Stem Cell Transplantation in Regenerative Medicine: From Foundational Concepts to Clinical Applications and Future Directions
This article provides a comprehensive overview of the rapidly evolving field of stem cell transplantation for regenerative medicine.
Stem Cell Transplantation in Regenerative Medicine: From Foundational Concepts to Clinical Applications and Future Directions
Abstract
This article provides a comprehensive overview of the rapidly evolving field of stem cell transplantation for regenerative medicine. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational knowledge on stem cell types and mechanisms with analysis of recent clinical breakthroughs, including newly FDA-approved therapies and advanced clinical trials. The content explores the methodological landscape, from established hematopoietic transplants to emerging iPSC and MSC-based applications in neurology, cardiology, and oncology. It critically addresses persistent challenges in safety, manufacturing, and regulation, while evaluating the comparative efficacy of different therapeutic approaches. By integrating current research, clinical trial data, and future prospects, this review serves as a strategic resource for navigating the translation of stem cell science into transformative clinical therapies.
Stem Cell Fundamentals: Mechanisms, Types, and Therapeutic Principles in Regeneration
Stem cells represent a foundational pillar of regenerative medicine, distinguished from traditional pharmaceuticals by their dynamic, biological nature. They are characterized by two defining biological properties: the capacity for self-renewal, which allows them to proliferate indefinitely, and differentiation potential, which enables them to develop into various specialized cell types [1] [2]. These characteristics underpin their classification as "living drugs" – therapeutic entities that are biologically active, can adapt to their environment, and potentially mediate complex therapeutic actions such as tissue repair and immune modulation [3]. This document outlines the core principles of stem cell biology and provides detailed protocols for their analysis and application in a therapeutic context, framing them within the advanced landscape of stem cell transplantation and regenerative medicine research.
Defining Biological Characteristics: Protocols for Analysis
Self-Renewal: Quantitative Assessment Protocols
Self-renewal is the process by which a stem cell divides to generate at least one copy of itself, thereby maintaining the stem cell pool throughout the life of an organism [1]. The following protocol details a standard in vitro method for quantifying this key characteristic.
Protocol 2.1.1: Colony-Forming Unit (CFU) Assay for Self-Renewal Potential
- Objective: To quantitatively assess the capacity of a single stem cell to proliferate and form a colony, demonstrating its self-renewal capability.
- Materials:
- Single-cell suspension of the stem cell population of interest.
- Appropriate culture medium (e.g., MesenCult for MSCs).
- Semi-solid medium (e.g., MethoCult for HSCs) or low-attachment culture vessels.
- Incubator (37°C, 5% CO₂).
- Staining solution (e.g., Crystal Violet or MTT).
- Methodology:
- Cell Seeding: Prepare a highly diluted single-cell suspension and seed cells into multi-well plates. For HSCs, mix the cell suspension with a semi-solid medium to immobilize daughter cells. The optimal cell density must be determined empirically to ensure well-separated colonies (e.g., 100-1,000 cells/cm² for MSCs).
- Culture: Incubate cells under optimal conditions for 7-14 days, without disturbing the cultures. Do not change the medium.
- Fixation and Staining: After the incubation period, carefully remove the medium. Fix cells with 4% paraformaldehyde (PFA) for 15-20 minutes, then stain with Crystal Violet for 30 minutes.
- Quantification and Analysis: Gently wash with water to remove excess stain. Count the number of colonies, where a colony is typically defined as a cluster of >50 cells. Calculate the colony-forming efficiency (CFE) as: (Number of Colonies / Number of Cells Seeded) x 100%.
- Data Interpretation: A higher CFE indicates a greater proportion of cells with self-renewal capacity within the population. Serial CFU assays can be performed to test for long-term self-renewal.
Differentiation Potential: Directed Differentiation and Quantitative Analysis
Differentiation potential refers to a stem cell's ability to develop into specialized cell types. This potential is categorized as totipotency, pluripotency, multipotency, and unipotency [1]. The protocol below is a generalized framework for directed differentiation and subsequent quality assessment.
Protocol 2.2.1: Directed Differentiation and Lineage Validation
- Objective: To guide stem cells toward a specific lineage and quantitatively validate the success of differentiation.
- Materials:
- Pluripotent Stem Cells (PSCs) or Multipotent Adult Stem Cells.
- Basal differentiation media.
- Lineage-specific growth factors and small molecules (e.g., BMP4 for mesoderm, Retinoic Acid for ectoderm, Activin A for endoderm).
- RNA/DNA extraction kits.
- Antibodies for immunocytochemistry (ICC) or flow cytometry.
- Facilities for RNA-Seq.
- Methodology:
- Directed Differentiation:
- Mesoderm (e.g., Cardiomyocytes): Culture PSCs and activate Wnt signaling with CHIR99021 for 24-48 hours. Subsequently, inhibit Wnt signaling with IWP-2 or IWR-1 to promote cardiac differentiation. Spontaneously beating cells should appear in 7-10 days [4].
- Ectoderm (e.g., Neurons): Culture PSCs in neural induction medium containing dual SMAD inhibitors (e.g., Noggin, SB431542) to suppress mesendodermal fates. Roster of neuronal subtypes can be generated with additional patterning factors like SHH or FGF8 [4].
- Validation of Differentiation:
- Gene Expression Analysis: Perform RT-qPCR to detect lineage-specific markers (e.g., TNNT2 for cardiomyocytes, TUBB3 for neurons).
- Protein Expression Analysis: Use ICC or flow cytometry to detect lineage-specific proteins.
- Functional Assays: Perform electrophysiological measurements for neurons or calcium transient assays for cardiomyocytes.
- Directed Differentiation:
- Advanced Quantitative Analysis: For a systems-level assessment of differentiation fidelity, tools like the Web-based Similarity Analytics System (W-SAS) can be employed. This algorithm calculates a quantitative similarity score (%) between the transcriptome of differentiated cells and the target human organ using organ-specific gene expression panels (Organ-GEPs) [5].
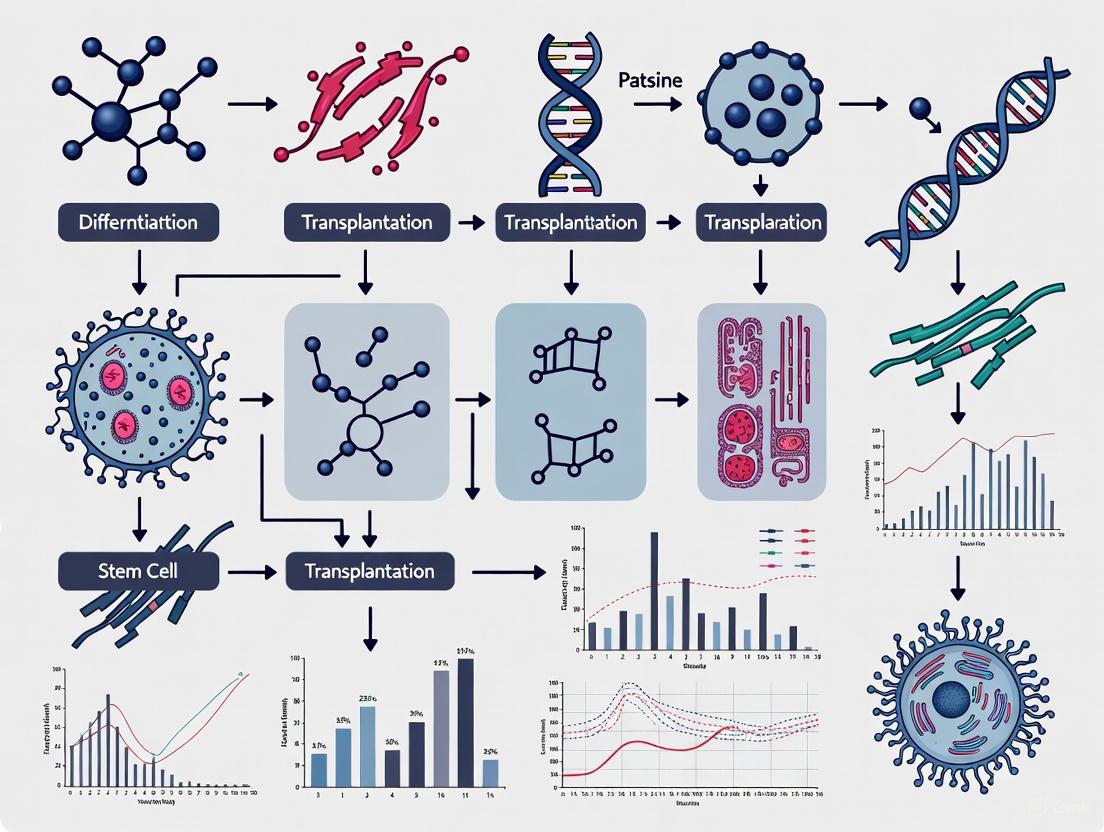
The relationships between stem cell types, their defining characteristics, and therapeutic applications are complex. The following diagram illustrates this logical framework.
The 'Living Drug' Concept: Clinical Applications and Trial Design
The "living drug" paradigm frames stem cells not as inert compounds but as dynamic biological agents that perform therapeutic functions in vivo. Their mechanisms are often complex, involving tissue integration, paracrine signaling, and immune modulation [1] [3].
Clinical Trial Protocols for 'Living Drugs'
Protocol 3.1.1: Phase I Trial Design for a Novel Stem Cell Therapy
- Objective: To assess the safety, tolerability, and preliminary dosing of a novel allogeneic MSC product in patients with steroid-refractory acute Graft-versus-Host Disease (SR-aGVHD).
- Trial Design:
- Type: Open-label, single-arm, dose-escalation study.
- Patient Population: Adults and children (≥2 months) with SR-aGVHD following allogeneic hematopoietic stem cell transplantation.
- Intervention: Intravenous infusion of allogeneic, bone marrow-derived MSCs. The dose is calculated based on patient body weight (e.g., 2 × 10^6 cells/kg). A series of multiple weekly infusions may be administered.
- Primary Endpoint: Incidence and severity of adverse events (AEs) and serious adverse events (SAEs) within 28 days post-infusion, with specific attention to infusion reactions and immunogenicity.
- Secondary Endpoints: Overall response rate (ORR) at Day 28, overall survival (OS) at 100 days and 1 year, and measurement of donor-specific antibodies.
- Key Considerations:
- Cell Source and Potency: The cell bank must be well-characterized. A potency assay measuring a key mechanism of action (e.g., T-cell suppression in vitro) is required [1].
- Immunosuppression: Concomitant immunosuppressive therapy for GVHD is permitted and should be recorded.
- Long-Term Follow-Up: Patients should be followed for at least 15 years to monitor for delayed adverse effects, such as tumorigenicity.
Quantitative Clinical Landscape
Recent regulatory milestones underscore the transition of stem cell "living drugs" from research to clinical reality. The table below summarizes key FDA-approved stem cell therapies, highlighting their diverse applications.
Table 1: Recently Approved Stem Cell-Based "Living Drugs" (2023-2025)
| Product Name (Approval Date) | Cell Type | Therapeutic Indication | Key Clinical Outcomes | Mechanism of Action (Living Drug Concept) |
|---|---|---|---|---|
| Ryoncil (Dec 2024) [3] | Allogeneic MSCs | Pediatric steroid-refractory acute Graft-versus-Host Disease (SR-aGVHD) | Improved survival in a life-threatening condition with limited options. | Immunomodulation via paracrine signaling; suppresses inflammation and promotes tissue repair. |
| Omisirge (Apr 2023) [3] | Cord Blood-Hematopoietic Progenitor Cells | Hematologic malignancies (post-umbilical cord blood transplant) | Accelerates neutrophil recovery, reducing infection risk. | "Living graft" that reconstitutes the patient's blood and immune system. |
| Lyfgenia (Dec 2023) [3] | Autologous CD34+ cells (gene-modified) | Sickle cell disease | 88% of patients achieved complete resolution of vaso-occlusive events. | A gene-modified living drug: patient's own cells are engineered to produce non-sickling hemoglobin. |
The Scientist's Toolkit: Essential Reagents and Platforms
Successful stem cell research and therapy development rely on a suite of specialized tools and platforms. The following table details key solutions for working with stem cells as living drugs.
Table 2: Research Reagent Solutions for Stem Cell Research and Therapy Development
| Research Tool / Reagent | Function / Description | Application in Protocol / Development |
|---|---|---|
| Briquilimab (Anti-CD117 Antibody) [6] | Monoclonal antibody that targets the CD117 receptor on hematopoietic stem cells. | Used in conditioning regimens to selectively clear host HSCs, replacing toxic chemotherapy/radiation for safer transplant preparation. |
| REPROCELL StemRNA Clinical Seed iPSC Clones [3] | GMP-compliant, clinically qualified human iPSC master cell banks. | Provides a standardized, scalable, and regulatable starting material for generating consistent, high-quality differentiated cell products for therapy. |
| Web-based Similarity Analytics System (W-SAS) [5] | Computational algorithm that calculates a quantitative similarity score (%) between differentiated cells and target human organs using Organ-GEPs. | Quality control protocol for assessing the fidelity of differentiated cells (e.g., cardiomyocytes, hepatocytes) for disease modeling and transplantation. |
| Alpha/Beta T-Cell Depletion [6] | A cell processing method that selectively removes αβ T-cells from a donor graft. | Reduces the risk of Graft-versus-Host Disease (GvHD) in allogeneic transplants, allowing for the use of haploidentical (partially matched) donors. |
Advanced Workflows: From Research to Clinical Application
The journey from a foundational stem cell discovery to a clinically approved therapy involves a highly regulated and multi-stage process. The following diagram maps this critical pathway, integrating key tools and decision points.
The advent of human Pluripotent Stem Cells (PSCs), encompassing both Embryonic Stem Cells (ESCs) and induced Pluripotent Stem Cells (iPSCs), has revolutionized biomedical research. These cells provide an unprecedented platform for modeling human diseases in vitro, enabling researchers to move beyond the limitations of traditional animal models, which often fail to fully recapitulate key aspects of human physiology and pathology [7]. The ability to generate patient-specific cellular models that harbor the exact genetic background of a disease has positioned PSCs as a cornerstone for elucidating disease mechanisms, discovering new biomarkers, and developing novel therapeutic strategies [8] [9]. This application note details the protocols and applications of ESCs and iPSCs in disease modeling, providing a practical toolkit for researchers and drug development professionals working within the broader field of regenerative medicine.
Pluripotent Stem Cells: A Comparative Analysis
Human pluripotent stem cells are defined by their capacity for unlimited self-renewal and their ability to differentiate into derivatives of all three primary germ layers: ectoderm, mesoderm, and endoderm. The two primary sources are ESCs and iPSCs.
Table 1: Comparison of Embryonic and Induced Pluripotent Stem Cells
| Feature | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of a blastocyst stage embryo [9] | Reprogrammed somatic cells (e.g., fibroblasts, blood cells) [8] |
| Reprogramming Method | N/A (naturally occurring) | Viral (retro/lenti) or non-viral (episomal, mRNA, Sendai virus) delivery of transcription factors [8] [9] |
| Key Transcription Factors | N/A | Oct4, Sox2, Klf4, c-Myc (OSKM) or Oct4, Sox2, Nanog, Lin28 [8] [9] |
| Pluripotency | Pluripotent | Pluripotent |
| Ethical Considerations | Associated with destruction of human embryos [10] [11] | Minimal ethical concerns; bypasses embryo use [10] |
| Immunological Compatibility | Allogeneic; potential for immune rejection | Can be autologous; minimal immune rejection [8] |
| Primary Application in Disease Modeling | Study of wild-type human development; isogenic control generation after gene editing | Patient-specific disease modeling; study of polygenic and sporadic diseases [8] [12] |
The groundbreaking discovery of iPSCs in 2006 by Yamanaka and colleagues, for which he was awarded a Nobel Prize, demonstrated that somatic cell fate could be reversed to a pluripotent state by forced expression of specific transcription factors [8] [9]. This innovation provided a critical, ethically acceptable alternative to ESCs and unlocked the potential for creating patient-specific disease models.
Disease Modeling Applications and Quantitative Outcomes
iPSCs, in particular, have become an indispensable tool for creating "disease-in-a-dish" models. The following table summarizes key disease areas where PSC modeling has demonstrated significant utility and quantitative outcomes.
Table 2: Quantitative Outcomes from PSC-Based Disease Modeling Studies
| Disease Area | PSC-Derived Cell Type | Modeled Pathology/Phenotype | Key Quantitative Readouts & Applications |
|---|---|---|---|
| Neurodegenerative [8] [12] | Dopaminergic Neurons (Parkinson's), Motor Neurons (ALS), Cortical Neurons (Alzheimer's) | α-synuclein aggregation, dopaminergic neuron degeneration, tau hyperphosphorylation, Aβ deposition | Phenotypic Screening: Identification of compounds rescuing neuronal function in vitro [12]. Mechanistic Studies: Recapitulation of dopaminergic neuron loss in substantia nigra [8]. |
| Cardiovascular [8] [12] | Cardiomyocytes | Arrhythmogenic disorders (e.g., KCNQ1 mutations), drug-induced cardiotoxicity | Functional Assays: Measurement of contractility and electrophysiology. Safety Screening: Used in regulatory safety initiatives (CiPA) for arrhythmia risk profiling [12]. |
| Metabolic [8] | Hepatocyte-like cells, Airway Epithelial Cells | Cystic fibrosis (defective CFTR chloride transport), Wilson's disease (copper accumulation), Familial Hypercholesterolemia | Drug Testing: Evaluation of correctors (e.g., lumacaftor) and potentiators (e.g., ivacaftor) for CFTR. Drug Repurposing: Identification of cardiac glycosides to reduce ApoB secretion [12]. |
| Autoimmune [8] | B/T Lymphocytes (SLE), Fibroblast-like Synoviocytes (RA), Oligodendrocytes (MS) | Dysregulated signaling, enhanced autoantibody production, pro-inflammatory phenotype, demyelination | Therapeutic Testing: Screening of targeted inhibitors for rheumatoid arthritis. Cell Therapy Development: Off-the-shelf, iPSC-derived CAR T-cell therapy (FT819) for SLE granted FDA RMAT designation [3]. |
| Oncology [3] | Natural Killer (NK) Cells, CAR T-cells | Gynecologic cancers, other malignancies | Cell Therapy Trials: Allogeneic, off-the-shelf NK cell therapy (FT536) derived from a clonal master hiPSC line is in clinical trials [3]. |
The global clinical trial landscape reflects this progress. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct PSC-derived products, with over 1,200 patients dosed and more than 10¹¹ cells administered, reporting no significant class-wide safety concerns [3].
Diagram 1: iPSC-based disease modeling and drug discovery workflow.
Detailed Experimental Protocols
Protocol: Generation of iPSCs from Somatic Cells
This protocol outlines the generation of iPSCs using a non-integrating Sendai viral vector system, which is preferred for its high efficiency and safety profile [8].
Key Research Reagent Solutions:
- Reprogramming Factors: Sendai virus particles encoding human OCT4, SOX2, KLF4, and c-MYC (CytoTune-iPS Sendai Reprogramming Kit).
- Source Somatic Cells: Human dermal fibroblasts, peripheral blood mononuclear cells (PBMCs), or urinary epithelial cells [8].
- Culture Medium: Feeder-free system using mTeSR1 or Essential 8 (E8) medium on recombinant laminin-521 or Matrigel-coated plates [8].
- Quality Control Reagents: Antibodies for flow cytometry/immunocytochemistry (SSEA-4, TRA-1-60, Nanog, Oct4); PCR kits for pluripotency gene expression; Karyostat+ kit for genomic integrity analysis.
Procedure:
- Cell Preparation: Isolate and expand source somatic cells. For fibroblasts, culture in DMEM + 10% FBS. For PBMCs, isolate via density gradient centrifugation and culture in media containing SCF, IL-3, and IL-6 [8].
- Viral Transduction: Plate 5 x 10⁴ to 1 x 10⁵ somatic cells. The next day, transduce with the Sendai virus cocktail at an appropriate Multiplicity of Infection (MOI). Centrifuge to enhance infection.
- Medium Change: 24 hours post-transduction, replace with fresh somatic cell medium.
- Switch to Pluripotency Medium: 7 days post-transduction, passage cells onto coated plates and switch to mTeSR1/E8 medium. Change medium daily.
- Colony Picking: Between days 21-28, manually pick emerging iPSC colonies based on hESC-like morphology (high nucleus-to-cytoplasm ratio, prominent nucleoli, compact colonies). Expand clonally.
- Quality Control:
- Pluripotency Validation: Confirm via PCR (endogenous OCT4, NANOG expression), immunocytochemistry (SSEA-4, TRA-1-60), and flow cytometry (>85% positive for pluripotency markers) [8].
- Genomic Integrity: Perform karyotype analysis (G-banding) or higher-resolution CNV analysis to rule out chromosomal abnormalities [8] [7].
- Vector Clearance: Confirm the absence of Sendai virus genome after several passages using RT-PCR.
Protocol: Directed Differentiation of iPSCs into Cortical Neurons for Alzheimer's Disease Modeling
This protocol generates cortical neurons to model pathologies like tau hyperphosphorylation and amyloid-beta deposition [8] [12].
Key Research Reagent Solutions:
- Neural Induction Medium: Commercially available kits (e.g., STEMdiff SMAD Neural Induction Kit) or custom N2/B27 supplements with dual SMAD inhibition (LDN-193189, SB431542) [12].
- Neuronal Maturation Factors: BDNF, GDNF, NT-3, cAMP, ascorbic acid.
- Characterization Reagents: Antibodies for PAX6 (neural progenitor), TBR1 (deep-layer cortical neuron), MAP2/β-III-Tubulin (mature neurons), p-Tau.
Procedure:
- Neural Induction: Dissociate iPSCs to single cells and aggregate into embryoid bodies in ultra-low attachment plates using neural induction medium with SMAD inhibitors for 7-10 days.
- Neural Progenitor Expansion: Plate resulting neural rosettes on coated dishes and expand in neural progenitor medium containing FGF2.
- Cortical Patterning: During neural induction, add ventralizing morphogens like retinoic acid and/or Wnt inhibitors to direct fate towards forebrain/cortical identity.
- Terminal Differentiation: Dissociate neural progenitors and plate on poly-ornithine/laminin-coated surfaces. Switch to neuronal maturation medium for 4-8 weeks, with half-medium changes every 2-3 days.
- Phenotypic Analysis:
- Immunocytochemistry: Confirm expression of cortical neuronal markers.
- Functional Assay: Use multi-electrode arrays (MEAs) to measure synaptic activity and network formation.
- Disease Phenotype: Treat with pro-aggregation agents or use neurons from AD patients to quantify Aβ42/40 ratio and p-Tau levels via ELISA.
Diagram 2: Differentiation and analysis workflow for cortical neuron disease modeling.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for PSC Culture, Differentiation, and Analysis
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Reprogramming Kits | CytoTune Sendai Virus Kit; Episomal Vectors | Non-integrating delivery of OSKM transcription factors for safe iPSC generation [8]. |
| Culture Media | mTeSR1, Essential 8 (E8) Medium | Chemically defined, xeno-free media for feeder-free maintenance of pluripotency [8]. |
| Culture Substrates | Recombinant Laminin-521, Matrigel | Extracellular matrix coatings that support iPSC/ESC attachment and growth [8]. |
| Differentiation Kits | STEMdiff Neural / Cardiac / Hepatocyte Kits | Standardized, optimized media and supplements for directed differentiation into specific lineages [12]. |
| Gene Editing Tools | CRISPR-Cas9 Systems (e.g., Lipofectamine CRISPRMAX) | Create isogenic control lines by correcting or introducing disease-specific mutations [7]. |
| Characterization Antibodies | Anti-OCT4, SOX2, SSEA-4 (Pluripotency); Anti-β-III-Tubulin, cTnT, AFP (Differentiation) | Validate pluripotent state and differentiation efficiency via immunostaining/flow cytometry [8]. |
| Functional Assay Kits | FLIPR Membrane Potential Dye (Cardiac Electrophysiology), Multi-Electrode Arrays (Neuronal Function) | Measure functional maturity and disease-specific functional deficits in derived cells [12]. |
Pluripotent stem cells have undeniably transformed disease modeling, offering a patient-specific, human-relevant, and scalable platform that bridges the gap between traditional preclinical models and clinical trials. The protocols and tools outlined here provide a foundation for generating robust and reproducible in vitro disease models. The future of the field lies in enhancing the maturity and complexity of these models through advanced 3D organoid and assembloid systems, bioengineering, and electrical stimulation [7] [13]. Furthermore, the ongoing clinical translation of PSC-derived therapies for conditions like Parkinson's disease and retinal degeneration underscores the tangible therapeutic potential of this technology [3]. As standardization, scalability, and functional maturation challenges are addressed, PSCs will continue to be powerhouse tools in the quest to understand and treat human disease.
In the landscape of regenerative medicine, mesenchymal stem cells (MSCs) and hematopoietic stem cells (HSCs) represent two pivotal populations of multipotent adult stem cells. Their capacity for self-renewal and differentiation is not intrinsically determined but is orchestrated by highly specialized microenvironments known as stem cell niches [14]. First proposed by Schofield in 1978 for HSCs, the niche concept defines a specific anatomical compartment that provides the structural, biochemical, and mechanical cues necessary to maintain stem cell quiescence, self-renewal, and lineage-specific differentiation [15] [14]. The therapeutic potential of these cells is inextricably linked to our understanding of their niches, which integrate signals from stromal neighbors, the extracellular matrix (ECM), vascular networks, and nervous inputs to govern stem cell fate decisions [14].
MSCs, initially identified in bone marrow, are non-hematopoietic, multipotent stromal cells defined by their adherence to plastic, specific surface marker expression (CD73, CD90, CD105), and capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [16]. Their therapeutic effects are largely mediated through paracrine release of bioactive molecules—growth factors, cytokines, and extracellular vesicles—that modulate the immune response, promote tissue repair, stimulate angiogenesis, and enhance cell survival [16]. HSCs, in contrast, reside at the apex of the hematopoietic hierarchy, responsible for lifelong production of all blood cell lineages. Their function is regulated by distinct bone marrow niche components, including the endosteal niche that maintains quiescence and the perivascular niche that supports proliferation and differentiation [14] [17]. This application note delineates the core properties, niche interactions, and clinical applications of MSCs and HSCs, providing detailed protocols for researchers leveraging these cells in regenerative medicine and drug development.
Core Cell Types: MSCs and HSCs
Mesenchymal Stem Cells (MSCs)
Origin and Sources: While first isolated from bone marrow (BM-MSCs), MSCs have since been obtained from multiple tissues, including adipose tissue (AD-MSCs), umbilical cord (UC-MSCs), dental pulp (DP-SCs), and placenta (P-MSCs) [16]. Each source confers distinct advantages: BM-MSCs exhibit high differentiation potential and strong immunomodulation, AD-MSCs are easily harvested in high yields, and UC-MSCs demonstrate enhanced proliferation capacity and lower immunogenicity, making them suitable for allogeneic transplantation [16].
Defining Characteristics and Markers: According to the International Society for Cellular Therapy (ISCT), MSCs must fulfill three criteria: (1) adherence to plastic under standard culture conditions; (2) expression of surface markers CD73, CD90, and CD105 (≥95% positive), while lacking expression of hematopoietic markers CD34, CD45, CD14 or CD11b, CD79α or CD19, and HLA-DR (≤2% positive); and (3) tri-lineage differentiation potential into osteoblasts, chondrocytes, and adipocytes in vitro [16]. CD105 (endoglin) is essential for cell migration and angiogenesis, CD90 mediates cell-cell and cell-ECM interactions, and CD73 functions as a 5'-exonuclease in purine metabolism [16].
Table 1: Comparative Characteristics of Primary MSC Sources
| Source Tissue | Key Advantages | Relative Yield | Primary Research & Clinical Applications |
|---|---|---|---|
| Bone Marrow (BM-MSC) | Gold standard, high differentiation potential, strong immunomodulation | Low | Graft-versus-host disease (GVHD), orthopedic repair, immune modulation |
| Adipose Tissue (AD-MSC) | Minimally invasive harvest, high cell yield, comparable therapeutic properties | High | Soft tissue regeneration, inflammatory conditions, cosmetic reconstruction |
| Umbilical Cord (UC-MSC) | High proliferation, low immunogenicity, ethically non-controversial | Medium | Allogeneic transplantation, pediatric regenerative applications |
| Dental Pulp (DP-SC) | Neural crest origin, accessible source | Low | Dental and craniofacial regeneration, neurogenic potential |
The Mechanisms of Action: MSCs mediate repair primarily through paracrine activity rather than direct differentiation. They secrete a diverse array of bioactive factors—including prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO), tumor necrosis factor-inducible gene 6 protein (TSG-6), and galectins—that collectively suppress T-cell proliferation, modulate dendritic cell maturation, and shift macrophages from a pro-inflammatory (M1) to an anti-inflammatory (M2) phenotype [16]. Furthermore, MSC-derived extracellular vesicles (EVs) carry proteins, lipids, and nucleic acids that can reprogram local cellular environments to promote survival and repair [16] [14].
Hematopoietic Stem Cells (HSCs)
Developmental Origin and Hierarchy: Definitive HSCs originate intra-embryonically from the dorsal aorta via an endothelial-to-hematopoietic transition (EHT) around week 4-5 of human gestation [18]. They subsequently migrate to the fetal liver for expansion and maturation before finally colonizing the bone marrow before birth [18]. In adults, HSCs sit at the apex of a tightly regulated hierarchy, giving rise to multipotent progenitors that further differentiate into all myeloid (erythrocytes, platelets, granulocytes, macrophages) and lymphoid (T cells, B cells, NK cells) lineages [17].
Niche Regulation and Key Markers: HSC function is regulated by two principal bone marrow niches. The endosteal niche, located near bone surfaces, maintains HSC quiescence through interactions with osteoblasts and low oxygen tension [14]. The perivascular niche, associated with sinusoidal blood vessels, promotes HSC proliferation and differentiation via signals from endothelial cells and perivascular stromal cells expressing CXCL12 [14] [17]. Key markers for human HSCs include CD34, CD59, Thy1, and CD133, while murine HSCs are commonly identified as Lineage⁻, Sca-1⁺, c-Kit⁺ (LSK) cells [17].
Table 2: Key Components of the Hematopoietic Stem Cell Niche
| Niche Component | Cell Type | Primary Function | Key Signaling Molecules |
|---|---|---|---|
| Endosteal Niche | Osteoblasts, Osteoclasts | Maintains HSC quiescence, long-term repopulating capacity | Ang-1, Osteopontin, BMP, Wnt |
| Perivascular Niche | Sinusoidal Endothelial Cells, CXCL12-abundant Reticular (CAR) Cells | Supports HSC proliferation, differentiation, and mobilization | CXCL12, SCF, VEGF, Notch |
| Neural | Sympathetic Neurons | Regulates circadian HSC mobilization | Norepinephrine |
| Mesenchymal | Leptin Receptor+ (LepR+) Stromal Cells, Nestin+ MSCs | Primary source of SCF and CXCL12 for niche maintenance | CXCL12, SCF, IL-6 |
The Stem Cell Niche: A Dynamic Regulatory Unit
The stem cell niche is a dynamic, hierarchical, and specialized microenvironment that localizes stem cells and regulates the balance between their quiescent, proliferative, and differentiated states [15] [14]. It comprises cellular constituents, an ECM scaffold, and a complex signaling milieu.
Cellular and Structural Architecture: Immediate stromal neighbors (osteoblasts in bone, fibroblasts in skin) provide juxtacrine and paracrine fate-determining signals [14]. Accessory populations—endothelial cells, pericytes, macrophages, adipocytes, and sympathetic neurons—integrate systemic and local demands to modulate niche activity [14]. The ECM provides structural lattice and biochemical cues; its composition (laminin, collagen, fibronectin, proteoglycans) and mechanical properties (stiffness, viscoelasticity) are translated via integrins and cadherins into intracellular signaling that directs stem cell behavior [14].
Conserved Signaling Axes: Three evolutionarily conserved signaling pathways are central to niche-stem cell crosstalk. The Wnt/β-catenin pathway promotes self-renewal and proliferation. Bone Morphogenetic Protein (BMP) signaling often opposes Wnt, driving differentiation and maintaining quiescence. The Notch pathway, activated by juxtacrine contact with neighboring cells, regulates fate decisions and maintains the stem cell pool [14]. These pathways, along with CXCL12/CXCR4 signaling for homing and retention, form the core molecular regulatory network of the niche [19] [17].
The following diagram illustrates the core signaling interactions within a generic stem cell niche.
Clinical Applications and Regulatory Landscape
The therapeutic application of MSCs and HSCs has achieved significant clinical milestones, with an expanding pipeline of regulated products.
FDA-Approved Therapies and Clinical Trials: As of December 2024, the FDA has approved several stem cell-based products. Ryoncil (remestemcel-L), approved in December 2024, is the first allogeneic bone marrow-derived MSC therapy for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD) [3]. Omisirge (omidubicel-onlv), approved in April 2023, is a nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cell therapy that accelerates neutrophil recovery in patients with hematologic malignancies [3]. The global clinical trial landscape for pluripotent stem cell (PSC)-derived products is also rapidly expanding, with 115 clinical trials identified as of December 2024 targeting ophthalmology, neurology, and oncology [3].
Emerging Trends and Platforms: A major innovation is the development of induced pluripotent stem cell-derived MSCs (iMSCs), which offer enhanced consistency, scalability, and a defined starting material compared to primary MSCs [3]. Clinical trials are ongoing for iMSCs in conditions like high-risk acute GvHD (NCT05643638) [3]. Furthermore, iPSC-derived therapies are entering advanced trials, such as Fertilo (the first iPSC-based therapy in a U.S. Phase III trial for oocyte maturation) and OpCT-001 (an iPSC-derived therapy for retinal degeneration) [3].
Regulatory Framework: All stem cell therapeutics require rigorous oversight. Investigational New Drug (IND) authorization from the FDA permits clinical trials, while full marketing approval requires a Biologics License Application (BLA) demonstrating safety, purity, and potency [3]. The International Society for Stem Cell Research (ISSCR) provides continuously updated guidelines to ensure ethical and scientific rigor in stem cell research and clinical translation [20].
Application Notes and Experimental Protocols
Protocol: Isolation and Expansion of Human Bone Marrow-Derived MSCs
Principle: This protocol isolates plastic-adherent, multipotent stromal cells from human bone marrow aspirate based on their defining characteristics [16].
Materials:
- Research Reagent Solutions:
- Ficoll-Paque PREMIUM: For density gradient separation of mononuclear cells.
- Complete Culture Medium: Alpha-MEM, 10% Fetal Bovine Serum (FBS), 1% L-glutamine, 1% penicillin/streptomycin.
- Trypsin-EDTA (0.25%): For cell detachment.
- Flow Cytometry Antibody Panel: Anti-CD73, CD90, CD105, CD34, CD45, HLA-DR.
- Tri-lineage Differentiation Kits: Osteogenic, chondrogenic, and adipogenic induction media.
Procedure:
- Density Gradient Centrifugation: Dilute bone marrow aspirate 1:1 with PBS. Carefully layer over Ficoll-Paque and centrifuge at 400 × g for 30 minutes at room temperature with brakes off.
- Mononuclear Cell Collection: Harvest the opaque interface layer containing mononuclear cells. Wash cells twice with PBS by centrifugation at 300 × g for 10 minutes.
- Primary Culture: Resuspend the cell pellet in complete culture medium and seed at a density of 50,000–100,000 cells/cm² in a tissue culture flask. Incubate at 37°C with 5% CO₂.
- Medium Change and Expansion: After 72 hours, replace the medium to remove non-adherent cells. Refresh the medium every 3–4 days thereafter.
- Passaging: At 70–80% confluence, detach cells using Trypsin-EDTA. Replate at a density of 1,000–5,000 cells/cm² for expansion.
- Phenotypic Verification (Flow Cytometry): At passage 3, analyze cells for surface markers. MSCs must be ≥95% positive for CD73, CD90, CD105 and ≤2% positive for CD34, CD45, HLA-DR.
- Functional Potency Assay (Tri-lineage Differentiation): Culture cells in commercial osteogenic, chondrogenic, and adipogenic induction media for 21 days. Confirm differentiation by Alizarin Red S (mineralization), Alcian Blue (proteoglycans), and Oil Red O (lipid droplets) staining, respectively.
Protocol: In Vitro Reconstruction of a 3D HSC Niche
Principle: This protocol creates a biomimetic 3D bone marrow organoid to study HSC-niche interactions, support HSC expansion, and model blood disorders [17].
Materials:
- Research Reagent Solutions:
- Gelatin-Methacryloyl (GelMA) Hydrogel: A photopolymerizable biomaterial providing a tunable 3D ECM scaffold.
- Stromal Cell Co-culture: Human bone marrow-derived MSCs (BM-MSCs) and human umbilical vein endothelial cells (HUVECs).
- Cytokine Cocktail: Recombinant human SCF, TPO, FLT3-L, and CXCL12.
- Long-term Culture Initiating Cell (LTC-IC) Assay: To quantify functional HSCs.
Procedure:
- Stromal Preparation: Expand BM-MSCs and HUVECs in standard 2D culture until 80% confluent.
- 3D Hydrogel Fabrication: a. Mix BM-MSCs and HUVECs (2:1 ratio) in a 5% (w/v) GelMA precursor solution containing a photoinitiator. b. Pipet the cell-GelMA suspension into a mold and crosslink via 30 seconds of UV light (365 nm). c. Transfer the polymerized hydrogel construct to a 24-well plate and culture in endothelial growth medium (EGM-2) for 7 days to form a pre-vascularized network.
- HSC Seeding and Culture: a. Isolate CD34⁺ HSCs from umbilical cord blood or mobilized peripheral blood using immunomagnetic beads. b. Seed the HSCs onto the surface of the pre-vascularized stromal construct. c. Culture the complete niche model in HSC expansion medium (StemSpan) supplemented with SCF (100 ng/mL), TPO (100 ng/mL), FLT3-L (100 ng/mL), and CXCL12 (50 ng/mL). d. Refresh half of the medium every 3 days.
- Analysis and Harvest: a. HSC Quantification: After 14-21 days, digest the hydrogel with collagenase to release cells. Count total nucleated cells and quantify CD34⁺CD38⁻ or CD34⁺CD45RA⁻ phenotypically primitive HSCs by flow cytometry. b. Functional Assay: Perform the LTC-IC assay or a colony-forming unit (CFU) assay to confirm the maintenance of functional, multipotent HSCs.
The workflow for this 3D HSC niche reconstruction is summarized below.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Stem Cell and Niche Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Ficoll-Paque | Density gradient medium for isolating mononuclear cells from whole blood or bone marrow. | Initial isolation of BM-MSCs or peripheral blood HSCs. |
| Defined Culture Media (e.g., StemSpan, MSCGM) | Serum-free or low-serum media optimized for expansion while maintaining stemness. | Supporting the growth of undifferentiated HSCs or MSCs. |
| Recombinant Cytokines (SCF, TPO, FLT3-L, CXCL12) | Key signaling molecules that regulate HSC survival, self-renewal, and retention in the niche. | Supplementing 3D HSC niche cultures and ex vivo expansion protocols. |
| GelMA Hydrogel | A tunable, biocompatible 3D polymer scaffold that mimics the native extracellular matrix. | Creating a biomimetic environment for 3D bone marrow organoids. |
| Flow Cytometry Antibodies (CD34, CD73, CD90, CD105, CD45) | Immunophenotyping for identification, purity assessment, and quantification of stem cell populations. | Verifying MSC (CD73+/CD90+/CD105+) and HSC (CD34+) phenotype. |
| Tri-lineage Differentiation Media | Induces osteogenic, chondrogenic, and adipogenic differentiation for functional MSC validation. | Confirming the multipotency of MSC cultures as per ISCT standards. |
MSCs and HSCs, guided by their intricate niches, are foundational to the current and future state of regenerative medicine. The transition from a purely cell-centric view to a niche-centric paradigm is critical for developing more effective therapies [14]. Future advancements will rely on high-resolution niche mapping, mechanobiologically informed biomaterial design, and the clinical translation of innovative platforms like engineered iMSCs and 3D bone marrow organoids [3] [17]. By treating the stem cell and its microenvironment as an inseparable functional unit, researchers and clinicians can unlock regenerative outcomes that surpass the capabilities of classical cell therapies alone.
Stem cell transplantation represents a cornerstone of regenerative medicine, offering promising therapeutic strategies for a range of debilitating conditions. The efficacy of these therapies is not attributed to a single mechanism but is instead driven by three core, interconnected biological processes: cellular differentiation, paracrine signaling, and immunomodulation [21] [22]. Historically, the regenerative potential of stem cells was primarily ascribed to their ability to differentiate and replace damaged cells. However, a paradigm shift has occurred, revealing that the secretion of bioactive molecules and profound modulation of the immune response are equally, if not more, critical for tissue repair [23] [24]. This application note details these key mechanisms, provides supporting experimental data and protocols, and outlines essential reagents for researchers in the field.
Cellular Differentiation: Direct Tissue Replacement
Stem cells possess the unique capacity to self-renew and differentiate into specialized cell types, providing a source for directly replacing lost or damaged tissues [21] [25].
- Pluripotent Stem Cells, including Embryonic Stem Cells (ESCs) and induced Pluripotent Stem Cells (iPSCs), can generate any cell type derived from the three germ layers (ectoderm, mesoderm, and endoderm) [22] [25].
- Multipotent Stem Cells, such as Mesenchymal Stem Cells (MSCs), exhibit a more restricted differentiation potential, typically giving rise to lineages of their tissue of origin, like osteoblasts, chondrocytes, and adipocytes [21] [26].
The following table summarizes the differentiation potential of key stem cell types:
Table 1: Stem Cell Types and Their Differentiation Potential
| Stem Cell Type | Potency | Key Differentiable Lineages | Sources |
|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Pluripotent | All somatic cell types [25] | Inner cell mass of blastocysts [25] |
| Induced Pluripotent Stem Cells (iPSCs) | Pluripotent | All somatic cell types [22] [10] | Genetically reprogrammed somatic cells [10] |
| Mesenchymal Stem Cells (MSCs) | Multotent | Osteoblasts, chondrocytes, adipocytes [21] [26] | Bone marrow, adipose tissue, umbilical cord [26] [22] |
| Hematopoietic Stem Cells (HSCs) | Multotent | All blood and immune cell types [25] | Bone marrow, peripheral blood [25] |
Figure 1: Stem Cell Differentiation Pathways. This diagram illustrates the hierarchical differentiation potential from a stem cell to specialized terminally differentiated cells through multipotent and pluripotent pathways.
Experimental Protocol: In Vitro Trilineage Differentiation of MSCs
This standard protocol assesses the multipotency of MSCs by inducing differentiation into osteocytes, adipocytes, and chondrocytes [26].
1. Materials:
- Confluent culture of human MSCs (e.g., bone marrow-derived).
- Control medium: Growth medium (e.g., DMEM with 10% FBS).
- Osteogenic Differentiation Medium: Control medium supplemented with 10 mM β-glycerophosphate, 50 µM ascorbate-2-phosphate, and 100 nM dexamethasone.
- Adipogenic Differentiation Medium: Control medium supplemented with 0.5 mM 3-isobutyl-1-methylxanthine (IBMX), 1 µM dexamethasone, 10 µM insulin, and 200 µM indomethacin.
- Chondrogenic Differentiation Medium: Serum-free high-glucose DMEM supplemented with 1% ITS+ premix, 100 nM dexamethasone, 50 µM ascorbate-2-phosphate, 40 µg/mL L-proline, and 10 ng/mL TGF-β3.
2. Method:
- Cell Seeding: Seed MSCs at appropriate densities (e.g., 2.1 x 10^4 cells/cm² for osteo/adipogenesis; 5 x 10^5 cells for chondrogenic pellet culture).
- Induction: Once cells reach confluence, replace the growth medium with the respective differentiation medium. Maintain control cells in growth medium.
- Medium Refreshment: Change the differentiation medium every 2-3 days for 21 days (osteogenic and adipogenic) or 14-28 days (chondrogenic).
- Analysis:
- Osteogenesis: Fix cells and stain with 2% Alizarin Red S to detect calcium deposits.
- Adipogenesis: Fix cells and stain with Oil Red O to visualize lipid vacuoles.
- Chondrogenesis: Fix pellet cultures, embed in paraffin, section, and stain with Alcian Blue or Toluidine Blue to detect sulfated glycosaminoglycans in the extracellular matrix.
Paracrine Signaling: Trophic Mediator of Repair
The therapeutic impact of stem cells is largely mediated by their secretome—a complex mixture of cytokines, growth factors, chemokines, and extracellular vesicles (exosomes) released in a paracrine manner [21] [24]. These factors influence the local microenvironment by:
- Promoting angiogenesis.
- Inhibing apoptosis and fibrosis.
- Stimulating proliferation and migration of resident progenitor cells.
- Modulating the immune response [23] [24].
Table 2: Key Paracrine Factors Secreted by Stem Cells and Their Functions
| Secreted Factor | Primary Functions in Regeneration | Evidence/Model System |
|---|---|---|
| VEGF | Angiogenesis, cardioprotection, neuroprotection [24] | Heart repair, wound healing models [24] |
| HGF | Inhibits T-cell proliferation, promotes angiogenesis, cytoprotection [24] | Immune modulation, cardiac repair [24] |
| TGF-β | Inhibits T-cell and NK cell proliferation, involved in bone formation, ECM homeostasis [24] | Immune modulation, bone repair models [24] |
| PGE2 | Shifts macrophages from pro-inflammatory M1 to anti-inflammatory M2 phenotype [23] | Osteoarthritis (OA) models, immune modulation [23] |
| TSG-6 | Potent anti-inflammatory protein, inhibits NF-κB pathway [23] | OA, intervertebral disc degeneration models [23] |
| Exosomes | Carry miRNAs, proteins, and lipids; can inhibit inflammatory factor release and promote cell proliferation [21] [23] | OA chondrocyte models, skin and bone healing [21] |
Experimental Protocol: Analyzing MSC Paracrine Actions via Conditioned Media
This protocol describes how to collect and test the bioactivity of the MSC secretome.
1. Materials:
- MSCs at 70-80% confluence.
- Serum-free basal medium.
- Ultracentrifuge tubes (for exosome isolation).
- ELISA or Luminex kits for specific cytokines (e.g., VEGF, HGF, TGF-β).
2. Method:
- Conditioned Media (CM) Collection:
- Wash MSCs twice with PBS to remove serum contaminants.
- Incubate cells with serum-free basal medium for 24-48 hours.
- Collect the medium and centrifuge at 2,000 x g for 10 minutes to remove cells and debris.
- (Optional) For exosome isolation, centrifuge the supernatant at 100,000 x g for 70 minutes.
- Concentrate the CM using centrifugal filter units (e.g., 3 kDa cutoff) if necessary. Aliquot and store at -80°C.
- Bioactivity Assay (e.g., Endothelial Cell Tube Formation):
- Pre-chill a 96-well plate and Matrigel at 4°C.
- Thaw Matrigel on ice and coat each well with 50 µL, then incubate at 37°C for 30 minutes to polymerize.
- Seed human umbilical vein endothelial cells (HUVECs) at 1-2 x 10^4 cells/well in the CM or control media.
- Incubate for 4-16 hours at 37°C.
- Image the tubes under a microscope and quantify total tube length, number of branches, or number of meshes using image analysis software (e.g., ImageJ). CM from MSCs will typically enhance tube formation compared to control media, indicating pro-angiogenic activity.
Immunomodulation: Controlling the Inflammatory Landscape
A critical mechanism of stem cell action, particularly for MSCs, is their potent ability to modulate both innate and adaptive immune responses [23] [27]. This creates an anti-inflammatory and pro-regenerative microenvironment conducive to healing.
MSCs achieve this through:
- Soluble Factors: Secretion of IDO, PGE2, TGF-β, and IL-10 [23] [27].
- Cell-Cell Contact: Interactions via surface molecules like programmed death ligand 1 (PD-L1) [27]. Their actions include suppressing T-cell and B-cell proliferation, inhibiting NK cell cytotoxicity, polarizing macrophages towards an anti-inflammatory M2 phenotype, and promoting the expansion of regulatory T cells (Tregs) [23] [27].
Figure 2: MSC-Mediated Immunomodulation. MSCs secrete soluble factors that act on various immune cells to suppress pro-inflammatory responses and promote an anti-inflammatory state.
Experimental Protocol: T-Cell Proliferation Suppression Assay
This protocol evaluates the immunomodulatory capacity of MSCs by measuring their effect on T-cell proliferation.
1. Materials:
- Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors.
- Mitogen (e.g., Phytohemagglutinin-P (PHA)) or CD3/CD28 T-cell activator beads.
- CFSE (Carboxyfluorescein succinimidyl ester) dye.
- Co-culture system (e.g., transwell inserts or direct contact in a well).
2. Method:
- PBMC and MSC Preparation:
- Isolate PBMCs from whole blood using density gradient centrifugation (e.g., Ficoll-Paque).
- Label PBMCs with CFSE according to manufacturer's instructions to track cell division.
- Co-culture Setup:
- Seed MSCs in a well of a 24-well plate and allow them to adhere overnight.
- Activate the CFSE-labeled PBMCs with PHA (e.g., 5 µg/mL) or CD3/CD28 beads.
- Add the activated PBMCs to the MSC monolayer. Include controls with activated PBMCs alone and non-activated PBMCs.
- Co-culture for 3-5 days.
- Analysis by Flow Cytometry:
- Harvest the non-adherent PBMCs.
- Analyze using a flow cytometer. The fluorescence intensity of CFSE decreases by half with each cell division.
- Gate on the T-cell population (CD3+). A reduction in the percentage of divided T-cells and a higher mean fluorescence intensity in the co-culture group compared to the activated PBMC-only control indicate suppression of T-cell proliferation by MSCs.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents required for investigating the mechanisms described above.
Table 3: Essential Research Reagents for Stem Cell Mechanism Studies
| Reagent / Material | Function / Application | Specific Examples |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Primary model system for multipotent stem cell research [26] | Bone marrow-derived MSCs, Adipose-derived MSCs [26] [22] |
| Trilineage Differentiation Kits | Standardized in vitro assessment of MSC multipotency [26] | Osteogenic, Adipogenic, Chondrogenic Induction Media Kits |
| Cytokine Detection Assays | Quantification of secreted paracrine factors [24] | ELISA Kits (VEGF, HGF, TGF-β), Luminex Multiplex Assays |
| Exosome Isolation Kits | Isolation and purification of extracellular vesicles from conditioned media | Polymer-based precipitation kits, Size-exclusion chromatography columns |
| Flow Cytometry Antibodies | Cell surface marker phenotyping and immunomodulation assays [26] [27] | Anti-CD73, CD90, CD105 (MSC positive); Anti-CD3, CD4, CD25, FoxP3 (T-cell/Treg analysis) |
| Immunomodulation Co-culture Systems | Tools for studying cell-contact dependent and independent mechanisms [27] | Transwell inserts (porous membrane) |
The therapeutic success of stem cell transplantation in regenerative medicine is a multifaceted process orchestrated by differentiation, paracrine signaling, and immunomodulation. A deep understanding of these interconnected mechanisms is paramount for optimizing existing therapies and developing novel, evidence-based treatments. As research progresses, leveraging the full potential of the stem cell secretome, including exosomes, and harnessing their immunomodulatory power represent the next frontier in developing safe and effective regenerative applications.
Stem cell transplantation has emerged as a cornerstone of regenerative medicine, demonstrating remarkable therapeutic potential across a spectrum of human diseases. The scope of this intervention extends far beyond structural tissue repair to encompass complex immunomodulatory functions, effectively "rebooting" a dysregulated immune system. This application note details the current clinical landscape, supported by quantitative data, and provides detailed experimental protocols for researchers and drug development professionals working in this field. The dual capacity of stem cells—particularly mesenchymal stem cells (MSCs)—for both tissue regeneration and immunomodulation positions them as uniquely powerful therapeutic agents for conditions ranging from orthopedic degeneration to life-threatening inflammatory syndromes [28] [29] [3].
Quantitative Landscape of Stem Cell Applications
The efficacy of stem cell therapy is highly indication-specific. Success rates, derived from clinical observations, laboratory tests, and patient-reported outcomes, vary significantly based on the pathological condition, cell source, and delivery protocol [28]. The following tables summarize key clinical and regulatory data.
Table 1: Therapeutic Success Rates of Stem Cell Therapies Across Indications
| Therapeutic Area | Specific Condition | Reported Success Rate / Efficacy | Cell Type / Product | Key Metric |
|---|---|---|---|---|
| Hematologic Malignancies | Blood Cancers (post-transplant) | 60-70% [28] | Hematopoietic Stem Cells | Success Rate of Transplant |
| Immunological | Pediatric Steroid-Refractory Acute GvHD | Approved (Dec 2024) [3] | Ryoncil (Allogeneic Bone Marrow MSCs) | FDA Approval for SR-aGVHD |
| Orthopedic & Regenerative | Joint Repair, Autoimmune/Inflammatory Conditions | ~80% [28] | Mesenchymal Stem Cells (MSCs) | Reported Success Rate |
| Ophthalmology | Retinal Degeneration (e.g., Retinitis Pigmentosa) | Phase I/IIa (IND Cleared 2024) [3] | OpCT-001 (iPSC-Derived Therapy) | Clinical Trial Phase |
| Genetic & Metabolic | Sickle Cell Disease | 88% achieved resolution of vaso-occlusive events [3] | Lyfgenia (Autologous Gene-Modified HSCs) | Clinical Trial Efficacy |
Table 2: Recent FDA-Approved Stem Cell Products (2023-2025)
| Product Name (Generic) | Brand Name | Approval Date | Cell Type | Indication |
|---|---|---|---|---|
| Omidubicel-onlv | Omisirge | April 17, 2023 [3] | Cord Blood-Derived Hematopoietic Progenitor Cells | Accelerate neutrophil recovery in hematologic malignancies |
| Lovotibeglogene autotemcel | Lyfgenia | December 8, 2023 [3] | Autologous Cell-Based Gene Therapy | Sickle Cell Disease |
| Remestemcel-L | Ryoncil | December 18, 2024 [3] | Allogeneic Bone Marrow MSCs | Pediatric Steroid-Refractory Acute Graft vs. Host Disease |
Detailed Experimental Protocols
Protocol: MSC Isolation and Expansion for Immunomodulation
This protocol is adapted for the production of MSCs for clinical applications in immune-mediated conditions like GvHD [28] [3].
- Objective: To isolate, culture-expand, and characterize allogeneic MSCs from bone marrow aspirate for intravenous administration.
- Materials: Refer to Section 5, "The Scientist's Toolkit," for key reagents.
- Procedure:
- Cell Isolation: Dilute human bone marrow aspirate with Dulbecco's Phosphate-Buffered Saline (DPBS) at a 1:1 ratio. Isolate the mononuclear cell fraction using density-gradient centrifugation with Ficoll-Paque PLUS (centrifuge at 400 × g for 30 minutes at room temperature).
- Plating and Expansion: Resuspend the cell pellet in complete growth medium (α-MEM supplemented with 10% FBS and 1% Penicillin-Streptomycin). Plate cells at a density of 5 × 10^4 cells/cm² in a CELLSTACK culture chamber. Incubate at 37°C with 5% CO₂.
- Medium Changes and Passaging: Replace the medium every 3 days. Upon reaching 80% confluence, passage cells using Trypsin-EDTA (0.25%). Use cells at passages 3-5 for all experiments and infusions to ensure potency and genomic stability.
- Quality Control and Characterization: Prior to release, confirm MSC identity via flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) surface markers. Assess differentiation potential by inducing osteogenic and adipogenic lineages in specific induction media for 21 days.
- Formulation and Administration: For clinical dosing, harvest MSCs and resuspend in a sterile infusion solution. The typical dose for SR-aGVHD is 2 × 10^6 cells per kilogram of patient body weight, administered via intravenous infusion over 30-60 minutes [3].
Protocol: Subretinal Transplantation of iPSC-Derived Retinal Pigment Epithelium (RPE)
This protocol outlines the critical steps for the treatment of retinal diseases such as Age-related Macular Degeneration (AMD) [29].
- Objective: To manufacture and surgically implant a monolayer of iPSC-derived RPE cells into the subretinal space.
- Materials: Refer to Section 5, "The Scientist's Toolkit."
- Procedure:
- RPE Differentiation: Differentiate human iPSCs into RPE cells using a directed, stepwise protocol involving small molecules and growth factors. Culture until a pure, pigmented, cobblestone morphology monolayer is evident.
- Graft Preparation (Sheets/Suspensions): Two formats can be used:
- Cell Suspension: Dissociate the RPE monolayer using Accutase to create a single-cell suspension. Concentrate to 100,000-200,000 cells/µl in a balanced salt solution.
- Monolayer Sheet: Harvest the RPE layer as a intact sheet using a thermoreversible hydrogel or enzymatic release, supported by a biodegradable polymer scaffold like PLGA.
- Surgical Delivery: Perform a standard 3-port pars plana vitrectomy. Create a localized retinal detachment (bleb) by injecting a balanced salt solution between the neural retina and the native RPE using a subretinal cannula. Subsequently, inject the cell suspension or implant the RPE sheet into the subretinal space.
- Post-operative Monitoring: Monitor patients for signs of graft rejection, proliferation, or retinal detachment. Assess graft viability and integration using non-invasive imaging techniques such as Spectral-Domain Optical Coherence Tomography (SD-OCT) and fundus autofluorescence. Evaluate functional outcomes through best-corrected visual acuity (BCVA) and microperimetry tests [29].
Visualizing Pathways and Workflows
The following diagrams, generated with Graphviz DOT language, illustrate core concepts in stem cell therapeutics.
Stem Cell Therapeutic Mechanisms
iPSC to Clinical Product Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Example Use in Protocol |
|---|---|---|
| Ficoll-Paque PLUS | Density gradient medium for isolation of mononuclear cells. | Isolation of MSCs from bone marrow aspirate (Protocol 3.1). |
| Mesenchymal Stem Cell Growth Medium | Serum-free or FBS-containing medium optimized for MSC expansion. | Culture and expansion of MSCs while maintaining differentiation potential (Protocol 3.1). |
| Trypsin-EDTA (0.25%) | Proteolytic enzyme for dissociating adherent cells from culture surfaces. | Passaging and harvesting of adherent MSCs (Protocol 3.1). |
| Flow Cytometry Antibody Panel | Antibodies against surface markers for cell population characterization. | Confirmation of MSC phenotype (CD73+, CD90+, CD105+, CD34-, CD45-) (Protocol 3.1). |
| StemRNA Clinical Seed iPSCs | GMP-compliant, clinically-grade induced Pluripotent Stem Cells. | Starting material for differentiation into therapeutic cells like RPE or dopaminergic neurons [3]. |
| Directed Differentiation Kits | Pre-defined media and factor combinations for specific cell lineage induction. | Efficient and reproducible differentiation of iPSCs into target cells like RPE (Protocol 3.2). |
| Biodegradable Scaffolds (e.g., PLGA) | 3D structural support for cell growth and transplantation. | Used as a carrier for implanting RPE monolayer sheets in subretinal transplantation (Protocol 3.2) [29] [30]. |
| GMP-Compliant Cytokines/Growth Factors | Recombinant proteins for directing cell fate and function during manufacturing. | Used in differentiation protocols (e.g., for RPE or neural progenitors) and to enhance cell potency [3]. |
Clinical Translation and Therapeutic Applications: From Bench to Bedside
Hematopoietic stem cell (HSC) therapy represents a cornerstone of regenerative medicine for patients with hematologic malignancies and blood disorders. These therapies are designed to reconstitute the blood-forming system in patients whose bone marrow has been damaged by disease, chemotherapy, or radiation. HSCs possess the unique capacities of self-renewal and multipotency, enabling them to differentiate into all blood cell lineages and restore normal hematopoiesis. The therapeutic use of these cells has been instrumental in treating a range of conditions—including malignant hematologic diseases such as leukemia and lymphoma, as well as inherited blood disorders and immunodeficiencies—thereby cementing its importance in modern medicine [31].
The clinical application of HSC therapy traces back several decades, with bone marrow transplantation representing the earliest form of cell therapy. Historically, HSC transplantation was the only FDA-approved stem cell therapy, and successive technological improvements have led to the commercialization and licensure of numerous cord blood and bone marrow-derived products [31]. This document provides application notes and experimental protocols for FDA-approved hematopoietic stem cell therapies, with a specialized focus on the recently approved advanced cell therapy, Omisirge (omidubicel-onlv), framing their use within the context of stem cell transplantation and regenerative medicine research.
FDA-Approved HSC Therapies: Landscape and Applications
The U.S. Food and Drug Administration (FDA) maintains a rigorous approval process for cellular therapies, requiring extensive preclinical data and phased clinical trials that demonstrate safety and efficacy. For HSC-based products, the FDA's Center for Biologics Evaluation and Research (CBER) is the reviewing authority, emphasizing the need for reproducible manufacturing processes and consistency between production batches [31]. As of 2025, the FDA has approved multiple hematopoietic progenitor cell products derived from cord blood for hematopoietic reconstitution [3] [32].
Table 1: FDA-Approved Hematopoietic Progenitor Cell (HPC) Products from Cord Blood
| Product Name | Manufacturer | Key Specifications |
|---|---|---|
| ALLOCORD | SSM Cardinal Glennon Children's Medical Center | HPC, Cord Blood; for intravenous infusion [32] |
| CLEVECORD | Cleveland Cord Blood Center | HPC, Cord Blood; ≥1.25×10^6 viable CD34+ cells/unit [31] [32] |
| Ducord | Duke University School of Medicine | HPC, Cord Blood; quantified minimum cell dose thresholds [31] [32] |
| HEMACORD | New York Blood Center | HPC, Cord Blood [32] |
| REGENECYTE | StemCyte, Inc. | HPC, Cord Blood; ≥1.25×10^6 viable CD34+ cells/unit [31] [32] |
| HPC, Cord Blood - MD Anderson | MD Anderson Cord Blood Bank | HPC, Cord Blood; dose expressed per kg of recipient [31] [32] |
| HPC, Cord Blood - Bloodworks | Bloodworks Northwest | HPC, Cord Blood; high pre-cryopreservation viability [31] [32] |
| HPC, Cord Blood - LifeSouth | LifeSouth Community Blood Centers, Inc. | HPC, Cord Blood [31] [32] |
These approved products are indicated for hematopoietic reconstitution in patients with hematologic malignancies such as acute leukemia and lymphoma, as well as inherited bone marrow failure syndromes and immunodeficiency disorders [31]. They are administered via intravenous infusion following myeloablative conditioning, which removes a patient's own stem cells to make room for the transplant but simultaneously weakens the immune system and increases infection risk [33].
A significant challenge in the field has been donor availability and suitability. Matched related donors are only available for about 30% of patients, and matched unrelated donor availability varies greatly by ethnicity, with racially and ethnically diverse donors being underrepresented in donor registries [34]. Cord blood stem cells offer a valuable alternative due to their greater immunologic tolerance, which reduces the risk of graft-versus-host disease (GvHD) in allogeneic transplant settings [31].
Omisirge (omidubicel-onlv): A Novel NAM-Modified Allogeneic Cell Therapy
Omisirge (omidubicel-onlv) is a significant innovation in the field of hematopoietic stem cell transplantation. Approved by the FDA on April 17, 2023, it is a nicotinamide (NAM)-modified allogeneic hematopoietic progenitor cell therapy derived from umbilical cord blood [33]. It is indicated for adults and pediatric patients 12 years and older with hematologic malignancies who are planned for umbilical cord blood transplantation following myeloablative conditioning. Its primary therapeutic aims are to reduce the time to neutrophil recovery and the incidence of infection [33].
Mechanism of Action and Technological Basis
Omisirge is composed of human allogeneic stem cells from umbilical cord blood that are processed and cultured with nicotinamide (NAM). The NAM modification technology is the key differentiator. By inhibiting culture-induced differentiation, NAM enhances the number and functionality of the targeted stem and progenitor cells during ex vivo expansion [34] [33]. This process is designed to yield a graft with a higher functional capacity for rapid and sustained engraftment compared to standard, unmanipulated cord blood units.
Clinical Efficacy Data
The approval of Omisirge was based on clinical trials demonstrating superior outcomes compared to standard umbilical cord blood transplantation. The pivotal trial showed statistically significant improvements in the primary efficacy endpoints.
Table 2: Key Clinical Efficacy Outcomes for Omisirge vs. Standard UCB [34] [33]
| Parameter | Omisirge | Standard Umbilical Cord Blood |
|---|---|---|
| Median Time to Neutrophil Recovery | Significantly Faster | Slower (Control) |
| Incidence of Bacterial or Fungal Infections | Significantly Reduced | Higher (Control) |
The accelerated neutrophil recovery is a critical clinical milestone, as it directly correlates with a reduced period of severe neutropenia, thereby lowering the risk of life-threatening infections and potentially reducing hospital stays [34] [33].
Administration Protocol
The administration of Omisirge is a carefully controlled process involving two distinct cellular fractions [33]:
- Premedication: Approximately 30 to 60 minutes prior to infusion, patients must receive premedication with an antihistamine, hydrocortisone, and acetaminophen to mitigate the risk of infusion reactions.
- Product Thawing and Preparation: The Omisirge graft is supplied as a cryopreserved suspension for infusion. The product consists of a patient-specific single dose with two components: a Cultured Fraction (CF) and a Non-cultured Fraction (NF). These must be thawed according to the manufacturer's precise instructions.
- Infusion Sequence:
- The CF bag is administered first via intravenous infusion.
- The NF bag is administered within 1 hour after the completion of the CF infusion.
Close monitoring of the patient during and after the infusion is mandatory for the early detection and management of adverse reactions.
Safety Profile and Black Box Warnings
Omisirge's product label carries a Boxed Warning for several serious risks [33]:
- Infusion Reactions: May occur during or shortly after infusion.
- Graft-versus-Host Disease (GvHD): Can be acute or chronic, and may be fatal.
- Engraftment Syndrome: A clinical constellation that can include fever, rash, and pulmonary edema.
- Graft Failure: Can result in severe infection or bleeding, and may be fatal.
Other Warnings and Precautions include the potential for malignancies of donor origin, transmission of serious infections, and transmission of rare genetic diseases from the donor cells [33]. The most common adverse reactions (incidence >20%) include infections, GvHD, and infusion reactions. This safety profile necessitates that Omisirge be administered only at experienced transplant centers capable of managing these complex complications.
Experimental and Research Protocols
In Vitro Functional Potency Assay for CD34+ Cell Characterization
Purpose: To quantify and qualify the hematopoietic progenitor cell population in a cord blood-derived product, which is a critical release criterion and predictor of in vivo engraftment potential.
Methodology:
- Sample Preparation: Thaw the cryopreserved cell product and wash to remove cryopreservant (e.g., DMSO). Resuspend in appropriate culture medium.
- Cell Staining: Aliquot cells and stain with fluorescently conjugated anti-human CD34 antibody and a viability dye. Use an isotype control for gating compensation.
- Flow Cytometry Analysis:
- Acquire data on a flow cytometer calibrated with fluorescence standards.
- Gate the live cell population based on viability dye exclusion.
- Within the live cell gate, identify the CD34+ cell population.
- Calculate the absolute count of viable CD34+ cells per kg of recipient body weight. This value is a key potency metric for HSC products [31].
- Colony-Forming Unit (CFU) Assay: Plate a defined number of viable cells in semi-solid methylcellulose media optimized for hematopoietic progenitors (e.g., MethoCult). Culture for 14 days at 37°C with 5% CO2. Score colonies (CFU-GEMM, BFU-E, CFU-GM) under an inverted microscope to assess clonogenic potential and lineage commitment.
Protocol for NAM-Modification of Cord Blood-Derived HSCs
Purpose: To replicate the core technology behind Omisirge by expanding a functionally enhanced population of hematopoietic stem and progenitor cells ex vivo.
Reagents and Materials:
- Cryopreserved human umbilical cord blood-derived CD34+ cells
- Nicotinamide (NAM) stock solution
- Serum-free hematopoietic cell expansion medium
- Recombinant human cytokines (SCF, TPO, FLT-3 ligand)
- Sterile tissue culture flasks or bags
- Controlled environment incubator (37°C, 5% CO2)
Procedure:
- Thaw and Enrich CD34+ Cells: Thaw cord blood unit and isolate CD34+ cells using immunomagnetic selection to a high purity (>90%).
- Initiate Culture: Seed cells at a density of 1-2 x 10^5 cells/mL in expansion medium supplemented with cytokines.
- Apply NAM Treatment: Add NAM to the experimental culture at a specified concentration (e.g., 0.1-1.0 mM). Maintain a control culture without NAM.
- Maintain Culture: Culture cells for 14-21 days, maintaining cell density and refreshing medium and cytokines every 3-4 days.
- Harvest and Analyze: At the end of the culture period, perform cell counts and viability analysis. Characterize the expanded product via flow cytometry for CD34+ content and perform CFU assays as described in Section 4.1. Compare the total nucleated cell (TNC) count, CD34+ cell count, and CFU capacity between NAM-treated and control cultures.
The Scientist's Toolkit: Essential Research Reagents
For researchers investigating hematopoietic stem cell biology and developing new expansion or engineering protocols, the following reagents and tools are essential.
Table 3: Key Research Reagent Solutions for HSC Research
| Research Reagent | Function in Experimental Protocol |
|---|---|
| Immunomagnetic CD34+ Selection Kits | Isolation and purification of hematopoietic stem and progenitor cells from complex mixtures like cord blood or bone marrow for downstream applications. |
| Serum-Free Hematopoietic Culture Media | Provides a defined, consistent environment for the ex vivo expansion and maintenance of HSCs, minimizing uncontrolled variables. |
| Recombinant Human Cytokines (SCF, TPO, FLT-3L) | Critical signaling molecules that promote HSC survival, proliferation, and maintenance of stemness in culture. |
| Flow Cytometry Antibodies (anti-CD34, CD45, CD38, etc.) | Enables phenotypic characterization, purity assessment, and tracking of HSCs and differentiated progeny. |
| Methylcellulose-based CFU Assay Media | A functional potency assay to quantify the frequency and lineage potential of clonogenic hematopoietic progenitors. |
| Nicotinamide (NAM) | A small molecule used to enhance ex vivo expansion by modulating cell differentiation pathways, as utilized in Omisirge manufacturing. |
Future Directions and Research Applications
The approval of Omisirge validates the approach of ex vivo manipulation and expansion of cord blood units to overcome the limitation of low cell dose. Furthermore, a supplementary Biologics License Application (sBLA) for omidubicel for the treatment of Severe Aplastic Anemia (SAA) has been accepted by the FDA with a target action date of December 10, 2025, indicating potential expansion of its indications [35].
Future research directions in this field include:
- Enhanced Cell Engineering: Genetic modification of HSCs to improve engraftment, add therapeutic genes, or enhance immunomodulatory properties [31].
- Optimization of Preconditioning Regimens: Developing less toxic conditioning regimens to reduce transplant-related morbidity while allowing effective engraftment [31].
- iPSC-Derived HSCs: Exploring induced pluripotent stem cells (iPSCs) as a scalable and customizable source for generating HSCs, though this remains largely in the research phase [3].
The field of regenerative medicine has reached a pivotal juncture with the recent approval of two groundbreaking therapies that exemplify the divergent yet complementary approaches in advanced cell-based treatments. The U.S. Food and Drug Administration (FDA) has approved Ryoncil (remestemcel-L) as the first mesenchymal stromal cell (MSC) therapy for steroid-refractory acute graft-versus-host disease (SR-aGVHD) in pediatric patients, and Lyfgenia (lovotibeglogene autotemcel), a lentiviral vector-based gene therapy for sickle cell disease (SCD) [36] [37]. These approvals represent significant regulatory milestones that validate nearly three decades of scientific research while establishing new standards for cell-based therapeutic development. This application note details the experimental protocols, clinical data, and mechanistic insights underlying these approvals to guide researchers and drug development professionals in advancing the next generation of regenerative medicines.
Ryoncil: The First FDA-Approved MSC Therapy
Mechanism of Action and Product Characterization
Ryoncil is an allogeneic bone marrow-derived mesenchymal stromal cell (MSC) therapy designed to modulate inflammatory responses in patients with SR-aGVHD [36]. Unlike traditional stem cells that primarily function through differentiation, MSCs act as "medicinal signaling cells" by secreting bioactive molecules that modulate the immune environment [38]. The therapy works through paracrine signaling whereby the infused cells release factors that suppress T-cell proliferation and downregulate pro-inflammatory cytokines and interferons, thereby mitigating the excessive immune response that characterizes aGVHD [36].
The evolution in understanding MSC biology has been crucial to Ryoncil's development. Originally termed "mesenchymal stem cells" in 1991 by Arnold Caplan, these cells were later redefined as "medicinal signaling cells" based on evidence that their therapeutic effects stem from immunomodulatory signaling rather than stem cell differentiation capabilities [38]. Single-cell RNA sequencing studies have further elucidated the transcriptomic heterogeneity of MSC populations, providing biomarkers for product characterization and quality control [38].
Clinical Protocol and Administration
The approved administration protocol for Ryoncil involves a standardized treatment course with specific handling requirements:
- Dosing Regimen: ( 2 \times 10^6 ) MSC/kg body weight per intravenous infusion [36] [39]
- Treatment Schedule: Twice weekly for four consecutive weeks (total of 8 infusions) [36] [39]
- Infusion Timing: Minimum of 3 days between infusions [39]
- Pre-medication: Administration of corticosteroids and antihistamines prior to infusion to minimize potential allergic reactions [36]
- Monitoring Parameters: Continuous assessment for hypersensitivity reactions, acute infusion responses, and infectious complications during and after administration [36]
Table 1: Ryoncil Clinical Administration Protocol
| Parameter | Specification |
|---|---|
| Cell Source | Allogeneic bone marrow from healthy adult donors |
| Recommended Dose | ( 2 \times 10^6 ) MSC/kg body weight |
| Administration Route | Intravenous infusion |
| Treatment Duration | 4 weeks |
| Total Infusions | 8 |
| Pre-medication | Corticosteroids and antihistamines |
| Critical Monitoring | Allergic reactions, infusion responses, infection signs |
Efficacy and Safety Data
The safety and efficacy of Ryoncil were established in a multicenter, single-arm study (NCT02336230) involving 54 pediatric patients with SR-aGVHD following allogeneic hematopoietic stem cell transplantation [36] [39]. Patients had Grade B-D SR-aGVHD (excluding Grade B skin-only involvement) according to the International Blood and Marrow Transplantation Registry Severity Index Criteria [39].
Table 2: Ryoncil Clinical Trial Outcomes (Day 28)
| Efficacy Parameter | Result | Statistical Significance |
|---|---|---|
| Overall Response Rate (ORR) | 70% | 95% CI: 56.4-82.0 |
| Complete Response (CR) Rate | 30% | 95% CI: 18.0-43.6 |
| Partial Response (PR) Rate | 41% | 95% CI: 27.6-55.0 |
| Median Duration of Response | 54 days | Range: 7-159+ days |
The most common adverse reactions (incidence ≥20%) included viral and bacterial infectious disorders, fever, hemorrhage, edema, abdominal pain, and hypertension [36] [39]. Serious potential complications include hypersensitivity reactions, transmission of infectious pathogens, and ectopic tissue formation [36].
Experimental Protocols for MSC Potency Assessment
For researchers developing MSC therapies, establishing robust potency assays is critical for regulatory approval. The following protocol outlines key assessment methods:
Protocol: MSC Potency and Characterization Assays
Immunomodulatory Potency Assay
- Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors
- Activate T-cells with anti-CD3/CD28 antibodies
- Co-culture with serial dilutions of MSCs at ratios from 1:1 to 1:10 (MSC:PBMC)
- Measure T-cell proliferation via 3H-thymidine incorporation or CFSE dilution
- Quantify cytokine production (IFN-γ, TNF-α, IL-10) via ELISA after 72 hours
Cell Surface Marker Characterization (Flow Cytometry)
- Stain 1×10^5 MSCs with antibodies against positive markers (CD73, CD90, CD105)
- Include negative markers (CD34, CD45, CD14, CD19, HLA-DR)
- Analyze using flow cytometry with ≥95% expression of positive markers and ≤2% expression of negative markers meeting ISCT criteria
Trilineage Differentiation Capacity
- Adipogenic differentiation: Culture in adipogenic induction medium for 21 days, assess with Oil Red O staining
- Osteogenic differentiation: Culture in osteogenic induction medium for 28 days, assess with Alizarin Red S staining
- Chondrogenic differentiation: Pellet culture in chondrogenic induction medium for 28 days, assess with Alcian Blue staining
Diagram 1: Ryoncil Mechanism of Action. The diagram illustrates the pathway from MSC administration to reduced inflammation and tissue repair through paracrine signaling and immunomodulation.
Lyfgenia: Gene Therapy for Sickle Cell Disease
Mechanism of Action and Genetic Engineering Approach
Lyfgenia (lovotibeglogene autotemcel) is a cell-based gene therapy that utilizes a lentiviral vector for genetic modification of autologous hematopoietic stem cells (HSCs) to treat sickle cell disease in patients 12 years and older with a history of vaso-occlusive events (VOEs) [37] [40]. Unlike CRISPR-based approaches, Lyfgenia employs a gene addition strategy wherein patients' own HSCs are genetically modified to produce HbAT87Q, a gene-therapy-derived hemoglobin that mimics the structure and function of normal adult hemoglobin (hemoglobin A) but contains a single amino acid substitution (threonine to glutamine at position 87) that prevents polymerization characteristic of sickling [37].
The therapeutic mechanism involves:
- Genetic Modification: Ex vivo introduction of a functional β-globin gene variant into CD34+ HSCs using a lentiviral vector
- Hemoglobin Expression: Production of HbAT87Q hemoglobin in red blood cell lineages
- Sickling Prevention: HbAT87Q hemoglobin inhibits polymerization under low oxygen conditions
- Oxygen Transport: Restoration of normal oxygen delivery to tissues
Clinical Protocol and Treatment Process
Lyfgenia administration involves a complex, multi-step treatment process requiring specialized infrastructure and expertise:
Protocol: Lyfgenia Treatment Process
HSC Collection (Week -8 to -6)
- Mobilize and collect CD34+ hematopoietic stem cells via apheresis
- Minimum collection target: 4.0×10^6 CD34+ cells/kg
Myeloablative Conditioning (Week -10 to -9 days)
- Administer busulfan-based myeloablative conditioning (3.2-4.0 mg/kg/day)
- Confirm adequate neutrophil and platelet count suppression prior to infusion
Genetic Modification (Week -7 to -1)
- Transduce CD34+ cells with lentiviral vector encoding βA-T87Q-globin gene
- Perform quality control testing including vector copy number, viability, and sterility
Product Infusion (Day 0)
- Thaw and administer Lyfgenia via central venous catheter
- Monitor for acute infusion reactions and adverse events
Engraftment Monitoring (Day +7 to +42)
- Track neutrophil and platelet engraftment
- Monitor for vector-derived hemoglobin expression
Long-term Follow-up (Years 1-15)
- Quarterly assessments for first year, then annually
- Monitor for insertional oncogenesis and other delayed adverse events
Table 3: Lyfgenia Treatment Timeline and Key Milestones
| Time Point | Activity | Key Parameters |
|---|---|---|
| Week -8 to -6 | HSC Collection | CD34+ cell count ≥4.0×10^6 cells/kg |
| Week -10 to -9 days | Myeloablative Conditioning | Busulfan administration |
| Week -7 to -1 | Genetic Modification | Vector copy number, viability, sterility |
| Day 0 | Product Infusion | Monitor infusion reactions |
| Day +7 to +42 | Engraftment Monitoring | Neutrophil/platelet recovery, HbAT87Q expression |
| Years 1-15 | Long-term Follow-up | Malignancy screening, VOE frequency, HbAT87Q stability |
Efficacy and Safety Data
The safety and efficacy of Lyfgenia were evaluated in a single-arm, 24-month multicenter study in patients with sickle cell disease and history of VOEs between ages 12-50 years [37]. Effectiveness was based on complete resolution of VOEs (VOE-CR) between 6 and 18 months after infusion.
Table 4: Lyfgenia Clinical Trial Outcomes
| Efficacy Parameter | Result | Patient Population |
|---|---|---|
| Complete Resolution of VOEs (VOE-CR) | 88% (28/32 patients) | Patients with history of vaso-occlusive events |
| Safety Parameter | Incidence | Management |
| Hematologic malignancy | Reported in clinical trials | Black box warning, lifelong monitoring required |
| Stomatitis | Common | Supportive care |
| Febrile neutropenia | Common | Standard management |
| Thrombocytopenia | Common | Monitoring and transfusion support |
The FDA included a black box warning for Lyfgenia regarding the risk of hematologic malignancy, requiring lifelong monitoring of patients for these malignancies [37]. Common adverse effects included stomatitis, low levels of platelets, white blood cells, and red blood cells, and febrile neutropenia, consistent with myeloablative conditioning and underlying disease [37].
Diagram 2: Lyfgenia Treatment Workflow. The diagram illustrates the key steps in the Lyfgenia treatment process from hematopoietic stem cell collection to therapeutic outcome.
Research Reagent Solutions for Cell and Gene Therapy Development
The development of advanced therapies like Ryoncil and Lyfgenia requires specialized reagents and platforms. The following table details essential research tools for scientists working in this field:
Table 5: Essential Research Reagents for Cell and Gene Therapy Development
| Reagent Category | Specific Product/Platform | Research Application | Example Use Case |
|---|---|---|---|
| Gene Delivery Systems | Lentiviral vectors (Lyfgenia) | Stable gene integration | HbAT87Q gene delivery to HSCs [37] |
| Celletto nano-mechanical platform | Non-viral gene delivery | Direct nuclear delivery of genetic material [41] | |
| LNP-SNAs (lipid nanoparticles) | CRISPR component delivery | Efficient Cas9/gRNA delivery with reduced toxicity [41] | |
| Cell Manufacturing | iDEM automated platform | Automated cell production | Closed-system MSC expansion [41] |
| Purified Exosome Product (PEP) | Cell-free therapeutic platform | Immune modulation and tissue repair [41] | |
| Analytical Tools | Single-cell RNA sequencing | Cell heterogeneity analysis | MSC subpopulation identification [38] |
| Flow cytometry panels | Cell surface marker analysis | ISCT criteria verification for MSCs [38] | |
| Cell Culture Systems | Trilineage differentiation media | Functional potency assessment | Adipogenic, osteogenic, chondrogenic differentiation [38] |
The approvals of Ryoncil and Lyfgenia represent transformative milestones in regenerative medicine, establishing new paradigms for treating severe inflammatory diseases and genetic disorders. Ryoncil validates the therapeutic potential of MSC-based immunomodulation, while Lyfgenia demonstrates the viability of ex vivo gene therapy for hereditary hematologic conditions. For researchers and drug development professionals, these successes highlight several critical considerations: the importance of understanding precise mechanisms of action, the need for robust potency assays and manufacturing controls, and the value of strategic regulatory engagement. As the field advances, emerging technologies such as nano-mechanical gene delivery, automated cell manufacturing, and single-cell analytics will further accelerate the development of next-generation regenerative therapies. These approved products not only provide new treatment options for patients but also establish regulatory precedents and technical roadmaps that will guide future innovation in stem cell and gene therapy research.
Application Notes: Clinical Landscape of iPSC-Derived Therapies
Induced pluripotent stem cell (iPSC) technology has emerged as a cornerstone of regenerative medicine, enabling the development of novel cell replacement and immunomodulatory therapies. By reprogramming adult somatic cells into a pluripotent state, researchers can generate patient-specific or off-the-shelf cells capable of differentiating into virtually any tissue type [9] [42]. This platform technology offers distinct advantages for clinical translation, including potential solutions for immune rejection and the capacity for unlimited expansion [43] [42]. The following application notes summarize three pioneering iPSC-derived therapies currently in clinical development for Parkinson's disease, primary photoreceptor diseases, and systemic lupus erythematosus (SLE), highlighting their therapeutic mechanisms, clinical progress, and quantitative outcomes.
Table 1: Overview of Pioneering iPSC-Derived Therapies in Clinical Development
| Therapeutic Candidate | Indication | Developer | Therapeutic Cell Type | Clinical Stage | Key Reported Outcomes |
|---|---|---|---|---|---|
| FT819 [44] | Systemic Lupus Erythematosus (SLE) | Fate Therapeutics | Off-the-shelf, CD19-targeted CAR T-cell | Phase 1 (NCT06308978) | - Significant SLEDAI-2K score reductions (e.g., 16-point reduction)- Complete renal response in lupus nephritis patients- Favorable safety profile with no dose-limiting toxicities |
| OpCT-001 [45] | Primary Photoreceptor Diseases (e.g., Retinitis Pigmentosa) | BlueRock Therapeutics | iPSC-derived photoreceptor cells | Phase 1/2a (IND Cleared) | - First iPSC-derived therapy for primary photoreceptor diseases to enter clinical trials |
| Bemdaneprocel (BRT-DA01) [45] | Parkinson's Disease | BlueRock Therapeutics | iPSC-derived dopaminergic neurons | Phase 1 (Completed), Advanced trials planned | - RMAT and Fast Track designation from FDA |
| iPSC-derived dopaminergic progenitors [42] | Parkinson's Disease | Multiple Institutions | iPSC-derived dopaminergic progenitors | Phase I/II (jRCT2090220384) | - Allogeneic cells survived transplantation and produced dopamine post-transplant |
The clinical data generated to date for these candidates demonstrates the versatile application of iPSC technology across diverse disease pathologies. For FT819, early clinical results indicate potent B-cell depletion and immune remodeling, leading to significant disease activity reduction in SLE patients [44]. The therapy has shown promising efficacy across different conditioning regimens, including a less-intensive regimen and a conditioning-free regimen for patients on standard-of-care maintenance therapy [44]. For OpCT-001, this first-in-class investigational therapy represents a novel approach to treating primary photoreceptor diseases by directly replacing degenerated photoreceptor cells in the retina [45]. In Parkinson's disease, multiple iPSC-derived dopaminergic neuron therapies have advanced to clinical testing, demonstrating successful engraftment, dopamine production, and acceptable safety profiles in early-stage trials [42] [45].
Experimental Protocols
Protocol 1: Manufacturing and Quality Control of iPSC-Derived Therapies
The transition from basic research to clinical application requires robust, reproducible manufacturing protocols conducted under current Good Manufacturing Practices (cGMP) [42] [45]. The following protocol outlines the general workflow for producing clinical-grade iPSC-derived cell therapies.
Starting Material and Reprogramming
- Somatic Cell Source Isolation: Obtain patient-specific (autologous) or healthy donor (allogeneic) somatic cells. Common sources include dermal fibroblasts, peripheral blood mononuclear cells, or urinary epithelial cells [46] [43]. For allogeneic approaches, select donors with homozygous HLA haplotypes to maximize immunologic compatibility [42].
- Reprogramming to iPSCs: Use non-integrating delivery systems to reprogram somatic cells into iPSCs. Preferred methods include:
- Sendai Viral Vectors: Efficient, non-integrating viral vectors based on the Sendai virus [42].
- Episomal Plasmid Vectors: Non-viral, plasmid-based systems that are gradually lost during cell divisions [42].
- Synthetic mRNA: Transfection with modified mRNAs encoding reprogramming factors (OCT4, SOX2, KLF4, c-MYC) [43] [42].
- Clonal Selection and Expansion: Isolate single-cell-derived iPSC colonies based on morphological criteria (tight, dome-shaped colonies with defined borders). Expand selected clones and establish master cell banks [44].
Genetic Engineering and Differentiation
- Genetic Modification (if applicable): For engineered therapies like FT819, introduce therapeutic transgenes (e.g., CAR constructs) into safe harbor loci (e.g., AAVS1) using CRISPR/Cas9 or other precise gene-editing tools [44] [42].
- Directed Differentiation: Differentiate iPSCs into target somatic cell types using staged protocols mimicking embryonic development. For example:
- Dopaminergic Neurons: Use dual SMAD inhibition, followed by activation of SHH and WNT pathways to pattern cells toward a floor-plate midbrain fate [47].
- Photoreceptor Precursors: Employ stepwise differentiation through retinal progenitor stages using combinations of growth factors (e.g., FGF, BMP, WNT inhibitors) [45].
- CAR T-cells: Differentiate iPSCs into hematopoietic progenitors, then into T-cell lineages using cytokines (SCF, FLT3L, IL-7, IL-2) and Notch signaling activation [44].
Purification and Formulation
- Cell Purification: Isolate target cell populations using fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) with cell-specific surface markers. For dopaminergic neurons, use markers like CORIN or LMX1A; for photoreceptor precursors, use CRX or OTX2 [47].
- Final Product Formulation: Wash and resuspend the final therapeutic cell product in an appropriate cryopreservation medium containing DMSO and human serum albumin. Fill vials at the specified cell density and cryopreserve using controlled-rate freezing [42].
Quality Control and Release Testing
- Sterility Testing: Perform tests for bacterial/fungal sterility, mycoplasma, and endotoxin according to pharmacopeial standards.
- Identity and Purity: Verify cell identity and differentiation status via flow cytometry for cell-type-specific markers. Assess purity and contamination with undifferentiated iPSCs (using markers like TRA-1-60) [42].
- Potency Assays: Develop functional assays relevant to the therapeutic mechanism (e.g., dopamine secretion for Parkinson's therapies, target cell killing for CAR T-cells) [44].
- Safety Testing: Perform karyotyping and genomic integrity analysis (e.g., SNP microarrays) to ensure the absence of chromosomal abnormalities or oncogenic mutations [42].
Protocol 2: Preclinical In Vivo Efficacy and Safety Assessment
Before initiating human trials, comprehensive preclinical testing in animal models is essential to demonstrate proof-of-concept, determine effective dosing, and assess potential risks.
Animal Model Selection
- Disease-Relevant Models: Select models that recapitulate key pathological features of the target disease:
- Parkinson's Disease: 6-hydroxydopamine (6-OHDA) lesioned rats or MPTP-treated non-human primates [47].
- SLE: Spontaneous lupus-prone mouse models (e.g., MRL/lpr, NZB/W F1) [46].
- Retinal Degeneration: Genetic models of photoreceptor degeneration (e.g., rd1, rd10 mice) or induced degeneration using light damage or chemical toxicity [45].
Cell Transplantation
- Delivery Route and Technique:
- Central Nervous System: Stereotactic injection into the target brain region (e.g., striatum or substantia nigra for Parkinson's disease) [47].
- Eye: Subretinal injection using a trans-scleral or trans-corneal approach with a fine glass micropipette [45].
- Systemic Administration: Intravenous infusion for immunomodulatory cells like CAR T-cells [44].
- Immunosuppression: Administer appropriate immunosuppressive regimens (e.g., tacrolimus, mycophenolate mofetil) for allogeneic cell transplants in immunocompetent animals, unless using immune-evasion technologies [42].
Efficacy and Safety Assessment
- Functional Recovery: Monitor disease-specific functional outcomes at regular intervals post-transplantation:
- Histological Analysis: At study endpoint, perform histological analysis to assess:
- Cell Survival and Integration: Identify transplanted cells (via human-specific antibodies or pre-labeling) and assess morphological integration into host tissue [47].
- Tumorigenicity: Thoroughly examine the transplantation site and major organs for any evidence of teratoma or other aberrant growth [42].
- Host Immune Response: Characterize local and systemic immune responses to the transplanted cells (e.g., T-cell infiltration, microglial activation) [42].
Table 2: Key Efficacy Parameters from Preclinical and Clinical Studies
| Therapeutic Area | In Vivo Functional Assays | Histological & Biomarker Endpoints | Clinical Efficacy Endpoints |
|---|---|---|---|
| Parkinson's Disease [47] | - Rotarod performance- Apomorphine-induced rotation- Cylinder test (forelimb use) | - Dopaminergic neuron survival (Tyrosine Hydroxylase+ cells)- Fiber outgrowth into striatum- Synaptic integration | - UPDRS Part III motor score |
| Retinal Disease [45] | - Optomotor response- Light-dark box transition | - Photoreceptor layer thickness on OCT- Synapse formation with host bipolar cells- Expression of opsins | - Visual acuity (BCVA)- Retinal sensitivity (microperimetry)- Visual field improvement |
| Autoimmunity (SLE) [46] [44] | - Proteinuria reduction- Survival prolongation- Autoantibody reduction | - Immune cell infiltration in kidneys (lupus nephritis)- Deposition of immune complexes | - SLEDAI-2K score reduction- Physician's Global Assessment (PGA)- Complete Renal Response (CRR) |
Signaling Pathways and Workflows
iPSC Differentiation and Therapeutic Application Workflow
Key Signaling Pathways in iPSC Differentiation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for iPSC-Derived Therapy Development
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Reprogramming Systems | Sendai Virus Vectors (CytoTune), Episomal Plasmids, Synthetic mRNA | Non-integrating delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC) to generate iPSCs from somatic cells [43] [42]. |
| Cell Culture Media | mTeSR, StemFlex, TeSR-E8 | Chemically defined, xeno-free media for maintenance and expansion of undifferentiated iPSCs [42]. |
| Differentiation Kits & Reagents | STEMdiff Dopaminergic Neuron Kit, Retinal Differentiation Kits, Hematopoietic Differentiation Kits | Specialized media and supplement formulations for directed differentiation of iPSCs into specific somatic cell lineages [47] [45]. |
| Small Molecule Inhibitors/Activators | SMAD Inhibitors (LDN-193189, SB431542), SHH Agonists (Purmorphamine), WNT Activators (CHIR99021) | Precisely control key signaling pathways during iPSC differentiation to steer cells toward desired fates [47]. |
| Cell Separation Markers | Anti-CORIN, Anti-LMX1A, Anti-CRX, Anti-CD19 | Antibodies for FACS or MACS to identify and purify specific cell populations during differentiation or from final products [44] [47]. |
| Gene Editing Tools | CRISPR/Cas9 Systems, AAVS1 Safe Harbor Targeting Vectors, TALEN | Precise genetic engineering for introducing therapeutic transgenes (e.g., CAR constructs) or correcting disease-causing mutations [44] [42]. |
| cGMP Manufacturing Components | cGMP-grade Cytokines, Vitronectin-XF, Recombinant Laminin | High-quality, traceable raw materials for manufacturing clinical-grade cell products under cGMP standards [42] [45]. |
Stem cell transplantation has evolved from a theoretical concept to a cornerstone of regenerative medicine, with significant advancements across various clinical specialties. This progress is marked by a deepening understanding of tissue-specific mechanisms, refined delivery protocols, and a growing number of advanced clinical trials and approved therapies. This document provides detailed application notes and experimental protocols for researchers and drug development professionals, focusing on four key therapeutic areas: neurology, ophthalmology, cardiology, and orthopedics. The content is framed within the broader context of translating foundational stem cell research into clinically viable regenerative treatments, highlighting both current achievements and future directions.
Neurology
Application Notes
The central nervous system (CNS) possesses a limited innate capacity for regeneration. Stem cell therapies aim to overcome this by replacing lost neurons and glial cells, providing neuroprotection, and modulating the hostile microenvironment of damaged neural tissue [48]. The therapeutic mechanisms are multifaceted, including neuroprotection (secretion of neurotrophic factors like BDNF and GDNF), immunomodulation (suppressing pro-inflammatory T cells and promoting anti-inflammatory cytokines like IL-10), and stimulation of angiogenesis (secretion of VEGF) [48]. Clinical targets primarily include neurodegenerative diseases and acute injuries, with a focus on replacing specific cell types, such as dopaminergic neurons in Parkinson's Disease (PD) or motor neurons in Amyotrophic Lateral Sclerosis (ALS) [48].
Table 1: Key Clinical Targets and Cellular Mechanisms in Neurological Applications
| Condition | Key Pathophysiology | Proposed Stem Cell Mechanism | Cell Types Used |
|---|---|---|---|
| Parkinson's Disease (PD) | Loss of dopaminergic neurons in the substantia nigra [48]. | Differentiation into dopamine-producing neurons; trophic support [48]. | MSCs, iPSC-derived dopaminergic progenitors [3] [48]. |
| Alzheimer's Disease (AD) | Amyloid-beta plaques, neurofibrillary tangles, neuronal loss [48]. | Reduction of amyloid-beta plaques, increased neurogenesis, immunomodulation [48]. | Neural Stem Cells (NSCs), MSCs [48]. |
| Spinal Cord Injury (SCI) | Disruption of axonal pathways, glial scar formation, inflammation [48]. | Axon regeneration, modulation of glial scar, immunomodulation, cell replacement [48]. | NSCs, MSCs, iPSC-derived neural progenitors [3] [48]. |
| Amyotrophic Lateral Sclerosis (ALS) | Degeneration of upper and lower motor neurons [48]. | Neuroprotection of motor neurons, immunomodulation, potential cell replacement [48]. | MSCs [48]. |
| Stroke | Ischemic or hemorrhagic brain tissue damage [48]. | Promotion of neuronal survival, angiogenesis, reduction of inflammation, cell replacement [48]. | NSCs, MSCs [48]. |
Experimental Protocol: Intrathecal Administration of Mesenchymal Stem Cells (MSCs) for Neurodegenerative Disease
This protocol outlines a standardized methodology for the intrathecal delivery of MSCs, a common route for treating diffuse neurological conditions like ALS and MS [48].
1. Cell Source and Preparation:
- Source: Isolate MSCs from bone marrow aspirate or adipose tissue (liposuction), or use pre-screened, GMP-grade umbilical cord tissue-derived MSCs from a certified cell bank [48] [49].
- Expansion: Culture cells in GMP-compliant, xeno-free medium. Passage cells at 70-80% confluence, do not exceed passage 5 to maintain genetic stability and potency [10].
- Quality Control (QC): Perform flow cytometry to confirm positive expression of CD73, CD90, CD105 and negative expression of CD34, CD45, CD11b. Test for mycoplasma, endotoxin, and sterility per regulatory guidelines [50].
- Formulation: On the day of administration, harvest cells using a gentle dissociation reagent. Wash and resuspend in sterile, clinical-grade normal saline or Plasmalyte-A at a final concentration of 10-50 million cells/mL. Maintain cells at 4°C and use within 4 hours of formulation [48].
2. Patient Preparation and Administration:
- Pre-medication: Consider pre-treatment with an antihistamine (e.g., diphenhydramine 25-50 mg IV/PO) to mitigate potential infusion reactions.
- Procedure: Position the patient in the lateral decubitus position. Under aseptic conditions and using fluoroscopic or ultrasound guidance, perform a lumbar puncture at the L3/L4 or L4/L5 interspace.
- Injection: Slowly inject the cell suspension (typical volume: 5-10 mL) into the intrathecal space over 2-5 minutes.
- Post-procedure: Have the patient remain supine for 1-2 hours. Monitor vital signs for any immediate adverse events (e.g., headache, nausea, changes in neurological status).
3. Safety and Efficacy Monitoring:
- Safety: Assess for adverse events (AEs) immediately post-procedure and at 24 hours, 1 week, 1 month, and 3 months. Key AEs to monitor include headache, back pain, meningismus, and any new neurological symptoms.
- Efficacy: Conduct baseline and follow-up assessments at 3, 6, and 12 months. Utilize standardized scales relevant to the disease (e.g., ALSFRS-R for ALS, UPDRS for PD, EDSS for MS), along with electrophysiological studies and MRI to track disease progression and potential structural changes [48].
Ophthalmology
Application Notes
The eye is an ideal target for stem cell therapy due to its immune privilege, accessibility, and compartmentalized anatomy that facilitates local delivery and reduces systemic exposure [51] [52]. Clinical progress has been most significant in retinal diseases, where the goal is to replace lost photoreceptors or retinal pigment epithelium (RPE) cells. As of December 2024, an analysis of 88 clinical trials in ophthalmology revealed that mesenchymal stem cells (MSCs) are the most frequently used (48.86%), followed by embryonic stem cell (ESC) and induced pluripotent stem cell (iPSC) derivatives [51]. The majority of trials target retinal diseases, with Age-related Macular Degeneration (AMD) and Retinitis Pigmentosa (RP) being the leading indications [51].
Table 2: Landscape of Ophthalmology Clinical Trials (Data up to Dec 2024)
| Trial Characteristic | Category | Number/Percentage of Trials |
|---|---|---|
| Total Analyzed Trials | - | 88 [51] |
| Geographical Distribution | United States | 37.50% (33 trials) [51] |
| China | 14.77% (13 trials) [51] | |
| United Kingdom | 9.09% (8 trials) [51] | |
| Cell Types Used | Mesenchymal Stem Cells (MSCs) | 48.86% (43 trials) [51] |
| Embryonic Stem Cells (ESCs) | Information missing | |
| Induced Pluripotent Stem Cells (iPSCs) | Information missing | |
| Primary Disease Targets | Age-Related Macular Degeneration (AMD) | Leading target [51] |
| Retinitis Pigmentosa (RP) | Second most common target [51] |
Experimental Protocol: Subretinal Transplantation of iPSC-Derived Retinal Pigment Epithelium (RPE) for Geographic Atrophy (GA)
This protocol details the surgical implantation of a monolayer of RPE cells, a leading approach for treating dry AMD with Geographic Atrophy [51] [52].
1. Cell Product Manufacturing:
- Reprogramming and Differentiation: Generate clinical-grade iPSCs from patient somatic cells (e.g., fibroblasts) or use a pre-qualified, allogeneic iPSC master cell bank. Differentiate iPSCs into RPE cells using a GMP-compliant, stepwise protocol involving defined growth factors and small molecules to recapitulate eye development [52].
- Maturation and Formatting: Culture the differentiated RPE cells on a biodegradable or non-biodegradable scaffold (e.g., a synthetic polyester membrane) to form a polarized, pigmented monolayer. Alternatively, prepare the cells as a suspension for injection.
- Release Testing: Perform rigorous QC including identity (RPE65 and bestrophin expression), purity (>95% RPE cells), viability (>80%), potency (phagocytosis of photoreceptor outer segments), and safety (sterility, mycoplasma, endotoxin, karyotyping, and tumorigenicity assay) [52].
2. Surgical Implantation:
- Anesthesia: Perform the procedure under local or general anesthesia.
- Access: Create a standard three-port pars plana vitrectomy.
- Retinal Detachment: Inject a balanced salt solution (BSS) through a custom cannula to create a localized bleb of neurosensory retinal detachment in the target subretinal area.
- Transplantation: Make a small retinotomy and carefully inject the RPE monolayer patch (typically 3x6 mm) or cell suspension (50-200k cells in ~0.1 mL) into the subretinal space using a specialized injector system.
- Closure: Ensure proper positioning of the graft. Close the sclerotomies and conjunctiva.
3. Post-operative Management and Monitoring:
- Immunosuppression: For allogeneic transplants, initiate a regimen of systemic and/or local immunosuppressants (e.g., tacrolimus and mycophenolate mofetil) to prevent rejection, typically starting pre-operatively and continuing for several months [52].
- Monitoring: Schedule follow-up visits at 1 day, 1 week, 1 month, 3 months, 6 months, and annually. Assessments should include:
- Visual Function: Best-corrected visual acuity (BCVA), microperimetry, and dark-adapted visual sensitivity.
- Structural Integrity: Spectral-domain Optical Coherence Tomography (SD-OCT) to assess graft integration, retinal architecture, and subretinal fluid. Fundus Autofluorescence (FAF) and Indocyanine Green Angiography (ICGA) to monitor RPE health and vascular integrity.
- Safety: Monitor for surgical complications (cataract, elevated intraocular pressure, retinal detachment, hemorrhage) and signs of immune rejection (intraocular inflammation, graft edema, pigment dispersion) [52].
Cardiology
Application Notes
Cardiovascular diseases, particularly heart failure post-myocardial infarction (MI), represent a massive unmet clinical need. Stem cell therapy aims to regenerate damaged cardiac tissue, improve perfusion, and reverse adverse remodeling [53] [49]. The therapeutic effect is now largely attributed to powerful paracrine signaling, where transplanted cells secrete bioactive molecules (growth factors, cytokines, extracellular vesicles) that promote angiogenesis, reduce apoptosis, and modulate the immune response, rather than large-scale engraftment and direct differentiation into new cardiomyocytes [49]. Key cell types under investigation include Mesenchymal Stem Cells (MSCs), cardiac progenitor cells (CPCs), and iPSC-derived cardiomyocytes [53] [49].
Table 3: Key Cell Types for Cardiac Regeneration
| Cell Type | Source | Mechanism of Action | Advantages & Challenges |
|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone Marrow, Adipose Tissue, Umbilical Cord [53] [49]. | Paracrine secretion (VEGF, FGF, HGF); immunomodulation; stimulation of angiogenesis; reduction of fibrosis [49]. | Adv: Ease of isolation, immunoprivileged, well-established safety profile [49]. Challenge: Modest functional improvements, poor engraftment [53]. |
| Induced Pluripotent Stem Cell (iPSC)-Derived Cardiomyocytes | Patient somatic cells (e.g., fibroblasts) [53]. | Direct remuscularization by forming new contractile tissue; paracrine effects [53]. | Adv: Patient-specific, unlimited supply, true regeneration potential [53]. Challenge: Risk of arrhythmogenicity, tumorigenicity, need for scaffolding [53]. |
| Cardiac Progenitor Cells (CPCs) | Heart tissue (atrial appendages, biopsies) [53]. | Differentiation into endothelial cells, smooth muscle cells, and potentially cardiomyocytes; paracrine signaling [53]. | Adv: Inherent cardiac commitment. Challenge: Very limited source, invasive procurement [53]. |
Experimental Protocol: Transendocardial Injection of MSCs for Ischemic Cardiomyopathy
This protocol describes a catheter-based, intramyocardial delivery method for precise administration of cells into the scarred and border-zone myocardium.
1. Cell Preparation:
- Use allogeneic or autologous MSCs from bone marrow or adipose tissue, expanded under GMP conditions as described in the neurology protocol.
- Final cell product: Resuspend 100-200 million MSCs in 5-10 mL of sterile saline or a proprietary buffer solution. Confirm viability >90% and absence of endotoxin prior to release.
2. Catheter-Based Delivery System:
- System: Employ a commercially available transendocardial injection system (e.g., NOGA StarTip Catheter with the NOGA XP Electromechanical Mapping System).
- Procedure:
- Mapping: Under fluoroscopic guidance, advance the mapping/injection catheter into the left ventricle. Create a real-time, 3D electromechanical map of the endocardial surface to identify areas of scar (low voltage, abnormal motion) and viable peri-infarct border zones.
- Target Selection: Select 15-20 injection sites within the scar and border zone, avoiding major coronary vessels and areas of extreme thinning.
- Injection: For each site, advance the needle from the catheter into the myocardium (typical depth: 4-8 mm). Slowly inject 0.5-1.0 mL of cell suspension. Withdraw the needle and proceed to the next site.
3. Post-Procedure Monitoring:
- Safety Monitoring: Monitor in-hospital for 24-48 hours for arrhythmias, pericardial effusion/tamponade, MI, or infection. Perform echocardiography post-procedure and at 24 hours to rule out pericardial effusion.
- Efficacy Endpoints: Assess at baseline, 6, and 12 months.
- Cardiac Function: Left Ventricular Ejection Fraction (LVEF) by cardiac MRI, the gold standard for volume and function assessment.
- Viability and Scar Size: Cardiac MRI with Late Gadolinium Enhancement (LGE) to quantify changes in infarct size.
- Functional Capacity: Six-minute walk test (6MWT) and New York Heart Association (NYHA) Class.
- Clinical Outcomes: Incidence of Major Adverse Cardiac Events (MACE) including mortality, recurrent MI, and heart failure hospitalizations [49].
Orthopedics
Application Notes
Orthopedic applications of stem cells primarily target the repair and regeneration of musculoskeletal tissues, with a major focus on osteoarthritis (OA) and cartilage defects [50]. The therapeutic strategy involves injecting cells to mitigate inflammation and promote the growth of new hyaline cartilage. Mesenchymal Stromal Cells (MSCs) are the dominant cell type, valued for their immunomodulatory properties and ability to differentiate into chondrocytes and osteoblasts [50]. Their mechanism is largely paracrine, secreting factors that counteract inflammation (e.g., IL-10, TGF-β) and stimulate resident progenitor cells [50]. Key molecular pathways, such as Toll-like Receptor (TLR) signaling, are critical modulators of the inflammatory environment and a key focus for optimizing therapy [50].
Experimental Protocol: Intra-Articular Injection of MSCs for Knee Osteoarthritis
This is a common, minimally invasive protocol for delivering MSCs directly into the osteoarthritic joint space.
1. Cell Harvesting and Preparation:
- Source: MSCs can be isolated from patient's (autologous) bone marrow or adipose tissue, or from allogeneic donor sources like umbilical cord tissue.
- Bone Marrow Aspirate: Aspirate bone marrow (typically 30-60 mL) from the posterior iliac crest. Isolate and concentrate the mononuclear cell fraction (containing MSCs) using a density gradient centrifugation system or a point-of-care concentrator.
- Adipose Tissue Harvest: Perform a mini-liposuction under local anesthesia to obtain adipose tissue. Process the tissue with enzymatic digestion (e.g., collagenase) to isolate the Stromal Vascular Fraction (SVF), which contains MSCs, for immediate use, or culture-expand the MSCs.
- Dosing: For autologous SVF or bone marrow concentrate, the entire product is typically injected. For culture-expanded MSCs, common doses range from 10 to 100 million cells per joint, suspended in 3-5 mL of platelet-rich plasma (PRP) or sterile saline to potentially enhance retention and efficacy.
2. Injection Procedure:
- Patient Positioning: Position the patient supine with the knee extended or slightly flexed.
- Asepsis and Anesthesia: Clean the knee with antiseptic solution. Use a local anesthetic (e.g., 1% lidocaine) to anesthetize the skin and subcutaneous tissue over the injection site.
- Landmark-Guided Injection: Using a sterile technique, insert a 21- or 22-gauge needle into the joint space, typically via a superolateral or anterolateral approach. Aspirate briefly to confirm intra-articular placement (may yield a small amount of synovial fluid).
- Cell Delivery: Slowly inject the cell preparation into the joint space.
3. Post-Procedure Rehabilitation and Assessment:
- Post-injection Care: Advise the patient to avoid strenuous activity and high-impact exercises for 2-4 weeks to allow for cell integration and early tissue repair.
- Rehabilitation: Implement a structured physical therapy program focusing on range of motion, progressive strengthening, and low-impact aerobic conditioning.
- Efficacy Monitoring: Use standardized patient-reported outcome measures at baseline, 3, 6, and 12 months. Key metrics include the Visual Analog Scale (VAS) for pain, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Knee Injury and Osteoarthritis Outcome Score (KOOS). Structural Assessment: Track changes in cartilage morphology and volume using MRI, ideally with quantitative sequences like T2 mapping or dGEMRIC.
Visualizations and Workflows
Signaling Pathway: TLR3 in Orthopedic Immunomodulation
The following diagram illustrates the role of Toll-like Receptor 3 (TLR3) in the inflammatory microenvironment of orthopedic diseases like osteoarthritis, and how it interacts with MSC-based therapies [50].
Experimental Workflow: iPSC-Derived RPE Cell Therapy
This workflow outlines the key stages from laboratory reprogramming to clinical implantation of a stem cell product for ophthalmology [52].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for Stem Cell Research & Development
| Reagent/Material | Function/Application | Specific Examples & Notes |
|---|---|---|
| GMP-Grade Cell Culture Media | Supports the expansion and maintenance of stem cells under clinically compliant conditions. | Xeno-free, defined formulations (e.g., TeSR-E8, StemFit); essential for iPSC/ESC culture to avoid animal-derived components [52]. |
| Differentiation Kits & Factors | Directs stem cell fate towards specific lineages (e.g., neuronal, cardiac, RPE). | Defined cytokine and small molecule kits for dopaminergic neurons, cardiomyocytes, or RPE cells. Key factors include FGF, BMP, Wnt, and RA pathway modulators [48] [52]. |
| Cell Separation & Characterization Kits | Isolates and identifies specific cell populations for research and QC. | Separation: FACS or MACS kits for CD34+, CD73+/90+/105+ MSCs. Characterization: Antibody panels for flow cytometry (e.g., Oct4, Nanog for pluripotency; RPE65 for RPE) [50]. |
| Biocompatible Scaffolds & Matrices | Provides a 3D structure for tissue engineering and supports cell delivery and integration. | Synthetic (PLGA, PCL) or natural (collagen, fibrin) hydrogels and membranes. Used for creating RPE patches, cardiac patches, or cartilage repair constructs [52] [50]. |
| In Vivo Tracking Agents | Enables non-invasive monitoring of cell fate, migration, and survival in animal models. | Superparamagnetic iron oxide nanoparticles (SPIONs) for MRI tracking; luciferase reporters for bioluminescence imaging (BLI); fluorescent dyes (e.g., DiR) for near-infrared imaging [49]. |
The field of regenerative medicine is increasingly pivoting towards novel manufacturing platforms designed to overcome the historical limitations of primary cell therapies. Among the most promising advances are allogeneic, off-the-shelf therapies derived from induced pluripotent stem cell-derived Mesenchymal Stem Cells (iMSCs). These platforms address critical challenges of scalability, consistency, and potency that have long hindered the widespread clinical application of stem cell-based treatments [3] [42]. Unlike primary MSCs, which exhibit donor-dependent variability and limited expansion capacity, iMSCs offer a renewable, standardized cell source capable of producing a uniform therapeutic product for a wide patient population [3]. This application note details the latest developments, protocols, and analytical tools underpinning this transformative technological shift.
Current Clinical and Regulatory Landscape
The period from 2023 to 2025 has marked a significant turning point for stem cell therapeutics, characterized by key regulatory milestones that highlight the viability of allogeneic and iPSC-derived approaches.
Recently Approved Stem Cell Therapies
The FDA's Approved Cellular and Gene Therapy Products list remains selective, with several recent approvals demonstrating the agency's willingness to license complex cellular products [3].
- Omisirge (omidubicel-onlv): Approved in April 2023, this nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cell therapy accelerates neutrophil recovery in patients with hematologic malignancies [3].
- Ryoncil (remestemcel-L): Approved in December 2024, Ryoncil is notable as the first FDA-approved MSC therapy, indicated for pediatric steroid-refractory acute graft-versus-host disease (SR-aGVHD). This approval validates the therapeutic potential of MSC-based modulation of immune responses [3].
FDA-Authorized Clinical Trials for Novel Platforms
The clinical pipeline features several pioneering iPSC-derived and allogeneic therapies, many supported by expedited FDA designations like RMAT (Regenerative Medicine Advanced Therapy) [3].
Table 1: Select Active Clinical Trials for Allogeneic and iPSC-Derived Therapies (2024-2025)
| Therapy/Product | Cell Type | Indication | Development Stage | Key Details |
|---|---|---|---|---|
| Fertilo [3] | iPSC-derived Ovarian Support Cells (OSCs) | In vitro oocyte maturation | Phase III (IND Cleared) | First iPSC-based therapy to enter U.S. Phase III trials (Feb 2025). |
| OpCT-001 [3] | iPSC-derived therapy | Retinal degeneration (e.g., retinitis pigmentosa) | Phase I/IIa | First iPSC-based therapy for primary photoreceptor diseases (IND Cleared Sep 2024). |
| FT819 [3] | Off-the-shelf, iPSC-derived CAR T-cell | Systemic lupus erythematosus (SLE) | Phase I | Granted FDA RMAT designation (Apr 2025). |
| iPSC-derived NPCs [3] | iPSC-derived neural progenitor cells | Parkinson’s disease, spinal cord injury, ALS | Phase I (IND Cleared) | Multiple off-the-shelf products for neurodegenerative conditions (Jun 2025). |
| MyoPAXon [3] | iPSC-derived CD54+ muscle progenitor cells | Duchenne muscular dystrophy (DMD) | Phase I | Allogeneic muscle progenitor cell therapy. |
| Cymerus iMSCs (CYP-001) [3] | iPSC-derived MSCs (iMSCs) | High-Risk Acute Graft-Versus-Host Disease | Clinical Trial | In combination with corticosteroids. |
Experimental Protocols for iMSC Generation and Characterization
Protocol 1: Generation of Clinical-Grade iMSCs
This protocol outlines a robust methodology for the derivation of iMSCs from human iPSCs, incorporating critical quality control checkpoints [42].
3.1.1 Materials and Reagents
- Starting Material: Clinical-grade human iPSC line, validated for pluripotency and genomic stability.
- Reprogramming Factors: OCT4, SOX2, KLF4, c-MYC (OSKM) via non-integrating delivery system (e.g., Sendai virus, episomal plasmids, or mRNA) [42].
- Culture Media: Commercially available MSC differentiation media, or in-house formulated media containing TGF-β, FGF, and PDGF signaling pathway modifiers.
- Supplements: Fetal Bovine Serum (FBS) or, preferably, defined, xeno-free supplements.
- Dissociation Reagents: Enzyme-free cell dissociation buffers or recombinant trypsin alternatives.
- Characterization Antibodies: Flow cytometry panels for CD73, CD90, CD105 (positive) and CD34, CD45, HLA-DR (negative).
3.1.2 Step-by-Step Workflow
- iPSC Culture and Quality Control: Maintain iPSCs in a pluripotent state. Confirm absence of differentiation and verify karyotype prior to initiation.
- Mesenchymal Induction: Seed iPSCs as single cells and initiate differentiation by switching to MSC-specific medium. Culture for 14-21 days, with medium changes every 2-3 days.
- Selection and Expansion: Harvest emerging spindle-shaped cells by mild dissociation. Re-plate and selectively expand adherent, MSC-morphology cells over multiple passages (P3-P5).
- Phenotypic Validation: At P3, confirm iMSC identity by flow cytometry. Cells must express standard MSC surface markers (≥95% positive for CD73, CD90, CD105; ≤5% positive for hematopoietic/endothelial markers) [10].
- Functional Potency Assays: Perform in vitro tri-lineage differentiation (osteogenesis, adipogenesis, chondrogenesis) to confirm multipotency. Conduct in vitro immunomodulation assays (e.g., T-cell suppression assay).
Protocol 2: Quantitative Assessment of iMSC Quality and Purity
A critical challenge is the quantitative assessment of iMSC quality beyond surface markers. This protocol utilizes a bioinformatic approach to evaluate molecular similarity to reference tissues or primary MSC benchmarks [5].
3.2.1 Materials and Reagents
- RNA Extraction Kit: High-quality, DNAse-treated total RNA extraction system.
- RNA-Seq Library Prep Kit: A kit compatible with low-input RNA for next-generation sequencing.
- Computational Resources: Access to a high-performance computing cluster or cloud-based analysis platform.
- Software: The Web-based Similarity Analytics System (W-SAS) or similar algorithm [5].
3.2.2 Step-by-Step Workflow
- RNA Isolation and Sequencing: Extract high-quality total RNA from the final iMSC product and from a reference sample (e.g., primary bone marrow MSCs). Prepare and sequence RNA-seq libraries.
- Data Preprocessing: Process raw sequencing reads (e.g., FASTQ files) through a standardized pipeline for quality control, alignment, and generation of transcript abundance values (e.g., TPM or FPKM).
- Similarity Score Calculation: Input the transcript abundance data into the W-SAS platform, which uses pre-defined organ/tissue-specific gene expression panels (Organ-GEPs) to compute a quantitative similarity score (%) [5].
- Data Interpretation: A high similarity score indicates that the iMSC transcriptome closely mirrors the reference MSC profile, providing a quantitative measure of successful differentiation and cellular identity.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful development of allogeneic off-the-shelf iMSC therapies relies on a suite of specialized reagents, platforms, and computational tools.
Table 2: Key Research Reagent Solutions for iMSC Therapy Development
| Item/Category | Function/Description | Example Application |
|---|---|---|
| Non-Integrating Reprogramming Vectors [42] | Generate iPSCs without genomic integration for improved safety. Sendai virus, episomal plasmids, or mRNA are common. | Derivation of clinical-grade iPSC master cell banks from donor somatic cells. |
| StemRNA Clinical Seed iPSCs [3] | Commercially available, clinically-compliant iPSC seed clones with a supporting Drug Master File (DMF). | Standardized, regulatory-friendly starting material for iMSC differentiation. |
| Defined, Xeno-Free Differentiation Media | Promote directed differentiation to the MSC lineage while reducing variability and safety concerns from animal sera. | Scalable and consistent manufacturing of iMSCs under GMP conditions. |
| Web-based Similarity Analytics System (W-SAS) [5] | A bioinformatic platform that calculates a quantitative score (%) for similarity between a sample and a target human organ/tissue. | Quality control and benchmarking of iMSC products against primary MSCs. |
| CRISPR-Cas9 Gene Editing Systems [42] | Precise genetic modification to enhance therapeutic properties (e.g., hypoimmunogenicity) or correct disease mutations. | Engineering "off-the-shelf" iMSCs with disrupted HLA expression to evade immune rejection. |
Discussion and Future Perspectives
The transition to allogeneic, off-the-shelf iMSC therapies represents a paradigm shift in regenerative medicine, moving from patient-specific, bespoke treatments towards scalable, standardized biological drugs. The recent regulatory approvals and burgeoning clinical trial pipeline are strong validators of this approach [3]. However, several challenges remain to be fully addressed. Tumorigenicity concerns, though mitigated by using differentiated iMSCs rather than pluripotent cells, require long-term monitoring [42]. Manufacturing scalability must be achieved without compromising cell quality or potency, necessitating advanced bioreactor systems and rigorous process control [11] [42]. Furthermore, the immunogenicity of allogeneic cells, even with HLA matching or engineering, is an area of active investigation [42].
Future progress will be driven by the integration of enabling technologies. CRISPR-Cas9 gene editing will allow for the precise engineering of iMSCs to enhance their survival, homing, and immunomodulatory functions, or to create universally compatible "off-the-shelf" cell products [42]. AI and machine learning are being deployed to improve the reproducibility of iPSC differentiation, predict batch outcomes, and optimize manufacturing parameters [42]. As these tools mature and quantitative assessment platforms like W-SAS become more widespread, the vision of a robust, scalable, and effective allogeneic iMSC therapy will move from the laboratory to the clinic, offering new hope for patients with a range of incurable diseases.
Navigating Clinical Hurdles: Safety, Manufacturing, and Regulatory Optimization
Addressing Tumorigenicity and Safety Concerns in Pluripotent Cell Therapies
The therapeutic potential of human pluripotent stem cells (PSCs), encompassing both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), is vast due to their capacity for self-renewal and differentiation into any cell type in the body [54]. However, their clinical translation is inherently linked to the critical challenge of ensuring safety, with tumorigenicity representing the most significant risk [42] [55]. Tumorigenic potential can arise from multiple sources, including the presence of residual undifferentiated PSCs in a final cell product, the proliferation of incompletely differentiated or genetically unstable cells, and the potential for ectopic tissue formation [55]. Addressing these concerns requires a multi-layered safety assessment strategy integrated throughout the entire development process, from cell line establishment to final product administration. This document outlines current standards and advanced protocols for mitigating tumorigenicity, providing a framework for researchers and drug development professionals to advance safer PSC-based therapies within the rigorous context of regenerative medicine.
Current Safety Landscape of PSC Clinical Trials
The clinical application of PSC-derived therapies is expanding rapidly. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct PSC-derived products, primarily targeting indications in ophthalmology, neurology, and oncology [3]. A significant milestone is that over 1,200 patients have been dosed with more than 10¹¹ cells, and the overall safety profile to date is encouraging, with no class-wide safety concerns observed [3]. This extensive clinical experience underscores the feasibility of PSC therapies while highlighting the continued importance of rigorous, product-specific safety monitoring.
The first iPSC-based therapy entered a U.S. Phase III trial in early 2025, and several other iPSC-derived products for retinal degeneration, Parkinson's disease, spinal cord injury, and ALS have recently received FDA IND clearance [3]. The safety data emerging from these pioneering trials are crucial for validating the risk-mitigation strategies discussed in this document.
Table 1: Recent FDA-Authorized Clinical Trials for Novel PSC-Derived Therapies (2024-2025)
| Therapy/Product Name | Cell Type | Indication | Development Stage | Key Safety Consideration |
|---|---|---|---|---|
| Fertilo [3] | iPSC-derived ovarian support cells | Supporting ex vivo oocyte maturation | Phase III (FDA IND cleared) | First iPSC-based therapy in U.S. Phase III; monitoring for potential off-target effects. |
| OpCT-001 [3] | iPSC-derived therapy | Retinal degeneration (retinitis pigmentosa) | Phase I/IIa | Local administration to immune-privileged site; monitoring for visual restoration and local reactions. |
| FT819 [3] | Off-the-shelf, iPSC-derived CAR T-cell | Systemic lupus erythematosus (SLE) | Phase I (RMAT designation) | Allogeneic source; risk of immune-mediated rejection or off-target cytotoxicity. |
| Neural progenitor cell therapies [3] | iPSC-derived neural progenitors | Parkinson's disease, spinal cord injury, ALS | Phase I (FDA IND cleared) | Risk of uncontrolled proliferation, ectopic tissue formation, and need for immunosuppression. |
| Autologous iPSC-derived Dopaminergic Neural Progenitor Cells [3] | Autologous iPSC-derived neural progenitors | Parkinson's Disease | Phase I | Autologous source reduces immune rejection risk; focus on genetic stability post-reprogramming. |
Comprehensive Safety Assessment Workflow
A robust safety assessment for PSC-derived products is not a single test but an integrated workflow that spans from initial cell banking to long-term post-transplantation monitoring. The following workflow diagram outlines the key stages and their primary safety objectives.
Diagram 1: Integrated workflow for comprehensive PSC therapy safety assessment, covering pre- and post-transplantation stages [55].
Experimental Protocols for Tumorigenicity Assessment
Protocol 1: In Vitro Soft Agar Colony Formation Assay
The Soft Agar Colony Formation Assay is a fundamental in vitro method for detecting anchorage-independent growth, a hallmark of cellular transformation [55]. This assay is used to evaluate the tumorigenic potential of PSC-derived populations or to assess the effects of genetic modifications.
4.1.1 Materials and Reagents
- PSC-derived cell population of interest
- Appropriate cell culture medium (e.g., Essential 8, StemFlex) [56]
- Low-melting-point agarose
- Base agarose
- Fetal Bovine Serum (FBS)
- 0.25% Trypsin-EDTA
- 6-well or 12-well cell culture plates
- Phosphate-Buffered Saline (PBS)
- Positive control cells (e.g., known tumorigenic cell line like HeLa)
- Negative control cells (e.g., primary fibroblasts)
4.1.2 Step-by-Step Procedure
- Prepare Base Agar Layer: Create a 0.6-1.0% solution of base agarose in culture medium. Autoclave and cool to approximately 40-45°C. Add 1.5-2 mL of this solution to each well of a 6-well plate to form a solid base layer. Allow it to solidify completely at room temperature or 4°C.
- Prepare Cell Suspension Layer: Trypsinize the test PSC-derived cells and prepare a single-cell suspension. Create a 0.3-0.4% solution of low-melting-point agarose in culture medium and cool to 37°C. Gently mix the cell suspension with the low-melting-point agarose solution to achieve a final density of 5,000-20,000 cells/mL. Ensure the mixture remains at 37°C to prevent premature gelling.
- Plate Cell Layer: Carefully overlay 1-1.5 mL of the cell-agarose mixture onto the solidified base agar layer in each well. Swirl gently to ensure an even distribution. Allow the top layer to solidify at room temperature for 15-20 minutes.
- Culture and Feed: Once solid, add 1-2 mL of complete culture medium on top of the soft agar layer to prevent drying. Incubate the plates at 37°C in a 5% CO₂ humidified incubator for 2-4 weeks. Refresh the overlay medium every 5-7 days.
- Stain and Quantify Colonies: After the incubation period, add 0.5-1 mL of 0.005% Crystal Violet or INT (iodonitrotetrazolium chloride) solution to each well and incubate for several hours or overnight. Colonies with a diameter >50-100 µm should be counted manually under a microscope or using an automated colony counter. Data should be presented as the number of colonies per well or the plating efficiency.
4.1.3 Data Interpretation and Troubleshooting
- A significant increase in colony formation compared to the negative control indicates anchorage-independent growth and potential tumorigenicity.
- A common issue is the failure of the top layer to solidify; ensure the agarose solutions are at the correct temperatures when mixing and plating.
- Low colony formation efficiency may require optimization of cell seeding density and culture duration.
Protocol 2: In Vivo Teratoma and Tumorigenicity Assay
The in vivo assay in immunodeficient mice is the gold standard for assessing the functional pluripotency of PSCs via teratoma formation and, critically, for evaluating the risk of tumor formation from a final differentiated cell product [55].
4.2.1 Materials and Reagents
- Test article: Undifferentiated PSCs (for pluripotency confirmation) or PSC-derived final product (for safety testing)
- Matrigel or similar basement membrane matrix
- Immunodeficient mice (e.g., NOD/SCID, NSG strains)
- Insulin syringes (0.5 mL, 27-29 gauge)
- Isoflurane anesthesia system
- 0.25% Trypsin-EDTA
- Appropriate cell culture medium and PBS
4.2.2 Step-by-Step Procedure
- Cell Preparation: Harvest the test cells using standard methods (e.g., enzymatic dissociation with trypsin for PSCs). Wash the cells with PBS and resuspend in an appropriate, cold, serum-free medium mixed 1:1 with Matrigel. Keep the cell suspension on ice to prevent Matrigel polymerization. The final cell concentration is typically (1 \times 10^7) cells/mL for PSCs (teratoma assay) and a clinically relevant dose for the differentiated product (safety assay).
- Animal Injection: Anesthetize the mice using an isoflurane chamber. For subcutaneous implantation, slowly inject 100-200 µL of the cell-Matrigel suspension into the flank or hind leg muscle. For intramuscular injection, target the tibialis anterior or gastrocnemius muscle. For testing cells intended for specific organs (e.g., intracerebral or intrahepatic), use stereotaxic injection systems.
- Post-Procedure Monitoring: Monitor animals daily for the first week and at least twice weekly thereafter. Palpate the injection site regularly to detect nodule formation. Monitor for signs of distress, weight loss, or morbidity.
- Study Endpoint and Necropsy: The study duration is typically 12-20 weeks for teratoma formation from PSCs and can be 6-12 months for tumorigenicity assessment of differentiated products. If a tumor exceeds 1.5-2.0 cm in diameter or the animal shows significant distress, euthanize the animal immediately. At the endpoint, perform a full necropsy.
- Histopathological Analysis: Excise the injection site and any suspicious lesions. Also, collect major organs (liver, lungs, spleen, kidneys, brain, and lymph nodes) for biodistribution assessment. Fix tissues in 10% neutral buffered formalin, process for paraffin embedding, section, and stain with Hematoxylin and Eosin (H&E). A qualified pathologist should examine the sections for the presence and composition of tumors (teratomas containing three germ layers vs. malignant tumors).
4.2.3 Data Interpretation and Troubleshooting
- For undifferentiated PSCs, a successful teratoma will show differentiated tissues from all three germ layers (e.g., cartilage/muscle for mesoderm, neural rosettes for ectoderm, gut epithelium for endoderm).
- For a PSC-derived product, the absence of teratomas or malignant tumors indicates a lower tumorigenic risk.
- High rates of animal mortality post-injection may be due to cell clumping or improper injection technique; ensure a smooth, single-cell suspension and proper surgical/anesthesia procedures.
Table 2: Key Research Reagent Solutions for PSC Safety Assessment
| Reagent/Category | Example Products | Function in Safety Protocol |
|---|---|---|
| Reprogramming Vectors | Sendai Viral Vectors, Episomal Plasmids [56] | Non-integrating reprogramming to generate iPSCs with reduced risk of insertional mutagenesis. |
| Cell Culture Media | Essential 8, StemFlex, MEF-conditioned Media [56] | Maintenance of pluripotent state under defined, feeder-free conditions, enhancing consistency and safety. |
| Characterization Kits | Pluripotency Marker Detection Kits, hPSC Scorecard Analysis [56] | Validation of pluripotent state and quantitative analysis of differentiation potential. |
| Differentiation Kits | PSC Neural Induction Medium, Cardiomyocyte Differentiation Kits [56] | Directed differentiation into specific lineages, ensuring high purity of the final product to reduce tumor risk. |
| Matrix & Support | Geltrex, Matrigel, Laminin-521 [55] [56] | Provides a defined extracellular matrix for cell growth and differentiation, used in both culture and in vivo assays. |
| Gene Editing Tools | CRISPR/Cas9 Systems [42] | Genetic modification for disease correction, introducing safety switches, or knocking out tumorigenic pathways. |
Advanced Strategies: "Safety-by-Design" and Novel Technologies
Moving beyond basic assessment, a "safety-by-design" approach integrates risk mitigation directly into the product development process. Key strategies include:
- Cell Sorting and Purging: Using fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) with antibodies against specific surface markers (e.g., SSEA-5, CD50) to deplete residual undifferentiated PSCs from the final differentiated cell product [55].
- Introduction of Suicide Genes: Engineering PSCs to express inducible suicide genes, such as the caspase-9 system (iCasp9) or herpes simplex virus thymidine kinase (HSV-TK). These genes remain inert until administration of a small-molecule drug, which then selectively triggers apoptosis in the transplanted cells if undesired proliferation occurs [42].
- CRISPR/Cas9 Genome Editing: Utilizing gene editing to create "fail-safe" mechanisms, such as knocking in inducible suicide genes or knocking out genes essential for cell cycle progression in undifferentiated states, but dispensable for the function of the mature, differentiated cell [42].
- AI and Machine Learning: Leveraging computational models to predict differentiation outcomes, identify key transcription factors, and classify cell colony morphology, thereby enhancing the standardization and quality control of PSC manufacturing [57] [42]. These tools can help identify subtle patterns predictive of genomic instability or aberrant differentiation.
The successful clinical translation of PSC-based therapies is inextricably linked to the rigorous and comprehensive addressing of tumorigenicity and other safety concerns. As evidenced by the growing number of clinical trials and the preliminary safety data from over 1,200 dosed patients, the field is making significant strides [3]. A multi-pronged strategy is essential, combining stringent pre-transplantation characterization and quality control, validated in vitro and in vivo tumorigenicity assays, and long-term post-transplant monitoring. The integration of novel "safety-by-design" approaches, such as suicide genes and advanced purification technologies, provides a promising path forward to further de-risk these powerful therapies. By adhering to these detailed protocols and embracing evolving best practices, researchers and clinicians can confidently advance the development of safe and effective pluripotent stem cell treatments, ultimately fulfilling their transformative potential in regenerative medicine.
Stem cell transplantation represents a frontier in regenerative medicine, offering potential solutions for a range of conditions from hematologic malignancies to degenerative diseases. However, the transition from laboratory research to clinically viable therapies is hampered by significant manufacturing challenges in scalability, standardization, and quality control. These hurdles must be overcome to ensure the consistent production of safe, effective, and accessible advanced therapy medicinal products (ATMPs). This document outlines the current landscape, detailed protocols, and strategic frameworks aimed at addressing these critical manufacturing challenges for researchers, scientists, and drug development professionals.
The Scalability Challenge
Scaling up stem cell manufacturing from laboratory scale to industrial production presents complex technical and logistical obstacles. The inherent variability of living cells, the need for precise environmental control, and the transition from 2D to 3D culture systems all contribute to this challenge.
Current Landscape and Quantitative Data
The global cell and gene therapy manufacturing market is experiencing rapid growth, with projections indicating it will reach $32.11 billion in 2025 and grow to $403.54 billion by 2035, representing a remarkable compound annual growth rate (CAGR) of 28.8% [58]. Autologous cell therapy manufacturing currently leads the global market with approximately 56% share [58]. This growth necessitates innovative approaches to scale up production while maintaining product quality and consistency.
Table 1: Scaling Modalities for Advanced Therapy Manufacturing
| Scaling Approach | Description | Key Challenges | Adopted Solutions |
|---|---|---|---|
| Scale-Up | Increasing volume in a single production unit (e.g., larger bioreactors) | Maintaining homogeneity, oxygen transfer, and nutrient distribution | Vertical-Wheel bioreactor systems for gentle, efficient mixing of shear-sensitive cells [59] |
| Scale-Out | Increasing capacity by adding multiple parallel production units | Inter-batch variability, increased operational complexity | Automated, closed-system processing units; decentralized manufacturing networks [60] [58] |
| Decentralized Manufacturing | Establishing point-of-care (POC) manufacturing facilities | Regulatory compliance across sites, quality consistency | Automated closed-system platforms; leveraging existing networks (e.g., blood centers) [58] |
Experimental Protocol: 3D Suspension Culture Scale-Up
Objective: To scale up human pluripotent stem cell (hPSC) expansion in 3D suspension culture using a bioreactor system.
Materials:
- TeSR-AOF 3D or similar defined, animal origin-free medium [59]
- PBS-MINI Bioreactor with Vertical-Wheel impeller [59]
- hPSC aggregates (single-cell passaged with eTeSR medium) [59]
- Metabolic supplements (e.g., glucose, glutamine)
Methodology:
- Inoculum Preparation:
- Dissociate hPSC colonies to single cells using appropriate enzyme-free dissociation reagent.
- Resuspend cells at 1-2 × 10^5 cells/mL in TeSR-AOF 3D medium supplemented with Rho-associated kinase (ROCK) inhibitor.
Bioreactor Setup:
- Assemble and sterilize the PBS-MINI Bioreactor according to manufacturer specifications.
- Add culture medium to the bioreactor and equilibrate to 37°C, 5% CO2.
- Implement environmental monitoring probes for pH (target: 7.2-7.4), dissolved oxygen (target: 30-50%), and temperature (target: 37°C ± 0.5°C).
Culture Initiation:
- Inoculate cells into the bioreactor at the recommended seeding density.
- Set impeller speed to 40-60 rpm to maintain aggregate suspension while minimizing shear stress.
Process Monitoring:
- Monitor key metabolic parameters (glucose, lactate, ammonia) daily.
- Perform daily sampling for cell count, viability assessment, and aggregate size measurement.
- Maintain aggregate size between 100-300 μm through mechanical dissociation if necessary.
Harvest:
- Harvest cells when target density (1-2 × 10^6 cells/mL) is achieved, typically after 5-7 days.
- Assess critical quality attributes (CQAs) including viability (>85%), pluripotency markers, and genetic stability.
The Standardization Imperative
Standardization across manufacturing processes is essential to ensure product consistency, comparability, and regulatory compliance. The complexity of stem cell biology and the influence of process parameters on product characteristics make standardization particularly challenging.
Process Parameters and Quality Attributes
Table 2: Critical Process Parameters and Their Impact on Quality Attributes
| Critical Process Parameter (CPP) | Target Range | Impacted Critical Quality Attribute (CQA) | Monitoring Method |
|---|---|---|---|
| Oxygenation Level | 30-50% dissolved oxygen | Differentiation potential, genetic stability, metabolic activity | Real-time sensor with feedback control [61] |
| pH | 7.2-7.4 | Cell viability, proliferation rate, differentiation efficiency | In-line pH sensor with automated CO2 or buffer control [61] |
| Glucose Concentration | 4-6 mM (maintained) | Cell viability, proliferation rate, lactate production | Automated sampling with biosensor or HPLC analysis [61] |
| Aggregate Size | 100-300 μm | Nutrient diffusion, differentiation homogeneity, viability | Automated image analysis with CNN algorithms [61] |
| Shear Stress | <1 Pa | Cell viability, membrane integrity, phenotypic stability | Computational fluid dynamics, impedance sensing [61] |
Experimental Protocol: Automated Quality Control Using AI
Objective: To implement real-time, non-invasive quality monitoring of stem cell cultures using artificial intelligence (AI).
Materials:
- Convolutional Neural Network (CNN) model for image analysis [61]
- High-resolution time-lapse imaging system
- Environmental sensors (pH, O2, metabolites) with IoT connectivity [61]
- Predictive modeling software platform
Methodology:
- System Configuration:
- Install time-lapse microscopy system with phase contrast and fluorescence capabilities.
- Calibrate environmental sensors for pH, dissolved oxygen, and metabolite monitoring.
- Implement data integration platform to combine imaging and sensor data streams.
AI Model Training:
- Train CNN on reference image datasets annotated for key morphological features:
- Colony morphology (compactness, border regularity)
- Differentiation status (emergent morphology changes)
- Contamination indicators (unusual patterns, debris)
- Validate model performance against manual assessments by expert biologists.
- Train CNN on reference image datasets annotated for key morphological features:
Real-Time Monitoring Workflow:
- Acquire images at 15-minute intervals from multiple culture vessels.
- Process images through trained CNN for feature extraction and classification.
- Integrate morphological data with real-time sensor readings.
- Apply predictive algorithms to forecast culture trajectories and detect anomalies.
Feedback Implementation:
- Program automated adjustments to culture parameters based on AI predictions:
- Medium exchange triggered by metabolic exhaustion prediction
- Agitation rate adjustment based on aggregate size distribution
- Early contamination detection leading to culture quarantine
- Document all interventions and predictions for regulatory compliance.
- Program automated adjustments to culture parameters based on AI predictions:
Quality Control Systems
Robust quality control systems are fundamental to ensuring the safety and efficacy of stem cell-based therapies. These systems must address multiple critical quality attributes throughout the manufacturing process.
Critical Quality Attributes (CQAs) and Monitoring Strategies
Table 3: Comprehensive Quality Control Testing Matrix
| Critical Quality Attribute (CQA) | Analytical Method | Acceptance Criteria | Testing Frequency |
|---|---|---|---|
| Cell Identity/Phenotype | Flow cytometry for surface markers | >90% expression of lineage-specific markers | In-process and final release |
| Viability | Automated cell counting with dye exclusion | >85% viability for release | In-process and final release |
| Potency | Functional assay (e.g., differentiation, secretion) | Meets product-specific specifications | Final release and stability |
| Genetic Stability | Karyotyping, SNP array, or whole genome sequencing | Normal karyotype, no major abnormalities | Pre-master cell bank, periodic during culture |
| Sterility | Microbial culture, mycoplasma testing, endotoxin testing | No growth, <0.25 EU/mL endotoxin | Final release |
| Tumorigenicity | Soft agar colony formation, in vivo teratoma assay (for PSCs) | No colony formation in soft agar | Pre-clinical lot testing |
| Purity | Flow cytometry for residual undifferentiated cells | <1% residual undifferentiated cells | In-process and final release |
Experimental Protocol: Genetic Stability Assessment During Long-Term Culture
Objective: To monitor and maintain genetic stability in human pluripotent stem cells during extended passaging.
Materials:
- eTeSR medium for enhanced genetic stability during single-cell passaging [59]
- Automated passaging system
- Genomic DNA extraction kit
- SNP microarray or next-generation sequencing platform
- Karyotyping reagents
Methodology:
- Culture Conditions:
- Maintain hPSCs in eTeSR medium optimized for single-cell passaging.
- Use defined, xeno-free culture matrices (e.g., STEMmatrix BME) [59].
- Implement automated, consistent passaging protocols to minimize selection pressure.
Sampling Schedule:
- Collect cells for genetic analysis at specific intervals:
- Every 10 passages for karyotyping
- Every 20 passages for high-resolution SNP analysis
- At critical manufacturing stages (master cell bank, working cell bank, end of production)
- Collect cells for genetic analysis at specific intervals:
Genetic Analysis:
- Perform G-band karyotyping to detect chromosomal abnormalities (>5-10 Mb).
- Conduct SNP microarray analysis to identify copy number variations (CNVs) and loss of heterozygosity (LOH).
- Analyze data for recurrent abnormalities associated with culture adaptation (e.g., 20q11.21 amplification).
Data Interpretation:
- Establish baseline genetic profile for the cell line.
- Monitor for emerging variants and assess potential functional impact.
- Implement predetermined action limits for genetic drift requiring intervention.
Integrated Manufacturing Solutions
Addressing the interconnected challenges of scalability, standardization, and quality control requires integrated approaches that leverage advanced technologies and systematic process design.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Reagents and Materials for Stem Cell Manufacturing
| Reagent/Material | Function | Example Product | Key Features |
|---|---|---|---|
| Defined Culture Medium | Supports expansion and maintenance of stem cells | TeSR-AOF 3D, eTeSR [59] | Xeno-free, chemically defined, optimized for 3D culture |
| Basement Membrane Matrix | Provides substrate for cell attachment and growth | STEMmatrix BME [59] | Soluble format, EHS-sourced, hPSC-qualified |
| Differentiation Kits | Directs differentiation to specific lineages | STEMdiff Cardiomyocyte Expansion Kit, STEMdiff Microglia Culture System [59] | Serum-free, optimized protocols, high purity |
| Cell Activation Systems | Enables genetic modification or expansion | ImmunoCult-XF T Cell Activators [59] | GMP-grade, serum-free, highly stable |
| Quality Control Assays | Assesses critical quality attributes | Maestro MEA System [59] | Functional assessment, multi-well format |
| Bioreactor Systems | Enables scalable 3D culture | PBS-MINI Bioreactor [59] | Vertical-Wheel technology, compact design |
Advanced Manufacturing Technologies
Recent advancements in manufacturing technologies are addressing key challenges in stem cell production:
Closed Automated Systems:
- Implement fully closed, automated processing systems to reduce contamination risk and improve consistency
- Utilize robotic liquid handling and integrated incubation for minimal manual intervention
- Achieve significant timeline reduction - some systems demonstrate 24-hour CAR-T cell manufacturing versus traditional 7-14 day processes [58]
Point-of-Care Manufacturing:
- Develop decentralized manufacturing models to improve patient access
- Establish standardized processes across multiple manufacturing sites
- Implement real-time release testing to ensure product quality at distributed locations [58]
The manufacturing challenges in stem cell transplantation regenerative medicine are substantial but not insurmountable. Through the implementation of advanced technologies such as AI-driven quality control, automated closed systems, and sophisticated process analytics, researchers and manufacturers can address the critical issues of scalability, standardization, and quality control. The protocols and frameworks outlined in this document provide a foundation for developing robust, reproducible manufacturing processes that will enable the translation of promising stem cell research into clinically viable therapies. Continued innovation in manufacturing technology, coupled with rigorous scientific approach and regulatory alignment, will be essential to realizing the full potential of stem cell-based regenerative medicine.
Within regenerative medicine, stem cell transplantation represents a frontier therapy for many otherwise incurable diseases. The fundamental biological principle unifying these therapies is the dependence on the administered cells' ability to survive, proliferate, and functionally integrate within the host [11]. The choice between autologous (using the patient's own cells) and allogeneic (using donor-derived cells) transplantation is pivotal, as it dictates the specific immune rejection risks and requisite management strategies. Autologous approaches largely circumvent adaptive immune rejection but face challenges related to cell quality and potential contamination. In contrast, allogeneic therapies hold the promise of an "off-the-shelf" product but require careful management of the host-versus-graft and graft-versus-host responses. This application note details the evidence, protocols, and reagent solutions for managing immune rejection across these distinct transplantation paradigms, providing a structured framework for researchers and drug development professionals.
Quantitative Evidence and Clinical Context
The adoption of different transplant strategies is guided by their distinct risk-benefit profiles, which are rooted in comparative clinical outcomes. The following tables summarize key efficacy and safety metrics from recent studies, providing a quantitative foundation for protocol selection.
Table 1: Evidence Base for Transplant Indications (ASTCT 2020 Guidelines) [62]
| Transplantation Type | Total Standard-of-Care (S) Indications | S Indications Supported by RCTs | Percentage of S Indications Supported by RCTs |
|---|---|---|---|
| Allogeneic | 43 | 3 | 7% |
| Autologous | 23 | 11 | 48% |
Table 2: Outcomes in Primary Plasma Cell Leukemia (pPCL) from a Japanese Registry (2006-2022) [63] [64]
| Outcome Measure | Autologous HCT (n=117) | Allogeneic HCT (n=65) |
|---|---|---|
| Median Overall Survival | 3.2 years | 1.4 years |
| Key Finding | Lower early mortality | Higher early mortality but potential for better long-term survival |
Table 3: Outcomes in Multiple Myeloma from an EBMT Registry Analysis (2002-2015) [65]
| Transplant Strategy | Patient Count (n=24,936) | Key Long-Term Benefit | Key Risk |
|---|---|---|---|
| Single Autologous (Auto-HCT) | 20,375 | Baseline for comparison | N/A |
| Tandem Autologous (Auto-Auto) | 3,683 | Limited but persistent advantage in OS/PFS | N/A |
| Tandem Auto-Allogeneic (Auto-Allo) | 878 | Clear long-term advantage for OS/PFS | Higher early mortality |
Immune Rejection Mechanisms and Management Pathways
The core challenge in allogeneic transplantation is navigating the host immune response directed against donor antigens, primarily HLAs. A successful outcome requires a careful balance between preventing rejection and minimizing collateral damage from over-immunosuppression.
Allogeneic Transplant Rejection Pathway
The diagram below outlines the primary immune activation cascade against allogeneic stem cells.
Core Management Strategies for Allogeneic Rejection
Management of the allogeneic response is multifaceted, aiming to induce a state of immune tolerance.
- Pharmacologic Immunosuppression: The cornerstone of rejection management, typically involving a calcineurin inhibitor (e.g., Tacrolimus), an antimetabolite (e.g., Mycophenolate Mofetil), and occasionally corticosteroids. These drugs inhibit T-cell activation and proliferation [11].
- T-cell Depletion: A powerful strategy to remove immunogenic cells from the graft ex vivo.
- Stem Cell Source and Manipulation: The use of umbilical cord blood is associated with a lower incidence and severity of GvHD due to the immunological naivety of its T-cells [3]. Emerging techniques involve generating induced Pluripotent Stem Cells (iPSCs) from donors with hypoimmunogenic genotypes, or genetically editing cells to delete HLAs, creating universal donor cells [3] [11].
Experimental Protocols for Rejection Assessment
Robust preclinical models and in vitro assays are critical for evaluating the immunogenicity of stem cell products and the efficacy of rejection mitigation strategies.
In Vitro T-cell Activation and Mixed Lymphocyte Reaction (MLR)
This protocol assesses the potential of donor cells to provoke an immune response from host T-cells.
Detailed Methodology:
- Peripheral Blood Mononuclear Cell (PBMC) Isolation: Isolate PBMCs from healthy human donors using density gradient centrifugation (e.g., Ficoll-Paque). These will serve as sources for "responder" (host) and "stimulator" (donor) cells.
- Stimulator Cell Preparation: Irradiate (e.g., 30-100 Gy) or treat with mitomycin C the donor-derived stem cells or PBMCs to halt their proliferation while retaining antigen-presenting capability.
- Co-culture Setup: Plate responder PBMCs with stimulator cells at varying ratios (e.g., 1:1 to 10:1 responder:stimulator) in a U-bottom 96-well plate. Include controls for responder-only and stimulator-only background.
- Incubation and Readout: Culture cells for 5-7 days. Measure T-cell proliferation using a standardized assay such as:
- 3H-thymidine Incorporation: Add 3H-thymidine for the final 16-18 hours of culture and measure incorporated radioactivity with a beta-counter.
- CFSE Dilution: Label responder cells with CellTrace CFSE dye prior to co-culture. Analyze dilution of fluorescence due to cell division by flow cytometry.
- Cytokine Analysis: Collect supernatant at day 3-5 and quantify pro-inflammatory cytokines (e.g., IFN-γ, TNF-α, IL-2) using ELISA or a multiplex bead-based assay.
In Vivo Assessment of Engraftment and Immune Response
Animal models are indispensable for studying the complex interplay of rejection in a physiological system.
Detailed Methodology:
- Model Selection: Use immunodeficient mice (e.g., NOD-scid IL2Rγ
nullor NSG) as baseline hosts for human cell engraftment. To test immunogenicity, use humanized mice (reconstituted with a human immune system) or fully immunocompetent mice for syngeneic/allogeneic murine cell transplants. - Cell Preparation and Delivery: Label stem cells with a luciferase reporter for bioluminescent imaging or a fluorescent protein (e.g., GFP). Administer cells via a clinically relevant route (e.g., intravenous, intramyocardial, intrathecal).
- Engraftment Monitoring: Track cell survival and location longitudinally using in vivo imaging systems (IVIS) for bioluminescent cells. For endpoint analysis, harvest target organs for histology and flow cytometry to quantify human cell presence and immune cell infiltration.
- Immune Monitoring: At sacrifice, analyze host immune organs (spleen, draining lymph nodes) and the graft site.
- Flow Cytometry: Characterize the composition of infiltrating immune cells (T-cells, B-cells, NK cells, macrophages) and their activation states (e.g., CD69, CD25).
- Histology: Perform H&E staining to visualize gross immune infiltration and specialized stains (e.g., immunohistochemistry for CD3) to identify specific cell types.
The Scientist's Toolkit: Key Research Reagents
The following table catalogues essential materials and their functions for conducting research in stem cell immune rejection.
Table 4: Research Reagent Solutions for Immune Rejection Studies
| Reagent / Material | Primary Function in Research | Example Application |
|---|---|---|
| Anti-human CD3/CD28 Dynabeads | Polyclonal activation of T-cells; positive control for MLR. | Validating T-cell responsiveness in in vitro assays [10]. |
| CellTrace CFSE / Cell Proliferation Dyes | Tracking and quantifying cell division by flow cytometry. | Measuring antigen-specific T-cell proliferation in MLR [10]. |
| Recombinant Human Cytokines (e.g., IL-2) | Supporting T-cell growth and survival in culture. | Expanding antigen-specific T-cell lines for co-culture experiments [10]. |
| Flow Cytometry Antibody Panels (CD3, CD4, CD8, CD25, CD69, HLA-DR) | Immunophenotyping and assessing activation status of immune cells. | Analyzing the composition and activation of infiltrating lymphocytes in grafted tissues [10]. |
| Immunodeficient Mouse Models (e.g., NSG) | Providing in vivo environment for human cell engraftment without T-cell-mediated rejection. | Initial studies of human stem cell survival and differentiation [10]. |
| CRISPR-Cas9 Gene Editing Systems | Genetically modifying stem cells to delete HLA molecules. | Creating "hypoimmunogenic" iPSC lines for universal transplantation [3] [11]. |
| ELISA / Luminex Kits (IFN-γ, TNF-α, IL-2) | Quantifying soluble protein biomarkers of immune activation. | Measuring T-cell response magnitude in MLR supernatant [10]. |
Integrated Experimental Workflow
A typical project evaluating a novel hypoimmunogenic stem cell line would integrate the protocols and reagents above into a coherent workflow, as visualized below.
The therapeutic success of stem cell-based regenerative medicine is fundamentally governed by the critical triad of delivery parameters: cell dosing, timing of administration, and route of delivery. These factors collectively determine the efficacy, safety, and clinical viability of cellular therapies by influencing engraftment, biodistribution, and functional integration. Within the broader context of stem cell transplantation research, optimizing these parameters is essential for translating promising preclinical results into consistent clinical outcomes. This protocol provides a structured framework for the systematic investigation and standardization of these delivery parameters, with the goal of enhancing the therapeutic potential of stem cell applications across a spectrum of cardiovascular, neurological, and inflammatory conditions.
Table 1: Comparative Efficacy of Intravenous (IV) vs. Non-IV Administration Routes in Stroke Treatment
A 2025 meta-analysis of 17 clinical studies provides quantitative evidence for the significant impact of administration route on therapeutic efficacy and the timing of functional recovery [66]. The data are summarized below:
| Parameter | IV Administration | Non-IV Administration | Statistical Significance |
|---|---|---|---|
| National Institutes of Health Stroke Scale (NIHSS) | Moderate improvement | Significant improvement | P < 0.05 (Non-IV groups showed greater improvement) |
| Barthel Index (BI) | Moderate improvement | Significant improvement | P < 0.05 (Non-IV groups showed greater improvement) |
| Modified Rankin Scale (mRS) | Moderate improvement | Significant improvement | P < 0.05 (Non-IV groups showed greater improvement) |
| Onset of Significant Functional Improvement | Earlier within 6 months | More pronounced long-term benefits at 12-month follow-up | Delayed but enhanced therapeutic efficacy in non-IV routes |
| Proposed Mechanism | Widespread systemic distribution | Enhanced cell delivery and integration at the target site | -- |
Key Findings: The analysis concluded that non-IV routes (which include intra-arterial, intracerebral, or intraventricular delivery) were associated with more significant long-term benefits in functional recovery for stroke patients, despite a potentially delayed response [66]. This underscores the necessity of extended follow-up periods in clinical trials to fully capture the therapeutic effect, particularly for localized delivery methods.
Experimental Protocols
Protocol 1: Systematic Comparison of Administration Routes
This protocol is designed to empirically evaluate the pharmacokinetics and functional efficacy of different administration routes for stem cell therapies, using stroke or acute myocardial infarction as a model system.
I. Materials and Reagents
- Cell Preparation: Mesenchymal Stem Cells (MSCs), Bone Marrow Mononuclear Cells (BM-MNCs), or Induced Pluripotent Stem Cell (iPSC)-derived progenitors [66] [67].
- Animal Model: Relevant animal model of the disease (e.g., rodent model of induced ischemic stroke or myocardial infarction).
- Imaging Agents: MRI contrast agents (e.g., Gadolinium-based), or fluorescent cell trackers (e.g., DiR or GFP-labeled cells).
- Functional Assessment Tools:
- For Stroke: National Institutes of Health Stroke Scale (NIHSS), Barthel Index (BI), modified Rankin Scale (mRS) [66].
- For Cardiac Repair: Cardiac MRI for Left Ventricular Ejection Fraction (LVEF), Left Ventricular End-Systolic Volume (LVESV), and Left Ventricular End-Diastolic Volume (LVEDV) measurements [68].
II. Methodology
- Cell Labeling and Preparation:
- Harvest and culture the chosen stem cell type under standard conditions.
- Label cells with a superparamagnetic iron oxide (SPIO) agent for MRI tracking or a fluorescent dye (e.g., CM-Dil) for histology. Confirm labeling efficiency and cell viability post-labeling via flow cytometry or trypan blue exclusion.
- Experimental Groups:
- Group 1 (IV): Cell suspension administered via tail vein or jugular vein.
- Group 2 (Non-IV): Cell suspension administered via a localized route. For stroke, this could be intra-arterial (via internal carotid artery) or intracerebral injection. For cardiac repair, this is typically an intracoronary or intramyocardial injection [66] [67].
- Group 3 (Control): Administration of vehicle solution only.
- In Vivo Administration:
- Standardize the cell dose (e.g., 1-5 x 10^6 cells) and injection volume across all groups.
- Perform administrations at a standardized time post-injury (e.g., 24-72 hours for acute MI [68]).
- Biodistribution and Engraftment Analysis (at 24h, 7d, 28d post-injection):
- In Vivo MRI Tracking: Anesthetize animals and perform T2*-weighted MRI scans to detect SPIO-labeled cells as hypointense signals in the target organ and off-target sites (e.g., lungs, liver, spleen).
- Ex Vivo Bioluminescence/Fluorescence Imaging: If using luciferase-expressing or fluorescently labeled cells, image excised organs to quantify signal intensity and calculate relative engraftment.
- Functional Outcome Assessment:
- Conduct functional tests (NIHSS, BI, mRS for stroke; echocardiography for cardiac function) at baseline and at regular intervals (e.g., 1, 2, 3, and 6 months) post-treatment.
- Histological Endpoint Analysis:
- At study endpoint, perfuse and harvest target tissues.
- Process tissues for cryosectioning and perform immunofluorescence staining for cell-specific markers (e.g., β-III tubulin for neurons, Troponin T for cardiomyocytes) and integration markers. Quantify cell survival and differentiation.
Diagram Title: Experimental Workflow for Administration Route Comparison
Protocol 2: Determining Optimal Cell Dosing
This protocol outlines a dose-escalation study to establish the minimum effective dose (MED) and maximum tolerated dose (MTD) for a stem cell therapy, a critical step in translational research.
I. Materials and Reagents
- Cell Source: Clinical-grade MSCs or other relevant stem cell type.
- Animal Model: Immunodeficient rodent model or a relevant large animal disease model.
- Safety Monitoring Tools: Automated hematology analyzer, clinical chemistry analyzer, histopathology equipment.
II. Methodology
- Dose Cohort Design:
- Establish at least four dosing cohorts plus a vehicle control group (n=8-10 per group).
- Example doses for MSCs in rodents: 1 x 10^5 (low), 5 x 10^5 (medium), 2 x 10^6 (high), 5 x 10^6 (very high) cells/kg.
- Administration:
- Administer cells via the predetermined optimal route from Protocol 1 at a fixed time post-injury.
- Efficacy Assessment:
- Monitor primary functional outcome measures (e.g., infarct size via MRI, LVEF, or neurological score) weekly for 8-12 weeks.
- The MED is defined as the lowest dose that produces a statistically significant improvement in the primary outcome compared to the control group.
- Safety and Toxicity Assessment:
- Clinical Observations: Monitor daily for signs of distress, morbidity, or abnormal behavior.
- Clinical Pathology: Collect blood samples pre-dose and at 1, 4, and 12 weeks post-dose for complete blood count (CBC) and serum chemistry to assess organ function.
- Gross Necropsy and Histopathology: At terminal endpoint, conduct a full necropsy. Weigh major organs and collect tissues (e.g., heart, brain, lungs, liver, spleen, kidneys) for histopathological examination to identify potential ectopic tissue formation or inflammatory responses.
- Data Analysis:
- Use non-linear regression models to analyze the dose-response relationship.
- The MTD is identified as the dose level immediately below that which causes dose-limiting toxicity.
Advanced Quality Control: Predicting Functional potency
Emerging technologies are shifting the paradigm from static, snapshot-based cell identification to dynamic prediction of functional quality. The following workflow integrates quantitative phase imaging (QPI) and machine learning to assess hematopoietic stem cell (HSC) diversity and predict potency based on temporal kinetics, a method that can be adapted for other stem cell types [69].
Table 2: The Scientist's Toolkit: Key Reagents for Potency Prediction
| Research Reagent / Technology | Function in Experiment |
|---|---|
| Quantitative Phase Imaging (QPI) | A label-free, non-invasive imaging technique that monitors live cell dynamics (e.g., division patterns, dry mass, morphology) in real-time without phototoxicity [69]. |
| Single-Cell Expansion Culture System | A specialized culture platform that supports the ex vivo expansion of stem cells (e.g., murine or human HSCs) while maintaining stemness, enabling long-term tracking of single cells and their progeny [69]. |
| Machine Learning Algorithms | Computational models (e.g., for UMAP analysis and clustering) that analyze high-dimensional kinetic data from QPI to classify cells and predict their functional potential (e.g., stemness, differentiation bias) [69]. |
| Flow Cytometry Antibody Panels | Antibodies for cell surface markers (e.g., CD201, CD150, CD48 for murine HSCs; CD34, CD38, CD90, CD201 for human HSCs) used to isolate pure phenotypic stem cell populations prior to kinetic analysis [69]. |
Diagram Title: Workflow for Predictive Stem Cell Potency Assessment
Clinical Translation and Regulatory Landscape
The optimization of delivery parameters is directly reflected in the evolving clinical trial landscape and recent regulatory approvals.
Dosing and Efficacy in Clinical Trials: Success rates for stem cell therapies are highly variable and depend on the specific condition. For example, stem cell transplants for blood cancers have success rates of 60-70%, while therapies for joint repair and inflammatory conditions report success rates around 80% [28]. A critical factor behind inconsistent efficacy in MSC trials is the optimization of the "transplant regimen," which includes cell dose, timing, and route of delivery [10].
Recent FDA Approvals and Trial Designs:
- Ryoncil: In December 2024, this allogeneic bone marrow-derived MSC therapy became the first FDA-approved MSC product for pediatric steroid-refractory acute graft-versus-host disease [3]. Its approval sets a precedent for the manufacturing and dosing standards required for regulatory success.
- Pluripotent Stem Cell (PSC) Trials: As of 2025, over 115 global clinical trials are using PSC-derived products. These trials typically progress through structured Phase I-III pathways and may be supported by expedited FDA designations like RMAT (Regenerative Medicine Advanced Therapy) to facilitate development [3].
- iPSC-Derived Therapies: The field is advancing rapidly, with the first U.S. Phase III trial for an iPSC-based therapy (Fertilo) commencing in 2025. Other iPSC-derived therapies for retinal degeneration, lupus, and Parkinson's disease have received FDA IND clearance, highlighting a trend towards more complex and scalable cell products [3].
The meticulous optimization of cell dosing, timing, and administration route is not merely a technical prerequisite but a foundational element for unlocking the full therapeutic potential of stem cell transplantation. Evidence indicates that the route of administration directly impacts the magnitude and timeline of functional recovery [66], while patient-specific factors and the quality of the cell product itself are critical determinants of success [28] [69]. The field is moving toward more sophisticated, data-driven approaches, including the use of machine learning to predict cell potency [69] and the standardization of protocols through pivotal clinical trials [3]. Future research must continue to integrate these parameters, developing personalized delivery regimens that account for disease etiology, patient pathophysiology, and the functional attributes of the cellular product to ensure the consistent and safe translation of stem cell therapies from the laboratory to the clinic.
The development of regenerative medicine therapies, particularly in the field of stem cell transplantation, is a rapidly advancing area of medical science. Recognizing the potential of these therapies to address serious and life-threatening conditions with unmet medical needs, regulatory agencies worldwide have established specialized pathways to expedite their development and review. These frameworks are designed to facilitate earlier patient access to promising therapies while maintaining rigorous standards for safety and efficacy. For researchers and drug development professionals, navigating this complex regulatory landscape is a critical component of successful product development.
In the United States, the Food and Drug Administration (FDA) offers several expedited programs for regenerative medicine therapies, including the Regenerative Medicine Advanced Therapy (RMAT) designation and Fast Track designation, which provide opportunities for enhanced FDA interactions and potential accelerated approval [70]. These programs were further clarified in a September 2025 draft guidance document, "Expedited Programs for Regenerative Medicine Therapies for Serious Conditions," which supersedes the February 2019 guidance and provides updated recommendations for sponsors [71] [72] [73]. Internationally, regulatory frameworks vary significantly, with countries like Mexico maintaining stringent oversight through agencies such as COFEPRIS, while navigating challenges with unproven stem cell clinics [74].
United States Regulatory Framework
Key Expedited Pathways and Designations
The FDA has established multiple expedited programs to facilitate the development of regenerative medicine therapies, each with distinct eligibility criteria and benefits. Understanding these pathways is essential for sponsors seeking to optimize their development strategy.
Table 1: FDA Expedited Programs for Regenerative Medicine Therapies
| Program | Year Established | Eligibility Criteria | Key Benefits |
|---|---|---|---|
| Fast Track | 1997 | Potential to address unmet medical need for serious condition based on nonclinical or clinical data [70] | Rolling review, early FDA interactions [70] |
| Breakthrough Therapy | 2012 | Preliminary clinical evidence demonstrates substantial improvement over available therapies on clinically significant endpoints [70] | Intensive FDA guidance, senior management involvement [70] |
| RMAT | 2016 (21st Century Cures Act) | Regenerative medicine therapy for serious condition; preliminary clinical evidence indicates potential to address unmet medical need [71] [70] | Same benefits as Breakthrough Therapy plus potential for accelerated approval [70] |
| Accelerated Approval | 1992 | Effect on surrogate or intermediate endpoint reasonably likely to predict clinical benefit [70] | Approval based on effect on surrogate endpoint; confirmatory trials required [70] |
| Priority Review | N/A | Potential to provide significant improvement in safety or effectiveness [70] | Review timeline reduced from 10 to 6 months [70] |
The RMAT designation, specifically created for regenerative medicine products, has demonstrated significant impact since its implementation. As of September 2025, the FDA has received almost 370 RMAT designation requests and approved 184, with 13 of these products ultimately receiving marketing approval [72]. This designation mirrors many elements of Breakthrough Therapy while being specifically tailored for cell, gene, and tissue-based modalities [70].
Recent FDA-Approved Stem Cell Therapies (2023-2025)
The regulatory pathways have facilitated the approval of several innovative stem cell therapies, demonstrating the tangible outputs of these expedited programs.
Table 2: Recently FDA-Approved Stem Cell Therapies (2023-2025)
| Product Name | Approval Date | Cell Type | Indication | Key Clinical Evidence |
|---|---|---|---|---|
| Omisirge (omidubicel-onlv) | April 17, 2023 | Cord blood-derived hematopoietic progenitor cells [3] | Accelerate neutrophil recovery in patients (12-65 years) with hematologic malignancies after cord blood transplantation [3] | Allogeneic nicotinamide-modified stem cell graft accelerates neutrophil recovery and reduces infection risk [3] |
| Lyfgenia (lovotibeglogene autotemcel) | December 8, 2023 | Autologous cell-based gene therapy [3] | Sickle cell disease in patients ≥12 years with history of vaso-occlusive events [3] | 88% of patients achieved complete resolution of vaso-occlusive events between 6-18 months post-treatment [3] |
| Ryoncil (remestemcel-L) | December 18, 2024 | Allogeneic bone marrow-derived MSCs [3] | Pediatric steroid-refractory acute graft versus host disease (SR-aGVHD) in patients ≥2 months [3] | First MSC therapy approved for SR-aGVHD; modulates immune response and mitigates inflammation [3] |
Clinical Trial Landscape for Pluripotent Stem Cells
The clinical application of pluripotent stem cells (PSCs), including induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs), has expanded significantly. As of December 2024, a major review identified 115 global clinical trials involving 83 distinct PSC-derived products targeting indications primarily in ophthalmology, neurology, and oncology [3]. Over 1,200 patients have been dosed with more than 10¹¹ cells, with no significant class-wide safety concerns reported, indicating a promising safety profile for these innovative therapies [3].
Notable recent FDA-authorized clinical trials include:
- Fertilo: In February 2025, received FDA IND clearance as the first iPSC-based therapy to enter U.S. Phase III trials. This therapy uses ovarian support cells derived from REPROCELL's StemRNA Clinical Seed iPSCs to support ex vivo oocyte maturation [3].
- OpCT-001: An iPSC-derived therapy targeting retinal degeneration that received FDA IND clearance in September 2024 for a Phase I/IIa trial [3].
- FT819: An off-the-shelf, iPSC-derived CAR T-cell therapy for systemic lupus erythematosus that received RMAT designation in April 2025 [3].
- Neural progenitor cell therapies: Three iPSC-based therapies targeting Parkinson's disease, spinal cord injury, and ALS received FDA IND clearance in June 2025 [3].
The RMAT Designation Process
The following workflow diagram illustrates the key stages in seeking and obtaining RMAT designation:
Emerging FDA Initiatives
In November 2025, the FDA unveiled the "Plausible Mechanism Pathway," a new approach targeting products for ultra-rare conditions where randomized trials are not feasible [75]. This pathway leverages the expanded access single-patient IND paradigm as a vehicle for future marketing applications and requires satisfaction of five core elements:
- Identification of a specific molecular or cellular abnormality
- The medical product targets the underlying biological alterations
- Well-characterized natural history of the disease
- Confirmation that the target was successfully drugged or edited
- Demonstration of improvement in clinical outcomes or disease course [75]
This initiative reflects FDA's ongoing efforts to adapt regulatory frameworks to the unique challenges of innovative therapies, particularly for rare diseases with small patient populations.
International Regulatory Frameworks
Regulatory Landscape in Mexico
Mexico's regulation of cell therapies operates within the framework of the General Health Law, with the Federal Commission for Protection against Sanitary Risk (COFEPRIS) serving as the primary regulatory authority [74]. COFEPRIS plays a role analogous to the U.S. FDA, enforcing safety and efficacy standards for biologics and novel treatments [74].
The country employs a multi-tiered oversight system for advanced therapies requiring COFEPRIS approval, ethics committee review, transplant committee approval, and monitoring by the National Center of Blood Transfusion (CNTS) [74]. Despite these regulatory layers, Mexico has faced challenges with private clinics exploiting regulatory gaps, particularly those holding stem cell banking licenses but administering unproven treatments beyond their authorization [74].
Mexico is currently developing a dedicated Official Mexican Standard (PROY-NOM-260-SSA1) to specifically regulate the disposition of stem cells for therapeutic and research purposes [74]. This proposed regulation, though not yet finalized, aims to establish clear rules for obtaining, processing, storing, and applying stem cells in therapy or trials.
Global Regulatory Perspectives
The International Society for Stem Cell Research (ISSCR) provides guidelines that address the international diversity of cultural, political, legal, and ethical issues associated with stem cell research and clinical translation [20]. These guidelines maintain widely shared principles calling for rigor, oversight, and transparency in all areas of practice [20].
In August 2025, the ISSCR released an update to its guidelines, specifically refining recommendations for stem cell-based embryo models (SCBEMs) in response to scientific and oversight developments [20]. Key revisions included retiring the classification of models as "integrated" or "non-integrated" in favor of the inclusive term "SCBEMs," and prohibiting the ex vivo culture of SCBEMs to the point of potential viability [20].
Application Notes and Experimental Protocols
Clinical Protocol: MSC Therapy for SR-aGVHD
Based on the recent approval of Ryoncil for steroid-refractory acute graft versus host disease, the following protocol outlines key methodological considerations for MSC-based therapies:
Objective: To evaluate the safety and efficacy of allogeneic bone marrow-derived mesenchymal stem cells (MSCs) for the treatment of steroid-refractory acute graft versus host disease (SR-aGVHD) in pediatric patients.
Investigational Product:
- Cell Source: Allogeneic bone marrow-derived MSCs from healthy donors [3]
- Characterization: Must express standard MSC surface markers (CD73+, CD90+, CD105+) and lack hematopoietic markers (CD34-, CD45-, CD14-)
- Dosage: 2 × 10^6 cells per kilogram of body weight [3]
- Administration: Intravenous infusion over 30-60 minutes
Patient Population:
- Pediatric patients ≥2 months of age with SR-aGVHD [3]
- Failure to respond to standard steroid treatment
- Appropriate organ function as defined by protocol
Study Endpoints:
- Primary Efficacy Endpoint: Overall response rate (complete + partial response) at Day 28
- Secondary Endpoints: Duration of response, overall survival at 100 days and 1 year
- Safety Endpoints: Incidence of infusion reactions, infections, and other adverse events
Statistical Considerations:
- Single-arm trial design may be acceptable given serious nature of condition and lack of effective alternatives
- Historical controls may be used for comparison
- Sample size justification based on feasibility and clinically meaningful effect size
Clinical Protocol: iPSC-Derived Therapy for Retinal Degeneration
Based on the OpCT-001 trial for retinal degeneration, this protocol outlines considerations for iPSC-derived therapies:
Objective: To assess the safety and tolerability of iPSC-derived photoreceptor progenitor cells in patients with retinitis pigmentosa and cone-rod dystrophy.
Investigational Product:
- Cell Source: Allogeneic iPSC-derived photoreceptor progenitor cells [3]
- Characterization: Pluripotency marker negative, expression of photoreceptor-specific markers
- Administration: Subretinal injection using specialized surgical technique
- Immunosuppression: Perioperative systemic immunosuppression to prevent rejection
Patient Population:
- Adults with genetically confirmed retinitis pigmentosa or cone-rod dystrophy
- Sufficient viable retina as determined by ocular imaging
- Adequate visual function in fellow eye
Study Endpoints:
- Primary Safety Endpoint: Incidence and severity of adverse events, including teratoma formation
- Efficacy Endpoints: Visual acuity, visual field testing, retinal structure on OCT
- Exploratory Endpoints: Quality of life measures, mobility performance
Research Reagent Solutions for Stem Cell Therapy Development
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent/Cell Line | Function | Application Example |
|---|---|---|
| REPROCELL StemRNA Clinical iPSC Seed Clones | GMP-compliant, clinically-grade iPSC master cell bank [3] | Starting material for iPSC-derived therapies (e.g., Fertilo) [3] |
| iPSC-Derived MSCs (iMSCs) | Enhanced consistency and scalability compared to primary MSCs [3] | Clinical trials for osteoarthritis, graft-versus-host disease [3] |
| CYP-001 iMSCs | Allogeneic iPSC-derived mesenchymal stem cells | Phase II trial for High-Risk Acute GvHD (NCT05643638) [3] |
| MyoPAXon | iPSC-derived CD54+ allogeneic muscle progenitor cells | Phase I trial for Duchenne Muscular Dystrophy (NCT06692426) [3] |
| FT536 | Allogeneic, off-the-shelf natural killer (NK) cell therapy from gene-edited clonal master hiPSC line | Clinical trials for gynecologic cancers (NCT06342986) [3] |
Regulatory Strategy and Compliance
Chemistry, Manufacturing, and Controls (CMC) Considerations
The September 2025 FDA draft guidance emphasizes that expedited clinical timelines must be paralleled by accelerated chemistry, manufacturing, and controls (CMC) readiness [70]. Regenerative medicine therapies with expedited development may face unique challenges in aligning product development with faster clinical timelines [72].
Key CMC considerations include:
- Early characterization of critical quality attributes (CQAs)
- Robust comparability protocols for manufacturing changes
- Implementation of quality-by-design principles
- Comprehensive process validation
The draft guidance specifically notes that if manufacturing changes are made after receiving RMAT designation, the post-change product may no longer qualify for the designation if comparability cannot be established with the pre-change product [72].
Clinical Trial Design Considerations
FDA encourages innovative trial designs for regenerative medicine therapies, particularly for rare diseases with small patient populations [72]. The September 2025 draft guidance highlights several approaches:
- Novel Trial Designs: Studies comparing several investigational agents to each other and a common control
- Natural History Data: Use as historical controls when treatment and control populations are adequately matched
- Multi-Site Collaborations: Multiple clinical sites investigating a therapy with intent to share combined data to support BLAs
- Patient-Focused Endpoints: Input from patient communities regarding clinically relevant endpoints
For cell and gene therapies targeting rare diseases, FDA has also released complementary guidance on "Innovative Designs for Clinical Trials of CGT Products in Small Populations" and "Postapproval Methods to Capture Safety and Efficacy Data for CGT Products" [76].
Postmarketing Requirements
Regenerative medicine therapies approved through expedited pathways typically have postmarketing requirements to gather additional evidence. The FDA recommends that monitoring plans for clinical trials include both short-term and long-term safety assessments [72]. For RMAT-designated products, confirmatory requirements may be met using real-world evidence (RWE), patient registries, or electronic health record data [70].
The "Plausible Mechanism Pathway" also includes a significant postmarket evidence-gathering component, requiring sponsors to collect real-world evidence to demonstrate: (1) preservation of efficacy, (2) no off-target edits, (3) effect of early treatment on childhood development milestones, and (4) detection of unexpected safety signals [75].
The regulatory landscape for stem cell therapies continues to evolve with the development of increasingly sophisticated expedited pathways. The RMAT designation and complementary programs like Fast Track have demonstrated tangible success in advancing regenerative medicine products to market, as evidenced by the approval of multiple stem cell therapies between 2023-2025. The recent FDA draft guidance and emerging initiatives like the "Plausible Mechanism Pathway" reflect ongoing efforts to balance accelerated access with rigorous evidence standards.
Globally, regulatory frameworks vary but show convergence toward pathways that address the unique challenges of stem cell-based therapies while maintaining patient safety as a paramount concern. For researchers and drug development professionals, early engagement with regulatory authorities, strategic use of expedited pathways, and careful attention to manufacturing and postmarketing requirements will be essential for successfully navigating this complex landscape and bringing innovative stem cell therapies to patients in need.
Evaluating Therapeutic Efficacy: Clinical Evidence, Comparative Analysis, and Future Modalities
Within the framework of stem cell transplantation and regenerative medicine research, the rigorous analysis of safety and efficacy data from Phase I-III clinical trials is paramount for translating novel therapies from the laboratory to the clinic. This document provides detailed application notes and protocols to support researchers, scientists, and drug development professionals in the systematic evaluation of clinical trial outcomes. The dynamic regulatory landscape, including expedited programs such as the Regenerative Medicine Advanced Therapy (RMAT) designation, further underscores the need for robust and standardized analytical approaches [72]. The following sections synthesize current evidence and methodologies, with a specific focus on stem cell-based interventions, to create a comprehensive guide for clinical data analysis.
Quantitative Data Analysis and Presentation
Transforming raw clinical trial data into meaningful insights requires a structured statistical approach. The primary goals are to summarize the fundamental characteristics of the data (descriptive statistics) and to make inferences or test hypotheses about a larger population based on the study sample (inferential statistics) [77].
Core Quantitative Data Analysis Methods
- Descriptive Statistics: These methods summarize and describe the core features of a dataset. Key measures include:
- Measures of Central Tendency: Mean (average), median (middle value), and mode (most frequent value).
- Measures of Dispersion: Range, variance, and standard deviation, which illustrate how spread out the data points are.
- Percentages and Frequencies: Essential for understanding the distribution of categorical data, such as patient demographics or response rates.
- Inferential Statistics: These techniques use sample data to make generalizations about a population. Common methods include:
- Hypothesis Testing (e.g., T-Tests, ANOVA): Used to determine if there are statistically significant differences between groups.
- Regression Analysis: Examines the relationship between a dependent variable (e.g., improvement in ejection fraction) and one or more independent variables (e.g., cell dose, patient age) to predict outcomes.
- Cross-Tabulation: Analyzes the relationship between two or more categorical variables, such as country and device usage in a clinical trial [77].
The following tables summarize key efficacy and safety outcomes from recent stem cell therapy trials, providing a template for data presentation.
Table 1: Efficacy Outcomes from a Meta-Analysis of Stem Cell Therapy for ST-Segment Elevation Myocardial Infarction (STEMI) [78]
| Outcome Measure | Follow-up Period | Mean Change (95% CI) or P-value | Statistical Significance |
|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | 12 months | +3.15% (1.01 to 5.29) | P < 0.01 |
| Left Ventricular End-Systolic Volume (LVESV) | 3-4 months | Favorable result | P ≤ 0.05 |
| Left Ventricular End-Diastolic Volume (LVEDV) | 3-4 months | Favorable result | P < 0.05 |
| Wall Mean Score Index (WMSI) | 6 months | Reduced | P = 0.01 |
| Infarct Size (IS) | 12 months | Decreased | P < 0.01 |
Table 2: Long-Term Safety Outcomes of iPS Cell-Derived Mesenchymal Stromal Cells (CYP-001) in Acute Steroid-Resistant Graft-versus-Host Disease [79]
| Safety Parameter | Result at 2-Year Follow-up |
|---|---|
| Overall Survival | 9 of 15 participants (60%) |
| Serious Adverse Events (related to CYP-001) | None identified |
| Tumors | None identified |
| Causes of Death (n=6) | Relapse of malignancy (n=2), Pneumonia (n=2), GvHD (n=1), Sepsis/Multi-organ dysfunction (n=1) |
| Investigator Assessment | No deaths or major safety concerns were related to CYP-001 treatment |
Experimental Protocols for Safety & Efficacy Analysis
Protocol for Analyzing Cardiac Function Efficacy Endpoints
This protocol outlines the methodology for assessing common cardiac efficacy endpoints, as utilized in the STEMI meta-analysis [78].
1. Objective: To quantitatively evaluate the improvement in cardiac structure and function following stem cell therapy in patients with STEMI. 2. Materials: - Cardiac Magnetic Resonance Imaging (MRI) or Echocardiography equipment. - Image analysis software (e.g., for calculating volumes and ejection fraction). - Statistical analysis software (e.g., R, SPSS, Python with Pandas/NumPy). 3. Methodology: - Image Acquisition: Acquire cardiac MRI or echocardiogram images at baseline (post-STEMI) and at predetermined follow-up intervals (e.g., 3-4 months, 6 months, 12 months). - Data Extraction: - Left Ventricular Ejection Fraction (LVEF): Calculate the percentage of blood pumped out of the left ventricle with each heartbeat. - Left Ventricular End-Systolic Volume (LVESV): Measure the volume of blood in the left ventricle at the end of systole (contraction). - Left Ventricular End-Diastolic Volume (LVEDV): Measure the volume of blood in the left ventricle at the end of diastole (relaxation). - Wall Mean Score Index (WMSI): Score segmental wall motion (e.g., 1=normal, 2=hypokinetic, 3=akinetic, 4=dyskinetic) and calculate the mean score. - Infarct Size: Quantify via delayed gadolinium enhancement on MRI. - Statistical Analysis: - Calculate the absolute change from baseline for each parameter for every patient. - For group comparisons, use a paired t-test to assess within-group changes and an independent samples t-test (or ANOVA for multiple groups) to compare changes between the treatment and control groups. - Employ a random-effects or fixed-effects model for meta-analysis, as appropriate, with heterogeneity assessed using the I² statistic.
Protocol for Long-Term Safety Monitoring in Cell Therapy Trials
This protocol is designed for extended safety follow-up, critical for regenerative medicine therapies, as demonstrated in the CYP-001 trial [79].
1. Objective: To monitor and evaluate the long-term safety and tolerability of stem cell therapies over a multi-year period. 2. Materials: - Electronic Data Capture (EDC) system for adverse event reporting. - Protocol for scheduled clinical assessments. - Digital health technologies (e.g., for remote patient monitoring) as recommended by recent FDA draft guidance [72]. 3. Methodology: - Study Visits: Schedule follow-up visits at regular intervals post-treatment (e.g., 6 months, 12 months, 18 months, 24 months). - Data Collection: - Survival Status: Record all-cause mortality. - Adverse Events (AEs) and Serious Adverse Events (SAEs): Document all AEs and SAEs, with investigator assessment of relatedness to the investigational product. - Disease-Specific Status: Monitor the underlying condition (e.g., GvHD grade, malignancy status). - Tumorigenicity: Actively screen for any new tumor formation via physical examination and appropriate imaging, given the theoretical risk associated with some cell therapies. - Data Analysis: - Summarize AEs: Present the frequency and severity of AEs and SAEs, stratified by relatedness. - Calculate Survival Rates: Use Kaplan-Meier analysis to estimate overall survival probabilities at key time points. - Report Key Outcomes: Clearly state the absence or presence of therapy-related tumors and other major safety concerns.
Workflow Visualization
The following diagram illustrates the integrated workflow for analyzing safety and efficacy data from a clinical trial, from data collection through to regulatory submission.
Clinical Data Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
The successful development and manufacturing of stem cell therapies rely on a foundation of high-quality, well-characterized biological and material resources. The following table details key reagents and their critical functions in this field.
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent / Material | Function & Application in Therapy Development |
|---|---|
| Bone Marrow Mononuclear Cells (BM-MNCs) | A mixed population of stem and progenitor cells used as an autologous or allogeneic therapy for conditions like STEMI; one of the most extensively studied cell types in early cardiac regenerative trials [78]. |
| Mesenchymal Stem/Stromal Cells (MSCs) | Adult stem cells with immunomodulatory properties; used in therapies for GvHD (e.g., Ryoncil) and other inflammatory conditions; can be derived from bone marrow, adipose tissue, or umbilical cord [79] [3]. |
| Induced Pluripotent Stem Cells (iPSCs) | Somatic cells reprogrammed to an embryonic-like pluripotent state; serve as a scalable, consistent starting material for generating differentiated cells (e.g., iMSCs, dopaminergic neurons, retinal cells) for a wide range of therapeutic applications [79] [3]. |
| iPSC Seed Clones | A master bank of clonally derived, characterized iPSCs; ensures consistency, reduces batch-to-batch variability, and supports regulatory compliance (e.g., via a submitted Drug Master File - DMF) for manufacturing multiple therapeutic doses [3]. |
| GMP-Grade Culture Media | Chemically defined, xeno-free media systems used for the expansion and differentiation of stem cells under Good Manufacturing Practice (GMP) conditions; critical for ensuring product quality and patient safety [79]. |
| Cell Sorting & Analysis Reagents | Fluorescently labeled antibodies and viability dyes used in flow cytometry for characterizing cell surface markers, assessing purity, and ensuring the absence of residual undifferentiated iPSCs in the final product [79]. |
The path to regulatory approval requires early and strategic planning. The U.S. Food and Drug Administration (FDA) encourages sponsors to engage with the Office of Therapeutic Products (OTP) early in product development [72]. Expedited programs like the RMAT designation are available for regenerative medicine products targeting serious conditions, offering intensive FDA guidance and potential use of accelerated approval pathways [71] [72]. Clinical trials must be designed and conducted in accordance with International Conference on Harmonisation (ICH) Good Clinical Practice (GCP) guidelines to ensure the protection of patient rights and the credibility of trial data [80]. Furthermore, manufacturing changes during development require a rigorous risk assessment to ensure product comparability, as changes may impact a product's qualification for an existing RMAT designation [72].
In conclusion, the analysis of clinical trial outcomes for stem cell therapies demands a meticulous, multi-faceted approach. By employing robust statistical methods, adhering to detailed safety and efficacy protocols, utilizing well-defined research reagents, and navigating the regulatory landscape with foresight, researchers can effectively demonstrate the therapeutic potential and safety of these innovative treatments, thereby advancing the field of regenerative medicine.
Within the rapidly advancing field of regenerative medicine, stem cell transplantation has emerged as a cornerstone therapeutic strategy for a range of debilitating diseases and injuries. The selection of an appropriate cell source is a fundamental determinant of clinical outcomes, dictating not only the therapeutic potential but also the complexity of the translational pathway. This analysis focuses on the two principal cell sourcing strategies: autologous (derived from the patient's own body) and allogeneic (derived from a healthy donor). The distinction between these sources influences every aspect of treatment, from immunological compatibility and manufacturing logistics to cost and scalability [81] [82]. Framed within the broader context of stem cell transplantation research, this document provides a detailed comparison of these paradigms, supported by structured data, experimental protocols, and analytical visualizations to guide researchers and drug development professionals.
The therapeutic premise of stem cell therapy lies in the unique properties of stem cells, including self-renewal and the ability to differentiate into specialized cell types [82]. These "living drugs" exert their effects through multiple mechanisms, such as direct differentiation to replace damaged cells, powerful paracrine signaling, and immunomodulation [22] [82]. The choice between autologous and allogeneic approaches fundamentally shapes how these mechanisms are harnessed and applied in a clinical setting.
Biological and Clinical Comparison
The core distinction between autologous and allogeneic transplantation lies in the origin of the stem cells. Autologous transplantation involves harvesting a patient's own cells, expanding them ex vivo if necessary, and re-infusing them back into the same patient. In contrast, allogeneic transplantation involves the transfer of stem cells from a genetically non-identical donor into a patient [81] [82]. This fundamental difference drives consequent variations in immunological response, therapeutic effect, and clinical risk profiles.
Key Comparative Characteristics
- Immunological Compatibility: Autologous cells are inherently self-compatible, presenting no risk of immune-mediated graft rejection and eliminating the need for immunosuppressive therapy. Allogeneic cells, however, are subject to recognition as foreign by the host immune system, creating a risk of immune rejection. Conversely, in certain oncological applications like allogeneic hematopoietic stem cell transplantation (HSCT), this immune reactivity can be beneficial, manifesting as a graft-versus-tumor effect where donor immune cells target residual cancer cells [83].
- Donor Availability and Cell Quality: Autologous sources guarantee a donor but are subject to the patient's health status, age, and disease history, which can compromise the quantity and quality of harvested cells. Allogeneic cells can be sourced from young, healthy donors, potentially offering more potent and pristine cells, but are limited by the need for a suitable human leukocyte antigen (HLA) match to minimize rejection risks [81] [83].
- Manufacturing and Logistics: Autologous therapies are inherently patient-specific, creating complex, decentralized logistics and high costs for individualized manufacturing batches. Allogeneic therapies offer a scalable, "off-the-shelf" model where a single donor's cells can be expanded to create a master cell bank capable of treating numerous patients, significantly streamlining production and reducing cost-per-dose [82].
- Key Risks: The principal risk of autologous therapy is the potential for contamination with the patient's diseased cells. For allogeneic therapy, the primary risks are Graft-versus-Host Disease (GvHD), where donor immune cells attack host tissues, and the requirement for often-toxic immunosuppression to prevent graft rejection [83].
Clinical Outcome Data
Recent large-scale meta-analyses and retrospective studies have provided quantitative insights into the performance of these two approaches in specific clinical indications, particularly in hematological malignancies.
Table 1: Comparative Clinical Outcomes in Hematological Cancers
| Outcome Measure | Autologous SCT | Allogeneic SCT | Context and Notes |
|---|---|---|---|
| Non-Relapse Mortality (36-mo) | 7.3% [83] | 27% [83] | Significantly higher early risk in allogeneic setting. |
| Relapse Incidence (36-mo) | 68.4% [83] | 45.9% [83] | Demonstrates graft-versus-tumor benefit of allogeneic. |
| Overall Survival (Median) | 33.5 months [83] | 17.5 months [83] | In pPCL; allogeneic has higher early mortality. |
| Therapeutic Mechanism | Tissue regeneration, immunomodulation [81] | Graft-versus-tumor effect, immunoreset [83] | |
| Primary Clinical Risk | Contamination with diseased cells, tumorigenicity [84] | Graft-versus-host disease, rejection, infection [83] |
A 2024 systematic review on multiple myeloma further reinforced that for patients relapsing after a first-line autologous transplant, a second autologous transplant resulted in superior overall and progression-free survival compared to an allogeneic transplant, which exhibited inferior outcomes despite its theoretical curative potential [85].
Experimental Protocols for Source Evaluation
To systematically evaluate autologous and allogeneic stem cell sources in a research setting, the following standardized protocols can be implemented. These methodologies are critical for generating comparable data on cell viability, functionality, and therapeutic potential.
Protocol 1: Isolation and Expansion of Mesenchymal Stem Cells (MSCs)
Objective: To isolate and expand MSCs from autologous (adipose tissue) and allogeneic (umbilical cord tissue) sources for comparative in vitro analysis.
Source Material Acquisition:
- Autologous (Adipose-derived): Obtain lipoaspirate tissue from patient under informed consent and IRB-approved protocols. Wash extensively with sterile phosphate-buffered saline (PBS) containing 1-2% antibiotic/antimycotic solution.
- Allogeneic (Umbilical Cord-derived): Obtain Wharton's jelly from donated umbilical cord tissue (post-birth, with maternal consent). Mechanically mince the tissue into a gelatinous consistency.
Cell Isolation:
- Enzymatic Digestion: Digest the tissue samples with 0.1% Collagenase Type I (or a blend of Collagenase IA/Dispase II) for 30-60 minutes at 37°C with gentle agitation.
- Neutralization and Filtration: Neutralize the enzyme with complete growth medium (α-MEM or DMEM/F12, supplemented with 10% Fetal Bovine Serum (FBS) or human platelet lysate, and 1% antibiotics). Filter the cell suspension through a 100μm strainer to remove debris.
- Centrifugation: Centrifuge the filtrate at 500 x g for 5 minutes. Resuspend the cell pellet in complete growth medium.
Cell Culture and Expansion:
- Plating: Seed the nucleated cell fraction into T175 culture flasks at a density of 5,000–10,000 cells/cm².
- Incubation: Maintain cultures at 37°C in a humidified 5% CO₂ incubator.
- Medium Changes: Replace the medium every 2-3 days to remove non-adherent cells.
- Passaging: Once cells reach 80-90% confluence (typically after 10-14 days), passage them using 0.25% Trypsin-EDTA. Culture cells to passage 3-5 for experimental use to maintain a relatively undifferentiated phenotype.
Quality Control:
- Immunophenotyping: Confirm MSC identity via flow cytometry. Cells must be ≥95% positive for CD73, CD90, CD105 and ≤2% positive for CD34, CD45, CD11b, CD19, and HLA-DR [86].
- Trilineage Differentiation: Validate multipotency by inducing differentiation into osteocytes (using osteogenic medium with β-glycerophosphate and ascorbic acid), adipocytes (using adipogenic medium with indomethacin and IBMX), and chondrocytes (using chondrogenic medium with TGF-β3) [22] [86].
Protocol 2: In Vivo Assessment of Engraftment and Immunogenicity
Objective: To compare the engraftment efficiency and immune response elicited by autologous versus allogeneic MSCs in an immunocompetent animal model.
Cell Preparation:
- Label early-passage (P3-P5) MSCs from both sources with a fluorescent cell tracker (e.g., CM-Dil or GFP-lentivirus) according to manufacturer instructions.
- Harvest and resuspend cells in sterile PBS at a concentration of 10,000 cells/μL for injection.
Animal Model and Injection:
- Utilize an immunocompetent murine model (e.g., C57BL/6 mice). For allogeneic cell tracking, MSCs from a Balb/c background can be used.
- Create a localized injury model (e.g., a subcutaneous lesion or a chemically-induced organ injury) to mimic a regenerative environment.
- Intradermally or intravenously inject 1 x 10⁶ labeled MSCs (in 100μL PBS) into the experimental mice. Include a control group injected with PBS only.
In Vivo Imaging and Analysis:
- Monitor cell retention and migration at designated time points (e.g., 1, 7, 14 days post-injection) using in vivo fluorescence imaging systems.
- At the endpoint, euthanize the animals and harvest the target organs (e.g., liver, lung, spleen) and the injection site.
Ex Vivo Histological Analysis:
- Process tissues for frozen or paraffin sectioning.
- Perform immunohistochemistry (IHC) or immunofluorescence (IF) staining on tissue sections.
- Staining Panels:
- For Engraftment: Identify labeled human MSCs (anti-human nuclear antigen).
- For Immune Response: Stain for host T-cells (anti-mouse CD3), macrophages (anti-mouse F4/80), and markers of activation (e.g., CD68, IFN-γ).
- Quantify the number of engrafted cells and the intensity of the peri-engraftment immune infiltrate.
The following diagram illustrates the logical workflow and key decision points for selecting and evaluating a stem cell source, from isolation to functional assessment.
The Scientist's Toolkit: Key Research Reagent Solutions
A robust and standardized toolkit is essential for conducting reproducible research in stem cell biology and therapy development. The following table outlines critical reagents and their functions for the isolation, characterization, and functional assessment of stem cells.
Table 2: Essential Reagents for Stem Cell Research
| Research Reagent | Function & Application | Key Considerations |
|---|---|---|
| Collagenase Type I/II | Enzymatic digestion of tissues (adipose, umbilical cord) to isolate stromal cells. | Type and concentration must be optimized for specific tissue type to maximize cell yield and viability. |
| Fetal Bovine Serum (FBS) / Human Platelet Lysate (hPL) | Serum supplement in basal media for cell growth and expansion. | hPL is increasingly favored as a xeno-free alternative to FBS to reduce immunogenicity for clinical applications. |
| Flow Cytometry Antibody Panels (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Immunophenotypic characterization of cell surface markers to confirm stem cell identity and purity (ISCT criteria). | Panels must include both positive and negative marker sets. Use isotype controls for validation. |
| Trilineage Differentiation Kits (Osteo, Adipo, Chondro) | Functional validation of multipotent differentiation potential per ISCT standards. | Different media formulations are required for each lineage. Staining with Alizarin Red, Oil Red O, and Alcian Blue is standard. |
| CRISPR-Cas9 Systems | Genome editing tool for gene knockout/knock-in studies; enhancing therapeutic properties or creating disease models. | Can be used with iPSCs to create corrected, patient-specific lines for autologous therapy with reduced disease risk. |
| Lentiviral Vectors (e.g., GFP) | Genetic modification of cells for stable gene expression; enables long-term tracking of transplanted cells in vivo. | Biosafety Level 2 practices are required. Consider potential for insertional mutagenesis in clinical applications. |
The choice between autologous and allogeneic stem cell sources presents a strategic trade-off for researchers and clinicians. The decision matrix is multifaceted, balancing safety, efficacy, and practicality.
- The autologous paradigm offers a superior safety profile by eliminating the risks of immune rejection and GvHD, making it a compelling choice for non-malignant, degenerative conditions. However, its patient-specific nature introduces significant challenges in cost, manufacturing scalability, and potential variability in cell potency due to patient-specific factors.
- The allogeneic paradigm offers the powerful advantage of an "off-the-shelf," scalable product derived from well-characterized, young, healthy donors. This is particularly valuable for acute conditions and for harnessing the graft-versus-tumor effect in oncology. Its primary limitations are the persistent risks of GvHD and immune rejection, necessitating often complex immunosuppressive regimens.
Future research directions will likely focus on overcoming the limitations of both approaches. For allogeneic therapies, strategies in immune modulation, including the use of HLA-haplobanked iPSCs or universal "off-the-shelf" cells engineered for immune evasion, are areas of intense investigation [25] [84]. For autologous therapies, optimizing ex vivo expansion and enhancing the potency of patient-derived cells through metabolic or genetic priming are key goals. The integration of gene-editing technologies like CRISPR-Cas9 to correct genetic defects in autologous cells or to enhance the therapeutic properties of allogeneic cells represents a revolutionary convergence of fields [25] [84]. Ultimately, the selection of a stem cell source will remain indication-specific, guided by a deepening understanding of disease mechanisms and the continuous refinement of enabling technologies.
1. Introduction Regenerative medicine is witnessing a paradigm shift from traditional cell-based therapies toward innovative cell-free approaches. Stem cell transplantation, particularly using Mesenchymal Stem Cells (MSCs), has demonstrated promise in treating degenerative diseases, injuries, and immune disorders by leveraging mechanisms like differentiation, immunomodulation, and paracrine signaling [11]. However, challenges related to safety, scalability, and standardization have prompted the exploration of secretome-based therapies—acellular products derived from MSC-conditioned media, comprising growth factors, cytokines, and extracellular vesicles (EVs) [87] [88]. This application note provides a structured comparison of these approaches, emphasizing quantitative data, experimental protocols, and practical workflows for researchers and drug development professionals.
2. Mechanism of Action and Therapeutic Components 2.1 Cell-Based Therapy Mechanisms MSCs exert therapeutic effects through direct differentiation into target cell types (e.g., osteocytes, chondrocytes) and complex paracrine interactions. Key mechanisms include:
- Direct Differentiation: Replacing damaged cells in tissues (e.g., cartilage, neurons) [11].
- Paracrine Signaling: Releasing bioactive molecules that modulate immune responses and promote angiogenesis [11] [88].
- Homing and Engraftment: Migrating to injury sites to facilitate tissue integration [11].
2.2 Secretome-Based Therapy Mechanisms The secretome, comprising soluble factors (e.g., VEGF, IL-10) and EVs, mediates regenerative effects without cellular presence. Primary mechanisms include:
- Immunomodulation: Suppressing pro-inflammatory cytokines and promoting anti-inflammatory responses via factors like TSG-6 and IL-10 [89] [88].
- Angiogenesis and Tissue Repair: Enhancing blood vessel formation and cell proliferation through VEGF, HGF, and IGF-1 [87] [90].
- Anti-apoptotic Effects: Reducing cell death via bFGF and GM-CSF [88].
Table 1: Quantitative Comparison of Therapeutic Components
| Parameter | Cell-Based Therapy | Secretome-Based Therapy |
|---|---|---|
| Key Components | Live MSCs, differentiated progeny | Soluble factors (cytokines, growth factors), extracellular vesicles (exosomes, microvesicles) |
| Critical Factors | CD105+, CD90+, CD73+ surface markers [88] | VEGF, HGF, IL-10, TSG-6, miRNAs [87] [88] |
| Typical Yield | 1–5 × 10^6 cells/mL (culture-dependent) [88] | 50–200 µg EV protein/mL (source-dependent) [91] |
| Primary Bioactivities | Differentiation, immunomodulation, engraftment | Anti-inflammatory, pro-angiogenic, anti-fibrotic [87] [89] |
3. Experimental Protocols for Secretome Production and Characterization 3.1 Secretome Production Workflow Protocol 1: Standardized Secretome Harvesting
- Cell Culture: Expand MSCs from sources like umbilical cord Wharton’s jelly (WJ-MSCs) or bone marrow (BM-MSCs) in serum-free media to avoid fetal bovine serum (FBS) contamination [91] [90].
- Conditioning: Culture cells to 80% confluency in hypoxic conditions (1–5% O₂) to enhance regenerative factor secretion (e.g., VEGF, HIF-1α) [91].
- Collection: Harvest conditioned media via centrifugation (2,000 × g, 20 min) to remove cells and debris.
- Concentration: Use tangential flow filtration (TFF) or ultrafiltration to concentrate secretome components [91].
- Storage: Lyophilize or store at –80°C in aliquots for stability [88].
Protocol 2: Functional Characterization
- ELISA: Quantify growth factors (e.g., VEGF, HGF) and cytokines (e.g., IL-10) using commercial kits [90].
- Nanoparticle Tracking Analysis: Determine EV size and concentration (e.g., 50–150 nm diameter) [91].
- Bioassays: Assess fibroblast migration (scratch assay) and macrophage polarization to M2 phenotype for immunomodulatory validation [90].
Figure 1: Workflow for Secretome Production and Storage
3.2 Cell-Based Therapy Protocol Protocol 3: MSC Transplantation Workflow
- Cell Sourcing: Isolate MSCs from bone marrow (BM-MSCs) or adipose tissue (AT-MSCs) using collagenase digestion and plastic adherence [90].
- Expansion: Culture in α-MEM medium with 10% FBS under normoxia (21% O₂) [90].
- Quality Control: Verify surface markers (CD73+/CD90+/CD105+) and differentiation potential [88].
- Administration: Deliver via intravenous or local injection (e.g., 1–2 × 10^6 cells/kg body weight) [3].
4. Comparative Efficacy and Applications 4.1 Preclinical and Clinical Evidence
- Cell-Based Therapy:
- Secretome Therapy:
- Wound Healing: WJ-MSC secretome accelerates fibroblast migration and VEGF expression in systemic sclerosis models [90].
- Chronic Pain: MSC secretome alleviates neuropathic pain by modulating glial cells and opioid receptors [89].
- Neonatal Care: Reduces lung injury in bronchopulmonary dysplasia (BPD) models via anti-inflammatory effects [88].
Table 2: Head-to-Head Comparison of Key Parameters
| Parameter | Cell-Based Therapy | Secretome-Based Therapy |
|---|---|---|
| Immunogenicity | Moderate (risk of immune rejection) | Low (acellular, reduced immunogenicity) |
| Tumorigenicity Risk | Present (cell proliferation concerns) | Negligible (no live cells) |
| Scalability | Limited by cell expansion capacity | High (lyophilized, stable formulations) |
| Standardization | Challenging (donor variability) | Moderate (batch-based quality control) |
| Regulatory Status | Multiple FDA approvals (e.g., Ryoncil) [3] | Preclinical/early clinical trials [89] [88] |
| Storage Requirements | Cryopreservation at –196°C | –80°C or lyophilized |
4.2 Signaling Pathways in Secretome Mechanisms
Figure 2: Signaling Pathways for Secretome-Mediated Repair
5. The Scientist’s Toolkit: Essential Research Reagents Table 3: Key Reagents for Secretome and Cell Therapy Research
| Reagent/Material | Function | Example Application |
|---|---|---|
| Serum-Free Media | Eliminates FBS contamination for secretome production [91] | MSC conditioning for EV harvest |
| Hypoxia Chambers | Maintains 1–5% O₂ to enhance regenerative factor secretion [91] | Upregulating VEGF/HIF-1α in MSC cultures |
| Tangential Flow Filtration (TFF) | Concentrates secretome components efficiently [91] | Industrial-scale EV biomanufacturing |
| ELISA Kits | Quantifies growth factors (e.g., VEGF, HGF) and cytokines [90] | Potency assessment of secretome batches |
| CD73/CD90/CD105 Antibodies | Validates MSC surface identity for cell therapy [88] | Quality control pre-transplantation |
| CRISPR-Cas9 Tools | Engineers MSCs for enhanced secretome payloads (e.g., miRNA-21) [88] | Generating programmed EVs for targeted therapy |
6. Discussion and Future Directions Cell-based therapies offer direct engraftment potential but face hurdles in safety and scalability. In contrast, secretome-based approaches provide a versatile, off-the-shelf alternative with lower risks, though standardization and large-scale production remain challenging [91]. For translational success, researchers should:
- Prioritize 3D culture systems (e.g., spheroids) and hypoxic conditioning to optimize secretome potency [91].
- Adopt TFF and lyophilization for scalable, stable secretome formulations [88].
- Leverage CRISPR-Cas9 to engineer MSCs for tailored secretome profiles [88].
7. Conclusion While cell-based therapies remain a cornerstone for conditions like SR-aGVHD, secretome-based strategies represent the next frontier in regenerative medicine, combining efficacy with enhanced safety. By employing the protocols, tools, and workflows outlined here, researchers can accelerate the development of both modalities toward clinical applications.
The field of regenerative medicine is undergoing a profound transformation, moving away from traditional palliative care models and toward potentially curative, cell-based interventions. This paradigm shift is most evident in the direct comparison, or benchmarking, of novel stem cell therapies against established standard of care (SoC) treatments. Conventional therapies for complex degenerative diseases, hematologic malignancies, and organ failure often focus on managing symptoms rather than addressing underlying pathophysiology. In contrast, stem cell-based therapies leverage the innate capacity of pluripotent and multipotent cells to regenerate damaged tissues, modulate immune responses, and restore physiological function [10]. This document provides a structured framework for benchmarking stem cell therapies against SoC through detailed application notes and experimental protocols designed for researchers and drug development professionals.
The benchmarking process must evaluate stem cell therapies across multiple dimensions: efficacy (measured by functional improvement and survival), safety (adverse event profiles), mechanistic novelty (regenerative versus symptomatic action), and clinical practicality (administration complexity and care requirements). The following sections provide standardized methodologies for this comparative assessment, with a focus on quantitative outcomes and reproducible experimental design.
Quantitative Benchmarking: Stem Cell Therapies vs. Standard of Care
Benchmarking requires systematic comparison of clinical outcomes, functional recovery, and procedural characteristics. The data presented below synthesizes findings from recent clinical studies and registry analyses [92] [93].
Table 1: Benchmarking Clinical Outcomes in Hematologic Malignancies
| Therapy Modality | Overall Survival (1-Year) | Treatment-Related Mortality | Major Complications | Therapeutic Mechanism |
|---|---|---|---|---|
| Allogeneic HSCT | 70-85% [92] | 10-20% [92] | Graft-versus-Host Disease, VOD [93] | Immune reconstitution, graft-versus-tumor |
| Autologous HSCT | 75-90% [92] | 2-5% [92] | Prolonged cytopenia, infections [93] | Myeloablation and immune reset |
| CAR-T Cell Therapy | 60-80% (varies by indication) | 1-3% [93] | CRS, ICANS, Neurotoxicity [93] | Genetically engineered targeted cytotoxicity |
| Conventional Chemotherapy | 30-60% (refractory diseases) | <2% | Myelosuppression, organ toxicity | Cytotoxic cell death |
Table 2: Benchmarking Functional and Care Complexity Outcomes
| Assessment Domain | Allogeneic HSCT | Autologous HSCT | CAR-T Therapy | Measurement Tool |
|---|---|---|---|---|
| Functional Independence (Discharge Score) | 65.2 [93] | 78.5 [93] | 59.8 [93] | Barthel Index (0-100) |
| Risk of Clinical Deterioration | Moderate [93] | Low [93] | High [93] | Modified Early Warning Score (MEWS) |
| Care Complexity | High [93] | Moderate [93] | Very High [93] | Index of Caring Complexity (ICC) |
| Pain at Discharge | Low [93] | Low [93] | Moderate [93] | Numerical Rating Scale (NRS) |
Experimental Protocols for Preclinical and Clinical Benchmarking
Protocol 1: In Vitro Screening of Stem Cell Therapeutic Potential
This protocol outlines the generation of patient-derived organoids (PDOs) for high-throughput screening of stem cell-derived molecules or direct cell therapies, benchmarking them against standard pharmaceutical compounds.
1. Patient-Derived Organoid (PDO) Generation
- Biopsy Processing: Obtain tumor or diseased tissue via biopsy. Mechanically dissociate and enzymatically digest (e.g., Collagenase/Dispase) to create a single-cell suspension [94].
- 3D Culture: Embed ~50,000 cells per well in Basement Membrane Extract (BME) or Matrigel. Overlay with specialized organoid growth medium containing Wnt3a, R-spondin 1, Noggin, and other niche-specific factors [94].
- Expansion and Biobanking: Culture for 7-14 days, passaging every 1-2 weeks. Cryopreserve established PDO lines in liquid nitrogen for future assays.
2. High-Throughput Compound Screening
- Experimental Arms:
- Arm A (Test): PDOs treated with stem cell-derived conditioned medium or co-cultured with MSC/iPSC-derived cells.
- Arm B (Positive Control): PDOs treated with standard-of-care chemotherapeutic agent.
- Arm C (Negative Control): PDOs in culture medium only.
- Assay Setup: Plate 5,000 organoid cells/well in 384-well plates. After 72-hour treatment, assess viability via ATP-based assays (e.g., CellTiter-Glo 3D) and high-content imaging for morphology and apoptosis (Caspase-3/7 activation) [94].
- Data Analysis: Calculate IC50 values for all arms. Compare dose-response curves of Test vs. Positive Control. A statistically significant (p<0.05) leftward shift in the Test arm curve indicates superior potency.
Protocol 2: Clinical Functional Benchmarking in Cell Therapy Patients
This protocol details the application of Dependence and Clinical-Social Fragility (DEP-CSF) indices to benchmark patient recovery and care burden following different cell therapies during hospitalization [93].
1. Patient Assessment Timeline
- T0 - Admission Assessment: Perform within 24 hours of hospital admission for cell therapy.
- T1 - Discharge Assessment: Perform within 24 hours prior to hospital discharge.
2. Standardized Metrics and Tools
- Functional Independence: Barthel Index (BI). Assesses 10 activities of daily living (e.g., feeding, bathing, mobility). Score: 0 (fully dependent) to 100 (fully independent) [93].
- Risk of Clinical Deterioration: Modified Early Warning Score (MEWS). Tracks vital parameters (SBP, HR, RR, temperature, AVPU score). A score ≥4 indicates high risk [93].
- Care Complexity: Index of Caring Complexity (ICC). Evaluates nursing time and skills required based on patient dependency and clinical support needs [93].
- Risk of Falling: Conley Scale. A score ≥2 indicates a significant risk of falling [93].
3. Data Integration and Benchmarking
- Data Collection: Incorporate assessments into electronic health records.
- Analysis: Compare mean scores and trends (T0 vs. T1) across therapy groups (Allo-HSCT, Auto-HSCT, CAR-T) using ANOVA or mixed-model analysis, adjusting for baseline characteristics.
- Interpretation: Therapies resulting in significantly higher BI scores and lower MEWS/ICC scores at T1 demonstrate a superior functional outcome profile and reduced care burden compared to others.
Visualization of Workflows and Signaling Pathways
Stem Cell Therapy Benchmarking Workflow
Mechanistic Pathways of Stem Cell Action
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Stem Cell and Organoid Research
| Reagent/Material | Function | Example Application |
|---|---|---|
| Human Pluripotent Stem Cells (hPSCs) | Self-renewing, pluripotent cells for differentiation into any cell type; foundation for disease modeling and therapy development [94]. | Generating isogenic cell lines via CRISPR-Cas9 to study disease mutations; source for differentiated cells. |
| Basement Membrane Extract (BME/Matrigel) | Extracellular matrix hydrogel providing a 3D scaffold for organoid growth, mimicking the in vivo niche [94]. | Supporting the formation and polarization of patient-derived intestinal, cerebral, and hepatic organoids. |
| Reprogramming Factors (Oct4, Sox2, Klf4, c-Myc) | Transcription factor cocktail for generating induced pluripotent stem cells (iPSCs) from somatic cells (e.g., fibroblasts) [94]. | Creating patient-specific iPSC lines for personalized disease modeling and drug screening. |
| Niche Factors (Wnt3a, R-spondin, Noggin) | Critical signaling molecules that maintain stemness and guide regional specification in organoid cultures [94]. | Long-term expansion of intestinal and gastric organoids by mimicking the stem cell niche. |
| CRISPR-Cas9 System | RNA-guided genome editing tool for introducing precise genetic modifications in stem cell lines [94]. | Creating knockout or knock-in mutation models in hPSCs to study genetic diseases and validate drug targets. |
| Defined Differentiation Media | Serum-free, chemically defined media combinations containing specific growth factors and small molecules to direct cell fate [94]. | Efficient and reproducible differentiation of hPSCs into cardiomyocytes, hepatocytes, or neurons. |
The Role of Advanced Trial Design and Biomarkers in Validating Therapeutic Impact
In the field of stem cell transplantation and regenerative medicine, the transition from promising preclinical results to validated clinical therapies presents significant challenges. A primary obstacle is the objective assessment of a therapy's biological activity and clinical impact in the complex in vivo environment. Advanced trial designs, coupled with rigorously validated biomarkers, are critical for de-risking this translation. Biomarkers—objectively measured indicators of biological processes, pathogenic states, or pharmacologic responses—provide the essential tools for confirming therapeutic mechanism, identifying responsive patient populations, and accurately measuring treatment efficacy [95]. Within stem cell applications for neurological disorders, spinal cord injury, and graft-versus-host disease (GvHD), biomarkers are moving beyond simple correlates to become integral components of modern clinical trial strategy, enabling dose selection, patient stratification, and early go/no-go decisions [96] [97] [95].
Biomarker Classification and Validation Pathways
Defining Biomarker Categories for Regenerative Medicine
Biomarkers are not a monolithic class; their intended use dictates the required stringency of validation. Regulatory bodies like the FDA and EMA have established precise definitions for biomarker categories crucial for therapeutic development [95].
- Diagnostic Biomarkers: Identify the presence or subtype of a disease. In stem cell therapy, this could help define the specific pathophysiology a cell product is intended to address.
- Prognostic Biomarkers: Provide information on the natural history of a disease, identifying patients with a higher likelihood of progression.
- Predictive Biomarkers: Forecast response to a specific therapeutic intervention, allowing for enrichment of clinical trials with patients most likely to benefit.
- Pharmacodynamic/Response Biomarkers: Indicate that a biological response has occurred in a patient after receiving a therapy, providing evidence of target engagement or biological activity [97] [95].
- Safety Biomarkers: Detect potential toxicity or adverse effects, a paramount concern with cell-based therapies.
The Fit-for-Purpose Validation Framework
The principle of "fit-for-purpose" is central to biomarker development. It stipulates that the level of analytical and clinical validation should be commensurate with the biomarker's intended application [97]. The validation pathway is a multi-stage process, evolving from exploratory research use to clinical decision-making tools.
Table 1: Stages of Biomarker Validation and Qualification
| Stage | Intended Use | Validation Level | Example in Stem Cell Therapy |
|---|---|---|---|
| Exploratory | Hypothesis generation; early discovery. | Minimal; identifies potential signals. | Identifying novel protein signatures in GvHD patient serum. |
| Probable Valid | Informed decision-making in preclinical or early clinical trials. | Demonstrated reproducibility and precision in defined matrices. | Measuring ST2 plasma levels to stratify GvHD risk in a Phase II trial. |
| Known Valid / Fit-for-Purpose | Critical decision points in late-phase trials or clinical care. | Rigorously validated accuracy, precision, sensitivity, and specificity across independent cohorts. | Using a validated ST2/Reg3α assay (e.g., MAGIC test) to guide GvHD therapy in practice [96] [98]. |
The key parameters for analytical validation of a biomarker assay include:
- Accuracy: The closeness of the measured value to the true value.
- Precision: The reproducibility of the assay under identical conditions.
- Sensitivity (LOD & LOQ): The lowest concentration that can be reliably detected or quantified.
- Specificity: The ability to distinguish the biomarker from other interfering substances.
- Robustness: The stability of assay performance under variable conditions [97].
Key Biomarker Applications in Stem Cell Transplantation
Predicting and Managing Graft-versus-Host Disease (GvHD)
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a cornerstone treatment for numerous hematologic malignancies. Its efficacy and toxicity are intimately linked to graft-versus-host disease (GvHD), a common and often fatal complication [96]. Biomarkers have shown tremendous progress in this area. The MAGIC (Mount Sinai Acute GvHD International Consortium) test is a prime example of a validated biomarker set moving toward clinical utility. It measures concentrations of two proteins, ST2 and Reg3α, in patient blood after transplant [98]. This test stratifies patients into risk groups, identifying those at high risk for severe GvHD complications and non-relapse mortality, thereby enabling preemptive or more aggressive therapeutic intervention [96] [98]. ST2, a receptor for IL-33, is involved in T-helper 2 immune responses and tissue repair, and its elevation is a strong indicator of treatment-resistant GvHD.
Assessing Mechanism of Action and Engraftment
For stem cell therapies targeting neurological conditions like Parkinson's disease or spinal cord injury, biomarkers are vital for confirming the therapy's mechanism of action. This is particularly true given that benefits may arise not only from direct cell replacement but also from powerful paracrine effects, including immunomodulation and stimulation of endogenous repair [99]. Proteomic and genomic analyses of serum or cerebrospinal fluid can detect secreted factors or donor-derived nucleic acids that serve as pharmacodynamic biomarkers, confirming that the transplanted cells are biologically active in the host. Furthermore, advanced imaging techniques can act as surrogate endpoints for engraftment and structural integration.
Monitoring Safety: Tumorigenicity and Immunogenicity
A primary safety concern with pluripotent stem cell-derived therapies (e.g., from ESCs or iPSCs) is the risk of tumor formation, such as teratomas [99] [100]. Safety biomarkers that detect early signs of aberrant cell growth are therefore essential. These could include serum proteins associated with cell proliferation or specific miRNA profiles. Similarly, for allogeneic cell products, biomarkers of immune activation can predict rejection, allowing for timely immunosuppression adjustment.
Detailed Experimental Protocols
Protocol 1: Validating a Protein Biomarker Assay for GvHD Risk Stratification
This protocol outlines the steps for developing and validating an ELISA-based assay to quantify a protein biomarker (e.g., ST2) in patient serum, based on the principles demonstrated by the MAGIC test [96] [98].
1. Sample Collection and Processing:
- Collection: Collect peripheral blood from patients at predetermined timepoints post-transplant (e.g., day 7, 14, 28). Use serum separator tubes.
- Processing: Allow blood to clot for 30 minutes at room temperature. Centrifuge at 1,500-2,000 x g for 10 minutes in a refrigerated centrifuge (4°C).
- Aliquoting and Storage: Immediately aliquot the supernatant serum into polypropylene cryovials. Flash-freeze aliquots in liquid nitrogen and store at -80°C. Avoid repeated freeze-thaw cycles.
2. Assay Procedure (ELISA):
- Reagent Preparation: Thaw all reagents and samples on ice. Prepare standards per the manufacturer's protocol with a serial dilution in the provided matrix to create a standard curve.
- Plate Setup: Add 100 µL of standard, control, or pre-diluted sample to the appropriate wells of the pre-coated microplate. Incubate for the specified time (e.g., 2 hours) on a plate shaker.
- Washing: Aspirate the liquid and wash each well 4 times with 300 µL of wash buffer.
- Detection Antibody: Add 100 µL of the prepared biotinylated detection antibody to each well. Incubate for 1 hour with shaking.
- Washing: Repeat the wash step as above.
- Enzyme Conjugate: Add 100 µL of Streptavidin-HRP solution to each well. Incubate for 30 minutes protected from light.
- Washing: Repeat the wash step.
- Substrate Development: Add 100 µL of TMB substrate solution to each well. Incubate for 10-20 minutes in the dark until optimal blue color develops.
- Stop Solution: Add 100 µL of stop solution (e.g., 1M H2SO4). The color will change from blue to yellow.
- Reading: Measure the absorbance at 450 nm with a wavelength correction of 570 nm or 630 nm within 30 minutes of adding the stop solution.
3. Data Analysis:
- Generate a standard curve by plotting the mean absorbance for each standard against its concentration. Use a 4- or 5-parameter logistic curve fit.
- Interpolate the sample concentrations from the standard curve. Samples yielding values above the highest standard must be re-assayed at a higher dilution.
4. Validation Steps:
- Precision: Assess intra-assay precision (repeatability) by testing ≥5 replicates of 3 QC samples in one run. Assess inter-assay precision (reproducibility) across ≥3 independent runs. %CV should be <15-20%.
- Accuracy/Recovery: Spike known quantities of the analyte into patient serum and calculate the percentage recovery (should be 85-115%).
- Linearity: Perform a serial dilution of a high-concentration sample and demonstrate linearity across the assay range.
- Stability: Perform freeze-thaw stability studies (e.g., 3 cycles) and short-term bench-top stability.
Protocol 2: Workflow for a Biomarker-Based Prospective Clinical Trial
This protocol describes the integration of a biomarker into a Phase II/III trial design for a stem cell therapy, using a "Biomarker-Stratified Design."
1. Pre-Trial: Biomarker Assay Validation
- Define Context of Use: Precisely state how the biomarker will be used (e.g., "to stratify patients into high-risk and low-risk groups for prophylactic treatment").
- Analytical Validation: Complete the full fit-for-purpose validation of the biomarker assay as described in Protocol 1.
- Protocol Finalization: Write the clinical trial protocol with embedded biomarker analysis, specifying timepoints for sample collection, analysis plan, and statistical considerations for the stratified groups.
2. Trial Execution:
- Screening and Consent: Screen potential participants and obtain informed consent for both the trial and biomarker testing.
- Baseline Sample Collection: Collect baseline samples (e.g., blood, tissue) before administration of the investigational therapy.
- Biomarker Testing and Stratification: Process samples and run the validated biomarker assay. Assign patients to biomarker-defined strata (e.g., Biomarker-High vs. Biomarker-Low).
- Randomization and Treatment: Randomize patients within each biomarker stratum to the experimental therapy or control arm. This allows for assessing the treatment effect within each biomarker group.
- Longitudinal Sampling: Collect additional samples at predefined post-treatment intervals to monitor pharmacodynamic changes and safety signals.
3. Data Analysis and Endpoint Assessment:
- Primary Analysis: Compare primary clinical endpoints (e.g., survival, response rate) between treatment arms within and across biomarker strata.
- Statistical Tests: Use appropriate methods (e.g., logistic regression for response, Cox proportional hazards for survival) including a term for the treatment-by-biomarker interaction to formally test if the treatment effect differs by biomarker status.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Biomarker Research in Stem Cell Therapy
| Research Reagent / Tool | Function and Application | Key Considerations |
|---|---|---|
| ELISA Kits (e.g., ST2, Reg3α) | Quantifying specific protein biomarkers in serum/plasma for GvHD risk stratification [98]. | Choose kits with validated performance for the specific sample matrix; critical for clinical grade assays. |
| Multiplex Immunoassay Panels (e.g., MSD, Luminex) | Simultaneously measuring dozens of analytes from a small sample volume for biomarker discovery and signature validation [96]. | Higher throughput than ELISA; requires careful normalization and validation of each analyte. |
| RNA Sequencing Kits | Profiling gene expression signatures in peripheral blood mononuclear cells (PBMCs) or sorted cell populations to identify prognostic patterns [96] [101]. | Bulk RNAseq provides an average profile; single-cell RNAseq reveals heterogeneity but is more complex. |
| Flow Cytometry Antibody Panels | Immunophenotyping immune cells (T cells, dendritic cells) to correlate cell populations with clinical outcomes (e.g., rejection, tolerance) [102]. | Requires extensive panel optimization and controls for high-dimensional data. |
| Exosome Isolation Kits | Isolating stem cell-derived exosomes from biofluids for analysis as therapeutic agents or biomarkers of cell activity and safety [100]. | Methods include precipitation, size-exclusion chromatography; choice affects yield and purity. |
Visualizing Workflows and Pathways
Biomarker Development and Validation Pathway
This diagram outlines the multi-stage pathway from biomarker discovery to clinical application, highlighting the iterative process of validation and qualification.
Key Signaling Pathways in GvHD Biomarker Biology
This diagram illustrates the simplified biological context of key GvHD biomarkers like ST2, showing their connection to critical immune pathways activated after transplantation.
Conclusion
Stem cell transplantation has unequivocally transitioned from a theoretical promise to a clinical reality, marked by significant FDA approvals and a robust pipeline of advanced trials. The field is now characterized by a diversification of cell sources, with iPSC-derived therapies gaining substantial momentum alongside established HSC and MSC platforms. Future progress hinges on systematically overcoming key challenges in manufacturing scalability, long-term safety monitoring, and precise immune management. The integration of gene-editing technologies, bioengineering solutions for tissue constructs, and a deeper understanding of paracrine mechanisms will further propel the field. For researchers and drug developers, the coming decade presents an opportunity to refine these 'living drugs' into standardized, accessible, and targeted therapies, ultimately fulfilling the transformative potential of regenerative medicine for a broad spectrum of incurable diseases.
References
- 1. Stem cell revolution: bridging the gap between research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12659346/]
- 2. Stem Cell Differentiation: Explained (2025) [https://www.dvcstem.com/post/stem-cell-differentiation]
- 3. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 4. Stem cell biology and drug discovery [https://bmcbiol.biomedcentral.com/articles/10.1186/1741-7007-9-42]
- 5. Development of a quantitative prediction algorithm for ... [https://www.nature.com/articles/s41467-021-24746-w]
- 6. Stem cell transplant without toxic preparation successfully ... [https://med.stanford.edu/news/all-news/2025/07/stem-cell-transplant.html]
- 7. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 8. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 9. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 10. Stem Cell Research: The Future of Regenerative Medicine ... [https://www.dvcstem.com/post/stem-cell-research]
- 11. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 12. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 13. Editorial: Role of induced pluripotent stem cells (iPSCs) in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1734717/full]
- 14. Stem-Cell Niches in Health and Disease: Microenvironmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249023/]
- 15. Stem Cell Niche Concept: Search for Current Expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429054/]
- 16. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 17. Reconstruction of Hematopoietic Stem Cell Niches In Vitro [https://www.sciencedirect.com/science/article/pii/S259000642501107X]
- 18. Editorial: Plasticity of the haematopoietic niche [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422902/]
- 19. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 20. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 21. Application of stem cells in regeneration medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276889/]
- 22. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 23. Immunoregulatory paracrine effect of mesenchymal stem ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1411507/full]
- 24. Stem cell paracrine actions and tissue regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2833273/]
- 25. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 26. Mesenchymal Stem/Stromal Cells and Their Paracrine Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875256/]
- 27. Mesenchymal stem cells and immunomodulation [https://www.nature.com/articles/cddis2015327]
- 28. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 29. Applications of Modern Cell Therapies: The Latest Data in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565404/]
- 30. Regenerative medicine: Current therapies and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4664309/]
- 31. How many FDA approved Hematopoietic stem cell therapy ... [https://synapse.patsnap.com/article/how-many-fda-approved-hematopoietic-stem-cell-therapy-are-there]
- 32. Approved Cellular and Gene Therapy Products [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/approved-cellular-and-gene-therapy-products]
- 33. Omisirge (omidubicel-onlv) FDA Approval History [https://www.drugs.com/history/omisirge.html]
- 34. OMISIRGE® (omidubicel-onlv) | Allogeneic Hematopoietic ... [https://omisirge.com/]
- 35. Ayrmid Ltd. Announces FDA Acceptance and Priority ... [https://www.gamida-cell.com/press_release/ayrmid-ltd-announces-fda-acceptance-and-priority-review-for-omidubicel-for-the-treatment-of-severe-aplastic-anemia-saa/]
- 36. 重磅!FDA批准首款“现货型”间充质干细胞药物上市 [https://ixcellbio.com/News/Industry/221.html]
- 37. FDA Approves First Gene Therapies to Treat Patients with ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease]
- 38. Ryoncil天价之谜:从"干细胞"到"基质细胞"的30年认知革命 [https://finance.sina.com.cn/roll/2025-03-17/doc-inepxuqr3618696.shtml]
- 39. 美国批准首款间充质干细胞药品上市 - ByDrug [https://bydrug.pharmcube.com/news/detail/aa74631b2434d2782d81741331656ca3]
- 40. LYFGENIA [https://www.fda.gov/vaccines-blood-biologics/lyfgenia]
- 41. 2025年9月干细胞研究和再生医学领域的行业动态 [https://www.ebiotrade.com/newsf/2025-11/20251106083912541.htm]
- 42. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 43. Induced pluripotent stem cells: applications in regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4313779/]
- 44. Fate Therapeutics Presents New Clinical Data at ACR ... [https://ir.fatetherapeutics.com/news-releases/news-release-details/fate-therapeutics-presents-new-clinical-data-acr-convergence]
- 45. OpCT-001 is the first iPSC-derived investigational cell ... [https://www.bluerocktx.com/bluerock-therapeutics-announces-fda-clearance-of-ind-application-for-investigational-ipsc-derived-cell-therapy-opct-001-for-the-treatment-of-primary-photoreceptor-diseases/]
- 46. Application potential of induced pluripotent stem cells in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511849/]
- 47. iPSC-based cell replacement therapy: from basic research ... [https://www.sciencedirect.com/science/article/pii/S1465324925000532]
- 48. Stem Cell Therapy for Neurological Disorders (2025) [https://www.dvcstem.com/post/stem-cell-therapy-for-neurological-disorders]
- 49. Stem Cell Therapy for Heart Failure (2025) [https://www.dvcstem.com/post/stem-cells-reverse-heart-disease]
- 50. Advances in cell therapy for orthopedic diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1567640/full]
- 51. Stem cell therapy in ophthalmology: emerging clinical trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12165522/]
- 52. Applications of Modern Cell Therapies: The Latest Data in ... [https://www.mdpi.com/2075-1729/15/10/1610]
- 53. Current status and new horizons in stem cell therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406451/]
- 54. Stem cells in regenerative medicine: Unlocking therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2667099225000283]
- 55. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 56. Pluripotent Stem Cell (PSC) Protocols [https://www.thermofisher.com/us/en/home/references/protocols/cell-culture/stem-cell-protocols/ipsc-protocols.html]
- 57. Editorial: Improving stem cell transplantation delivery using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11931077/]
- 58. Contract Manufacturing Outsourcing Trends For Advanced ... [https://www.outsourcedpharma.com/doc/contract-manufacturing-outsourcing-trends-for-advanced-therapies-in-and-beyond-0001]
- 59. ISSCR 2025: Quality Is Our Common Language [https://www.stemcell.com/virtual-conference-exhibition/isscr]
- 60. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 61. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 62. Comparison of Classification of Indications for Allogeneic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424524/]
- 63. Comparison of autologous and allogeneic hematopoietic ... [https://pubmed.ncbi.nlm.nih.gov/40930225/]
- 64. Comparison of autologous and allogeneic hematopoietic ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725014022]
- 65. Outcomes following different upfront stem cell ... [https://www.nature.com/articles/s41409-025-02675-2]
- 66. Stem Cell–Based Therapies via Different Administration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808770/]
- 67. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 68. Mesenchymal Stem Cell Therapy for Acute Myocardial ... [https://www.researchprotocols.org/2025/1/e60591]
- 69. Quantitative phase imaging with temporal kinetics predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12260078/]
- 70. Expedited FDA Approval of Stem Cell Therapies - FDAMap [https://www.fdamap.com/blog/expedited-fda-approval-of-stem-cell-therapies/]
- 71. Expedited Programs for Regenerative Medicine Therapies ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/expedited-programs-regenerative-medicine-therapies-serious-conditions-0]
- 72. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 73. Expedited Programs for Regenerative Medicine Therapies ... [https://www.federalregister.gov/documents/2025/09/25/2025-18653/expedited-programs-for-regenerative-medicine-therapies-for-serious-conditions-draft-guidance-for]
- 74. SCA LRA Update - April 2025: Regulatory Landscape of ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/04/09/sca-lra-update-april-2025-regulatory-landscape-of]
- 75. FDA's New “Plausible Mechanism Pathway” and Other ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-plausible-mechanism-pathway-and-other-initiatives-drugs-for-ultra-rare-conditions]
- 76. FDA Releases Three Biotherapies Guidance Documents [https://www.aabb.org/news-resources/news/article/2025/09/24/fda-releases-three-biotherapies-guidance-documents]
- 77. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 78. Clinical efficacy and safety of autologous stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4975151/]
- 79. Two-year safety outcomes of iPS cell-derived ... [https://www.nature.com/articles/s41591-024-02990-z]
- 80. ICH Guidance Documents [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/ich-guidance-documents]
- 81. Stem Cell Therapy: Overview, Benefits & Risks (2025) [https://www.dvcstem.com/post/stem-cell-therapy]
- 82. Stem cells as biological drugs for incurable diseases [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04632-8]
- 83. Comparison of autologous and allogeneic hematopoietic ... [https://haematologica.org/article/view/haematol.2021.280568]
- 84. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 85. Allogeneic versus autologous stem cell transplantation ... [https://pubmed.ncbi.nlm.nih.gov/40334055/]
- 86. Regenerative medicine applications: An overview of ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.942750/full]
- 87. Therapeutic Potential on Wound Healing and Cell-Free ... [https://pubmed.ncbi.nlm.nih.gov/40076553/]
- 88. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 89. Cell-Free Therapies for Chronic Pain: The Rise of ... [https://www.mdpi.com/2076-3425/15/12/1263]
- 90. Cell-free regenerative medicine: identifying the best source ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1518412/full]
- 91. Method standardization of secretome production, collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423684/]
- 92. Benchmarking [https://www.ebmt.org/benchmarking]
- 93. Dependence and clinical fragility in hematopoietic stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464104/]
- 94. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 95. Discovery and validation of biomarkers to aid the ... [https://www.nature.com/articles/s41582-020-0362-2]
- 96. for posttransplantation outcomes Biomarkers [https://pubmed.ncbi.nlm.nih.gov/29622549/]
- 97. Biomarker Assay Development and Validation in Precision ... [https://protocolsandsolutions.com/blogs/news/biomarker-assay-development-and-validation-in-precision-medicine]
- 98. Biomarkers & MAGIC - predicting patient outcomes after a ... [https://www.anthonynolan.org/blog/2017/03/biomarkers-magic-predicting-patient-outcomes-after-a-stem-cell-transplant]
- 99. for neurological disorders: current progress... Stem cell therapies [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-024-01987-1]
- 100. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 101. Biomarkers for posttransplantation outcomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5958654/]
- 102. Frontiers | Regulated cell death and DAMPs as biomarkers and... [https://www.frontiersin.org/journals/transplantation/articles/10.3389/frtra.2025.1575703/full]