Stem Cell Therapy Clinical Outcomes: A Systematic Review and Meta-Analysis of Efficacy and Safety Across Medical Specialties
This systematic review and meta-analysis synthesizes current evidence on the clinical outcomes of stem cell therapies across cardiovascular, neurological, and hepatic diseases.
Stem Cell Therapy Clinical Outcomes: A Systematic Review and Meta-Analysis of Efficacy and Safety Across Medical Specialties
Abstract
This systematic review and meta-analysis synthesizes current evidence on the clinical outcomes of stem cell therapies across cardiovascular, neurological, and hepatic diseases. Drawing from recent clinical trials and meta-analyses published through 2025, we evaluate efficacy endpoints including left ventricular ejection fraction (LVEF), National Institutes of Health Stroke Scale (NIHSS) scores, Model for End-Stage Liver Disease (MELD) scores, and quality of life metrics. Our analysis reveals condition-specific efficacy patterns, with significant functional improvements observed in stroke and liver failure patients, while highlighting the safety profile of mesenchymal stem cell therapies. We critically examine methodological challenges in trial design, address optimization strategies for cell sourcing and delivery routes, and discuss the imperative for standardized outcome reporting to advance the field of regenerative medicine.
The Current Landscape of Stem Cell Clinical Trials: Efficacy Evidence and Therapeutic Mechanisms
Global Disease Burden and Unmet Medical Needs Driving Stem Cell Research
The global burden of disease has undergone a significant transformation over recent decades, creating substantial unmet medical needs that are driving innovation in regenerative medicine. Non-communicable diseases (NCDs) now account for nearly two-thirds of the world's total mortality and morbidity, with ischemic heart disease, stroke, and diabetes leading this global health challenge [1]. This shift occurs alongside persistent infectious diseases and a growing burden of age-related disorders, creating complex healthcare demands that conventional treatments struggle to address.
Amidst these challenges, stem cell research has emerged as a promising therapeutic avenue, particularly for conditions with limited treatment options. The alignment between disease burden and research focus, however, remains imperfect. A comprehensive analysis of 8.6 million disease-specific publications revealed significant divergence between research efforts and global health needs, with some high-burden conditions receiving disproportionately little scientific attention [2]. This misalignment highlights the importance of strategically directing research toward areas of greatest unmet need, where stem cell therapies may offer transformative potential.
Analysis of Stem Cell Clinical Outcomes Across Therapeutic Areas
Cardiovascular Diseases
Cardiovascular diseases remain the leading cause of death globally, with heart failure representing a particularly challenging condition despite advances in pharmacological therapy. Mesenchymal stem cell (MSC) therapy has been investigated as a promising intervention for heart failure with reduced ejection fraction (HFrEF), targeting left ventricular pressure and improving wall thickness [3].
Table 1: Clinical Outcomes of MSC Therapy for Heart Failure with Reduced Ejection Fraction
| Outcome Measure | Effect Size (Hedges' g) | P-value | Statistical Significance | Heterogeneity (I²) |
|---|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | 0.096 | 0.18 | Not Significant | 0.5% |
| Quality of Life (QoL) | -0.518 | 0.01 | Significant | - |
| Major Adverse Cardiac Events (MACE) | No increased risk | - | Not Significant | - |
A systematic review of clinical trials published from 2018 onwards demonstrated that while MSC therapy was safe and improved quality of life for HFrEF patients, it did not significantly improve LVEF or other efficacy outcomes [3]. These findings suggest that MSC therapy may provide symptomatic benefits without directly reversing the underlying cardiac dysfunction, highlighting the need for further research into mechanisms and protocols.
Beyond cell therapy, recent research has explored extracellular vesicles (EVs) as potential alternatives for cardiac repair. These cell-derived, nano-sized particles carry therapeutic cargo and have demonstrated cardioprotective effects in animal models of acute myocardial infarction, including reduced inflammation, apoptosis, smaller infarct size, and improved cardiac functionality [4].
Cerebrovascular Diseases
Ischemic stroke represents the second leading cause of death globally, with over 63 million years of healthy life lost annually due to stroke-related death and disability [5]. Stem cell therapy has gained increasing attention since the 1990s as a potential treatment, with MSCs, bone marrow mononuclear cells, and bone marrow progenitor cells primarily employed for their immunomodulatory, anti-inflammatory, and neuroregenerative effects.
Table 2: Efficacy Outcomes of Stem Cell Therapy for Acute/Subacute Ischemic Stroke
| Time Point | Outcome Measure | Risk Ratio (RR) | 95% Confidence Interval | P-value | Statistical Significance |
|---|---|---|---|---|---|
| 90 days | mRS score 0-2 | 1.31 | 1.01-1.70 | 0.044 | Significant |
| 1 year | mRS score 0-1 | 1.74 | 1.09-2.77 | 0.020 | Significant |
| Overall | Serious Adverse Events | 0.85 | 0.70-1.04 | 0.11 | Not Significant |
| Overall | Mortality | 0.72 | 0.49-1.08 | 0.12 | Not Significant |
A systematic review of 13 randomized controlled trials involving 872 patients found that stem cell therapy for acute/subacute ischemic stroke within one month of onset significantly improved long-term functional outcomes without increasing serious adverse events or mortality [5]. The 1-year incidence of excellent functional outcome (modified Rankin Scale score 0-1) was significantly higher in the cell therapy group (45/195) compared to controls (23/179), indicating meaningful clinical benefits.
Autoimmune and Rheumatic Diseases
Autoimmune and rheumatic diseases rank as the third most significant threat to human health after cardiovascular diseases and cancer, affecting approximately 10% of individuals globally and posing substantial economic challenges [6]. MSC transplantation has shown promise in treating these conditions through its immunomodulatory properties, which include modulating anti-inflammatory factors and promoting immune tolerance.
Table 3: Efficacy of MSC Transplantation for Autoimmune and Rheumatic Diseases
| Disease Condition | Outcome Measure | Effect Size | 95% Confidence Interval | P-value | Statistical Significance |
|---|---|---|---|---|---|
| Osteoarthritis (BM-MSC) | VAS | SMD = -0.95 | -1.55 to -0.36 | 0.002 | Significant |
| Osteoarthritis (UC-MSC) | VAS | SMD = -1.25 | -2.04 to -0.46 | 0.002 | Significant |
| Osteoarthritis (AD-MSC) | VAS | SMD = -1.26 | -1.99 to -0.52 | 0.0009 | Significant |
| Systemic Lupus Erythematosus | SLEDAI | SMD = -2.32 | -3.59 to -1.06 | 0.0003 | Significant |
| Inflammatory Bowel Disease | Clinical Efficacy | RR = 2.02 | 1.53 to 2.67 | <0.00001 | Significant |
A systematic review of 42 randomized controlled trials with 2,183 participants demonstrated that MSC transplantation significantly improved symptoms in patients with osteoarthritis, systemic lupus erythematosus, and inflammatory bowel disease without increasing adverse events [6]. The safety profile across studies supports MSC transplantation as a viable alternative treatment option for autoimmune and rheumatic diseases.
Experimental Protocols and Methodologies
MSC Characterization and Quality Control
The International Society for Cellular Therapy has established minimum criteria for defining MSCs. These cells must: (a) express specific cell surface markers (CD73, CD90, and CD105) while lacking expression of CD14, CD34, CD45, and HLA-DR; (b) exhibit plastic adherence in standard culture conditions; and (c) demonstrate capacity for in vitro differentiation into adipocytes, chondrocytes, and osteoblasts [3]. These standardized criteria ensure consistent characterization across research studies and clinical applications.
Clinical Trial Design Considerations
Recent meta-analyses have employed rigorous methodology to assess stem cell efficacy. Typical approaches include comprehensive searches of multiple databases (PubMed, Scopus, EBSCO Medline, Cochrane Library), systematic screening processes following PRISMA guidelines, and statistical analysis using random-effects models to account for clinical variations in MSC preparation [3] [6]. Risk of bias assessment is typically conducted using Cochrane Risk of Bias tools, with sensitivity analyses to validate findings.
For stroke trials, recent research has emphasized the importance of aligning the timing of stem cell administration and functional evaluation to minimize heterogeneity. Most successful trials have initiated stem cell therapy within one month of stroke onset, with functional assessments at standardized timepoints (90 days, 180 days, and 1 year) to capture both short-term and long-term outcomes [5].
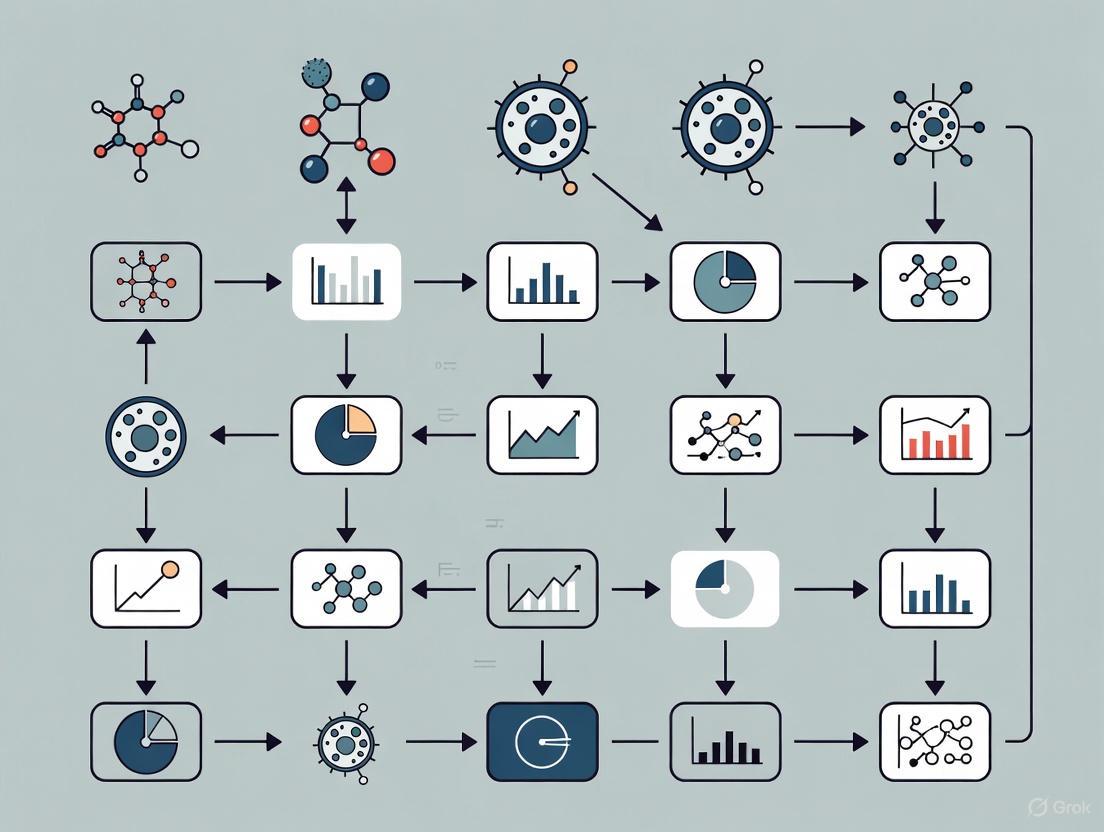
Diagram 1: Relationship between global health needs and stem cell research development. The flow demonstrates how population health trends drive research priorities and ultimately clinical applications.
Outcome Assessment Strategies
Success rates in stem cell therapy are measured through comprehensive evaluations encompassing clinical observations, laboratory tests, patient-reported outcomes, and long-term follow-up. Clinical observations include physical examinations and imaging studies; laboratory tests monitor biomarkers such as inflammatory markers; patient-reported outcomes evaluate changes in symptoms and quality of life; and long-term follow-up assesses the durability of response [7]. This multi-faceted approach ensures thorough assessment of therapeutic impact.
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Reagents for Stem Cell Investigations
| Reagent/Material | Function | Application Examples |
|---|---|---|
| CD73, CD90, CD105 Antibodies | MSC surface marker identification | Flow cytometry, immunocytochemistry for MSC characterization |
| CD14, CD34, CD45, HLA-DR Antibodies | Negative marker confirmation | Purity assessment and exclusion of hematopoietic contaminants |
| Adipogenic Differentiation Media | Induces adipocyte differentiation | In vitro trilineage differentiation potential verification |
| Chondrogenic Differentiation Media | Induces chondrocyte differentiation | In vitro trilineage differentiation potential verification |
| Osteogenic Differentiation Media | Induces osteoblast differentiation | In vitro trilineage differentiation potential verification |
| Tissue Culture Plasticware | Provides adherent surface | MSC expansion and maintenance |
| ELISA Kits for Inflammatory Markers | Quantifies cytokine levels | Assessment of immunomodulatory effects (IL-6, TNF-α) |
| Exosome Isolation Kits | Extracts extracellular vesicles | Preparation of cell-free therapeutic agents |
These research reagents enable standardized characterization of MSCs across different laboratories and clinical trials, facilitating comparison of results and ensuring cell population consistency. The International Society for Cellular Therapy guidelines have been instrumental in establishing these standardized approaches [3].
Mechanisms of Action and Signaling Pathways
Stem cells, particularly MSCs, exert their therapeutic effects through multiple mechanisms rather than direct cell replacement alone. These include paracrine signaling, immunomodulation, and trophic support. Anti-apoptotic action is exerted on injured cardiomyocytes through the transfer of healthy mitochondria via tunneling nanotubes and the secretion of exosomes carrying regenerative signals [3]. MSCs activate survival pathways under low-oxygen conditions, strengthening their therapeutic potential in ischemic conditions.
In cardiac repair, MSC-mediated benefits primarily occur through paracrine mechanisms rather than direct differentiation into cardiomyocytes. These paracrine effects include protective and reparative actions on existing tissue, modulation of inflammatory responses, and promotion of angiogenesis [3] [4]. Similarly, in neurological applications, MSCs demonstrate immunomodulatory, anti-inflammatory, and neuroregenerative effects that contribute to functional recovery after stroke [5].
Diagram 2: Key therapeutic mechanisms of mesenchymal stem cell therapy. The diagram illustrates how multiple mechanisms converge to produce functional improvements in treated patients.
The evolving global disease burden, characterized by the rising prevalence of non-communicable diseases alongside persistent infectious challenges, continues to drive stem cell research toward areas of greatest unmet medical need. Current evidence suggests that MSC therapy demonstrates favorable safety profiles across multiple conditions, with significant functional improvements in specific applications such as acute/subacute ischemic stroke and certain autoimmune diseases.
Future research directions include optimizing cell delivery methods, standardizing protocols for cell preparation and dosage, developing engineered extracellular vesicles with enhanced cardiac targeting and prolonged circulation, and identifying patient selection criteria to maximize therapeutic benefits [5] [4]. Additionally, addressing the psychological aspects of stem cell therapy participation through monitoring and intervention for treatment-emergent emotional distress may improve trial compliance and retention [8].
As the field advances, strategic alignment of research priorities with global health needs, strengthened international collaborations, and open science policies will be essential to fully realize the potential of stem cell therapies in addressing the world's most pressing health challenges.
Mesenchymal stem cells (MSCs) have emerged as a highly promising strategy in regenerative medicine due to their self-renewal, pluripotency, and immunomodulatory properties [9]. These nonhematopoietic, multipotent stem cells can differentiate into various mesodermal lineages and significantly modulate the immune system [9]. The therapeutic potential of MSCs from different tissues has been widely explored in preclinical models and clinical trials for human diseases, ranging from autoimmune diseases and inflammatory disorders to neurodegenerative diseases and orthopedic injuries [9]. According to the International Society for Cellular Therapy (ISCT), MSCs are defined by three key criteria: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, and CD105 ≥95%) while lacking expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [9] [10].
The therapeutic effects of MSCs are primarily mediated through the release of bioactive molecules, including growth factors, cytokines, and extracellular vesicles, which play crucial roles in modulating the local cellular environment, promoting tissue repair, angiogenesis, and cell survival, and exerting anti-inflammatory effects [9]. MSCs can also interact with various immune cells, such as T cells, B cells, dendritic cells, and macrophages, modulating the immune response through both direct cell-cell interactions and the release of immunoregulatory molecules [9]. This comprehensive review delves into the molecular mechanisms, signaling pathways, and regulatory factors underpinning the therapeutic effects of MSCs, while objectively comparing their performance across different tissue sources within the context of clinical outcomes meta-analysis research.
MSCs can be isolated from a diverse range of adult and perinatal tissues, each with distinct biological characteristics, advantages, and limitations for clinical applications. The selection of MSC source significantly influences cell yield, proliferation capacity, differentiation potential, and ultimately, therapeutic efficacy [9] [11] [12].
Table 1: Comparative Analysis of Primary MSC Sources
| Source Tissue | Key Markers | Isolation Yield | Proliferation Rate | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Bone Marrow (BM-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- | Limited (0.01-0.001% of nucleated cells) [11] | Moderate | Gold standard, well-characterized, high differentiation potential [9] | Invasive harvesting, donor age-dependent quality [11] |
| Adipose Tissue (AD-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- | High (~1 billion cells from 300g tissue) [11] | Fast | Abundant tissue, less invasive harvesting, superior in bone regeneration/skin healing [11] | Donor metabolic health influences quality |
| Umbilical Cord (UC-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- | High concentration in Wharton's jelly [11] | Very High | Enhanced proliferation, low immunogenicity, suitable for allogeneic transplantation [9] [11] | Perinatal source only, ethical considerations |
| Umbilical Cord Blood (UCB-MSCs) | CD73+, CD90+, CD105+, CD45-, CD34- | Variable | High | Biological advantages, delayed senescence, enhanced anti-inflammatory function [11] | Limited volume, low frequency of MSCs |
| Placenta (PMSCs) | CD73+, CD90+, CD105+, CD45-, CD34- | High | Very High (superior to UC-MSCs) [11] | Pronounced immunosuppressive effects [11] | Complex composition, challenging isolation |
| Menstrual Blood (MenSCs) | CD29+, CD73+, CD90+, CD105+, CD45-, CD34- | Moderate | Very High (doubles every 20 hours) [11] | Easy non-invasive collection, high proliferation, minimal ethical concerns [11] | Limited to female donors, newer source requiring more research |
Table 2: Differentiation Potential and Clinical Applications by MSC Source
| Source Tissue | Osteogenic Potential | Chondrogenic Potential | Adipogenic Potential | Prominent Clinical Applications |
|---|---|---|---|---|
| Bone Marrow | High (original lineage) [9] | High (original lineage) [9] | High (original lineage) [9] | Graft-versus-host disease, orthopedic repairs, myocardial infarction [9] [10] |
| Adipose Tissue | Moderate | Moderate | High (native tissue) [12] | Bone regeneration, wound healing, plastic surgery [11] |
| Umbilical Cord | Moderate | High | Moderate | Allogeneic transplantation, inflammatory disorders, clinical trials for Crohn's disease [9] [13] |
| Placenta | Moderate to High | Moderate to High | Moderate to High | Immunological disorders, ongoing research for multiple indications [11] |
| Dental Pulp | Low to Moderate | Moderate | Low | Dental and craniofacial applications [9] |
The biological properties and therapeutic performance of MSCs vary significantly based on their tissue origin. Bone marrow-derived MSCs (BM-MSCs) represent the most extensively studied type and are considered the "gold standard" known for their high differentiation potential and strong immunomodulatory effects [9]. However, their clinical use is constrained by invasive harvesting procedures and declining cell quality with donor age [11]. Comparatively, adipose tissue-derived MSCs (AD-MSCs) offer practical advantages with easier harvesting through liposuction and significantly higher yields, while demonstrating comparable therapeutic properties to BM-MSCs [9] [11].
Perinatal tissues such as umbilical cord, cord blood, and placenta have emerged as valuable MSC sources with enhanced proliferation capacities and lower immunogenicity, making them particularly suitable for allogeneic transplantation [9] [11]. Umbilical cord-derived MSCs (UC-MSCs) specifically exhibit significantly higher proliferative and migratory capacities compared to BM-MSCs, characterized by high safety, low immunogenicity, and low application risk [11]. More novel sources like menstrual blood-derived MSCs (MenSCs) demonstrate exceptionally high proliferation rates—doubling every 20 hours, twice the rate of BM-MSCs—while offering minimal ethical concerns and non-invasive collection [11].
Biological Mechanisms of Action: Paracrine Signaling and Immunomodulation
The therapeutic efficacy of MSCs primarily operates through two fundamental biological mechanisms: paracrine signaling and immunomodulation. Rather than directly replacing damaged tissues through differentiation and engraftment, evidence indicates that MSCs predominantly function through the secretion of bioactive factors that modulate the host environment and promote endogenous repair processes [10].
Paracrine Signaling and Tissue Repair
MSCs generate a microenvironment that supports regeneration through the secretion of factors that induce other cells to regenerate tissue [10]. These paracrine effects are mediated through the release of numerous biologically active molecules, including cytokines, chemokines, growth factors, extracellular matrix, and extracellular vesicles (EVs) [10]. These molecules collectively exert broad therapeutic effects, including stimulating tissue regeneration and angiogenesis, modulating the innate and adaptive immune system, regulating apoptosis, and influencing fibrosis/scar formation [10].
The paracrine effects of MSCs have been largely attributed to extracellular vesicles, particularly exosomes, which demonstrate bioactivity capable of treating fibrosis, promoting tissue regeneration, and reducing inflammation [10] [14]. These double-layer phospholipid membrane vesicles mediate cell-to-cell communication through their cargo of proteins, lipids, carbohydrates, and nucleic acids (e.g., microRNA, mRNA), representing a potential cell-free therapeutic alternative [10] [14]. In cardiac repair, for instance, MSCs exert beneficial effects through paracrine mechanisms including anti-apoptotic actions on injured cardiomyocytes due to the transfer of healthy mitochondria via tunneling nanotubes and the secretion of exosomes carrying regenerative signals [3].
Diagram 1: MSC Therapeutic Mechanisms. This diagram illustrates the two primary therapeutic mechanisms of MSCs: paracrine signaling through extracellular vesicles, growth factors, cytokines, and other bioactive molecules; and immunomodulation through regulation of various immune cells including T-cells, macrophages, dendritic cells, and B-cells. These mechanisms collectively contribute to tissue repair, angiogenesis, and creation of an anti-inflammatory environment.
Immunomodulatory Properties
MSCs possess remarkable immunomodulatory capabilities that enable them to interact with and regulate virtually all immune cells [9]. Through both direct cell-cell contact and secretion of immunoregulatory molecules, MSCs can suppress activation and maturation of innate immune cells while skewing early innate reactions toward an anti-inflammatory phenotype [10]. This immunomodulatory function has become a key factor in developing MSC-based treatments for conditions including rheumatoid arthritis, Crohn's disease, and graft-versus-host disease (GVHD) [9].
The immunomodulatory effects of MSCs are not constitutive but are rather activated by inflammatory cytokines such as interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α) in a process called "licensing" [10]. Once activated, MSCs secrete various factors that modulate immune responses, including prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO), transforming growth factor-beta (TGF-β), and interleukin-10 (IL-10) [10]. These molecules collectively suppress T-cell proliferation and activation, inhibit dendritic cell maturation, promote the generation of regulatory T-cells (Tregs), and shift macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes [9] [10].
Experimental Protocols for MSC Characterization
Standardized experimental protocols are essential for characterizing MSCs and ensuring reproducible research outcomes and therapeutic applications. The International Society for Cellular Therapy (ISCT) has established minimal criteria for defining MSCs, which form the basis for most characterization protocols [9] [10].
Surface Marker Characterization by Flow Cytometry
Flow cytometry represents the gold standard technique for confirming MSC surface marker expression patterns according to ISCT criteria [9].
Protocol Details:
- Cell Preparation: Harvest MSCs at 70-80% confluence (passage 3-5), wash with PBS, and dissociate using non-enzymatic cell dissociation solution or low-concentration trypsin-EDTA to preserve surface markers [12].
- Antibody Staining: Resuspend 1×10⁶ cells in flow cytometry buffer (PBS with 1% FBS). Incubate with fluorochrome-conjugated antibodies against CD73, CD90, CD105 (positive markers) and CD34, CD45, CD14/CD11b, CD79α/CD19, HLA-DR (negative markers) for 30 minutes at 4°C in the dark [9] [11].
- Analysis: Analyze stained cells using a flow cytometer. A population is considered positive for a specific marker if ≥95% express positive markers and ≤2% express negative markers [9] [10].
- Quality Control: Include appropriate isotype controls for each antibody to account for non-specific binding and establish gating parameters [12].
Trilineage Differentiation Assays
The functional capacity of MSCs to differentiate into osteogenic, chondrogenic, and adipogenic lineages represents a critical component of their characterization [9].
Table 3: Trilineage Differentiation Protocol Specifications
| Differentiation Lineage | Induction Media Components | Differentiation Period | Staining Methods | Key Molecular Markers |
|---|---|---|---|---|
| Osteogenic | Dexamethasone, β-glycerophosphate, ascorbic acid-2-phosphate [9] | 21-28 days | Alizarin Red S (mineralized matrix) [9] | Osteocalcin, Runx2, Alkaline Phosphatase |
| Chondrogenic | TGF-β3, dexamethasone, ascorbic acid-2-phosphate, insulin-transferrin-selenium, proline [9] | 21-28 days | Alcian Blue (sulfated proteoglycans) [9] | Collagen type II, Aggrecan, SOX9 |
| Adipogenic | Dexamethasone, isobutylmethylxanthine, indomethacin, insulin [9] [12] | 14-21 days | Oil Red O (lipid droplets) [9] | PPAR-γ, FABP4, Leptin |
Protocol Details:
- Base Media: Use high-glucose Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) for all differentiation assays [12].
- Cell Seeding Density: Optimal densities vary by lineage: 2.1×10⁴ cells/cm² for osteogenic differentiation, 1.6×10⁷ cells/mL in micromass culture for chondrogenic differentiation, and 2.1×10⁴ cells/cm² for adipogenic differentiation [12].
- Media Refreshment: Change differentiation media every 3-4 days throughout the differentiation period [12].
- Quality Control: Include undifferentiated MSCs maintained in growth media (DMEM with 10% FBS without induction factors) as negative controls for all staining procedures [9].
Diagram 2: MSC Characterization Workflow. This diagram outlines the standardized experimental workflow for characterizing mesenchymal stem cells, beginning with isolation and expansion, followed by surface marker characterization through flow cytometry and plastic adherence assessment, evaluation of trilineage differentiation potential, and concluding with functional assays including immunomodulatory, secretome, and migration analyses.
Research Reagent Solutions for MSC Studies
The selection of appropriate research reagents is critical for ensuring reproducible and reliable MSC research outcomes. The following table details essential materials and their specific functions in MSC experimental workflows.
Table 4: Essential Research Reagents for MSC Studies
| Reagent Category | Specific Products | Experimental Function | Application Notes |
|---|---|---|---|
| Cell Culture Media | Dulbecco's Modified Eagle Medium (DMEM), Alpha-MEM, Fetal Bovine Serum (FBS) [12] | Supports MSC expansion and maintenance | Serum lot consistency critical; consider platelet lysate alternatives [12] |
| Dissociation Reagents | Trypsin-EDTA, Collagenase, Non-enzymatic cell dissociation solutions [12] | Cell harvesting and passaging | Enzyme concentration and exposure time affect surface marker preservation [12] |
| Characterization Antibodies | Anti-CD73, CD90, CD105, CD34, CD45, HLA-DR [9] [11] | Flow cytometry surface marker analysis | Fluorochrome conjugates should be titrated for optimal signal-to-noise [12] |
| Differentiation Kits | Osteo-, Chondro-, Adipogenic Induction Media [9] [12] | Trilineage differentiation assessment | Media components must be freshly supplemented; include undifferentiated controls [9] |
| Analysis Reagents | Alizarin Red S, Alcian Blue, Oil Red O [9] | Detection of differentiation outcomes | Quantification possible via dye extraction and spectrophotometry [9] |
| Cryopreservation Media | DMSO, FBS, Culture Media [12] | Long-term cell storage | Controlled-rate freezing preserves cell viability and functionality [12] |
Clinical Translation and Outcomes Analysis
The clinical translation of MSC therapies has demonstrated both promising outcomes and significant challenges. While MSC safety has been consistently established across numerous clinical trials, efficacy results have been variable, leading to only a limited number of regulatory approvals despite extensive clinical testing [10].
Regulatory Approval Landscape
To date, sixteen MSC-based therapies have received marketing authorization worldwide, with ten derived from bone marrow, three from umbilical cord, two from adipose tissue, and one from umbilical cord blood [11]. These approved products target conditions including acute graft-versus-host disease, acute myocardial infarction, complex anal fistulas in Crohn's disease, osteoarthritis, and amyotrophic lateral sclerosis [11]. Notably, 2024 marked the first FDA approval of an MSC therapy in the United States with Ryoncil (remestemcel-L) for pediatric steroid-refractory acute graft-versus-host disease [13].
Clinical Efficacy Across Indications
The therapeutic efficacy of MSCs varies considerably across different clinical indications and patient populations. In cardiac applications, a recent systematic review and meta-analysis of clinical trials investigating MSC therapy for heart failure with reduced ejection fraction (HFrEF) demonstrated only small, non-significant improvements in left ventricular ejection fraction (LVEF), though significant quality of life improvements were observed [3]. This analysis encompassed 12 clinical trials and found no increased risk of major adverse cardiac events, supporting the safety profile of MSC therapy despite limited efficacy in functional cardiac parameters [3].
In neurological applications, MSC trials for conditions such as multiple sclerosis, stroke, and spinal cord injury have shown more promising results, with studies reporting improvements in functional outcomes and disease stabilization [10]. Similarly, in orthopedic applications, MSC therapies for osteoarthritis and cartilage defects have demonstrated pain reduction and functional improvement, though structural repair outcomes remain variable [10].
The clinical performance of MSCs is influenced by multiple factors including cell source, donor characteristics, passage number, culture conditions, delivery route, and timing of administration [10] [12]. These variables contribute to the heterogeneity in therapeutic outcomes observed across clinical trials and represent significant challenges in standardizing MSC-based therapies for routine clinical use [10].
Mesenchymal stem cells represent a promising therapeutic modality with diverse applications in regenerative medicine and immunology. The comparative analysis of MSC sources reveals that each tissue origin offers distinct advantages and limitations, with bone marrow MSCs representing the best-characterized population, adipose tissue providing practical advantages in harvesting and yield, and perinatal sources offering superior proliferation capacity and lower immunogenicity for allogeneic applications.
The biological properties of MSCs—including their paracrine activity, immunomodulatory capacity, and differentiation potential—underpin their therapeutic mechanisms across a spectrum of diseases. However, challenges remain in standardization, manufacturing, and clinical protocol optimization. Future directions in MSC therapeutics include the development of improved potency assays, standardization of manufacturing protocols, optimization of delivery strategies, and exploration of novel approaches such as iPSC-derived MSCs and preconditioning strategies to enhance therapeutic efficacy.
As the field advances, the comprehensive understanding of MSC sources and biological properties will continue to inform clinical applications and research directions, ultimately enhancing the therapeutic potential of these remarkable cells in treating human diseases.
Heart failure with reduced ejection fraction (HFrEF) remains a major global health burden, characterized by significant morbidity, mortality, and impaired quality of life [3]. While guideline-directed medical therapy (GDMT) has improved outcomes, a residual risk persists, driving investigation into regenerative approaches including stem cell therapy [3]. This comparison guide objectively evaluates the performance of mesenchymal stem cell (MSC) therapy against conventional care in HFrEF patients, focusing on two critical endpoints: left ventricular ejection fraction (LVEF) changes and quality of life (QoL) outcomes. The analysis is framed within a broader thesis on stem cell clinical outcomes meta-analysis reviews, providing researchers and drug development professionals with synthesized experimental data and methodological insights.
Tabular Comparison of Clinical Outcomes
Table 1: Efficacy Outcomes of MSC Therapy in HFrEF from Meta-Analysis
| Outcome Measure | Intervention Group (MSC) | Control Group | Effect Size (Hedges' g) | P-value | Statistical Significance |
|---|---|---|---|---|---|
| LVEF Change | Not Significantly Improved | - | 0.096 | 0.18 | No |
| Quality of Life (QoL) | Significantly Improved | - | -0.518 | 0.01 | Yes |
| Global Circumferential Strain | Not Significantly Improved | - | - | - | No |
| 6-Minute Walk Test | Not Significantly Improved | - | - | - | No |
| Major Adverse Cardiac Events | No Increased Risk | - | - | - | No (Safe) |
Source: Systematic review and meta-analysis of clinical trials (2018–2025) [3].
Table 2: Quality of Life Assessment Tools in Heart Failure Research
| Instrument Name | Type | Domains Measured | Score Range | Mode of Administration |
|---|---|---|---|---|
| Kansas City Cardiomyopathy Questionnaire (KCCQ) | Disease-specific | Physical limitation, Symptoms, QoL, Social limitation | 0–100 (worst to best) | Self-administered |
| Minnesota Living with Heart Failure Questionnaire (MLHFQ) | Disease-specific | Physical, Emotional | 0–105 (best to worst) | Self-administered |
| EuroQol five-dimensional questionnaire (EQ-5D) | Non-disease-specific | Mobility, Self-care, Usual activities, Pain/Discomfort | -0.594–1.000 (worst to best) | Self-administered |
| The MOS 36-Item Short-Form Health Survey (SF-36) | Non-disease-specific | Physical & Social activities, Mental health, Vitality | 0–100 (worst to best) | Self-administered |
Source: Scientific Statement on Quality of Life in Heart Failure [15].
Experimental Protocols and Methodologies
Cell Therapy Administration Protocols
Clinical trials investigating MSC therapy for HFrEF employ standardized yet distinct protocols for cell preparation and delivery. The primary cell type used is mesenchymal stem cells, which are multipotent adult stem cells characterized by plastic adherence, specific surface markers (CD73+, CD90+, CD105+), and capacity for in vitro differentiation into adipocytes, chondrocytes, and osteoblasts [3] [6]. These cells are typically sourced from bone marrow (BM-MSCs) or umbilical cord tissue (Wharton's Jelly).
The delivery methods commonly utilized in featured experiments include:
- Intracoronary Infusion: Delivery via catheter into the coronary arteries.
- Transendocardial Injection: Direct injection into the myocardial tissue using a specialized catheter system.
- Intravenous Infusion: Systemic delivery through a peripheral vein.
- Intramyocardial Injection: Direct injection into the heart muscle during open-heart surgery (less common in recent trials).
Dosages in cited trials typically range from 20 to 200 million cells, with preparation following Good Manufacturing Practice (GMP) standards. Most trials utilize allogeneic MSCs from healthy donors rather than autologous cells from HFrEF patients, as the latter may have impaired cell function due to disease and aging [3].
Endpoint Assessment Methodologies
The assessment of LVEF and QoL outcomes follows rigorous standardized protocols in clinical trials:
LVEF Measurement Protocol: LVEF is primarily quantified using transthoracic echocardiography performed according to the American Society of Echocardiography guidelines. Measurements are taken at baseline (pre-treatment) and at predetermined follow-up intervals (e.g., 3, 6, and 12 months). The biplane method of disks (modified Simpson's rule) is the preferred technique for LVEF calculation. Core laboratories blinded to treatment assignment typically analyze images to minimize bias [3] [16].
Quality of Life Assessment Protocol: QoL is measured using validated patient-reported outcome (PRO) instruments, primarily the Kansas City Cardiomyopathy Questionnaire (KCCQ) and Minnesota Living with Heart Failure Questionnaire (MLHFQ). These are administered at baseline and follow-up visits. The KCCQ-23 covers seven domains over a 2-week recall period: symptom frequency, symptom burden, physical limitations, social limitations, QoL, self-efficacy, and symptom stability. A 5-point change in the overall KCCQ score is considered clinically significant [15].
Visualized Pathways and Workflows
MSC Therapeutic Mechanisms in HFrEF
Clinical Trial Workflow for HFrEF Cell Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Cardiac Stem Cell Research
| Research Tool | Specific Function | Application Context |
|---|---|---|
| Mesenchymal Stem Cells | Multipotent progenitor cells with immunomodulatory properties | Primary therapeutic agent; sourced from bone marrow or umbilical cord |
| Late Gadolinium Enhancement CMR | Quantification of myocardial fibrosis and scar tissue | Pre-treatment assessment of myocardial viability [17] |
| Flow Cytometry Antibodies | Characterization of MSC surface markers (CD73, CD90, CD105) | Quality control of cell products pre-transplantation [3] [6] |
| Echocardiography System | Non-invasive assessment of cardiac structure and function | Primary method for LVEF measurement pre- and post-treatment [16] |
| Validated QoL Questionnaires | Standardized assessment of patient-reported outcomes | KCCQ and MLHFQ for quantifying symptomatic improvement [15] |
| Surgical Adhesive | Biocompatible tissue adhesive for patch fixation | Securing engineered heart patches in minimally invasive procedures [18] |
| Cell Culture Media | Expansion and maintenance of MSCs in vitro | Pre-transplantation cell culture and preparation [3] |
This comparison guide demonstrates the differential effects of MSC therapy in HFrEF, highlighting a clear dissociation between structural and functional cardiac parameters versus patient-reported outcomes. While MSC therapy does not significantly improve LVEF, it provides clinically relevant benefits in quality of life without increasing major adverse cardiac events. For researchers and drug development professionals, these findings suggest that regenerative therapies may target aspects of heart failure beyond simple contractile improvement, possibly through paracrine-mediated symptomatic relief. Future work should focus on standardizing cell products, delivery methods, and identifying patient subgroups most likely to benefit from this therapeutic approach.
Stroke remains a leading cause of long-term adult disability worldwide, with only a small proportion (approximately 14%) of stroke survivors achieving full recovery of activities of daily living (ADLs), while 25%-50% require some assistance, and approximately half experience long-term dependency [19]. The prediction and measurement of functional outcomes after ischemic stroke is therefore critically important for setting realistic treatment goals, informing patients and their relatives, facilitating discharge planning, and assessing the effectiveness of new therapeutic interventions [19]. Within the specific context of emerging stem cell therapies for stroke, the critical challenge lies in accurately quantifying therapeutic efficacy through validated, standardized outcome measures.
The National Institutes of Health Stroke Scale (NIHSS), modified Rankin Scale (mRS), and Barthel Index (BI) have emerged as the three predominant instruments for evaluating neurological deficit, functional disability, and independence in daily activities, respectively [19] [20] [21]. Their combined application provides a multidimensional assessment framework that is particularly vital for evaluating complex, restorative therapies like stem cell transplantation, where the mechanisms of recovery extend beyond acute salvage to encompass neural repair and plasticity [22] [23] [5]. This guide provides a comparative analysis of these scales and details their application in the field of stem cell research for ischemic stroke.
Comparative Analysis of Stroke Outcome Measures
The following table provides a systematic comparison of the three key outcome measures, detailing their primary focus, structure, and interpretation.
Table 1: Comparative Overview of Primary Stroke Outcome Measures
| Feature | NIHSS | mRS | Barthel Index (BI) |
|---|---|---|---|
| Primary Domain Assessed | Neurological impairment | Global disability/Functional independence | Activities of Daily Living (ADLs) |
| Scale Type & Range | Ordinal; 0-42 points [21] | Ordinal; 0-6 grades [19] | Ordinal; 0-100 points [19] |
| Administration | Clinical examination by trained healthcare professional [21] | Structured interview or clinical assessment | Structured interview or patient report |
| Key Strengths | - Objective, quantitative [21]- Strong predictor of outcome [21]- Widely used in acute trials | - Captures global disability [24]- Intuitive and widely grasped [25]- Standard for stroke trials [25] | - Focuses on functional independence [20]- Sensitive to change [20] |
| Key Limitations | - Language barrier reduces validity [21]- Poor reliability for some items (e.g., ataxia) [21] | - Requires training for reliability [25] | - Less sensitive to specific motor changes |
| Interpretation of Scores | ≤5: Mild stroke [21]5-14: Moderate stroke [21]≥15: Severe stroke [21] | 0-2: Functional independence [25]3-5: Varying degrees of disability6: Death | ≥95: Functional independence [20]60-90: Moderate disability<60: Severe disability |
Experimental Protocols for Outcome Assessment
Protocol for NIHSS Assessment
The NIHSS is a systematic, quantitative assessment tool designed to be administered in less than 10 minutes by trained physicians, nurses, or therapists [21]. The protocol involves a 15-item neurological examination where a trained observer rates the person's ability to answer questions and perform activities without coaching. Ratings for each item are scored on a 3- to 5-point scale, with 0 as normal, and there is an allowance for untestable items [21]. The examination evaluates:
- Levels of consciousness
- Visual-field loss
- Extra-ocular movement
- Motor strength (arm and leg)
- Limb ataxia
- Sensory loss
- Language
- Dysarthria
- Neglect [21]
Certification through formal training is recommended to ensure reliability, as overall scoring can be inconsistent without proper training [21].
Protocol for mRS Assessment
The mRS is a global disability scale typically assessed through a structured interview or questionnaire. The assessment focuses on the patient's level of independence in daily activities rather than specific neurological symptoms. The protocol involves:
- Structured Interview: Asking standardized questions about the patient's function in daily life.
- Clinical Assessment: Evaluating the patient's need for assistance with personal care, activities, and physical tasks.
- Grading: Assigning a single integer from 0 to 6 based on predefined criteria, where 0 indicates no symptoms and 6 indicates death [19] [24] [25].
A single point change on the mRS is considered clinically important, and it is the top recommended scale for assessing global disability and clinically meaningful change in function in stroke recovery trials [25].
Protocol for Barthel Index Assessment
The BI assessment is performed through a structured interview or direct observation to evaluate ten core activities of daily living. The protocol involves:
- Item-Specific Scoring: Each of the 10 items is scored based on the patient's level of independence, with weighting for different activities.
- Performance-Based Assessment: Evaluating actual performance rather than capacity.
- Direct Observation or Patient Report: Can be conducted in person or via telephone by trained staff [20].
The final score is the sum of all item scores, with higher scores indicating greater independence. The BI has demonstrated reliability in telephone assessments, making it suitable for long-term follow-up in clinical trials [20].
Workflow for Functional Outcome Measurement in Clinical Trials
The following diagram illustrates the standard workflow for applying these outcome measures in a stem cell therapy clinical trial for ischemic stroke.
Application in Stem Cell Therapy: Efficacy Data and Meta-Analysis Findings
Recent meta-analyses of randomized controlled trials (RCTs) have specifically employed these scales to quantify the effect of stem cell therapy for acute and subacute ischemic stroke. The consolidated findings demonstrate the utility of these measures in capturing treatment benefits.
Table 2: Stem Cell Therapy Efficacy Based on mRS, NIHSS, and BI Outcomes (Meta-Analysis Data)
| Outcome Measure | Timepoint | Risk Ratio (RR) or Mean Difference | 95% Confidence Interval | P-value | Significance |
|---|---|---|---|---|---|
| mRS 0-1 [5] | 90 days | RR = 1.15 | 0.72 - 1.84 | 0.55 | Not Significant |
| mRS 0-1 [5] | 1 year | RR = 1.74 | 1.09 - 2.77 | 0.020 | Significant |
| mRS 0-2 [5] | 90 days | RR = 1.31 | 1.01 - 1.70 | 0.044 | Significant |
| NIHSS Score [5] | 180 days | Mean Difference = -0.80 | -1.54 - -0.05 | < 0.05 | Significant |
| Barthel Index [5] | 1 year | Mean Difference = 5.67 | -1.17 - 12.51 | 0.10 | Not Significant |
A 2025 meta-analysis of 13 RCTs involving 872 patients found that stem cell therapy for acute/subacute ischemic stroke within one month of onset significantly improved the likelihood of achieving excellent functional outcomes (mRS 0-1) at one year and good functional outcomes (mRS 0-2) at 90 days, without increasing serious adverse events or mortality [5]. This underscores the importance of long-term follow-up, as the full benefits of regenerative therapies may not be captured at the traditional 90-day endpoint.
Decision Framework for Outcome Measure Selection
The choice of outcome measures in a clinical trial depends on the primary research question, phase of the trial, and specific domain of recovery being targeted. The following logic diagram aids in selecting the most appropriate scale.
Table 3: Key Research Reagent Solutions for Stroke Recovery Trials
| Tool / Reagent | Primary Function | Application Context |
|---|---|---|
| Certified NIHSS Training | Ensures reliable, consistent scoring of neurological deficits by multiple raters. | Mandatory for all clinical site personnel involved in acute assessment to maintain data integrity [21]. |
| Structured mRS Interview | Standardizes the process of assigning the global disability score to minimize rater variability. | Critical for primary outcome assessment at 90 days and 1 year; improves reliability [24] [25]. |
| Standardized BI Protocol | Provides a consistent framework for evaluating activities of daily living across sites. | Used for assessing functional independence, often as a secondary outcome measure [20] [5]. |
| Diffusion Tensor Imaging (DTI) | Assesses white matter integrity, specifically damage to the corticospinal tract. | Serves as a prognostic biomarker; damage predicts motor recovery limits and can stratify patients [19] [26]. |
| CT Angiography (CTA) | Visualizes large vessel occlusion and collateral circulation. | Provides predictive information on outcome independent of clinical scores like NIHSS [19]. |
| Electroencephalography (EEG) | Measures brain electrical activity and interhemispheric imbalance post-stroke. | Used as a neurophysiological biomarker to predict individual recovery potential [26]. |
The rigorous assessment of functional recovery using the NIHSS, mRS, and BI provides the critical evidence base needed to evaluate the therapeutic potential of stem cell therapies for ischemic stroke. While the NIHSS excels in quantifying initial neurological deficit and the BI details independence in daily activities, the mRS has proven to be a robust global disability measure and primary endpoint for pivotal trials. Meta-analyses of RCTs demonstrate that the concerted application of these scales can successfully detect significant, clinically meaningful improvements in functional outcomes associated with stem cell therapy, particularly at later time points such as one year. The continued standardization of these assessment protocols, combined with the integration of novel neuroimaging and molecular biomarkers, will further enhance the precision and predictive power of future clinical trials in this promising field.
Liver failure, particularly Acute-on-Chronic Liver Failure (ACLF), represents a significant global health burden characterized by rapid clinical deterioration, organ failure, and high short-term mortality rates exceeding 15% at 28 days [27]. The Model for End-Stage Liver Disease (MELD) score, ranging from 6 to 40, has been the cornerstone for assessing disease severity and prioritizing liver transplantation, the only definitive treatment for advanced cases [28]. However, the persistent shortage of donor organs and the limited eligibility of many patients for transplantation have created an urgent need for effective alternative therapies [27] [29]. Among emerging treatments, stem cell therapy, particularly using Mesenchymal Stem Cells (MSCs), has shown promising potential for improving survival and liver function, thereby bridging the critical gap in liver failure management [30] [27]. This review comprehensively analyzes the efficacy of MSC therapy against standard care and other alternatives, focusing on survival benefits and MELD score improvements through meta-analyses of randomized controlled trials.
Stem Cell Therapy: Mechanisms and Protocols
Therapeutic Mechanisms of Mesenchymal Stem Cells
MSCs exert their therapeutic effects through multiple interconnected mechanisms that target both liver regeneration and systemic inflammation. These cells possess a strong potential for regulating the body's immune response and reducing the intense systemic inflammation characteristic of ACLF [29]. The pathogenesis of ACLF involves extensive hepatic necrosis triggered by intense systemic inflammation, which causes an inflammatory cytokine storm, resulting in portal hypertension, organ dysfunction, and organ failure [27]. MSCs function as seed cells to remodel and repair damaged liver tissues through paracrine signaling and direct cell-to-cell interactions [27]. They ameliorate hepatic dysfunction and improve liver regeneration after hepatectomy acute liver failure by paracrine mechanisms, making them promising therapeutic alternatives for patients with chronic liver disease who are ineligible for transplantation [27].
Experimental Protocols and Methodologies
The standard protocols for MSC therapy in liver failure have been refined through numerous randomized controlled trials. The following workflow illustrates the typical experimental and treatment process:
Figure 1: Experimental Workflow for MSC Therapy in ACLF
Population and Inclusion Criteria: Clinical trials typically enroll patients diagnosed with ACLF, with most studies focusing on HBV-related liver failure [31] [27]. Participants are adults with confirmed chronic liver disease experiencing acute deterioration, organ failure, and high short-term mortality risk [27].
Intervention Protocols: The intervention groups receive MSC therapy alongside standard medical treatment (SMT). The most common cell sources are allogeneic MSCs derived from umbilical cord tissue (UC-MSCs) or bone marrow (BM-MSCs) [31] [27]. Administration routes include intravenous infusion or hepatic artery injection, with total doses ranging from 1×10⁶ to 1×10⁸ cells per kilogram of body weight [27]. Multiple injections may be administered based on clinical response.
Control Groups: Control participants receive standard medical treatment (SMT) alone, which typically includes nutritional support, management of complications, and treatment of precipitating factors [30] [27]. In some studies, control groups may receive SMT combined with plasma exchange (PE) [31].
Outcome Measures and Timing: Primary outcomes include changes in MELD scores, survival rates, and albumin levels. Secondary outcomes encompass improvements in international normalized ratio (INR), total bilirubin (TBIL), alanine aminotransferase (ALT) levels, and monitoring of adverse events [30] [27]. Assessments are typically conducted at 2, 4, and 24 weeks post-therapy to evaluate short-term and medium-term efficacy [27].
Comparative Efficacy Analysis: Stem Cell Therapy vs. Alternatives
MELD Score Improvements Across Interventions
The MELD score serves as a crucial objective indicator for quantifying liver disease severity and predicting mortality risk. The following table summarizes MELD score improvements across different therapeutic interventions for liver failure:
Table 1: MELD Score Improvements Across Liver Failure Interventions
| Intervention | Patient Population | MELD Score Change | Timeframe | Study Details |
|---|---|---|---|---|
| MSC Therapy | ACLF patients | Significant decrease [30] [27] | 4-24 weeks | 7 RCTs, n=363; combined with SMT [30] [27] |
| Stem Cell Therapy + Plasma Exchange | Liver failure patients | Enhanced reduction [31] | Not specified | Superior to SMT alone; allogeneic cells most effective [31] |
| Liver Transplantation | ESLD patients | N/A (MELD replaced) | Post-transplant | 79% lower mortality risk vs. candidates (MELD 18-40) [32] |
| Steroid Therapy | Severe Alcoholic Hepatitis | Limited efficacy with high MELD [33] | 7 days (Lille score) | Effective only with MELD <39; efficacy decreases as MELD rises [33] |
| Standard Medical Treatment | ACLF patients | Minimal improvement | 4-24 weeks | Control group in MSC trials [30] [27] |
Survival Outcomes and Secondary Efficacy Endpoints
Survival benefit remains the ultimate endpoint for evaluating liver failure interventions. The table below compares survival outcomes and secondary efficacy measures across different treatment modalities:
Table 2: Survival Outcomes and Secondary Efficacy Measures in Liver Failure
| Intervention | Survival Benefit | Secondary Efficacy Measures | Key Limitations |
|---|---|---|---|
| MSC Therapy | Improved survival with decreased MELD [30] | ↑ Albumin, ↓ INR, ↓ ALT; No significant adverse events [30] [27] | Standard protocols not yet established [27] |
| Liver Transplantation | 79% lower mortality risk vs. waitlist [32] | Gold standard for ESLD | Donor shortage, eligibility restrictions, surgical risks [27] |
| Steroid Therapy | 75% response rate in SAH (Lille score <0.45) [33] | Bridge to transplantation | 25% non-response; contraindicated with infection [33] |
| G-CSF Therapy | Improved 90-day survival in SAH [33] | Rescue therapy for steroid non-responders | Limited data; not for patients with active sepsis [33] |
| Standard Medical Treatment | Baseline survival | Nutritional support, complication management | Limited efficacy in severe cases [30] [27] |
Advanced MELD Scoring Systems in Prognostication
Recent advancements in MELD scoring have improved mortality prediction and transplant prioritization. MELD 3.0, implemented in the United States in 2023, incorporates sex and albumin alongside traditional parameters (bilirubin, INR, creatinine, sodium), addressing historical disadvantages for female patients [34] [35]. Germany recently transitioned to reMELD-Na in 2025, featuring refined coefficients and clinically meaningful bounds for creatinine, bilirubin, INR, and sodium to reduce disproportionate influence of renal dysfunction [34]. Validation studies demonstrate superior predictive performance for both systems compared to original MELD, with MELD 3.0 without albumin showing the best overall performance for predicting survival in males (c-index 0.827), while reMELD-Na performed best in females (c-index 0.705) [34].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for MSC Therapy in Liver Failure
| Reagent/Material | Specification | Research Application |
|---|---|---|
| Mesenchymal Stem Cells | Allogeneic UC-MSCs or BM-MSCs [27] | Primary therapeutic agent; tissue regeneration and immunomodulation |
| Cell Culture Media | Serum-free, xeno-free formulations | MSC expansion and maintenance under GMP conditions |
| Flow Cytometry Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR [27] | MSC characterization and purity verification |
| MELD Score Components | Bilirubin, INR, Creatinine assays [28] | Primary efficacy endpoint measurement |
| Liver Function Assays | Albumin, ALT, AST, TBIL kits [30] [27] | Secondary efficacy endpoint assessment |
| Cytokine Panels | IL-6, TNF-α, TGF-β, PGE2 [27] | Mechanistic studies of immunomodulatory effects |
The meta-analyses of randomized controlled trials demonstrate that MSC therapy significantly improves MELD scores and survival outcomes in patients with liver failure, particularly ACLF, without increasing adverse events [30] [27]. When combined with standard medical treatment or plasma exchange, MSC therapy enhances patient survival and reduces MELD scores more effectively than conventional approaches alone [31]. The superior efficacy of allogeneic stem cells and optimal administration routes such as deep vessel injection further refine the therapeutic potential of this emerging modality [31].
While liver transplantation remains the definitive treatment for end-stage liver disease, with recipients experiencing up to 79% lower mortality risk compared to waitlist candidates [32], MSC therapy represents a promising bridge or alternative for transplant-ineligible patients. The ongoing evolution of MELD scoring systems to MELD 3.0 and reMELD-Na further enhances prognostic accuracy and equitable organ allocation [34] [35].
Future research should focus on standardizing treatment protocols, identifying optimal cell sources and administration routes, and conducting large-cohort randomized controlled trials with longer follow-up periods [30] [27]. As the field of regenerative medicine advances, MSC therapy holds significant potential to address the critical unmet need in liver failure treatment, potentially reducing dependency on organ transplantation and improving survival for patients with limited therapeutic options.
The foundational premise of stem cell therapy has undergone a significant evolution. Originally, the therapeutic potential was attributed primarily to the ability of stem cells to differentiate into target cell types, thereby replacing damaged tissues [36] [37]. However, a paradigm shift has emerged, suggesting that the beneficial effects are not restricted to cell replacement alone but are largely mediated through paracrine actions and immunomodulation [36] [37]. It is now clear that stem cells function as sophisticated "living drugs," secreting a potent combination of trophic factors that modulate the molecular composition of their environment [38]. These secreted biomolecules evoke responses from resident cells, leading to cytoprotection, angiogenesis, and modulation of immune responses, which collectively facilitate tissue regeneration [36] [39]. This guide objectively compares the performance of these primary mechanisms—paracrine effects, immunomodulation, and direct tissue regeneration—by synthesizing experimental data and detailing the methodologies used to investigate them.
Comparative Analysis of Key Mechanisms
The following table summarizes the core mechanisms, their primary functions, and key experimental findings that demonstrate their efficacy.
Table 1: Comparative Analysis of Stem Cell Mechanisms of Action
| Mechanism | Primary Functions | Key Experimental Findings | Cell Types Studied |
|---|---|---|---|
| Paracrine Signaling | Secretion of cytokines, growth factors, and extracellular vesicles to promote cell survival, angiogenesis, and reduce inflammation [36] [37]. | Conditioned medium from MSCs reduced infarct size and improved cardiac function in rodent MI models, recapitulating benefits of whole cells [37]. | Mesenchymal Stem Cells (MSCs), Cardiac Progenitor Cells (CPCs) [37] [39]. |
| Immunomodulation | Suppression of pro-inflammatory responses; promotion of anti-inflammatory phenotypes in immune cells like T lymphocytes and macrophages [36] [40]. | MSCs switched macrophage phenotype from pro-inflammatory M1 to anti-inflammatory M2, associated with improved musculoskeletal repair [40]. Co-culture with MSCs inhibited CD4+ T lymphocyte proliferation [41]. | MSCs, Periodontal Ligament-derived MSCs (hPDL-MSCs) [40] [41]. |
| Tissue Regeneration & Differentiation | Direct differentiation into functional tissue-specific cells to replace damaged ones [38]. | Hematopoietic Stem Cell Transplantation (HSCT) successfully reconstitutes the immune and hematopoietic systems in patients [38]. | Hematopoietic Stem Cells (HSCs), Embryonic Stem Cells (ESCs) [38]. |
Detailed Experimental Protocols for Key Mechanisms
Investigating Paracrine Mechanisms
Objective: To isolate and characterize the therapeutic effects of factors secreted by stem cells, independent of cell engraftment and differentiation.
- Cell Conditioning: Mesenchymal Stem Cells (MSCs) are cultured under standard conditions or preconditioned with stimuli such as hypoxia to enhance secretion of trophic factors [36] [37].
- Collection of Conditioned Medium (CM): The culture medium is replaced with a serum-free option. After 24-72 hours, the CM is collected and centrifuged to remove cells and debris. This CM contains the secreted paracrine factors [37] [39].
- In Vitro Bioactivity Assays:
- Cytoprotection: Cardiomyocytes are subjected to hypoxia-reoxygenation injury. Groups are treated with either MSC-CM or control medium. Apoptosis is quantified by measuring caspase-3 activity and TUNEL staining [37].
- Angiogenesis: Human umbilical vein endothelial cells (HUVECs) are cultured with CM and assessed for tube formation on Matrigel, a measure of angiogenic potential [36].
- In Vivo Validation: In a rodent model of myocardial infarction, the left anterior descending coronary artery is ligated. Animals receive intramyocardial injections of either MSC-CM, control medium, or whole MSCs. Functional outcomes are assessed via echocardiography (e.g., Left Ventricular Ejection Fraction, LVEF), and infarct size is measured histologically [37].
Evaluating Immunomodulatory Effects
Objective: To determine the ability of stem cells to modulate the activity of immune cells through paracrine and cell-contact-dependent pathways.
- Co-culture Models: Three primary in vitro setups are used to dissect the mechanism [41]:
- Indirect with Insert: MSCs and immune cells (e.g., CD4+ T cells) are cultured in the same well but separated by a semi-permeable membrane (e.g., 0.4 µm pores), allowing exchange of soluble factors but preventing cell-to-cell contact. This isolates the paracrine mechanism [41].
- Direct with Insert: MSCs are attached to the bottom side of a porous membrane, and immune cells are added to the opposite side, allowing for limited contact.
- Direct without Insert: Immune cells are added directly to plastic-adherent MSCs, enabling full cell-to-cell contact in addition to paracrine signaling [41].
- Immune Cell Activation: CD4+ T lymphocytes are activated using mitogens or anti-CD3/CD28 antibodies [41].
- Outcome Measures:
- Proliferation: T-cell proliferation is quantified using methods like CFSE dilution followed by flow cytometry [41].
- Phenotype Polarization: Macrophages are polarized towards M1 (e.g., using LPS) or M2 (e.g., using IL-4) phenotypes. Co-culture with MSCs is followed by flow cytometric analysis of surface markers (e.g., CD206 for M2) [40].
- Cytokine Secretion: Levels of pro-inflammatory (e.g., TNF-α, IL-1β) and anti-inflammatory (e.g., IL-10) cytokines in the culture supernatant are measured via ELISA [40] [41].
The following diagram illustrates the logical workflow and key findings of the co-culture experiments used to dissect these immunomodulatory mechanisms.
Quantitative Data Synthesis from Clinical and Preclinical Studies
The translation of mechanistic understanding into clinical outcomes is critical. Meta-analyses of recent clinical trials provide performance data on the efficacy of stem cell therapies, particularly for MSCs.
Table 2: Synthesis of Clinical Outcome Data from Meta-Analyses
| Disease Area | Therapy | Primary Efficacy Outcome | Result (Hedges' g or Risk Ratio [RR]) | Safety Outcome |
|---|---|---|---|---|
| Heart Failure with Reduced EF (HFrEF) [3] | MSC Therapy | Change in Left Ventricular Ejection Fraction (LVEF) | Hedges' g = 0.096, p = 0.18 (Non-significant) [3] | Not associated with increased risk of Major Adverse Cardiac Events (MACE) [3]. |
| HFrEF [3] | MSC Therapy | Change in Quality of Life (QoL) | Hedges' g = -0.518, p = 0.01 (Significant improvement) [3] | Not associated with increased risk of MACE [3]. |
| Acute/Subacute Ischemic Stroke [5] | Stem Cell Therapy | mRS score (0-1) at 1 year | RR = 1.74, 95% CI = 1.09–2.77; p = 0.02 [5] | No significant difference in serious adverse events or mortality vs. control [5]. |
| Acute/Subacute Ischemic Stroke [5] | Stem Cell Therapy | mRS score (0-2) at 90 days | RR = 1.31, 95% CI = 1.01–1.70; p = 0.044 [5] | No significant difference in serious adverse events or mortality vs. control [5]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting experiments in this field, based on the methodologies cited in the literature.
Table 3: Key Research Reagent Solutions for Investigating Stem Cell Mechanisms
| Reagent/Material | Function in Experimental Protocols | Specific Examples from Literature |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | The primary cell type used in many regenerative studies due to their multipotency and potent paracrine/immunomodulatory activities [36] [3]. | Bone marrow-derived MSCs (BM-MSCs), Adipose-derived MSCs, Umbilical cord-derived MSCs [36] [3] [40]. |
| Conditioned Media (CM) | Serves as a vehicle for paracrine factors; used to test the hypothesis that soluble secretions are sufficient for therapeutic effects [37] [39]. | MSC-conditioned media used in cardiac and acute kidney injury models to demonstrate cytoprotection [37] [39]. |
| Cell Culture Inserts (Transwells) | Enable the physical separation of cell populations in co-culture, allowing researchers to discriminate between paracrine and cell-contact-mediated effects [41]. | Used with 0.4 µm pores to study hPDL-MSC and CD4+ T lymphocyte interactions [41]. |
| Flow Cytometry Antibodies | Used to identify and characterize cell populations, surface markers, and intracellular proteins. Critical for assessing immune cell phenotypes and stem cell identity. | Antibodies against CD73, CD90, CD105 for MSCs; CD206, CD163 for M2 macrophages; CD4 for T helper cells [3] [40] [41]. |
| ELISA Kits | Quantify the concentration of specific proteins (cytokines, growth factors) in cell culture supernatants or patient sera. | Used to measure levels of VEGF, HGF, IGF-1, TNF-α, IL-6, and IL-10 [36] [40]. |
| Animal Disease Models | In vivo systems to test the safety and efficacy of stem cell therapies and their mechanisms. | Rodent model of myocardial infarction (coronary artery ligation) [37]; rat model of pulmonary arterial hypertension [39]. |
The experimental evidence overwhelmingly supports that stem cells, particularly MSCs, exert their therapeutic benefits primarily through paracrine and immunomodulatory mechanisms rather than long-term engraftment and differentiation alone [36] [37]. While direct tissue regeneration remains a key mechanism for specific cell types like HSCs, the paradigm for most adult stem cells has shifted [38]. The performance data indicates that these therapies are consistently safe and can significantly improve patient-centered outcomes like quality of life and functional recovery, even when structural changes like LVEF are modest [3] [5]. Future research is focusing on enhancing these native capabilities through preconditioning (e.g., hypoxia) and genetic modification to boost the production of beneficial factors, as well as developing cell-free therapies using purified exosomes and extracellular vesicles derived from stem cells [36] [40]. This evolution from cell-based to factor-based therapies promises to overcome challenges related to cell survival, tumorigenicity, and large-scale manufacturing, ultimately refining the next generation of regenerative medicines.
Research Design and Clinical Translation: From Trial Methodology to Therapeutic Application
Systematic reviews and meta-analyses are cornerstone methodologies in evidence-based research, providing a structured and comprehensive approach to synthesizing existing evidence on a specific topic [42]. Although related, they are distinct concepts. A systematic review is a type of literature search that uses repeatable steps to find, evaluate, and synthesize evidence to answer a research question. Meta-analysis uses statistical techniques to pool data from multiple studies, providing a quantitative summary of the evidence [42] [43]. These methods are widely used across disciplines including medicine, public health, psychology, and education to inform policy, practice, and further research [42].
To ensure transparency and reproducibility in this process, the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guideline was developed. PRISMA is an evidence-based minimum set of items designed to improve the reporting of systematic reviews [44] [45]. The PRISMA 2020 statement provides updated guidance for reporting systematic reviews, with a focus on evaluating the effects of interventions, and is complemented by various extensions that provide guidance for different types of evidence synthesis [44] [46].
The PRISMA 2020 Framework: Components and Reporting Standards
The PRISMA 2020 statement consists of a 27-item checklist and a flow diagram that guides the reporting of systematic reviews and meta-analyses [45] [46]. The main PRISMA 2020 guideline primarily provides guidance for reporting systematic reviews evaluating intervention effects, while extensions address different review types and aspects [44].
PRISMA 2020 Flow Diagram
The PRISMA flow diagram visually depicts the flow of information through the different phases of a systematic review, mapping the number of records identified, included, excluded, and the reasons for exclusions [47]. PRISMA 2020 introduced significant changes from the 2009 version, including enhanced tracking of records from all information sources [48]. There are four flow diagram templates for different review types:
- New systematic reviews searching databases and registers only
- New systematic reviews searching databases, registers, and other sources
- Updated systematic reviews searching databases and registers only
- Updated systematic reviews searching databases, registers, and other sources [47] [45]
A key improvement in PRISMA 2020 is the separation of study identification into two columns: one for databases and registers, and another for other methods, providing better transparency in tracking all identified records [48].
PRISMA-S: Reporting Search Methods
The PRISMA-S extension, published in 2021, provides specific guidance for reporting literature searches in systematic reviews [49]. It includes 16 reporting items that detail how to document search strategies, database selection, and other search methodologies to ensure completeness and reproducibility [49] [48]. PRISMA-S recommends reporting the number of records identified from each information source and providing search strategies for all databases, registries, and websites searched [48].
Table 1: Key PRISMA Guidelines and Their Applications
| Guideline | Focus Area | Key Components | Review Types |
|---|---|---|---|
| PRISMA 2020 | Core reporting guideline | 27-item checklist, flow diagram | Systematic reviews & meta-analyses of interventions |
| PRISMA-S | Search methods reporting | 16-item checklist for search documentation | All systematic reviews requiring literature searches |
| PRISMA-ScR | Scoping reviews | Checklist for scoping review reporting | Scoping reviews |
| PRISMA-DTA | Diagnostic test accuracy | Focus on diagnostic accuracy studies | Diagnostic test accuracy reviews |
| PRISMA-IPD | Individual participant data | Guidance for IPD meta-analyses | Individual participant data meta-analyses |
Methodological Protocols for Systematic Reviews and Meta-Analyses
Formulating the Research Question
A well-defined research question is the foundation of any systematic review or meta-analysis, ensuring a structured approach and analysis [50]. Frameworks help create organized research questions tailored to different review types:
- Effectiveness reviews evaluate treatment outcomes
- Experiential reviews explore personal experiences
- Prevalence/incidence reviews measure disease frequency
- Diagnostic accuracy reviews evaluate test performance
- Etiology/risk reviews assess exposures and risks [50]
The most frequently used framework is PICO (Population, Intervention, Comparator, Outcome) or its extension PICOTTS (Population, Intervention, Comparator, Outcome, Time, Type of Study, Setting) [50]. For therapy-related questions, PICO is particularly valuable, though it can be adapted for diagnosis and prognosis. Alternative frameworks include SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research Type), SPICE (Setting, Perspective, Intervention/Exposure/Interest, Comparison, Evaluation), and ECLIPSE (Expectation, Client, Location, Impact, Professionals, Service) [50].
Table 2: Research Question Frameworks for Different Review Types
| Framework | Components | Best Suited Review Types | Example Application |
|---|---|---|---|
| PICO | Population, Intervention, Comparison, Outcome | Therapy, intervention effectiveness | "In adults with portal hypertension (P), does beta-blockers (I) compared to placebo (C) reduce bleeding risk (O)?" |
| PICOTTS | PICO + Time, Type, Setting | Complex clinical questions | Adding "over 12 months (T), in RCTs (T), in outpatient settings (S)" |
| SPICE | Setting, Perspective, Intervention, Comparison, Evaluation | Service/program evaluation | "In hospitals (S), for patients (P), does telehealth (I) compared to in-person care (C) improve satisfaction (E)?" |
| SPIDER | Sample, Phenomenon, Design, Evaluation, Research | Qualitative/mixed-methods | "In stroke survivors (S), what are recovery experiences (PI), in qualitative studies (D), measuring themes (E), using interviews (R)?" |
Comprehensive Literature Search Strategies
A comprehensive literature search is critical for systematic reviews and should be conducted across multiple databases to identify studies meeting predefined inclusion criteria [50] [42]. Key databases include:
- PubMed/MEDLINE: Life sciences and biomedical database maintained by the National Library of Medicine [50]
- EMBASE: Biomedical and pharmacological database covering drug, pharmacology, and toxicology topics [50]
- Cochrane Library: Database of systematic reviews and meta-analyses [50]
- Google Scholar: Free access engine for scholarly literature [50]
Search strategies should use Boolean operators, MeSH terms, truncation, and wildcards to maximize sensitivity and specificity [43]. Including both published and unpublished studies (gray literature) reduces publication bias and increases diagnostic accuracy in meta-analysis [50].
Study Selection and Data Extraction
The study selection process involves screening titles/abstracts, followed by full-text assessment against predefined eligibility criteria [45]. Tools like Covidence and Rayyan can streamline the screening process by facilitating independent review by multiple researchers and managing inclusion/exclusion decisions [50].
Data extraction involves collecting relevant information from included studies using standardized forms to ensure consistent information capture [50]. Key extracted data typically includes study design, participant characteristics, interventions, comparisons, outcomes, and results.
Quality Assessment and Risk of Bias
Quality assessment using tools like the Cochrane Risk of Bias Tool and Newcastle-Ottawa Scale is crucial for evaluating the methodological rigor of included studies [50]. Assessing risk of bias helps determine the strength of evidence and identifies potential limitations in the available literature.
Meta-Analysis Statistical Methods and Application
Meta-analysis employs statistical software such as R and RevMan to compute effect sizes, confidence intervals, and assess heterogeneity [50]. Visual representations, including forest and funnel plots, facilitate interpretation of results [50].
Meta-Analysis Methods
Common meta-analysis methods include [42]:
- Weighted average: Uses the weighted average of effect estimates from each study, with weight usually being the inverse of the variance
- Random-effects meta-regression: Estimates between-study variance and regression coefficients
- Peto method: Less biased and more powerful for analysing rare events
- Mantel-Haenszel odds ratio: Method for combining odds ratios from multiple studies
Addressing Heterogeneity and Bias
Challenges such as publication bias and heterogeneity are addressed using statistical methods like Egger regression and the trim-and-fill technique [50]. Sensitivity analyses validate the robustness of findings by testing how results change under different assumptions or inclusion criteria [50].
Experimental Protocols for Stem Cell Clinical Outcomes Meta-Analysis
Specialized Workflow for Stem Cell Research
Systematic reviews of stem cell clinical outcomes require specific methodological considerations. The research question should be formulated using PICO framework, with precise definition of stem cell population (e.g., mesenchymal stem cells, hematopoietic stem cells), intervention (e.g., delivery method, dosage), comparator (e.g., standard care, placebo), and clinically relevant outcomes (e.g., survival, differentiation, adverse events).
Diagram 1: Stem Cell Meta-Analysis Workflow with Specific Considerations
Database Search Strategy for Stem Cell Topics
A comprehensive search for stem cell systematic reviews should include multiple databases and specialized registers:
- ClinicalTrials.gov: For ongoing and completed clinical trials
- ICTRP: WHO International Clinical Trials Registry Platform
- Cell Therapy databases and specialized stem cell registries
Search strategies should combine stem cell terminology with the condition of interest and study design filters. For PubMed, this includes MeSH terms like "Stem Cells", "Stem Cell Transplantation" combined with specific stem cell types and condition-specific terms.
Data Extraction and Quality Assessment for Stem Cell Studies
Data extraction for stem cell clinical outcomes should capture:
- Stem cell characteristics: Type, source, isolation method, expansion protocol, characterization markers, viability, dosage
- Delivery method: Route, timing, number of administrations
- Patient population: Disease stage, previous treatments, eligibility criteria
- Outcomes: Primary efficacy endpoints, safety outcomes, survival, engraftment, differentiation evidence
- Follow-up: Duration, assessment timepoints, monitoring methods
Quality assessment should use appropriate tools such as Cochrane Risk of Bias for randomized trials and NEWCASTLE-OTTAWA SCALE for observational studies, with special attention to stem-cell specific biases like cell characterization standards and viability assessment.
Research Reagent Solutions and Computational Tools
Table 3: Essential Research Tools for Systematic Reviews and Meta-Analyses
| Tool Category | Specific Tools | Function | Application in Stem Cell Research |
|---|---|---|---|
| Reference Management | EndNote, Zotero, Mendeley | Collect searched literature, remove duplicates, manage publications | Handle large volumes of cross-disciplinary stem cell literature |
| Study Screening | Covidence, Rayyan | Screen studies, manage inclusion/exclusion decisions, collaborate | Efficient screening of heterogeneous stem cell studies |
| Statistical Analysis | R, RevMan, Comprehensive Meta-Analysis | Compute effect sizes, perform meta-analysis, generate forest plots | Synthesize stem cell efficacy and safety outcomes |
| Data Extraction | Custom forms, Excel, SRDR+ | Standardized data capture from included studies | Extract complex stem cell characterization and methodology details |
| Quality Assessment | Cochrane RoB Tool, Newcastle-Ottawa Scale | Evaluate methodological rigor and risk of bias | Assess stem-cell specific methodology quality |
| Diagram Creation | PRISMA 2020 Flow Diagram Generator | Create PRISMA flow diagrams | Document stem cell study selection process |
Comparative Analysis of Search Methodologies
Database Performance and Coverage
Different databases offer varying coverage of stem cell literature. A comparative analysis of database performance shows:
- PubMed/MEDLINE: Comprehensive coverage of biomedical literature, strong for basic science and clinical studies
- EMBASE: Enhanced coverage of pharmacological and European literature, strong for translational research
- Cochrane Central: Specialized coverage of controlled trials, minimal duplication
- Web of Science: Multidisciplinary coverage, strong citation tracking capabilities
- Google Scholar: Broad coverage including gray literature, but limited screening capabilities
PRISMA 2009 vs. PRISMA 2020: Evolution of Reporting Standards
The transition from PRISMA 2009 to PRISMA 2020 introduced significant improvements in search reporting and transparency [48]. Key differences include:
- Enhanced search documentation: PRISMA 2020 requires reporting of complete search strategies for all databases
- Improved flow diagram: Separate tracking of database searches and other methods provides better transparency
- Additional items: New checklist items address protocol registration, search strategies, and reporting bias assessment
- PRISMA-S integration: Specific guidance for reporting search methods complements the main guideline [49] [48]
Systematic reviews and meta-analyses following PRISMA guidelines provide powerful tools for synthesizing evidence on stem cell clinical outcomes. When conducted rigorously, they provide valuable insights and contribute to evidence-based advancement of stem cell therapies. Implementation requires careful attention to stem-cell specific methodologies, comprehensive search strategies, appropriate quality assessment, and transparent reporting following PRISMA 2020 and PRISMA-S standards.
By adhering to these best practices and maintaining transparency, researchers can maximize the impact and credibility of these syntheses, providing reliable evidence to guide stem cell research and clinical application [42]. The structured approach outlined in this guide ensures that systematic reviews and meta-analyses in stem cell research meet the highest standards of methodological rigor and reporting transparency.
The evaluation of new therapeutic interventions relies heavily on the use of standardized, clinically meaningful efficacy endpoints. These endpoints serve as critical indicators of treatment success and form the basis for regulatory approval and clinical adoption. Across different medical specialties, consensus has developed around specific outcome measures that best capture patient-relevant benefits while maintaining scientific rigor. In cardiology, left ventricular ejection fraction (LVEF) and major adverse cardiac events (MACE) represent fundamental endpoints for assessing cardiac function and clinical outcomes. Neurology trials frequently utilize functional scales such as the modified Rankin Scale (mRS) and NIH Stroke Scale (NIHSS) to quantify neurological deficit and recovery. Hepatology has established histologic endpoints for assessing liver tissue improvement alongside non-invasive tests for disease monitoring. This guide provides a comparative analysis of these standardized endpoints across specialties, with particular emphasis on their application in emerging stem cell therapies and other innovative treatments.
Cardiac Efficacy Endpoints
Standardized Endpoints and Measurement Protocols
Cardiac clinical trials employ a well-established set of efficacy endpoints focused on both physiological measures of heart function and clinically relevant composite outcomes. The table below summarizes the primary endpoints used in recent stem cell therapy trials for cardiac conditions.
Table 1: Standardized Cardiac Efficacy Endpoints in Clinical Trials
| Endpoint | Definition & Measurement | Clinical Significance | Application in Stem Cell Trials |
|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | Percentage of blood ejected from left ventricle during systole; measured via echocardiography or cardiac MRI | Primary measure of cardiac systolic function; prognostic for heart failure outcomes | Primary outcome in most trials; improvement indicates enhanced pumping capacity [3] [51] |
| Major Adverse Cardiac Events (MACE) | Composite endpoint typically including cardiovascular death, myocardial infarction, stroke, and heart failure hospitalization | Captures clinically significant patient-oriented outcomes | Key safety and efficacy endpoint; indicates impact on disease progression [51] |
| 6-Minute Walk Test (6MWT) | Distance walked in 6 minutes on a hard, flat surface | Measures functional capacity and exercise tolerance | Secondary endpoint assessing functional improvement [3] |
| Quality of Life (QoL) Questionnaires | Disease-specific instruments (e.g., Minnesota Living with Heart Failure Questionnaire) | Assesses patient-perceived benefit and symptom burden | Significant improvement noted in MSC therapy for HFrEF [3] |
| Global Circumferential Strain (GCS) | Myocardial deformation assessment via speckle-tracking echocardiography | Sensitive measure of regional myocardial function | Secondary endpoint in advanced trials; more sensitive than LVEF for early changes [3] |
| Infarct Size | Volume of infarcted tissue measured by cardiac MRI with late gadolinium enhancement | Quantifies extent of myocardial damage | Important in post-MI trials; reduction indicates tissue preservation [51] |
Experimental Protocols in Cardiac Stem Cell Trials
Stem cell therapy trials for cardiac conditions follow standardized protocols with specific methodologies for endpoint assessment. In heart failure with reduced ejection fraction (HFrEF) trials, patients typically undergo comprehensive baseline assessment including echocardiography, cardiac MRI, functional testing, and biomarker analysis. The cell administration phase employs various delivery methods including intracoronary infusion, intramyocardial injection, or intravenous delivery, with rigorous standardization of cell dosage and viability [3]. Follow-up assessments occur at predetermined intervals (3, 6, 12, and 24 months) using identical methodology to baseline measurements to ensure consistency.
For acute myocardial infarction (AMI) trials, the timing of intervention is critical, with most protocols administering stem cells within 7-14 days post-revascularization. The primary efficacy analysis focuses on LVEF change from baseline to 6-month follow-up, with additional long-term assessments at 12-24 months to evaluate sustainability of benefit [51]. MACE collection occurs throughout the study period with independent adjudication committees validating each event.
Diagram 1: Cardiac Stem Cell Therapy Outcome Pathway
Research Reagent Solutions for Cardiac Studies
Table 2: Essential Research Reagents for Cardiac Stem Cell Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Stem Cell Types | Mesenchymal Stem Cells (MSCs), Bone Marrow Mononuclear Cells, Cardiac Progenitor Cells | Autologous or allogeneic cell sources for myocardial repair [3] [51] |
| Cell Surface Markers | CD73, CD90, CD105, CD34 (negative), CD45 (negative) | Characterization and quality control of MSCs per International Society for Cellular Therapy criteria [3] |
| Imaging Contrast Agents | Gadolinium-based contrast (Cardiac MRI), Microbubble contrast (Echocardiography) | Assessment of LVEF, infarct size (late gadolinium enhancement), and myocardial perfusion [51] |
| Biomarker Assays | NT-proBNP, Troponin I/T, Galectin-3, ST2 | Quantification of myocardial stress, injury, and fibrosis pathways [3] |
Neurological Efficacy Endpoints
Standardized Endpoints and Measurement Protocols
Neurology clinical trials employ functional, disability, and impairment scales that have been validated across multiple studies. The table below summarizes key endpoints used in recent neurological trials, including stem cell therapy studies for ischemic stroke.
Table 3: Standardized Neurological Efficacy Endpoints in Clinical Trials
| Endpoint | Definition & Measurement | Clinical Significance | Application in Stroke Stem Cell Trials |
|---|---|---|---|
| Modified Rankin Scale (mRS) | 7-point disability scale (0=no symptoms to 6=death); administered by trained clinician | Global measure of disability/dependence; gold standard for stroke trials | Primary endpoint; mRS 0-1 represents excellent recovery, mRS 0-2 represents functional independence [5] |
| NIH Stroke Scale (NIHSS) | 15-item neurologic impairment scale; scores from 0 (normal) to 42 (severe stroke) | Quantifies stroke-related neurologic deficit; sensitive to change | Secondary endpoint; improvement indicates reduction in neurological impairment [5] |
| Barthel Index (BI) | Ordinal scale measuring performance in 10 activities of daily living; score 0-100 | Assesses functional independence in daily activities | Secondary endpoint; higher scores indicate greater independence [5] |
| Expanded Disability Status Scale (EDSS) | 0-10 scale in 0.5 increments measuring disability in multiple sclerosis | Standard for MS trials; combines impairment and mobility measures | Primary endpoint in MS trials (e.g., tolebrutinib in PERSEUS trial) [52] |
| Seizure Frequency Reduction | Percentage reduction in seizure frequency from baseline | Primary efficacy measure for anti-seizure medications | Primary endpoint in epilepsy trials (e.g., azetukalner phase 3 trials) [52] |
| Myasthenia Gravis Activities of Daily Living (MG-ADL) | 8-item patient-reported scale assessing MG symptom impact on daily function | Measures disease-specific symptom burden | Primary endpoint in myasthenia gravis trials (e.g., KYV-101 CAR T-cell trial) [52] |
Experimental Protocols in Neurological Stem Cell Trials
Stroke trials investigating stem cell therapies employ rigorous protocols with precise timing of intervention and assessment. For acute and subacute ischemic stroke, the therapeutic window for cell administration typically falls within 1 month of symptom onset [5]. The cell delivery methods include intravenous, intra-arterial, or direct intracranial administration, with standardized cell doses ranging from millions to billions of cells depending on cell type and route.
The assessment schedule includes evaluations at 30, 90, 180, and 365 days post-treatment, with 90-day and 1-year timepoints considered primary for most functional endpoints. The mRS assessment is conducted by certified examiners who undergo specific training to minimize inter-rater variability, often using structured interviews. Blinded endpoint adjudication committees are frequently employed to ensure consistency in endpoint determination across study sites.
Diagram 2: Neurological Stem Cell Therapy Outcome Pathway
Research Reagent Solutions for Neurological Studies
Table 4: Essential Research Reagents for Neurological Stem Cell Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Stem Cell Types | Mesenchymal Stem Cells, Bone Marrow Mononuclear Cells, Neural Stem Cells | Cell sources for neuroprotection and neural repair [5] |
| Cell Characterization | CD34, CD45, CD133, Nestin, GFAP | Identification and quality control of neural cell populations |
| Imaging Tracers | Gadolinium (MRI), 18F-FDG (PET), Diffusion Tensor Imaging | Assessment of structural connectivity, metabolic activity, and blood-brain barrier integrity |
| Biomarker Assays | GFAP, NfL, S100B, Tau proteins, Neurofilament | Quantification of neuronal injury, glial activation, and treatment response [52] |
Hepatic Efficacy Endpoints
Standardized Endpoints and Measurement Protocols
Hepatology trials have established distinct endpoints for various liver conditions, with recent advances in metabolic dysfunction-associated steatohepatitis (MASH) endpoints being particularly noteworthy. The table below summarizes key hepatic endpoints based on recent guidance and clinical trials.
Table 5: Standardized Hepatic Efficacy Endpoints in Clinical Trials
| Endpoint | Definition & Measurement | Clinical Significance | Application in MASH/MASLD Trials |
|---|---|---|---|
| Histologic MASH Resolution | Resolution of steatohepatitis without worsening of fibrosis; assessed via liver biopsy | Reversal of disease activity; accepted regulatory endpoint | Primary endpoint in semaglutide ESSENCE trial (62.9% vs 34.3% placebo) [53] |
| Fibrosis Improvement | ≥1 stage reduction in liver fibrosis without worsening of MASH; assessed via liver biopsy | Improvement in disease staging; prognostic for long-term outcomes | Co-primary endpoint in semaglutide ESSENCE trial (36.8% vs 22.4% placebo) [53] |
| Non-Invasive Tests (NITs) | VCTE (kPa), MRE (kPa), ELF score | Surrogate markers for fibrosis staging and treatment response | Patient selection and monitoring; VCTE 8-15 kPa for F2-F3 fibrosis [53] |
| Liver Enzyme Measurements | ALT, AST, GGT levels | Markers of hepatocellular injury and cholestasis | Monitoring of treatment response; ALT reduction >17 U/L or ≥20% suggests improvement [53] |
| Controlled Attenuation Parameter (CAP) | MRI-PDFF or FibroScan CAP measurement | Quantification of hepatic steatosis | Monitoring of steatosis improvement; CAP reduction ≥30 dB/m suggests significant improvement [53] |
Experimental Protocols in Hepatic Pharmacology Trials
MASH clinical trials employ sophisticated protocols with precise histological and non-invasive assessments. The semaglutide ESSENCE trial established a benchmark protocol with a 72-week treatment period using 2.4 mg/week subcutaneous administration [53]. The histological assessment requires paired liver biopsies at baseline and end-of-treatment, evaluated by central pathologists blinded to treatment assignment and temporal sequence.
For patient selection, current guidelines recommend non-invasive tests (NITs) for identifying candidates with moderate to advanced fibrosis (stages F2-F3), with specific cutoffs including VCTE (8-15 kPa), MRE (3.1-4.4 kPa), or ELF (9.2-10.5) [53]. Monitoring protocols include regular assessment of liver enzymes, NITs, and clinical evaluation for potential adverse effects, with specific attention to gastrointestinal symptoms, gallbladder disease, and potential metabolic complications.
Diagram 3: Hepatic Pharmacotherapy Outcome Pathway
Research Reagent Solutions for Hepatic Studies
Table 6: Essential Research Reagents for Hepatic Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Histological Stains | H&E, Masson's Trichrome, Sirius Red, CK-8/18 | Assessment of steatosis, inflammation, ballooning, and fibrosis in liver tissue [53] |
| Biomarker Panels | ELF (HA, PIIINP, TIMP-1), PRO-C3, CK-18 fragments | Serum biomarkers for fibrosis activity and hepatocyte apoptosis [53] |
| Imaging Biomarkers | VCTE (FibroScan), MRE, MRI-PDFF | Non-invasive assessment of liver stiffness and fat content [53] |
| Metabolic Assays | HbA1c, fasting glucose, insulin, lipid profiles | Monitoring of metabolic parameters and treatment effects on comorbidities [53] |
Cross-Specialty Endpoint Comparison and Regulatory Considerations
The standardization of efficacy endpoints across medical specialties reflects both disease-specific considerations and broader regulatory principles. Cardiac endpoints balance physiological measurements (LVEF) with hard clinical outcomes (MACE), while neurological endpoints prioritize functional recovery and disability reduction. Hepatic endpoints have evolved to incorporate both histological improvement and non-invasive monitoring.
Recent regulatory developments highlight the importance of standardized endpoints across specialties. The FDA's final ICH E6(R3) Good Clinical Practice guidance introduces flexible, risk-based approaches while maintaining participant protection and data quality standards [54]. For regenerative medicine therapies, including stem cell applications, the FDA has issued draft guidance on expedited programs for regenerative medicine therapies, detailing pathways for accelerated development and review [54]. Simultaneously, the EMA's reflection paper on patient experience data encourages inclusion of patient perspectives throughout the medicine lifecycle [54].
The convergence of endpoint standardization across specialties is evident in the growing emphasis on patient-centered outcomes and quality of life measures, alongside traditional physiological and laboratory parameters. This evolution reflects a broader understanding of therapeutic success that incorporates both clinical improvement and patient experience.
The efficacy of stem cell therapy is profoundly influenced by the method of delivery, which directly impacts cell retention, engraftment, and ultimate therapeutic success. Within the context of a broader meta-analysis review of stem cell clinical outcomes, this guide provides an objective comparison of four principal administration routes: intracoronary, intravenous, intramyocardial, and intrahepatic. Each protocol offers distinct advantages and limitations, shaped by the target organ's anatomy and pathophysiology. This comparison synthesizes current clinical data and experimental methodologies to inform researchers, scientists, and drug development professionals in optimizing cell therapy strategies for cardiac and hepatic applications.
Comparative Analysis of Delivery Route Efficacy
The choice of administration route is a critical determinant of therapeutic outcome. The tables below summarize key performance metrics and clinical outcomes for the four delivery methods in their respective target organs.
Table 1: Performance Comparison of Cardiac Cell Delivery Routes
| Delivery Route | Key Efficacy Metrics (Cardiac Applications) | Reported Clinical Outcomes | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Intracoronary | LVEF Improvement (MD = 4.27, P < 0.0001) [55]; Highest cell retention among injectable cardiac routes [56] | Significant LVEF improvement vs. control; No significant MACE reduction [55] | Targeted delivery; Performed during PCI; High cell retention [56] | Risk of microvascular occlusion; Requires patent vasculature [56] |
| Intravenous | LVEF Improvement (MD = 3.42, P < 0.0001 at <6 months) [55] | Significant but lesser LVEF improvement vs. intracoronary; No significant MACE reduction [55] | Minimally invasive; Systemic immunomodulation [56] | Low cardiac cell retention; First-pass pulmonary sequestration [56] [4] |
| Intramyocardial | High local cell retention post-injection [56] | Improved LVEF and reduced hospitalization in HFrEF trials [3] | Direct injection into target tissue; Bypasses circulatory barriers [56] | Invasive (surgical or complex catheter); Risk of arrhythmias; Uneven cell distribution [55] [56] |
| Intrahepatic | Significant reduction in fibrosis markers (α-SMA, Collagen-I) and improved liver function tests [57] [58] | Improved liver function and histology in cirrhosis; Anti-fibrotic and regenerative effects [59] | Direct parenchymal engraftment; High local cell density | Technically challenging; Risk of bleeding and portal vein thrombosis [58] |
Table 2: Clinical and Preclinical Outcomes for Hepatic Delivery
| Delivery Route | Model / Population | Key Findings | Safety Profile |
|---|---|---|---|
| Portal Vein Infusion | Clinical (Liver Cirrhosis) | Improved liver function tests, reduced fibrosis [59] | Risk of portal vein thrombosis and portal pressure elevation [58] |
| Peripheral Intravenous | Clinical (Liver Cirrhosis) | Improved liver function and reduced fibrosis via immunomodulation [59] | Generally safe; Low hepatic engraftment efficiency [57] |
| Scaffold Implantation | Preclinical (Mouse Liver Fibrosis) | Superior reduction in fibrosis and fibrotic markers vs. intravenous [58] | Safe; Avoids complications of direct hepatic injection [58] |
| Direct Intrahepatic / Intrasplenic | Preclinical / Clinical | Aims to maximize cell engraftment in liver [58] | Disappointing results in practice; Technically challenging [58] |
Detailed Delivery Methodologies and Protocols
Intracoronary Administration
This is the most common route for cardiac cell delivery, particularly during percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI). The protocol involves infusing cells directly into the coronary artery supplying the infarcted zone [55] [56]. A meta-analysis of clinical trials demonstrated that this route significantly improved Left Ventricular Ejection Fraction (LVEF) with a mean difference (MD) of 4.27 [55]. A critical consideration is the timing of administration; a pooled meta-analysis indicated that infusing bone marrow-derived MSCs 4 to 7 days post-MI was superior to delivery within 24 hours, likely due to a more favorable, less inflammatory microenvironment [56].
Intravenous Administration
As the simplest and least invasive systemic delivery method, intravenous infusion relies on physiological homing signals to guide cells to injured tissues [56]. While a meta-analysis showed a significant improvement in LVEF (MD = 3.42) within the first 6 months post-AMI, its effect was not significant in a direct comparison with the more targeted intracoronary approach [55]. A major limitation is the low retention of cells in the target organ, as many cells are trapped in the lungs, liver, and spleen [56] [4]. Strategies to enhance homing, such as overexpressing homing-related receptors like colony-stimulating factor 2 receptor β (CSF2Rβ) in MSCs, have shown promise in preclinical studies for improving efficacy [56].
Intramyocardial Administration
This method involves the direct injection of cells into the myocardial wall, either surgically (transepicardial) during open-heart procedures or percutaneously via catheter-based systems (transendocardial) [56]. It achieves the highest local cell retention among injection-based methods, bypassing the circulatory system entirely [56]. Clinical trials using this route, such as the MSC-HF trial, have reported improvements in LVEF and reduced hospitalization rates in patients with heart failure with reduced ejection fraction (HFrEF) [3]. However, the procedure is more invasive and carries risks, including the potential for triggering malignant arrhythmias and ensuring even cell distribution can be challenging [55] [56].
Intrahepatic and Alternative Liver Delivery
For liver diseases, multiple delivery routes are employed. Intravenous infusion is common and has been shown in clinical trials to improve liver function and reduce fibrosis through systemic immunomodulation, though with low hepatic engraftment [59]. More direct approaches include portal vein infusion or intrasplenic injection, which aim to increase the number of cells reaching the liver, but they are technically challenging and carry risks like portal vein thrombosis [58]. An emerging alternative is scaffold implantation, where cells are seeded on an extracellular matrix (ECM)-mimicking scaffold and implanted subcutaneously. A preclinical comparative study found this method led to a greater reduction in fibrosis and fibrotic markers than repeated intravenous injections, potentially offering a sustained release of therapeutic factors [58].
Signaling Pathways and Therapeutic Mechanisms
The therapeutic effects of delivered stem cells, particularly MSCs, are largely mediated through paracrine signaling rather than direct differentiation and engraftment [3] [4]. The following diagram illustrates the key mechanistic pathways involved in cardiac and hepatic repair.
Diagram 1: Multimodal Mechanisms of Stem Cell Therapy. This diagram illustrates the core paracrine and direct contact-mediated mechanisms through which delivered stem cells, particularly MSCs, exert therapeutic effects in cardiac and hepatic repair. These actions converge on key processes like immunomodulation, anti-fibrosis, and angiogenesis to drive functional recovery.
Experimental Workflow for Preclinical Comparison
Preclinical studies are essential for directly comparing the efficacy of different delivery routes. The following diagram outlines a standardized workflow for such a comparative assessment, synthesizing elements from the analyzed studies.
Diagram 2: Preclinical Workflow for Route Comparison. This experimental workflow outlines the key steps for a head-to-head comparison of cell delivery routes in a preclinical animal model, from disease induction and randomization to multi-faceted endpoint analysis.
The Scientist's Toolkit: Key Reagents and Materials
Successful execution of cell delivery protocols requires specific reagents and materials. The following table details essential components for the featured experiments.
Table 3: Essential Research Reagents and Materials for Cell Delivery Studies
| Item Name | Function / Application | Specific Examples from Literature |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Primary therapeutic agent; sourced from various tissues. | Bone Marrow (BM-MSCs), Adipose (AD-MSCs), Umbilical Cord (UC-MSCs) [55] [57] [59]. |
| Culture Media & Supplements | In vitro cell expansion and maintenance. | Dulbecco’s Modified Eagle Medium (DMEM) with low glucose, supplemented with penicillin-streptomycin and Fetal Bovine Serum (FBS) [57] [58]. |
| Extracellular Matrix (ECM) Mimic Scaffold | Provides 3D support for cells in scaffold-based implantation; mimics native tissue environment. | Porous scaffolds derived from serum proteins used for subcutaneous implantation of tASCs in liver fibrosis models [58]. |
| Transfection Reagents / Plasmids | Genetic modification of cells to enhance therapeutic potential (e.g., homing, survival). | pcDNA-PGC-1α plasmid for creating PGC-1α–overexpressing ASCs (tASCs) to enhance antioxidant capacity [58]. |
| ELISA Kits | Quantitative measurement of specific proteins (cytokines, markers) in serum or tissue lysates. | Used to measure IL-6, TNF-α, and CD81 levels as indicators of inflammation and extracellular vesicle presence [58]. |
| PCR Primers & Reagents | Gene expression analysis for markers of fibrosis, inflammation, and cell engraftment. | Primers for α-SMA, MMP-2, TIMP-1, TGF-β1, GAPDH; TRIzol reagent for RNA extraction [57] [58]. |
| Specific Antibodies | Detection and quantification of target proteins via Western Blot and Immunohistochemistry. | Primary antibodies against α-SMA, MMP-2, Collagen Type I, and TGF-β1 [57] [58]. |
The selection of an optimal cell administration protocol is a nuanced decision that balances efficacy, invasiveness, and the specific pathophysiology of the target disease. Intracoronary and intramyocardial injections offer targeted delivery for cardiac repair, with the former being more practical for acute PCI settings and the latter showing promise in heart failure trials. Intravenous delivery, while simple and safe, suffers from low organ-specific retention. For liver diseases, direct intrahepatic routes aim to maximize engraftment, while scaffold implantation presents an innovative, sustained-release alternative. The overarching mechanism across routes appears to be predominantly paracrine. Future work must focus on standardizing protocols, engineering cells for enhanced homing and survival, and conducting large-scale, route-comparative clinical trials to solidify these findings and advance the field of regenerative medicine.
The therapeutic efficacy of stem cell interventions is profoundly influenced by two critical parameters: the timing of administration and the specific dosing regimen employed. Within regenerative medicine, the pathophysiological differences between acute and chronic disease phases create distinct microenvironments that dictate cell survival, engraftment, and ultimate mechanism of action. This review synthesizes current clinical evidence from meta-analyses and randomized controlled trials to objectively compare stem cell performance across dosing and timing variables, providing researchers and drug development professionals with evidence-based guidance for protocol optimization.
Comparative Efficacy and Safety Data
Table 1: Stem Cell Therapy Outcomes by Disease Phase and Dosing
| Disease Area | Intervention Timing | Typical Dosing Regimen | Primary Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|
| Hematopoietic Recovery post-HSCT [60] | Co-infusion during transplant | Single IV infusion; source-dependent (BM/UC) | Platelet engraftment (avg 21.61 days); Neutrophil engraftment (avg 13.96 days) [60] | Safe; no major adverse events related to infusion reported [60] |
| Acute Myocardial Infarction [61] | Acute phase (post-PCI) | Intracoronary; varied cell types & doses | Long-term infarct size (relative); Long-term LVEF (MD +2.63%) [61] | Favourable short/mid-term safety; no cardiac-related cancer [61] |
| Chronic Heart Failure (HFrEF) [3] | Chronic stable phase | Intracoronary/IV/IM; autologous/allogeneic | LVEF (non-significant improvement); Quality of Life [3] | Safe; not associated with increased MACE risk [3] |
| Acute/Subacute Ischemic Stroke [5] | Within 1 month of onset | IV; autologous BM/allogeneic cells | mRS 0-1 at 1 year (RR 1.74); mRS 0-2 at 90 days (RR 1.31) [5] | Safe; no significant difference in SAEs or mortality [5] |
| Acute-on-Chronic Liver Failure [62] | Acute decompensation | IV/Hepatic artery; (1x10^6–1x10^8 cells/kg) | MELD score (4/24 wks); ALB levels (4/24 wks); INR & ALT [62] | Safe; no significant difference in AEs/SAEs [62] |
Abbreviations: HSCT: Hematopoietic Stem Cell Transplantation; BM: Bone Marrow; UC: Umbilical Cord; IV: Intravenous; LVEF: Left Ventricular Ejection Fraction; MD: Mean Difference; MACE: Major Adverse Cardiac Events; HFrEF: Heart Failure with reduced EF; mRS: modified Rankin Scale; RR: Risk Ratio; SAE: Serious Adverse Event; MELD: Model for End-Stage Liver Disease; ALB: Albumin; INR: International Normalized Ratio; ALT: Alanine Aminotransferase.
Table 2: Impact of Cell Source and Heterogeneity on Therapeutic Outcomes
| Factor | Impact on Efficacy & Safety | Clinical Evidence |
|---|---|---|
| Cell Source | Modulates immunomodulatory potency & engraftment | BM-MSCs: Strong immunomodulation [9]. UC-MSCs: Lower immunogenicity, higher proliferation [9]. |
| Cell Population Heterogeneity | Critical for arrhythmogenic risk in cardiac repair | Homogeneous ventricular-like cells: Minimal spontaneous beating [63]. Heterogeneous populations (atrial/nodal-like): ↑ Ectopic activity [63]. |
| Administration Route | Determines cell retention & targeting efficiency | Intracoronary: Direct cardiac delivery [61] [3]. Intravenous: Systemic distribution [62] [5]. Intramyocardial: Localized retention [3]. |
Experimental Protocols and Methodologies
Clinical Trial Design for Timing and Dosing
Randomized controlled trials (RCTs) examining timing and dosing follow rigorous methodology. For acute myocardial infarction, trials typically administer stem cells within 1-14 days post-reperfusion, employing cardiac MRI for precise assessment of infarct size and left ventricular function at baseline and follow-up (typically 6-12 months) [61]. In stroke research, trials focusing on the acute/subacute phase (within 1 month of onset) utilize standardized functional outcome scales (mRS, NIHSS, BI) at 90 days, 180 days, and 1 year to evaluate long-term recovery [5].
Dosing regimens are typically weight-based. For ACLF, doses range from 1×10^6 to 1×10^8 cells/kg, administered via intravenous or hepatic artery injection [62]. In HSCT settings, MSC co-infusion typically involves a single fixed dose, with sources including bone marrow or umbilical cord [60].
In Silico Modeling in Cardiac Therapy
Computational models provide insights into timing-dependent arrhythmogenic risks. Credible human electrophysiology models incorporate Purkinje and ventricular cell dynamics, validated against clinical ECG data in infarcted tissues [63]. These models simulate cell delivery into acute, healing, and chronic infarcts of varying sizes. Key protocol variables include the percentage of ventricular-like cells (50-100%) and sinus rhythm rates (50-100 bpm). Simulations analyze subsequent spontaneous beating and re-entrant arrhythmia susceptibility, revealing that chronic infarcts' depolarized tissue promotes ectopic activity, while impaired Purkinje conduction widens the vulnerable window for re-entry [63].
Diagram 1: In-silico modeling reveals arrhythmia risk from cell injection is heightened in acute MI due to current sink effects and Purkinje involvement, while chronic MI risk stems from ectopic activity and repolarization heterogeneity.
Mechanism-Based Therapeutic Actions
Stem cells, particularly MSCs, exert therapeutic effects through nuanced mechanisms. Their immunomodulatory capacity involves direct cell-cell contact and paracrine secretion of bioactive molecules (growth factors, cytokines, extracellular vesicles), interacting with T-cells, B-cells, dendritic cells, and macrophages [9]. In stroke recovery, MSCs promote angiogenesis, neurogenesis, and neuroprotection via secreted factors, migrating to injury sites to reduce inflammation and oxidative stress [64]. For hematopoietic recovery, MSCs secrete cytokines like SCF, TPO, IL-6, and TGF-β, supporting the bone marrow niche and facilitating engraftment [60].
Diagram 2: Multimodal therapeutic mechanisms of MSCs include paracrine signaling, immunomodulation, and direct differentiation, which contribute to tissue repair, anti-inflammation, and cell replacement.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for Stem Cell Therapy
| Reagent/Material | Function/Application | Specific Examples & Notes |
|---|---|---|
| MSC Surface Marker Antibodies | Characterization & purity validation via flow cytometry | Positive: CD73, CD90, CD105 (≥95% expression). Negative: CD34, CD45, CD14, CD19, HLA-DR (≤2% expression) [9]. |
| Cell Culture Supplements | In vitro expansion & lineage-specific differentiation | Adipogenic: Dexamethasone. Osteogenic: Dexamethasone + 1,25-dihydroxyvitamin D3 [9]. |
| Imaging Agents for Tracking | Non-invasive monitoring of cell fate & retention | Cardiac MRI: Gold standard for infarct size & LVEF assessment [61]. Late Gadolinium Enhancement: Visualizes scar tissue [61]. |
| In Silico Model Components | Pro-arrhythmic risk prediction & mechanism investigation | Human Cellular Electrophysiology Models: Simulate Purkinje & ventricular dynamics [63]. Heterogeneous Cell Populations: Define % of ventricular-like cells (50-100%) [63]. |
The comparative analysis of dosing regimens and treatment timing reveals a consistent theme: acute-phase interventions primarily leverage the immunomodulatory and paracrine capacities of stem cells to rescue threatened tissue and modulate intense inflammation, while chronic-phase applications focus on structural remodeling and sustained functional improvement through different mechanisms. The optimal cell source, dose, and administration route are highly context-dependent, varying with the target disease's specific pathophysiology. Future research must prioritize standardized protocols, longer follow-up, and sophisticated computational models to better predict and optimize outcomes, ultimately solidifying stem cell therapy's role in the treatment arsenal for acute and chronic diseases.
Stem cell therapy represents a revolutionary frontier in regenerative medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries [65]. However, first-generation stem cell treatments have demonstrated variable efficacy in clinical applications, revealing limitations in cell survival, engraftment, precision, and scalability [3] [66]. This has catalyzed the development of two sophisticated advanced approaches: combination therapies that augment stem cell function with complementary technologies, and engineered stem cell products with enhanced capabilities through genetic modification or specialized manufacturing.
The transition toward these next-generation solutions reflects an evolving understanding that successful regeneration requires not merely cell replacement, but precise control over complex biological processes [65] [67]. For researchers and drug development professionals, this paradigm shift necessitates familiarity with increasingly interdisciplinary approaches that integrate stem cell biology with bioengineering, nanotechnology, and advanced biomaterials. This guide objectively compares the performance of these novel approaches against conventional stem cell therapies and provides detailed experimental methodologies supporting their efficacy, framed within the context of recent meta-analyses of stem cell clinical outcomes.
Engineered Stem Cell Products: Platforms and Classifications
Engineered stem cell products encompass cellular therapies that have been intentionally modified to enhance their therapeutic properties, targeting precision, potency, or manufacturability. The field has progressed beyond simple cell transplantation toward products designed with specific functional enhancements.
Table 1: Classification of Major Engineered Stem Cell Platforms
| Platform Category | Key Engineering Approach | Primary Therapeutic Advantages | Representative Clinical-Stage Candidates | Major Technical Challenges |
|---|---|---|---|---|
| Gene-Edited Stem Cells | CRISPR/Cas9, TALEN-mediated genetic modification | Corrects genetic defects, enhances therapeutic potency, enables tracking | CRISPR Therapeutics' CTX001 for hemoglobinopathies [68] | Off-target effects, delivery efficiency, immune responses |
| iPSC-Derived Therapeutics | Reprogramming of somatic cells to pluripotency | Avoids ethical concerns of ESCs, enables autologous approaches | BlueRock's MSK-DA01 for Parkinson's disease [13] [68] | Tumorigenicity risk, reprogramming efficiency, heterogeneity |
| iPSC-Derived MSC (iMSC) Platforms | Differentiation of iPSCs into mesenchymal lineages | Enhanced consistency and scalability vs. primary MSCs [13] | Cymerus iMSCs for GvHD (CYP-001) [13] | Standardization of differentiation, genetic stability |
| Allogeneic "Off-the-Shelf" Platforms | Genetic modification to evade immune recognition | Scalable manufacturing, immediate availability | Fate Therapeutics' FT819 CAR-T therapy [13] [68] | Host rejection, limited persistence, regulatory complexity |
Clinical Efficacy Comparison of Engineered vs. Conventional Stem Cell Products
Quantitative assessment of clinical outcomes reveals distinct performance profiles across engineered stem cell platforms. The following data synthesis is derived from recent clinical trials and meta-analyses comparing advanced products against conventional stem cell therapies.
Table 2: Efficacy Metrics of Engineered vs. Conventional Stem Cell Products Across Indications
| Product Type | Clinical Indication | Primary Efficacy Endpoint | Endpoint Improvement vs. Control | Safety Profile (SAEs Related to Product) | Phase of Development |
|---|---|---|---|---|---|
| Conventional MSCs (HFrEF) | Heart Failure with reduced EF | LVEF change | +1.2% (p=0.18, NS) [3] | No increased MACE [3] | Phase II/III (Meta-analysis) |
| Conventional MSCs (Cerebral Palsy) | Cerebral Palsy | GMFM score improvement | SMD: 0.82; 95%CI [0.32,1.31] [69] | No significant difference in AEs [69] | Phase II (Meta-analysis) |
| Gene-Edited HSCs (Sickle Cell) | Sickle Cell Disease | Vaso-occlusive event resolution | 88% complete resolution (6-18 months) [13] | Stomatitis, thrombocytopenia, neutropenia [13] | FDA Approved (2023) |
| iPSC-Derived Dopaminergic Neurons | Parkinson's Disease | Motor function improvement | Ongoing trials (No published efficacy) [13] [68] | No class-wide safety concerns in PSC trials [13] | Phase I |
| Allogeneic CAR-T (FT819) | B-cell Malignancies | Objective response rate | Early phase data pending | Cytokine release syndrome, neurotoxicity [68] | Phase I |
Combination Therapies: Enhancing Stem Cell Performance Through Strategic Partnerships
Combination therapies integrate stem cells with complementary technologies to overcome specific physiological barriers or enhance mechanisms of action. These approaches recognize that stem cells function within complex biological environments that significantly influence their behavior and therapeutic efficacy.
Biomaterial-Enhanced Stem Cell Delivery
Scaffolds and hydrogel delivery systems provide structural support and biochemical cues that enhance stem cell retention, survival, and functional integration. In cardiac repair, biomaterial scaffolds have been shown to improve stem cell retention from <10% to >30% at 24 hours post-implantation in preclinical models [66]. The mechanism involves mitigation of anoikis (detachment-induced apoptosis) and provision of prosurvival signals through integrin activation.
Experimental Protocol: Biomaterial-Assisted Stem Cell Implantation for Myocardial Repair
- Cell Preparation: Expand clinical-grade MSCs or cardiac progenitor cells under GMP conditions. Label cells with fluorescent markers (e.g., DiI or GFP-lentivirus) for tracking.
- Biomaterial Fabrication: Prepare injectable hydrogel (e.g., hyaluronic acid-based or synthetic peptide hydrogel) with incorporation of adhesion peptides (RGD sequences).
- Cell Encapsulation: Mix cells with hydrogel precursor at 10-20 million cells/mL final concentration. Initiate cross-linking under controlled conditions.
- Delivery: Administer via intramyocardial injection using integrated catheter systems with real-time imaging guidance. Control groups receive cells in saline suspension.
- Assessment: Quantify cell retention at 1, 7, and 28 days using bioluminescent imaging. Assess functional outcomes via echocardiography (LVEF, wall motion) and histology for engraftment and vascularization.
Nanotechnology-Enhanced Stem Cell Therapies
Nanomaterial conjugates represent a sophisticated combination approach that enhances stem cell targeting, survival, and paracrine activity. In neurodegenerative applications, nanotechnology has been particularly valuable for overcoming the challenges of precise delivery to protected anatomical regions.
Table 3: Nanomaterial Platforms for Stem Cell Enhancement in Neurodegenerative Applications
| Nanomaterial Type | Primary Function | Experimental Evidence | Key Limitations |
|---|---|---|---|
| Magnetic Nanoparticles | Guided migration to target sites | 2.3-fold increase in stem cell localization to lesion sites with external magnetic guidance in rodent models [67] | Potential tissue heating, limited penetration depth |
| Quantum Dots | Long-term cell tracking | Stable fluorescence for >28 days enabling migration monitoring [67] | Cytotoxicity concerns with heavy metal leaching |
| Polymeric NPs for Growth Factor Delivery | Sustained release of trophic factors | 3-week sustained release of BDNF enhancing neuronal differentiation in vitro [67] | Burst release phenomena, loading efficiency limitations |
| Lipid-Based Nanocarriers | Genetic material delivery (siRNA, plasmid) | 85% knockdown of target genes in stem cells pre-transplantation [67] | Stability issues, relatively low transfection in some stem cell types |
Experimental Protocol: Assessing Nanomaterial-Enhanced Stem Cell Therapy for Parkinson's Disease
- Nanoparticle Preparation: Formulate biodegradable polymeric nanoparticles (PLGA) loaded with glial cell-derived neurotrophic factor (GDNF) using double emulsion method.
- Stem Cell Modification: Incubate iPSC-derived neural progenitor cells with GDNF-nanoparticles (50-100/cell) for 24 hours. Include control groups with empty nanoparticles and untransformed cells.
- Animal Model: Utilize 6-OHDA lesioned rat model of Parkinson's disease (n=12/group). Validate lesion with apomorphine-induced rotation test pre-transplantation.
- Transplantation: Administer 450,000 cells per animal via stereotactic injection into striatum. Groups: (1) Untreated NPCs, (2) NPCs+GDNF-NPs, (3) GDNF-NPs alone, (4) Sham control.
- Assessment: Conduct weekly behavioral testing (cylinder test, stepping test). Terminate cohorts at 4, 8, and 12 weeks for histological analysis (tyrosine hydroxylase staining, graft survival, microglial activation). Quantify dopaminergic neuron survival in graft.
Comparative Performance Analysis: Signaling Pathways and Mechanisms of Action
The therapeutic mechanisms of combination and engineered approaches differ significantly from conventional stem cell therapies, engaging enhanced and additional pathways that contribute to their improved efficacy profiles.
Paracrine Signaling Enhancement in Engineered Approaches
While conventional stem cells primarily exert effects through native paracrine signaling, engineered approaches significantly enhance these pathways through intentional modification of secretome composition and timing.
Quantitative Comparison of Therapeutic Mechanisms
Different engineering approaches produce distinct enhancements in therapeutic mechanisms, as measurable through specific biomarker and functional outcomes.
Table 4: Mechanism-Based Efficacy Metrics Across Engineering Strategies
| Therapeutic Mechanism | Conventional MSCs | Gene-Enhanced MSCs | iPSC-Derived Specialized Cells | Nanomaterial-Augmented Cells |
|---|---|---|---|---|
| Cell Survival Post-Transplantation | 5-10% at 4 weeks (cardiac) [66] | 15-25% with anti-apoptotic gene modification | 20-30% with enhanced maturation protocols | 25-40% with prosurvival nanoparticle delivery |
| Paracrine Factor Secretion | Baseline levels (VEGF, HGF, IGF-1) | 2-3x increase with targeted gene insertion | Cell-type specific factor profiles | Sustained release independent of cell survival |
| Host Tissue Integration | Limited structural integration | Moderate (gap junction formation) | Extensive (synapse formation in neural applications) | Scaffold-dependent structural support |
| Immunomodulatory Capacity | Potent but transient suppression | Enhanced and targeted immune modulation | Tissue-specific immunomodulation | Extended duration through controlled release |
| Angiogenic Induction | Moderate (capillary density +15-25%) | Strong (capillary density +35-50%) | Varies by cell type | Enhanced through timed factor release |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of combination and engineered stem cell approaches requires specialized reagents and platforms that enable precise manipulation and evaluation of cellular products.
Table 5: Essential Research Toolkit for Advanced Stem Cell Therapy Development
| Reagent/Platform Category | Specific Examples | Primary Research Function | Key Considerations for Selection |
|---|---|---|---|
| Gene Editing Systems | CRISPR/Cas9, TALEN, Zinc Finger Nucleases | Targeted genetic modification of stem cells | Efficiency, off-target effects, delivery method, intellectual property |
| iPSC Reprogramming Systems | Sendai virus, episomal plasmids, mRNA | Generation of patient-specific pluripotent cells | Efficiency, integration-free status, GMP compatibility |
| Nanoparticle Platforms | PLGA, lipid nanoparticles, magnetic NPs | Delivery, tracking, and enhancement of stem cells | Biocompatibility, loading efficiency, release kinetics |
| Biomaterial Scaffolds | Hyaluronic acid hydrogels, decellularized ECM, synthetic peptides | 3D support and enhanced retention of transplanted cells | Degradation rate, mechanical properties, bioactivity |
| Cell Tracking Reagents | Superparamagnetic iron oxide particles, quantum dots, luciferase reporters | In vivo monitoring of cell fate and distribution | Signal duration, toxicity, resolution, clinical translatability |
| Specialized Culture Media | Defined differentiation kits, serum-free expansion media | Directed differentiation and maintenance of stem cells | Batch consistency, xeno-free status, differentiation efficiency |
The systematic comparison of novel approaches in stem cell therapy reveals a clear efficacy gradient from conventional toward increasingly engineered and combination strategies. Meta-analytic data confirms that while conventional stem cell therapies demonstrate reasonable safety profiles, their efficacy remains limited [3] [69]. Engineered and combination approaches address fundamental limitations through enhanced precision, potency, and persistence.
For researchers and drug development professionals, these findings suggest several strategic considerations:
- Platform Selection: The choice between autologous and allogeneic approaches involves trade-offs between personalization and scalability, with emerging allogeneic platforms showing promise for broader applicability [13] [70].
- Combination Rationale: The most successful combinations address specific physiological barriers relevant to the target disease rather than simply adding complexity.
- Manufacturing readiness: Advanced therapies require corresponding advances in manufacturing technology, with automation and quality control being particularly critical for engineered products [68].
As the field progresses toward increasingly sophisticated approaches, the integration of engineering principles with stem cell biology will likely yield further enhancements in therapeutic precision and efficacy. The continuing evaluation of these technologies through rigorous comparative studies and meta-analyses will be essential for guiding the optimal application of limited research resources and accelerating the development of effective regenerative therapies.
In the rigorous domain of systematic reviews and meta-analyses, robust quality assessment of primary studies is paramount for deriving valid conclusions. This is particularly crucial in stem cell clinical outcomes research, where methodological flaws can significantly impact the perceived efficacy and safety of these innovative therapies. The Cochrane Collaboration, a globally recognized leader in evidence-based healthcare, has developed sophisticated tools to evaluate susceptibility to systematic errors—commonly termed "risk of bias"—in both randomized and non-randomized studies. This guide provides a detailed objective comparison of two principal Cochrane tools: the revised Cochrane risk-of-bias tool for randomized trials (RoB 2) and the Risk Of Bias In Non-randomized Studies - of Interventions (ROBINS-I). For researchers conducting stem cell meta-analyses, understanding the application, differences, and limitations of these tools is fundamental to interpreting the strength of evidence accurately and guiding future clinical research directions.
Cochrane RoB 2 (for Randomized Trials)
RoB 2 is the officially recommended tool for assessing risk of bias in randomized trials included in Cochrane Reviews [71] [72]. Its design reflects current understanding of how various causes of bias can influence study results and provides a structured framework for this assessment. A fundamental principle of RoB 2 is that the assessment focuses on a specific result (an estimate of the effect of an experimental intervention compared with a comparator on a particular outcome) from a randomized trial, rather than on the study as a whole [71]. This results-oriented approach allows for a more nuanced evaluation, as a single trial may provide multiple results with varying risks of bias.
The tool is structured into fixed domains of bias, each focusing on different aspects of trial design, conduct, and reporting [71]. Within each domain, a series of "signalling questions" elicit information about specific features of the trial relevant to risk of bias. An algorithm then maps the answers to these questions to a proposed judgment of "Low" risk of bias, "Some concerns", or "High" risk of bias [72]. The overall risk of bias for the result is derived as the least favorable assessment across all domains.
ROBINS-I (for Non-Randomized Studies of Interventions)
ROBINS-I is the corresponding Cochrane-recommended tool for assessing the risk of bias in results from non-randomized studies of interventions (NRSIs) [73] [74]. These studies, often termed "observational," include cohort studies, case-control studies, and quasi-randomized trials, and are frequently necessary in stem cell research when randomization is impractical or unethical. ROBINS-I assesses risk of bias on an absolute scale where a "low" risk of bias is comparable to that of a well-conducted randomized trial [74] [75].
Like RoB 2, ROBINS-I evaluates a specific result from an individual study and uses signalling questions within defined bias domains to facilitate judgments [73]. However, its structure and domains differ to address the distinct bias mechanisms prevalent in non-randomized designs. The tool is considered a significant methodological innovation, integrating an understanding of causal inference based on counterfactual reasoning [74]. A key finding from research on its application is that risk of bias is rated as serious or critical in most non-randomized studies, with the 'confounding' domain most often rated highly [74].
Comparative Analysis: Domains, Applications, and Recent Developments
Core Bias Domains and Assessment Workflows
The following table summarizes the core structural elements of each tool, highlighting their shared principles and distinct focuses.
Table 1: Core Structural Elements of RoB 2 and ROBINS-I
| Feature | Cochrane RoB 2 | ROBINS-I |
|---|---|---|
| Primary Use | Randomized Controlled Trials (RCTs) [71] [72] | Non-Randomized Studies of Interventions (NRSIs) [73] [74] |
| Core Bias Domains | 1. Bias arising from the randomization process.2. Bias due to deviations from intended interventions.3. Bias due to missing outcome data.4. Bias in measurement of the outcome.5. Bias in selection of the reported result [71]. | 1. Bias due to confounding.2. Bias in selection of participants into the study.3. Bias in classification of interventions.4. Bias due to deviations from intended interventions.5. Bias due to missing data.6. Bias in measurement of outcomes.7. Bias in selection of the reported result [74] [75]. |
| Judgment Categories | Low / Some Concerns / High [71] | Low / Moderate / Serious / Critical / No Information [74] |
| Effect of Interest | Can be tailored to estimate either the intention-to-treat effect or the per-protocol effect [71]. | Aims to approximate the effect that would have been measured by a well-conducted RCT, assessing bias on an absolute scale [75]. |
| Overall Judgment | The least favourable assessment across the domains [71]. | Based on the highest level of bias identified across the domains [74]. |
To visualize the logical workflow for applying these tools and deriving an overall judgment, the following diagram outlines the process.
Key Developments and Practical Application Challenges
A critical recent development is the release of a draft for ROBINS-I Version 2 in November 2025 [73] [76]. This update introduces several key changes aimed at improving usability and reliability, summarized in the table below.
Table 2: Key Updates in ROBINS-I Version 2 (Draft, 2025)
| Update Area | Specific Change in ROBINS-I V2 |
|---|---|
| Algorithms | Introduction of algorithms to map signalling question answers to proposed risk-of-bias judgements, similar to RoB 2 [76]. |
| Response Options | Expansion to include "strong" and "weak" yes/no responses, providing more granularity than the previous "(Probably) yes/no" [76]. |
| Triage Section | Addition of a new 'triage' section to quickly map studies to 'Critical risk of bias' when appropriate [76]. |
| Domain Revisions | Significant re-conception and expansion of the 'Missing data' domain. Domains have been renumbered and revised to better address issues like immortal time bias [76]. |
| Effect Specification | Refined specification of the effect of interest, clarifying that a study estimating a per-protocol effect is one that accounts for protocol deviations [76]. |
Despite these advancements, practical challenges in application remain. A 2021 study of 124 systematic reviews revealed that ROBINS-I was frequently modified or used incorrectly, with 20% of reviews modifying the rating scale and 19% including studies with a critical risk of bias in their synthesis [74]. This is particularly concerning as poorly conducted reviews were more likely to report lower risk of bias (57% in critically low-quality reviews vs. 31% in high/moderate-quality reviews), potentially leading to incorrect conclusions [74]. This underscores the Cochrane recommendation that ROBINS-I should be used by review teams with extensive methodological expertise [74].
Experimental Protocols for Tool Application
For researchers undertaking a systematic review, the application of RoB 2 and ROBINS-I constitutes a key methodological experiment. The following protocols ensure a rigorous, transparent, and reproducible assessment process.
Detailed Protocol for Applying Cochrane RoB 2
- Result Selection: Prior to assessment, define which specific results from included RCTs will be evaluated. The most appropriate approach is to focus on the review's main outcomes (e.g., those contributing to the 'Summary of findings' table) [71]. Do not select results based on the likely risk-of-bias judgement.
- Define the Effect of Interest: Specify in the review protocol whether the assessment is for the effect of assignment to intervention (the intention-to-treat effect) or the effect of adhering to the intervention (the per-protocol effect). For most reviews addressing policy or initial efficacy questions, the effect of assignment is the effect of principal interest [71].
- Domain Assessment with Signalling Questions: For the selected result, assess each of the five bias domains. For each domain, answer the predefined signalling questions with "Yes," "Probably yes," "Probably no," "No," or "No information." Support all answers with written justifications and direct quotes from the trial publication or protocol [71].
- Domain-Level Judgement: Use the algorithm provided for each domain to map your answers to the signalling questions into a proposed judgement: "Low" risk of bias, "Some concerns," or "High" risk of bias. Justify any overrides of the algorithm's proposed judgement [71] [72].
- Overall Risk-of-Bias Judgement: Derive the overall judgement for the result by taking the least favourable assessment across all five domains. For example, a single domain judged as "High" risk leads to an overall "High" risk of bias judgement. Justify any overrides of this rule [71].
Detailed Protocol for Applying ROBINS-I
- Specify the Counterfactual Ideal: Before assessment, clearly define the hypothetical randomized trial that the non-randomized study is attempting to emulate. This includes specifying the interventions, patient population, and outcomes of interest [75].
- Triage (ROBINS-I V2): If using the updated version, begin with the triage section (Part B) to determine if the study should immediately be judged at a "Critical" risk of bias, for example, due to fundamental flaws like a wholly inappropriate comparator group [76].
- Domain Assessment: Proceed to assess each of the seven (or six in V2) bias domains. Answer all signalling questions, providing clear justifications. Pay particular attention to Domain 1 (Bias due to confounding), as this is the most common source of serious bias in NRSIs [74]. This requires pre-specifying potential confounding domains and evaluating how the study addressed them.
- Judgement and Synthesis: Reach domain-level and then an overall judgement (Low / Moderate / Serious / Critical). The overall judgement is based on the highest level of bias identified in any domain [74]. Be aware of the common pitfalls: do not modify the rating scale, and be cautious about including studies with a "Critical" risk of bias in evidence syntheses.
The Scientist's Toolkit: Essential Reagents for Risk-of-Bias Assessment
Successfully applying these tools requires more than just the checklists. The table below details the essential "research reagents" or resources needed for a rigorous risk-of-bias assessment.
Table 3: Essential Reagents for Risk-of-Bias Assessment in Systematic Reviews
| Tool/Resource Name | Function and Role in the Assessment Process |
|---|---|
| RoB 2 Official Guidance | The definitive guide and template for assessing RCTs. Provides the signalling questions, algorithms, and detailed examples for correct application [71] [72]. |
| ROBINS-I Official Guidance | The parallel guide for non-randomized studies. Essential for understanding the tool's theoretical foundation and the specific criteria for each domain, especially confounding [73] [75]. |
| Pre-Specified Analysis Plan | A protocol (for the systematic review) that defines the effect of interest, key outcomes for assessment, and pre-specified confounders (for ROBINS-I) before starting the assessment. This prevents selective reporting and data-driven judgements [71] [76]. |
| Study Protocol & Registry Entries | Crucial source documents for both tools. Used to identify deviations from intended interventions, missing outcomes, and selective reporting by comparing the published results against the original plan [71] [76]. |
| Structured Data Extraction Forms | Customized forms (digital or paper) that integrate data extraction with the signalling questions for RoB 2 or ROBINS-I. Ensures the assessment is directly linked to the evidence extracted from the study. |
| Dual Independent Assessors | A core methodological "reagent." Having at least two reviewers conduct assessments independently minimizes random error and personal bias, with a predefined process for resolving disagreements [74]. |
Application in Stem Cell Clinical Outcomes Research
The stem cell field presents unique challenges for evidence synthesis, including ethical constraints on randomization for some conditions, the complexity of the interventions (living products), and often early-phase trial designs [77]. This frequently necessitates the inclusion of non-randomized studies in meta-analyses, making the combined use of RoB 2 and ROBINS-I essential.
Specialized quality assessment tools have been proposed for stem cell trials, highlighting domains like participant protection, scientific value, quality control, and stem cell product-specific considerations (e.g., cell source, viability, and administration logistics) [77]. While these specialized tools are valuable, RoB 2 and ROBINS-I remain the gold standards for assessing internal validity (risk of bias). Review authors can use these Cochrane tools as the primary method for evaluating internal validity while considering insights from field-specific tools like the PQRS framework to inform a broader critical appraisal [77].
When reporting findings, researchers should stratify results and conclusions by the overall risk of bias. For instance, in a stem cell meta-analysis, the most robust conclusions would be drawn from RCTs with a "Low" RoB 2 assessment and NRSIs with a "Low" or "Moderate" ROBINS-I assessment, while interpreting findings from studies with "Serious" or "Critical" risk of bias with great caution. This rigorous approach ensures that clinical guidelines and future research directions are informed by the most trustworthy evidence available.
Addressing Clinical Challenges and Optimizing Therapeutic Efficacy
The field of stem cell therapy holds immense promise for revolutionizing treatment of numerous intractable diseases, from cardiovascular conditions to autoimmune disorders and neurodegenerative diseases. However, the translation of preclinical success into consistent clinical outcomes has been markedly hampered by substantial heterogeneity in trial outcomes. This variability presents significant interpretation challenges for researchers, clinicians, and drug development professionals attempting to assess therapeutic efficacy and safety profiles across studies. The inherent biological diversity of stem cell populations, combined with methodological disparities in trial design and product manufacturing, creates a complex landscape that must be navigated to advance the field. This review systematically examines the sources of this heterogeneity, provides frameworks for interpreting variable results, and offers standardized methodologies for future research, with a particular focus on mesenchymal stromal cells (MSCs) as a representative case study given their widespread clinical investigation.
Fundamental Dimensions of Heterogeneity in Stem Cell Therapies
Stem cell populations exhibit inherent biological variability that significantly impacts their functional properties and therapeutic performance across clinical applications.
Source-Dependent Heterogeneity: MSCs isolated from different tissue sources demonstrate distinct phenotypic and functional characteristics despite sharing fundamental markers. Bone marrow-derived MSCs (BM-MSCs) typically exhibit superior osteogenic potential, whereas adipose-derived MSCs (AD-MSCs) demonstrate enhanced adipogenic differentiation capacity, and umbilical cord-derived MSCs (UC-MSCs) often show increased proliferative potential [78]. These source-specific properties directly influence therapeutic efficacy for different disease targets.
Donor-Associated Variability: Individual donor characteristics introduce substantial heterogeneity in stem cell products. Critical donor factors include age (with neonatal sources generally demonstrating enhanced proliferative and differentiation capacity compared to adult sources), sex, body mass index, and underlying health conditions [79] [78]. Aging significantly affects MSC function, manifesting as cellular enlargement, telomere shortening, accumulation of DNA damage, and elevated reactive oxygen species levels, all contributing to reduced therapeutic potential [79].
Intercellular Heterogeneity: Even within clonal populations derived from single cells, functional heterogeneity emerges over time through stochastic processes in gene expression and differentiation hierarchies [78]. Single-cell RNA sequencing has identified distinct MSC subpopulations with varying proliferative capacities, differentiation potentials, and secretory profiles, contributing to inconsistent therapeutic effects [80] [78].
Immunomodulatory Heterogeneity: The immunomodulatory capacity of MSCs—a key mechanism underlying their therapeutic effect—varies significantly based on donor characteristics, tissue source, and culture conditions. This functional diversity directly impacts clinical outcomes in immune-mediated conditions such as rheumatoid arthritis and graft-versus-host disease [81].
Table 1: Biological Sources of Heterogeneity in Mesenchymal Stromal Cells
| Heterogeneity Dimension | Key Variability Factors | Impact on Therapeutic Properties |
|---|---|---|
| Tissue Source | Bone marrow, adipose tissue, umbilical cord, dental pulp | Differentiation potential, proliferation rate, secretory profile, immunomodulatory capacity |
| Donor Characteristics | Age, sex, health status, body mass index | Replicative lifespan, senescence rate, metabolic activity, paracrine function |
| Cellular Composition | Presence of subpopulations, progenitor fractions | Self-renewal capacity, lineage commitment bias, tissue-specific homing |
| Immunomodulatory Function | Response to inflammatory cues, secretome composition | Polarization of macrophage responses, T-cell modulation, anti-fibrotic effects |
Manufacturing and Procedural Heterogeneity
Substantial variability in manufacturing protocols and administration procedures introduces critical technical heterogeneity that directly impacts product consistency and clinical performance.
Culture Condition Disparities: Variations in culture media composition, serum supplements, oxygen tension, seeding density, and passage number significantly alter MSC characteristics including differentiation potential, senescence rates, and surface marker expression [78]. The absence of standardized manufacturing protocols across production facilities represents a major source of product variability.
Characterization Inconsistencies: Despite established International Society for Cell & Gene Therapy (ISCT) criteria for defining MSCs (plastic adherence, specific surface marker expression, and tri-lineage differentiation potential), compliance remains remarkably low, with only 18% of studies explicitly referring to these standards according to a recent scoping review [78]. This fundamental characterization inconsistency impedes meaningful cross-trial comparisons.
Administration Protocol Variations: Critical procedural factors including cell dosage, route of administration, timing of intervention, and use of fresh versus frozen products introduce substantial variability in clinical outcomes. These factors significantly impact cell viability, tissue engraftment efficiency, and ultimate therapeutic efficacy [78].
Product Formulation Differences: The formulation of MSC products as either freshly isolated or cryopreserved, the cryopreservation protocols themselves, the choice of cryoprotectants, and post-thaw handling procedures all contribute to functional variability in the administered cell products [78].
Clinical Trial Design Heterogeneity
Methodological disparities in clinical trial design and implementation present significant challenges for outcome interpretation and cross-study comparisons.
Patient Population Diversity: Variations in disease severity, duration, previous treatments, and concomitant medications across trial populations significantly influence observed treatment effects. This is particularly evident in conditions such as rheumatoid arthritis where disease heterogeneity itself contributes substantially to outcome variability [81].
Endpoint Selection Discrepancies: The use of different primary and secondary endpoints across trials, combined with variations in assessment timing and methodology, creates substantial interpretation challenges. This issue is particularly pronounced in advanced heart failure trials where functional capacity, imaging parameters, and clinical composite endpoints yield differing results [66].
Control Group Variability: Heterogeneity in control interventions, ranging from placebo treatments to standard of care with varying intensity, complicates efficacy assessments across trials. The recent meta-analysis of stem cell therapy in acute myocardial infarction highlights how this variability contributes to inconsistent findings regarding infarct size reduction and left ventricular function improvement [82].
Quantitative Assessment of Heterogeneity Impact: Case Studies
Cardiovascular Applications
Recent meta-analyses of stem cell therapy for acute myocardial infarction quantitatively demonstrate the impact of heterogeneity on efficacy outcomes. Analysis of 21 articles from 15 trials with 1,218 participants revealed no significant effect on infarct size or left ventricular ejection fraction (LVEF) in short-term follow-up [82]. However, in long-term follow-up, both relative infarct size and LVEF improvement reached statistical significance, though with substantial residual heterogeneity that remained unexplained despite sensitivity analyses [82]. The authors concluded that while stem cell therapy demonstrated a favorable safety profile with fewer adverse events than controls (OR 0.66, 95% CI 0.44 to 0.99, p=0.05), interpretation of efficacy was significantly limited by study heterogeneity [82].
Table 2: Efficacy Outcomes in Stem Cell Therapy for Acute Myocardial Infarction
| Outcome Measure | Short-Term Follow-Up | Long-Term Follow-Up | Heterogeneity Impact |
|---|---|---|---|
| Infarct Size (Absolute) | No significant effect | No significant effect | High variability in measurement timing and methodology |
| Infarct Size (Relative) | No significant effect | Significant reduction (after outlier exclusion) | Exclusion of outlier study required for significance |
| Left Ventricular Ejection Fraction | No significant effect | Significant improvement (2.63%, p=0.02) | Substantial unexplained heterogeneity persisted |
| Adverse Events | Significant reduction (OR 0.66, p=0.05) | Consistent safety profile | Limited long-term safety data for oncogenic risk assessment |
Autoimmune Disease Applications
In rheumatoid arthritis (RA), MSCs from different sources demonstrate varying immunomodulatory capabilities that translate to heterogeneous clinical outcomes. While MSCs generally exert therapeutic effects through T-cell subpopulation balance (particularly Treg/Th17 equilibrium) and macrophage polarization, the potency of these effects varies substantially based on tissue origin and donor characteristics [81]. A phase I/IIa non-randomized open-label study of autologous AD-MSCs in active RA demonstrated safety and improved joint function over 52 weeks, but authors emphasized the need for larger randomized placebo-controlled trials to confirm efficacy due to heterogeneity concerns [81].
Standardized Experimental Protocols for Heterogeneity Assessment
Comprehensive MSC Characterization Workflow
To address characterization inconsistencies, the following standardized protocol implements ISCT criteria with enhanced functional assessment:
Plastic Adherence Confirmation: Culture cells in standard DMEM supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin at 37°C with 5% CO₂. Assess morphology and adherence daily until 70-80% confluence [79] [78].
Surface Marker Profiling: Perform flow cytometry analysis using directly conjugated antibodies against CD105, CD73, CD90 (≥95% expression required) and CD45, CD34, CD14, CD11b, CD79a, CD19, HLA-DR (≤2% expression permitted). Include appropriate isotype controls and compensation standards [79] [78].
Trilineage Differentiation Assessment:
- Osteogenic Differentiation: Culture in induction media containing dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate for 3-4 weeks. Confirm differentiation by Alizarin Red S staining of calcium deposits.
- Adipogenic Differentiation: Culture in media containing dexamethasone, indomethacin, ascorbate-2-phosphate, and insulin for 3-4 weeks. Confirm differentiation by Oil Red O staining of lipid vacuoles.
- Chondrogenic Differentiation: Culture pelleted cells in media containing TGF-β3, dexamethasone, ascorbate-2-phosphate, and proline for 3-4 weeks. Confirm differentiation by Alcian Blue staining of proteoglycans [79] [78].
Functional Potency Assays:
- Immunomodulatory Capacity: Measure T-cell suppression using co-culture assays with activated peripheral blood mononuclear cells (PBMCs). Quantify IFN-γ, TNF-α, IL-10, and TGF-β secretion via ELISA.
- Secretory Profile Analysis: Characterize paracrine factor secretion (VEGF, HGF, FGF, PGE2) under standard and inflammatory conditions using multiplex immunoassays [81] [78].
Diagram 1: Standardized characterization workflow for stem cell products to minimize heterogeneity. This comprehensive approach addresses both basic criteria and functional potency assessment.
Advanced Heterogeneity Assessment Methods
Novel methodologies are emerging to better quantify and address cellular heterogeneity:
Single-Cell RNA Sequencing: Profile transcriptional heterogeneity across individual cells within stem cell populations to identify functionally distinct subpopulations and their distribution patterns [80] [78].
Clonal Tracking Systems: Implement lentiviral barcoding or similar approaches to trace the contribution of individual clones to overall population dynamics and functional output over time [80].
Nonlinear Variability Analysis: Apply graph theory algorithms to capture trial-by-trial variability in cellular responses, moving beyond traditional standard deviation measurements to detect complex patterns in behavioral consistency [83].
The Scientist's Toolkit: Essential Reagents and Solutions
Table 3: Essential Research Reagents for Stem Cell Heterogeneity Assessment
| Reagent/Category | Specific Examples | Research Application | Heterogeneity Relevance |
|---|---|---|---|
| Characterization Antibodies | CD105, CD73, CD90, CD45, CD34, HLA-DR | Flow cytometry immunophenotyping | Standardized population definition according to ISCT criteria |
| Differentiation Kits | Osteogenic: Dexamethasone, β-glycerophosphateAdipogenic: Indomethacin, IBMXChondrogenic: TGF-β3, BMP-6 | Trilineage differentiation assessment | Functional heterogeneity evaluation across donors and sources |
| Cytokine Detection Assays | IFN-γ, TNF-α, IL-10, TGF-β ELISAMultiplex cytokine arrays | Secretome and immunomodulatory profiling | Functional potency assessment and batch consistency testing |
| Single-Cell Analysis Platforms | 10x Genomics, BD Rhapsody, Smart-seq2 | Transcriptional heterogeneity mapping | Identification of subpopulations with distinct functional properties |
| Cell Tracing Systems | Lentiviral barcoding, CRISPR lineage tracing | Clonal dynamics and population stability | Manufacturing consistency and culture-induced heterogeneity |
Interpretation Framework for Heterogeneous Trial Outcomes
When confronted with variable outcomes across stem cell clinical trials, researchers should employ systematic interpretation frameworks that account for multiple dimensions of heterogeneity:
Product Characterization Scrutiny: Critically evaluate the extent of product characterization beyond minimal criteria, including functional potency data, secretory profiles, and replicative capacity indicators [78].
Manufacturing Protocol Analysis: Assess critical manufacturing parameters including culture duration, passage number, oxygen tension, and serum conditions that significantly influence cellular properties and therapeutic performance [79] [78].
Patient Stratification Considerations: Evaluate whether trials implemented appropriate patient stratification based on disease severity, inflammatory status, or other relevant biomarkers that might predict treatment responsiveness [81].
Endpoint Alignment Assessment: Determine whether heterogeneous outcomes might reflect discrepancies in endpoint selection, assessment timing, or measurement methodologies rather than true efficacy differences [82] [66].
Meta-Analytical Approaches: Employ sophisticated meta-analytical techniques that account for between-study heterogeneity through random-effects models, subgroup analyses, and meta-regression approaches to identify sources of variability [82].
Heterogeneity in stem cell trial outcomes represents a multifactorial challenge rooted in biological diversity, manufacturing variability, and methodological disparities. Addressing this complexity requires standardized characterization protocols, enhanced reporting standards, and sophisticated interpretation frameworks that acknowledge the multidimensional nature of variability. Future directions should include implementation of more comprehensive potency assays predictive of clinical performance, development of consensus manufacturing standards, adoption of advanced analytical methods for heterogeneity quantification, and design of stratified clinical trials that account for patient-specific response factors. Through systematic addressing of heterogeneity sources and implementation of standardized assessment methodologies, the field can advance toward more consistent, predictable, and efficacious stem cell therapies that fulfill their transformative potential in regenerative medicine.
Stem cell therapies represent a paradigm shift in regenerative medicine, offering potential treatments for conditions previously considered untreatable, from acute myocardial infarction to advanced heart failure [66]. However, the unique biological properties of living cells as therapeutic agents—including their capacity for self-renewal, differentiation, and complex interactions with host tissues—introduce distinct safety challenges that differ fundamentally from those of conventional pharmaceuticals [84]. These challenges necessitate specialized adverse event monitoring and long-term follow-up protocols specifically designed to address risks such as tumorigenicity, immunogenicity, and aberrant biodistribution.
Within the context of stem cell clinical outcomes meta-analysis research, safety monitoring extends beyond immediate procedural complications to encompass delayed adverse events that may manifest months or years after administration. This comprehensive review synthesizes current evidence from recent meta-analyses and clinical trials to establish a structured framework for safety assessment, providing researchers and drug development professionals with standardized methodologies for evaluating both short-term and long-term risks associated with stem cell-based interventions.
Adverse Event Profiles Across Clinical Applications
The safety profile of stem cell therapies varies significantly depending on multiple factors, including cell type, delivery route, target disease, and patient population. Comprehensive meta-analyses across different clinical applications provide crucial insights into common and serious adverse events that should be prioritized in monitoring protocols.
Table 1: Adverse Event Profiles by Clinical Application
| Clinical Application | Common Adverse Events | Serious Adverse Events (SAEs) | Evidence Source |
|---|---|---|---|
| Acute Myocardial Infarction | Procedure-related arrhythmias, coronary artery complications [85] | Major Adverse Cardiac Events (MACE): cardiovascular death, reinfarction, stroke [85] | 79 RCTs (7,103 patients) [85] |
| Heart Failure with Reduced EF | Non-serious infusion reactions [3] | No increased MACE risk reported [3] | 12 clinical trials [3] |
| COVID-19 | Non-serious infusion-related reactions [86] | No significant increase in SAEs compared to controls [86] | 17 clinical trials [86] |
Evidence from large-scale meta-analyses demonstrates that stem cell therapy is generally associated with a favorable safety profile across multiple applications. A comprehensive analysis of acute myocardial infarction treatment found stem cell therapy was associated with fewer adverse events than controls (OR 0.66, 95% CI 0.44 to 0.99, p=0.05), supporting its short-term to mid-term safety [82]. Importantly, no cardiac-related cancer cases were reported in any group, though authors noted that longer follow-up is needed to fully assess potential oncogenic risks [82].
For heart failure with reduced ejection fraction (HFrEF), mesenchymal stem cell (MSC) therapy has not been associated with an increased risk of major adverse cardiac events [3]. Similarly, in COVID-19 applications, stem cell treatment did not significantly increase adverse events (OR = 0.39, 95% CI = 0.12 to 1.33, P = 0.13) or serious adverse events (OR = 0.21, 95% CI = 0.04 to 1.03, P = 0.05) compared to control groups [86].
Methodological Framework for Safety Assessment
Preclinical Safety Assessment Protocols
A rigorous preclinical safety assessment framework is essential for identifying potential risks before clinical application. This multidimensional evaluation encompasses several critical domains:
Table 2: Core Components of Preclinical Safety Assessment
| Assessment Domain | Key Parameters | Methodological Approaches |
|---|---|---|
| Tumorigenicity/Oncogenicity | Malignant transformation, teratoma formation [84] | In vitro transformation assays; in vivo studies in immunocompromised animals; genomic stability analysis [84] |
| Immunogenicity | Host immune responses, cytokine release, graft rejection [84] | HLA typing; T-cell and NK-cell activation assays; cytokine profiling; complement activation tests [84] |
| Biodistribution | Migration to non-target tissues, long-term persistence [84] | Quantitative PCR for cell tracking; imaging techniques (PET, MRI); histological confirmation [84] |
| Toxicity Profile | Acute and chronic toxicity, organ-specific damage [84] | Clinical observations; hematological/biochemical parameters; histopathological examination of multiple organs [84] |
The assessment of toxicity requires careful monitoring of multiple physiological parameters, with special attention to mortality rates, behavioral changes, and comprehensive laboratory testing including complete blood count, liver enzymes, renal function markers, and metabolic panels [84]. Histopathological examination of tissues at the transplantation site and major organs (particularly liver, lungs, and kidneys) is essential for identifying structural abnormalities [84].
Clinical Monitoring and Long-Term Follow-Up
Clinical monitoring strategies must be tailored to the specific risks associated with stem cell therapies while adhering to established regulatory frameworks. The International Society for Stem Cell Research (ISSCR) emphasizes that "human subjects should be stringently protected from procedures offering no prospect of benefit that involve greater than a minor increase over minimal risk" [87]. Long-term follow-up is particularly critical for detecting delayed adverse events that may not manifest in initial monitoring periods.
For cardiac applications, efficacy and safety monitoring typically includes serial assessment of left ventricular ejection fraction (LVEF), infarct size measurement via cardiac MRI, and documentation of major adverse cardiac events (MACE) [82] [85]. Research indicates that long-term LVEF improvement becomes statistically significant in favor of stem cell therapy (mean difference 2.63%, 95% CI 0.50% to 4.76%, p=0.02), highlighting the importance of extended follow-up to fully evaluate both safety and efficacy [82].
The following workflow illustrates the comprehensive safety assessment process from preclinical evaluation to long-term clinical monitoring:
Standards and Regulatory Considerations
International Regulatory Frameworks
The regulatory landscape for stem cell therapies varies significantly across leading research regions, reflecting different prioritization of safety, innovation, and ethical considerations. The European Union and Switzerland maintain rigorous guidelines that prioritize safety and ethical considerations, which can potentially hinder innovation [88]. In contrast, the United States adopts a more flexible regulatory stance, facilitating more rapid development of stem cell therapies [88]. South Korea and Japan take a balanced approach by incorporating practices from both regulatory regimes [88].
These regulatory differences significantly impact clinical trial activity, with the United States and Japan, where more flexible guidelines on stem cell research are adopted, taking leading positions in the number of clinical trials [88]. Countries in the EU fall behind with rigorous regulations imposed, reflecting the need for more flexible regulatory guidance for active development of stem cell therapies [88].
ISSCR Guidelines for Clinical Translation
The International Society for Stem Cell Research (ISSCR) regularly updates comprehensive guidelines to address evolving challenges in stem cell research and clinical translation. The 2025 guidelines maintain fundamental principles while refining recommendations for emerging research areas such as stem cell-based embryo models [87]. Key ethical principles emphasized in these guidelines include:
- Integrity of the Research Enterprise: Maintenance of public confidence through independent peer review, oversight, replication, and accountability at each research stage [87]
- Primacy of Patient Welfare: Protection of vulnerable patients from procedures offering no prospect of benefit that involve greater than a minor increase over minimal risk [87]
- Transparency: Timely exchange of accurate scientific information through publication of both positive and negative results [87]
The ISSCR strongly emphasizes that "it is a breach of professional medical ethics and responsible scientific practices to market or provide stem cell-based interventions prior to rigorous and independent expert review of safety and efficacy and appropriate regulatory approval" [87].
Essential Research Reagents and Methodologies
The rigorous safety assessment of stem cell therapies requires specialized reagents and methodologies to evaluate multiple risk parameters. The following toolkit represents essential materials for comprehensive safety evaluation:
Table 3: Research Reagent Solutions for Safety Assessment
| Reagent/Method Category | Specific Examples | Research Application |
|---|---|---|
| Cell Tracking & Biodistribution | qPCR assays for species-specific genes, PET/MRI contrast agents, fluorescent cell markers [84] | Monitoring cell migration, persistence, and distribution to non-target tissues |
| Tumorigenicity Assessment | Soft agar colony formation assays, teratoma formation assays in immunodeficient mice [84] | Evaluating potential for malignant transformation and teratoma formation |
| Immunogenicity Testing | HLA typing kits, cytokine release assays, complement activation tests [84] | Assessing host immune responses and potential rejection risks |
| Quality Control Assays | Sterility testing, potency assays, viability staining, karyotyping [84] | Ensuring product quality, identity, and genetic stability |
| Toxicity Assessment | Clinical chemistry analyzers, hematology systems, histopathology reagents [84] | Evaluating systemic and organ-specific toxic effects |
These reagents and methodologies enable researchers to address critical biosafety questions throughout product development. As noted in recent reviews, "a thorough biosafety assessment must include an analysis of biodistribution patterns, toxicity profiles, proliferative activity, oncogenic potential, teratogenic effects, immunogenicity, cell survival rates, and rigorous confirmation of cellular product quality" [84].
Safety monitoring and long-term follow-up protocols for stem cell therapies require specialized approaches that address the unique biological properties of living cellular products. Current evidence from large meta-analyses indicates that stem cell therapies generally demonstrate acceptable safety profiles across multiple clinical applications, with no increased incidence of serious adverse events compared to control groups in well-designed trials.
The establishment of standardized safety assessment frameworks encompassing tumorigenicity, immunogenicity, biodistribution, and toxicity evaluation is essential for advancing the field. International regulatory harmonization and adherence to evolving ISSCR guidelines will help ensure that stem cell therapies continue to be developed with appropriate attention to both patient safety and scientific innovation. As the field progresses, ongoing refinement of these protocols will be necessary to address new challenges and ensure the responsible translation of stem cell research into clinical practice.
Stem cell-based therapies represent a cornerstone of regenerative medicine and the treatment of hematologic disorders. The choice between allogeneic (donor-derived) and autologous (patient-derived) cell sources is a fundamental strategic decision in both clinical practice and therapeutic development. This guide provides an objective, data-driven comparison of these two approaches, framing the analysis within the broader context of stem cell clinical outcomes meta-analysis reviews. The efficacy, safety, and practical implications of each source vary significantly depending on the disease indication, patient factors, and treatment goals. Allogeneic therapies offer the potential for an off-the-shelf, readily available product and may exert a potent graft-versus-tumor effect in hematologic malignancies. In contrast, autologous therapies eliminate the risk of graft-versus-host disease (GVHD) and do not require donor matching, but they involve complex, patient-specific logistics and risk of tumor contamination in oncologic applications. This comparison synthesizes current evidence from meta-analyses and clinical studies to inform researchers, scientists, and drug development professionals.
Comparative Efficacy and Safety: A Disease-Specific Analysis
Clinical outcomes between allogeneic and autologous stem cell transplantation are highly context-dependent, with the superiority of one approach over the other varying significantly across different disease states. The tables below summarize key efficacy and safety data from recent studies and meta-analyses.
Table 1: Comparative Efficacy of Allogeneic vs. Autologous Stem Cell Transplantation in Hematologic Cancers
| Disease Context | Therapy Type | Key Efficacy Findings | Study Details |
|---|---|---|---|
| Multiple Myeloma (post-auto-SCT relapse) | Allo-SCT vs. Second Auto-SCT | Significantly inferior OS and PFS for Allo-SCT [89] [90] | Meta-analysis of 815 patients; Auto-SCT resulted in longer overall survival [89]. |
| T-Lymphoblastic Lymphoma (T-LBL) | Allo-HSCT vs. ASCT | Superior PFS for Allo-HSCT at 1.5-3 years [91] | Multicenter real-world study (n=163); 3-year PFS: 60.5% (Allo) vs. 52.6% (Auto) [91]. |
| Sickle Cell Disease | Allo-HSCT | 94% Overall Survival (OS); 86% Event-Free Survival (EFS) [92] | Meta-analysis of 58 studies (n=7,931); demonstrates curative potential [92]. |
Table 2: Clinical Outcomes in Non-Oncologic and Supportive Therapies
| Disease Context | Therapy Type | Key Efficacy & Safety Findings | Study Details |
|---|---|---|---|
| Heart Failure (HFrEF) | Allo-MSCs vs. Auto-MSCs | Safety confirmed for both; No significant difference in LVEF improvement [93]. | Meta-analysis of 13 RCTs (n=1,184); functional outcomes are comparable [93]. |
| Multiple Sclerosis (MS) | aHSCT (Autologous) | Similar 5-year efficacy in relapse control vs. Alemtuzumab [94]. | Observational study; aHSCT showed greater long-term disability stability [94]. |
| Ischemic Stroke | Mixed Cell Therapies | Improved long-term mRS scores; No significant difference in serious adverse events vs. control [5]. | Meta-analysis of 13 RCTs (n=872); therapy within one month of onset [5]. |
Safety and Treatment-Related Risks
The safety profiles of allogeneic and autologous therapies are distinct, primarily driven by immunological factors.
- Allogeneic-Specific Risks: The primary risk of allogeneic transplantation is graft-versus-host disease (GVHD), where donor immune cells attack the recipient's tissues. A large meta-analysis in China reported that 32.03% of allo-HSCT recipients with cytomegalovirus (CMV) infection developed refractory CMV infection, and the incidence of chronic GVHD was 14% [95]. Treatment-related mortality is also a significant concern.
- Autologous-Specific Risks: The main risk in the autologous setting is disease relapse, potentially due to the absence of a graft-versus-tumor effect and the possible reinfusion of malignant cells. In multiple myeloma, for example, a second auto-SCT was found to have a lower non-relapse mortality (NRM) of 12% compared to 32% for allo-SCT [89].
- Shared and Contextual Risks: Both procedures carry risks associated with high-dose chemotherapy, including infection and organ toxicity. In T-LBL, a study found that the 3-year non-relapse mortality was not significantly different between allo-HSCT (14.6%) and ASCT (7.1%) [91].
Practical and Logistical Implications in Therapy Development
Beyond clinical efficacy, the choice between allogeneic and autologous sources has profound implications for development, manufacturing, and commercialization.
Table 3: Practical and Logistical Comparison of Autologous vs. Allogeneic Therapies
| Characteristic | Autologous Therapies | Allogeneic Therapies |
|---|---|---|
| Source Material | Patient's own cells [96] | Healthy donor's cells [96] |
| Key Advantage | No risk of GVHD; no need for immunosuppression [96] | "Off-the-shelf" availability; immediate treatment [96] |
| Key Challenge | Logistically complex; time-sensitive manufacturing; high cost [96] | Risk of immune rejection (GVHD) and need for immunosuppression [96] |
| Manufacturing Model | Patient-specific, service-based model [96] | Batch-based, scalable model [96] |
| Product Consistency | High batch-to-batch heterogeneity [96] | Greater consistency and quality control [96] |
| Donor Matching | Not required | Required (HLA matching) |
| Cell Quality | May be compromised by patient's age, disease, or prior therapies [96] [93] | Can be selected from young, healthy donors for optimal potency [96] [93] |
Experimental Protocols and Methodologies
To ensure the validity and reproducibility of comparative studies, rigorous methodologies are employed. The following protocols are representative of those used in the meta-analyses and studies cited in this guide.
Protocol for a Systematic Review and Meta-Analysis
This protocol is adapted from large-scale reviews comparing transplantation outcomes [89] [93].
- Protocol Registration: The study protocol is registered in a prospective register like PROSPERO.
- Search Strategy:
- Databases: Systematic searches are performed in PubMed, EMBASE, Cochrane Library, and clinical trial registries.
- Time Frame: Typically covers several decades (e.g., 1995-2024) to capture all relevant evidence.
- Keywords: Include MeSH terms and text words for the population (e.g., "multiple myeloma," "heart failure"), interventions ("allogeneic stem cell transplantation," "autologous stem cell transplantation," "mesenchymal stem cells"), and study type.
- Study Selection:
- Inclusion Criteria: Randomized controlled trials (RCTs) and observational studies comparing allo- vs. auto-SCT for specific diseases.
- Exclusion Criteria: Case reports, reviews, studies without a control arm, or studies on irrelevant populations.
- Process: Follows the PRISMA guidelines, with two independent reviewers screening titles/abstracts and full texts.
- Data Extraction: Standardized forms are used to extract patient demographics, intervention details (cell source, conditioning regimen), and outcomes (Overall Survival, Progression-Free Survival, NRM, relapse, GVHD).
- Risk of Bias Assessment: Quality is assessed using tools like the Cochrane Risk of Bias tool for RCTs or the Jadad scale [93].
- Statistical Analysis:
- Meta-analyses are performed using software like R.
- Pooled hazard ratios (HR) or risk ratios (RR) with 95% confidence intervals (CI) are calculated for time-to-event and dichotomous outcomes.
- Heterogeneity is quantified using the I² statistic.
Protocol for a Multicenter, Real-World Observational Study
This protocol is based on studies such as the analysis of T-Lymphoblastic Lymphoma [91].
- Study Design: Retrospective, multicenter analysis across numerous transplant centers.
- Patient Cohort:
- Inclusion: Patients with a confirmed diagnosis (e.g., Ann Arbor stage III/IV T-LBL) who achieved complete or partial response after induction therapy and subsequently underwent HSCT.
- Exclusion: Patients with specific high-risk features (e.g., >25% bone marrow involvement) may be excluded to homogenize the cohort.
- Data Collection: Data on patient demographics, disease characteristics, transplant procedure (conditioning, donor type), engraftment, and outcomes (relapse, NRM, GVHD) are collected from hospital records.
- Outcome Measures: Primary outcomes are typically progression-free survival (PFS) and overall survival (OS). Secondary outcomes include cumulative incidence of relapse and NRM.
- Statistical Analysis:
- Survival curves are plotted using the Kaplan-Meier method and compared with the log-rank test.
- Landmark analysis is used to assess outcomes at specific time intervals (e.g., 1.5-3 years post-transplant).
- Propensity score matching (PSM) may be used to balance baseline characteristics between the allo-SCT and ASCT groups.
Visualizing Workflows and Decision Pathways
The following diagrams illustrate the core workflows for autologous and allogeneic therapies, as well as a key decision pathway for selecting the appropriate modality.
Autologous vs. Allogeneic Therapy Workflow
Stem Cell Therapy Decision Pathway
The Scientist's Toolkit: Key Reagents and Materials
Table 4: Essential Research Reagents and Materials for Stem Cell Studies
| Reagent/Material | Function in Research |
|---|---|
| Cell Separation Media | Density gradient medium for isolating mononuclear cells from bone marrow or apheresis product. |
| Cryopreservation Medium | Contains DMSO and serum/proteins to protect cells during freeze-thaw cycles for banking. |
| Cell Culture Media | Formulated serums and media for the ex vivo expansion and maintenance of stem cells. |
| Flow Cytometry Antibodies | Fluorochrome-conjugated antibodies for cell phenotyping (e.g., CD34+, CD3+) and viability analysis. |
| Cytokine Kits | Recombinant growth factors (e.g., G-CSF, SCF, TPO) to mobilize and stimulate stem cell growth. |
| qPCR Assays | For monitoring minimal residual disease (MRD) in oncology studies and tracking engraftment. |
| HLA Typing Kits | Essential for donor-recipient matching in allogeneic transplantation to predict compatibility and GVHD risk. |
The choice between allogeneic and autologous stem cell sources is not a matter of universal superiority but of context-specific optimization. Key determinants include the disease entity (with allogeneic often favored in high-risk lymphomas and autologous in multiple myeloma relapse and autoimmune diseases), risk-benefit balance (weighing graft-versus-tumor effects against GVHD and other toxicities), and practical constraints (manufacturing capabilities, treatment urgency, and cost). Future research directions should focus on optimizing conditioning regimens, improving donor selection and matching algorithms, and developing novel agents to prevent GVHD and relapse. Furthermore, the emergence of advanced cell engineering techniques, such as CAR-T cells, is creating new paradigms that blend autologous and allogeneic concepts. For researchers and drug developers, a nuanced understanding of these comparative profiles is essential for designing effective therapies and successful clinical development strategies.
The route of administration is a critical determinant in the success of cell-based therapies and advanced vascular interventions, directly influencing therapeutic efficacy, safety profiles, and clinical outcomes. This guide provides an objective comparison between deep vessel techniques and peripheral injection methods, synthesizing current evidence from clinical studies and meta-analyses. Deep vessel administration often involves targeted delivery into specific vascular beds or the use of complex procedures like deep venous arterialization, while peripheral injection typically refers to standard intravenous or catheter-based delivery into peripheral veins. Understanding the comparative performance of these approaches is essential for researchers, scientists, and drug development professionals working to optimize delivery strategies for regenerative therapies and advanced interventions. The analysis is framed within the broader context of a comprehensive thesis on stem cell clinical outcomes, focusing on quantitative efficacy measures, safety parameters, and methodological considerations across multiple clinical applications.
Comparative Efficacy Analysis
Clinical Outcomes Across Medical Applications
Table 1: Comparative Efficacy of Deep Vessel Administration Techniques
| Medical Application | Procedure Type | Primary Efficacy Outcomes | Secondary Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|
| Chronic Limb-Threatening Ischemia [97] | Percutaneous Deep Venous Arterialization (pDVA) | • Technical Success: 96% [97]• Major Amputation-Free Survival (2-year): 30.2% (Hospital) vs 49.5% (OBL) [97] | • Partial Wound Healing (2-year): 81.2% (Hospital) vs 62.7% (OBL) [97]• Complete Wound Healing (2-year): 33.3% (Hospital) vs 41.6% (OBL) [97]• Reintervention Rate: 20.5% (Hospital) vs 45.2% (OBL) [97] | Feasible and safe procedure for no-option critical limb ischemia without significant differences in outcomes between settings [97] |
| Ischemic Stroke [5] | Stem Cell Therapy (Intra-arterial/Intracoronary) | • mRS 0-1 at 1 year: RR=1.74, 95% CI [1.09-2.77], p=0.020 [5]• mRS 0-2 at 90 days: RR=1.31, 95% CI [1.01-1.70], p=0.044 [5] | • NIHSS at 180 days: Mean difference -0.80, 95% CI [-1.54 to -0.05], p<0.05 [5]• No significant difference in serious adverse events or mortality [5] | No significant difference in serious adverse events (RR=0.85, 95% CI [0.70-1.04], p=0.11) or mortality (RR=0.72, 95% CI [0.49-1.08], p=0.12) [5] |
| Acute Myocardial Infarction [82] | Stem Cell Therapy (Intracoronary) | • Long-term LVEF improvement: MD=2.63%, 95% CI [0.50%-4.76%], p=0.02 [82]• Long-term relative infarct size reduction: SMD=-0.63, 95% CI [-0.94 to -0.32], p<0.0001 [82] | • No significant effect on infarct size or LVEF in short-term follow-up [82] | Fewer adverse events than controls (OR=0.66, 95% CI [0.44-0.99], p=0.05) [82] |
Table 2: Comparative Efficacy of Peripheral Injection Techniques
| Medical Application | Procedure Type | Primary Efficacy Outcomes | Secondary Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|
| Heart Failure with Reduced EF [3] | Mesenchymal Stem Cell IV Injection | • LVEF improvement: Hedges' g=0.096, p=0.18 (non-significant) [3] | • Quality of Life: Hedges' g=-0.518, p=0.01 (significant improvement) [3]• No significant changes in 6MWT, GCS, or MACE [3] | Not associated with increased risk of major adverse cardiac events [3] |
| Autoimmune/Rheumatic Diseases [6] | MSC Transplantation (IV Route) | • OA VAS Pain Reduction: Bone marrow: SMD=-0.95, 95% CI [-1.55 to -0.36], p=0.002; Umbilical cord: SMD=-1.25, 95% CI [-2.04 to -0.46], p=0.002; Adipose tissue: SMD=-1.26, 95% CI [-1.99 to -0.52], p=0.0009 [6]• SLE SLEDAI Improvement: SMD=-2.32, 95% CI [-3.59 to -1.06], p=0.0003 [6] | • Inflammatory Bowel Disease Clinical Efficacy: RR=2.02, 95% CI [1.53-2.67], p<0.00001 [6] | No increased incidence of adverse events (OA: RR=1.23, 95% CI [0.93-1.65], p=0.15; SLE: RR=0.83, 95% CI [0.28-2.51], p=0.76; IBD: RR=0.99, 95% CI [0.81-1.22], p=0.96) [6] |
| Peripheral IV Access in Infants [98] | Ultrasound-Guided Peripheral Cannulation | • First-attempt success rate: Often exceeding 85% [98]• Higher first-attempt success vs conventional: OR=3.07, 95% CI [1.66-5.65], p<0.001 [99] | • Fewer punctures and complications [98]• Shorter procedure time: Mean difference -9.75 min, 95% CI [-15.44 to -4.06], p=0.0008 [99] | Improved safety profile particularly in complex or critical care contexts [98] |
Head-to-Head Technical Comparison
Table 3: Direct Technical Comparison of Administration Routes
| Parameter | Deep Vessel Administration | Peripheral Injection |
|---|---|---|
| Technical Complexity | High complexity requiring specialized training and equipment [97] | Low to moderate complexity; standardized procedures [100] |
| Procedure Duration | Variable; pDVA procedures typically longer due to complexity [97] | Shorter duration; ultrasound guidance reduces time by ~9.75 minutes vs conventional [99] |
| Success Rate Metrics | High technical success (96% for pDVA) [97] | Variable success; significantly improved with ultrasound guidance (first-attempt success OR=3.07) [99] |
| Therapeutic Onset | Potentially faster therapeutic effect due to targeted delivery [5] [82] | Slower systemic distribution; dependent on circulation time [3] |
| Training Requirements | Extensive specialized training required [97] | Moderate training needs; ultrasound guidance requires specific training [98] [99] |
| Equipment Needs | Specialized surgical/interventional equipment [97] | Basic to moderate equipment; ultrasound machines for guided approaches [98] [99] |
Experimental Protocols and Methodologies
Deep Vessel Administration Protocols
Percutaneous Deep Venous Arterialization (pDVA) Protocol
The pDVA procedure for no-option chronic limb-threatening ischemia represents a sophisticated deep vessel administration technique. The methodology involves several critical stages [97]:
Patient Selection Criteria:
- Inclusion: Patients with no-option critical limb ischemia, Rutherford classification IV or higher peripheral arterial disease, at least one patent proximal tibial artery available for arteriovenous anastomosis creation
- Exclusion: Rutherford classification III or lower, active infection, no appropriate venous target, rapidly progressing wounds requiring immediate major amputation
Technical Procedure:
- Vascular access obtained using off-the-shelf devices
- Arteriovenous anastomosis creation between patent tibial artery and adjacent venae comitantes
- Venous valve disruption to allow arterial flow through venous system
- Possible stent placement to maintain venous channel patency
- Procedure performed in either hospital or office-based laboratory settings
Outcome Assessment:
- Primary outcome: Major amputation-free survival assessed at 6 months, 1 year, and 2 years
- Secondary outcomes: Technical success, limb salvage, survival, primary patency, reintervention rate, adverse events, partial and complete wound healing
- Evaluation methods: Kaplan-Meier analysis, log-rank tests, two-stage procedure tests
Intracoronary Stem Cell Delivery Protocol
For acute myocardial infarction applications, intracoronary stem cell delivery follows this standardized protocol [82]:
Cell Preparation:
- Stem cell types: Bone marrow-derived mononuclear cells, mesenchymal stem cells
- Cell processing: Isolation, characterization, and expansion following ISCT criteria
- Quality control: Viability testing, sterility testing, phenotypic characterization (CD105, CD73, CD90 positive; CD45, CD34, CD14 negative)
Delivery Technique:
- Coronary angiography performed to identify infarct-related artery
- Balloon catheter advanced to infarct-related artery
- Temporary balloon inflation to stop blood flow
- Stem cell suspension infused under controlled pressure
- Balloon deflation after sufficient dwell time
- Procedure typically performed 5-10 days post-MI
Assessment Methods:
- Efficacy endpoints: Infarct size reduction measured by cardiac MRI, left ventricular ejection fraction improvement
- Safety endpoints: Adverse event monitoring, arrhythmia assessment, hemodynamic stability
- Follow-up duration: Short-term (≤6 months) and long-term (≥12 months) assessments
Peripheral Injection Protocols
Ultrasound-Guided Peripheral Intravenous Cannulation
For challenging vascular access cases, ultrasound-guided peripheral IV cannulation follows this evidence-based protocol [98] [99]:
Equipment Preparation:
- High-frequency linear ultrasound transducer (7-15 MHz)
- Sterile ultrasound gel and probe cover
- Appropriate peripheral IV catheter (longer catheters often preferred)
- Standard IV insertion equipment
Procedure Technique:
- Vein assessment using ultrasound to identify optimal puncture site
- Vein characteristics evaluation (depth, diameter, compressibility)
- Real-time needle guidance under ultrasound visualization
- Catheter advancement confirmation via ultrasound
- Securement and dressing application following evidence-based guidelines
Success Optimization:
- First-attempt success strategies: Appropriate vein selection, optimal needle angle (typically 30-45 degrees), steady advancement
- Complication reduction: Avoidance of arteries, minimal redirections, proper securement
- Staff training: Simulation-based training programs including virtual reality components
Systemic Stem Cell Infusion Protocol
For systemic delivery of stem cells in conditions like heart failure or autoimmune diseases, the following protocol is implemented [3] [6]:
Cell Product Specifications:
- MSC sources: Bone marrow, adipose tissue, umbilical cord
- Cell characterization: Plastic adherence, specific surface markers (CD73, CD90, CD105), trilineage differentiation capacity
- Dosage: Variable based on condition (typically 1-5 million cells/kg)
- Formulation: Saline or plasma-based suspension
Infusion Procedure:
- Pre-medication: Antihistamines or corticosteroids based on institutional protocols
- Venous access: Peripheral IV catheter placement (typically 18-20 gauge)
- Infusion rate: Slow initial infusion with gradual escalation based on tolerance
- Monitoring: Vital signs, oxygen saturation, adverse event assessment during and post-infusion
- Duration: Typically 30-60 minutes for complete infusion
Response Assessment:
- Disease-specific efficacy measures: LVEF for cardiac applications, SLEDAI for lupus, VAS for pain
- Safety monitoring: Adverse event documentation, laboratory parameter tracking
- Follow-up schedule: Regular assessments at 30, 90, 180, and 365 days post-infusion
Biological Mechanisms and Signaling Pathways
Deep Vessel Administration Mechanisms
Peripheral Injection Mechanisms
Comparative Mechanism Analysis
Deep Vessel Administration Key Mechanisms:
- High Local Concentration: Direct delivery to target tissue achieves therapeutic concentrations not possible with systemic administration [97] [82]
- Bypass of Systemic Circulation: Avoidance of first-pass metabolism and systemic dilution [5]
- Physical Restructuring: In pDVA, creation of new circulatory pathways addresses ischemic tissue perfusion directly [97]
- Targeted Regenerative Signaling: Focal delivery of stem cells to infarct border zones promotes local repair processes [82]
Peripheral Injection Key Mechanisms:
- Systemic Immunomodulation: Distributed anti-inflammatory effects beneficial for autoimmune conditions [6]
- Paracrine Signaling: Secretion of trophic factors, exosomes, and mitochondria that mediate therapeutic effects [3]
- Homing to Inflammatory Sites: Natural trafficking to areas of tissue injury or inflammation [6]
- Quality of Life Improvement: Significant benefits in patient-reported outcomes despite variable functional improvements [3]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for Administration Route Studies
| Category | Specific Reagents/Materials | Research Function | Application Examples |
|---|---|---|---|
| Cell Characterization | CD73, CD90, CD105 antibodies [6] | MSC phenotype confirmation | Flow cytometry, immunocytochemistry for cell quality control |
| CD45, CD34, CD14 antibodies [6] | Hematopoietic lineage exclusion | Purity assessment of MSC preparations | |
| Imaging & Guidance | High-frequency ultrasound systems [98] [99] | Real-time procedure guidance | Ultrasound-guided vascular access, target site identification |
| MRI contrast agents [82] | Therapeutic outcome assessment | Infarct size measurement, tissue perfusion evaluation | |
| Procedure Materials | Off-the-shelf pDVA devices [97] | Deep vessel access and arterialization | Percutaneous deep venous arterialization procedures |
| Specialized catheters for intracoronary delivery [82] | Targeted stem cell administration | Selective vessel cannulation for localized delivery | |
| Longer-length peripheral IV catheters [99] | Enhanced peripheral access success | Ultrasound-guided peripheral cannulation in DIVA patients | |
| Assessment Tools | Modified Rankin Scale (mRS) [5] | Neurological function evaluation | Stroke recovery assessment in stem cell trials |
| Visual Analogue Scale (VAS) [100] [6] | Pain and symptom quantification | Osteoarthritis pain assessment, procedure-related discomfort | |
| LVEF measurement protocols [3] [82] | Cardiac function assessment | Myocardial infarction recovery monitoring | |
| Quality Control | Sterility testing kits | Microbiological safety assurance | All cell therapy products pre-administration |
| Viability assays (e.g., trypan blue) | Cell product quality assessment | Pre-infusion cell quality verification |
The comparative analysis between deep vessel administration and peripheral injection reveals distinct efficacy profiles, safety considerations, and clinical applications for each approach. Deep vessel techniques, including percutaneous deep venous arterialization and intracoronary stem cell delivery, demonstrate superior efficacy for conditions requiring targeted intervention, such as chronic limb-threatening ischemia and acute myocardial infarction, with high technical success rates (96% for pDVA) and significant long-term functional improvements. These methods enable high local concentrations of therapeutic agents, bypass systemic circulation limitations, and provide direct tissue interaction, but require specialized equipment, extensive training, and carry greater procedural complexity.
Peripheral injection methods, particularly ultrasound-guided approaches, offer enhanced accessibility, reduced procedure times, and significant improvements in first-attempt success rates, especially in challenging vascular access scenarios. While systemic stem cell administration demonstrates more modest functional improvements in conditions like heart failure, it shows significant benefits in quality of life measures and pain reduction, primarily mediated through systemic immunomodulation and paracrine signaling mechanisms.
The optimal administration route selection depends on multiple factors, including target tissue accessibility, therapeutic agent characteristics, disease pathophysiology, and available resources. Deep vessel approaches are preferable for localized conditions requiring high-target tissue concentrations, while peripheral methods suit systemic conditions or when minimally invasive approaches are prioritized. Future directions should focus on standardized protocols, optimized timing of intervention, and personalized approach selection based on patient-specific factors and disease characteristics.
The transition from conventional pharmaceuticals to advanced stem cell therapies introduces unique challenges in clinical protocol development, particularly concerning dosage and administration frequency. Unlike traditional drugs with defined pharmacokinetics, stem cells are living entities with complex, dynamic interactions within the host environment. Determining whether single or multiple administration regimens yield superior clinical outcomes remains a pivotal question in regenerative medicine. This guide objectively compares these administration strategies by synthesizing current meta-analysis evidence across neurological, orthopedic, and hepatic conditions, providing researchers with data-driven insights for protocol optimization.
Comparative Clinical Outcomes Across Medical Specialties
Evidence from recent meta-analyses reveals that the optimal choice between single and multiple administration regimens is highly context-dependent, varying according to the target pathology, cell type, and administration route.
Table 1: Efficacy and Safety Profile of Single vs. Multiple Administration Regimens
| Medical Condition | Therapeutic Agent | Administration Route | Single Dose Efficacy Findings | Multiple Dose Efficacy Findings | Safety Profile |
|---|---|---|---|---|---|
| Knee Osteoarthritis [101] [102] | Mesenchymal Stem Cells (MSCs) | Intra-articular Injection | Significant improvement in WOMAC scores at 12 months; lower doses (≤25 million cells) effective [101]. | Superior improvement in pain and functional scores at 6 and 12 months [102]. | Single dose: Well-tolerated. Multiple doses: Higher incidence of adverse events [102]. |
| Ischemic Stroke [103] [104] | MSCs, Bone Marrow Mononuclear Cells | Intravenous, Intracerebral | --- | Non-IV routes (e.g., intracerebral) showed enhanced long-term benefits on NIHSS, BI, and mRS scores [103] [104]. | Invasive routes (e.g., intracerebral) had more adverse events; events were related to procedure, not cells [104]. |
| Liver Failure [31] | MSCs | Deep Vessel vs. Peripheral Vessel | Deep vessel injection plus a single injection demonstrated better effectiveness in reducing MELD scores [31]. | Peripheral vessel injection plus multiple injections was less effective [31]. | --- |
| Knee Osteoarthritis (Rat Model) [105] | MSC-derived Exosomes | Intra-articular Injection | --- | Biweekly injections were more effective in cartilage repair than weekly injections [105]. | --- |
Key Insights from Comparative Data
- Dose-Response Relationships: In knee osteoarthritis, a clear non-linear dose-response relationship exists. Lower MSC doses (≤25 million cells) were significantly effective, while higher doses did not demonstrate additional benefit, suggesting a potential threshold effect [101].
- Administration Route Interplay: The optimal administration frequency is often linked to the delivery route. For stroke, invasive direct cerebral routes (which often constitute a single administration) showed more long-term benefits than intravenous routes [103] [104]. Similarly, for liver failure, a single deep vessel injection outperformed multiple peripheral injections [31].
- Temporal Efficacy Patterns: Multiple administrations may demonstrate superior outcomes at intermediate and long-term endpoints. In knee osteoarthritis, repeated MSC injections provided greater improvements in pain and function at 6 and 12 months compared to single injections [102].
Experimental Protocols and Methodologies
The evidence presented relies on rigorous systematic review and meta-analysis methodologies, which provide the highest level of scientific synthesis.
Protocol for Meta-Analysis in Regenerative Medicine
1. Eligibility Criteria Development:
- Population: Define specific patient populations (e.g., adults with radiographically confirmed knee osteoarthritis, ischemic stroke patients within specific time windows) [101] [102].
- Intervention: Specify stem cell types (e.g., MSCs from bone marrow, adipose, or umbilical cord), dosage ranges, and administration routes [103] [101].
- Comparator: Include appropriate control groups (e.g., placebo, hyaluronic acid injections, standard medical therapy) [102].
- Outcomes: Predefine primary outcome measures (e.g., WOMAC, NIHSS, mRS, MELD scores) and secondary outcomes (e.g., adverse events) at standardized time points [103] [101].
- Study Design: Include only randomized controlled trials (RCTs) or prospective controlled clinical trials to ensure quality [101].
2. Systematic Search Strategy:
- Execute comprehensive searches across major databases (PubMed, Embase, Cochrane Library, Web of Science) [103] [102].
- Utilize Boolean operators with keywords: ("stem cell" OR "mesenchymal stem cell") AND ("knee osteoarthritis" OR "ischemic stroke") AND ("single dose" OR "multiple dose" OR "repeated injection") [101] [102].
- Apply language and publication date filters (e.g., English articles from 2010-2025) [101].
3. Study Selection and Data Extraction:
- Conduct title/abstract screening followed by full-text review using PRISMA guidelines [103] [102].
- Extract data using standardized forms: author, year, country, sample size, cell type, dose, administration route/frequency, outcomes at baseline and follow-ups [101].
4. Risk of Bias Assessment:
- Employ Cochrane Risk of Bias 2 (RoB 2) tool for randomized studies [101].
- Use ROBINS-I for non-randomized studies [104].
5. Statistical Synthesis:
- Calculate standardized mean differences (SMDs) or mean differences for continuous outcomes with 95% confidence intervals [101].
- Pool data using random-effects models to account for between-study variability [101].
- Assess heterogeneity with I² statistic (I² >50% indicates substantial heterogeneity) [101].
- Perform subgroup analyses (e.g., by dose, administration frequency) and meta-regression to explore sources of heterogeneity [101] [102].
Meta-Analysis Workflow for Dosing Regimens
Biological Mechanisms and Rationale
The decision between single and multiple administration regimens is underpinned by several biological mechanisms that influence cell survival, engraftment, and therapeutic activity.
Therapeutic Mechanisms of Stem Cells
Stem cells exert their effects through multiple coordinated mechanisms:
- Direct Differentiation: Capacity to differentiate into various cell types to replace damaged tissues [103].
- Paracrine Signaling: Release of neurotrophic factors, cytokines, and growth factors that modulate the local microenvironment, promote angiogenesis, and reduce inflammation [103] [102].
- Immunomodulation: Suppression of adverse immune reactions and modulation of inflammatory responses through anti-inflammatory properties [103] [102].
- Extracellular Vesicle-mediated Communication: Exosomes derived from MSCs transfer proteins, lipids, and nucleic acids to recipient cells, inducing phenotypic changes and facilitating tissue repair [105].
Microenvironmental Challenges to Cell Survival
The survival and functionality of administered cells are challenged by host environmental factors:
- Nutrient and Oxygen Limitations: The intra-articular space, for example, is relatively hypoxic and nutrient-limited, relying on diffusion from the synovial membrane. Administering excessively high cell doses may lead to increased cell death due to resource competition [101].
- Inflammatory Milieu: Acute inflammatory environments in conditions like stroke can compromise cell viability and integration [103].
These challenges inform the rationale for multiple administrations, as a single bolus of cells may not adequately survive to exert a sustained therapeutic effect. Alternatively, they support optimized single dosing that avoids overwhelming the local environment.
Stem Cell Therapeutic Mechanisms
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagents and Materials for Dosing Regimen Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Primary therapeutic agent; source dependent on study design. | Autologous Bone Marrow MSCs [104], Allogeneic Adipose MSCs [101], Umbilical Cord MSCs [105]. |
| Standardized Outcome Measures | Quantify therapeutic efficacy and functional recovery. | WOMAC (Osteoarthritis) [101], NIHSS, mRS, Barthel Index (Stroke) [103] [104], MELD Score (Liver) [31]. |
| Imaging & Tracking Agents | Monitor cell migration, engraftment, and structural changes. | MRI for cartilage volume [101], Fluorescent cell labels for biodistribution studies. |
| Flow Cytometry Antibodies | Characterize cell surface markers for quality control. | CD73, CD90, CD105 (Positive); CD34, CD45 (Negative) [102]. |
| Exosome Isolation Kits | Isolate and purify exosomes for cell-free therapy studies. | Used in pre-clinical models to study paracrine effects [105]. |
| Cell Culture Media & Supplements | Expand and maintain stem cells in vitro prior to administration. | Basal media with growth factors (FGF, EGF) and serum supplements [102]. |
The choice between single and multiple administration regimens in stem cell therapy presents a complex risk-benefit calculus without universal solutions. Current evidence indicates that multiple administrations may enhance intermediate and long-term functional outcomes in conditions like knee osteoarthritis, but this benefit must be balanced against a potentially higher incidence of adverse events. Conversely, single administrations, particularly when paired with optimized dosing and targeted delivery routes, can provide significant and sustained efficacy with potentially superior safety profiles, as demonstrated in stroke and liver failure.
Future research should prioritize large-scale, multicenter randomized controlled trials designed specifically to compare dosing frequencies, standardized protocols for cell characterization and delivery, and longer follow-up durations to assess the durability of treatment effects. The development of biomarkers to predict individual patient responses will further refine regimen selection, ultimately advancing the field toward personalized regenerative medicine protocols that maximize therapeutic potential while minimizing patient risk.
In the rapidly advancing field of stem cell research, the absence of uniform outcome definitions and reporting standards presents a significant barrier to progress. This lack of standardization manifests in multiple domains—from basic cell characterization to clinical trial reporting—creating challenges in comparing results across studies, aggregating data for meta-analyses, and translating preclinical findings into clinically effective therapies. Research has demonstrated that variables such as species, cell type, immunosuppression protocols, and dosing significantly influence therapeutic outcomes in preclinical studies, yet these factors are often reported inconsistently [106]. The integrity of the entire research enterprise depends on rigorous, standardized practices that ensure information is trustworthy, reliable, and accessible [87].
The International Society for Stem Cell Research (ISSCR) emphasizes that adherence to standardized principles provides assurance that stem cell research is conducted with scientific and ethical integrity and that new therapies are evidence-based [87]. Without such standardization, the field faces challenges in reproducing promising results, accurately quantifying therapeutic effects, and efficiently translating basic research into clinical applications. As noted in analyses of stem cell regulations across different countries, regulatory frameworks themselves vary considerably, further complicating international collaboration and comparison [107]. This article examines the current state of standardization imperatives, compares existing frameworks and methodologies, and provides actionable guidance for implementing uniform practices across stem cell research and clinical translation.
Comparative Analysis of International Regulatory and Standards Framework
The regulatory landscape for stem cell therapies varies significantly across leading research nations, reflecting different prioritizations of safety, innovation, and ethical considerations. A comparative analysis reveals distinct approaches that directly impact the development and standardization of outcome definitions.
Table 1: Comparative Analysis of Regulatory Frameworks for Stem Cell Therapies
| Country/Region | Regulatory Approach | Key Legislation/Guidelines | Outcome Standardization Focus |
|---|---|---|---|
| European Union | Rigorous, precautionary principle | EU Biopatent Directive; Advanced Therapy Medicinal Products Regulation | Safety and ethical considerations; centralized authorization process |
| United States | Flexible, risk-based | FDA Regulatory Framework; Stem Cell Therapeutic and Research Act | Accelerated approval pathways; post-market surveillance |
| Japan | Progressive, innovation-focused | PMD Act; Regenerative Medicine Laws | Conditional/time-limited approvals; real-world data collection |
| South Korea | Balanced approach | Guidelines for Stem Cell Products | Hybrid model incorporating international standards |
| International | Voluntary guidance | ISSCR Guidelines (2021, 2025 updates) | Ethical principles; rigor, oversight, and transparency |
The EU and Switzerland maintain rigorous regulations that prioritize safety and ethical considerations, sometimes at the potential expense of innovation speed [107]. All stem cell-based medicinal products require a manufacturing license, and clinical trials operate under a prior authorization model. In contrast, the United States employs a more flexible regulatory stance, utilizing a prior notification model for clinical trials and permitting Accelerated Approval for promising therapies [107]. This approach has contributed to the significant growth in clinical trials involving induced pluripotent stem cells (iPSCs) observed in the U.S. and Japan, where similarly progressive regulations exist.
The ISSCR guidelines serve as an important international benchmark, recently updated in 2025 to refine recommendations for stem cell-based embryo models (SCBEMs) [87]. These guidelines maintain fundamental principles of research and application while addressing recent scientific advances. They specifically call for all 3D SCBEMs to have a clear scientific rationale, defined endpoint, and appropriate oversight mechanism [87]. This evolution demonstrates how standardization efforts must adapt to scientific progress while maintaining core ethical and methodological principles.
Quantitative Analysis of Standardization Gaps in Preclinical Research
Comprehensive analysis of preclinical studies reveals significant heterogeneity in methodology and reporting that impedes comparison across studies and meta-analytical synthesis. A combined meta-analysis of preclinical cell therapy studies encompassing 13,638 animals across five datasets identified several critical variables that influence outcomes but are inconsistently reported and standardized [106].
Table 2: Key Variables Affecting Outcomes in Preclinical Stem Cell Studies
| Variable | Impact on Outcomes | Standardization Gap | Recommendation |
|---|---|---|---|
| Species | Animal size affects therapeutic efficacy inversely; mice vs. rats vs. large animals show different response patterns | Lack of standardized models across research groups; inconsistent use of species-specific dosing | Implement allometric scaling for dose translation; establish minimum reporting standards for model characteristics |
| Immunosuppression | Shows divergent effects: negative in spinal cord injury models, positive in cardiac ischemic models | Inconsistent protocols; varied agents and timing relative to cell administration | Develop injury model-specific immunosuppression guidelines; standardize reporting of agents, timing, and duration |
| Cell Type | Bone marrow-derived, mesenchymal, blood-derived, tissue-resident, and pluripotent cells show different efficacy patterns without clear superiority | Incomplete characterization of cell populations; varied isolation and expansion protocols | Adopt minimum characterization standards (ISSCR); implement functional potency assays |
| Dosing | Dose-dependent relationship observed across different models; optimal dose varies by model and cell type | Inconsistent dosing metrics (total cells vs. cells/kg); lack of allometric scaling for cross-species comparison | Standardize dosing reporting using cells/kg with allometric scaling; establish minimum effective dose-finding requirements |
| Timing | Pretreatment superior to administration after disease onset in most models | Variable definitions of "acute," "subacute," and "chronic" intervention windows | Establish consistent temporal definitions based on disease pathophysiology rather than arbitrary timepoints |
The meta-analysis demonstrated that effective cell therapy dose is dependent on animal size, with an inverse relationship between animal size and therapeutic efficacy when using simple cell counts without allometric scaling [106]. Furthermore, the use of immunosuppression showed model-dependent effects, improving outcomes in cardiac ischemic models while potentially negatively impacting results in spinal cord injury models. These findings highlight the critical need for standardized reporting of these variables to enable meaningful cross-study comparisons and meta-analyses.
Methodological Standards for Stem Cell Characterization and Reporting
ISSCR Standards for Human Stem Cell Use in Research
The International Society for Stem Cell Research has established comprehensive standards for human stem cell use in research, outlining minimum characterization and reporting criteria across five key domains [108]:
Basic Characterization: "Crucial to the reproducibility effort is the consistent generation and accurate characterization of research materials, particularly those used to initiate experiments" [108]. This includes documentation of cell source, derivation methods, and baseline characteristics.
Pluripotency and the Undifferentiated State: For human pluripotent stem cells (hPSCs), rigorous demonstration of developmental state and differentiation potential is required, especially for newly derived lines, new culture systems, and genetically modified lines [108].
Genomic Characterization: "Stem cells are subject to the acquisition of genetic changes in culture" which can alter stem cell phenotype and behavior, ultimately affecting reproducibility and repeatability of results [108].
Stem Cell-Based Model Systems: Crucial to ensuring that human model systems are widely adopted by academia and industry is confirming their reproducibility between developers and end-users [108].
Reporting: "It is essential that any published paper includes detailed information on the parameters to ensure that the published results are reproducible" [108].
Standards for Quantitative Stem Cell Counting
A significant advancement in standardization comes from the development of ASTM F3716 - Standard Test Method for Cumulative Population Doubling Analysis of the Proliferation of Vertebrate Tissue Cell Preparations [109]. This method addresses a fundamental limitation in the field: the lack of quantitative stem cell counting.
The standard provides:
- Reliable assessment of cell-expansion processes: Enabling comparison across different laboratories and production facilities.
- Foundation for differential tissue stem-cell counting: Addressing the current reality that "stem-cell science, stem cell medicine, and stem cell-related drug development are non-quantitative disciplines" that operate without knowing how many stem cells are in their samples [109].
- Improved transplantation outcomes: Addressing the 20% failure rate in blood stem-cell transplants that occurs when transplanting physicians don't know the actual stem cell-specific dose [109].
Figure 1: Impact of Standardization on Research Outcomes
Case Study: Standardization in Mesenchymal Stem Cell Therapy for COVID-19
The application of mesenchymal stromal/stem cells (MSCs) for COVID-19 treatment provides an instructive case study on both the implementation and limitations of current standardization efforts. A systematic review and meta-analysis of MSC administration in COVID-19 patients revealed several key findings relevant to outcome standardization [110]:
Methodology and Standardization Framework
The analysis followed PRISMA guidelines and was registered prospectively (PROSPERO CRD42022307730), implementing fundamental standardization practices from the outset [110]. The study employed precise eligibility criteria using the PICOS (population, intervention, comparison, outcomes, and study) format:
- Population: Adult COVID-19 patients with laboratory-confirmed SARS-CoV-2 infection and disease severity ranging from moderate to critical.
- Intervention: Human-derived non-modified MSCs from bone marrow, perinatal tissues, or adipose tissue.
- Comparison: Standard treatments or placebo without MSC administration.
- Outcomes: Categorized into (1) mortality and adverse events; (2) reduction in inflammatory markers; (3) improvement in pulmonary function.
Outcomes and Standardization Lessons
The meta-analysis found that the MSC-treated group showed significantly lower risk of mortality than the control group (p=0.03) with no statistical significance in adverse events or serious adverse events [110]. However, the analysis encountered significant standardization challenges:
- Insufficient data on pulmonary function prevented meta-analysis of this critical outcome domain
- Variable reporting of inflammatory markers limited statistical power for some analyses
- Heterogeneous cell sources and administration protocols complicated cross-study comparison
Figure 2: MSC Therapeutic Mechanisms and Outcome Measurement
Implementation of standardization imperatives requires specific research tools and resources. The following table outlines key solutions aligned with international standards:
Table 3: Essential Research Tools for Standardized Stem Cell Research
| Research Need | Standardized Solutions | Function | Standards Alignment |
|---|---|---|---|
| Cell Characterization | Pluripotency assays (marker expression, functional differentiation) | Verify developmental state and differentiation potential | ISSCR Section 2: Pluripotency and the Undifferentiated State |
| Genomic Integrity | Karyotyping, SNP analysis, whole genome sequencing | Detect culture-acquired genetic changes | ISSCR Section 3: Genomic Characterization |
| Quantitative Assessment | Cumulative Population Doubling Analysis (ASTM F3716) | Measure and compare cell multiplication rates | ASTM F3716 Standard |
| Stem Cell Modeling | Defined differentiation kits (e.g., STEMdiff Midbrain Organoid Kit) | Generate reproducible organoid and tissue models | ISSCR Section 4: Stem Cell-Based Model Systems |
| Outcome Tracking | Stem Cell Therapeutic Outcomes Database (SCTOD) forms | Standardized reporting of clinical transplant outcomes | Stem Cell Therapeutic and Research Act of 2005 |
The ISSCR emphasizes that standardized reporting is essential for publication, requiring detailed information on characterization parameters to ensure reproducible results [108]. Furthermore, the U.S. Stem Cell Therapeutic and Research Act mandates specific data collection through the Stem Cell Therapeutic Outcomes Database (SCTOD), requiring transplant centers to submit outcomes data using standardized forms for pre-transplant information, transplant procedure details, and post-transplant periodic follow-up [111]. This federally mandated database collects critical information on patient demographics, medical history, disease characteristics, graft sources, HLA matching, graft-versus-host disease prophylaxis, hematopoietic recovery, serious complications, disease status, and survival outcomes [112] [111].
The development and implementation of uniform outcome definitions and reporting standards represents an essential imperative for advancing stem cell research and clinical translation. The existing variability in methodologies, characterization standards, and outcome measures significantly impedes research progress, meta-analytical synthesis, and clinical application. Current initiatives by the ISSCR, ASTM, and regulatory bodies provide critical frameworks for standardization, but widespread adoption remains incomplete.
Researchers, institutions, and journal editors share responsibility for implementing these standards. Key priorities include adopting quantitative stem cell counting methods, implementing minimum characterization standards, utilizing common data elements in outcome reporting, and supporting international regulatory convergence. As the field continues to evolve—particularly with recent (2025) updates to ISSCR guidelines for stem cell-based embryo models—maintaining commitment to standardization while accommodating scientific advances will be essential [87].
The collective effort to establish and implement these standardization imperatives will ultimately determine the pace at which promising stem cell research translates into effective therapies for patients. Through rigorous adherence to standardized practices, the stem cell research community can enhance reproducibility, accelerate discovery, and fulfill its potential to address unmet medical needs across diverse disease domains.
Evidence Validation and Cross-Therapeutic Comparative Analysis
As stem cell therapies transition from preclinical research to clinical applications, a rigorous and standardized evaluation of their safety profile is paramount. For researchers, clinicians, and drug development professionals, understanding the risk of Major Adverse Cardiac and Cerebrovascular Events (MACCE) is a critical component of therapeutic development and risk-benefit assessment. This review synthesizes evidence from recent meta-analyses and clinical trials to objectively validate the safety profile of stem cell therapies across three primary indications: chronic heart failure, acute myocardial infarction, and ischemic stroke. By compiling comparative safety data and delineating underlying biological mechanisms, this analysis aims to inform future clinical trial design and safety monitoring protocols in the field of regenerative medicine.
Comparative Safety Profiles Across Clinical Indications
Chronic Heart Failure
In patients with chronic heart failure, stem cell therapy demonstrates a promising safety profile with no significant increase in MACCE. A 2024 meta-analysis of 36 randomized controlled trials (RCTs) involving 2,801 patients provided robust safety validation for both bone-marrow mononuclear cells (BMMNCs) and mesenchymal stem cells (MSCs) [113].
Key Safety Findings in Heart Failure:
- No significant difference in MACE: The risk ratio for major adverse cardiovascular events was 0.83 (95% CI: 0.67-1.06), indicating no statistically significant increase in adverse events compared to control groups [113].
- Potential mortality benefit: A marginally decreased risk of all-cause death was observed (RR: 0.82, 95% CI: 0.68-0.99) [113].
- Reduced hospitalization risk: Heart failure hospitalization rates were lower in stem cell therapy groups (RR: 0.77, 95% CI: 0.61-0.98) [113].
- No difference between cell types: Subgroup analyses revealed no statistically significant differences in safety outcomes between BMMNCs and MSCs (between-subgroup p > 0.05) [113].
Table 1: Safety Outcomes of Stem Cell Therapy in Chronic Heart Failure
| Safety Outcome | Risk Ratio (95% CI) | Number of Studies | Number of Patients | Between-Subgroup P-value (BMMNC vs. MSC) |
|---|---|---|---|---|
| Major Adverse Cardiovascular Events | 0.83 (0.67-1.06) | 36 | 2,801 | 0.12 |
| All-Cause Mortality | 0.82 (0.68-0.99) | 36 | 2,801 | >0.05 |
| Hospitalization for Heart Failure | 0.77 (0.61-0.98) | 36 | 2,801 | >0.05 |
| Left Ventricular Ejection Fraction Improvement | BMMNC: 3.05% (1.11-4.99); MSC: 2.82% (1.19-4.45) | 36 | 2,801 | 0.86 |
Acute Myocardial Infarction
For patients with acute myocardial infarction (AMI), recent evidence confirms the safety of stem cell interventions without excess adverse events. A comprehensive meta-analysis of 48 RCTs concluded that stem cell-based therapies did not lead to significant increases in serious adverse events compared to control treatments [114].
Key Safety Findings in Acute Myocardial Infarction:
- Comparable serious adverse events: The risk ratio for serious adverse events was 0.93, with no statistically significant difference between groups [114].
- No mortality benefit observed: Risk ratio for all-cause mortality was 0.73, which was not statistically significant [114].
- No increased cerebrovascular risk: The risk of stroke was comparable between groups (RR: 0.81) [114].
- No oncogenic concern: No increased risk of cancer was observed following stem cell administration (RR: 0.82) [114].
Table 2: Safety Outcomes of Stem Cell Therapy in Acute Myocardial Infarction
| Safety Outcome | Risk Ratio (95% CI) | Number of Studies | Number of Patients |
|---|---|---|---|
| All-Cause Mortality | 0.73 | 48 | Not reported |
| Serious Adverse Events | 0.93 | 48 | Not reported |
| Recurrent Myocardial Infarction | 0.67 | 48 | Not reported |
| Heart Failure Hospitalization | 0.79 | 48 | Not reported |
| Cancer Incidence | 0.82 | 48 | Not reported |
| Stroke | 0.81 | 48 | Not reported |
Ischemic Stroke
The safety profile of stem cell therapy in ischemic stroke patients has been extensively validated across multiple meta-analyses, with consistent findings of no significant increase in serious adverse events. A 2025 analysis of 18 RCTs involving 1,026 patients demonstrated comparable safety between stem cell and control groups [115].
Key Safety Findings in Ischemic Stroke:
- No excess mortality: A 2025 meta-analysis of 13 RCTs (872 patients) found no significant difference in all-cause mortality between stem cell therapy and control groups (RR: 0.72, 95% CI: 0.49-1.08) [5].
- Comparable serious adverse events: The incidence of serious adverse events was similar between groups (RR: 0.85, 95% CI: 0.70-1.04) [5].
- Functional improvement: Significant improvements in modified Rankin Scale scores were observed at 1-year follow-up (RR for mRS 0-1: 1.74, 95% CI: 1.09-2.77) [5].
- Differential efficacy by cell type: Network meta-analysis revealed that umbilical cord blood MSCs (UCB-MSCs) ranked highest for neurological recovery, while BMMNCs excelled in improving motor function and daily living activities [116].
Table 3: Safety and Efficacy Outcomes of Stem Cell Therapy in Ischemic Stroke
| Outcome Measure | Stem Cell Type | Effect Size (95% CI) | SUCRA Value (%) |
|---|---|---|---|
| NIHSS (Neurological Function) | UCB-MSC | Not applicable | 69.4% |
| Peripheral Blood SC | Not applicable | 29.2% | |
| BM-MSC | Not applicable | 0.8% | |
| mRS (Disability) | BMMNC | Not applicable | 66.8% |
| Peripheral Blood SC | Not applicable | 31.7% | |
| Progenitor Cells | Not applicable | 1.3% | |
| FMA (Motor Function) | BMMNC | Not applicable | 79.3% |
| BM-MSC | Not applicable | 17.3% | |
| UCB-MSC | Not applicable | 3.4% | |
| MBI (Daily Living) | BMMNC | Not applicable | 56.3% |
| Progenitor Cells | Not applicable | 34.2% | |
| BM-MSC | Not applicable | 9.5% |
Methodological Approaches for Safety Assessment
Standardized Experimental Protocols
The consistent safety profile observed across indications reflects methodological standardization in clinical trial design and safety monitoring.
Core Methodological Components:
- Cell Preparation and Characterization: All studies included precise characterization of cell populations using flow cytometry for specific surface markers (CD34, CD45, CD90, CD105) and viability assessment via dye exclusion tests [117].
- Delivery Protocols: Standardized delivery approaches included intracoronary infusion for cardiac applications (over 30 seconds to 2 minutes with balloon occlusion) and intravenous or intra-arterial injection for stroke applications [113] [114].
- Safety Endpoint Adjudication: Pre-specified safety endpoints included MACE (typically a composite of death, myocardial infarction, stroke, and revascularization), heart failure hospitalization, and serious adverse events, adjudicated by blinded clinical events committees [113] [5].
- Follow-up Duration: Systematic follow-up ranging from 6 months to 5 years, with most studies reporting 12-month safety data [113] [114].
Figure 1: Methodological Workflow for Stem Cell Therapy Safety Assessment
Mechanisms Underlying Safety Profile
The favorable safety profile of stem cell therapies, particularly the lack of excess MACCE, can be attributed to several biological mechanisms that have emerged from preclinical and clinical studies.
Key Safety Mechanisms:
- Paracrine Signaling: Rather than replacing damaged tissue through direct differentiation, stem cells primarily exert effects through paracrine signaling, releasing vesicles and factors that modulate inflammation, apoptosis, and endogenous repair processes [118] [66].
- Immunomodulatory Properties: MSCs specifically demonstrate potent immunomodulatory effects, suppressing pro-inflammatory T-cell responses and promoting regulatory T-cell activity, which may mitigate inflammatory damage without triggering excessive immune activation [117].
- Metabolic Regulation: Preclinical evidence suggests stem cells can improve pathological metabolic remodeling in ischemic tissues by normalizing glucose utilization, fatty acid oxidation, and mitochondrial function, potentially reducing arrhythmic complications [118].
- Angiogenic Potential: Controlled enhancement of angiogenesis through VEGF and other angiogenic factor secretion may improve perfusion without promoting pathological neovascularization or plaque instability [118].
Figure 2: Biological Mechanisms Contributing to Stem Cell Therapy Safety
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for Stem Cell Safety Studies
| Reagent/Material | Primary Function | Application Context |
|---|---|---|
| Flow Cytometry Antibodies (CD34, CD45, CD90, CD105) | Cell population characterization and purity assessment | Quality control for manufactured cell products; verification of cell identity |
| Viability Assays (Trypan blue, Methylene blue exclusion) | Determination of cell viability prior to administration | Ensuring minimum viability thresholds (>70-80%) for clinical use |
| Cell Culture Media (X-VIVO 10, Plasma-Lyte A) | Maintenance of cell function during processing and delivery | Preservation of cell viability and function during transportation and administration |
| Cryopreservation Solutions (DMSO-based) | Long-term storage of cell products | Maintenance of cell bank inventories and stability studies |
| PCR and ELISA Kits (Cytokine profiling) | Assessment of secretory profile and potency | Lot-to-lot consistency testing; mechanism of action studies |
| Sterility Testing Kits (Mycoplasma, endotoxin) | Safety testing for microbial contamination | Final release criteria for clinical cell products |
The comprehensive safety validation across multiple indications and cell types provides reassuring evidence for the continued clinical development of stem cell therapies. The consistent demonstration of no excess MACCE risk, coupled with potential functional benefits, supports the feasibility of larger Phase III trials aimed at definitive efficacy evaluation.
Critical Research Gaps and Future Directions:
- Long-term Safety Data: Follow-up beyond 5 years remains limited, necessitating extended monitoring for late adverse events.
- Standardized Dosing Protocols: Optimal cell doses, timing of administration, and delivery methods require further refinement through dose-finding studies.
- Predictive Safety Biomarkers: Development of biomarkers to identify patient subgroups with heightened risk for adverse events would enhance patient selection.
- Comparative Effectiveness Research: Direct comparisons between cell types and with established therapies would better position stem cell interventions in treatment algorithms.
The accumulating safety evidence summarized in this review provides a robust foundation for the rational design of future clinical trials and supports the careful expansion of stem cell therapies into broader clinical practice within appropriately structured regulatory frameworks.
Within regenerative medicine, stem cell therapy has emerged as a promising intervention for a range of diseases traditionally managed by conventional pharmacological and surgical treatments. This review synthesizes current evidence from clinical studies and meta-analyses to objectively compare the efficacy of stem cell therapy against standard medical treatments. The analysis is framed within a broader thesis on stem cell clinical outcomes, focusing on quantitative measures of functional improvement, safety profiles, and methodological considerations crucial for researchers and drug development professionals. The comparative assessment spans multiple therapeutic areas, including cardiovascular diseases, neurological disorders, and endocrine conditions, providing a data-driven foundation for evaluating the clinical potential of stem cell-based interventions.
Quantitative Efficacy Comparisons Across Conditions
Cardiovascular Disease
Table 1: Efficacy Outcomes in Heart Disease Treatment
| Outcome Measure | Stem Cell Therapy Group | Conventional Therapy Group | P-value |
|---|---|---|---|
| LVEF Improvement | 30.2% ± 8.4% to 43.6% ± 9.7% | 32.5% ± 7.9% to 36.8% ± 8.1% | < 0.01 |
| 6-Minute Walk Test | 80 meters improvement | 30 meters improvement | < 0.001 |
| Quality of Life (MLHFQ) | 56.2 ± 15.3 to 38.5 ± 12.1 | 54.7 ± 14.5 to 48.6 ± 13.2 | < 0.001 |
| Hospitalization Rates | 10.6% | 27.1% | 0.03 |
Data sourced from a prospective cohort study at Nottingham University Hospital (2024) comparing 47 patients receiving stem cell therapy with 48 patients receiving conventional therapy for heart disease [119].
In cardiac applications, a 2024 prospective cohort study demonstrated significant advantages for stem cell therapy in improving left ventricular ejection fraction (LVEF), functional capacity, and quality of life compared to conventional pharmacological treatments, surgical procedures, or implantable devices [119]. The stem cell group showed a markedly greater improvement in LVEF (13.4% absolute increase versus 4.3% in conventional therapy), along with superior gains in exercise capacity and significantly reduced hospitalization rates [119].
Conversely, a 2025 systematic review and meta-analysis focusing specifically on mesenchymal stem cell (MSC) therapy for heart failure with reduced ejection fraction (HFrEF) reported more modest findings, with only small, non-significant improvements in LVEF (Hedges' g = 0.096, p = 0.18) but significant quality of life improvements (Hedges' g = -0.518, p = 0.01) [3]. This discrepancy highlights the importance of cell type and patient selection in determining therapeutic outcomes.
Neurological Disorders
Table 2: Functional Outcomes in Ischemic Stroke Treatment
| Outcome Measure | Time Point | Stem Cell Therapy Group | Control Group | Risk Ratio [95% CI] |
|---|---|---|---|---|
| mRS Score 0-1 | 365 days | 45/195 (23.1%) | 23/179 (12.8%) | 1.74 [1.09-2.77] |
| mRS Score 0-2 | 90 days | 105/322 (32.6%) | 67/257 (26.1%) | 1.31 [1.01-1.70] |
| NIHSS Score | 180 days | - | - | -0.80 [-1.54 to -0.05] |
| Serious Adverse Events | Overall | 119/330 (36.1%) | 114/279 (40.9%) | 0.85 [0.70-1.04] |
Data compiled from a 2025 meta-analysis of 13 randomized controlled trials involving 872 patients with acute/subacute ischemic stroke [5].
For ischemic stroke, a 2025 systematic review and meta-analysis of 13 randomized controlled trials demonstrated that stem cell therapy significantly improved long-term functional outcomes, with a higher proportion of patients achieving favorable modified Rankin Scale (mRS) scores at 90 days and 1 year post-treatment [5]. The analysis found no significant differences in serious adverse events or mortality between groups, supporting the safety of stem cell interventions in the neurological domain [5].
The therapeutic window and administration route appear critical for optimal outcomes in neurological applications. Current evidence supports stem cell administration within the acute and subacute phases of ischemic stroke (within 1 month of onset), with functional benefits becoming more pronounced at long-term follow-up points [5] [120].
Other Therapeutic Areas
In endocrine applications, a meta-analysis on premature ovarian failure demonstrated that stem cell transplantation significantly improved ovarian function parameters, including increased estradiol levels (SMD: -0.47, 95% CI: -0.73 to -0.21, p < 0.01) and follicle count (P = 0.0255), along with achieving pregnancy (combined proportion: 0.09, 95% CI: 0.03 to 0.15) and live birth outcomes (SMD: 0.09, 95% CI: 0.03 to 0.15) [121].
For diabetic foot ulcers, an overview of systematic reviews suggested potential benefits of stem cell therapy in promoting wound healing and reducing amputation rates, though the supporting evidence was graded as critically low to moderate quality due to methodological limitations in the available studies [122].
Experimental Protocols and Methodologies
Stem Cell Preparation and Delivery Protocols
The methodologies employed in stem cell therapy trials vary significantly across clinical applications, reflecting disease-specific requirements and mechanistic considerations:
Cell Types and Sources: Mesenchymal stem cells (MSCs) represent the most frequently investigated cell type across cardiovascular and neurological applications, sourced primarily from bone marrow (BM-MSCs), adipose tissue (AD-MSCs), or umbilical cord (UC-MSCs) [3] [123]. The International Society for Cellular Therapy defines MSCs by specific surface markers (CD73, CD90, CD105 positive; CD14, CD34, CD45, HLA-DR negative), plastic adherence, and tri-lineage differentiation potential [3].
Delivery Methods: Cardiovascular trials typically employ intracoronary, intravenous, or intramyocardial injection routes [3] [124]. Neurological applications utilize intravenous, intra-arterial, or intranasal administration, with the choice influenced by the target lesion and blood-brain barrier considerations [120]. Optimal dosing regimens remain under investigation, with cardiovascular studies typically employing 20-100 million cells and stroke trials utilizing up to 109 cells for intravenous administration [119] [120].
Timing Considerations: The therapeutic time window significantly influences outcomes. In stroke applications, intervention within the acute and subacute phases (within 1 month of onset) demonstrates superior functional recovery compared to later administration [5]. Cardiovascular applications typically target patients with chronic heart failure who remain symptomatic despite guideline-directed medical therapy [3].
Figure 1: Experimental Workflow for Stem Cell Therapy Clinical Trials
Assessment Methodologies
Standardized assessment protocols enable meaningful comparison between stem cell and conventional therapies:
Cardiac Function: LVEF measured by echocardiography or cardiac MRI serves as the primary quantitative endpoint, supplemented by functional capacity assessments (6-minute walk test) and disease-specific quality of life questionnaires (Minnesota Living with Heart Failure Questionnaire) [119] [3].
Neurological Function: The modified Rankin Scale (mRS) represents the primary disability measure in stroke trials, with secondary endpoints including the National Institutes of Health Stroke Scale (NIHSS) for neurological deficit and Barthel Index (BI) for activities of daily living [5].
Advanced Imaging Techniques: Magnetic resonance imaging (MRI) modalities provide objective biomarkers of treatment efficacy, including diffusion tensor imaging (DTI) for white matter integrity, functional MRI (fMRI) for functional connectivity, and magnetic resonance spectroscopy (MRS) for metabolic changes [120].
Mechanisms of Action and Signaling Pathways
Stem cell therapies exert therapeutic effects through mechanisms distinct from conventional pharmacological approaches:
Paracrine Signaling: Rather than primarily replacing damaged cells, MSCs predominantly secrete bioactive molecules (growth factors, cytokines, exosomes) that modulate the local tissue environment, inhibit apoptosis, and promote endogenous repair mechanisms [3] [120].
Immunomodulation: MSCs demonstrate significant anti-inflammatory properties through T-cell modulation, macrophage polarization toward anti-inflammatory phenotypes, and reduction of pro-inflammatory cytokine production [3] [123].
Angiogenic Potential: Stem cells promote neovascularization in ischemic tissues through secretion of vascular endothelial growth factor (VEGF), angiopoietin-1, and other pro-angiogenic factors, enhancing tissue perfusion and viability [124].
Mitochondrial Transfer: Emerging evidence indicates that MSCs can transfer healthy mitochondria to damaged cells, restoring cellular bioenergetics and promoting survival in ischemic tissues [120].
Figure 2: Comparative Mechanisms: Stem Cell vs. Conventional Therapies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Stem Cell Therapy Investigations
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Stem Cell Markers | CD73, CD90, CD105, CD14, CD34, CD45, HLA-DR | Characterization and purity assessment according to ISCT criteria [3] |
| Differentiation Media | Adipogenic, chondrogenic, osteogenic induction kits | Validation of multilineage differentiation potential [3] |
| Cell Tracking Agents | GFP labeling, superparamagnetic iron oxide nanoparticles (SPIOs) | In vivo cell fate monitoring and migration studies [120] |
| Functional Assays | Transwell migration, tube formation, cytokine arrays | Evaluation of paracrine and functional capacities [3] [123] |
| Animal Models | Myocardial infarction (rodent), middle cerebral artery occlusion (stroke) | Preclinical efficacy and safety assessment [124] [120] |
The comparative analysis of stem cell therapy versus standard medical treatments reveals a complex efficacy landscape characterized by promising functional improvements in specific clinical contexts alongside methodological challenges that require resolution. Current evidence suggests that stem cell therapy, particularly MSC-based approaches, demonstrates superior outcomes in quality of life measures and certain functional parameters compared to conventional treatments in cardiovascular and neurological applications. However, the field requires further standardization of cell products, delivery protocols, and patient selection criteria to validate and optimize these therapeutic benefits. For drug development professionals and researchers, the evolving evidence base supports continued investment in large-scale, well-controlled clinical trials to establish the definitive role of stem cell therapy within the therapeutic arsenal for degenerative diseases.
Stem cell therapy has emerged as a revolutionary frontier in regenerative medicine, demonstrating potential across a wide spectrum of debilitating diseases and injuries [65]. These therapies leverage the unique properties of stem cells, including self-renewal and differentiation into specialized cell types, making them indispensable for therapeutic applications targeting tissue repair and regeneration [65]. As the field evolves, a critical need exists to objectively evaluate and compare the relative efficacy of these treatments across different disease states to guide research priorities and clinical application.
This comparative guide synthesizes current evidence from randomized controlled trials and meta-analyses to evaluate the performance of stem cell therapies, primarily focusing on mesenchymal stem cells (MSCs), across neurological, cardiovascular, and autoimmune conditions. MSCs are particularly attractive therapeutic agents due to their multipotency, immunomodulatory properties, and availability from various tissues, including bone marrow, adipose tissue, and umbilical cord [9] [6]. We present structured quantitative data, detailed methodological protocols, and analytical frameworks to provide researchers, scientists, and drug development professionals with a comprehensive evidence synthesis for cross-condition efficacy assessment.
Comparative Efficacy Tables Across Disease States
Primary Efficacy Outcomes for Major Disease Categories
The table below summarizes the relative improvement magnitudes of stem cell therapy across different disease conditions based on recent meta-analyses of randomized controlled trials.
Table 1: Cross-Condition Efficacy Analysis of Stem Cell Therapies
| Disease Category | Specific Condition | Primary Efficacy Endpoint | Relative Improvement (vs. Control) | Statistical Significance | Number of RCTs/Participants |
|---|---|---|---|---|---|
| Neurological | Acute/Subacute Ischemic Stroke | mRS score 0-1 at 1 year | Risk Ratio: 1.74 (95% CI: 1.09-2.77) [5] | P = 0.020 | 13 RCTs (872 participants) [5] |
| mRS score 0-2 at 90 days | Risk Ratio: 1.31 (95% CI: 1.01-1.70) [5] | P = 0.044 | 13 RCTs (872 participants) [5] | ||
| Cardiovascular | Heart Failure with Reduced Ejection Fraction (HFrEF) | Left Ventricular Ejection Fraction (LVEF) | Hedges' g = 0.096 [3] | P = 0.18 (NS) | 12 RCTs (Systematic Review) [3] |
| Quality of Life (QoL) | Hedges' g = -0.518 [3] | P = 0.01 | 12 RCTs (Systematic Review) [3] | ||
| Autoimmune & Rheumatic | Osteoarthritis (OA) - Pain (VAS) | Bone Marrow MSCs: SMD = -0.95 [6] | P = 0.002 | 42 RCTs (2,183 participants) [6] | |
| Umbilical Cord MSCs: SMD = -1.25 [6] | P = 0.002 | 42 RCTs (2,183 participants) [6] | |||
| Adipose Tissue MSCs: SMD = -1.26 [6] | P = 0.0009 | 42 RCTs (2,183 participants) [6] | |||
| Systemic Lupus Erythematosus (SLEDAI) | SMD = -2.32 [6] | P = 0.0003 | 42 RCTs (2,183 participants) [6] | ||
| Inflammatory Bowel Disease (Clinical Efficacy) | Risk Ratio: 2.02 (95% CI: 1.53-2.67) [6] | P < 0.00001 | 42 RCTs (2,183 participants) [6] | ||
| Multiple Sclerosis | Not Significant [6] | NS | 42 RCTs (2,183 participants) [6] |
Safety Profile Comparison Across Conditions
The safety profile of stem cell therapies is a critical consideration for clinical translation. The table below compares adverse event rates across different medical conditions.
Table 2: Safety Profile of Stem Cell Therapies Across Conditions
| Condition | Serious Adverse Events (Risk Ratio) | Mortality (Risk Ratio) | Statistical Significance |
|---|---|---|---|
| Acute/Subacute Ischemic Stroke [5] | RR = 0.85 (95% CI: 0.70-1.04) | RR = 0.72 (95% CI: 0.49-1.08) | P = 0.11 (NS) |
| Osteoarthritis [6] | RR = 1.23 (95% CI: 0.93-1.65) | - | P = 0.15 (NS) |
| Systemic Lupus Erythematosus [6] | RR = 0.83 (95% CI: 0.28-2.51) | - | P = 0.76 (NS) |
| Inflammatory Bowel Disease [6] | RR = 0.99 (95% CI: 0.81-1.22) | - | P = 0.96 (NS) |
| Multiple Sclerosis [6] | RR = 1.12 (95% CI: 0.81-1.53) | - | P = 0.50 (NS) |
Experimental Protocols and Methodologies
Common Methodological Framework for Stem Cell Clinical Trials
Stem Cell Source and Characterization Clinical trials included in this analysis primarily utilized mesenchymal stem cells (MSCs) from various sources, including bone marrow (BM-MSCs), adipose tissue (AD-MSCs), and umbilical cord (UC-MSCs) [9] [6]. According to International Society for Cellular Therapy (ISCT) standards, MSCs were defined by three key criteria: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, and CD105 ≥95%; lack of expression of hematopoietic markers CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [9] [6].
Cell Processing and Delivery Protocols Processing methods varied across studies but shared common elements. For neurological applications such as ischemic stroke, stem cells were typically administered via intravenous infusion or direct intracranial injection [5]. For cardiovascular conditions like HFrEF, intracoronary infusion or intramyocardial injection were common delivery routes [3]. In autoimmune diseases, intravenous infusion was the predominant administration method [6].
Advanced processing techniques included:
- CD34 positive selection for stem cell isolation (with 25-50% reduction in total stem cell yield)
- Selective T-cell removal in allogeneic transplants to reduce graft-versus-host disease
- Genetic engineering approaches, including CXCR4 overexpression to enhance cell homing to ischemic regions
- Neural stem cells loaded with superparamagnetic iron oxide nanoparticles to increase proliferation rates [125]
Dosage and Timing Parameters The specific doses and timing of interventions varied substantially across studies. For ischemic stroke, interventions occurred within 1 month of stroke onset [5]. In chronic conditions like osteoarthritis and autoimmune diseases, treatment timing was more flexible, with follow-up periods ranging from 6 months to 3.5 years across various studies [5] [6].
Efficacy Assessment Methodologies
Neurological Function Assessment For stroke trials, the modified Rankin Scale (mRS) was the primary outcome measure, assessing disability and functional independence [5]. Additional measures included the National Institutes of Health Stroke Scale (NIHSS) for neurological impairment and the Barthel Index (BI) for activities of daily living [5].
Cardiac Function Assessment For HFrEF, the primary efficacy measure was the change in left ventricular ejection fraction (LVEF) measured by echocardiography or cardiac MRI [3]. Secondary outcomes included the 6-Minute Walk Test (6MWT) for functional capacity and quality of life questionnaires [3].
Autoimmune Disease Activity Assessment Disease-specific indices were employed for autoimmune conditions: the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) for osteoarthritis, Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) for SLE, and clinical efficacy rates for inflammatory bowel disease [6].
Signaling Pathways and Mechanisms of Action
Multimodal Mechanistic Framework of Mesenchymal Stem Cells
Figure 1: Multimodal Mechanistic Framework of MSCs
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Stem Cell Types | Mesenchymal Stem Cells (MSCs), Bone Marrow Mononuclear Cells, Induced Pluripotent Stem Cells (iPSCs) [65] [5] [107] | Therapeutic agents with regenerative and immunomodulatory properties |
| Characterization Markers | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) [9] [6] | MSC identification and purity verification per ISCT standards |
| Culture Components | Plastic-adherent culture flasks, Specific serum formulations [9] | MSC expansion and maintenance while preserving differentiation potential |
| Differentiation Media | Osteogenic, Chondrogenic, Adipogenic induction cocktails [9] | Verification of multilineage differentiation capacity |
| Engineering Tools | CXCR4 overexpression vectors, Superparamagnetic iron oxide nanoparticles [125] | Enhancement of homing capability and tracking ability |
| Delivery Systems | CD34+ selection devices, Intracoronary catheters, Stereotactic injection apparatus [5] [125] | Targeted administration of cellular products |
| Tracking Reagents | Iron oxide nanoparticles, Fluorescent labels [125] | In vivo monitoring of cell migration and engraftment |
Analytical Framework for Cross-Condition Efficacy Evaluation
Efficacy- Effectiveness Translation Considerations
The translation of efficacy demonstrated in controlled trials to effectiveness in real-world settings varies across conditions and healthcare systems [126]. Understanding the "efficacy-effectiveness gap" requires consideration of biological factors (genetics, age, comorbidities, disease severity) and behavioral factors (adherence to treatment regimens) [126]. Furthermore, system-level factors including healthcare organization, resources, and patient management protocols significantly influence long-term outcomes [126].
The health production function framework provides a systematic approach for identifying and quantifying determinants of relative effectiveness and sources of variation between populations [126]. This approach classifies inputs into three main levels: patient, provider, and healthcare environment or system, enabling more accurate prediction of real-world outcomes across different jurisdictions [126].
Statistical Considerations for Cross-Condition Comparison
Appropriate statistical methodology is crucial for valid cross-condition efficacy comparisons. Parametric methods (t-tests, ANOVA, linear mixed models) are efficient under well-defined assumptions of normality and homogeneity of variance [127]. Nonparametric techniques (Friedman test, Brunner-Munzel test) provide robust alternatives for skewed, ordinal, or non-normal data distributions commonly encountered in clinical outcomes [127]. Bayesian approaches enable incorporation of prior knowledge and uncertainty quantification, particularly valuable in rare diseases with limited sample sizes [127].
For missing data, which are almost unavoidable in clinical research, appropriate handling based on the missingness mechanism (MCAR, MAR, MNAR) is essential for validity [127]. Likelihood-based estimation and multiple imputation can provide valid inference under missing-at-random assumptions, while specialized models (selection models, pattern-mixture models) are required for data missing not at random [127].
Mesenchymal stem cells (MSCs) have emerged as a cornerstone of regenerative medicine due to their multipotent differentiation capacity, immunomodulatory properties, and potential for self-renewal [9]. Originally identified in bone marrow, MSCs have since been isolated from numerous tissue sources, each exhibiting distinct biological characteristics and therapeutic potentials [9] [128]. The International Society for Cellular Therapy (ISCT) establishes minimum criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73, CD90, CD105 positive; CD34, CD45, HLA-DR negative), and in vitro tri-lineage differentiation potential (osteogenic, chondrogenic, and adipogenic) [9] [3].
Among the various sources, bone marrow-derived MSCs (BM-MSCs), umbilical cord-derived MSCs (UC-MSCs), and adipose tissue-derived MSCs (AD-MSCs) represent the most extensively studied and clinically relevant populations [128]. The selection of an optimal MSC source is critical for therapeutic success, as the tissue of origin significantly influences functional characteristics including proliferation rate, secretome composition, differentiation potential, and immunomodulatory capacity [128]. This review provides a comprehensive, data-driven comparison of BM-MSCs, UC-MSCs, and AD-MSCs to inform research applications and clinical translation in regenerative medicine.
Bone Marrow-derived MSCs (BM-MSCs) were the first discovered and remain the most extensively characterized MSC population [9]. Harvested primarily from iliac crest aspirates, BM-MSCs represent the reference standard against which other MSC sources are compared [128]. They are particularly noted for their strong osteogenic potential and robust immunomodulatory effects [9].
Adipose Tissue-derived MSCs (AD-MSCs) are obtained from lipoaspirate or resected adipose tissue [128]. These cells share similarities with BM-MSCs but offer practical advantages including higher tissue availability and less invasive harvesting procedures [128]. AD-MSCs demonstrate enhanced proliferation rates compared to BM-MSCs, with donor age having less impact on their expansion potential [128].
Umbilical Cord-derived MSCs (UC-MSCs) are isolated from various umbilical cord compartments, including Wharton's jelly, perivascular region, and cord tissue itself [128]. As neonatal-derived cells, UC-MSCs exhibit primitive properties with higher proliferation capacity and lower immunogenicity compared to adult-derived sources [9] [128]. Their collection poses no donor risk and raises fewer ethical concerns [128].
Table 1: Comparative Characteristics of Primary MSC Sources
| Parameter | BM-MSCs | AD-MSCs | UC-MSCs |
|---|---|---|---|
| Tissue Source | Iliac crest bone marrow aspirate | Lipoaspirate or adipose tissue | Wharton's jelly, perivascular region, or cord tissue |
| Harvesting Procedure | Invasive, painful | Minimally invasive | Non-invasive, no donor risk |
| Cell Yield | Low (0.001-0.01% of nucleated cells) | High (∼500,000 cells/gram fat) | High (substantial tissue amount) |
| Proliferation Capacity | Moderate | High, less influenced by donor age | Highest among sources |
| Immunogenicity | Low | Low | Very low (suitable for allogeneic use) |
| Primary Research Applications | Bone regeneration, immunomodulation | Angiogenesis, fat grafting, osteoarthritis | Neurological disorders, cardiac repair, immunomodulation |
Secretome and Functional Protein Profiles
The therapeutic effects of MSCs are increasingly attributed to their paracrine activity rather than direct differentiation and engraftment [9] [129]. Comparative analysis of secretory profiles reveals significant differences between MSC sources that inform their therapeutic specialization.
Table 2: Comparative Secretome Profile of MSC Sources
| Secreted Factor | BM-MSCs | AD-MSCs | UC-MSCs | Functional Significance |
|---|---|---|---|---|
| IL-6 | Lower secretion | Intermediate | Highest secretion | Pleiotropic inflammatory mediator |
| IL-8 | Lower secretion | Intermediate | Highest secretion | Neutrophil chemotaxis and angiogenesis |
| VEGF | Moderate | Higher levels | Moderate | Angiogenesis induction |
| BDNF | Moderate | Higher levels | Moderate | Neuronal survival and differentiation |
| TGF-β | Moderate | Moderate | Higher levels | Immunoregulation and fibrosis |
| MMP-1 | Lower secretion | Higher secretion | Intermediate | Collagen degradation |
| MMP-3 | Lower secretion | Higher secretion | Intermediate | Extracellular matrix remodeling |
| IL-1RA | Moderate | Moderate | Highest secretion | Anti-inflammatory (IL-1 receptor antagonist) |
BM-MSCs secrete lower concentrations of pro-inflammatory cytokines such as IL-6 and IL-8 compared to AD-MSCs and UC-MSCs [128]. They also produce lower levels of matrix metalloproteinases (MMPs) including MMP-1 (collagenase 1) and MMP-3 (stromelysin 1), and notably do not secrete MMP-13 (collagenase 3) [128]. This reduced proteolytic enzyme profile makes BM-MSCs strong candidates for regeneration of bone, cartilage, and tendons [128].
UC-MSCs from Wharton's jelly demonstrate a stronger anti-inflammatory profile compared to other sources, secreting higher levels of IL-1RA and IFN-α, along with the highest levels of IL-6, IL-8, TGF-β2, and PDGF-AA [128]. This enhanced immunomodulatory capacity positions UC-MSCs favorably for treating inflammatory and autoimmune conditions.
AD-MSCs exhibit superior angiogenic potential, likely attributable to their higher secretion of vascular endothelial growth factor (VEGF) and brain-derived neurotrophic factor (BDNF) [128]. In comparative preclinical studies of spinal cord injury, AD-MSCs demonstrated greater potential for enhancing angiogenesis compared to BM-MSCs [128].
Experimental Methodologies for MSC Comparison
Standardized Isolation and Culture Protocols
BM-MSC Isolation Protocol: Bone marrow aspirates are collected into heparinized tubes and diluted with phosphate-buffered saline (PBS). Mononuclear cells are isolated via density gradient centrifugation using Ficoll-Paque (1.077 g/mL) at 400-800 × g for 30 minutes [9]. The interface layer containing mononuclear cells is collected, washed, and resuspended in complete culture medium: α-MEM or DMEM/F-12 supplemented with 10-15% fetal bovine serum (FBS), 2 mM L-glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin [9]. Cells are plated at 1-5 × 10^5 cells/cm² and maintained at 37°C with 5% CO₂. Non-adherent cells are removed after 48-72 hours, and medium is changed twice weekly [9]. Upon reaching 70-80% confluence, cells are detached using 0.25% trypsin/EDTA and subcultured at 1:3 ratios.
AD-MSC Isolation Protocol: Adipose tissue samples are washed extensively with PBS containing 5% antibiotic-antimycotic solution [128]. The extracellular matrix is digested with 0.1-0.3% collagenase type I or II at 37°C with agitation for 45-90 minutes [128]. Enzyme activity is neutralized with complete culture medium (DMEM/F12 with 10% FBS), and the digest is centrifuged at 600-1200 × g for 10 minutes. The resulting stromal vascular fraction (SVF) pellet is resuspended, filtered through 70-100μm mesh, and plated in culture vessels [128]. Expansion medium typically consists of DMEM/F12 with 10% FBS, 2 mM L-glutamine, and antibiotics. Cells are cultured at 37°C with 5% CO₂ with medium changes twice weekly.
UC-MSC Isolation Protocol: Umbilical cords are collected in sterile PBS or saline with antibiotics [128]. Blood vessels are removed, and Wharton's jelly tissue is minced into 1-2mm³ fragments. Explants are either placed directly on culture surfaces or digested enzymatically with collagenase type IV (0.5-1mg/mL) and hyaluronidase (30μg/mL) for 2-4 hours at 37°C [128]. For explant culture, tissue pieces are allowed to adhere to plastic for 5-7 days before adding complete medium (DMEM/F12 with 10% FBS, 2mM L-glutamine, antibiotics). Migrated cells are harvested upon confluence. UC-MSCs typically exhibit faster population doubling times and can be maintained for more passages before senescence compared to adult sources [128].
Differentiation Capacity Assessment
Osteogenic Differentiation: Confluent MSC cultures (P3-P5) are induced with osteogenic medium: basal medium supplemented with 10mM β-glycerophosphate, 50μM ascorbic acid-2-phosphate, and 100nM dexamethasone for 21-28 days [9] [3]. Differentiation is confirmed by Alizarin Red S staining detecting calcium deposits and expression of osteogenic markers (alkaline phosphatase, osteocalcin, RUNX2).
Adipogenic Differentiation: Confluent MSCs are treated with adipogenic induction medium: DMEM with 10% FBS, 1μM dexamethasone, 0.5mM isobutylmethylxanthine (IBMX), 10μg/mL insulin, and 200μM indomethacin for 14-21 days [9] [3]. Lipid accumulation is visualized by Oil Red O staining, with adipogenic commitment confirmed by PPAR-γ and FABP4 expression.
Chondrogenic Differentiation: 2.5×10^5 MSCs are pelleted in conical tubes and cultured in chondrogenic medium: DMEM containing 1% ITS+ premix, 100nM dexamethasone, 50μg/mL ascorbic acid-2-phosphate, 40μg/mL proline, and 10ng/mL TGF-β3 for 21-28 days [9] [3]. Cartilage matrix production is assessed by Alcian blue or Safranin O staining for proteoglycans, with collagen type II expression confirming chondrogenic differentiation.
Therapeutic Performance Across Disease Models
Neurological Applications
In neurological disorders including spinal cord injury, multiple sclerosis, and stroke, MSC sources demonstrate distinct therapeutic profiles. Comparative studies in spinal cord injury models indicate that UC-MSCs and BM-MSCs show similar efficacy in inducing symptom relief, but UC-MSCs demonstrate higher survival rates post-transplantation, suggesting that fewer cells may be required to achieve therapeutic effects [128].
When comparing AD-MSCs and BM-MSCs in spinal cord injury models, both cell types survived, migrated to the injury site, and improved locomotor function while reducing lesion cavity size [128]. However, AD-MSCs produced superior functional outcomes, attributed to their greater angiogenic potential mediated by higher BDNF and VEGF secretion [128].
In multiple sclerosis, clinical trials have demonstrated that high doses of UC-MSCs improved quality of life and prevented disease progression, whereas lower doses of BM-MSCs provided limited functional benefits [128]. This suggests potential dose-response differences between MSC sources in inflammatory neurological conditions.
Cardiac and Metabolic Applications
In heart failure with reduced ejection fraction (HFrEF), MSC therapy has demonstrated safety and improvement in quality of life, though effects on left ventricular ejection fraction (LVEF) have been inconsistent across studies [3]. Meta-analysis of clinical trials shows MSC therapy results in only small, non-significant improvements in LVEF (Hedges' g = 0.096, p = 0.18), with low heterogeneity between studies (I² = 0.5%) [3]. However, quality of life measures showed significant improvement (Hedges' g = −0.518, p = 0.01) [3].
Notably, umbilical cord-derived MSCs have demonstrated particular promise in cardiac applications. One study reported that UC-MSCs improved both left ventricular function and quality of life in HFrEF patients [3]. The therapeutic mechanisms primarily involve paracrine effects rather than direct differentiation, with MSC-secreted factors promoting angiogenesis, reducing apoptosis, and modulating inflammatory responses [3].
In metabolic diseases like type 2 diabetes mellitus (T2DM), MSC-based therapies have significantly improved glycemic control, reduced insulin requirements, and enhanced β-cell function in both clinical and preclinical settings [130]. Safety profiles have been favorable, with primarily transient and self-limiting adverse effects reported [130]. Both autologous and allogeneic MSC approaches have shown efficacy, suggesting that donor source may be flexible for metabolic applications.
Orthopedic Applications
In orthopedic conditions such as knee osteoarthritis (KOA), MSC therapy has demonstrated significant impacts on pain reduction and functional improvement [131]. When combined with arthroscopy, MSC treatment promotes regeneration of articular cartilage, subchondral bone, and joint-space width, as measured by WOMAC, VAS, KOOS, and ICRS scoring systems, along with radiological improvement on MRI [131].
The selection between BM-MSCs and AD-MSCs for orthopedic applications involves important trade-offs. While BM-MSCs have extensive therapeutic features and high affinity during treatment, their harvest is associated with increased pain and morbidity due to the invasive aspiration procedure [131]. Conversely, AD-MSCs are increasingly viewed as a safer and effective alternative, accessible from waste tissues following liposuction or abdominoplasties with less donor site morbidity [131].
Signaling Pathways and Molecular Mechanisms
The therapeutic effects of different MSC sources are mediated through distinct signaling pathways that reflect their tissue-specific origins and functional specializations.
UC-MSCs demonstrate particularly strong activity in the Wnt/β-catenin and Hippo signaling pathways, which contribute to their enhanced proliferative capacity and tissue-regenerative properties [132]. When transfected with miRNA-21, UC-MSCs further enhance their therapeutic potential through inhibition of the PTEN/AKT/FOXO3a signaling pathway [132].
AD-MSCs exhibit potent effects on mitochondrial function through activation of the AMPK/NR4A1 signaling axis, reducing oxidative stress and inhibiting excessive autophagy [132]. This mitochondrial regulation capability enables AD-MSCs to improve oocyte quality and fertility in aged animal models via mitochondrial transfer [132].
BM-MSCs show robust activity in the TGF-β1/Smad3 signaling pathway, contributing to their immunomodulatory potency and connective tissue regeneration capacity [132]. This pathway activation underpins the effectiveness of BM-MSCs in modulating immune responses in conditions like graft-versus-host disease and autoimmune disorders [9].
Research Reagent Solutions
Table 3: Essential Research Reagents for MSC Studies
| Reagent Category | Specific Products | Research Application | Technical Notes |
|---|---|---|---|
| Isolation Enzymes | Collagenase Type I, II, IV; Hyaluronidase | Tissue dissociation and stromal cell liberation | Concentration and incubation time vary by tissue source (0.1-0.3% for adipose, 0.5-1% for umbilical cord) |
| Culture Media | α-MEM, DMEM/F12, DMEM-LG | MSC expansion and maintenance | Supplement with 10-15% FBS or defined serum alternatives; avoid high glucose for certain applications |
| Serum Supplements | Fetal Bovine Serum (FBS), Platelet Lysate, Serum-free Formulations | Cell growth and proliferation | Batch testing critical for consistent performance; consider defined serum-free options for clinical translation |
| Differentiation Kits | Osteogenic, Adipogenic, Chondrogenic Induction Media | Multilineage differentiation assessment | Follow standardized induction protocols with appropriate positive controls |
| Characterization Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR | Immunophenotyping by flow cytometry | Use ≥95% positive for CD73, CD90, CD105; ≤2% positive for hematopoietic markers |
| Functional Assays | CFU-F Assay, Transwell Migration, Mixed Lymphocyte Reaction | Clonogenicity, migration, and immunomodulation assessment | Establish donor-specific baseline values for comparative studies |
The comparative analysis of BM-MSCs, AD-MSCs, and UC-MSCs reveals a complex landscape where each source offers distinct advantages for specific research and clinical applications. BM-MSCs remain the most extensively characterized source with proven utility in bone regeneration and immunomodulation, though their invasive harvest and age-dependent quality represent limitations. AD-MSCs provide practical advantages of accessibility and yield, demonstrating superior angiogenic potential that positions them favorably for vascularized tissue engineering and osteoarthritis applications. UC-MSCs offer the highest proliferation capacity and strongest immunomodulatory profile, making them ideal candidates for allogeneic banking and inflammatory disorder treatment.
Future research directions should prioritize the development of standardized isolation and characterization protocols to reduce heterogeneity in MSC populations [128] [129]. Additionally, investigation into preconditioning strategies and combination therapies may further enhance the therapeutic efficacy of all MSC sources [132]. As single-cell transcriptomic analyses advance, more precise functional subpopulations within each MSC source will likely be identified, enabling refined selection for specific applications [133]. The growing understanding of MSC-derived extracellular vesicles as potential cell-free therapeutics represents another promising avenue that may circumvent challenges associated with whole-cell transplantation [129] [132].
The selection of optimal MSC source ultimately depends on the specific research or clinical context, weighing factors including target tissue, disease pathophysiology, practical constraints, and desired mechanism of action. This comparative analysis provides an evidence-based framework to guide researchers and clinicians in making informed decisions regarding MSC source selection for regenerative medicine applications.
The evaluation of stem cell therapies relies heavily on robust clinical evidence to confirm their safety and efficacy. Within this evidence hierarchy, Randomized Controlled Trials (RCTs) and Non-Randomized Controlled Trials (nRCTs) represent two fundamental study designs, each with distinct methodological strengths and limitations. RCTs are traditionally considered the gold standard for establishing the efficacy of medical interventions because the random assignment of participants to intervention or control groups minimizes selection bias and controls for both known and unknown confounding variables [134] [135]. This process is intended to ensure that any differences in outcomes can be attributed to the intervention itself, thus providing high internal validity [136] [137].
Conversely, nRCTs are clinical trials where investigators allocate participants to different groups without random assignment [138] [139]. These studies, which include observational cohort, case-control, and quasi-experimental designs, are often employed when RCTs are prohibitively expensive, time-consuming, ethically problematic, or impractical to conduct [136] [135]. While nRCTs can offer valuable real-world evidence and greater external validity, they are more susceptible to biases, particularly selection bias and confounding, which can threaten the validity of their causal inferences [138] [140].
In the rapidly advancing field of stem cell therapeutics, where clinical outcomes are often measured through complex meta-analyses, understanding the impact of study design on outcome estimates is paramount. This guide provides a comparative assessment of RCTs and nRCTs, focusing on their methodological quality and the consequent effects on reported outcomes within stem cell research.
Quantitative Outcome Comparisons in Meta-Analyses
Empirical evidence from meta-analyses directly comparing RCTs and nRCTs reveals that the choice of study design can lead to clinically relevant differences in outcome estimates.
Table 1: Summary of Meta-Analytic Comparisons of RCTs vs. nRCTs
| Field of Medicine | Nature of Discrepancy | Reported Magnitude/Proportion of Differences | Source |
|---|---|---|---|
| Breast Cancer Surgery | Clinically relevant differences in effect estimates for surgical procedures. | 20-40% of topics showed clinically relevant differences [140]. | Meta-analysis |
| Digestive System Surgery | Comparison of effects between RCTs and nRCTs. | ~25% of nRCTs gave different results from RCTs [140]. | Meta-analysis |
| General Medical Literature | Greater than two-fold difference in odds ratios. | 33% of topics examined showed significant differences [140]. | Meta-analysis |
A specific example from stem cell research for liver disease illustrates how outcome measures can vary. A 2018 meta-analysis in Translational Medicine reported that stem cell therapy for acute-on-chronic liver failure (ACLF) showed significant improvement in certain biochemical markers compared to controls, but the degree of improvement and the significance of results were influenced by the mix of included study designs (both RCTs and nRCTs) [141]. This underscores the necessity of considering design when interpreting meta-analytic results.
Methodological Protocols: A Side-by-Side Comparison
The fundamental difference between RCTs and nRCTs lies in their approach to participant allocation and the subsequent methods used to ensure validity.
Table 2: Core Methodological Protocols for RCTs and nRCTs
| Methodological Feature | Randomized Controlled Trial (RCT) | Non-Randomized Controlled Trial (nRCT) |
|---|---|---|
| Allocation Sequence | Computer-generated random sequence [137]. | Investigator-determined or participant preference-based allocation [139]. |
| Allocation Concealment | Mandatory to prevent foreknowledge of treatment assignment. | Not applicable, as allocation is often open. |
| Control for Confounding | Primarily achieved through randomization (balances known and unknown confounders at baseline) [134]. | Achieved statistically in the analysis phase using multivariable regression, propensity score matching, or other causal inference methods [136]. |
| Blinding | Often implemented (single, double, or triple-blind) to reduce performance and detection bias. | Frequently difficult or impossible to implement, increasing risk of performance and detection bias. |
| Primary Analysis | Often Intent-to-Treat (ITT) analysis, which maintains the benefits of randomization [135]. | Often Per-Protocol or As-Treated analysis, which can introduce bias. |
Detailed Experimental Workflow: RCT
The following diagram illustrates the standard workflow for a parallel-group RCT, the most common design in clinical research [134].
RCT Participant Flow
Detailed Experimental Workflow: nRCT
The following diagram illustrates a common nRCT workflow, such as an observational cohort study, where groups are formed based on exposure or preference.
nRCT Participant Flow
The Impact of Design on Evidence and Interpretation in Stem Cell Research
The methodological differences between RCTs and nRCTs directly shape the level of evidence they generate and how that evidence should be interpreted, especially in a complex field like stem cell therapy.
Internal Validity versus Generalizability
- RCTs Excel in Internal Validity: The primary strength of a well-conducted RCT is its high internal validity. For instance, in a meta-analysis of stem cell therapy for cardiovascular diseases, high-certainty evidence from RCTs supported improvements in left ventricular end-systolic volume and ejection fraction in acute myocardial infarction [142]. This strong causal inference is possible because randomization minimizes confounding.
- nRCTs Offer Broader Generalizability: nRCTs often include a more diverse patient population that is representative of "real-world" clinical practice, including patients with comorbidities who are frequently excluded from RCTs [136] [135]. This enhances the external validity and applicability of the findings to broader patient populations, answering questions about effectiveness rather than just efficacy.
Navigating the Evidence Hierarchy
The following diagram illustrates the logical relationship between study design, its methodological attributes, and the strength of evidence it contributes within a meta-analytic framework.
Evidence Generation Logic
The Scientist's Toolkit: Key Reagents and Materials
The conduct of both RCTs and nRCTs in stem cell research requires specialized reagents and solutions. The table below details several key components.
Table 3: Research Reagent Solutions for Stem Cell Clinical Trials
| Reagent/Material | Function in Clinical Research | Application Example |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | The primary investigational biologic product; multipotent cells with immunomodulatory and regenerative potential. | Used in trials for ACLF [141], cardiovascular diseases [142], and chronic low back pain [143]. |
| Bone Marrow Mononuclear Cells (BM-MNCs) | A mixed population of unsorted bone marrow cells, including hematopoietic and mesenchymal stem cells. | Investigated as a therapy for ACLF and decompensated liver cirrhosis [141]. |
| Placebo (e.g., Saline Injection) | An inert substance administered to the control group to blind participants and investigators, mitigating placebo effects. | Serves as the control intervention in double-blind RCTs for chronic low back pain [143] and other conditions. |
| Propensity Score Matching Algorithms | A statistical method used in nRCTs to simulate randomization by creating comparable intervention and control groups based on observed covariates. | Reduces selection bias in observational studies comparing surgical outcomes or drug effectiveness [136] [135]. |
| Validated Patient-Reported Outcome (PRO) Measures | Standardized tools (e.g., VAS, ODI) to quantify subjective outcomes like pain and functional status. | Critical for assessing efficacy in chronic low back pain trials [143]. |
| Cryopreservation Media | Solutions containing cryoprotectants (e.g., DMSO) to maintain cell viability during frozen storage and transport. | Essential for the logistics of cell-based therapies, ensuring consistent product quality in multi-center trials. |
The dichotomy between RCTs and nRCTs is not a simple matter of one being universally superior to the other. Rather, each design answers different but equally important questions. RCTs provide the most reliable evidence for efficacy under controlled conditions, while nRCTs generate crucial insights into effectiveness in routine clinical practice [136] [135]. In stem cell research, where interventions are complex and patient populations heterogeneous, a comprehensive evidence base must incorporate both.
Methodological innovations such as pragmatic clinical trials (PrCTs), which incorporate randomization within real-world settings, and advanced causal inference methods for observational data, are blurring the lines between these designs [136] [135]. The goal for researchers, clinicians, and developers is not to prioritize one design over the other, but to critically appraise the methodology of each study, understand the potential biases, and recognize that triangulation of evidence from multiple study types offers the most robust foundation for evaluating the true clinical value of stem cell therapies [136] [140].
The reproducibility of scientific results is a cornerstone of the research enterprise, serving as a critical mechanism for verifying findings, controlling for error and fraud, and assessing the generalizability of results [144]. In recent decades, what has been termed a "reproducibility crisis" has emerged across multiple scientific fields, with large-scale replication projects frequently failing to reproduce published findings [145] [144]. This crisis encompasses several interconnected problems: the virtual absence of replication studies in many fields, widespread failures to reproduce published results, evidence of publication bias, a high prevalence of questionable research practices that inflate false-positive rates, and insufficient transparency in reporting methods, data, and analyses [144].
Within translational stem cell research, these challenges take on particular significance. As regenerative medicine advances toward clinical applications, ensuring the validity and reproducibility of preclinical findings becomes paramount for patient safety and research progress. This guide examines the current evidentiary strength in stem cell research through the critical lenses of publication bias and reproducibility, providing researchers with methodological frameworks to assess and enhance the reliability of scientific findings in this rapidly evolving field.
Clinical Evidence Assessment: Stem Cell Therapies Across Conditions
The clinical evidence for stem cell therapies varies considerably across medical conditions. The tables below summarize key efficacy and safety findings from recent meta-analyses, highlighting both promising results and ongoing limitations in the evidence base.
Table 1: Clinical Outcomes of Stem Cell Therapy for Knee Osteoarthritis
| Outcome Measure | Number of Comparative Studies | Studies Favoring MSC Group | Studies Exceeding MCID | Evidence Quality (GRADE) |
|---|---|---|---|---|
| Patient-Reported Outcomes | 10 | 7 | 4 | Low to Very Low |
| Pain VAS | Multiple | 7 of 10 | 4 of 10 | Low to Very Low |
| Functional Scores (WOMAC, KOOS) | Multiple | 7 of 10 | 4 of 10 | Low to Very Low |
Source: Adapted from [146]
Table 2: Cardiac and Neurological Outcomes of Stem Cell Therapy
| Medical Condition | Primary Outcome | Effect Size | Statistical Significance | Safety Profile |
|---|---|---|---|---|
| Heart Failure with Reduced EF (HFrEF) | Left Ventricular EF | Hedges' g = 0.096 | p = 0.18 (NS) | No increased MACE risk |
| HFrEF | Quality of Life | Hedges' g = -0.518 | p = 0.01 | No increased MACE risk |
| Acute/Subacute Ischemic Stroke | mRS 0-1 at 1 year | RR = 1.74 | p = 0.020 | No significant difference in SAEs or mortality |
| Acute/Subacute Ischemic Stroke | mRS 0-2 at 90 days | RR = 1.31 | p = 0.044 | No significant difference in SAEs or mortality |
Sources: Adapted from [3] [5] Abbreviations: EF = Ejection Fraction; MACE = Major Adverse Cardiac Events; mRS = modified Rankin Scale; NS = Not Significant; RR = Risk Ratio; SAEs = Serious Adverse Events
The evidence for mesenchymal stem cell (MSC) therapy in knee osteoarthritis demonstrates a concerning pattern: while the majority of comparative studies report favorable outcomes, fewer than half show improvements exceeding the minimum clinically important difference (MCID) [146]. The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) assessment rates this evidence as low to very low quality, typically due to small sample sizes, short follow-up durations, use of concomitant treatments, and publication bias [146].
In cardiac applications, MSC therapy for HFrEF shows a dissociation between objective functional measures and patient-reported outcomes. While left ventricular ejection fraction—the primary efficacy measure—showed no significant improvement, quality of life demonstrated statistically and potentially clinically significant enhancement [3]. This pattern highlights the complexity of assessing "efficacy" in stem cell therapies and the importance of multiple outcome domains.
The most promising results emerge from neurological applications, particularly ischemic stroke. A 2025 meta-analysis of 13 randomized controlled trials demonstrated statistically significant improvements in functional outcomes (measured by mRS scores) at both 90 days and 1 year post-treatment, without increased serious adverse events or mortality [5]. This suggests that timing of intervention may be critical, as this analysis specifically focused on acute and subacute ischemic stroke (within 1 month of onset).
Methodological Framework: Assessing Reproducibility and Bias
Typologies of Replication Studies
Replication efforts serve distinct epistemic functions in scientific research. Schmidt (2009) identifies five primary functions: controlling for sampling error, controlling for artifacts (internal validity), controlling for fraud, enabling generalizability, and enabling verification of the underlying hypothesis [144]. These functions are achieved through different replication designs:
- Direct Replications attempt to repeat a study as closely as possible to verify its specific findings
- Conceptual Replications test the same underlying hypothesis using different methods or conditions
The continuum between these approaches allows researchers to address different questions about the reliability and validity of original findings [144].
Publication Bias and Questionable Research Practices
Publication bias represents a significant threat to the validity of systematic reviews and meta-analyses. This bias manifests through multiple mechanisms:
- Selective Publication: Statistically significant results are more likely to be published than null findings [145] [144]
- Time-Lag Bias: Significant results tend to be published more rapidly
- Language and Location Biases: Positive results may be published in higher-impact journals
Empirical evidence suggests alarming rates of bias across scientific fields. In economics, approximately 70% of significant results would not have been statistically significant in a bias-free world [145]. In biomedical literature between 1990 and 2015, 96% of studies using P values claimed at least some statistically significant results [145], indicating a strongly skewed publication record.
Questionable research practices that contribute to irreproducibility include small sample sizes leading to "power failure," selective reporting of outcomes, post-hoc narrative building, P-hacking, and lack of protocol registration or data sharing [145]. These practices collectively inflate false-positive rates throughout the scientific literature.
Experimental Protocols and Methodologies
Standardized Protocols for Stem Cell Clinical Trials
The most reliable evidence for stem cell therapies comes from randomized controlled trials with standardized protocols. For stroke applications, the recent meta-analysis by Tanaka et al. (2025) established specific methodological criteria [5]:
- Population: Patients with acute or subacute ischemic stroke within 1 month of onset
- Intervention: Stem cell transplantation (mesenchymal, bone marrow mononuclear, or progenitor cells)
- Comparison: Standard care (rehabilitation with/without placebos)
- Outcomes: Primary - modified Rankin Scale (mRS); Secondary - NIH Stroke Scale, Barthel Index, serious adverse events, mortality
- Timing: Assessments at 90 days, 180 days, and 1 year
This protocol alignment across studies enabled meaningful meta-analysis and contributed to the more robust findings in this domain compared to other applications [5].
MSC Characterization and Delivery Protocols
For mesenchymal stem cell therapies, standardization of cell characterization and delivery is methodologically critical. The International Society for Cellular Therapy has established minimum criteria for defining MSCs [3]:
- Plastic adherence in standard culture conditions
- Specific surface marker expression (CD73+, CD90+, CD105+; CD14-, CD34-, CD45-, HLA-DR-)
- In vitro differentiation capacity into osteoblasts, adipocytes, and chondrocytes
Delivery protocols vary significantly across clinical applications:
- Orthopedic Applications: Typically intra-articular injection for knee osteoarthritis, often using bone marrow-derived MSCs or adipose-derived stromal vascular fraction [146]
- Cardiac Applications: Intracoronary, intravenous, or intramyocardial delivery routes [3]
- Neurological Applications: Intracerebral or intravenous transplantation [5]
This methodological diversity contributes to challenges in comparing outcomes across studies and conditions.
Signaling Pathways and Experimental Workflows
Mesenchymal Stem Cell Mechanism of Action
The therapeutic effects of MSCs are mediated through multiple interconnected biological pathways. The diagram below illustrates the key mechanisms through which MSCs exert their effects in conditions like osteoarthritis, cardiac failure, and stroke.
Diagram 1: MSC Therapeutic Mechanisms
MSCs primarily exert their effects through two principal mechanisms: differentiation potential and immune modulation [146]. The multipotent nature of MSCs allows differentiation into various tissue lineages including osteoblasts, chondrocytes, and adipocytes, potentially contributing directly to tissue regeneration [146]. Additionally, MSCs possess significant paracrine and immunomodulating effects through the release of growth factors, cytokines, and exosomes, resulting in reduced inflammation and activation of survival pathways in injured cells [146] [3]. The relative contribution of these mechanisms varies across different disease contexts and may help explain the condition-specific efficacy patterns observed in clinical studies.
Research Workflow for Reproducibility Assessment
Implementing a systematic approach to reproducibility assessment is methodologically essential for evaluating stem cell research. The following workflow outlines key stages in this process:
Diagram 2: Reproducibility Assessment Workflow
This workflow emphasizes the systematic, protocol-driven approach necessary for robust reproducibility assessment. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) framework provides a standardized methodology for identifying, selecting, and critically appraising relevant research [3] [5]. At each stage, specific methodological safeguards against bias must be implemented, including comprehensive search strategies, predefined inclusion/exclusion criteria, independent study selection by multiple reviewers, and standardized data extraction forms.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents for Stem Cell Investigations
| Reagent/Material | Function/Application | Specification Requirements |
|---|---|---|
| Mesenchymal Stem Cells | Primary therapeutic agent; experimental material | ISCT criteria: CD73+, CD90+, CD105+; CD14-, CD34-, CD45-; plastic adherence; trilineage differentiation [3] |
| Cell Culture Media | In vitro expansion and maintenance of MSCs | Serum-free or FBS-containing formulations with appropriate growth factors |
| Flow Cytometry Antibodies | Characterization of cell surface markers | Conjugated antibodies against CD73, CD90, CD105, CD14, CD34, CD45, HLA-DR |
| Differentiation Kits | Verification of multilineage potential | Osteogenic, adipogenic, and chondrogenic induction media |
| Cytokine/Growth Factor Arrays | Analysis of paracrine secretion profiles | Multiplex assays for VEGF, HGF, IGF, FGF, etc. |
| Exosome Isolation Kits | Isolation and characterization of extracellular vesicles | Ultracentrifugation or commercial kit-based methods |
The reagents and materials listed in Table 3 represent core components of standardized stem cell research protocols. Adherence to International Society for Cellular Therapy (ISCT) criteria for MSC characterization is methodologically essential for ensuring consistent cell populations across experiments and laboratories [3]. This standardization is particularly important given the diverse tissue sources of MSCs, including bone marrow, adipose tissue, umbilical cord, and amniotic fluid [146]. Variations in source material and isolation protocols represent significant challenges to reproducibility in the field.
The current evidence base for stem cell therapies presents a mixed picture regarding both efficacy and reproducibility. While promising results exist in specific applications like stroke treatment, widespread methodological limitations and evidence quality issues persist across the field. The assessment of publication bias and reproducibility reveals several critical areas for improvement: standardization of cell characterization and delivery protocols, implementation of preregistered study designs with publicly available protocols, increased data sharing and transparency, and deliberate pursuit of replication studies.
The scientific community's growing recognition of these challenges has spurred development of potential solutions, including enhanced reproducibility practices through open science frameworks, improved statistical training and methodology, and more rigorous peer review processes focused on methodological soundness rather than novelty alone [145] [144]. For stem cell research to fulfill its translational potential, the field must continue advancing toward more reproducible, transparent, and rigorously validated scientific practices that can support robust clinical applications.
Conclusion
This comprehensive analysis demonstrates that stem cell therapy, particularly using mesenchymal stem cells, presents a favorable safety profile across multiple clinical applications while showing variable efficacy outcomes. Significant functional improvements are evident in neurological and hepatic conditions, whereas cardiovascular applications show more modest benefits primarily in quality of life. Critical gaps remain in standardization of outcome measures, optimization of delivery protocols, and understanding long-term effects. Future directions should prioritize large-scale, rigorously controlled trials with standardized endpoints, exploration of combination therapies, and development of personalized approaches based on patient-specific factors and disease mechanisms. The evolving regulatory landscape and ethical framework will continue to shape the responsible translation of these promising therapies into clinical practice.
References
- 1. New Global Burden of Disease Study: mortality declines ... [https://www.healthdata.org/news-events/newsroom/news-releases/new-global-burden-disease-study-mortality-declines-youth-deaths]
- 2. Global distribution of research efforts, disease burden, and ... [https://www.nature.com/articles/s41591-025-03923-0]
- 3. Cardiac Repair and Clinical Outcomes of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109878/]
- 4. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 5. Efficacy and safety of stem cell therapy for acute and ... [https://www.nature.com/articles/s41598-025-04405-6]
- 6. Efficacy and safety of mesenchymal stromal cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04184-x]
- 7. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 8. Clinical observational studies of potential participants ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020729/]
- 9. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 10. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 11. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 12. Mesenchymal stem cells biological and biotechnological ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299924004072]
- 13. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 14. Exosomes vs Stem Cells: Differences & Utility (2025) [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 15. Quality of life in heart failure. The heart of the matter. A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370584/]
- 16. New Joint Scientific Statement on Ejection Fraction ... [https://www.escardio.org/The-ESC/Press-Office/Press-releases/new-joint-scientific-statement-on-ejection-fraction-released-by-leading-heart-failure-organisations]
- 17. What's new in heart failure? September 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502451/]
- 18. Mayo Clinic researchers identify a new stem cell patch to ... [https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-researchers-identify-a-new-stem-cell-patch-to-gently-heal-damaged-hearts/]
- 19. Imaging for Prediction of Functional Outcome and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3981064/]
- 20. Long-term functional recovery after first ischemic stroke [https://pmc.ncbi.nlm.nih.gov/articles/PMC2830874/]
- 21. NIH Stroke Scale [https://www.physio-pedia.com/NIH_Stroke_Scale]
- 22. A review and meta-analysis of stem cell therapies in stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10761518/]
- 23. Revolutionizing Stroke Recovery: Unveiling the Promise of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10986404/]
- 24. Variability of the Modified Rankin Scale Score Between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8382369/]
- 25. Effect of inpatient rehabilitation facility care on ninety day ... [https://www.sciencedirect.com/science/article/abs/pii/S1052305723001325]
- 26. Biomarkers for prognostic functional recovery poststroke [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1062807/full]
- 27. Efficacy and safety of mesenchymal stem cell therapy in acute ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04303-8]
- 28. MELD (model for end-stage liver disease) score [https://www.mayoclinic.org/tests-procedures/meld-score-liver-disease/about/pac-20590545]
- 29. Could Stem Cells Help Treat Acute-on-Chronic Liver Failure? [https://cells4life.com/2025/07/could-stem-cells-treat-acute-on-chronic-liver-failure/]
- 30. Efficacy and safety of mesenchymal stem cell therapy in ... [https://pubmed.ncbi.nlm.nih.gov/40254564/]
- 31. A comprehensive meta-analysis of stem cell therapy for ... [https://www.sciencedirect.com/science/article/pii/S1665268124003697]
- 32. The Survival Benefit of Liver Transplantation [https://www.sciencedirect.com/science/article/pii/S160061352203550X]
- 33. Stratification and selection of therapies to improve survival ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476741/]
- 34. Validation of MELD 3.0 and ReMELD-Na scoring systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464064/]
- 35. The Development and Appraisal of MELD 3.0 in Liver ... [https://www.xiahepublishing.com/m/2310-8819/JCTH-2024-00303]
- 36. Stem cell paracrine actions and tissue regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2833273/]
- 37. Emerging Concepts in Paracrine Mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4874329/]
- 38. Stem cells as biological drugs for incurable diseases [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04632-8]
- 39. Exploiting paracrine mechanisms of tissue regeneration to ... [https://transplantationresearch.biomedcentral.com/articles/10.1186/2047-1440-2-10]
- 40. The Role of Paracrine Regulation of Mesenchymal Stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.587052/full]
- 41. Paracrine- and cell-contact-mediated immunomodulatory ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03759-4]
- 42. Systematic review and meta-analysis in clinical trials [https://www.sciencedirect.com/science/article/pii/S1357303925000775]
- 43. Meta-Analytic Methodology for Basic Research: A Practical ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2019.00203/full]
- 44. PRISMA statement [https://www.prisma-statement.org/]
- 45. LibGuides: Creating a PRISMA flow diagram: PRISMA 2020 [https://guides.lib.unc.edu/prisma]
- 46. An updated guideline for reporting systematic reviews [https://www.equator-network.org/reporting-guidelines/prisma/]
- 47. PRISMA 2020 flow diagram [https://www.prisma-statement.org/prisma-2020-flow-diagram]
- 48. PRISMA 2020 and PRISMA-S: common questions on tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014944/]
- 49. PRISMA-Search [https://www.prisma-statement.org/prisma-search]
- 50. A comprehensive guide to conduct a systematic review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366998/]
- 51. Systematic Review and Meta-Analysis of Stem Cell ... [https://www.medrxiv.org/content/10.1101/2025.08.25.25334375v1.full]
- 52. Eyeing Neurology Drug Development: 2H Trial Readouts ... [https://www.neurologylive.com/view/eyeing-neurology-drug-development-2h-trials-watch-for-in-2025]
- 53. November 2025 updates to AASLD Practice Guidance [https://pubmed.ncbi.nlm.nih.gov/41201884/]
- 54. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 55. Impact of mesenchymal stem cell therapy on cardiac function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322349/]
- 56. Injectable Stem Cell-Based Therapies for Myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12111900/]
- 57. Stem cells harvested from different sources ameliorate liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577378/]
- 58. Scaffold implantation vs. intravenous delivery [https://astr.or.kr/DOIx.php?id=10.4174/astr.2025.108.3.186]
- 59. Mesenchymal stem cell therapy as a game-changer in liver ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04127-y]
- 60. Mesenchymal stem cell infusion to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500263X]
- 61. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207128/]
- 62. Efficacy and safety of mesenchymal stem cell therapy in acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010635/]
- 63. In silico evaluation of cell therapy in acute versus chronic ... [https://www.nature.com/articles/s41598-024-67951-5]
- 64. Stem Cell Therapy: A Stroke Recovery Breakthrough in ... [https://www.dvcstem.com/post/stem-cell-therapy-stroke]
- 65. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 66. A comprehensive review of clinical trials and progress in ... [https://www.sciencedirect.com/science/article/pii/S2352320425001944]
- 67. Harnessing nanotechnology for stem-cell therapies ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1630475/full]
- 68. Revealing the Top 25 Innovative Stem Cell Companies in ... [https://www.scispot.com/blog/top-innovative-stem-cell-companies-in-the-us]
- 69. Evaluation of stem/stromal cell transplantation safety and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04550-9]
- 70. Engineered Cell Therapy Market Outlook from 2025 to 2035 [https://www.futuremarketinsights.com/reports/engineered-cell-therapy-market]
- 71. Chapter 8: Assessing risk of bias in a randomized trial [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-08]
- 72. RoB 2: A revised Cochrane risk-of-bias tool for randomized ... [https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials]
- 73. ROBINS-I | Cochrane Bias [https://methods.cochrane.org/bias/risk-bias-non-randomized-studies-interventions]
- 74. Cochrane's risk of bias tool for non-randomized studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8809341/]
- 75. Risk of bias tools - Read more [https://sites.google.com/site/riskofbiastool/welcome/home/read-more]
- 76. Risk of bias tools - ROBINS-I V2 tool [https://www.riskofbias.info/welcome/robins-i-v2]
- 77. Improving Stem Cell Clinical Trial Design and Conduct [https://pmc.ncbi.nlm.nih.gov/articles/PMC7671799/]
- 78. The issue of heterogeneity of MSC-based advanced ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1400347/full]
- 79. The heterogeneity of mesenchymal stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734083/]
- 80. Stem cell heterogeneity, plasticity, and regulation [https://www.sciencedirect.com/science/article/abs/pii/S0024320523008755]
- 81. Review: progression and heterogeneity of multiple sources of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04515-y]
- 82. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pubmed.ncbi.nlm.nih.gov/40579230/]
- 83. Capturing trial-by-trial variability in behaviour [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368238/]
- 84. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 85. Mid- to long-term efficacy and safety of stem cell therapy for ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03891-1]
- 86. Safety and efficiency of stem cell therapy for COVID-19 [https://ghrp.biomedcentral.com/articles/10.1186/s41256-022-00251-5]
- 87. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 88. focusing on induced pluripotent stem cell (iPSC)-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11583560/]
- 89. Allogeneic versus autologous stem cell transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057802/]
- 90. Allogeneic versus autologous stem cell transplantation ... [https://pubmed.ncbi.nlm.nih.gov/40334055/]
- 91. Allogeneic versus autologous hematopoietic stem cell ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525002307]
- 92. Efficacy and Safety of Allogeneic Hematopoietic Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/40953733/]
- 93. a systematic review and meta-analysis of RCTs | Stem Cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04209-5]
- 94. Multiple Sclerosis and Related Disorders [https://www.sciencedirect.com/science/article/abs/pii/S2211034825002846]
- 95. Epidemiology, clinical outcomes, and treatment patterns of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1518275/full]
- 96. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 97. Comparison of outcomes of percutaneous deep venous ... [https://www.sciencedirect.com/science/article/abs/pii/S0741521424012308]
- 98. Peripheral Vascular Access in Infants: Is Ultrasound-Guided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387647/]
- 99. Recent Advances in Ultrasound-Guided Peripheral ... [https://www.mdpi.com/2039-4403/15/10/359]
- 100. Comparison of peripheral intravenous catheterization applied ... [https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-02979-0]
- 101. Efficacy of a single intra-articular injection of mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398016/]
- 102. Efficacy and safety of single versus repeated injections ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465953/]
- 103. Stem Cell–Based Therapies via Different Administration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808770/]
- 104. Comparison of the Administration Route of Stem Cell ... [https://www.mdpi.com/2077-0383/12/7/2735]
- 105. Mesenchymal stem cell-derived exosomes for the ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1588841/full]
- 106. Combined meta-analysis of preclinical cell therapy studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647619/]
- 107. Comparative analysis of regulations and studies on stem cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04065-9]
- 108. ISSCR Standards for Human Stem Cell Use in Research [https://www.stemcell.com/psc-cell-quality/isscr-standards]
- 109. Standards and the Future of Stem Cell Research [https://www.astm.org/news/standards-and-the-future-of-stem-cell-research]
- 110. Systematic review and meta-analysis of mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10140776/]
- 111. Agency Information Collection Activities: Proposed ... [https://www.federalregister.gov/documents/2025/05/16/2025-08703/agency-information-collection-activities-proposed-collection-public-comment-request-information]
- 112. SCTOD Requirements [https://cibmtr.org/CIBMTR/Data-Operations/Center-Membership/SCTOD-Requirements]
- 113. of mesenchymal Comparative versus... effectiveness stem cell [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03829-7]
- 114. Efficacy & safety of stem cell therapy for treatment of acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550445/]
- 115. Safety and Efficacy of Stem Cell Therapy in Ischemic Stroke [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943215/]
- 116. The efficacy and safety of stem cell therapy for ischemic stroke [https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-025-04246-w]
- 117. matched-pair cohort Comparative of the short-term analysis ... clinical [https://jeo-esska.springeropen.com/articles/10.1186/s40634-020-00310-1]
- 118. Metabolic regulation for the treatment of ischemic heart ... [https://www.nature.com/articles/s44325-025-00089-z]
- 119. Comparison of Conventional Therapies With Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/41018340/]
- 120. Clinical trials and advanced MRI techniques with stem cell ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07054-5]
- 121. Meta-analysis highlight the therapeutic potential of stem ... [https://www.sciencedirect.com/science/article/pii/S2352320424001299]
- 122. Efficacy of stem cell therapy for diabetic foot [https://pmc.ncbi.nlm.nih.gov/articles/PMC10961866/]
- 123. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 124. Therapeutic effects of stem cells in different body systems, a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8554700/]
- 125. Stem Cell Therapy Success Rates Hit 78%: New Research ... [https://globalrph.com/2025/03/stem-cell-therapy-success-rates-hit-78-new-research-reveals-breakthrough-results/]
- 126. UNDERSTANDING VARIATIONS IN RELATIVE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4824958/]
- 127. Efficacy Analysis in Clinical Trials [https://arxiv.org/html/2511.04903v1]
- 128. Mesenchymal stem cells in neurological disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636885/]
- 129. Umbrella review of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554768/]
- 130. Autologous and allogeneic mesenchymal stem cell-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305282/]
- 131. The Effectiveness of Mesenchymal Stem Cell (MSCs ... [https://orthopedicreviews.openmedicalpublishing.org/article/137660]
- 132. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 133. Unveiling distinctions between mesenchymal stromal cells ... [https://www.sciencedirect.com/science/article/pii/S2405844025006917]
- 134. Randomized controlled trials – The what, when, how and why [https://www.sciencedirect.com/science/article/pii/S147751312400617X]
- 135. Comparing Randomized Controlled Trials and Real-World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7276323/]
- 136. Rethinking the pros and cons of randomized controlled trials ... [https://bmcproc.biomedcentral.com/articles/10.1186/s12919-023-00285-8]
- 137. Randomized Controlled Trials: Overview, Benefits and ... [https://www.clinicaltrials.astellas.com/what-is-a-randomized-clinical-trial]
- 138. Nonrandomized control: understanding study design, ... [https://www.sciencedirect.com/science/article/pii/B9780323905091000540]
- 139. What Is A Non-Randomized Controlled Clinical Trial? [https://www.allclinicaltrials.com/blog/non-randomized-controlled-trials]
- 140. Meta-analytic comparison of randomized and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3364302/]
- 141. Clinical performance of stem cell therapy in patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5946490/]
- 142. Stem cells for treatment of cardiovascular diseases [https://www.sciencedirect.com/science/article/abs/pii/S1568163721000040]
- 143. Clinical efficacy and safety of somatic cell therapy for chronic ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04628-4]
- 144. Reproducibility of Scientific Results [https://plato.stanford.edu/archives/win2018/entries/scientific-reproducibility/]
- 145. Transparency, bias, and reproducibility across science: a meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11563668/]
- 146. What Is the Evidence for the Clinical Use of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7170666/]