or embryonal carcinoma components may indicate potential malignancy and would preclude therapeutic use [41].
Experimental Protocol and Methodological Variations
The standard teratoma assay protocol involves several critical steps, though significant variation exists between laboratories [39] [41]:
Cell Preparation: Undifferentiated pluripotent stem cells are harvested and prepared for injection. The number of cells injected typically ranges from 1×10^5 to 1×10^7 cells, though the minimum number required for teratoma formation varies by cell line and injection site [43].
Host Selection: Immunodeficient mouse strains are essential to prevent rejection of human cells. Common strains include SCID (severe combined immunodeficient), NOD (non-obese diabetic), NOG (NOD.Cg-Prkdcscid Il2rgtm1Sug), and NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl) mice [44] [42].
Injection Site: Cells are typically implanted into one of several anatomical locations:
- Subcutaneous space
- Intramuscular
- Renal capsule
- Testis
Observation Period: The time between cell injection and tumor analysis typically ranges from 6 to 20 weeks, depending on the cell line, number of cells injected, and site of implantation [41].
Histological Analysis: Following tumor formation, teratomas are excised, fixed, sectioned, and stained with hematoxylin and eosin for histological examination. The critical endpoint is the confirmed presence of differentiated tissues representing all three germ layers [39] [41].
A standardized workflow for the teratoma assay is presented in Figure 1 below:
Figure 1. Teratoma Assay Workflow. This diagram illustrates the key steps in performing a teratoma assay, from cell preparation through histological analysis.
Key Research Reagents and Materials
Table 1: Essential Reagents for Teratoma Formation Assays
| Reagent/Category | Specific Examples | Function/Purpose | Considerations |
|---|---|---|---|
| Immunodeficient Mice | SCID, NOD, NOG, NSG strains | Host organisms that accept xenogeneic cell transplants without rejection | Different strains vary in degree of immunodeficiency; NSG and NOG typically show superior engraftment [44] |
| Extracellular Matrix | Matrigel, Basement Membrane Extract | Provides structural support for injected cells, enhancing teratoma formation | Essential for certain injection sites; promotes cell survival and organization [43] |
| Cell Culture Media | Pluripotent stem cell maintenance media | Expands undifferentiated cell population prior to injection | Typically contain FGF2 and TGF-β; specific formulations vary by cell line [39] |
| Histological Stains | Hematoxylin and Eosin (H&E) | Visualizes tissue architecture and differentiated structures in teratomas | Standard method for identifying derivatives of three germ layers [39] [41] |
| Immunohistochemistry Reagents | Antibodies against germ layer-specific markers | Confirms identity of differentiated tissues within teratomas | Optional validation beyond H&E staining; provides molecular confirmation [41] |
Directed Differentiation Assays: In Vitro Alternatives
Fundamental Principles and Methodological Approaches
Directed differentiation encompasses in vitro techniques that steer pluripotent stem cells toward specific lineages through controlled exposure to morphogens, growth factors, and small molecules that mimic developmental signaling pathways [39] [40]. Unlike spontaneous differentiation approaches (e.g., embryoid body formation), directed differentiation employs precisely timed sequences of signaling cues to recapitulate embryonic development and generate well-defined cell populations [40].
These assays have gained prominence due to their reproducibility, scalability, and avoidance of animal use, while also providing quantitative data on differentiation efficiency [40]. The underlying principle involves stepwise manipulation of key developmental pathways—including TGF-β, BMP, WNT, and FGF signaling—to guide cells through intermediate developmental stages toward target phenotypes [40].
Experimental Protocol for Trilineage Differentiation
A standard directed differentiation protocol for assessing pluripotency involves trilineage differentiation toward definitive endoderm, mesoderm, and ectoderm lineages:
Baseline Characterization: Confirmation of undifferentiated state through morphology and pluripotency marker expression (OCT3/4, NANOG, SOX2, SSEA-4) [40].
Definitive Endoderm Differentiation: Activation of Nodal/TGF-β signaling using factors like Activin A, often combined with WNT pathway activation in the initial stages [40].
Mesoderm Differentiation: Primarily driven by BMP4 and FGF2 signaling, with specific pathway inhibitors used to pattern different mesodermal subtypes [40].
Ectoderm Differentiation: Dual SMAD inhibition (using SB431542 and LDN193189) to suppress mesendodermal differentiation and promote neural induction [40].
Analysis Phase: Assessment of differentiation efficiency through:
- Flow cytometry for surface markers (CXCR4 for endoderm, PDGFRβ for mesoderm, PAX6 for ectoderm)
- qPCR analysis of lineage-specific genes
- Immunocytochemistry for protein expression [40]
A standardized workflow for directed trilineage differentiation is presented in Figure 2 below:
Figure 2. Directed Trilineage Differentiation Workflow. This diagram illustrates the key steps in performing directed differentiation to assess pluripotent potential.
Advanced Molecular Tools for In Vitro Assessment
Recent advances in directed differentiation include the development of sophisticated molecular tools for more precise quantification of differentiation outcomes. The hiPSCore scoring system represents one such innovation—a machine learning-based approach that utilizes 12 validated genes to classify pluripotent and differentiated states with high accuracy [40]. This system employs markers including:
- Pluripotency: CNMD, NANOG, SPP1
- Endoderm: CER1, EOMES, GATA6
- Mesoderm: APLNR, HAND1, HOXB7
- Ectoderm: HES5, PAMR1, PAX6 [40]
Long-read nanopore transcriptome sequencing has further enabled the identification of 172 genes associated with specific differentiation states not adequately covered by current guidelines, highlighting the continuous evolution of in vitro assessment capabilities [40].
Key Research Reagents and Materials
Table 2: Essential Reagents for Directed Differentiation Assays
| Reagent/Category | Specific Examples | Function/Purpose | Considerations |
|---|---|---|---|
| Growth Factors/Cytokines | Activin A, BMP4, FGF2, VEGF | Direct lineage specification through developmental pathway activation | Concentration and timing critically influence differentiation outcomes [40] |
| Small Molecule Inhibitors | SB431542, LDN193189, CHIR99021 | Precise modulation of signaling pathways (TGF-β, BMP, WNT) | Enable more reproducible differentiation than protein factors alone [40] |
| Cell Culture Matrices | Matrigel, Laminin-521, Vitronectin | Provide structural support and influence cell fate decisions | Defined matrices preferred for clinical applications [40] |
| Lineage-Specific Antibodies | Anti-CXCR4, Anti-SOX17, Anti-PAX6, Anti-T/Brachyury | Detection and quantification of differentiated cells | Essential for flow cytometry and immunocytochemistry validation [40] |
| qPCR Assays | Pluripotency and germ layer-specific gene panels | Quantitative assessment of differentiation efficiency at transcriptional level | Newer panels (e.g., hiPSCore) show improved specificity over traditional markers [40] |
Comparative Analysis: Key Parameters for Assay Selection
Technical and Performance Metrics
Table 3: Direct Comparison of Teratoma and Directed Differentiation Assays
| Parameter | Teratoma Assay | Directed Differentiation |
|---|---|---|
| Assay Type | In vivo | In vitro |
| Time Required | 6-20 weeks [41] | 1-4 weeks [40] |
| Cost Factors | High (animal maintenance, long duration) [41] [42] | Moderate (reagents, culture materials) [40] |
| Detection Sensitivity | ~1 in 10^4 - 10^6 (for residual undifferentiated cells) [44] | Variable; highly efficient culture assays can approach teratoma assay sensitivity [44] |
| Primary Readout | Histological identification of tissues from three germ layers [39] [41] | Molecular and immunophenotypic markers of germ layer commitment [40] |
| Standardization Status | Poorly standardized; significant inter-laboratory variability [41] | Moderately standardized; commercial kits available [40] |
| Regulatory Acceptance | Still required for safety assessment of hPSC-derived medicinal products [41] | Accepted for characterization but may not replace teratoma for safety studies [41] |
| Malignancy Detection | Can identify malignant elements (teratocarcinoma) [41] | Cannot directly assess tumorigenic potential [41] |
| Quantitative Capacity | Primarily qualitative (presence/absence of tissues) [39] | Highly quantitative (flow cytometry, qPCR) [40] |
| Ethical Considerations | Significant animal use concerns; classified as moderate to severe procedure [41] [42] | No animal use required; more ethically acceptable [40] [42] |
Advantages and Limitations in Research and Development Contexts
Teratoma Assay Advantages:
- Provides the most rigorous in vivo evidence of developmental pluripotency through formation of complex, organized tissues [39] [41]
- Simultaneously evaluates both pluripotency and potential malignancy in a single assay [41]
- Remains the regulatory "gold standard" for safety assessment of hPSC-derived products [44] [41]
- Can detect functional pluripotency that might be missed by molecular markers alone [39]
Teratoma Assay Limitations:
- Time-consuming, labor-intensive, and expensive due to animal maintenance requirements [41] [42]
- Poorly standardized with significant protocol variability between laboratories [41]
- Raises ethical concerns regarding animal use and is classified as a moderate to severe procedure [41] [42]
- Primarily qualitative with limited capacity for quantitative comparison between cell lines [39]
- Results can be influenced by numerous variables including injection site, cell number, and mouse strain [41]
Directed Differentiation Advantages:
- Faster results (typically weeks instead of months) [40]
- More ethically acceptable as no animals are required [40] [42]
- Highly quantitative through flow cytometry, qPCR, and other molecular methods [40]
- More easily standardized across laboratories, especially with commercial kits [40]
- Enables high-throughput screening of multiple cell lines or conditions [40]
Directed Differentiation Limitations:
- Cannot assess tumorigenic potential or detect malignant elements [41]
- May not fully recapitulate the complexity of in vivo differentiation [39]
- Results can be highly protocol-dependent and vary between cell lines [40]
- May not be universally accepted by regulatory authorities for safety assessment [41]
- Requires extensive validation to ensure markers specifically identify target lineages [40]
Emerging Trends and Future Directions
The field of stem cell potency assessment is evolving toward increasingly sophisticated in vitro methods that may eventually reduce or replace teratoma assays. Several emerging trends are particularly noteworthy:
Advanced Molecular Tools: Technologies like the hiPSCore machine learning scoring system represent a significant advancement in quantitative pluripotency assessment [40]. By leveraging validated gene marker sets and computational analysis, these approaches provide objective, standardized metrics for evaluating differentiation potential that correlate well with functional outcomes.
Enhanced Sensitivity Detection: Novel in vitro methods such as digital PCR and highly efficient culture (HEC) assays now approach or surpass the sensitivity of teratoma assays for detecting residual undifferentiated cells in differentiated products [44]. These technologies offer detection sensitivities sufficient for safety screening while avoiding animal use.
Regulatory Science Advancements: While teratoma assays remain part of regulatory requirements for hPSC-derived medicinal products, there is growing recognition of the need for validated in vitro alternatives [44] [41]. International consortia are working toward harmonized procedures for evaluating teratoma formation risk, which may facilitate broader acceptance of in vitro methods [44].
Microenvironment-Based Safety Studies: Recent research suggests that the teratoma-forming potential of pluripotent stem cells is significantly influenced by cellular microenvironment and dissemination [43]. Studies demonstrate that disseminated iPSCs administered intravenously do not form teratomas, while congregated cells in confined spaces do, highlighting the importance of delivery method in safety assessments [43].
Both teratoma formation assays and directed differentiation approaches provide valuable, complementary information for assessing stem cell potency. The teratoma assay remains indispensable for evaluating the tumorigenic potential of pluripotent stem cells and their derivatives, particularly in regulatory contexts requiring safety assessment [41]. Meanwhile, directed differentiation assays offer powerful, quantitative tools for characterizing differentiation capacity in a more efficient, ethical, and standardized manner [40].
For research and drug development professionals, strategic implementation of these assays should consider the specific application context. Basic research and initial cell line characterization may benefit from comprehensive in vitro assessment using directed differentiation coupled with modern molecular tools like hiPSCore [40]. In contrast, preclinical development of cell therapies destined for clinical trials may still require teratoma formation data to satisfy regulatory requirements [44] [41].
As the field advances, continued refinement and validation of in vitro methods will likely expand their applications in safety assessment, potentially reducing reliance on animal-based testing. The optimal approach for many organizations will involve leveraging the strengths of both methodologies—using directed differentiation for rapid screening and initial characterization, while reserving teratoma assays for final safety assessment of clinical candidates. This balanced strategy ensures rigorous evaluation of stem cell products while adhering to ethical principles and practical research constraints.
In the field of stem cell research and therapy development, robust potency assays are critical for assessing the quality, functionality, and therapeutic potential of cellular products. These assays are essential for ensuring product consistency, manufacturing stability, and ultimately, clinical efficacy [15] [17]. Among the various analytical techniques available, flow cytometry, ELISA, and PCR have emerged as cornerstone methodologies for the rapid quantification of biomarkers and surrogate endpoints in both in vitro and in vivo research settings.
The selection of appropriate analytical techniques is guided by several factors, including the specific biological questions, required throughput, sensitivity, and regulatory considerations. This guide provides a comparative analysis of flow cytometry, ELISA, and PCR methodologies, supported by experimental data and protocols, to assist researchers in selecting the optimal approach for their stem cell potency assay requirements.
Technical Comparison of Core Methodologies
The table below provides a systematic comparison of the key technical parameters for flow cytometry, ELISA, and PCR in the context of biomarker analysis and potency assessment.
Table 1: Technical Comparison of Flow Cytometry, ELISA, and PCR
| Parameter | Flow Cytometry | ELISA | PCR/qPCR |
|---|---|---|---|
| Primary Application | Multiplexed protein/cell surface marker analysis, cell phenotyping [45] [46] | Soluble protein/cytokine quantification [17] | Gene expression analysis, vector copy number (VCN) [47] [17] |
| Throughput | High (624 samples in 2 hours for antibody detection) [48] | Moderate to High | High |
| Multiplexing Capacity | High (13-plex bead panels demonstrated) [48] [49] | Low (typically single-plex) | Moderate (with digital PCR) |
| Sensitivity | High (detects low-abundance cell populations) | High (pg/mL range) | Very High (single copy detection) |
| Reproducibility (CV) | Intra-plate: 3.16-6.71%; Inter-plate: 3.33-5.49% [48] | Typically <15% | Typically <10% for qPCR [47] |
| Key Strengths | Single-cell resolution, functional assays, high-parameter data | Standardized protocols, wide availability, quantitative | Absolute quantification, high sensitivity, functional genomic insights |
| Limitations | High instrument cost, complex data analysis | Limited multiplexing, requires specific antibodies | Only measures nucleic acids, not protein function |
Detailed Experimental Protocols and Applications
Flow Cytometry for Antibody and Neutralization Detection
Protocol: Multiplex Bead-Based Assay for Antibody Detection [48]
- Bead Preparation: Carboxyl-coated multiplex beads are barcoded with different fluorescent intensities. Recombinant antigens (e.g., SARS-CoV-2 S-RBD) are covalently immobilized onto the beads using EDC/sulfo-NHS chemistry.
- Assay Setup: Antigen-coupled beads are incubated with diluted serum samples or purified antibodies in a 96-well plate for 30 minutes at 4°C with gentle shaking.
- Detection: After washing, a cocktail of fluorochrome-conjugated detection antibodies (e.g., anti-human IgG, IgM, IgA) is added and incubated for 30 minutes.
- Analysis: Beads are washed and analyzed using a flow cytometer. The bead identity (determined by size and barcode fluorescence) and the presence of bound antibodies (determined by detection antibody fluorescence) are quantified simultaneously.
Application Example: A high-throughput bead-based flow cytometry assay was developed to simultaneously detect human IgM, IgG, and IgA antibodies against the SARS-CoV-2 spike RBD. This assay enabled the measurement of three antibody isotypes across 624 samples within 2 hours, demonstrating high reproducibility with intra-plate coefficients of variation (CVs) ranging from 3.16 to 6.71% [48].
Protocol: Cell-Free Flow Cytometric Neutralization Assay [49]
- Bead Coating: Streptavidin-coated beads are coupled with biotinylated viral antigens (e.g., RBD from different SARS-CoV-2 variants).
- Blocking Incubation: Coated beads are incubated with serum samples containing potential neutralizing antibodies. During this step, neutralizing antibodies in the serum bind to the RBD on the beads.
- ACE2 Receptor Addition: A recombinant human ACE2 receptor fused to a murine IgG1 Fc tag (rhACE2-mIgG1) is added. If neutralizing antibodies have blocked the RBD, ACE2 binding is inhibited.
- Detection: The bound ACE2-mIgG1 is detected using a fluorochrome-conjugated anti-mouse IgG antibody.
- Analysis: Flow cytometry is used to measure the fluorescence intensity on the beads, which is inversely proportional to the neutralizing capacity of the serum antibodies.
ELISA for Functional Potency Assessment
Protocol: IFN-γ Release Assay for CAR T-Cell Potency [47] [17]
- Coating: A monoclonal antibody specific for IFN-γ is coated onto a microtiter plate.
- Stimulation & Incubation: CAR T-cells are co-cultured with target cells expressing the cognate antigen. The supernatant is then collected and added to the coated ELISA plate, allowing IFN-γ to be captured.
- Detection: A detection antibody (biotin-conjugated anti-IFN-γ) is added, followed by an enzyme-conjugated streptavidin (e.g., Horseradish Peroxidase, HRP).
- Signal Development: A substrate solution (e.g., TMB) is added, which produces a colorimetric change catalyzed by the enzyme.
- Quantification: The reaction is stopped, and the absorbance is measured. The intensity of color is proportional to the concentration of IFN-γ in the supernatant, serving as a measure of CAR T-cell activation and potency.
PCR for Genomic and Transcriptomic Analysis
Protocol: Vector Copy Number (VCN) Quantification by ddPCR [47] [17]
- DNA Extraction: Genomic DNA is isolated from the cell therapy product (e.g., CAR T-cells).
- Digestion: The DNA is digested with a restriction enzyme to reduce viscosity and improve partition efficiency.
- Partitioning: The digested DNA is mixed with PCR mastermix and loaded into a droplet generator, which partitions the sample into thousands of nanoliter-sized droplets.
- Amplification: The droplets undergo PCR amplification with target-specific probes (e.g., for the CAR transgene) and reference gene probes (e.g., for a single-copy endogenous gene like RPP30).
- Analysis: The droplet reader counts the positive and negative droplets for both target and reference. The VCN is calculated using the formula: VCN = (Concentration of target gene) / (Concentration of reference gene).
Table 2: Key Research Reagent Solutions for Potency Assays
| Reagent Type | Specific Example | Function in Assay |
|---|---|---|
| Recombinant Antigens | SARS-CoV-2 Spike RBD [48] [49] [46] | Capture antigen for detecting specific antibodies in serological assays. |
| Fluorochrome-Conjugated Antibodies | Anti-human IgG-PE, IgM-V450, IgA-B488 [48] | Multiplexed detection of different antibody isotypes in flow cytometry. |
| Capture/Detection Antibody Pairs | Matched anti-IFN-γ antibody pair [17] | Quantification of cytokine release in ELISA-based potency assays. |
| qPCR/ddPCR Reagents | Probes for CAR transgene and reference gene [47] [17] | Absolute quantification of vector copy number and genetic modification. |
| Bead Platforms | RayPlex Multiplex Beads, BD CBA Beads [48] [49] | Solid support for multiplexed antigen or antibody binding in flow assays. |
Integrated Workflows and Data Analysis
The application of these techniques in tandem provides a comprehensive picture of product characteristics. The following diagram illustrates a potential integrated workflow for profiling an advanced therapy medicinal product (ATMP), such as CAR T-cells, leveraging the strengths of each technology.
Integrated Workflow for CAR T-Cell Potency Profiling
For data interpretation, flow cytometry provides high-content data at the single-cell level, enabling the identification of rare populations and complex phenotyping. ELISA offers straightforward, quantitative data on soluble factors, which is often easily benchmarked against release criteria. PCR and ddPCR provide absolute quantification of specific nucleic acid sequences, which is critical for safety (e.g., VCN) and understanding genetic modification efficiency.
Flow cytometry, ELISA, and PCR each offer distinct advantages for the quantification of biomarkers in stem cell and cell therapy research. The choice of technique is dictated by the specific analyte—be it a cell surface marker, a secreted protein, or a genetic marker. As the field advances toward more complex and targeted therapies, the integration of data from these complementary platforms will be essential for developing robust potency assays that accurately predict the in vivo therapeutic efficacy of cellular products. The ongoing harmonization of quality control tests, particularly in academic settings, underscores the importance of standardized, validated applications of these core technologies [47].
Advanced in vivo models, particularly those involving chimera formation and engraftment studies, provide critical platforms for evaluating the functional potency and therapeutic potential of stem cells. These models allow researchers to observe how human stem cells behave in a living, complex physiological environment—integrating into host tissues, responding to in vivo signals, and contributing to functional repair. For cell therapies targeting neurological disorders, chimeric brain models enable the study of human cell pathophysiology within functional neural circuits, offering insights that are not possible with in vitro systems alone [50]. The ability of human neural cells to mature, form synapses, and functionally integrate into host animal brains provides a powerful assay for assessing therapeutic cell quality and predictive clinical outcomes.
A critical component of these studies is chimerism analysis—the precise measurement of donor cell engraftment levels within host tissues. Next-generation sequencing (NGS) has emerged as a highly sensitive method for this monitoring, enabling detection of microchimerism (<1% donor chimerism) that may have clinical utility in early relapse detection and allograft monitoring for various cellular therapies [51]. This guide compares the performance of current technologies for engraftment monitoring and provides detailed experimental protocols for implementing these advanced models in stem cell research and development.
Comparative Analysis of Engraftment Monitoring Technologies
Monitoring donor cell engraftment is essential for evaluating the success of chimerism studies. The table below compares the performance characteristics of the primary technologies used for chimerism analysis.
Table 1: Performance Comparison of Engraftment Monitoring Technologies
| Technology | Analytical Sensitivity | Key Strengths | Key Limitations | Ideal Applications |
|---|---|---|---|---|
| NGS-based Chimerism Analysis | 0.2% for single donor [51] | High sensitivity and reproducibility; quantitative across full chimerism range; compatible with multiple donor scenarios [51] | Requires specialized bioinformatics; higher cost per sample than STR-PCR | Microchimerism detection; minimal residual disease monitoring; multi-donor transplantation [51] |
| STR-PCR (Short Tandem Repeat) | Typically 1-5% [51] | Well-established methodology; widely available; lower cost | Limited sensitivity; semi-quantitative at low chimerism levels | Routine monitoring where high sensitivity is not critical; institutional standards where validated |
| qPCR (Quantitative PCR) | 0.1-1% depending on markers [51] | High sensitivity for specific markers; rapid turnaround | Limited to known markers; requires pre-selection of informative polymorphisms | Tracking specific cell populations; known genetic markers |
The selection of an appropriate monitoring technology depends on the specific research requirements. NGS-based methods offer superior sensitivity and are particularly valuable for detecting microchimerism in advanced therapy applications, while STR-PCR may suffice for routine engraftment monitoring where high sensitivity is not critical [51].
Experimental Protocols for Chimera Formation and Engraftment Assessment
Generating Human-Animal Chimeric Brain Models
Human-animal chimeric brain models can be generated through several approaches, each with distinct advantages and applications:
Neonatal Transplantation: Transplant human pluripotent stem cell (hPSC)-derived neural progenitor cells (NPCs) or fetal brain cell-derived NPCs into the brains of postnatal day 0-3 immunodeficient mice [50].
- Procedure: Inject 50,000-100,000 cells in 1-2 μL of sterile PBS into the lateral ventricle or specific brain regions using a precision stereotactic apparatus. Allow cells to integrate for 6-13 months for complete maturation and widespread CNS distribution [50].
- Applications: Studying human cell development, migration, and integration into neural circuits; modeling neurological disorders [50].
Adult Transplantation: Transplant hPSC-derived neural cells or cerebral organoids into the brains of adult immunodeficient mice [50].
- Procedure: Use stereotactic surgery to deliver cells to specific brain regions. Typically results in lower chimerism than neonatal transplantation but offers opportunities for cell therapy testing in disease models.
- Applications: Evaluating regenerative cell therapies for neurodegenerative conditions; disease modeling in adult contexts [50].
Blastocyst Complementation: Microinject hPSCs into pre-implantation blastocysts of genetically engineered animals where genes necessary for specific tissue development are disrupted [50].
- Procedure: Inject 10-15 hPSCs into the blastocoele cavity of E3.5-4.5 mouse blastocysts. Transfer these blastocysts into the uterus of a pseudopregnant maternal surrogate.
- Applications: Generating high degrees of chimerism across multiple organ systems; studying human cell development in specific niches [50].
NGS-Based Engraftment Monitoring Protocol
The following protocol details the steps for implementing NGS-based chimerism analysis:
Sample Preparation: Extract genomic DNA from peripheral blood or tissue samples using standard methods. Assess DNA quality and quantity via spectrophotometry (A260/280 ratio of 1.8-2.0) and fluorometry [51].
Whole Genome Amplification (for low-input samples): When working with limited DNA, select an appropriate WGA platform based on analytical endpoints:
- For quantitative accuracy in chimerism or copy number variation analysis, use modified MALBAC-based platforms (e.g., PicoPLEX, SurePlex) [52].
- For allelic fidelity, use primary template-directed amplification (PTA)-based platforms (e.g., ResolveDNA) which show lower allelic dropout rates [52].
- Input DNA can be as low as 100 pg with appropriate WGA methods [52].
Library Preparation and Sequencing: Utilize commercial NGS-based chimerism kits that employ both single-nucleotide polymorphisms and insertions/deletions as genetic markers. Follow manufacturer protocols for library preparation. Sequence on an appropriate NGS platform (e.g., Illumina) to achieve minimum coverage of 100x across targeted loci [51].
Data Analysis: Use specialized bioinformatics pipelines (e.g., custom scripts or commercial software) to calculate donor chimerism percentages based on informative genetic markers. Establish quality metrics for sequencing performance and data analysis [51].
Interpretation: Report percentage donor chimerism with assay sensitivity limits (typically 0.2% for single donor, 0.5% for double donors) [51]. Monitor trends over time rather than single timepoints for most applications.
Research Reagent Solutions for Engraftment Studies
Successful implementation of chimera formation and engraftment studies requires specific reagents and platforms optimized for these applications. The following table details key solutions and their functions.
Table 2: Essential Research Reagents and Platforms for Engraftment Studies
| Reagent/Platform | Function | Key Considerations |
|---|---|---|
| Immunodeficient Mouse Strains | Host organisms for human cell engraftment | Select based on specific immune deficiencies (e.g., NSG, NOG) to maximize human cell acceptance and survival [50] |
| Whole Genome Amplification Kits | Amplify minimal DNA inputs for analysis | REPLI-g (Qiagen) for high yield; PicoPLEX (Takara Bio) for quantitative accuracy; ResolveDNA (BioSkryb) for allelic fidelity [52] |
| NGS-based Chimerism Assays | Detect and quantify donor cell engraftment | Assess sensitivity (0.2% for single donor), accuracy across chimerism range, and multi-donor capability [51] |
| Stereotactic Injection Apparatus | Precise delivery of cells to specific brain regions | Critical for neonatal and adult transplantation models; requires specialized training and calibration [50] |
| Cell Culture reagents for NPC differentiation | Generate neural progenitor cells from hPSCs | Use defined, xeno-free media for clinical translation; ensure batch-to-batch consistency [50] |
| Single-cell RNA-seq Platforms | Characterize engrafted cell phenotypes | Enables paired analysis of transcriptional phenotypes and TCR repertoire in engrafted cells [17] |
Advanced in vivo models utilizing chimera formation and sophisticated engraftment monitoring provide indispensable tools for assessing stem cell potency and therapeutic potential. NGS-based chimerism analysis offers significant advantages in sensitivity and accuracy over traditional methods, enabling detection of microchimerism that may be crucial for predicting clinical outcomes. The selection of appropriate chimera models—whether neonatal, adult, or blastocyst complementation—should be guided by specific research objectives, balancing chimerism levels with practical and ethical considerations. As these technologies continue to evolve, they will enhance our ability to translate stem cell research into effective clinical therapies, particularly for neurological disorders where human-specific disease mechanisms are paramount.
Overcoming Challenges: Strategies for Developing Robust and Reproducible Assays
Addressing Product Heterogeneity and Donor-to-Donor Variability
In the development of cell-based therapies, product heterogeneity and donor-to-donor variability represent significant challenges that can compromise therapeutic efficacy and consistency. For Advanced Therapy Medicinal Products (ATMPs), potency assays are fundamental quality control tools required to ensure that each product batch possesses the biological activity necessary for its intended clinical effect [53]. These assays are particularly crucial for stem cell therapies, where inherent biological variability can obscure clinical efficacy signals during regulatory evaluation [54]. The growing stem cell assay market, projected to reach US$13.5 billion by 2034 at a 17.55% CAGR, reflects the increasing importance of these characterization tools in therapeutic development [6].
A comprehensive analysis of FDA-approved cell therapy products reveals that manufacturers employ an average of 3.4 potency tests per product, with the most common being viability/count measurements (52%) and expression markers (27%) [55]. However, as the field advances, more sophisticated functional bioassays are being implemented to better address product heterogeneity. This guide systematically compares the current technologies and methodologies for quantifying and standardizing stem cell potency, providing researchers with actionable frameworks for addressing variability challenges in therapeutic development.
Comparative Analysis of Stem Cell Potency Assay Technologies
Technology Performance Comparison
Table 1: Comparison of Major Potency Assay Technologies for Stem Cell Characterization
| Technology Platform | Key Measurable Parameters | Throughput Capacity | Donor Variability Assessment | Regulatory Acceptance | Key Limitations |
|---|---|---|---|---|---|
| Flow Cytometry | Surface marker expression, Intracellular proteins, CAR expression [53] [55] | Medium to High | Quantitative for phenotypic heterogeneity | Well-established for identity/potency [55] | Single endpoint measurement; Limited functional data |
| Functional Bioassays (Cytotoxicity, Differentiation) | Cytolytic activity, Differentiation potential, Secreted factors [53] [56] | Low to Medium | Functional assessment of potency variation | Required for most ATMPs [53] | Time-consuming; Complex standardization |
| Molecular Assays (qPCR, ddPCR, NGS) | Gene expression, Vector copy number, TCR repertoire [17] [53] | Medium to High | Genomic-level donor differences | Accepted with validation [17] | May not reflect functional protein activity |
| Bioelectronic Assays (Impedance) | Real-time cytolysis, Kinetic monitoring [56] | Medium | Continuous functional assessment | Emerging for potency testing [56] | Specialized equipment required |
| Multi-omics Approaches | Transcriptomics, Epigenomics, Proteomics [17] | Low | Comprehensive molecular profiling | Developing regulatory framework [17] | Data complexity; High cost |
Quantitative Assessment of Donor Variability Impact
Table 2: Documented Donor Variability Across Stem Cell Types and Assay Readouts
| Stem Cell Type | Assay Category | Variability Range Reported | Key Influencing Factors | Clinical Relevance |
|---|---|---|---|---|
| Mesenchymal Stem/Stromal Cells (MSCs) | Immunomodulation (IDO-1 expression) [54] | 10-90% between donors | Donor age, tissue source | Direct correlation with T-cell suppression efficacy (R>0.9) [54] |
| CAR T-cells | Cytokine Release (IFN-γ) [17] [53] | Significant inter-donor differences | TCR repertoire diversity, Differentiation state [17] | Correlates with clinical response and persistence |
| Adipose-Derived Stem Cells (ASCs) | Differentiation Potential [57] | Varies by lineage commitment | Donor health status, Isolation method | Impacts regenerative capacity in tissue engineering |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogramming Efficiency [9] [5] | Source cell-dependent | Epigenetic memory, Reprogramming method | Affects differentiation propensity and safety profile |
Experimental Approaches for Addressing Variability
Establishing a Comprehensive Potency Assay Matrix
For mesenchymal stem cell products, researchers have developed a multi-parameter potency matrix to address manufacturing consistency challenges. This approach measures multiple factors critical to therapeutic function:
- IDO-1 expression: Quantified via enzymatic activity or PCR to assess activated lymphocyte suppression capability [54]
- M-CSF production: Measured by ELISA to evaluate macrophage polarization capacity [54]
- Extracellular vesicle (EV) secretion: Characterized by nanoparticle tracking analysis to determine Treg induction potential [54]
This matrix approach establishes correlations between potency factor levels and biological activity, enabling setting of thresholds for product release. For example, a threshold of 75% IDO-1 expression has been correlated with effective in vitro T-cell suppression (R>0.9, P<0.001) [54]. Similar matrix approaches can be adapted for other stem cell types by identifying key mechanism-of-action markers.
Protocol: Standardized Potency Assay for Immunomodulatory Capacity
Title: Assessment of MSC Immunosuppressive Potential via IDO-1 Activity Measurement
Principle: This protocol measures indoleamine 2,3-dioxygenase 1 (IDO-1) activity, which catalyzes tryptophan degradation and correlates with MSC immunosuppressive capacity [54].
Reagents and Equipment:
- Test MSC population (cryopreserved or fresh)
- IFN-γ for priming (100-500 U/mL)
- Tryptophan solution (100 μM in PBS)
- HPLC system with fluorescence detector or colorimetric assay reagents
- T-cell suppression assay components (optional correlation)
Procedure:
- Cell Preparation: Seed MSCs at 5×10^4 cells/well in 24-well plates and culture until 80% confluent.
- IFN-γ Priming: Stimulate with IFN-γ (100-500 U/mL) for 24 hours to induce IDO-1 expression.
- Reaction Incubation: Add tryptophan solution (100 μM) and incubate for 4-6 hours at 37°C.
- Metabolite Quantification: Collect supernatant and measure kynurenine production via HPLC (fluorescence detection at 360 nm excitation/460 nm emission) or colorimetric assay.
- Data Analysis: Calculate IDO-1 activity as kynurenine production rate (μM/hour/10^6 cells).
- Correlation with Functional Activity: Parallel samples can be used in T-cell suppression assays to establish correlation between IDO-1 activity and immunosuppressive function.
Validation Parameters:
- Establish inter-donor variability range using multiple donor sources
- Determine correlation coefficient between IDO-1 activity and T-cell suppression
- Set minimum potency threshold based on clinical lot data
Protocol: Bioelectronic Real-Time Cytotoxicity Monitoring for CAR T-Cells
Title: Functional Potency Assessment of CAR T-Cells via Impedance-Based Killing Assay
Principle: This label-free method continuously monitors tumor cell killing by engineered immune cells through measurement of electrical impedance, providing kinetic data on cytolytic activity [56].
Reagents and Equipment:
- Maestro Z system (Axion BioSystems) or equivalent impedance platform
- CAR T-cell test article (cryopreserved or fresh)
- Target tumor cells (appropriate antigen-positive line)
- 96-well bioelectronic assay plates
- Cell culture medium and supplements
Procedure:
- Target Cell Seeding: Plate tumor cells in bioelectronic plates (5×10^3 - 2×10^4 cells/well based on size) and culture for 24-48 hours to establish adhesion.
- Baseline Measurement: Record initial impedance values for each well.
- Effector Cell Addition: Add CAR T-cells at various effector-to-target ratios (e.g., 0.1:1 to 10:1).
- Continuous Monitoring: Record impedance every 15-60 minutes over 3-9 days under controlled culture conditions (37°C, 5% CO2).
- Data Analysis: Calculate cytolysis percentage based on impedance reduction normalized to target-only controls.
- Kinetic Parameters: Determine time to 50% cytolysis (T50) and maximum killing rate from kinetic curves.
Validation Parameters:
- Establish donor-specific kinetic profiles for multiple CAR T-cell lots
- Correlate impedance data with traditional cytotoxicity measures (e.g., chromium release)
- Determine inter-donor variability in killing kinetics and potency
Figure 1: Stem Cell Potency Assay Technology Landscape. This diagram illustrates the relationships between major assay technologies, the specific types of variability they address, and their primary applications in therapeutic development.
The Scientist's Toolkit: Essential Reagents and Technologies
Table 3: Key Research Reagent Solutions for Stem Cell Potency Assessment
| Reagent/Category | Specific Examples | Primary Function in Potency Assessment | Variability Mitigation Role |
|---|---|---|---|
| Cell Culture Reagents | mTeSR1TM medium, Defined media supplements [9] | Maintain stemness or direct differentiation | Reduces batch-to-batch variability in cell maintenance |
| Differentiation Inducers | Activin A, BMP4, bFGF, VEGF [9] | Direct lineage-specific differentiation | Standardizes differentiation efficiency assessment |
| Flow Cytometry Reagents | Antibodies to OCT4, NANOG, SSEA-4, TRA-1-60 [9] [5] | Pluripotency marker detection | Quantifies phenotypic heterogeneity between donors |
| Molecular Assay Kits | ddPCR for VCN, TCR sequencing kits [17] | Genomic and transcriptomic profiling | Identifies genetic-level donor differences |
| Bioelectronic Plates | Impedance-based microtiter plates [56] | Real-time functional monitoring | Provides kinetic data on donor-dependent functional variation |
| Cytokine Detection | IFN-γ ELISA, Multiplex cytokine panels [17] [53] | Secreted factor quantification | Measures functional immunomodulatory capacity |
Emerging Technologies and Future Directions
Advanced Analytical Approaches
The field of stem cell potency assessment is rapidly evolving beyond traditional methods. Multi-omics approaches - including genomics, epigenomics, transcriptomics, proteomics, and metabolomics - are providing unprecedented resolution in characterizing donor-specific attributes [17]. For CAR T-cell products, profiling of TCR repertoire diversity and vector integration sites has revealed correlations with clinical outcomes, enabling better donor selection [17]. Epigenomic analysis, particularly DNA methylation profiling, has identified distinct epigenetic loci associated with in vivo persistence and potency in CD19 CAR T-cell products [17].
Artificial intelligence integration is enhancing stem cell assay capabilities through improved classification of stem cell types and prediction of differentiation behavior. AI models are being developed to improve stem cell potency assessment and reduce analytical errors, potentially transforming how donor variability is quantified and managed [6].
Protocol: Multi-Omic Donor Profiling for Stem Cell Selection
Title: Comprehensive Donor Stratification via Integrated Genomic and Functional Profiling
Principle: This integrated protocol combines genomic stability assessment, epigenetic profiling, and functional potency evaluation to establish donor qualification criteria.
Procedure:
- Genomic Stability Assessment:
Epigenetic Profiling:
Functional Potency Correlation:
- Correlate genomic/epigenetic markers with in vitro functional outcomes
- Establish donor eligibility criteria based on multi-parameter assessment
Application: This approach enables prediction of donor-specific performance potential before manufacturing commitment, reducing failure rates due to inherent biological variability.
Figure 2: Comprehensive Donor Qualification Workflow. This decision framework illustrates the multi-parameter approach to donor stratification based on integrated genomic, epigenetic, functional, and secretory profiling to address inherent biological variability.
Addressing product heterogeneity and donor-to-donor variability requires a systematic, multi-parametric approach to potency assessment. The most effective strategies combine traditional functional assays with emerging molecular and bioelectronic technologies to create comprehensive product profiles. As regulatory expectations evolve, manufacturers should implement potency assay matrices that measure multiple mechanism-based attributes rather than relying on single-parameter tests [55] [54].
Successful variability management involves early donor screening using genomic and epigenetic tools, process controls to minimize manufacturing-induced variability, and comprehensive release testing that reflects clinical mechanism of action. The integration of real-time functional assessments like bioelectronic assays provides kinetic data that can detect subtle potency differences between donors [56]. As the field advances, the adoption of standardized potency assessment frameworks will be crucial for demonstrating consistent product quality and achieving regulatory approval for stem cell-based therapies.
For advanced cell therapies, demonstrating biological function through potency assays is a mandatory regulatory requirement for late-stage clinical trials and commercial approval [58]. However, the development of these assays is significantly complicated by the pleiotropic nature of cellular products, such as mesenchymal stromal cells (MSCs), which deploy a plurality of immunomodulatory and regenerative functions in response to host environmental cues [58] [59]. A single effector pathway cannot serve as a reliable surrogate for the overall therapeutic potential, as it may lead to misleading conclusions about product quality and consistency [58].
This guide objectively compares the assay matrix approach, a strategy endorsed by the International Society for Cell Therapy (ISCT), against conventional single-mechanism assays [58]. We summarize experimental data demonstrating how a multi-analyte matrix more accurately captures biological complexity and correlates with clinical outcomes. The content is framed within a broader thesis on stem cell potency, underscoring that overcoming assay complexity is pivotal for successful clinical translation.
The Assay Matrix Approach: A Multi-Parameter Solution
The assay matrix approach is founded on the principle that the potency of a complex cell therapy product is best defined by the summation of its multiple effector pathways [58]. Instead of relying on a single readout, this strategy employs a panel of complementary assays designed to capture the major biological activities significant to the product's mechanism of action, such as immunomodulation, homing, and trophic support [58] [59].
Rationale and Regulatory Context
Regulatory authorities, including the U.S. FDA and EMA, require robust potency assays for advanced-phase clinical trials of cell-based products, which are classified as more than minimally manipulated cellular and gene therapy products [58]. The core challenge is that the mechanisms of action in humans are often not fully defined, and there is a lack of reference standards [58]. Furthermore, the biological activity of MSCs is not constitutive but is induced by inflammatory signals from the host microenvironment [58] [60]. Therefore, a potency assay must measure the dynamic response of MSCs to physiological inflammatory cues rather than merely quantifying a baseline state.
Key Components of an Assay Matrix
A comprehensive matrix often integrates two or more of the following analytical systems [58] [17]:
- Secretome Analysis: Quantifying the profile of cytokines, chemokines, and growth factors secreted by the cells upon activation.
- Transcriptome Analysis: Measuring RNA expression of genes related to immunomodulation and homing.
- Functional Co-culture Assays: Assessing the suppression of immune cell (e.g., T cell, macrophage) proliferation or activation.
- Multi-omics Profiling: Using genomics, epigenomics, proteomics, and metabolomics to deeply characterize product attributes [17].
Table 1: Comparative Analysis of Potency Assay Platforms
| Assay Platform | Key Measured Parameters | Therapeutic Context | Correlation with Clinical Suppression | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Secretome + PBMC Suppression [58] | Downregulated cytokines (TNF-α, IFNγ); Upregulated cytokines (VEGF, GCSF); T cell proliferation (Ki67+) | Crohn's disease, GvHD | Strong correlation (R² ≥ 0.5) with T cell suppression for key cytokines | Captures bidirectional interaction; Functional output | Uses surrogate cells (donor PBMC variability) |
| Macrophage Co-culture (IL-1RA) [60] | Secreted IL-1RA from MSCs; Macrophage markers (CD36, CD80); TNF-α release | Macrophage-driven diseases | Defines maximum MSC capacity; Therapeutically relevant pathway | Robust, reproducible, and straightforward | Focused on a single, specific inflammatory axis |
| On-Chip 3D System [32] | 24 immunomodulatory/trophic proteins (e.g., cytokines, chemokines, MMPs) | Osteoarthritis (Phase 3 trial) | Improved prediction of patient pain scores (VAS, KOOS) vs. 2D culture | Enhanced clinical predictive validity; Microphysiological environment | Higher complexity and cost; Emerging technology |
| CAR T-Cell Multi-Omics [17] | Vector copy number, integration sites, TCR repertoire, DNA methylation, metabolite levels | CAR T-cell immunotherapy | Associates product attributes with persistence and efficacy | Unprecedented depth of product characterization | Highly complex data; Lack of standardized cut-offs |
Experimental Protocols for Key Assay Matrix Systems
Protocol 1: Secretome Analysis and PBMC Suppression Assay
This protocol measures the effect of MSCs on immune cell proliferation and the accompanying cytokine signature [58].
Detailed Methodology:
- Cell Preparation: Obtain MSCs from the manufacturing process. Isolate Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors.
- Stimulation and Co-culture: Activate PBMCs with Staphylococcal Enterotoxin B (SEB). Co-culture activated PBMCs with MSCs at varying MSC:PBMC ratios (e.g., from 1:8 to 1:2). Include controls for PBMCs alone and MSCs alone.
- Proliferation Measurement: After a suitable incubation period (e.g., 3-5 days), assess T-cell proliferation by flow cytometry using a Ki67 antibody to label proliferating cells within the CD3+ T cell population.
- Secretome Collection and Analysis: Collect supernatant from co-cultures. Analyze a focused panel of 29+ cytokines (e.g., TNF-α, IFNγ, IL-13, VEGF, GCSF, CXCL10) using a multiplex immunoassay (e.g., Luminex) or ELISA.
- Data Analysis: Perform linear regression analysis to correlate the suppression of CD3+Ki67+ T cells with the up- or down-regulation of specific cytokines. Cytokines with a correlation coefficient (R²) ≥ 0.5 are considered robust predictors of MSC-mediated suppression [58].
Protocol 2: Macrophage Co-culture Potency Assay
This protocol measures the anti-inflammatory capacity of MSCs in an M1 macrophage-dominated environment via IL-1RA secretion [60].
Detailed Methodology:
- Macrophage Differentiation and Polarization: Differentiate THP-1 monocytes into macrophages using Phorbol 12-myristate 13-acetate (PMA). Polarize the macrophages to an M1 phenotype using a cytokine cocktail (e.g., IFN-γ and LPS).
- Co-culture Setup: Co-culture ABCB5+ MSCs (or other MSC types) with the M1-polarized macrophages at a pre-optimized ratio (determined by titrating a wide range of MSC/macrophage ratios). Use a transwell system to separate cell types if needed.
- Validation of Macrophage Phenotype: Confirm successful M1 polarization by flow cytometry analysis of surface markers CD36 and CD80, and by measuring the release of proinflammatory TNF-α.
- Potency Readout: Quantify the amount of Interleukin-1 Receptor Antagonist (IL-1RA) secreted into the co-culture supernatant using a validated enzyme-linked immunosorbent assay (ELISA).
- Assay Validation: The ELISA method must demonstrate guideline-concordant selectivity, accuracy, and precision over a relevant concentration range for use in batch release testing.
Protocol 3: On-Chip 3D Potency Assay
This protocol describes a microphysiological system for evaluating the potency of bone marrow aspirate concentrate (BMAC) with enhanced clinical predictive power [32].
Detailed Methodology:
- Device and Hydrogel Preparation: Use a poly(dimethylsiloxane) (PDMS) microfluidic device. Synthesize a PEG-4MAL hydrogel functionalized with RGD peptide and cross-linked with a protease-degradable peptide.
- Cell Encapsulation and Perfusion: Thaw and encapsulate the BMAC clinical sample within the hydrogel. Incorporate the cell-laden hydrogel into the microfluidic device and perfuse with media at a rate of 1.0 μL/min for 24 hours.
- Simulated Synovial Fluid Challenge: For osteoarthritis applications, culture cells in a defined OA simulated synovial fluid (simSF) containing abundant proteins and glycosaminoglycans to mimic the pathological joint environment.
- Multiplexed Secretory Analysis: After the perfusion period, analyze the conditioned media for the secretion of 24+ immunomodulatory and trophic proteins (cytokines, chemokines, MMPs) using a multiplex protein array.
- Model Building for Clinical Prediction: Use secreted analyte levels as inputs to build linear regression prediction models for patient-matched clinical outcomes (e.g., VAS pain scores). Validate the model's predictive power through cross-validation.
Visualizing the Assay Matrix Strategy
The following diagram synthesizes the core concepts of the assay matrix approach, illustrating how multiple assay systems converge to provide a comprehensive potency profile.
The Scientist's Toolkit: Key Research Reagent Solutions
The successful implementation of a potency assay matrix relies on specific biological reagents and tools. The following table details essential materials and their functions.
Table 2: Essential Research Reagents for Potency Assay Development
| Reagent / Tool | Function in Potency Assay | Example Application |
|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Serve as responder immune cells to measure the immunomodulatory capacity of the test product. | Used as stimulator/responder cells in co-culture suppression assays with MSCs [58] [32]. |
| Interferon-gamma (IFN-γ) | A critical inflammatory cue used to pre-activate or "license" MSCs, inducing their immunosuppressive functions. | Used as a surrogate for activated PBMCs to trigger MSC effector pathways in simplified assays [58]. |
| PEG-4MAL Hydrogel | A synthetic, tunable hydrogel that provides a 3D scaffold for cell encapsulation, mimicking aspects of the native extracellular matrix. | Used in on-chip 3D systems to support BMAC or MSC culture and function [32]. |
| Multiplex Cytokine Array | Allows simultaneous quantification of dozens of analytes (cytokines, chemokines) from a small volume of conditioned media. | Used for secretome analysis to define cytokine signatures correlated with potency [58] [32]. |
| THP-1 Cell Line | A human monocytic cell line that can be differentiated into macrophages, providing a consistent and renewable cell source. | Differentiated into M1 macrophages for co-culture potency assays measuring IL-1RA production [60]. |
| Validated ELISA Kits | Provide a highly specific, accurate, and precise method for quantifying a single, therapeutically relevant protein. | Used for batch release testing of specific analytes like IL-1RA [60]. |
The growing complexity of cell-based medicinal products demands equally sophisticated tools for quality control. The evidence compared in this guide demonstrates that the assay matrix approach consistently outperforms single-parameter assays by more accurately capturing the multi-mechanistic biology of cells like MSCs and CAR-T cells. The integration of secretome analysis, functional co-cultures, and advanced platforms like 3D on-chip systems provides a robust correlative power with clinical outcomes, as seen in phase 3 trial data [32]. While the development and validation of these matrix assays present significant challenges, they are indispensable for de-risking clinical translation, ensuring product consistency, and ultimately fulfilling regulatory requirements for the next generation of transformative cell therapies.
In stem cell research, the journey from fundamental discovery to clinical therapy is paved with challenges, chief among them being the control of technical variability. For stem cell potency assays—the definitive tests that measure a cellular product's biological activity and therapeutic potential—uncontrolled variability in culture conditions and reagent sourcing can compromise data integrity, obscure true biological signals, and ultimately hinder clinical translation [61] [62]. Potency assays are not merely research tools; they are regulatory requirements for Advanced Therapy Medicinal Products (ATMPs), making their reproducibility paramount [16] [17]. This guide objectively compares how choices in culture reagents and protocols introduce variability and provides experimentally-supported methodologies to control these factors, ensuring that potency data for both in vitro and in vivo research is reliable, meaningful, and compliant.
Quantitative Impact of Reagent Sourcing on Cellular Phenotype
Even minor, often unconsidered variations in growth media and serum can significantly alter critical cellular parameters, directly impacting the readouts of potency assays.
Systematic Comparison of Media and Serum Effects
A comprehensive 2025 study quantitatively demonstrated how 12 different fetal bovine sera (FBS) and eight growth media brands affected five distinct cell types, including models relevant to therapeutic development like neuroblastoma (SH-SY5Y) and embryonic kidney (HEK-293T) cells [63]. Using high-throughput imaging and functional analyses, the research revealed that proliferation and morphological changes occurred independently of one another, meaning that a culture might appear healthy by growth rate yet possess an altered, potentially therapeutically compromised phenotype [63].
Table 1: Impact of Serum and Media Variation on Key Cell Parameters [63]
| Cell Parameter | Observed Effect of Reagent Variation | Experimental Method |
|---|---|---|
| Cell Proliferation | Varied significantly across different FBS and media brands. | Automated cell counting and confluence analysis. |
| Cell Morphology | 44 morphological parameters were affected, independently from proliferation changes. | High-throughput imaging and morphological profiling of 561,519 cells. |
| Drug Sensitivity | Cellular response to pharmaceutical compounds was altered. | Dose-response assays following drug treatment. |
| Mitochondrial Function | Mitochondrial membrane potential was shifted. | Fluorescence-based measurement of mitochondria potential. |
| Differentiation Capacity | The ability of cells to differentiate into specialized lineages was impacted. | Induction of differentiation and assessment of marker expression. |
The most drastic differences were surprisingly observed in serum-free conditions, where the choice of basal medium alone determined cell survival and response to growth factors like EGF [63]. This finding is critical for the stem cell field, where defined, serum-free media are increasingly the standard for manufacturing cell therapies. The study provides an online resource (Shinyapp) for researchers to explore the effects of 28 distinct growth conditions, underscoring the need for meticulous reagent selection and documentation [63].
Consequences for Potency Assay Outcomes
This reagent-induced variability directly threatens the validity of potency assays. For example, a potency assay for "ProtheraCytes" (expanded CD34+ cells) is based on the quantification of secreted Vascular Endothelial Growth Factor (VEGF), which promotes revascularization of damaged heart tissue [16]. If the culture medium or serum lot inadvertently influences the cells' secretory profile, the measured VEGF level may not reflect the product's true therapeutic potency but rather an artifact of the reagent batch. Another review on potency assays for human adipose-derived stem cells (hASCs) in wound healing emphasizes that variability due to "different lots or types of reagents" can introduce "non-negligible inconsistency" in the product's critical quality attributes, such as its ability to modulate inflammation or induce angiogenesis [62]. Consequently, controlling this variability is not just about good science—it is a regulatory necessity for batch release certification [62].
Experimental Protocols for Controlling Variability
Implementing standardized, monitored protocols is the primary defense against the variability introduced by complex biological systems and reagents.
Protocol for Tracking Culture Performance During Scale-Up
Successful scale-up of mammalian cell cultures requires vigilant monitoring of key performance indicators to detect minor deviations before they become failures. The following metrics and actions are recommended for labs transitioning from small-scale flasks to multi-liter systems [64]:
- Metric 1: Early-Stage Growth Kinetics. Track doubling time from P0 to P2 and lag phase duration after each expansion. Consistent growth in early passages predicts stable performance at larger scales.
- Actionable Protocol: Record growth data at the same time daily. Use a single, consistent viability method (e.g., trypan blue exclusion with automated cell counting) across all technicians. Review doubling times in short weekly intervals.
- Metric 2: Metabolic Load Indicators. Monitor daily glucose and lactate trends and ammonia concentration between feeds. Shifts in metabolic byproducts can predict downstream viability loss.
- Actionable Protocol: Increase sampling frequency during transitions between culture vessels (e.g., from flask to spinner to bioreactor). Compare metabolic profiles against a reference control lot rather than relying on a fixed threshold.
- Metric 3: Phenotypic and Expression Consistency. Document morphology changes relative to the master cell bank and expression levels per cell at multiple time points.
- Actionable Protocol: Capture images at fixed magnifications and standardized timepoints. Use simple assays like ELISA or flow cytometry to validate expression drift. Confirm phenotypic consistency at each expansion stage before proceeding to the next scale.
Diagram 1: A workflow for monitoring key metrics during cell culture scale-up to control variability.
Longitudinal Study on Seeding Density and Feeding Regimes
A 2021 systematic investigation into culturing a human embryonic carcinoma reference cell line (2102Ep) highlights how subtle protocol ambiguities introduce variability. The study compared long-term effects by altering two parameters: seeding density (20,000 vs. 66,667 cells/cm²) and feeding regime (medium exchange after 48h vs. 96h) over multiple passages [61].
Experimental Protocol:
- Cell Culture: 2102Ep cells were maintained in DMEM high glucose with GlutaMAX, supplemented with 10% FBS.
- Variable Application:
- Route A1 (Control): P55 cells seeded at 20,000 cells/cm², fed every 48h, and reseeded at 72h.
- Route B1: P57 cells seeded at 66,667 cells/cm² with a 96h feeding/reseeding cycle.
- Route B2: P59 cells seeded at 20,000 cells/cm² with a 48h feeding/72h reseeding cycle.
- Data Collection: Specific Growth Rate (SGR), viability, and specific metabolite rates (SMR) for glucose were tracked over ten passages.
Key Findings: The results revealed that SGR and viability could be maintained at similar levels under different protocols (e.g., Route B2 had a marginally higher average SGR than A1). However, the specific metabolite rates for glucose differed significantly between routes B1 and B2 [61]. This indicates that interactions between phenotype, metabolism, and feeding regime may not be reflected in growth rates alone, highlighting a hidden layer of variability. The study concludes that the common use of split ratios and subjective confluency assessments in place of defined seeding densities and precise feeding schedules is a major source of uncontrolled inconsistency [61].
The Scientist's Toolkit: Essential Reagent Solutions
Selecting the right tools is fundamental to controlling variability. The table below details key reagent types and their functions, curated from the cited experimental data and industry resources.
Table 2: Key Research Reagent Solutions for Controlling Variability
| Reagent / Material | Function & Rationale | Experimental Evidence & Examples |
|---|---|---|
| Defined, Serum-Free Media | Eliminates lot-to-lot variability of animal sera; supports reproducible cell growth and function. | Studies show serum-free medium choice critically affects cell survival and signaling [63]. Commercially available: eTeSR, StemSpan-AOF, TeSR-AOF 3D [65]. |
| Quality-Controlled FBS | When serum is required, rigorously tested lots provide greater consistency for critical cell culture. | Systematic screening of 12 FBS brands showed profound effects on morphology, drug sensitivity, and differentiation [63]. |
| Synthetic Hydrogels | Provide a defined, reproducible 3D extracellular matrix for organoid and co-culture studies. | Alternatives to animal-derived Matrigel (e.g., GrowDex, Peptimatrix) reduce biological variability [66]. |
| GMP-Grade Cell Activators | Ensure consistent, robust activation and expansion of cells for therapy, like T-cells for CAR-T products. | GMP ImmunoCult-XF T Cell Activators are designed for stable, soluble, and consistent performance [65]. |
| Potency Assay Kits | Quantitatively measure biological activity linked to the mechanism of action for batch release. | Automated ELLA system used for VEGF potency assay of CD34+ cells showed high precision (CV ≤ 10%) [16]. |
Signaling Pathways and Molecular Mechanisms in Potency
Understanding the molecular mechanisms underlying potency is essential for designing relevant assays. For cellular immunotherapies like CAR T-cells, potency is a multi-faceted attribute driven by complex intracellular signaling.
Diagram 2: Key signaling and functional pathways defining potency in cell therapies like CAR T-cells.
The mechanism of action begins with antigen recognition by the chimeric antigen receptor (CAR), triggering T-cell activation [17]. This activation initiates a cascade of cellular responses, which potency assays are designed to measure. The critical functions include:
- Immediate Effector Function: Measured by cytotoxicity against target cells and the release of cytokines like IFN-γ, TNF-α, and IL-2 [17].
- Viability and Expansion: Assessed through cell proliferation and viability assays, ensuring the product can expand after administration [17].
- Persistence: Evaluated by analyzing T-cell phenotypes (e.g., the proportion of stem-cell memory T-cells) and tracking long-term survival in vivo [17]. This complex mechanism is vulnerable to variability at multiple points. Culture conditions that drive T-cells toward an exhausted phenotype or that fail to support robust expansion will result in a less potent product, underscoring the need for controlled processes from the lab bench to the clinic.
Navigating the Transition from Research-Grade to GMP-Compliant Potency Assays
For researchers and drug development professionals in the field of stem cell therapies, potency assays represent far more than a regulatory checkbox—they are the definitive link between laboratory research and clinical success. Potency assays quantitatively measure the biological activity of a cellular product, providing essential evidence of its specific ability to achieve the intended therapeutic effect as defined by regulatory bodies including the FDA and EMA [14] [67]. These assays are legally mandated for each batch of cellular therapy products where the molecular structure cannot be fully defined, making them indispensable for clinical translation [62].
The transition from research-grade assays to Good Manufacturing Practice (GMP)-compliant methods represents a critical juncture in therapeutic development. This process involves transforming exploratory, flexible assays into standardized, validated tests that can consistently ensure product quality, safety, and efficacy across manufacturing batches [68]. For stem cell-based therapies, this transition is particularly complex due to the inherent variability of biological systems and the multifaceted mechanisms of action through which these therapies exert their effects [69] [62]. A well-executed transition strategy not only satisfies regulatory requirements but can significantly accelerate overall development timelines by guiding process decisions and ensuring consistent efficacy [67].
Key Differences Between Research and GMP Potency Assays
Understanding the fundamental distinctions between research-grade and GMP-compliant potency assays is essential for successful transition planning. Research assays are designed for discovery and mechanism elucidation, while GMP assays must deliver standardized, reproducible results suitable for quality control and batch release decisions.
Table: Comparative Analysis of Research-Grade vs. GMP-Compliant Potency Assays
| Characteristic | Research-Grade Assays | GMP-Compliant Assays |
|---|---|---|
| Primary Purpose | Mechanistic investigation, proof-of-concept | Batch release, quality control, regulatory compliance |
| Standardization | Flexible, adaptable protocols | Fixed, rigorously standardized protocols |
| Validation Requirements | Limited or no formal validation | Full validation for accuracy, precision, specificity, linearity, and robustness |
| Reagent Quality | Research-grade, minimal documentation | GMP-grade, full traceability with Certificates of Analysis |
| Data Output | Qualitative or semi-quantitative | Fully quantitative with established acceptance criteria |
| Documentation | Laboratory notebooks, basic protocols | Extensive documentation, including SOPs and validation reports |
| Scalability | Often low-throughput, manual processes | Designed for high-throughput, routine testing |
The regulatory definitions underscore these distinctions. The US FDA defines potency as "the specific ability or capacity of the product, as indicated by appropriate laboratory tests or by adequately controlled clinical data obtained through the administration of the product in the manner intended, to effect a given result" (21 CFR 600.3(s)) [68]. Furthermore, regulations stipulate that potency tests must be "specifically designed for each product so as to indicate its potency in a manner adequate to satisfy the interpretation of potency" (21 CFR 610.10) [68]. The ICH Q6B guidance further emphasizes that potency should be a "quantitative measure of biological activity based on the attribute of the product which is linked to the relevant biological properties" [68].
Common research techniques such as Western blotting and immunoprecipitation often fall short of GMP requirements due to their semi-quantitative nature and variability [68]. Similarly, complex experimental designs using advanced technologies like AlphaLISA, NanoBRET, or mass spectrometry, while powerful for mechanistic studies, may be impractical for routine GMP testing due to their complexity and specialized equipment requirements [68].
Strategic Framework for Transitioning to GMP-Compliant Assays
The Three-Stage Transition Process
Successful transition from research to GMP-compliant potency assays follows a phased approach that aligns with product development milestones [68]. This systematic progression ensures that assay readiness matches regulatory expectations at each development stage.
Development Stage: During preclinical research, the initial assay is designed to represent the product's mechanism of action (MOA) under a limited set of conditions. For stem cell therapies, this typically involves identifying the most relevant biological functions that correlate with therapeutic activity. For example, in human adipose-derived stem cells (hASCs) for wound healing, this might involve measuring secretion of pro-angiogenic factors like VEGF or immunomodulatory capabilities [62].
Optimization Stage: As the product enters early clinical trials, the assay is prepared for expanded use in a commercial setting. This involves defining specifications for critical reagents and considering the availability of materials and specialized equipment [68]. At this stage, developers should address reagent qualification and begin assessing assay performance characteristics.
Qualification/Validation Stage: Prior to Phase 3 trials or submission of Marketing Authorization Applications, the assay undergoes protocol-driven evaluation of reproducibility, accuracy, precision, specificity, robustness, and range [68]. This stage is crucial for setting acceptance criteria for commercial manufacturing.
The following workflow illustrates this systematic transition process:
Analytical Validation Parameters for GMP Compliance
For a potency assay to be considered GMP-compliant, it must demonstrate consistent performance across key validation parameters. These parameters establish the assay's reliability for quality control decision-making.
Table: Essential Validation Parameters for GMP-Compliant Potency Assays
| Validation Parameter | Acceptance Criteria | Application Example |
|---|---|---|
| Accuracy | Mean recoveries between 85-115% | VEGF quantification in CD34+ cell supernatants showed recoveries of 85-105% [16] |
| Precision | CV ≤10-20% for repeatability | Automated VEGF ELISA demonstrated CVs ≤10% for repeatability and ≤20% for intermediate precision [16] |
| Specificity | No interference from matrix components | VEGF assay showed maximal concentration in unspiked medium below LLOQ (2 pg/mL vs 20 pg/mL LLOQ) [16] |
| Linearity | R² ≥0.95 across working range | VEGF assay demonstrated linear range of 20-2800 pg/mL with R²=0.9972 [16] |
| Robustness | Insensitive to minor procedural variations | Consistent performance across operators, equipment, and reagent lots |
Case Studies and Experimental Approaches
CD34+ Cell Therapy Potency Assay Validation
A validated potency assay for ProtheraCytes (expanded autologous CD34+ cells) demonstrates the complete transition from research to GMP-compliant method. The mechanism of action involves promoting cardiac regeneration through angiogenesis mediated by vascular endothelial growth factor (VEGF) secretion [16].
Experimental Protocol:
- Cell Culture: CD34+ cells expanded for 9 days under GMP-compliant conditions
- Sample Collection: Supernatants collected after expansion period
- Analysis Method: Quantitative VEGF measurement using automated ELLA system (Bio-Techne) with microfluidic cartridge design
- Controls: Inclusion of high/low positive controls and negative controls (culture medium alone)
- Validation Parameters: Specificity, linearity, accuracy, precision (repeatability and intermediate precision), and robustness
Key Results: The transition from traditional ELISA to an automated system reduced coefficients of variation (CVs) from >30% to below 15%, demonstrating improved precision required for GMP compliance [16]. The validated method showed a linear response across 20-2800 pg/mL (R²=0.9972), with mean recoveries of 85-105% demonstrating accuracy, and CVs ≤10% for repeatability and ≤20% for intermediate precision confirming precision [16].
Stem Cell Potency Assay Strategies for Wound Healing Applications
For human adipose-derived stem cells (hASCs) in wound healing, potency assay strategies must capture the multifaceted mechanism of action across inflammatory, proliferative, and remodeling phases of healing [62].
Experimental Approaches:
- Biological Assays: In vivo models measuring T-cell infiltration reduction, collagen formation, angiogenesis, and scar reduction
- Surrogate Assays: Quantitative measurements of specific secreted factors (VEGF, HGF, TGF-β) or gene expression markers
- Matrix Approach: Combination of multiple assays to fully characterize product functionality
Key Methodology: When developing potency assays for hASCs, researchers must select methods that reflect the product's relevant mechanisms of action. For immunomodulatory effects, this may include measuring the reduction of pro-inflammatory cytokines (IFN-γ, TNF-α) or increased anti-inflammatory factors (IL-10, PGE2) in co-culture systems [62]. For angiogenic potential, direct measurement of VEGF secretion or endothelial tube formation assays provide quantitative potency measures.
Essential Reagents and Research Tools
The successful transition to GMP-compliant potency assays requires careful selection and qualification of critical reagents. The following toolkit outlines essential materials and their functions in potency assay development and validation.
Table: Research Reagent Solutions for Potency Assay Development
| Reagent Category | Specific Examples | Function in Potency Assessment |
|---|---|---|
| Detection Systems | ELLA automated immunoassay system (Bio-Techne), ELISA kits | Quantitative measurement of secreted factors (VEGF, cytokines) |
| Cell Culture Reagents | GMP-grade culture media, serum-free supplements, expansion cytokines | Maintenance of stem cell phenotype and function during testing |
| Reference Materials | Custom cell mimics (TruCytes), standardized target cells | Assay standardization and reduction of variability |
| Flow Cytometry Reagents | GMP-grade antibodies for surface markers (CD34, CD45, CD73, CD90, CD105) | Phenotypic characterization and purity assessment |
| Molecular Biology Tools | ddPCR for vector copy number, TCR sequencing | Genetic modification quantification and cellular repertoire analysis |
Analysis of FDA-Approved Cell Therapy Potency Tests
Reviewing potency tests used for FDA-approved cell therapy products provides valuable insights for developers designing their own assays. An analysis of 31 approved CTPs revealed that a matrix approach is common, with an average of 3.4 potency tests per product [15].
Frequency of Potency Test Types:
- Viability and Count: 37 tests (52%) - Used by 19 of 31 CTPs (61%)
- Expression Markers: 19 tests (27%) - Used by 20 of 31 CTPs (65%)
- Bioassays: 7 tests (7%) - Functional activity measurements
- Genetic Modification: 6 tests (9%) - Vector copy number, transgene expression
- Histology: 2 tests (3%) - Tissue organization and cell viability
Notably, "Viability and Count" and "Expression" are the two tests most frequently used together, occurring for 16 CTPs (52%) [15]. This combination approach allows for both quantitative cellular metrics and functional characterization.
For CAR-T cell therapies specifically, common potency measurements include:
- CAR expression by flow cytometry
- Interferon-γ production in response to target cells (e.g., Kymriah, Yescarta) [15]
- Cytotoxic activity against target cells (e.g., Tecelra) [15]
Emerging Technologies and Future Directions
The field of potency assessment is rapidly evolving with new technologies enhancing our ability to characterize complex cell therapy products meaningfully.
Multi-Omics Approaches: Advanced profiling methods including genomics, epigenomics, transcriptomics, proteomics, and metabolomics are providing unprecedented insights into cell therapy products at the molecular level [17]. For CAR-T cells, these approaches have identified key characteristics associated with clinical responses, such as:
- Vector Integration Sites: Monitoring for potential genotoxicity and clonal expansion
- TCR Repertoire: Assessing diversity as a potential potency marker
- Epigenetic Profiles: Evaluating differentiation states that impact persistence
- Metabolic Profiles: Characterizing energy pathways influencing function
Novel Analytical Platforms: Automated systems like the ELLA platform used in the CD34+ cell case study demonstrate how technological advances can address GMP requirements for precision, reproducibility, and practical implementation in quality control environments [16]. These systems reduce operator-dependent variability and provide the standardized operating procedures essential for GMP compliance.
The integration of artificial intelligence and machine learning for potency assay data analysis represents the next frontier in cell therapy characterization, potentially enabling more predictive correlations between in vitro potency measurements and clinical outcomes [69].
Ensuring Quality and Compliance: Validation Parameters and Comparative Analysis
In the development of stem cell therapies, demonstrating therapeutic efficacy through robust potency assays is a critical regulatory and scientific requirement. These assays are essential for confirming that a cellular product possesses the biological activity required for its intended clinical effect, as defined by its mechanism of action (MoA) [17] [55]. For Advanced Therapy Medicinal Products (ATMPs), regulators require a "potency strategy" that ideally uses quantitative assays to measure biological activity, ensuring batch-to-batch consistency, manufacturing control, and product stability [70] [55]. The validation of these methods ensures that the results generated are reliable and fit for their intended purpose, guiding critical decisions in both research and clinical development.
The core validation parameters—specificity, accuracy, precision, linearity, and robustness—form the foundation of this process. These parameters are evaluated during a structured method qualification, which confirms the assay is appropriate before proceeding to full validation [70]. This guide examines these core parameters through the lens of stem cell potency, providing a comparative analysis of experimental approaches and technical standards essential for researchers and drug development professionals.
Defining the Core Validation Parameters
Specificity
Specificity is the ability of an assay to unequivocally assess the analyte of interest in the presence of other components, such as impurities, matrix elements, or other interfering substances. In the context of potency, it confirms that the measured signal is directly and solely related to the intended biological activity [16]. For a stem cell therapy whose MoA involves secretion of a specific factor, the potency assay must specifically quantify that factor without cross-reactivity or interference from the culture medium or other secreted proteins.
Accuracy
Accuracy expresses the closeness of agreement between the measured value and a value accepted as either a conventional true value or an accepted reference value. It indicates how correct the results are. Accuracy is often assessed by measuring the recovery of a known amount of the analyte (spike) added to a sample matrix [70] [16]. In cell-based assays, where a "true value" is often elusive, accuracy can be evaluated by comparing results to those from a validated reference method or by using standards of known activity [71].
Precision
Precision describes the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions. It is a measure of reproducibility and is typically examined at three levels:
- Repeatability: Precision under the same operating conditions over a short interval of time (intra-assay).
- Intermediate Precision: Precision within laboratories, such as between different days, analysts, or equipment.
- Reproducibility: Precision between different laboratories (often not assessed until validation) [70].
Precision is usually expressed as the coefficient of variation (CV) (%)(CV)(CV) of a series of measurements [16].
Linearity
Linearity of an analytical method is its ability to elicit test results that are directly proportional to the concentration of analyte in the sample within a given range. This range, the "linear range," is the interval of concentrations over which the method performs with acceptable accuracy, precision, and linearity. The assessment involves preparing and analyzing a series of samples with known analyte concentrations across the expected range and evaluating the relationship, often via linear regression resulting in a correlation coefficient (R²) [16].
Robustness
Robustness is a measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters. It indicates the reliability of an method during normal usage. Parameters to test can include incubation times, temperatures, reagent lots, or analyst technique. A robust method will show minimal variability in results when these operational parameters are slightly altered [70] [71].
Experimental Data and Comparative Analysis
The following sections present experimental data from qualified and validated cell-based potency assays, illustrating how these core parameters are evaluated in practice.
Case Study: Flow Cytometry-Based Cytotoxicity Potency Assay
A study detailing the qualification of a flow cytometry-based method for assessing the potency of an allogeneic Natural Killer (NK) cell product, GTA002 (oNKord/inaleucel), provides a clear template for evaluating core parameters [70]. The method quantitatively determines effector and target cell counts and qualitatively expresses potency as a percentage of cytotoxicity.
Table 1: Qualification Results for a Flow Cytometry-Based Cytotoxicity Assay [70]
| Validation Parameter | Experimental Approach | Result | Pre-defined Acceptance Criteria |
|---|---|---|---|
| Accuracy | Comparison of measured bead concentration to known value using counting beads. | Mean recovery of 100.2% | Recovery within 80–120% |
| Precision (Repeatability) | 10 replicates of one sample in one run by one analyst. | CV ≤ 10% for effector and target cell counts | CV ≤ 15% for cell count; CV ≤ 20% for cytotoxicity |
| Precision (Intermediate Precision) | Multiple replicates over different days by different analysts. | CV ≤ 20% for cytotoxicity | CV ≤ 20% for cytotoxicity |
| Linearity & Range | Serial dilutions of counting beads and effector cells across expected E:T ratios. | Linear response (R² > 0.95) across all tested ranges | R² ≥ 0.95 |
| Specificity | Use of fluorochrome-conjugated antibodies and viability dye to distinguish effector and target cells in co-culture. | Effector and target cell populations were effectively resolved. | Clear discrimination of cell populations |
| Robustness | Deliberate variation in incubation time and staining volume. | CV within acceptable precision limits | Method performance maintained despite variations |
Case Study: VEGF ELISA Potency Assay for CD34+ Cell Therapy
For ProtheraCytes, an expanded autologous CD34+ cell therapy, the mechanism of action involves revascularization via secretion of Vascular Endothelial Growth Factor (VEGF). Consequently, a potency assay was developed and validated based on the quantification of VEGF secreted during cell expansion using an automated immunoassay system (ELLA) [16].
Table 2: Validation Results for a VEGF ELISA Potency Assay [16]
| Validation Parameter | Experimental Approach | Result | Acceptance Criteria |
|---|---|---|---|
| Accuracy (Recovery) | Spiking of known concentrations of VEGF into the cell culture medium (StemFeed). | Mean recovery between 85% and 105% for all concentrations | 80–120% |
| Precision (Repeatability) | Multiple replicates of three control levels within one run. | CV ≤ 10% | CV ≤ 15% or 20% |
| Precision (Intermediate Precision) | Multiple replicates of three control levels across different days and analysts. | CV ≤ 20% | CV ≤ 20% |
| Linearity | Analysis of 8 spiked VEGF concentrations across the range of 20–2800 pg/mL. | R² = 0.9972 | R² > 0.95 |
| Specificity | Measurement of VEGF in unspiked StemFeed culture medium. | VEGF concentration < 2 pg/mL (below the Lower Limit of Quantification (LLOQ) of 20 pg/mL) | Concentration in blank below LLOQ |
| Robustness | Not explicitly detailed, but the automated ELLA platform reduces manual handling variability. | N/A | N/A |
Experimental Protocols for Key Assays
Protocol: Flow Cytometry-Based Cell Potency/Cytotoxicity Assay
This protocol is adapted from the qualification of the NK cell potency assay [70].
1. Principle: Effector cells (e.g., NK, CAR-T cells) are co-cultured with target cells (e.g., leukemic K562 cell line). After co-culture, cells are stained with fluorochrome-conjugated antibodies and a viability dye. Flow cytometry is used to quantitatively distinguish and count live effector and target cells, from which percentage cytotoxicity is calculated.
2. Materials:
- Effector Cells: The cellular therapy product (e.g., GTA002 NK cells).
- Target Cells: Pre-stained K562 chronic myelogenous leukemia cell line.
- Staining Antibodies: Fluorochrome-labelled antibodies against effector cell markers (e.g., anti-CD45) and target cell markers.
- Viability Dye: 7-AAD or propidium iodide (PI).
- Culture Medium: Appropriate medium, often supplemented with cytokines (e.g., IL-2, IL-15).
- Flow Cytometer: A calibrated instrument with capabilities for the chosen fluorochromes.
3. Procedure:
- Step 1: Preparation. Thaw and wash effector and target cells if cryopreserved. Resuspend in culture medium.
- Step 2: Co-culture. Plate effector and target cells at multiple Effector:Target (E:T) ratios (e.g., 10:1, 3:1, 1:1) in a multi-well plate. Include controls for effector cells alone and target cells alone to determine background.
- Step 3: Incubation. Incubate the co-culture plates for a specified duration (e.g., 4-24 hours) in a 37°C, 5% CO₂ incubator.
- Step 4: Staining. Harvest cells from the co-culture. Stain with predetermined concentrations of antibodies and viability dye for 15 minutes at room temperature in the dark. Do not wash after staining if using 7-AAD/PI direct staining.
- Step 5: Acquisition. Acquire samples on the flow cytometer, collecting a sufficient number of events for statistical analysis.
- Step 6: Analysis. Using flow cytometry analysis software, gate on live (viability dye-negative) cells. Further gate on effector cell and target cell populations based on their specific markers. The percentage cytotoxicity can be calculated using formulas that account for the natural death of target cells in the control sample.
Protocol: VEGF Quantification Potency Assay
This protocol is adapted from the validated method for ProtheraCytes [16].
1. Principle: The concentration of VEGF secreted by CD34+ cells into the culture supernatant is quantified using a sandwich-type quantitative immunoassay. The assay uses specific antibodies against VEGF-A, and the resulting fluorescence is proportional to the amount of VEGF present.
2. Materials:
- Cell Culture Supernatant: Supernatant collected from expanded CD34+ cell cultures after a defined period (e.g., 9 days).
- Automated Immunoassay System: ELLA system (Bio-Techne).
- VEGF Cartridge: Simple Plex Cartridge Kit containing VEGF-A.
- Controls: High, low, and negative controls for system suitability.
3. Procedure:
- Step 1: Sample Collection. Centrifuge the CD34+ cell culture to pellet cells. Collect the supernatant without disturbing the cell pellet.
- Step 2: Sample Loading. Load the supernatant samples and controls into the designated wells of the VEGF cartridge according to the manufacturer's instructions.
- Step 3: Run. Insert the cartridge into the ELLA instrument and start the pre-programmed run. The system is fully automated, performing all incubation, washing, and detection steps.
- Step 4: Data Analysis. The instrument software automatically generates a standard curve and calculates the VEGF concentration in each sample, reported in pg/mL.
Visualization of Validation Workflows and Concepts
Potency Assay Validation Pathway
This diagram outlines the sequential process of developing and validating a fit-for-purpose potency assay.
Accuracy vs. Precision in Measurement
This conceptual diagram illustrates the fundamental difference between accuracy and precision, a critical concept in assay validation.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and instruments critical for implementing and validating cell-based potency assays.
Table 3: Essential Research Reagent Solutions for Potency Assay Development
| Item | Function / Application | Example Use Case |
|---|---|---|
| Fluorochrome-conjugated Antibodies | Label specific cell surface markers (e.g., CD45, CD3) for identification and enumeration via flow cytometry. | Distinguishing effector cells from target cells in a co-culture cytotoxicity assay [70]. |
| Viability Dyes (7-AAD, PI, Annexin V) | Identify dead or apoptotic cells by penetrating compromised membranes, crucial for accurate live cell counting. | Determining the viability of cellular products pre- and post-co-culture; part of the gating strategy in flow cytometry [70] [72]. |
| Automated Immunoassay System (e.g., ELLA) | Perform fully automated, microfluidic-based sandwich ELISAs. Reduces hands-on time and variability. | Quantifying secreted potency markers (e.g., VEGF) from cell culture supernatants with high precision [16]. |
| Cell Culture Media & Supplements | Support the growth and function of cells during in vitro potency assays. Cytokines (e.g., IL-2, IL-15) can maintain effector cell activity. | Maintaining NK cell potency during the cytotoxicity co-culture period [70]. |
| Reference Materials & Controls | Calibrate instruments, validate methods, and serve as in-process controls to assure measurement quality. | Using counting beads for flow cytometry accuracy checks; using high/low VEGF controls for assay qualification [70] [71] [16]. |
| Cryopreservation Solutions (e.g., CryoStor) | Protect cells from cryo-injury during frozen storage, preserving viability and potency for later testing. | Storing standardized batches of effector or target cells for use in repeat potency assays over time [73]. |
The rigorous application of core validation parameters—specificity, accuracy, precision, linearity, and robustness—is non-negotiable for developing stem cell potency assays that are both scientifically sound and regulatory compliant. As demonstrated by the case studies, a "fit-for-purpose" qualified method forms the foundation for reliable product characterization, lot release, and stability studies. The evolving regulatory landscape, which now increasingly considers advanced profiling like genomic and epigenomic characteristics, underscores the need for robust and potentially multi-parametric potency assays [17]. By adhering to these fundamental validation principles and leveraging modern tools like automated immunoassay platforms and highly standardized flow cytometry, developers can ensure their stem cell therapies are characterized with the highest level of confidence, ultimately accelerating the translation of these promising treatments from the laboratory to the clinic.
Potency assays are critical quality control tests required by regulatory bodies like the U.S. Food and Drug Administration (FDA) to ensure that cell therapy products (CTPs) can consistently deliver their intended biological effect. These assays serve to confirm that a product's proposed mechanism of action will translate into clinical efficacy, assess manufacturing consistency, and evaluate product stability [15]. For Advanced Therapy Medicinal Products (ATMPs), including those based on CD34+ hematopoietic stem cells and mesenchymal stromal cells (MSCs), developing appropriate potency tests remains a significant challenge for developers [15]. An analysis of the 31 FDA-approved CTPs reveals that products typically employ multiple potency tests, with an average of 3.4 tests per product [55]. This guide provides a comprehensive comparison of validated potency assays for CD34+ and MSC-based therapies, summarizing experimental data and methodologies to support researchers and drug development professionals in this critical area.
CD34+ Hematopoietic Stem Cell Therapy Potency Assays
Validated Assays and Key Metrics
CD34+ hematopoietic stem cells are crucial for reconstituting the hematopoietic system in patients with disorders affecting blood cell production. The potency assays for these therapies focus on quantifying viable stem cells and demonstrating their functional capacity for proliferation and differentiation.
Table 1: Validated Potency Assays for CD34+ Hematopoietic Stem Cell Therapies
| Product Category | Potency Tests Employed | Key Metrics Measured | Regulatory Reference |
|---|---|---|---|
| Cord Blood Units (Hemacord, Allocord, etc.) | Total Nucleated Cells (TNC) | Total cell count | [15] |
| Viability of CD45+ or total nucleated cells | Cell vitality | [15] | |
| Viable CD34+ Cell Count (flow cytometry) | Stem cell quantity | [15] | |
| Colony Forming Unit (CFU) Assay | Functional differentiation potential | [15] | |
| Cultured Cord Blood (Omisirge) | CD34+ Cell Fold-Increase | Expansion potential | [15] |
| Genetically Modified HSCs (Zynteglo, Skysona) | Vector Copy Number (qPCR) | Genetic modification level | [15] |
| Percent Lentiviral Vector-Positive Cells | Transduction efficiency | [15] | |
| Colony Forming Cells (CFC) | Clonogenic potential | [15] |
Advanced Functional Potency Assays
Beyond basic characterization, novel functional potency assays have been developed to better predict the in vivo performance of CD34+ cell products. The IL-3-pSTAT5 phospho flow cytometry assay represents one such advanced method that has undergone rigorous validation [74].
Experimental Protocol: IL-3-pSTAT5 Phospho Flow Cytometry Assay
- Sample Preparation: Cryopreserved cord blood units (CBUs) are thawed and processed for analysis [74].
- Stimulation: CD34+ cells are stimulated with interleukin-3 (IL-3) to activate the STAT-5 signaling pathway [74].
- Fixation and Permeabilization: Cells are fixed and permeabilized to allow intracellular staining.
- Antibody Staining: Cells are stained with fluorescently labeled antibodies against CD34, CD45, and phosphorylated STAT5 (pSTAT5) [74].
- Flow Cytometry Analysis: Samples are analyzed using flow cytometry to quantify the percentage of CD34+CD45+pSTAT5+ cells [74].
- Data Interpretation: Results are compared against an established threshold of 50% CD34+CD45+pSTAT5+, which provides 100% sensitivity and 98.3% specificity for predicting unit potency [74].
This assay demonstrated excellent correlation with the traditional Colony-Forming Unit (CFU) assay (r² = 0.82, n = 56) while offering significantly faster turnaround time [74]. The validation study confirmed robust intra-assay precision (average CV of 7.3%), inter-user and inter-laboratory agreement, and stability under varying post-thaw incubation and staining conditions [74].
Expanded Flow Cytometric Panels for Enhanced Characterization
Modern flow cytometric approaches have evolved beyond basic CD34 enumeration to include additional parameters critical for product characterization. The International Society of Hematotherapy and Graft Engineering (ISHAGE) protocol has been the gold standard for stem cell enumeration, but expanded panels now provide more comprehensive product profiling [75].
Experimental Protocol: Expanded Flow Cytometric Panel
- Panel Design: A pre-formulated dried antibody panel containing CD45 FITC, CD34 PE, CD3 Pacific Blue, CD19 APC, and viability dye 7-AAD [75].
- Sample Staining: The dried reagent format ensures improved standardization and reliability compared to liquid antibody formulations [75].
- Flow Cytometry Analysis: Using counting beads for absolute quantification [75].
- Multi-Parameter Analysis: Simultaneous enumeration of leucocytes (CD45+), stem cells (CD34+), T-cells (CD3+), and B-cells (CD19+) with viability assessment [75].
This validated approach demonstrates high linearity (r² ≥ 0.95 for all populations), sensitivity, and accuracy across various sample types including peripheral blood, fresh leukapheresis products, and cryopreserved stem cell products [75]. The inclusion of T-cell and B-cell enumeration is particularly valuable for products such as donor lymphocyte infusions, TCR α/β- and CD19-depleted haploidentical allogeneic stem cell grafts, and various ATMPs [75].
Figure 1: Workflow of the IL-3-pSTAT5 phospho flow cytometry potency assay for CD34+ hematopoietic stem cells [74].
MSC-Based Therapy Potency Assays
MSC Characterization and Critical Quality Attributes
Mesenchymal stromal cells (MSCs) represent a promising therapeutic option for diverse conditions including osteoarthritis, graft-versus-host disease, and cardiovascular diseases [76]. According to the International Society for Cell and Gene Therapy (ISCT), MSCs must meet three key criteria: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, CD105 ≥95%; lack of CD45, CD34, CD14/CD11b, CD79α/CD19, HLA-DR ≤2%); and (3) capacity for in vitro differentiation into osteogenic, chondrogenic, and adipogenic lineages [77] [76].
Table 2: Critical Quality Attributes for MSC-Based Therapies
| Category | Parameter | Measurement Technique | Significance |
|---|---|---|---|
| Dosage | Cell Count | Automated cell counters | Determines therapeutic dose |
| Cell Viability | Trypan blue, flow cytometry with viability dyes | Ensures product quality and safety | |
| Identity | Immunophenotype | Flow cytometry for CD73, CD90, CD105 (positive) and CD45, CD34, CD14, CD19, HLA-DR (negative) | Confirms MSC identity per ISCT criteria |
| Potency | Trilineage Differentiation | Osteogenic, chondrogenic, adipogenic induction with histological staining | Demonstrates multipotency |
| Secretome Analysis | ELISA, multiplex arrays for growth factors, cytokines | Measures paracrine activity | |
| Immunomodulatory Activity | T-cell suppression assays, IDO activity | Quantifies immune modulation capacity |
Addressing MSC Heterogeneity in Potency Assessment
MSC therapies face significant challenges in potency assessment due to high donor-to-donor and batch-to-batch variability [76]. This heterogeneity necessitates robust, standardized manufacturing processes and analytical methods to ensure consistent product quality. As MSC therapies advance, there is increasing emphasis on implementing Quality-by-Design (QbD) approaches to identify Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs) [76].
For MSC manufacturing, key quality attributes consistently measured include cell number and viability, immunophenotype, and differentiation potential [76]. The transition from two-dimensional to three-dimensional bioreactor systems for MSC expansion introduces additional complexity in potency assessment, requiring careful monitoring of process parameters including pH, dissolved oxygen, and nutrient supply [76].
Emerging Approaches for MSC Potency Assessment
Recent advances in MSC potency testing focus on mechanism-based assays that reflect the proposed therapeutic mechanism of action. For MSC-derived extracellular vesicle (MSC-EV) therapies, which were a highlighted topic at the ISCT 2025 Annual Meeting, potency assay development faces unique challenges [78].
Key considerations for MSC-EV potency assays include:
- Pinpointing the "active ingredient" in context-specific settings [78]
- Aligning manufacturing with Critical Quality Attributes (CQAs) and potency assays [78]
- Implementing single-vesicle analytics for comprehensive characterization [78]
- Engaging regulators early to align on mechanism-driven product definitions [78]
The field is moving toward embedding potency assays into early process development and manufacturing protocols, with analytics directly linked to clinical relevance [78].
Comparative Analysis of Signaling Pathways
The therapeutic effects of both CD34+ and MSC-based therapies are mediated through specific signaling pathways that can be leveraged for potency assessment.
Figure 2: Key signaling pathways utilized in potency assays for CD34+ hematopoietic stem cells and MSC-based therapies [74] [77].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell Potency Assays
| Reagent Category | Specific Examples | Application | Experimental Function |
|---|---|---|---|
| Flow Cytometry Antibodies | Anti-CD34, CD45, CD3, CD19, CD73, CD90, CD105 | Cell surface marker identification | Phenotypic characterization and purity assessment |
| Intracellular Staining Reagents | Anti-pSTAT5, fixation/permeabilization buffers | Phospho flow cytometry | Detection of intracellular signaling activation |
| Viability Assessment | 7-AAD, trypan blue, propidium iodide | Viability staining | Discrimination of live/dead cells |
| Cell Culture Reagents | Colony-Stimulating Factors, Mesenchymal Stem Cell Media, Differentiation Kits (osteogenic, chondrogenic, adipogenic) | Functional assays | Support of cell growth and differentiation potential |
| Molecular Biology Tools | qPCR reagents, ELISA kits, multiplex cytokine arrays | Molecular analysis | Gene expression, protein quantification, secretome analysis |
Validated potency assays for CD34+ and MSC-based therapies encompass a range of techniques from basic cell quantification to sophisticated functional assessments. The IL-3-pSTAT5 phospho flow cytometry assay represents a robust, validated approach for CD34+ cell potency assessment that correlates well with traditional CFU assays while offering improved speed and standardization [74]. For MSC-based therapies, potency assessment requires a multi-parameter approach addressing immunophenotype, differentiation potential, and immunomodulatory activity [77] [76]. The field is increasingly moving toward mechanism-based potency tests that directly reflect the proposed biological activity of the product, with an emphasis on standardization and quality-by-design principles to ensure consistent manufacturing of safe and effective therapies [76] [15]. As stem cell science continues to advance, potency assays will likely evolve toward greater physiological relevance, potentially incorporating multi-omics approaches and functional assessments that better predict in vivo performance.
For researchers and drug development professionals working with stem cells and other advanced therapy medicinal products (ATMPs), potency assays are not merely a regulatory checkbox; they are a fundamental Critical Quality Attribute (CQA) that defines the biological activity of the product. Potency represents the therapeutic activity of the drug product as indicated by appropriate laboratory tests or by adequately developed and controlled clinical data, serving as a legal requirement for lot release testing of biologics [79]. As the field of cell therapy continues to expand—with the US FDA approving 31 cell therapy products between 2010 and 2024—the strategic selection of appropriate potency assays has never been more critical for ensuring product safety, efficacy, and manufacturing consistency [55].
The central challenge in potency assay development lies in creating a quantitative measure that accurately reflects the drug's intended mechanism of action (MoA) while being practically implementable within manufacturing and quality control constraints. For stem cell therapies and other complex biologics, this often requires a matrix of assays that collectively capture the multifaceted nature of biological activity. This comparative analysis examines the landscape of available potency assay technologies, their applications in stem cell research, and strategic considerations for selecting the optimal approach for your product development pipeline.
Current Landscape: Analysis of FDA-Approved Cell Therapy Products
A comprehensive review of the 31 US FDA-approved cell therapy products reveals critical patterns in potency assay implementation. These products collectively employ 104 potency tests, averaging 3.4 tests per product (standard deviation 2.0), with a median of 3.0 tests [55]. This data underscores the common regulatory acceptance of a potency assay matrix rather than relying on a single test method.
Table 1: Distribution of Potency Test Types for 31 FDA-Approved Cell Therapy Products
| Test Category | Number of Tests | Percentage of Non-Redacted Tests | Example Applications |
|---|---|---|---|
| Viability and Count | 37 | 52% | Cell viability, total nucleated cell count |
| Expression | 19 | 27% | CAR expression, surface marker expression |
| Bioassays | 7 | 7% | Cytotoxicity, cytokine release |
| Genetic Modification | 6 | 9% | Vector copy number, transgene expression |
| Histology | 2 | 3% | Tissue structure assessment |
The distribution of potency test types reveals that relatively simple "Viability and Count" measurements dominate current regulatory strategies, followed by "Expression" assays [55]. However, it is important to note that 32% of potency tests (33 of 104) were redacted in regulatory documents, potentially obscuring the complete picture, particularly for more complex bioassays which may be underrepresented in public data [55].
When analyzed by product class, hematopoietic stem cell-cord blood products utilized the highest number of potency tests per product (4.4 ± 0.7), while tissue-engineered products and CAR T-cell therapies employed fewer tests (1.8 ± 1.1 and 1.9 ± 0.9 respectively) [55]. This variability highlights how assay selection must be tailored to product-specific characteristics and mechanisms of action.
Comparative Analysis of Major Potency Assay Platforms
In Vivo vs. In Vitro Assay Systems
The fundamental division in potency assay approaches lies between traditional in vivo systems and increasingly sophisticated in vitro alternatives. In vivo assays, which measure immune response or protection in animal models, have historically been the gold standard for many vaccine products [23]. However, these assays present significant ethical concerns under the 3Rs principles (Replacement, Reduction, and Refinement), require substantial resources, exhibit high variability (%CV of 34% to 125%), and necessitate lengthy experimental periods [23] [80].
In contrast, in vitro methods address many of these limitations by providing results with lower variability (%GCV below 10% for some platforms), faster turnaround times, reduced ethical concerns, and lower operational costs [23]. The transition to in vitro alternatives is particularly relevant for stem cell therapies, where in vivo models may poorly predict human physiological responses.
Table 2: In Vivo vs. In Vitro Potency Assay Comparison
| Parameter | In Vivo Assays | In Vitro Assays |
|---|---|---|
| Variability | High (%CV 34-125%) [23] | Low (%GCV <10%) [23] |
| Duration | Weeks to months | Hours to days |
| Ethical Considerations | Significant animal use | Minimal animal use |
| Resource Intensity | High (housing, feeding, space) | Moderate (specialized equipment) |
| Physiological Relevance | Whole-system response | Isolated mechanism |
| Regulatory Precedent | Well-established | Increasingly accepted |
Advanced In Vitro Assay Technologies
Bioelectronic Assays
Bioelectronic assays represent a cutting-edge approach that enables real-time, label-free monitoring of cell activity through impedance-based systems. These platforms use microtitre plates with embedded electrodes to measure cellular impedance, which correlates with cell viability and status [56]. As cells attach to the well surface, they cover more electrode area, increasing impedance; cell death causes detachment and decreased impedance [56].
This technology provides continuous kinetic data on cytolysis, enabling researchers to determine not just if cells are killed, but when and how rapidly the killing occurs. A study investigating GD2-targeted CAR-T cells for glioblastoma demonstrated the power of this approach, revealing exhaustion patterns where cell killing never reached 100% despite initial effectiveness [56]. The GxP-compliant versions of these systems are increasingly valuable for regulatory submissions as developers must provide more comprehensive potency data [56].
Live-Cell Imaging Platforms
Live-cell imaging systems, such as the Incucyte platform, provide visual documentation of cell behavior over days to months under controlled environmental conditions [56]. These systems enable direct observation of cell-cell interactions and temporal dynamics, offering rich qualitative and quantitative data. However, they present technical challenges including potential occlusion when immune cells are plated atop target cells, the need for differentiating dyes that may alter cellular behavior, and complex data analysis requiring subjective interpretation [56].
Endpoint Assay Methods
Traditional endpoint methods continue to play important roles in potency assessment. The chromium release assay, despite being a longtime gold standard, is increasingly being replaced due to safety concerns regarding radioactive materials [56]. Colorimetric alternatives like lactate dehydrogenase (LDH) and MTT assays provide non-radioactive options but share limitations of being time-consuming, technically demanding, and providing only single timepoint measurements [56]. These methods may miss critical kinetic events such as shifts in kill curves or immune cell exhaustion followed by tumor regrowth [56].
Emerging Multi-Omics Approaches in Potency Assessment
Advanced analytical technologies are enabling more comprehensive product characterization through multi-omics approaches. Genomic profiling now extends beyond basic vector copy number (VCN) analysis to include vector integration sites and T-cell receptor (TCR) repertoire sequencing [17]. The recent FDA investigation into secondary malignancies following CAR T-cell therapy highlights the importance of monitoring vector integration sites for safety assessment [17].
Epigenomic profiling provides insights into CAR T-cell differentiation states, which are critically important for therapeutic efficacy [17]. Carlos et al. analyzed DNA methylation profiles in 114 CD19 CAR T-cell products and identified 18 distinct epigenetic loci associated with clinical outcomes [17]. Similarly, transcriptomic, proteomic, and metabolomic analyses at both bulk and single-cell resolution are enhancing our understanding of CAR T-cell function at the molecular level [17].
Table 3: Multi-Omics Technologies for Potency Assessment
| Technology Type | Key Measurements | Applications in Potency Assessment |
|---|---|---|
| Genomics | Vector copy number, integration sites, TCR repertoire | Safety, clonal expansion, persistence |
| Epigenomics | DNA methylation, chromatin accessibility | Differentiation state, memory potential |
| Transcriptomics | RNA expression patterns | Functional subset identification, exhaustion markers |
| Proteomics | Surface marker expression, intracellular signaling | Activation status, effector molecules |
| Metabolomics | Energy metabolism, metabolic intermediates | Metabolic fitness, persistence capacity |
Experimental Design and Methodologies
Core Experimental Protocols
Cytotoxicity Bioassay Protocol
A well-designed cytotoxicity assay should quantify immune cell-mediated killing at physiologically relevant cell ratios to provide insight into functionality [56]. A representative protocol for impedance-based cytotoxicity assessment includes:
- Plate Preparation: Seed target cells (e.g., tumor cells) in a 96-well bioelectronic plate at optimal density (e.g., 10,000-50,000 cells/well depending on cell size) and culture for 24-48 hours to establish monolayer [56].
- Baseline Measurement: Record initial impedance values using bioelectronic system after target cell adhesion [56].
- Effector Cell Addition: Add therapeutic cells (e.g., CAR-T cells, stem cells) at effector-to-target ratios spanning physiological range (e.g., 0.1:1 to 10:1) [56].
- Continuous Monitoring: Maintain plates in controlled environment (37°C, 5% CO2) with impedance measurements taken at regular intervals (e.g., every 15 minutes) for duration of experiment (typically 3-9 days) [56].
- Data Analysis: Calculate cytolysis metrics including time to 50% killing (KT50), maximum kill rate, and area under the curve for kinetic response [56].
Two-Stage Serological Assay Protocol
For products where immune activation is the mechanism of action, a two-stage serological approach may be appropriate:
- Immunization Phase: Administer set doses of reference and test batches to subject groups (in vivo) or immune cell cultures (in vitro) [23].
- Serum Collection: After predetermined period (typically 2-4 weeks), collect serum samples or culture supernatants [23].
- Antibody Titration: Create dilution series from each sample and determine antibody titer through ELISA or similar immunoassay [23].
- Dose-Response Modeling: Plot titer against original dose and use parallel line analysis to estimate relative potency [23].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Potency Assays
| Reagent/Platform | Function | Application Context |
|---|---|---|
| Bioelectronic Plates (e.g., Maestro Z) | Label-free, real-time impedance monitoring | Continuous cytotoxicity kinetics |
| Live-Cell Imaging Systems (e.g., Incucyte) | Visual monitoring of cell interactions | Morphological assessment, adhesion |
| Flow Cytometry Panels | Multiplexed surface and intracellular marker analysis | Phenotypic characterization, purity |
| ddPCR/qPCR Reagents | Vector copy number quantification, gene expression | Genetic modification assessment |
| Cytokine Detection Assays | Multiplexed cytokine quantification (IFN-γ, IL-2, etc.) | Functional activation assessment |
| Metabolic Assay Kits | Glycolytic rates, mitochondrial function | Metabolic fitness profiling |
| Epigenetic Modifiers | DNMT/HDAC inhibitors, CRISPR-epigenetic tools | Differentiation state manipulation |
Strategic Implementation and Regulatory Considerations
Assay Validation and Variability Management
Potency assays demonstrate significantly higher variability compared to physicochemical methods, necessitating careful validation and control strategies [79]. Relative Potency (RP) measurement, derived from pairwise comparison of dose-response curves between reference standard and test samples, helps control intra-lab and interlab variability [79]. The four-parameter logistic (4PL) fit is most commonly used, though other models (5PL, linear fit with parallel line analysis) may be appropriate depending on experimental setup [79].
A robust assay validation strategy should include:
- Analytical Quality by Design (AQbD): Implementing design of experiments (DoE) to find optimal parameter ranges and identify interactions [79].
- Replication Strategy: Incorporating multiple dilution series within assay runs to improve precision and enable outlier identification [79].
- Run Number Optimization: Determining appropriate number of assay runs for reportable potency value based on variability assessment [79].
Diagram 1: Integrated Potency Assay and Manufacturing Development Timeline
Regulatory Expectations and Documentation
Regulators expect potency tests to assure manufacturing consistency, product stability, and intended biological activity [55]. The potency test is typically performed on the final manufactured product after packaging as part of release testing for licensure [55]. As revealed in the analysis of FDA-approved products, a matrix approach is common, with 65% of products using gene or protein expression measurements and 61% using cell viability or count as potency tests [55].
For novel stem cell therapies, developers should anticipate increased regulatory scrutiny on demonstrating that potency assays adequately capture the relevant biological mechanisms. The integration of multi-omics data into potency arguments is becoming increasingly valuable, though the transition from characterization assays to validated potency methods requires substantial bridging data [17].
Selecting the appropriate potency assay requires balancing scientific rigor with practical implementation within manufacturing constraints. Based on our analysis of approved products and emerging technologies, we recommend:
Adopt a Matrix Approach: Implement multiple complementary assays that collectively capture critical mechanism(s) of action, following the pattern of approved products averaging 3.4 potency tests each [55].
Prioritize Physiological Relevance: Select assays that most closely mirror the intended therapeutic mechanism, even when simpler surrogate assays are available [79].
Incorporate Kinetic Measurements: Where possible, utilize real-time platforms like bioelectronic assays that provide rich kinetic data beyond single endpoint measurements [56].
Plan for Regulatory Evolution: Anticipate increasing expectations for comprehensive potency data by building robust datasets during development that support later-stage submissions [17] [56].
Balance Innovation and Practicality: While emerging multi-omics technologies offer unprecedented characterization depth, ensure that release methods are practical for GMP implementation and stability monitoring [17] [79].
The optimal potency assay strategy is product-specific and stage-appropriate, evolving from early research focus on mechanism elucidation to commercial emphasis on robustness and reproducibility. By applying these principles and learning from approved products, developers can create potency assessment strategies that adequately characterize their product's biological activity while meeting regulatory expectations for market approval.
The Role of Reference Standards and Controls in Ensuring Batch-to-Batch Consistency
In the field of advanced therapy medicinal products (ATMPs), including stem cell therapies, ensuring consistency between manufacturing batches is a paramount yet challenging endeavor. Batch-to-batch variability can significantly impact product quality, safety, and ultimately, clinical efficacy. For cell-based therapies, this variability presents a substantial obstacle to clinical translation and commercial success. Reference standards and analytical controls serve as critical tools to mitigate this variability, providing benchmarks against which product quality and biological activity can be measured. Without these essential tools, even minor variations in raw materials, manufacturing processes, or environmental conditions can lead to significant differences in the critical quality attributes of the final product. This guide explores the pivotal role of reference standards and controls in managing batch-to-batch variation, with a specific focus on their application in stem cell potency assays spanning in vitro and in vivo research contexts.
The Critical Need for Standardization in Cell Therapy
Biological treatments, including stem cell therapies, represent one of the most significant medical breakthroughs of the 21st century. However, the initial enthusiasm has been tempered by challenges in achieving consistent clinical outcomes. In the cardiovascular regenerative medicine field specifically, over two decades of research in cell-based therapies have yielded promising results that have proven difficult to translate reliably to the clinical scenario [81]. A key factor contributing to this translational challenge is the inherent variability of living cell products.
Cell-based therapies present greater complexity than traditional small-molecule drugs, with characteristics including higher inherent variability, more limited stability, and greater molecular and mechanistic complexity [81]. Their biological activity depends heavily on their source, processing, and storage conditions. Viable cells may lose biological function during processing or storage, or change properties in response to their environment, with potentially significant functional and safety consequences. Regulatory agencies including the FDA and EMA have emphasized that merely confirming cell identity and viable cell number at product release does not necessarily correlate with biological activity measurements [81].
The potency assay—a quantitative measure of biological activity—serves as a critical quality attribute that must be controlled to ensure consistent dosing and therapeutic effect [23]. For stem cell therapies, potency measurement is particularly challenging due to complex, often multifactorial mechanisms of action that may not be fully understood. Development of adequate potency assays that reproducibly measure the ability of cell-based ingredients to produce a given bioactivity represents a crucial step forward in standardizing these treatments [81].
Table 1: Sources of Batch-to-Batch Variability in Biological Products
| Variability Source | Impact on Product | Examples from Literature |
|---|---|---|
| Raw Material Differences | Altered processability and performance | Variation in 5-aminosalicylic acid API requiring different granulation liquid [82] |
| Manufacturing Process | Changes in critical quality attributes | Differences in secretory profiles of BMAC samples [32] |
| Analytical Method Variability | Inconsistent potency measurements | High variability in in vivo potency assays (%CV of 34-125%) [23] |
| Storage and Handling | Product stability issues | Loss of mRNA integrity and potency under thermal stress [22] |
Reference Standards: Cornerstones of Comparability
Reference standards serve as established benchmarks of known quantity and quality against which test samples can be compared. These standards are essential for demonstrating comparability when manufacturing changes occur, and for ensuring consistency across multiple production lots. The importance of using relative potency measurements, which compare test samples to a reference standard, cannot be overstated in biological systems where experimental conditions can significantly influence results [23].
The development of appropriate reference materials for cell therapies presents unique challenges. According to regulatory perspectives, reference materials and standards must be highly characterized and sufficiently homogeneous and stable to guarantee consistency [81]. However, the heterogeneity and complexity of living cells complicate the development of a reference cell line or "cell-ruler" to normalize potency measurements across batches [81]. This challenge is particularly pronounced for autologous therapies, where each batch is manufactured from a different donor, introducing inherent variability that cannot be eliminated through standardized starting materials.
Implementing Reference Standards in Potency Assays
The use of reference standards is exemplified in a validated potency assay for CD34+ cell-based therapy (ProtheraCytes). In this approach, the potency assay measuring VEGF secretion was validated according to international guidelines, with performance characteristics including linearity, precision, accuracy, and specificity rigorously demonstrated [16]. The implementation of such standardized assays allows for meaningful comparison of potency across different manufacturing batches, which is essential for quality control and lot release.
For the CD34+ cell therapy validation, the assay demonstrated a linear response across the range of 20 pg/mL to 2800 pg/mL with a correlation coefficient (R²) of 0.9972 [16]. Method precision was evidenced by coefficients of variation for repeatability precision ≤10% and intermediate precision ≤20%, while accuracy was confirmed through mean recoveries between 85% and 105% for each concentration level [16]. These performance characteristics provide confidence that the assay can reliably detect meaningful changes in product potency across different batches.
Controls in Experimental and Manufacturing Workflows
Controls serve different but complementary functions to reference standards in ensuring batch-to-batch consistency. While reference standards provide a continuous scale for comparison, controls typically represent fixed points that verify assay performance, validate methods, and monitor processes. In cell therapy manufacturing, multiple types of controls are implemented throughout the production process.
The importance of controls is particularly evident in complex potency assays. For example, in the development of a 3D on-chip potency assay for bone marrow aspirate concentrate (BMAC) samples used in a Phase 3 trial for osteoarthritis, appropriate controls were essential for establishing the predictive validity of the platform [32]. The study utilized a simulated synovial fluid (simSF) control that mimicked the composition and viscosity of OA patient-derived synovial fluid, providing a uniform test condition for BMAC samples [32]. This approach allowed for meaningful comparison across different batches by controlling for environmental variables that might otherwise confound results.
Types of Controls in Potency Testing
The validation of the VEGF potency assay for CD34+ cell therapy illustrates the critical role of controls in quality assurance [16]. The implementation included:
- Positive controls: Verified assay performance across predetermined ranges (high control: 1108-2274 pg/mL; low control: 24.4-42.0 pg/mL)
- Negative controls: Confirmed assay specificity (StemFeed medium with VEGF concentration <2 pg/mL, below the lower limit of quantification of 20 pg/mL)
- System suitability controls: Ensured proper assay operation with each run
This systematic approach to controls provides assurance that the potency assay is performing as expected when testing therapeutic batches, thereby generating reliable results that support batch release decisions.
Quantitative Approaches to Batch Consistency
Modern approaches to ensuring batch-to-batch consistency increasingly rely on quantitative, data-driven methods. Multivariate analysis has proven particularly valuable for understanding complex relationships between material attributes and processability. A study investigating 131 full-scale batches of 5-aminosalicylic acid demonstrated that interactions between particle size, specific surface area, and packing behavior caused variation that was mistakenly considered unimportant when variables were evaluated individually [82]. Only through multivariate analysis could the combined effect of these factors be understood and controlled.
The power of advanced analytical approaches is further demonstrated in the development of a 3D on-chip potency assay for BMAC samples [32]. This platform utilized linear regression prediction models based on secreted analyte information from in vitro assays and patient-matched clinical data. The 3D system demonstrated improved clinical prediction compared to traditional 2D culture, with assay metrics displaying higher correlative power with patient pain scores [32]. This approach represents a significant advancement in quantitatively linking product attributes to clinical outcomes.
Table 2: Comparison of Potency Assay Platforms for Cell Therapies
| Assay Platform | Key Advantages | Limitations | Batch Consistency Application |
|---|---|---|---|
| In Vivo Assays | Measures biological response in whole organism | High variability (%CV 34-125%), ethical concerns, resource-intensive [23] | Traditionally used but increasingly replaced |
| Traditional 2D Culture | Established methodology, relatively simple | Limited clinical predictive value [32] | Moderate ability to predict batch performance |
| 3D On-Chip Systems | Enhanced clinical prediction, better simulation of in vivo environment [32] | More complex implementation, requires specialized equipment | Superior correlation with clinical outcomes |
| Automated Immunoassays (ELLA) | High precision (CV ≤10%), rapid, reproducible [16] | Measures surrogate markers rather than direct function | Excellent for quantitative batch release |
Experimental Protocols for Potency Assessment
VEGF Potency Assay for CD34+ Cell Therapy
The validation of the VEGF potency assay for CD34+ cell-based therapy provides a comprehensive protocol for ensuring batch-to-batch consistency [16]. The detailed methodology includes:
Sample Preparation:
- Culture CD34+ cells for 9 days under standardized expansion conditions
- Collect cell culture supernatants by centrifugation
- Store samples at -80°C if not testing immediately
VEGF Quantification:
- Utilize the ELLA automated immunoassay system (Bio-Techne) with Simple Plex cartridges for VEGF-A
- Load samples and standards following manufacturer specifications
- Run the automated assay protocol (approximately 90 minutes duration)
- Measure relative fluorescence units (RFU) proportional to VEGF concentration
Quality Control:
- Include high and low positive controls with predetermined acceptable ranges
- Include negative controls (culture medium alone)
- Verify standard curve correlation coefficient (R² > 0.95)
- Document all control results for batch release decisions
This protocol demonstrates how a standardized, validated method provides consistent measurement of a critical quality attribute across manufacturing batches.
3D On-Chip Potency Assay Protocol
The microfluidic on-chip 3D system for BMAC potency assessment represents a more complex but potentially more predictive approach [32]:
Device Preparation:
- Utilize poly(dimethylsiloxane) (PDMS) microfluidic device with specific design parameters
- Incorporate synthetic PEG-4MAL hydrogel functionalized with RGD peptide
- Crosslink with protease-degradable peptide and non-degradable dithiothreitol
Cell Encapsulation and Culture:
- Thaw BMAC samples and determine viability (typically 75% ± 10%)
- Encapsulate cells in hydrogel at standardized density
- Incorporate cell-laden hydrogel into microfluidic device
- Perfuse with media at 1.0 μL/min for 24 hours (simulating physiological interstitial fluid velocity)
Analysis:
- Collect perfusate and measure 24 immunomodulatory and trophic proteins
- Utilize multiplexed analysis platform for secretory profiling
- Apply linear regression models to predict clinical outcomes
- Compare secretory profiles to reference standards for batch assessment
This protocol highlights how advanced platforms can provide more physiologically relevant environments for potency assessment, potentially offering better prediction of clinical performance across batches.
Visualizing Experimental Workflows
Reference Standard Implementation Workflow
Reference Standard Implementation Workflow
3D Potency Assay Process
3D Potency Assay Process
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Potency Assays
| Reagent/Equipment | Function in Potency Testing | Application Example |
|---|---|---|
| ELLA Automated Immunoassay System | Automated, high-precision protein quantification | VEGF measurement in CD34+ cell therapy [16] |
| Microfluidic 3D Culture Devices | Physiologically relevant cell culture environment | BMAC potency assessment [32] |
| PEG-4MAL Hydrogel | Synthetic extracellular matrix for 3D culture | Cell encapsulation in on-chip assays [32] |
| Reference Standard Materials | Calibration and normalization of potency measurements | Relative potency calculations [23] |
| Multiplex Cytokine Arrays | Simultaneous measurement of multiple secretory factors | Profiling immunomodulatory proteins [32] |
| Validated Antibody Panels | Specific detection of target antigens | Immunoassay development for potency [22] |
Reference standards and controls serve as indispensable tools in the pursuit of batch-to-batch consistency for stem cell therapies and other advanced medicinal products. As the field continues to evolve, these tools will play an increasingly important role in bridging the gap between in vitro characterization and in vivo performance. The development of more predictive potency assays, coupled with appropriately characterized reference materials and rigorously implemented controls, provides a path toward more reliable and effective cell-based therapies. By adopting systematic approaches to quality control—including multivariate analysis, advanced assay platforms, and data-driven prediction models—researchers and manufacturers can better ensure that each batch of therapeutic product delivers consistent, predictable clinical performance.
Conclusion
Stem cell potency assays are indispensable for bridging the gap between basic research and clinical application, ensuring that cell-based therapies are characterized by their definitive biological function rather than mere phenotypic markers. A well-defined Mechanism of Action is the essential foundation for developing a relevant potency assay, which often requires a multi-faceted 'assay matrix' to fully capture a product's complexity. The future of potency testing lies in the continued development of more predictive, clinically relevant, and robust assays that can keep pace with the innovation in stem cell biology, ultimately accelerating the delivery of safe and effective advanced therapies to patients.
References
- 1. Cell potency [https://en.wikipedia.org/wiki/Cell_potency]
- 2. What Is Cell Potency And Why Does It Matter In Therapy? [https://stemshealthregenerativemedicine.com/blog/what-is-cell-potency-and-why-does-it-matter-in-therapy/]
- 3. Totipotent vs Pluripotent Stem Cells (2025) [https://www.dvcstem.com/post/totipotent-vs-pluripotent]
- 4. Describing the Stem Cell Potency: The Various Methods of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5118841/]
- 5. Describing the Stem Cell Potency: The Various Methods of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2016.00134/full]
- 6. Stem Cell Assay Market 2025 Rapid Growth with 17.55% ... [https://www.towardshealthcare.com/insights/stem-cell-assay-market]
- 7. Hallmarks of Totipotent and Pluripotent Stem Cell States [https://pmc.ncbi.nlm.nih.gov/articles/PMC10939785/]
- 8. Stem cells: a comprehensive review of origins and ... [https://orthopedicreviews.openmedicalpublishing.org/article/37498-stem-cells-a-comprehensive-review-of-origins-and-emerging-clinical-roles-in-medical-practice]
- 9. In vitro and in vivo differentiation of induced pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5829497/]
- 10. 5. Standards in Stem Cell Research [https://www.isscr.org/guidelines/standards-in-stem-cell-research]
- 11. Mechanism of action, potency and efficacy - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11067168/]
- 12. Mechanism of action, potency and efficacy: considerations for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05179-7]
- 13. A Checklist For Mechanism-Based Potency Testing In Cell ... [https://www.cellandgene.com/doc/a-checklist-for-mechanism-based-potency-testing-in-cell-therapy-0001]
- 14. Potency Assays for Cell and Gene Therapy [https://insights.forgebiologics.com/how-potency-assays-support-gene-therapy-success]
- 15. Analysis of the measurements used as potency tests ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11877884/]
- 16. Validation of a potency assay for CD34 + cell based therapy [https://www.nature.com/articles/s41598-025-14828-w]
- 17. New insights on potency assays from recent advances and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597888/full]
- 18. Strategies for Developing Mechanism of Action and ... [https://www.marinbio.com/strategies-for-developing-mechanism-of-action-and-potency-assays-for-ai-generated-advanced-therapy-medicinal-products-atmps/]
- 19. Potency assays and biomarkers for cell-based advanced ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1186224/full]
- 20. How Potency Testing Can Delay Advanced Therapies [https://biobridgeglobal.org/industry/how-potency-testing-can-delay-advanced-therapies/]
- 21. Advancing Potency Assay Development for ... [https://pubmed.ncbi.nlm.nih.gov/40257954/]
- 22. Establishing correlation between in vitro potency and in ... [https://www.nature.com/articles/s41541-025-01181-2]
- 23. In Vitro vs In Vivo Potency Assays: Modern Vaccine Batch ... [https://www.quantics.co.uk/blog/in-vitro-vs-in-vivo-potency-assays-modern-vaccine-batch-release/]
- 24. The Oct protein: more than a magic stemness 4 - PMC marker [https://pmc.ncbi.nlm.nih.gov/articles/PMC4163606/]
- 25. Sox2, a key factor in the regulation of pluripotency and neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4131272/]
- 26. Role of Oct in maintaining and regaining 4 pluripotency stem cell [https://stemcellres.biomedcentral.com/articles/10.1186/scrt39]
- 27. SOX2, a persistent marker for multipotential neural stem cells ... [https://pubmed.ncbi.nlm.nih.gov/15711057/]
- 28. Sox2+ Adult Stem and Progenitor Cells Are Important for ... [https://www.sciencedirect.com/science/article/pii/S1934590911004322]
- 29. Nanog, as a key cancer stem cell marker in tumor ... [https://pubmed.ncbi.nlm.nih.gov/35337852/]
- 30. Expression of the pluripotency markers Oct3/4, Nanog and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3506717/]
- 31. Analysis of the measurements used as potency tests for ... [https://pubmed.ncbi.nlm.nih.gov/40038737/]
- 32. On-chip 3D potency assay for prediction of clinical ... [https://www.nature.com/articles/s41467-025-60158-w]
- 33. Need for standardization of cytokine profiling in CAR T cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11403224/]
- 34. Simplified flow cytometry-based assay for rapid multi-cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245854/]
- 35. High-Throughput Cytokine Detection Platform for ... [https://www.sciencedirect.com/science/article/pii/S2472630325001050]
- 36. Multi-assay assessment of cytotoxicity reveals multiple ... [https://www.nature.com/articles/s41598-025-86792-4]
- 37. Advances in Cytotoxicity Testing: From In Vitro Assays to In ... [https://www.mdpi.com/1422-0067/26/22/11202]
- 38. A review of cytotoxicity testing methods and in vitro study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534221/]
- 39. Evaluating Strategies to Assess the Differentiation Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762643/]
- 40. Reassessment of marker genes in human induced ... [https://www.nature.com/articles/s41467-024-52922-1]
- 41. Teratoma Assay for Testing Pluripotency and Malignancy ... [https://www.mdpi.com/1422-0067/24/4/3879]
- 42. Reconsidering pluripotency tests: Do we still need teratoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7615844/]
- 43. Direct in vivo application of induced pluripotent stem cells ... [https://www.thno.org/v09p0290.htm]
- 44. Evaluating teratoma formation risk of pluripotent stem cell- ... [https://www.sciencedirect.com/science/article/pii/S146532492500684X]
- 45. Comparative analysis of RT-qPCR, flow cytometry, and Di- ... [https://www.sciencedirect.com/science/article/pii/S2405580825003127]
- 46. Flow cytometric analysis of the SARS coronavirus 2 ... [https://www.nature.com/articles/s41598-025-92389-8]
- 47. Harmonisation of quality control tests for academic ... [https://www.nature.com/articles/s41409-025-02637-8]
- 48. A Novel Flow Cytometry Array for High Throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567774/]
- 49. A flow cytometry-based neutralization assay for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1014309/full]
- 50. Emerging Human Pluripotent Stem Cell-Based Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11365908/]
- 51. Performance Characteristics of Next-Generation ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157824001818]
- 52. Performance Evaluation of Whole-Genome Amplification ... [https://pubmed.ncbi.nlm.nih.gov/41277018/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=10MSL6XygFtCE0XpaQpog-pEt8342fXkY9lzrR7q6H0wVRyEa2&fc=None&ff=20251124065242&v=2.18.0.post22+67771e2]
- 53. Potency assays and biomarkers for cell-based advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288881/]
- 54. 221 A Potency Assay Matrix for Establishing Consistency of ... [https://www.sciencedirect.com/science/article/pii/S2666636725002854]
- 55. Analysis of the measurements used as potency tests for the 31 ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06253-4]
- 56. Bioelectronic assays: Setting a standard for potency ... [https://www.axionbiosystems.com/resources/news/bioelectronic-assays-setting-standard-potency-measurement]
- 57. Stem cells: their source, potency and use in regenerative ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975018300624]
- 58. Potency Analysis of Mesenchymal Stromal Cells Using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5855117/]
- 59. Potency Assays for Mesenchymal Stromal Cell Secretome ... [https://www.mdpi.com/1422-0067/24/11/9379]
- 60. Potency assay to predict the anti-inflammatory capacity of a ... [https://www.sciencedirect.com/science/article/pii/S1465324924000501]
- 61. The importance of cell culture parameter standardization [https://pmc.ncbi.nlm.nih.gov/articles/PMC8806261/]
- 62. Potency assays for human adipose-derived stem cells as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9188073/]
- 63. Systematic Comparison of FBS and Medium Variation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898771/]
- 64. Reducing Variability: 3 Key Metrics for Successful Scale- ... [https://cellculturecompany.com/reducing-variability-3-key-metrics-for-successful-scale-up-and-expansion-of-custom-cell-cultures/]
- 65. ISSCR 2025: Quality Is Our Common Language [https://www.stemcell.com/virtual-conference-exhibition/isscr]
- 66. The Complete Guide to Cell-Based Assays [https://www.sptlabtech.com/the-complete-guide-to-cell-based-assays]
- 67. How Potency Assay Strategy Can Accelerate Cell Therapy ... [https://slingshotbio.com/how-potency-assay-strategy-can-accelerate-cell-therapy-development/]
- 68. GMP Potency Assays for PROTACs. Molecular Glues and ... [https://www.marinbio.com/precision-in-efficacy-developing-robust-gmp-potency-assays-for-protacs-molecular-glues-and-other-targeted-protein-degradation-tpd-drugs/]
- 69. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 70. Qualification of a flow cytometry-based method for the ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10830575/]
- 71. Understanding and managing sources of variability in cell ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/451/Understanding-and-managing-sources-of-variability-in-cell-measurements]
- 72. Assessment and Comparison of Viability Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10872314/]
- 73. Key quality parameter comparison of mesenchymal stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1412811/full]
- 74. of a rapid Validation for cord blood potency using... assay stem cells [https://pubmed.ncbi.nlm.nih.gov/36196510/]
- 75. Widely applicable, extended flow cytometric stem enumeration... cell [https://www.nature.com/articles/s41598-022-22339-1?error=cookies_not_supported&code=a75ef72d-0912-4455-8659-752a4ec37a04]
- 76. Identification of critical process parameters and quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408662/]
- 77. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 78. A Thematic Synthesis for Advancing MSC EV Therapies [https://www.sciencedirect.com/science/article/pii/S1465324925009120]
- 79. Potency Assay Variability Estimation in Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788244/]
- 80. Research progress on substitution of in vivo method(s) by ... [https://pubmed.ncbi.nlm.nih.gov/36779650/]
- 81. The Essential Need for a Validated Potency Assay for Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8599250/]
- 82. Identifying sources of batch to batch variation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0032591007003683]