Strategies for Improving Reprogramming Efficiency: From Somatic Cells to Functional iPSCs
This article provides a comprehensive guide for researchers and drug development professionals on the latest strategies to enhance the efficiency and safety of induced pluripotent stem cell (iPSC) generation.
Strategies for Improving Reprogramming Efficiency: From Somatic Cells to Functional iPSCs
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the latest strategies to enhance the efficiency and safety of induced pluripotent stem cell (iPSC) generation. It covers foundational principles, including the core reprogramming factors and their mechanisms, explores advanced methodological approaches like non-integrating delivery systems and chemical reprogramming, and offers practical solutions for common troubleshooting and optimization challenges. Furthermore, it discusses critical validation frameworks and comparative analyses of different reprogramming techniques, synthesizing key insights to accelerate robust iPSC generation for research and clinical applications.
Decoding the Blueprint: Core Reprogramming Factors and Molecular Mechanisms
The Yamanaka Factors (OSKM) and Alternative Cocktails (OSNL)
Core Concepts: Understanding the Factors
What are the Yamanaka Factors (OSKM)?
The Yamanaka factors, officially known as the OSKM combination, are four transcription factors identified by Shinya Yamanaka and Kazutoshi Takahashi in 2006 as sufficient to reprogram somatic cells back into a pluripotent state. This groundbreaking discovery demonstrated that adult cells could be reprogrammed to behave like embryonic stem cells, creating what are known as induced pluripotent stem cells (iPSCs) [1] [2] [3].
The OSKM acronym stands for:
- OCT4 (Octamer-binding transcription factor 3/4): A POU-family transcription factor critical for maintaining pluripotency and self-renewal. It inhibits the expression of genes associated with ESC differentiation [4] [5].
- SOX2 (SRY-box transcription factor 2): A high-mobility group (HMG) box transcription factor that works cooperatively with OCT4 to regulate pluripotency-associated genes [4] [5].
- KLF4 (Krüppel-like factor 4): A transcription factor with a dual role, both suppressing somatic cell-specific genes and activating pluripotency-associated genes [4] [5].
- c-MYC (Cellular Myelocytomatosis): A proto-oncogene that enhances reprogramming efficiency by promoting global histone acetylation, which facilitates the binding of OCT4 and SOX2 to their target loci. It also accelerates cell proliferation [4] [5].
What is the OSNL alternative cocktail?
In 2007, simultaneously with Yamanaka's human cell reprogramming, James Thomson's group identified an alternative combination of factors sufficient for reprogramming human somatic cells to pluripotency [4] [2] [5]. The OSNL cocktail consists of:
- OCT4: Serves the same critical pluripotency function as in the OSKM combination.
- SOX2: Functions identically to its role in the OSKM cocktail.
- NANOG: A homeodomain-containing transcription factor that functions as a key regulator for maintaining pluripotency alongside OCT4 and SOX2 [4] [5].
- LIN28: An RNA-binding protein that promotes cell proliferation during the early phase of iPSC generation, functioning similarly to c-MYC [4] [5].
Comparative Table: OSKM vs. OSNL Reprogramming Factors
| Factor | OSKM Cocktail | OSNL Cocktail | Primary Function | Safety Considerations |
|---|---|---|---|---|
| OCT4 | ✓ | ✓ | Master pluripotency regulator; inhibits differentiation genes | Essential for reprogramming |
| SOX2 | ✓ | ✓ | Partners with OCT4; maintains pluripotent state | Essential for reprogramming |
| KLF4 | ✓ | ✗ | Dual role: suppresses somatic genes, activates pluripotency | Generally safe |
| c-MYC | ✓ | ✗ | Promotes histone acetylation; accelerates cell proliferation | Proto-oncogene; tumor risk concern |
| NANOG | ✗ | ✓ | Reinforces pluripotency network; not strictly essential | Safe; enhances quality |
| LIN28 | ✗ | ✓ | Promotes proliferation; regulates microRNAs | Safer alternative to c-MYC |
Troubleshooting Common Reprogramming Issues
FAQ: Low Reprogramming Efficiency
Q: Our reprogramming efficiency remains consistently low despite using validated protocols. What factors should we investigate?
A: Low reprogramming efficiency can result from multiple factors. Consider these troubleshooting steps:
- Factor Stoichiometry: The ratio of reprogramming factors is critical. Research indicates that an OCT4highSOX2low stoichiometry is particularly important for efficient reprogramming [3]. Optimize your factor ratios rather than simply increasing total factor load.
- Cell Source Selection: The starting somatic cell type significantly impacts efficiency. Dermal fibroblasts remain the most common source, but peripheral blood mononuclear cells (PBMCs) have shown excellent results with certain protocols [6]. Primary cells from older donors may require additional factors or longer reprogramming periods.
- Epigenetic Barriers: Enhance efficiency with epigenetic modifiers. Studies show that histone deacetylase inhibitors (e.g., Valproic Acid, Sodium Butyrate, Trichostatin A) and DNA methyltransferase inhibitors (e.g., 5'-aza-cytidine) can significantly improve reprogramming rates [4]. For example, combining 8-Br-cAMP with Valproic Acid increased human fibroblast reprogramming efficiency by up to 6.5-fold [4].
- Metabolic Optimization: Ensure proper metabolic conditions. The transition from oxidative phosphorylation to glycolysis is a crucial early reprogramming event [3]. Maintain optimal nutrient conditions and consider hypoxia (5% O2) to enhance efficiency.
FAQ: Genomic Integration Concerns
Q: We need to minimize genomic integration of reprogramming factors for clinical applications. What delivery systems should we consider?
A: Safety concerns regarding genomic integration have prompted development of multiple non-integrating delivery systems:
- Episomal Plasmids: DNA-based vectors that remain separate from the host genome and are gradually diluted through cell divisions. Effective but typically lower efficiency than viral methods [4].
- Sendai Virus: An RNA virus that replicates in the cytoplasm without genomic integration. Provides high efficiency and is eventually cleared from the cells [4].
- Synthetic mRNA: In vitro transcribed mRNA that directly translates into protein without risk of integration. Requires careful optimization to avoid triggering innate immune responses [4].
- Recombinant Protein: Direct delivery of the reprogramming factors as proteins. Completely avoids genetic material but has very low efficiency [4].
For clinical applications, Sendai virus and synthetic mRNA systems currently offer the best balance of efficiency and safety.
FAQ: Teratoma Formation and Incomplete Differentiation
Q: Our iPSCs consistently form teratomas in differentiation assays or show incomplete differentiation. How can we address this?
A: Teratoma formation indicates persistent undifferentiated pluripotent cells:
- Improve Characterization: Implement rigorous pluripotency assessment beyond standard markers. Include transcriptional analysis, epigenetic profiling, and in vivo teratoma formation assays [6] [2].
- Enhance Differentiation Protocols: Implement sequential differentiation with stage-specific markers rather than direct differentiation. Consider 3D organoid systems that better recapitulate developmental cues [2].
- Cell Sorting: Use fluorescence-activated cell sorting (FACS) with surface markers specific to your target cell type to eliminate residual undifferentiated cells.
- Alternative Cocktails: Consider using the OSNL combination, which may produce higher-quality iPSCs in some systems, as NANOG enhances the stability of the pluripotency network [5].
Quantitative Data and Optimization Parameters
Table: Efficiency Comparison of Reprogramming Methods
| Delivery Method | Integration Risk | Relative Efficiency | Clearance Timeline | Best Application Context |
|---|---|---|---|---|
| Retrovirus | High (integrates) | High | Permanent | Basic research; robust cell lines |
| Lentivirus | Medium (integrates) | High | Permanent | Basic research; difficult-to-transfect cells |
| Sendai Virus | None (cytoplasmic) | High | 10-20 passages | Clinical applications; high-efficiency needs |
| Episomal Plasmids | Low (non-integrating) | Medium | 5-15 passages | Clinical applications; GMP production |
| Synthetic mRNA | None | Medium-High | 3-7 days | Clinical applications; minimal manipulation |
| Recombinant Protein | None | Low | Immediate | Specialized applications with efficiency concerns |
Table: Enhancing Reprogramming Efficiency with Small Molecules
| Small Molecule | Concentration Range | Mechanism of Action | Efficiency Improvement | Key Considerations |
|---|---|---|---|---|
| Valproic Acid (VPA) | 0.5-2 mM | Histone deacetylase inhibitor | Up to 6.5-fold (with 8-Br-cAMP) [4] | Cytotoxic at high concentrations |
| Sodium Butyrate | 0.5-1 mM | Histone deacetylase inhibitor | Significant improvement | Requires concentration optimization |
| 5'-aza-cytidine | 0.5-5 µM | DNA methyltransferase inhibitor | Moderate improvement | Can induce genomic instability |
| RepSox | 2-10 µM | Replaces SOX2; TGF-β pathway inhibition | Enables factor minimization | Specific cell type responses vary |
| 8-Br-cAMP | 0.1-0.5 mM | cAMP analog; enhances signaling | 2-fold improvement alone [4] | Synergistic with other enhancers |
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagents for iPSC Reprogramming
| Reagent Category | Specific Examples | Function | Protocol Notes |
|---|---|---|---|
| Reprogramming Factors | OSKM, OSNL combinations | Induce pluripotency | Optimize ratios for specific cell types |
| Delivery Systems | Sendai virus, episomal plasmids, mRNA | Introduce factors into cells | Match to application (research vs. clinical) |
| Culture Media | mTeSR Plus, TeSR media | Maintain pluripotent state | Use consistently for reproducible results |
| Enhancement Molecules | Valproic Acid, Sodium Butyrate | Improve efficiency | Titrate carefully to avoid cytotoxicity |
| Characterization Tools | Pluripotency antibodies, PCR panels | Verify iPSC quality | Use multiple validation methods |
| Differentiation Media | STEMdiff systems | Direct lineage specification | Follow stage-specific protocols |
Experimental Workflows and Visualization
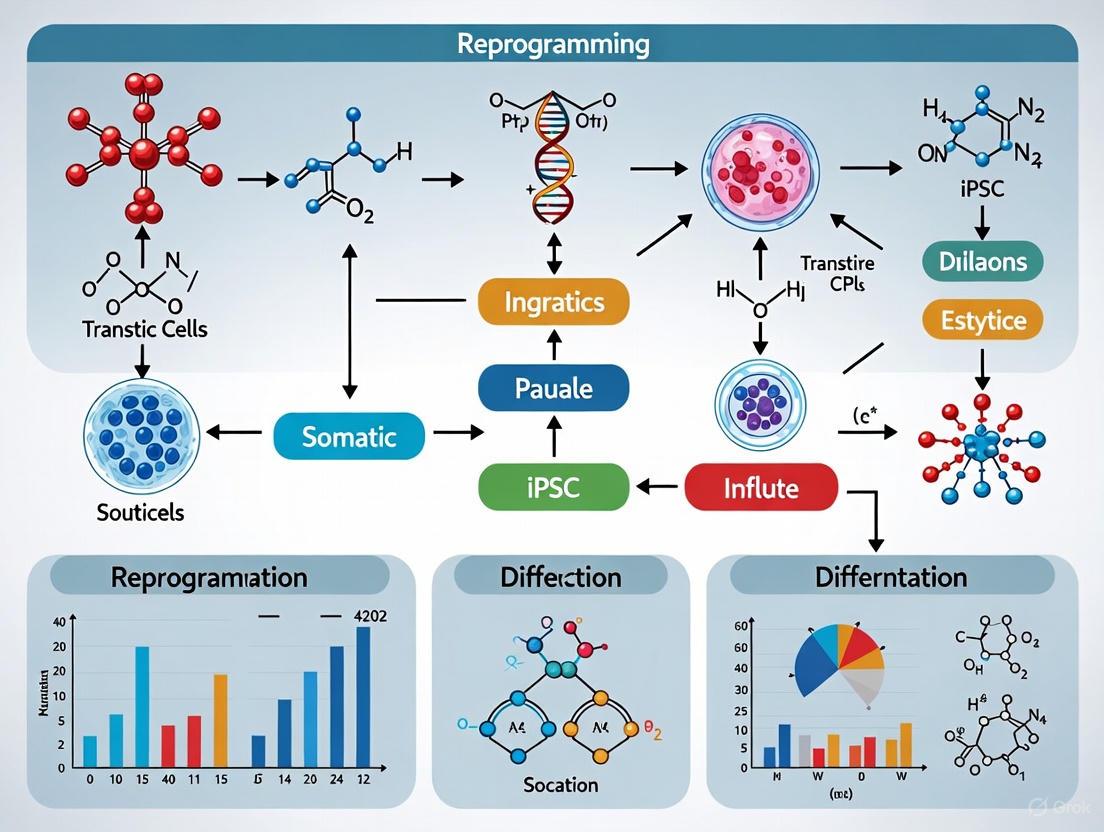
Diagram: OSKM Reprogramming Workflow and Mechanisms
Diagram: Molecular Mechanism of Yamanaka Factors
Advanced Technical Protocols
Detailed Methodology: mRNA-Based Reprogramming
For researchers requiring non-integrating methods suitable for clinical applications, synthetic mRNA reprogramming provides an excellent option:
Day 0: Plating Somatic Cells
- Isolate and culture source cells (e.g., fibroblasts or PBMCs) in appropriate medium
- Plate 5×10⁴ cells per well in a 6-well plate coated with suitable matrix
- Ensure cells are 70-80% confluent at time of transfection
Days 1-5: Daily mRNA Transfection
- Prepare mRNA cocktail containing OSKM or OSNL factors plus B18R protein
- Transfect using lipid-based transfection reagent optimized for mRNA
- Include modified nucleotides (e.g., pseudouridine) to reduce innate immune response
- Change medium 4-6 hours post-transfection to reduce cytotoxicity
Days 6-18: Transition and Colony Growth
- Reduce transfection frequency to every other day
- Switch to iPSC culture medium (e.g., mTeSR Plus or equivalent)
- Monitor for emergence of embryonic stem cell-like morphology
Days 19-30: Colony Picking and Expansion
- Manually pick well-defined colonies based on ESC-like morphology
- Transfer to feeder-free culture conditions
- Expand and bank validated iPSC lines
Critical Optimization Parameters:
- mRNA quality and purity is essential - use HPLC-purified transcripts
- Include B18R protein to suppress interferon response
- Maintain strict RNAse-free conditions throughout the process
- Monitor for complete mRNA clearance post-reprogramming (typically 3-7 days after final transfection)
Partial vs. Full Reprogramming for Different Applications
Recent advances have demonstrated that partial reprogramming through transient expression of Yamanaka factors can reverse age-associated phenotypes without completely resetting cell identity [1] [7]. This approach has shown promise in reversing epigenetic aging markers, restoring vision in old mice, and enhancing cognitive function in aged mouse models [1].
For full reprogramming to pluripotency, the complete epigenetic reset is necessary, making it ideal for disease modeling and differentiation to various cell types. The OSNL combination may produce higher-quality iPSCs for certain applications, particularly when avoiding proto-oncogenes like c-MYC is a priority [4] [5].
The choice between OSKM and OSNL, and between full versus partial reprogramming, should be guided by the specific research goals, with careful consideration of the trade-offs between efficiency, safety, and the desired cellular phenotype.
FAQ: Oncogenes in Cell Reprogramming
Q1: Why is c-Myc considered a liability in iPSC generation for therapeutic applications? c-Myc is a powerful transcription factor that acts as an oncogene, with its constitutive overexpression contributing to tumor formation. This poses significant risks to the long-term safety and stability of induced pluripotent stem cells (iPSCs), as it can enhance the tumorigenic potential of the resulting cells, making them unsuitable for clinical therapies [4] [8].
Q2: What are the primary strategies for reducing tumorigenic risk in reprogramming? The main strategies involve moving away from integrating viral vectors and finding substitutes for potentially oncogenic factors like c-Myc. Researchers focus on:
- Using non-integrating delivery systems (e.g., Sendai virus, episomal plasmids, synthetic mRNA).
- Employing safer factor combinations, such as replacing c-Myc with L-Myc or Glis1.
- Developing fully chemical reprogramming methods that avoid exogenous genetic material altogether [4] [8] [9].
Q3: Can pluripotency be achieved without using c-Myc? Yes, seminal work by Takahashi and Yamanaka demonstrated that somatic cell reprogramming into iPSCs could be achieved by expressing only OCT4, SOX2, and KLF4, without c-Myc, proving it is not an absolute requirement. However, its absence often results in lower reprogramming efficiency [4].
Q4: Besides L-Myc and Glis1, what other factors can replace c-Myc in reprogramming? Research has shown that other family members, such as N-Myc, can substitute for c-Myc. Furthermore, genes not belonging to the Myc family, including SALL4 and Esrrb, have also been identified as functional alternatives that can mitigate tumorigenic risk [4] [9].
Q5: How do the reprogramming efficiencies of safer alternatives compare to c-Myc? While most alternatives to c-Myc exhibit significantly lower reprogramming efficiency, specific optimizations can improve outcomes. For instance, L-Myc has been reported to maintain reprogramming efficiency while reducing the tumorigenic risk. The table below provides a comparative overview.
Table 1: Comparison of c-Myc and Safer Alternatives in iPSC Reprogramming
| Factor | Key Characteristics | Reported Impact on Efficiency | Tumorigenic Risk | Key References |
|---|---|---|---|---|
| c-Myc | Proto-oncogene; accelerates cell cycle; global histone acetylation | High | High | [4] [8] [5] |
| L-Myc | Myc family member; promotes reprogramming | Similar to c-Myc, with reports of high-quality iPSC generation | Lower | [4] [10] |
| Glis1 | Pioneer transcription factor; activates pluripotency genes | Promotes reprogramming; used in high-efficacy protocols | Lower | [4] [10] |
| SALL4 | Transcription factor; can replace c-Myc in OSKM combo | Successful reprogramming demonstrated | Lower | [4] |
| Esrrb | Nuclear receptor; can substitute for c-Myc | Comparable effectivity reported | Lower | [4] [9] |
Troubleshooting Guides
Issue 1: Low Reprogramming Efficiency After Replacing c-Myc
Problem: After substituting c-Myc with a safer alternative like L-Myc or Glis1, the number of successfully generated iPSC colonies is unacceptably low.
Solutions:
- Optimize Factor Ratios: The stoichiometry (ratio) of reprogramming factors is critical. Titrate the amounts of OCT4, SOX2, KLF4, and your chosen c-Myc alternative. Research indicates that the specific ratio of SOX2 and OCT4 significantly affects both efficiency and colony quality [5].
- Combinatorial Approach: Use a combination of supplementary factors. For example, a protocol successfully used a cocktail including L-Myc, LIN28, and Glis1 alongside OSK to efficiently reprogram challenging senescent and pathologic human fibroblasts [10].
- Supplement with Small Molecules: Enhance efficiency by adding small molecules to the culture medium. Molecules like Valproic Acid (VPA) and 8-Bromoadenosine 3′,5′-cyclic monophosphate (8-Br-cAMP) have been shown to increase reprogramming efficiency. One study found that combining 8-Br-cAMP with VPA increased human fibroblast reprogramming efficiency by up to 6.5-fold [4].
- Modulate p53 Activity: Transiently inhibiting the p53 pathway can boost efficiency, as p53 is a major barrier to reprogramming that eliminates cells with DNA damage. However, this must be done carefully. Research shows that overexpressing the p53 isoform Δ133p53 can both inhibit apoptosis and promote DNA repair during reprogramming, leading to a 4-fold increase in efficiency and better genetic quality in the resulting iPSCs [11].
Issue 2: Genomic Instability and Persistent Tumorigenic Concern
Problem: Even with non-integrating methods, the reprogramming process itself can induce DNA damage, leading to concerns about the genomic integrity of the final iPSCs.
Solutions:
- Employ Non-Integrating Delivery Systems: To avoid insertional mutagenesis, use methods such as Sendai virus, episomal plasmids, or synthetic self-replicating RNA. These systems do not integrate into the host genome and are gradually diluted out over cell divisions, producing "transgene-free" iPSCs [8] [12] [10].
- Monitor DNA Damage Response: Actively check for markers of DNA damage during reprogramming, such as γH2AX foci. Using factors that enhance DNA repair, like Δ133p53, can help maintain genomic stability. Overexpression of Δ133p53 was shown to promote DNA double-strand break repair and reduce chromosomal aberrations in resulting iPSC clones [11].
- Rigorous Post-Reprogramming Characterization: Implement thorough quality control checks, including karyotyping and whole-genome sequencing, to select iPSC clones without deleterious mutations for downstream applications [8] [11].
Experimental Protocol: High-Efficacy Reprogramming Using Safer Factors
This protocol is adapted from studies that successfully generated iPSCs from senescent and pathologic human cells using a optimized factor combination [10].
Objective: To generate integration-free human iPSCs from somatic fibroblasts using a cocktail of reprogramming factors that excludes c-Myc.
Materials and Reagents:
- Source Cells: Human dermal or myocardial fibroblasts.
- Reprogramming Factors: OCT4, SOX2, KLF4, L-MYC, LIN28, Glis1, and a short hairpin RNA (shRNA) for p53 knockdown.
- Delivery System: A non-integrating Sendai virus vector or episomal system to deliver the factor cocktail.
- Basal Medium: DMEM/F12 or equivalent.
- Essential Supplements: TGF-β or the TGF-β inhibitor SB431542, depending on the protocol phase.
- Characterization Reagents: Antibodies for TRA-1-60, alkaline phosphatase staining kit.
Method:
- Cell Seeding: Plate fibroblasts at an appropriate density and culture until they reach 70-80% confluency.
- Factor Transduction: Transfert the cells with the cocktail of reprogramming factors (OCT4, SOX2, KLF4, L-MYC, LIN28, Glis1, sh-p53).
- Media Optimization:
- Protocol 1: Culture the transfected cells in medium containing TGF-β.
- Protocol 2 (Recommended): Culture the transfected cells in medium containing the TGF-β inhibitor SB431542 (without TGF-β). This protocol has demonstrated superior efficiency in generating iPSC colonies from aged and pathologic cells [10].
- Colony Expansion: Monitor for the emergence of embryonic stem cell-like colonies between days 14-28. Manually pick and expand candidate colonies.
- Validation: Confirm pluripotency through:
- Immunofluorescence staining for markers like TRA-1-60.
- Alkaline phosphatase staining.
- In vitro differentiation into all three germ layers.
Signaling Pathways and Molecular Mechanisms
The diagram below illustrates the core molecular interplay between the Yamanaka factors, the p53 pathway, and the role of safer alternatives like L-Myc and Glis1 during the reprogramming process.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Oncogene-Safe iPSC Reprogramming
| Reagent / Tool | Function in Reprogramming | Example & Notes |
|---|---|---|
| Non-Integrating Vectors | Delivers reprogramming factors without genomic integration, reducing mutagenesis risk. | Sendai Virus, Episomal Plasmids, Synthetic Self-Replicating RNA (e.g., VEE-RF RNA) [12] [10]. |
| Safer Factor Cocktails | Replaces oncogenic c-Myc to maintain efficiency while lowering tumorigenic potential. | Combinations including L-Myc, Glis1, LIN28, or SALL4 [4] [10]. |
| Small Molecule Enhancers | Modulates signaling pathways and epigenetics to boost reprogramming efficiency. | Valproic Acid (VPA) (HDAC inhibitor), 8-Br-cAMP (signaling activator), SB431542 (TGF-β inhibitor) [4] [10]. |
| p53 Pathway Modulators | Temporarily overcomes the p53-mediated barrier to reprogramming without permanent knockout. | shRNA for p53 knockdown, or overexpression of Δ133p53 to inhibit apoptosis and promote DNA repair [10] [11]. |
| Pluripotency Validation Kits | Confirms the successful generation and quality of iPSC colonies. | TRA-1-60 Antibody (surface marker), Alkaline Phosphatase Live Stain [10]. |
The reprogramming of somatic cells into induced pluripotent stem cells (iPSCs) requires overcoming significant epigenetic barriers that stabilize the differentiated cell state. Chromatin remodeling—the dynamic alteration of chromatin structure—is a fundamental molecular mechanism that enables this dramatic cell fate change. This technical support center document details the key epigenetic barriers and provides troubleshooting guidance for researchers aiming to improve reprogramming efficiency.
FAQs: Core Concepts of Chromatin in Reprogramming
What are the main epigenetic barriers that resist reprogramming to pluripotency? The main epigenetic barriers include repressive histone modifications such as H3K9me3 (histone H3 lysine 9 trimethylation) and H3K27me3 (histone H3 lysine 27 trimethylation), which create condensed, inaccessible chromatin regions. These marks must be actively removed to activate the pluripotency network. Specifically, H3K9me3 constitutes a major barrier by locking somatic genes in an active state and silencing pluripotency genes. Similarly, DNA methylation patterns specific to the somatic cell type must be erased to allow for re-establishment of the pluripotent epigenome [13] [14].
What is the role of "pioneer factors" in initiating chromatin remodeling? Pioneer transcription factors, such as OCT4 and SOX2, are crucial for the initial steps of reprogramming. Unlike conventional transcription factors, they possess the unique ability to bind directly to condensed chromatin. Their binding initiates a series of chromatin remodeling events that lead to chromatin decondensation and increased accessibility. This process occurs progressively during cell division, exposing specific gene promoters and enabling other transcription factors to bind and activate the pluripotency network [15].
How does the chromatin state of a somatic cell influence the reprogramming trajectory? The initial chromatin state of the somatic cell determines the efficiency and kinetics with which reprogramming factors can access their target sites. Genes with an "open" chromatin state (e.g., with active H3K4me2/3 marks) are bound by reprogramming factors immediately. In contrast, core pluripotency genes like NANOG are often located in refractory heterochromatic regions enriched for repressive H3K9me3 marks, requiring extensive chromatin remodeling for activation. This creates a sequential and often inefficient reprogramming process [13].
What are the key chromatin-related checkmarks for high-quality iPSCs? High-quality iPSCs should exhibit:
- Erasure of Somatic Memory: Successful removal of repressive marks (e.g., H3K9me3, H3K27me3) from key pluripotency gene promoters.
- Establishment of Bivalent Domains: Presence of both activating (H3K4me3) and repressive (H3K27me3) marks at developmental gene promoters, poising them for future differentiation [13] [14].
- X-Chromosome Reactivation: In female somatic cells, the inactivated X chromosome should be reactivated [13].
- Activation of Endogenous Pluripotency Network: Sustained expression of core pluripotency factors like OCT4 and NANOG driven by their own promoters, without reliance on exogenous transgenes.
Troubleshooting Guide: Overcoming Epigenetic Barriers
Problem 1: Low Reprogramming Efficiency
Possible Causes and Solutions:
| Possible Cause | Recommended Solution | Key Reagents & Mechanisms |
|---|---|---|
| Repressive H3K9me3 marks | Inhibit H3K9 methyltransferases (e.g., SUV39H1) or overexpress H3K9 demethylases (e.g., KDM4B). | KDM4B: Removes H3K9me3, facilitating the activation of pluripotency genes like NANOG [14]. |
| Closed chromatin at pluripotency loci | Utilize histone deacetylase (HDAC) inhibitors to increase chromatin accessibility. | Valproic Acid (VPA): An HDAC inhibitor that increases global histone acetylation, promoting an open chromatin state and enhancing reprogramming efficiency [4] [14]. |
| Inefficient MET | Ensure the culture conditions support MET, an early reprogramming step. | The OSKM factors inherently drive MET; optimizing media (e.g., using specific growth factors) can support this transition [2]. |
| Inadequate pioneer factor activity | Use an optimized reprogramming factor cocktail that includes potent pioneer factors. | OCT4/SOX2: The core pioneer factors. SALL4 or NR5A2 can substitute for c-MYC or OCT4, respectively, in some cocktails to improve safety and efficiency [4] [15]. |
Problem 2: Incomplete Silencing of Somatic Genes
Possible Causes and Solutions:
| Possible Cause | Recommended Solution | Key Reagents & Mechanisms |
|---|---|---|
| Persistent active chromatin marks | Promote the activity of complexes that deposit repressive marks on somatic genes. | PRC2 Complex: Catalyzes H3K27me3, silencing somatic genes. Its recruitment is facilitated by OSKM factors [13]. |
| Insufficient DOT1L inhibition | Inhibit DOT1L, a histone methyltransferase that places the active H3K79me2/3 mark. | DOT1L Inhibitors: Loss of DOT1L enhances the downregulation of somatic genes early in reprogramming [13]. |
Problem 3: Heterogeneous iPSC Populations with Incomplete Pluripotency
Possible Causes and Solutions:
| Possible Cause | Recommended Solution | Key Reagents & Mechanisms |
|---|---|---|
| Incomplete establishment of bivalent domains | Ensure culture conditions and factors support the function of chromatin modifiers that establish bivalency. | PRC2 and Trithorax Complexes: Work in concert to establish H3K27me3 and H3K4me3 marks, respectively, at developmental promoters. UTF1 has been implicated in regulating bivalency and can substitute for some reprogramming factors [13]. |
| Inadequate activation of core pluripotency genes | Extend the reprogramming timeline and confirm the activation of endogenous OCT4 and NANOG. | The switch from exogenous to endogenous factor expression is a key hallmark of successful, stable reprogramming [13]. |
The Scientist's Toolkit: Essential Reagents for Modifying Chromatin
The following table details key reagents used to manipulate the epigenetic landscape during reprogramming.
Table: Key Research Reagents for Epigenetic Modulation
| Reagent / Tool | Function / Mechanism in Reprogramming | Example Application |
|---|---|---|
| Valproic Acid (VPA) | HDAC inhibitor; increases histone acetylation, promoting an open chromatin state. | Used in combination with reprogramming factors to significantly increase iPSC generation efficiency [4] [14]. |
| KDM4B | Histone demethylase; specifically removes repressive H3K9me3 marks. | Overexpression facilitates the activation of silenced pluripotency genes like NANOG [14]. |
| DOT1L Inhibitors | Inhibits H3K79 methylation, an active mark that maintains somatic gene expression. | Enhances the early phase of reprogramming by silencing the somatic program [13]. |
| RepSox | Small molecule; replaces SOX2 in the reprogramming cocktail by inhibiting TGF-β signaling. | Simplifies the reprogramming cocktail, potentially improving safety and efficiency [4]. |
| 5'-Azacytidine | DNA methyltransferase inhibitor; promotes DNA demethylation. | Can be used to erase somatic DNA methylation patterns, though requires careful titration due to toxicity [13]. |
| Pioneer Factors (OCT4, SOX2) | Initiate reprogramming by binding closed chromatin and initiating remodeling. | The foundational components of most reprogramming cocktails [15]. |
Experimental Protocols & Workflows
Protocol: Assessing Chromatin Accessibility During Reprogramming via Chromatin Immunoprecipitation (ChIP)
This protocol is critical for troubleshooting epigenetic barriers by analyzing histone modifications at specific gene loci (e.g., NANOG promoter) during the reprogramming process.
Key Materials:
- Crosslinking Buffer (1% formaldehyde)
- Cell Lysis Buffer
- Micrococcal Nuclease (for enzymatic shearing) or Sonication equipment
- Protein A/G Magnetic Beads
- ChIP-validated Antibodies (e.g., anti-H3K9me3, anti-H3K4me3)
- DNA Purification Kit
- qPCR Primers for target genomic regions
Detailed Methodology:
- Crosslinking: Fix approximately 1-2 x 10^7 cells at your desired reprogramming time point with 1% formaldehyde for 10 minutes at room temperature to preserve protein-DNA interactions. Quench with glycine [16] [17].
- Cell Lysis: Harvest cells and lyse them using an appropriate ice-cold lysis buffer supplemented with protease inhibitors. Perform all steps at 4°C to prevent protein degradation [17].
- Chromatin Shearing (Fragmentation):
- Enzymatic Shearing (Recommended): Digest chromatin with Micrococcal Nuclease to yield fragments of 150-900 bp. This step must be optimized. Perform a pilot experiment with different enzyme concentrations to achieve the desired fragment size [16].
- Sonication: As an alternative, use a sonicator. Perform a time-course experiment to determine the optimal number of cycles/duration to achieve a DNA smear with the majority of fragments below 1 kb, avoiding over-sonication [16].
- Immunoprecipitation: Pre-clear the chromatin lysate with protein A/G beads. Incubate the pre-cleared chromatin (5-10 µg per reaction) with 3-5 µg of your target-specific antibody (e.g., anti-H3K9me3) and a control IgG overnight at 4°C with rotation. The next day, add beads to capture the antibody-chromatin complexes [16] [17].
- Washing and Elution: Wash the beads sequentially with low-salt, high-salt, and LiCl buffers, followed by a TE buffer to remove non-specifically bound chromatin. Elute the immunoprecipitated protein-DNA complexes from the beads [17].
- Reverse Crosslinking and DNA Purification: Reverse the crosslinks by incubating with NaCl at 65°C. Treat with RNAse A and Proteinase K. Purify the DNA using a commercial kit or phenol-chloroform extraction [16].
- Analysis: Analyze the purified DNA by quantitative PCR (qPCR) using primers specific for your genomic regions of interest. Compare the enrichment in your specific antibody sample to the control IgG sample.
Troubleshooting Common ChIP Issues:
- High Background: Ensure chromatin is properly fragmented. Add pre-clearing and additional wash steps. Optimize antibody concentration to prevent non-specific binding [17].
- Weak or No Signal: Confirm cell lysis is complete. Increase the amount of starting material and/or antibody. Verify the antibody is validated for ChIP and is suitable for the target [16] [17].
- Low DNA Recovery: Avoid over-crosslinking. Re-optimize cell lysis and fragmentation steps. Ensure you are using an effective ChIP-grade antibody with high affinity [17].
Workflow: A Strategic Roadmap for Enhancing Reprogramming Efficiency
The following diagram visualizes a logical workflow for diagnosing and overcoming epigenetic barriers in iPSC generation.
Diagram: A troubleshooting workflow for diagnosing and overcoming major epigenetic barriers to improve iPSC reprogramming efficiency.
This technical support center provides targeted troubleshooting guides and FAQs to help researchers overcome common challenges in improving the efficiency of somatic cell reprogramming to induced pluripotent stem cells (iPSCs).
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ: My reprogramming efficiency remains low despite using the OSKM factors. What are the primary strategic enhancers I can use? The core OSKM (OCT4, SOX2, KLF4, c-MYC) factors are often insufficient for high efficiency. You can augment them with three main classes of enhancers:
- Small Molecules: Compounds like Valproic Acid (VPA) and Sodium Butyrate (HDAC inhibitors) can increase efficiency by up to 6.5-fold when used in combination [4]. These modulators open chromatin structure, facilitating access to pluripotency genes.
- MicroRNAs (miRNAs): miRNAs such as the miR-302/367 cluster or gga-miR-1811 (in avian models) are potent enhancers. They promote critical steps like the Mesenchymal-to-Epithelial Transition (MET), significantly boosting efficiency [4] [18].
- Epigenetic Modulators: Target repressive marks like H3K9me3. Using inhibitors for enzymes like SUV39H1 or overexpressing erasers like KDM4B can remove these barriers, resetting the epigenetic landscape to a pluripotent state [14] [19].
FAQ: How do I choose between a viral and non-viral reprogramming method for a therapy-oriented project? The choice is critical for clinical translation. Non-integrating methods are strongly recommended for therapeutic applications to avoid insertional mutagenesis.
- Sendai Virus (SeV): This is a non-integrating viral method that offers significantly higher reprogramming success rates compared to episomal methods [20]. A key advantage is that it is naturally diluted and cleared from the host cell over several passages.
- Episomal Vectors: These are non-integrating DNA-based methods but typically yield lower success rates than SeV [20]. They are a good choice when any viral component must be avoided.
- Chemical Reprogramming: This is a completely non-genetic method using only small molecules. Recent advances have drastically reduced the reprogramming timeline to as little as 16 days, making it a highly promising and safe alternative [21].
FAQ: I am observing high levels of differentiation in my emerging iPSC colonies. What could be the cause? This is often related to the balance of reprogramming factors and culture conditions.
- Factor Imbalance: The relative ratios of reprogramming factors are critical. Research indicates that specific ratios of SOX2 and OCT4 significantly impact both efficiency and final colony quality [5].
- Incomplete Epigenetic Remodeling: The persistence of repressive epigenetic marks (e.g., H3K27me3) can prevent full activation of the pluripotency network and lead to spontaneous differentiation. Ensure your protocol includes epigenetic enhancers like HDAC or DOT1L inhibitors [4] [14].
- Culture Conditions: Suboptimal feeding schedules, low colony density during passaging, or inadequate use of ROCK inhibitor (Y-27632) during single-cell passaging can increase differentiation pressure [20].
Quantitative Data on Reprogramming Enhancers
The following tables summarize key quantitative data on various enhancers to aid in experimental design.
Table 1: Efficiency of Small Molecule and Epigenetic Enhancers
| Enhancer Class/Name | Specific Example | Reported Impact on Efficiency | Key Mechanism of Action |
|---|---|---|---|
| HDAC Inhibitor | Valproic Acid (VPA) | Up to 6.5-fold increase (with 8-Br-cAMP) [4] | Increases histone acetylation, opens chromatin |
| cAMP Activator | 8-Br-cAMP | 2-fold increase [4] | Activates cAMP signaling pathways |
| DNA Methylation Inhibitor | 5-aza-cytidine, RG108 | Enhances robustness [4] | Reduces DNA methylation, derepresses genes |
| H3K9me3 Targeting | SUV39H1 inhibition | Enhances induction efficiency [19] | Reduces repressive H3K9me3 chromatin mark |
Table 2: Comparison of Non-Integrating Reprogramming Methods
| Method | Type | Genomic Integration? | Relative Success Rate | Key Considerations |
|---|---|---|---|---|
| Sendai Virus (SeV) | Viral | No | Significantly higher [20] | Effective, but requires clearance confirmation |
| Episomal Vectors | DNA/Vector | No | Lower [20] | Virus-free; lower efficiency |
| Chemical Reprogramming | Small Molecules | No | Highly efficient and rapid [21] | No genetic material; protocol can be complex |
Detailed Experimental Protocols
Protocol 1: Enhancing Reprogramming with HDAC Inhibitors This protocol uses Valproic Acid (VPA) to improve efficiency.
- Reprogramming Initiation: Transduce/transfect somatic cells (e.g., fibroblasts, PBMCs) with your chosen OSKM factor delivery system (e.g., Sendai virus, episomal vectors).
- VPA Treatment: 24-48 hours post-transduction, supplement the culture medium with 0.5 - 2 mM VPA. Prepare a 100 mM stock solution in DMSO and dilute in fresh medium.
- Medium Refreshment: Refresh the VPA-containing medium every day for the next 10-12 days.
- Monitoring: Observe for the appearance of compact, ESC-like colonies. The presence of VPA should increase the number of such colonies.
- Colony Picking: After 3-4 weeks, manually pick individual colonies for expansion and characterization.
Protocol 2: Confirmatory Assay for Pluripotency and Characterization Rigorous quality control is essential for any generated iPSC line.
- Immunofluorescence for Pluripotency Markers:
- Culture iPSCs on glass coverslips in a 12-well plate until ~70% confluent.
- Fix with 4% Paraformaldehyde (PFA) for 15 minutes.
- Permeabilize and block with 0.1% Triton X-100 and 5% normal serum for 1 hour.
- Incubate with primary antibodies against OCT4, SOX2, and NANOG overnight at 4°C.
- The next day, incubate with fluorescently-labeled secondary antibodies for 1 hour at room temperature.
- Mount and image. Nuclei should show strong positive staining for these key pluripotency transcription factors [6].
- Sendai Virus Clearance Check (if applicable):
Molecular Mechanisms and Workflows
Diagram 1: Molecular Mechanism of Epigenetic Enhancers in Reprogramming
Diagram 2: Enhanced Reprogramming Workflow with Key Checkpoints
The Scientist's Toolkit: Key Research Reagents
| Item | Function in Reprogramming | Example/Note |
|---|---|---|
| Sendai Virus (SeV) Vectors | Non-integrating delivery of OSKM factors. | Higher success rates than episomal methods [20]. |
| Valproic Acid (VPA) | HDAC inhibitor; opens chromatin. | Can dramatically improve efficiency in combination [4]. |
| ROCK Inhibitor (Y-27632) | Improves survival of dissociated iPSCs. | Critical during passaging and freezing [20]. |
| miR-302 Mimics | Promotes MET and enhances reprogramming. | Can be transfected alongside OSKM factors [4] [18]. |
| TeSR mTeSR Plus Medium | Defined, xeno-free medium for iPSC maintenance. | Supports robust growth of established lines [6]. |
| Antibodies (OCT4, SOX2, NANOG) | Immunocytochemistry for pluripotency confirmation. | Essential part of quality control [6]. |
The Impact of Somatic Cell Source on Reprogramming Efficiency
The choice of somatic cell source is a critical experimental variable in induced pluripotent stem cell (iPSC) research, significantly impacting reprogramming efficiency, kinetics, and the quality of resulting cell lines. Since the initial discovery that somatic cells could be reprogrammed into pluripotent stem cells using defined factors, researchers have explored a wide range of somatic cell types as starting materials [2]. The original iPSC studies utilized mouse and human fibroblasts reprogrammed with the Yamanaka factors (OCT4, SOX2, KLF4, and c-MYC) [5]. Since then, the field has expanded to include diverse somatic cell sources, each with distinct advantages and challenges for reprogramming experiments.
The developmental origin, epigenetic landscape, and proliferation capacity of the starting somatic cell population profoundly influence the reprogramming process [4]. Somatic cells can be obtained from various tissue sources, including skin, blood, and other accessible tissues, with varying levels of donor invasiveness during collection [22]. This technical resource provides troubleshooting guidance and detailed protocols to help researchers select and optimize somatic cell sources for their specific reprogramming applications, with the goal of maximizing efficiency and reproducibility while minimizing technical artifacts.
Quantitative Analysis of Reprogramming Efficiencies
Extensive research has revealed significant variations in reprogramming efficiency across different somatic cell types. The table below summarizes key efficiency data for commonly used somatic cell sources in iPSC generation:
Table 1: Reprogramming Efficiency Across Different Somatic Cell Sources
| Somatic Cell Source | Reprogramming Efficiency | Key Advantages | Notable Limitations |
|---|---|---|---|
| Human Fibroblasts | Typically <1% of transfected cells [23] | Well-established protocols; Extensive characterization | Invasive collection; Slow proliferation |
| Human Cord Blood Cells | Highly efficient with optimized chemical methods [24] | Non-invasive collection; Immature epigenetics | Limited donor availability; Cord blood-specific |
| Human Peripheral Blood Cells | Efficient with chemical reprogramming; >100 hCiPS colonies from single fingerstick drop [24] | Minimally invasive; Renewable source | Lower efficiency with viral methods; Requires specific culture conditions |
| Mouse Spleen Leukocytes | ~30% of surviving cells after low pH stimulus (STAP) [25] | Rapid reprogramming with certain methods | High cell death with stimulus; Limited human application data |
| Neural Stem Cells | Achievable with OCT4 alone [4] | Endogenous stemness factors; High intrinsic plasticity | Limited availability; Specialized isolation requirements |
Beyond conventional cell sources, researchers have explored specialized somatic cells with unique reprogramming properties:
Neural Stem Cells: These cells represent a special case where exogenous expression of OCT4 alone can successfully generate iPSCs, highlighting the significant role of endogenous stemness factors in the reprogramming process [4]. This contrasts with most somatic cell types that require multiple transcription factors for efficient reprogramming.
Blood Cell Populations: Recent advances in chemical reprogramming have dramatically improved the efficiency of generating human chemically induced pluripotent stem (hCiPS) cells from blood sources [24]. This approach has demonstrated high reproducibility across different donors using both fresh and cryopreserved blood cells.
Multiple Murine Tissue Sources: Research on stimulus-triggered acquisition of pluripotency (STAP) demonstrated that cells from diverse mouse tissues including brain, lung, muscle, adipose, liver, and cartilage could be reprogrammed with 10-30% efficiency among surviving cells after low-pH treatment [25].
Troubleshooting Guides: Cell Source-Specific Reprogramming Challenges
Frequently Asked Questions
Q1: Why do my blood-derived reprogramming cultures show poor adherence and eventual senescence?
A: This common issue occurs when standard reprogramming conditions optimized for fibroblasts are applied to blood cells without modification. Blood cells require specific cytokine pre-treatment and culture conditions to enable successful reprogramming. Solution: Implement a 7-day expansion phase in erythroid progenitor cell (EPC) media containing SCF, EPO, IL-3, and IL-6 before initiating chemical reprogramming [24]. This preconditioning step promotes the transition from suspension to adherent culture and prevents senescence.
Q2: How can I improve the low efficiency of fibroblast reprogramming?
A: Fibroblast reprogramming efficiency can be enhanced through several strategies:
- Utilize small molecule enhancers such as 8-Bromoadenosine 3′,5′-cyclic monophosphate (8-Br-cAMP), which can improve human fibroblast reprogramming efficiency by approximately 2-fold [4].
- Combine 8-Br-cAMP with valproic acid (VPA) to increase iPSC generation efficiency by up to 6.5-fold [4].
- Consider p53 inhibition in combination with different reprogramming factors, which has been shown to markedly increase iPSC generation efficiency [4].
Q3: What is the minimum blood volume required for successful reprogramming?
A: Recent chemical reprogramming advances have significantly reduced blood volume requirements. Studies demonstrate that a single drop of fingerstick blood (approximately 20-30 μL) is sufficient to generate an average of over 100 hCiPS colonies when using optimized chemical reprogramming methods [24]. This represents a substantial improvement over earlier blood reprogramming protocols that required larger venous blood draws.
Q4: How does donor age impact reprogramming efficiency across different cell sources?
A: Donor age inversely correlates with reprogramming efficiency for most somatic cell sources, though the magnitude of this effect varies:
- Fibroblasts from older donors typically show reduced reprogramming efficiency and slower kinetics compared to neonatal sources [5].
- Blood cells from older donors may require extended preconditioning or modified cytokine combinations to achieve efficiency comparable to cord blood sources [24].
- Optimization with alternative transcription factor combinations (e.g., OSKMNL with six factors) has demonstrated success in reprogramming fibroblasts from old donors where standard methods failed [5].
Detailed Experimental Protocols
Chemical Reprogramming of Human Blood Cells
This protocol describes an optimized method for generating human chemically induced pluripotent stem (hCiPS) cells from peripheral blood mononuclear cells (PBMCs) with high efficiency [24].
Table 2: Key Reagents for Blood Cell Chemical Reprogramming
| Reagent Category | Specific Examples | Function in Reprogramming |
|---|---|---|
| Cytokines for Preconditioning | SCF, EPO, IL-3, IL-6 | Promote erythroid progenitor expansion and adherence |
| Epigenetic Modulators | Sodium butyrate, Trichostatin A, 5-aza-cytidine | Enhance chromatin accessibility; Facilitate epigenetic remodeling |
| Signaling Pathway Modulators | RepSox, CHIR99021, BMP4 | Regulate key reprogramming pathways; Replace transcription factors |
| Metabolic Regulators | 8-Br-cAMP, VPA | Alter cellular metabolism to support pluripotency acquisition |
Step-by-Step Workflow:
PBMC Isolation and Preconditioning
- Isolate mononuclear cells from fresh or cryopreserved peripheral blood using density gradient centrifugation.
- Culture PBMCs in EPC expansion medium containing SCF (100 ng/mL), EPO (10 U/mL), IL-3 (10 ng/mL), and IL-6 (10 ng/mL) for 7 days.
- Maintain cells at a density of 1-2×10^6 cells/mL in tissue culture-treated plates at 37°C with 5% CO₂.
Chemical Reprogramming Induction
- Plate preconditioned cells on Matrigel-coated plates at a density of 5×10^4 cells/cm² in chemical reprogramming medium.
- Implement a staged chemical cocktail approach with sequential exposure to specific small molecule combinations as detailed in recent studies [24].
- Replace medium every 2 days and monitor for morphological changes indicating transition to adherent state.
Emergence and Expansion of hCiPS Colonies
- First adherent colonies typically appear between day 10-14 of chemical treatment.
- Manually pick well-defined colonies with clear iPSC morphology between days 18-21.
- Transfer selected colonies to feeder-free culture conditions and expand using standard hPSC culture methods.
Quality Control and Characterization
- Confirm pluripotency marker expression (OCT4, SOX2, NANOG, TRA-1-60, TRA-1-81) via immunocytochemistry.
- Perform karyotype analysis to ensure genomic integrity.
- Validate trilineage differentiation potential through embryoid body formation assays.
Figure 1: Experimental workflow for chemical reprogramming of human blood cells to pluripotency, highlighting key stages from cell isolation through quality control.
Fibroblast Reprogramming with Efficiency Enhancers
This protocol enhances standard fibroblast reprogramming through small molecule supplementation to significantly improve efficiency [4].
Enhanced Reprogramming Procedure:
Fibroblast Culture Preparation
- Culture human dermal fibroblasts in DMEM/F12 medium supplemented with 10% FBS and 1% GlutaMAX.
- Plate fibroblasts at 70-80% confluence in tissue culture-treated dishes 24 hours before reprogramming initiation.
Factor Delivery with Small Molecule Enhancement
- Deliver OSKM factors using your preferred method (lentiviral, Sendai virus, or mRNA-based).
- Simultaneously add efficiency-enhancing small molecules:
- 8-Br-cAMP (250 µM) to improve reprogramming approximately 2-fold
- Valproic acid (0.5-1 mM) to potentially increase efficiency up to 6.5-fold when combined with 8-Br-cAMP
- Alternative epigenetic modulators such as Sodium butyrate (0.5 mM) or Trichostatin A (50 nM)
Monitoring and Colony Selection
- Monitor cultures for emergence of embryonic stem cell-like morphology beginning around day 7-10.
- Manually pick colonies based on compact morphology and well-defined borders between days 18-28.
- Expand colonies in feeder-free conditions for further characterization.
Figure 2: Key molecular events in enhanced fibroblast reprogramming showing how small molecule enhancers target specific stages of the process.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Optimizing Reprogramming Efficiency
| Reagent Category | Specific Products | Application Function | Cell Source Specificity |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM); OCT4, SOX2, NANOG, LIN28 (OSNL) | Core transcription factor combinations for pluripotency induction | Universal application with efficiency variations |
| Chemical Enhancers | 8-Br-cAMP, Valproic acid, Sodium butyrate, RepSox, CHIR99021 | Improve efficiency; Replace transcription factors; Modulate signaling | Blood cells (8-Br-cAMP + VPA); Fibroblasts (all) |
| Cytokines/Growth Factors | SCF, EPO, IL-3, IL-6, FGF2, BMP4 | Preconditioning; Enhance survival and adherence | Blood cells (SCF, EPO, IL-3, IL-6); Universal (FGF2) |
| Culture Matrices | Matrigel, Vitronectin, Laminin-521 | Provide optimal substrate for reprogramming and iPSC expansion | Blood cells (Matrigel); Fibroblasts (all matrices) |
| Epigenetic Modulators | 5-aza-cytidine, RG108, Trichostatin A, DZNep | Facilitate epigenetic remodeling; Enhance chromatin accessibility | Universal application with concentration optimization needed |
| Metabolic Regulators | DMEM/F12, N2/B27 supplements, L-ascorbic acid | Support metabolic transition during reprogramming | Universal application |
The selection of an appropriate somatic cell source remains a fundamental decision in experimental design for iPSC generation, with significant implications for reprogramming efficiency, experimental timeline, and clinical applicability. Blood-derived cells have emerged as particularly promising starting materials due to their minimally invasive collection and recent efficiency improvements through chemical reprogramming methods [24]. Fibroblasts continue to be valuable for research applications, especially when enhanced with small molecule cocktails that address their inherent efficiency limitations [4].
Future directions in somatic cell source optimization include the development of universal chemical reprogramming platforms that can efficiently reprogram diverse cell types with minimal protocol modifications [26]. Additionally, research into the molecular mechanisms underlying the varying reprogramming competencies of different somatic cell types will continue to inform the rational selection of starting materials for specific applications [9]. As the field advances toward clinical translation, considerations of donor accessibility, scalability, and safety profiles will increasingly guide the selection of somatic cell sources for both basic research and therapeutic development [22] [5].
Advanced Reprogramming Technologies: Delivery Systems and Novel Platforms
The generation of induced pluripotent stem cells (iPSCs) from somatic cells represents one of the most significant advancements in regenerative medicine and biomedical research. Since the initial discovery by Takahashi and Yamanaka that somatic cells could be reprogrammed using defined factors, the field has rapidly evolved to encompass numerous delivery strategies for introducing reprogramming factors into target cells. The core challenge lies in selecting an appropriate delivery system that balances reprogramming efficiency with safety profile, particularly regarding genomic integrity. This technical guide examines the spectrum of available delivery systems—from early integrating retroviruses to modern non-integrating methods—within the broader context of improving reprogramming efficiency for both basic research and clinical applications.
The fundamental process involves the ectopic expression of key pluripotency factors, typically OCT4, SOX2, KLF4, and c-Myc (OSKM), though alternative combinations exist. The delivery method significantly influences not only the success rate but also the molecular characteristics of the resulting iPSCs, their differentiation potential, and ultimately their suitability for therapeutic use. This resource provides researchers with practical guidance for selecting, optimizing, and troubleshooting these critical methodologies.
The table below provides a comprehensive comparison of the primary delivery systems used in iPSC generation, summarizing key characteristics to guide method selection.
Table 1: Comprehensive Comparison of iPSC Delivery Systems
| Delivery Method | Mechanism of Action | Reprogramming Efficiency | Genomic Integration | Primary Advantages | Primary Limitations |
|---|---|---|---|---|---|
| MMLV Retrovirus | Integrating viral vector | High [27] [28] | Yes | Efficient, stable transgene expression [28] | Insertional mutagenesis, transgene reactivation [29] [30] |
| Lentivirus | Integrating viral vector | High [27] | Yes | Infects dividing & non-dividing cells [27] | Insertional mutagenesis, residual expression [20] [30] |
| Sendai Virus (SeV) | Non-integrating RNA virus | Medium to High [20] [27] | No | High efficiency, no genomic integration [20] | Difficult to fully remove from cells [27] |
| Episomal Vectors | Non-integrating plasmid | Medium [20] [27] | No (Low risk) | Non-viral, simple to implement [27] | Low efficiency, requires verification of episome loss [20] |
| Adenovirus | Non-integrating viral vector | Low [27] [31] | No | No genomic integration, transgene-free cells [27] [31] | Very low reprogramming efficiency [31] |
| Synthetic mRNA | DNA-free RNA transfection | High [27] [32] | No | Highly safe, no genetic footprint [32] | Multiple transfections required, requires stringent culture [27] |
| Protein Transduction | Direct protein delivery | Low [27] [31] | No | Maximum safety, no genetic material [27] [31] | Very low efficiency, difficult protein purification [27] |
| piggyBac Transposon | Excisable integrating vector | Medium [27] | Yes (but excisable) | Footprint-free excision after reprogramming [27] [31] | Must verify excision didn't introduce mutations [27] |
Decision Framework: Selecting a Delivery System
The following workflow diagram outlines a logical decision-making process for selecting the most appropriate delivery system based on research goals and experimental constraints.
Troubleshooting Common Experimental Challenges
This section addresses specific, frequently encountered problems during iPSC generation, providing evidence-based solutions to improve experimental outcomes.
FAQ 1: Low Viral Transduction Efficiency
- Problem: Low viral titer or poor infectivity leads to insufficient reprogramming factor delivery.
- Possible Causes:
- Suboptimal transfection efficiency in packaging cells.
- Low plasmid quality for virus production.
- Improper viral harvesting or storage conditions.
- Target cells not actively dividing (for retroviruses).
- Solutions:
- Optimize Packaging: Use high-quality, endotoxin-free plasmids and optimize transfection reagent ratios for packaging cells (e.g., HEK293T). [28]
- Concentrate Virus: Concentrate viral supernatant by ultracentrifugation or PEG precipitation to achieve a higher multiplicity of infection (MOI). [28]
- Enhance Infection: Use polybrene to facilitate viral entry. For difficult-to-transduce cells, use "spinoculation" (centrifugation during infection). [28] [30]
- Confirm Cell Status: Ensure target cells are healthy, low-passage, and actively proliferating at the time of transduction. [28]
FAQ 2: Poor Cell Survival Post-Transduction/Transfection
- Problem: Significant cell death occurs following the introduction of reprogramming factors.
- Possible Causes:
- Cytotoxicity from transfection reagents or viral particles.
- Stress induced by the reprogramming process itself.
- Over-proliferation and senescence triggered by oncogenic factors like c-Myc.
- Solutions:
- Use ROCK Inhibitor: Add a ROCK inhibitor (Y-27632) to the culture medium for the first 24-48 hours post-transduction to enhance cell survival. [20] [28]
- Adjust Polybrene: Reduce polybrene concentration or shorten exposure time to minimize toxicity. [28]
- Co-culture with Feeders: For fragile cell types, use a feeder layer (e.g., irradiated MEFs) during the early stages of reprogramming for additional support. [28]
FAQ 3: Delayed or Absent Colony Formation
- Problem: Reprogramming colonies fail to appear or are significantly delayed beyond the expected timeframe (typically 3-4 weeks).
- Possible Causes:
- Insufficient expression of reprogramming factors.
- Epigenetic barriers in the starting somatic cell population.
- Suboptimal culture conditions.
- Solutions:
- Confirm Factor Expression: Use qPCR or immunostaining to verify the expression of OCT4, SOX2, KLF4, and c-Myc. [28]
- Add Small Molecules: Enhance reprogramming efficiency by adding small-molecule enhancers such as valproic acid (VPA), sodium butyrate, or the GSK3 inhibitor CHIR99021. [4] [28]
- Modify Culture Conditions: Lower oxygen tension (to 5% O₂) to mimic physiological hypoxia, which can promote reprogramming. [28]
- Select Optimal Cells: Use starting somatic cells with high reprogrammability, such as keratinocytes or peripheral blood mononuclear cells (PBMCs), which can offer higher efficiency than fibroblasts. [29] [20]
FAQ 4: Partially Reprogrammed or Morphologically Abnormal Colonies
- Problem: Emerging colonies do not exhibit the tight, dome-shaped morphology of true iPSCs and may show signs of differentiation.
- Possible Causes:
- Incomplete epigenetic remodeling.
- Persistent expression or premature silencing of transgenes.
- Overgrowth and spontaneous differentiation.
- Solutions:
- Stringent Morphological Selection: Manually pick only colonies that are compact, with defined borders and a high nuclear-to-cytoplasmic ratio. Avoid colonies with a flat or differentiated appearance. [28]
- Timely Passaging: Passage colonies before they become over-confluent and begin to differentiate in the center. [20] [28]
- Verify Pluripotency: Rigorously characterize candidate lines through immunostaining for pluripotency markers (OCT4, NANOG, SSEA-4, TRA-1-60) and trilineage differentiation assays. [20] [28]
Essential Research Reagents and Materials
The table below lists key reagents and materials critical for successful iPSC generation and culture, regardless of the delivery method chosen.
Table 2: Essential Reagent Toolkit for iPSC Generation
| Reagent/Material | Function/Purpose | Example Use Cases |
|---|---|---|
| Packaging Cell Line | Produces viral particles for gene delivery. | HEK293T cells for lentiviral/retroviral production. [28] |
| Polybrene | A cationic polymer that enhances viral transduction efficiency. | Added to viral supernatant to neutralize charge repulsion between virus and cell membrane. [28] |
| ROCK Inhibitor (Y-27632) | Improves survival of single pluripotent stem cells by inhibiting apoptosis. | Added to medium after passaging or thawing to increase cell survival. [20] [28] |
| bFGF (Basic Fibroblast Growth Factor) | Key cytokine for maintaining pluripotency and self-renewal in human iPSC culture. | Added daily to iPSC culture medium to sustain an undifferentiated state. [28] |
| Extracellular Matrix Substrates | Provides a scaffold for cell attachment and growth, replacing feeder layers. | Matrigel, Vitronectin, or Laminin-521 for feeder-free culture. [20] [28] |
| Small Molecule Enhancers | Compounds that improve reprogramming efficiency by modulating signaling pathways and epigenetics. | Valproic acid (HDAC inhibitor), CHIR99021 (Wnt activator), RepSox (TGF-β inhibitor). [4] [31] |
| Pluripotency Marker Antibodies | Used to confirm the successful reprogramming to a pluripotent state via immunostaining or flow cytometry. | Antibodies against OCT4, SOX2, NANOG, SSEA-4, TRA-1-60. [20] [28] |
Core Experimental Workflow
The following diagram illustrates the generalized step-by-step workflow for generating iPSCs, highlighting stages that are common across most delivery methods and where key quality control checks should be implemented.
The evolution of iPSC delivery systems from integrating retroviruses to sophisticated non-integrating and footprint-free methods reflects the field's dual focus on enhancing efficiency and ensuring safety. The choice of delivery system remains a fundamental determinant of experimental success and clinical translatability. While retroviral and lentiviral systems offer robust efficiency for basic research, the clear trend is toward non-integrating methods like Sendai virus and synthetic mRNA for preclinical and therapeutic applications due to their superior safety profiles. [20] [32]
Future improvements will likely focus on standardizing protocols, further increasing the efficiency of non-integrating methods, and developing more sophisticated chemical reprogramming approaches that eliminate the need for genetic material altogether. [4] [2] By carefully considering the trade-offs between efficiency, safety, and practical experimental requirements outlined in this guide, researchers can strategically select and optimize their reprogramming methodology to advance both fundamental knowledge and therapeutic innovation.
Chemical reprogramming represents a paradigm shift in regenerative medicine, offering a fundamentally innovative approach for generating human induced pluripotent stem cells (iPSCs) using small molecules instead of genetic factors. This non-genetic methodology provides a more flexible, standardized, and clinically promising pathway for cell fate manipulation. By targeting key signaling and epigenetic pathways, chemical reprogramming enables precise control over the pluripotency acquisition process while avoiding the risks associated with viral vectors and genomic integration. This technical support center guide addresses the most common experimental challenges and provides proven solutions to optimize chemical reprogramming protocols for somatic cells.
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Encountered Issues and Solutions
Q: My somatic cells are not transitioning from suspension to an adherent state during the initial reprogramming phase. What could be causing this?
A: Failure of cellular adhesion often indicates suboptimal culture conditions or incorrect cell state. Research on blood cell reprogramming showed that standard erythroid progenitor cell (EPC) conditions failed to support adhesion, requiring protocol modification.
- Solution: Implement a "bridge" culture medium that transitions cells toward a mesenchymal state prior to reprogramming. For cord blood mononuclear cells (hCBMCs) or peripheral blood mononuclear cells (PBMCs), use specialized expansion media containing SCF, IL-3, and IL-6 for 7 days before applying chemical reprogramming cocktails [24].
- Additional verification: Ensure your starting cell population is viable and properly characterized. For blood cells, use fresh or properly cryopreserved samples with >90% viability [24].
Q: I observe extensive cellular senescence or apoptosis shortly after applying chemical reprogramming cocktails. How can I improve cell survival?
A: This common challenge occurs when somatic cells experience excessive stress during the initial reprogramming transition.
- Solution: Incorporate ROCK inhibitor (Y27632) or RevitaCell Supplement during the first 48-72 hours of reprogramming [33]. For confluent cultures (>85%), always include ROCK inhibitor during passaging.
- Protocol adjustment: For blood cell reprogramming, research indicates that inhibition of the H3K79 histone methyltransferase Dot1L – either via shRNA or small molecule inhibitors (EPZ004777) – can significantly reduce senescence barriers and enhance reprogramming efficiency [34].
- Timing consideration: Apply senescence-inhibiting treatments during the first week of reprogramming, as this window is critical for overcoming initial epigenetic barriers [34].
Q: The reprogramming efficiency is low compared to published results. Which factors most significantly impact efficiency?
A: Reprogramming efficiency depends on multiple interdependent variables that must be optimized for your specific cell type.
- Key efficiency enhancers:
- Epigenetic modulation: Dot1L inhibition increases reprogramming efficiency 3-6 fold across multiple human fibroblast lines (IMR-90, MRC-5) and can substitute for Klf4 and c-Myc in factor-based protocols [34].
- Cell density: Passage cells at 40-85% confluency. Overly confluent cultures demonstrate poor survival after passaging [33].
- Donor variability: Account for inherent differences between cell donors by including positive control lines (e.g., H9 or H7 ESC lines) in your experiments [33].
Q: How long should I maintain cells in reprogramming conditions before seeing iPSC colonies?
A: The timeline varies by cell type and protocol efficiency.
- Blood cells: Under optimized chemical conditions, initial adherent transitions appear within 2 weeks, with distinct hCiPS colonies emerging by week 3 [24].
- General indicators: Successful reprogramming shows accelerated emergence of Tra-1-60-positive cell clusters by days 10-14 when using optimized protocols [34].
- Troubleshooting: If no colonies appear after 4 weeks, verify your small molecule concentrations and refresh stocks, as some compounds degrade more quickly than others.
Advanced Technical Challenges
Q: Can I use cryopreserved cells for chemical reprogramming, and are there special considerations?
A: Yes, both fresh and cryopreserved cells can be successfully reprogrammed.
- Blood cells: The chemical reprogramming approach has been validated with both fresh and cryopreserved cord blood and peripheral blood cells across different donors [24].
- Best practices: Thaw cells quickly (<2 minutes at 37°C) and transfer to pre-rinsed tubes before adding medium drop-wise to prevent osmotic shock [33]. Do not use PBS, DPBS, or HBSS for rinsing as they lack necessary proteins.
- Viability check: Always count cell viability with trypan blue after thawing. For successful reprogramming, seed at least 1 × 10^5 viable cells/cm² for most somatic cell types [33].
Q: What are the critical quality control checkpoints for successful chemical reprogramming?
A: Implement these verification steps throughout your protocol:
- Starting material: Ensure your somatic cells have minimal differentiation and are proliferating normally before reprogramming initiation.
- Day 7-10: Check for morphological changes from suspension to adherent (for blood cells) or increased nuclear-to-cytoplasmic ratio (for fibroblasts).
- Day 14-21: Monitor for emergence of tight, dome-shaped colonies with defined borders.
- Endpoint validation: Verify pluripotency through immunostaining for OCT4, SOX2, NANOG, TRA-1-60, and TRA-1-81, followed by functional differentiation into all three germ layers [24] [34].
Quantitative Data and Experimental Protocols
Key Small Molecule Cocktails for Enhanced Reprogramming
Table 1: Experimentally Validated Chemical Cocktails for Reprogramming Enhancement
| Component | Concentration Range | Primary Mechanism | Experimental Impact |
|---|---|---|---|
| Dot1L Inhibitor (EPZ004777) | 1-10 μM | H3K79 histone methyltransferase inhibition | 3-4 fold increase in efficiency; enables OS (Oct4-Sox2) only reprogramming [34] |
| ROCK Inhibitor (Y27632) | 10 μM | Inhibition of Rho-associated kinase; reduces apoptosis | Markedly improves cell survival during early reprogramming and single-cell passaging [33] |
| Valproic Acid | 0.5-2 mM | Histone deacetylase (HDAC) inhibitor | Enhances epigenetic remodeling; more effective with integrating viral systems [33] |
| Bridge Medium Components | Varies by protocol | Promotes mesenchymal transition | Enables blood cell adhesion and dramatically improves chemical reprogramming response [24] |
Optimized Chemical Reprogramming Workflow for Human Blood Cells
Essential Research Reagent Solutions
Table 2: Key Materials for Chemical Reprogramming Experiments
| Reagent/Cell Type | Specific Function | Application Notes |
|---|---|---|
| Human Cord Blood Mononuclear Cells (hCBMCs) | Primary somatic cell source | Highly accessible; reprogramming efficiency confirmed across donors [24] |
| Peripheral Blood Mononuclear Cells (PBMCs) | Patient-specific cell source | Minimally invasive collection; compatible with fingerstick blood samples [24] |
| Essential 8 Medium | Feeder-free pluripotent stem cell culture | Supports chemical iPSC expansion and maintenance; compatible with VTN-N coating [33] |
| Geltrex Matrix | Basement membrane matrix for cell attachment | Provides optimal surface for adherent transition during reprogramming [33] |
| NCC Reporter System | Age and senescence monitoring | Distinguishes young/old cells via nucleocytoplasmic compartmentalization [35] |
Molecular Mechanisms and Pathway Diagrams
Epigenetic Regulation in Chemical Reprogramming
Critical Timing for Reprogramming Interventions
Table 3: Optimal Time Windows for Key Reprogramming Interventions
| Intervention | Critical Period | Observed Effect | Mechanistic Insight |
|---|---|---|---|
| Dot1L Inhibition | Days 1-14 | 3-fold enhancement; enables 2-factor (OS) reprogramming | Facilitates early epigenetic remodeling; loss of H3K79me from fibroblast-specific genes [34] |
| ROCK Inhibition | First 48 hours post-passaging | Significantly improves cell survival | Prevents anoikis during single-cell dissociation [33] |
| Bridge Culture Medium | 7 days pre-reprogramming | Enables blood cell adhesion and response | Promotes mesenchymal transition necessary for chemical reprogramming competence [24] |
| Temperature Shift (38-39°C) | After passage 10 (Sendai systems) | Clears residual c-Myc and KOS vectors | Exploits temperature-sensitive mutations in reprogramming vectors [33] |
Chemical reprogramming technology has evolved from a promising concept to a robust, clinically relevant platform for generating human iPSCs. The troubleshooting guidelines and experimental protocols outlined here address the most significant technical barriers to implementation. As research advances, further optimization of small molecule cocktails and timing regimens will continue to enhance efficiency and reliability. The non-genetic nature of this approach, combined with its compatibility with minimally invasive cell sources like blood, positions chemical reprogramming as a cornerstone technology for personalized regenerative medicine and drug development applications.
Frequently Asked Questions (FAQs)
FAQ 1: What are the main advantages of using biomaterials over traditional viral methods for cell reprogramming? Biomaterial-based methods offer several key advantages over viral reprogramming. They avoid the risk of genomic integration and insertional mutagenesis associated with viral vectors, thereby enhancing the safety profile of the resulting induced pluripotent stem cells (iPSCs) [36]. Furthermore, engineered biomaterials provide a way to precisely control the biophysical and biochemical microenvironment, which can significantly improve reprogramming efficiency and guide more accurate cell fate transitions [23] [37].
FAQ 2: Why is the 3D genome structure important for generating high-quality iPSCs? Research indicates that the 3D folding of DNA within the nucleus (the genome's architecture) directly influences gene expression. High-resolution mapping has revealed that iPSCs do not always perfectly replicate the genome folding patterns found in gold-standard embryonic stem cells (ESCs). Instead, they can retain traces of the 3D configuration from the original somatic cell, a phenomenon linked to incomplete reprogramming and potential difficulties in subsequent differentiation. Modifying the culture environment, such as the growth medium, can help correct these folding patterns [38].
FAQ 3: My iPSC cultures are showing high levels of spontaneous differentiation (>20%). What could be the cause? Excessive differentiation in pluripotent stem cell cultures can be attributed to several factors related to culture conditions and handling. Using culture medium that has been stored for too long or allowing the culture plate to remain outside the incubator for extended periods can trigger differentiation. Additionally, allowing colonies to become over-confluent, generating uneven or overly large cell aggregates during passaging, and failing to physically remove differentiated areas before passaging are common procedural errors that contribute to this problem [39].
FAQ 4: How can synthetic polymer scaffolds address the limitations of natural matrices like Matrigel? Natural matrices suffer from batch-to-batch variability, undefined composition, and limited tunability, which hinder experimental reproducibility and clinical translation [40]. Synthetic scaffolds, such as thermoresponsive terpolymers, offer precisely controllable biochemical and mechanical properties. They ensure consistent quality, can be functionalized with specific bioactive peptides (e.g., RGD), and are scalable, providing a more reliable and customizable platform for stem cell expansion and differentiation [37] [40].
Troubleshooting Common Experimental Challenges
Problem: Low Reprogramming Efficiency
Potential Causes and Solutions:
- Cause 1: Suboptimal Substrate Stiffness. The mechanical properties of the culture substrate are a critical factor in directing cell fate.
- Solution: Utilize biomaterials with a stiffness tailored for pluripotency. Research suggests that very soft substrates (e.g., around 0.1 kPa) can enhance the initiation of reprogramming to iPSCs [36]. Test a range of stiffnesses to optimize for your specific cell type and reprogramming method.
- Cause 2: Inconsistent Surface Topography. The physical nano- and micro-scale features of the culture surface influence cell signaling.
- Solution: Implement engineered surfaces with defined topographies. For example, nanogrooves have been shown to promote the direct reprogramming of fibroblasts into neurons [36]. Consistency in fabricating these topographical cues is key to achieving reproducible results.
- Cause 3: Inefficient Delivery of Reprogramming Factors. Viral methods, while efficient, pose safety risks.
- Solution: Adopt non-viral delivery systems. Techniques such as electroporation of mRNA or the use of chitosan nanoparticles and gold nanoparticles for delivering plasmid DNA have been successfully used for reprogramming somatic cells into iPSCs [36].
Problem: Differentiated Cells Exhibit Immature or Fetal-like Characteristics
Potential Causes and Solutions:
- Cause: Lack of Maturation Cues in the Culture System. The standard 2D environment may not provide the necessary complex signals for full functional maturation.
- Solution: Transition to 3D culture systems using advanced biomaterial scaffolds. For example, a synthetic thermoresponsive terpolymer functionalized with RGD peptides and vitronectin demonstrated a statistically significant increase in the expression of mature cardiac-specific markers (cTnT ~65% and cTnI ~25%) in differentiated cardiomyocytes compared to those cultured on traditional Matrigel [40]. This shows how tailored synthetic environments can drive greater maturity.
The following tables summarize key quantitative relationships between biomaterial properties and cellular outcomes, as reported in the literature.
Table 1: Influence of Substrate Stiffness on Cell Differentiation and Reprogramming
| Cell Type | Substrate Stiffness | Cell Fate Outcome | Key Signaling Pathways | Citation |
|---|---|---|---|---|
| Human Mesenchymal Stromal Cells (hMSCs) | ~0.5 kPa | Adipocyte Differentiation | YAP/TAZ Inactivation [41] | [36] |
| Human Mesenchymal Stromal Cells (hMSCs) | ~64 kPa | Osteoblast Differentiation | YAP/TAZ Activation, ROCK [41] | [36] |
| Mouse Embryonic Fibroblasts (MEFs) | ~0.1 kPa | Enhanced iPSC Reprogramming | Integrin/FAK, YAP/TAZ [23] | [36] |
| Neural Stem Cells (NSCs) | Stiff ECM | Impaired Neurogenesis | YAP/β-catenin [41] | [41] |
Table 2: Performance of a Synthetic Thermoresponsive Scaffold for Cardiac Differentiation
| Culture Matrix | Cardiac Troponin T (cTnT) Expression | Cardiac Troponin I (cTnI) Expression | Key Features |
|---|---|---|---|
| Synthetic Terpolymer (with bioactive molecules) | ~65% | ~25% | Tunable stiffness, thermoresponsive, functionalizable, xeno-free [40] |
| Matrigel (Traditional Natural Matrix) | Lower than synthetic polymer | Lower than synthetic polymer | Batch variability, undefined composition, animal-derived [40] |
Detailed Experimental Protocols
Protocol 1: Reprogramming on Soft Substrates to Enhance iPSC Generation
This protocol outlines the use of hydrogels with tunable stiffness to improve the efficiency of somatic cell reprogramming.
Substrate Preparation:
- Select a tunable hydrogel system (e.g., PEG-based, polyacrylamide).
- Prepare the hydrogel solution to achieve a final elastic modulus of approximately 0.1 kPa, as this stiffness has been shown to favor reprogramming initiation [36].
- Coat culture plates with the polymer solution and allow it to crosslink according to the manufacturer's instructions.
Cell Seeding and Transfection:
- Plate the source somatic cells (e.g., human dermal fibroblasts) onto the soft hydrogel substrate at an appropriate density.
- Deliver the reprogramming factors (e.g., OSKM genes) using a non-viral method such as electroporation of mRNA or nucleofection with minicircle DNA to enhance safety [36].
Culture and Monitoring:
- Culture the cells in a defined medium supportive of pluripotency.
- Monitor the emergence of iPSC colonies over 2-3 weeks. Colonies on optimal soft substrates should appear more compact and homogeneous.
Protocol 2: Using Synthetic Thermoresponsive Scaffolds for Cardiomyocyte Differentiation
This protocol details the use of a synthetic, functionalized polymer for the efficient differentiation of hPSCs into mature cardiomyocytes [40].
Scaffold Functionalization and Cell Seeding:
- Synthesize the thermoresponsive terpolymer composed of NiPAAm, VPBA, and PEGMMA via free-radical polymerization [40].
- Functionalize the polymer by incorporating RGD peptides, vitronectin, or fibronectin to enhance cell adhesion and signaling.
- Plate human iPSCs or ESCs onto the functionalized terpolymer scaffold in both 2D and 3D culture configurations.
Maintenance and Differentiation:
- Maintain the cells in pluripotency medium to ensure robust expansion.
- Initiate cardiac differentiation by switching to a specialized differentiation medium. The tailored biochemical and mechanical cues provided by the functionalized scaffold promote robust lineage specification.
Analysis of Differentiated Cardiomyocytes:
- After differentiation, analyze cells using flow cytometry and immunofluorescence for cardiac-specific markers like cardiac Troponin T (cTnT) and Troponin I (cTnI).
- Perform gene expression analysis (e.g., qPCR) to confirm the maturity of the derived cardiomyocytes. Expect significant increases in marker expression compared to natural matrices.
Key Signaling Pathways in Mechanotransduction
The following diagram illustrates the core mechanotransduction pathway by which cells sense and respond to the stiffness of their extracellular matrix (ECM), ultimately influencing cell fate decisions like reprogramming and differentiation [23] [41].
Diagram Title: Core Mechanotransduction Pathway from ECM Stiffness to Cell Fate
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomaterial-Mediated Cell Reprogramming and Differentiation
| Reagent / Material | Function / Description | Example Application |
|---|---|---|
| Vitronectin XF | A defined, recombinant human protein used as a substrate for feeder-free culture of pluripotent stem cells. | Coating tissue culture plates to support the attachment and growth of human iPSCs in a xeno-free condition [39]. |
| Synthetic Terpolymer (NiPAAm-based) | A thermoresponsive scaffold with tunable stiffness and functionality. Allows for non-invasive cell harvesting due to its temperature-dependent solubility [40]. | Serving as a synthetic, customizable matrix for the expansion and cardiac differentiation of hPSCs, outperforming natural matrices in producing mature cardiomyocytes [40]. |
| RGD Peptide | A short peptide sequence (Arg-Gly-Asp) that mimics cell adhesion sites in the ECM by binding to integrin receptors. | Functionalizing synthetic polymers to enhance cell adhesion, spreading, and downstream signaling critical for survival and directed differentiation [40]. |
| mTeSR Plus Medium | A chemically defined, serum-free medium optimized for the maintenance and expansion of human pluripotent stem cells. | Providing essential nutrients and signaling molecules to maintain iPSCs in a pluripotent state during culture and expansion on biomaterial substrates [39]. |
| Non-Viral Delivery Vectors | Materials such as chitosan nanoparticles, gold nanoparticles, or electroporation systems for introducing reprogramming factors without viral integration. | Safely delivering OSKM transcription factors or other genetic material into somatic cells to initiate reprogramming with reduced risk of genomic alteration [36]. |
3D Culture Systems and Microenvironments for Enhanced Reprogramming
Frequently Asked Questions (FAQs)
FAQ 1: How does a 3D culture system improve reprogramming efficiency compared to traditional 2D culture? 3D culture systems bridge the gap between 2D cell cultures and animal models by providing a reproducible, controlled microenvironment that mimics in vivo conditions [42]. In the context of reprogramming somatic cells into induced pluripotent stem cells (iPSCs), dynamic 3D culture has been shown to significantly improve efficiency. One study demonstrated that applying orbital shaking (a form of dynamic culture) to adherent reprogramming cells during the middle phase prevented cell cycle arrest by suppressing the expression of the cell cycle inhibitor p57, resulting in a twofold increase in reprogramming efficiency [43]. In 2D cultures, over-confluency can upregulate p57 and inhibit proliferation, which is detrimental to the reprogramming process [43].
FAQ 2: What are the main types of 3D culture systems available for reprogramming experiments? 3D culture systems can be broadly classified into scaffold-based and non-scaffold based (scaffold-free) systems [42].
- Scaffold-Based Systems utilize a physical structure to support 3D growth. Examples include:
- Polymeric Hard Scaffolds: Pre-fabricated scaffolds designed to mimic the in vivo extracellular matrix (ECM).
- Biological Scaffolds: Use natural components like collagen, fibronectin, or laminin, often reconstituted into hydrogels.
- Micropatterned Surface Microplates: Feature micrometer-sized compartments on the well bottom to control spheroid size and growth.
- Non-Scaffold Based Systems facilitate self-assembly of cells. Examples include:
- Hanging Drop Microplates: Use gravity to encourage cells to aggregate into spheroids in suspended droplets.
- Spheroid Microplates with Ultra-Low Attachment (ULA) Coating: Special well coatings and geometries minimize cell adhesion, promoting the formation of a single, consistent spheroid per well.
- Microfluidic 3D Cell Culture: Incorporates a perfusive flow of culture medium to continuously supply nutrients and remove waste, allowing for more complex, long-term cultures [42].
FAQ 3: My 3D bioprinted constructs show low cell viability. What are the primary factors to check? Low viability in 3D bioprinted constructs can be attributed to several variables related to the bioprinting process itself [44]. You should investigate:
- Needle Type and Print Pressure: Smaller needle diameters and higher print pressures increase the shear stress experienced by cells during extrusion, which can damage them. Test different combinations of tapered needles and lower pressures to optimize viability.
- Print Time: The total duration of the printing session can affect viability, especially for sensitive bioinks. Conduct studies to determine the maximum allowable print time for your specific cell-material combination.
- Bioink Crosslinking: The crosslinking method (e.g., exposure to UV light or harsh chemicals) can be cytotoxic. Ensure the crosslinking process is as gentle as possible and that cells are not exposed for prolonged periods.
- Cell Concentration: Both excessively high and low cell densities within the bioink can lead to apoptosis or low proliferation. Perform encapsulation studies to identify the optimal cell concentration for your specific cell type and material [44].
Troubleshooting Guides
Problem: Low Reprogramming Efficiency in 3D Culture
Potential Causes and Solutions:
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Cell Cycle Arrest | Check for over-confluency and assay for upregulation of p57. | Implement dynamic culture conditions (e.g., orbital shaking) during the middle phase of reprogramming (days 7-16) to suppress p57 and maintain proliferation [43]. |
| Suboptimal Starting Cell Density | Test different seeding densities in a pilot experiment. | Seed cells at a high density to avoid low proliferation rates, but use dynamic culture to prevent the inhibitory effects of over-confluency [43]. |
| Inefficient Reprogramming Method | Compare the success rates of different non-integrating methods for your cell type. | Use the Sendai virus (SeV) reprogramming method, which has been shown to yield significantly higher success rates than episomal vectors in various somatic cell types [20]. |
| Poor Nutrient/Waste Exchange | Assess viability in the core of 3D structures via sectioning and live/dead staining. | For thick constructs (>0.2 mm), introduce microchannels through bioprinting or use perfused microfluidic systems to improve transport [44]. |
Problem: Poor Viability in 3D Cultures and Bioprinted Constructs
Potential Causes and Solutions:
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| High Shear Stress | Perform a 24-hour viability study testing different needle types and pressures. | Use tapered needle tips and the lowest possible print pressure that allows for consistent extrusion [44]. |
| Improper Crosslinking | Create thin-film controls with your crosslinking method to isolate its effects. | Optimize the degree of crosslinking and explore alternative, gentler crosslinking mechanisms (e.g., ionic, enzymatic) [44]. |
| Material Toxicity or Contamination | Use a pipetted thin film control with your material to assess its inherent toxicity. | Test new material batches and ensure sterile handling during bioink preparation [44]. |
| Incorrect Cell Concentration | Run an encapsulation study with a range of cell densities. | Identify and use the optimal cell concentration for your specific cell type and material permeability [44]. |
Experimental Protocols
Detailed Protocol: Improving Reprogramming Efficiency with Dynamic 3D Culture
This protocol is adapted from research demonstrating that orbital shaking can prevent cell cycle arrest and enhance iPSC generation [43].
Key Research Reagent Solutions:
| Item | Function in the Protocol |
|---|---|
| Orbital Shaker | Provides dynamic culture conditions through gentle, continuous shaking. |
| Fibroblasts with Doxycycline-inducible OSKM Genes | Allows synchronized initiation of reprogramming upon doxycycline addition. |
| Reprogramming Medium | Contains essential supplements and factors to support the induction of pluripotency. |
| Doxycycline | Induces the expression of OSKM reprogramming factors (Oct4, Sox2, Klf4, Myc). |
| Mouse Embryonic Fibroblast (MEF) Media / Matrigel | Provides a feeder layer or substrate for adherent cell culture. |
Methodology:
- Cell Seeding: Seed neonatal skin fibroblasts (or other somatic cells) at a high density of 3000 cells/cm² on an appropriate substrate (e.g., Matrigel). Allow cells to attach overnight.
- Reprogramming Initiation: Add reprogramming medium containing doxycycline to induce the expression of the OSKM factors.
- Dynamic Culture Application: Begin orbital shaking the day after doxycycline addition. Continue shaking throughout the reprogramming process.
- Factor Withdrawal: On day 16, withdraw doxycycline from the culture medium to cease forced expression of reprogramming factors.
- Colony Analysis: On day 20, fix the cultures and count the number of Nanog-positive colonies to quantify reprogramming efficiency. A significant (e.g., twofold) increase in efficiency is expected in dynamic versus static cultures [43].
Detailed Protocol: Sendai Virus (SeV) Reprogramming for High-Efficiency iPSC Generation
This protocol summarizes the use of non-integrating Sendai virus vectors, a method known for high success rates [20].
Key Research Reagent Solutions:
| Item | Function in the Protocol |
|---|---|
| CytoTune Sendai Reprogramming Kit | Contains SeV vectors expressing OSKM factors and EmGFP. |
| Amaxa Nucleofector II Device | Enables high-efficiency transduction for some cell types (alternative to viral transduction). |
| ROCK Inhibitor (Y-27632) | Improves cell survival after thawing and passaging. |
| mTeSR1 Medium | A defined medium for the maintenance and expansion of iPSCs. |
Methodology:
- Transduction: Transduce fibroblasts or Peripheral Blood Mononuclear Cells (PBMCs) with the CytoTune Sendai Virus vectors.
- Monitoring: Refresh the medium 24 hours post-transduction. Culture for approximately 6 more days, feeding every other day. Monitor transduction efficiency by examining GFP-positive cells.
- Replating: Approximately 7 days (for fibroblasts) or 3 days (for PBMCs) after transduction, harvest and replate the cells onto fresh plates.
- Colony Picking: After 2-3 weeks, manually pick at least 24 individual colonies that have reached an appropriate size for transfer and expansion.
- Expansion and Banking: Expand the picked clones. Cryopreserve a master bank (MB) at passage 10, followed by further expansion and creation of a distribution bank (DB) [20].
Essential Diagrams
Diagram 1: Dynamic 3D Culture Workflow for Enhanced Reprogramming
Diagram 2: Signaling Pathway in Dynamic vs. Static Reprogramming
Integrating CRISPR-Cas9 for Precision Genome Editing in iPSCs
Frequently Asked Questions (FAQs)
1. What are the major challenges when using CRISPR-Cas9 in iPSCs? iPSCs are notoriously difficult to edit genetically compared to other cell types. Key challenges include low editing efficiency, high sensitivity to manipulation, and a tendency to spontaneously differentiate during culture. Furthermore, the homology-directed repair (HDR) pathway, which is necessary for precise knock-in edits or mutation corrections, occurs even less frequently in iPSCs than in immortalized cell lines [45].
2. How can I improve the efficiency of CRISPR-Cas9 editing in my iPSC culture? Improving efficiency involves optimizing several factors. Using high-fidelity Cas9 variants and highly specific guide RNAs (gRNAs) can minimize off-target effects [46]. For delivery, ribonucleoprotein (RNP) electroporation has been shown to achieve high cleavage efficiency (>80%) in iPSCs [47]. Synchronizing the cell cycle of your iPSC population can also enhance HDR efficiency, as this repair mechanism is active only during specific cell cycle stages [45].
3. What are unintended "on-target" effects, and why are they a concern for iPSC editing? A significant concern is the generation of large, on-target structural variants (SVs) that standard PCR and Sanger sequencing can miss [48]. These can include large deletions, insertions, and even loss of heterozygosity. One study found that 33% of analyzed iPSC clones had acquired such detrimental defects that escaped standard quality controls [48]. These SVs can alter the genotype and potentially corrupt research results or compromise therapeutic safety [49].
4. My edited iPSCs are differentiating spontaneously. How can I prevent this? Maintaining pluripotency requires constant attention. You should image cells daily to identify and manually remove any differentiated areas, passage cells during the log phase of growth, and keep culture media fresh [45]. Using media like Essential 8 and supplements such as ROCK inhibitor (Y-27632) during passaging and thawing can significantly improve cell survival and help maintain an undifferentiated state [47].
5. What is the advantage of using CRISPR activation (CRISPRa) for reprogramming somatic cells into iPSCs? Conventional reprogramming methods use forced expression of transcription factors, which can lead to off-target gene activation and heterogeneous, aberrant iPSCs. CRISPRa, which uses a catalytically inactive Cas9 (dCas9) to activate endogenous genes, offers a more precise alternative. It results in reprogramming with higher fidelity and less heterogeneity by directly activating the endogenous promoters of pluripotency factors like OCT4 and SOX2 [50] [51].
Troubleshooting Guides
Common Problems and Solutions for CRISPR-Cas9 in iPSCs
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Low Editing Efficiency [46] [45] | Poor gRNA design, inefficient delivery method, low Cas9/gRNA expression. | Redesign gRNA for specificity and on-target score; Use RNP electroporation instead of transfection; Validate with a positive control gRNA (e.g., HPRT) [47]. |
| High Cell Death / Toxicity [46] | High concentration of CRISPR components, electroporation/transfection stress. | Titrate CRISPR components to find the lowest effective dose; Use a Cas9 protein with a nuclear localization signal; Include ROCK inhibitor (Y-27632) in media post-transfection [47]. |
| Spontaneous Differentiation [45] | Suboptimal culture conditions, over-confluence, inadequate daily maintenance. | Passage cells at 75-85% confluency; Perform daily imaging and removal of differentiated areas; Use quality matrix (e.g., Geltrex) and fresh, pre-warmed media [45] [47]. |
| Mosaicism (Mixed Edited/Unedited Cells) [46] | Editing occurred after cells have already divided; prolonged Cas9 activity. | Synchronize the cell cycle before editing; Use single-cell cloning to isolate fully edited clones; Employ inducible Cas9 systems for tighter temporal control. |
| Unintended On-Target Structural Variants [49] [48] | Improper repair of double-strand breaks; limited detection methods. | Implement advanced quality control (QC) beyond Sanger sequencing, such as long-range PCR, TPCR, and qPCR for copy number assessment [48]. |
Quantitative Data on Editing Efficiencies and Outcomes
| Experimental Metric | Typical Range / Outcome | Notes & Context |
|---|---|---|
| HDR Efficiency in iPSCs | Very Low [45] | A major bottleneck; significantly lower than in immortalized cell lines. |
| RNP Electroporation Efficiency | >80% Cleavage [47] | Achieved using the Neon Transfection System with an HPRT control gRNA. |
| Lipofection Efficiency | >50% Cleavage [47] | Achieved using Lipofectamine CRISPRMAX with an HPRT control gRNA. |
| Incidence of On-Target SVs | 33% of Clones [48] | Found in a study of 27 iPSC clones edited at 9 different genomic loci. |
| CRISPRa Reprogramming Boost | 8-fold increase [50] | Achieved by adding EEA and miR-302/367 (CRISPRa+ME) targeting to basal CRISPRa. |
Advanced Quality Control for Edited iPSC Clones
Standard genotyping methods like PCR and Sanger sequencing are insufficient for detecting large on-target defects [48]. The following workflow is recommended to ensure genomic integrity of your edited iPSC lines:
Detailed Experimental Protocols
This protocol uses the Neon Transfection System for high-efficiency delivery.
Key Reagents:
- Gibco Human Episomal iPSC Line
- Essential 8 Medium
- TrypLE Express Enzyme
- GeneArt Platinum Cas9 Nuclease
- GeneArt gRNA (e.g., HPRT control for optimization)
- Neon Transfection System with 10μL Kit
- RevitaCell Supplement or ROCK inhibitor (Y-27632)
Methodology:
- Cell Preparation: Culture iPSCs in Essential 8 Medium on Geltrex-coated plates. On the day of electroporation, detach cells using TrypLE Express to create a single-cell suspension. Count cells and wash with PBS.
- RNP Complex Assembly: For one reaction, combine 0.5 μL of Cas9 nuclease (3 μg/μL) and 300 ng of gRNA in a tube with 5 μL of Resuspension Buffer R. Mix gently and incubate at room temperature for 10 minutes.
- Cell Electroporation: Resuspend 1 x 10^6 cells in 50 μL Resuspension Buffer R. Transfer 5 μL of this cell suspension to the 6 μL of prepared RNP complex. Pipette the 10 μL mixture into a Neon tip and electroporate using the pre-set protocol 7 (1,200 V, 30 ms, 1 pulse).
- Recovery and Analysis: Immediately transfer the electroporated cells into a 24-well plate containing 0.5 mL of pre-warmed Essential 8 Medium with 1X RevitaCell Supplement. Change the medium to fresh Essential 8 the next day. Analyze cleavage efficiency 48-72 hours post-electroporation using a cleavage detection kit or sequencing.
This protocol describes boosting reprogramming efficiency by targeting non-coding regulatory elements.
Key Reagents:
- Primary human somatic cells (e.g., fibroblasts, LCLs)
- dCas9VP192 activator plasmid
- gRNA plasmids targeting:
- Basal reprogramming factors (OCT4, SOX2, KLF4, MYC, LIN28A)
- EEA motif (using a combination of five guides)
- Promoter of the miR-302/367 cluster (MIR302CHG)
Methodology:
- gRNA Design: Design gRNAs to target the promoters of the endogenous pluripotency genes OCT4, SOX2, KLF4, MYC, and LIN28A. Additionally, design five 14 nt gRNAs targeting the conserved 36 bp EEA motif and gRNAs for the promoter of the MIR302CHG gene.
- Cell Transfection: Co-transfect the somatic cells with the dCas9VP192 activator plasmid and the combination of gRNA plasmids (basal + EEA + miR-302/367) using an appropriate method like nucleofection.
- Culture and Observation: Plate transfected cells on feeder layers or in feeder-free conditions suitable for emerging iPSCs. For suspension cells like LCLs, attached reprogramming intermediates can be observed by day 10. Remove non-attached cells to enrich for reprogramming cells.
- Colony Picking and Validation: Emerging iPSC colonies typically become visible and can be manually picked after 2-3 weeks. Accelerated reprogramming kinetics and larger colony sizes are observed with the optimized CRISPRa + ME condition. Expand clones and validate pluripotency through standard methods (e.g., immunostaining for NANOG/TRA-1-60, trilineage differentiation, karyotyping).
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function / Application | Example Products / Notes |
|---|---|---|
| Synthetic gRNA | Defines CRISPR-Cas9 target specificity; synthetic versions offer high purity and consistency. | GeneArt Precision gRNA Synthesis Kit; Predesigned gRNAs from various suppliers. |
| High-Fidelity Cas9 | Reduces off-target editing effects; engineered variant of wild-type Cas9. | HiFi Cas9, eSpCas9, other commercial high-fidelity Cas9 nucleases. |
| ROCK Inhibitor (Y-27632) | Improves survival of iPSCs after dissociation (e.g., during passaging or electroporation). | A critical supplement in culture media post-thaw and post-transfection. |
| Essential 8 Medium | A defined, xeno-free culture medium optimized for the feeder-free growth of iPSCs. | Gibco Essential 8; helps maintain a uniform, undifferentiated state. |
| Geltrex/Matrigel | A solubilized basement membrane preparation used as a substrate to coat culture vessels for iPSCs. | Provides a scaffold for cell attachment and growth in feeder-free systems. |
| dCas9 Activator (VP192) | The core enzyme for CRISPRa; a deactivated Cas9 fused to a transcriptional activator (VP192). | Used with gRNAs to activate endogenous gene expression without cutting DNA [51]. |
| Neon Transfection System | An electroporation system optimized for high-efficiency delivery of molecules (like RNPs) into iPSCs. | Often yields higher editing efficiency than lipid-based transfection methods [47]. |
Overcoming Practical Hurdles: Maximizing Efficiency and Ensuring Quality
The transition to feeder-free and chemically defined culture systems represents a critical advancement in induced pluripotent stem cell (iPSC) research. These systems eliminate the variability and safety concerns associated with mouse feeder cells and animal-derived components, providing a standardized platform that enhances experimental reproducibility and clinical translation potential. This technical support center provides comprehensive guidance for researchers navigating this transition, offering troubleshooting advice and detailed protocols to optimize reprogramming efficiency and culture stability.
Media Formulations: A Comparative Analysis
Chemically defined media provide a standardized environment for iPSC derivation and maintenance. The table below summarizes key media formulations and their reported performance.
Table 1: Composition and Key Features of Selected Chemically Defined Media
| Media Name | Key Components | Reported Reprogramming Efficiency | Notable Features & Applications | Key References |
|---|---|---|---|---|
| E8 Medium | DMEM/F12, Insulin, Selenium, Transferrin, L-ascorbic acid, FGF2, TGF-β (or NODAL) | Improved efficiency over feeder-based systems; supports integration-free iPS derivation [52]. | Albumin-free; eliminates batch variability; supports long-term self-renewal [52]. | [52] |
| StemFit (AK03) | Proprietary, Xeno-free | Effective for maintaining pluripotency on rLN511E8; supports high split ratios (up to 1:100) [53]. | Commercial xeno-free medium; used with recombinant laminin-511 E8 fragment for robust culture [53]. | [53] |
| B8 Medium | In-lab generated FGF2, TGF-β3, Neuregulin 1, and other defined components | Suitable for derivation and long-term culture (>100 passages) of hiPSC lines [54]. | Negligible cost (3% of commercial media); enables weekend-free feeding without compromising pluripotency [54]. | [54] |
| XF-hEPS Derivation Media | DF12, Neurobasal, Insulin, Transferrin, Selenium, hLif, small molecules (ChIR, etc.), Xeno-free KSR | 46% efficiency in deriving human extended pluripotent stem (hEPS) cell lines from discarded blastocysts [55]. | For specialized derivation of hEPS cells; includes ROCK inhibitor (Y27632) for cell survival [55]. | [55] |
| Chemical Reprogramming System | Small molecule cocktails (e.g., BeiCell 2nd Gen Kit) | Up to 38% efficiency; reduces reprogramming time to 10-16 days [56]. | Non-integrating, genetically safe; applicable across diverse donor backgrounds and ages [56]. | [56] |
Essential Research Reagent Toolkit
The successful implementation of a feeder-free system relies on a core set of defined reagents.
Table 2: Key Reagents for Feeder-Free, Chemically Defined iPSC Culture
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Defined Substrates | Recombinant Laminin-511 E8 (rLN511E8), Recombinant Laminin-521 (LN521), Vitronectin (VTN-NC) | Supports robust cell attachment, survival, and long-term self-renewal; replaces Matrigel and feeder cells [53] [57]. |
| Growth Factors | bFGF (FGF2), TGF-β1/TGF-β3, Neuregulin 1 | Critical for maintaining pluripotency and self-renewal. In-lab generation of recombinant proteins can drastically reduce costs [54]. |
| Small Molecule Inhibitors/Enhancers | ROCK inhibitor (Y-27632), CHIR99021 (GSK-3 inhibitor), (S)-(+)-dimethindene maleate, minocycline hydrochloride | Enhances cell survival after passaging (ROCKi) and can be used to establish or modulate pluripotency states (e.g., in hEPS cells) [55] [57]. |
| Lipid & Trace Element Supplements | Chemically Defined Lipid Concentrate, Selenium | Supports membrane integrity and provides essential cofactors for metabolic processes and antioxidant defense. |
| Cell Dissociation Reagents | Accutase, EDTA, TrypLE Select | Enzymatic (Accutase, TrypLE) or non-enzymatic (EDTA) passaging methods for gentle cell dissociation as clumps or single cells [55] [53]. |
Troubleshooting Common Experimental Issues
Problem: Low Cell Attachment Survival After Passaging
- Potential Causes: Inadequate coating with substrate, improper handling of single cells, outdated or inactivated ROCK inhibitor.
- Solutions:
- Ensure the recombinant laminin (e.g., LN521) coating is fresh and uniform [53].
- Always use a ROCK inhibitor (e.g., Y-27632) in the medium for the first 24-48 hours after passaging, especially when cells are dissociated into single cells [55] [52].
- Confirm the pH and osmolality of the dissociation reagent and culture medium are within specification.
Problem: High Rate of Spontaneous Differentiation
- Potential Causes: Suboptimal concentration of key growth factors (FGF2, TGF-β), over-confluent cultures, microbial contamination, or inconsistent medium changes.
- Solutions:
- Manually remove differentiated areas from the culture daily.
- Titrate growth factors to ensure they are at effective concentrations; avoid over-diluting medium supplements [54].
- Maintain cells at an appropriate density and adhere to a strict feeding schedule. The B8 medium format allows for weekend-free feeding, which can improve schedule consistency [54].
- Check for mycoplasma contamination.
Problem: Low Reprogramming Efficiency
- Potential Causes: Poor condition of starting somatic cells, inefficient delivery of reprogramming factors, suboptimal culture conditions for the emergence of iPSC colonies.
- Solutions:
- Use early-passage, healthy somatic cells. For fibroblasts, ensure robust proliferation in defined media like E8 with added factors before reprogramming [52] [57].
- Optimize the reprogramming method. Consider non-integrating methods like episomal vectors or sendai virus on defined LN521 substrate, which can achieve efficiencies of 0.15–0.3% [57].
- For chemical reprogramming, strictly follow the staged medium protocol, as the process involves precise epigenetic modulation over 10-20 days [56].
Problem: Inconsistent Results Between Experiments
- Potential Causes: Batch-to-batch variability in key reagents, even within defined systems.
- Solutions:
Detailed Protocol: Derivation of Transgene-Free iPSCs on LN521
This protocol is adapted from established methods for deriving clinical-grade iPSCs [57].
Workflow Overview:
Materials:
- Somatic Cells: Human dermal fibroblasts (e.g., from ATCC or Coriell).
- Reprogramming Vector: Excisable polycistronic lentiviral vector expressing OSKM [57].
- Culture Substrate: Recombinant human Laminin-521 (LN521).
- Media: Defined xeno-free medium (e.g., TeSR2, E8, or NutriStem).
- Supplements: ROCK inhibitor (Y-27632).
Method:
- Prepare Somatic Cells: Culture human fibroblasts in DMEM supplemented with 10% human serum until they are 70-80% confluent and actively dividing [57].
- Viral Transduction: Transduce fibroblasts with the excisable lentivirus at an appropriate multiplicity of infection (MOI). Include a polybrene-like reagent to enhance transduction efficiency.
- Initiate Reprogramming Culture: 24-48 hours post-transduction, harvest the fibroblasts and plate them onto LN521-coated plates in xeno-free medium supplemented with ROCK inhibitor.
- Medium Management: Change the medium daily. Colonies with embryonic stem cell-like morphology will begin to appear between 20 and 30 days.
- Isolate and Expand Clones: Mechanically pick or dissociate well-defined colonies and transfer them to new LN521-coated wells for expansion.
- Remove Reprogramming Transgenes: Once stable iPSC lines are established, treat them with Cre recombinase to excise the integrated reprogramming cassette. Confirm excision via genomic PCR [57].
- Characterization: Validate the resulting transgene-free iPSC lines for pluripotency marker expression (e.g., OCT4, SOX2, NANOG), normal karyotype, and the ability to differentiate into all three germ layers.
Signaling Pathways in a Defined Culture System
The maintenance of pluripotency in defined media is governed by a core set of activated signaling pathways. The following diagram illustrates the key pathways and their interactions.
Frequently Asked Questions (FAQs)
Q1: Why is it critical to remove albumin from chemically defined media? Albumin, often derived from bovine serum (BSA), is a major source of batch-to-batch variability because it can bind lipids, growth factors, and other impurities inconsistently. Its removal, as achieved in E8 medium, eliminates this variability and enhances culture consistency and reproducibility [52]. Research revealed that the toxicity of β-mercaptoethanol (BME) in the absence of BSA was a key factor, and removing BME made BSA unnecessary [52].
Q2: Can I switch my existing iPSC lines from feeder-dependent to feeder-free conditions? Yes, most established iPSC lines can be successfully adapted. The standard protocol involves dissociating the cells from feeders and plating them directly onto a defined substrate like recombinant laminin-511 E8 fragment in a defined medium like StemFit or E8. The cells typically adapt within 2-3 passages [53].
Q3: What are the primary advantages of chemical reprogramming over factor-based methods? Chemical reprogramming uses only small molecules to induce pluripotency, which offers a primary advantage of being non-integrating and genetically safe, eliminating the risk of insertional mutagenesis [56]. Furthermore, the process using modern kits can be very rapid (as little as 10-16 days) and highly efficient (up to 38%), and it is applicable to somatic cells from a wide range of donor backgrounds [56].
Q4: How does the choice of extracellular matrix impact reprogramming efficiency? The extracellular matrix provides critical signals for cell survival, proliferation, and identity. Laminin isoforms 521 and 511 E8 have been shown to support significantly higher reprogramming efficiencies and better long-term culture of pluripotent cells compared to other matrices like Matrigel or vitronectin, as they more closely mimic the natural stem cell niche [53] [57]. One study reported a 15–30 fold increase in reprogramming efficiency using LN521 over conventional systems [57].
Preventing and Managing Spontaneous Differentiation in iPSC Cultures
Spontaneous differentiation is a common challenge in induced pluripotent stem cell (iPSC) research that can compromise experimental results and therapeutic applications. Maintaining high-quality, undifferentiated cultures is essential for improving the overall efficiency of somatic cell reprogramming and for generating reliable tools for drug development. This technical support center article provides researchers with targeted FAQs and evidence-based troubleshooting strategies to identify, prevent, and manage spontaneous differentiation in iPSC cultures, thereby enhancing the reproducibility and success of reprogramming initiatives.
FAQs: Understanding Spontaneous Differentiation
What is spontaneous differentiation and why is it problematic?
Spontaneous differentiation occurs when iPSCs prematurely begin developing into specialized cell types without deliberate induction. This is problematic because it:
- Reduces Reprogramming Efficiency: Differentiated cells do not contribute to expanding pluripotent cultures.
- Compromises Experimental Consistency: Introduces uncontrolled variables in disease modeling and drug screening.
- Risks Therapeutic Applications: Undetected differentiated cells could lead to unpredictable outcomes in cell therapies.
What are the visual indicators of spontaneous differentiation?
Healthy iPSC colonies appear compact with well-defined borders and prominent nucleoli. Signs of spontaneous differentiation include:
- Flat, Spread-Out Colonies: Loss of tight colony morphology.
- Irregular Borders: Fuzzy or uneven colony edges.
- Changes in Cell Morphology: Appearance of elongated, spindle-shaped, or large flattened cells within colonies.
- Increased Cytoplasmic/Nuclear Ratio: Visible changes in cell structure.
Troubleshooting Guide: Common Differentiation Problems and Solutions
Problem 1: Excessive Differentiation (>20%) in Cultures
Potential Causes and Solutions:
- Old Culture Medium: Ensure complete cell culture medium kept at 2-8°C is less than 2 weeks old [39].
- Inadequate Differentiation Removal: Physically remove differentiated areas prior to passaging [39].
- Prolonged Plate Exposure: Avoid having culture plates out of the incubator for more than 15 minutes at a time [39].
- Overgrown Cultures: Passage cultures when majority of colonies are large and compact with dense centers, before they overgrow [39].
- Excessive Colony Density: Decrease density by plating fewer cell aggregates during passaging [39].
- Oversensitive Cell Lines: Reduce incubation time with passaging reagents like ReLeSR if your cell line is particularly sensitive [39].
Problem 2: Low Cell Attachment After Plating
Potential Causes and Solutions:
- Insufficient Initial Plating: Plate 2-3 times more cell aggregates initially and maintain a more densely confluent culture [39].
- Delayed Processing: Work quickly after treatment with passaging reagents to minimize time cell aggregates spend in suspension [39].
- Over-Dissociation: Do not excessively pipette to break up cell aggregates; instead increase incubation time with passaging reagent by 1-2 minutes [39].
- Incorrect Plate Selection: Ensure non-tissue culture-treated plates are used with Vitronectin XF coating, while tissue culture-treated plates are used with Corning Matrigel [39].
Problem 3: Differentiated Cells Detaching with Colonies
Potential Causes and Solutions:
- Excessive Reagent Exposure: Decrease incubation time with ReLeSR by 1-2 minutes [39].
- Elevated Temperature: Decrease incubation temperature to room temperature (15-25°C) [39].
Table 1: Culture Conditions and Their Impact on Differentiation
| Factor | Optimal Range | Effect Outside Range | Citation |
|---|---|---|---|
| Medium age | <2 weeks (2-8°C) | Increased differentiation | [39] |
| Plate exposure time | <15 minutes | Morphological changes | [39] |
| Colony density | Appropriate split ratios | Multi-layering & differentiation | [39] [33] |
| Passaging confluency | ~85% confluency | Poor cell health & differentiation | [33] |
| Aggregate size | 50-200 μm | Poor survival or differentiation | [39] |
Table 2: Reagent-Based Solutions for Differentiation Management
| Reagent | Function | Application Notes | Citation |
|---|---|---|---|
| ROCK inhibitor/RevitaCell | Enhances single-cell survival | Recommended when passaging overly confluent cells | [33] |
| CEPT/polyamines | Improves cell survival | Use for passaging single cell suspensions; change medium 24-48h later | [58] |
| Accutase | Generates single cell suspension | Ideal for counting cells or collecting pellets | [58] |
| ReLeSR | Standard passaging | Reduces need for physical removal of differentiated cells | [58] |
| Matrigel | Extracellular matrix | Critical for proper attachment; do not let dry out | [58] |
Experimental Protocols for Differentiation Management
Routine Maintenance Feeding Schedule
Materials:
- StemMACS iPS-Brew XF or similar defined medium [58]
- D-PBS without Ca++ and Mg++ [39]
- Appropriate matrix (Matrigel, Vitronectin XF, Geltrex) [39] [58] [33]
Protocol:
- Feed cells with iPS-Brew medium every other day.
- Implement "double feeding" (1.5x volume) on Fridays to avoid weekend feeding.
- Use these volumes for normal feeding:
- 10 cm dish: 10 mL medium
- 6-well plate: 2 mL/well
- 12-well plate: 1 mL/well
- 24-well plate: 500 μL/well
- 96-well plate: 200 μL/well
- Change medium 24-48 hours after passaging to remove CEPT/polyamines when used [58].
Passaging with ReLeSR for Standard Maintenance
Materials:
Protocol:
- Wash iPSCs with DPBS to completely remove medium.
- Add sufficient ReLeSR to cover cells (same volume as Matrigel used for coating).
- Let sit 30-60 seconds at room temperature.
- Aspirate ReLeSR completely.
- Incubate at 37°C for 5-7 minutes (varies by cell line).
- Add iPS-Brew to well and detach colonies by triturating carefully.
- Break up colonies without creating single cell suspension.
- Passage at 1:20-1:40 ratio when using iPS Brew/CEPT/polyamines.
- Shake plate well to distribute cells evenly [58].
CEPT Preparation for Enhanced Cell Survival
Materials:
- Chroman 1 (MedChem Express HY-15392)
- Emricasan (SelleckChem S7775)
- Polyamine supplement (Sigma-Aldrich P8483)
- Trans-ISRIB (R&D Systems 5284)
- DMSO (Life Technologies A1516401)
Stock Solutions Preparation:
- Chroman 1 (0.5 mM, 10,000X stock): Dissolve 5 mg in 22.91 mL DMSO
- Emricasan (50 mM, 10,000X stock): Dissolve 5 mg in 0.1756 mL DMSO
- Trans-ISRIB (7 mM, 10,000X stock): Dissolve 10 mg in 3.165 mL DMSO, gently warming at 45-60°C
- Storage: Store stocks at 4°C for up to one month or -20°C for up to 1 year
Working Solution:
- Dilute Chroman, Emricasan, and trans-ISRIB at 1:10,000 and polyamine supplement at 1:1,000 into desired medium [58].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for iPSC Culture and Differentiation Management
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Culture Media | StemMACS iPS-Brew XF, Essential 8 Medium, mTeSR Plus | Supports pluripotency | Use defined, feeder-free formulations |
| Dissociation Reagents | ReLeSR, Accutase, Gentle Cell Dissociation Reagent | Detaches cells for passaging | ReLeSR for clump passaging; Accutase for single cells |
| Extracellular Matrices | Corning Matrigel, Vitronectin XF, Geltrex | Provides attachment surface | Match matrix with media system |
| Survival Enhancers | CEPT cocktail, ROCK inhibitor (Y27632) | Reduces apoptosis after passaging | Critical for single-cell passaging |
| Quality Control Tools | Alkaline phosphatase kits, Pluripotency markers (OCT4, NANOG, SOX2, TRA-1-60) | Assess pluripotent state | Regular monitoring essential |
Signaling Pathways in iPSC Pluripotency and Differentiation
The maintenance of pluripotency and prevention of spontaneous differentiation involves coordinated signaling pathways that can be visualized through the following workflow:
Advanced Techniques: Biomaterial Engineering for Differentiation Control
Emerging research indicates that engineered biomaterials with tailored biophysical properties can significantly influence cell fate transitions during reprogramming [23]. Key approaches include:
- Matrix Stiffness Optimization: Tuning substrate stiffness to mimic natural stem cell niches
- 3D Culture Systems: Implementing three-dimensional scaffolds that better replicate in vivo microenvironments
- Microtopographical Cues: Using surface patterning to guide pluripotency maintenance
- Mechanotransduction Modulation: Leveraging integrin-mediated signaling pathways that influence chromatin states and epigenetic regulation
These advanced biomaterial approaches work through critical signaling pathways including integrins/FAK, PI3K/Akt, YAP/TAZ, Hippo, Rock, Bmp, Erk, Wnt and Notch, which collectively regulate the cell reprogramming process [23].
Effective prevention and management of spontaneous differentiation in iPSC cultures requires diligent monitoring, proper technique, and systematic troubleshooting. By implementing the protocols and strategies outlined in this technical guide, researchers can significantly improve the quality and consistency of their iPSC cultures, thereby enhancing the overall efficiency of somatic cell reprogramming research. Regular quality control assessments, including verification of pluripotency markers and genomic stability, should complement these culture management practices to ensure reproducible results across experiments and applications.
Strategies to Improve Low HDR Rates in CRISPR-iPSC Workflows
The combination of induced pluripotent stem cell (iPSC) technology and CRISPR-based gene editing has revolutionized biomedical research and therapeutic development [4] [59]. However, a significant technical challenge persists: achieving efficient homology-directed repair (HDR) in iPSCs [45] [60]. Unlike error-prone non-homologous end joining (NHEJ), which dominates DNA repair in these cells, HDR enables precise genome modifications essential for creating accurate disease models and performing gene correction [60] [61]. This guide addresses the specific factors contributing to low HDR rates in iPSC workflows and provides evidence-based troubleshooting strategies to enhance precision editing efficiency.
Frequently Asked Questions (FAQs)
Why is HDR inherently inefficient in iPSCs compared to other cell types?
iPSCs present unique challenges for HDR-mediated editing. Firstly, the HDR pathway is naturally less frequent in iPSCs compared to immortalized cell lines, with DSBs predominantly repaired by the NHEJ pathway [45] [60]. Reports indicate initial HDR efficiencies in iPSCs can be as low as 2-5% in many cases [60] [62]. Furthermore, iPSCs are particularly sensitive to the cytotoxicity caused by double-strand breaks (DSBs) induced by CRISPR nucleases, which can trigger apoptosis and reduce the survival of successfully edited cells [45] [62]. This cellular stress response further limits the pool of cells available for HDR.
What are the consequences of low HDR efficiency for my experiments?
Low HDR efficiency directly translates to an immense practical burden. When the desired HDR event is rare, researchers must screen hundreds or even thousands of single-cell clones to identify a few with the correct modification [60]. This process is time-consuming, resource-intensive, and can take months. Furthermore, even cells that undergo HDR are susceptible to repeated cutting by the CRISPR machinery if the original target site remains intact, leading to unwanted indels that corrupt the precise edit [60]. This problem is exacerbated in iPSCs, which often require multiple precise edits to model complex diseases [45].
Can I use alternative editing technologies to bypass HDR altogether?
Yes, for certain types of edits, newer technologies can circumvent the need for traditional HDR. Base editing achieves single-base conversions (e.g., C→T or A→G) by fusing a deaminase enzyme to a Cas9 nickase, avoiding DSBs and the associated cellular toxicity [59]. Prime editing offers even greater versatility, using a reverse transcriptase and a prime editing guide RNA (pegRNA) to directly write new genetic information into a target site, enabling precise insertions, deletions, and all 12 possible base-to-base conversions without requiring DSBs or donor templates [59]. These systems are ideal for point mutations but may have limitations on the size of the insertion.
Troubleshooting Guide: Key Strategies to Enhance HDR
Optimize the HDR Donor Template
The design of the donor template is a critical factor for successful HDR. Key parameters include template type, strand polarity, homology arm length, and strategic modifications.
Table 1: HDR Donor Template Design Guidelines
| Parameter | Recommendation | Impact on HDR Efficiency |
|---|---|---|
| Template Type | Use single-stranded DNA (ssODN) for small edits (<200 nt); long ssDNA for larger inserts [61]. | Reduces toxicity and random integration compared to dsDNA [61]. |
| Template Polarity | For Cas12a, always use the non-targeted strand sequence for the donor. For Cas9, the effect is less pronounced, but testing both is advised [63] [61]. | Using the non-targeted strand with Cas12a prevents interference with nuclease binding and can dramatically improve HDR [63]. |
| Homology Arm Length | 30-40 nt for ssODNs; 350-700 nt for long ssDNA templates [63] [61]. | Longer arms (≥350 nt) show an exponential relationship with knock-in efficiency in iPSCs [61]. |
| 5' End Modifications | Incorporate 5'-biotin or 5'-C3 spacers on the donor DNA [64]. | 5'-C3 spacer can produce a 20-fold rise in correctly edited mice; 5'-biotin increases integration up to 8-fold [64]. |
| Stabilizing Mods | Add phosphorothioate (PS) linkages at the 5' and 3' ends of ssODNs [63]. | Protects the donor from exonuclease degradation, crucial in high-nuclease environments like iPSCs [63]. |
Implement Cellular and Molecular Interventions
Manipulating cellular states and repair pathways can create a more favorable environment for HDR.
Table 2: Cellular and Molecular Interventions to Boost HDR
| Intervention | Method | Mechanism & Outcome |
|---|---|---|
| p53 Suppression | Co-transfect with p53 shRNA or use chemical inhibitors [62]. | Prevents CRISPR-induced apoptosis. Combined with pro-survival molecules, increased HDR from ~3% to >90% in some iPSC lines [62]. |
| HDR Enhancers | Use commercial small molecule blends like Alt-R HDR Enhancer [63] [65]. | Biases the DSB repair pathway towards HDR and away from NHEJ. HDR rates >50% observed in challenging Jurkat cells [63]. |
| RAD52 Supplementation | Add human RAD52 protein to the CRISPR injection mix [64]. | Enhances ssDNA integration. Increased precise HDR by >3-fold (from 8% to 26%) in a mouse model, though it may increase template multiplication [64]. |
| Pro-survival Cocktails | Use supplements like CloneR and RevitaCell during and after transfection [62]. | Improves cell viability post-electroporation, increasing the number of cells that survive to complete HDR [62]. |
Refine CRISPR System and Target Site Selection
The choice of nuclease, guide RNA, and target site geometry profoundly influences the HDR outcome.
Block Re-cutting with Silent Mutations: Introduce silent "blocking mutations" in the repair template to alter the PAM site or the seed region of the gRNA binding site. This prevents the CRISPR complex from recognizing and re-cutting the successfully edited allele, allowing pure HDR clones to proliferate. This strategy can increase editing accuracy by up to 100-fold for biallelic edits [60] [61].
Minimize Cut-to-Mutation Distance: The efficiency of incorporating a mutation via HDR drops rapidly as the distance from the Cas9 cut site increases. For optimal results, design gRNAs so the cut site is within 10 nucleotides of the intended edit. A distance of just 10 bp can reduce incorporation efficiency by half [60].
Choose the Right Nuclease and Concentration: While Cas9 is widely used, the Cas12a (Cpf1) nuclease, especially hyperactive variants like Cas12a Ultra, can be highly effective. When using Cas12a, keep RNP concentrations moderate (1-2 µM) to avoid degradation of ssDNA donors [63].
The following diagram summarizes the strategic framework and key components of a highly efficient CRISPR-iPSC HDR workflow:
Detailed Experimental Protocol
The following is a detailed methodology, adapted from a high-efficiency protocol that achieved HDR rates exceeding 90% in human iPSCs [62].
Materials and Reagents
Table 3: Essential Research Reagent Solutions
| Reagent | Function | Example Product/Catalog |
|---|---|---|
| Alt-R S.p. HiFi Cas9 Nuclease V3 | High-fidelity nuclease to minimize off-target effects. | IDT #108105559 [62] |
| Modified ssODN Donor | Repair template with blocking mutations and phosphorothioate modifications. | Ultramer DNA Oligo (IDT) [63] |
| p53 shRNA Plasmid | Knocks down p53 to inhibit apoptosis and improve editing efficiency. | [62] |
| CloneR | Supplement that improves survival of dissociated iPSCs. | STEMCELL Technologies #05888 [62] |
| Alt-R HDR Enhancer | Small molecule that biases repair toward HDR. | Integrated DNA Technologies [63] |
| Electroporation/Nucleofection System | Device for efficient intracellular delivery of RNP complexes. | e.g., Lonza 4D-Nucleofector [62] |
Step-by-Step Workflow
- iPSC Culture: Maintain iPSCs in feeder-free conditions (e.g., on Matrigel) in media such as mTeSR Plus or Stemflex. Culture until cells are 80-90% confluent in a 6-well plate [62].
- Reagent Preparation:
- RNP Complex: Combine 0.6 µM crRNA (with tracrRNA) with 0.85 µg/µL of HiFi Cas9 protein. Incubate at room temperature for 20-30 minutes.
- Final Mix: To the RNP complex, add 0.5 µg of a GFP reporter plasmid (for tracking transfection efficiency), 5 µM of the modified ssODN donor template, and 1 µg of p53 shRNA plasmid [62].
- Nucleofection:
- Change the cell culture media to a "cloning media" (e.g., Stemflex supplemented with 1% RevitaCell and 10% CloneR) one hour before nucleofection.
- Dissociate the cells using Accutase for 4-5 minutes.
- Resuspend 1x10^6 cells in the nucleofection solution containing the prepared RNP/donor mix.
- Perform nucleofection using a predefined program (e.g., CA-137 for Lonza 4D-Nucleofector) [62].
- Post-Transfection Recovery:
- Immediately after nucleofection, transfer the cells to a plate pre-coated with Matrigel and containing the pre-warmed cloning media.
- After 48 hours, replace the cloning media with standard iPSC culture media.
- Allow the edited cell pool to expand for 5-7 days before analysis [62].
- Validation and Quality Control:
- HDR Efficiency: Assess initial editing efficiency in the bulk cell population using T7EI assay or NGS-based methods like ICE analysis (Synthego) or rhAmpSeq (IDT) [65] [62].
- Single-Cell Cloning: Isolate single cells to generate clonal lines. Screen these clones via PCR and Sanger sequencing to identify those with the correct HDR edit.
- Safety Validation: Perform karyotyping (e.g., G-banding) to confirm genomic integrity. Conduct off-target analysis using targeted NGS or whole-genome sequencing on final clones [59] [62].
Achieving high HDR rates in CRISPR-iPSC workflows is challenging but attainable through a multi-faceted approach. Success hinges on the synergistic optimization of donor template design, cellular state manipulation, and precise CRISPR system engineering. By implementing the detailed strategies and protocols outlined in this guide—such as using modified donors, suppressing p53, and adding pro-survival factors—researchers can dramatically improve the efficiency of precise genome editing. This enables the rapid generation of high-quality isogenic iPSC lines, thereby accelerating disease modeling, drug discovery, and the development of regenerative therapies.
Monitoring and Preserving Genomic and Epigenetic Integrity
Troubleshooting Guide: FAQs for iPSC Researchers
What are the most common genomic instability issues in iPSCs, and how can I detect them?
Human pluripotent stem cells (hPSCs) can acquire recurrent, non-random genetic abnormalities during culture. The most common chromosomes affected are 1, 8, 10, 12, 17, 18, 20, and X [66]. These changes often confer a growth advantage, leading to their expansion in culture. Furthermore, exome sequencing has revealed recurrent acquisition of dominant negative P53 mutations [66].
The following table summarizes key detection methods and their limitations [66]:
| Method | Detects | Key Limitation |
|---|---|---|
| G-banding Karyotyping | Gross chromosomal abnormalities | Detection limit ~5-20% mosaicism |
| FISH (Fluorescence in situ Hybridization) | Specific, known abnormalities (e.g., trisomy 12) | Only tests for pre-specified anomalies; detection limit ~5-20% |
| Digital Droplet PCR (ddPCR) | Specific, known copy number variations | Highly sensitive for known targets but not a broad screen |
Recommendation: Employ a combination of methods for comprehensive screening. Be aware that a culture deemed "karyotypically normal" may harbor low-level mosaicism undetectable by routine analysis [66].
How can my cell culture practices minimize the appearance of genetic variants?
Specific culture conditions can significantly impact genetic and epigenetic stability. Research indicates that single-cell passaging and feeder-free conditions are associated with a higher chance of cytogenetic changes compared to bulk passaging methods [66]. Genetically variant cells often bypass the growth bottlenecks that restrict karyotypically normal cells, giving them a selective advantage [66].
Mitigation Strategies:
- Limit Single-Cell Passaging: Use bulk passaging methods (e.g., using small clumps of cells) where possible to reduce cell death and selective pressure.
- Monitor Growth Rates: Be cautious of cultures that suddenly exhibit enhanced growth rates and plating efficiencies, as this can indicate the emergence of adapted, potentially abnormal cells [66].
- Characterize Cultures Regularly: Perform genetic characterization at early and late passages to monitor for the appearance of variants.
What are the major epigenetic concerns during reprogramming and culture, and how can I ensure data quality?
Reprogramming involves massive epigenetic remodeling, and incomplete resetting can result in aberrant DNA methylation or histone modification patterns that reflect the cell of origin or the reprogramming process itself [67]. For downstream assays like RNA-seq or ATAC-seq, poor sample quality can severely skew results and mask true biological signals.
The table below outlines key quality control metrics for common epigenomic and transcriptomic assays [67]:
| Assay | Critical QC Metric | Passing Threshold | Mitigation for Failed QC |
|---|---|---|---|
| ATAC-seq | TSS (Transcription Start Site) Enrichment | ≥ 6 | Pre-treat cells with DNase; sort viable cells; indicates poor sample prep. |
| ATAC-seq | Fraction of Reads in Peaks (FRIP) | ≥ 0.1 | Repeat transposition step; ensure high cell viability. |
| Bulk RNA-seq | Sequencing Depth | ≥ 25M reads | Remove sources of sample degradation; repeat library prep. |
| MethylationEPIC | Percentage of Failed Probes | ≤ 1% | Ensure optimal input DNA for bisulfite conversion kit. |
| scRNA-seq | Median Unique Molecular Identifiers (UMIs) per Cell | Assay-dependent | Increase initial cell input; concentrate sample. |
General Best Practice: Avoid sample degradation at any step, as PCR amplification during library construction will only occur on non-degraded sequences, creating a false representation of the original sample [67].
Experimental Protocols for Integrity Assessment
Protocol 1: Quick and Efficient CRISPR-Cas9 Genome Editing in iPSCs
This protocol allows for rapid genome editing in iPSCs using electroporation of a plasmid-based CRISPR/Cas9 system, minimizing the time Cas9 is expressed and reducing the risk of off-target effects and genomic integration [68].
Workflow Overview:
Detailed Methodology [68]:
- sgRNA and Plasmid Design: Design your sgRNA using online tools (e.g., crisprscan.org). Clone the annealed oligos into the BbsI site of the PX459V2.0-eSpCas9(1.1) plasmid (Addgene #108292), which contains a puromycin resistance marker.
- Cell Culture: Culture human iPSCs on Matrigel-coated plates in StemFlex medium. Use cells at ~80% confluence for electroporation.
- Electroporation: Use the Neon Transfection System. Transfert 1 x 10^6 iPSCs with 5 μg of the constructed CRISPR plasmid and 0.5 μg of a GFP plasmid (as a tracer) using the following condition: 1200 V, 30 ms, 1 pulse.
- Selection and Recovery: 16 hours after electroporation, replace the medium with puromycin-containing medium (10 μg/mL). After 24 hours of selection, return to normal culture medium and allow cells to recover and form colonies for 4 days.
- Clonal Isolation: Use sterile cloning disks to pick single-cell clones and transfer them to a 48-well plate for expansion.
- Validation: Screen expanded clones by PCR, sequencing, and functional assays (e.g., Western blot). Confirm the absence of Cas9 plasmid integration by PCR on genomic DNA.
Protocol 2: Enhancing Reprogramming Efficiency and Safety with Small Molecules
Using small molecules to replace reprogramming factors can enhance efficiency and safety by reducing the reliance on genetic manipulation [4] [69].
Key Small Molecule Applications:
- Replacing Transcription Factors: The small molecule RepSox (a TGF-β pathway inhibitor) can replace Sox2 in the reprogramming cocktail [4].
- Improving Efficiency: Combining small molecules can significantly boost reprogramming yields. For example, combining 8-Bromoadenosine 3′,5′-cyclic monophosphate (8-Br-cAMP) with the histone deacetylase inhibitor Valproic Acid (VPA) increased human fibroblast reprogramming efficiency by up to 6.5-fold [4].
- Specific Examples:
- To reprogram mouse embryonic fibroblasts (MEFs) transduced with only Oct4 and Klf4, treat with 10 μM CHIR99021 (a GSK-3 inhibitor) for four weeks [69].
- To reprogram certain human breast cancer cells, use a combination of rapamycin (an mTOR inhibitor) and 2 μM Y-27632 (a ROCK inhibitor) for seven days [69].
The Scientist's Toolkit: Essential Reagents for Genomic and Epigenetic Integrity
| Reagent / Tool | Function | Key Consideration |
|---|---|---|
| Y-27632 (ROCK inhibitor) | Improves survival of single iPSCs during passaging and freezing/thawing. | Reduces apoptosis but does not address the underlying selective pressure for genetic variants [69]. |
| CHIR99021 (GSK-3 inhibitor) | Enhances reprogramming; maintains self-renewal. | Can be used to reduce the number of required transcription factors (e.g., substitute for Sox2) [69]. |
| Valproic Acid (VPA) | Histone deacetylase inhibitor; improves reprogramming efficiency. | Works synergistically with other molecules like 8-Br-cAMP [4]. |
| Puromycin | Antibiotic for selection of transfected cells. | Used in CRISPR protocols to select for cells that have taken up the Cas9/sgRNA plasmid [68]. |
| Matrigel | Basement membrane matrix for feeder-free culture. | Associated with a higher risk of cytogenetic changes compared to feeder layers; requires careful monitoring [66] [68]. |
| CRISPR/Cas9 System | For precise genome editing in iPSCs. | Plasmid-based, transient delivery methods minimize the risk of Cas9 genomic integration [68]. |
Core Integrity Monitoring Pathway
The following diagram summarizes the core strategy for monitoring and preserving genomic and epigenetic integrity in iPSC cultures, integrating concepts from the troubleshooting guide and protocols.
Scalable Manufacturing and Automation for Clinical-Grade iPSCs
Frequently Asked Questions (FAQs) on iPSC Reprogramming and Manufacturing
Q1: What are the major bottlenecks in scaling up iPSC manufacturing for clinical trials?
Scaling iPSC manufacturing presents significant technical and financial challenges. A primary bottleneck is the high cost and labor-intensive nature of current processes, which are difficult to scale for wider patient access [70]. Furthermore, achieving consistent quality is hampered by high variability in starting materials and the fact that many manufacturing processes are not adaptive enough to normalize these differences [70]. There is also a shortage of specialized professionals capable of operating within complex GMP (Good Manufacturing Practice) environments [70]. Finally, a major hurdle is understanding how manufacturing conditions—such as expansion protocols and culture conditions—directly impact the therapeutic efficacy, persistence, and functionality of the final cell product [70].
Q2: How can automation address the challenges of clinical-grade iPSC production?
Automation is a strategic enabler for overcoming key challenges in iPSC production. It directly enhances process reproducibility and robustness by reducing human error and variability, which is crucial for products with complex living cells [71]. It helps manage the high costs of manufacturing by reducing long-term operational costs and labor inputs [70] [71]. Automated systems, especially closed systems, also contribute to better control over the culture environment, ensuring tight monitoring and maintenance of critical process parameters [72]. This is vital for ensuring batch-to-batch consistency and product quality.
Q3: What are the critical quality control checks for a clinical-grade iPSC line?
Ensuring the quality of a clinical-grade iPSC line involves a multi-faceted approach. Key checks are summarized in the table below.
Table 1: Critical Quality Control Checks for Clinical-Grade iPSCs
| Quality Attribute | Key Checks & Assays | Purpose & Importance |
|---|---|---|
| Pluripotency & Identity | Expression of surface markers (CD73, CD90, CD105); lack of hematopoietic markers (CD45, CD34); demonstration of trilineage differentiation (osteocytes, adipocytes, chondrocytes) [73]. | Verifies the cell population is a true MSC and possesses the required differentiation potential. |
| Genomic Integrity | Karyotyping; testing for genomic stability; screening for acquired mutations [74]. | Ensures genetic stability and identifies variants that could pose safety risks, such as tumorigenicity. |
| Safety Profile | Sterility, mycoplasma, and endotoxin testing; tumorigenicity assays (e.g., in vivo teratoma formation or in vitro alternatives) [73] [74]. | Confirms the product is free from microbial contamination and has an acceptable tumorigenic risk profile. |
| Viability & Potency | Cell viability and morphology; functional potency assays tailored to the target cell type [74]. | Assesses cell health and the biological functional capacity of the cells, which is a key indicator of clinical efficacy. |
Q4: What is the difference between research-grade and GMP-grade cells and materials?
The distinction lies in the rigor of documentation, testing, and the environment in which they are produced. For cells, the process and quality control for research-grade and GMP-grade may be similar, but GMP-grade manufacturing occurs within a B-grade clean room and includes more extensive testing, such as for chromosomal stability [73]. For raw materials, terms like "GMP-grade" indicate compliance with manufacturing standards, but developers must still assess each material for its origin, purity, and safety for clinical use. There is often a need for greater transparency and standardized nomenclature from suppliers [74].
Troubleshooting Common iPSC Reprogramming and Manufacturing Issues
Problem 1: Low Reprogramming Efficiency
Potential Causes and Solutions:
- Cause: Suboptimal Transcription Factor Delivery or Ratio. The efficiency and quality of reprogramming are highly dependent on the delivery method and the precise ratios of reprogramming factors [5].
- Solution: Utilize optimized factor combinations. While the original Yamanaka factors (OSKM) are foundational, research shows that enhancing retinoic acid signaling by co-expressing RAR-γ (Rarg) and Lrh-1 with OSKM can dramatically accelerate reprogramming and improve the quality of iPSC colonies [75]. Consider non-integrating delivery methods (e.g., episomal plasmids, mRNA) for improved clinical safety [76].
- Solution: Employ engineered biomaterials. Biomaterials with tailored biophysical properties (e.g., specific matrix stiffness, surface topography) can guide cell fate transitions and significantly enhance reprogramming efficiency by modulating gene expression and epigenetic states [23].
Problem 2: High Batch-to-Batch Variability in Final Product
Potential Causes and Solutions:
- Cause: Inconsistency in Raw Materials. Variability in growth factors, media, and reagents can introduce inconsistencies that compromise clinical outcomes [74].
- Solution: Implement a rigorous raw material qualification strategy. This includes early assessment and control in material selection, parallel testing of GMP versions, and qualifying multiple batches to demonstrate manufacturing consistency [74].
- Cause: Manual and Open Process Steps. Highly manual processes are a primary source of unwanted variability [71].
- Solution: Integrate automation and closed systems. Automated manufacturing platforms standardize processes, reduce human intervention, and enable real-time monitoring, which is essential for maintaining batch-to-batch consistency [70] [72] [71]. Adopting a "fit-for-purpose" manufacturing model with patient-adjacent, regionalized manufacturing can also better address the variability inherent in patient-specific supply chains [70].
Problem 3: Difficulties in Scaling Up from Research to Clinical-Commercial Scale
Potential Causes and Solutions:
- Cause: Legacy Manufacturing Processes. Complex, resource-intensive, and difficult-to-scale legacy processes create a bottleneck that inflates costs and limits patient access [70].
- Solution: Plan for scale-up early in development. Delaying automation until late stages can lead to major bottlenecks. A strategic, early-stage plan for automation lays a strong foundation for future growth and demonstrates commercial viability to investors [74] [71].
- Solution: Leverage scalable technologies like bioreactors. Transitioning from 2D culture flasks to 3D bioreactor systems is essential for producing the large cell numbers required for clinical trials and commercial therapy [77]. These systems offer better control and monitoring capabilities.
Key Signaling Pathways in Cell Reprogramming
The following diagram illustrates the key molecular mechanisms and signaling pathways that are critical during the cell reprogramming process, particularly in response to engineered biomaterials.
Key Signaling Pathways in Reprogramming
Standardized Workflow for Scalable iPSC Generation
This workflow outlines a modern, scalable process for generating clinical-grade iPSCs, integrating automation and quality control from the start.
Scalable Clinical-Grade iPSC Workflow
Research Reagent Solutions for iPSC Reprogramming
The following table details essential materials and their functions for setting up a robust iPSC reprogramming and manufacturing workflow.
Table 2: Key Research Reagents for iPSC Reprogramming and Culture
| Reagent / Material | Function & Application | Key Considerations for Scalability |
|---|---|---|
| GMP-Grade Reprogramming Factors | Proteins or mRNAs for non-integrating reprogramming (e.g., OCT4, SOX2, KLF4, c-MYC) [76]. | Ensure xeno-free production and documented traceability for regulatory compliance [74]. |
| Chemically Defined Culture Medium | Supports iPSC expansion and maintenance without animal sera [73]. | Scalable production format; batch-to-batch consistency is critical for process reproducibility [74]. |
| Matrix Stiffness-Tunable Hydrogels | 3D biomaterial scaffolds that provide biophysical cues to enhance reprogramming efficiency and guide cell fate [23]. | Compatibility with closed-system bioreactors and automation for scalable 3D culture. |
| Closed-Automated Bioprocessing System | Integrated equipment for automated cell culture, expansion, and differentiation in a closed environment [72] [77]. | Reduces manual labor and variability; essential for scaling up and ensuring GMP compliance [71]. |
Detailed Experimental Protocol: Enhancing Reprogramming with RAR-γ and Lrh-1
This protocol is based on a study demonstrating that co-expression of Rarg and Lrh-1 with the Yamanaka factors enables rapid and efficient reprogramming towards ground-state pluripotency [75].
Objective: To rapidly generate high-quality mouse iPSC colonies from embryonic fibroblasts (MEFs) using a six-factor combination.
Materials:
- Cells: MEFs isolated from Oct4-GFP transgenic reporter mice.
- Vectors: piggyBac (PB) transposon vectors PB-CAG-OCKS (carrying Oct4, c-Myc, Klf4, Sox2) and PB-CAG-RL (carrying Rarg, Lrh-1).
- Reagents: Transfection reagent, PB transposase expression plasmid, mouse iPSC/ESC culture medium.
Methodology:
- Cell Seeding: Plate Oct4-GFP MEFs in appropriate culture vessels and incubate until they reach 70-80% confluency.
- Co-transfection: Co-transfect the MEFs with the PB-CAG-OCKS and PB-CAG-RL vectors, along with the plasmid transiently expressing PB transposase.
- Culture and Monitoring:
- After transfection, culture the cells in mouse iPSC/ESC medium.
- Monitor the cultures daily for the appearance of compact, ES-like colonies under a bright-field microscope.
- Simultaneously, monitor for activation of the endogenous Oct4 locus using GFP fluorescence.
- Observation and Analysis:
- Key Outcome: With the six-factor combination (OCKS + RL), rapidly emerging GFP-positive colonies (indicating true iPSCs with activated endogenous pluripotency network) can be observed as early as 4 days post-transfection.
- Compare the efficiency and speed with a control transfected with only the four factors (PB-CAG-OCKS).
- Colony Picking and Expansion: Pick individual GFP-positive colonies and expand them to establish stable iPSC lines.
Benchmarking Success: Quality Control, Safety, and Translational Potential
Frequently Asked Questions (FAQs)
Pluripotency and Characterization
Q1: What are the essential quality control checks for a new human induced pluripotent stem cell (hiPSC) line? A new hiPSC line should undergo a panel of quality control checks to confirm its identity, pluripotency, and safety before use in downstream applications. The essential checks are summarized in the table below.
Table 1: Essential Quality Control Checks for a New hiPSC Line
| Test Category | Specific Test | Method(s) | Acceptance Criteria |
|---|---|---|---|
| Pluripotency | Expression of Pluripotency Markers | Immunocytochemistry for OCT3/4, SOX2, NANOG [2] | >90% expression of key markers [78] |
| Trilineage Differentiation Potential | Directed differentiation into endoderm, mesoderm, ectoderm (e.g., using a trilineage differentiation kit) [78] | Successful generation of cells from all three germ layers | |
| Genetic Integrity | Karyotype Analysis | G-banding or equivalent [20] | Normal karyotype without major abnormalities |
| Genetic Mutations | Copy Number Variant (CNV) analysis, Whole Genome Sequencing [20] | Absence of clinically significant mutations acquired during reprogramming | |
| Identity | Short Tandem Repeat (STR) Profiling | PCR-based STR analysis [20] | Matches the parental somatic cell line |
| Sterility | Mycoplasma Testing | PCR or culture-based detection [20] | Negative for mycoplasma contamination |
Q2: My hiPSC cultures are showing excessive spontaneous differentiation (>20%). What could be the cause and how can I fix it? Excessive differentiation often stems from suboptimal culture conditions or handling. Below is a troubleshooting guide for this common issue.
Table 2: Troubleshooting Excessive Spontaneous Differentiation in hiPSC Cultures
| Potential Cause | Recommended Action |
|---|---|
| Old or Improper Medium | Ensure complete culture medium is less than 2 weeks old when stored at 2-8°C [39]. |
| Overgrown Colonies | Passage cultures when colonies are large and compact but before the centers become overly dense and begin to differentiate [39]. |
| Prolonged Time Outside Incubator | Minimize the time culture plates are out of the incubator to less than 15 minutes at a time [39]. |
| High Colony Density | Decrease the colony density by plating fewer cell aggregates during passaging [39]. |
| Incomplete Removal of Differentiated Areas | Manually remove areas of differentiation using a pipette tip or scraping prior to passaging [39] [79]. |
Potency Assay Development
Q3: What is a "matrix approach" to potency assays for cell therapies, and why is it necessary? For complex biological products like iPSC-derived therapies, a single potency assay is often insufficient. The matrix approach involves using two or more complementary assays that together reflect the product's critical mechanism of action (MoA) [80] [81]. This is necessary because iPSC-derived therapies often have multiple modes of action that may not be fully captured by one test. Regulators, including the FDA, advocate for this approach to ensure a comprehensive assessment of product quality [80].
Q4: What are the major challenges in developing potency assays for iPSC-derived therapies, and how can they be overcome? Developing robust potency assays is one of the most significant hurdles in translational iPSC research. Key challenges and mitigation strategies include:
- Product Complexity: iPSC-derived products are living entities with multiple MoAs. Solution: Adopt a matrix approach early in development, focusing on assays reflective of key MoAs [81].
- Lack of Reference Standards: Unlike traditional drugs, individualized therapies often lack a universal reference standard. Solution: Use a well-characterized in-house assay control to monitor performance and bridge different product lots [81].
- Inherent Variability: Donor-to-donor variability in starting materials can confound assay results. Solution: Implement rigorous controls to distinguish between true product variability and assay variability [81].
- Need for Rapid Release: Many cell therapies have short shelf lives. Solution: Develop a streamlined testing process and, if justified, use surrogate markers for release while longer functional assays are ongoing [81].
Tumorigenicity Assessment
Q5: What methods are available to assess the tumorigenic risk of an iPSC-derived therapeutic product? The gold standard for tumorigenicity assessment is the in vivo tumor formation assay in immunocompromised mice (e.g., NSG mice), with monitoring recommended for 4-7 months [82]. However, this is lengthy and expensive. Several in vitro methods offer faster turnaround and are suitable for batch-to-batch screening.
Table 3: Comparison of Tumorigenicity Assessment Methods for iPSC-Derived Products
| Method | Principle | Sensitivity | Turnaround Time | Key Considerations |
|---|---|---|---|---|
| In Vivo Animal Model [82] | Injection of cells into immunocompromised mice to monitor for tumor formation. | Can detect 100 - 10,000 undifferentiated cells per million [82]. | 4 - 7 months [82] | Considered the gold standard but slow and costly. |
| Soft Agar Colony Formation [82] | Measures anchorage-independent growth, a hallmark of transformation. | Varies based on protocol. | 2 - 4 weeks | A classic in vitro method for assessing malignant potential. |
| Flow Cytometry [82] | Detects and quantifies specific cell surface markers (e.g., TRA-1-60, SSEA-4) on residual undifferentiated iPSCs. | High (can approach 0.001%) [82]. | 1 - 2 days | Fast and quantitative, but only detects known markers. |
| PCR (qRT-PCR or ddPCR) [82] | Measures the expression of pluripotency-associated genes (e.g., OCT4, NANOG). | Very high (can detect single transcripts). | 1 - 2 days | Highly sensitive, but does not confirm the presence of live, tumorigenic cells. |
| Microfluidics [82] | Captures and analyzes single cells or small clusters in miniaturized chambers. | Potentially very high (single-cell resolution). | 1 - 2 days | Emerging technology; allows for high-throughput screening. |
Q6: What is the threshold of undifferentiated cells that poses a tumorigenic risk? The exact threshold is not definitively established, but studies indicate that the injection of as few as 100 undifferentiated ESCs spiked into a population of differentiated cells can form teratomas in immunocompromised mice [82]. Therefore, a tumorigenicity assay should aim for a high sensitivity, ideally able to detect 100 undifferentiated cells per million (0.01%) or fewer [82].
Troubleshooting Guides
Troubleshooting hiPSC Reprogramming Efficiency
Problem: Low reprogramming efficiency using non-integrating methods.
- Potential Cause 1: Source cell type. The type of somatic cell being reprogrammed can impact efficiency.
- Potential Cause 2: Critical starting cell quality.
- Solution: Ensure the somatic cells are healthy, proliferating, and free of contamination before initiating reprogramming.
- Potential Cause 3: Suboptimal culture conditions post-reprogramming.
- Solution: After transduction/nucleofection, maintain cells in hypoxic conditions (5% O₂) if possible, as it can enhance efficiency [20]. Use high-quality media and matrices. The addition of a ROCK inhibitor (Y-27632) is crucial for enhancing the survival of single cells and newly emerging iPSC colonies [20] [79].
Troubleshooting hiPSC-Derived Cardiomyocyte Differentiation
Problem: No beating cardiomyocytes observed by Day 15 of differentiation.
- Potential Cause 1: Starting hiPSCs were not of high quality or were too differentiated.
- Solution: Always start with high-quality hiPSCs (e.g., >90% expression of OCT3/4, TRA-1-60) and remove any differentiated areas before initiating the protocol [78]. Use low-passage cells and avoid letting cultures become over-confluent during maintenance.
- Potential Cause 2: Cells did not reach sufficient confluency at the start of differentiation.
- Solution: It is critical that hiPSCs reach >95% confluency within 48 hours after seeding as single cells before starting the differentiation protocol [78]. Titrate the seeding density for your specific cell line.
- Potential Cause 3: Use of an inappropriate extracellular matrix.
- Solution: The differentiation protocol may require a specific matrix. For example, some cardiomyocyte differentiation kits perform best with Corning Matrigel, and switching from another matrix (e.g., Vitronectin) may require a transition period [78].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for hiPSC Reprogramming and Quality Control
| Reagent / Kit | Function | Example Use Case |
|---|---|---|
| Sendai Virus Vectors [20] [79] | Non-integrating viral delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC). | Reprogramming somatic cells (e.g., fibroblasts, PBMCs) into hiPSCs with high efficiency. |
| Episomal Vectors [20] [83] | Non-integrating plasmid-based delivery of reprogramming factors. | Integration-free reprogramming, often used for clinical applications. |
| ROCK Inhibitor (Y-27632) [20] [79] | Improves survival of single hiPSCs and cryopreserved cells. | Added to culture medium during passaging, thawing, and after reprogramming to enhance cell survival. |
| Gentle Cell Dissociation Reagent [39] [78] | Enzyme-free solution for dissociating hiPSC colonies into small clusters. | Used for routine passaging of hiPSCs while maintaining high viability. |
| Trilineage Differentiation Kit [78] | Directed differentiation of hiPSCs into endoderm, mesoderm, and ectoderm lineages. | Functional validation of hiPSC pluripotency during quality control. |
| hPSC Genetic Analysis Kit [78] | Detects common genetic abnormalities in hiPSCs. | Routine monitoring of genomic stability in master cell banks. |
Experimental Workflows and Pathways
Workflow 1: Quality Control Pipeline for a New hiPSC Line
This diagram outlines the key steps and decision points in establishing and qualifying a new hiPSC line for research or therapeutic development.
Pathway 2: Molecular Mechanisms of Somatic Cell Reprogramming
This diagram illustrates the key molecular and cellular stages a somatic cell undergoes during reprogramming to pluripotency.
Workflow 3: The Matrix Approach to Potency Assay Development
This diagram visualizes the multi-faceted strategy for developing a robust potency testing matrix for an iPSC-derived cell therapy product.
Analyzing Donor-Specific Genetic and Epigenetic Variation in iPSC Lines
Within the broader goal of improving reprogramming efficiency in somatic cell to iPSC research, a significant hurdle is the inherent variability between individual iPSC lines. A primary source of this heterogeneity is the genetic and epigenetic legacy of the donor somatic cell. This technical support center provides targeted guidance to help researchers identify, troubleshoot, and mitigate the challenges posed by donor-specific variation in their experimental systems.
FAQ: Core Concepts
1. What is the fundamental difference between genetic and epigenetic variation in this context?
- Genetic Variation refers to differences in the primary DNA sequence itself (e.g., single nucleotide polymorphisms (SNPs), insertions, deletions) that are inherited from the donor and are present in all their cells [84]. These can influence disease predisposition and general cellular functions.
- Epigenetic Variation involves heritable changes in gene expression that do not alter the DNA sequence, including DNA methylation, histone modifications, and chromatin accessibility [85] [86]. The somatic cell from which an iPSC is reprogrammed carries an epigenetic "memory" of its original tissue type, which can be partially retained in the resulting iPSC line [85].
2. Why does donor-specific variation matter for my iPSC experiments? Donor-specific variation can directly impact key aspects of your research:
- Reprogramming Efficiency: The epigenetic landscape of the starting somatic cell influences the accessibility of pluripotency gene promoters to reprogramming factors like OSKM (Oct4, Sox2, Klf4, c-Myc), thereby affecting how easily it can be reprogrammed [87] [85].
- Differentiation Bias: iPSCs may retain an epigenetic memory of their somatic cell of origin, leading to a preferential differentiation tendency back into that lineage [85]. This can skew results in disease modeling or when generating specific cell types.
- Experimental Reproducibility: Significant genetic and epigenetic differences between donor lines can confound results, making it difficult to distinguish true disease-specific phenotypes from background donor variation [32].
3. What are the main sources of genetic instability in iPSC lines? The primary sources are the original donor genome and potential mutations acquired during the reprogramming process or subsequent cell culture. Some reprogramming methods, particularly those using integrating viruses, carry a risk of insertional mutagenesis that can disrupt tumor suppressor genes [88]. Furthermore, the rapid proliferation of iPSCs can select for clones with spontaneous mutations that confer a growth advantage.
Troubleshooting Guides
Problem: Low Reprogramming Efficiency
Potential Cause: The epigenetic state of the donor somatic cell is restrictive, preventing the binding of reprogramming factors to key pluripotency gene promoters [87] [85].
Solutions:
- Optimize the Reprogramming Method: Use non-integrating methods (e.g., episomal vectors, mRNA reprogramming) to reduce genomic disruption and improve the likelihood of generating solid iPSC clones [88].
- Incorporate Small Molecules: Supplement the reprogramming cocktail with small molecules that modulate epigenetic barriers. For instance, inhibitors of DNA methyltransferases (DNMTs) can promote a more open chromatin state at pluripotency loci like OCT4 and NANOG, facilitating their activation [86].
- Select an Optimal Donor Cell Type: If possible, choose a starting cell type with a more open chromatin configuration, as some cell types reprogram more efficiently than others [85].
Problem: Inconsistent Differentiation Outcomes Between iPSC Lines
Potential Cause: Residual epigenetic memory from the donor somatic cell or genetic differences between donors are causing lineage-specific biases [85] [32].
Solutions:
- Extended Passaging: Culture the iPSCs for multiple passages. In some cases, particularly with murine iPSCs, epigenetic marks can be gradually reset over time, diminishing the lineage bias [85].
- Use Clones with Minimal Memory: Select iPSC clones that have been rigorously characterized to have minimal residual epigenetic memory for your target differentiation lineage.
- Leverage Isogenic Controls: For genetic variants, use genome editing (e.g., CRISPR/Cas9) to correct or introduce a specific mutation in a control iPSC line, creating an isogenic pair. This allows you to study the mutation's effect against an identical genetic background [84].
Problem: Poor Performance in Disease Modeling or Drug Screening
Potential Cause: iPSC-derived cells exhibit an immature, fetal-like phenotype rather than an adult phenotype, limiting their relevance for modeling late-onset diseases [32]. Furthermore, donor variability can affect the response to drug compounds.
Solutions:
- Screen Multiple Clones: Use several iPSC clones per donor to account for clonal variation and identify the most functionally relevant model for your disease [32].
- Improve Differentiation Protocols: Develop or adopt protocols that include maturation steps to push the cells toward a more adult-like state.
- Utilize HLA and KIR Genotyping: For studies where immune response is relevant, select donor lines with specific HLA (human leukocyte antigen) and KIR (killer-cell immunoglobulin-like receptor) profiles to control for immune compatibility [32].
The tables below consolidate key quantitative information from recent studies to aid in experimental planning and benchmarking.
Table 1: Comparison of Non-Integrating iPSC Reprogramming Methods
| Method | Reported Advantages | Reported Challenges / Notes |
|---|---|---|
| Episomal Vectors | - Rapid transgene clearance (∼17-21 days) [88]- Deemed clinically ideal by Global Alliance for iPSC Therapies [88] | - Low base efficiency (∼0.0006%) [88]- Often requires p53 suppression or oncogenes (c-Myc/Lin28) for colony formation [88] |
| Sendai Vectors | - Robust and popular method [88] | - Requires extensive passaging to dilute viral components [88]- Requires careful screening for residual viral elements [88] |
| Self-Replicating RNA | - Mimics cellular mRNA, no DNA intermediate [88] | - Requires co-agents to suppress immune response [88]- Retains viral RNA for several passages [88] |
| mRNA Reprogramming | - Non-integrating and safe [88] [32] | - Laborious (requires daily transfections for up to 17 days) [88]- Can trigger interferon response [88] |
Table 2: High-Efficiency CRISPR Genome Editing in iPSCs [84]
| Experimental Condition | Homology-Directed Recombination (HDR) Efficiency | Fold Increase vs. Base Protocol |
|---|---|---|
| Base Protocol | 2.8% | (Baseline) |
| + p53 shRNA | 30.8% | 11x |
| + p53 shRNA + Pro-survival supplements (CloneR, etc.) | 59.5% - >90% (in some clones) | 21x |
Detailed Experimental Protocols
Protocol 1: High-Efficiency Precision Genome Editing in iPSCs
Based on the method by [84] for introducing point mutations with high HDR efficiency.
Key Reagents:
- Cell Line: Human iPSCs maintained in feeder-free conditions (e.g., on Matrigel) with mTeSR Plus or Stemflex medium.
- Nucleofection System: (e.g., Lonza 4D-Nucleofector)
- CRISPR Components: Alt-R S.p. HiFi Cas9 Nuclease V3, target-specific guide RNA (IDT).
- Repair Template: Single-stranded oligonucleotide (ssODN) with desired mutation and silent mutations in the PAM site to prevent re-cutting.
- Plasmid: pCXLE-hOCT3/4-shp53-F (Addgene #27077) for transient p53 knockdown.
- Pro-survival Supplements: CloneR (STEMCELL Technologies), RevitaCell (Gibco).
Workflow:
- Culture and Preparation: Maintain iPSCs in high-quality condition. One hour before nucleofection, change the medium to a "cloning media" composed of Stemflex with 1% RevitaCell and 10% CloneR.
- RNP Complex Formation: Combine 0.6 µM guide RNA with 0.85 µg/µL of HiFi Cas9 protein. Incubate at room temperature for 20-30 minutes to form the ribonucleoprotein (RNP) complex.
- Nucleofection Mixture: For one reaction, combine the pre-formed RNP complex with 0.5 µg of a GFP reporter plasmid (e.g., pmaxGFP), 5 µM of ssODN repair template, and 50 ng/µL of the p53 shRNA plasmid.
- Nucleofection: Dissociate iPSCs into single cells using Accutase. Mix 1x10^6 cells with the nucleofection mixture and electroporate using an appropriate stem cell nucleofection program.
- Recovery and Culture: Plate the nucleofected cells immediately into cloning media. Culture for 3-5 days before transitioning to standard medium without pro-survival supplements.
- Clone Isolation and Validation: After 7-10 days, pick individual colonies for expansion. Screen for the desired edit using PCR and sequencing. Karyotype analysis is recommended to confirm genomic stability.
The following diagram illustrates the core workflow and key boosting factors for this protocol:
Protocol 2: Assessing Epigenetic Memory via DNA Methylation Analysis
Based on studies investigating epigenetic resetting during reprogramming [85] [86].
Objective: To evaluate the DNA methylation status at key lineage-specific gene promoters in your iPSC line compared to the donor somatic cell and a reference ESC line.
Methodology:
- Sample Collection: Extract genomic DNA from the donor somatic cells, the derived iPSCs (at early and late passages), and a reference ESC line.
- DNA Methylation Analysis: Perform genome-wide DNA methylation profiling using methods like Whole Genome Bisulfite Sequencing (WGBS) or targeted analysis using bisulfite sequencing PCR.
- Data Analysis:
- Focus on the promoter regions of genes that are highly expressed in the donor somatic cell type.
- Identify CpG sites that are highly methylated in the donor cell. Successful epigenetic reprogramming should lead to significant demethylation of these sites in the iPSCs, making their profile similar to the ESC reference.
- Persistent high methylation at these loci in the iPSCs indicates residual epigenetic memory.
- Functional Correlation: Correlate the methylation findings with gene expression data (e.g., from RNA-seq) and functional differentiation assays toward the lineage of the donor cell versus other lineages.
The relationship between epigenetic states and reprogramming is summarized below:
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Managing Donor Variation
| Reagent / Tool | Primary Function | Example Use-Case |
|---|---|---|
| p53 shRNA Plasmid | Transient inhibition of p53 pathway | Boosts survival and HDR efficiency during CRISPR genome editing [84]. |
| Pro-survival Supplements (CloneR, ROCKi) | Inhibits apoptosis in dissociated cells | Improves cell recovery after single-cell cloning or nucleofection [84]. |
| Non-Integrating Reprogramming Kits (e.g., mRNA, Episomal) | Generates footprint-free iPSCs | Produces clinical-grade iPSCs without vector integration, reducing genetic variability [88] [32]. |
| DNMT Inhibitors | Reduces DNA methylation | Added during reprogramming to open chromatin and improve efficiency by demethylating pluripotency gene promoters [86]. |
| HLA & KIR Genotyping Services | Determines immune cell receptor profiles | Selects immunologically matched donor lines for cell therapy or transplantation studies [32]. |
Technical Support Center
Troubleshooting Guides
Issue: Low Reprogramming Efficiency
- Problem: The conversion rate of somatic cells to iPSCs is extremely low.
- Solution:
- Optimize Factor Delivery: Ensure high transfection efficiency. If using viral vectors, check viral titer. For non-viral methods like mRNA, confirm the quality and concentration of the nucleic acids [4] [89].
- Use Small Molecule Enhancers: Supplement the culture medium with small molecules known to enhance reprogramming, such as Valproic Acid (VPA) or Sodium Butyrate, which act as histone deacetylase inhibitors. The combination of 8-Br-cAMP with VPA has been shown to increase iPSC generation efficiency by up to 6.5-fold [4].
- Co-delivery of Helper mRNAs: Include mRNAs encoding indirect NHEJ inhibitors (e.g., HDR-Enh01) and anti-apoptotic proteins (e.g., Via-Enh01) during electroporation to improve Homology-Directed Repair (HDR) frequency and cell viability, particularly under GMP-compatible conditions [90].
- Validate Somatic Cell Source: Ensure the starting somatic cells are healthy and at an appropriate passage number. Some cell types, like neural stem cells, may have higher innate reprogramming potential and require fewer factors [4].
Issue: High Cell Death Post-Transfection/Transduction
- Problem: A significant proportion of cells die following the introduction of reprogramming factors.
- Solution:
- Optimize Electroporation Parameters: If using electroporation for mRNA or DNA delivery, systematically test voltage, pulse length, and cell density to find the least cytotoxic conditions [90].
- Mitigate P53-Mediated Toxicity: The DNA damage response during reprogramming can trigger apoptosis. Using a p53 inhibitor or co-delivering anti-apoptotic signals (Via-Enh01) can significantly improve cell survival and engraftment capacity [90].
- Use Gentle Viral Vectors: If using viruses, compare the cytotoxicity of different types. Sendai virus, a non-integrating RNA virus, is often less cytotoxic than integrating viral vectors [91].
Issue: Incomplete Reprogramming or Partially Reprogrammed Cells
- Problem: iPSC colonies fail to fully silence somatic genes or activate the full pluripotency network.
- Solution:
- Extend Reprogramming Timeline: Some somatic cell types require a longer period for complete epigenetic remodeling. Do not pick colonies too early.
- Analyze Pluripotency Markers: Use rigorous validation methods beyond morphology, including immunostaining for core pluripotency transcription factors (OCT4, SOX2, NANOG) and demethylation of pluripotency gene promoters [2].
- Ensure Factor Persistence: For mRNA-based methods, repeated transfections are necessary as the mRNA is transient. Ensure a consistent and sustained delivery of reprogramming factors throughout the critical early phase [4].
Issue: Genomic Instability and Tumorigenic Risk
- Problem: Concerns about insertional mutagenesis from integrating vectors or mutations in oncogenes/tumor suppressors.
- Solution:
- Prioritize Non-Integrating Methods: Use reprogramming methods that do not integrate into the host genome, such as Sendai virus, synthetic mRNA, episomal plasmids, or recombinant proteins [89] [91].
- Substitute Oncogenic Factors: Replace the proto-oncogene c-MYC with its family member L-MYC or other non-tumorigenic factors like GLIS1 or SALL4, which can maintain efficiency while reducing tumorigenic risk [4].
- Rigorous Genomic Quality Control: After iPSC generation, perform whole-genome sequencing or karyotyping to check for chromosomal abnormalities and use PCR to confirm the absence of residual reprogramming vectors [91].
Frequently Asked Questions (FAQs)
Q1: What is the most efficient reprogramming method available today? A1: No single method is universally "best," as the choice involves trade-offs. Viral methods (like Lentivirus) traditionally offer high efficiency, especially for hard-to-transfect cells, but pose safety risks due to genomic integration [4]. Non-integrating methods like mRNA reprogramming now achieve high efficiencies, are highly scalable, and eliminate integration concerns, making them a top choice for clinical applications [89] [92]. Sendai virus is also highly efficient and non-integrating, but requires effort to clear the virus from the final cell product [91]. The highest efficiency is achieved by optimizing the entire system—factor combination, delivery, and culture conditions—rather than relying on a single component [4].
Q2: How can I improve the safety profile of my generated iPSCs for potential clinical use? A2: A multi-pronged approach is key:
- Use Non-Integrating Delivery Systems: mRNA, Sendai virus, and episomal plasmids are preferred to avoid insertional mutagenesis [91].
- Employ Safer Factor Combinations: Use L-MYC instead of c-MYC and consider small molecule substitutes for certain transcription factors (e.g., RepSox for SOX2) [4].
- Implement Chemical Reprogramming: Fully defined small-molecule cocktails can reprogram somatic cells without any genetic material, representing the ultimate in safety, though protocols are still being refined [4] [2].
- Incorporate Suicide Genes: For allogeneic therapies, engineering an inducible caspase-9 (iC9) "suicide switch" allows for the elimination of transplanted cells in case of adverse events, a strategy already being implemented in GMP-compatible protocols [93].
Q3: Why is my reprogramming efficiency so low, and how can I track the process? A3: Low efficiency often stems from suboptimal delivery, poor cell health, or an inhospitable culture environment. Beyond the troubleshooting steps above, you can track the reprogramming process by monitoring the emergence of distinct morphological changes and intermediate cell states. Molecularly, the process involves an early stochastic phase where somatic genes are silenced, followed by a more deterministic activation of the pluripotency network. Single-cell RNA sequencing can be used to track these transcriptional waves and identify where your protocol is failing [2].
Q4: What are the primary cost drivers in iPSC generation, and how can they be managed? A4: The main costs are:
- Reagents and Kits: Commercial reprogramming kits and high-quality culture media can be expensive [89].
- Instrumentation: Automated bioreactors and cell sorters represent a significant capital investment [89] [92].
- Labor: The process is often labor-intensive and requires highly skilled personnel [89].
- Quality Control: Extensive safety testing (e.g., genomic stability, sterility) adds to the cost [91]. Cost management strategies include adopting automation to reduce labor and improve consistency, transitioning to defined, xeno-free culture media to reduce batch variability, and leveraging AI-driven predictive modeling to optimize protocols and reduce costly trial-and-error experiments [89] [92].
Data Presentation
Table 1: Comparison of Key Reprogramming Delivery Systems
| Delivery System | Genetic Material | Genomic Integration? | Relative Efficiency | Relative Safety | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Retro/Lentivirus | DNA | Yes (Permanent) | High | Low | High efficiency for many cell types; stable transgene expression. | High risk of insertional mutagenesis; transgene silencing. |
| Sendai Virus | RNA | No (Transient) | High | Medium-High | High efficiency; non-integrating; broad cell tropism. | Viral clearance required; potential immunogenicity. |
| Episomal Plasmid | DNA | No (Very low risk) | Low-Medium | High | Non-integrating; simple production. | Low efficiency; requires repeated transfections. |
| Synthetic mRNA | RNA | No | High | High | Non-integrating; high efficiency; no viral components. | Requires multiple transfections; can trigger innate immune response. |
| Recombinant Protein | Protein | No | Very Low | Very High | No genetic material; safest profile. | Very low efficiency; difficult to produce and deliver. |
Source: Data synthesized from [4] [91]
Table 2: Cost and Market Analysis Factors
| Factor | Impact on Cost & Accessibility | Market Trend |
|---|---|---|
| Reprogramming Kits & Reagents | Major recurring cost; commercial kits simplify process but are expensive. | Shift towards small molecule & chemical reprogramming kits for cost-efficiency [92]. |
| Automation & Instrumentation | High initial investment (bioreactors, workstations) but lowers long-term per-batch costs. | Automation is a key trend to reduce labor and improve scalability [89]. |
| End-User Market | Pharmaceutical & Biotech companies drive demand for high-throughput, standardized models. | This segment is expected to show the most rapid growth [92]. |
| Regional Dynamics | North America leads in market share; Asia-Pacific is the fastest-growing region due to heavy R&D investment [89] [92]. | Government initiatives in China and South Korea are accelerating market expansion [92]. |
Source: Data synthesized from [89] [92]
Experimental Protocols
Detailed Methodology: TALEN-Mediated Gene Correction with Non-Viral DNA Template
This protocol, adapted from a 2024 Nature Communications study, details an efficient and GMP-compatible method for correcting the sickle cell mutation in Hematopoietic Stem and Progenitor Cells (HSPCs), showcasing a modern non-viral editing approach [90].
1. Design of Editing Components:
- TALEN Construction: Design two TALE nucleases (TALENs) targeting the specific mutation site in exon 1 of the HBB gene (e.g., TALEN-HBBss for mutant, TALEN-HBBββ for wild-type).
- ssODN Repair Template: Design a single-stranded oligodeoxynucleotide (ssODN) repair template containing the corrective sequence (sickle-to-wild type) flanked by homologous arms. Include silent mutations to prevent re-cleavage by the TALENs after correction [90].
2. Optimization of Electroporation Conditions:
- Cell Preparation: Isolate and pre-stimulate mobilized CD34+ HSPCs from a healthy donor or patient in a cytokine-rich, GMP-compatible medium for 24-48 hours.
- mRNA and ssODN Delivery: Electroporate the cells using a clinically relevant system (e.g., Lonza 4D-Nucleofector) with a pre-optimized buffer. Co-deliver three key components as mRNAs:
- TALEN-encoding mRNA (specific dose determined by titration).
- HDR-Enh01 mRNA: An indirect NHEJ inhibitor to boost HDR efficiency and reduce indels.
- Via-Enh01 mRNA: An anti-apoptotic protein to improve cell viability post-electroporation.
- Simultaneously, introduce the ssODN repair template during electroporation [90].
3. Culture and Differentiation:
- After electroporation, culture the cells in a specialized erythroid differentiation medium. This typically involves a multi-phase protocol using cytokines like SCF, EPO, and IL-3 to support the development of mature red blood cells (RBCs) from the edited HSPCs [90].
4. Assessment of Editing Outcomes:
- Efficiency: Use digital droplet PCR (ddPCR) or Amplicon Sequencing (AmpliconSeq) to quantify the percentage of HBB alleles that have been precisely corrected via HDR.
- Phenotypic Rescue: Analyze the resulting RBCs using HPLC or flow cytometry to measure the expression of normal adult hemoglobin (HbA), confirming functional correction of the sickle cell phenotype.
- Safety: Perform transcriptomic analysis (e.g., RNA-seq) to assess the activation of DNA damage response pathways (like P53) and ensure the preservation of long-term hematopoietic stem cell (LT-HSC) signatures, which is critical for successful engraftment [90].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item | Function in Reprogramming/Editing | Example/Specification |
|---|---|---|
| Sendai Virus Vectors | Non-integrating viral vector for delivering OSKM transcripts; high efficiency. | CytoTune-iPS Sendai Reprogramming Kit [91]. |
| mRNA Reprogramming Kit | Synthetic mRNA for OSKM factors; non-integrating, high efficiency. | Requires modified nucleotides to evade immune detection [92]. |
| HDAC Inhibitors (e.g., VPA) | Small molecule epigenetic modifiers that enhance reprogramming efficiency by opening chromatin. | Used in chemical reprogramming cocktails [4] [2]. |
| HDR-Enh01 mRNA | mRNA encoding a protein that indirectly inhibits NHEJ, favoring precise HDR during gene editing. | Critical for improving the ratio of precise correction to indels [90]. |
| Via-Enh01 mRNA | mRNA encoding an anti-apoptotic protein; improves viability of sensitive cells post-electroporation. | Essential for maintaining HSPC fitness in GMP-compatible protocols [90]. |
| GMP-compatible Culture Media | Defined, xeno-free media essential for clinical-grade iPSC generation and differentiation. | e.g., TeSR-E8; supports feeder-free culture [90]. |
| CRISPR-Cas9 RNP | Pre-complexed Ribonucleoprotein of Cas9 protein and guide RNA; enables precise, transient editing with reduced off-target effects. | Preferred over plasmid DNA for higher efficiency and lower toxicity [93]. |
Workflow and Pathway Diagrams
Diagram 1: Reprogramming Method Selection Workflow
Diagram 2: iPSC Safety & Tumorigenicity Risk Assessment
Regulatory Landscapes and Harmonization for iPSC-Based Therapies
Regulatory Requirements for Clinical-Grade iPSC Manufacturing
Advancing induced pluripotent stem cell (iPSC) research from the laboratory to clinical trials requires adherence to stringent quality and regulatory standards established by major authorities like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) [94]. The establishment of clinical-grade master cell banks (MCBs) is a foundational step, and manufacturers are increasingly adapting International Council for Harmonisation (ICH) guidelines for biological products to ensure safety, purity, and potency [94].
Key Regulatory and Quality Requirements for Master Cell Banks
The table below summarizes the core requirements for manufacturing clinical-grade iPSC Master Cell Banks, highlighting areas where further harmonization is needed [94].
Table: Key Quality and Regulatory Requirements for Clinical-Grade iPSC Master Cell Banks
| Requirement Area | Key Considerations | FDA & EMA Perspectives |
|---|---|---|
| Reprogramming Vectors | Safety profile of delivery method (viral, non-viral); clearance of reprogramming factors [4] [94]. | Guidance needed on authorized vectors; preference for non-integrating methods [94] [74]. |
| Identity Testing | Confirmation of cell line uniqueness and pluripotency markers (e.g., OCT4, SOX2) [4] [94]. | Minimum identity testing standards require harmonization [94]. |
| Purity Testing | Freedom from adventitious agents (viruses, mycoplasma); monitoring for microbial contaminants [94]. | Minimum purity testing standards, including adventitious agent testing, need harmonization [94]. |
| Genomic Stability | Karyotype analysis; monitoring for mutations during reprogramming and expansion [94] [74]. | Oversampling and banking DNA at key stages for retrospective analysis is recommended [74]. |
| Potency Assays | Demonstration of ability to differentiate into target cell types; challenge in defining clinically relevant surrogates [74]. | A lack of clarity exists around critical quality attributes; robust, standardized assays are needed [74]. |
| Tumorigenicity Safety | Risk from residual undifferentiated cells; use of in vivo (e.g., teratoma formation) and in vitro assays [95] [74]. | Traditional in vivo assays are lengthy; orthogonal approach using multiple assay types is recommended [74]. |
| Stability Testing | Demonstrating stability of iPSC banks under defined storage conditions [94]. | ICH guidelines for stability should be extended to cover cell therapy banks [94]. |
Troubleshooting Common iPSC Workflow Challenges
This section addresses frequent operational hurdles in iPSC research and development, from reprogramming to differentiation.
Reprogramming and Culture
Problem: Low Reprogramming Efficiency
- Cause: Suboptimal delivery of reprogramming factors or poor starting cell health.
- Solution: Use a cocktail of small molecules to enhance efficiency. Combining 8-Bromoadenosine 3′,5′-cyclic monophosphate (8-Br-cAMP) with valproic acid (VPA) has been shown to increase human fibroblast reprogramming efficiency by up to 6.5-fold [4]. Ensure somatic cells are healthy and at low passage before reprogramming.
Problem: Excessive Differentiation in Cultures (>20%)
- Cause: Old culture medium, overgrown colonies, or prolonged time outside the incubator.
- Solution: Use fresh, cold cell culture medium less than two weeks old. Remove differentiated areas before passaging and avoid having culture plates out of the incubator for more than 15 minutes. Passage cultures when colonies are large and compact but before they overgrow [39].
Problem: Poor Cell Survival After Thawing or Passaging
- Cause: Cells are overly confluent or sensitive to dissociation.
- Solution: For passaging, use cells between 40-85% confluency. If cells are overly confluent, include a ROCK inhibitor (e.g., Y-27632) during passaging to improve survival. After thawing, ensure correct seeding density and use of a ROCK inhibitor [33].
Characterization, Differentiation, and Safety
Problem: Failure of Neural Induction from iPSCs
- Cause: Low quality of starting iPSCs or incorrect plating density.
- Solution: Remove all differentiated and partially differentiated iPSCs before induction. Plate cell clumps (not a single-cell suspension) at a recommended density of 2–2.5 x 10⁴ cells/cm². Overnight treatment with 10 µM ROCK inhibitor Y27632 at the time of splitting can prevent extensive cell death [33].
Problem: Difficulty Defining Potency Assays for iPSC-Derived Products
- Cause: The biological attributes predicting clinical efficacy are not fully understood, and assays are highly variable.
- Solution: Develop phase-appropriate, biologically relevant surrogate markers. For example, enzyme activity can be a stand-in for long-term clinical improvement. Employ a tiered analytical approach, collecting extensive data for product understanding without making all data part of rigid release criteria [74].
Problem: Managing Tumorigenicity Risk
- Cause: Presence of residual undifferentiated iPSCs or mutations acquired during reprogramming.
- Solution: Implement orthogonal safety testing. This includes sensitive in vitro assays for residual pluripotent cells (e.g., proliferation assays, oncogene panels) alongside genomic integrity testing. Clearance of reprogramming vectors, such as using temperature-sensitive Sendai virus mutants, is also critical [4] [74].
FDA Authorization vs. Approval and the Clinical Trial Landscape
Understanding the regulatory pathway from initial trials to market approval is crucial for researchers.
Key Regulatory Definitions
- FDA IND Authorization: An Investigational New Drug (IND) application must clear a 30-day FDA review before human trials can begin. This authorization means the FDA has no objections to the proposed study but does not mean the therapy is proven safe and effective [96].
- FDA Approval: Formal marketing approval under a Biologics License Application (BLA) is granted only after successful large-scale trials demonstrate a product is safe, pure, and potent for its intended use [96].
Recent iPSC Clinical Trial Milestones (2023-2025)
The field is experiencing rapid growth, with over 115 global clinical trials involving 83 distinct pluripotent stem cell (PSC)-derived products as of December 2024, targeting ophthalmology, neurology, and oncology [96]. The overall safety profile is encouraging, with no class-wide concerns observed after more than 1,200 patients have been dosed [96].
Table: Select Advanced iPSC-Derived Clinical Trials (2023-2025)
| Therapy/Product | Indication | Development Stage (as of 2025) | Key Regulatory Milestone |
|---|---|---|---|
| Fertilo (Gameto) | Infertility | Phase III | First FDA IND clearance for a U.S. Phase III iPSC-based therapy (Feb 2025) [96]. |
| CYP-004 (Cynata) | Osteoarthritis | Phase III | Represents the world's first Phase 3 clinical trial for an iPSC-derived cell therapeutic [22]. |
| OpCT-001 | Retinal Degeneration | Phase I/IIa | FDA IND clearance (Sep 2024); first iPSC-based therapy for primary photoreceptor diseases [96]. |
| FT819 | Systemic Lupus Erythematosus | Phase I | FDA RMAT designation (Apr 2025) [96]. |
| iPSC-derived NPCs | Parkinson's Disease, ALS, Spinal Cord Injury | Phase I | FDA IND clearance for multiple off-the-shelf products (Jun 2025) [96]. |
| FT536 | Gynecologic Cancers | Clinical Trials | An allogeneic, off-the-shelf natural killer (NK) cell therapy from a master iPSC line [96]. |
Workflow for iPSC Therapy Development
The journey from research to a clinically approved iPSC therapy is a multi-stage process requiring close attention to regulatory and manufacturing scale-up. The diagram below outlines the key stages and critical requirements.
Strategies for Global Regulatory Harmonization
A fragmented global regulatory environment is a significant barrier to the efficient development of iPSC therapies [74]. Variations in how different jurisdictions evaluate safety, potency, and product quality create uncertainty for developers.
Key challenges and proposed solutions include:
- Challenge: Lack of clarity on Critical Quality Attributes (CQAs). Expectations for potency assays, tumorigenicity screening, and genomic stability remain ambiguous with limited regulatory precedent [74].
Solution: Establish global harmonization initiatives and multi-stakeholder forums where regulators, scientists, and industry professionals can collaboratively define best practices and clear CQA criteria [94] [74].
Challenge: Regulatory uncertainty for innovative manufacturing. The use of novel genome editing or manufacturing outside strict GMP cleanrooms creates technical "grey areas" [74].
- Solution: Encourage early, iterative engagement between regulators and developers through workshops or pilot programs to clarify expectations and reduce development risks [74].
The Scientist's Toolkit: Essential Reagents and Materials
Successful and reproducible iPSC research relies on a suite of core reagents and materials. The following table details key components.
Table: Essential Research Reagents for iPSC Workflows
| Reagent Category | Example Products | Function and Application |
|---|---|---|
| Reprogramming Kits | CytoTune -iPS Sendai 2.0 Reprogramming Kit [33] | Delivers reprogramming factors (OSKM) using a non-integrating Sendai virus vector to convert somatic cells into iPSCs. |
| Culture Media | mTeSR Plus, Essential 8 Medium [39] [33] | Defined, feeder-free media formulations that support the growth and maintenance of undifferentiated pluripotent stem cells. |
| Culture Matrices | Geltrex, Vitronectin XF, Corning Matrigel [39] [33] | Synthetic or basement membrane extracts that provide a substrate for attachment and growth of iPSCs in culture. |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent, EDTA [39] [33] | Enzymatic or non-enzymatic solutions used to detach cells from culture vessels for sub-culturing (passaging). |
| ROCK Inhibitor | Y-27632 [33] | A small molecule that significantly improves cell survival after thawing or single-cell passaging by inhibiting apoptosis. |
| Small Molecule Enhancers | Valproic Acid (VPA), 8-Br-cAMP, RepSox [4] | Chemicals that improve reprogramming efficiency; some, like RepSox, can act as substitutes for specific reprogramming factors. |
| Differentiation Kits | ReproCardio (iPSC-derived cardiomyocytes), various neural differentiation kits [22] [33] | Pre-optimized media and protocol systems for directing the differentiation of iPSCs into specific somatic cell lineages. |
| Characterization Antibodies | Kits for OCT4, SOX2, NANOG, SSEA-4 [94] [33] | Antibodies used in flow cytometry or immunostaining to confirm pluripotency and identity of iPSCs and their derivatives. |
Clinical Trial Case Studies
The translation of induced pluripotent stem cell (iPSC) technologies from research to clinical applications has progressed significantly, with several pioneering trials demonstrating safety and efficacy. The table below summarizes key clinical case studies.
Table 1: Summary of Clinical Trials for iPSC-Derived Products
| Clinical Indication | Product / Trial Sponsor | Cell Type Derived | Clinical Trial Phase | Key Outcomes and Status |
|---|---|---|---|---|
| Age-Related Macular Degeneration (AMD) | Eyecyte-RPE / RIKEN Center [22] [91] | Retinal Pigment Epithelium (RPE) | IND Approved (2024) [91] | First iPSC transplant into humans (2013); IND approval in India for geographic atrophy [22] [91]. |
| Graft-versus-Host Disease (GvHD) & Osteoarthritis | CYP-001 / Cynata Therapeutics [22] | Mesenchymal Stem Cells (MSCs) | Phase 3 (Osteoarthritis) [22] | Met clinical endpoints in steroid-resistant acute GvHD; Advanced to Phase 3 for osteoarthritis in 440 patients [22]. |
| Parkinson's Disease | Allogeneic Dopaminergic Progenitors [91] | Dopaminergic Neuron Progenitors | Phase I/II (jRCT2090220384) [91] | Cells survived transplantation, produced dopamine, and no tumor formation was reported [91]. |
| Parkinson's Disease | Autologous Dopaminergic Neurons / Mass General Brigham [91] | Dopaminergic Neurons | Clinical Trial (HPSC, 2024) [91] | Uses patient's own blood-derived iPSCs, eliminating the need for immunosuppression [91]. |
Troubleshooting Common iPSC Culture Issues
Successful clinical application depends on robust laboratory practices. Below are common issues and solutions when working with iPSCs and their derivatives.
Excessive Differentiation in Cultures
- Problem: Over 20% of the culture shows signs of spontaneous differentiation.
- Solutions: [39]
- Ensure culture medium is fresh (less than 2 weeks old when stored at 2-8°C).
- Physically remove differentiated areas from colonies before passaging.
- Minimize the time culture plates are outside the incubator to less than 15 minutes.
- Avoid overgrowth by passaging when colonies are large, compact, and dense in the center.
- Optimize passaging by ensuring even cell aggregate size and decreasing colony density.
Low Cell Attachment After Plating
- Problem: Cells fail to attach properly after passaging or thawing.
- Solutions: [39] [33]
- Plate 2-3 times the number of cell aggregates initially to maintain a densely confluent culture.
- Work quickly after cells are treated with passaging reagents to minimize suspension time.
- Reduce incubation time with passaging reagents if the culture is particularly sensitive.
- Ensure the use of correct cultureware (e.g., non-tissue culture-treated for Vitronectin XF coating).
Challenges in Neural Differentiation from iPSCs
- Problem: Low efficiency in deriving neural stem cells (NSCs) or neurons.
- Solutions: [33]
- Start with High-Quality iPSCs: Remove all differentiated and partially differentiated cells before beginning neural induction.
- Optimize Seeding Density: Plate cell clumps (not single cells) at a recommended density of 2–2.5 x 10^4 cells/cm².
- Use a ROCK Inhibitor: Treating with 10 µM ROCK inhibitor Y27632 during plating can prevent extensive cell death.
- Check Reagents: Use fresh, correctly stored neural induction supplements like B-27, which is stable for only 2 weeks at 4°C after preparation.
FAQs on iPSC-Derived Products and Clinical Translation
Q1: What are the major safety concerns for clinical application of iPSC-derived products? The primary safety concerns include the risk of tumor formation from residual undifferentiated pluripotent cells, genomic instability introduced during reprogramming, and immune responses to allogeneic cells. Recent advances in non-integrating reprogramming methods and rigorous quality control are mitigating these risks [91].
Q2: How can reprogramming efficiency and safety be improved? Efficiency and safety can be enhanced by:
- Safer Reprogramming Factors: Using L-Myc instead of c-Myc, or alternative factors like SALL4 and Glis1, to reduce tumorigenic risk [4].
- Non-Integrating Delivery Systems: Using Sendai virus or episomal plasmids to avoid permanent genetic alterations [4] [91].
- Small Molecule Enhancers: Using compounds like valproic acid (VPA) or 8-Br-cAMP to significantly boost reprogramming efficiency [4].
- Chemical Reprogramming: Using entirely non-genetic methods with small molecule combinations [4].
Q3: Our iPSC-derived neurons are not maturing or functioning correctly. What could be wrong? This is a common challenge. Ensure that:
- The differentiation protocol includes precise signaling molecules (e.g., specific growth factors and small molecules) at correct concentrations and timing. For midbrain dopaminergic neurons, this is critical for safety and efficacy [97].
- The base iPSC line is of high quality and genetically stable, as line-to-line variability can affect differentiation potential [33] [98].
- You are using a validated protocol and high-quality, fresh reagents, particularly specialized supplements like B-27 [33].
Q4: What is the significance of "off-the-shelf" versus autologous iPSC therapies?
- Autologous Therapies: Use the patient's own cells (e.g., from blood or skin), which eliminates the risk of immune rejection but is patient-specific, time-consuming, and costly [91].
- Allogeneic ("Off-the-Shelf") Therapies: Use cells from a healthy, matched donor. These can be manufactured in large, standardized batches, making them more scalable and cost-effective. Immune rejection is a potential risk, which may be managed with mild immunosuppression or gene editing to create universal donor cells [22] [45].
Research Reagent Solutions
The table below lists key reagents and their functions critical for successful iPSC reprogramming, differentiation, and clinical application.
Table 2: Essential Research Reagents for iPSC Work
| Reagent / Tool | Function in iPSC Research |
|---|---|
| OSKM Factors | The core transcription factors (OCT4, SOX2, KLF4, c-MYC) for initiating somatic cell reprogramming [4]. |
| RepSox | A small molecule that can replace the Sox2 and c-Myc genes in reprogramming, enhancing safety [4] [99]. |
| Sendai Virus Vectors | A non-integrating, viral vector system for delivering reprogramming factors; can be cleared from the cells [33]. |
| ROCK Inhibitor (Y-27632) | Dramatically improves survival of iPSCs after passaging, thawing, or single-cell dissociation [33]. |
| Valproic Acid (VPA) | A histone deacetylase inhibitor that enhances reprogramming efficiency [4]. |
| B-27 Supplement | A serum-free supplement essential for the survival and maturation of many neural cell types [33]. |
| CRISPR-Cas9 | Genome editing tool used to correct disease-causing mutations in patient-derived iPSCs or to create isogenic control lines [91] [45]. |
| Vitronectin / Geltrex | Defined substrates used for feeder-free culture of iPSCs, promoting attachment and growth under xeno-free conditions [39] [33]. |
Workflow: From Somatic Cell to Clinical Application
The following diagram illustrates the key stages involved in developing an iPSC-derived product for clinical use, highlighting critical quality control checkpoints.
Signaling Pathway for Dopaminergic Neuron Differentiation
A key clinical success has been generating dopaminergic neurons for Parkinson's disease. The diagram below outlines the core signaling pathways manipulated during this differentiation.
Conclusion
Enhancing reprogramming efficiency is a multi-faceted challenge that requires a synergistic approach, combining optimized factor cocktails, advanced non-integrating delivery methods, and precisely engineered culture environments. The move towards chemical reprogramming and biomaterial-based strategies offers promising avenues for generating safer, clinical-grade iPSCs. However, the path to clinical translation depends on rigorous validation through standardized quality control assays and a clear regulatory framework. Future progress will hinge on integrating automation for scalable manufacturing and deepening our understanding of epigenetic memory, ultimately unlocking the full potential of iPSCs in regenerative medicine, sophisticated disease modeling, and drug discovery.
References
- 1. Yamanaka Factors And Cellular Reprogramming [https://www.lifespan.io/topic/yamanaka-factors/]
- 2. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 3. The occurrence and development of induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11063328/]
- 4. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 5. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 6. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 7. In vivo cyclic overexpression of Yamanaka restricted to... factors [https://www.nature.com/articles/s42003-024-06328-w?error=cookies_not_supported&code=acf55589-af0f-4571-a249-f96251e91e2b]
- 8. Possible Strategies to Reduce the Tumorigenic Risk of ... [https://www.mdpi.com/1422-0067/25/10/5177]
- 9. Cell reprogramming: methods, mechanisms and applications [https://cellregeneration.springeropen.com/articles/10.1186/s13619-025-00229-x]
- 10. Development of a High-Efficacy Reprogramming Method ... [https://www.mdpi.com/1422-0067/21/18/6764]
- 11. p53 isoform Δ133p53 promotes efficiency of induced ... [https://www.nature.com/articles/srep37281]
- 12. Efficient Generation of Human iPSCs by a Synthetic Self- ... [https://www.sciencedirect.com/science/article/pii/S1934590913002592]
- 13. Chromatin Dynamics during Cellular Reprogramming - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4216318/]
- 14. Epigenetic regulation of reprogramming and pluripotency [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1559183/full]
- 15. Understanding the molecular mechanisms of reprogramming [https://www.sciencedirect.com/science/article/abs/pii/S0006291X1530989X]
- 16. Chromatin Immunoprecipitation Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/chip-troubleshooting-guide?srsltid=AfmBOopHFDshWg7VmuoJRYciYrRJ6hEU1q4FaOFfs4-HpRP1S-oeibfc]
- 17. Troubleshooting of Chromatin Immunoprecipitation (ChIP) [https://www.antibody-creativebiolabs.com/troubleshooting-of-chromatin-immunoprecipitation.htm]
- 18. Synergistic Role of miRNA-1811 and miRNA-302 in ... [https://www.sciencedirect.com/science/article/pii/S0032579125009058]
- 19. Genome-Wide Silencer Screening Reveals Key ... [https://pubmed.ncbi.nlm.nih.gov/40112175/]
- 20. Human iPSC Reprogramming Success: The Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 21. Highly efficient and rapid generation of human pluripotent ... [https://www.sciencedirect.com/science/article/pii/S1934590923000693]
- 22. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 23. Regulation of cell reprogramming by engineered ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525008793]
- 24. Chemical reprogramming of human blood cells to ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925002607]
- 25. Low pH reprograms somatic murine cells into pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4049782/]
- 26. Improving chemical reprogramming strategies [https://www.nature.com/articles/s41580-025-00836-1]
- 27. Delivery Methods for Generating iPSCs [https://blog.addgene.org/delivery-methods-for-generating-ipscs]
- 28. Retrovirus-mediated Reprogramming of Stem Cells [https://www.creative-biolabs.com/stem-cell-therapy/retrovirus-mediated-reprogramming-of-stem-cells.htm]
- 29. Gene-delivery systems for iPS cell generation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2811526/]
- 30. All Roads Lead to Induced Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4046204/]
- 31. New strategies to generate induced pluripotent stem cells [https://www.sciencedirect.com/science/article/abs/pii/S0958166909001074]
- 32. Key Challenges in Clinical iPSC Applications [https://www.reprocell.com/blog/key-challenges-in-clinical-ipsc-applications-how-reprocell-helps-you-succeed]
- 33. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 34. Chromatin modifying enzymes as modulators of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3501145/]
- 35. Chemically induced reprogramming to reverse cellular aging [https://www.aging-us.com/article/204896/text]
- 36. A biomaterial approach to cell reprogramming and differentiation [https://pmc.ncbi.nlm.nih.gov/articles/PMC5616208/]
- 37. Bottom-up Biomaterial strategies for creating tailored stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1581292/full]
- 38. Penn Bioengineers Show Why Lab-made Stem Cells Might Fail [https://penntoday.upenn.edu/news/penn-bioengineers-show-why-lab-made-stem-cells-might-fail-errors-dna-folding]
- 39. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 40. Synthetic thermoresponsive scaffolds for the expansion and ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04674b?page=search]
- 41. The Role of Stiffness in Cell Reprogramming: A Potential ... [https://www.mdpi.com/2073-4409/8/9/1036]
- 42. 3D Cell Culture Guide [https://www.creative-bioarray.com/support/3d-cell-culture-guide.htm]
- 43. Dynamic culture improves cell reprogramming efficiency [https://www.sciencedirect.com/science/article/abs/pii/S0142961216300540]
- 44. Troubleshooting Guide: 3D Bioprinted Culture Viability - Allevi [https://www.allevi3d.com/troubleshooting-issues-with-3d-viability/]
- 45. Overcoming Barriers of CRISPR Gene Editing in iPS Cells [https://www.synthego.com/blog/ipsc-crispr-editing/]
- 46. Troubleshooting Guide for Common CRISPR-Cas9 Editing ... [https://synapse.patsnap.com/article/troubleshooting-guide-for-common-crispr-cas9-editing-problems]
- 47. CRISPR-Cas9 Genome Editing In Human Induced ... [https://www.thermofisher.com/us/en/home/life-science/genome-editing/genome-editing-learning-center/genome-editing-resource-library/genome-editing-application-notes/protocol-crispr-cas9-genome-editing-human-induced-pluripotent-stem-cells.html]
- 48. CRISPR/Cas9 editing in iPSCs results in detrimental on ... [https://www.sciencedirect.com/science/article/pii/S2213671122000972]
- 49. Unintended CRISPR-Cas9 editing outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10182114/]
- 50. CRISPR activation enables high-fidelity reprogramming into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8828555/]
- 51. Human pluripotent reprogramming with CRISPR activators [https://www.nature.com/articles/s41467-018-05067-x]
- 52. Chemically defined conditions for human iPS cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3084903/]
- 53. A novel efficient feeder-free culture system for the ... [https://www.nature.com/articles/srep03594]
- 54. Negligible-Cost and Weekend-Free Chemically Defined ... [https://www.sciencedirect.com/science/article/pii/S2213671119304461]
- 55. Chemically defined and xeno-free media enables the ... [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-025-01410-0]
- 56. Human Chemical Reprogramming Kit (2nd Gen) [https://stem-immune.com/hCiPSc-kit2?srsltid=AfmBOopUVkTp81YjQW_CGglbRNKd4pvoUAuyfdVyUX9NRXsToHhUIrIi]
- 57. A defined xeno-free and feeder-free culture system for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961213015342]
- 58. Protocol for Maintaining iPSC Cultures [https://www.protocols.io/view/protocol-for-maintaining-ipsc-cultures-g788bzrzx.html]
- 59. Application Of CRISPR Technology In iPSC Gene Correction [https://www.cellandgene.com/doc/application-of-crispr-technology-in-ipsc-gene-correction-0001]
- 60. 3 Tips to Improve HDR Efficiency for CRISPR Editing in ... [https://blog.addgene.org/3-tips-for-improving-hdr-efficiency-for-editing-human-cells-with-crispr]
- 61. Homology-directed repair FAQs [https://www.takarabio.com/learning-centers/gene-function/gene-editing/crisprcas9-knockins/homology-directed-repair-faqs?srsltid=AfmBOoo76w8HmcsyqXQghGCnPaAI4sUd8ceFTH7nFeflztzO5Z8OqwDf]
- 62. A high efficiency precision genome editing method with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11061145/]
- 63. Guidelines for achieving high rates of HDR with CRISPR Ca [https://www.lubio.ch/blog/hdr-crispr-cas12]
- 64. CRISPR-Cas9 HDR optimization: RAD52, denatured, and 5 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616026/]
- 65. STANDARDIZED METHODS IN IPSC FOR CRISPR ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924005589]
- 66. Genomic Integrity [https://www.stemcell.com/genomic-integrity]
- 67. Comprehensive guide for epigenetics and transcriptomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11799959/]
- 68. A simple, quick, and efficient CRISPR/Cas9 genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7656785/]
- 69. iPSC reprogramming [https://www.abcam.com/en-us/technical-resources/guides/pluripotent-stem-cells/ipsc-eprogramming]
- 70. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 71. Is Early Automation The Key To Scalable Cell Therapy ... [https://www.cellandgene.com/doc/is-early-automation-the-key-to-scalable-cell-therapy-manufacturing-0001]
- 72. Automating iPSC culture: scalable workflows [https://www.insights.bio/cell-and-gene-therapy-insights/webinars/739/automating-ipsc-culture-scalable-workflows]
- 73. FAQ - Clinical MSCs [https://www.reprocell.com/clinical-stem-cell-services/faq-mscs]
- 74. From nascent to mainstream: Overcoming barriers in iPSC ... [https://ct.catapult.org.uk/news/from-nascent-to-mainstream-overcoming-barriers-in-ipsc-therapy-development]
- 75. Rapid and efficient reprogramming of somatic cells to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3215025/]
- 76. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 77. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 78. Troubleshooting Guide for STEMdiff™ Cardiomyocyte Kits [https://www.stemcell.com/troubleshooting-guide-for-human-pluripotent-stem-cell-derived-cardiomyocytes.html]
- 79. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/hk/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 80. How To Overcome Potency Assay Development ... [https://www.cellandgene.com/doc/how-to-overcome-potency-assay-development-challenges-for-gene-therapies-0001]
- 81. Navigating Challenges in Cell Therapy Potency Assays [https://www.biopharminternational.com/view/navigating-challenges-in-cell-therapy-potency-assays]
- 82. Assessing Tumorigenicity in Stem Cell-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376867/]
- 83. Impelling force and current challenges by chemicals in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789182/]
- 84. A high efficiency precision genome editing method with ... [https://www.nature.com/articles/s41598-024-60766-4]
- 85. Their Role in iPSC Reprogramming and Differentiation [https://www.reprocell.com/blog/epigenetic-modifications-their-role-in-ipsc-reprogramming-and-differentiation]
- 86. The dynamics of chromatin states mediated by epigenetic ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1097780/full]
- 87. Epigenetics of reprogramming to induced pluripotency - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3602907/]
- 88. The Challenges to Advancing Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 89. Cell Reprogramming Market to Hit USD 715.6 Million by ... [https://www.biospace.com/press-releases/cell-reprogramming-market-to-hit-usd-715-6-million-by-2032-driven-by-growing-regenerative-medicine-demand-coherent-market-insights]
- 90. Non-viral DNA delivery and TALEN editing correct the ... [https://www.nature.com/articles/s41467-024-49353-3]
- 91. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 92. Cellular Reprogramming Tools Market Rises with USD 480 ... [https://www.biospace.com/press-releases/cellular-reprogramming-tools-market-rises-with-usd-480-million-forecast-in-2025-and-global-r-d-investments]
- 93. CMN Weekly (19 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-19-september-2025-your-weekly-crispr-medicine-news/]
- 94. Quality and Regulatory Requirements for the Manufacture ... [https://pubmed.ncbi.nlm.nih.gov/39821060/]
- 95. Induced Pluripotent Stem Cell (iPSC) Therapy Market Size, ... [https://www.precedenceresearch.com/induced-pluripotent-stem-cell-therapy-market]
- 96. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 97. iPSC-based cell replacement therapy: from basic research ... [https://www.sciencedirect.com/science/article/pii/S1465324925000532]
- 98. Reprogramming biology: iPSCs and the future of predictive ... [https://www.jax.org/news-and-insights/2025/november/reprogramming-biology-ipscs-and-the-future-of-predictive-research]
- 99. New steps forward in cell reprogramming [https://www.hsci.harvard.edu/new-steps-forward-cell-reprogramming]