Stem Cell Secretome Characterization and Exosome Isolation: A Comprehensive Guide for Translational Research
This article provides a comprehensive overview of the current landscape, methodologies, and challenges in stem cell secretome and exosome research.
Stem Cell Secretome Characterization and Exosome Isolation: A Comprehensive Guide for Translational Research
Abstract
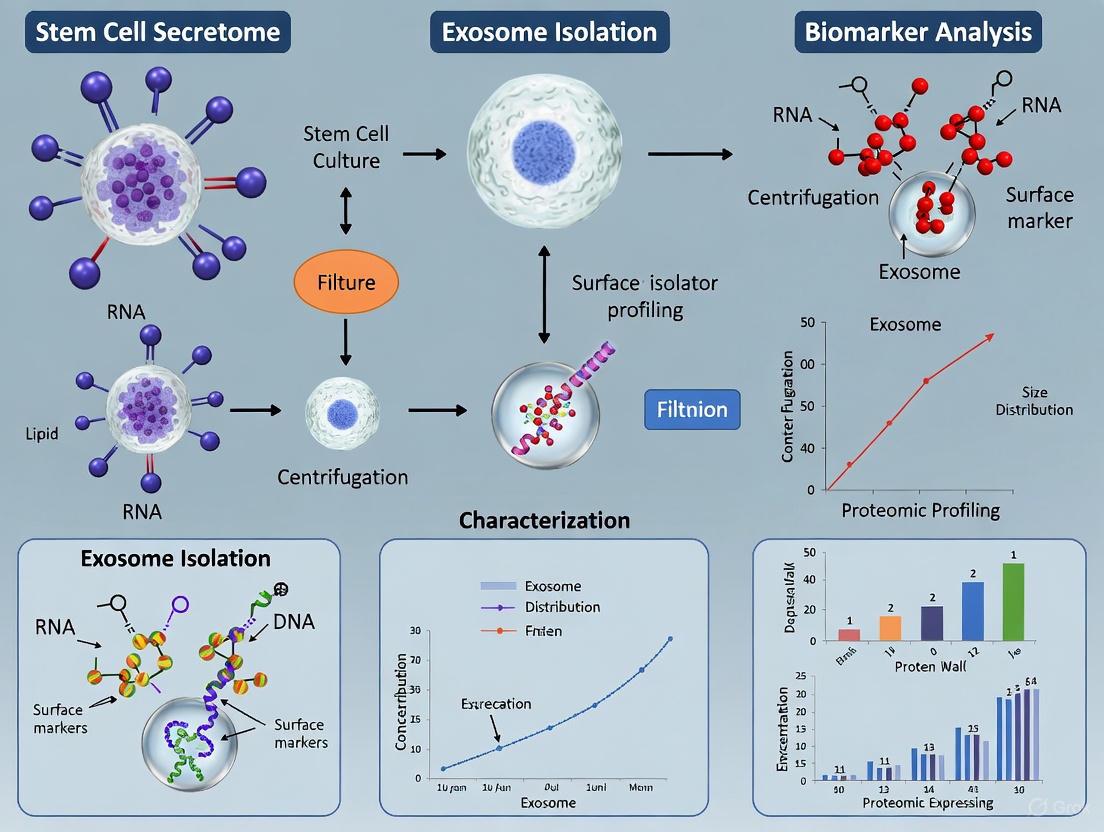
This article provides a comprehensive overview of the current landscape, methodologies, and challenges in stem cell secretome and exosome research. Tailored for researchers, scientists, and drug development professionals, it explores the foundational biology of mesenchymal stem cell (MSC) secretomes and extracellular vesicles (EVs), including exosomes. It details standardized and emerging protocols for isolation, purification, and characterization, addressing critical bottlenecks in production and analysis. The content further covers troubleshooting common pitfalls, optimizing protocols for clinical translation, and validating findings through comparative analysis of EVs from different MSC sources. By synthesizing the latest advances from recent clinical trials and research, this guide aims to bridge the gap between basic research and clinical application of these promising cell-free therapeutics.
The Secretome and Exosomes: Unraveling the Biology of MSC Paracrine Signaling
The secretome encompasses the complete set of molecules secreted by cells into the extracellular space, representing a critical functional component of cellular communication and therapeutic action. In stem cell research, particularly involving mesenchymal stem cells (MSCs), the secretome has emerged as a primary mediator of regenerative effects, shifting the therapeutic paradigm from cell differentiation to paracrine signaling [1]. This complex mixture includes soluble factors (growth factors, cytokines, metabolites) and membrane-bound vesicles (extracellular vesicles, including exosomes) that collectively modulate immune responses, promote tissue repair, and regulate cellular homeostasis [2] [1].
The composition of the secretome is not static but is dynamically "personalized" according to local microenvironmental cues, making its precise characterization essential for therapeutic development [1]. For MSC-based therapies, the secretome's regenerative potential is attributed to its immunomodulatory factors, trophic factors, and capacity to empower resident cells to regenerate damaged tissue [1]. Understanding how to properly define, isolate, and characterize these components is fundamental for advancing secretome-based cell-free therapies in regenerative medicine.
Secretome Production and Collection
Standardized protocols for secretome production are crucial for ensuring reproducible and therapeutically consistent products. The process begins with careful cell culture management and progresses through multiple clarification steps to yield a defined secretome preparation.
Cell Culture and Conditioning
Cell Sources: Mesenchymal stem cells can be isolated from various tissues, including bone marrow (BMSCs), adipose tissue (ASCs), and umbilical cord (UC-MSCs) [3] [1]. Each source may yield a secretome with distinct compositional and functional properties.
Culture Conditions: Cells are typically expanded in standard culture media supplemented with fetal bovine serum (FBS), human platelet lysate (PL), or serum/xeno-free (S/X) chemically-defined media [2]. Recent trends favor PL and S/X media to eliminate xenogenic contaminants and reduce immunologic risks [2].
Starvation Period: Before secretome collection, cells are washed with PBS to remove residual serum contaminants and incubated in serum-free medium for 24-48 hours [2]. This starvation phase minimizes contamination from serum-derived proteins while allowing accumulation of cell-secreted factors.
Collection and Clarification
The following workflow outlines the standard process for secretome collection and initial processing:
This sequential centrifugation process effectively removes cells, cellular debris, and large particles while preserving soluble factors and smaller extracellular vesicles [2]. The final filtration step ensures sterility before storage or downstream processing.
Extracellular Vesicle Isolation Techniques
Extracellular vesicles (EVs), particularly exosomes (30-150 nm), are key secretome components that facilitate intercellular communication by transferring proteins, lipids, and nucleic acids between cells [3] [4]. Multiple isolation techniques have been developed, each with distinct advantages and limitations.
Comparison of Isolation Methods
Table 1: Techniques for Extracellular Vesicle Isolation
| Method | Principle | Purity | Yield | Scalability | Instrumentation | Applications |
|---|---|---|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation based on size/density | High | Medium | Medium | Ultracentrifuge | Research, proteomics |
| Size-Exclusion Chromatography (SEC) | Separation by size through porous matrix | Medium-High | Medium | High | Chromatography system | Functional studies, diagnostics |
| Tangential Flow Filtration (TFF) | Size-based separation through membranes | Medium | High | High | Filtration apparatus | Large-scale production, therapeutics |
| Polymer-based Precipitation | Polymer reduces EV solubility | Low | High | High | Centrifuge | RNA analysis, biomarker discovery |
| Immunoaffinity Capture | Antibody binding to surface markers | Very High | Low | Low | Antibody-conjugated surfaces | Subtype-specific isolation, diagnostics |
| Density Gradient Ultracentrifugation | Separation by buoyant density | Very High | Low | Low | Ultracentrifuge | High-purity research applications |
Ultracentrifugation remains the most widely used method due to its high purity, but it requires costly equipment and lengthy procedures [5] [3]. Precipitation methods offer advantages in simplicity and yield but typically result in lower purity with co-precipitated contaminants [5] [3]. Recent advancements include microfluidic and immunoaffinity technologies that enable high-throughput and specific exosome isolation by targeting surface markers like CD9, CD63, and CD81 [4].
Detailed Protocol: Ultracentrifugation for EV Isolation
For researchers requiring high-purity EVs for mechanistic studies or therapeutic development, ultracentrifugation provides a reliable isolation method:
Sample Preparation: Begin with clarified secretome (prepared as in Section 2.2) in ultracentrifuge tubes. For plasma samples, dilute 100 μL with 11.9 mL PBS before ultracentrifugation [6].
First Ultracentrifugation: Centrifuge at 150,000×g for 3 hours at 4°C to pellet EVs and larger particles [6].
Wash Step: Carefully aspirate supernatant and resuspend pellet in 12 mL PBS.
Second Ultracentrifugation: Centrifuge at 120,000×g for 3 hours at 4°C to further purify EVs from co-precipitated proteins [6].
Resuspension: Resuspend final EV pellet in 100-500 μL PBS (volume dependent on initial sample size) [6].
Storage: Aliquot and store at -80°C until use. Avoid multiple freeze-thaw cycles.
For enhanced purity, particularly from complex biofluids like plasma, density gradient ultracentrifugation can be employed as a secondary purification step, effectively separating EVs from contaminating lipoproteins and protein aggregates [6].
Secretome Characterization and Quantification
Comprehensive characterization of the secretome and its components is essential for quality control and understanding biological activity. The following diagram illustrates the relationship between secretome components and their analysis techniques:
Quantitative Analysis of Secretome Components
Table 2: Secretome Characterization Techniques and Applications
| Analysis Type | Technique | Parameters Measured | Sample Requirements | Applications |
|---|---|---|---|---|
| EV Concentration & Size | Nanoparticle Tracking Analysis (NTA) | Particle size distribution, concentration | 1×10^8 - 1×10^9 particles/mL | Quality control, dose standardization |
| EV Surface Markers | Flow Cytometry (MACSPLEX) | Tetraspanins (CD9, CD63, CD81), cell-specific markers | 1×10^9 - 1×10^10 particles | EV characterization, subtype identification |
| Protein Composition | Proteomics (LC-MS/MS) | Global protein identification and quantification | 10-100 μg protein | Biomarker discovery, mechanistic studies |
| Soluble Factors | Multiplex Immunoassays | Cytokines, growth factors, inflammatory mediators | 25-100 μL sample | Functional potency, immunomodulatory assessment |
| Lipid Mediators | ELISA | PGE2, other eicosanoids | 50-100 μL sample | Anti-inflammatory activity evaluation |
| EV Morphology | Electron Microscopy | Vesicle structure, size confirmation | 1×10^9 - 1×10^10 particles | Visual validation of EV preparation |
Recent studies emphasize the importance of evaluating both soluble factors and EVs, as they may target different therapeutic pathways. For instance, soluble factors below 5 kDa (including PGE2) have been shown to inhibit NF-κB and IRF activation in innate immune pathways, while components larger than 100 kDa regulate T cell proliferation [7].
Functional Potency Assays
Beyond physical characterization, functional assays are critical for evaluating secretome bioactivity:
Immunomodulatory Assays: Measure inhibition of T-cell proliferation using PBMCs stimulated with PHA/IL-2, assessed via dye dilution and flow cytometry [7].
Anti-inflammatory Activity: Evaluate NF-κB and IRF pathway modulation using reporter cell lines (e.g., THP-1 dual cells) treated with secretome fractions [7].
Chondroprotective Effects: Assess anti-inflammatory properties in an in vitro OA model using inflamed chondrocytes, with gene expression evaluated by qRT-PCR [2].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Secretome Research
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cell Culture Media | DMEM/F12, StemPro MSC SFM XenoFree | MSC expansion and secretome production | Serum-free/xeno-free formulations reduce contaminants |
| Supplementation | Fetal Bovine Serum (FBS), Human Platelet Lysate (PL) | Provides growth factors and nutrients | PL reduces xenogenic risks but has batch-to-batch variation |
| EV Isolation Kits | qEVsingle columns, MagCapture exosome isolation kit, Total exosome isolation kit | Rapid, standardized EV isolation | Kit selection depends on required purity, yield, and downstream applications |
| Characterization Antibodies | Anti-CD9, anti-CD63, anti-CD81, anti-Alix, anti-TSG101 | EV marker detection and validation | Follow MISEV guidelines for mandatory and suggested markers |
| Protein Quantitation | Qubit Protein Assay, ProCartaPlex Immunoassays | Quantifying soluble factors and EV cargo | Multiplex arrays enable comprehensive secretome profiling |
| Analysis Instruments | NanoSight NTA, CytoFLEX flow cytometer, Ultracentrifuges | EV physical characterization | Multi-method approach provides complementary data |
Applications in Regenerative Medicine
The therapeutic potential of MSC secretome has been demonstrated across multiple disease models, including respiratory, hepatic, and neurological conditions [1]. In osteoarthritis treatment, secretomes from BMSCs expanded in different media conditions exhibited significant anti-inflammatory effects on chondrocytes, with FBS-expanded secretome showing the most pronounced therapeutic potential despite high molecular similarity across conditions [2]. These findings highlight that subtle differences in secretome composition, particularly in miRNA content of EVs, can significantly influence therapeutic outcomes.
The future of secretome-based therapies lies in engineering strategies to modulate secretome content according to specific disease and tissue needs [1]. Preconditioning of MSCs with inflammatory cytokines, hypoxia, or 3D culture systems can enhance the therapeutic potential of their secretome [1]. Furthermore, development of standardized, GMP-compliant protocols for secretome production and characterization will be essential for successful clinical translation [2] [8].
As research progresses, the clarity around secretome mechanisms of action will improve, enabling more targeted and effective cell-free therapies for a wide range of conditions that currently lack adequate treatment options.
Extracellular vesicles (EVs) are a heterogeneous group of phospholipid bilayer-surrounded particles released by nearly all cell types that play crucial roles in intercellular communication and maintaining homeostasis [9] [10]. These nanoparticles mediate the transfer of bioactive molecules between cells, influencing diverse biological processes including immune modulation, tissue regeneration, and pathological progression [11] [10]. Among EVs, exosomes and microvesicles represent two distinct populations that differ fundamentally in their biogenesis, physical characteristics, and cargo composition despite their shared role as cellular messengers [9]. Understanding these differences is particularly critical in the context of stem cell secretome characterization, where exosome isolation and analysis form the foundation for developing novel regenerative therapies and drug delivery systems [12] [13].
The research community has increasingly recognized that many therapeutic effects previously attributed to stem cells are actually mediated through their secretome - the totality of substances released by cells, which includes exosomes, microvesicles, proteins, and cytokines [12]. This paradigm shift has accelerated interest in characterizing exosomes and microvesicles, particularly for their potential as cell-free therapeutic agents that offer reduced immunogenicity and tumorigenicity risks compared to whole-cell therapies [13] [14]. This Application Note provides a structured comparison of exosomes and microvesicles, detailed experimental protocols for their isolation and characterization, and practical guidance for incorporating these vesicles into stem cell secretome research.
Comparative Analysis: Exosomes versus Microvesicles
Biogenesis and Release Pathways
The fundamental distinction between exosomes and microvesicles lies in their biogenesis pathways. Exosomes originate from the endosomal system through the formation of multivesicular bodies (MVBs) [9] [15]. During exosome biogenesis, early endosomes mature into late endosomes, and the inward budding of the endosomal membrane generates intraluminal vesicles (ILVs) within MVBs [13] [15]. These ILVs are subsequently released into the extracellular space as exosomes when MVBs fuse with the plasma membrane [14]. This process can be regulated by the endosomal sorting complex required for transport (ESCRT) machinery, though ESCRT-independent mechanisms involving sphingomyelinases, phospholipase D2, and ARF6 have also been documented [9].
In contrast, microvesicles (also called ectosomes) are formed through the direct outward budding and fission of the plasma membrane [9] [10]. This process is regulated by aminophospholipid translocases such as flippases and scramblases that mediate phospholipid rearrangement, along with RhoA and Rho-associated coiled-coil-containing protein kinase (ROCK) and LIM Kinase (LIMK) that control actin dynamics and cytoskeletal reorganization [9] [16]. Microvesicle formation typically occurs at sites of membrane overcrowding or in tight spaces where cytoskeletal protein contraction facilitates membrane bending and vesicle release [9].
Physical Characteristics and Molecular Markers
Exosomes and microvesicles exhibit distinct physical properties and carry different molecular markers that serve as identifiers for their characterization and isolation.
Table 1: Physical Characteristics of Exosomes and Microvesicles
| Characteristic | Exosomes | Microvesicles |
|---|---|---|
| Size Range | 30-150 nm [11] [13] | 100-1000 nm [9] [10] |
| Origin | Endosomal system (MVBs) [9] [15] | Plasma membrane budding [9] [10] |
| Density | 1.13-1.19 g/mL [11] | Not well-defined |
| Shape | Cup-shaped in TEM [16] | Heterogeneous, often irregular |
| Key Markers | Tetraspanins (CD63, CD81, CD9), ALIX, TSG101, HSP70/90 [9] [10] | Integrins, selectins, CD40, phosphatidylserine [9] [10] |
Table 2: Cargo Composition of Exosomes and Microvesicles
| Cargo Type | Exosomes | Microvesicles |
|---|---|---|
| Proteins | Tetraspanins, ESCRT components (ALIX, TSG101), heat shock proteins, Rab proteins [9] | Membrane proteins (receptors, ligands, adhesion molecules), cytoskeletal proteins, integrins [9] |
| Nucleic Acids | mRNA, miRNA, long non-coding RNA, tRNA, mitochondrial DNA [9] [15] | DNA, mRNA, miRNA, other non-coding RNAs [9] |
| Lipids | Cholesterol, sphingomyelin, ceramide, phosphatidylserine [15] | Cholesterol, phosphatidylserine, diacylglycerol [10] |
The following diagram illustrates the key differences in biogenesis pathways and cellular release mechanisms for exosomes and microvesicles:
Experimental Protocols for Isolation and Characterization
Isolation of Exosomes from Stem Cell Secretome
The following protocol describes two primary methods for exosome isolation from stem cell conditioned media: size-exclusion chromatography (SEC) and ultracentrifugation (UC). SEC is increasingly recognized as producing higher purity exosomes with better preserved physical and functional properties [17].
Size-Exclusion Chromatography Protocol
Principle: SEC separates particles based on their hydrodynamic diameter using a column packed with porous beads. Larger particles (such as exosomes) elute first as they cannot enter the pores, while smaller proteins and contaminants are retained longer in the column [11] [17].
Materials:
- qEV Original SEC Columns (35 nm or 70 nm, Izon Science)
- Phosphate-buffered saline (PBS), pH 7.4
- Stem cell conditioned media (centrifuged to remove cells and debris)
- Automated fraction collector (optional)
- 0.22 μm syringe filters
Procedure:
- Prepare stem cell conditioned media by centrifugation at 2,000 × g for 30 minutes to remove cells and large debris.
- Filter the supernatant through 0.22 μm filters to remove remaining particulates.
- Equilibrate the SEC column with 15-20 mL of PBS according to manufacturer instructions.
- Load 0.5-1.0 mL of filtered conditioned media onto the column.
- Add PBS as elution buffer and collect sequential fractions (0.5 mL each).
- Fractions 2-4 typically contain the highest concentration of exosomes with minimal protein contamination [17].
- Analyze exosome concentration and size distribution using nanoparticle tracking analysis.
- Clean the column with 0.5 M NaOH and store in PBS with 0.05% sodium azide.
Advantages: Preserves exosome integrity, high purity, quick processing (approximately 20 minutes), suitable for various biological fluids [17]. Disadvantages: Lower throughput, requires specialized columns, may not completely separate exosomes from similar-sized particles.
Ultracentrifugation Protocol
Principle: UC separates particles based on density, size, and shape through sequential centrifugation steps at increasing forces, ultimately pelleting exosomes at high gravitational forces [14].
Materials:
- Ultracentrifuge with fixed-angle or swinging-bucket rotor
- Polycarbonate or polyallomer centrifuge tubes
- PBS, pH 7.4
- Stem cell conditioned media
Procedure:
- Centrifuge conditioned media at 300 × g for 10 minutes to remove live cells.
- Transfer supernatant to new tubes and centrifuge at 2,000 × g for 20 minutes to remove dead cells and large debris.
- Transfer supernatant and centrifuge at 10,000 × g for 30 minutes to remove larger vesicles and organelles.
- Filter the supernatant through 0.22 μm filters.
- Ultracentrifuge at 100,000 × g for 70 minutes to pellet exosomes.
- Carefully discard supernatant and resuspend the exosome pellet in PBS.
- For higher purity, repeat the ultracentrifugation step (optional).
- Resuspend the final exosome pellet in an appropriate buffer for downstream applications.
Advantages: Considered the "gold standard", high throughput, no specialized reagents required. Disadvantages: Time-consuming, may cause exosome aggregation or damage, co-pellets protein aggregates and other contaminants [17].
Characterization and Validation
Comprehensive characterization of isolated exosomes and microvesicles is essential for validating isolation efficiency and confirming vesicle identity.
Nanoparticle Tracking Analysis (NTA):
- Principle: Measures Brownian motion of individual particles to determine size distribution and concentration [16]
- Protocol: Dilute samples in PBS to achieve 20-100 particles per frame. Acquire three 60-second videos using appropriate camera settings. Analyze data with NTA software to determine size distribution and concentration.
Transmission Electron Microscopy (TEM):
- Principle: Visualizes vesicle morphology and structure at high resolution [16]
- Protocol: Adsorb vesicles to Formvar-carbon coated grids, fix with glutaraldehyde, contrast with uranyl acetate, and image using TEM.
Western Blot Analysis:
- Principle: Detects specific protein markers characteristic of exosomes or microvesicles [17]
- Protocol: Lyse vesicles in RIPA buffer, separate proteins by SDS-PAGE, transfer to membrane, and probe with antibodies against CD63, CD81, ALIX (exosome markers) or specific surface receptors (microvesicle markers).
The following workflow diagram illustrates the complete process from sample preparation to characterization:
The Scientist's Toolkit: Essential Research Reagents
Successful isolation and characterization of exosomes and microvesicles requires specific reagents and equipment. The following table outlines essential materials for conducting experiments in stem cell secretome research.
Table 3: Research Reagent Solutions for EV Isolation and Characterization
| Category | Specific Product/Kit | Application | Key Features |
|---|---|---|---|
| Isolation Kits | qEV SEC Columns (Izon) | Size-based separation of exosomes | Preserves vesicle integrity, high purity, rapid processing |
| Total Exosome Isolation Reagent (Thermo Fisher) | Precipitation-based isolation | Simple protocol, suitable for various sample types | |
| ExoQuick-TC (System Biosciences) | Culture media exosome isolation | Optimized for conditioned media | |
| Characterization Antibodies | Anti-CD63 | Exosome marker detection | Tetraspanin surface marker |
| Anti-CD81 | Exosome marker detection | Tetraspanin surface marker | |
| Anti-ALIX | Exosome marker detection | ESCRT pathway component | |
| Anti-TSG101 | Exosome marker detection | ESCRT pathway component | |
| Cell Culture | Mesenchymal Stem Cell Media | Production of stem cell secretome | Defined formulations for MSC culture |
| Serum-free Media | Production of contaminant-free EVs | Eliminates fetal bovine serum exosomes | |
| Analysis Instruments | ZetaView (Particle Metrix) | Nanoparticle tracking analysis | Size distribution and concentration |
| Exosome ELISA Kits | Quantification of specific exosomes | Sensitive detection of exosome subpopulations |
Applications in Stem Cell Research and Therapeutics
Exosomes and microvesicles derived from stem cells have demonstrated significant therapeutic potential across various medical applications. Mesenchymal stem cell-derived exosomes (MSC-Exos) have shown efficacy in modulating immune responses, promoting angiogenesis, and facilitating tissue repair in neurological disorders, cardiovascular diseases, and autoimmune conditions [13] [15]. The therapeutic effects are largely mediated through the transfer of bioactive cargo, including growth factors, cytokines, and regulatory miRNAs that influence recipient cell behavior [18] [15].
In regenerative medicine, stem cell-derived exosomes have demonstrated remarkable wound healing capabilities by modulating macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes, enhancing angiogenesis, and promoting re-epithelialization [9]. Dental stem cell-derived exosomes have shown particular promise in craniofacial and neural tissue regeneration due to their enriched cargo of osteogenic and neuroprotective miRNAs [11]. Furthermore, the emerging field of engineered exosomes offers opportunities to enhance targeting specificity and therapeutic efficacy through surface modifications and customized cargo loading [13] [14].
For drug development professionals, exosomes represent promising drug delivery vehicles due to their natural biocompatibility, low immunogenicity, and ability to cross biological barriers such as the blood-brain barrier [11] [13]. Both passive and active loading strategies have been developed to incorporate therapeutic agents into exosomes, including small molecules, proteins, and nucleic acids [11]. The development of standardized isolation protocols and comprehensive characterization workflows, as outlined in this Application Note, is essential for advancing exosome-based therapeutics toward clinical applications.
The therapeutic benefits of mesenchymal stem cells (MSCs) are now largely attributed to their paracrine activity rather than direct cell replacement, with secreted exosomes serving as primary mediators of intercellular communication [19] [20] [21]. Exosomes are nanoscale (30-200 nm), lipid-bilayer enclosed extracellular vesicles that transport functional biomolecules—including proteins, lipids, mRNAs, and microRNAs—from donor to recipient cells [19] [3] [21]. This transfer orchestrates complex therapeutic processes such as anti-inflammatory responses, angiogenesis promotion, and tissue regeneration [19] [20]. Adipose-derived stem cell exosomes (ADSC-Exos) offer distinct advantages due to their accessibility, high yield from abundant adipose tissue, low immunogenicity, and absence of tumorigenic risks [19]. This application note details the key bioactive components of MSC-derived exosomes and provides standardized protocols for their characterization and functional validation.
Comprehensive Characterization of Exosomal Cargo
Protein Cargo
Exosomes carry a specific subset of cellular proteins that facilitate their biogenesis, targeting, and biological activity. These include tetraspanins (CD9, CD63, CD81), heat shock proteins (HSP70, HSP90), and proteins involved in endosomal biogenesis (ALIX, TSG101) [19] [3]. Beyond these structural proteins, exosomes encapsulate numerous therapeutic proteins and cytokines that modulate recipient cell behavior.
Table 1: Key Protein Components in MSC-Derived Exosomes
| Protein Category | Specific Examples | Documented Functions |
|---|---|---|
| Tetraspanins | CD9, CD63, CD81 | Exosome structure, cargo sorting, cellular uptake [19] [3] |
| Biogenesis Machinery | ALIX, TSG101 | Formation of multivesicular bodies (MVBs) [19] [21] |
| Heat Shock Proteins | HSP70, HSP90 | Protein folding, cell protection, immunomodulation [19] |
| Growth Factors | VEGF, FGF, HGF, IGF-1 | Angiogenesis, fibroblast proliferation, tissue repair [19] [20] |
| Anti-inflammatory Factors | TSG-6, IL-10, HO-1 | Suppression of excessive inflammation, macrophage polarization [20] |
Nucleic Acid Cargo
The nucleic acid content, particularly microRNAs (miRNAs) and mRNAs, constitutes a critical mechanism through which exosomes alter gene expression in recipient cells. The sorting of non-coding RNAs into exosomes is a regulated process controlled by RNA-binding proteins (RBPs) like hnRNPA2B1, which recognize specific structural motifs on the RNAs [19].
Table 2: Nucleic Acid Components in MSC-Derived Exosomes
| Nucleic Acid Type | Key Examples | Therapeutic Functions |
|---|---|---|
| microRNAs (miRNAs) | miR-21, miR-146a, miR-524-5p | Anti-inflammatory effects, angiogenesis, fibrosis attenuation [19] [20] |
| mRNAs | Angiogenic mRNAs, NORAD lncRNA | Protein expression in recipient cells, tissue regeneration [19] [21] |
| Other ncRNAs | tRNAs, lncRNAs | Gene regulation, cellular metabolism [3] |
Lipid Composition
The exosomal membrane is enriched in specific lipids, including cholesterol, ceramide, phosphoglycerides, and fatty-acyl chains, which contribute to membrane stability, rigidity, and fusion with target cells [3]. Lipid-mediated mechanisms, such as ceramide-induced membrane curvature, are also involved in the ESCRT-independent biogenesis of exosomes [19].
Experimental Protocols for Isolation and Characterization
Protocol 1: Standardized Isolation of Exosomes from Adipose-Derived MSCs
Principle: This protocol utilizes precipitation-based isolation, which provides higher efficiency and purity compared to other methods and does not require specialized, costly equipment [3].
Materials:
- Adipose tissue from healthy donors (obtained with ethical approval)
- Low-glucose Dulbecco's Modified Eagle's Medium (DMEM)
- Phosphate Buffered Saline (PBS)
- Exosome precipitation solution (e.g., polyethylene glycol)
- Centrifuge and rotors
- Sterile cell culture flasks and containers
Procedure:
- ADSC Culture: Isolate ADSCs from human adipose tissue samples via collagenase digestion and plastic adherence. Culture cells in low-glucose DMEM supplemented with 10% exosome-depleted FBS and 1% penicillin/streptomycin at 37°C and 5% CO₂ [19] [3].
- Conditioned Medium Collection: At 70-80% confluence, wash cells with PBS and culture in serum-free medium for 24-48 hours. Collect the conditioned medium (CM).
- Precipitation: Centrifuge the CM at 2,000 × g for 30 minutes to remove cells and debris. Mix the supernatant with exosome precipitation solution (e.g., 0.5 volumes) and incubate overnight at 4°C.
- Pellet Exosomes: Centrifuge the mixture at 1,500 × g for 30 minutes at 4°C to pellet the exosomes.
- Resuspension: Resuspend the exosome pellet in a suitable buffer, such as PBS, for downstream applications [3].
Validation: The isolated exosomes can be characterized using transmission electron microscopy (TEM) for morphology, nanoparticle tracking analysis (NTA) for size and concentration, and Western blotting for surface markers (CD9, CD63, CD81, TSG101) [3].
Protocol 2: Cargo Profiling and Functional Analysis
Principle: To identify and quantify the key bioactive components (proteins, mRNAs, miRNAs) within the isolated exosomes and validate their functional roles.
Materials:
- Isolated exosomes (from Protocol 1)
- Lysis buffer (e.g., RIPA buffer)
- Proteinase K and RNase inhibitors
- TRIzol reagent or similar for RNA isolation
- cDNA synthesis and qPCR kits
- Mass spectrometry system
- ELISA kits for specific proteins (e.g., VEGF, TSG-6)
Procedure: A. Protein Profiling via Mass Spectrometry: 1. Lyse exosomes using a suitable lysis buffer. 2. Digest proteins with trypsin. 3. Analyze peptide mixtures using liquid chromatography-tandem mass spectrometry (LC-MS/MS). 4. Identify proteins by searching against relevant databases (e.g., Swiss-Prot) [20] [8].
B. RNA Cargo Analysis: 1. Extract total RNA from exosomes using TRIzol, ensuring the addition of RNase inhibitors to prevent degradation. 2. For miRNA analysis, use reverse transcription followed by quantitative PCR (qPCR) with specific stem-loop primers for miRNAs of interest (e.g., miR-21, miR-146a). 3. For mRNA analysis, perform cDNA synthesis and qPCR to detect specific transcripts (e.g., VEGF mRNA, NORAD lncRNA) [19].
C. Functional Uptake and Validation Assay: 1. Label isolated exosomes with a lipophilic dye (e.g., PKH67). 2. Incubate labeled exosomes with target cells (e.g., human umbilical vein endothelial cells (HUVECs) for angiogenesis studies) for 24 hours. 3. Fix cells and visualize uptake using confocal microscopy. 4. Assess functional outcomes: - Angiogenesis: Perform tube formation assay on Matrigel with HUVECs. - Anti-inflammatory effect: Measure levels of TNF-α and IL-10 in macrophage cultures using ELISA after inflammatory stimulation [19] [20].
Visualizing Signaling Pathways and Workflows
Exosome Biogenesis, Cargo Sorting, and Uptake
Experimental Workflow for Exosome Analysis
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Exosome Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Isolation Kits | Polyethylene glycol-based precipitation kits | Efficient exosome precipitation from conditioned medium [3] |
| Characterization Antibodies | Anti-CD9, Anti-CD63, Anti-CD81, Anti-TSG101 | Western blot validation of exosomal markers [3] [21] |
| Visualization Dyes | PKH67, PKH26 | Fluorescent labeling of exosomes for uptake studies [21] |
| RNA Protection | RNase inhibitors | Preservation of exosomal RNA integrity during isolation [19] |
| Cell Culture Supplements | Exosome-depleted FBS | Prevents contamination with bovine exosomes during cell culture [3] |
| Analysis Kits | ELISA kits (VEGF, TSG-6, IL-10), BCA assay | Quantification of specific exosomal proteins and total protein [20] |
Mesenchymal stromal cells (MSCs) have emerged as a cornerstone of regenerative medicine due to their multipotent differentiation capacity, self-renewal properties, and powerful immunomodulatory functions [22]. While initially identified in bone marrow, MSCs have since been isolated from virtually all adult tissues, with adipose tissue and dental pulp emerging as two of the most clinically valuable and readily accessible sources [23]. The therapeutic efficacy of MSCs is now largely attributed to their paracrine activity rather than direct cell replacement, mediated through the release of a complex mixture of bioactive molecules collectively known as the secretome, which includes soluble factors and extracellular vesicles (EVs) such as exosomes [24] [22].
This application note provides a structured comparison of MSC tissue sources, focusing on bone marrow, adipose tissue, and dental pulp, with an emphasis on their differential secretome profiles and implications for clinical translation. We present standardized protocols for the isolation and characterization of MSC-derived exosomes to support researchers in developing reproducible, potent cell-free therapies.
Biological Characteristics and Regenerative Potentials
MSCs from different tissue sources exhibit distinct biological properties influenced by their ontogeny and niche microenvironment [24] [23]. The table below summarizes key characteristics of MSCs derived from bone marrow, adipose tissue, and dental pulp.
Table 1: Comparative Analysis of MSC Biological Properties from Different Tissue Sources
| Parameter | Bone Marrow-MSCs (BM-MSCs) | Adipose Tissue-MSCs (AD-MSCs) | Dental Pulp-MSCs (DPSCs) |
|---|---|---|---|
| Tissue Origin | Medullary stroma of bone marrow [23] | Subcutaneous adipose tissue [25] | Dental pulp tissue [26] |
| Isolation Method | Gradient separation or plastic adherence [23] | Enzymatic digestion (SVF) or mechanical fragmentation (MF) [24] | Mechanical fragmentation of pulp tissue [24] |
| Key Markers | CD73, CD90, CD105, STRO-1, CD271 [23] | CD73, CD90, CD105 [24] [25] | CD73, CD90, CD105, Nestin [24] [26] |
| Proliferation Rate | Moderate [25] | High [25] | Very high [24] [26] |
| Osteogenic Potential | High [23] [25] | Moderate [23] [25] | High (superior to AD-MSCs) [26] |
| Adipogenic Potential | High [25] | High [25] | Low/absent [24] |
| Neurogenic Potential | Limited | Limited | High (neural crest origin) [26] |
| Immunomodulatory Effect | Potent [25] | Highly potent [25] | Potent, with low immunogenicity [26] |
Secretome and Exosome Profiles
The composition of the MSC secretome varies significantly based on the tissue of origin, impacting its therapeutic potential [24]. These differences manifest in both soluble factors and extracellular vesicles.
Table 2: Comparative Secretome and Exosome Profiles of Different MSC Sources
| Component | Bone Marrow-MSCs (BM-MSCs) | Adipose Tissue-MSCs (AD-MSCs) | Dental Pulp-MSCs (DPSCs) |
|---|---|---|---|
| Key Soluble Factors | High SDF-1, HGF [25] | High bFGF, IGF-1, IFN-γ [25] | Variable cytokines/chemokines; context-dependent [24] |
| Exosome Size & Yield | Comparable EV number [24] | Higher number of small exosomes [24] | Comparable EV number [24] |
| Distinct miRNA Cargo | Regulatory functions under investigation | Predominant role in cell cycle and proliferation regulation [24] | Enriched in oxidative stress and apoptosis pathway regulation [24] |
| Therapeutic Implications | Preferable for bone and cartilage regeneration [23] [25] | Ideal for soft tissue repair, angiogenesis, immunomodulation [25] | Promising for neural regeneration and oral/dental applications [24] [26] |
Experimental Protocols for Secretome and Exosome Analysis
Protocol 1: Isolation of MSCs from Adipose Tissue and Dental Pulp
Principle: MSCs are isolated from tissues using enzymatic digestion or mechanical fragmentation, followed by expansion in culture [24].
Reagents:
- Collagenase Type I or IV
- Basic Medium (BM): αMEM supplemented with L-glutamine, penicillin/streptomycin
- Fetal Bovine Serum (FBS) or Human Platelet Lysate (hPL)
- Phosphate-Buffered Saline (PBS)
- Trypsin-EDTA
Procedure for Adipose-derived MSCs (ADSCs):
- Wash & Digest: Wash lipoaspirate tissue with PBS. Digest with 0.2% collagenase type IV in BM for 30 minutes at 37°C with agitation [24] [25].
- Isolate Stromal Vascular Fraction (SVF): Centrifuge digest at 300-1200 g for 10 minutes. Collect the cell pellet (SVF) [24].
- Plate & Culture: Resuspend SVF in BM supplemented with 10% FBS or 5% hPL. Plate in culture dishes and incubate at 37°C with 5% CO₂ [24] [25].
- Expand Cells: Refresh medium twice weekly. At 80-90% confluence, detach cells with trypsin-EDTA and passage at a density of 2,000 cells/cm² [25].
Procedure for Dental Pulp-derived MSCs (DPSCs):
- Extract & Fragment: Isolate pulp from teeth (e.g., third molars). Cut into 1-2 mm³ fragments using a scalpel [24].
- Explant Culture: Wash fragments by centrifugation. Seed fragments directly onto culture dishes in BM with 10% FBS [24].
- Cell Outgrowth: Maintain cultures for 2-4 weeks, allowing cells to migrate from explants. Refresh medium twice weekly [24].
- Expand Cells: At 80% confluence, detach cells with trypsin-EDTA and passage at 2.5 × 10³ cells/cm² [24].
Protocol 2: Collection and Processing of Conditioned Medium (Secretome)
Principle: Conditioned medium (CM) containing the MSC secretome is collected from subconfluent cultures to avoid differentiation effects [24].
Reagents:
- Serum-free basal medium
- Ultracentrifugation tubes
Procedure:
- Prepare Cells: Culture MSCs until 70-80% confluence.
- Wash & Incubate: Wash cell layer twice with PBS to remove serum contaminants. Add serum-free basal medium.
- Collect CM: Incubate for 24-48 hours. Collect CM and centrifuge at 2,000 g for 20 minutes to remove dead cells and debris [24].
- Concentrate (Optional): Concentrate CM using ultrafiltration units (e.g., 3 kDa cutoff) if necessary.
- Store: Aliquot and store CM at -80°C. Avoid multiple freeze-thaw cycles.
Protocol 3: Isolation and Purification of Exosomes
Principle: Exosomes are isolated from CM based on their size and density, using sequential centrifugation and size-exclusion chromatography (SEC) for high purity [27].
Reagents:
- Ultracentrifuge and fixed-angle rotor
- PBS (filtered, 0.22 µm)
- Size-exclusion chromatography columns
Procedure:
- Clarify CM: Centrifuge CM at 2,000 g for 30 minutes, then at 10,000 g for 45 minutes at 4°C to remove large vesicles and apoptotic bodies.
- Ultracentrifuge: Transfer supernatant to ultracentrifuge tubes. Pellet exosomes at 100,000-120,000 g for 70-120 minutes at 4°C [27].
- Wash: Resuspend pellet in a large volume of filtered PBS. Ultracentrifuge again at 100,000-120,000 g for 70-120 minutes.
- Purify (Optional): Resuspend final pellet in PBS and further purify using a size-exclusion chromatography column to isolate exosomes from non-vesicular contaminants [27].
- Resuspend & Store: Resuspend pure exosomes in a small volume of PBS. Characterize immediately or store at -80°C.
Workflow Visualization
The following diagram illustrates the integrated workflow from MSC isolation to secretome and exosome characterization:
Integrated Workflow for MSC Secretome Analysis
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their functions for MSC culture, secretome collection, and exosome isolation, as featured in the protocols above.
Table 3: Essential Research Reagent Solutions for MSC Secretome Studies
| Reagent / Kit | Function / Application | Key Considerations |
|---|---|---|
| Collagenase Type I/IV | Enzymatic digestion of tissues (AT, BM) to isolate MSCs [24] [25] | Concentration and incubation time are tissue-dependent; activity testing recommended. |
| Human Platelet Lysate (hPL) | Xeno-free supplement for clinical-scale MSC expansion [25] | Superior growth-promoting properties vs. FBS; requires heparin addition. |
| Size-Exclusion Chromatography (SEC) Columns | High-purity isolation of exosomes from conditioned medium [27] | Preserves vesicle integrity and function; ideal for downstream applications. |
| Nanoparticle Tracking Analysis (NTA) | Characterizes exosome size distribution and concentration [27] [28] | Requires instrument calibration; provides particle size and count. |
| CD63/CD81/CD9 Antibodies | Exosome detection and characterization via Western Blot or flow cytometry [27] [28] | Tetraspanins are common positive markers for exosome identification. |
| TEM & SEM | Visualizes exosome morphology and ultrastructure [27] [28] | Requires specialized equipment and expertise for sample preparation. |
| Trilineage Differentiation Kits | Confirms MSC multipotency (osteogenic, adipogenic, chondrogenic) [24] [22] | Quality control step; essential for validating MSC identity per ISCT criteria. |
The selection of an MSC tissue source is a critical determinant of therapeutic efficacy in regenerative medicine. Bone marrow, adipose tissue, and dental pulp each yield MSCs with distinct biological profiles and secretome signatures, making them uniquely suited for different clinical applications. BM-MSCs demonstrate superior osteogenic capacity, AD-MSCs excel in proliferation and immunomodulation, while DPSCs show remarkable neurogenic potential. The provided protocols for secretome collection and exosome isolation establish a foundation for standardized, reproducible research, enabling the development of potent, cell-free regenerative therapies tailored to specific disease pathologies.
From Bench to Bedside: Standardized Protocols for Isolation, Characterization, and Clinical-Scale Production
The stem cell secretome, particularly its rich cargo of exosomes, has emerged as a primary mediator of therapeutic effects in regenerative medicine, offering a cell-free alternative to whole-cell therapies. Exosomes are nanoscale extracellular vesicles (30-150 nm) bounded by a lipid bilayer and loaded with bioactive molecules—including proteins, lipids, and nucleic acids—from their parent cells [29] [18]. Their role in intercellular communication, influencing processes such as immune modulation, angiogenesis, and tissue remodeling, makes them invaluable for therapeutic and diagnostic applications [29] [30]. Isolating these vesicles with high purity and yield from complex biological fluids or cell culture supernatants is therefore a critical first step in secretome characterization and the development of exosome-based therapeutics [5] [4].
This article provides a detailed technical overview of four cornerstone isolation techniques: ultracentrifugation, precipitation, size-exclusion chromatography, and microfluidics. The selection of an appropriate method represents a fundamental trade-off between yield, purity, scalability, and the specific requirements of downstream applications [5]. For researchers in drug development, understanding these nuances is essential for ensuring the consistency, potency, and safety of exosome-based products, ultimately accelerating their translation from the laboratory to the clinic [31].
Comparative Analysis of Isolation Techniques
Choosing an optimal exosome isolation method requires balancing multiple performance metrics against practical experimental constraints. The table below summarizes the key characteristics of the four primary techniques.
Table 1: Performance Comparison of Major Exosome Isolation Methods
| Isolation Method | Purity | Yield | Scalability | Technical Complexity | Primary Applications |
|---|---|---|---|---|---|
| Ultracentrifugation | High [5] | Medium [5] | Medium [5] | High (requires specialized equipment) [5] | Gold-standard for research, proteomic studies [5] |
| Precipitation | Low [5] | High [5] | High [5] | Low (simple protocol) [5] | Rapid diagnostics, RNA analysis [5] |
| Size-Exclusion Chromatography (SEC) | Medium–High [5] | Medium [5] | High [5] | Medium [5] | High-integrity exosomes for functional studies, therapeutic development [5] |
| Microfluidics | Very High (with affinity) [32] | Varies | Developing | High (device design/fabrication) [31] | Point-of-care diagnostics, specific subpopulation isolation [4] [32] |
Beyond these core metrics, each method presents unique advantages and limitations. Ultracentrifugation, while considered the benchmark, is time-consuming and the high g-forces can potentially damage exosomes [5]. Precipitation is simple and efficient but co-precipitates contaminants like lipoproteins, which can interfere with downstream analyses [5]. SEC excels at preserving exosome integrity and biological activity, making it increasingly popular for therapeutic applications [5]. Microfluidic platforms represent a paradigm shift, offering rapid, automated isolation with minimal sample volumes, often by combining size-based and immunoaffinity-based separation for high specificity [31] [32].
Detailed Protocols for Key Isolation Methods
Protocol 1: Differential Ultracentrifugation
Differential ultracentrifugation remains the most widely cited method for exosome isolation, separating vesicles based on their size and density through sequential centrifugation steps [5].
Materials and Reagents
- Refrigerated ultracentrifuge and fixed-angle or swinging-bucket rotors
- Polycarbonate or polyallomer ultracentrifuge tubes
- Phosphate-buffered saline (PBS), sterile and pre-cooled (4°C)
- 0.22 µm filter unit
- Source material (e.g., conditioned cell culture media from stem cell cultures)
Step-by-Step Procedure
- Sample Pre-Clearance: Centrifuge the cell culture supernatant or biofluid at 300 × g for 10 minutes at 4°C to pellet intact cells.
- Debris Removal: Transfer the supernatant to a new tube and centrifuge at 2,000 × g for 20 minutes at 4°C to remove dead cells and large debris.
- Filtration (Optional): Carefully filter the supernatant through a 0.22 µm filter to remove larger particles and microvesicles.
- Ultracentrifugation: Transfer the filtered supernatant to ultracentrifuge tubes. Pellet exosomes by ultracentrifugation at ≥100,000 × g for 70-120 minutes at 4°C.
- Wash/Resuspension: Carefully decant the supernatant. Resuspend the often invisible pellet in a large volume of PBS (e.g., 10-30 mL). Perform a second ultracentrifugation step under the same conditions to wash the exosomes.
- Final Resuspension: Completely decant the supernatant and resuspend the final exosome pellet in a small volume (50-200 µL) of PBS or a suitable buffer for storage at -80°C.
Critical Steps and Troubleshooting
- Rotor Selection: Swinging-bucket rotors provide a more uniform pellet but often require longer run times than fixed-angle rotors.
- Pellet Visibility: The exosome pellet may not be visible. When discarding the supernatant after the final spin, do so carefully and consider leaving a small volume of liquid to avoid disturbing the pellet.
- Contamination: Adherence to a strict cleaning protocol for ultracentrifuge tubes is essential to avoid cross-contamination and lipid contamination.
Protocol 2: Size-Exclusion Chromatography (SEC)
SEC separates exosomes from smaller contaminating proteins and aggregates based on their hydrodynamic radius, offering excellent preservation of vesicle structure and function [5].
Materials and Reagents
- Size-exclusion chromatography columns (e.g., qEV columns, Sepharose CL-2B, Sephacryl S-400)
- Fraction collector (optional but recommended)
- PBS or other isotonic elution buffer
- Concentrated exosome sample (pre-cleared by centrifugation at 10,000 × g for 30 min)
Step-by-Step Procedure
- Column Equilibration: Follow manufacturer instructions to equilibrate the SEC column with at least two column volumes of elution buffer (e.g., PBS).
- Sample Application: Carefully load the pre-cleared sample onto the top of the resin bed. The sample volume should typically not exceed 0.5-2% of the total column volume for optimal resolution.
- Elution and Fraction Collection: Allow the sample to enter the resin, then add elution buffer and begin collecting sequential fractions. The void volume (containing exosomes) will elute first, followed by smaller proteins and other contaminants.
- Fraction Analysis: Identify exosome-rich fractions using nanoparticle tracking analysis (NTA), UV-vis spectrophotometry (absorbance at ~280 nm), or protein assays. Pool the exosome-positive fractions.
- Concentration (Optional): If a higher concentration is required, the pooled fractions can be concentrated using ultrafiltration devices with a 100-kDa molecular weight cut-off.
Critical Steps and Troubleshooting
- Sample Volume: Overloading the column with too large a sample volume is a common mistake that severely compromises resolution and purity.
- Flow Control: For gravity-flow columns, maintain a consistent hydrostatic pressure to ensure a stable flow rate. Automated systems provide better reproducibility.
- Buffer Compatibility: Ensure the elution buffer is compatible with downstream applications (e.g., avoid azide in cell-based assays).
Protocol 3: Microfluidic Immunoaffinity Capture
Microfluidic immunoaffinity capture isolates exosomes with high specificity by leveraging antibodies immobilized on a chip to target specific exosomal surface markers (e.g., CD9, CD63, CD81) [32].
Materials and Reagents
- Microfluidic chip with integrated anti-CD63 (or other target) antibodies (e.g., ExoChip)
- Syringe pump or peristaltic pump for precise flow control
- Binding and wash buffers (e.g., PBS with 1% BSA)
- Low-pH elution buffer (e.g., glycine-HCl) or a neutral buffer with a competing ligand
- Pre-cleared biofluid or cell culture supernatant
Step-by-Step Procedure
- Chip Priming: Prime the microfluidic channels with PBS or a suitable binding buffer to remove air bubbles and condition the surface.
- Sample Loading: Dilute the pre-cleared sample with binding buffer if necessary. Use a syringe pump to infuse the sample through the chip at a slow, controlled flow rate (e.g., 5-20 µL/min) to maximize antibody-antigen binding.
- Washing: After sample loading, wash the chip channels extensively with wash buffer to remove unbound and non-specifically bound contaminants.
- Elution: Introduce an elution buffer to release the captured exosomes from the immobilized antibodies. Collect the eluate in small fractions into neutralization buffer (if using low-pH elution) to maintain exosome viability.
- Chip Regeneration (Optional): For reusable chips, a regeneration buffer can be applied to prepare the surface for the next run.
Critical Steps and Troubleshooting
- Flow Rate Optimization: A slower flow rate increases interaction time with the antibody-coated surface, improving capture efficiency and yield.
- Antibody Specificity: The purity and subpopulation of the isolated exosomes are directly determined by the specificity of the immobilized antibody.
- Sample Clogging: Pre-clearing the sample via centrifugation (e.g., 10,000 × g for 30 min) and filtration (0.22 µm) is critical to prevent clogging of the microchannels.
Workflow and Decision Pathway
The following diagram illustrates a generalized experimental workflow for exosome isolation and analysis, integrating the techniques discussed.
Diagram 1: General Exosome Isolation Workflow
For researchers, the choice of the primary isolation path depends heavily on the experimental goal. The following decision pathway can guide method selection.
Diagram 2: Method Selection Decision Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of exosome isolation and characterization protocols requires specific reagents and instruments. The following table details key solutions for the featured techniques.
Table 2: Essential Research Reagents and Materials for Exosome Isolation
| Reagent/Material | Function/Application | Example Specifics |
|---|---|---|
| Polycarbonate Ultracentrifuge Tubes | Withstand high g-forces during ultracentrifugation without cracking. | Compatible with specific rotor types (e.g., Type 70 Ti, Type 45 Ti). |
| Size-Exclusion Chromatography Columns | Separate exosomes from contaminating proteins based on size. | qEV original columns, Sepharose CL-2B. |
| PBS (Phosphate-Buffered Saline) | Universal buffer for sample dilution, washing, and exosome resuspension. | Sterile, calcium- and magnesium-free for cell culture applications. |
| Protease/Phosphatase Inhibitor Cocktails | Preserve the protein and phosphoprotein cargo of exosomes during isolation. | Added to lysis buffers for downstream western blot or mass spectrometry. |
| Anti-Tetraspanin Antibodies (CD63, CD81, CD9) | Key reagents for immunoaffinity capture and characterization of exosomes. | Used immobilized on microfluidic chips [32] or for flow cytometry. |
| Polyethylene Glycol (PEG) | Polymer used in precipitation kits to force exosomes out of solution. | Component of commercial kits (e.g., ExoQuick, Total Exosome Isolation kits). |
| DMEM/F12 Medium | Base medium for stem cell culture and production of conditioned media for secretome analysis. | Often supplemented with vitamin C to enhance secretome production [33]. |
| Synthemax / Matrigel / Vitronectin | Defined substrates for coating culture vessels to support the growth of pluripotent stem cells. | Provides a scaffold for cell attachment and growth, influencing secretome composition [33]. |
| Nanoparticle Tracking Analyzer (NTA) | Instrument for determining exosome concentration and size distribution. | Measures Brownian motion (e.g., Malvern Nanosight). |
The isolation of exosomes from the stem cell secretome is a rapidly evolving field where methodological choice directly dictates the validity and translational potential of research outcomes. While ultracentrifugation remains a robust benchmark, SEC has gained prominence for its balance of purity and preservation of biological function. Precipitation offers unmatched simplicity for screening, and microfluidics represents the cutting edge for high-specificity, clinical-grade isolation. As the field progresses, the integration of these methods, such as combining SEC with microfluidic affinity capture, and the standardisation of protocols in line with MISEV guidelines, will be crucial for overcoming current challenges in yield and reproducibility [5]. For researchers and drug development professionals, a nuanced understanding of these techniques is indispensable for harnessing the full therapeutic potential of stem cell-derived exosomes.
Within stem cell secretome research, particularly for therapeutic applications, the precise characterization of isolated exosomes is a critical step to ensure the quality, purity, and functionality of these extracellular vesicles (EVs). The heterogeneity of EVs and the presence of co-isolated contaminants necessitate a multi-parametric analytical approach. This Application Note details a core suite of characterization techniques—Nanoparticle Tracking Analysis (NTA), Transmission Electron Microscopy (TEM), Flow Cytometry for tetraspanins (CD9/CD63/CD81), and Proteomics—framed within the context of stem cell secretome research. We provide standardized protocols and data interpretation guidelines to facilitate the rigorous characterization essential for robust and reproducible research outcomes in drug development [34] [11].
Core Characterization Techniques: Principles and Applications
A combination of techniques is mandatory to comprehensively assess the key physical and biochemical properties of isolated exosomes. The following table summarizes the primary application and measured parameters for each core method.
Table 1: Overview of Core Exosome Characterization Techniques
| Technique | Primary Measured Parameters | Key Application in Secretome Research |
|---|---|---|
| Nanoparticle Tracking Analysis (NTA) | Particle size distribution (in nm) and concentration (particles/mL) [35]. | Quantifying yield and confirming exosomal size range (typically 30-150 nm) [36] [35]. |
| Transmission Electron Microscopy (TEM) | Morphology, structural integrity, and bilayer membrane visualization [35] [37]. | Visual confirmation of classic cup-shaped, spherical vesicle morphology. |
| Flow Cytometry (CD9/CD63/CD81) | Surface protein expression and semi-quantification of tetraspanin markers [28]. | Phenotypic confirmation of exosomal identity using established protein markers [28] [35]. |
| Proteomics | Global protein identification and cargo composition [35]. | Validating presence of exosomal markers (e.g., Flotillin-1, TSG101) and assessing therapeutic cargo [35]. |
Technical Considerations and Limitations
Each technique provides unique insights but also has inherent limitations. NTA, while excellent for size and concentration, may struggle to distinguish exosomes from similar-sized impurities [28]. TEM provides definitive morphology but requires specialized equipment and expertise, and the vacuum environment can alter vesicle structure. Flow cytometry for exosomes is challenging due to their small size, often requiring capture on beads for analysis. Proteomics is powerful for cargo profiling but requires sophisticated instrumentation and data analysis, and results can be confounded by non-exosomal protein contaminants [35] [11]. Therefore, the integration of data from all these methods is essential for a confident assessment of exosome preparations.
Detailed Experimental Protocols
Nanoparticle Tracking Analysis (NTA)
Principle: NTA utilizes light scattering and Brownian motion to determine the size distribution and concentration of particles in a liquid suspension [35].
Protocol:
- Sample Preparation: Thaw the isolated exosome sample on ice. Dilute the sample in sterile, particle-free phosphate-buffered saline (PBS) to achieve a concentration within the ideal detection range of the instrument (typically 20-100 particles per frame). Optimal dilution factors must be determined empirically and are critical for accurate results [35].
- Instrument Calibration: Calibrate the NTA instrument (e.g., Malvern NanoSight NS300) using silica microspheres of known size (e.g., 100 nm) according to the manufacturer's instructions.
- Data Acquisition: Using a syringe pump to ensure a consistent flow:
- Load the diluted sample into the instrument.
- Record three to five 60-second videos for each sample, ensuring the camera level is adjusted to visualize particles as sharp, distinct points.
- Maintain a constant temperature (e.g., 25°C) during all measurements.
- Data Analysis: Process the captured videos using the integrated software (e.g., NTA 3.4 Software). Report the mean, mode, and D10/D50/D90 values for particle size and the estimated concentration (particles/mL). Results from multiple recordings should be averaged.
Transmission Electron Microscopy (TEM)
Principle: TEM employs a beam of electrons to visualize the ultrastructure of exosomes, confirming their spherical or cup-shaped morphology and bilayer membrane [35] [37].
Protocol (Negative Staining):
- Grid Preparation: Glow-discharge a carbon-coated Formvar grid (200-400 mesh) to render it hydrophilic.
- Sample Application: Pipette 3-5 µL of the exosome suspension onto the grid. Allow it to adsorb for 1-2 minutes in a humidified chamber.
- Staining and Washing:
- Wick away excess liquid carefully with filter paper.
- Immediately add a drop of 1-2% uranyl acetate solution to the grid and stain for 1 minute.
- Wick away the stain and wash by applying a drop of deionized water, which is then immediately wicked away. Repeat the wash step.
- Drying and Imaging: Allow the grid to air-dry completely. Image the samples using a TEM operated at 80-100 kV. Capture images at various magnifications to assess morphology and homogeneity.
Flow Cytometry for Tetraspanin Profiling (CD9/CD63/CD81)
Princique: This protocol uses antibody-conjugated magnetic beads to capture exosomes, enabling their subsequent detection and characterization via flow cytometry [28].
Protocol (Bead-Based Capture Assay):
- Exosome Capture:
- Incubate 10-20 µL of aldehyde/sulfate latex beads with 10-50 µg of exosome protein in a total volume of 100 µL PBS. Rotate this mixture for 15 minutes at room temperature.
- Stop the reaction by adding 100 mM glycine in PBS and incubate for an additional 30 minutes.
- Pellet the beads (5,000 x g, 5 minutes) and wash twice with 0.1% BSA in PBS (PBS-BSA).
- Antibody Staining:
- Resuspend the exosome-coated beads in 100 µL PBS-BSA.
- Add fluorochrome-conjugated antibodies against CD9, CD63, and CD81 (or relevant isotype controls). Use titrated antibody concentrations as per manufacturer recommendations.
- Incubate for 30-45 minutes at 4°C in the dark.
- Pellet the beads and wash twice with PBS-BSA to remove unbound antibodies.
- Flow Cytometry Acquisition: Resuspend the final bead pellet in 300-500 µL PBS-BSA. Analyze the samples on a flow cytometer equipped with appropriate lasers and filters. Collect a minimum of 10,000 bead events. The median fluorescence intensity (MFI) of the stained sample versus the isotype control is used to determine tetraspanin expression.
Proteomic Analysis by Mass Spectrometry
Principle: Liquid chromatography with tandem mass spectrometry (LC-MS/MS) enables the global identification and quantification of proteins in an exosome preparation, confirming identity and revealing functional cargo [35].
Protocol:
- Protein Extraction and Digestion:
- Lyse the exosome pellet in a suitable lysis buffer (e.g., RIPA buffer). Determine the protein concentration using an assay compatible with detergents (e.g., BCA assay).
- Reduce and alkylate proteins using dithiothreitol (DTT) and iodoacetamide (IAA), respectively.
- Digest the proteins into peptides using sequencing-grade trypsin (typically at a 1:50 enzyme-to-protein ratio) overnight at 37°C.
- LC-MS/MS Analysis:
- Desalt the resulting peptides using C18 solid-phase extraction tips.
- Separate the peptides via reversed-phase nano-liquid chromatography (nano-LC).
- Elute peptides directly into a high-resolution tandem mass spectrometer (e.g., Q-Exactive HF-X, TimsTOF).
- Operate the MS in data-dependent acquisition (DDA) mode, automatically switching between MS1 and MS2 to fragment the most intense ions.
- Data Processing:
- Search the raw MS/MS data against a relevant protein sequence database (e.g., Swiss-Prot Human) using search engines like MaxQuant or FragPipe.
- Use standard false discovery rate (FDR) thresholds (<1%) for protein identification.
Table 2: Key Protein Markers for Characterization of Stem Cell-Derived Exosomes
| Protein Category | Example Markers | Function / Significance |
|---|---|---|
| Tetraspanins | CD9, CD63, CD81 [28] [35] | Classical exosome surface markers; involved in vesicle biogenesis and cargo sorting. |
| Endosomal Sorting Complexes | TSG101, Alix [35] | Proteins associated with the ESCRT pathway, crucial for exosome biogenesis. |
| Heat Shock Proteins | HSP70, HSP90 | Stress proteins often enriched in exosomes. |
| Membrane Transport & Fusion | Flotillin-1, Annexins [35] | Involved in membrane organization and vesicle fusion processes. |
| Stem Cell-Specific Markers | CD44, CD73, CD90 [11] [38] | Markers indicative of the mesenchymal stem cell origin of the vesicles. |
Research Reagent Solutions
The following table lists essential reagents and kits commonly used in the characterization of stem cell-derived exosomes.
Table 3: Essential Research Reagents for Exosome Characterization
| Reagent / Kit | Function / Application | Example Vendor / Citation |
|---|---|---|
| Total Exosome Isolation Reagent | Precipitation-based isolation of exosomes from cell culture supernatant or biofluids prior to characterization [37]. | Thermo Fisher Scientific [37] |
| Anti-CD9/CD63/CD81 Antibodies | Fluorochrome-conjugated antibodies for the flow cytometric phenotyping of exosomes (typically in a bead-based assay) [28]. | Multiple (e.g., Santa Cruz Biotechnology [37]) |
| Aldehyde/Sulfate Latex Beads | Beads for capturing exosomes via surface proteins for subsequent antibody staining and analysis by flow cytometry [28]. | Thermo Fisher Scientific |
| Uranyl Acetate | Heavy metal salt used for negative staining of exosomes to provide contrast for imaging by TEM [37]. | Electron Microscopy Sciences |
| Protease Inhibitor Cocktail | Added to lysis buffers during protein extraction for proteomics to prevent degradation of the protein cargo [35]. | Promega [35] |
Integrated Data Analysis and Workflow
The power of this characterization strategy is realized through the integration of data from all four techniques. The following diagram illustrates the sequential workflow and how data from each method contributes to a comprehensive conclusion.
A multi-parametric approach integrating NTA, TEM, flow cytometry, and proteomics is non-negotiable for the rigorous characterization of exosomes within stem cell secretome research. The protocols and frameworks provided in this Application Note offer a standardized pathway for researchers to validate their isolations, assess batch-to-batch consistency, and build a solid foundation for subsequent functional studies and therapeutic development. By adhering to these detailed strategies, scientists can enhance the reliability and translational potential of their exosome-based research.
Within the rapidly advancing field of stem cell secretome characterization, the isolation of pure, functional exosomes is a fundamental prerequisite for their successful application in therapeutic development and basic research. The presence of co-isolated contaminants—such as protein aggregates, non-exosomal vesicles, and residual media components—can severely compromise experimental results and therapeutic efficacy, leading to unreliable data and potential safety concerns. This application note details a robust, orthogonal analytical workflow that integrates Size Exclusion Chromatography-High Performance Liquid Chromatography (SEC-HPLC) with complementary protein assays to provide a critical assessment of exosome purity. Designed for researchers, scientists, and drug development professionals, the protocols herein are framed within the context of a broader thesis on stem cell secretome research, offering detailed methodologies to overcome the significant challenge of contaminants in exosome isolation.
The Central Role of SEC-HPLC in Purity Analysis
SEC-HPLC, also known as molecular sieve chromatography, is a powerful technique that separates macromolecules based on their hydrodynamic volume or size in solution [39]. The principle relies on the differential access of molecules to the pores of a chromatographic column's stationary phase: larger molecules, such as exosomes, are excluded from most pores and elute first, while smaller molecules and soluble proteins penetrate the pores and elute later [39]. This mechanism makes SEC-HPLC exceptionally well-suited for resolving desired exosome populations from smaller, non-vesicular contaminants that are prevalent in stem cell-conditioned media.
The application of SEC-HPLC for troubleshooting in bioprocessing underscores its critical value. A key study investigating low yield in Protein A chromatography for monoclonal antibodies and Fc-fusion proteins demonstrated that SEC-HPLC analysis of the column load and flow-through was indispensable for identifying the root cause: the presence of non-binding protein aggregates that were missed by SDS-PAGE analysis alone [40]. This finding highlights that contaminant interference is not merely a theoretical concern but a practical issue that can significantly impact downstream processing efficiency and product quality. Applying this analytical rigor to secretome analysis is therefore paramount.
Diagram 1: SEC Separation Principle. Larger particles are excluded from column pores and elute first, while smaller molecules penetrate pores and have longer retention times.
Comprehensive Experimental Protocols
SEC-HPLC Analysis of Secretome Samples
This protocol is adapted from established SEC-HPLC methods for macromolecular analysis [39] [41] and is designed for the characterization of exosome-containing samples.
Materials and Reagents
- Mobile Phase: 150 mM phosphate-buffered saline (PBS), pH 7.0. Filter through a 0.22 µm nylon membrane filter and degas via ultrasonication before use [39].
- SEC Column: A biocompatible SEC column, such as an AdvanceBio SEC column or an Ultra-hydrogel DP column, suitable for separating nanoparticles and biopolymers [39] [41].
- HPLC System: An Agilent 1260 Infinity Bio-inert Quaternary LC System or equivalent, equipped with a UV/Vis detector [39].
- Sample Preparation: Concentrate the stem cell-conditioned medium or isolated exosome sample to approximately 1 mg/mL. Filter through a 0.22 µm nylon membrane filter immediately before injection to remove particulates [39].
Methodology
- System Equilibration: Install the SEC column and equilibrate with the degassed mobile phase at a flow rate of 0.5 mL/min for 30-60 minutes, or until a stable baseline is achieved [39].
- Sample Injection: Place the filtered sample in a vial on the autosampler. Set the injection volume, typically 20 µL, and the detection wavelength (e.g., 280 nm for protein detection) [39].
- Chromatographic Run: Initiate the sequence using an isocratic elution with the PBS mobile phase at 0.5 mL/min. Monitor the elution profile for 30-40 minutes.
- Data Analysis: Identify peaks corresponding to exosomes (early eluting), protein aggregates (variable elution), and soluble proteins (late eluting). Collect fractions for further analysis.
Orthogonal Protein Assays for Contaminant Detection
To complement the SEC-HPLC profile, perform the following assays on the starting material and collected SEC fractions.
Total Protein Quantification (BCA Assay)
- Principle: The bicinchoninic acid (BCA) assay measures total protein concentration, which is useful for normalizing samples but cannot distinguish exosomal from contaminating proteins.
- Procedure: Use a commercial BCA kit according to the manufacturer's instructions. Measure the absorbance of standards and unknown samples at 562 nm.
- Data Interpretation: A high total protein-to-particle ratio (as determined by NTA) in a sample or fraction indicates significant soluble protein contamination.
Specific Marker Analysis (Western Blot)
- Principle: Immunoblotting detects the presence of specific exosomal markers and potential contaminants.
- Procedure: Separate proteins from whole secretome and SEC fractions by SDS-PAGE. Transfer to a membrane and probe with antibodies against:
- Data Interpretation: Purer exosome preparations will show strong signals for exosomal markers and weak or absent signals for contaminant markers.
Research Reagent Solutions
The following table details essential materials for implementing the described purity assessment workflow.
Table 1: Key Research Reagents and Materials for Purity Assessment
| Item | Function/Description | Example Product/Criteria |
|---|---|---|
| SEC-HPLC Column | Separates particles by size; core of the purity assessment. | AdvanceBio SEC Column; Ultra-hydrogel DP Column [39] [41] |
| Biocompatible HPLC System | Reduces non-specific adsorption of biomolecules. | Agilent 1260 Infinity Bio-inert System [39] |
| Mobile Phase Buffer | Provides the liquid phase for SEC separation. | 150 mM Phosphate Buffered Saline (PBS), pH 7.0 [39] |
| Filtration Membranes | Removes particulates from mobile phase and samples. | 0.22 µm Nylon Membrane Filter [39] |
| Antibody Panel | Detects exosomal markers and contaminants via Western Blot. | Anti-CD63, Anti-CD81, Anti-Alix, Anti-Apolipoprotein [3] [11] |
| Protein Assay Kit | Quantifies total protein content (e.g., BCA Assay). | Commercial BCA Protein Assay Kit |
Integrated Workflow and Data Interpretation
Combining SEC-HPLC with protein assays provides a multi-dimensional view of sample purity. The typical workflow begins with preparing the stem cell-conditioned medium, which is then analyzed by SEC-HPLC. The resulting chromatogram guides the collection of fractions, which are subsequently characterized using protein quantification and Western blotting. This integrated approach is crucial for identifying and quantifying contaminants that can skew functional assays and impede therapeutic development.
Diagram 2: Integrated Purity Assessment Workflow. The orthogonal approach combines size-based separation with specific biochemical assays for a comprehensive analysis.
Table 2: Interpreting SEC-HPLC and Protein Assay Data for Purity Assessment
| Analysis Method | Observation | Interpretation | Recommended Action |
|---|---|---|---|
| SEC-HPLC Profile | A single, sharp peak in the exclusion volume. | High purity exosome fraction. | Proceed to functional assays. |
| Broad or multiple peaks in the inclusion volume. | Significant contamination with soluble proteins/aggregates. | Optimize initial isolation (e.g., use SEC as a clean-up step). | |
| BCA Assay | Low total protein in exosome SEC fraction. | Good separation from soluble contaminants. | Correlate with Western blot and NTA data. |
| High total protein in exosome SEC fraction. | Poor separation; co-elution of proteins. | Re-optimize SEC method or use a different column. | |
| Western Blot | Strong CD63/CD81 signal in exosome fraction. | Successful isolation of exosomes. | Confirm absence of contaminant markers. |
| Presence of apolipoprotein signals. | Contamination with serum-derived proteins. | Switch to serum-free culture conditions. |
The rigorous characterization of stem cell-derived exosomes is a critical step in translating their potential into reliable research and safe, effective therapies. The orthogonal strategy outlined here—leveraging the size-based separation power of SEC-HPLC alongside quantitative and specific protein assays—provides researchers with a comprehensive toolkit for critical purity assessment. By systematically identifying and quantifying contaminants, this workflow enables scientists to overcome a major hurdle in the field, ensuring that subsequent functional studies and therapeutic applications are built upon a foundation of well-characterized, high-quality exosome preparations.
The clinical translation of stem cell secretomes and extracellular vesicles (EVs) faces a critical manufacturing bottleneck: transitioning from laboratory-scale production to robust, reproducible processes that meet regulatory standards for clinical applications. As these biological products advance toward clinical trials, implementing Good Manufacturing Practice (GMP)-compliant processes becomes essential to ensure product safety, identity, purity, and potency [43]. The inherent biological variability of mesenchymal stem/stromal cells (MSCs) from different tissue sources and donors further complicates this transition, necessitating standardized approaches to manufacturing and quality control [44].
This article outlines scalable bioreactor platforms and quality control frameworks for GMP-compliant production of stem cell secretomes and EVs, with a focus on standardized protocols for clinical translation. We present a systematic approach to critical process parameters (CPPs) and critical quality attributes (CQAs) that align with the Quality-by-Design (QbD) principles endorsed by regulatory authorities [45] [44]. By integrating recent advances in bioreactor technology with comprehensive characterization methods, we provide a roadmap for researchers to bridge the gap between benchtop discovery and clinical-scale manufacturing of secretome-based therapeutics.
Bioreactor Systems for Scalable Secretome Production
Comparative Analysis of Bioreactor Platforms
Stirred-tank bioreactors and hollow fiber systems represent the two most promising platforms for scaling up secretome and EV production under GMP-compliant conditions. Each system offers distinct advantages for different stages of process development and manufacturing.
Table 1: Comparison of Bioreactor Systems for MSC Secretome Production
| Bioreactor Type | Working Volume | Max Cell Concentration | Scalability | Key Applications | Reference |
|---|---|---|---|---|---|
| Stirred-Tank (Microcarrier-based) | 0.1-3L | 1.0-2.3 × 10^6 cells/mL | High | Large-scale EV production for ARS treatment | [46] |
| Hollow Fiber Bioreactor | 200mL (intracapillary space) | 5 × 10^8 total cells | Medium-High | Clinical-scale EV production, LPS-primed EVs | [43] [46] |
| DASGIP Parallel System | 125-200mL | 2.1-4.7 × 10^6 cells/mL | Medium | Process optimization, parameter screening | [45] |
| PBS MINI Vertical-Wheel | 60-300mL | 1.26 × 10^6 cells/mL | Medium | Aggregate-based cultures, 3D expansion | [45] |
Hollow Fiber Bioreactor Protocol for Clinical-Scale EV Production
The hollow fiber bioreactor system enables high-density cell culture in a closed, controlled environment suitable for GMP compliance. The following protocol has been successfully implemented for producing EVs approved for a Phase I clinical trial for heart failure [43] and for acute radiation syndrome [46].
Materials:
- Quantum Cell Expansion System (Terumo BCT) or similar hollow fiber bioreactor
- GMP-grade human platelet lysate (hPL) or xeno-free media supplements
- Serum-free medium (SFM) compatible with MSCs
- GMP-compatible human MSC working cell bank
- Lipopolysaccharide (LPS) for priming (if applicable)
- Ultracentrifugation equipment or tangential flow filtration system
Procedure:
Bioreactor Preparation:
- Coat the hollow fiber bioreactor with 0.005% human fibronectin in PBS for 4 hours
- Perform a systemic washout with culture media to remove coating solution
- Verify integrity of the closed system and aseptic connections
Cell Seeding and Expansion:
- Seed 3.0 × 10^7 MSCs into the bioreactor's extracapillary space
- Allow cells to attach for 24 hours with minimal circulation
- Initiate continuous media perfusion through the intracapillary space
- Monitor cell growth via glucose consumption and lactate production rates
- Expand cells for approximately 6 days until reaching approximately 5 × 10^8 total cells [46]
Serum-Free Conditioning and EV Induction:
- Wash out expansion media with PBS
- Replace with 200mL SFM supplemented with 1.0 µg/mL LPS for primed EV production [46]
- Collect conditioned media at 24-hour intervals for up to 96 hours
- Maintain physiological parameters: pH 7.2-7.4, dissolved oxygen 20-60%, temperature 37°C
EV Harvest and Concentration:
- Pool conditioned media and perform low-speed centrifugation (2,000 × g, 20 min, 4°C)
- Concentrate using tangential flow filtration (TFF) with 100-500kDa MWCO membranes [43]
- Perform final purification through ultracentrifugation (100,000 × g, 2h, 4°C) or size-exclusion chromatography
- Formulate EVs in PBS with trehalose as a cryoprotectant [46]
- Store final product at -65°C to -85°C [43]
Figure 1: GMP-Compliant Workflow for Bioreactor-Based EV Production
Quality Control and Characterization of Secretome Products
Critical Quality Attributes (CQAs) for Secretome and EV Products
Implementing a robust quality control strategy is essential for GMP-compliant manufacturing of secretome-based products. The following CQAs should be evaluated for both in-process testing and final product release.
Table 2: Critical Quality Attributes for Secretome and EV Products
| Quality Attribute | Testing Method | Release Criteria | Frequency | Reference |
|---|---|---|---|---|
| Particle Concentration & Size | Nanoparticle Tracking Analysis | 30-200 nm diameter, <20% PDI | Each batch | [43] [46] |
| EV-Specific Markers | Western Blot, Flow Cytometry | Positive: CD9, CD63, CD81, TSG101; Negative: Calnexin | Each batch | [47] [48] |
| Protein Content | BCA Assay | Batch-consistent profile | Each batch | [47] [46] |
| Sterility | BacT/ALERT, Mycoplasma PCR | No microbial growth | Each batch | [43] |
| Endotoxin | LAL Assay | <0.5 EU/mL | Each batch | [43] |
| Purity | Protein:Particle Ratio | Consistent with reference batch | Each batch | [43] |
| Identity (Proteomics) | LC-MS/MS | Tissue-specific signature | Reference batch | [48] [49] |
| Potency (in vitro) | Cell-based assays (angiogenesis, immunomodulation) | EC50 within specification | Each batch | [44] [49] |
| Potency (in vivo) | Disease-relevant animal models | Significant efficacy vs. control | Process changes | [43] [46] |
Comprehensive Characterization Protocol
A. Nanoparticle Characterization:
- Sample Preparation: Dilute EV samples 1:100-1:1000 in sterile, filtered PBS
- NTA Analysis:
- Transmission Electron Microscopy:
B. Proteomic Characterization (LC-MS/MS):
- Protein Extraction:
- Trypsin Digestion:
- Reduce with 5mM DTT, 30min, 56°C
- Alkylate with 11mM iodoacetamide, 24°C, darkness
- Digest with trypsin (50:1 ratio), 16h, 37°C
- Desalt with C18 columns [48]
- LC-MS/MS Analysis:
C. Functional Potency Assays:
- Angiogenesis Assay:
- Seed HUVECs (5×10^3 cells/well) in matrigel-coated 96-well plates
- Treat with secretome samples (1-100μg/mL)
- Quantify tube formation after 6-8h
- Include VEGF (50ng/mL) as positive control [49]
- Immunomodulation Assay:
- Isolate human PBMCs from healthy donors
- Activate with CD3/CD28 beads (1:1 ratio)
- Treat with EVs (1×10^9 particles/mL)
- Measure IFN-γ and IL-10 secretion after 48h by ELISA [46]
Figure 2: Quality Control Testing Strategy for Secretome Products
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for GMP-Compliant Secretome Production
| Reagent Category | Specific Products | Function | GMP-Compliant Alternatives |
|---|---|---|---|
| Cell Culture Media | StemPro MSC SFM, mTeSR, DMEM/F12 | Cell expansion and conditioning | Xenofree formulations with hPL supplementation |
| Bioreactor Systems | Quantum Cell Expansion System, DASGIP, PBS MINI | Scalable cell culture platform | Closed-system, sterilizable bioreactors |
| EV Isolation Kits | Ultracentrifugation, TFF systems, Size-exclusion chromatography | EV purification and concentration | GMP-compatible TFF cartridges |
| Characterization Tools | NanoSight NTA, Malvern Zetasizer, LC-MS/MS systems | Physical and molecular characterization | Qualified methods with reference standards |
| QC Assay Kits | BCA protein assay, LAL endotoxin test, Flow cytometry panels | Quality control testing | Validated kits with certificates of analysis |
The successful clinical translation of stem cell secretomes and EVs requires careful integration of scalable bioreactor systems with robust quality control frameworks. The protocols outlined herein provide a foundation for implementing GMP-compliant manufacturing processes that can consistently produce therapeutic-grade secretome products. By adopting a QbD approach that identifies and monitors critical process parameters and quality attributes, researchers can enhance process robustness while ensuring product safety and efficacy.
As evidenced by recent clinical advancements, including the approval of an EV-enriched secretome for a Phase I cardiac trial [43], these manufacturing strategies are already enabling the transition from preclinical research to clinical applications. Continued refinement of bioreactor technologies, analytical methods, and regulatory frameworks will further accelerate the clinical translation of secretome-based therapies for a wide range of degenerative, inflammatory, and ischemic conditions.
Within the evolving paradigm of stem cell-derived secretome and exosome therapies, the route of administration is a critical determinant of therapeutic success. This document provides detailed application notes and protocols for comparing intravenous (IV) infusion and aerosolized inhalation, framing this investigation within a broader thesis on stem cell secretome characterization and exosome isolation. The therapeutic potential of mesenchymal stem cell (MSC)-derived secretomes, which include extracellular vesicles like exosomes, growth factors, and cytokines, is now well-established for their abilities to modulate immune responses, promote tissue repair, and enhance regeneration [3] [50]. However, the translational efficacy of these "cell-free" therapeutics is profoundly influenced by their delivery method, which governs biodistribution, target organ concentration, and systemic exposure. This document provides standardized protocols for preclinical assessment of these routes, ensuring that data on pharmacokinetics (PK), pharmacodynamics (PD), and dose optimization are collected systematically for robust comparison, in alignment with modern clinical trial protocol standards like SPIRIT 2025 [51].
Comparative Pharmacokinetic & Pharmacodynamic Data
The administration route directly impacts key PK/PD parameters, dictating the required dosing regimen and therapeutic potential. Table 1 summarizes quantitative data from a comparative preclinical study, illustrating the profound impact of route selection on drug exposure and retention.
Table 1: Pharmacokinetic Comparison of Intravenous vs. Inhaled Administration
| Parameter | Intravenous (IV) Injection | Aerosolized Inhalation | Implication for Therapy |
|---|---|---|---|
| Lung Cmax & AUC | Baseline (1x) | ~20x higher than IV [52] | Vastly increased drug exposure in the lung tissue. |
| Lung Drug Half-Life | Shorter half-life | ~2x longer than IV [52] | Prolonged therapeutic effect in the lungs. |
| Time above MEC in Lung | < 24 hours [52] | 168 hours [52] | Supports less frequent dosing. |
| Systemic Distribution | Widespread (Liver > Spleen ≥ Lungs) [53] | Primarily localized to lungs; 45% lower in liver/kidney [52] | Reduced potential for systemic toxicity. |
| Proposed Dosing | Daily IV dosing [52] | Potential for weekly dosing [52] | Improved patient compliance and convenience. |
The data demonstrates that inhalation provides superior target engagement for pulmonary conditions with a favorable safety profile, while IV infusion leads to broader systemic distribution.
Experimental Protocols
The following protocols are designed for a head-to-head comparison of administration routes for MSC-derived products in rodent models.
Protocol: Preclinical PK/PD Study for Route Comparison
Objective: To compare the lung exposure and systemic distribution of a therapeutic agent (e.g., MSC-derived exosomes or a small molecule drug like caspofungin) following IV and inhaled administration.
Materials:
- Therapeutic Agent (e.g., characterized MSC-exosomes, fluorescently labeled if needed)
- Animal Model (e.g., Sprague-Dawley rats, 200-250g)
- IV Administration Setup (Syringe pump, catheter)
- Aerosol Delivery System (Nose-only inhalation chamber, nebulizer)
- HPLC-MS-MS system for drug quantification [52]
Method:
- Dosing:
- Sample Collection: At predetermined time points (e.g., 0.25, 0.5, 1, 2, 4, 8, 24, 72, 168h post-dose), collect plasma and tissue samples (lungs, liver, kidney, spleen).
- Bioanalysis: Homogenize tissue samples. Analyze drug/exosome concentrations in plasma and tissue homogenates using HPLC-MS-MS for drugs or appropriate assays (e.g., ELISA, particle analysis) for exosomal markers [52].
- Data Analysis: Calculate PK parameters (C~max~, T~max~, AUC, t~1/2~) for plasma and each tissue. Compare lung-to-systemic ratios between the two cohorts.
Protocol: Isolation of MSC-Derived Exosomes for Administration
Objective: To obtain a purified and characterized exosome population from MSC-conditioned medium for use in administration studies.
Materials:
- Human Adipose-Derived MSCs (AD-MSCs) [3]
- Conditioned Medium (CM) from MSC cultures
- Ultracentrifugation equipment [3] [54]
- Polymeric Precipitation Kit (e.g., Total Exosome Isolation reagent) [3] [54]
- Phosphate Buffered Saline (PBS)
- Trehalose solution for cryopreservation [54]
Method:
- CM Collection: Culture AD-MSCs until 70-80% confluent. Replace medium with serum-free or exosome-depleted FBS medium. Collect CM after 48 hours [3] [54].
- CM Pre-Clearing: Centrifuge CM at 300 × g for 10 min (remove cells) and 2,000 × g for 20 min (remove cell debris). Filter through a 0.22 µm filter [54].
- Exosome Isolation (Precipitation Method):
- Concentrate the pre-cleared CM using an ultrafiltration device (e.g., 50 kDa MWCO) [54].
- Mix the concentrate with a volume of precipitation reagent as per manufacturer's instructions (e.g., 1:2 sample:reagent ratio).
- Incubate overnight at 4°C.
- Centrifuge at 10,000 × g for 1 hour at 4°C. Discard the supernatant.
- Resuspend the exosome pellet in PBS/trehalose and store at -80°C [54].
- Characterization: Validate exosome isolates using Nanoparticle Tracking Analysis (size/concentration), Transmission Electron Microscopy (morphology), and Western Blotting for markers (CD63, CD81, TSG101, Alix) [3] [11].
The experimental workflow for the complete process, from exosome isolation to administration and analysis, is depicted below.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of these protocols relies on specific reagents and equipment. Table 2 lists key materials and their functions.
Table 2: Essential Research Reagents and Materials
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Total Exosome Isolation Reagent | Polymer-based precipitation for high-yield exosome isolation from cell culture media. | Sold by Invitrogen; used for rapid, equipment-light isolation [54]. |
| Size Exclusion Chromatography (SEC) Columns | High-purity exosome purification post-concentration; separates EVs from soluble proteins. | qEV columns (Izon); EVsecond SEC columns (ImmunoStep) [11] [54]. |
| Ultracentrifugation Equipment | Traditional "gold-standard" method for exosome pelleting; requires significant equipment. | Beckman Coulter Optima XPN series with fixed-angle rotors [3]. |
| Trehalose in PBS | A cryoprotectant solution for resuspending and storing exosome pellets to maintain vesicle integrity. | 25 mM concentration in PBS is commonly used for storage at -80°C [54]. |
| Nose-only Inhalation System | Precisely delivers aerosolized therapeutics to the respiratory tract of rodent models. | Enables controlled dosing and minimizes test article waste [52]. |
| Nanoparticle Tracking Analyzer | Characterizes the size distribution and concentration of isolated exosome preparations. | Malvern Panalytical NanoSight NS300 [3] [11]. |
The data and protocols presented herein underscore a fundamental principle in therapeutic development: the administration route is not merely a delivery mechanism but a core component of the therapeutic strategy. For pulmonary indications like aspergillosis, asthma, or COPD, the evidence is overwhelmingly in favor of aerosolized inhalation. It achieves superior drug levels at the disease site with prolonged retention, while minimizing systemic exposure and enabling less frequent dosing [52]. This targeted approach aligns with the goals of personalized medicine and can be particularly advantageous for potent biologics like MSC-exosomes, where controlling systemic distribution is desirable.
Conversely, intravenous infusion remains indispensable for treating systemic conditions or when the therapeutic target is outside the pulmonary system, ensuring widespread distribution via the circulatory system [53]. The choice between routes must be guided by the pathophysiology of the target disease, the mechanism of action of the therapeutic, and the overall benefit-risk profile.
Integrating these comparative assessments early in the therapeutic development pipeline, using standardized protocols like those described, is crucial. Furthermore, the design of subsequent clinical trials must be informed by this preclinical data, adhering to modern guidelines like the SPIRIT 2025 statement, which emphasizes detailed protocol descriptions for interventions, outcomes, and data sharing to enhance reproducibility and transparency [51] [55]. By systematically evaluating and optimizing administration routes, researchers can fully leverage the immense potential of stem cell secretome and exosome therapies, ensuring they deliver the right dose to the right place at the right time.
Navigating Roadblocks: Solutions for Purity, Yield, and Functional Consistency in EV Research
The therapeutic potential of stem cell secretomes, particularly their exosome component, has positioned them as a leading candidate in regenerative medicine and drug development [56] [20]. These extracellular vesicles (EVs) mediate intercellular communication by transporting proteins, nucleic acids, and lipids, influencing processes from tissue repair to immunomodulation [57]. However, the transition from research to clinical application is hindered by a central, unresolved challenge: the efficient isolation of these nanoscale particles from complex biological media with high yield and purity [58] [59] [50]. Current methods often involve compromises, where increases in yield can sacrifice purity and vice versa, leading to inconsistent experimental results and unreliable therapeutic products [59] [57]. This application note details standardized, optimized protocols and strategic insights to overcome these inefficiencies, enabling the reproducible production of high-quality exosomes for downstream applications.
Comparative Analysis of Isolation Techniques
Selecting an isolation method is a critical decision that dictates the quality and functionality of the resulting exosomes. The table below provides a quantitative comparison of the most common techniques, highlighting the inherent trade-offs.
Table 1: Quantitative Comparison of sEV/Exosome Isolation Methods
| Method | Reported sEV Concentration (Particles/mL) | Reported Particle Size (nm) | Purity (Relative Particle-to-Protein Ratio) | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| PEG-based Precipitation (CP) | Saliva: 2.43E+11Plasma: 1.76E+11Media: 1.46E+10 [59] | 76.13 - 86.90 [59] | Low [59] | Simple protocol; high yield; minimal equipment [59] | Low purity; co-precipitation of contaminants [59] |
| PEG-Precipitation with Ultrafiltration (CPF) | Successively lower than CP, but higher than UC [59] | ~94.13 (Plasma) [59] | Moderate (Higher than CP) [59] | Good balance of yield and purity; specified CD9 expression [59] | Requires additional filtration equipment [59] |
| Ultracentrifugation (UC) | Saliva: 1.74E+09Plasma: 1.02E+10Media: 1.30E+09 [59] | 88.13 - 97.83 [59] | High [59] | Considered the "gold standard"; good reproducibility [59] [57] | Time-consuming; low yield; requires expensive equipment; risk of vesicle damage [59] [57] |
| Size-Exclusion Chromatography (SEC) | Lower than CP/CPF; higher than UC (but fraction-dependent) [59] | 84.97 - 95.50 (high size variation) [59] | High [59] | High purity; preserves vesicle integrity [59] [57] | Lower yield; sample dilution; requires optimization for different fluids [59] |
| Tangential Flow Filtration (TFF) | Information not explicitly quantified in results | Information not explicitly quantified in results | High [20] | Scalable; suitable for GMP biomanufacturing; gentle on vesicles [20] | Can be complex to set up; requires specialized systems [57] |
| Microfluidic Devices (e.g., BEST) | Information not explicitly quantified in results | Information not explicitly quantified in results | High (Biologically intact) [57] | High purity; rapid isolation; potential for automation and integration [57] | Low throughput; not yet widely adopted for large-scale production [58] |
Detailed Experimental Protocols
Integrated Chemical Precipitation and Ultrafiltration (CPF) Protocol
This protocol combines precipitation and filtration to offer a balanced approach for labs without access to ultracentrifugation equipment [59].
3.1.1 Research Reagent Solutions
Table 2: Essential Reagents for the CPF Protocol
| Reagent/Material | Function | Notes for Standardization |
|---|---|---|
| Polyethylene Glycol (PEG) | Drives exosomes out of solution via volume exclusion [59] | Use a consistent molecular weight (e.g., PEG 8000) and concentration. |
| 0.22 µm Pore Syringe Filter | Removes large debris and particles [59] | Use low-protein-binding PVDF or PES filters. |
| Ultrafiltration Device (e.g., 100 kDa MWCO) | Concentrates the sample and removes residual PEG and soluble proteins [59] | Ensures final sample is in a desired buffer (e.g., PBS). |
| Phosphate-Buffered Saline (PBS) | Washing and resuspension buffer | Use sterile, particle-free PBS. |
3.1.2 Step-by-Step Procedure
- Sample Preparation: Centrifuge cell culture media (conditioned for 48-72 hours in FBS-free media to eliminate serum-derived vesicle interference) at 2,000 × g for 30 minutes to remove cells and large debris [56] [59].
- PEG Precipitation: Mix the clarified supernatant with PEG solution to a final concentration of 8-10%. Incubate the mixture overnight at 4°C with gentle agitation [59].
- Initial Pellet Formation: Centrifuge the PEG-sample mixture at 10,000 × g for 1 hour at 4°C to pellet the crude exosome preparation. Carefully discard the supernatant.
- First Resuspension: Resuspend the pellet in a minimal volume of PBS.
- Pre-filtration: Pass the resuspended pellet through a 0.22 µm syringe filter to remove large aggregates and improve sample homogeneity [59].
- Ultrafiltration: Load the filtered suspension into a 100 kDa molecular weight cut-off (MWCO) ultrafiltration device. Centrifuge according to the manufacturer's instructions until the volume is significantly reduced.
- Buffer Exchange/Wash: Add fresh PBS to the concentrator and repeat centrifugation. This step removes residual PEG and contaminants. Repeat this wash step twice.
- Final Concentration: Concentrate the sample to the desired volume (e.g., 100-200 µL). The final isolate, now in a pure PBS buffer, can be aliquoted and stored at -80°C.
Optimized Ultracentrifugation Protocol with Density Gradient
This protocol enhances purity over standard differential ultracentrifugation and is recommended for applications requiring the highest quality, such as therapeutic development [59] [57].
3.2.1 Research Reagent Solutions
- Iodixanol or Sucrose Density Gradient: A pre-formed continuous or discontinuous gradient (e.g., 5%-40%) to separate particles based on buoyant density [57].
- Ultra-Clean PBS.
- Optimal Cutting Density (OCD) Ultracentrifuge Tubes.
3.2.2 Step-by-Step Procedure
- Sample Preparation & Pelletting: Begin with steps 1-4 from the CPF protocol (Sections 3.1.2.1-3.1.2.4) to obtain a crude exosome pellet.
- Density Gradient Layering: Carefully layer the resuspended crude exosome pellet on top of a pre-formed iodixanol density gradient in an ultracentrifuge tube.
- Isopycnic Centrifugation: Ultracentrifuge at 100,000 - 120,000 × g for 18 hours at 4°C. During this run, exosomes will migrate to the region of the gradient matching their own buoyant density (~1.10-1.14 g/mL) [57].
- Fraction Collection: Gently collect the gradient from the top in 1 mL fractions. The exosome-rich fractions can be identified by measuring the density or via protein/nanoparticle tracking analysis.
- Dilution and Washing: Pool the exosome-rich fractions and dilute them in a large volume of PBS (typically 1:3 or 1:4) to reduce the density medium concentration.
- Final Pelletting: Ultracentrifuge the diluted pool at 100,000 - 120,000 × g for 2 hours at 4°C to form a pure exosome pellet.
- Final Resuspension: Discard the supernatant completely. Resuspend the final, high-purity pellet in a small volume of PBS (e.g., 50-100 µL). Aliquot and store at -80°C.
Strategic Workflow and Decision Pathways
The following workflow diagram synthesizes the protocols and strategic considerations into a logical pathway for optimizing exosome isolation, from sample preparation to characterization.
Diagram 1: A strategic workflow for selecting an exosome isolation protocol based on research goals and scale.
Pre-Isolation Strategy: Cell Culture Optimization
The quality of the isolation is fundamentally determined by the quality of the starting material. Optimizing cell culture conditions can significantly enhance secretome and exosome yield and functionality [56] [50].
- 3D Culture Systems: Culturing mesenchymal stem cells (MSCs) in 3D formats (e.g., spheroids, hydrogels) more closely mimics their physiological environment and can enhance the production of therapeutic factors, such as interleukin-10, compared to standard 2D culture [56].
- Hypoxic Conditioning: Mimicking physiological oxygen levels (1-10% O₂, vs. standard 21%) upregulates HIF-1α, leading to increased production of pro-angiogenic and regenerative factors like VEGF and angiotensin [56].
- Biochemical Priming: Pre-conditioning MSCs with inflammatory cytokines like IFN-γ and TNF-α can steer the secretome towards a more potent immunomodulatory profile, increasing the release of factors like TSG-6, IL-10, and PGE2 [56] [50].
Post-Isolation Characterization and Quality Control
Rigorous characterization is non-negotiable for validating isolation success. The following table outlines the essential techniques.
Table 3: Essential Characterization Techniques for Isolated Exosomes
| Technique | Parameter Measured | Protocol Summary | Expected Outcome for sEVs |
|---|---|---|---|
| Nanoparticle Tracking Analysis (NTA) | Particle size distribution and concentration [59] | Dilute sample in PBS; inject into NTA chamber; analyze Brownian motion of particles with laser scattering. | Peak size mode of 30-150 nm; high particle concentration confirms yield [59]. |
| Transmission Electron Microscopy (TEM) | Ultrastructural morphology and membrane integrity [59] | Adsorb sample to grid; negative stain with uranyl acetate; image under TEM. | Cup-shaped, spherical vesicles with intact lipid bilayer [59]. |
| Western Blot | Presence of exosomal protein markers [59] | Lyse sample; separate proteins via SDS-PAGE; transfer to membrane; probe with antibodies against exosomal markers. | Positive for Tetraspanins (CD9, CD63, CD81), TSG101, Flotillin-1. Negative for Calnexin/GM130 [59]. |
| BCA Assay | Total protein content [59] | Mix sample with BCA working reagent; incubate at 37°C; measure absorbance at 562 nm. | Used with NTA data to calculate particle-to-protein ratio, a key metric for purity (higher ratio = higher purity) [59]. |
Efficiently isolating exosomes from complex media is an achievable goal through strategic method selection and rigorous optimization. No single method is universally superior; the choice must align with the specific downstream application, balancing the need for yield, purity, and scalability. The integrated CPF protocol provides an accessible and balanced solution for many research settings, while density-gradient ultracentrifugation and Tangential Flow Filtration offer paths to higher purity and clinical translation. By adopting the standardized protocols and quality control measures outlined here, researchers can significantly improve the reproducibility and reliability of their stem cell secretome and exosome research, accelerating the development of these promising biotherapeutics.
The therapeutic potential of the stem cell secretome, particularly extracellular vesicles (EVs) like exosomes, is immense. However, the full translation of these cell-free therapies into clinical applications is hampered by two significant technical challenges: achieving high-resolution characterization in the low nanometer range (30-200 nm) and ensuring high specificity in biomarker detection. The lack of standardized, reproducible protocols for isolation and characterization leads to inconsistent results across studies and complicates the reliable evaluation of these therapeutics in clinical trials [34] [50]. This application note details advanced methodologies and integrative approaches designed to overcome these critical limitations, providing a robust framework for researchers in stem cell and drug development.
Comparative Analysis of Exosome Isolation Techniques
Selecting the appropriate isolation technique is paramount, as the method directly impacts the size profile, purity, and subsequent biomarker analysis of the isolated vesicles. The choice involves a trade-off between yield, purity, and the preservation of biological integrity.
Table 1: Performance Metrics of Key Exosome Isolation Methods
| Method | Principle | Purity | Yield | Advantages | Limitations | Impact on Characterization |
|---|---|---|---|---|---|---|
| Differential Ultracentrifugation | Sequential centrifugation based on size/density [57] | High [5] | Medium [5] | Considered the "gold standard"; economical for consumables [57] | Time-consuming; may cause exosome damage due to high forces; requires expensive equipment [57] [60] | Can compromise nanometer resolution due to particle deformation/aggregation [57] |
| Density Gradient Centrifugation | Separation based on buoyant density in a gradient medium [57] | High [60] | Low [60] | Superior separation efficiency; prevents re-mixing of components [57] | Cumbersome preparation; lengthy process; low yield [57] [60] | Higher purity improves biomarker specificity by reducing contaminants [57] |
| Size-Exclusion Chromatography (SEC) | Separation based on hydrodynamic size [5] | Medium-High [5] | Medium [5] | Maintains structural integrity and biological function; highly reproducible [5] [4] | Requires specialized chromatography system [5] | Preserves native size, enhancing nanometer resolution accuracy [4] |
| Tangential Flow Filtration (TFF) | Size-based separation using parallel flow to prevent clogging [57] [5] | Medium [5] | High [5] | Excellent scalability for high-volume applications [5] | Pressure and shear force may damage vesicle morphology [60] | High yield is beneficial for downstream assays, but may include some co-isolates [57] |
| Immunoaffinity Capture | Antibody-based binding to specific surface markers (e.g., CD63, CD81) [5] [4] | Very High [5] | Low [5] | High specificity for exosome subpopulations [4] | Limited throughput; high cost; antibody-dependent [5] | Maximizes biomarker specificity by isolating specific vesicle subtypes [4] |
| Polymer-based Precipitation | Use of polymers (e.g., PEG) to precipitate vesicles [5] | Low [5] | High [5] | Fast and simple; requires only a centrifuge [5] | Co-precipitates contaminants like lipoproteins [5] | Low purity severely compromises biomarker specificity [5] |
Advanced Protocols for High-Resolution Characterization
Integrated Protocol for Isolation and Purity Assessment
This protocol combines SEC and TFF to achieve high-yield isolation of mesenchymal stem cell-derived EVs (MSC-EVs) with minimal damage, ideal for subsequent high-resolution characterization.
Materials:
- Conditioned media from MSC cultures
- Ultracentrifugation equipment
- Size-exclusion chromatography system
- Tangential Flow Filtration system
- Phosphate-Buffered Saline (PBS)
Methodology:
- Pre-clearing: Centrifuge the conditioned media at 2,000 × g for 30 minutes to remove cells and apoptotic debris [60].
- Concentration: Use a TFF system with a 100-kDa molecular weight cut-off membrane to concentrate the pre-cleared supernatant. This step reduces processing volumes while maintaining vesicle integrity [57] [60].
- High-Resolution Size Separation: Load the concentrated sample onto a SEC column (e.g., qEVoriginal). Elute with PBS and collect the vesicle-rich fractions based on UV absorbance or pre-determined elution volumes [5].
- Purity Assessment: Analyze the SEC fractions using nanoparticle tracking analysis (NTA) and protein assays.
- Determine particle concentration by NTA.
- Measure total protein concentration using a BCA or similar assay.
- Calculate a purity index (Particle-to-Protein ratio). A higher ratio indicates a lower level of soluble protein contaminants and higher preparation purity [5].
Protocol for Enhanced Biomarker Specificity via Multiplexed Nanosensing
This protocol employs a label-free electrochemical immunosensor for the specific detection of neuron-specific enolase (NSE), demonstrating a approach that can be adapted for stem cell exosome surface biomarkers.
Materials:
- Screen-printed carbon electrode (SPCE)
- Inorganic nanomaterials (e.g., Gold Nanoparticles, Graphene Oxide)
- Primary antibodies against target biomarkers (e.g., anti-NSE)
- Bovine Serum Albumin (BSA)
- Electrochemical analyzer
Methodology:
- Electrode Functionalization:
- Drop-cast a suspension of inorganic nanomaterials (e.g., graphene oxide/gold nanoparticle nanocomposite) onto the SPCE surface and dry. This enhances the electrode's surface area and electrical conductivity [61] [62].
- Immobilize the primary antibody onto the functionalized electrode surface via physical adsorption or covalent coupling. Incubate for 2 hours at room temperature.
- Surface Blocking: Wash the electrode and incubate with a 1% BSA solution for 1 hour to block non-specific binding sites [61].
- Sample Incubation and Detection:
- Incubate the prepared electrode with the isolated exosome sample or a solution containing the target biomarker for 30 minutes.
- Wash thoroughly to remove unbound material.
- Perform electrochemical measurements (e.g., electrochemical impedance spectroscopy). The binding of the target biomarker to the antibody insulates the electrode surface, increasing the electrical impedance. The change in impedance is proportional to the biomarker concentration, allowing for highly specific and sensitive quantification [61].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Exosome Characterization
| Item/Category | Function | Application Note |
|---|---|---|
| CD63, CD81, CD9 Antibodies | Immunoaffinity capture and surface phenotype validation [5] | Essential for confirming exosomal identity and isolating specific subpopulations via kits or in-house columns. |
| PBS (Phosphate-Buffered Saline) | Washing buffer and diluent [60] | Used throughout isolation and characterization protocols to maintain physiological pH and osmolarity. |
| Iodixanol / Sucrose | Density gradient medium [57] | Used for high-purity isolation of EVs based on their buoyant density. |
| Polyethylene Glycol (PEG) | Polymer for precipitating exosomes [5] | Enables quick, equipment-light isolation, though with lower purity. |
| Gold Nanoparticles (AuNPs) | Signal amplification in biosensors [61] [63] | Enhance conductivity and allow for label-free detection in electrochemical immunosensors. |
| Screen-Printed Electrodes (SPE) | Transducer platform for electrochemical sensing [61] | Provide a portable, low-cost platform for developing point-of-care biomarker detection devices. |
| Protein Assay Kits (e.g., BCA) | Quantification of total protein [5] | Used with particle concentration data to calculate sample purity indices. |
Workflow and Pathway Visualizations
Integrated Strategy for Overcoming Characterization Challenges
This diagram outlines a holistic workflow that combines advanced isolation, high-resolution characterization, and data analysis to tackle the core challenges.
Biosensor Mechanism for Specific Biomarker Detection
This diagram illustrates the working principle of a nanomaterial-enhanced electrochemical immunosensor, a key technology for achieving high biomarker specificity.
In the rapidly advancing field of stem cell research, the therapeutic potential of the stem cell secretome and its exosome components has emerged as a promising cell-free alternative to whole-cell therapies. The secretome, comprising the complete set of molecules and biological factors secreted by cells into the extracellular space, includes cytokines, chemokines, growth factors, and extracellular vesicles (EVs) such as exosomes [64]. These components mediate therapeutic effects through paracrine signaling, demonstrating significant potential for regenerative medicine, immunomodulation, and tissue repair [8] [65]. However, the translational of these findings from laboratory research to clinical applications faces a substantial obstacle: the lack of standardized, unified protocols for the isolation and dosing of secretome and exosome products. This methodological heterogeneity compromises data reproducibility, hinders comparative analysis across studies, and ultimately delays clinical adoption [8] [66] [67]. This Application Note addresses these critical standardization challenges and provides detailed protocols to enhance methodological consistency within the stem cell secretome and exosome research community.
The Standardization Imperative: Challenges and Consequences
The absence of standardized protocols creates significant variability in both the production of secretome and the isolation of exosomes, directly impacting the quality, potency, and safety of the final product.
- Challenge 1: Reproducibility and Optimization. Standard methods for secretome production, collection, and characterization remain a major challenge, affecting the reproducibility, optimization, and bulk production of these therapeutics [8] [65]. This lack of standardization extends to exosome research, where the dynamic homeostasis of biological systems leads to variable yields and compositions across different laboratories and protocols [67].
- Challenge 2: Dosing and Therapeutic Efficacy. The complex nature of the secretome, which includes RNA, proteins, and EVs with short circulation half-lives, poses a significant challenge for delivery and accurate dosing [64]. The biological activity of the final product is highly dependent on the isolation technique, making it difficult to establish reliable dose-response relationships and compare therapeutic efficacy across clinical trials [66] [5].
- Challenge 3: Purity and Contaminant Profile. Different isolation methods co-purity various non-exosomal components, such as lipoproteins, protein aggregates, and other EVs, which can interfere with downstream analysis and therapeutic application [5]. The table below summarizes the performance metrics of common exosome isolation methods, illustrating the trade-offs between purity, yield, and scalability that researchers must navigate in the absence of a gold standard.
Table 1: Comparative Performance Metrics of Major Exosome Isolation Protocols
| Method | Purity | Yield | Scalability | Key Instrumentation |
|---|---|---|---|---|
| Differential Ultracentrifugation | High | Medium | Medium | Ultracentrifuge |
| Size-Exclusion Chromatography (SEC) | Medium–High | Medium | High | Chromatography system |
| Tangential Flow Filtration (TFF) | Medium | High | High | Filtration apparatus |
| Polymer-based Precipitation | Low | High | High | Centrifuge |
| Immunoaffinity Capture | Very High | Low | Low | Antibody-conjugated surfaces |
Detailed Experimental Protocols for Secretome and Exosome Processing
To address these challenges, the following sections provide detailed, actionable protocols for key stages of secretome and exosome workflow.
Protocol 1: Mesenchymal Stem Cell (MSC) Secretome Production and Collection
This protocol outlines the standardized production and collection of the whole secretome from Mesenchymal Stem Cells (MSCs), a common source for regenerative applications [8] [64].
- Step 1: Cell Culture and Expansion. Culture human MSCs from a validated source (e.g., bone marrow, adipose tissue) in appropriate growth medium. Maintain cells at 37°C with 5% CO₂ and passage at 80-90% confluence. Use cells between passages 3-6 for consistency.
- Step 2: Pre-conditioning and Serum Starvation. Once the cells reach 80% confluence, wash them three times with phosphate-buffered saline (PBS) to remove serum contaminants. Replace the growth medium with a serum-free basal medium. Pre-conditioning may involve incubating cells under specific experimental conditions (e.g., hypoxia, inflammatory cytokine stimulation) to modulate secretome composition [8].
- Step 3: Secretome Collection. Incubate the cells in serum-free medium for 24-48 hours. Following incubation, collect the conditioned medium into sterile centrifuge tubes.
- Step 4: Clarification and Concentration. Centrifuge the conditioned medium at 2,000 × g for 30 minutes at 4°C to remove cellular debris. Filter the supernatant through a 0.22 µm PES filter. The clarified secretome can be concentrated using tangential flow filtration (TFF) or ultrafiltration units with a 3-5 kDa molecular weight cut-off, as required for downstream applications [5].
- Step 5: Storage. Aliquot the concentrated secretome and store at -80°C. Avoid multiple freeze-thaw cycles to preserve bioactive component integrity.
Protocol 2: Exosome Isolation via Size-Exclusion Chromatography (SEC)
This protocol describes exosome isolation using SEC, which offers a strong balance of purity, structural integrity, and reproducibility [66] [5].
- Step 1: Sample Preparation. Begin with clarified cell culture supernatant or biofluid (e.g., plasma, serum). For biofluids, a preliminary low-speed centrifugation (2,000 × g for 20 minutes) is essential. Avoid samples with high viscosity or particulate matter.
- Step 2: Column Equilibration. Pack a chromatography column (e.g., Sepharose CL-2B, Sephacryl S-400) and equilibrate it with at least 2 column volumes (CV) of particle-free PBS or a similar isotonic buffer (pH 7.4).
- Step 3: Sample Loading and Elution. Load a sample volume not exceeding 0.5-2% of the total column CV. Elute the sample with the same equilibration buffer at a constant, slow flow rate (e.g., gravity flow or a pump-controlled rate of 0.5-1 mL/min). Collect sequential fractions (typically 0.5-1 mL each).
- Step 4: Fraction Analysis and Pooling. The first eluted fractions (void volume) will contain exosomes and similarly sized vesicles. Identify exosome-rich fractions by measuring absorbance at 280 nm or by using nanoparticle tracking analysis (NTA). Pool the fractions containing the highest concentration of exosomes (typically fractions corresponding to the peak eluting just after the void volume).
- Step 5: Concentration and Storage. Concentrate the pooled exosome fractions using centrifugal filters with a 100 kDa molecular weight cut-off. Resuspend the final exosome pellet in PBS and store at -80°C. Characterize the isolate using NTA, transmission electron microscopy (TEM), and western blot for markers (e.g., CD9, CD63, CD81) [66] [67].
Protocol 3: Full Incorporation of Secretome into Lipid Bicontinuous Cubic Phases
For advanced therapeutic delivery, this protocol details the encapsulation of the entire MSC secretome into lipid bicontinuous cubic phases, which can serve as precursors to cubosome nanoparticles for controlled release [64].
- Step 1: Lipid Film Preparation. Weigh 10-50 mg of monoolein or phytantriol into a glass vial. Dissolve the lipid in a minimal volume of chloroform. Gently evaporate the chloroform under a stream of inert gas (e.g., nitrogen or argon) while rotating the vial to form a thin, uniform lipid film on the walls. Further dry the film under vacuum overnight to remove any residual solvent.
- Step 2: Hydration with Secretome. Hydrate the dry lipid film with the prepared, concentrated MSC secretome (from Protocol 1). Use a lipid-to-secretome ratio that yields a final lipid concentration of 5-10% w/w. The secretome serves as the aqueous phase.
- Step 3: Cubic Phase Formation. Seal the vial and incubate the mixture at a temperature above the lipid's phase transition temperature (typically 20-60°C) for 24-48 hours. Periodically vortex or gently mix the sample to facilitate homogeneous cubic phase formation.
- Step 4: Characterization. Verify the formation and structure of the lipid bicontinuous cubic phase using Small-Angle X-ray Scattering (SAXS). A successful encapsulation will show SAXS patterns dominated by bicontinuous cubic phases (e.g., gyroid, diamond, primitive) with structural parameters confirming the incorporation of secretome components without phase separation [64].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table catalogs key reagents and materials critical for implementing the protocols described and advancing research in this field.
Table 2: Essential Research Reagents and Materials for Secretome and Exosome Workflows
| Reagent/Material | Function/Application |
|---|---|
| Monoolein/Phytantriol | Lipids used to form bicontinuous cubic phases and cubosomes for whole secretome encapsulation and delivery [64]. |
| Sepharose CL-2B | Matrix for Size-Exclusion Chromatography (SEC), enabling high-purity exosome isolation based on size [5]. |
| Tangential Flow Filtration (TFF) System | For scalable concentration and buffer exchange of secretome and exosome samples [5]. |
| CD63/CD81/CD9 Antibodies | Specific surface markers used for immunophenotyping exosomes via flow cytometry or western blot, and for immunoaffinity capture [66] [5]. |
| Nanoparticle Tracking Analyzer | Instrument for determining exosome concentration and size distribution by tracking Brownian motion [66] [67] [5]. |
| Polyethylene Glycol (PEG) | Polymer used for precipitating exosomes from large sample volumes; a key component in precipitation kits [5]. |
| Serum-Free Basal Medium | Essential for producing contaminant-free secretome during the collection phase [8]. |
Workflow and Decision Pathways
The following diagrams outline the logical workflow for secretome processing and the decision pathway for selecting an appropriate exosome isolation method.
Secretome Processing Workflow
Exosome Isolation Decision Chart
Characterization and Quantification Guidelines
Robust characterization is non-negotiable for validating any isolation protocol. The table below summarizes the primary techniques used to assess exosome yield, purity, and identity, which are critical for establishing accurate dosing parameters.
Table 3: Key Techniques for Exosome Characterization and Quantification
| Technique | Parameter Measured | Role in Standardization |
|---|---|---|
| Nanoparticle Tracking Analysis (NTA) | Particle size distribution and concentration [5]. | Provides critical quantitative data for dosing, ensuring consistent particle numbers between preparations. |
| Transmission Electron Microscopy (TEM) | Morphological visualization and size confirmation [66] [67]. | Verifies the isolation of intact, cup-shaped vesicles and rules out gross contamination or aggregation. |
| Western Blot | Detection of exosomal marker proteins (CD9, CD63, CD81, TSG101) and absence of negative markers (e.g., Calnexin) [67]. | Confirms exosomal identity and assesses sample purity, a key metric for protocol validation. |
| Resistive Pulse Sensing (RPS) | Highly precise, particle-by-particle quantification [5]. | Alternative to NTA for accurate concentration measurement, useful for cross-validation. |
| UV-Vis/Protein Assay | Total protein concentration [5]. | Must be interpreted cautiously alongside particle data to assess protein contamination levels. |
The path to clinical application of stem cell secretome and exosome-based therapies is inextricably linked to resolving the current lack of unified protocols. Standardization in production, isolation, and characterization is not merely a methodological preference but a fundamental requirement for ensuring product safety, efficacy, and reproducibility. By adopting detailed, community-vetted protocols such as those outlined herein, leveraging appropriate reagent toolkits, and implementing rigorous quantification and characterization standards, researchers can overcome these critical hurdles. Concerted efforts toward standardization, potentially guided by frameworks like the MISEV guidelines, will accelerate the transition of these promising cell-free therapeutics from the laboratory to the clinic, unlocking their full potential in regenerative medicine and drug development [8] [5].
The field of regenerative medicine is experiencing a significant paradigm shift, moving away from whole mesenchymal stem/stromal cell (MSC) transplantation toward cell-free therapeutic strategies utilizing MSC-derived secretomes [20]. This transition is largely driven by the recognition that most therapeutic benefits of MSCs are mediated through their paracrine secretions rather than direct cell replacement or long-term engraftment [68]. The secretome, comprising a complex mixture of bioactive factors including soluble proteins, cytokines, growth factors, and extracellular vesicles (EVs) such as exosomes, demonstrates remarkable therapeutic potential for modulating immune responses, promoting angiogenesis, and facilitating tissue repair [20].
Despite this promise, the clinical translation of secretome-based therapies faces substantial challenges, primarily due to inconsistencies in secretome composition and the absence of standardized production protocols [56] [8]. This Application Note addresses these challenges by providing detailed, evidence-based methodologies for optimizing culture conditions through tailored priming strategies and advanced 3D bioreactor systems. By implementing these protocols, researchers can significantly enhance the potency, yield, and reproducibility of MSC secretomes for both basic research and clinical applications.
Priming Strategies for Enhanced Secretome Potency
Conceptual Framework and Key Priming Modalities
Priming, also known as preconditioning, involves the exposure of MSCs to specific physiological, pharmacological, or environmental stimuli to direct the secretome toward a desired therapeutic profile [69]. This process leverages the inherent adaptability of MSCs to modify their secretory output in response to changing microenvironmental conditions [70]. The table below summarizes the primary priming modalities and their key effects on secretome composition and function.
Table 1: Key Priming Modalities and Their Effects on Secretome Composition
| Priming Modality | Key Signaling Pathways | Major Secretome Alterations | Therapeutic Implications |
|---|---|---|---|
| Hypoxic Conditioning (1-5% O₂) | HIF-1α stabilization [56] | ↑ Angiogenic factors (VEGF, Angiopoietin) [56]↑ Immunomodulatory factors [69] | Enhanced neovascularizationImproved tissue regeneration [56] |
| Inflammatory Priming (IFN-γ, TNF-α) | NF-κB, JAK-STAT [56] | ↑ IDO1, IL6, PGE2, TSG-6 [69] [56] | Potent immunomodulationM2 macrophage polarization [56] |
| 3D Spheroid Culture | Altered mechanotransduction | ↑ EV production [69]↑ Anti-inflammatory factors (e.g., IL-10) [56] | Improved homing & bioactivity [70] |
| Biochemical Stimuli (H₂O₂, LPS) | Nrf2, MAPK [56] | ↑ Pro-angiogenic proteins (VEGF, HGF) [56] | Enhanced cytoprotectionOxidative stress resistance |
The following diagram illustrates the workflow for developing a tailored priming strategy, integrating the modalities described above to achieve a specific therapeutic objective.
Figure 1: Workflow for developing a tailored priming strategy for secretome enhancement.
Detailed Experimental Protocols for MSC Priming
Protocol 1: Hypoxic Priming for Angiogenic Secretome Enhancement
Objective: To enhance the angiogenic and regenerative potential of the MSC secretome through controlled hypoxic conditioning.
Materials:
- Hypoxia Workstation/Chamber: Capable of maintaining 1-5% O₂, 5% CO₂, and 37°C.
- Gas Mixer: For precise control of O₂, N₂, and CO₂ concentrations.
- Anaerobic Chamber: (Optional) For sample processing in low-oxygen environments to prevent reoxygenation.
- Cell Culture Media: Serum-free, chemically defined (e.g., RoosterCollect EV-Pro [70]).
Procedure:
- Cell Preparation: Seed MSCs at a density of 5,000-8,000 cells/cm² in standard culture flasks. Allow cells to adhere for 24 hours under normoxic conditions (21% O₂, 5% CO₂, 37°C).
- Media Exchange: After 24 hours, carefully aspirate the growth media and wash the cell monolayer twice with PBS to remove serum residues. Add serum-free, low-particulate collection media.
- Hypoxic Exposure: Transfer the culture flasks to the pre-equilibrated hypoxia chamber set to 1-3% O₂ and 5% CO₂ at 37°C. Incubate for 24-72 hours. Note: The optimal duration may vary by MSC source and should be determined empirically.
- Conditioned Media Collection: After the priming period, collect the conditioned media (CM). For optimal results, perform this step inside the hypoxia workstation to prevent reoxygenation effects.
- Processing: Centrifuge the CM at 2,000 × g for 10 minutes at 4°C to remove cellular debris. Aliquot the supernatant (the primed secretome) and store at -80°C or proceed immediately to EV isolation.
Validation: Assess priming efficacy by measuring the upregulation of HIF-1α via Western blot and quantifying the increased concentration of VEGF and HGF in the CM using ELISA [56].
Protocol 2: Pro-inflammatory Cytokine Priming for Immunomodulation
Objective: To boost the immunomodulatory capacity of the MSC secretome through stimulation with pro-inflammatory cytokines.
Materials:
- Priming Cocktail: Recombinant human IFN-γ (10-50 ng/mL) and TNF-α (10-30 ng/mL).
- Control Solution: Phosphate-Buffered Saline (PBS) containing a equivalent concentration of Bovine Serum Albumin (BSA) as the cytokine stocks.
- Serum-Free Collection Media.
Procedure:
- Cell Preparation: Culture MSCs to 70-80% confluence in standard flasks.
- Media Exchange: Aspirate the growth media, wash twice with PBS, and add fresh serum-free media.
- Cytokine Addition: Add the prepared IFN-γ and TNF-α priming cocktail to the experimental group. Add the BSA/PBS control solution to the control group.
- Incubation: Incubate the cells for 24-48 hours at 37°C and 5% CO₂.
- Conditioned Media Collection: Collect the CM and centrifuge at 2,000 × g for 10 minutes at 4°C to remove cell debris.
- Cytokine Removal (Optional): For downstream functional assays requiring the removal of the priming cytokines, use desalting columns or dialysis. Aliquot and store the primed secretome at -80°C.
Validation: Confirm priming success by evaluating the gene expression of IDO1 and TSG-6 via qPCR, and by measuring the protein level of PGE2 or the increased immunosuppressive capacity in a T-cell proliferation assay [69] [56].
3D Culture Systems for Scalable Secretome Production
Comparative Analysis of 3D Culture Platforms
Moving from two-dimensional (2D) monolayers to three-dimensional (3D) culture systems represents a fundamental advancement in biomanufacturing MSCs, as 3D environments more closely mimic the native tissue milieu [56]. The choice of 3D system significantly impacts the quantity and quality of the resulting secretome. The table below provides a comparative analysis of common 3D culture platforms based on recent research.
Table 2: Quantitative Comparison of 3D Culture Systems for MSC Secretome Production
| Culture System | Proliferation Fold vs 2D | EV Production Change | Key Functional Outcomes | Scalability & Practical Notes |
|---|---|---|---|---|
| 2D Monolayer | 1.0 (Baseline) | Baseline | Standard mineralization, baseline angiogenic potential [70] | High simplicity, low cost, but limited secretome yield [70] |
| Spheroids | ~0.5-0.7 fold [70] | Decreased 30-70% [70] | Enhanced mineralization homogeneity [56]; May induce endothelial cell senescence [70] | Simple formation; limited by diffusion, leading to core hypoxia & necrosis [56] |
| Matrigel | ~0.6-0.9 fold [70] | Decreased ~30% [70] | Not specified in results | Poorly defined composition, batch-to-batch variability, limited scalability [70] |
| Bio-Block Hydrogel | ~2.0 fold increase [70] | Increased ~44% [70] | Preserved trilineage differentiation; EVs enhance endothelial cell function [70] | Tunable properties, "puzzle-piece" design facilitates scaling and mass transport [70] |
The decision-making process for selecting an appropriate 3D culture system, based on research objectives and practical constraints, is visualized below.
Figure 2: A decision tree for selecting the most appropriate 3D culture system based on research goals.
Protocol for 3D Spheroid Culture and Secretome Harvest
Objective: To generate a potent MSC secretome by culturing cells as 3D spheroids, which mimic cell-cell and cell-matrix interactions more accurately than 2D cultures.
Materials:
- Low-Adhesion Plates: 96-well or 384-well round-bottom plates.
- Spheroid Formation Matrix: (Optional) Methylcellulose-based hydrogel or other inert polymers to enhance spheroid uniformity.
- Serum-Free Media.
Procedure:
- Cell Suspension: Harvest MSCs using standard trypsinization. Count and resuspend cells in serum-free media at a concentration of 1 × 10⁶ cells/mL.
- Spheroid Seeding:
- With Matrix: Mix the cell suspension with a spheroid formation matrix according to the manufacturer's instructions. Aliquot the cell-matrix mixture into the wells of a low-adhesion plate.
- Without Matrix: Pipette the cell suspension directly into the wells of a low-adhesion plate. A common seeding density is 5,000-10,000 cells per well for a 96-well plate.
- Spheroid Formation: Centrifuge the plate at 200 × g for 5 minutes to aggregate cells at the bottom of the wells. Incubate the plate for 24-48 hours at 37°C and 5% CO₂ to allow for compact spheroid formation.
- Priming in 3D: For enhanced effects, combine 3D culture with other priming strategies. After spheroids form, carefully replace the media with fresh serum-free media containing desired priming agents (e.g., cytokines for inflammatory priming) and incubate further.
- Conditioned Media Collection: Pool the CM from the wells. Centrifuge sequentially at 300 × g for 5 min to remove spheroids, then at 2,000 × g for 10 minutes, and finally at 10,000 × g for 30 minutes at 4°C to eliminate debris and large vesicles.
- Concentration (Optional): Concentrate the CM using ultrafiltration centrifugal devices (e.g., 3 kDa MWCO). The resulting supernatant is the 3D-primed secretome, ready for analysis or storage at -80°C.
Validation: Use nanoparticle tracking analysis (NTA) to confirm increased particle concentration and size distribution profile typical for EVs. Functional assays should show enhanced anti-inflammatory activity or pro-angiogenic potential compared to 2D controls [69] [70].
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of the protocols outlined in this document requires high-quality, consistent reagents and specialized materials. The following table catalogues key solutions recommended for priming and 3D culture workflows.
Table 3: Research Reagent Solutions for Secretome Enhancement Protocols
| Product Category | Specific Examples | Key Function | Protocol Application |
|---|---|---|---|
| Chemically Defined Media | RoosterCollect EV-Pro [70] | Serum-free, xeno-free media for EV production | Critical for all secretome collection to avoid FBS contamination |
| MSC Expansion Media | RoosterNourish MSC-XF [70] | Serum-free expansion media | Pre-culture expansion of MSCs prior to priming experiments |
| Priming Cytokines | Recombinant Human IFN-γ & TNF-α | Potent inflammatory priming agents | Immunomodulatory secretome priming protocol |
| 3D Culture Substrates | Low-adhesion U-bottom plates [56] | Facilitates spheroid self-assembly | 3D spheroid formation protocol |
| Hydrogel Systems | Bio-Block platform [70] | Tunable, biomimetic 3D scaffold | Scalable 3D culture for high-potency secretome production |
| Isolation Kits | Exosome Isolation Kits (e.g., based on precipitation) | Rapid isolation of EVs from conditioned media | Downstream processing of primed secretome |
| Characterization Tools | Antibody arrays for exosomal markers (CD9, CD63, CD81) [28] | Confirmation of exosome identity and profiling | Validation of EV quantity and quality post-isolation |
Concluding Remarks
The strategic optimization of MSC culture conditions through tailored priming and advanced 3D bioreactor systems is no longer an enhancement but a necessity for realizing the full therapeutic potential of secretome-based therapies. The protocols and data presented herein provide a robust framework for researchers to systematically enhance secretome potency, functionality, and yield. The integration of hypoxic conditioning, inflammatory priming, and biomimetic 3D culture environments can collaboratively shape a secretome with a targeted and powerful regenerative signature.
As the field progresses, future efforts must focus on the integration of these optimized processes with GMP-compliant biomanufacturing and rigorous potency assay development to ensure batch-to-batch consistency and clinical efficacy. By adopting these standardized yet flexible protocols, the scientific community can accelerate the translation of MSC secretomes from a promising research tool to a reliable, off-the-shelf therapeutic for a wide range of degenerative and inflammatory diseases.
In the rapidly advancing field of stem cell secretome and exosome research, establishing robust functional assays represents a pivotal challenge in translating physical characterization into meaningful biological understanding. The secretome—comprising soluble proteins, growth factors, and extracellular vesicles including exosomes—mediates the therapeutic effects of mesenchymal stem cells (MSCs) through paracrine signaling rather than direct cell engraftment [20]. This paradigm shift toward cell-free therapeutics underscores the critical need for assay methodologies that can reliably connect the physical attributes of secretome components (such as particle concentration, size, and surface marker expression) to their pharmacological activity in biologically relevant systems.
Functional assay development serves as the essential bridge between descriptive analytics and therapeutic application, enabling researchers to quantify the bioactivity of secretome components, validate their mechanisms of action, and establish potency metrics for quality control. As the field moves toward clinical applications, particularly in neonatal care for conditions like bronchopulmonary dysplasia (BPD) and necrotizing enterocolitis (NEC), the implementation of standardized, functionally relevant assays becomes increasingly crucial for ensuring batch-to-batch consistency and predicting therapeutic efficacy [20]. This application note provides detailed protocols and methodologies for establishing a comprehensive functional assay framework that effectively links physical characterization to biological activity in stem cell secretome research.
Physical Characterization of Secretome Components
Isolation and Basic Characterization
Efficient isolation of small extracellular vesicles (sEVs), including exosomes, from conditioned cell culture media forms the foundation of secretome analysis. A novel cocktail strategy integrating chemical precipitation and ultrafiltration with a two-step filtering process (CPF method) has demonstrated superior performance in achieving high purity and homogeneous vesicle populations compared to traditional methods like PEG-based precipitation (CP), ultracentrifugation (UC), and size-exclusion chromatography (SEC) [59]. This method simplifies operative procedures, reduces costs, and maintains high efficiency without requiring high-cost reactants or extensive processing time [71].
The initial physical characterization typically employs a triad of complementary techniques to establish baseline vesicle properties:
- Nanoparticle Tracking Analysis (NTA): Quantifies concentration and size distribution of vesicles in scatter mode [59]
- Transmission Electron Microscopy (TEM): Visualizes ultrastructural morphology and confirms lipid bilayer integrity [59]
- Western Blot Analysis: Validates expression of sEV surface biomarkers (CD63, CD9, Flotillin-1, TSG101) [59]
Table 1: Comparative Analysis of sEV Isolation Methods for Functional Studies
| Method | Particle Yield (particles/mL) | Peak Size (nm) | Purity Assessment | Practical Considerations |
|---|---|---|---|---|
| CPF Method (Chemical Precipitation + Ultrafiltration) | 2×10⁶ (cell media) [71] | 110 [71] | High purity, minimal non-vesicular particles [59] | Simplified procedure, low cost, high efficiency [71] |
| PEG-based Precipitation (CP) | 1.46×10¹⁰ (cell media) [59] | 76.13±4.4 (cell media) [59] | Lowest purity by particle-to-protein ratio [59] | High yield but compromised purity |
| Ultracentrifugation (UC) | 1.3×10⁹ (cell media) [59] | 88.13±5.1 (cell media) [59] | Highest purity by particle-to-protein ratio [59] | Time-consuming, requires specialized equipment |
| Size-Exclusion Chromatography (SEC) | Lower than CPF [59] | 84.97±8.2 (cell media) [59] | High purity but heterogeneous population [59] | Fraction-dependent concentration variations |
Advanced Characterization Workflow
The following workflow diagram illustrates the integrated approach to secretome characterization from isolation through functional validation:
Diagram 1: Integrated Secretome Characterization Workflow. This workflow outlines the sequential process from stem cell culture through comprehensive physical and functional characterization, culminating in integrated data analysis for potency assessment.
Functional Assay Development: Linking Metrics to Biology
Biochemical Assay Principles and Strategies
Biochemical assay development is the process of designing, optimizing, and validating methods to measure biological activity, binding interactions, or functional outcomes [72]. In the context of secretome research, these assays serve as crucial tools for quantifying the functional potency of isolated components. Effective assay development follows a structured sequence: defining biological objectives, selecting appropriate detection methods, optimizing components, validating performance, and scaling for reproducibility [72].
Universal assay platforms offer significant advantages for secretome analysis, particularly when investigating multiple targets within enzyme families or pathway components. These assays detect common products of enzymatic reactions or binding events, enabling researchers to study various targets with the same assay system. For example, universal ADP assays can monitor multiple kinase targets, while aptamer-based TR-FRET assays can quantify methyltransferase activities [72]. The fundamental concept involves competitive direct detection with various antibody and tracer modifications providing multiple fluorescent formats (FI, FP, TR-FRET).
Mix-and-read homogeneous assays simplify workflows by directly detecting biological activities without separation steps, making them particularly suitable for high-throughput screening applications. After the biological reaction is complete, researchers simply add detection reagents, incubate, and read the plate [72]. This configuration is amenable to automation and produces robust results, making it ideal for quantifying secretome activities across multiple samples.
Advanced Technologies for Target Engagement
Novel assay technologies are emerging that address key challenges in functional characterization of secretome components. The Structural Dynamics Response (SDR) assay, developed by NIH scientists, leverages the natural vibrations of proteins to detect ligand binding interactions [73]. This technique measures changes between the motion of a protein's ligand-free and its ligand-bound states by altering the light output of a sensor protein, typically NanoLuc luciferase (NLuc) [73].
The SDR assay offers several advantages for secretome research:
- Works without need for target-specific reagents or specialized instruments [73]
- Detects compounds binding at both active and allosteric sites [73]
- Requires minimal protein amounts compared to standard methods [73]
- Functions across a wide range of protein classes and structures [73]
For researchers investigating the mechanisms underlying secretome activities, Cellular Thermal Shift Assay (CETSA) has emerged as a leading approach for validating direct target engagement in intact cells and tissues [74]. This method provides quantitative, system-level validation of drug-target interactions, helping bridge the gap between biochemical potency and cellular efficacy [74].
Experimental Protocols for Functional Characterization
Protocol 1: Angiogenesis Assay for Pro-angiogenic Factor Activity
Purpose: To quantify the angiogenic potential of secretome components through their stimulation of vascular endothelial growth factor (VEGF) and other pro-angiogenic factors.
Materials:
- Human umbilical vein endothelial cells (HUVECs)
- Endothelial cell basal medium
- Matrigel matrix
- Secretome samples (sEVs and conditioned media)
- VEGF-positive control
- Anti-VEGF neutralizing antibody (negative control)
- 96-well tissue culture plates
- Inverted microscope with imaging capability
Procedure:
- Matrigel Preparation: Thaw Matrigel overnight at 4°C. Pre-chill pipettes and 96-well plates.
- Matrix Coating: Add 50 μL of Matrigel to each well of a 96-well plate. Incubate at 37°C for 30 minutes to allow polymerization.
- Cell Preparation: Harvest HUVECs at 80-90% confluence. Wash with PBS and resuspend in endothelial cell basal medium at 1.0×10⁵ cells/mL.
- Treatment Application: Add 100 μL of cell suspension to each Matrigel-coated well.
- Secretome Addition: Add secretome samples at standardized concentrations (e.g., 10-100 μg/mL sEV protein). Include VEGF (50 ng/mL) as positive control and basal medium as negative control.
- Incubation: Incubate plates at 37°C, 5% CO₂ for 6-18 hours.
- Imaging and Analysis: Capture images (4-5 fields per well) using an inverted microscope at 100× magnification.
- Quantification: Measure total tube length, number of branch points, and number of meshes per field using image analysis software (e.g., ImageJ Angiogenesis Analyzer).
Validation Parameters:
- Z'-factor >0.5 indicates robust assay performance [72]
- VEGF positive control should show at least 3-fold increase in tube formation versus negative control
- Include anti-VEGF antibody to confirm specificity
Protocol 2: Anti-inflammatory Activity Assessment
Purpose: To evaluate the immunomodulatory capacity of MSC-derived secretomes by quantifying their effect on macrophage polarization and inflammatory cytokine production.
Materials:
- THP-1 monocytic cell line or primary human monocytes
- Phorbol 12-myristate 13-acetate (PMA) for THP-1 differentiation
- Lipopolysaccharide (LPS) for inflammatory stimulation
- Secretome samples (sEVs and conditioned media)
- ELISA kits for TNF-α, IL-6, IL-10
- Flow cytometry antibodies for CD86 (M1 marker) and CD206 (M2 marker)
- RPMI-1640 medium with 10% FBS
Procedure:
- Macrophage Differentiation: Differentiate THP-1 cells (1.0×10⁵ cells/mL) with 100 nM PMA for 48 hours in 24-well plates.
- Inflammatory Stimulation: Stimulate differentiated macrophages with 100 ng/mL LPS for 6 hours to induce M1 polarization.
- Secretome Treatment: Add secretome samples (20-100 μg/mL sEV protein) to stimulated macrophages. Include untreated and LPS-only controls.
- Incubation: Incubate cells for 24 hours at 37°C, 5% CO₂.
- Supernatant Collection: Collect culture supernatants for cytokine analysis by ELISA.
- Cell Harvesting: Detach cells using accutase and stain for CD86 and CD206 markers for flow cytometry analysis.
- Data Analysis: Quantify cytokine concentrations and calculate M2/M1 macrophage ratio.
Key Anti-inflammatory Mediators to Assess:
- TNF-α-stimulated gene/protein 6 (TSG-6)
- Interleukin-10 (IL-10)
- Heme oxygenase-1 (HO-1) [20]
Protocol 3: Barrier Integrity and Wound Healing Assay
Purpose: To evaluate the protective and regenerative effects of secretome components on epithelial barrier function, particularly relevant for NEC applications.
Materials:
- Caco-2 intestinal epithelial cells or other relevant epithelial line
- Transwell inserts (0.4 μm pore size, 12-mm diameter)
- Electric cell-substrate impedance sensing (ECIS) instrumentation (optional)
- Fluorescein isothiocyanate (FITC)-dextran (4 kDa)
- Secretome samples
- Tumor necrosis factor-alpha (TNF-α) for barrier disruption
Procedure:
- Barrier Formation: Seed Caco-2 cells at 1.0×10⁵ cells/insert on Transwell filters. Culture for 14-21 days, changing medium every 2-3 days until transepithelial electrical resistance (TEER) exceeds 500 Ω×cm².
- Pre-treatment: Add secretome samples (50-100 μg/mL sEV protein) to both apical and basolateral compartments for 24 hours.
- Barrier Challenge: Add TNF-α (50 ng/mL) to basolateral compartment to induce barrier disruption.
- TEER Measurement: Measure TEER values at 0, 6, 12, 24, and 48 hours post-challenge using volt-ohm meter.
- Paracellular Permeability: Add FITC-dextran (1 mg/mL) to apical compartment at 48 hours. Collect basolateral medium after 2 hours and measure fluorescence (excitation 490 nm, emission 520 nm).
- Data Analysis: Calculate percentage protection in TEER reduction and FITC-dextran flux compared to TNF-α-only controls.
Quantitative Data Integration and Analysis
Correlating Physical and Functional Parameters
Successful functional assay development requires systematic correlation of physical characterization data with biological activity measurements. The following table illustrates key parameters to monitor and their proposed correlations:
Table 2: Correlation Matrix Linking Physical Properties to Functional Outcomes
| Physical Parameter | Measurement Technique | Functional Assay | Expected Correlation | Quality Threshold |
|---|---|---|---|---|
| sEV Concentration | NTA [59] | Angiogenesis (tube formation) | Positive correlation with pro-angiogenic activity | >2×10⁶ particles/mL for significant effect [71] |
| sEV Size Distribution | NTA [59] | Anti-inflammatory (cytokine modulation) | 80-120 nm peak associated with optimal activity [59] | Peak size: 110 nm [71] |
| CD63/CD9 Expression | Western Blot [59] | Barrier Integrity (TEER protection) | Positive correlation with restorative capacity | Strong band intensity at ~50 kDa [59] |
| TSG101/Flotillin-1 | Western Blot [59] | Macrophage Polarization (M2/M1 ratio) | Presence enhances immunomodulation | Detectable bands at expected molecular weights [59] |
| Particle-to-Protein Ratio | NTA + BCA Protein [59] | All functional assays | Higher ratio indicates better purity and potency | >3.0×10¹⁰ particles/mg [59] |
Data Normalization and Potency Units
To enable meaningful comparisons across different secretome preparations and donor sources, implement standardized normalization approaches:
- Vesicle-based normalization: Dose functional assays based on particle count (e.g., particles/cell)
- Protein-based normalization: Standardize to total secretome protein (μg/mL)
- Cell equivalence normalization: Express doses as secretome yield per originating cell number
For potency assessment, calculate specific activity units:
- Angiogenic units: mm tube length/10⁹ sEVs
- Anti-inflammatory units: % reduction in TNF-α/μg secretome protein
- Barrier protective units: % TEER maintenance/10⁹ sEVs
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Secretome Functional Analysis
| Reagent/Material | Function | Application Examples | Considerations |
|---|---|---|---|
| Transcreener ADP Assay | Universal detection of ADP-generating enzymes [72] | Kinase activity profiling in secretome-treated cells | Homogeneous, mix-and-read format suitable for HTS |
| AptaFluor SAH Assay | Detection of methyltransferase activity [72] | Epigenetic modifications mediated by secretome components | Aptamer-based TR-FRET detection |
| NanoLuc Luciferase (NLuc) | Sensor protein for SDR assays [73] | Detection of target engagement by secretome factors | High sensitivity, compatible with structural dynamics measurements |
| CETSA Platform | Cellular target engagement validation [74] | Confirming direct binding of secretome factors to molecular targets | Works in intact cells and tissues |
| Matrigel Matrix | Extracellular matrix for 3D culture | Angiogenesis tube formation assays | Lot-to-lot variability requires batch testing |
| TEM Grids | Ultrastructural visualization of sEVs [59] | Quality control of secretome preparations | Requires specialized equipment and expertise |
| CD63/CD9/Flotillin-1 Antibodies | sEV marker validation [59] | Western blot confirmation of sEV identity | Essential for MSC-derived vesicle characterization |
| TNF-α/IL-10 ELISA Kits | Cytokine quantification | Anti-inflammatory activity assessment | Include both pro- and anti-inflammatory markers |
Pathway Mapping and Mechanistic Integration
Understanding the signaling pathways modulated by secretome components provides deeper insight into their mechanisms of action. The following diagram maps key pathways relevant to neonatal applications:
Diagram 2: Secretome Signaling Pathways in Neonatal Applications. This map illustrates the key mechanistic pathways through which MSC-derived secretomes exert therapeutic effects in bronchopulmonary dysplasia (BPD) and necrotizing enterocolitis (NEC), highlighting anti-inflammatory, angiogenic, and barrier-protective activities.
Developing robust functional assays that effectively link physical characterization to biological activity is essential for advancing stem cell secretome research toward clinical applications. By implementing the protocols and methodologies outlined in this application note, researchers can establish a comprehensive framework for quantifying the therapeutic potential of secretome components. The integrated approach—combining rigorous physical characterization with biologically relevant functional assessments—provides the necessary foundation for standardizing secretome-based therapeutics, ultimately enabling more predictive potency assessment and quality control for regenerative medicine applications.
As the field continues to evolve, emphasis should be placed on further assay refinement, validation across multiple laboratory settings, and correlation with in vivo efficacy outcomes. Through continued development and implementation of these functional assay systems, the promise of secretome-based therapies for conditions such as BPD and NEC moves closer to widespread clinical realization.
Ensuring Efficacy and Safety: Source Comparison, Functional Assays, and Clinical Trial Insights
Within the broader scope of a thesis on stem cell secretome characterization, this application note provides a focused comparative analysis of the proteomic profiles of bone marrow-mesenchymal stem cell (BM-MSC) and adipose-derived MSC (AD-MSC) exosomes. The therapeutic potential of MSCs is increasingly attributed to their paracrine activity, predominantly mediated by their secretome, which includes extracellular vesicles like exosomes [75]. Exosomes, nano-sized vesicles (30-200 nm), carry a functional cargo of proteins, lipids, and nucleic acids, playing a pivotal role in intercellular communication and tissue repair [48]. Critical to their translational application is the understanding that the composition and function of these exosomes are not universal; they exhibit significant heterogeneity based on the tissue origin of the parent MSCs [76]. This document delineates the distinct proteomic signatures and functional biases of BM-MSC and AD-MSC-derived exosomes, providing researchers with a rationale for selecting the optimal cell source for specific therapeutic applications, alongside detailed protocols for exosome isolation and characterization.
Quantitative Proteomic Comparison
A comparative label-free proteomic analysis of BM-MSC and AD-MSC exosomes reveals distinct protein profiles and functional specializations [48]. The following tables summarize the key quantitative and functional differences.
Table 1: Proteomic Profile Overview and Exosome Characteristics
| Parameter | Bone Marrow (BM)-MSC Exosomes | Adipose (AD)-MSC Exosomes |
|---|---|---|
| Total Proteins Identified | 771 proteins [48] | 457 proteins [48] |
| Particle Concentration | Lower than AD-MSC exosomes [48] | Higher than BM-MSC exosomes [48] |
| Key Upregulated Proteins | - CD9, CD81, TSG101 [48]- Matrix proteins (e.g., Collagens) [77] | - CD9, CD81, TSG101 [48] |
| Key Functional Cargo | Proteins enriched in regeneration pathways [48] | Proteins involved in immune regulation [48] |
Table 2: Functional Pathway Enrichment and Therapeutic Potential
| Functional Category | Bone Marrow (BM)-MSC Exosomes | Adipose (AD)-MSC Exosomes |
|---|---|---|
| Primary Functional Bias | Tissue regeneration & extracellular matrix (ECM) remodeling [48] | Immunomodulation [48] |
| Enriched Pathways | - ECM-receptor interaction [48]- Focal adhesion [48] | - Platelet activation [76]- Endocytosis [76] |
| Therapeutic Implications | - Bone repair [48]- Cartilage regeneration [48] | - Graft-versus-host disease [78]- Inflammatory condition [77] |
| Response to Inflammatory Licensing | Secretome shifts towards immunomodulatory profile (e.g., increased IDO) [77] | Secretome shifts towards immunomodulatory profile (e.g., increased IDO) [77] |
Experimental Protocols for Exosome Research
To ensure the reproducibility of comparative exosome studies, standardized protocols for production, isolation, and characterization are essential [8].
Protocol: Exosome Isolation via Ultracentrifugation
Principle: This method uses high-speed centrifugal forces to separate exosomes from other components in the cell culture supernatant based on their size and density [75]. Applications: Gold-standard method for research-scale exosome preparation for downstream proteomic and functional analysis [75]. Procedure:
- Cell Culture: Culture BM-MSCs or AD-MSCs in serum-free medium or medium with exosome-depleted FBS for 48 hours [48].
- Harvesting Supernatant: Collect the conditioned medium and perform a series of differential centrifugations:
- 300 × g for 10 min to pellet cells.
- 2,000 × g for 10 min to remove dead cells.
- 10,000 × g for 30 min to remove cell debris and large vesicles [48].
- Filtration: Filter the supernatant through a 0.45 μm or 0.22 μm membrane to remove remaining particulates [48].
- Ultracentrifugation: Transfer the filtered supernatant to ultracentrifuge tubes and centrifuge at 120,000 × g for 70 minutes at 4°C to pellet the exosomes [48].
- Washing: Resuspend the exosome pellet in a large volume of phosphate-buffered saline (PBS) and perform a second ultracentrifugation at 120,000 × g for 70 minutes to wash the exosomes [48].
- Resuspension: Resuspend the final, purified exosome pellet in a small volume of PBS and aliquot for storage at -80°C [48].
Protocol: Proteomic Profiling via LC-MS/MS
Principle: Proteins extracted from exosomes are digested into peptides, which are then separated by liquid chromatography and identified by tandem mass spectrometry [48]. Applications: Comprehensive, unbiased identification and quantification of the protein cargo of exosomes. Procedure:
- Protein Extraction: Lyse exosomes in a strong denaturant (e.g., 8 M urea buffer) supplemented with a protease inhibitor. Use ultrasonication to aid lysis [48].
- Protein Quantification: Determine protein concentration using a bicinchoninic acid (BCA) assay kit [48].
- Digestion: Reduce disulfide bonds with dithiothreitol (e.g., 5 mM at 56°C for 30 min), alkylate with iodoacetamide (e.g., 11 mM in darkness), and digest proteins into peptides using trypsin overnight at a 50:1 protein-to-trypsin ratio [48].
- Peptide Desalting: Desalt the digested peptides using a C18 solid-phase extraction column [48].
- LC-MS/MS Analysis:
- Chromatography: Separate the peptides by reverse-phase UHPLC using a C18 column with a gradient of increasing acetonitrile.
- Mass Spectrometry: Ionize peptides using an electrospray ionization (ESI) source and analyze them in a high-resolution mass spectrometer (e.g., Q Exactive Plus). Perform a full MS scan (e.g., m/z 350-1800) followed by data-dependent MS/MS scans on the most intense ions [48].
- Data Analysis: Process the raw MS data using search engines (e.g., MaxQuant) against a human protein database (e.g., Swiss-Prot). Perform bioinformatic analysis (GO, KEGG) to interpret the biological functions of the identified proteins [48].
The following workflow diagram integrates these two core protocols, providing a visual guide from cell culture to data analysis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Exosome Isolation and Proteomics
| Reagent / Kit | Function | Application Note |
|---|---|---|
| Exosome-Depleted FBS | Fetal bovine serum processed to remove contaminating bovine exosomes, ensuring clean background for secreted vesicle studies. | Critical for producing exosomes intended for therapeutic or diagnostic research without foreign contamination [47]. |
| Ultracentrifugation Equipment | Equipment capable of generating forces >100,000 × g to pellet nanoscale exosomes from solution. | The gold-standard isolation method; requires fixed-angle or swinging-bucket rotors (e.g., Beckman Ti70) [75] [48]. |
| BCA Protein Assay Kit | Colorimetric assay for quantifying total protein concentration based on bicinchoninic acid reaction. | Used to normalize exosome protein content before proteomic analysis or functional experiments [48]. |
| Trypsin, Sequencing Grade | Protease enzyme that cleaves peptide bonds at the C-terminal side of lysine and arginine residues. | Essential for digesting exosomal proteins into peptides for subsequent LC-MS/MS analysis [48]. |
| CD9, CD63, CD81 Antibodies | Antibodies against canonical exosome surface tetraspanin markers. | Used in Western blotting to confirm the identity and purity of isolated exosome preparations [79] [48]. |
| TSG101 Antibody | Antibody against Tumor Susceptibility Gene 101, a protein involved in the endosomal sorting complex required for transport (ESCRT) pathway. | Serves as a positive marker for exosomes in Western blot analysis, confirming their endosomal origin [48]. |
Functional Cargo and Signaling Pathways
The distinct protein cargo of BM-MSC and AD-MSC exosomes directs their engagement in unique biological pathways, which underpins their specialized therapeutic effects.
BM-MSC Exosomes: A Regeneration-Promoting Profile. The proteome of BM-MSC exosomes is significantly enriched for proteins involved in extracellular matrix (ECM)-receptor interaction and focal adhesion pathways [48]. This includes various collagens, fibronectin, and integrins, which are crucial for providing structural support and signaling cues that facilitate tissue repair and regeneration [77]. This molecular signature aligns with their observed superior potential in applications such as bone and cartilage repair.
AD-MSC Exosomes: An Immunomodulatory Profile. Exosomes derived from AD-MSCs carry a protein cargo biased towards immune regulation [48]. Pathway analysis shows enrichment for processes like platelet activation and endocytosis, which are intimately linked to cell-cell communication and immune signaling [76]. This makes AD-MSC exosomes particularly promising for treating inflammatory and autoimmune conditions.
It is crucial to note that the secretome and exosomal cargo are dynamic. Upon exposure to an inflammatory microenvironment (e.g., licensing with IFN-γ and TNF-α), both BM-MSCs and AD-MSCs undergo a functional shift towards a potent immunosuppressive phenotype (MSC2). This is characterized by a marked upregulation of factors like Indoleamine 2,3-dioxygenase (IDO) in their secretome, enhancing their immunomodulatory capacity regardless of source [77]. The following diagram summarizes these functional specializations and the impact of inflammatory licensing.
This application note establishes a clear functional dichotomy between exosomes derived from BM-MSCs and AD-MSCs based on their proteomic cargo. BM-MSC exosomes, enriched in ECM and adhesion proteins, are predisposed for tissue regeneration and repair. In contrast, AD-MSC exosomes, carrying a profile conducive to immune regulation, are better suited for modulating inflammatory responses. This foundational knowledge empowers researchers and drug developers to make an informed, rationale-based selection of MSC source for exosome-related therapeutic programs. Furthermore, the plasticity of the MSC secretome in response to inflammatory cues offers a strategic avenue for potentiating exosome function through pre-conditioning, thereby enhancing their efficacy for specific clinical applications. Future work will focus on standardizing isolation protocols and validating these functional specializations in advanced disease models.
Within the broader context of stem cell secretome and exosome isolation research, functional in vitro validation is a critical step to confirm the therapeutic potential of isolated components. This document provides detailed application notes and protocols for assessing three core biological functions: immunomodulation, anti-apoptotic effects, and pro-migratory activity. These assays are essential for researchers and drug development professionals seeking to characterize the functional profile of stem cell-derived secretomes and exosomes before advancing to in vivo studies or clinical applications. The protocols are designed to be integrated into a standardized workflow for secretome characterization, ensuring robust and reproducible data generation.
Experimental Workflows and Signaling Pathways
The following diagram outlines the sequential workflow for the comprehensive functional validation of stem cell-derived secretomes and exosomes, from cell culture to data analysis.
Key Signaling Pathways in Functional Assays
The therapeutic effects of secretomes and exosomes are mediated through specific signaling pathways, as illustrated below.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential reagents and materials for functional validation assays.
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Source Cells | Secretome/exosome production | MSCs (bone marrow, umbilical cord), Dental Stem Cells (DPSCs, SHED), Hair Follicle Stem Cells [11] [80] [20] |
| Isolation Kits | Secretome/exosome purification | Ultracentrifugation, Size-Exclusion Chromatography (SEC), Polymer-based precipitation, Immunoaffinity capture (e.g., anti-CD63, CD81, CD9) [27] [11] |
| Characterization Instruments | Quality control of isolates | Nanoparticle Tracking Analysis (NTA), Transmission Electron Microscopy (TEM), Flow Cytometry, Western Blot [27] [80] |
| Cell Lines for Assays | Target cells for functional testing | Macrophages (e.g., THP-1), Lymphocytes, Human Umbilical Vein Endothelial Cells (HUVECs), Keratinocytes (HaCaT), Fibroblasts [81] [80] |
| Assay Kits | Quantifying cell responses & viability | PrestoBlue/MTT for viability, Annexin V/PI for apoptosis, ELISA for cytokines (IL-10, TNF-α, IFN-γ), Scratch assay tools [80] |
Detailed Experimental Protocols and Data Analysis
Protocol for Immunomodulation Assays
Objective: To evaluate the ability of secretomes/exosomes to modulate immune cell responses, including macrophage polarization and T-cell proliferation.
Background: Immunomodulation is a cornerstone of secretome therapy. MSC-derived secretomes and exosomes contain factors like IL-10, TSG-6, and HO-1 that can suppress pro-inflammatory responses and promote regulatory pathways, which is crucial for treating inflammatory diseases and supporting tissue regeneration [81] [20].
Materials:
- Isolated secretome/exosome samples from MSCs or DSCs.
- Immune cells: THP-1 cell line (human monocytes) or primary peripheral blood mononuclear cells (PBMCs).
- Culture media: RPMI-1640 for immune cells.
- Inducing agents: Phorbol 12-myristate 13-acetate (PMA) for THP-1 differentiation, Lipopolysaccharide (LPS) for M1 polarization, IL-4 for M2 polarization.
- Antibodies for Flow Cytometry: Anti-CD86 (M1 marker), Anti-CD206 (M2 marker).
- ELISA Kits: For TNF-α, IFN-γ, IL-10, and IL-4.
Method:
- Macrophage Differentiation and Polarization:
- Culture THP-1 cells in RPMI-1640 medium supplemented with 10% FBS.
- Differentiate THP-1 monocytes into macrophages by treating with 100 ng/mL PMA for 48 hours.
- Polarize macrophages towards the M1 phenotype by adding 100 ng/mL LPS for 24 hours.
- Treatment with Test Samples:
- After M1 polarization, replace the medium with fresh medium containing the secretome/exosome sample (e.g., 50-100 µg/mL protein content). Use untreated M1 macrophages as a negative control and M2 macrophages (induced with 20 ng/mL IL-4) as a positive control.
- Incubate for 24-48 hours.
- Flow Cytometry Analysis:
- Harvest the cells and stain with fluorescently labeled anti-CD86 and anti-CD206 antibodies.
- Analyze using flow cytometry to determine the percentage of CD86+ (M1) and CD206+ (M2) populations. A successful immunomodulatory effect is indicated by a decrease in CD86 and an increase in CD206.
- Cytokine Profiling:
- Collect cell culture supernatants after treatment.
- Perform ELISA for pro-inflammatory (TNF-α, IFN-γ) and anti-inflammatory (IL-10) cytokines according to the manufacturer's instructions.
Troubleshooting Tip: If the polarization shift is weak, optimize the secretome/exosome concentration and treatment duration. Using primary macrophages instead of THP-1 cells can sometimes yield more physiologically relevant results.
Protocol for Anti-Apoptotic Assays
Objective: To assess the protective effect of secretomes/exosomes against induced apoptosis in vulnerable cell lines.
Background: The anti-apoptotic potential is conferred by factors such as HGF, IGF-1, and bFGF present in the secretome, which activate pro-survival pathways like Akt and Erk, protecting cells from programmed cell death in injury models [20].
Materials:
- Target cells: A sensitive cell line such as H9c2 (cardiac myoblasts) or a neuronal cell line.
- Apoptosis inducer: Hydrogen peroxide (H₂O₂) or serum starvation.
- Staining Kit: Annexin V-FITC / Propidium Iodide (PI) Apoptosis Detection Kit.
- Viability Assay: PrestoBlue or MTT reagent.
- Caspase-3 Activity Assay Kit.
Method:
- Cell Plating and Pre-treatment:
- Plate target cells in a 24-well plate at a density of 5 x 10⁴ cells/well and allow them to adhere overnight.
- Pre-treat the cells with the secretome/exosome sample (e.g., 50-100 µg/mL) for 4-6 hours. Include a vehicle control (PBS).
- Induction of Apoptosis:
- Induce apoptosis by adding a predetermined concentration of H₂O₂ (e.g., 200-500 µM) or by replacing the growth medium with serum-free medium.
- Incubate for 16-24 hours.
- Assessment of Apoptosis by Flow Cytometry:
- Harvest the cells (both adherent and floating) and resuspend in binding buffer.
- Stain the cells with Annexin V-FITC and PI according to the kit protocol.
- Analyze by flow cytometry within 1 hour. Viable cells are Annexin V-/PI-, early apoptotic cells are Annexin V+/PI-, and late apoptotic/necrotic cells are Annexin V+/PI+.
- Cell Viability Measurement:
- In a separate 96-well plate, set up identical treatment conditions.
- After the apoptosis induction period, add PrestoBlue reagent (10% of well volume) and incubate for 1-2 hours.
- Measure the fluorescence (Ex/Em: 560/590 nm). Viability is expressed as a percentage relative to the untreated control.
Troubleshooting Tip: The concentration of the apoptosis inducer (H₂O₂) must be titrated for each cell line to achieve ~50% cell death in the control group, ensuring a dynamic range for detecting protective effects.
Protocol for Pro-Migratory (Wound Healing) Assays
Objective: To determine the effect of secretomes/exosomes on cell migration, a key process in wound healing and tissue repair.
Background: Pro-migratory effects are driven by the activation of pathways such as HGF/IGF1, which stimulate Akt, Erk, and Stat3 signaling. Furthermore, exosomes can activate specific pathways like SMAD6/BMP2 to promote processes like angiogenesis, which is integral to migration and repair [81] [80].
Materials:
- Target cells: Keratinocytes (HaCaT), fibroblasts, or Human Umbilical Vein Endothelial Cells (HUVECs).
- Culture Plates: 12-well or 24-well plates.
- Mitomycin C: (Optional) To inhibit cell proliferation and isolate migration.
- Imaging Equipment: Inverted microscope with camera.
- Image Analysis Software: ImageJ with "MRI Wound Healing Tool" plugin.
Method:
- Cell Plating and Wound Creation:
- Plate cells in a 12-well plate at a high density to form a confluent monolayer overnight.
- Scratch a straight line in the monolayer using a sterile 200 µL pipette tip.
- Gently wash the well with PBS to remove dislodged cells.
- Treatment and Imaging:
- Add fresh medium containing the secretome/exosome sample. If proliferation inhibition is desired, pre-treat cells with 10 µg/mL Mitomycin C for 2 hours before scratching [80].
- Take an image of the scratch at 0 hours (T=0h) at several predefined locations.
- Incubate the plate and take images of the same locations at 12, 18, and 24 hours (T=12h, 18h, 24h).
- Quantification of Migration:
- Measure the width of the scratch at each time point using ImageJ software.
- Calculate the percentage of wound closure using the formula:
% Wound Closure = [(Width at T=0h - Width at T=Xh) / Width at T=0h] * 100.
Troubleshooting Tip: For consistency, mark the bottom of the plate to ensure the same areas are imaged over time. Using Mitomycin C is critical if the secretome has strong proliferative effects, as it allows you to distinguish between migration and proliferation.
Quantitative Data Presentation and Interpretation
Table 2: Expected quantitative outcomes from functional validation assays.
| Functional Assay | Key Measurable Parameters | Expected Result with Active Secretome | Typical Data Range (from literature) |
|---|---|---|---|
| Immunomodulation | CD206+ M2 Macrophages (% of population) | > 2-fold increase vs. M1 control | 25-40% M2 macrophages [20] |
| Secreted IL-10 (pg/mL) | Significant increase | 150-350 pg/mL [20] | |
| Secreted TNF-α (pg/mL) | > 50% decrease | 50-80% reduction vs. control [81] | |
| Anti-Apoptotic | Viable Cells (Annexin V-/PI-, % of population) | > 30% increase vs. injured control | 60-80% viable cells vs. 40-50% in control [20] |
| Caspase-3 Activity (% of control) | > 40% decrease | 50-70% of control activity [20] | |
| Pro-Migratory | Wound Closure at 18h (% of initial area) | > 50% increase vs. control | 70-90% closure vs. 40-50% in control [80] |
| Angiogenesis (Tube Formation, % of control) | Significant enhancement | 2- to 3-fold increase in tube length [81] |
The protocols detailed herein provide a robust framework for the functional validation of stem cell-derived secretomes and exosomes. By systematically assessing immunomodulation, anti-apoptotic, and pro-migratory activities, researchers can generate quantitative, reproducible data that confirms the therapeutic potential of their isolates. Integrating these validated functional assays into the broader secretome characterization pipeline is essential for advancing promising cell-free therapies from bench to bedside.
Dental Stem Cells (DSCs) are a distinct subpopulation of mesenchymal stem cells (MSCs) that have gained significant recognition in regenerative medicine for their unique therapeutic properties [82]. Recent paradigm shifts have redefined MSCs as "medical signaling cells," with their primary biological effects mediated through paracrine secretion, particularly via exosomes [82]. DSC-derived exosomes (DSC-Exos) are nanoscale extracellular vesicles (30-150 nm) that encapsulate a complex cargo of lipids, proteins, RNA, and metabolites, serving as crucial mediators of intercellular communication [82] [83]. These vesicles replicate the therapeutic effects of their parent cells while offering superior benefits including reduced immunogenicity, minimal side effects, excellent biocompatibility, and high drug-loading capacity [82] [84]. This application note provides a comprehensive comparative analysis of DSC-Exos, detailing their unique regenerative profiles and providing standardized protocols for their isolation, characterization, and functional validation.
Comparative Analysis of DSC-Exos vs. Conventional MSC-Exos
Origin and Source Advantages
DSCs offer several distinct advantages over conventional MSC sources such as bone marrow or adipose tissue. They can be obtained through minimally invasive procedures from routinely discarded dental tissues, mitigating ethical concerns and minimizing donor-site morbidity [82]. Multiple DSC subpopulations have been characterized for exosome production, including:
- Stem cells from apical papilla (SCAPs)
- Stem cells from human exfoliated deciduous teeth (SHEDs)
- Dental follicle stem cells (DFSCs)
- Gingival mesenchymal stem cells (GMSCs)
- Periodontal ligament stem cells (PDLSCs)
- Dental pulp stem cells (DPSCs) [82]
Molecular and Functional Distinctions
Molecular profiling studies have revealed significant variations in the bioactive cargo of DSC-Exos compared to conventional MSC-Exos. DSC-Exos contain a distinct repertoire of miRNAs, growth factors, and extracellular matrix proteins that contribute to their specialized regenerative effects [82]. The table below summarizes key comparative characteristics:
Table 1: Comparative Analysis of DSC-Exos versus Conventional MSC-Exos
| Characteristic | DSC-Exos | Conventional MSC-Exos | Significance/References |
|---|---|---|---|
| Origin & Procurement | Minimally invasive from dental tissues | Bone marrow aspiration, liposuction | Reduced ethical concerns, lower donor-site morbidity [82] |
| Proliferation Rate | Higher proliferation potential | Standard proliferation | Enhanced expansion capacity [82] |
| Neurogenic Capacity | Superior neurogenic differentiation | Moderate neurogenic capacity | Ideal for neural repair applications [82] [85] |
| Immunological Profile | Enhanced immunoprivileged status | Moderate immunogenicity | Lower risk of immune rejection [82] |
| miRNA Enrichment | miRNAs associated with osteogenesis, neuroprotection, angiogenesis | Different miRNA profile | Specialized regenerative effects [82] |
| Retention at Injury Sites | Enhanced retention | Standard retention | Improved therapeutic efficacy [82] |
| Angiogenic Potential | Strong promotion of angiogenesis | Variable angiogenic capacity | Enhanced vascularization [83] [84] |
| Odontogenic/Osteogenic Capacity | Superior dentinogenesis and osteogenesis | Moderate osteogenic capacity | Ideal for craniofacial regeneration [82] [83] |
Immunoprivileged Properties
DSC-Exos exhibit a favorable immunological profile with studies suggesting a lower risk of eliciting immune rejection compared to MSC-Exos from other sources. This enhanced immunoprivileged status increases their feasibility for allogeneic transplantation without requiring extensive immunosuppression [82]. The immunological safety of DSC-Exos is further demonstrated in studies showing their effectiveness in modulating inflammatory responses without triggering significant immune activation [83].
DSC-Exos in Regenerative Applications
Neuroregeneration
Dental pulp stem cells, owing to their neural crest origin, exhibit superior neuroregenerative potential compared to MSCs from other sources [84]. Research has demonstrated that exosomes derived from human DPSCs (hDPSCs) promote neuroprotection and neural repair through multiple mechanisms:
- Secretion of neurotrophic factors including NGF and BDNF [84]
- Reduction of neuronal apoptosis and stimulation of axonal regeneration [84]
- Enhancement of Schwann cell proliferation, motility, and neurotrophic factor secretion [84]
- Promotion of axonal growth and remyelination via modulation of the miR-122-5p/p53 pathway [84]
A recent study on peripheral nerve injury demonstrated that neurodifferentiated hDPSCs at early passages (P4) secreted higher levels of neurotrophic, angiogenic, and immunomodulatory factors including FGF-2, IL-6, IL-8, and PDGF-AA compared to undifferentiated cells [85]. Furthermore, exosomes from early-passage undifferentiated cells showed a more abundant and relevant neuroregenerative mRNA cargo, highlighting the importance of passage number in therapeutic efficacy [85].
Pulp-Dentine Complex Regeneration
In regenerative endodontics, DSC-Exos facilitate multiple regenerative functions for pulp-dentine complex restoration:
- Promoting odontoblastic differentiation and dentine mineralization [83]
- Enhancing angiogenesis through activation of the Cdc42/p83 MARK signaling pathway [84]
- Regulating inflammation and immune responses [83]
- Supporting neuroprotection and neuroregeneration [83]
Studies using immunostaining for CD31 in HUVECs demonstrated that treatment with DPSC-Exos leads to significantly greater neovascularization and capillary formation in vivo, accompanied by elevated CD31 expression [84]. Additionally, exosomes from odontogenically differentiated DPSCs (OD-Exo) showed enhanced odontogenic potential compared to exosomes from undifferentiated cells, with miR-27a-5p elevated by nearly eleven-fold in OD-Exo [84].
Bone Regeneration
DSC-Exos play a significant role in osteogenesis through several mechanisms:
- Activation of Wnt/β-catenin and BMP/Smad signaling pathways [84]
- Dynamic changes in miRNA profiles under osteogenic conditions [84]
- Upregulation of osteogenesis-related miRNAs (miR-29c-5p, miR-10b-5p, miR-378a-5p, miR-9-3p) [84]
- Downregulation of inhibitory miRNAs (miR-31-3p, miR-221-3p, miR-183-5p, miR-503-5p) [84]
In rat mandibular defect models, administration of DPSC-Exos led to significant bone regeneration, reduced defect area, and increased bone surface density [84]. Integration of DPSC-Exos with biomaterials such as PLGA-PEG-PLGA microspheres incorporated into nanofiber PLA scaffolds has shown enhanced bone regeneration through facilitated endogenous cell recruitment and differentiation [84].
Table 2: Regenerative Mechanisms of DSC-Exos in Specific Tissue Types
| Tissue Type | Key Mechanisms | Functional Outcomes |
|---|---|---|
| Neural Tissue | Secretion of NGF, BDNF; Modulation of miR-122-5p/p53 pathway; Enhanced Schwann cell function | Neuroprotection, reduced apoptosis, axonal regeneration, remyelination [85] [84] |
| Pulp-Dentine Complex | Activation of Cdc42/p83 MARK pathway; TGFβ1/Smad signaling; Enhanced miR-27a-5p expression | Angiogenesis, odontoblastic differentiation, dentin mineralization [83] [84] |
| Bone Tissue | Wnt/β-catenin & BMP/Smad activation; Osteogenic miRNA regulation | Osteogenic differentiation, bone formation, mineralization [84] |
| Vascular Tissue | Upregulation of VEGFA, FGF-2, MMP-9; CD31 enhancement | Neovascularization, capillary formation, improved perfusion [84] |
Experimental Protocols
Isolation and Purification of DSC-Exos
The following protocol details the standard methodology for isolating exosomes from dental stem cells:
Cell Culture and Conditioned Media Collection
- Culture DSCs (DPSCs, SHEDs, SCAPs, etc.) in serum-free media to avoid bovine exosome contamination [50]
- Collect conditioned media after 24-48 hours during the logarithmic growth phase [50]
- Remove cells and debris by centrifugation at 2,000 × g for 30 minutes [82]
- Concentrate the media using tangential flow filtration or ultrafiltration [82]
Exosome Isolation Methods
- Ultracentrifugation: Gold standard method involving sequential centrifugation steps culminating at 100,000-120,000 × g for 70 minutes [82] [84]
- Size-Exclusion Chromatography (SEC): Separates exosomes based on size, providing high purity preserves vesicle integrity [82]
- Precipitation Kits: Polymer-based precipitation offering high yield but potential impurity [84]
- Microfluidic-based Techniques: Emerging approaches including alternating current electroosmosis for improved efficacy [82]
Purification and Concentration
- Purify crude exosome preparations using SEC or ultrafiltration [82]
- Resuspend the final exosome pellet in phosphate-buffered saline (PBS)
- Store at -80°C in small aliquots to avoid freeze-thaw cycles
Characterization of DSC-Exos
Characterization should follow the guidelines established by the International Society for Extracellular Vesicles (ISEV) [85]:
Nanoparticle Tracking Analysis (NTA)
- Determine particle size distribution and concentration [85]
- Confirm diameter range of 30-150 nm [85]
Electron Microscopy
- Visualize exosome morphology using transmission electron microscopy (TEM) or scanning electron microscopy (SEM) [85] [84]
- Confirm classic cup-shaped morphology [85]
Protein Marker Analysis
- Detect positive markers (CD9, CD63, CD81) via western blot [84]
- Confirm absence of negative markers (e.g., calnexin) [85]
Functional Cargo Analysis
- Extract RNA and profile miRNA content using RNA sequencing [86]
- Analyze protein composition via mass spectrometry [82]
Figure 1: Workflow for the isolation and characterization of DSC-Exos
Functional Validation Assays
Cellular Proliferation and Viability
- Treat target cells (e.g., HUVECs, neuronal cells) with isolated DSC-Exos
- Assess viability using MTT or WST-1 assays at 24, 48, and 72 hours [87] [88]
- Both iMSC-EVs and ADMSC-EVs significantly increased HDF viability at 48 and 72 hours (p ≤ 0.01, p ≤ 0.05) [87] [88]
Apoptosis Assay
- Induce apoptosis in target cells using appropriate stressors (e.g., H₂O₂)
- Treat with DSC-Exos and measure apoptosis levels using flow cytometry with Annexin V/PI staining [87] [88]
- Both iMSC-EVs and ADMSC-EVs significantly reduced apoptosis levels (p ≤ 0.01) in both HDFs and ADMSCs [87] [88]
Migration Assay
- Use transwell or scratch wound assay to evaluate cell migration [87] [88]
- Image at 0, 12, and 24 hours to quantify migration rate
- iMSC-EVs significantly enhanced ADMSC migration (p < 0.0001) [87] [88]
Angiogenesis Assay
- Plate HUVECs on Matrigel and treat with DSC-Exos
- Quantify tube formation by measuring tube length, branch points, and loop numbers [84]
- DPSC-Exo treatment leads to significantly greater neovascularization and capillary formation [84]
Neurite Outgrowth Assay
- Differentiate PC12 cells or primary neuronal cultures
- Treat with DSC-Exos and measure neurite length and branching after 24-48 hours [85]
- DPSC-Exos promote axonal growth and remyelination [84]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for DSC-Exos Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Culture Media | Serum-free MSC media, αMEM with GlutaMAX | Supports DSC expansion without foreign exosome contamination [87] [50] |
| Isolation Kits | ExoQuick-TC, Total Exosome Isolation | Polymer-based precipitation for high-yield exosome isolation [84] |
| Characterization Antibodies | Anti-CD9, CD63, CD81, TSG101 | Positive exosome marker detection via western blot or flow cytometry [85] [84] |
| Negative Marker Antibodies | Anti-calnexin, GM130 | Confirming absence of intracellular contaminants [85] |
| Visualization Reagents | PKH67, DiI lipophilic dyes, CFSE | Exosome labeling for uptake and tracking studies [87] |
| Scaffold Materials | HPCH/CW hydrogel, PLGA-PEG-PLGA, PLA nanofibers | Exosome delivery vehicles for controlled release [84] |
Signaling Pathways Mediating DSC-Exos Effects
Research has elucidated several key signaling pathways through which DSC-Exos exert their regenerative effects:
Figure 2: Key signaling pathways mediated by DSC-Exos
DSC-Exos represent a promising frontier in regenerative medicine, offering unique therapeutic advantages including enhanced immunoprivileged properties, specialized regenerative capabilities, and minimal ethical concerns. Their distinct molecular profiles, particularly their unique miRNA signatures, underlie their superior performance in neuroregeneration, pulp-dentine complex restoration, and bone regeneration compared to conventional MSC-Exos. The protocols and methodologies outlined in this application note provide researchers with standardized approaches for isolating, characterizing, and functionally validating DSC-Exos. As the field advances, addressing challenges related to scalable production, standardization of isolation techniques, and comprehensive safety profiling will be essential for clinical translation. DSC-Exos hold significant potential to revolutionize regenerative therapies across multiple tissue systems, particularly in neural, dental, and craniofacial applications.
The field of regenerative medicine is increasingly shifting from cell-based therapies toward cell-free therapeutic agents, with extracellular vesicles (EVs) derived from mesenchymal stromal cells (MSCs) emerging as particularly promising candidates [89] [90]. These nanoscale vesicles mediate therapeutic effects through intercellular communication, transferring bioactive molecules that modulate immune responses, promote tissue repair, and regulate inflammation [91] [92]. However, the clinical translation of MSC-EV therapies faces significant challenges related to donor variability, finite expansion capacity of primary MSCs, and batch-to-batch inconsistencies [93] [94].
Induced pluripotent stem cell-derived MSCs (iPSC-MSCs or iMSCs) represent a transformative approach to overcoming these limitations [95]. By deriving MSCs from a clonally defined iPSC source, this platform offers a renewable, scalable, and standardized cell source for EV production [93]. This Application Note details the methodologies for generating, characterizing, and utilizing iMSCs for the production of consistent, high-quality EV preparations, providing researchers with standardized protocols to advance therapeutic EV development.
Comparative Advantages of iMSC-EVs
Overcoming Limitations of Primary MSCs
Traditional MSC sources, including bone marrow and adipose tissue, exhibit inherent biological diversity that introduces variability in growth characteristics, potency, and therapeutic activity [95]. Primary MSCs have finite expansion capabilities and demonstrate phenotypic drift during in vitro passaging, creating significant challenges for manufacturing scalable EV batches with consistent quality [93]. iMSCs circumvent these limitations through their origin from a single, clonally defined iPSC line, enabling the creation of a stable master cell bank that provides a nearly limitless, uniform supply of starting material [95].
Functional and Manufacturing Advantages
iMSCs retain the therapeutic hallmarks of primary MSCs while offering enhanced manufacturing capabilities. Functionally, iMSC-EVs have demonstrated comparable efficacy to primary MSC-EVs in disease models such as bleomycin-induced pulmonary fibrosis, significantly reducing Ashcroft fibrosis scores and bronchoalveolar lavage fluid protein levels [93]. From a manufacturing perspective, iMSCs achieve significantly higher expansion rates in bioreactor systems, with one platform demonstrating expansion for up to 20 days in 3D culture, yielding >5×10⁸ cells per batch and producing approximately 1.2×10¹³ EV particles daily in a fixed-bed bioreactor [93].
Table 1: Quantitative Comparison of EV Production Platforms
| Parameter | Primary MSC-EVs | iMSC-EVs |
|---|---|---|
| Starting Material | Multiple donors, biological diversity | Single clonal iPSC line, uniform source |
| Expansion Potential | Finite (limited population doublings) | Essentially unlimited |
| Batch Consistency | Variable due to donor differences | High due to clonal origin |
| Scalability | Limited by donor cell availability | High, suitable for bioreactor systems |
| Reported EV Yield | Variable, donor-dependent | ~1.2×10¹³ particles/day in fixed-bed bioreactor [93] |
| Genetic Engineering Potential | Limited due to transfection challenges | High (edits can be introduced at iPSC stage) [95] |
Experimental Protocols
iPSC to iMSC Differentiation Protocol
This standardized protocol enables the efficient derivation of iMSCs from iPSCs, generating a consistent cell source for EV production.
Materials and Reagents
- iPSC Line: Clinically qualified iPSC line with normal karyotype and validated differentiation potential [94]
- Basal Media: iPS Brew XF medium or equivalent defined iPSC maintenance medium [94]
- Induction Supplement: CHIR99021 (WNT pathway activator) [94]
- Matrix Substrate: iMatrix-511 or laminin for cell attachment [94]
- Dissociation Enzyme: Accutase or TrypLE Select [94]
- MSC Medium: α-MEM supplemented with 5% human platelet lysate (HPL) [93]
Step-by-Step Procedure
Day -1: iPSC Seeding
- Culture iPSCs to 70-80% confluency in defined maintenance medium.
- Dissociate cells using TrypLE or Accutase and resuspend in medium containing 10 µM Y-27632 (ROCK inhibitor).
- Seed cells onto iMatrix-511-coated plates at a density of 3×10³ cells/cm².
- Incubate at 37°C with 5% CO₂ overnight.
Day 0: MSC Induction Initiation
- Replace medium with MSC induction medium (iPS Brew XF + 4 µM CHIR99021).
- Ensure complete medium replacement to remove residual maintenance factors.
Days 1-6: Induction Phase
- Maintain cells in MSC induction medium with daily medium changes.
- Monitor morphological changes daily; emerging MSC-like cells typically appear as partially detaching clusters.
Day 6: Medium Transition
- Switch cultures to complete MSC medium (α-MEM + 5% HPL).
- Do not passage detaching cell clusters; allow MSC-like cells to grow out from attached clusters.
Days 7-14: MSC Outgrowth and Expansion
- Continue culture in MSC medium with every-other-day medium changes.
- Once cultures reach full confluence (typically 7-10 days after induction), dissociate with Accutase.
- Replate at 1:2 split ratio on iMatrix-511-coated plates; designate this as passage 1 (P1).
Quality Control Checkpoints:
- At P4, assess cells for homogeneous MSC morphology.
- Validate MSC surface marker expression (CD44, CD73, CD90, CD105, CD166) and absence of hematopoietic markers (CD34, CD45, HLA-DR) by flow cytometry [93] [94].
- Confirm absence of pluripotency markers (OCT4, NANOG, SOX2) to ensure complete differentiation.
Bioreactor Scale-Up and EV Production
For large-scale EV production, transition from flask-based culture to bioreactor systems to achieve higher cell densities and increased EV yields.
Bioreactor Setup and Operation
- System Selection: Implement a fixed-bed bioreactor system for adherent iMSC culture, providing uniform nutrient perfusion and minimal shear stress [93].
- Inoculation: Seed iMSCs at a density of 1×10⁴ cells/cm² into the bioreactor system.
- Process Parameters: Maintain temperature at 37°C, dissolved oxygen at 40-60%, and pH at 7.2-7.4 with continuous perfusion.
- Harvesting: Collect conditioned medium continuously or at scheduled intervals for EV isolation.
EV Isolation and Purification
- Clarification: Remove cells and large debris by centrifugation at 2,000 × g for 20 minutes.
- Concentration: Use tangential flow filtration with 100-500 kDa membranes to concentrate the clarified supernatant.
- Isolation: Employ size-exclusion chromatography (SEC) for high-purity EV isolation [92] [29].
- Sterilization: Filter purified EVs through 0.22 µm filters for sterilization.
- Concentration Adjustment: Concentrate to desired final concentration using centrifugal filter units.
Table 2: EV Characterization Assays and Specifications
| Characterization Parameter | Recommended Method | Target Specifications |
|---|---|---|
| Size Distribution | Nanoparticle Tracking Analysis (NTA) | 70-150 nm, monomodal distribution [93] |
| Morphology | Transmission Electron Microscopy (TEM) | Cup-shaped vesicles, intact membranes [92] [93] |
| Surface Markers | Flow cytometry, Western blot | CD63, CD81, TSG101 positive [93] |
| Concentration | NTA, tunable resistive pulse sensing | Variable based on production scale |
| Protein Contamination | BCA assay, specific marker tests | Absence of apolipoproteins |
| Potency | Context-specific functional assays | Defined based on intended application |
Analytical and Quality Control Methods
Comprehensive EV Characterization
Rigorous characterization is essential to ensure EV quality, consistency, and functionality across production batches.
Physical Characterization
- Nanoparticle Tracking Analysis: Dilute EV preparations in filtered PBS to achieve 20-100 particles per frame. Acquire multiple 60-second videos and analyze with appropriate software to determine particle size distribution and concentration [92].
- Transmission Electron Microscopy: Apply 5-10 µL of purified EV sample to formvar/carbon-coated grids. Negative stain with 2% uranyl acetate and image at 80-100 kV to assess morphology and membrane integrity [92] [93].
Molecular Characterization
- Surface Marker Analysis: Use flow cytometry with capture beads (e.g., Annexin V or CD63 beads) or Western blot to confirm presence of tetraspanins (CD9, CD63, CD81) and absence of cellular contaminants [92] [93].
- Cargo Analysis: Extract RNA and protein for miRNA sequencing and proteomic analysis to characterize therapeutic cargo and monitor batch-to-batch consistency [29].
Functional Potency Assays
Develop context-specific potency assays aligned with intended therapeutic applications to ensure biological activity.
Immunomodulatory Activity
- T-cell Proliferation Assay: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors, label with CFSE, and activate with CD3/CD28 antibodies. Co-culture with iMSC-EVs (dose range: 10⁸-10¹⁰ particles/well) for 3-5 days. Analyze T-cell proliferation by flow cytometry and cytokine production by ELISA [94].
- Macrophage Polarization Assay: Differentiate monocyte-derived macrophages with M-CSF, then treat with iMSC-EVs in the presence of IFN-γ and LPS. Assess M2 polarization markers (CD206, IL-10) versus M1 markers (CD86, TNF-α) by flow cytometry and cytokine analysis [81].
Tissue Repair Models
- In Vitro Wound Healing Assay: Create scratch wounds in confluent fibroblast or epithelial cell monolayers. Treat with iMSC-EVs and monitor wound closure over 24-48 hours using live-cell imaging [91] [90].
- Angiogenesis Assay: Seed endothelial cells on Matrigel and treat with iMSC-EVs. Quantify tube formation parameters (number of nodes, branches, total tube length) after 6-18 hours [81].
Applications and Therapeutic Evidence
iMSC-EVs have demonstrated therapeutic potential across diverse disease models, leveraging their immunomodulatory and regenerative properties.
Documented Efficacy in Disease Models
- Pulmonary Fibrosis: In a bleomycin-induced pulmonary fibrosis mouse model, iMSC-EVs significantly reduced Ashcroft fibrosis scores and bronchoalveolar lavage fluid protein levels, demonstrating efficacy comparable to primary MSC-EVs [93].
- Anterior Cruciate Ligament (ACL) Repair: EVs modulate the injury microenvironment by attenuating inflammation, promoting neovascularization, inhibiting fibrotic scar formation, and directing osteochondral differentiation at the tendon-bone interface [91].
- Orthopedic Applications: EVs show promise in managing degenerative disorders including osteoarthritis, intervertebral disc degeneration, osteoporosis, and tendinopathy through their effects on inflammation modulation and tissue regeneration [92].
Clinical Translation Considerations
Early clinical trials delivering MSC-EVs via topical, intra-articular, or inhalation routes have reported acceptable safety and encouraging therapeutic signals [90]. Route of administration significantly influences effective dosing, with nebulization therapy achieving therapeutic effects at approximately 10⁸ particles, significantly lower than intravenous routes [96]. For clinical development, engage regulators early to align on mechanism-driven product definitions, critical quality attributes, and appropriate potency assays [89].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for iMSC-EV Production
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| iPSC Maintenance | iPS Brew XF, mTeSR, StemFlex | Defined, xeno-free media for pluripotent cell culture |
| iMSC Differentiation | CHIR99021, Y-27632 | WNT activation for MSC induction; ROCK inhibition to enhance viability |
| Cell Attachment | iMatrix-511, laminin, vitronectin | Recombinant proteins for consistent cell adhesion and growth |
| iMSC Expansion | α-MEM + 5% HPL, MSC Brew | Serum-free or human platelet lysate-supplemented media |
| EV Isolation | Size-exclusion columns, TFF systems, ultracentrifugation | High-purity isolation with minimal vesicle damage |
| EV Characterization | NTA systems, TEM reagents, flow cytometry | Comprehensive physical and molecular analysis |
| Functional Assays | CFSE, cytokine ELISA kits, Matrigel | Potency assessment for specific therapeutic applications |
Technical Diagrams
iMSC-EV Bioprocessing Workflow
EV Biogenesis and Cargo Loading Mechanisms
Challenges and Future Directions
Despite the considerable advantages of iMSC-EV platforms, several challenges require attention for successful clinical translation. Batch-to-batch functional variability persists even with clonally derived iMSCs, necessitating robust functional testing of each EV batch [94]. Variations in EV-specific protein profiles among independent iMSC-EV preparations highlight the need for comprehensive characterization and quality control [94].
Future development should focus on establishing standardized potency assays linked to clinical relevance, integrating artificial intelligence for quality prediction, and implementing GMP-compliant, automated manufacturing processes [89] [93]. Genetic engineering of iMSCs at the iPSC stage offers opportunities to enhance EV targeting, loading, and therapeutic potency, creating customized EV products for specific clinical applications [95]. As the field advances, proactive engagement with regulatory agencies will be essential to establish appropriate frameworks for iMSC-EV characterization, manufacturing, and clinical evaluation [89] [95].
The transition from characterizing stem cell secretomes to interpreting clinical trial data represents a critical juncture in therapeutic development. Research has demonstrated that the therapeutic effects of stem cells are largely mediated by their paracrine secretions, particularly the secretome and exosomes, offering a promising cell-free regenerative strategy [8]. The efficacy and safety of these advanced therapies, as with all drug candidates, must ultimately be validated through rigorously designed clinical trials. This application note provides a structured framework for analyzing dose-effect relationships and safety profiles from registered clinical studies, with specific consideration for therapies derived from stem cell secretomes and exosomes. Understanding these relationships is fundamental to determining the minimum effective dose, the maximum tolerated dose, and the therapeutic index—the ratio that defines a drug's safety window [97].
Core Concepts in Dose-Response and Safety Analysis
Fundamental Parameters of Dose-Response Relationships
Dose-response data are typically graphed with the dose (or its logarithm) on the x-axis and the measured effect on the y-axis, depicting the relationship independent of time. These curves reveal several critical parameters [97]:
- Potency: The location of the curve along the dose axis, representing the dose required to produce a given effect.
- Maximal Efficacy (Ceiling Effect): The greatest attainable response, regardless of dose.
- Slope: The change in response per unit dose, which indicates the variability in patient sensitivity.
- Therapeutic Index: The ratio between the minimum toxic concentration and the median effective concentration (TD50/ED50), which helps determine a drug's efficacy and safety profile.
Table 1: Key Parameters of Dose-Response Relationships
| Parameter | Definition | Clinical Significance |
|---|---|---|
| Potency | Dose required to produce 50% of maximal effect (ED50) | Determines dosing frequency and amount; lower potency requires higher doses |
| Maximal Efficacy | Greatest attainable biological response | Determines the therapeutic ceiling and ultimate effectiveness |
| Slope | Steepness of the dose-response curve | Predicts the safety margin and potential for small dose changes to cause large effects |
| Therapeutic Index | Ratio of TD50 (toxic dose) to ED50 (effective dose) | Quantifies drug safety; a small index indicates narrow safety window |
Safety Profile Assessment and Adverse Event Collection
Safety analysis in clinical trials involves identifying untoward medical occurrences after drug exposure, known as Adverse Events (AEs). A significant challenge in this process is the reliance on participant reports for subjective symptoms, where the method of eliciting this information substantially influences the data collected [98]. Research indicates that more specific questioning (e.g., checklists) detects more AEs compared to general enquiries, though open questions may better identify severe or bothersome AEs. This methodological variation complicates comparisons between studies and pooled analyses [98].
Experimental Protocols for Data Generation and Analysis
Protocol for Cell Type-Specific Exosome Isolation and Characterization
The following protocol, adapted from recent methodologies, enables the isolation of cell type-specific exosomes from complex tissues, which is crucial for understanding the active components in stem cell secretome therapies [28].
Phase 1: Genetic Labeling of Cell Type-Specific Exosomes
- Step 1: Design plasmids encoding cell type-specific promoter-driven tetraspanins (CD9, CD63, CD81) fused with "in frame" fluorescent reporters (e.g., GFP).
- Step 2: Deliver constructs via appropriate methods (e.g., Tissue Nanotransfection - TNT) for in vivo application.
- Step 3: Validate specificity by confirming reporter gene expression is restricted to target cells.
Phase 2: Isolation of Labeled Exosomes
- Step 1: Homogenize tissue and perform differential centrifugation (300 × g for 10 min, 2,000 × g for 20 min, 10,000 × g for 30 min).
- Step 2: Ultracentrifuge supernatant at 100,000 × g for 70 min to pellet crude EVs.
- Step 3: Resuspend pellet and incubate with anti-GFP magnetic agarose beads for immunocapture.
- Step 4: Wash beads and elute bound exosomes.
Phase 3: Characterization of Isolated Exosomes
- Step 1: Nanoparticle Tracking Analysis (NTA) to determine size distribution (30-150 nm expected).
- Step 2: Transmission Electron Microscopy (TEM) to confirm vesicular morphology.
- Step 3: Antibody array for exosomal markers (CD9, CD63, CD81, TSG101, Alix).
- Step 4: Protein quantification and functional analysis of cargo.
This labeling and isolation protocol spans 2-3 days and enables the study of exosome-mediated communication from specific cell types in vivo [28].
The following structured protocol addresses the challenges in AE data collection, ensuring comprehensive and comparable safety data [98].
Phase 1: Study Design and Instrument Development
- Step 1: Define AE terminology and grading criteria in the study protocol.
- Step 2: Develop a structured data collection instrument combining:
- Open-ended general enquiry: "How have you been feeling since your last visit?"
- Targeted symptom checklist (include expected AEs based on mechanism of action).
- Memory aids for participants to record symptoms between visits.
- Step 3: Train study staff in consistent administration of AE questions.
Phase 2: Implementation During Trial Visits
- Step 1: At each study visit, begin with open-ended questioning.
- Step 2: Follow with structured checklist for comprehensive coverage.
- Step 3: For all identified AEs, document:
- Onset date, duration, and temporal relationship to dosing
- Severity (using standardized grading scales)
- Action taken regarding study treatment
- Outcome and relationship to investigational product
- Step 4: Ascertain AEs between visits using patient diaries or electronic prompts.
Phase 3: Data Analysis and Reporting
- Step 1: Categorize AEs by body system and severity.
- Step 2: Compare AE rates between treatment and control groups.
- Step 3: Conduct dose-response analyses for AE incidence.
- Step 4: Report specific methods used for AE elicitation in publications to enable cross-study comparisons.
This systematic approach mitigates the under-detection of AEs while capturing clinically significant symptoms, providing a more complete safety profile [98].
Diagram 1: Dose-Response Clinical Data Analysis Workflow
Data Presentation and Analysis Framework
Comparative Analysis of Therapeutic Candidates
When comparing multiple drug candidates, dose-response curves provide critical information for candidate selection. As illustrated in the comparison of Drugs X, Y, and Z [97]:
- Drug X demonstrates greater potency than Drugs Y or Z, producing greater biological activity per dosing equivalent.
- Drugs X and Z show equal maximal efficacy, despite differences in potency.
- Drug Y is more potent than Drug Z but has lower maximal efficacy, making it unsuitable where high efficacy is required.
Table 2: Hypothetical Dose-Response Comparison of Stem Cell-Derived Therapeutics
| Therapeutic Candidate | ED50 (Effective Dose 50%) | Maximal Efficacy (% Wound Closure) | Therapeutic Index | Key Advantages |
|---|---|---|---|---|
| Whole Secretome | 5.2 μg/mL | 92% | 8.5 | Broad spectrum of bioactive factors |
| Purified Exosomes | 2.1 μg/mL | 88% | 12.3 | Standardized composition, lower immunogenicity |
| rHFSC-Exosomes | 1.8 μg/mL | 95% | 15.7 | Enhanced skin regeneration potential [80] |
| SynthEVs (Biomimetic) | 3.7 μg/mL | 82% | 6.2 | Precisely engineered cargo |
Biomarker Analysis in Secretome and Exosome Preparations
Comparative analysis of secretome and exosome components reveals differential enrichment of bioactive molecules. Studies of rat hair follicle stem cell (rHFSC) derivatives show distinct biomarker profiles between unfractionated secretome and purified exosomes [80]. For instance, certain biomolecules demonstrate significantly higher concentrations in exosomes, suggesting selective packaging mechanisms, while others are more abundant in the general secretome. This differential packaging has implications for therapeutic activity and should be considered when interpreting dose-response relationships.
Table 3: Methodological Comparison for AE Elicitation in Clinical Trials
| Elicitation Method | AE Detection Rate | Strength | Limitation | Recommended Context |
|---|---|---|---|---|
| General Enquiry | Lower (RR: 0.12-0.64) [98] | Identifies bothersome/severe AEs | Under-detects less salient symptoms | Initial screening at study visits |
| Structured Checklist | Higher | Comprehensive coverage | May capture trivial symptoms | Systematic assessment at predefined intervals |
| Patient Diary | Intermediate | Captures transient symptoms between visits | Compliance issues | Between-visit monitoring |
| Clinical Interview | Highest | Detailed contextual information | Resource-intensive | For serious AEs |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Exosome Isolation and Characterization
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Anti-Tetraspanin Magnetic Beads (CD9/CD63/CD81) | Immunoaffinity capture of exosomes | Preferred for specific subpopulation isolation; use according to MISEV guidelines [28] |
| GFP-Trap Magnetic Agarose | Immunocapture of GFP-tagged exosomes | Essential for cell type-specific exosome isolation from reporter systems [28] |
| Protein Quantification Assays | Measurement of cargo content | Critical for dose standardization in functional studies [80] |
| Exosome Antibody Arrays | Multiplexed biomarker profiling | Enables comprehensive characterization of vesicle content [28] [80] |
| RNA Isolation Kits | Nucleic acid cargo extraction | Quality control through RNA integrity measurement [28] |
| Ultracentrifugation Systems | Size-based EV separation | Remain the gold standard for bulk isolation; requires standardization [28] [80] |
| Nanoparticle Tracking Analyzer | Size and concentration measurement | Validates exosome preparation quality (30-150 nm) [28] [80] |
Diagram 2: Exosome Characterization to Clinical Application Pipeline
The rigorous interpretation of clinical trial data for stem cell secretome and exosome therapies requires specialized methodologies at every stage—from the precise isolation and characterization of therapeutic vesicles to the systematic collection and analysis of dose-response and safety data. By implementing the protocols and frameworks outlined in this application note, researchers can generate robust, comparable data that accurately characterizes both the efficacy and safety profiles of these innovative therapeutics. This approach facilitates the rational development of dosing strategies that maximize therapeutic benefit while minimizing risks, ultimately accelerating the translation of promising stem cell-derived therapies from bench to bedside.
Conclusion
The characterization of the stem cell secretome and the isolation of exosomes represent a paradigm shift toward effective cell-free regenerative therapies. While significant progress has been made in understanding their biology and therapeutic potential, the field is constrained by a lack of standardized, reproducible protocols for isolation, characterization, and dosing, hindering clinical translation. Future efforts must prioritize the establishment of universal standards, scalable GMP production, and rigorous functional validation. Bridging these gaps through global collaboration and deeper mechanistic studies will be crucial to fully harnessing the power of MSC-derived secretomes and exosomes, ultimately unlocking their transformative potential in precision medicine, regenerative therapy, and drug delivery.
References
- 1. Mesenchymal stem cell secretome for regenerative medicine [https://www.sciencedirect.com/science/article/pii/S2090123224001814]
- 2. Secretome and extracellular vesicle signatures in bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367461/]
- 3. Isolation and characterization of exosomes from adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8053584/]
- 4. Exosome isolation and characterization for advanced ... [https://www.sciencedirect.com/science/article/pii/S2590006425001711]
- 5. Exosome Isolation Protocols and Quantification Guidelines [https://www.sepscience.com/exosome-isolation-protocols-and-quantification-guidelines-12144]
- 6. Comprehensive Comparison of Methods for Isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150312/]
- 7. Size-dependent immunomodulation by MSC secretome ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04670-2]
- 8. Method standardization of secretome production, collection ... [https://www.sciencedirect.com/science/article/pii/S2352320425000811]
- 9. Comparative Analysis of Exosomes and Extracellular ... [https://www.mdpi.com/1420-3049/29/15/3681]
- 10. Extracellular microvesicles/exosomes: discovery, disbelief ... [https://www.nature.com/articles/s41375-020-01041-z]
- 11. Isolation methods of exosomes derived from dental stem cells [https://www.nature.com/articles/s41368-025-00370-y]
- 12. What is a Stem Cell Secretome? What are Exosomes [https://anova-irm.com/en/stem-cell-therapy/secretome-exosomes-therapy]
- 13. Stem Cell-Derived Exosomes: A Comprehensive Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417880/]
- 14. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 15. Biogenesis, Composition and Potential Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276992/]
- 16. Characterization of size distribution and markers for ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1497795/full]
- 17. Comparative Proteomics of Seminal Exosomes Reveals ... [https://www.mdpi.com/2227-9059/13/10/2459]
- 18. Exosomes vs Stem Cells: Differences & Utility (2025) [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 19. Adipose-derived stem cell exosomes - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181847/]
- 20. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 21. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 22. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 23. Different Sources of Mesenchymal Stem Cells for Tissue ... [https://www.mdpi.com/1422-0067/23/11/6356]
- 24. Comparative analysis of human Mesenchymal Stromal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616983/]
- 25. Comparative analysis of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4453294/]
- 26. Comparative analysis of dental-derived stem cells and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1717849/full]
- 27. Clinical applications of extracellular vesicles [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1671963/full]
- 28. Labeling, isolation, and characterization of cell type-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505222/]
- 29. Isolation methods of exosomes derived from dental stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170887/]
- 30. Adipose-derived stem cell exosomes: multifaceted therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527763/]
- 31. Microfluidic Devices for Manufacture of Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12287800/]
- 32. 2.5. Microfluidic Based Isolation Techniques [https://bio-protocol.org/exchange/minidetail?id=8068622&type=30]
- 33. Protocol for differentiation of human pluripotent stem cells into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205342/]
- 34. Updated protocols for cell lysate, secretome, and exosome ... [https://pubmed.ncbi.nlm.nih.gov/40058715/]
- 35. A streamlined method for isolating and characterizing small ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-025-00040-9]
- 36. Nanotechnology-Enhanced Extracellular Vesicles [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361355/]
- 37. Transmission Electron Microscopy-based characterization of ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02383-w]
- 38. Continuous map of early hematopoietic stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11889232/]
- 39. SEC-HPLC Protocol [https://neutab.creative-biolabs.com/sec-hplc-analysis.htm]
- 40. SEC-HPLC analysis of column load and flow-through ... [https://www.sciencedirect.com/science/article/abs/pii/S1046592823001894]
- 41. A SIMPLE SIZE-EXCLUSION CHROMATOGRAPHIC ... [https://chemrxiv.org/engage/chemrxiv/article-details/67b4a4066dde43c9086aa36d]
- 42. Characterization of the Secretome from Spheroids ... [https://www.mdpi.com/2227-9059/12/8/1842]
- 43. GMP‐Compliant Process for the Manufacturing of an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365392/]
- 44. Identification of critical process parameters and quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408662/]
- 45. Critical Analysis of cGMP Large-Scale Expansion Process ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8561684/]
- 46. Large-scale bioreactor production of extracellular vesicles ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03688-2]
- 47. Proteomic Analysis of the Secretome and Exosomes of Feline ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7912403/]
- 48. Comprehensive proteomic analysis of exosomes derived from ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02032-8]
- 49. Proteomic analysis of human mesenchymal stromal cell ... [https://www.nature.com/articles/s41536-019-0070-y]
- 50. Updated protocols for cell lysate, secretome, and exosome ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000568]
- 51. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 52. Pharmacokinetic and Pharmacodynamic Comparison of ... [https://pubmed.ncbi.nlm.nih.gov/32985935/]
- 53. Article Biodistribution and pharmacokinetics of aerosol and ... [https://www.sciencedirect.com/science/article/pii/S1525001603001771]
- 54. Enrichment protocols for human conjunctival extracellular ... [https://www.nature.com/articles/s41598-024-79481-1]
- 55. SPIRIT 2025 Statement: Defining standard protocol items ... [https://www.equator-network.org/reporting-guidelines/spirit-2013-statement-defining-standard-protocol-items-for-clinical-trials/]
- 56. Method standardization of secretome production, collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423684/]
- 57. Efficient methods of isolation and purification of extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463815/]
- 58. Recent advances in scalable exosome production [https://www.sciencedirect.com/science/article/pii/S2096691125000196]
- 59. A simplified and efficient method for isolating small ... [https://www.nature.com/articles/s41598-025-99822-y]
- 60. Mesenchymal stem cell-derived extracellular vesicles [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1626996/full]
- 61. Advances and Challenges in Nanomaterial-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785636/]
- 62. Recent applications and challenges of inorganic ... [https://www.sciencedirect.com/science/article/pii/S2773045X25000032]
- 63. High-sensitivity nanosensors for biomarker detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3629948/]
- 64. Whole secretome of mesenchymal stem cells is fully ... [https://www.frontiersin.org/journals/medical-engineering/articles/10.3389/fmede.2025.1397406/full]
- 65. Method standardization of secretome production, collection ... [https://pubmed.ncbi.nlm.nih.gov/40951916/]
- 66. A comprehensive review on recent advances in exosome ... [https://www.sciencedirect.com/science/article/pii/S1936523324002481]
- 67. A state-of-the-art review of the recent advances in exosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10829349/]
- 68. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 69. Optimizing mesenchymal stromal cells priming strategies ... [https://www.sciencedirect.com/science/article/pii/S0753332225004123]
- 70. Comparison of 3D culture systems on mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562725/]
- 71. New way to isolate cultured cell exosomes [https://pubmed.ncbi.nlm.nih.gov/40709977/]
- 72. Biochemical Assay Development: Strategies to Speed Up ... [https://bellbrooklabs.com/accelerate-biochemical-assay-development/?srsltid=AfmBOopwAcs87CEURaFz5mxveJKXT_QDaxMepVSqcEOwQ9eVptJvrvrK]
- 73. New Assay Technology Could Reshape Approach to Drug ... [http://ncats.nih.gov/news-events/news/new-assay-technology-could-reshape-approach-drug-discovery]
- 74. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 75. Mesenchymal stem cell derived-exosomes [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02622-3]
- 76. Understanding molecular characteristics of extracellular ... [https://www.sciencedirect.com/science/article/pii/S2773041724000015]
- 77. Proteomic profiling of iPSC and tissue-derived MSC ... [https://www.nature.com/articles/s41536-024-00382-y]
- 78. Human bone marrow- and adipose-mesenchymal stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4529699/]
- 79. Bone Marrow Mesenchymal Stem Cell-Derived Exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299787/]
- 80. Rat Hair Follicle Stem Cell-Derived Exosomes [https://www.mdpi.com/1422-0067/26/11/5081]
- 81. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 82. methods of Isolation derived from exosomes dental stem cells [https://www.nature.com/articles/s41368-025-00370-y?error=cookies_not_supported]
- 83. Mechanistic insights into dental stem cells‐derived exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339802/]
- 84. Exosomes Derived from Dental Pulp Stem Cells in Tissue ... [https://doi.org/10.54254/2753-8818/2025.AU27275]
- 85. Neuronal Differentiation and Exosome Profiling of Dental Pulp Stem ... [https://www.preprints.org/manuscript/202509.0245/v1]
- 86. Potential of Dental Pulp Stem Cell Exosomes [https://www.sciencedirect.com/science/article/pii/S0020653924014886]
- 87. Comparative analysis of extracellular vesicles from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12136449/]
- 88. Comparative analysis of extracellular vesicles from induced ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0325065]
- 89. A Thematic Synthesis for Advancing MSC EV Therapies [https://www.sciencedirect.com/science/article/pii/S1465324925009120]
- 90. iPSC-, MSC- and iMSC-Derived Exosome Therapeutics [https://www.reprocell.com/blog/ipsc-msc-and-imsc-derived-exosome-therapeutics-the-cell-free-future-of-regenerative-medicine]
- 91. Decoding the exosomal secretome: stem cell-elicted ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1691651/full]
- 92. Clinical Status of Exosomes: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357840/]
- 93. A scalable platform for EPSC-Induced MSC extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04507-y]
- 94. EV products obtained from iPSC-derived MSCs show batch ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1282860/full]
- 95. Solving The Stem Cell Consistency Conundrum With iMSCs [https://www.cellandgene.com/doc/solving-the-stem-cell-consistency-conundrum-with-imscs-0001]
- 96. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 97. Dose-Response Relationships - Clinical Pharmacology [https://www.merckmanuals.com/professional/clinical-pharmacology/pharmacodynamics/dose-response-relationships]
- 98. Eliciting adverse effects data from participants in clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC7098080/]